Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 16/19/02. The contractual start date was in October 2017. The draft report began editorial review in July 2022 and was accepted for publication in December 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Hollis et al. This work was produced by Hollis et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Hollis et al.
Chapter 1 Introduction
Some sections of this chapter have been reproduced from the online remote behavioural intervention for tics (ORBIT) trial protocol, which has been published. 1
Scientific background
Tourette syndrome (TS) and chronic tic disorders (CTDs) are common, disabling, childhood-onset conditions characterised by motor and vocal tics (i.e. involuntary, repetitive movements or vocalisations) that have been present for at least 1 year. 2 Affecting approximately 1% of young people (an estimated 70,000 people aged 7–17 years in England), they are associated with significant distress, psychosocial impairment and reduced quality of life (QoL). 3 In many cases, symptoms decline in severity during late adolescence and into early adulthood,4 leading to lower rates in adult populations. 5
Tourette syndrome and CTDs rarely occur alone, and it is estimated that around 85% of people with TS or a CTD experience one or more co-occurring psychiatric conditions. 6 The most common comorbidities are attention deficit hyperactivity disorder (ADHD) and obsessive–compulsive disorder (OCD), both affecting approximately 50% of the TS population across the lifetime. 6 Symptoms associated with anxiety disorders, disruptive behaviour and ‘episodic rage’, depression, self-injurious behaviour and autism spectrum disorders are also frequently experienced in this patient group. 7,8 The extent of overlap with other diagnostic categories and symptoms has led many to argue that TS belongs to a broader spectrum of neurodevelopmental disorders with shared risk factors and overlapping behavioural, cognitive and social-emotional features. 9 Furthermore, additional comorbidities are often associated with greater functional impairment and distress than tics themselves10 and may contribute to difficulties managing tics in daily life. Therefore, tic treatment can be complex, and it is important to take the impact of comorbid conditions on the child and their tics into account.
Current treatment options
To date, in the UK there are still no National Institute for Health and Care Excellence (NICE) guidelines on the management of tics in children and young people (CYP), though evidence-based pharmacological and behavioural therapy (BT) treatments exist,3,11–13 together with consensus and evidence-based treatment guidelines. 11,14 For many years, pharmacological treatments were considered the first-line treatments, with randomised controlled trials (RCTs) of both antipsychotics and noradrenergic agents demonstrating effectiveness with small effect sizes (see Hollis et al. 3 for a review). However, such drugs are often associated with significant adverse effects such as weight gain and sedation,3 and there has been accumulating evidence for the efficacy of BTs as a viable alternative. Recognising this, recent European guidelines,11 North American guidelines15 and a Health Technology Assessment (HTA) Evidence Synthesis3 all recommend that BT should be offered as the first-line treatment for tics in children and adolescents in a stepped-care approach. These guidelines universally highlight two key BT approaches for their notable evidence base: habit reversal training (HRT) and exposure and response prevention (ERP). 11,12 The comprehensive behavioural intervention for tics (CBIT) package, which is based on HRT with additional components, shows similar efficacy to medication. 12 However, it is noteworthy that the evidence base for ERP is weaker than that for HRT/CBIT.
Behavioural therapy for tics
Clinical data and background
The effectiveness of BT for reducing tics is now well established,3 with systematic reviews demonstrating a similar magnitude of effect for HRT/CBIT as for pharmaceutical interventions. 3,11,12 With numerous larger-scale RCTs having been conducted to date, CBIT in particular is supported by a strong evidence base regarding its efficacy and safety. 11 ERP is also endorsed, though ‘to a lesser degree of certainty’11 than HRT/CBIT, owing to its more limited evidence base to date. Systematic reviews of the literature also highlight that psychoeducation, whilst shown to be inferior to BT for tics as a standalone treatment in numerous RCTs, should always be offered as an initial component in BT, regardless of subsequent therapeutic approach. 11
Whilst BT models differ in their therapeutic processes, they share similar rationales, theoretical underpinnings and goals. There are various theories highlighting different mechanisms that may be involved in BT for tics. For instance, one theory suggests that HRT/CBIT and ERP work on an underlying principle that motor and vocal tics are linked to a ‘premonitory urge’ (a somatosensory discomfort that occurs before a tic). Tics are then reinforced over time through their association with the premonitory urge, creating an urge–tic cycle. A core aim of BTs for tics is to disrupt the urge–tic reinforcement cycle. This theory also posits that other internal stressors (e.g. emotional distress) and external or situational factors (e.g. environmental stressors, such as noise or social context) may maintain or worsen tics, and so the therapist will also work with patients to address these factors. However, the exact mechanisms involved in BT for tics remain unclear.
Detailed session-by-session guidance on the delivery of HRT/CBIT and ERP can be found in published treatment manuals, but we provide a brief overview of these approaches below. To date there has been no specific research into which BT is preferable for whom or when either HRT/CBIT or ERP in particular may be indicated. From clinical experience alone, Verdellen et al. 16 posit that patients with a large number of tics may obtain greater benefit from ERP, as the model addresses multiple (all) tics simultaneously. There is also some clinical or theoretical rationale to applying ERP where there is comorbid OCD, as ERP is the primary evidence-based therapy for OCD symptoms. However, more studies are needed to clarify which BT works best for whom and when. In clinical practice, clinicians often report combining approaches.
Habit reversal training
In HRT, the core aim of therapy is to break the urge–tic–relief cycle by developing alternative or ‘competing’ responses to the premonitory urge. The process of HRT comprises two main components: (1) awareness training, which involves strategies and techniques to increase awareness of both premonitory urges and tics themselves and (2) competing response training, where physically incompatible actions are identified and performed to disrupt/block tic expression. Competing response training only commences for each tic once the individual has developed good awareness of the tic occurring and the ‘tic signal’ preceding it. This process is followed for each tic individually, such that tics are treated one by one in a hierarchy, usually starting with the most bothersome. Working sequentially through each tic in the hierarchy, treatment involves competing response practice and mastery in-session, followed by continued practice at home.
Comprehensive behavioural intervention for tics
Comprehensive behavioural intervention for tics, which is supported by the largest trials to date,17 is simply an extended package of HRT with additional therapeutic components. These include relaxation training, contingency management and functional analyses to identify and address contextual factors that may exacerbate tics, as well as working with families/schools to promote social support. Though there is some uncertainty as to the ‘active’ components of CBIT, several RCTs have consistently demonstrated the superiority of CBIT to psychoeducation-based treatment in young people and adults, with reductions in tic severity maintained at up to 6 months. 3,11 An 11-year naturalistic follow-up of the original CBIT trial17 showed reduced tic severity was maintained in those who had received CBIT. 18 A recent pilot trial also provided preliminary evidence for the efficacy of a modified form of CBIT with play-based adaptations and significant parent involvement for young children with tics. 19
Exposure and response prevention
Exposure and response prevention also aims to break the urge–tic–relief cycle of reinforcement, but instead of developing a competing response to individual tics, the patient learns to tolerate premonitory urges and suppress tic expression altogether. As such, all tics are addressed simultaneously. During therapy sessions, the patient is supported in practicing suppressing tics for prolonged periods (i.e. ‘response prevention’), and strategies are then used to increase ‘exposure’ to the premonitory urge and tic-inducing environmental factors. This typically includes practice focusing on the urge and gradually increasing exposure to situations and activities that typically elicit tics, whilst at all times resisting the urge to tic.
Randomised controlled trial evidence for ERP is more limited, though the available studies suggest that it may be as effective as HRT in reducing tics. One study directly compared HRT with ERP for children with tics and found no statistically significant difference in the reduction of symptoms in terms of tic frequency and a slightly favourable response to ERP on the Yale Global Tic Severity Scale (YGTSS). 20 Another study involving both children and adults (n = 43; 7–55 years of age) randomised to either ERP or HRT also demonstrated comparable effects maintained up to the 3-month follow-up. 16 Other naturalistic studies have provided supplementary evidence that ERP can be implemented in clinical settings, with comparable effect sizes to those seen in trials to date. 11 Though larger-scale trials of ERP-based interventions are needed, these findings highlight the potential for BTs as effective and safe first-line treatments for tics.
Access to BTs for tics
Despite an increasingly clear evidence base and guidelines consistently recommending BT as a first-line treatment approach, access to BTs remains limited. Estimates suggest that only around one in five young people with TS are currently able to access BT for tics in the UK,21 contrasting with approximately 50% receiving medication, despite their more significant risks of adverse effects. 12,13 Furthermore, those young people who manage to access BT typically receive four or fewer face-to-face therapy sessions, which is under half the recommended number. 21
Research also suggests that families prefer and request better access to BT for tics and are often unsatisfied with current treatment options. Qualitative analysis collated from interviews with 42 young people with TS and a survey of 295 parents of children with TS identified that many families felt health-care professionals were not knowledgeable about TS. 21 Specifically, respondents noted the struggle to access limited BT resources, with 76% of parents saying they would like BT to be available for their child, highlighting the need for improved access to behavioural interventions for TS.
Though various factors are likely at play, the ongoing lack of expert therapists trained to deliver behavioural interventions for tics is a considerable barrier to provision. At present, Tourettes Action (https://www.tourettes-action.org.uk) lists fewer than 10 endorsed NHS behavioural therapists for young people with TS throughout the UK. In England, this equates to approximately one therapist to every 10,000 CYP with TS. This lack of provision is compounded by an uneven geographical distribution of therapists, with the majority located in London and surrounding areas. As a result, many families face long-distance travel to national specialist centres for support, which is expensive, disruptive and time-consuming, creating further inequity of access. There is therefore a desperate need for solutions to improve access to specialist treatment for tics, including scaling up provision of BTs.
Digital therapy and internet-based cognitive–behavioural therapy
Over the last decade, internet-based cognitive–behavioural therapy (iCBT) has been developed, which can enable effective and often less therapist-intensive interventions to be delivered over long distances and at reduced cost. 22 The potential for internet-delivered treatments to widen access and meet treatment needs more flexibly has been further highlighted throughout the COVID-19 pandemic, with many services increasing their remote and online therapy options through necessity. However, research with service users and staff during this period has also highlighted the importance of appropriate therapist training and technology for online delivery and the need to minimise digital exclusion of the most vulnerable groups. 23
The first substantial evidence for iCBT as an effective delivery approach was in the treatment of adults with depression and anxiety disorders, and there is now a large literature indicating that iCBT, in various forms, can be effective and have lasting impact. 24–26 Across diagnostic conditions, studies have now shown the efficacy of iCBT compared to no-treatment control conditions and results comparable to face-to-face treatment in terms of symptom reduction,26,27 which could also result in as much as 50% cost savings. 26
There is also now a growing literature on digital therapies for mental health difficulties in CYP. Reflecting findings with adult iCBT, effect sizes for short- to medium-term outcomes appear broadly equivalent to those seen in face-to-face treatment. 3 Recognising this evidence, NICE now recommend digitally delivered CBT in the treatment of mild to moderate depression in CYP,28 and there has been growing interest in the potential utility of online platforms for a wide range of patient groups and therapeutic approaches; these include iCBT-based programmes for post-traumatic stress disorders (PTSD), OCD and eating disorders, parenting programmes for behavioural support and interventions designed for use with specific physical health or neurodevelopmental problems. 22
Therapist-guided iCBT
Research has demonstrated that an important factor in the efficacy and cost-effectiveness of iCBT, mediated by engagement/adherence with therapy, is the provision of therapist guidance. Though self-guided programmes may seem superficially attractive due to their very low implementation costs, data indicate that low adherence is a major drawback. 29 Overall, research has shown that therapist-supported platforms perform better in terms of engagement and adherence; moreover, they deliver higher effect sizes and are more cost-effective than pure self-help. 25,30 Supporting a low-intensity model of practitioner involvement, even a ‘minimal’ amount of therapist support can be of significant benefit. 31 Importantly, service users themselves also report a preference for online interventions that integrate some traditional face-to-face or telephone support. 23
One multi-diagnostic, therapist-supported platform of note is the ‘BIP’ [Barninternetprojektet (Child Internet Project; Swedish digital platform)] iCBT programme developed by researchers at the Karolinska Institutet in Sweden. Delivered via a secure, password-protected internet platform that enables the presentation of different treatment content to different paediatric populations, the BIP research platform has been used to deliver iCBT for a range of conditions, including phobias,32 anxiety33 and OCD. 34 Similar to models adopted by improving access to psychological therapies (IAPT) in the UK, where graduate mental health workers support adults through manualised, evidence-based iCBT treatment for mild to moderate depression, anxiety and obsessive–compulsive symptoms, the BIP-iCBT treatment content is presented in chapters, like a self-help book, but with interactive materials and videos.
There are some clinical data to support the use of the BIP system for therapist-guided iCBT. A RCT using the BIP system compared participants who received BIP OCD therapy with a waiting-list control and found a significant reduction in OCD symptoms at 3 months post-treatment. 34 Additionally, there were no adverse events (AEs) reported, and participants were generally satisfied with the delivery of treatment, with only 4% stating they would have preferred face-to-face therapy. Qualitative interviews with participants in this trial also demonstrated support for the online delivery of the therapy. Specifically, they noted that iCBT allowed them to control the pace and intensity of the therapy and facilitated self-disclosure, whilst still allowing them to feel supported by a clinician. 35 Symptom reduction was also noted in a RCT using the BIP system for anxiety,36 social anxiety disorder37 and OCD,38 and in a pilot study using BIP for specific phobia,32 demonstrating the potential diversity of this platform. Whilst the evidence base for the BIP system has primarily derived from Swedish studies, recent research has demonstrated its generalisability to youth populations in the UK and Australia. 39
Remote delivery of BT for tics
Despite the growing literature on iCBT using BIP and other systems, there is little research evidence with regards to the effectiveness of the online treatment of TS. In a recent review of digital health interventions (DHIs), Hollis et al. 40 found that the majority of online interventions have been designed to help CYP at risk of developing or with a diagnosis of an anxiety and/or depression, with neurodevelopmental disorders such as TS/CTDs being largely overlooked to date.
Innovations in remote BT for tics to date have primarily focused on video conference delivery, using software such as Skype, with two pilot RCTs providing some support for this approach in CYP. 41,42 Himle et al. 41 compared video conference-delivered CBIT to traditional face-to-face treatment (8–17 years of age; N =20) and found equivalent reductions in tic severity in both groups, which were sustained at the 4-month follow-up. Ricketts et al. 42 compared CBIT delivered over Skype to a wait list control group (N= 20) and reported greater reductions in tic severity in the video conference group. Though both studies were small, ratings from patients indicated high levels of satisfaction with the treatment and a strong therapeutic alliance. Despite some technical challenges (e.g. video/audio disruption, difficulties viewing homework), video conference delivery was generally rated as highly acceptable by the participants. 41 Another related pilot RCT also evaluated DVD-supported HRT, where young people (7–13 years of age, N = 44) were guided through a HRT programme with the support of a parent. The results showed the equivalence of DVD-supported HRT and face-to-face treatment, though large drop-out rates make these findings difficult to interpret.
Similarly, there have been two preliminary studies of internet-delivered BT for tics to date, using interactive self-help programmes with therapist support (text/phone). In one pilot study using the BIP system in Sweden, children (8–16 years of age, N =23) were randomised to either an ERP-based or a HRT-based intervention delivered online via the BIP system. 43 Participants in both intervention groups showed improvement 3 months after treatment completion in terms of tic-related impairment and parent-rated tic severity; however, only those in the ERP arm showed significant reductions in clinician-rated tic severity as measured with the Yale Global Tic Severity Scale-total tic severity score (YGTSS-TTSS). Furthermore, therapeutic gains were maintained at the 12-month follow-up, and no severe adverse events (SAEs) were reported. Although this was not a study powered to compare efficacy, the findings show that ERP treatment delivered online via a therapist-supported platform such as BIP may be effective in reducing tics and provide some support for an ERP-based format over HRT when delivering BT for tics online. Engagement with and acceptability of the treatment were good, with no dropouts or data loss at any of the assessment points, and 83% of users rated the treatment as good or very good. The researchers in Sweden also noted that the online treatment format demanded less therapist time (approximately 25 minutes/week per participant) than face-to-face BT using primarily text-based support.
Most recently, an Israeli RCT randomised young people (7–18 years of age; N = 45) to either internet-delivered CBIT or a wait list control. 44 The results showed a significant reduction in total tic severity (YGTSS-TTSS) in the CBIT group relative to the control condition, with therapeutic benefits maintained at the 6-month follow-up. Again, this study highlighted the potential for considerable time- and cost-saving benefits relative to traditional face-to-face treatment, with therapists spending on average just 7 minutes per participant per week providing telephone support.
Summary and study rationale
There is now reasonable RCT evidence to support the clinical effectiveness of BT for treating tics in CYP. Overall, findings demonstrate the equal effectiveness of BT compared to pharmacological alternatives, with considerably reduced risks of side effects. Whilst most trial data relate to HRT/CBIT, which has the broadest evidence base at present, there are promising clinical and pilot trial data on the acceptability and benefits of ERP and its suitability for adaptation to online delivery. Reflecting the current evidence base, BTs are now recommended as first-line treatment approaches in the treatment of tics in CYP, though there is a need for more research focusing on longer-term outcomes and larger-scale RCT evaluations of ERP. 11
Despite growing support for BT in terms of both its evidence base and acceptability amongst service users, access to BT for tics remains very limited, with geographical barriers and a lack of trained therapists noted as key ongoing issues. Qualitative research underlines patient dissatisfaction with the lack of behavioural treatment availability for tics and the need for improved access to treatment. This has led to an increased focus on training, dissemination and adapted treatment delivery in recent years. Particularly in light of the COVID-19 pandemic and the necessity to deliver patient care remotely where possible to maintain existing service provisions, harnessing digital technologies and service innovations is becoming an increasingly important part of NHS policy for the UK. 45
There is now a sizeable evidence base supporting internet-delivered treatments or iCBT more broadly, with research showing treatment effects comparable to face-to-face interventions for a growing range of conditions and groups. 40 Significant cost-saving potential is indicated, particularly for therapist-guided platforms that bolster better engagement, adherence and efficacy. However, research to date has largely focused on common mental health conditions such as anxiety and depression, with less attention given to online BT for tics or other more ‘specialist’ interventions. Most studies to date have also evaluated treatments outside of the UK, with many being conducted in Sweden using the BIP platform. Whilst a limited number of small RCTs have recently provided preliminary support for internet-delivered BT for tics, larger-scale (adequately powered) RCTs and clarifications on the generalisabilty of internet-delivered BT to the UK population are needed. There is evidence that uptake and use of DHIs (such as BIP TIC) are highly context dependent,46,47 and it would therefore be unwise to assume that a delivery package that works in Sweden will work equally well in the UK.
Study aims and design
The aim of this study was to evaluate the clinical and cost-effectiveness of a therapist-guided, parent-assisted ERP BT intervention for tics in young people with TS/CTDs. The interventions were delivered remotely via the BIP technical platform. Building on previous evidence from a Swedish pilot trial,43 the study compared an online ERP-based behavioural intervention and online tic-related psychoeducation. Our primary hypothesis was that remotely delivered, therapist-supported ERP-based BT would be superior to an active comparator intervention of online tic-related psychoeducation in reducing tic severity.
The study design was a single-blind, parallel-group, randomised controlled superiority trial, with an internal pilot and strict ‘stop–go’ progression criteria. The primary clinical outcome (tic severity) was measured via blind-assessed, clinician-rated YGTSS-TTSS. 4 A range of secondary clinician-, parent- and child-completed outcome measures were also implemented, addressing tic-related impairment, behavioural and emotional difficulties and global improvement. Measures of QoL, service use and treatment credibility and satisfaction were also obtained. Details of all primary and secondary measures, including their psychometric properties, can be found in the ‘Trial methods’ section.
The overarching aim of this study was to address the BT treatment gap for young people with tic disorders in a cost-effective manner that can be feasibly scaled up to provide widespread and equitable access to evidence-based treatment for tics across the NHS. In particular, the study aimed to add to the currently limited evidence base relating to online BT for tics by implementing an adequately powered RCT of an ERP-based, therapist-supported online intervention compared with an appropriate (psychoeducation-based) active control intervention. As the therapist role in guided iCBT is to encourage uptake and adherence to the programme, not to deliver highly specialised therapy, the skill set required is easily acquired, as demonstrated by the successful low-intensity IAPT programme, which uses graduate mental health workers to facilitate use of self-help materials by patients. Hence, if the acceptability and efficacy of the proposed therapist-guided behavioural intervention for tics is demonstrated in this trial, it should be feasible to roll it out and adopt it at scale in the NHS, IAPT BT for CYP with tics.
Chapter 2 Intervention development
Some sections of this chapter have been reproduced from the ORBIT trial protocol, which has been published. 1
The interventions were hosted on BIP, a Swedish web-based research platform that has been specifically designed for use by CYP and their parents, with an age-appropriate appearance, animations and interactive scripts (http://www.bup.se/BIP/). Both the ERP and psychoeducation interventions consisted of 10 chapters, to be completed over 10–12 weeks.
Both the interventions had a ‘child’ and ‘supporter’ component – the child and supporter had separate logins to access their respective interventions. The content that the supporter accessed reflected/aligned with the content in their child’s intervention. Both the child and supporter received remote access from a therapist via the BIP platform. Please note that the term ‘supporter’ was used in both interventions to reflect the child’s caregiver involved in the trial. This typically meant their parent but could also mean another caregiver.
Exposure with response prevention intervention
The ERP intervention was based on ERP techniques with functional analyses and social support. The first case study of ERP was reported in an adult by Bullen and Hemsley. 48 Since then, ERP for tic management has been shown to be effective in children and adults. 16,43,49 ERP as a component of BT for tics has also been advocated within the recently published European guidelines for psychological interventions for tics. 11
Most children can relate to a pattern of feeling a premonitory urge (a sensation that lets them know a tic is coming), which causes a tic and then results in relief. Over time, this pattern results in a negative reinforcement cycle that helps to maintain the tics. The ERP model serves to disrupt this cycle. During the initial phase of treatment, participants are instructed to practice suppressing their tics: this is known as ‘response prevention’. Then, with the help of another person, typically a therapist or carer/parent, the participant is instructed to provoke premonitory urges and control the need to express the tic: this is known as ‘exposure with response prevention’. The child feels the urge and does not respond, and so the cycle between urge, tic and relief is broken. There are various hypotheses on why ERP breaks the pattern and results in reduced tics. Previously, it was thought that habituation to the premonitory urge occurs and therefore the urge reduces,50 as do the tics. More recent research has suggested that for many individuals the urge remains despite not expressing the tics. 51,52 It may be that, similar to changes in cognitions in anxiety during treatment following extinction learning,53 the tic is evaluated differently, and previous cognitions such as ‘I dislike or fear the urge/I cannot control my tics’ are disproven, and, with practice, the child becomes more effective at controlling their tics and tolerating the urge. The basic ERP technique described in the ORBIT treatment is drawn from a published manual for face-to-face treatment for children. 54 However, the intervention has been successfully adapted for delivery in different formats including group-based treatment55,56 and therapist-supported online self-help. 43
The Swedish team did an in-house translation of all the ERP intervention content (text from chapters, scripts for videos) from Swedish to English and shared this with us as MS Word documents. This content was reviewed and edited by E. Bethan Davies and Tara Murphy for clarity and to keep relevant terminology consistent and understandable within an English context. The chapter content is described in Table 1.
| Chapter | Child intervention | Parent/supporter intervention |
|---|---|---|
| 1 | Learn about tics Introduction to ERP, learn about different types of tics and child asked to think about tics they have |
Introduction Introduction to ERP, learn about their role as supporter in intervention and how to use a credit and reward system for child’s practice |
| 2 | More about tics Child learns about tic signals (premonitory urge), creates a list of their own tics and ranks how personally bothersome the tics are for them |
Thoughts and behaviours of supporters Supporter learns about tic signals (premonitory urge), learns about importance of not commenting on tics, common thoughts and feelings parents/caregivers have about their child’s tics and how emotions are linked to behaviours |
| 3 | Practising stopping your tics Child learns about how to gain some control of tics via tic signal and ERP practice, how their supporter will help them do this and how to use tic stopwatch within the programme to practice ERP |
Praise Supporter learns how to support their child with ERP practice, the importance of providing praise with practice and how to prompt their child to engage with ERP practice |
| 4 | Making the practice more challenging Child learns how to increase tic signals (premonitory urge), how to practise in different situations/places and to use tic stopwatch to practice in different situations/places |
Prompts Parent/supporter learns effective ways to prompt and encourage their child with ERP practice and to plan specific times to do ERP practice |
| 5 | Continued practice Child to continue doing ERP practice and to heighten their premonitory urge for practice |
Situations and reactions Supporter learns about changing situations that impact frequency of tics, about changing their reactions that may trigger tics and about influence of external factors in maintaining tics |
| 6 | School Child learns about how tics may interfere with school and strategies they could use in school to help with tics. Child is asked if they can talk to their teacher about their tics and learns about bullying, if they are affected by it and to talk to an adult if so |
Troubleshooting Supporter learns to solve potential problems they may face in ERP, which areas to focus on if child’s ERP practice is not going as well as intended and to contact child’s school about tics (if appropriate) |
| 7 | Talk about your tics Child learns to talk to other people about their tics; they will write an explanation about tics that they can use to tell other people; optional task to tell their class at school about tics |
Continued practice Supporter reviews all strategies learnt so far and to evaluate how they feel their child’s ERP practice is progressing |
| 8 | Continued practice Child to continue doing ERP practice in different situations/places |
Continued practice Supporter to assist child in doing ERP practice as much as possible |
| 9 | The final sprint Child to learn/plan how to manage tics once ERP finishes and to decide what is most important for them to focus on in future practice |
Continued practice Supporter to continue assisting child in doing ERP practice and to highlight key areas to focus on in remaining treatment |
| 10 | Plan for the future Child to make plan on how to continue working on tics in future, asked for feedback on what they liked and did not like about ERP and asked for feedback on what aspects of ERP they found helpful |
Plan for the future Supporter to make plan on how to work with child to continue working on tics in future, asked to review information learnt in ERP and asked for positive and negative feedback about ERP |
Psychoeducation intervention
Psychoeducation about tics has been shown to be useful for improving the knowledge and attitudes of children with tic disorders and other people around them. 57 Research suggests helping carers develop positive attitudes and expert knowledge on tics can help them support the individual with the condition to better manage their tics and associated symptoms. Psychoeducation has been used as a comparator in several RCTs in tic interventions to date. 17,58–60
The psychoeducation content was created in-house by Tara Murphy and E. Bethan Davies. This consisted of psychoeducational information about TS and co-occurring conditions (chapter contents are described in Table 2). Information and activities ranged from reviewing the definition of tics, natural history, common presentations and co-occurring conditions, prevalence, aetiology, risk and protective factors and strategies for describing tics to other people. Development of expertise and a positive perspective on tic disorders were emphasised. The psychoeducation chapters included strategies for promoting positive behaviours that are rewarded by a carer or parent as a parallel element to the tic control practice in ERP. There was no information on tic control within the psychoeducational intervention. The material for psychoeducation was modified and adapted from the supportive psychotherapy intervention for children, used within the RCT to evaluate CBIT17 and relevant self-help psychoeducation for parents. 61
| Chapter | Child intervention | Parent/supporter intervention |
|---|---|---|
| 1 | Learn about tics Introduction to psychoeducation, learn about different types of tics and child asked to think about tics they have |
Introduction Introduction to psychoeducation, learn about their role as supporter in intervention and how to use a credit and reward system for child’s engagement with psychoeducation |
| 2 | Tics and tic list Child learns about tic signals (premonitory urge), creates a list of their own tics and ranks how personally bothersome the tics are for them |
Praise Supporter learns how to support their child with psychoeducation and how to prompt their child to engage with psychoeducation |
| 3 | Learning about tics Child learns more information about tics and how their supporter will help them during the next phase of psychoeducation |
Prompts Parent/supporter learns effective ways to prompt and encourage their child to use the new knowledge they have learnt in psychoeducation |
| 4 | More than tics Child learns about common comorbid conditions and other challenges that occur with tics and to practice their research skills through finding out information about a chosen comorbid condition |
More than tics Supporter learns about common comorbid conditions and other challenges that occur with tics and to think about whether any of these conditions affect their child |
| 5 | Healthy habits Child to learn about healthy habits, including habits they already do, and whether they can put any more into practice |
Healthy habits for your child Supporter learns about healthy habits to ensure their child is as strong as possible to cope with their tics and to think of daily routine changes for their child to help with tic management |
| 6 | School Child learns about how tics may interfere with school and strategies they could use in school to help with tics. Child is asked if they can talk to their teacher about their tics and learns about bullying, if they are affected by it and to talk to an adult if so |
School Supporter learns to solve potential problems they may face in psychoeducation, which areas to focus on if child’s engagement with psychoeducation is not going as well as intended and to contact child’s school about tics (if appropriate) |
| 7 | Talking about tics with your class Child learns to talk to other people about their tics; optional task to tell their class at school about tics |
Thoughts and behaviours of supporters Supporter learns about tic signals (premonitory urge), about importance of not commenting on tics and common thoughts and feelings parents/caregivers have about their child’s tics |
| 8 | Risk and protective factors Child learns about risk and protective factors in relation to tics and about resiliency in relation to tics |
Risk and protective factors Supporter learns about risk and protective factors for tics and to identify factors that may help their child cope better with their tics |
| 9 | Tics and the future Child learns about some recent research about tics and about what happens to tics and coexisting conditions as people get older |
Looking after yourself Supporter reviews all strategies so far and learns about ways to look after themselves so they are able to support child as best they can |
| 10 | Plan for the future Child to make plan on how to continue working on tics in future, asked for feedback on what they liked and did not like about psychoeducation and asked for feedback on what aspects of psychoeducation they found helpful |
Plan for the future Supporter to make plan on how to work with child to continue being educated on tics in future, asked to review information learnt in psychoeducation and asked for positive and negative feedback about psychoeducation |
The role of the therapist
Patients had regular contact with a therapist during the 10-week period via messages that could be sent inside the treatment platform (resembling an email). The therapist could directly comment on exercises that the patient had been working on and give specific feedback to motivate the patient. The patient typically had contact with the therapist at least once a week. The therapist role was to support the participant in completing the intervention; they did not deliver any therapeutic content and were not trained in how to deliver BT. Key tasks included troubleshooting, technical support and promoting engagement with the intervention.
If necessary, it was possible to allow the therapist-guided treatment to be given over a 12-week period if the therapist only offered support for a maximum of 10 weeks during the 12-week period. This may have been needed if the participant was unable to engage with the ORBIT treatment for reasons such as holidays, exam periods, illness or bereavement. Access to the BIP system was granted for 1 year.
If any circumstance occurred meaning that the child was unable to log in and access the ORBIT treatment for 5 days or more, therapist support and access to the intervention were paused for that week, until the child was able to fully engage in the treatment again. Treatment and therapist support could be paused for a maximum of 2 weeks. Therapists consulted with the trial manager and their clinical supervisor in these cases.
During the screening/baseline assessment (prior to starting the therapy), participants were introduced to the therapy platform and, where possible, met their therapist. During the treatment, the participants received remote contact with this therapist via an in-built text message function in the system (similar to an email); at the same time, an SMS reminder was delivered to their phone through the BIP system each time they received a new message from their therapist inside the BIP platform. Phone calls to the family were made when the participants/therapists felt it was necessary. Therapists logged in to the system to provide the participants with feedback, answer questions or remind them to complete the next chapter/module if required. The amount of contact the therapist had with the family was determined on an individual basis as the therapist deemed necessary. Any phone calls made outside the BIP system were not logged in the BIP system but recorded manually in a data file. All therapist activity was logged in the system. Additionally, therapists kept their own log of contacts in an Excel file. This file allowed them to keep track of when a chapter/module was opened to check progress and provide a brief log of messages/contacts with the family. The therapists were able to log in at least every 48 hours of a working week but were advised to log in daily to check for messages/inactivity.
Chapter 3 Trial methods
Some sections of this chapter have been reproduced from the ORBIT trial protocol, which has been published1 under the CC-BY-4.0 licence.
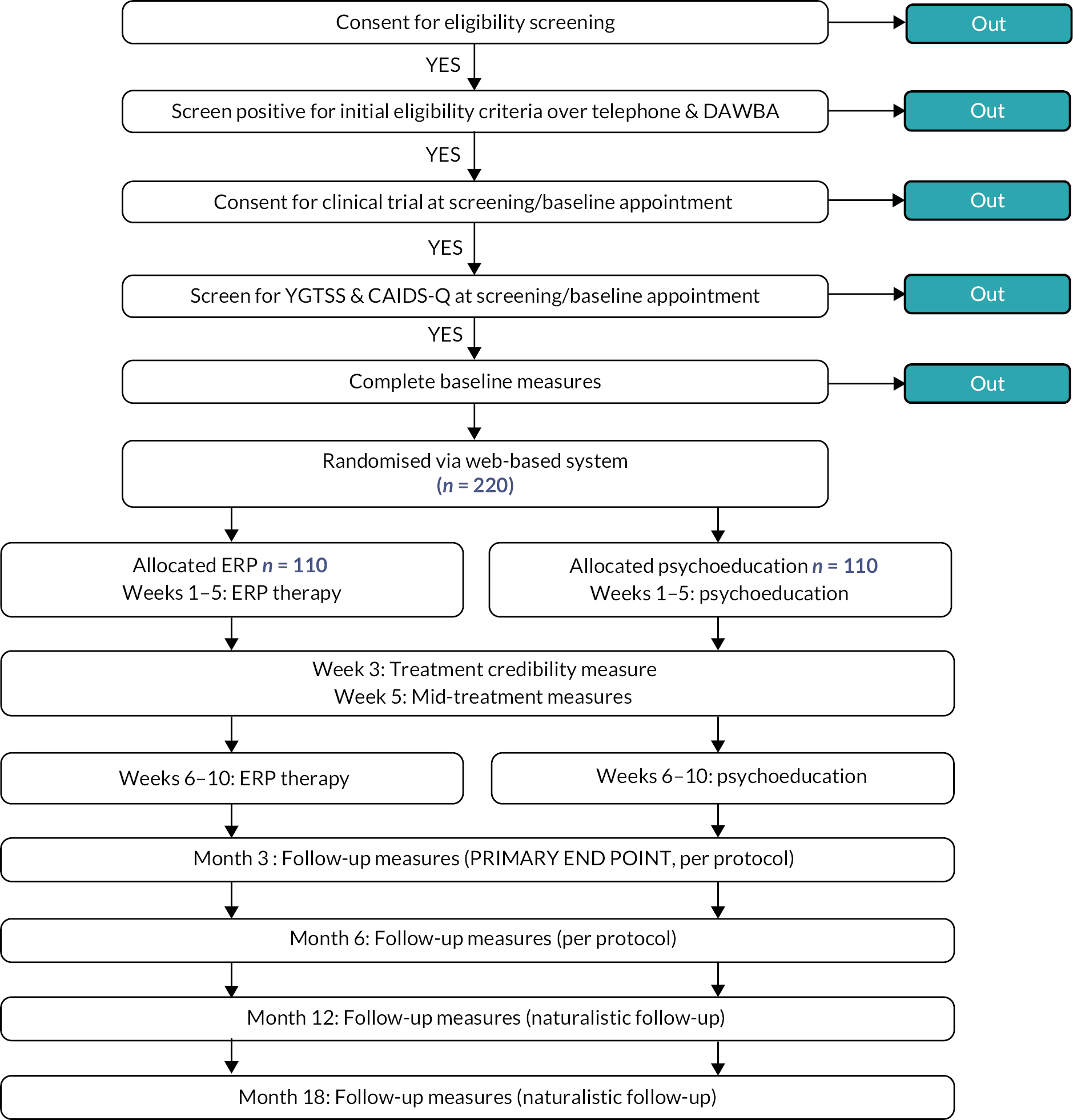
Trial design
ORBIT was a parallel-group, single-blind, non-commercial, randomised controlled superiority trial with an internal pilot for CYP with tics. Participants were randomised in a 1 : 1 ratio to receive 10 weeks of treatment of either online, remotely delivered, therapist-supported BT for tics or online, remotely delivered, therapist-supported psychoeducation on tics. Participants were followed-up at mid-treatment and at 3, 6, 12 and 18 months post-randomisation. Months 3 and 6 were per-protocol follow-ups in which participants were encouraged not to change medication or start alternative therapies for tics. Months 12 and 18 were naturalistic follow-ups where participants might be using alternative treatments in accordance with standard practice recommended by their usual treating clinician. A sub-sample of participants and parents were purposively selected to participate in process evaluation interviews after the 3-month follow-up time point. A flow chart of the study design is shown in Figure 1.
Internal pilot
The objective of the internal pilot was to determine whether recruitment, engagement with the intervention and retention to the trial were sufficient to allow the trial to progress and provide a definitive answer on the effectiveness of the intervention. The internal pilot ran for the first 9 months of recruitment. Allowing for a staggered start to recruitment, the stop–go rules for the internal pilot were as follows:
-
The study needed to have recruited 66 patients by the end of the ninth month of recruitment.
-
At least 60% of participants needed to have completed the intervention (with completion defined as completing at least the first four child chapters).
-
80% of participants who had reached the relevant time window needed to have completed the primary outcome measure (YGTSS) at the primary end point (3 months) within the specified time frame for measure completion.
The success of the internal pilot was judged by the independent Trial Steering Committee (TSC) and Data Monitoring Committee (DMC).
Ethical approval and research governance
The trial was conducted in compliance with the principles of the Declaration of Helsinki (1996), the principles of good clinical practice (GCP) and in accordance with all applicable regulatory requirements including but not limited to the Research Governance Framework and the Mental Capacity Act 2005.
Ethical and Health Research Authority (HRA) approval was received from Northwest Greater Manchester Research Ethics Committee on 23 March 2018 (protocol v2.0; ref.: 18/NW/0079). The published trial protocol1 was approved by an independent TSC and DMC. Two substantial amendments were made and approved; these are described below. The trial was prospectively registered with the ISRCTN (ISRCTN70758207) and ClinicalTrials.gov (NCT03483493).
Substantial amendments
One subsequent amendment was made to the protocol (v.3.0, 16 April 2018) after initial Research Ethics Committee (REC)/HRA approval. This amendment was to allow the 10-week intervention to be delivered over a 12-week period to account for periods of therapist absence during bank holidays or unforeseen circumstances. The amendment was approved by the committee on 15 May 2018. There was one further subsequent substantial amendment; however, this was not to trial protocol. An amendment was submitted on 28 June 2018 to give REC/HRA approval for the interview schedules as part of the process evaluation; this was approved on 2 July 2018 for interview schedules. The limited number of amendments from the original protocol is testament to the fidelity to the original proposal and indicates that the study procedures and interventions could be successfully delivered within the ORBIT trial.
Study oversight
The study was overseen by three groups.
Trial Management Group
The full Trial Management Group (TMG) consisted of all the co-investigators listed on the protocol and a representative from the patient and public involvement (PPI) group when possible. The TMG met at least every 6 months to discuss study progress and overall conduct of the trial.
Trial Steering Committee
The role of the TSC was to provide overall supervision of the trial on behalf of the Trial Sponsor and Trial Funder and to ensure that the trial was conducted to the rigorous standards set out in the Medical Research Council’s (MRC) Guidelines for GCP. The TSC met every year, with an additional meeting to review the internal pilot.
Data Monitoring Committee
The DMC assessed whether there were any ethical or safety reasons why the trial should not continue. The DMC met annually and reviewed the internal pilot.
Participants
The study sought to recruit CYP with tic disorders.
Inclusion criteria
-
Aged 9–17 years: patient confirmed through screening.
-
Suspected or confirmed TS/chronic tic disorder:
-
- Including moderate/severe tics: score > 15 on the YGTSS-TTSS; TTSS score > 10 if motor or vocal tics only: researcher confirms at screening appointment.
-
-
Competent to provide written informed consent (parental consent for child aged < 16 years): researcher confirms at screening appointment.
-
Broadband internet access and regular PC/laptop/Mac user, with mobile phone SMS: patient confirmed through screening.
Exclusion criteria
-
Previous structured behavioural intervention for tics (e.g. HRT/CBIT or ERP) within last 12 months: patient confirmed through screening.
-
Change to medication for tics (start or stop of tic medication) within the previous 2 months: patient confirmed through screening, and subsequent medication/interventions commenced throughout the trial recorded at each time point for analysis.
-
Diagnoses of alcohol/substance dependence, psychosis, suicidality or anorexia nervosa: confirmed through parent development and well-being assessment (DAWBA).
-
Moderate/severe intellectual disability: confirmed through qualitative judgement of the assessor at the telephone screen [and confirmed at baseline through child and adolescent intellectual disability screening questionnaire (CAIDS-Q)] through questions relating to type of school the child attends and previous diagnoses.
-
Immediate risk to self or others: confirmed through screening questions and DAWBA.
-
Parent or child not able to speak or read/write English: patient confirmed through screening by the assessor.
Recruitment procedures
Participant identification
There were three streams to participant identification. Patients could be identified via previous or current referrals at (1) one of the two study sites or (2) the patient identification centres (PICs). For both instances, a member of the usual care team identified potential participants from the patient records or current referrals held at the two study sites. Patients were provided with a brief information sheet and ‘consent to contact’ (C2C) form, which was passed to the research team once completed.
The third stream was through public recruitment campaigns. Specifically, the study advertised for participant recruitment via the Tourettes Action website (a national charity for people with tics) and a study website. A brief information sheet and a C2C form were hosted online.
Screening and baseline appointment
Once C2C had been established, patients were contacted by a member of the research team to go through the telephone screening questionnaire. The screening questionnaire was developed by the research team to understand the patient’s eligibility for the trial and took approximately 20–30 minutes to complete.
Patients who met the eligibility requirements were invited to attend a screening/baseline appointment. The appointment was held at one of the two study sites. All patients were reimbursed for their travel costs to attend this appointment. Before participants attended the screening/baseline appointment parents were asked to complete an online DAWBA. 62 Further details on the DAWBA are described under the Measures section.
At the screening/baseline appointment the researcher took informed consent and went through the eligibility criteria. As part of the eligibility check, the YGTSS assessment and the CAIDS-Q63 were conducted. Further details on measures are described under the Measures section.
After completion of baseline measures, patients were randomised into the study by the researcher via the web-based system hosted on a secure server by Sealed Envelope. At this appointment participants were introduced to the ORBIT therapy platform and provided with login details. Participants set their own start date for therapy but were encouraged to make it with 24–48 hours of their baseline appointment.
Consent
All participants provided written informed consent before completion of screening measures. For young people under 16 years old legal consent was sought from parents/carers and verbal or written assent from the young person. At 16 years of age or over written consent was sought from both the young person and their parent/carer. The original signed and dated consent forms were held securely as part of the trial site file, with copies sent to the participant, their general practitioner (GP) and the referring site (if applicable) for their records.
Randomisation, concealment and blinding
Randomisation was conducted using the Sealed Envelope online randomisation system and managed by Priment Clinical Trials Unit. Participants were randomised online by an outcome assessor. Randomisations were on ratio 1 : 1 and stratified by study site using block randomisation with varying block sizes.
The outcome assessor, statisticians, health economists, trial manager and chief investigator were blind to the treatment allocation, and the therapist was notified by the randomisation system of the treatment allocation. Although participants were not directly informed of their treatment allocation, it was likely that they would have been able to guess their allocation once the intervention had started.
Interventions
The two interventions have been described in detail in Chapter 2. The experimental arm consisted of 10 weeks of online, therapist-supported ERP therapy and the control arm consisted of 10 weeks of online, therapist-supported psychoeducation for tics.
Follow-up
Follow-up measures were completed at the mid-treatment point (5 weeks) and at 3 and 6 months (this formed phase 1, per-protocol design). For phase 2 (a naturalist design), follow-up measures were obtained at 12 and 18 months. Follow-up measures were completed remotely (via videoconferencing or telephone) and via an online database.
Measures
Primary outcome measure
The primary outcome was the severity of tics as measured by the TTSS (0–50) on the YGTSS. 4 The primary end point was 3 months post-randomisation. The primary outcome (YGTSS-TTSS) was measured at baseline (pre-intervention; face-to-face), at 3 months (primary end point) and at 6, 12 and 18 months post-randomisation (online via videoconferencing or telephone where this was not possible).
The YGTSS was administered by a blinded assessor as an investigator-based semistructured interview focusing on motor and vocal tic frequency, severity and tic-related impairment over the previous week.
In this study, four index YGTSS scores were obtained: Total Motor Tic Score, Total Phonic Tic Score, TTSS (primary outcome) and Overall Impairment Rating (secondary outcome). The Total Motor Tic Score is derived by adding the five items pertaining to motor tics (range 0–25); the Total Phonic Tic Score is derived by adding the five items pertaining to phonic tics (range 0–25); the TTSS (range 0–50) is derived by adding the Total Motor Tic Score and the Total Phonic Tic Score.
The YGTSS takes between 15 and 35 minutes to administer.
All outcome assessors underwent training alongside 6-month rater-agreement checks in the YGTSS (see Appendix 1, Table 31).
Secondary outcome measures
Yale Global Tic Severity Scale: impairment scale4
The impairment scale forms one of the four index YGTSS scores described above. The impairment rating is on a 50-point scale ranging from 0 (no impairment) to 50 (severe impairment). The rating focuses on distress and impairment experienced in interpersonal, academic and occupational realms.
Parent tic questionnaire64
The parent tic questionnaire (PTQ) assesses the number, frequency and intensity of motor and vocal tics. Frequency ratings are made on a 1–4 scale (constantly, hourly, daily and weekly) and intensity ratings are made on a 1–4 scale. A separate score for each tic is calculated by adding the frequency and intensity ratings, giving a score ranging from 0 to 8. Motor and vocal tic severity scores are computed by summing the scores for all motor and vocal tics respectively and a severity score computed by summing the two sub-scores. The PTQ was completed by parents/carers at all measurement time points (baseline, mid-treatment, 3-, 6-, 12- and 18-month follow-up) via the online web-based data platform.
Clinical Global Impressions-Improvement Scale65
The Clinical Global Impressions-Improvement Scale (CGI-I) provides an overall clinician-determined summary measure that takes into account all available information to determine improvement since initiation of the intervention. The CGI-I consists of one item scored on a seven-point scale from 1 (very much improved) to 7 (very much worse). The measure was completed online via the online data platform at each follow-up time point after treatment (3, 6, 12, 18 months) by the outcome assessor who completed the YGTSS.
Children’s Global Assessment Scale66
The Children’s Global Assessment Scale (CGAS) is a 0–100 scale that integrates psychological, social and academic functioning in children as a measure of psychiatric disturbance. Scores above 70 indicate functioning in a normal range. The CGAS was completed by the researcher who completes the YGTSS via the online data platform at baseline and at 3, 6, 12 and 18 months of follow-up.
Strengths and difficulties questionnaire (parent completed)67
The strengths and difficulties questionnaire (SDQ) is a brief measure of behavioural and emotional difficulties. The SDQ consists of 25 items that are rated on a three-point Likert scale (not true, somewhat true and certainly true). The items are designed to be divided between five sub-scales, each consisting of five items, which can be used to create scores for emotional symptoms, conduct problems, hyperactivity–inattention, peer problems and pro-social behaviour. The items for all but pro-social behaviours can be summed to generate a ‘total difficulties score’. 68 The standard SDQ can be supplemented with a brief impact supplement that assesses the impact of the child’s difficulties in terms of distress, social impairment, burden and chronicity. 67 The SDQ was completed by parents/carers as part of the DAWBA at baseline and via the online data platform at 3, 6, 12 and 18 months of follow-up.
The mood and feelings questionnaire (child-completed version)69
The moods and feelings questionnaire (MFQ) is a 33-item questionnaire designed to report depressive symptoms. The items are rated on a three-point scale (0 = not true, 1 = sometimes, 2 = true). The MFQ is scored by summing together the values for each item. The MFQ was completed by the child/young person at each time point (baseline, mid-treatment, 3, 6, 12 and 18 months of follow-up) via the online data platform. The measure was used to check for side effects as well as outcomes in this trial.
Spence Child Anxiety Scale (self-report)70
The Spence Child Anxiety Scale (SCAS) is a child self-report measure designed to evaluate symptoms relating to anxiety. The SCAS consists of 44 items. Children are asked to rate on a four-point scale (0 = never, 1 = sometimes, 2 = often, 3 = always) the frequency with which they experience each symptom. The ratings are summed from the 38 anxiety items to provide a total score (maximum = 114), with high scores reflecting greater anxiety. The SCAS was completed by the child/young person at baseline and at 3, 6, 12 and 18 months of follow-up via the online data platform.
Child health utility 9D (parent- and child-completed versions)71
The CHU9D is a paediatric QoL measure for use in health-care resource-allocation decision-making. The questionnaire consists of nine items, each with a five-level response category. There are two versions of the questionnaire: a self-report measure and a proxy measure, which can be completed by the parent/carer of the child. The CHU9D was completed at baseline and at 3, 6, 12 and 18 months of follow-up via the Swedish BASS data platform (online) by the parent/carer and the child/young person.
The Child and Adolescent Gilles de la Tourette Syndrome Quality of Life Scale72
The Child and Adolescent Gilles de la Tourette Syndrome Quality of Life Scale (CandA-GTS-QoL) is a disease-specific measure of health-related QoL (HRQoL) designed for children and adolescents with TS. There are two versions of the measure: one for children aged 6–12 years and one for young people aged 13–18 years. The questionnaire consists of 27 items, each with a five-level response category. The CandA-GTS-QoL was completed at baseline and at 3, 6, 12 and 18 months of follow-up via the online data platform by the child/young person.
Client service receipt inventory73
The client service receipt inventory (CSRI) is a flexible research instrument developed to collect information on service receipt, service-related issues and income. The questions of the CSRI are largely structured in a multiple-choice format, but, to contend with the complexity of community care arrangements, a few open-ended questions are also asked. The measure also asks about school attendance since the last measure completion time point (3/6 months). A modified version of the CSRI was to be completed at baseline and at 3, 6, 12 and 18 months of follow-up via the BASS platform (online). This modified version also combines elements of the child and adolescent service use schedule (CA-SUS). 74 The questionnaire takes < 15 minutes to complete.
Adverse events/side effects
Adverse events/side effects were recorded on a modified version of the side effects scale developed by Hill and Taylor. 75 The scale consists of 17 short items relating to common side effects (such as headaches, anxiety, sleep and low mood). The participant is asked to respond on a five-point scale ranging from ‘not at all’ to ‘all the time’ to describe the presence of each item. The scale was completed at baseline (to ascertain the presence of these symptoms prior to treatment), mid-treatment and at 3 and 6 months of follow-up via the BASS platform (online) by the parent/carer, with input from the child/young person.
Treatment credibility
To assess treatment credibility, we administered a short questionnaire created by the research team. The questionnaire consisted of two items that are scored on a five-point scale. The questionnaire asks how well the internet treatment suits children for managing tics and how much improvement they expect from the treatment. The questionnaire was completed 3 weeks into the treatment by parents/carers and CYP via the online data platform.
Treatment satisfaction and need for further treatment
To assess treatment satisfaction, the research team created a brief questionnaire consisting of seven items. Six of the seven items are scored on a five-point scale and ask how helpful the treatment was and whether the participant would recommend it to others. The seventh item is a three-choice option asking whether the families would prefer face-to-face treatment, had no preference or would prefer internet treatment. The need for further treatment questionnaire consists of one item that asks the CYP and parents/carers and to rate whether they feel they/their child needs more treatment for their tics. This is rated on a five-point scale ranging from ‘I/my child doesn’t need any more treatment’ to ‘I/my child needs a lot more treatment’. Both the satisfaction and need for further treatment questionnaires were completed online at the 3-month follow-up point by parents/carers and CYP.
Concomitant interventions
Parents completed a short questionnaire that asked about other treatments/interventions/medications in progress. This was completed at baseline and then again at 3, 6, 12 and 18 months of follow-up with the researcher via online videoconferencing/telephone.
Screening measures
Two measures were used as screening measures.
Development and well-being assessment
The DAWBA is a package of interviews and questionnaires completed by parents and teachers and designed to generate International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)/Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) psychiatric diagnoses for CYP. The DAWBA computer algorithm estimates the probability of having a psychiatric disorder in bands of < 0.1%, 0.5%, 3%, 15%, 50% and > 70% based on large community-based population studies. 62 DAWBA was used to exclude people who are rated as being likely (50–70%) to experience self-harm, psychosis and anorexia nervosa or suicidality. If the DAWBA indicated a high likelihood of suicidality, the participant’s GP or usual treating clinician would be informed.
Child and adolescent intellectual disability screening questionnaire76
The CAIDS-Q determines the presence of intellectual disability and was used at baseline only. The questionnaire contains seven items answered in a yes/no format by someone who knows the person well. A total score is calculated and a cut-off (by age group) indicates whether the child is likely to have an intellectual disability or not. The score can also be used as a proxy for IQ in situations where only an approximate indication of intellectual ability is needed, and it was used to exclude participants who were likely to have an intellectual disability.
Sample size
To detect a clinically important average difference of 0.5 of a standard deviation (SD) between intervention and comparator with 90% power at p < 0.05 (two-sided), after making an allowance of 20% for dropout, requires a total sample size of 220 participants. Our systematic review77 found the average estimate for the SD of the YGTSS-TTSS from 19 trials of behavioural intervention for tics was 6.6. Thus, the trial was powered to detect an average change of 3.3 on the YGTSS, which was sufficient to ensure the risk of missing a clinically significant effect in the trial was low.
Analysis
Statistical analyses were conducted using Stata® (version 16; StataCorp LP, College Station, TX, USA) in line with a predefined statistical analysis plan (SAP) approved by the TSC. The SAP stated that confidence intervals (CIs) rather than p-values were to be reported. Analysis was performed on a modified intention-to-treat basis, in which participants were analysed according to their allocated group for cases where data were available. Baseline demographic characteristics of participants, as well as their clinical and mental health outcomes at baseline and at 3 and 6 months of follow-up, were summarised by randomised group using mean (SD) or count (percentage), respectively, for continuous and categorical data.
Phase 1 analysis
This analysis has been described and published; sections have been reproduced from the Hollis et al. 78 publication under the CC-BY 4.0 Licence.
The primary outcome was estimated using a linear regression model with YGTSS-TTSS at 3 months as the outcome and study group as the main explanatory variable, adjusting for YGTSS-TTSS at baseline and site (Nottingham/London).
Linear regression models were also fitted to estimate the effect of the intervention on secondary outcomes at mid-treatment and at 3 and 6 months of follow-up (post-randomisation). The statistical model for the CGI-I did not adjust for baseline as this is a measure of change. Using CGI-I to indicate response to treatment, the scale was dichotomised to define response as ‘improved’ or ‘much improved’ versus non-response as ‘minimally improved’, ‘stayed the same’, ‘worse’ or ‘very much worse’. Two unplanned subgroup analyses explored whether the effect of the intervention on the primary outcome was modified by either anxiety diagnosis or ADHD diagnosis. The statistical models were the same as for the main analysis of the primary outcome, with the addition of a fixed effect of the comorbidity (anxiety or ADHD) and an interaction between the comorbidity and the study arm. All statistical analyses were conducted on complete cases. This analysis has been described in Hollis et al. 78
Phase 2 analysis
For the phase 2 follow-up, a sample power calculation was not specified. Outcomes at 12 and 18 months were summarised by randomised group, for continuous data using mean (SD) or for categorical data using count (percentage). A single linear mixed model was fitted for each outcome, with measures from all available time points (at mid-treatment and at 3, 6, 12 and 18 months of follow-up) as the repeated-measures outcome and a random effect of participant to account for correlations between the repeated measures on each individual at different time points. The main explanatory variables were treatment, time and the treatment by time interaction, adjusting for site and the baseline measure of the outcome. Since correlations are commonly smaller over longer time periods, we adjusted for baseline through an interaction with time, which allowed correlations with baseline to differ between follow-up times. The effect of the intervention at 12 and 18 months was estimated from this model.
As with the phase 1 analysis, the statistical model for CGI-I did not adjust for baseline as this is a measure of change. Response to treatment was compared between study arms using separate logistic regression models at 12 and 18 months, adjusting for site. Estimated effects are reported with 95% CIs.
We summarised changes in other (non-trial) tic treatments (medication or therapy) between 6 and 12 months and between 6 and 18 months by study arm and for the sample overall using counts (N) and percentages (%). The phase 2 analysis is currently under peer review with the Journal of Child Psychology and Psychiatry. 79
Chapter 4 Trial results
Participant flow
In total, 445 individuals registered their interest in taking part in the trial between 8 May 2018 and 30 September 2019. Figure 2 presents the recruitment and screening flow diagram for the trial, summarising information for exclusion at both the initial telephone screen and the baseline appointment through to randomisation. Phase 1 of the trial was considered complete on 30 April 2020 when the last participant completed the 6-month follow-up. Phase 2 and the trial overall were considered complete on 12 April 2021 when the last participant completed the 18-month follow-up. Retention to follow-up data during phase 1 (3-month primary end point and 6-month follow-up) and phase 2 (12- and 18-month follow-ups) are shown in the CONSORT flow diagram in Figure 3.
FIGURE 2.
Recruitment and screening flow.

Internal pilot
The TSC met on 28 January 2019 to judge the success of the internal pilot against the three targets. The TSC judged that all three targets had been met; a summary is provided in Table 3. As a result, the trial was recommended to continue.
| Criteria | Target | Achievement |
|---|---|---|
| Recruitment | 66 by month 6 | 67 by month 6 |
| Intervention completion | 66% | 96% |
| Primary outcome completion | 80% | 88% |
Baseline characteristics
Baseline characteristics of the sample are presented in Table 4 and show that characteristics and scores on the primary outcome and secondary outcomes were similar between the two arms. Participants had a mean age of 12 years, were predominately male (177/224; 79%) and defined their ethnicity as white (195/224; 87%). It is interesting to note that very few participants (30/224; 13%) were receiving medication for tics at baseline. Given that the phase 1 and phase 2 results were analysed at separate time points, the findings are reported separately for each phase.
| Psychoeducation (N = 112) n (%) |
ERP (N = 112) n (%) |
|
|---|---|---|
| Age at randomisation (years) – mean (SD) | 12.4 (2.1) | 12.2 (2.0) |
| Sex | ||
| Male | 87 (78%) | 90 (80%) |
| Female | 25 (22%) | 22 (20%) |
| Ethnicity | ||
| White | 99 (88%) | 96 (86%) |
| Asian | 3 (3%) | 7 (6%) |
| Black | 0 (0%) | 1 (1%) |
| Mixed | 7 (6%) | 3 (3%) |
| Other | 1 (1%) | 0 (0%) |
| Not given | 2 (2%) | 5 (4%) |
| Main caregiver in trial | ||
| Mother | 101 (90%) | 93 (83%) |
| Father | 10 (9%) | 16 (14%) |
| Grandmother | 1 (1%) | 1 (1%) |
| Other | 0 (0%) | 2 (2%) |
| Mother’s highest educational level | ||
| No qualifications | 1 (1%) | 3 (3%) |
| Mandatory secondary education (e.g. GCSEs) | 17 (15%) | 16 (14%) |
| Further education (e.g. A levels, BTEC, NVQ) | 32 (29%) | 33 (29%) |
| Higher education (e.g. BA, BSc) | 46 (41%) | 46 (41%) |
| Postgraduate education (e.g. MA, MSc, PhD) | 16 (14%) | 14 (13%) |
| Father’s highest educational level | ||
| No qualifications | 5 (4%) | 2 (2%) |
| Mandatory secondary education (e.g. GCSEs) | 29 (26%) | 29 (26%) |
| Further education (e.g. A levels, BTEC, NVQ) | 33 (29%) | 35 (31%) |
| Higher education (e.g. BA, BSc) | 34 (30%) | 32 (29%) |
| Postgraduate education (e.g. MA, MSc, PhD) | 11 (9%) | 14 (13%) |
| Mother’s occupational status | ||
| Not in work/unemployed | 22 (20%) | 19 (20%) |
| Lower occupational statusa | 26 (23%) | 24 (21%) |
| Higher occupational statusb | 57 (51%) | 65 (58%) |
| Other | 7 (6%) | 4 (4%) |
| Father’s occupational status | ||
| Not in work/unemployed | 4 (4%) | 2 (2%) |
| Lower occupational statusa | 30 (27%) | 33 (29%) |
| Higher occupational statusb | 67 (60%) | 65 (58%) |
| Other | 10 (9%) | 12 (11%) |
| Tic typology | ||
| Both motor and vocal tics | 106 (95%) | 103 (92%) |
| Motor tics only | 6 (5%) | 9 (8%) |
| Vocal tics only | 0 (0%) | 0 (0%) |
| Comorbidities | ||
| Anxiety disorder | 27 (24%) | 34 (30%) |
| ADHD | 25 (22%) | 26 (23%) |
| Oppositional defiant disorder | 23/111 (21%) | 26/110 (24%) |
| Autism spectrum disorders | 4/112 (4%) | 9/111 (8%) |
| OCD | 3 (3%) | 8 (7%) |
| Major depression | 6 (5%) | 2 (2%) |
| Conduct disorder | 2/111 (2%) | 3/110 (3%) |
| Taking any tic medicationc | 16 (13%) | 14 (13%) |
| Centre | ||
| Nottingham | 57 (51%) | 57 (51%) |
| London | 55 (49%) | 55 (49%) |
Instances of unblinding
Four occasions of unblinding occurred throughout the entire trial. Each instance was reported to the trial manager and reviewed by the independent TSC and DMC for monitoring. For all occasions, the young person disclosed information about their treatment to the outcome assessor at the end of the follow-up assessment. When this occurred, all remaining follow-ups were conducted by an alternative, blinded assessor.
Phase 1 results
The phase 1 results were published in Hollis et al. 78
Losses to follow-up
The sample size calculation allowed for 20% missing data; however, data from the primary outcome measure (YGTSS-TTSS) at the primary end point (3 months) were collected from 99/112 participants (88.4%) in the intervention group and 105/112 participants (93.7%) in the psychoeducation group. Thus, retention to follow-up was better than anticipated. Data from the primary measure at 6 months were obtained from 93/112 participants (84.5%) for each group. The only predictor of missingness was site, which was included as a covariate in the statistical models.
Primary outcome
The mean scores for the primary outcome – the YGTSS-TTSS at 3 months – were lower in the ERP group (23.9, SD 8.2) than in the psychoeducation group (26.8, SD 7.3). When comparing to baseline scores, the mean total decrease in the YGTSS-TTSS was greater in the ERP group (4.5; 16%) than the psychoeducation group (1.6; 6%). Table 5 shows the results of the adjusted (for baseline and site) difference in mean scores when comparing the ERP group with the psychoeducation group. The results showed that the ERP intervention reduced the YGTSS-TTSS by −2.29 points (95% CI −3.86 to −0.71) in comparison to psychoeducation, with an effect size of −0.31 (95% CI −0.52 to −0.10).
At 6 months, this adjusted effect on tics (YGTSS-TTSS) was slightly increased (estimated difference −2.64, 95% CI −4.56 to −0.73), with an effect size of −0.36 (95% CI −0.62 to −0.10).
Effect sizes for the primary and secondary outcomes are presented in Figure 4.
FIGURE 4.
Effect sizes for primary and secondary outcomes up to the 6-month follow-up. Note: Figure published in Hollis et al. 78

Secondary outcomes
Figure 4 shows the forest plot of effect sizes for secondary outcomes.
Secondary tic measures
An additional measure of tic symptoms was recorded through the PTQ. The findings supported that of the primary outcome: that is, participants in the ERP group showed greater tic reduction than those in the psychoeducation group at 3 months (−9.44, 95% CI −15.37 to −3.51) and 6 months (−8.60, 95% CI −14.43 to −2.77). However, the findings from the YGTSS impairment scale did not show any statistically significant difference in tic-related impairment at either time point (see Table 5).
| Psychoeducation mean (SD) |
ERP mean (SD) |
Estimated difference (95% CI) |
Standardised effect size | |
|---|---|---|---|---|
| Baseline | ( N = 112) | ( N = 112) | ||
| Primary outcome | ||||
| TTSS on the YGTSS | 28.4 (7.1) | 28.4 (7.7) | ||
| Secondary outcomes | ||||
| Impairment score on the YGTSS | 22.9 (9.9) | 23.8 (10.3) | ||
| PTQ | 53.1 (26.1) | 54.7 (29.9) | ||
| CGAS | 72.1 (11.8) | 70.7 (13.7) | ||
| SDQ | 16.3 (6.2) | 18.0 (6.5) | ||
| MFQ | 15.9 (11.5) | 16.3 (11.3) | ||
| SCAS | 30.5 (17.9) | 32.9 (20.2) | ||
| CandA-GTS-QoL | 35.0 (17.2) | 36.6 (16.4) | ||
| 3 months | ||||
| Patients analysed for primary outcome | ( N = 100) | ( N = 101) | ||
| Primary outcome | ||||
| TTSS on the YGTSS | 26.8 (7.3) | 23.9 (8.2) | −2.29 (−3.86 to −0.71) | −0.31 (−0.52 to −0.10) |
| Secondary outcomes | ||||
| Impairment score on the YGTSS | 19.1 (10.9) | 16.7 (10.4) | −2.24 (−4.82 to 0.33) | |
| PTQ | 45.7 (25.5) | 34.7 (26.4) | −9.44 (−15.37 to −3.51) | |
| CGI-I | 3.37 (1.11) | 2.96 (1.1) | −0.41 (−0.71 to −0.11) | |
| CGAS | 75.2 (12.6) | 75.9 (12.6) | 0.96 (−1.48 to 3.41) | |
| SDQ | 14.2 (6.3) | 14.7 (6.1) | −0.38 (−1.62 to 0.85) | |
| MFQ | 12.6 (11.1) | 10.7 (11.1) | −1.36 (−3.75 to 1.02) | |
| SCAS | 28.2 (18.3) | 27.2 (19.0) | −2.80 (−6.52 to 0.93) | |
| CandA-GTS-QoL | 31.8 (17.7) | 25.7 (18.0) | −4.81 (−8.79 to −0.83) | |
| 6 months | ||||
| Patients analysed for primary outcome | ( N = 93) | ( N = 93) | ||
| Primary outcome | ||||
| TTSS on the YGTSS | 25.0 (7.6) | 21.5 (8.8) | −2.64 (−4.56 to −0.73) | −0.36 (−0.62 to −0.10) |
| Secondary outcomes | ||||
| Impairment score on the YGTSS | 17.0 (10.5) | 14.7 (10.7) | −1.95 (−4.68 to 0.78) | |
| PTQ | 40.6 (24.3) | 31.1 (21.6) | −8.60 (−14.43 to −2.77) | |
| CGI-I | 3.1 (1.1) | 2.8 (1.3) | −0.31 (−0.66 to 0.03) | |
| CGAS | 76.8 (12.3) | 77.5 (14.7) | 0.60 (−2.24 to 3.44) | |
| SDQ | 13.3 (6.1) | 15.3 (6.2) | 0.57 (−0.93 to 2.07) | |
| MFQ | 11.4 (11.2) | 11.4 (12.1) | −0.61 (−3.85 to 2.64) | |
| SCAS | 25.9 (18.7) | 25.7 (19.6) | −5.10 (−9.70 to −0.50) | |
| CandA-GTS-QoL | 28.9 (18.3) | 27.4 (16.5) | −2.91 (−7.60 to 1.78) | |
Other secondary measures
There was no statistically significant difference in young person-reported anxiety (SCAS) at 3 months; however, at 6 months there was a greater reduction in SCAS scores in the ERP group than in the psychoeducation group (−5.10, 95% CI −9.70 to −0.50). Conversely, the young person-reported tic-specific QoL (CandA-GTS-QoL) and the outcome assessor-completed perception of global improvement (CGI-I) showed greater improvement in the ERP group than in the psychoeducation group at 3 months (CGI-I −0.41, 95% CI −0.71 to −0.11; CandA GTS-QoL −4.81, 95% CI −8.79 to −0.83) but no statistically significant difference at 6 months.
FIGURE 5.
Forest plot of standardised effect sizes for primary and secondary outcomes at 12- and 18-month follow-ups. Note: Figure in Hollis et al. 79
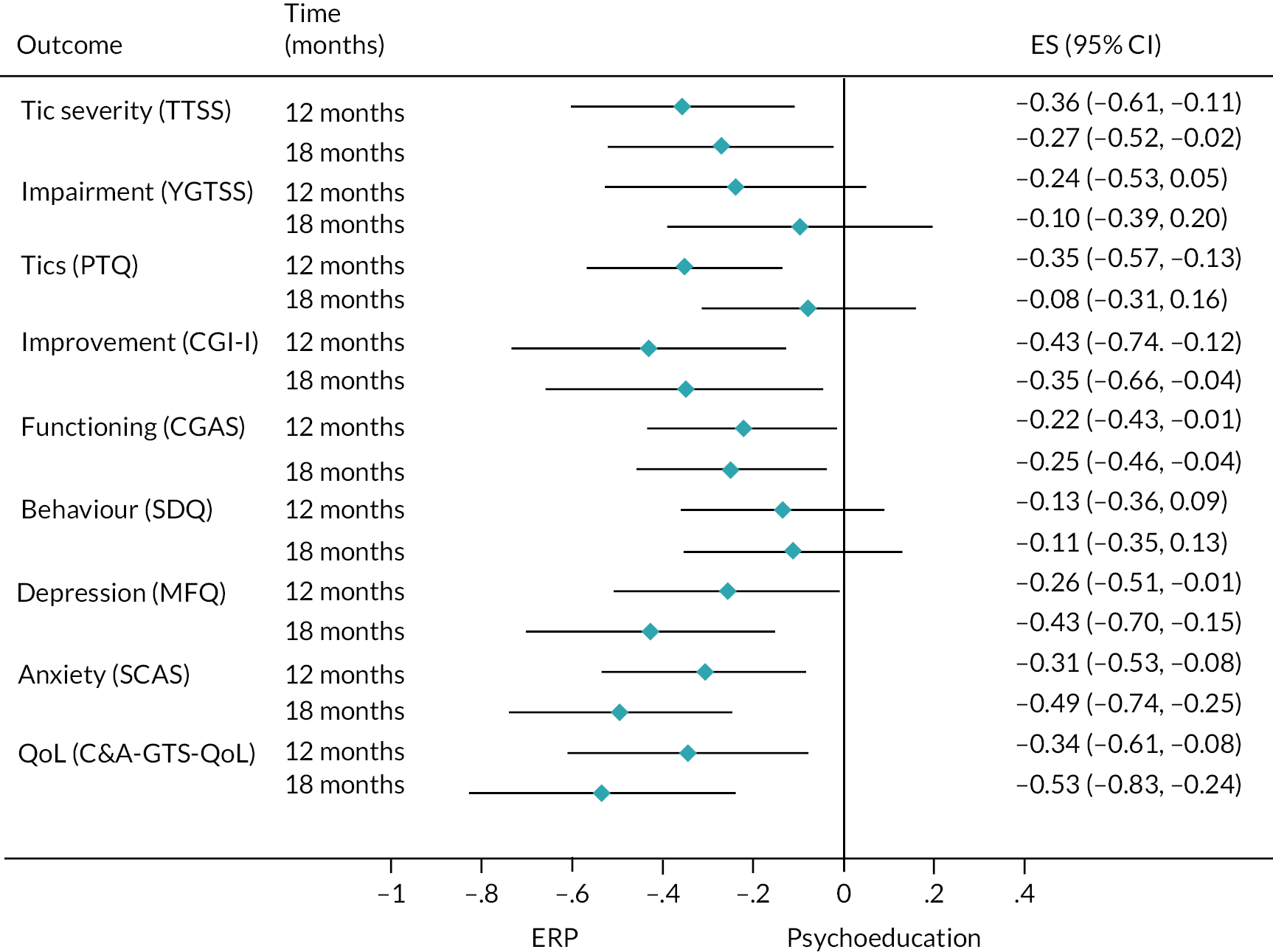
There was no statistically significant difference at either 3 or 6 months in the other secondary outcomes of parent-reported general emotional and behavioural functioning (SDQ), young person-reported low mood (MFQ) and outcome assessor-reported overall functioning (CGAS).
Effect of the intervention at the intervention mid-point
Table 6 shows there was no statistical difference in scores on the MFQ or the PTQ at the mid-point of the intervention.
| Control (psychoeducation) (N = 112) mean (SD) |
Intervention (ERP) (N = 112) mean (SD) |
Estimated difference (95% CI) |
|
|---|---|---|---|
| PTQ | 45.3 (24.3) | 42.8 (27.0) | −3.58 (−8.33 to 1.16) |
| MFQ | 14.4 (10.6) | 12.7 (12.0) | −0.56 (−3.54 to 0.41) |
Unplanned analysis
An unplanned post hoc analysis investigated whether the interventions had a differential effect on participants with or without comorbid anxiety or ADHD. Table 7 shows that there was no evidence to support this.
| Control (psychoeducation) (N = 112) |
Intervention (ERP) (N = 112) |
3-month follow-up | ||||
|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | Estimated difference (95% CI) |
Interaction p-value |
|
| Anxiety disorder | ||||||
| No anxiety disorder | 77 | 25.9 (7.3) | 71 | 23.2 (8.2) | −1.78 (−3.61 to 0.05) | 0.204 |
| Anxiety disorder | 23 | 29.8 (6.4) | 30 | 25.5 (8.1) | −4.10 (−7.18 to −1.02) | |
| ADHD | ||||||
| No ADHD | 78 | 26.4 (7.5) | 79 | 23.3 (8.3) | −2.24 (−4.03 to −0.45) | 0.906 |
| ADHD | 22 | 28.3 (6.5) | 22 | 25.8 (7.6) | −2.47 (−5.85 to 0.92) | |
Treatment responders
An additional unplanned analysis was also conducted to compare treatment responders between the two groups. A positive treatment response was defined by a rating of 1 or 2 (very much/much improved) on the CGI-I. Table 8 shows that there were more people classified as treatment responders at both 3 and 6 months in the ERP group than the psychoeducation group. The analysis demonstrated significantly greater treatment response with ERP at 3 months [36% (95% CI 26 to 45); N = 101] than for psychoeducation [20% (95% CI 12 to 28); N = 100], odds ratio (OR) 2.22 (95% CI 1.17 to 4.20). This superior treatment response was sustained at 6 months for ERP [47% (95% CI 37 to 57); N = 93] compared to psychoeducation [29% (95% CI 20 to 39); N = 93], OR 2.20 (95% CI 1.20 to 4.04).
| Psychoeducation N (%) |
ERP N (%) |
OR (95% CI) | |
|---|---|---|---|
| 3 months | ( N = 100) | ( N = 101) | |
| CGI-I score indicating ‘much’ or ‘very much’ improved (responded to treatment) | 20 (20%) | 36 (36%) | 2.22 (1.17 to 4.20) |
| 6 months | ( N = 93) | ( N = 93) | |
| CGI-I score indicating ‘much’ or ‘very much’ improved (responded to treatment) | 27 (29%) | 44 (47%) | 2.20 (1.20 to 4.04) |
| Change in response between 3 and 6 months | ( N = 93) | ( N = 90) | |
| No response to treatment at either time | 56 (60%) | 37 (41%) | |
| Response at both times | 9 (10%) | 23 (26%) | |
| New responder at 6 months | 18 (19%) | 20 (22%) | |
| Relapsed responder at 6 months | 10 (11%) | 10 (11%) |
Treatment adherence
The minimum treatment was specified as completion of the first four chapters for both groups. This minimum treatment was selected as the first four chapters contained the main principles of the intervention, with the subsequent chapters used to reinforce the theory and strategies. This was achieved for 88% (99/112) in the ERP group and 94% (105/112) in the psychoeducation group, indicating high engagement rate for both treatments. The results of engagement are shown in Table 9.
| Psychoeducation (control) (N = 112) |
ERP (intervention) (N = 112) |
|
|---|---|---|
| Young person met therapist – N (%) | 86 (77%) | 80 (71%) |
| Treatment suitability and expectation of improvement (credibility) – median (25th to 75th centiles) | ||
| Young person | 6 (5 to 7) | 7 (6 to 8) |
| Supporting parent/caregiver | 5 (4 to 6) | 6 (5 to 7) |
| Completion of first four chapters of intervention (adherence) – N (%) | ||
| Young person | 105 (94%) | 99 (88%) |
| Supporting parent/caregiver | 103 (92%) | 95 (85%) |
| Number of chapters of intervention completed (dose) – median (25th to 75th centiles) | ||
| Young person | 9 (7 to 10) | 8 (6 to 10) |
| Supporting parent/caregiver | 10 (8 to 10) | 9 (5 to 10) |
| Number of logins – median (25th to 75th centiles) | ||
| Young person | 13 (10 to 18) | 19 (10 to 28) |
| Parent/carer | 17 (12 to 24) | 18 (12 to 27) |
| Therapist time on platform in minutes – mean (SD) | ||
| Young person | 55.6 (27.1) | 59.2 (29.2) |
| Parent/carer 1 | 74.2 (34.4) | 83.9 (42.8) |
| Parent/carer 2 | 0.4 (2.1) | 1.0 (7.2) |
| Therapist time on phone in minutes – mean (SD) | ||
| Young person | 0.1 (0.3) | 0.2 (1.8) |
| Parent/carer 1 | 3.5 (7.5) | 3.7 (6.4) |
| Parent/carer 2 | 0.3 (2.0) | 0.2 (1.9) |
| Total therapist time in minutes – mean (SD) | 133.9 (55.1) | 148.2 (64.9) |
| Platform logins – mean (SD) | ||
| Young person | 14.6 (8.6) | 19.8 (10.9) |
| Parent/carer 1 | 18.1 (9.0) | 20.4 (11.5) |
| Parent/carer 2 | 1.6 (2.6) | 6.8 (8.7) |
The numbers of times participants logged in to the intervention were similar across both groups, although there was a slightly higher number of logins for the participants in the ERP group.
There was slightly more therapist time required to support the ERP intervention compared to the psychoeducation intervention by approximately 15 minutes. However, it is noteworthy that the overall therapist contact time per family (combined parent/carer and young person) was 2.5 hours, which equates to 15 minutes a week; this is much lower than that of face-to-face therapy. Parent/carer and young person perceptions of treatment suitability and credibility are explored in Chapter 6, but Table 9 demonstrates that they were high across both groups.
Adverse events
Adverse events were recorded up until 6 months (phase 1). Table 10 shows the number of AEs recorded throughout the trial. There were slightly fewer AEs in the ERP group compared to psychoeducation (359 vs. 431), and fewer participants in the ERP group experienced one or more AEs (n = 88/112; 79%) than in the psychoeducation group (n = 94/112; 84%). The most commonly occurring AEs were low mood, increased tics and anger/irritability.
| Psychoeducation (control group) (N = 112) |
ERP (intervention group) (N = 112) |
|
|---|---|---|
| Number of events | n | n |
| SAEs | 2 | 0 |
| All AEs (including SAEs) | 433 | 359 |
| Expected AEs (including SAEs) by type | ||
| Low mood/depressed | 78 | 57 |
| Increased tics | 47 | 36 |
| Increased anger/outbursts/disruptive behaviours | 37 | 21 |
| Increased irritability | 41 | 45 |
| Increased anxiety/stress | 21 | 26 |
| Increased tiredness/fatigue | 2 | 2 |
| Headaches | 13 | 16 |
| Increased/decreased sleep | 52 | 38 |
| Unexpected AEs (including SAEs) by type | ||
| Daydreaming | 22 | 14 |
| Increased OCB/OCD-type behaviours | 1 | 1 |
| Excited | 35 | 32 |
| Nightmares | 11 | 12 |
| Unsteady | 10 | 1 |
| Poor appetite | 13 | 15 |
| Talks less to/less interested in other children | 35 | 27 |
| Stomachache | 11 | 16 |
| Restlessness | 1 | 0 |
| Changes in focus | 2 | 0 |
| Unspecified | 1 | 0 |
| Sex differences | ||
| AEs – male | 311 | 289 |
| AEs – female | 120 | 70 |
| SAEs – male | 1 | 0 |
| SAEs – female | 1 | 0 |
| Number of participants | n (%) | n (%) |
| Experiencing a SAE | 2 (2%) | 0 (0%) |
| Experiencing any AE (including SAEs) | 94 (84%) | 88 (79%) |
There were two SAEs throughout the trial, which affected two participants who were both in the psychoeducation group. The SAEs were judged as unrelated to the trial by the TSC and DMC. One of the SAEs was a male participant collapsing and being admitted to hospital as a result of a functional movement disorder. The other SAE involved a female participant attending accident and emergency as a result of a ‘tic attack’. The independent clinicians on the TSC and DMC agreed with the chief investigator that waxing and waning of tics is part of the natural course of the disorder and should not be considered related to the intervention. Both participants were discharged from hospital with no further action. The parents informed the trial team that they had not recently been engaging with ORBIT at the time of the event and they did not consider the events to be related to their participation.
Phase 2 results
The findings from phase 2 are currently under review.
On 12 April 2021, the final 18-month follow-up was completed (see Figure 3).
Missing data
There was no primary outcome for the phase 2 results; however, the YGTSS-TTSS (the primary outcome for phase 1) was a key outcome of interest. Completion of this YGTSS-TTSS was good throughout the trial. At 12 months, data were collected from 91/112 participants (81%) in both the ERP group and the psychoeducation group, and at 18 months data were collected from 89/112 participants (80%) from the ERP group and from 90/112 participants (80%) from the psychoeducation group. The only predictor of missingness was site, which was included as a covariate in the statistical models. Other measures that were completed by the outcome assessor, including the CGI-I and the CGAS, also sustained good completion rates (see Table 11).
| 12-month follow-up | 18-month follow-up | |||
|---|---|---|---|---|
| Psychoeducation (N = 112) n (%) |
ERP therapy (N = 112) n (%) |
Psychoeducation (N = 112) n (%) |
ERP therapy (N = 112) n (%) |
|
| TTSS on the YGTSS | 21 (19%) | 21 (19%) | 22 (20%) | 23 (21%) |
| Impairment score on the YGTSS | 21 (19%) | 21 (19%) | 22 (20%) | 23 (21%) |
| PTQ | 46 (41%) | 46 (41%) | 58 (52%) | 60 (54%) |
| CGI-I | 21 (19%) | 21 (19%) | 22 (20%) | 23 (21%) |
| CGAS | 21 (19%) | 21 (19%) | 22 (20%) | 23 (21%) |
| SDQ | 47 (42%) | 46 (41%) | 59 (53%) | 60 (54%) |
| MFQ | 51 (46%) | 53 (47%) | 63 (56%) | 67 (60%) |
| SCAS | 51 (46%) | 53 (47%) | 63 (56%) | 68 (61%) |
| CandA-GTS-QoL | 51 (46%) | 53 (47%) | 64 (57%) | 68 (61%) |
However, data from measures that the parent/carer or young person completed online into the database, which were not directly collected or supported by the outcome assessors (e.g. PTQ, MFQ, SCAS, SDQ, CandA-GTS-QoL), were less well completed, with a large amount of missing data (ranging from 41% to 61% missing). Thus, the results from these measures should be interpreted with caution. In all cases, the quantities of missing data were similar for each randomised group.
Key outcome of interest
At 12 months, the mean YGTSS-TTSS in the ERP group was 21.7 (SD 8.8) compared to 24.9 (SD 7.3) in the psychoeducation group. The analysis, which adjusted for tic severity at baseline and site, demonstrated that the ERP intervention reduced TTSS by −2.64 points (95% CI −4.48 to −0.79), with an effect size of −0.36 (95% CI −0.61 to −0.11), compared to the psychoeducation group.
At 18 months, the mean YGTSS-TTSS in the ERP group was 21.5 (SD 9.0) and 23.9 (SD 8.4) in the psychoeducation group. The analysis indicated that the ERP intervention reduced the TTSS by −2.01 points (95% CI −3.86 to −0.15), with an effect size of −0.27 (95% CI −0.52 to −0.02), in comparison to the psychoeducation group (see Table 12).
| 12-month follow-up | 18-month follow-up | |||||
|---|---|---|---|---|---|---|
| Psychoeducation (N = 112) mean (SD) |
ERP therapy (N = 112) mean (SD) |
Estimated difference (95% CI) |
Psychoeducation (N = 112) mean (SD) |
ERP therapy (N = 112) mean (SD) |
Estimated difference (95% CI) |
|
| Outcomes | ||||||
| TTSS on the YGTSS | 24.9 (7.3) | 21.7 (8.8) | −2.64 (−4.48 to −0.79) |
23.9 (8.4) | 21.5 (9.0) | −2.01 (−3.86 to −0.15) |
| Impairment score on the YGTSS | 17.5 (11.1) | 14.8 (11.6) | −2.41 (−5.35 to 0.53) |
16.9 (12v1) | 15.8 (11.5) | −0.97 (−3.93 to 1.99) |
| PTQ | 43.0 (25.3) | 30.7 (23.8) | −9.89 (−16.01 to −3.77) |
35.9 (25.6) | 28.1 (19.1) | −2.15 (−8.83 to 4.53) |
| CGI-I | 3.07 (0.9) | 2.67 (1.09) | −0.43 (−0.75 to −0.10) |
2.86 (1.1) | 2.49 (1.36) | −0.38 (−0.71 to −0.05) |
| CGAS | 75.0 (12.9) | 77.4 (13.3) | 2.85 (0.15 to 5.56) |
77.3 (12.6) | 79.3 (13.5) | 3.18 (0.47 to 5.90) |
| SDQ | 14.6 (6.4) | 14.4 (5.6) | −0.86 (−2.31 to 0.58) |
13.8 (5.4) | 13.6 (6.1) | −0.71 (−2.26 to 0.84) |
| MFQ | 14.3 (11.6) | 11.4 (10.4) | −2.93 (−5.77 to −0.09) |
16.0 (14.6) | 10.9 (10.0) | −4.87 (−8.00 to −1.75) |
| SCAS | 29.9 (19.1) | 25.3 (17.1) | −6.11 (−10.41 to −1.81) |
32.6 (20.4) | 24.3 (18.6) | −9.41 (−14.11 to −4.70) |
| CandA-GTS-QoL | 32.2 (16.8) | 25.5 (16.8) | −5.79 (−10.28 to −1.30) |
36.8 (21.1) | 26.0 (16.6) | −9.00 (−13.98 to −4.01) |
The standardised effect sizes for all outcomes in phase 2 are presented in Figure 5.
Other measures
The parent-reported measure of tics (PTQ) also showed that the ERP group had less tic severity than the psychoeducation group at 12 months (−9.89, 95% CI −16.01 to −3.77), but this was not found at 18 months (see Figure 5 and Table 12). There was no statistically significant difference between the two groups on the YGTSS impairment scale at either time point.
The young person-reported MFQ (mood) and SCAS (anxiety) showed larger reductions in symptoms at 12 months (MFQ −2.93, 95% CI −5.77 to −0.09; SCAS −6.11, 95% CI −10.41 to −1.81) and 18 months (MFQ −4.87, 95% CI −8.00 to −1.75; SCAS −9.41, 95% CI −14.11 to −4.70) in the ERP group compared to the psychoeducation group.
At both time points, young person-reported tic-specific QoL showed greater improvement in the ERP group compared to the psychoeducation group (12 months −5.79, 95% CI −10.28 to −1.30; 18 months −9.00, 95% CI −13.98 to −4.01).
The same was also true for the outcome assessor-completed CGAS (12 months 2.85, 95% CI 0.15 to −5.56; 18 months 3.18, 95% CI 0.47 to −5.90) and CGI-I (12 months −0.43, 95% CI −0.75 to −0.10; 18 months 0.38, 95% CI −0.71 to −0.05). However, there was no statistically significant difference in parent-reported general emotional and behavioural functioning (SDQ) at either time point (see Table 12).
Unplanned analysis
After 6 months (phase 2), participants were allowed to start other tic treatments (behavioural or pharmacological) outside the trial interventions. However, between 6 and 12 months only 11 (6%) started a new tic medication and only 6 (3%) started a new tic therapy. Between 6 and 18 months only 7 (4%) started a new tic medication and only 2 (1%) started a new tic therapy (see Table 13).
| Changes between 6 and 12 months | Changes between 6 and 18 months | |||||
|---|---|---|---|---|---|---|
| Psychoeducation (N = 86) n |
ERP therapy (N = 86) n |
Total (N = 172) n (%) |
Psychoeducation (N = 86) n |
ERP therapy (N = 84) n |
Total (N = 170) n (%) |
|
| Tic medication | ||||||
| None at either time point | 79 | 76 | 155 (90%) | 81 | 76 | 157 (92%) |
| At both time points | 1 | 1 | 2 (1%) | 1 | 0 | 1 (1%) |
| Started after 6 months | 5 | 6 | 11 (6%) | 3 | 4 | 7 (4%) |
| Stopped after 6 months | 1 | 3 | 4 (2%) | 1 | 4 | 5 (3%) |
| Tic therapy | ||||||
| None at either time point | 84 | 78 | 162 (94%) | 83 | 81 | 164 (96%) |
| At both time points | 0 | 1 | 1 (1%) | 0 | 0 | 0 |
| Started after 6 months | 1 | 5 | 6 (3%) | 2 | 0 | 2 (1%) |
| Stopped after 6 months | 1 | 2 | 3 (2%) | 1 | 3 | 4 (2%) |
Most participants were not using tic medication (90% at 12 months, 92% at 18 months) or other tic therapy (94% at 12 months, 96% at 18 months) during phase 2. The number of participants who changed their medication or therapy status was too small to conduct a sensitivity analysis on the YGTSS-TTSS.
We conducted the same unplanned post hoc analysis conducted in phase 1 that compared treatment response on the CGI-I. Comparable to phase 1, the analysis revealed greater treatment responses with ERP at 12 months (2.27, 95% CI 1.23 to 4.22) and 18 months (1.80, 95% CI 0.99 to 3.27). Furthermore, we demonstrated that participants who responded at 6 months were more likely to continue to respond at later follow-up and less likely to relapse if they were in the ERP group than the psychoeducation group (see Table 14).
| 12-month follow-up | 18-month follow-up | |||||
|---|---|---|---|---|---|---|
| Psychoeducation (N = 91) n (%) |
ERP therapy (N = 91) n (%) |
Odds ratio (95% CI) |
Psychoeducation (N = 90) n (%) |
ERP therapy (N = 89) n (%) |
Odds ratio (95% CI) |
|
| CGI-I score indicating much or very much improved from baseline (responded to treatment) | 25 (27%) | 42 (46%) | 2.27 (1.23 to 4.22) |
37 (41%) | 49 (55%) | 1.80 (0.99 to 3.27) |
| Responders at 6 months | ||||||
| Continued response at later follow-up | 13/26 (50%) | 26/40 (65%) | – | 14/26 (54%) | 30/39 (77%) | – |
| Relapsed responder at later follow-up | 13/26 (50%) | 14/40 (35%) | 12/26 (46%) | 9/39 (23%) | ||
| Non-responders at 6 months | ||||||
| Continued non-response at later follow-up | 51/62 (82%) | 33/46 (72%) | – | 38/60 (63%) | 29/45 (64%) | – |
| New responder at later follow-up | 11/62 (18%) | 13/46 (28%) | 22/60 (37%) | 16/45 (36%) | ||
Chapter 5 Cost-effectiveness analysis
There were two components to the cost-effectiveness analysis. The primary analysis was an analysis alongside the RCT described in Chapters 3 and 4. The secondary analysis was a decision model, using trial data to project the costs and quality-adjusted life-years (QALYs) associated with ERP therapy and psychoeducation over 10 years. The decision model includes a synthetic arm so that the potential costs and QALYs of a face-to-face CBIT could be incorporated into the analysis. CBIT is considered to be the ‘gold standard’ treatment for tics but is not currently widely available in the NHS in England.
Cost of the intervention
The intervention cost is made up of two components. Firstly, there is the BIP platform, which delivers the ERP intervention. Secondly, there is the therapist time cost to support the delivery of the intervention. Therapist time was available in the ERP therapy as well as in the psychoeducation arm.
Cost of the BIP platform
The cost of the BIP platform is split into a fixed cost per participant and a variable cost based on platform use.
Fixed cost
A yearly cost of the platform was provided by the Swedish team in SEK. This was translated into Great Britain pounds (GBP) using the exchange rate at the time of the analysis (September 2020). This cost is divided by the number of participants in the intervention group to a conservative estimate of the fixed cost per participant: it is likely that there will be a higher caseload of people using the platform if it were to be rolled out and hence it is likely the cost per patient would be less in such circumstances.
Variable cost
Every time a participant logs in to the BIP platform they are sent a text message. To account for this an average of the cost of sending a text with different UK network providers has been calculated. This has then been multiplied by the number of logins to the platform by participants and their supporters.
Cost of delivering therapist support
The cost of therapist support is also broken down into a fixed and variable cost.
Fixed cost
The fixed cost of therapist support is made up of the cost of training and supervision for the therapists. Most of the therapists were trained in supervision, which occurred every week over the course of the intervention for 1 hour. The hourly cost of therapists and those providing supervision is used to calculate the total cost of supervision and training. This cost is also divided by the number of participants in the intervention arm to provide an average fixed cost of therapist support per participant. It is also likely that this is a conservative estimate (the true cost per patient is likely to be less as the number of patients per therapist may be higher in the real world).
Variable cost
Total therapist time per participant is collected as part of the platform. This is broken down into therapist time for the child, parent 1 and parent 2 and phone time with the therapist for the child, parents and parents and child together. A patient-level variable cost of therapist support is calculated for each participant based on therapist time reported and the grade of the therapist they are reported to have interacted with.
Economic evaluation methods
Perspective, discounting and time horizon
In line with NICE Technology Assessment guidelines,80 both the primary analysis alongside the RCT and secondary decision model analysis took an NHS and personal social services cost perspective. A secondary analysis from a wider societal cost perspective was also conducted for the analysis alongside the RCT. All costs and QALYs after 12 months were discounted at a rate of 3.5% per annum. 80 The analysis alongside the RCT reports costs and QALYs at 6 and 18 months to take into account the naturalistic observation that occurs after 6 months. The decision model has a time horizon of 10 years.
Outcome measures
Both the analysis alongside the RCT and the decision models estimate costs and QALYs.
The primary outcome measure was the incremental cost-effectiveness ratio (ICER), calculated as the mean incremental cost per QALY gained calculated from the parent-completed CHU9D at 18 months.
The analysis alongside the RCT also reports the incremental cost per change in YGTSS-TTSS.
Primary analysis: analysis alongside the RCT
The analysis alongside the RCT incorporated the costs incurred and health benefits accrued over the 18-month time horizon of the trial. All statistical analysis was conducted in Stata version 17. 81
Costs and resource use
The costs that each young person incurred included the cost of the intervention, including the cost of the BIP platform for each participant randomised to ERP therapy, and the cost of delivering therapist support for both ERP therapy and psychoeducation groups (see above) and resource use collected during the trial using an adapted version of the CA-SUS. 82–84
The primary analysis was from a health and social care cost perspective. Resource use was collected on specialist tic services, contacts with professionals in the community, inpatient contacts, emergency contacts and medication use at baseline and at 3, 6, 12 and 18 months asking about resource use since last follow-up or in the previous 3 months at baseline using the CA-SUS. Unit costs used in the health and social care cost perspective analysis are reported in Table 15 and are in 2019 GBP.
| Item | Unit cost (GBP) | Source |
|---|---|---|
| Tic disorder clinic | ||
| Specialist assessment | 949 | Cost provided by clinicians at GOSH and NHCFT |
| Treatment session in clinic | 67 | Cost provided by clinicians at GOSH and NHCFT |
| CAMHS | ||
| Multidisciplinary team | 119 | Cost from PSSRU 2016 adjusted using NHS cost inflation index |
| Paediatrician (hospital) | 180 | Average of consultant- and non-consultant-led hospital paediatrician from PSSRU 2019 |
| Paediatrician (community) | 176 | Average of consultant- and non-consultant-led community paediatrician PSSRU 2019 |
| Child and adolescent psychiatrist | 292 | Weighted average of child and adolescent psychiatry national reference costs 2019 |
| Neurologist | 109 | Medical consultant, hospital-based doctors (PSSRU 2019) |
| Psychologist | 54 | Band 7 community-based clinical psychologist (PSSRU 2019) |
| Speech and language therapist | 54 | Band 7 community-based speech and language therapist (PSSRU 2019) |
| Occupational therapist | 45 | Band 6 community-based occupational therapist (PSSRU 2019) |
| Rheumatologist | 354 | Paediatric rheumatology (national reference costs) |
| ENT | 105 | Weighted average ear, nose and throat attendances (national reference costs) |
| Geneticist | 368 | Geneticist (national reference costs) |
| Counsellor | 54 | Band 7 community scientific and professional staff (PSSRU 2019) |
| School counsellor | 49 | School-based children’s health services (PSSRU 2019) |
| School-based speech and language intervention | 91 | Average of group-based and one-to-one session (PSSRU 2019) |
| School nurse | 59 | School-based children’s health services (PSSRU 2019) |
| Podiatry | 67 | Weighted average podiatry attendances (PSSRU 2019) |
| Cardiologist | 179 | Weighted average paediatric attendances (national reference costs) |
| Psychiatric nurse | 55 | Nurse (mental health clinic) (PSSRU 2019) |
| Orthotic services | 86 | Weighted average orthotics attendances (national reference costs) |
| Orthopaedics | 128 | Weighted average paediatric orthopaedics (national reference costs) |
| Dentist | 133 | Dentist patient contact (PSSRU 2019) |
| Endocrinologist | 228 | Weighted average paediatric endocrinologist (national reference costs) |
| GP | ||
| Clinic | 39 | 9-minute GP appointment (PSSRU 2019) |
| Nurse (GP practice) | ||
| Clinic | 6 | 10-minute GP nurse appointment (PSSRU 2019) |
| Social worker | 50 | Children’s services (PSSRU 2019) |
| Special education needs coordinator | 21 | Cost per hour based on average salary from National Careers Service, 37-hour work week and 46.4 working weeks per year |
| Educational psychologist | 54 | Band 7 community psychologist |
| Parental group | 26 | Average of cost per session from different parental groups in PSSRU 2019 |
| Play/art/music/drama therapist | 54 | Band 7 art therapist in community-based scientific and professional staff (PSSRU 2019) |
| Physiotherapist | ||
| Group session | 81 | NHS costs for children’s health services (PSSRU 2019) |
| One-to-one | 100 | |
| Dietitian | 90 | National reference costs |
| Osteopath | 40 | NHS England website on osteopaths |
| Orthodontics | 137 | Weighted average of orthodontic attendances (national reference costs) |
| Eye specialist | 117 | Paediatric ophthalmologist (national reference costs) |
| Urologist | 133 | Weighted average of urology attendances (national reference costs) |
| Paediatric inpatient stay | ||
| Rotavirus complications | 566 | Weighted average of paediatric gastroenteritis elective inpatient attendances (national reference costs) |
| Minor injuries | 1032 | Weighted average of paediatric minor injury inpatient attendances (national reference costs) |
| Cardiology | 1551 | Weighted average of paediatric cardiology inpatient attendances (national reference costs) |
| Accident and emergency | 218 | Weighted average of accident and emergency attendances (national reference costs) |
Wider societal costs include out-of-pocket costs, the cost of education support, voluntary services and the cost of days off from school, also collected using the CA-SUS. When reporting days off from school we report total days off as well as the number of days off that participants attributed as being related to TS.
Out-of-pocket costs are calculated using the amount reported by parents in the CA-SUS. The costs of days off from school are calculated using a human capital approach based on the cost of child care for each day a participant has reported taking off school. Unit costs used in the wider societal cost perspective analysis are reported in Table 16 and are in 2019 GBP.
| Item | Unit cost (GBP) | Source |
|---|---|---|
| Education support | ||
| Individual tuition at home | 31 | Per-hour average collected from survey of 2000 tutors run by ‘thetutor.com’ |
| Individual tuition in a special unit | 21 | Cost per hour based on average annual salary from National Careers Service (NCS), a 37-hour work week and 46.4 working weeks in a year |
| Education welfare officer | 18 | Cost per hour based on average annual salary from NCS, a 37-hour work week and 46.4 working weeks in a year |
| Classroom assistant | 9 | Cost per hour based on Office for National Statistics (ONS) Standard Occupational Classification (SOC) 2019 weekly wage and a 37-hour work week |
| Support from learning mentor | 9 | Cost per hour based on ONS SOC 2019 weekly wage and a 37-hour work week |
| Voluntary services | ||
| Tourettes Action | 10 | Unit cost for any average contact provided by Tourettes Action |
| Day care centre | 38 | PSSRU 2019 cost per day |
| Early years support worker | 10 | Cost per hour based on average annual salary from NCS, a 37-hour work week and 46.4 working weeks in a year |
| Local self-help group | 26 | Assumed cost to be the same as parent support groups in the community |
| Days off school | 83 | Daily wage of a childminder based on ONS SOC 2019 |
Utilities
Health-related QoL utility tariffs are calculated from responses to the CHU9D,85 a child-specific patient-reported outcome measure validated for use in the calculation of QALYs and applying the algorithm developed by Stevens. 86 NICE does not recommend specific measures of HRQoL in CYP but that the choice of measure should be informed by evidence of psychometric performance, evidence that it is valid in the age ranges being studied and the quality and availability of value sets. The CHU9D has been validated for use in child and adolescent mental health services, is designed for those aged 7–17 years in line with our inclusion criteria and has a UK value set.
The CHU9D was completed as a patient-reported outcome by the young person and a proxy reported outcome asking about the young person completed by a parent/carer at baseline and at 3, 6, 12 and 18 months. The parent-completed version of the measure was pre-specified as the primary analysis in the health economics analysis plan (HEAP) based on the assumption that we would have better completion rates for the parent-completed rather than young person-completed version.
Cost–utility analysis
Analyses were pre-specified in the HEAP.
We calculated complete case descriptive statistics for the percentage of participants that used each type of resource and the mean number of contacts for the participants that used them. The mean difference in costs and 95% CIs for each resource use type was calculated using regression analysis adjusting for baseline costs, with site as a covariate and bias-corrected bootstrapping with 1000 iterations for complete cases (complete resource use at baseline and at 3-, 6-, 12- and 18-month follow-ups).
The mean difference in QALYs at 6 and 18 months and 95% CIs were calculated using regression analysis adjusting for baseline utility, with site as a covariate and bias-corrected bootstrapping with 1000 iterations for complete cases (complete CHU9D at baseline and at 3-, 6-, 12- and 18-month follow-ups).
We assumed data were missing at random. Predictors of missingness were explored, with site identified as the only predictor of missingness. In line with the statistical analysis of the primary outcome we have conducted a complete case analysis adjusting for predictors of missingness.
Incremental cost-effectiveness ratio
We explore the mean incremental cost per QALY gained and the mean cost per point reduction in YGTSS-TTSS comparing ERP and psychoeducation from the health and social care cost perspective at 18 months. Costs include total health-care resource use per participant and variable costs per participant for both trial arms. For the intervention arm, costs include the costs for the platform, therapist time, supervision and training. For the control arm, we do not include any platform or training and supervision costs, as we assume that the psychoeducation information could be provided without the need to use the platform (i.e. on a standalone website). However, therapist time is included given that this was provided as part of the active psychoeducation arm. The ICERs were calculated using seemingly unrelated regression (SUR; Stata command SUREG) to account for any potential correlation between costs and outcomes.
Cost-effectiveness acceptability planes and cost-effectiveness acceptability curves
The adjusted, bootstrapped SUR QALYs, TTSS and cost data were used to calculate the probability that ERP is cost-effective compared to psychoeducation for a range of cost-effectiveness threshold values. A cost-effectiveness plane of the bootstrapped results is also reported for both the YGTSS-TTSS and QALY analyses.
Sensitivity analyses
Sensitivity analyses were conducted to explore the impact of different assumptions regarding the cost of the intervention. Three assumptions were changed:
-
Applying a licence fee per participant instead of a fixed cost per year based on a UK iCBT digital intervention. 87 We apply different licence fees starting at £25 to explore how this impacts the probability of cost-effectiveness.
-
Assuming fortnightly supervision instead of weekly supervision of therapists delivering the intervention.
-
Adding the cost of the platform to the psychoeducation group to reflect how this might be rolled out in practice.
Secondary analysis: 10-year decision analytic model
A 10-year decision model allows us to project the costs incurred and health benefits accrued beyond the time horizon of the trial. Moreover, the decision model allows us to include an additional arm for CBIT, which is considered to be the ‘gold standard’ treatment for tics but is not currently widely available. Health service costs and QALYs were calculated for the 10 years following the trial, drawing on data from the trial and available literature where needed.
Design
In the model, cost-effectiveness is estimated by calculating which of three options – (1) online psychoeducation, (2) online ERP and (3) CBIT – has the highest net monetary benefit (NMB) for a range of QALY cost-effectiveness thresholds. The model was designed following a rapid review of the literature and informed by expert clinical input.
Cycle duration is 6 months, with 20 cycles in total to project the results forward 10 years to estimate how costs and outcomes might change for this patient group going into adulthood. The duration of 10 years was chosen to adequately capture long-term costs and QALYs, but such an analysis does not project so far into the future that the results might no longer hold. In line with NICE guidelines, costs and QALYs have been discounted at the recommended rate of 3.5% per year. 80 There are associated costs and utility values for each of three health states of mild, moderate and severe tics.
Transition probabilities for ERP and psychoeducation were obtained during the trial follow-up between 6 and 18 months to measure the natural progression of tics following the intervention, as using data from baseline to 6 months would have overestimated the long-term impact by including the initial decrease in tic severity in the transition probabilities. Transition probabilities for CBIT were calculated from the literature (Markov model structure; Table 17). The mean utilities and costs associated with each health state were calculated using the patient-level data for the study.
| To very mild | To mild | To moderate | To severe | To very severe | |
|---|---|---|---|---|---|
| Online ERP and CBIT | |||||
| From very mild | 0.600 | 0.200 | 0.200 | 0.000 | 0.000 |
| From mild | 0.273 | 0.273 | 0.318 | 0.045 | 0.091 |
| From moderate | 0.023 | 0.279 | 0.535 | 0.070 | 0.093 |
| From severe | 0.000 | 0.000 | 0.214 | 0.786 | 0.000 |
| From very severe | 0.000 | 0.043 | 0.087 | 0.043 | 0.826 |
| Online psychoeducation | |||||
| From very mild | 0.250 | 0.750 | 0.000 | 0.000 | 0.000 |
| From mild | 0.143 | 0.643 | 0.071 | 0.071 | 0.071 |
| From moderate | 0.039 | 0.118 | 0.667 | 0.176 | 0.000 |
| From severe | 0.000 | 0.100 | 0.250 | 0.400 | 0.250 |
| From very severe | 0.000 | 0.000 | 0.043 | 0.217 | 0.739 |
The patient population in the model is assumed to be the same as that in the trial, including in terms of sample size and demographics.
The model was designed in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA), with inputs calculated in Stata version 17. 81
Markov model structure
Following our rapid review of the literature, searching for tics/Tourette’s, young people/adolescents and economic evaluations, we were unable to identify any previous decision models for the treatment of tics in young people. Our review also identified that there is no official definition for what categorises mild to severe tics. We decided to base the model on the commonly referenced structure of severity suggested by Bloch and Leckman,88 where tics are categorised based on the TTSS on the YGTSS as very mild (0–9), mild (10–19), moderate (20–29), severe (30–39) or very severe (40–50). It is possible for individuals to go from any severity level to another each cycle within a relatively short period of time, although the probability of going from a very mild state to very severe and vice versa is close to zero (see Figure 6).
FIGURE 6.
Markov model structure.
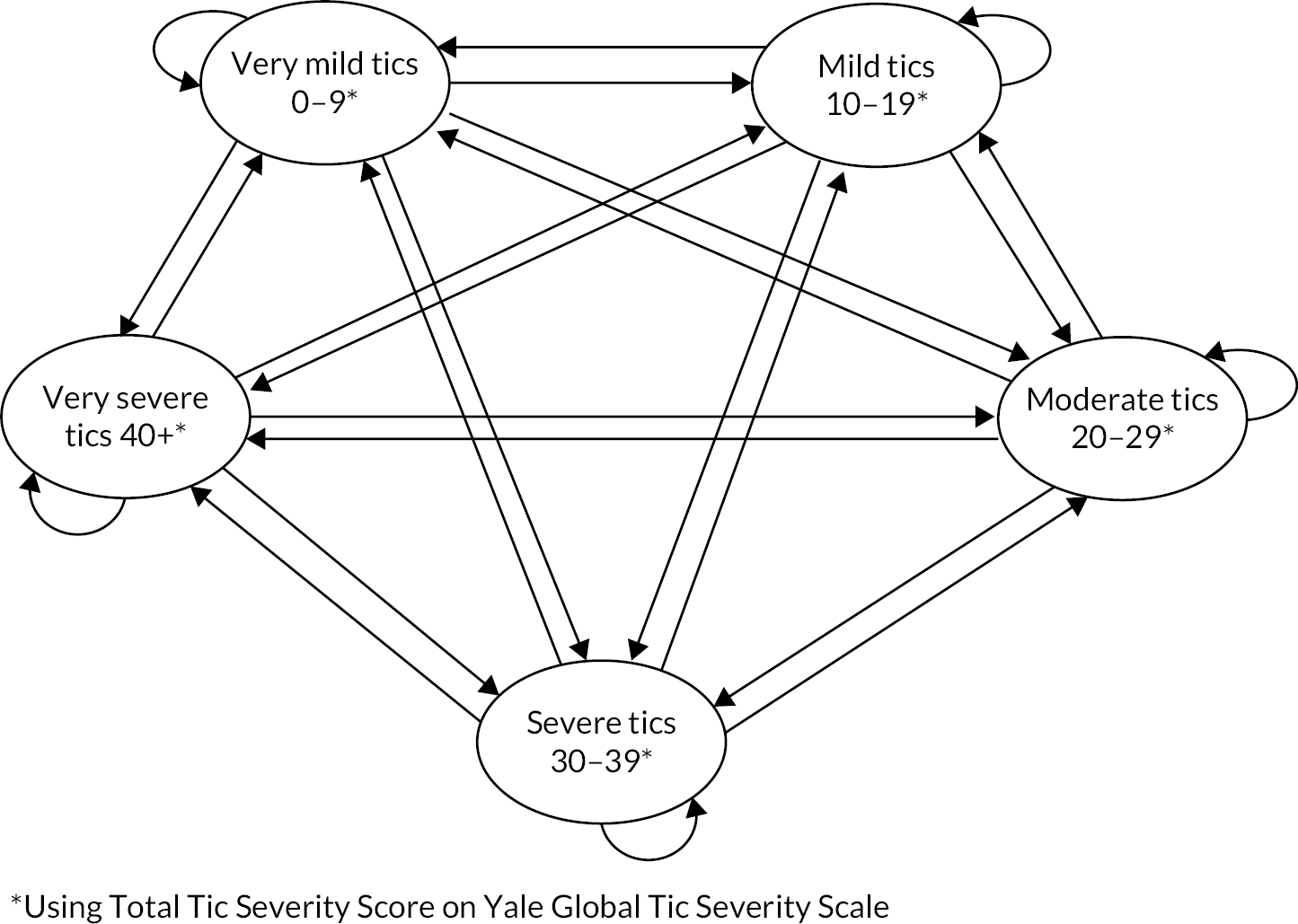
Figure 7 shows tic progression over the course of the trial for online psychoeducation and ERP. Discussions with clinicians led us to conclude that it was feasible to simulate a decrease in tic severity in the CBIT group at 6 months from the trial literature data, shown by the dashed line in Figure 7, and then assume a similar tapering to ERP, shown in Figure 7 after 6 months. For this reason, the transition probabilities applied to the CBIT arm after 6 months are the same as those drawn from the trial for the ERP arm.
FIGURE 7.
Tic progression over time by group.

Figures 8 and 9 show the proportions of participants in each group that fell into each health state at baseline and at 6 months, respectively. These results illustrate patients moving into lower-severity health state and tic scores falling over time. Table 18 reports the proportions of participants in each group when they enter the model and begin moving through the health states using the transition probabilities reported in Table 17. For the probabilistic sensitivity analysis (PSA), transition probabilities were sampled using the Dirichlet distribution. 89 Values for CBIT were obtained by combining data from the available literature on CBIT effectiveness for young people at 6 months. 17,59,90,91
FIGURE 8.
Proportions of participants in each tic severity health state by group at baseline.
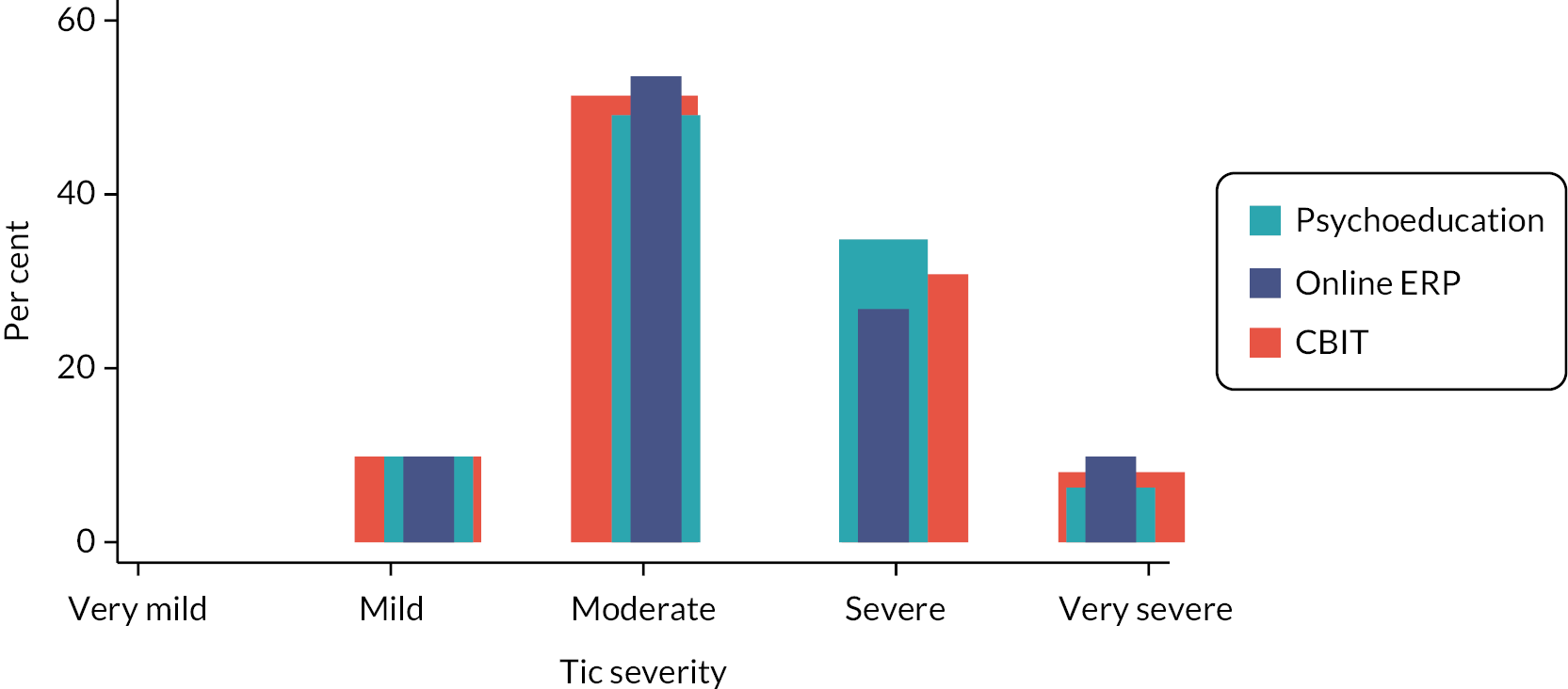
FIGURE 9.
Proportions of participants in each tic severity health state by group at 6 months.

| Online ERP (18 months) (%) |
Online psychoeducation (18 months) (%) |
Face-to-face CBIT (6 months) (%) |
|
|---|---|---|---|
| Very mild | 12 | 4 | 10 |
| Mild | 19 | 18 | 38 |
| Moderate | 33 | 37 | 42 |
| Severe | 14 | 21 | 9 |
| Very severe | 22 | 21 | 1 |
Calculating health-care costs and utilities
Cost of online ERP
The mean cost per participant of ERP came from the trial results reported above. In the base case scenario this is the same as what is reported in the trial analysis: £155. This includes £104.57 for the online platform and supervision and a mean variable cost of £50.43 per participant for therapist time in the trial.
Cost of online psychoeducation
In the trial analysis the cost of the platform was not included for the psychoeducation arm as it was assumed in practice that this was unlikely to be delivered online. The cost of therapist support was included to reflect the additional support that these patients received compared to what would be available in usual care. This led to a mean cost per participant of £43.76, which is what was used as the base case in the model.
Cost of face-to-face CBIT
In the available literature, CBIT is consistently referred to as consisting of eight sessions, two lasting 90 minutes for the purpose of building rapport and six 60-minute sessions. 59,91 This was confirmed by specialist tic clinics, which also provided information on who normally delivers CBIT in the UK. Based on this, CBIT was assumed to be delivered by a grade 8a clinical psychologist over the course of 9 hours, resulting in a cost per simulated participant of £675.
Health state costs
Health state costs associated with each level of tic severity included costs associated with the use of specialist tic services as these were the only costs collected as part of the trial that had a significant relationship with tic severity. The average cost per participant at each severity level was calculated adjusting for age, comorbidities using the DAWBA and sex.
Costs for patients in the online psychoeducation arm and online ERP between 0 and 18 months were calculated using information on tic severity available in the trial. These patients then enter the model at 18 months. Those in the CBIT arm effectively enter the model at 6 months based on their level of tic severity after the simulated decrease between baseline and 6 months.
Health state utilities
The relationship between tic severity and HRQoL is not clear. Some studies have found a positive relationship between tic severity and factors relating to QoL, such as functional impairment and psychosocial scores in children. 92,93 A few studies have found that tic severity only has a small impact on HRQoL, if any, and that a greater contributor is comorbidities. Some studies have found a significant relationship between tic severity and HRQoL. 94–97 We therefore included key significant comorbidities using the DAWBA data from the trial as well as age and sex when calculating CHU9D utility values for tic health states.
Analysis of the trial data showed that transitioning from one of the mild-severity health states to a moderate-severity health state had a significant impact on costs and utility values, but there was no statistically significant difference between a very-mild-severity and a mild-severity health state. Similarly, there was a significant difference in costs and utilities between a moderate-severity health state and the severe health states, but there was no difference between severe and very severe tics. Therefore, costs and utilities are allocated as illustrated by Figure 10. Means, standard errors and distributions calculated from the trial data for use in the model are reported in Table 19. Utilities were divided by two when applied to health states to reflect the 6-month cycle duration.
FIGURE 10.
Allocation of costs and utilities according to health states.
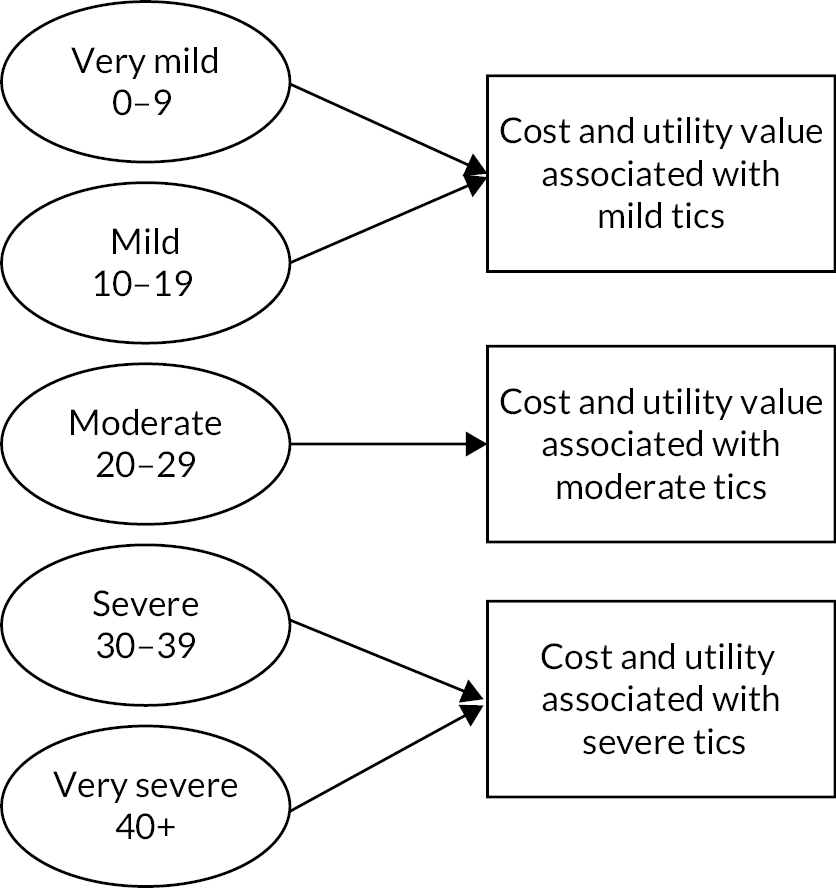
| Value | SE | Distribution | |
|---|---|---|---|
| 6-month health-care costs | |||
| Mild | £129 | 15.21 | Gamma |
| Moderate | £133 | 12.63 | Gamma |
| Severe | £194 | 19.02 | Gamma |
| Utility weights on CHU9D | |||
| Utility | SE | Distribution | |
| Mild | 0.867 | 0.006 | Beta |
| Moderate | 0.839 | 0.004 | Beta |
| Severe | 0.814 | 0.005 | Beta |
Cost-effectiveness analysis
We calculated the total costs and QALYs for patients treated with online ERP compared with online psychoeducation and face-to-face CBIT. We calculated an individual ICER for ERP compared with psychoeducation and ERP compared with CBIT. We also calculated the NMB of each intervention to be able to more easily compare all three options. Any costs and QALYs obtained after 12 months were discounted at 3.5% in line with NICE guidance. 80
Sensitivity analysis
Deterministic analysis and PSA were used to explore the uncertainty regarding our results.
Deterministic analysis
We varied the input variables, either in combination or alone, while other inputs were held at a constant value. We used this to explore how changing assumptions regarding the cost components of the different interventions may impact the results. We implemented:
-
a licence fee for the platform of £25 per participant based on the sensitivity analysis we conducted for the main trial analysis
-
including the cost of the platform for the online psychoeducation arm to reflect how much it would cost to roll out this intervention in this manner
-
setting the cost of online psychoeducation to £0 to provide a conservative estimate of how cost-effective online ERP would be compared with a ‘do nothing’ approach
-
applying the same transition probabilities to the online psychoeducation arm as were applied to the online ERP and CBIT arms.
Probabilistic sensitivity analysis and cost-effectiveness acceptability curve
We computed 5000 replications of the model in our PSA, varying the values as set out in Tables 17 and 19. The 5000 replications were then used to construct cost-effectiveness acceptability curves (CEACs) showing the probability that online ERP was cost-effective compared with online psychoeducation and face-to-face CBIT for a range of cost-effectiveness threshold values using the NMB approach, where NMB equals total QALYs multiplied by a cost-effectiveness threshold minus total costs.
Results
Costs of the intervention
The fixed and variable costs of the BIP platform and therapist support are reported in Tables 20–23. For variable login costs, the mean cost per patient was £1.25 higher (95% CI £0.46 to £2.04) for the intervention arm compared to the control. For variable therapist support costs, the mean cost per patient was £5.03 higher (95% CI £0.88 to £9.97) for ERP compared to psychoeducation.
| Item | Data |
|---|---|
| Cost per year in SEK | 96,000 |
| Cost per year in GBP September 2020 | 8494 |
| N of participants in online ERP arm using platform | 111 |
| Fixed cost of platform per participant in GBP | 77 |
| ERP therapy | Psychoeducation | |||
|---|---|---|---|---|
| Mean (£) | SD (£) | Mean (£) | SD (£) | |
| Child | 3.36 | 1.85 | 2.54 | 1.46 |
| Parent 1 | 3.46 | 1.95 | 3.07 | 1.52 |
| Parent 2 | 0.04 | 0.33 | 0.01 | 0.10 |
| Total | 6.87 | 3.54 | 5.62 | 2.62 |
| Item | Description | Grade | Total costs (£) |
|---|---|---|---|
| Independent training | Total of 10 hours of independent time reported | 1 grade 4 research assistant 1 grade 5 nurse |
177 |
| Therapist time to attend supervision | Weekly supervision lasting 1 hour over 108 weeks | 1 grade 4 research assistant 3 grade 5 nurses |
7825 |
| Delivery of supervision | Weekly supervision lasting 1 hour over the 108 weeks | 1 grade 8c clinician 1 grade 7 nurse practitioner |
6894 |
| ERP therapy | Psychoeducation | |||
|---|---|---|---|---|
| Mean (£) | SD (£) | Mean (£) | SD (£) | |
| Therapist time | ||||
| Child | 18 | 9 | 16 | 9 |
| Parent 1 | 25 | 13 | 22 | 10 |
| Parent 2 | 0.29 | 2 | 0.09 | 1 |
| Total | 43 | 20 | 38 | 17 |
| Phone cost | ||||
| Child | 0.01 | 0.14 | 0 | 0.02 |
| Parents | 0.29 | 1 | 0.27 | 1 |
| Parent and child | 0.02 | 0.16 | 0.02 | 0.16 |
| Total | 0.33 | 1 | 0.29 | 1 |
| Total therapist cost | 43 | 20 | 38 | 17 |
Primary analysis: analysis alongside the RCT
Resource use and costs
Table 24 reports the mean number of contacts and SDs for the reported numbers and percentages who have used the specialist tic service. Other service uses and medication uses are reported in Tables 25 and 26. There was no significant difference in costs between the two groups, with means per-patient differences in total resource use cost (excluding intervention costs) at 6 months of £63 (95% CI −£158 to £284) and £192.79 (95% CI −£251.74 to £637.32) at 18 months for the intervention arm compared with the control (see Table 27). School-related information is reported in the separate health economic analysis document.
| ERP therapy | Psychoeducation | |||
|---|---|---|---|---|
| N (%) | Meana (SD) | N (%) | Meana (SD) | |
| Specialist tic clinic | ||||
| Baseline | 9 (8%) | 1 (0) | 5 (4%) | 1 (0) |
| 3 months | 6 (6%) | 1 (1) | 3 (3%) | 2 (1) |
| 6 months | 0 (0%) | 0 (0) | 6 (6%) | 2 (1) |
| 12 months | 6 (7%) | 3 (2) | 6 (7%) | 3 (3) |
| 18 months | 7 (8%) | 1 (0) | 8 (9%) | 1 (0) |
| CAMHS | ||||
| Baseline | 34 (30%) | 3 (3) | 28 (25%) | 2 (2) |
| 3 months | 19 (19%) | 3 (3) | 24 (24%) | 2 (2) |
| 6 months | 20 (22%) | 3 (4) | 25 (27%) | 3 (3) |
| 12 months | 22 (24%) | 3 (2) | 28 (31%) | 4 (6) |
| 18 months | 21 (24%) | 3 (3) | 26 (29%) | 4 (6) |
| Paediatrician in hospital | ||||
| Baseline | 18 (16%) | 1 (1) | 15 (13%) | 1 (0) |
| 3 months | 9 (9%) | 1 (0) | 9 (9%) | 1 (0) |
| 6 months | 12 (13%) | 1 (0) | 8 (9%) | 1 (0) |
| 12 months | 10 (11%) | 1 (1) | 8 (9%) | 2 (1) |
| 18 months | 7 (8%) | 1 (1) | 10 (11%) | 1 (0) |
| Paediatrician in the community | ||||
| Baseline | 5 (4%) | 1 (0) | 5 (4%) | 1 (0) |
| 3 months | 5 (5%) | 1 (0) | 3 (3%) | 1 (0) |
| 6 months | 2 (2%) | 2 (1) | 2 (2%) | 1 (0) |
| 12 months | 1 (1%) | 2 (0) | 0 (0%) | 0 (0) |
| 18 months | 2 (2%) | 1 (0) | 1 (1%) | 1 (0) |
| Child and adolescent psychiatrist | ||||
| Baseline | 2 (2%) | 2 (1) | 4 (4%) | 2 (1) |
| 3 months | 2 (2%) | 2 (1) | 4 (4%) | 3 (4) |
| 6 months | 2 (2%) | 4 (2) | 4 (4%) | 1 (1) |
| 12 months | 1 (1%) | 2 (0) | 4 (4%) | 1 (0) |
| 18 months | 2 (2%) | 1 (0) | 0 (0%) | 0 (0) |
| Neurologist | ||||
| Baseline | 2 (2%) | 1 (0) | 4 (4%) | 1 (0) |
| 3 months | 0 (0%) | 0 (0) | 3 (3%) | 1 (0) |
| 6 months | 6 (6%) | 3 (4) | 3 (3%) | 1 (0) |
| 12 months | 5 (6%) | 1 (0) | 4 (4%) | 1 (1) |
| 18 months | 4 (4%) | 2 (1) | 1 (1%) | 1 (0) |
| Child and adolescent psychologist | ||||
| Baseline | 1 (1%) | 2 (0) | 2 (2%) | 6 (6) |
| 3 months | 2 (2%) | 0 (0) | 2 (2%) | 1 (0) |
| 6 months | 2 (2%) | 2 (1) | 2 (2%) | 2 (1) |
| 12 months | 2 (2%) | 6 (1) | 3 (3%) | 2 (1) |
| 18 months | 0 (0%) | 0 (0) | 2 (2%) | 2 (1) |
| Speech and language therapist | ||||
| Baseline | 3 (3%) | 1 (1) | 2 (2%) | 1 (0) |
| 3 months | 6 (6%) | 2 (1) | 2 (2%) | 7 (7) |
| 6 months | 3 (3%) | 6 (5) | 0 (0%) | 0 (0) |
| 12 months | 4 (4%) | 4 (4) | 1 (1%) | 20 (0) |
| 18 months | 1 (1%) | 20 (0) | 0 (0%) | 0 (0) |
| Occupational therapist | ||||
| Baseline | 2 (2%) | 1 (0) | 2 (2%) | 3 (2) |
| 3 months | 4 (4%) | 1 (0) | 3 (3%) | 1 (0) |
| 6 months | 4 (4%) | 7 (9) | 0 (0%) | 0 (0) |
| 12 months | 5 (6%) | 4 (4) | 2 (2%) | 11 (13) |
| 18 months | 3 (3%) | 7 (11) | 1 (1%) | 2 (0) |
| ERP therapy | Psychoeducation | |||
|---|---|---|---|---|
| N (%) | Meana (SD) | N (%) | Meana (SD) | |
| Other primary care contacts | ||||
| Baseline | 75 (67%) | 4 (6) | 69 (62%) | 6 (9) |
| 3 months | 58 (57%) | 3 (5) | 58 (58%) | 3 (3) |
| 6 months | 46 (49%) | 4 (5) | 61 (66%) | 3 (4) |
| 12 months | 46 (53%) | 4 (8) | 52 (58%) | 4 (5) |
| 18 months | 46 (53%) | 6 (16) | 52 (58%) | 3 (3) |
| Accident and emergency contacts | ||||
| Baseline | 6 (5%) | 1 (0) | 11 (10%) | 1 (0) |
| 3 months | 2 (2%) | 1 (0) | 7 (7%) | 1 (1) |
| 6 months | 5 (5%) | 2 (1) | 5 (5%) | 1 (0) |
| 12 months | 10 (11%) | 1 (0) | 12 (13%) | 2 (2) |
| 18 months | 7 (8%) | 1 (0) | 7 (8%) | 1 (0) |
| Other secondary care contacts | ||||
| Baseline | 3 (3%) | 1 (1) | 1 (1%) | 1 (0) |
| 3 months | 1 (1%) | 5 (0) | 1 (1%) | 1 (0) |
| 6 months | 0 (0%) | 0 (0) | 1 (1%) | 1 (0) |
| 12 months | 0 (0%) | 0 (0) | 0 (0%) | 0 (0) |
| 18 months | 3 (3%) | 9 (10) | 1 (1%) | 1 (0) |
| ERP therapy | Psychoeducation | |
|---|---|---|
| N (%) | N (%) | |
| Clonidine | ||
| Baseline | 4 (4%) | 9 (8%) |
| 3 months | 3 (3%) | 10 (10%) |
| 6 months | 4 (4%) | 7 (8%) |
| 12 months | 3 (3%) | 6 (7%) |
| 18 months | 1 (1%) | 5 (6%) |
| Risperidone | ||
| Baseline | 0 (0%) | 3 (3%) |
| 3 months | 0 (0%) | 2 (2%) |
| 6 months | 0 (0%) | 1 (1%) |
| 12 months | 1 (1%) | 2 (2%) |
| 18 months | 2 (2%) | 3 (3%) |
| Aripiprazole | ||
| Baseline | 7 (6%) | 1 (1%) |
| 3 months | 5 (5%) | 1 (1%) |
| 6 months | 5 (5%) | 0 (0%) |
| 12 months | 6 (7%) | 1 (1%) |
| 18 months | 4 (5%) | 2 (2%) |
| Any tic medication a | ||
| Baseline | 14 (13%) | 16 (14%) |
| 3 months | 12 (12%) | 15 (15%) |
| 6 months | 15 (16%) | 8 (9%) |
| 12 months | 15 (18%) | 11 (12%) |
| 18 months | 11 (12%) | 12 (13%) |
| ERP therapy | Psychoeducation | Adjusted differencea (95% CI) |
p-value | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Specialist tic services | ||||
| Baseline | 128 (248) | 91 (168) | ||
| 3 months | 158 (314) | 121 (242) | ||
| 6 months | 200 (384) | 192 (414) | ||
| 12 months | 149 (271) | 209 (506) | ||
| 18 months | 145 (305) | 102 (192) | ||
| 18 months discounted | 140 (295) | 99 (186) | ||
| Total | 719 (988) | 643 (1046) | −3.28 (−284.66 to 278.1) | 0.982 |
| Community services | ||||
| Baseline | 73 (166) | 82 (178) | ||
| 3 months | 68 (149) | 55 (104) | ||
| 6 months | 94 (277) | 93 (183) | ||
| 12 months | 66 (213) | 95 (164) | ||
| 18 months | 159 (657) | 83 (131) | ||
| 18 months discounted | 153 (635) | 80 (127) | ||
| Total | 478 (1259) | 381 (432) | 91.04 (−131.43 to 313.52) | 0.423 |
| Hospital services | ||||
| Baseline | 10 (107) | 14 (147) | ||
| 3 months | 28 (282) | 9 (87) | ||
| 6 months | 0 (0) | 6 (59) | ||
| 12 months | 0 (0) | 0 (0) | ||
| 18 months | 99 (529) | 32 (305) | ||
| 18 months discounted | 96 (511) | 31 (295) | ||
| Total | 141 (658) | 58 (347) | 90.58 (−46.8 to 227.96) | 0.196 |
| Accident and emergency | ||||
| Baseline | 8 (41) | 21 (77) | ||
| 3 months | 6 (37) | 24 (92) | ||
| 6 months | 19 (89) | 14 (63) | ||
| 12 months | 0 (0) | 0 (0) | ||
| 18 months | 19 (68) | 14 (49) | ||
| 18 months discounted | 18 (66) | 14 (48) | ||
| Total | 43 (113) | 78 (185) | −15.18 (−52.42 to 22.05) | 0.424 |
| Medication costs | ||||
| Baseline | 13 (31) | 13 (32) | ||
| 6 months | 15 (44) | 9 (30) | ||
| 12 months | 64 (146) | 50 (122) | ||
| 18 months | 69 (145) | 44 (130) | ||
| 18 months discounted | 66 (140) | 42 (125) | ||
| Total | 168 (309) | 134 (291) | 48.17 (−21.8 to 118.15) | 0.177 |
| Total healthcare resource use costs | ||||
| Baseline | 231 (361) | 221 (333) | ||
| 3 months | 280 (542) | 227 (342) | ||
| 6 months | 328 (565) | 314 (502) | ||
| 12 months | 279 (475) | 354 (575) | ||
| 18 months | 491 (1104) | 275 (446) | ||
| 18 months discounted | 474 (1067) | 266 (431) | ||
| Total health-care costs | 1549 (2340) | 1294 (1434) | 192.79 (−251.74 to 637.32) | 0.395 |
There were no significant differences in total wider costs (excluding intervention costs) at 6 months (mean difference of £117.07 per participant, 95% CI −£205.95 to £440.09) and 18 months (mean difference of £302.73 per participant, 95% CI −£327.26 to £932.72). The mean differences in costs also were not significant when total health-care costs were added to the wider societal costs [£203.16 (95% CI −£241.03 to £647.34) at 6 months and £576.77 (95% CI −£413.55 to £1567.10) at 18 months].
Utilities and QALYs
The follow-up rate for the CHU9D was lower than for the CA-SUS, as this was collected separately online from the other questionnaires. At 6 months, QALYs for the young-person self-completed CHU9D were 0.011 (95% CI 0.000 to 0.022) higher for those in the ERP group compared to those in the psychoeducation group (see Table 28). There were no statistically significant differences between arms for the parent proxy-completed CHU9D at 6 months (0.007, 95% CI −0.002 to 0.017) or at 18 months for the young-person (0.036, 95% CI −0.015 to 0.087) or proxy parent/carer (0.036, 95% CI −0.006 to 0.008) CHU9D.
| ERP therapy | Psychoeducation | Adjusted differencea (95% CI) | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | |||
| Parent-completed | ||||||||
| Baseline | 112 | 0.832 | 0.085 | 112 | 0.845 | 0.088 | ||
| 3 months | 89 | 0.853 | 0.091 | 92 | 0.822 | 0.107 | ||
| 6 months | 64 | 0.849 | 0.106 | 76 | 0.841 | 0.110 | ||
| 12 months | 66 | 0.857 | 0.124 | 65 | 0.816 | 0.115 | ||
| 18 months | 52 | 0.838 | 0.117 | 54 | 0.834 | 0.113 | ||
| 18 months discounted | 52 | 0.810 | 0.113 | 54 | 0.806 | 0.109 | ||
| QALYs at 6 months | 63 | 0.425 | 0.039 | 74 | 0.417 | 0.040 | 0.007 (−0.002 to 0.017) | 0.140 |
| QALYs at 12 months | 52 | 0.858 | 0.087 | 54 | 0.834 | 0.083 | ||
| QALYs at 18 months | 46 | 1.285 | 0.126 | 41 | 1.246 | 0.118 | 0.036 (−0.006 to 0.077) | 0.094 |
| Young person-completed | ||||||||
| Baseline | 112 | 0.815 | 0.097 | 112 | 0.827 | 0.094 | ||
| 3 months | 86 | 0.866 | 0.102 | 89 | 0.831 | 0.117 | ||
| 6 months | 63 | 0.853 | 0.118 | 66 | 0.814 | 0.122 | ||
| 12 months | 60 | 0.856 | 0.102 | 61 | 0.810 | 0.127 | ||
| 18 months | 45 | 0.840 | 0.100 | 49 | 0.811 | 0.133 | ||
| 18 months discounted | 45 | 0.812 | 0.096 | 49 | 0.784 | 0.129 | ||
| QALYs at 6 months | 59 | 0.425 | 0.049 | 65 | 0.418 | 0.043 | 0.011 (0.000 to 0.022) | 0.048a |
| QALYs at 12 months | 47 | 0.842 | 0.103 | 46 | 0.825 | 0.092 | ||
| QALYs at 18 months | 38 | 1.264 | 0.132 | 33 | 1.236 | 0.134 | 0.036 (−0.015 to 0.087) | 0.169 |
Primary analysis: mean incremental cost per QALY gained of ERP compared to psychoeducation at 18 months based on proxy parent/carer responses to the CHU9D
From a health and social care cost perspective at 18 months, accounting for the correlation between costs and QALYs using SUR and adjusting for baseline utility and site, the mean incremental cost per participant of ERP compared to psychoeducation was £662 (95% CI −£59 to £1384), with a mean incremental QALY calculated using the parent-completed CHU9D of 0.040 (95% CI −0.004 to 0.083) per participant and an incremental cost per QALY gained of £16,708. The cost-effectiveness acceptability plane (CEAP) is shown in Figure 11. At a cost-effectiveness threshold of £20,000 per QALY there is a 65% probability that ERP is cost-effective, increasing to 79% at a threshold value of £30,000 per QALY (see Figure 12).
FIGURE 11.
Cost-effectiveness acceptability plane QALY analysis using parent-completed CHU9D. Note: Figure in Hollis et al. 79

FIGURE 12.
Cost-effectiveness acceptability curve QALY analysis using parent-completed CHU9D. Note: Figure in Hollis et al. 79
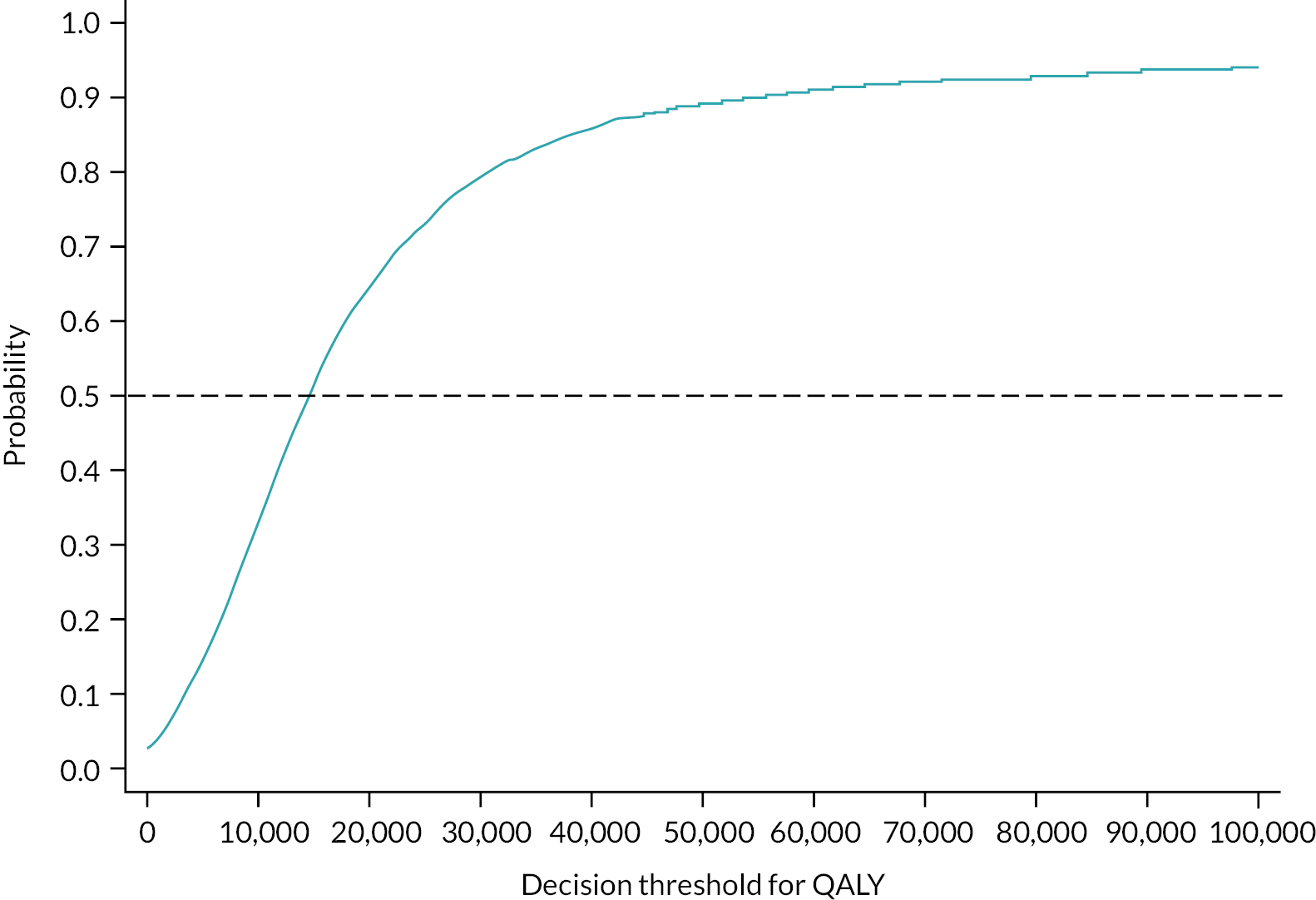
From a wider cost perspective, the mean incremental cost per participant of ERP compared to psychoeducation was £1080 (95% CI −£351 to £2510), with a mean incremental QALY calculated using the parent-completed CHU9D of 0.035 (95% CI −0.004 to 0.083) per participant and an incremental cost per QALY gained of £16,708. The incremental cost per QALY gained was £30,480, with a 53% probability of being cost-effective compared with the control at a cost-effectiveness threshold of £30,000 per QALY.
Figure 13 reports the CEAP using incremental QALYs calculated from young person self-completed CHU9D responses. The mean incremental cost per participant of ERP compared to psychoeducation was £156 (95% CI −£637 to £950), with a mean incremental QALY calculated using the young person-completed CHU9D of 0.038 (95% CI −0.015 to 0.090) per participant and an incremental cost per QALY gained of £4139. At a cost-effectiveness threshold of £20,000 the ERP intervention has an 84% probability of being cost-effective, increasing to 88% at a threshold of £30,000 per QALY gained. The CEAC for this analysis is reported in Figure 14.
FIGURE 13.
Cost-effectiveness acceptability plane QALY analysis using young person-completed CHU9D. Note: Secondary analysis: mean incremental cost per QALY gained of ERP compared to psychoeducation at 18 months is based on young person self-completed responses to the CHU9D.

FIGURE 14.
Cost-effectiveness acceptability curve QALY analysis using young person-completed CHU9D. Note: Secondary analysis: probability that ERP is cost-effective compared to psychoeducation at 18 months is based on young person self-completed responses to the CHU9D.
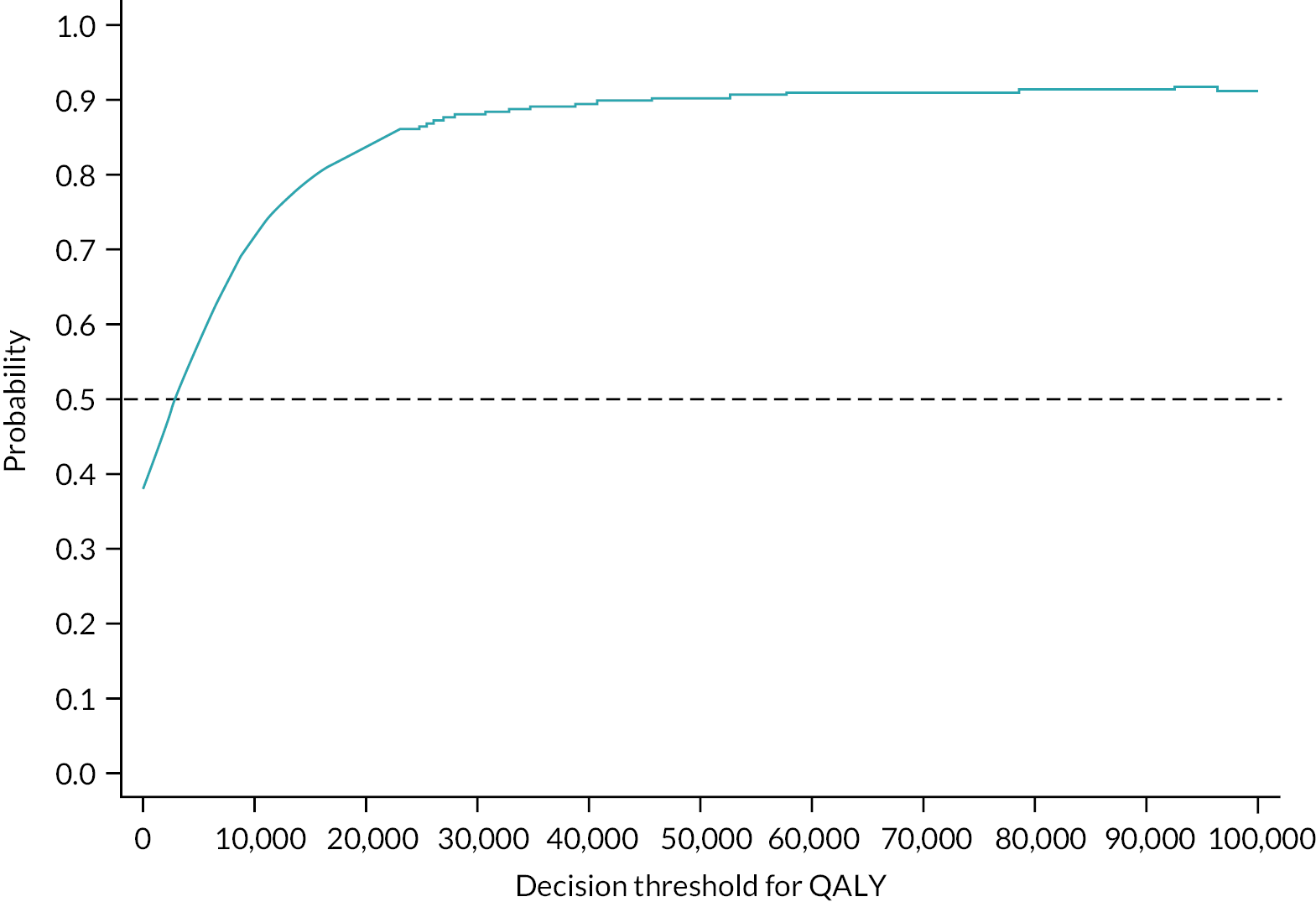
From a wider cost perspective, the incremental cost per QALY gained at 18 months is £10,053 (mean incremental cost of £381, 95% CI −£950 to £1713). The probability of the ERP intervention being cost-effective compared to psychoeducation from a wider cost perspective at a threshold of £20,000 per QALY gained is 69%, and it is 79% at £30,000 per QALY gained.
At 18 months, the incremental mean cost per patient of ERP compared with psychoeducation, including intervention costs, was £305 (95% CI −£136 to £746), with a mean reduction of −1.68 points on the YGTSS-TTSS (95% CI −3.79 to −0.43) and an incremental cost per reduction in YGTSS-TTSS (YGTSS-TTSS multiplied by −1) of £182 from a health and social care cost perspective. The ICER is reported in the CEAP in Figure 15. There is a 90% probability that ERP is cost-effective compared with psychoeducation for cost-effectiveness thresholds > £1000 per point reduction in YGTSS-TTSS (see Figure 16).
FIGURE 15.
Cost-effectiveness acceptability plane for TTSS analysis. Note: Figure in Hollis et al. 79
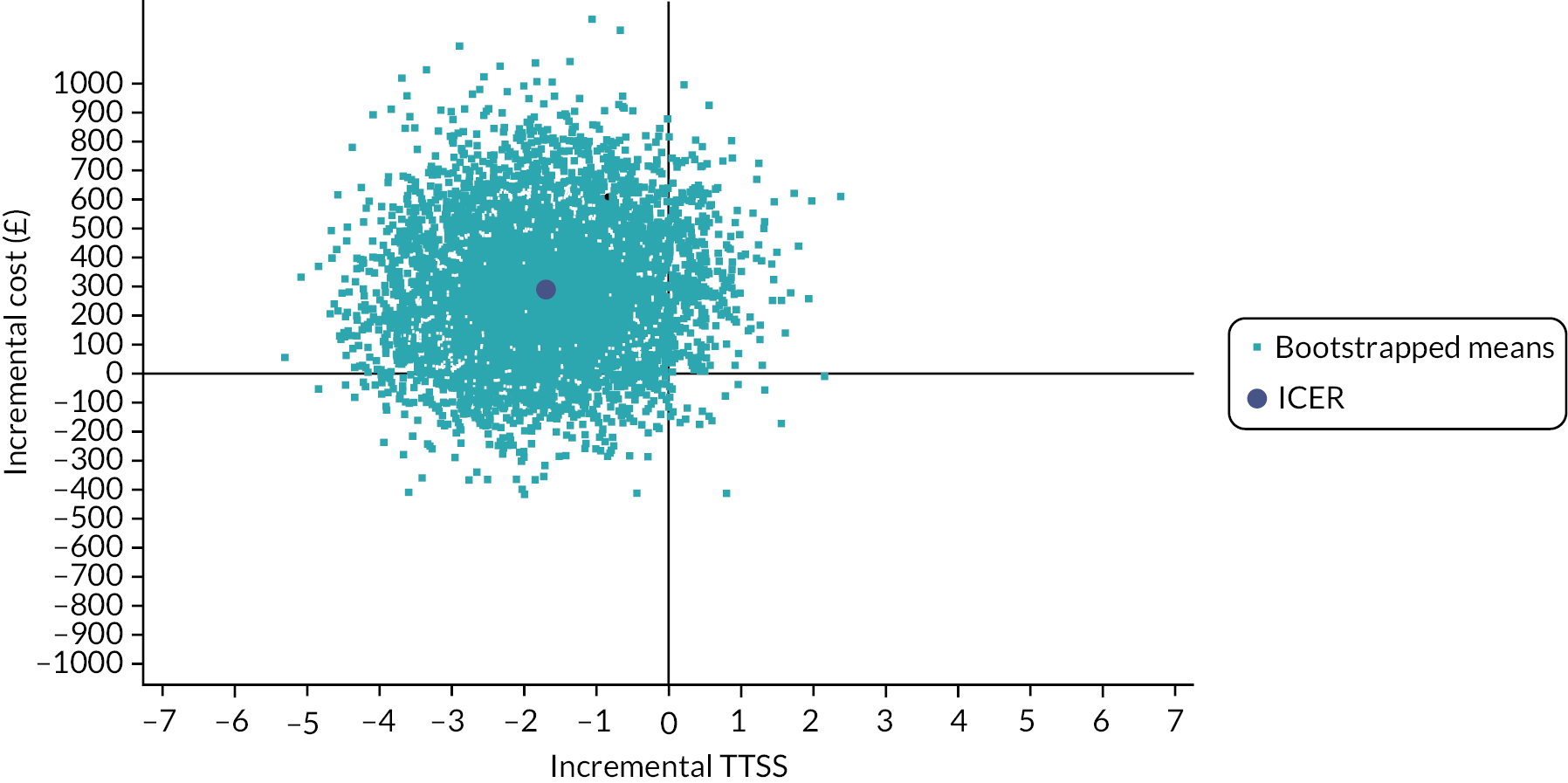
FIGURE 16.
Cost-effectiveness acceptability curve for a cost per point reduction on the TTSS. Note: Secondary analysis: mean incremental cost per unit change on the TTSS of ERP compared to psychoeducation at 18 months. Figure in Hollis et al. 79
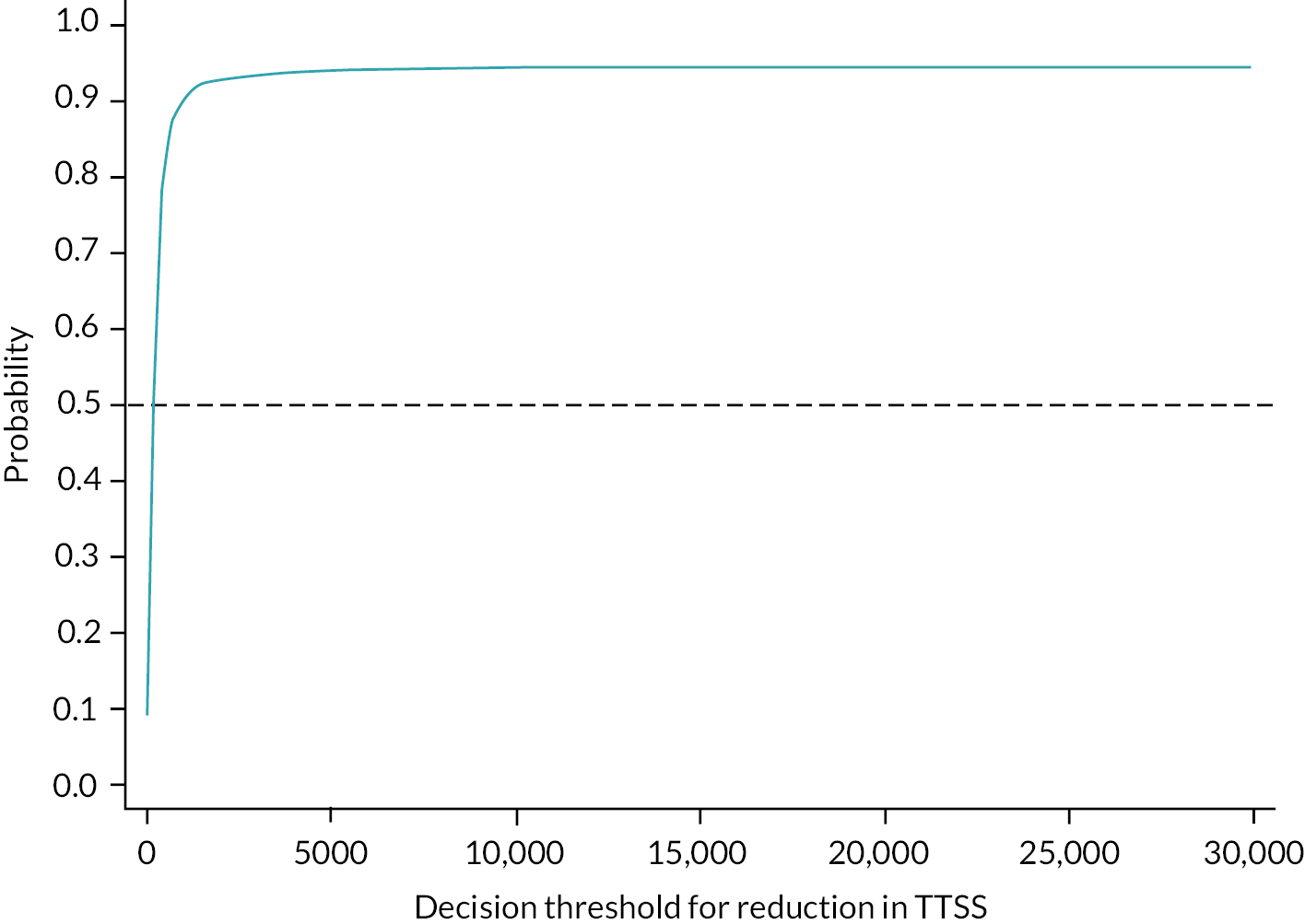
From a wider cost perspective, the incremental cost per point reduction in YGTSS-TTSS was £346.3, with an 86% probability of being cost-effective compared with the control at a cost-effectiveness threshold of £1000 per point reduction in YGTSS-TTSS. (Please note the ICER has not been multiplied by −1 so the interpretation of the plane is reversed.)
Sensitivity analysis
In order to explore how different costing models for the platform impact the cost-effectiveness of the intervention we applied a licence fee starting at £25 per participant and increasing by £10 increments up to £165. Figure 17 shows that at a licence fee of £25 per participant ERP has an 82% chance of being cost-effective at a threshold value of £30,000 per QALY gained; this falls to 77% when the licence fee was set to £165 per participant. This small range would suggest that at a threshold value of £30,000 per QALY gained there is little uncertainty around ERP being cost-effective compared with psychoeducation, even if the cost of rolling out the intervention was marginally more expensive than expected from the trial.
FIGURE 17.
Impact of different licence fees on probability of cost-effectiveness at a threshold of £30,000 per QALY gained. Note: Figure in Hollis et al. 79
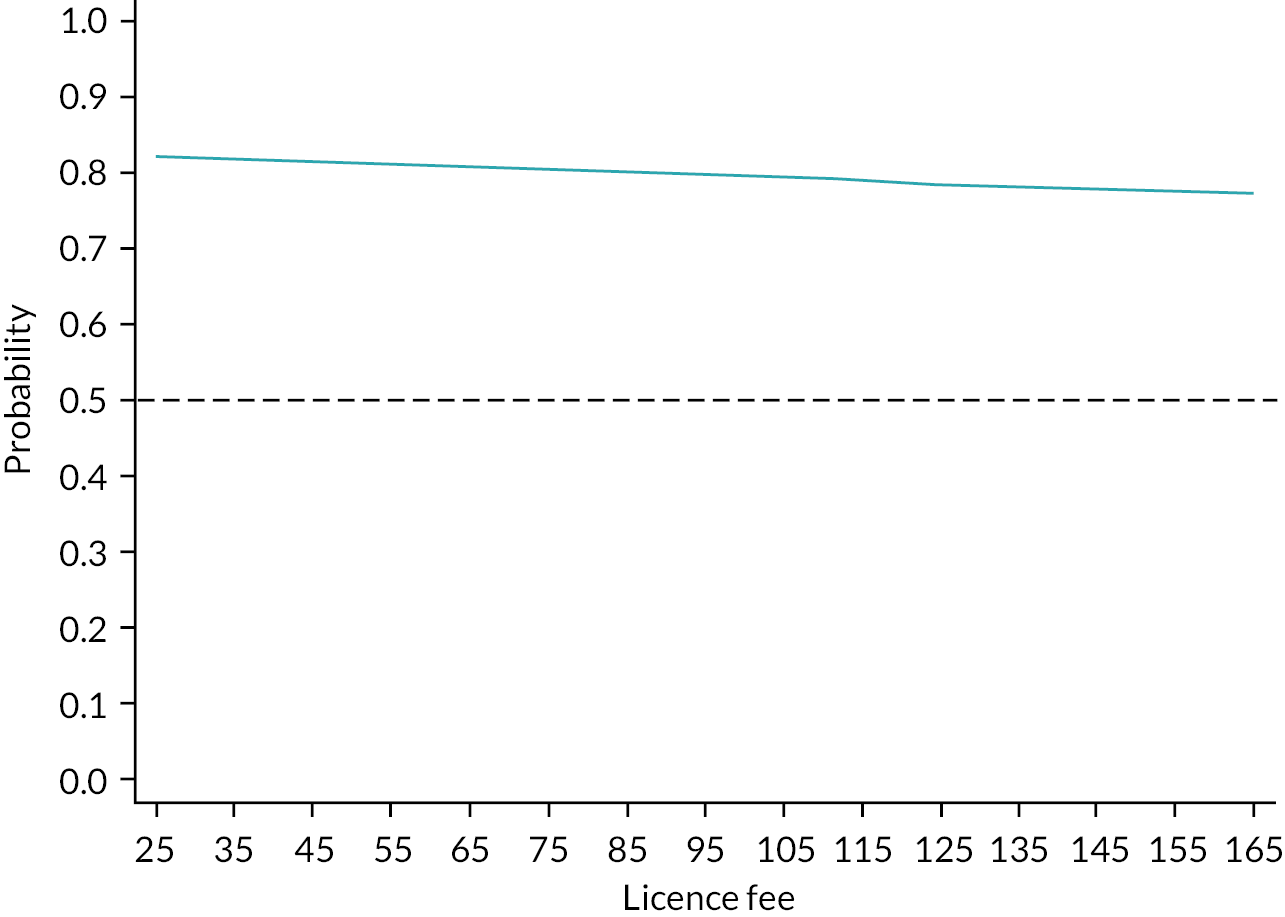
We see similar results at a threshold value of £1000 per point reduction in YGTSS-TTSS. As there is no official threshold for a point reduction in YGTSS-TTSS we also conducted this for a threshold value of £200 per point reduction in YGTSS-TTSS and found that the probability of cost-effectiveness falls below 50% at a licence fee per participant of £155 or more.
As therapists were trained during supervision, it is feasible to assume that once fully trained and familiar with the delivery of the intervention only fortnightly supervision would be necessary. When applying fortnightly supervision, the fixed cost of the intervention falls from £104 to £71. This results in an ICER of £162 per point reduction in YGTSS-TTSS and a probability of 90% of being cost-effective compared with psychoeducation at a threshold of £1000 per point reduction in YGTSS-TTSS.
Using the parent-completed CHU9D, when supervision is assumed to be fortnightly this results in an ICER of £15,885 per QALY gained, and there is an 81% probability that ERP is cost-effective compared with psychoeducation at a threshold of £30,000 per QALY gained.
Given psychoeducation was also delivered through the platform and the possibility of trying to provide this as an alternative intervention side by side with ERP but without the requirement of therapist support, an alternative sensitivity analysis added the fixed platform cost to the psychoeducation arm. This increased the probability of cost-effectiveness to 71% using parent-completed CHU9D at a threshold value of £20,000 per QALY gained and 83% at a threshold value of £30,000 per QALY gained.
Secondary analysis: 10-year decision analytic model
We report the mean total cost and QALYs accrued per participant over the course of the 10 years in the model for each intervention. After 5000 replications, online ERP cost an additional £70.76 per participant compared with psychoeducation and resulted in an additional 0.009 QALYs per participant. This resulted in an ICER of £8276 per QALY gained. CBIT cost an additional £537.38 per participant compared to online ERP and led to an additional 0.018 QALYs per participant.
Figure 18 shows the probability that each intervention is cost-effective at different cost-effectiveness threshold values. At cost-effectiveness thresholds below than £10,000 per QALY gained, psychoeducation has the highest probability of being cost-effective. ERP is cost-effective compared with CBIT at cost-effectiveness threshold values below £30,000 per QALY gained. Figure 19 shows the CEAC for ERP compared with CBIT alone; there is a > 94% chance that ERP is cost-effective compared with CBIT at threshold values of £20,000 per QALY gained or below.
FIGURE 18.
Cost-effectiveness acceptability curve showing the probability each intervention is cost-effective at a range of threshold values.

FIGURE 19.
Cost-effectiveness acceptability curve showing the probability that ERP is cost-effective compared with CBIT.
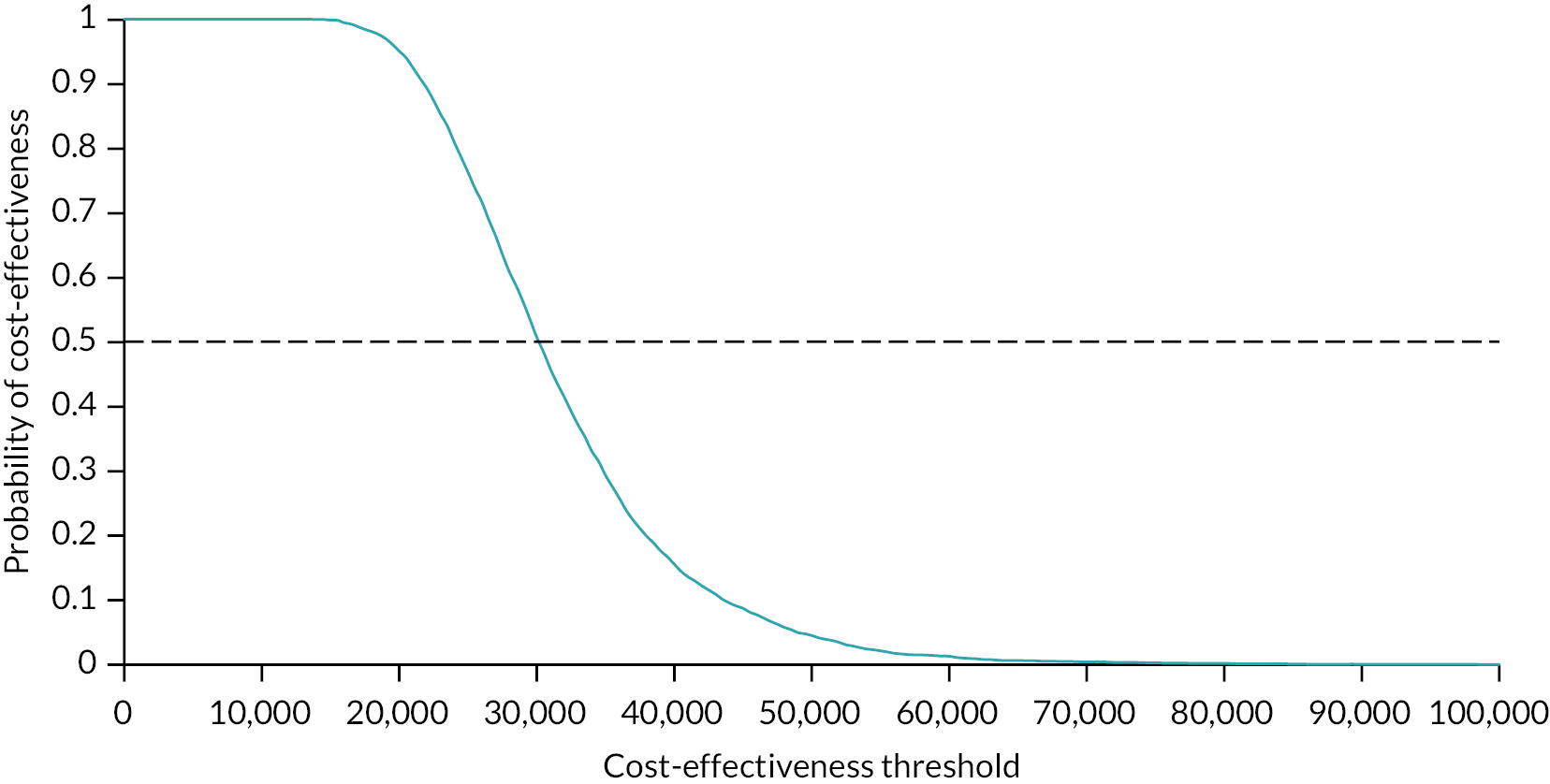
Figure 20 shows that there is a > 50% chance that online ERP is cost-effective compared with psychoeducation from threshold values of £10,000 per QALY gained or more.
FIGURE 20.
Cost-effectiveness acceptability curve showing the probability that online ERP is cost-effective compared with online psychoeducation.
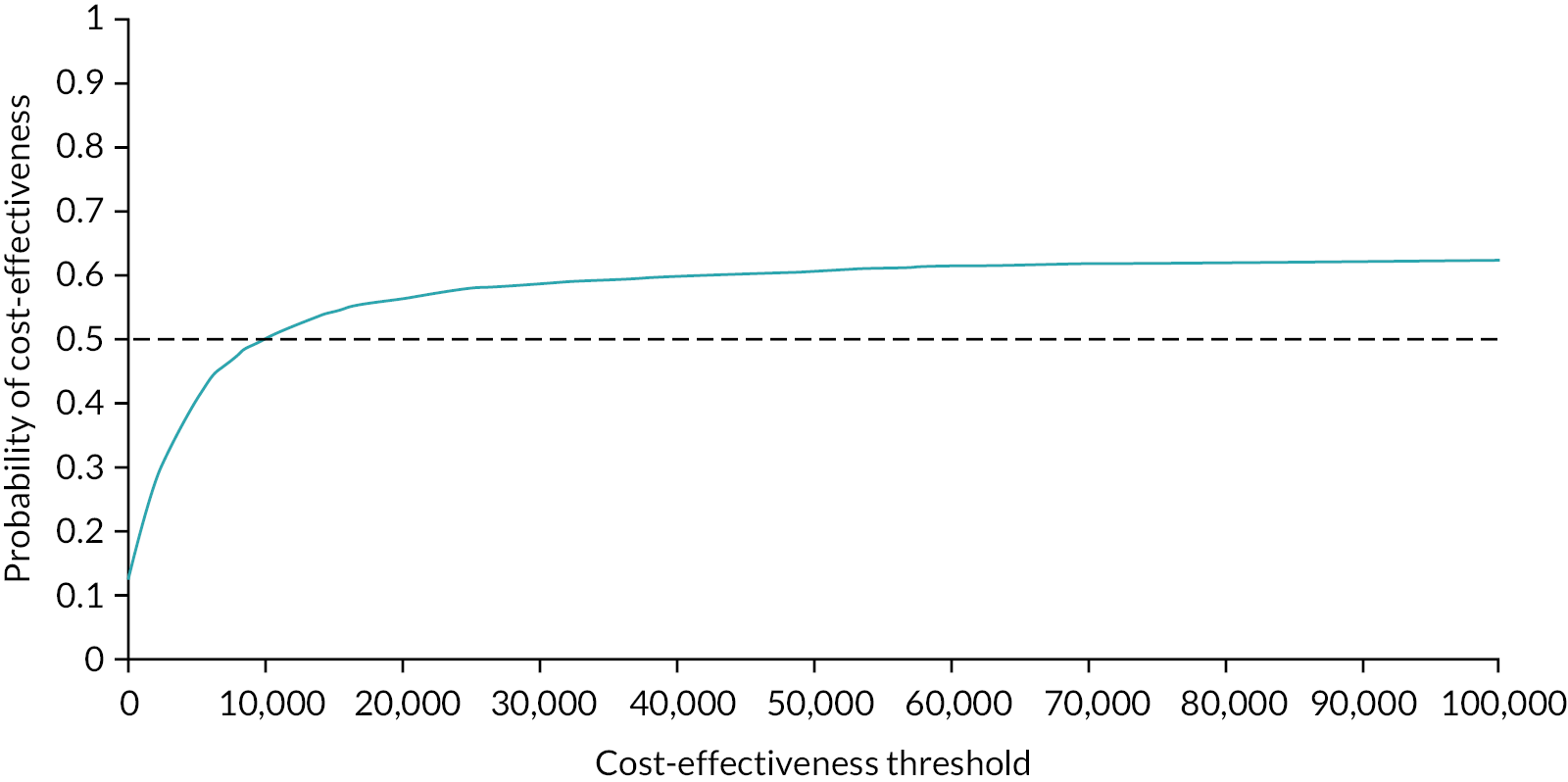
Sensitivity analysis
When the platform was assumed to work on a licence fee basis, online ERP was cost-effective compared with online psychoeducation from threshold values of £4000 per QALY gained. This analysis had little impact on the probability of being cost-effective compared with CBIT; online ERP became cost-effective up to values of £31,000 per QALY gained.
When the cost of psychoeducation was assumed to include the platform cost, online ERP is cost-effective compared with psychoeducation from threshold values of £5000 per QALY gained.
In a sensitivity analysis in which we applied a cost of £0 to online psychoeducation, online ERP was cost-effective from threshold values of £13,000 per QALY gained or more.
Applying the same transition probabilities to all of the groups also lowered the threshold at which online ERP is cost-effective compared with online psychoeducation to £3000 per QALY gained.
Conclusion
The 18-month time horizon is long enough to be able to conduct a full economic evaluation and we found that ERP has a 79% chance of being cost-effective compared with psychoeducation at a cost-effectiveness threshold of £30,000 per QALY gained. This is likely to be conservative given that psychoeducation is already better than what is widely available as treatment as usual. Moreover, the cost of the platform is not included for this group in the trial analysis as it was assumed that this information would normally be available elsewhere. When this cost is included the probability of cost-effectiveness goes up to 83%.
Most of the sensitivity analyses conducted have little impact on the results, suggesting that we can be reasonably confident that these results accurately reflect the cost-effectiveness of ERP compared with psychoeducation at 18 months. The initial naturalistic follow-up suggests that benefits of the intervention can be maintained past the initial intervention.
There was a higher probability that the intervention was cost-effective when the young person self-completed responses to the CHU9D are used to calculate QALYs, with a significant difference in QALYs in favour of ERP at 6 months. We pre-specified in the HEAP that the proxy parent/carer-completed CHU9D would be used to calculate QALYs in the primary analysis. This was due to the assumption that we might have a larger number of young people who might not compete the CHU9D, as did indeed happen. Further work is required to determine the suitability of proxy parent/carer-reported CHU9D for tics. Our work on determining health states for the model demonstrated that there was a significant difference in CHU9D proxy utility scores between mild, moderate and severe YGTSS-TTSS, suggesting that the changes in the CHU9D do correspond to the key clinical mechanism of interest in this trial: reducing tics.
The results of the long-term decision model suggest that online ERP is more than 50% cost-effective compared with the active control of online psychoeducation at threshold values considered acceptable by NICE. When we account for the cost of the platform in the online psychoeducation arm, online ERP becomes cost-effective at threshold values of £5000 per QALY gained, suggesting that if the NICE threshold is higher than this for a QALY gained it is more cost-effective to roll out online ERP than online psychoeducation using a similar platform. Even under the assumption that the cost of the active control is £0, which will be underestimating the cost-effectiveness given that it is still accounting for the benefit of online psychoeducation without the cost, online ERP is over 50% cost-effective from threshold values of £13,000 per QALY gained.
Online ERP has a > 50% chance of being cost-effective compared with CBIT at threshold values below £30,000 per QALY gained and a > 94% probability of cost-effectiveness at threshold values of £20,000 per QALY gained or below. Given research showing that the opportunity cost is likely to be closer to £13,000 than £30,000 per QALY gained, the more cost-effective intervention appears to be online ERP. 98 Moreover, even in a situation in which we were able to pay £30,000 per QALY gained for CBIT, this would not resolve the lack of therapists available in the UK to deliver this intervention. The results of the decision model suggest that the remotely delivered ERP intervention can provide an alternative to face-to-face CBIT therapy, with only minimal impact on HRQoL.
Chapter 6 Process evaluation
The information presented in this chapter has been published elsewhere. 99–102
Introduction
Parallel to the main ORBIT RCT, a process evaluation was undertaken, which followed the guidelines as recommended by the MRC’s framework on process evaluations of complex interventions. 103 ORBIT is regarded as a complex intervention because it is composed of multiple components with the potential for interactions between them and with several possible outcomes. 104 The MRC guidelines stipulate that in order to carry out a process evaluation of a complex intervention the following three key functions must be examined: (1) implementation (identifying what was delivered and how this was done or achieved), (2) mechanisms of impact (factors that contributed to the delivered intervention producing or not producing change) and (3) context (contextual factors external to the intervention that affected implementation, intervention mechanisms and outcomes).
Implementation fidelity
Implementation can refer to how an intervention can be implemented within routine clinical practice. However, this can only be achieved once an intervention has shown efficacy in an outcome evaluation. Implementation can also refer to how the delivery of an intervention was achieved within the context of a RCT and the structures and processes through which an intervention was delivered as intended. 103 This is often termed ‘implementation fidelity’. In short, implementation fidelity refers to the degree to which a study was implemented according to design or protocol. If an intervention is designed according to well-established theoretical and empirical underpinnings, including identifying ‘essential ingredients’ and their subsequent relationships with the intended outcomes, implementation fidelity is seen as crucial. 105
There are multiple benefits to a trial that rigorously assesses implementation fidelity. These include improving the validity of intervention outcomes,106,107 enabling replicability108 and aiding in the understanding of why an intervention succeeded or failed in its intended outcome (e.g. symptom reduction). 109 For example, a study may erroneously determine that the lack of impact of an intervention was caused by elements of the programme itself if no process measures were evaluated (i.e. a type III error). 110 Therefore, it is essential that a RCT that includes a process evaluation should contain a rigorous analysis of implementation fidelity.
Mechanisms of impact
The second key component involves exploring the mechanisms through which the intervention produces change. This is crucial to understanding how the effects of the intervention occurred and how these effects might be replicated in future iterations of similar interventions. 111 By exploring the mechanisms of potential impact of an intervention, a process evaluation can provide a better understanding of the causal pathways and identify any unexpected consequences. 112 Mechanisms of impact include mediators, moderators and contextual factors associated with change.
Mediators
Part of the MRC guidance for conducting an analysis of impact involves assessing the extent to which the causal assumptions underpinning the intervention can be tested through mediation. Mediator analysis refers to the examination of the mechanisms underlying an intervention’s theory of change. This means extending the fundamental assumptions from ‘if intervention A is implemented then B will occur’ to ‘if intervention A is implemented, this will lead to a change in the mediating variable or variables, which will lead to a change in outcome B’. 113 Mediator analysis is useful as it can uncover how an intervention produces change, and mediators generally have an impact during treatment.
Moderators
Moderator analysis typically involves assessing who benefits from an intervention, and a moderator generally precedes treatment. This involves an assessment of any pre-existing characteristics of the sample that may predict who will gain the most from an intervention. In the ORBIT trial, child and parent participants’ as well as therapists’ backgrounds, beliefs and circumstances may have dictated the way in which they interacted with the intervention. 102 Thus, it is important to the evaluation of an intervention to pursue contextual factors and moderator configurations in order to understand any potential variability in outcomes.
Overall, mediator and moderator analyses are key to understanding how and for whom an intervention does or does not work, which allows for an identification of ‘essential ingredients’. This will ensure that an intervention is implemented on a wider scale with only the essential components being delivered and targeted at the people who will benefit most.
Context
The final component is context, which refers to any factors external to the intervention that may have acted as barriers or facilitators to the way it is implemented or to the outcomes. The uptake and use of DHIs are largely dependent on context; thus, understanding the context is crucial to interpreting the findings and making generalisations from the results. In conclusion, a process evaluation of a complex intervention such as ORBIT is crucial to explaining trial outcomes and will aid in understanding its overall implementation.
Aims and objectives
The aims of the ORBIT process evaluation were to understand the causes of the observed behaviour change data obtained from the RCT, to explore the fidelity of intervention delivery, acceptability of the intervention and reasons for observed variations in uptake and use and to consider the resources and implementation processes required. 102
Specific objectives were:
-
to assess the fidelity, reach and dose of intervention delivery
-
to explore whether any of the intervention features were tailored for individual needs, enabling potential recommendations for adaptations
-
to explore the intervention from the perspectives of children, parents, therapists and clinicians in order to gain a deeper understanding of potential mechanisms underlying participant behaviour change whilst probing for any unexpected consequences
-
to evaluate any factors external to ORBIT that may have affected delivery (i.e. the environment and its characteristics) or whether its mechanisms of impact worked as intended
-
to consider the resources and implementation processes required for effective implementation, uptake and use of the intervention.
In this chapter, we present a planned, mixed-methods, two-phase process evaluation of the ORBIT trial following the MRC’s 2015 guidelines103 to explore the fidelity of delivery and the contextual factors influencing engagement with the intervention (phase 1) and the impact of the intervention and mediators, contextual factors and moderators of this impact (phase 2). 101
Phase 1: fidelity of delivery and contextual factors influencing children’s level of engagement with ORBIT
The phase 1 results were published in Khan et al. 99
Here we report phase 1 of the process evaluation of ORBIT. The aim of this study was to conduct the first phase of a two-stage process evaluation of ORBIT as outlined in the protocol. 101 Phase 1 focuses on intervention implementation by exploring the fidelity of delivery experienced by participants through usage statistics, reach and the acceptability of the intervention. It also investigates contextual factors associated with the observed variation in uptake and usage by examining the components specified in MRC guidelines. 103
Introduction
The MRC have developed guidelines for conducting process evaluations of complex interventions such as ORBIT. 103 In order to evaluate intervention implementation, MRC guidelines for process evaluations suggest researchers assess (1) reach (the extent to which a target audience encounters the intervention), (2) dose (how much intervention is delivered and received), (3) fidelity (the quality of what was delivered) and (4) adaptations (any modifications made to an intervention in order to achieve better contextual fit). 102 The intended target audience for ORBIT was CYP with tic disorders; however, there were pertinent questions that could be asked, such as whether there were socioeconomic biases in who was reached. In terms of dosage, the ORBIT protocol1 states that the intervention should consist of 10 individual intervention chapters following a suggested frequency and total duration of 10–12 weeks. There were four core chapters (chapters 1–4), and this was deemed the minimum requirement for treatment completion. There were six additional chapters offering information regarding reinforcement, further practise and relapse prevention. For DHIs, the fidelity of delivery of the intervention is assured by the online delivery platform. However, the intervention that is experienced by the user is highly dependent on the extent to which they engage with the intervention and use it as intended. Hence, in this process evaluation, the focus is on usage and the proportion of participants receiving the predefined ‘minimum effective dose’ of four or more chapters. 102 Finally, understanding adaptations to the intended intervention involves exploring whether these improve its contextual fit or compromise its functioning,114 or whether they represent innovation or intervention drift. 115 Participants were able to make modifications to various components of the intervention, such as the ‘tic stopwatch’, which was used to self-time the length of tic control.
Methods
Study design
This study followed MRC guidelines103 for the process evaluation of complex interventions and used a mixed-methods, longitudinal design to explore the implementation fidelity of an online intervention for CYP with tics1 and the contextual factors that influenced their level of engagement. Here, an overview of the methodology of the process evaluation, including study-specific outcome measures, is given as context to the main trial.
Participants
The sample included in the quantitative component of the process evaluation consisted of key information from all participants (N = 112) from the intervention arm of the RCT. The sample included in the qualitative component of the process evaluation consisted of interviews with child and parent participants (target n ≥ 20), interviews with all therapists delivering the intervention or supervising the therapists and interviews with referring clinicians (target n > 5).
Participants were only contacted if they gave explicit written consent to participate in an interview for the ORBIT trial and, for a child under 16, parental assent was obtained.
There were two therapists at the Nottingham study site and two at the London study site, with one supervisor at each site. The therapists were educated to graduate level and were not required to have previous experience in treating tic disorders but were trained on the platform and its contents and received regular expert supervision. Therapists received training in BT for tics during the trial. ‘Clinician’ refers to any health-care professional (usually a doctor) who was responsible for referring participants to the ORBIT trial and was purposively selected from the PIC sites. Whilst these clinicians were not explicitly involved in the ORBIT trial, the main purpose of interviewing them was to gain their views on potential implementation in routine care.
Measures
Demographic and clinical data
Demographic and clinical information was recorded from a baseline demographics questionnaire. These data included the child’s age, residence (full postcode), gender, ethnicity, parental education level and occupation, all current suspected or confirmed diagnoses and interventions and medication use.
Index of multiple deprivation
The index of multiple deprivation (IMD) is a relative measure of deprivation across seven different domains: income deprivation, employment deprivation, education, skills and training deprivation, health deprivation and disability, crime, barriers to housing and services and living environment deprivation (https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019). Based on the postcode, a rank of deprivation associated with participants’ area of residence was calculated from 32,844 small areas or neighbourhoods in England, with higher ranks indicating greater deprivation. Ranks were recoded into quintiles, with quintile 1 being the most deprived and quintile 5 being the least deprived.
Usage metrics
Online usage data were collected and recorded from participants throughout the trial. These included the following measures: number of chapters completed per child and per parent; total therapists’ time per child and per parent; individual therapists’ telephone time with participants; volume of written communication (total number of characters) submitted by child and parent via the online system; total number of logins for child and for parent; average time between each login (in days) for child and for parent; and average pages visited per login for child and for parent. 102
Satisfaction and treatment credibility
At the 3-week post-randomisation point of treatment, all participants were asked to rate treatment credibility. Two questions were asked: one relating to how well suited the participant felt the intervention was for helping the CYP to manage their tics and the other about how much better they expected to feel as a result of the intervention. The responses were on a Likert scale of 0–4 for each question, with higher scores indicating higher treatment credibility. At the primary end point, all participants were asked to rate their satisfaction with the intervention. Eight satisfaction questions were asked, with responses rated on 0–4 scales, meaning the overall satisfaction score was out of 32. 102
Semistructured interviews
In line with previous literature,116,117 four semistructured interview schedules were developed. The child and parent interview schedules were drafted and underwent revision from the main process evaluation researcher and three academics. Participant interviews aimed to elicit information regarding why they took part, their views of the content and chapters, impact of the therapy, what they found helpful or not, barriers to participation and their views of their assigned therapist. The revised drafts were sent to two dyads of the PPI group – including two children with tics – for feedback and were revised accordingly. The PPI input was invaluable, as it ensured the questions were understood by children as young as 9 years of age. 102
The therapist interview schedules were drafted and underwent revision from the main researcher and the same three academics, as well as with input from a therapist and a clinical researcher with specific expertise in the field. Therapist interviews aimed to elicit information about their role on the trial, what specific skills they felt they needed, any training needs identified, experiences of supervision and their perceptions of their interactions with participants. 102
The clinician interview schedules were drafted and underwent revision from the same team as above and were guided by normalisation process theory (NPT). 118,119 NPT attempts to identify factors that promote and inhibit the routine incorporation of complex interventions into routine practice. It also attempts to explain how such interventions work, looking not only at early implementation, but also beyond it, whereby an intervention becomes so embedded into routine practice that it is normalised. 119 As the purpose of the clinician interviews was to explore their views about the feasibility of integrating the intervention into everyday practice, including any potential barriers to or facilitators of this, the NPT framework approach seemed the most appropriate. The clinician interview schedule questions aimed at eliciting information on how they got involved in the ORBIT trial and why, their experience of recruiting for the trial, including factors that affected recruitment, and how the NHS could incorporate the intervention into everyday practice. 102
Data collection
Quantitative process data were collected simultaneously along with enrolment, intervention delivery and outcome data collection in the main RCT. Qualitative process data were collected at various time points. Interviews with therapists involved in the ORBIT trial were conducted early in the study and near the end of recruitment to gain an understanding of their experience at different time points. Interviews with referring clinicians were conducted at the end of recruitment. Interviews with CYP and parents were conducted following completion of the intervention at the 3-month follow-up assessment (primary end point) in the main RCT to minimise the risk of bias in outcomes. Recruitment for the interviews began in August 2018 and ended in October 2019.
All interviews were conducted either face to face, by telephone or via videoconferencing (Webex or Skype). Younger children were interviewed together with their parents, while older children were interviewed separately. Participants were purposively sampled so that a diverse range of views on the intervention were voiced. This included ensuring perspectives were heard from participants of a range of ages, genders, ethnicities and levels of interaction with the intervention. The overall sample enabled a diversity of views of the intervention to be expressed and ensured that data reached a level of saturation. In addition to the interviews, at the end of treatment all participants were asked to give their overall feedback on the intervention, in which they could provide open-ended responses.
Data analysis
The quantitative data set was presented with total numbers and percentages and means with SDs or medians (ranges), if not normally distributed. Data were tested for normality using the Kolmogorov–Smirnov test. A principal component analysis was run to determine a composite measure of level of engagement. Correlations between variables were examined using bivariate Spearman correlations, and t-tests were conducted to explore any significant differences between groups with chi-squared tests to explore for differences between categorical variables. A multiple linear regression was calculated to identify predictors of engagement with independent variables. All statistical analyses used a significance level of p < 0.05 and were conducted using IBM SPSS Statistics version 27 (IBM Corporation, Armonk, NY, USA).
All interviews were recorded either by videoconferencing software or by Dictaphone and were then transcribed verbatim. Transcripts were checked for accuracy against the recordings, with any corrections made as appropriate and anonymised for confidentiality purposes. As the process evaluation was a combination of exploration and description, the framework method120 of analysis was used to identify, analyse and report patterns within the transcribed interviews. Moreover, the steps outlined by Gale et al. 121 were systematically followed to create an overall framework matrix using categories of engagement and contextual factors. Consistency of analysis was ensured throughout using a codebook and through frequent meetings between researchers. Researcher bias was minimised through regular cross-checking of data and outcomes by members of the research team.
The software package QSR NVivo 12 (QSR International, Warrington, UK) was used to analyse the interview data. In addition, the end-of-treatment feedback questionnaire was exported into an Excel spreadsheet and quantitative content analysis122 was performed. Overall, the findings from the qualitative analysis were linked to relevant quantitative adherence outcomes and contextual factors to assess which potential variables might have influenced implementation fidelity and in what way, in an approach termed ‘triangulation’. 123
Ethical considerations
Ethical approval for the process evaluation was obtained from North West–Greater Manchester Central Research Ethics Committee as part of the ORBIT trial (REC: 18/NW/0079). All child and parent participants provided written informed consent and all interview participants provided oral consent for audio-recording.
Results
Overview of qualitative sample
From the intervention group, 38 children and their parents were contacted to participate in semistructured interviews. Eighteen of these did not respond or declined to participate. Overall, semistructured interviews were conducted with children (n = 20) and parents (n = 20), therapists (n = 4) and clinicians (n = 6). The average age of child interviewees was 12 years (range 9–16 years) with 16 (80%) of the sample being male and four (20%) being female. Most of the sample was white (n = 18, 90%). The mean YGTSS-TTSS was 28.8 (SD 7.2), with a range of 13–45 for child interviewees. All 20 of the interviews with the parents were with the CYP’s mother, with all 20 having completed at least further education. One of the therapist interviewees was a therapist’s supervisor and half of the clinicians were consultant psychiatrists (n = 3, 50%).
Reach
A total of 445 families expressed an interest in taking part in the study either through self-referral via Tourettes Action’s website (n = 251) or via clinic referral (n = 194); however, 47 were subsequently uncontactable and 90 were ineligible to take part for reasons such as having had BT in the last 12 months or being due to start BT, living outside of England or being an immediate risk to self/others. 102 Of the 308 potentially eligible CYP, 84 families (27.3%) declined to take part due to the child not wanting to participate, the family not wanting to attend the baseline appointment, having insufficient time or no specific reason given. Thus, 112/224 CYP (90 male, 22 female) with an average age of 12.2 years (range 9–17; see Table 4 for baseline characteristics of sample) were randomised to the intervention arm of the ORBIT trial and were included in the process evaluation. The sample was predominantly white (n = 96, 85.7%) and well educated, with just over half (n = 60, 53.5%) of the participants’ mothers having completed university/higher education. 102
The median IMD rank was 19,318, with a range of 147–32,668 (out of 32,844). Of the 112 participants, 8 (7.1%) were in the most deprived quintile (1), 31 (27.7%) in quintile 2, 18 (16%) in quintile 3, 26 (23.3%) in quintile 4 and 29 (25.6%) in the least deprived quintile (5). Although the reach of the intervention was not limited geographically, for the purposes of the research participants did have to attend a baseline screening assessment at either the Nottingham study site (n = 57, 50.9%) or the London study site (n = 55, 49.1%) depending on personal preference and/or location of residence. All participants were based in England, with 63 (56.3%) participants living in towns, 30 (26.7%) in cities and 19 (17%) in villages. 102
In terms of clinical characteristics, the intervention reached a moderately severe symptomatic sample with a mean YGTSS-TTSS of 28.4 (SD 7.7) out of a maximum of 50, with a range of 12–50. Most participants (n = 98, 87.5%) were not on any medication for their tics, and just under half of the overall intervention sample had no diagnosed or suspected comorbidities (n = 51, 45.5%). Of those who did have a comorbid diagnosis, the most common was anxiety disorder (n = 34, 30.4%) followed by ADHD (n = 26, 23.2%). An assessment of depressive symptoms by the MFQ showed a mean score of 16.3 (SD 11.3) out of 66, with 14 (12.5%) participants scoring above the cut-off (≥ 29), suggesting clinically significant depression. 124
It was not possible to interview people who had not taken part in the study, so the qualitative data threw little light on reach; however, one clinician identified that some families were worried about the level of commitment involved and associated travel to one of the study sites under the category ‘Initial response to ORBIT’ and theme clinician perceptions of and contribution to recruitment:102
So children quite often with autism … other kind of family reasons where I think they were just worried about the level of that kind of commitment to … an intervention to be able to kind of travel to Nottingham or London for the initial assessment.
(Clinician 3, psychiatrist)
Dose
Child participants completed an average of 7.5 (SD 2.7) out of 10 chapters of the intervention and their parents completed an average of 7.6 (SD 2.8), indicating high engagement. Only 13 (11.6%) child participants and 17 (15.2%) parents failed to meet the criteria for treatment completion (i.e. minimum of first four chapters completed as per protocol), with a total of 99 (88.4%) child participants and 95 (84.8%) parents completing their treatment, meaning that adherence to the intervention was high. Indeed, 46 (41%) CYP and 52 (46.4%) parents completed all 10 chapters of the intervention and only one child participant failed to complete any chapters. Child participants logged on to the online treatment platform an average of 19.8 (SD 10.9) times throughout the 10–12 weeks, with an average of 4.2 (SD 2.6) days between logins. In terms of total interactions with their assigned therapist, child participants required their therapist’s online assistance for an average of 59 minutes and 14 seconds (SD 29 minutes and 8 seconds) over the course of treatment, which results in approximately 6 minutes per child per week. Parents interacted online with their assigned therapist for an average of 1 hour, 23 minutes and 55 seconds (SD 42 minutes and 45 seconds), which results in approximately 8 minutes per parent per week. Of 112 CYP, only 2 (1.8%) were contacted by telephone by their assigned therapist. Of 112 parents, 49 (43.7%) were contacted by telephone by their assigned therapist.
Interview data relating to participants’ perceptions of ORBIT organisation (category: ‘ORBIT programme content’) covered the implementation component of dose. Although most participants felt that the intervention was just the right length, some CYP wished to have a longer period in which to access their therapist:
I just liked doing the whole bit of ORBIT and chatting to my therapist, but I think it was too short. Cause I could only chat to my therapist for 10 weeks, but then we had a full year logging on to ORBIT but we could not chat to our therapist which I found a bit annoying.
(Child 20, 12 years old)
Fidelity
At the 3-week point of post-randomisation, participants were asked to rate treatment credibility. Treatment credibility was rated highly by child participants, with a mean score of 6.4 (SD 1.5) out of 8. Furthermore, at the primary end point, participants were asked to rate their overall satisfaction with the intervention. Child participants were highly satisfied with the intervention, with a mean score of 24.8 (SD 5.2) out of a total of 32. At the end of treatment, participants were asked to give their feedback on the intervention within the online platform and they were able to give open-ended responses. Only 67 (59.8%) child participants provided this feedback. From the quantitative content analysis conducted, four categories were generated relating to implementation fidelity, namely: ‘limitations of ORBIT’ (n = 51), which captured how participants felt that overall ORBIT was helpful but was limited by certain factors; ‘ORBIT as a suitable treatment’ (n = 49), which suggested that participants felt that the online delivery of treatment for tic disorders was suitable; ‘problems with using ORBIT’ (n = 20), which captured those participants who stated that they felt ORBIT was not helpful to them or was associated with negative factors; and ‘feeling supported’ (n = 19), where participants mentioned that they felt supported in a way that they had never been before (e.g. by their therapist). 102
Although satisfaction was rated as high, some participants felt that the role of the therapist was somewhat misleading. This was captured by the theme expectations of role of the therapist (category: ‘Initial response to ORBIT’). Some felt that a therapist was not needed for the delivery of the intervention:
Like that just I don’t like emailing so I think I felt a bit awkward cause I didn’t really know how to write back but I felt most of the comments were quite generic … I don’t know just I’d say something and [therapist] be like ‘oh well done’ … but I don’t think [therapist] necessarily has to be there. I think you could have done it on your own.
(Child 21, 15 years old)
The therapists themselves concurred with this, suggesting that perhaps they should not have been called ‘therapists’ within the ORBIT study:
I think part of it would come down to whether we would want to use the word ‘therapist’ within ORBIT because there’s a lot of semantics and meaning about that word and I’m not sure off the top of my head if therapist or … what’s the lay meaning of therapist basically? Does that mean psychotherapist, does that mean someone who’s got a doctorate, who knows? So, everyone could … participants come into that with their own meaning, and it also assumes that I … they’ve got expectations about what a therapist is, it assumes that I’m the expert and I really felt like I wasn’t in this. My supervisors were experts.
(Therapist 1)
Adaptations
Regarding adaptations, the intervention did not appear to evolve in any way from the original plans. There appeared to be consistency in the way the intervention was delivered and received. Interviews with therapists confirmed how consistency was maintained in delivery. For example, they created a list of standardised responses to common queries (theme: ‘Strategies to support therapists’):
We had standardised documents, of like a collection of standardised responses so any time we’d come across something unique or difficult or not immediately obvious to answer, after sort of emailing around and reviewing potential answers we’d obviously say how to come up with an answer to send to the participant and once I’d done so, I’d add a section into the collection of responses and add it in. So basically, we had something we could look at and call upon when we see someone and go ‘look, we’re not sure how to answer that, let me check this document’ and then you can see if there was anything similar, or it’s been answered before, umm, that was very useful …
(Therapist 2)
Parts of the intervention were designed to be adapted by the user and tailored to their needs and preferences, such as the ‘tic stopwatch’ and ‘tic ladder’ (hierarchy of exposure exercises). For instance, on the ‘tic stopwatch’ participants could modify the difficulty levels of the given exercises, such as the ‘focusing on tic signals’ task, which could be altered depending on how difficult the participant found it. The ‘tic ladder’ could also be modified so that participants could add their own places to the hierarchy depending on where they tic the most frequently. This was captured by the theme ‘Adaptations’:
I had to answer questions in the chapters and when I finished it, I could go back and change it and I could change my ladder when I do my tics and where I do my tics most often and my tic list of what I have. I liked the idea that I could change it. And it helped me.
(Child 20, 12 years old)
Contextual factors influencing intervention implementation
Engagement with a complex intervention is seen as crucial in determining the effective implementation of the intervention. Thus, in order to establish a measure of intervention implementation that captured both the breadth and depth of participants’ usage, a principal component analysis with Varimax (orthogonal) rotation was conducted on the seven items relating to the dose of intervention received. The analysis suggested a two-factor model. The strongest factor accounted for 47% of the variance (eigenvalue 3.3) and seemed to capture strength of engagement with the intervention. Factor scores ranged from −2.65 to 2.26, with a mean of 0.001 (SD 0.99), and these scores were used as the engagement measure. 102
Data met assumptions of independence and linearity and did not deviate substantially from normality; therefore, parametric tests were conducted. A two-tailed t-test found that participants who were enrolled at the London site (mean 0.25, SD 0.90) scored significantly higher on engagement compared to those enrolled at the Nottingham site (mean −0.22, SD 1.03), t(109) = −2.58, p = 0.011. Moreover, those who were self-referred (mean 0.16, SD 0.94) scored higher on engagement than those who were referred through clinics (mean −0.24, SD 1.04), t(109) = −2.06, p = 0.041. Spearman’s rho correlations were run to determine the associations between engagement and various contextual factors. CYP’s engagement factor score was strongly correlated with parents’ chapter completion (ρ = 0.73, n = 111, p < 0.001) and moderately correlated with therapist time with parents (ρ = 0.46, n = 111, p < 0.001). There were no significant relationships between CYP’s engagement factor score and age, parental education, IMD, YGTSS-TTSS at baseline or MFQ baseline score. There were also no statistically significant relationships between a child’s gender, comorbidities or use of tic medication and CYP’s engagement. 102
A multiple linear regression was conducted with CYP’s engagement factor score as the dependent variable and site, child’s age, child’s gender, IMD, YGTSS-TTSS at baseline, method of referral, parental education, therapist time with parents and parents’ chapter completion as the independent variables. The results of the simultaneous regression indicated that collectively the independent variables accounted for a significant amount of variance in the CYPs engagement factor score, F(10,100) = 20.84, p < 0.001, R2 = 0.64. There was no evidence of multicollinearity, with all tolerances above 50% and all variance inflation factors below 2. Only parents’ chapter completion [β = 0.69, t(110) = 10.18, p < 0.001] and therapist time with parents [β = 0.19, t(110) = 2.96, p = 0.004] were significant independent predictors in the model. 102
Under the framework category ‘participant contextual factors’, the theme of parental persuasiveness was generated. Many of the parents interviewed outlined that they were often the main motivating force behind their child’s level of engagement by reminding their child to practise the learnt techniques:
If he’s got a really bad tic and I’ll say to him you know, [child’s name] use your tic timer in your head, try and see how long you can do he will then do it … but he doesn’t really use the techniques himself without being reminded to … So I suppose that was a little bit of a disappointment.
(Parent 15, mother)
Discussion
This first phase of a two-stage process evaluation used a mixed-methods approach to investigate the extent to which the ORBIT intervention was implemented as planned within the context of an RCT and to explore participants’ experiences with the intervention and the contextual factors influencing children’s engagement. 102 In doing so, this made it possible to identify reasons for variation in uptake, usage and engagement, to reflect on how implementation may ultimately give greater confidence in the outcomes and to outline lessons for potential future implementation within routine care. Uptake of the intervention was high, with nearly 90% of participants receiving the predefined minimum effective dose of the first four chapters completed. The median uptake was eight chapters, and only one child failed to access any chapters. Fidelity of delivery was also excellent, with participants reporting high levels of satisfaction and acceptability. 102
The intended sample of CYP with a diagnosed tic disorder was reached, with 7.1% of families residing in the most deprived areas (IMD quintile 1) and over a quarter (25.6%) of the families residing in the least deprived areas (IMD quintile 5). As over half (53.5%) of the CYP’s mothers had completed graduate-level education against a UK average of 42%,125 it seems that more advantaged families may have been over-represented. This is a concern, as one of the aims of ORBIT was to increase access to evidence-based therapeutic interventions for CYP with tic disorders,100 particularly as access to services is generally limited for those from lower socioeconomic status backgrounds. 126 Although the initial baseline visit with associated travel may have been a disincentive to more disadvantaged families, this would not be relevant if ORBIT was delivered entirely remotely in routine care rather than as part of a RCT. Moreover, there was no evidence that socioeconomic factors influenced CYP’s engagement with ORBIT. Furthermore, a child’s age, severity of tics, well-being and comorbidities did not appear to influence their level of engagement with the intervention, providing further evidence that the intervention would have a wide reach within routine clinical care. However, due to the various factors relating to this RCT specifically as opposed to routine care, caution should be taken when interpreting the results from this study concerning reach. 102
London study site, self-referral and higher parental engagement were all associated with higher levels of child engagement. The London site is a world-renowned centre of excellence for paediatric care, which may have increased parents’ motivation for treatment. However, the only independent predictor of child engagement in the multivariate analysis was level of parental engagement with the intervention, as measured by their chapter completion and by parent time with the therapist. This is consistent with previous literature,127–129 which found that parental involvement was particularly key for younger CYP to assist with their engagement with therapeutic interventions, which in turn leads to better outcomes. 130–132 It has been shown in the literature that parental engagement may impact a provider’s ability to implement parent- and family-focused evidence-based treatment with fidelity. 130 Therefore, it is crucial to understand the role of parental support for the implementation of DHIs for children, as without attention to the key processes of child and family engagement efforts to improve the effectiveness and efficiency of the treatment are less likely to succeed. 100
An interesting finding relates to the usage and interactions with the therapist within this study. Therapists interacted online with their assigned child participants for an average of approximately 6 minutes per child per week, which is lower than the 24‐minute average time per week participants interacted with their therapists in the Swedish pilot trial of the BIP platform. 43 In the UK, study therapists were encouraged to use pre-prepared scripts to respond to participants. Their responsibilities involved reinforcing the ORBIT treatment material, with the aim of spending approximately 6 minutes per week responding to each child, which was in the therapist guidance given by supervisors. It was also apparent from qualitative interviews that many participants felt that the term ‘therapist’ was somewhat misleading. Some participants felt that ‘therapist’ had connotations of a clinically trained individual delivering an intervention. This may have limited their reliance on the therapist. Therefore, in any implementation of this intervention within routine health care, it would be sensible to alter this title to ‘coach’, ‘guide’ or ‘mentor’ to better reflect the role of the therapist. 102
Conclusions
In conclusion, the intervention had high fidelity of delivery and was evaluated positively by CYP, although some participants suggested some minor improvements, and reach may have been constrained by the nature of the RCT. Parental engagement was a strong, independent predictor of intervention implementation, which has important implications for the design and implementation of digital therapeutic interventions into CAMHS. 102
Phase 2: factors influencing the effectiveness of ORBIT
The phase 2 findings have been published in Khan et al. 100 and also Khan. 102
Here we report phase 2 of the process evaluation of ORBIT. The aim of this study was to conduct the second phase of a two-stage process evaluation of ORBIT as outlined in the protocol. 101 Phase 2 focuses on the impact and contextual factors influencing effectiveness as well as factors moderating and mediating the relationship between implementation of the intervention (child engagement) and the impact of the intervention on tic severity and clinical improvement. 102
Introduction
Although BT is effective and avoids the unpleasant side effects associated with medication, access to therapy is limited due to insufficient numbers of specialists and the uneven geographical distribution of services relative to demand. 21 DHIs have been shown to be effective for a range of neurodevelopmental disorders in CYP, including tic disorders, and thus offer potential to widen access to evidence-based behavioural treatments. 133 However, despite an expanding body of evidence to support the acceptability and effectiveness of online therapy, uptake of DHIs into clinical practice has been disappointing. 134 Previous research has focused on intervention outcomes, with little attention given to the mechanisms of impact: the way in which the intervention components and participants’ responses to the intervention produce change. Knowledge of how and why a DHI works increases the potential for replication across contexts. 103 Furthermore, understanding mechanisms of impact is crucial for assessing core components of an intervention (e.g. ‘essential ingredients’), which helps with defining the minimum therapeutic dose. 102
There are no studies in the tic disorder literature assessing mechanisms of impact of digital interventions; however, studies of face-to-face BT for tics have suggested that clinical factors can moderate the effectiveness of behavioural treatment. Sukhodolsky et al. 135 found that the presence of tic medication significantly moderated impact. For participants receiving 10 weeks of BT, medication status did not impact on effectiveness. In contrast, participants in the psychoeducation and supportive therapy group who were receiving medication showed significantly greater tic reductions than participants not on medication. Tic phenomenology, age, gender, family functioning, treatment expectancy and comorbidities did not moderate response to treatment. A more recent study that examined moderators of treatment outcome after adolescents with CTD received either individual or group therapy found that a higher level of anxiety and a higher premonitory urge to tic favoured treatment in groups, whereas increased sensitivity and higher depression symptomology favoured individual treatment. 55
This second phase of the process evaluation study uses qualitative and quantitative data to explore the contextual factors influencing effectiveness and the factors moderating and mediating the relationship between implementation of the intervention (level of child engagement) and the impact of the intervention on tic severity and clinical improvement. 102 This provides insight into how and why outcomes occurred under given circumstances and what mechanisms underlie these impacts. To the best of our knowledge, this is the first study to examine potential mediators and moderators of an online intervention delivered to CYP with tic disorders. 102
Methods
Study design
This study used a mixed-method, longitudinal design to explore the mechanisms of impact of an online, therapist-supported, parent-assisted ERP intervention for CYP with tics delivered via the BIP TIC platform. 43 The study used quantitative analyses to explore contextual factors, mediators and moderators of impact and qualitative analyses to illuminate those relationships in more depth.
Participants
Participants were CYP randomised to receive the active intervention (N = 112) and their parents. Participants were purposively sampled to represent views from a range of ages, genders, ethnicities and levels of interaction with the intervention. Four therapists and six referring clinicians agreed to participate in semistructured interviews.
Measures
Outcomes
The primary outcome for assessing impact was the tic severity change score as measured by the YGTSS-TTSS4 at the primary end point (3-month post-randomisation) minus the YGTSS-TTSS at baseline. In this trial, the range of YGTSS-TTSS scores at baseline was 12–50. Hence, possible scores on the tic severity change measure could range from 38 (maximum possible deterioration) to −50 (maximum possible improvement in tic severity). The secondary outcome measure used was the CGI-I. 65
Child engagement factor score
In order to establish a comprehensive measure of child’s level of engagement with the intervention, a principal component analysis with Varimax (orthogonal) rotation found that seven variables loaded on the engagement factor representing higher dose of intervention received more logins, more chapters completed, more therapist time for child (SMS-based support), greater total number of characters submitted to therapist within the online platform, fewer days between logins, fewer number of pages visited per login and less telephone contact by the therapist (engagement prompts). 99
Contextual, mediator and moderator variables
Based on previous research on BT for tic disorders and theoretical assumptions,135,136 as well as recommendations about the domains that should be included when conducting moderator and mediator analyses in paediatric RCTs,137 the following four potential mediator variables were selected: depression change (as measured on the MFQ),7 anxiety change (as measured on the SCAS),138 treatment satisfaction (Likert scale: overall satisfaction 0–32) and treatment credibility (Likert scales: how well suited and how much better do you expect to be from treatment 0–8). Treatment satisfaction and credibility scales were constructed by the research team. The following seven potential moderator variables were selected that would potentially influence the strength of the relationship between intervention (level of engagement) and efficacy: medication use, comorbidity, parental support (number of chapters completed), baseline tic severity (as measured on the YGTSS-TTSS), age, deprivation (as measured on the IMD) and mother’s level of education. Contextual variables are those that directly influence level of effectiveness, and they were selected based on findings from phase 1 of the process evaluation and outcomes from the exploratory correlational analyses. 102
Data collection
The data collection is described in detail in the process evaluation protocol101 and elsewhere within this monograph.
Data analysis
Data were tested for normality using the Kolmogorov–Smirnov test. A repeated-measures analysis of variance (ANOVA) was initially run to determine an effect on tic severity over time. The effect size of the intervention was calculated using Cohen’s d. 139 Spearman correlations were used to analyse relationships between the outcome variables (YGTSS-TTSS change and CGI-I) and all contextual, mediator and moderator variables. This was done to establish whether a relationship between the variables existed prior to the next stage of analysis. Mediator analyses were conducted using the bootstrapping indirect effects method using the PROCESS macro in SPSS. 140 Contextual variables were examined in a multiple linear regression model. Moderators were examined using regression models. Each potential moderator variable was considered in turn. To formally assess the statistical significance of any observed effect moderation, a multiple linear regression model was fitted with the inclusion of an interaction term between the child engagement factor score and the moderator variable. 102
Each variable was centred prior to its inclusion in the mediator and moderator models; continuous variables were centred at their respective means, while binary variables were recoded as −0.5 and 0.5 (rather than 0 or 1). Centring refers to the subtraction of the overall mean from each observation. Therefore, each variable is ‘zeroed’ at its own mean. Centring the data aids interpretation of mediator and moderator analyses and diminishes the effects of multicollinearity. 141 Given the exploratory nature of the mediator and moderator analyses, we did not correct for multiple comparisons. 142 All data used a significance level of p < 0.05. All statistical analyses were conducted using IBM SPSS Statistics version 27.
Results
Impact
Primary outcome
A repeated-measures ANOVA with a Greenhouse–Geisser correction determined that mean YGTSS-TTSS statistically significantly differed between baseline and the primary end point [F(1,100) = 39.71, p < 0.001]. There was a reduction in YGTSS-TTSS from baseline (mean 27.92, SD 7.17) to the primary end point (mean 23.87, SD 8.18) in the group that had received the intervention, and this was statistically significant (p < 0.001). Cohen’s d for the pre–post change in YGTSS-TTSS was 0.5, indicating a moderate effect. 102
Secondary outcome
Of 101 participants in the active intervention group, 36 (36%) were classified as ‘responders’, with their condition rated as being ‘very much improved’ or ‘much improved’ on the CGI-I. Thirty-seven (37%) were rated as ‘minimally improved’, 18 (18%) were rated as having no change in their condition and 10 (9%) were rated as being minimally worse. No participants were rated as being much or very much worse in their condition since the initiation of treatment. 102
Correlations
Spearman’s rank correlations were used to analyse associations between all contextual, mediator and moderator variables and the primary (YGTSS-TTSS change) and secondary (CGI-I) outcomes. Only YGTSS-TTSS at baseline (ρ = −0.26, p < 0.001) was statistically significantly correlated with YGTSS-TTSS change so that higher scores at baseline were associated with a greater decrease in tic severity at the primary end point. Child engagement factor score (ρ = −0.23, p = 0.02) and parental chapter completion (ρ = −0.25, p = 0.01) were statistically significantly negatively correlated with CGI-I, suggesting that CYP with high levels of engagement with the intervention and CYP with parents who completed more chapters showed better overall clinical improvement at the primary end point.
Table 29 shows the intercorrelations between YGTSS-TTSS change score, CGI-I and contextual, mediator and moderator variables.
| Variable | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. TTSS change | 0.51** | −0.05 | 0.11 | 0.07 | −0.05 | −0.08 | 0.09 | 0.05 | 0.01 | −0.26** | 0.13 | −0.04 | −0.02 |
| 2. CGI-I | – | −0.23* | 0.04 | 0.02 | −0.12 | −0.06 | 0.05 | −0.25 | −0.25* | 0.05 | 0.03 | 0.00 | 0.13 |
| 3. Child engagement factor score | – | −0.01 | 0.08 | 0.47** | 0.31** | 0.04 | −0.19* | 0.73** | 0.08 | −0.14 | 0.18 | −0.01 | |
| 4. MFQ at baseline | – | 0.63** | −0.25* | 0.05 | −0.15 | 0.02 | −0.12 | 0.30** | 0.06 | 0.03 | 0.03 | ||
| 5. SCAS at baseline | – | 0.04 | 0.11 | −0.07 | 0.24* | −0.07 | 0.26** | 0.02 | 0.06 | −0.04 | |||
| 6. Treatment satisfaction | – | 0.56** | 0.08 | −0.21 | 0.23* | −0.13 | −0.19 | 0.08 | −0.21 | ||||
| 7. Treatment credibility | – | 0.12 | −0.14 | 0.24* | 0.01 | −0.34** | 0.24* | 0.05 | |||||
| 8. Medication status | – | 0.03 | 0.00 | −0.04 | 0.02 | 0.00 | −0.08 | ||||||
| 9. Comorbidity status | – | −0.13 | 0.10 | −0.14 | 0.04 | −0.20* | |||||||
| 10. Parent-completed chapters | – | −0.01 | −0.22* | 0.16 | −0.02 | ||||||||
| 11. TTSS at baseline | – | −0.02 | −0.16 | −0.06 | |||||||||
| 12. Age | – | −0.08 | −0.07 | ||||||||||
| 13. IMD | – | 0.21* | |||||||||||
| 14. Mother level of education | – |
Contextual factors influencing impact
Following on from the correlational analysis, we explored whether parental engagement was an independent contextual predictor of YGTSS-TTSS change and overall clinical improvement (CGI-I). Multiple linear regressions were conducted with parental chapter completion, IMD and maternal level of education as the independent variables. There was no evidence of multicollinearity, with all tolerances above 50% and all variance inflation factors below 2. The results of the simultaneous regression indicated that collectively the independent variables did not predict YGTSS-TTSS change. However, the independent variables did explain a statistically significant amount of variance on CGI-I, F(3,97) = 3.14, p = 0.029, R2 = 0.09. Parental chapter completion [β = −0.10, t(100) = −2.41, p = 0.018] was the only significant independent predictor in the model. 102
Mediators
Simple mediation analyses found that the relationship between child’s level of engagement (child engagement factor score) and either tic severity change (YGTSS-TTSS change) or CGI-I was not mediated by depression change (MFQ change), anxiety change (SCAS change), treatment satisfaction or treatment credibility. 102
Moderators
A moderator analysis was conducted to assess whether medication use, comorbidity, parental chapter completion, YGTSS-TTSS at baseline, age, deprivation (IMD) or mother’s level of education moderated the relationship between child’s level of engagement (child engagement factor score) and either of the outcome variables YGTSS-TTSS change or CGI-I. No variables were found that moderated the relationship between child engagement factor score and outcome in terms of either YGTSS-TTSS change or CGI-I. 102
Framework categories
From the analysis of the qualitative data, three categories were generated relating to participants’ perceptions of the impact of the ORBIT intervention: ‘Mechanisms of impact’, ‘Intervention outcomes’ and ‘ORBIT programme content’ (see Appendix 2, Table 32 for full analytic framework categories and themes).
Mechanisms of impact
This framework category tried to determine how the intervention had worked. Within the theme features of online therapy to support tic reduction, CYP highlighted the need to practise and how the interactive aspects of the intervention had helped with their tics (quote 1, see Appendix 3, Table 33). Others mentioned that the extent to which they were able to visualise how the treatment and ‘tic cycle’ worked had helped them (quote 2). This visualisation also enabled child participants to see how and which tics were increasing or decreasing in severity or frequency.
Other participants felt that the use of the reward system motivated them to complete the practices within ERP (quote 3). Parents explained how during the middle of treatment their children began to disengage with the intervention and thus introduced the reward system, which reignited their motivation levels (quote 4).
Conversely, some participants felt that the nature of online therapy posed certain barriers that might have impeded its impact, with some CYP saying that they would have preferred face-to-face therapy. This was captured by the theme limitations of online therapy (quote 5). This theme also captured the frustration some felt at not receiving an immediate response from their assigned therapist (quote 6). One parent spoke about how their internet connection was substandard and found it quite frustrating whenever the treatment programme could not be accessed (quote 7). 102
Parental chapter completion was a contextual factor that was significantly associated with clinical improvement. Qualitative analysis also highlighted the importance of the extent to which CYP received support from their parents in completing the treatment. CYP appreciated being able to complete the therapeutic activities and chapters with their family members. This was captured by the strong theme working together (quote 8). Parents also seemed to appreciate this time spent working together as a team, which they felt may have led to more positive outcomes (quote 9). One parent explained how the added complication of comorbid ADHD meant that she had to arrange a suitable time and place to enable her child to feel sufficiently relaxed to complete the chapters (quote 10). Although the working together theme was largely related to the parent-and-child relationship, some parents did appreciate having therapist support. They particularly seemed to appreciate having an expert on hand if they required their assistance on anything that they were unsure about (quote 11). Finally, one of the clinicians suggested that parental support seemed to be the key factor of this online intervention (quote 12). 102
Intervention outcomes
From this category, various themes were gathered that outlined the impact that the intervention had on CYP and parents. The theme improvement in tics showed how participants felt that the intervention had allowed the severity and frequency of their tics to dissipate (quote 13). For one child participant in particular, the intervention did not have an impact on the overall severity and frequency of their tics; however, it did allow them to better understand their premonitory urges (referred to as ‘tic signals’; quote 14). 102
From the theme expectations versus reality, some parents thought that the intervention would be more effective than it had been and were somewhat disappointed by the outcome (quote 15). Finally, from the theme improved self-esteem and confidence, some parents also noticed how there was an improvement in their child’s related psychological symptoms because of the intervention (quote 16). 102
Online treatment content
In terms of what are known as ‘essential ingredients’, these were captured by the theme useful and enjoyable program resources. This theme elucidated how participants found certain components of the intervention to be the most impactful. Most CYP found the ‘tic stopwatch’ (timing how long they can suppress their tics) and ‘tic ladder’ (hierarchy of tics) to be the most useful to them (quote 17). Many participants were also attracted to the videos and animations, which some found to be engaging and an effective alternative to large quantities of text presenting key information (quote 18). Parents also stated that they liked the videos, as they clarified the ways in which they should deliver the therapeutic techniques to their children (quote 19). 102
Finally, under the theme lack of fit between content and child, some older participants found the content and presentation of some of the materials in the intervention to be ‘child-like’ and aimed more towards younger children (quote 20). One of the therapists agreed with this sentiment but felt that due to the large age range involved in ORBIT they had to cater to all participants (quote 21). 102
Discussion
In this second phase of the process evaluation, we examined the impact of the intervention in terms of reduction in tic severity and global clinical improvement. Within the active intervention group, tic severity was reduced by four points from baseline to 3-month follow-up with a Cohen’s d effect size of 0.5, and 36% were rated as ‘very much improved’ or ‘much improved’ on the CGI-I. A further 37% showed some improvement. This process evaluation, which aimed to understand mechanisms of impact, found that only tic severity at recruitment was associated with reduction of tic severity post-intervention. Level of usage as captured by the child engagement factor score99 was not associated with improvement in tic severity; however, higher levels of child engagement and higher parental chapter completion were associated with higher levels of overall clinical improvement. Only parental chapter completion was independently associated with CGI-I scores. No mediators or moderators were identified for either reduction in tic severity or clinical improvement. There may have been a lack of power to detect mediators and moderators for the relationship between usage and impact of the intervention due to the high level of overall uptake and the relatively modest impact compared to face-to-face therapy. 3
Engagement and parental support
Although child engagement with the intervention led to better overall improvement at the primary end point only on one of our outcome measures, the CGI-I, the findings of this study are broadly consistent with the literature. 143 Additionally, the association between parental chapter completion and positive outcomes is also consistent with previous research. 130,132,144 The findings from this study suggest that parental involvement worked through encouraging CYP’s engagement, which led to positive outcomes, as CYP who were interviewed in the qualitative component of the current study emphasised that parental support was key to their levels of engagement. As parents had their own chapters to work through, they appeared to gain more knowledge of their child’s tics and were able to understand them better. Furthermore, both CYP’s and parents’ accounts of their experiences frequently cited being able to work together as a team as one of the main drivers of how they conducted their time on ORBIT. It was clear from the interviews that ORBIT managed to facilitate a symbiotic relationship between child and parent, which may have led to its impact. 102
In terms of what are known as ‘essential ingredients’, this study appeared to shed some light on what these may constitute. Specific features such as the video demonstrations of therapy, animations, the ability to visualise which tics were increasing or decreasing in severity and frequency on the ‘tic ladder’ and the ‘tic stopwatch’ were all highlighted in interviews as important mechanisms of impact. Indeed, these interactive components were identified as key features of the intervention that seemed to be used most. This is consistent with evidence that interactive elements, including attractive audio-visual material, are amongst the most highly used features of DHIs as they tend to maintain users’ interest. 145,146 This would be especially important to younger children whose concentration levels would not be maintained with material that was simply presented in writing, for example. Whilst many of the younger children appreciated the graphics and animations, older children felt they were somewhat ‘child-like’. However, there was no evidence from the quantitative data that child age influenced engagement99 or efficacy. 102
Mediators and moderators
The absence of significant findings in the mediator and moderator analyses in this study suggests that treatment efficacy was not significantly affected by the sociodemographic or clinical characteristics of participants. Furthermore, interviews with parents, children and therapists also failed to reveal any perceptions of clinical factors influencing outcomes. Therefore, the findings from this study suggest that ORBIT is appropriate for a wide demographic of CYP with tic disorders, regardless of parental education or deprivation, age, baseline tic severity, tic medication use, anxiety or depression levels or comorbidities. The lack of statistically significant findings is encouraging for clinical practice, suggesting that health-care specialists can confidently recommend this digital intervention to most families. 102
There may be some potential explanations as to why no significant mediators or moderators were found. As a process evaluation, this study only included participants in the active intervention arm. Thus, we explored factors moderating the relationship between level of engagement and outcomes rather than the relationship between group membership and outcome. This meant that the sample size was diminished, thus creating low statistical power. It is well established that large sample sizes and substantial power are necessary to be able to detect mediator and moderator effects. 147
Conclusions
Overall, the intervention had a positive impact on participants as it reduced the severity of their tics and improved overall clinical condition. This study found that parental engagement was a significant contextual predictor of overall improvement of tics; however, there was no evidence of mediators or moderators of outcomes of the online ERP intervention delivered to CYP with tic disorders. The results of these analyses suggest that engaging parents is a key factor in successful outcomes and that whilst online therapy seems to be an effective alternative to face-to-face therapy for CYP with tic disorders there is no subgroup that is more or less likely to find this treatment beneficial. This is a positive finding from a clinical perspective, as it suggests that ORBIT can be implemented within routine health care for a broad range of CYP with tic disorders. However, more research needs to be carried out in this area with larger sample sizes and with a primary focus on the potential mediators and moderators of impact in order to fully understand the mechanisms through which online therapy has its desired effect. 102
Overall discussion
The aims were to conduct a mixed-methods process evaluation of an ERP intervention for CYP with tics delivered online with therapist and parental support. Specific objectives were to assess the extent to which the intervention was implemented as part of a trial and the contextual factors that influenced child participants’ level of engagement, as well as to evaluate the overall impact of the intervention, the mechanisms through which it achieved its impact and the factors influencing its overall efficacy. 102 In doing so, this process evaluation aimed to contribute to the wider understanding of how online BTs for CYP can improve outcomes and, more broadly, the factors influencing CYP’s engagement with DHIs and the potential resources needed in order to implement online ERP for CYP within routine clinical practice.
Overall, these findings contribute to our understanding of the way in which DHIs work and what is required to make their impact more successful. As some studies have shown that digital technology can be used to reduce symptoms in CYP with tic disorders, this process evaluation contributes to the wider knowledge of the underpinnings of their mechanisms of action. 102 Table 30 provides a summary of the key findings from the process evaluation and their potential application to practice.
| Key finding | Application to practice |
|---|---|
| - Minimal contact time with therapist | - Therapists could be employed on a part-time basis in any future roll out, thus cutting costs |
| - High fidelity | - Greater confidence in trial outcomes and the intervention is acceptable and satisfactory to patients |
| - Level of parental engagement predicted child level of engagement and better overall improvement in symptoms | - In future roll out, ensure parents are involved as much as possible |
| - ‘Therapist’ name misleading | - Alter the name of ‘therapist’ to ‘e-coach’, ‘guide’ or ‘mentor’ |
| - Interactive components such as the video demonstrations of therapy, animations, ‘tic ladder’ and the ‘tic stopwatch’ were all identified as ‘essential ingredients’ | - Utilise these components more frequently in future roll out |
| - No significant findings in the mediator and moderator analyses | - Suggests that the intervention is appropriate for a wide demographic of patients with tic disorders, regardless of parental education or deprivation, age, baseline tic severity, tic medication use, anxiety or depression levels or comorbidities |
Strengths and limitations
This study marks a comprehensive evaluation of a digital intervention delivered to CYP with tic disorders. This understanding is important in order to fully understand the circumstances under which such interventions are likely to be effective, for whom and maximise their efficacy. 148 In addition to explaining intervention-specific processes, the findings also contribute to the currently limited knowledge regarding how CYP and their parents engage with digital interventions to manage complex symptoms. Furthermore, it provides evidence of the feasibility and utility of digital interventions amongst a youth population. 102
There are several strengths within the design of this process evaluation, which was carried out concurrently with the ORBIT trial. A particular strength was that the methodology was based on a peer-reviewed published protocol,101 which is considered ‘best practice’ within process evaluation research. The sample involved in the semistructured interviews and within the intervention group was comparable in terms of age, gender and baseline YGTSS-TTSS. As stipulated in MRC guidelines,103 a mixed-methods approach was undertaken in the form of an integrative mixed-methods design. Moreover, the qualitative data offered a more in-depth evaluation to participants, therapists and referring clinicians’ perceptions and experiences with ORBIT and were able to capture outcomes that the quantitative data set could not. 102 Furthermore, the analysis of intervention usage data provided a detailed and objective insight into the important features and underlying determinants central to the implementation and effectiveness of this intervention. As recommended,103 process evaluation data were analysed prior to the trial findings being known, thus avoiding a biased interpretation of the data.
Another major strength of this study is the use of an objective, comprehensive measure of a child’s level of engagement with the intervention. By using a principal component analysis of dose of intervention received, we were able to capture an innovative measure of engagement, which could be replicated in future designs of such studies. Several strategies were utilised to strengthen the validity of the qualitative analyses. A multidimensional perspective was achieved by considering both CYP’s and parents’ as well as therapists’ and referring clinicians’ perceptions. 149 A subset of the transcripts was also double coded and disagreements in coding were discussed, strengthening the validity and reliability of the qualitative data. A further strength of the qualitative data was the use of PPI in guiding the semistructured interview questions. 102
Despite these strengths, this study and the subsequent findings should be interpreted with caution due to several limitations. Firstly, it was difficult to recruit participants for interview who had either dropped out of the ORBIT trial early or were not deemed treatment completers, and thus the data may have been skewed towards more positive experiences of the intervention. Limitations relating to the quantitative data set must also be considered. This study was embedded within a trial, which limited the sampling frame. Although the ORBIT trial was one of the largest in online tic disorder research, for the purposes of the mediator and moderator analyses in particular the sample size was somewhat underpowered. Therefore, the lack of statistically significant findings within these analyses may have been due to the lack of power, and so such results should be considered as exploratory. Finally, whilst process evaluations tend not to assess the control arm, doing so might have strengthened the generalisability of the overall findings while giving a more holistic view of ORBIT. 102
Implications for research and practice
The findings of this process evaluation have implications for potential research in this area. Primarily, it would be important for any future work to overcome the limitations highlighted above. 102 Indeed, a more intensive effort to recruit participants who did not engage satisfactorily with digital interventions or dropped out early would be welcome. This would enable researchers to gain a more holistic understanding of the implementation and mechanisms of action and prevent the findings from being skewed towards more positive experiences. 102
Future RCTs of complex interventions should consider the integration of quantitative process data from the outset, which could then provide further insight. More broadly, it would be valuable for future studies of complex interventions for CYP to include process evaluations. These should include objective usage metrics and longitudinal qualitative data. Finally, and most crucially of all, future research should consider how this evidence-based online ERP intervention can be made deliverable in routine NHS care, thus giving more people access to much-desired non-pharmacological treatments. 102
As discussed, tic disorders and associated conditions are highly debilitating, having a profound impact on both CYP and their parents. A range of tic-related difficulties with academic work and social and emotional well-being in CYP have been reported. Considering these tic‐related impairments and implications for future life, knowledge of the best treatment options for tic disorders in CYP is clinically important. 102 Children and their parents generally prefer BT over medication due to the fewer associated adverse effects;21 however, the most widespread mode of treatment is pharmacotherapy. 12
Therefore, the findings from this process evaluation have important implications for practice in a myriad of ways. They show how CYP engage with complex interventions and the importance of parental support and motivation, identify those who benefit the most from such interventions and, more broadly, show how DHIs can be designed and implemented in order to maximise their efficacy. 102 Most importantly of all, the findings demonstrate that an online intervention is effective, can be delivered with high fidelity and is highly acceptable to CYP with tic disorders, and that there is no subgroup who benefits the most. This has important implications for how this intervention could be delivered to patients within the UK. An online intervention that could be deployed to large numbers of patients at a relatively low cost is a much-needed and seemingly acceptable means of providing patients with access to an evidence-based treatment. It could provide immediate access to ORBIT for those who otherwise would not have access due to long waiting lists or their geographical location, which could also potentially free up existing resources and services for those requiring more complex treatment and assessment. 102 Such cutting of costs and waiting times would represent a two-fold benefit for the NHS and patients alike.
In addition, one of the barriers to reach identified was the associated travel to the baseline assessment. It would therefore be sensible to have an initial remote assessment. As the use of remote medical assessments has increased due to the COVID-19 pandemic, this flexible approach would allow even more people to benefit from this intervention. 102 As already discussed, it is also recommended that the term ‘therapist’ should be altered to avoid high expectations of their role. Furthermore, the ‘therapists’ could be employed on a part-time basis and would require very little training, which would cut costs even further. As the findings indicate, ‘therapists’ should engage the parents as much as possible to achieve successful outcomes.
Conclusions
This mixed-methods study is a comprehensive assessment of the processes underlying a complex online intervention delivered to CYP with tic disorders using MRC guidelines as a framework. 150 Overall, ORBIT is an effective and acceptable means of delivering an evidence-based ERP treatment to CYP with tic disorders and supporting them in overcoming barriers to accessing this therapy. Whilst some CYP may require additional support from their parents to enhance their level of engagement with the intervention, there is substantial evidence that this online intervention is a promising means through which these debilitating and complex symptoms can be addressed. 102
Chapter 7 Patient and public involvement
Aim
The overarching aim of the PPI work in the ORBIT trial was to collaboratively involve CYP with tic disorders and their parent/carers at all stages of the ORBIT trial. Specific objectives included:
-
to inform the refinement of the intervention from Swedish to English
-
to incorporate the experiences of young people and their parent/carers to inform patient-facing documents
-
to advise on how to maintain patient and public interest in the trial throughout its lifespan
-
to assist in interpretation and presentation of the data to the public.
Method
We partnered with Tourettes Action [Tourettes Action (tourettes-action.org.uk)], a national charity, in order to facilitate PPI in this study.
As part of this, we developed a core PPI panel, consisting of four young people with TS and their parent (in all instances, the parent was the mother). The panel was recruited via Tourettes Action and known by contacts through clinical co-applicant.
As the initial step, the method in which the families wanted to be involved was established. All families wanted to remote contact, which was partially driven by concerns of ‘ticcing’ in front of other families/new people, and partially driven by the fact the PPI group were geographically spread over England. Although a budget was provided for PPI travel, the families stated they would find it difficult to find the time.
There were no specified meetings with the PPI group, although they received a monthly update from the trial manager to ensure they were kept informed of progress.
The PPI group were invited by the trial manager to contribute to all relevant tasks. The tasks were outlined via emails, with suggested deadlines for response to agree/decline the request. If they agreed to provide feedback/support to the task, the trial manager either setup a phone/videoconference or emailed further details (mode of contact was chosen by the families). Most contact was arranged for the evenings and/or weekends to avoid conflicting with school/work time. The task was then discussed in more detail, with opportunities for questions. Feedback on the task was either provided to the trial manager in real-time (i.e. a discussion over phone/videoconference) or in written form at a later agreed date. In all instances, the trial manager provided summary feedback explaining how their support had informed the development or design of the trial documents/materials/procedures.
The families were informed they could decline any request and they would still be part of the PPI group, unless they decided they did not want to have continued involvement. No families withdrew from PPI support.
PPI input was conducted throughout the trial, from start to finish. The key areas of input were:
-
refining the therapy from Swedish to English
-
advising on how to deal with Christmas and other holiday breaks in providing continuing access to the ORBIT intervention
-
developing patient-facing documents and reviewing outcome measures
-
advising on promoting continued engagement/recruitment to the trial (with specific input from Tourettes Action)
-
inputting into interview schedules as part of the process evaluation
-
supporting analysis of interview data
-
reviewing dissemination plan and contributing to lay dissemination materials.
We also had a lay member on our TSC, Neelam Gurvav, a parent of a young person with tics, attended all of our TSC meetings, and she provided excellent input throughout.
Results
The resulting impacts of PPI will be discussed in relation to each objective.
Refining the therapy
Once the initial content of the interventions had been finalised, both interventions were sent out to review with two parent–child dyads from the PPI panel and two members of the MindTech Involvement team.
The two parent–child dyads were given a login respectively to the child and parent/supporter interventions. Each PPI member was provided with a feedback form (Microsoft Word format) to complete alongside going through the intervention. They were provided with 4 weeks to review the intervention.
Several changes were made to the two interventions (child and parent/supporter) based on feedback:
-
inclusion of a ‘warning’ at the beginning of both interventions that the intervention would be about tics, therefore potentially making the child tic more when engaging with it (suggestibility of tics)
-
reducing length of some videos and/or cutting one video into two videos
-
ensuring all audio on videos was the same volume
-
reducing text on lengthy webpages
-
correcting spelling errors/typos and clarifying sentences and text lost in translation
-
both interventions having three ‘characters’ with tics – feedback suggested that these were better as cartoons and not as photos.
These changes resulted in the final versions of the ERP and psychoeducation interventions described in Chapter 2.
Therapy breaks
As a result of consultation with our PPI panel, there was unanimous agreement that continuing therapy over festive periods such as Christmas would be too difficult for families. Issues around changes in routine, family visits and festive activities would make it difficult for families to log in. As a result of this, we placed a substantial amendment for REC/HRA approval in April 2018, which allowed the 10-week intervention to be delivered over a 12-week period, with a maximum of 10 weeks of therapist support. This allowed families to take a holiday or deal with unexpected life events.
Developing patient-facing documents and outcome measures
Our PPI panel reviewed all of our patient-facing documents, such as participant information sheets, therapy manuals and supporting documents. The main feedback was to make these as brief as possible; as such, where possible, information was removed or shortened and subheadings were put in to break up the information.
Our PPI panel also reviewed our chosen outcome measures. The group was informed as to which documents were standardised and so changes to wordings or removing specific items were not possible and which measures had been created by the trial team and were able to be changed. The group was supportive of all of the chosen outcome measures, indicating that they felt they were all important. The group particularly commented on the need to measure other outcomes (such as anxiety and low mood). As such, no changes to outcome measures were made based on the PPI review.
Encouraging engagement and study uptake
As noted previously, potential participants could register their interest in the trial through the Tourettes Action webpage as well as through our own study webpage. Thus, our PPI partners were a key part of trial recruitment. Indeed, 251/445 (56%) people who registered interest in the trial were self-referred.
Alongside our charity partners, Tourettes Action, we developed a social media strategy to ensure that the ORBIT trial was maintained in the public eye. Consultation with our PPI panel indicated that families would rather view/listen to a video blog than read a written blog.
Our research team created monthly video blogs and ‘spotlight on researcher’ profiles that were hosted on the Tourettes Action webpage. Each member of the research team completed their blog, and in their blog they informed the public what it is like being a researcher/therapist/trial manager.
This approach kept the public informed about ORBIT and served to educate on what research entails. Anecdotally, the team noticed an increase in self-referrals to the trial after a blog was posted, suggesting that the approach may be successful in promoting recruitment to trials.
When we reached key milestones, such as finishing recruitment, we also created video blogs to inform the public and wider audience of this. These were hosted on the Tourettes Action webpage and on our study webpage.
Interview schedules
As part of the process evaluation, we developed interview schedules in order to carry out interviews with a subset of children and parents involved in the trial. The interview schedules were drafted and underwent initial revision from the process evaluation research team. The team then sent the revised drafts to parent–child dyads of the PPI group – including two young people with tics – for feedback. Most of the comments from the young people related to making sure the questions asked were simple enough to be understood by the younger participants. After their feedback, the schedules were revised accordingly. The PPI input at this stage was invaluable, as it ensured that the questions were understood by children as young as 9 years of age.
Analysing data
We also approached two members of our PPI group to help analyse a proportion of the interview data emanating from the process evaluation; however, due to time constraints and the COVID-19 pandemic, they were not able to do this task. Moreover, the young people from our PPI group felt that the analysis would be too complex to carry out with no formal training.
Dissemination
Members from our PPI group – including two young people with tics – have provided extensive feedback on aspects of our dissemination strategy.
This PPI panel supported our researcher in co-creating a lay summary of the main trial findings. This summary document has been emailed to all participating ORBIT families and includes a link to an online video blog. The video blog provides a brief, spoken summary of the results aimed at a lay audience.
The PPI panel also advised that video blogs were again preferable over written summaries for wider dissemination. The PPI panel reviewed draft video scripts, provided feedback and approved the final product. To achieve this wider dissemination, the video blogs were hosted on the Institute of Mental Health social media accounts (Twitter, webpage) and on those of Tourettes Action.
We had planned to host a free, online event to be held on an evening and aimed at families to discuss the findings of ORBIT. However, on advice of our PPI panel, this has been placed on hold. The PPI group felt that until the intervention was closer to being offered outside the trial, families may be disappointed or frustrated to learn that this clinically effective intervention is not available in routine care. We have thus postponed this event until we are closer to achieving this aim. The agenda is drafted and includes one of our PPI parent–child dyads giving a short talk where they will discuss their experiences of being involved in the ORBIT trial.
We also invited ORBIT PPI members to the MindTech National Symposium in December 2021 as part of their continued development and training on digital technologies in mental health. At this event, there was a talk provided by Seonaid Anderson (formally of Tourettes Action) that was dedicated to the PPI activities. The talk detailed the methods of involvement and outcomes/impacts on the trial and was well received.
Equality, diversity and inclusion
Participant representation
Our participants were predominately white, British; however, this is reflective of the clinical population presenting to clinical services with tics in England. We adopted a wide approach to recruitment, including self-referral via adverts from national charities. By allowing referrals from people not being seen by specialist services we hoped to broaden the range and characteristics of people who could participate. We also noted that although our participants did encompass a range of socioeconomic groups, overall our group was of slightly higher socioeconomic status than the general population. We anticipate that this may be due to having one of our research sites in London, where people are likely to have higher earning status than those in rural/northern areas. We did, however, have patient identification sites in the north to try to ensure wider representation. Our process evaluation revealed that treatment outcome was not significantly affected by the sociodemographic or clinical characteristics of participants. Thus, participant characteristics did not mediate/moderate the study outcome. 100
Research team
Our research team included patients, public members and research members of different ethnicities and socioeconomic backgrounds and with representation from all areas of England. Our PPI activities have been described. Our team also included a mixture of male and female clinicians and academics, including senior and junior members. Junior members were provided with training and experience in clinical trial design, management and PPI.
Discussion
Patient and public involvement was an integral part of the ORBIT trial, integrated from start to finish and involved in all key steps.
Our two core channels of PPI involvement were through the national charity Tourettes Action and through our panel of PPI parents and young people. We believe combining both was a particularly effective approach in PPI. Tourettes Action allowed us to reach a larger audience and to develop a national profile with regards to the trial. This platform was pivotal in not only facilitating recruitment, but also educating the public on the aims and outcomes of the trial. In contrast, our PPI panel allowed us to get in-depth critical opinions and advice on key study documents and dissemination materials, as well as informing our dissemination strategy. Both approaches bought a different but complimentary angle to our PPI.
The key areas where PPI was particularly important were recruitment, retention and dissemination. Facilitating self-referrals into the study via Tourettes Action contributed over half of the total number of initial referrals into the trial and was a key part in achieving the recruitment target within time. Furthermore, not only did our PPI provide direct input into the patient-facing documents, they also co-developed the strategies for engagement/retention and dissemination. The success of this is likely to be reflected in our excellent recruitment rate and retention to the primary outcome, continuing until the 18-month follow-up.
We would have liked to have had face-to-face communication with our families as well as attendance at our team meetings. Although we did offer this, it was not taken up by any of our PPI members. Reasons for this included issues with time to travel, taking time away from school/work and not feeling comfortable with ‘ticcing’ during meetings or around strangers. However, by being flexible in our communication style with families we were able to keep our original PPI panel throughout the trial. We believe that offering the mode of communication that suited them at a time that suited them (usually outside traditional work hours) and providing sufficient time and feedback on tasks were key to facilitating this. It is also important to note that the members of our PPI group were reimbursed for all of their activities in line with INVOLVE guidelines on PPI payments.
There were some limitations in what we achieved with regards to PPI involvement in terms of analysis. As mentioned, we approached members of our PPI team to analyse a subset of interview transcripts for the process evaluation; however, this was not feasible as a result of the COVID-19 pandemic, lack of training for the young people and time constraints. There have been studies in which PPI members have been formally trained in qualitative analysis and in which the analysis is conducted collaboratively with researchers in face-to-face workshops. Due to the pandemic and time constraints, such an approach was not feasible. In hindsight, we could have conducted workshops via videoconferencing; however, this would have been difficult to achieve due to the complexity of the qualitative analyses.
Despite this, the PPI involvement in ORBIT was largely successful. Dr Seonaid Anderson, who supported the trial as part of her previous role in Tourettes Action as well as her position as a freelance neurodiversity consultant (Neuro-Diverse | Dr Seonaid Anderson, neurodiversity consultant), summarised the PPI on ORBIT:
-
HUGE collective research AND clinical expertise in the ORBIT team
-
genuinely include people in the different stages of their research, not just to have them as participants
-
actively listened to my expertise in terms of how to reach potential participants
-
were creative and adaptable in their style of reaching an audience
-
innovative in creating videos to explain what the study was about and videos about results.
Dr Seonaid Anderson, December 2021
Reflections
Overall, PPI has been a crucial element of the ORBIT trial, which has been integral to the study’s design, delivery and dissemination. The impact of this involvement was overwhelmingly positive, and there were no negative outcomes associated with PPI; however, we note the limitation regarding the involvement of the PPI in the analysis of the intervention. Having an adequately costed PPI budget was crucial to support the delivery of this important aspect of the work.
Our research team consisted of a combination of researchers with previous experience of PPI (such as the trial manager), alongside more junior members with limited or no experience. Utilising the trial manager as the main point of contact enabled junior members of staff to learn about PPI involvement and thus supported their development as researchers. In the initial application, we had suggested that co-applicant S. Brown would facilitate most of the PPI activities. Brown provided support and guidance on PPI where needed; however, given the level of involvement that our PPI group had, it was more efficient and effective for this to be led by the trial manager, who had a more comprehensive understanding of the trial progress and need for PPI.
Although we did not have any set meeting dates, we still were able to facilitate and benefit from regular PPI input, and the use of monthly newsletters ensured that the PPI families were kept abreast of the trial progress. This approach of more flexibility with meetings/task involvements was novel to our research team, with previous research following more specified meetings and areas for input. However, we feel that ORBIT was a good example of true PPI collaboration that facilitated meaningful involvement. The fluid approach was preferred by our PPI families, which may be a result of the characteristics of our group (i.e. young children with tics and potential anxiety regarding participating in group meetings).
Our PPI partner, Tourettes Action, particularly our key contact, Dr Seonaid Anderson, provided the expertise in the topic area and lived experience of the population to facilitate PPI involvement. The charity played a key role in PPI and in offering a route to identify families to form the PPI panels. This meant that PPI was straightforward, present and meaningful.
Chapter 8 Discussion
Sections of this chapter have been reproduced from Hollis et al. ,78 under licence CC-BY-4.0.
To our knowledge, ORBIT is the first adequately powered RCT of ERP BT for tics. ORBIT also represents the largest trial of any behavioural treatment for tics and the first trial to examine the effectiveness of an online, internet-delivered behavioural intervention for tics in CYP compared to an active control condition. A key driver of the ORBIT trial is the lack of access to face-to-face BT for CYP with tics due to a lack of highly trained expert therapists. The overarching aim of ORBIT was to develop a clinically effective and cost-effective digital online behavioural intervention to close this treatment gap.
Key findings
The trial results support the clinical and cost-effectiveness of the online delivery of therapist-supported ERP for tics. Analysis of the primary outcome (tic severity at 3 months post-randomisation) indicated a significant effect in favour of therapist-supported ERP compared to supported psychoeducation (effect size = −0.31). Importantly, the therapeutic effect was durable, with a slightly increased effect size at the 6-month follow-up (−0.36). Compared with the psychoeducation comparator, participants were twice as likely to show a positive treatment response with the ERP intervention, with just under half (47%) having responded positively by the 6-month follow-up. In the ERP arm the YGTSS-TTSS was reduced by 16% at 3 months and by 25% at 6 months. Consensus clinical opinion is that these reductions are clinically important, as is the doubling of clinical response within the online ERP arm compared to psychoeducation. The reduction in tics associated with the ERP behavioural intervention was similar in those with and without coexisting anxiety and ADHD diagnoses. Additionally, secondary outcomes indicate that online ERP for tics also had a beneficial impact on anxiety, low mood and overall functioning, although caution is needed in interpreting these secondary outcomes, which involved significant amounts of missing data.
Long-term follow-up studies of any treatments for chronic tics have been exceedingly rare. This is the first controlled study to demonstrate the long-term effectiveness (beyond 6 months) of ERP for tics. The extended naturalistic follow-up showed sustained long-term effects of the ERP intervention for tics for up to 18 months after the start of treatment. The effect size of online ERP compared with psychoeducation was larger at 12 months (−0.36) than at the end-of-treatment 3-month primary end point. At 12 months, 46% were classed as responders to online ERP, with this increasing to 55% at 18 months. In addition, extended follow-up showed those receiving online ERP compared with online psychoeducation had reduced scores for low mood and anxiety at 12 and 18 months and superior tic-specific QoL, with the largest effects seen at 18 months.
In the naturalistic follow-up beyond 6 months, participants were free to access tic medication and therapy as clinically required. However, very few participants (< 10%) started new treatments during the extended follow-up period, although at least half were classed as non-responders. This highlights the lack of availability of behavioural treatment for tics in the UK outside this trial, with so few receiving treatments during the extended follow-up, although many needed it. Hence, this naturalistic follow-up essentially represents an intention-to-treat, parallel-group, long-term 18-month follow-up of online ERP for tics in CYP.
The total therapist contact time in the current trial was approximately 2.5 hours compared to 9–10 hours in comparable evidence-based face-to-face BT for tics.
The health economic analysis showed that the ICER for the cost per QALY analysis falls below the NICE cost-effectiveness threshold commonly used in health technology assessments of £20,000 per QALY gained. There is a 65% probability that the ERP intervention is cost-effective at this threshold.
The process evaluation showed that the ERP intervention had high fidelity of delivery and was evaluated positively by CYP, although some participants suggested some minor improvements and reach may have been constrained by the nature of the RCT. Only parental chapter completion was independently associated with clinical improvement. No other mediators or moderators were identified for either reduction in tic severity or clinical improvement.
Study successes
The trial recruited ahead of time and target, reflecting a significant unmet treatment need in the population. Acceptability and safety of the intervention were high. Retention rates to the 3-month primary outcome end point (90%) and 6-month follow-up (> 80%) were excellent. Retention rates to the primary outcome measure remained high at 12 months (81% in both arms) and 18 months (> 79% in both arms). Treatment adherence was high in both groups, with 88% in the ERP group and 94% in the psychoeducation group achieving the minimum treatment ‘dose’ specified as completion of the first four chapters for both interventions.
The participants in this trial had a moderate to severe level of baseline tic severity (mean YGTSS-TTSS 28.4, SD 7.7), which is approximately 0.5 SD higher than reported in previous face-to-face behavioural treatment trials2,5 and is representative of caseloads seen in routine care. The trial design minimised the clinical comorbidity exclusions, resulting in a sample broadly representative of real-world clinical practice, and included participants with autism spectrum disorder, a group usually excluded in similar behavioural intervention trials. In the behavioural intervention group, just under a third had a coexisting anxiety disorder and just under a quarter had ADHD. A relatively small proportion of participants (13%) were concurrently receiving tic medication. A particular strength of the design was the inclusion of an active comparator arm controlling for non-specific effects of therapist contact, homework assignments and online access. PPI has been a crucial element of the ORBIT trial, which has been integral to the study’s design, delivery and dissemination.
Limitations
The study has several limitations. First, despite being the largest trial to date of a behavioural intervention for tics, it is also the first adequately powered trial of therapist-supported, online ERP, and further replications are required. Second, it is not possible in this trial to separate the effects of digital online delivery and ERP. In future, clinical and cost-effectiveness comparisons of digital online versus face-to-face ERP/CBIT will be needed. Third, there remains the question of the ‘digital divide’, whereby some people do not have sufficient access to the internet and smartphones. This could have potentially limited the reach of this internet-delivered ERP intervention. While this does not appear to be an issue in the UK, with 90% of households having access to the internet and 98% of young people owning a smartphone according to the Office for National Statistics,151 it may be an important consideration when generalising these findings to other countries or vulnerable groups with lower levels of online access. Fourth, whilst the sex distribution is typical of a tic disorder population, a large proportion of the sample was white, which may limit the generalisability of the findings with regards to ethnicity. Fifth, the levels of tic medication use and comorbid OCD diagnoses were lower than in comparable studies conducted in the USA, which may limit generalisability to these populations. Sixth, while the level of tic severity in ORBIT is higher than in comparable studies and is representative of tic severity seen in ‘real-world’ practice, the findings may not be generalisable to those young people with tics outside the severity range of this study population. Finally, it is important to note that the delivery of this study was via two study centres with expertise in tics. Although the therapeutic content was delivered online, it is important for safeguarding that there is adequate supervision of the therapists supporting the intervention. It would be important in the future to evaluate the best model for national roll-out, including the benefits and cost-effectiveness of decentralising the therapist role and providing training to each site to support local delivery or to operate as a central remote delivery hub accepting referrals from local services.
Results in context
The magnitude of effect of this online ERP is about half the size reported from previous superiority trials of face-to-face HRT/CBIT for tics. 152 However, it is difficult to make direct comparisons of therapeutic efficacy with previous trials of face-to-face BT given that this trial had a higher level of baseline tic severity, fewer comorbidity exclusions, a lower proportion of participants receiving tic medication, longer follow-up and a potent active comparator. In practice, the direct comparison of efficacy may also be misleading with respect to implementation because the purpose is not to replace face-to-face therapy but to allow this scarce resource to be better targeted to those who need it most (e.g. children with the most severe tics such as eye poking) and to offer an effective digitally enabled intervention to a much larger population of children/adolescents who are currently unable to access any behavioural treatment for tics.
Major differences between online delivery and face-to-face BT for tics are the reduced amount of therapist time, required skill level of the therapist and cost.
Interpretation of findings
In summary, the findings from this trial suggest that online therapist-supported ERP is a clinically effective and cost-effective BT for reducing tic symptoms in CYP that has durable and sustained long-term benefits. These benefits extend over the longer term beyond tic reduction to improved mood, anxiety and psychosocial functioning. The intervention required approximately a quarter of the therapist time that is required for face-to-face therapy and less highly trained therapists. In health-care settings where tic treatments are difficult to access and with few highly trained expert therapists, therapist-supported online ERP could greatly increase the availability and reach of this durable and cost-effective behavioural treatment for CYP with tic disorders.
Implications for future research and health care
We identify four key areas of future research. First, further research is needed to determine the optimum care pathways with respect to the sequencing and integration of digital and face-to-face BT for tics in CYP and how best to integrate online BT for tics within treatment pathways. Within care pathway research we suggest two delivery models that would be worthy of further study. The first is a ‘stepped care’ model, in which digital/online delivery may be delivered as a first-line behavioural intervention with non-responders or poor responders being ‘stepped up’ to more intensive face-to-face therapy. It is important to note that such a model would not suit all patients, particularly those with complex needs or limited online access, and as such should not be a mandatory first-line treatment before escalation to face-to-face services. We also acknowledge that such a model would require appropriate oversight of dropouts or treatment failures. However, given that the majority of patients currently do not receive any therapeutic support, this model is likely to increase access to evidence-based care. The second model to evaluate is the ‘blending’ of online and face-to-face therapy for more complex cases, thereby reducing the overall number of face-to-face sessions required. These models could be evaluated for their clinical and cost-effectiveness using further RCT designs, including ‘field trials’ or real-world evaluations exploring implementation in clinical practice. Alongside this, it would be important to evaluate whether the models would best be delivered by a specialist centre accepting outside referrals or by training local sites to deliver the intervention.
Second, we did not provide participants with the opportunity to select how they interacted with their therapist. Further research designs could explore the impact of personalisation on effectiveness and engagement, providing opportunities for participants to choose the mode and frequency with which they engage with their therapist.
Third, the value of including parental chapters could be extended and explored in online CYP mental health interventions more widely beyond the ORBIT trial intervention, such as in interventions aimed at other mental health disorders such as low mood and anxiety. The value of including parental chapters was demonstrated by the process evaluation, which showed that parental chapter completion was the only independent predictor of clinical improvement within the ERP intervention arm. Future trials could compare a parent-supported versus non-parent-supported arm.
Fourth, the costs and benefits of online ERP for CYP with tic disorders are likely to extend beyond these 18-month trial data, and hence further health economic analysis is required to project the findings over a longer time horizon using decision modelling. This would also make it possible to include other comparators, such as face-to-face therapy, to evaluate any cost savings of relatively cheap but effective online behavioural interventions compared to ‘gold standard’ best practice. Given the costs of conducting a lengthy RCT, we suggest that this may be best explored using a budget impact assessment as part of a real-world evaluation.
Given the shortage of highly trained therapists with expertise in tic disorders and limited access to BT, online delivery of ERP for tics has the potential to greatly expand the reach of effective behavioural interventions. From a public health perspective, with more efficient use of therapist time it should be possible to treat four people for every one person treated with face-to-face therapy. In addition, the requirement for less experienced therapists to support online BT should expand the potential pool of therapists and thereby further extend the availability of online-delivered BT for tics. A further strength of the online delivery model is that fidelity of therapeutic content is built into the intervention, making transfer to real-world effectiveness much less susceptible than in traditional face-to-face therapy to therapeutic drift and to being impacted by the skill level of individual therapists.
Given that the intervention was developed initially by the Karolinska Team in Sweden and refined by our team in the UK there are implications regarding intellectual property. The ORBIT team, including Nottinghamshire Healthcare NHS Foundation Trust, University of Nottingham, Great Ormond Street Hospital Trust and Karolinska Institute (Sweden), are working with the University of Nottingham Technology Transfer Office to facilitate these matters. Background intellectual property (software and know-how) is held by the Karolinska Institute inventors, while the UK-based parties have all contributed variously to adapting ORBIT for UK users. All parties have agreed a plan leading towards the generation of a vehicle to make the intervention available within the UK.
Acknowledgements
This research was funded by the NIHR Heath Technology Assessment (Ref 16/19/02). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. CH, CLH, EBD and CG acknowledge the financial support of the NIHR Nottingham Biomedical Research Centre and NIHR MindTech MedTech Co-operative. We thank additional members who supported the ORBIT team at University College London and University of Nottingham. We would like to thank Tourettes Action for their support of the trial. We would like to thank our PPI members for their help. We thank members of our TSC, chaired by Edmund Sonuga-Barke, and the members of our DMC, chaired by Stephen Scott. We would also like to thank Angela Summerfield for her continued administrative support and help. We acknowledge that all research at Great Ormond Street Hospital NHS Foundation Trust and University College London Great Ormond Street Institute of Child Health is made possible by the NIHR Great Ormond Street Hospital Biomedical Research Centre. This work used services from the eHealth Core Facility at Karolinska Institutet, which is supported by the Strategic Research Area Healthcare Science.
We would also like to thank our patient identification centres, which recruited patients into the ORBIT study: Guys and St Thomas NHS Foundation Trust (Dr Tammy Hedderly), Oxford Health NHS Foundation Trust (Dr Wendy Woodhouse), North East London NHS Foundation Trust (Dr Ana Mendes and Alex Gaskill), Pennine Care NHS Foundation Trust (Prof Prathiba Chitsabesan), Sussex Partnership NHS Foundation Trust (Dr Anne Marie Skarstam), Central Manchester University Hospitals NHS Foundation Trust (Dr Rachel Elvins), Cumbria Partnership NHS Foundation Trust (Dr Barry Chipchase), Leicestershire Partnership NHS Trust (Rebekah Pole), United Lincolnshire Hospitals NHS Trust (Dr Julie Clarke), East Kent Hospitals University NHS Foundation Trust (Dr Femi Ogunbona), Northern Lincolnshire and Goole NHS Foundation Trust [Dr Suresh Nelapatla (Lisa-Jayne Cottam, Caroline Burnett)], Northumberland Tyne and Wear NHS Foundation Trust (Dr Nadine Mushet), Nottingham University Hospitals NHS Trust (Dr Dilip Nathan), Birmingham Women’s and Children’s NHS Foundation Trust (Dr Ashley Liew) and Northamptonshire Healthcare NHS Foundation Trust (Dr Felicity Larson and Liz Sabin).
Contributions of authors
Chris Hollis (https://orcid.org/0000-0003-1083-6744) was the chief investigator and co-conceived and cowrote the study, the trial protocol (with input from all authors), was responsible for study implementation and general project management. Hollis wrote the discussion and the conclusion (see Chapter 8) and is the guarantor.
Charlotte L Hall (https://orcid.org/0000-0002-5412-6165) co-conceived and cowrote the study design, wrote the trial protocol with input from all authors, was responsible for study implementation and general project management. Hall oversaw trial management and contributed to the conception of the mixed-methods process evaluation and developed the interview guides for qualitative analysis. Hall provided supervision for the process evaluation and wrote the introduction chapter (1). Hall wrote all other chapters and sections.
Kareem Khan (https://orcid.org/0000-0003-3836-2827) was responsible for recruitment and follow-ups. Khan contributed to the conception of the mixed-methods process evaluation and developed the interview guides for qualitative analysis. Khan conducted the data collection and initial analysis of both the quantitative and qualitative data. Khan wrote the process evaluation chapter (6) and supported writing of all other chapters and sections.
Marie Le Novere (https://orcid.org/0000-0002-9479-8599) wrote the health economic analysis plan, conducted the economic evaluation and cowrote the economic evaluation chapter (5).
Louise Marston (https://orcid.org/0000-0002-9973-1131) co-conceived and cowrote the study design, designed and wrote the statistical analysis plan, conducted the analysis, and designed the tables and graphs.
Rebecca Jones (https://orcid.org/0000-0001-6924-0924) co-conceived and cowrote the study design, designed and wrote the statistical analysis plan, conducted the analysis, and designed the tables and graphs.
Rachael Hunter (https://orcid.org/0000-0002-7447-8934) co-conceived and cowrote the study design, designed the economic evaluation, wrote the health economic analysis plan, conducted the economic evaluation, cowrote the economic evaluation chapter (5).
Beverley J Brown (https://orcid.org/0000-0002-1026-278X) was responsible for study implementation, general project management, recruitment, and follow-ups.
Charlotte Sanderson (https://orcid.org/0000-0001-6324-3112) was responsible for study implementation, general project management, recruitment, and follow-ups.
Per Andrén (https://orcid.org/0000-0003-1358-0166) co-conceived and cowrote the study design.
Sophie D Bennett (https://orcid.org/0000-0002-1076-7112) was responsible for study implementation and general project management.
Liam R Chamberlain (https://orcid.org/0000-0002-0432-9415) was a trial therapist.
E Bethan Davies (https://orcid.org/0000-0003-3134-0879) was a trial therapist, contributed to the conception of the mixed-methods process evaluation and developed the interview guides for qualitative analysis. Davies provided supervision for the process evaluation and cowrote the intervention development chapter (2).
Amber Evans (https://orcid.org/0000-0003-2232-3495) was a trial therapist.
Natalia Kouzoupi (https://orcid.org/0000-0002-1748-7156) was a trial therapist.
Caitlin McKenzie (https://orcid.org/0000-0001-7832-4388) was responsible for recruitment and follow-ups.
Isobel Heyman (https://orcid.org/0000-0001-7358-9766) co-conceived and cowrote the study design.
Joseph Kilgariff (https://orcid.org/0000-0002-7195-7753) provided therapist supervision.
Cristine Glazebrook (https://orcid.org/0000-0002-7459-9445) co-conceived and cowrote the study design, conceived and wrote the initial process evaluation design in the trial protocol. Glazebrook contributed to the conception of the mixed-methods process evaluation, developed the interview guides for qualitative analysis and provided supervision for the process evaluation.
David Mataix-Cols (https://orcid.org/0000-0002-4545-0924) co-conceived and cowrote the study design.
Eva Serlachius (https://orcid.org/0000-0001-7115-6422) co-conceived and cowrote the study design.
Elizabeth Murray (https://orcid.org/0000-0002-8932-3695) co-conceived and cowrote the study design and was responsible for study implementation and general project management.
Tara Murphy (https://orcid.org/0000-0003-1759-3562) co-conceived and cowrote the study design, was responsible for study implementation and general project management. Murphy provided therapist supervision and cowrote the intervention development chapter (2).
All authors contributed to the interpretation of the data and re-drafts. All authors had full access to all data in the study and had final responsibility for the decision to submit for publication.
Publications
This monograph draws upon several published peer-reviewed papers, including:
Hall CL, Davies EB, Andrén P, Murphy T, Bennett S, Brown BJ, et al. Investigating a therapist-guided, parent-assisted remote digital behavioural intervention for tics in children and adolescents – ‘online remote behavioural intervention for tics’ (ORBIT) trial: protocol of an internal pilot study and single-blind randomised controlled trial. BMJ Open 2019;9(1):e027583.
Hollis C, Hall CL, Jones R, Marston L, Le Novere M, Hunter R, et al. Therapist-supported online remote behavioural intervention for tics in children and adolescents in England (ORBIT): a multicentre, parallel group, single-blind, randomised controlled trial. The Lancet Psychiatry 2021;8(10):871–82.
Hollis C, Hall CL, Khan K, Jones R, Marston L, Le Novere M, et al. Long term clinical and cost-effectiveness of a therapist-supported online remote behavioural intervention for tics (ORBIT) in children and adolescents: extended 12 and 18-month follow-up of a single-blind randomised controlled trial. J Child Psychol Psychiatry 2023;64(6):941–51.
Khan K, Hollis C, Hall CL, Davies EB, Mataix-Cols D, Andrén P, et al. Protocol for the process evaluation of the online remote behavioural intervention for tics (ORBIT) randomized controlled trial for children and young people. Trials 2020;21:1–10.
Khan K, Hollis C, Hall CL, Murray E, Davies EB, Andrén P, et al. Fidelity of delivery and contextual factors influencing children’s level of engagement: process evaluation of the online remote behavioral intervention for tics trial. J Med Internet Res 2021;23(6):e25470.
Khan K, Hollis C, Hall CL, Davies EB, Murray E, Andrén P, et al. Factors influencing the efficacy of an online behavioural intervention for children and young people with tics: process evaluation of a randomised controlled trial. J Behav Cogn Ther 2022;3:197–206.
Khan K. Process Evaluation for Online Remote Behavioural Intervention (ORBIT) Trial. PhD thesis. Nottingham: University of Nottingham; 2021.
Ethics statement
Ethical and Health Research Authority approval was received from Northwest Greater Manchester Research Ethics Committee on 23 March 2018 (ref.: 18/NW/0079) and thus the study was conducted in line with the Declaration of Helsinki.
Data-sharing statement
Individual participant data that underlie the results reported in this article, after de-identification (text, tables, figures, data dictionary and appendices), will be available. All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review and appropriate agreements being in place.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Hall CL, Davies E, Andrén P, Murphy T, Bennett S, Brown BJ, et al. Investigating a therapist-guided, parent-assisted remote digital behavioural intervention for tics in children and adolescents – ‘online remote behavioural intervention for tics’ (ORBIT) trial: protocol of an internal pilot study and single-blind randomised controlled trial. BMJ Open 2019;9.
- Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Arlington, VA: American Psychiatric Association; 2013.
- Hollis C, Pennant M, Cuenca J, Glazebrook C, Kendall T, Whittington C, et al. Clinical effectiveness and patient perspectives of different treatment strategies for tics in children and adolescents with Tourette syndrome: a systematic review and qualitative analysis. Health Technol Assess 2016;20:1-450.
- Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson JO, et al. The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry 1989;28:566-73.
- Schlander M, Schwarz O, Rothenberger A, Roessner V. Tic disorders: administrative prevalence and co-occurrence with attention-deficit/hyperactivity disorder in a German community sample. Eur Psychiatry 2011;26:370-4.
- Hirschtritt ME, Lee PC, Pauls DL, Grados MA, Illmann C, King RA, et al. Lifetime prevalence, age of risk, and genetic relationships of comorbid psychiatric disorders in Tourette syndrome. JAMA Psychiatry 2015;72:325-33.
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry 2003;60:837-44.
- Kious BM, Jimenez-Shahed J, Shprecher DR. Treatment-refractory Tourette syndrome. Prog Neuropsychopharmacol Biol Psychiatry 2016;70:227-36.
- Cukier HN, Dueker ND, Slifer SH, Lee JM, Whitehead PL, Lalanne E, et al. Exome sequencing of extended families with autism reveals genes shared across neurodevelopmental and neuropsychiatric disorders. Molecular Autism 2014;5.
- Bernard BA, Stebbins GT, Siegel S, Schultz TM, Hays C, Morrissey MJ, et al. Determinants of quality of life in children with Gilles de la Tourette syndrome. Mov Disord 2009;24:1070-3.
- Andrén P, Jakubovski E, Murphy TL, Woitecki K, Tarnok Z, Zimmerman-Brenner S, et al. European clinical guidelines for Tourette syndrome and other tic disorders – version 2.0. Part II: psychological interventions. Eur Child Adolesc Psychiatry 2022;31:403-23.
- Whittington C, Pennant M, Kendall T, Glazebrook C, Trayner P, Groom M, et al. Practitioner review: treatments for Tourette syndrome in children and young people – a systematic review. J. Child Psychol Psychiatry 2016;57:988-1004.
- Roessner V, Plessen KJ, Rothenberger A. ESSTS Guidelines Group . European clinical guidelines for Tourette syndrome and other tic disorders. Part II: pharmacological treatment. Eur Child Adolesc Psychiatry 2011;20:173-96.
- Hollis C, Pennant M, Cuenca J, Glazebrook C, Kendall T, Whittington C, et al. Clinical effectiveness and patient perspectives of different treatment strategies for tics in children and adolescents with Tourette syndrome: a systematic review and qualitative analysis. Health Technol Assess 2016;20:1-450.
- Pringsheim T, Okun MS, Müller-Vahl K, Martino D, Jankovic J, Cavanna AE, et al. Practice guideline recommendations summary: treatment of tics in people with Tourette syndrome and chronic tic disorders. Neurology 2019;92:896-90.
- Verdellen CW, Keijsers GP, Cath DC, Hoogduin CA. Exposure with response prevention versus habit reversal in Tourettes’s syndrome: a controlled study. Behav Res Ther 2004;42:501-11.
- Piacentini J, Woods DW, Scahill L, Wilhelm S, Peterson AL, Chang S, et al. Behavior therapy for children with Tourette disorder: a randomized controlled trial. JAMA 2010;303:1929-37.
- Espil FM, Woods DW, Specht MW, Bennett SM, Walkup JT, Ricketts EJ, et al. Long-term outcomes of behavior therapy for youth with Tourette disorder. J Am Acad Child Adolesc Psychiatry 2021;61:764-71.
- Bennett SM, Capriotti M, Bauer C, Chang S, Keller AE, Walkup J, et al. Development and open trial of a psychosocial intervention for young children with chronic tics: the CBIT-JR study. Behav Ther 2020;51:659-69.
- Verdellen C, Van De Griendt J, Hartmann A. ESSTS Guidelines Group . European clinical guidelines for Tourette syndrome and other tic disorders. Part III: behavioural and psychosocial interventions. Eur Child Adolesc Psychiatry 2011;20:197-20.
- Cuenca J, Glazebrook C, Kendall T, Hedderly T, Heyman I, Jackson G, et al. Perceptions of treatment for tics among young people with Tourette syndrome and their parents: a mixed methods study. BMC Psychiatry 2015;15.
- Sanderson C, Kouzoupi N, Hall CL. Technology matters: the human touch in a digital age – a blended approach in mental healthcare delivery with children and young people. Child Adolesc Ment Health 2020;25:120-2.
- Vera San Juan N, Shah P, Schlief M, Appleton R, Nyikavaranda P, Birken M, et al. Service user experiences and views regarding telemental health during the COVID-19 pandemic: a co-produced framework analysis. PLOS ONE 2021;16.
- Andersson G, Wagner B, Cuijpers P. Guided Internet-Based Treatments in Psychiatry. Berlin: Springer; 2016.
- Johansson R, Andersson G. Internet-based psychological treatments for depression. Expert Rev Neurother 2012;12:861-9.
- Hedman E, Ljótsson B, Lindefors N. Cognitive behavior therapy via the internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev Pharm Out 2012;12:745-64.
- Andersson G, Cuijpers P, Carlbring P, Riper H, Hedman E. Guided internet‐based vs. face‐to‐face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta‐analysis. World Psychiatry 2014;13:288-95.
- National Institute for Health and Care Excellence (NICE) . Depression in Children and Young People: Identification and Management (NICE Guideline 134) 2009. https://www.nice.org.uk/guidance/ng134 (accessed 12 May 2021).
- Karyotaki E, Furukawa TA, Efthimiou O, Riper H, Cuijpers P. Guided or self-guided internet-based cognitive–behavioural therapy (iCBT) for depression? Study protocol of an individual participant data network meta-analysis. BMJ Open 2019;9.
- Cuijpers P, Donker T, Johansson R, Mohr DC, van Straten A, Andersson G. Self-guided psychological treatment for depressive symptoms: a meta-analysis. PLOS ONE 2011;6.
- Grist R, Croker A, Denne M, Stallard P. Technology delivered interventions for depression and anxiety in children and adolescents: a systematic review and meta-analysis. Clin Child Fam Psychol Rev 2019;22:147-71.
- Vigerland S, Thulin U, Ljótsson B, Svirsky L, Öst LG, Lindefors N, et al. Internet-delivered CBT for children with specific phobia: a pilot study. Cogn Behav Ther 2013;42:303-14.
- Vigerland S, Lenhard F, Bonnert M, Lalouni M, Hedman E, Ahlen J, et al. Internet-delivered cognitive behavior therapy for children and adolescents: a systematic review and meta-analysis. Clin Psychol Rev 2016;50:1-10.
- Lenhard F, Vigerland S, Andersson E, Rueck C, Mataix-Cols D, Thulin U, et al. Internet-delivered cognitive behavior therapy for adolescents with obsessive–compulsive disorder: an open trial. PLOS ONE 2014;9.
- Lenhard F, Vigerland S, Engberg H, Hallberg A, Thermaenius H, Serlachius E. ‘On my own, but not alone’ – adolescents’ experiences of internet-delivered cognitive behavior therapy for obsessive–compulsive disorder. PLOS ONE 2016;11.
- Vigerland S, Ljótsson B, Thulin U, Öst LG, Andersson G, Serlachius E. Internet-delivered cognitive behavioural therapy for children with anxiety disorders: a randomised controlled trial. Behav Res Ther 2016;76:47-56.
- Nordh M, Wahlund T, Jolstedt M, Sahlin H, Bjureberg J, Ahlen J, et al. Therapist-guided internet-delivered cognitive behavioral therapy vs internet-delivered supportive therapy for children and adolescents with social anxiety disorder: a randomized clinical trial. JAMA Psychiatry 2021;78:705-13.
- Aspvall K, Andersson E, Melin K, Norlin L, Eriksson V, Vigerland S, et al. Effect of an internet-delivered stepped-care program vs in-person cognitive behavioral therapy on obsessive–compulsive disorder symptoms in children and adolescents: a randomized clinical trial. JAMA 2021;325:1863-73.
- Aspvall K, Lenhard F, Melin K, Krebs G, Norlin L, Näsström K, et al. Implementation of internet-delivered cognitive behaviour therapy for pediatric obsessive–compulsive disorder: Lessons from clinics in Sweden, United Kingdom and Australia. Internet Interventions 2020;20.
- Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, et al. Annual research review: digital health interventions for children and young people with mental health problems – a systematic and meta‐review. J Child Psychol Psychiatry 2017;58:474-503.
- Himle MB, Freitag M, Walther M, Franklin SA, Ely L, Woods DW. A randomized pilot trial comparing videoconference versus face-to-face delivery of behavior therapy for childhood tic disorders. Behav Res Ther 2012;50:565-70.
- Ricketts EJ, Goetz AR, Capriotti MR, Bauer CC, Brei NG, Himle MB, et al. A randomized waitlist-controlled pilot trial of voice over internet protocol-delivered behavior therapy for youth with chronic tic disorders. J Telemed Telecare 2016;22:153-62.
- Andrén P, Aspvall K, de la Cruz LF, Wiktor P, Romano S, Andersson E, et al. Therapist-guided and parent-guided internet-delivered behaviour therapy for paediatric Tourette’s disorder: a pilot randomised controlled trial with long-term follow-up. BMJ Open 2019;9.
- Rachamim L, Zimmerman-Brenner S, Rachamim O, Mualem H, Zingboim N, Rotstein M. Internet-based guided self-help comprehensive behavioral intervention for tics (ICBIT) for youth with tic disorders: a feasibility and effectiveness study with 6 month-follow-up. Eur Child Adolesc Psychiatr 2022;31:275-87.
- NHS England . NHS Long Term Plan 2019. https://www.longtermplan.nhs.uk/ (accessed 29 January 2022).
- Lau R, Stevenson F, Ong BN, Dziedzic K, Treweek S, Eldridge S, et al. Achieving change in primary care – causes of the evidence to practice gap: systematic reviews of reviews. Implement Sci 2016;11.
- Kaplan HC, Brady PW, Dritz MC, Hooper DK, Linam WM, Froehle CM, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q 2010;88:500-59.
- Bullen J, Hemsley D. Sensory experience as a trigger in Gilles de la Tourette’s syndrome. J Behav Ther Exp Psychiatry 1983;14:197-201.
- van de Griendt JM, van Dijk MK, Verdellen CW, Verbraak MJ. The effect of shorter exposure versus prolonged exposure on treatment outcome in Tourette syndrome and chronic tic disorders – an open trial. Int J Psychiatry Clin Pract 2018;22:262-7.
- Verdellen CW, Hoogduin CA, Kato BS, Keijsers GP, Cath DC, Hoijtink HB. Habituation of premonitory sensations during exposure and response prevention treatment in Tourette’s syndrome. Behav Modif 2008;32:215-27.
- Specht MW, Woods DW, Nicotra CM, Kelly LM, Ricketts EJ, Conelea CA, et al. Effects of tic suppression: ability to suppress, rebound, negative reinforcement, and habituation to the premonitory urge. Behav Res Ther 2013;51:24-30.
- Houghton DC, Capriotti MR, Scahill LD, Wilhelm S, Peterson AL, Walkup JT, et al. Investigating habituation to premonitory urges in behavior therapy for tic disorders. Behav Ther 2017;48:834-46.
- Craske MG, Treanor M, Conway CC, Zbozinek T, Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behav Res Ther 2014;58:10-23.
- Verdellen C, Van De Griendt J, Kriens S. Tics – Therapist Manual. Amsterdam: Boom Publishers; 2011.
- Nissen JB, Kaergaard M, Laursen L, Parner E, Thomsen PH. Combined habit reversal training and exposure response prevention in a group setting compared to individual training: a randomized controlled clinical trial. Eur Child Adolesc Psychiatry 2019;28:57-68.
- Heijerman-Holtgrefe A, Verdellen C, van de Griendt J, Beljaars LP, Kan KJ, Cath D, et al. Tackle your Tics: pilot findings of a brief, intensive group-based exposure therapy program for children with tic disorders. Eur Child Adolesc Psychiatry 2021;30:461-73.
- Nussey C, Pistrang N, Murphy T. How does psychoeducation help? A review of the effects of providing information about Tourette syndrome and attention‐deficit/hyperactivity disorder. Child Care Health Dev 2013;39:617-27.
- Wilhelm S, Peterson AL, Piacentini J, Woods DW, Deckersbach T, Sukhodolsky DG, et al. Randomized trial of behavior therapy for adults with Tourette syndrome. Arch Gen Psychiatry 2012;69:795-803.
- Rizzo R, Pellico A, Silvestri PR, Chiarotti F, Cardona F. A randomized controlled trial comparing behavioral, educational, and pharmacological treatments in youths with chronic tic disorder or Tourette syndrome. Front Psychiatry 2018;9.
- Yates R, Edwards K, King J, Luzon O, Evangeli M, Stark D. Habit reversal training and educational group treatments for children with Tourette syndrome: a preliminary randomised controlled trial. Behav Res Ther 2016;80:43-50.
- Chowdhury U, Murphy T. Tic Disorders: A Guide for Parents and Professionals. London: Jessica Kingsley Publishers; 2016.
- Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry 2000;41:645-55.
- McKenzie K, Murray GC, Murray AL. The validity of the child and adolescent intellectual disability screening questionnaire (CAIDS-Q) with children aged 6–7 years, 11 months: a brief report. Psychiatry Res 2013;210:675-7.
- Chang S, Himle MB, Tucker BT, Woods DW, Piacentini J. Initial psychometric properties of a brief parent-report instrument for assessing tic severity in children with chronic tic disorders. Child Fam Behav Ther 2009;31:181-91.
- Guy W. ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Rockville, MD: Institute of Mental Health, Psychopharmacology Research Branch; 1976.
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A children’s global assessment scale (CGAS). Arch Gen Psychiatry 1983;40:1228-31.
- Goodman R. The extended version of the strengths and difficulties questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry 1999;40:791-9.
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40:1337-45.
- Angold A, Costello EJ, Messer SC, Loeber R, Van Kammen W, Stouthamer-Loeber M, et al. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res 1995;5:237-49.
- Spence SH. A measure of anxiety symptoms among children. Behav Res Ther 1998;36:545-66.
- Stevens K. The child health utility 9D (CHU9D) – a new, paediatric, preference-based measure of health related quality of life. PRO Newsletter 2010;43:11-2.
- Su MT, McFarlane F, Cavanna AE, Termine C, Murray I, Heidemeyer L, et al. The English version of the Gilles de la Tourette Syndrome – Quality of Life Scale for Children and Adolescents (CandA-GTS-QoL). J Child Neurol 2017;32:76-83.
- Beecham J, Knapp M. Measuring Mental Health Needs. London: Gaskell; 2001.
- Byford S, Barrett B, Roberts C, Wilkinson P, Dubicka B, Kelvin RG, et al. Cost-effectiveness of selective serotonin reuptake inhibitors and routine specialist care with and without cognitive–behavioural therapy in adolescents with major depression. Br J Psychiatry 2007;191:521-7.
- Hill P, Taylor E. An auditable protocol for treating attention deficit/hyperactivity disorder. Arch Dis Child 2001;84:404-9.
- McKenzie K, Murray GC, Murray AL. The validity of the child and adolescent intellectual disability screening questionnaire (CAIDS-Q) with children aged 6–7 years, 11 months: a brief report. Psychiatry Res 2013;210:675-7.
- Hollis C, Falconer CJ, Martin JL, Whittington C, Stockton S, Glazebrook C, et al. Annual research review: digital health interventions for children and young people with mental health problems – a systematic and meta‐review. J Child Psychol Psychiatry 2017;58:474-503.
- Hollis C, Hall CL, Jones R, Marston L, Le Novere M, Hunter R, et al. Therapist-supported online remote behavioural intervention for tics in children and adolescents in England (ORBIT): a multicentre, parallel group, single-blind, randomised controlled trial. Lancet Psychiatry 2021;8:871-82.
- Hollis C, Hall CL, Khan K, Jones R, Marston L, Le Novere M, et al. Long term clinical and cost-effectiveness of a therapist-supported online remote behavioural intervention for tics (ORBIT) in children and adolescents: extended 12 and 18-month follow-up of a single-blind randomised controlled trial. J Child Psychol Psychiatry 2023;64:941-51.
- National Institute for Health and Care Excellence (NICE) . NICE Health Technology Evaluations: The Manual: Process and Methods 2022. https://www.nice.org.uk/process/pmg36 (accessed 20 May 2022).
- StataCorp . Stata Statistical Software: Release 17 2021.
- Byford S, Harrington R, Torgerson D, Kerfoot M, Dyer E, Harrington V, et al. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves: results of a randomised controlled trial. Br J Psychiatry 1999;174:56-62.
- Harrington R, Peters S, Green J, Byford S, Woods J, McGowan R. Randomised comparison of the effectiveness and costs of community and hospital based mental health services for children with behavioural disorders. BMJ 2000;321.
- Barrett B, Byford S, Chitsabesan P, Kenning C. Mental health provision for young offenders: service use and cost. Br J Psychiatry 2006;188:541-6.
- Furber G, Segal L. The validity of the child health utility instrument (CHU9D) as a routine outcome measure for use in child and adolescent mental health services. Health Qual Life Outcomes 2015;13.
- Stevens K. Assessing the performance of a new generic measure of health-related quality of life for children and refining it for use in health state valuation. Appl Health Econ Health Policy 2011;9:157-69.
- Richards D, Enrique A, Eilert N, Franklin M, Palacios J, Duffy D, et al. A pragmatic randomized waitlist-controlled effectiveness and cost-effectiveness trial of digital interventions for depression and anxiety. Npj Digital Med 2020;3:1-10.
- Bloch MH, Leckman JF. Clinical course of Tourette syndrome. J Psychosom Res 2009;67:497-501.
- Briggs AH, Ades A, Price MJ. Probabilistic sensitivity analysis for decision trees with multiple branches: use of the Dirichlet distribution in a Bayesian framework. Med Decis Making 2003;23:341-50.
- Chen CW, Wang HS, Chang HJ, Hsueh CW. Effectiveness of a modified comprehensive behavioral intervention for tics for children and adolescents with Tourette’s syndrome: a randomized controlled trial. J Adv Nurs 2020;76:903-15.
- Haas M, Jakubovski E, Kunert K, Fremer C, Buddensiek N, Häckl S, et al. ONLINE-TICS: internet-delivered behavioral treatment for patients with chronic tic disorders. J Clin Med 2022;11.
- Conelea CA, Woods DW, Zinner SH, Budman CL, Murphy TK, Scahill LD, et al. The impact of Tourette syndrome in adults: results from the Tourette syndrome impact survey. Community Ment Health J 2013;49:110-20.
- Pringsheim T, Lang A, Kurlan R, Pearce M, Sandor P. Understanding disability in Tourette syndrome. Dev Med Child Neurol 2009;51:468-72.
- Cavanna AE, David K, Orth M, Robertson MM. Predictors during childhood of future health-related quality of life in adults with Gilles de la Tourette syndrome. Eur J Paediatr Neurol 2012;16:605-12.
- Eddy C, Rizzo R, Gulisano M, Agodi A, Barchitta M, Calì P, et al. Quality of life in young people with Tourette syndrome: a controlled study. J Neurol 2011;258:291-30.
- Storch EA, Merlo LJ, Lack C, Milsom VA, Geffken GR, Goodman WK, et al. Quality of life in youth with Tourette’s syndrome and chronic tic disorder. J Clin Child Adolesc Psychol 2007;36:217-27.
- Cutler D, Murphy T, Gilmour J, Heyman I. The quality of life of young people with Tourette syndrome. Child Care Health Dev 2009;35:496-504.
- Claxton K, Martin S, Soares M, Rice N, Spackman E, Hinde S, et al. Methods for the estimation of the National Institute for Health and Care Excellence cost-effectiveness threshold. Health Technol Assess 2015;19:1-503.
- Khan K, Hollis C, Hall CL, Murray E, Davies EB, Andrén P, et al. Fidelity of delivery and contextual factors influencing children’s level of engagement: process evaluation of the online remote behavioral intervention for tics trial. J Med Internet Res 2021;23.
- Khan K, Hollis C, Hall CL, Davies EB, Murray E, Andrén P, et al. Factors influencing the efficacy of an online behavioural intervention for children and young people with tics: process evaluation of a randomised controlled trial. J Behav Cogn Ther 2022;3:197-206.
- Khan K, Hollis C, Hall CL, Davies EB, Mataix-Cols D, Andrén P, et al. Protocol for the process evaluation of the online remote behavioural intervention for tics (ORBIT) randomized controlled trial for children and young people. Trials 2020;21:1-10.
- Khan K. Process Evaluation of Online Remote Behavioural Intervention for Tics (ORBIT). PhD Thesis 2021.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350.
- Richards DA, Hallberg IR. Complex Interventions in Health: An Overview of Research Methods. Abingdon: Routledge; 2015.
- Bragstad LK, Bronken BA, Sveen U, Hjelle EG, Kitzmüller G, Martinsen R, et al. Implementation fidelity in a complex intervention promoting psychosocial well-being following stroke: an explanatory sequential mixed methods study. BMC Med Res Methodol 2019;19.
- Hulscher MEJL, Laurant MGH, Grol RPTM. Process evaluation on quality improvement interventions. Qual Saf Health Care 2003;12:40-6.
- Carroll C, Patterson M, Wood S, Booth A, Rick J, Balain S. A conceptual framework for implementation fidelity. Implement Sci 2007;2.
- Montgomery P, Underhill K, Gardner F, Operario D, Mayo-Wilson E. The Oxford Implementation Index: a new tool for incorporating implementation data into systematic reviews and meta-analyses. J Clin Epidemiol 2013;66:874-82.
- Hasson H. Systematic evaluation of implementation fidelity of complex interventions in health and social care. Implement Sci 2010;5.
- Dobson D, Cook TJ. Avoiding type III error in program evaluation: results from a field experiment. Eval Program Plan 1980;3:269-76.
- Grant A, Treweek S, Dreischulte T, Foy R, Guthrie B. Process evaluations for cluster-randomised trials of complex interventions: a proposed framework for design and reporting. Trials 2013;14.
- Bonell C, Fletcher A, Morton M, Lorenc T, Moore L. Realist randomised controlled trials: a new approach to evaluating complex public health interventions. Soc Sci Med 2012;75:2299-306.
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173-82.
- Hawe P, Shiell A, Riley T. Complex interventions: how ‘out of control’ can a randomised controlled trial be?. BMJ 2004;328:1561-3.
- Bumbarger B, Perkins D. After randomised trials: issues related to dissemination of evidence‐based interventions. J Child Serv 2008;3:55-64.
- Partridge SR, Allman-Farinelli M, McGeechan K, Balestracci K, Wong AT, Hebden L, et al. Process evaluation of TXT2BFiT: a multi-component mHealth randomised controlled trial to prevent weight gain in young adults. Int J Behav Nutr Phys Act 2016;13.
- Young DR, Steckler A, Cohen S, Pratt C, Felton G, Moe SG, et al. Process evaluation results from a school- and community-linked intervention: the trial of activity for adolescent girls (TAAG). Health Educ Res 2008;23:976-86.
- May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: normalization process theory. Implement Sci 2009;4.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8.
- Ritchie J, Spencer L. Analyzing Qualitative Data. Abingdon: Routledge; 2002.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13.
- Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277-88.
- O’Cathain A, Murphy E, Nicholl J. Three techniques for integrating data in mixed methods studies. BMJ 2010;341.
- Burleson Daviss W, Birmaher B, Melhem NA, Axelson DA, Michaels SM, Brent DA. Criterion validity of the mood and feelings questionnaire for depressive episodes in clinic and non‐clinic subjects. J Child Psychol Psychiatry 2006;47:927-34.
- ONS . UK Population 2017 2017. https://www.ons.gov.uk/aboutus/transparencyandgovernance/freedomofinformationfoi/ukpopulation2017 (accessed 30 June 2022).
- Packness A, Waldorff FB, Christensen R, Hastrup LH, Simonsen E, Vestergaard M, et al. Impact of socioeconomic position and distance on mental health care utilization: a nationwide Danish follow-up study. Soc Psychiatry Psychiatr Epidemiol 2017;52:1405-13.
- Lyneham HJ, Rapee RM. Evaluation of therapist-supported parent-implemented CBT for anxiety disorders in rural children. Behav Res Ther 2006;44:1287-300.
- Pennant ME, Loucas CE, Whittington C, Creswell C, Fonagy P, Fuggle P, et al. Computerised therapies for anxiety and depression in children and young people: a systematic review and meta-analysis. Behav Res Ther 2015;67:1-18.
- Thirlwall K, Cooper PJ, Karalus J, Voysey M, Willetts L, Creswell C. Treatment of child anxiety disorders via guided parent-delivered cognitive–behavioural therapy: randomised controlled trial. Br J Psychiatry 2013;203:436-44.
- Haine-Schlagel R, Walsh NE. A review of parent participation engagement in child and family mental health treatment. Clin Child Fam Psychol Rev 2015;18:133-50.
- Nock MK, Ferriter C. Parent management of attendance and adherence in child and adolescent therapy: a conceptual and empirical review. Clin Child Fam Psychol Rev 2005;8:149-66.
- Vernon TW, Koegel RL, Dauterman H, Stolen K. An early social engagement intervention for young children with autism and their parents. J Autism Dev Disord 2012;42:2702-17.
- Khan K, Hall CL, Davies EB, Hollis C, Glazebrook C. The effectiveness of web-based interventions delivered to children and young people with neurodevelopmental disorders: systematic review and meta-analysis. J Med Internet Res 2019;21.
- Bennion MR, Hardy G, Moore RK, Millings A. E-therapies in England for stress, anxiety or depression: what is being used in the NHS? A survey of mental health services. BMJ Open 2017;7.
- Sukhodolsky DG, Woods DW, Piacentini J, Wilhelm S, Peterson AL, Katsovich L, et al. Moderators and predictors of response to behavior therapy for tics in Tourette syndrome. Neurology 2017;88:1029-36.
- Nissen JB, Parner ET, Thomsen PH. Predictors of therapeutic treatment outcome in adolescent chronic tic disorders. BJPsych Open 2019;5.
- Burns BJ, Hoagwood K, Mrazek PJ. Effective treatment for mental disorders in children and adolescents. Clin Child Fam Psychol Rev 1999;2:199-254.
- Spence SH. A measure of anxiety symptoms among children. Behav Res Ther 1998;36:545-66.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Cambridge, MA: Academic Press; 2013.
- Hayes AF. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr 2009;76:408-20.
- Kraemer HC, Blasey CM. Centring in regression analyses: a strategy to prevent errors in statistical inference. Int J Methods Psychiatr Res 2004;13:141-51.
- Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt 2014;34:502-8.
- Bennett GG, Glasgow RE. The delivery of public health interventions via the internet: actualizing their potential. Annu Rev Public Health 2009;30:273-92.
- Brigden A, Anderson E, Linney C, Morris R, Parslow R, Serafimova T, et al. Digital behavior change interventions for younger children with chronic health conditions: systematic review. J Med Internet Res 2020;22.
- Brouwer W, Kroeze W, Crutzen R, de Nooijer J, de Vries NK, Brug J, et al. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J Med Internet Res 2011;13.
- Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of web-based vs. non-web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res 2004;6.
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 2002;7:83-104.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- Mason J. Mixing methods in a qualitatively driven way. Qual Res 2006;6:9-25.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350.
- Office for National Statistics . Exploring the UK’s Digital Divide 2021. https://www.ons.gov.uk/peoplepopulationandcommunity/householdcharacteristics/homeinternetandsocialmediausage/articles/exploringtheuksdigitaldivide/2019-03-04 (accessed 28 June 2022).
- Whittington C, Pennant M, Kendall T, Glazebrook C, Trayner P, Groom M, et al. Practitioner review: treatments for Tourette syndrome in children and young people – a systematic review. J Child Psychol Psychiatry 2016;57:988-1004.
- Jeon S, Walkup JT, Woods DW, Peterson A, Piacentini J, . Detecting a clinically meaningful change in tic severity in Tourette syndrome: a comparison of three methods. Contemp Clin Trials 2013;36:414-20.
Appendix 1 Yale Global Tic Severity Scale
Some sections of this appendix have been reproduced from the ORBIT trial protocol, which has been published. 1
The primary outcome for the ORBIT trial is the severity of tics as measured by the TTSS (0–50) on the YGTSS. The YGTSS is administered by a blinded outcome assessor as an investigator-based semistructured interview focusing on motor and vocal tic frequency, severity and tic-related impairment over the previous week. The YGTSS symptom checklist lists 46 tic disorder symptoms, including 12 simple motor tics (e.g. eye blinking), 19 complex motor tics (e.g. facial expressions), 7 simple vocal tics (e.g. coughing) and 8 complex vocal tics (e.g. words), with 4 of these items designated on the instrument as ‘other’ symptoms. The YGTSS generates a TTSS (0–50) and an impairment score (0–50).
Five index scores are obtained: Total Motor Tic Score, Total Phonic Tic Score, Total Tic Score, Overall Impairment Rating and Global Severity Score. The Total Motor Tic Score is derived by adding the five items pertaining to motor tics (range: 0–25); the Total Phonic Tic Score is derived by adding the five items pertaining to phonic tics (range: 0–25); the Total Tic Score is derived by adding the Total Motor Tic Score and the Total Phonic Tic Score; and the Overall Impairment Rating is rated on a 50-point scale anchored by 0 (no impairment) and 50 (severe impairment). A Global Severity Score (range: 0–100) is derived by summing the Total Motor Tic Score, Total Phonic Tic Score and Overall Impairment Rating. The TTSS (0–50) is the primary outcome.
YGTSS rater training
For ORBIT, rater training of our YGTSS assessors consisted of the following steps:
-
Researchers training on the YGTSS will be supervised by Dr Tara Murphy the expert rater (ER).
-
Training will consist of reading Tara Murphy’s slides on YGTSS, which include the background and basic instructions for using the YGTSS.
-
They are also required to read the pivotal Leckman et al. (1988) paper. 4
-
Assessors are asked to view at least three pre-recorded YGTSS assessment sessions. They will be asked to rate these; however, this will be solely for training purposes, with discussions afterwards, and scores will not be used to calculate reliability or agreement. Assessors are encouraged to make a list of any questions/queries and rationale behind their decision-making.
-
They then discuss their scores on this with Tara Murphy.
-
Assessors then undergo a live test score with Tara Murphy (i.e. the score a dummy patient) and also shadow a live assessment of YGTSS with an experienced assessor and score the patient. These scores are then discussed with Tara Murphy/an experienced assessor to compare scores and discuss the rationale behind the scoring.
-
The next step will be a testing phase in which three different YGTSS assessments will be used against an ER to determine the extent of agreement with the ER.
-
In line with the methodology reported by in DSM-5,153 the raters have to be within 15% of the ER for the Total Motor Tic Score, the Total Vocal Tic Score and the Total Tic Score on the three recordings.
-
The 15% will always be rounded up in cases where 15% of a score results in a score that is not a whole integer (i.e. 15% of 25 = 3.75 points; this would be rounded up to 4 points). The 15% can be in either direction of the score.
-
Assessors who do not meet the criteria will be given additional training and asked to score the recordings again until the specified agreement criteria are met.
-
The assessor’s agreement with the ER will be assessed every 6 months during the trial. Up to a total of four new YGTSS assessment videos will be used to check agreement at follow-up (i.e. after initial agreement within the specified range has been established). The videos will be recordings from YGTSS conducted on ORBIT patients at baseline or follow-up assessments. Each of the trial assessors will submit at least one video.
-
If any assessors fall outside this 15% agreement with the ER they will be required to engage in further training as and when this is appropriate during the trial.
-
Assessors also participate in monthly conference calls with the ER and trial manager. These calls provided a forum for discussing cases and developing a common approach to conducting assessments across sites. Additional reviewing of videos and discussion with the assessors about scoring will be provided by the ER via email on an ad hoc basis. The ER will keep a record of these supervision meetings. 4,153
| TTS | TTS 15 low | TTS 15 high | Motor total | Motor 15 low | Motor 15 high | Vocal total | Vocal 15 low | Vocal 15 high | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Rater baseline training scores | ||||||||||
| Video 1 | ||||||||||
| ER | 26 | 22.1 | 29.9 | 15 | 12.8 | 17.3 | 11 | 9.4 | 12.7 | |
| A1 | 29 | 22.1 | 29.9 | 15 | 12.8 | 17.3 | 14 | 9.4 | 12.7 | |
| A2 | 30 | 22.1 | 29.9 | 17 | 12.8 | 17.3 | 13 | 9.4 | 12.7 | |
| A3 | 29 | 22.1 | 29.9 | 16 | 12.8 | 17.3 | 13 | 9.4 | 12.7 | |
| A4 | 30 | 22.1 | 29.9 | 17 | 12.8 | 17.3 | 13 | 9.4 | 12.7 | |
| A5 | 26 | 22.1 | 29.9 | 13 | 12.8 | 17.3 | 13 | 9.4 | 12.7 | |
| Video 2 | ||||||||||
| ER | 27 | 22.9 | 31.1 | 15 | 12.8 | 17.3 | 12 | 10.2 | 13.8 | |
| A1 | 28 | 22.9 | 31.1 | 16 | 12.8 | 17.3 | 12 | 10.2 | 13.8 | |
| A2 | 30 | 22.9 | 31.1 | 16 | 12.8 | 17.3 | 14 | 10.2 | 13.8 | |
| A3 | 33 | 22.9 | 31.1 | 20 | 12.8 | 17.3 | 13 | 10.2 | 13.8 | |
| A4 | 27 | 22.9 | 31.1 | 16 | 12.8 | 17.3 | 11 | 10.2 | 13.8 | |
| A5 | 28 | 22.9 | 31.1 | 17 | 12.8 | 17.3 | 11 | 10.2 | 13.8 | |
| Video 3 | ||||||||||
| ER | 26 | 22.1 | 29.9 | 11 | 9.4 | 12.7 | 15 | 12.8 | 17.3 | |
| A1 | 26 | 22.1 | 29.9 | 12 | 9.4 | 12.7 | 14 | 12.8 | 17.3 | |
| A2 | 39 | 22.1 | 29.9 | 19 | 9.4 | 12.7 | 20 | 12.8 | 17.3 | |
| A3 | 35 | 22.1 | 29.9 | 19 | 9.4 | 12.7 | 16 | 12.8 | 17.3 | |
| A4 | 32 | 22.1 | 29.9 | 17 | 9.4 | 12.7 | 15 | 12.8 | 17.3 | |
| A5 | 36 | 22.1 | 29.9 | 19 | 9.4 | 12.7 | 17 | 12.8 | 17.3 | |
| Video 4 | ||||||||||
| ER | 22 | 18.7 | 25.3 | 15 | 12.8 | 17.3 | 7 | 6.0 | 8.0 | |
| A1 | 24 | 18.7 | 25.3 | 17 | 12.8 | 17.3 | 7 | 6.0 | 8.0 | |
| A2 | Left position on trial – no further YGTSS conducted | |||||||||
| A3 | 25 | 18.7 | 25.3 | 18 | 12.8 | 17.3 | 7 | 6.0 | 8.0 | |
| A4 | 23 | 18.7 | 25.3 | 15 | 12.8 | 17.3 | 8 | 6.0 | 8.0 | |
| A5 | 24 | 18.7 | 25.3 | 17 | 12.8 | 17.3 | 7 | 6.0 | 8.0 | |
| Rater expert agreement check, January 2019 | ||||||||||
| ER | 34 | 28.9 | 39.1 | 17 | 14.5 | 19.6 | 17 | 14.5 | 19.6 | |
| A1 | 37 | 28.9 | 39.1 | 21 | 14.5 | 19.6 | 16 | 14.5 | 19.6 | |
| ER | 10 | 8.5 | 11.5 | 10 | 8.5 | 11.5 | 0 | 0 | 0.2 | |
| A3 | 11 | 8.5 | 11.5 | 11 | 8.5 | 11.5 | 0 | 0 | 0.2 | |
| ER | 29 | 24.7 | 33.4 | 13 | 11.1 | 15.0 | 16 | 13.6 | 18.4 | |
| A4 | 29 | 24.7 | 33.4 | 13 | 11.1 | 15.0 | 16 | 13.6 | 18.4 | |
| ER | 31 | 26.4 | 35.7 | 15 | 12.8 | 17.3 | 16 | 13.6 | 18.4 | |
| A5 | 29 | 26.4 | 35.7 | 14 | 12.8 | 17.3 | 15 | 13.6 | 18.4 | |
| Rater expert agreement check, June 2019 | ||||||||||
| ER | 35 | 29.8 | 40.3 | 17 | 14.5 | 19.6 | 18 | 15.3 | 20.7 | |
| A1 | 33 | 29.8 | 40.3 | 18 | 14.5 | 19.6 | 15 | 15.3 | 20.7 | |
| ER | 30 | 25.5 | 34.5 | 16 | 13.6 | 18.4 | 14 | 11.9 | 16.1 | |
| A3 | 29 | 25.5 | 34.5 | 17 | 13.6 | 18.4 | 12 | 11.9 | 16.1 | |
| ER | 20 | 17.0 | 23.0 | 10 | 8.5 | 11.5 | 10 | 8.5 | 11.5 | |
| A4 | 23 | 17.0 | 23.0 | 13 | 8.5 | 11.5 | 10 | 8.5 | 11.5 | |
| ER | 47 | 39.9 | 54.1 | 23 | 19.6 | 26.5 | 24 | 20.4 | 27.6 | |
| A5 | 45 | 39.9 | 54.1 | 23 | 19.6 | 26.5 | 22 | 20.4 | 27.6 | |
| Rater expert agreement check, December 2019 (A3–A4 no longer actively conducting YGTSS) | ||||||||||
| ER | 34 | 28.9 | 39.1 | 18 | 15.3 | 20.1 | 16 | 13.6 | 18.4 | |
| A1 | 31 | 28.9 | 39.1 | 18 | 15.3 | 20.1 | 13 | 13.6 | 18.4 | |
| ER | 22 | 18.7 | 35.3 | 13 | 11.1 | 14.9 | 9 | 7.7 | 10.4 | |
| A1 | 28 | 18.7 | 35.3 | 17 | 11.1 | 14.9 | 11 | 7.7 | 10.4 | |
| ER | 33 | 28.1 | 37.9 | 17 | 14.5 | 19.6 | 16 | 13.6 | 18.4 | |
| A5 | 33 | 28.1 | 37.9 | 17 | 14.5 | 19.6 | 16 | 13.6 | 18.4 | |
| ER | 25 | 21.3 | 28.8 | 16 | 13.6 | 18.4 | 9 | 7.7 | 10.4 | |
| A5 | 25 | 21.3 | 28.8 | 15 | 13.6 | 18.4 | 10 | 7.7 | 10.4 | |
| Retraining given to R1 and scores on new videos, December 2019 | ||||||||||
| ER | 34 | 28.9 | 39.1 | 18 | 15.3 | 20.7 | 16 | 13.6 | 18.4 | |
| A1 | 31 | 28.9 | 39.1 | 18 | 15.3 | 20.7 | 15 | 13.6 | 18.4 | |
| ER | 22 | 18.7 | 25.3 | 13 | 11.1 | 14.9 | 9 | 7.7 | 10.4 | |
| A1 | 25 | 18.7 | 25.3 | 15 | 11.1 | 14.9 | 10 | 7.7 | 10.4 | |
| Rater expert agreement check, June 2020 | ||||||||||
| ER | 24 | 20.4 | 27.6 | 14 | 11.9 | 16.1 | 10 | 8.5 | 11.5 | |
| A1 | 25 | 20.4 | 27.6 | 16 | 11.9 | 16.1 | 9 | 8.5 | 11.5 | |
| ER | 12 | 10.2 | 13.8 | 12 | 10.2 | 13.8 | 0 | 0 | 0 | |
| R1 | 12 | 10.2 | 13.8 | 12 | 10.2 | 13.8 | 0 | 0 | 0 | |
| ER | 19 | 16.2 | 21.9 | 11 | 9.4 | 12.7 | 8 | 6.8 | 9.2 | |
| A5 | 19 | 16.2 | 21.9 | 10 | 9.4 | 12.7 | 9 | 6.8 | 9.2 | |
| ER | 41 | 34.9 | 47.2 | 21 | 17.9 | 24.2 | 20 | 17.0 | 23.0 | |
| A5 | 38 | 34.9 | 47.2 | 18 | 17.9 | 24.2 | 20 | 17.0 | 23.0 | |
Appendix 2 Analytical framework
| Description | |
|---|---|
| Category 1: Motivation for participating | |
| To remove tics | Participants stated that they wanted to participate so that their or their child’s tics will be gone completely or decrease in severity and frequency |
| To help others/research | Altruistic reasons for participating |
| Some sort of support | Lack of support from services, therefore looking for any type of support available |
| Hoped to learn more about tics | Lack of information and knowledge of tics, so wanted to learn more to help themselves/their child |
| Due to it being done online | Participants’ motivating factor was because it was online |
| Category 2: Initial response to ORBIT | |
| Participant responsiveness | How participants and therapists initially responded to ORBIT; includes assessments by participants about the outcomes and relevance of ORBIT |
| Quality of ORBIT trial description | Degree to which the ORBIT trial was sufficiently and clearly described |
| Quality of delivery | Concerns whether the intervention was delivered in a way appropriate to achieving what was intended, including participants’ thoughts on therapists |
| Strategies to support therapists | Refers to strategies such as provision of manuals, guidelines, training and supervision |
| Clinician perceptions of and contribution to recruitment | Refers to consistency of recruitment procedures, perceptions of reasons for non-participation among potential participants and subgroups less likely to participate |
| Perception of initial recruitment strategies | Includes participants’ views on the initial telephone screening and baseline assessment |
| Relevance of questionnaires | Participants’ views on the relevance of the questionnaires to themselves |
| Expectations of role of the therapist | Perception that ‘therapist’ was a misleading name |
| Category 3: ORBIT programme content | |
| Perceptions of ORBIT organisation | Includes views on whether ORBIT was an appropriate length, the structure of sessions and frequency of therapist contact |
| Lack of fit between content and child | Includes judgement on the videos, animations, appropriateness to child’s age and missions |
| Useful and enjoyable programme resources | What participants felt they have learnt from ORBIT (e.g. strategies parents have made as a result) and what were the most useful and enjoyable resources used |
| Ease of use | The ability to use ORBIT even if you lack IT skills |
| ORBIT recommendations | What participants and therapists feel could be added to or removed from ORBIT to improve the programme |
| Category 4: Mechanisms of impact | |
| Features of online therapy to support tic reduction | Perception of online therapy working to help reduce tics and related behaviours, including acceptability and satisfaction with ORBIT |
| Perceived benefits of therapist support | Having a therapist provided continued focus and motivation and the ability to answer any queries |
| Limitations of online therapy | ORBIT was limited by being delivered online and participants would have preferred face-to-face therapy |
| Working together | Instances of parent and child going through ORBIT together and the impact on how ORBIT was used and their relationship |
| Unanticipated consequences | This captures anything that happened unexpectedly as a result of ORBIT |
| Category 5: Intervention outcomes | |
| Level of control | The child has better control over their tics in their daily life |
| Expectations vs. reality | Considering the participants’ expectations of ORBIT, what the reality has been in outcomes |
| Long-term outcomes | Going forward, what the future holds for participants; this includes anything the participant has said about future plans regarding use of services and whether they will continue to use ORBIT |
| Routine clinical practice | This refers to what clinicians feel are the main enablers or barriers to implementation of ORBIT in clinical practice (e.g. lack of funding) |
| Improved self-esteem and confidence | The intervention improved the child’s sense of self, confidence and QoL |
| Improvement in tics | The intervention improved the frequency and severity of the child’s tics |
| Impact on parent | The intervention had a positive impact on the parent in caring for their child |
| Category 6: Intervention characteristics that enabled implementation | |
| Flexibility of online therapy | Being able to do online therapy at your own time and pace is seen as a positive |
| Therapist support | Having therapist support was seen as essential |
| Use of computers | CYP prefer using computers over face-to-face contact |
| Perceived impact of therapy | If the participant started to perceive the intervention as having a positive impact, they were more likely to engage |
| Adaptations | Participants tailoring the intervention by making modifications to suit their needs |
| Category 7: Trial-related enablers to implementation | |
| Opportunity to discuss tics | This captures how children could open up and talk about their tics to someone other than their family members for the first time |
| Follow-ups | Having continuous support through follow-up appointments had a positive impact |
| Financial reimbursement | The use of vouchers as a reward for completing each follow-up aided implementation, as well as expenses being reimbursed for initial baseline assessment |
| Trust in experts | Refers to how participants felt positive about the therapy as it was conceptualised and delivered by tic experts |
| Category 8: Trial-related barriers to implementation | |
| Staffing resources | Staffing issues and demands placed on the ORBIT team affected quality of implementation |
| Demand on participants | Trial-related demands on participants (e.g. travelling long distances for baseline assessment and ability to participate in follow-ups) |
| Therapists’ workload | Overworking of therapists affected quality of implementation |
| Therapeutic relationship | Therapists struggled to build an alliance with participants due to a lack of visibility |
| Therapists’ background and confidence | Therapists did not feel confident in their qualifications or ability to carry out their role expertly |
| Category 9: Intervention characteristics that supported tic reduction | |
| Visualisation of progress | Participants were more likely to engage better as they could see the progress they were making and competing to beat their times on tasks |
| Use of rewards | Children were more likely to engage as they knew they would be receiving a reward for completing the tasks and practises |
| Category 10: Intervention characteristics that hindered engagement | |
| Repetitiveness | Participants found the content highly repetitive and therefore would lose motivation and disengage |
| Perceived lack of utility | Participants would disengage if they did not see an immediate impact on their tics |
| Lack of interaction | Participants wanted more face-to-face contact with therapists even if this was via videoconferencing and were more likely to stop persisting with ORBIT if they did not receive this |
| Negative impact on tics | As can be an effect of ERP, tics began to worsen and therefore participants would disengage |
| Lack of relevance | If participants began to feel some of the components of the intervention were not relevant to them, they would disengage |
| Perceptions of lack of engagement | Reasons clinicians and therapists felt that some may have not engaged as well as others |
| Category 11: Participant contextual factors | |
| Perceived utility | Participants who expected long-term benefit of ORBIT persisted to complete the chapters and tasks |
| High motivation levels | Participants who were highly motivated to engage in ORBIT continued to engage with it |
| Parental persuasiveness | Parents were the main motivating force behind their child’s level of engagement |
| Category 12: Family contextual factors | |
| Life stressors | This captures how families struggled with ORBIT due to various stressors (e.g. child about to move to a new school) |
| Busy lives | The context of how families fit ORBIT into their everyday lives despite being busy (e.g. work, extracurricular activities) |
| Family dynamics | Parents with other children who also have neurodevelopmental or health issues |
| School life | How the exam period or holidays affected participation in ORBIT |
Appendix 3 Qualitative quotes (mechanisms of impact)
| Quote number | Verbatim quote | Framework category | Theme |
|---|---|---|---|
| 1 | ‘I thought the therapy would help and I was hoping that it would help if I put some effort in and practise in. But I did not know how it was going to help like I didn’t know that there was going to be tic stopwatches in there, videos, and chapters in there’ (Child 20, 12 years old) | Mechanisms of impact | Features of online therapy to support tic reduction |
| 2 | ‘It was like a circle, a vicious circle, where it was like urge, tics, it goes away, urge, tic, go away [“tic cycle”]. And that helps you visualise what goes on and there was another one that was like, the urge, then tic, resist, urge, tic, resist. That helped you visualise what you needed to do’ (Child 4, 11 years old) | Features of online therapy to support tic reduction | |
| 3 | ‘I liked the … reward thing because it was like a constant practising, you’ll get a reward so it was like the motivation to do the practise’ (Child 27, 13 years old) | Features of online therapy to support tic reduction | |
| 4 | ‘We did get into a bit of a lull midway through which is when we implemented the rewards which was … he’s a saver … he likes pocket money so we kind of factored the rewards into his pocket money and … that gave him a bit more impetus because we did hit a bit of lull … I don’t know maybe midway through? Maybe just afterwards and implemented and we had all the rewards stuff and knew about it but in the beginning, he was so focused on it and so into it that we didn’t need to do it. So we implemented that side of it later’ (Parent 6, mother) | Features of online therapy to support tic reduction | |
| 5 | ‘I guess with face to face, it’s easier to connect with my therapist. It’s easier to work through something with them. It’s easier to make sure I understood the ORBIT stuff so yeah I would have probably have preferred face to face’ (Child 18, 14 years old) | Limitations of online therapy | |
| 6 | ‘You don’t get an instant response from the therapist. Obviously they don’t work after 5 or 6 o’clock at night … but sometimes they’re in every 3 days or so. So if he didn’t get a response the next day, there wasn’t an immediate answer to his questions, which again for kids, they want something a little more immediate. And in the same, when you’re having a particularly rough time, you’d email, you know, make a comment and because the therapist only works 3 days a week, you didn’t get a response straight away … and that can be a bit frustrating’ (Parent 5, mother) | Limitations of online therapy | |
| 7 | ‘Well our internet connection is not great so it kept cutting out or freezing now and again. That was annoying’ (Parent 18, mother) | Limitations of online therapy | |
| 8 | ‘I did the chapters with my mum and with my brothers and the tic stopwatch I had my mum or my brothers looking for my tics if I did the tic or not. And like I said that like made it harder for me if I wanted them to or just cheered me on’ (Child 20, 12 years old) | Working together | |
| 9 | ‘I think … I do this is just from judging from our perspective I do think [child’s name] needed to have me guide him if you like on it. So this is what we’re going to do and we’re going to sit down and I explained to him I’ve already watched those bits I need to do but you need to watch this section and if you got any questions you can ask me. I think it was nice. I think [child’s name] we kind of felt like a team working together on this’ (Parent 11, mother) | Working together | |
| 10 | ‘There was some times when he was tired and he didn’t particularly want to do it but I think because we did it together it then become oh actually I’ve got the computer out we go on the nice sofa and sit together. So I tried to make it at times when he was reasonably relaxed and receptive because I know what he’s like … in terms of prevarication with ADHD. So most of the time it ended up being a nice time that we ended up spending together doing something that was just the two of us’ (Parent 21, mother) | Working together | |
| 11 | ‘I don’t think I could have done it without [name of therapist] … being there. Because … you know therapy … if I just had access to videos its similar to watching YouTube you know. There are plenty of therapists out there on YouTube but knowing the right questions to ask and where you’re struggling and the support behind it, that they know about tics, it does help’ (Parent 27, mother) | Working together | |
| 12 | ‘My experience of the cognitive behavioural therapy tended to be you know probably 13 plus that they would have to have fairly committed parents who I think there needs to be a fair bit of encouragement in all these things’ (Clinician 6, psychiatrist) | Working together | |
| 13 | ‘Yeah I think it has helped. It’s helped me with supressing my tics. Like stopping me ticcing and also like it’s stopped me like how much I actually tic’ (Child 27, 13 years old) | Intervention outcomes | Improvement in tics |
| 14 | ‘I think it would have had an impact if I didn’t struggle so much with noticing my tic signals. Because you know I can’t even remember not ticcing so if I did have any tic signals they’re just how I feel normally so I didn’t pick up on them. And because I didn’t pick up on them I really struggled to know when my tics are coming. I mean because I didn’t know my tics were coming I couldn’t stop them. So I think it helped me realise more that there is a tic signal and I think with particularly strong tics’ (Child 21, 15 years old) | Improvement in tics | |
| 15 | ‘I thought we’d have an 80–90% reduction … but yeah I was expecting it to be a lot more than it was so I think I was expecting him to be just a little calmer and a little nicer around the house. But it didn’t really work quite that well’ (Parent 5, mother) | Expectations vs. reality | |
| 16 | ‘It’s affected his self-esteem positively. It’s affected his outlook on himself … you know sort of being more positive about what he’s got. And I think things like that are essential and … so even now that they haven’t been limited and I think with his age they’ll start to increase’ (Parent 8, mother) | Improved self-esteem and confidence | |
| 17 | ‘I think the one where we had to make a list of all the tics [tic ladder]. I engaged quite well with that one I think. I think it was a nice method like getting all the tics and putting them in an organised list’ (Child 27, 13 years old) | ORBIT programme content | Useful and enjoyable programme resources |
| 18 | ‘I liked the videos because I didn’t have to read it. And they were telling you it’ (Child 16, 10 years old) | Useful and enjoyable programme resources | |
| 19 | ‘I really enjoyed the videos like when you see the therapist delivering the therapy in the sessions because to me it just kind of shows … because I’m very visual, I like to see things and you know be reassured that actually what I’m doing is right’ (Parent 25, mother) | Useful and enjoyable programme resources | |
| 20 | ‘Some of it was really a bit young for me because I am on the older end of the test study but … some of it was good to like go over the basics. Some of the like tasks like dragging facts into boxes were maybe a bit young for my age’ (Child 22, 15 years old) | Lack of fit between content and child | |
| 21 | ‘I think the older children tend to get less out of it, because obviously we’ve got quite a wide age range from 9 to 17, so inevitably the older children, I’ve got quite a lot of feedback that they felt it was a bit too young for them, so there’s that’ (Therapist 3) | Lack of fit between content and child |
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- AE
- adverse event
- BIP
- Barninternetprojektet (Child Internet Project; Swedish digital platform)
- BT
- behavioural therapy
- C2C
- consent to contact
- CA-SUS
- child and adolescent service use schedule
- CAIDS-Q
- child and adolescent intellectual disability screening questionnaire
- CandA-GTS-QoL
- Child and Adolescent Gilles de la Tourette Syndrome Quality of Life Scale
- CBIT
- comprehensive behavioural intervention for tics
- CEAC
- cost-effectiveness acceptability curve
- CEAP
- cost-effectiveness acceptability plane
- CGAS
- Children’s Global Assessment Scale
- CGI-I
- Clinical Global Impressions-Improvement scale
- CHU9D
- child health utility 9D
- CI
- confidence interval
- CSRI
- client service receipt inventory
- CYP
- children and young people
- DAWBA
- development and well-being assessment
- DMC
- Data Monitoring Committee
- ER
- expert rater
- ERP
- exposure and response prevention
- GBP
- Great Britain pounds
- GCP
- good clinical practice
- HEAP
- health economics analysis plan
- HRQoL
- health-related quality of life
- HRT
- habit reversal training
- IAPT
- improving access to psychological therapies
- iCBT
- internet-based cognitive–behavioural therapy
- ICER
- incremental cost-effectiveness ratio
- IMD
- index of multiple deprivation
- MFQ
- moods and feelings questionnaire
- NMB
- net monetary benefit
- OCD
- obsessive–compulsive disorder
- OR
- odds ratio
- ORBIT
- online remote behavioural intervention for tics
- PIC
- patient identification centre
- PPI
- patient and public involvement
- PSA
- probabilistic sensitivity analysis
- PTQ
- parent tic questionnaire
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- SAE
- serious adverse event
- SCAS
- Spence Child Anxiety Scale
- SD
- standard deviation
- SDQ
- strengths and difficulties questionnaire
- SUR
- seemingly unrelated regression
- TMG
- Trial Management Group
- TS
- Tourette syndrome
- TSC
- Trial Steering Committee
- TTSS
- total tic severity score
- YGTSS
- Yale Global Tic Severity Scale