Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number NIHR130694. The contractual start date was in January 2021. The final report began editorial review in September 2022 and was accepted for publication in February 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the final manuscript document. However, they do not accept liability for damages or losses arising from material published in this manuscript.
Permissions
Copyright statement
Copyright © 2024 Gkiouleka et al. This work was produced by Gkiouleka et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Gkiouleka et al.
Chapter 1 Background
Since the COVID-19 pandemic, discussions about health inequalities in the UK have intensified. The disproportionately higher numbers of COVID-19 infections and deaths among the poorer segments of the population, ethnic minorities and multiply disadvantaged groups revealed a destructive synergy between entrenched socio-economic inequalities, structural racism and the unequal social impact of lockdowns on these groups. 1–3 This has driven public health bodies, healthcare professionals, researchers and patient advocacy groups to acknowledge the magnitude of the problem and the urgent need for services and interventions that can reduce health inequalities. 4,5 However, socio-economic inequalities in health are not a new problem and neither do they concern communicable diseases only. Rather, they have been on the national public health discourse since at least the early ’80s with the publication of the Black Report,6 which summarised the evidence and brought to the public attention the extent to which ill-health and death were unequally distributed among the country’s population.
Today, almost 40 years later after the publication of the report, and after a multitude of relevant studies, reports7–9 and policy plans, children aged 10–14 in the poorest areas of the country are still expected to live 18 fewer years in good health than children of the same age living in more affluent areas. 10 The gap in life expectancy between people living in the most deprived areas and those in the least deprived is increasing because of significant gains in life expectancy only among the latter in the period between 2014 and 2019. 11 Notably life expectancy has declined over the last 10 years for women living in the poorest regions of the country. 9 Evidence shows that inequalities in life expectancy are primarily driven by inequalities in chronic conditions such as cancer and cardiovascular and respiratory disease. 12,13 In the most deprived areas of the country, patients with cardiovascular disease (CVD) deal with a four times higher possibility of premature death than patients in the least deprived areas. 14 Similarly, inequalities in cancer incidence and survival burden the most disadvantaged groups with an excess of 19,000 deaths per year. 15
There is a consensus that the causes of health inequalities are traced mostly outside the healthcare system and involve the conditions in which people grow, live and work, what we call the social determinants of health (SDH). 16 However, the healthcare system, and especially general practice, has still an important role to play in mitigating the impact of those determinants and defining the range of health inequalities. 17–19 The work of general practitioners (GPs) focuses on dealing with people rather than diseases20 and people appear with a multitude of physical, social and psychological problems before any other interaction with the healthcare system. Moreover, general practice as a system can contribute significantly to the recording and management of risk factors (e.g. hypertension) and behaviours (e.g. smoking) that are directly linked with conditions like diabetes, CVD and respiratory disease. 21,22 Given that these conditions are among the leading causes of death for both men and women and even more so in socio-economically disadvantaged areas,23 the role of general practice in prevention and in closing the socio-economic gap is magnified. From this perspective, general practice is seen as a key place where the impact of SDH and health inequalities can be addressed and mitigated,20 for example via enabling access to a series of health and social services. For the same reasons though, general practice risks inadvertently sustaining or even increasing inequalities, for example, via unequal workforce distribution between deprived and non-deprived areas. 19,24 Also, it can increase inequalities due to interventions and services that benefit disadvantaged groups less than those with a socio-economic advantage. 25 International evidence indicates that public health interventions that are delivered without accounting for socio-economic differences among recipients can have differential outcomes and increase inequalities [i.e. intervention-generated inequalities (IGIs)]. 26 Although evidence about intervention-generated inequalities in general practice is currently limited, we should not assume that they are absent or irrelevant.
At the same time, the healthcare system as an institution (i.e. an organisation founded for a social purpose and involving formal rules, procedures, resources and cultural elements) and general practice as part of it are subject to the broader social, economic and political climate. Therefore, established social inequalities result in inequalities in healthcare as well. Since at least the early ’70s, when the GP Julian Tudor-Hart introduced the ‘inverse care law’,27 people with the greatest need for good medical care have been those who are the least likely to receive it. 28,29 Despite a variety of national policies that aimed at making general practice more equitable in the last 30 years, inequalities in the provision of general practice services are still vast. 30,31 People registered with practices serving the most deprived areas have an overall worse experience of making an appointment or communicating with their practice via phone, while older patients experience less continuity of care. 32 In a similar pattern, in urban inner areas with multiply disadvantaged populations, hypertension cases remain worryingly uncontrolled and CVD-related prescriptions are given to only half of those eligible for them. 33,34 In a recent paper, Todd et al. 35 showed that these patterns are not explained by how far people live from GP premises, as almost 98% of the people in deprived areas live within a 20-minute walk of GP premises. Looking a bit deeper, we find that practices in more deprived areas are disadvantaged by the NHS funding formula, especially since the reduction in the inequalities weighting in 2012, ending up with smaller budgets, decreased workforce and increased workloads. 31,36 A report published in 2020 by the Health Foundation showed that when adjusting for increased health needs in poorer areas, practices serving more deprived populations receive 7% less funding per registered patient compared with practices serving less deprived populations. 37 In such a complex context and with puzzling findings regarding the impact of general practice on health inequalities, identifying the type of services and interventions that can effectively reduce inequalities becomes a challenging task.
This realist review examined the evidence on interventions and aspects of routine care in general practice that are likely to increase or decrease health inequalities in chronic conditions and produced an evidence synthesis and a framework for the design and delivery of equitable general practice. The current report discusses the aims, background and context of the study, the analytical framework that informed the research process, and the realist methodology used. Moreover, it provides a synthesis of the main findings as well as recommendations for policy, practice and future research.
Research context: interventions aiming to reduce health inequalities in general practice
The last systematic review of the evidence on health service interventions that can reduce inequalities was published more than two decades ago. 38 The study concluded that health services either alone or through sharing initiatives with other agencies can implement interventions to reduce health inequalities. Characteristics of successful interventions included a systematic, intensive and multidisciplinary approach, and enhanced access and service utilisation, addressing the needs of the target populations and community involvement. Since then, the evidence base has expanded, and the healthcare landscape has changed substantially.
A significant milestone was the development of the PROGRESS-Plus conceptual framework for the understanding of inequality based on multiple criteria. 39 Proposed by Campbell and Cochrane Collaborations, the framework encouraged researchers to adopt a more systematic approach to equity by considering multiple social categories that stratify social and health opportunities and outcomes. The criteria include place of residence; race/ethnicity/culture/language; occupation; gender/sex; religion; education; socio-economic status; social capital as well as social categories associated with discrimination (e.g. disability and age); features of relationships (e.g. smoking parents); and time-dependent relationships (e.g. being a carer). Attwood and colleagues explored equity in primary-care-based physical activity interventions across PROGRESS-Plus criteria. 40 They found that the majority of randomised controlled trials (RCTs) of physical activity interventions in primary care do record information on selected PROGRESS-Plus criteria. However, only a few of them finally report details of relevant analyses to determine which groups may benefit or be further disadvantaged by such interventions. 40 Moreover, Terens and colleagues41 reviewed trials of quality-improvement interventions aimed to reduce health inequities among people with diabetes in primary care and explored the extent to which experimental studies addressed and reported equity issues. Among the reviewed studies almost all reported the age, gender/sex and race distribution of participants. Most of them also reported on at least one additional PROGRESS-Plus criterion, mostly education and income. Finally, although only a few studies examined differential intervention effects by PROGRESS-plus criteria, they showed that a quality-improvement strategy improves care for older and less educated people and African Americans. 41
Another review of the evidence on the impact of CVD primary prevention on health inequalities42 showed that adopting a high-risk approach (i.e. screening and treating high-risk individuals only) increases socio-economic inequalities in screening, healthy diet advice, smoking cessation, statin and anti-hypertensive prescribing, and adherence. The authors stressed that interventions targeted at high-risk patients usually focus on individual action either of patients or healthcare professionals. Instead, they suggested a shift towards an approach that integrates policy and population exposure to risk factors. These findings point to what we call IGIs. 25 Such inequalities emerge when public health interventions, although benefiting health overall, increase health inequalities by disproportionately benefitting socio-economically privileged groups or unintentionally harming disadvantaged groups. 25 Interventions with such unintended aggravating impact on health inequalities tend to be those that require considerable individual material or psychosocial resources without accounting for pre-existing inequalities in such resources across socio-economic groups. 25,26,40 In contrast, a review study on the impact of shared decision-making in primary and secondary care showed that relevant interventions reduce socio-economic inequalities by particularly benefitting disadvantaged groups through increased knowledge, informed choice, participation and reduced decisional conflict. 43
Despite the significance of the findings, the evidence regarding interventions that can effectively reduce health inequalities in general practice is still limited and disparate. Most of the available evidence reviews focus on research trials with often small samples and variant study quality. Further, they often exclude interventions that target the SDH and/or IGIs. Acknowledging these gaps, our study provides up-to-date, extended and integrated evidence on aspects of care and interventions in general practice that decrease inequalities in health and healthcare. Also, it identifies which groups are more likely to benefit and, finally, suggests a framework for the design and delivery of equitable general practice.
Social context: general practice in the times of the COVID-19 pandemic
General practice in the UK consists of 6000–7000 small- to medium-sized businesses that are contracted by the NHS to provide a programme of core services. 44 They are primarily funded through a mixture of capitation via a contractual reimbursement formula (commonly known as the Carr-Hill Formula), nationally directed financial incentives and provision of national or local enhanced services (e.g. immunisation, minor surgery). In addition, practices can receive income from a range of other activities, such as dispensing medication, participating in research and undertaking teaching and training. 45,46 In 2019, Primary Care Networks (PCNs) were established and incentivised practices to form around local populations of 30,000 to 50,000 patients. 47 The workforce within general practice has become increasingly multidisciplinary, with the incentivisation of additional roles provided through PCNs; these include social prescribers, physician associates, paramedics and pharmacists. 48 Most practices are run and owned by a group of two or more GPs called a partnership. However, several practices are owned by single-handed GPs or large limited multi-national companies. Decisions are generally made by the partnership usually in collaboration with a practice manager, who is sometimes part of the partnership. 44 The partnership model is being increasingly debated because of financial and time commitments coupled with a workforce and workload crisis. 49
The pandemic occurred when general practice as a sector was already affected by shortages in workforce, substantial workloads and funding pressures. 50–52 Evidence shows that these problems have been affecting practices in deprived areas more, with fewer GPs, direct patient care (DPC) staff and paramedics per 10,000 patients employed in disadvantaged areas31 and funding which does not sufficiently account for deprivation levels. 53 In the aftermath of the COVID-19 pandemic, general practice has been faced with an immense backlog of routine long-term condition care due to the redirection of workforce and resources to the vaccination programmes. 54,55 Falling numbers of qualified full-time GPs and record high numbers of appointment bookings have resulted in an increase of 300 patients per practitioner since 2015. 56,57 In parallel, the systematic demoralisation of the profession in the public discourse during the pandemic58 coupled with remote working conditions59 and increased pressure has left GPs struggling with feelings of frustration and loss in terms of autonomy and control over their working lives. 60 As expected, these challenges are even harder for practices in socio-economically disadvantaged areas with pre-existing shortages in workforce and resources. 31
During these challenging times, there have been also some changes in response to the pandemic which do not immediately look negative or positive but rather warrant a thorough evaluation in terms of their impact on inequalities. One of them has been the increase in remote consultations to limit the transmission of COVID-19. 2 Evidence shows that within a few weeks, GPs achieved at least an 80% increase in remote consultations compared with fewer than 10% before the pandemic. 61 The use of technology enabled this shift and has certainly made GPs and patients more confident to use available telephone services and online tools for the purpose of triage and consultation. 61 However, careful evaluation is needed to assess the extent to which remote services and the use of technology increase access to general practice services and if so for whom. 62 Data show that more than 10 million people in the UK have limited digital literacy and large groups of the population live without consistent access to the internet. 63 At the same time, many minors, women and migrants live in contexts where privacy and safety are not guaranteed and this makes a remote consultation with a healthcare professional often impossible. 1 So, it is likely that a change which was introduced out of necessity and is understood as positive, at least to some extent, could have a worsening impact on some already disadvantaged groups if adopted as a general undifferentiated strategy. A qualitative study on primary care staff working in the most deprived areas of the country during the COVID-19 pandemic stresses how digital poverty and limited IT literacy should be seriously considered in future NHS plans to expand the use of digital care. 64
Finally, during the same period there have also been some examples of positive and promising practice. These concerned mostly an increased sense of community that emerged in several places through the implementation of vaccination programmes and public health initiatives which brought together general practices, local councils, faith leaders, community groups and charity organisations. 65 The ‘Everyone In’ initiative for rough sleepers is such an example: GPs worked together with local councils and other actors to protect those experiencing or being at risk of rough sleeping from the spread of COVID-19. 66 Similarly, vaccination programmes across Crawley, east Surrey and mid-Sussex run by the GP Federation, Alliance for Better Care (ABC), included an explicit orientation towards equity in vaccination uptake, local partnerships with small voluntary sector organisations and charities, and a mentality of working with people to reach populations who have been historically marginalised by healthcare services (e.g. refugees, people in poverty, Gypsy Roma Travellers). 67 The success of such initiatives demonstrates that given the mandate and funding, general practice can play a vital role in achieving public health goals and be a cornerstone of intersectoral collective initiatives for the equitable distribution of SDH like housing, safety and care. 66,67
Together with the negative impact of the COVID-19 pandemic on services’ capacity and the well-being of the healthcare workforce, there are important lessons to be learned from this period in terms of the role of general practice in reducing health inequalities and mitigating their impact on people’s health. Although it seems that we have reached a post-peak pandemic period, the health, social and economic consequences of the pandemic are still experienced by large shares of the population and especially by disadvantaged individuals and groups. 1 Moreover, the latest cost of living crisis aggravates even further the deterioration of life conditions for increasing numbers of people. 68 In this context and against a backdrop of alarming unmet need,55 it is urgent that general practice be supported to play its important role in promoting health for all and protecting the most vulnerable. Currently, there are voices which talk about general practice as a ‘sinking ship’69 but at the same time, others talk about the things we can do to secure general practice’s future as healthier, more equitable and effective for its people and its patients. 60,65 Our work aims to strengthen these latter voices by providing evidence on aspects of routine care and interventions in general practice that can reduce health inequalities in chronic conditions specifically and also inform general practice more broadly in terms of providing equitable care.
Conceptual framework: understanding health inequalities in their complexity
Health inequalities is not a one-dimension concept, and neither is it necessarily understood in the same way by healthcare professionals, researchers and policy-makers. The same applies for the drivers and causes of health inequalities. A recent study by Olivera and colleagues70 suggests that local healthcare systems in England lack a clear conceptual framework for addressing health inequalities and rather use a series of value judgements which are not linked to concrete action. However, consistency and transparency regarding the way we understand the problem and its causes are necessary for suggesting solutions. Thus, this section briefly discusses the different conceptualisations of health inequalities used among public health researchers and professionals, including GPs. Also, we clarify which of these conceptualisations have informed the current study.
Understandings of health inequalities and ways to tackle them
Health inequalities include inequalities in relation to health outcomes (e.g. morbidity and mortality) and healthcare at the patient level (e.g. access, experience, diagnosis) and system level (e.g. workforce and funding). 71 Contrary to the mainstream and narrow focus on socio-economic disadvantage, health inequalities emerge on the basis of multiple social categories, including gender, ethnicity, race, migration status, sexuality, religion, disability and the intersections of those categories (e.g. migrant women with low socio-economic status). 72
As for the fundamental causes and driving mechanisms of health inequalities, approaches vary across a spectrum from individualisation to politicisation. 73–76 At one end of the spectrum, we find approaches which focus on the extent to which individual risk factors and behaviours drive health inequalities. 77,78 According to these approaches, interventions to tackle health inequalities should be targeted at vulnerable groups and should focus on lifestyle and behaviour change. Such approaches aim to close the inequality gap by supporting only disadvantaged individuals to maintain or improve their health. Hence, they either focus on strengthening individuals through providing education, advice or counselling or by strengthening disadvantaged communities to work together in order to achieve better health outcomes. 77,78
In the middle of the spectrum, approaches focus on the ways that living conditions affect health and how living conditions are systematically different across groups based on social categories like socio-economic status and/or gender. The suggested interventions resulting from these approaches emphasise the need for improving the living conditions that affect health and reducing structural inequalities (e.g. in income or education). 79 In most cases, these approaches focus on the gradient of inequalities. Hence, they promote interventions and measures that benefit the population in general but the lower individuals and groups stand on the socio-economic gradient, the greater benefit they experience. 77 Finally, at the other end of the spectrum, we find approaches that frame health inequalities as a political issue. These approaches consider that health inequalities result from the unequal distribution of SDH, which in their turn are the consequence of public policy, economic and political structures, and ultimately of unequal power distributions. 9 As expected, these approaches suggest interventions that focus on addressing the unequal distribution of resources and power and on policy decisions and change. 73–76 Such interventions also focus on the gradient and the population as a whole but they cut across multiple sectors from macro-economic and labour-market policies, environmental policies, to cultural values and human rights. 77
A recent study in Scotland showed that among GPs there are two prevalent conceptualisations regarding the drivers of health inequalities which are also linked both with the way GPs understand their own role in tackling health inequalities and with the way they perceive their patients. 74 On the one hand, there are GPs who see health inequalities as the outcome of unequal living conditions shaped by specific public policies and the socio-economic structures. These GPs tend to perceive their patients as victims of social injustice and express empathy and understanding of the patients’ difficulty to follow a healthy lifestyle. According to them, decreasing inequalities in wealth distribution is key for the reduction of health inequalities. On the other hand, there are GPs who identify behaviours and cultural issues as the main drivers of health inequalities. They perceive their patients as responsible for failing to develop healthy habits and according to them the answer to health inequalities lies in behavioural interventions. Another study on English GPs from various areas in Southern England19 showed that what they tend to associate with health inequalities has to do with patients’ access to health services in primary and secondary care and elsewhere. They acknowledge the need for delivery of care proportionate to patient need. In identifying what they can do to reduce health inequalities, they exclusively focus on service-related aspects and, specifically, organisation of their time, continuity of care and integration of services, which, however, are shaped by structural factors such as organisational changes and their cultural distance from their patients. These views seem to be consistent with views of the overall NHS staff, who tend to engage more in action against health inequalities if inequalities are framed around healthcare and the specific aspects of care for which they are responsible and have power to influence. 80
These views demonstrate a lack of consensus regarding the form of inequalities (e.g. risk factors vs. access to care), their driving mechanisms and effective actions to tackle them. 70 Moreover, they reflect a narrow action scope for healthcare professionals and especially GPs which does not expand far beyond the clinical encounter. However, this lack should not be understood as the outcome of uninformed healthcare professionals. Rather it should be perceived as a call for an agreed conceptual framework at the national level to guide healthcare policy-makers and professionals in addressing and reducing health inequalities.
Health inequalities in the context of this study
In the context of this study, we adopt the broad definition of health inequalities that includes social inequalities in health outcomes and healthcare at the patient and system level. 71 As for understanding the drivers of health inequalities, we stand with approaches at the politicisation end of the spectrum which focus on the impact of social structures, political environments and power distributions on the SDH and the emergence of health inequalities. 8,9,81–87
Our conceptualisation is informed by intersectionality, an analytical approach introduced by black feminist scholars and activists, which conceptualises power as a phenomenon with multiple dimensions. 88,89 Intersectionality suggests that social categories like gender, race, class or sexuality are not individual characteristics but rather the reflection of power hierarchies which inform each other and are context-specific. 90–92 The experience and social position of individuals are the outcome of the synergy between these hierarchies. This has three implications: first, that social disadvantage is something more nuanced than the direct effect of socio-economic position. 93 Second, it implies that multiple disadvantage (e.g. being a poor woman of an ethnic minority background) is something qualitatively different from the sum of its parts (e.g. disadvantage across socio-economic position, gender and ethnicity). 94 Third, the boundaries between the macro-level and individual factors are permeable, which means that individuals are not only shaped by structural forces, but they are also capable of resisting, challenging and shaping them. 94,95
From this perspective, inequalities in health outcomes and healthcare are the reflection of social inequalities as these emerge through multiple layers of privilege and disadvantage across categories including socio-economic status, gender, race, migration, ethnicity, disability and sexuality. 72 Additionally, general practice is understood as embedded within the power distribution system that produces social and health inequalities. 95 This implies that the power hierarchies that are effective in the society at large (e.g. across gender or race) are effective within general practice as well and they inform internal institutional hierarchies (e.g. across seniority or professional role). Finally, individuals, including patients and employees, are affected by these hierarchies according to their position in the general practice context and at the same time have the potential to entrench or challenge them. 96
As the evidence presented in the previous section shows, people working in general practice are not always aware of the impact of structural forces on their work. Even when they are, they do not often feel capable of challenging them if they are not able to see their direct link with specific aspects of care. Therefore, in this study we focus on interventions and aspects of care that have the potential to decrease or increase health inequalities while we put our findings and conclusions in the context of power organisation. Building on intersectional understandings of power, we have two aims. First, we aim to enable people working in general practice to acknowledge the links between their everyday practice and the structural forces that produce health inequalities. Second, we aim to offer them a conceptual tool to acknowledge their own and their patients’ intersectional position within their context and their resulting capabilities to challenge inequalities in general practice. This way people involved in general practice will be more able to engage in effective coordinated action against health inequalities across the system. Finally, they will acknowledge that this action should shift from the binary approach between prioritising individuals versus populations97 to one that emphasises that populations are made of individuals who are different.
Review questions and objectives
Our study aims to answer the following research questions:
What types of interventions and aspects of routine care in general practice decrease or increase inequalities in healthcare and outcomes among people with or at risk of CVD, cancer, diabetes and/or chronic obstructive pulmonary disease (COPD)?
For whom do these interventions and aspects of care work best, why, and in what circumstances?
Our main objective is to synthesise this evidence to produce specific guidance and a framework for healthcare professionals and decision-makers at a local and national level about how best to tackle health inequalities in general practice services.
Chapter 2 Review methods
Since the start of this study, we have been aware that we needed a methodology which would allow us to account for the complexity of health inequalities as a problem and the way that routine care and interventions in general practice have a differential impact across different contexts and patient groups. Therefore, we chose to adopt a realist review approach. Realist review and evidence synthesis builds on the idea that contexts act on mechanisms to produce specific outcomes. The realist analysis is based on identifying a series of context–mechanism–outcome configurations (CMOCs). 98–100 CMOCs are statements that represent causal relationships, or, in other words, relationships between particular elements of context, mechanism and outcome with reference to the data. The concept of context involves social, geographical or other features affecting the implementation of interventions, as well as the characteristics of the people involved and their circumstances. A mechanism refers to a force that causes things to happen: an outcome (intended or not). 98
In contrast to systematic reviews which aim to assess the effectiveness of distinct interventions, realist reviews focus on the mechanisms that link context with specific outcomes. A realist review is less concerned with if an intervention is effective and more with understanding why it is or isn’t. 101 Moreover, it explores the specific groups for which an intervention is more likely to have impact and under which circumstances. 101 Using realist methodology enabled us to decipher underlying processes and principles that are common in effective interventions against health inequalities in general practice and extract evidence-based conclusions which are transferrable across contexts.
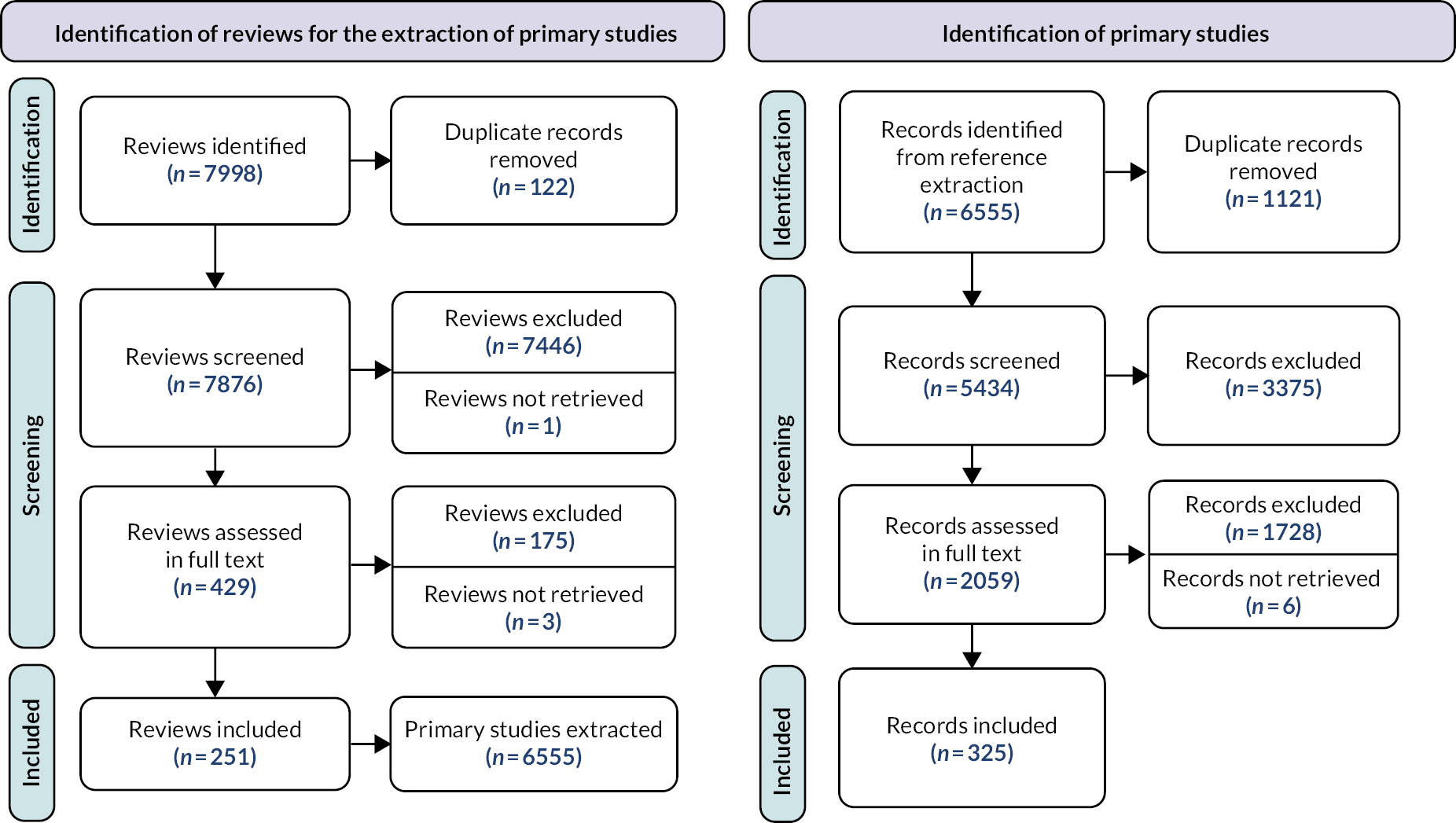
Our review was informed by Pawson’s five iterative steps: (1) locating existing theories, (2) searching for evidence, (3) selecting articles, (4) extracting and organising data and (5) synthesising the evidence. 99 To conduct the review within the study’s timeline, we combined steps 3 and 4 to speed up the process (see Figure 1). At the stage of evidence synthesis (step 5), we conducted a deliberative workshop with relevant stakeholders (n = 13) to refine our findings and the programme theory. The review ran for 20 months, from January 2021 until September 2022. The protocol was originally registered with PROSPERO (registration number: CRD42020217871) and published after peer review in 2021. 102 In the following sections, we elaborate on all the steps of the review process including study identification and selection, data extraction and synthesis. No ethics clearance was required since the review included only secondary data.
FIGURE 1.
Flow diagram of the project.

Expert panel
An expert panel was recruited for the EQUALISE (Reducing Health Inequalities through General Practice: A Realist Review) study to provide content expertise for the development and refinement of the programme theory. The panel consisted of 12 experts including academics, clinicians (recruited mainly through regional clinical research networks) and patient representatives and met twice: once in March 2021 at the stage of developing the initial programme theory (IPT), and once in May 2022 for the refinement of the results and programme theory. Additional communications with some of the expert panel members took place via e-mails throughout the study for the exchange of relevant information or material. The two meetings were held virtually on the Microsoft Teams platform due to COVID-19-related restrictions and lasted for 2 hours each. More details about the meetings are available in Table 1.
| Date | Participants | Key topics discussed |
|---|---|---|
| 14 January 2021 |
|
Introduction to the project and discussion on the role of the PPI group throughout the study |
| 10 March 2021 |
|
Introduction to the study and discussion on the drivers of health inequalities in general practice for the refinement of the IPT |
| 24 March 2022 |
|
Discussion on findings and their implications for practice |
| 5 May 2022 |
|
Discussion on findings and suggested framework |
| 11 May 2022 |
|
Discussion on findings, suggested framework, and implications for policy and practice |
Ahead of the meetings, we provided the participants with an agenda and preparatory material (e.g. the aim and objectives of the study, progress update). The meetings started with a brief slide-presentation by our team to introduce the participants to the topic(s) of the discussions. The discussions focused on the relevance and effectiveness of the programme theory and were facilitated by members of our team (AG, JF or GW) to ensure that all attendants would have the time and space to share their input. Notes from the meetings were used to inform the progress of the review and refine the programme theory. The expert panel members who required a reimbursement for their organisations were offered the appropriate payment according to the University’s guidance.
Patient and public involvement
Patient and public involvement (PPI) was strong and consistent across all the steps of the study. The project team included three regular patient representatives, AM, SM and RH. All of them were recruited through pre-existing connections with the research team, they contributed to research design and the writing of the research funding proposal, and participated (all or in rotation) in every project meeting. Additionally, patient representatives recruited through the Healthwatch and the Patients Association participated in the expert panel (n = 2) and the deliberative workshop (n = 2). All the patient representatives are women involved in patient and carer advocacy coming from the East of England. They are affected by social disadvantage that cuts across gender, ethnic minority status, age, religion, neurodiversity, socio-economic position and being a carer. AG led the PPI component of the review. At the beginning of the project, she invited the three regular PPI members to attend an initial meeting during which they discussed the scope and terms of their involvement. At the end of that initial meeting the PPI members signed a letter of engagement to be used as a point of reference and mutual commitment. At least one of the regular PPI members attended the monthly project meetings. Before each project meeting, AG contacted PPI members separately to address any potential questions or issues related to the meetings’ agenda.
Two additional separate meetings for the regular PPI members took place in November 2021 (virtual) and in March 2022 (face to face). In the meeting held in November, AG and the PPI members discussed the process of data extraction and coding with some examples from the included literature. The meeting lasted for almost an hour and at the end the PPI members agreed to contribute to the coding and data-extraction process. The PPI members were sent five papers each, which they coded on their own time and then sent their codes and thoughts on the process to AG via e-mail. This enabled AG to expand and enhance her scope during the coding and data-extraction process and also provided the PPI members with an insight into the data-extraction process, which was necessary for a better understanding of the included literature, the review process and the evidence synthesis. The meeting held in March 2022 was a day workshop that took place at the Cambridge Biomedical Campus. Two of the regular PPI members attended together with AG. The focus of the day was the relevance of the findings and the resulting suggestions for practice. The PPI members had been sent the relevant material in advance and had the opportunity to share their thoughts and feedback during their meeting. The meeting took place in an informal setting and functioned as an opportunity for AG to express her appreciation of the PPI contribution to the project. AG used the notes of the meeting to refine the findings by integrating the PPI members’ suggestions. All the PPI members (regular or not) were reimbursed for their contribution to the project, including meeting attendance and preparatory work, on a set hourly rate (£25) according to the Cambridge University guidance and were reimbursed for any other costs related to their involvement to the project (e.g. travel expenses).
Deliberative workshop
The deliberative workshop took place in May 2022 at the Pitt building in Cambridge. It included health professionals recruited mainly through regional clinical research networks and specifically GPs (n = 4), social prescribers and care coordinators (n = 2), patient representatives (one member of the regular PPI group and two additional PPI representatives), one well-being coach, and academics (n = 3) together with three members of the research team (AG, JF and GW). The aim of the workshop was the discussion of the study findings and the suggested framework and practice qualities for equitable general practice. The meeting was facilitated by a professional facilitator. It involved a presentation of the study and findings by members of the research team (AG and JF) at the beginning, and three subsequent sessions focusing on the relevance and effectiveness of findings, missing elements from the results, and suggested ways to translate the findings into practice. During every session, the participants worked in small groups and added their collective reflections and comments in flipchart sheets provided by the facilitator. At the end of every session each working group shared their input and there was an open discussion among all the participants. At the end of the day, all the sheets with participants’ notes were collected by the facilitator and given to AG, who integrated them into a summary document. The document informed a discussion on the refinement of results held by AG and JF.
Locating existing theories
Our first step was to identify the key theories that explain how, for whom, why and in what circumstances interventions or care delivered in general practice may increase or decrease health inequalities. We achieved this through three inter-connected processes. (1) We conducted an exploratory background search to get familiarised with the relevant literature (including literature on IGIs). This search was deliberately conducted using informal methods (i.e. snowballing and citation tracking)103 to ensure that the scope would be adequately broad. (2) We organised a panel discussion with key content experts (details on the panel and the participants are available in Appendix 1) during which we had the opportunity to explore relevant theories and explanations. (3) We refined our findings from the literature review and the experts’ input through iterative discussions within the project team. This process revealed that the elements involved in the production of health inequalities in general practice cover a broad range of interventions, areas of interest and levels of analysis (e.g. individual or practice level), and the literature mostly focuses on outcomes (e.g. patterns of inequalities in accessing services) rather than driving mechanisms. We used our discussions within the expert panel and the research team to reflect on the potential mechanisms that may link elements of the general practice context with certain outcomes, and came up with an IPT. The programme theory reflected the breadth of the relevant elements of context, mechanisms and outcomes, and included a series of interventions that have the potential to increase or decrease inequalities. The interventions were focused on either context or mechanisms. The programme theory served as a theoretically informed evaluative framework to inform our formal literature search and evidence collection. 99 Figure 2 shows the IPT and the different areas which were later populated with evidence. The areas of interest were not organised at that stage beyond CMO groupings but, as reflected in Figure 2, they covered different domains from individual characteristics like staff beliefs, skills and knowledge to structural factors like GP distribution, funding and power hierarchies.
FIGURE 2.
Initial programme theory.

Search strategy
Our search strategy was set with the guidance of an experienced librarian (IK). Given the broad scope of our research questions, we decided to run an initial search of systematic reviews of interventions delivered in general practice and focused on CVD, cancer, diabetes and/or COPD. Driven by the IPT, we undertook electronic searches of MEDLINE, EMBASE, CINAHL, PsychINFO, the Web of Science and the Cochrane Library. The original search was undertaken on 7 April 2021, and it was updated on 23 March 2022. More details on our search strategy are available in Appendix 2. We decided that our search scope should include studies focusing on contexts outside the UK to account for contextual differences and identify the circumstances under which mechanisms can lead to specific outcomes.
All the identified titles and abstracts of reviews were screened for eligibility by AG and 20% were independently screened by JF to check for systematic errors. Wherever there was a disagreement, it was solved through discussion. The screening was conducted using Rayyan. 104 The inclusion and exclusion criteria for reviews were:
Inclusion criteria:
-
reviews that used a comprehensive search strategy and appropriate quality-appraisal tool;
-
reviews of interventions or care which targeted CVD, cancer, diabetes or COPD or their risk factors, namely, smoking, hypertension, diet, exercise and cholesterol;
-
reviews of interventions or care delivered in general practice;
-
reviews including clinical outcomes relating to the type of care (acute, chronic and preventive), function of care (diagnosis, screening and prevention, follow-up and continuity, treatment) and domain of care (effective, efficient, timely, patient-centred and safe);105
-
reviews undertaken in high-income countries, as defined by the Organisation for Economic Co-operation and Development (OECD), with no language restrictions.
In a slight deviation from our published protocol,102 we decided to include review studies regardless of whether they were reporting on the differential effectiveness of care/intervention across groups or interventions aimed at disadvantaged groups. Given that at the stage of developing the programme theory we found that driving mechanisms of health inequalities are less discussed in the literature, we thought that broader inclusion criteria for the reviews could increase our chances of accessing relevant literature which could be useful for answering our research question.
Exclusion criteria:
-
reviews of studies focusing on drug effectiveness or efficacy;
-
reviews of interventions focusing on children, mental health or disease areas not listed above;
-
reviews superseded by more recent reviews.
As a next step, two researchers (AG, RT) extracted all the primary studies included in the systematic reviews which met our inclusion criteria. One researcher (AG) screened all the titles and abstracts and a second researcher (JF) screened 5% of the articles to check for systematic errors. The inclusion and exclusion criteria for the primary studies were:
Inclusion criteria:
-
interventions which reported on clinical or care-related outcomes by socio-economic group, or other PROGRESS-Plus criteria, relating to the type of care (acute, chronic and preventive), function of care (diagnosis, screening and prevention, follow-up and continuity, and treatment) and domain of care (effective, efficient, timely, patient-centred and safe);
-
studies on interventions targeted at disadvantaged groups;
-
general practice interventions or care targeting CVD, cancer, diabetes or COPD or their risk factors, namely, smoking, hypertension, diet, exercise and cholesterol;
-
interventions focusing on clinical outcomes (e.g. mortality and myocardial infarction) or clinical measures of risk factors (e.g. change in blood pressure) or behavioural outcomes (e.g. physical activity) or care-related outcomes (e.g. screening uptake);
-
studies undertaken in high-income countries, as defined by the OECD, with no language restrictions.
Exclusion criteria:
-
studies focusing on drug effectiveness or efficacy;
-
studies focusing on children, mental health or disease areas not listed above.
Again, shifting slightly from our published protocol102 instead of including only studies with an experimental study design, we decided to include studies of other designs (e.g. qualitative studies or surveys) in order to increase our possibilities to access data about interventions that target the SDH or IGIs.
Article selection
As per realist methodology, documents were selected according to the extent that they could contribute to the development and refinement of the programme theory – that is, they contain relevant data. 100 During screening the full text of the included primary studies, AG grouped the studies into six groups according to their focus and the country the study took place. The six groups were then classified in terms of relevance in the following order: (1) studies which focused on inequalities in the UK were deemed of the highest relevance, followed by (2) studies discussing interventions targeted at disadvantaged groups in the UK, (3) studies on interventions in the UK without an inequality focus, (4) studies on inequalities outside the UK, (5) studies on interventions targeted at disadvantaged groups outside the UK and (6) studies on interventions outside the UK without an inequality focus. We anticipated that studies focusing on settings outside the UK were likely to be less relevant but were selected for data extraction when we judged that they included information transferrable to the UK context.
Quality-assessment checklist criteria were not used as per realist methods,99 rather the rigour of the extracted data was taken into account during the coding and synthesis phase. Given that the literature did not provide rich information on inequality-producing mechanisms, we considered that even if studies were judged to be of limited rigour, they could still be used for the data synthesis if they contributed to the refinement of the programme theory. 100 To conduct the review within the study timeline, the selection of articles took place at the same time as the data extraction to speed up the process. This meant that AG uploaded the included studies by priority group in QRS NVivo (NVivo qualitative data analysis software, version 12; QSR International, Warrington, UK)106 and coded relevant useful data. When no useful data were available in the article, the article was then removed from the NVivo sources list. The data extraction stopped when sufficient iteration was achieved.
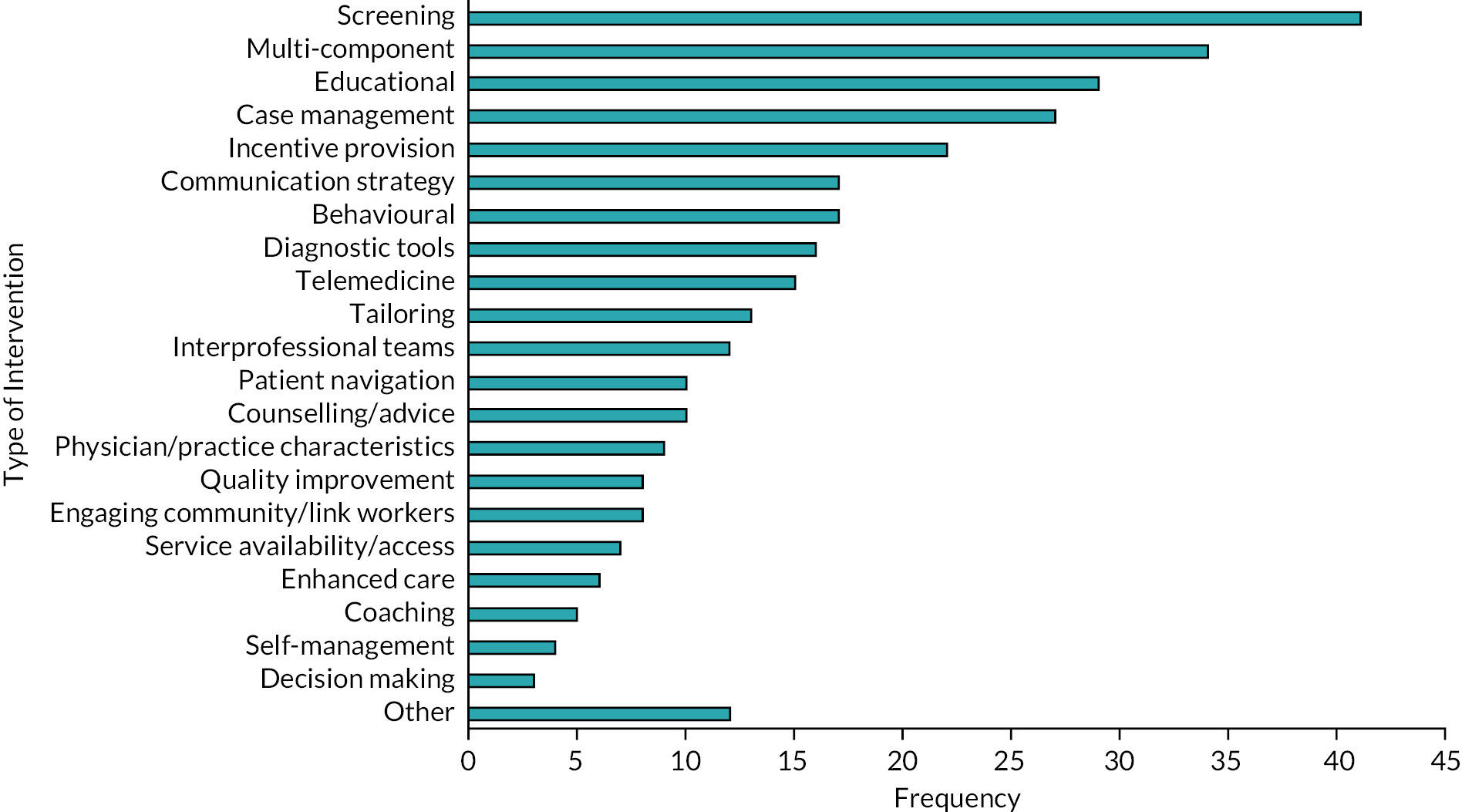
Data extraction and organisation
Key characteristics of all the included studies including the country the study took place, condition of focus, dimension of inequality (e.g. socio-economic status or other PROGRESS-Plus criteria), domain and form of intervention were extracted using an Excel spreadsheet by AG and RT. More details on these data are available in Figure 4 and Table 2.
| Study design | Number of studies |
|---|---|
| RCT or other experimental design | 157 |
| Cross-sectional, survey or population studies | 61 |
| Cohort studies | 25 |
| Longitudinal or time series | 12 |
| Qualitative studies | 11 |
| Mixed methods | 8 |
| Quasi experimental | 3 |
| Other | 48 |
| Country | |
| USA | 143 |
| UK | 102 |
| Australia and New Zealand | 17 |
| Netherlands | 15 |
| Canada | 14 |
| Scandinavian countries | 14 |
| Spain | 6 |
| Italy | 5 |
| Other | 9 |
| Health problem | |
| Diabetes | 114 |
| Cancer | 77 |
| CVD | 69 |
| General care for chronic conditions | 43 |
| Hypertension | 27 |
| Behavioural risk factors (e.g. smoking) | 19 |
Next, AG coded the data with feedback on the process by members of the research team (JF, GW) and the PPI group (AM, RH, SM). In the beginning of the data-coding process, a random sample of approximately 5% was additionally and independently coded by JF to check for systematic errors. Shifting slightly from the published protocol which mentioned the independent coding of a random sample of 10%, JF and AG discussed codes regularly, while another random sample of approximately 5% was independently coded by the three regular members of the PPI group to ensure the breadth and accuracy of the scope of the data extraction process.
Coding was based on the following two questions:
-
Does the text refer to any of the elements included in the IPT?
-
Does the text refer to the unequal effectiveness of care services or interventions?
Codes were chosen with an open-minded approach to reflect the themes that were emerging from the data, they were inductive (i.e. created to categorise data reported in included studies), deductive (i.e. ones that came from the IPT) or retroductive (i.e. created based on an interpretation of data to infer what the hidden causal forces might be for outcomes). They were refined regularly throughout the data analysis and were finally organised across 14 broader themes: namely, access to care, communication, community engagement, competing priorities, cultural understanding, differences between practices, interprofessional cooperation, patient education and behaviour change, patient enablement, patient perceived risk, resources distribution, the role of the GP in intervention success, time constraints, and workforce. We also created two additional categories for codes referring to theories of interventions and descriptive codes that did not refer to processes of inequalities.
Data synthesis
The data were synthesised by AG with the input of the research team (JF, GW, RH, AM) based on a realist logic and in light of the IPT. Having organised our coded data in themes, we worked on forming CMOCs (i.e. statements of causal relationships)98 within and also across themes. Given the diversity of the included articles in terms of studied condition, intervention type, outcome and PROGRESS-Plus criteria, our synthesis aimed to elicit common patterns and generalisable messages. Therefore, instead of specific characteristics of interventions, we focused on the underlying principles that informed care and interventions and the ways they can be employed to achieve equitable care in general practice. To meet this goal, CMOCs (see Figures 5–9) were refined and abstracted to a higher level so that they would enable us to understand what the broader qualities of care and interventions are that are likely to decrease or increase inequalities in general practice. This entailed using where necessary some or all of the following questions to inform the interrogation of our data:107
Relevance:
-
Are the data included in an excerpt of an included document relevant to programme theory development?
Judgements about trustworthiness and rigour:
-
Are the data sufficiently trustworthy to warrant making changes or additions to the programme theory?
Interpretation of meaning:
-
If the answer to the previous questions is yes, can these data be interpreted as being elements of context, mechanism or outcome?
Interpretations and judgements about CMOCs:
-
What is the CMOC (partial or complete) for the specific data?
-
Are there more data in this or in other documents to inform CMOCs contained in this document?
-
How does this CMOC relate to those already developed?
Interpretations and judgements about programme theory:
-
How do CMOCs relate to programme theory?
-
Are there data within and across documents that inform how specific CMOCs relate to the programme theory?
-
In light of the CMOCs and the supporting data, does the programme theory need to be changed?
Summarising, the evidence synthesis was implemented by the following processes:107–109
-
juxtaposition of data sources: comparing and contrasting data available in different sources;
-
reconciling ‘contradictory’ or disconfirming data: finding explanations about why outcomes differ in apparently similar circumstances;
-
consolidation of sources of evidence: defining whether similarities between findings presented in different sources are adequate to form patterns in the development of CMOCs and programme theory.
Chapter 3 Results
Our literature search and screening revealed that there is limited research on interventions that aim to decrease inequalities in general practice or evidence about the effect of general practice interventions by PROGRESS-Plus criteria. Even studies focusing on inequalities tend to report outcomes by groups (e.g. by level of socio-economic deprivation) without elaborating on the rationale of the studied intervention or the mechanisms leading to the observed outcomes. There are more studies discussing the impact of interventions targeted at disadvantaged groups. These studies tend to report results without considering the impact of the studied intervention on inequalities. Moreover, in these studies disadvantaged groups tend to combine a series of characteristics linked with social marginalisation (e.g. ethnic minorities living in deprived neighbourhoods). However, the authors do not discuss how the different dimensions of disadvantage (i.e. ethnicity or race and deprivation) inform each other in the emergence of the reported outcomes. This reflects the reality of social and health disadvantage being the result of multiple intersecting social hierarchies but at the same time offers limited information about the ways that specific groups can be supported. For these reasons, we focused on aspects of care and interventions that can make primary care more equitable or – when dysfunctional – are more likely to affect more severely groups who experience social and/or economic disadvantage.
In the following sections, we discuss the results of the review elaborating on the numbers and key characteristics of the included studies and we present the synthesis of our evidence.
Details of included studies
We identified 7998 review studies, of which 251 met the inclusion criteria. From the included reviews, we retrieved 6555 primary studies and proceeded with a second round of screening. In total, 325 studies met the inclusion criteria for primary studies. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagrams for the identification of reviews and the review of primary studies are available in Figure 3.
FIGURE 3.
PRISMA diagrams. Our PRISMA diagrams do not report reasons for exclusion of studies because often studies were excluded for multiple reasons. Our diagrams are consistent with Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES) publication standards for realist syntheses. 98
The included primary studies (n = 325) covered a period of approximately 30 years, from 1989 until 2021, and most of them were conducted in the USA (n = 143) and the UK (n = 102). The studies were grouped into three categories: those focusing primarily on inequalities (n = 56), those focusing on an intervention or an aspect of care targeted at specific disadvantaged groups (n = 137) and those focusing on an intervention without an inequality focus but reporting results by at least one PROGRESS-Plus criterion (n = 132). The studies also involved a wide range of designs, with almost half of them being RCTs or other experimental design (n = 157). Most of the studied interventions concerned diabetes (n = 114), followed by studies on cancer (n = 77) and CVD (n = 49). The reported outcomes included clinical outcomes (n = 139), service uptake (n = 88), care quality (n = 73) and behavioural outcomes (n = 25). The most-studied type of intervention was screening (n = 41), followed by interventions with multiple components (e.g. tailored information material and counselling) (n = 34) and educational interventions (n = 29). In most studies, more than one PROGRESS-Plus criteria were addressed. Ethnicity was addressed most often (n = 145), together with sex or gender (n = 98) and/or socio-economic position (n = 99, measured by proxies of socio-economic status, occupational status, social capital or social class), and/or age (n = 96) and/or geography (n = 38). Other PROGRESS-Plus criteria including education, migration, disability, language and HIV stigma were addressed on their own or in combination with other criteria only in 25 studies. More detailed information about the included studies is available in Figure 4 and Table 2.
FIGURE 4.
Studied interventions.
Evidence synthesis
Our data extraction and organisation resulted in the final selection of 159 articles (details available in Appendix 3) and a series of CMOCs (n = 21) covering a broad range of topics, interventions and affected groups. In line with the IPT, our data revealed that inequalities in general practice emerge through complex processes that take place in different domains, for example, in the clinical encounter between physicians and patients but also during communication between a local practice and the population it serves, and in the process of funding allocation. What we also noticed was that although interventions seemed to focus on one aspect of care (e.g. invitations to screening programmes), the intervention effectiveness was affected by different aspects (e.g. the availability of patient contact details or the extent to which patients could engage with written material). This stressed how inequality-producing processes are not only complex but also inter-related and, at the same time, made structuring and organising our evidence a complicated task.
We realised that, on the one hand, organising our evidence vertically across levels (e.g. individual, practice, macro-level) would not allow us to effectively capture how inequality-producing mechanisms cut across levels. On the other hand, organising our findings across aspects of care (e.g. service accessibility, care quality, care outcomes) would hinder our ability to produce transferrable conclusions. To deal with this puzzle, we had to return to our conceptualisation of health inequalities and the aims of our study. As stressed earlier, we understand health inequalities as the result of power imbalance across a series of intersecting hierarchies cutting across the individual and structural levels. What we aim is to contextualise individual action and aspects of care within the power organisation to enable people working in general practice to understand the links between structural factors and their practice, and engage in meaningful action against health inequalities. Therefore, we decided that the most efficient way to organise our findings was by building on the way power is organised. To do this, we drew upon intersectional understandings of power organisation, and specifically on the Domains of Power Framework. 110
The framework, developed by the sociologist P.H. Collins, suggests that for each power hierarchy (i.e. class, gender or race), power is organised through four interrelated domains: the structural domain, which involves social structures like public policy, laws, religion, economy, and relevant institutions; the disciplinary domain, which involves all the bureaucratic procedures which aim to control and organise behaviour (e.g. protocols, routines, rules and regulations used in everyday life); the cultural domain, which involves the dominant ‘worldviews’ as well as narratives and counter-narratives regarding inequalities, their causes, and solutions, language, ideas, images and values; the interpersonal domain, which involves the experience of individuals within the power structure, including relationships and interactions of the everyday life. The framework does not promote the significance of one domain over the others but highlights the importance of their synergy in the organisation of power and the emergence of inequality in any social context. 110,111
In the following sections we present the CMOCs that emerged from the reviewed literature organised across the four power domains. We consider that this is a useful framework because, while it allows us to understand processes and their resulting outcomes in specific domains, at the same time by highlighting the synergy between the domains it captures the complexity of inequalities and the action to reduce them within general practice.
Structural domain – structures and politics
Funding of general practice
A key structural factor is the distribution of funding, including financially incentivised quality-assessment strategies, such as the Quality and Outcomes Framework (QOF) and contractual reimbursement using the Carr-Hill formula. QOF was introduced in 2004 as a system which links financial incentives with the quality of care in general practice. 112,113 It aimed to improve the overall quality of care provided and decrease variations of care across practices by resourcing and rewarding best practice. Evidence shows that in the UK inequalities in the quality of the provided care related to deprivation decreased during the first 3 years of QOF. During this period an additional budget of £2 billion was allocated to primary care, which was associated among other things with a 12% increase in the number of GPs and the recruitment of additional administrative and nursing staff. During its first 3 years, QOF seemed to reduce inequalities in the delivery of clinical care between less and more deprived patients through a standardisation of care (see Figure 5, CMOC 1). 114,115 However, later studies suggest that this impact has not been sustained across time116 and, despite the improvements in quality of care, inequalities across age, ethnicity and socio-economic deprivation persist. 29,117,118
FIGURE 5.
CMOCs in the structural domain.
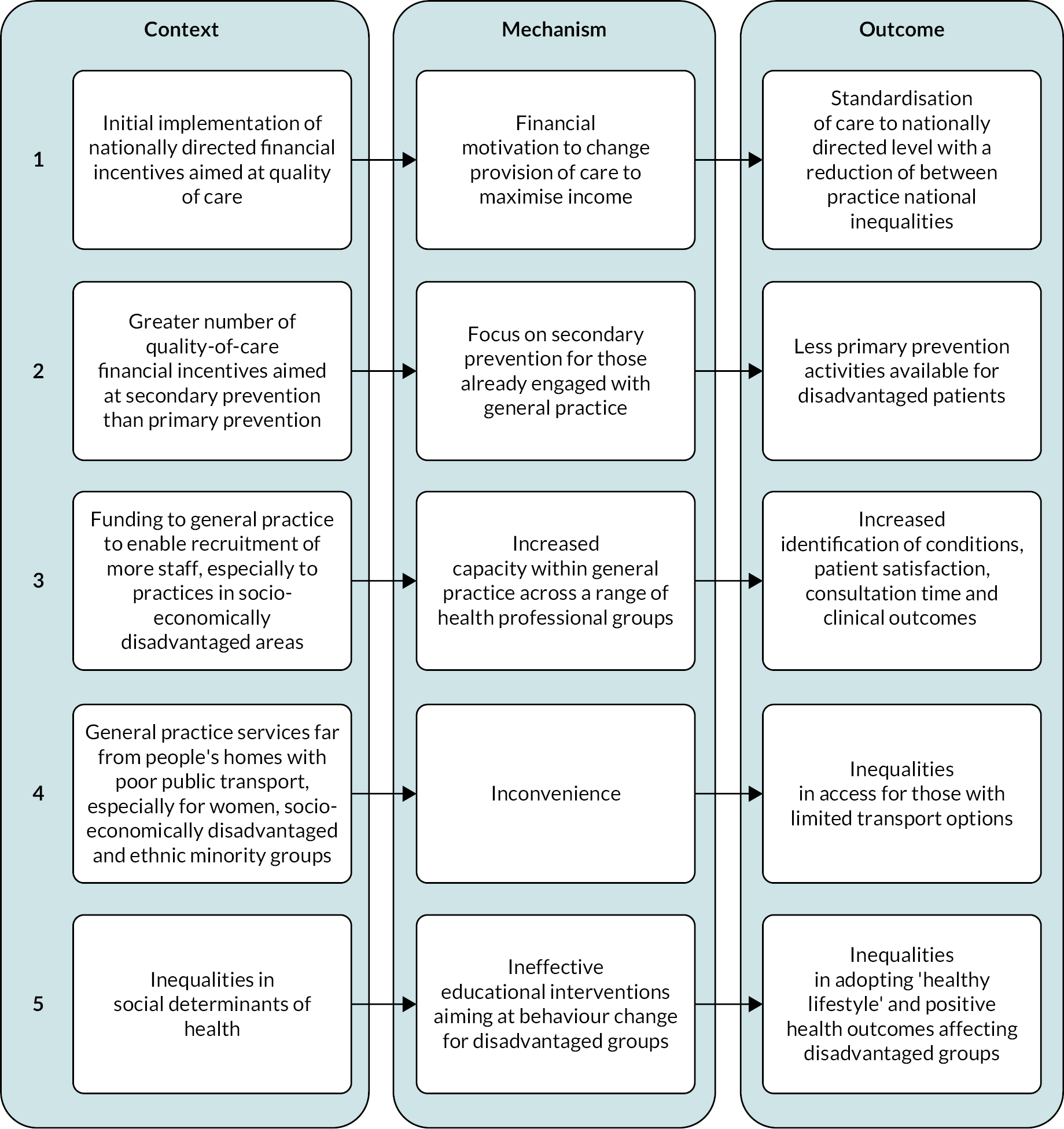
Moreover, a series of studies show that a structural aspect of QOF programmes that is relevant to health inequalities concerns the prioritisation of tasks and activities in standard care (see Figure 5, CMOC 2). 29,115,119–122 There is evidence suggesting that financial incentives can effectively drive physicians to conduct certain activities. 117 For example, after the introduction of QOF, recording of smoking status increased from 55.5% to 64.3% for men (p < 0.001) and from 67.9% to 75.8% for women (p < 0.001), which linked with improvements in smoking outcomes. 117 However, within the public health domain of QOF, almost 75% of the incentivised indicators are aimed at patients who already suffer from smoking-related diseases (secondary prevention) and only 25% of the incentivised indicators are aimed at primary prevention for people who may be at risk but have not yet developed a smoking-related disease. 115 In the context of local practices, where workload is usually high and resources limited, this imbalance interferes with the prioritisation of the incentivised activities over those not incentivised. 95–98 In the case of prevention, this can maintain or even increase inequalities in preventive service utilisation. This is because poorer and socially disadvantaged people tend to use less preventive healthcare when they don’t face immediate pain or disability. 123,124 In later sections, we discuss how disciplinary aspects of the QOF also link with inequalities against socially and economically disadvantaged groups.
Moreover, the data indicate that funding allows local general practices to increase their capacity through the recruitment of additional staff (see Figure 5, CMOC 3). 125–132 One of the included studies126 shows that practices with higher numbers of full-time equivalent GPs per 1000 patients record higher numbers of patients in their hypertension registers. The authors estimated that an extra GP per thousand patients would be associated with 6% increase in detected hypertension and a 33% increase in the patients who would be able to get an appointment quickly. 126 Another study set in a single practice in an urban area of extreme socio-economic deprivation in Glasgow128 showed that funding for the appointment of an additional part-time salaried GP for five sessions per week allowed the increase of consultation time for patients with complex needs, which in turn was associated with higher patient enablement. In addition, there is evidence that patients from practices with fewer medical staff have higher haemoglobin A1c concentrations,129 while smaller practices are generally found in deprived or remote areas. 130,131 Importantly, even after the introduction of the QOF poorly performing practices are still concentrated in more deprived areas. 119,125
Service convenience and inequalities in social determinants of health
The location of services together with the availability of transport options can lead to inequalities in access to general practice through increasing or decreasing service convenience (see Figure 5, CMOC 4). 129,133–140 For example, a study on the quality of general practice in remote and very remote areas in Scotland133 for people with coronary heart disease (CHD), diabetes and stroke showed that despite the higher prevalence of CVD and diabetes, rates of statin prescribing were lower than in urban areas. A study on British Bangladeshi patients with diabetes showed that geographical barriers in the places where people live (e.g. high-rise flats with no working lifts) discourage patients from leaving their home. 138 Evidence from non-UK contexts also shows that transportation plays an important role in the effectiveness of weight-management interventions by enabling attendance. 137 This is particularly relevant for ethnic minority groups with low socio-economic status who encounter additional barriers in accessing services, such as unreliable or unaffordable transportation. 139
What is also alarming is that within disadvantaged patients, women are likely to be even more severely affected by the inconvenience of service delivery due to increased mobility or transportation barriers. The included studies do not offer evidence regarding potential gendered effects of geographical or environmental barriers and time constraints on accessing general practice. However, they highlight the fact that women and especially those belonging to deprived and/or ethnic minority communities are more likely to be financially or practically dependent for their transport on other members of their household, deal with increased time constraints due to increased caring responsibilities, and feel afraid to go out alone. 129,140
Apart from accessing general practice services, inequalities in SDH link with inequalities in the effectiveness of educational interventions aiming at behaviour change and the reduction of behavioural risk factors (e.g. smoking). 129,137,138,141–146 People living in deprived areas or ethnic minorities face practical barriers in their attempts to develop what is called ‘healthy lifestyle’, which probably affects their ability to achieve and sustain their health-related goals (see Figure 5, CMOC 5). 129,137,138,141–146 Studies in the USA146,147 and the UK111,114 highlight the impact of language barriers, insufficient or unaffordable transportation and budget or time limitations, which are only some of the SDHs that interfere with the effectiveness of educational interventions aiming to improve care outcomes among disadvantaged groups. As an answer to these constraints, interventions aiming to encourage and sustain healthy behaviours among African Americans with diabetes in the USA integrate free food prescriptions for healthy foods and free access to exercise facilities acknowledging the importance of SDH. 146,147
Cultural domain – ideas and knowledge(s)
Cultural understanding and tailoring of services
The literature highlights in different ways the importance of cultural understanding in providing effective and equitable general practice services (see Figure 6, CMOC 1). 135,138,139,142,147–153 Many of the studies conducted mostly in the USA discuss interventions focused on the cultural tailoring of provided services to African American or Latino populations. In most cases, tailoring means adjusting interventions or messages so that they align with targeted groups’ cultural norms, health beliefs and lifestyle habits and eventually become more effective. 29,115–120,142 Cultural influences are relevant to how people think about their health and the origins of their disease, what is appropriate in a clinical encounter, and the extent to which they endorse health promotion or treatment activities. 138,154,155 Further, evidence shows that culturally tailored telecommunication systems can help urban African Americans with hypertension to adhere to their medication and evidence-based guidelines for dietary behaviour and physical activity. 139 Tailored education combined with shared decision-making has been found to increase empowerment and self-care among African Americans. 146 Moreover, tailored interactive digital educational material is associated with greater satisfaction with medication information and lower levels of diabetes distress among low-income Latino and African American adults compared to non-tailored educational material. 156,157 Similarly, tailored multicomponent interventions about diabetes increase the sense of control over condition self-management among ethnic minority patients and improve their behavioural outcomes. 150
FIGURE 6.
CMOCs in the cultural domain.
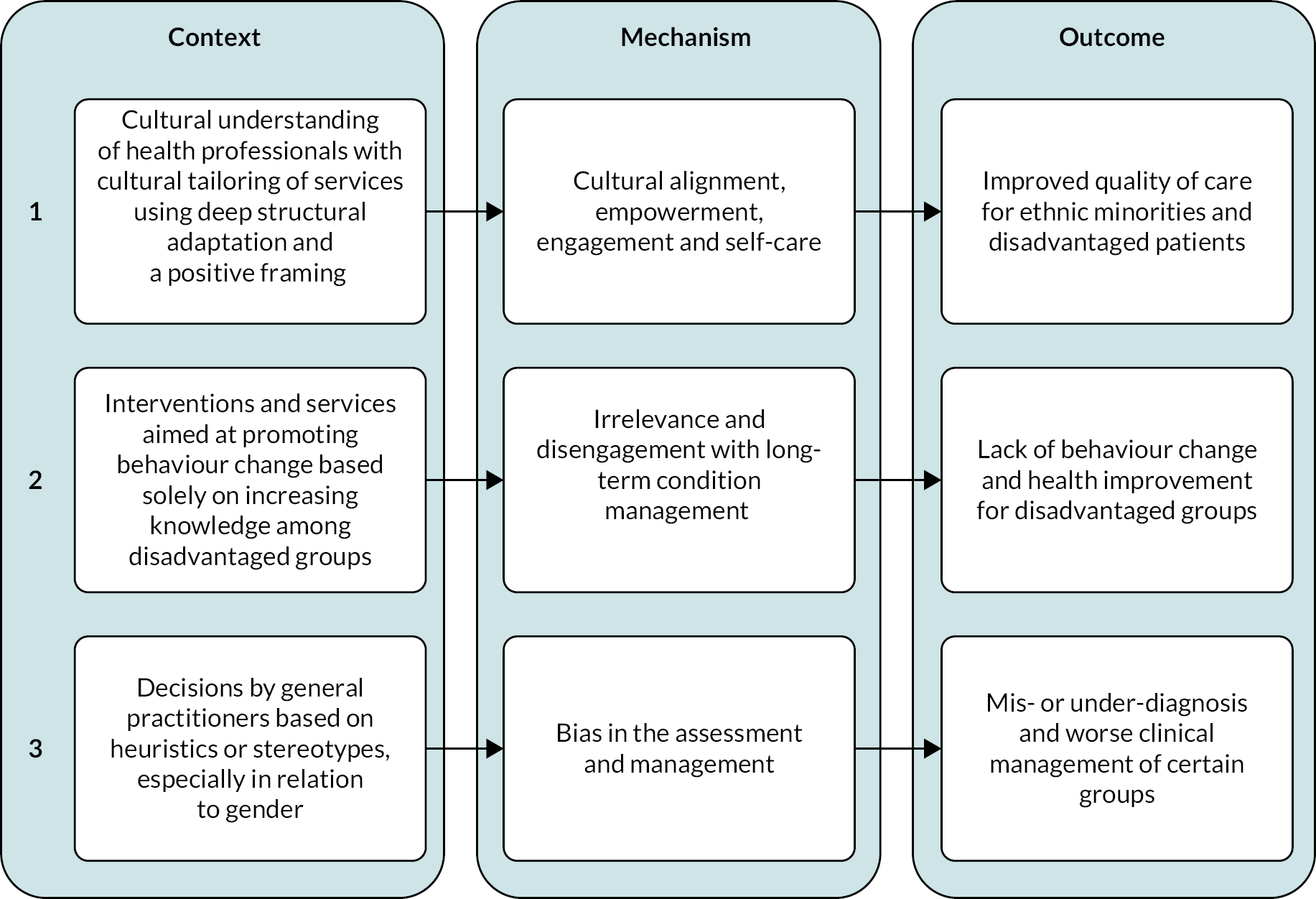
However, cultural tailoring is a multi-component process. 139,158,159 It can involve a surface structure adaptation (i.e. matching intervention materials and messages to observable characteristics of a target population) and/or deep structure adaptation (i.e. developing intervention materials that are aligned with the cultural values and social, historical and psychological forces that affect how health behaviours are viewed). 139 Therefore, it implies much more than translation or name-matching and demands the developing of a deep understanding of patients’ beliefs and needs. Starting from translation, evidence highlights that translation services to be effective need to be chosen and provided carefully158 based on knowledge about the languages used within targeted communities and possible inequalities within these communities in terms of literacy in the language of translation. 159
Research in the UK focuses on what culturally sensitive care and interventions entail. A study on a lifestyle intervention on weight change in South Asian people at high risk of diabetes shows that adopting a family focus was especially important for the success of the intervention in the specific group due to the strong cultural emphasis on family life and collective eating. 158 Another study focusing on interventions to promote physical activity among South Asian women with CHD and diabetes152 highlights that instead of overemphasising barriers of cultural difference, which often promote defeatist attitudes among professionals, health-promotion strategies should focus on a positive framing of what is meaningful for this group. They should also address possible misconceptions around the benefit of exercise, respect for the women’s experience of their ‘body limits’ and an understanding of their own motivation for physical activity. 152
Similarly, a study on the beliefs and folk models of diabetes among British Bangladeshis shows that perceptions about food’s ‘nourishing power’ interfere with what Western science defines as healthy eating (e.g. white sugar or lamb are perceived as energy and health-giving nutrients), and exercise is not a relatable concept nor does it have positive connotations within these groups. 138 The authors conclude that health educational interventions need to align with people’s lay epidemiology and folk models to be effective. In the same line, gender norms are another component of cultural understanding. Often the importance of gender is discussed in relation to religious ethnic minority women, who within the context of Western societies are perceived to be (and in some cases are) sensitive about interacting with men or exposing their bodies in front of others in healthcare contexts or physical activity spaces. 152 However, our data show that what people believe about what constitutes proper male or female behaviour interferes with the effectiveness of their care. 152,153 Characteristic examples include South Asian women believing that exercise is a ‘selfish’ behaviour for a woman who should be caring for her family instead of spending time on herself,152 or Turkish men being less likely to adopt health-promoting behaviours when relevant advice is offered by women educators. 153
To increase the cultural alignment between health professionals and groups who sit outside what we perceive as ‘the norm’, interventions are often based on integrating community members in care either as link workers, peer educators, community health workers or patient navigators. 160,161 It is understood that community members can provide health practitioners with the necessary cultural understanding that the latter may lack. They can also make patient experience smoother in terms of communication and more appropriate in terms of approach. 143 It follows almost naturally that these mechanisms can enhance the trust between patients and general practices, bridge communication gaps and enhance overall care quality. 160,162 For example, it has been found that link workers traditionally working in community outreach and education improve adherence to care plans among Mexican American populations in the USA,150 as well as patients of South Asian origin in the UK. 163 In a similar manner, increasing the concordance between health workers – from physicians to receptionists – and general practice users has also been found to contribute to achieving more culturally appropriate care in various settings. 164,165
Increasing knowledge alone does not decrease health inequalities
Inequalities in care (e.g. accessing screening services) and care outcomes either clinical (e.g. type 2 diabetes) or behavioural (e.g. self-management) are associated with people’s level of knowledge around health and how this knowledge affects their behaviour. 166,167 In the context of public health, it is often assumed that inequalities in health and healthcare result from the fact that socio-economically disadvantaged groups lack health knowledge and literacy compared to more privileged groups who tend to have greater access to education and knowledge resources. 129,168,169 Therefore, educational interventions are often seen as an effective way to decrease inequalities in care outcomes, especially behavioural outcomes like self-management of chronic conditions and adoption of healthy lifestyles. 158,170,171 However, the studies included in this review draw quite a different picture. They highlight that although inequalities in health literacy and knowledge are relevant to health inequalities, educational interventions or training on their own are not enough to close the gap in health outcomes (see Figure 6, CMOC 2). 135,141,151,168 A pilot randomised trial on knowledge, awareness and self-management among South Asians with diabetes in Manchester found that interventions focusing on questionnaires and educational packages do not increase knowledge or self-management behaviours. 141 Additional evidence shows that enhanced diabetes care, including training and educational support, does not necessarily improve outcomes among South Asians in the UK, even though they172 value education and have high regard for knowledge acquired from an ‘educated person’. 135
A study on breast cancer screening among Asian women in the UK suggests that relevant educational interventions should focus on increasing awareness of the purpose and relevance of screening services because limited understanding in these domains reduces attendance in this group. 149 Also, as described earlier, the content and goals of educational interventions should be consistent with the everyday reality of the targeted populations as this is shaped by culture and structural inequalities. 138,150–152 Moreover, studies hint at the fact that the extent to which people perceive themselves as capable of achieving certain goals can also interfere with the effectiveness of educational interventions. 150,173–175 Often in literature, such perceptions are described with the psychological concept of self-efficacy. 176 However, we know that the social position that people occupy within their contexts informs the way they perceive the world, themselves and their capabilities. 90 Disadvantaged groups, beyond practical barriers, are more likely to encounter perceptional barriers in their attempts to adopt healthier behaviours and engage with their care plans. 143,146,154,177 For example, evidence shows that they often tend to have fatalistic beliefs about disease and perceive barriers in accessing services as higher than what they are. 154
Biases among healthcare staff
Evidence suggests that GPs often tend to make decisions in their everyday work routine based on heuristics or mental short-cuts (e.g. that men have a higher index of suspicion for CVD). This can lead to patients deviating from the ‘typical’ clinical picture being excluded from care because of implicit bias (see Figure 6, CMOC 3). 117,165,178–180 Meta-analyses have shown that the risk of cardiovascular mortality is two times higher among men and three times higher among women with type 2 diabetes compared to men and women without diabetes. 181–183 The gender inequality observed is attributed to less effective monitoring of risk factors among women. An observational survey among GPs in Paris178 showed that information regarding CVD risk factors was regularly less available in the files and risk assessment could be performed significantly less often for women seeing male physicians. The authors highlight that although women are generally assessed for CVD risk less often than men, gender inequalities decrease when women patients are seen by women physicians. They attribute these results partly to physicians understanding the guidelines about risk assessment differently according to their patient’s gender (i.e. men are seen as more susceptible to CVD risk), partly to women being more likely to follow guidelines more consistently.
In the UK, findings as such may be particularly relevant for gender inequalities in remote and very remote areas because practices there tend to have a significantly lower number of women GPs. 133 This has also been linked with reduced choice for patients and poor access to some forms of treatment. 133 Additionally, evidence from 14 general practices in London showed that South Asian patients had better blood pressure and total cholesterol recording than white patients, while those with no records for ethnicity had the poorest recorded outcomes. 164 The authors attributed this inequality partially to risk factor recording being considered more relevant in the case of South Asian patients because they are perceived to be at greater risk of CVD.
Disciplinary domain – rules and practices
Excluding patients from quality standards
We have already discussed how certain structural aspects of financial incentive schemes can contribute to the increase of within-practice inequalities. Here, we elaborate on how the way that such schemes are implemented in day-to-day practice is an additional driver of health inequalities in general practice. The included literature focuses on the QOF and suggests that its main caveat concerns the fact that practices are allowed to exclude from the measurement of achievement targets patients who are unsuitable for chronic disease management. 29 According to the national guideline these patients include those who refuse or fail to attend a review, those who should not receive treatment due to comorbidity, those who have been recently registered with a practice, those with drug-related limitations, patients who refuse investigation or treatment, and/or those for whom further investigation or treatment is unavailable or it is inappropriate to attend a review due to specific circumstances (e.g. terminal illness). 29 The purpose of excluding certain patients from these assessments is to avoid penalising practices for the characteristics of the population they serve.
However, the way this exclusion process is used maintains and conceals inequalities in service provision. 29,119–122,125,169,184 This is especially true for diagnostic indicators like foot and eye screening in diabetes and spirometry and record of forced expiratory volume in 1 second (FEV1) in COPD as well as treatment indicators for CHD, stroke and diabetes which are associated negatively with levels of deprivation. 29 One of the included studies114 shows that performance as measured by the QOF is higher in practices with higher rates of patients excluded from QOF indicators. Specifically, a 1% higher rate of exception reporting was associated with a 0.35% higher rate of achievement in the second year of the framework and a 0.16% higher rate in the third year. However, practices serving the most deprived population had an exception-reporting rate that was 0.55% higher than the rate in practices serving the least deprived population in year 2, while in the third year the difference in the rate reached 0.67%. This means that approximately 630 more people are likely to be excluded in a practice of 9000 patients (which is the average list size for practices in June 202256) in the most deprived areas compared to the least deprived. Additional evidence suggests that exception-reporting rates are higher among disadvantaged groups at higher risk of diabetes complications and poorer health outcomes. 120 This evidence suggests that in more deprived areas there are either more patients who can be formally exempted from QOF indicators (e.g. due to limited attendance or increased comorbidities) or there are more patients who are treated as exceptions so that the practices can maximise their income. 120,169 In other words, it means that patients perceived as less likely to engage or respond to treatment (e.g. due to complex psychosocial problems) are less likely to be provided with ongoing support by their practice due to the effort of the practice to achieve certain performance targets (see Figure 7, CMOC 1). 29,119–122,125,169,184 It is also likely that both explanations can be true at the same time, while evidence on this remains inconclusive.
FIGURE 7.
CMOCs in the disciplinary domain (1).
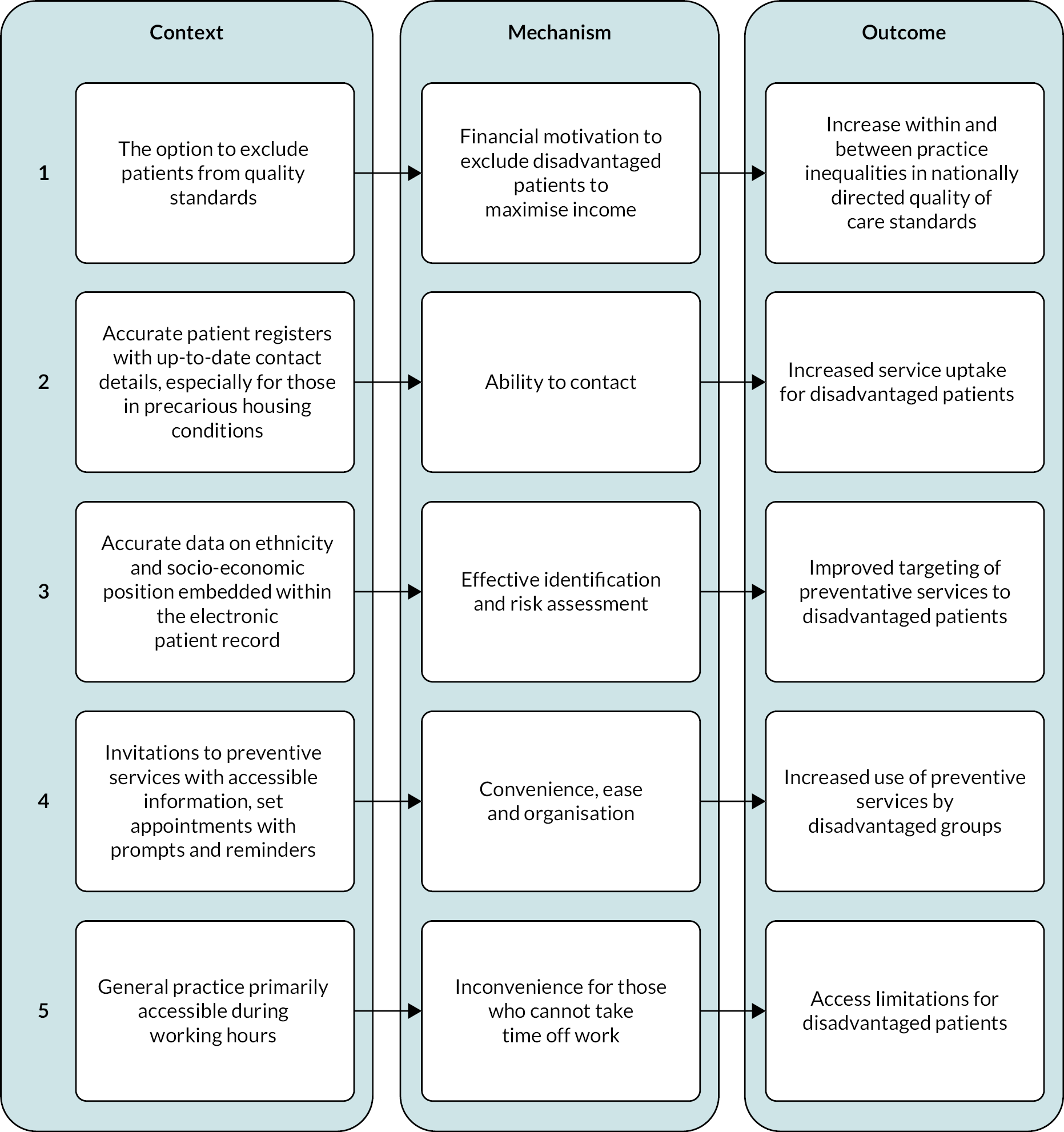
Regardless of the justification for exceptions, the increased exception rates among disadvantaged groups have two serious implications. The first is that QOF through the way the exception reporting is used in day-to-day practice probably excludes disadvantaged patients from accessing necessary care including preventive and diagnostic services. 185 Importantly, this exclusion is not considered in the overall assessment of service delivery. While evidence shows that the introduction of the QOF narrowed the gap between least and most deprived populations, at least during the first three years of its use in terms of care quality,114,115 it is likely that it has sustained or even increased the gap in terms of unmet need within and between practices. The second implication is that by not accounting for the extra effort that practices in disadvantaged areas need to put to achieve quality targets and maintain income, the framework reinforces the misuse of the exception process and at the same time maintains or even widens inequalities between practices by entrenching the inverse care law. 29
Accurate patient contact details and demographic information in electronic patient records
Additional procedures that increase inequalities especially in terms of service uptake are relevant with the collection, use and maintenance of patient information. Evidence shows this is particularly true for screening services. 127,149 Maintaining accurate patient registers with up-to-date contact details enables effective contact and this links to higher rates of screening uptake and quick delivery of interventions (see Figure 7, CMOC 2). 127,149,164,186,187 However, maintaining accurate patient registries is not equally easy for all patients. Practices often have inaccurate contact details and telephone numbers of people in precarious housing, or those who live in inner city urban areas, migrants and older patients. 127,136,188–190
The optimal collection and use of patient socio-demographic data is also linked with inequalities in care effectiveness (see Figure 7, CMOC 3). 191,192 Studies on the effectiveness of CVD screening and the Health Checks programme in the UK highlight the lack of socio-demographic information especially for patients in more deprived areas. 164,193 A study across 14 general practices in Ealing published in 2010 showed that South Asian patients had better blood pressure and total cholesterol recording than white patients, while those with no records for ethnicity had the poorest data records. 164 As stressed earlier, the authors suggested that this inequality may be attributed to implicit bias that patients of ethnicity other than South Asian are not at high risk of CVD. However, other potential explanations include either that South Asian patients visit their practice more often, or there is greater ethnic concordance between South Asian patients and GPs enabling better exchange of information. This kind of evidence does not allow the effective assessment of the direction and size of inequalities but hints at the fact that in these practices there is an unspecified number of unidentified patients who may be at risk of CVD.
A prospective cohort study from 1993 to 2008 across 531 general practices in England and Wales showed that using a CVD risk algorithm which allowed adjustment for patient level of deprivation, ethnicity and clinical conditions improved the accuracy of identification of those at high risk compared to the Framingham score. 194 The authors suggested that this benefit was particularly relevant for South Asian women and for patients with type 2 diabetes and that it demonstrated the utility of linked electronic data for the development of tools that will enable physicians to make better decisions. The importance of collecting and using sociodemographic characteristics has also been highlighted in relation to the identification of lung cancer at an early stage. 195 Further, two studies on the impact of QOF on intermediate outcomes for diabetes and the quality of chronic disease management stress the importance of integrating patient data in the assessment of interventions and the need for differentiation within broader patient groups. 114,196 Both studies highlight that suboptimal use of patient data, like merging distinct ethnic groups (e.g. Indians, Pakistanis and Bangladeshis) or social classes (e.g. skilled and unskilled workers) into single undifferentiated categories (e.g. South Asians or manual classes), carries the danger of masking inequalities within disadvantaged groups.
Invitation methods to preventive services
Invitation methods to services involve additional bureaucracies through which inequalities in service uptake can increase or decrease. A study from the UK found that invitation letters with predetermined appointments are effective in increasing health checks among patients with severe mental illness and that a reminder letter has also a positive effect among non-attendants (see Figure 7, CMOC 4). 191,197,198 The authors suggest that this increase is driven by the fact that set appointments remove the difficulties entailed in making an appointment, which might be a particularly relevant factor affecting this category of patients due to increased anxiety levels and fluctuations of symptoms. In contrast, if invitations to screening programmes are sent in the form of extensive written material, they are likely to be dismissed and overlooked by disadvantaged patients and especially those with limited language or literacy skills. It is important to note that this is true even if the information is in plain everyday language and it applies whenever the communication between a practice and its patients is based on written material. 197,198
Using prompts and reminders also has a positive impact on screening uptake especially for disadvantaged groups (see Figure 7, CMOC 4). 134,154,189,190,197,199 ‘Forgetting to go to the appointment’ is a popular reason for not attending189 and reminders such as text-messages one or two days before the appointment date seem to help patients to organise their programme in a way that benefits their attendance. A study on reminders for routine cancer screening in London189 used mobile-phone contact records available in general practice registers to send text-message reminders two days before women were scheduled for routine breast cancer screening. The intervention increased overall uptake but, importantly, women living in the most deprived areas, despite having the least complete and up-to-date contact details,189 benefitted the most, with an absolute increase in attendance of 13.6% and a relative increase of 28%. However, an intervention focusing on sending text-message reminders for bowel-cancer screening with the involvement of primary care did not have an effect on gender inequalities or the socio-economic gradient in uptake. 190 Such findings highlight how intervention effects differ across disease types and patient groups.
Service hours and contact time
The studied literature shows that time is an important factor linked with inequalities in general practice; either this refers to the actual opening times of services,134,200 the length of clinical consultation, or the frequency of contact between patients and practice staff. 128,165,201,202 Evidence suggests that patients from ethnic minority backgrounds and people who cannot take time off work have increased difficulty in accessing their GP or screening services if these are available only during working hours (see Figure 7, CMOC 5). 134,200 Importantly, the challenges are the same in the case of telephone services if those are offered only during usual working hours. 200
Beyond flexible opening times, increased contact time in terms of both consultation duration and follow-ups has a serious impact on the overall communication during the clinical encounter and is associated with better patient experience and effectiveness of care (see Figure 8, CMOC 6). 128,129,142,165,201–203 Longer consultation times allow practitioners to work without feeling stressed and this improves their communication skills as well as the outcome of their communication with their patient because there is more space for information exchange. 128 Similarly, it has been shown that regular-follow up benefits information exchange about medication, diet and exercise and gives the opportunity to adjust the care plan or its goals. 129,142,203 Better communication has been found to be associated with more feelings of enablement and satisfaction for patients and confidence for practitioners, who feel that they do their work effectively. 201,202 These are beneficial qualities of care for everybody. However, they are even more so for patients who live in deprived areas and ethnic minorities. This is because these patients are more likely to deal with increased language and literacy limitations139 or have complex physical, social and psychological problems and therefore need more time to communicate their situation and understand what they need to do. 128
FIGURE 8.
CMOCs in the disciplinary domain (2).
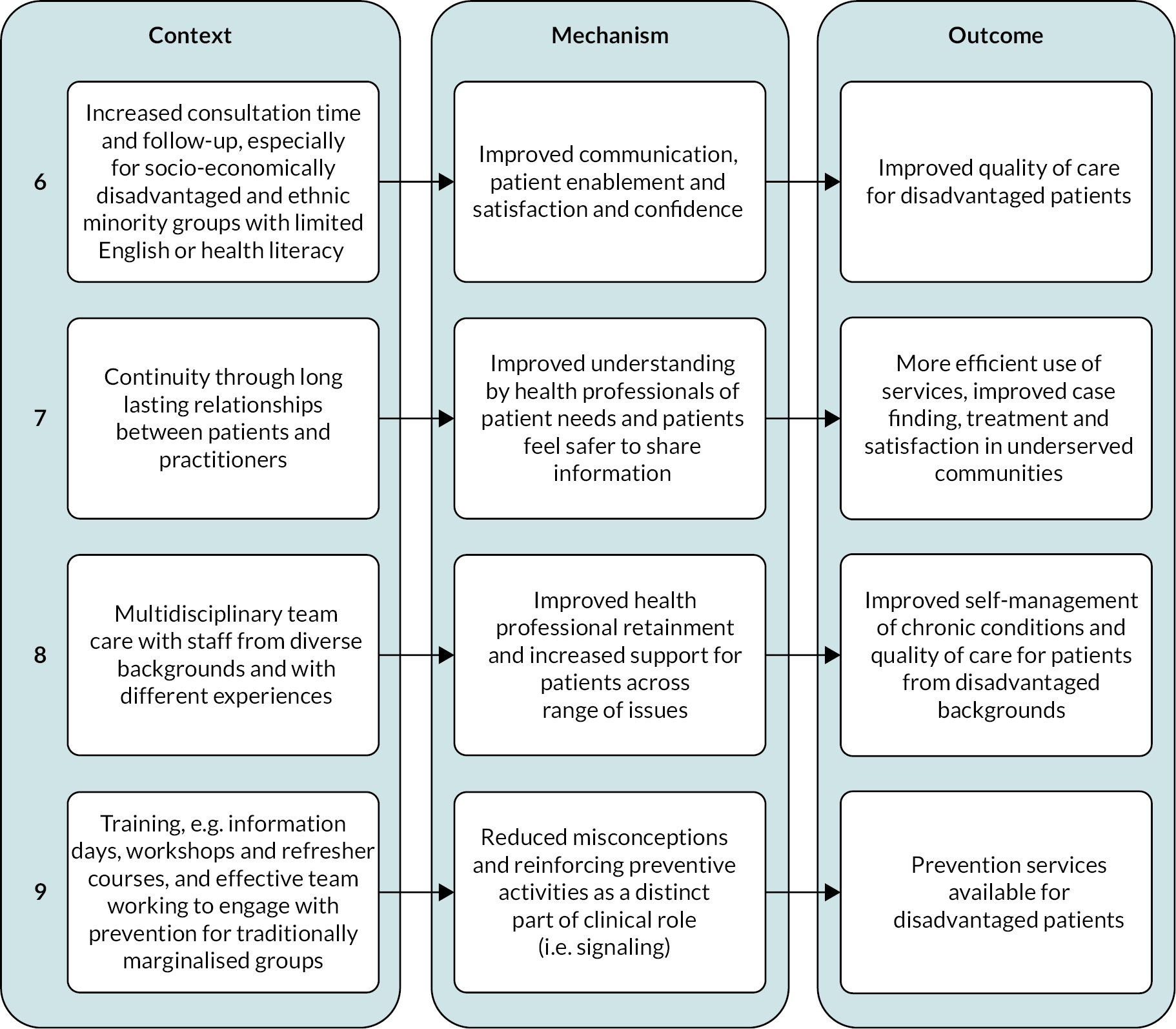
Continuity
Continuity emerges as an additional procedural element that links with improved care effectiveness because it improves the understanding of patient needs, especially for elderly or under-served patients and those with complex physical and psychosocial problems (see Figure 8, CMOC 7). 143,204–206 A qualitative study on the lessons learned through the Health Checks programme in the UK stresses that the existence of long-lasting relationships between patients and practitioners enabled the latter to know what type of approach would work best for their population and this benefitted the delivery of the programme, especially among patients who are under-served. 206 Additional evidence128 shows that continuity of care is higher for complex consultation, hinting at the fact that complex problems can be more effectively addressed in the context of an ongoing relationship between patients and physicians either because patients may feel safer sharing information or because physicians can develop a better understanding of their patients or both.
In a qualitative study on the effectiveness of cancer detection in primary care,204 GPs were found to value interpersonal continuity as key for the effectiveness of cancer detection. According to their testimonies, trusting relationships allow GPs to identify those patients who need to be referred for further investigation from those who don’t. According to them, relationship continuity is threatened by the existence of multiple points of provision (e.g. walk-in centres) and the use of part-time or locum cover GPs. A study conducted in the USA echoes these findings and adds on the importance of continuity between primary care physicians and oncologists during cancer treatment for the better effectiveness of care and the higher satisfaction of patients in under-served communities. 207
Multidisciplinary team care
Organising care in a way that involves supportive roles is associated with the effectiveness of care and inequalities in care outcomes (see Figure 8, CMOC 8). 161,208–212 Evidence shows that programmes led by nurse practitioners improve patient management and health outcomes compared to usual care among African Americans with diabetes in rural areas. 210 Specifically, integrating in care a certified nurse practitioner who, instead of being constantly based in the practice, rotates in the rural site to provide necessary support and training works particularly well for people who face more logistic challenges in remote settings. In one of the studies, it is highlighted how nurses practically help with the use of the telehealth service for patients who face accessibility difficulties and how this links with improvements in diabetes self-management. 157 Another study from the USA also highlights the cost-effectiveness of chronic disease management by nurse practitioners and their important role in addressing health inequalities in under-served minority populations. 213
In Canada, a study showed that the presence of nurses allowed GPs to focus on their preferred domains, improved the overall communication in the practice, and increased job satisfaction among physicians, which in turn increased their desire to remain in their work. 161 Nurse practitioners were described as ‘bridges between administration staff and physicians’ because they enabled a better exchange of information. Their presence was associated with creating shared care plans, increasing access to primary care for under-served patients, and delivering new services outside the practice (e.g. home visits for frail patients). Other studies hint at the same direction by highlighting the effectiveness of interprofessional teams including nurses, health assistants and pharmacists in improving care quality for under-served people with diabetes, cancer and CVD. 207,212,214
Supporting staff to engage with prevention for traditionally marginalised groups
Availability of preventive services increases when all members of staff in a practice including healthcare assistants and nurses are supported to engage in prevention. A qualitative study on identifying best practice in England’s Health Checks programme206 found that healthcare assistants consider that training, such as information days, workshops and refresher courses, enables them to engage more effectively in the delivery of the Health Checks programme. Additionally, effective team working based on the allocation of specific tasks and responsibilities to named individuals within practices was also mentioned as a key for the successful delivery of the programme. Another study215 on the role of practice nurses in screening and preventive activities for CVD among patients with severe mental health problems showed that providing relative training to the nurses increases the level of screening and lifestyle advice given to this group of patients. It is believed that training activities for nurses and healthcare assistants decrease their misconceptions and help them understand preventive activities as a distinct part of their role (i.e. through the process of signalling). Hence, they are more likely to undertake such activities and increase the overall service availability within a practice (see Figure 8, CMOC 9). 159,170,201,206,215 Importantly, if this is targeted at disadvantaged groups it can decrease inequalities in prevention services that negatively impact traditionally marginalised people within society and healthcare. 159,215
Interpersonal domain – relationships and experiences
Relationships between practice staff and patients
Many of the included studies refer to the importance of the quality of clinical encounters and the relationship between practice staff and patients. 142,201,203,204,206 However, there are only limited studies examining specific aspects of this relationship and their impact on health inequalities. Evidence shows that when patients perceive their healthcare providers as empathetic, with good communication skills and an interest in their symptoms and their overall concerns, they feel supported to ask questions and engage with decision-making and care management. This in turn leads to more effective and long-term person-centred condition management (see Figure 9, CMOC 1). 150,170,202,216–218 We know that shared decision-making is associated with many positive outcomes and especially better control of diabetes. 146,219 This is particularly important for improving care quality among ethnic minority and socio-economically disadvantaged patients who might be less assertive, or may have limited health literacy. 138,143,206 Studies show that British Bangladeshis tend to view their GP as a busy authoritative person and tend to engage less in information exchange, while patients across different South Asian communities in Britain know less about diabetes and its management compared to white British. 138
FIGURE 9.
CMOCs in the interpersonal domain.
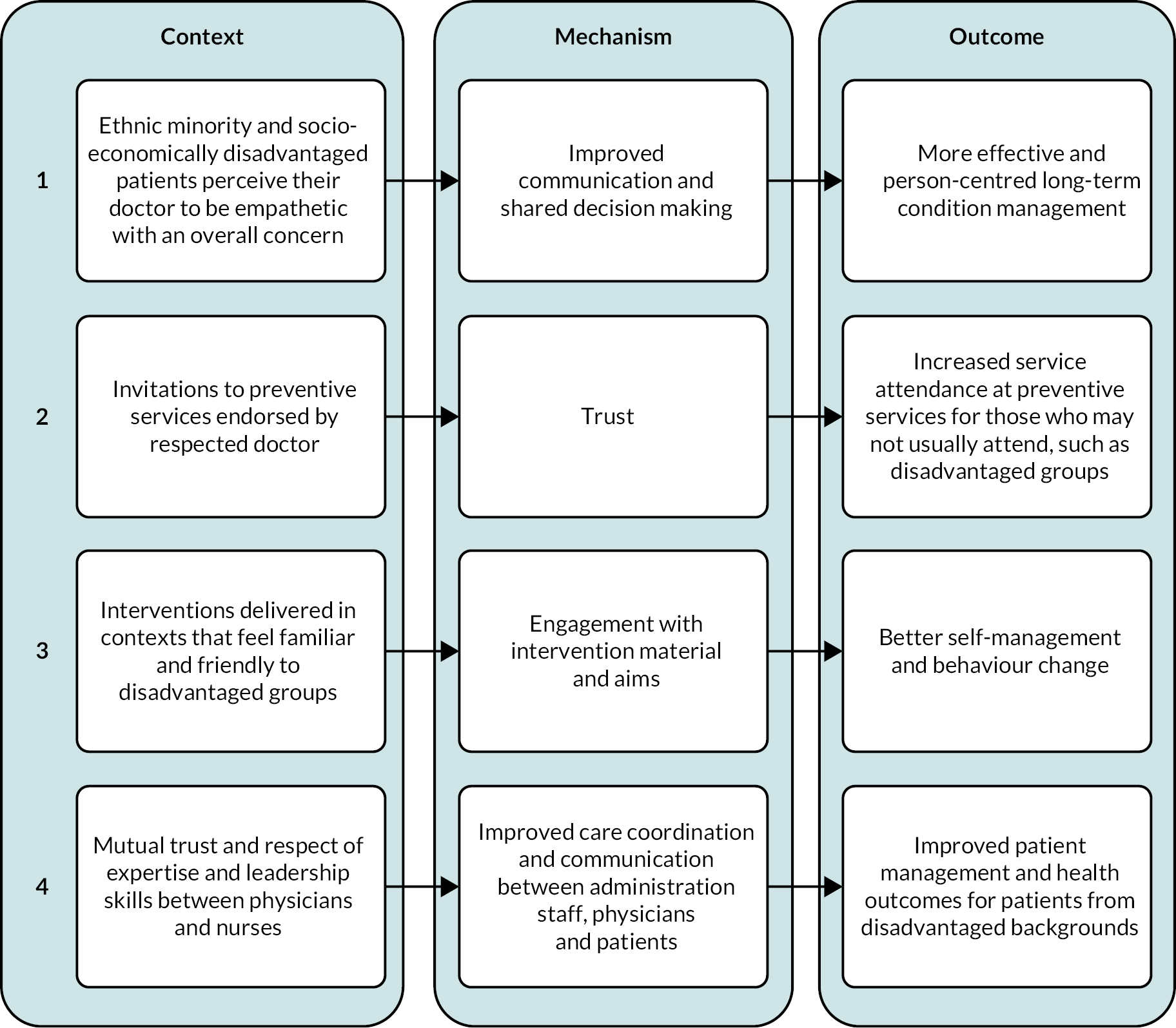
Further, a study on breast-cancer screening uptake among ethnic minority women in inner-city Cardiff general practices highlights the importance of trust between patients and their physicians for the decrease of inequalities in prevention (see Figure 9, CMOC 2). 136 The study shows that when women received an endorsement letter from their doctor they decided to attend the programme because of trusting their doctor and their opinion. A study in the USA points towards a similar direction, showing that physician recommendation for screening mammography can increase screening uptake among 65+ and low-income women. 220 Additionally, supportive relationships emerge as a key factor for the success of educational interventions among disadvantaged groups (see Figure 9, CMOC 3). 146,158,161,217 A study on an educational intervention for African Americans with diabetes highlights how creating a familiar feeling within the intervention groups (including group leaders) was key for the success of the intervention, which led to decreases in hemoglobin A1c and HDL cholesterol. 146 The positive impact of a supportive atmosphere is also highlighted in a study conducted in Canada on medical group visits in primary care and their impact on diabetes patients with low socio-economic status. 217
Effective team working among practice staff
In previous sections, we discussed how multidisciplinary care teams can contribute to the decrease of inequalities in care effectiveness as well as the importance of supporting all practice staff to engage with prevention activities for disadvantaged patients. Additionally, those studies stress that achieving improvements through integrating additional roles in care (including nurse practitioners) is subject to effective team working among practice staff. Effective teamwork involves effective communication regarding allocated responsibilities to individuals, trust between practitioners, and respect for the expertise and leadership skills of the non-physician members of staff. This eventually links with improved management and health outcomes, especially among disadvantaged patients (see Figure 9, CMOC 4). 161,206,208,209,212
Five qualities of equitable general practice: an action framework
The overarching question of our study was which types of interventions or aspects of care can decrease or increase inequalities in general practice for chronic diseases. In the previous section, we discussed a wide and diverse range of evidence related to inequalities across different domains. In this section, we discuss our findings with reference to the IPT, and we suggest an action framework for equitable general practice (see Figure 10). The framework identifies that equitable general practice has five key qualities (represented by the multicolour concentric rings in the figure): connected, intersectional, flexible, inclusive and community-centred. Also, it highlights areas of relevant action in the structural, cultural, disciplinary and interpersonal domains.
FIGURE 10.
Action framework for equitable general practice.
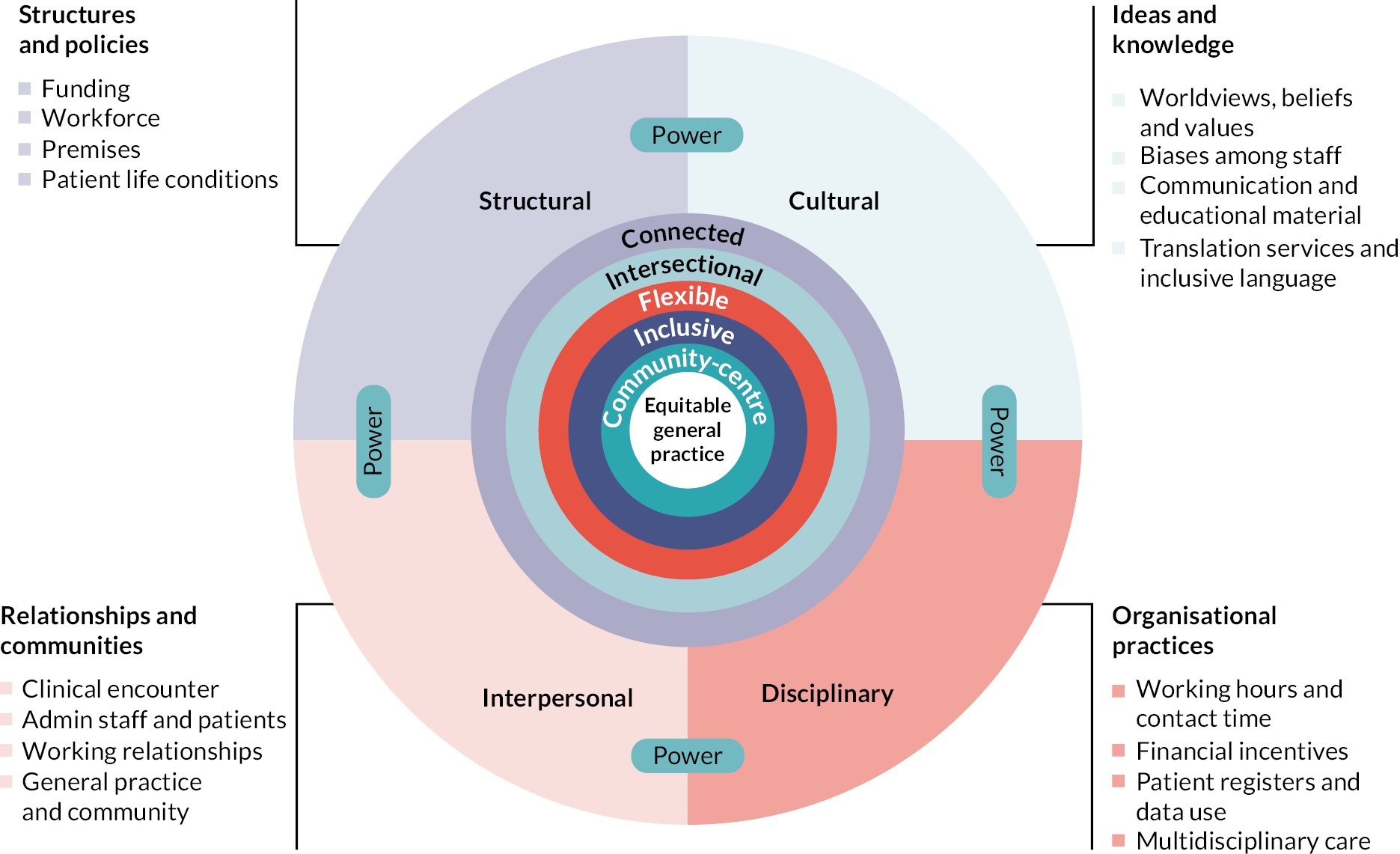
This framework is the outcome of discussions within our research team and the integration of feedback we got from our PPI colleagues and the expert panel, and through a deliberative workshop with health professionals and academic GPs as described in the methods section. It incorporates the components of the IPT that were found in the evidence and refined through CMOCs and maps them as relevant areas of action across the four different domains of power organisation. This means that the framework is not exhaustive as there might be series of other elements relevant to health inequalities in general practice that are simply not discussed in the literature. As one of the deliberative workshop participants stressed, not everything that happens is measured. Moreover, the framework provides guidance, but our analysis has expressed this at the level of abstraction that enables people involved in general practice to use it (and, where necessary, adapt it) according to the particularities of their context.
The main message we aim to convey with this framework is that action to reduce health inequalities demands shifting our focus from the GP as an individual to general practice as a heterogeneous multidimensional system. Within this system all the involved actors, from the position they occupy, need to challenge established power dynamics. It does not imply that everyone can push for change to the same extent across all the domains nor that action should always focus on all the four domains. Rather, it aims to enable people involved in general practice to become aware of their opportunities and limitations in contributing to the reduction of health inequalities, but also of their interconnections, so that they can meaningfully engage in collective coordinated action. Below, we present the action framework for equitable general practice, and we discuss what it means for general practice to be connected, intersectional, flexible, inclusive and community-centred.
Connected
Our evidence synthesis highlights the fact that health inequalities in general practice are connected in linear and non-linear ways. For example, in what looks like a linear process, in socio-economically disadvantaged areas, the ineffective collection and use of patient information links with ineffective patient risk assessment and screening uptake, and eventually with disadvantaged patients at risk of CVD or cancer not receiving the necessary care. 127,149,164,186,187 At the same time, disadvantaged patients are also excluded from receiving necessary care because they are disproportionately affected by the exception reporting within QOF. 29,119–122,125,169,184 To top it all, it is likely that physicians’ biased perceptions regarding patient risk can interfere with their decisions and adherence to prevention guidelines, resulting in certain individuals within disadvantaged groups being further excluded from appropriate care. 117,165,178–180 Though connected in non-linear ways, regulated procedures such as using patient information and achieving quality standards together with stereotypes about which patient is at risk affect disadvantaged patients simultaneously. Therefore, the range of inequalities in receiving appropriate care is the outcome of the synergy between these procedures and domains (i.e. disciplinary and cultural).
The reviewed studies provide a series of juxtapositions of health inequalities in general practice, but our evidence synthesis describes a continuous process through which decisions and activities across different time points, operational levels and power domains operate in tandem to shape a landscape of inequalities where disadvantaged groups are affected by multiple forces. In this landscape, the consequences of dysfunctions in certain procedures or activities rarely stay limited in the ‘areas’ they emerge. Rather, they spread out across a series of other interconnected procedures, activities or functions and across time. Therefore, interventions to reduce health inequalities should be understood, designed and delivered as the connected components of coordinated action towards equitable general practice.
Intersectional
The second important conclusion that emerges from our evidence synthesis is that none of the discussed interventions or aspects of care works the same way for everybody. We saw, for example, that educating patients about their condition and its management can improve self-management behaviour and related health outcomes but importantly this is only true for some patients. It is less true for patients with adverse living conditions for whom practical barriers interfere with the effectiveness of educational interventions. 135,141,151,168
Further, our findings stress multiple times that interventions targeted at disadvantaged groups of patients often fail to account for differences within these groups. For example, we saw that translating written communication to engage with patients who have limited English-language skills without accounting for differences in literacy or dialects used within groups excludes certain patients from engaging with information material. 158,159 Such examples highlight how general practice needs to incorporate an intersectional perspective to be able to recognise the differential needs of patients and deliver compatible and effective services. Importantly, they show how an intersectional perspective is a necessary tool for the design and delivery of interventions which will not generate or increase inequalities due to the unintended exclusion of disadvantaged patients. 25,26
Services need to account for differences across not only socio-economic status, but also gender, ethnicity and religion. They need to be designed and delivered in perspective of patients’ social reality and life conditions in order to acknowledge other dimensions of social positioning that are related to health inequalities. The reviewed studies do not offer information regarding the impact of sexual orientation or disability but we know that these are social categories which link with both socio-economic and health disadvantage. 72 Similarly, across different contexts there might be other social categories (e.g. caste)221 that are meaningful for the understanding of health inequalities and action against them.
Adopting an intersectional perspective in the design and delivery of general practice will provide people involved in the sector with the conceptual tools to understand that inequality-producing mechanisms are connected across time, organisational levels and power domains. It will enable them to acknowledge the relevance of structural factors with their everyday work, identify specific opportunities and limitations in challenging inequality-producing mechanisms according to their own position in the system, and engage in meaningful collective action that builds on difference instead of dismissing it.
Flexible
To achieve nuanced approaches and to develop interventions that account for difference within groups there is a need for flexibility. Our findings stress that different patients have different needs and that socially disadvantaged individuals are likely to need additional support in terms of accessing care and also in terms of making the best out of it. For example, they may need extra encouragement to get involved in decision-making138,143,206 or some practical assistance with visiting their practice146,147 or using a telehealth service157 or translation services. 159 Developing equitable care and interventions means that healthcare workers will be asked to make allowances for differences in patient needs and be flexible in terms of care delivery. The reviewed literature shows that flexibility concerns the optimal use of resources in terms of employees and their skills and knowledge (e.g. cultural understanding provided by nurses and non-clinical staff),161,208–212 opening hours (e.g. offering services outside usual opening hours),134,200 contact time (e.g. longer sessions for patients with complex physical and psychosocial problems)128,165,201,202 and communication material (e.g. choosing between written and non-written material and inclusive language/translation). 159 Moreover, it concerns an overall mindset among employees and decision-makers who can think outside the norm and adjust their decisions and actions based on their ability to understand their patients within the context of their culture and social position.
Inclusive
Our evidence stresses at multiple instances the importance of cultural understanding between practitioners and their patients, and the difference services can make when designed and delivered in a way that aligns with patient worldviews, preferences and needs. 135,138,141,142,147–153 Beyond language, our findings show that culture influences how disease and health are understood, and what is perceived as healthy behaviour, the role of family as a supportive or interfering factor, and what is considered ‘appropriate’ male or female behaviour. 138,152,154,155,158 Although not extensively discussed in the literature, our findings hint at the fact that practitioners’ decisions are affected by their perceptions of their patients. We saw, for example, that considering women as being less at risk of CVD may exclude them from optimal risk assessment,117,168,178–180 or perceiving patients as being less able to reach care goals may link with these patients being excluded from QOF assessments. 91–94,95,138,151 This evidence highlights that besides being flexible, equitable general practice is also inclusive. This means care designed and delivered in a way that it does not exclude people based on assumptions about who they are, what they need and how they ‘should’ behave. Importantly, inclusivity concerns interpersonal relationships and interactions that involve all the actors in general practice from decision-makers to GPs, nurses, supportive and administrative staff and patients. 161,206,208,209,212
Community-centred
The fifth quality of equitable general practice is being community-centred. Community-centred general practice means designing and delivering care with people and not for people. Building long-lasting relationships of trust with communities and tailoring services to local need are discussed in our findings as ways to improve care for disadvantaged patients. 145,160–165 Suggested ways to achieve this include integrating community members in care, increasing ethnic and language concordance between patients and practice staff,143,160–165 and supporting all the practice staff including non-clinical employees to engage with the provision of care. 159,170,201,206,215 For example, we saw how training nurses and trusting them as leaders in the delivery of interventions links with improved outcomes for people with serious mental illness or people in remote areas. 161,206,208,209,212 Our evidence highlights that the sense of community concerns a multitude of elements that cut across all the domains of power. These include proximate premises, up-to-date patient contact details, interventions delivered in familiar contexts, cultural understanding, trusting relationships between GPs and patients, multidisciplinary care teams, and mutual respect among practice employees across professional hierarchies.
Chapter 4 Discussion
Statement of principal findings
Our review revealed that research on general practice interventions that can decrease health inequalities is limited and lacks detail and in-depth focus. The studies addressing inequalities mostly document the problem and its range but they do not investigate the elements of interventions or care that link with the reported outcomes. Focusing on the transferrable qualities of interventions and building on intersectional analyses of power organisation,91,110 we suggested an action framework for equitable general practice. The suggested framework identifies five key qualities of equitable general practice as being connected, intersectional, flexible, inclusive and community-centred. These qualities should inform interventions and action across four domains. In the structural domain the areas of action include funding, premises, workforce distributions and patient life conditions. In the cultural domain, relevant areas involve patient and healthcare staff beliefs and organisational culture, biases among healthcare staff, communication and training material, translation services and inclusive language. In the disciplinary domain (organisational practices) areas of action involve working hours and contact time, financial incentives and quality assessment, patient registers and data use, and multidisciplinary care. Finally, in the interpersonal domain, areas of action cover the quality of clinical encounter, the interaction between practice administration staff and patients, as well as the relationship between practices and the broader communities they serve.
In the following sections, we provide a discussion on the interpretation of the findings in relation to existing literature, and we discuss the strengths and limitations of our study as well as the implications of our findings for research, practice and policy.
Interpretation of findings
Our review revealed that inequalities in general practice are studied more often in terms of clinical outcomes like levels of cholesterol, blood pressure and haemoglobin A1c and service uptake, including mostly the utilisation of screening and other preventive services. Fewer studies focus on inequalities in quality of care including the effectiveness of quality assessment tools like the QOF, practitioner behaviour (e.g. following guidelines) and patient satisfaction. Even fewer studies focus on behavioural outcomes involving adherence to treatment and medication, self-management, smoking, eating habits and physical activity. There were no studies focusing on inequalities in recovery from disease, life expectancy or mortality, which reveals an important gap since all the studied conditions are among the leading causes of death and drivers of inequality in early death. 222 Diabetes was the condition studied most often, followed by cancer and CVD. None of the included studies focused exclusively on patients with COPD, which is quite alarming given that poverty is a known risk factor for COPD. 223 Finally, in terms of dimensions of inequality, we noticed that disadvantaged groups in the included studies combined a multitude of categories associated with socio-economic marginalisation. These most often involved deprivation or other proxies of low socio-economic status, having an ethnic minority heritage, which was often conflated with race and/or migration, being a woman, and living in geographically remote or socio-economically deprived areas. Despite the differences that these categories imply within disadvantaged groups,72 they are rarely considered or explored in the included studies. Moreover, other dimensions associated with marginalisation and stigma like mental illness, HIV stigma, sexual orientation or homelessness fall outside the focus of the included studies.
Our findings revealed that inequalities in general practice emerge through multiple interconnected processes. To account for this complexity while identifying specific focus areas in care and interventions which link with inequalities, we organised our findings across different domains of power organisation. 110 We found that in the structural domain, which involves social structures, policy and institutions, the implementation of nationally directed financial incentives to improve quality of care increases the motivation to provide better care among practitioners. 112–115 This leads to more standardised care, which in turn decreases inequalities between practices at the initial stages of implementation,114,115 without coherent evidence regarding the sustainability of the decrease across time. 29,116–118 However, incentivising secondary over primary prevention links to the disproportionate focus on secondary prevention for those already engaged with general practice. This results in fewer primary prevention activities for disadvantaged patients. 29,115,117,119–123
Further, increasing funding for general practices especially in socio-economically disadvantaged areas may enable staff increase where appropriate and improvement in the capacity of general practices overall. This links to a series of positive outcomes, including the identification of disadvantaged patients at risk, and patient satisfaction as well as clinical outcomes. 125–132 Moreover, inequalities in SDH, including remote location of services and limited transport options, increase inconvenience and inequalities in accessing screening and other services. 129,133–140 This is especially the case for disadvantaged ethnic minority women, who also tend to be dependent on other members of their household for their mobility. 129,140 Additionally, inequalities in SDH reduce the effectiveness of educational interventions for disadvantaged groups who experience increased material barriers in participating and adhering to interventions. This eventually increases inequalities in the adoption of ‘healthy lifestyle’ and health outcomes. 129,137,138,141–147
In the cultural domain, which involves ideas, beliefs and knowledge(s), our findings showed that cultural understanding is a fundamental quality of care for the reduction of health inequalities. 135,138,139,142,147–155 Increased cultural understanding between healthcare providers and patients and tailoring of services that involves deep structural adaptation and positive framing increases the alignment of the offered services with patient worldviews and preferences. This in turn improves overall quality of care for ethnic minorities and disadvantaged patients through increased empowerment and engagement with care. 121,122,156–165 Additionally, our findings highlight that increasing knowledge among disadvantaged groups does not necessarily decrease inequalities. Designing interventions with a narrow focus on education and training often produces the opposite of the desired outcomes and increases inequalities in behaviour change and health improvement affecting disadvantaged groups. 135,141,151,168,172 This is because targeted disadvantaged groups often find such interventions not relatable and/or difficult to engage with. Finally, our findings show that when practitioners tend to take decisions based on heuristics or stereotypes, such as, for example, that men are more susceptible to CVD risk, they are likely to contribute to inequalities in effective diagnosis and clinical management due to implicit bias. 117,165,178–180 We saw that CVD risk factors were regularly less available in the files of women and risk assessment could be performed significantly less often for women seeing male physicians. 178
Our findings also highlight the importance of routines, bureaucracies and other standardised procedures within general practice in inequalities in unmet need, service uptake and care quality. These aspects of care, located in what we call the disciplinary domain, involve the use of the exception reporting in the frame of the QOF, which can motivate practitioners to exclude disadvantaged patients on the assumption that these patients are less likely to achieve targeted outcomes to maximise their local practice income. 29,119–122,125,169,184,185 Such ‘manipulations’ of exception reporting are difficult to capture; however, they are likely to increase inequalities within and between local practices in quality of care as well as unmet need. 29,187 We also found that when practices operate only during usual opening hours it can contribute to inequalities in access because they set access barriers for disadvantaged groups who are less likely to be able to take time off work. 134,200 The collection, maintenance and use of patient information is another aspect of care in this domain that is associated with inequalities. We found that accurate and up-to-date information of patient contact details increases the chances of contact with patients and this links to increased uptake of screening services among disadvantaged groups. 127,149,166,186,187 Moreover, the integration of ethnicity and socio-economic position in risk assessments improves the targeting of preventive services to disadvantaged groups through effective identification of patients at risk. 164,191–194
Increased contact time between healthcare professional and patient in terms of consultation and follow-up frequency can improve quality of care for disadvantaged patients through a series of mechanisms that involve improved communication, increased patient satisfaction and enablement. 128,165,201,202 This is especially true for those with communication and language difficulties and psychosocial problems, including neurodiverse patients. Similarly, long-lasting relationships between patients and practitioners can improve care effectiveness for disadvantaged groups because they enable a better understanding of patient needs and a safer environment for information-sharing. 143,204–207 These mechanisms lead to improved case-finding, more efficient use of services and improved quality of care and satisfaction among patients in under-served communities.
Finally, in terms of care organisation, our review revealed that when care involves multidisciplinary teams with staff from diverse backgrounds and expertise, it improves health professional retention and broadens the availability of patient support. This in turn leads to improved self-management of chronic conditions among geographically and/or socio-economically marginalised patients. 161,208–212 Related to this, supporting practice staff (including nurses and administrative staff) to engage with preventive activities targeted at disadvantaged groups can also decrease inequalities in prevention. 159,170,201,206,215 Support can take the form of training as a way to increase staff’s awareness that prevention is part of their duties and solve their misconceptions around their work and also around patients’ needs. 184–186
In the interpersonal domain, which involves individual experience and everyday interactions among people and communities, when disadvantaged groups perceive their doctor as empathetic and concerned with their overall issues, they achieve better outcomes. 150,170,202,216–218 Empathy creates space for effective communication and shared decision-making which lead to improved chronic-condition management. Similarly, trust between patient and doctor is a useful mechanism to increase uptake of preventive services among multiply disadvantaged groups. 136 For example, ethnic minority or 65+ women with low income are more likely to use screening services if they know that this is something that their doctor endorses. 220 Further, creating a familiar atmosphere in general practice and particularly in the spaces used for the delivery of interventions encourages disadvantaged groups to engage with the aims and the material of interventions and improves their health outcomes. 116,127,217 Finally, effective teamwork based on mutual trust and respect among professionals across roles and hierarchies is an additional key for the improvement of patient management. 161,208,208,209,212 This is especially true for local practices which deal with disadvantaged populations because it improves care coordination and information exchange among staff.
Our study highlights the multitude of different elements and aspects of care that link with inequalities in general practice and the interconnectedness of processes. It also makes clear that although action can be taken in specific areas and domains, to decrease inequalities we need coordinated and collective action across domains. However, coordinated and collective action within the highly diverse context of general practice is not a straightforward task. Our findings show that the context and the differences within disadvantaged groups as well as the small details of interventions can make a difference in terms of increasing or decreasing inequalities. This means that there is a need for standard high quality of care which nevertheless accounts for differences across contexts and targeted populations. Therefore, instead of suggesting specific interventions, it makes more sense to aim for common overarching principles for equitable care which will benefit everyone but even more so disadvantaged patients. 224
Equitable general practice has five key qualities. It is connected, intersectional, flexible, inclusive and community-centred. These qualities ensure the adoption of an integrative perspective with enough nuance to account for differences across people and contexts. Importantly, they are qualities of care that enable us to shift from understanding intervention effectiveness in binary terms between the individual and the population97 and rather focus more on the inherent connection between the two. Finally, they highlight that equality, inclusion and collective action are cornerstones for effective action and should be addressed at all levels and in every opportunity rather than being treated as a relevant yet distinct aspect of effective care.
Comparison with existing literature
Our findings reveal how broad the field of health inequalities is, the multitude of outcomes it involves as well as the diversity of groups affected. This once again underlines the need for a better collective understanding of the forms and the driving mechanisms of health inequalities and effective ways to tackle them. 70 In line with Attwood et al.,40 we found that although studied interventions record or even control for some of the PROGRESS-Plus criteria, only a very limited number of them report results by one or more criteria. However, our study highlights that beyond reporting results by different criteria, there is also need for research that accounts for the combination(s) of these criteria. Our study has clearly shown that disadvantage in terms of health services and outcomes emerges across the intersection of multiple aspects of social position beyond what we strictly understand as socio-economic. 72 Also, it has shown that gender is a crucial difference within disadvantaged groups, implying different forms of challenges for men and women but also different understandings of what is appropriate behaviour225 in the context of health promotion.
Our findings agree with the previous systematic review of the effectiveness of health service interventions aimed at reducing inequalities in health38 in terms of characteristics of successful interventions. We found that interdisciplinary teams improve health professional retention and increase the support for patients across a range of issues which lead to improvement in self-management and quality of care for disadvantaged patients with chronic conditions. 161,208–212 We further revealed that interdisciplinary teams need to be diverse in terms of expertise and background while working relationships between team members need to be based on mutual respect across professional roles and hierarchies. 159,170,201,206,215 Like Arblaster et al.,38 we also found that access to services, especially preventive, is linked with inequalities in service utilisation and the identification of patients at risk. Further, we revealed that access is affected through processes related to data collection and maintenance of patient records,127,149,164,186,187 invitation methods,134,154,189,190,197,199 convenience129,133–140 and working hours of services134,200 as well as with inequalities in SDH across socio-economic status and gender. 129,140 Finally, we found that community is a key principle in developing equitable general practice and thus it should cut across all the relevant interventions developed across domains from policies, dominant knowledge, bureaucracies and procedures to interpersonal interaction.
Moreover, our findings are partially in line with those of Terens et al.,41 which showed that quality-improvement strategies improve care for those older and/or less-educated and African Americans. Specifically, we found that the QOF decreased inequalities between socio-economic groups but only during the first three years of its implementation. 112–115 Further, we revealed that the QOF is likely to increase inequalities in primary prevention services due to the disproportionate number of quality-of-care financial incentives aimed at secondary prevention. 29,115,119–122 This is in line with Capewell and Graham,42 who showed that high-risk approaches to prevention increase inequality. We have shown that the implementation of the QOF and specifically the exception reporting can also increase inequalities in unmet need within and between practices. 29,119–122,125,169,184 Such findings have two serious implications. First, interventions aiming to improve quality of care or care outcomes can generate inequalities which are often undocumented. Second, IGIs25,26 can emerge due to intervention design (i.e. offering more incentives for secondary prevention) but also due to the intervention’s implementation in the every-day (i.e. manipulating the exclusion process of the QOF to maximise impact at the expense of disadvantaged patients). Finally, in contrast to previous findings which show that shared decision-making in primary and secondary care reduces socio-economic inequalities,43 our findings do not offer conclusions exclusively relevant to shared decision-making in general practice. In line with those findings, we have also found that engagement with intervention materials, patient enablement and empowerment, improved communication and shared decision-making are all mechanisms which lead to positive health outcomes for disadvantaged groups. 150,170,202,216–218
Strengths and limitations of the study
Strengths
The first strength of our study concerns the breadth of the studies included for data extraction. By reviewing studies with non-experimental designs we traced information related to the SDH,129,137,138,141–146 and aspects of care particularly important for disadvantaged groups. 201,206,207 Moreover, we explored the meaning of certain concepts, such as, for example, cultural understanding. 139 Also, we revealed the extent of existing gaps in the current evidence base especially in relation to driving mechanisms of health inequalities in general practice and the underpinning rationales of the studied interventions.
The study benefitted from the consistent involvement of researchers with a diverse background (i.e. clinical and non-clinical, public health, sociology), patient and public representatives with personal experience of health inequalities, as well as experts in the field through the expert panel and the deliberative workshop. By receiving feedback from different people and at different time points throughout the research process we managed to achieve a fine balance between research and academic rigour on the one hand, and relevance with everyday practice on the other. Therefore, we are confident that the conclusions of the study and the suggested principles of the framework are sufficiently robust and transferable.
Further, framing health inequalities in general practice in the context of power inequalities and organising our findings, and the suggested framework across the four domains of power organisation,110 is a unique strength of this study for multiple reasons. First, with this conceptualisation we shifted our focus from how individual GPs can reduce health inequalities. Instead, we focused on how general practice as a system can operate in order to challenge inequality-producing processes which affect the populations it aims to serve as well as its own people. We have effectively captured the complexity of the problem, while at the same time we have suggested specific areas of action and qualities that should inform care in the structural, cultural, disciplinary and interpersonal domain. Importantly, we have shown how structural mechanisms like funding and service distribution set the ‘rules’ for the operation of general practice, while these rules affect patients in different ways because of pre-existing inequalities in SDH. 29,119–122,125,169,184 This is an important acknowledgement in the current climate because it underlines that the answer to health inequalities requires political initiative and structural change. 226
Importantly, with our power-informed framework and realist methodology, we have highlighted that health inequalities often emerge or increase not because of the services and interventions available but because of the way these services and interventions are implemented. The CMOCs in the disciplinary domain demonstrate exactly how regulated procedures like patient data collection and maintenance, quality-assessment programmes, risk-assessment guidelines, working hours, invitation methods to preventive services all aim to improve care quality. However, the way they are implemented (e.g. manipulating exception reporting in the QOF, or not recording CVD risk factors because of misperceptions of patient risk, or invitations involving extensive written material) often creates ‘cracks’ through which disadvantaged patients fall. 29,119–122,125,127,149,164,169,184,186,187,194 This helps us understand better how interventions can potentially generate or increase inequalities either because of how their design does not account for pre-existing inequalities in SDH (e.g. working hours excluding disadvantaged groups who cannot take time off work), or because their implementation leaves space for discriminatory treatment against disadvantaged groups (e.g. the exception-reporting process in the QOF in some cases may lead to the exclusion of disadvantage patients from quality-standards assessments). These examples highlight that service/intervention design and implementation should always take place in the context of the targeted populations with the cultural, material and psychosocial realities it entails. Furthermore, our findings show how a multidisciplinary agency that overcomes hierarchical structures is required.
While the review highlights how organisational implementation of policies can increase inequalities, it also shows that organisation development is required to address inequalities through the proposed framework. Adapted organisational learning, a process by which organisations’ learning from their experiences leads to behaviour change,227 is important in addressing inequalities. General practice staff modifying organisational routines through feedback loops, partnership working and strategic planning are key. This organisational change is required not only within local general practices, but also across and between comparable contexts, such as PCNs, and requires the sharing of transferable learning and experiences. Our study and suggested framework encourage all those working in general practice to think of themselves as power actors within a system where everyone has a role to play in the reduction of health inequalities.
Limitations
Limitations of this study concern the fact that the reviewed evidence does not contain the detail needed for us to clearly understand how and the extent to which specific interventions increase or decrease inequalities. Rather, it focuses more on interventions and aspects of care that have a benefitting impact on disadvantaged groups in terms of health outcomes, service utilisation and care quality. Further, the evidence is silent on the underpinning rationales of interventions, the mechanisms through which they produced observed outcomes, and the differential ways that individuals are affected within and between disadvantaged groups.
To deal with the limitations imposed by the available information, we decided first to focus on aspects of care and interventions that are relevant with good quality and equitable care and to highlight the particular ways they link with inequality. Second, we formed CMOCs abstracted to a higher level, in order to compensate for the lack of in-depth and detailed information while producing a series of meaningful and also transferrable conclusions. Although specific criteria for transferrable learning were not used at the point of evidence review or data extraction, we are confident that our findings are transferrable based on the use of a realist approach. One of the key realist ontological assumptions is that mechanisms are inherent, widespread and context-sensitive causal processes. Hence, they may be operating even in – strictly speaking – different contexts (e.g. the USA and the UK) but with the same circumstances being present (e.g. offering general practice services to disadvantaged communities in circumstances of limited resources, increased workloads, language differences etc.).
In other words, whilst the information available did not enable us to produce highly specific explanations of how each individual intervention increased or decreased inequalities and to what extent, we were able to analyse and interpret these data to develop CMOCs that broadly explain the underpinning causal process that was common across individual interventions. Based on these broad explanations, we identified five qualities of equitable general practice and specific areas in which relevant action can and should be taken. The extent to which the suggested qualities can reduce inequalities in general practice is subject to the context in which they will be implemented and the particularities of the targeted populations. However, they are highly likely to contribute to the design and delivery of equitable care.
An additional limitation concerns the fact that the concept of intersectionality and power organised across four interrelated domains was not directly integrated in the inclusion and exclusion criteria of our review, which may have limited the reviewed evidence base. However, by including studies that focused on interventions targeted at disadvantaged groups which often experience multiple disadvantages (although this is not sufficiently addressed in the literature), we have captured the ways that people are differentially affected by interventions because of their intersectional social position, which can lead to sustained or widened inequalities. Further, by developing a broad IPT that included structural, cultural, organisational and individual elements of context, we have achieved a wide scope for our review.
Recommendations for future research
The vast majority of studies on general practice do not disaggregate findings by disadvantaged groups, meaning that the impact of interventions on inequalities remains unknown. Research in general practice should prioritise inequalities and apply a health-inequalities lens to all research and evaluation work. Studies on intervention evaluation need to disaggregate their data by dimensions of inequality more systematically. This implies a shift from reporting average scores across intervention groups and elaborating on the differential impact that interventions may have on the basis of differences across socio-economic status, gender, age, ethnicity and also sexuality and disability. Equally important is the systematisation of this evidence and the development of platforms which will allow us to access it easily and use it effectively. In this research a large volume of time was spent reviewing the full text of included studies to identify inequalities data. Electronic databases and journals should develop easier processes to identify inequalities evidence. Machine learning techniques could be useful for the development of such platforms.
Importantly, future research should focus on effective ways to integrate and operationalise intersectionality, moving beyond the simple interpretation of intersectionality as an interaction of disadvantage. We need more studies that account for the intersection of social categories (e.g. gender and race) and explore inequalities between and also within (disadvantaged) groups. This will reveal relationships of inequalities that are systematically ignored and will offer specific guidance for action targeted at groups who experience multiple vulnerabilities. 72 Research should focus more on the role of carers (paid or unpaid) in the effective delivery of interventions aiming to tackle inequalities as well as on health inequalities affecting carers themselves. A gender focus would be particularly useful in this kind of research as women are significantly more likely to undertake caregiving roles, often unpaid, and with a significant burden on their general health. 228
In terms of using the PROGRESS-Plus criteria as a way to capture disadvantaged groups, research needs to question more the selection and operationalisation of the criteria. Selecting criteria which are relevant to inequalities in specific contexts would require some exploratory preparatory work and engaging in dialogue with community members and experts. The same applies to the operationalisation of the criteria. In the UK, the Index of Multiple Deprivation is commonly used as a proxy for socio-economic status and studies on health inequalities often report their outcomes between the most and least deprived groups. Although this approach reflects some general patterns, it is likely that it masks the accurate range of health inequalities which would be revealed if individual measures of socio-economic status were used. From another perspective, binary or categorical operationalisations that do not account for nuances within groups need also to be abandoned. This concerns gender, since studies in the field are still using the binary operationalisation which only sees males/men and females/women and excludes trans* and non-binary persons, and also ethnicity, which tends to be operationalised with a few broad categories which include multiple different ethnic subgroups (e.g. South Asian, black, white).
Importantly, the evidence base needs to be expanded with detailed information about the transferable evidence-based principles behind specific interventions. Also, it should capture upstream drivers of inequalities in SDH which interfere with access to services and intervention effectiveness. This implies that experimental designs should not be regarded as the only way to achieve robust conclusions nor should they necessarily be prioritised over other designs when it comes to funding. Mixed-methods and qualitative studies employing interviews and focus groups, and also ethnographic and observational studies, and document analyses can offer rich and in-depth information in these areas. This means that studies with non-experimental designs should also be included in systematic reviews and evidence syntheses.
Additionally, research needs to focus more on COPD as it is closely associated with levels of deprivation and two-thirds of the affected people are not diagnosed. 229 This among other factors implies studies on inequalities in the diagnosis and management of COPD, especially across gender, ethnicity and occupational status (which are strongly associated with smoking) and their intersections, as well as on ways that general practice interventions can address inequalities in housing and exposure to air pollution. 230
There is also need for more research on effective types of GP organisation from a health-inequalities perspective. There are different models of ownership, management and leadership across local general practices in the country which seem to benefit continuity of care and access to services. 231 More research is needed to expand the evidence on relevant models and also to evaluate the extent to which the achieved improvements translate into a decrease in inequalities.
Research should also focus on the cultural domain. The NHS often takes pride in being one of the most diverse institutions in the country. However, there is increasing evidence suggesting that this diversity is not reflected in governance and leadership. 232 The latest alarming findings of the British Medical Association also suggest that there is a concerning level of racism in the medical profession affecting black, Asian and mixed-race doctors and medical students which stems from fellow doctors, other NHS staff and patients. 233 An earlier report by the NHS Race and Health Observatory234 revealed overwhelming evidence for consistent ethnic inequalities across a multitude of services as well. In our study, we found that lack of cultural understanding and implicit bias can increase health inequalities in general practice. Evidence as such highlights the need for more studies on the interconnection(s) between structural racism, healthcare worker and patient experiences of discrimination, and care outcomes in general practice. There is also a need for more regular and thorough assessment of equality and inclusion strategies and their impact on inequalities in health outcomes. Further, more studies need to explore effective ways to increase cultural understanding in general practice. This kind of research should start from exploring what cultural understanding involves across different contexts, how religion and faith interfere with cultural competence, and to what extent cultural differences affecting the quality and effectiveness of care might stem from differences not in terms of ethnicity but in terms of social class and sexuality. 235,236
Further, more research is needed to evaluate existing interventions from a health-inequalities perspective. Specifically, we need up-to-date evidence regarding the long-term effects of the QOF and its impact on inequalities in chronic conditions between and within practices. Quantitative analysis across time could also reveal potential changes in rates of exception reporting in QOF, while qualitative and ethnographic research could offer evidence on the way the exception-reporting process is implemented across general practices. Case studies should also explore successful examples of engaging patients with complex psychosocial needs in care and to what extent this might be associated with changes in exception reporting and quality target achievement. Finally, more research is needed on the development of effective tools for collecting, storing and integrating patient socio-demographic information in care.
Research topics
-
Organisational models of care in general practice effective in addressing inequalities.
-
Evaluation of the impact of existing policies on health inequalities, such as funding mechanisms and recruitment and retention interventions.
-
Shifting research from describing the problem of inequalities in general practice to identifying what works.
-
Interventions and policies which seek to make general practice more culturally competent.
-
Conditions and risk factors which are intrinsically linked with disadvantage, such as COPD and smoking.
Methodology research priorities
-
Disaggregate routine research and evaluation data in general practice by socio-economic status, gender, age and ethnicity, plus any other relevant aspects of disadvantage.
-
Use machine learning techniques to help leverage and navigate the existing health inequalities literature.
-
Adopt an intersectionality approach to understand how the interaction of multiple individual and community characteristics leads to disadvantage or privilege.
-
Develop and refine the PROGRESS-Plus criteria to capture more accurately the different aspects of disadvantage and their intersection.
-
Use qualitative and mixed-methods research designs to study the impact of the SDH on inequalities in general practice and the effectiveness of relevant interventions.
Implications for practice and policy
A major implication for practice and policy concerns exploring and developing ways in which the identified key qualities of equitable general practice can be integrated in the organisational development of future general practice. In this section we aim to integrate our framework into a series of specific suggestions for practice and policy to be considered by relevant stakeholders.
There are four main target audiences for our policy implications and practice recommendations:
-
National general practice policy-makers, such as NHS England.
-
Local and regional health systems, such as Integrated Care Systems or regional NHS England teams.
-
Workforce, training and education organisations, such as Health Education England and medical schools.
-
Individual local general practices.
While there is usually one target organisation for the policy implications or practice recommendations, there are often other organisations that are important system partners and we have sought to highlight these too.
Policy implication and practice recommendation 1
Target organisation: national general practice policy-makers
Other relevant organisations: individual local general practices, and local and regional health systems.
Create a positive vision: health inequalities in general practice emerge through complex processes and ways to tackle them require thorough long-term, multi-level action, rather than attempting to tackle complex problems with simple solutions. During our deliberative workshop, experts and public representatives suggested that policy-makers could start by articulating a positive vision of what equitable general practice looks like. This among other factors implies using conceptualisations of health inequalities which build on intersectionality and interrogate disadvantage across a series of context-specific dimensions beyond socio-economic status. We consider it important that reducing health inequalities remains high in the policy-makers’ agenda and solutions are planned based on a long-term perspective and the integration of different policy domains. This may include social policy for the mitigation of inequalities in SDH. It may also involve the engagement of front-line workers in general practice and disadvantaged groups in the development of health-inequality-related strategy in a consistent and meaningful manner. Public face-to-face and online forums at the local, regional and national level, the presence of delegations of workers and disadvantaged communities in high-level meetings, as well as clear, transparent and accessible channels of communication between people in the field and decision-makers are some of the ways that such involvement could be achieved.
Policy implication and practice recommendation 2
Target organisation: workforce, training and education organisations and individual local general practices
Other relevant organisations: national general practice policy-makers and local and regional health systems:
-
Make effective use of diversity: the reviewed evidence highlights the importance of diversity but also shows that it needs to be employed in ways that promote equity in care outcomes. Through discussions with experts and our PPI group we reached the conclusion that effective use of diversity implies fighting structural racism and sexism, as well as inclusion work for staff members and patients related to sexual orientation, religion, disability and caring responsibilities. Some effective measures to be considered in this direction include ensuring equality in career progression; closing the gender and ethnic gaps in senior management; cultivating an organisational culture that is less ethnocentric and Western-centric; including social sciences and humanities modules in medical training that will focus on the cultural aspects of health and care; increasing cultural competence at the practice level with the recruitment and progression of local clinical and non-clinical staff; active engagement with local and community social and cultural initiatives; increasing availability and accessibility of translation services; creating safe and inclusive care and work places within general practice with the use of appropriate language, visible markers (e.g. LGBTQI+ flags, reasonable adjustments) and information material; encouraging staff to engage with equality, diversity and inclusion networks and initiatives at their workplace by allocating an amount of their time or offering relevant incentives.
Policy implication and practice recommendation 3
Target organisation: workforce, training and education organisations
Other relevant organisations: local and regional health systems and individual local general practices:
-
Support the general practice workforce in disadvantaged areas: during the iterative discussions within the research team to refine our findings, it often became clear that to deliver equitable care, general practice staff in disadvantaged areas need to be supported with material and educational resources. Relevant stakeholders could consider workforce schemes to promote the recruitment and retention of staff in disadvantaged and remote areas, with people who, ideally, are representative of the local population. This could be achieved by providing financial or training incentives, especially to less experienced employees, and medical school placements. Further, developing a subspecialty related to providing care to disadvantaged patients with suitable incentives to encourage uptake (such as career development roles or financial incentives) could also increase the workforce ability to provide equity-focused care.
Policy implication and practice recommendation 4
Target organisation: national general practice policy-makers
Other relevant organisations: local and regional health systems:
-
Ensure a more equitable distribution of funding: as with workforce resources, funding also emerged as a key factor for achieving equitable general practice both through the reviewed evidence and during the deliberative workshop for the refinement of the study findings. People involved with general practice could all work together to identify ways in which funding across general practices will better account for differences in need of the served populations and the extra effort needed to achieve quality targets in practices in disadvantaged areas. This may involve the reconsideration of contractual reimbursement for provision of activity. Through discussions with experts, we concluded that more equitable funding distribution could be achieved by updating the Carr-Hill formula so that it integrates patient socio-economic status and ethnicity; higher patient list weights for practices operating in disadvantaged areas; updating the QOF so that it includes indicators related to achieving equity; offering primary prevention; achieving targets related to conditions intrinsically associated with disadvantage, such as COPD.
Policy implication and practice recommendation 5
Target organisation: individual local general practices
Other relevant organisations: national general practice policy-makers and local and regional health systems:
-
Tackle accessibility barriers: the findings highlight that general practice services need to be accessible in terms of location, and to develop processes which will enable patients to overcome transportation barriers. To achieve this, relevant stakeholders could consider co-locating practices with local services such as foodbanks or citizen advice offices, or locating them close to community landmarks such as schools, libraries, cultural or recreational centres and worship buildings. Similarly, contributing to the development of community transport options, providing targeted home visits and remote consultation options could help people deal with transportation barriers. The evidence also points to the importance of physical and psychological safety as an element to be seriously considered when such initiatives are taken. It also points to the importance of support for the use of technology when telemedicine options are adopted as a way to increase accessibility.
Policy implication and practice recommendation 6
Target organisation: individual local general practices
Other relevant organisations: national general practice policy-makers and local and regional health systems:
-
Invest in high-quality data: the evidence and our expert panels stressed that collecting and using high-quality data are paramount to recognising and acting against inequalities. We concluded that special attention could be paid to the collection and maintenance of patient data including health-related and socio-economic information. This could imply securing the necessary time before or during the consultation for data collection; making data collection and maintenance a specific part of the professional role of clinical and non-clinical staff; using IT resources for the development and maintenance of accurate and up-to-date patient registers; and investing in training on data-collection tools and data-sharing policies. Our public representatives stressed that acquiring high-quality data would also require increasing trust between general practices and communities for the exchange of sensitive information. Similarly, procedures related to risk-assessment tools and evaluation of programmes and interventions could integrate health-related and socio-economic information for the identification of disadvantaged patients at risk.
Policy implication and practice recommendation 7
Target organisation: individual local general practices
Other relevant organisations: national general practice policy-makers and local and regional health systems:
-
Increase continuity of care: reflecting on the study findings, experts highlighted that enhancing continuity between patient and healthcare professionals could also contribute to equitable general practice. This can involve providing incentives (e.g. financial, training, social) for staff to remain in their post and improving working conditions; focusing on continuity between micro-teams and patients instead of individual GPs and patients; involving GP teams in invitation to prevention services (e.g. Health Check or smear tests); encouraging regular staff meetings within practices during which staff can exchange information about vulnerable patients and agree on the care plan.
Policy implication and practice recommendation 8
Target organisation: national general practice policy-makers
Other relevant organisations: local and regional health systems and individual local general practices:
-
Balance autonomy with standardised care: the reviewed evidence showed that interventions like the QOF demonstrate that standardisation of care improves overall quality, however, when it comes to inequality there is a need for flexibility as well. Public representatives and social prescribers who participated in the deliberative workshop suggested that local general practices could have relative autonomy to decide how to do their work better in terms of reducing inequalities. Some of the suggested ways to achieve this included increasing the time that GPs have at their disposal for patient consultation; translation services specific to the needs of the served population; working hours that work better for the community; developing and delivering interventions in spaces that feel familiar and friendly to the target groups; making the most of the available budget and human resources to engage disadvantaged patients with care.
Equality, diversity and inclusion
We tried to ensure that our study would include the voices of those who are often marginalised within the healthcare system and are affected by health inequalities in general practice. For this, we have worked consistently with a PPI group consisting of three women who have experience in patient advocacy and are themselves affected by social disadvantage that cuts across gender, ethnic minority status, age, religion, neurodiversity, socio-economic position and being a carer. Their input has been very valuable during the whole project but especially during the stages of development of the IPT, findings refinement, and the development of the framework for equitable general practice. They particularly helped us to highlight important gaps in the reviewed literature, refine the CMOCs, and link our findings to specific aspects of care in general practice. Moreover, in our deliberative workshop we had additional members of the public combining intersectional disadvantage across gender, disability, sexual orientation and socio-economic status. Their voice has helped us not only refine our findings but also acknowledge the strengths and limitations of our study. Further, in our expert panel we included individuals who work in charity organisations for homeless people and in patient advocacy.
Our research team includes people with different characteristics, and it is relatively diverse in terms of the ethnicity, language and cultural background of its members. Men and women are balanced although people identifying as non-binary or trans persons are underrepresented. The team is inclusive of sexual diversity, while a few of our members have experiences of migration and/or are members or allies of disadvantaged communities. In terms of geographical representation, although the study and meetings were mainly conducted in Cambridge, our team also includes members (SS and CB) based in Newcastle who have a long experience in research, clinical work and public health policy on health inequalities in north-east England and the north-south health divide. Their input on the interconnectedness of processes in general practice, the impact of social determinants on intervention effectiveness, and the translation of our findings into policy and practice has been particularly valuable. Also, GW works academically and clinically in London and broader south-east England. Apart from providing guidance in terms of realist methodology he significantly contributed to contextualising the findings in the setting of general practice in the UK. In terms of expertise, our team also combines people with clinical experience, public health researchers, as well as interdisciplinary social scientists working at the interface of public health, social policy, geography, sociology, epidemiology and behavioural sciences. There has been a good balance between junior and senior members of the team. AG as the most junior member has been offered opportunities to engage with general practice in south-east and north-east England and health inequalities work previously undertaken by Public Health England. She has also been supported to expand her network with international public health and health service researchers and clinicians.
Chapter 5 Conclusions
Inequalities in general practice are the outcome of complex processes and power imbalances across four different domains that include structures, ideas, regulations and bureaucracies, and relationships among individuals and communities. More research is needed to unravel the impact of interventions on inequalities across these domains. However, to reduce inequalities and achieve equitable care, there is a need to understand general practice as a system in which everyone involved has a role to play in resisting inequality-producing mechanisms. In this context, services and interventions in general practice should be designed and delivered with the vision to be connected, intersectional, flexible, inclusive and community-centred.
Additional information
Acknowledgements
This study was conducted with the support from the National Institute for Health and Care Research (NIHR) Health Services and Delivery Research Programme, award number NIHR130694. We are especially grateful to Annie Moseley, Rebecca Harmston and Sukaina Manji for their support as patient and public representatives and consistent contribution during the study. We would like to thank Fiona Head for her contribution to the study design and her comments on this report, Rachel Talbot for her assistance in literature screening and data extraction, Joao Rocha for his contribution to our research team meetings, and all the experts who participated in our expert panel and shared their input on the initial programme theory and the interpretation of the findings. Also, we would like to thank all the participants in the deliberative workshop for a fruitful discussion that helped us refine our findings.
Contributions of authors
Anna Gkiouleka (https://orcid.org/0000-0003-3543-4418) (Research Associate, Health Inequalities) carried out the review, contributed to the interpretation of the results and prepared the results for publication, led PPI activity, co-organised and co-facilitated research expert panel meetings and the deliberative workshop, and is the leading author of the current report.
Geoff Wong (https://orcid.org/0000-0002-5384-4157) (Associate Professor, Primary Care) is co-principal investigator, contributed to the study design, provided methodological guidance in realist approach, overviewed the research process, co-organised and co-facilitated research expert panel meetings and the deliberative workshop, contributed to and edited this report.
Sarah Sowden (https://orcid.org/0000-0001-9359-3463) (Clinical Lecturer and Hon Consultant, Public Health), contributed to the study design, initial programme theory, interpretation of results and editing this report.
Isla Kuhn (https://orcid.org/0000-0002-2879-4020) (Head of Medical Library Services, Librarianship), contributed to the study design, initial programme theory, interpretation of results, conducted the literature searches and edited this report.
Annie Moseley (https://orcid.org/0000-0001-9990-1834) (Patient and Public Involvement Representative), contributed to the study design, initial programme theory, interpretation of the results, deliberative workshop and editing this report.
Sukaina Manji (https://orcid.org/0000-0003-0086-811X) (Patient and Public Involvement Representative), contributed to the study design, initial programme theory, interpretation of the results and editing this report.
Rebecca R Harmston (https://orcid.org/0000-0002-4765-367X) (Patient and Public Involvement Representative), contributed to the study design, initial programme theory, interpretation of the results and editing this report.
Rikke Siersbaek (https://orcid.org/0000-0003-3223-1420) (Post-doc Researcher, Inclusion Health) contributed to the study design, programme theory, interpretation of the results and editing this report.
Clare Bambra (https://orcid.org/0000-0002-1294-6851) (Professor, Public Health) contributed to the study design and editing this report.
John A Ford (https://orcid.org/0000-0001-8033-7081) (Clinical Lecturer, Public Health) conceived the idea and drafted the initial funding application, is co-principal investigator, contributed to the study design and review process, co-organised and co-facilitated research expert panel meetings and the deliberative workshop, contributed to and edited this report; he is the guarantor.
Data-sharing statement
All requests for data should be sent to the corresponding author. Access to available anonymised data may be granted following review.
Ethics statement
No ethical approval is required for this study because it only uses secondary data.
Information governance statement
This study did not handle any personal information.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HSDR programme or the Department of Health and Social Care.
Publication
Ford JA, Gkiouleka A, Kuhn I, Sowden S, Head F, Siersbaek R, et al. Reducing health inequalities through general practice: protocol for a realist review (EQUALISE). BMJ Open 2021;11(6):e052746.
Disclaimers
This manuscript presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Bambra C, Lynch J, Smith KE. The Unequal Pandemic: COVID-19 and Health Inequalities. Bristol: Policy Press; 2021.
- Anderson M, Pitchforth E, Asaria M, Brayne C, Casadei B, Charlesworth A, et al. LSE-Lancet Commission on the future of the NHS: re-laying the foundations for an equitable and efficient health and care service after COVID-19. Lancet 2021;397:1915-78. https://doi.org/10.1016/S0140-6736(21)00232-4.
- Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 2020;74:964-8. https://doi.org/10.1136/jech-2020-214401.
- Local Government Association . Health Inequalities: Deprivation and Poverty and COVID-19 2021. www.local.gov.uk/health-inequalities-deprivation-and-poverty-and-covid-19 (accessed 16 December 2022).
- NHS England . Action Required to Tackle Health Inequalities in Latest Phase of COVID-19 Response and Recovery 2020. www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/what-are-healthcare-inequalities/action-required-to-tackle-health-inequalities-in-latest-phase-of-covid-19-response-and-recovery/ (accessed 16 December 2022).
- Black SD. Inequalities in Health: The Black Report 1982.
- Acheson D. Independent Inquiry into Health Inequalities: The Acheson Report 1998.
- The Marmot Review . Fair Society, Healthy Lives - Executive Summary. Fair Society, Healthy Lives 2010;32. www.instituteofhealthequity.org/projects/fair-society-healthy-lives-the-marmot-review (accessed 16 December 2022).
- Marmot M. Health equity in England: the Marmot review 10 years on. BMJ 2020;368. https://doi.org/10.1136/bmj.m693.
- McKeown R. The First Comprehensive Map of Young People’s Health Inequalities in the UK. London: The Health Foundation; 2022.
- Raleigh V. What is Happening to Life Expectancy in England. The King’s Fund; 2021.
- Bennett JE, Pearson-Stuttard J, Kontis V, Capewell S, Wolfe I, Ezzati M. Contributions of diseases and injuries to widening life expectancy inequalities in England from 2001 to 2016: a population-based analysis of vital registration data. Lancet Publ Health 2018;3:e586-97.
- Dugravot A, Fayosse A, Dumurgier J, Bouillon K, Rayana TB, Schnitzler A, et al. Social inequalities in multimorbidity, frailty, disability, and transitions to mortality: a 24-year follow-up of the Whitehall II cohort study. Lancet Publ Health 2020;5:e42-50.
- Waterall J. Health Matters: Preventing Cardiovascular Disease. London: Public Health Matters, Public Health England; 2019.
- National Cancer Intelligence Network . Cancer by Deprivation in England: Incidence, 1996–2010 and Mortality, 1997–2011 2014.
- Dahlgren G, Whitehead M. The Dahlgren-Whitehead model of health determinants: 30 years on and still chasing rainbows. Publ Health 2021;199:20-4. https://doi.org/10.1016/j.puhe.2021.08.009.
- Starfield B. Primary care: an increasingly important contributor to effectiveness, equity, and efficiency of health services. SESPAS report 2012. Gac Sanit 2012;26:20-6. https://doi.org/10.1016/j.gaceta.2011.10.009.
- Maguire D, Buck D. Inequalities in Life Expectancy-Changes over Time and Implications for Policy. London: The King’s Fund; 2015.
- Exworthy M, Morcillo V. Primary care doctors’ understandings of and strategies to tackle health inequalities: a qualitative study. Prim Health Care Res Dev 2019;20. https://doi.org/10.1017/S146342361800052X.
- Allen M, Allen J, Hogarth S, Marmot M. Working for Health Equity: The Role of Health Professionals. London: UCL Institute of Health Equity; 2013.
- Lee S, Shafe AC, Cowie MR. UK stroke incidence, mortality and cardiovascular risk management 1999–2008: time-trend analysis from the General Practice Research Database. BMJ Open 2011;1.
- Hippisley-Cox J, Pringle M. Prevalence, care, and outcomes for patients with diet-controlled diabetes in general practice: cross sectional survey. Lancet 2004;364:423-8.
- Steel N, Ford JA, Newton JN, Davis ACJ, Vos T, Naghavi M, et al. Changes in health in the countries of the UK and 150 English Local Authority areas 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018;392:1647-61. https://doi.org/10.1016/S0140-6736(18)32207-4.
- Barr B, Bambra C, Whitehead M. The impact of NHS resource allocation policy on health inequalities in England 2001-11: longitudinal ecological study. BMJ 2014;348.
- White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations?. Soc Ineq Publ Health 2009;65:65-81. https://doi.org/10.1332/policypress/9781847423207.001.0001.
- McGill R, Anwar E, Orton L, Bromley H, Lloyd-Williams F, O’Flaherty M, et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Publ Health 2015;15. https://doi.org/10.1186/s12889-015-1781-7.
- Hart JT. The inverse care law. Lancet 1971;297:405-12.
- Mercer SW, Guthrie B, Furler J, Watt GC, Hart JT. Multimorbidity and the inverse care law in primary care. Br Med J 2012;344.
- McLean G, Sutton M, Guthrie B. Deprivation and quality of primary care services: evidence for persistence of the inverse care law from the UK Quality and Outcomes Framework. J Epidemiol Commun Health 2006;60:917-22. https://doi.org/10.1136/jech.2005.044628.
- Fisher R, Allen L, Malhotra AM, Alderwick H. Tackling the Inverse Care Law: Analysis of Policies to Improve General Practice in Deprived Areas Since 1990. London: The Health Foundation; 2022.
- Nussbaum C, Massou E, Fisher R, Morciano M, Harmer R, Ford J. Inequalities in the distribution of the general practice workforce in England: a practice-level longitudinal analysis. BJGP Open 2021;5. https://doi.org/10.3399/BJGPO.2021.0066.
- Saunders CL, Flynn S, Massou E, Lyratzopoulos G, Abel G, Burt J. Sociodemographic inequalities in patients’ experiences of primary care: an analysis of the General Practice Patient Survey in England between 2011 and 2017. J Health Serv Res Policy 2021;26:198-207. https://doi.org/10.1177/1355819620986814.
- Wu AS, Dodhia H, Whitney D, Ashworth M. Is the rule of halves still relevant today? A cross-sectional analysis of hypertension detection, treatment and control in an urban community. J Hypertens 2019;37:2470-80.
- Curtis HJ, Walker AJ, MacKenna B, Croker R, Goldacre B. Prescription of suboptimal statin treatment regimens: a retrospective cohort study of trends and variation in English primary care. Br J Gen Pract 2020;70:e525-33. https://doi.org/10.3399/bjgp20X710873.
- Todd A, Copeland A, Husband A, Kasim A, Bambra C. Access all areas? An area-level analysis of accessibility to general practice and community pharmacy services in England by urbanity and social deprivation. BMJ Open 2015;5.
- Ashworth M, L’Esperance V, Round T. Primary care funding entrenches health inequalities: time for a rethink. Br J Gen Pract 2021;71:102-4. https://doi.org/10.3399/bjgp21X714965.
- Fisher R, Dunn P, Asaria M, Thorlby R. Level or Not? Comparing General Practice in Areas of High and Low Socioeconomic Deprivation in England. London: The Health Foundation; 2020.
- Arblaster L, Lambert M, Entwistle V, Forster M, Fullerton D, Sheldon T, et al. A systematic review of the effectiveness of health service interventions aimed at reducing inequalities in health. J Health Serv Res Policy 1996;1:93-103. https://doi.org/10.1177/135581969600100207.
- O’Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol 2014;67:56-64. https://doi.org/10.1016/j.jclinepi.2013.08.005.
- Attwood S, van Sluijs E, Sutton S. Exploring equity in primary-care-based physical activity interventions using PROGRESS-Plus: a systematic review and evidence synthesis. Int J Behav Nutr Phys Act 2016;13. https://doi.org/10.1186/s12966-016-0384-8.
- Terens N, Vecchi S, Bargagli AM, Agabiti N, Mitrova Z, Amato L, et al. Quality improvement strategies at primary care level to reduce inequalities in diabetes care: an equity-oriented systematic review. BMC Endocr Disord 2018;18. https://doi.org/10.1186/s12902-018-0260-4.
- Capewell S, Graham H. Will cardiovascular disease prevention widen health inequalities?. PLOS Med 2010;7. https://doi.org/10.1371/journal.pmed.1000320.
- Durand M-A, Carpenter L, Dolan H, Bravo P, Mann M, Bunn F, et al. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLOS ONE 2014;9.
- Beech J, Baird B. GP Funding and Contracts Explained. London: The King’s Fund; 2020.
- NHS England . Primary Care Commissioning n.d. www.england.nhs.uk/contact-us/privacy-notice/how-we-use-your-information/our-services/primary-care-commissioning/ (accessed 16 December 2022).
- Monitor . Improving GP Services: Commissioners and Patient Choice 2015.
- NHS England . Primary Care Networks n.d. www.england.nhs.uk/primary-care/primary-care-networks/ (accessed 16 December 2022).
- NHS England . Expanding Our Workforce n.d. www.england.nhs.uk/gp/expanding-our-workforce/ (accessed 16 December 2022).
- Mathew R. Is partnership what the next generation of GPs want?. BMJ Opin 2019. https://blogs.bmj.com/bmj/2019/01/21/rammya-mathew-is-partnership-what-the-next-generation-of-gps-want/ (accessed 16 December 2022).
- Orton P, Orton C, Pereira Gray D. Depersonalised doctors: a cross-sectional study of 564 doctors, 760 consultations and 1876 patient reports in UK general practice. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2011-000274.
- Thompson M, Walter F. Increases in general practice workload in England. Lancet 2016;387:2270-2.
- Hobbs FR, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–14. Lancet 2016;387:2323-30.
- Levene LS, Baker R, Bankart J, Walker N, Wilson A. Socioeconomic deprivation scores as predictors of variations in NHS practice payments: a longitudinal study of English general practices 2013–2017. Br J Gen Pract 2019;69:e546-54. https://doi.org/10.3399/bjgp19X704549.
- Jameel F. The primary care backlog is a ticking time bomb. BMJ 2022;376. https://doi.org/10.1136/bmj.o294.
- Reed S, Schlepper L, Edwards N. Health System Recovery from COVID-19 International Lessons for the NHS. London: Nuffield Trust; 2022.
- British Medical Association . Pressures in General Practice Data Analysis 2022.
- NHS . Patients Registered at a GP Practice – May 2022: Totals (GP Practice-All Persons) 2022.
- Mroz G, Papoutsi C, Greenhalgh T. UK newspapers ‘on the warpath’: media analysis of general practice remote consulting in 2021. Br J Gen Pract 2022;72:e907-15.
- Murphy M, Scott LJ, Salisbury C, Turner A, Scott A, Denholm R, et al. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract 2021;71:e166-77.
- Jefferson L, Holmes M. GP workforce crisis: what can we do now?. Br J Gen Pract 2022;72:206-7. https://doi.org/10.3399/bjgp22X719225.
- NHS England . Important—for Action—Second Phase of NHS Response to COVID19 2020.
- Parker R, Figures E, Paddison C, Matheson J, Blane D, Ford J. Inequalities in general practice remote consultations: a systematic review. BJGP Open 2021;5.
- Serafino P. Exploring the UK’s Digital Divide. London: Office for National Statistics; 2019.
- Norman C, Wildman JM, Sowden S. COVID-19 at the deep end: a qualitative interview study of primary care staff working in the most deprived areas of England during the COVID-19 pandemic. Int J Environ Res Publ Health 2021;18. https://doi.org/10.3390/ijerph18168689.
- Ashwell G, Blane D, Lunan C, Matheson J. General practice post-COVID-19: time to put equity at the heart of health systems?. Br J Gen Pract 2020;70. https://doi.org/10.3399/bjgp20X712001.
- Local Government Association . Lessons Learnt from Councils’ Response to Rough Sleeping During the Covid-19 Pandemic 2020.
- NHS . GP Teams Work Together With Members of Health Inequality Groups to Expand Their COVID-19 Vaccine Equity Project 2022.
- Finch D. The Cost-of-Living Crisis is a Health Emergency Too. London: The Health Foundation; 2022.
- Russell P. NHS ‘Sinking Ship’ Warning to Health Secretary Over GP Retention Crisis. London: Medscape; 2022.
- Olivera JN, Ford J, Sowden S, Bambra C. Conceptualisation of health inequalities by local healthcare systems: a document analysis. Health Soc Care Commun 2022;30:e3977-84. https://doi.org/10.1111/hsc.13791.
- Ford J, Sowden S, Olivera J, Bambra C, Gimson A, Aldridge R, et al. Transforming health systems to reduce health inequalities. Future Healthc J 2021;8:e204-9. https://doi.org/10.7861/fhj.2021-0018.
- Gkiouleka A, Huijts T, Beckfield J, Bambra C. Understanding the micro and macro politics of health: Inequalities, intersectionality and institutions: a research agenda. Soc Sci Med 2018;200:92-8. https://doi.org/10.1016/j.socscimed.2018.01.025.
- Raphael D. A discourse analysis of the social determinants of health. Crit Publ Health 2011;21:221-36.
- Babbel B, Mackenzie M, Hastings A, Watt G. How do general practitioners understand health inequalities and do their professional roles offer scope for mitigation? Constructions derived from the deep end of primary care. Crit Publ Health 2017;29:168-80. https://doi.org/10.1080/09581596.2017.1418499.
- Mackenzie M, Hastings A, Babbel B, Simpson S, Watt G. Tackling and mitigating health inequalities: policymakers and practitioners ‘talk and draw’ their theories. Soc Pol Admin 2017;51:151-70. https://doi.org/10.1111/spol.12154.
- Brassolotto J, Raphael D, Baldeo N. Epistemological barriers to addressing the social determinants of health among public health professionals in Ontario, Canada: a qualitative inquiry. Crit Publ Health 2014;24:321-36. https://doi.org/10.1080/09581596.2013.820256.
- Whitehead M. A typology of actions to tackle social inequalities in health. J Epidemiol Commun Health 2007;61:473-8. https://doi.org/10.1136/jech.2005.037242.
- Sowden S, Nezafat-Maldonado B, Wildman J, Cookson R, Thomson R, Lambert M, et al. Interventions to reduce inequalities in avoidable hospital admissions: explanatory framework and systematic review protocol. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-035429.
- Blane D, Bartley M, Smith GD. Disease aetiology and materialist explanations of socioeconomic mortality differentials. Eur J Publ Health 1997;7:385-91.
- Ford J. Director’s appointment should be used to reframe the debate around health inequalities. Health Serv J 2020. www.hsj.co.uk/leadership/directors-appointment-should-be-used-to-reframe-the-debate-around-health-inequalities/7028959.article (accessed 16 December 2022).
- Whitehead M, Popay J. Swimming upstream? Taking action on the social determinants of health inequalities. Soc Sci Med 2010;71:1234-6. https://doi.org/10.1016/j.socscimed.2010.07.004.
- Katikireddi SV, Higgins M, Smith KE, Williams G. Health inequalities: the need to move beyond bad behaviours. J Epidemiol Commun Health 2013;67:715-6. https://doi.org/10.1136/jech-2012-202064.
- Bambra C, Smith KE, Garthwaite K, Joyce KE, Hunter DJ. A labour of Sisyphus? Public policy and health inequalities research from the Black and Acheson Reports to the Marmot Review. J Epidemiol Commun Health 2011;65:399-406. https://doi.org/10.1136/jech.2010.111195.
- Raphael D. Social determinants of health: present status, unanswered questions, and future directions. Int J Health Serv 2006;36:651-77. https://doi.org/10.2190/3MW4-1EK3-DGRQ-2CRF.
- Beckfield J, Krieger N. Epi plus demos plus cracy: linking political systems and priorities to the magnitude of health inequities-evidence, gaps, and a research agenda. Epidemiol Rev 2009;31:152-77. https://doi.org/10.1093/epirev/mxp002.
- Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav 1995;35:80-94. https://doi.org/10.2307/2626958.
- Bambra C, Fox D, Scott-Samuel A. Towards a politics of health. Health Promot Int 2005;20:187-93. https://doi.org/10.1093/heapro/dah608.
- Crenshaw K. Mapping the margins: identity politics, intersectionality, and violence against women. Stanford Law Rev 1991;43:1241-99.
- Collective CR. The Combahee river collective statement. Home Girls: Black Fem Anthol 1983;1:264-74.
- Crenshaw K. Whose story is it, anyway? Feminist and antiracist appropriations of Anita Hill. Sex, Violence, Work and Reproduction 1992:826-44. www.jstor.org/stable/j.ctt14bs8md.61 (accessed 16 December 2022).
- Collins PH. Black Feminist Thought: Knowledge, Consciousness, and the Politics of Empowerment. London: Routledge; 2002.
- Yuval-Davis N. Situated intersectionality and social inequality. Rais Politiq 2015;58:91-100.
- Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med 2014;110:10-7.
- Collins P, Bilge S. Intersectionality. New York: John Wiley & Sons; 2016.
- Weber L, Parra-Medina D. Gender Perspectives on Health and Medicine: Key Themes. Amsterdam: Elsevier; 2003.
- Beckfield J, Olafsdottir S, Sosnaud B. Healthcare systems in comparative perspective: classification, convergence, institutions, inequalities, and five missed turns. Annu Rev Sociol 2013;39:127-46. https://doi.org/10.1146/annurev-soc-071312-145609.
- Rose GA, Khaw K-T, Marmot M. Rose’s Strategy of Preventive Medicine: The Complete Original Text. Oxford: Oxford University Press; 2008.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review: a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34. https://doi.org/10.1258/1355819054308530.
- Wong G. Doing Realist Research. London: SAGE; 2018.
- Wong G, Westhorp G, Greenhalgh J, Manzano A, Jagosh J, Greenhalgh T. Quality and reporting standards, resources, training materials and information for realist evaluation: the RAMESES II project. Health Serv Deliv Res 2017;5:1-108.
- Ford JA, Gkiouleka A, Kuhn I, Sowden S, Head F, Siersbaek R, et al. Reducing health inequalities through general practice: protocol for a realist review (EQUALISE). BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-052746.
- Greenhalgh T, Peacock R. Information in practice. Building 2005;19.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan – a web and mobile app for systematic reviews. Syst Rev 2016;5. https://doi.org/10.1186/s13643-016-0384-4.
- Ramalho A, Castro P, Goncalves-Pinho M, Teixeira J, Santos JV, Viana J, et al. Primary health care quality indicators: an umbrella review. PLOS ONE 2019;14. https://doi.org/10.1371/journal.pone.0220888.
- NVivo (Version 12). Warrington: QSR International; 2018.
- Wong G, Brennan N, Mattick K, Pearson M, Briscoe S, Papoutsi C. Interventions to improve antimicrobial prescribing of doctors in training: the IMPACT (IMProving Antimicrobial presCribing of doctors in Training) realist review. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2015-009059.
- Carrieri D, Pearson M, Mattick K, Papoutsi C, Briscoe S, Wong G, et al. Interventions to minimise doctors’ mental ill-health and its impacts on the workforce and patient care: the Care Under Pressure realist review. Health Serv Deliv Res 2020;8:1-132.
- Price T, Wong G, Brennan N, Withers L, Cleland J, Wanner A, et al. Remediation programmes for practising doctors to restore patient safety: the RESTORE realist review. Health Serv Deliv Res 2021;9.
- Collins PH. The Palgrave Handbook of Intersectionality in Public Policy. Cham: Springer; 2019.
- Collins PH, Bilge S. Intersectionality. London: John Wiley & Sons; 2020.
- Roland M. Linking physicians’ pay to the quality of care: a major experiment in the United Kingdom. N Engl J Med 2004;351:1448-54.
- Crawley D, Ng A, Mainous AG, Majeed A, Millett C. Impact of pay for performance on quality of chronic disease management by social class group in England. J R Soc Med 2009;102:103-7. https://doi.org/10.1258/jrsm.2009.080389.
- Fullwood C, Doran T, Reeves D. The effect of financial incentives on inequalities in the quality of primary care. J Epidemiol Community Health 2008;62.
- Laverty AA, Bottle A, Majeed A, Millett C. Blood pressure monitoring and control by cardiovascular disease status in UK primary care: 10 year retrospective cohort study 1998-2007. J Public Health 2011;33:302-9. https://doi.org/10.1093/pubmed/fdq078.
- Hamilton FL, Bottle A, Vamos EP, Curcin V, Ng A, Molokhia M, et al. Impact of a pay-for-performance incentive scheme on age, sex, and socioeconomic disparities in diabetes management in UK primary care. J Ambul Care Manage 2010;33:336-49. https://doi.org/10.1097/JAC.0b013e3181f68f1d.
- Hamilton FL, Laverty AA, Huckvale K, Car J, Majeed A, Millett C. Financial incentives and inequalities in smoking cessation interventions in primary care: before-and-after study. Nicotine Tob Res 2016;18:341-50. https://doi.org/10.1093/ntr/ntv107.
- Alshamsan R, Lee JT, Majeed A, Netuveli G, Millett C. Effect of a UK pay-for-performance program on ethnic disparities in diabetes outcomes: interrupted time series analysis. Ann Fam Med 2012;10:228-34. https://doi.org/10.1370/afm.1335.
- Calvert M, Shankar A, McManus RJ, Lester H, Freemantle N. Effect of the quality and outcomes framework on diabetes care in the United Kingdom: retrospective cohort study. BMJ 2009;338. https://doi.org/10.1136/bmj.b1870.
- Dalton AR, Alshamsan R, Majeed A, Millett C. Exclusion of patients from quality measurement of diabetes care in the UK pay-for-performance programme. Diabet Med 2011;28:525-31. https://doi.org/10.1111/j.1464-5491.2011.03251.x.
- McGovern MP, Williams DJ, Hannaford PC, Taylor MW, Lefevre KE, Boroujerdi MA, et al. Introduction of a new incentive and target-based contract for family physicians in the UK: good for older patients with diabetes but less good for women?. Diabet Med 2008;25:1083-9. https://doi.org/10.1111/j.1464-5491.2008.02544.x.
- Doran T, Fullwood C, Gravelle H, Reeves D, Kontopantelis E, Hiroeh U, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med 2006;355:375-84. https://doi.org/10.1056/NEJMsa055505.
- Cookson R, Propper C, Asaria M, Raine R. Socio-economic inequalities in health care in England. Fisc Stud 2016;37:371-403. https://doi.org/10.1111/j.1475-5890.2016.12109.
- Goddard M, Smith P. Equity of access to health care services: theory and evidence from the UK. Soc Sci Med 2001;53:1149-62.
- Doran T, Fullwood C, Kontopantelis E, Reeves D. Effect of financial incentives on inequalities in the delivery of primary clinical care in England: analysis of clinical activity indicators for the quality and outcomes framework. Lancet 2008;372:728-36. https://doi.org/10.1016/S0140-6736(08)61123-X.
- Atherton H, Dalton A, Fleming S, Hirst J, Nunan D, Selwood M, et al. Are there enough GPs in England to detect hypertension and maintain access?. Br J Gen Pract 2013;63:346-7.
- Baker D, Middleton E. Cervical screening and health inequality in England in the 1990s. J Epidemiol Commun Health 2003;57:417-23. https://doi.org/10.1136/jech.57.6.417.
- Mercer SW, Fitzpatrick B, Gourlay G, Vojt G, McConnachie A, Watt GCM. More time for complex consultations in a high-deprivation practice is associated with increased patient enablement. Br J Gen Pract 2007;57:960-6. https://doi.org/10.3399/096016407782604910.
- Mold F, While A, Forbes A. The management of type 2 diabetes care: the challenge within primary care. Pract Diab Int 2008;25:28-36.
- Modell M, Wonke B, Anionwu E, Khan M, Tai SS, Lloyd M, et al. A multidisciplinary approach for improving services in primary care: randomised controlled trial of screening for haemoglobin disorders. BMJ 1998;317:788-91. https://doi.org/10.1136/bmj.317.7161.788.
- Millett C, Car J, Eldred D, Khunti K, Mainous AG, Majeed A. Diabetes prevalence, process of care and outcomes in relation to practice size, caseload and deprivation: national cross-sectional study in primary care. J R Soc Med 2007;100:275-83. https://doi.org/10.1177/014107680710000613.
- Saxena S, Car J, Eldred D, Soljak M, Majeed A. Practice size, caseload, deprivation and quality of care of patients with coronary heart disease, hypertension and stroke in primary care: national cross-sectional study. BMC Health Serv Res 2007;7. https://doi.org/10.1186/1472-6963-7-96.
- McLean G, Guthrie B, Sutton M. Differences in the quality of primary medical care services by remoteness from urban settlements. Qual Saf Health Care 2007;16:446-9. https://doi.org/10.1136/qshc.2006.020875.
- Lantz P, Stencil D, Lippert M, Beversdorf S, Jaros L, Remington P. Erratum: breast and cervical cancer screening in a low-income managed care sample: the efficacy of physician letters and phone calls. Am J Public Health 1995;85:834-6.
- Stone M, Pound E, Pancholi A, Farooqi A, Khunti K. Empowering patients with diabetes: a qualitative primary care study focusing on South Asians in Leicester, UK. Fam Pract 2005;22:647-52. https://doi.org/10.1093/fampra/cmi069.
- Bell TS, Branston LK, Newcombe RG, Barton GR. Interventions to improve uptake of breast screening in inner city Cardiff general practices with ethnic minority lists. Ethn Health 1999;4:277-84.
- Mayer-Davis EJ, D’Antonio AM, Smith SM, Kirkner G, Levin Martin S, Parra-Medina D, et al. Pounds off with empowerment (POWER): a clinical trial of weight management strategies for black and white adults with diabetes who live in medically underserved rural communities. Am J Public Health 2004;94:1736-42. https://doi.org/10.2105/ajph.94.10.1736.
- Greenhalgh T, Helman C, Chowdhury AM. Health beliefs and folk models of diabetes in British Bangladeshis: a qualitative study. BMJ 1998;316:978-83. https://doi.org/10.1136/bmj.316.7136.978.
- Migneault JP, Dedier JJ, Wright JA, Heeren T, Campbell MK, Morisky DE, et al. A Culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African-Americans: a randomized controlled trial. Ann Behav Med 2012;43:62-73. https://doi.org/10.1007/s12160-011-9319-4.
- Hippisley-Cox J, Yates J, Pringle M, Coupland C, Hammersley V. Sex inequalities in access to care for patients with diabetes in primary care: questionnaire survey. Br J Gen Pract 2006;56:342-8.
- Vyas A, Haidery AZ, Wiles PG, Gill S, Roberts C, Cruickshank JK. A pilot randomized trial in primary care to investigate and improve knowledge, awareness and self-management among South Asians with diabetes in Manchester. Diabet Med 2003;20:1022-6. https://doi.org/10.1046/j.1464-5491.2003.01082.x.
- Martin PD, Rhode PC, Dutton GR, Redmann SM, Ryan DH, Brantley PJ. A primary care weight management intervention for low-income African-American women. Obesity 2006;14:1412-20. https://doi.org/10.1038/oby.2006.160.
- Thompson JR, Horton C, Flores C. Advancing diabetes self-management in the Mexican American population: a community health worker model in a primary care setting. Diabetes Educ 2007;33:159S-65. https://doi.org/10.1177/0145721707304077.
- Bennett GG, Foley P, Levine E, Whiteley J, Askew S, Steinberg DM, et al. Behavioral treatment for weight gain prevention among black women in primary care practice: a randomized clinical trial. JAMA Intern Med 2013;173:1770-7. https://doi.org/10.1001/jamainternmed.2013.9263.
- Robinson S, Baron RB, Cooper B, Janson S. Does health service use in a diabetes management program contribute to health disparities at a facility level? Optimizing resources with demographic predictors. Populat Health Manag 2009;12:139-47.
- Peek ME, Harmon SA, Scott SJ, Eder M, Roberson TS, Tang H, et al. Culturally tailoring patient education and communication skills training to empower African-Americans with diabetes. Transl Behav Med 2012;2:296-308. https://doi.org/10.1007/s13142-012-0125-8.
- Beune EJ, Moll van Charante EP, Beem L, Mohrs J, Agyemang CO, Ogedegbe G, et al. Culturally adapted hypertension education (CAHE) to improve blood pressure control and treatment adherence in patients of African origin with uncontrolled hypertension: cluster-randomized trial. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0090103.
- Philis-Tsimikas A, Fortmann A, Lleva-Ocana L, Walker C, Gallo LC. Peer-led diabetes education programs in high-risk Mexican Americans improve glycemic control compared with standard approaches: a Project Dulce promotora randomized trial. Diab Care 2011;34:1926-31. https://doi.org/10.2337/dc10-2081.
- Hoare T, Thomas C, Biggs A, Booth M, Bradley S, Friedman E. Can the uptake of breast screening by Asian women be increased? A randomized controlled trial of a linkworker intervention. J Pub Health 1994;16:179-85.
- Vincent D. Culturally tailored education to promote lifestyle change in Mexican Americans with type 2 diabetes. J Am Acad Nurse Pract 2009;21:520-7. https://doi.org/10.1111/j.1745-7599.2009.00439.x.
- Bhopal RS, Douglas A, Wallia S, Forbes JF, Lean MEJ, Gill JMR, et al. Effect of a lifestyle intervention on weight change in south Asian individuals in the UK at high risk of type 2 diabetes: a family-cluster randomised controlled trial. Lancet Diab Endocrinol 2014;2:218-27. https://doi.org/10.1016/S2213-8587(13)70204-3.
- Sriskantharajah J, Kai J. Promoting physical activity among South Asian women with coronary heart disease and diabetes: what might help?. Fam Pract 2007;24:71-6.
- Uitewaal PJM, Voorham AJJ, Bruijnzeels MA, Berghout A, Bernsen RMD, Trienekens PH, et al. No clear effect of diabetes education on glycaemic control for Turkish type 2 diabetes patients: a controlled experiment in general practice. Neth J Med 2005;63:428-34.
- Raine R, Moss SM, von Wagner C, Atkin W, Hans IK, Howe R, et al. A national cluster-randomised controlled trial to examine the effect of enhanced reminders on the socioeconomic gradient in uptake in bowel cancer screening. Br J Cancer 2016;115:1479-86. https://doi.org/10.1038/bjc.2016.365.
- Percac-Lima S, Ashburner JM, Bond B, Oo SA, Atlas SJ. Decreasing disparities in breast cancer screening in refugee women using culturally tailored patient navigation. J Gen Intern Med 2013;28:1463-8. https://doi.org/10.1007/s11606-013-2491-4.
- Weinstock RS, Teresi JA, Goland R, Izquierdo R, Palmas W, Eimicke JP, et al. IDEATel Consortium . Glycemic control and health disparities in older ethnically diverse underserved adults with diabetes: five-year results from the Informatics for Diabetes Education and Telemedicine (IDEATel) study. Diabet Care 2011;34:274-9. https://doi.org/10.2337/dc10-1346.
- Carter EL, Nunlee-Bland G, Callender C. A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspect Health Inf Manag 2011;8.
- Baradaran HR, Knill-Jones RP, Wallia S, Rodgers A. A controlled trial of the effectiveness of a diabetes education programme in a multi-ethnic community in Glasgow [ISRCTN28317455]. BMC Publ Health 2006;6. https://doi.org/10.1186/1471-2458-6-134.
- Atri J, Falshaw M, Gregg R, Robson J, Omar RZ, Dixon S. Improving uptake of breast screening in multiethnic populations: a randomised controlled trial using practice reception staff to contact non-attenders. BMJ 1997;315:1356-9. https://doi.org/10.1136/bmj.315.7119.1356.
- McElmurry BJ, McCreary LL, Park CG, Ramos L, Martinez E, Parikh R, et al. Implementation, outcomes, and lessons learned from a collaborative primary health care program to improve diabetes care among urban Latino populations. Health Promot Pract 2009;10:293-302. https://doi.org/10.1177/1524839907306406.
- Roots A, MacDonald M. Outcomes associated with nurse practitioners in collaborative practice with general practitioners in rural settings in Canada: a mixed methods study. Hum Resour Health 2014;12. https://doi.org/10.1186/1478-4491-12-69.
- Allen JK, Dennison-Himmelfarb CR, Szanton SL, Bone L, Hill MN, Levine DM, et al. Community Outreach and Cardiovascular Health (COACH) Trial: a randomized, controlled trial of nurse practitioner/community health worker cardiovascular disease risk reduction in urban community health centers. Circ Cardiovasc Qual Outcomes 2011;4:595-602. https://doi.org/10.1161/CIRCOUTCOMES.111.961573.
- O’Hare JP, Raymond NT, Mughal S, Dodd L, Hanif W, Ahmad Y, et al. UKADS Study Group . Evaluation of delivery of enhanced diabetes care to patients of South Asian ethnicity: the United Kingdom Asian Diabetes Study (UKADS). Diabet Med 2004;21:1357-65. https://doi.org/10.1111/j.1464-5491.2004.01373.x.
- Dalton AR, Bottle A, Okoro C, Majeed A, Millett C. Implementation of the NHS Health Checks programme: baseline assessment of risk factor recording in an urban culturally diverse setting. Fam Pract 2011;28:34-40. https://doi.org/10.1093/fampra/cmq068.
- Dalton AR, Bottle A, Okoro C, Majeed A, Millett C. Uptake of the NHS Health Checks programme in a deprived, culturally diverse setting: cross-sectional study. J Public Health 2011;33:422-9. https://doi.org/10.1093/pubmed/fdr034.
- Batterham RW, Hawkins M, Collins PA, Buchbinder R, Osborne RH. Health literacy: applying current concepts to improve health services and reduce health inequalities. Publ Health 2016;132:3-12. https://doi.org/10.1016/j.puhe.2016.01.001.
- Volandes AE, Paasche-Orlow MK. Health literacy, health inequality and a just healthcare system. Am J Bioeth 2007;7:5-10. https://doi.org/10.1080/15265160701638520.
- Valdez A, Napoles AM, Stewart SL, Garza A. A randomized controlled trial of a cevical cancer education intervention for Latinas delivered through interactive, multimedia kiosks. J Cancer Educ 2018;33:222-30. https://doi.org/10.1007/s13187-016-1102-6.
- Sigfrid LA, Turner C, Crook D, Ray S. Using the UK primary care Quality and Outcomes Framework to audit health care equity: preliminary data on diabetes management. J Publ Health 2006;28:221-5. https://doi.org/10.1093/pubmed/fdl028.
- Whittemore R, Melkus GD, Sullivan A, Grey M. A nurse-coaching intervention for women with type 2 diabetes. Diabetes Educ 2004;30:795-804. https://doi.org/10.1177/014572170403000515.
- De Lusignana S, Gallagher H, Jones S, Chan T, Van Vlymen J, Tahir A, et al. Audit-based education lowers systolic blood pressure in chronic kidney disease: the Quality Improvement in CKD (QICKD) trial results. Kidney Int 2013;84:1289-20.
- Bellary S, O’Hare JP, Raymond NT, Gumber A, Mughal S, Szczepura A, et al. UKADS Study Group . Effectiveness of enhanced diabetes care to patients of South Asian ethnicity: the United Kingdom Asian Diabetes Study (UKADS): a cluster randomised controlled trial. Lancet 2008;371:1769-76.
- Jandorf L, Braschi C, Ernstoff E, Wong CR, Thelemaque L, Winkel G, et al. Culturally targeted patient navigation for increasing African Americans’ adherence to screening colonoscopy: a randomized clinical trial – navigation to increase colon cancer screening for minorities. Cancer Epidemiol Biom Prev 2013;22:1577-87.
- McCann S, Weinman J. Empowering the patient in the consultation: a pilot study. Patient Educ Couns 1996;27:227-34. https://doi.org/10.1016/0738-3991(95)00830-6.
- McCleary-Jones V. Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus. ABNF Journal 2011;22:25-32.
- Bandura A. The explanatory and predictive scope of self-efficacy theory. J Soc Clin Psychol 1986;4:359-73. https://doi.org/10.1521/jscp.1986.4.3.359.
- Muggah E, Dahrouge S, Hogg W. Access to primary health care for immigrants: results of a patient survey conducted in 137 primary care practices in Ontario, Canada. BMC Fam Pract 2012;13. https://doi.org/10.1186/1471-2296-13-128.
- Delpech R, Ringa V, Falcoff H, Rigal L. Primary prevention of cardiovascular disease: more patient gender-based differences in risk evaluation among male general practitioners. Eur J Prev Cardiol 2016;23:1831-8. https://doi.org/10.1177/2047487316648476.
- Hippisley-Cox J, Coupland C. Identifying patients with suspected colorectal cancer in primary care: derivation and validation of an algorithm. Br J Gen Pract 2012;62:e29-37. https://doi.org/10.3399/bjgp12X616346.
- Hyun KK, Redfern J, Patel A, Peiris D, Brieger D, Sullivan D, et al. Gender inequalities in cardiovascular risk factor assessment and management in primary healthcare. Heart 2017;103:492-8. https://doi.org/10.1136/heartjnl-2016-310216.
- Hendriks SH, van Hateren KJ, Groenier KH, Houweling ST, Maas AH, Kleefstra N, et al. Sex differences in the quality of diabetes care in the Netherlands (ZODIAC-45). PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0145907.
- Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ 2006;332:73-8. https://doi.org/10.1136/bmj.38678.389583.7C.
- Lee WL, Cheung AM, Cape D, Zinman B. Impact of diabetes on coronary artery disease in women and men: a meta-analysis of prospective studies. Diabet Care 2000;23:962-8. https://doi.org/10.2337/diacare.23.7.962.
- Ashworth M, Armstrong D. The relationship between general practice characteristics and quality of care: a national survey of quality indicators used in the UK Quality and Outcomes Framework, 2004–5. BMC Fam Pract 2006;7:1-8.
- Kontopantelis E, Springate DA, Ashcroft DM, Valderas JM, van der Veer SN, Reeves D, et al. Associations between exemption and survival outcomes in the UK’s primary care pay-for-performance programme: a retrospective cohort study. BMJ Qual Saf 2016;25:657-70. https://doi.org/10.1136/bmjqs-2015-004602.
- Exeter D, Moss L, Zhao J, Kyle C, Riddell T, Jackson R, et al. The distribution and frequency of blood lipid testing by sociodemographic status among adults in Auckland, New Zealand. J Prim Health Care 2015;7:182-91.
- Bush K, Thomas R, Raymond NT, Sankar S, Barker PJ, O’Hare JP. Cluster randomised controlled trial evaluation of a link worker-delivered intervention to improve uptake of diabetic retinopathy screening in a South Asian population. Diab Vasc Dis Res 2014;11:294-7. https://doi.org/10.1177/1479164114532964.
- Millward K. Who uses NHS health checks? Investigating the impact of ethnicity and gender and method of invitation on uptake of NHS health checks. Int J Equity Health 2016;15.
- Kerrison RS, Shukla H, Cunningham D, Oyebode O, Friedman E. Text-message reminders increase uptake of routine breast screening appointments: a randomised controlled trial in a hard-to-reach population. Br J Cancer 2015;112:1005-10. https://doi.org/10.1038/bjc.2015.36.
- Hirst Y, Skrobanski H, Kerrison RS, Kobayashi LC, Counsell N, Djedovic N, et al. Text-message Reminders in Colorectal Cancer Screening (TRICCS): a randomised controlled trial. Br J Cancer 2017;116:1408-14. https://doi.org/10.1038/bjc.2017.117.
- Hardy S, Gray R. Is the use of an invitation letter effective in prompting patients with severe mental illness to attend a primary care physical health check?. Prim Health Care Res Develop 2012;13:347-52.
- Chin M, Cook S, Drum M, Jin L, Guillen M, Humikowski C, et al. Erratum: improving diabetes care in midwest community health centers with the Health Disparities Collaborative. Diabet Care 2004;27.
- Lang SJ, Abel GA, Mant J, Mullis R. Impact of socioeconomic deprivation on screening for cardiovascular disease risk in a primary prevention population: a cross-sectional study. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009984.
- Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:1475-82. https://doi.org/10.1136/bmj.39609.449676.25.
- Iyen-Omofoman B, Tata LJ, Baldwin DR, Smith CJP, Hubbard RB. Using socio-demographic and early clinical features in general practice to identify people with lung cancer earlier. Thorax 2013;68:451-9. https://doi.org/10.1136/thoraxjnl-2012-202348.
- Millett C, Netuveli G, Saxena S, Majeed A. Impact of pay for performance on ethnic disparities in intermediate outcomes for diabetes: a longitudinal study. Diabet Care 2009;32:404-9. https://doi.org/10.2337/dc08-0912.
- Wardle J, von Wagner C, Kralj-Hans I, Halloran SP, Smith SG, McGregor LM, et al. Effects of evidence-based strategies to reduce the socioeconomic gradient of uptake in the English NHS Bowel Cancer Screening Programme (ASCEND): four cluster-randomised controlled trials. Lancet 2016;387:751-9. https://doi.org/10.1016/S0140-6736(15)01154-X.
- Siddiqui AA, Sifri R, Hyslop T, Andrel J, Rosenthal M, Vernon SW, et al. Race and response to colon cancer screening interventions. Prev Med 2011;52:262-4. https://doi.org/10.1016/j.ypmed.2011.01.005.
- McDermott L, Wright AJ, Cornelius V, Burgess C, Forster AS, Ashworth M, et al. Enhanced invitation methods and uptake of health checks in primary care: randomised controlled trial and cohort study using electronic health records. Health Technol Assess 2016;20:1-92. https://doi.org/10.3310/hta20840.
- Warren FC, Calitri R, Fletcher E, Varley A, Holt TA, Lattimer V, et al. Exploring demographic and lifestyle associations with patient experience following telephone triage by a primary care doctor or nurse: secondary analyses from a cluster randomised controlled trial. BMJ Qual Saf 2015;24:572-82. https://doi.org/10.1136/bmjqs-2015-003937.
- Riley R, Coghill N, Montgomery A, Feder G, Horwood J. Experiences of patients and healthcare professionals of NHS cardiovascular health checks: a qualitative study. J Publ Health 2016;38:543-51. https://doi.org/10.1093/pubmed/fdv121.
- Mead N, Bower P, Roland K. Factors associated with enablement in general practice: cross-sectional study using routinely-collected data. Br J Gen Pract 2008;58:346-52. https://doi.org/10.3399/bjgp08X280218.
- Nielsen AB, de Fine Olivarius N, Gannik D, Hindsberger C, Hollnagel H. Structured personal diabetes care in primary health care affects only women’s HbA1c. Diabet Care 2006;29:963-9. https://doi.org/10.2337/diacare.295963.
- Green T, Atkin K, Macleod U. Cancer detection in primary care: insights from general practitioners. Br J Cancer 2015;112:S41-9. https://doi.org/10.1038/bjc.2015.41.
- Hong JS, Kang HC, Kim J. Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea. J Korean Med Sci 2010;25:1259-71. https://doi.org/10.3346/jkms.2010.25.9.1259.
- Ismail H, Kelly S. Lessons learned from England’s Health Checks Programme: using qualitative research to identify and share best practice. BMC Fam Pract 2015;16. https://doi.org/10.1186/s12875-015-0365-z.
- Shen MJ, Binz-Scharf M, D’Agostino T, Blakeney N, Weiss E, Michaels M, et al. A mixed-methods examination of communication between oncologists and primary care providers among primary care physicians in underserved communities. Cancer 2015;121:908-15. https://doi.org/10.1002/cncr.29131.
- Majumdar SR, Guirguis LM, Toth EL, Lewanczuk RZ, Lee TK, Johnson JA. Controlled trial of a multifaceted intervention for improving quality of care for rural patients with type 2 diabetes. Diabet Care 2003;26:3061-6. https://doi.org/10.2337/diacare.26.11.3061.
- Everett CM, Thorpe CT, Palta M, Carayon P, Gilchrist VJ, Smith MA. Division of primary care services between physicians, physician assistants, and nurse practitioners for older patients with diabetes. Med Care Res Rev 2013;70:531-41. https://doi.org/10.1177/1077558713495453.
- Bray P, Cummings DM, Morrissey S, Thompson D, Holbert D, Wilson K, et al. Improved outcomes in diabetes care for rural African Americans. Ann Fam Med 2013;11:145-50. https://doi.org/10.1370/afm.1470.
- Fann JR, Fan MY, Unutzer J. Improving primary care for older adults with cancer and depression. J Gen Intern Med 2009;24:S417-24. https://doi.org/10.1007/s11606-009-0999-4.
- Hutchison RW. Treating diabetes in underserved populations using an interprofessional care team. J Interprof Care 2014;28:568-9. https://doi.org/10.3109/13561820.2014.917408.
- Allen JK, Dennison Himmelfarb CR, Szanton SL, Frick KD. Cost-effectiveness of nurse practitioner/community health worker care to reduce cardiovascular health disparities. J Cardiovasc Nurs 2014;29:308-14. https://doi.org/10.1097/JCN.0b013e3182945243.
- Sellors J, Kaczorowski J, Sellors C, Dolovich L, Woodward C, Willan A, et al. A randomized controlled trial of a pharmacist consultation program for family physicians and their elderly patients. Can Med Assoc J 2003;169:17-22.
- Hardy S, Hinks P, Gray R. Does training practice nurses to carry out physical health checks for people with severe mental illness increase the level of screening for cardiovascular risk?. Int J Soc Psychiatry 2014;60:236-42.
- Mercer SW, Jani BD, Maxwell M, Wong SY, Watt GC. Patient enablement requires physician empathy: a cross-sectional study of general practice consultations in areas of high and low socioeconomic deprivation in Scotland. BMC Fam Pract 2012;13. https://doi.org/10.1186/1471-2296-13-6.
- Thompson C, Meeuwisse I, Dahlke R, Drummond N. Group medical visits in primary care for patients with diabetes and low socioeconomic status: users’ perspectives and lessons for practitioners. Can J Diabetes 2014;38:198-204. https://doi.org/10.1016/j.jcjd.2014.03.012.
- Phelan EA, Balderson B, Levine M, Erro JH, Jordan L, Grothaus L, et al. Delivering effective primary care to older adults: a randomized, controlled trial of the senior resource team at group health cooperative. J Am Geriatr Soc 2007;55:1748-56. https://doi.org/10.1111/j.1532-5415.2007.01416.x.
- Hull S, Chowdhury TA, Mathur R, Robson J. Improving outcomes for patients with type 2 diabetes using general practice networks: a quality improvement project in east London. BMJ Qual Saf 2014;23:171-6. https://doi.org/10.1136/bmjqs-2013-002008.
- Michielutte R, Sharp PC, Foley KL, Cunningham LE, Spangler JG, Paskett ED, et al. Intervention to increase screening mammography among women 65 and older. Health Educ Res 2005;20:149-62. https://doi.org/10.1093/her/cyg108.
- Kapilashrami A, Hill S, Meer N. What can health inequalities researchers learn from an intersectionality perspective? Understanding social dynamics with an inter-categorical approach?. Soc Theor Health 2015;13:288-307.
- Institute of Health Equity . Social Inequalities in the Leading Causes of Early Death: A Life Course Approach 2015.
- Lee YS, Oh JY, Min KH, Lee SY, Kang KH, Shim JJ. The association between living below the relative poverty line and the prevalence of chronic obstructive pulmonary disease. J Thorac Dis 2019;11:427-37. https://doi.org/10.21037/jtd.2019.01.40.
- Benach J, Malmusi D, Yasui Y, Martinez JM. A new typology of policies to tackle health inequalities and scenarios of impact based on Rose’s population approach. J Epidemiol Commun Health 2013;67:286-91. https://doi.org/10.1136/jech-2011-200363.
- Stanistreet D, Bambra C, Scott-Samuel A. Is patriarchy the source of men’s higher mortality?. J Epidemiol Commun Health 2005;59:873-6.
- Fisher R. Levelling Up General Practice in England: What Should Government Prioritise. London: Health Foundation; 2021.
- Greve HR. Oxford Research Encyclopedia of Business and Management. Oxford: Oxford University Press; 2017.
- Stokes P. Full Story. The Gender Gap in Unpaid Care Provision: Is There an Impact on Health and Economic Position. London: ONS; 2013.
- The National Institute for Health and Care Excellence . Chronic Obstructive Pulmonary Disease in Adults 2016.
- British Lung Foundation . Briefing: Health Inequalities and Lung Disease 2017.
- Nuffield Trust . General Practice: Case Studies of GP Organisations Working at Scale to Deliver Access and Continuity 2022.
- King’s Fund . Making the Difference: Diversity and Inclusion in the NHS 2015.
- British Medical Association . Racism in Medicine 2022.
- NHS Race and Health Observatory . Ethnic Inequalities in Healthcare: A Rapid Evidence Review 2022.
- Kraus MW, Callaghan B, Ondish P. Handbook of Cultural Psychology. New York: Guilford Press; 2019.
- Smalley KB, Warren JC, Barefoot KN. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol 2016;35:103-14. https://doi.org/10.1037/hea0000231.
Appendix 1 Expert panel members
| Prof. Ann Louise Kinmonth | Emerita Professor of General Practice | University of Cambridge |
| Dr Amy Dehn Lunn | National Medical Director’s Clinical Fellow | Primary Care Team NHS England |
| Dr John Paterson | GP and Clinical Chair | Oldham CCG |
| Bola Owolabi | GP and Director Health Inequalities | NHS England and Improvement |
| Dr James Matheson | GP and Health Inequalities Standing Group lead | NHS England |
| Prof. Kurt Strange | Family Doctor and Director of the Center for Community Health Integration | Case Western Reserve University |
| Ms Sandie Smith | Chief Executive | HealthWatch Cambridgeshire and Peterborough |
| Dr David Blane | Research Fellow in General Practice and Primary Care | University of Glasgow |
| Prof. Mike Kelly | Honorary Senior Fellow | University of Cambridge, PHPC |
| Ms Rachel Power | Chief Executive | The Patients Association |
| Mr Steven Platts | CEO | Groundswell |
| Dr Julia Oni | GP, Trailblazer Fellow and Visiting Researcher | Fair Health, University of Cambridge |
Appendix 2 Search strategy
EQUALISE – all the databases
23 March 2022
Contents
Search numbers
MEDLINE
EMBASE
CINAHL
Web of Science
Scopus
ASSIA
Search numbers
| 1st version | Total (revised strategy) | 2010 onwards | Additional papers: April 2021–23 March 2022 | |
|---|---|---|---|---|
| MEDLINE via OVID | 3239 | 3229 | 1755 | 252 |
| EMBASE via OVID | 858 | 813 | 640 | 110 |
| Web of Science Core Collection | 3453 | 3441 | 3457 | 321 |
| Scopus | 6912 | 6917 | 3993 | 541 |
| CINAHL via EBSCO | 979 | 959 | 703 | 71 |
| ASSIA via Proquest | 459 | 464 | 273 | 31 |
| Total | 15,900 | 9821 | 1005 | |
| Total deduplicated | 11,813 | 7204 | 802 |
Using Prady for Heath Inequalities: https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-018-0567-x
Using Cochrane filter for LMIC: https://epoc.cochrane.org/lmic-filters
Revisions run 28 April 2021
Updates run 23 March 2022
Publication limit – 2010 onwards
MEDLINE
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review and Other Non-Indexed Citations, Daily and Versions(R) <1946 to April 27, 2021>
-
Meta-Analysis as Topic/ or meta analy$.tw. or metaanaly$.tw. or Meta-Analysis/ or (systematic adj (review$1 or overview$1)).tw. or exp Review Literature as Topic/ or cochrane.ab. or embase.ab. or (psychlit or psyclit).ab. or (psychinfo or psycinfo).ab. or (cinahl or cinhal).ab. or science citation index.ab. or bids.ab. or cancerlit.ab. or reference list$.ab. or bibliograph$.ab. or hand-search$.ab. or relevant journals.ab. or manual search$.ab. or ((selection criteria or data extraction).ab. and Review/) or (review or systematic review).pt. or review*.ti. (3,162,808)
-
(primary care or primary health care or primary healthcare or (general practi* or family practi* or family medicine or GP)).mp. or exp primary health care/ or exp general practice/ or exp family practice/ or exp physicians, family/ or exp general practitioners/ (400,484)
-
cardiovascular.mp. or exp heart failure/ or exp myocardial infarction/ or ((heart or cardiac or myocardial) adj2 (failure or infarc$ or attack$)).tw. or exp hypertension/ or hypertens$.tw. or exp blood pressure/ or (blood pressure or bloodpressure).tw. (1,581,094)
-
exp Neoplasms/ or (cancer$ or neoplas$ or tumo$ or carcinoma$ or hodgkin$ or nonhodgkin$ or adenocarcinoma$ or leuk?emia$1 or metasta$ or malignan$ or lymphoma$ or sarcoma$ or melanoma$ or myeloma$ or oncolog$).tw. (4,634,209)
-
exp Diabetes Mellitus/ or diabet$.tw,ot. or (IDDM or NIDDM or MODY or T1DM or T2DM or T1D or T2D).tw,ot. or (non insulin$ depend$ or non insulin$ depend$ or non insulin?depend$ or non insulin?depend$).tw,ot. or (insulin$ depend$ or insulin?depend$).tw,ot. (728,342)
-
Lung Diseases, Obstructive/ or exp Pulmonary Disease, Chronic Obstructive/ or emphysema$.mp. or (chronic$ adj3 bronchiti$).mp. or (obstruct$ adj3 (pulmonary or lung$ or airway$ or airflow$ or bronch$ or respirat$)).mp. or COPD.mp. or COAD.mp. or COBD.mp. or AECB.mp. (165,269)
-
or/3-6 (6,705,868)
-
Residence Characteristics/ or Environment design/ or exp Marital status/ or neighbo?rhood*.mp. or residential environment*.mp. or rural*.mp. or inner?city.mp. or housing instability.mp. or housing insecurity.mp. or housing strain.mp. or housing security.mp. or mortgage problems.mp. or foreclosure.mp. or eviction*.mp. or housing loss.mp. or home repossession*.mp. or home ownership.mp. or (repossess* adj3 hous*).mp. or (repossess* adj3 propert*).mp. or mortgage delinquency.mp. or mortgage arrears.mp. or mortgage debt*.mp. or overcrowding.mp. or (living adj1 (outside or inside or near* or adjacent)).mp. or (household adj2 size).mp. or (marital status or marriage status).mp. or (widow* or cohabit* or divorce* or single parent* or live* alone).mp. (311,172)
-
Cultural Deprivation/ or Acculturation/ or Culture/ or Cross-Cultural Comparison/ or Cultural Characteristics/ or Cultural Diversity/ or Language/ or “Transients and Migrants”/ or exp “Emigrants and Immigrants”/ or Minority groups/ or Minority health/ or Prejudice/ or Racism/ or Xenophobia/ or Social Discrimination/ or exp Race Relations/ or exp Ethnic Groups/ or exp Continental Population Groups/ or Refugees/ or minorit*.mp. or migration background.mp. or racial.mp. or racism.mp. or ethnology.mp. or race.mp. or ethnic*.mp. or non?English.mp. or language other than.mp. or latino*.mp. or latina*.mp. or hispanic*.mp. or whites.mp. or caucasian*.mp. or non?white.mp. or Torres Strait Islander.mp. or aboriginal.mp. or native american.mp. or inuit.mp. or eskimo.mp. or first nation*.mp. or indigenous.mp. or english as a second language.mp. or foreign language.mp. (794,191)
-
Occupations/ or Unemployment/ or occupations.mp. or unemployment.mp. (60,330)
-
exp Gender Identity/ or Women’s Health/ or gender differences.mp. or (sex disparit* or sex difference?).mp. or gender identity.mp. or sex role.mp. or wom#n* role?.mp. or m#n* role?.mp. or gender* role?.mp. or servicewomen.mp. or Sex factors/ (369,763)
-
exp Educational status/ or Education/ or Schooling.mp. or educational status.mp. or (education* adj2 level?).mp. or ((higher or better or worse or less) adj educated).mp. or ((higher or better or worse or less) adj level? of education).mp. (129,018)
-
Religion/ or religi*.mp. (65,444)
-
Social determinants of Health/ or Psychosocial Deprivation/ or Sociological Factors/ or Working Poor/ or Hierarchy, Social/ or disparit*.mp. or inequalit*.mp. or inequit*.mp. or equity.mp. or deprivation.mp. or gini.mp. or concentration index.mp. or Socioeconomic Factors/ or Social Welfare/ or exp Social Class/ or exp Poverty/ or Income/ or Social class*.mp. or social determinants.mp. or social status.mp. or social position.mp. or social background.mp. or social circumstance*.mp. or socio-economic.mp. or socioeconomic.mp. or sociodemographic.mp. or socio-demographic.mp. or SES.mp. or disadvantaged.mp. or impoverished.mp. or poverty.mp. or economic level.mp. or assets index.mp. or income*.mp. (680,103)
-
Social Stigma/ or social capital/ or Social Control, Informal/ or exp Social Support/ or exp Social Environment/ or Trust/ or Social conditions/ or Social isolation/ or Social marginalization/ or Anomie/ or social participation/ or social exclusion.mp. or (social adj (capital or cohes* or organis* or organiz*)).mp. or (community adj3 (cohes* or participa*)).mp. or ((neighbourhood or neighborhood) adj cohes*).mp. or social relationships.mp. or social network*.mp. or collective efficacy.mp. or civil society.mp. or informal social control.mp. or neighbo*rhood disorder.mp. or social disorgani?ation.mp. or anomie.mp. or social support.mp. or social participation.mp. or trust.mp. or emotional support.mp. or psychosocial support.mp. or community capital.mp. or neighbo*rhood cohesion.mp. or social influence.mp. or (soci*context* or soci*-context*).mp. (290,007)
-
Health Status Disparities/ or Health Services Accessibility/ or Health Equity/ or health*care disparit*.mp. or health care disparit*.mp. or health status disparit*.mp. or health disparit*.mp. or health inequalit*.mp. or health inequit*.mp. or medically underserved.mp. (128,342)
-
(potential determinants or significant correlates of or (independent correlates or independent association*) or variables associated with or determinants of or factors associated with or identif* determinants or (more likely or less likely or just as likely) or risk factors for or (significantly related to or significant predictor) or (also adj2 associated with) or (at increased risk or at decreased risk) or association* between or (positively associated or negatively associated) or differed by or (were high* amongst or were low* amongst) or (inverse relationship with or inversely associated with or inversely related to) or reverse association or differentially affects or evidence of a link between or (significantly adj3 likelihood of) or protective factors for or (differ* adj2 according to) or (inverse adj2 gradient) or (positive adj2 gradient) or (negative adj2 gradient) or (trends were adj3 across) or (related to adj3 variable*) or (differences were adj3 explained by) or (significant among or no# significant among)).mp. (2,188,102)
-
or/8-17 (3,807,319)
-
1 and 2 and 7 and 18 (3504)
-
(afghanistan or albania or algeria or american samoa or angola or “antigua and barbuda” or antigua or barbuda or argentina or armenia or armenian or aruba or azerbaijan or bahrain or bangladesh or barbados or republic of belarus or belarus or byelarus or belorussia or byelorussian or belize or british honduras or benin or dahomey or bhutan or bolivia or “bosnia and herzegovina” or bosnia or herzegovina or botswana or bechuanaland or brazil or brasil or bulgaria or burkina faso or burkina fasso or upper volta or burundi or urundi or cabo verde or cape verde or cambodia or kampuchea or khmer republic or cameroon or cameron or cameroun or central african republic or ubangi shari or chad or chile or china or colombia or comoros or comoro islands or iles comores or mayotte or democratic republic of the congo or democratic republic congo or congo or zaire or costa rica or “cote d’ivoire” or “cote d’ ivoire” or cote divoire or cote d ivoire or ivory coast or croatia or cuba or cyprus or czech republic or czechoslovakia or djibouti or french somaliland or dominica or dominican republic or ecuador or egypt or united arab republic or el salvador or equatorial guinea or spanish guinea or eritrea or estonia or eswatini or swaziland or ethiopia or fiji or gabon or gabonese republic or gambia or “georgia (republic)” or georgian or ghana or gold coast or gibraltar or greece or grenada or guam or guatemala or guinea or guinea bissau or guyana or british guiana or haiti or hispaniola or honduras or hungary or india or indonesia or timor or iran or iraq or isle of man or jamaica or jordan or kazakhstan or kazakh or kenya or “democratic people’s republic of korea” or republic of korea or north korea or south korea or korea or kosovo or kyrgyzstan or kirghizia or kirgizstan or kyrgyz republic or kirghiz or laos or lao pdr or “lao people’s democratic republic” or latvia or lebanon or lebanese republic or lesotho or basutoland or liberia or libya or libyan arab jamahiriya or lithuania or macau or macao or republic of north macedonia or macedonia or madagascar or malagasy republic or malawi or nyasaland or malaysia or malay federation or malaya federation or maldives or indian ocean islands or indian ocean or mali or malta or micronesia or federated states of micronesia or kiribati or marshall islands or nauru or northern mariana islands or palau or tuvalu or mauritania or mauritius or mexico or moldova or moldovian or mongolia or montenegro or morocco or ifni or mozambique or portuguese east africa or myanmar or burma or namibia or nepal or netherlands antilles or nicaragua or niger or nigeria or oman or muscat or pakistan or panama or papua new guinea or new guinea or paraguay or peru or philippines or philipines or phillipines or phillippines or poland or “polish people’s republic” or portugal or portuguese republic or puerto rico or romania or russia or russian federation or ussr or soviet union or union of soviet socialist republics or rwanda or ruanda or samoa or pacific islands or polynesia or samoan islands or navigator island or navigator islands or “sao tome and principe” or saudi arabia or senegal or serbia or seychelles or sierra leone or slovakia or slovak republic or slovenia or melanesia or solomon island or solomon islands or norfolk island or norfolk islands or somalia or south africa or south sudan or sri lanka or ceylon or “saint kitts and nevis” or “st. kitts and nevis” or saint lucia or “st. lucia” or “saint vincent and the grenadines” or saint vincent or “st. vincent” or grenadines or sudan or suriname or surinam or dutch guiana or netherlands guiana or syria or syrian arab republic or tajikistan or tadjikistan or tadzhikistan or tadzhik or tanzania or tanganyika or thailand or siam or timor leste or east timor or togo or togolese republic or tonga or “trinidad and tobago” or trinidad or tobago or tunisia or turkey or turkmenistan or turkmen or uganda or ukraine or uruguay or uzbekistan or uzbek or vanuatu or new hebrides or venezuela or vietnam or viet nam or middle east or west bank or gaza or palestine or yemen or yugoslavia or zambia or zimbabwe or northern rhodesia or global south or africa south of the sahara or sub-saharan africa or subsaharan africa or africa, central or central africa or africa, northern or north africa or northern africa or magreb or maghrib or sahara or africa, southern or southern africa or africa, eastern or east africa or eastern africa or africa, western or west africa or western africa or west indies or indian ocean islands or caribbean or central america or latin america or “south and central america” or south america or asia, central or central asia or asia, northern or north asia or northern asia or asia, southeastern or southeastern asia or south eastern asia or southeast asia or south east asia or asia, western or western asia or europe, eastern or east europe or eastern europe or developing country or developing countries or developing nation? or developing population? or developing world or less developed countr* or less developed nation? or less developed population? or less developed world or lesser developed countr* or lesser developed nation? or lesser developed population? or lesser developed world or under developed countr* or under developed nation? or under developed population? or under developed world or underdeveloped countr* or underdeveloped nation? or underdeveloped population? or underdeveloped world or middle income countr* or middle income nation? or middle income population? or low income countr* or low income nation? or low income population? or lower income countr* or lower income nation? or lower income population? or underserved countr* or underserved nation? or underserved population? or underserved world or under served countr* or under served nation? or under served population? or under served world or deprived countr* or deprived nation? or deprived population? or deprived world or poor countr* or poor nation? or poor population? or poor world or poorer countr* or poorer nation? or poorer population? or poorer world or developing econom* or less developed econom* or lesser developed econom* or under developed econom* or underdeveloped econom* or middle income econom* or low income econom* or lower income econom* or low gdp or low gnp or low gross domestic or low gross national or lower gdp or lower gnp or lower gross domestic or lower gross national or lmic or lmics or third world or lami countr* or transitional countr* or emerging economies or emerging nation?).ti,ab,sh,kf. (2,043,021)
-
19 not 20 (3229)
-
limit 21 to yr=“2010 -Current” (1755)
EMBASE
EMBASE <1974 to 2021 April 26>
-
exp Meta Analysis/ or ((meta adj analy$) or metaanalys$).tw. or (systematic adj (review$1 or overview$1)).tw. or cancerlit.ab. or cochrane.ab. or embase.ab. or (psychlit or psyclit).ab. or (psychinfo or psycinfo).ab. or (cinahl or cinhal).ab. or science citation index.ab. or bids.ab. or reference lists.ab. or bibliograph$.ab. or hand-search$.ab. or manual search$.ab. or relevant journals.ab. or ((data extraction or selection criteria).ab. and review.pt.) (520,210)
-
(primary care or primary health care or primary healthcare or (general practi* or family practi* or family medicine or GP)).ti,ab. or exp *primary health care/ or exp *primary medical care/ or exp *general practice/ or exp *general practitioner/ (369,563)
-
cardiovascular.ti,ab. or exp *cardiovascular disease/ or exp *heart failure/ or exp *heart disease/ or exp *heart infarction/ or ((heart or cardiac or myocardial) adj2 (failure or infarc$ or attack$)).ti,ab. or exp *hypertension/ or hypertens$.ti,ab. or exp *blood pressure/ or (blood pressure or bloodpressure).ti,ab. (3,482,073)
-
exp *Neoplasm/ or (cancer$ or neoplas$ or tumo$ or carcinoma$ or hodgkin$ or nonhodgkin$ or adenocarcinoma$ or leuk?emia$1 or metasta$ or malignan$ or lymphoma$ or sarcoma$ or melanoma$ or myeloma$ or oncolog$).ti,ab. (5,574,124)
-
exp *Diabetes Mellitus/ or diabet$.ti,ab. or (IDDM or NIDDM or MODY or T1DM or T2DM or T1D or T2D).ti,ab. or (non insulin$ depend$ or non insulin$ depend$ or non insulin?depend$ or non insulin?depend$).ti,ab. or (insulin$ depend$ or insulin?depend$).ti,ab. (1,044,969)
-
exp *chronic Obstructive Lung Disease/ or exp *chronic bronchitis/ or exp *emphysema/ or (chronic$ adj3 bronchiti$).ti,ab. or (obstruct$ adj3 (pulmonary or lung$ or airway$ or airflow$ or bronch$ or respirat$)).ti,ab. or (COPD or COAD or COBD or AECB).ti,ab. or (emphysema or chronic obstructive pulmonary disease or chronic bronchitis or chronic asthma).ti,ab. or exp *Asthma/ (368,977)
-
or/3-6 (9,656,917)
-
demography/or environmental planning/or marriage/or divorce/or cohabitation/or widow/or exp “single (marital status)”/or neighbo?rhood*.mp. or residential environment*.mp. or rural*.mp. or inner?city.mp. or housing instability.mp. or housing insecurity.mp. or housing strain.mp. or housing security.mp. or mortgage problems.mp. or foreclosure.mp. or eviction*.mp. or housing loss.mp. or home repossession*.mp. or home ownership.mp. or (repossess* adj3 hous*).mp. or (repossess* adj3 propert*).mp. or mortgage delinquency.mp. or mortgage arrears.mp. or mortgage debt*.mp. or overcrowding.mp. or (living adj1 (outside or inside or near* or adjacent)).mp. or (household adj2 size).mp. or (marital status or marriage status).mp. or (widow* or cohabit* or divorce* or single parent* or live* alone).mp. (615,953)
-
exp cultural deprivation/ or cultural factor/ or cultural anthropology/ or cultural diversity/ or exp migrant/ or minority group/ or minority health/ or prejudice/ or exp social discrimination/ or exp race relation/ or exp ethnic group/ or exp ancestry group/ or exp refugee/ or minorit*.mp. or migration background.mp. or racial.mp. or racism.mp. or ethnology.mp. or race.mp. or ethnic*.mp. or non?English.mp. or language other than.mp. or latino*.mp. or latina*.mp. or hispanic*.mp. or whites.mp. or caucasian*.mp. or non?white.mp. or Torres Strait Islander.mp. or aboriginal.mp. or native american.mp. or inuit.mp. or eskimo.mp. or first nation*.mp. or indigenous.mp. or english as a second language.mp. or foreign language.mp. (1,026,416)
-
exp employment status/ or job characteristics/ or occupations.mp. or unemployment.mp. (57,789)
-
exp gender identity/ or women’s health/ or sex difference/ or (sex disparit* or sex difference?).mp. or gender identity.mp. or sex role.mp. or wom#n* role?.mp. or m#n* role?.mp. or gender* role?.mp. or servicewomen.mp. (459,352)
-
exp educational status/ or schooling.mp. or educational status.mp. or (education* adj2 level?).mp. or ((higher or better or worse or less) adj educated).mp. or ((higher or better or worse or less) adj level? of education).mp. (154,356)
-
religion/ or religi*.mp. (92,451)
-
“social determinants of health”/ or social aspect/ or working poor/ or exp social hierarchy/ or socioeconomics/ or disparit*.mp. or inequalit*.mp. or inequit*.mp. or equity.mp. or deprivation.mp. or gini.mp. or concentration index.mp. or social welfare/ or social class/ or poverty/ or social status/ or social background/ or social class*.mp. or social determinants.mp. or social status.mp. or social position.mp. (656,251)
-
(social background or social circumstance* or socio-economic or socioeconomic or sociodemographic or socio-demographic or SES or disadvantaged or impoverished or poverty or economic level or assets index or income*).mp. (491,973)
-
exp social isolation/ or social capital/ or social stigma/ or social support/ or social environment/ or trust/ or exp social exclusion/ or anomie/ or social participation/ or social exclusion.mp. or (social adj (capital or cohes* or organis* or organiz*)).mp. or (community adj3 (cohes* or participa*)).mp. or ((neighbourhood or neighborhood) adj cohes*).mp. or social relationships.mp. or social network*.mp. or collective efficacy.mp. or civil society.mp. or informal social control.mp. or neighbo*rhood disorder.mp. or ocial disorgani?ation.mp. or anomie.mp. or social support.mp. or social participation.mp. or trust.mp. or emotional support.mp. or psychosocial support.mp. or community capital.mp. or neighbo*rhood cohesion.mp. or social influence.mp. or (soci*context* or soci*-context*).mp. (322,503)
-
health disparity/ or health equity/ or health care access/ or health*care disparit*.mp. or health care disparit*.mp. or health status disparit*.mp. or health disparit*.mp. or health inequalit*.mp. or health inequit*.mp. or medically underserved.mp. (125,245)
-
(potential determinants or significant correlates of or (independent correlates or independent association*) or variables associated with or determinants of or factors associated with or identif* determinants or (more likely or less likely or just as likely) or risk factors for or (significantly related to or significant predictor) or (also adj2 associated with) or (at increased risk or at decreased risk)).mp. (1,614,601)
-
(association* between or (positively associated or negatively associated) or differed by or (were high* amongst or were low* amongst) or (inverse relationship with or inversely associated with or inversely related to) or reverse association or differentially affects or evidence of a link between or (significantly adj3 likelihood of) or protective factors for or (differ* adj2 according to) or (inverse adj2 gradient) or (positive adj2 gradient) or (negative adj2 gradient) or (trends were adj3 across) or (related to adj3 variable*) or (differences were adj3 explained by) or (significant among or no# significant among)).mp. (994,983)
-
or/8-19 (4,596,535)
-
1 and 2 and 7 and 20 (900)
-
(afghanistan or albania or algeria or american samoa or angola or “antigua and barbuda” or antigua or barbuda or argentina or armenia or armenian or aruba or azerbaijan or bahrain or bangladesh or barbados or republic of belarus or belarus or byelarus or belorussia or byelorussian or belize or british honduras or benin or dahomey or bhutan or bolivia or “bosnia and herzegovina” or bosnia or herzegovina or botswana or bechuanaland or brazil or brasil or bulgaria or burkina faso or burkina fasso or upper volta or burundi or urundi or cabo verde or cape verde or cambodia or kampuchea or khmer republic or cameroon or cameron or cameroun or central african republic or ubangi shari or chad or chile or china or colombia or comoros or comoro islands or iles comores or mayotte or democratic republic of the congo or democratic republic congo or congo or zaire or costa rica or “cote d’ivoire” or “cote d’ ivoire” or cote divoire or cote d ivoire or ivory coast or croatia or cuba or cyprus or czech republic or czechoslovakia or djibouti or french somaliland or dominica or dominican republic or ecuador or egypt or united arab republic or el salvador or equatorial guinea or spanish guinea or eritrea or estonia or eswatini or swaziland or ethiopia or fiji or gabon or gabonese republic or gambia or “georgia (republic)” or georgian or ghana or gold coast or gibraltar or greece or grenada or guam or guatemala or guinea or guinea bissau or guyana or british guiana or haiti or hispaniola or honduras or hungary or india or indonesia or timor or iran or iraq or isle of man or jamaica or jordan or kazakhstan or kazakh or kenya or “democratic people’s republic of korea” or republic of korea or north korea or south korea or korea or kosovo or kyrgyzstan or kirghizia or kirgizstan or kyrgyz republic or kirghiz or laos or lao pdr or “lao people’s democratic republic” or latvia or lebanon or lebanese republic or lesotho or basutoland or liberia or libya or libyan arab jamahiriya or lithuania or macau or macao or “macedonia (republic)” or macedonia or madagascar or malagasy republic or malawi or nyasaland or malaysia or malay federation or malaya federation or maldives or indian ocean islands or indian ocean or mali or malta or micronesia or federated states of micronesia or kiribati or marshall islands or nauru or northern mariana islands or palau or tuvalu or mauritania or mauritius or mexico or moldova or moldovian or mongolia or montenegro or “montenegro (republic)” or morocco or ifni or mozambique or portuguese east africa or myanmar or burma or namibia or nepal or netherlands antilles or nicaragua or niger or nigeria or oman or muscat or pakistan or panama or papua new guinea or new guinea or paraguay or peru or philippines or philipines or phillipines or phillippines or poland or “polish people’s republic” or portugal or portuguese republic or puerto rico or romania or russia or russian federation or ussr or soviet union or union of soviet socialist republics or rwanda or ruanda or samoa or pacific islands or polynesia or samoan islands or navigator island or navigator islands or “sao tome and principe” or saudi arabia or senegal or serbia or seychelles or sierra leone or slovakia or slovak republic or slovenia or melanesia or solomon island or solomon islands or norfolk island or norfolk islands or somalia or south africa or south sudan or sri lanka or ceylon or “saint kitts and nevis” or “st. kitts and nevis” or saint lucia or “st. lucia” or “saint vincent and the grenadines” or saint vincent or “st. vincent” or grenadines or sudan or suriname or surinam or dutch guiana or netherlands guiana or syria or syrian arab republic or tajikistan or tadjikistan or tadzhikistan or tadzhik or tanzania or tanganyika or thailand or siam or timor leste or east timor or togo or togolese republic or tonga or “trinidad and tobago” or trinidad or tobago or tunisia or turkey or “turkey (republic)” or turkmenistan or turkmen or uganda or ukraine or uruguay or uzbekistan or uzbek or vanuatu or new hebrides or venezuela or vietnam or viet nam or middle east or west bank or gaza or palestine or yemen or yugoslavia or zambia or zimbabwe or northern rhodesia or global south or africa south of the sahara or “sub saharan africa” or subsaharan africa or africa, central or central africa or africa, northern or north africa or northern africa or magreb or maghrib or sahara or africa, southern or southern africa or africa, eastern or east africa or eastern africa or africa, western or west africa or western africa or west indies or indian ocean islands or caribbean region or caribbean islands or caribbean or central america or latin america or “south and central america” or south america or asia, central or central asia or asia, northern or north asia or northern asia or asia, southeastern or southeastern asia or south eastern asia or southeast asia or south east asia or asia, western or western asia or europe, eastern or east europe or eastern europe or developing country or developing countries or developing nation? or developing population? or developing world or less developed countr* or less developed nation? or less developed population? or less developed world or lesser developed countr* or lesser developed nation? or lesser developed population? or lesser developed world or under developed countr* or under developed nation? or under developed population? or under developed world or underdeveloped countr* or underdeveloped nation? or underdeveloped population? or underdeveloped world or middle income countr* or middle income nation? or middle income population? or low income countr* or low income nation? or low income population? or lower income countr* or lower income nation? or lower income population? or underserved countr* or underserved nation? or underserved population? or underserved world or under served countr* or under served nation? or under served population? or under served world or deprived countr* or deprived nation? or deprived population? or deprived world or poor countr* or poor nation? or poor population? or poor world or poorer countr* or poorer nation? or poorer population? or poorer world or developing econom* or less developed econom* or lesser developed econom* or under developed econom* or underdeveloped econom* or middle income econom* or low income econom* or lower income econom* or low gdp or low gnp or low gross domestic or low gross national or lower gdp or lower gnp or lower gross domestic or lower gross national or lmic or lmics or third world or lami countr* or transitional countr* or emerging economies or emerging nation?).ti,ab,sh,kw. (2,341,497)
-
21 not 22 (813)
-
limit 23 to yr=“2010 -Current” (640)
CINAHL
| # | Query | Results |
|---|---|---|
| S22 | s19 not s20 Limiters – Published Date: 20100101-20211231 |
703 |
| S21 | s19 not s20 | 959 |
| S20 | (afghanistan OR albania OR algeria OR american samoa OR angola OR “antigua and barbuda” OR antigua OR barbuda OR argentina OR armenia OR armenian OR aruba OR azerbaijan OR bahrain OR bangladesh OR barbados OR republic of belarus OR belarus OR byelarus OR belorussia OR byelorussian OR belize OR british honduras OR benin OR dahomey OR bhutan OR bolivia OR “bosnia and herzegovina” OR bosnia OR herzegovina OR botswana OR bechuanaland OR brazil OR brasil OR bulgaria OR burkina faso OR burkina fasso OR upper volta OR burundi OR urundi OR cabo verde OR cape verde OR cambodia OR kampuchea OR khmer republic OR cameroon OR cameron OR cameroun OR central african republic OR ubangi shari OR chad OR chile OR china OR colombia OR comoros OR comoro islands OR iles comores OR mayotte OR democratic republic of the congo OR democratic republic congo OR congo OR zaire OR costa rica OR “cote d’ivoire” OR “cote d’ ivoire” OR cote divoire OR cote d ivoire OR ivory coast OR croatia OR cuba OR cyprus OR czech republic OR czechoslovakia OR djibouti OR french somaliland OR dominica OR dominican republic OR ecuador OR egypt OR united arab republic OR el salvador OR equatorial guinea OR spanish guinea OR eritrea OR estonia OR eswatini OR swaziland OR ethiopia OR fiji OR gabon OR gabonese republic OR gambia OR “georgia (republic)” OR georgian OR ghana OR gold coast OR gibraltar OR greece OR grenada OR guam OR guatemala OR guinea OR guinea bissau OR guyana OR british guiana OR haiti OR hispaniola OR honduras OR hungary OR india OR indonesia OR timor OR iran OR iraq OR isle of man OR jamaica OR jordan OR kazakhstan OR kazakh OR kenya OR “democratic people’s republic of korea” OR republic of korea OR north korea OR south korea OR korea OR kosovo OR kyrgyzstan OR kirghizia OR kirgizstan OR kyrgyz republic OR kirghiz OR laos OR lao pdr OR “lao people’s democratic republic” OR latvia OR lebanon OR lebanese republic OR lesotho OR basutoland OR liberia OR libya OR libyan arab jamahiriya OR lithuania OR macau OR macao OR “macedonia (republic)” OR macedonia OR madagascar OR malagasy republic OR malawi OR nyasaland OR malaysia OR malay federation OR malaya federation OR maldives OR indian ocean islands OR indian ocean OR mali OR malta OR micronesia OR federated states of micronesia OR kiribati OR marshall islands OR nauru OR northern mariana islands OR palau OR tuvalu OR mauritania OR mauritius OR mexico OR moldova OR moldovian OR mongolia OR montenegro OR “montenegro (republic)” OR morocco OR ifni OR mozambique OR portuguese east africa OR myanmar OR burma OR namibia OR nepal OR netherlands antilles OR nicaragua OR niger OR nigeria OR oman OR muscat OR pakistan OR panama OR papua new guinea OR new guinea OR paraguay OR peru OR philippines OR philipines OR phillipines OR phillippines OR poland OR “polish people’s republic” OR portugal OR portuguese republic OR puerto rico OR romania OR russia OR russian federation OR ussr OR soviet union OR union of soviet socialist republics OR rwanda OR ruanda OR samoa OR pacific islands OR polynesia OR samoan islands OR navigator island OR navigator islands OR “sao tome and principe” OR saudi arabia OR senegal OR serbia OR seychelles OR sierra leone OR slovakia OR slovak republic OR slovenia OR melanesia OR solomon island OR solomon islands OR norfolk island OR norfolk islands OR somalia OR south africa OR south sudan OR sri lanka OR ceylon OR “saint kitts and nevis” OR “st. kitts and nevis” OR saint lucia OR “st. lucia” OR “saint vincent and the grenadines” OR saint vincent OR “st. vincent” OR grenadines OR sudan OR suriname OR surinam OR dutch guiana OR netherlands guiana OR syria OR syrian arab republic OR tajikistan OR tadjikistan OR tadzhikistan OR tadzhik OR tanzania OR tanganyika OR thailand OR siam OR timor leste OR east timor OR togo OR togolese republic OR tonga OR “trinidad and tobago” OR trinidad OR tobago OR tunisia OR turkey OR “turkey (republic)” OR turkmenistan OR turkmen OR uganda OR ukraine OR uruguay OR uzbekistan OR uzbek OR vanuatu OR new hebrides OR venezuela OR vietnam OR viet nam OR middle east OR west bank OR gaza OR palestine OR yemen OR yugoslavia OR zambia OR zimbabwe OR northern rhodesia OR global south OR africa south of the sahara OR “sub saharan africa” OR subsaharan africa OR africa, central OR central africa OR africa, northern OR north africa OR northern africa OR magreb OR maghrib OR sahara OR africa, southern OR southern africa OR africa, eastern OR east africa OR eastern africa OR africa, western OR west africa OR western africa OR west indies OR indian ocean islands OR caribbean region OR caribbean islands OR caribbean OR central america OR latin america OR “south and central america” OR south america OR asia, central OR central asia OR asia, northern OR north asia OR northern asia OR asia, southeastern OR southeastern asia OR south eastern asia OR southeast asia OR south east asia OR asia, western OR western asia OR europe, eastern OR east europe OR eastern europe OR developing country OR developing countries OR developing nation? OR developing population? OR developing world OR less developed countr* OR less developed nation? OR less developed population? OR less developed world OR lesser developed countr* OR lesser developed nation? OR lesser developed population? OR lesser developed world OR under developed countr* OR under developed nation? OR under developed population? OR under developed world OR underdeveloped countr* OR underdeveloped nation? OR underdeveloped population? OR underdeveloped world OR middle income countr* OR middle income nation? OR middle income population? OR low income countr* OR low income nation? OR low income population? OR lower income countr* OR lower income nation? OR lower income population? OR underserved countr* OR underserved nation? OR underserved population? OR underserved world OR under served countr* OR under served nation? OR under served population? OR under served world OR deprived countr* OR deprived nation? OR deprived population? OR deprived world OR poor countr* OR poor nation? OR poor population? OR poor world OR poorer countr* OR poorer nation? OR poorer population? OR poorer world OR developing econom* OR less developed econom* OR lesser developed econom* OR under developed econom* OR underdeveloped econom* OR middle income econom* OR low income econom* OR lower income econom* OR low gdp OR low gnp OR low gross domestic OR low gross national OR lower gdp OR lower gnp OR lower gross domestic OR lower gross national OR lmic OR lmics OR third world OR lami countr* OR transitional countr* OR emerging economies OR emerging nation?) | 568,828 |
| S19 | S1 AND S2 AND S7 AND S18 | 1,045 |
| S18 | S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 | 2,976,766 |
| S17 | TI ((“potential determinants” or “significant correlates of” or (“independent correlates” or “independent association*”) or “variables associated with” or “determinants of” or “factors associated with” or “identif* determinants” or (“more likely” or “less likely” or “just as likely”) or “risk factors for” or (“significantly related to” or “significant predictor”) or (also n2 “associated with”) or (“at increased risk” or “at decreased risk”) or “association* between” or (“positively associated” or “negatively associated”) or “differed by” or (“were high* amongst” or “were low* amongst”) or (“inverse relationship with” or “inversely associated with” or “inversely related to”) or “reverse association” or “differentially affects” or “evidence of a link between” or (significantly n3 “likelihood of”) or “protective factors for” or (differ* n2 “according to”) or (inverse n2 gradient) or (positive n2 gradient) or (negative n2 gradient) or (“trends were” n3 across) or (“related to” n3 variable*) or (“differences were” n3 “explained by”) or (“significant among”)) or AB ((“potential determinants” or “significant correlates of” or (“independent correlates” or “independent association*”) or “variables associated with” or “determinants of” or “factors associated with” or “identif* determinants” or (“more likely” or “less likely” or “just as likely”) or “risk factors for” or (“significantly related to” or “significant predictor”) or (also n2 “associated with”) or (“at increased risk” or “at decreased risk”) or “association* between” or (“positively associated” or “negatively associated”) or “differed by” or (“were high* amongst” or “were low* amongst”) or (“inverse relationship with” or “inversely associated with” or “inversely related to”) or “reverse association” or “differentially affects” or “evidence of a link between” or (significantly n3 “likelihood of”) or “protective factors for” or (differ* n2 “according to”) or (inverse n2 gradient) or (positive n2 gradient) or (negative n2 gradient) or (“trends were” n3 across) or (“related to” n3 variable*) or (“differences were” n3 “explained by”) or (“significant among”)) | 1,123,275 |
| S16 | TI (health*care disparit* or health status disparit* or health disparit* or health inequalit* or health inequit* or medically underserved) or AB (health*care disparit* or health status disparit* or health disparit* or health inequalit* or health inequit* or medically underserved) or (MH “Health Status Disparities”) OR (MH “Healthcare Disparities”) OR (MH “Health Services Accessibility+”) OR (MH “Health Services Needs and Demand+”) | 136,051 |
| S15 | TI (social exclusion or (social n1 (capital or cohes* or organis* or organiz*)) or (community n3 (cohes* or participa*)) or ((neighbourhood or neighborhood) n1 cohes*) or social relationships or social network* or collective efficacy or civil society or informal social control or neighbo*rhood disorder or social disorgani?ation or anomie or social support or social participation or trust or emotional support or psychosocial support or community capital or neighbo*rhood cohesion or social influence or (soci*context* or soci*-context*)) or AB (social exclusion or (social n1 (capital or cohes* or organis* or organiz*)) or (community n3 (cohes* or participa*)) or ((neighbourhood or neighborhood) n1 cohes*) or social relationships or social network* or collective efficacy or civil society or informal social control or neighbo*rhood disorder or social disorgani?ation or anomie or social support or social participation or trust or emotional support or psychosocial support or community capital or neighbo*rhood cohesion or social influence or (soci*context* or soci*-context*)) or (MH “Stigma”) OR (MH “Social Capital”) OR (MH “Social Control+”) OR (MH “Social Responsibility+”) OR (MH “Trust”) OR (MH “Social Isolation+”) OR (MH “Social Behavior+”) OR (MH “Social Participation”) | 602,044 |
| S14 | TI (disparit* or inequalit* or inequit* or equity or deprivation or gini or concentration index or Social class* or social determinants or social status or social position or social background or social circumstance* or socio-economic or socioeconomic or sociodemographic or socio-demographic or SES or disadvantaged or impoverished or poverty or economic level or assets index or income*) or AB (disparit* or inequalit* or inequit* or equity or deprivation or gini or concentration index or Social class* or social determinants or social status or social position or social background or social circumstance* or socio-economic or socioeconomic or sociodemographic or socio-demographic or SES or disadvantaged or impoverished or poverty or economic level or assets index or income*) or (MH “Social Determinants of Health”) OR (MH “Psychosocial Deprivation”) OR (MH “Socioeconomic Factors+”) OR (MH “Social Welfare+”) OR (MH “Social Class+”) OR (MH “Poverty+”) or (MH “Income+”) | 534,993 |
| S13 | TI (religi*) or AB (religi*) or (MH “Religion and Religions+”) | 57,447 |
| S12 | TI (Schooling or educational status or (education* n2 level*) or ((higher or better or worse or less) n1 educated) or ((higher or better or worse or less) n1 level* of education) or AB (Schooling or educational status or (education* n2 level*) or ((higher or better or worse or less) n1 educated) or ((higher or better or worse or less) n1 level* of education) or (MH “Educational Status”) OR (MH “Education+”) | 980,898 |
| S11 | TI (sex disparit* or sex difference* or gender identity or sex role or wom#n* role? or m#n* role? or gender* role* or servicewomen or gender differences) or AB (sex disparit* or sex difference* or gender identity or sex role or wom#n* role? or m#n* role? or gender* role* or servicewomen or gender differences) or (MH “Gender Identity+”) OR (MH “Women’s Health”) OR (MH “Sex Factors”) | 177,618 |
| S10 | TI (occupations or unemployment) or AB (occupations or unemployment) or (MH “Occupations and Professions+”) OR (MH “Unemployment”) | 120,826 |
| S9 | TI (minorit* or migration background or racial or racism or ethnology or race or ethnic* or non#English or “language other than” or latino* or latina* or hispanic* or whites or caucasian* or non?white or Torres Strait Islander or aboriginal or native american or inuit or eskimo or first nation* or indigenous or “english as a second language” or foreign language) or AB (minorit* or migration background or racial or racism or ethnology or race or ethnic* or non#English or “language other than” or latino* or latina* or hispanic* or whites or caucasian* or non?white or Torres Strait Islander or aboriginal or native american or inuit or eskimo or first nation* or indigenous or “english as a second language” or foreign language) or (MH “Cultural Deprivation”) OR (MH “Acculturation”) OR (MH “Culture+”) OR (MH “Cultural Diversity”) OR (MH “Language+”) OR (MH “Transients and Migrants”) OR (MH “Immigrants+”) OR (MH “Emigration and Immigration”) OR (MH “Minority Groups”) OR (MH “Prejudice+”) OR (MH “Racism”) OR (MH “Cultural Bias”) OR (MH “Discrimination”) OR (MH “Race Relations+”) OR (MH “Ethnic Groups+”) OR (MH “Refugees+”) | 476,652 |
| S8 | TI (neighbo?rhood* or residential environment* or inner?city or housing instability or housing insecurity or housing strain or housing security or mortgage problems or foreclosure or eviction* or housing loss or home repossession* or home ownership or (repossess* n3 hous*) or (repossess* n3 propert*) or mortgage delinquency or mortgage arrears or mortgage debt* or overcrowding or (living n1 (outside or inside or near* or adjacent)) or (household n2 size) or (marital status or marriage status) or (widow* or cohabit* or divorce* or single parent* or live* alone)) or AB (neighbo?rhood* or residential environment* or inner?city or housing instability or housing insecurity or housing strain or housing security or mortgage problems or foreclosure or eviction* or housing loss or home repossession* or home ownership or (repossess* n3 hous*) or (repossess* n3 propert*) or mortgage delinquency or mortgage arrears or mortgage debt* or overcrowding or (living n1 (outside or inside or near* or adjacent)) or (household n2 size) or (marital status or marriage status) or (widow* or cohabit* or divorce* or single parent* or live* alone)) or (MH “Residence Characteristics+”) OR (MH “Social Environment+”) OR (MH “Community Living+”) OR (MH “Marital Status+”) | 223,604 |
| S7 | S3 OR S4 OR S5 OR S6 | 1,694,516 |
| S6 | TI (cancer* or neoplas* or tumo* or carcinoma* or Hodgkin* or nonhodgkin* or adenocarcinoma* or leuk#emia* or metasta* or malignan* or lymphoma* or sarcoma* or melanoma* or myeloma* or oncolog*) or AB (cancer* or neoplas* or tumo* or carcinoma* or Hodgkin* or nonhodgkin* or adenocarcinoma* or leuk#emia* or metasta* or malignan* or lymphoma* or sarcoma* or melanoma* or myeloma* or oncolog*) or (MH “Neoplasms+”) | 794,229 |
| S5 | TI (emphysema* or asthma* or (chronic* n3 bronchiti*) or (obstruct* n3 (pulmonary or lung* or airway* or airflow* or bronch* or respirat*)) or COPD or COAD or COBD or AECB) or AB (emphysema* or (chronic* n3 bronchiti*) or (obstruct* n3 (pulmonary or lung* or airway* or airflow* or bronch* or respirat*)) or COPD or COAD or COBD or AECB) or (MH “Pulmonary Disease, Chronic Obstructive+”) OR (MH “Lung Diseases, Obstructive+”) OR (MH “Emphysema+”) OR (MH “Bronchitis, Chronic”) OR (MH “Asthma+”) | 80,609 |
| S4 | TI(diabet* or IDDM or NIDDM or MODY or T1DM or T2DM or T1D or T2D or non insulin* depend* or non insulin* depend* or non insulin#depend* or non insulin#depend* or insulin* depend* or insulin#depend*) or AB(diabet* or IDDM or NIDDM or MODY or T1DM or T2DM or T1D or T2D or non insulin* depend* or non insulin* depend* or non insulin#depend* or non insulin#depend* or insulin* depend* or insulin#depend*) or (MH “Diabetes Mellitus+”) | 244,035 |
| S3 | TI (cardiovascular or ((heart or cardiac or myocardial) n2 (failure or infarc* or attack*)) or hypertens* or blood pressure or bloodpressure) or AB(cardiovascular or ((heart or cardiac or myocardial) n2 (failure or infarc* or attack*)) or hypertens* or blood pressure or bloodpressure) or (MH “Cardiovascular Diseases+”) OR (MH “Myocardial Infarction+”) OR (MH “Hypertension+”) OR (MH “Blood Pressure+”) or (MH “Heart Failure+”) | 744,420 |
| S2 | TI ((primary care or primary health care or primary healthcare) or (general practi* or family practi* or family medicine or GP)) or AB ((primary care or primary health care or primary healthcare) or (general practi* or family practi* or family medicine or GP)) or (MH “Primary Health Care”) OR (MH “Physicians, Family”) OR (MH “Family Practice”) | 159,547 |
| S1 | (TI (systematic* n3 review*)) or (AB (systematic* n3 review*)) or (TI (systematic* n3 bibliographic*)) or (AB (systematic* n3 bibliographic*)) or (TI (systematic* n3 literature)) or (AB (systematic* n3 literature)) or (TI (comprehensive* n3 literature)) or (AB (comprehensive* n3 literature)) or (TI (comprehensive* n3 bibliographic*)) or (AB (comprehensive* n3 bibliographic*)) or (TI (integrative n3 review)) or (AB (integrative n3 review)) or (JN “Cochrane Database of Systematic Reviews”) or (TI (information n2 synthesis)) or (TI (data n2 synthesis)) or (AB (information n2 synthesis)) or (AB (data n2 synthesis)) or (TI (data n2 extract*)) or (AB (data n2 extract*)) or (TI (medline or pubmed or psyclit or cinahl or (psycinfo not “psycinfo database”) or “web of science” or scopus or embase)) or (AB (medline or pubmed or psyclit or cinahl or (psycinfo not “psycinfo database”) or “web of science” or scopus or embase)) or (MH “Systematic Review”) or (MH “Meta Analysis”) or (TI (meta-analy* or metaanaly*)) or (AB (meta-analy* or metaanaly*)) OR TI(review*) | 351,975 |
Web of Science
| # 22 | 2457 | #19 not #20 Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=2010-2021 |
| # 21 | 3441 | #19 not #20 Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 20 | 4,244,311 | TS=(afghanistan OR albania OR algeria OR “american samoa” OR angola OR “antigua and barbuda” OR antigua OR barbuda OR argentina OR armenia OR armenian OR aruba OR azerbaijan OR bahrain OR bangladesh OR barbados OR “republic of belarus” OR belarus OR byelarus OR belorussia OR byelorussian OR belize OR “british honduras” OR benin OR dahomey OR bhutan OR bolivia OR “bosnia and herzegovina” OR bosnia OR herzegovina OR botswana OR bechuanaland OR brazil OR brasil OR bulgaria OR “burkina faso” OR “burkina fasso” OR “upper volta” OR burundi OR urundi OR “cabo verde” OR “cape verde” OR cambodia OR kampuchea OR “khmer republic” OR cameroon OR cameron OR cameroun OR “central african republic” OR “ubangi shari” OR chad OR chile OR china OR colombia OR comoros OR “comoro islands” OR “iles comores” OR mayotte OR “democratic republic of the congo” OR “democratic republic congo” OR congo OR zaire OR “costa rica” OR “cote divoire” OR “cote d ivoire” OR “cote divoire” OR “cote d ivoire” OR “ivory coast” OR croatia OR cuba OR cyprus OR “czech republic” OR czechoslovakia OR djibouti OR “french somaliland” OR dominica OR “dominican republic” OR ecuador OR egypt OR “united arab republic” OR “el salvador” OR “equatorial guinea” OR “spanish guinea” OR eritrea OR estonia OR eswatini OR swaziland OR ethiopia OR fiji OR gabon OR “gabonese republic” OR gambia OR “georgia (republic) “ OR georgian OR ghana OR “gold coast” OR gibraltar OR greece OR grenada OR guam OR guatemala OR guinea OR “guinea bissau” OR guyana OR “british guiana” OR haiti OR hispaniola OR honduras OR hungary OR india OR indonesia OR timor OR iran OR iraq OR” isle of man” OR jamaica OR jordan OR kazakhstan OR kazakh OR kenya OR “democratic peoples republic of korea” OR “republic of korea” OR “north korea” OR “south korea” OR korea OR kosovo OR kyrgyzstan OR kirghizia OR kirgizstan OR “kyrgyz republic” OR kirghiz OR laos OR “lao pdr” OR “lao people’s democratic republic” OR latvia OR lebanon OR “lebanese republic” OR lesotho OR basutoland OR liberia OR libya OR “libyan arab jamahiriya” OR lithuania OR macau OR macao OR “macedonia (republic) “ OR macedonia OR madagascar OR “malagasy republic” OR malawi OR nyasaland OR malaysia OR “malay federation” OR “malaya federation” OR maldives OR “indian ocean islands” OR “indian ocean” OR mali OR malta OR micronesia OR “federated states of micronesia” OR kiribati OR “marshall islands” OR nauru OR “northern mariana islands” OR palau OR tuvalu OR mauritania OR mauritius OR mexico OR moldova OR moldovian OR mongolia OR montenegro OR “montenegro (republic) “ OR morocco OR ifni OR mozambique OR “portuguese east africa” OR myanmar OR burma OR namibia OR nepal OR “netherlands antilles” OR nicaragua OR niger OR nigeria OR oman OR muscat OR pakistan OR panama OR “papua new guinea” OR “new guinea” OR paraguay OR peru OR philippines OR philipines OR phillipines OR phillippines OR poland OR “polish people’s republic” OR portugal OR “portuguese republic” OR puerto rico OR romania OR russia OR “russian federation” OR ussr OR “soviet union” OR “union of soviet socialist republics” OR rwanda OR ruanda OR samoa OR “pacific islands” OR polynesia OR “samoan islands” OR “navigator island” OR “navigator islands” OR “sao tome and principe” OR “saudi arabia” OR senegal OR serbia OR seychelles OR “sierra leone” OR slovakia OR “slovak republic” OR slovenia OR melanesia OR “solomon island” OR “solomon islands” OR “norfolk island” OR “norfolk islands” OR somalia OR “south africa” OR “south sudan” OR “sri lanka” OR ceylon OR “saint kitts and nevis” OR “st. kitts and nevis” OR “saint lucia” OR “st. lucia” OR “saint vincent and the grenadines” OR “saint vincent” OR “st. vincent” OR grenadines OR sudan OR suriname OR surinam OR “dutch guiana” OR “netherlands guiana” OR syria OR “syrian arab republic” OR tajikistan OR tadjikistan OR tadzhikistan OR tadzhik OR tanzania OR tanganyika OR thailand OR siam OR “timor leste” OR “east timor” OR togo OR “togolese republic” OR tonga OR “trinidad and tobago” OR trinidad OR tobago OR tunisia OR turkey OR “turkey (republic) “ OR turkmenistan OR turkmen OR uganda OR ukraine OR uruguay OR uzbekistan OR uzbek OR vanuatu OR “new hebrides” OR venezuela OR vietnam OR “viet nam” OR “middle east” OR “west bank” OR gaza OR palestine OR yemen OR yugoslavia OR zambia OR zimbabwe OR “northern rhodesia” OR “global south” OR “africa south of the sahara” OR “sub saharan africa” OR “subsaharan africa” OR “africa, central” OR “central africa” OR “africa, northern” OR “north africa” OR “northern africa” OR magreb OR maghrib OR sahara OR “africa, southern” OR “southern africa” OR “africa, eastern” OR “east africa” OR “eastern africa” OR “africa, western” OR “west africa” OR “western africa” OR “west indies” OR “indian ocean islands” OR “caribbean region” OR “caribbean islands” OR caribbean OR “central america” OR “latin america” OR “south and central america” OR “south america” OR “asia, central” OR “central asia” OR “asia, northern” OR “north asia” OR “northern asia” OR “asia, southeastern” OR “southeastern asia” OR “south eastern asia” OR “southeast asia” OR “south east asia” OR “asia, western” OR “western asia” OR “europe, eastern” OR “east europe” OR “eastern europe” OR “developing country” OR “developing countries” OR “developing nation?” OR “developing population?” OR “developing world” OR “less developed countr*” OR” less developed nation?” OR “less developed population?” OR “less developed world” OR “lesser developed countr*” OR “lesser developed nation?” OR “lesser developed population?” OR “lesser developed world” OR “under developed countr*” OR “under developed nation?” OR “under developed population?” OR “under developed world” OR “underdeveloped countr*” OR “underdeveloped nation?” OR “underdeveloped population?” OR “underdeveloped world” OR “middle income countr*” OR “middle income nation?” OR “middle income population?” OR “low income countr*” OR “low income nation?” OR “low income population?” OR “lower income countr*” OR “lower income nation?” OR “lower income population?” OR “underserved countr*” OR “underserved nation?” OR “underserved population?” OR “underserved world” OR “under served countr”* OR “under served nation?” OR “under served population?” OR “under served world” OR “deprived countr*” OR “deprived nation?” OR “deprived population?” OR “deprived world” OR “poor countr*” OR “poor nation?” OR “poor population?” OR “poor world” OR “poorer countr*” OR “poorer nation?” OR “poorer population?” OR “poorer world” OR “developing econom*” OR “less developed econom*” OR “lesser developed econom*” OR “under developed econom*” OR “underdeveloped econom*” OR “middle income econom*” OR “low income econom*” OR “lower income econom*” OR “low gdp” OR “low gnp” OR “low gross domestic” OR” low gross national” OR “lower gdp” OR “lower gnp” OR “lower gross domestic” OR “lower gross national” OR lmic OR lmics OR “third world” OR “lami countr*” OR “transitional countr*” OR “emerging economies” OR “emerging nation*”) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 19 | 3855 | #18 AND #7 AND #2 AND #1 Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 18 | 6,520,328 | #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 17 | 1,664,398 | TS= (“potential determinants” or “significant correlates of” or (“independent correlates” or “independent association*”) or “variables associated with” or “determinants of” or “factors associated with” or “identif* determinants” or (“more likely” or “less likely” or “just as likely”) or “risk factors for” or (“significantly related to” or “significant predictor”) or (also near/2 “associated with”) or (“at increased risk” or “at decreased risk”) or “association* between” or (“positively associated” or “negatively associated”) or “differed by” or (“were high* amongst” or “were low* amongst”) or (“inverse relationship with” or “inversely associated with” or “inversely related to”) or “reverse association” or “differentially affects” or “evidence of a link between” or (significantly near/3 “likelihood of”) or “protective factors for” or (differ* near/2 “according to”) or (inverse near/2 gradient) or (positive near/2 gradient) or (negative near/2 gradient) or (“trends were” near/3 across) or (“related to” near/3 variable*) or (“differences were” near/3 “explained by”) or (“significant among”)) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 16 | 31,052 | TS= (“health*care disparit*” or “health status disparit*” or “health disparit*” or “health inequalit*” or “health inequit*” or “medically underserved” or “health services accessibilty”) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 15 | 482,724 | TS= (“social exclusion” or (social near/1 (capital or cohes* or organis* or organiz*)) or (community near/3 (cohes* or participa*)) or ((neighbourhood or neighborhood) near/1 cohes*) or “social relationship*” or “social network*” or “collective efficacy” or “civil society” or “informal social control” or “neighbo*rhood disorder” or “social disorgani?ation” or anomie or “social support” or “social participation” or trust or “emotional suppor”t or “psychosocial support” or “community capital” or “neighbo*rhood cohesion” or “social influence” or (soci*context* or soci*-context*)) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 14 | 1,276,321 | TS=(disparit* or inequalit* or inequit* or equity or deprivation or gini or “concentration index” or “Social class*” or “social determinant*” or “social status” or “social position” or “social background” or “social circumstance*” or socio-economic or socioeconomic or sociodemographic or socio-demographic or SES or disadvantaged or impoverished or poverty or “economic level” or “assets index” or income*) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 13 | 231,859 | TS= (religi*) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 12 | 798,113 | TS=(Schooling or “educational status” or (education* near/2 level*) or ((higher or better or worse or less) near/1 educated) or ((higher or better or worse or less) near/1 level* of education)) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 11 | 192,026 | TS= (“sex disparit*” or “sex difference*” or “gender identity” or “sex role” or “sex factor*”or “wom?n* role*” or “m?n* role*” or “gender* role*” or servicewomen or “gender difference*”) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 10 | 296,306 | TS= (occupation* or unemploy*) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 9 | 2,599,763 | TS=(minorit* or “migration background” or racial or racism or ethnology or race or ethnic* or non?English or “language other than” or latino* or latina* or hispanic* or whites or caucasian* or non?white or “Torres Strait Islander “ or aboriginal or “native american “ or inuit or eskimo or “first nation* “ or indigenous or “english as a second language “ or “foreign language” or “cultural deprivation” or acculturation or “cultural diversity” or transient* or migrant* or emigra* or immigra* or “minority group*” or prejudic* or “cultural bias” or discriminat* or refugee*) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 8 | 204,758 | TS= (neighbo?rhood* or “residential environment* “ or inner?city or “housing instability “ or “housing insecurity “ or “housing strain “ or “housing security “ or “mortgage problems “ or foreclosure or eviction* or “housing loss “ or “home repossession* “ or “home ownership “ or (repossess* near/3 hous*) or (repossess* near/3 propert*) or “mortgage delinquency “ or “mortgage arrears “ or “mortgage debt* “ or overcrowding or (living near/1 (outside or inside or near* or adjacent)) or (household near/2 size) or (“marital status “ or “marriage status “) or (widow* or cohabit* or divorce* or single parent* or live* alone)) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 7 | 7,057,470 | #6 OR #5 OR #4 OR #3 Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 6 | 343,492 | TS= (emphysema* or asthma* or (chronic* near/3 bronchiti*) or (obstruct* near/3 (pulmonary or lung* or airway* or airflow* or bronch* or respirat*)) or COPD or COAD or COBD or AECB) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 5 | 849,488 | TS=(diabet* or IDDM or NIDDM or MODY or T1DM or T2DM or T1D or T2D or non insulin* depend* or non insulin* depend* or non insulin?depend* or non insulin?depend* or insulin* depend* or insulin?depend*) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 4 | 4,694,313 | TS= (cancer* or neoplas* or tumo* or carcinoma* or Hodgkin* or nonhodgkin* or adenocarcinoma* or leuk?emia* or metasta* or malignan* or lymphoma* or sarcoma* or melanoma* or myeloma* or oncolog*) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 3 | 1,602,108 | TS=(cardiovascular or ((heart or cardiac or myocardial) near/2 (failure or infarc* or attack*)) or hypertens* or blood pressure or bloodpressure) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 2 | 279,490 | TS=((“primary care “ or “primary health care “ or “primary healthcare “) or (“general practi* “ or “family practi* “ or “family medicine “ or GP)) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
| # 1 | 3,086,781 | TS= (review* or (literature near/4 search*) or meta-analys* or metaanalys*) Indexes=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan=All years |
Scopus
-
((Title-abs-key(review* or (literature w/4 search*) or meta-analys* or metaanalys*)) and (Title-abs-key((“primary care “ or “primary health care “ or “primary healthcare “) or (“general practi* “ or “family practi* “ or “family medicine “ or GP))) and (Title-abs-key(cardiovascular or ((heart or cardiac or myocardial) w/2 (failure or infarc* or attack*)) or hypertens* or blood pressure or bloodpressure) OR TITLE-ABS-KEY((cancer* or neoplas* or tumo* or carcinoma* or Hodgkin* or nonhodgkin* or adenocarcinoma* or leuk#emia* or metasta* or malignan* or lymphoma* or sarcoma* or melanoma* or myeloma* or oncolog*)) OR TITLE-ABS-KEY((diabet* or IDDM or NIDDM or MODY or T1DM or T2DM or T1D or T2D or “non insulin* depend*” or “non insulin* depend*” or “non insulin#depend*” or “non insulin#depend*” or “insulin* depend*” or insulin#depend*)) OR TITLE-ABS-KEY((emphysema* or asthma* or (chronic* w/3 bronchiti*) or (obstruct* w/3 (pulmonary or lung* or airway* or airflow* or bronch* or respirat*)) or COPD or COAD or COBD or AECB))) and ((TITLE-ABS-KEY(neighbo?rhood* or “residential environment*” or inner?city or “housing instability” or “housing insecurity” or “housing strain” or “housing security” or “mortgage problems” or foreclosure or eviction* or “housing loss” or “home repossession*” or “home ownership” or (repossess* w/3 hous*) or (repossess* w/3 propert*) or “mortgage delinquency” or “mortgage arrears” or “mortgage debt*” or overcrowding or (living w/1 (outside or inside or near* or adjacent)) or (household w/2 size) or (“marital status” or “marriage status”) or (widow* or cohabit* or divorce* or single parent* or live* alone))) or (TITLE-ABS-KEY(minorit* or “migration background” or racial or racism or ethnology or race or ethnic* or non#English or “language other than” or latino* or latina* or hispanic* or whites or caucasian* or non?white or “Torres Strait Islander” or aboriginal or “native american” or inuit or eskimo or “first nation*” or indigenous or “english as a second language” or “foreign language” or “cultural deprivation” or acculturation or “cultural diversity” or transient* or migrant* or emigra* or immigra* or “minority group*” or prejudic* or “cultural bias” or discriminat* or refugee*) OR TITLE-ABS-KEY((occupation* or unemploy*))) or (TITLE-ABS-KEY((“sex disparit*” or “sex difference*” or “gender identity” or “sex role” or “sex factor*” or “wom#n* role*” or “m#n* role*” or “gender* role*” or servicewomen or “gender difference*”)) OR TITLE-ABS-KEY(Schooling or “educational status” or (education* w/2 level*) or ((higher or better or worse or less) w/1 educated) or ((higher or better or worse or less) w/1 level* of education)) OR TITLE-ABS-KEY((religi*))) or (TITLE-ABS-KEY(disparit* or inequalit* or inequit* or equity or deprivation or gini or “concentration index” or “Social class*” or “social determinant*” or “social status” or “social position” or “social background” or “social circumstance*” or socio-economic or socioeconomic or sociodemographic or socio-demographic or SES or disadvantaged or impoverished or poverty or “economic level” or “assets index” or income*) OR TITLE-ABS-KEY(“social exclusion” or (social w/1 (capital or cohes* or organis* or organiz*)) or (community w/3 (cohes* or participa*)) or ((neighbourhood or neighborhood) w/1 cohes*) or “social relationship*” or “social network*” or “collective efficacy” or “civil society” or “informal social control” or “neighbo*rhood disorder” or “social disorgani?ation” or anomie or “social support” or “social participation” or trust or “emotional support” or “psychosocial support” or “community capital” or “neighbo?rhood cohesion” or “social influence” or (soci?context* or soci*-context*))) or (TITLE-ABS-KEY((“health?care disparit*” or “health status disparit*” or “health disparit*” or “health inequalit*” or “health inequit*” or “medically underserved” or “health services accessibilty”)) OR TITLE-ABS-KEY(“potential determinants” or “significant correlates of” or (“independent correlates” or “independent association*”) or “variables associated with” or “determinants of” or “factors associated with” or “identif* determinants” or (“more likely” or “less likely” or “just as likely”) or “risk factors for” or (“significantly related to” or “significant predictor”) or (also w/2 “associated with”) or (“at increased risk” or “at decreased risk”) or “association* between” or (“positively associated” or “negatively associated”) or “differed by” or (“were high* amongst” or “were low* amongst”) or (“inverse relationship with” or “inversely associated with” or “inversely related to”) or “reverse association” or “differentially affects” or “evidence of a link between” or (significantly w/3 “likelihood of”) or “protective factors for” or (differ* w/2 “according to”) or (inverse w/2 gradient) or (positive w/2 gradient) or (negative w/2 gradient) or (“trends were” w/3 across) or (“related to” w/3 variable*) or (“differences were” w/3 “explained by”) or (“significant among”))))) and not (Title-abs-key (afghanistan OR albania OR algeria OR “american samoa” OR angola OR “antigua and barbuda” OR antigua OR barbuda OR argentina OR armenia OR armenian OR aruba OR azerbaijan OR bahrain OR bangladesh OR barbados OR “republic of belarus” OR belarus OR byelarus OR belorussia OR byelorussian OR belize OR “british honduras” OR benin OR dahomey OR bhutan OR bolivia OR “bosnia and herzegovina” OR bosnia OR herzegovina OR botswana OR bechuanaland OR brazil OR brasil OR bulgaria OR “burkina faso” OR “burkina fasso” OR “upper volta” OR burundi OR urundi OR “cabo verde” OR “cape verde” OR cambodia OR kampuchea OR “khmer republic” OR cameroon OR cameron OR cameroun OR “central african republic” OR “ubangi shari” OR chad OR chile OR china OR colombia OR comoros OR “comoro islands” OR “iles comores” OR mayotte OR “democratic republic of the congo” OR “democratic republic congo” OR congo OR zaire OR “costa rica” OR “cote divoire” OR “cote d ivoire” OR “cote divoire” OR “cote d ivoire” OR “ivory coast” OR croatia OR cuba OR cyprus OR “czech republic” OR czechoslovakia OR djibouti OR “french somaliland” OR dominica OR “dominican republic” OR ecuador OR egypt OR “united arab republic” OR “el salvador” OR “equatorial guinea” OR “spanish guinea” OR eritrea OR estonia OR eswatini OR swaziland OR ethiopia OR fiji OR gabon OR “gabonese republic” OR gambia OR “georgia (republic) “ OR georgian OR ghana OR “gold coast” OR gibraltar OR greece OR grenada OR guam OR guatemala OR guinea OR “guinea bissau” OR guyana OR “british guiana” OR haiti OR hispaniola OR honduras OR hungary OR india OR indonesia OR timor OR iran OR iraq OR” isle of man” OR jamaica OR jordan OR kazakhstan OR kazakh OR kenya OR “democratic peoples republic of korea” OR “republic of korea” OR “north korea” OR “south korea” OR korea OR kosovo OR kyrgyzstan OR kirghizia OR kirgizstan OR “kyrgyz republic” OR kirghiz OR laos OR “lao pdr” OR “lao people’s democratic republic” OR latvia OR lebanon OR “lebanese republic” OR lesotho OR basutoland OR liberia OR libya OR “libyan arab jamahiriya” OR lithuania OR macau OR macao OR “macedonia (republic) “ OR macedonia OR madagascar OR “malagasy republic” OR malawi OR nyasaland OR malaysia OR “malay federation” OR “malaya federation” OR maldives OR “indian ocean islands” OR “indian ocean” OR mali OR malta OR micronesia OR “federated states of micronesia” OR kiribati OR “marshall islands” OR nauru OR “northern mariana islands” OR palau OR tuvalu OR mauritania OR mauritius OR mexico OR moldova OR moldovian OR mongolia OR montenegro OR “montenegro (republic) “ OR morocco OR ifni OR mozambique OR “portuguese east africa” OR myanmar OR burma OR namibia OR nepal OR “netherlands antilles” OR nicaragua OR niger OR nigeria OR oman OR muscat OR pakistan OR panama OR “papua new guinea” OR “new guinea” OR paraguay OR peru OR philippines OR philipines OR phillipines OR phillippines OR poland OR “polish people’s republic” OR portugal OR “portuguese republic” OR puerto rico OR romania OR russia OR “russian federation” OR ussr OR “soviet union” OR “union of soviet socialist republics” OR rwanda OR ruanda OR samoa OR “pacific islands” OR polynesia OR “samoan islands” OR “navigator island” OR “navigator islands” OR “sao tome and principe” OR “saudi arabia” OR senegal OR serbia OR seychelles OR “sierra leone” OR slovakia OR “slovak republic” OR slovenia OR melanesia OR “solomon island” OR “solomon islands” OR “norfolk island” OR “norfolk islands” OR somalia OR “south africa” OR “south sudan” OR “sri lanka” OR ceylon OR “saint kitts and nevis” OR “st. kitts and nevis” OR “saint lucia” OR “st. lucia” OR “saint vincent and the grenadines” OR “saint vincent” OR “st. vincent” OR grenadines OR sudan OR suriname OR surinam OR “dutch guiana” OR “netherlands guiana” OR syria OR “syrian arab republic” OR tajikistan OR tadjikistan OR tadzhikistan OR tadzhik OR tanzania OR tanganyika OR thailand OR siam OR “timor leste” OR “east timor” OR togo OR “togolese republic” OR tonga OR “trinidad and tobago” OR trinidad OR tobago OR tunisia OR turkey OR “turkey (republic) “ OR turkmenistan OR turkmen OR uganda OR ukraine OR uruguay OR uzbekistan OR uzbek OR vanuatu OR “new hebrides” OR venezuela OR vietnam OR “viet nam” OR “middle east” OR “west bank” OR gaza OR palestine OR yemen OR yugoslavia OR zambia OR zimbabwe OR “northern rhodesia” OR “global south” OR “africa south of the sahara” OR “sub saharan africa” OR “subsaharan africa” OR “africa, central” OR “central africa” OR “africa, northern” OR “north africa” OR “northern africa” OR magreb OR maghrib OR sahara OR “africa, southern” OR “southern africa” OR “africa, eastern” OR “east africa” OR “eastern africa” OR “africa, western” OR “west africa” OR “western africa” OR “west indies” OR “indian ocean islands” OR “caribbean region” OR “caribbean islands” OR caribbean OR “central america” OR “latin america” OR “south and central america” OR “south america” OR “asia, central” OR “central asia” OR “asia, northern” OR “north asia” OR “northern asia” OR “asia, southeastern” OR “southeastern asia” OR “south eastern asia” OR “southeast asia” OR “south east asia” OR “asia, western” OR “western asia” OR “europe, eastern” OR “east europe” OR “eastern europe” OR “developing country” OR “developing countries” OR “developing nation?” OR “developing population?” OR “developing world” OR “less developed countr*” OR” less developed nation?” OR “less developed population?” OR “less developed world” OR “lesser developed countr*” OR “lesser developed nation?” OR “lesser developed population?” OR “lesser developed world” OR “under developed countr*” OR “under developed nation?” OR “under developed population?” OR “under developed world” OR “underdeveloped countr*” OR “underdeveloped nation?” OR “underdeveloped population?” OR “underdeveloped world” OR “middle income countr*” OR “middle income nation?” OR “middle income population?” OR “low income countr*” OR “low income nation?” OR “low income population?” OR “lower income countr*” OR “lower income nation?” OR “lower income population?” OR “underserved countr*” OR “underserved nation?” OR “underserved population?” OR “underserved world” OR “under served countr”* OR “under served nation?” OR “under served population?” OR “under served world” OR “deprived countr*” OR “deprived nation?” OR “deprived population?” OR “deprived world” OR “poor countr*” OR “poor nation?” OR “poor population?” OR “poor world” OR “poorer countr*” OR “poorer nation?” OR “poorer population?” OR “poorer world” OR “developing econom*” OR “less developed econom*” OR “lesser developed econom*” OR “under developed econom*” OR “underdeveloped econom*” OR “middle income econom*” OR “low income econom*” OR “lower income econom*” OR “low gdp” OR “low gnp” OR “low gross domestic” OR” low gross national” OR “lower gdp” OR “lower gnp” OR “lower gross domestic” OR “lower gross national” OR lmic OR lmics OR “third world” OR “lami countr*” OR “transitional countr*” OR “emerging economies” OR “emerging nation*”))
ASSIA
-
(ti((review* OR (literature NEAR/4 search*) OR meta-analys* OR metaanalys*)) OR ab((review* OR (literature NEAR/4 search*) OR meta-analys* OR metaanalys*))) AND (ti(((“primary care “ OR “primary health care “ OR “primary healthcare “) OR (“general practi* “ OR “family practi* “ OR “family medicine “ OR GP))) OR ab(((“primary care “ OR “primary health care “ OR “primary healthcare “) OR (“general practi* “ OR “family practi* “ OR “family medicine “ OR GP)))) AND (ti((emphysema* OR asthma* OR (chronic* NEAR/3 bronchiti*) OR (obstruct* NEAR/3 (pulmonary OR lung* OR airway* OR airflow* OR bronch* OR respirat*)) OR COPD OR COAD OR COBD OR AECB) OR (diabet* OR IDDM OR NIDDM OR MODY OR T1DM OR T2DM OR T1D OR T2D OR non insulin* depend* OR non insulin* depend* OR non insulin?depend* OR non insulin?depend* OR insulin* depend* OR insulin?depend*) OR (cancer* OR neoplas* OR tumo* OR carcinoma* OR Hodgkin* OR nonhodgkin* OR adenocarcinoma* OR leuk?emia* OR metasta* OR malignan* OR lymphoma* OR sarcoma* OR melanoma* OR myeloma* OR oncolog*) OR (cardiovascular OR ((heart OR cardiac OR myocardial) NEAR/2 (failure OR infarc* OR attack*)) OR hypertens* OR blood pressure OR bloodpressure)) OR ab((emphysema* OR asthma* OR (chronic* NEAR/3 bronchiti*) OR (obstruct* NEAR/3 (pulmonary OR lung* OR airway* OR airflow* OR bronch* OR respirat*)) OR COPD OR COAD OR COBD OR AECB) OR (diabet* OR IDDM OR NIDDM OR MODY OR T1DM OR T2DM OR T1D OR T2D OR non insulin* depend* OR non insulin* depend* OR non insulin?depend* OR non insulin?depend* OR insulin* depend* OR insulin?depend*) OR (cancer* OR neoplas* OR tumo* OR carcinoma* OR Hodgkin* OR nonhodgkin* OR adenocarcinoma* OR leuk?emia* OR metasta* OR malignan* OR lymphoma* OR sarcoma* OR melanoma* OR myeloma* OR oncolog*) OR (cardiovascular OR ((heart OR cardiac OR myocardial) NEAR/2 (failure OR infarc* OR attack*)) OR hypertens* OR blood pressure OR bloodpressure)))
Appendix 3 List of studies included in evidence synthesis
| Authors | Year | Title | Journal | Volume | Issue | Pages |
|---|---|---|---|---|---|---|
| H. R. Baradaran; R. P. Knill-Jones; S. Wallia; A. Rodgers | 2006 | A controlled trial of the effectiveness of a diabetes education programme in a multi-ethnic community in Glasgow [ISRCT28317455] | BMC Public Health | 6 | ||
| J. P. Migneault; J. J. Dedier; J. A. Wright; T. Heeren; M. K. Campbell; D. E. Morisky; P. Rudd; R. H. Friedman | 2012 | A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African-Americans: a randomized controlled trial | Annals of Behavioral Medicine | 43 | 1 | 62–73 |
| M. J. Shen; M. Binz-Scharf; T. D'Agostino; N. Blakeney; E. Weiss; M. Michaels; S. Patel; M. D. McKee; C. L. Bylund | 2015 | A mixed-methods examination of communication between oncologists and primary care providers among primary care physicians in underserved communities | Cancer | 121 | 6 | 908–915 |
| M. Modell; B. Wonke; E. Anionwu; M. Khan; S. S. Tai; M. Lloyd; B. Modell | 1998 | A multidisciplinary approach for improving services in primary care: randomised controlled trial of screening for haemoglobin disorders | British Medical Journal | 317 | 7161 | 788–791 |
| R. Raine; S. M. Moss; C. Von Wagner; W. Atkin; I. K. Hans; R. Howe; F. Solmi; S. Morris; N. Counsell; A. Hackshaw; S. Halloran; G. Handley; R. F. Logan; S. Rainbow; S. Smith; J. Snowball; H. Seaman; M. Thomas; S. G. Smith; L. M. McGregor; G. Vart; J. Wardle; S. W. Duffy | 2016 | A national cluster-randomised controlled trial to examine the effect of enhanced reminders on the socioeconomic gradient in uptake in bowel cancer screening | British Journal of Cancer | 115 | 12 | 1479–1486 |
| R. Whittemore; G. D. e. Melkus; A. Sullivan; M. Grey | 2004 | A nurse-coaching intervention for women with type 2 diabetes | The Diabetes Educator | 30 | 5 | 795–804 |
| E. L. Carter; G. Nunlee-Bland; C. Callender | 2011 | A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities | Perspectives in Health Information Management / AHIMA, American Health Information Management Association | 8 | 1 | 101–106 |
| A. Vyas; A. Z. Haidery; P. G. Wiles; S. Gill; C. Roberts; J. K. Cruickshank | 2003 | A pilot randomized trial in primary care to investigate and improve knowledge, awareness and self-management among South Asians with diabetes in Manchester | Diabetic Medicine | 20 | 12 | 1022–1026 |
| G. Ogedegbe; W. Chaplin; A. Schoenthaler; D. Statman; D. Berger; T. Richardson; E. Phillips; J. Spencer; J. P. Allegrante | 2008 | A practice-based trial of motivational interviewing and adherence in hypertensive African Americans | American Journal of Hypertension | 21 | 10 | 1137–1143 |
| P. D. Martin; P. C. Rhode; G. R. Dutton; S. M. Redmann; D. H. Ryan; P. J. Brantley | 2006 | A primary care weight management intervention for low-income African-American women | Obesity | 14 | 8 | 1412–1420 |
| F. D. R. Hobbs; D. A. Fitzmaurice; J. Mant; E. Murray; S. Jowett; S. Bryan; J. Raftery; M. Davies; G. Lip | 2005 | A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) vs. routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study | Health Technology Assessment | 9 | 40 | 609–620 |
| A. Valdez; A. M. Napoles; S. L. Stewart; A. Garza | 2018 | A randomized controlled trial of a cervical cancer education intervention for Latinas delivered through interactive, multimedia kiosks | Journal of Cancer Education | 33 | 1 | 222–230 |
| J. Sellors; J. Kaczorowski; C. Sellors; L. Dolovich; C. Woodward; A. Willan; R. Goeree; R. Cosby; K. Trim; R. Sebaldt; M. Howard; L. Hardcastle; J. Poston | 2003 | A randomized controlled trial of a pharmacist consultation program for family physicians and their elderly patients | CMAJ. Canadian Medical Association Journal | 169 | 1 | 17–22 |
| R. E. Myers; R. Sifri; T. Hyslop; M. Rosenthal; S. W. Vernon; J. Cocroft; T. Wolf; J. Andrel; R. Wender | 2007 | A randomized controlled trial of the impact of targeted and tailored interventions on colorectal cancer screening | Cancer | 110 | 9 | 2083–2091 |
| B. J. Turner; C. S. Hollenbeak; Y. Liang; K. Pandit; S. Joseph; M. G. Weiner | 2012 | A randomized trial of peer coach and office staff support to reduce coronary heart disease risk in African-Americans with uncontrolled hypertension | Journal of General Internal Medicine | 27 | 10 | 1258–1264 |
| E. Muggah; S. Dahrouge; W. Hogg | 2012 | Access to primary health care for immigrants: results of a patient survey conducted in 137 primary care practices in Ontario, Canada | BMC Family Practice | 13 | 4 | 128–128 |
| M. C. Gulliford; M. Ashworth; D. Robotham; A. Mohiddin | 2007 | Achievement of metabolic targets for diabetes by English primary care practices under a new system of incentives | Diabetic Medicine | 24 | 5 | 505–511 |
| J. R. Thompson; C. Horton; C. Flores | 2007 | Advancing diabetes self-management in the Mexican American population: a community health worker model in a primary care setting | Diabetes Educator | 33 | Suppl. 6 | 221–230 |
| R. E. Jordan; R. J. Lancashire; P. Adab | 2011 | An evaluation of Birmingham Own Health telephone care management service among patients with poorly controlled diabetes. A retrospective comparison with the General Practice Research Database | BMC Public Health | 11 | 21 | 1988–1995 |
| D. C. Ziemer; J. P. Doyle; C. S. Barnes; W. T. Branch; C. B. Cook; I. M. El-Kebbi; D. L. Gallina; P. Kolm; M. K. Rhee; L. S. Phillips | 2006 | An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes (IPCAAD) 8 | Archives of Internal Medicine | 166 | 5 | 507–513 |
| C. A'Court; H. Atherton; A. Dalton; S. Fleming; J. Hirst; D. Nunan; M. Selwood; R. J. McManus | 2013 | Are there enough GPs in England to detect hypertension and maintain access? | British Journal of General Practice | 63 | 612 | 346–347 |
| S. de Lusignana; H. Gallagher; S. Jones; T. Chan; J. van Vlymen; A. Tahir; N. Thomas; N. Jain; O. Dmitrieva; I. Rafi; A. McGovern; K. Harris | 2013 | Audit-based education lowers systolic blood pressure in chronic kidney disease: the Quality Improvement in CKD (QICKD) trial results | Kidney International | 84 | 3 | 609–620 |
| G. G. Bennett; P. Foley; E. Levine; J. Whiteley; S. Askew; D. M. Steinberg; B. Batch; M. L. Greaney; H. Miranda; T. H. Wroth; M. G. Holder; K. M. Emmons; E. Puleo | 2013 | Behavioral treatment for weight gain prevention among black women in primary care practice: a randomized clinical trial | JAMA Internal Medicine | 173 | 19 | 1770–1777 |
| A. A. Laverty; A. Bottle; A. Majeed; C. Millett | 2011 | Blood pressure monitoring and control by cardiovascular disease status in UK primary care: 10 year retrospective cohort study 1998–2007 | Journal of Public Health | 33 | 2 | 302–309 |
| P. M. Lantz; D. Stencil; M. T. Lippert; S. Beversdorf; L. Jaros; P. L. Remington | 1995 | Breast and cervical cancer screening in a low-income managed care sample: the efficacy of physician letters and phone calls | American Journal of Public Health | 85 | 6 | 834–836 |
| S. A. Berkowitz; S. Percac-Lima; J. M. Ashburner; Y. Chang; A. H. Zai; W. He; R. W. Grant; S. J. Atlas | 2015 | Building equity improvement into quality improvement: reducing socioeconomic disparities in colorectal cancer screening as part of population health management | Journal of General Internal Medicine | 30 | 942–949 | |
| T. Hoare; C. Thomas; A. Biggs; M. Booth; S. Bradley; E. Friedman | 1994 | Can the uptake of breast screening by asian women be increased? A randomized controlled trial of a linkworker intervention | Journal of Public Health | 16 | 2 | 179–185 |
| T. Green; K. Atkin; U. Macleod | 2015 | Cancer detection in primary care: insights from general practitioners | British Journal of Cancer | 112 | 6 | S41–S49 |
| F. Gany; C. Trinh-Shevrin; A. Aragones | 2008 | Cancer screening and Haitian immigrants: the primary care provider factor | Journal of Immigrant and Minority Health | 10 | 3 | 255–261 |
| D. P. Peiris; A. A. Patel; A. Cass; M. P. Howard; M. L. Tchan; J. P. Brady; J. De Vries; B. A. Rickards; D. J. Yarnold; N. E. Hayman; A. D. Brown | 2009 | Cardiovascular disease risk management for Aboriginal and Torres Strait Islander peoples in primary health care settings: findings from the Kanyini Audit | Medical Journal of Australia | 191 | 6 | 304–309 |
| D. Baker; E. Middleton | 2003 | Cervical screening and health inequality in England in the 1990s | Journal of Epidemiology and Community Health | 57 | 6 | 417–423 |
| P. J. Fagan; A. B. Schuster; C. Boyd; J. A. Marsteller; M. Griswold; S. M. E. Murphy; L. Dunbar; C. B. Forrest | 2010 | Chronic care improvement in primary care: evaluation of an integrated pay-for-performance and practice-based care coordination program among elderly patients with diabetes | Health Services Research | 45 | 6 PART 1 | 1763–1782 |
| K. Bush; R. Thomas; N. T. Raymond; S. Sankar; P. J. Barker; J. P. O'Hare | 2014 | Cluster randomised controlled trial evaluation of a link worker-delivered intervention to improve uptake of diabetic retinopathy screening in a South Asian population | Diabetes and Vascular Disease Research | 11 | 4 | 294–297 |
| J. K. Allen; C. R. Dennison-Himmelfarb; S. L. Szanton; L. Bone; M. N. Hill; D. M. Levine; M. West; A. Barlow; L. Lewis-Boyer; M. Donnelly-Strozzo; C. Curtis; K. Anderson | 2011 | Community Outreach and Cardiovascular Health (COACH) trial: a randomized, controlled trial of nurse practitioner/community health worker cardiovascular disease risk reduction in urban community health centers | Circulation: Cardiovascular Quality and Outcomes | 4 | 6 | 595–602 |
| V. Champion; M. Maraj; S. Hui; A. J. Perkins; W. Tierney; U. Menon; C. S. Skinner | 2003 | Comparison of tailored interventions to increase mammography screening in nonadherent older women | Preventive Medicine | 36 | 2 | 150–158 |
| E. Banks; V. Beral; R. Cameron; A. Hogg; N. Langley; I. Barnes; D. Bull; G. Reeves; R. English; S. Taylor; J. Elliman; C. L. Harris | 2002 | Comparison of various characteristics of women who do and do not attend for breast cancer screening | Breast Cancer Research | 4 | 1 | 893–898 |
| P. Bray; D. Thompson; J. D. Wynn; D. M. Cummings; L. Whetstone | 2005 | Confronting disparities in diabetes care: the clinical effectiveness of redesigning care management for minority patients in rural primary care practices | Journal of Rural Health | 21 | 4 | 317–321 |
| J. S. Hong; H. C. Kang; J. Kim | 2010 | Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea | Journal of Korean Medical Science | 25 | 9 | 1259–1271 |
| G. Worrall; J. Knight | 2011 | Continuity of care is good for elderly people with diabetes: retrospective cohort study of mortality and hospitalization | Canadian Family Physician | 57 | 1 | 275–283 |
| S. R. Majumdar; L. M. Guirguis; E. L. Toth; R. Z. Lewanczuk; T. K. Lee; J. A. Johnson | 2003 | Controlled trial of a multifaceted intervention for improving quality of care for rural patients with type 2 diabetes | Diabetes care | 26 | 11 | 3061–3066 |
| R. De Mil; E. Guillaume; L. Guittet; O. Dejardin; V. Bouvier; C. Pornet; V. Christophe; A. Notari; H. Delattre-Massy; C. De Seze; J. Peng; G. Launoy; C. Berchi | 2018 | Cost-effectiveness analysis of a navigation program for colorectal cancer screening to reduce social health inequalities: a French cluster randomized controlled trial | Value in Health | 21 | 6 | 685–691 |
| J. K. Allen; C. R. Dennison Himmelfarb; S. L. Szanton; K. D. Frick | 2014 | Cost-effectiveness of nurse practitioner/community health worker care to reduce cardiovascular health disparities | Journal of Cardiovascular Nursing | 29 | 4 | 308–314 |
| G. Ogedegbe; J. N. Tobin; S. Fernandez; A. Cassells; M. Diaz-Gloster; C. Khalida; T. Pickering; J. E. Schwartz | 2014 | Counseling African Americans to control hypertension: cluster-randomized clinical trial main effects | Circulation | 129 | 20 | 2044–2051 |
| E. J. A. J. Beune; E. P. Moll Van Charante; L. Beem; J. Mohrs; C. O. Agyemang; G. Ogedegbe; J. A. Haafkens | 2014 | Culturally adapted hypertension education (CAHE) to improve blood pressure control and treatment adherence in patients of African Origin with uncontrolled hypertension: cluster-randomized trial | PLOS ONE | 9 | 3 | 182–191 |
| D. Vincent | 2009 | Culturally tailored education to promote lifestyle change in Mexican Americans with type 2 diabetes | Journal of the American Academy of Nurse Practitioners | 21 | 9 | 520–527 |
| M. E. Peek; S. A. Harmon; S. J. Scott; M. Eder; T. S. Roberson; H. Tang; M. H. Chin | 2012 | Culturally tailoring patient education and communication skills training to empower African-Americans with diabetes | Translational Behavioral Medicine | 2 | 3 | 296–308 |
| L. Jandorf; C. Braschi; E. Ernstoff; C. R. Wong; L. Thelemaque; G. Winkel; H. S. Thompson; W. H. Redd; S. H. Itzkowitz | 2013 | Culturally targeted patient navigation for increasing African Americans’ adherence to screening colonoscopy: a randomized clinical trial | Cancer Epidemiology Biomarkers and Prevention | 22 | 9 | 1577–1587 |
| R. E. Myers; B. Stello; C. Daskalakis; R. Sifri; E. T. Gonzalez; M. DiCarlo; M. B. Johnson; S. E. Hegarty; K. Shaak; A. Rivera; L. Gordils-Molina; A. Petrich; B. Careyva; R. De-Ortiz; L. Diaz | 2019 | Decision support and navigation to increase colorectal cancer screening among Hispanic patients | Cancer Epidemiology Biomarkers and Prevention | 28 | 2 | 384–391 |
| S. Percac-Lima; J. M. Ashburner; B. Bond; S. A. Oo; S. J. Atlas | 2013 | Decreasing disparities in breast cancer screening in refugee women using culturally tailored patient navigation | Journal of General Internal Medicine | 28 | 11 | 1463–1468 |
| E. A. Phelan; B. Balderson; M. Levine; J. H. Erro; L. Jordan; L. Grothaus; N. Sandhu; P. J. Perrault; J. P. Logerfo; E. H. Wagner | 2007 | Delivering effective primary care to older adults: a randomized, controlled trial of the senior resource team at group health cooperative | Journal of the American Geriatrics Society | 55 | 11 | 1748–1756 |
| G. McLean; M. Sutton; B. Guthrie | 2006 | Deprivation and quality of primary care services: evidence for persistence of the inverse care law from the UK Quality and Outcomes Framework | Journal of Epidemiology and Community Health | 60 | 11 | 917–922 |
| P. J. M. Uitewaal; M. A. Bruijnzeels; R. M. D. Bernsen; A. J. J. Voorham; A. W. Hoes; S. Thomas | 2004 | Diabetes care in Dutch general practice: differences between Turkish immigrants and Dutch patients | European Journal of Public Health | 14 | 1 | 15–18 |
| C. Millett; J. Car; D. Eldred; K. Khunti; A. G. Mainous; A. Majeed | 2007 | Diabetes prevalence, process of care and outcomes in relation to practice size, caseload and deprivation: national cross-sectional study in primary care | Journal of the Royal Society of Medicine | 100 | 6 | 275–283 |
| G. McLean; B. Guthrie; M. Sutton | 2007 | Differences in the quality of primary medical care services by remoteness from urban settlements | Quality and Safety in Health Care | 16 | 6 | 446–449 |
| C. M. Everett; C. T. Thorpe; M. Palta; P. Carayon; V. J. Gilchrist; M. A. Smith | 2013 | Division of primary care services between physicians, physician assistants, and nurse practitioners for older patients with diabetes | Medical Care Research and Review | 70 | 5 | 531–541 |
| S. Robinson; R. B. Baron; B. Cooper; S. Janson | 2009 | Does health service use in a diabetes management program contribute to health disparities at a facility level? optimizing resources with demographic predictors | Population Health Management | 12 | 3 | 139–147 |
| S. Hammouche; R. Holland; N. Steel | 2011 | Does quality of care for hypertension in primary care vary with postcode area deprivation? An observational study | BMC Health Services Research | 11 | 12 | 1015–1051 |
| S. Hardy; P. Hinks; R. Gray | 2014 | Does training practice nurses to carry out physical health checks for people with severe mental illness increase the level of screening for cardiovascular risk? | International Journal of Social Psychiatry | 60 | 3 | 236–242 |
| R. S. Bhopal; A. Douglas; S. Wallia; J. F. Forbes; M. E. J. Lean; J. M. R. Gill; J. A. McKnight; N. Sattar; A. Sheikh; S. H. Wild; J. Tuomilehto; A. Sharma; R. Bhopal; J. B. E. Smith; I. Butcher; G. D. Murray | 2014 | Effect of a lifestyle intervention on weight change in south Asian individuals in the UK at high risk of type 2 diabetes: a family-cluster randomised controlled trial | The Lancet Diabetes and Endocrinology | 2 | 3 | 218–227 |
| R. Alshamsan; J. T. Lee; A. Majeed; G. Netuveli; C. Millett | 2012 | Effect of a UK pay-for-performance program on ethnic disparities in diabetes outcomes: interrupted time series analysis | Annals of Family Medicine | 10 | 3 | 228–234 |
| T. Doran; C. Fullwood; E. Kontopantelis; D. Reeves | 2008 | Effect of financial incentives on inequalities in the delivery of primary clinical care in England: analysis of clinical activity indicators for the quality and outcomes framework | The Lancet | 372 | 9640 | 728–736 |
| M. Ashworth; J. Medina; M. Morgan | 2008 | Effect of social deprivation on blood pressure monitoring and control in England: A survey of data from the quality and outcomes framework | BMJ | 337 | 7680 | 1215–1218 |
| M. Calvert; A. Shankar; R. J. McManus; H. Lester; N. Freemantle | 2009 | Effect of the quality and outcomes framework on diabetes care in the United Kingdom: retrospective cohort study | BMJ (Online) | 338 | 7707 | 1366–1370 |
| J. Wardle; C. Von Wagner; I. Kralj-Hans; S. P. Halloran; S. G. Smith; L. M. McGregor; G. Vart; R. Howe; J. Snowball; G. Handley; R. F. Logan; S. Rainbow; S. Smith; M. C. Thomas; N. Counsell; S. Morris; S. W. Duffy; A. Hackshaw; S. Moss; W. Atkin; R. Raine | 2016 | Effects of evidence-based strategies to reduce the socioeconomic gradient of uptake in the English NHS Bowel Cancer Screening Programme (ASCEND): four cluster-randomised controlled trials | The Lancet | 387 | 10020 | 751–759 |
| M. Stone; E. Pound; A. Pancholi; A. Farooqi; K. Khunti | 2005 | Empowering patients with diabetes: a qualitative primary care study focusing on South Asians in Leicester, UK | Family Practice | 22 | 6 | 647–652 |
| S. McCann; J. Weinman | 1996 | Empowering the patient in the consultation: a pilot study | Patient Education and Counseling | 27 | 3 | 227–234 |
| S. Bellary; J. P. O'Hare; N. T. Raymond; A. Gumber; S. Mughal; A. Szczepura; S. Kumar; A. H. Barnett | 2008 | Enhanced diabetes care to patients of south Asian ethnic origin (the United Kingdom Asian Diabetes Study): a cluster randomised controlled trial | The Lancet | 371 | 9626 | 1769–1776 |
| L. McDermott; A. J. Wright; V. Cornelius; C. Burgess; A. S. Forster; M. Ashworth; B. Khoshaba; P. Clery; F. Fuller; J. Miller; H. Dodhia; C. Rudisill; M. T. Conner; M. C. Gulliford | 2016 | Enhanced invitation methods and uptake of health checks in primary care: randomised controlled trial and cohort study using electronic health records | Health Technology Assessment | 20 | 84 | Jan-92 |
| S. F. McLendon; F. G. Wood; N. Stanley | 2019 | Enhancing diabetes care through care coordination, telemedicine, and education: evaluation of a rural pilot program | Public Health Nursing | 36 | 3 | 310–320 |
| C. Millett; J. Gray; M. Wall; A. Majeed | 2009 | Ethnic disparities in coronary heart disease management and pay for performance in the UK | Journal of General Internal Medicine | 24 | 1 | Aug-13 |
| J. Gray; C. Millett; S. Saxena; G. Netuveli; K. Khunti; A. Majeed | 2007 | Ethnicity and quality of diabetes care in a health system with universal coverage: population-based cross-sectional survey in primary care | Journal of General Internal Medicine | 22 | 9 | 1317–1320 |
| S. Honeycutt; R. Green; D. Ballard; A. Hermstad; A. Brueder; R. Haardörfer; J. Yam; K. J. Arriola | 2013 | Evaluation of a patient navigation program to promote colorectal cancer screening in rural Georgia, USA | Cancer | 119 | 16 | 3059–3066 |
| J. P. O'Hare; N. T. Raymond; S. Mughal; L. Dodd; W. Hanif; Y. Ahmad; K. Mishra; A. Jones; S. Kumar; A. Szczepura; E. W. Hillhouse; A. H. Barnett | 2004 | Evaluation of delivery of enhanced diabetes care to patients of South Asian ethnicity: the United Kingdom Asian Diabetes Study (UKADS) | Diabetic Medicine | 21 | 12 | 1357–1365 |
| A. R. H. Dalton; R. Alshamsan; A. Majeed; C. Millett | 2011 | Exclusion of patients from quality measurement of diabetes care in the UK pay-for-performance programme | Diabetic Medicine | 28 | 5 | 525–531 |
| R. Riley; N. Coghill; A. Montgomery; G. Feder; J. Horwood | 2016 | Experiences of patients and healthcare professionals of NHS cardiovascular health checks: a qualitative study | Journal of Public Health (United Kingdom) | 38 | 3 | 543–551 |
| F. C. Warren; R. Calitri; E. Fletcher; A. Varley; T. A. Holt; V. Lattimer; D. Richards; S. Richards; C. Salisbury; R. S. Taylor; J. L. Campbell | 2015 | Exploring demographic and lifestyle associations with patient experience following telephone triage by a primary care doctor or nurse: secondary analyses from a cluster randomised controlled trial | BMJ Quality and Safety | 24 | 9 | 572–582 |
| S. Attwood; K. Morton; S. Sutton | 2016 | Exploring equity in uptake of the NHS Health Check and a nested physical activity intervention trial | Journal of Public Health (United Kingdom) | 38 | 3 | 560–568 |
| N. Mead; P. Bower; M. Roland | 2008 | Factors associated with enablement in general practice: cross-sectional study using routinely-collected data | British Journal of General Practice | 58 | 550 | 346–352 |
| S. Eilat-Tsanani; M. Sorek; N. Gay; O. Chaimovitch; L. Kulton; H. Tabenkin | 2001 | Family physicians' initiative to increase compliance with screening mammography - an innovative community project | Israel Medical Association Journal | 3 | 12 | 920–924 |
| P. Uitewaal; M. Bruijnzeels; T. De Hoop; A. Hoes; S. Thomas | 2004 | Feasibility of diabetes peer education for Turkish type 2 diabetes patients in Dutch general practice | Patient Education and Counseling | 53 | 3 | 359–363 |
| K. Khunti; S. Ganguli; R. Baker; A. Lowy | 2001 | Features of primary care associated with variations in process and outcome of care of people with diabetes | British Journal of General Practice | 51 | 466 | 356–360 |
| F. L. Hamilton; A. A. Laverty; K. Huckvale; J. Car; A. Majeed; C. Millett | 2016 | Financial incentives and inequalities in smoking cessation interventions in primary care: before-and-after study | Nicotine and Tobacco Research | 18 | 3 | 341–350 |
| K. K. Hyun; J. Redfern; A. Patel; D. Peiris; D. Brieger; D. Sullivan; M. Harris; T. Usherwood; S. MacMahon; M. Lyford; M. Woodward | 2017 | Gender inequalities in cardiovascular risk factor assessment and management in primary healthcare | Heart | 103 | 7 | 500–506 |
| J. McGinn; C. Davis | 2006 | Geographic variation, physician characteristics, and diabetes care disparities in a metropolitan area, 2003–2004 | Diabetes Research and Clinical Practice | 72 | 2 | 162–169 |
| R. S. Weinstock; J. A. Teresi; R. Goland; R. Izquierdo; W. Palmas; J. P. Eimicke; S. Ebner; S. Shea | 2011 | Glycemic control and health disparities in older ethnically diverse underserved adults with diabetes: five-year results from the Informatics for Diabetes Education and Telemedicine (IDEATel) study | Diabetes Care | 34 | 2 | 274–279 |
| C. Thompson; I. Meeuwisse; R. Dahlke; N. Drummond | 2014 | Group medical visits in primary care for patients with diabetes and low socioeconomic status: users’ perspectives and lessons for practitioners | Canadian Journal of Diabetes | 38 | 3 | 198–204 |
| T. Greenhalgh; C. Helman; A. M. m. Chowdhury | 1998 | Health beliefs and folk models of diabetes in British Bangladeshis: a qualitative study | British Medical Journal | 316 | 7136 | 978–983 |
| G. Stapleton; P. Schröder-Bäck; H. Brand; D. Townend | 2014 | Health inequalities and regional specific scarcity in primary care physicians: ethical issues and criteria | International Journal of Public Health | 59 | 3 | 449–455 |
| V. McCleary-Jones | 2011 | Health literacy and its association with diabetes knowledge, self-efficacy and disease self-management among African Americans with diabetes mellitus | The ABNF Journal : Official Journal of the Association of Black Nursing Faculty in Higher Education, Inc | 22 | 2 | 25–32 |
| J. Hippisley-Cox; Coupl; C. | 2012 | Identifying patients with suspected colorectal cancer in primary care: derivation and validation of an algorithm | British Journal of Medical Practice | 62 | 594 | e29–e37 |
| C. Millett; J. Gray; S. Saxena; G. Netuveli; A. Majeed | 2007 | Impact of a pay-for-performance incentive on support for smoking cessation and on smoking prevalence among people with diabetes | CMAJ. Canadian Medical Association Journal | 176 | 12 | 1705–1710 |
| F. L. Hamilton; A. Bottle; E. P. Vamos; V. Curcin; Anthea; M. Molokhia; A. Majeed; C. Millett | 2010 | Impact of a pay-for-performance incentive scheme on age, sex, and socioeconomic disparities in diabetes management in UK primary care | Journal of Ambulatory Care Management | 33 | 4 | 336–349 |
| R. Raine; S. W. Duffy; J. Wardle; F. Solmi; S. Morris; R. Howe; I. Kralj-Hans; J. Snowball; N. Counsell; S. Moss; A. Hackshaw; C. Von Wagner; G. Vart; L. M. McGregor; S. G. Smith; S. Halloran; G. Handley; R. F. Logan; S. Rainbow; S. Smith; M. C. Thomas; W. Atkin | 2016 | Impact of general practice endorsement on the social gradient in uptake in bowel cancer screening | British Journal of Cancer | 114 | 3 | 321–326 |
| C. Millett; S. Saxena; G. Netuveli; A. Majeed | 2009 | Impact of pay for performance on ethnic disparities in intermediate outcomes for diabetes: a longitudinal study | Diabetes Care | 32 | 3 | 404–409 |
| D. Crawley; A. Ng; A. G. Mainous; A. Majeed; C. Millett | 2009 | Impact of pay for performance on quality of chronic disease management by social class group in England | Journal of the Royal Society of Medicine | 102 | 3 | 103–107 |
| S. J. Lang; G. A. Abel; J. Mant; R. Mullis | 2016 | Impact of socioeconomic deprivation on screening for cardiovascular disease risk in a primary prevention population: a cross-sectional study | BMJ Open | 6 | 3 | S417–S424 |
| C. R. Simpson; P. C. Hannaford; L. D. Ritchie; A. Sheikh; D. Williams | 2011 | Impact of the pay-for-performance contract and the management of hypertension in Scottish primary care: a 6–year population-based repeated cross-sectional study | British Journal of General Practice | 61 | 588 | 1123–1129 |
| A. R. H. Dalton; A. Bottle; C. Okoro; A. Majeed; C. Millett | 2011 | Implementation of the NHS Health Checks programme: baseline assessment of risk factor recording in an urban culturally diverse setting | Family Practice | 28 | 1 | 34–40 |
| B. J. McElmurry; L. L. McCreary; C. G. Park; L. Ramos; E. Martinez; R. Parikh; K. Kozik; L. Fogelfeld | 2009 | Implementation, outcomes, and lessons learned from a collaborative primary health care program to improve diabetes care among urban Latino populations | Health Promotion Practice | 10 | 2 | 293–302 |
| P. Bray; D. M. Cummings; S. Morrissey; D. Thompson; D. Holbert; K. Wilson; E. Lukosius; R. Tanenberg | 2013 | Improved outcomes in diabetes care for rural African Americans | Annals of Family Medicine | 11 | 2 | 145–150 |
| S. Hull; T. A. Chowdhury; R. Mathur; J. Robson | 2014 | Improving outcomes for patients with type 2 diabetes using general practice networks: a quality improvement project in east London | BMJ Quality and Safety | 23 | 2 | 171–176 |
| J. R. Fann; M. Y. Fan; J. Unützer | 2009 | Improving primary care for older adults with cancer and depression | Journal of General Internal Medicine | 24 | SUPPL. 2 | 1083–1089 |
| J. Atri; M. Falshaw; R. Gregg; J. Robson; R. Z. Omar; S. Dixon | 1997 | Improving uptake of breast screening in multiethnic populations: a randomised controlled trial using practice reception staff to contact non-attenders | British Medical Journal | 315 | 7119 | 1356–1359 |
| R. E. Myers; R. Sifri; C. Daskalakis; M. DiCarlo; P. R. Geethakumari; J. Cocroft; C. Minnick; N. Brisbon; S. W. Vernon | 2014 | Increasing colon cancer screening in primary care among African Americans | Journal of the National Cancer Institute | 106 | 12 | 734–746 |
| A. Wennerstrom; T. Bui; J. Harden-Barrios; E. G. Price-Haywood | 2015 | Integrating community health workers into a patient-centered medical home to support disease self-management among Vietnamese Americans: lessons learned | Health Promotion Practice | 16 | 1 | 72–83 |
| R. Michielutte; P. C. Sharp; K. L. Foley; L. E. Cunningham; J. G. Spangler; E. D. Paskett; L. D. Case | 2005 | Intervention to increase screening mammography among women 65 and older | Health Education Research | 20 | 2 | 149–162 |
| T. S. Bell; L. K. Branston; R. G. Newcombe; G. R. Barton | 1999 | Interventions to improve uptake of breast screening in inner city Cardiff general practices with ethnic minority lists | Ethnicity and Health | 4 | 4 | 277–284 |
| M. P. McGovern; D. J. Williams; P. C. Hannaford; M. W. Taylor; K. E. Lefevre; M. A. Boroujerdi; C. R. Simpson | 2008 | Introduction of a new incentive and target-based contract for family physicians in the UK: good for older patients with diabetes but less good for women? | Diabetic Medicine | 25 | 9 | 1083–1089 |
| S. Hardy; R. Gray | 2012 | Is the use of an invitation letter effective in prompting patients with severe mental illness to attend a primary care physical health check? | Primary Health Care Research & Development | 13 | 4 | 347–352 |
| H. Ismail; S. Kelly | 2015 | Lessons learned from England’s Health Checks Programme: using qualitative research to identify and share best practice | BMC Family Practice | 16 | 1 | 428–434 |
| S. W. Mercer; B. Fitzpatrick; G. Gourlay; G. Vojt; A. McConnachie; G. C. M. Watt | 2007 | More time for complex consultations in a high-deprivation practice is associated with increased patient enablement | British Journal of General Practice | 57 | 545 | 960–966 |
| J. Robson; I. Dostal; V. Madurasinghe; A. Sheikh; S. Hull; K. Boomla; C. Griffiths; S. Eldridge | 2017 | NHS Health Check comorbidity and management: an observational matched study in primary care | British Journal of General Practice | 67 | 655 | e86–e93 |
| P. J. M. Uitewaal; A. J. J. Voorham; M. A. Bruijnzeels; A. Berghout; R. M. D. Bernsen; P. H. Trienekens; A. W. Hoes; S. Thomas | 2005 | No clear effect of diabetes education on glycaemic control for Turkish type 2 diabetes patients: a controlled experiment in general practice | Netherlands Journal of Medicine | 63 | 11 | 428–434 |
| A. Roots; M. MacDonald | 2014 | Outcomes associated with nurse practitioners in collaborative practice with general practitioners in rural settings in Canada: a mixed methods study | Human Resources for Health | 12 | 1 | 45–52 |
| J. Wright; D. Martin; S. Cockings; C. Polack | 2006 | Overall Quality of Outcomes Framework scores lower in practices in deprived areas | British Journal of General Practice | 56 | 525 | 277–279 |
| S. W. Mercer; B. D. Jani; M. Maxwell; S. Y. S. Wong; G. C. M. Watt | 2012 | Patient enablement requires physician empathy: a cross-sectional study of general practice consultations in areas of high and low socioeconomic deprivation in Scotland | BMC Family Practice | 13 | 2 | 123–129 |
| K. E. Lasser; K. S. Kenst; L. M. Quintiliani; R. S. Wiener; J. Murillo; L. Pbert; Z. Xuan; D. J. Bowen | 2013 | Patient navigation to promote smoking cessation among low-income orimary care patients: a pilot randomized controlled trial | Journal of Ethnicity in Substance Abuse | 12 | 4 | 374–390 |
| T. Doran; C. Fullwood; H. Gravelle; D. Reeves; E. Kontopantelis; U. Hiroeh; M. Roland | 2006 | Pay-for-performance programs in family practices in the United Kingdom | New England Journal of Medicine | 355 | 4 | 375–384 |
| M. M. Safford; S. Andreae; A. L. Cherrington; M. Y. Martin; J. Halanych; M. Lewis; A. Patel; E. Johnson; D. Clark; C. Gamboa; J. S. Richman | 2015 | Peer coaches to improve diabetes outcomes in rural Alabama: a cluster randomized trial | Annals of Family Medicine | 13 | 1 | S18–S26 |
| A. Philis-Tsimikas; A. Fortmann; L. Lleva-Ocana; C. Walker; L. C. Gallo | 2011 | Peer-led diabetes education programs in high-risk Mexican Americans improve glycemic control compared with standard approaches: a Project Dulce promotora randomized trial | Diabetes Care | 34 | 9 | 1926–1931 |
| C. S. Skinner; V. J. Strecher; H. Hospers | 1994 | Physicians' recommendations for mammography: do tailored messages make a difference? | American Journal of Public Health | 84 | 1 | 43–49 |
| E. J. Mayer-Davis; A. M. D'Antonio; S. M. Smith; G. Kirkner; S. L. Martin; D. Parra-Medina; R. Schultz | 2004 | Pounds off with empowerment (POWER): a clinical trial of weight management strategies for black and white adults with diabetes who live in medically underserved rural communities | American Journal of Public Health | 94 | 10 | 1736–1742 |
| S. Saxena; J. Car; D. Eldred; M. Soljak; A. Majeed | 2007 | Practice size, caseload, deprivation and quality of care of patients with coronary heart disease, hypertension and stroke in primary care: national cross-sectional study | BMC Health Services Research | 7 | 10 | 1137–1143 |
| J. Hippisley-Cox; C. Coupland; Y. Vinogradova; J. Robson; R. Minhas; A. Sheikh; P. Brindle | 2008 | Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2 | BMJ | 336 | 7659 | 1475–1482 |
| M. Exworthy; V. Morcillo | 2019 | Primary care doctors’ understandings of and strategies to tackle health inequalities: a qualitative study | Primary Health Care Research and Development | 20 | ||
| R. Delpech; V. Ringa; H. Falcoff; L. Rigal | 2016 | Primary prevention of cardiovascular disease: more patient gender-based differences in risk evaluation among male general practitioners | European Journal of Preventive Cardiology | 23 | 17 | 1831–1838 |
| J. S. Haas; A. L. Jeffrey; R. P. Elyse; G. Irina; A. R. Nancy; V. K. Elissa; Z. K. Emily; M. Z. Alan; B. Phyllis; X. M. Lucasc; S. H. Stella; W. F. Eric; R. W. David | 2015 | Proactive tobacco cessation outreach to smokers of lowsocioeconomic status: a randomized clinical trial | JAMA Internal Medicine | 175 | 2 | 218–226 |
| A. Farooqi; M. Bhavsar | 2001 | Project Dil: a co-ordinated primary care and community health promotion programme for reducing risk factors of coronary heart disease amongst the South Asian community of Leicester – experiences and evaluation of the project | Ethnicity and Health | 6 | 03-Apr | 265–275 |
| S. P. Tu; V. Taylor; Y. Yasui; A. Chun; M. P. Yip; E. Acorda; L. Li; R. Bastani | 2006 | Promoting culturally appropriate colorectal cancer screening through a health educator: a randomized controlled trial | Cancer | 107 | 5 | 959–966 |
| J. Sriskantharajah; J. Kai | 2007 | Promoting physical activity among South Asian women with coronary heart disease and diabetes: What might help? | Family Practice | 24 | 1 | 71–76 |
| A. A. Siddiqui; R. Sifri; T. Hyslop; J. Andrel; M. Rosenthal; S. W. Vernon; J. Cocroft; R. E. Myers | 2011 | Race and response to colon cancer screening interventions | Preventive Medicine | 52 | 03-Apr | 262–264 |
| H. B. Bosworth; M. K. Olsen; J. M. Grubber; B. J. Powers; E. Z. Oddone | 2011 | Racial differences in two self-management hypertension interventions | American Journal of Medicine | 124 | 5 | e731–e738 |
| C. Griffiths; J. Motlib; A. Azad; J. Ramsay; S. Eldridge; G. Feder; R. Khanem; R. Munni; M. Garrett; A. Turner; J. Barlow | 2005 | Randomised controlled trial of a lay-led self-management programme for Bangladeshi patients with chronic disease | British Journal of General Practice | 55 | 520 | 831–837 |
| T. L. Gary; L. R. Bone; M. N. Hill; D. M. Levine; M. McGuire; C. Saudek; F. L. Brancati | 2003 | Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans | Preventive Medicine | 37 | 1 | 23–32 |
| M. C. Rosal; I. S. Ockene; A. Restrepo; M. J. White; A. Borg; B. Olendzki; J. Scavron; L. Candib; G. Welch; G. Reed | 2011 | Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income Latinos: Latinos en control | Diabetes Care | 34 | 4 | 838–844 |
| E. Kontopantelis; D. Reeves; J. M. Valderas; S. Campbell; T. Doran | 2013 | Recorded quality of primary care for patients with diabetes in England before and after the introduction of a financial incentive scheme: a longitudinal observational study | BMJ Quality and Safety | 22 | 1 | 53–64 |
| J. Broomfield; N. Schieda; S. M. Sullivan; L. W. Chambers; J. Kaczorowski; T. Karwalajtys | 2008 | Recording blood pressure readings in elderly patients’ charts: what patient and physician characteristics make it more likely? | Canadian Family Physician | 54 | 2 | 222–230 |
| L. M. McGregor; C. Von Wagner; W. Atkin; I. Kralj-Hans; S. P. Halloran; G. Handley; R. F. Logan; S. Rainbow; S. Smith; J. Snowball; M. C. Thomas; S. G. Smith; G. Vart; R. Howe; N. Counsell; A. Hackshaw; S. Morris; S. W. Duffy; R. Raine; J. Wardle | 2016 | Reducing the social gradient in uptake of the NHS colorectal cancer screening programme using a narrative-based information leaflet: a cluster-randomised trial | Gastroenterology Research and Practice | 2016 | 2 | 135–145 |
| E. G. Eakin; S. S. Bull; K. M. Riley; M. M. Reeves; P. McLaughlin; S. Gutierrez | 2007 | Resources for health: a primary-care-based diet and physical activity intervention targeting urban Latinos with multiple chronic conditions | Health Psychology | 26 | 4 | 392–400 |
| D. A. Fitzmaurice; F. D. R. Hobbs; S. Jowett; J. Mant; E. T. Murray; R. Holder; J. P. Raftery; S. Bryan; M. Davies; G. Y. H. Lip; T. F. Allan | 2007 | Screening vs. routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial | British Medical Journal | 335 | 7616 | 383–386 |
| G. Journath; M. L. Hellénius; U. Petersson; H. Theobald; P. M. Nilsson | 2008 | Sex differences in risk factor control of treated hypertensives: a national primary healthcare-based study in Sweden | European Journal of Preventive Cardiology | 15 | 3 | 258–262 |
| S. H. Hendriks; K. J. J. Van Hateren; K. H. Groenier; S. T. Houweling; A. H. E. M. Maas; N. Kleefstra; H. J. G. Bilo | 2015 | Sex differences in the quality of diabetes care in the Netherlands (ZODIAC-45) | PLOS ONE | 10 | 12 | 40–51 |
| M. Strong; R. Maheswaran; J. Radford | 2006 | Socioeconomic deprivation, coronary heart disease prevalence and quality of care: a practice-level analysis in Rotherham using data from the new UK general practitioner Quality and Outcomes Framework | Journal of Public Health | 28 | 1 | 39–42 |
| A. B. S. Nielsen; N. De Fine Olivarius; D. Gannik; C. Hindsberger; H. Hollnagel | 2006 | Structured personal diabetes care in primary health care affects only women’s HbA1c | Diabetes Care | 29 | 5 | 963–969 |
| T. W. Kenealy; K. S. Eggleton; E. M. Robinson; N. F. Sheridan | 2010 | Systematic care to reduce ethnic disparities in diabetes care | Diabetes Research and Clinical Practice | 89 | 3 | 256–261 |
| R. M. Davis; A. D. Hitch; M. M. Salaam; W. H. Herman; I. E. Zimmer-Galler; E. J. Mayer-Davis | 2010 | TeleHealth improves diabetes self-management in an underserved community: Diabetes TeleCare | Diabetes Care | 33 | 8 | 1712–1717 |
| Y. Hirst; H. Skrobanski; R. S. Kerrison; L. C. Kobayashi; N. Counsell; N. Djedovic; J. Ruwende; M. Stewart; C. Von Wagner | 2017 | Text-message Reminders in Colorectal Cancer Screening (TRICCS): a randomised controlled trial | British Journal of Cancer | 116 | 11 | 1408–1414 |
| R. S. Kerrison; H. Shukla; D. Cunningham; O. Oyebode; E. Friedman | 2015 | Text-message reminders increase uptake of routine breast screening appointments: a randomised controlled trial in a hard-to-reach population | British Journal of Cancer | 112 | 6 | 1005–1010 |
| D. J. Exeter; L. Moss; J. Zhao; C. Kyle; T. Riddell; R. Jackson; S. Wells | 2015 | The distribution and frequency of blood lipid testing by sociodemographic status among adults in Auckland, New Zealand | Journal of Primary Health Care | 7 | 3 | 182–191 |
| M. P. McGovern; M. A. Boroujerdi; M. W. Taylor; D. J. Williams; P. C. Hannaford; K. E. Lefevre; C. R. Simpson | 2008 | The effect of the UK incentive-based contract on the management of patients with coronary heart disease in primary care | Family Practice | 25 | 1 | 33–39 |
| J. T. Lee; G. Netuveli; A. Majeed; C. Millett | 2011 | The effects of pay for performance on disparities in stroke, hypertension, and coronary heart disease management: interrupted time series study | PLOS ONE | 6 | 12 | 123–133 |
| F. Mold; A. While; A. Forbes | 2008 | The management of type 2 diabetes care: the challenge within primary care | Practical Diabetes International | 25 | 1 | 28–36 |
| M. Ashworth; D. Armstrong | 2006 | The relationship between general practice characteristics and quality of care: a national survey of quality indicators used in the UK Quality and Outcomes Framework, 2004–5 | BMC Family Practice | 7 | 11 | 1408–1414 |
| R. W. Hutchison | 2014 | Treating diabetes in underserved populations using an interprofessional care team | Journal of Interprofessional Care | 28 | 6 | 568–569 |
| Y. Van Mourik; L. C. M. Bertens; M. J. M. Cramer; J. W. J. Lammers; J. B. Reitsma; K. G. M. Moons; A. W. Hoes; F. H. Rutten | 2014 | Unrecognized heart failure and chronic obstructive pulmonary disease (COPD) in frail elderly detected through a near-home targeted screening strategy | Journal of the American Board of Family Medicine | 27 | 6 | 811–821 |
| A. R. H. Dalton; A. Bottle; C. Okoro; A. Majeed; C. Millett | 2011 | Uptake of the NHS Health Checks programme in a deprived, culturally diverse setting: cross-sectional study | Journal of Public Health | 33 | 3 | 422–429 |
| B. Iyen-Omofoman; L. J. Tata; D. R. Baldwin; C. J. P. Smith; R. B. Hubbard | 2013 | Using socio-demographic and early clinical features in general practice to identify people with lung cancer earlier | Thorax | 68 | 5 | 451–459 |
| L. A. Sigfrid; C. Turner; D. Crook; S. Ray | 2006 | Using the UK primary care Quality and Outcomes Framework to audit health care equity: preliminary data on diabetes management | Journal of Public Health | 28 | 3 | 221–225 |
| E. J. Cook; C. Sharp; G. Randhawa; A. Guppy; R. Gangotra; J. Cox | 2016 | Who uses NHS health checks? Investigating the impact of ethnicity and gender and method of invitation on uptake of NHS health checks | International Journal for Equity in Health | 15 | 1 | Jan-17 |
Glossary
- Context
- Settings, structures, environments, conditions or circumstances which lead to behavioural and/or emotional responses for individuals affected.
- Context–mechanism–outcome configurations
- Relationships between the building blocks of realist analysis (i.e. how mechanisms are triggered under specific contexts to cause specific outcomes).
- Equity
- Fair opportunity; in the context of healthcare, it suggests fair opportunity to receive appropriate and effective care.
- General practice
- The system of providers, commissioners, professionals and organisations that together provide non-specialised medical care in the community.
- General practitioner
- Doctor who treats all medical conditions of patients in a community and refers them to hospitals, specialist treatment or other medical services.
- Intersectionality
- The concept which suggests that people’s experience and social position is affected by multiple inter-related social categories like gender, race or class. Social categories reflect interconnected systems of social power organisation which are context-specific and lead to complex social inequalities.
- Intervention-generated inequalities
- Unintentional variations in outcomes for individuals or groups which result from any health-related intervention and generate or increase inequalities.
- Local general practices
- Local healthcare organisations that provide non-specialised medical care in the community. In the UK, the majority of these organisations are run with independent contracts and have an organisational partnership model. These organisations are sometimes referred to as GP surgeries or GP practices.
- Mechanism
- The way in which individuals and groups respond to, and reason about, the resources, opportunities or challenges offered by a particular programme, intervention or process. Mechanisms are triggered in specific contexts and lead to changes in behaviour.
- Outcome
- The impact or behaviours resulting from the interaction between mechanisms and contexts.
- Power organisation
- The ways that power relations are organised in a society to maintain the status quo. They are rooted in socially constructed concepts such as race, gender and class and involve beliefs, cultural norms and practices that shape institutions and people’s experience.
- Programme theory
- A set of theoretical explanations or assumptions about how a particular programme, process or intervention is expected to work.
- Rayyan QCRI
- A web application used to facilitate the screening process for a literature review.
- Social determinants of health
- The conditions in which people are born, live, grow and work.
List of abbreviations
- CHD
- coronary heart disease
- CMO
- context–mechanism–outcome
- CMOC
- context–mechanism–outcome configuration
- COPD
- chronic obstructive pulmonary disease
- CVD
- cardiovascular disease
- DPC
- direct patient care
- GP
- general practitioner
- IGIs
- intervention-generated inequalities
- IPT
- initial programme theory
- OECD
- Organisation for Economic Co-operation and Development
- PCN
- Primary Care Network
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QOF
- Quality and Outcomes Framework
- RCT
- randomised controlled trial
- SDH
- social determinants of health
