Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 16/117/03. The contractual start date was in June 2018. The final report began editorial review in November 2021 and was accepted for publication in October 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Hughes et al. This work was produced by Hughes et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Hughes et al.
Chapter 1 Background
Sexual assault referral centres (SARCs) are a single point of access for the treatment of people who have experienced sexual assault. They bring together criminal justice and health services to address the multiple needs of someone reporting a sexual assault as a recent or non-recent event. SARCs are commissioned by NHS England and provision includes forensic medical examinations (to collect evidence for a prosecution), physical and mental health assessment, safeguarding and risk assessment, and psychosocial support. SARCs also refer to other agencies in the local area should a need be identified.
Mental health problems are common in people who attend SARCs. In the Netherlands,1 the United States2 and England,3 approximately 40% of SARC attendees have been estimated to have a mental health problem. In a recent audit of Thames Valley SARCs, Brooker and Tocque4 found that 69% of attendees could be defined as experiencing a mental health problem, 20% had a history of admission to a psychiatric unit, 32% were drinking at ‘hazardous’ levels and 45% had previously self-harmed. In a secondary analysis of data from the Adult Psychiatric Morbidity Survey, Brooker and Tocque4 found that there was a consistent relationship between risk of mental health and substance use problems and the level of sexual violence experienced. While the national service specification for SARCs5 acknowledges that mental health issues are common among people attending SARCs, it states only that SARCs should ensure the provision of appropriate psychosocial support according to need, and where this exceeds what NHS talking therapies can support, then people will be referred to secondary mental health services.
In the first national survey of SARCs, Brooker and Durmaz6 reported that only half of the SARCs routinely assessed mental health needs of attendees and, where it was assessed, it was completed by a forensic medical examiner (FME). Substance misuse issues were not always included. Almost two-thirds of SARC services reported problems in referring on to mental health services for a variety of reasons. The paper argued that more research was needed in this important area, and that NHS England should fully describe the skills required to undertake a mental health risk assessment when someone has been the victim of rape or sexual assault.
Rationale
Despite the elevated levels of mental health and substance use needs of those who attend SARCs, there is limited evidence regarding the specific needs of people who attend SARCs, what works for whom, in what context, and where resources could be allocated to obtain maximum benefit. To do this, there is a need to identify models of identifying and assessing mental health and/or substance use problems; what subsequent referral pathways are available for a range of people; the views and preferences of people who use SARCs; the workforce needs, not only for SARC staff but for the network of agencies that work with survivors (including mental health, third sector counselling and substance use services); and the costs and benefits of different models of service provision.
The aim of the Mixed Methods of SARCs study (MiMoS) study was to generate evidence related to how SARCs identify and address mental health and substance use issues, through the following questions:
-
What programmes are identified in published and grey literature to inform how mental health and substance use can be best addressed in SARCs?
-
What models can be identified across the SARC services in terms of addressing mental health and substance use?
-
What is the prevalence and nature of mental health and substance use among people who attend SARCs?
-
What types of services are accessed by people with a range of needs following attendance at a SARC, and how satisfied are they with those services?
-
What are the barriers and facilitators to accessing the right support at the right time for people who have attended a SARC?
-
How do outcomes differ between a bespoke psychological therapies service at a SARC and mainstream mental health?
Research objectives
-
To undertake an evidence review of global SARC provision for health outcomes (including mental health and substance use) – work package (WP) 1.
-
To identify what models of SARCs currently exist in England (WP2).
-
To identify the mental health and substance use needs of attendees of SARCs in England (WP3).
-
To identify what services are available in SARCs in England and to explore satisfaction with care, barriers to access and gaps in provision (WPs 2, 3 and 4).
-
To understand, from the perspective of the SARC workforce, their current practice, skills and training needs in terms of recognition of, and referral for, mental health and substance use issues (WP4).
-
To obtain the survivors’ views on how they felt their emotional well-being was addressed by the SARC, as well as by external services (WP4).
-
To compare health outcomes for people who experience sexual assault and access bespoke SARC psychological therapies provision compared with those who experience sexual assault and are in mainstream mental health services (WP5).
-
To produce a range of lay and academic outputs that will aim to identify and share good practice in SARC services related to substance use and mental health to have an impact on care delivery.
To address these questions and objectives, a three-year multimethod study was undertaken, comprising five WPs of research and an additional WP (WP6) for co-production of outputs with key stakeholders and dissemination (Figure 1). The first WP was a systematic review of the literature7 to identify models of good practice in working with mental health and substance use (WP1). An additional realist synthesis was conducted to identify initial programme theories, which would be refined in subsequent WPs.
FIGURE 1.
Study flow chart.
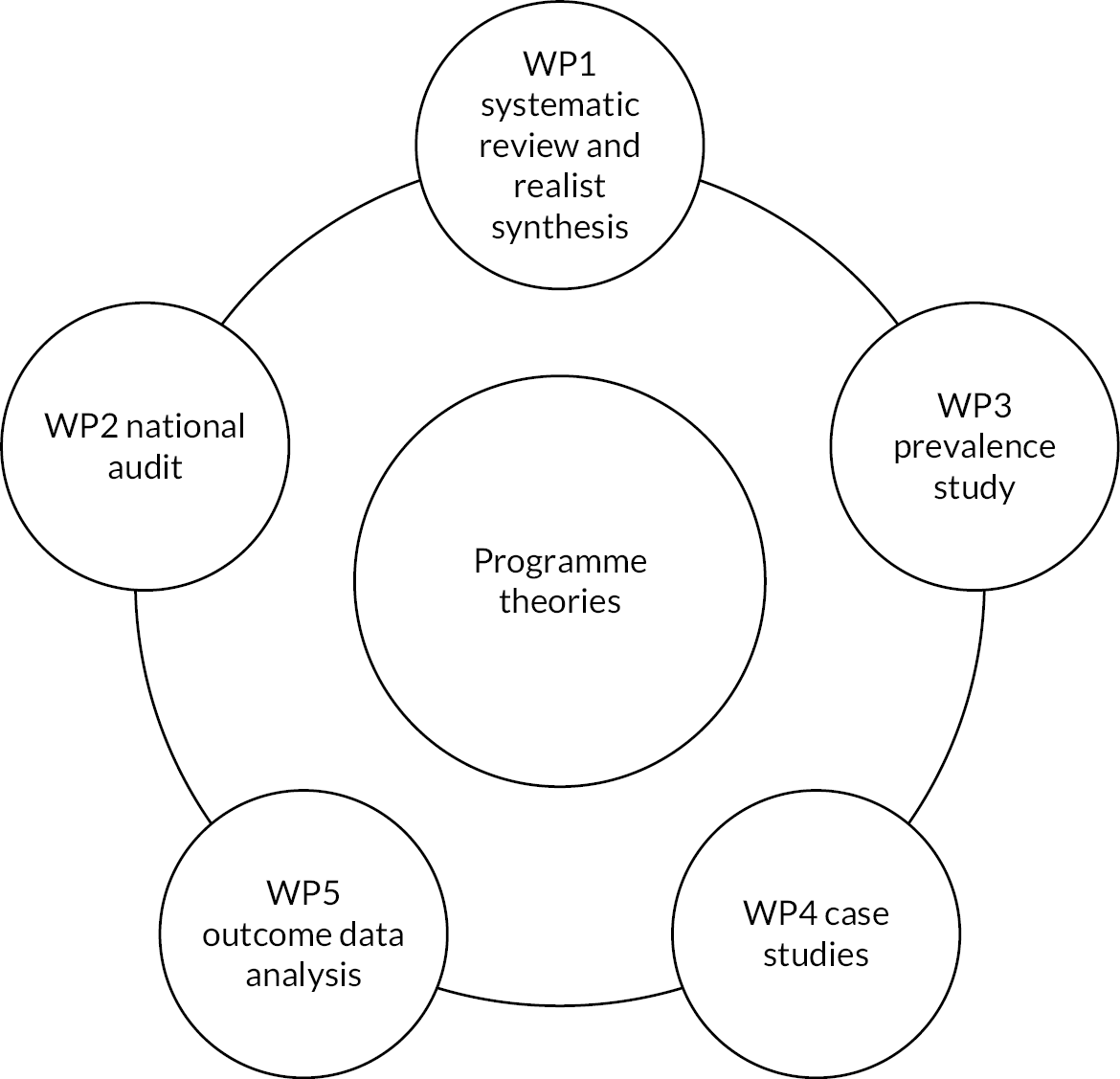
WP2 was a national survey of SARCs to identify the ways in which they are recognising and addressing mental health and substance use. This was completed as an audit and the findings were used to undertake a cluster analysis to identify a typology of SARCs (three typology clusters were identified). This typology was then used as a sampling framework for six case studies using the SARC as the case ensuring we had examples of all three clusters.
WP3 was intended to be a prospective study of mental health and substance use needs of people attending SARCs across the range of typologies, where informed consent was obtained then participants completed a set of screening tools in the immediate period after attending a SARC (more than one week up to six weeks post SARC attendance). WP3 was modified because of the pause to research in 2020 resulting from the COVID-19 pandemic and the continuing impact of social restrictions.
In WP4, two activities were undertaken: a realist analysis of local documentation,8 which provided contextual information to inform theory development and refinement through group and individual interviews. Three main groups of informants were interviewed: staff who worked in the SARC; people who attended the SARC to report a sexual assault (survivors) and respondents from ‘partner agencies’ consisting of key informants from local primary and secondary mental health providers; rape counselling agencies and drug and alcohol treatment services.
In WP5, analysis of anonymised datasets: (1) South London and Maudsley Foundation NHS Trust Clinical Record Interactive Search (CRIS) dataset comparing outcomes of people with and without a reported sexual assault who accessed mainstream mental health services for specific psychological treatments; (2) a SARC clinical dataset comparing outcomes of SARC clients who received different forms of therapeutic support via in-house SARC therapeutic pathways.
Through a process of iteration, synthesis and consultation with key stakeholders, data from the WPs were used to develop and refine programme theories and provide evidence about; how services work for certain groups of people, what are the contexts that influence outcomes and the mechanisms by which outcomes are realised. Findings include recommendations for policy, practice and further research in relation to mental health and substance use needs. The findings were presented in online consultation events with survivors and practitioner advisors and the recommendations further refined as a result.
Patient and public involvement
The survivor voice and perspective is especially important to the MiMoS study. From WP1, it was noted how little survivor-focused research existed. We worked in partnership with survivors for all aspects of the study and we had a person who led this aspect as the lead coordinator (Dr Sarah Kendal). Fay Maxted (FM) is one of the MiMoS study co-investigators and she is chief executive of the Survivors Trust. She is a high-profile activist for the rights of survivors of abuse. Fay has been an active member of the project group and offers the survivor perspective to all aspects of the study including the interpretation of data and developing recommendations for the report and other outputs. In addition to FM, a lived-experience advisory group (LEAG) was convened. Advertisements for group members were placed in SARC services and on the project website, and some individuals were introduced to the group via contacts of the project team. Four group members were young people (age range 18–25 years).
The LEAG worked closely with the researcher(s) on all aspects of the study – planning and data collection, and were part of the analysis phases. A flexible and individualised approach was undertaken to meet the needs and comfort of the individuals. This involved having options to contribute including face-to-face meetings (prior to COVID-19 restrictions), telephone calls, Skype/Microsoft Teams® video calls and email. The involvement of survivors was influenced by the Survivors Voices Charter ‘Turning Pain into Power: A Charter for Organizations Engaging Abuse Survivors in Projects, Research and Service Development’. 9 Concetta Perot from Survivor’s Voices was a key contributor and advisor to the research study and provided training on working with survivors of abuse to the research team prior to recruitment and data collection. Concetta Perot facilitated a training session on working with survivors as part of our researcher training in July 2019 as well as attending some of the study steering groups.
Limited personal information was collected from the members around their demographics, and it is summarised in Table 1.
| Route into group | Adult men | Adult women | Young people |
|---|---|---|---|
| Via project team contact | 1 | 1 | |
| Via project team contact | 1 | ||
| Via project team contact | 1 | ||
| Via project team contact | 1 | 1 | |
| Via project team contact | 1 | ||
| Responded to advert | 1 | ||
| Responded to advert | 1 | 1 | |
| Responded to advert | 1 | 1 | |
| Responded to advert | 1 | ||
| Introduced by LEAG member | 1 | ||
| Total | 2 | 8 | 4 |
In May 2019, a LEAG meeting took place in Huddersfield to scrutinise draft study protocol documents prior to NHS ethics application. Three LEAG members were able to attend in person and provided comprehensive input into the plans to recruit and collect data including safety issues. Two more members were able to provide detailed written feedback by email.
In June 2020, a virtual LEAG meeting to respond to documents produced by WP3. Comments were also received via email from three further LEAG members. Owing to the impact of the COVID-19 pandemic, the LEAG members have been less responsive; however, a small core group remains in contact with us. A survivor-focused meeting was planned for September 2021 to present the initial findings as part of the stakeholder involvement but it was cancelled as no one signed up. This was despite widely circulating the invitation to many survivor groups around the UK and promotion on social media.
Research ethics and governance
Ethical approval process
Recruiting people who have recently experienced violence and abuse to research studies needs to be conducted sensitively and in conjunction with those with lived experience. While there is a risk of adding an additional burden during a difficult time, there is also evidence to suggest that survivors of abuse find participating in research helpful. Survivors Voices produced a charter ‘Pain into Power’, which aims to promote the engagement of survivors in research and this survivor-led document provides a useful framework to inform the design and implementation of research. 9
There were three main risks to the MiMoS study. The LEAG was mostly concerned with protecting anonymity of participants and the risks that could be posed to participants if they lived with their perpetrator. The LEAG stressed the importance of using a range of methods of communication according to the preference of each potential participant. We also implemented a code-word scheme so that if during a phone or online conversation a participant gave us the code word we would know that they were no longer able to have a private conversation. The LEAG felt that it would be helpful to have information that signposted all participants and potential participants to a range of relevant helplines and resources. This information was on a page of our study website as well as on participant information sheets. We additionally identified that participation may exacerbate emotional distress and there may be disclosures of self-harm or suicidality. To mitigate these risks, we were very clear in our written and verbal communication exactly what the study was about and the nature of the participation. We excluded anyone who was already in acute distress (as evidenced by admission to a mental health unit and/or having been in contact with mental health crisis team). All researchers underwent training prior to data collection and this was facilitated by Concetta Perot from Survivors Voices regarding how to work with people who experience trauma and we had a robust standard operating procedure (SOP), which included detailed protocol for handling any issues that arose during recruitment and data collection (see Report Supplementary Material 1).
WP3, 4 and 5 required NHS ethical and Health Research Authority (HRA) approval. We co-produced the recruitment strategy and data collection methods with the LEAG. NHS Ethics Committee Favourable opinion was obtained on 6 December 2019 (IRAS 238440 REC reference 19/NW/0663).
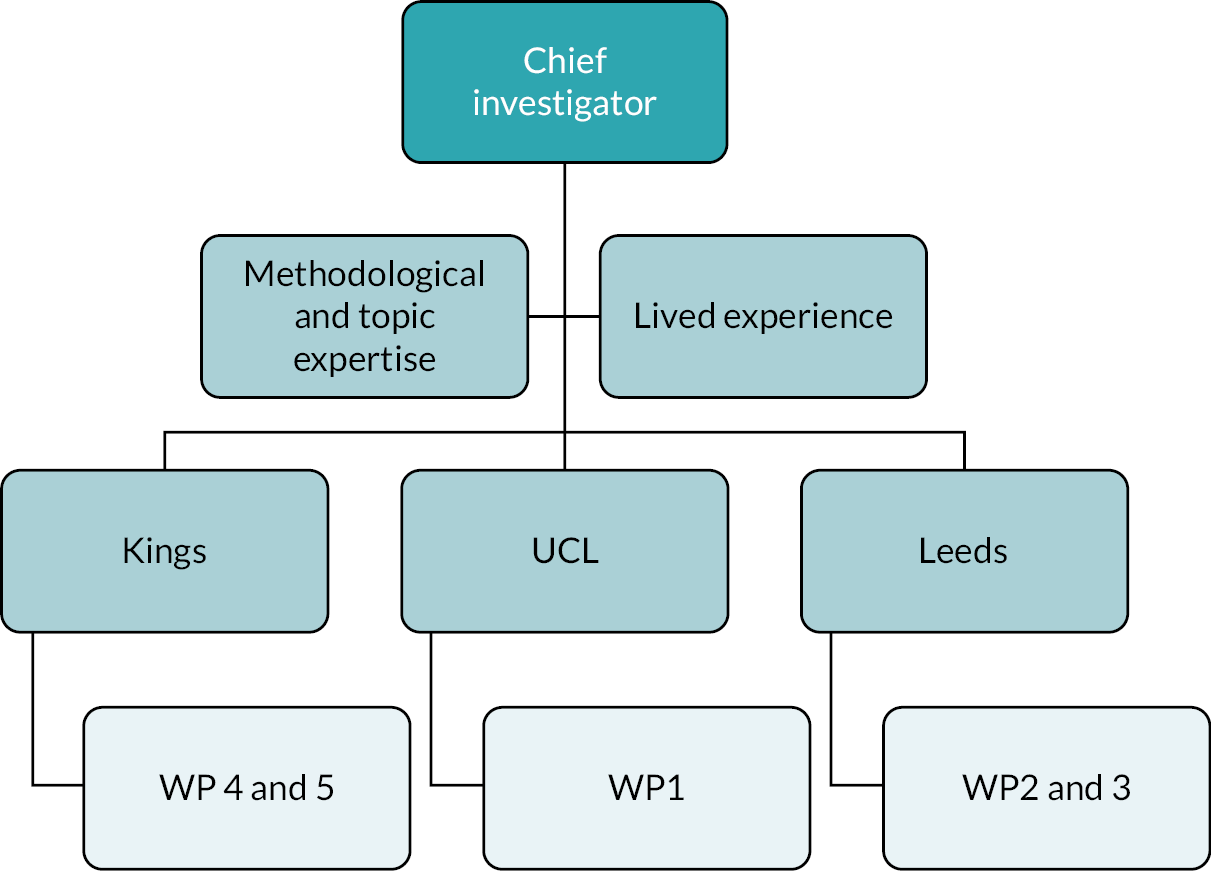
Project governance
The chief investigator, Professor Elizabeth Hughes, had overall responsibility for the delivery of the study. Each WP had a named academic lead. There were three main centres with an associated lead academic and researchers . In addition, we had additional senior academics and a lay co-investigator who brought topic and methodological expertise to the project team.
The core project team met weekly throughout the project, which was operationally focused and discussed progress of WPs against milestones. In addition to these meetings, we had steering group meetings; these groups had a wider membership, including members of the LEAG and external stakeholders, including SARC managers, forensic medical experts and psychologists (Figure 2). The purpose of the steering group was more strategic and included stakeholder input into the development of the study phases and reflecting on the implications of emerging findings. We also had an independent oversight group, which met once per year to review progress and provide independent advice about any issues that emerged including the disruption caused by the COVID-19 pandemic.
FIGURE 2.
Project management structure.
Impact of COVID-19
The study was greatly impacted by the COVID-19 pandemic in a number of ways:
-
The prevalence study had to be halted in March 2020 just as we were starting to recruit actively. There was a national pause to NHS research that was not COVID-19 related. The research was restarted in stages in the summer of 2020 using remote methods to collect data. We moved to WP4 staff focus groups ahead of WP3 (survivors) first then recommenced WP3 in autumn 2020, but not all SARCs were able to support this particular WP, because of new ways of working, as indicated in point 2. By early 2021, it was clear that we would not be reaching our target of 360 people recruited for the baseline and we made the difficult decision to remove the six-month follow-up and concentrate on maximising the responses for the baseline screening questionnaires. This was done in agreement with National Institute for Health and Care Research (NIHR) and the independent oversight group. The other issue this impacted was recruitment to survivor interviews in WP4, as WP3 was a route to recruit people for that aspect of the study. We also found that many survivors did not wish to participate in our study due to feeling the challenges of the impact of COVID-19 lockdowns.
-
SARCs changed their mode of delivery. The SARCs in our case study sites moved to remote working, apart from the forensic examinations. This impacted on the staff capacity to support research when it restarted, as they were working in difficult circumstances themselves, such as working from home, home schooling and staff sickness. The SARCs also reported that there was a drop in footfall at the SARCs and this was possibly due to under-reporting due to lockdown and the ban on social mixing. This reduced the population from which to recruit.
-
The MiMoS team moved to working remotely. The whole team worked from home during the pandemic and all meetings, recruitment and data collection occurred using telephone and video meetings (Microsoft Teams). Some of the researchers lived alone and we recognised that the team missed the peer support from being in an office with colleagues, as well as support from their line managers. Undertaking research into interpersonal violence can have an impact on a person’s well-being. To address this issue as much as possible, there was a senior member of the team ‘on call’ during data collection and researchers could call the person after an interview for advice and support even if there was no safeguarding issue to be addressed. We had weekly meetings for all the researchers and welfare was always on the agenda. In order to support the team, the chief investigator sought permission from the NIHR to use some of the underspend in the budget (unused travel and subsistence) to have a weekly group yoga session online. At the end of the six sessions, the researchers gave feedback and here is a summary:
-
‘The sessions offered me a much-needed diversion/break from the lockdown routine of sitting on my desk working. As it was my first time, I must say I was surprised how the sessions were a good form of exercise’.
-
‘The sessions helped me to relax and not think of anything else during that moment, so much that afterwards I could switch back to my usual routine feeling refreshed’.
-
‘I have recently taken up running, but needed something else to go with it, and as the swimming pools are currently closed (still so in my area!) yoga is a good alternative. It’s something I need to build into my “self-care” routine and continue as a good habit for the rest of my life’.
-
‘Thanks so much for offering these yoga sessions. It was great to be able to have these regularly as it really helps to acknowledge the impact of this work on us’.
-
‘I particularly liked the sessions where we moved more (as opposed to the more yin-style ones). I think this is because I spend so much time sitting at my desk! Therefore, it felt really good to move around and get my body in different positions’.
-
‘For me, there was something important about having a shared experience with the team all together where we were not “talking shop” and getting out of our heads and into our bodies and being in the moment. Scheduling in a session in the middle of the day was a reminder how important it is to be able to take breaks from sitting, thinking and feeling usual level of stress that comes as part of the job’.
-
‘These yoga sessions were a good opportunity to move and have a break from sitting at my desk and staring at a screen. I very much enjoyed the more dynamic sessions and thought it was a fun way for the team to bond over a non-work related activity’.
-
Chapter 2 Systematic literature review (work package 1)
Systematic review aims
A systematic review7 was conducted to identify the evidence informing the identification and treatment of mental health and substance misuse in UK SARCs and equivalent services internationally. For the purposes of the review, SARCs and (equivalent services internationally) were defined as specialist services providing both health care and the collection of forensic evidence within a single service. The review addressed the following three questions:
-
What are the approaches to identification and treatment of mental health and substance misuse problems in different SARC service models?
-
What models of care in SARCs are effective regarding service users’ mental health and substance misuse outcomes?
-
What are stakeholders’ views and policy recommendations about how SARCs should address the mental health and substance misuse needs of service users?
To our knowledge, this is the first systematic review examining mental health and substance misuse provision in SARCs.
Methodology
The systematic review protocol was registered at PROSPERO (CRD42018119706) and the review followed guidance from the Centre for Reviews and Dissemination on undertaking reviews in health care and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 10
Eligibility criteria
There were three subsearches within the review and each one related to the main questions and as such had specific inclusion criteria. Some papers had information that addressed more than one review question.
Inclusion criteria
-
Question 1: Any service description with information about mental health and drug and/or alcohol conditions (journal articles, doctoral theses, conference proceedings and book chapters were eligible for inclusion).
-
Question 2: Comparison studies; SARC service users; mental health and drug and/or alcohol conditions outcomes (compared SARCs with standard care; different SARC service models; or two different interventions/packages of care within a SARC).
-
Question 3: Qualitative interviews, focus groups or surveys of sexual assault service stakeholders.
Search strategy
The review team searched for relevant studies through four electronic databases (PsycINFO, MEDLINE, the International Bibliography of the Social Sciences and the Cumulative Index to Nursing and Allied Health Literature), conference proceedings, government websites and Google Scholar. The search was restricted to humans and to records published from 1975 onwards. This is because the first one-stop service for sexual assault (SANE: sexual assault nurse examiner) model was introduced in the mid-1970s. The last search was conducted in August 2018, and was refreshed for the realist review in 2020. The paper relating to the initial systematic review has been published. 7
Data were extracted from studies relevant to each research question. A narrative synthesis was conducted according to economic and social care research guidelines. 11 Members of the review team extracted the data using a data extraction schedule designed and piloted for the purposed of this review. Ten per cent of the data extraction was checked by another team member to control for selection bias.
The Mixed Methods Appraisal Tool12 was applied to assess the quality of the included studies for review questions 2 and 3. The quality assessment was undertaken by members of the review team. Papers were not excluded because of low-quality scores but quality scores were reported and considered in the narrative synthesis.
Findings
A total of 107 papers were included in the review. The PRISMA diagram (Figure 3) illustrates study screening and selection.
FIGURE 3.
PRISMA diagram.
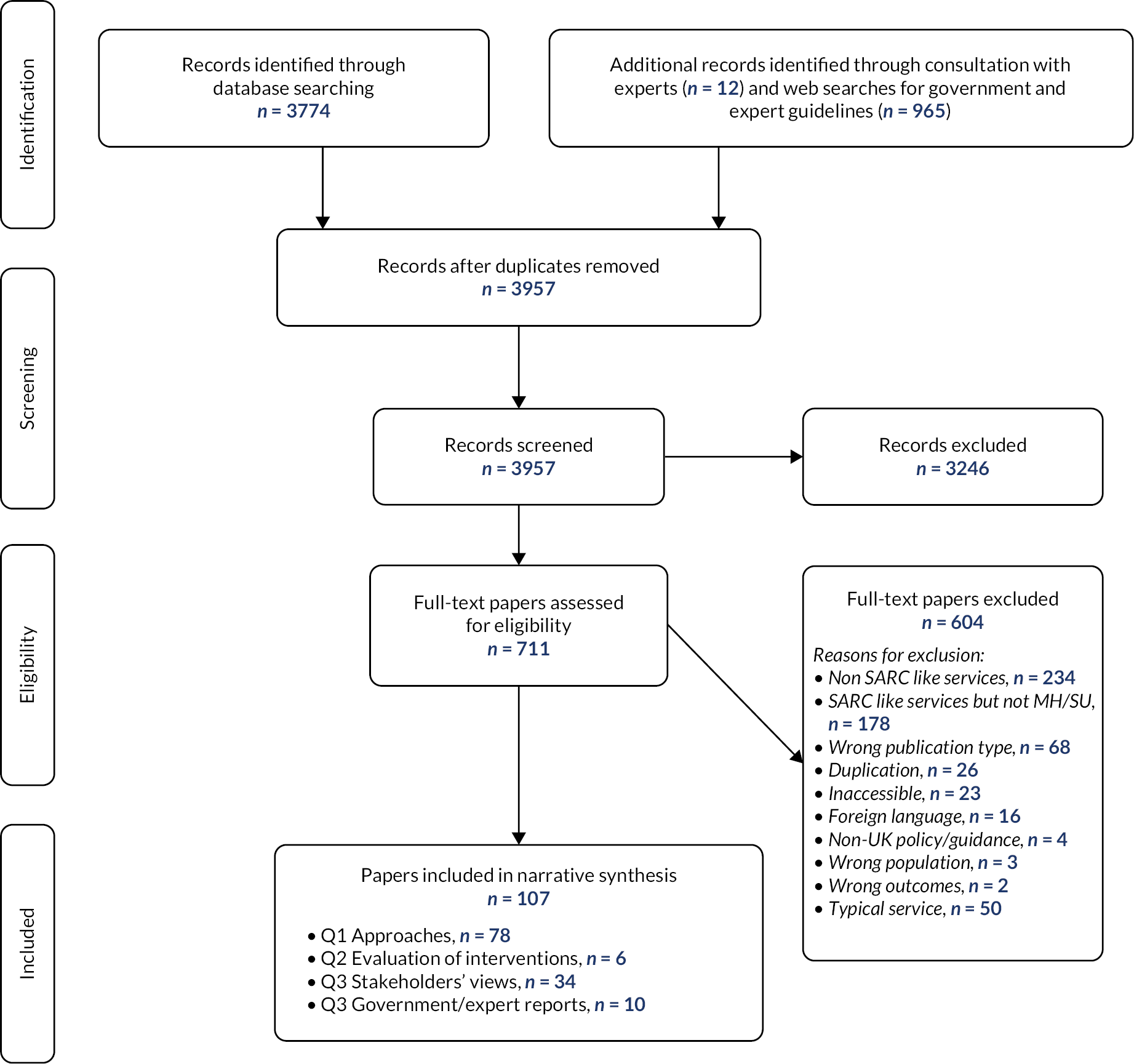
The included papers were published between 1979 and 2019 and covered services around the world. Some of the papers were relevant to more than one research question.
Question 1: approaches to mental health and substance misuse
We found 78 papers that provided information on how SARCs identify and treat mental health/substance misuse problems. These were published between 1979 and 2019, with 64 being journal articles and 14 retrieved through searches of grey literature. Based on extracted data from these 78 papers, we developed a provisional service typology for three domains of service provision as shown in Figure 4.
FIGURE 4.
Approaches to mental health and substance use.
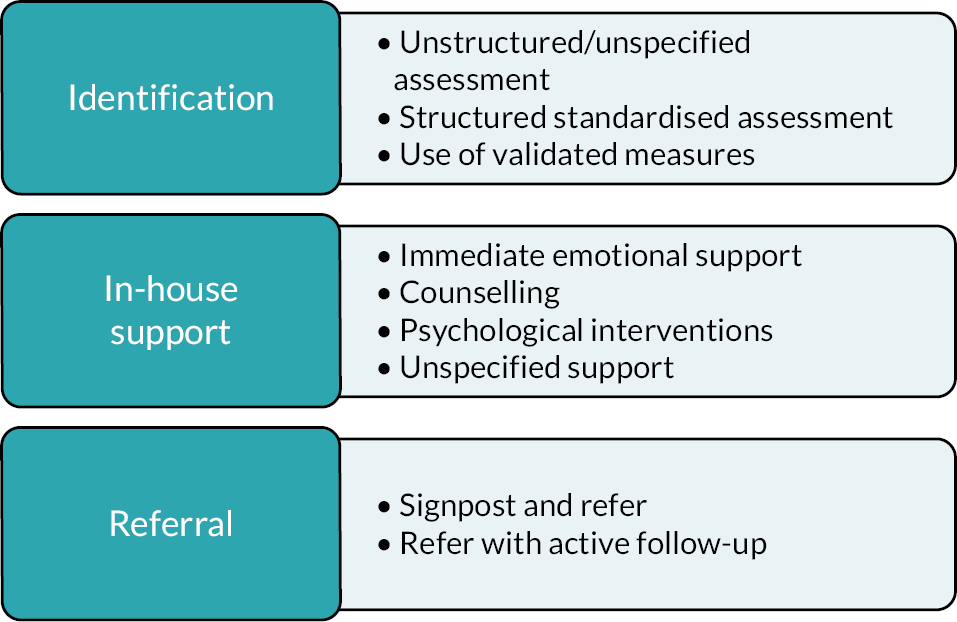
The most common approach to identification was unstructured assessment, which included professional judgement, casual observation, medical history-taking, self-reported disclosure and one-off questions about mental health. Unstructured approaches to identification were the most reported across all service models, and especially in UK SARCs, and the equivalent model in the United States. The most common approach to in-house support was the provision of supportive or unspecified counselling. That included any type of counselling provided from the sexual assault team that was not specified as a structured psychological therapy; for example, crisis counselling, supportive counselling and unspecified counselling. Finally, referral to other services was most reported to involve signposting and/or referral without active follow-up. Overall, there was a wide variation in mental health and substance misuse service provision in SARCs. The included papers had minimal information on how drug and/or alcohol was identified or addressed.
Question 2: evaluation of interventions
The review identified five studies evaluating psychological interventions for people attending SARCs. The studies were all randomised controlled trials (RCTs) published between 2003 and 2017, and set in the United States and the UK. Four of these studies evaluated brief psychoeducational video interventions compared with standard care and one study evaluated a brief six-session ‘cognitive processing therapy’ compared with standard care. The assessed outcomes were substance use and abuse, anxiety, depression and post-traumatic stress disorder (PTSD). Video interventions were shown before or after the forensic medical examination. They included information on what would happen during the examination, as well as psycho-educational material about self-management to prevent post-assault distress and substance misuse. These RCTs provided mixed evidence of moderate quality. They had significant methodological shortcomings, including small sample sizes and high attrition rates. In summary, there is a lack of robust empirical evidence to guide interventions for mental health and drug and/or alcohol conditions provision in SARCs.
Question 3: stakeholder views and policy recommendations
The review identified 34 papers (relating to 32 studies) that reported stakeholder views on how SARCs should identify and respond to mental health/substance use for people following sexual assault. Of these, 25 were peer-reviewed publications and 9 were identified from grey literature searches. They were published between 1980 and 2018; 11 studies included staff from sexual assault services as participants, 5 included service users, 2 included carers, 1 included staff from partner agencies working closely with sexual assault services, and 13 included a mix of stakeholders. The included studies consisted of surveys, interviews and quantitative questionnaires. Of the total, 13 studies were set in the United States, 12 in the UK, 4 in Canada, 2 in South Africa and 1 in each of 7 European countries.
The main recommendations included (Table 2):
-
accessibility, flexibility and continuity of care
-
SARCs to systematically assess for mental health and drug/alcohol needs
-
provision of in-house counselling/psychological support for both adult and child service users
-
clear referral pathways and closer links with mental health/substance misuse services
-
SARC staff to facilitate and encourage the take-up of follow-up services
-
SARC staff to receive training in assessing and managing mental health and drug/alcohol needs; how to support people who identify as lesbian, gay, bisexual, transgender, queer (LGBTQ+) plus pansexual, asexual, non-binary, and intersex LGBTQ+ and people with learning difficulties.
| Included papers, N (dates) | Main recommendations | |
|---|---|---|
| Stakeholders’ views | 34 (1980–2018) | Systematic assessment of mental health/SM In-house counselling/psychological support Clear referral pathways Refer with active follow-up SARC staff trained in mental health/substance misuse; LGBT and learning difficulties training |
| Policy documents | 10 (2004–18) | Some assessment of mental health/substance misuse Refer when needs are greater than IAPT level 3 support Absence of guidance about substance misuse Cognitive behavioural therapy for clients with PTSD Specialist support for LGBT people Counselling to friends and family |
A total of 10 policy documents from government and expert bodies published between 2004 and 2018 were retrieved, including 6 UK government documents, 3 European policy documents reporting on the European Union-funded Comparing Sexual Assault Interventions (COSAI) project, and 1 research project commissioned by the UK Home Office. 7 The main recommendation that consistently emerged from the synthesis of the policy documents was that there was a need to assess for mental health and substance use issues at the SARC. Older guidance suggested this should be in the form of a comprehensive assessment; however, more recent guidance recommended assessing risk of self-harm and vulnerability but did not specify how this should be done.
In the UK, there is a stepped approach to the provision of psychological treatment. NHS talking therapy services offer steps 2 and 3 of the stepped model of care, in which step 1 is delivered in primary care. Step 2 comprises low-intensity interventions for mild to moderate depression and anxiety delivered by psychological well-being practitioners, and step 3 comprises high-intensity interventions delivered by specialist therapists. Step 4 is treatment for severe and recurrent anxiety and depression, and is delivered by senior therapists. National Institute for Health and Care Excellence (NICE) guidance13 recommends that people with a diagnosis of PTSD should receive step 3 therapy within one month of the traumatic event and does not recommend low-intensity interventions due to the lack of evidence that they are effective. People with more complex and multiple mental health needs above NHS talking therapies level 3 should be referred to community mental health teams (CMHT) or acute mental health services. The role that SARCs play in providing support for survivors with mental health needs at or below this severity threshold is not specified. From the review of the policy documents, it was noted that there was a lack of guidance about how to address the drug and alcohol needs of people who attend SARCs.
European Union COSAI guidance recommendations were broadly similar to the UK SARC specifications but they included more specific guidance in directing SARCs to aim to actively engage people with mental health problems, ensuring provision of cognitive behaviour therapies (CBTs) to treat clients with symptoms of PTSD, advocating the provision of counselling support for families and close friends of the SARC client where needed, as well as access to specialist counselling support for people who identify as LGBTQ+.
Limitations of the review
Many of the included papers did not focus specifically on mental health and drug and/or alcohol conditions and so may lack detail in terms of these issues. Moreover, many of the studies had small sample sizes and high attrition rates and therefore risk being underpowered to detect differences, so their findings are not reliable. It was interesting to note that most of the qualitative studies reported staff views only, and there was a distinct lack of the survivor perspective regarding care and treatment related to mental health and alcohol/drug needs. Finally, while policy guidance was identified to inform SARC service provision, such guidance lacked specific detail on how this should be done, and this may reflect the lack of evidence.
Conclusions
The issues related to mental health and drug/alcohol use issues for those who attend a sexual assault centre have received little research or policy attention. There is a limited evidence base on interventions to address mental health needs within sexual assault services, and significant variation in how sexual assault services identify and assess mental health and substance misuse service needs. The review7 highlights the urgent need for high-quality evidence to inform service development.
The subsequent chapters report on the research conducted in UK SARC services from 2019 to 2021. Chapter 3 reports on a national survey conducted to establish the ways in which SARCs address mental health and substance use (WP2).
Chapter 3 National sexual assault referral centre survey (work package 2)
Design and setting
This was a service-level audit that aimed to describe how SARCs across England identified, assessed and responded to mental health and alcohol/drug use in people who attended their services.
Procedure
The MiMoS team joined with the other NIHR commissioned study (NIHR 16/117/04) to undertake a single survey that addressed both project aims. A set of questions were developed in Qualtrics (Qualtrics XM, London, UK) online survey platform and were piloted by a sample of SARC stakeholders prior to distribution. The survey met the HRA criteria for a ‘service evaluation/audit’ and therefore did not require NHS ethics approval but did receive an internal ethics review at Coventry University.
The survey was completed by a SARC manager and aimed to collect information in relation to SARCs themselves, their workforce and service delivery. For the purposes of meeting the aims of the MiMoS study, data were collected on mental health interventions [nature of mental health/substance misuse screening, provision of any mental health service on site (e.g. counselling, trauma focused), any special requirements for mental health/substance misuse]; mental health/substance misuse pathways (formally commissioned, locally negotiated, local data on numbers referred and outcome, nature of inequality data routinely obtained); and mechanisms for local victim–survivor engagement (satisfaction questionnaires, involvement in managing the service, recruiting/training staff; a copy of the survey is available as a project upload).
SARC managers across England were contacted via email distribution lists. The email explained the purpose of the survey and provided a link to the electronic survey. Responses were monitored and reminder emails were sent out to SARCs who had not responded. The data collection period remained open between March and April 2019.
Analysis
The data were exported to Microsoft Excel® and analysed using IMB SPSS Statistics v25 and summarised using descriptive statistics. For the cluster analysis, usable data for the five variables selected for the cluster analysis were used. The ‘best fit’ natural grouping revealed by a two-step cluster analysis was three clusters. As validation, this cluster solution was compared with all cluster solutions derived from hierarchical and K–means methods and reruns of the two-step method for forced solutions with two to five clusters and was accepted as the optimal solution by the research team. The three-cluster solution was then presented to a stakeholder group of SARC staff to check that these had face validity.
In summary, there was an overall response rate of 77% (36 of a possible 47 SARCs). The responses to each item within the survey was variable within the respondents so the denominator is the total number of responders to that item rather than the overall response of N = 36. As previously reported, this survey was done in conjunction with the other commissioned research study (NIHR 16/117/04 MESARCH) and for the purposes of addressing the MiMoS study aim, only the variables relating to mental health and substance use will be reported here.
Findings
Mental health background of sexual assault referral centre staff
A full set of descriptive statistics can be found in Appendix 1. The responses indicated that there is overall limited mental health experience in the core SARC skill mix. It is interesting to note that just under half reported that the counsellor had a mental health background or qualification. As seen in Table 3, this question was left blank by some respondents. It is therefore difficult to know whether a non-response indicates no mental health staff in that SARC or that those roles are not present in that SARC. The table presents the percentage ‘yes’ of those who responded to the question but also the percentage ‘yes’ of the total respondents to the survey.
| Yes, where answered (%) | Yes (n) | No (n) | Staff (N) | Yes, of all 32 (%) | |
|---|---|---|---|---|---|
| Counsellor | 45 | 5 | 6 | 11 | 16 |
| Crisis worker | 32 | 7 | 15 | 22 | 22 |
| ISVA | 29 | 4 | 10 | 14 | 13 |
| Consultant/clinical lead | 25 | 2 | 12 | 16 | 13 |
| SARC manager | 20 | 5 | 20 | 25 | 16 |
| Deputy manager | 15 | 2 | 11 | 13 | 6 |
| Paediatrician | 14 | 2 | 12 | 14 | 6 |
| Children’s ISVA | 10 | 1 | 9 | 10 | 3 |
| Administrator | 4 | 1 | 25 | 26 | 3 |
| Play therapist | 0 | 0 | 7 | 7 | 0 |
Assessment of mental health and substance use needs
The respondents were asked to indicate the method (e.g. professional judgement, standardised screening tools) used to assess a set of common additional needs that survivors may present with including depression, anxiety, suicide, drugs and/or alcohol and PTSD. From Table 4, it is noted that just over one-third of SARCs reported using standardised tools for any diagnosis (38%) and this seemed to be mainly for screening for drugs and or alcohol use (24%) and PTSD (21%).
| We use professional judgement and open questions within routine assessment (N) | We use standardised screening tools e.g. PHQ-9 to assess depression (N) | SARCs using screening tools (%) | |
|---|---|---|---|
| Depression | 24 | 5 | 17 |
| Anxiety | 25 | 4 | 14 |
| Suicide risk | 24 | 5 | 17 |
| Drugs and/or alcohol | 22 | 7 | 24 |
| PTSD | 22 | 6 | 21 |
| Use standardised tools (any diagnosis) | – | 11 | 38 |
Mental healthcare provision
Only 7% (2/28) of SARCs stated that a talking therapy service was provided or co-located within the SARC (even if the provider was a different organisation). One-fifth of respondents (21%, N = 6 of 29) reported that they had access to a clinical psychologist, either in-house or co-located within the SARC (even if the provider was a different organisation) and half (46%, n = 13 of 28) reported that they had a counselling service provided within or co-located at the SARC (even if provided externally). Only 10% (n = 3) indicated that they had some form of in-house or co-located substance use service provided by an external organisation. Only one SARC stated that they had an ‘other mental health or substance misuse service’ provided or co-located within the SARC (even if the provider was a different organisation). This was indicated to be a ‘mental health nurse on an 18-hour per week contract’ and their role was to undertake assessments, manage and follow up referrals.
One question asked respondents to consider a range of follow-up services that would likely to be involved in mental health and substance use care and indicate whether there was a pathway agreement in place, whether it was informal and ad hoc, whether there were discussions in place but not yet implemented, and finally if none and no plans for formalised onward referral (Table 5). The majority of SARCs reported that they had formal pathways to child protection and counselling for children and young people, but for adults it appears to be less formalised and variable between SARCs. Just under half of the respondents indicated that they had a written referral pathway agreed to single point of access (48%) and community mental health services (48%), and only 40% to the local mental health crisis teams. Only 36% had a formal pathway to drug and/or alcohol teams and 19% had a formal pathway to talking therapy services.
| Written referral pathway agreement (%) | Informal and ad hoc only (%) | Formal discussions to improve pathways taking place, but no implementation as yet (%) | No, and none planned (%) | |
|---|---|---|---|---|
| Single point of access to mental health services | 48 | 37 | 7 | 7 |
| CMHTs | 46 | 36 | 11 | 7 |
| Child and adolescent mental health services | 52 | 26 | 15 | 7 |
| IAPT service | 19 | 54 | 12 | 15 |
| Drug and alcohol teams | 36 | 54 | 0 | 11 |
| Mental health crisis teams (adult) | 40 | 52 | 4 | 4 |
| Mental health crisis team (CAMHS) | 44 | 36 | 12 | 8 |
| Counselling for adults | 76 | 20 | 4 | 0 |
| Counselling for children | 84 | 8 | 0 | 8 |
| Child protection services | 74 | 19 | 7 | 0 |
| Domestic violence services | 57 | 36 | 7 | 0 |
| Other | 26 |
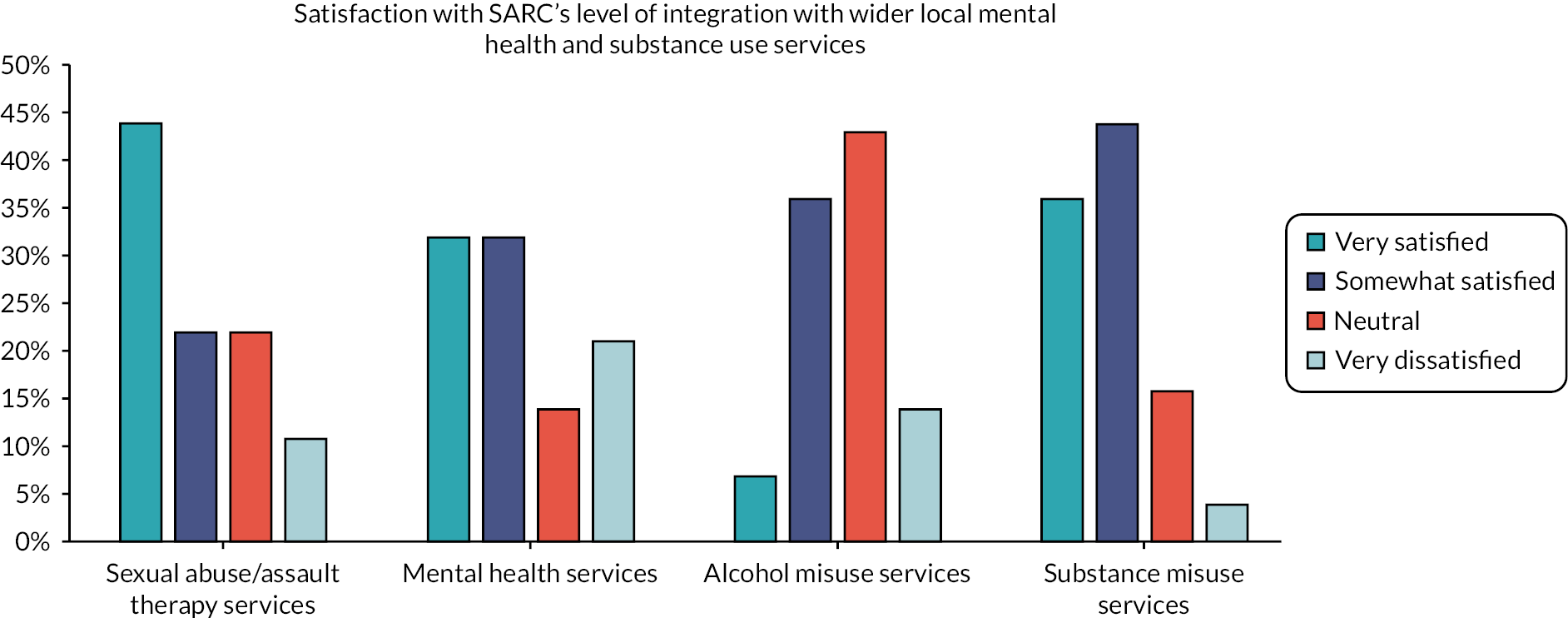
Sexual assault referral centre respondents were asked to rate how satisfied they were with the level of integration with external agencies. Figure 5 indicates that SARCs are most satisfied with integration with external sexual abuse/assault therapy services, and 64% were very satisfied/somewhat satisfied with mental health services. However, satisfaction was most positive in relation to substance use services with 80% of respondents indicating very satisfied/somewhat satisfied with integration.
FIGURE 5.
Satisfaction with level of integration.
At the end of the survey, a free-text question asked respondents to make suggestions about what could improve integrated mental health support. The free-text responses were grouped thematically as follows (with the number of related responses in brackets):
-
SARCs having more ‘resource’ (n = 5).
-
Additional training and development occurring in SARCs (n = 6).
-
Additional training and development occurring together with external mental health services (n = 7).
-
Improved pathways when making referrals to external agencies (n = 10).
-
Improved responses when making referrals to external agencies (n = 12).
-
Provision of specialist mental health services on SARC sites (n = 17).
Cluster analysis
There were usable data for the five variables selected for the cluster analysis from 28 SARCs (just under 60% of the total number of SARCs). The ‘best fit’ natural grouping revealed by a two-step cluster analysis was three clusters. As validation, this cluster solution was compared with all cluster solutions derived from hierarchical and K–means methods and reruns of the two-step method for forced solutions with two to five clusters and was accepted as the optimal solution by the research team (Table 6).
| Cluster | SARCs (N) | Name | Description |
|---|---|---|---|
| Type 1 | 8 | Some support, not integrated | No written pathways to mental health services No drug and alcohol support Variable staffing, use of structured assessment and provision of in-house counselling |
| Type 2 | 8 | Clinicians and pathways | All have mental health staff All have written referral pathways to mental health services Least likely to offer in-house counselling |
| Type 3 | 12 | Integrated and holistic | All have written referral pathways to mental health services Nearly all provide structured assessment and drug and alcohol support Most likely to provide in-house counselling |
We then presented the three-cluster solution to a stakeholder group to sense check that these clusters and their characteristics had face validity. The cluster analysis identified three broad types of service models and ways of working in relation to mental health. Cluster 1 ‘some support, not integrated’ were SARCs that had limited mental health staffing, no formal care pathways to mental health services and variable methods of assessment. Cluster 2 ‘clinicians and pathways’ tended to have staff with a mental health background in the team, written referral pathways to other relevant external agencies but did not provide in house counselling. Cluster 3 SARCs provided an integrated mental health and alcohol/drug offer among their other work. All three clusters had referral pathways, structured assessment and were most likely to offer in-house counselling.
Conclusion
The survey was useful in that it provided a national snapshot of how SARCs addressed mental health and alcohol/drug use. However, there are several limitations to the data. First, the surveys were completed by one person at each SARC (typically the SARC manager) who may not have all the information about what happens within various parts of the service. Second, not all SARCs participated in the study so there is a risk that this does not represent all the mental health and drug/alcohol approaches. However, the response rate was reasonable and there was a range of providers and geographical spread in the responding SARCs.
The findings broadly concur with the systematic review in that there was a lack of structured tools for assessing mental health and substance use; there was limited evidence that there were any psychological therapies provided in-house in SARCs and mostly informal or ad hoc referral pathways to external or partner agencies for mental health and alcohol/drug issues. Using the variables, a cluster analysis was performed, which identified three clusters into which the SARCs who responded fitted. However, the cluster analysis was limited by the quality of the responses to the survey and the fact that not all SARCs provided data. The analysis also demonstrated that while there was some clustering of variables into three types, there was considerable variability between SARCs. The clusters were presented to a group of SARC staff stakeholders, who verified that the clusters have some face validity. However, it was helpful as a rudimentary guide to inform the sampling of SARCs across the range of types of provision for the subsequent case studies.
Chapter 4 Prevalence study (work package 3)
The aim of this study was to collect data on mental health and substance use needs to the be able to estimate the prevalence of mental health and substance use difficulties of people attending SARCs. It was a cross-sectional design.
Setting and sample
The setting was participating SARCs at six sites across England, which were selected with examples from each of the three clusters identified in WP2. The target sample was adults over the age of 18 years who attend SARCs and who consent to participate. The inclusion criteria were as follows:
-
aged 18 years or older
-
able to read and understand English (or there are suitable confidential translation services available).
The exclusion criteria are as follows:
-
lack of capacity to provide informed consent
-
participation was deemed to significantly increase risk to self or others (e.g. being in an acute mental health crisis as evidenced by being admitted to a psychiatric inpatient unit at the time of recruitment)
-
attendee of a SARC that was not participating in the study.
A priori sample size calculation
The sample size of n = 360 across the six sites were calculated based on the following: an estimated population of 4000 across six sites per year and 40–60 referrals per site, per month. Based on a previous audit of mental health needs at a single SARC in England, the SARC staff obtained consent and collected data on 42% of attendees and 38% declined to participate (with limited support to recruit). It should, therefore, have been feasible to obtain consent from 50% of attendees to participate, which meant 20–30 per site, per month. However, because of the impact of COVID-19, several factors impeded recruitment and the target sample was not achieved.
Measures
The measures were selected as they have good reliability and validity and are appropriate for the setting and sample:
-
demographics questionnaire designed for the study which covered gender, sexuality ethnicity, age, socioeconomic status (by post code) previous contact with mental health services and pre-existing self-reported mental health and drug/alcohol issues (see Report Supplementary Material 1)
-
Clinical Outcome in Routine Evaluation 10 (CORE-10) covering anxiety, depression, trauma, physical problems, functioning and risk to self14
-
alcohol screening tool: Alcohol Use Disorders Identification Test (AUDIT-C)15
-
the PC-PTSC-516
-
Recovering Quality of Life (ReQoL): a quality-of-life measure developed specifically for those with mental health conditions17
-
drug use screening tool: Drug Abuse Screen Tool (DAST)18
-
Structured Assessment of Personality Abbreviated Scale (SAPAS): a brief screening tool for personality disorder. 19
Information on each outcome measure cut-off scores is provided in Appendix 2.
Data management
The information provided by participants was treated as confidential and, in accordance with the Data Protection Act 2018 and General Data Protection Regulations, any personal data (identifiable details) were stored separately from the research data (i.e. answers given during on the questionnaire). Research data were anonymised using a study number. The only exception to this confidentiality was if the research team had concerns about current or future risk of serious harm to the participant or to anybody else. Similarly, confidentiality was broken if participants disclosed details of intention to commit a crime or if participants shared details of a crime for which they had not been convicted. If that happened, the research team followed SOPs, which covered things like informing the participant’s GP or other relevant services (on a need-to-know basis only). Researchers always tried to discuss this with participants first where possible.
A data management plan (MiMoS_23240_Data Management Plan_v1_16.08.2019) was developed for WP3, 4 and 5 to complement this protocol.
Recruitment and enrolment
The recruitment strategy was informed by a trauma-informed approach aiming to empower participants to have control over decisions to participate in research. 9 The research team worked with the LEAG group to develop a range of options for people to opt to engage with the study and they designed our recruitment materials and participant information sheet.
Sexual assault referral centre staff mentioned the study to people during their attendance at the SARC. Because of the pandemic, some of this contact was via telephone so the staff emailed PDF versions of the leaflet and obtained consent to be contacted by the research team. More details of this procedure can be found in the study protocol. Participants could also refer themselves to the study via the study website. Once consent to be contacted was received, the MiMoS researcher made contact via the potential participant’s preferred contact method. A total of five attempts at contact were made, after which the potential participant was not contacted again. If the researchers were able to make contact, they would then provide the information necessary for the participant to make a fully informed decision to participate or not. Participants were given at least 24 hours (or longer if needed or requested) to consider the information before deciding whether to take part. Once consent was obtained, the baseline study questionnaire was sent via a link emailed to the participant using the University of Leeds online survey (Online Survey). There was also an option to complete a paper version of the questionnaire. A further option for completing the questionnaires was over the phone with a researcher. In this instance, the researcher completed the online consent form and questionnaire over the phone with the participant, obtaining text or email confirmation of consent.
The participants received a £10 e-voucher for participation in the prevalence study.
Welfare checks and safeguarding
The MiMoS researcher was able to log into the Online Survey and review the responses. If any of the responses indicated risk to self/others, a welfare call would be undertaken as per the SOP. All MiMoS researchers had access to an on-call senior team member (EH, ML, BLE) if they required advice about risk and action to be taken. All action was documented using identity numbers to protect anonymity recorded in the secure shared Microsoft Teams folder.
The demographics of our prevalence study sample, both non-recent and recent cases, was initially compared with routine data collected from the six sites over the course of the national survey (WP2) to assess the representativeness of our sample. The final dataset was then weighted for demographics (e.g. age, sex, deprivation).
Analysis
A direct estimate of the prevalence of mental health within SARC attendees was determined from the sample and weighted estimates produced for the SARC sites. Additionally, a further weighted national estimate was produced (if demographic data could be obtained for all 47 SARC sites; see Appendix 3). Analysis of other health, well-being and behavioural measures followed the same principle to produce direct (and site-specific and national weighted) estimates. Prior to producing these estimates, the dataset was analysed to determine how or whether demographics, site or method of data collection influenced prevalence measures.
Findings
WP3 was an aspect of the MiMoS study that was most affected by the COVID-19 pandemic. The target sample of 360 was not achieved due to challenges related to the COVID-19 pandemic. Recruitment started in the spring of 2020 and was almost immediately suspended due to the first lockdown in March 2020 (all NHS research was suspended at that time unless it was COVID-19-related) and restarted in September 2020). Once the study was able to restart data collection, it continued to be affected by the continuing pandemic during the autumn, winter and to the spring of 2021, with to the third wave and second national lockdown. For this reason, the study remained open to recruitment from September 2020 to the end of May 2021, extending the original six-month recruitment window. A decision was made to end recruitment rather than extend it further as there was no indication in the spring that it was going to be possible to recruit anywhere near our target in a reasonable period of time. Even with extending the recruitment window there was no sign that recruitment was picking up to the expected pre-COVID-19 estimated pace. It is also important to note that of the original six SARCs, recruitment only occurred from four of the services due to changes to services during the COVID-19 pandemic at some of the SARCs, which made additional recruitment difficult. In addition, some SARCs saw a dramatic drop in attendees during the lockdown periods. The decision to end recruitment was agreed by an independent study oversight group and with the funder. The decision to remove the planned six-month follow-up was also approved and the amendment made to the NHS ethics protocol.
Recruitment
Participants were recruited from four of the six case study sites. A total of 236 consents to contact were received from people who had recently attended a SARC, of which 157 (67%) were contacted by a member of the MiMoS team. Of those contacted, 78 (50%) gave informed consent to participate and completed the online screening (Figure 6). Two were excluded from the analysis as they were under 18 years of age, leaving 76 to be included in the analysis.
FIGURE 6.
Participant flow.

Sample characteristics
The sample was recruited mostly from the London SARC. However, on comparing sample characteristics from London and non-London, there were very few demographic differences except that in London:
-
there were slightly fewer people who identified as white
-
participants had slightly higher educational attainment, were more employed and fewer were living in temporary accommodation
-
slightly lower mental health needs were identified and lower prescription of medication for mental health and alcohol/drug treatment.
Most of these differences were not statistically significant except for those living outside London who were more likely to state that they were prescribed medication for mental health or substance use difficulties (64%) than participants living in London (36%) (Pearson Chi-square p ≤ 0.05). Therefore, the sample was not disaggregated by London/not-London.
London and the south were less affected by the impact of autumn local area lockdowns compared with the north of England, and this is one of the reasons why recruitment was more successful in these areas. Most of the sample (80%) were in the 18–24 years and 25–34 years age groups. The vast majority were women (91%), with 6% identifying as male and 3% identified as trans/non-binary. In terms of sexuality, most (73%) identified as straight; 8% as gay/lesbian and 19% as bisexual. Most (65%) of the sample identified as white; 13% as Asian/Asian British and 13% as Black Caribbean, African, British.
The survey demographics were compared with national data from the 2018–19 Sexual Assault Referral Centre Indicators of Performance (SARCIP) returns. This showed that the survey was broadly representative of the overall SARC population in 2018–19, with a slightly lower proportion of people identifying as white due to the dominance of participants from London and slightly more participants aged 25–34 years.
Prevalence of mental health, alcohol and drug needs
A series of standardised screening tools were used to measure mental health, well-being and substance use needs. The moderate to severe cut-off score for the CORE-10 is above 2 and the clinical cut-off (indicating those in need of psychological therapy compared to a non-clinical population is 1). We are deliberately reporting the percentage of those scoring in the higher severity range and therefore likely to be experiencing an elevated level of psychological distress requiring specialist mental health assessment and support (Table 7).
| n | CORE-10 | AUDIT-C | PTSD-5 | ReQoL-10 | Health problems | DAST-10 | SAPAS | ||
|---|---|---|---|---|---|---|---|---|---|
| Moderate – severe (%) | Increasing risk (%) | Likely PTSD (%) | Clinical range (%) | Moderate – severe (%) | Moderate – severe (%) | Likely PD (%) | |||
| Age-group (years) | 18–24 | 31 | 84 | 10 | 93 | 90 | 48 | 33 | 67 |
| 25–34 | 33 | 64 | 15 | 94 | 80 | 30 | 17 | 52 | |
| 35+ | 12 | 91 | 8 | 100 | 100 | 75 | 33 | 82 | |
| Ethnicity | White | 49 | 73 | 16 | 94 | 85 | 47 | 34 | 64 |
| Non-white | 25 | 80 | 4 | 95 | 90 | 42 | 13 | 58 | |
| Sexa | Female | 68 | 78 | 13 | 97 | 87 | 49 | 28 | 63 |
| Male | 5 | 40 | 0 | 60 | 75 | 20 | 20 | 40 | |
| Total | 76 | 76 | 12 | 94 | 87 | 45 | 26 | 63 | |
| 95% CI | 65% to 85% | 6% to 21% | 86% to 98% | 77% to 94% | 33% to 57% | 17% to 39% | 50% to 74% | ||
These results showed an overall prevalence (95% CI) of:
-
76% (65–85%) with moderate–severe psychological distress (CORE-10)
-
12% (6–21%) scored between 8–15, indicating ‘increasing risk of alcohol problems’ (AUDIT-C)
-
94% (86–98%) PTSD (PC-PTSC-5)
-
87% (77–94%) were in the clinical range for low quality of life (Re-QoL-10)
-
45% (33–57%) moderate to severe health problems (Re-QoL)
-
26% (17–39%) moderate to severe drug problems (DAST)
-
63% (50–74%) personality disorder (SAPAS).
In 2018–19, 14,357 adults (aged 18 years or over) attended SARCs across England. By applying the unadjusted prevalence of mental health or substance use conditions to this total (Table 8) we estimate that, of these 14,357:
-
10,911 had moderate–severe psychological distress
-
1700 had increasing alcohol risk
-
13,548 had likely PTSD
-
12,511 had clinically low quality of life
-
6423 had moderate to severe health problems
-
3800 had moderate to severe drug problems
-
8973 had a probable personality disorder.
| CORE-10 moderate to severe (n) | AUDIT-C increasing risk (n) | PTSD – possible PTSD (n) | ReQoL-10 clinical range (n) | ReQoL health problems – moderate to severe (n) | DAST 10 – moderate to severe (n) | SAPAS –possible PD (n) | |
|---|---|---|---|---|---|---|---|
| Unadjusted from survey | 10,911 | 1700 | 13,548 | 12,511 | 6423 | 3800 | 8973 |
| Weighted by age | 11,615 | 1528 | 13,655 | 12,960 | 7415 | 4212 | 9668 |
| Weighted by ethnicity | 10,668 | 2114 | 13,491 | 12,357 | 6654 | 4506 | 9063 |
| Weighted by gender | 10,581 | 1691 | 13,341 | 12,353 | 6507 | 3926 | 8723 |
The prevalence of each mental health condition or substance misuse varied slightly by various demographics (age, ethnicity, sex/gender) – but disaggregated sample sizes were relatively small. When applying the disaggregated prevalence to the disaggregated national SARC population for 2018–19 (see Appendix 3), the weighted estimates show broadly similar numbers of SARC attendees with identified mental health issues, alcohol and/or drug use.
Although sample sizes are small, a cross-tabulation between outcomes shows that there is some tendency for dual diagnosis of mental health and substance misuse (Table 9). These differences were statistically significant only for 72% of individuals with moderate to severe drug misuse who also had health problems (compared with 38% of those with no/low drug misuse).
| CORE-10 | AUDIT-C | PTSD-5 | ReQoL-10 | Health problems | DAST-10 | SAPAS | |||
|---|---|---|---|---|---|---|---|---|---|
| (n) | Moderate – severe | Increasing risk | Likely PTSD | Clinical range | Moderate – severe | Moderate – severe | Likely PD | ||
| DAST-10 | Moderate – severe | 18 | 83% | 11% | 94% | 78% | 72% | 89% | |
| No/low risk | 50 | 76% | 14% | 86% | 82% | 38% | 48% | ||
| Pearson chi-squared test of association | p = 0.52 | p = 0.76 | p = 0.89 | p = 0.42 | p < 0.05 | p < 0.05 | |||
| AUDIT-C | Increasing risk | 9 | 100% | 100% | 100% | 33% | 22% | 50% | |
| Lower risk | 66 | 73% | 89% | 79% | 47% | 24% | 62% | ||
| Pearson chi-squared test of association | p = 0.72 | p = 0.46 | p = 0.22 | p = 0.46 | p = 0.76 | p = 0.44 | |||
Summary
The analysis indicated consistently elevated levels of psychological distress across the sample recruited. All participants completed the scales in the immediate period after visiting a SARC but at least one week was allowed prior to data collection to allow the initial and acute reaction to trauma to subside. Elevated levels of PTSD were also identified. These results are not surprising considering the recent sexual assault experience but illustrate the importance of using standardised screening tools to identify need and inform what sort of follow-up and access to trauma-specific psychological therapy may be needed. There was some tendency for substance use concerns to co-occur with psychological distress. A larger sample could explore this trend with more certainty; however, accessing effective treatment for co-occurring mental health and substance use can be a challenge, especially psychological therapies (which can exclude those who have active alcohol or drug issues). There are limits to this study because the sample size required was not reached due to impact of the COVID-19 pandemic. However, the sample is representative of people who attend SARCs as well as the rates broadly concur with previous prevalence studies of mental health of SARC attendees. 1,3
Realist synthesis of literature review
Realist methodology
The mixed-methods study was informed by an iterative programme of realist inquiry, which used realist evaluation20,21 and realist synthesis approaches22 to develop and refine programme theories and provide an increasingly evidence-informed theoretical framework to understand emerging findings.
The initial programme theories explained how the SARCs, and related services are intended or expected to achieve specific outcome patterns. As the project proceeded, further theories were developed and refined to encapsulate the diversity of experiences and explain what works, for whom, in what circumstances and why. The programme theories were developed and refined iteratively using tools such as logic models, if–then statements and context, mechanism and outcome configurations (CMOCs) and supported by data from a range of sources including WPs 1–5.
While each WP produced its own discreet outputs, an iterative approach was taken; each stage was informed by the findings of the previous stages, as well as within each stage (e.g. qualitative interview schedules were modified as patterns were identified, and theories were developed which were tested at the subsequent interviews).
We used a comparative realist evaluation approach comprising detailed investigation of the relationship between organisational processes and contexts,23 which generated a holistic understanding of the phenomenon under investigation. 24 Using this methodology, the study sought to explain and understand current SARC service provision by considering how variations in service provision and processes interplay with important aspects of individual service users, thereby influencing how mechanisms work and produce different outcome patterns. 21 This was achieved by developing, refining and testing hypotheses (programme theories) that described how various outcome patterns (O) were observed depending on whether the contexts (C) allowed specific mechanisms (M) to operate. These hypotheses are called CMOCs. A simple example could be the following:
-
Mechanism (resource) – identification of need and referral to external mental health services.
-
Context – previous positive/negative experience of mental health services.
-
Mechanism (response) – service-user decision to take up the referral.
-
Outcome patterns – attending/not attending mental health services, which influences longer-term expected outcomes such as improved wellbeing and reduced risk of further assault.
A CMOC incorporating these elements could be constructed as follows. It is expected that identifying a mental health need and subsequent referral to external mental health services (M) will result in improved wellbeing (O). However, if the service user has had previous adverse or unsatisfactory experiences of these services (C) and as a result decides not to take-up the referral (M) then the anticipated desirable mechanism (decision to take-up the referral) will fail to ‘fire’. Not only will the anticipated benefits of attending these services not be realised (O), but the service user might experience adverse outcomes such as despair or lack of hope (O), thereby potentially leading to worsening of psychological state and higher risk of further assault.
In this CMOC, the key elements that influence outcome patterns (O) are the referral process mechanisms (M) and whether they operate as expected, which is dependent on the context (C) of previous experiences of referral to these (or similar) services.
Realist review
To generate initial programme theories that would then be refined and tested in the case studies and other WPs, a realist review was undertaken. This used outputs identified in the WP1 systematic review. In line with realist methodology,20 the review aimed to create an initial framework for understanding how SARCs respond to mental health/substance misuse while identifying gaps in knowledge and key areas of interest. The review aimed to address the following question:
-
What are the theoretical explanations relating immediate and longer-term outcomes to the identification and treatment of mental health and substance misuse problems in SARCs?
The review was based on international literature. However, the findings were prioritised for relevance to the UK sexual assault service models.
Methodology
The review protocol was registered on PROSPERO (CRD42020182808) and the review follows the RAMESES publication standards for realist reviews. 22
The realist review included papers from the systematic review and built on its searches. 7 We updated the search in the PsycINFO and MEDLINE databases (20 March 2020) using broad search terms and synonyms for SARCs. The search was limited to humans but there were no language restrictions. We also consulted experts in the field to identify additional key papers. The purpose of the review was to develop a theoretical framework and initial programme theories that were specific to the SARC setting, which would then be further refined through the research activities of the other work streams. 25 Therefore, a single comprehensive search, specifically focused on SARCS, rather than iteratively developing additional theoretically driven searches was considered appropriate for the purposes of the programme as a whole.
All retrieved records were independently screened for relevance by two reviewers in a web-based review management system (Covidence, Melbourne, Victoria, Australia). Any disagreements were resolved by discussion and, where necessary, after discussions with a third researcher. A data extraction schedule was drafted, piloted and further developed. We extracted data using Microsoft Excel®.
A separate row was used for each theory, whether this was a complete theory or fragment, rather than for each paper. This approach ensured that theory-rich papers did not result in theory-dense outputs and allowed more precise categorisation and comparison of theories. Data were extracted in the form of form of context (C), mechanisms (M) and outcomes (O), and included ‘if–then, leading to’ statements. This approach ensured that relevant details were extracted for theory development and the relationships between C, M and O were articulated. Training sessions and workshops were held for the team to develop skills and knowledge in realist synthesis. However, where members of the data extraction team were less comfortable with describing theoretical relationships, the ‘if–then’ statement column was completed later, by more experienced members of the team using the extracted data and with reference to the original sources.
Extracted information also included theory description, position in pathway, intervention, expected outcomes, for whom, in what setting; generalisability for UK SARCs, usefulness, plausibility, relevance and trustworthiness of the theory. We extracted data for all included papers, found both from the original and the updated search. Most members of the review team extracted data and were involved in discussions around theory generation.
Microsoft Word® was used to collate extracted data according to their position in the pathway. The extracts were then compiled into themes and subthemes that were relevant to these pathway positions. These documents were then reviewed and the contents synthesised into further refined ‘if–then’ statements and CMOCs. Regular discussions among the review team facilitated theory generation. During this process, consideration was given to associations with existing mid-range theories or the development of bespoke theories.
An example of the development of synthesised CMOCs is provided below. This example is positioned at the ‘pre-SARC’ point in the process pathway.
Initial ‘if–then’ statements
The following ‘if–then’ statements were constructed directly from the literature by extracting CMOCs from the source documents and then formulating the relationships between these elements in the extraction form.
49: If sexual assault service staff members (i.e. forensic nurses) are educated and trained appropriately, then they can carry out public health/preventative activities, resulting in a safer community. 26
87: If someone attends a SARC they will benefit from the multi-agency model because of the joined up approach between bureaucratic systems. If they do not trust statutory services however then they may be wary of the SARC because of its perceived links with the police and health system. 27
126: if the services and structures around sexual assault support and the legal system are perceived as fair and supportive, then a higher proportion of assaults would probably be reported. 28
144: If survivors are unaware of SARCs or don’t think they fit the criteria, then they will either not present at all or may present outside the forensic window. This may be because e.g. they think their injuries aren’t serious enough, they are too traumatised to help-seek, or they have internalised rape myths. Therefore, SARCS should aim info strategies specifically at those at risk and should ensure it’s clear who is eligible for support. 29
Extracts and synthesised statements retained their extracted theory ID number at every stage, to allow referral back to the extraction form and source documents. This ensured that important meaning was not lost and allowed clarification of details. Table 10 demonstrates how this specific information extracted from the source documents was synthesised. This stage of the process produced less detailed, yet generally applicable key principles, which could be used to guide the other work streams and potentially be tailored for implementation in any SARC setting.
| Position in pathway | Theme | Subtheme | Context | Mechanism | Outcome | References |
|---|---|---|---|---|---|---|
| Pre-SARC | Role of the SARC in supporting engagement | SARC role in raising awareness about their service | If SARCs raise awareness about their service and provide outreach to the community | Survivors will know about the SARC and understand why, how and when to access it | More survivors will access the service in a timely manner, thus providing an opportunity to improve mental health outcomes | 49, 87, 126, 144, 171, 221, 247 |
Findings
The initial programme theories were developed from the study proposal and discussions with the study team. For instance, the prevalence of unmet needs indicated problems with the start of the pathway, such as access, referral, and case-finding issues. Rates of mental health service-use, PTSD and substance use are also known to be high in users of SARC services. However, it was not clear how well these needs were being assessed or met during first contact or subsequently (e.g. through referral pathways or follow-up). A process/logic model was developed, which included assumptions about what good-quality care would look like, possible decisions at key points in the pathway and important questions for the study to answer.
Initial hypotheses were developed, which assumed that attending a SARC would be a good thing for those with mental health and/or alcohol/drug use needs. In theory, attending a SARC means that:
-
Survivors can have their mental health and/or alcohol/drug needs assessed; can be referred to talking therapies or drug and alcohol services where needed; can be supported to access other services to have their healthcare needs met, which might otherwise cause stress; that is, SARC attendance provides a point from which formal support services can be accessed.
and
-
In the immediate aftermath of assault, survivors can gain reassurance that they will be believed; they can have negative appraisals about blame challenged by SARC staff; can regain a sense of control and safety. That is, SARC attendance might reduce risk for developing/exacerbating MH/SU difficulties through informal (trauma-informed) ways that survivors are treated, which increase sense of safety.
These two processes may also interact – survivors are more likely to disclose difficulties and take up services where they have experienced trauma-informed care. The synthesis aimed to develop initial programme theories that begin to describe how these formal and informal processes impact on outcomes for people with histories of mental health problems and substance use.
The findings were grouped into three time points to reflect the journey of service users through support services and to highlight places in this journey that can facilitate or impede improved outcomes. Within each section is a theory statement, developed from CMOCs that provide an explanatory interpretation of the synthesised literature. The sections are titled as followed:
-
Pre-SARC – this includes awareness of the SARC service, what is known about its purpose, how it is accessed (via police, third party service, self-referral).
-
Within the SARC – first attendance and initial impressions, process and procedures, assessments and methods of assessment, the forensic examination (consent, capacity, being informed, psychosocial support, physical environment), follow-up support, appointments, signposting and information giving.
-
Post SARC – how referrals to external agencies are conducted, follow-up support (e.g. for legal processes), satisfaction with support, gaps in onward service provision.
These are presented below and in summary form in Table 10.
Pre-sexual assault referral centre
Sexual assault referral centre role in raising awareness and supporting system integration of such centres
SARCs have only been introduced recently and therefore there is variable awareness of their existence within the general population and referral agencies. UK service specification (2018) says that SARC services and what they provide are not well known. Therefore, raising awareness and promoting SARC provision and ease of access to services is a priority. One area of interest is how SARCs work with other agencies and the communities they serve to raise awareness of their existence, what services are offered and how to access them.
All local areas should ensure that there is an opportunity for survivors to access SARC services as self-referrals. Lack of awareness of services is raised in literature from a range of international settings. For instance, a study in the Congo concluded that fear and lack of awareness were the two most important barriers to uptake of services. 30
If SARCs raise awareness about their service and provide outreach to the community, then more survivors will access the service in a timely manner, thus providing an opportunity to improve equality of access and improve mental health outcomes. This is because survivors will know about the SARC and what it offers. They may be more likely to recognise that their experience constitutes a sexual assault and have more confidence this will be treated seriously and sympathetically in SARCs and have reduced fear or uncertainty about attending. This may especially be the case for those with pre-existing mental health needs. Awareness-raising may include explaining the definition of sexual assault, the function of the SARC for both forensic and non-forensic cases, who is eligible for support, and the option of self-referral without police input.
SARC role in reducing barriers for vulnerable groups
A strong theme in the literature relates to the under-representation of specific groups within SARC services. This can be at odds with estimates of the demographic profiles of people in the general population that experience sexual assault. For instance, services experience under-representation of people with serious mental illness,31 ethnic minorities32 and people with learning disabilities. 33
Specific groups face additional barriers to attending a SARC, including physical and intellectual disabilities and a perception that SARCs are not for their use or cannot meet their needs. Other groups may also face barriers. Men may only report if they have physical injuries and may be put off by the perception that SARCs are primarily for females. Similarly, LGBTQ+ survivors may perceive SARCs as not being for them, and there may be a lack of knowledge and skills among staff, service provision might be gender binary, and there could be a minimisation of experiences of abuse. If SARC staff are aware of the needs and challenges for specific vulnerable groups, then they may be able to reduce barriers and increase the likelihood of SARC attendance. This is because they can direct marketing at specific groups and direct resources to ensure equal access.
Although [service] will provide an excellent service for males … it was felt by one service provider, their publicity is not explicit enough in male society. Marketing needs to be available in pharmacies, GUM clinics, drug services. The marketing needs to state that men do not have to report a crime to the police, as this would put a lot of them off visiting [service] for help. However, since 28th February 2011 there is a separate page dedicated to men on the [service] website also on poster cards and on buses that has made a difference.
(Winters et al.)34
Within the sexual assault referral centre
The experience that the service user has within the SARC can impact on mental health outcomes in several ways. SARCs need to promote service users’ safety, choice and control, to reduce potentially re-traumatising experiences (e.g. Du Mont et al. 35). This can include having processes in place to promote trauma-informed care that are influenced by the structure of the service as well as the behaviours of staff members. Furthermore, successfully identifying and responding to mental health and substance-use needs, depends upon the assessment procedures in place and how these are enacted.
Mental health and substance use provision
Identification of mental health and substance use needs
The literature did not highlight consistent approaches across SARCs to identification of need regarding mental health and substance use. However, the development of theory indicated that having standardised processes would improve identification of needs and provide more equal access to therapies and continuing support.
If SARCs use consistent structured assessments that are adapted for specific groups (i.e. psychosocial vulnerabilities, learning difficulties) to identify mental health and substance use needs, then needs and risk will be identified successfully, more equally and in a timely manner. However, identification of need is only the first stage in the process. Appropriate responses then rely on other elements of service provision, such as training, resources, a consistent approach between staff and access to further services. A consistent approach to assessment might be particularly useful in supporting other positive mechanisms, such as helping staff to feel more comfortable asking clients about mental health problems and substance intake. Successful identification is important in addressing symptoms early which is in turn crucial in the progression of mental illness.
Mental health prevention and intervention
If SARCs provide early and timely post assault intervention and in-house psychological support, then attendees might experience improved mental health outcomes. This is because early intervention can reduce immediate and long-term distress and specialist services can tailor support and facilitate disclosure to the police.
Trauma-informed care
Trauma-informed care provision is particularly relevant for SARC service users. The literature is divided into two categories: first regarding the provision of training and second regarding trauma-informed interactions. There is a theoretical link between training in trauma-informed care and subsequent trauma-informed interactions. However, there are other potential areas that could be explored for contexts and mechanisms that contribute towards trauma informed interactions, for instance the culture of the service, staff recruitment strategies, service delivery procedures and even the layout or design of the physical space.
Trauma-informed ways of working include empowering service users, offering choice and understanding when it is declined, sensitivity and being attentive to signs and symptoms of trauma. Trauma-informed interactions are described as being proactive in offering support, empowerment, dignity and respect, care and compassion. Members of staff should listen, provide choices, explain things carefully, be aware of and attentive to service-users’ needs, take steps to respond to emotional needs, provide continuity of care and acknowledge a range of emotions.
If staff members are trained to have a specialism in sexual assault and how to work specifically to support the needs of survivors then the risk of secondary victimisation is reduced. This, in turn can impact on the survivor accessing appropriate services and, ultimately, their recovery. This is because having a sense of control and clarity means that detrimental situations such as fear of unknown procedures are mitigated. These improved outcomes are also found because this specific training can raise awareness of a survivor’s emotional distress and challenge assumptions about sexual assault. It can mean that members of staff are more likely to ask with sensitivity about the assault and refer to appropriate evidence-based treatments.
If SARC staff provide trauma-informed interactions, this can improve help-seeking, support steps to recovery, reduce psychological harm, lead to increased participation in the legal process and have longer term impacts on physical and mental health. This is because survivors feel respected, cared for, and supported, feel calmer and safer, listened to, in control and informed and are less likely to feel dehumanised, confused and frightened. It reduces denial and self-blame, creates a sense of safety, and creates an environment that will be more psychologically supportive.
Service organisation
Collocation of services
If a multidisciplinary set of staff are co-located in the SARC, this can have advantages for the speed, quality, and variety of care. It can reduce the potential for negative consequences resulting from lack of coordination and continuity of care. This could be more important for attendees with complex needs (such as substance use problems and PTSD risk factors) so that risk factors are recognised and packages of care are coordinated.
Role clarity and integration
Role clarity and integration in the literature is focused on the differentiation of crises workers (or advocates) from the nursing and medical roles involved in forensic medical examinations. While clear role separation is considered broadly beneficial and lack of clarity can lead to confusion and variability of services, there is also an argument for blurring boundaries between roles; specifically, that nurses should be trained to deal with emotional needs as well as completing forensic medical examinations.
Relationships with non-co-located services
There are advantages to working closely with non-co-located services. This can help to expand the services available to SARC attendees and offer specialist support for specific groups. However, this requires ongoing commitment and resources to sustain momentum. There is an indication that if positive communication and relationships are not effectively and consistently maintained, then this might even have a negative effect.
Quality improvement
The literature explicitly discussed the use of data for developing evidence-based services. There are many ways in which the collection, analysis and reporting of routinely collected data can be used to evaluate the performance of the SARC and to inform quality improvement activities, for instance in identifying training needs, providing tailored care and addressing underrepresentation of certain groups.
Post sexual assault referral centre
Staff role in supporting service users to take up follow-up services
If SARC staff offer patient-centred, holistic support at the initial appointment then service users will be more likely to attend further appointments. This is because they will trust service providers, recognise their own needs and be empowered to take the next steps. Additionally, if follow-up appointments are clearly documented and there is a specific staff member to coordinate long-term support then uptake will be improved because service users will not have to arrange their own referrals at a time of distress.
Referral to mental health services
Survivors from underserved groups including males and people from the black and minority ethnic community face barriers in engaging with mental health care following a SARC appointment, which can negatively impact mental health outcomes. These barriers include gaps in provision, limited support (leading to more travelling and expense), long waiting lists, dismissive or alienating attitudes from providers and internalised stigmas or negative views of the services.
If SARCs face barriers when referring into mental health services, then service users may not receive the support that they require to meet their needs. This is due to a lack of effective resources at mental health services which can lead to SARC staff addressing the issues themselves, delays in referrals due to ineffective pathways or because the support that is offered by the mental health team is not specialised enough, or too variable in its approach to meet the service user’s needs.
Conclusion
The realist synthesis provided a theoretical framework for the wider study, which was organised around stages in the visual process model. This followed the service-user pathway from access routes, through to initial contact with the service and on to follow-up and referral to other services. Also considered was the likelihood of repeat contact with services.
The findings described how SARCs were intended to work as well as synthesising findings from empirical studies, which described how aspects of SARC services worked for certain groups of users and which recognised unintended consequences. Findings also articulated key concerns about difficulties in providing high quality services and highlighted areas that would benefit from further investigation.
Barriers to access
Important barriers to accessing services are related to lack of understanding and awareness about the existence of services, what they provide and how they are organised. Even when SARC services were known about, fear and anxiety about the consequences of contacting the services could be a significant barrier, especially when considering the prevalence of mental health problems and post-traumatic stress in this cohort. The relationship with the justice system could also be off-putting for certain potential service-users, for instance those with substance use problems.
This lack of awareness applies to the general population as well as organisations and agencies that might be in a position to signpost or refer service-users. There was a lack of evidence about the best ways to organise and deliver awareness-raising activities and where responsibility should lay.
There are further concerns that specific, vulnerable groups might face additional barriers to access, and that (partially as a consequence of low levels of exposure to or identification of these groups) SARC staff might be lacking in skills or knowledge about providing appropriate services.
Identifying and responding to mental health and substance-use needs
The literature suggests that consistent, systematic assessment processes are beneficial, both directly to identify and respond appropriately to unmet needs and indirectly to raise the profile of mental health and substance use problems in the cohort, thereby creating a more supportive culture.
Training in trauma-informed care and the promotion of trauma-informed interactions are also viewed as important elements in the provision of appropriate care. These can reduce distress, prevent re-traumatisation, improve long-term outcomes and potentially improve access through reputation and prior experience, in the case of repeat victimisation.
Service organisation
Multidisciplinary teams could have many advantages, including speed, quality and variety, coordination and continuity of care. A critical area that would benefit from further exploration is the integration or differentiation of roles. Potentially, this could be addressed by initiating a set of core competencies and responsibilities, such as FMEs being trained to deal with emotional needs. However, some elements of role clarity are important to maintain to reduce confusion and variability of service provision.
While relationships with non-co-located services can expand the services available to SARC attendees and provide access to specialist services, maintaining these relationships and positive communication requires resources and ongoing commitment.
There were several ways in which the systematic collection and use of route data could be used to improve and monitor services. For instance, in identifying training needs, providing tailored care, and addressing underrepresentation of certain groups.
Post sexual assault referral centre services
As discussed earlier, attendance at further appointments can be influenced by experiences at the initial appointment. Key mechanisms in the literature associate good outcomes with positive experiences, leading to service-users’ trust, recognition of their own needs and feeling empowered. Practical support can also be important to help coordinate follow-up support, particularly when service users have difficulties in arranging their own care through experiencing distress. There can be significant barriers in accessing mental health services, particularly regarding availability of appropriate services. This can lead to additional pressure being experienced by SARC staff members, particularly when the SARC does not have appropriate resources for mental health support.
Summary
The review identified problems with access that are largely rooted in population education, effectively targeted marketing, and system integration. Key issues are allocation of roles, responsibilities, and resources for addressing these problems, for instance whether the responsibility sits with the SARCs or other agencies.
Specific vulnerable groups might face access barriers and might also not be recognised within the services, unless systematic assessments and routine data capture and monitoring are carried out. This can lead to under-representation of required skills, knowledge and approaches to address the diversity of service-users’ needs. Systematic assessment of needs and good quality routine data capture and analysis could be important for local quality improvement activities that are context-specific and address system-level complexities.
The elements of trauma-informed care that are important in the SARC setting and the ways that these approaches can improve outcomes are clearly articulated in the literature. This review has extended evidence in the field by drawing together various elements into detailed hypotheses.
Questions remain, regarding the ideal make-up of multidisciplinary teams and the differentiation and sharing of roles, responsibilities, and competencies. Continuing coordination and follow-up by the SARC has benefits but clearly relies on the availability of appropriate resources. The extent to which a range of services (especially follow-on services) should be provided in-house or by external organisations is a complex issue, which is associated with system-level integration, available services and resources devoted to the initiation and maintenance of interorganisational relationships.
Chapter 5 Work package 4 case studies
This WP consisted of a case study analysis of six SARC sites identified from the cluster analysis, undertaken from service data gathered by the national SARC survey (WP2), which represented differing models of service provision.
The case studies included two main elements:
-
Documentary review of SARC guidelines, policies, protocols and procedures on mental health and substance use problems.
-
Realist interviews with SARC service users, and interviews and focus groups with SARC staff and partner agencies.
Full details of the documentary analysis methods and how it contributed to the realist evaluation have been published. 8
Documentary analysis
To review documentation from the six case study SARCs and extract information related to the identification, referral and provision of care for people with mental health and substance use needs. The document review examined critically the policies, protocols and procedures on mental health and substance use problems and explored how they related to the CMOCs being developed through the study.
Identification of data sources
Service managers and personnel were asked for their consent to support the identification of eligible documentation during WP2 (national survey of SARCs). During the case study site visits, SARC staff and/or researchers identified eligible materials through hand searches and SARC service intranet searches. In addition, internet searches identified documents such as Care Quality Commission reports and published journal articles related to the sites.
Data extraction
Data from all relevant documentation were extracted by a researcher using a standardised extraction form developed by researchers and based on SARC national service and NHS England guidance. This form was used to extract data on any policies, procedures and guidelines related to mental health and substance use (e.g. assessment protocols, referral pathways, intervention strategies). A second reviewer (another member of the research team) independently extracted data from a random sample of 20% of documents to verify intersubjectivity of decision-making, eliminate ambiguity and improve communicability of key concepts. All data were extracted into a Microsoft Excel spreadsheet.
These data were then used to create a ‘journey map’ for each site, providing a condensed and chronological representation of how SARC pathways identify and respond to mental health and substance use needs.
Programme theory development
The journey maps were used to refine initial programme theories identified in the realist review and through stakeholder consultation. This was done by examining evidence relating to the complex patterns of contexts, mechanisms and outcomes;21 for example, identifying potential blocks or aids to receiving appropriate support. Journey maps were also used to inform staff and service user interviews in WP4 by identifying any points of clarification needed about SARC processes and any opportunities for emerging theories to be tested. This process was supported by the LEAG, who reviewed one of the journey maps and suggested questions for staff based on this review.
Journey maps
Journey maps for each of the case study sites were created using a realist methodology and has subsequently been published. 8 These journey maps were used to orientate the researcher to the emerging context–mechanism–outcomes and inform the topic guides for each focus group and interview that was subsequently conducted.
Case study qualitative interviews (work package 4)
Sample and setting
A purposive sample of service users across the six identified SARC case study sites was recruited to ensure diversity with respect to gender, age, ethnicity, mental health status and timing of assault (recent or non-recent). The case studies were chosen to represent the three types of SARC models of working with mental health and/or drug and alcohol use that were identified from a cluster analysis of variables from the WP2 national audit of SARCs.
Survivor inclusion:
-
aged 18 years or over
-
able to read and understand English or there are suitable confidential translation services available
-
had an identified mental health or substance use need to take part in the interview.
Exclusion:
-
lacks capacity to provide informed consent
-
where participation is deemed to significantly increase risk to self or others.
SARC and partner agencies’ staff were also purposively recruited across the six study sites to ensure representation within the workforce; for example, within SARCs to ensure representation from management, FMEs and nurses, independent sexual violence advisors (ISVA), and within external agencies to ensure representation from relevant third-sector partners including sexual and domestic violence sector services and sexual violence counsellors, NHS mental health services and local substance use treatment providers. Where SARCs provided in-house or co-located therapeutic services, these staff were also approached.
Recruitment
Recruitment took place between July 2020 and April 2021. Service users were primarily recruited through WP3 three from those who had substance use consented to be contacted about other aspects of the study. Additionally, staff at the SARC sites were asked to identify any service users who may wish to take part in the interview. Researchers emailed or texted to make initial contact (using a method preferred by the person) and provided written information about the study (PIS). Where service users agreed to take part, a convenient time was arranged to undertake the interview.
Staff within the sites were informed about the study through emails, video calls, and face to face meetings (prior to COVID-19 restrictions). They were provided with written information (participant information sheet) and asked to contact the researchers with any questions. Where researchers had met members of staff, these staff were contacted directly to ask about willingness to participate. In other cases, emails were sent to groups of staff asking for volunteers. Staff within the SARC were asked to suggest colleagues from linked services who may be willing to participate. The researchers also approached research and development in linked mental health trusts to support recruitment of staff in these services. Individuals in these services were then contacted about participation.
For those who agreed to take part, researchers arranged a convenient time and location for the interview and obtained informed consent for data collection.
Topic guides
The topic guides were developed from a combination of theory-seeking, theory-refining and theory-testing questions and were developed iteratively with our increased understanding, to move from open (seeking) questions to explicitly refine hypotheses. Overall, the interviews sought to understand the mechanisms by which interventions are intended to achieve certain outcomes and the individual and organisational contexts that modify these outcomes.
The topic guides for staff in SARCs and partner agencies sought to understand how staff work with a range of mental health issues, to explore staff experiences of offering support to people who may have (or are at risk of developing) mental health problems, how those who have a high risk of mental health problems or pre-existing mental health problems are identified, how SARCs ensure service users get access to appropriate continuing care, and to explore the workforce training and skills needs in regard to supporting people with mental health needs, substance use and experiences of trauma. The topic guide was adapted for different staff groups and also for each site. Adaptations were based on data from analysis of site documents, which indicated the different activities undertaken at each site.
The service user topic guides sought to identify and explore their perceived needs in relation to mental health and substance use, how they view the identification and assessment of mental health problems and/or substance use, their views on the referral pathway, satisfaction with the services they received, and outcomes. Topic guides can be located in Report Supplementary Material 2.
Procedure
Following recruitment, researchers arranged a convenient time for the interview and obtained informed consent. Interviews and focus groups were conducted online (using video-call in Microsoft Teams). The interviews and focus groups were recorded in Teams and transcribed verbatim by a third-party transcription service with a confidentiality agreement with the University of Leeds. The transcripts were then de-anonymised to remove any names of people or places and were uploaded into NVivo (QSR International, Warrington, UK). Service user participants were sent an electronic £20 voucher to thank them for their participation.
In line with the realist approach to interviews,36 transcripts were analysed while data collection was continuing so that the content of interviews could be informed by previous findings. The research team met regularly (weekly) during the analysis process to discuss emerging theories and consider additional questions that may help to test and refine these theories. This included describing the content of recent interviews, comparing this content with data from other workstreams, considering the implications for the wider study aims and refining the topic guides to explore potential contexts, mechanisms and outcomes. In addition, three half-day workshops were held with the wider study team to discuss findings and refine theories. Members of the LEAG also contributed to these discussions, both in person and through email correspondence (further information on coding in NVivo is provided as a project upload).
Analysis
A within- and between-case analysis was conducted for SARC staff, partner agencies and service user interviews to identify and explore themes that are the same across services and those which vary between services. A deviant case analysis, where individual transcripts or site transcripts were interrogated for information that seems discrepant with the overall analysis, was also undertaken.
A separate NVivo file was created for each site and the site data were analysed in NVivo in two stages. For the first stage, an a priori coding frame was created from other data sources and used to organise the data from each site within overarching themes. A mixture of a deductive and inductive approach was used to develop the coding frame.
Initially, the coding frame was developed by considering data from the evidence review7 and realist synthesis, from the documentary analysis8 and from research meetings with the wider study team, including the LEAG. Unlike some realist analysis,37 the initial broad codes were created as themes rather than initial programme theories. This is because the study design meant that there was not a clear set of initial programme theories at the beginning of data collection; instead, they were developed throughout the project, including from the qualitative interview data. However, the codes captured themes that related to initial programme theories which had emerged throughout the wider study. In particular, the coding frame was intended to maintain the concept of a ‘journey’ through the service, in line with previous data collection. As such, it included themes related to accessing the SARC, to services provided within the SARC and to onward referral to other services. This approach supported the identification of potential blockages compared with potential opportunities in identifying and supporting mental health and substance use needs. Data from the transcripts were coded using this a priori framework.
In addition to this deductive approach, novel themes from the interviews were also derived. For example, where participants discussed contexts or mechanisms which were not captured in the coding frame, these themes were added either as another theme or as a subtheme to narrow the focus further. This added an inductive element to the analysis. Both the a priori themes and the new themes/subthemes were integrated to generate an overall description of the data.
In stage two, each code/theme was scrutinised to identify initial programme theories/CMOCs.
Ensuring rigour
Several researchers undertook the coding. Therefore, prior to coding, researchers undertook training to identify key features in the data (i.e. contexts, mechanisms, and outcomes), with all researchers then coding the same transcript and comparing findings to assess intercoder agreement. Additionally, a code book was developed, which included descriptions of all the codes and which was regularly updated, ensuring that all researchers were using the codes consistently. Similarly, at the stage of developing theories, all researchers explored the data within one theme/node and then met to discuss findings. This process ensured that all researchers were confident in the method of analysis and had opportunities to discuss any challenges. The research team met regularly during the analysis process to discuss emerging theories and consider additional questions that may help to test and refine these theories.
In addition to weekly researcher meetings, three whole-team meetings were held (October 2019, September 2020, May 2021) to discuss emerging findings and plan the next stages of data collection and analysis. These meetings included co-applicants, researchers, and lay representatives. Members of the LEAG contributed both in person and by email correspondence. These meetings helped to ensure that the study aims were being met and that data from other WPs were being considered alongside the data from WP4.
Consensus across the study team workstreams was sought at key points in the investigation; for instance, development of initial theories to be refined and tested and construction of the coding framework. This was achieved through a combination of workshops, meetings and discussion documents circulated by email.
Findings
Recruitment and demographics: sexual assault referral centre staff and partner agencies
A total of 26 interviews and focus groups were conducted with SARC staff, representing 31 individuals, and 17 interviews and focus groups were conducted with staff from partner agencies, representing 20 individuals. See Table 11 for demographic details. Interviews were conducted with staff and partner agencies from all six SARC sites and were purposively selected to represent the range of roles at each SARC based on the information obtained via the national survey (WP2) and documentary analysis (WP4).
| SARC staff (N = 31) (n) | Partner agency staff (N = 20) (n) | ||
|---|---|---|---|
| Sex | Female | 30 | 15 |
| Male | 1 | 5 | |
| Ethnicity | White British | 15 | 8 |
| Irish | 2 | 1 | |
| White European | 4 | 0 | |
| Black British | 1 | 0 | |
| Mixed | 0 | 2 | |
| Missing | 9 | 9 | |
| Age (years) | 18–35 | 4 | 3 |
| 36–45 | 6 | 2 | |
| 46–55 | 8 | 3 | |
| 55+ | 1 | 2 | |
| Missing | 12 | 10 | |
| Years at service | < 2 | 6 | 1 |
| 2–5 | 6 | 3 | |
| 6–15 | 6 | 4 | |
| 15+ | 2 | 3 | |
| Missing | 11 | 9 | |
| Role | FME | 5 | 6a |
| FNE | 6 | 2b | |
| Crisis worker | 7 | 5c | |
| Manager | 5 | 3d | |
| ISVA | 2 | 2e | |
| Counsellor/psychologist/psychotherapist | 4 | 0 | |
| Other | 0 | 2 |
Within sexual assault referral centre analysis
In this next section, data are presented on the within-case analysis from SARC staff and partner agency care providers in each of the six case study sites. Four central themes generated from the programme theory have been identified where there is strong and consistent data emerging:
-
Access to the SARC and initial engagement.
-
Identification and assessment of mental health and alcohol/drug use needs.
-
Care and treatment for mental health and psychological distress that is provided within the SARC service.
-
Care and treatment that is provided by partner agencies.
Sexual assault referral centre 1 (NHS London, in-house psychology)
Case study 1 is a multisite NHS SARC service covering the city of London.
Increasing access to the sexual assault referral centre
If the person lives a long way from one of the SARC1 bases, then they may have to spend a long time on public transport (as it is a major city) to attend. In addition, the person may be on a low income, which prevents them from buying a travel ticket or using a taxi. Sex workers may feel discriminated against or may not trust the police, which acts as a barrier. The SARC staff talked about workable solutions to increasing access to under-served groups, including having a male crisis worker. In addition, if appointments can be offered online this reduces ‘did not attend’ rates, improves access and offers more flexibility for appointments.
Sometimes, coming from a borough that is really far away from one of the sites can be a deterrent because you can spend a lot of time on public transport which would obviously impact on being able to access the service. But now working online, that is one of the barriers that in a way has been made a lot better, has improved access. However, there are other issues obviously, those clients with no internet or who may not have the privacy, they still require to be seen face-to-face.
(SARC1 staff member)
Assessment of mental health and alcohol/drug use
If someone calls the SARC to make initial contact, there is a variation in how the initial assessment is completed with some crisis workers sticking rigidly to the proforma and others tailoring the assessment to the individual needs or situation.
There are two strands to assessment: standardised questions and an assessment of risk using professional judgement. If forensic examiners are completing mental health risk assessments as part of the FME appointment, this may add additional time to what is already a lengthy procedure, and when someone has multiple needs it can become even more time consuming to collect the information. A solution suggested is that this assessment could be performed by another member of staff (on the same day). If the person requires emotional support during the forensic medical examination, the FME will provide some reassuring responses but tends to refer to another member of staff (crisis worker) as they are perceived as ‘more qualified to support them’ and that FMEs are not ‘mental health trained’.
If SARC staff or police ask about drug and/or alcohol use, especially if asking without compassion, this can be perceived as ‘victim blaming’ and may result in the person not wishing to disclose their substance use.
All cases are reviewed within 24 hours. A decision is made jointly with the person about what interventions may be suitable (i.e. to offer counselling or clinical psychologist). However, if the person is currently actively suicidal then they would not be offered the in-house option and referred to hospital emergency department psychiatric liaison and crisis intervention.
Interventions
If there is a clear policy on when and how to triage and refer people with complex needs to external agencies, including mental health, then the person is supported to get their needs met. This process is supported by weekly case reviews in the multidisciplinary team meeting. The decisions are made as to whether in-house support or onward referral is the most appropriate option for the person.
If a SARC service provides in-house therapies, this is seen as beneficial because they can obtain all their support post assault in one place. It also improves engagement in therapies, as having to work with multiple external agencies can be overwhelming. However, if people have multiple and complex needs then the SARC in-house support staff do not feel that they have the expertise to address these needs (as their focus is ‘on trauma not complex mental health needs’) and therefore they ask for psychiatric consultation from external mental health provider. However, if the SARC refers to an external mental health service, they find that the waiting lists are long and often the person is left with no support. SARC staff report that they spend considerable time ensuring that their referral forms are accurately completed to meet the remit and threshold of the service. Staff also report barriers to having some referrals accepted by external mental health services due to what is perceived as extremely high thresholds of mental distress needing to be demonstrated to be accepted. However, if the SARC can offer a range of options for psychological support, such as single sessions or group sessions, they can tailor the offer to the individual and ensure they receive some form of support even if the waiting lists for more intensive therapies are long.
In addition, immediate psychological support could work as preventative in terms of reducing the impact of the trauma, thereby reducing the need for long-term interventions that may be required if someone is not able to access immediate support, but this has not been formally evaluated.
If the person is referred from the SARC to an external mental health service, the service may lack knowledge or awareness of the constraints on what types of interventions can be offered in the pre-trial phase. The SARC staff can advise on the requirements for pretrial therapy as well as supporting the mental health staff in how they can integrate the trauma into their continuing mental healthcare plan so that the person achieves optimal outcomes.
So there are gaps in the knowledge [in other mental health services] and perhaps sometimes not feeling as skilled to address the trauma of rape and sexual assault, which obviously in SARCs is our bread and butter.
(SARC staff member)
If SARCs wish to develop better referral pathways with mental health services, this would require considerable time especially in a large capital city (where SARC1 is based) with multiple providers to navigate. However, closer relationships with partner agencies (such as being able to have an informal chat about a referral before sending it over) and having a specific person who acts as a point of contact in the partner agency improves the chances of the person being connected to the right service and reduces the chance of the referral being rejected by the partner agency.
In terms of substance use, the SARC reported minimal barriers to referring people who identified as needing help with their use. The SARC reported that this is because they have good working relationships with local substance use services. From a drug/alcohol external partner perspective, they will try to see a person referred from the SARC on the same day if possible and not put them on a waiting list. There is no specific link worker to the SARC in the drug/alcohol service team. The drug and alcohol partners report they routinely assess for domestic violence, but not sexual violence, and some staff may not feel confident to undertake routine enquiry. However, if drug/alcohol staff are aware of the role of the SARC they are more likely to make people who disclose sexual violence aware of the role of the SARC and make a referral.
Sexual assault referral centre 2 (private provider, town in northern England covering a mainly urban, ethnically diverse regional area)
SARC 2 covers an urban, densely populated, socially deprived and ethnically diverse area of the north, which includes post-industrial towns and cities. The forensic examinations are conducted by forensic nurse examiners (FNEs; qualified adult nurses). The crisis workers work alongside the FNEs and make the initial contact with a person, usually over the phone. The SARC reaches out to local services via email to make services aware of their service. More recently, the crisis workers have been contacting local services that support marginalised groups to encourage more people to come forward and report sexual assaults (this includes people from black and ethnic minorities, LGBTQ+ and student support services). They also offer online training to external agencies to raise awareness of sexual assault, and what the SARC can offer. However, staff also acknowledge that this kind of outreach is hard to do when the service is really busy.
Assessment
At first contact the crisis worker will undertake a brief interview to collect information and assess capacity to undertake a forensic examination, which includes asking about mental state and intoxication. The FNE would undertake a full assessment at the time of the attendance at the SARC and the crisis worker would be present throughout that appointment. However, it was acknowledged that the FNEs are not mental health professionals and therefore if a formal mental health assessment is needed, then there are limited options but to call 999 or assessment at a hospital emergency department:
it’s really difficult because as nurses, although we’re trained to recognise that somebody needs mental health support, we’re not trained to carry out Mental Health Act assessments. So sometimes, I suppose, when we feel that that’s needed, it’s … our options really, if the crisis team can’t intervene at that point … our options are 999 or A&E which are … I don’t really think are the most suitable options for our patients.
(SARC 2, SARC manager)
There is a SOP for alcohol and drugs. Withdrawals are assessed using standardised tools, such as the Clinical Institute Withdrawal Alcohol (CIWA) scale, and the person is constantly assessed during their time at the SARC. SARC staff noted that they were surprised at the level of needs of people who came to the SARC in terms of mental health and at time this felt quite ‘frightening’ to be making decisions about whether someone was safe to go home or needed further support from mental health. To address this, SARC2 staff have been able to access training to address this deficit in knowledge and confidence.
Intervention
SARC2 did not offer any in-house interventions apart from a six-week follow-up call.
Onward referral
The SARC has a range of information on local services to pass on to people for them to follow up for themselves. However, if there is a mental health concern or crisis, the staff will phone the mental health crisis team on the persons’ behalf.
When you’ve got somebody in crisis; that’s when we seem to struggle, or when you need somebody to have a mental health review. So, for example, they’re in psychosis, you don’t think that they can consent to a medical. You’ll send them away to be mentally health assessed and then they’ll come back the next day and they’ve not seen any mental health professionals.
(SARC2 staff member)
The SARC staff talked about how challenging it was to access urgent mental health support for people that they felt concerned about. When they would contact the person’s mental health worker, often they would say that the person was fine to go home without actually assessing them and the SARC staff expressed concern about this:
They always say this she’ll be fine, just send her home, part of me is thinking wait a minute, they’ve just experienced a really bad trauma … this could exacerbate any pre-existing conditions … and I’m not happy just to let that person go
They also talked about the length of time it takes to get a crisis response from the mental health team if they did not feel that the person was safe to go home after the SARC. In one example, a FNE described how they were with someone for eight hours while they were trying to figure out a plan, and in the end the person was taken to the local hospital emergency department for a psychiatric assessment.
I was with this patient nearly eight hours because I didn’t feel that it was safe to let her go, but we didn’t have a safety plan in place because nobody would see the patient. It was just like hot potato with the patient – until eventually we could get … because we couldn’t even get her in a car so that the police take her to A&E for her safety. So, in the end we still didn’t have a correct safety plan in place but at least we could get her into a car to get her to A&E, which then she was sectioned after that.
(SARC2 FNE)
The other complication in accessing the mental health crisis team is the geographical boundaries that the SARC spans. For instance, the manager described how difficult it was to get a mental health crisis visit to the SARC because the survivor was from another town with a different mental health service to the one that covers the city where the SARC is based.
Follow-up
Every person who comes to the SARC is entered on a ‘safeguarding tracker’ and this is where referrals to other agencies are logged and the outcomes of those referrals. SARC2 staff undertake a six-week follow-up call and, in this call, they check the progress of any referral that has been made, whether they have experienced any trauma symptoms and if there is any further support that they need. If needs are identified, staff would signpost to a variety of services, depending on the need. Outcomes of referrals are logged in the safeguarding tracker and if the person has not heard anything from the referral at this stage, the SARC staff will chase it up with the external agency.
We’re very client-led, we very much go at their pace … We don’t have anything like if they don’t answer the phone three times, their case is closed and stuff like that, we’ll be there whenever someone needs us to be there basically, and even if they shut the door 20 times, the 21st we’ll still be there kind of thing. So yeah, I just think we’re lucky enough to work within a framework that allows us to be really flexible and responds to the clients’ needs really, as opposed to them needing to fit with us.
(SARC3 ISVA)
Sexual assault referral centre 3 (security provider, private sector, urban and rural area south of England)
There is no in-house psychological support such as psychologist or counselling at SARC3. The crisis worker interviewed has a counselling background.
Access
The SARC is actively involved in raising awareness of service to external agencies such as GPs, police and social care. However, they also note that if the service is short staffed then there is less time to be able to do the outreach which reduces the chances of underserved groups engaging in the SARC. The SARC are seeing more males attending and recognise that they have specific needs, so there is a plan to recruit a male crisis worker who will also be able to do outreach with LGBTQ+ community.
Assessment
On initial contact, the crisis worker (who has a counselling background) completes an initial set of questions on an in house proforma. If this is conducted over the phone, it is harder for the crisis worker to notice mental health or substance use issues because they are not able to see non-verbal behaviours and other visual cues.
The main assessment undertaken by the crisis worker (face-to-face or over the telephone) involves asking about mental health issues and how they are managed. Further assessments are undertaken by the doctors and nurses, who use their clinical judgement to make assessments of mental health and substance use need as opposed to using standardised mental health screening tools, like the crisis worker. However, if a screening tool is used then the onwards referral may have more impact because it provides a meaningful score that the partner agencies understand.
If you use a screening tool, then when you’re referring someone, you can actually give a concrete, you know, so and so’s score is actually 8. So that person who will be familiar with the score will sit up and listen. Whereas if you’re just giving a clinical assessment without the backup of the screening tool, it’s not so impactful.
(SARC3 FME)
There is no consistent approach to the assessment of substance use issues because every case is different; therefore it is difficult to have a set protocol for this. According to SARC3 FMEs, people are more open about their mental health than their drug/alcohol use and often reported that their use was ‘under control.’
Intervention
If someone attends SARC3 with mental health problems, then they are signposted to their GP or an external counselling agency. The person attending the SARC is asked to give consent for information sharing with other agencies such as mental health, safeguarding team, drug and alcohol service. If a referral is required, the SARC staff make initial contact on behalf of the person which means they do not have to make contact themselves and to avoid them getting ‘lost in the system.’ If a person has existing mental health problems, SARC staff notify their mental health team to inform them that their client has attended the SARC. SARC3 has limited contact with GPs but with the person’s consent the SARC will ring the GP and talk directly to them, as email and telephone messages may take too long to action if there is an urgent concern.
If the person is not in an acute mental health crisis, SARC3 staff find it difficult to meet the person’s needs as there is limited local support except for an external counselling service. Other provision locally includes talking therapies and trauma therapy (six to eight sessions). There is no formal referral to rape counselling services and people need to self-refer. If a person has significant mental health needs, they may be able to access the external mental health provider for six to eight weeks of therapy then, if needed, they can move on to waiting lists for more long-term therapy. The waiting list at that time was three months.
Withdrawal from drugs or alcohol can be a barrier to attendance as the examination takes several hours and the person is unable to cope with this while withdrawing. SARC3 has no provision to manage opiate or alcohol withdrawals during attendance.
We’re in quite a difficult position at the moment in the SARC. Most SARCs, and I will talk about our service, in that we don’t have any medication within the site to help with drug or alcohol withdrawal … And we need to know whether they are going to be withdrawing, for instance, when they come to us because they’re with us for a long time.
(SARC3 FME)
There are no formalised procedures for the care of people with mental health needs and staff feel that more could be done to support those needs. There are no formal referral pathways and decisions about need for referral are made based on clinical judgement of the person’s needs. People who are not in crisis are given information about how to make contact themselves.
The SARC3 staff make follow-up calls to check on how the person is, and inform about what referrals have been made, and progress on those referrals. If the SARC has any concerns about the well-being of the person at that stage, they have limited options other than refer to the GP or other partner agency. Referrals are hampered by the lack of concrete connections to local partner agencies.
There are no formal referral pathways to substance use. One worker said that they had so far not encountered anyone who needed help with this issue but said that they would ask as colleagues if they needed information about local services. According to the manager, the crisis workers have good knowledge of local services. One SARC worker has created a resource list that can be printed and given to people to pursue their own self-referral. SARC will make the initial contact with external agency to make it easier for the person to then make contact.
We do hand out telephone numbers and email addresses for some different agencies, but that’s really left to the client to contact them independently, rather than for us to be making the referrals. So, it would be quite nice to have a specific, okay, we’ve identified that someone has mental health issues, so this is the process or procedure that we’re going to follow.
(Crisis worker)
Sexual assault referral centre 4 (private provider, North Midlands city and area)
SARC4 uses a range of strategies to increase awareness of their service including social media (Twitter), outreach to GP practices, universities (such as freshers’ week stalls) and have worked with the human trafficking team, but the women they met at that point did not want to engage. An open day was planned for all the local LGBTQ+ specific agencies to promote the service to this community. SARC4 has a quarterly operations meeting where all partner agencies are invited but it was noted that, despite an invitation, there has yet to be any representation from the local mental health provider.
Sex workers access are less likely to engage with the SARC, for fear of judgment and lack of understanding. If the SARC works closely with the local sex worker support service then the women will be able to get to know the SARC worker, form a relationship and trust them. This means they are more likely to engage with the SARC should they need that service.
If external agencies can physically accompany vulnerable people to the SARC then engagement will be increased.
Assessment
The nurse undertakes an assessment based on the interview and makes decisions regarding onward referral using professional judgement.
Intervention
There is no in-house mental health provision. The SARC liaises with local mental health services if a need is identified. There is a single point of access in the mental health service and from this point the referral is referred onto the most appropriate service. If someone needs psychological therapies they are referred to that service and, for more complex needs, they may be referred to a psychiatrist and have a care coordinator. If a person presents to the SARC in an acute mental health crisis they are referred immediately to local emergency department for emergency mental health assessment. However, this is perceived as not a suitable option for someone who is traumatised as it is busy and noisy, and seen as a last resort when they have no other option.
We send them there because we don’t know what else to do in the SARC … we don’t see SARC as a place of safety for somebody.
Onward referral
There are no specific referral pathways as external services change a lot. Most people who come to SARC4 are already known to mental health services so the SARC staff tend to call the crisis team who can then link up with their named worker.
If person is directly involved in decisions about follow-up care, then they feel more empowered and more likely to engage with the referral process. The SARC staff receive timely feedback in terms of outcomes of referrals they make to mental health including receiving an email within 24 hours to acknowledge receipt of the referral and the mental health team contact the person themselves within 48 hours. If SARC staff check that referrals are being followed through, then the person is less likely to get lost in the system.
SARC 4 offers follow-up calls by the nurse at six weeks post visit to see how people are getting on, whether they have managed to engage with other services and whether their referral has been actioned. If there has been no action, the nurse will offer to follow it up on their behalf if they wish. The lack of geographical co-location is mentioned as a barrier to access to mental health services – one SARC staff member said that in five years they had never seen the mental health crisis team come to the SARC.
Sexual assault referral centre 5 (private provider, south-east England, semi-rural and provincial area, in-house mental health pathway)
SARC5 provides a bespoke in-house, stepped-care, talking therapies service in partnership with the local mental health NHS trust and two third-sector organisations. Having a clinical psychologist with expertise in trauma influences the trauma-informed culture of the entire SARC. They role model the use of non-pathologising language and reconceptualise presenting issues in team meetings through the lens of complex trauma. In addition to improving the approach that people receive in the SARC, the psychologist also supports the understanding of vicarious trauma that is, the impact of working with trauma on the SARC staff.
I am very clear and very animated about ensuring that we don’t pathologize trauma and we are very careful with our language that we use in discussions around sexual trauma.
(Clinical psychologist)
Assessment
The SARC uses trauma screening scales and work is in relation to a person’s own understanding of what is happening to them and their goals for therapy, not a focus on symptom reduction and not work in a medical model (i.e. diagnosis of disorders). Through the continuing work on the psychology pathway, the psychologist can feed back to the SARC team about the positive things that people say about their experience of attending the SARC and informs the team that their compassionate and caring approach is likely to have prevented secondary trauma.
without you, the client would come with even more secondary trauma or another experience that felt very sort of powerless or traumatising in some way.
(SARC5 clinical psychologist)
Intervention
Sexual assault referral centre 5 has an in-house psychological therapies service including counselling and clinical psychology service that NICE offers recommended trauma therapy – eye movement desensitisation and reprocessing (EMDR) therapy and CBT. This was established in partnership with the mental health provider and emerged from a recognition that there was a gap in service provision for trauma.
Despite the in-house provision, SARC5 staff are aware of gaps in the mental health services. An example given is women in later life who have experienced a non-recent trauma that is affecting them now. They do not meet the criteria for CMHTs despite their levels of distress and risk being high. The psychologist also mentioned holding a lot of risk and complexity without the support of being within a mental health multidisciplinary team.
The SARC team can provide consultancy and specialist assessment to the CMHT, and this can improve the quality of the intervention that the person receives as well as reducing the sense of fragmentation that can occur across various parts of mental health care. If SARCs refer to many other agencies, the person must talk about their issues repeatedly and there is a risk that the person will disengage as they feel overwhelmed and that no one is supporting them.
Trauma is experienced as fragmented and non-linear, and the psychological therapy pathway offers a timeline and by being embedded in the SARC provides the person with ‘real safety’. In contrast, usual care (referral to an anonymous clinician in a separate service) seems very disconnected from the safety of the SARC and may result in secondary trauma, especially if it is a complex process and the other service is not operating in a trauma-informed way.
People with complex mental health needs who do not get what they need from other services may turn back to the SARC for help, especially if they have not heard back about onward referrals. Chasing up referrals to external agencies can be time-consuming for the SARC staff.
Sexual assault referral centre 6 (NHS provider, no in-house clinical psychology, no standardised tools)
Increasing access to sexual assault referral centre for vulnerable groups
Sexual assault referral centre 6 monitors the diversity of the people who attend and actively outreach to key services for the under-represented groups to increase awareness in those services about what the SARC offers and how to access. Both the SARC staff and external agencies are aware that services need to be able to address the specific needs of diverse groups, including men (who are less likely to report a sexual assault because of the perception that it is a gendered crime and the heightened levels of shame that men feel). The male survivor agency pointed out that the lack of diversity in SARC team (staffed by white middle-class cis-gendered women) may be a barrier to engagement as it does not reflect the diversity of the potential attendees (underserved groups such as people who identify as cis-male, LGBQT+, people from black and ethnic minorities). To address this, SARC staff reported that they engage in outreach activities to target under-served groups.
An important example is that the SARC delivers training to the police on how to work with vulnerable people who report a sexual assault, and this training helps police to provide a sensitive response to those who may be presenting with multiple needs. This helps the person to feel more comfortable in the interactions with the police and they may be more likely to access the SARC and get their needs met.
The external sex worker agency recognised that fears of drug withdrawal can prevent some women from contemplating attending the SARC. Flexibility is important for people who are dependent on substance use. If the SARC can be flexible with appointment times to fit in with treatment (such as methadone pick up times) or allow people to bring their own alcohol to stave off withdrawals, then the person is more able to engage with the SARC process.
Mental health and substance use assessment
The SARC manager, crisis workers and forensic examiner all commented that many people who attended the SARC had pre-existing mental health and other needs, and it was their impression that the complexity was increasing over time, and that there was a need to take time to undertake a comprehensive assessment. One person mentioned that this was especially important when the SARC was unable to access information and medical notes from other service providers.
If you went to your GP, you’d have a bit of background. And if you went to A&E, they can at least access your hospital letters. We don’t know anything about the clients who come, but you’re with them, sort of, many hours, and I think that’s why our history has just, sort of, got longer and longer.
(SARC5 FME)
CMO configuration
If the SARC staff use their professional judgement as well as good interpersonal skills (non-judgement, person centred; context) to undertake a more detailed and accurate assessment (mechanism) of the complexity of need then this would improve identification of need (outcome). One contextual aspect that was mentioned was that the FME had an interest or background of safeguarding or domestic violence. In terms of the mechanism of assessment, this was performed using a proforma developed in-house. Psychological screening tools were not used. Professional judgement was seen as safer and more accurate and that use of screening tools with their cut-off scores were seen as too limiting in giving a ‘black and white’ response. If the person is assessed too soon after the assault, their feelings are often numbed or in an acutely distressed state and this will not provide an accurate picture of their mental state.
Substance use
The crisis worker would ask about substance use, but the FME would assess more fully as part of the medical history. A pro forma is used to assess drug and alcohol use at the time of assault and a toxicology screen would show what drugs had been used up to 14 days before. Once again, the importance of using non-judgemental and sensitive approach was stressed to help the survivor feel more comfortable about answering questions. However, there was some element of dilemma about the gathering of information on drug and alcohol use – that the forensic examination notes are admissible in court and disclosure of substance use could impact on the case. However, there were also comments about the importance of ‘honesty at the time of the examination as this would be a better strategy should the case go to court.’ If the client is reassured that the police will not prosecute for illegal drug use, then this will be a better strategy if the sexual assault case comes to court.
Interventions
Sexual assault referral centre 6 has an in-house counselling service, which people can access directly or as part of aftercare. They reported that they offer pretrial ‘stabilisation therapy’ approved by the criminal justice system as ‘CBT and EMDR are not recommended as pretrial therapy.’ Pretrial therapy guidance stipulates that the person should not discuss details of the assault as this can impact on the outcome of the court case. The pretrial therapy guidance also makes it clear that no one should be denied the treatment that they really need while waiting for a court case. However, if the person is not allowed to discuss the trauma this is an obstacle to processing and recovery, especially if there are delays in the case coming to court (especially as an impact of COVID-19).
The SARC is commissioned to provide short- to medium-term therapy, which may not address complex trauma but can help with symptom management and coping.
I think with complex trauma, what we’d be hoping for, is to be able to provide that psychoeducation to help clients unshame in that way, that they can understand why they feel like they do. And then it can begin with some coping strategies, some ways of managing how they feel.
(SARC counsellor)
Psychoeducation is offered as a group and survivors can gain peer support and share strategies to help them cope. However, if a person is deemed too ‘unstable’ they would not be offered in-house counselling as there needs to be some level of stability to cope and benefit from counselling.
The SARC also provides support for significant others – if they can learn about trauma and how it impacts on a person then they are in a better position to support them.
SARC staff see ‘little trauma’ being able to be dealt with by in-house counselling and ‘big’ trauma by local talking therapy services.
External agencies/onward care
Counsellors may refer on if they feel that the person needs specialist help. Onward referral tends to be via GP; however, some GPs encourage self-referral to single point of access or talking therapies. GPs are perceived as gatekeepers, not as direct referrals to CMHT. However, people who are feeling very mentally unwell may struggle with self-referral. Some people may already be under the care of mental health and/or substance use services. Some people may perceive the referral onwards as negative or punitive; for example, there may be fears around referral onwards for substance use issues (feeling blamed for their choice of coping mechanism). However, if they can be reassured that the referral is supportive not punitive then they are more likely to engage.
The FME talked about the variety of thresholds of risk that doctors at the SARC have and this can lead to inconsistencies in action in relation to risk assessment. Therefore, if doctors had more training in mental health and risk, they would feel more confident in managing mental health rather than focusing on risk. Safeguarding referrals were made to protect the doctor by erring on the side of caution.
Mental health and social care have ‘astronomically’ high thresholds; if SARCs do not refer people as they are worried about not meeting these thresholds, then this will reduce the metrics of need for that service. It is important to refer despite the high thresholds.
There may be many third-sector services that could be useful to the person, but the SARC staff may not be aware of them or have the time to develop relationships with the services. External agencies providing support include NHS psychotherapy, which specialises in treating people with complex mental health and personality problems, some of whom have experienced sexual violence. The city-based sex worker charity offers EMDR/CBT, which is useful in terms of access, as NHS services have long waiting lists. The local rape counselling service offers counselling, as well as more directive therapy such as CBT and other adjunct complementary therapies, such as massage and walking groups, to promote well-being. However, if someone has complex needs (which many attendees of SARC6 do) then their presenting issues may not be a neat fit for external agencies, and they end up being passed from one place to another thereby not receiving the right care.
Between-case analysis
In WP2, a cluster analysis was performed on the mental health-related variables and three clusters of SARC respondents emerged. While this was useful in informing the purposive sampling of the SARCs for the case studies, there are some considerable differences between the SARCs even within the same cluster as well as between clusters. This next section focuses on the crosscutting similarities as well as some divergencies that have been identified with reference to the programme theories identified in the realist review.
The importance of an effective interface between sexual assault referral centres and external agencies
An effective interface relates both to SARCs’ knowledge of external agencies who can provide support and/or treatment for mental health and/or alcohol/drug issues as well as these agencies having awareness of SARCs, what they offer and what is involved. As well as knowledge, SARC and partner agency respondents talked about the importance of having a two-way relationship that involves being able to discuss potential referrals and offer joint consultation and advice in a timely way. The SARCs varied in how close their relationships were for a variety of reasons. The SARCs based in cities and regional areas have multiple mental health and alcohol/drug providers that they could potentially refer to (depending on the person’s postcode). To navigate this complex landscape, there needs to be time and resource to do this. One SARC (SARC2) is planning to create a role within the team to act as mental health liaison to address this need. The other example of building awareness and relationships was mentioned by SARC6, which offers open days to partner agencies on a regular basis. SARC4 regularly invites partner agencies to quarterly operational meetings but have yet to have anyone from the mental health service attend. In the partner agency interviews, many mentioned that they had a lack of knowledge about what their local SARC offered and in some cases, there was a misunderstanding of the range of ongoing psychological support offered by the SARC. An example of this was where an NHS psychotherapist assumed that their local SARC offered all levels of psychological therapy for trauma when in fact they only offered short-term counselling. This lack of understanding and awareness of the local SARC also meant that if a person disclosed a sexual assault to a worker in the partner agency, they would not necessarily suggest contacting the SARC. This represents a missed opportunity to receive some immediate care and response from those with expertise in sexual violence, the opportunity to pursue a criminal prosecution, and missed opportunities for referral to trauma therapy if that need was identified.
Outreach work that targets people who are often ‘underserved’ such as sex workers, LBGTQ+ and trafficked people was mentioned. SARC6 monitors the demographics of who attends and actively outreaches to groups that are not attending. They have a strong relationship with the local sex worker organisation. SARCs 2 and 4 also have relationships with local sex worker agencies. However, despite the high levels of people who attend the SARCs who are already in receipt of care from mental health and substance use services, there was limited evidence of the SARCs engaging in outreach to these services specifically. Conversely, the rates of sexual assault experienced by those in mental health services is high yet when the mental health partner agencies were interviewed there was limited evidence that there was an effective pathway to SARCs from these services and a lack of routine enquiry.
Identification of mental health and alcohol/drug needs
Sexual assault referral centres reported that mental health assessment in general consists of semi-structured interview (usually by the FME, with some input from the crisis worker) as opposed to the use of standardised screening tools. SARC3 FME and crisis workers make decisions as to what the needs are based on their professional judgement. It is important to note that there is limited mental health expertise or training in the SARC workforce so this ‘professional judgement’ may be inconsistent. The psychologist at SARC5 emphasised the importance of taking a non-pathologising approach when working and assessing people who are experiencing a normal reaction to a trauma. To work in this way, those who assess the mental health needs should have a good grounding in the ways in which trauma manifests in individuals. Some SARCs have described feeling concerned about the safety and well-being of a person attending the SARC and sending the person to a hospital emergency department for an emergency psychiatric assessment while also acknowledging that this is a completely unsuitable environment for someone who is in mental distress after a trauma. They see this as their only option, and one SARC mentioned that despite contacting the local mental health crisis team they had never once attended the SARC to see an attendee.
Drug and alcohol use is assessed by asking about past and current use as part of the overall assessment interview. Some SARCs mentioned a reluctance to mention substance use due to the concern they might be perceived as ‘victim blaming.’ Others mentioned that they felt most people would not be very forthcoming about any alcohol or drug use issues, but another felt it was better to be honest in the assessment as it may affect their sexual assault court case if it came to light that they did have a drug or alcohol issue and they had not mentioned it at the forensic examination. Other FMEs were concerned about exploring too much about substance use as the examination records were admissible in court.
The other area where substance use was mentioned was in the assessment of capacity to consent to a forensic examination if the person was intoxicated. There was no standardised approach to this assessment, and it was undertaken on an individual basis and using professional judgement. This means that some examinations were conducted even if the person was intoxicated, if the examiner was satisfied that the person had capacity, whereas other exams might not take place if the person had taken any drugs and/or alcohol. There is a window of opportunity for the collection of forensic samples and for some survivors; missing this window could mean that the prosecution cannot proceed if the examination is delayed due to any kind of intoxication. However, ensuring capacity to consent to an invasive lengthy and traumatic procedure is essential to avoid re-traumatising the person and there needs to be clearer guidance on how to manage the issue of capacity to consent when substance use have been consumed.
Another barrier faced by those who have drug or alcohol dependency is that the SARCs in the six case studies did not have the capacity to assess withdrawals and offer opiate substitution therapy, such as methadone or offer treatment for alcohol withdrawals. Withdrawals are likely to happen during a SARC appointment due to the length of time required (which can be several hours) and often such a visit is unplanned, and the person may have been in another service prior to the SARC, such as at the police station. SARC2 can assess alcohol withdrawals using the CIWA which uses objective signs (sweating, tremor, restlessness) and symptoms (anxiety) to assess severity of alcohol withdrawal. If the CIWA score indicates withdrawals, then they can offer some alcohol to consume to reduce withdrawals and prevent harmful outcomes of withdrawal (such as seizures). However, SARC2 is not able to assess for opiate withdrawal and offer opiate substitution therapy. Both SARCs and external agencies recognise that the concerns over withdrawals will be a significant barrier to attendance at the SARC for anyone who is dependent on alcohol or drugs who has been sexually assaulted.
In-house psychological support and external mental health and drug and alcohol support
Sexual assault referral centre 5 has an in-house psychological therapies pathway, which is the most comprehensive service within the six SARC case study sites. This is led by a clinical psychologist who is an expert in trauma. There are two benefits to this service. First, the person will receive an expert triage of their psychological needs and timely access to appropriate support, either in-house counselling delivered by two local non-government organisation (NGO) rape counselling services, or in-house trauma therapy delivered in partnership with the local mental health provider. The second benefit of this service is the impact that the clinical psychologist has to the ethos of the SARC team by promoting the trauma informed care approach in team meetings and other informal discussions. The input of the clinical psychologist also supports the SARC staff in managing the vicarious trauma they may experience. This was also seen as a benefit in the other SARCs that had in-house provision (SARCs 1 and 6).
Whilst we have training in understanding the role of vicarious trauma, our nursing colleagues won’t. And I think it’s just really important that we are always just checking in with that really, in a very informal basis. We don’t provide clinical supervision but I think that those discussions go some way to just normalising some of the experiences that our nurse colleagues may be having.
(SARC 5 clinical psychologist)
However, there are also some challenges too. Despite the comprehensive in-house offer, there are some people who are identified as having too complex needs for the in-house service, and they are then referred to the mainstream mental health services. There are gaps in provision for people who are too complex for the in-house offer yet not crossing the threshold for secondary care. The other barrier is long waiting lists even if the person crosses the threshold (NICE recommends that trauma therapy should commence within four weeks of the event). The only other SARC with clinical psychology is SARC1 (London). As in SARC 5, the presence of the clinical psychologist impacts on the assessment and triage of the person who presents at the SARC, and every case is reviewed in a multidisciplinary meeting. SARC1 does not, however, offer the same level of in-house support as SARC5 and will refer to partner agencies for trauma therapy and other mental health support. SARC1 also report challenges in referrals due to high thresholds and long waiting lists and even stated that they offer some form of support to people they feel have high needs rather than leave them with no support at all. There was a suggestion that low level and immediate support may be helpful and potentially prevent a longer-term psychological problem. SARC6 has an in-house counselling service, which can offer supportive interventions that can help stabilise trauma reactions but does not offer trauma therapy and does not work with people with severe or complex needs; however, there is no formalised psychological assessment at SARC6 to inform decisions about whether someone needs higher-intensity therapies.
In the rest of the SARCs in the study, the crisis workers offer most of the emotional support at first contact, the main examination and via some form of follow-up calls and appointments; the nature and purpose of the ‘follow-up’ is inconsistent across SARCs. In some SARCs, the crisis workers are involved alongside the FME in undertaking a mental health assessment, including risk assessment as well as enquiry about drug and alcohol. Crisis workers and FMEs come with a variety of backgrounds, and few have a mental health practitioner background and/or training. Without the presence of a mental health expert (such as in SARCs 5 and 1) they report a lack of understanding of what types of mental health and other psychological support is available and how to refer. There is also a lack of use of standardised tools to screen for mental health and substance use needs. Use of standardised screening tools can be helpful in facilitating referrals to external agencies, as well as providing a consistent way of identifying needs, as variability of assessment of risk and mental health between practitioners has been mentioned.
There is no evidence of any support offered in relation to substance use. SARCs will either signpost the person to their local drug and alcohol service or the person must self-refer. In some examples, SARC1 reports a positive relationship with local drug and alcohol services and if they refer someone to them, the drug and alcohol service will see them, if possible, on the same day and will fast track them into treatment rather than go on a waiting list. The drug and alcohol partner agencies interviewed do not report a close relationship with the local SARC and also do not routinely ask about sexual assault.
Summary
As found in the literature review7 and in the national SARC survey, there is limited formal mental health expertise within the SARC skill mix. Assessment of mental health needs is often completed by people who have limited training in mental health including the FMEs (although it is important to note that some crisis workers and FMEs may have relevant backgrounds from previous roles). Therefore, there is variability of practice both within and between SARCs. There was limited evidence of the routine use of screening tools for PTSD and other mental health issues in assessment processes. Substance use issues were not formally assessed using screening tools (such as AUDIT-C), and there was limited evidence of drug and alcohol expertise or in-house support for substance use issues in the SARC, even though concern about withdrawal is a recognised barrier to accessing the SARC.
In SARCs that had a clinical psychologist providing in-house interventions, this was perceived as having three positive outcomes: improving assessment and triage of psychological support, providing seamless and timely care in a coherent way, and providing expertise on trauma to the general SARC team. However even with the provision of co-located service, there were still examples where some people were not able to access appropriate support. This tended to be people who were described as having more complex needs beyond the scope of what could be provided in the SARC. Staff who provided in-house mental health provision felt isolated from the external mental health services and this made them feel less able to take on people with more severe or complex needs. Many people who attended a SARC were already engaged in mental health services, so this made connecting to mental health services easier. In some cases, SARCs were able to offer advice to mental health staff about how to integrate the trauma into the care plan.
All SARCs reported challenges in referral to external mental health services, including not having a clear pathway, high thresholds for acceptance and long waiting lists. Some of the SARCs described engaging in outreach work to increase uptake by ‘underserved’ groups (such as sex workers, LGBTQ+ community) but this outreach did not include engagement with the local mental health service. Some SARCs reported offering people low-intensity support even though the person’s needs were greater than indicated for such an intervention as they were concerned that the person would be left without support. However, there is no evidence to support low-intensity interventions for people with complex trauma such as this from the literature. Many SARCs indicated that they would take people to a hospital emergency department in an acute crisis as they thought they had no other option, even though this was felt to be an inappropriate place for a traumatised person to be.
Survivor interviews recruitment and demographics
A total of 12 service user interviews were undertaken between September 2020 and April 2021. Of those approached from the prevalence study participation, 22% consented to be interviewed.
It was challenging to recruit people who attended a SARC for the reasons outlined in Chapter 7. Most of the people recruited for the qualitative interviews were drawn from those who had previously participated in the prevalence study (WP3) and recruited from four of the six case study sites. Owing to under-recruiting in WP3, there was a much smaller pool for WP4. Survivors were not recruited from SARC 5 or 6 despite efforts to promote the recruitment by the MiMoS team, the services were under strain due to impact of COVID-19 and not able to undertake the promotion of WP3 or 4.
There were 10 female, 1 male and 1 trans male recruited. Most had self-reported mental health issues (Table 12).
| Variable | N (%) | |
|---|---|---|
| Gender | Cis female | 10 (84) |
| Cis male | 1 (8) | |
| Trans male | 1 (8) | |
| Age (years) | < 30 | 2 (16) |
| 30–39 | 3 (25) | |
| 40–49 | 3 (25) | |
| Missing | 4 (33) | |
| Ethnicity | White British | 7 (58) |
| European | 1 (8) | |
| Mixed | 1 (8) | |
| Asian | 1 (8) | |
| Missing | 2 (6) | |
| Employment status | Employed | 4 (33) |
| Unemployed | 5 (41) | |
| In education | 1 (8) | |
| Missing | 2 (16) | |
| Education | Degree | 3 (25) |
| NVQ/BTech | 3 (25) | |
| No formal qualification | 1 (8) | |
| Missing | 5 (41) | |
| Disability | Yes | 4 (33) |
| No | 6 (50) | |
| Missing | 2 (16) | |
| Mental health (self-reported) | Yes | 9 (75) |
| No | 1 (8) | |
| Missing | 2 (16) |
Analysis of survivor interviews
‘Pre sexual assault referral centre’ expectations and accessibility
Most of the survivors did not know about the SARC prior to the assault. Most were made aware of the SARC after reporting the assault to the police. One person mentioned that she had ‘Googled’ the SARC and had then self-referred (female 1 SARC1) and she had expected the experience to be ‘horrifying but it wasn’t, it was fine’ (female 1 SARC1).
If people were more aware of the SARC and what happens there prior to assault via local promotional campaigns, then people would be less deterred about the thought of attendance and therefore increase likelihood of engaging (outcome). Another survivor also mentioned specifically dreading the examination and said: ‘I think it would be the actual physical examination part of it that might be a bit deterring’ (female 2 SARC3). As she had been raped many years ago, she was also worried that people would not believe that it had happened to her again. She also felt that the initial police contact had inferred that as she had been intoxicated with alcohol at the time of the assault that it had been her fault (victim blaming).
Attending the SARC is presented as a choice, but people also reported feeling a moral obligation to report the offence both internally and communicated externally too. Having a forensic examination was strongly advised by the police to whom they reported the offence:
if I wanted to get this person to not repeat his offending … then I had to go through with it didn’t I?
(Male 1, SARC1)
I didn’t want someone to go through what I’d been through. So, I knew I had to do it even though I was afraid.
(Female 2 SARC3)
A female survivor felt that, overall, she received a positive initial experience from police and SARC but felt that her hopes were unrealistically raised about the possibility of a prosecution and wishes that people had been more realistic about the low levels of cases currently being taken to court:
‘I am a bit concerned about other people getting their hopes up [about a conviction] … it’s been on the news that case get dropped’. The police later informed her that they were dropping the investigation.
Another survivor (female 1, SARC4) expressed her dissatisfaction with the police because she felt they were very quick to say that they did not have enough evidence to take to the Crown Prosecution Service and that the abrupt way they interacted with her contrasted with the way in which the SARC staff (and subsequently the ISVA) had worked with her.
Experience of the sexual assault referral centre
The overwhelming impression from all the survivors was that despite the examination not being a pleasant thing to go through, the way the SARC staff treated them made a difficult thing bearable. One survivor described it as ‘life changing’:
I have been through same sort of things before with different people and they have not made me feel as comfortable as what [SARC] has.
(Female 2 SARC5)
The staff there made me feel really comfortable. They were really empathetic, showed a lot of compassion and made me feel relaxed.
(Female 1, SARC4)
Qualities that the survivors mentioned were staff that were non-judgemental, kind, and believed their disclosures. Many mentioned that the kind, patient and supportive approach they received really helped them to calm down. They found that they were placed in control of the process by being informed about what was to happen and that they could stop at any time.
Some people valued the SARC staff taking time and offering support through the process, and others described wanting to get it ‘over and done with’ as quickly as possible. One survivor described how important it was that the SARC staff took their time and did not rush through the process, as the whole thing was overwhelming, and if the SARC process had been rushed she did not feel she could have gone through with it. Thus, working with an individual’s pace and preferences is clearly important.
she was like talking to me … and like they didn’t rush you or anything, they were so patient.
(Female 2 SARC5)
One of the survivors interviewed identified as a trans male and felt that the SARC experience had been ‘totally cis-centric’ but felt that overall, the experience was positive:
its [the cis-gendered] more likely who they’re going to be dealing with … well, they weren’t bad about it you know, Because I deal with a lot of agencies that are completely ignorant and nasty when it comes to trans.
(Trans male SARC3)
He appreciated that the SARC ensured they used the correct pronouns:
well it’s the simple things like not calling me she … it’s always appreciated when people are good to you in that way.
(Trans male SARC3)
Survivors talked about the visit to the SARC as ‘being a bit of a blur’ (male 1 SARC1). One female survivor described her emotions as ‘all over the place because it was the same day … the same night as the assault’ (female 2 SARC5).
A male survivor talked about how the examination ‘wasn’t very nice, it was quite embarrassing really’ but that ‘they were nice enough, the people who examined me’ (male 1 SARC1).
If the SARC staff make people feel at ease by explaining what they are going to do, and offer the option to stop the process at any time, it then it makes the examination more bearable for the survivor:
It gives you like a sense of you’ve still control even though you have been through what you going through and you didn’t have the control when the assault took place, you still have control after the aftermath.
(Female 2, SARC5)
The clinical environment and experience of forensic examination
The clinical aspect of the examination was mentioned by survivors. They understood the need for the forensic examination to be undertaken in a very clinical environment, some found that environment quite triggering. One person described that the whiteness, sounds and lights of the clinic room induced an extreme panic attack.
It was just too white … the centre was too long; the hallway went on forever. Yeah and like what they were wearing. I don’t know if it was because of COVID, I don’t know, everything seemed really scary … they were lovely though. If it weren’t for the way they spoke, like, I don’t think I could have managed it.
(Female 1 SARC3)
This survivor described having an intense panic attack during the exam and did not have a crisis worker in the examination. This same survivor felt out of control during the examination because she says she finds it hard to say no especially in the emotional state she was in, so she consented and complied even though she was struggling to cope with the experience.
Having someone else to offer emotional support and advocacy during the examination itself is important to monitor the person’s non-verbal cues, offer regular check-ins, and suggest breaks and so on. A survivor at SARC1 said having the crisis worker in the forensic examination:
it’s quite nice to have someone there who is for emotional support.
(Female 1 SARC1)
Another survivor described how important it had been to have built up a rapport with the crisis worker prior to the examination:
The whole experience is quite daunting and long, so you know [if] you’ve got a good rapport with people working there, it makes it a lot easier.
(Female 2 SARC1)
Another survivor described that as the initial assessment was completed in the same room as the physical forensic examination, they were distracted by the examination bed:
it’s a bit weird, you are sat there and then you see the bed and you know in a minute you’ve got to do whatever on the bed … I suppose it would have been better had it [assessment] been in another room.
(Male 1, SARC1)
One survivor mentioned the cold temperature of the clinic room:
That place is freezing, absolutely freezing … yeah numbing, that building is numbing.
(Female 2 SARC5)
One person described their own behaviour during the examination as quite ‘robotic’ and stoical and suggested that she was dissociating during the examination. In fact, the survivor described his ability to dissociate when:
things are difficult, or people are difficult I have a very robotic approach and it works for me. It works for me that he [FME?] did that to my dissociative body. I wasn’t there …
(Trans male SARC3)
Onward support and care
A survivor (female 1 SARC3) who had panicked during the forensic examination recalled that the SARC staff and examiner were concerned about her immediate well-being, and as she was under the care of the local mental health services, the SARC called the care coordinator and waited for a call back. However, the survivor recalls that:
They [mental healthcare coordinator] did call back and said send her home, obviously that is why they had to say okay we have done our bit, we don’t think you should be going, you know our options are tied now … they were good like in the way … they worked out I was under them [mental health service] and yeah tried to do their best.
(Female 1 SARC3)
While many remembered discussions about their support needs, they found it hard to take in and retain information. Some remember being given a pack of information to take home, and how they were not able to start to digest the information until a few days later:
I didn’t take it all in … I just took the leaflet from her … weren’t til a few days later that I sat with the leaflet that’s when I took in more.
(Female 2 SARC5)
They made sure I knew there would be options of different types of therapies available, like group sessions or counselling or whatever and I’d get a say in what that looks like. There, obviously, is waiting lists for these things.
(Female 1 SARC1)
Another survivor recalls leaving the appointment with a ‘stack of A4’ with lots of information. The SARC was also able to connect her to a women’s project and she was at the end of eight weeks of group therapy at the time of the interview, and that she expected to receive one to one therapy from the same organisation after the groups ended. This survivor was unable to access the in-house support that SARC1 usually offers because of the limited service running at the time of the pandemic. She was asked if she would have preferred this support to be offered by the SARC or externally:
I think I would have preferred that a little bit because obviously you kind of … like I had got along with people that I had worked with so if I got it [psychological support] from there I would feel a bit more comfortable, yeah.
(Female 2 SARC1)
She also said that she was grateful that the SARC had facilitated the referral to the women’s counselling service as she saw self-referral as a bit daunting.
One survivor at SARC1 stated that it was hard to think about what sort of continuing support would be useful at the time of the SARC appointment, as she was still processing what had just happened to her. At the time of the interview, she was still waiting to hear the outcome of referrals for support but stated that the delay was not such an issue as it had given her time to process what had happened.
Survivors mentioned receiving follow-up calls from the SARCs. In this conversation, survivors recalled that SARCs were able to check on progress of referrals or whether any other support needs had arisen. This is also useful as many survivors talked about not being able to think clearly about what support they may need at the time of the main SARC appointment, so having follow-up contact also allows a chance to consider what they need after the acute reactions had subsided.
Survivors mentioned that they also appreciated the follow-up calls from the SARCs because it helped them feel that there was someone who genuinely cared about them.
yes they are quite good at just you know every now and then they’d give you a ring just to see how I was and that I am doing ok. Which you know at least makes it seem like they care.
(Female survivor 1 SARC1)
In contrast, another survivor spoke about how the lack of a follow-up call after visiting SARC5 was very disappointing:
It’s very disheartening, very disheartening to think that you have gone to a service and you feel deflated on the situation that’s happened to you, and they haven’t checked on you necessarily mentally, emotionally, and obviously physically but it’s kind of tough.
(Female 3, SARC5)
One survivor talked positively about being referred to an ISVA and that she was able to access specialist sexual violence counselling as a result.
this is one of the best things to come out of the SARC … they referred me to that [ISVA] … And then through my ISVA I’ve accessed counselling, like specialist counselling around sexual violence …
(Female 1 SARC4)
She only had to wait five weeks to access the specialist counselling and was offered up to 30 sessions. Owing to COVID-19 restrictions, the counselling was being offered via Skype. However, despite the short waiting time, she felt that it would have been good to have had it when the incident actually happened ‘because I was struggling with quite a few things at that time’. The survivor also mentioned exactly why specialist counselling was important as she had been worrying that she had imagined the incident and trying to rationalise it in her head, but the counsellor had normalised her reactions as part of the trauma response.
speaking to my counsellor about that, she said that’s a very normal response to trauma, thinking did it actually happen …
(Female 1 SARC4)
One survivor was referred to an external agency for rape and sexual assault counselling and when she received a follow-up call from the SARC, she was asked by the SARC if the external agency had been in touch and they hadn’t, so, she was advised to go to the website and self-refer (and after that, she had a contact within three days). The survivor mentioned that someone else had helped to complete the online self-referral. In addition, the SARC also helped her to get other mental health support which she found very beneficial:
I don’t think to be honest I would be here today. I wouldn’t be how I am today. I can go out now on my own and feel comfortable but before [the services helped her] I couldn’t go out at all.
(Female survivor SARC5)
it definitely does help going to counselling that is for sexual assault and rape … because they know how to word things so that you are not going to get offended … they’re brilliant they know what they are doing.
(Female survivor 1, SARC5)
One survivor had been receiving therapy at the in-house provision at SARC5 and found it contrasted significantly with previous help she had received:
literally, every sort of type of healthcare professional that I have ever spoken to or any referral places that I have been advised about or whatever, they have never wanted to help. They don’t seem to listen, and they don’t get what is going through your head. But with [SARC] they listen to you as a person not what you are struggling with, and they treat you as an individual which you are. Then they work out how to help you based on what you personally need rather than what they think everybody suffering with the same thing needs.
(Female 2 SARC5)
She also mentioned that the SARC therapist made her feel that she mattered because she felt listened to and not just offered medication.
a lot of people I have seen before, even like doctors, you go there with … anxiety or depression and they think everyone suffers the same and has the same triggers and medication will work ... they treat you as a blanket rather than you are an individual.
(Female 2 SARC5)
The difference between the experiences seems to hinge on feeling that the person is not being judged, treating the person as an individual, and that the counsellor or therapist understands issues related to sexual assault (context).
One survivor at SARC1 was receiving counselling online after waiting six months (this was during the 2020 COVID-19 pandemic) and found it useful to access this online as she didn’t need to leave home and go anyway, and this felt safe: ‘in a safe space at your home … but then it can feel a bit weird trying to, you know, have these certain conversations through a screen’ (female 1, SARC1).
In contrast to the positive impact of specialist sexual violence counselling (either in-house or external agency) survivors generally talked despondently about accessing continuing support for their mental health and/or drug and alcohol needs, and the lengthy waiting lists for NHS therapies. One survivor described how he struggled to find support because he had mental health and alcohol/drug use issues and therefore did not fit the criteria for existing services due to his multiple needs:
I’ve had a real long battle with substance and mental health … so it’s all a bit of a nightmare, so we don’t get picked up by anyone really.
(Male 1 SARC5)
Others mentioned long waiting lists for NHS-provided therapies:
I’ve been on the waiting list for NHS therapy since October 2019 and no idea where that is.
(Female 2 SARC1; interview conducted in Autumn 2020)
In contrast to the language used to describe how they were treated in the SARCs and other specialist sexual violence services, the survivors talked about their perceptions of mainstream mental health including the lack of understanding and feeling judged.
I’ve had talking therapy … that was on the NHS, and I thought I am never going to go again … I just didn’t like her. I felt she was judging me, so I said I didn’t need it and walked out’ and ‘other services they [SARC] send you to that are nothing to do with what you have been through [sexual assault] like they were speaking to you, you think what the … hang on a minute, you aint a clue what you’re talking about. This ain’t how I felt … or this ain’t how it happened, you’re judging me.
(Female 1, SARC5)
I think the NHS can be really poor sometimes … I think GPs can be quite insensitive towards mental health problems, so I think [the SARC] was better.
(Female 2 SARC1)
The impact of receiving a less than positive experience from external mental health services often lead to disengagement.
Those who were already under the care of the mental health services found that the lack of a response in a crisis meant they were less likely to ask for help in the future:
that’s the story of the mental health team, you know sometimes they are good and other days they leave you to it … they [therapy group] rang them [mental health team] on the Friday to say look [name deleted] is in a bad way and literally got told we’ll contact her at the beginning of next week and then my daughter found me on the floor, and I’d taken an overdose. So, it’s kind of a bit like I won’t bother to ask for help because what’s the point you end up getting upset and let down.
(Female 1, SARC3)
And in addition,
no the crisis team aren’t very good in this area. I’ve only had one experience with them where we actually spoke, and we got on well. The rest of the time I’ve found them quite rude, dismissive.
(Female 1 SARC3)
One survivor who has bipolar affective disorder was admitted to mental health ward shortly after the visit to the SARC, but it was not described as a helpful experience, and they took their own discharge:
My CPN [community psychiatric nurse] doesn’t realise how horrible the [mental] hospital is … people were attempting to bully me … so, it’s not just the patients trying to bully you, it is often the staff. So as soon as I had the opportunity, I walked out of there.
(Trans female, SARC3)
It is not clear whether the bullying mentioned was due to transphobia but experiences of transphobia from other agencies (not specified) had been mentioned earlier in the interview.
Summary
Overall, the experience of attending a SARC was a positive one for the survivors who took part in the interview. Despite many not having prior knowledge of the SARC and being naturally wary of the thought of a forensic examination, the way that they were greeted by SARC staff, put at ease, and had everything explained to them prior to it happening really made a difference. Survivors talked powerfully about the importance of being believed and being given choice and control (trauma-informed interactions). They talked about being overwhelmed at the time, so having information to take away and digest when they were ready was useful. Many SARCs undertook follow-up calls, which the survivors really valued, and the follow-up calls were also an opportunity to check progress on referrals or check if any new needs had arisen. The survivors who had received mental health care did not find this as ‘trauma informed’ as the SARC, and indeed those who had received psychological support at the SARC or in a sexual violence counselling service felt that it was important to their recovery to work with someone who was familiar with issues related to sexual trauma. However, there was evidence that some people had to wait a long time for therapy due to the long waiting lists in the NHS.
Chapter 6 Secondary data analysis psychological therapies outcomes (work package 5)
The original aim of this work package was to assess changes in psychological well-being among people with experiences of sexual assault who receive psychological treatments from a mainstream mental health service compared with people who received psychological treatments from a SARC. We sought to answer this question by comparing two clinical datasets – one from a mainstream mental health service and one from a SARC. To compare the groups, we aimed to match cases from each dataset on key clinical and demographic information and then compare changes in measures of psychological distress between the groups. However, upon obtaining the datasets, it became clear that there was insufficient clinical and demographic information in the SARC dataset to allow us to determine whether cases were comparable (e.g. presence of mental health needs prior to treatment, history of contact with psychiatric services). In addition, the SARC dataset had a small sample size with respect to the primary outcome (i.e. CORE outcome measure psychological well-being score at the end of treatment; n = 110). These issues meant that it was not appropriate or feasible to compare outcomes between the datasets, and so a within-group analysis was undertaken. We also identified challenges with respect to extracting some data from the mental health dataset (e.g. type of therapy received, number of sessions of therapy received) and it was not possible to obtain data on some key data items (e.g. timing of assault). The within-group analyses followed the objectives outlined in the original study protocol, which aimed to describe the sociodemographic and clinical characteristics of the two samples, and to examine changes in psychological wellbeing pre- and post-therapeutic treatment in each service setting. As a team, we explored further ways that we might use the clinical datasets to answer important related questions about our areas of investigation. We established that for the mainstream mental health dataset it was possible to build a cohort of service users who had received psychological therapies and then split the cohort into two distinct groups: group 1 – service users who had experienced a sexual assault, and group 2 – service users who had not experienced a sexual assault. This dataset would allow us to directly examine whether psychological treatment outcomes differ among mental health service users who have and have not been exposed to sexual assault. Despite published literature on differences in the clinical and sociodemographic characteristics of these two groups, there was a dearth of evidence comparing the psychological treatment outcomes of mental health service users who had and had not experienced sexual assault. Our project aim for this add-on analyses was therefore to explore and compare the characteristics and outcomes of those who have received psychological therapy in a mainstream mental health service and either have or have not experienced sexual assault.
Study design
This is a retrospective cohort study using anonymised data.
Setting and study population
Participants were drawn from two anonymised clinical databases: a mainstream mental health service in southeast London and a specialist sexual assault service in south-east England (SARC5). For the mainstream mental health service dataset, inclusion criteria were people who had received psychological therapy between January 2016 and December 2019, and who had completed a self-report outcome measure, specifically the Clinical Outcome in Routine Evaluation Outcome Measure (CORE-OM) or CORE-10. For the SARC dataset, inclusion criteria were people who had attended the SARC and who received the SARC’s in-house psychological therapies service between January 2016 and December 2020, and who had completed a self-report outcome measure, the CORE-OM. In addition, to meet aim 2, a cohort was extracted from the mental health service database who had no documented experience of sexual assault but who met the other criteria.
Description of sexual assault referral centre 5 database
Sexual assault referral centre 5 provides a bespoke in-house, stepped-care, talking therapies service in partnership with the local mental health NHS trust and two third-sector organisations. This service provides specialist trauma-focused talking therapies for males and females reporting recent and non-recent sexual assault. The stepped-care model is divided in to four tiers. In tiers 1 and 2, specialist counselling is provided to SARC attendees aged 13 years and above. They aim to contact people referred to them within 48 hours and to assess their needs within 7 days from initial contact. These services can offer up to 12 sessions of specialist counselling. In tiers 3 and 4, the NHS clinical psychologists who work with the SARC 5 provide up to 20 sessions of NICE-compliant specialist psychological interventions (e.g. EMDR, CBT) to SARC attendees aged 18 years and above. These psychologists start treatment between one and three months post attendance at the SARC; treatment is focused on addressing trauma related solely to the sexual assault, so clients with additional complexities (e.g. those with severe mental illness, severe personality disorders) are referred on for coordination by other mental health services. The anonymised clinical dataset that we received from this SARC comprised the demographic and clinical information on people who had received either the talking therapies service via the mental health NHS trust or via the Family Matters third-sector organisation.
The SARC service and its partners have established a standardised clinical database system for the reporting of key demographic and clinical data of the SARC service users. The database includes detailed demographic and clinical information, including before- and after-therapy CORE-OM mean scores. The database was established in 2016 and also includes textual summaries of reasons for discharge from therapy.
Description of clinical record interactive search database
The South London and Maudsley NHS Foundation Trust (SLaM) is a large mental healthcare provider in south-east London, covering a catchment of over 1.2 million residents in four South London boroughs, as well as some national specialist services.
The SLaM Biomedical Research Centre case register and CRIS application were developed in 2008. 38 The CRIS system provides a research repository of real-time, de-identified, structured and open-text data from SLaM’s bespoke electronic health record system. 39 It comprises comprehensive records of all clinical information recorded throughout patients’ journeys, including demographic information, details of referrals and transfers, detailed clinical assessments and care plans. Over 250,000 patient records can be accessed through CRIS.
To establish a cohort within CRIS that met our inclusion criteria, we developed initial search terms and subsequent methods for validating our searches. Details of this process can be seen in Appendix 5. Through this process, we established a sample of 265 individuals who had received psychological therapy between January 2016 and December 2019, who had completed a pre- and post-therapy self-report outcome measure, and who had a documented sexual assault, and 257 individuals with no documented sexual assault but who met the other criteria.
Pilot work
Pilot searches of the clinical dataset for the mental health service (CRIS system), since its year of inception in 2006 to the end of 2016, indicate that there are CORE-OM data on more than 3000 women who have been raped or have experienced other forms of sexual assault. From this information, we estimate that around 300 women per year receive psychological treatment who have a document of sexual assault on the CRIS system; therefore, approximately 900 cases for 2016 to 2019.
Pilot searches of the referral rates with the SARC5 indicated that around four to six referrals per week were referred to the psychological treatment pathway (approximately 16–20 per month); before- and after-treatment assessment are taken for everyone in treatment.
Permissions and ethical approval
The CRIS received ethical approval as an anonymised data resource for secondary analyses from the Oxford C Research Ethics Committee (reference: 08/H0606/71+5). Approval for use of CRIS for the current study was obtained from the CRIS oversight committee (project number 19-085).
The SARC service already has in place permission agreements from service users to the sharing of their anonymised data for research purposes. For this study, we received approval from a South East NHS trust (name omitted) to obtain an anonymised version of their database (with names and contact details removed) with data from inception up until January 2020. We similarly received approval from one third-sector counselling service to obtain an anonymised database with data from inception to January 2021, but not from the other service.
Measures
Demographic and clinical characteristics in the Clinical Record Interactive Search
Gender, age (calculated using date of birth and date last seen) and ethnicity were extracted from structured fields. Social deprivation was measured using the 2019 Index of Multiple Deprivation (IMD), a measure of relative deprivation for neighbourhoods in England termed lower super output areas (LSOAs). IMD was derived from the LSOA associated with the patient’s most recent address, and converted into quintiles (1 – most deprived, 5 – most affluent).
Diagnoses are recorded in CRIS using the International Classification of Diseases, revision 10. Individuals are assigned a primary diagnosis when in contact with a SLaM service. As patients may have several spells of care under SLaM (defined as a continuous period of care) and therefore may have been assigned multiple diagnoses, we explored several related variables:
-
all primary diagnoses given between 2000 and 2019, extracting the percentage of individuals who had been assigned each major classification
-
the most recent primary diagnoses assigned to the patient, extracting the percentage of individuals who had been assigned each major classification
-
the number of different diagnoses that individuals were given between 2000 and 2019.
Level of risk was assessed using a structured risk assessment tool, which is completed by clinicians during assessment if the patient is deemed to be at risk either to oneself, to others or from others. This tool specifies several risk clusters, including self-harm/suicide, violence, self-neglect, physical health, and adult safeguarding. In addition, it specifies triggers and protective factors that may be present for the individual. Under each of these seven headings, the clinician completes checklists about the presence of current and historic risk factors which may contribute towards each one (e.g. social isolation, alcohol misuse).
Completion of the structured assessment is dependent on staff behaviour and, therefore, may not identify all those with risk factors. Nevertheless, a pragmatic approach was taken, assuming that, in general, where the tool has been completed, this is due to a higher level of risk being identified.
To measure risk, the proportion of sexual assault group and controls who had a completed tool was used to indicate the likelihood of full risk assessment being undertaken. In addition, within each of the risk clusters, the percentage of individuals who had been identified as having the current and/or historic risk factor was determined to identify the level of each risk.
Demographics and clinical characteristics in sexual assault referral centre 5
The two standardised clinical datasets from the talking therapies service at the NHS trust and from the third-sector organisation were combined into a single dataset for analysis.
The following demographic and clinical variables were used in the analysis of the SARC dataset: gender (categorical variable), age at referral (continuous variable), ethnicity (categorical variable), marital status (categorical variable), relationship to assailant (categorical variable) and number of therapy sessions received by discharge (continuous variable). A site code (i.e. NHS or third sector) was added to the combined dataset so that analyses could explore demographic and clinical differences between the sites.
Psychological distress
The CORE-OM is a 34-item self-report measure of psychological distress. It comprises four domains: wellbeing, symptoms, functioning and risk. Users rate how they have been feeling over the last week on a five-point scale ranging from 0 (not at all) to 4 (most or all of the time). The south-east dataset reported data exclusively based on the CORE-OM 34-item measure.
The CORE-10 is a brief, 10-item version of the CORE-OM. Items cover depression, anxiety, trauma, physical problems, functioning and risk to self. The same 0–4 scale is used to rate items. The mental health dataset reported data based on the CORE-OM 34-item measure and the CORE-10 outcome measure.
Responses on both the CORE-OM 34-item and the CORE-10 measures are averaged to produce a mean score between 0 and 4 indicating the level of current psychological distress. Scores above 1 are considered to be in the clinical range, with the following scores indicating levels of clinical severity (≤ 1.5 mild; > 1.5–2 moderate; > 2–2.5 moderate to severe; > 2.5 severe).
The CORE OM can be converted to the six-item CORE-6D40 and used to calculate a preference-based index for use in economic evaluations to calculate quality-adjusted life years. Psychological therapy attendances were costed using the NHS national schedule of costs41 at £71 per appointment.
Analysis
Sexual assault referral centre 5 dataset
All data were analysed using StataMP16 (Stata Corp., College Station, TX, USA) statistics software. Descriptive statistics of demographic data, proportions and Pearson chi-square tests for categorical data and means and standard deviations for continuous data, were calculated for the entire sample and also stratified by site (i.e. NHS NGO, counselling). Tests of associations on clinical data were calculated, using means, standard deviations, 95% confidence intervals and t-tests for all normally distributed data and for non-normally distributed data using medians and non-parametric Mann–Whitney U-tests.
A thematic analysis of the brief textual summaries of reasons for discharge from therapy was also conducted, to provide further details on peoples’ treatment journeys.
Clinical record interactive search dataset
All variables were analysed using IMB SPSS (IBM, Armonk, NY, USA) statistics software, version 26 for Windows. Pearson chi-square tests were used to compare categorical variables and Mann–Whitney U-tests were used to compare means of continuous variables.
Descriptive statistics – proportional for categorical variables and means and standard deviations for continuous variables – were calculated to describe the sociodemographic and clinical characteristics of the sample.
Main statistical analyses examined changes in psychological well-being (based on CORE outcome assessments before and after treatment) following psychological treatment from a mainstream mental health service compared with a SARC. We examined the sociodemographic and clinical characteristics of the cohorts to explore whether there are systematic differences for example, history of previous psychiatric contact such as admission. We then addressed these differences using appropriate statistical techniques.
Findings
Between 1 April 2016 and 31 December 2020, the NGO counselling service received a total of 467 referrals via SARC5. Between 1 July 2016 and 31 January 2020 the NHS therapies service received 229 referrals via the SARC5.
South-east England sample characteristics
As can be seen in Table 13, both NGO counselling and the NHS supported mostly female service users; the NHS supported significantly more male service users than the NGO (p < 0.05). NGO counselling services were significantly more likely to support service users of a younger age (p < 0.001) and service users of Asian and black ethnicities (p < 0.05) compared with the NHS services. The marital status of service users was similar across the two services, as was the service users’ relationship to the perpetrator.
| NGO counselling | NHS therapy | p-value | Total | ||||
|---|---|---|---|---|---|---|---|
| (n) | (%) | (n) | (%) | (n) | (%) | ||
| Gender | 0.004a,b | ||||||
| Total | 464 | 100 | 29 | 693 | |||
| Female | 445 | 96.0 | 206 | 90.0 | 651 | 94.0 | |
| Male | 19 | 4.0 | 22 | 9.6 | 41 | 5.9 | |
| Transgender | – | – | 1 | 0.4 | 1 | 0.1 | |
| Ethnicity | |||||||
| Total | 393 | 100 | 221 | 0.05a | N (614) | ||
| White | 358 | 91.1 | 210 | 95.0 | 568 | 92.5 | |
| Mixed/multiple ethnic group | 9 | 2.3 | 7 | 3.2 | 16 | 2.6 | |
| Asian | 12 | 3.0 | 1 | 0.5 | 13 | 2.1 | |
| Black | 14 | 3.6 | 3 | 1.3 | 17 | 2.8 | |
| Marital status | |||||||
| Total | 374 | 100 | 199 | 100 | 0.13a | 573 | 100 |
| Single | 244 | 65.2 | 134 | 67.3 | 378 | 66.0 | |
| Partnered/cohabiting | 90 | 24.1 | 34 | 17.1 | 124 | 21.6 | |
| Married/civil partnered | 26 | 7.0 | 21 | 10.6 | 47 | 8.2 | |
| Separated/divorced/widowed | 14 | 3.7 | 10 | 8.3 | 24 | 4.2 | |
| Relationship to perpetrator | |||||||
| Total | 395 | 100 | N (207) | 0.14a,d | 602 | 100 | |
| Stranger | 108 | 27.3 | 69 | 33.3 | 177 | 29.5 | |
| Acquaintance | 159 | 40.2 | 85 | 41.1 | 244 | 40.5 | |
| Ex-partner | 46 | 11.7 | 15 | 7.2 | 61 | 10.1 | |
| Partner | 41 | 10.4 | 12 | 5.8 | 53 | 8.8 | |
| Family member | 39 | 9.9 | 20 | 9.7 | 59 | 9.8 | |
| Not specified | 2 | 0.5 | 6 | 2.9 | 8 | 1.3 | |
| Age (years), N; mean (SD) | 453 | 26.1 (11.5) | 229 | 28.5 (10.2) | 0.001c | 682 | 26.9 (11.1) |
Assessment of psychological distress pretreatment
Of the 467 referrals that NGO counselling received between 1 April 2016 and 31 December 2020, a total of 227 (49%) completed a CORE-OM assessment prior to starting treatment. Of the 229 referrals that the NHS therapies service received between 1 July 2016 and 31 January 2020, 76 (33%) completed a CORE-OM assessment prior to starting treatment.
The 76 SARC service users in the NHS therapies pathway (M = 1.87; SD 0.66 CI 1.72 to 2.02) compared with the 227 SARC service users in the NGO counselling therapy pathway (M = 1.63; SD 0.86 CI 1.52 to 1.74) reported statistically significant higher mean levels of psychological distress prior to starting treatment t (166) = 2.5, p < 0.01.
These findings highlight that, on average, SARC service users on both the NHS therapies pathway and the NGO counselling pathway had symptoms of moderate psychological distress within the clinical range prior to receiving therapy. In addition, SARC service users on the NHS therapies pathway had higher baseline levels of psychological need (prior to starting treatment) than SARC service users on the NGO counselling therapy pathway. These observations align with the tiered model of the SARC5 therapies pathway, whereby SARC service users with greater psychological needs are triaged to the NHS therapies pathway and those with lower psychological needs are directed to the NGO counselling therapies pathway.
Number of therapeutic sessions
Data were available on the number of therapeutic sessions offered by both the NHS therapies pathway (n = 23) and NGO counselling pathway (n = 156). The mean number of sessions offered to SARC service users in the NHS therapies pathway was 13.35 (SD 7.61, CI 3.00 to 20.00). The mean number of sessions offered to SARC service users in the NGO counselling therapies pathway was 8.3 (SD 4.23, CI 1.00 to 12.00).
Assessment of psychological distress post-treatment
A total of 88/227 (39%) SARC service users on the NGO counselling therapies pathway completed a CORE-OM assessment at the end of treatment. A total of 22/76 (28%) SARC service users on the NHS therapies pathway completed a CORE-OM assessment at the end of treatment.
Post-treatment analyses revealed that overall SARC service users on the NHS therapies pathway (median 0.50; SD 0.34, CI 0.00 to 0.91) and SARC service users on the NGO counselling therapies pathway (median 0.41; SD 0.60, CI 0.00 to 1.88) reported considerable reductions in psychological distress, bringing their scores (on average) below the clinical range. No statistically significant differences were observed on levels of post-treatment psychological distress between SARC service users on the KMPT therapies pathway and the SARC service users on the NGO counselling therapy pathway (z = –0.78, p = 0.43; Mann–Whitney U-test). All 22 (100%) SARC service users on the NHS therapies pathway and 66 (75%) of SARC service users on the NGO counselling therapy pathway achieved reliable change (i.e. ≥ 0.5 mean change score before and after treatment) in levels of psychological distress post-treatment.
SARC service users on the NHS therapies pathway on average received a greater number of therapeutic sessions than SARC service users on the NGO counselling therapy pathway. All SARC service users on the NHS therapies pathway showed a reliable improvement in CORE score post-treatment, compared with 75% of SARC service users on the NGO counselling therapy pathway. A note of caution around these findings; there was a high percentage of missing data on CORE-OM post-treatment psychological assessments, particularly in the NHS therapies pathway group (missingness around 70%, n = 22 CORE-OM post-treatment data), and this impacts on our interpretations around the data.
Thematic analysis of reasons for discharge from therapy
We conducted a thematic analysis of summary textual data from the NGO counselling therapy pathway, concerning the reasons service users did not undertake therapy or stopped therapy prematurely. The analysis demonstrated that the main reasons for not undertaking therapy were due to not being able to find the time to attend whilst balancing various other commitments in their lives (e.g. university attendance, work schedules, exams, childcare commitments) and service users not responding to contacts by the service. Another barrier was service users not feeling ready to undertake therapy. Transportation difficulties were also raised as a barrier to engagement, with service users reporting being unable to travel alone to therapy sessions, raising concerns about traffic issues or reporting that they lived in a geographically remote area which presented challenges in travelling to the service for sessions. In response to the COVID-19 pandemic, the service temporarily changed the format of their therapy sessions to remote online delivery, which may have resolved some of the barriers raised by service users in the previous sentence. However, this format change did not facilitate engagement for all, and some service users elected to wait to undertake therapy until face-to-face sessions were reinstated. Further additional reasons for service users not undertaking therapy were that some had complex presentations that required support beyond what the service could offer and that some service users were already undertaking therapy with another provider. With respect to reasons for ending treatment early, some service users decided to stop early because they felt better, and others moved outside of the catchment area. A few service users ended therapy early stating that they wanted to move on and start with a new chapter in their lives, and a few others cited problems related to family issues (including domestic abuse, death/sickness of a family member/relative).
We conducted a thematic analysis of summary textual data from the NHS therapeutic pathway, concerning the reasons service users did not undertake therapy or stopped therapy prematurely. There were less textual descriptions for this dataset, so the richness of our analysis was more limited than for the NGO counselling dataset. The analysis demonstrated that the main reason for not undertaking therapy were that service users were not suitable for the service, either due to having greater mental health needs than could be sufficiently supported by the service or by having fewer mental health needs or additional relational needs that fell outside the scope of the service. In these instances, service users with greater mental health needs were referred on to CMHTs and other NHS tier-4 mental health services and those with lower needs or additional relational needs were referred on to NGO counselling or other third-sector specialist abuse organisations. The second biggest barrier was service users failing to attend sessions or disengaging from treatment (no additional details were given to indicate the possible reasons for disengagement). Further additional reasons for service users not undertaking therapy were that a few were already engaged with a CMHT and a few refused to have an initial therapeutic assessment (no additional details were given to indicate why service users refused these assessments).
Discussion
This analysis provides important insights into the impact of in-house SARC specialist therapeutic treatments in improving clinical outcomes among SARC services users. Prior to treatment, service users accessing both the NHS therapies pathway and the NGO counselling pathway reported moderate levels of psychological distress. Post treatment, service users accessing both pathways reported considerable reductions in psychological distress. Indeed, psychological distress scores fell on average to below the clinical range in both groups, despite service users on the NHS therapies pathway reporting considerably higher levels of distress at pretreatment. These findings highlight that SARC service users on the NHS therapies pathway achieve comparable improvements in post-treatment levels of psychological distress to service users on the NGO counselling pathways. One reason for this finding may be due to the fact that service users on the NHS therapies pathway receive more therapy sessions than those on the NGO counselling pathway.
The textual data in this clinical dataset allowed us to identify the main reasons why SARC service users do not undertake therapy. One important finding was that several service users were not suitable for the service, either due to having greater mental health needs than could be sufficiently supported by the service or additional relational needs that fell outside the scope of the service. These findings highlight that SARC services support people with considerable mental health and social needs, which require input from other relevant organisations (e.g. NHS mental health services, substance use services). Another reason why some service users did not take up the treatment was that they did not feel ready to engage in therapy or that they struggled to commit to this work alongside the other commitments in their lives. The result suggests that some service users may feel the need to access therapeutic support at a later date in time and this may mean that they are only able to access therapeutic support via NHS services, which may or may not have access to specialist trauma focused treatments.
Strengths and limitations
To our knowledge, SARC5 is unique in its provision of a bespoke in-house, stepped-care talking therapies service in partnership with a local mental health NHS trust and third-sector organisations. By examining SARC5’s clinical dataset we were able to examine the impact of this in-house therapeutic service in improving the psychological well-being outcomes of SARC users. We were also able to explore differences in therapeutic treatment outcomes among service users accessing two different therapeutic pathways in this stepped-care levels in this model (i.e. the NHS therapeutic pathway and the NGO counselling pathway).
This clinical database uses a robust and validated measure of psychological well-being to examine pre and post treatment changes among SARC users. It also includes detailed demographic and clinical information about SARC clients receiving the therapies service, as well as textual summaries of reasons for discharge from therapy. Despite these strengths, we observed a high percentage of missing data on CORE-OM post-treatment psychological assessments, particularly in the NHS therapies pathway group which impacts on our overall interpretations of the data.
We originally intended to use this dataset to compare changes in psychological well-being outcomes among people who received psychological treatments from this SARC with people who received psychological treatments from a mainstream mental health service. However, when we obtained the SARC dataset it contained insufficient clinical and demographic information to allow us to determine whether the SARC clinical sample was comparable to the mainstream mental health sample (e.g. presence of mental health needs prior to treatment, history of contact with psychiatric services). In addition, the SARC dataset had a small sample size with respect to the primary outcome, which meant it was not appropriate or feasible to compare outcomes between the datasets. For this reason, we undertook a within group analysis for the SARC dataset.
Clinical record interactive search analysis
To establish a cohort within CRIS that met our inclusion criteria, we developed initial search terms and subsequent methods for validating our searches. Details of this process can be seen in Appendix 4, Box 1. Through this process, we established a sample of 265 individuals who had received psychological therapy between January 2016 and December 2019, who had completed a pre- and post-therapy self-report outcome measure, and who had a documented sexual assault, and 257 individuals with no documented sexual assault but who met the other criteria (control).
Sample characteristics
The sexual assault group were significantly more likely to be female (76%) and significantly less likely to be of white ethnic origin (62%) than the control group (55% and 70%, respectively; Table 14). There was no difference in age distribution or in mean age but the those in the sexual assault group were more likely to live in more deprived areas than the controls.
| Variable | SA group (n = 265) | Control group (n = 257) | p-valuea |
|---|---|---|---|
| Gender, n (%) | < 0.001 | ||
| Female | 202 (76) | 141 (55) | |
| Male | 62 (23) | 116 (45) | |
| Age group (years), n (%) | 0.452 | ||
| < 40 | 116 (44) | 120 (47) | |
| 40+ | 149 (56) | 137 (53) | |
| Age (mean ± SD) | 43.8 ± 14.0 | 45.0 ± 17.5 | 0.871b |
| Ethnic group, n (%) | |||
| White | 154 (62) | 155 (70) | < 0.001 |
| Asian/Asian mix | 15 (6) | 18 (6) | |
| Black/black mix | 69 (28) | 30 (28) | |
| Other | 12 (5) | 19 (5) | |
| Not known (excluded above) | – (6) | – (14) | |
| IMD 2019 quintile, n (%) | < 0.001 | ||
| 1 - most deprived | 73 (28) | 35 (14) | |
| 2 | 120 (47) | 114 (45) | |
| 3 | 47 (18) | 59 (23) | |
| 4 | 12 (5) | 26 (10) | |
| 5 - most affluent | 5 (2) | 18 (5) | |
| Not known (excluded above) | – (3) | – (2) | |
| Mean IMD score ± SD | 27.9 ± 9.3 | 23.4 ± 9.6 | < 0.001b |
Outcomes (validated)
Analysis of CORE assessments that were validated to have been associated with a period of psychological therapy showed that both pre- and post-therapy the sexual assault group had a significantly higher mean score (2.3 ± 0.79 and 1.59 ± 0.88, respectively) than controls (1.87 ± 0.81 and 1.22 ± 0.81; Table 15). The number of weeks between pre- and post-therapy COREs, the number of sessions delivered and the average number of sessions per week were also significantly higher in the sexual assault group than in the control groups. However, the average CORE change during therapy did not differ significantly between the two groups. Overall, 62% of sexual assault group showed a reliable improvement in CORE score with an average change of –0.71 ± 0.77, compared with 58% of controls showing reliable change with an average change of –0.64 ± 0.70.
| Variable | SA group (n = 265) | Control group (n = 257) | p-value |
|---|---|---|---|
| Pre-therapy CORE (mean ± SD) | 2.3 ± 0.79 | 1.87 ± 0.81 | < 0.001a |
| Post-therapy CORE (mean ± SD) | 1.59 ± 0.88 | 1.22 ± 0.81 | < 0.001a |
| CORE change (mean ± SD) | –0.71 ± 0.77 | –0.64 ± 0.70 | 0.183a |
| Weeks between pre and post (mean ± SD) | 45.2 ± 27.2 | 32.7 ± 22.2 | < 0.001a |
| Number of sessions (mean ± SD) | 22.0 ± 16.6 | 16.0 ± 10.1 | < 0.001a |
| Sessions/week (mean ± SD) | 0.54 ± 0.27 | 0.57 ± 0.30 | 0.157a |
| Cost @ £71/session (mean ± SD) | £1564 ± 1178 | £1138 ± 719 | < 0.001a |
| CORE change pre to post therapy | 0.197 | ||
| –2+ | 17 (6) | 10 (4) | |
| –1 to < –2 | 82 (31) | 70 (27) | |
| –0.5 to < –1 | 65 (25) | 68 (26) | |
| Reliable improvement | 164 (62) | 148 (58) | |
| –0.1 to < –0.5 | 54 (20) | 57 (22) | |
| 0 to < ± 0.1 | 10 (4%) | 15 (6) | |
| 0.1 to < 0.5 | 22 (8) | 28 (11) | |
| No reliable change | 86 (32) | 100 (39) | |
| 0.5 to < 2 | 15 (6) | 9 (4) | |
| Deterioration | 15 (6) | 9 (4) | |
| Clinical outcome | < 0.05 | ||
| Recovered (reliably improved to non-clinical) | 65 (25) | 87 (34) | |
| Not recovered (details below) | 200 (75) | 170 (66) | |
| Not reliable – non-clinical | 12 (5) | 36 (14) | |
| Reliably improved to mild | 35 (13) | 26 (10) | |
| Not reliable – mild | 18 (7) | 19 (7) | |
| Reliably improved to moderate | 53 (20) | 32 (12) | |
| Not reliable – moderate | 35 (13) | 33 (13) | |
| Reliably improved still severe | 11 (4) | 3 (1) | |
| Not reliable still severe | 36 (14) | 21 (8) |
Figure 7 shows the differences in clinical severity identified by the CORE assessments pre- and post-therapy between the sexual assault and control groups. There was a significantly greater proportion of people in the sexual assault group with severe psychological distress pre-therapy (45%) than in the control group (25%), whereas, post-therapy, the distribution of outcomes had shifted towards milder clinical categories, such that a significantly greater proportion of the control group were non-clinical (48%) than the sexual assault group (29%).
FIGURE 7.
CORE measures grouped by severity.
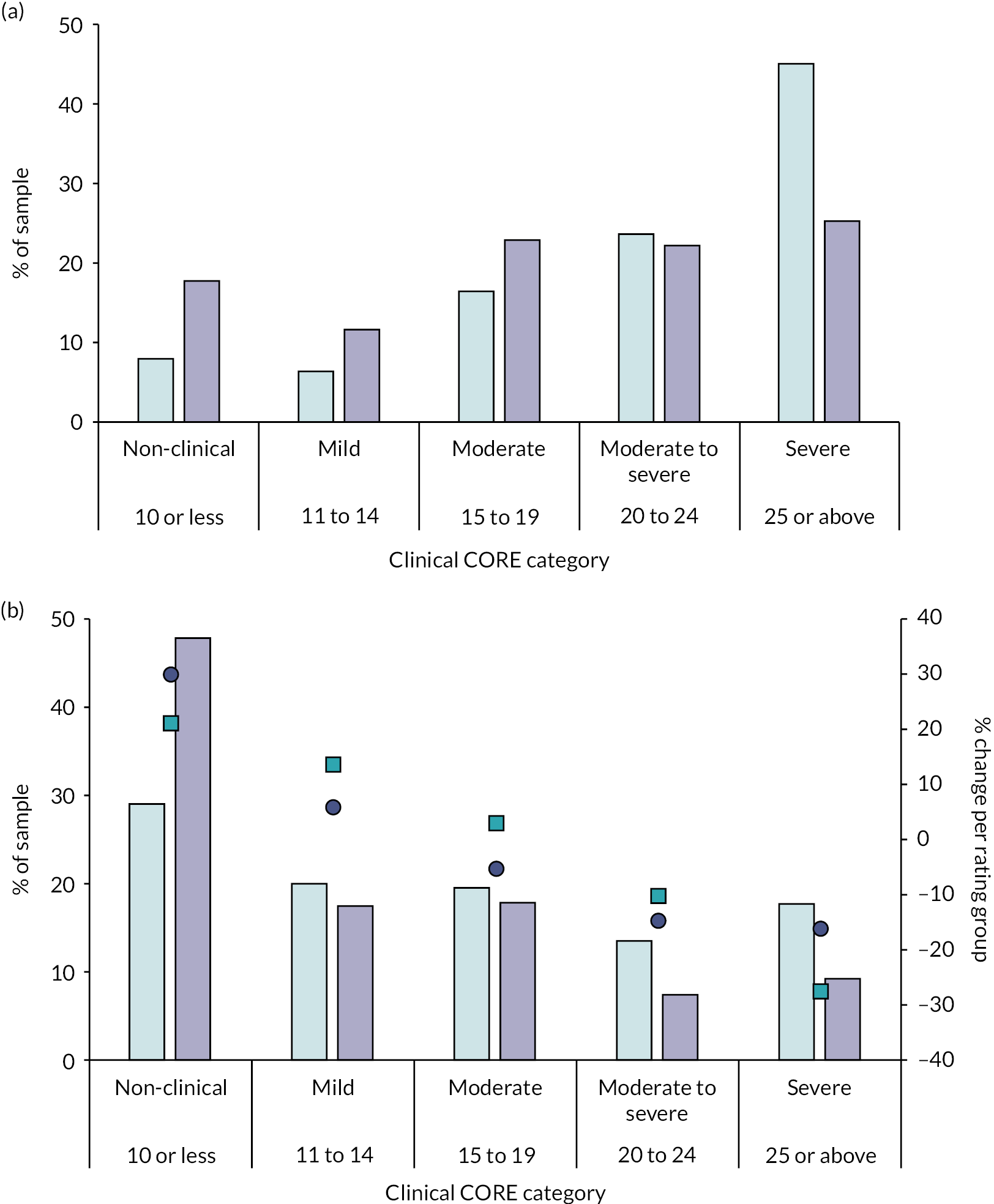
Clinical Outcomes in Routine Evaluation Outcome Measure or CORE-10 findings were grouped into levels of clinical severity: (A) pre-therapy assessments; (B) post-therapy assessments. In Figure 7, aqua bars show the percentage of the sexual assault group and purple bars show the percentage of the control group in each clinical category. Aqua squares show the change in percentage of the sexual assault group post-therapy in each clinical category. Purple circles show the change in percentage of control group in each clinical category. Pearson chi-square comparing the two groups for severe and not-severe pre-therapy (A) was p < 0·001 and for non-clinical compared with clinical post-therapy (B) was p < 0·001.
Clinical contacts/resource use
For all measures of clinical contact, the sexual assault group had significantly greater levels of service use than the control group (see Appendix 5, Table 17). That is, those in the sexual assault group were twice as likely (36% in total) to have had more than three spells of care than those in th control group (17%); they were nearly three times as likely to have had more than four CORE assessments during 2015–20 (32%) compared with the control group (12%); first contact with services was significantly earlier in the sexual assault group; the number of psychological therapy sessions attended in 2016–19 was greater in this group (mean 28.4 ± 13.7) than in the control group (mean 19.2 ± 21.3) and 62% of the sexual assault group received more than 20 therapy sessions compared with 33% of the control group; the year of first diagnosis was earlier in the sexual assault group and they received significantly more diagnoses (mean 7.7 ± 7.7) than controls (mean 4.3 ± 4.3); overall, 45% of the sexual assault group received four or more diagnoses compared with 22% of controls.
The full list of diagnoses across all year 2000–19 (see Appendix 5, Table 18) showed that the sexual assault group was more likely (23%) to have schizophrenia, schizotypal, delusional and other non-mood psychotic disorders than the control group (15%) whereas those in the control group were more likely to have mood (affective) disorders (31%) than the sexual assault group (21%).
Appendix 5, Table 19 shows that 82% of the sexual assault group had previously received at least one full risk assessment and this was significantly higher than in the control group (65%). A higher proportion of people in the sexual assault group compared with those in the control group scored positively for all the current and historic trigger risk factors recorded. These differences were statistically significant for triggers relating to relationship/family conflicts, adverse life events, historic drug and alcohol abuse and transitions in care. Furthermore, a higher proportion of people in the sexual assault group compared with the control group scored positively for most of the self-harm/suicide risk factors recorded. These differences were statistically significant for risk relating to previous suicide attempt/accidental overdose, historic acts of deliberate self-harm, alcohol/substance misuse, current deteriorating depression with distress and significant anniversary.
Health costs
We calculated the CORE-6D preference-based index and cost of therapy for patients who had CORE-OM questionnaire responses available (Table 16). As a result, this analysis is on a smaller sample than the main analysis as not all patients have CORE-OM responses and the CORE-6D cannot be calculated from the CORE-10.
| Variable | SA group | Control group | ||
|---|---|---|---|---|
| N | Mean (95% CI) | N | Mean (95% CI) | |
| Pre-therapy CORE-6D | 117 | 0.521 (0.485 to 0.556) | 85 | 0.605 (0.563 to 0.647) |
| Post-therapy CORE-6D | 103 | 0.667 (0.627 to 0.708) | 78 | 0.768 (0.730 to 0.806) |
| Cost @ £71/session (validated) | 103 | 1793 (1487 to 2101) | 78 | 1304 (1140 to 1264) |
| Cost @ £71/session (all sessions) | 103 | 2216 (1840 to 2591) | 78 | 1509 (1279 to 1739) |
The sexual assault group had a significantly lower preference-based index both pre therapy (the control group had an index 0.082 greater; 95% CI 0.022 to 0.142) and post therapy (control group index 0.101 greater; 95% CI 0.042 to 0.160) and significantly higher costs for validated (control group cost £490 lower, 95% CI –836 to –144) and all sessions (control group cost £707 lower, 95% CI –1144 to –270).
The sexual assault group had a particularly low preference-based index. There are few instances where the CORE-6D has been used, but a recent prison sample had a CORE-6D preference-based index of 0.75 to 0.713 on enrolment to a trial for common mental health problems,1 with people in prison with a common mental health problem more like community controls than sexual assault.
Individuals who had been sexually assaulted highlighted the importance of equity considerations in economic evaluations: even though there is evidence that they benefit from therapy, potentially as much as the control group, they have a lower preference-based index and cost significantly more than controls. As a result, treatment for this group is less likely to be cost-effective unless equity considerations are included in the analysis, potentially including a weighting for patients who had been sexually assaulted.
Discussion
This study is one of the first to directly compare the psychological treatment outcomes of psychiatric service users who have and have not reported a sexual assault. Our findings indicate that service users with experiences of sexual assault appear to have greater levels of mental health care need than those without experiences of sexual assault. Despite greater levels of pre-therapy psychological distress among those with experiences of sexual assault, similar post-treatment reductions in distress are observed compared with service users without experiences of sexual assault. Our findings indicate that service users who have experienced a sexual assault may be less likely to achieve clinical recovery post psychological treatment, when compared with service users who have not experienced sexual assault. These findings suggest that further mental health care may be needed for service users with abuse histories, and that more research is required on how to evaluate the cost-effectiveness of these services.
Strengths and limitations
Owing to limitations within the SARC clinical dataset, with respect to a lack of clinical and sociodemographic information and missingness on the primary outcome (i.e. psychological distress scores post treatment), we needed to deviate from some aspects of our original protocol. We were not able to directly compare this mainstream mental health dataset to the SARC clinical dataset, as we could not determine if the two populations were comparable and were unable to conduct the health economics analysis as we had planned. We, therefore, conducted a within-group analysis of the primary research question and looking at healthcare cost within this mainstream mental health dataset.
We found that the way in which sexual assault was documented in clinical records varied considerably (e.g. a lack of specification around the type, frequency or severity of violence experienced). This meant that we were unable to extract and analyse data on some assault-related variables that we had pre-specified in our protocol.
As we had access to one of the most well-established anonymised health records system in England, we decided to include an additional add-on analysis as part of our within-group comparison. We sought to explore and compare the characteristics and outcomes of those who had received psychological therapy in a mainstream mental health service and either had or had not experienced sexual assault. We were aware that there was an evidence base comparing the clinical and sociodemographic characteristics of these two groups, but an absence of data directly comparing the psychological treatment outcomes of mental health service users who had and had not experienced sexual assault.
Our inclusion criteria were restricted to people who had attended a psychological therapy session and had a recorded CORE outcome, which suggests that our sample had at least some level of engagement with therapeutic work. Our sample is not, therefore, representative of the entire population of interest. In addition, our cohort inevitably missed people who had experienced sexual assault but who had not been asked about this by clinicians or who had not had a disclosure documented in their clinical notes. In addition, completion of structured risk assessment tools was dependent on individual staff perceptions and behaviours about service users’ presenting risks, which resulted in missing data on this variable for several service users.
Finally, we were required to undertake multiple manual validation checks on key study variables to ensure correct data classification. Although these manual checks strengthen our methodology and confidence in the data it inevitably limits the sample size that we could include for the analyses, as we could only include a number that was feasible for us to manually validate.
Chapter 7 Protocol changes
Work package 3 (prevalence study) had opened to recruitment in February 2020 and the COVID-19 pandemic was just escalating. We recruited six people to the point that we decided to halt recruitment due to the impact of the national lockdown and the challenges of undertaking safety and welfare protocols while in lockdown with the additional challenges of being able to contact mental health and primary care should we have concerns about any of the participants. In addition, a halt was called to all non-COVID-19 research by the HRA in 2020. The MiMoS team focused on working on desk-based activity during the pause. The following activities were undertaken:
-
realist review of the literature
-
documentary analysis and journey mapping of the six case study sites
-
developing the topic guides based on 1 and 2
-
setting up the WP 5 secondary data analysis.
By July 2021, we were given permission by the Clinical Research Network to recommence data collection for staff in the WP4 case studies as long as the services agreed that this activity did not affect them delivering the services (which were operating differently under COVID-19 restrictions). WP3 (prevalence study) recommenced recruitment from October 2020.
Changes to protocol:
-
Pause research – informed HRA (March 2020).
-
Recommence research – notified HRA and permission to move data collection to remote methods only. We already had ethical approval to collect WP3 prevalence data using an online survey and to recruit and consent via remote methods such as telephone and text messaging. The main change was for the WP4 (qualitative focus groups and interviews). The original plan for WP4 was to conduct focus groups in person. We changed this to use Microsoft Teams. Focus groups and interviews were recorded within the Teams facility and downloaded for transcription.
-
After trying to recruit to the target for WP3, it was proving difficult due to the impact of the rising second wave in the autumn/winter of 2020 and the subsequent second lockdown in the first quarter of 2021. We discussed in the independent oversight group and with the funders and, with their permission, we altered the protocol to halt data collection on the 31 May 2021, and to omit the six-month follow-up aspect of this part of the study. It would have taken many more months to recruit 360 as a target (in fact it was hard to estimate at that stage as the continuing impact of COVID-19 was hard to predict), as well as needing to keep the study open potentially for a further year (with additional costs) to collect the follow-up data. This would have needed to be costed by NIHR but there was no certainty that even with the extra costing it would yield the original targets. In addition, we had been able to spend more time on the secondary data analysis in WP5, which was yielding useful data on outcomes of psychological therapies for people with a sexual assault history compared with those without such a history.
Chapter 8 Synthesis
Logic model
The initial logic model (Figure 8) was developed from discussions with stakeholders (including those with lived experience) and MiMoS team from the findings of the literature review (WP1) and national survey (WP2). Figure 8 represents the journey into and out from the SARC. The purple areas represent the three areas of focus for the data collection and the navy is the expected outcomes should the system fire. A realist review was undertaken to identify programme theories that were then tested in WP4 case study interviews. The data have been synthesised across all the WPs and logically set out along the care pathway (‘pre-SARC’ or the journey into SARC; what happens within the SARC and ‘post-SARC’ onward referral and treatment).
FIGURE 8.
Logic model. A&E, accident and emergency.
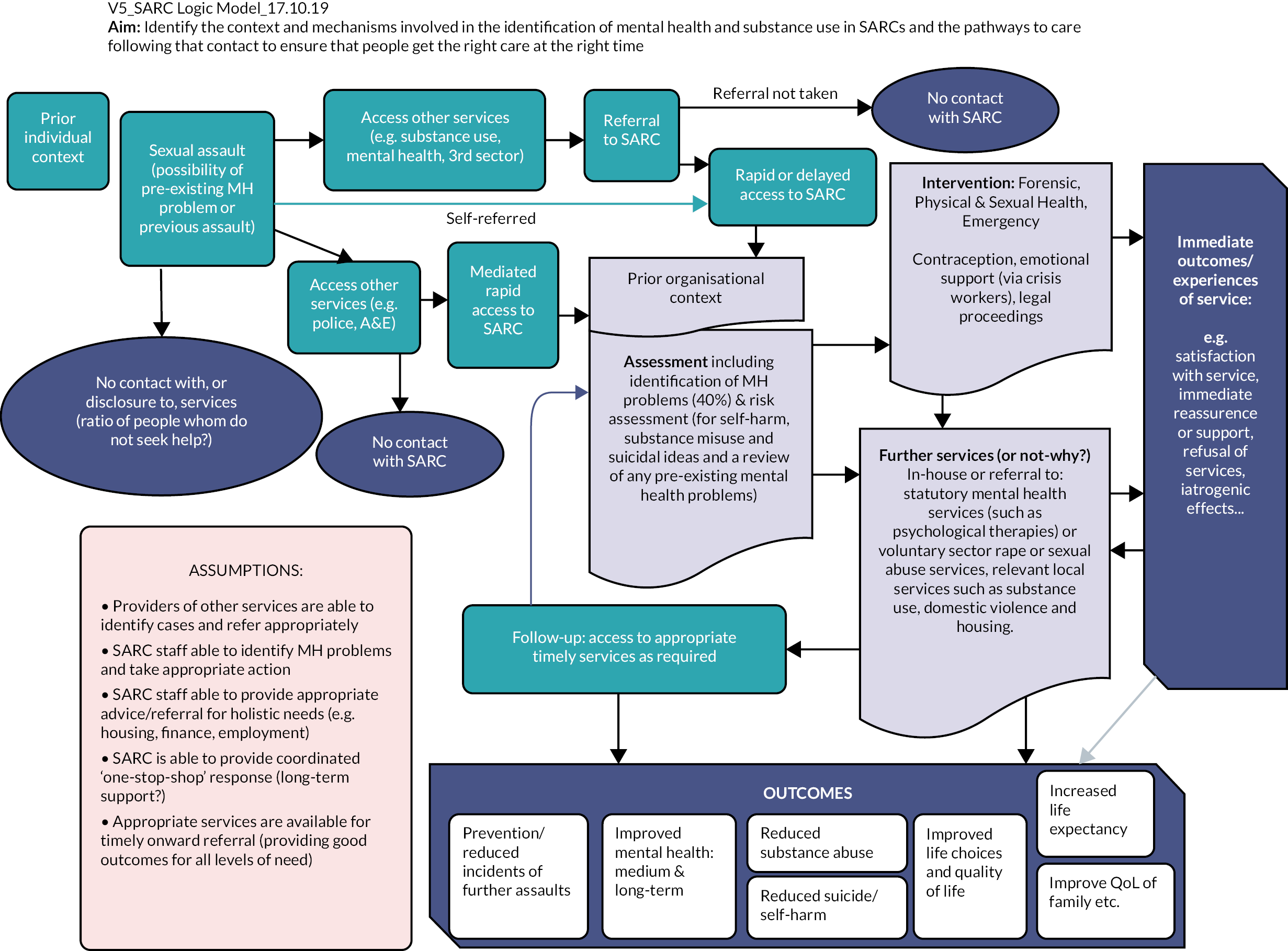
Synthesis
Pre-sexual assault referral centre: lack of prior awareness of sexual assault referral centre and its functions
Most of our survivor interviewees were not aware of SARCs prior to their assault. Most heard about the SARC from reporting to the police and the police then accompanying them to the site. One person found out from a search on the internet. The lack of awareness of the SARC and what happens at a SARC could deter people from attending because they do not know that it exists or have concerns about not knowing what will happen there. This lack of awareness also featured in the partner agency interviews. There were some misconceptions from partner agencies as to what was offered at the local SARC, including one NHS mental health interviewee thinking that SARCs offered every level of psychological therapy for sexual trauma when in fact their local SARC only offered a limited number of sessions of supportive counselling. Some partner agency informants indicated that a mental health referral for therapy may be rerouted to the SARC if there was recent sexual assault rather than offer an assessment. Some SARCs had run open days prior to the pandemic so that external agencies could attend and learn about the nature of their offer. SARC staff recalled the value of being able to run external training to partner agencies but that due to having less time and resource, because of increasing footfall, this awareness raising work often did not happen.
There is a high prevalence of sexual assault experienced by people with mental health issues; however, very few mental health services have reported a pathway to SARCs following a disclosure of a sexual assault. 44 In addition, in WP5 we identified that, over a period of 10 years in one NHS mental health trust alone, 3000 women who had received some form of psychological therapy input (as indicated by CORE-10 outcome data) had a case note indication that they had experienced sexual assault. It is not known whether the psychological therapy was because of the impact of sexual assault or other reasons and, even if it was related to the sexual assault, whether it was the correct therapy (i.e. trauma therapy). It is also not known whether they had any contact with the local SARC. A free-text search was conducted for any reference to SARCs and there was an absence of any references to attendance or referral to a SARC in the case notes which could indicate a lack of awareness of attendance on the part of the mental health staff, or the group that had experienced had not reported it officially.
If SARCs were able to promote the work of the SARC, by discussing what a SARC is and what it offers (mechanism) with general population, as well with key local organisations that work with underserved groups such as mental health, substance use and so on, then this would mean that more people were aware of their existence as well as knowing in advance what the SARC offers and therefore there would be more uptake from underserved groups (outcome) and improvements in the working relationships between SARC and partner agencies (outcome).
At the sexual assault referral centre
The survivors consistently spoke highly of the non-judgemental and compassionate care they received from initial phone contact right through to follow-up contact. This was noted across all the SARCs where survivors attended. SARC staff interviews also discussed examples of compassionate care that they delivered. The survivors appreciated working with staff who ‘got’ trauma as opposed to some less positive experiences they had at other agencies (such as NHS mental health and psychological therapies). The context of trauma informed interactions may well be boosted by the presence of a mental health professional such as the clinical psychologists in SARCs 1 and 5 who can bring this into internal training and team discussions.
If SARCs and other relevant agencies adopt a trauma informed approach (context) using trauma informed interactions such as believing the survivor, non-judgement and compassion, dispelling victim blaming myths, offering choice and control (mechanism), then this improves engagement with that service (outcome) and potentially aids recovery (outcome).
The forensic examination
The systematic review identified studies that have evaluated the impact of giving people prior information about what would be involved in a forensic examination and found that this intervention reduced distress. In the interviews, some survivors expressed that the forensic examination was the thing they most dreaded, yet they felt that the actual experience was not as bad as expected because they had been fully briefed prior to the exam by the SARC staff. The other important issue was giving the survivor choice and control both before the examination and during which is something they had not had during the assault itself. The assumption that could be made is that prior information and giving choice and control serves to prevent re-traumatisation.
If survivors are prepared in advance for the forensic examination (by a priori briefing) and given choice and control (mechanism, and have someone accompany them to provide emotional support; e.g. SARC crisis worker) by staff who understand trauma and able to use a trauma-informed approach (context) then they can cope much better with the experience and the experience is less likely to exacerbate trauma (outcome).
Assessment and response to mental health and substance use
Within the systematic review and national survey there was variations identified in the approach to assessment. Mental health assessment is conducted using professional opinion following an interview. It is also important to note that from the data including the national survey and staff interviews, many of the people who work in the SARCs including the crisis workers and forensic examiners do not have a background in mental health and so the issue of consistency and quality of ‘professional opinion’ in relation to assessment of mental health is also in question. In SARCs that had a clinical psychology presence, there was evidence of the use of screening for PTSD, as well as a triage assessment of need led by the clinical psychologist, in conjunction with the rest of the multi-disciplinary team. Having a mental health practitioner in the team also offered a secondary benefit in advising others in the team on the impact of trauma (including issues of vicarious trauma among staff) and more generally about mental health issues experienced by service users.
If survivors receive an assessment of mental health needs (mechanism) that is informed by having people with specific mental health expertise within the team (context), then their needs are more accurately identified, and they can therefore be referred to the right care at the right time (outcome).
There was limited evidence of the use of screening tools, and some suggestion that screening tools were too ‘black and white’ and felt impersonal like a ‘tick-box exercise’. Some responders did feel that using standardised screening tools could support referrals, serving as objective evidence of level of need. In WP3 a suite of mental health screening tools was administered in the form of an online survey to those who had presented to the SARC after a sexual assault no earlier than a week after attendance and no later than 6 weeks of attendance. Of those who consented to participate, all completed the online questionnaires (see Chapter 3). The respondents were broadly representative of the population of people who attend SARCs nationally. Most of the participants had previous contact with mental health services prior to attendance at the SARC. Most (94%) scored positive on the trauma checklist. It was estimated from 2017–18 SARC service use data that of 14,357 people who used a SARC over one year; 13,584 were likely to score above threshold for PTSD. NICE guidance indicates that where someone has been assessed as having PTSD after a trauma then they should be offered trauma therapy within a month. However, based on the findings from the review, the national SARC survey and interviews in the case studies, routine screening for PTSD is not currently routine practice in SARCs.
We only found two SARCs that screen for PTSD and the south-east SARC has a specific triage system where the person is discussed as a team and placed either in a NGO counselling service or if more complex, referred to the therapy service provided by the local mental health service (WP5) From the analysis of the routinely collected data at this service, we noted that the levels of severity of baseline symptoms (CORE) were higher for those who referred to the mental health provider service compared with the third sector supportive therapy, but the two groups of survivors did equally well as a result. While there are limitations of analysing routine data from a small data set it is a promising finding and suggests that future research is needed to evaluate the benefits of global screening for PTSD and stepped care interventions for survivors of sexual trauma.
If SARCs adopt the use of standardised screening tools for PTSD (context) as a part of their assessment (mechanism) then this would ensure that people were effectively identified (outcome), provided consistency of practice across SARCs in the identification of PTSD (outcome) as well as identifying those who require evidence-based therapies and therefore improve their mental health (outcome).
In terms of continuing psychological support, many people who came through the SARCs often only accessed in-house counselling, external counselling or were referred to a variety of mental health care. Some SARCs can and do facilitate referrals to relevant external agencies as they have good knowledge of the range of services available, as well as their referral criteria. However, in some SARCs who cover a wide area that also involves several mental health and substance use care providers (such as in Yorkshire, London and Manchester), it is less clear and transparent about how to refer when each service has a different offer and routes into treatment. SARC staff noted that it is sometimes easier to connect a person to mental health support. We found that in SARCs where there was a lack of mental health expertise in the team, this impacted on how effectively and confidently the team identified and responded to mental health and drug/alcohol needs. It was also noted that when a SARC offered more than simply signposting people to external services (such as facilitating a referral and checking in on progress and outcomes of the referral) that this lead better engagement with that service as survivors often felt overwhelmed with information or too daunted to instigate a self-referral.
IF SARCs have good relationships with external agencies (context) and therefore more clarity around referral criteria and processes, then the referral process (mechanism) would run effectively and therefore survivors would receive more timely and appropriate aftercare.
The importance of survivor-centred care
The survivors that we interviewed could articulate consistently the qualities of the interactions that they received by a range of staff from the crisis workers over the phone or face to face to the FME/FNE and the ISVA. Most of our survivor interviewees had also had a range of experiences receiving care and treatment from external agencies especially NHS mental health services. They described dissatisfaction with mental health services including waiting lists and negative attitudes. Some of the qualities the survivors mentioned are simply good practice, but there were some elements mentioned that are the components of ‘trauma-informed care’. 42 These include the staff seeing and understanding the manifestations of distress through the lens of trauma, clearly making sure that the person has choice and control at every step and actively seeks consent to continue each aspect of the forensic examination. The other aspect that is important is that the survivors felt believed by the SARC staff and some even gave examples where they were clearly told that they were not to blame for what had happened and that the responsibility lay with the perpetrator. This is important as victim blaming, and self-blame and shame are common reactions to sexual violence;43 it is the only interpersonal crime where the victim is cross-examined. Even narratives in the media perpetuate this idea that somehow the victim placed themselves in a situation and therefore carries some of the responsibility for what happened. This shaming and blaming are extremely damaging for someone’s recovery and in fact may prohibit disclosure and reporting for fear of not being believed or being blamed/shamed. This is even more apparent in mental health care where some evidence that due to the nature of mental illness disclosures of sexual violence could be dismissed as a manifestation of someone’s delusional thinking. In addition, it is now known that disclosures and recounting of a traumatic event are often inconsistent and at times incoherent and this is related to the functioning of memory and recall of an event that was deeply traumatic.
Chapter 9 Discussion
Main findings
This is the first comprehensive programme of research to examine what works for whom under what circumstances for people with mental health and/or drug/alcohol needs who attend SARCs. In the original protocol, the study aimed to establish the following:
-
What programmes are identified in published and grey literature to inform how mental health and substance use can be best addressed in SARCs?
-
What models can be identified across the SARC services in terms of addressing mental health and substance use?
-
What is the prevalence and nature of mental health and substance use in people who attend SARCs?
-
What types of services are accessed by people with a range of needs following attendance at a SARC, and how satisfied are they with those services?
-
What are the barriers and facilitators to accessing the right support at the right time for people who have attended a SARC?
-
How do outcomes differ between a bespoke psychological therapies service at a SARC and mainstream mental health?
Despite the impact of the COVID-19 pandemic and the subsequent disruption to research, social distancing requirements and lockdowns, the data obtained from a range of sources have been able to address the six research questions. The implications of the findings are discussed, followed by a discussion of the robustness and limitations of these findings. In light of this, we then set out the recommendations for policy, practice and further research.
Nature of the needs of people who attend sexual assault referral centres
It is firstly important to state that the trauma response to a sexual assault is normal and expected and can manifest in people in a myriad of ways. This trauma response should not be immediately pathologised and ‘diagnosed’ as there is a risk of imposing potentially damaging and stigmatizing psychiatric labels on people. In many cases of trauma, a significant percentage of people do not go on to develop PTSD or other mental health conditions. 43
Previous research has tried to identify predisposing risk factors for PTSD and other mental health issues following a sexual trauma but failed to find specific factors that correlate with this and Dworkin and colleagues43 suggest that it is more useful to explore the multilevel social context of survivors and the impact of these on recovery. Many survivors experience feelings of shame and self-blame after an assault in part due to internalising societal ‘rape myths’ which leads to a reluctance to seek help or report the assault. SARC services have shown that their trauma informed approaches have a powerful and positive impact on the experience of the survivor and their future recovery. Indeed, the survivors in the interviews talked about the importance of being believed, as well as being told that they were not to blame for what had happened. These seem to be really key messages that promote the start of recovery. Some of the survivors had also had contact with mental health services and described receiving a less trauma-informed approach including feeling judged and blamed for the assault and stated that it made a real difference if they worked with someone who really understood sexual assault and its impact including psychological therapies and/or counselling delivered at a SARC or counselling delivered by a sexual violence service specifically. An accurate assessment of need can only be useful if it opens the door to someone getting the kind of help that will support them to move forward with their life.
In terms of thinking about mental health needs, it is important to distinguish between those who attend a SARC who have prior mental health needs as well as those with no prior mental health needs. We have identified a third group who struggle to find the right care at the right time. They present with mental health and/or alcohol/drug issues needs that are perceived by SARCs (if they provide in-house counselling) as too ‘complex’ for the in-house support (if it exists), and not meeting the threshold for secondary mental health or NHS psychological therapies, or they face long waiting lists to get help. There were examples of SARCs struggling to access crisis mental health support if they had immediate and significant concerns about the safety of a person and often the only option was to take someone in acute distress to the local emergency department.
In WP5, those with a history of assault presented with higher levels of psychological distress at start of therapy as well as scoring higher on risk assessments especially in relation to self-harm and suicidality. However, the group with a history of sexual assault did just as well in treatment as the comparison group. While it is unclear how many people were accessing therapy in relation to the sexual assault, it does indicate that while those who have experienced sexual assault experience significant mental distress, accessing therapy can improve their symptoms. However, owing to having more complex needs and severity of distress at baseline, the people in the sexual assault group tended to require more sessions of therapy. Any assessment of cost-effectiveness should address this to ensure that there is equity in comparing different groups.
Models of care
The cluster analysis performed using data from the survey served to identify three ways of working in relation to the responses to the mental health questions in the national survey. This informed the sampling strategy and ensured we had SARCs that represented the three clusters. However, it was clear from the richer case study data that the clusters lacked specificity and accuracy. The survey was completed typically by a SARC manager who may not have all the specific details on how mental health was managed at the micro levels. Overall, it became clear from the case studies that a more sensible grouping of SARCs were ones that had in-house clinical psychology (SARCs 1 and 5) which meant that survivors were reviewed and triaged in discussions led by an experienced mental health professional (clinical psychologist). Survivors appreciated receiving therapy in a setting with expertise in trauma related to sexual assault. The second model of care was one SARC (SARC6) that provided in-house counselling. This was provided by trained counsellors who were not necessarily mental health practitioners. Unfortunately, we were unable to recruit survivors from this SARC, so we are unable to present the survivor perspective on that service. The third group of SARCs did not have any mental health provision in the team, and variable relationships with relevant external agencies. It was notable that where there was a lack of mental health expertise in the skill mix, the staff identified this as a deficit and one SARC (SARC2) is planning to recruit a mental health nurse to work in the SARC and be able to take on the liaison role with the local mental health services.
Contexts and mechanisms facilitate identification, care and treatment for mental health and substance use issues within and beyond sexual assault referral centres
Several contextual issues were identified: the presence or not of a mental health professional in the SARC, the quality of relationships with external agencies and capacity within the local therapy provision. Contextual issues identified clustered around the presence of a mental health professional within the team. This had the benefit of helping assess need and triage survivors according to that need, developing the ethos of trauma-informed care in the team by role modelling, informal teaching and within multidisciplinary team discussions. Another important contextual issue was the quality of external relationships with external agencies. If there were positive communication channels (usually a single point of contact) then it facilitated the referral process. Where these relationships did not exist, the referral process became confusing and fragmented and often led to the survivor not getting their needs met. The third important contextual issue was whether there was local capacity in the systems to be able to provide timely and appropriate therapies. Waiting lists and limited sessions were mentioned by both SARC staff and survivors as contextual issues that inhibited recovery and added to the stress felt by both the SARC staff (who felt responsible for the continuing well-being of the people that they saw but also felt that it was beyond their role and expertise to offer continuing mental health support) and for the survivors who struggled to advocate for themselves due to feeling overwhelmed by what they were going through, and felt rejected by the system if they didn’t meet the referral criteria or experienced a long wait for treatment.
Robustness and limitations
From its inception the team worked with survivors on the design and procedures and this he findings. Training all the research team in working with survivors in a trauma-informed care approach. The programme theories have been informed, developed and refined by using and synthesising data from a range of sources including working with survivor and SARC stakeholders throughout the process.
While we conducted a national survey of SARCs regarding their practice, this was not in-depth. However, this assisted in generating clusters of responses that were used as a sampling framework to ensure the case study sites selected represented a range of ways of working. In addition to this, SARCs represented a range of providers (NHS, private health and private security) and geographical locations including 3 SARCs in the north and northwest and London and the south.
Limitations of the study are in relation to under-recruiting the target of survivors both for the prevalence study and the case study interviews. This was as a direct impact of the COVID-19 pandemic. The other limitation was that as the mental health data were collected during local and national lockdowns, it is possible that the high rates of mental distress could partly be a reflection of more general mental health impacts of COVID-19 in the general population. The intention was to follow up the survivors in the prevalence study at six months after completion of the screening tools to repeat those tools again and collect information on what treatment and support (or not) they had been able to access. Owing to slow and low recruitment to this part of the study, the six-month follow up was not feasible within the period of the study and was removed. However, mapping service use and mental health distress over time will be important in terms of identifying need and unmet need following attendance at the SARC and should be considered as a research study at a future point in the post-pandemic era.
Impact of COVID
As with all other NHS research, the MiMoS study was impacted in 2020–21 by the COVID-19 pandemic. Specific details of the ways in which aspects of the study have already been addressed. As the data were collected during unprecedented social change (lockdown and social distancing measures) and there were changes to how services can be delivered (remote and home working, use of telephone and online appointments) the data may be additionally impacted by these issues.
Recommendations for future research
We have observed and described the variation in SARCs’ service delivery and organisation and have theorised mechanisms by which service users’ outcomes and experience can be optimised – but we still lack robust quantitative evidence about effective models of SARC care. For example:
-
Does routine screening for mental health conditions improve access to mental health care and mental health outcomes for SARC service users?
-
What should be offered in terms of in-house counselling (style, format, intensity) and does this provision of in-house counselling (rather than relying on referrals to mental health services) improve users’ experience and outcomes?
-
Do routine follow-up calls from the SARC improve continuity of care and take-up of referrals/signposting to mental health services?
There is also a compelling case for research which aims to develop and evaluating a specific care pathway for the identification and treatment of PTSD for people who come to a SARC, involving routine screening using validated, structured measures and in-house provision or clear referral pathways/service level agreements to NICE-recommended treatment.
A review of the types of in-house counselling/therapy provided and what they can achieve. For example, if only short-term counselling is available in-house then it limits what can be addressed. The concern is always if a service user is seen to be receiving/having received something, then it is assumed they don’t need anything else. While short-term in-house supportive counselling may be helpful, including helping the service user through the legal process, evidence-based therapy for PTSD may still needed. There were examples of a range of supportive interventions delivered within the SARC including brief follow-up support, through to ‘stabilisation therapy’, peer support groups and ‘counselling’ which was ill defined and described. Therefore, a further recommendation for research would be to evaluate the impact of a range of interventions that vary both in type and intensity.
In the secondary data analysis of CRIS, it was incredibly labour-intensive to text mine and verify sexual assault because of a lack of routine enquiry. While cases were identified in CRIS, there was little mention of police or SARC involvement. Brooker and colleagues44 found, from a review of literature and a request for information from mental health NHS trusts, that the relationship between mental health services and SARCs is not well established. Further research should explore the prevalence and risk factors for sexual assault in people who use secondary mental health services and evaluate effective ways of facilitating routine enquiry, and pathways to SARC when a disclosure is made.
Conclusions
SARCs were established to be a single setting where survivors could get all their needs met including forensic examination and other health needs. It is well established that many people who report a sexual assault have pre-existing mental health (and other needs such as drug and alcohol conditions) and a sexual assault can be a trigger for acute distress in the short term, and (for some) longer-term impact on mental health. However, despite this high prevalence, it is clear from the data from a variety of sources (literature review as well as data from this study) that there is great variability in what kinds of mental health and substance use assessment and care pathways are available in English SARCs (and similar services in other countries.
SARCs play a significant role not just in the collection of vital forensic evidence to pursue a conviction but a significant role in supporting a survivor through the use of trauma-informed interactions and immediate psychosocial support. There is much work to do to improve the quality of care pathways from SARCs to mainstream mental health (and drug and alcohol services), which includes a greater understanding of each other’s roles and remit, effective methods of identifying those most in need of mental health and substance use treatment while at the SARC, as well as establishing the evidence for effective care pathways and timely services. The data suggest that mental health services may need more support to be able to offer a service that understands and responds to the specific needs of people who experience sexual trauma, and that there are clear opportunities for SARCs and mental health to share their expertise. Further research is needed to evaluate the effectiveness of new ways of working, and to evaluate the effectiveness of low-intensity supportive counselling for trauma, as there is no evidence to support this currently.
Acknowledgements
First, we would like to acknowledge the survivors who contributed to this study as LEAG members and as participants. Being able to include and involve survivors was a key ambition and we thank them all for taking the time to support our study and for bravely sharing their experiences with us. We thank the NIHR for recognising the topic as important, and for funding us to undertake the study and working flexibly with us through the more challenging two years of the COVID-19 pandemic. Next, we would like to thank the SARC staff that took part in the study while undertaking their usual business especially in a time of COVID-19. It was remarkable and humbling that so many people who worked within the SARCs and the local partner agencies gave up their valuable time to participate in the study.
We want to give thanks to many people who acted as advisors to the study including Dr Sheila Paul (GP and forensic physician); Concetta Perot (researcher and co-founder of Survivors Voices), Esther Silva (lead for national implementation at NHS England), and Kate Davis (national director for commissioning SARCs at NHS England).
A data sharing agreement can be found in the supplementary material. All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
We would also like to acknowledge the work of Professor Charlie Brooker, who has been working in the field of sexual assault and mental health for many years. It was his drive and energy that raised awareness of the need to attend to the mental health needs of people who had experienced sexual trauma, and his work directly influenced the commissioning brief for the study.
We also thank members of the independent oversight group, chaired by Professor Hannah Bows (University of Durham), who gave up their time to sit on this group and provided input as critical friends during the life of the project.
Finally, we would like to pay tribute to the whole of the MiMoS research team who undertook a challenging study while in lockdown themselves, working from home and isolated from the usual peer support that comes from working at the office. They were committed to this project and worked relentlessly through the various challenges that COVID-19 threw at us with fortitude and professionalism.
Contributions of authors
Elizabeth Hughes (https://orcid.org/0000-0002-4480-0806), chief investigator, oversaw the delivery of the study and was involved in analysis as well as leading the writing of the report.
Jill Domoney (https://orcid.org/0000-0001-8157-621X), researcher on the project, data collection and analysis and contribution to writing the report.
Nicky Knights (https://orcid.org/0000-0003-2703-4609), researcher on the project, data collection and analysis and contribution to writing the report.
Holly Price (https://orcid.org/0000-0001-7806-1477), researcher on the project, data collection and analysis and contribution to writing the report.
Sibongile Rutsito (https://orcid.org/0000-0002-9155-840X), researcher on the project, data collection and analysis and contribution to writing the report.
Theodora Stefanidou (https://orcid.org/0000-0002-3172-2685), researcher on the project, systematic review, data collection and analysis and contribution to writing the report.
Rabiya Majeed-Ariss (https://orcid.org/0000-0003-0892-4710), researcher on the project, data collection and analysis and contribution to writing the report.
Alexandra Papamichail (https://orcid.org/0000-0002-8589-6648), researcher on the project, data collection and analysis and contribution to writing the report.
Steven Ariss (https://orcid.org/0000-0002-5557-4613), co-investigator, realist methodology, analysis and contributed to writing the report.
Gail Gilchrist (https://orcid.org/0000-0002-5616-6283), co-investigator, methodological advice, analysis and writing of report.
Rachael Hunter (https://orcid.org/0000-0002-7447-8934), co-investigator, health economics, analysis, contribution to writing report.
Sarah Kendal (https://orcid.org/0000-0001-8557-5716), co-investigator, lived-experience lead, contributed to analysis and writing report.
Brynmor Lloyd-Evans (https://orcid.org/0000-0001-9866-788X), co-investigator, WP1 lead, contributed to analysis and writing report.
Mike Lucock (https://orcid.org/0000-0003-0968-5475), co-investigator, contributed to psychological assessment in WPs 3 and 5, interpretation and contributed to writing the report.
Fay Maxted (https://orcid.org/0000-0002-1599-1412), co-investigator, lay representative, contributed to the involvement of lived experience across the study, contributed to interpretation of findings and writing report.
Rebekah Shallcross (https://orcid.org/0000-0003-4764-0411), co-investigator, WP3 lead, protocol development, contributed to analysis and writing report.
Karen Tocque (https://orcid.org/0000-0002-5249-6891), co-investigator, statistician, contributed to statistical WPs 2, 3 and 5 analysis and writing report.
Kylee Trevillion (https://orcid.org/0000-0001-5865-4726), co-investigator, WPs 4 and 5 lead, contributed to analysis and writing report.
Ethical approval
This study obtained favourable opinion from Preston NHS research ethics committee, reference 6 December 2019 (REC reference 19/NW/0663).
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Bicanic I, Snetselaar H, De Jongh A, Van de Putte E. Victims’ use of professional services in a Dutch sexual assault centre. Eur J Psychotraumatol 2014;5.
- Brown R, Du Mont J, Macdonald S, Bainbridge D. A comparative analysis of victims of sexual assault with and without mental health histories: acute and follow-up care characteristics. J Forensic Nurs 2013;9:76-83.
- Brooker C, Tocque K, Paul S. Assessment of the mental health status of a one year cohort attending a two Sexual Assault Referral Centres in England. J Forensic Leg Med 2018;54:44-9.
- Brooker C, Tocque K. Mental health risk factors in sexual assault: what should Sexual Assault Referral Centre staff be aware of?. J Forensic Leg Med 2016;40:28-33.
- NHS England . Commissioning Framework for Adult and Paediatric Sexual Assault Referral Centre (SARC) Services 2015.
- Brooker C, Durmaz E. Mental health, sexual violence and the work of Sexual Assault Referral Centres (SARCs) in England. J Forensic Leg Med 2015;31:47-51.
- Stefanidou T, Hughes E, Kester K, Edmondson A, Majeed-Ariss R, Smith C, et al. The identification and treatment of mental health and substance misuse problems in sexual assault services: a systematic review. PLoS ONE 2020;15.
- Price H, Domoney J, Ariss S, Hughes E, Trevillion K. Documentary analysis within a realist evaluation: recommendations from a study of Sexual Assault Referral Centres. Int J Qual Methods 2021;20.
- Survivors Voices . The Charter for Engaging Survivors n.d. https://survivorsvoices.org/charter (accessed 12 July 2022).
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Mark R, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Lancaster: Lancaster University; 2006.
- Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract 2018;24:459-67.
- National Institute for Health and Care Excellence . Post-Traumatic Stress Disorder 2018.
- Connell J, Barkham M. CORE-10 User Manual. Version 1.1. 2007. www.coresystemtrust.org.uk (accessed 31 May 2023).
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP) – Alcohol Use Disorders Identification Test. Arch Intern Med 1998;158:1789-95.
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, et al. The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a Veteran Primary Care sample. J Gen Intern Med 2016;31:1206-11.
- Keetharuth AD, Brazier J, Connell J, Bjorner JB, Carlton J, Taylor Buck E, et al. Recovering Quality of Life (ReQoL): a new generic self-reported outcome measure for use with people experiencing mental health difficulties. Br J Psychiatry 2018;212:42-9.
- Skinner HA. The drug abuse screening test. Addict Behav 1982;7:363-71.
- Moran P, Morven L, Tennyson L, Walters P, Thornicroft G, Mann A. Standardised Assessment of Personality – Abbreviated Scale (SAPAS): preliminary validation of a brief screen for personality disorder. Br J Psychiatry 2003;183:228-32.
- Pawson RT. Realist Evaluation. London: Sage; 1997.
- Pawson RT. Realist Evaluation 2004 n.d. www.betterevaluation.org/en/approach/realist_evaluation (accessed 12 July 2022).
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11.
- Baker GR. The contribution of case study research to knowledge of how to improve quality of care. BMJ Qual Safe 2011;20:i30-5.
- Easton G. Critical realism in case study research. Ind Mark Manage 2010;39:118-28.
- Shearn K, Allmark P, Piercy H, Hirst J. Building realist program theory for large complex and Messy Interventions. Int J Qual Methods 2017;16.
- Esteves RB, Lasiuk GC, Cardoso L, Kent-Wilkinson A. Toward the establishment of a forensic nursing specialty in Brazil: an integrative literature review. J Forensic Nurs 2014;10:189-98.
- Rheingold AA, Zinzow H, Hawkins A, Saunders BE, Kilpatrick DG. Prevalence and mental health outcomes of homicide survivors in a representative US sample of adolescents: data from the 2005 National Survey of Adolescents. J Child Psychol Psychiatry 2012;53:687-94.
- Hansen M, Stefansen K, Skilbrei M-L. Non-reporting of sexual violence as action: acts, selves, futures in the making. Nord J Criminol 2021;22:42-57.
- Mukhtar SA, Smith DA, Phillips MA, Kelly MC, Zilkens RR, Semmens JB. Capturing sexual assault data: an information system designed by forensic clinicians and healthcare researchers. Health Inform Manag J 2017;47:46-55.
- Loko Roka J, Van den Bergh R, Au S, De Plecker E, Zachariah R, Manzi M, et al. One size fits all? Standardised provision of care for survivors of sexual violence in conflict and post-conflict areas in the Democratic Republic of Congo. PLOS ONE 2014;9.
- Nesvold H, Friis S, Ormstad K. Sexual assault centers: attendance rates, and differences between early and late presenting cases. Acta Obstet Gynecol Scand 2008;87:707-15.
- Nelson DD. An Examination of Predictors of Sexual Assault Mental Health Treatment Utilization in Asian American, Native Hawaiian, and Caucasian Sexual Assault Survivors. PhD Dissertation 2016.
- Olsen A, Majeed-Ariss R, Teniola S, White C. Improving service responses for people with learning disabilities who have been sexually assaulted: an audit of forensic services. Br J Learn Disab 2017;45:238-45.
- Winters L. Sexual Violence Needs Assessment for Merseyside. Observatory Report Series No. 85 2011.
- Du Mont J, Macdonald S, White M, Turner L, White D, Kaplan S, et al. Client satisfaction with nursing-led sexual assault and domestic violence services in Ontario. J Forensic Nurs 2014;10:122-34.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60.
- Power J, Gilmore B, Vallieres F, Toomey E, Mannan H, McAuliffe E. Adapting health interventions for local fit when scaling-up: a realist review protocol. BMJ Open 2019;9.
- Stewart R, Soremekun M, Perera G, Broadbent M, Callard F, Denis M, et al. The South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLAM BRC) case register: development and descriptive data. BMC Psychiatry 2009;9.
- Perera G, Broadbent M, Callard F, Chang CK, Downs J, Dutta R, et al. Cohort profile of the South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLaM BRC) Case Register: current status and recent enhancement of an Electronic Mental Health Record-derived data resource. BMJ Open 2016;6.
- Mavranezouli I, Brazier JE, Rowen D, Barkham M. Estimating a preference-based index from the Clinical Outcomes in Routine Evaluation-Outcome Measure (CORE-OM): valuation of CORE-6D. Med Decis Making 2013;33:381-95.
- NHS England . National Schedule of NHS Costs 2021 2021. www.england.nhs.uk/costing-in-the-nhs/national-cost-collection (accessed 12 July 2022).
- Sweeney A, Filson B, Kennedy A, Collinson L, Gillard S. A paradigm shift: relationships in trauma-informed mental health services. BJPsych Adv 2018;24:319-33.
- Dworkin ER, Menon SV, Bystrynski J, Allen NE. Sexual assault victimization and psychopathology: a review and meta-analysis. Clin Psychol Rev 2017;56:65-81.
- Brooker C, Edmondson A, Hughes L. The contribution of mental health services to a new strategic direction for sexual assault and abuse services. J Forensic Leg Med 2019;64:45-8.
Appendix 1 Work package 2 – descriptive analysis
Response summary
Expected number of SARCs (from 2018/19 SARCIP submissions): 49.
Actual responses to survey: 36; which is a response rate of 73%. From Q20 onwards, there were 32 responses – a response rate of 65%.
Service provision
| Q4 | What organisation or company has lead responsibility for the day-to-day management of your SARC? (Please select the one that most closely resembles your management model) |
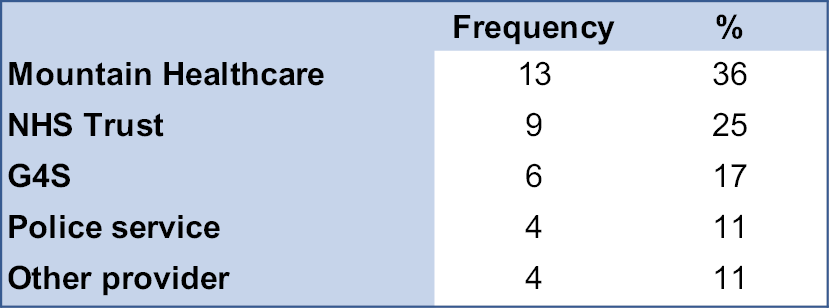
Others:
-
Care UK until 31 March 2019 then G4S.
-
First light.
-
Safe in Tees Valley.
-
SV2 – Supporting victims of sexual violence. Charity no 1,077,863.
Around one-third of SARCs are managed by Mountain Healthcare, with one-quarter managed by the NHS and the others equally by G4S, the police or another provider. On average, SARCs are based on 1.4 (range: 1–3) sites.
Almost all SARCs (35/36; 97%) provide 24-hours-a-day, 7-days-a-week service for police referrals but around half (17/36; 47%) provide the same for self-referrals. Where 24/7 is not provided, opening times were stated.
The majority (28/36) of respondents did not know the total annual budget for the SARC or what proportion was provided by the Office of the Police and Crime Commissioner.
| Q19 | Which of the following client group(s) does your SARC support? |
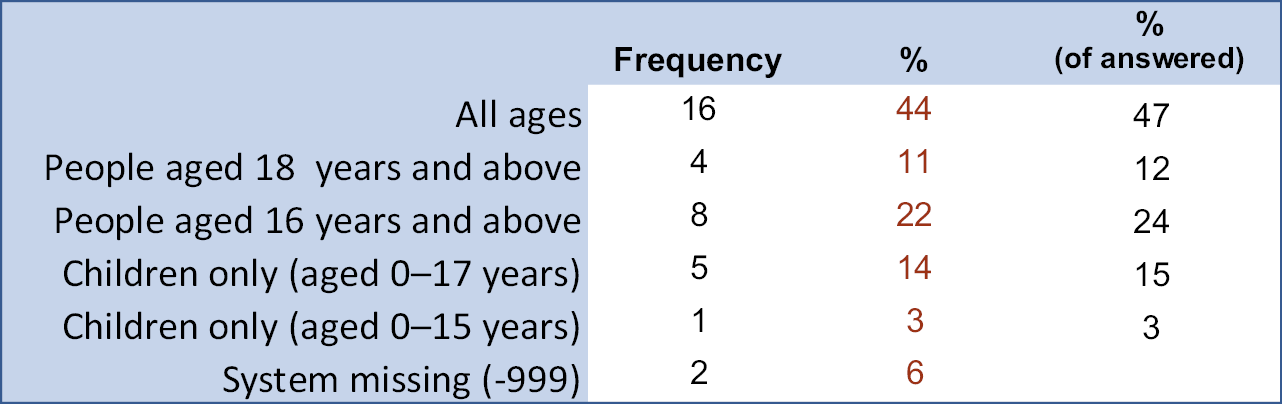
Around half of SARCs (16/34; 47%) provide service to all age groups. Another one-third provide service to people aged 16/18 years and above (12/34; 36%) and 18% (6/34) to children aged under 16/18 years.
Staffing
| Q20 | Please complete the grid below for full- and part-time staff, including hours per week or whole time equivalent (WTE), and any vacant posts. Number of staff and WTE/hours per week (e.g. one member of staff working half of the week could be 1 × 0.5 WTE or 1 × 18 hours) |
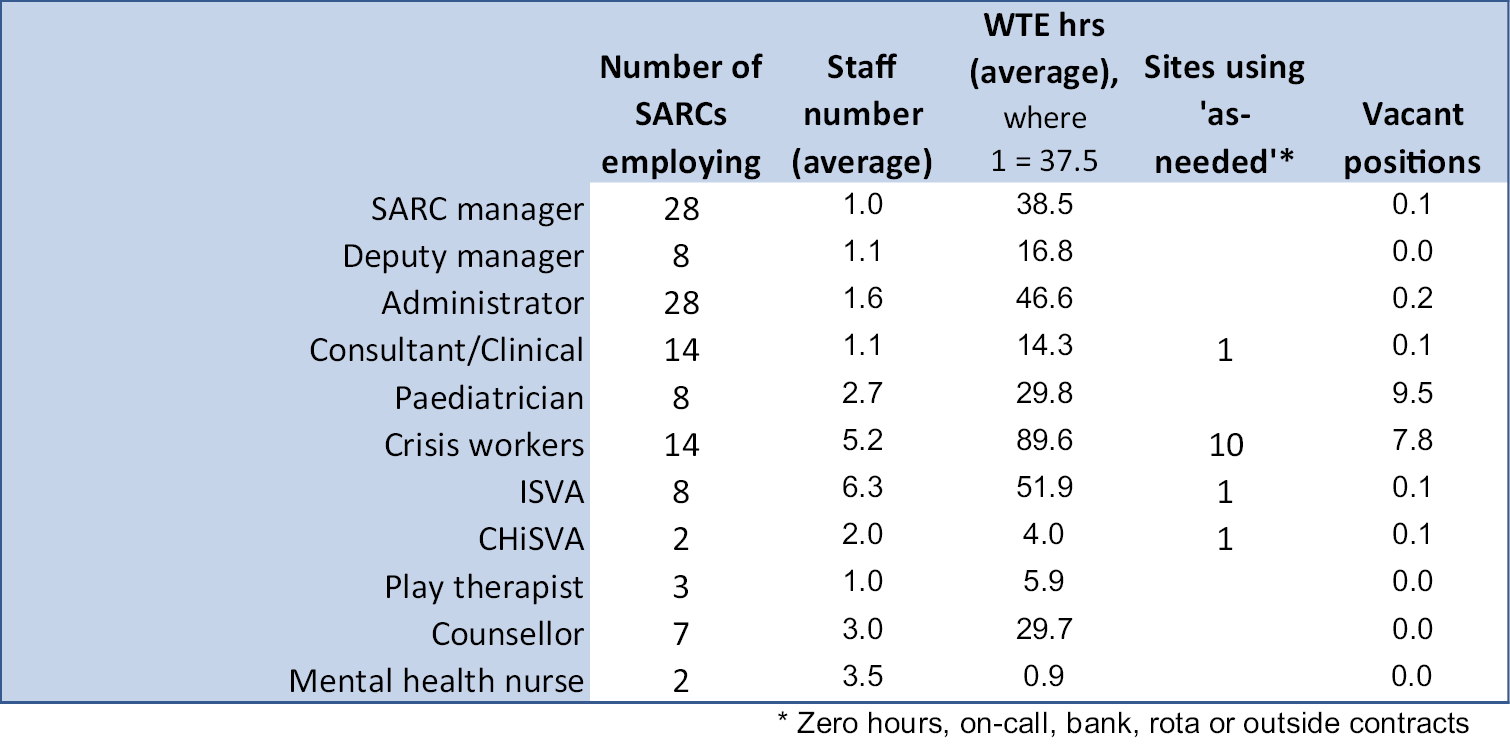
| Q21 | Please complete the grid below for staff that work at the SARC on an as-needed basis (e.g. on-call, zero-hours contracts) indicating what those arrangements are and if staffing needs are currently being met. Number of staff and contract arrangements |
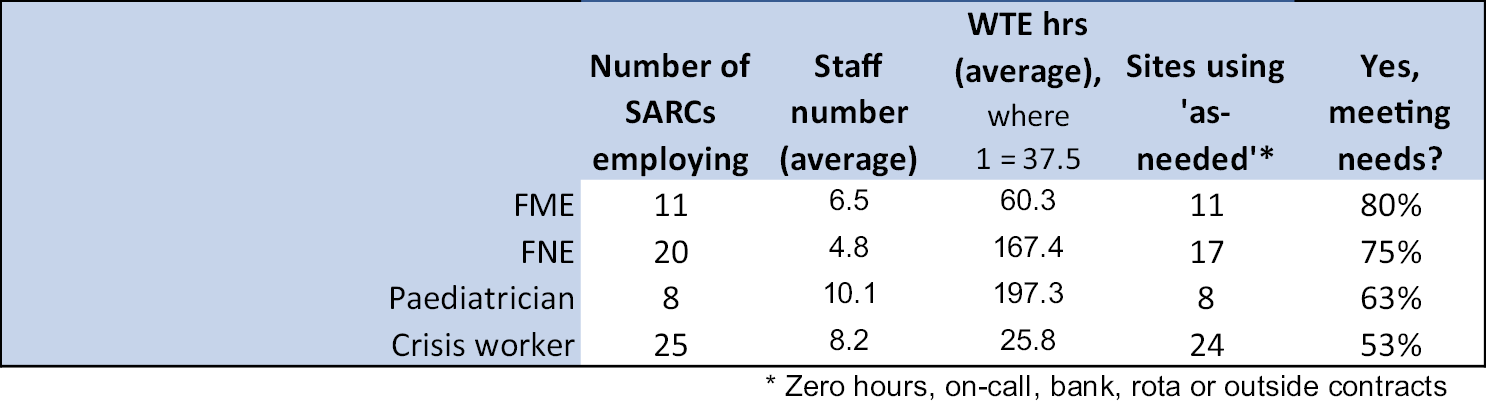
| Q22 | Of the FMEs, FNEs and paediatricians indicated above, how many have completed national qualifications and training (e.g. MMFLM)? |
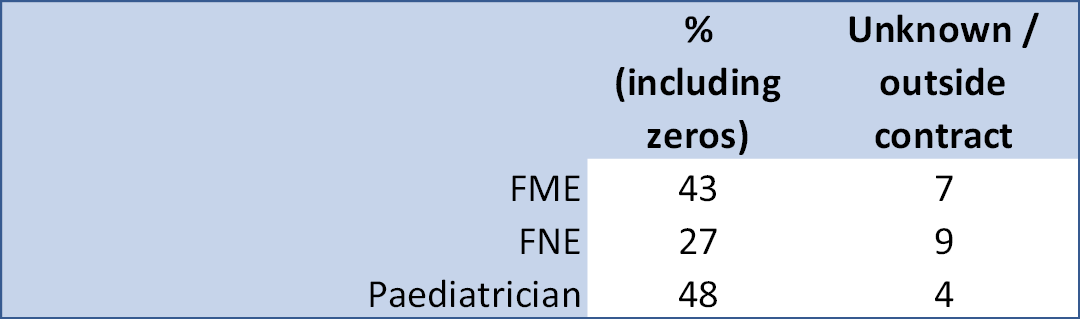
| Q23 | What is the approximate ratio of FMEs to FNEs in your SARC? |
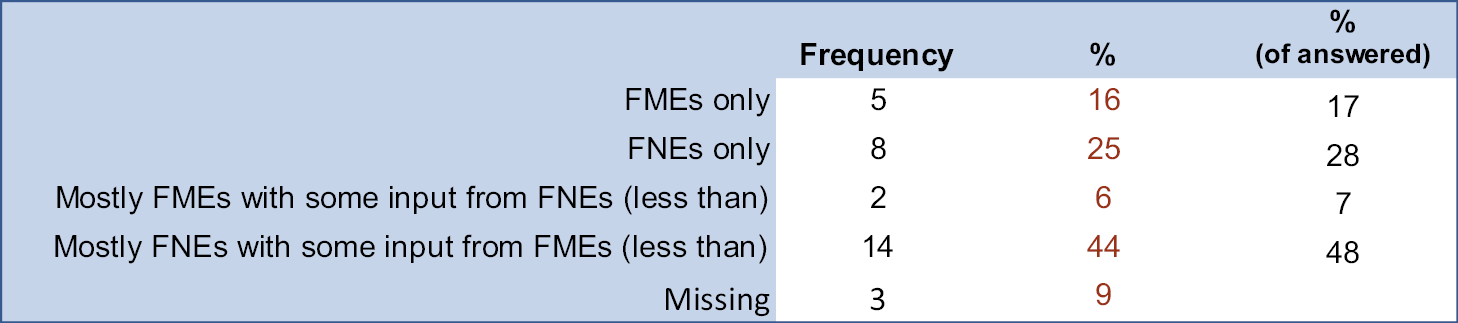
| Q24 | Is your service able to offer all service users the option of a male or female forensic practitioner for the forensic examination? (Please only select ‘not applicable’ if you do not offer the service) |
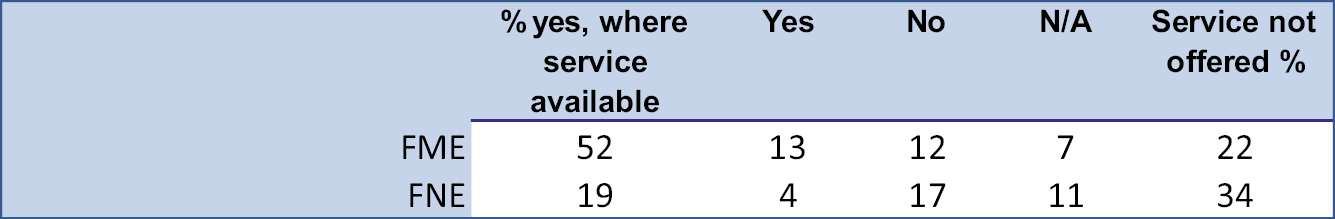
From this point onwards, only 32 SARCs responded. Some 94% (29/31) stated that there was a named person within the facility with responsibility for ensuring a suitable forensic environment.
Service delivery
| Q26 | What methods do you use for recording access to forensic rooms? (Please tick all that apply) |
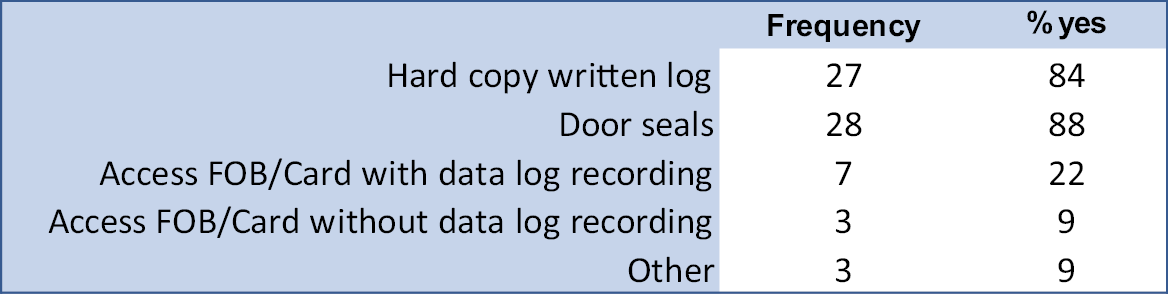
Only four SARCs (13%) said that FMEs/FNEs covered both SARC cases and custody examinations. Three stated how this was managed:
-
FME contract managed through Derbyshire Police.
-
One FNE – shifts separated; does not see alleged perpetrator and victim in the same case.
-
The FME will not see a suspect of sexual assault in custody.
| Q29 | How many of the following services are offered at the SARC? (Please tick all that apply) |
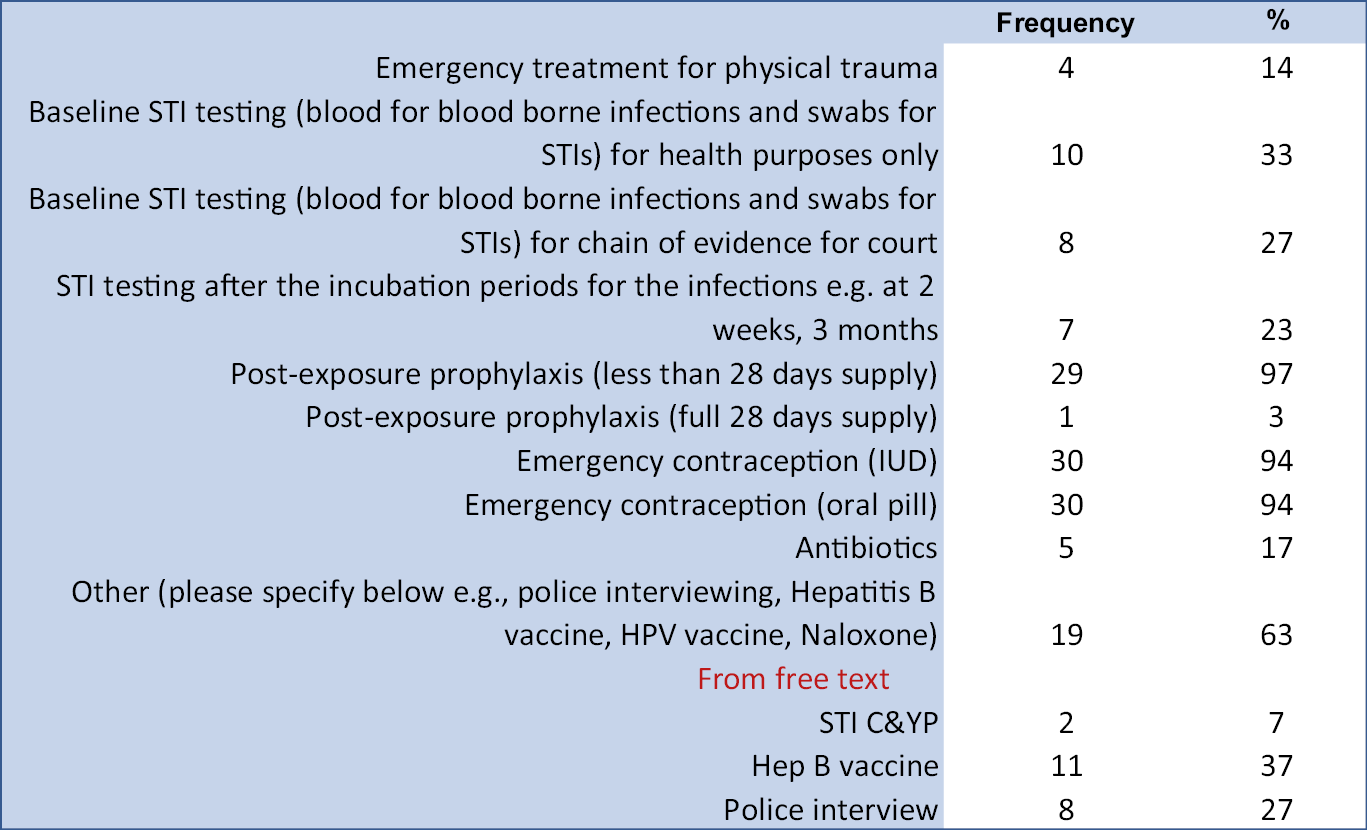
| Q30 | Which best describes the way your SARC is integrated with other professionals/services? |
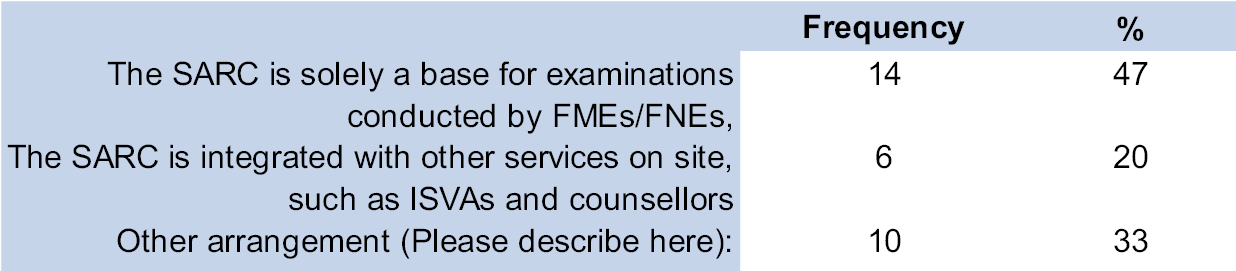
| Q31 | Do any of the SARC staff have a professional mental health qualification (e.g. background or training in mental health nursing, psychology, psychiatry or other recognised degree or qualification)? |
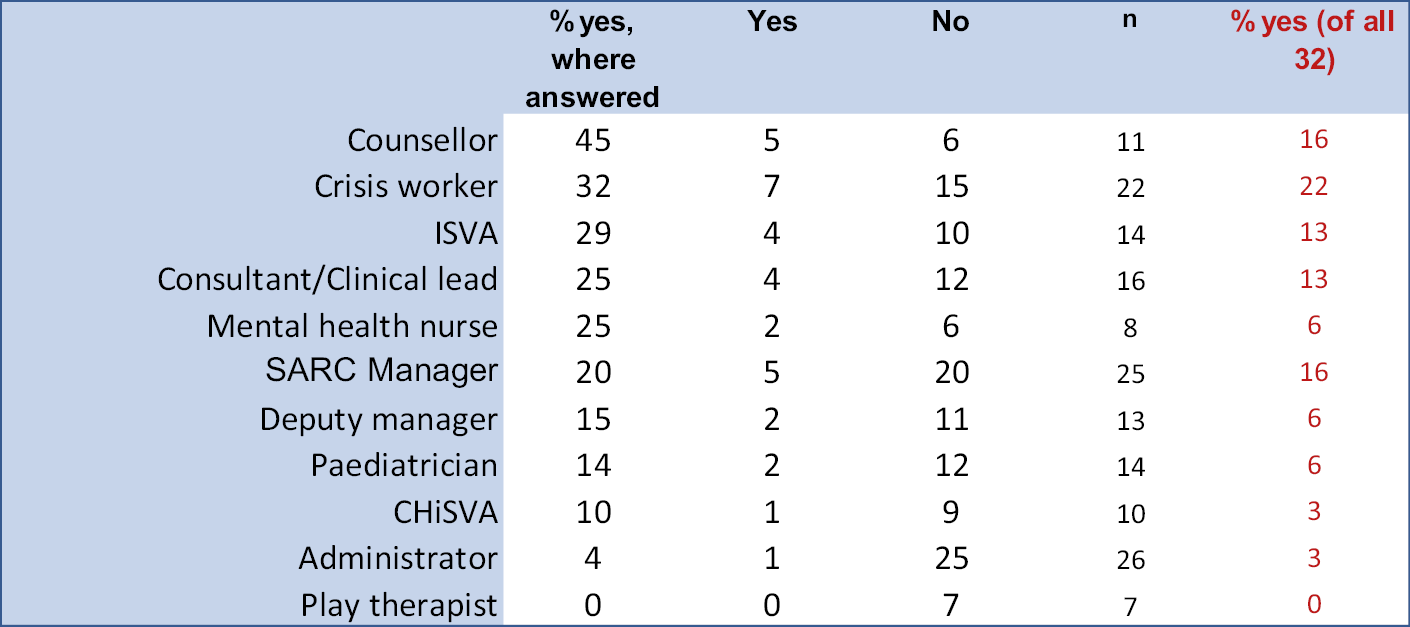
| Q32 | How do you identify and assess for mental health and substance use issues in people who attend the SARC (please tick any that apply)? |
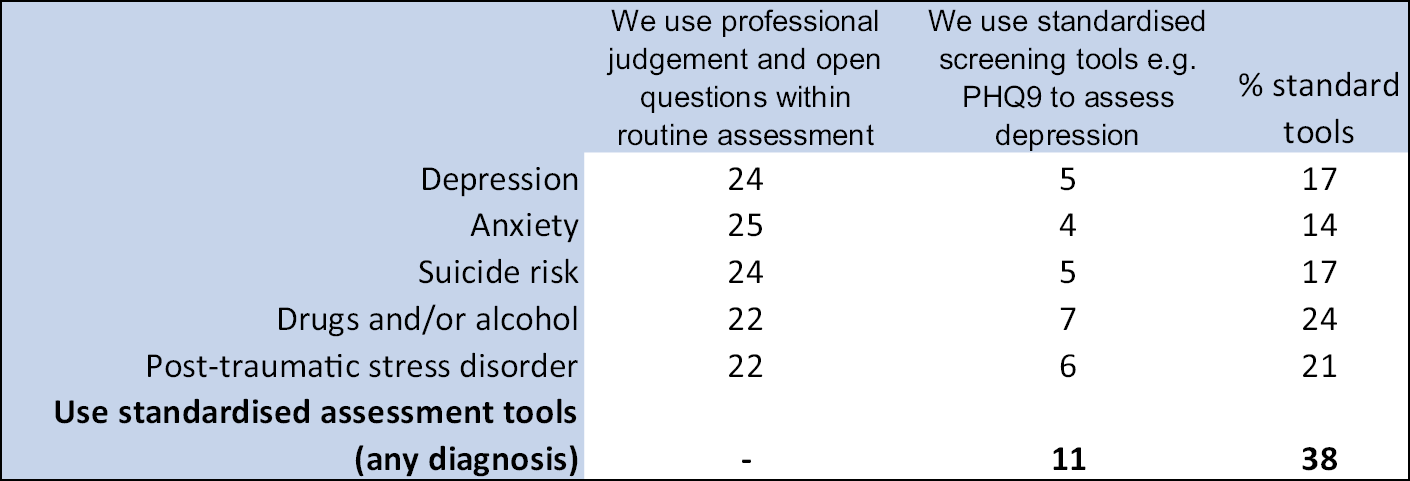
Only 7% (2/28) stated that a talking therapy service was provided or co-located within the SARC (even if the provider is a different organisation). Further, 21% (6/29) stated that access to a clinical psychologist was provided or co-located within the SARC (even if the provider is a different organisation).
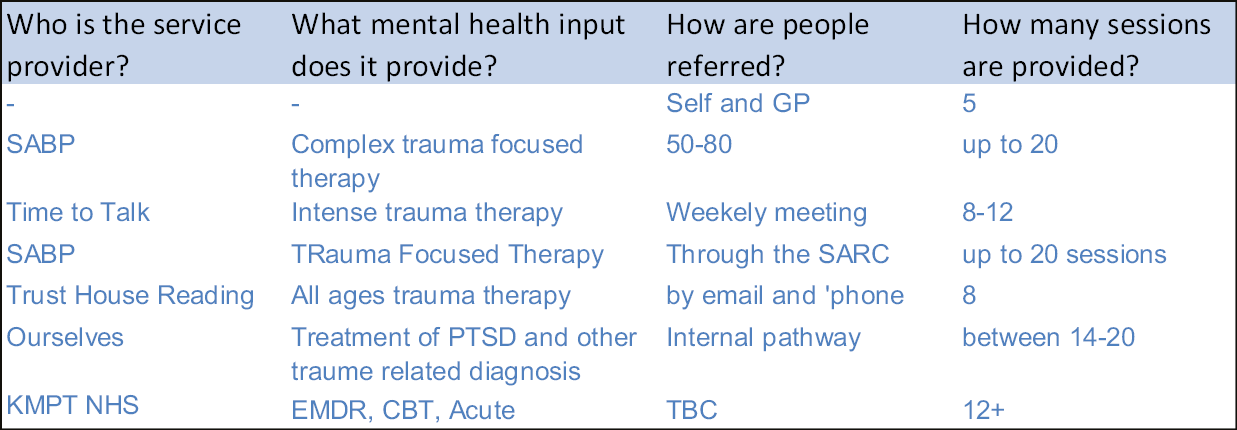
Over half (15/28; 54%) stated that a specialist counselling service was provided or co-located within the SARC (even if provider is a different organisation).
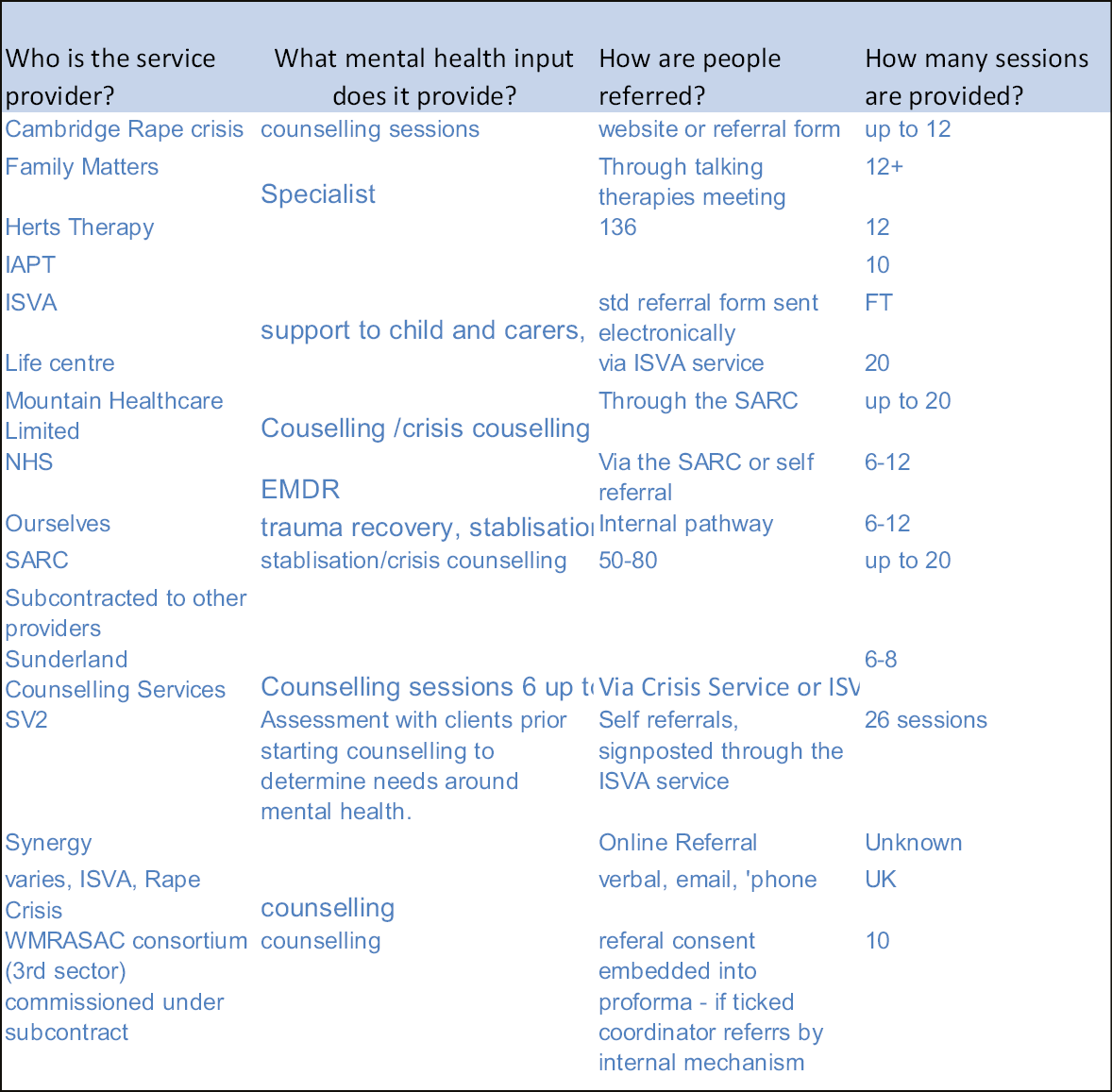
IAPT, Increasing Access to Psychological Therapies
Some 10% (3/30) stated that a drug or alcohol service provided or co-located within the SARC (even if provider is a different organisation);
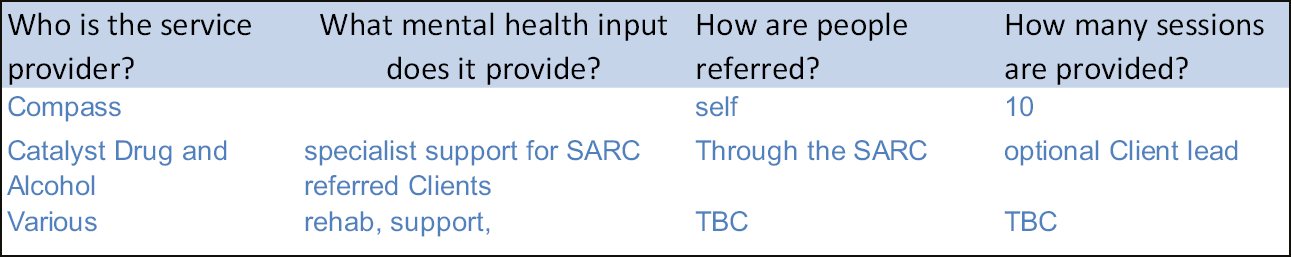
18% (5/28) stated that single session debriefing was provided or co-located within the SARC (even if provider is a different organisation).
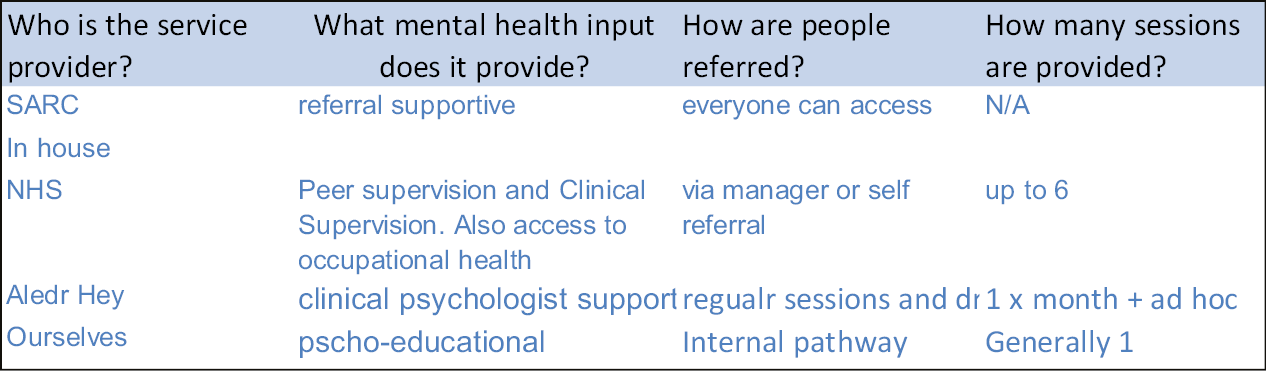
Only one SARC stated that other mental health or substance misuse services were provided or co-located within the SARC (even if the provider is a different organisation). This was indicated to be a ‘mental health nurse – 18 hours per week contract’.
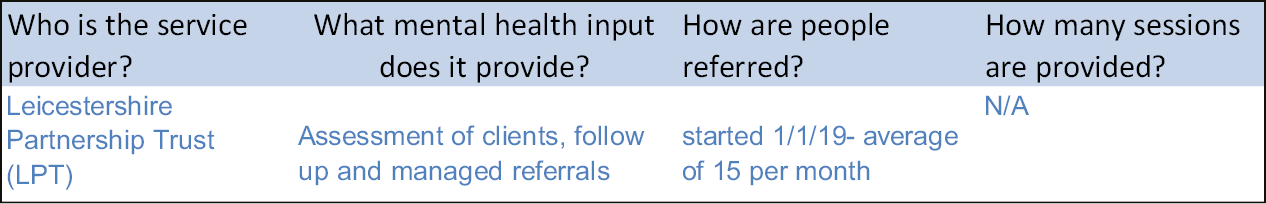
Final questions
| Q46 | Please indicate if you have the following in terms of onward referrals to other services |
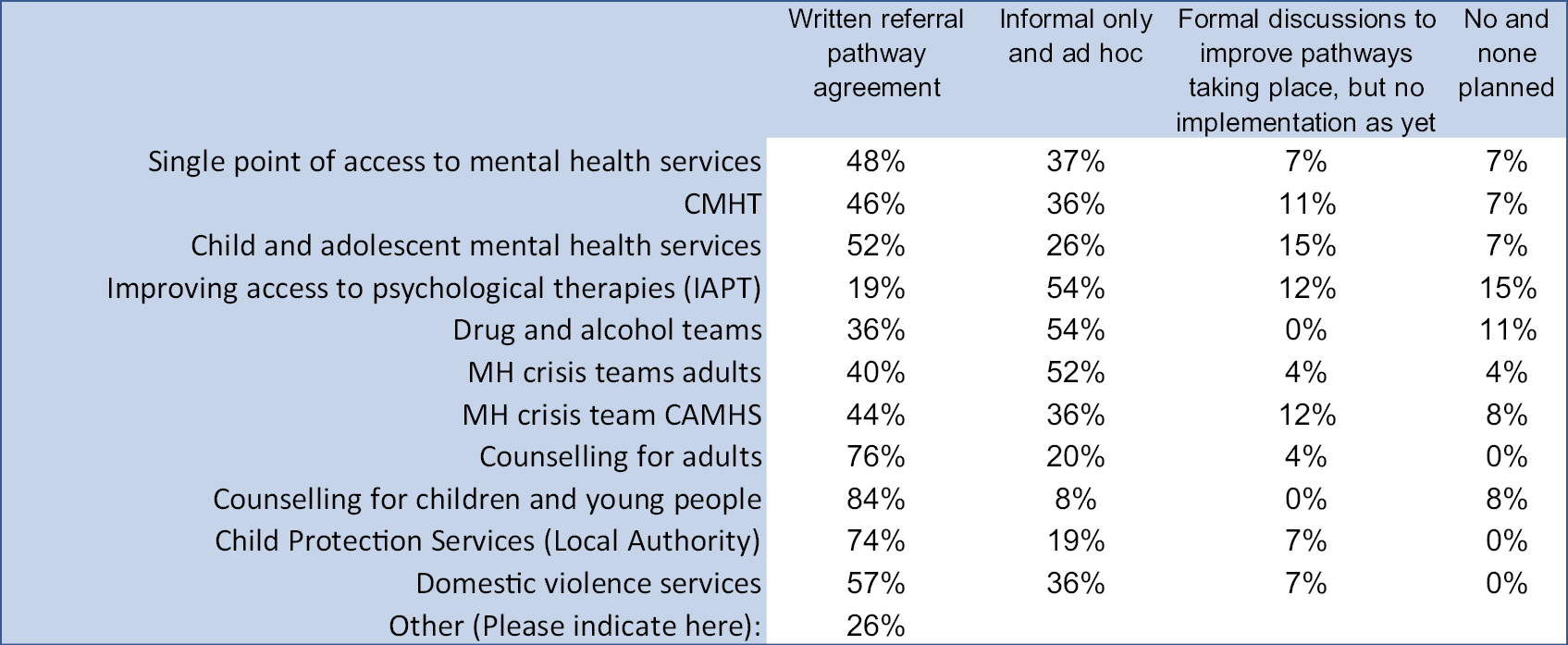
IAPT, Increasing Access to Psychological Therapies
| Q47 | How satisfied are you with the level of integration of your service within the wider local services context? |
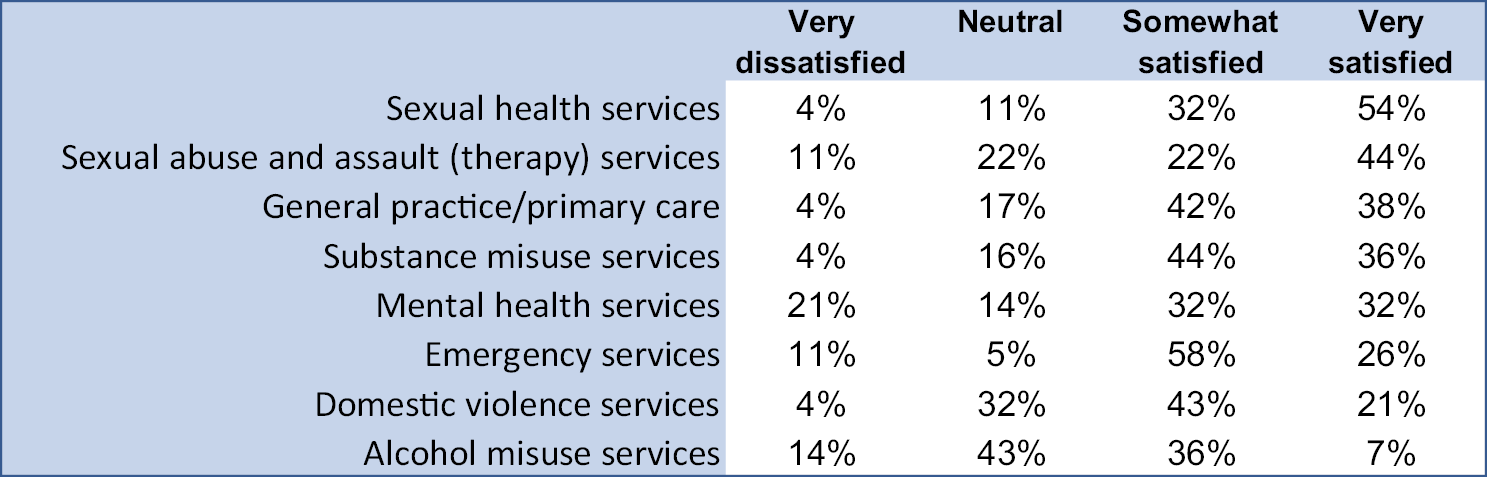

Appendix 2 Cut-off scores for the work package 3 prevalence study
| CORE-10 | ≥ 15 |
|---|---|
| ≤ 10 – non-clinical | |
| 11–14 – mild psychological distress | |
| 15–19 – moderate psychological distress | |
| 20–24 – moderate-to-severe psychological distress | |
| ≥ 25 – severe psychological distress | |
| AUDIT-C | ≥ 8 |
| 0–7 Lower risk – no intervention required | |
| 8–15 Increasing risk – brief advice 1 | |
| 16–19 Higher risk – brief advice and/or extended brief advice | |
| 20+ Possible dependence – referral to services | |
| PC-PTSC-5 | ≥ 3 |
| Screening tool 3 + indicates likely PTSD | |
| ReQoL-10 | ≥ 25 |
| A ReQoL-10 score between 0 and 24 is considered as falling within the clinical range | |
| A score of 25 and above is considered as falling within the range of the general population | |
| ReQoL_physical health | ≥ 2 |
| Please describe your physical health (problems with pain, mobility, difficulties caring for yourself or feeling physically unwell) over the last week | |
| 0 (no problems) | |
| 1 (slight problems) | |
| 2 (moderate problems) | |
| 3 (severe problems) | |
| 4 (very severe problems) | |
| DAST-10 | ≥ 3 |
| 0 No problems reported (none at this time) | |
| 1–2 low level (monitor, reassess at a later date) | |
| 3–5 moderate level (further investigation) | |
| 6–8 substantial level (intensive assessment) | |
| 9–10 severe level (intensive assessment) | |
| SAPAS | ≥ 3 |
| 3+ indicates likely personality disorder |
Appendix 3 Prevalence estimates weighting methodology
The prevalence of mental health and substance misuse problems determined from the survey sample (see Table 3) was disaggregated by demographics (age, ethnicity and gender a–f). This was multiplied by the estimated demographics of all attendees of SARCs from the SARCIPs 2018–19 returns (h) to obtain an estimated of the number of attendees likely to show the various mental health and substance misuse problems. The overall weighted prevalence was determined as the sum of each demographic category by the total number of attendees in 2018/19; n = 14,357.
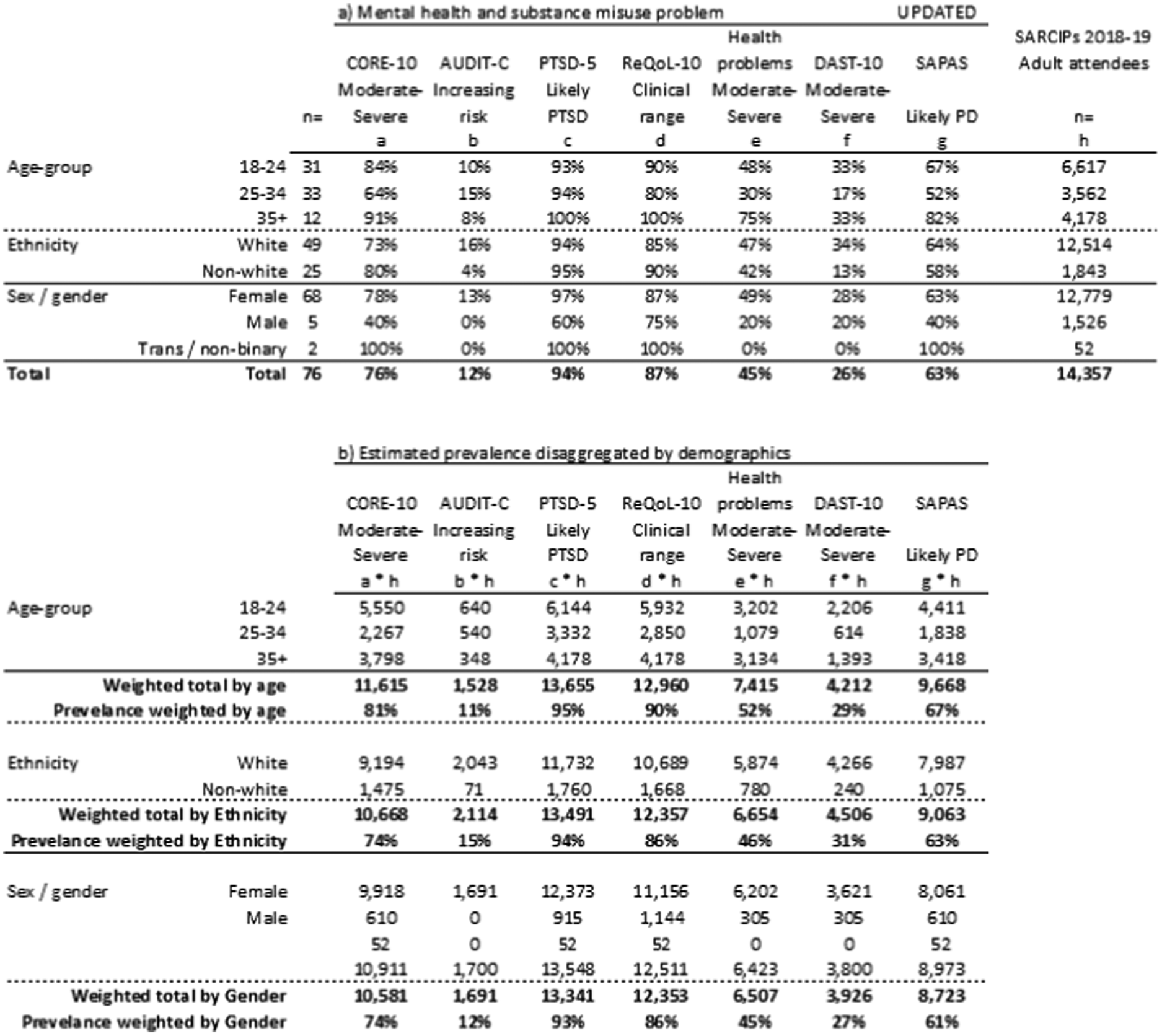
Appendix 4 Work package 5: establishing the cohort in clinical record interactive search
We aimed to extract a cohort of people who had experienced a sexual assault anytime in their lifetime, had received psychological therapy in SLaM (at least one face-to-face contact labelled as psychological therapy) between January 2016 and December 2019, and who had completed pre- and post-therapy CORE assessments. Lower date restrictions were selected to match the dates of the Kent database, which was established in 2016. We also aimed to extract a cohort of people who had no documented experience of sexual assault but who met the remaining criteria. To do this, we first established a group of users from the CRIS system that had a documented face-to-face psychological therapy attendance during the 2016–19 period, totalling 21,965 people (search criteria used can be seen in Box 1).
Received psychological therapy
Within events:
-
Note type = psychological therapy AND
-
Type of contact = Face to face AND
-
Event was = attended
between 2016 and 2019 (i.e. > 31/12/2015 and < 1/01/2020)
AND has CORE outcome
Any CORE recorded between 2016 and 2019 (i.e. after 31 December 2015 and before 1 January 2020)
Both CORE-10 and CORE-OM are eligible
With at least one ‘Last’ or ‘Follow-up’ rating period
AND has one or more of the following sexual assault terms in free text (event notes and/or attachments/correspondence) at any time:
-
‘*Sexual violence*’
-
‘*Rape*’
-
‘*Sexual abuse*’
-
‘*Sexually abused*’
-
‘*Sexual assault*’
-
‘*Sexually assaulted*’
-
‘*Child sexual abuse*’
A further group of users were established who had a documented CORE measurement during the same period, totalling 15,342 individuals. Of these, 11,929 individuals had both a CORE measurement and a face-to-face psychological therapy attendance during 2016–19.
We established a further cohort of 64,110 individuals who were identified as having terms for sexual assault in the free-text fields related to their clinical notes and/or medical correspondence at any time period. Search terms included: sexual violence, rape, sexual abuse, sexually abused, sexual assault, sexually assaulted, child sexual abuse.
By linking these two cohorts together, we identified two groups of users:
-
Individuals who had both a CORE measurement and a face-to-face psychological therapy attendance during 2016–19 and who had sexual assault terms in free-text fields; a total of 6059 people.
-
Individuals who had both a CORE measurement and a face-to-face psychological therapy attendance during 2016–19 and who did not have sexual assault terms in free-text fields; a total of 5870 people.
In the CRIS system, CORE assessments are labelled as to the time-point when they are taken: initial assessment, first session, mid-session, last session, follow-up. To limit the sample to those who had pre- and post-therapy scores on the CORE, we searched for people who had more than one CORE measure, one of which was labelled as a last session or follow-up measure. This produced samples of:
-
2555 individuals who had a documented sexual assault term (sexual assault positive)
-
2456 who did not have sexual assault terms (sexual assault negative).
Validating that the sample met our criteria
The presence of sexual assault terms in the free-text fields did not necessarily mean that the individual had experienced sexual violence. For example, these terms were present in cases where the individual was a perpetrator, or where another family member had been a victim of sexual assault. Therefore, a random sample of 520 sexual assault cases (approximately 20%) were manually checked to establish whether the classification was correct.
Of the 520 sexual assault cases, 26 cases were excluded where the notes/correspondence could not be accessed (too long or corrupted) and five cases were excluded where they had been extracted due to a typographic error (e.g. ‘neccsarry’, ‘hecsays’, ‘medicsal’). Of the remaining 489 sexual assault cases, 305 (62%) were correct. Owing to the substantial number of false positives (38%) and the fact that it was not feasible to manually check all 2555 cases, the 305 validated cases were used as a representative sample for further analysis.
One hundred cases without a documented sexual assault term were also checked for accuracy. Of these, 98 (98%) cases were correct. Owing to the high percentage of correct classifications, further checks were not undertaken on this sample. Excluding the two cases identified as incorrect, a random sample of 305 individuals (including the 98 checked for negative validity) were selected from the 2456 non-sexual-assault group to act as a control sample.
Our selection criteria included those cases that had more than one CORE measure, one of which was a last session/follow-up assessment and had a face-to-face psychological therapy attendance within the specified dates. However, these data needed further interrogation to identify whether the CORE measures represented pre- and post-therapy scores related to the psychological therapy attendance. For example, in some cases, CORE assessments were recorded on dates that were in a different year to the documented therapy attendance. Therefore, further manual validation was undertaken on the 610 cases to identify those cases with an episode of therapy that had associated outcome measures. During this validation, the number of therapy sessions attended within the pre- and post-CORE date range was counted, providing a measure of dosage.
Of the 610 cases, 522 (85%) had identifiable episodes of therapy with associated CORE measurements – 265 sexual assault and 257 no sexual assault. This therefore represented our final sample for subsequent analysis.
Appendix 5 Work package 5 clinical record interactive search analysis
| Variable | SA (n = 265) | Non-SA (n = 257) | p-value |
|---|---|---|---|
| Spell number (2015–19), n (%) | < 0.001 | ||
| 1 | 80 (30) | 112 (44) | |
| 2 | 38 (14) | 57 (22) | |
| 3 | 50 (19) | 40 (19) | |
| 4 | 33 (12) | 18 (7) | |
| 5 | 25 (9) | 10 (4) | |
| 6 | 9 (3) | 7 (3) | |
| 7+ | 28 (11) | 9 (4) | |
| Not known (excluded above) (%) | 1 | 2 | |
| Spell number (mean ± SD) | 3.3 ± 2.4 | 2.3 ± 1.8 | < 0.001* |
| Number of CORE assessments (2015–20), n (%) | < 0.001 | ||
| 2 | 58 (22) | 119 (46) | |
| 3 | 64 (24) | 55 (21) | |
| 4 | 58 (22) | 53 (21) | |
| 5 | 33 (12) | 13 (5) | |
| 6 | 21 (8) | 8 (3) | |
| 7 | 11 (4) | 4 (2) | |
| 8+ | 20 (8) | 5 (2) | |
| Number of COREs (mean ± SD) | 4.8 ± 2.6 | 3.5 ± 2.6 | < 0.001* |
| Year first CORE (mean ± SD) | 2016.4 ± 1.2 | 2016.8 ± 1.2 | < 0.005* |
| Year first ever CORE (2006+) (mean ± SD) | 2014.4 ± 3.7 | 2015.6 ± 3.1 | < 0.001* |
| Number of psychological therapy attendances (2016–19), n (%) | < 0.001 | ||
| 1–10 | 39 (15) | 67 (26) | |
| 11–20 | 63 (24) | 106 (41) | |
| 21–30 | 79 (30) | 48 (19) | |
| 31–40 | 31 (12) | 22 (9) | |
| 40+ | 53 (20) | 14 (5) | |
| Number of attendances, mean ± SD | 28.4 ± 13.7 | 19.2 ± 21.3 | < 0.001* |
| Cost @£71/attendance, mean ± SD | £2018 ± 1512 | £1358 ± 972 | < 0.001* |
| Number of diagnoses (2000–19), n (%) | < 0.001 | ||
| 1 | 41 (16) | 72 (28) | |
| 2–3 | 48 (18) | 70 (28) | |
| 4–5 | 46 (17) | 50 (20) | |
| 6–7 | 39 (15) | 20 (8) | |
| 8–10 | 30 (11) | 22 (9) | |
| 11–15 | 24 (9) | 12 (5) | |
| 16+ | 36 (14) | 7 (3) | |
| Number of diagnoses, mean ± SD | 7.7 ± 7.7 | 4.3 ± 4.3 | < 0.001* |
| Year of first diagnosis, mean ± SD | 2010.2 ± 5.4 | 2012.7 ± 5.2 | < 0.001* |
| ICD-10 block | Primary ICD-10 diagnosisa | SA (n = 265) | Controls (n = 257) |
|---|---|---|---|
| n (%) | n (%) | ||
| F20–F29 | Schizophrenia, schizotypal, delusional, and other non-mood psychotic disorders | 475 (23) | 167 (15) |
| F30–F39 | Mood [affective] disorders | 429 (21) | 332 (31) |
| F40–F48 | Anxiety, dissociative, stress-related, somatoform and other nonpsychotic mental disorders | 284 (14) | 148 (14) |
| F60–F69 | Disorders of adult personality and behaviour | 252 (12) | 42 (4) |
| F99–F99 | Unspecified mental disorder | 231 (11) | 123 (11) |
| F10–F19 | Mental and behavioural disorders due to psychoactive substance use | 196 (10) | 100 (9) |
| F50–F59 | Behavioural syndromes associated with physiological disturbances and physical factors | 91 (4) | 66 (6) |
| XXXX | Other diagnosis not F-codes | 46 (2) | 56 (5) |
| F00–F01 | Dementia in Alzheimer’s disease | 18 (1) | 13 (1) |
| F01–F09 | Mental disorders due to known physiological conditions | 15 (1) | 17 (2) |
| F70–F79 | Intellectual disabilities | 0 (0) | 0 (0) |
| F80–F89 | Pervasive and specific developmental disorders | 0 (0) | 0 (0) |
| F90–F98 | Behavioural and emotional disorders with onset usually occurring in childhood and adolescence | 0 (0) | 10 (1) |
| F specified | [sum of highlighted above] | 0 (0) | 0 (0) |
| 178 (9) | 171 (16) |
| SA group | Control group | p-value | ||||
|---|---|---|---|---|---|---|
| Current risk | Historic risk | Current risk | Historic risk | Current risk | Historic risk | |
| A: Trigger factors a | ||||||
| Relationship/family conflicts | 79 (28) | 98 (34) | 42 (20) | 45 (21) | < 0.05 | < 0.01 |
| Adverse life events | 46 (17) | 83 (29) | 21 (10) | 40 (18) | < 0.05 | < 0.01 |
| Dysfunctional coping mechanisms | 65 (23) | 66 (23) | 37 (17) | 39 (18) | 0.116 | 0.126 |
| Drug and alcohol abuse | 25 (9) | 60 (22) | 13 (6) | 28 (14) | 0.241 | < 0.05 |
| Poor social network | 59 (21) | 58 (21) | 36 (17) | 32 (15) | 0.182 | 0.081 |
| Physical health problems | 67 (25) | 50 (19) | 37 (18) | 28 (13) | 0.059 | 0.111 |
| Employment/housing/financial difficulties | 61 (22) | 45 (17) | 33 (16) | 22 (11) | 0.077 | 0.055 |
| Disengagement/poor concordance | 30 (11) | 41 (16) | 14 (7) | 23 (11) | 0.093 | 0.148 |
| Transitions in care | 21 (8) | 20 (8) | 7 (3) | 5 (2) | < 0.05 | < 0.05 |
| B: Self-harm and suicide b | ||||||
| Previous suicide attempt/accidental overdose | – | 114 (63) | – | 47 (39) | – | < 0.01 |
| Acts of deliberate self-harm | 45 (23) | 106 (55) | 28 (23) | 54 (43) | 0.994 | < 0.05 |
| Alcohol/substance misuse | 48 (25) | 87 (47) | 15 (13) | 36 (31) | < 0.05 | < 0.01 |
| Expressed plans to end life | 40 (20) | 69 (36) | 23 (18) | 38 (30) | 0.633 | 0.273 |
| Experience of loss (financial, relationship) | 57 (30) | 65 (35) | 24 (20) | 32 (26) | 0.051 | 0.111 |
| Feelings of hopelessness | 66 (34) | 62 (33) | 37 (29) | 35 (28) | 0.436 | 0.328 |
| Social isolation | 75 (39) | 59 (32) | 41 (33) | 34 (28) | 0.265 | 0.461 |
| Physical illness | 68 (36) | 53 (29) | 32 (26) | 32 (26) | 0.061 | 0.506 |
| Psychotic symptoms including command hallucinationsc | 4 (14) | 8 (27) | 0 (0) | 3 (18) | – | 0.482 |
| Deteriorating depression with distress | 59 (30) | 44 (24) | 18 (15) | 24 (20) | < 0.01 | 0.324 |
| Poor engagement with services/treatment | 24 (13) | 33 (18) | 16 (13) | 16 (13) | 0.916 | 0.304 |
| Command hallucinations (voices telling them to kill themselves) | 16 (9) | 28 (16) | 7 (6) | 13 (11) | 0.393 | 0.299 |
| Significant anniversary | 17 (9) | 21 (12) | 4 (3) | 2 (2) | 0.051 | < 0.01 |
| Family history of suicide | – | 18 (10) | – | 8 (7) | – | 0.372 |
| Experiencing significant stress | 99 (48) | – | 50 (40) | – | 0.153 | – |
List of abbreviations
- AUDIT-C
- Alcohol Use Disorders Identification Test
- CBT
- cognitive behaviour therapy
- CIWA
- Clinical Institute Withdrawal Alcohol
- CMHT
- community mental health team
- CMOC
- context, mechanism and outcome configuration
- COSAI
- Comparing Sexual Assault Interventions
- CRIS
- Clinical Record Interactive Search
- DAST
- Drug Abuse Screen Test
- EMDR
- eye movement desensitization and reprocessing
- FME
- forensic medical examiner
- FNE
- forensic nurse examiner
- IMD
- Index of Multiple Deprivation
- ISVA
- independent sexual violence adviser
- LEAG
- Lived Experience Advisory Group
- LGBTQ+
- lesbian, gay, bisexual, transgender, intersex, queer/questioning, asexual and many other terms (such as non-binary and pansexual)
- LSOA
- lower super output area
- MiMoS
- Mixed Methods of SARCs Study
- NGO
- non-government organisation
- NICE
- National Institute for Health and Care Excellence
- PC-PTSC-5
- Primary Care PTSD Screen for DSM-5
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-analyses
- PTSD
- post-traumatic stress disorder
- RCT
- randomised controlled trial
- ReQoL
- Recovering Quality of Life
- SAPAS
- Structured Assessment of Personality Abbreviated Scale
- SARC
- sexual assault referral centre
- SARCIP
- Sexual Assault Referral Centre indicators of performance
- SLaM
- South London and Maudsley NHS Foundation Trust
- SOP
- standard operating procedure
- WP
- work package
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/YTRW7448).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
