Notes
Article history
The contractual start date for this research was in November 2019. This article began editorial review in August 2023 and was accepted for publication in June 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health and Social Care Delivery Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Akdur et al. This work was produced by Akdur et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Akdur et al.
Background
The COVID-19 pandemic highlighted the need for standardised metrics for care home residents and it is now a policy priority to have a fully digitalised social care sector. 1,2 However, what constitutes a minimum data set (MDS) to support care home residents is not well established in the UK. 1 The Developing research resources And minimum data set for Care Homes’ Adoption and use (DACHA) study, funded from 2019 to 2024, aims to synthesise existing data sources with resident data from care homes for older people in England, to deliver a core set of data. We describe a MDS as ‘a comprehensive, standardised account of the characteristics and needs and ongoing care of residents living in long-term care (care home) settings’. 3
Focusing on quality of life
There are MDS systems, such as interRAI4 and the Minimum Data Set 3.0 Resident Assessment Instrument5 that are widely used in several OECD (Organisation for Economic Co-operation and Development) countries and regions such as the USA, Canada, Japan, New Zealand and continental Europe. 1,6 Often, these MDS prioritise data on resident health over social care and quality of life (QoL). 1 There is no international consensus on collecting data on QoL in an established way that can be considered equivalent to the consensus for health and functioning measures. The aim of the DACHA consultation work presented in this paper was to address the call from a wide range of stakeholders using resident data to develop consensus on the ‘what’ and ‘how’ to measure QoL of residents in care homes.
A series of consultation events were held in 2021 about the use and the sharing of care home data during the COVID-19 pandemic. 7 Forty individuals identified through DACHA research team’s networks with local authorities, care homes and health and social care professionals from various professional groups (local authority and government officials, researchers, data researchers, primary health care professionals, care home staff and care home managers) participated. They commented on the DACHA study’s early findings and discussed the challenges with their access to care home resident data during the COVID-19 pandemic. A specific issue that was raised was the difficulty in obtaining meaningful and consistent data on resident QoL in care homes. 7 These views were corroborated by an online national survey of care homes,8,9 to identify the range and the method of data collection on care home residents. The survey found that, in England, only 31% of care homes systematically collected QoL information on their residents, with little evidence of standardised measures being used. 8,9 These results informed our decision to focus on QoL measurement in the DACHA 2022 consultation. 7–9 Here, we describe the design, execution and findings of our consultation on QoL in care homes.
The overall DACHA study, and in particular our work on QoL measures, is significant given the government’s current policy focus on creating a data set for social care providers. 10 This paper highlights the importance of ensuring that a focus is maintained on data that can provide actionable insights, such as QoL measures.
Understanding and measuring quality of life
Quality of life is a multidimensional construct. It includes those aspects related to physical and psychological health [health-related QoL (HRQoL)],11 disease-specific QoL (aspects of QoL affected by a health condition or disease)12 and social care-related QoL (SCRQoL). 13 SCRQoL measures the aspects of QoL most impacted by person-centred social care; for example, being able to maintain social relationships or engage in meaningful and enjoyable activities. There are various QoL measures used in long-term care settings that could be included in a MDS, such as those identified in Siette et al.’s review. 14 The QoL measures that are dominantly used in policy and practice tend to be those that capture HRQoL. The relative absence and limited scope of social care variables in the care records is partly due to the health-oriented focus of most resident data sets available for regional or national use, even when older people are living in social care settings. 1 Historically, it is healthcare disciplines that have led work on the identification and development of measures and metrics in long-term care facilities.
There are, however, multiple users and stakeholders of MDS and QoL data, and therefore there are different priorities and interests in how these data can be captured. Our consultation involves a diverse set of stakeholder groups (care home staff, managers, commissioners, care providers, regulatory bodies, clinical or researcher old-age specialists, primary care professionals, relatives/family carers of care home residents, care home managers). Some social care voices are often obscured in stakeholder conversations. This study aims to consider/include seldom heard and overlooked stakeholders, such as care home staff and residents, relatives and family carers, as well. 15–17
Aims and objectives
Our aims were to explore with stakeholders (including a range of people using care home resident data):
-
Which principles and aspects/domains are the most important to capture in QoL assessments in care homes?
-
Given the opportunity, why and how the stakeholders would or would not use the data from different QoL measures.
We then synthesised these responses from stakeholders to make informed decisions about the measures to be included in the DACHA MDS.
To establish more social care inclusion, we considered health-related, dementia-specific (due to the prevalence of dementia or severe memory problems in care homes18,19), and SCRQoL measures, to capture the QoL of care home residents as impacted by the care they receive.
The consultation aimed to establish whether including the shortlisted QoL measures in an MDS would be supported by those who would use the information for planning, care, review and decision-making.
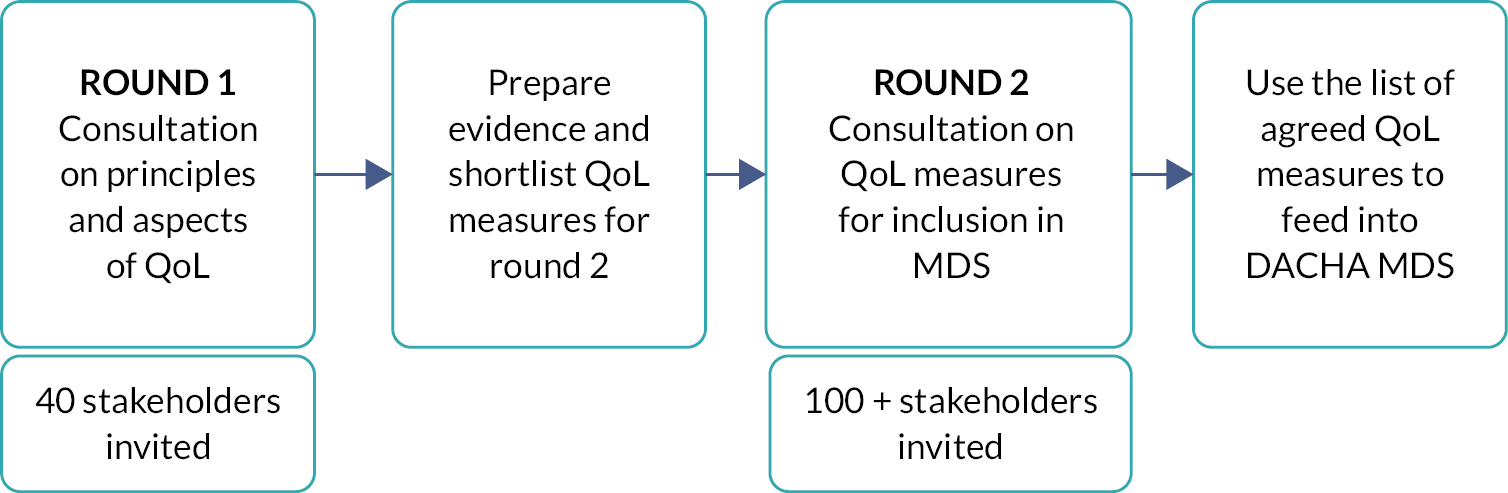
Methods
The underlying premise of the consultation was that individuals or groups involved in or affected by how residents’ data are used, should inform the development of the MDS. It was hoped that recruiting representatives of different stakeholder groups could support the uptake and use of the QoL section of the MDS. A recent review of MDS implementation established the importance of those who complete and use MDS recognising the relevance of the data for their work and residents’ well-being. 20 There were two online consultation rounds to address our objectives (rounds 1 and 2, as above; see Figure 1).
FIGURE 1.
Flowchart design for the consultation.
The assumptions of the Delphi technique informed the consultation approach. 21,22 Specifically, we purposefully recruited people knowledgeable about living, working in and with care homes, and caring for someone who is a care home resident, ranking of strength of agreement and sharing of group preferences. The stakeholders belonged to one of the six expert groups listed below and were able and willing to rate and review factors and measurement tools in the consultation. These abilities and/or experiences formed the inclusion criteria. While we knew directly the invited experts from round 1 (smaller group), their expression of opinions in the survey were collected in an anonymous way that was not attributable to their identities. Round 1 invitees were from a wide range of regions in England and Wales and had a good spread of genders. In round 2 (larger group), due to the survey being public, we neither knew the identities of the invited experts nor could attribute any response to any identity. The process began with a set of selected items (the principles and aspects of QoL); this approach has been noted in some modified Delphi studies. 22,23 In the first phase of the process, we listed these items of QoL measurement by gathering evidence from literature and from DACHA study. In the second phase, we conducted a two-step consultation exercise – the second building on the first – to generate consensus both on the most important factors to capture and about which QoL measures are the best suited for care homes.
The Thiscovery (www.thiscovery.org) platform (a bespoke online platform for remote collaboration, engagement, and research) facilitated the above specifications using the principles of the Delphi technique. It provided a useful interface, specifically designed for research, that prompted the individuals to engage in the DACHA study by laying out the specifics of the QoL factors and measures and providing optional external links for further information to inform the stakeholders. For both rounds, we recruited participants from those stakeholder groups who need to use care home data for practice, research, audit and regulation. We used purposive sampling to identify individual stakeholders in England and Wales through the individual networks of DACHA study steering committee and the research team members. These stakeholders belonged to these expert groups:
-
care home staff member
-
senior operations/care home manager
-
old-age specialist (clinical or research)
-
relative/family carer of a care home resident
-
primary care/hospital health care professional
-
service commissioner, provider, or regulator (such as local authority and Care Quality Commission officials).
We invited all the participants from DACHA consultation events held in 2021, which focused on the views of the stakeholders (who work in, for and with care homes) about their use and sharing of care home date during the COVID-19 pandemic. We worked with Thiscovery to create briefing notes, design a two-stage consultation and conduct analysis on the results.
For round 1, we created lists of 12 principles and 9 domains of QoL for stakeholders to rank (see Appendices 1 and 2 for definitions). These principles and domains – for example, resident inclusivity (regardless of the dementia status), informing day-to-day care, physical health, environment – were derived from DACHA’s MDS principles by Burton et al. 1 and a recent systematic review of QoL measures by Siette et al. 14 Please refer to Appendix 3 for Burton et al.’s MDS principles. 1
Round 1 had two overarching questions:
-
What should a measure of QoL be able to do?
-
What domains of QoL are most important to measure?
We ran a small pilot test of the surveys to check question clarity and technical or process issues among several members of the DACHA research team and study steering committee, and some members from the DACHA patient and public involvement and engagement (PPIE) group, prior to launching the consultation.
To participate, stakeholders registered on the Thiscovery website. Participant information was provided in the invitation e-mail and at the start of the survey. Informed consent was obtained at the start of the online survey. The first survey had an explainer video, describing the consultation aims and tasks. Stakeholders ranked the perceived importance of each factor between 1 (the least important) and 9 (the most important), with 5 as the neutral score. Responses were anonymised and stored on Thiscovery.
Based on the findings from round 1, the DACHA team shortlisted QoL measures (which measure HRQoL, SCRQoL and dementia-specific QoL) that met the highest ranked factors from round 1. To create this shortlist, we gathered evidence from DACHA’s internal evaluation of QoL measures, including those used in existing minimum data sets (MDS), and Siette et al.’s systematic review. 14 We considered the following criteria when shortlisting instruments:
-
The measures will have evidence of use or feasibility for use in residential long-term care settings in the UK.
-
The instruments will be outcome measures, and not process measures, to be suitable for quantitative data analysis.
-
The measures will take no longer than 10 minutes to complete.
-
The measures will be relatively new: produced 2000 onwards.
-
The measures will have sufficient psychometric properties.
Please refer to Appendices 4 and 5 for a list of measures that were reviewed internally by the DACHA team and the measures included in Siette et al.’s review (2021). 14
In the second consultation exercise (round 2), we invited participants from round 1 and also extended invitation to others within the same stakeholder groups via social media, NHS CHAIN Network (www.chain-network.org.uk) bulletin and targeted invitations using the DACHA research team’s social care networks and links via social care representative organisations and social care research/practitioner groups (e.g. National Care Forum, NIHR Applied Research Collaboration Care Home network).
Via Thiscovery, round 2 participants watched an explainer video prior to answering the questions. They were given a summary of the shortlisted measures with the option to click to view the full measure on a separate window. One measure [EuroQol-5 Dimensions, five-level version (EQ-5D-5L) proxy version 2] could not be shared in full, due to licensing restrictions, so only a summary was shared with the participants (see Appendix 6 for the summaries that the research team has created and provided in the consultation for each measure).
Participants were asked to comment on and rank:
-
Their familiarity with the measures (yes/no).
-
Their confidence in and perceived usefulness of the measures on a scale from 1 (not confident at all) to 9 (very confident).
-
How they would use the information provided by the measures.
-
Preference for one of the two dementia-specific QoL measure (QUALIDEM or DEMQOL).
Free-text questions focused on the perceived advantages and challenges of using the shortlisted QoL measures. All participants received a feedback e-mail through the Thiscovery platform, which shared the findings of the consultation24 and thanked them for their participation. There was an option to comment further on their experience of using the online platform.
Results
Round 1
Round 1 took place between 8 June and 25 July 2022 and attracted 30 responses. The stakeholder numbers from each group are shown in Table 1.
| Stakeholder group | Stakeholders (n) |
|---|---|
| Care home manager | 8 |
| Care home staff | 2 |
| Commissioner/provider/regulator | 7 |
| Old-age specialist (research/clinical) | 8 |
| Primary care professional | 4 |
| Relative/carer of a care home resident | 1 |
The highest ranked principles to have in a QoL measure were (1) resident inclusion, (2) ease of completion, and (3) potential to shape the day-to-day care (see Table 2). The highest ranked domains were (1) mental health items, (2) emotional state items and (3) social interaction items (see Table 3).
| Rank | Principle | Mean score | Standard deviation |
|---|---|---|---|
| 1 | Resident inclusion | 8.57 | 0.90 |
| 2 | Easy to complete | 7.93 | 1.48 |
| 3 | Inform day to day care | 7.77 | 1.10 |
| 4 | Completion by residents | 7.60 | 1.96 |
| 5 | Sensitive to change | 7.43 | 1.94 |
| 6 | Inform decisions | 7.30 | 1.73 |
| 7 | External access | 7.23 | 1.68 |
| 8 | Reflect differences in care received | 7.00 | 1.84 |
| 9 | Quick to complete | 6.90 | 1.97 |
| 10 | Written in notes | 6.70 | 2.52 |
| 11 | Have a numeric score | 6.50 | 1.46 |
| 12 | Completion by staff | 6.03 | 1.77 |
| Rank | Aspect/domain | Mean score | Standard deviation |
|---|---|---|---|
| 1 | Mental health | 8.27 | 0.91 |
| 2 | Emotional state | 8.27 | 0.94 |
| 3 | Social connection | 8.20 | 1.10 |
| 4 | Physical health | 8.03 | 1.00 |
| 5 | Personhood | 8.00 | 1.51 |
| 6 | Autonomy | 7.93 | 1.46 |
| 7 | Environment | 7.70 | 1.34 |
| 8 | Overall quality of life | 7.57 | 1.74 |
| 9 | Spiritual connection | 7.33 | 1.71 |
Round 2
Five QoL measures met the criteria identified as important to stakeholders in round 1. Two of these measures were dementia-specific proxy measures of QoL.
Shortlisted proxy or self-report measures of HRQoL or SCRQoL were:
-
ASCOT-Proxy (Adult Social Care Outcomes Toolkit, proxy report version)25
-
ICECAP-O (ICEpop CAPability measure for Older people)26 (self-report)
-
EQ-5D-5L proxy version 2. 27
Shortlisted dementia-specific proxy-report measures of QoL were:
-
DEMQOL-CH (Dementia Quality of Life: Care Home)28 (proxy)
-
QUALIDEM (Quality of Life for People with Dementia)29 (proxy).
As well as satisfying the round 1 criteria, these measures met the following internal criteria:
-
The shortlisted measures have evidence on their use or on feasibility for their use in the UK residential long-term care settings. 17–22
-
The measures take 10 minutes or less time to complete. We excluded instruments that take over 10 minutes based on Siette et al.’s review. 14
-
The shortlisted instruments are outcome measures, and not process measures, and are suitable for quantitative data analysis.
-
The measures are relatively new – developed in 2000 or later. Note: even though EQ-5D was launched in 1990, EQ-5D-5L was produced in 2009 and is within the inclusion criteria.
-
The measures have sufficient psychometric properties. 14
Owing to the similarity in use and research evidence between two dementia-specific QoL measures, stakeholders were asked to choose between QUALIDEM and DEMQOL-CH. This was based on how they might use the results of the measures to inform their decision-making.
The online survey was open between 12 and 30 September 2022 and attracted 72 responses. Responses from relatives of care home residents and care home staff represented almost a third of all round 2 responses, with old-age specialists (clinical/research) being one quarter of the round 2 stakeholders. The stakeholder numbers from each group are given in Table 4.
| Stakeholder group | Stakeholders (n) |
|---|---|
| Care home manager | 9 |
| Care home staff | 6 |
| Commissioner/provider/regulator | 9 |
| Old-age specialist | 19 |
| Primary care professional | 6 |
| Relative/carer of a care home resident | 16 |
| Other | 7 |
Half of the stakeholders were familiar with (i.e. heard of or used) at least one of the shortlisted QoL measures (see Table 5). ASCOT-Proxy and DEMQOL-CH were the most recognised measures. All the measures were perceived to be useful by stakeholders, ASCOT-Proxy perceived to have the most useful information by 50 stakeholders, followed by EQ-5D-5L (n = 47; see Table 6). Stakeholders ranked all the QoL outcome measures from 1 (not confident at all) to 9 (very confident) in the measure’s perceived ability to capture QoL in care homes. The mean confidence levels for all measures were above 5 (the neutral score) (see Table 7).
| Stakeholder group | Familiar (n) | Not familiar (n) |
|---|---|---|
| Care home manager | 4 | 5 |
| Care home staff | 2 | 4 |
| Commissioner/provider/regulator | 6 | 3 |
| Old-age specialist | 16 | 3 |
| Primary care and hospital professionals | 0 | 8 |
| Relative/carer of a care home resident | 5 | 11 |
| Measure | Yes | No | Not sure |
|---|---|---|---|
| ASCOT | 50 | 6 | 16 |
| EQ5D5L | 47 | 8 | 17 |
| ICECAP-O | 43 | 8 | 21 |
| QUALIDEM | 45 | 7 | 20 |
| DEMQOL-CH | 42 | 7 | 23 |
| Measure | Mean | Median | Standard deviation |
|---|---|---|---|
| QUALIDEM | 5.97 | 6 | 1.94 |
| ASCOT | 5.79 | 6 | 1.76 |
| ICECAP-O | 5.77 | 6 | 2.19 |
| DEMQOL-CH | 5.72 | 6 | 1.94 |
| EQ-5D-5L | 5.59 | 6 | 1.93 |
For health or social care-related QoL measures, care home staff and old-age specialists had the highest mean confidence level scores for ASCOT, whereas care home managers and commissioners/providers/regulators scored ICECAP-O the highest. Relatives of care home residents scored both ASCOT and ICECAP-O the highest.
Consensus for the dementia-specific QoL measures was less clear, with four of the stakeholder groups scoring QUALIDEM higher of the two, and three groups scoring DEMQOL-CH higher (see Table 8).
| Care home staff | Care home managers | Commissioners/providers/regulators | Old-age specialists | Primary care and hospital professionals | Resident relatives | |
|---|---|---|---|---|---|---|
| ASCOT-Proxy | 5.17 | 5.33 | 5.33 | 5.84 | 5.63 | 6.31 |
| EQ-5D-5L Proxy 2 | 5 | 5.89 | 5.22 | 5.68 | 5.75 | 6.13 |
| ICECAP-O | 4.17 | 6.44 | 5.67 | 6 | 5.13 | 6.31 |
| Dementia-specific proxy measures | ||||||
| DEMQOL-CH | 5.83 | 5.33 | 5.67 | 5.16 | 5.38 | 6.27 |
| QUALIDEM | 5.17 | 6.11 | 5.56 | 6.21 | 5.38 | 6.47 |
Additionally, more stakeholders favoured QUALIDEM (n = 26, 36%) over DEMQOL-CH; 21% favoured DEMQOL-CH (n = 15) and 43% (n = 31) were not sure.
An optional comment box was provided for stakeholders to capture qualitative data on how they would, or would not, use the information provided by each measure in their role. This question received responses that focused predominantly on the opportunities and challenges of the measures, rather than specific ways in which the measures would be used by stakeholders. In these responses, proxy bias and the length of the questionnaire were noted the most often as barriers for some of the measures. Table 9 shows a summary of perceived challenges and advantages of the five QoL measures.
| Perceived advantages | Perceived challenges | |
|---|---|---|
| ASCOT-Proxy | Holistic approach Basis for care planning and quality improvement |
Repetition/duplication of work in care plans Limited in its range of questions Proxy report |
| EQ-5D-5L Proxy | Good documenting of changes An early warning system to avoid escalation |
Focusing on the wrongs more than positives Too health centric Too task oriented Proxy report |
| ICECAP-O | Simple documenting of how residents are feeling A positive exploration of resident’s own state of mind and feelings about everyday life Very quick to complete due to being short |
Vague More appropriate for older adults in the community |
| QUALIDEM | Better understanding of residents and their care needs Understanding the quality of life of residents with dementia from a regulator view Easier to report than DEMQOL-CH due to its layout |
Too much information Length Proxy report |
| DEMQOL-CH | Useful evaluation of interventions aimed at improving mood, anxiety, and memory Mood assessment for medication optimisation or deprescribing |
Too much information Length Proxy report Overemphasis on emotional wellbeing |
Discussion and conclusions
This consultation aimed to establish what different stakeholders working in/with and visiting care homes thought QoL measurement should capture to inform planning, care, review and decision-making. It then asked participants to rank the shortlisted QoL measures for possible inclusion in a MDS. Based on evidence and consultation findings, the MDS pilot in participating care homes included four QoL outcome measures from the consultation: ASCOT-Proxy, ICECAP-O, EQ-5D-5L Proxy Version 2, and QUALIDEM. All the shortlisted measures have been used in UK settings as valid and reliable tools for data collection in care home research. 30–35 We acknowledge that a high number of stakeholders in this consultation were ‘unsure’ about selecting between two dementia-specific proxy measures. However, we selected QUALIDEM as it was rated higher than DEMQOL-CH by participants. We chose not to include both measures in our final list due to resource limitations of the participating care homes and the digital care system providers: it was not feasible to trial both measures in care homes simultaneously as part of the DACHA pilot study.
The consultation indicated neutral to positive scores for all QoL measures from all stakeholder groups (mean and median scores around 5–6 from a possible maximum of 9). Qualitative responses revealed concerns about proxy reporting of the assessments by care home staff. Self-report was reported as a perceived advantage. Evidence shows that self-report assessments can be used by people with mild to moderate dementia,36 but they are not feasible for people with severe cognitive impairment where proxy reporting would be preferred. 37 It is estimated that 80% of the UK care home population have either dementia or severe memory problems affecting their ability to self-report even with support. 18,19 Not all care home residents have relatives or family carers, and proxy report by relatives/family carers is often unfeasible, yielding a high percentage of missing data. 38 Self-report is the ideal;39 however, these principles have to be balanced against collecting data from those residents unable to self-report via proxy report consistently and fairly. 38,40 Proxy completion can offer a consistent way of capturing QoL data for all residents and specially adapted measures for proxy report (such as two of the included measures: EQ-5D-5L and ASCOT-Proxy) are designed to limit proxy reporting biases in their design.
Initially, the pre-pandemic plan had been to have region-based face-to-face small group consultations, but this was then substituted with online consultations. This two-stage process engaged a wide range of stakeholder groups in our research. It demonstrated the ability to gather input from different stakeholder groups in a limited period using an online platform. Responses from the two often underrepresented and seldom-heard groups (relatives and family carers of care home residents, and care home staff) formed almost one third of all round 2 responses. Voices from care home staff15,16 and family carers17 are often represented by senior care staff and a few carers. These groups’ input on the outcome measures and perceived advantages and challenges were instrumental in prompting important discussions. Compared with other groups, care home staff and relatives or family carers of residents ranked either one or both of the dementia-specific proxy measures as the highest within their groups. The reason why they favoured these measures might be indicative of their direct experience of the daily lives of older people, living with dementia or memory problems, for whom they provide care and support. This is important and new knowledge in this area.
Strengths and limitations
The level of engagement and the comments on the five QoL measures from those stakeholders that participated was indicative of the interest and importance placed on the topic. It also demonstrated that people with no history of using standardised measures were confident commenting on their respective challenges and benefits for assessing residents’ QoL.
We recognise an important limitation of using online consultations is that we could not capture the viewpoint of a key stakeholder: care home residents themselves. However, the consultation is complementary to DACHA’s research and PPIE activities, which have involved people living in care homes, families of people living in care homes and care home staff (including managers). The DACHA PPIE team are collaborating with the National Activity Providers Association41 to listen to the voices of residents using one-to-one or group discussions, facilitated by activity coordinators working in the homes and who are known to the residents. The inclusion of QoL measures in the DACHA MDS has been discussed in these sessions and fed back into the study. In these sessions, care home residents advocated for the importance of capturing data on resident QoL. 42 This consultation focuses on stakeholders other than care homes residents, who work in and/or have an interest in care homes. The opinions and perspectives of the stakeholders are of relevance as potential end users of an MDS system if a MDS were to be operationalised in the UK. We are confident in the number of participants who took part in the consultation (30 in round 1 and 72 in round 2) due to representation of different stakeholder groups pertinent to our study, and the sense-checking nature of this consultation. The qualitative data from within the same expertise groups were convergent.
We are also cognisant of the underrepresentation of relatives/family carers in round 1 (n = 1) and the imbalance this might have caused in the selection of the QoL principles and domains. We could not predict which principles and domains might have been the highest ranked if more relatives participated in round 1, as we cannot extrapolate the responses from one relative to a group level. This imbalance in the composition of stakeholders was rectified in round 2.
During round 2, Queen Elizabeth II’s mourning period in September 2022 impacted the levels of participation, because of an institutional embargo on public dissemination activities. This affected engagement, and it is reasonable to believe that more stakeholder representatives would have participated if the consultation had occurred at a different time.
Further, a two-step registration process was required to participate in the surveys on the Thiscovery platform. While it was advantageous to have the functionality on Thiscovery to send reminders and thank you messages to the registered users, some stakeholders with NHS e-mail addresses could not complete the registration and had to use alternative e-mail addresses. We only became aware of this technical issue towards the end date of round 2 and this platform-wide issue was fixed after the end date.
Future research should focus on actively involving care home residents in stakeholder consultations. Insights into the actual experiences of residents can ensure that the delivery of a prototype or services is directly reflective of resident perspectives. We applied the above learnings from this consultation to later stages of the DACHA study when we undertook further consultation exercises in 2023–4.
Conclusion
This study informed the inclusion of four QoL measures in the longitudinal pilot study with care homes in 2023. Interviews and focus groups will collect further data about the perceptions of care home staff who completed measures during the pilot study and about the usefulness of the data collected via these measures. We will also collect data on who completed the questions, so that we can control for and consider this in the analyses. The QoL section of DACHA MDS can contribute to informing similar care home data sets internationally.
Additional information
CRediT contribution statement
Gizdem Akdur (https://orcid.org/0000-0001-7326-4750): Conceptualisation (equal), Data curation (equal), Formal analysis (lead), Investigation (lead), Methodology (equal), Project administration (equal), Resources (equal), Visualisation (lead), Writing – original draft (lead), Writing – reviewing and editing (lead).
Lisa Irvine (https://orcid.org/0000-0003-1936-3584): Conceptualisation (equal), Data curation (equal), Formal analysis (lead), Funding acquisition (lead), Investigation (lead), Methodology (equal), Project administration (equal), Resources (equal), Visualisation (equal), Writing – original draft (equal), Writing – reviewing and editing (equal).
Stacey Rand (https://orcid.org/0000-0001-9071-2842): Investigation (equal), Methodology (equal), Validation (equal), Writing – original draft (equal), Writing – reviewing and editing (equal).
Ann-Marie Towers (https://orcid.org/0000-0003-3597-1061): Funding acquisition (lead), Investigation (equal), Methodology (equal), Validation (equal), Writing – original draft (equal), Writing – reviewing and editing (equal).
Lucy Webster (https://orcid.org/0000-0001-9152-4990): Investigation (equal), Methodology (equal), Writing – original draft (equal), Writing – reviewing and editing (supporting).
Karen Spilsbury (https://orcid.org/0000-0002-6908-0032): Funding acquisition (lead), Investigation (supporting), Writing – reviewing and editing (equal).
Liz Jones (https://orcid.org/0009-0007-1063-5025): Funding acquisition (lead), Investigation (supporting), Writing – reviewing and editing (equal).
Claire Goodman (https://orcid.org/0000-0002-8938-4893): Conceptualisation (equal), Data curation (equal), Funding acquisition (lead), Investigation (lead), Methodology (equal), Project administration (lead), Resources (lead), Supervision (lead), Validation (equal), Writing – original draft (lead), Writing – reviewing and editing (equal).
Acknowledgements
We thank Jordan Moxey, Ruth Cousens, Luke Steer, Sam Minter, Glyn Cannon, Andy Paterson, Sophie Machin and André Sartori from the Thiscovery (www.thiscovery.org) team for their support in building this project.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
This study was reviewed by the University of Hertfordshire’s Health, Science, Engineering and Technology Ethics Committee with Delegated Authority (ECDA). Reference number: HSK/SF/UH/05009; approval date: 30 May 2022.
Information governance statement
The DACHA team is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, Thiscovery is the Data Processor; University of Hertfordshire is the Data Controller, and we process personal data in accordance with their instructions. You can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for University of Hertfordshire’s Data Protection Officer at dataprotection@herts.ac.uk or 01707 286215.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/NPYT7562.
Primary conflicts of interest: This consultation is part of the DACHA study, which is funded by the National Institute for Health and Care Research (NIHR) Health Service Research and Delivery programme (HS&DR NIHR127234) and supported by the NIHR Applied Research Collaborations (ARC) East of England, Kent, Surrey and Sussex, and Yorkshire and Humber. Claire Goodman and Karen Spilsbury are NIHR Senior Investigators. Ann-Marie Towers is active in the following panels: NIHR Research for Social Care Panel, NIHR School for Social Care Panel, Panel for NIHR Three School’s Dementia Awards. Karen Spilsbury is part of the following panels and committees: HSDR funding committee (2014–8), PRP Core committee member (2022–current), DLAF panel member, REF Sub-panel. Claire Goodman is part of the following panels and committees: Alzheimer’s Research Strategy Council, Dementia UK Research Strategy Committee, NIHR Social Care Research Advisory Group, Assessment Panel Welsh Government for Welsh Adult Social Care Research Centre (2022), Senior Investigator 15 and 16 selection committee (social care subcommittee), NIHR HS&DR Panel (2010–7).
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the Health and Social Care Delivery Research programme or the Department of Health and Social Care.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Health and Social Care Delivery Research programme as award number NIHR127234.
This article reports on one component of the research award Developing research resources And minimum data set for Care Homes’ Adoption and use (the DACHA study). For more information about this research please view the award page (https://www.fundingawards.nihr.ac.uk/award/NIHR127234).
About this article
The contractual start date for this research was in November 2019. This article began editorial review in August 2023 and was accepted for publication in June 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health and Social Care Delivery Research editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Copyright
Copyright © 2024 Akdur et al. This work was produced by Akdur et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- ASCOT
- Adult Social Care Outcomes Toolkit
- DACHA
- Developing research resources And minimum data set for Care Homes’ Adoption and use
- DEMQOL-CH
- Dementia Quality of Life: Care Home
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- HRQoL
- health-related quality of life
- ICECAP-O
- ICEpop CAPability measure for Older people
- MDS
- minimum data set
- PPIE
- patient and public involvement and engagement
- QoL
- quality of life
- QUALIDEM
- Quality of Life for People with Dementia
- SCRQoL
- social care-related quality of life
References
- Burton JK, Wolters AT, Towers AM, Jones L, Meyer J, Gordon AL, et al. Developing a minimum data set for older adult care homes in the UK: exploring the concept and defining early core principles. Lancet Healthy Longev 2022;3:e186-93.
- Thompson R. Government Announces Plans to Digitalise Social Care by 2024. Care England; 2022.
- Musa MK, Akdur G, Hanratty B, Kelly S, Gordon A, Peryer G, et al. Uptake and use of a minimum data set (MDS) for older people living and dying in care homes in England: a realist review protocol. BMJ Open 2020;10.
- interRAI . InterRAI Long-Term Care Facilities (LTCF) Assessment Form and User’s Manual (Standard English Edition), 10.0 2020.
- US Centers for Medicare and Medicaid Services . Minimum Data Set (MDS) 3.0 Resident Assessment Instrument (RAI) Manual 2024. www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/MDS30RAIManual (accessed 16 January 2023).
- Bernabei R, Landi F, Onder G, Liperoti R, Gambassi G. Second and third generation assessment instruments: the birth of standardization in geriatric care. J Gerontol Med Sci 2008;63A:308-13.
- DACHA . Feedback on DACHA Study’s 2021 Consultation Events 2021. http://dachastudy.com/wp-content/uploads/2021/10/Report-DACHA-consultation-2021.pdf (accessed 16 January 2023).
- Hanratty B, Liddle J, Warmoth K, Irvine L, Akdur G, Burton J, et al. Data collection in care homes for older adults: a national survey in England. J Long Term Care 2023;2023:288-96. https://doi.org/10.31389/jltc.199.
- Hanratty B. Developing Research Resources and Minimum Data Set for Care Homes’ Adoption and Use: Update on Progress from the DACHA Study. International Long-term Care Policy Network ILPN; 2022.
- Department of Health and Social Care . Care Data Matters: A Roadmap for Better Data for Adult Social Care – GOV.UK 2023. www.gov.uk/government/publications/care-data-matters-a-roadmap-for-better-data-for-adult-social-care/care-data-matters-a-roadmap-for-better-data-for-adult-social-care (accessed 13 July 2023).
- Centers for Disease Control and Prevention . Health-Related Quality of Life (HRQOL) 2022. https://archive.cdc.gov/www_cdc_gov/hrqol/index.htm#:~:text=Health%2Drelated%20quality%20of%20life%20(HRQOL)%20is%20an%20individual's,role%20in%20public%20health%20practice.&text=How%20Are%20You%20Doing%3F (accessed 18 January 2023).
- Bowling A, Rowe G, Adams S, Sands P, Samsi K, Crane M, et al. Quality of life in dementia: a systematically conducted narrative review of dementia-specific measurement scales. Aging Ment Health 2015;19:13-31.
- Netten A, Burge P, Malley J, Potoglou D, Towers AM, Brazier J, et al. Outcomes of social care for adults: developing a preference-weighted measure. Health Technol Assess 2012;16:1-166.
- Siette J, Knaggs GT, Zurynski Y, Ratcliffe J, Dodds L, Westbrook J. Systematic review of 29 self-report instruments for assessing quality of life in older adults receiving aged care services. BMJ Open 2021;11.
- Care England . Hidden and Unheard Voices from the Care Home 2017.
- Stephens M, Knight A. ‘Things won’t improve if they’re just left to fester’: a qualitative study exploring how UK care home staff perceive and experience engagement in health research. J Long-Term Care 2022;2022:268-76.
- Knowles S, Combs R, Kirk S, Griffiths M, Patel N, Sanders C. Hidden caring, hidden carers? Exploring the experience of carers for people with long‐term conditions. Health Soc Care Community 2016;24:203-13.
- NHS England . Providing Proactive Care for People Living in Care Homes: Enhanced Health in Care Homes Framework 2023. www.england.nhs.uk/long-read/providing-proactive-care-for-people-living-in-care-homes-enhanced-health-in-care-homes-framework/ (accessed 1 May 2024).
- Alzheimer’s Society . Dementia UK: Update 2014.
- Musa MK, Akdur G, Brand S, Killett A, Spilsbury K, Peryer G, et al. The uptake and use of a minimum data set (MDS) for older people living and dying in care homes: a realist review. BMC Geriatr 2022;22.
- Jones J, Hunter D. Qualitative research: consensus methods for medical and health services research. BMJ 1995;311:376-80.
- Woodcock T, Adeleke Y, Goeschel C, Pronovost P, Dixon-Woods M. A modified Delphi study to identify the features of high quality measurement plans for healthcare improvement projects. BMC Med Res Methodol 2020;20.
- Brauer P, Desroches S, Dhaliwal R, Li A, Wang Y, Conklin AI, et al. Modified Delphi process to identify research priorities and measures for adult lifestyle programs to address type 2 diabetes and other cardiometabolic risk conditions. Can J Diabetes 2022;46:411-8.
- DACHA . DACHA 2022 Quality of Life Consultation Feedback Report 2022. http://dachastudy.com/wp-content/uploads/2022/12/DACHA-2022-Consultation-report-FINAL-.pdf (accessed 19 January 2023).
- Personal Social Services Research Unit . ASCOT: Adult Social Care Outcomes Toolkit 2018. www.pssru.ac.uk/ascot (accessed 18 January 2023).
- University of Bristol . ICECAP-O n.d. www.bristol.ac.uk/population-health-sciences/projects/icecap/icecap-o (accessed 25 June 2024).
- EuroQoL . EQ-5D-5L n.d. https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/ (accessed 18 January 2023).
- Brighton and Sussex Medical School . DEMQOL n.d. www.bsms.ac.uk/research/neuroscience/cds/research/demqol.aspx (accessed 18 January 2023).
- Dichter MN, Ettema TP, Schwab CGC, Meyer G, Bartholomeyczik S, Halek M, et al. QUALIDEM User Guide. Amsterdam: German Center for Neurodegenerative Diseases; 2016.
- Towers AM, Smith N, Palmer S, Welch E, Netten A. The acceptability and feasibility of using the Adult Social Care Outcomes Toolkit (ASCOT) to inform practice in care homes. BMC Health Serv Res 2016;16.
- Rand S, Caiels J, Collins G, Forder J. Developing a proxy version of the Adult social care outcome toolkit (ASCOT). Health Qual Life Outc 2017;15.
- Perry-Duxbury M, Van Exel J, Brouwer W, Sköldunger A, Gonçalves-Pereira M, Irving K, et al. Actifcare Consortium . A validation study of the ICECAP-O in informal carers of people with dementia from eight European countries. Qual Life Res 2020;29:237-51.
- Toh HJ, Yap P, Wee SL, Koh G, Luo N. Feasibility and validity of EQ-5D-5L proxy by nurses in measuring health-related quality of life of nursing home residents. Qual Life Res 2021;30:713-20.
- Dichter M, Bartholomeyczik S, Nordheim J, Achterberg W, Halek M. Validity, reliability, and feasibility of a quality of life questionnaire for people with dementia. Z Gerontol Geriatr 2011;44:405-10.
- Hoben M, Banerjee S, Beeber AS, Chamberlain SA, Hughes L, O’Rourke HM, et al. Feasibility of routine quality of life measurement for people living with dementia in long-term care. J Am Med Dir Assoc 2022;23:1221-6.
- Trigg R, Jones RW, Skevington SM. Can people with mild to moderate dementia provide reliable answers about their quality of life?. Age Ageing 2007;36:663-9.
- Ekström MP, Palmqvist S, Currow DC, Sjøgren P, Kurita GP, Jakobsen G, et al. Mild to moderate cognitive impairment does not affect the ability to self-report important symptoms in patients with cancer: a prospective longitudinal multinational study (EPCCS). J Pain Symptom Manage 2020;60:346-54.e2.
- Towers AM, Smith N, Allan S, Vadean F, Collins G, Rand S, et al. Care home residents’ quality of life and its association with CQC ratings and workforce issues: the MiCareHQ mixed-methods study. Health Serv Deliv Res 2021;9:1-188.
- Rand S, Caiels J. Using Proxies to Assess Quality of Life: A Review of the Issues and Challenges. Canterbury: Personal Social Services Research Unit, University of Kent; 2015.
- Robertson S, Cooper C, Hoe J, Hamilton O, Stringer A, Livingston G. Proxy rated quality of life of care home residents with dementia: a systematic review. Int Psychogeriatr 2017;29:569-81.
- NAPA . NAPA Activities n.d. https://napa-activities.co.uk/about-us (accessed 17 May 2023).
- Micklewright K, Akdur G, Biswas P, Blades P, Irvine L, Jones L, et al. Activity provider-facilitated patient and public involvement with care home residents. Health Expect 2024;10.
- Preference Based Living . PELI-Nursing Home Full Version 2.0 2022. www.preferencebasedliving.com/for-practitioners/practitioner/assessment/peli-questionnaires/peli-nursing-home-full-version-2-0 (accessed 7 May 2024).
- Faulkner M, Davies S, Nolan M, Brown‐Wilson C. Development of the combined assessment of residential environments (CARE) profiles. J Adv Nurs 2006;55:664-77.
Appendix 1
Definitions for QoL principles (consultation round 1). The principles were created by the DACHA team.
| Quality of life principles |
|---|
| Sensitive to change: QoL measures need to measure changes in care home residents’ needs and circumstances over time. |
| Reflect differences in care received: QoL measures need to be sensitive to the impact of care received (differences in care models/quality of care etc.). |
| Inform day to day care: QoL measures need to have the potential to inform direct care when included in digital care records. |
| Have a numeric score: QoL measures in an MDS need to be suitable for quantitative/numeric analysis. |
| Resident inclusion: QoL measures need to be for all residents, including those with dementia. QoL measures need to be feasible to collect about all residents, not only those who can self-report. |
| Completion by staff: QoL measures need to be completed by the staff providing care to residents. |
| Completion by residents: QoL measures need to be completed directly by residents receiving care, if they are able to do so. |
| External access: QoL measures need to be useful to commissioners and external organisations working with care homes (e.g. Care Quality Commission) to inform decision-making. |
| Quick to complete: Each QoL measure needs to be completed in less than 10 minutes by the staff providing care. |
| Easy to complete: QoL questions need to be clear, unambiguous and not upsetting to residents or staff. |
| Inform decisions: QoL measures need to be able inform the decisions of visiting healthcare professionals. |
| Written in notes: QoL measures need to include descriptive notes on residents (e.g. notes on how the resident’s day was, what they ate). |
Appendix 2
Definitions for QoL aspects/domains (consultation round 1).
| Quality of life aspects/domains |
|---|
| Physical health: refers to functional status, physical conditions and their related symptoms, pain and perceptions of overall health. |
| Mental health: refers to items that capture mental and cognitive health conditions, as well as clinical symptoms that would indicate mental health problems. |
| Emotional state: refers to items which capture experiences of positive and negative emotions which are not obviously symptoms of mental health. This includes items which explore feelings of peace, calm, happiness and loneliness, among others. |
| Social connection: refers to items addressing the frequency and quality of social interactions. Items addressing feelings of belonging, friendship and support were also categorised under this domain. |
| Environment: refers to items addressing living conditions and deployable resources. Included in this domain are items addressing satisfaction with social care services, as well as items which ask respondents to reflect on the emotional, psychological and physical effects of living conditions. |
| Personhood: relates to items addressing levels of satisfaction with personally and culturally meaningful activities which provide joy and a sense of identity. This domain also refers to items that address identity continuity, and effects of ageing on identity and sense of self. |
| Autonomy: relates to items addressing capacity and satisfaction with one’s ability to manage activities of daily living. Emotion-centric items associated with dependence and autonomy are also categorised as relating to autonomy. |
| Spiritual connection: covers feelings of faith, and inner peace, as well as involvement in religious or spiritual practices such as prayer. |
| Overall quality of life: relates to single items asking respondents to rate their QoL as a whole. |
Appendix 3
Early core principles for a UK minimum data set for older-adult care home residents, reproduced with permission from Burton et al. (2021). 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0. The text below includes minor additions and formatting changes to the original text.
-
The MDS must primarily focus on measuring what matters most to support those living in care homes through systematic data collection and sharing.
-
The MDS must be evidence-based in design and contents, requiring co-production with key stakeholders.
-
The MDS must reduce data burden and duplication of effort for the care home. This will be achieved through piloting, collaboration and ongoing engagement with homes.
-
The MDS will be most effective when underpinned by digital care planning and care records systems, within the care home, serving the day-to-day needs of residents, staff, families and friends. This requires digital infrastructure and investment to deliver at scale.
-
The MDS will include information on the care home service, individual-level data on residents and information on the model of staffing that supports them, but will not include individual-level data identifying the workforce in each home.
-
The MDS should bring together data from within the care home, coupled with data held externally about residents and care services.
-
Data sharing with external users of the MDS must have an agreed purpose. Data sharing pathways must be defined and formalised in data sharing agreements, using secure environments for access where appropriate. Care home residents’ privacy rights must be protected.
-
Care homes should be supported to access and use the data they collect and share using electronic dashboards.
-
The MDS requires national infrastructure and integration with existing data systems.
Appendix 4
The list of QoL measures internally reviewed by DACHA team, grouped by type.
Appendix 5
List of 29 quality of life measures reviewed by Siette et al. (2021); table reproduced with permission from Siette et al. (2021). 14 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) licence, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0. The text below includes minor additions and formatting changes to the original text.
| Instrument (year) | Items, n (length, minutes) |
|---|---|
| 15D (1992) | 15 (5) |
| ADRQOL (1997) | 40 (10–15) |
| A-QoL-8D (2011) | 35 (5) |
| ASCOT-SCT4 (2012) | 9 (5–10) |
| CAD-EOLD (2001) | 14 (N/A) |
| COMQOL (1991) | 44 (45) |
| DEMQOL (2005) | 29 (< 10) |
| DUKE (1990) | 17 (10) |
| DQOL (1999) | 29 (10) |
| EQ-5D (1990) | 6 (2–5) |
| HUI (1996) | 8 (3) |
| ICECAP-O (2006) | 5 (5–10) |
| interRAI (LTCF) (2008) | 50 (40–60) |
| JoLS (2019) | 13 (N/A) |
| MANSA (1999) | 25 (30) |
| NHP (1980) | 45 (10) |
| NHVQOL (2007) | 57 (10–15) |
| OHIP (1993) | 49 (17) |
| OPQOL (2009) | 13 (N/A) |
| PGCMS41(1975) | 17 (10 minutes) |
| QOL-AD (1999) | 26 (10–15) |
| LTC-QOL (2005) | 9 (N/A) |
| QUALID (2000) | 11 (5) |
| QUALIDEM (2007) | 40 (10) |
| SF-36 (1992) | 36 (10) |
| SWLS (1985) | 7 (1–3) |
| WHOQOL-AGE (2013) | 13 (N/A) |
| WHOQOL-BREF (1996) | 32 (15–20) |
| WHOQOL-OLD (2006) | 24 (N/A) |
Appendix 6
Summaries of QoL as provided during the consultation (round 2). Summaries were created by the DACHA team.
ASCOT-proxy
The Adult Social Care Outcomes Toolkit (ASCOT) is a suite of tools designed to measure the aspects of QoL most affected by social care. We propose to use the ASCOT-Proxy, which is designed to be completed by staff on behalf of people who struggle with self-report (e.g. due to cognitive impairment).
There are eight domains of SCRQoL in ASCOT and one question per domain. The care worker is asked to rate the resident’s SCRQoL in two ways: (1) how they rate the resident’s SCRQoL is in that domain; and (2) how they think the resident would rate themselves, if they were able (so 16 responses in total).
The eight domains of SCRQoL are:
-
food and drink
-
accommodation (cleanliness and comfort)
-
personal (cleanliness and comfort)
-
social participation
-
occupation (spending their time doing things they value and enjoy)
-
control over daily life
-
safety
-
dignity.
EQ-5D-5L proxy
EuroQol-5 Dimensions, five-level version is designed to measure health-related quality of life. EQ-5D-5L asks carers to rate the resident’s health today on five dimensions, each with five levels of severity. There is also a final question about overall quality of life.
There are six questions in total, which relate to:
-
mobility – problems in walking
-
self-care – problems in washing/dressing oneself
-
problems in doing usual activities
-
level of pain/discomfort
-
level of anxiety/depression
-
scoring overall health (scale 0–100).
ICECAP-O
ICEpop CAPability measure for Older people (ICECAP-O) is designed to measure of capability in older people, and focuses on well-being defined in a broader sense, rather than health. ICECAP-O asks the resident to rate own quality of life ‘at the moment’, with four levels of severity.
There are five questions in total which relate to:
-
attachment (love and friendship)
-
security (thinking about the future without concern)
-
role (doing things that make you feel valued)
-
enjoyment (enjoyment and pleasure)
-
control (independence).
QUALIDEM
Quality of Life for People with Dementia (QUALIDEM) is designed to measure dementia-related quality of life. QUALIDEM asks how the carer would rate the residents based on observations during the past week. There are 40 questions in total, which relate to:
-
relationship with caregivers (7 questions)
-
positive and negative feelings (9 questions)
-
restless tense behaviour (3 questions)
-
positive self-image (3 questions)
-
social relationships (6 questions)
-
social isolation (3 questions)
-
feeling at home (4 questions)
-
having something to do (2 questions)
-
other (enjoy meals, does not want to eat, likes to lie down) (3 questions).
DEMQOL-CH
Dementia Quality of Life: Care Home (DEMQOL-CH) is designed to measure dementia-related QoL. DEMQOL asks the carer how their resident felt during the past week. There are 32 questions in total, which relate to:
-
Positive and negative feelings (11 questions) – Are they cheerful? Frustrated? Sad? Content? Lively? Irritable?
-
Memory or forgetfulness (9 questions) – Do they forget people’s names? Where they are? What day it is? Muddled thoughts?
-
Everyday life (11 questions) – Keeping clean? Getting in touch with people? Playing a useful part in things? Things taking longer than they used to?
-
Overall quality of life (1 question).
