Notes
Article history
The research reported in this issue of the journal was funded by the HSDR programme or one of its preceding programmes as project number 17/08/25. The contractual start date was in September 2018. The final report began editorial review in February 2021 and was accepted for publication in November 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HSDR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 McDermott et al. This work was produced by McDermott et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 McDermott et al.
Chapter 1 Background and literature
Introduction
This chapter explores both the policy background and what is known from the literature about skill mix change in primary care. First, we explore the policy context in the UK at present, setting out the policy drivers at work and the assumptions underlying the policy solutions proposed. Second, we conducted a scoping literature review to explore what we know from the international literature about these assumptions and the implementation and impact of skill mix.
The workforce crisis in general practice in England
The current workforce crisis in general practice has been described in terms of a shortage of general practitioners (GPs), which is creating unsustainable GP workload pressures. It is claimed that heavy workloads for a limited supply of GPs are exacerbated by increasing complexity of patient caseloads due to frailty amongst an ageing population, population growth and declining NHS investment. In addition, a desire among new GPs for a better work–life balance, reticence about business risks associated with the partnership model and pension caps can further deplete the workforce through decisions to reduce time commitments and retire early.
Alternative approaches to managing demand in primary care range from self-care and team-based care to online consultations and the use of artificial intelligence to improve problem-screening, diagnosis, treatment and monitoring. 1–5 In recent years, attention has also focused on changing the skills and occupational mix of the general practice workforce through the employment of practitioners from a wide range of health-care disciplines to assist limited numbers of GPs in keeping pace with population growth and the changing health-care needs of an ageing population. 6
It has been observed that what has been framed as a shortage of doctors is a demand–capacity mismatch, which needs to be addressed by increasing the supply of staff able to deliver primary care. 6 However, it has been estimated that current strategies to increase GP recruitment will fall short of government targets and will not be sufficient to address demand. 7–9 Therefore, this recruitment and retention difficulty raises concern that primary care services could reach saturation point unless additional workers are employed to undertake some of the work that is traditionally carried out by GPs.
A national vision for a transformed NHS based on new models of care was set out in the NHS Five Year Forward View in 201410 and refreshed in 2017. 11 Both the NHS Five Year Forward View and the Primary Care Workforce Commission report12 [i.e. a report by an independent commission established by Health Education England (HEE) in 2014] recommended that primary care services be redesigned to support the development of multidisciplinary teams of highly skilled health-care staff. 10–12 The details are set out in the General Practice Forward View (GPFV), which was published in April 2016. 13 The GPFV proposed the creation of a minimum of 5000 new non-medical roles in general practices in England where ‘wider members of the practice-based team will play an increasing role in providing day-to-day coordination and delivery of care’ (contains public sector information licensed under the Open Government Licence v3.0). 13 This model is further endorsed in a report by the House of Lords Select Committee on the long-term sustainability of the NHS in 2017. 14
These recommendations are reflected in ‘skill mix’ changes in primary care, as the proportion of non-GPs to GPs in the workforce has been increasing in recent years. 15 Understanding the effects of these workforce changes requires clarity on what it means to change skill mix in general practice, what factors affect the uptake of skill mix and the impact of skill mix on health outcomes and costs.
Definition of skill mix and a framework of possibilities
There are variations in the meaning attributed to the term ‘skill mix’. Skill mix has been used in the literature to refer to the range of competencies possessed by an individual health-care worker, the senior (supervisory) staff to junior (supervised) staff ratio within a particular discipline or the mix of different types of staff in a team/health-care setting. 16
Conceptualising skill mix can be difficult because it cannot be considered in isolation from the broader organisational and health-care system contexts in which people work, or from other concurrent policy initiatives and organisational developments. 17 Therefore, there is a need to consider contextual factors that influence skill mix, which are often neglected in the literature. 17–20
Using skill mix change to address a demand–capacity imbalance would require tasks to be reallocated from GPs to non-GPs. Task reallocation refers to ‘a broad spectrum of shifting tasks and responsibilities, ranging from minimal delegation to complete substitution and also the introduction of complementary care’. 21 Therefore, skill mix changes can be seen to be occurring at both the role level and the service interface level and, as such, have been described as involving enhancement, substitution, delegation and/or innovation. 16 Two studies (a recent review of skill mix change and a qualitative comparison of three 'new' non-medical roles, which features skill mix change) have enabled further clarification and refinement of these categories of skill mix changes. 22,23 These studies suggest an overlap and a mixing of objectives in the four changes mentioned above (i.e. enhancement, substitution, delegation and/or innovation). Instead, it is suggested that enhancement and innovation should be seen as expressing different aspects of change from those related to delegation and substitution. Likewise, it is suggested that substitution is also discussed in relation to supplementation.
Of the four changes identified above, enhancement and innovation most clearly delineate the means through which skill mix can change. For example, nurses may extend their skills and lead clinics (i.e. enhancement). At the same time, the introduction of physiotherapists trained to deliver first-contact physiotherapy in general practices is an example of skill mix change through innovation. Likewise, delegation and substitution most accurately describe how skill mix change has led to task transfers between occupational groups. For example, nurses act as non-medical prescribers, enabling this core GP task to be transferred to nurse prescribers without supervision (i.e. substitution). Tasks can also be transferred to those who require supervision (i.e. delegation); for example, GPs may transfer tasks to physician associates (PAs) or health-care assistants (HCAs). Last, it is necessary to make a distinction between substitution and supplementation. Substitution implies explicit full substitution of a GP by an alternative (non-GP) practitioner, whereas studies indicate that general practices often aim at supplementing GPs to extend the range of services to patients. 24
The next section indicates how skill mix has changed over time in general practice, thereby contextualising the most recent workforce changes.
Skill mix changes in general practice in the UK
Since the introduction of the NHS in 1948, GPs have been contractually committed to providing primary and personal medical care for every patient on their registered list. Traditionally, many GPs worked in small or single-handed community-based practices, in contrast to consultant physicians and surgeons working in hospitals. They were seen as ‘gatekeepers’ because they select which patients to refer to specialist services available through hospitals or other health and social care services.
In 1966, doctors’ dissatisfaction over pay and conditions in the NHS led to a revised GP contract whereby GPs could be reimbursed for 70% of the cost of employing ancillary staff. 25 This led to the first skill mix change through innovation, that is, the rapid employment of practice nurses to carry out basic nursing tasks, such as recording health screening measurements, dressing wounds and administering injections. 26
General practitioner contract changes in 1990 and 2004 led to enhanced roles for general practice nurses in managing long-term conditions, such as diabetes, asthma and chronic obstructive pulmonary disease, as well as health promotion. 27 Although general practice has remained predominantly staffed by doctors and nurses, subsequent enhancement of nursing roles has enabled the transfer of tasks through a mixture of delegation and substitution. General practice nurses are now involved in broader aspects of patient care, such as minor surgical procedures, the treatment of minor injuries, health screenings, family planning, giving lifestyle advice and running vaccination programmes. 28 In addition, some nurses have undertaken training in the diagnosis and management of undifferentiated cases, developments now recognised in the role of advanced nurse practitioners (ANPs). 29 The employment of HCAs in general practice has also enabled the transfer of former nursing tasks through delegation. 30 HCAs are usually locally trained staff, with no standard training programme or agreed scope of practice. HCAs are not regulated and they perform their roles under the supervision of registered professionals.
Policy context underpinning skill mix changes in general practice in England
Although changes to skill mix in UK primary care have been happening gradually for some time, it is only in the past 5 years that policy has explicitly addressed this issue. Understanding how skill mix is perceived and implemented is vital to understanding the policy-drivers and mechanisms being put in place to realise the policy. To do this, we analysed the GPFV and the Network Contract Directed Enhanced Services (DES). 13,31 This analysis identified both the mechanisms that have been put in place and the outcomes expected from the implementation of employing additional roles in general practice.
The GPFV (published in April 2016) commits to an extra investment of £2.4B a year by 2020/21 to support general practice workforce expansion, moving from the two traditional occupational groups (i.e. GPs and nurses) to a more diverse and multidisciplinary workforce. 13 The programme also proposes investment to support a minimum of 5000 other staff working in general practice by 2020/21. In 2018, the government announced additional funding of £20.5B by 2023/24, and The NHS Long Term Plan (published in January 2019) sets out key ambitions for the next 10 years. 32 The ‘plan’ proposed a new service model with £4.5B of new investment to fund expanded community multidisciplinary teams aligned with primary care networks (PCNs). The PCNs were to be formed by general practices working together to deliver ‘fully integrated community-based healthcare’ (contains public sector information licensed under the Open Government Licence v3.0) for 30,000–50,000 people. 32 The implementation plan for this is set out in the Interim NHS People Plan (published in June 2019)33 and the subsequent We are the NHS: People Plan for 2020/21 (published in July 2020). 34
Although a gradual increase in the employment of non-GPs by general practices has preceded the formation of PCNs, these networks have become important as one of several mechanisms to increase skill mix and improve the recruitment and retention of doctors and nurses by the employment of additional primary care staff through the Additional Roles Reimbursement Scheme (ARRS) (with the investment of £891M). Through the Network Contract DES, which is an add-on contract to the existing General Medical Services (GMS) contract, network member practices are contracted to deliver seven national service specifications and are expected to achieve locally agreed schemes. 35 Five roles were initially selected: (1) clinical pharmacists (CPs), (2) PAs, (3) paramedics, (4) physiotherapists and (5) social prescribers. The focus on these five roles was based on the availability of practitioners, on the strength of practice demand and on confidence that these newer roles can reduce GP workload and create additional capacity.
Based on the historical ‘success’ of a 70% reimbursement of staff costs model in establishing roles for nurses and receptionists under the Charter for General Practice in 1965,25 a similar model was initially proposed under the ARRS for PCNs (i.e. 70% reimbursement to support staff employed in newer roles). From April 2020, the reimbursement has increased to 100% and a further six roles have been added: (1) pharmacy technicians, (2) care co-ordinators, (3) health and well-being coaches, (4) dieticians, (5) podiatrists and (6) occupational therapists. 36
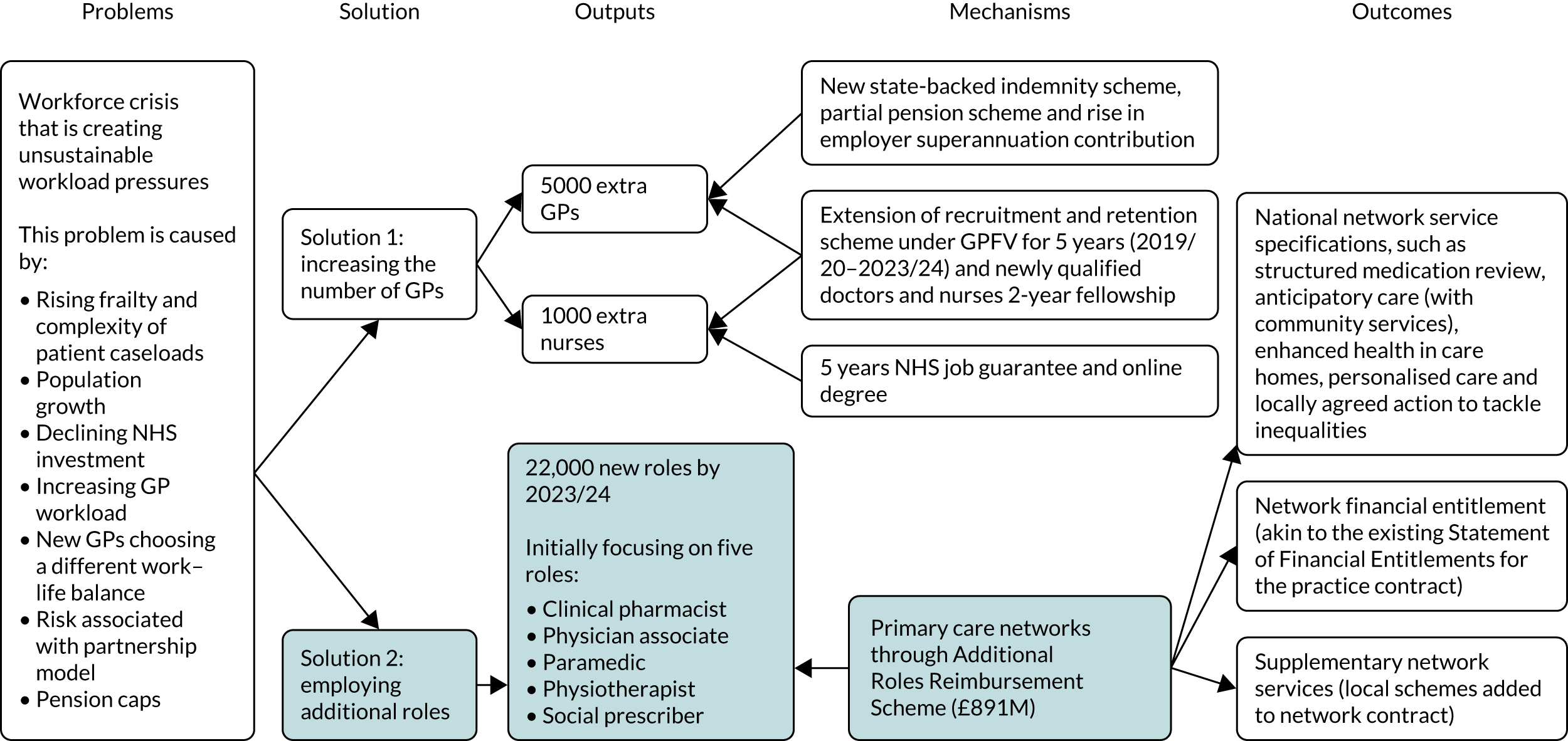
The policy intention is that workers in these newer roles become part of general practice teams rather than provide supporting services. The ARRS, therefore, adds impetus to increasing skill mix employment in primary care. However, because there is currently limited evidence about how changing the workforce composition works, this research provides evidence to fill that gap. In this context, a study of the scale and nature of the expansion of multidisciplinary work in general practice and the impact of these changes on outcomes are particularly important, and both are discussed below. Our summary of the current policy context, including the mechanisms that have been put in place and the anticipated outcomes, is set out in Figure 1. The relevant immediate context for this study is highlighted.
FIGURE 1.
Skill mix policy context.
Rationale for employing newer roles
The rationale for employing newer roles, as set out in policy documents and research evaluations, is influenced by perceptions of what practitioners in these roles can contribute, the time taken to embed newer roles and costs associated with implementing new ways of working. The contribution of newer roles is more evident for some roles than for others. For example, CPs can deal with medication-related tasks, such as medication reviews, repeat prescribing and monitoring safe or financially incentivised prescribing practices. 9,37–39 On the other hand, PAs have been described as being able to safely attend to ‘less complex’ patients. 40
In addition to perceptions about the contributions made by practitioners in newer roles, financial incentives have been shown to influence GPs’ willingness to adopt skill mix. For example, in Germany, GPs were willing to delegate home visit-related tasks to PAs if reimbursed by health insurers. In addition, in France, GPs were willing to delegate tasks to nurses when they shared a lower proportion of the cost of employing them. 41,42
Research has shown that the expansion of nursing in primary care has primarily been driven by a need to transfer work to manage GP workload. 43 Similarly, the introduction of CPs into English general practice has been done to reduce the burden on existing staff. 44 In the case of ANPs, variation in how ANPs were trained and supported has been shown to influence their ability to deal with acute ‘same-day’ care to manage high patient demand while complex patients are seen by GPs. 45
Multidisciplinary working
Team-based care has been shown to enable doctors to work more collaboratively and reflexively. 46 Evidence suggests that team-based care could improve continuity of care, with patients more likely to get the care they need. 47,48 However, the contexts in which multidisciplinary teams operate are important and facilitating factors include co-location; a stable organisational structure; clearly defined roles and workflow; good communication through ‘huddles’, team meetings and informal ‘handoffs’ of patients; shared goals; and mutual respect and trust. 23,49–54
Trust in non-GPs’ abilities has been shown to be key for acceptance by both GPs and patients. 21,55 For GPs, trust in non-GPs can be gained over time and influenced by the doctors’ belief that non-GP colleagues know when to seek help. 21,49,55–59 Established trust also facilitates the expansion of jurisdictional boundaries and reduced supervision. 56
Much of the evidence about skill mix changes in practice derives from secondary care contexts where established hierarchies and organisational structures support a structured approach to task-shifting and delegation. In UK primary care, by contrast, GPs act as both lead clinicians and organisational owner/employers. 60,61 In this context, the renegotiation of boundaries between professionals working together in a multidisciplinary team may be complicated by the fact that one professional is the employer of the other and, therefore, holds overarching responsibility and liability for what happens within the practice.
Research has long highlighted the issue of interprofessional competition and professionals’ attempts to protect occupational jurisdiction in their work, and many of these issues are pertinent when considering skill mix in primary care. 62–65 Studies have also revealed tensions between staff relating to authority, legitimacy, expertise and efforts made to gain professional recognition. 43,66–68
Within primary care, we know that when doctors’ expectations of a new role are not met (e.g. an expectation that non-GP autonomous practitioners, such as PAs, would reduce their workload), then they are less inclined to accept other professionals as part of the primary care team. 24,67 Others have noted that the concept of PAs as substitutes for GPs affect acceptance of such staff. 24 It has also been highlighted elsewhere that there is a need for a ‘paradigm shift’ among staff to accept CPs extending their role beyond dispensing. 56,69
Impact on outcomes
Most studies of increased skill mix employment have found no reductions in costs. In some cases, skill mix employment has resulted in lower productivity and adverse consequences for practitioners, such as increased workload for those taking on new tasks and lowered staff morale. 70 Some studies have reported cost reductions only when practitioners’ skill levels are appropriately matched to the severity of patients’ conditions, whereas other studies have reported mixed findings on the impact of skill mix on costs. 58,71–73 A few studies have reported cost reductions as a result of implementing skill mix changes. 71,74,75 However, when GPs are replaced by less expensive workers, estimations of cost should consider whether the same tasks take significantly longer to carry out, as this might explain why expected cost savings are not achieved. 70,76 It is also possible that ‘new’ roles may extend the scope of general practice (i.e. widening the health-care offering and meeting an unmet need). In doing so, the costs of additional work may not be fully compensated. 77
Patient outcomes, such as the safety and quality of care, are not consistently defined across the literature. Studies58,71–77 on the outcome of skill mix on patients have mainly focused on how patterns of care and service utilisation have been affected by the availability of newer types of practitioners in primary care, alongside an investigation of patient attitudes to particular service innovations and consultations with individual practitioner types.
Research indicated that changing skill mix increased patients’ ability to get an appointment, which led to increased acceptability of skill mix and positive experiences. 55,59,73,75,78,79 However, accommodating patient choice of practitioner is essential, and evidence suggests that patients’ overall evaluation of their care, as well as their trust and confidence, decrease if they do not have access to the practitioner of their choice (e.g. for those who want to see a GP but see a nurse instead). 80 Furthermore, the trust of patients in non-GP roles was influenced by factors such as the severity of their condition and desire for continuity of care, with increased severity associated with a preference for more highly qualified health-care professionals. 40,81 Generally, patients can find it more challenging to understand and navigate access to care when confronted with extensive and diverse primary care teams. 82
Why is this research needed now?
Several factors make it imperative to research the current skill mix changes in general practice.
First, changes in skill mix are occurring at a rapid pace, but have undergone limited evaluation. Therefore, it is vital that early evaluation of the operationalisation of skill mix policy and the impact of skill mix change on outcomes, costs and experiences of health care in England are undertaken. The complexity of the policy environment, variation in how general practices make and implement local managerial decisions, a wide range of clinically active professionals and the vital interests of patients experiencing health care mean that a multidisciplinary research approach is needed to gather coherent and useful information [work package (WP) 1].
Second, improvements in data collection [e.g. NHS Digital, Workforce Minimum Data Set (wMDS)] mean that data are now available for a detailed analysis of changes in workforce composition. This provides a platform to estimate staff costs and look for associations between skill mix changes and multiple outcomes (WP1).
Third, there is a lack of evidence about factors motivating changes in skill mix. General practices have traditionally been independently owned and operated businesses. The manner in which practices deliver services in accordance with the terms of their NHS contract is scrutinised by the Care Quality Commission, but management styles and structures are not standardised. 83,84 Moreover, organisational arrangements are transforming in many areas with the emergence of new models of care. 10 Given this diversity and the current period of change, it is crucial to explore GPs’ and practice managers’ motivations for employing different practitioners, as well as what these practitioners can bring to primary care and the financial viability of skill mix implementation for GPs as business owners (WP2 and WP3).
Fourth, there can be ambiguity about which practitioners perform which roles in general practice. The MUNROS (iMpact on practice, oUtcomes and costs of New roles for health pROfeSsionals) study85 observed that lack of clarity about practitioner roles and variation in the scope of practice of individuals within the same practitioner type could impede the smooth transfer of work and add confusion for patients seeking care. 10 This is, therefore, an area in which this research can reduce ambiguity and potentially increase acceptance and operational efficiency (WP2 and WP3).
Finally, the expansion of skill mix in primary care is gaining impetus with developing the PCN ARRS. 31 Under this scheme, practitioners are expected to work across networks, as opposed to being situated in single practices. As these roles are rapidly rolled out, it is imperative that we understand the factors that affect the successful integration of newer roles into practice teams because this knowledge can inform the design and operation of the scheme. Understanding the factors that support smooth team working and the requirements for supervision will support PCNs in supporting and managing newer practitioners.
In summary, we know that the implementation of skill mix change is not unproblematic and there may be unintended adverse consequences, such as increased workload for practitioners taking on new tasks, higher costs, lower staff morale and productivity, and concern about continuity of care for patients. 15,56,70,86–88 Variation in approaches to skill mix change across primary care providers and in what different types of practitioner contribute in general practice settings can now be evaluated using more detailed national- and practice-level data. These data, about the scale of skill mix deployment, its effectiveness and impact on costs, and about quality and patterns of care, are urgently needed to inform future workforce and resource planning. Furthermore, as access to timely and safe health care is vital for patients, the evidence from this research is needed to provide patients with practical and locally relevant guidance about making the best use of the options available, and to provide practices and PCNs with information about the factors most likely to support the successful integration of newer types of workers into general practice.
Aims and objectives
This study aims to investigate evolving patterns of skill mix in primary care, examine how and why skill mix changes are implemented, explore practitioner and patient experiences of these changes, and estimate the overall impact on outcomes and costs associated with a broader spectrum of practitioner types.
We identified three research questions and related WPs to address these aims.
Research question 1 (work package 1): what is the scale and distribution of skill mix changes in primary care and how is skill mix change associated with outcomes and costs?
-
How has the workforce changed and where has any change occurred?
-
How are compositional changes to the workforce associated with later changes in a range of outcomes, including patient and practitioner satisfaction?
-
How are workforce changes associated with later changes in costs and practice efficiency?
Research question 2 (work packages 2 and 3): what motivations drive skill mix deployment at the practice level and what is delivered by the deployment of different practitioner types?
-
What motivates practices to choose/not choose increased skill mix deployment? (WP2.)
-
Which aspects of health care are undertaken by different practitioner types? (WP3.)
Research question 3 (work package 3): how do skill mix changes affect the experiences of employers, practitioners and patients?
-
How are new ways of working being negotiated in general practices where skill mix changes have occurred?
-
How is the implementation of change in skill mix associated with the achievement of organisational objectives at practice level?
-
How does increased skill mix affect patients’ experiences when accessing primary care services? (WP1 and WP3.)
Work package 4 drew together data from all WPs to develop a comprehensive understanding of the implementation of skill mix changes in general practices and the consequences of these changes.
Summary
This chapter has set out the policy context underlying current skill mix changes in general practice in England and briefly summarised the relevant literature. In the rest of this report, we describe our methods and set out our findings. This was a complex project, and the organisation of our results chapters seeks to lead the reader through the study, considering, in turn, what is happening to skill mix in practice, why practices are opting to change the skill mix of their practice teams, how they are operationalising such changes and what the outcomes associated with skill mix change might be. Therefore, Chapter 3 addresses the first part of research question 1, providing the first in-depth quantitative exploration of the scale of skill mix changes in England. Chapter 4 addresses the first part of research question 2, exploring the motivations for employing a wider range of practitioners as reported by practice managers. Chapter 5 addresses the second part of research question 2 and research question 3, exploring how practices have accommodated newer types of workers and examining patient-reported experiences. Chapter 6 addresses the second part of research question 1, considering the outcomes associated with skill mix change in practices. Chapter 7 looks across the WPs to triangulate our findings. Finally, Chapter 8 provides an overall discussion and conclusions.
Chapter 2 Methods
Design
The study adopts a multimethod strategy to understand the breadth and depth of changes affecting general practice in England. Quantitative analysis of national data sets on workforce and other aspects of care quality and experience (WP1) is used to capture the extent and impact of skill mix changes. A large-scale survey of general practice managers (WP2) was designed to explore motivations for the employment of non-GPs across general practice in England. In parallel, exploration of issues such as definitional ambiguity in roles, variation in how the same role is implemented in different settings and variation in how work is experienced requires a methodological approach that interrogates roles and settings in depth and in situ. Here, the study employs a complementary comparative case study approach (WP3) to examine conduct and practice using in-depth qualitative methods in a way that is sensitive to important differences in context.
NHS Digital data (work package 1)
We used data about the range of practitioners employed in practices across England, which were available from NHS Digital. Using panel data regression techniques, we estimated practice-level associations between changes in patterns of skill mix and changes in costs and outcomes measured using national data sets.
Growth in the number and range of different workforce professionals employed by practices in recent years has facilitated new ways to deliver services for patients and offered the potential to lower costs and improve outcomes. 89 As practices are primarily small, employee-owned enterprises, they are likely able to respond to these changes more rapidly than larger organisations, such as hospitals, to contain costs and prioritise specific outcomes.
Details of data sources and a full account of our analysis are described in Chapters 3 and 6. In broad terms, we created and analysed a longitudinal practice-level workforce data set using the practice-level wMDS available from NHS Digital for 2015–19. The resulting workforce composition data were analysed against selected outcome data sets to look for associations between workforce composition and outcomes, including overall costs.
In addition to examining workforce changes by geographical region and over time, we looked for indications of potential substitution between the staff groups. Modelling was used to generate scenarios about potential variation in outcomes produced by changes in the number of practitioners employed.
Practice manager survey (work package 2)
We conducted an online survey with practice managers in general practices in England between August and December 2019. We targeted practice managers because it is typically their responsibility to report workforce data to NHS England, and they are generally involved in implementing decisions about staff employment.
Our initial plan was to conduct a postal survey to be sent to all general practices in England using publicly available practice addresses, but negotiated an agreement to conduct an online survey for the following reasons.
First, by using an online platform, we were able to use data that practices had previously supplied to NHS Digital to prepopulate the survey with practice-specific workforce data for managers to confirm or correct according to their current workforce. This allowed us to adapt survey questions so that they were appropriate for each general practice and to avoid duplication or unnecessary questions. For example, we asked participants to indicate the reasons for employing the types of practitioners in their current workforce.
Second, it became evident that local clinical research networks (LCRNs) were interested in supporting us in distributing the survey. The online version was seen as the most effective and appropriate way to reach practice managers.
Third, the use of an online survey was a more cost-effective way of gathering and extracting data for analysis.
We developed and pilot-tested an online questionnaire to be completed by practice managers. In addition to facilitating a check for accuracy of the NHS Digital wMDS, managers were asked about motivations for hiring staff from selected practitioner groups, their future workforce plans and their ideal workforce.
Survey administration
We worked with 15 LCRNs to e-mail the survey link to practice managers in England. Practices that had not opted out of receiving research invitations from their LCRNs were invited to participate in the study, receiving three e-mail invitations/reminders to participate in the study. We requested assistance from the Practice Management Network and used social media to publicise the survey to reach additional practices.
Practice managers were asked to enter a practice identification (ID) (Figure 2), which prevented duplication and allowed the survey software to automatically assign numerical IDs based on the order in which the respondent had started to complete the questionnaire. We did not store the response data with the practice IDs and the key was stored separately. All data were stored on our secured servers. The practice’s identity was needed to ensure that we presented the practice with appropriate questions related to their current staff and provided information for LCRN records about responding practices.
FIGURE 2.
Practice manager survey front page.
The online questionnaire was created using Lighthouse Studio (version 9.7.2; Sawtooth Software Inc., Provo, UT, USA) and was hosted on University of Manchester (Manchester, UK) servers. Data analysis was conducted using Stata® 15.1 (StataCorp LP, College Station, TX, USA).
Survey content
The study focused on six practitioners (ANPs, specialist nurses, HCAs, PAs, paramedics and CPs) because they represented a mix of:
-
staff whose employment in practices largely predates the new GP contract (e.g. HCAs and advanced nurses)
-
staff whose employment has often been linked to financial incentives (e.g. CPs)
-
staff whose employment can be used to offer additional services (e.g. specialist nurses and CPs)
-
additional roles that can also be funded through PCNs (e.g. PAs and paramedics).
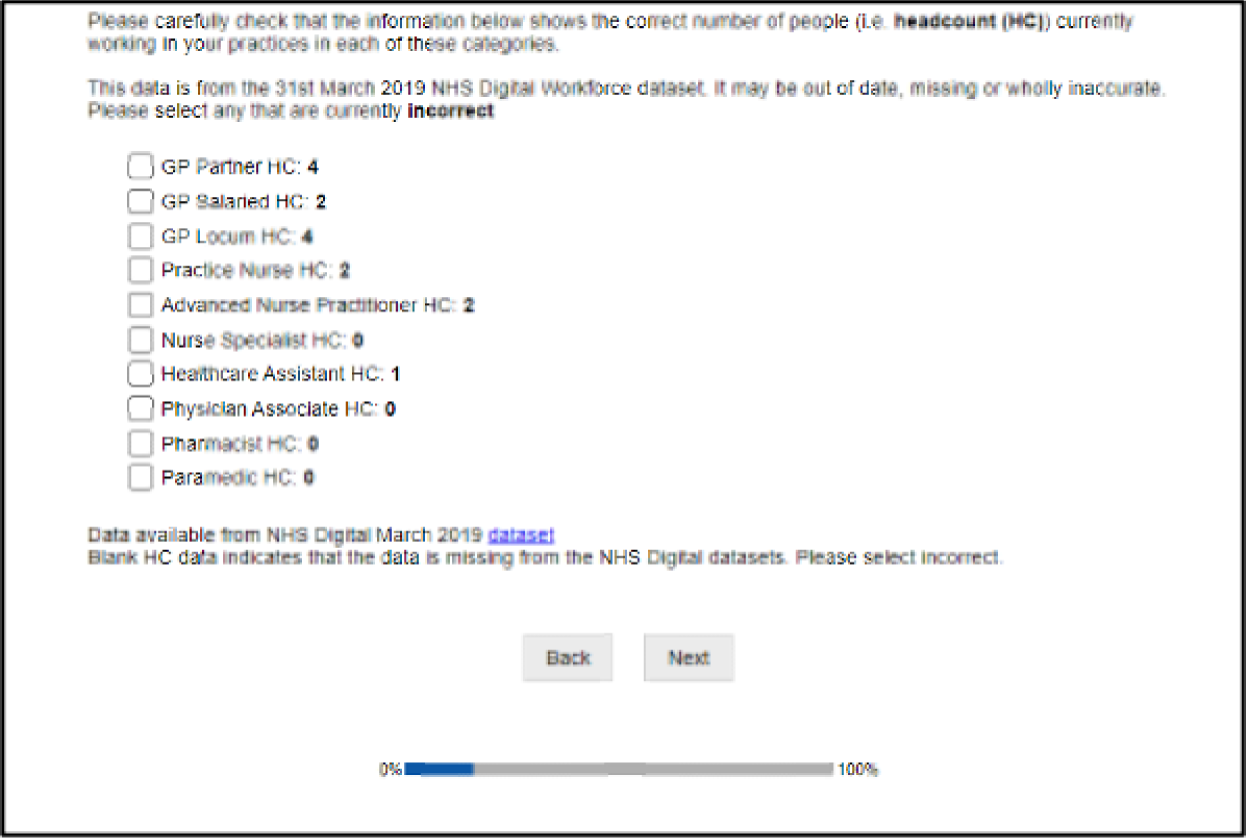
The questionnaire consisted of three sets of questions. The first set of questions focused on verifying publicly available practice workforce data. Practice managers were shown the workforce data [both headcount and full-time equivalent (FTE)] that NHS Digital released for their practice, as of 31 March 2019. This question is shown in Figure 3.
FIGURE 3.
Practice manager questionnaire: is the data correct?
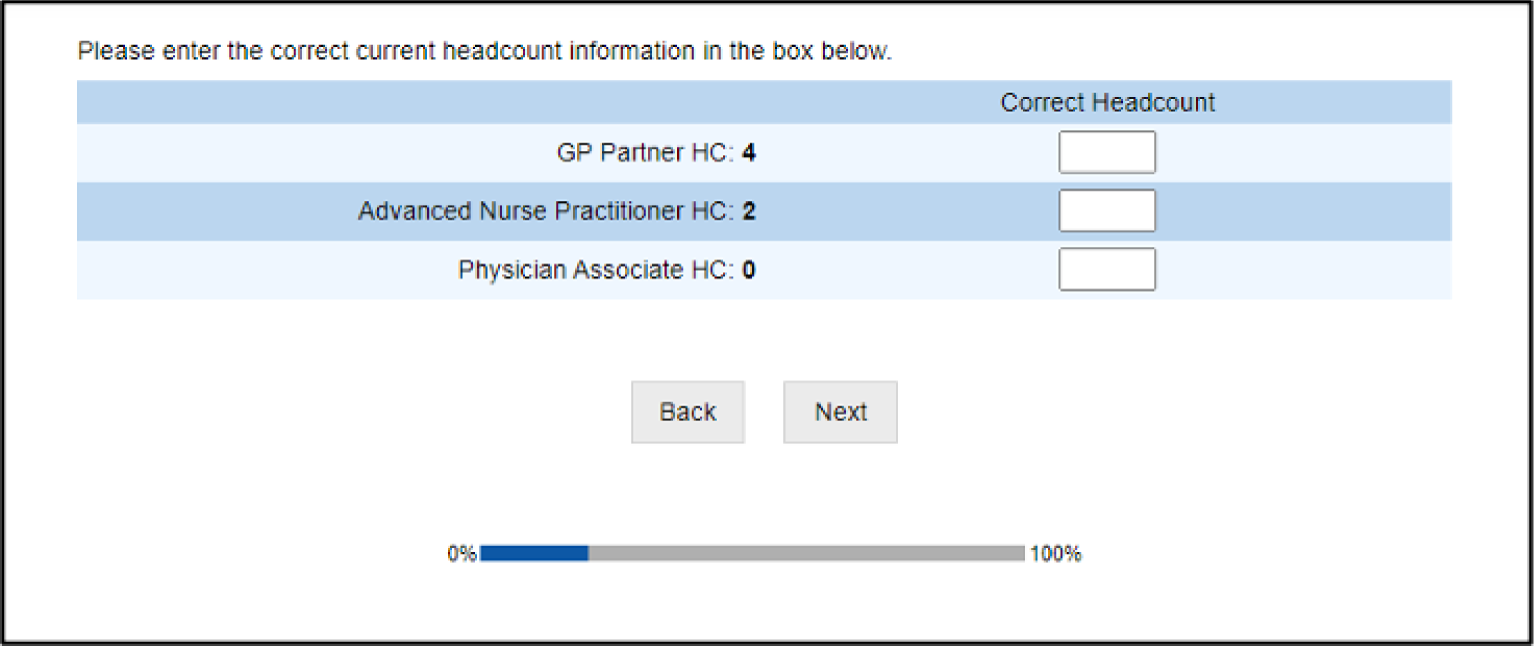
Practice managers were then asked to enter the correct current headcount or FTE figures for any incorrect practitioner groups (Figure 4).
FIGURE 4.
Practice manager questionnaire: entering correct data.
The second set of questions asked those who employed staff in one of the six roles of interest what factors influenced their decision to employ staff in that role. Respondents were presented with a list of 12 predefined factors, the selection of which was informed by our knowledge of the literature and previous workforce research. Respondents were also permitted to add factors not captured in the list using free text. They were asked to select all factors that applied to their decision for each type of worker. They were then asked if any additional funding was explicitly supplied to support the employment of these staff, from which funding organisation and whether or not they were still receiving funding.
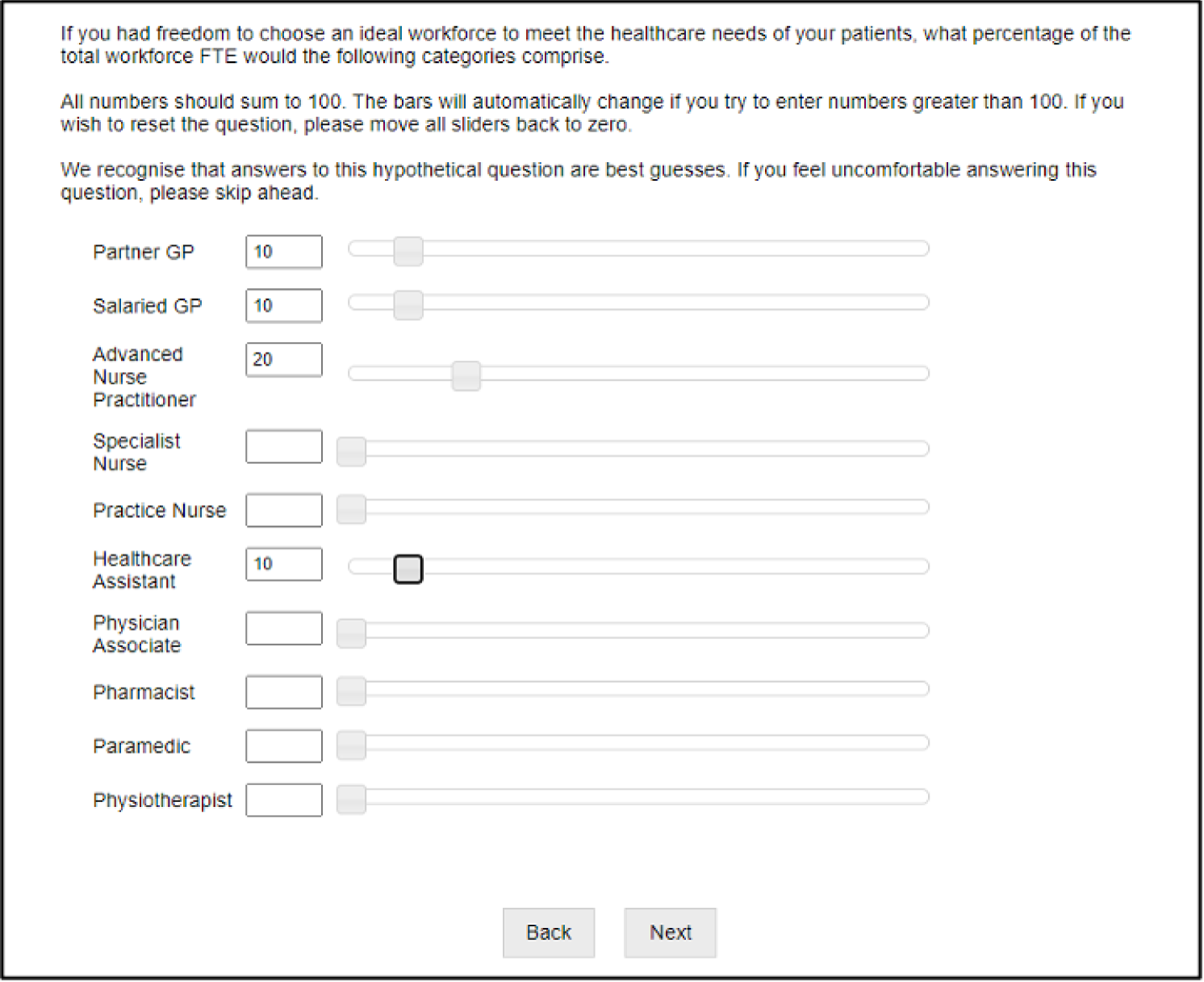
Regardless of their current workforce composition, the final set of questions asked all participants whether or not they would wish to employ additional staff from a list of roles in the future and, if so, whether they would prefer them to be directly employed by the practice or through a PCN. Finally, participants were asked to indicate their ideal workforce composition by selecting the percentage of their total clinical workforce made up of each of the listed roles. GPs were included in the list of roles for this question. Respondents were required to use slider bars to indicate the percentages for each worker group (Figure 5). These bars were programmed so that total percentages were automatically adjusted to 100%.
FIGURE 5.
Practice manager questionnaire: ideal workforce slider bars.
Case study (work package 3)
Multiple case studies
Aware of the need to generate rich research findings in their practical context, we used Yin’s multiple case study approach. 90 This enabled us to understand issues where there is limited prior knowledge and/or complex organisational conditions. Our claims to generalisability from the case studies rest on theoretical generalisation rather than on representativeness. In other words, our use of theory to structure both site selection and data collection allowed us to further refine and develop theory in this area, providing the opportunity for generalisation beyond the cases studied. 91
We conducted in-depth case studies of five purposively selected general practices using an appropriate mix of qualitative methods, including interviews with staff members and observations of consultations with GP and non-GPs. In case study research, the decision as to how many cases to include represents a balance of breadth (i.e. the need to recruit enough cases to make sure that there is the requisite variety between sites to capture the phenomenon of interest) and depth (i.e. the need to limit the number of sites to be able to collect data in sufficient depth to ensure a full understanding of each case site). Our experience of similar studies suggests that five case studies represent a broad enough sample to capture variation across the key dimensions of interest, while at the same time ensuring that we can undertake the requisite data collection to gain an in-depth understanding of the detailed local context and experiences of the full range of relevant staff, as well as patients. 92–94
Two primary considerations guided the selection of general practice sites for the case studies. First, we were interested in comparing the experiences of practices with a wide range of practitioner types with practices with a narrower range. Second, we were interested in comparing practices that have had a long experience of skill mix diversity with practices that have only recently become more diverse.
Selection of case studies
Sampling was informed by data from WP1 (i.e. data on employment of different practitioner types based on NHS Digital 2018 submission and insights from Expert Advisory Group members). Practices were chosen based on the following criteria:
-
Diversity of practitioners employed. This refers to the number of different types of practitioners in a general practice. From NHS Digital data, we were able to identify practices employing each of the individually listed practitioner types. This allowed us to select practices with more diverse teams (i.e. a larger number of different roles) and those with fewer roles other than GP and practice nurse. In addition, analysis of the scale of employment of specific types of practitioner allowed us to select those sufficiently prevalent in national data sets to be associated with having greater influence on workload or working practices. As a result, we selectively recruited practices based on their diversity of practitioners whose skills are likely to have greater operational impact.
-
Duration/maturity of skill mix implementation. This refers to the period during which a practice has been engaged in implementation of skill mix. We categorised general practices as being early adopters or late adopters. Early adopters refers to practices that have adopted skill mix in or before 2016 and late adopters refers to practices that have adopted skill mix since 2018. These dates were determined by availability of data (as a result of changes in NHS Digital data collection and publication).
-
Whether a practice has a large or small number of practitioners employed within a role. We selected this based on headcount rather than FTE. We focused on how practitioners work rather than the level of work that the practitioner undertakes.
-
Whether a practice has increased or reduced the number of practitioners employed within a role.
Data collection
Case study data were collected between August and December 2019. We initially planned to conduct case studies in six general practices, but, in early 2020, a sixth site withdrew to focus on another initiative. Our recruitment of an alternative site was interrupted by the COVID-19 pandemic. However, realising that we had a rich and extensive data set, we followed the advice of the Study Steering Committee to abandon this plan and focus on data already gathered. Moreover, following a review of the qualitative data collected, we concluded that we had reached data saturation.
We conducted observations of GP and non-GP consultations at each site and face-to-face interviews with practice staff, focus groups and patient surveys. We conducted a total of 38 interviews and 27 observations (totalling 1620 minutes). Observational field notes provided insight into discrepancies between what people do and say, which pointed to tensions and new areas of interest that we explored in subsequent interviews.
We conducted focus groups with Patient Participation Group (PPG) members (n = 29) in four out of five sites. One of the sites (i.e. site C) did not have an active PPG and we were not able to recruit patients for a focus group at that site. We contacted all patients who indicated in the patient survey that they were willing to participate in a focus group. However, only patients at site D agreed to participate.
Survey sheets were distributed to patients as they attended the practices during site visits. Most survey sheets were distributed by our researchers and a total of 125 patient surveys were collected across five sites. The survey asked patients about which practitioner they had seen and how satisfied they were with how the consultation was conducted. Patients were also asked to provide their contact details (e.g. name, telephone number and/or e-mail address) if they were willing to participate in a focus group. For those patients who gave their contact details, these details were physically separated from the survey sheet and assigned study IDs to maintain anonymity.
Interviews and focus groups were transcribed verbatim by a transcriber approved by the University of Manchester.
To add information about how skill mix changes have been affected by, or facilitated, responses to COVID-19, we carried out follow-up telephone interviews with GP partners and/or practice managers at all general practices in our case study sites between September 2020 and January 2021.
Data analysis
Initial thematic codes identified by Imelda McDermott from reviews of the literature and research questions were reviewed, adapted and refined by the research team following initial data collection and a series of team discussions. For patient surveys, Elizabeth Dalgarno identified thematic codes based on literature reviews, research questions and free coding. Data from patient surveys and focus groups were compared across sites, and findings were reviewed with public contributors who were members of our Expert Advisory Group.
Anonymity
All participants were anonymised using study IDs, pseudonyms and/or vague job titles. Research sites were also anonymised and contextual details that might identify sites were disguised. All personal data that potential patient participants shared with us were stored in the University of Manchester’s Research Data Storage Service, which provides robust, managed and secure replicated storage and is accessible by members of the research team only. The pseudonymisation key was held separately and securely in the Research Data Storage Service (password protected) and was accessible to Sharon Spooner [study principal investigator (PI)] and Imelda McDermott.
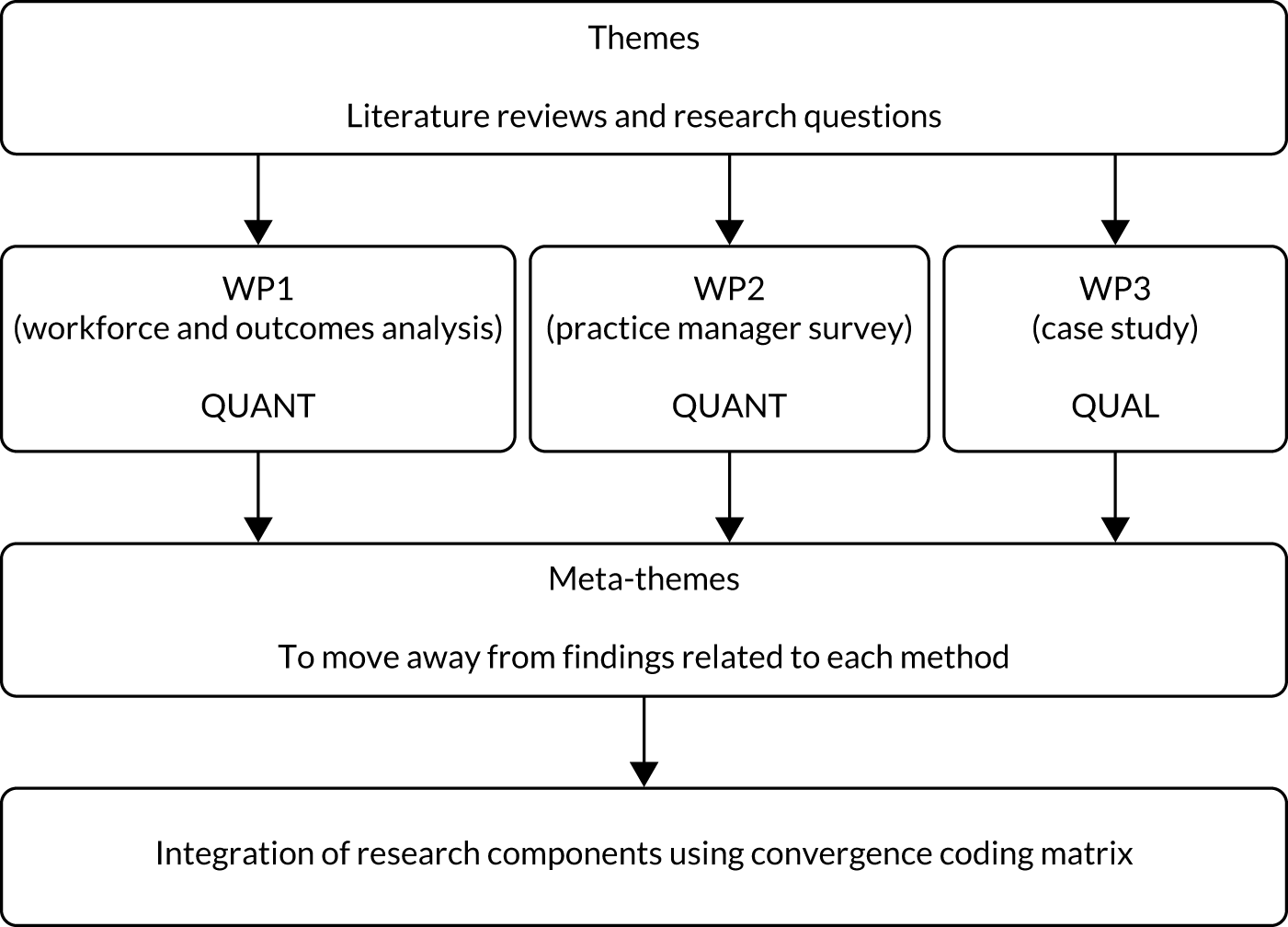
Triangulation (work package 4)
Our methodological approaches have been combined using the principle of ‘triangulation’. 95,96 In this context, the term triangulation describes a process that employs mixed methods to gain a complete picture of a problem. 97 Qualitative and quantitative data are not only used to cross-corroborate findings (i.e. to confirm descriptions of how particular roles are implemented); qualitative findings are also used to complement the quantitative analysis. For example, qualitative elements of the research are used to inform the measurements or analyses undertaken in the quantitative research, providing context to assist interpretation while at the same time inductively generating insights into the way in which phenomena are related in practice. 96 In this way, qualitative and qualitative research work together to facilitate a richer understanding of the phenomenon, generating a multifaceted portrayal of a complex social situation with breadth and depth. 98
Although the WPs (i.e. WP1, WP2 and WP3) were analysed separately, ongoing engagement between researchers on each WP was maintained during ad hoc conversations and monthly team meetings throughout the project to ensure that findings were integrated as specified in WP4. For example, insights from study sites and clinical members of the research team helped shape analysis and interpretation of how the employment of CPs may influence prescribing patterns.
As more structured support for this engagement, one researcher (IM) produced thematic codes based on a review of literature and the research questions. Themes were used to help structure an iterative dialogue between members of the research team, with regular meetings held to share findings as they emerged in each of the WPs. The thematic codes were grouped into meta-themes that cut across findings from different methods and integrated using a ‘convergence coding matrix’. 99 Meta-themes were considered for agreement and disagreement based on convergence (i.e. where findings directly agree), complementarity (i.e. where findings offer complementary information on the same issue), dissonance (i.e. where findings appear to contradict one another) and silence (i.e. where themes arise from one component study but not others). 100 Figure 6 depicts the triangulation process.
FIGURE 6.
Triangulation process.
Patient and public involvement
Members of Primary Care Research in Manchester Engagement Resource (PRIMER) (Manchester, UK) and a PPG that liaises with their practice team on matters related to GP services provided comments on our proposal. In addition, these members contributed to the research design, including case studies and the patient survey, in terms of patient experiences of care navigation, choice, confidence and understanding practitioner roles.
Two PRIMER representatives were members of the Expert Advisory Group to bring patient and public involvement perspectives to all aspects of research activity. The representatives contributed to the development of patient surveys and focus group topic guides and provided feedback on patient survey findings. Anne McBride supported PRIMER representatives to be fully involved throughout the research project. We are continuing to work through ideas for resources that may improve patients’ understanding of what less familiar practitioners do in general practice settings.
Ethics
Ethics approval was obtained following review by NHS Health Research Authority and North West- Greater Manager South Research Ethics Committee (reference 18/NW/0650).
Reimbursement
Following discussions and advice from the Greater Manchester Clinical Research Network, we obtained funder agreement to provide incentives to encourage participation in WP2 (i.e. the Practice Manager Survey) and WP3 (i.e. the case studies).
For WP2, general practices that completed and returned the survey were entered into a prize draw in which five winners of £50 were randomly selected. An ID key was used to identify the winning practices, which were then contacted to arrange for the prize to be sent to them (addressed to the practice manager). We were informed that some LCRNs offered supplementary funding to practices to cover the costs of completing the survey. The prize was payable to the practice to be spent on staff development.
For WP3, we reimbursed general practices for staff time that was diverted due to participation in interviews and observations.
Project management and governance
The project was managed by the PI with a project manager from the National Institute for Health and Care Research Collaboration for Leadership in Applied Health Research and Care. However, owing to employment changes, the project manager left the project in month 13 of the project and a replacement administrator was appointed in month 16. Team meetings were conducted monthly, chaired by the PI and attended by the project manager/administrator and the research team. Minutes recorded in discussions and progress with key activities are listed in the timetable [see the NIHR Journals Library. URL: www.journalslibrary.nihr.ac.uk/programmes/hsdr/170825/#/ (accessed 31 January 2022)]. Project risks were discussed, and actions agreed to optimise smooth running and coordination of the project.
Issues arising in WP1 included delays due to unanticipated difficulties with data access. This was discussed with our Study Steering Committee and the National Institute for Health and Care Research Health and Social Care Delivery Research project manager, who confirmed continuing support for our proposed plans to accommodate these difficulties. Specifically, we experienced the following unanticipated problems in gaining access to routinely collected data sets.
Workforce data
As a result of changes made by NHS Digital to their collection, analysis and publication of the wMDS, our analysis was delayed while NHS Digital revised statistics from the earlier period of analysis.
GP Patient Survey
Changes in access requirements prevented access to the most detailed level of the most recent GP Patient Survey. We were, however, able to analyse data suitable for addressing our original research questions.
Hospital Episode Statistics
Delays in the processes necessary to obtain access to Hospital Episode Statistics after 2016–17 have not been resolvable within the study period. Nonetheless, our analysis of these data makes a useful contribution to our proposed overall analysis of outcomes.
Adjustments in WP2 to change from a postal to online survey, as described above, gained momentum following initial contact with the lead Clinical Research Network. Imelda McDermott set up contacts with LCRNs. Jon Gibson managed the running of the Practice Manager Survey and responded to queries from the LCRNs.
For WP3, the team involved in this WP (i.e. IM, SS, MG, KC, AM and DH) met fortnightly during the data analysis period and shared nuanced findings across the remaining members of the research team.
Meetings of the Study Steering Committee were arranged at the intended 6-monthly intervals. Full attendance was achieved on each occasion using virtual platforms, and minutes were produced and agreed.
Expert Advisory Group meetings were similarly arranged at 6-monthly intervals, but it proved challenging to maintain attendance by individuals from different practitioner groups. However, those who attended these meetings made valuable contributions and our patient and public involvement representatives remained engaged with the project throughout.
Chapter 3 Understanding the patterns of skill mix in England
In Chapter 1 we have seen that the strong policy push towards diversifying the skill mix of general practice in England is primarily driven by an ongoing workforce crisis and also underpinned by an aspiration to provide more comprehensive services for an ageing population. In this chapter, we explore how far those policy aspirations are reflected in the workforce’s current (up to 2019) composition.
To do this, we analysed national data on the workforce employed by general practices in England, particularly focusing on trends in the employment of different health-care professionals. Findings on the regional distribution of the workforce were published in the British Journal of General Practice in January 2020. 101 In this section, we expand upon these findings to examine how the workforce has changed over time, which provides insight into whether or not other worker groups have diminished in numbers as the variety of workforce groups has increased. The analysis was directed to answer research question 1(i) with regard to how the workforce has changed and where any change has occurred.
Data
We obtained data from NHS Digital on the range of practitioners employed in practices across England. We created a longitudinal practice-level workforce data set using the practice-level general practice workforce data sets (completed by practices as part of their wMDS obligations). These data contain both headcounts and numbers of FTEs for 38 categories of staff [GP categories, n = 5; nurse categories, n = 8; direct patient care (DPC) categories, n = 16; administration categories, n = 9]. For the purpose of this analysis, we focus on categories of staff who are responsible for directly providing health care to patients. These categories of staff are reported in three groups: (1) the GP group, including GP partners, salaried GPs and locum GPs, (2) the nurse’s group, including practice nurses, ANPs and specialist nurses, and (3) the DPC group, including HCAs, PAs, CPs, physiotherapists, paramedics and other allied health professionals.
We used data from 2015 to 2019. The most recent data we report is from the quarterly update that reports data to September 2019.
This is an evolving data collection, with different staff members being added at different times and a dedicated payment now offered to recognise the costs involved in reporting the data. 102 We worked closely with NHS Digital to understand the properties of the data. In data from September 2019, there were usable data for 6296 practices out of the 6867 practices for whom workforce data were made available.
Methods
To describe the practice workforce and its changing nature, we summarised workforce composition by year, by practice size and by region. We used data from the General Practice Workforce data sets from NHS Digital between September 2015 and September 2019. In addition to plotting the geographical distribution of the workforce, we estimated regression models to further examine the association between workforce and practice characteristics. We estimated separate equations for GP, nurse and DPC FTE per 1000 patients (PTP). However, workforce decisions relating to these groups are likely to be associated with practice workforce decisions for the other groups. Therefore, the equation error terms are likely correlated and any cross-equation hypothesis testing will be biased. To account for this correlation, we estimated the models as a seemingly unrelated regression system that has contemporaneous cross-equation error correlation. 103 We estimated the models using the sureg command in Stata 15.1.
Research question 1(i): how has the workforce changed and where has any change occurred?
Composition of the practice workforce
Since September 2015, for the sample practices with usable data, there has been an increase in total workforce FTE from around 47,600 to 51,600 (Table 1). Within that increase in workforce FTE, there has been a decline in the FTE of partner GPs and an increase in the FTE of advanced nurse roles and newer DPC roles, such as CPs and PAs. Table 1 also presents figures for workforce FTE PTP. These figures highlight workforce change in relation to the number of registered patients to whom the workforce are delivering health care, with implications for the capacity of the workforce to deal with changing levels of workload. For example, where an unchanging workforce has to serve an increasing number of patients, then this potentially reduces the practitioner time that can be focused on the needs of each patient. Table 1 shows that, although the number of FTEs in these workforce roles has increased by 8.44%, FTEs PTP have increased by 2.87% after accounting for the growing number of patients. These figures show the same pattern as the raw workforce figures. The number of GP partner FTEs PTP are declining, whereas salaried GPs and locum FTEs are increasing. The number of practice nurse FTEs PTP remains roughly constant, whereas the number of ANP FTEs PTP is increasing. This confirms a gradual shift in the overall workforce composition during this period. Graphical representations of this analysis can be found in Appendix 1, Figures 28–30.
| Date | Measure | Staff type | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GP: partner | GP: salaried | GP: locum | Nurse: practice | Nurse: advanced | HCA | PA | Pharmacist | Physiotherapist | Paramedic | Total | ||
| September 2015 | FTE | 20,719 | 6554 | 578 | 10,745 | 3336 | 5463 | 12 | 165 | 19 | No data | 47,591 |
| September 2016 | FTE | 20,621 | 7168 | 693 | 11,204 | 3705 | 5995 | 35 | 396 | 21 | 57 | 49,895 |
| September 2017 | FTE | 19,849 | 7479 | 1187 | 11,086 | 4103 | 5508 | 49 | 534 | 23 | 184 | 50,002 |
| September 2018 | FTE | 18,692 | 7829 | 1154 | 11,026 | 4409 | 5758 | 81 | 777 | 22 | 335 | 50,083 |
| September 2019 | FTE | 18,028 | 8319 | 1321 | 11,136 | 4737 | 6194 | 207 | 1097 | 41 | 529 | 51,609 |
| % change in total FTE between 2015 and 2019 | 8.44% | |||||||||||
| September 2015 | FTE PTP | 0.3642 | 0.1152 | 0.0102 | 0.1889 | 0.0586 | 0.0960 | 0.0002 | 0.0029 | 0.0003 | No data | 0.8365 |
| September 2016 | FTE PTP | 0.3566 | 0.1240 | 0.0120 | 0.1938 | 0.0641 | 0.1037 | 0.0006 | 0.0068 | 0.0004 | 0.0010 | 0.8630 |
| September 2017 | FTE PTP | 0.3384 | 0.1275 | 0.0202 | 0.1890 | 0.0700 | 0.0939 | 0.0008 | 0.0091 | 0.0004 | 0.0031 | 0.8524 |
| September 2018 | FTE PTP | 0.3150 | 0.1319 | 0.0194 | 0.1858 | 0.0743 | 0.0970 | 0.0014 | 0.0131 | 0.0004 | 0.0056 | 0.8439 |
| September 2019 | FTE PTP | 0.3005 | 0.1387 | 0.0220 | 0.1857 | 0.0790 | 0.1033 | 0.0035 | 0.0183 | 0.0007 | 0.0088 | 0.8605 |
| % change in total FTE PTP between 2015 and 2019 | 2.87% | |||||||||||
There has been an expansion of skill mix in a greater proportion of practices in some regions than in others. Table 2 shows the proportion of practices in each region with at least some FTE of the workforce roles. This demonstrates that, for instance, paramedics have been hired predominantly by practices in the south of England, whereas CPs are more evenly geographically distributed but have the highest uptake by practices in the east of England, North East and Yorkshire and the Midlands. ANPs are employed by 57% of practices in the east of England, but are employed by only 23% of practices in London. Paramedics are employed by 12% of practices in the south-east of England, but are employed by only 1% of practices in the north of England. These results highlight the variation in workforce composition across England.
| Region of England | Staff type (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| GP: partner | GP: salaried | GP: locum | Nurse: practice | Nurse: advanced | HCA | PA | Pharmacist | Physiotherapist | Paramedic | |
| East | 93 | 67 | 30 | 95 | 57 | 79 | 4 | 20 | 1 | 11 |
| London | 93 | 67 | 23 | 89 | 23 | 56 | 2 | 10 | 0 | 1 |
| Midlands | 94 | 64 | 30 | 94 | 50 | 77 | 3 | 20 | 1 | 4 |
| Midlands and east | 93 | 60 | 15 | 93 | 46 | 73 | 1 | 9 | 0 | 2 |
| North-east and Yorkshire | 92 | 67 | 23 | 95 | 58 | 85 | 3 | 22 | 1 | 3 |
| North-west | 85 | 63 | 25 | 92 | 43 | 65 | 2 | 16 | 1 | 2 |
| North | 89 | 60 | 10 | 91 | 43 | 71 | 0 | 10 | 0 | 1 |
| South-east | 94 | 73 | 18 | 95 | 45 | 57 | 2 | 12 | 0 | 12 |
| South-west | 95 | 77 | 19 | 98 | 52 | 85 | 0 | 16 | 2 | 9 |
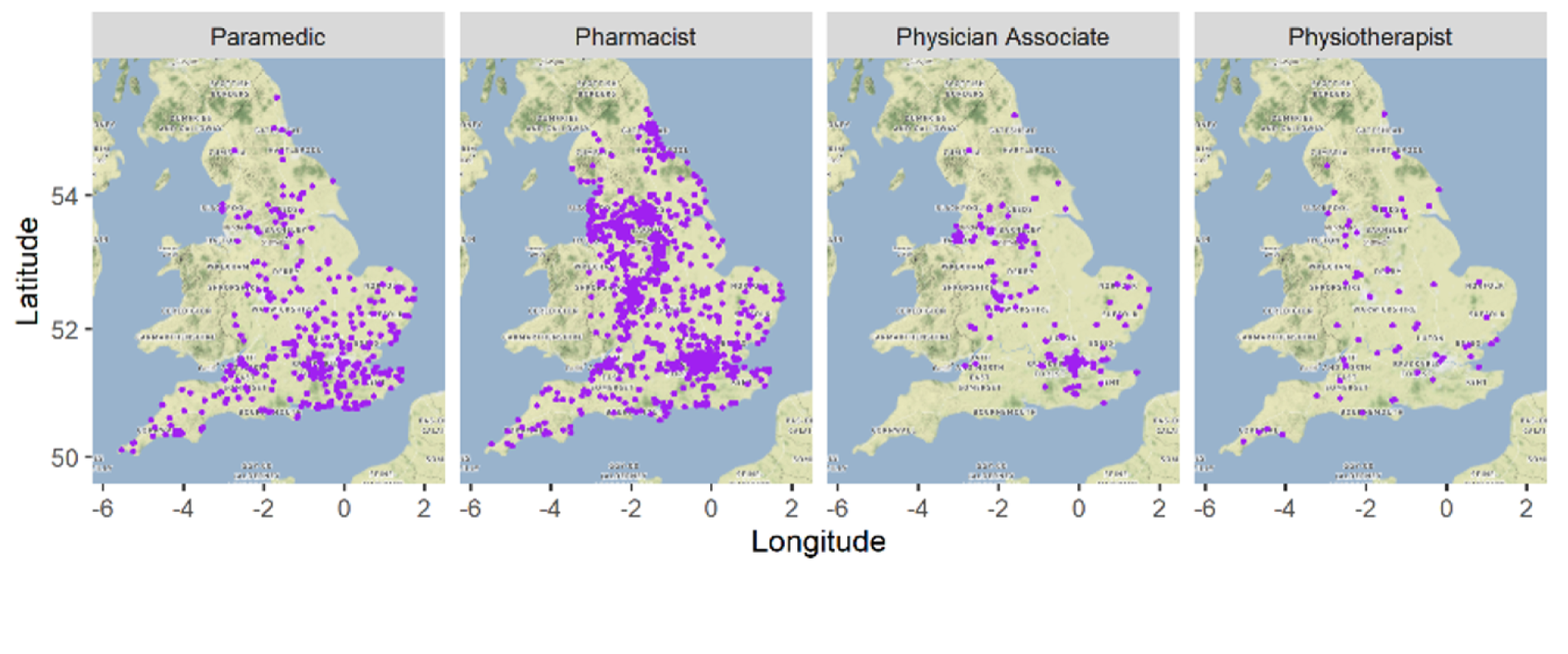
Figure 7 presents a map of England, highlighting practices that employ the different workforce roles. In addition to the pattern of paramedic and CP employment described above, Figure 7 shows that the practices employing PAs are located in the main population centres (i.e. London, the Midlands and the north-west of England) and, also, that there are a very small number of practices currently employing physiotherapists.
FIGURE 7.
Maps of England highlighting practices that employ different workforce roles. Map data ©2021 Google.
Modelling workforce
In addition to plotting the geographical distribution of the workforce, we estimated regression models to further examine the association between workforce and practice characteristics.
Our statistical analyses were based on a sample of 6287 general practices. Despite not being able to analyse data for all practices in England, our core sample was highly representative and allowed us to confidently extrapolate our results to the situation of English primary care more broadly. The characteristics of the typical practice in our sample are described in Table 3, which indicates that the mean number of GP FTE PTP is 0.57, whereas the mean numbers of nurse and other DPC (i.e. pharmacists, paramedics, PAs and physiotherapists) FTE PTPs are 0.27 and 0.20 respectively. The mean distance to the nearest hospital for a practice was 8.57 km and 17% of the practices in our sample were in rural areas. Moreover, 16% of practices in the sample were dispensing practices and 72% were on a GMS contract. The mean percentage of patients aged ≥ 65 years in the sample was 17.73%.
| Variable | Observed, n | Mean | SD |
|---|---|---|---|
| GP FTE PTP | 6287 | 0.57 | 0.27 |
| Nurse FTE PTP | 6287 | 0.27 | 0.15 |
| DPC FTE PTP | 6287 | 0.20 | 0.22 |
| Patients (thousands) | 6287 | 9.08 | 5.82 |
| Distance to nearest hospital (km) | 6287 | 8.57 | 8.38 |
| Distance to nearest medical school (km) | 6287 | 19.67 | 16.32 |
| Proportion (%) of patients aged ≥ 65 years | 6287 | 17.73 | 6.95 |
| MPIG per patient | 6287 | 0.66 | 2.17 |
| Rural (1 = yes; 0 = no) | 6287 | 0.17 | 0.38 |
| Market forces factor | 6287 | 1.18 | 0.11 |
| Income deprivation | 6287 | 0.14 | 0.07 |
| GMS (1 = yes; 0 = no) | 6287 | 0.72 | 0.45 |
| Dispensing practice (1 = yes; 0 = no) | 6287 | 0.16 | 0.37 |
| Extended hours payments (per patients) | 6287 | 1.21 | 1.19 |
To study the association between staffing and practice-level characteristics, we estimated a seemingly unrelated regressions model. We opted for a seemingly unrelated regressions model instead of a set of independent standard linear regressions because the employment decisions for the three workforce groups are likely to be connected. For instance, employing extra GPs is likely to reduce the workforce budget for employing staff from the other groups. In this case, the three separate models will likely have a correlated error term. The seemingly unrelated regressions model accounts for this contemporaneous correlation. 103 The Breusch–Pagan test is a test for independence of residual vectors between the model equations. As shown in Table 3, the null hypothesis of independence of residuals is rejected and, therefore, our model choice is justified.
Patient list size enters these models in several ways. First, the outcome variables are workforce FTE PTP to ensure comparability across practices with different catchment populations. Second, patient list size is included as covariates as a cubic function to capture non-linearities in the effect of patient population on staffing (e.g. if the contribution to the practice drops or jumps above a certain patient number for certain roles). The parameter estimates, shown in Table 4, suggest that the number of patients is not significantly associated with workforce PTP. This relationship is presented differently in Figure 8, which shows that the level of staff PTP is stable across different patient population sizes.
| Outcome variable | Practice workforce FTE PTP | ||
|---|---|---|---|
| GP | Nurse | DPC | |
| Number of patients (thousands) | 0.001 (0.002) | 0.001 (0.001) | 0.002 (0.001) |
| Number of patients (thousands)2 | –0.000 (0.000) | 0.000 (0.000) | –0.000 (0.000) |
| Number of patients (thousands)3 | 0.000 (0.000) | –0.000 (0.000) | –0.000 (0.000) |
| Distance to nearest hospital (km) | 0.000 (0.001) | 0.001*** (0.000) | 0.002*** (0.000) |
| Distance to nearest medical school (km) | –0.001*** (0.000) | 0.001*** (0.000) | 0.001*** (0.000) |
| Proportion (%) of patients aged ≥ 65 years | 0.008*** (0.001) | 0.003*** (0.000) | 0.003*** (0.000) |
| MPIG per patient | 0.007*** (0.002) | 0.000 (0.001) | 0.003*** (0.001) |
| Rural (1 = yes; 0 = no) | 0.033*** (0.012) | 0.014** (0.006) | 0.094*** (0.008) |
| Market forces factor | 0.061 (0.039) | –0.346*** (0.021) | –0.122*** (0.026) |
| Income deprivation | 0.117* (0.063) | 0.304*** (0.034) | 0.329*** (0.042) |
| GMS (1 = yes; 0 = no) | –0.006 (0.008) | –0.024*** (0.004) | –0.022*** (0.005) |
| Dispensing practice (1 = yes; 0 = no) | 0.055*** (0.012) | 0.016*** (0.006) | 0.238*** (0.008) |
| Extended hours payments (per patients) | 0.010*** (0.003) | 0.002 (0.001) | 0.003 (0.002) |
| Constant | 0.325*** (0.059) | 0.546*** (0.032) | 0.161*** (0.040) |
| Observations | 6287 | 6287 | 6287 |
| R 2 | 0.065 | 0.198 | 0.369 |
| Breusch–Pagan test of independence | χ2(6) = 884.098 | p < 0.001 | |
FIGURE 8.
Workforce predictive margins of patient list size.
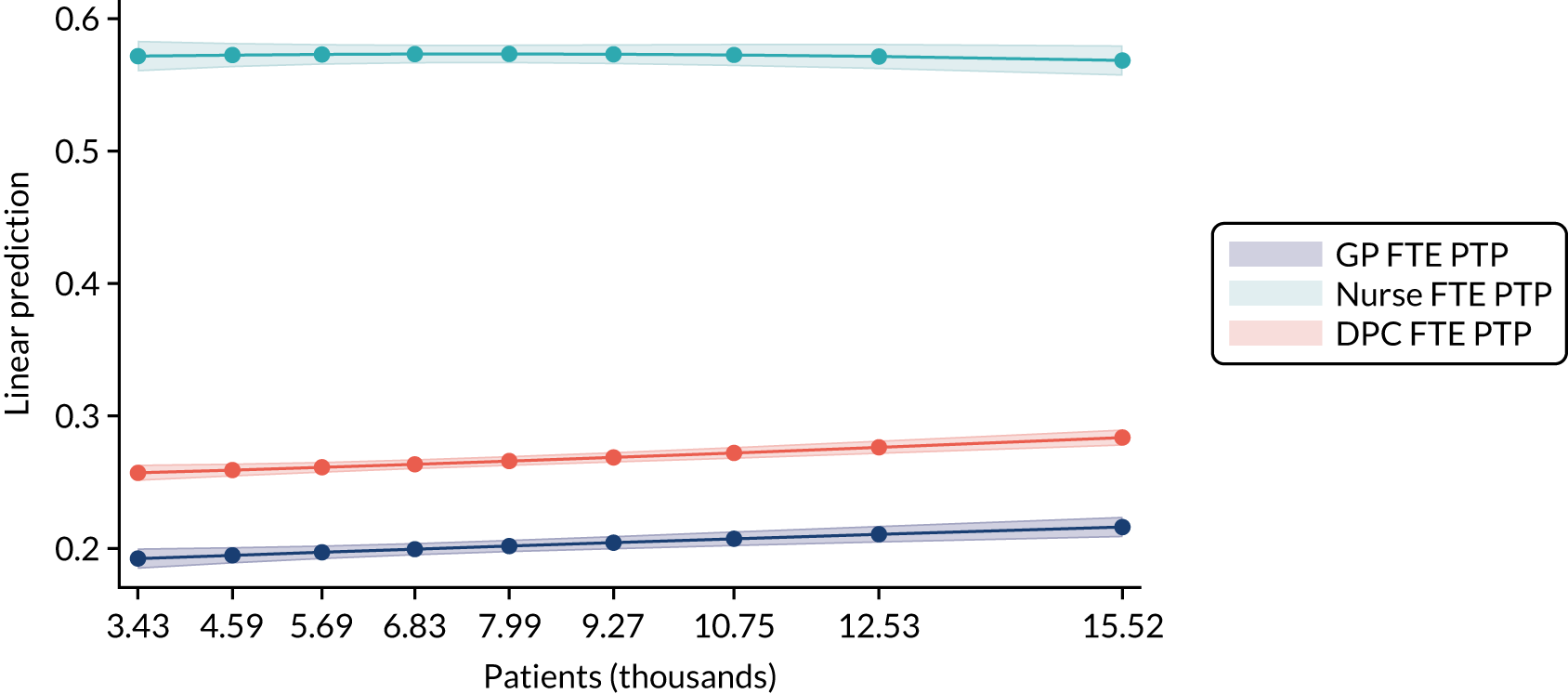
Table 4 also shows that distance to the nearest hospital and medical school (in kilometres) are both positively associated with nurse and DPC FTE PTP, whereas distance to nearest medical school (in kilometres) is negatively associated with GP workforce. Distance to nearest medical school is potentially a supply effect where newly qualified GPs are more likely to locate near to where they have trained, whereas the distance to nearest hospital is a measure of the availability of secondary care. Practices that are located further away from a hospital have more nursing and DPC staff employed.
The proportion of patients aged ≥ 65 years, the amount of payments received through the minimum practice income guarantee (MPIG), rurality, patient income deprivation, the payments for extended hours access and being a dispensing practice are positively associated with workforce groups. These factors indicate that patient demand factors and income payments are positively associated with staff employment.
The market forces factor, which measures the unavoidable cost differences between geographical locations, is negatively associated with nurse and DPC workforce, but is not significantly different from zero for GPs. This is potentially a supply factor where staff on lower salaries (e.g. DPC/nurses) are unable to locate to more expensive areas. Alternatively, there could be a greater demand for GP services in more expensive locations and less demand for appointments with DPC and nursing staff.
Summary
Skill mix change in general practice has been expanding since 2015 to include roles such as CPs and paramedics. However, these roles still represent a small proportion of the workforce. The roll-out of these roles in general practice has not been uniform across the country, with paramedics mainly employed by practices in the south of England and PAs employed by practices in the larger cities. A more detailed workforce analysis shows a range of demand and supply factors associated with the practice workforce. These factors range from geographical factors (e.g. distance to the nearest hospital that may provide initial training for health professionals), supply factors (e.g. the market forces factor, which may affect the affordability of living near the practice for lower-paid workers) and demand factors (e.g. the proportion of patients aged ≥ 65 years whose health-care needs are likely to increase). These contextual differences are an important step in understanding the motivating factors behind the expansion of skill mix and, therefore, any subsequent analysis of the impact on service delivery.
Chapter 4 Practice manager survey
The main objectives of this WP were to investigate practice preferences for different workforce practitioner groups and to ascertain the accuracy of the workforce data collected by NHS Digital through the National Workforce Reporting System, focusing on practice-level data.
In our protocol, we stated that we would also explore ‘Which aspects of healthcare are undertaken by different practitioner types?’ Following reflection on previous work in this area (e.g. the MUNROS study85), we decided that this research question was too nuanced for an online survey and these issues were instead explored using qualitative methods in WP3. Therefore, in this chapter, we address research question 2(i) with regard to what motivates practices to choose/not choose increased skill mix deployment.
In workforce planning, and in appraising the effectiveness of workforce policies, it is vital to have accurate practice-level workforce data as submitted by practices to fulfil their contractual requirements and populate the wMDS. The wMDS was established in 2011 by the then Department of Health (now the Department of Health and Social Care) to support workforce planning and the commissioning of education and training.
Survey questionnaire
The first set of questions presented practices with data about their workforce composition that were retrieved from the wMDS. Respondents were asked to confirm or correct these data.
The second set of questions selectively asked practices about factors influencing their decision to employ staff in specific roles that they had just confirmed. Questions focused on six practitioner categories: (1) ANP, (2) specialist nurse, (3) HCA, (4) PA, (5) paramedic and (6) CP. As indicated in Chapter 2, these categories were chosen to include established practitioner types, employment supported by financial incentives, staff providing additional services and staff available through PCN funding. Respondents were presented with a list of 12 predefined motivating factors drawn from our knowledge of workforce policy and literature and insights from GP members of the research team. Respondents were permitted to add additional factors not captured in the list. Practices were asked to select all that applied to their decision. Those practices that employed staff in one of the six roles of interest were then asked if they had received external funding to support staff employment in that role and, if so, from which organisation and if they were still receiving funding.
The third set of questions was posed to all practices regardless of the workforce they currently employed. Practices were asked if they wanted to employ additional staff from a list of roles in the future and, if so, if they wished for them to be directly employed by the practice or through a PCN.
Finally, practices were asked to select their ideal workforce by selecting the percentage of their workforce that should be made up of different roles. Respondents used slider bars to indicate the percentage for each worker group. Bars were programmed to adjust to 100% total.
For the second and third sets of questions, we presented statistics for the variables of interest. These statistics were the percentage or proportion of practices selecting each option. For continuous variables, we presented a standard deviation (SD). Factors that affected the likelihood of the practice responding to the questionnaire could introduce bias if the characteristics and responses of the responding practices were systematically different from non-responding practices. Therefore, we used inverse probability weighting (see Mansournia and Altma104) to reduce this potential for bias. 64 To calculate these weights, we estimated a logistic regression model for the binary variable of whether or not a practice responded, using the workforce, region and registered population characteristics as explanatory variables. We predicted the probability of responding for each practice using this regression model and took the reciprocal of this fitted value as a weight.
Response and sample
Survey responses were submitted by 1261 practice managers. Workforce data from NHS Digital contained records for 7012 practices, as of December 2019. Our sample accounted for around 17% of this total population of general practices.
After exclusions due to missing data both in the submission and in the NHS Digital data (from responders and non-responders), responses from 1205 (i.e. 96% of 1261) practices were used for this analysis. The sample contained at least one respondent from 174 of 191 (91%) Clinical Commissioning Groups (CCGs).
Practices in the sample were larger than non-responding practices in terms of both workforce and patient list size. Mean GP FTE for the sample practices was 5.94 FTE compared with a mean of 4.84 FTE for non-responding practices (i.e. a difference of 1.1 FTE). Sample practices also employed more FTEs across the other three workforce groups (i.e. nurses, DPC and administration). Sample practices had, on average, larger patient list sizes than the total population, with a mean of 10,219 patients compared with a mean of 8702 patients (i.e. a difference of 1517 patients). The results from the logistic regression are presented in Table 5.
| Response (1 = yes, 0 = no) | Coefficient | SE | 95% CI |
|---|---|---|---|
| Practice GP FTE | 0.05 | 0.01 | 0.03 to 0.07 |
| Practice DPC FTE | 0.05 | 0.01 | 0.03 to 0.08 |
| Income deprivation | –2.34 | 0.56 | –3.45 to –1.24 |
| Region | |||
| London | 0.40 | 0.12 | 0.17 to 0.63 |
| Midlands | –0.59 | 0.13 | –0.84 to –0.34 |
| North East and Yorkshire | –0.17 | 0.13 | –0.41 to 0.08 |
| North West | –0.42 | 0.14 | –0.69 to –0.15 |
| South east of England | –0.58 | 0.13 | –0.84 to –0.31 |
| South west of England | –0.08 | 0.14 | –0.34 to 0.19 |
| Constant | –1.36 | 0.12 | –1.60 to –1.12 |
| n | 6447 | ||
| Pseudo-R2 | 0.04 | ||
| Log-likelihood | –2991.24 | ||
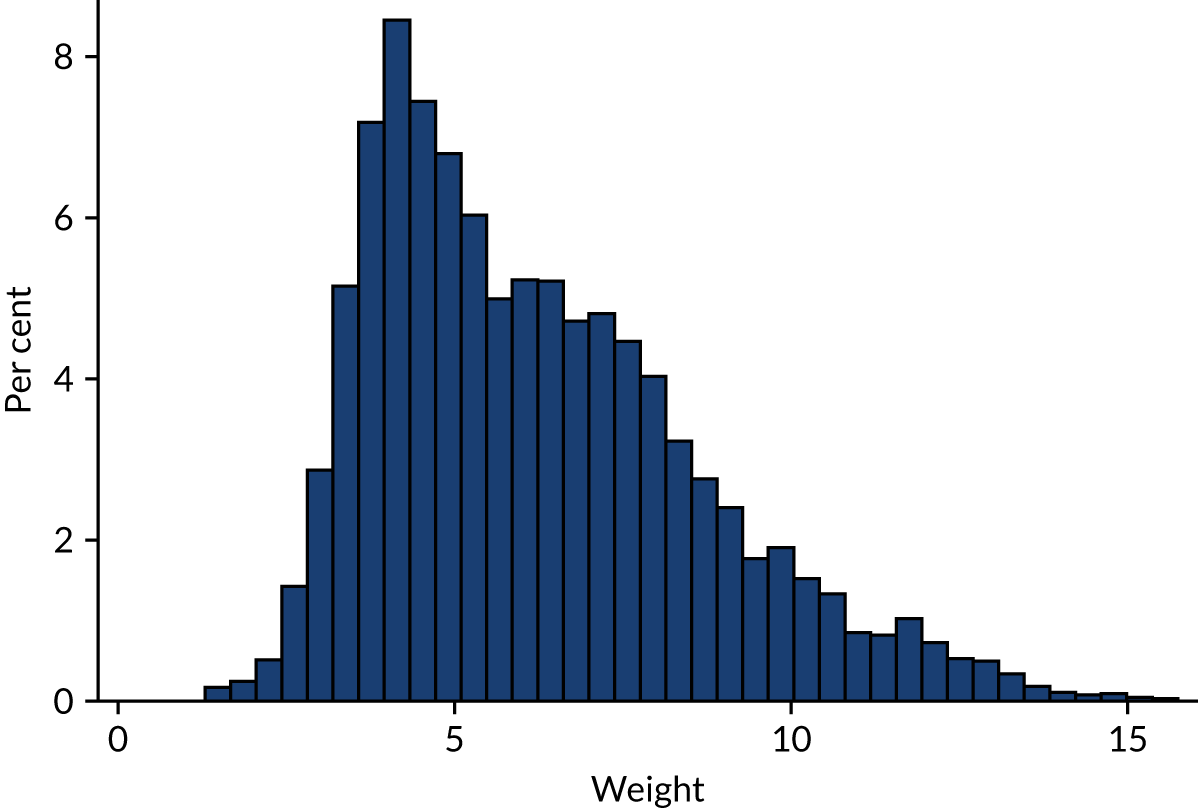
The distribution of the resulting weights is shown in Figure 9.
FIGURE 9.
Histogram of inverse probability weights.
Workforce data
Table 6 shows the number of practices that indicated that workforce data from NHS Digital were incorrect for the different staff groups. Around 30% of practices indicated that the FTE data were incorrect for the GP partner, GP salaried, practice nurse and HCA categories. Nurse specialists, PAs and paramedics had the lowest rates of data labelled as incorrect.
| Category | Practices, n | Practices selected incorrect, n | % incorrect |
|---|---|---|---|
| GP partner | 1247 | 394 | 31.6 |
| GP salaried | 1247 | 409 | 32.8 |
| GP locum | 1247 | 189 | 15.2 |
| Practice nurse | 1232 | 363 | 29.5 |
| Nurse advanced | 1232 | 291 | 23.6 |
| Nurse specialist | 1232 | 56 | 4.5 |
| HCA | 1218 | 374 | 30.7 |
| PA | 1218 | 34 | 2.8 |
| CP | 1218 | 247 | 20.3 |
| Paramedic | 1218 | 67 | 5.5 |
The practitioner categories with the largest percentage of incorrect data, such as GP, practice nurse and HCA, were the most commonly employed practitioners. Therefore, there was more chance of the FTE being incorrect relative to some of the other categories, such as paramedic or PA, where the vast majority of practices did not employ any FTE. Table 7 separated practices that employed some staff from the group (i.e. FTE > 0) and practices that did not (i.e. FTE = 0)
| Category | FTE | NHS Digital, n (%) | Indicated incorrect, n (%) | NHS Digital | Corrected | |||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | n (%) | Mean | SD | ||||
| GP partner | FTE = 0 | 83 (6.7) | 19 (22.9) | 0.00 | 0.00 | 76 (6.0) | 0.00 | 0.00 |
| FTE > 0 | 1164 (93.3) | 375 (32.2) | 3.39 | 2.28 | 1181 (94.0) | 3.29 | 2.17 | |
| All | 1247 (100.0) | 394 (31.6) | 3.16 | 2.36 | 1257 (100.0) | 3.09 | 2.24 | |
| GP salaried | FTE = 0 | 337 (27.0) | 60 (17.8) | 0.00 | 0.00 | 303 (24.1) | 0.00 | 0.00 |
| FTE > 0 | 910 (73.0) | 349 (38.4) | 1.96 | 1.82 | 952 (75.9) | 2.01 | 1.83 | |
| All | 1247 (100.0) | 409 (32.8) | 1.43 | 1.78 | 1255 (100.0) | 1.52 | 1.81 | |
| GP locum | FTE = 0 | 884 (70.9) | 107 (12.1) | 0.00 | 0.00 | 852 (68.2) | 0.00 | 0.00 |
| FTE > 0 | 363 (29.1) | 82 (22.6) | 0.64 | 0.78 | 397 (31.8) | 0.69 | 0.75 | |
| All | 1247 (100.0) | 189 (15.2) | 0.19 | 0.51 | 1249 (100.0) | 0.22 | 0.53 | |
| Practice nurse | FTE = 0 | 64 (5.2) | 21 (32.8) | 0.00 | 0.00 | 52 (4.2) | 0.00 | 0.00 |
| FTE > 0 | 1168 (94.8) | 342 (29.3) | 2.03 | 1.69 | 1196 (95.8) | 2.13 | 1.99 | |
| All | 1232 (100.0) | 363 (29.5) | 1.92 | 1.71 | 1248 (100.0) | 2.04 | 2 | |
| Nurse advanced | FTE = 0 | 713 (57.9) | 117 (16.4) | 0.00 | 0.00 | 632 (51.2) | 0.00 | 0.00 |
| FTE > 0 | 519 (42.1) | 174 (33.5) | 1.36 | 0.96 | 603 (48.8) | 1.59 | 2.39 | |
| All | 1232 (100.0) | 291 (23.6) | 0.57 | 0.92 | 1235 (100.0) | 0.77 | 1.85 | |
| Nurse specialist | FTE = 0 | 1122 (91.1) | 25 (2.2) | 0.00 | 0.00 | 1115 (90.4) | 0.00 | 0.00 |
| FTE > 0 | 110 (8.9) | 31 (28.2) | 1.01 | 1.06 | 118 (9.6) | 1.02 | 1.01 | |
| All | 1232 (100.0) | 56 (4.5) | 0.09 | 0.43 | 1233 (100.0) | 0.1 | 0.43 | |
| HCA | FTE = 0 | 252 (20.7) | 91 (36.1) | 0.00 | 0.00 | 168 (13.6) | 0.00 | 0.00 |
| FTE > 0 | 966 (79.3) | 283 (29.3) | 1.38 | 1.08 | 1069 (86.4) | 1.53 | 1.92 | |
| All | 1218 (100.0) | 374 (30.7) | 1.09 | 1.11 | 1237 (100.0) | 1.32 | 1.86 | |
| PA | FTE = 0 | 1183 (97.1) | 26 (2.2) | 0.00 | 0.00 | 1166 (95.5) | 0.00 | 0.00 |
| FTE > 0 | 35 (2.9) | 8 (22.9) | 1.33 | 0.99 | 55 (4.5) | 1.29 | 0.87 | |
| All | 1218 (100.0) | 34 (2.8) | 0.04 | 0.277 | 1221 (100.0) | 0.06 | 0.32 | |
| CP | FTE = 0 | 989 (81.2) | 189 (19.1) | 0 | 0 | 815 (66.3) | 0.00 | 0.00 |
| FTE > 0 | 229 (18.8) | 58 (25.3) | 1.02 | 0.77 | 415 (33.7) | 0.93 | 1.34 | |
| All | 1218 (100.0) | 247 (20.3) | 0.19 | 0.52 | 1230 (100.0) | 0.32 | 0.89 | |
| Paramedic | FTE = 0 | 1136 (93.3) | 43 (3.8) | 0.00 | 0.00 | 1100 (90.1) | 0.00 | 0.00 |
| FTE > 0 | 82 (6.7) | 24 (29.3) | 1.23 | 0.77 | 121 (9.9) | 1.27 | 0.72 | |
| All | 1218 (100.0) | 67 (5.5) | 0.08 | 0.37 | 1221 (100.0) | 0.13 | 0.44 | |
Table 7 shows that practices that employed some practitioners (i.e. a FTE > 0) were larger, at between 22.6% (GP locums) and 38.4% (GP salaried), than the full sample, which ranges between 2.8% (PAs) and 32.8% (GP salaried). Table 7 also shows the mean FTE in the NHS Digital data and the data that the practice managers had corrected.
Figure 10 presents histograms of these differences for each of the staff groups. The histograms present the NHS Digital FTE for the staff group minus the FTE that the practice manager corrected. A positive value indicated that the NHS Digital FTE value was an overestimate, whereas a negative value indicated that the NHS Digital FTE value was an underestimate. These values were presented for the practices that indicated that the published FTE values were incorrect.
FIGURE 10.
Full-time equivalent difference.
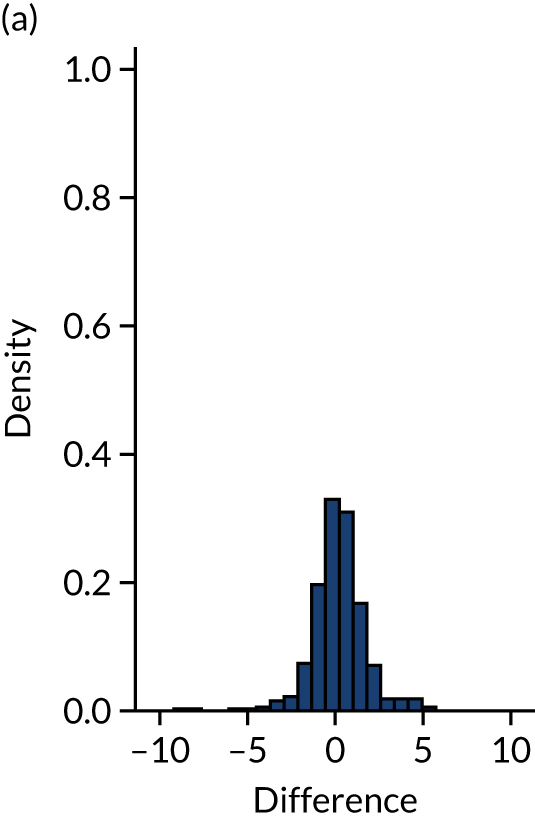
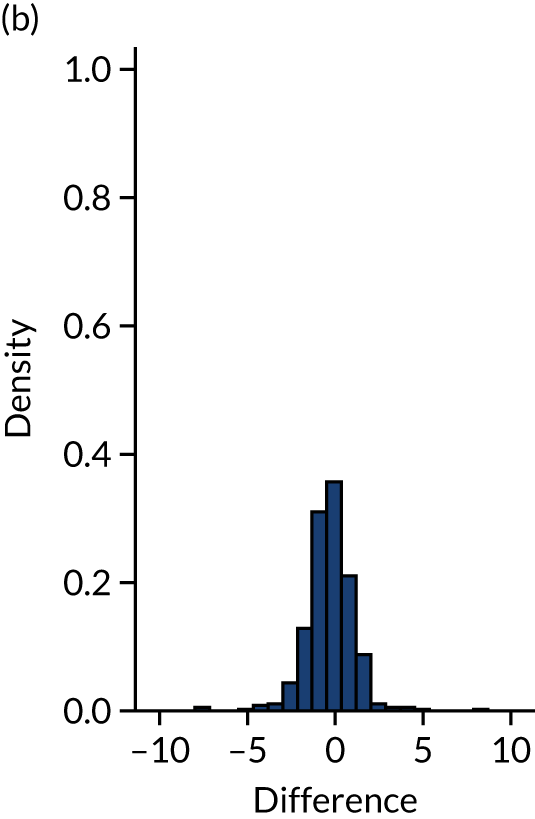
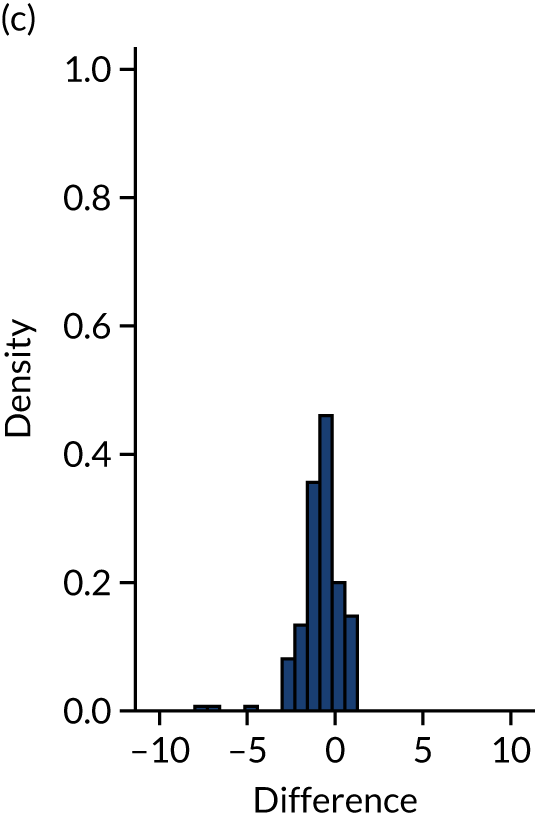
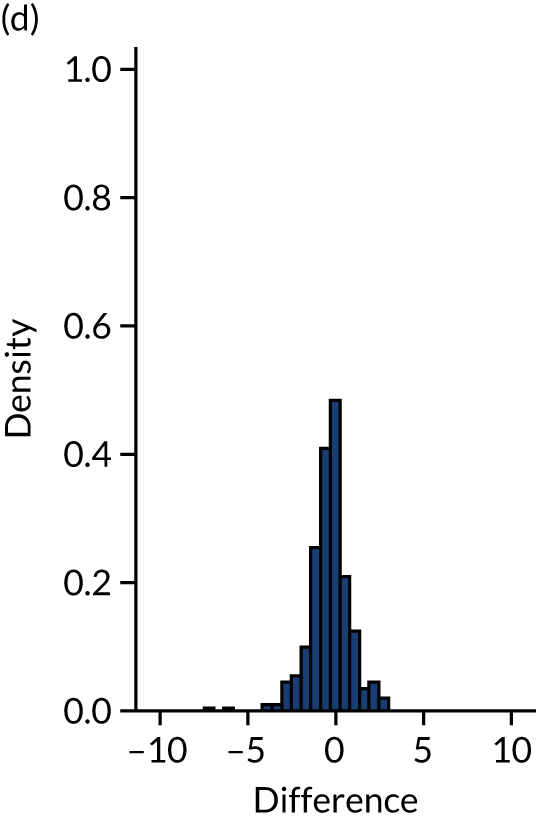
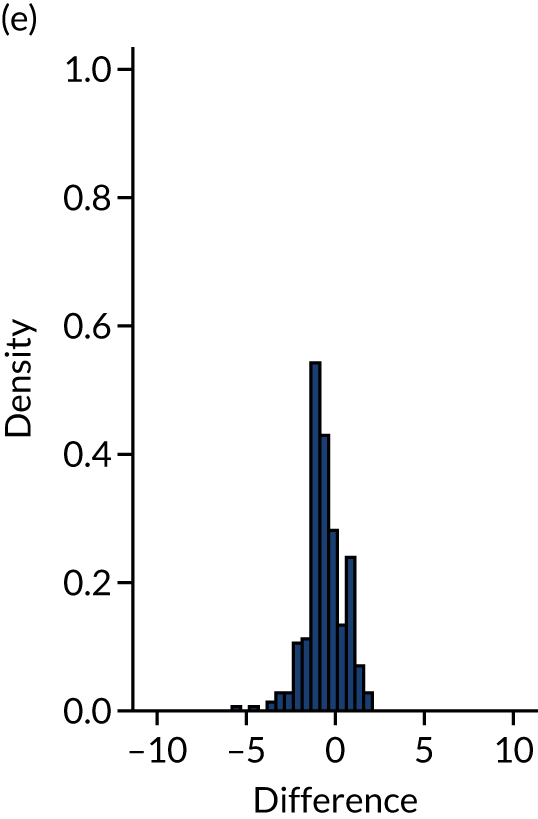
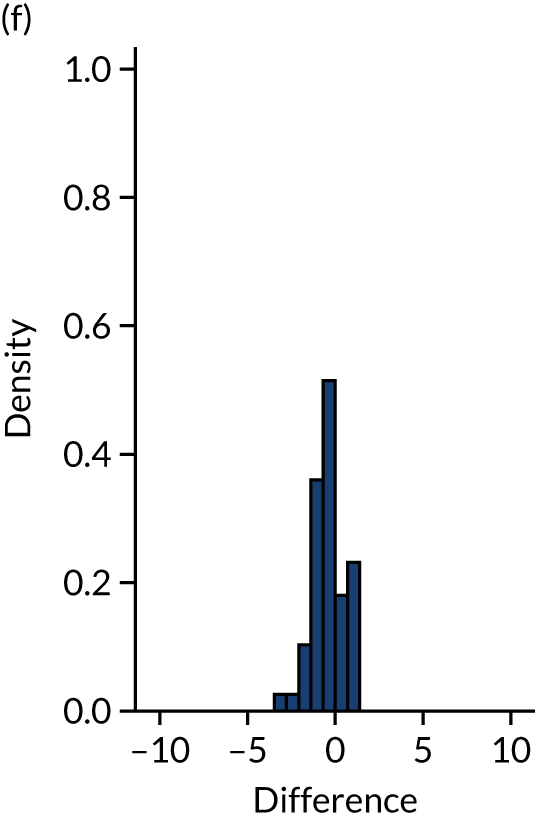
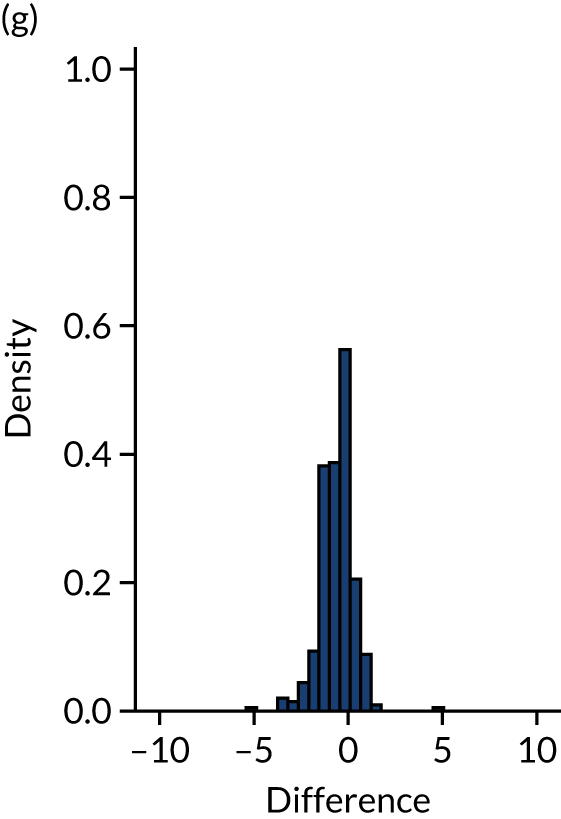
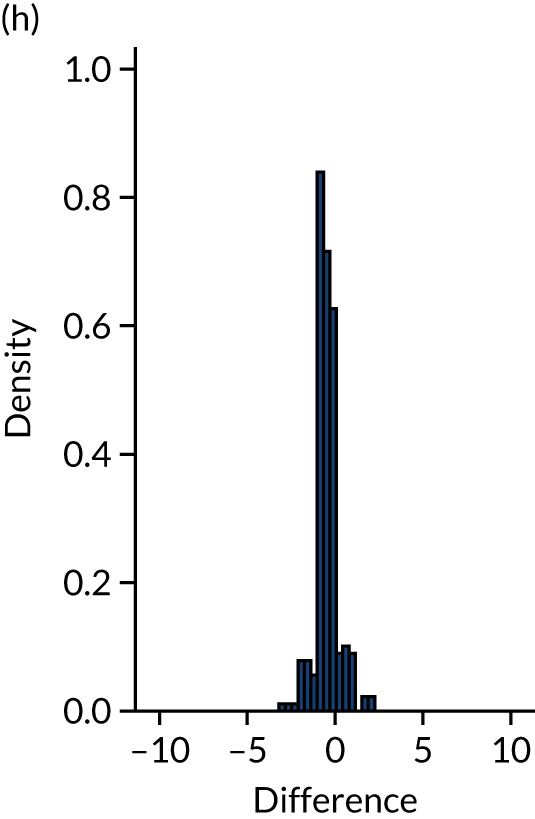
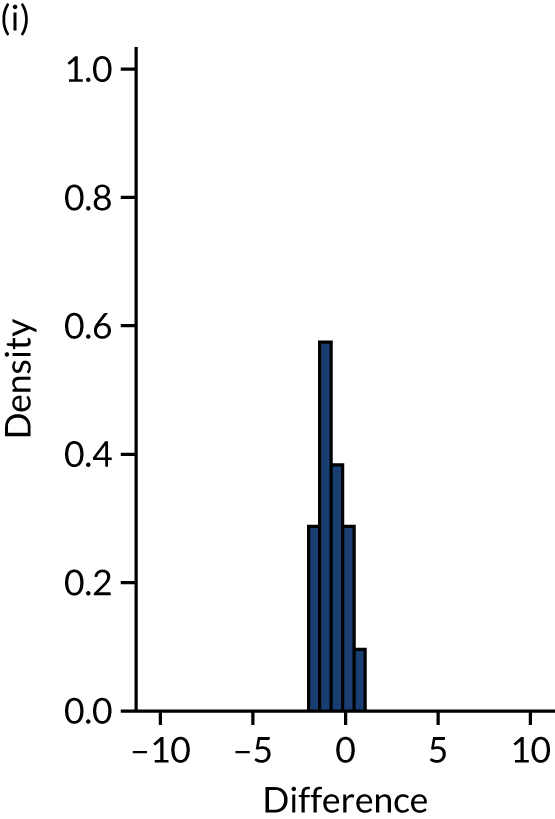
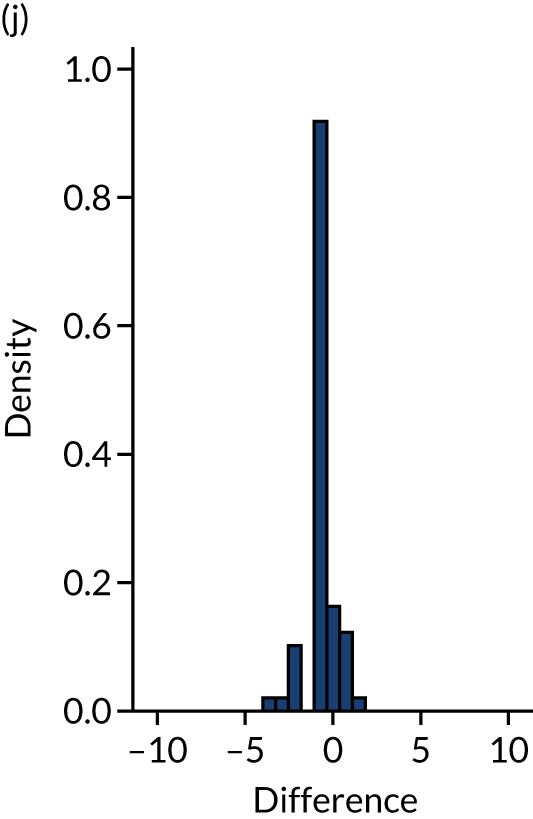
The histograms for each group are approximately centred on zero, with broadly symmetrical density above and below zero and the majority of the density within the range ± 5 FTE. These characteristics of the histograms suggest that there are no systematic biases in the data. Given that there are no skews and given the relatively small sizes, the differences could be characterised as random measurement error. Although the exact reason for any differences would require further investigation, these results suggest that the workforce data released by NHS Digital are not limited by systematic bias and are, therefore, appropriate for analysis of associations between practitioner composition of the workforce and the activity and outcomes data set used in WP1.
Research question 2(i): what motivates practices to choose/not choose increased skill mix deployment?
Alongside the list of motivating factors, Table 8 shows that the most commonly selected motivating factor for employing advanced nurses and PAs was ‘To increase overall appointment availability’. For employers of CPs and paramedics it was ‘Desire to release GP time’. The most commonly selected motivating factor for employing specialist nurses and HCAs was ‘Desire to achieve a better match between what patients need and what the practitioner team can deliver’ (Figure 11).
| Motivating factor | Percentage of practices with practitioner type | |||||
|---|---|---|---|---|---|---|
| ANP (n = 615) | Specialist nurse (n = 125) | HCA (n = 1087) | PA (n = 61) | CP (n = 486) | Paramedic (n = 125) | |
| To increase overall appointment availability | 75.58 | 48.43 | 67.38 | 75.90 | 51.20 | 68.58 |
| Desire to release GP time | 69.97 | 56.74 | 23.94 | 65.95 | 78.27 | 81.25 |
| Desire to achieve a better match between what patients need and what the practitioner team can deliver | 69.04 | 78.92 | 67.48 | 66.36 | 70.02 | 66.42 |
| Desire to move forward with national policy for skill mix (i.e. different types of practitioners) | 55.13 | 46.67 | 47.04 | 58.72 | 62.92 | 57.92 |
| Desire to improve cost-effectiveness | 53.37 | 40.81 | 62.37 | 51.19 | 54.62 | 46.31 |
| To provide additional or improved services to patients, such as increased access beyond what is currently available | 52.46 | 52.49 | 49.62 | 36.90 | 52.83 | 47.64 |
| Desire to improve working conditions for practice staff | 40.79 | 27.21 | 38.35 | 35.42 | 35.30 | 32.45 |
| Unable to recruit a GP | 37.40 | 15.50 | 2.90 | 31.00 | 13.20 | 35.70 |
| To cope with recruitment issues (i.e. our choices are limited by the availability of suitable practitioners) | 31.71 | 15.44 | 7.81 | 40.03 | 21.33 | 41.21 |
| To keep pace with the range of services offered by other local practices | 15.09 | 15.19 | 25.23 | 12.29 | 22.62 | 11.49 |
| To make use of specific services, funding or incentives provided by a local CCG, federation, GP network, etc. | 7.90 | 16.41 | 12.18 | 14.98 | 39.26 | 12.45 |
| To fit with local policy decisions (e.g. funding for specific types of practitioner through an incentive scheme) | 7.29 | 8.72 | 6.05 | 11.79 | 31.90 | 5.80 |
Other commonly selected factors across the staff groups were ‘Desire to improve cost-effectiveness’, ‘Desire to move forward with national policy for skill mix (i.e. different types of practitioners)’ and ‘To provide additional or improved services to patients such as increased access beyond what is currently available’. Supply factors such as ‘To cope with recruitment issues (i.e. our choices are limited by the availability of suitable practitioners)’ and ‘Unable to recruit a GP’ were not as frequently selected, but were most commonly selected by employers of ANPs, paramedics and PAs. Few practices added additional motivating practices, which suggests that the predefined list covered most motivations.
FIGURE 11.
Motivating factors: proportion of practices with practitioner types who selected motivating factor. Note that responses are weighted by inverse probability weights. (a) ANP; (b) specialist nurse; (c) HCA; (d) PA; (e) CP; and (f) paramedic.
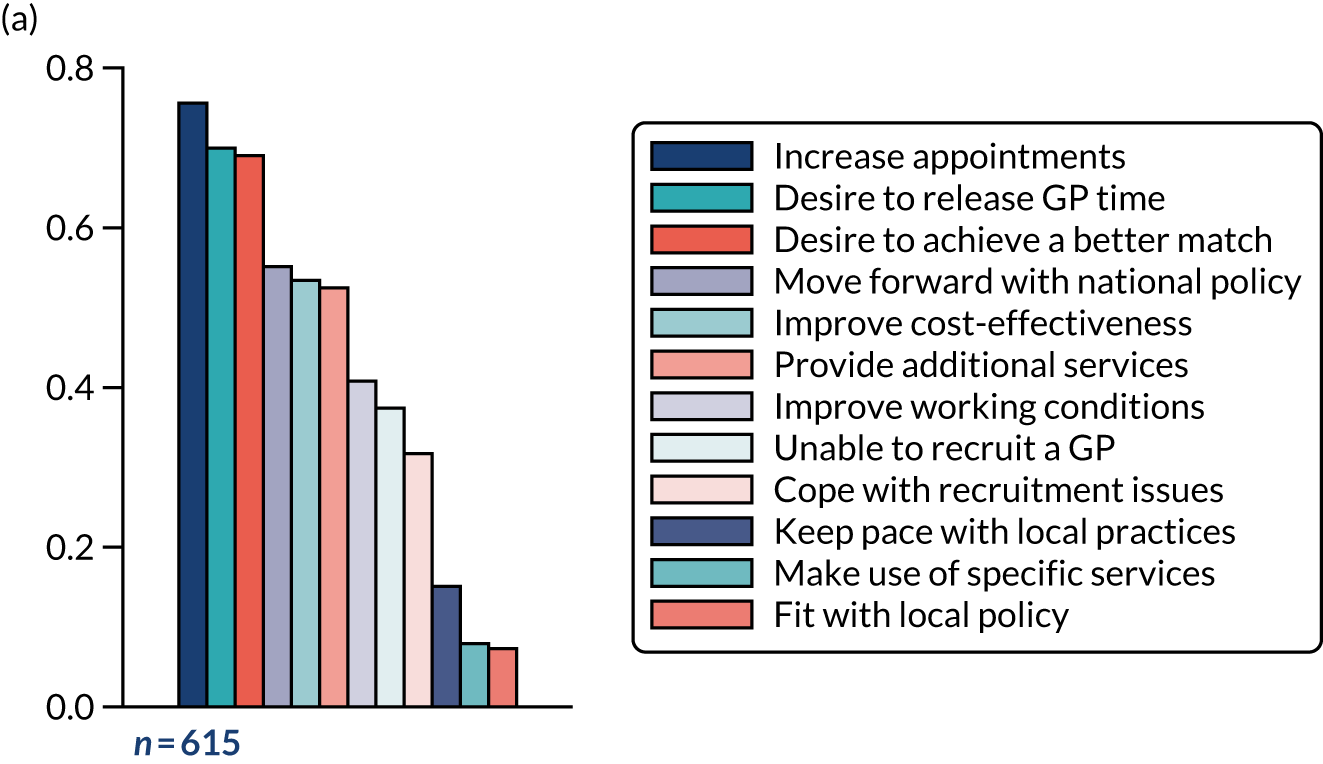
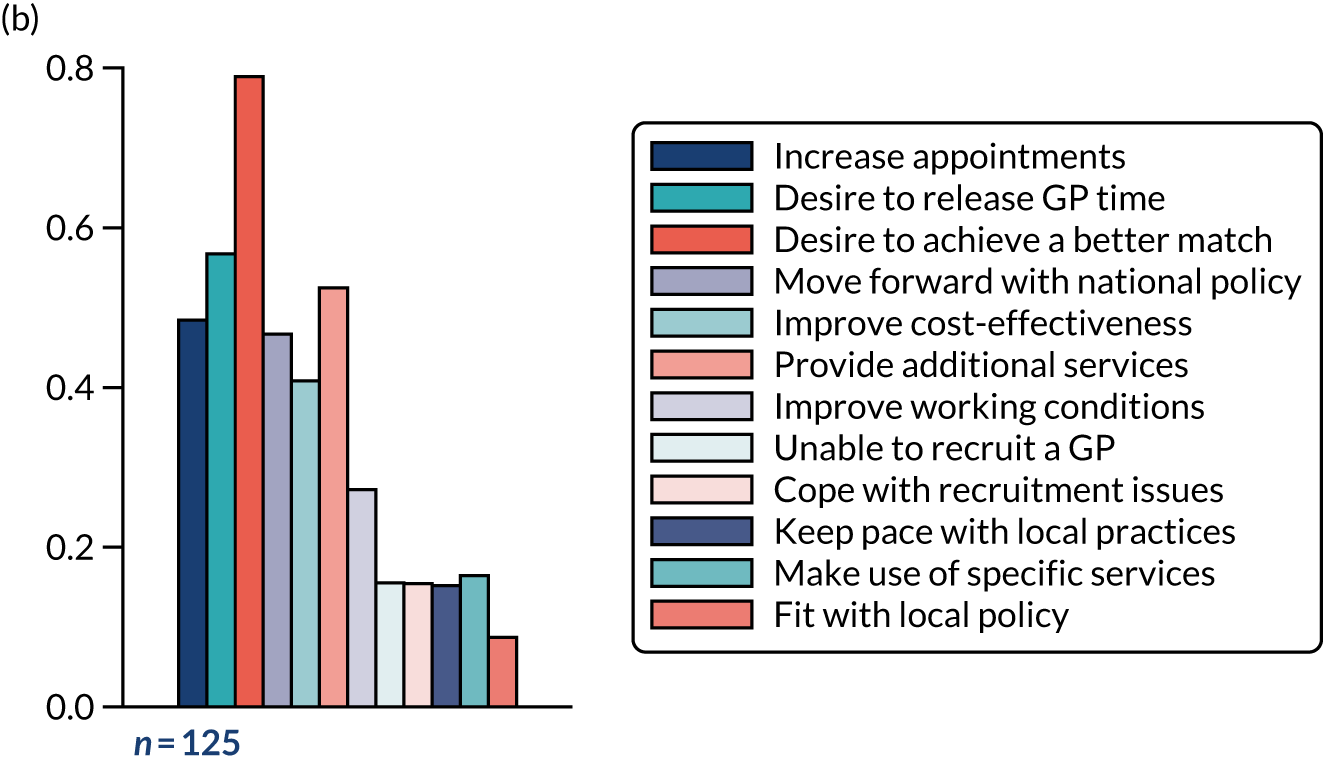

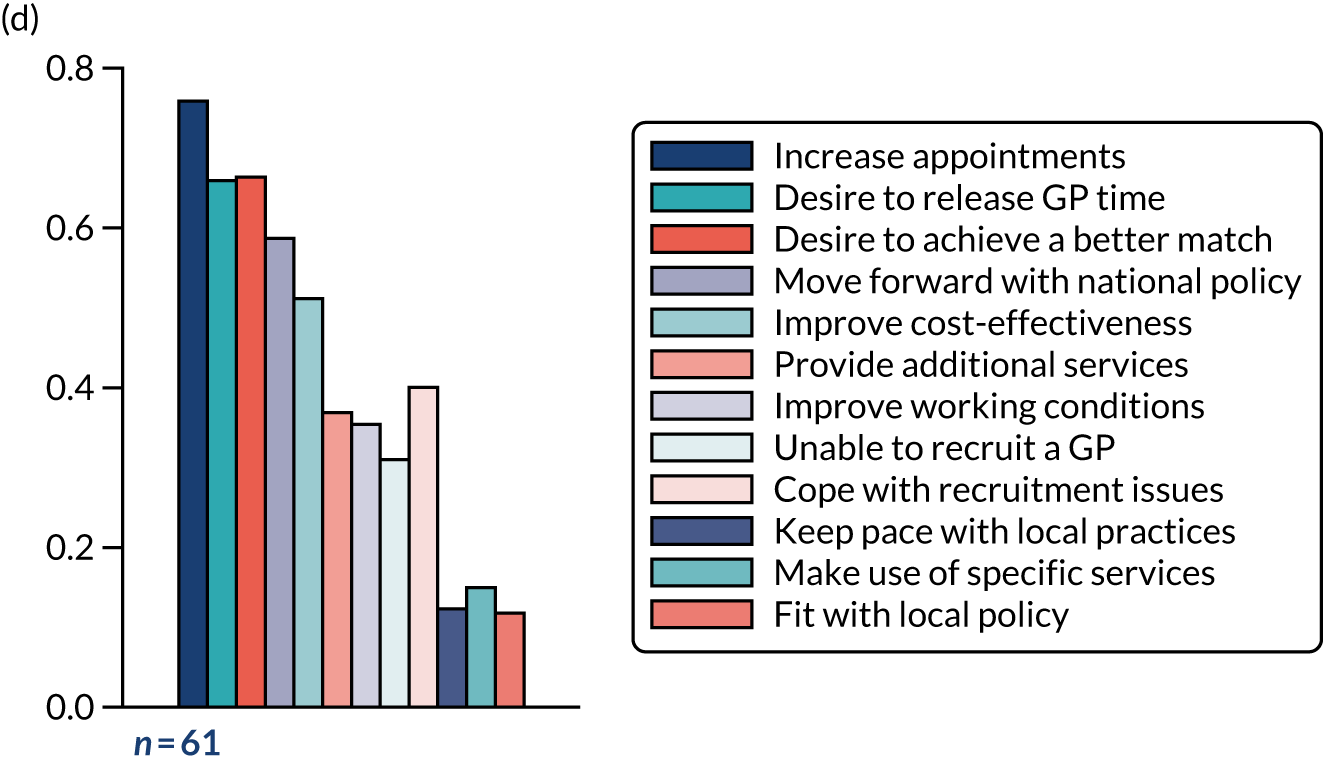
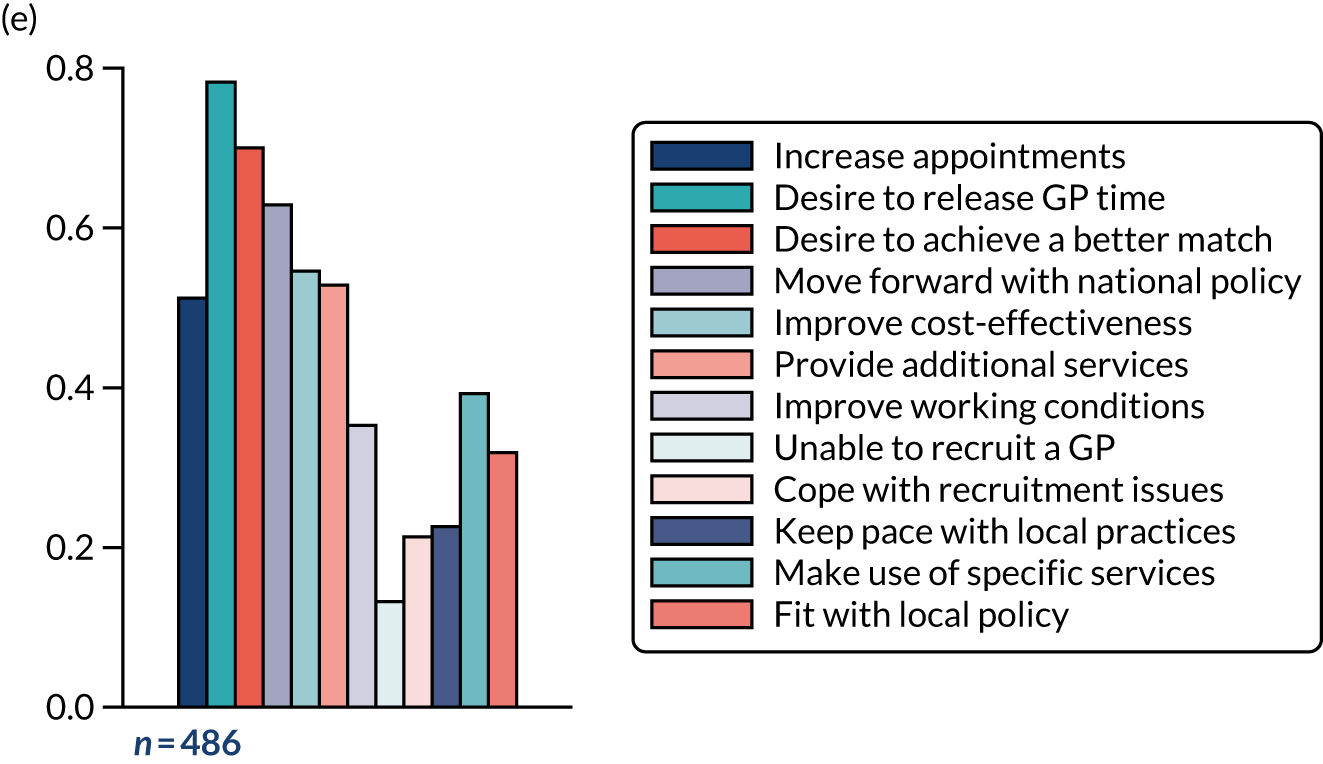
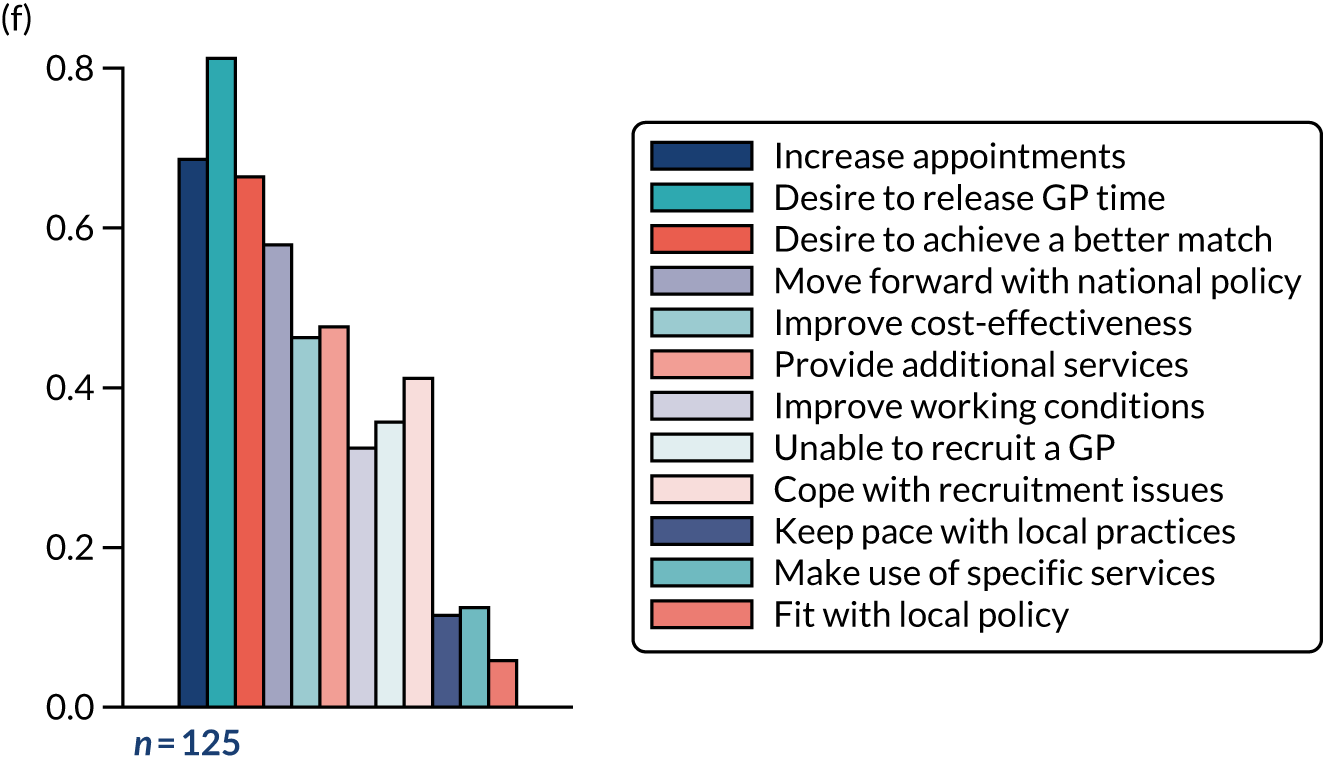
External funding as factor influencing workforce composition
Table 9 shows the percentages of practices that receive external funding to support staff employment in the six roles of interest. CPs’ and PAs’ employment was most commonly supported by specific additional funding, with 63% and 34% of practices that employ them, respectively, receiving funding. Of the 486 practices that employed CPs, 31% reported receiving funding from NHS England and 18% reported receiving funding from local providers, such as the PCN or a GP federation (which is a group of general practices forming an organisational entity to work together within a local health economy). Of the 61 practices that employed PAs, 19% had received funding from HEE and 10% had received funding from their CCG. Around 16% of practices that employed paramedics and specialist nurses had received additional funding to support their employment. Twenty-four per cent of the practices that employed CPs reported that they were still receiving additional funding at the time of completing the questionnaire.
| Financial support | Staff type (%) | |||||
|---|---|---|---|---|---|---|
| ANP (n = 615) | Specialist nurse (n = 125) | HCA (n = 1087) | PA (n = 61) | CP (n = 486) | Paramedic (n = 125) | |
| Do not know | 5.7 | 5.4 | 5.6 | 6.6 | 4.7 | 3.0 |
| None | 73.7 | 64.1 | 72.4 | 45.8 | 27.4 | 72.6 |
| CCG | 3.5 | 11.0 | 3.5 | 9.8 | 15.0 | 7.8 |
| Local | 1.7 | 1.6 | 1.5 | 0.7 | 18.2 | 4.6 |
| HEE | 3.2 | 1.8 | 2.8 | 18.7 | 3.3 | 1.4 |
| NHS England | 0.8 | 0.0 | 0.7 | 3.3 | 31.0 | 0.3 |
| Other | 1.0 | 2.0 | 0.8 | 5.2 | 2.7 | 2.9 |
| Any financial incentive? | 7.9 | 16.4 | 7.6 | 34.2 | 63.4 | 16.7 |
| Still receive? | 1.9 | 4.4 | 1.5 | 14.9 | 23.6 | 5.7 |
Desire for future access to additional practitioners
Table 10 shows the number of practices from the full sample that indicated that they would like to have access to additional practitioners from the listed roles, either through direct employment or through a PCN or federation. The most commonly selected staff were the more traditional roles (i.e. salaried GPs, ANPs, GP partners and practice nurses). Of the practices that indicated that they would like more staff from newer primary care roles (e.g. PAs, CPs, paramedics or physiotherapists), the majority indicated that they wished to access these staff through a network, federation or other existing organisation. In total, 57.7% of practices indicated that they would like access to physiotherapists through a PCN or other organisation, whereas only 25.9% of practices indicated that they would like access to additional PAs in the same way.
| Additional practitioner | Employed through our own practice (%) | Access through a network, federation or similar organisation (%) |
|---|---|---|
| Salaried GP | 41.3 | 14.0 |
| ANP | 33.2 | 21.6 |
| Partner GP | 32.0 | 3.5 |
| Practice nurse | 28.3 | 10.0 |
| CP | 23.5 | 53.3 |
| HCA | 22.6 | 9.7 |
| Physiotherapist | 16.0 | 57.7 |
| Paramedic | 14.3 | 45.2 |
| PA | 14.0 | 25.9 |
| Specialist nurse | 11.5 | 25.9 |
Preferred ideal workforce composition
General practitioner partners formed 28% of the mean ideal workforce, with some level of GP workforce selected by 91% of respondents (Table 11 and Figure 12). Practice nurses formed 15.3% of the mean ideal workforce and were selected by 90% of respondents. Among other roles, CPs were most commonly selected to be part of the workforce (by 78% of respondents) and formed 7.6% of the mean ideal workforce. This compared with 25% of the responding practices currently employing CPs. PAs were selected by 26% of respondents and formed 2.2% of the mean ideal workforce. As highlighted in Figure 12, newer roles, such as CPs, physiotherapists, PAs and paramedics, formed a greater proportion of the ideal workforce relative to the current workforce employed by the practice.
| Staff type | Ideal workforce | Current workforce | Correlation between means | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| % selecting > 0 | Mean % of ideal workforce | SD | % FTE > 0 | Mean % of workforce (FTE) | SD | |||
| Partner GP | 89.8 | 28.1 | 19.28 | 92.4 | 37.3 | 19.59 | 0.34 | < 0.001 |
| Salaried GP | 76.8 | 14.8 | 12.94 | 73.3 | 15.7 | 15.28 | 0.39 | < 0.001 |
| ANP | 76.2 | 10.9 | 9.49 | 48.3 | 7.0 | 9.35 | 0.37 | < 0.001 |
| Specialist nurse | 36.5 | 2.9 | 5.22 | 10.0 | 0.8 | 3.32 | 0.17 | < 0.001 |
| Practice nurse | 90.0 | 15.4 | 8.87 | 96.6 | 22.7 | 10.83 | 0.12 | < 0.001 |
| HCA | 87.3 | 11.3 | 8.31 | 83.1 | 13.2 | 9.58 | 0.23 | < 0.001 |
| PA | 26.3 | 2.2 | 4.88 | 5.3 | 0.4 | 2.30 | 0.25 | < 0.001 |
| CP | 78.2 | 7.6 | 6.99 | 25.4 | 2.2 | 5.12 | 0.16 | < 0.001 |
| Paramedic | 45.4 | 3.2 | 4.39 | 8.1 | 0.6 | 2.45 | 0.35 | < 0.001 |
| Physiotherapist | 54.9 | 3.7 | 4.35 | 2.6 | 0.02 | 0.31 | 0.07 | 0.031 |
FIGURE 12.
Current and ideal workforce composition (%).
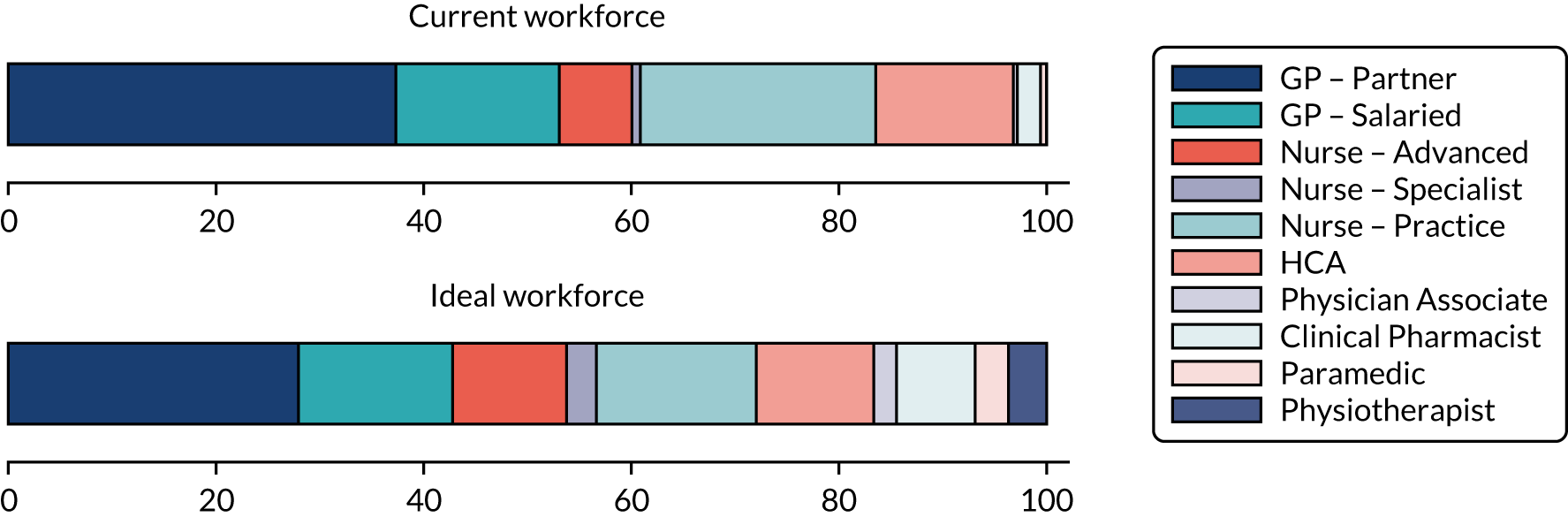
Summary
The practice manager survey confirms a lack of systematic bias in the NHS Digital primary care workforce data sets. Furthermore, it confirms variation in the reasons driving employment of different practitioner types and the employment models preferred by practices for different practitioner groups. Exploration of the notion of an ideal future workforce demonstrated that practice managers would predominantly employ GPs and nurses, but wished to have increased input from other selected practitioner groups.
Three factors motivated the largest proportion of practices to employ non-GPs, which differed between types of practitioners. The most common motivating factor for employing ANPs and PAs was to increase overall appointment availability. For CPs and paramedics, the most common motivating factor was to release GP time. For specialist nurses and HCAs, the most common motivating factor was to provide a better match between what patients need and what the general practice team can deliver. The survey also shows that CPs and PAs were most commonly supported by specific additional funding. However, this funding was not reported to be a key motivating factor for their current employment.
The ideal practice workforce would comprise > 70% GPs and nurses, containing, on average, fewer GPs than the current workforce. Newer roles comprised < 20% the ideal practice workforce, with CPs the most commonly selected. Practices’ decisions to employ practitioners directly or externally, such as through the PCN, were dependent on the type of practitioners. Practices preferred to directly employ additional GPs, ANPs or practice nurses. Those practices interested in employing PAs, CPs, paramedics or physiotherapists would prefer to access them through a PCN, federation or other similar networks.
Chapter 5 Case studies
The main objectives of this WP were to examine how new working arrangements have been introduced by employers and practitioners and how patients and staff experience service delivery using a broader range of diverse practitioner types. We explored the background and working relationships that contextualise findings from the Practice Manager Survey (i.e. WP2). We also examined the aspirations held by practices for the work carried out by newer practitioners and how these aspirations translated into practice. We drew on our development of Sibbald et al. ’s16 skill mix framework to explore if practices (1) were changing skill mix through enhancement of existing roles or introducing newer roles (i.e. innovation), (2) were transferring tasks from GPs to non-GPs primarily through delegation or substitution and (3) were motivated by the potential to substitute GPs or increase the number of alternative practitioners as a way of service improvement or supplementation of GPs.
This chapter is structured around the following research questions:
-
Research question 2(ii): which aspects of health care are undertaken by different practitioner types?
-
Research question 3(i): how are new ways of working being negotiated in general practices where skill mix changes have occurred?
-
Research question 3(ii): how is the implementation of change in skill mix associated with the achievement of organisational objectives at practice level?
-
Research question 3(iii): how does increased skill mix affect patients’ experiences when accessing primary care services?
Site descriptions
Case study sites were purposively selected to provide a diversity of practitioners employed (i.e. both large and small numbers of each), a range in the duration/maturity of skill mix implementation and any recent changes in the employment of practitioners. Table 12 provides an overview of key characteristics of each site, with richer context descriptions provided textually below.
| Characteristic | Site | ||||
|---|---|---|---|---|---|
| A | B | C | D | E | |
| Maturity of skill mix | Early adopter | Late adopter | Early adopter | Early adopter | Early adopter |
| Registered patients, n | 11,100 | 13,600 | 58,700 | 17,200 | 10,100 |
| Index of Multiple Deprivation decile (1 = more deprived, 10 = less deprived) | 10 | 9 | 8 | 8 | 6 |
| Location | Small town, semi-rural | One of two practices in a small town, semi-rural | City, a multisite practice | The only practice in a small town, semi-rural | City |
| Workforce |
GP partners, n = 7 GP registrars, n = 3 ACPs, n = 4 (paramedic trainee, n = 1; nurse trainee, n = 1) CP, n = 1 (employed by the CCG) Others: HCAs, midwife and health visitors |
GP partners, n = 6 Salaried GPs, n = 3 ACPs, n = 2 (one had a care home background and one was a district nurse) CP, n = 1 Practice nurses, n = 4 Others: HCAs and a community midwife |
GP partners and salaried GPs, n = > 20 Urgent care practitioners, n = 2 (one a trainee ACP) PA, n = 1 First contact musculoskeletal practitioner, n = 1 CPs, n = 5 ANPs, n = 2 Social prescriber employed by a voluntary sector, n = 1 Others: HCAs, specialist nurses and a phlebotomist |
GP partners, n = 8 Salaried GP, n = 4 Nurse lead, n = 1 ANPs, n = 4 Practice nurses, n = 2 Treatment room nurses, n = 4 Research nurse, n = 1 Others: HCAs, phlebotomists and a medicine management team |
GP partners, n = 3 Salaried GPs, n = 5 CP, n = 1 PAs, n = 2 ANP, n = 1 Practice nurses, n = 2 Others: HCAs, community nurses and health visitors |
Site A was a traditional practice in a small town with an ageing population for whom frailty was a big issue. As a major part of the work at the practice was visiting patients at home or in residential care homes, the practice had made a strategic decision to recruit advanced clinical practitioners (ACPs) with backgrounds in nursing and paramedic practice. The practice also had one CP, who was employed by the local CCG but based at the practice. The practice was an early adopter of skill mix changes that predominantly expanded the number of regulated occupational groups within the practice.
Site B was similar to site A in terms of being a traditional practice in a small town, but with a less affluent patient population. The practice was a late adopter, and skill mix changes predominantly related to the expansion of regulated practitioners, such as the CP. The practice employed two ACPs from nursing backgrounds as part of a local project to reduce hospital admissions. The remit of the ACPs was to care for frail elderly patients, including those in care homes, which involved collaboration and coordination with GPs and the district nurses who were co-located on the practice’s premises.
Site C was a multisite practice that was located in a major city; it was an early adopter of skill mix changes. The site had the widest range of occupational groups employed across practice sites, including regulated practitioners (i.e. a CP and a first contact musculoskeletal practitioner) and non-regulated practitioners (i.e. a PA and a social prescriber). A designated GP was responsible for workforce planning and auditing of practitioner performance. The practice had a central reception team with > 20 staff dealing with calls from patients registered at all practice sites. This team was located on the main site and organised like a call centre, with most of the staff having customer service experience.
Site D was the only practice in a town after several mergers over the last few years. The practice was co-located with a community hospital, a step-down facility from the acute hospital for rehabilitation. The practice employed nurses to deal with minor illnesses, such as dressings for their ageing population. The practice also provided care for minor injuries, as it was located at some distance from a hospital with accident and emergency (A&E) capacity. The practice was an early adopter of skill mix and had employed PAs in the past, but now operated with a mix of doctors, nurses and HCAs at the practice.
Site E was a practice in the suburbs of a large post-industrial city. The practice was an early adopter of skill mix and increased skill mix through regulated (CP) and non-regulated (PA) additions. Space at the premises was at a premium, which meant that staff did not have dedicated consultation rooms and had to change rooms daily depending on staffing. The practice participated in a local ‘care navigation’ scheme, involving the reception team in directing patients internally (to different practitioners within the practice) and externally (to several other primary care services such as opticians).
Table 12 describes the workforce composition at case study sites. Owing to the fast-changing nature of skill mix changes, workforce composition was correct at the time of data collection and may have changed following the completion of our fieldwork.
Data collection
We conducted a total of 38 interviews and 27 clinical observations across the case study sites. Table 13 summarises the data collected at the sites and indicates the range of different practitioners who were interviewed and observed. This was in addition to data collected from patients through surveys or focus groups (Table 14). Survey sheets were distributed to patients as they attended the practices during site visits. PPG members were invited to participate in a focus group via the general practice.
| Role | Site, n | Total, n | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | ||||||||
| Interview | Observation | Interview | Observation | Interview | Observation | Interview | Observation | Interview | Observation | Interview | Observation | |
| GP | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 9 | 7 |
| Practice nurse | 1 | 2 | 1 | 2 | ||||||||
| ANP | 1 | 2 | 1 | 1 | 1 | 2 | 1 | 4 | 5 | |||
| ACP (including trainees) | 1 | 1 | 1 | 2 | 2 | 4 | 3 | |||||
| PA | 1 | 1 | 2 | 2 | 3 | 3 | ||||||
| CP | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 5 | 2 | |||
| Paramedic | 1 | 1 | 1 | 1 | ||||||||
| Social prescriber | 1 | 1 | ||||||||||
| Reception | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 5 | 4 | |
| Practice manager | 1 | 1 | 2 | 1 | 5 | |||||||
| Total | 9 | 8 | 6 | 4 | 9 | 6 | 7 | 4 | 7 | 5 | 38 | 27 (totalling1620 minutes) |
| Activity | Site | Total | ||||
|---|---|---|---|---|---|---|
| A | B | C | D | E | ||
| PPG/Patient Focus Group | 7 | 2 | 0 | 12 | 8 | 29 |
| Patient survey | 16 | 17 | 20 | 54 | 18 | 125 |
The above data are now discussed in relation to the aforementioned research questions examined in this WP.
Research question 2(ii): which aspects of health care are undertaken by different practitioner types?
This section starts by describing the perceived recent changes in the work of GPs and nurses. This is followed by a discussion of the roles and work undertaken by other regulated (e.g. paramedics and CPs) and non-regulated (e.g. PAs and social prescribers) occupational groups.
General practitioners
During site visits, we observed that most GPs were predominantly engaged in providing health care directly to patients. GPs were also supplying supervision and support to other practitioners who were conducting separate consultations with patients, as well as providing advice to reception staff and attending to a wide variety of clinical and non-clinical responsibilities. The increase in skill mix was perceived as changing the role of some GPs in that non-GP practitioners tended to deal with less complex cases, whereas GPs dealt with the more complex cases. This led GPs to comment that they were increasingly operating in a similar manner to hospital consultants (i.e. seeing more complex cases as if they were ‘GP consultants’ whereas non-GPs selectively took on less complex tasks that would formerly have been part of a more varied GP caseload):
But because we’ve got so many nurse practitioners it means that us GPs see all the much more complicated things and [. . . ] we are becoming more like a GP consultant.
ID44: site D, GP partner (bold text highlights the relevance of the quote)
However, not every GP was sufficiently experienced to take on the consultant role. Experienced GPs recognised that less experienced colleagues needed proper support and time for development to progress their careers within general practice:
So our new GP can’t jump into that complex multimorbidity role; and that’s a real challenge for us, so we’re having to create tiers now of GPs, which is where the GP consultant role comes in, actually I can support . . . the junior GP has the training to deal with the complexity but perhaps not the experience; now how can we work with them to support them.
ID28: site C, GP partner (bold text highlights the relevance of the quote)
In addition, although GPs were traditionally always available to provide advice for non-GPs, with the addition of newer roles, some practices in our study decided to allocate an on-call/triage GP who did not see patients face to face but who was fully available to support non-GPs (e.g. providing advice or signing prescriptions on behalf of practitioners, such as PAs, who were not able to prescribe).
Owing to multiple different responsibilities and a lack of designated time for each task, GPs indicated that they found it difficult or impossible to complete all their work and responsibilities within office hours.
Nurses (including advanced nurse practitioners)
As noted in Chapter 1, the employment of practice nurses represented an early change in general practice skill mix some decades ago and, for many practice nurses, their roles have not changed from dealing with chronic disease management and care. Subsequently, different nurse roles have developed, such as specialist nurses and ANPs.
In our sites, ANPs were often responsible for the initial assessment of patients requesting health care for a wide range of problems. ANPs often dealt with same-day care, sometimes as part of dedicated acute illness teams, with a remit for minor illnesses and ‘low-end’ mental health issues, with more complex health issues excluded (particularly at site E). Many ANPs would request tests and assess blood results as part of managing same-day caseloads or in relation to regular reviews of patients with chronic diseases. Some ANPs were responsible for reviewing hospital letters and thereby reduced pressure on GPs who might otherwise review them. In an evolving hierarchy of diverse practitioners, less qualified staff could escalate problems they were unable to deal with to ANPs, whereas ANPs themselves sometimes escalated problems to GPs. Some ANPs, as senior nurses, had an educational role in training or supervising other nurses and HCAs.
The ability to prescribe was seen as an essential component of ANPs’ scope of practice, enabling them to deal with minor illnesses independently and reduce the need to interrupt GP/patient consultations to get prescriptions signed. Of particular interest in this study was that this enabled some ANPs to see patients with undifferentiated symptoms in the same way as GPs, rather than being delegated specific tasks. Therefore, some ANPs viewed themselves as ‘generalists’ and engaged in a patient-facing work very similar to that of GPs. In recognition of this, the ANP in site C was deployed on a GP rota and paid at the same rate as GPs. In another site, ANPs were regarded as ‘80% of a doctor’ (ID43: site D, managing partner), with the distinction that GPs also did managerial work and GP partners had legal responsibilities.
As noted in the next section, some practices preferred to recruit advanced practitioners from a range of different occupations, noting that they were not appointing to a particular occupational role, but appointing the ‘right person’ who could be upskilled and moulded into how the practice wanted them to work. As illustrated below, this meant that, although an advanced nurse might be appointed as an advanced practitioner, the practice preferred to name the role as an ACP. Consequently, the non-occupational specific role title of ‘ACP’ introduced some opaqueness about which regulatory body the role-holder was working under (such as nursing, paramedic or allied health professional) and which was relevant for their individual requirements of advanced practice.
Advanced clinical/care practitioners
Three of our sites (i.e. sites A, B and C) employed ACPs. Site A had two ACPs (one was a trained nurse and the other a trained paramedic). Both ACPs were employed by a community health service as part of a local pilot to put advanced practitioners into various surgeries. Commitment to complete ACP training was attached to the job and, as such, both ANPs were in the process of completing the master’s-level course to attain ACP qualification. The practice received funding to mentor these two practitioners in exchange for their training in primary care. The nurse ACP dealt with frail and elderly patients and patients in care homes, particularly those at risk of hospital admission, whereas the paramedic ACP dealt with same-day appointments at the practice and urgent home visits.
The paramedic ACP at site A had a remit to look after patients with frailty and those aged ≥ 65 years. The practice served four nursing homes, at which the ACP attended for half a day each week in rotation. From care homes, she received advance notification of patients who needed to be seen, but encouraged patients who were mobile enough to come into the surgery for minor treatments, such as ear syringing (which the nurses would do). The paramedic ACP deferred women’s health issues to colleagues because she lacked experience in this area. Similarly, the paramedic ACP did not deal with asthma or diabetic reviews or any other chronic illness and, as a consequence, experienced a lack of variation in her role. Owing to the demand for same-day appointments, the paramedic ACP was involved in seeing mainly acute cases and claimed that her paramedic training meant that she had experiences of dealing with whatever she was presented with, although, as noted above, this did not include the treatment of certain conditions.
Site B had two ACPs from nursing backgrounds employed as part of a local project to reduce hospital admissions. The remit of the ACPs was to care for frail elderly patients, including those in care homes, which involved collaboration and coordination with GPs and the district nurses co-located at the practice site. One ACP nurse dealt with patients aged ≥ 55 years and the other ACP focused on frailty for older patients (i.e. mostly patients aged ≥ 65 years, but with an increasing number of patients aged > 85 or 90 years). The nurse ACP who dealt with frailty for older patients previously worked as a district nurse and then a community matron before training as an ACP and joining the practice. Her work was supported by telephone triage that she carried out early each morning to assess all requests for home visits by older adults. She dealt with home visits for housebound older people (‘domiciliary care’) and ward rounds at care homes, which included medication reviews, symptom management, care plan updates, blood pressure checks and monitoring for delirium.
Site C had one trainee ACP who was doing a master’s in advanced clinical practice and another staff member about to begin training. Both staff had background experience in urgent care and worked in an urgent care setting to deal with same-day urgent appointments.
Clinical pharmacists
The new title of CP was introduced in 2015 as part of an NHS pilot to address the scarcity of GPs and nurses when there was an oversupply of qualified pharmacists. 105
Clinical pharmacists in our case study sites were allocated medication-related work. We found variation across CPs and sites regarding the broad range of activities that CPs were performing (listed in Box 1).
Face-to-face or telephone consultation for medication reviews (particularly for polypharmacy).
Home visit reviews for patients who are housebound, elderly or post-discharge.
Medication-specific clinics, such as warfarin clinics.
Medication audits.
Changing medications as recommended in hospital discharge letters.
Responding to medication queries from practice staff and community pharmacists.
Providing medication advice to patients and staff.
Repeat prescription re-authorisation.
Monitoring and improving prescribing adherence to guidelines from the Medicines and Healthcare products Regulatory Agency, CCG medicines guidance and QOF recommendations.
Managed controlled drug monitoring.
Disseminating changes to prescribing guidelines within the practice.
QOF, Quality and Outcomes Framework.
Prior qualifications and experience allowed CPs to form links between general practices and community pharmacies. For example, CPs could readily identify and redirect appropriate patients to community pharmacists for help with symptom control (e.g. for coughs and colds) and signpost patients to services, such as smoking cessation services. Experienced CPs also managed a group of medicine management pharmacists working within nearby practices and acted in a supervisory role by managing and/or overseeing less experienced pharmacists and training and supporting pharmacy technicians. CPs consulted with the GPs about more complex areas of medicine, such as mental health, and did not generally perform physical examinations of patients.
Clinical pharmacists’ roles generally evolved to fit the practice’s needs and this could involve exploring different configurations of work in terms of how CPs balance time in various clinical and non-clinical aspects of the role (as seen, for example, in the appointment of the CP at site C as education lead for the practice).
The role of each CP reflected who employed them and to what extent their role and time were split between different organisations. The CP at site E was employed directly by the practice, whereas at sites A and B the CPs were employed by the local CCGs but based at the practice. Therefore, at sites A and B, the CPs’ roles were split between doing CCG work and practice work. CPs who were employed by CCGs were able to exploit their access to wider knowledge of best practice and the latest evidence gained from this boundary-spanning network and apply this to clinical reviews with patients. However, one of the challenges of being employed by the CCG while working and based at a practice was balancing competing time and work requirements.
The CP at site D was employed by an on-site pharmacy owned by the GP partners. Therefore, arrangements were made for them to carry out work, such as NHS health checks, on behalf of the practice, in addition to running the pharmacy. By accessing patients’ records, the CPs could ensure that patients had the appropriate clinical checks and blood tests. CPs also delivered same-day care for minor ailments, such as urinary tract infections and simple skin infections. Site D also envisaged that their CP would in future (i.e. after training) handle prescribing, prescription reauthorisations and care home medications management.
Paramedics: urgent care practitioners
Site A employed one paramedic and site C employed two urgent care practitioners. These practitioners were referred to using the non-occupational specific role title of ‘advanced clinical/care practitioners’ in all sites (see Advanced clinical/care practitioners).
Physiotherapists
To date, there are limited numbers of physiotherapists delivering ‘first-contact physiotherapy’ in general practice with a potential role in the assessment and independent management of patients with musculoskeletal conditions. Although site C had a physiotherapist, access was through GP referral rather than direct access and, therefore, it was not within the remit of this study.
Physician associates
Physician associates are a non-regulated profession. This means that there is no centrally agreed scope of practice and no regulatory body overseeing their training. Therefore, it is up to each practice to negotiate the work carried out by the PAs that they employ. The patient-facing work carried out by PAs in our study appeared similar to much of the patient-facing work carried out at the first point of contact by GPs and ANPs, with a focus on being the first point of contact for acute problems. PAs did not generally deal with the long-term management of health conditions, palliative care and ‘behind the scenes’ work (such as administrative work, home visits and ‘on-call’ work) that GPs do in addition to their acute work.
An exception was that site E employed two PAs whose remit included medication reviews and chronic disease management, in addition to seeing patients with mental health problems. The more experienced PA also reviewed test results and hospital letters. However, much of the PA’s work involved dealing with acute conditions and minor illnesses. These PAs were not as involved in long-term management; however, for some patients, they attempted to provide continuity of care through follow-up appointments and, in one case, specifically employing skills gained through prior experience of working in a hospital psychiatric unit.
The PAs in site E claimed that they could spend more time with their patients because they felt under less time pressure and had fewer responsibilities than GPs. The PAs perceived that this allowed their care to be more effective, thorough and more ‘holistic’ than care provided by GPs. However, as PAs were unable to prescribe, their ability to progress through consultations was hampered by the need to ask GPs to sign prescriptions, reducing their consulting rate.
Others often viewed PAs as non-independent practitioners who had been fast-tracked in their training for their role, but who had limited experience in health care. To build knowledge and confidence, PAs in site E regularly asked for help and spoke of picking up ‘tips and tricks’ from more experienced practitioners. As their clinical experience developed, PAs had gradually been able to see more ‘complex’ patients. As such, the scope of their practice was defined in terms of GPs’ level of confidence in their perceived abilities.
At site D, the role of the GPs in determining the contribution of PAs resulted in a less favourable assessment of this role. Site D’s experience of employing PAs in the past was that they needed a lot of support, particularly during training. GPs who reported poor opinions of PAs perceived them as highly protocol driven and lacking in clinical experience. In addition, PAs were believed to offer limited value to the practice because of their inability to prescribe or request imaging investigations and, therefore, they were unable to independently manage a significant proportion of their cases. As a result of these difficulties, PAs were no longer employed at this practice.
Health-care assistants
In general practice, HCAs/health-care support workers are employed to carry out a wide range of duties. The work of HCAs often involves background tasks (e.g. sterilising equipment, restocking clinical rooms), but can also involve work with patients, including conducting health checks, phlebotomy and health promotional activities. 106 The work of HCAs supports the delivery of the Quality and Outcomes Framework (QOF) and health promotion. 106 However, as HCAs have limited training or qualifications, their work is supervised and supported by qualified nurses or other professional staff.
Social prescribers and care co-ordinators
The social prescriber role was non-regulated, and work was delegated by referrals from GPs. Site C was the only site to employ a social prescriber and their remit was to work with patients to identify support for social problems that were barriers to their health and well-being. In particular, the social prescriber dealt with social isolation, loneliness and mental health, which tended to overlap with other co-existing medical issues. This overlap meant that part of the social prescriber’s role was to clarify ways of approaching difficulties that crossed the boundaries of health and social care:
And we take a holistic approach to social prescribing, in that we gather background information and then work in a client-centred way to identify goals in collaboration with the client. And identifying barriers to their well-being in terms of isolation or loneliness, or identifying positive activities, meaningful activity that might help their well-being. Or identifying sources of, potential sources, my advice or support that might help their well-being. So it’s quite open ended in terms of what we provide.
ID31: site C, social prescriber
At sites A and B, the roles of ‘care coordinators’ had much in common with elements of the social prescriber role, and their work was practice-based, although they were employed by a local community health service. The care coordinators worked to coordinate with and/or signpost patients to social care and community services and resources, and sought to address the social dimensions of health directly and indirectly through preventing or ameliorating associated clinical conditions. Improving coordination between primary care and social care organisations and addressing social care needs were addressed, reducing the need for GPs to be personally involved in these issues.
Although these roles are increasing the skill mix in the practice, they are not taking tasks away from the GP and are an illustration of a service improvement.
Summary
Discussion of the above roles indicates the extent to which general practices have become more multidisciplinary, with practitioners from a more diverse range of disciplinary backgrounds. Our research confirmed the continuing development and enhancement of nursing roles that sees many nurses now working at an advanced level. In addition, some newer practitioner types, such as CPs and paramedics, work independently within their regulated scope of practice (i.e. innovation). The introduction of newer non-regulated roles, such as the PA and social prescriber, further broadens the diversity of workers within general practice.
Although these skill mix changes increase opportunities to distribute work differently within general practices, decisions must now be made about which tasks to transfer from GPs to non-GPs. Training, supervision and regulatory arrangements are all different for each occupational group, and often for each individual; therefore, there is no automatic association between one occupation group and whether the transfer of tasks is through substitution or delegation. In addition, as indicated above, a number of these roles appear to be providing service improvements and role supplementation rather than the role substitution of GPs.
The increased diversity of practitioners makes it more challenging to effectively match practitioners with conditions and problems appropriate for their role and experience. The next section indicates the processes of categorisation that practices used to meet this challenge and the flexibility and adaptability required to achieve effective matching and resolve instances of unsuccessful matching.
Research question 3(i): how are new ways of working being negotiated in general practices where skill mix changes have occurred?
As noted in Chapter 1, general practices have traditionally been staffed by a mix of doctors and nurses and supported by staff responsible for administrative and managerial duties. This research question examines how the addition of newer occupational groups to general practice has led to new ways of working and how any changes have been negotiated and implemented. The findings that follow focus on the manner in which the case study practices enabled the patient-based workload to be distributed among a more diverse practice workforce and the associated transfer of tasks from GPs to others. There is less focus on interprofessional competition and the protection of occupational jurisdiction by GPs. This is not to say that interprofessional competition was not raised in the case study sites, or that it would not evolve over time between different occupational groups, but it did not appear to have led to the blocking of task transfer from GPs. Instead, these practices (mostly early adopters) had accepted the need for an increased skill mix, and issues raised about new ways of working were primarily focused on the extra work associated with skill mix change.
Our study shows that to match a patient’s problems with a practitioner requires the effective application of processes of categorisation (of practitioners’ skills and patient’s problems), matching patients’ problems with the skills of a practitioner, and (short-term) flexibility and (longer-term) adaptability (in how the practice is organised, how practitioners work and how patients act) to make adjustments when these are necessary.
This section describes how tasks are distributed in the evolving multidisciplinary practice teams and leads into a presentation of how practices have enabled the matching of the skill sets brought by a broader range of practitioners to individual patient needs. Several structures and processes that support this matching are also highlighted.
Categorisation
Practitioner categorisation refers to how practices categorised their practitioners to effectively match a practitioner with a patient. The detailed study of these categorisation processes within five general practices indicates the complexity of determining an effective categorisation at the first point of contact between the patient and the practice.
The first challenge relates to the need to consider the difference between competencies gained through training qualifications and those gained through acquired previous experience and developing expertise in the role. Practitioner categorisation rests on the notion that different practitioners are trained/qualified to deal with a subset of work, which we would call ‘role competencies’. However, our studies also indicated that practitioners can become experts in an area of work because of upskilling, specialisation and/or past experiences, which we would refer to as ‘role-holder competencies’ (i.e. competencies that go beyond role competencies derived from the original training course). For example, site E employed two PAs who had received training around specific role competencies. Both PAs, therefore, had the same qualifications and were largely trained in the same way. However, although both PAs dealt with same-day appointments, one had an interest in mental health and had gained expertise when working in psychiatry (i.e. role-holder competencies). Therefore, patients with mental health problems would preferentially be offered appointments with this PA.
Likewise, some practitioners have expertise that is separate from their current role. For example, site A employed two ACPs (one ACP with a background in nursing and one ACP with a background as a paramedic). The ACP qualification (i.e. role competencies) confirmed a set of standards for both practitioners to work at an advanced level. However, as one ACP was a nurse and the other a paramedic, the ACPs had different specialisations and past experiences (i.e. role-holder competencies) and dealt with different types of patients.
Our study indicated that the broader the spectrum of practitioner competencies, the greater the need for a more sophisticated process categorise practitioners and to address the differences between role competencies and role-holder competencies. This spectrum requires practices to utilise knowledge of role competencies and individual strengths and interests when evaluating role-holder competencies.
A second challenge arose if broad practitioner categorisations led to duplication of work. This GP describes the difficulty with avoiding duplication and managing overlaps between practitioners:
I think there’s a fair amount of duplication going on [ . . . ] I think there’s duplication sometimes with pharmacists and nurses, and we’re trying to get that rationalised. We keep working on it, to make sure that people aren’t being seen too many times, and talk to too many people. But I think you do often end up talking through something on the phone, that you realise halfway through, that somebody else is doing it, or you know, there’s really nothing to do, until something else happens, and it’s that kind of thing. And I don’t quite know how to reduce that [ . . . ] so that’s a difficult balance.
ID11: site A, GP partner (bold text highlights the relevance of the quote)
Although it may be possible to have an agreed overlap for minor tasks, there is a risk that practitioners feel that they have infringed on someone else’s role, as described by our participants:
So, I know certainly there’ve been times where I felt like I’ve stepped on one of the practice nurse’s toes because I’m getting . . . you know, I’ve got a diabetic patient coming in to see me and I’m doing their med[ication] review but then they’re still booking in, you know, to have their feet checked, and those bits are the sort of overlap of how we do it.
ID17: site B, CP (bold text highlights the relevance of the quote)
A separate process within the matching exercise, but equally important to effective matching, was the patient and problem categorisation. Again, our study indicated the changes that practices had made to ensure that this was as accurate as possible.
To facilitate problem categorisation, the role of receptionists had significantly changed and expanded, as they no longer simply booked appointments, but also guided patients to appointments with different types of practitioners. This required receptionists to explain to patients why they needed to ask about their symptoms or health issues and reassure them that this was to get them to the right appointment. Receptionists needed to acquire new knowledge and skills and use more complex processes than had previously been required, developing a nuanced understanding of practitioners’ changing skills and competencies. Provision of clinically informed advice from doctors or other practitioners to assist reception staff when these decisions were unclear was part of the previously mentioned supporting mechanisms.
Matching
For many patients, receptionists quickly understood what was required and confidently guided them to a suitable problem. However, matching did not always lead to an appropriate appointment (even in cases that appeared straightforward):
There’s always going to be the odd error in the system but that’s where you look and you think, well I can’t prescribe something for that infected toe, it needs to be seen by someone else.
ID13: site A, practice nurse
Accurate categorisation of problems also depended on how patients articulated the problem. In the context of primary care, the innumerable array of undifferentiated symptoms and unfiltered health and other concerns that were routinely encountered could make categorisation difficult. Although experienced receptionists could develop and apply tacit knowledge, as well as formal training, incidents would occur where patients had appointments with practitioners unable to deal with their problem:
. . . with the pressure of appointments and the demand of the patient, just sometimes the receptionist will book an inappropriate appointment. And we learn, you know. So where that came from was the nurses’ meeting last week . . . where the reception manager was in there and the nurses were saying, well, you know, this appointment was made, and it wasn’t right, you know, so we learn.
ID3: site A, practice manager
In some cases, an apparently simple problem becomes recognised as a more serious problem or complex issue. Whatever the reason, prompt resolution of the mismatching of problem and practitioner is particularly important for the patient. Such situations highlight the need for short-term flexibility and longer-term adaptability within the organisation and in how practitioners work.
Flexibility and adaptability
The use of processes of categorisation and matching can have an impact on patients seeking health care. Instead of simply booking an appointment with the practitioner of their choice, they will be asked to explain the problems behind their request. Based on this information, a receptionist will propose a course of action that may be different from their expectations, such as the type of practitioner or appointment. A more detailed exploration of these elements is explored in Research question 3(iii): how does increased skill mix affect patients’ experiences when accessing primary care services?.
In addition, general practices, as organisations, needed to facilitate longer-term adaptability by setting up and revising processes and procedures that accommodate and keep pace with changes in categorisation and matching. Adaptations vary from reviews of changes in care that are deliverable by individual practitioners to ‘work arounds’ that are necessary to accommodate the requirements of medical indemnity insurance cover for advanced practitioners delivering specific services:
. . . so for example we’ve got all these different skill mixes and some of them going out to see vulnerable people at home; and then there were daft things like the insurance didn’t cover certain health professionals doing a flu jab, they could do it in practice but not at home; and it’s little bits like that that suddenly then you’ve now got to send out a second health professional.
ID28: site C, GP partner
We observed other examples of organisational adaptability in the different systems general practices put in place to monitor whether or not categorisation ‘works’ (i.e. whether or not patients were or would be booked in with the ‘right’ practitioners). Site C designated a GP as workforce lead with responsibility for such monitoring. In other sites, recognising this issue was dependent on individual staff raising it at staff meetings rather than through a more systematic process at an organisational level. Further details of the longer-term organisational adaptability are provided in Supporting mechanisms.
Last, practitioners needed to demonstrate short-term flexibility by, for example, finding solutions for patients when a mismatch of problems and practitioners occurred. This required organisations to consider supporting mechanisms that facilitated practitioners seeking advice or needing to transfer patients to other practitioners. Similarly, the need for staff flexibility and adaptability extended to reception staff. In some sites, reception staff carried out some administrative duties. In others sites, administrative duties were the responsibility of back-office administrative staff. In site D, rotation of front-desk and back-office staff ensured greater operational flexibility. Allocation of duties at other sites demonstrated various processes and working practices, as non-clinical tasks were variously allocated to receptionists, medical secretaries and others.
To reduce pressure on GPs and other clinicians, site C adopted a ‘lean journey’ approach whereby an administrative team followed a protocol to deal with prescription management and blood pressure checks, with provision for alerting GPs about abnormal results from tests (i.e. an exception handling approach that takes much of the work of processing results away from GPs). The administrative team were also responsible for the arrangement of pre-appointment blood pressure checks and selecting those patients who were suitable for face-to-face consultations.
Supporting mechanisms
Organisations had made some longer-term adjustments to their processes to support categorisation processes, matching and addressing any mid-matching. These supporting mechanisms are discussed under Managerial and administrative processes, Training, Supervision and Team meetings and information.
Managerial and administrative processes
On a very practical level, the categorisation of practitioners and patient problems required the development of processes that identified and captured the range of clinical competencies within the practice team and defined the services that each practitioner could provide. ‘Skill matrices’ were used by reception staff to triage patients and allocate them to practitioners with the requisite skills to deal with them. Parallel online triage systems were also in use, allowing information collected through an online template to match with a suitable practitioner. To cope with the volume of work involved in dealing with operational issues, site D created a new role. The new role was an operational manager whose role included ensuring that information in the skill matrix kept pace with practitioners’ progression and development. Incidents of serious mismatching became the subject of informal reminders or formal case reviews for discussion and learning.
Training
Implementation of the processes underpinning skill mix changes required training, and practitioners were encouraged to enhance their skills through, for example, becoming independent prescribers or upskilling to replace departing colleagues (e.g. in chronic disease management). Practices looked to address the organisation’s key skills/care gaps, enabling practitioners to take on more work to free up GP time and better match practice populations’ needs.
General practice funding allocated to external training was framed in terms of investment of time and money in developing practitioners. All general practices in our study supported practitioners doing training and attending courses, particularly if it supported being able to better address the needs of certain patient cohorts in-house.
Some funding was provided by local CCGs. In site E, the local CCG organised regular training for PAs to cover topics such as paediatrics and mental health conditions. In site C, the CPs attended monthly training sponsored by the pharmaceutical industry. Site C also recruited practitioners supported by a training bursary from HEE. In addition, site C tapped into funding via local training practices for ACP training.
However, funding support for training was not always universally available. For example, the CP in site C described how some training was available for pharmacists employed only by the PCN, which meant that pharmacists directly employed by the practice could not access those training courses. Another example was provided by the PA in site E who felt that ‘because the PA role is quite new it’s not always apparent what those opportunities are and you sometimes have to create those opportunities’. Therefore, it could be argued that allocated funding influenced which practitioners the practice felt inclined to ‘experiment’ with without taking on additional financial risk. Subsequently, the availability of funding could affect how practices decided which practitioners to employ.
The reception teams were not only trained to identify ‘red flags’ as indicators of potentially serious health problems, but all teams also had training in care navigation (i.e. in how to ask questions to ensure that patients were booked in with the ‘right’ clinicians using a skill mix matrix or internal directory of services). In site E, care navigation training was provided as part of a local initiative to signpost patients to internal and external services. In site C, call handling by reception staff was assessed and reviewed to identify additional training needs.
Supervision
Formal and informal supervision covered various activities and provided supervising GPs with insights into how practitioners work and their level of skill. This enabled GPs to identify issues arising with patient care that needed to be addressed as learning opportunities and to ensure the effectiveness of categorisation and matching processes. In addition, supervision was used to ensure that newer practitioners were working safely with patients and provide support for junior and less experienced staff.
Formal supervision took the form of protected debrief time, ranging from once a week to two or three times a week to, sometimes, daily. As practitioners’ clinical knowledge and confidence increased, and supervising GPs’ trust in them increased, the need for formal debriefs decreased and practitioners were trusted to ask for help when they needed it. Formal debriefs also provided newer practitioners with validation of their clinical decisions, helped to build team relationships and added evidence for appraisal during their monthly review.
Practices adapted rotas to facilitate supervision for newer GPs and other newer practitioners by allocating experienced GPs as ‘duty’ doctors. The timetables of these duty doctors were less structured and meant that ‘duty’ doctors could help and advise other staff. For example, if during consultations non-GPs were unsure of diagnosis or treatment, they could immediately ask the duty doctor for advice. If necessary, the duty doctor could then do a joint consultation with the practitioner, adding to the practitioner’s knowledge and skills while also properly addressing the patient’s problems.
For newer practitioners, such as PAs, our participants claimed that, although the safety-oriented clinical supervision they had with GPs was useful, they found a lack of an external support network to provide more pastoral supervision.
Informal supervision and support also took place during daily coffee/lunch breaks, allowing people to get advice and share an understanding of guidelines and best practice. Shared breaks also strengthened horizontal relationships and openness between staff members, which facilitated informal advice-seeking. Participants felt that co-location was an important facilitator in informal supervision, which would be less easily achieved through supervision carried out collaboratively with neighbouring practices. This could create difficulties for practitioners employed through the PCN:
If they’ve got any concerns about a patient they talk to the doctors, they stop them in the corridor, they’re here so they stop them in the corridor and that’s the beauty of them being here. [ . . . ] it’s [location] massively important, it wouldn’t work if they weren’t based here, I can’t imagine working remotely with them, I really can’t. And that’s going to be a potential problem with the PCNs.
ID18: site B, practice manager
Supervision could also create tensions between GPs and newer practitioners because of the considerable experience and expertise of practitioners being supervised:
There was a little bit of initial tension around some of those discussions because you’re not dealing with trainees, you’re dealing with very experienced people. So it took perhaps a little bit of time for everyone to become comfortable with that dynamic and for them to understand that we respected their expertise in their area. But that the work they were doing was work which would traditionally have been done by GPs and we wanted to make sure that the aspects of it that we had more experience in were being done in the right way.
ID28 site B, GP partner
However, the effectiveness of supervision depended on the receptiveness and responsiveness of supervised practitioners. Some GPs found practitioners to be defensive about feedback on their practice, which may have been a reflection of how the practitioner perceived their level of expertise or the expertise of their supervisor:
I think it’s very dependent on the allied professional, but I see that a lot, where you’ve been seen by one of the more junior allied professionals with reassurance given, review is needed and they come back and you think, actually, they need this, this, this done and I try in a very, sort of, constructive way, say, what’s the learning from here? Actually, can find that sometimes there’s quite a defensive reaction, which you wouldn’t get sometimes from GPs, we’re very used to being self, you know, critical, how can we improve? Reflect on things, how can we improve?
ID33: site C, GP partner (bold text highlights the relevance of the quote)
There was a perception among GPs and other staff that PAs needed supervision at a level expected during on-the-job training, which they perceived as necessary to compensate for lack of clinical/medical experience or because PAs had been fast-tracked. In contrast, a GP partner at site C viewed musculoskeletal practitioners as ‘independent’ and needing minimal supervision and, therefore, the easiest of all the allied professionals to transition into primary care.
Experienced GPs also noted the high level of support and reassurance that trainee GPs now require. Some practices found that trainee/new GPs were not ready to oversee other practitioners, as they were unprepared for the level of responsibility and needed to build up their confidence to grow into this role.
The use of debriefs with newer practitioners had prompted practice nurses who did not have debriefs in the past to request them as a means of addressing a long-standing need to get advice and reassurance on their practice.
In different ways, in each of these supervisory activities, there was clear potential for improving the skills, knowledge and confidence of practitioners, therefore, easing the need for practitioners to ask GPs for advice during consultations. However, arrangements needed to be in place to allocate appropriate time to this activity, as there was a danger that it would increase the workload of GPs and other senior practitioners if they were expected to provide debrief time on top of their usual day-to-day work.
Team meetings and information exchange
Our participants claimed that the relatively isolated mode of working in primary care compared with secondary care meant that making an effort to meet regularly is essential, particularly for individual well-being and support. These meetings can be both formal and informal.
Examples of formal meetings included clinical meetings or multidisciplinary team meetings. GPs at site A met once a week to discuss issues such as work delegation, and the nursing team met once a month. For multidisciplinary team meetings in site D, the clinical team met with staff working closely with the practice, such as the district nurses and a frailty coordinator. Site E had fortnightly clinical meetings on two different days to allow people working on different days to attend. Sites B and D had palliative care meetings (fortnightly in site B) to review active cases.
Site E had plenary meetings, which were attended by somebody from each team within the practice and would be attended by at least one GP. Following the plenary meeting, the practice manager met with nurses, HCAs, reception staff and secretaries to discuss how to implement plans that had been discussed. Site E also adopted a team huddle approach for the reception team, whereby all reception staff would meet at lunchtime (lasting from a few minutes to half an hour) to catch up on general issues or communicate any new changes being implemented by the practice.
The organisation of team meetings was challenging because clinicians were often caught up in busy days or working at different sites and practitioners could be employed by different organisations. It was also challenging to ensure that all staff were consulted in the decision-making process. For example, reception staff were generally excluded from clinical and multidisciplinary team meetings and only received information cascaded to them by the practice manager.
Examples of informal meetings included lunchtime and/or coffee break meetings that were considered as de facto team meetings. Our analysis shows that these informal meetings were used for knowledge-sharing and learning across multiprofessional teams and, particularly, for newer practitioners with less clinical experience getting support. Other functions of informal meetings included getting clinical advice from a GP or the team, developing a more sociable and less siloed team, creating a site identity (especially in site C, which was a multisite practice), providing an informal debrief and creating time for doctors to recover from the morning session. A GP partner at site C claimed that friction in the team developed when coffee break meetings did not happen. Site E used to have coffee meetings, but these meetings had been replaced by lunchtime meetings because of heavy workloads.
The practice manager in site E attempted to create a ‘family-friendly atmosphere’ and a ‘laid-back’ environment where everyone was on first-name terms. Similarly, colleagues in site A made their new CP feel like part of the team by inviting her to social events. Another trainee appreciated the simple routine of tea making in the morning because ‘Just silly things like making the tea in the morning, it just brings everyone together’ (ID26: site C, trainee ACP).
Overall, our participants highlighted that practices benefited from a relatively stable workforce and from having several long-standing staff members who met regularly and were supportive and willing to help each other. This also enabled informal team meetings to serve their purpose.
Summary
Against a background of gradual change in the composition of the primary care workforce, the recent introduction of financial support for workforce expansion through PCNs is set to accelerate the employment of a more diverse workforce.
Our in-depth exploration of observed clinical consultations (both GP and non-GP consultations) and interviews with staff working at general practices found variation in the degree to which roles are established and the familiarity of patients, GPs and other staff with newer roles. We also found variation in practitioners’ scope of practice within particular roles due to the inconsistency of individuals’ competencies and familiarity with general practice.
The generalist nature of general practice means that categorisation is needed to allow non-clinical reception staff to distribute work effectively. In our study, practice staff attempted to match the ‘right’ patients to the ‘right’ clinicians. However, in practice, the accuracy of categorisation is dependent of patients ‘correctly’ reporting their problem and the receptionist ‘correctly’ understanding and matching the problem with the ‘right’ practitioner. Improved outcomes from categorisation and matching can be achieved where organisational structures, staff training, practitioner flexibility and patient acceptance work effectively together to resolve deficiencies. Underpinning the implementation of skill mix, we identified adaptations in how practitioners are supported by management and administration, training, supervision, and formal and informal interactions.
Implementation of skill mix is an evolving process rather than an end in itself. Our study suggests that, rather than attempting to achieve an ‘optimal’ skill mix, general practices need to engage in ongoing management of the skills of their workforce using the processes outlined above. The next section describes several unintended consequences of new ways of working, including the risk of duplication of work and the impact on GP workloads of ongoing supervision for newer roles, which can adversely affect their work–life balance.
Research question 3(ii): how is the implementation of change in skill mix associated with the achievement of organisational objectives at practice level?
As noted in Chapter 1, two main programme theories were identified for the introduction of additional roles in general practice. Skill mix was seen as a means of enabling tasks to be transferred from the ‘unsustainably heavy workload of GPs’ and creating additional capacity in a sector in the midst of a workforce crisis. The first section below highlights the rationale expressed at a local level for contemporary changes. Consideration is then given to the extent to which the skill mix changes have enabled the achievement of objectives at practice level. The section is completed by considering the impact on practice staff and the unintended consequences of skill mix changes identified in the case study sites.
Motivations driving skill mix change
Participants at our study sites reported two dominant motivations for implementing skill mix change: (1) increasing capacity and (2) achieving cost-efficiencies. This GP partner articulates the manner in which some participants linked these two motivations:
The motivation was partly around trying to find a more efficient way of doing some of the work. [ . . . ] So part of it’s about dealing with the workload efficiently. [ . . . ] recruiting doctors can sometimes be difficult. We’ve never failed to do it when we needed to, but sometimes we’ve had to work quite hard to get someone of the quality we want. And obviously, lots of other practices have struggled. Part of it’s about dealing with the workload efficiently. [ . . . ] part of it is workforce, part of it is efficiency, both in terms of cost and clinically. And part of it is that the NHS system is encouraging things like this, and so there’s the ability to access funding and support for it.
ID21: site B, GP partner
Practice managers tended to focus on the need for cost-efficiencies. However, the examples provided related to potential cost-efficiencies for task transfer in particular cases, rather than for the practice overall. For example, the practice manager at site A thought that for some tasks the GPs in their practice were working below their licence, such as doing care home visits that could be carried out by ‘lesser-qualified staff’, such as an ANP. Therefore, the transfer of home care visits was an explicit substitution (for that task) of an ANP for a GP. Another explicit substitution was the transfer of patients from GPs to physiotherapists and CPs who could use their specialist knowledge to deal with ‘complex’ cases, thereby releasing GPs to do other work. Therefore, increased skill mix was conceptualised as supporting cost-efficient patient interactions while also enabling the provision of additional services and high quality of care for patients.
Some of those participants expressing these motivations also referred to the consultant GP model as the future model of general practice workforce, whereby GPs develop specialist skills (as in hospitals) and retain the value of long-term relationships with patients and the provision of ‘holistic’ care.
In addition to direct employment of newer practitioners, our participants argued that employing practitioners through PCNs could support practices by providing PCN-employed practitioners to cover sickness or periods of leave, thereby enabling a more standardised approach to doing things. However, these respondents could also envisage a risk that practitioners working in and across different practices would need to juggle different, and possibly conflicting, priorities. Moreover, our participants highlighted a potential tension between PCNs and general practices in relation to establishing the ‘most efficient way of providing care’ (ID21: site B, GP partner).
Notwithstanding the above, it must be noted that these were not universally accepted views. Many GP partners expressed that they would still like to have more GPs and, therefore, viewed recruitment of non-GPs as a pragmatic response and short-term solution to GP recruitment difficulties.
The next section discusses the extent to which practices indicated that they had achieved their objectives by increasing skill mix.
Meeting objectives of increasing capacity and achieving cost-efficiencies (while improving the quality of the service)
All case study sites claimed that skill mix changes had improved access to appointments [see also Research question 3(iii): how does increased skill mix affect patients’ experiences when accessing primary care services?]. Participants said that the introduction of newer practitioners had enabled new ways of organising care and increasing capacity. In addition, the introduction of newer practitioners had allowed practices to move away from firefighting, or ‘just getting by’ in the context of heavy demand, to operating at a more sustainable pace.
Our participants claimed that skill mix could enable a ‘better’ standard of care for particular groups, such as frail elderly people, people who need same-day appointments or people who need medication reviews. ‘Better’ was defined as making use of a practitioner who has more specialist skills in a particular area (e.g. medication reviews or specialist care for chronic illness) than GPs and who is able to perform the task thoroughly because they have more time to devote to the exercise. Medication safety was identified by our participants as an area of clear improvement in the quality of care when practices had a CP.
Cost-efficiencies were described in site C enabling them to deliver services differently, including making sure that GPs were only dealing with ‘complex’ cases and not just about taking out chunks of GP work and replacing GPs with a ‘specialist’. Site C had undertaken internal modelling and looked at CPs in terms of the administrative prescription changes CPs made and how much work was being taken away from GPs. The practice noted that significant extra hours were added to the GPs’ working time when their CPs were absent. From this, the practice was confident that its model was working, although the practice found it difficult to describe in economic terms:
. . . we know it’s working, but if you are speaking to a health economist, I would struggle to give the absolute in-depth figures.
ID28: site C, GP partner
The practice manager in site D claimed that, although it was cheaper to employ non-GPs such as ANPs, the practice would need to reinvest the money elsewhere. Therefore, skill mix was not about saving money, but about using existing resources and potentially employing another ANP. As the practice manager put it:
. . . it’s purely just been redeployment of skills.
ID36: site D, practice manager
The efficiencies noted above appear to depend on finding the right ‘place’ for staff (i.e. the fit between the skills of staff and their work). For example, upskilling staff enabled staff to do more, but practice managers were aware that this could result in demands for higher pay and/or staff leaving to work elsewhere. Practices found it challenging to determine the cost-efficiencies of skill mix because of unanticipated extra work and uncertainty about how sustainable certain roles would be. For example, a GP partner in site E felt that there were many unknown costs in terms of throughput of patients. The GP partner felt that she was doing extra work due to unnecessary additional work generated by PAs bringing people back too often and using up appointments. Likewise, several GPs noted that, although some tasks were taken away from GPs, additional workload arose from the requirements that GPs must authorise prescriptions generated by non-prescribing colleagues, make referrals and make decisions based on letters from specialists or investigation results (see Supervision). Such comments demonstrate that multiple additional factors and consequences should also be considered alongside the calculation of cost-efficiencies.
Impact on practice staff
Practice staff needed to manage uncertainties and anxieties surrounding their own and their patients’ lack of understanding of what newer practitioners could do. Limited understanding of roles and the performance of similar tasks by different practitioners made it difficult for patients to distinguish between practitioner types and patients would find themselves being corrected when they mistakenly referred to newer practitioners as ‘doctors’:
But there obviously will be times during the consultation, especially with the elderly or anyone with mental health issues, that they might say, doctor, thank you. And I’ll be like, no, you can only correct people so many times without it being a bit, no, I’m not. And sometimes they call me nurse and sometimes I try and say, oh, actually I’m not a nurse, it all depends whether I’m in a bad mood.
ID26: site C, trainee ACP
Skill mix had also increased the need for staff to legitimise their roles in relation to others. This particularly affected newer roles, such as urgent care practitioners and PAs. A trainee ACP with a paramedic background described it as being caught between the doctors’ and nurses’ ‘camps’ (ID26: site C, trainee ACP).
Other practitioners viewed PAs as seeing themselves as similar to a GP. This was attributed to the need to defend their newly acquired status in primary care and being ‘ambassadors’ for their role (ID34: site C, PA). As a consequence, PAs were often viewed less favourably by other practitioners:
I think it’s possibly more problematic for physician associates because they’re non-clinicians [ . . . ]. But the problem is they have no clinical experience which is very tricky for them I think, the differences in the way that they’re regulated and under the purview of a doctor so to speak. [ . . . ] they really do believe they’re almost equal, which I find, you know, completely disagreeable [ . . . ] PAs have trained in the medical schools, and I think some of the golden mantle effect rubs off on them, we’re almost a doctor, we’re almost that confident, we’re almost that good, but they’re only nurses, so there’s a perception of status amongst the PAs going, well, we’re equal. In reality, you know, I think there’s always a situation of they don’t know what they don’t know, but I think that profession will mature over time [ . . . ] You know, the difficulty is you read a physician associate’s notes and fantastic assessment, but then the plan is then discussed with the doctor or more likely is dictated by the doctor.
ID32: site C, ANP (bold text highlights the relevance of the quotation)
Unintended implications for general practitioners
In addition to the impact on staff, several unintended implications of skill mix changes were observed specifically for GPs in the case study sites.
First, the need for ongoing GP supervision of other practitioners created a new and, for many, unexpected workload that was found onerous by some, particularly where there were fewer GPs performing this role and where there was a lack of peer support. GPs found that supervision could be particularly demanding when several practitioners needed support simultaneously. This caused ‘debrief fatigue’ (ID1: site A, GP partner):
There can be times when I have about three or four people queued up just waiting for my time really, and sometimes I just get them all in and say, look, let’s just take this as a learning opportunity, come in and listen to what’s going on with the debrief.
ID33: site C, GP partner
Our GP participants noted an increased need to provide safety nets when working with more non-GPs. Patient safety was protected when each practitioner took a cautious approach to care, knew when to ask for help, and used debriefing/supervision. Patient safety was also assured through processes that provided checks and balances, including a policy for GPs to review patient cases.
The supervisory role meant that GPs needed to juggle their clinical work with the need to review that of other practitioners and with responding to instant messages requesting help, which, consequently, affected GPs’ work–life balance:
So I’m constantly supporting even throughout the lunch break, so it’s very rare that I even get to look at any of my own clinical workload until the end of the day [ . . . ] And then, unfortunately, you get your . . . [newly qualified] GPs who are staying late, because they can’t keep on top of just the clinical workload from the day, who then come in with a list of questions and you’re trying to support them and you’re thinking, I’m trying to get them home, but I might be here another hour later. [ . . . ] it doesn’t affect work, but home life I’ve had to set up a laptop that I take home with me, so that I can see the kids and then I can log on and I can do all my clinical work. But, occasionally, I’ll come across something and it’ll make me cross, because I thought, I should have seen that earlier today and if the patient is going to need a phone call and it’s 8 o’clock at night now, it’s just . . . that’s not right.
ID33: site C, GP partner
Second, a GP partner in site C argued that GPs were feeling pressure in a ‘squeezed middle’:
I feel very much in the squeezed middle group, so I’m an experienced clinician but I’m not close to retirement, it’s not an option, so I need to support everybody, so I’ll need to try and prevent my partners from retiring too early, so you’re protecting the retiring cohort, you’re trying to support the newly trained. I wasn’t trained to do the job I’m now doing, so it’s evolved.
ID28: site C, GP partner
Last, with practitioners upskilling and specialising in some areas, our participants highlighted the risk of GPs being de-skilled because of the reduced range of issues they would deal with. Moreover, our case study sites had supported experienced practitioners to undertake such training only to have them request higher salaries or take their skills elsewhere, exacerbating local workforce retention. Upskilling could also increase the duplication of work. This was an area where some practices struggled to get a clear idea of how to avoid and manage overlaps between practitioners dealing with the same patient.
Summary
General practitioners most often stated that their motivation for skill mix change was a shortage of GPs. In contrast, practice managers tended to focus on the need for cost-efficiencies and saw skill mix as enabling new ways of organising care, which benefited the quality of care.
Skill mix was also said to improve access to appointments; however, as noted below, this requires that patients are happy with the choice of practitioners they are offered. Reference was made to the tension between enabling continuity of care (i.e. seeing the same practitioners) and prompt access to appointments with practitioners who might not be their ‘usual’ practitioner or their practitioner of choice.
Changing the skill mix in the case study sites has enabled the transfer of tasks from GPs to others (e.g. through either enhancement or innovation). However, whether this is through delegation or role substitution is sometimes unclear when specialists or advanced practitioners are taking on these tasks wholly unsupervised.
In terms of achieving cost-efficiencies from skill mix, this was difficult for practice managers to evaluate in purely economic terms because of unanticipated extra work, such as GP supervision for non-GPs. In terms of safety and quality of care, skill mix also created a need to provide more safety nets through ongoing GP supervision. The extra work for GPs associated with skill mix change was frequently discussed.
These case studies also raise questions about whether practices are transferring tasks as a means of role substitution or supplementation. Where a specialist is involved, or a discrete cohort of patients (e.g. frail and elderly patients) are concerned, it would appear that there is an explicit full substitution of tasks. For other interventions, however, such as the first contact appointment, it appears that skill mix increases the number of occupational groups who could perform that task, with GPs continuing to do so too (unless a practice was operating a consultant GP model). If the GPs continue to perform these tasks, the practices arguably operate an explicit role supplementation approach to improve timely access. Again, this appears to be achieved through explicit supplementation, where there is no intention that an alternative practitioner will take up all of the GPs’ tasks. Therefore, practices enable task substitution rather than role substitution, with associated implications for extra work for GPs.
Research question 3(iii): how does increased skill mix affect patients’ experiences when accessing primary care services?
This section provides insights into patient experiences in general practices with an increased skill mix, including accessing appointments and consultation experience. The section presents findings from patient surveys (completed by 125 patients) and focus groups with the PPG members in four sites, including a patient group in one of the sites. Overall, the section indicates the additional efforts (or ‘work’) of patients accessing appointments in a practice with an expanded skill mix, the factors that facilitate patient acceptance of skill mix changes and the issues that remain challenging to address. The section begins with an overview of survey responses concerning the usefulness of appointments and the appropriateness of the practitioner. The section then examines the patient experience of the new triage and sorting processes developed to categorise and match practitioners and patients [see Research question 3(i): how are new ways of working being negotiated in general practices where skill mix changes have occurred?].
Usefulness of patient consultation
Patients were asked to complete a survey based on their consultation on that same day. Survey questions included asking how useful the appointment was, whether or not the patient thought they saw the right practitioner to deal with their problem and whether or not it was the type of practitioner they wanted. Half of the respondents (63/125) had consulted with a non-GP. As noted in Table 15, a large majority of patients indicated that everything had been dealt with (82%), that the health practitioner was definitely or probably the right practitioner (94%) and that they had seen the type of practitioner they wanted (77%), with 23% of respondents indicating no preference. In addition, 5% of respondents reported that their practitioner had ‘dealt with something they had not intended to discuss’.
| Question | Response | Number of responses (N = 125), n (%) |
|---|---|---|
| How useful was your appointment today? | Dealt with everything | 102 (82) |
| Unanswered | 5 (4) | |
| Most things were dealt with | 7 (6) | |
| A little was dealt with | 5 (4) | |
| Some things were dealt with | 6 (5) | |
| Do you think that the health practitioner you saw today was the right one to deal with your problem(s)? | Definitely yes | 96 (77) |
| Probably yes | 22 (18) | |
| Probably no | 1 (1) | |
| Possibly | 2 (2) | |
| Unanswered | 4 (3) | |
| Is this the type of practitioner you wanted?’ | Yes | 93 (74) |
| No preference | 29 (23) | |
| No | 3 (2) |
The focus groups provided further information about the accessibility of appointments at these practices. As noted above, 77% of patient respondents indicated that they had seen the practitioner they wanted. Patients in the focus groups reported their perception that appointments were more readily available because of skill mix. However, these findings need to be supplemented with reference to the ‘work’ required by patients in booking appointments in practices with a diverse workforce, which is identified below as (1) information-gathering, (2) navigating information technology (IT) and telephone appointment systems, (3) making compromises and (4) developing new relationships.
Patient experience of categorisation and matching
Information gathering
As noted above, matching a patient’s problems with the appropriate practitioner requires a categorisation process of practitioner skills. In addition to practices facing the challenge of determining an effective categorisation of practitioners [see Research question 3(i): how are new ways of working being negotiated in general practices where skill mix changes have occurred?], this research indicates the information-gathering that patients need to undertake in the matching process. The patient survey showed that patients had a limited understanding of newer practitioner types and their capabilities. Some 67% (84/125) of patients indicated not knowing how to find information about the problems/conditions dealt with by each type of practitioner. Of those patients who indicated knowing where to find this information, 13% (16/125) stated they would do so online, 8% (10/125) said that they would look at the ‘waiting room information board’, 4% (5/125) would ‘ask receptionists’ and 2% (2/125) would look at the ‘waiting room screen’.
Members of the PPG claimed that patients’ lack of awareness of the new systems was a result of poor communication about what different practitioners can offer. At one practice, this had created so much confusion that the practice had adopted the inclusive term of ‘clinicians’ for GPs and non-GPs. Focus group members viewed this change as a way to minimise name ambiguity, but this change also appeared to remove opportunities for an informed choice of type of practitioner.
Furthermore, PPG members reported that minimal and/or unclear communication was initially given about how access to appointments was changing. In addition, reference was made to a limited choice about these changes, which were felt to be changes imposed by the CCGs.
Navigating information technology and telephone appointment systems
Patients were required to navigate IT and telephone appointment systems in the new matching processes. The focus groups reported that patients had difficulties navigating the new online and telephone triage systems to access an appointment because there were often several ways to do so and because the processes were unclear and confusing to navigate. The focus groups also reported that success varied depending on which type of access was required, with the following quote indicating concerns about the potential for differentiated access:
If you go online and look at the appointment system it’s generally, I would say from my experience, 3 or 4 weeks before you can get an appointment . . . I thought the idea of the apps [applications] was actually to reduce that pressure on the receptionists. Well, in that case, it’s not doing that is it because if you want an appointment, you’re not going to use the app. It does make it hard work . . . it seems a little bit unfair because people like us, if you’re quite happy doing things online, you can sort of play the system, if you like, you can look on one, look on another and find an appointment. But there are a lot of people who can’t do that.
ID46: site D, PPG focus group
Members of the PPG were particularly keen to indicate that if they found the new systems and roles confusing to navigate, it would be even more difficult for patients who were not PPG members or regular attendees. Focus group participants also raised particular concerns for how certain groups (e.g. vulnerable groups, such as those with learning difficulties or language barriers and older people who do not access the internet) would be made aware of changes.
Making compromises
Although focus group patients reported their perception that appointments were more readily available because of skill mix, this was qualified with reference to several compromises that focus groups raised.
The first compromise was expressed in the view that waiting times were reduced only if patients were willing to forgo having a choice of practitioners, which meant accepting appointments with someone other than a GP. Group participants indicated that they felt that patients had little choice but to accept and adjust to these changes, which they saw as being a consequence of broader changes within the NHS, which they themselves also had to accept. Therefore, acceptance was viewed as inevitable and skill mix was not necessarily seen as an opportunity to enhance the choice of practitioner.
A second compromise related to the extent to which skill mix practices could provide continuity of care. The majority of patients in the survey (65/125, 52%) reported that they received better health care overall when they were always, or mostly, seen by the same practitioner. This echoed the focus group data, where PPG members reported that continuity (defined as seeing the same practitioner) was desirable and important for patient satisfaction and maintaining and/or developing an ongoing relationship between patient and practitioner. In the focus groups, patients felt that skill mix did not always accommodate continuity of care and reported facing difficulties with this and with accessing the same practitioner for follow-up appointments when this was made more difficult by the new access systems. This had a negative impact on patient satisfaction and led to patients having to compromise choice and continuity to gain access to an appointment.
A third compromise reported by PPG members related to concerns regarding patients disclosing their medical conditions to receptionists and the robustness of the training/expertise of the receptionists doing the triage.
Developing new relationships
Notwithstanding the above lack of information and some patient compromises, focus group patients indicated that, although patients were often unsure about what skills different practitioners had, once patients had experienced a consultation with a newer practitioner, they reported being happy with non-GP consultations. This change in patient perceptions could be an illustration of patient adaptability [noted in earlier findings in Research question 3(i): how are new ways of working being negotiated in general practices where skill mix changes have occurred?] and also represents the fourth source of patient ‘work’ (i.e. developing new relationships with a range of newer practitioners).
Discussions within the Patient Focus Groups indicated that patients made sense of the newer roles by deconstructing their past relationships with GPs. The following quotation is an illustration of this change in attitudes, which also indicates a perception that non-GPs can provide longer and more ‘holistic’ consultations:
My experiences have been very good. In fact with the physician associate, I found her very good because I have a . . . quite a lot of ailments, a lot of things wrong with me, and she’s more understanding of looking at me as a whole rather than just dealing with an isolated ailment, which I find the GPs tend to only want to talk to you about that one thing. And I find that she’s been very, very good at dealing with everything and joining the dots up a little bit. And the nurse, senior nurse . . . I think the nurse, the senior nurse, is very, very thorough, and so is the physician associate as well. That’s what I’ve found. In fact I prefer to go and see them rather than go and see the GP.
ID55: site E, PPG focus group (bold text highlights the relevance of the quotation)
However, this deconstruction of relationships with GPs was not without concerns. Focus group patients were concerned about any adverse consequences for patients, particularly older patients, of disrupting long-established relationships.
Given the need for patients to invest time in developing new relationships with newer practitioners, it is useful to note that at sites A and E (both of which were early adopters of skill mix) it was felt that newer practitioners had begun to provide this continuity for some patients, which improved patient satisfaction and increased trust in and acceptance of the newer roles. Continuity was noted as particularly important for vulnerable groups. For example, in Site E, a PA took the lead for patients with learning disabilities. These developments in early adopters indicate that there are opportunities to both facilitate access to, and improve the patient experience of, practices with diverse skill mix.
Factors facilitating and improving the patient experience of skill mix changes
If patients are required to invest time and effort in more information-gathering, navigate new and sometimes complex IT and telephone appointment systems, make compromises and develop new relationships, then addressing any of the issues discussed above at a practice level could improve the patient experience. A couple of factors highlighted by PPG members as improving the patient experience of the consultation and gaining access to practitioners are noted below.
First, of considerable concern to PPG members was the development of patient communication to ensure patient understanding of the newer roles and systems and the acceptability of skill mix changes more broadly. Again, we see evidence that greater patient knowledge does evolve over time. This may also reflect reports from site A focus groups that the practice had recently improved information regarding the role changes and the online triage processes, and that the practice’s updated website had helped inform patients of the newer roles and systems.
Members of the PPG felt that practices should pay more attention to making sure that patients could access information to understand how the practice was changing. However, there was no consensus about how best to communicate the newer practitioner roles to patients, whether this should be via screens in surgeries (which informs only those attending), by the internet, by text messages or by mailouts.
Receptionists were often cited as key facilitators of information transfer and, when suitably trained, could act as key patient communicators. However, there was an acknowledgement of the great responsibility being placed on receptionists to educate patients while simultaneously matching the unwell person to an appropriate practitioner:
It is difficult because that means you’re putting a lot on the receptionist to explain in great detail the difference between a physician’s assistant . . . associate, sorry, and a GP, or a senior nurse practitioner and they will say, oh, you can see the physician’s assist . . . you know, associate, and people probably think, oh, that’s a nurse. Now if you’re feeling distressed or, you know, upset, you think, you know, I hardly ever come and now I can’t even see a doctor. That’s what people think.
ID55: site E, PPG focus group
Educating the infrequent visitor is likely to remain a challenge because, as the above illustration indicates, the time at which the visitor needs to know of any changes is a time when the visitor is likely to be less responsive to new information.
Another challenge that remains is how to provide practitioner information that usefully categorises practitioner competencies for patients. Patient representative members in our study were keen to develop such a list as a useful output of the project and suggested that the list include information such as training, qualifications, skills and competences. However, as indicated in Research question 3(i): how are new ways of working being negotiated in general practices where skill mix changes have occurred?, practitioners within the same occupational group are often further distinguished both by their qualification-based competencies and role-holder competencies. In addition, as indicated in the case studies, several practitioners broadened their scope of practice over time. For these reasons, it was decided that it would not be possible to develop such a standardised list for dissemination.
Second, reference was made to how patients were often reassured when non-GPs acknowledged their limitations and referred or escalated patients to more senior staff (e.g. GPs) or practitioners with relevant specialist skills. The contribution made by the visibility of what focus group participants referred to as GP ‘supervision’ appeared to be a pivotal point in patients’ acceptance of changes, improving trust in the newer roles and increasing acceptance of skill mix more broadly:
I think one of the things about seeing the PA is the fact that if they’re not comfortable you will be referred to a GP and I think that’s really important for patients to know. They don’t just bumble along doing things by the rule but if they’re not happy they’ll put their hand up and say, ‘I’m out of my depth, you need to go and see a doctor,’ and ‘you . . . well stay there and I’ll go and talk to them’. I’ve seen that happen and I think that gives you enormous sense of relief in some respects that they’re a cog in the wheel.
ID55: site E, PPG focus group
It is useful to note that a small number of patient respondents to the survey (12/125, 10%) reported that their practitioner had ‘involved another practitioner’ in their consultation.
Summary
A large majority (77%) of patients surveyed believed that their appointment had been useful and that they had seen the right practitioner to deal with their problem(s). However, the focus groups did raise concerns about the patient ‘work’ required to understand, access and develop relationships with new practitioners. The introduction of newer roles had brought new systems of access/triage systems to practices, but changes were not communicated well, and concerns were raised about how less-informed patients, particularly older adults, infrequent attendees and vulnerable groups, could navigate the new system. Although patients had limited understanding of newer practitioner types and their capabilities, many patients were reassured after they had consulted with a new non-GP. A contributing factor in this was that a longer appointment slot provided time for more ‘holistic’ consultations than was typically available with GPs, which does have implications for costs. In addition, the visibility and availability of GP ‘supervision’, when needed, improved trust in, and acceptance of, the newer roles among patients.
Follow-up interviews during COVID-19 pandemic
Realising the extent to which ‘normal’ work in general practice was disrupted in response to the COVID-19 pandemic, we resumed contact with our case study sites to explore how their practice responded to the challenges presented by the pandemic and how the pandemic might have brought about changes in how practices implemented skill mix or their future plans. We conducted telephone interviews with participants (i.e. GP partners and/or practice managers) at all five case study sites.
Structure
In March 2020, at the beginning of the pandemic, support work was needed to keep up to date with rapidly changing guidelines and operating procedures to allow general practices to continue working safely. Practices reported that this included procuring laptops and setting up IT systems to allow staff to work from home. Deficient communication through official channels meant that GP partners and practice managers would watch evening news bulletins for government announcements about what must be carried out the next day with regard to contacting shielding patients (i.e. patients who had been identified as clinically extremely vulnerable by NHS England, which may not be the same list of patients as identified by local general practices). The support provided by local organisations varied and often related to the meeting of IT needs.
At the practice, reception staff had to manage the throughput of patients differently. Entrances to practices were colour coded to manage patient flow. In site E, the reception team kept a record every 30 minutes of how many people were in the waiting room to ensure that social distancing was maintained. Although site E had concern over space during our fieldwork, during COVID-19 it managed to designate rooms for (potential) COVID-19 cases. However, the site also set up an in-hours and out-of-hours COVID-19 hub with neighbouring general practices.
All sites encouraged their staff to work from home. However, some staff were less comfortable with making full use of digital technology than others. For example, in site E, older GPs were judged to be ‘stuck in their ways’ and worried about how they would manage home visits if only a limited number of GPs were in the building. In site B, nurses were doing relatively fewer remote consultations than GPs. In site C, non-GPs were generally less comfortable when dealing with risks associated with telephone triage and consultations.
Processes
During the pandemic, there was a move towards total triage and remote consultations to prevent the spread of the virus by people coming to general practices. A GP partner in site C described this as ‘COVID medicine’:
I think best practice medicine outwith a pandemic would’ve been to go and see the patient but you’re all the time we’re weighing up the risk that we pose by exposing them to more clinicians and having more footfall either through the surgery or going out to the nursing home.
Site C
For triage, all practices used COVID-19 screening questions as part of a process to determine which patients needed a consultation via telephone/video and which patients could be seen face to face. Site C prepared a complete list of specialist skills within the team and booked patients based on skills rather than practitioners’ roles (e.g. in relation to women’s health or mental health). The system was described as similar to a hospital referral letter, which provides information about the nature of the patient’s problem. In site D, the receptionist did a basic triage in terms of whether the patient’s problem was ongoing or new. Patients were then allocated to the on-call list of practitioners. When the practitioner did an initial telephone consultation, they decided whether or not patients needed to be seen, and those requiring a face-to-face consultation were generally seen on the same day. In sites A, B and D, doctors dealt with telephone triage. However, in site B, triage for frail and elderly patients, home visits and care home visits were carried out by the ACPs, as was the case before COVID-19 started. In site E, the site had a ‘doctor first’ triage model where all patients were triaged by a GP. The GP would speak to the patient on the telephone and would decide whether or not the patient needed to be seen face to face.
For remote consultations, all general practices used software that enabled two-way text messaging and video consultations. Patients were able to attach photographs in a text message or upload several pictures to e-mails and images were then attached to the patient’s record.
In terms of supervision, staff could not meet with a wider group of colleagues. Informal meetings were staggered or arranged in shifts, allowing only four to six practitioners in a room together. However, GPs were more available for debriefing or advice, as they were mostly using the telephone rather than seeing patients face to face.
Outcomes
Practices reported variation in patients’ acceptance of remote consultations. Site D found that the elderly population in its area was not averse to using technology and site B found less resistance from elderly patients than expected. In site C, remote consultations worked well for working-age adults, as they did not have to take time off work to see their GP. Site A had not carried out many video consultations, but found that photographs and telephone consultations worked well.
Remote consultations worked for different groups of patients in different sites. Site C found that remote consultations worked well for patients with mental health conditions. Most mental health examinations were based on verbal communication, rather than requiring examinations, and were, therefore, suitable for a video or telephone consultation. Site B found that remote consultations worked well for children when parents only needed reassurance. Site A developed a way of conducting ward rounds at care home:
. . . it’s very useful for care homes, so they’re finding they’re doing their ward rounds at care homes by a video. So, basically somebody at the care home is walking round with a tablet and showing the doctor at that patient’s bedside the wound or whatever the issue is, and then walking onto the next patient. So it works very well with care homes and that’s what the video consultations is an improvement for, and that’s great – care homes.
Site A
However, there were challenges with the use of remote consultations. Video consultations were described as ‘a little bit of an uphill battle’ and ‘cumbersome’ because of difficulty with coordinating the doctor, patient and functioning video cameras. There were also difficulties with connectivity. Despite having Wi-Fi connections in site C, video-consulting was streamed through practitioners’ telephones. Some practice rooms had a worse connection than others, and unreliable connectivity adversely affected video quality. Similar problems were encountered by practitioners working from home. Site C found it difficult for practitioners to communicate complex issues digitally or on the telephone, especially for elderly patients with multiple comorbidities.
When asked about arrangements made during COVID-19 that will stay in the future, all practices envisaged continuing with total triage whereby patients were assessed in terms of whether they need to be seen face to face or remotely (using telephone or video) and whether or not they need to be seen by a GP.
Reflecting generally on their COVID-19 experiences, site A spoke about introducing a shift change conversation where all staff had a 5-minute uninterrupted catch-up, which is similar to a handover in hospitals, to help practice staff feel like they are part of a multidisciplinary team. Site B had learned more about managing patient demand and shifting patient expectations and had thought about which non-GPs they will need in the future. Initially, site B had wanted to recruit a paramedic to deal with home visits; however, as the number of home visits had declined following firmer demand management, the site decided that it wanted to invest more in practitioners who can deal with mental health, specifically a community psychiatric nurse, because the site had seen an increase in low-grade mental health issues related to COVID-19, rather than chronic mental health issues per se. Site C was moving towards a total triage model using artificial intelligence to ensure that it can meet what are assessed as the clinical needs of patients, rather than responding to what could be perceived as patient demands. The proposed change was based on shifting patients’ expectations from access because they wanted to be seen to access because they were telling practices why they needed to be seen. The practice will then decide the ‘right’ next step, which may be a telephone call, advice-giving, signposting elsewhere or face-to-face appointments. Although previously the practice’s reception team did not do any clinical or health navigation, with the new tool, receptionists will be gathering clinical information, including an assessment of urgency, which will then be forwarded to a clinician to assess the appropriateness of the appointment. Site D found that it had carried out more shared decision-making during COVID-19 regarding if and how they should see patients, which brought staff closer together. Site E envisaged that there would be more flexible working from home than in the past, with doctors doing telephone triage and issuing prescriptions from home while practitioners and attached staff (e.g. midwives) who do hands-on treatments would return to working in the practice. Staff at site E had also started communicating more with their neighbouring practices, could access each other’s systems (for practices within the same PCN) and had learned about what activities can be amalgamated and coordinated with neighbouring practices and what activities can be done in-house.
During the COVID-19 pandemic, all sites had daily online and/or socially distanced meetings in the reception area. Site A had moved all meetings online, whereas site C had a daily online meeting to convey information from an announcement made by the government the previous evening. Every morning staff at site C met to discuss issues, such as the workforce problems caused by many of the non-clinical managers working from home, daily statistics on COVID-19 rates, nursing home issues and any changes in government announcements. Their regular monthly face-to-face meetings had been replaced with an hour-long weekly ‘power catch-up’ between clinicians and the management team.
Our study participants also highlighted specific concerns following the move to ‘COVID medicine’. Practitioners felt that they could not build up the face-to-face rapport with patients via remote consultations, which they felt was a cornerstone of GP work. A GP partner in site C reported feeling anonymous to patients, a situation that was described as similar to patients telephoning into NHS 111. This GP further argued that it was hard to measure the unintended consequences of remote consultations.
Practitioners also reported concerns about patients delaying seeking help for conditions such as cancer, heart attack, stroke and chronic obstructive pulmonary disease. In addition, practitioners were unable to do preventative health checks or face-to-face components of health checks for patients with long-term conditions and were dealing with a 6-month backlog of these routine appointments.
Chapter 6 Outcomes associated with skill mix changes
In Chapter 3, we set out how skill mix is distributed across England and highlighted regional differences in skill mix employment. In Chapter 4, we described motivations for skill mix change, as articulated by practice managers. In Chapter 5, we explored in some depth the day-to-day realities of skill mix change in practice, including patient experiences. In this chapter, we return to the quantitative data to examine whether or not there are any discernible changes in outcomes associated with skill mix as currently operationalised in England. To do this, we linked workforce data to a wide range of patient, population and practitioner outcomes reflecting health-care activity, quality and expenditure. This section addresses research question 1(ii) (i.e. how are compositional changes to the workforce associated with later changes in a range of outcomes, including patient and practitioner satisfaction?) and research question 1(iii) (i.e. how are workforce changes associated with later changes in costs and practice efficiency?).
Data
Workforce data
As in Chapter 3, we used the workforce data obtained from NHS Digital on the range of practitioners employed in practices across England. We created a longitudinal, practice-level workforce data set using the wMDS. 107 As of October 2020, the data sets are available monthly; however, for the duration of the analysis we present here, data were available annually or quarterly. We use data from 2015 to 2019.
As with 2019 data, these data contain both headcounts and numbers of FTEs for 35 categories of staff (i.e. 11 categories of GPs, 7 categories of nurses and 17 categories of DPC staff). We did not consider variations in other types of staff, as our focus was to look at the outcomes for patients as a consequence of clinical decisions made by and direct interactions with different types of practitioners.
The practice-level workforce data sets are an evolving data collection, with different staff members being added at different times and a dedicated payment now offered to recognise the costs involved in reporting the data. Table 16 presents a list of workforce roles included in the data sets in 2015 and in 2019. The number of roles recorded in the DPC categories has expanded from nine categories to 17 categories, plus eight categories for trainees and apprentices to better reflect the expanding skill mix in general practice. Detailed descriptions of the categories are provided in the National Workforce Reporting System data entry guidance document. 108 We worked closely with NHS Digital to understand the properties of the data. We identified some errors that were fixed and some observations that contained imputed values. Out of the 6867 practices for whom workforce data were made available in the September 2019 data set, there were usable data for 6296 practices.
| GPs | Nurses | DPC | |||
|---|---|---|---|---|---|
| 2015 | 2019 | 2015 | 2019 | 2015 | 2019 |
| All GPs | All GPs | All nurses | All nurses | All DPC | All DPC |
| Senior partners | Senior partners | Practice nurse | Practice nurse | Dispenser | Dispenser |
| Partner Providers | Partner Providers | ANP | ANP | Health care assistant | Health care assistant |
| Salaried (practice) | Salaried (practice) | Specialist nurse | Specialist nurse | Phlebotomists | Phlebotomists |
| Salaried (other) | Salaried (other) | Nurse with extended role | Nurse with extended role | Pharmacists | Pharmacists |
| ST3–4 | ST1–4a | Trainee nurse | Trainee nurse | Physiotherapists | Physiotherapists |
| F1–F2b | F1–F2 | District nurse | Nurse dispenser | Podiatrists | Podiatrists |
| Retainer | Retainer | Research nurse | Nurse partner | PAs | PAs |
| Locum (vacancy) | Locum (vacancy) | Nurse dispenser | Therapist counsellor | Therapist counsellor | |
| Locum (absence) | Locum (absence) | Nurse partner | DPC other | Occupational therapist | |
| Locum (other) | Locum (other) | Therapist (other) | |||
| Locum (not stated) | Locum (not stated) | Nurse associate | |||
| Paramedic | |||||
| Pharmacy technician | |||||
| Social prescribing link worker | |||||
| High intensity therapist | |||||
| Psychological well-being practitioner | |||||
| DPC other | |||||
| Trainee and apprentice roles (n = 8) | |||||
Outcomes data
We obtained outcomes from the following range of sources:
-
the GP Patient Survey (GPPS)
-
QOF
-
prescribing data
-
Hospital Episode Statistics
-
NHS payments to general practices
-
the GP Worklife Survey.
With the exception of the GP Worklife Survey, all of these sources have universal coverage of practices in England and we obtained them at practice level. The GP Worklife Survey includes data from a sample of individual GP respondents. The outcomes are listed in Table 17. 109
| Data source | Data point | Measure |
|---|---|---|
| GPPS | 2015, 2017 and 2019 |
|
| QOF | 2015 and 2019 |
|
| Prescribing | 2016 and 2019 |
|
| Hospital Episode Statistics | 2011/15 and 2017/18 |
|
| NHS payments to general practice | 2015 and 2019 |
|
| GP Worklife Survey | 2015 and 2019 |
|
The GP Patient Survey
The GPPS is a recurring and independently administered survey that has been sent to > 2 million people across the UK on behalf of NHS England. The survey asks patients how they feel about various aspects of services delivered by their general practice. Weighted and unweighted data are available at practice level and GPPS data are widely used by national organisations (e.g. by NHS England to provide comparative data across CCGs and by the Care Quality Commission to monitor practices’ performance).
To look for associations between workforce composition and patient satisfaction, we obtained data on how respondents reported their overall experience and satisfaction with making an appointment and how recently respondents had seen a GP and a nurse at the practice. In the absence of data reliably reporting the number of consultations delivered by a general practice, data reporting the interval since patients had seen a GP or nurse allowed us to generate a proxy measure of the number of appointments provided (based on the principle that respondents will tend to report less time since their last visit at practices that offer more consultations). Owing to subsequent changes to survey questions, the latest year for which the measures on time since last visited the practice were available was 2017.
Respondents were asked to classify their responses into five bands: (1) within the last 3 months, (2) between 3 and 6 months, (3) between 6 and 12 months, (4) over 12 months ago or (5) never seen a GP/nurse at this practice. We converted the proportions reported in the different categories into a single summary measure of average time since patients last saw a GP and/or last saw a nurse. To do so, we estimated a constant-only interval regression model and assumed that the times since the last visit were normally distributed. We estimated average values within each category by taking predictions from the interval regression model and then taking the mean of these to arrive at a single measure of time since the last visit for each practice.
Quality and Outcomes Framework
Since the introduction of the 2004 GP contract, the QOF has been a voluntary, but largely accepted, element within the GMS contract held by NHS GPs in England. The QOF was established as a pay-for-performance scheme, awarding financial incentives to general practices for delivering interventions and achieving patient outcomes with selected health conditions. Evidence-based indicators were informed by the National Institute for Health and Care Excellence and have been revised at intervals. 110 From the QOF, we obtained data on the total number of points in the clinical domains awarded to the practice as a global marker of the technical quality of patient care.
Prescribing in general practice
Definitions of what constitutes good quality in prescribing are contested and entangled with issues (e.g. effectiveness, risks, costs and patient choices) that are difficult to evaluate in national-level data. 111
However, as part of global efforts to reduce the emergence of antibiotic resistance, measures of the relative frequency with which prescriptions for broad and narrow-spectrum antibiotics are issued are among recognised markers of quality of general practice prescribing (i.e. lower usage of broad-spectrum antibiotics indicates higher-quality prescribing habits). 112
Prescribing expenditure in general practice constitutes a significant portion of the £9.08B expenditure on community-dispensed prescriptions in England in 2019. The overall number of prescription items dispensed in the community in England in 2019 was 1.12 billion. 113 Practice-level data on volume and cost are typically standardised by the number of age, sex and temporary resident originated prescribing units (ASTRO-PUs). ASTRO-PUs are weightings reported by the NHS Business Services Authority (Newcastle upon Tyne, UK) for age, sex and temporary residents that can be applied to practice populations.
From the prescribing data, we obtained three indicators. As an indicator of prescribing quality, we used the percentage of prescribed antibiotics that were broad spectrum. We measured prescribing volume using a number of items prescribed per ASTRO-PU. We measured prescribing cost as net ingredient cost divided by the number of prescribed items.
Hospital Episode Statistics
Hospital Episode Statistics is a database containing a wide range of data about services accessed by patients at all NHS hospitals in England. 114 To examine whether or not general practice workforce composition is associated with variation in the use of hospital services, we obtained annual counts of admissions (i.e. elective and non-elective), outpatient attendances (i.e. first attendances only, attended appointments only) and A&E attendances.
NHS payments to practices series
The NHS payment to practices data series provides information on NHS payments to individual providers of general practice services in England. 115 The data includes payments under the Global Sum, Personal Medical Services (PMS) contracts, QOF and local incentive schemes at practice level. These figures do not include expenditure on prescriptions or use of secondary care. Therefore, these payments represent only a proportion of the expenditure of the NHS on services delivered or generated by general practices.
Total NHS expenditure on activity delivered or generated by general practices
We calculated the total NHS expenditure for each practice using payments made to practices, prescribing expenditure and expenditure on the different forms of hospital care. For payments to practices, we used ‘total payments’, which includes the Global Sum and MPIG, balance of PMS expenditure, QOF, DES, local incentive schemes premises, Primary Care Organisation administered, information management and technology, non-DES items, GPFV, PCNs and prescribing. 115 Prescribing expenditure is ‘actual costs’, which are the net ingredient costs less discount, payment for consumables (previously known as container allowance), payment for containers plus out-of-pocket expenses. 116 Expenditure on hospital care was calculated using NHS tariffs for A&E attendances and unit costs from the Personal Social Services Research Unit for admissions and outpatient attendances. 117
We considered NHS expenditure rather than costs to practices. Therefore, we did not estimate staff costs separately. These costs are largely borne by the practice and data for each practice are not available. As practices pay these costs from the income they receive from the NHS, the costs are included in the total payments to practices.
National GP Worklife Surveys
A series of National GP Worklife Surveys have reported on GPs’ experiences of their working lives. In addition to information about colleagues working in their practice, GPs are asked about their overall satisfaction with work, hours of work and the potential for delegation of work. 109 From the 2015, 2017 and 2019 waves of the GP Worklife Survey, we obtained levels of overall GP job satisfaction, the number of hours worked in a typical week and (from 2017 and 2019) perceptions of the proportion of work that could be delegated to one of the newer types of practitioner now working in general practice.
Data on characteristics of practices and populations
We obtained data on registered populations from NHS Digital. We used the proportions of registered patients in the following age categories: 0–4 years, 5–14 years, 15–44 years, 45–64 years, 65–74 years, 75–84 years and ≥ 85 years. We attached statistics from the Index of Multiple Deprivation to data on the distribution of registered patients across lower-layer super output areas and calculated the mean deprivation of each practice’s registered population. We used a binary indicator for a rural location, which was available from the NHS payments to practices data sets.
Methods
We used multivariate regression models to examine the relationships between organisational factors, inputs, outputs and expenditure. We examined how workforce composition affects the production of health care for patients, the working lives of GPs and NHS expenditure on activity delivered or generated by practices.
We measured the levels of input of different types of staff using numbers of FTEs PTP. We grouped staff into three broad groups: (1) GPs, (2) nurses and (3) other practitioners providing DPC. It was not possible to separate the DPC group into separate professions because the numbers in each group were too small. In addition, the way in which data are collected make it difficult to clearly distinguish between, for example, a HCA and a PA. For the prescribing outcomes, we also separated out the CPs from the other DPC professionals because it might be assumed that such professionals’ impact on prescribing will differ from other professionals.
We adopted the specification used by Delhy et al. 118 to model outcomes as a function of staffing levels. Based on the seminal work of Carey,119 these outcomes include cubic functions of the levels of input of each different type of staff. This has been shown to be an acceptable alternative to the more flexible translog specification and one that involves fewer interaction terms and, therefore, is less likely to suffer from multicollinearity in applied work.
To display the effects intuitively, we estimated marginal effects for each input, showing how outcomes and input levels are associated with holding other variables at their mean values. These are presented as margin plots and are evaluated at decile points in the actual distributions of staff input. We also present goodness-of-fit statistics for the regression models and tests of joint significance of the parameters for the different workforce groups.
Covariates
From the payments to general practices data set, we obtained figures on the weighted population for each practice. By dividing by the total population from the same source, we created a measure of per-capita workload. We also obtained the amount paid to the practice under the MPIG scheme from this same source. The MPIG payment is an additional payment to the practice over what would be expected under the capitation formula because the practice historically received this level of payment. We divided the payment by the registered population.
We classified practices by contract type as PMS practices tend to have higher payment levels than practices holding the General Medical Services (GMS) contract and may have a wider scope of services than GMS practices. We also identified practices that could dispense for at least some of their patients because of a lack of pharmacies in their area of residence.
We obtained the Market Forces Factor index for each practice from the NHS England CCG allocations 2019/20 to 2023/24 technical documents. 120 This is a measure of relative wages in the local area and is used in the capitation formula to compensate practices for variations in expected input prices due to cost of living.
Scenario analysis
In addition to the margin plots, we also present the results as scenario analysis. We calculated how each outcome would change if the average practice (i.e. with average population size and an average staff level mix) was to increase the number of FTE of each staff type by one unit. We undertook the same exercise for expenditure, using the estimated function for practice payments plus prescribing costs and the unit costs applied to the estimated effects on the volumes of hospital care.
Longitudinal analysis
We estimated long differences using differences between the first and last periods available in the data. This approach has two main advantages. First, it examines the effect of more substantial differences in staffing at the level of practices. Second, this differencing eliminates time-invariant practice characteristics, which may affect efficiency and quality. The coefficients estimated are, therefore, more likely to isolate the independent association between outcomes and staffing levels, reducing the risk of bias due to unobserved heterogeneity.
The longitudinal analysis is presented in Appendix 2 (see Table 23 and Figures 31–42). Owing to limited availability of data, in the longitudinal analysis, we assessed changes in outcomes and expenditure PTP as functions of polynomials of staffing indicators (i.e. changes in levels of FTE staffing PTP, plus interaction terms between GPs and nurses and between GPs and DPC, as well as total number of FTE). For the analysis of changes in the logarithm of total costs, we used the following explanatory variables: polynomials of changes in staffing with interaction terms (GP with nurses and DPC FTE), total FTE and total number of patients.
Estimation
We used Stata for the analyses. We weighted all analyses by the denominator of the dependent variable (most often, the size of the registered population). We used robust standard errors to allow for heteroscedasticity.
Results
Research question 1(ii): how are compositional changes to the workforce associated with later changes in a range of outcomes, including patient and practitioner satisfaction?
Descriptive statistics for each of the outcomes used in the cross-sectional analysis are provided in Table 18. These are shown only for the 6287 practices on which usable workforce data were available. The median practice was awarded 98.49% of the total QOF points available. One-quarter of practices were awarded < 96% of available QOF points. Descriptive statistics for the staffing variables and other covariates are shown in Table 19.
| Outcome | n | Mean | SD | p10 | p25 | p50 | p75 | p90 |
|---|---|---|---|---|---|---|---|---|
| GPPS (2018) | ||||||||
| Months since last saw GP | 5404 | 5.41 | 0.66 | 4.61 | 4.96 | 5.38 | 5.83 | 6.25 |
| Months since last saw nurse | 5404 | 7.96 | 1.18 | 6.52 | 7.12 | 7.86 | 8.7 | 9.5 |
| GPPS (2019) | ||||||||
| Satisfaction with appointment | 6238 | 0.7 | 0.15 | 0.5 | 0.6 | 0.7 | 0.8 | 0.88 |
| Satisfaction with practice | 6238 | 0.84 | 0.1 | 0.7 | 0.78 | 0.85 | 0.91 | 0.95 |
| QOF (2019) | ||||||||
| QOF achievement (%) | 6238 | 96.6 | 5.69 | 91.8 | 96 | 98.49 | 99.78 | 100 |
| Prescribing (2019) | ||||||||
| Percentage of broad- to narrow-spectrum antibiotics | 6099 | 4.51 | 2.31 | 1.86 | 2.88 | 4.19 | 5.77 | 7.52 |
| Total items prescribed per ASTRO-PU | 6238 | 0.12 | 0.04 | 0.08 | 0.1 | 0.12 | 0.15 | 0.17 |
| Cost (£) per item | 6234 | 27.00 | 5.18 | 21.08 | 23.36 | 26.24 | 30.26 | 34.15 |
| Hospital Episode Statistics (2018) | ||||||||
| A&E attendances PTP | 5404 | 257.08 | 81.58 | 162.49 | 197.93 | 247.61 | 306.83 | 361.55 |
| Admissions PTP | 5404 | 97.93 | 24.53 | 69.75 | 81.97 | 96.19 | 112.3 | 128.35 |
| Outpatient attendances PTP | 5404 | 1572.54 | 390.31 | 1160.02 | 1318.29 | 1524.66 | 1773.43 | 2042.63 |
| GP Worklife Survey (2019) | ||||||||
| GP job satisfaction (1–7 scale) | 1282 | 4.43 | 1.53 | 2 | 3 | 5 | 6 | 6 |
| GP working hours per week | 1227 | 41.01 | 14.46 | 23 | 33 | 40 | 50 | 60 |
| Potential delegation to new roles | 1202 | 26.91 | 17.63 | 5 | 12.5 | 25 | 35 | 50 |
| Expenditure (2019) | ||||||||
| Expenditure (prescribing + payments) | 6287 | 29,0538.9 | 72,859.7 | 209,815.0 | 245,141.9 | 285,494.9 | 324,851.1 | 370,855.5 |
| n (%) | Mean | SD | p10 | p25 | p50 | p75 | p90 | |
|---|---|---|---|---|---|---|---|---|
| Staff | ||||||||
| GP FTE | 6238 | 5.11 | 3.72 | 1.36 | 2.32 | 4.27 | 7.04 | 9.83 |
| Nurse FTE | 6238 | 2.49 | 2.33 | 0.56 | 1.00 | 1.89 | 3.27 | 4.96 |
| DPC FTE | 6238 | 1.86 | 2.34 | 0.00 | 0.53 | 1.11 | 2.43 | 4.42 |
| Total FTE | 6238 | 9.47 | 7.16 | 2.64 | 4.49 | 7.97 | 12.54 | 17.73 |
| Patients | ||||||||
| Total patients | 6238 | 9095.51 | 5836.89 | 3435 | 5144 | 8011 | 11,602 | 15,559 |
| Age (years) (%) | ||||||||
| 0–4 | 6238 | 5.41 | 1.42 | 3.80 | 4.51 | 5.30 | 6.20 | 7.13 |
| 5–14 | 6238 | 11.86 | 2.58 | 9.21 | 10.45 | 11.68 | 13.12 | 14.95 |
| 15–44 | 6238 | 39.20 | 9.49 | 29.49 | 33.27 | 37.47 | 43.05 | 50.03 |
| 45–64 | 6238 | 25.87 | 4.18 | 20.88 | 24.08 | 26.65 | 28.48 | 30.08 |
| 65–74 | 6238 | 9.57 | 3.57 | 4.78 | 7.05 | 9.69 | 11.97 | 14.11 |
| 75–84 | 6238 | 5.78 | 2.47 | 2.52 | 4.01 | 5.75 | 7.42 | 8.96 |
| ≥ 85 | 6238 | 2.32 | 1.13 | 0.89 | 1.50 | 2.27 | 3.00 | 3.72 |
| Average needs weighting | 6236 | 1.01 | 0.10 | 0.89 | 0.94 | 1.00 | 1.08 | 1.14 |
| Practice | ||||||||
| Market Forces Factor | 6238 | 1.00 | 0.04 | 0.96 | 0.96 | 0.98 | 1.02 | 1.06 |
| MPIG payment per patient | 6238 | 0.66 | 2.18 | 0.00 | 0.00 | 0.00 | 0.81 | 2.22 |
| Income deprivation | 6238 | 0.14 | 0.07 | 0.06 | 0.08 | 0.12 | 0.18 | 0.24 |
| Rural (1 = rural) | 6238 (16.74) | |||||||
| Dispensing (1 = dispensing) | 6238 (15.93) | |||||||
| GMS (1 = GMS) | 6238 (71.87) | |||||||
| Region of England | ||||||||
| Midlands | 1246 (19.97) | |||||||
| London | 1085 (17.39) | |||||||
| North-east and Yorkshire | 992 (15.90) | |||||||
| North-west | 915 (14.67) | |||||||
| South-east | 825 (13.23) | |||||||
| East | 653 (10.47) | |||||||
| South-west | 522 (8.37) | |||||||
Table 20 presents the fit statistics for the outcome regression models. In addition, tests of joint significance (F-tests) for the workforce parameters are also presented. The p-values for these tests show that for the majority of outcomes the staff variables are significant at p < 0.05 and mostly at p < 0.01. The interaction terms between the GP and nurse/DPC categories are generally not significant.
| Outcome | n | Fit statistics | Workforce parameters: tests of joint significance (F-tests) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R 2 | Root MSE | GP terms (n = 3) | Nurse terms (n = 3) | DPC terms (n = 3)a | Interaction terms (n = 2) | All staff terms (n = 11)a | |||||||
| F-value | p-value | F-value | p-value | F-value | p-value | F-value | p-value | F-value | p-value | ||||
| GPPS (2018) | |||||||||||||
| Months since last saw GP | 5400 | 0.10 | 0.62 | 14.71 | < 0.01 | 6.62 | < 0.01 | 0.16 | 0.92 | 0.78 | 0.46 | 20.42 | < 0.01 |
| Months since last saw nurse | 5400 | 0.27 | 1.00 | 0.37 | 0.77 | 77.25 | < 0.01 | 26.70 | < 0.01 | 0.46 | 0.63 | 50.41 | < 0.01 |
| GPPS (2019) | |||||||||||||
| Satisfaction with appointment | 6232 | 0.21 | 0.13 | 44.55 | < 0.01 | 1.74 | 0.16 | 15.94 | < 0.01 | 0.38 | 0.68 | 32.43 | < 0.01 |
| Satisfaction with practice | 6232 | 0.25 | 0.08 | 62.92 | < 0.01 | 1.96 | 0.12 | 18.41 | < 0.01 | 1.22 | 0.30 | 40.82 | < 0.01 |
| QOF (2019) | |||||||||||||
| QOF achievement (%) | 6232 | 0.06 | 5.43 | 8.34 | < 0.01 | 0.75 | 0.52 | 4.61 | < 0.01 | 2.42 | 0.09 | 4.01 | < 0.01 |
| Prescribing (2019) | |||||||||||||
| Percentage of broad- to narrow-spectrum antibiotics | 6093 | 0.12 | 1.98 | 0.69 | 0.56 | 0.05 | 0.98 | 3.26 | < 0.01 | 0.39 | 0.76 | 1.66 | 0.05 |
| Total items prescribed per ASTRO-PU | 6232 | 0.53 | 0.03 | 0.35 | 0.79 | 1.28 | 0.28 | 48.15 | < 0.01 | 1.03 | 0.38 | 22.92 | < 0.01 |
| Cost per item | 6232 | 0.26 | 4.3939 | 4.0909 | < 0.0101 | 0.6868 | 0.5757 | 3.3434 | < 0.01 | 4.2020 | < 0.0101 | 6.4040 | < 0.01 |
| Hospital Episode Statistics (2018) | |||||||||||||
| A&E attendances PTP | 5400 | 0.41 | 58.09 | 2.34 | 0.07 | 3.49 | 0.02 | 2.68 | 0.05 | 4.49 | 0.01 | 1.69 | 0.07 |
| Admissions PTP | 5400 | 0.55 | 16.16 | 0.53 | 0.66 | 0.96 | 0.41 | 3.03 | 0.03 | 0.37 | 0.69 | 3.41 | < 0.01 |
| Outpatient attendances PTP | 5400 | 0.31 | 329.81 | 5.56 | < 0.01 | 2.01 | 0.11 | 1.85 | 0.14 | 0.11 | 0.89 | 6.42 | < 0.01 |
| GP Worklife Survey (2019) | |||||||||||||
| GP job satisfaction (scale 1–7) | 1282 | 0.05 | 1.50 | 1.65 | 0.18 | 0.81 | 0.49 | 0.80 | 0.49 | 0.13 | 0.88 | 1.66 | 0.08 |
| GP working hours per week | 1227 | 0.04 | 14.20 | 0.44 | 0.72 | 1.11 | 0.34 | 2.03 | 0.11 | 0.03 | 0.97 | 1.33 | 0.20 |
| Potential delegation to new roles | 1202 | 0.07 | 17.09 | 1.47 | 0.22 | 0.58 | 0.63 | 3.34 | 0.02 | 0.63 | 0.54 | 5.61 | < 0.01 |
| Expenditure (2019) | |||||||||||||
| Prescribing + practice payments | 6285 | 0.73 | 35666.0 | 9.48 | < 0.01 | 8.12 | < 0.01 | 20.78 | < 0.01 | 0.99 | 0.37 | 43.01 | < 0.01 |
In the following sections, we discuss the results of the regression models. Each figure (see Figures 13–27) has three or four subgraphs that plot the effect of workforce on the outcome measure. For instance, an upwards sloping curve would signify a positive relationship between the amount of workforce PTP in that staff category and the outcome measure. Figures 13–27 present 95% confidence intervals and the relationship between workforce and the outcome across the range of workforce levels. Given the different scales of outcomes, we focus here on the direction of the relationship before focusing on the magnitude of the relationship in the next section (see Scenario analysis).
How is time since last practice visit with a specific practitioner type associated with workforce composition?
Our analysis of GPPS data on the time since patients last saw a GP (Figure 13) and a nurse (Figure 14) show that practices with more GPs have shorter time periods since respondents last saw a GP, whereas practices with more nurses have lengthier time periods since respondents last saw a GP. Practices with more nurses and DPC staff have shorter times since respondents last saw a nurse.
FIGURE 13.
Estimated effects of staff levels on average time (months) since last saw a GP. (a) GPs; (b) nurses; and (c) DPC staff.

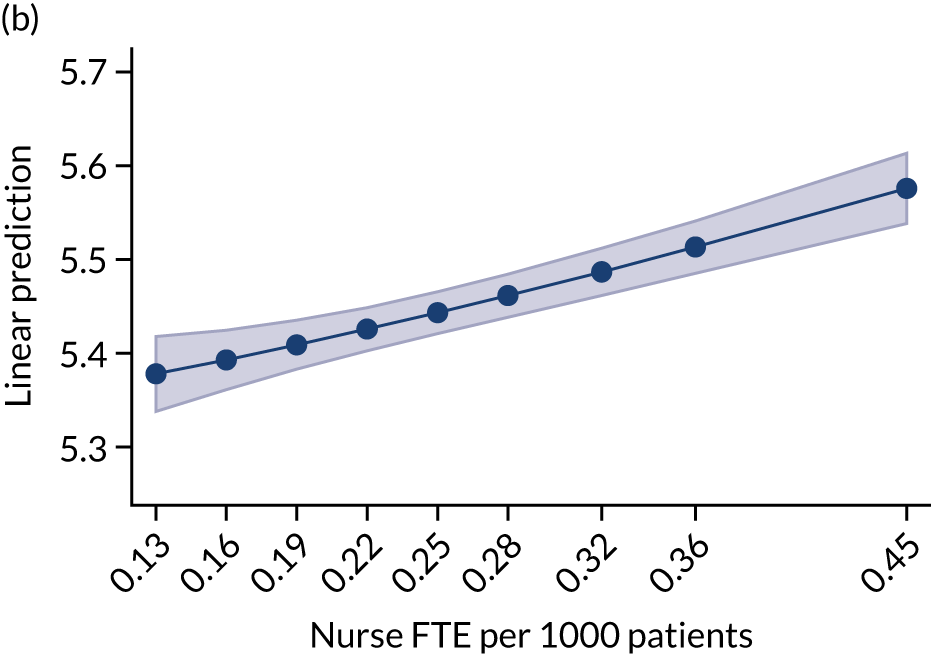

FIGURE 14.
Estimated effects of staff levels on average time (months) since last saw a nurse. (a) GPs; (b) nurses; and (c) DPC staff.
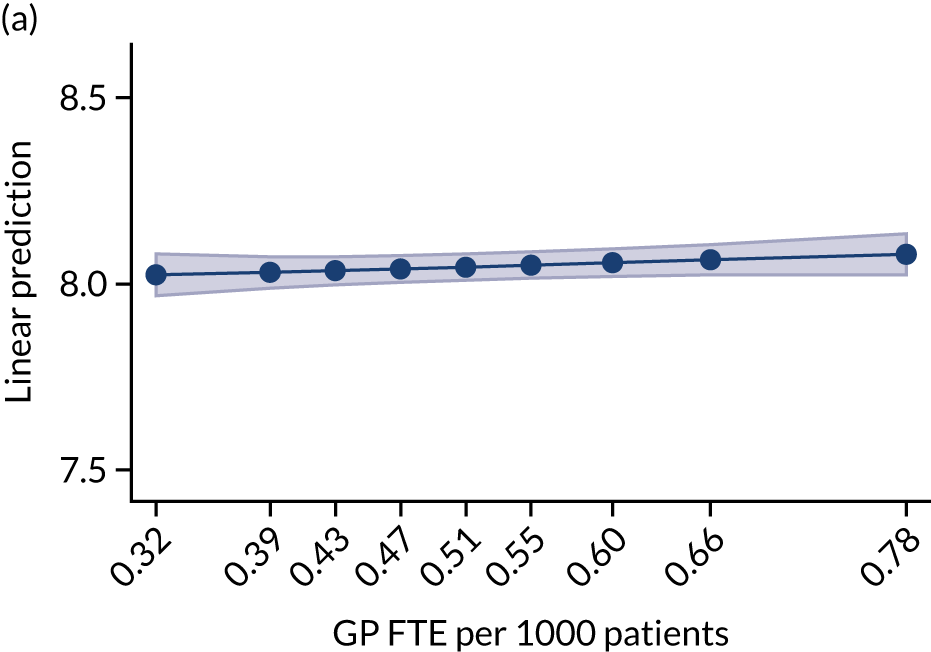
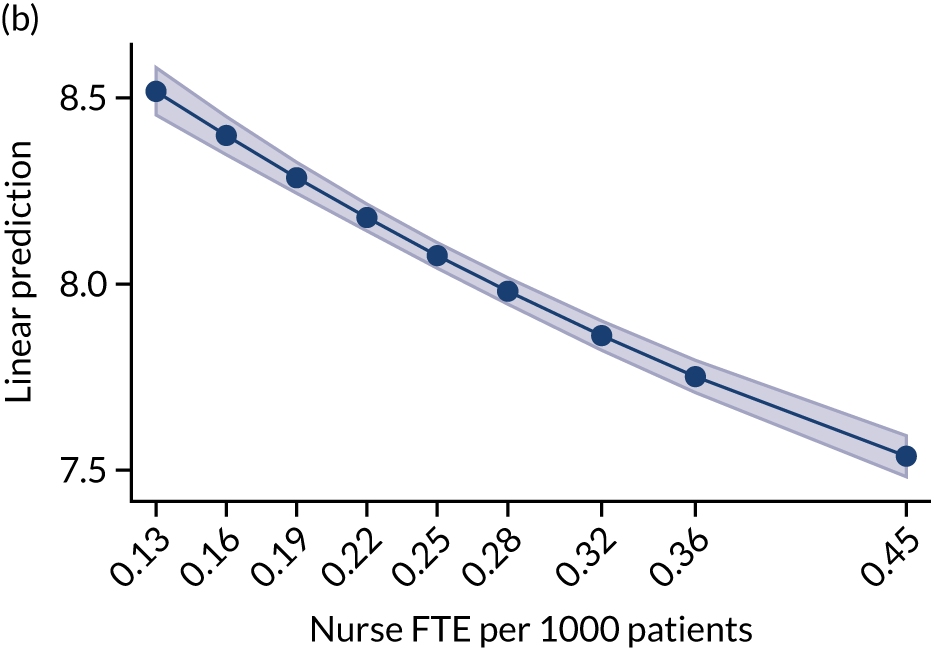
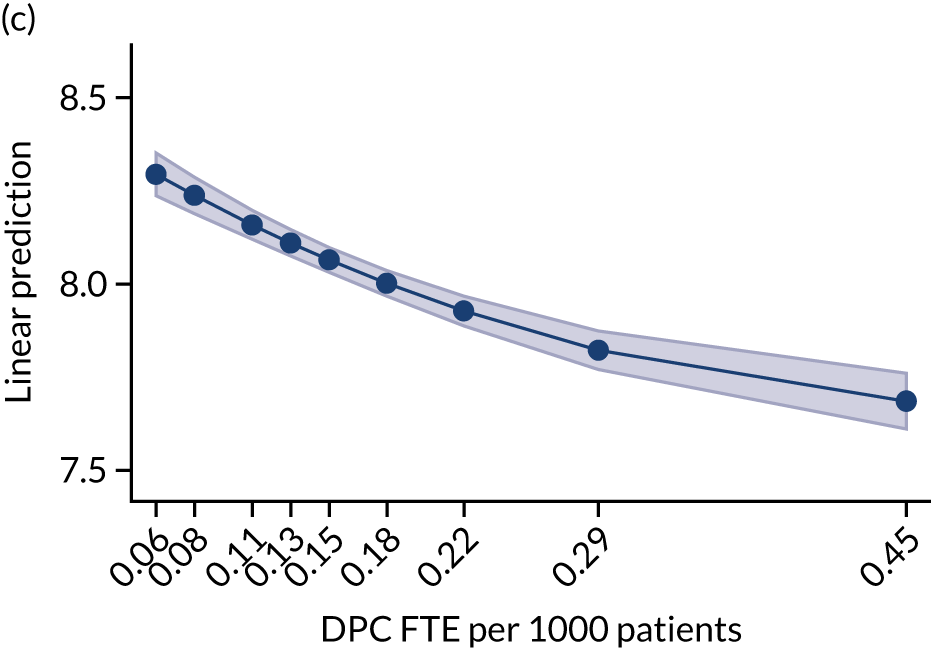
How is patient satisfaction associated with workforce composition?
Practices with more GP FTE PTP have a higher proportion of respondents reporting having had a very good or fairly good experience of making an appointment. Figures 15 and 16 show that the other two broad workforce groups (i.e. nurse and DPC staff) show an initial decline in the proportion of patients selecting the two good responses, followed by a levelling off. Respondents were more likely to report very good or fairly good overall experience of their general practice in practices with more GP FTE PTP. Practices with more DPC staff had lower proportions of respondents indicating a good overall experience.
FIGURE 15.
Question 18 of the GPPS: overall experience of making an appointment. (a) GPs; (b) nurses; and (c) DPC staff.
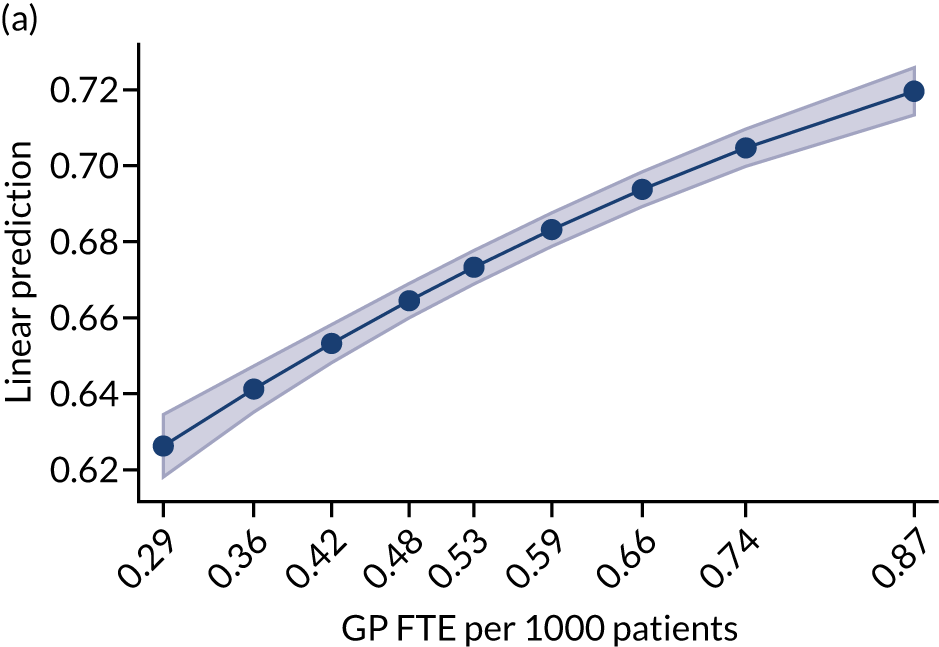
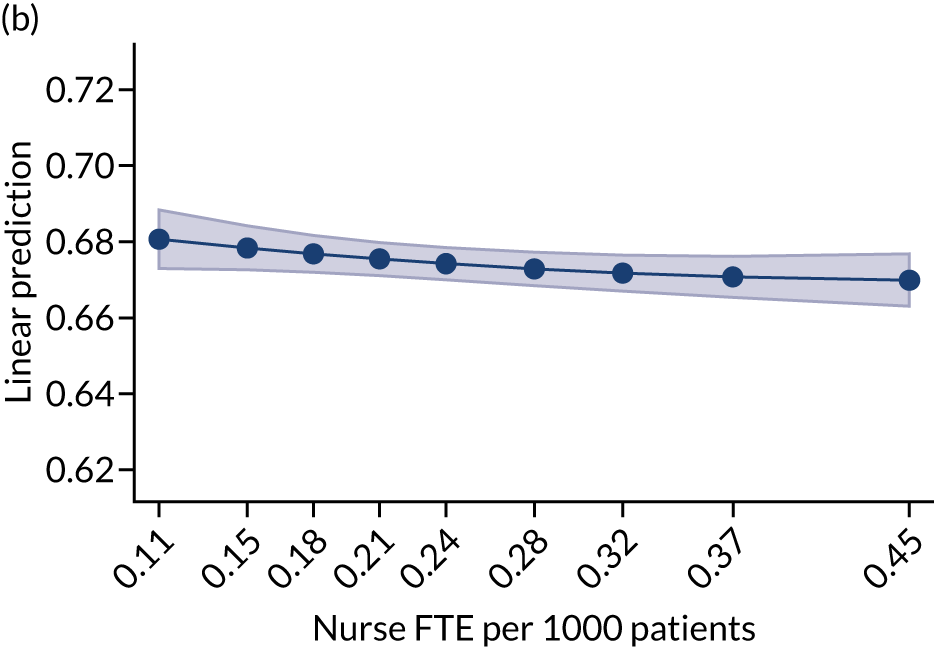
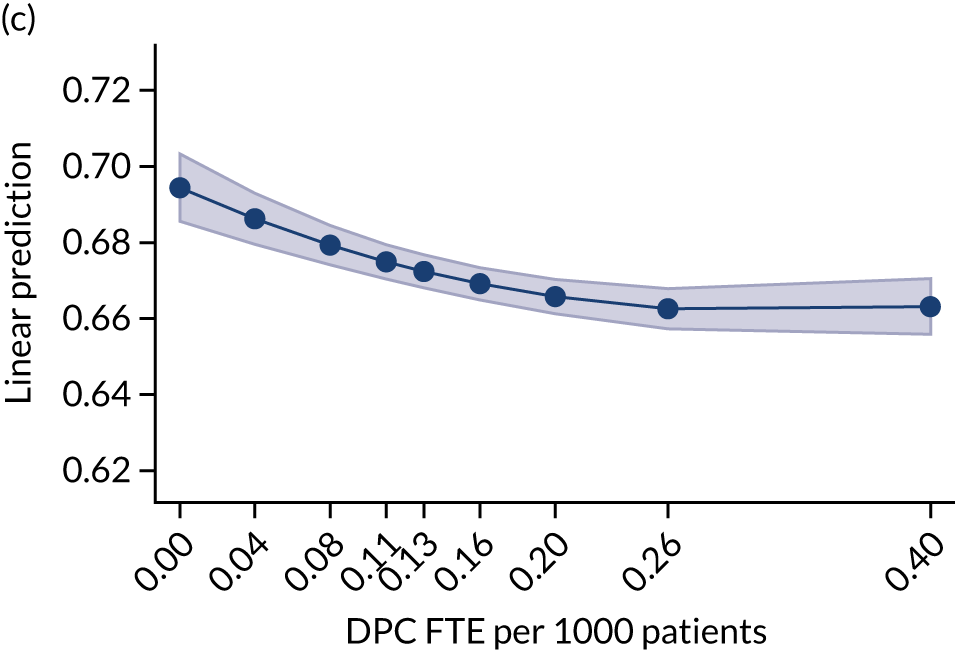
FIGURE 16.
Question 28 of the GPPS: overall experience. (a) GPs; (b) nurses; and (c) DPC staff.
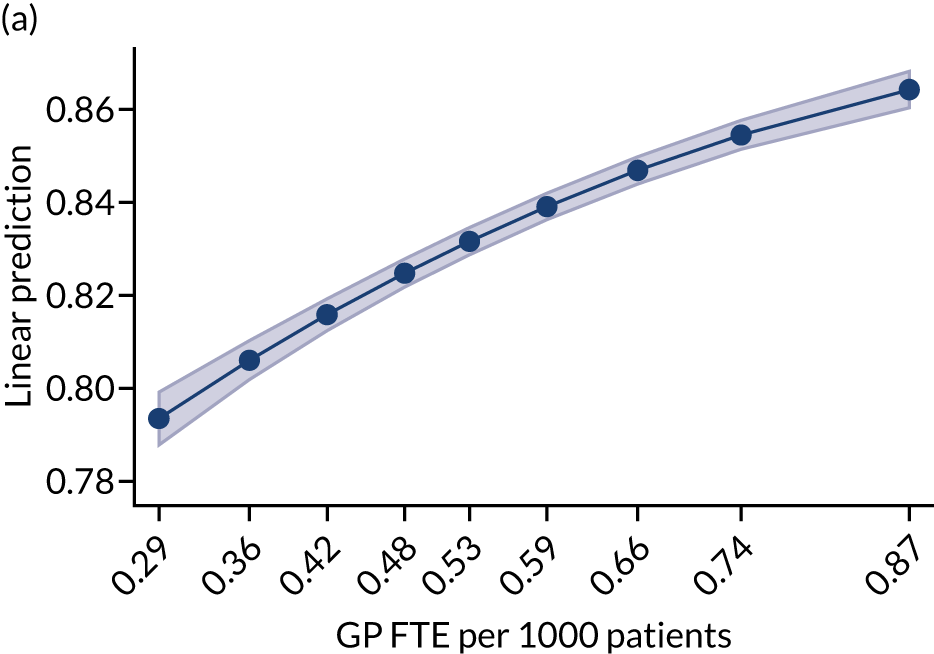
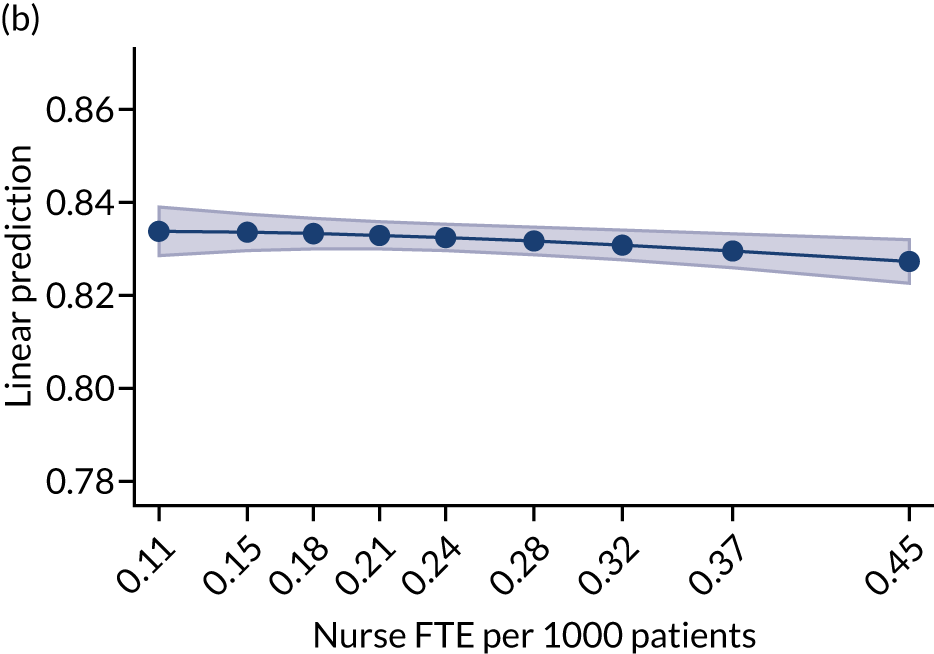
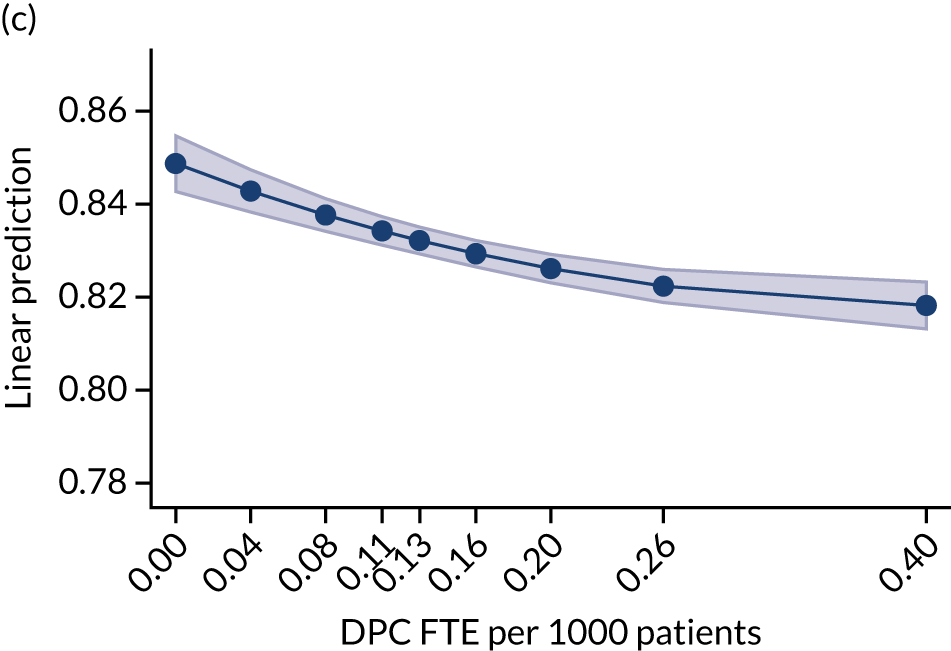
How is achievement across the clinical sections of Quality and Outcomes Framework associated with workforce composition?
Our analysis looked at the association of the QOF points achieved by practices and their workforce composition PTP. Figure 17 shows increasing and then levelling off trends for all three worker groups. This indicates that practices with more staff FTE PTP achieve, on average, a higher percentage of QOF points.
FIGURE 17.
Quality and Outcomes Framework: total achievement (%). (a) GPs; (b) nurses; and (c) DPC staff.
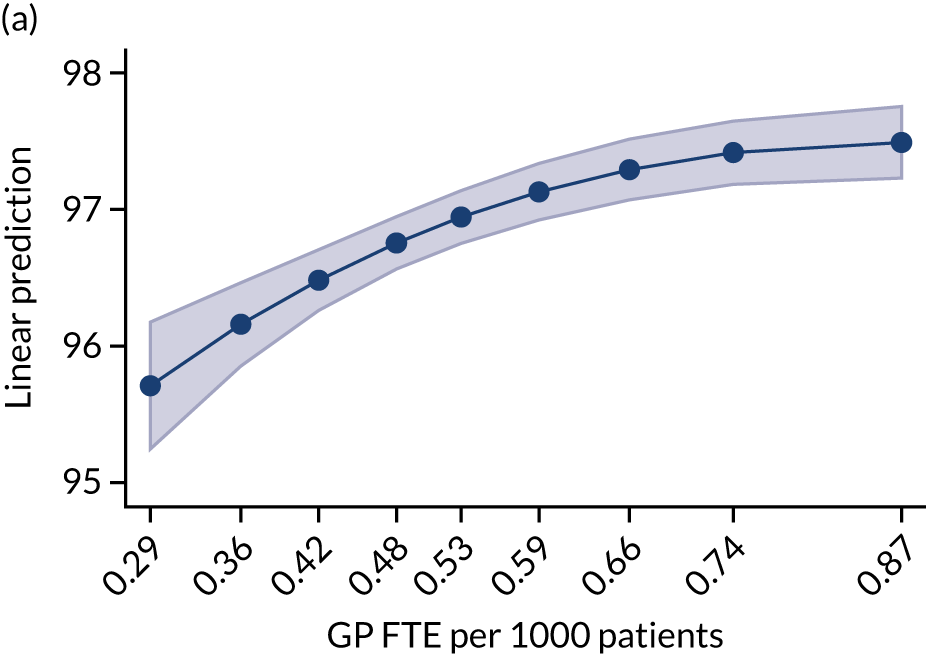
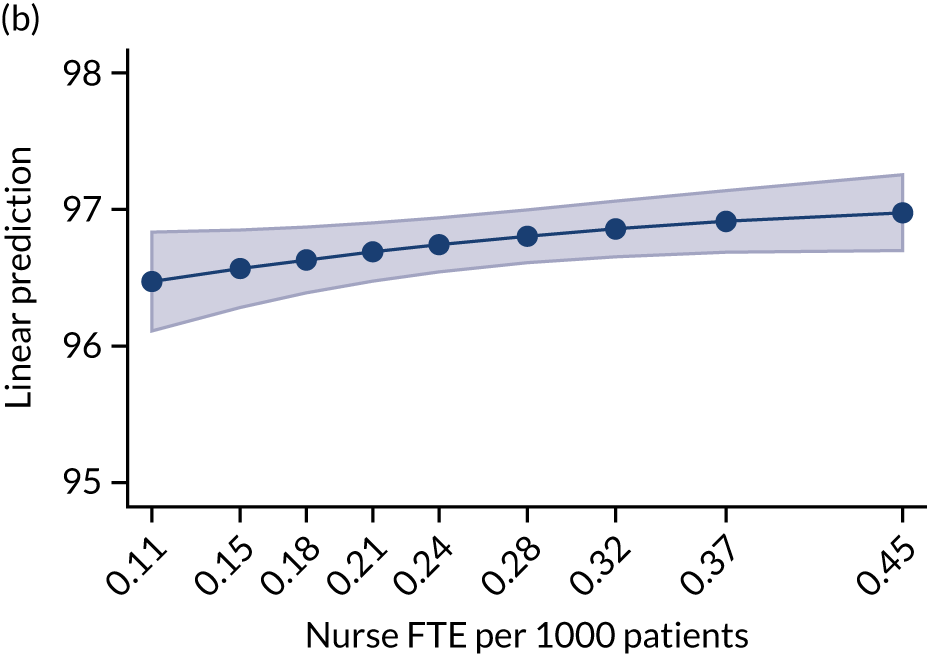
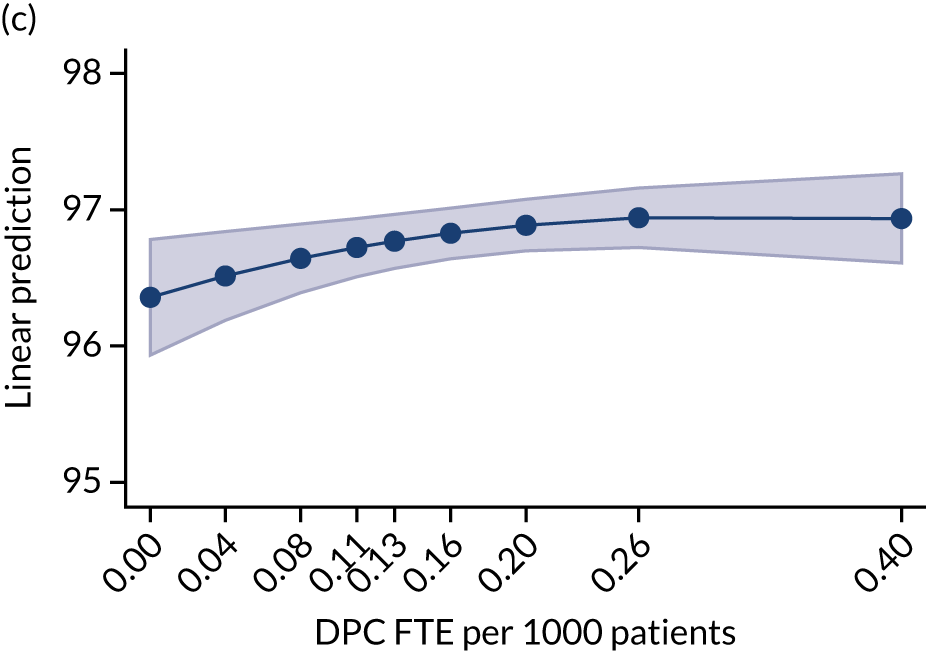
How are selected prescribing measures associated with workforce composition?
A larger number of CPs PTP is associated with a lower ratio of broad- to narrow-spectrum antibiotics (Figure 18), fewer total items prescribed per ASTRO-PU (Figure 19) and lower average costs per item (Figure 20). There is no significant relationship between the level of GP staffing PTP and the three prescribing outcome measures.
FIGURE 18.
Percentage of broad- to narrow-spectrum antibiotics. (a) GPs; (b) nurses; (c) DPC staff (without pharmacists); and (d) pharmacists.
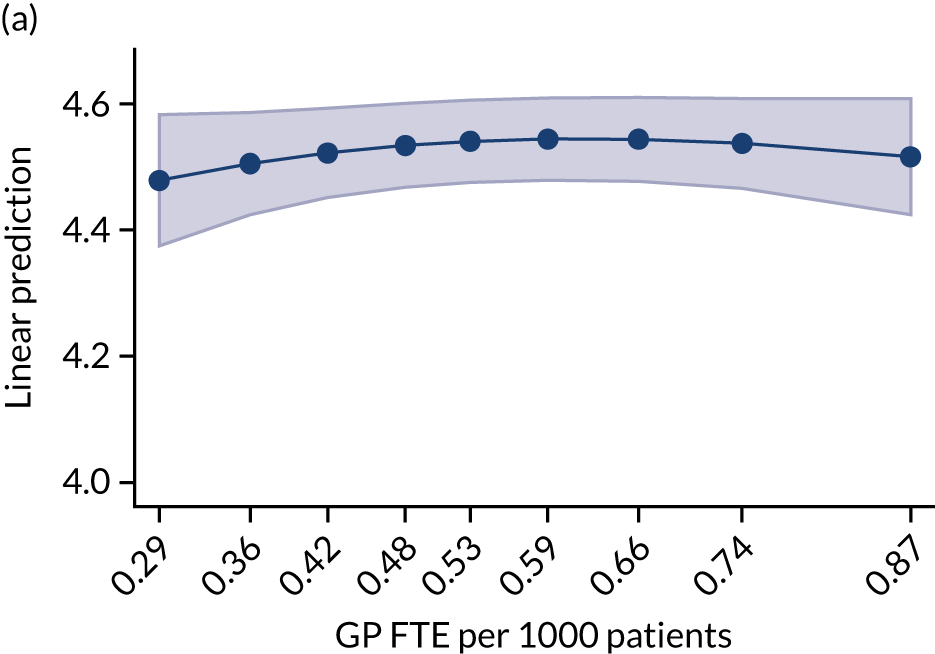

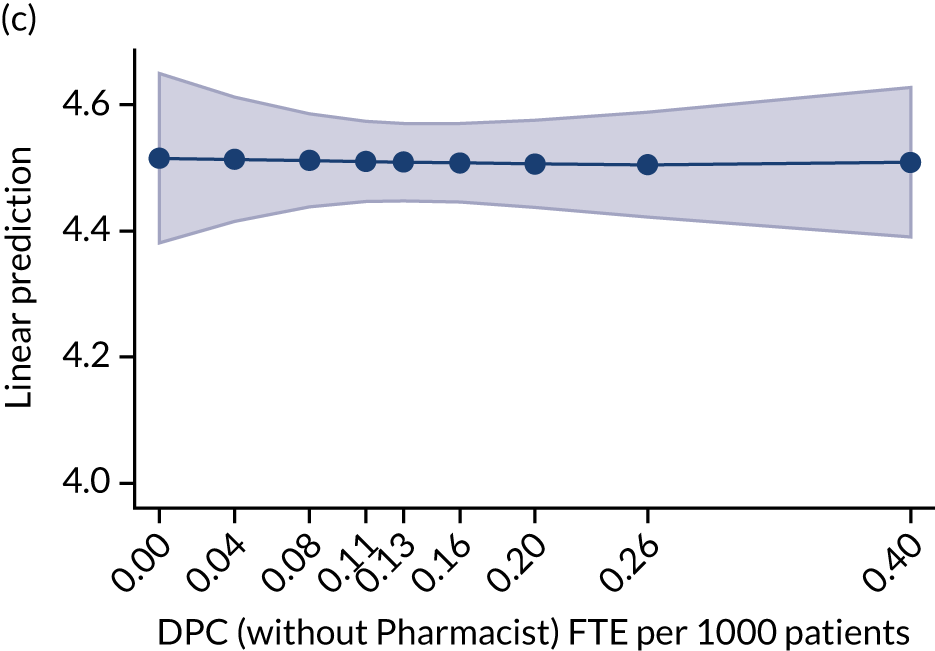
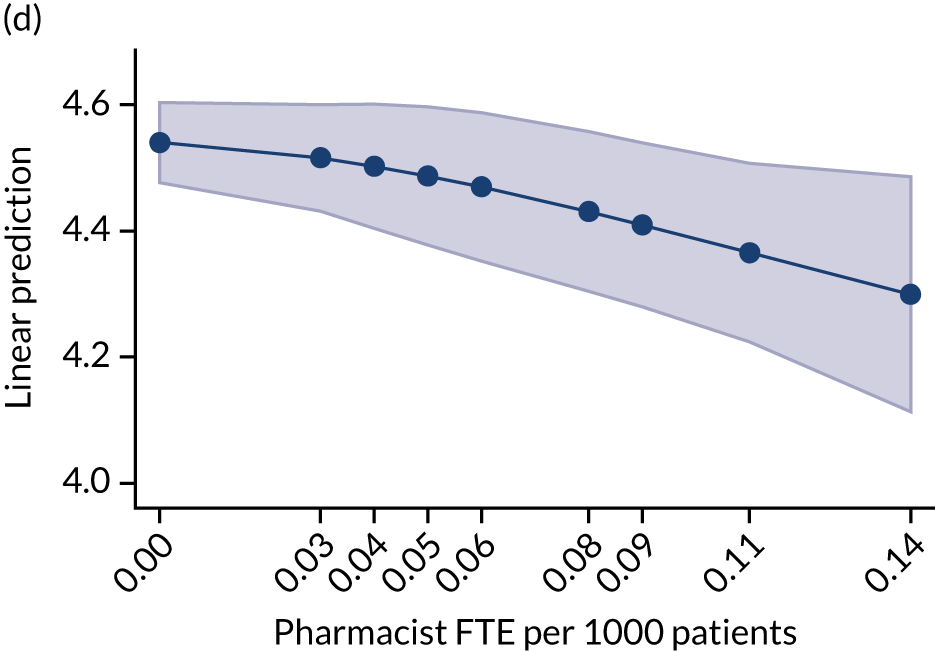
FIGURE 19.
Volume of prescribing: total items prescribed per ASTRO-PUs. (a) GPs; (b) nurses; (c) DPC staff (without pharmacists); and (d) pharmacists.


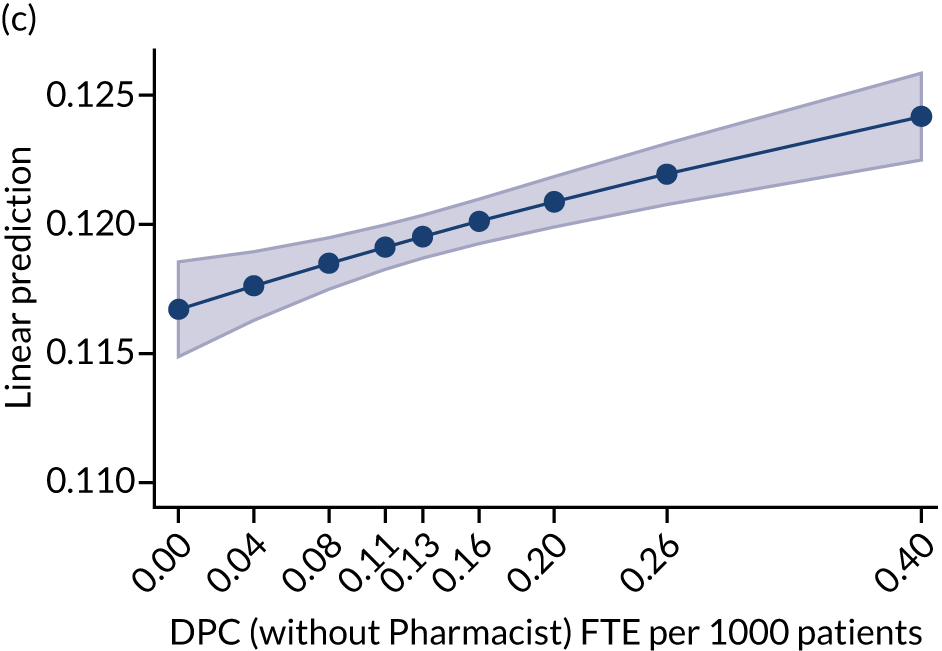
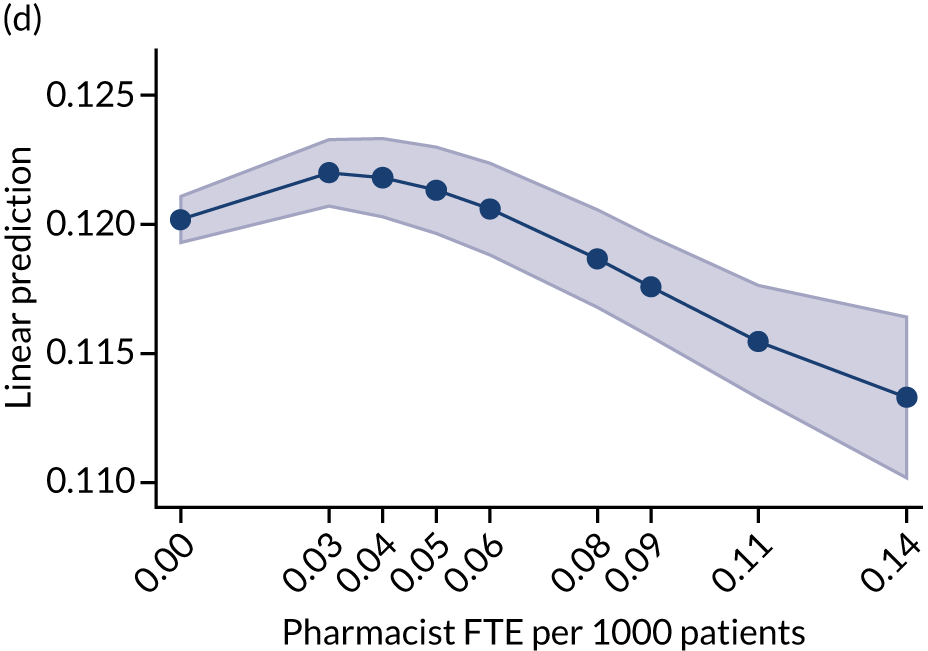
FIGURE 20.
Prescribing cost per item ( = cost per ASTRO-PU/items per ASTRO-PU). (a) GPs; (b) nurses; (c) DPC staff (without pharmacists); and (d) pharmacists.
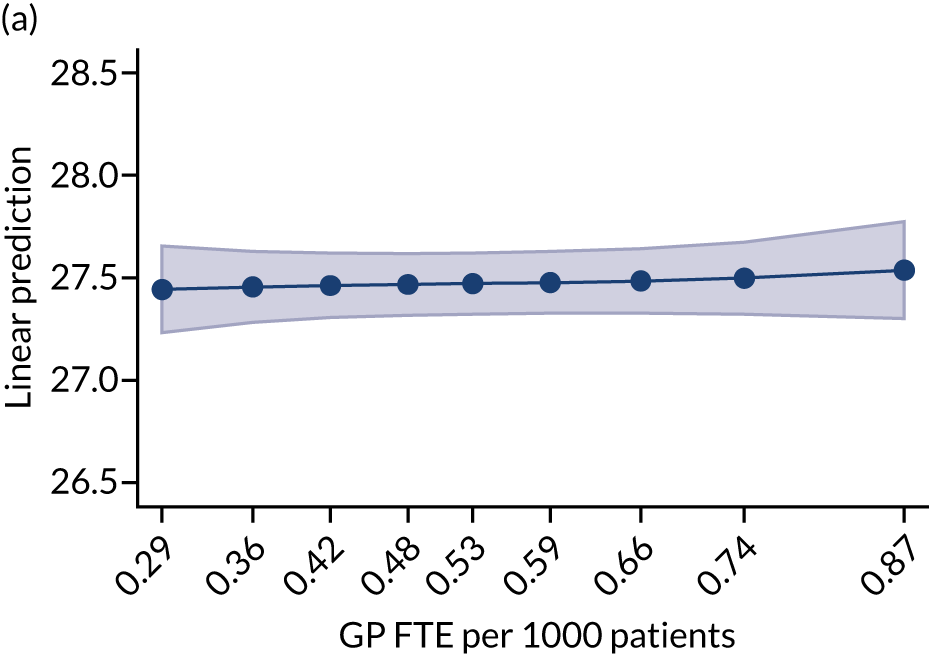
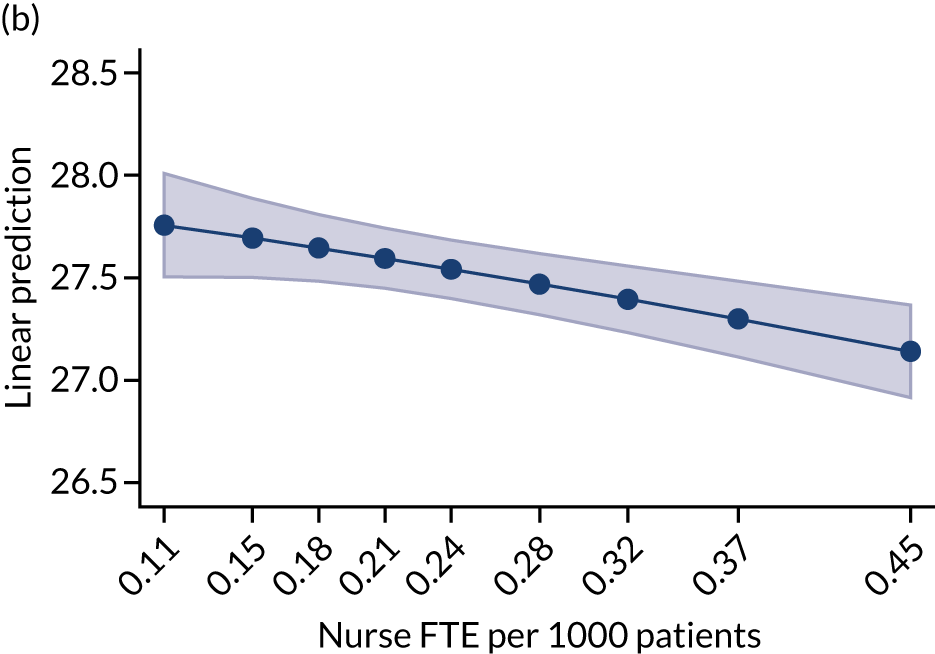
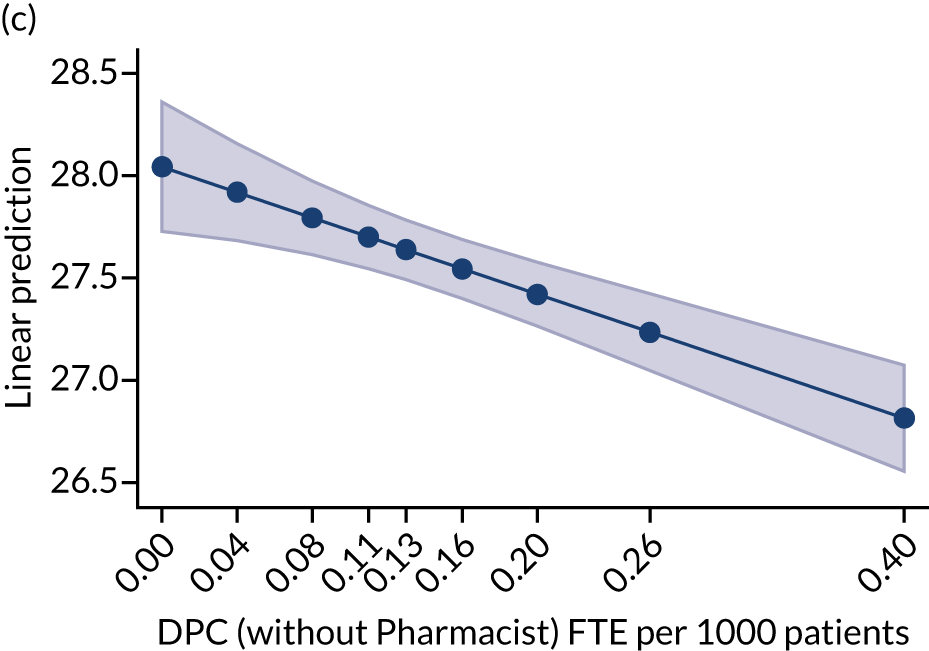
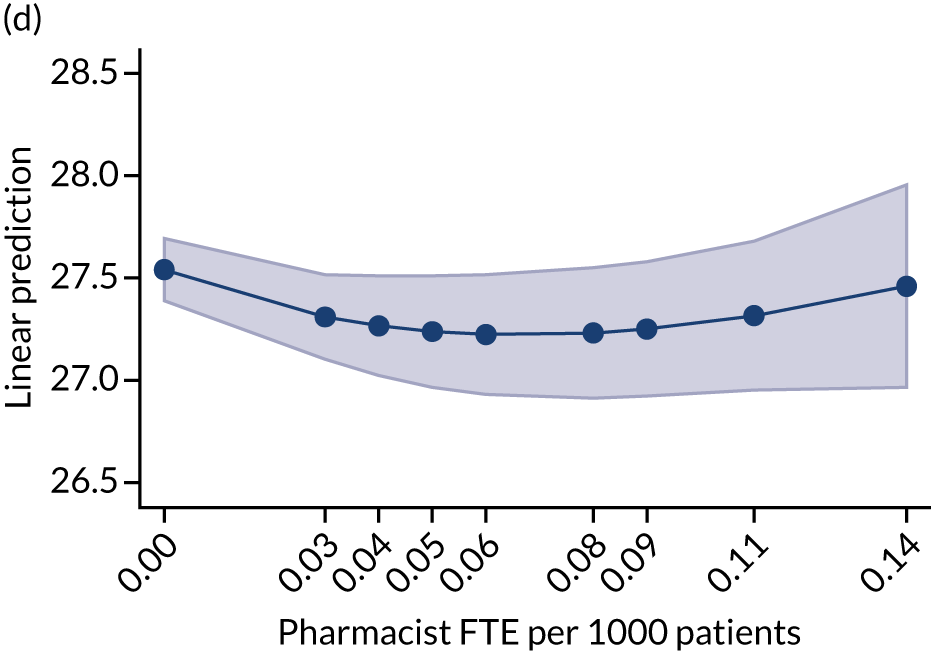
How is practice population utilisation of hospital services associated with workforce composition?
Analysis of secondary care activity (using Hospital Episode Statistics data) shows that the relationship between GPs and nurses FTE and A&E attendances is relatively flat, whereas increased numbers of DPC staff is associated with higher levels of A&E attendance (Figure 21). There is a positive relationship for GP and nursing staff and hospital admissions (i.e. elective and emergency), whereas there is a negative relationship with DPC staff (Figure 22). There is a positive relationship with GP staffing for outpatient appointments, but a negative relationship with both nursing and DPC staff (Figure 23).
FIGURE 21.
Accident and emergency attendances PTP. (a) GPs; (b) nurses; and (c) DPC staff.
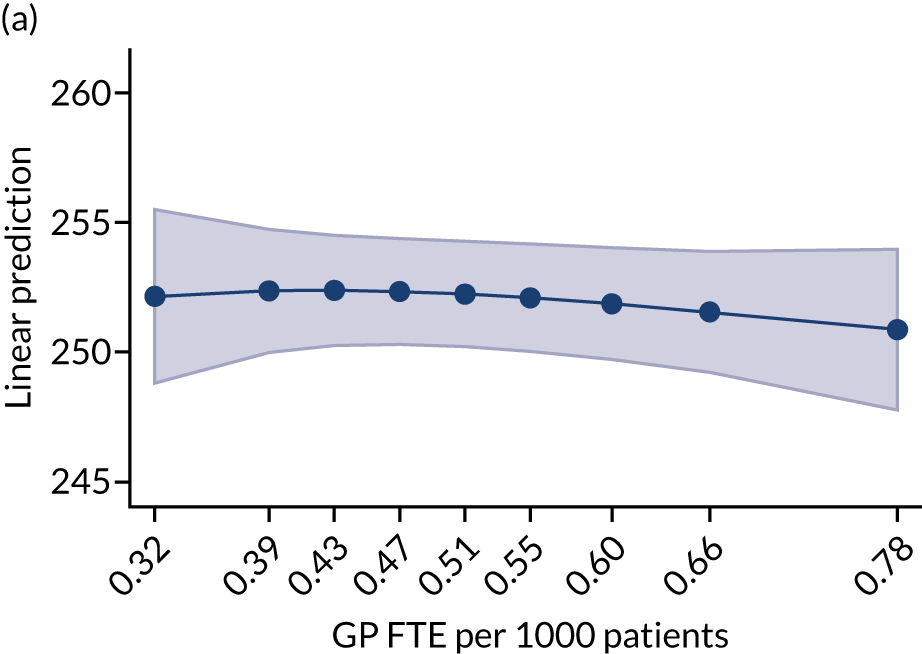
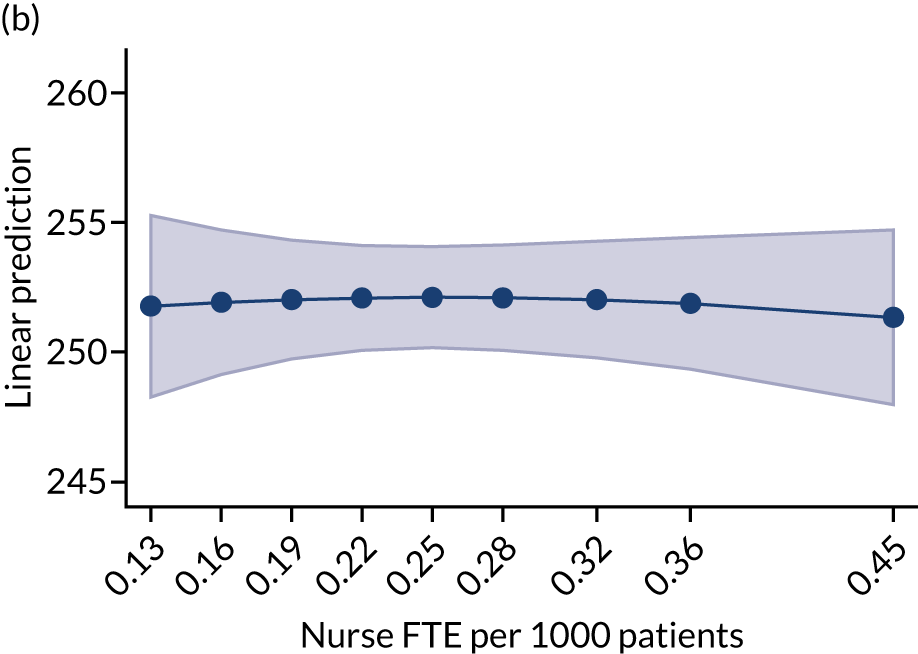

FIGURE 22.
Admissions PTP. (a) GPs; (b) nurses; and (c) DPC staff.
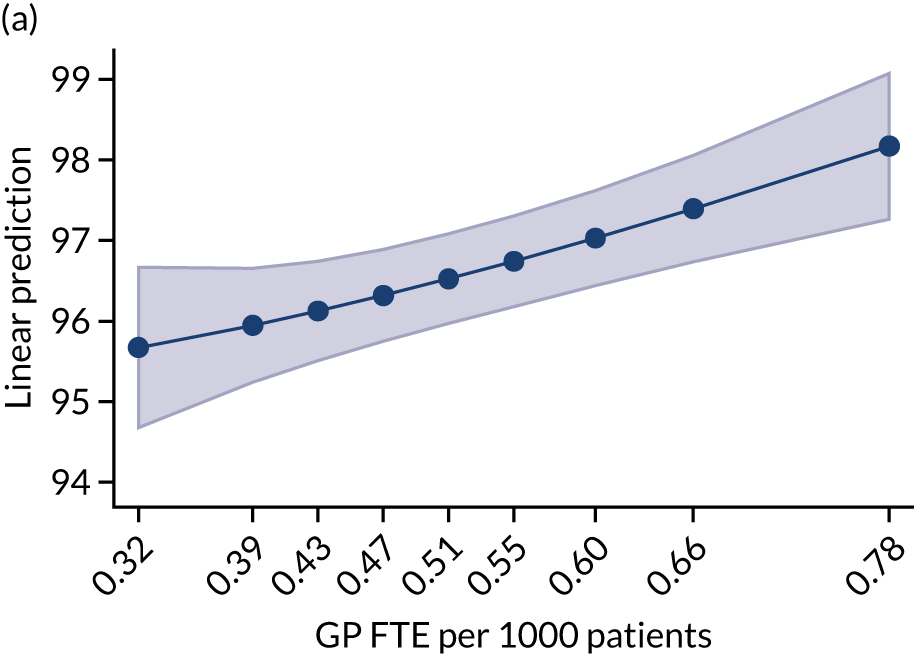
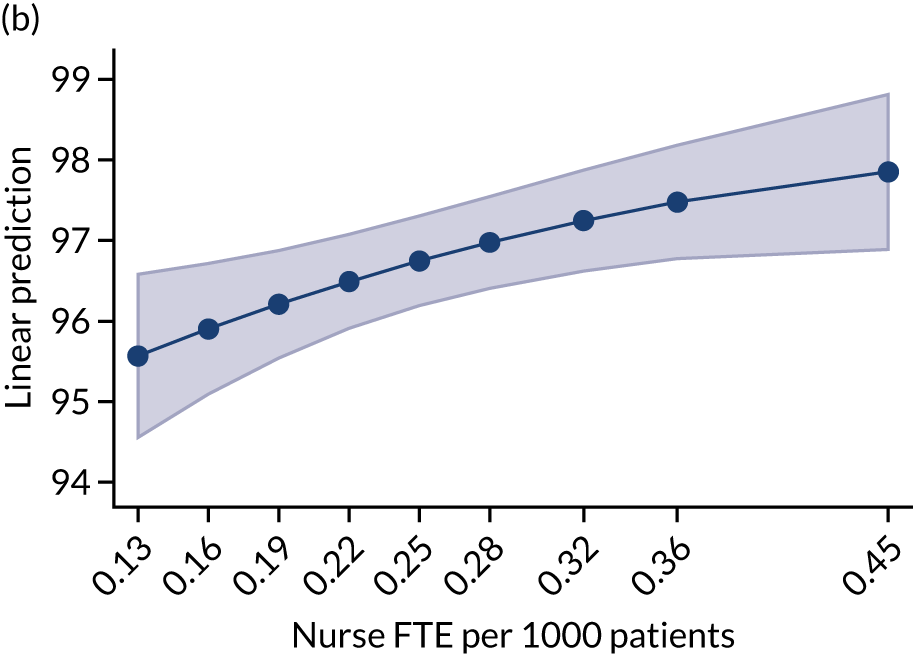
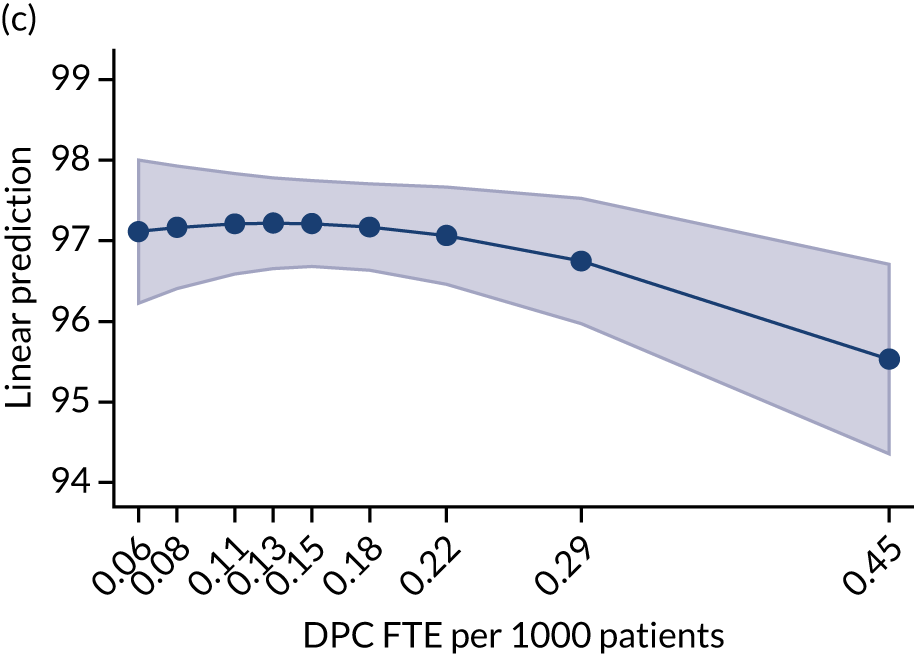
FIGURE 23.
Outpatient attendances PTP. (a) GPs; (b) nurses; and (c) DPC staff.
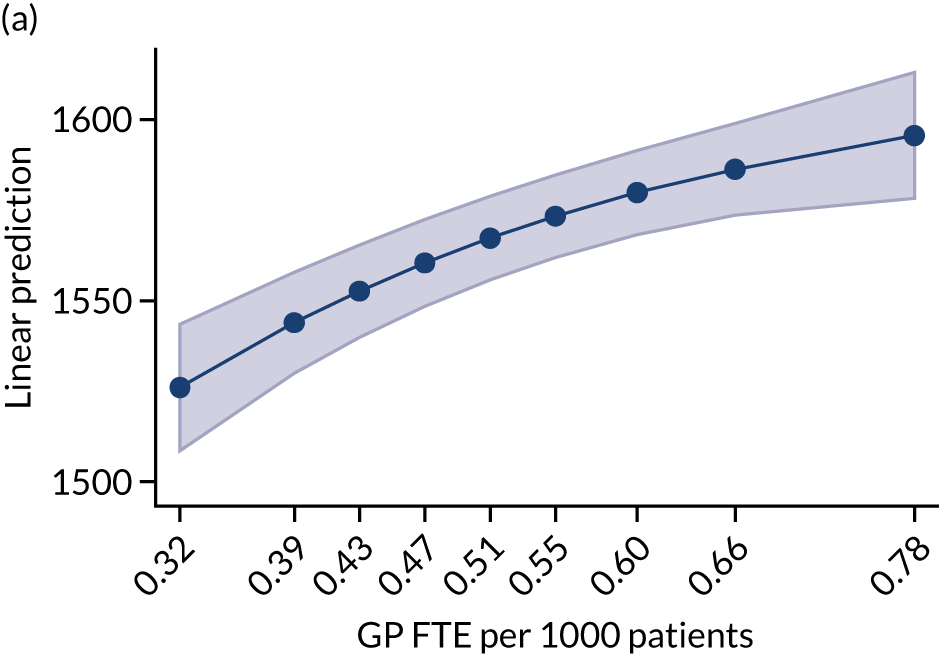
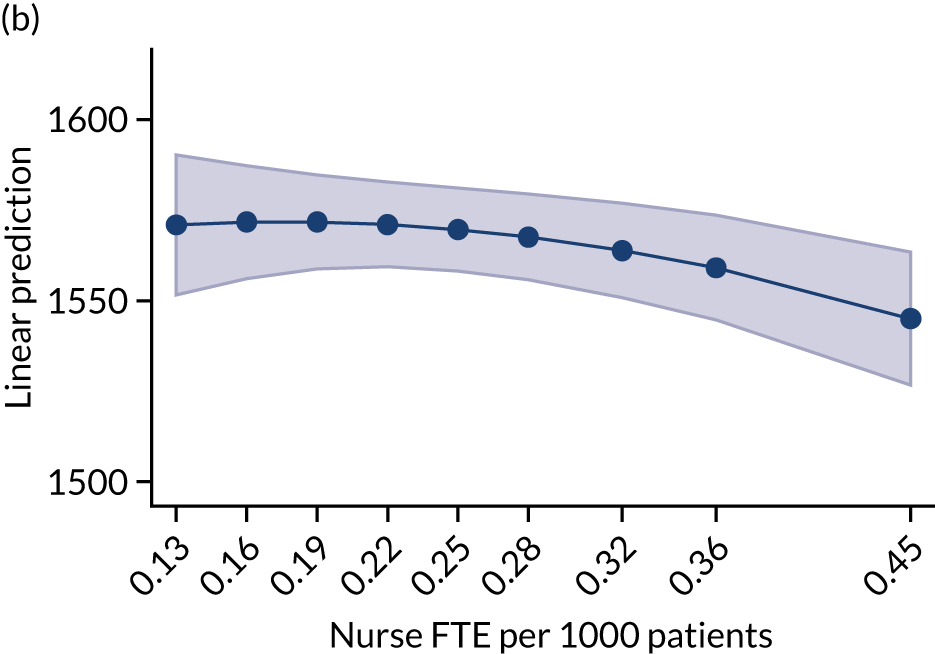

How are general practitioners’ working lives associated with workforce composition?
The analysis of GP Worklife Survey (looking at GP job satisfaction, hours of work and percentage of work that could be delegated) shows that GP job satisfaction is positively associated with the number of GPs PTP at the respondent’s practice. The relationship between GP job satisfaction and the other two staff categories is slightly negative, but not statistically significant (Figure 24), indicating that GP job satisfaction is unaffected by an increase in the number of these staff. There is a negative relationship between the number of GPs PTP at the respondent’s practice and the number of hours that the respondent GP reports working, which suggests that GPs work longer hours in practices where there are fewer GPs PTP (Figure 25). The association between GP working hours and the two other staff categories is flat or slightly negative, suggesting that the employment of the two other staff has a limited impact on the workload undertaken by GPs (Figure 26).
FIGURE 24.
General practitioner job satisfaction. (a) GPs; (b) nurses; and (c) DPC staff.
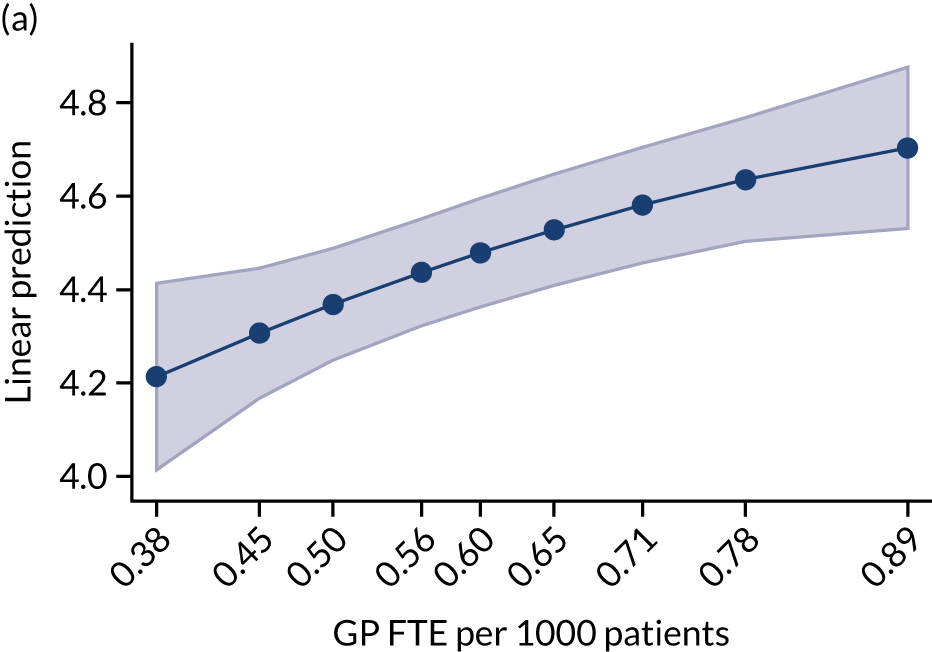
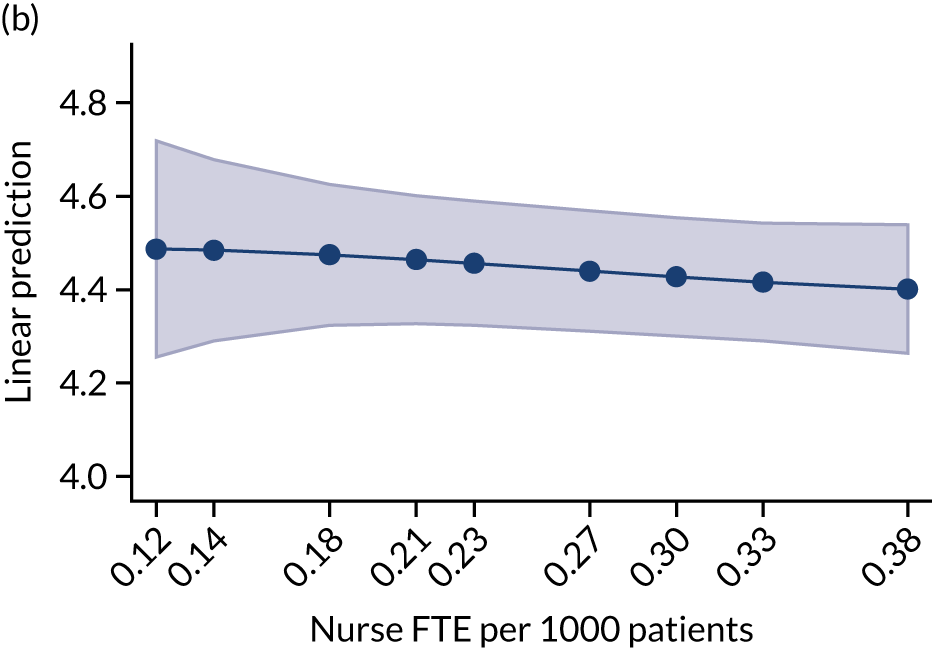
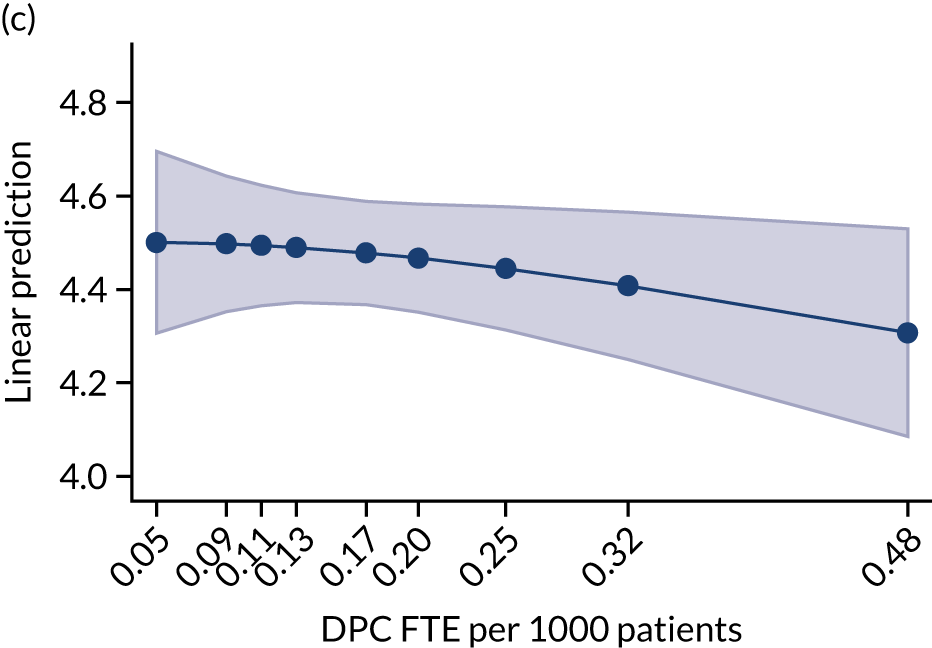
FIGURE 25.
General practitioner hours of work per week. (a) GPs; (b) nurses; and (c) DPC staff.
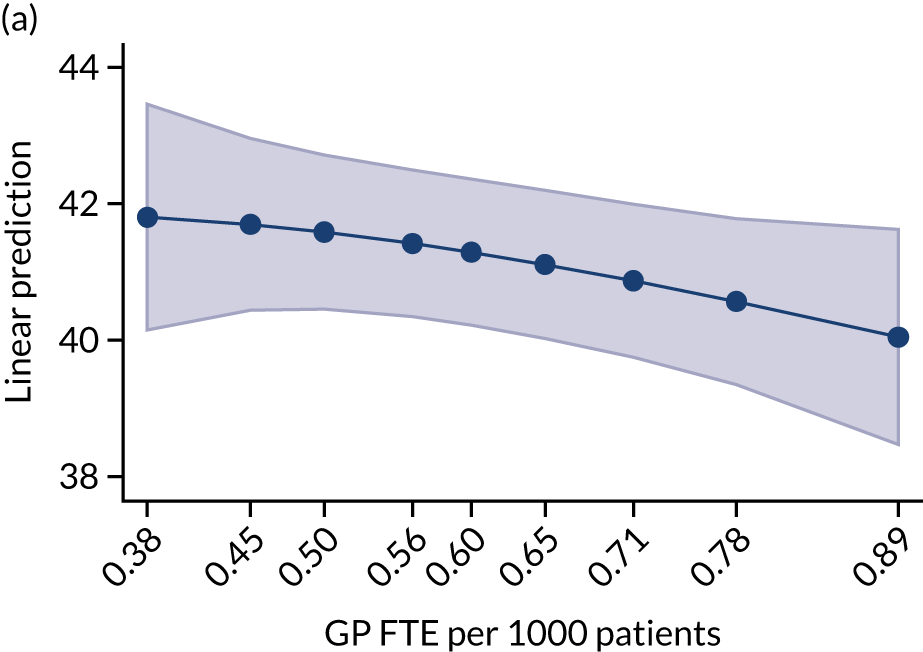
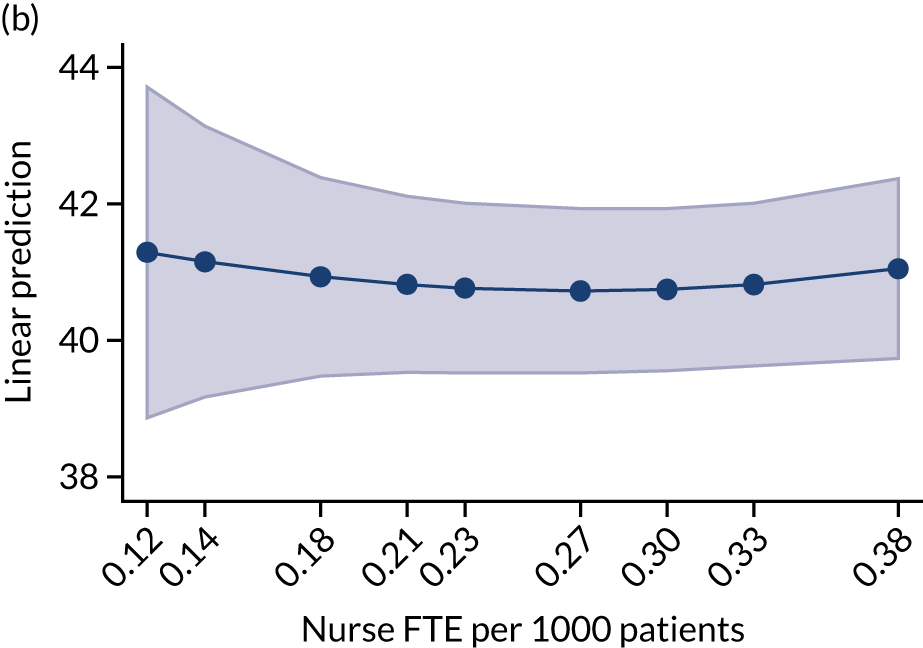
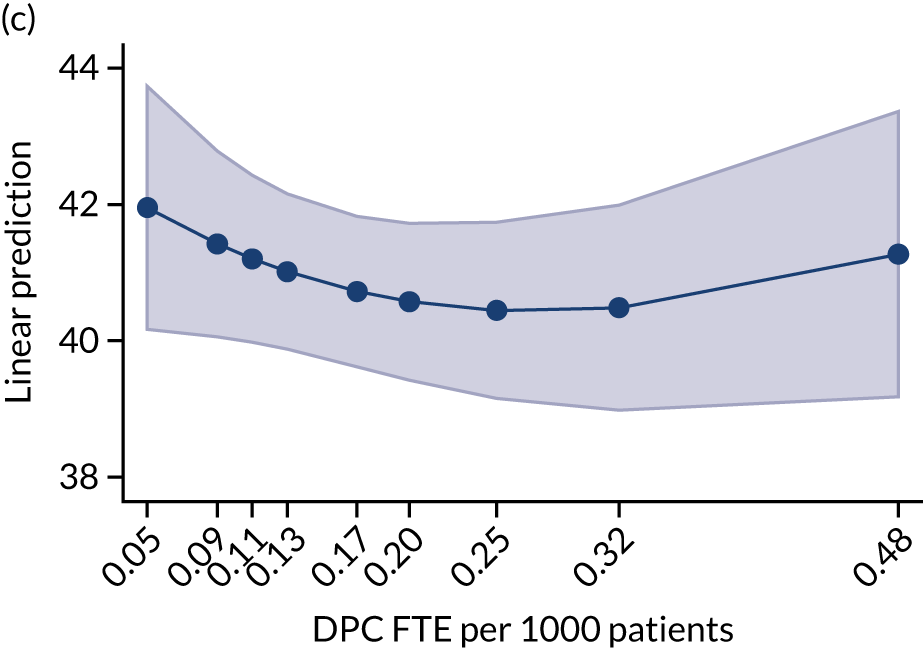
FIGURE 26.
Percentage of work that could be delegated to new roles. (a) GPs; (b) nurses; and (c) DPC staff.
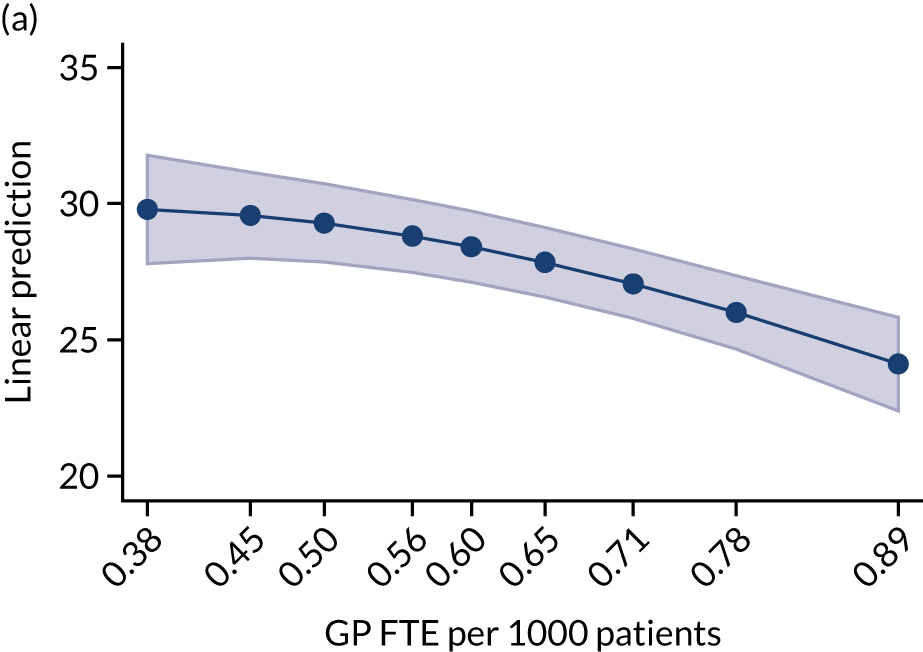
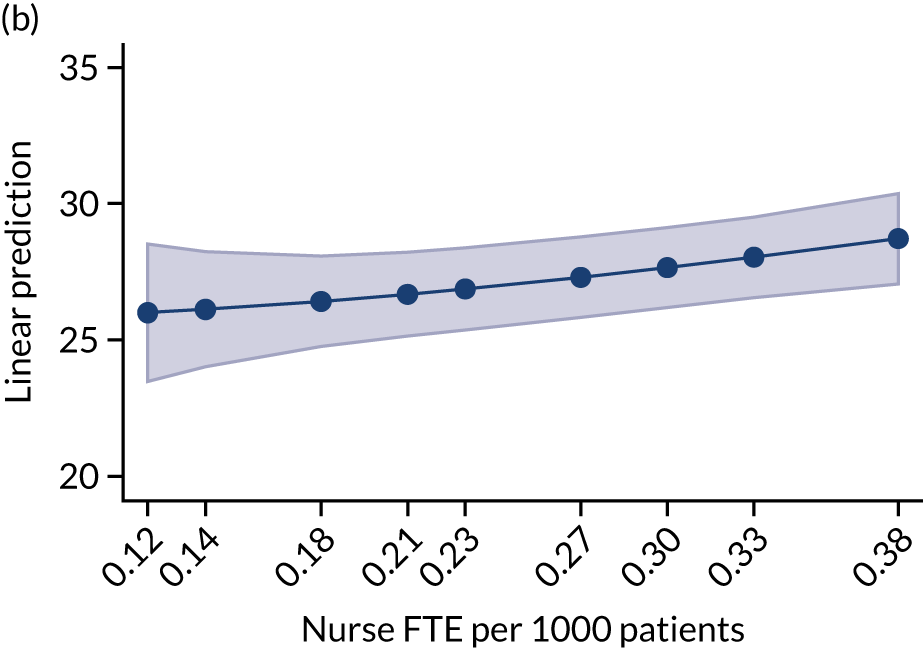
Research question 1(iii): how are workforce changes associated with later changes in costs and practice efficiency?
Our analysis of the association between workforce changes and changes in costs and efficiency looked at NHS expenditure in the form of payments to practices and prescribing costs. In Figure 27, we report the analysis for both total NHS expenditure PTP and for log-transformed values of total NHS expenditure. On the one hand, rescaling the NHS expenditure by the number of patients allows the comparison of practices of different size. On the other hand, the analysis on the log-transformed variable help adjusting the skewness in distribution of (raw) total NHS expenditure, and to allow an intuitive interpretation of distances on the scale of the vertical axis as percentage changes in total NHS expenditures. There is a positive association between the log of total NHS expenditure on activity delivered or generated by general practices and levels of staffing in all three workforce groups (i.e. GPs, nurses and DPC staff). The result is not entirely surprising, as it suggests that additional staff generally increase the total NHS expenditure for the practice. Therefore, our cross-sectional analysis does not show a clear pattern of cost savings related to differences in skill mix.
FIGURE 27.
Expenditure (payments to practice + prescribing costs) PTP. (a) GPs; (b) nurses; and (c) DPC staff.
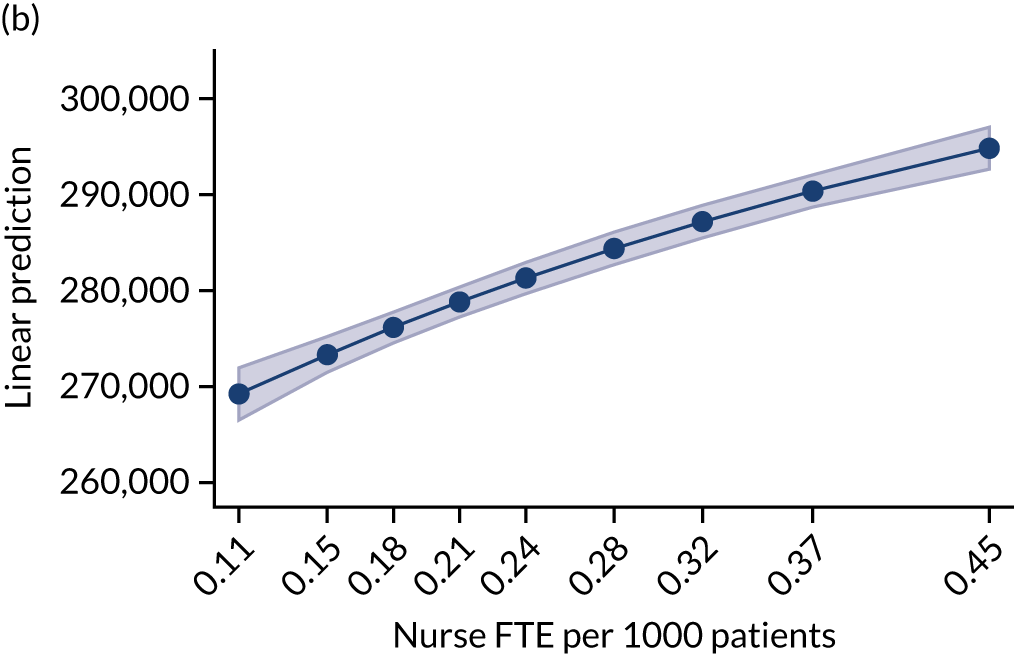
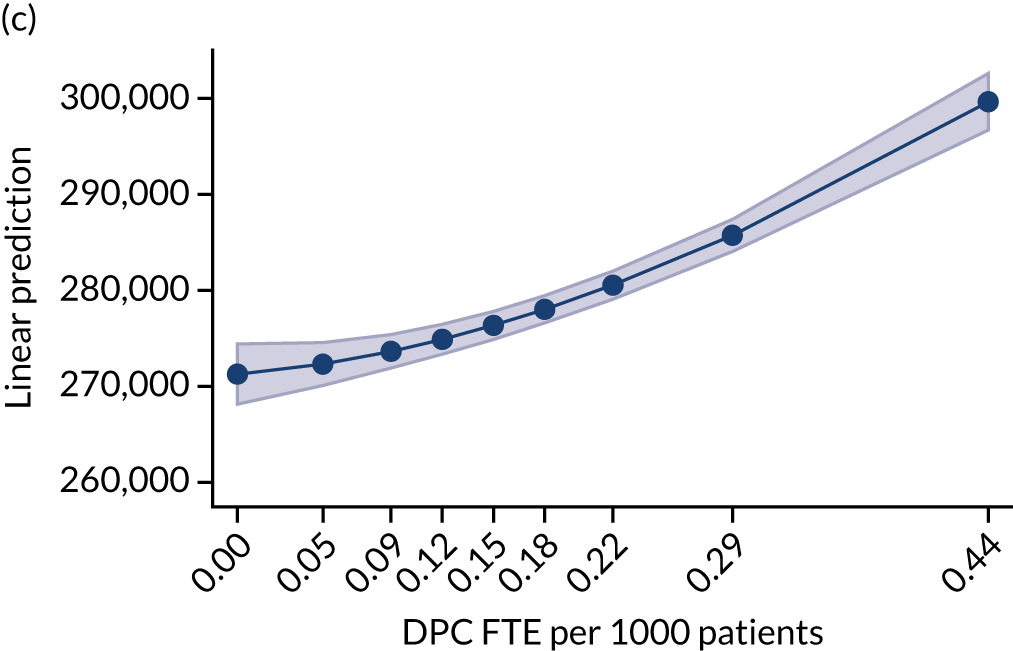
Scenario analysis
Table 21 shows the results from the scenario analysis. Data in the different columns of Table 21 show the average effects of increases in 1 FTE of the worker on the outcome measure for the median practice in our cross-sectional sample, based on the same regression models used to produce the Figures 13–27. We also present the impact on overall expenditure. To achieve this, we have applied tariff costs onto the hospital service use and added these expenditures onto the NHS payments to practices and prescribing costs. 117 The analysis shows that a 1 FTE increase in GPs results in the largest increase in expenditure, followed by DPC and nursing.
| Outcome | Staff group | ||||
|---|---|---|---|---|---|
| GP | Nurse | DPC | DPC (no pharmacists) | Pharmacist | |
| Patient satisfaction with making appointments | 0.008 | –0.013 | –0.010 | ||
| Patient satisfaction with general practice | 0.008 | –0.007 | –0.008 | ||
| QOF achievement | 0.315 | 0.027 | 0.133 | ||
| Prescribing | |||||
| Percentage of broad- to narrow-spectrum antibiotics | 0.021 | 0.009 | –0.005 | –0.173 | |
| Total items prescribed per ASTRO-PU | 0.000 | 0.002 | 0.002 | –0.007 | |
| Cost per item | 0.122 | –0.128 | –0.225 | 0.126 | |
| Hospital Episode Statistics | |||||
| A&E attendances | –0.613 | 0.113 | 2.290 | ||
| Admissions | 0.411 | 0.601 | –0.130 | ||
| Outpatient attendances | 12.951 | –11.249 | –12.214 | ||
| Activity | |||||
| Time (months) since last saw a GP | –0.051 | 0.087 | 0.022 | ||
| Time (months) since last saw a nurse | 0.077 | –0.244 | –0.126 | ||
| GP Worklife Survey | |||||
| Job satisfaction | 0.049 | –0.018 | –0.060 | ||
| Working hours per week | –0.037 | 0.401 | 0.007 | ||
| Delegation | –0.603 | 1.144 | 1.652 | ||
| Costs | 1805.380 | 2973.551 | 5967.940 | ||
| Log(costs) | 0.010 | 0.017 | 0.019 | ||
| Hospital costs | 3049.144 | 544.969 | –1724.945 | ||
| Total costs (costs + hospital costs) | 4854.524 | 3518.520 | 4242.995 | ||
For patient satisfaction with the overall experience of their practice, an increase of 1 GP FTE increases satisfaction, at the median practice, by 0.8%, whereas an increase in 1 DPC FTE decreases satisfaction by the same amount (see Figures 15 and 16). Practices with smaller decreases in GP FTE PTP have a greater improvement in the proportion of patients reporting a very good or fairly good experience of making an appointment and with the overall experience at the general practice. On the other hand, changes in nurse and DPC FTE PTP do not appear to show any association with patients’ satisfaction.
The analysis of the change in percentage of QOF points achieved also shows results consistent with those illustrated in the Figure 15. An increase in 1 GP FTE increases QOF outcomes by 0.315%, whereas an increase of 1 nurse FTE increases the same outcome by 0.027%. GP and nurse FTE show a slight positive association. This means that, on average, increases in these staff FTE PTP are associated with a higher increase in percentage of QOF points. On the other hand, the effect for 1 additional DPC FTE for this outcome is ambiguous.
With regard to the prescription of broad- to narrow-spectrum antibiotics, increases in nurse FTE PTP seem to be associated with the largest reductions in the ratio of prescription of broad- to narrow-spectrum antibiotics (0.009% vs. 0.021% in GP FTE PTP).
Regarding the changes in volume of prescribing, increases in nurse and DPC (with no CPs) FTE are positively associated with increases in numbers of items prescribed (both 0.002). On the other hand, a 1 FTE increase in CP employment is associated with a reduction in the number of prescribed items (–0.007).
Changes in prescribing costs per item (see Figures 18–20) show similar reductions of 0.122 and 0.126 for increases of 1 FTE GP and pharmacist employed, respectively. On the other hand, for additional nurse and other DPC we find reductions in prescribing costs of 0.128 and 0.225, respectively.
Interestingly, changes in A&E attendance, admissions PTP and outpatient attendances PTP show varied associations with changes in staffing. An 1-unit increase in GP FTE is associated with a reduction in A&E attendances, additional nurse and DPC FTEs are associated with outpatient attendance reductions, and an increase in DPC FTE is associated with a reduction in admissions. For all other scenarios, there are associated increases in activity.
An increase in GP FTE is associated with a reduced period of time since patients reported seeing a GP and an increase in the time since patients reported seeing a nurse. Similarly, an increase in nurse FTE is associated with a reduction in the time since patients saw a nurse, but an increase since patients saw a GP. An increase in DPC FTE was associated with an increase in the reported time since patients saw a GP, but a reduction in the time since patients saw a nurse.
The patterns for NHS expenditures suggest that the strongest increases per additional staff FTE are related to DPC (5697.9).
Contrary to the findings from the cross-sectional analysis, GP job satisfaction, although improved overall with the addition of 1 FTE GP (0.049), does not show improvement with changes in the FTE of other staff FTE PTP.
Discussion
Summary of findings
Our approach represents a cross-sectional assessment of associations between different levels of employment of different types of professionals and a variety of outcome indicators, followed by a scenario analysis modelling potential changes that may be associated with marginal changes in employment mix.
We have found associations in a wide range of indicators associated with different levels of skill mix employment in primary care. Figures 13–27 demonstrate levels of outcomes associated with differing levels of employment of particular types of practitioners, controlling for a range of contextual factors (as listed in Methods and in Table 19). We found that, unsurprisingly, a larger number of FTE of GPs or nurses PTP is associated with a lower reported time since seeing a GP or a nurse. Perhaps more interestingly, we found that a higher FTE of nurses PTP is associated with a longer reported time since seeing a GP. This suggests that there is at least some degree of substitutability between these two groups. Similarly, a higher FTE of GPs PTP is associated with a slightly longer time since last seeing a nurse.
In terms of patient satisfaction with making an appointment, we have shown that a higher FTE of GPs PTP is associated with relatively higher patient satisfaction with their experience of making an appointment, whereas a higher FTE of both nurses and other DPC staff is associated with lower satisfaction. We found that a higher FTE of GPs PTP is associated with a higher level of overall satisfaction with a general practice, whereas a higher FTE of other DPC staff is associated with a relatively lower overall satisfaction. A higher FTE of nurses PTP is not associated with any difference in overall satisfaction. These findings may reflect the issues, which we have described in Chapter 5, relating to the complexity of the systems required to support the categorisation of patients to see appropriate professionals. It would appear that, notwithstanding their satisfaction with their individual clinical encounters, patients may find these processes burdensome. Furthermore, patients’ limited awareness of what newer types of practitioners could provide could contribute to lower satisfaction with a more diverse workforce and their desire to achieve continuity of care from the same practitioner would be likely to be less achievable.
In terms of clinical quality, we found that a higher FTE PTP of GPs, nurses and other DPC staff are all associated with higher levels of total QOF performance, with the highest level associated with a higher FTE of GPs PTP. This is interesting, as it is often nurses who undertake the majority of QOF-related work. It might be expected that a higher FTE of nurses might be the biggest driver of increase in QOF performance. However, our study suggests that having more GPs PTP supports better QOF performance, perhaps due to GPs in such practices having more time to spend overseeing the QOF process.
Because of their role in monitoring and influencing prescribing, we separated CPs from other DPC staff when examining prescribing. We found that a higher FTE of CPs PTP was associated with relatively higher prescribing quality (as measured by the percentage of broad- to narrow-spectrum antibiotics prescribed), with no change associated with higher FTE of GPs, nurses or other DPC staff. In terms of prescribing volume, we found that a higher FTE of GPs PTP is not associated with any difference in numbers of items prescribed per weighted population, whereas a higher FTE PTP of both nurses and other DPC staff (excluding CPs) is associated with more items prescribed. A higher FTE of CPs PTP is associated with fewer items prescribed per weighted population.
Finally, in terms of prescribing costs, we found that a higher FTE of GPs PTP is associated with a higher cost per item prescribed, whereas a higher FTE of nurses and other DPC staff is associated with a lower cost per item. A higher FTE of CPs PTP is not associated with any difference in cost per item. Therefore, it would seem that employing more CPs is associated with better prescribing quality and lower prescribing volume, with no association with cost per item. A higher employment level of nurses and other DPC staff has no association with prescribing quality, but is associated with higher prescribing volume, albeit of lower-cost items. This may relate to the discovery of unmet needs or an improvement in chronic disease management. However, if so, one might expect that a higher FTE of GPs PTP would also be associated with higher prescribing volume. Alternatively, this finding may reflect the complex processes, which we have described in Research question 3(i): how are new ways of working being negotiated in general practices where skill mix changes have occurred?, by which non-prescribing professionals seek support from GPs or other prescribers. If a nurse, PA or HCA without prescribing rights feels that a patient needs a prescription, then they have to request that a GP or other prescriber authorise the script. It is possible that such prescribing activity is subject to less scrutiny or inclination to consider a non-pharmaceutical alternative (e.g. counselling, physiotherapy) than is the case when a GP personally initiates a prescription, leading to a relative increase in prescribing overall.
Considering hospital utilisation, we found that a higher FTE of GPs or nurses PTP was associated with a relatively lower rate of A&E attendances, but a higher FTE of other DPC staff PTP was associated with a relatively higher rate of A&E attendances. This may be related to the increased complexity of making an appointment or could reflect a feeling among patients that consulting a non-GP did not bring them sufficient assurance or resolution of their problem. In addition, owing to perceived or formal constraints on which practitioners are permitted to refer patients to hospital departments, some non-GPs may recommend that patients attend A&E as a self-referral for the same (and possibly appropriate) reasons as a GP would process a formal referral to an A&E or non-A&E department. Associations between changes in workforce composition and hospital admissions and outpatient attendances are difficult to interpret. Higher FTE of GPs PTP would seem to be associated with more admissions and outpatient attendances, perhaps reflecting the uncovering of unmet need, whereas higher FTE of nurses PTP is associated with more admissions but fewer outpatient attendances. Higher FTE of other DPC staff PTP is, similarly, associated with a lower outpatient activity. It may be that increasing the available nursing workforce and DPC workforce allows practices to more effectively manage patients with chronic diseases, such as diabetes or asthma, and thereby reduce acute events requiring hospital care. Similarly, effective delivery of health promotion may reduce patients’ requirements from hospital services.
We explored associations between the FTE of different professionals with GP satisfaction using GP Worklife Survey data. We found that higher FTE of GPs PTP is associated with higher overall GP job satisfaction, but higher FTE of nurses and other DPC staff is associated with slightly lower overall GP satisfaction. In terms of GP hours of work, higher FTE of GPs PTP is associated with a slightly smaller number of hours of work, whereas higher FTE of both nurses and other DPC staff is associated with a negative and then positive relationship with GP hours of work (i.e. a slight U-shaped curve). This suggests that there may be an optimum ratio of other professionals to GPs and that there is a threshold of employment of other types of practitioners beyond which higher levels of employment are associated with a larger number of hours of work for GPs, perhaps reflecting higher supervision requirements. GPs were asked what proportion of their workload could be safely delegated to other professionals. GPs working in practices with a higher FTE of both nurses and other DPC staff suggested a higher percentage of work that they felt could be delegated, perhaps indicating that experience of working alongside other types of professionals increases confidence in delegation.
Finally, we explored costs for GP-based prescribing and payable to practices (including QOF, salaries and business) costs associated with higher FTE PTP of all types of professionals and found that higher FTE of GPs, nurses and other DPC staff are all associated with higher costs.
Overall, the patterns identified with the longitudinal analysis are broadly consistent with the cross-sectional results. This is reassuring, as it attenuates concerns regarding potential unobserved practice characteristics driving the cross-sectional results. The most interesting exceptions are represented by A&E attendances, overall admissions and outpatient admissions, which have been found to grow stronger in facilities showing higher increases in FTE across all staff categories (i.e. GP, nurse and DPC). Total cost also reveals an interesting longitudinal pattern, growing less in practices where GP FTE PTP increased the most.
Strengths and limitations
Our analysis is based on national data. We used the most up-to-date data available, although we did not use data for 2020 because the COVID-19 pandemic has had profound impacts on health-care activity levels and patient outcomes. It would be of future interest to consider whether or not practices with some forms of skill mix were more resilient to the pandemic and could adapt and respond more flexibly. It would also be interesting to discover if workforce composition helped practices to maintain high performance on quality indicators and if skill mix contributed to a more rapid recovery of performance.
No national data are available at the practice level on the volume of consultations delivered. The appointments in general practice series currently provides data at only the CCG level. We created a measure of how recently a practice’s patients had seen a GP and how recently they had seen a nurse based on data from the 2017 GPPS. This is based on a sample of patients’ responses about each practice and is only a crude proxy for the utilisation of primary care.
There is potential for skill mix to be endogenous in the outcome equations if there are unmeasured factors associated with both skill mix and outcomes. This would occur, for example, if a broader skill mix was associated with innovation and if innovation led to better patient care. We included a range of measured characteristics of practices and their populations to minimise the risk of omitted variable bias. We also examined changes over time, which controls for unmeasured but time-invariant characteristics of practices. Nonetheless, the risk of confounding from time-varying factors remains. We experimented with potentially exogenous variables (i.e. whether or not the CCG has offered incentives to employ new staff types, local labour and housing market conditions) in an instrumental variables framework, but these variables were not sufficiently predictive to provide accurate results. The results should be interpreted with this limitation in mind, and future work should focus on identifying better exogenous predictors of variation in skill mix.
Implications
We will consider the wider implications of these findings in our discussion. However, our quantitative findings would appear to align with the qualitative findings from our case studies. In particular, we find that patient satisfaction with their overall interaction with their practices would seem to be sensitive to changes in skill mix, which may reflect the increasing complexity of appointment systems that we have described. This may also be one of the underlying mechanisms driving the association between higher FTE of other DPC staff and higher A&E attendances. CPs are associated with better prescribing quality and lower volumes, suggesting a particular role in medication management, whereas higher levels of employment of both nurses and other professionals are associated with higher prescribing volume. In our case studies, we found that non-GPs may respond to patients’ needs by generating a prescription that is then presented to a colleague who is a prescriber for authorisation/signing. It is possible that this split responsibility (between indicating to the patient that a prescription is indicated, generating a request for a prescription and signing off the prescription) drives the higher prescribing volume that we found. Alternatively, it may represent a more direct effect of nurses and other professionals undertaking chronic disease management and identifying unmet needs. More worrying for current policy in England, we found that higher FTE of the non-GP workforce is associated with lower GP job satisfaction, which suggests that, although the current policy is driven by difficulties in recruiting and retaining GPs, it is not a forgone conclusion that increasing skill mix provides an answer to the problem. Overall costs are higher when the number of practitioners PTP is larger, and our findings suggest that these differences are only marginally smaller for professionals other than GPs.
Chapter 7 Triangulation
The main objective of this WP is to triangulate the findings from WP1, WP2 and WP3. All WPs were analysed separately, and findings were integrated and considered for agreement and disagreement based on convergence, complementarity, dissonance and silence.
Table 22 displays findings from the different WPs and their convergence coding. For a small number of themes, as might be expected given the different focuses of each WP, there is no intersection between the findings of different WPs (hence, silence). For most themes, however, we see a degree of complementarity in findings where different WP findings offer complementary information and insights on the same issue. Complete convergence in findings was rare, as the case studies typically allowed for deeper exploration of particular issues identified in the quantitative WPs. This generated a richer understanding of the themes. Dissonance was also rare, but where a degree of dissonance was identified, investigating this often resulted in valuable refinements to our interpretation of the research findings. We will examine this following the structure of the meta-themes of motivation, funding, ideal workforce, new ways of working and outcomes/impacts (see Table 22).
| Meta-theme | Theme | WP findings | |||
|---|---|---|---|---|---|
| 1 | 2 (practice manager survey) | 3 (case study) | 4 (convergence coding) | ||
| Motivation | Overall motivation regarding changes in skill mix employment | Not measured |
Top three reasons: (1) desire to release GP time, (2) desire to achieve a better match and (3) increase appointments Minority: unable to recruit a GP or cope with recruitment issues |
GP partners and practice managers have different views For GP partners, shortage of GPs/inability to recruit or retain GPs For practice managers, the need to control costs to the practice |
There is an element of convergence between the findings from the survey and the case studies. Both findings identified the difficulty in recruiting GPs as a motivation for skill mix, albeit a minority view in the survey and a majority view in the case studies. In a rare instance of dissonance, the inability to recruit GPs came up regularly in the case studies (i.e. WP3), despite ‘unable to recruit a GP’ not being frequently selected as a motivation for skill mix in the survey (i.e. WP2). Therefore, the case studies offer a degree of complementarity to the national practice manager survey by revealing a difference between the view of practice managers and GP partners. Although the majority of GP partners interviewed quoted the shortage of GPs as a motivation for skill mix change in the general practice, practice managers tended to focus on the need for cost-efficiencies and, hence, seeing skill mix as enabling new ways of organising care The move to employ newer practitioners across practices via PCNs requires further exploration |
| Motivation for employing ANPs | Not measured | To increase appointment availability | Some ANPs’ roles had been expanded because of their experience, allowing them to see patients with undifferentiated symptoms in the same way as GPs. One ANP was deployed on a GP rota and paid the same rate as GPs | Complementarity | |
| Motivation for employing PAs | Not measured | To increase appointment availability | PAs saw patients with relatively undifferentiated problems, but dealt with ‘less complex’ patients. PAs had a longer appointment time and were unable to prescribe, reducing the number of patients they can see | Complementarity: PAs offer a particular type of appointment (i.e. appointments for patients with less complex problems), requiring high-quality categorisation and matching processes at the point of making an appointment | |
| Motivation for employing CPs | Not measured | To release GP time | To deal with all aspects of medicine-related activities | Complementarity | |
| Motivation for employing paramedics | Not measured | To release GP time | To deal with on-the-day appointments | Complementarity | |
| Motivation for employing ACPs | Not measured | Not measured | Depending on their background, some ACPs (i.e. nurses) dealt with frail and elderly patients and care home patients, whereas others (i.e. paramedics) dealt with same-day urgent appointments | Silence | |
| Motivation for employing social prescribers | Not measured | Not measured | In one site, this role was a service enhancement, rather than taking work away from GPs, as the service was accessible only through GP referral. In two other sites, the sites employed ‘care coordinators’ who were not reception staff, but a new role employed by a local community health service based at the general practice. Social prescribers enabled better coordination between primary care and social care organisations, taking this work away from GPs | Silence | |
| Funding | Not measured |
Most additional/external funding available was for CPs and PAs Source of funding: |
CPs: directly employed by the practice or by a local CCG PAs: local CCGs and small bursaries from HEE ACPs: local community health services Social prescribers: local integrated care organisations and community health services |
Complementarity | |
| Ideal workforce | GPs in the GP Worklife Survey reported that up to 30% of their work could be transferred to other types of practitioners. Working in an environment in which more of these other types of practitioners were employed is associated with a higher per cent of work deemed transferable, suggesting that experience of new roles builds confidence in them. However, higher FTE of other types of practitioners is associated with lower GP satisfaction and potentially higher hours of work when the proportion increases above a certain level |
Practice managers wanted more staff in traditional roles (i.e. salaried GPs, ANPs, GP partners and practice nurses) New roles comprised < 20% of their ideal practice workforce, with CPs the most commonly selected. |
GP partners wanted more GPs. Recruitment of non-GPs was a pragmatic response and a short-term solution to GP recruitment difficulties. However, practice managers tended to focus on the need for cost-efficiencies and a new way of organising care | Complementarity/dissonance: on the surface, there is dissonance, as in the survey a majority of practice managers’ motivation for employing non-GPs was not because of the difficulty of finding GPs. The case studies explain the dissonance by showing that GPs and practice managers have different views. Therefore, the case studies have provided complementarity to the survey findings. The quantitative work shows that having a higher FTE of GPs is associated with higher job satisfaction. This shows complementarity with the case studies findings | |
| A new way of working | Mechanisms to support a new way of working | The quantitative analysis shows that higher FTE of practitioners other than GPs is associated with lower satisfaction with appointment-making procedures and that higher FTE of other DPC staff is associated with lower satisfaction with the surgery as a whole. There is lower GP satisfaction associated with higher FTE of other professionals | Not measured | There is a need for general practices to be engaged in categorisation work by matching the ‘right’ patients to the ‘right’ clinicians. Different holders of particular roles may have different personal skills and competencies. This means that those staff responsible for matching patients to practitioners need to have a good understanding of each role-holder’s personal competencies. In practice, staff recognised incidents of inaccurate matching. Good outcomes (for patients, practitioners and the practice) are dependent on good categorisation and matching, and flexibility and longer-term adaptability on several levels:
|
Complementarity: the case studies provide evidence that may, in part, explain some elements of the quantitative findings. Patients may find the categorisation and matching processes burdensome and may feel dissatisfied if flexibility and longer-term adaptability are not demonstrated in practitioners’ responses or the practice. GPs’ job satisfaction may be affected by their changing roles, including the requirement to supervise other practitioners coupled with the expectation that they continue to carry wider responsibility for the actions of others |
| Changing roles | The finding that the employment of newer types of practitioners may be associated with lower GP satisfaction raises some concerns, suggesting that it is not a forgone conclusion that the changes under way with regard to skill mix will increase GP satisfaction with their jobs | Not measured |
GP partners: becoming GP consultants with responsibilities for supervision Receptionists: operating as care navigators, implementing the categorisation and matching process Nurses: gradually advancing personal skills and competencies over time |
Complementarity: the quantitative findings raise some concerns about the overall impact of the change in roles associated with skill mix change in the context of a GP recruitment/retention crisis. This may require further research to explore in more depth | |
| Employment of newer roles | Not measured | Practice managers wished to access newer roles through a network, federation or other existing organisation | Greater support can be received when accessing newer roles via a PCN, but there is a risk of conflicting priorities and tension between PCNs and general practices |
Convergence: the case studies show that both GPs and practice managers welcome the potential support of PCNs in employing newer types of practitioners. Both groups expressed some concern over the risk of conflicting priorities and tension between PCNs and general practices Dissonance: the case studies reveal the complex processes required to incorporate newer types of practitioners into practices’ organisational routines. Employment by an external agency (i.e. the PCN) may make this more difficult, something that practice managers do not seem to have taken into account in their consideration of optimum future employment mechanisms. Further research will be required to explore this issue |
|
| Reflection on changes during the COVID-19 response | Not measured | Not measured | More flexible working, total triage and increasing remote consultations | Silence | |
| Unintended consequences | The lower GP satisfaction associated with the employment of newer types of practitioners is concerning | Not measured |
Supervision increases GP workload Implications for their own skill set |
Complementarity: our study suggests that this issue requires further investigation to understand in more depth how GPs experience these changes | |
| Outcomes/impacts | Overall service delivery | Higher FTE of other DPC staff is associated with overall lower patient satisfaction with their general surgery | Not measured |
Patients in the case studies expressed a degree of resignation when faced with skill mix changes. Patients accepted that such changes were inevitable, but highlighted that they would need time to adjust their expectations and to understand what newer types of practitioners could do. Those patients with experience of newer types of practitioners suggested that satisfaction improves with familiarity and is helped by continuity (i.e. seeing the same practitioner more than once) Our study highlights the evolving nature of service delivery by newer types of practitioners, as their skills improve over time and with specific training activities |
Complementarity: both the case studies and the quantitative analysis suggest that the employment of newer types of practitioners requires adjustment by both professionals and patients. Such adjustments take time and work by both parties, and there may be an initial decline in overall satisfaction. Further research is required to explore whether or not, after a period of adjustment, satisfaction improves with increased familiarity and as practitioners’ skills develop |
| Patient safety | Employment of CPs is associated with better prescribing quality | Not measured | Case studies suggested that the complex patchwork of regulatory oversight of newer types of practitioners may raise safety issues. In particular, PAs are not regulated and require oversight. The visible availability of supervision enhances patient perceptions of safety by more experienced practitioners, but this may burden those required to supervise | Complementarity: case studies and quantitative findings highlight the complex picture relating to safety and skill mix change. Different types of practitioners offer different advantages and/or risks, and clarity over regulation and supervision requirements would be helpful | |
| Quality of care | Higher employment of GPs, nurses and other DPC staff are all associated with higher QOF performance. This difference is greatest for the employment of more GPs | Not measured | Not measured | Silence | |
| Access to appointments | Higher FTE of nurses and other DPC practitioners is associated with lower satisfaction in the appointment-making process | Some of the newer roles (i.e. ANPs and PAs) were employed to increase access to appointments |
Although newer roles can increase overall appointment availability and release GP time, some of the newer roles required longer appointment times, therefore reducing the number of patients they can see Patients told us that, although newer types of practitioners had increased the availability of appointments, they had to adjust their expectations as this meant that they were not always able to see the type of practitioner of their choice |
Dissonance between practice managers’ survey and other WPs Convergence and complementarity between case studies and quantitative findings. The complex appointment-making processes that are required to categorise and match patients may be burdensome to patients and the provision of additional appointments does not straightforwardly improve patient experiences. Simply providing more appointments may not be enough to improve patients’ perceptions of access |
|
| Continuity of care | Not measured | The majority of patients we surveyed reported that they received better health care overall when always or mostly seen by the same practitioner. The focus group expanded on this by defining continuity as seeing the same practitioner and that continuity was desirable and important for patient satisfaction | |||
| Patient experiences | Higher employment of other DPC staff is associated with a lower overall patient satisfaction | Not measured | Patient satisfaction with skill mix changes was related to improved waiting times for access to appointments. However, there were concerns over how less-informed patients, particularly older adults, infrequent attendees and vulnerable groups, could navigate the new system. A contributing factor for increased patient satisfaction was a longer appointment slot for new roles, patient education/communication and availability of GP supervision | Complementarity: case studies and quantitative findings confirm that the implementation of skill mix change has complex impacts on patient experiences, which may change over time as newer practitioners become more familiar to patients | |
| Cost-effectiveness/efficiencies |
Higher levels of employment of all types of practitioner is associated with higher primary care costs, as measured by payments to practices and prescribing costs. The higher costs that are associated with higher levels of employment of DPC practitioners or nurses are not much lower than the costs associated with higher levels of employment of GPs The employment of pharmacists is associated with a lower volume of prescribing and cost/item. The employment of more nurses and other DPC staff is associated with higher prescribing volume and overall cost |
Not measured |
Difficult to measure the cost-effectiveness of skill mix because of the need for GPs to provide supervision for non-GPs, therefore increasing GP workload Many newer types of practitioners cannot issue prescriptions, leading to inefficiencies, as authorisation must be individually obtained |
Convergence: both WPs confirm that higher levels of employment of non-GPs is not necessarily cheaper than higher levels of GP employment [as demonstrated by overall costs (WP1) and the relative reduction in availability for consultations due to longer consultations and supervision activities (WP3)] Complementarity: the higher prescribing volume and costs associated with higher levels of employment of nurses and other DPC staff may be explained by the splitting of responsibility for initiating a prescription and signing it off, or it may reflect prescribing associated with increased chronic disease management. Further research is required to understand this in more depth. There may also be less inclination for non-GPs to explore non-pharmaceutical treatments because of limited training/experience |
|
| Impact on practice staff | Higher levels of employment of other professionals is associated with lower GP satisfaction. There appears to be a U-shaped curve between GP hours of work and employment of other types of professionals, suggesting that there may be a threshold above which a larger number of other professionals acts to increase GP workload | Not measured | Practice staff needed to manage uncertainties and anxieties surrounding what newer practitioners can do because of limited understanding of different roles and nuanced differences between different role-holders | Convergence: case studies and quantitative work confirm that the impact of skill mix change is complex. It seems likely that skill mix will evolve over time and that familiarity and trust are important factors. Further research is required to understand how these factors are developed if practitioners are employed by a third party, such as a PCN, and move between practices | |
The triangulation of our findings has confirmed the value of our mixed-methods approach. Looking across each of the WPs in this way has broadened and deepened our understanding of the complex and evolving impact of skill mix change in practice and has highlighted important issues for further research. In addition, our consideration of complementarity, convergence, dissonance and silence has confirmed that triangulation does not simply reflect a process by which different research approaches offer ‘checking’ of findings against one another to converge on some ‘truth’. Rather, the interplay between our WPs has generated new insights and has suggested new avenues for future research. 121
Chapter 8 Discussion
Summary of findings
This research adopted a mixed-methods approach to investigate evolving patterns of skill mix in primary care, examine how and why skill mix changes are implemented, explore practitioner and patient experiences of these changes, and estimate the overall impact on outcomes and costs associated with a broader spectrum of practitioner types.
The context in which skill mix change occurs in general practice is one in which the current workload in general practice is regarded as unsustainable because of changing demographics (i.e. increasing numbers of frail elderly patients with complex needs). At the same time, the number of GPs in the workforce has been decreasing. The assumption underlying policies driving changes in skill mix is that the workforce crisis can be addressed by bringing additional types of practitioners into the general practice workforce. It is intended that these newer practitioners will (1) see patients with undifferentiated problems and will, therefore, relieve pressure on practices, while maintaining patient satisfaction, or (2) bring specific skills useful for relieving workload pressure in other ways. Current policy mechanisms accelerate the implementation of skill mix change via a new GP contract that includes a Network Contract DES. The contract supports groups of practices to employ an increasing number and wider range of newer types of practitioners across the network, with an initial focus on the following five new roles: (1) CPs, (2) PAs, (3) paramedics, (4) physiotherapists and (5) social prescribers. The contract has been added on to the existing GMS contract, and it provides 100% reimbursement for the employment of practitioners in the newer roles. Crucially, under this contract, the practitioners may be deployed across any/all of the network practices rather than in a single practice. Our study took place before, and in the early stages of, the implementation of this contract. Therefore, we focused on newer types of practitioners employed by practices rather than practitioners employed by a network. This provided an opportunity to explore in depth the factors driving and supporting skill mix employment and to consider the implications of this for the employment of practitioners across a network.
How has the workforce changed and where has any change occurred?
Skill mix in general practice has been expanding to include roles such as CPs and paramedics. However, these roles still represent a very small proportion of the workforce recorded during the study period (i.e. 2015–19). The roll-out of these roles into general practice has not been uniform across the country, with paramedics mainly employed by practices in the south of England and PAs being employed by practices in larger cities. Analysis of practice-level workforce data shows that a range of demand and supply factors are associated with the practice workforce. These factors include geographical factors (e.g. distance to the nearest hospital that may provide initial training for health professionals), supply factors (e.g. the market forces factor, which may affect the affordability of living near the practice for less highly paid workers) and demand factors (e.g. the proportion of patients aged ≥ 65 years whose health-care needs are likely to increase).
Practice managers’ reasons for implementing skill mix changes and vision for the future
Our national practice manager survey, which received 1205 responses (approximately 17% of all general practices in England) between August and December 2019, showed that the motivation for employing new roles varied between types of practitioners. In addition, the range of motivations included to increase overall appointment availability, release GP time and provide a better match between what patients need and what the general practice team can deliver. Funding was not reported to be a key motivating factor for practices’ current employment choices. The survey also showed that the ideal practice workforce would comprise > 70% GPs and nurses, whereas newer practitioners would make up < 20% of the ideal practice workforce. Our case studies showed that practice managers held different views from many interviewed practitioners, which may explain why ‘unable to recruit a GP’ was not frequently selected in the online survey (WP2) by practice managers as a motivation for skill mix. Our case study findings added more nuance around these motivations, suggesting that the recruitment of new roles was a pragmatic response and a short-term solution to GP recruitment difficulties. Moreover, although accessing new roles via PCNs was broadly welcomed, practices expressed concern over the potential for conflicting priorities between PCNs and practices. During our case studies, details of how practitioners would be employed via PCNs continued to emerge and develop. Many of the arrangements were complex and variable, and it was unclear how this would work in practice. We return to this issue below.
New ways of working
The case studies explored in depth the way in which skill mix change has been accommodated in five practices. Our findings further complemented the survey by showing that, although newer roles can increase overall appointment availability and release GP time, some of the newer roles required longer appointment times, reducing the number of patients who can be seen. Moreover, we found that most roles required some ongoing GP supervision, creating an unexpected new workload for GPs and raising questions about the cost-effectiveness of skill mix. The case studies further described the processes that general practices had put in place to organise new ways of working and gathered the experiences of practice staff and patients in navigating the new system. There was variability in the breadth of practitioners’ scope of practice, in the degree to which roles were established and in the familiarity of patients, GPs and other staff with new roles. There was also variability of staff holding these roles in terms of the consistency of competencies they held and their familiarity with general practice. Role competencies (i.e. those competencies derived from training programmes) often differed from role-holder competencies (i.e. those competencies derived from individuals’ personal experiences and acquired skills). This means that practices cannot assume that practitioners holding the same title, qualifications and training will necessarily undertake the same tasks. In our case study sites, general practices engaged in categorisation (of practitioner and problem) to inform appointment matching. Practices categorised their practitioners according to their qualifications, training, upskilling, specialisation and/or past experiences. Categorisation took the form of a competency framework, skill mix matrix or internal directory of services. Receptionists used these categories to match patients’ problems with what practitioners could deal with. However, the problem(s) patients presented to receptionists during triage could be different from those which patients subsequently presented during consultations. This could lead to imperfect matching and required practices to put in place an adaptable system to allow practitioners to respond with flexibility when patients’ needs demanded a prompt resolution of mismatching. Practices also needed to monitor, review and adjust processes where necessary. Patient education/communication and availability of GP supervision for new roles were important in ensuring patient acceptance of skill mix change. Patients reflected that relational continuity (i.e. seeing the same practitioner more than once) was helpful in developing trust and confidence.
The arrival of the COVID-19 pandemic changed the way in which practices delivered care. All practices adopted a total triage approach to determine if a telephone/video consultation was adequate or if patients needed to be seen face to face. In various ways, general practices also changed the way in which they categorised their practitioners and problems. The inevitable and accelerating use of remote consultations brought challenges in terms of accessibility of equipment and IT connectivity and also created difficulties for patients and staff in adjusting to consultations using technology. It was envisaged that, in future, a greater proportion of work would be carried out from home and that increased use of remote consultations would continue. The format of meetings also changed, with more regular, shorter meetings with the wider team and more shared decision-making and coordination of work with neighbouring practices.
Outcomes and expenditure
Our quantitative analysis utilised a production function approach. This approach explores associations between an increase in FTE of particular practitioner groups and a range of outcomes, controlling for factors such as deprivation, practice size and patient demographics. We also modelled change in expenditure associated with increases in FTE of different practitioners and changes in outcomes associated with a unit change in FTE of different practitioner groups.
We found that higher FTE PTP of nurses and other DPC staff are associated with relatively lower patient satisfaction with their experience of making an appointment, perhaps reflecting the complexities associated with categorisation and matching, which we have elucidated. Higher levels of employment of other DPC staff are also associated with a relatively lower overall satisfaction with the practice. We found that a higher FTE PTP of GPs was associated with higher GP satisfaction, whereas a higher FTE PTP of other DPC staff and nurses is associated with a slightly lower overall GP satisfaction. GP hours of work describe a U-shaped curve, with an apparent threshold effect where a higher FTE of other DPC staff PTP above a certain level is associated with larger number of GP hours of work.
Clinical pharmacists would seem to have a particular role in improving prescribing quality and reducing prescribing volume, reflecting their particular skills and the ways in which we found their time being used in practices. We found evidence of a higher prescribing volume associated with higher FTE of both nurses and other DPC staff. This may reflect increasing chronic disease management, but it may also reflect a loosening of control of prescribing associated with the separation that we observed between prescription initiation and signing when practitioners do not hold prescribing qualifications. In terms of health services use, higher FTE of other DPC staff is associated with a slightly higher A&E attendance. Higher levels of employment of all practitioner types PTP is associated with higher costs, with the largest increase associated with higher numbers of GPs. However, the magnitude of the differences between types of practitioners observed is not large.
In summary, we have shown an increase in skill mix diversity in general practices, with an increasing proportion of practices employing a wide range of newer types of practitioners. Patients are generally accepting of these changes, but their implementation is not straightforward and does not necessarily result in overall increases in efficiency because of the complicated matching processes required to make sure patients see the right practitioners, the inefficiencies associated with mismatching and the need for ongoing supervision of some of the newer practitioners. There is some evidence of lower patient satisfaction with the practical steps of making an appointment that are a necessary part of matching their problem with a suitable practitioner. However, our qualitative work also reveals the dynamic nature of skill mix change, with practices, practitioners and patients all adapting over time to the changes that are occurring. Therefore, any evaluation of their impact will represent only a snapshot of an evolving situation.
The complexity of the task of skill mix implementation, and the need for ongoing negotiation and adaptation over time, raises important questions for the implementation of skill mix change via PCNs. In particular, our findings suggest that practitioners who work across multiple practices may find themselves working in different ways in different practices and that the supportive mechanisms required to facilitate the necessary adaptations over time may be more difficult to implement with practitioners who move between practices. Therefore, it is possible that the complex ongoing adaptive work required to make these changes work in practice may be difficult to achieve with practitioners who spend short periods of time in more than one practice.
Comparison with previous research
Conceptualisation
There are various definitions attributed to the term ‘skill mix’. Moreover, the plethora of role titles and inconsistency in the definition of roles have created confusion, for both patients and practice staff, in terms of what health-care workers can deliver in practice. 67,122–125 To counter this, it has been suggested that skill mix should be considered within the broader organisational and health-care system contexts. 17 Our study offers a complementary view by suggesting that skill mix should be seen as an evolving process rather than an end in itself. Rather than attempting to achieve an ‘optimal’ skill mix, general practices need to engage in ongoing categorisation work (of practitioner and problem) to match each problem with a suitable practitioner and to maintain flexibility and adaptability of organisational processes. Our study also suggests that the ultimate expression of skill mix in general practices will be one of diversity, in which different practitioners work in different ways in different contexts. Although this brings with it some complications, it is in fact consonant both with the historical experience of practices with the employment of practice nurses in general practice (in that practice nurses have always undertaken varied and developing roles) and specialist nurses in hospital settings. 126,127 What is crucial in all settings is that appropriate organisational processes exist for the induction and supervision of staff and that processes allow flexibility over time so that staff acquiring new skills can adapt their scope of practice.
Task reallocation
In their early work on this topic, Sibbald et al. 16 delineated skill mix change in terms of enhancement, substitution, delegation and/or innovation. Enhancement refers to individuals increasing the scope of their role, whereas substitution references the ideal that practitioners will be interchangeable, with a newer type of worker substituting for a GP. It is this formulation that, to a large extent, underpins the assumptions of the policy context that we have elucidated (i.e. newer types of practitioners will compensate for the shortage of GPs, both by direct substitution and also by delegation, with GPs passing on some tasks, thereby freeing them up to undertake more complex work). However, recent studies have suggested that enhancement and innovation most appropriately refer to whether changes are through existing or new roles, and delegation and substitution refer to how tasks are transferred. 16,20,21 Our study shows that non-GPs, specifically CPs and PAs, viewed themselves as providing work that is complementary to GPs’ work rather than as acting GP substitutes.
The potential for skill mix change to complement or supplement existing roles (to improve services) is not new and has been referenced over the last couple of decades. 24,128 This study, however, has enabled us to see how these outcomes of supplementation (rather than substitution) emerge from the complexity of multidisciplinary working where patients presenting with (often) undifferentiated symptoms need to be seen in a time-critical environment and multiple practitioners are enabled to do a range of tasks for them. This apparent (and relative) openness to performing the same tasks across professions is arguably different from other studies in which resistance to changing skill mix and transferring tasks has been seen as emerging from the protection of more specialist professional boundaries, and maybe this too will evolve over time in general practice. 64
The study has confirmed the benefits (identified in Chapter 1) of developing Sibbald et al. ’s16 framework to better delineate whether skills are changed through enhancement of someone’s existing role or innovation of a new role (with associated training), the basis on which tasks are transferred (substitution or delegation), and how the GP and alternative practitioner are subsequently deployed (substitution or supplementary).
The need for supervision, which we observed in the case studies, suggests that strict substitution will rarely be possible. Furthermore, the continued evolution of service delivery, as staff develop new skills and practices adapt to accommodate a wider range of professionals, suggests that it is unlikely ever to be possible to straightforwardly distinguish between these categories.
Our quantitative work indicates that larger numbers of other DPC staff may be associated with larger numbers of GP hours of work. This finding requires further elucidation; however, taken together, these findings suggest that the assumptions underlying the current skill mix change policy may be overly simplistic.
Other studies reviewing the implementation of skill mix have commented on the lack of clear role definitions and several studies have called for clearer role definitions for practitioners. 22,23,49,88,89,129 Our study shows that attempts to delineate roles between practitioners need to be seen as part of an ongoing process that will be locally specific and contingent. Moreover, we would suggest that roles will continue to adapt over time as newer practitioners settle into their roles, undertake additional training and learn from their colleagues. Importantly, we have highlighted that role competencies and role-holder competencies may differ, requiring practices to adapt to the evolving capabilities of different practitioners over time.
It has also been proposed that much of the time GPs spend on administrative tasks could be freed up by transferring such tasks to administrative staff. 9 Administrative staff were found to be able to deal with referrals and results-chasing if supported by simplified processes. 37 Studies have suggested that non-clinical staff should be responsible for e-prescribing and dealing with technical difficulties. 130 However, it is difficult to clearly distinguish between ‘administrative’ and ‘clinical’ tasks, with many so-called administrative tasks requiring a degree of clinical knowledge. 131 General practices in our study had identified elements of work that had formerly fallen to GPs, but could be carried out by other practitioners or non-clinical staff (e.g. administrative or reception staff), such as signing prescriptions, reviewing blood test results and reviewing hospital letters. However, other studies have highlighted the realities of how complex these tasks can be, with practices developing quite convoluted routines that are also context specific. 132 This suggests that it may not be straightforward to identify a general category of work that can be transferred in every situation. Moreover, our finding that higher levels of employment of other DPC staff is associated with a higher number of GP hours of work suggests that changing skill mix may not straightforwardly reduce the workloads of GPs.
Factors such as legal limits in the scope of practice (e.g. around prescribing) and lack of trust in non-GPs’ abilities have been found to affect task reallocation. 21 Our study shows that the lack of prescribing rights for some new roles, specifically PAs, could disrupt the consultations’ flow and may be associated with increased prescribing volume. On the other hand, the availability of GPs to provide supervision for non-GPs increased patients’ trust and confidence in consultations with non-GPs, albeit at the expense of hoped-for increased efficiency.
Multidisciplinary working in general practice
Issues of interprofessional competition and professionals’ attempts to protect occupational jurisdiction in their work are well documented. 62–65 Studies have revealed tensions between staff in relation to authority, legitimacy, expertise and efforts made to gain professional recognition in multidisciplinary working. 43,66–68 Earlier studies found that the following factors facilitated multidisciplinary working in primary care: co-location, a stable organisational structure, having clearly defined roles and workflow, good communication through ‘huddles’, team meetings, informal ‘handoffs’ of patients, shared goals, respect and trust. 49–54 Our study adds to the existing literature by providing a detailed description of different ways in which meetings can be conducted and the purpose of these meetings. In addition, our study has highlighted a significant degree of variation in approaches to professional boundaries in practice. Although some practitioners defended boundaries in traditional ways by, for example, explaining how and why their role was different from others, at the same time we found a willingness to be flexible and an acknowledgement that professional work may change over time.
Incentives
Earlier studies found that financial incentives influence the willingness to adopt skill mix. 41,42,89,129 Although additional funding to encourage new ways of working can incentivise skill mix change, such changes could be unsustainable without longer-term funding. 42,133 Our survey shows that funding and incentives were not the main reasons for employing non-GPs. With the exception of CPs and, to a much lesser extent, PAs, most general practices employed advanced nurses, specialist nurses, paramedics or HCAs without incentives. However, our case studies show that the source of funding determined which practitioners the practice could ‘experiment’ with without taking on additional financial risk. Therefore, the availability of funding could affect how practices categorised their practitioners.
Care navigation
The availability of wider practitioners in general practice required reception staff to have training about their various capabilities, and some were more highly trained than others in care navigation. Care navigation was seen as an extension to a receptionist’s job whereby they signposted individual patients to external non-clinical services. This could include generating personalised action plans linked with resources in the community to support patients using local groups and support services to address their non-medical needs. 134,135 HEE developed three levels for care navigation competencies, with the receptionist at the ‘essential’ level, the social prescriber at the ‘enhanced’ level and the navigator team leader at the ‘expert’ level. 136 In our study, care navigation was carried out by either receptionists or social prescribers. Although receptionists signposted patients internally to different practitioners or externally to other primary care services, social prescribers coordinated and/or signposted patients to social care and community services and resources. In addition, social prescribers sought to address the social dimensions of health directly and also indirectly through preventing or ameliorating associated clinical conditions.
Supervision
Studies have identified GP supervision as an unintended consequence of skill mix. 137 Our study provides a detailed description of what supervision involves and the importance of informal coffee break meetings for knowledge exchange and staff development. The purpose of these informal meetings was to provide supervision, develop less siloed working and facilitate multidisciplinary working. For this to work, it requires practices to have a relatively stable staff make up with several longstanding staff. Our study also found that supervision created a new additional workload for GPs that was causing ‘debrief fatigue’. Our quantitative work suggests reduced work-related satisfaction for GPs in practices with higher employment of other professionals. This finding requires further study.
Cost-effectiveness
There were mixed views about whether non-GPs provided good value for money. The perceived cost-effectiveness of employing ACPs was found to be pertinent to its sustainability. 45 However, non-GPs may take longer to complete tasks than GPs, as was the case for practice-employed CPs. 138 There was also evidence of increased transaction costs and a decrease in the continuity of care as staff spent increasing amounts of time conferring with each other and, therefore, had less time available for DPC. 139 Although cost-effectiveness did not prompt change, without careful attention from managers skill mix changes might lead to service improvements at a greater overall cost. 128 If this is the case, a proportion of these additional costs will require continuous funding through realignment of budgets for populations rather than within practices. Moreover, our interview participants claimed that cost-effectiveness of skill mix was difficult to measure in economic terms because of unanticipated extra work (e.g. GP supervision) involved when employing new roles, which has created an additional workload for GPs. This is consistent with our finding that higher FTE of all types of practitioners is associated with higher expenditures. The perceived cost-effectiveness of employing ACPs was found to be pertinent to its sustainability. 45
Patient experiences
Patient experiences of skill mix were referred to in the literature in terms of patterns of care, service utilisation, patient attitudes or consultations with single practitioner types. 140–143 Although patients reported having limited knowledge of what new roles can deliver, patient acceptability of non-GPs was influenced by patients’ expectation of what new roles can deliver, practitioners’ accessibility and promotion of the role. 43,144 Skill mix has been associated with increased access to appointments, longer consultation times and improvement in patient satisfaction, quality of life, follow-up appointments and continuity of practitioners (with non-GPs, as they were more available than GPs). 55,57,58,72,73,75,144,145 Similar to these studies, we found that patient-reported satisfaction with skill mix changes was related to improved waiting times for access to appointments. However, our quantitative work suggests that overall satisfaction with the process of obtaining an appointment is lower when there are more different types of practitioners employed. Patients in our study also had a limited understanding of newer practitioner types and their capabilities. However, some patients reported being happy with their non-GP consultations and contributing factors included longer appointment slots, which were seen as providing patients with more ‘holistic’ consultations than with GPs, and, consequently, improved trust in and acceptance of the new roles among patients. Patients in our study appreciated practitioner accessibility, indicating a trade-off for some between access to care and seeing their preferred practitioner. The introduction of new roles resulted in new systems of access/triage, which could raise issues for less informed patients, particularly older adults, vulnerable groups and infrequent attendees. Therefore, patient communication was highlighted in our study as an important factor in gaining patients’ acceptance and understanding of new roles. In addition, respondents in our focus groups told us that their acceptance of skill mix change was enhanced by a feeling that newer practitioners were well supported, and that GPs were available for expert advice if required. This suggests that, although surveys of patient satisfaction provide important evidence about patient experiences, the picture may be somewhat more nuanced than it initially appears. Qualitative interviews provide an important avenue for exploring in more depth the factors that underpin satisfaction with different types of appointments and, most importantly, the work involved for patients in skill mix changes in general practice.
Impact on outcomes
Although our own research (see Chapter 5) and previous research141,146 have shown that patients are generally satisfied with their encounters with nurses and other professionals, our study suggests that a higher FTE of professionals other than GPs is associated with overall lower satisfaction with patients’ interaction with their practices. 141,146 This may reflect the increasingly complex organisational processes required to ensure that patients are categorised correctly and matched with the correct professional. As we have described in Research question 3(iii): how does increased skill mix affect patients’ experiences when accessing primary care services?, such processes may also be burdensome for patients.
A study examining the correlation between nurse staffing and a range of indicators from the QOF, using data from the second year of the scheme, found that a higher level of nursing staff was associated with better performance on several clinical domains of the QOF. 147 We examined more recent data from the QOF and included a wider range of staff. Although we did not examine QOF achievement in particular disease areas, we considered a wider range of outcomes.
We found that a higher FTE of CPs is associated with higher prescribing quality and lower prescribing volume. There is a considerable volume of previous research (see Rationale for employing newer roles) exploring the role of CPs in primary care practices. Our findings are in accord with a Cochrane review148 from 2010, which explored the evidence relating to the impact of pharmacist-led interventions in outpatient and community settings. The review148 found that pharmacist-led services reduced the total number of medications prescribed and therapeutic duplication. Ethnographic research into influences on prescribing in general practice found that practice-level ‘macro’ policies (e.g. practice-wide policies about what to prescribe in certain circumstances) effectively improved prescribing quality, and it may be that the presence of CPs supports the development of such policies. 149 An evaluation of a programme in one CCG in the West Midlands found that CPs employed in practices were able to undertake activities such as medication reviews, audits and planned medication changes to improve cost-effectiveness. 150 These interventions were deemed to have both saved money and saved GPs time. However, data collection was subjective (relying on practice reports). Estimations of cost were based solely on cost reductions arising out of medication changes, rather than taking into account potential later costs associated with those changes (e.g. hospital admissions or need for new prescribing). A Cochrane review151 of interventions to reduce polypharmacy in older adults found no clear evidence of a beneficial effect of pharmaceutical care delivered by physicians, pharmacists or geriatricians. A realist synthesis of the conduct of post-discharge medication reviews by pharmacists in primary care concluded that such programmes work best when they are designed to promote collaboration and trust between professionals and when pharmacists take responsibility for outcomes. 152 This suggests (in keeping with our qualitative evidence) that the value of employing CPs in general practice is context dependent and requires careful service design.
Previous research153 has shown that increasing access to primary care may be associated with a decline in A&E attendance. Our study suggests that, although an increase in access to GPs and nurses is associated with a reduction in A&E attendances, the same is not true for other DPC staff.
Although we are not aware of any previous research that has looked at the association of GP satisfaction with the employment of a wider range of professionals, previous research154,155 has considered associations between GP burnout and other aspects of their practices. Workplace factors, such as workload and perceived control, were found to be drivers of primary care physician burnout. 154 Feeling unsupported and having a higher burden of administrative tasks were associated with an increased risk of burnout. 155 Our findings are congruent with this, in that it is likely that GPs working in an environment with a larger number of FTE GPs PTP will feel more supported, driving increased satisfaction. Moreover, it is possible that GPs working in an environment with a wider variety of DPC staff and fewer GPs have a relatively higher burden of administrative work (e.g. dealing with clinical decisions arising from patient letters and blood test results), which cannot be eased by delegation.
In terms of costs, previous research156 has suggested that employing ANPs may reduce costs and health-care utilisation; however, we are not aware of any other studies that have looked at overall primary care costs.
Strengths and limitations
Study overall
Our study took place at a time when, as we have demonstrated, skill mix in general practice is changing rapidly. Therefore, it may be that both our case studies and our outcomes analysis are capturing the effects of early turbulence as practices and individuals get used to new ways of working. However, some of our case study practices had been working with a more diverse workforce for several years, and we found that the need for adaptation and flexibility were ongoing. Delays in obtaining outcomes data limited our ability to undertake more in-depth analyses of change over time. Our study also took place when general practice was on the cusp of a change from having newer types of practitioner predominantly employed by practices to a policy-driven shift towards financially supported, centrally employed staff moving between practices. Although we are unable to offer direct evidence about the impact of this shift, we can make some inferences, which are discussed below. In addition, this means that our examination of outcomes associated with different levels of skill mix may be capturing outcomes associated with newly employed practitioners. We have shown that there is a development over time as practitioners settle into their roles and develop new skills, and it will be important in future to explore whether or not this has an impact on outcomes.
Workforce data sets and outcomes data
Our analysis is based on national data, although we did not use data for 2020 because the COVID-19 pandemic had profound impacts on health-care activity levels and patient outcomes. No national data are currently available at practice level on the volume of consultations delivered. We created a measure of how recently a practice’s patients had seen a GP and how recently they had seen a nurse, on average, based on data from the 2017 GPPS. This is based on a sample of patients’ responses about each practice and is only a crude proxy for the utilisation of primary care.
There is potential for skill mix to be endogenous in the outcome equations if there are unmeasured factors associated with both skill mix and outcomes. We included a range of measured characteristics of practices and their populations to minimise the risk of omitted variable bias. We also examined changes over time, which controls for unmeasured but time-invariant characteristics of practices. Nonetheless, the risk of confounding from time-varying factors remains. We experimented with potentially exogenous variables (e.g. whether or not the CCG has offered incentives to employ new staff types, local labour and housing market conditions) in an instrumental variables framework, but these were not sufficiently predictive to provide accurate results. The results should be interpreted with this limitation in mind, and future work should focus on identifying better exogenous predictors of variation in skill mix.
Practice managers’ survey
The strengths of this study are in the collection of large-scale data on general practices’ motivation for employing skill mix and a detailed description of how skill mix policy is enacted in practice.
A limitation of the national practice manager survey was the response rate (i.e. 17%). However, we have implemented weighting to minimise any bias.
Another limitation is in the suspected inaccuracy of wMDS. However, our analysis has demonstrated that systematic bias is not present in our sample. 157
Case studies
As with all case study approaches, our aim was not for generalisation based on representativeness. Rather, our aim was to use theory to support generalisation from the particulars of our case study sites to the wider context of the NHS. Using this approach, we have shown how the particularities of each case required the development of locally specific routines, and we have drawn out from this a number of broader issues that practices need to consider in implementing skill mix, including categorisation and maintaining adaptability. The strength of this work lies in the multifaceted and in-depth data collected from observation in both clinical and administrative areas, which allowed us to capture a fully rounded picture of the implementation task.
A practical limitation of the case study work was the difficulty in getting patients involved with the study. We did not manage to collect as many patient surveys as planned, despite seeking practices’ support in distributing the survey. There was variable capacity and/or willingness within practices for getting reception staff to do this. Moreover, many patients needed the questions read out to them or more explanation of the purpose of the survey than reception staff were able to give. In addition, one of the sites (i.e. site C) did not have an active PPG nor were we able to recruit patients for a focus group at that site. We contacted all patients who indicated in the survey that they were willing to participate in the focus groups. However, only patients in site D agreed to participate in the focus group.
Conclusions
We have provided an in-depth, multifaceted exploration of the implementation of skill mix change in general practices in England. Our study highlights the inherent complexity of skill mix change and the associated need for adaptability from practitioners, practice staff, practice organisational processes and patients. We have also demonstrated the evolving nature of skill mix change, showing how practitioners develop new competencies over time and expand their scope of practice. Although others23 have called for greater clarity about the scope of new roles, our study has highlighted the distinction between role competencies and role-holder competencies. Practitioners coming into general practice from other disciplines bring their existing skills and abilities, whereas role-holders develop new skills with training and experience. This pattern mirrors the development of practice nursing in the 1980s and 1990s, during which time practice nurses significantly expanded their skills and scope of practice. 158 The result of such piecemeal development is a workforce that is highly variable in skills, experience and competencies, even when ostensibly occupying the same role. 158 Our study suggests that the implementation of skill mix change in general practice will follow a similar pattern and that practices will need to remain adaptable and flexible, with processes in place to accurately gauge the abilities and potential scope of practice of new employees, as well as good organisational structures to support them in their development. 159
We have also shown that, although concepts such as substitution and delegation are useful in orientating thinking about skill mix change, in practice the reality is messy and variable. 16 Individual practitioners may, during the course of a single clinic, perform some tasks that straightforwardly substitute for work that would otherwise have been carried out by a GP, requiring supervision and support in carrying out other tasks. Outcomes analysis does not seem to suggest that increasing the FTE of some groups of professionals necessarily improves the working environment for others. Introducing newer practitioners into general practice changes roles in complex ways, and it cannot be assumed that the process will be straightforward for practitioners or patients alike. Reassuringly, we found that patients are generally happy to be seen by newer types of practitioners, but patients highlighted the value of continuity and the importance of feeling that practitioners were adequately supported and supervised. The complex processes that general practices needed to implement to ensure that categorisation and matching of patients to practitioners is appropriate may explain the lower satisfaction with appointment-making processes reported by patients in practices with higher proportions of other professionals. This is something that practices need to consider as they develop their workforce. There is clear potential for such processes to add to the burden of treatment experienced by patients with chronic ill health, and it is important that practices act to reduce this as far as possible. 158 We found that increased employment of CPs is associated with clear benefits in improved prescribing quality and lower prescribing volume. Increasing the employment of other types of practitioners has a variable impact on outcomes. The higher rates of A&E attendance associated with higher rates of employment of other DPC practitioners need further exploration, as does the apparent lower GP satisfaction associated with higher employment of these other practitioners. Employing newer types of practitioners would not seem to be straightforwardly more cost-efficient than employing more GPs.
In summary, our study has shown that the assumptions underlying current policy in England may be overly simplistic. Although there is clear potential for newer types of practitioners to provide high-quality holistic primary health care, skill mix change is not a straightforward or easily implementable solution to the current GP workforce crisis, and it will require careful management.
Implications for health care
Our study suggests that it is unlikely to be possible to specify any ‘ideal’ balance of skill mix for general practices, as the value that different practitioners contribute in the workforce will change over time and will vary depending on the precise needs of local populations. Practice managers responding to our survey and GPs in our case studies valued the contribution of advanced practitioners, particularly nurses. There is also some evidence from our quantitative work that higher levels of employment of nurses are associated with better outcomes in some areas, in particular lower rates of A&E attendance and lower outpatient attendances. This suggests that nurse training may need to take account of increased demand for nurses working in general practice. This may require, for example, adjustments to current nurse training programmes. The employment of CPs would seem to have clear benefits in terms of prescribing quality and volume. Again, this may require adjustments to current pharmacy training programmes. Working in hospital settings is quite different from working in primary care, as practitioners can feel isolated when working alone in primary care and, therefore, training of these and other professionals needs to take this into account. In addition, GP training may need to be adjusted to consider the need for supervision and oversight of other types of practitioners. Furthermore, as newly qualified GPs cannot necessarily deal with high proportions of complex cases, they may require access to additional training and support as they gain experience and build clinical confidence to function as GP consultants.
More generally, our study highlights the need for ongoing training within practices once newer practitioners are employed. This may have implications for those employed to work across PCNs. Practices’ needs for a balance of particular skills will change over time, and our study suggests that active management will be required, iteratively assessing current practice capabilities and working with colleagues across PCNs to ensure that the supply of staff meets demand.
Our study also suggests that the relationship between GP satisfaction and the skill mix of their workforce is complex. It is not clear that increasing skill mix will increase GPs’ job satisfaction and thereby enhance recruitment and retention. It may be that, in our study, we are capturing the early impacts of skill mix changes and that this may improve as GPs become accustomed to working in more diverse teams. However, this cannot be assumed and this issue requires careful monitoring and research over time.
The growing scale of skill mix implementation in primary care is accompanied by changes in how health care is delivered and in the organisational structures and managerial responsibilities that are needed:
-
The distribution of undifferentiated work is a complex task that requires sufficient understanding of the presenting problem(s) and the capabilities of each practitioner to support safe and effective categorisation and matching.
-
The distribution of work will change over time as practitioners settle into roles and expand their capabilities, and practices need to adapt to these changes. Staff turnover will be complicated, as it is unlikely that newly recruited practitioners will have exactly the same skills and capabilities as those that have left.
-
Deficiencies in categorisation and matching are inevitable, but can be accommodated if system design and the approach of practitioners are sufficiently flexible to make timely adjustments.
-
Scope of practice for many practitioners remains ill-defined and is not uniform. Practitioners are, therefore, not interchangeable, deployment is contextually embedded and progressive career development (e.g. upskilling, additional qualifications) alters whole-team capability.
-
Regulation of practitioners is important and currently somewhat confused. For example, ACPs have similar master’s-level training and potential scope of practice, but those from physiotherapy, nursing or paramedic backgrounds will be subject to regulation by different professional bodies. CPs are also separately regulated, but it remains unclear how far GPs are responsible for the actions of those they employ if CPs or other practitioners go beyond their level of competence or scope of practice. Employer’s liability in these circumstances has not been tested, and this may be more complex if practitioners are employed by a third party, such as a PCN. PAs are currently unregulated, which may be problematic in the longer run, particularly if they are accorded prescribing rights.
-
A different type of practice management is required. Practice managers now work with GPs and other practitioners on how work is distributed across a broader range of practitioner types. In contrast to former hierarchical structures and traditional roles of business management, practice managers need to work more closely with diverse clinical teams and should engage with skill management across the clinical and administrative team.
-
Clinical staff across all disciplines generally undertake most of their early training in specialist departments and hospital settings. Training to prepare all types of practitioners for the broad caseloads of general practice is not universally available, but is necessary to ensure a continuing supply of appropriately trained practitioners. Robust training standards are needed for all practitioners progressing to independent practice. We also noted that, as proposals for PAs to become prescribers have been delayed, PAs remain unable to work independently.
-
Case studies confirmed that GPs undertake a wide range of duties that are largely hidden from view. Increasing skill mix employment brings an increased need for supervision of others’ work that may not be allocated sufficient time or resources.
-
Senior clinicians expressed concerns about wider issues arising from skill mix implementation. These included concerns about ensuring that all practitioners work within the limitations of their training and experience, challenges when discussing case management with less qualified practitioners and uncertainty about who is ultimately responsible for care quality.
-
Team interactions (including allocated time and physical space) need to be recognised as part of the working day, as staff need to get to know each other; their knowledge base; their individual skills, expertise and experience; and their strengths and weakness beyond formal training and role allocation. Heavy workloads and staggered working hours already make this difficult. It seems likely that team interactions will become more challenging as practices need to engage with PCN ARRS-employed practitioners.
-
Communication with patients is key. Good categorisation of the problem for which patients request help is essential, but clear communication is hampered by many organisational, societal and idiosyncratic factors. It would be advantageous if patients were knowledgeable about which problems are ideally suited to the skills of a particular type of practitioner, but there are limited ways for patients to acquire information about this to make an informed choice.
-
All of these findings mean that implementing skill mix across groups of practices via PCNs may be challenging. In particular, practices will need to put in place structures and processes that ensure that peripatetic staff moving between practices get the opportunity to engage with practice staff. Such staff must be prepared to potentially work differently in each practice they visit. Cross-network meetings may help in harmonising expectations of staff and roles, and this is something that should be prioritised.
Implications
We collected reflections on working during the COVID-19 pandemic through a small number of interviews with participants in case study sites. However, the following recommendations are based on a study that was conducted pre-COVID 19 and, therefore, did not consider issues that emerged because of the pandemic.
For research
-
Further research is required to analyse changes in outcomes (and related overall costs) over time as larger numbers of newer practitioners settle into practice and develop their skills. It will be particularly important to track impacts on other measures of overall health service use.
-
It will be important to monitor closely the implementation of skill mix via PCNs, with a close examination of the ways in which practices are adapting to staff who are only present for short periods of time, and identify factors that support this process and monitor the impact on outcomes.
-
There is a need to track GP job satisfaction over time and to consider the factors affecting this. We have highlighted that newly qualified GPs may not feel ready to take on the required supervisory roles and other responsibilities.
-
There is some evidence that the experience of working in a more diverse workforce affects attitudes, and it seems likely that GPs and managers exposed to newer practitioners may adjust their expectations about what their workforce should look like. These changes need to be explored over time, as they have implications for training and the supply of workers.
-
The current ARRS offers incentives to employ a more diverse workforce at group level. Future research should consider the impact of ARRS in comparison with more direct investment in practices.
-
Wider professional issues that have been identified in previous research (see Multidisciplinary working) and surfaced in our research remain partially understood:
-
Further research should explore the mechanisms that help mixed groups of professionals retain what is valued in their own professional identities and maintain engagement and motivation while working across professional boundaries.
-
It has been proposed that some GPs prefer to continue in roles closer to the comprehensive, generalist roles that attracted them to general practice, rather than working in roles more typical of consultants with an emphasis on dealing with complex cases, supervision, etc. Further research is needed to explore how different caseload preferences may be accommodated in GP settings.
-
The processes by which newly qualified but relatively inexperienced GPs progress to become more experienced and eventually capable of senior clinical roles are unclear. Further information about this is needed to inform the development of appropriate career pathways.
-
Further research is needed to determine how the categorisation of patients’ problems can be improved. It has been suggested that artificial intelligence may offer some solutions for this issue. However, our study suggests that patients may express their problems in ways that do not facilitate categorisation and, therefore, it is possible that artificial intelligence-based solutions will make this worse. The impact of such innovations in practice needs to be carefully studied.
-
For policy
Current policy is driving the implementation of skill mix across groups of practices within PCNs via a direct subsidy of the employment of a variety of newer types of practitioners. Our study demonstrates that there are complex challenges associated with the implementation of skill mix when it occurs at the practice level. It is not at all clear how these challenges will be managed when practitioners are employed centrally to work across more than one practice. Specific issues which will need to be considered:
-
Policy should not assume that the deployment of newer practitioners across PCNs will provide a straightforward or complete solution to the current GP workforce and workload crisis. GPs in practices will need to supervise peripatetic workers carefully and the benefits for practices in terms of workload reduction are not currently clear.
-
General practices need to manage the distribution of work through, for example, categorisation and matching of their practitioners and patients. Greater adaptability of various practitioners can be supported by having both formal and informal meetings (e.g. regular coffee breaks) between practitioners. However, this may be more challenging for peripatetic practitioners, such as PCN-employed staff who are only present in each practice on 1 or 2 days per week. PCNs could seek to limit the number of practices with which each practitioner interacts by, for example, deploying practitioners over a small number of closely linked practices rather than across the whole group. Moreover, PCNs should prioritise retaining staff so that there is time for practices and patients to adapt. It takes time for new roles to bed in, and this is likely to take longer when practitioners are only present in the practice for short periods of time.
-
In facilitating the management of staff, there will need to be close interactions between practices and PCNs. Practices will need to agree on how individual practitioners will be expected to work, including their responsibilities and scope of practice, with close liaison if the scope of practice is to be changed. Line management and the respective responsibilities of practices and the PCN for oversight and performance management of staff will need to be clearly worked out and managed. There will need to be a clear understanding of who is liable with regard to practitioner performance. Regulation of new roles needs to be clarified. Moreover, dedicated funding or development support for PCN management should be prioritised.
-
Change in outcomes associated with the ARRS will be very difficult to determine. The wMDS needs to clearly capture these new roles and demarcate the length of time that each practitioner employed across the PCN spends in each practice.
-
Patients value continuity of practitioner and satisfaction may be affected by complex categorisation and matching processes. There may, therefore, be a trade-off between patient and practice satisfaction with new arrangements. Moreover, our study found increased attendance levels at A&E for practices with higher levels of non-GPs. It is important that policy allows time for adjustments to be made and accommodations reached before making changes in response to this.
-
There is stronger evidence of benefit from the deployment of CPs and ACPs, suggesting that these roles should be prioritised.
For practice
-
General practices need to understand how they can choose between practitioner types (if there is sufficient supply in their locality) and how they can gain the greatest benefit from skill mix.
-
Practice managers need to understand how to manage a diverse skill mix workforce and develop functional processes to optimise categorisation and matching. Practice managers may require additional training for this. PCNs could play a role in training practice managers and working with practices to support them in integrating new roles into their practice, but PCNs will require dedicated management resources to achieve this.
-
The training and development of newer types of practitioners needs to be carefully managed and optimised over time. Those responsible for training different practitioners need to work together, understanding the difference between role competencies and role-holder competencies. Preparation for working in an isolated setting and for working collaboratively within a diverse team need to be prioritised.
-
Regulatory arrangements need to be clarified and made more transparent, particularly in relation to practitioners employed across more than one practice.
-
Practices need dedicated time to allow training and team development. It is unclear how this will work with regard to peripatetic members of staff who may need to attend meetings in multiple practices. The creation of small locality groups of two to three practices within PCNs may help this.
For practitioners
-
Practitioners need to communicate about, and feel comfortable with, their scope of practice, and practices should seek to generate an ethos in which it feels ‘safe’ for each individual to be candid about knowledge, skills and aptitudes.
-
In the context of dealing with undifferentiated caseloads, practitioners in all roles need to recognise their strengths and limitations. Practitioners may find it difficult to identify unconscious gaps, but participation in sensitive and supportive case reviews can be used to reveal deficits and improve future performance.
-
Both acceptability of seeking assistance from colleagues and the practicalities of getting assistance need to be fully supported by all practitioners to make this a normal and everyday practice that underpins patient safety.
-
Experiential learning is a long-established facet of clinical work. The value and service enhancement of such learning should be recognised and appropriately rewarded for all practitioners.
For patients
-
Increasing diversification of the practitioner workforce will, in time, become more familiar to patients. Discussions with our patient and public involvement representatives about how this might look have recognised that the deeply contextual nature of how individual practitioners work in specific settings makes it difficult to design a universally applicable solution. Individual practices will need to work closely with their PPG to generate ways of effectively communicating how appointment booking systems work or what different practitioners can do.
-
Categorisation depends on effective communication by patients of the nature of their problem, which is likely to present greater difficulties for those not familiar with medical conditions and a more significant problem for patients who, for any reason, are more vulnerable to increased health inequalities. Systems to identify such patients should be considered for inclusion in the initial assessment. Once such difficulties have been confirmed, they can be allocated to a receptionist with enhanced training for an individually tailored assessment.
-
Building patients’ satisfaction, confidence and trust in new systems requires time and the willingness of both practitioners and patients to adapt to the new arrangements. Factors that can increase patient confidence and trust include longer appointment times and ensuring that non-GPs have access to advice from more experienced colleagues when uncertain of how to proceed.
Dissemination
The COVID-19 pandemic significantly curtailed dissemination opportunities, severely affecting plans to disseminate to international conference audiences. Nonetheless, through a combination of planned and substitute activities, we have found ways to reach key audiences in primary care workforce planning and strategy, practice managers, GPs and other practitioners, and patient representatives.
We published two articles in the British Journal of General Practice101,160 and submitted another paper to the same journal. We contributed to a policy engagement activity by contributing to a publication On Primary Care: General Practice, Pharmacy and Workforce organised by Policy@Manchester. 161 The publication was distributed to policy-makers and we subsequently engaged in a follow-up virtual event with selected policy audiences. We also presented at various conferences throughout the project. Appendix 3 lists past and future publications and events.
We contacted each participating practice to offer feedback that best suited their preference and scheduling requirements and arranged individually tailored virtual presentations and discussion sessions for four of the five practices.
We also produced a video animation162 that highlights key findings for the future delivery of primary care. The animation has been sent to practice managers by the Practice Managers Association (Alderley Edge, UK) and has been well received. Publication and dissemination of our animation was accompanied by invitations to policy-makers and leading NHS England/HEE contacts to engage in discussion about the evidence behind our findings and recommendations.
We engaged with PRIMER representatives to explore how the study findings could be developed to guide patients’ decision-making through a better understanding of how to gain benefits from a wider skill mix. However, the inherent complexities that have been highlighted by this research mean that significant additional resources would be required to translate current knowledge into practical recommendations for implementation at practice level and to enhance patients’ experience. To partially bridge this gap, and for the information of our various stakeholders [the Practice Managers Association; the Association of Medical Secretaries, Practice Managers, Administrators and Receptions (London, UK); and the Royal College of General Practitioners (London, UK)], we have published two blogs. 163,164
We had an excellent platform to present selected findings from our research to delegates at the Royal College of General Practitioners Annual Conference in February 2021 and also presented at key 2021 conferences, such as the Health Services Research UK and Society for Academic Primary Care Annual Scientific Meeting.
Acknowledgements
Contributions of others
Participants
We would like to thank all the patients and staff who took time out of their extremely busy workdays to participate in our study.
Academic colleagues
We would like to acknowledge the collaborative engagement and support of academic colleagues, particularly whose expertise and specialist knowledge have assisted our quantitative analysis.
Expert Advisory Group
We would like to thank members of the Expert Advisory Group who offered support and feedback on the content and progress of the study: Kirsty Roberts (Workforce Lead for Primary Care, Greater Manchester Health and Social Care Partnership), Stephen Heaney (Practice Manager, Oldham CCG Board Member), Myra Upton (President of the Association of Medical Secretaries, Practice Managers, Administrators and Receptionists), Rachel Souter (Head of the General Practice Workforce Programme, NHS England), Dan Smith (Paramedic Practitioner, Manchester), Kellie Johnson (Practice Nursing and Care Navigation Training and Deployment, Stoke CCG), Zoe Ahearne (ANP), Sunil Aggarwal (deputy for Drew Tarmey, PA Training Course, Manchester), Ceinwen Mannall (National Lead for the General Practice Pharmacist Training Pathway), Judith Hogg (PRIMER member) and Ailsa Donnelly (PRIMER member).
Patient and public involvement
We would like to thank PRIMER and the PPG for providing a patient and public perspective. We would especially like to thank two PRIMER representatives, Ailsa Donnelly and Judith Hogg, for providing feedback throughout the project.
Administrative support
Kevin Sanderson Shortt (project manager) provided project management support (September 2018–September 2019).
Danielle Harris (project support administrator) provided administrative support (December 2019–December 2020).
Contributions of authors
Imelda McDermott (https://orcid.org/0000-0002-1949-2362) (Research Fellow) led and conducted the qualitative WP, contributed to interpretation of the case study, managed the ethics and governance of the project, and led the final report writing.
Sharon Spooner (https://orcid.org/0000-0001-6965-3673) (Clinical Lecturer) was the PI and designed and led the study, with contributions to report preparation and other outputs.
Mhorag Goff (https://orcid.org/0000-0003-4936-2881) (Research Associate) conducted the qualitative WP, contributed to interpretation of the case study, managed the literature and contributed to report writing.
Jon Gibson (https://orcid.org/0000-0003-4177-8049) (Research Fellow) conducted quantitative analysis and modelling, and contributed to report writing.
Elizabeth Dalgarno (https://orcid.org/0000-0002-3639-6268) (Research Associate) contributed to the initial updating of the literature, the data analysis of the patient survey/focus group and to the first draft of the section of the report on patient experiences (Research question 3(iii): how does increased skill mix affect patients’ experiences when accessing primary care services?).
Igor Francetic (https://orcid.org/0000-0002-2481-3749) (Research Fellow) assisted with quantitative analysis and presentation of the outcomes data.
Mark Hann (https://orcid.org/0000-0002-4508-5584) (Research Fellow) contributed to the development and interpretation of quantitative analysis and outputs.
Damian Hodgson (https://orcid.org/0000-0002-9292-5945) (Professor of Organisation Studies) contributed to the overall study design, interpretation of the study and report writing.
Anne McBride (https://orcid.org/0000-0003-1047-1319) (Professor of Employment Relations) contributed to the overall study design, interpretation of the study and report writing.
Katherine Checkland (https://orcid.org/0000-0002-9961-5317) (Professor of Health Policy and Primary Care) contributed to the overall study design, interpretation of the study and report writing.
Matt Sutton (https://orcid.org/0000-0002-6635-2127) (Chairperson in Health Economics) led the design and the delivery of the quantitative WP and contributed to report writing.
Publications
McDermott, I. Multidisciplinary teams in primary care: lessons from the development of skill mix in general practice. In Bradley LK, Warwick-Giles L, Checkland K, Coleman A, Schafheutle E, Willis S, et al. , editors. On Primary Care: General Practice, Pharmacy, Workforce. Manchester: Policy@Manchester; 2020. pp. 42–4.
Spooner S, Gibson J, Checkland K, McBride A, Hodgson DE, Hann M, et al. Regional variation in practitioner employment in general practices in England: a comparative analysis. Br J Gen Pract 2020;70:e164–71.
McDermott I, Spooner S, Checkland K. Achieving the Right Mix of Skills in General Practice: It's a Process Not a Destination. 2021. URL: https://blog.policy.manchester.ac.uk/posts/2021/10/achieving-the-right-mix-of-skills-in-general-practice-its-a-process-not-a-destination/ (accessed 4 March 2022).
Spooner S, McDermott I and Checkland K. Managing Changes in the General Practice Workforce. 2021. URL: https://blog.policy.manchester.ac.uk/posts/2021/06/managing-changes-in-the-general-practice-workforce/ (accessed 4 March 2022).
University of Manchester Faculty of Biology, Medicine and Health. Who Should I See? Managing Changes in the General Practice Workforce. 2021. URL: https://www.youtube.com/watch?v=-wEvQtgpkAE (accessed 4 March 2022).
Gibson J, Francetic I, Spooner S, Checkland K, Sutton M. Associations of primary care workforce composition with population, professional and system outcomes: retrospective cross-sectional analysis [published online ahead of print January 17 2022]. Br J Gen Pract 2022.
Data-sharing statement
The terms under which consent was sought and obtained mean that there is no access to raw data from the study. Further information can be obtained from the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HSDR programme or the Department of Health and Social Care.
References
- Chapple A, Rogers A. ‘Self-care’ and its relevance to developing demand management strategies: a review of qualitative research. Health Soc Care Community 1999;7:445-54. https://doi.org/10.1046/j.1365-2524.1999.00212.x.
- Greaves CJ, Campbell JL. Supporting self-care in general practice. Br J Gen Pract 2007;57:814-21. https://doi.org/10.3399/096016407782605018.
- Baird B, Charles A, Honeyman M, Maguire D, Das P. Understanding Pressures in General Practice. London: The King’s Fund; 2016.
- Royal College of General Practitioners (RCGP) . The 2022 GP: A Vision for General Practice in the Future NHS 2013.
- Panch T, Szolovits P, Atun R. Artificial intelligence, machine learning and health systems. J Glob Health 2018;8. https://doi.org/10.7189/jogh.08.020303.
- Bodenheimer TS, Smith MD. Primary care: proposed solutions to the physician shortage without training more physicians. Health Aff 2013;32:1881-6. https://doi.org/10.1377/hlthaff.2013.0234.
- Hobbs FDR, Bankhead C, Mukhtar T, Stevens S, Perera-Salazar R, Holt T, et al. Clinical workload in UK primary care: a retrospective analysis of 100 million consultations in England, 2007–2014. Lancet 2016;387:2323-30. https://doi.org/10.1016/S0140-6736(16)00620-6.
- Primary Care Workforce Commission . The Future of General Practice: Creating Teams for Tomorrow 2015. https://napc.co.uk/wp-content/uploads/2017/09/Future_of_primary_care.pdf (accessed 27 January 2022).
- Beech J, Bottery S, Charlesworth A, Evans H, Gershlick B, Hemmings N, et al. Closing the Gap: Key Areas for Action on the Health and Care Workforce. London: The Health Foundation, The King’s Fund and The Nuffield Trust; 2019.
- NHS England . Five Year Forward View 2014.
- NHS England . Next Steps on the NHS Five Year Forward View 2017.
- Primary Care Workforce Commission . The Future of Primary Care: Creating Teams for Tomorrow 2015.
- NHS England . General Practice Forward View 2016.
- House of Lords Select Committee on Long-term Sustainability of the NHS . The Long-Term Sustainability of the NHS and Adult Social Care Report of Session 2016–17 2017.
- National Audit Office . Improving Patient Access to General Practice 2017.
- Sibbald B, Shen J, McBride A. Changing the skill-mix of the health care workforce. J Health Serv Res Policy 2004;9:28-3. https://doi.org/10.1258/135581904322724112.
- Buchan J, O’May F. Determining Skill Mix: Practical Guidelines for Managers and Health Professionals n.d. www.who.int/hrh/en/HRDJ_4_2_07.pdf (accessed 9 February 2022).
- Buchan J, Ball J, O’May F. If changing skill mix is the answer, what is the question?. J Health Serv Res Policy 2001;6:233-8. https://doi.org/10.1258/1355819011927549.
- Cunningham J, O’Toole T, White M, Wells JSG. Conceptualizing skill mix in nursing and health care: an analysis. J Nurs Manag 2019;27:256-63. https://doi.org/10.1111/jonm.12673.
- Dubois CA, Singh D. From staff-mix to skill-mix and beyond: towards a systemic approach to health workforce management. Hum Resour Health 2009;7. https://doi.org/10.1186/1478-4491-7-87.
- Niezen MG, Mathijssen JJ. Reframing professional boundaries in healthcare: a systematic review of facilitators and barriers to task reallocation from the domain of medicine to the nursing domain. Health Policy 2014;117:151-69. https://doi.org/10.1016/j.healthpol.2014.04.016.
- Nelson PA, Martindale A, McBride A, Hodgson D. Greater Manchester Primary Care Workforce Strategy: Rapid Literature Review. Manchester: NIHR Collaboration for Leadership in Applied Health Research and Care Greater Manchester; 2017.
- Nelson PA, Bradley F, Martindale AM, McBride A, Hodgson D. Skill-mix change in general practice: a qualitative comparison of three ‘new’ non-medical roles in English primary care. Br J Gen Pract 2019;69:e489-e498. https://doi.org/10.3399/bjgp19X704117.
- van der Biezen M, Derckx E, Wensing M, Laurant M. Factors influencing decision of general practitioners and managers to train and employ a nurse practitioner or physician assistant in primary care: a qualitative study. BMC Fam Pract 2017;18. https://doi.org/10.1186/s12875-017-0587-3.
- Charter for general practice. Br Med J 1965;1. https://doi.org/10.1136/bmj.1.5436.669.
- Cartwright A, Scott R. The work of a nurse employed in a general practice. Br Med J 1961;1:807-13. https://doi.org/10.1136/bmj.1.5228.807.
- Audit Commission . A Focus on General Practice 2002.
- The Queen’s Nursing Institute . General Practice Nurses. General Practice Nurses Work in a GP Surgery As Part of a Primary Healthcare Team n.d. www.qni.org.uk/nursing-in-the-community/work-of-community-nurses/general-practice-nurse/ (accessed 27 January 2022).
- King R, Tod A, Sanders T. Development and regulation of advanced nurse practitioners in the UK and internationally. Nurs Stand 2017;32:43-50. https://doi.org/10.7748/ns.2017.e10858.
- Robertson G. Sharing the care. Nurs Stand 2006;21:22-5. https://doi.org/10.7748/ns.21.1.22.s26.
- NHS England and NHS Improvement . Network Contract Directed Enhanced Service: Additional Roles Reimbursement Scheme Guidance 2019.
- NHS England . The NHS Long Term Plan 2019.
- NHS England . Interim NHS People Plan 2019.
- NHS England . We Are the NHS: People Plan for 202021 – Action for Us All n.d. www.england.nhs.uk/publication/we-are-the-nhs-people-plan-for-2020-21-action-for-us-all/ (accessed 27 January 2022).
- NHS England and NHS Improvement . Network Contract Directed Enhanced Service: Contract Specification 2020 21 – PCN[0] Requirements and Entitlements 2020. www.england.nhs.uk/wp-content/uploads/2020/03/Network-Contract-DES-Specification-PCN-Requirements-and-Entitlements-2020-21-October-FINAL.pdf (accessed 27 January 2022).
- NHS England and NHS Improvement . Primary Care Networks Additional Roles Reimbursement Scheme: Update to Commissioner. Letter 2020.
- Salisbury H. What should GPs stop doing?. BMJ 2018;363. https://doi.org/10.1136/bmj.k4976.
- Singh C. What tasks can physicians delegate to pharmacists?. Br J Gen Pract 2019;69. https://doi.org/10.3399/bjgp19X700649.
- Yeung EY, Mohammed RS. What tasks can physicians delegate to pharmacists?. Br J Gen Pract 2018;68. https://doi.org/10.3399/bjgp18X699509.
- Drennan VM, de Lusignan S, Gage H, Gabe J, Halter M. Building an evidence base for the primary care workforce. BMJ 2018;360. https://doi.org/10.1136/bmj.k248.
- Dini L, Sarganas G, Boostrom E, Ogawa S, Heintze C, Braun V. German GPs’ willingness to expand roles of physician assistants: a regional survey of perceptions and informal practices influencing uptake of health reforms in primary health care. Fam Pract 2012;29:448-54. https://doi.org/10.1093/fampra/cmr127.
- Combes J-B, Paraponaris A, Videau Y. French GPs’ Willingness to Delegate Tasks: May Financial Incentives Balance Risk Aversion? 2019. https://ideas.repec.org/p/eru/erudwp/wp19-09.html (accessed 27 January 2022).
- Rashid C. Benefits and limitations of nurses taking on aspects of the clinical role of doctors in primary care: integrative literature review. J Adv Nurs 2010;66:1658-70. https://doi.org/10.1111/j.1365-2648.2010.05327.x.
- Nabhani-Gebara S, Fletcher S, Shamim A, May L, Butt N, Chagger S, et al. General practice pharmacists in England: integration, mediation and professional dynamics. Res Social Adm Pharm 2020;16:17-24. https://doi.org/10.1016/j.sapharm.2019.01.014.
- Evans C, Pearce R, Greaves S, Blake H. Advanced clinical practitioners in primary care in the UK: a qualitative study of workforce transformation. Int J Environ Res Public Health 2020;17. https://doi.org/10.3390/ijerph17124500.
- Baird B, Reeve H, Ross S, Honeyman M, Nosa-Ehima M, Sahib B, et al. Innovative Models of General Practice. London: The King’s Fund; 2018.
- Schottenfeld L, Petersen D, Peikes D, Ricciardi R, Burak H, McNellis R, et al. Creating Patient-Centered Team-Based Primary Care. Rockville, MD: Agency for Healthcare Research and Quality; 2016.
- Wagner EH. The role of patient care teams in chronic disease management. BMJ 2000;320:569-72. https://doi.org/10.1136/bmj.320.7234.569.
- Burrows KE, Abelson J, Miller PA, Levine M, Vanstone M. Understanding health professional role integration in complex adaptive systems: a multiple-case study of physician assistants in Ontario, Canada. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05087-8.
- Academy of Medical Royal Colleges . Developing Professional Identity in Multi-Professional Teams 2020.
- Feindel A, Rosenberg G, Steinhäuser J, Mozr C, Goetz K. Primary care practice assistants’ attitudes towards tasking shifting and their perceptions of the challenges of task shifting – development of a questionnaire. Health Soc Care Community 2019;27:e323-e333. https://doi.org/10.1111/hsc.12736.
- Miller R, Weir C, Gulati S. Transforming primary care: scoping review of research and practice. J Integr Care 2018;26:176-88. https://doi.org/10.1108/JICA-03-2018-0023.
- NHS Wales . All Wales Guidelines for Delegation 2010.
- Einola K, Alvesson M. The making and unmaking of teams. Hum Relat 2019;72:1891-919. https://doi.org/10.1177/0018726718812130.
- Norful AA, de Jacq K, Carlino R, Poghosyan L. Nurse practitioner–physician comanagement: a theoretical model to alleviate primary care strain. Ann Fam Med 2018;16:250-6. https://doi.org/10.1370/afm.2230.
- Drennan VM, Gabe J, Halter M, de Lusignan S, Levenson R. Physician associates in primary health care in England: a challenge to professional boundaries?. Soc Sci Med 2017;181:9-16. https://doi.org/10.1016/j.socscimed.2017.03.045.
- Joyce P, Arnett R, Hill A, Hooker RS. Patient willingness to be seen by a physician associate in Ireland. Int J Healthc 2018;4:41-50. https://doi.org/10.5430/ijh.v4n2p41.
- Lovink MH, Persoon A, Koopmans RTCM, Van Vught AJAH, Schoonhoven L, Laurant MGH. Effects of substituting nurse practitioners, physician assistants or nurses for physicians concerning healthcare for the ageing population: a systematic literature review. J Adv Nurs 2017;73:2084-102. https://doi.org/10.1111/jan.13299.
- Karimi-Shahanjarini A, Shakibazadeh E, Rashidian A, Hajimiri K, Glenton C, Noyes J, et al. Barriers and facilitators to the implementation of doctor–nurse substitution strategies in primary care: a qualitative evidence synthesis. Cochrane Database Syst Rev 2019;4. https://doi.org/10.1002/14651858.CD010412.pub2.
- Hyde P, McBride A, Young R, Walshe K. Role redesign: new ways of working in the NHS. Pers Rev 2005;34:697-712. https://doi.org/10.1108/00483480510623475.
- Rivett G. From Cradle to Grave: Fifty Years of the NHS. London: The King’s Fund; 1998.
- Abbott A. The System of Professions: An Essay on the Division of Expert Labor. Chicago, IL: University of Chicago Press; 1988.
- Nancarrow SA, Borthwick AM. Dynamic professional boundaries in the healthcare workforce. Sociol Health Illn 2005;27:897-919. https://doi.org/10.1111/j.1467-9566.2005.00463.x.
- Currie G, Finn R, Martin G. Professional competition and modernizing the clinical workforce in the NHS. Work Employ Soc 2009;23:267-84. https://doi.org/10.1177/0950017009102858.
- Quinlan E, Robertson S. Mutual understanding in multi-disciplinary primary health care teams. J Interprof Care 2010;24:565-78. https://doi.org/10.3109/13561820903520385.
- Jakimowicz M, Williams D, Stankiewicz G. A systematic review of experiences of advanced practice nursing in general practice. BMC Nurs 2017;16. https://doi.org/10.1186/s12912-016-0198-7.
- Lindblad E, Hallman EB, Gillsjö C, Lindblad U, Fagerström L. Experiences of the new role of advanced practice nurses in Swedish primary health care – a qualitative study. Int J Nurs Pract 2010;16:69-74. https://doi.org/10.1111/j.1440-172X.2009.01810.x.
- McMurray R. The struggle to professionalize: an ethnographic account of the occupational position of advanced nurse practitioners. Hum Relat 2010;64:801-22. https://doi.org/10.1177/0018726710387949.
- Hazen AC, Wal AW, Sloeserwij VM, Zwart DL, Gier JJ, Wit NJ, et al. Controversy and consensus on a clinical pharmacist in primary care in the Netherlands. Int J Clin Pharm 2016;38:1250-60. https://doi.org/10.1007/s11096-016-0360-z.
- Sibbald B, McBride A, BIrch S. Labour Substitution and Efficiency in Healthcare Delivery: General Principles and Key Messages. London: Centre for Workforce Intelligence; 2011.
- Anthony BF, Surgey A, Hiscock J, Williams NH, Charles JM. General medical services by non-medical health professionals: a systematic quantitative review of economic evaluations in primary care. Br J Gen Pract 2019;69:e304-e313. https://doi.org/10.3399/bjgp19X702425.
- Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev 2018;7. https://doi.org/10.1002/14651858.CD001271.pub3.
- Randall S, Crawford T, Currie J, River J, Betihavas V. Impact of community based nurse-led clinics on patient outcomes, patient satisfaction, patient access and cost effectiveness: a systematic review. Int J Nurs Stud 2017;73:24-33. https://doi.org/10.1016/j.ijnurstu.2017.05.008.
- Fuller JD, Perkins D, Parker S, Holdsworth L, Kelly B, Fragar L, et al. Systematic Review on Service Linkages in Primary Mental Health Care: Informing Australian Policy and Practice. Acton, ACT: Australian Primary Health Care Research Institute; 2009.
- Cawley JF, Hooker RS. Determinants of the physician assistant/associate concept in global health systems. Int J Healthc 2018;4:50-6. https://doi.org/10.5430/ijh.v4n1p50.
- Birch S, McBride. A, Gibson J, Sutton M. Workforce Planning: Modelling and Planning a Changing Workforce. Report Prepared for European Union As Part of MUNROS Project 2017.
- Ferrante JM, Cohen DJ, Crosson JC. Translating the patient navigator approach to meet the needs of primary care. J Am Board Fam Med 2010;23:736-44. https://doi.org/10.3122/jabfm.2010.06.100085.
- Martínez-González NA, Djalali S, Tandjung R, Huber-Geismann F, Markun S, Wensing M, et al. Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Serv Res 2014;14. https://doi.org/10.1186/1472-6963-14-214.
- Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care review. Cochrane Database Syst Rev 2005;2. https://doi.org/10.1002/14651858.CD001271.pub2.
- Paddison CAM, Abel GA, Burt J, Campbell JL, Elliott MN, Lattimer V, et al. What happens to patient experience when you want to see a doctor and you get to speak to a nurse? Observational study using data from the English General Practice Patient Survey. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-018690.
- Morris L, Moule P, Pearson J, Foster D, Walsh N. Patient views on the advanced practitioner role in primary care: a realist review. Physiotherapy 2019;105. https://doi.org/10.1016/j.physio.2018.11.089.
- Zwar N, Dennis S, Griffiths R, Perkins D, May J, Hasan I, et al. Optimising Skill-mix in the Primary Health Care Workforce for the Care of Older Australians: A Systematic Review. Acton, ACT: Australian Primary Health Care Research Institute; 2007.
- Checkland K, McDermott I, Coleman A, Warwick-Giles L, Bramwell D, Allen P, et al. Planning and managing primary care services: lessons from the NHS in England. Public Money Manag 2018;38:261-70. https://doi.org/10.1080/09540962.2018.1449467.
- Checkland K. Management in general practice – the challenge of new GMS contract. Br J Gen Pract 2004;54:734-9.
- Bond C, Bruhn H, de Bont A, van Exel J, Busse R, Sutton M, et al. The iMpact on practice, oUtcomes and costs of New roles for health pROfeSsionals: a study protocol for MUNROS. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010511.
- NHS England . Clinical Pharmacists in General Practice Pilot 2015.
- Clay H, Stern R. Making Time in General Practice. London: Primary Care Foundation and NHS Alliance; 2015.
- Nelson PA, Martindale A, McBride A, Hodgson D. Salford Primary Care Workforce Strategy: Contribution to a Safer Salford Rapid Literature Review. Manchester: NIHR Collaboration for Leadership in Applied Health Research and Care Greater Manchester; 2017.
- Freund T, Everett C, Griffiths P, Hudon C, Naccarella L, Laurant M. Skill mix, roles and remuneration in the primary care workforce: who are the healthcare professionals in the primary care teams across the world?. Int J Nurs Stud 2015;52:727-43. https://doi.org/10.1016/j.ijnurstu.2014.11.014.
- Yin RK. Case Study Research: Design and Methods. Thousand Oaks, CA: SAGE Publications Ltd; 2009.
- Stake RE. The Art of Case Study Research. Thousand Oaks, CA: SAGE Publications Ltd; 1995.
- Segar J, Checkland K, Coleman A, McDermott I, Russell J, Greenhalgh T, et al. Case Study Evaluation: Past, Present and Future Challenges. Bingly: Emerald Group Publishing Ltd; 2015.
- McDermott I, Checkland K, Coleman A, Osipovič D, Petsoulas C, Perkins N. Engaging GPs in commissioning: realist evaluation of the early experiences of Clinical Commissioning Groups in the English NHS. J Health Serv Res Policy 2017;22:4-11. https://doi.org/10.1177/1355819616648352.
- Checkland K, McDermott I, Coleman A, Perkins N. Complexity in the new NHS: longitudinal case studies of CCGs in England. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010199.
- Denzin NK. The Research Act: A Theoretical Introduction to Sociological Methods. Chicago, IL: Aldine; 1970.
- Bell E, Bryman A. The ethics of management research: an exploratory content analysis. Br J Manage 2007;18:63-77. https://doi.org/10.1111/j.1467-8551.2006.00487.x.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341. https://doi.org/10.1136/bmj.c4587.
- Hammersley M. The Politics of Social Research. Thousand Oaks, CA: SAGE Publications Ltd; 1995.
- Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res 2006;16:377-94. https://doi.org/10.1177/1049732305285708.
- Heslehurst N, Dinsdale S, Sedgewick G, Simpson H, Sen S, Summerbell CD, et al. An evaluation of the implementation of maternal obesity pathways of care: a mixed methods study with data integration. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0127122.
- Spooner S, Gibson J, Checkland K, McBride A, Hodgson DE, Hann M, et al. Regional variation in practitioner employment in general practices in England: a comparative analysis. Br J Gen Pract 2020;70:e164-e71. https://doi.org/10.3399/bjgp20X708185.
- NHS England . Outcome of 2017 18 GMS Contract Negotiations 2017.
- Zellner A. An efficient method of estimating seemingly unrelated regressions and tests for aggregation bias. J Am Stat Assoc 1962;57:348-68. https://doi.org/10.1080/01621459.1962.10480664.
- Mansournia MA, Altman DG. Inverse probability weighting. BMJ 2016;352. https://doi.org/10.1136/bmj.i189.
- NHS England . Clinical Pharmacists 2019.
- Health Careers . Healthcare Assistant n.d. www.healthcareers.nhs.uk/explore-roles/healthcare-support-worker/roles-healthcare-support-worker/healthcare-assistant (accessed 5 January 2021).
- NHS Digital . General Practice Workforce 2019. https://digital.nhs.uk/data-and-information/publications/statistical/general-and-personal-medical-services (accessed 5 February 2021).
- NHS Digital . NWRS User Guidance. Data Entry Module Frequently Asked Questions (FAQs) 2020. www.gmthub.co.uk/wp-content/uploads/2021/03/nwrs-dataentrymodulefaqsv3.pdf (accessed 1 February 2022).
- Gibson J, Sutton M, Spooner S, Checkland K. Ninth National GP Worklife Survey. Manchester: University of Manchester; 2018.
- Sutcliffe D, Lester H, Hutton J, Stokes T. NICE and the Quality and Outcomes Framework (QOF) 2009–2011. Qual Prim Care 2012;20:47-55.
- Barber N. What constitutes good prescribing?. BMJ 1995;310:923-5. https://doi.org/10.1136/bmj.310.6984.923.
- Pont LG, Morgan TK, Williamson M, Haaijer FM, van Driel ML. Validity of prescribing indicators for assessing quality of antibiotic use in Australian general practice. Int J Pharm Pract 2017;25:66-74. https://doi.org/10.1111/ijpp.12318.
- NHS Business Services Authority . Prescribing Costs for 2019 2019. www.nhsbsa.nhs.uk/prescribing-costs-2019-published (accessed 6 January 2021).
- NHS Digital . Hospital Episode Statistics (HES) n.d. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics (accessed 6 January 2021).
- NHS Digital . NHS Payments to General Practice Series 2019 20 n.d. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-payments-to-general-practice (accessed 26 January 2021).
- NHS Digital . Practice Level Prescribing – Glossary of Terms n.d. https://digital.nhs.uk/data-and-information/areas-of-interest/prescribing/practice-level-prescribing-in-england-a-summary/practice-level-prescribing-glossary-of-terms#actual-cost (accessed 26 January 2021).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2019. Canterbury: PSSRU, University of Kent; 2019.
- Delhy R, Dor A, Pittman P. The impact of nursing staff on satisfaction scores for U.S. hospitals: a production function approach. Med Care Res Rev 2020;78:672-83. https://doi.org/10.1177/1077558720950572.
- Carey K. A panel data design for estimation of hospital cost functions. Rev Econ Stat 1997;79:443-53. https://doi.org/10.1162/003465300556850.
- NHS England . Technical Guide to CCG Allocations 2019–20 to 2023 24: Spreadsheet Files for CCG Allocations 2019–20 to 2023 24 2019. www.england.nhs.uk/publication/technical-guide-to-ccg-allocations-2019-20-to-2023-24-spreadsheet-files-for-ccg-allocations-2019-20-to-2023-24 (accessed 28 February 2022).
- Pollitt C, Harrison S, Hunter DJ, Marnoch G. No hiding place: on the discomforts of researching the contemporary policy process. J Soc Policy 1990;19:169-90. https://doi.org/10.1017/s0047279400001987.
- Booker M, Voss S. Models of paramedic involvement in general practice. Br J Gen Pract 2019;69:477-8. https://doi.org/10.3399/bjgp19X705605.
- Limb M. Physician assistants can lighten doctors’ workload but are a challenge to professional boundaries. BMJ 2016;354. https://doi.org/10.1136/bmj.i4664.
- Spilsbury K, Meyer J. Defining the nursing contribution to patient outcome: lessons from a review of the literature examining nursing outcomes, skill mix and changing roles. J Clin Nurs 2001;10:3-14. https://doi.org/10.1046/j.1365-2702.2001.00423.x.
- Eaton G, Wong G, Williams V, Roberts N, Mahtani KR. Contribution of paramedics in primary and urgent care: a systematic review. Br J Gen Pract 2020;70:e421-e426. https://doi.org/10.3399/bjgp20X709877.
- Phillips CB, Pearce C, Hall S, Kljakovic M, Sibbald B, Dwan K, et al. Enhancing care, improving quality: the six roles of the general practice nurse. Med J Aust 2009;191:92-7. https://doi.org/10.5694/j.1326-5377.2009.tb02701.x.
- Dury C, Hall C, Danan JL, Mondoux J, Aguiar Barbieri-Figueiredo MC, Costa MA, et al. Specialist nurse in Europe: education, regulation and role. Int Nurs Rev 2014;61:454-62. https://doi.org/10.1111/inr.12123.
- Richardson G, Maynard A, Cullum N, Kindig D. Skill mix changes: substitution or service development?. Health Policy 1998;45:119-32. https://doi.org/10.1016/S0168-8510(98)00038-4.
- Bienkowska-Gibbs T, King S, Saunders C, Henham M-L. New Organisational Models of Primary Care to Meet the Future Needs of the NHS: A Brief Overview of Recent Reports 2015.
- Gagnon MP, Nsangou vÉR, Payne-Gagnon J, Grenier S, Sicotte C. Barriers and facilitators to implementing electronic prescription: a systematic review of user groups’ perceptions. J Am Med Inform Assoc 2014;21:535-41. https://doi.org/10.1136/amiajnl-2013-002203.
- Holten Møller, NLaV S, Dugdale JCM, Grasso MA, Boujut JF, Hassanaly P. From Research to Practice in the Design of Cooperative Systems: Results and Open Challenges. London: Springer London; 2012.
- Grant S, Checkland K, Bowie P, Guthrie B. The role of informal dimensions of safety in high-volume organisational routines: an ethnographic study of test results handling in UK general practice. Implement Sci 2017;12. https://doi.org/10.1186/s13012-017-0586-8.
- Bailey S, Checkland K, Hodgson D, McBride A, Elvey R, Parkin S, et al. The policy work of piloting: mobilising and managing conflict and ambiguity in the English NHS. Soc Sci Med 2017;179:210-17. https://doi.org/10.1016/j.socscimed.2017.02.002.
- Tierney S, Wong G, Mahtani KR. Current understanding and implementation of ‘care navigation’ across England: a cross-sectional study of NHS clinical commissioning groups. Br J Gen Pract 2019;69:e675-e681. https://doi.org/10.3399/bjgp19X705569.
- Havard J. How Care Navigation Can Help GP Practices Manage Demand 2019. www.gponline.com/care-navigation-help-gp-practices-manage-demand/article/1522712 (accessed 1 February 2022).
- Health Education England . Care Navigation: A Competency Framework 2016.
- Cardozo LJ, Steinberg J, Lepczyk MB, Binns-Emerick L, Cardozo Y, Aranha AN. Improving preventive health care in a medical resident practice. Arch Intern Med 1998;158:261-4. https://doi.org/10.1001/archinte.158.3.261.
- Duncan P, Ridd MJ, McCahon D, Guthrie B, Cabral C. Barriers and enablers to collaborative working between GPs and pharmacists: a qualitative interview study. Br J Gen Pract 2020;70:e155-e163. https://doi.org/10.3399/bjgp20X708197.
- Bohmer RM, Imison C. Lessons from England’s health care workforce redesign: no quick fixes. Health Aff 2013;32:2025-31. https://doi.org/10.1377/hlthaff.2013.0553.
- Bornhöft L, Larsson ME, Thorn J. Physiotherapy in primary care triage – the effects on utilization of medical services at primary health care clinics by patients and sub-groups of patients with musculoskeletal disorders: a case–control study. Physiother Theory Pract 2015;31:45-52. https://doi.org/10.3109/09593985.2014.932035.
- Desjardins-Charbonneau A, Roy JS, Thibault J, Ciccone VT, Desmeules F. Acceptability of physiotherapists as primary care practitioners and advanced practice physiotherapists for care of patients with musculoskeletal disorders: a survey of a university community within the province of Quebec. BMC Musculoskelet Disord 2016;17. https://doi.org/10.1186/s12891-016-1256-8.
- Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ 2003;327:1219-21. https://doi.org/10.1136/bmj.327.7425.1219.
- Halter M, Drennan VM, Joly LM, Gabe J, Gage H, de Lusignan S. Patients’ experiences of consultations with physician associates in primary care in England: a qualitative study. Health Expect 2017;20:1011-19. https://doi.org/10.1111/hex.12542.
- Morris L, Moule P, Pearson J, Foster D, Walsh N. Patient acceptability of the physiotherapy first contact practitioner role in primary care: a realist informed qualitative study. Musculoskeletal Care 2021;19:38-51. https://doi.org/10.1002/msc.1505.
- Imison C, Castle-Clarke S, Watson R. Reshaping the Workforce to Deliver the Care Patients Need. London: Nuffield Trust; 2016.
- McDevitt J, Melby V. An evaluation of the quality of emergency nurse practitioner services for patients presenting with minor injuries to one rural urgent care centre in the UK: a descriptive study. J Clin Nurs 2015;24:523-35. https://doi.org/10.1111/jocn.12639.
- Griffiths P, Murrells T, Maben J, Jones S, Ashworth M. Nurse staffing and quality of care in UK general practice: cross-sectional study using routinely collected data. Br J Gen Pract 2010;60:36-48. https://doi.org/10.3399/bjgp10X482086.
- Nkansah N, Mostovetsky O, Yu C, Chheng T, Beney J, Bond CM, et al. Effect of outpatient pharmacists’ non-dispensing roles on patient outcomes and prescribing patterns. Cochrane Database Syst Rev 2010;7. https://doi.org/10.1002/14651858.CD000336.pub2.
- Grant A, Sullivan F, Dowell J. An ethnographic exploration of influences on prescribing in general practice: why is there variation in prescribing practices?. Implement Sci 2013;8. https://doi.org/10.1186/1748-5908-8-72.
- Bush J, Langley CA, Jenkins D, Johal J, Huckerby C. Clinical pharmacists in general practice: an initial evaluation of activity in one English primary care organisation. Int J Pharm Pract 2018;26:501-6. https://doi.org/10.1111/ijpp.12426.
- Rankin A, Cadogan CA, Patterson SM, Kerse N, Cardwell CR, Bradley MC, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev 2018;9. https://doi.org/10.1002/14651858.CD008165.pub4.
- Luetsch K, Rowett D, Twigg MJ. A realist synthesis of pharmacist-conducted medication reviews in primary care after leaving hospital: what works for whom and why?. BMJ Qual Saf 2021;30:418-30. https://doi.org/10.1136/bmjqs-2020-011418.
- Whittaker W, Anselmi L, Kristensen SR, Lau YS, Bailey S, Bower P, et al. Associations between extending access to primary care and emergency department visits: a difference-in-differences analysis. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1002113.
- Gregory ST, Menser T. Burnout among primary care physicians: a test of the areas of worklife model. J Healthc Manag 2015;60:133-48. https://doi.org/10.1097/00115514-201503000-00009.
- Hall LH, Johnson J, Watt I, O’Connor DB. Association of GP wellbeing and burnout with patient safety in UK primary care: a cross-sectional survey. Br J Gen Pract 2019;69:e507-e514. https://doi.org/10.3399/bjgp19X702713.
- Tsiachristas A, Wallenburg I, Bond CM, Elliot RF, Busse R, van Exel J, et al. Costs and effects of new professional roles: evidence from a literature review. Health Policy 2015;119:1176-87. https://doi.org/10.1016/j.healthpol.2015.04.001.
- NHS England . General and Personal Medical Services, England – Data Quality Statement (Historic) 2018.
- Atkin K, Lunt N. Negotiating the role of the practice nurse in general practice. J Adv Nurs 1996;24:498-505. https://doi.org/10.1046/j.1365-2648.1996.02179.x.
- Crossman S, Pfeil M, Moore J, Howe A. A case study exploring employment factors affecting general practice nurse role development. Prim Health Care Res Dev 2016;17:87-9. https://doi.org/10.1017/S1463423615000304.
- Gibson J, Francetic I, Spooner S, Checkland K, Sutton M. Primary care workforce composition and population, professional, and system outcomes: a retrospective cross-sectional analysis. Br J Gen Pract 2022. https://doi.org/10.3399/BJGP.2021.0593.
- Bradley LK, Warwick-Giles L, Checkland K, Spooner S, McDermott I, . On Primary Care: General Practice, Pharmacy, Workforce. Manchester: Policy@Manchester; 2020.
- University of Manchester Faculty of Biology, Medicine and Health . Who Should I See? Managing Changes in the General Practice Workforce 2021. https://www.youtube.com/watch?v=-wEvQtgpkAE (accessed 4 March 2022).
- Spooner S, McDermott I, Checkland K. Managing Changes in the General Practice Workforce 2021. https://blog.policy.manchester.ac.uk/posts/2021/06/managing-changes-in-the-general-practice-workforce/ (accessed 4 March 2022).
- McDermott I, Spooner S, Checkland K. Achieving the Right Mix of Skills in General Practice: It’s a Process Not a Destination 2021. https://blog.policy.manchester.ac.uk/posts/2021/10/achieving-the-right-mix-of-skills-in-general-practice-its-a-process-not-a-destination/ (accessed 4 March 2022).
Appendix 1 Composition of practice workforce
FIGURE 28.
Total FTE by practitioner type.
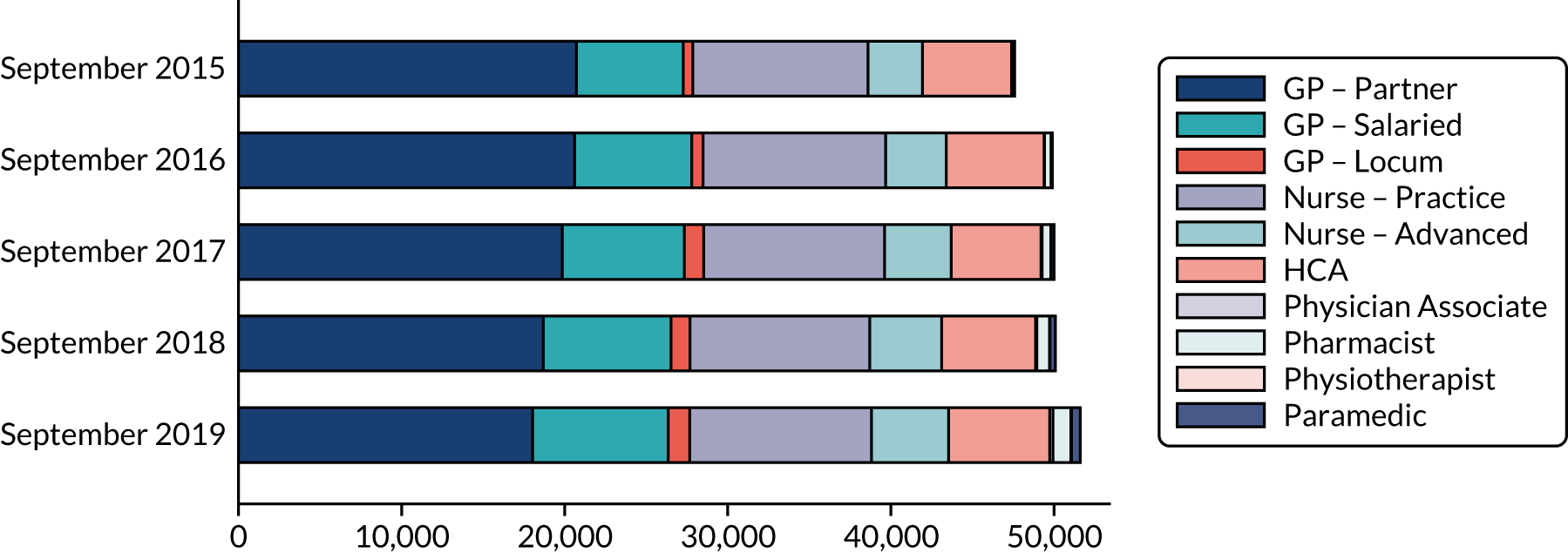
FIGURE 29.
Full-time equivalent by practitioner type PTP.
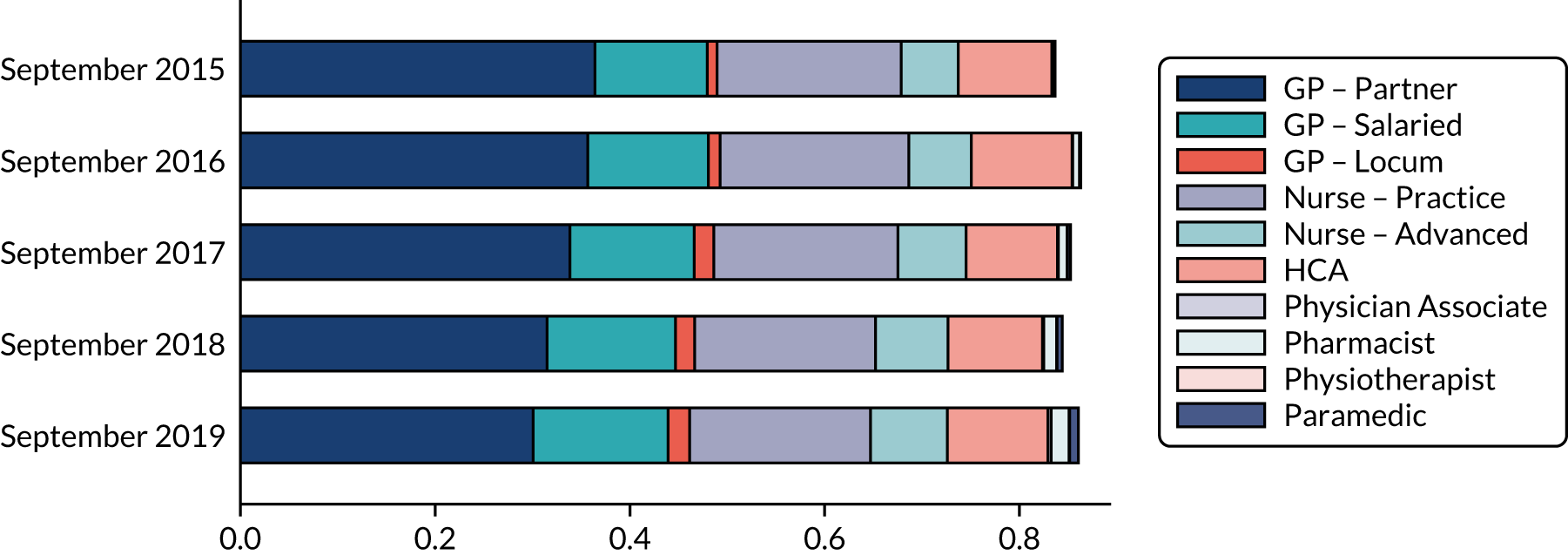
FIGURE 30.
Proportion of practice with worker role (September 2019).

Appendix 2 Longitudinal analysis
This section presents the results of the analyses for the different outcomes.
How is patient satisfaction associated with workforce composition?
Similarly to the cross-sectional results (Table 23 and Figure 31), Figure 32 shows that practices with smaller decreases in GP FTE PTP have a greater improvement in the proportion of patients reporting very good or fairly good experience of making an appointment and with the overall experience at the general practice. On the other hand, changes in nurse and DPC FTE PTP do not appear to show any association with patients’ satisfaction.
| Staff | n | Mean | SD | p10 | p25 | p50 | p75 | p90 |
|---|---|---|---|---|---|---|---|---|
| Change in GP FTE | 4334 | 0.78 | 2.32 | –1.36 | –0.40 | 0.39 | 1.70 | 3.24 |
| Change in nurse FTE | 4334 | 0.42 | 1.52 | –0.77 | –0.19 | 0.13 | 0.81 | 1.71 |
| Change in DPC FTE | 4334 | 0.57 | 1.58 | –0.52 | 0.00 | 0.16 | 0.93 | 2.05 |
| Change in total FTE | 4334 | 1.77 | 4.01 | –1.21 | –0.16 | 1.04 | 2.82 | 5.22 |
FIGURE 31.
Change in question 18 of the GPPS: overall experience of making an appointment – 2015–19. (a) GPs; (b) nurses; and (c) DPC staff.

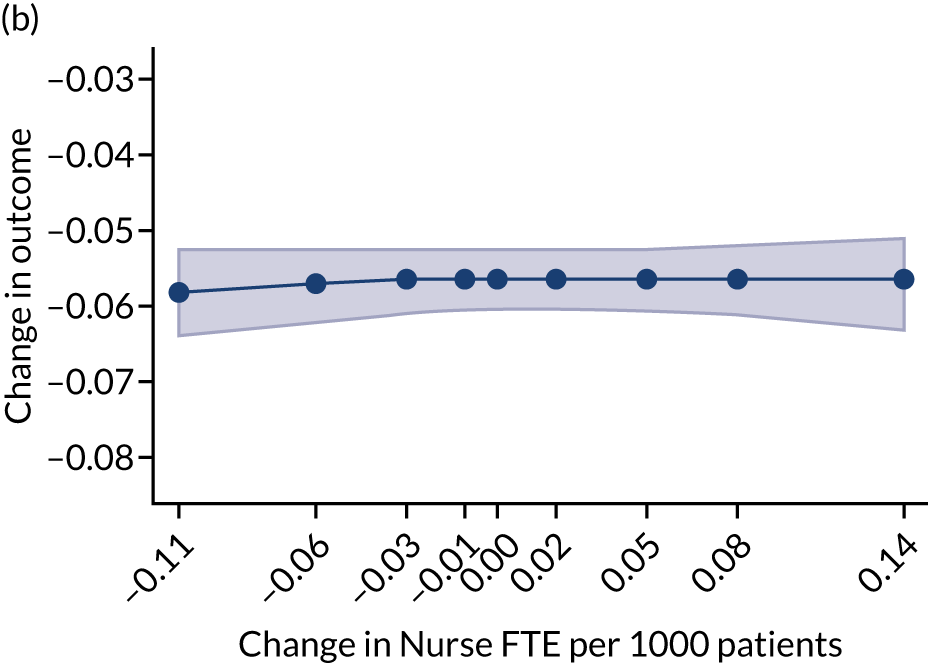
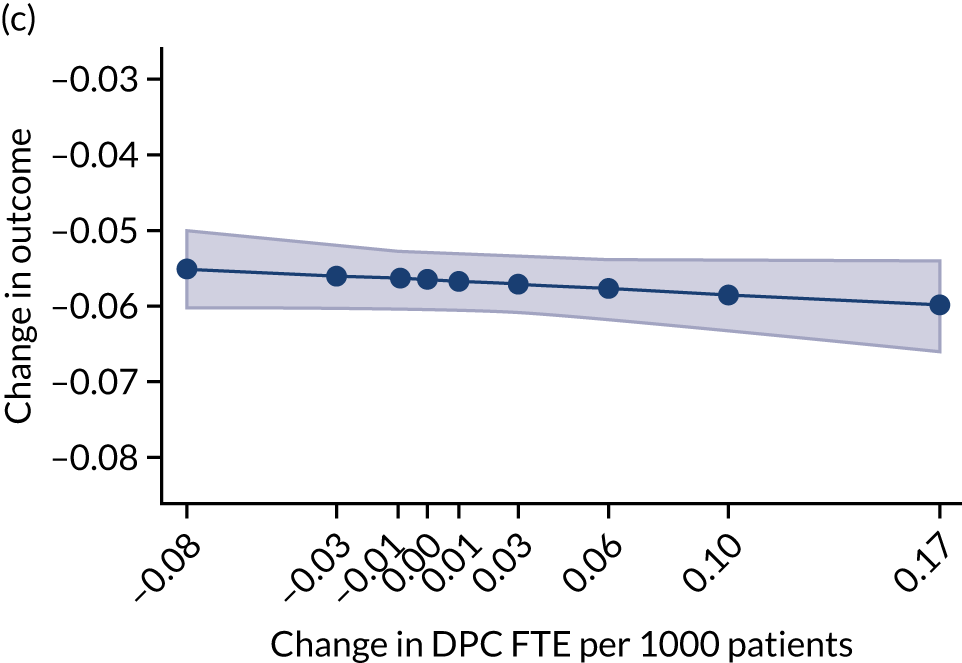
FIGURE 32.
Change in question 28 of the GPPS: overall experience of general practice – 2015–19. (a) GPs; (b) nurses; and (c) DPC staff.

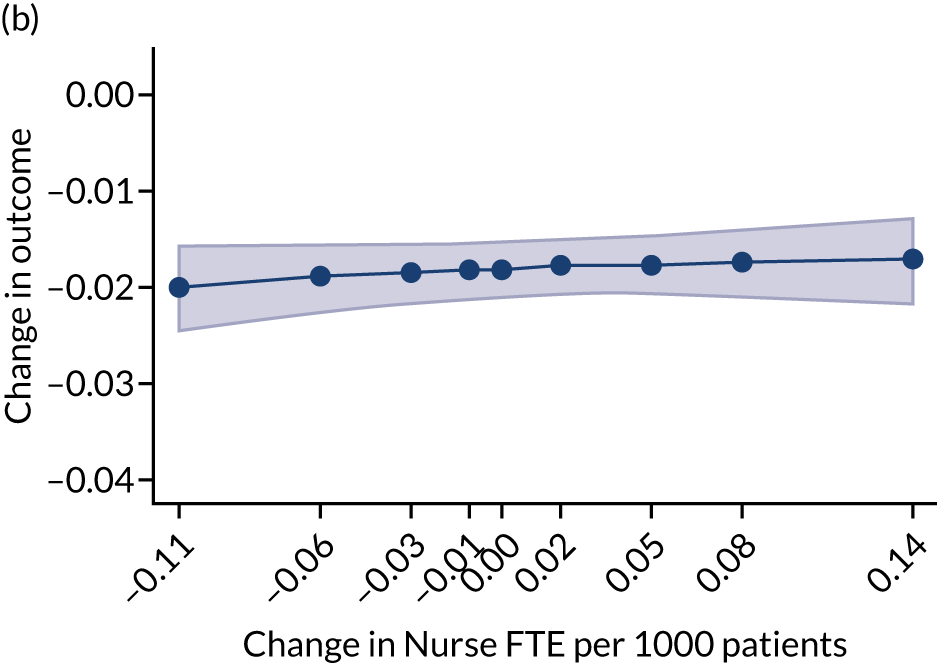
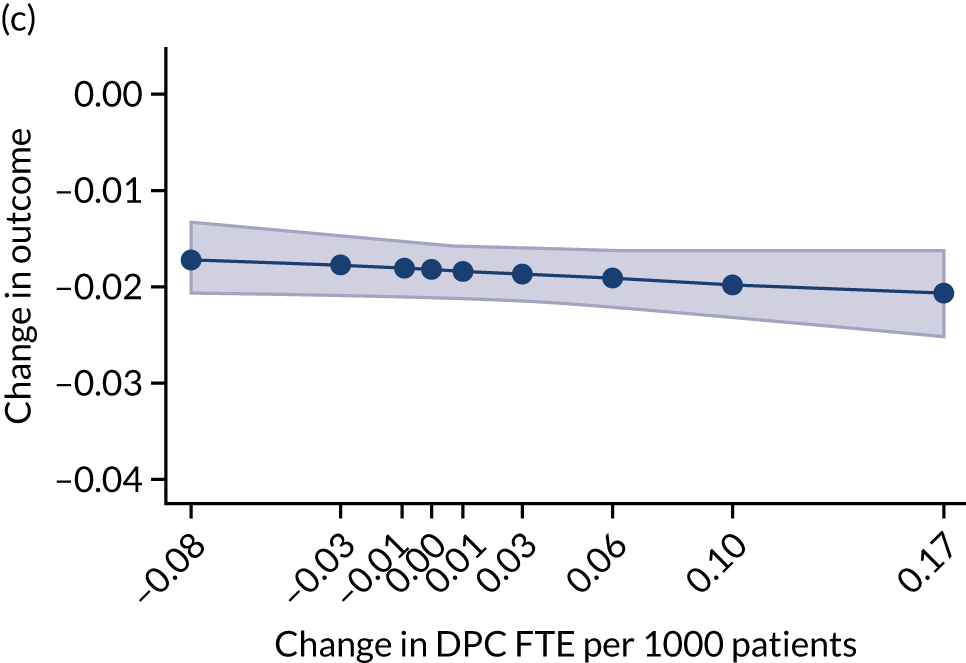
How is achievement across the clinical sections of Quality and Outcomes Framework associated with workforce composition?
The analysis on the change in percentage of QOF points achieved also shows results consistent with those obtained for the cross-sectional analysis. GP and nurse FTE show a slight positive association, meaning that, on average, increases in staff FTE PTP are associated with a higher increase in percentage of QOF points. The analysis does not reveal clear patterns in relation to DPC FTE for this outcome (Figure 33).
FIGURE 33.
Change in QOF: total achievement (%) – 2015–19. (a) GPs; (b) nurses; and (c) DPC staff.
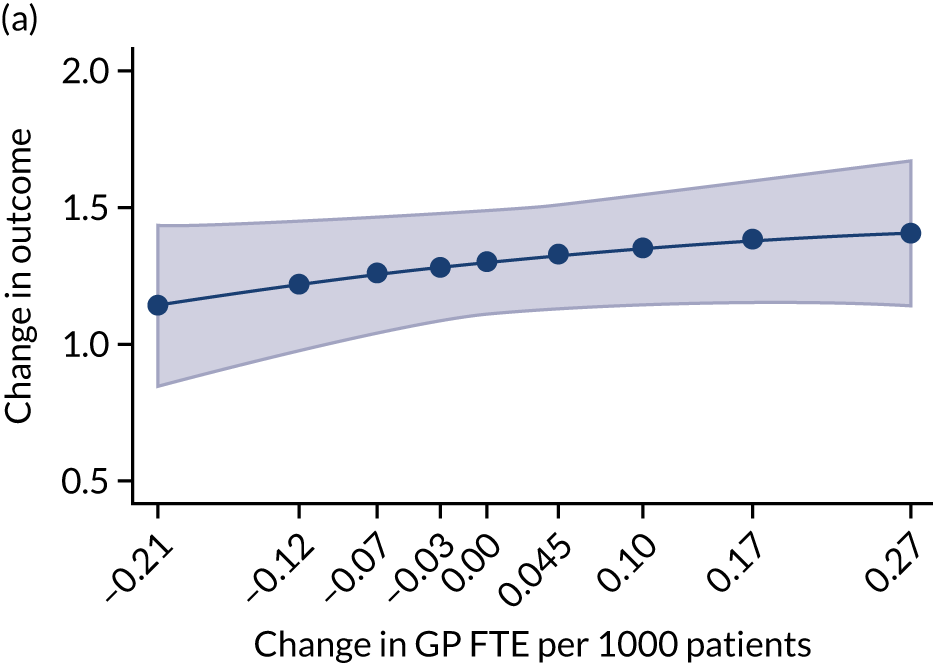
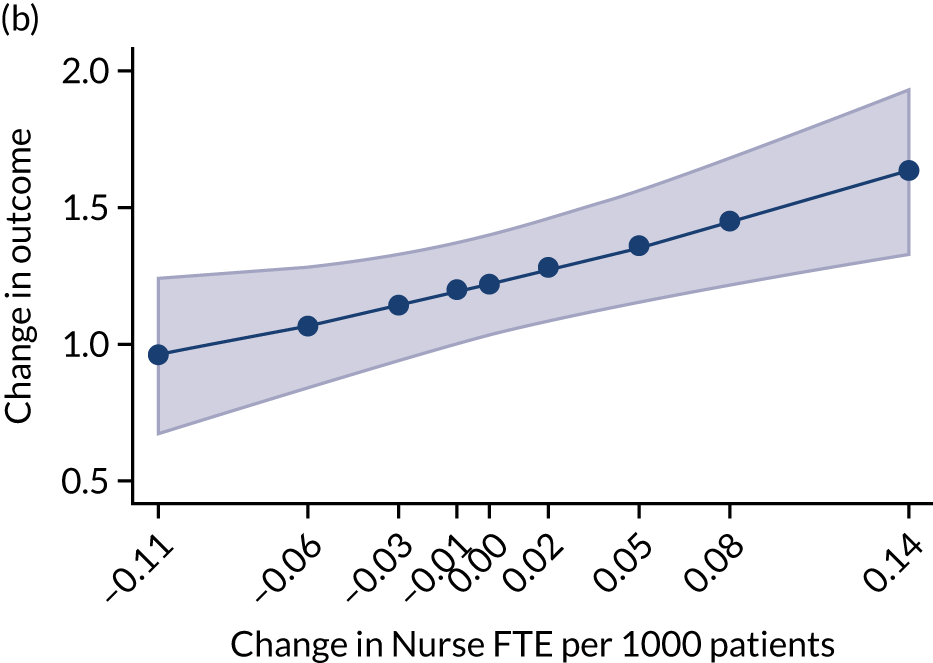
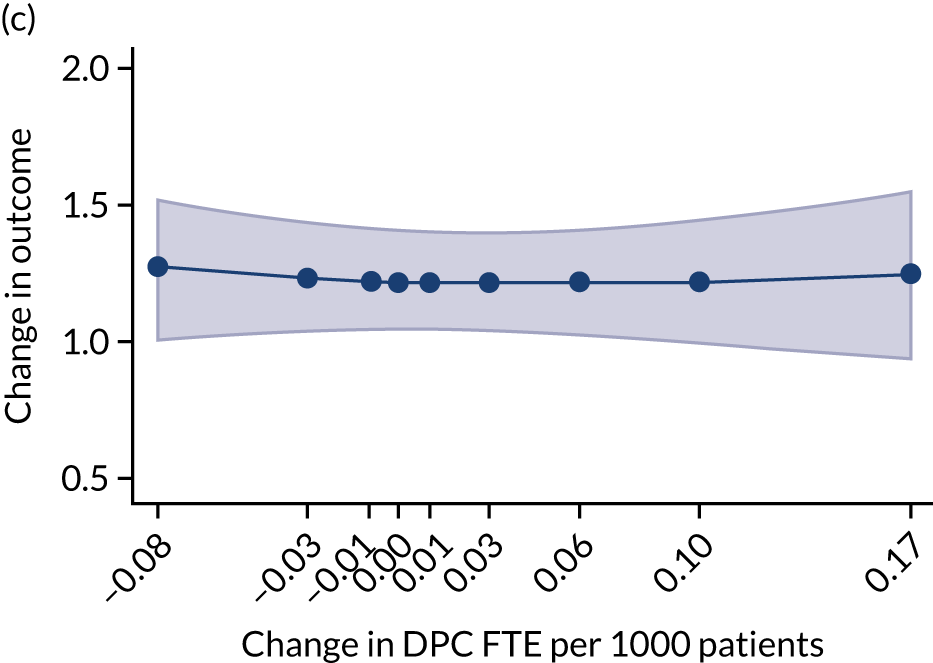
How are selected prescribing measures associated with workforce composition?
With regard to the prescription of broad- to narrow-spectrum antibiotics (Figure 34), the longitudinal patterns seem to depart slightly from the cross-sectional results. In fact, increases in nurse FTE PTP seem to be associated with stronger reductions in prescription of antibiotics.
FIGURE 34.
Change in percentage of broad- to narrow-spectrum antibiotics: 2016–19. (a) GPs; (b) nurses; (c) DPC staff (without pharmacists); and (d) pharmacists.
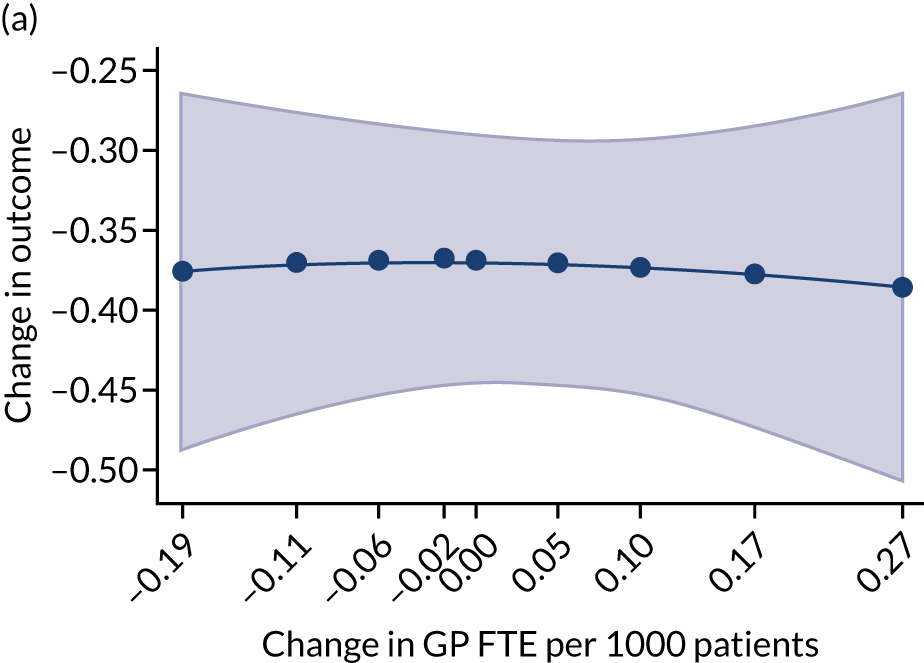
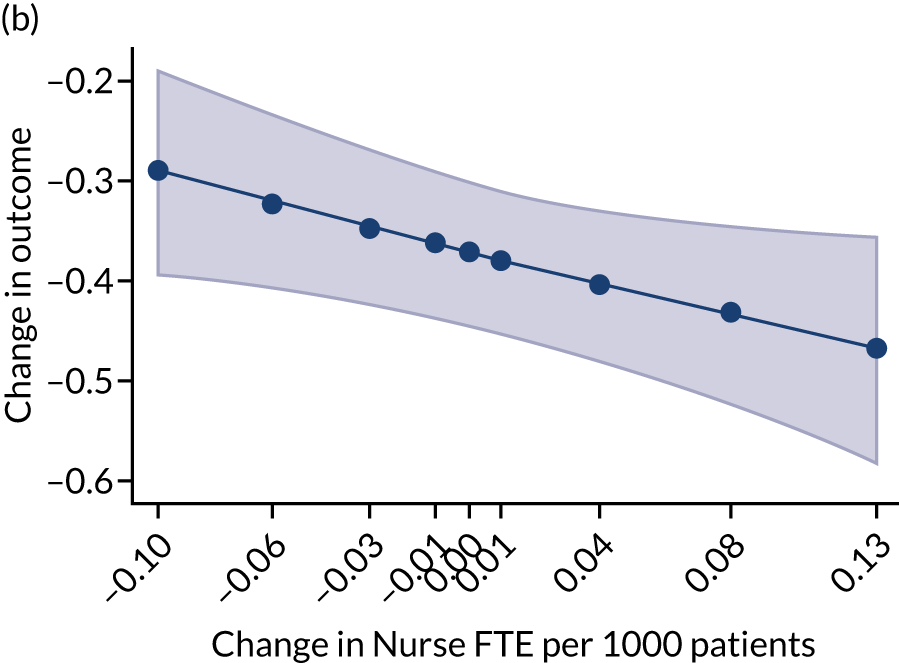
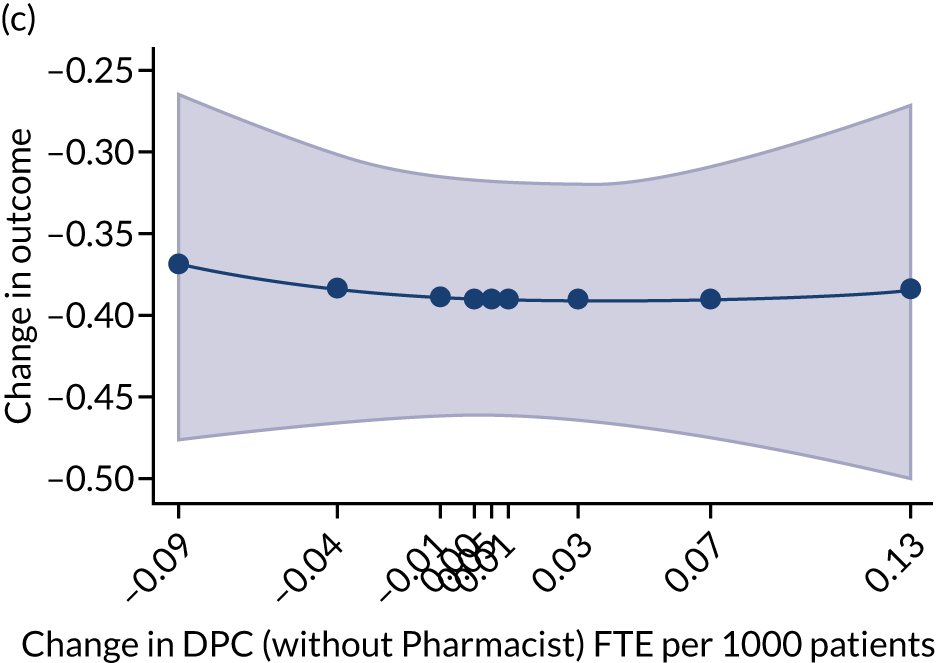
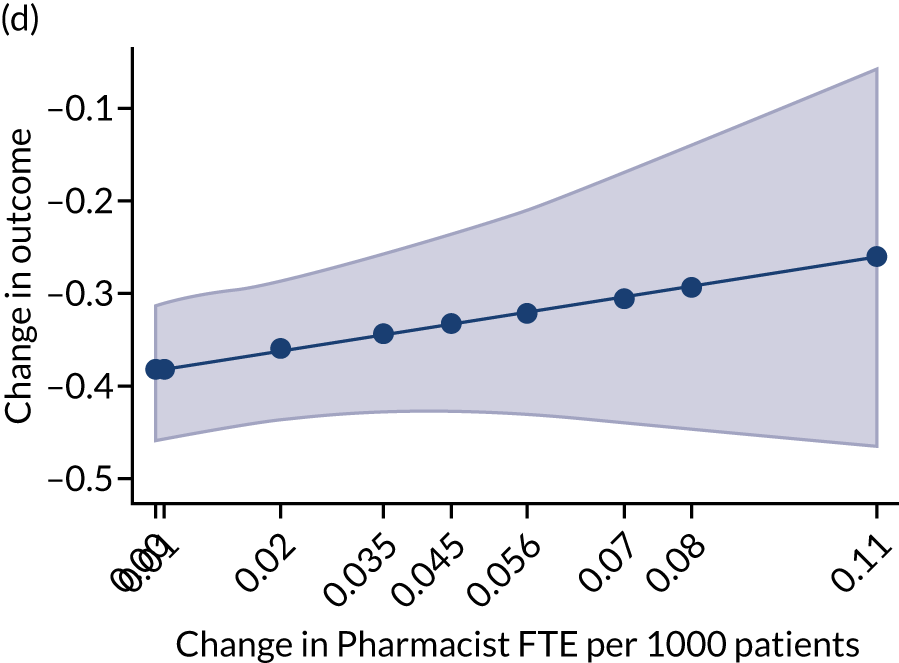
Regarding the changes in volume of prescribing (Figure 35), the main difference with the static cross-sectional analysis is related to an association between increases in GP FTE and total items prescribed per ASTRO-PU. Similar to the results of the cross-sectional analysis, increases in nurse and DPC staff (without pharmacists) FTE are positively associated to increases in prescribing. On the other hand, higher increases in CP FTE seems to reduce prescribing slightly more strongly, overall.
FIGURE 35.
Change in volume of prescribing: total items prescribed per ASTRO-PU – 2016–19. (a) GPs; (b) nurses; (c) DPC staff (without pharmacists); and (d) pharmacists.
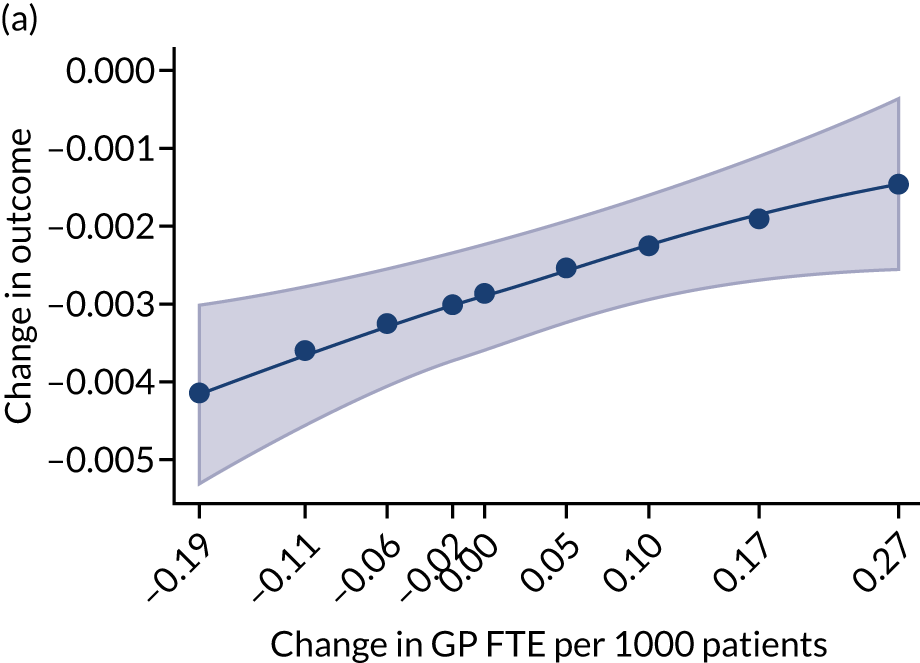
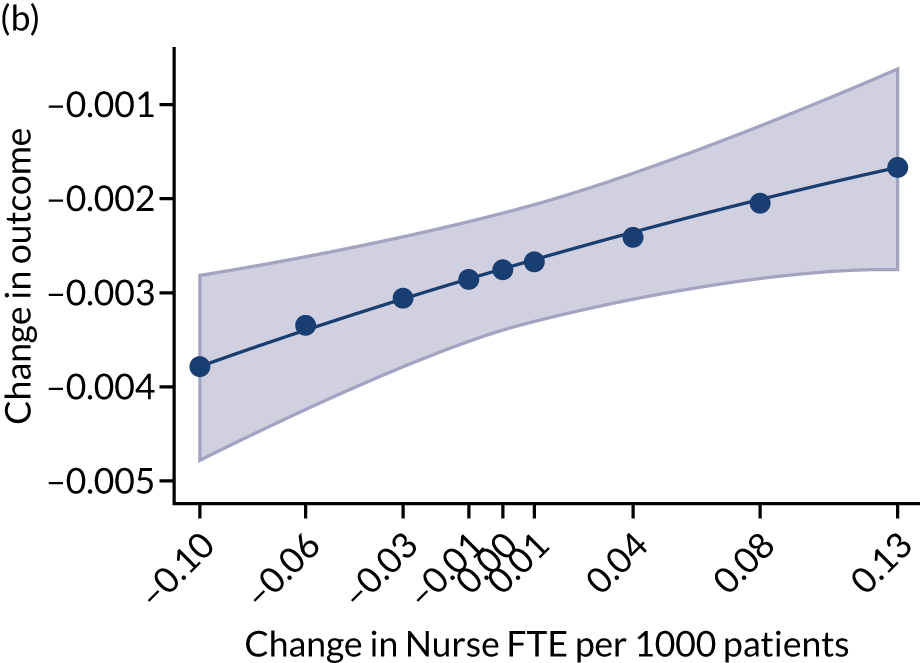
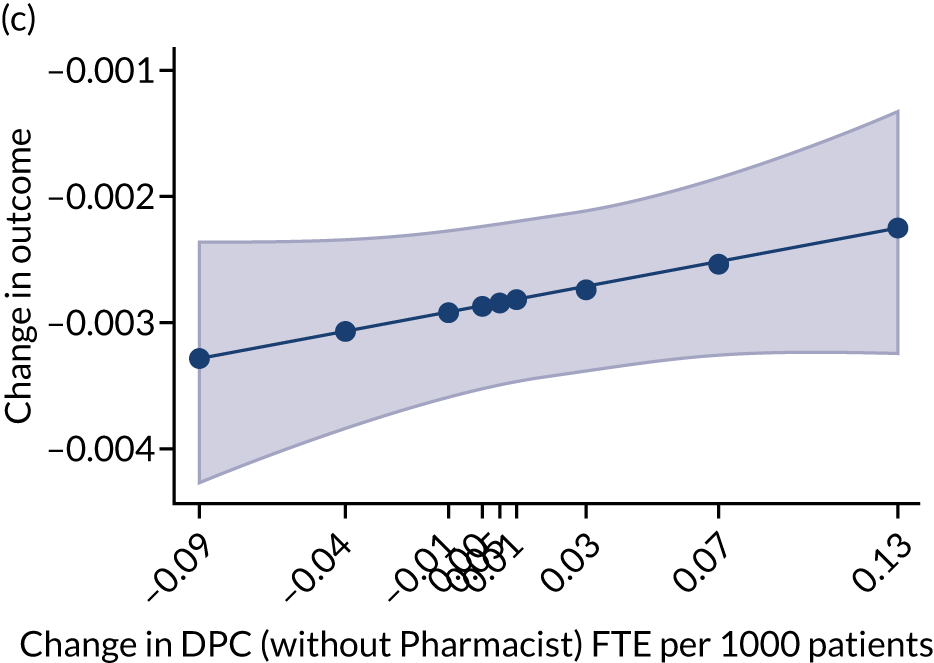
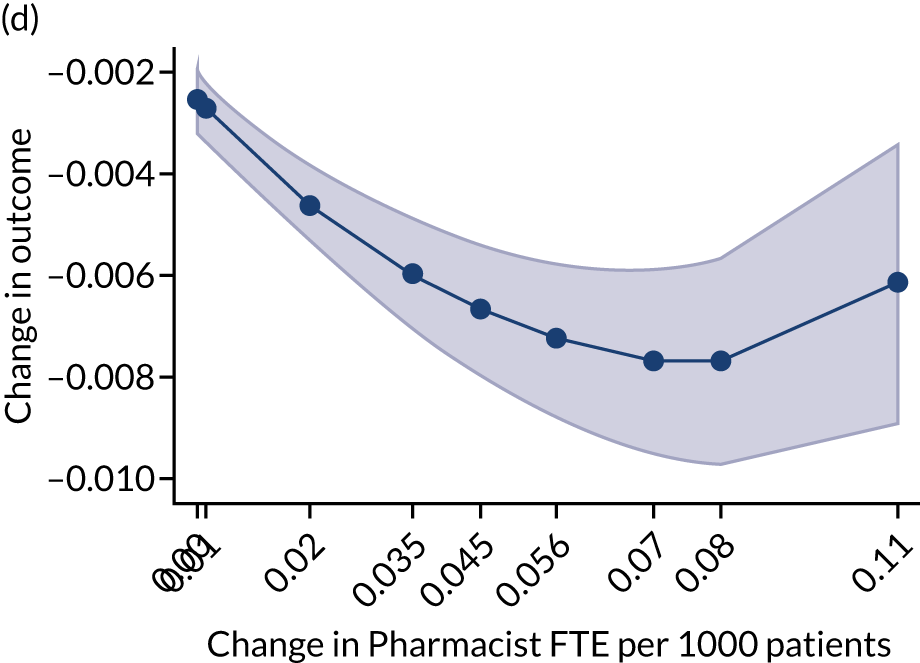
Changes in prescribing costs per item (Figure 36) show a negative association with changes in all categories of staff FTE PTP. This diverges from the cross-sectional results, which showed a slightly positive association between costs per item prescribed and nurse and DPC staff (without pharmacists) FTE PTP.
FIGURE 36.
Change in prescribing cost per item ( = cost per ASTRO-PU/items per ASTRO-PU): 2016–19. (a) GPs; (b) nurses; (c) DPC staff (without pharmacists); and (d) pharmacists.
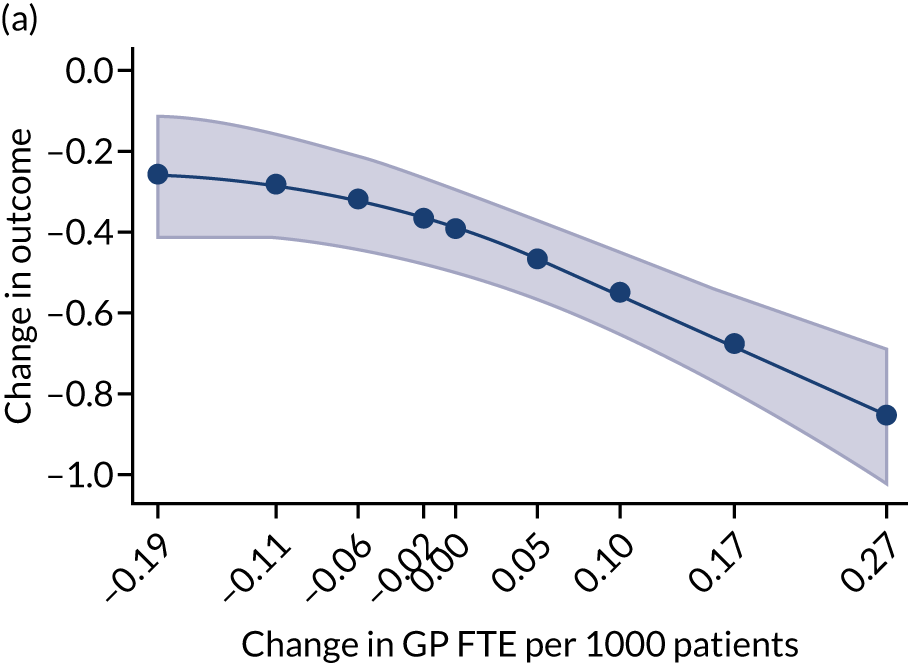
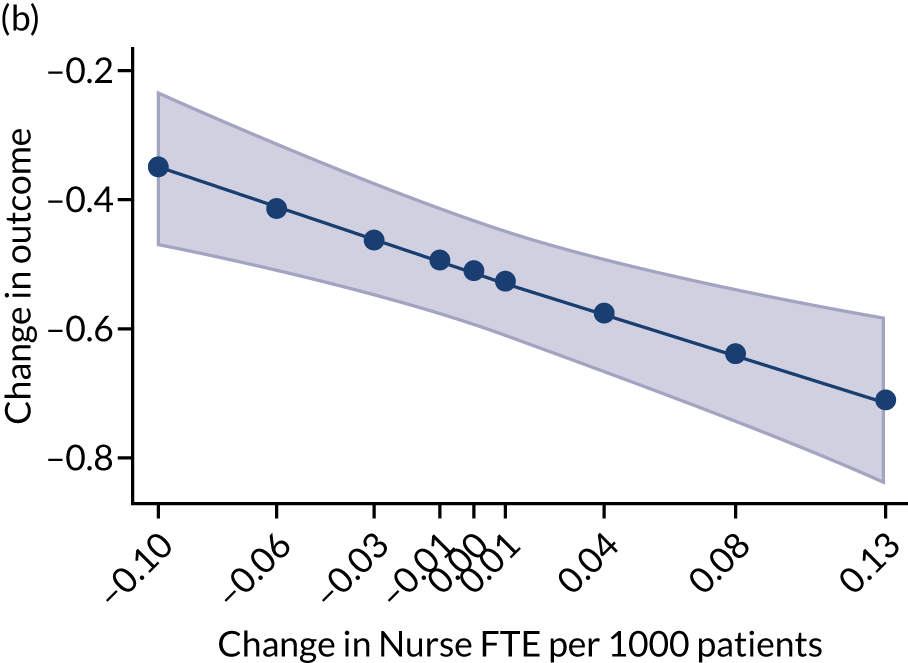
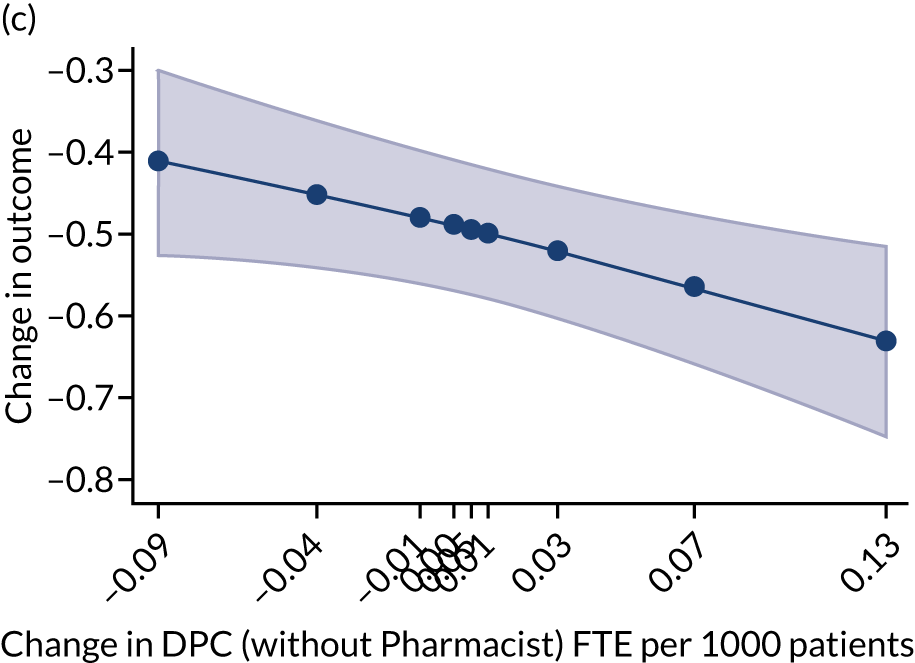
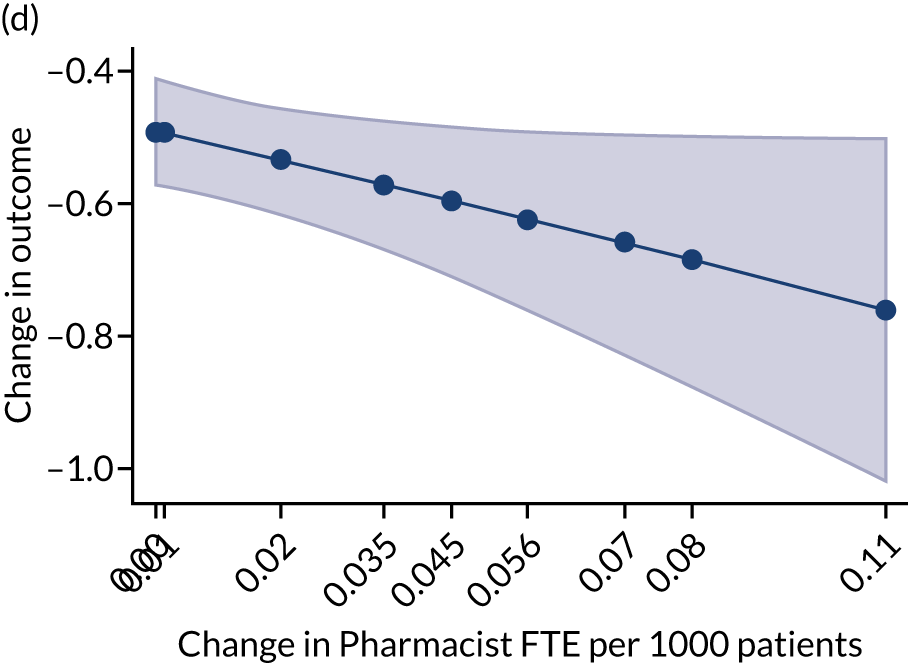
How is practice population utilisation of hospital services associated with workforce composition?
Interestingly, the changes in A&E attendance PTP (Figure 37), admissions PTP (Figure 38) and outpatient attendances PTP (Figure 39) all show positive associations with changes in staffing. This means that across all categories of staff (i.e. GP, nurse and DPC), higher increases in FTE PTP are associated over time with higher increases in attendances and admissions. The longitudinal analysis on these outcomes seems to offer starkly different results compared with the cross-sectional results, which are more prone to suffer from bias from unobserved heterogeneity.
FIGURE 37.
Change in A&E attendances PTP: 2015–17. (a) GPs; (b) nurses; and (c) DPC staff.
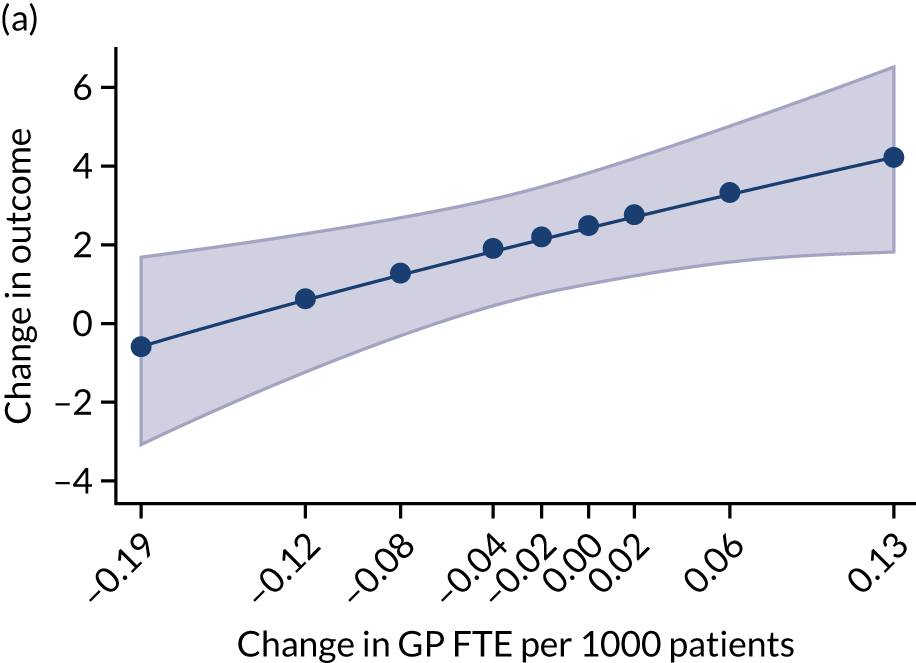
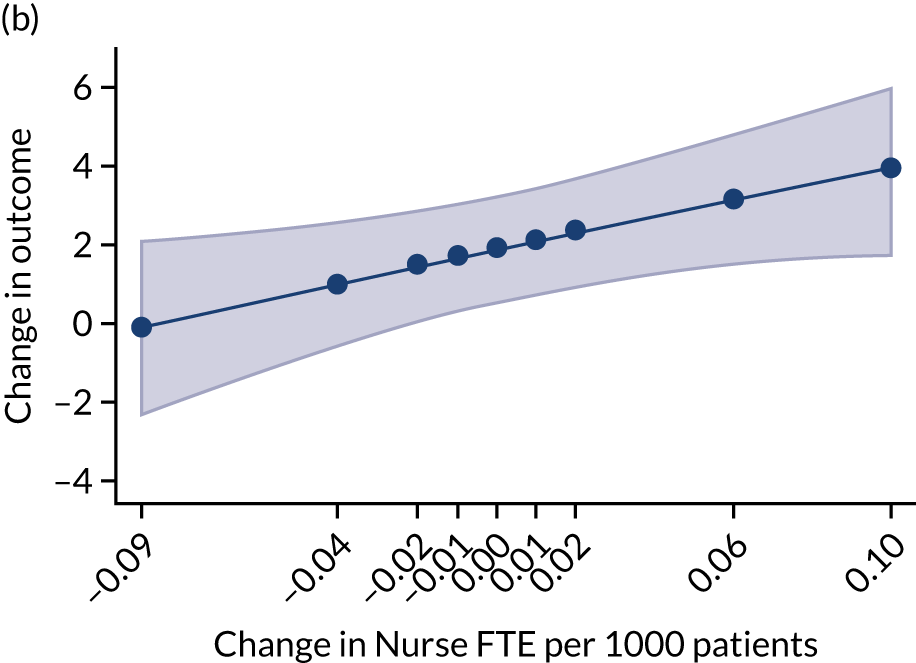
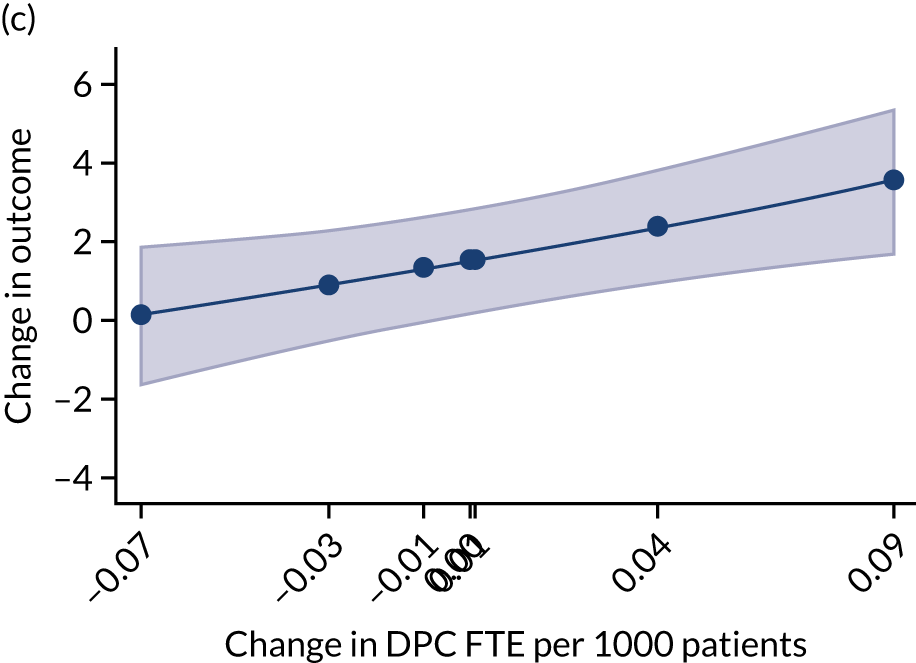
FIGURE 38.
Change in admissions PTP: 2015–17. (a) GPs; (b) nurses; and (c) DPC staff.
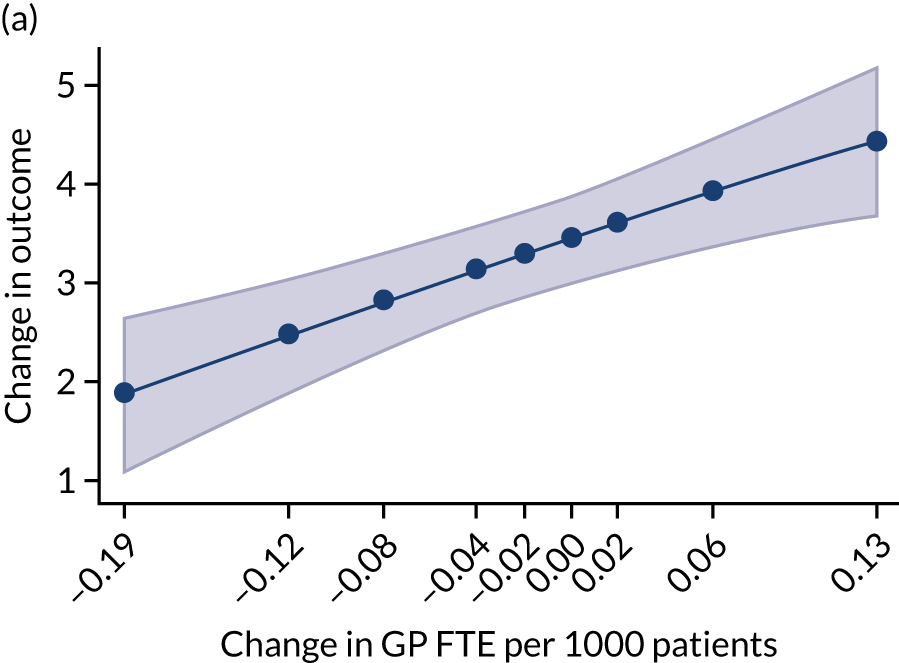

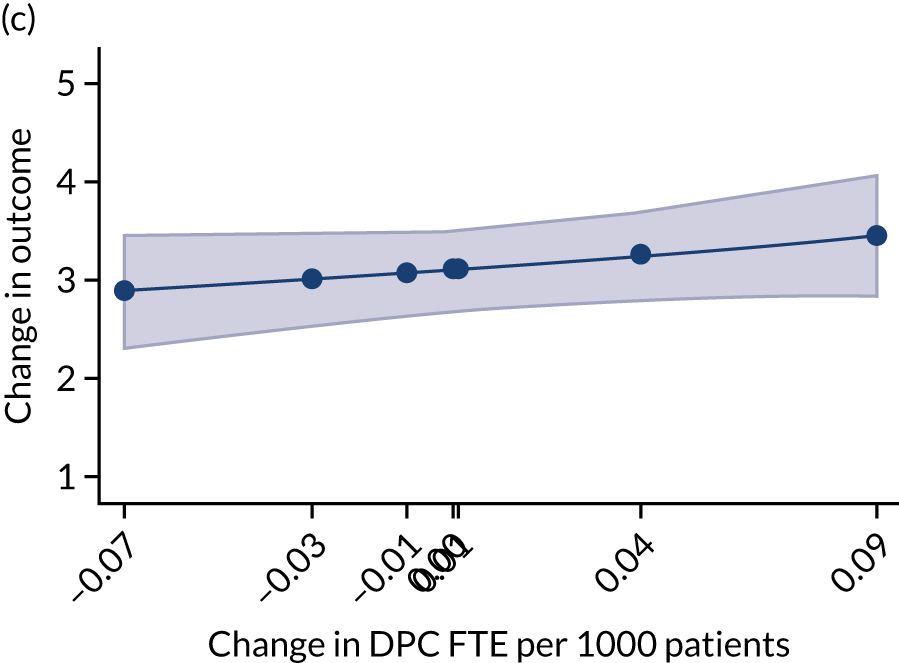
FIGURE 39.
Change in outpatient attendances PTP: 2015–17. (a) GPs; (b) nurses; and (c) DPC staff.
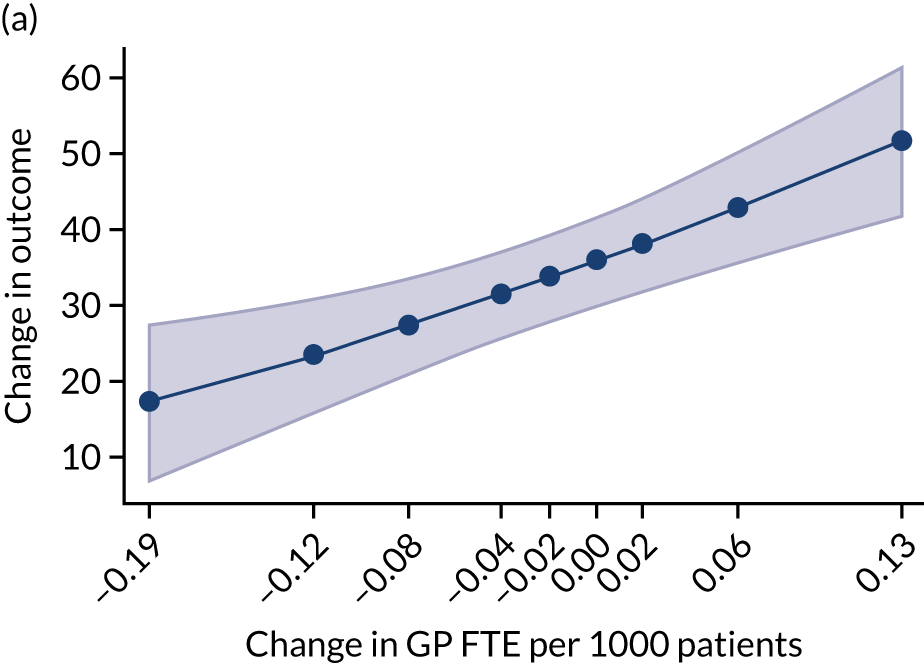

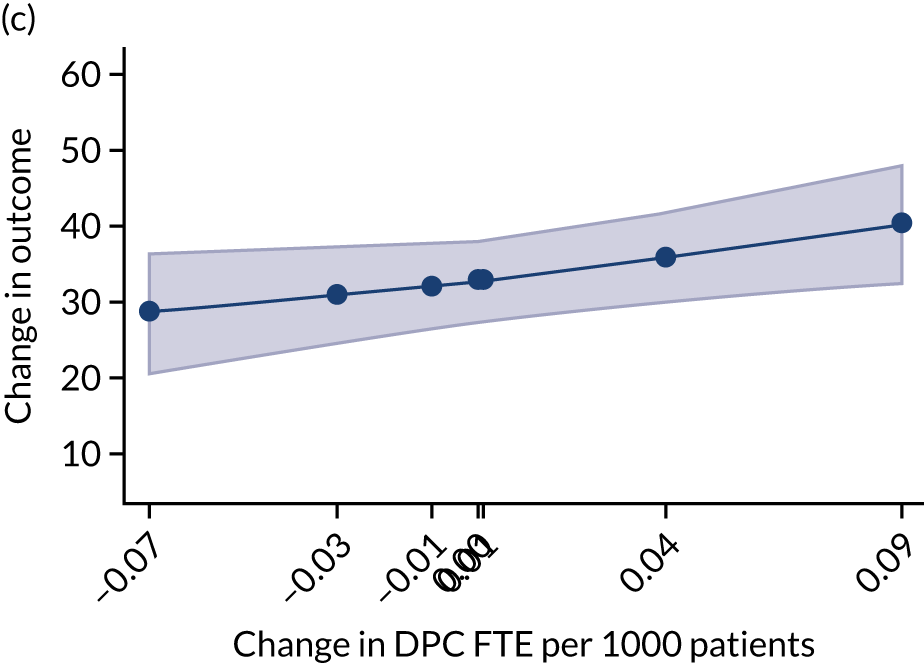
How are workforce changes associated with later changes in costs and practice efficiency?
The longitudinal patterns for costs PTP (Figure 40) are consistent with the cross-sectional results. Increases in staff FTE PTP are associated with stronger increases in costs. On the other hand, when looking at changes in log-total costs, higher increases in GP FTE PTP show a negative association with changes in costs. As the difference in log-total costs approximates the growth rate of total costs, this latter result suggests that increases in GP FTE PTP may result in milder increases in costs overall (Figure 41).
FIGURE 40.
Change in costs PTP: 2016–19. (a) GPs; (b) nurses; and (c) DPC staff.
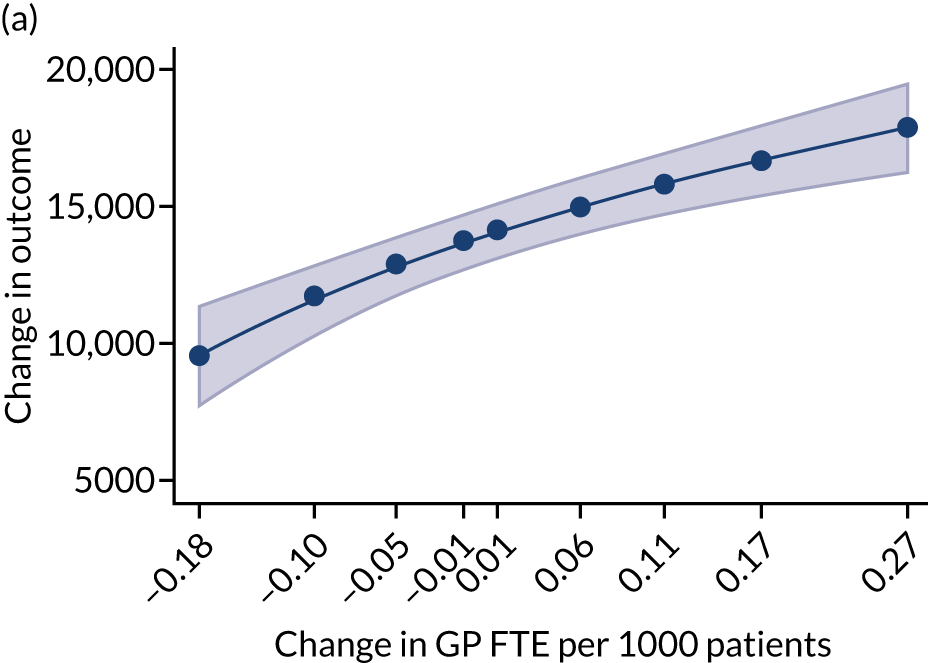
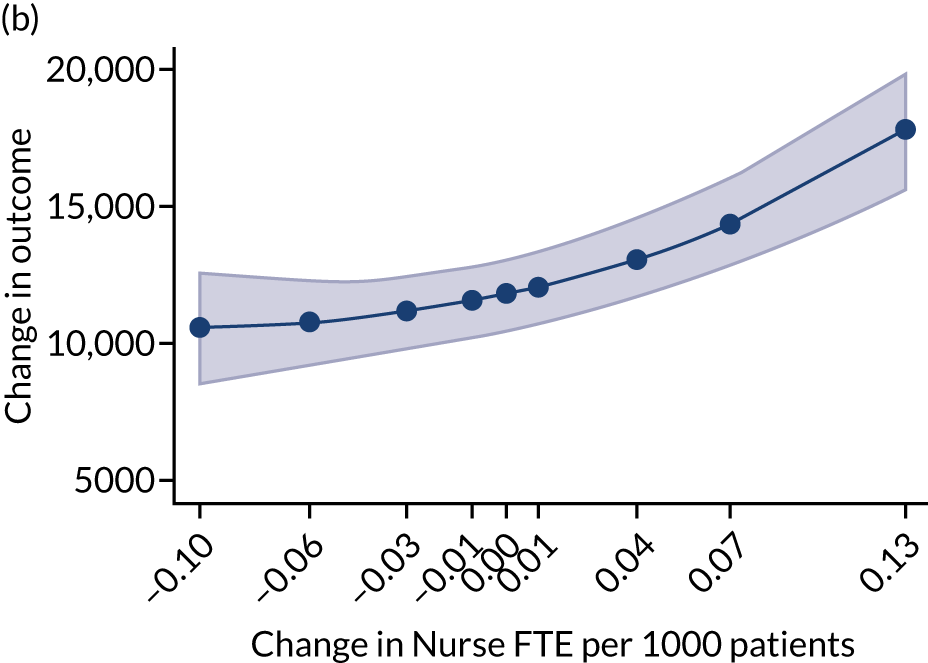
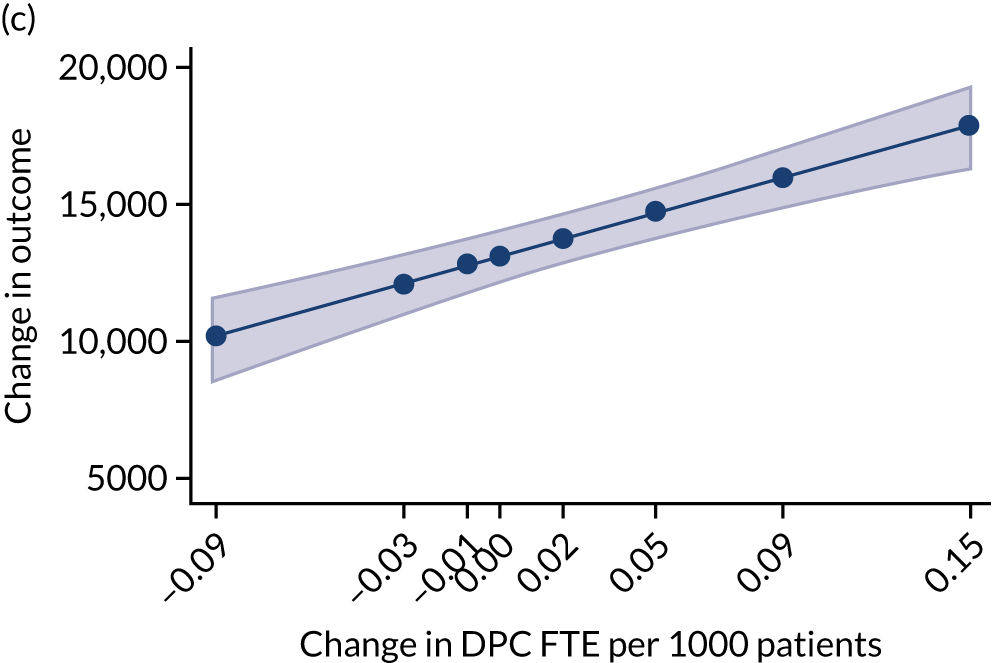
FIGURE 41.
Change in log-total costs: 2016–19. (a) GPs; (b) nurses; and (c) DPC staff.
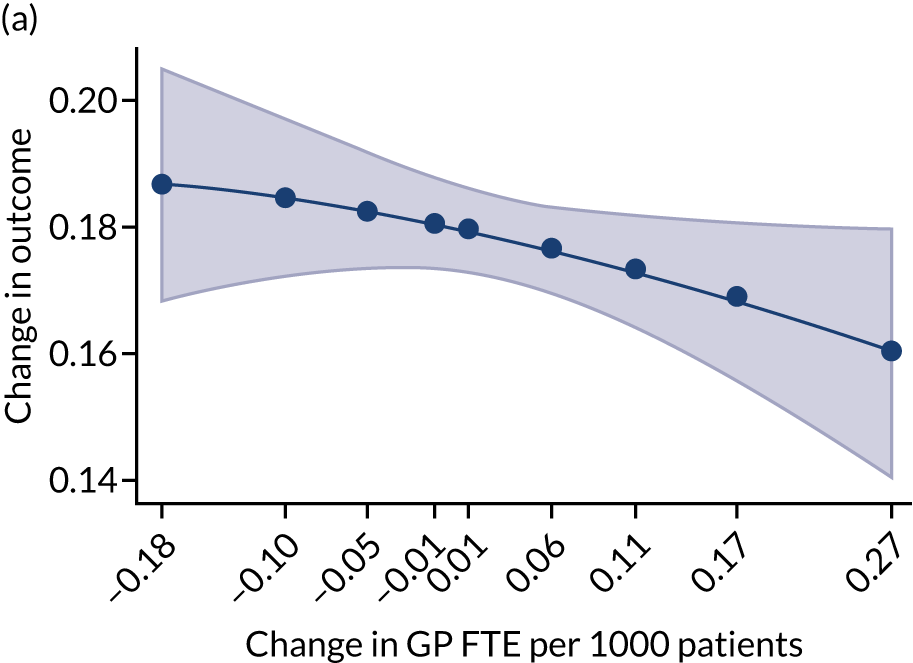
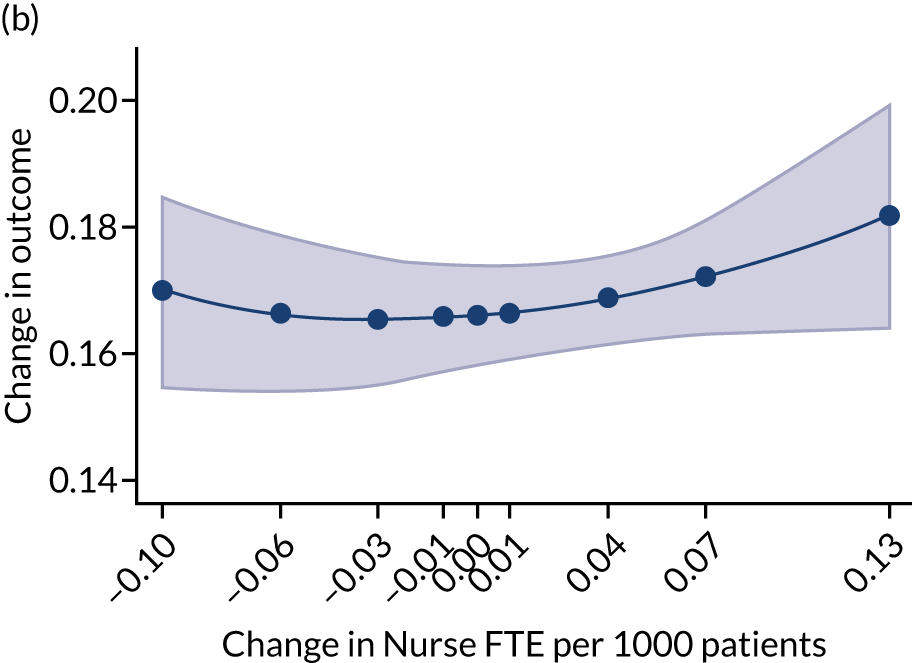
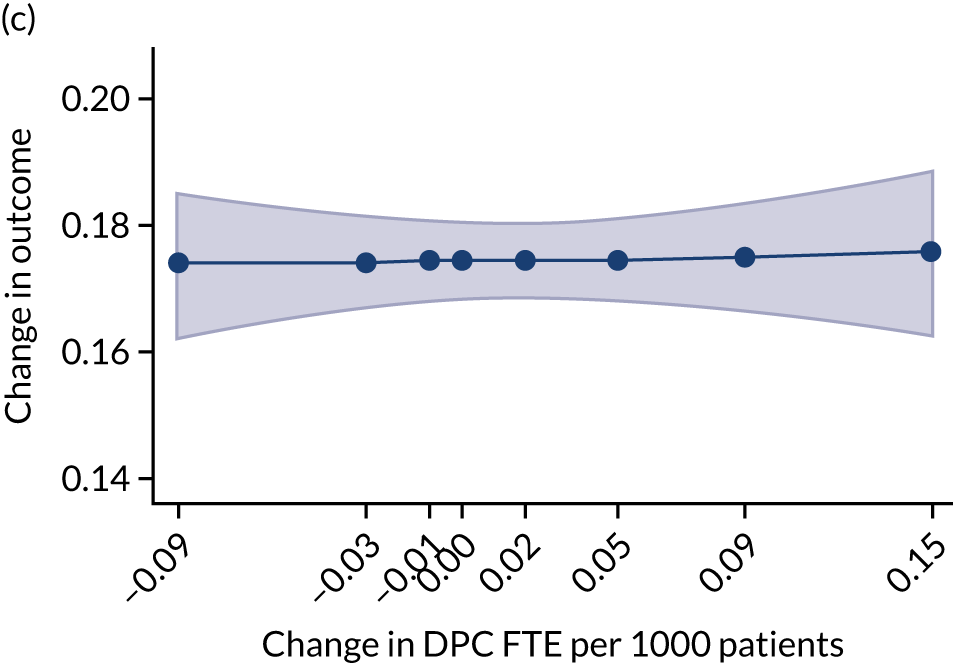
How is general practitioner job satisfaction associated with workforce composition?
Contrary to the findings from the cross-sectional analysis, GP job satisfaction, although improved overall, does not show associations with changes in staff FTE PTP over time (Figure 42).
FIGURE 42.
Change in GP job satisfaction (from the GP Worklife Survey): practice median level. (a) GPs; (b) nurses; and (c) DPC staff.
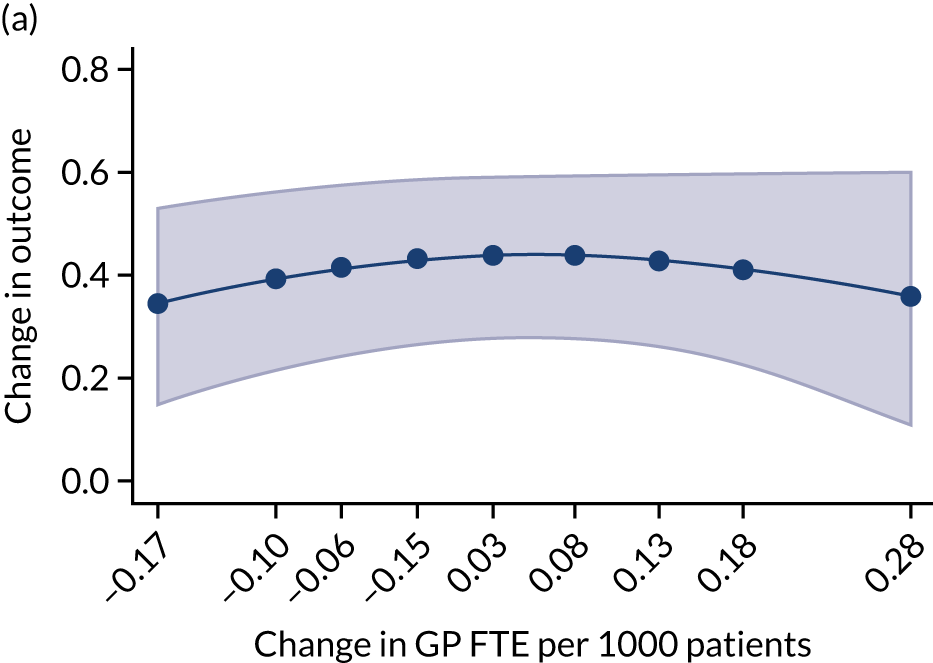
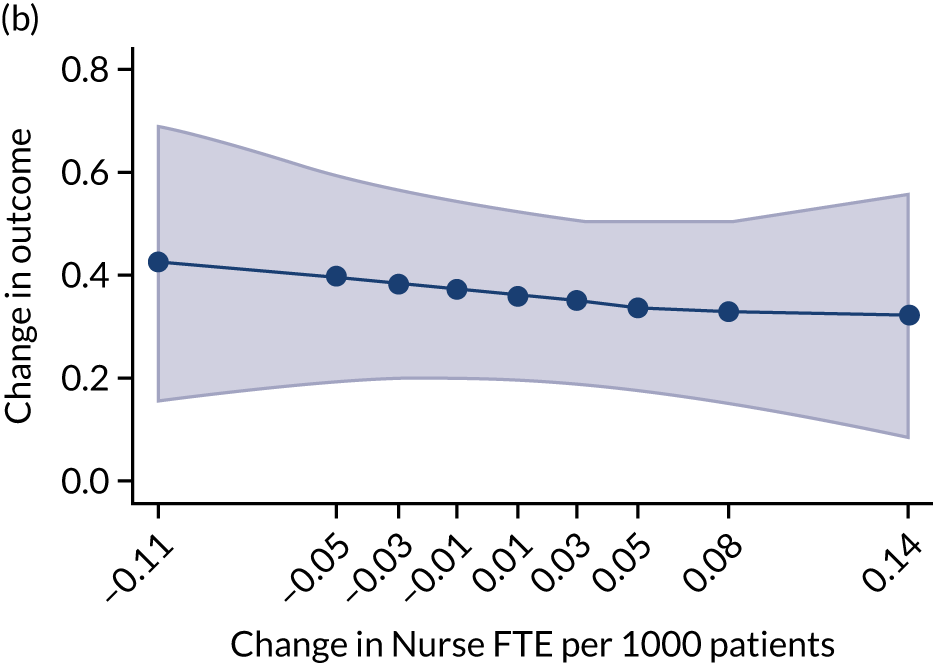
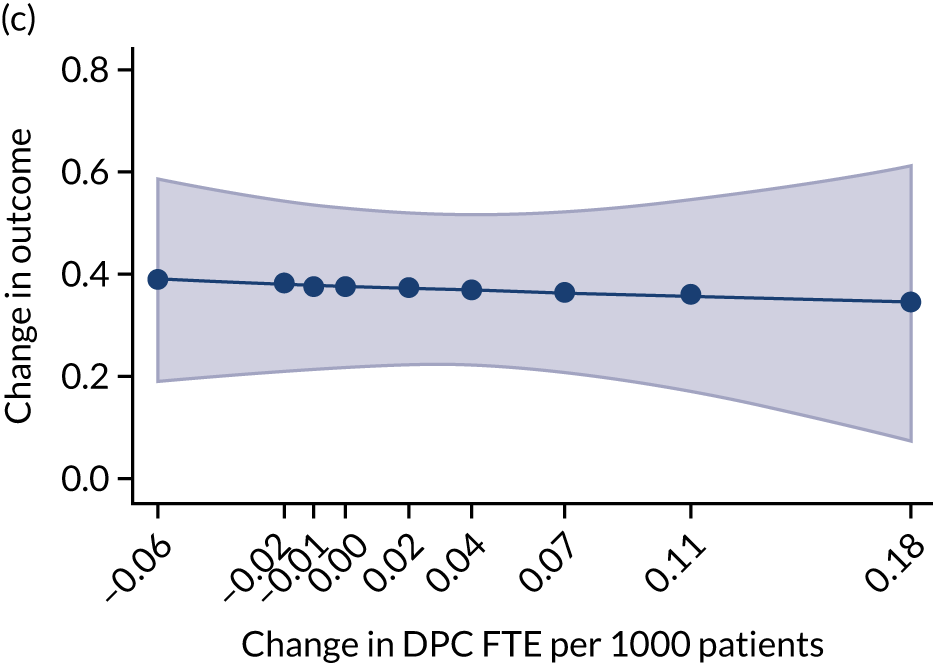
Appendix 3 List of publications and events
| Date | Publication/event | Type | Title |
|---|---|---|---|
| February 2020 | British Journal of General Practice | Journal article | Regional variation in practitioner employment in general practices in England: a comparative analysis101 |
| March 2019 | British Journal of General Practice Annual Conference | Oral presentation | Skill mix in primary care: the scale and distribution of skill mix in GP practice across England (IM) |
| July 2019 | The Second National Primary Care Dataset Workshop | Oral presentation | An investigation of the scale, scope and impact of skill mix change in primary care (JG) |
| June 2019 | Royal College of General Practice North West Faculty Meeting | Oral presentation | Closing the gaps in GP recruitment and retention – evidence for action (SS, KC and JG) |
| July 2019 | Health Services Research UK Annual Conference | Oral presentation | Changing skill mix in primary care: an analysis of the employment of a wider range of practitioners in GP practices (SS) |
| September 2019 | Health Policy and Politics Network Annual Conference | Oral presentation | Solving the ‘crisis’ in general practice: a case study of how history can be used to improve policymaking (IM) |
| February 2020 | The National Primary Care Dataset Workshop | Workshop | Determinants of primary care workforce variation in England (JG) |
| March 2020 | British Journal of General Practice Annual Conference | Oral presentation |
Determinants of primary care workforce variation in England (JG) Motivating factors behind skill mix change: results from a practice managers’ survey in England (JG) |
| April 2020 | Health Organisation, Policy and Economics (HOPE) Research Seminar | Oral presentation | Skill mix in primary care (MG) |
| July 2020 | Health Services Research UK Annual Conference | Oral presentation |
Conceptualising skill mix: theory vs. practice (IM) Motivating factors behind skill mix change: results from a survey of practice managers in England (JG) |
| September 2020 | Policy@Manchester | Online publication and virtual event | On primary care: general practice, pharmacy and workforce (IM, SS and KC) |
| October 2020 | Health Organisation, Policy and Economics (HOPE) Research Seminar | Oral presentation | Overview of emerging results from skill mix project (JG) |
| November 2020 | Greater Manchester Workforce Collaboration Summit | Oral presentation | Building effective skill mix in primary care (IM and SS) |
| February 2021 | Royal College of General Practice Annual Conference | Poster and oral presentations |
Poster: From the practice manager’s desk – a 2020 vision of skill mix in the future general practice workforce (SS) Oral presentation: Making sense of skill mix in general practice: an overview of where and how newer types of practitioners are delivering health care in GP practices (SS) |
| January 2022 | British Journal of General Practice | Journal article | Primary care workforce composition and population, professional, and system outcomes: a retrospective cross-sectional analysis160 |
List of abbreviations
- A&E
- accident and emergency
- ACP
- advanced clinical practitioner
- ANP
- advanced nurse practitioner
- ARRS
- Additional Roles Reimbursement Scheme
- ASTRO-PU
- age, sex and temporary resident originated prescribing unit
- CCG
- Clinical Commissioning Group
- CP
- clinical pharmacist
- DES
- Directed Enhanced Services
- DPC
- direct patient care
- FTE
- full-time equivalent
- GMS
- General Medical Services
- GP
- general practitioner
- GPFV
- General Practice Forward View
- GPPS
- General Practitioner Patient Survey
- HCA
- health-care assistant
- HEE
- Health Education England
- ID
- identification
- IT
- information technology
- LCRN
- local clinical research network
- MPIG
- minimum practice income guarantee
- MUNROS
- iMpact on practice, oUtcomes and costs of New roles for health pROfeSsionals
- PA
- physician associate
- PCN
- primary care network
- PI
- principal investigator
- PMS
- Personal Medical Services
- PPG
- Patient Participation Group
- PRIMER
- Primary Care Research in Manchester Engagement Resource
- PTP
- per 1000 patients
- QOF
- Quality and Outcomes Framework
- SD
- standard deviation
- wMDS
- Workforce Minimum Data Set
- WP
- work package
