Notes
Article history
The contractual start date for this research was in June 2022. This article began editorial review in November 2023 and was accepted for publication in March 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health and Social Care Delivery Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 King et al. This work was produced by King et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 King et al.
Background
Health visiting services in the United Kingdom
Child health programmes (CHPs) in the UK offer every child and their family an evidence-based programme of screening tests, immunisations, developmental reviews, information and advice. Successive Health for All Children Reports have developed the evidence-based foundations for these programmes. 1–6 They place a clear emphasis on parenting support, public health priorities such as breastfeeding and obesity prevention, and integrated services with the health visitor as the lead. They adopt a model of progressive universalism, recognising there are different levels of need, with specific tailoring required to meet the needs of individual families. The overarching aim is to give every baby and child the best start in life to ensure they reach their full potential. 7
The early years are crucial for a baby’s future health and development. 8 Between conception and age 2 years, an individual’s cognitive, emotional and physical development will influence their life chances into adulthood. 9 Deprivation in childhood negatively impacts life chances. 10–16 Babies’ and young children’s health, development and safety are affected by a wide range of factors including caregiver interaction, diet, sleeping arrangements, home conditions, dental hygiene and opportunities for play. Too many babies also experience physical, sexual and psychological abuse, neglect, exposure to domestic violence, substance abuse, parental mental illness, loss of a parent and poor attachment relationships with parents or carers. Health visitors play an important role in identifying the support that a new family needs and are key to delivering CHPs for babies and pre-school children. They deliver a universal service, intended to take account of the different dynamics and needs of all families, and provide a suitable platform for enabling early intervention and reducing inequalities in health. Health visitors are specialist public health nurses who are qualified nurses or midwives who have undergone additional training. 17 They are the only professionals who proactively and systematically reach all families with babies and young children from the antenatal period up to school entry.
Difference in different United Kingdom countries
Political devolution in the UK has enabled devolved institutions to influence national policy for early child health and development. 18 The specific delivery of CHPs across the UK varies depending on each country’s policy and strategic frameworks. Key differences are summarised in Table 1. However, there is little detailed knowledge about how health visiting services are organised and delivered in the four countries. Within England, where a range of providers are commissioned by local authorities, data suggest significant variation in delivery/uptake of mandated contacts between local areas, and variation in who completes them. 19,20 A recent survey conducted in 2018,21 which attempted to map the variety of ways in which teams and caseloads are configured in different areas, garnered 584 responses from individual health visitor practitioners, but the majority of these (n = 531) were working in England. The survey found that health visiting teams and their caseloads are organised in a variety of ways across the UK, with various pros and cons of different caseload management approaches, and a mixed and complex picture.
| England | Northern Ireland | Scotland | Wales | |
|---|---|---|---|---|
| Key legislation | Health and Social Care Act 2012 | Health and Social Care (Reform) Act (Northern Ireland) 2009 | Children and Young People (Scotland) Act 2014 | Social Services and Wellbeing (Wales) Act 2014 |
| Child Health Policy | Healthy Child Programme 0–19 years (2009, 2016, 2018, 2021, 2023) | Health Child, Healthy Future Programme (2010) | Getting It Right For Every Child (GIRFEC) Policy (2010) and Universal Health Visiting Programme (2015) | Healthy Child Wales Programme 0–7 years (2016) |
| Over-arching model | ‘Universal in reach, personalised in response’ | UNOCINI Thresholds of Need Model22 | SHANARRI model of well-being23 | ‘All Wales approach’ |
| Who commissions CHP? (Purchaser) | One hundred and fifty-three upper-tier and unitary local authorities | Department of Health and executive agency Public Health Agency | No purchaser–provider split | No purchaser–provider split |
| Who delivers CHP? (Provider) | Range of providers including NHS bodies, local authorities, private healthcare providers, charities or community interest companies | Six Health and Social Care Trusts | Fourteen territorial NHS Boards, working with 32 local authorities via 30 integrated joint boards and one joint monitoring committee | Seven local health boards |
| Working and employment models | Health visitors expected to lead on mandated reviews, but can delegate any aspect of their work to other staff members, including community staff nurses and nursery nurses | Health visitors managed by Health and Social Care Trusts. Assessments led by health visitors, but opportunities for skill mix at local level encouraged24 | Health visitors employed by NHS, except in Highland (employed by Highland Council). All visits to be undertaken by health visitors in the home | Health visitors provide expert clinical leadership to a multidisciplinary team where skill mixing is used ‘as an enhancement’ to the professional role of health visitor |
| Scheduled assessments in universal service | 5 (+ 2 suggested) Antenatal: 1 Birth to 1 year: 3 (+ 2 suggested) 1–5 years: 1 |
7 Antenatal: 1 Birth to 1 year: 4 1–5 years: 2 |
11 Antenatal: 1 Birth to 1 year: 7 1–5 years: 3 |
8 Antenatal: 0 (unless targeted) Birth to 1 year: 5 1–5 years: 3 |
Health visiting in the United Kingdom during the pandemic
The UK Government’s Coronavirus Action Plan (March 2020) set out measures to respond to the COVID-19 outbreak and detailed the government’s four-stage strategy: contain, delay, research and mitigate. It also set out changes to legislation necessary for giving public bodies across the UK the tools and powers they need to carry out an effective response. Across the UK, initial lockdown restrictions from March 2020 saw all non-urgent healthcare services stopped and capacity focused on the COVID-19 response. 25,26 Providers of community services were generally requested to ‘release capacity’ to support the acute sector, and health visiting services in many areas were reduced to a partial service incorporating a significantly reduced number of contacts. 27 The timing, duration and stringency of COVID-19 responses across the four nations of the UK diverged, highlighting their autonomy and legislative powers as devolved nations. 28 These responses included school closures, movement and gathering restrictions, self-isolation and the use of personal protective equipment (PPE). Initially, very little consideration was given to the wider impacts of the pandemic on babies and young children, or the health visiting service that supports them. The Institute of Health Visiting reported that service leads and commissioners lacked information and guidance on issues such as redeployment, PPE and infection control, and acceptable adaptations of the health visiting service delivery model (iHV, personal communication).
While the precise guidance from governments differed across the UK, all NHS managers had to support prioritisation of the workforce as part of the resilience response, and health visitors everywhere had to think differently about the prioritisation of support to families. Guidance emphasised the importance of some home visits (e.g. the first postnatal assessment), but there was a general presumption that most contacts would be virtual, with face-to-face contacts (with PPE) only where an individual assessment identifies a compelling need. 29 Where aspects of services were paused, the rate at which they were reinstated varied considerably. 30 The increased workload and pressures of working during the COVID-19 pandemic had significant negative impacts on the mental and physical health and well-being of health visiting staff. 31–33
Throughout the pandemic response, practitioners expressed concerns about the impacts of reduced/differently delivered services on babies and families, particularly in relation to safeguarding and neglect, but also the impact of missed needs on the baby’s growth and development, parental mental health, breastfeeding and wider determinants of health exacerbated by COVID-19. 31–36 An estimated 1.4 million women would have experienced maternity and child health care between March 2020 and March 2022 under some level of COVID-19 restrictions. 25,37 Changes to maternity services, including restrictions on birth partners, reduced in-person appointments and increased virtual care provision, have led to increased stress, depression and anxiety among new mothers, which might have then impacted on health visitors’ caseloads. 38–41 Some restrictions continued beyond March 2022, such as limits to antenatal/postnatal hospital visits and some play and stay groups remaining closed. Reports of parents’ experiences show a mixed picture both in terms of different families’ ability to cope and the support they were given. Many parents felt unsupported, were cut off from family and community networks and with reduced access to formal services. 40,42–44 Existing inequalities were exacerbated for those in poorer, less educated and ethnic minority households and those facing issues of overcrowding, temporary housing, mental ill-health, lack of access to digital technologies or substance abuse within their families. 45–50 Prior to the start of the review we developed an initial programme theory (PT), drawing on this background literature (see Appendix 1, Figure 3).
Aim and objectives
The aim of the study was to identify and analyse literature related to health visiting, published since the start of the COVID-19 pandemic response, to better understand how the pandemic was experienced by health visiting services. As stated in our protocol, the study sought to answer the question: ‘How can the organisation and delivery of health visiting services in the UK be improved in light of the COVID-19 pandemic, to provide equitable, effective and efficient services for young children and their families?’51 To be able to address this question, we identified four sub-questions:
-
What are the mechanisms that explain variation in and mitigation of impacts of the COVID-19 pandemic in different contexts?
-
What are the important contexts that influence whether the different mechanisms produce the outcomes that have been identified in the literature?
-
In what circumstances are the (positive and negative) impacts likely to be most (and least) profound?
-
What can we learn from the way health visiting services have responded to the COVID-19 pandemic to improve their organisation and delivery?
Objectives
-
To conduct a realist review of the literature to examine what the impacts (both positive and negative) of the COVID-19 pandemic have been on health visiting services in the UK, for whom, in different contexts.
-
To engage with key policy, practice and research stakeholders in England, Scotland, Wales and Northern Ireland to understand important contextual differences across the UK in relation to the planning, organisation and delivery of health visiting services.
-
To identify recommendations for improving the organisation and delivery and ongoing post-pandemic recovery of health visiting services in different settings, for different groups. 51
Methods
Since March 2020, there has been a profusion of literature describing the experiences and impact of the COVID-19 pandemic on health services delivery. 42,52–55 This literature comes from a range of academic researchers, practitioners, advocacy organisations, policy-makers and other commentators, and is published not just in academic journals but also as reports, working papers, presentations and other documents. It contains important learning at a time when services, and the contexts in which they are delivered, were undergoing an unusual amount of change. Our review of this literature capitalises on the opportunity to learn new things about health visiting services and what works, for whom and in what circumstances. Given the complexity of health visiting as a programme of work and the variety of relevant literature and its sources, we chose to conduct a realist review. A realist review is a systematic and theory-driven approach to synthesising and analysing evidence. It focuses on understanding how complex interventions work in particular contexts by examining the underlying mechanisms and contextual factors. 56,57 The involvement of stakeholders in a realist review is crucial.
People with lived experience and stakeholder engagement
The engagement of professional stakeholders and people with lived experience of caring for babies during the pandemic in the design, conduct and dissemination of this study has ensured recommendations are meaningful and outputs are accessible to parents/carers, the wider public, commissioners, providers and policy-makers. Our patient and public involvement (PPI) lead (MB) has worked as a key member of the research team from inception to completion. We recruited a group of eight people with lived experienced of health visiting (who have had cause to access health visiting services during the pandemic period) to work alongside us. The group of eight comprised two people from each of the four UK countries, sampled to ensure diversity of the number of children and deprivation levels. The group met online four times during the study, facilitated by our PPI lead. Members also contributed additional feedback outside of meetings (by e-mailing or telephoning our PPI lead or researcher). This is described in more detail in our synopsis paper.
To form a separate professional stakeholder group, we invited 26 professionals (policy leads, commissioners, practitioners and policy advocates), with representatives from each of the four UK nations. In a change to our original protocol, stakeholders met five times throughout the study, rather than the planned six, and contributed additional feedback outside of meetings (by reviewing and commenting on documents). This was to make best use of their time and involvement.
Realist review methods
Our realist review methodology followed Pawson’s five iterative steps,58 and is described in more detail in our protocol. 60 This manuscript is reported following the RAMESES publication standards for realist synthesis. 59
The steps, and the involvement of our stakeholder group and people with lived experience group in each step, are summarised in Table 2.
| Step | Aim | Approach |
|---|---|---|
| Step 1: locate existing theories | To locate underlying programme theories for health visiting service delivery during the COVID-19 pandemic | Early discussion and literature scoping to inform an initial PT Informal exploratory searching of published literature and current policy documents Further development of the PT with our stakeholder group |
| Step 2: search for evidence | To conduct a formal search of literature related to health visiting during the COVID-19 pandemic | Searches conducted in five databases (see Appendix 2) Grey literature identified from relevant websites Literature provided by stakeholders Citation chaining E-mail alerts of relevant material ongoing throughout Documents screened against inclusion/exclusion criteria |
| Step 3: article selection | To select full-text documents for inclusion in the review based on an assessment of relevance | Documents selected for inclusion when they contained data that could inform the PT A random sample of 10% independently assessed for relevance |
| Step 4: extracting and organising data | To organise and describe relevant documents To code data and make interpretations and judgements |
Characteristics of included studies extracted into an Excel spreadsheet Full texts of documents coded deductively, inductively and retroductively Theories and interpretations included in additional memos Initial interpretations and judgements discussed with team and with stakeholder and lived experience groups |
| Step 5: synthesising the evidence and drawing conclusions | To apply a realist logic to analyse the extracted data To construct propositions represented through CMOCs |
Propositions represented through CMOCsa with evidence for justification Draft set of CMOCs presented to full project team in January 2023 for discussion and refinement CMOCs presented to stakeholder and lived experience groups in February 2023. Groups helped provide a richer understanding of contexts and mechanisms in different localities Regular meetings between EG and EK to discuss and iteratively develop these CMOCs Extended project team meeting September 2023 to refine the themes found and discuss/develop the final PT. The CMOCs were mapped onto themes and then recommendations, which were presented to the stakeholder group, who suggested refinements and highlighted areas of uncertainty |
Our search strategy involved formal searches (in October 2022) of MEDLINE, CINAHL, EMBASE, HMIC and Google Scholar using combinations of free text and subject heading terms describing health visiting and relevant UK policies and programmes with terms describing the COVID-19 pandemic. The searches were limited to identifying literature published from 2020 onwards to capture material produced from the beginning of the COVID-19 pandemic response. This main search was augmented by searches for grey literature conducted in November and December 2022, to identify relevant reports, position papers, policy and programme documentation and other non-research material that was not identified in the main searches. This search focused on material available via relevant organisational websites identified by the project team, using a combination of searching and browsing to explore published material. Our strategy was further supplemented by forward and backward citation searching in May 2023, by a Google Scholar search alert active throughout the project, and by requests to our professional stakeholder group.
Documents were screened for inclusion by EK by title and abstract (where available), and then in full text (see published protocol for more detail60). At each stage, a 10% random sample of records was screened in duplicate by EG for quality control purposes. Eligibility criteria were applied as follows:
Inclusion
-
Type of intervention: health visiting
-
Study design: all study designs
-
Types of settings: any setting providing health visiting services
-
Types of participants: all families eligible for universal health visiting services
-
Outcome measures: all outcome measures related to health visiting services
Exclusion
-
Health visiting type models or programmes run in countries other than the UK
-
Specialist or targeted health visiting services for select populations only
As the project progressed, we made minor deviations and additions to our original protocol.
In step 1, we analysed the similarities and differences in health visiting services across the four UK nations. We created a table detailing CHPs across the different UK nations and shared it with our stakeholder group for feedback and refinement (summarised in Table 1).
In step 2, we conducted an additional search in April 2023 to address the limited data on responses to the COVID-19 pandemic at local management level. To avoid missing relevant material and potential pandemic-related insights, we devised a new search to uncover recently published content related to health visiting services, even if it did not explicitly mention the pandemic. We refined our search by removing COVID-19-related terms and repeated it in the same databases, focusing on material published from 2021 onwards. A relatively small number of included papers were found in this search. They predominantly referred to data collected prior to the COVID-19 pandemic or with different or unclear populations (e.g. midwives). Although these papers were re-reviewed at a later stage in our iterative methods, none were found to contribute further to our PT.
We did not undertake the potential option of other purposive searching, for example looking at other countries, or at closely aligned services. Our original searches identified several articles from other countries, but they were deemed ineligible due to the unique nature of the health visitor role within the UK’s settings. The team felt there was sufficient data focusing on health visiting to refine the PT, without the need to look at other services such as social work.
In step 3, we selected documents for inclusion based on assessment of their relevance, in terms of their contribution to theory building and/or testing. However, we did not assess the methods used to generate the data. This is because most documents were either first-person accounts of health visiting or documents from organisations whose primary purpose is advocacy. We reflected on this advocacy/first-person perspective during our data analysis.
In step 4, we also used the KUMU software [Kumu, Kumu Relationship Mapping Software, 2023. URL: https://kumu.io (accessed 31 October 2023)] to visually draw links between different areas of interest, to add reflections from stakeholder and lived experience groups, and to visually present these at team and stakeholder meetings.
In step 5, themes from the data were presented as draft context, mechanism, outcome configurations (CMOCs) and discussed at a face-to-face team meeting. Through further discussion with the team, regular meetings between EK and EG, and the input of our lived experience and stakeholder groups these CMOCs were iteratively refined. We wrote narratives for the CMOCs based on themes and underlying propositions, checking for consistency against our data and uncovering gaps and overlaps. Finally, each CMOC was translated into a finding and draft recommendation, which was subsequently refined by our stakeholder group. During the stakeholder meeting, the attendees were also asked to indicate how ‘do-able’ they felt these recommendations would be to implement, with a group discussion on this.
Equality, diversity and inclusion
Our expression of interest form for recruiting the lived experience group included optional questions on ethnicity and postcode. From the postcodes, we calculated the relevant index of deprivation and attempted to achieve a spread of deprivation levels and geographical areas, albeit within a small group. Group meetings were held online to allow those from across the UK to attend without travel time. Group members discussed their own preferred time for meetings, to fit around child care and existing commitments.
We had little control over the diversity of our professional stakeholder group, who were recruited for the professional roles that they occupy. We did not collect any personal information from these members. All meetings were held online to reduce travel.
We did not receive any notifications about additional accessibility requirements from either group. A more thorough discussion of equality, diversity and inclusion (EDI) issues, particularly in relation to the data, is included in our accompanying synopsis paper.
Statistical analysis
There was no statistical analysis performed in this realist review.
Data sources (for systematic reviews)
Full details of search strategies and data sources are shown in Appendix 2.
Ethics
General University Ethics Panel approval was obtained from the University of Stirling (reference 7662).
Results
Documents included in the review
A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram showing the identification, screening and inclusion of documents is provided in Figure 1. A total of 118 documents contributed data to the review, with full details shown in Table 3, Appendix 3.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses61 diagram showing the identification, screening and inclusion of documents. a, Google Scholar and website search results screened ‘on screen’; see Appendix 2 for details.
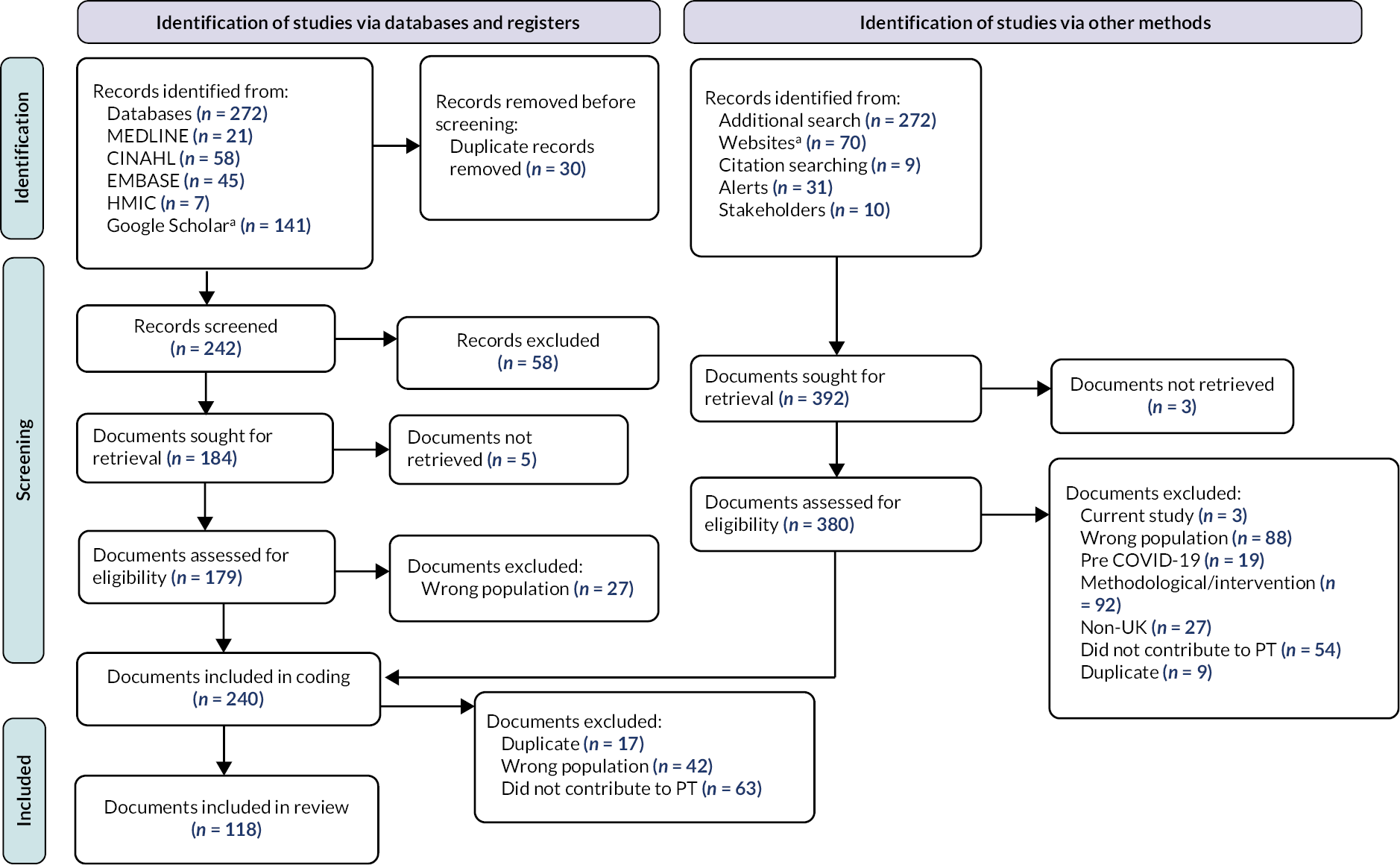
The majority of included documents were from either an advocacy perspective (33%) or the perspectives of practitioners (28%). Most documents were from England (n = 51) or the UK (n = 37), with very few specifically focused on Scotland (n = 4), Wales (n = 7) or Northern Ireland (n = 1). Our stakeholder group discussions sought to counter this English bias in the literature. A more detailed analysis and discussion of both the primary perspective and the country of focus for documents included in the review can be found in our synopsis paper.
Working definitions of terms
Various terminology is used across the devolved nations in relation to health visiting and the CHPs. Following guidance from stakeholders, we developed working definitions of terms which we use throughout the results and discussion. These can be found in the Glossary.
Review findings
Our findings are grouped into three categories: health visiting contacts, health visiting connections and the health visiting workforce. Tables of CMOCs with quotes are shown in Appendix 4. The full relationships between CMOCs, findings and recommendations are included in our synopsis paper.
Health visiting contacts
The practice of health visiting rests on the conduct of ongoing holistic assessments of family needs, conducted by experienced professionals, so that the families and practitioners can identify any support required for the baby/family to thrive. Our findings highlight the importance of these universal assessment reviews, particularly in terms of ensuring potential needs are not missed, and enabling the team to provide a proactive and personalised response to the changing needs of babies, young children and families. While a proportion of reviews was always missed prior to the pandemic (national data sets on this are poor but all highlight gaps), the COVID-19 pandemic meant many more were either missed or were conducted differently. Across our data, practitioners and families express concerns about potential needs not being identified in good time (CMOC01). An increased number of contacts were made remotely, for example, via telephone or with questionnaires sent by post, and using a wider staff skill mix. Our data suggest that such contacts can sometimes enable useful information to be gathered, and that this information can support an assessment of needs (CMOC02). However, face-to-face contacts play a crucial role since they can gather information through physical observations and interactions which might otherwise be missed (CMOC03). Our data highlighted practitioners’ concerns about not being able to assess a family properly remotely. This was recognised to have an impact on other parts of the healthcare system, for example, when issues were picked up later by other healthcare professionals.
Our findings also illustrate the role face-to-face universal assessment reviews play in building trusting relationships with families (CMOC08). From the health visitor’s perspective, these universal assessment reviews enable them to identify problems which parents might have missed, to intervene early, to tailor advice and support for each family and to have sensitive conversations with families. The need for this appeared to be heightened when more families were under considerable pressure (e.g. caused by the pandemic response and cost of living crisis).
From the parents’/carers’ perspective, our data suggest that families feel more supported when they have an opportunity to build a relationship through face-to-face contacts; such contacts facilitate a better understanding of the family context (CMOC09), and families are more likely to disclose their concerns. However, outside the universal assessment reviews, remote contacts can be useful for certain families at certain times. For example, when health visiting teams use remote contacts to proactively maintain open and responsive channels of communication, parents can feel supported (CMOC12). During the difficult times of the pandemic response, some families found a quick ‘check-in’ (e.g. by phone or video call) by the health visitor made them feel that somebody was interested in them, and had remembered them, even if they didn’t receive a longer face-to-face contact.
From the health visitors’ perspective, practitioners might successfully use remote connections to keep in touch with families on their caseloads, when it is appropriate to do so (CMOC11). With no travel time required, remote connections can allow practitioners to be in more regular contact with multiple families, for example using WhatsApp groups to disseminate information. Some families, however, do not have the resources or desire to engage meaningfully with remote consultations and the substitution of face-to-face contacts accentuates the disparities between individuals who struggle with non-face-to-face interactions, and those who are accustomed to and excel in an online environment. The needs of babies and young children are an important consideration in the choice of method of contact, since they are generally excluded from any remote form of interaction (CMOC10); in face-to-face contact, health visitors can directly observe mother–baby interaction, development, play and feeding.
During the pandemic, urgent and immediate needs took precedence, resulting in less time for providing families with holistic, preventive support. Our data highlight health visitors’ concerns around not being able to fulfil their health promotion and wider support role adequately, given demand and caseloads (CMOC04). The pandemic exacerbated issues already seen with high workloads. From the families’ perspective, regular contacts with the health visiting team enable the building of supportive relationships and increase opportunities to explore aspects of family/infant health and well-being, particularly as families’ needs change over time (CMOC05). With fewer face-to-face contacts, there were missed opportunities to provide tailored support that benefits from physical presence, for example, demonstrating or role-modelling activities. However, the pandemic experience also highlights that some forms of information, guidance and support can be usefully delivered by health visiting teams in a digital format (e.g. apps, videos, links to support groups) (CMOC06). Digital/remote provision is only useful for some support, for some people, some of the time. New digital resources were created during the pandemic, continuing a trend that had begun prior. While this gives health visiting teams useful new ways of delivering information and support, there is little evidence of evaluation of these resources, and there appears to be duplication across different local areas (CMOC07).
Health visiting connections
Health visitors are only able to support families in a holistic way by making connections to other services and to the wider community. This relies on a sound understanding of the communities they work in, an up-to-date knowledge of local services and good relationships with other professionals working in their communities. The COVID-19 pandemic response disrupted the continuity of care, with greater mobility of staff within and between health visiting teams, and redeployment of staff to more acute services. Community contexts were also disrupted, with many services closing, reducing capacity or becoming less accessible, for example by increasing their thresholds for support. Our findings highlight that when other services in the community close, or change their provision, then health visitors cannot perform a vital part of their role, signposting and referring families for additional help (CMOC13). Health visitors may assume additional responsibilities in situations where other forms of support are lacking. This may include managing cases that would previously have been handled by children’s social care, or assisting children who are awaiting a diagnosis for special educational needs or disability support. Furthermore, health visitors may go beyond their usual duties to help families with tasks such as translation, form filling and accessing food banks, which are typically supported by local charities (CMOC14).
Some aspects of the wider community provision could not be easily replaced during the pandemic, such as local peer support and socialising groups for babies. Our findings suggest that children and families missed out on opportunities to socialise and take part in different activities (particularly those that support learning and development), which potentially increased the risk of social isolation and stress on parents (CMOC15). From the families’ perspective, our data highlight the concerns of parents regarding children’s lack of contact with other people outside their close family, and particularly opportunities to socialise with children of their own age. Fun activities/groups also provide a useful structure to parents’ days, enabling them to venture out of the house, connect with other parents and experts and try new ideas for engaging their children.
During the pandemic response, informal contact was generally restricted between members of health visiting teams and others, such as clinicians. Our findings highlight that these connections are important for staff well-being and development. Data point to issues of workforce stress and isolation related to this lack of connection, and fewer opportunities for informal discussion, support and peer review, alongside formal clinical supervision and reflection (CMOC16). There are indications that the increased stress and isolation resulted in mental and physical health impacts for some health visitors, including reduced self-care, burnout and lack of compassion for families on their caseload (compassion fatigue).
Digital and remote technologies were increasingly used as a substitute for face-to-face interaction between staff. Our findings suggest that the use of such technologies can enable peer discussions, team meetings and delivery of some types of education, and can increase access to training and networks that may not be available locally. They can also be an efficient use of time when combined with more traditional communication and education routes (CMOC17).
The health visitor role depends on good interagency working, particularly with regard to safeguarding which relies on the appropriate sharing of information between professionals and agencies. Our data highlight the importance of the health visitor’s role in making connections with other agencies such as social services and general practitioner (GP) surgeries. During the pandemic response, many other agencies, schools and child-care settings were not seeing children face-to-face. Health visitors’ connections to other agencies were disrupted, at a time of increased concerns regarding parental mental health, domestic abuse and issues of child safeguarding. In some areas, due to redeployment and workforce shortages, there were not enough health visitors to meet the scale of need (CMOC18).
Health visiting workforce
Health visiting work relies on skilled practitioners, able to exercise professional judgement to identify and respond to needs in an appropriate and tailored way. Health visitors and other members of health visiting teams had varied experiences during the COVID-19 pandemic in relation to the guidance they were given, the procedures they were asked to follow and the restructuring of provision. There was also considerable variation in the extent to which health visiting team members were redeployed to support other parts of the healthcare system, and the extent to which health visiting teams were protected, or even enhanced, during the height of the pandemic. Across our data, being or feeling valued as a highly trained specialist is an important theme. Findings highlight that top-down guidance, updates and restructures often did not reflect the policy and professional commitments to babies, children, families and health visitors. When health visitors in some areas were seen as dispensable and able to be redeployed, they felt particularly devalued (CMOC19).
A related theme is the extent to which government policy focused on managing acute care during the COVID-19 pandemic, with a focus on babies and young children being largely absent. Much literature reflects that younger children were not considered a priority for policy and decision-makers during the pandemic response. The divergence in policy across the devolved nations, and across local authorities within England, also led to different models of support for parents with babies and young children (CMOC20). This situation exacerbated pre-existing workforce pressures, sometimes pushing health visiting services close to breaking point, with a range of negative consequences being reported within the literature for staff, families and children (CMOC21). Understaffing, redeployments, staff illness and health visitors leaving contributed to increased workload and work-related stress for remaining health visitors.
Discussion
The COVID-19 pandemic rapidly and dramatically altered the context in which health visiting services are delivered. The impact of the pandemic on babies and families has been far-reaching, uneven and enduring. Health visiting staff rapidly adapted, finding new ways to ensure that babies and families continued to receive support in different contexts. However, the variation in practice and service delivery across the UK has been amplified, and there are important and ongoing implications of the pandemic response for future service delivery.
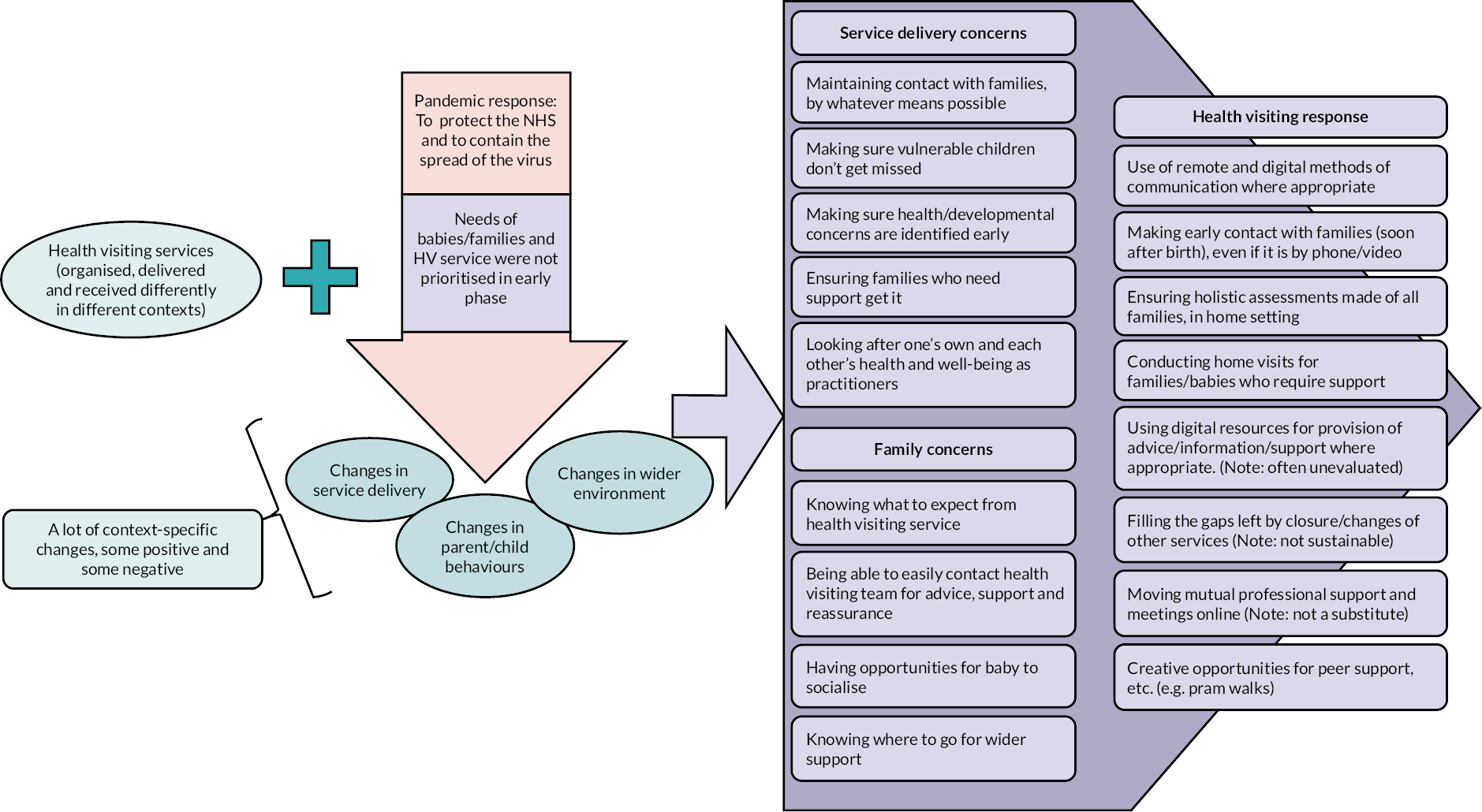
This study sought to answer the question: How can the organisation and delivery of health visiting services in the UK be improved in light of the COVID-19 pandemic, to provide equitable, effective and efficient services for young children and their families? The 118 documents included in our study reported on aspects of changes made to services during the pandemic in different contexts. Our realist review of these documents, together with the input and guidance from our professional stakeholder and lived experience groups, has revealed a new understanding of the mechanisms by which health visiting outcomes occur. In terms of providing equitable, effective and efficient services, our findings highlight the importance of relationships (built via contacts) between health visitors and families, and holistic assessments for early intervention (facilitated by connections to other staff and support services). They also point to the variety of health visiting work and illustrate how, during a very challenging time, practitioners made adaptations in the way they practised, driven by core motivations: to maintain contact with families by whatever means possible; to make sure vulnerable children don’t get missed; to make sure health/developmental concerns are identified early; to ensure families who need support get it; and to look after one’s own and each other’s health and well-being as practitioners. These points (relationships, holistic assessments and health visiting work) are discussed further below.
In terms of improving the organisation and delivery of health visiting services in the UK, our study found very little evidence detailing disruptions at this managerial level, and consequently no new insights into how teams or caseloads might be organised, for example, for greater efficiency. However, findings suggest that the complexity and variety of health visiting work in different and constantly changing contexts call for requisite variety in turn, with skilled professionals (and their managers) having the flexibility and capacity to assess the appropriateness of their services for the environment they operate in. Such situations do not suit standardisation, but instead, they require good communication and information flow.
Our final PT diagram summarises our findings and is presented in Figure 2 below.
FIGURE 2.
Final PT.
Importance of relationships
The concerns of practitioners throughout the pandemic response highlighted the importance of relationships between health visitors and families. Practitioners recognised the need to build and maintain trusting relationships with families by any means possible, even when home visits were not advised. Research has consistently shown that establishing positive relationships between parents and health visitors is crucial for achieving desired outcomes in child health. 10,62 A good relationship allows a health visitor to assess the needs of an individual family and provide tailored support, and facilitates disclosure from family members, for example regarding domestic violence or mental health. 1 It is particularly important for enabling access to support for those families who might otherwise find such support hard to access. 10,63–65 During the pandemic response, many contacts between health visitors and families were stopped or were no longer face-to-face. While families missed the face-to-face contact for the mandated reviews, many were also positive about other methods of maintaining contact, such as WhatsApp messages or phone calls. When regular contact was maintained, families felt reassured that they had not been forgotten, encouraging them to reach out to their health visitors with queries. Our lived experience group shared mixed experiences of the health visiting service, before and during the COVID-19 pandemic. One frustration was with health visitors who appeared to be focused on a tick-box exercise rather than building a real relationship with families. This, and our review findings, demonstrate that the skill of relationship building is the priority, whether the contact is face-to-face or online.
Holistic assessments for early intervention
Health, developmental and other problems within a family can be identified early and mitigated with the help of skilled practitioners. Our findings show that maintaining this role is a key concern for health visitors. It is important to conduct holistic assessments and identify needs soon after every baby is born. However, family situations and child vulnerability are dynamic. The assessment of needs by health visitors is articulated in other research as an ongoing process, with repeated iterations facilitated by the continuous provision of a comprehensive service that covers the period from pregnancy to starting school. 10 While face-to-face contact is critical for holistic assessments, remote contact can be a useful way of keeping in touch with families and making sure emerging needs are not missed. They can also help families keep in touch with the health visiting service and feel less isolated.
When the need for support is identified, practitioners are then concerned with ensuring that those needs are met. In a context that was rapidly changing, the importance of a health visitor’s role in signposting and making referrals was highlighted. 66,67 Where other services and/or informal support becomes less available or accessible, this presents additional challenges for health visiting teams. 68–70 Health visitors, as skilled public health practitioners and as a key part of a local child/family health and social care system, tailor their advice and support within a particular context. Some forms of support rely on face-to-face contact. However, the pandemic has shown that some support can be provided to some families using remote methods. Digital technologies, if evaluated, can provide a quick and acceptable mechanism for providing information to multiple families at once. Parent–peer support can also sometimes be facilitated in creative ways.
Health visiting work: varieties of human work
Our findings highlight the wide variation in health visiting service delivery and the range of ways in which the COVID-19 pandemic impacted health visiting work. A recent review of literature on health visitor workloads noted the complexity of health visitors’ work and the difficulties in capturing its diversity. 71 Reflecting on our own findings, particularly with our lived experience group, we uncovered significant disparities in the perception of how health visiting is practised and its actual implementation. Our understanding of the processes at work is drawn from Shorrock’s concept of ‘varieties of human work’, borrowed from psychology and ergonomics science literature. 72–74 This concept has been useful in other areas of UK health care to explain the influences of human and organisational characteristics. 75,76 It helps us to elaborate the distinction between work-as-imagined, work-as-prescribed, work-as-disclosed and work-as-done, each of which has areas of overlap and areas of difference.
The pandemic experience exposed a partial understanding of health visiting work-as-imagined by policy-makers and the public. It highlighted a disconnect between an imagined, abstract system and a lived, experienced one, where the envisioned work represented a strong perception of what should be happening in the health visiting service. Some decisions affecting health visiting work during the pandemic were made on the basis of an incomplete imagined view of the work. Moreover, the lack of clarity and communication with families regarding health visiting work means they often do not know what to expect. This can mean families’ expectations are not met.
We obtained some documents describing how the formalised work of health visitors (work-as-prescribed) was disrupted at a national level during the pandemic response. Our data and stakeholder group discussions revealed that work was also significantly disrupted at the subnational level, with local service managers adopting varying approaches to service organisation and delivery. However, there was a dearth of evidence describing these changes. Our findings highlight many of the problems with work-as-prescribed that are articulated by Shorrock: there are many ways in which the work of health visitors can be done; much health visiting work is impossible to capture in prescribed work; and the conditions of work (such as staffing levels and time) are not guaranteed and are usually suboptimal in practice.
Within the many documents we reviewed that discussed health visiting during the COVID-19 pandemic, it is important to observe how health visiting work is described and by whom. What was disclosed or explained in the data is not a complete expression of how work is really done. Some work-as-disclosed might be explicitly designed to reassure, in terms of demonstrating an alignment with work-as-prescribed. Other work-as-disclosed might amplify the differences between work-as-done and work-as-prescribed, perhaps as part of an advocacy agenda that is fighting to preserve or increase resources in a difficult financial climate. 77–79
Work-as-done is actual activity that takes place in an environment that is inevitably more complex and constrained than imagined. The pandemic introduced additional variety in work-as-done across different health visiting teams and within different families. It has been reported that variations in the interpretation of COVID-19 rules led to different local restrictions,80 resulting in greater variety in health visiting work. This variety reflects the degree of flexibility that health visitors need to tailor support for individual families and to meet the needs of different populations. 81 While it is impossible to fully describe work-as-done and how that changed during the pandemic, it is useful to draw attention to the motivations, expressed in the literature, for the adaptations that health visitors made during the pandemic.
Implications for policy and practice
In October 2023, we discussed draft recommendations, identified from our CMOCs, with our professional stakeholder group and separately with the lived experience group. Professional stakeholders present at that final meeting took part in a poll on the ‘do-ability’ of these recommendations. Stakeholders not able to attend sent responses separately via e-mail. This feedback led to refinements, particularly in terms of specificity, resulting in the implications for policy and practice listed below.
Health visiting contacts
-
Health visiting contacts are vital opportunities to gather information for an assessment of the needs of babies, children and their families. All families should know what to expect and what to receive as part of a prescribed schedule of universal reviews that are sufficient to identify their needs. Since assessment is a continuous process, some light-touch contact/check-ins are important between universal assessment reviews. All relevant forms of contact with families are useful, but the additional benefits of face-to-face contact over remote connections must be recognised.
-
Health visiting contacts provide an opportunity for preventive, holistic support. Health visiting teams must have sufficient capacity to provide this service, beyond responding to immediate needs.
-
Health visiting contacts are an opportunity to build relationships and provide reassurance. Universal assessment reviews should be conducted face-to-face by a qualified health visitor, with whom families can build a relationship over time.
-
Remote contacts can prove beneficial for some families during particular periods and can provide a means of establishing open communication channels and offering assistance or information when needed. However, practitioners must consider inclusivity in relation to remote service delivery, and the potential to disadvantage some families.
-
Digital resources can be a useful way of providing additional support; however, practitioners must be assured that such resources are of high quality. Furthermore, alternatives should be in place to meet the needs of families living with digital poverty, to avoid inadvertently widening inequalities in access and outcomes.
Health visiting connections
-
Connecting families with other services is an important part of the health visitor’s role. Health visitors should be supported to highlight where local service provision is missing and to advocate for additional local investment to strengthen the system of support for families across a range of health, education and social needs.
-
Connecting with other health visitors is important for staff well-being and development. Digital and remote technologies might be considered for certain staff training and team meetings, but these should be combined with more traditional communication and education routes.
-
Interagency work is an important part of the health visitor role. Health visiting and other services/agencies involved in safeguarding children must support each other and co-ordinate service delivery, to maintain the visibility of children during times of crisis.
Health visiting workforce
-
Health visiting should be appropriately valued for its impact on child and family health and for longer-term public health outcomes. Universal home visiting services, dedicated to new parents and children, are ‘vital services’ and should therefore be protected in any future emergency. The long-term repercussions of the pandemic response for certain children and for health visiting teams remain partially understood. Additional organisational support may be required to mitigate its impacts.
Future research
The RReHOPE study forms an important piece of a jigsaw of evidence, alongside several others funded by NIHR. 19,82–85 Completed and ongoing studies are bringing together additional evidence, which combines primary and administrative data, to examine the variations in health visiting organisation and delivery throughout England. These studies also aim to assess the resulting impacts on outcomes and experiences for babies, children and parents. This collective body of research will provide a much stronger evidence base for future policy and practice.
This realist review presents several areas for future research. First, it is imperative to explore how health visiting teams can optimise their use of limited resources and manage their workload to enhance their capacity to identify and tackle health needs within the community. This is consistent with another recent review that highlighted the urgent need to assess the complexity of health visitor workload activity and the quality of service provided. 71 Second, further research could explore differences and changes in health visiting service organisation at the local management level and the implications for both staff and service users. Case study research here might further explore how access, delivery and uptake of health visiting and related services vary across regions, and how and why different population groups are affected by changes in services. Third, it is necessary to enhance the theoretical understanding of how alterations in service organisation and delivery can influence outcomes, translating evidence into a plausible narrative that explains how changes can be implemented effectively in a specific locality. Such research might also consider how the measurement and collection of outcomes at the local level can be improved. Fourth, support is needed for national funding of large cohort studies of babies born since 2020 to look at the effect of health visiting input over time on outcomes for children. Fifth, this realist review highlighted the English-centric bias in the current health visiting literature and the need for future work to be focused on other UK nations. Finally, the current work with our lived experience group highlighted the value of their perspectives and input. Further research should explore how parents can actively participate in improving service delivery in their localities. A further step could be to identify health visiting as a James Lind Alliance topic area for prioritisation of specific domains of research, which will inform policy and practice over the next 5–10 years.
Strengths and limitations
Our realist review has looked across the four UK countries and has synthesised and analysed data from 118 documents that informed our PT of health visiting during the COVID-19 pandemic. We have incorporated the insights of people with lived experience, and professional stakeholders from across the UK, who have helped us to identify implications for policy and practice, with the aim of improving the organisation and delivery of health visiting services in the UK.
The review was limited by the lack of specific evidence from Scotland, Wales and Northern Ireland. This limited our ability to analyse the evidence in a comparative way, and inevitably led to findings and conclusions that might be more significant for the English setting than for other countries. However, our stakeholder group helped us to consider the differences in context, policy and service delivery, and the impact of the pandemic across the four countries of the UK. They have also helped us to tailor our recommendations to different countries, which will be further reflected in additional country-specific outputs.
A further limitation was the lack of data focusing on pandemic-related changes at a local management level. Our extensive searching and communications with professional stakeholders suggest that such information was not formally recorded. This meant our review could not fully uncover local variability, for example in service organisation and workload/caseload management.
The number of mandated universal assessment reviews varies between each country, from 5 in England to 11 in Scotland. While the evidence in our review demonstrated the value of face-to-face universal assessment reviews, it did not enable us to comment further on the optimum number of reviews.
Conclusions
During the COVID-19 pandemic, health visiting teams adapted service delivery in different contexts in order to continue providing support for families with babies, and to ensure families remained visible to them in very challenging circumstances. They prioritised the need to build and maintain trusting relationships with families and used a range of methods to communicate and interact with families. However, the lack of face-to-face contact and home visits posed a considerable threat to this important part of a health visitors’ role. Health visitors also prioritised holistic needs assessments; they placed considerable importance on the postnatal assessment review and used remote contacts to try to keep in touch with families’ changing needs within a dynamic context. The experience reinforced the importance of scheduled home-based assessment reviews, conducted by a health visitor in the home setting, throughout the baby’s first 3 years. These home visits must be long enough to enable the health visitor to build trusting relationships, and to offer proactive and holistic support. The pandemic experience also highlighted that a health visitor, in optimally fulfilling their role, depends significantly on their connections with other support services in the local community. As these were impacted by the pandemic, so too were health visitors.
Given the gaps in evidence highlighted above, there is still a great deal to learn about the equitable, effective and efficient organisation and delivery of health visiting services in the UK. However, this study has culminated in some important implications for policy and practice and will usefully inform future research.
Additional information
CRediT contribution statement
Emma King (https://orcid.org/0000-0003-3611-9647): Methodology, Project Administration, Investigation, Writing – original draft.
Erica Gadsby (https://orcid.org/0000-0002-4151-5911): Conceptualisation, Funding acquisition, Methodology, Supervision and Writing – reviewing and editing.
Madeline Bell (https://orcid.org/0000-0003-2846-7318): Conceptualisation, Funding Acquisition, Methodology, Writing – reviewing and editing.
Geoff Wong (https://orcid.org/0000-0002-5384-4157): Conceptualisation, Funding acquisition, Methodology, Writing – reviewing and editing.
Sally Kendall (https://orcid.org/0000-0002-2507-0350): Conceptualisation, Funding acquisition, Methodology, Writing – reviewing and editing.
Acknowledgements
We would like to acknowledge Claire Duddy, specialist librarian, for undertaking the formal searches, initial drafting of the PRISMA diagram and contribution of Appendix 2. With thanks also to Alison Morton, Institute of Health Visiting, and the people with lived experience and professional stakeholders involved in this study for their enthusiasm, commitment, guidance and input.
Data-sharing statement
This realist review uses secondary data and therefore the data generated are not suitable for sharing beyond that contained within the manuscript. Further information can be obtained from the corresponding author.
Ethics statement
Ethical approval was obtained from the University of Stirling, application reference RReHOPE 7662 on 26 April 2022.
Information governance statement
The University of Stirling is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, the University of Stirling is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: www.stir.ac.uk/about/professional-services/student-academic-and-corporate-services/policy-and-planning/legal-compliance/data-protectiongdpr/privacy-notices/
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/MYRT5921.
Primary conflicts of interest: Madeline Bell is an employee of an NIHR Local Clinical Research Network. Sally Kendall was a Trustee of the Institute of Health Visiting 2012–18. Geoff Wong was a member of the HTA Prioritisation Committee 2015–22, HTA Remit and Competitiveness Committee 2015–21, and HTA Post-Funding Committee 2018–21. No further disclosure of interests to declare.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practices and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Study registration details
This study is registered as PROSPERO CRD42022343117.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research programme as award number NIHR134986.
This article reports on one component of the research award Realist Review: Health visiting in light Of the COVID-19 Pandemic Experience (RReHOPE). For more information about this research please view the award page (https://fundingawards.nihr.ac.uk/award/NIHR134986).
About this article
The contractual start date for this research was in June 2022. This article began editorial review in November 2023 and was accepted for publication in March 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health and Social Care Delivery Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Copyright
Copyright © 2024 King et al. This work was produced by King et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
Glossary
- Face-to-face
- Health visitors or other practitioners seeing a child in person, in the child’s home, in a clinic, at a health visitor-led baby group, etc.
- Remote connections
- Synchronous or asynchronous connections made using a variety of technology, for example phone calls, text messages, phone-based helplines and WhatsApp. These are generally brief connections between service users and members of the health visiting team, who may or may not be a qualified health visitor. They may be initiated by either the health visiting team or the service user.
- Remote consultations
- Synchronous consultations using telephone, or internet-based voice or video calls, to relay specific information to service users. This may be a one-to-one call or a group call with other service users. This might include breastfeeding support, classes on baby massage, or other additional support from a health visitor. They are different from the universal assessment reviews. Delivery is by a member of the health visiting team, or appropriately qualified role outside the health visiting team.
- Remote outreach
- Asynchronous outreach by the health visiting team is designed to deliver non-personalised information to many people. Examples of methods used include blanket e-mails, photocopied letters and posts on social media. Examples of information shared include meningitis symptoms, who to contact if you need medical help, ideas for play and interaction with your child.
- Remote universal assessment review
- Synchronous telephone or internet-based voice or video consultation involving direct interaction between a service user and a health visitor or member of the health visiting team. It is a direct replacement for one or more of the universal assessment reviews set out in the Child Health Programme for that nation.
- Universal assessment reviews
- Reviews of child development set out in the Child Health Programme for each nation of the United Kingdom. Offered to all families and ideally carried out face-to-face by a qualified health visitor.
List of abbreviations
- CHP
- Child Health Programme
- CMOC
- context, mechanism, outcome configuration
- PPE
- personal protective equipment
- PPI
- patient and public involvement
- PT
- programme theory
References
- Health for All Children. Oxford: Oxford University Press; 1989.
- Health for All Children. Oxford: Oxford University Press; 1992.
- Health for All Children. Oxford: Oxford University Press; 1996.
- Health for All Children. Oxford: Oxford University Press; 2003.
- Health for All Children. Oxford: Oxford University Press; 2006.
- Health for All Children. Oxford: Oxford University Press; 2019.
- Hackett A, Clarke K, Wilkinson J. Health Visiting: Specialist Community Public Health Nursing. Amsterdam: Elsevier; 2022.
- Rosenthal DM, Ucci M, Heys M, Hayward A, Lakhanpaul M. Impacts of COVID-19 on vulnerable children in temporary accommodation in the UK. Lancet Public Health 2020;5:e241-2. https://doi.org/10.1016/S2468-2667(20)30080-3.
- HM Government . The Best Start for Life: A Vision for the 1,001 Critical Days. The Early Years Healthy Development Review Report CP419 (25 March 2021) 2021. www.gov.uk/government/publications/the-best-start-for-life-a-vision-for-the-1001-critical-days (accessed 10 November 2023).
- Cowley S, Whittaker K, Malone M, Donetto S, Grigulis A, Maben J. Why health visiting? Examining the potential public health benefits from health visiting practice within a universal service: a narrative review of the literature. Int J Nurs Stud 2015;52:465-80. https://doi.org/10.1016/j.ijnurstu.2014.07.013.
- Wickham S, Anwar E, Barr B, Law C, Taylor-Robinson D. Poverty and child health in the UK: using evidence for action. Arch Dis Child 2016;101:759-66. https://doi.org/10.1136/archdischild-2014-306746.
- Taylor-Robinson D, Lai ETC, Wickham S, Rose T, Norman P, Bambra C, et al. Assessing the impact of rising child poverty on the unprecedented rise in infant mortality in England, 2000–2017: time trend analysis. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-029424.
- Galster G, Marcotte DE, Mandell M, Wolman H, Augustine N. The influence of neighborhood poverty during childhood on fertility, education, and earnings outcomes. Hous Stud 2007;22:723-51. https://doi.org/10.1080/02673030701474669.
- Featherstone B, Morris K, Daniel B, Bywaters P, Brady G, Bunting L, et al. Poverty, inequality, child abuse and neglect: changing the conversation across the UK in child protection?. Child Youth Serv Rev 2019;97:127-33. https://doi.org/10.1016/j.childyouth.2017.06.009.
- Cecil-Karb R, Grogan-Kaylor A. Childhood body mass index in community context: neighborhood safety, television viewing, and growth trajectories of BMI. Health Soc Work 2009;34:169-77. https://doi.org/10.1093/hsw/34.3.169.
- Bandyopadhyay A, Whiffen T, Fry R, Brophy S. How does the local area deprivation influence life chances for children in poverty in Wales: a record linkage cohort study. SSM Popul Health 2023;22. https://doi.org/10.1016/j.ssmph.2023.101370.
- Bryar RM, Cowley DS, Adams CM, Kendall S, Mathers N. Health visiting in primary care in England: a crisis waiting to happen?. Br J Gen Pract 2017;67:102-3. https://doi.org/10.3399/bjgp17X689449.
- Black M, Barnes A, Baxter S, Beynon C, Clowes M, Dallat M, et al. Learning across the UK: a review of public health systems and policy approaches to early child development since political devolution. J Public Health (Oxf) 2019;42:224-38. https://doi.org/10.1093/pubmed/fdz012.
- Fraser C, Harron K, Woods G, Shand J, Kendall S, Woodman J. Variation in health visiting contacts for children in England: cross-sectional analysis of the 2–2½ year review using administrative data (Community Services Dataset, CSDS). BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-053884.
- Woodman J, Harron K, Hancock D. Which children in England see the health visiting team and how often?. J Health Visit 2021;9:282-4. https://doi.org/10.12968/johv.2021.9.7.282.
- Whittaker K, Appleton JV, Peckover S, Adams C. Organising health visiting services in the UK: frontline perspectives. J Health Visit 2021;9:68-75. https://doi.org/10.12968/johv.2021.9.2.68.
- Department of Health . Thresholds of Need Model 2010. www.health-ni.gov.uk/publications/thresholds-need-model (accessed 15 November 2023).
- Cabinet Secretary for Education and Skills . Getting It Right for Every Child (GIRFEC): Wellbeing (SHANARRI) n.d. www.gov.scot/policies/girfec/wellbeing-indicators-shanarri/ (accessed 13 November 2023).
- Nursing, Midwifery and Allied Health Professional Directorate . Healthy Child, Healthy Future – A Framework for the Universal Child Health Promotion Programme in Northern Ireland 2010. www.health-ni.gov.uk/publications/healthy-child-healthy-future (accessed 13 November 2023).
- Singh A, Shah N, Mbeledogu C, Garstang J. Child wellbeing in the United Kingdom following the COVID-19 lockdowns. Paediatr Child Health (Oxford) 2021;31:445-8. https://doi.org/10.1016/j.paed.2021.09.004.
- Jackson C, Brawner J, Ball M, Crossley K, Dickerson J, Dharni N, et al. Being pregnant and becoming a parent during the COVID-19 pandemic: a longitudinal qualitative study with women in the Born in Bradford COVID-19 research study. Res Sq 2023;23. https://doi.org/10.21203/rs.3.rs-2317422/v1.
- Conti G, Dow A. Using FOI Data to Assess the State of Health Visiting Services in England Before and During COVID-19. London: UCL Department of Economics; 2021.
- Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav 2021;5:529-38. https://doi.org/10.1038/s41562-021-01079-8.
- Institute of Health Visiting . 24 March – Morning Update: COVID-19 2020. https://ihv.org.uk/news-and-views/news/24-march-morning-update-covid-19/ (accessed 16 November 2023).
- Morton A, Adams C. Health visiting in England: the impact of the COVID-19 pandemic. Public Health Nurs 2022;39:820-30. https://doi.org/10.1111/phn.13053.
- Conti G, Dow A. The Impacts of Covid-19 on Health Visiting in England: First Results. London: UCL Department of Economics; 2020.
- Institute of Health Visiting . State of Health Visiting in England: Are Babies and Their Families Being Adequately Supported in England in 2020 to Get the Best Start in Life? 2020.
- Barlow J, Bach-Mortensen A, Homonchuk O, Woodman J. The Impact of the COVID-19 Pandemic on Services from Pregnancy through Age 5 Years for Families Who Are High Risk of Poor Outcomes or Who Have Complex Social Needs 2020. www.ucl.ac.uk/children-policy-research/projects/impact-covid-19-pandemic-services-pregnancy-through-age-5-years (accessed 15 November 2023).
- Institute of Health Visiting . State of Health Visiting in England: ‘We Need More Health Visitors!’ 2021.
- The Child Safeguarding Review Panel . Annual Report 2020: Patterns in Practice, Key Messages and 2021 Work Programme 2021. https://assets.publishing.service.gov.uk/media/609945c78fa8f56a3e32f9a3/The_Child_Safeguarding_Annual_Report_2020.pdf (accessed 15 November 2023).
- The Child Safeguarding Review Panel . Child Protection in England: National Review into the Murders of Arthur Labinjo-Hughes and Star Hobson 2022. www.gov.uk/government/publications/national-review-into-the-murders-of-arthur-labinjo-hughes-and-star-hobson (accessed 15 November 2023).
- Office for National Statistics . How People Spent Their Time After Coronavirus Restrictions Were Lifted, UK: March 2022 2022. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/howpeoplespenttheirtimeaftercoronavirusrestrictionswerelifteduk/march2022 (accessed 20 March 2024).
- Irvine LC, Chisnall G, Vindrola-Padros C. The impact of maternity service restrictions related to COVID-19 on women’s experiences of giving birth in England: a qualitative study. Midwifery 2024;128. https://doi.org/10.1016/j.midw.2023.103887.
- Kasaven LS, Raynaud I, Jalmbrant M, Joash K, Jones BP. The impact of the COVID-19 pandemic on perinatal services and maternal mental health in the UK. BJPsych Open 2023;9. https://doi.org/10.1192/bjo.2022.632.
- Silverio SA, De Backer K, Easter A, von Dadelszen P, Magee LA, Sandall J. Women’s experiences of maternity service reconfiguration during the COVID-19 pandemic: a qualitative investigation. Midwifery 2021;102. https://doi.org/10.1016/j.midw.2021.103116.
- Sanders J, Blaylock R. Anxious and traumatised’: users’ experiences of maternity care in the UK during the COVID-19 pandemic. Midwifery 2021;102. https://doi.org/10.1016/j.midw.2021.103069.
- Saunders B, Hogg S. Babies in Lockdown: Listening to Parents to Build Back Better 2020. https://parentinfantfoundation.org.uk/our-work/campaigning/babies-in-lockdown/#fullreport (accessed 17 May 2022).
- McKinnell C. The Impact of Covid-19 on Maternity and Parental Leave: First Report of Session 2019–21: Report, Together with Formal Minutes Relating to the Report. London: House of Commons; 2020.
- UNICEF United Kingdom . Early Moments Matter: Guaranteeing the Best Start in Life for Every Baby and Toddler in England 2022. www.unicef.org.uk/wp-content/uploads/2022/10/EarlyMomentsMatter_UNICEFUK_2022_PolicyReport.pdf (accessed 15 November 2023).
- Holt L, Murray L. Children and Covid 19 in the UK. Child Geogr 2022;20:487-94. https://doi.org/10.1080/14733285.2021.1921699.
- Baker C, Hutton G, Christie L, Wright S. COVID-19 and the Digital Divide. UK Parliament; 2020.
- Lemkow-Tovías G, Lemkow L, Cash-Gibson L, Teixidó-Compañó E, Benach J. Impact of COVID-19 inequalities on children: an intersectional analysis. Sociol Health Illn 2023;45:145-62. https://doi.org/10.1111/1467-9566.13557.
- Co-POWeR . Co-POWeR Animation Video 2022. https://mymedia.leeds.ac.uk/Mediasite/Play/49c3e27d80eb4ea6895c07ad90e00d7b1d (accessed 13 November 2023).
- Cattan S, Lloyd E, Montacute R, Shorthouse R. Early Years Inequalities in the Wake of the Pandemic. London: IFS; 2021.
- Watts G. COVID-19 and the digital divide in the UK. Lancet Digit Health 2020;2:e395-6. https://doi.org/10.1016/S2589-7500(20)30169-2.
- King E, Gadsby E, Bell M, Duddy C, Kendall S, Wong G. Health visiting in the UK in light of the COVID-19 pandemic experience (RReHOPE): a realist review protocol. BMJ Open 2023;13. https://bmjopen.bmj.com/content/13/3/e068544 (accessed 21 November 2023).
- Gadsby EW, Christie-de Jong F, Bhopal S, Corlett H, Turner S. Qualitative analysis of the impact of the SARS-CoV-2 pandemic response on paediatric health services in North of Scotland and North of England. BMJ Open 2022;12. https://doi.org/10.1136/bmjopen-2021-056628.
- Institute of Health Visiting . Making History: Health Visiting During Covid-19 2020. https://ihv.org.uk/news-and-views/news/spotlighting-the-vital-safety-net-that-health-visitors-have-provided-for-babies-and-young-children-during-the-current-pandemic/ (accessed 15 November 2023).
- Lewis R, Pereira P, Thorlby R, Warburton W. Understanding and Sustaining the Health Care Service Shifts Accelerated by COVID-19 2020. www.health.org.uk/publications/long-reads/understanding-and-sustaining-the-health-care-service-shifts-accelerated-by-COVID-19 (accessed 15 November 2023).
- Wilson H, Waddell S. COVID-10 and Early Intervention: Understanding the Impact, Preparing for Recovery. London: Action for Children; 2020.
- Pawson R. Evidence-Based Policy: A Realist Perspective. Thousand Oaks, CA: SAGE Publications Ltd; 2006.
- RAMESES . Realist Synthesis: RAMESES Training Materials 2013. www.ramesesproject.org/media/Realist_reviews_training_materials.pdf (accessed 20 March 2024).
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist Synthesis: An Introduction 2004.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. https://doi.org/10.1186/1741-7015-11-21.
- King E, Gadsby E, Bell M, Duddy C, Kendall S, Wong G. Health visiting in the UK in light of the COVID-19 pandemic experience (RReHOPE): a realist review protocol. BMJ Open 2023;13. https://doi.org/10.1136/bmjopen-2022-068544.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372. https://doi.org/10.1136/bmj.n71.
- Bidmead C. Health Visitor/Parent Relationships: A Qualitative Analysis – Appendix 1. London: National Nursing Research Unit, King’s College London; 2013.
- Cowley S, Malone M, Whittaker K, Donetto S, Grigulis A, Maben J. What makes health visiting successful—or not? 2. The service journey. J Health Visit 2018;6:404-12. https://doi.org/10.12968/johv.2018.6.8.404.
- de la Cuesta C. Relationships in health visiting: enabling and mediating. Int J Nurs Stud 1994;31:451-9. https://doi.org/10.1016/0020-7489(94)90015-9.
- Chalmers KI, Luker KA. The development of the health visitor-client relationship. Scand J Caring Sci 1991;5:33-41. https://doi.org/10.1111/j.1471-6712.1991.tb00079.x.
- Institute of Health Visiting . Professional Advice to Support Best Practice: The Antenatal Contact 2020. https://ihv.org.uk/wp-content/uploads/2020/03/Antenatal-Visit-FINAL-VERSION-27.3.20.pdf (accessed 15 November 2023).
- Public Health Agency . Impact of the Covid-19 Pandemic on Breastfeeding Support 2021. www.publichealth.hscni.net/sites/default/files/2021-12/20-104030%20PHA%20breastfeeding%20research%20report%20V7%2021.05.2021%20client%20use%20only.pdf (accessed 30 April 2024).
- Health visitor’s projects for vulnerable families go above and beyond. Prim Health Care 2022;32. https://doi.org/10.7748/phc.32.3.5.s1.
- NHS Confederation, NHS Providers Community . Hidden Waits. The Lasting Impact of the Pandemic on Children’s Services in the Community 2022.
- Boddy B. Newly qualified health visitor: adapting practice in difficult times. J Health Visit 2020;8:282-3. https://doi.org/10.12968/johv.2020.8.7.282.
- Reid B, Tracey J. Health visitor workload: an integrative review of the literature. Prim Health Care 2023;34:36-42. https://doi.org/10.7748/phc.2023.e1804.
- Moppett IK, Shorrock ST. Working out wrong-side blocks. Anaesthesia 2018;73:407-20. https://doi.org/10.1111/anae.14165.
- Shorrock S. The Varieties of Human Work 2016. https://humanisticsystems.com/2016/12/05/the-varieties-of-human-work/ (accessed 15 November 2023).
- Hollnagel E. Can We Ever Imagine How Work Is Done? 2017. www.skybrary.aero/sites/default/files/bookshelf/3934.pdf (accessed 15 November 2023).
- Holt J. Reflection on the Varieties of Human Work and How They Apply to Healthcare 2020. www.pslhub.org/learn/improving-patient-safety/human-factors-improving-human-performance-in-care-delivery/reflection-on-the-varieties-of-human-work-and-how-they-apply-to-healthcare-r3328/#:~:text=Shorrock%20discussed%20the%20four%20varieties,and%20work%2Das%2Ddone (accessed 15 November 2023).
- Royal College of Obstetricians and Gynaecologists . Each Baby Counts: Safety Thinking Toolkit: Work As Imagined Versus Work As Done 2022. www.rcog.org.uk/about-us/quality-improvement-clinical-audit-and-research-projects/each-baby-counts-learn-support/safety-thinking-toolkit/ (accessed 30 November 2023).
- First 1001 Days Movement . Why Health Visitors Matter: Perspectives on a Widely Valued Service 2022. https://parentinfantfoundation.org.uk/wp-content/uploads/2022/05/Why-Health-Visitors-Matter.pdf (accessed 10 November 2023).
- Ryan A. Early Years Recovery Briefing. National Children’s Bureau; 2020.
- Appleton JV. Vulnerable children and early intervention – what about health visiting?. Child Abuse Rev 2021;30:89-97. https://doi.org/10.1002/car.2686.
- Reed J, Hogg S. Working for Babies. Listening to Local Voices for a Better Recovery. First 1001 Days Movement, ISOS Partnership, Local Government Association; 2021.
- Seaman HE. Establishing health visitors’ professional identity. J Health Visit 2022;10:334-46. https://doi.org/10.12968/johv.2022.10.8.334.
- Woodman J. Research Award: Which Health Visiting Models in England Are Most Promising for Mitigating the Harms of Maternal Related Adverse Child Experiences?. National Institute for Health and Care Research; 2022.
- Harron K. Research Award: Evaluation of the 0–5 Public Health Investment in England: A Mixed Methods Study Integrating Analyses of National Linked Administrative Data with In-depth Case Studies. National Institute for Health and Care Research; 2022.
- Cavallaro F, Kendall S, van der Meulen J, Kennedy E, Howarth E, Gilbert R, et al. Evaluation of the real-world implementation of the Family Nurse Partnership in England: an observational cohort study using linked data from health, education and children’s social care. Int J Popul Data Sci 2022;7. https://doi.org/10.23889/ijpds.v7i3.1831.
- Woodman J. Measuring Child Development at the 2–2½ Year Health Review in England: Available Tools, Stakeholder Priorities and Feasibility of Implementation. National Institute for Health and Care Research; 2022.
- First 1001 Days Movement – Joint Statement in Response to COVID-19 2020. https://5e0ce443-5301-4ac7-91aa-e6b8f500afdc.usrfiles.com/ugd/5e0ce4_c15afecdf5a44e558f1e0c3c1a406e07.pdf (accessed 10 November 2023).
- Action for Children, ACP, Best Beginnings, First Days Movement, Home Start, Institute of Health Visiting . The Future of Public Health – Giving Every Child the Best Start in Life 2020. https://childpsychotherapy.org.uk/sites/default/files/civicrm/persist/contribute/files/Future%20of%20Public%20Health%20-%20Best%20Start%20in%20Life_6_.pdf (accessed 10 November 2023).
- Action for Children . Parenting Services under Pressure: Unequal Access to Early Years Support in England 2022. https://media.actionforchildren.org.uk/documents/Parenting_services_under_pressure.pdf (accessed 10 November 2023).
- Aquino MRJ, Gilroy V, Jackson V, Arnott A, Swinson S, Murning M, et al. A Mixed-Methods Exploration of Health Visiting Service Provision and Innovations in England During COVID-19. Växjö: Linnéuniversitetet; 2022.
- Baldwin S, Stephen R, Bishop P, Kelly P. Development of the Emotional Wellbeing at Work Virtual Programme to support UK health visiting teams. J Health Visit 2020;8:516-22. https://doi.org/10.12968/johv.2020.8.12.516.
- Baldwin S, Stephen R, Kelly P, Bishop P. Learning and reflections from the iHV Emotional Wellbeing at Work Champions Programme. J Health Visit 2022;10:420-7. https://doi.org/10.12968/johv.2022.10.10.420.
- Bear L, James D, Simpson N, Alexander E, Bazambanza C, Bhogal JK, et al. A Right to Care: The Social Foundations of Recovery from Covid-19. London: London School of Economics and Political Science; 2020.
- Best Beginnings, Home Start, Parent-Infant Foundation . Babies in Lockdown: Listening to Parents to Build Back Better 2020. https://babiesinlockdown.files.wordpress.com/2020/08/babies-in-lockdown-main-report-final-version.pdf (accessed 10 November 2023).
- Parent-Infant Foundation . No One Wants to See My Baby: Challenges to Building Back Better for Babies 2021.
- Boddy B. Newly qualified health visitor: COVID-19 – a public health crisis. J Health Visit 2020;8:146-7. https://doi.org/10.12968/johv.2020.8.4.146.
- Boddy B. Newly qualified health visitor: looking to the future for children and families. J Health Visit 2020;8:234-6. https://doi.org/10.12968/johv.2020.8.6.234.
- Boddy B. Newly qualified health visitor: the evidence to support home visiting. J Health Visit 2020;8:188-9. https://doi.org/10.12968/johv.2020.8.5.188.
- Boddy B. Health visiting services during the pandemic: the changes and challenges ahead. J Health Visit 2021;9:16-8. https://doi.org/10.12968/johv.2021.9.1.16.
- Boddy B. Health visitor workforce numbers. J Health Visit 2022;10:390-2. https://doi.org/10.12968/johv.2022.10.9.390.
- Boddy B. Covid 2 years on: what is the evidence?. J Health Visit 2022;10:128-30. https://doi.org/10.12968/johv.2022.10.3.128.
- Brook J. Redesigning the health visiting service offer. J Health Visit 2020;8:261-2. https://doi.org/10.12968/johv.2020.8.6.261.
- McTier A, Sills R. The Impact of COVID-19 on Children and Families in Scotland: Understanding Needs and Services Through Local Social Work Data. Scottish Government Children and Families Collective Leadership Group; 2021.
- Commissioner for England . Lockdown Babies: Children Born During the Coronavirus Crisis (Briefing) 2020. https://assets.childrenscommissioner.gov.uk/wpuploads/2020/05/cco-lockdown-babies.pdf (accessed 30 April 2024).
- Cole E. It was a chance for us to remember why we became health visitors in the first place. Prim Health Care 2022;32:14-6. https://doi.org/10.7748/phc.32.3.14.s4.
- COVID-19 reflections. Community Pract 2020;93:24-5.
- Anonymous . Checking the baby blind spot: babies in lockdown. Community Pract 2021;94.
- McQueen F, White J. Put children and families first in ‘perfect storm’. Community Pract 2020;94.
- Holland A. Showcasing health visiting in Wales part 2. Community Pract 2022;95:40-3.
- Griffin F. New ways of working. Community Pract 2022;95.
- Holland A. Part 1: showcasing health visiting in Wales. Community Pract 2022;95:40-3.
- Conti G, Dow A. The Impacts of COVID-19 on Health Visiting Services in England: FOI Evidence for the First Wave. London: UCL Department of Economics; 2020.
- De Backer K, Brown JM, Easter A, Khazaezadeh N, Rajasingam D, Sandall J, et al. Precarity and preparedness during the SARS-CoV-2 pandemic: a qualitative service evaluation of maternity healthcare professionals. Acta Obstet Gynecol Scand 2022;101:1227-37. https://doi.org/10.1111/aogs.14438.
- Driscoll J, Lorek A, Kinnear E, Hutchinson A. Multi-agency safeguarding arrangements: overcoming the challenges of Covid-19 measures. J Child Serv 2020;15:267-74. https://doi.org/10.1108/JCS-07-2020-0035.
- Driscoll J, Hutchinson A, Lorek A, Kiss K, Kinnear E. Hearing the voice of the child through the storm of the pandemic: the impact of COVID-19 measures on the detection of and response to child protection concerns. Int J Child Rts 2021;29:400-25. https://doi.org/10.1163/15718182-29020005.
- Durand C, Kane C, McIlroy H, Verhoeff F. Infants attending the paediatric emergency department with feeding difficulties & referrals to nurse led infant feeding clinic. Arch Dis Child 2021;106:A392-3. https://doi.org/10.1136/archdischild-2021-rcpch.682.
- Entwistle F. Infant feeding: the COVID effect. Community Pract 2020;93:48-9.
- Evans N. What will the ‘new normal’ look like for children’s services?. Nurs Child Young People 2020;32:8-10. https://doi.org/10.7748/ncyp.32.5.8.s8.
- Feger H. Securing the digital future. Community Pract 2021;94:48-9.
- Forbes L. A new normal for health visiting. J Health Visit 2020;8. https://doi.org/10.12968/johv.2020.8.4.150.
- Gill B, Hampton T, Geary R, Whittaker K. Greater support, recognition, and research for health visiting post-pandemic. Br J Gen Pract 2022;72:368-9. https://doi.org/10.3399/bjgp22X720221.
- Halnan B. Attend anywhere. Community Pract 2022;95:28-31.
- Hancock D. What will children’s services look like in the future?. J Health Visit 2020;8:290-3. https://doi.org/10.12968/johv.2020.8.7.290.
- Hancock D. How has Covid-19 affected health visiting teams. J Health Visit 2021;9:460-2. https://doi.org/10.12968/johv.2021.9.11.460.
- Hanley J. That pesky nucleic acid molecule in a protein coat. J Health Visit 2020;8. https://doi.org/10.12968/johv.2020.8.4.172.
- Hanley J. Collaboration in a changed world. J Health Visit 2021;9:172-4. https://doi.org/10.12968/johv.2021.9.4.172.
- Hanley J. Are health visitors valued after all?. J Health Visit 2022;10:41-2. https://doi.org/10.12968/johv.2022.10.1.41.
- Harding R, Paechter C. Effects of Covid-19 on Families with Children under Five in Nottingham. Report Prepared for Small Steps, Big Changes. Nottingham: Nottingham Centre for Children, Young People and Families; 2020.
- Launder M. Child health checks failed to recover after Covid, figures show. Health Serv J 2023.
- Healthwatch South Gloucestershire . Lessons from Health Visiting During COVID-19: The Experiences of South Gloucestershire Residents 2022.
- Hefferon C, Taylor C, Bennett D, Falconer C, Campbell M, Williams JG, et al. Priorities for the child public health response to the COVID-19 pandemic recovery in England. Arch Dis Child 2021;106:533-8. https://doi.org/10.1136/archdischild-2020-320214.
- House of Commons Petitions Committee . The Impact of Covid-19 on New Parents: One Year On 2021.
- Institute of Health Visiting . Health Visiting During COVID-19: An IHV Report 2020.
- Institute of Health Visiting . The Early Years Commission – Call for Evidence – Written Evidence Submitted by the Institute of Health Visiting 2020.
- Waters C, Lewis A, Childs L, Martin P, Smith J. Remaining Responsive During the COVID-19 Pandemic: Developing New Ways of Delivering Public Health Nursing Services. London: Institute of Health Visiting; 2020.
- Institute of Health Visiting . State of Health Visiting in England: Are Babies and Their Families Being Adequately Supported in England in 2020 to Get the Best Start in Life? 2020.
- Morton A. Health Visiting During COVID-19 and Beyond: The Impact on Children and Families (Presentation). London: Institute of Health Visiting, Local Government Association; 2020.
- Adams C. Is a Secondary Pandemic on the Way?. London: Institute of Health Visiting; 2020.
- Institute of Health Visiting . The Impact of COVID-19 on Education and Children’s Services: Submission to Parliamentary Education Committee By: Institute of Health Visiting 2020.
- Institute of Health Visiting . Making History: Health Visiting During COVID-19 2020. https://ihv.org.uk/wp-content/uploads/2021/07/Health-visiting-making-history-case-studies-FINAL-VERSION-updated-14.7.21.pdf (accessed 17 May 2022).
- Institute of Health Visiting . Health Visiting During COVID-19: Unpacking Redeployment Decisions and Support for Health Visitors’ Wellbeing 2020.
- Institute of Health Visiting . Professional Advice to Support Best Practice: Family Perinatal Mental Health 2020.
- Institute of Health Visiting . Professional Advice to Support Best Practice: Family Perinatal Mental Health (Version 2) 2020.
- Institute of Health Visiting . Professional Advice to Support Best Practice: The Antenatal Visit (Version 2) 2020.
- Institute of Health Visiting . Professional Advice to Support Best Practice: The New Birth Visit 2020.
- Institute of Health Visiting . Professional Advice to Support Best Practice: The New Birth Visit (Version 2) 2020.
- Institute of Health Visiting . Professional Advice to Support Best Practice: Virtual Contacts by Health Visitors 2020.
- Institute of Health Visiting . Professional Advice to Support Best Practice: Virtual Contacts by Health Visitors (Version 2) 2020.
- Institute of Health Visiting . Professional Advice to Support Best Practice: Working With Vulnerable Families 2020.
- Institute of Health Visiting . Professional Advice to Support Best Practice: Working With Vulnerable Families (Version 2) 2020.
- Institute of Health Visiting . State of Health Visiting, UK Survey Report. A Vital Safety Net under Pressure: 9th IHV Annual Health Visiting Survey: Data Year Ending November 2022 2023.
- Jackson L, De Pascalis L, Harrold JA, Fallon V, Silverio SA. Postpartum women’s experiences of social and healthcare professional support during the COVID-19 pandemic: a recurrent cross-sectional thematic analysis. Women Birth 2022;35:511-20. https://doi.org/10.1016/j.wombi.2021.10.002.
- Kombe B. Born in a Pandemic 2020. https://ihv.org.uk/news-and-views/voices/born-in-a-pandemic/ (accessed 30 April 2024).
- Harrogate and District NHS Foundation Trust . 0–19 Services Business Continuity – Briefing for All 0–19 Staff 2020.
- Harrogate and District NHS Foundation Trust . Update to 0–19 Teams on HDFT Prioritisation of Face to Face Contact at Primary Visit: Suzanne Lamb, Head of Safeguarding and Lead Nurse for Public Health and Quality 2020.
- Manning JC, Bramley L, Coad J, Evans C, Evans K, Tinkler L, et al. Priorities for Research During the Coronavirus SARS-CoV-2 (COVID-19) Pandemic and Beyond: A Survey of Nurses, Midwives and Health Visitors in the United Kingdom. J Res Nurs 2021;26:442-54.
- Moltrecht B, Dalton LJ, Hanna JR, Law C, Rapa E. Young parents’ experiences of pregnancy and parenting during the COVID-19 pandemic: a qualitative study in the United Kingdom. BMC Public Health 2022;22. https://doi.org/10.1186/s12889-022-12892-9.
- Morton A. Who is providing a safety net for babies and young children?. J Health Visit 2020;8:276-8. https://doi.org/10.12968/johv.2020.8.7.276.
- Morton A. Health visiting: lockdown stories may prompt change: resources are needed where damage to early years support has been greatest, says Institute of Health Visiting. Nurs Childr Young People 2021;33. https://doi.org/10.7748/ncyp.33.4.9.s3.
- NHS England, NHS Improvement . COVID-19 Restoration of Community Health Services for Children and Young People: Second Phase of NHS Response (Letter) 2020.
- NHS England . Important – For Action – Second Phase of NHS Response to COVID 19 (Letter) 2020.
- Scottish Executive . National Clinical Guidance for Nursing and AHP Community Health Staff During COVID-19 Pandemic (v. 1.3) 2020.
- Russell MJ. Coping alone. Nurs World 2022;2022:32-3. https://doi.org/10.12968/nuwa.2022.7.32.
- Health visitor diaries: harrowing disclosures and safeguarding in a sector beset by cuts. Nurs Childr Young People 2021;33:11-3. https://doi.org/10.7748/ncyp.33.6.11.s4.
- How we rose to the leadership challenges of COVID-19. Nurs Stand 2021;36:40-3. https://doi.org/10.7748/ns.36.6.40.s17.
- Oldman C. The right to healthy housing. J Health Visit 2021;9. https://doi.org/10.12968/johv.2021.9.2.86.
- Oldman C. A depleted workforce. J Health Visit 2022;10:348-50. https://doi.org/10.12968/johv.2022.10.8.348.
- Oldman C. Redeployment: the work left undone. J Health Visit 2020;8. https://doi.org/10.12968/johv.2020.8.5.218.
- Papworth R, Harris A, Durcan G, Wilton J, Sinclair C. Maternal Mental Health During a Pandemic: A Rapid Evidence Review of Covid-19’s Impact Centre for Mental Health March 2021. https://maternalmentalhealthalliance.org/mmhpandemic/ (accessed 1 June 2023).
- Perez A, Panagiotopoulou E, Curtis P, Roberts R. Barriers and facilitators to mood and confidence in pregnancy and early parenthood during COVID-19 in the UK: mixed-methods synthesis survey. BJPsych Open 2021;7.
- Powell J, Taylor J. Safeguarding children and families during the pandemic. J Health Visit 2021;9:154-6. https://doi.org/10.12968/johv.2021.9.4.154.
- Adams C. Health visitors must stay on the front line for families. Prim Health Care 2020;30. https://doi.org/10.7748/phc.30.6.11.s5.
- Public Health England, NHS, Local Government Association . Winter Planning: Support to Children and Families (Letter) 2020.
- Public Health Scotland . COVID-19 Early Years Resilience and Impact Survey (CEYRIS): Report 4 – Full Findings 2020.
- Royal College of Nursing . Remote Consultations Guidance under COVID-19 Restrictions 2020.
- Moseley M. Choosing to Challenge. London: Royal College of Nursing; 2021.
- Rhodes A, Kheireddine S, Smith AD. Experiences, attitudes, and needs of users of a pregnancy and parenting app (Baby Buddy) during the COVID-19 pandemic: mixed methods study. JMIR Mhealth Uhealth 2020;8. https://doi.org/10.2196/23157.
- Riley V, Ellis N, Mackay L, Taylor J. The impact of COVID-19 restrictions on women’s pregnancy and postpartum experience in England: a qualitative exploration. Midwifery 2021;101. https://doi.org/10.1016/j.midw.2021.103061.
- Rooke N. The big switch. Community Pract 2021;94:32-5.
- Salisbury T, Qurashi N, Mansoor Q. Change in incidence and severity of abusive head trauma in the paediatric age group pre- and during COVID-19 lockdown in the north east of England. Br Ir Orthop J 2022;18:101-10. https://doi.org/10.22599/bioj.265.
- Seaman HE. Health Visitors’ Professional Identity and Their Lived Experience of Service Change. Hatfield: University of Hertfordshire; 2021.
- Singh A, Shah N, Mbeledogu C, Garstang J. Child wellbeing in the United Kingdom following the COVID-19 lockdowns. Paediatr Child Health (Oxford) 2021;31:445-8. https://doi.org/10.1016/j.paed.2021.09.004.
- Stiles C. Health visitor prescribing during the Covid-19 pandemic. Case Rep Womens Health 2021;31.
- Thomson G, Cook J, Nowland R, Donnellan WJ, Topalidou A, Jackson L, et al. Resilience and post-traumatic growth in the transition to motherhood during the COVID-19 pandemic: a qualitative exploratory study. Scand J Caring Sci 2022;36:1143-55. https://doi.org/10.1111/scs.13087.
- Watson M, Sarica S, Wason D, Mitchell R, Parkinson J. COVID-19 Early Years Resilience and Impact Survey (CEYRIS). Report 3 – The Experience of Parents and Carers of 2–7-Year-Olds in Scotland During COVID-19. Edinburgh; 2020.
- Welsh Government . Professional Advice to Support Best Practice: The Birth Visit 2020.
- Wilkinson E. Health visitor shortages are risking child health and piling pressure on other services. BMJ 2022;378. https://doi.org/10.1136/bmj.o2189.
- Williams S. The Horror, Hope and Future of Healthcare: Health Visiting and COVID-19. Institute of Health Visiting; 2021.
Appendix 1 Initial programme theory
FIGURE 3.
Initial PT summarising background material.
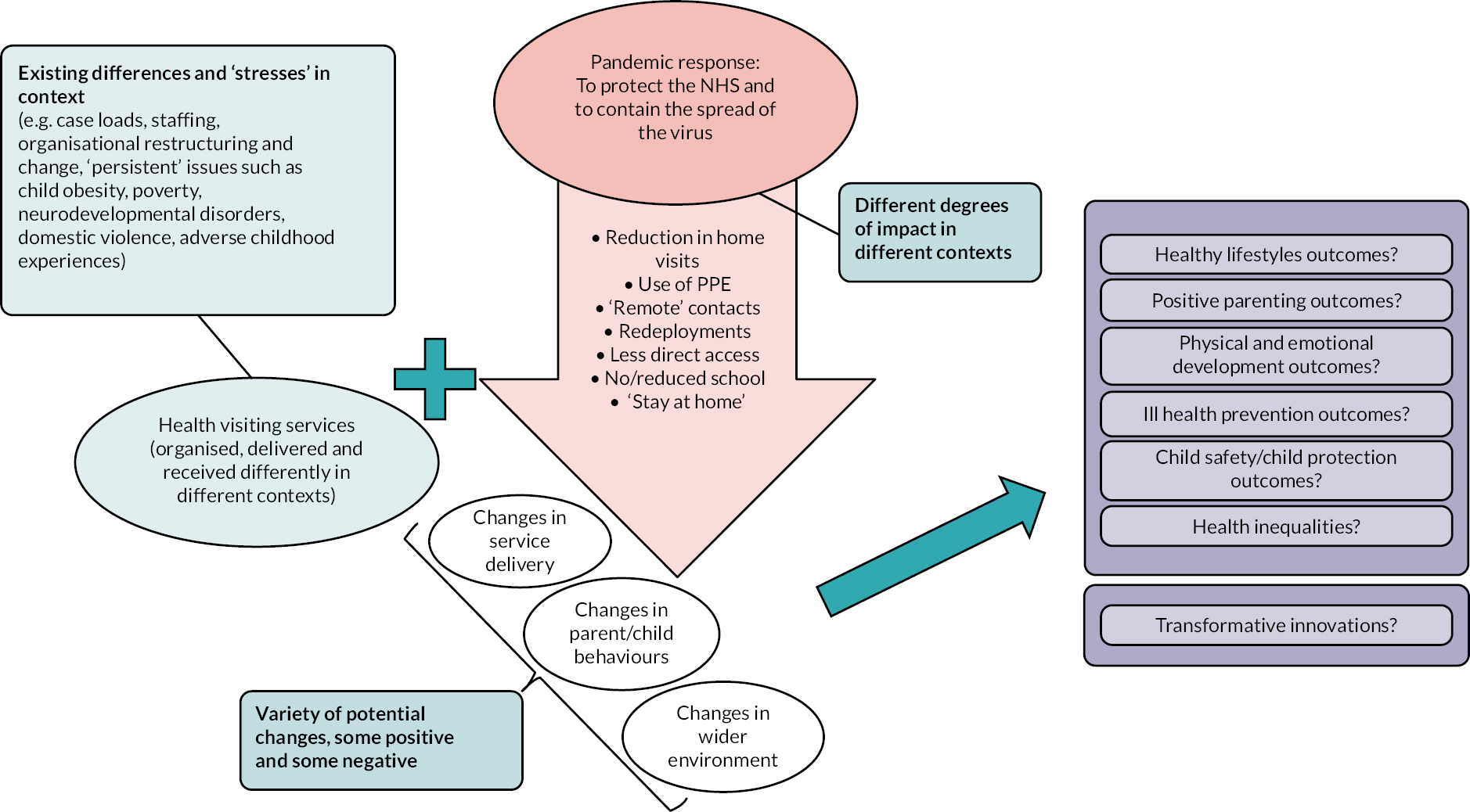
Appendix 2 Search strategies
Searches to inform initial PT development (June 2022)
PubMed
Host: US National Library of Medicine (https://pubmed.ncbi.nlm.nih.gov/)
Date range searched: 2009–22
Date searched: 29 June 2022
Searcher: CD
Hits: n = 19
| 1 | “health visitor*”[Title] OR “health visiting”[Title] | 1675 |
| 2 | “child health program*”[Title] | 148 |
| 3 | “healthy child program*”[Title] | 5 |
| 4 | “healthy child wales”[Title] | 0 |
| 5 | “getting it right for every child”[Title] | 0 |
| 6 | “healthy child healthy future”[Title] | 0 |
| 7 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 | 1828 |
| 8 | Publication year 2009–22 | 346 |
| 9 | Filters applied: Review, Systematic Review; English language | 19 |
CINAHL
Host: EBSCOhost
Date range searched: 2009–22
Date searched: 29 June 2022
Searcher: CD
Hits: n = 29
| S1 | “health visitor*”[Title] OR “health visiting”[Title] | 2253 |
| S2 | “child health program*”[Title] | 64 |
| S3 | “healthy child program*”[Title] | 14 |
| S4 | “healthy child wales”[Title] | 0 |
| S5 | “getting it right for every child”[Title] | 4 |
| S6 | “healthy child healthy future”[Title] | 1 |
| S7 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 | 2336 |
| Publication year 2009–22 | 874 | |
| Filters applied: English | 869 | |
| Filters applied: Clinical queries: Review – Best Balance | 29 |
Google Scholar
Host: Google (scholar.google.com; Google Chrome, incognito window)
Date range searched: 2009–22
Date searched: 29 June 2022
Searcher: CD
Hits: n = 24 (First 100 hits screened on screen; 24 identified to consider for inclusion)
| “health visitor” OR “health visiting” OR “healthy child programme” OR “healthy child wales” OR “getting it right for every child” OR “healthy child healthy future” | |
| Limits applied: 2009–22 | c 19,700 |
Host: Google (google.com; Google Chrome, incognito window)
Date range searched: Unknown
Date searched: 30 June 2022
Searcher: CD
Hits: n = 19 (Up to 100 hits for each limiter screened on screen; 19 identified to consider for inclusion)
| “health visiting” | |
| “health visitor*” | |
| “healthy child programme” | |
| “healthy child wales” | |
| “getting it right for every child” | |
| “healthy child healthy future” | |
| Limits | site:gov.uk |
| site:gov.scot | |
| site:gov.wales | |
| northern-ireland.gov.uk |
Main searches (October 2022)
MEDLINE
Host: Ovid
Data parameters: MEDLINE® Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE® Daily and Ovid MEDLINE® 1946–present
Date range searched: 2020–current (Daily update)
Date searched: 5 October 2022
Searcher: CD
Hits: n = 21
| 1 | (health visitor* or health visiting).ti,ab,kw. | 3416 |
| 2 | child health program*.ti,ab,kw. | 645 |
| 3 | healthy child program*.ti,ab,kw. | 30 |
| 4 | healthy child wales.ti,ab,kw. | 2 |
| 5 | getting it right for every child.ti,ab,kw. | 3 |
| 6 | healthy child healthy future.ti,ab,kw. | 0 |
| 7 | or/1-6 | 4080 |
| 8 | SARS-CoV-2/ or COVID-19/ or exp COVID-19 Testing/ or exp COVID-19 Vaccines/ | 193,669 |
| 9 | (corona* adj1 (virus* or viral*)).ti,ab,kw,kf. | 5543 |
| 10 | (coronavirus* or coronoravirus* or coronaravirus* or coronovirus* or 2019nCoV* or 19nCoV* or “2019 novel*” or Ncov* or “n-cov” or “SARSCoV-2*” or “SARSCoV-2*” or SARSCoV2* or “SARS-CoV2*” or “severe acute respiratory syndrome*” or COVID*2).ti,ab,kw,kf. | 296,260 |
| 11 | (covid* or pandemic).ti,ab,kw,kf. | 304,389 |
| 12 | (CoV not (Coefficien* or “co-efficien*” or covalent* or Covington* or covariant* or covarianc* or “cut-off value*” or “cutoff value*” or “cut-off volume*” or “cutoff volume*” or “combined optimi?ation value*” or “central vessel trunk*” or CoVR or CoVS)).ti,ab,kw,kf. | 102,362 |
| 13 | or/8-12 | 345,607 |
| 14 | limit 13 to yr=“2020-current” | 309,865 |
| 15 | 7 and 14 | 21 |
CINAHL
Host: EBSCOhost
Date range searched: 2020–current (update date unknown)
Date searched: 5 October 2022
Searcher: CD
Hits: n = 58
| S1 | TI (“health visitor*” OR “health visiting”) OR AB (“health visitor*” OR “health visiting”) OR SU (“health visitor*” OR “health visiting”) | 5440 |
| S2 | TI “child health program*” OR AB “child health program*” OR SU “child health program*” | 276 |
| S3 | TI “healthy child program*” OR AB “healthy child program*” OR SU “healthy child program*” | 68 |
| S4 | TI “healthy child wales” OR AB “healthy child wales” OR SU “healthy child wales” | 5 |
| S5 | TI “getting it right for every child” OR AB “getting it right for every child” OR SU “getting it right for every child” | 12 |
| S6 | TI “healthy child healthy future” OR AB “healthy child healthy future” OR SU “healthy child healthy future” | 3 |
| S7 | (MH “English National Board for Nursing, Midwifery and Health Visiting”) | 17 |
| S8 | (MH “Community Practitioners’ and Health Visitors’ Association”) | 450 |
| S9 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 | 5773 |
| S10 | (MH “COVID-19”) OR (MH “COVID-19 Testing”) OR (MH “COVID-19 Vaccines”) OR (MH “COVID-19 Pandemic”) | 66,413 |
| S11 | (MH “SARS-CoV-2”) | 1101 |
| S12 | TI ((corona* N1 (virus* or viral*))) OR AB ((corona* N1 (virus* or viral*))) OR SU ((corona* N1 (virus* or viral*))) | 765 |
| S13 | TI (coronavirus* or coronoravirus* or coronaravirus* or coronovirus* or 2019nCoV* or 19nCoV* or “2019 novel*” or Ncov* or “n-cov” or “SARSCoV-2*” or “SARSCoV-2*” or SARSCoV2* or “SARS-CoV2*” or “severe acute respiratory syndrome*” or COVID*2) OR AB (coronavirus* or coronoravirus* or coronaravirus* or coronovirus* or 2019nCoV* or 19nCoV* or “2019 novel*” or Ncov* or “n-cov” or “SARSCoV-2*” or “SARSCoV-2*” or SARSCoV2* or “SARS-CoV2*” or “severe acute respiratory syndrome*” or COVID*2) OR SU (… | 30,557 |
| S14 | TI ((covid* or pandemic)) OR AB ((covid* or pandemic)) OR SU ((covid* or pandemic)) | 120,190 |
| S15 | TI ((CoV NOT (Coefficien* or “co-efficien*” or covalent* or Covington* or covariant* or covarianc* or “cut-off value*” or “cutoff value*” or “cut-off volume*” or “cutoff volume*” or “combined optimi?ation value*” or “central vessel trunk*” or CoVR or CoVS))) OR AB ((CoV NOT (Coefficien* or “co-efficien*” or covalent* or Covington* or covariant* or covarianc* or “cut-off value*” or “cutoff value*” or “cut-off volume*” or “cutoff volume*” or “combined optimi?ation value*” or “central vessel trunk*” or CoVR or CoVS))).ti,ab,kw,kf. | 0 |
| S16 | S10 OR S11 OR S12 OR S13 OR S14 OR S15 (Published Date 20200101-) | 115,470 |
| S17 | S9 AND S16 | 58 |
EMBASE
Host: Ovid
Date range searched: 2020–current (Daily update)
Date searched: 5 October 2022
Searcher: CD
Hits: n = 45
| 1 | (health visitor* or health visiting).ti,ab,kw. | 3318 |
| 2 | child health program*.ti,ab,kw. | 600 |
| 3 | healthy child program*.ti,ab,kw. | 38 |
| 4 | healthy child wales.ti,ab,kw. | 1 |
| 5 | getting it right for every child.ti,ab,kw. | 8 |
| 6 | healthy child healthy future.ti,ab,kw. | 0 |
| 7 | health visitor/ | 1704 |
| 8 | or/1-7 | 4942 |
| 9 | exp severe acute respiratory syndrome coronavirus 2/ or coronavirus disease 2019/ or experimental coronavirus disease 2019/ or exp sars-cov-2 vaccine/ | 280,505 |
| 10 | (corona* adj1 (virus* or viral*)).ti,ab,kw,kf. | 5826 |
| 11 | (coronavirus* or coronoravirus* or coronaravirus* or coronovirus* or 2019nCoV* or 19nCoV* or “2019 novel*” or Ncov* or “n-cov” or “SARSCoV-2*” or “SARSCoV-2*” or SARSCoV2* or “SARS-CoV2*” or “severe acute respiratory syndrome*” or COVID*2).ti,ab,kw,kf. | 321,736 |
| 12 | (covid* or pandemic).ti,ab,kw,kf. | 334,900 |
| 13 | (CoV not (Coefficien* or “co-efficien*” or covalent* or Covington* or covariant* or covarianc* or “cut-off value*” or “cutoff value*” or “cut-off volume*” or “cutoff volume*” or “combined optimi?ation value*” or “central vessel trunk*” or CoVR or CoVS)).ti,ab,kw,kf. | 110,761 |
| 14 | or/9-13 | 394,047 |
| 15 | limit 14 to yr=“2020-current” | 350,818 |
| 16 | 8 and 15 | 45 |
HMIC (Health Management Information Consortium)
Host: Ovid
Date range searched: 2020–current (July 2022 update)
Date searched: 5 October 2022
Searcher: CD
Hits: n = 7
| 1 | (health visitor* or health visiting).ti,ab. | 3699 |
| 2 | child health program*.ti,ab. | 14 |
| 3 | healthy child program*.ti,ab. | 72 |
| 4 | healthy child wales.ti,ab. | 0 |
| 5 | getting it right for every child.ti,ab. | 1 |
| 6 | healthy child healthy future.ti,ab. | 0 |
| 7 | health visiting/ or health visitor assistants/ or health visitor service/ or health visitors/ or liaison health visitors/ | 2544 |
| 8 | or/1-7 | 4246 |
| 9 | (corona* adj1 (virus* or viral*)).ti,ab. | 3 |
| 10 | (coronavirus* or coronoravirus* or coronaravirus* or coronovirus* or 2019nCoV* or 19nCoV* or “2019 novel*” or Ncov* or “n-cov” or “SARSCoV-2*” or “SARSCoV-2*” or SARSCoV2* or “SARS-CoV2*” or “severe acute respiratory syndrome*” or COVID*2).ti,ab. | 2153 |
| 11 | (covid* or pandemic).ti,ab. | 3394 |
| 12 | (CoV not (Coefficien* or “co-efficien*” or covalent* or Covington* or covariant* or covarianc* or “cut-off value*” or “cutoff value*” or “cut-off volume*” or “cutoff volume*” or “combined optimi?ation value*” or “central vessel trunk*” or CoVR or CoVS)).ti,ab. | 50 |
| 13 | or/9-12 | 3658 |
| 14 | limit 13 to yr=“2020-current” | 2158 |
| 15 | 8 and 14 | 7 |
Google Scholar
Host: Google (scholar.google.com; Google Chrome, incognito window)
Date range searched: 2020–22
Date searched: 5 October 2022
Searcher: CD
Hits: n = c 1820 (First 500 hits screened on screen; 141 identified to consider for inclusion)
| (“health visitor” OR “health visiting” OR “healthy child programme” OR “healthy child wales” OR “getting it right for every child” OR “healthy child healthy future”) AND (covid OR sars-cov-2 OR pandemic) | |
| Limits applied: 2020–22 | c 1820 |
Grey literature searches (November 2022)
The following websites were explored using a combination of searches and browsing. Full details of the search strings used and dates that searches were conducted are provided. Results were screened ‘on screen’ to identify potentially relevant material that had not already been captured by the main searches outlined above.
Department of Health and Social Care
Host: www.gov.uk/government/organisations/department-of-health-and-social-care
Date range searched: Updated after 1 January 2020–present
Date searched: 6 November 2022
Searcher: CD
Hits: 36
| “health visitor” OR “health visitors” OR “health visiting” | |
| Updated after 1 January 2020 | 36 |
Public Health Scotland
Host: Searched via Google as search bar on web page produced an error message
Date range searched: 1 January 2020–present
Date searched: 21 November 2022
Searcher: CD
Hits: 9
| (“health visitor” OR “health visitors” OR “health visiting”) site: publichealthscotland.scot | |
| From date 1 January 2020 to today | 9 |
Public Health Wales
Host: Searched via Google as search on website is very sensitive
Date range searched: 1 January 2020–present
Date searched: 16 November 2022
Searcher: CD
Hits: 47
| (“health visitor” OR “health visitors” OR “health visiting”) site:https://phw.nhs.wales/ | |
| From date 1 January 2020 to today | 47 |
Public Health Agency NI
Host: Searched via Google as search on website produced an error message
Date range searched: 1 January 2020–present
Date searched: 16 November 2022
Searcher: CD
Hits: 41
| (“health visitor” OR “health visitors” OR “health visiting”) site: www.publichealth.hscni.net/ | |
| From date 1 January 2020 to today | 41 |
Institute of Health Visiting
Host: https://ihv.org.uk/
Date range searched: No limit
Date searched: 18 November 2022
Searcher: CD
Hits: 35
| covid OR “covid-19” OR “covid19” OR “coronavirus” OR “pandemic” | 35 |
Royal College of Nursing
Host: https://rcn.org.uk
Date range searched: January 2020–present
Date searched: 18 November 2022
Searcher: CD
Hits: 32
| “health visitor” (since January 2020) | 14 |
| “health visitors” (since January 2020) | 11 |
| “health visiting” (since January 2020) | 7 |
Royal College of Paediatrics and Child Health
Host: www.rcpch.ac.uk/
Date range searched: January 2020–present
Date searched: 18 November 2022
Searcher: CD
Hits: 11
| health visitor OR “health visitors” OR “health visiting” | 11 |
Patient Experience Library
Host: http://patientlibrary.net
Date range searched: January 2020–current
Date searched: 7 December 2022
Searcher: CD
Hits: 405
| “health visitor” + limit January 2020–December 2022 | 250 |
| NB Screened first 100 results (after approximately page 5, documents contained a single HV mention; excluded generic Healthwatch patient feedback surveys) | |
| “health visiting” + limit January 2020–December 2022 | 155 |
Additional search (March 2023)
Note: To increase the specificity of this additional search, the search term ‘child health program*’ was removed as it retrieved a significant volume of international literature that was not relevant and this search aimed to identify material focused on UK settings.
MEDLINE
Host: Ovid
Data parameters: MEDLINE® Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE® Daily and Ovid MEDLINE® 1946–present
Date range searched: 2021–current (Daily update)
Date searched: 31 March 2023
Searcher: CD
Hits: n = 113
| 1 | (health visitor* or health visiting).ti,ab,kw. | 3439 |
| 2 | healthy child program*.ti,ab,kw. | 32 |
| 3 | healthy child wales.ti,ab,kw. | 2 |
| 4 | getting it right for every child.ti,ab,kw. | 3 |
| 5 | healthy child healthy future.ti,ab,kw. | 0 |
| 6 | or/1-5 | 3462 |
| 7 | limit 6 to yr=“2021 -Current” | 113 |
CINAHL
Host: EBSCOhost
Date range searched: 1 January 2021–31 March 2023
Date searched: 31 March 2023
Searcher: CD
Hits: n = 152
| S1 | TI (“health visitor*” OR “health visiting”) OR AB (“health visitor*” OR “health visiting”) OR SU (“health visitor*” OR “health visiting”) | 5458 |
| S2 | TI “healthy child program*” OR AB “healthy child program*” OR SU “healthy child program*” | 69 |
| S3 | TI “healthy child wales” OR AB “healthy child wales” OR SU “healthy child wales” | 5 |
| S4 | TI “getting it right for every child” OR AB “getting it right for every child” OR SU “getting it right for every child” | 12 |
| S5 | TI “healthy child healthy future” OR AB “healthy child healthy future” OR SU “healthy child healthy future” | 4 |
| S6 | (MH “English National Board for Nursing, Midwifery and Health Visiting”) | 17 |
| S7 | (MH “Community Practitioners’ and Health Visitors’ Association”) | 453 |
| S8 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 | 5519 |
| Limiters Published Date: 20210101-20230331; Language: English | 152 |
EMBASE
Host: Ovid
Date range searched: 2021–current (Daily update)
Date searched: 31 March 2023
Searcher: CD
Hits: n = 148
| 1 | (health visitor* or health visiting).ti,ab,kw. | 3366 |
| 2 | healthy child program*.ti,ab,kw. | 41 |
| 3 | healthy child wales.ti,ab,kw. | 1 |
| 4 | getting it right for every child.ti,ab,kw. | 8 |
| 5 | healthy child healthy future.ti,ab,kw. | 0 |
| 6 | or/1-5 | 3402 |
| 7 | limit 6 to yr=“2021 -Current” | 148 |
HMIC (Health Management Information Consortium)
Host: Ovid
Date range searched: 2021–current (March 2023 update)
Date searched: 31 March 2023
Searcher: CD
Hits: n = 8
| 1 | (health visitor* or health visiting).ti,ab. | 3703 |
| 2 | healthy child program*.ti,ab. | 72 |
| 3 | healthy child wales.ti,ab. | 0 |
| 4 | getting it right for every child.ti,ab. | 1 |
| 5 | healthy child healthy future.ti,ab. | 0 |
| 6 | health visiting/ or health visitor assistants/ or health visitor service/ or health visitors/ or liaison health visitors/ | 2547 |
| 7 | or/1-6 | 4240 |
| 8 | limit 7 to yr=“2021 -Current” | 8 |
Google Scholar
Host: Google (scholar.google.com; Google Chrome, incognito window)
Date range searched: 2021– current
Date searched: 5 April 2023
Searcher: CD
Hits: n = c 4160 (First 200 hits screened on screen; 72 identified to consider for inclusion)
| (“health visitor” OR “health visiting” OR “healthy child programme” OR “healthy child wales” OR “getting it right for every child” OR “healthy child healthy future”) | |
| Limits applied: 2021–23 | c 4160 |
Search alert (Google Scholar)
A search alert was created in Google Scholar in October 2022, using the main search string. The alert aimed to capture any newly published and indexed material relating to health visiting services.
Appendix 3
| Study ID | Year published | Type of document | Country | Overall document aim | Perspective | Overall study design |
| 1001Days-202086 | 2020 | Statement | UK | Calls on the government to act to protect babies. | Advocacy | N/A |
| 1001Days-202180 | 2021 | Report | England | Captures the need for national and local action to prioritise the first 1001 days. | Advocacy | Qualitative |
| 1001Days-202277 | 2022 | Report | England | Compilation of short testimonies about why health visitors are important in ensuring our children are safe, healthy and able to thrive. | Advocacy | N/A |
| Action for Children-202087 | 2020 | Statement | England | Sets out what government must put in place to improve the health of babies, children and their families across England. | Advocacy | N/A |
| Action for Children-202288 | 2022 | Report | England | Presents a survey of parents on accessing parenting support in the early years. | Advocacy | Mixed methods |
| Action for Children-2020a78 | 2020 | Briefing | England | Sets out what government must put in place to improve the health of babies, children and their families across England. | Advocacy | N/A |
| Appleton-202179 | 2021 | Editorial | UK | Synthesises papers in the same issue that discuss vulnerable children and the importance of early intervention. | Academic | N/A |
| Aquino-202289 | 2022 | Original research | England | Explores the provision of, and innovations in, HV services in the North East and North Cumbria, during COVID-19. | Academic | Mixed methods |
| Baldwin-202090 | 2020 | Case study | UK | Discusses a virtual programme developed to support the emotional well-being of health visiting teams in the UK. | Academic | Case study |
| Baldwin-202291 | 2022 | Original research | UK | Presents the evaluation, learning and reflections from the Emotional Wellbeing at Work programme. | Academic | Evaluation |
| Bear-202092 | 2020 | Report | UK | Presents key findings from a 6-month ethnographic study on the impact of the COVID-19 pandemic on disadvantaged households and communities across the UK. | Academic | Qualitative |
| Best Beginnings-202093 | 2020 | Report | UK | Reveals the disproportionate impact of COVID-19 and subsequent measures on those pregnant, giving birth or at home with a baby or toddler. | Advocacy | Survey |
| Best Beginnings-202194 | 2021 | Report | UK | Highlights a ‘baby blind spot’ in COVID-19 recovery efforts and a shortage of funding for voluntary sector organisations and core services like health visiting to offer the level of support required to meet families’ needs. | Advocacy | Qualitative |
| Boddy-202095 | 2020 | Opinion piece | England | Explores the fast-changing public health emergency of COVID-19 and the health visitor response. | Practitioner | N/A |
| Boddy-2020a70 | 2020 | Opinion piece | England | Reflects on the changes and challenges faced by health visitors during the coronavirus pandemic. | Practitioner | N/A |
| Boddy-2020b96 | 2020 | Opinion piece | UK | Reflects on the role of the health visitor. | Practitioner | N/A |
| Boddy-2020c97 | 2020 | Opinion piece | UK | Reflects on the importance of home visiting by the health visitor for children and parents. | Practitioner | N/A |
| Boddy-202198 | 2021 | Opinion piece | England | Reflects on the findings of the State of Health Visiting survey alongside current evidence of the impact of the COVID-19 pandemic on children and families. | Practitioner | N/A |
| Boddy-202299 | 2022 | Opinion piece | England | Discusses where the low numbers of health visitors leave the profession and what changes need to be implemented. | Practitioner | N/A |
| Boddy-2022a100 | 2022 | Article | UK | Presents evidence on the impact on maternal, infant and child health in the 2 years since the start of the pandemic. | Practitioner | N/A |
| Brook-2020101 | 2020 | Opinion piece | UK | Discusses the importance of evaluating changes that have been made in practice during the pandemic. | Practitioner | N/A |
| Celcis-2021102 | 2021 | Report | Scotland | Reports on the impact of COVID-19 on children and families. | Policy | Mixed methods |
| Children’s Commissioner-2020a69 | 2020 | Report | England | Sets out the widening inequalities over children and young people’s community services. | Policy | N/A |
| Children’s Commissioner-2020103 | 2020 | Briefing | England | Highlights the need for policy-makers to put families with young children, and especially those with newborns, at the heart of coronavirus planning. | Policy | N/A |
| Cole-2022104 | 2022 | Case study | England | Showcases award-winning projects to support isolated families during the pandemic. | Academic | N/A |
| Community Practitioner-2020105 | 2020 | Diary | UK | Reveals the experiences of a community nursery nurse in England and a health visitor in Scotland working during the pandemic. | Practitioner | N/A |
| Community Practitioner-2021106 | 2021 | Conference report | England | Synopsis of Sally Hogg’s presentation at the Unite- Community Practitioners and Health Visitors Association conference talking about the baby blind spot in mental health policy. | Advocacy | N/A |
| Community Practitioner-2021a107 | 2021 | Conference report | England | Presents a conference session on the impact of COVID-19 on children and families and the need to prioritise them in future. | Practitioner | N/A |
| Community Practitioner-2022108 | 2022 | Report | Wales | Provides examples of innovations to health visiting to share outstanding work done during the pandemic. | Practitioner | N/A |
| Community Practitioner-2022a109 | 2022 | Diary | England | A health visitor reveals how she coped and thrived while in post (and shielding) during the pandemic. | Practitioner | N/A |
| Community Practitioner-2022b110 | 2022 | Report | Wales | Presents small examples/case studies of how health visitors in Wales are developing new services and workarounds as a result of pandemic restrictions. | Practitioner | N/A |
| Conti-2020111 | 2020 | Report | England | Presents new evidence on the state of health visiting services before the pandemic and on the redeployment of staff. | Academic | Secondary data analysis |
| Conti-2020a31 | 2020 | Report | England | Presents the first findings from new survey data providing concerning evidence on the impacts of COVID-19 on the ability of health visitors to deliver benefits for young children and families. | Academic | Quantitative |
| Conti-202127 | 2021 | Report | England | Presents an evaluation of the state of health visiting services prior to COVID-19 and the exact scale and variation in redeployment of health visiting staff during the first COVID-19 wave. | Academic | Quantitative |
| De Backer-2022112 | 2022 | Original research | England | Explores the experiences of maternity services staff who provided maternity care during the SARS-CoV-2 pandemic to inform future improvements in care. | Academic | Evaluation |
| Driscoll-2020113 | 2020 | Original research | England | Presents a study on how different agencies are responding to the challenges of safeguarding during COVID. | Academic | Mixed methods |
| Driscoll-2021114 | 2021 | Original research | England | Presents interview data from professionals with child protection responsibilities in 24 London Boroughs. | Academic | Mixed methods |
| Durand-2021115 | 2021 | Original research | England | Assesses the presentation and management of infant feeding problems in the local paediatric population. | Academic | Secondary data analysis |
| Entwistle-2020116 | 2020 | Opinion piece | UK | Presents results from the survey into infant feeding during COVID-19. | Policy | Survey |
| Evans-2020117 | 2020 | Article | England | Presents some of the strategies employed during the pandemic and discusses that some of these are likely to stay beyond the pandemic. | Writer | N/A |
| Feger-2021118 | 2021 | Case study | UK | Discusses the rapid rise of online consultations and the greater scrutiny needed to keep health care safe and accessible. | Policy | N/A |
| Forbes-2020119 | 2020 | Opinion piece | England | Discusses the role of community-based workers during the COVID-19 pandemic. | Policy | N/A |
| Gill-2022120 | 2022 | Article | UK | Discusses what health visiting is and how it looks post pandemic. | Academic | N/A |
| Government-20219 | 2021 | Report | England | Reviews the 1001 critical days through pregnancy to the age of 2. | Policy | Qualitative |
| Halnan-2022121 | 2022 | Original research | England | Presents views on using digital technology to maintain a Healthy Child Programme service during lockdown. | Practitioner | Survey |
| Hancock-2020122 | 2020 | Article | UK | Presents examples of the impact of mental health on infants. | Writer | N/A |
| Hancock-2021123 | 2021 | Article | England | Presents a detailed picture of the effects of the pandemic on health visiting services in England. | Writer | N/A |
| Hanley-2020124 | 2020 | Opinion piece | UK | Presents some of the effects of the pandemic on the emotional well-being of parents and health professionals. | Practitioner | N/A |
| Hanley-2021125 | 2021 | Opinion piece | UK | Discusses health visitors and healthcare practitioners collaborating with other clinicians and researchers to establish how COVID-19 has affected their practice and their clients. | Practitioner | N/A |
| Hanley-2022126 | 2022 | Opinion piece | UK | Presents the value of health visitors and the hope that this will be recognised post COVID. | Practitioner | N/A |
| Harding-2020127 | 2020 | Report | England | Discusses how families with young children under the age of 5 have found life under the COVID-19 lockdown. | Advocacy | Qualitative |
| Health Services Journal-2023128 | 2023 | Report | UK | Highlights that the number of mandated health visiting reviews has still not returned to pre-pandemic levels. | Practitioner | N/A |
| Healthwatch South Gloucester-2020129 | 2020 | Report | England | Reports the experiences of women who had transitioned from maternity care to health visiting during the period of 2020–2. | Advocacy | Qualitative |
| Hefferon-2021130 | 2021 | Original research | England | Outlines key impacts of COVID-19 on children in England. | Advocacy | Mixed methods |
| House of Commons-202043 | 2020 | Report | UK | Reports a government enquiry into extending maternity leave by 3 months during the pandemic. | Policy | Qualitative |
| House of Commons-2021131 | 2021 | Report | UK | Examines a range of issues affecting new parents during the pandemic. | Policy | N/A |
| iHV-2020132 | 2020 | Report | UK | Makes recommendations to support the health visiting workforce maximise their contribution and impact as part of the wider COVID-19 response. | Advocacy | Qualitative |
| iHV-2020a133 | 2020 | Statement | England | Presents evidence submitted by iHV in response to a Call for Evidence from the Early Years Commission. | Advocacy | N/A |
| iHV-2020b134 | 2020 | Blog | Wales | Shares blogs from the devolved UK Countries as part of UK Maternal Mental Health Awareness Week. | Advocacy | N/A |
| iHV-2020c135 | 2020 | Report | England | Reports the findings from 862 health visitors in practice in England and highlights the range of issues facing the profession. | Advocacy | Survey |
| iHV-2020d136 | 2020 | Conference report | England | Presents key messages from a webinar on supporting the development of babies and young children during the COVID-19 outbreak. | Advocacy | N/A |
| iHV-2020e137 | 2020 | Opinion piece | UK | Highlights how redeployment and the lack of face-to-face visiting are creating a perfect storm of vulnerable children. | Advocacy | N/A |
| iHV-2020f138 | 2020 | Statement | England | Presents evidence submitted to the government enquiry on the impact of COVID-19 on education and children’s services. | Advocacy | N/A |
| iHV-2020g139 | 2020 | Case study | England | Presents a set of case studies, family stories and creative submissions gathered to help tell the health visiting COVID-19 story. | Advocacy | Case study |
| iHV-2020h140 | 2020 | Report | England | Presents the impact of redeployment that was found in the working under COVID report | Advocacy | N/A |
| iHV-2020i141 | 2020 | Clinical guidance | England | Professional advice to describe best practice in supporting family perinatal mental health and well-being by health visitor teams during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-2020j142 | 2020 | Clinical guidance | England | Professional advice to describe best practice in supporting family perinatal mental health and well-being by health visitor teams during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-2020k66 | 2020 | Clinical guidance | England | Professional advice to describe the new process for delivery of antenatal visits by health visitor teams during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-2020l143 | 2020 | Clinical guidance | England | Professional advice to describe the new process for delivery of antenatal visits by health visitor teams during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-2020m144 | 2020 | Clinical guidance | England | Professional advice to describe the new process of delivery of new birth visits by health visitors during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-2020n145 | 2020 | Clinical guidance | England | Professional advice to describe the new process of delivery of new birth visits by health visitors during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-2020o146 | 2020 | Clinical guidance | England | Professional advice to describe the new process of delivery of heath visiting contacts using virtual methods during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-2020p147 | 2020 | Clinical guidance | England | Professional advice to describe the new process of delivery of heath visiting contacts using virtual methods during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-2020q148 | 2020 | Clinical guidance | England | Professional advice to describe the new process for delivery of safeguarding vulnerable families by health visitor teams during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-2020r149 | 2020 | Clinical guidance | England | Professional advice to describe the new process for delivery of safeguarding vulnerable families by health visitor teams during the COVID-19 pandemic. | Advocacy | N/A |
| iHV-202134 | 2021 | Report | England | Presents specific information about the state of health visiting in England. | Advocacy | Survey |
| iHV-2023150 | 2023 | Report | UK | Presents Health Visiting Survey data for the year ending November 2022. | Advocacy | Survey |
| Jackson-2022151 | 2021 | Original research | UK | Explores UK women’s postnatal experiences of social and healthcare professional support during the COVID-19 pandemic. | Academic | Qualitative |
| Jackson-2022a26 | 2022 | Original research | England | Discusses women’s experience of pregnancy, childbirth and caring for a baby during the pandemic. | Academic | Qualitative |
| Kombe-2020152 | 2020 | Blog | England | Highlights a film that has been produced to capture experiences of children during the pandemic. | Practitioner | N/A |
| Lamb-2020153 | 2020 | Clinical guidance | England | Presents 0–19 Services Business Continuity – Briefing for all 0–19 staff in Harrogate and District Foundation Trust. | Practitioner | N/A |
| Lamb-2020a154 | 2020 | Clinical guidance | England | Update to 0–19 teams on Harrogate and District Foundation Trust Prioritisation of Face to Face Contact at Primary Visit. | Practitioner | N/A |
| Manning-2021155 | 2021 | Original research | UK | Identified priorities for research in relation to the COVID-19 pandemic and ‘beyond’. | Academic | Mixed methods |
| Moltrecht-2022156 | 2022 | Original research | UK | Investigates young parents’ experiences during the pandemic, including their perceived challenges and needs. | Academic | Qualitative |
| Morton-2020157 | 2020 | Opinion piece | England | Considers the consequences of redeployment for children, families and health visitors. | Advocacy | N/A |
| Morton-2021158 | 2021 | Opinion piece | UK | Sets out the situation for HV services due to the pandemic and years of cuts to services. | Advocacy | N/A |
| Morton-202230 | 2022 | Original research | England | Considers the impact of the pandemic in 2020 on families with children under 5 years in England. | Advocacy | Secondary data analysis |
| NHS England-2020159 | 2020 | Letter | England | Guidance on the restoration of community health services for children and young people. | Policy | N/A |
| NHS England-F2020a160 | 2020 | Letter | England | Thank you to teams for everything achieved in securing the NHS COVID-19 response. | Policy | N/A |
| NHS Scotland-2020161 | 2020 | Clinical guidance | Scotland | Clinical guidance for all NHS staff working in the community and Health and Social Care Partnerships during COVID-19. | Practitioner | N/A |
| Nursery World-2022162 | 2022 | Report | UK | Reports how the pandemic has increased parental stress and how this can be passed to their children. | Advocacy | N/A |
| Nursing children and young people-2021163 | 2021 | Diary | England | Diaries of two health visitors in England. | Practitioner | N/A |
| Nursing Standard-2020164 | 2020 | Opinion piece | England | Descriptions from five black nursing professionals of how the pandemic affected their work. | Practitioner | N/A |
| Oldman-2021165 | 2021 | Opinion piece | UK | Presents how health visitors are ideally placed to advise government on the impact of homelessness on the health of children. | Practitioner | N/A |
| Oldman-2022166 | 2022 | Opinion piece | England | Calls for a workforce plan to address decline of health visiting workforce. | Practitioner | N/A |
| Oldman-2022a167 | 2020 | Opinion piece | UK | Discusses how the world of nursing, midwifery and health visiting has changed during COVID-19. | Practitioner | N/A |
| Papworth-2021168 | 2021 | Original research | UK | Explores the challenge the pandemic placed on perinatal mental health and the services that support women and families. | Advocacy | Mixed methods |
| Perez-2021169 | 2021 | Original research | UK | Investigates how COVID-19 and associated restrictions influence mood and parenting confidence. | Academic | Mixed methods |
| Powell-2021170 | 2021 | Case study | England | Highlights the multiagency responses to the impact that the pandemic had on safeguarding. | Policy | N/A |
| Primary Healthcare-2020171 | 2020 | Opinion piece | UK | Highlights the importance of the health visitor ‘front line’ in tackling the impact of COVID on parents. | Advocacy | N/A |
| Public Health Agency-202167 | 2021 | Report | Northern Ireland | Explores experiences of mothers and service providers in accessing and providing breastfeeding support. | Policy | Qualitative |
| Public Health England-2020172 | 2020 | Letter | England | Short letter from Public Health England stating that health visitors should no longer be redeployed. | Policy | N/A |
| Public Health Scotland-2020173 | 2020 | Report | Scotland | Full report of the COVID-19 Early Years Resilience and Impact Survey into early years resilience during COVID. | Academic | Survey |
| RCN-2020174 | 2020 | Clinical guidance | UK | Guidance to support health visitors to seeing patients through remote consultation processes. | Policy | N/A |
| RCN-2021175 | 2021 | Opinion piece | Wales | Presents the need for more investment in early intervention to prevent child abuse. | Policy | N/A |
| Rhodes-2020176 | 2020 | Original research | UK | Presents the impact of the COVID-19 pandemic for users of the Baby Buddy app. | Academic | Mixed methods |
| Riley-2021177 | 2021 | Original research | England | Reports the impact of COVID-19 restrictions on women’s pregnancy and postpartum experience. | Academic | Qualitative |
| Rooke-2021178 | 2021 | Case study | Wales | Discusses experience of undertaking the safeguarding module virtually. | Practitioner | Scoping exercise |
| Salisbury-2022179 | 2022 | Original research | England | Investigates whether there is a change in the incidence or severity of abusive head trauma pre- and during COVID-19 lockdown. | Practitioner | Secondary data analysis |
| Seaman-2021180 | 2021 | Original research | England | Explores health visitors’ perceptions of their professional identity and their experience of living through a time of significant service change. | Academic | Qualitative |
| Singh-2021181 | 2021 | Article | UK | Considers the impact of lockdowns on child well-being based on the experience of paediatricians. | Practitioner | N/A |
| Stiles-2021182 | 2021 | Editorial | UK | Discusses the options of health visitors to prescribe. | Practitioner | N/A |
| Sylvester-202268 | 2022 | Editorial | England | Reports some of the innovative ways that health visitors coped with the pandemic restrictions. | Practitioner | N/A |
| Thomson-2022183 | 2022 | Original research | UK | Explores how women have adapted to becoming a new parent during the pandemic. | Academic | Mixed methods |
| Watson-2020184 | 2020 | Report | Scotland | Presents the experiences of parents and carers during the COVID-19 pandemic in Scotland. | Academic | Survey |
| Welsh Government-2020185 | 2020 | Clinical guidance | Wales | Describes the delivery of new birth visits by health visitors during the COVID-19 pandemic. | Policy | N/A |
| Wilkinson-2022186 | 2022 | Article | England | Reports the significant consequences of understaffing. | Writer | N/A |
| Williams-2021187 | 2021 | Blog | Wales | Reports experiences of health visiting on different COVID-19 frontlines. | Practitioner | N/A |
Appendix 4 Context, mechanism and outcome configurations and example quotes
Health visiting contacts
Health visiting contacts are an opportunity to gather information for an assessment of need for babies, young children and their families
CMOC01: When health visiting teams are not picking up issues through routine surveillance (C) educators and health professionals might see differences in their cases (O) because issues (e.g. developmental issues) are not recognised in a timely way (M)
Vicky Thomas, consultant paediatrician at Newcastle Hospitals NHS Foundation Trust, says that the lack of health visitors has affected children they have seen, especially in the pandemic.
‘The particularly striking issues we’ve seen have been around developmental issues; several children have presented much later than we would have hoped because the routine surveillance of all aspects of development was one of the major casualties of the pandemic’ (Wilkinson-2022). 186
Routine enquiry is more difficult through virtual or telephone methods. It is recommended that health visitors explore open questions about relationships and support networks if they are unable to see a new mother in person (Boddy-2020a). 100
Thomas’s department has also seen a lot of anxious parents bringing their children to the emergency department with the sort of concerns that would be better dealt with in primary care or that maybe don’t even need any medical attention.
‘Health visitors have a vital role in supporting families with these sorts of anxieties and signposting them to appropriate resources’, she says. […] Thomas is most concerned about vulnerable people who have lost an important line of protection or support, including those with complex medical needs or living in poverty, or whose parents aren’t fluent English speakers, or are suffering from mental health problems or addiction. ‘At worst I think there has been a significant risk that children across the country who were vulnerable to neglect or abuse by their parents have been invisible to professionals’ (Wilkinson-2022). 186
Service providers also highlighted this issue, noting that the lack of physical proximity to mother and baby had hampered their ability to identify potential tongue ties and that, during the pandemic, often they only diagnosed this because of how badly damaged the mothers’ nipples had become and how it impacted the emotional well-being of breastfeeding mothers (Public Health Agency-2021). 67
CMOC02: When a family is contacted by phone/video soon after the birth (C) health visiting staff might be able to detect concerns that they can raise with the health visitor (O) because some forms of assessment are relatively easy to do remotely (M)
We are only doing home visits if absolutely required. All contacts are by phone, for NBV calls are made day 4–7, 7–10, and day 10–14. We rotate into hubs to provide HV telephone support daily and offer one clinic a week which is risk assessed by HV and they have to have an appointment. We are being very well protected and the feedback from clients is very positive too (iHV-2020). 132
And, after months of online delivery, there is a good deal of clear thinking on the ground about what a successful hybrid model of online and in-person family support might look like, and the circumstances in which to most effectively deploy different online tools. Most professionals and service leaders foresee an expanded role for virtual family support, but also acknowledge that a blanket approach risks excluding some families, or failing to fully identify and respond to their needs (1001Days-2021). 80
CMOC03: When there are fewer face-to-face contacts between a health visitor and the family (C) health visitors might miss important information or cues related to needs (O) because physical observations are an important part of assessing needs (M)
I was recently talking to a student health visitor who told me about new ways of working remotely where she is placed. The part of the job that she found most difficult was not being able to see the home setting and make a comprehensive assessment of the environment. She worried that she was not going to be able to detect issues around safety or safeguarding as easily (Brook-2020). 101
Ensuring the privacy and safety of service users; assessing children’s development; identifying safeguarding concerns; identifying parental mental health concerns; and building trusting relationships and rapport with parents. Whilst these issues are a concern for many service users, they are particularly concerning for babies, who are especially vulnerable and can be invisible in online contacts. Digital and telephone contact is also challenging for assessing early childhood development, as a report by Action for Children observed, ‘It can be more difficult to engage younger children through digital methods. Activities focused on development for young children are often reliant on things like eye contact, direct speech and the manipulation of objects, which are harder to implement in digital delivery’. When working with a baby, professionals must also engage with the parents and with the relationships between the parents and the baby. Observing the different individuals and their interactions is an incredibly important part of work with the family and is difficult in the absence of face-to-face contact (Best Beginnings-2021). 94
There has been an increase in home working [by health visitors] since the pandemic which may have added to this reduced visibility. At the same time, ‘the retraction of universal services’ and reduced face-to-face contacts have affected the ability of professionals to identify ‘ “new” or increased need, and safeguarding issues’, despite health visitors working very hard to adopt some new and innovative ways of working during the pandemic (Appleton-2021). 79
Between March and early June, NHS England advised providers of community services to release capacity to support the COVID-19 by reducing health visitor contacts from 5 mandated contacts to 2 virtual contacts, with additional contacts available for those previously identified as vulnerable. In this period, there is an increased possibility that perinatal mental health issues may not have been identified, and this is particularly concerning for assessing infant mental health and safeguarding concerns, given that cues will likely be non-verbal and dependant [SIC] on professional skill and knowledge (Action for Children-2020a). 78
Face-to-face contacts should be prioritised for families who are not known to services to mitigate known limitations of virtual contacts and support effective assessment of needs/risks (NHS England-2020). 159
Health visiting contacts are an opportunity to provide information and support
CMOC04: When Health Visitors have a manageable workload (C) they are more able to provide holistic support to the family (O) because they are not just in ‘fire-fighting’ mode (responding to most immediate/high priority needs amongst prioritised families) (M)
Joanne Gill, an experienced health visitor in Somerset, says that they are really just firefighting. ‘We used to be able to do much more one-to-one work; there’s not enough staff for what we really want to do’. She has seen the effect of the pandemic first hand on the mental health of families and children’s development, and the thought that children might be falling through the net ‘is a constant fear’ (Wilkinson-2022). 186
When Phillippa Guillou had her daughter in 2020, she was determined to breastfeed, but it was painful and there were problems with latching. She tried calling and texting her health visitor for help but got nowhere. Two months later she received a response and a referral for tongue tie, but by then she’d had to start using formula milk. ‘I was really upset about breastfeeding. I didn’t have any friends or a network that could help me – and when I called a charity, they said there aren’t any services locally, can you pay for a private consultation? But it was £200, and I didn’t have the money. I’m still sad about it’ (Wilkinson-2022). 186
The health visiting staff provided us with many sad and worrying accounts. Respondents expressed feelings of panic and anxiety, of feeling overwhelmed and being exhausted. We received reports of extremely low morale and finding the job demoralising. Feeling undervalued by managers and their employer was cited by a number of respondents – one individual told us that ‘the job is now, more than ever, about ticking boxes and not assessing and determining health needs’ (Conti-2020a). 31
CMOC05: When there are very few or no contacts between health visiting teams and families (C) some families will feel less supported (O) because they feel they have been ‘abandoned’ by the health visiting service (M)
I had my twins 6 weeks ago, 2 weeks into lockdown they was in NICU for 10 day as I was 34 weeks and 5 days when they born. Just under 4 lbs for both …. Since having the care from NICU I had seen one midwife and one health visitor, I feel like we was just given the babies and basically keep them alive … (Best Beginnings-2020). 93
Many families felt their health visitor was less accessible at this time, while children under two experienced disproportionately high levels of harm due to pandemic measures that were designed to protect the nation, research found (Cole-2022). 104
In particular, the value of an effective health visiting service is being recognised, with families speaking out on social media about the effects on them and their children when they miss out on this vital support. …Frustrated parents have criticised health visitors for a lack of face-to-face contact, with suggestions that they have been ‘allowed to bow out’ during the pandemic. Some stories on social media are heartbreaking. …To be clear: health visitors have not bowed out. They should feel proud of all they have achieved against the odds. The Institute of Health Visiting (iHV) has been overwhelmed by how services have adapted to support as many families as possible (Morton-2021). 158
CMOC06: When a family is contacted by phone/video (C) staff might be able to direct families to digital interventions or other support (O) because some forms of information and guidance are easy to give this way (M)
The guidance supports blended models, stating that ‘health visitors should use their clinical judgement to identify whether virtual, other digital or blended approaches can be used to support the needs of a child or family’ (Best Beginnings-2021). 94
Possible solutions showing utility are digital interventions. Digital interventions have been effective in reducing postnatal anxiety around parenting practices and improving infant health outcomes pre-pandemic. Future research should aim to examine the feasibility and acceptability of psycho-educational interventions to help reduce maternal anxiety, to dissipate misconceptions about attending essential hospital appointments through the remainder of the global COVID-19 pandemic (Jackson-2022). 151
Quality-assured digital interventions such as the NHS-approved Baby Buddy app provide a vital source of 24/7 support for parents and caregivers of all backgrounds, encouraging them to access frontline services. Digital and online services can benefit families in many ways, and, in some cases, the ‘digital pivot’ of services that would usually be face-to-face has led to innovation and the development of new delivery models which bring clear benefits for service-users and organisations. There clearly are benefits of online and hybrid models of service delivery (which use a mix of digital and face-to-face models) in some contexts. Research during the pandemic has shown how digital services, when delivered alongside face-to-face public services, can improve outcomes for babies and their parents (Best Beginnings-2021). 94
As well as the switch to phone and video therapeutic work, The Little Minds Matter: Bradford Infant Mental Health Service have recognised the stress facing families, and have worked at pace with local partners, like Public Health, to create a video to help parents who were struggling to care for a crying baby which has been widely accessed via social media (Best Beginnings-2020). 93
CMOC07: When Covid-19 prompted the creation of new digital resources (C) health visitors had different opportunities to provide information and support to families (O) because such resources are easily shared via remote contacts (M)
Mothers considered WhatsApp an excellent tool in providing an instant source of breastfeeding support, vital when they could not wait for the next scheduled online support group or one-to-one video call. […] ‘WhatsApp group is fantastic. You don’t need to wait for the call, but someone will come back to you. Some things you don’t want to wait for an answer on and mums always have the answers’. […] The platform itself was considered very convenient, in that, mothers did not need to seek or research the information, or the support they needed, as they knew they could get this quickly and via their phone. It was also helpful that mothers could use WhatsApp to call service providers, could send texts, as well as share photos, videos and voice notes. This flexibility meant that mothers felt they received well-rounded support on this platform. […] Mothers enjoyed the mix of professional and peer facilitation (Public Health Agency-2021). 67
As COVID-19 struck and lockdown meant that expectant and new parents were cut-off from their family and support networks, Baby Buddy stepped up as a ‘digital best friend’, with personalised daily information, 300 + films and 24/7 access to the Baby Buddy Crisis Messenger. Pre-pandemic, most parents were recommended to use Baby Buddy by their midwife, health visitor or GP. So, with lockdown and the resulting reduction in face-to-face appointments, we were expecting fewer new registrations. Instead, we have seen 16.7k new registered users during the ‘core’ lockdown period (23 March–4 July 2020). This is a 9.3% uplift on the same period in 2019 (Best Beginnings-2020). 93
She (CNN) first phoned me a couple weeks ago to check in on how I was doing with feeding my baby. It was so nice to hear from someone with useful tips and support & even though I couldn’t have anyone visit my home they provided me with links, images & videos to help with breastfeeding which I found useful. My sister also had a positive experience with the team … (iHV-2020b). 134
Health visiting contacts are an opportunity to build relationships and provide reassurance
CMOC08: When assessing babies and very young children face-to-face (C) parents are potentially less anxious/more reassured (O1) because assessments are more thorough and being carried out by a trained professional (M)
Not having face-to-face visits with health visitors or midwives in the weeks following the birth, makes me anxious that she hadn’t been “checked” for any potential health concerns which may have arisen after birth. i.e. skin conditions, feeding, weight gain or loss (Best Beginnings-2020). 93
Six months on and how has my way of practising changed? It’s completely different. I’m doing behaviour visits and other contacts with parents and carers over the phone. I’ve always understood that only 7% of communication comes from the words we use. The rest is made up from intonation, body language and other non-verbal cues – that’s harder now. Perhaps the biggest challenge for me is that the child’s voice is lost. You are only conversing with a parent/carer. Over the years, I have really developed the skill of understanding what children are trying to tell me, even when they cannot yet speak. Even non-verbal children are communicating all the time. … I worry about the reduction in breastfeeding rates without any support. What is being missed with developmental reviews? (Community Practitioner-2020). 105
New mothers particularly missed the reassurance that their baby was developing satisfactorily, and that they were ‘doing a good job’. They also wanted advice on feeding, weaning and sleeping. Several women mentioned wanting to have their baby weighed, with a few recalling the drop-in clinics they had attended with previous children. Some women reported seeking informal support and information from other sources including Google, Facebook groups for parents, friends and family members with children and a few weighed the baby themselves for ‘peace of mind’. Women who mentioned this self-help approach generally said they would have preferred professional input (Jackson-2022a). 26
CMOC09: When there are fewer face-to-face health visiting contacts (C) some families will feel less supported (O) because they do not have the opportunity to build a relationship with their health visitor (M)
For many families, the increase in online support has been valuable, enabling greater flexibility and removing the need for travel time. But the risks of fully online provision have also been raised. These include challenges in identifying safeguarding issues, building positive and trusting relationships with families, and judging children’s development and parental mental health issues. Babies have been identified as being particularly vulnerable to being ‘invisible’ during online contact (Action for Children-2022). 88
Unsurprisingly, the impacts of social distancing, isolation, loneliness and an inability – or greater difficulty – in building relationships via a digital platform proved to be some of the emerging themes. There appeared to be only a few examples of families feeling as if they really knew their HV or SN, coupled with an overwhelming number of examples of families not knowing where to turn or how to contact the service for support or guidance (Halnan-2022).And further research is needed to understand their impact and any unintended consequences before any changes are adopted more permanently. The value of face-to-face work, the importance of relationships, and the significance of professionals observing a baby and parent–infant interaction must not be forgotten (Hancock-2020). 122
Remote contacts ‘work’ for certain families at certain times
CMOC10: When support is offered online (C) some families may not be able to engage meaningfully (O) because they do not have the resources or desire to do so (M)
Those experiencing poverty, chaotic homes or more significant difficulties have been particularly disadvantaged, often lacking the devices, data, WiFi and/or safe, calm space to engage. Some families have thrived in the virtual space, where it is easier for them to ‘attend’ appointments. Many young parents find the increased use of WhatsApp and other text or video-based services familiar and welcome (Best Beginnings-2020). 93
Particularly noticeable is the reduction in services for new and expecting mothers, there has been a dramatic decrease in pre- and postnatal check-ups, including the removal of regular appointments to check the baby’s health and weight. Some appointments, including check-ups for women in their third trimester (usually weekly) have been moved online, although there are certain measurements and checks that cannot be taken remotely. Moreover, women without access to devices or smartphones are left at a serious disadvantage here and mother and baby’s health will suffer as a result. In-person services at hospitals, including newborn hearing screening, face considerable backlogs and some new parents are falling through the cracks (Bear-2020). 92
Digital exclusion also remains a concern, with low-income families more likely to lack the equipment or connectivity to enable engagement with digitally delivered services and, therefore, most likely to miss out on care and support. […] Although digital service delivery may have worked as a back-up during the pandemic, this should not be confused with it being a sustainable delivery mechanism in a different context. As Action for Children have observed, during the lockdown families had fewer distractions and therefore more time to commit to services, alongside more reasons to seek support – increased engagement in services that pivoted to digital delivery at this point may have reflected these wider factors, rather than the change in delivery mechanism (Best Beginnings-2021). 94
CMOC11: When Health Visitors judge it is appropriate (C) they may use remote connections (O) because this is a way to keep in touch with all their case load in a safe way (M)
For many families, the increase in online support has been valuable, enabling greater flexibility and removing the need for travel time. But the risks of fully online provision have also been raised. These include challenges in identifying safeguarding issues, building positive and trusting relationships with families, and judging children’s development and parental mental health issues. Babies have been identified as being particularly vulnerable to being ‘invisible’ during online contact. Our own report with the Early Intervention Foundation in June 2020 explored some of the benefits and drawbacks of virtual delivery (Action for Children-2022). 88
One of the biggest changes has been the delivery of contacts, which have changed from being face-to-face, often in the family home, to either virtual or telephone contacts for both the safety of professionals and families. The iHV has published advice on the use of virtual contacts (iHV, 2020b). 134
The benefits are that it is a good option for families who are shielding, and it reduces travel time, especially in more rural locations where health visitors have a large geographical area to cover. However, there are recognised limitations to virtual contacts in relation to effective assessments of needs and risks, as well as accessibility to virtual methods and the choice of families, who prefer to have a telephone consultation rather than a virtual one (Boddy-2020a). 70
The iHV found (2021) 88.6% of practitioners agreed or strongly agreed that video enabled contacts can be used effectively to provide families with quick access to straightforward concerns. […] However, there continue to be safety concerns with the majority of practitioners reporting that video contacts could not safely or effectively replace in-person universal assessments (Boddy-2022). 99
CMOC12: When health visiting teams use remote connections to maintain an open and responsive channel of communication with parents (C) parents feel supported (O) because they feel somebody is taking an interest in them (M)
One of my successes has been the ability to give far more time to breastfeeding mothers and to help with feeding issues. A great deal more video or phone contact has been possible and just to offer a call can be very reassuring – a mother or father can feel that someone has remembered them (Community Practitioner-2022a). 109
Most positive was the experience frequently described that some families appeared readier to engage and to speak frankly remotely, and that meetings could become more collaborative and less fraught. Similarly, some young people seemed to access services – including mental health services – more readily remotely and to find disclosure easier on the phone or online. A ‘mixed economy’ (independent chair) of direct and virtual engagement was seen as the way forward (Driscoll-2020). 113
As the pandemic developed, innovative solutions emerged to support families with breastfeeding, including the use of telemedicine. Effective telehealth requires planning and proactive participation and, throughout the pandemic, it enabled families and specialists to connect (Boddy-2022a). 100
Consider offering families a 9-5 health visitor telephone advice service, if not already available, as many families are suffering heightened anxiety and are unsure how they can get the essential information they need, when they need it (Welsh Government-2020). 185
Health visiting connections
Connecting families with other services is an important part of the health visitor role
CMOC13: When there is closure of other local services/groups/organisations that health visitors can refer families to (C) health visitors cannot perform a vital part of their role (e.g. signpost/refer onwards) (O) because they have limited access to do so (M)
Many walk-in baby clinics have now closed, which cuts off another route for health visitors to offer advice and identify families that might need more support or a new parent who is struggling with mental health (Wilkinson-2022). 186
With partners working outside of the home, and mothers unable to physically meet friends, family or wider support networks, the emotional, educational and household burdens were often exacerbated. […] Particularly for new mothers, Post Natal Depression (PND) and other mental health concerns have not been met with support. There was very little support from local council-run family centres, or any other formal institutions after six weeks. At this stage, mothers have been discharged from active Midwife care and Health Visitor checks. […] The lack of kin support networks affected many new mothers’ ability to care for themselves and virtual support was not as readily available or easy to access. For instance, breastfeeding clinics online were less accessible than going to the family centre to meet with a clinician or asking a grandmother or friend for advice or help. Local council support was seen as a gap in institutional care capacities (Bear-2020). 92
In our interviews, one parent felt strongly about the reduction in open-access, baby and toddler-type groups he had noticed in his local area. The children’s centre he had attended regularly with his older daughters for Stay and Play sessions has since closed, so he was unable to access it with his third daughter. He felt that nothing had replaced this in his local area, saying that there is now a ‘definite lack there’, with ‘nothing, no similar type of free service or support available’. Even without taking account for the pandemic, he felt that ‘there’s been a complete lack of those services’ (Action for Children-2022). 88
CMOC14: When there is closure of other local services/groups/organisations that health visitors can refer families to (C) health visitors will potentially feel compelled to do more ‘extracurricular’ tasks (O) because they feel professionally obliged to do so (M)
While the health visiting service attempts to continue as normal, local community groups and services have closed their doors and moved to telephone appointments, yet many do not provide interpreting services. Over the past 10 weeks I’ve contacted emergency dentists, registered children at school, walked to pharmacies to collect prescriptions, and arranged various appointments on behalf of families (Community Practitioner-2020). 105
Emma Carey (featured on our front cover) won the NHS England sponsored Community and General Practice Nursing category of the 2021 RCN Nursing Awards for going above and beyond to support isolated families. Seeing first-hand how COVID-19 lockdowns were affecting babies and young families inspired her to create a walking scheme for health visitors and families, and a community recipe book, Bites from the Breadline, for those on low incomes. The walking group aimed to replace the informal contact, support and advice parents usually got from drop-in clinics, reduce social isolation and improve mental and physical well-being. It meant health visitors could go out to meet people, deliver public health messages and chat to parents. Everyone had access to green spaces and exercise (Sylvester-2022). 68
The Institute of Health Visiting (iHV) developed the Emotional Wellbeing at Work (EWW) programme to support health visiting services to deal with the increased demands placed on them during the COVID-19 pandemic (Baldwin-2022). 91
CMOC15: When there is closure of other local services/groups/organisations that HV can refer families to (C) families may become concerned that some of their chid(ren)’s development may be affected (O), because they are unable to socialise with other children and access different activities (M)
‘My 4 months old has only seen his brother, father and my face. I’m worried about his development also, I planned to take him to various classes, meet other mums with babies – this is also not possible at the moment’ (Best Beginnings-2020). 93
Parents are struggling to access baby and toddler groups. Our research, like others, found that many services remain unavailable for parents and their babies. Several parents told us baby and toddler groups aren’t operating or are not operating as they normally would. Even if groups are running, restrictions and booking systems make it hard for parents to access them. The flexible, drop-in nature of these groups was a key part of what made them attractive and accessible for parents and their babies. The absence and/or inaccessibility of community baby and toddler groups is likely to continue to exacerbate feelings of loneliness and isolation that have been reported over the pandemic. […] Professionals in our survey made similar observations; only 12% of respondents told us that baby and toddler groups in their area were ‘back to normal’ and 66% reported they were operating with some restrictions. Worryingly, 12% of respondents said baby and toddler groups were no longer operating in their area (Best Beginnings-2021). 94
Many parents were concerned that their babies were missing out on developmental opportunities through these classes and groups. We were reassured by both the Institute for Health Visiting and Professor Elizabeth Meins, a developmental psychologist and professor of psychology from the University of York, that it was nurturing interactions with their caregivers that contributed the most to baby development. However, the groups are still valuable, not least because of the support and interaction they provide for parents (House of Commons-2020). 43
Connecting with other health visitors is important for staff well-being and development
CMOC16: When HVs have reduced informal contact with other HVs and clinicians (e.g. with social distancing or online working) (C) they are under more stress and isolation (O) because they have reduced opportunity for informal discussion, feedback, and debriefing within HVs, and between HVs and other colleagues (e.g. GPs).
COVID-19 has made informal support from peers (in the office/over lunch) almost impossible and this is one of the hardest things to deal with over the last 6 months especially being a newly qualified HV (iHV-2020c). 135
This has been tremendously challenging, with 75% of health visitors reporting an increase in stress as health visitors have had to adapt to a very different way of working, often in isolation from colleagues as office space capacity is reduced for safety (Boddy-2021). 98
The alarm goes off for another day out in practice. I don’t actually start until 8.30 a.m. and, with no office to drive to, working from home can feel odd and tiring. I’m getting up earlier than I am used to for my 12-hour shifts in the hospital as a midwife. […] I wish we could be working together in the office and car sharing to visits. Being separate has brought home how much learning gets done talking things through on the car ride. […] It has been challenging to go from the office, with lots of informal peer support, to more lone working, which can make the role feel isolating at times. […] Team meeting: we meet online for 15–30 minutes every day to check in, catch up and talk about our day. With more remote working it’s important to ensure there is a plan in place so all whereabouts are known at the end of the day (Nursing children and young people-2021). 163
Remote delivery and home-working can affect workforce health and well-being. Risk of burnout can be mitigated by: ensuring staff have ‘down time’ between contacts to process information, adequate supervision and services do not set unattainable targets based on any disproportionate calculation of clinical time to be saved from virtual interventions. Look after yourself and follow the Government’s COVID-19 guidance on social distancing and self-isolation as needed and employ strategies which help you manage your own mental health and well-being during this time (iHV-2020n). 145
CMOC17: When HVs have the option of using online meetings to work or train with colleagues and other health and care professionals (C) this can save them time (O) because they do not have to travel to these (M).
As well as the switch to phone and video therapeutic work, The Little Minds Matter: Bradford Infant Mental Health Service have recognised the stress facing families, and have worked at pace with local partners, like Public Health, to create a video to help parents who were struggling to care for a crying baby which has been widely accessed via social media. Connecting with other professionals has continued, virtually. For example, in June they ran a webinar with an international expert, attended by over 200 people (Best Beginnings-2020). 93
The virtual world we now live in has opened up new channels of communication. Previously, it was difficult to access individuals who could support and help with new projects and research, primarily because arranging face-to-face meetings was almost impossible. With the popularity of webinars and internet meetings, that difficulty has become a thing of the past. New channels of communication are opened up, making regular contact easier and problems that might have been challenges are able to be resolved more quickly (Hanley-2021). 125
The most frequently identified benefits related to remote multiagency working arrangements, which were regarded by most participants as increasing efficiency. Attendance at meetings by professionals was frequently reported to be much higher, particularly for those such as general practitioners (GPs) who had previously struggled to take time out of clinics to attend child protection conferences and for professionals more generally in relation to short notice events such as strategy meetings (Driscoll-2020). 113
Interagency working is an important part of the health visitor role
CMOC18: When multi-agency working was reduced and outside agencies closed (C) health visitors struggled to safeguard children (O) because there were fewer opportunities for children to be seen and assessed (M)
Many professionals expressed a renewed recognition of the fact that the families who need extra help are not always the ones ‘on the list’. Efforts to engage all families during lockdown allowed professionals to identify and respond to the needs of families with babies not previously known to services, and many would like to see the role of universal and open-to-all services reinvigorated for this reason. In some areas services are already actively pursuing this, for example making additional health visits (which go beyond the mandatory checks) and bolstering programmes of open-to-all family support groups (1001Days-2021). 80
There has been talk recently of ‘ghost children’ but perhaps it is our services, not our children, who have become ghosts of their former selves. The pandemic – on top of years of austerity – has led to the withdrawal of many services from our communities. As a result, many young children do not see public services, and their needs and vulnerabilities are not known (1001Days-2022). 77
‘We are being asked to flag families that are Child Protection, Child in Need and also “cause for concern”. This is so the skeleton team left after redeployment can prioritise these cases. This seems an impossible task as our assessment of these families is only a reflection of how things stand at the time, and isn’t robust enough in a fast moving situation. Also we have no tool to inform this decision making, so it’s unlikely to be applied consistently throughout the service. What if we haven’t highlighted a family as a cause for concern and they spiral into crisis? Who will be accountable and what organisational risk assessment is in place to help protect us?’ […] ‘Those vulnerable children, now shielded from the eyes of early years provision and schools, are the ones we strive to make contact with. When the parents of these children decline our support (citing the need to be in isolation) the judgements we are forced to make weigh heavily on our shoulders’ (iHV-2020). 132
The health visiting workforce
Health visiting should be valued appropriately for its impact on child and family health
CMOC19: When some of the health visitor workforce is moved into other roles (C) this leads to increased service delivery challenges for the remaining health visitors (O1) and a feeling of HVs being devalued (O2) due to increased workloads when HVs are already spread thinly (M1) and when HVs are seen as dispensable and able to move to other roles (M2)
…for God’s sake, you’ve got to give us credit, we are the people on the frontline. I’ve got really helpful information, I see clients and I see them regularly and I feel like people… yes, I feel a bit dismissed sometimes (De Backer-2022). 112
The COVID-19 pandemic has resulted in a crisis in the NHS and Social Care, unlike anything experienced before. This crisis has been acutely felt in Public Health Nursing (PHN) where large numbers of the workforce were prepared for redeployment to inpatient physical health wards to help care for the influx of patients suffering from COVID-19. […] Approximately 30% of the PHN workforce were assigned for redeployment or were self-isolating in recent weeks, with additional staff prepared for redeployment to help manage the predicted peak in hospital admissions (iHV-2020b). 134
‘I realise other services are struggling but I really worry about these vulnerable children, hidden away in dangerous homes, away from professionals who safeguard them. I will support other services but are the families on my caseload now insignificant?’ (iHV-2020)132
CMOC20: When the response by policy and decision makers to COVID was focused on short term acute issues and not longer-term public health support (C), this led to health visiting and younger children being largely ignored for policy and funding decisions (O) because they were not considered a priority (M)
We have identified three specific policy calls for the UK Government: The UK Government must support local authorities to invest in and rebuild health visiting services; Babies and the services that support them must be included in COVID-19 recovery policy and investment at a national and local level. This must include investment in community and voluntary sector support; An evidence-based approach must be taken to ensure the appropriate use of digital and phone-based service delivery, and investment in relational, face-to-face support where this is needed (Best Beginnings-2021). 94
Despite the huge pressures the pandemic has placed on families with young children, the Government’s immediate response to the current crisis has shown that 0–5s are forgotten or an afterthought (Action for Children-2020a). 78
Until recently, children in the UK have been considered inconsistently throughout the pandemic. […] During the pandemic, I have been concerned that the plight of children has been overshadowed by the Government and media spotlight being mostly on adult deaths and efforts to reduce the rampant spread of COVID-19 amongst the community. Little attention has been given to babies and young children – did most people assume they were unaffected? (Kombe-2020). 152
CMOC21: With the HV service close to breaking point pre-COVID (C) there were negative consequences for staff, families, and children during the pandemic (O) because it did not have the capacity to manage any additional pressures (M)
How did we let this happen? This state of affairs took hold long before COVID-19. It is not the failure of a single health visitor, provider or commissioner but is the predicted consequence of years of cuts to the service which the pandemic has only made worse. Councils in England have seen a reduction of £700 million in real terms in public health funding between 2014-15 and 2020-21 (Morton-2021). 158
This report focuses on the impact of COVID-19 on families, but many of the problems discussed existed before the pandemic (Best Beginnings-2020). 93
Child health in England was already at crisis point, and research has identified that the pandemic changed the way that people live and access health care (Boddy-2022a). 100
I start documenting the day’s visits and think about the referrals I did not get done this morning that I need to do. The need is high at the moment and we work hard to ensure that all families are seen, and their support needs are assessed – every family that we miss is a family that may need help, support and signposting. We desperately need more health visitors to be able to do our job to the best of our abilities, to build relationships and to identify concerns as early as possible so we can put in interventions to help families (Nursing children and young people-2021). 163
