Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as award number NIHR130396. The contractual start date was in September 2020. The draft manuscript began editorial review in November 2022 and was accepted for publication in March 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2023 Prieto et al. This work was produced by Prieto et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Prieto et al.
Chapter 1 Introduction and background
The risk of developing a urinary tract infection (UTI) rises as people age. It is more common in postmenopausal women and older men with prostatic disease. The presence of an indwelling urinary catheter (IUC) increases the risk of catheter-associated urinary tract infection (CAUTI) and up to 50% of women in long-term care may have asymptomatic bacteriuria (ASB). Bloodstream infection (BSI) is a serious consequence of UTI and can result in significant morbidity and mortality. The inappropriate treatment of UTI in older people in long-term residential care is an important driver for antimicrobial resistance.
This realist synthesis draws together evidence from research and grey literature and from stakeholder contributions by residents and family carers, care home staff and managers, primary care clinicians, specialist practitioners and commissioners of care to inform how interventions to prevent and recognise UTI and CAUTI can be delivered effectively by staff working in care homes.
Aim and objectives
The aim of the realist synthesis is to produce evidence-informed theoretical explanations of which strategies are effective (or not) in preventing older people in care homes from acquiring UTI.
The objectives are to:
-
identify which interventions could be effective, the mechanisms by which these strategies work (or why they fail), for whom and under what circumstances
-
understand what needs to be in place for the implementation of programmes to support the prevention of UTI and its recurrence in older people with and without a urinary catheter living in care homes in the UK.
Background
Care homes in the UK provide long-term residential or nursing care for a range of people who are vulnerable and have health and social support needs, in particular the frail elderly. In 2022, there were 408,371 people living in care homes in the UK. The population was higher in England than in any other part of the UK. 1 The number of registered care homes in the UK in 2022 was reported as 17,079, many of which were owned and managed by the independent sector. 2 Care homes are licensed and regulated in each of the devolved nations and funding of places ranges from fully privately funded, a mix of private and local authority funding and full local authority funding.
The workforce in care homes is similarly diverse with few professionally qualified staff. In 2022, data from England illustrated the low numbers of healthcare professionals (HCPs) working in the health and social care sector. 3 Around 80,000 (5%) of the 1.62 million adult social care workforce were regulated professionals, of which 32,000 (2%) were registered nurses, with most of these (30,000) working in residential care establishments. 3 In addition, care homes face a high turnover of staff, with a turnover rate of 34% in a 12-month period among registered nurses. 3 This combination of factors makes the care home sector a complex environment in which to co-ordinate and manage infections.
Research suggests that a high proportion of people living in care homes have a degree of frailty, but that a further 40% are at risk of becoming frail. 4 Care and nursing home residents have varying degrees of frailty, including levels of immunocompromise (a reduced ability to fight infections and other diseases), which make them more vulnerable to adverse events such as infection and falls.
The knowledge and skills required to respond to and manage outbreaks of infection in care homes are compromised by the paucity of training opportunities and limited resources available. Although care is often under the supervision of a registered nurse, staff working in care homes are likely to have limited knowledge of infection prevention. For the majority of the unqualified care home workforce across the UK, basic training includes minimal content on infection prevention and control (IPC) underpinned by a Care Certificate for staff recruited in recent years. 5 In addition, evidence suggests that leadership at both a strategic and operational level within care homes has a significant effect on the way that care is delivered. 6
Urinary tract infection
Urinary tract infection is the most commonly diagnosed infection in older people. It is caused by the multiplication of micro-organisms within the urinary tract and can result in a number of clinical syndromes, including pyelonephritis, cystitis and urethritis. Infection can also spread to the bloodstream. Consequences of UTI can range from a mild self-limiting illness to severe sepsis with a mortality rate of 20–40%. 7,8 Inadequate antimicrobial therapy significantly increases the risk of infection spreading to the bloodstream. Resistance to antibiotics normally used to treat UTI is now common in the UK, with 40% of uropathogens now resistant to trimethoprim. 9 Older people who experience repeated episodes of UTI, and therefore frequent exposure to antibiotics, are at greater risk of acquiring resistant pathogen-associated BSI. 10,11 UTI accounts for more than 50% of antibiotic prescriptions in long-term care settings. 12
The incidence of UTI increases with age in both men and women and is highest among those living in long-term care facilities at 44–58 infections per 100 person-years at risk. 8 Several factors predispose older people to UTI, including genitourinary tract disorders, increased susceptibility to ASB (bacteria in the urine), cognitive impairment and incontinence. 12,13 Older people living in care homes are more likely to have these comorbidities and are therefore at particular risk of acquiring UTI. In a cohort and nested case–control study undertaken in six long-term care facilities in Norway, the incidence of UTI was 2 per 1000 resident days [95% confidence interval (CI) 1.8 to 2.2] and they accounted for 40% of infections acquired by residents. 14 Risk factors for UTI included being confined to bed [odds ratio (OR) 2.7], an IUC (OR 2.0), skin ulcers (OR 1.8) and urinary incontinence (OR 1.5). 14
Although most UTIs in this setting are not associated with an invasive device, the presence of an IUC provides a route for bacteria colonising the perineum to gain access to the bladder and increases the risk of UTI by 3–8% per day. 15,16 A prevalence survey of 425 care homes in the UK found 6.9% of the 12,827 resident population had a urinary catheter. 17 This study also provided evidence of variation in practice both in relation to discharge from hospital with an IUC and its removal once in the care home, suggesting there is room for a more proactive approach to reducing IUC use.
Urinary tract infection is one of the most common reasons for hospitalisation accounting for one-third of the admissions from care homes. 15 In those admitted with BSI, half occur as a result of a urinary source. 15 In a study of community-acquired infections in older people admitted to hospital, residents in care home were found to have more comorbidities (p = 0.048) and higher rates of resistant bacteria (70% vs. 36%, p = 0.026) compared to people resident in their own homes. 18 Improving understanding of the strategies that could be effective in preventing UTI in in long-term care settings is a priority given the increased susceptibility of this population, the frequency with which UTI occur and the impact on the wider population in terms of acute care resources and increasing antimicrobial resistance.
Prevention strategies
Although the predominant cause of infection among older people is UTI, guidance about strategies for prevention in care homes is limited and mainly focused on urinary catheters. 19,20 Guidance does not account for the varying contexts in which care is delivered,21 the challenges presented by residents with complex health needs or the demands of care delivery by unqualified staff with limited supervision. 22,23 A systematic review by Lee et al. 24 explored evidence for the impact of different components of infection prevention programmes on practice and infection outcomes. Education, monitoring and feedback were identified as essential components in strategies for affecting behavioural changes in healthcare workers at long-term care facilities. However, little is known about the practicality of implementing these approaches in UK care homes.
A recent systematic review of interventions to reduce UTI in nursing home residents identified 19 studies, most of which were small scale, non-randomised before and after studies. 25 The majority of these were focused on prevention of infection related to urinary catheters, for example, by replacing indwelling catheters with intermittent or condom catheterisation, ensuring appropriate indication for the catheter and improving management to reduce the risk of UTI. Six studies were focused on improving continence care and bladder training.
Optimising the care of urinary catheters and the use of alternatives to a catheter are key strategies for preventing UTI. Duration of catheterisation is the most important modifiable risk factor for CAUTI16 and so timely review and removal of catheters is imperative. Urinary catheters are commonly inserted in older people while they are in hospital but can remain in place following discharge from hospital when there is no clear plan for review and removal. A recent prevalence survey of patients with an IUC on district nursing caseloads in the UK found a high proportion of newly placed catheters (those placed within 4 weeks in patients without a catheter previously) originated in hospital, with only half having an active management plan likely to result in early removal of the catheter. 26 Most patients with a newly placed catheter were men aged 70 years or older, of whom 11% were in residential care or on an assisted living unit.
In residents without a catheter, studies have focused on strategies to reduce the risk of recurrent UTI (RUTI; at least two UTI in 6 months or three in 12 months) using a range of non-antibiotic agents that prevent uropathogens adhering to epithelial tissue in the urinary tract (D-mannose), create an antiseptic environment in the bladder (methenamine hippurate, cranberry) and support natural defences against UTI (probiotics and oestrogen). There is a body of evidence from small-scale trials and systematic reviews, although the efficacy and feasibility of using such approaches in a care home setting are important considerations. 27
Recognising urinary tract infection and residents at increased risk in care homes
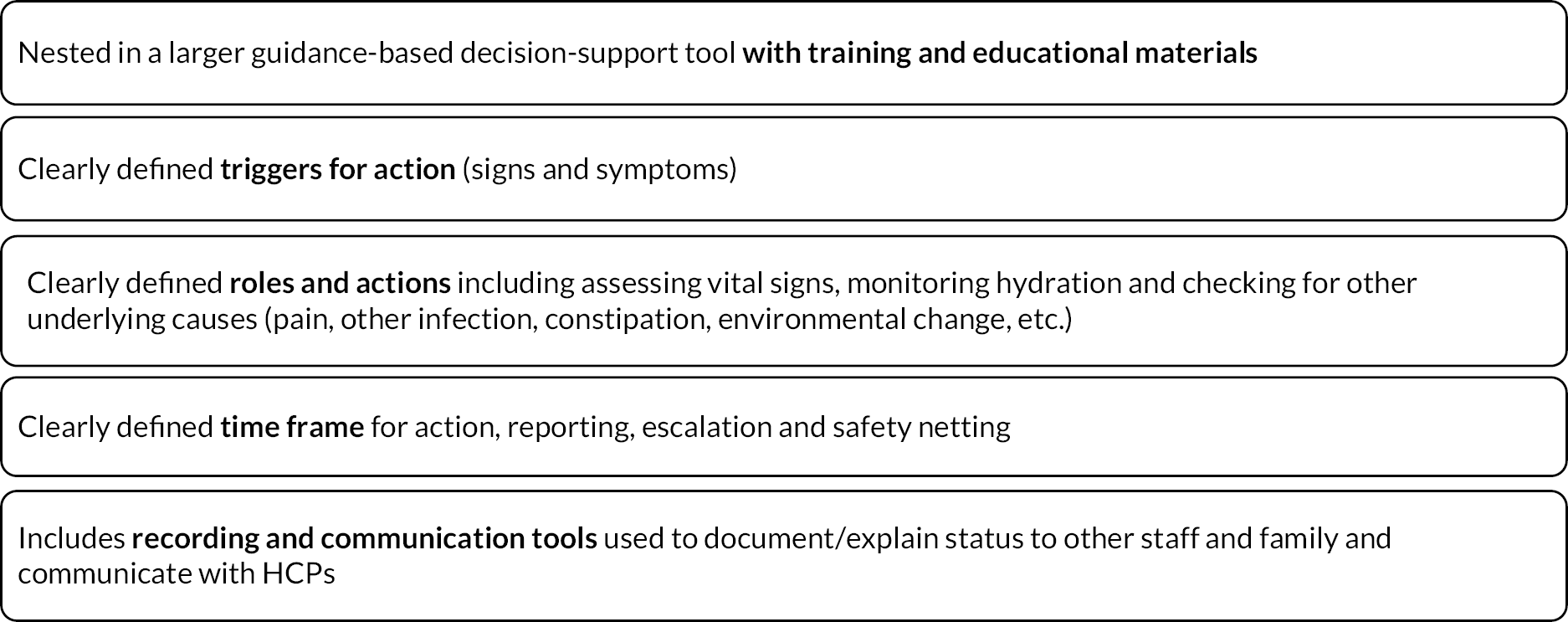
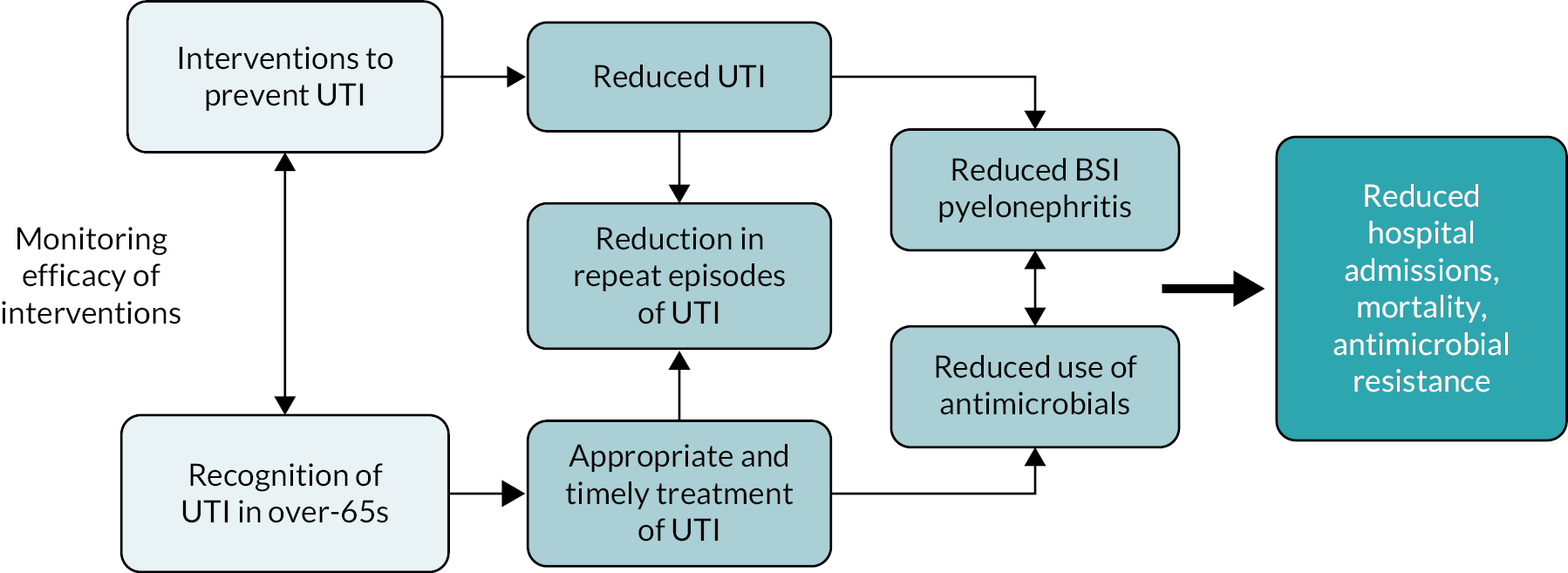
Mechanisms that support accurate recognition of UTI by care home staff, nurse practitioners and general practitioners (GPs) are critical to driving improvements in UTI prevention as they enable informed assessment of individual residents and monitoring of the effectiveness of prevention strategies (Figure 1). Overdiagnosis of UTI is a known problem in care homes,28–30 and without accurately distinguishing infection from ASB, it is not possible to measure the impact of prevention strategies. Targeting prevention strategies at those residents at greatest risk of UTI may be a useful approach, but this also requires reliable mechanisms to identify residents who experience recurrent infections. 8,25
FIGURE 1.
How recognition of UTI is integral to its prevention.
Accurate recognition of UTI in long-term care is problematic. Many adults over 65 years have ASB and discriminating those who have a UTI when this may present as generalised symptoms such as abdominal or back pain can be difficult. 31 In addition, a high proportion of care home residents are living with cognitive impairment or dementia and may not be able to communicate symptoms. Reagent strip tests (dipsticks) are commonly used by care home staff and clinicians as a UTI diagnostic tool despite their unreliability in older people and recommendations in national guidelines to cease their use in this group. 20,32,33 Use of urine dipsticks may drive unnecessary antibiotic prescribing for ASB,13 placing individuals at risk of adverse drug effects and more recurrent infections with antibiotic-resistant bacteria. 31
Significant resources within primary care would be required to provide full clinical assessments for all suspected UTI cases in care homes and therefore GPs rely on care staff to make clinically accurate observations. Staff working in care homes for older people may have limited ability to distinguish relevant signs and symptoms and limited access to specialist advice. Also, recent emphasis on the importance of early recognition of deterioration and sepsis may bring about an overly cautious approach to escalating concerns to the GP for fear of missing an infection. This creates a tension between reducing unnecessary use of antibiotics in line with antimicrobial stewardship (AMS) and early recognition and treatment of infection, with GPs often providing prescriptions over the phone.
Rates of emergency hospital admissions due to UTI are reported to have increased markedly in England since 2001,34 and one-third of admissions to hospital from care homes are due to UTI. 15 UTI prevention is therefore an important driver for reducing admission rates. Older people, particularly those in care homes, are the most vulnerable to UTI; yet, guidance on effective prevention strategies is limited and mostly not directed at this setting. Consequently, there is an urgent need for coherent, evidence-based programmes to support the prevention of UTI that are both relevant and practical to implement in care homes in the UK.
High rates of resistance to antibiotics used to treat UTI have emerged as a major public health problem, with a high proportion of urinary Escherichia coli (E. coli) isolates now resistant to trimethoprim. 9 Up to 50% of antibiotics administered in care homes for older people are prescribed for UTI. 15,35 However, because UTI is difficult to diagnose accurately in this population, a high proportion of antimicrobial prescriptions is unnecessary,13,36 while if UTI is present, inadequate antimicrobial therapy significantly increases the risk of BSI. 7 In the last decade, there has been a rapid, year-on-year, increase in incidence of invasive infections caused by the most common uropathogen, E. coli, with more than 43,000 cases reported in England in 2019. 37 The majority of these infections occur as a result of UTI, 68% originate outside acute healthcare settings, 70% occur in adults over 65,11,18 and cases associated with substantial antimicrobial resistance and increases in ambient temperatures. 10
In recognition of the important threat to public health presented by these trends in E. coli infections and resistance in uropathogens, a national target was set to reduce the number of Gram-negative BSI by 50% by 2021. 38 Since most of these infections occur because of UTIs in elderly people, identifying strategies that prevent UTI and understanding how to implement them effectively are essential to address this target.
The next chapter of the report describes the methods used in the realist synthesis.
Chapter 2 Review methods
Rationale for using realist synthesis
Realist synthesis was considered the most appropriate method to use for this review in order to provide a theory-driven understanding of what needs to be included in UTI prevention programmes to support their successful implementation in care homes for older people in the UK. Previous systematic and literature reviews on UTI prevention have established what is known about UTI prevention strategies but have not addressed how the active components of intervention programmes work in care homes. Moreover, the evidence base for some of these strategies (e.g. promoting hydration) is heterogeneous with few randomised controlled trials (RCTs) to include in a systematic review,39 necessitating a more inclusive approach to sourcing evidence.
A realist synthesis was therefore undertaken, employing a systematic approach to the searching of evidence, since this has an explanatory focus and seeks to understand how complex programmes work in particular contexts and settings. 40 The review examined the relationship between interventions to prevent UTI and the context in which they were applied to identify causal explanations of phenomena of interest, their mechanisms of action and what outcomes they produced. 41 Different sources of evidence were sought to construct a programme theory through a process that included several rounds of stakeholder engagement, an overview of relevant extant theory42 and examination of primary research relating to the topic.
In realist terms, a programme theory represents the underpinning mechanism of action, rather than the intervention40 and realist synthesis results in context–mechanism–outcome configurations (CMOcs) that explain how an intervention might or might not work. These configurations ensure external validity as they enable theory building to a level of abstraction that means the theories are useful in other contexts. 43
Context–mechanism–outcome configurations are often referred to as mid-range theories and afford the appropriate level of closeness to practice enabling the testing of initial programme theory propositions. 44 Providing a clear account of the mechanisms of action was considered essential to understanding how interventions to prevent UTI can and should be delivered in UK care homes. This is because mechanisms of action explain the way in which the resource element of an intervention might work. In scientific realism, mechanisms are a combination of the resources offered by an intervention (e.g. a risk assessment tool) and the reasoning or behaviour that is required to implement them (e.g. how this changed the reasoning of stakeholders to bring about the desired outcome). 40 CMOcs therefore provide explanations of what works, for whom and in which contexts and circumstances.
Changes in the review process
Minor changes were made to the published protocol relating to adaptations required to its delivery during the COVID-19 pandemic. More specifically, the project team and advisory group meetings were held online rather than in person and for shorter time periods than originally planned. The quality of communications and interactions may therefore have been affected by the limitations of online communication, although meeting virtually did facilitate attendance. Members of the core research team were able to meet in person at key points during the study to deliberate on theory development, which enhanced theory formulation. Similarly, the stakeholder workshops and teacher–learner interviews were held virtually rather than in person and for a shorter duration than planned, which may have affected the nature and quality of interactions.
Our original intention was to create a range of resources to support the prevention and recognition of UTI and CAUTI in the care home setting, such as care planning and decision-support tools. Our consideration of the literature and engagement with stakeholders helped us to identify a wide range of resources that were already in use in this setting and led us to question the value of adding further tools. Instead, we conducted a gap analysis (see Appendix 7, Table 5) to identify what types of resource are already in use in the care home setting and whether or where additional resources might be useful.
Review strategy
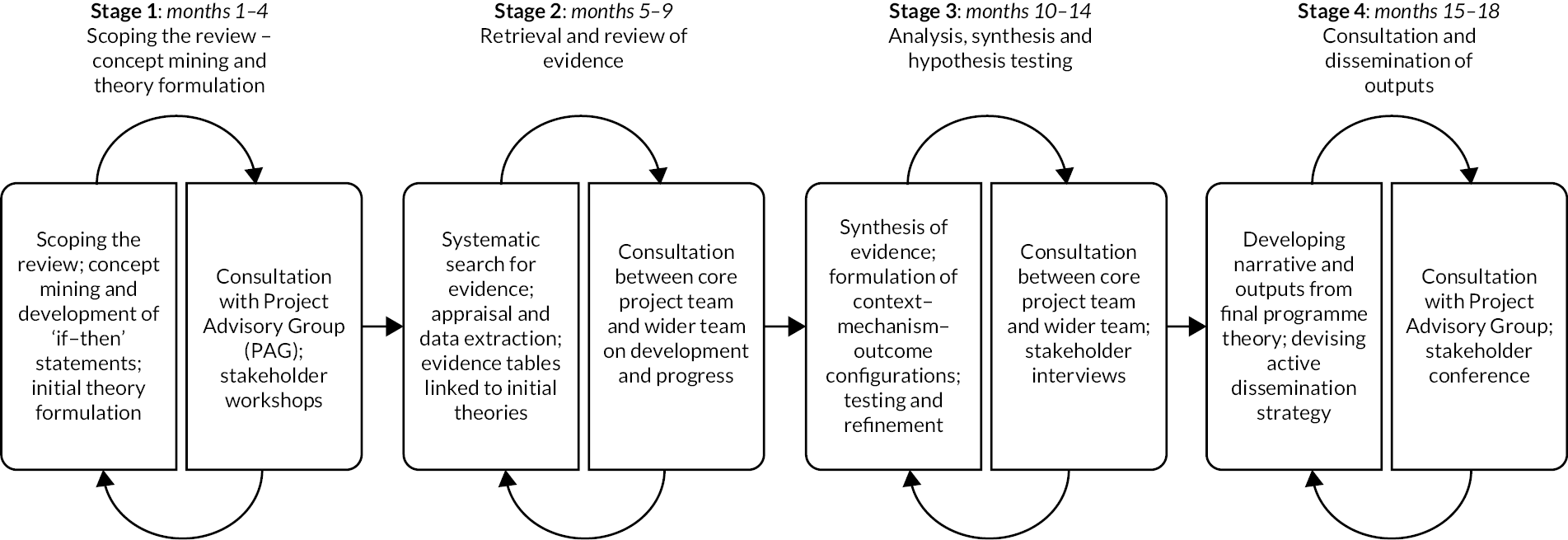
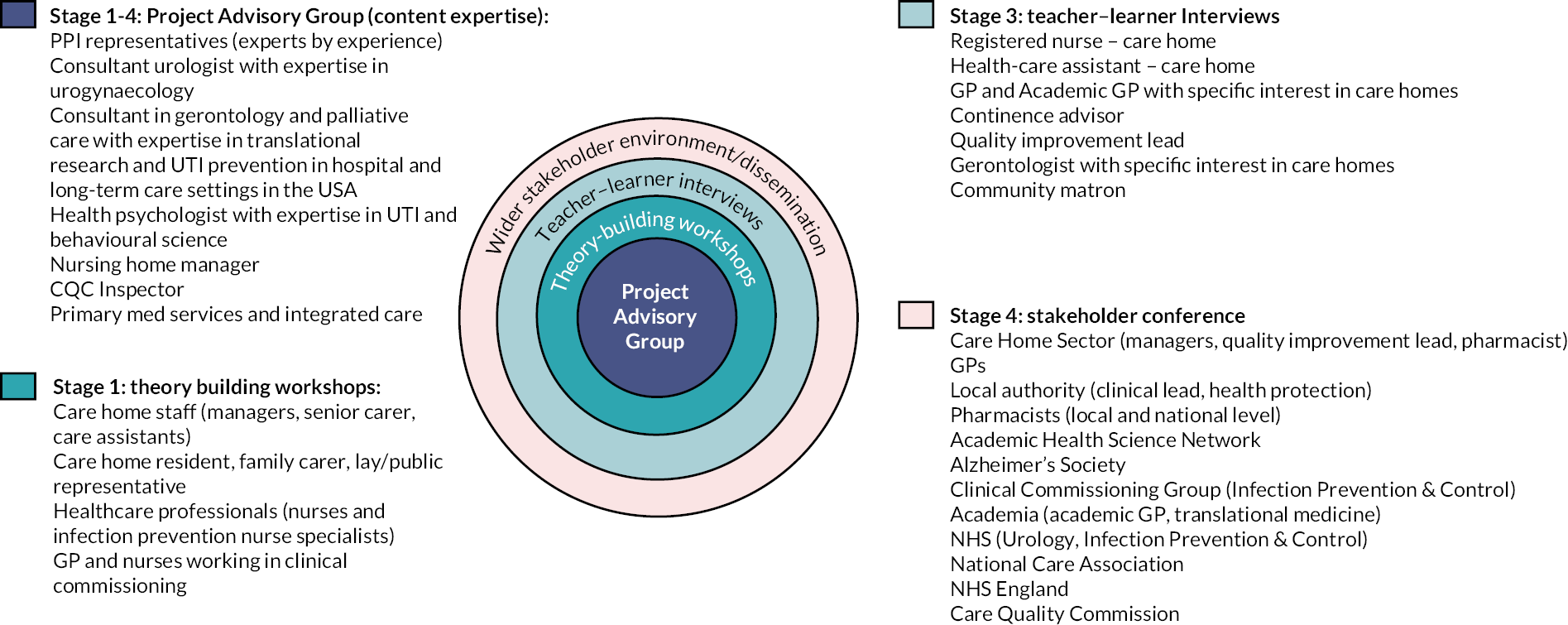
The review drew on evidence from health and social care, including primary research relating to UTI prevention and recognition in older people in care homes and improvement project reports in grey literature. It was conducted in an iterative rather than linear way over four stages (Figure 2).
FIGURE 2.
Stages of the project. Reproduced from Prieto et al. 45 Published by the BMJ Publishing Group Limited. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/.
Project advice and oversight
A Project Advisory Group (PAG) was established, comprising three patient and public involvement (PPI) representatives with experience of supporting older people living in care homes and individuals with relevant subject or professional expertise, including HCPs, a nursing home manager, a representative of the independent regulator for health and social care in England and researchers in the field of UTI/CAUTI prevention. The PAG was chaired by one of the PPI members and met on four occasions during the project to advise on priority issues within the review theory areas, comment on iterations of the plausible hypotheses and CMOcs and to provide challenge to the research team through their expert and lay perspectives.
The research team met at scheduled meetings to discuss progress and undertake in-depth discussions. Due to the restrictions imposed during the COVID-19 pandemic in 2020 and 2021, most of these meetings were via Microsoft TeamsTM.
Ethics
The study was identified as a service evaluation/service development following submission to the UK Health Research Authority and subsequent review by the University of Southampton Faculty Ethics Committee. However, we sought ethics approval from the University of Southampton Faculty Ethics Committee to engage with and interview stakeholders, which was granted on 15 October 2020 (submission ID 53942.A1).
Stage 1: concept mining and theory development
This stage of the realist synthesis used input from content experts in the research team, the PAG and stakeholders in addition to the preliminary scoping search.
Stakeholder engagement, including patient and public involvement
The project was supported by stakeholders, including PPI representatives, throughout the process to inform the development of initial and refined programme theories (CMOc) and establish their practical relevance and real-world potential.
A stakeholder analysis was undertaken by the research team and the PAG to identify a range of people who needed to be involved in the various aspects of the review process to impact on its success (Figure 3). This informed our approach to engaging with stakeholders in our initial theory-building workshops and at different points during the research to guide its development.
FIGURE 3.
Stakeholder matrix.
Stakeholders contributed to development and refinement of the programme theory, advising on the applicability of evidence and its relevance in specific contexts. In so doing, they helped to ensure that the synthesis was underpinned by multiple perspectives and focused upon what is important to care home residents and those who provide care.
Scoping interviews
Our initial plan was to conduct three face-to-face workshops with key stakeholders, in three separate locations across the country, to gain an insight into how the prevention and recognition of UTI/CAUTI was currently managed, the barriers and facilitators, decision-making processes, multidisciplinary involvement and staff and resident perspectives on the impact of UTI/CAUTI. However, the impact of the COVID-19 pandemic on the residential care sector resulted in us conducting the workshops online and undertaking one-to-one interviews with a small number of carers and residents. The interviews were conducted by three members of the research team via Microsoft Teams. They were recorded digitally and transcribed. An interview schedule was developed to ensure that all relevant aspects of the prevention and recognition of UTI/CAUTI were addressed. It covered the following areas:
-
residents and their family’s experience and involvement:
-
what are their priorities.
-
-
importance of ‘knowing’ the resident
-
experiences of caring for residents to prevent UTI/CAUTI:
-
what influences best practice
-
identification of residents at risk
-
recognition/communication of subtle changes in a resident’s condition
-
levers and drivers, for example, policies, pathways, guidance followed
-
experience–intuition–knowledge–training–peer influences.
-
-
involvement of GPs and other members of the multidisciplinary primary care team:
-
how the care team communicate between each other on residents’ symptoms.
-
-
what consequences people see in missing a UTI/CAUTI.
Interview with resident and family
An approach was made by the project lead to the PPI liaison officer in Wessex. They agreed for members of the research team to present the study at one of their PPI coffee group meetings to see if there were members of the PPI coffee group who may have experience as a relative of someone within a home. Two interviews were secured with members of this group.
An interview with a care home resident was secured following one of the care home workshops. The resident was interviewed with the support of the care home manager and a member of the care home staff.
Workshops
Workshops with care home managers and staff
Our initial approach to recruiting care homes was through the Research Delivery Manager for Social Care and Patient and Public Engagement [National Institute for Health and Care Research (NIHR) Clinical Research Network Wessex] and the Deputy Director of Quality and Nursing for West Hampshire Clinical Commissioning Group (CCG). It was agreed by them that the research team could present the study to care home managers at one of their regular virtual CCG meetings in January 2021. We asked care home managers who attended if they were interested in participating to share their details with the team, who would make contact to arrange a dedicated workshop with their home.
Two care homes were recruited via this route. The first was a residential home with a 33-bed capacity, which at the time of the workshop had 25 residents. The workshop was held via Microsoft Teams, with four members of the home in January 2021. The second care home was a 20-bed residential home with dementia specialist care. A workshop was held via Microsoft Teams, with five members of the home in March 2021.
Workshops with infection prevention and control practitioners
A member of the research team contacted the co-ordinator for the Infection Prevention Society Care Home Special Interest Group (IPS SIG), who agreed that the research team could deliver a workshop at an upcoming SIG meeting. This was delivered virtually by two members of the team and recorded digitally via Microsoft Teams in February 2021. Twenty members of the SIG contributed to the discussion.
Workshop with healthcare practitioners in clinical commissioning
A workshop was convened in April 2021 via Microsoft Teams with seven representatives from CCGs across Hampshire. The aim was to capture system-level perspectives from individuals working in commissioning. Initial contact was through a colleague working as a commissioning manager for NHS West Hampshire CCG. Through their contacts, others in similar roles were recruited from across four CCGs (NHS Southampton, Fareham and Gosport, North Hampshire and West Hampshire).
Discussions with continence advisors and general practitioners
The issue of RUTI and its management in the care home setting required discussion with clinicians working in the field of urology and bladder and bowel continence. These were conducted in a series of conversations held via Microsoft Teams by a member of the research team.
Analysis of scoping interviews and workshops
The recordings of stakeholder interviews and workshops in stage 1 were transcribed and organised thematically using the topic guide areas and a modified qualitative descriptive process. This involved familiarisation, constructing themes and defining and naming themes aligned with the topic areas. This analysis informed initial theory formulation (see ‘Conceptualising what happens’ and ‘If … then tentative hypotheses’).
Literature scoping
Search methods
We conducted a broad scoping search to identify literature on UTI and CAUTI in care homes (or similarly termed facilities) using the two concepts of disease and environment. English language and 10-year date limits were used, as the focus on UTI/CAUTI in the care home sector has been more prominent in the imperative to prevent antimicrobial resistance and prevent BSI caused by Gram-negative organisms. Articles were stored in EndNoteTM reference management software and transferred to CovidenceTM review management software, where they were deduplicated prior to screening.
The starting point for the review was a scoping or ‘background’ search,46 which extended a preliminary search of MEDLINE, CINAHL and grey literature undertaken during development of the research proposal. This extended generic topic-based multipurpose search was undertaken in September 2020 and focused on evidence that directly addressed the prevention and recognition of UTI in older people in long-term care facilities. Additional databases searched at this stage were EMBASE, Cochrane Library, Web of Science Core Collection (including the Social Sciences Citation Index), Sociological Abstracts, Bibliomap and NIHR Journals Library. Supplementary searches, for example, using key index studies (highly cited) to find ‘sibling’ studies/papers (contemporaneous papers/studies that share a context), were also undertaken at this stage, using Google Scholar and ‘Publish or Perish’ software. 47 In addition, an exploratory search was undertaken in October 2020 for relevant literature relating to the US Agency for Healthcare Research and Quality (AHRQ) Safety Program to reduce CAUTI in long-term care given its relevance to the review.
The scoping search identified key empirical studies, systematic and narrative reviews and guidelines, organisations with grey literature of interest and reports of quality improvement initiatives (e.g. interventions to increase fluid intake in older people living in care homes). The results of the searches are reported in Chapter 3 with details of the search strategy in Appendix 1.
Screening and appraisal
Title and abstract screening of each article was undertaken by two project team members independently of each other to identify articles within scope and out of scope for the review (Box 1). Any conflicts were resolved by the cochief investigators.
Older people (60 years plus) in care homes or other long-term care settings (not learning disability).
Study design-
Primary quantitative and qualitative studies such as intervention studies, surveys of knowledge/practice, observation of practice, interviews/focus groups, case studies.
-
Systematic reviews.
-
Guidelines, recommendations, policy.
-
Narrative review, commentaries, case reports, regulatory inquiries.
-
Address other aspects of care or service delivery that influence or inform UTI/CAUTI prevention, for example, quality, safety, workforce, antimicrobial stewardship.
-
Epidemiological or antimicrobial resistance data that provide context and background to the topic.
Tags were applied to those articles screened as relevant to assist in organising the data into the following broad categories:
-
UTI/CAUTI prevention
-
UTI/CAUTI recognition
-
AMS intervention
-
quality, safety, workforce or cultural context
-
other tentative theory elicitation.
The research team worked as two subgroups to identify key papers from each of the categories for theory building. From these papers, key terms, concepts and potential explanations about UTI/CAUTI prevention and recognition among older people living in care homes were identified as possible mechanisms and outcomes and data were extracted (Box 2).
-
What is the intervention (nature and content)?
-
In what circumstance or context has it been used?
-
What are its policy intentions and objectives?
-
What terms and concepts are articulated?
-
What was the outcome?
-
What explanations are offered for its success or failure?
-
What appears to be the active ingredients of the intervention?
-
What questions/issues are there in relation to the intervention?
-
Possible theory areas (broad)
Concept mining and theory development
A process of concept mining48 was used to map evidence about approaches to recognising and preventing UTI in older people living in care homes, how they might work and any reported enablers or barriers to their successful implementation. This involved searching different bodies of evidence and consulting with stakeholders to develop the scope of the study and identify information, key terms and concepts that could help with theory building.
Research team meetings
Through group discussion, we drew up a list of questions about interventions to recognise and prevent UTI/CAUTI and sought to clarify the meaning of terms and concepts used. This assisted our thinking in bringing together evidence on the efficacy of interventions to prevent UTI with evidence on the context-dependent active elements of intervention programmes in care homes. It also informed our ideas around alignment with external programmes, services and the wider policy context.
Project Advisory Group consultation
Consultation with our PAG and stakeholders was vital to defining the scope of the review to reflect practice and priorities in the real world. We met with the PAG in stage 1 to seek their feedback on our first iteration of programme theory areas and to gain their advice on additional stakeholders to involve and further evidence to include.
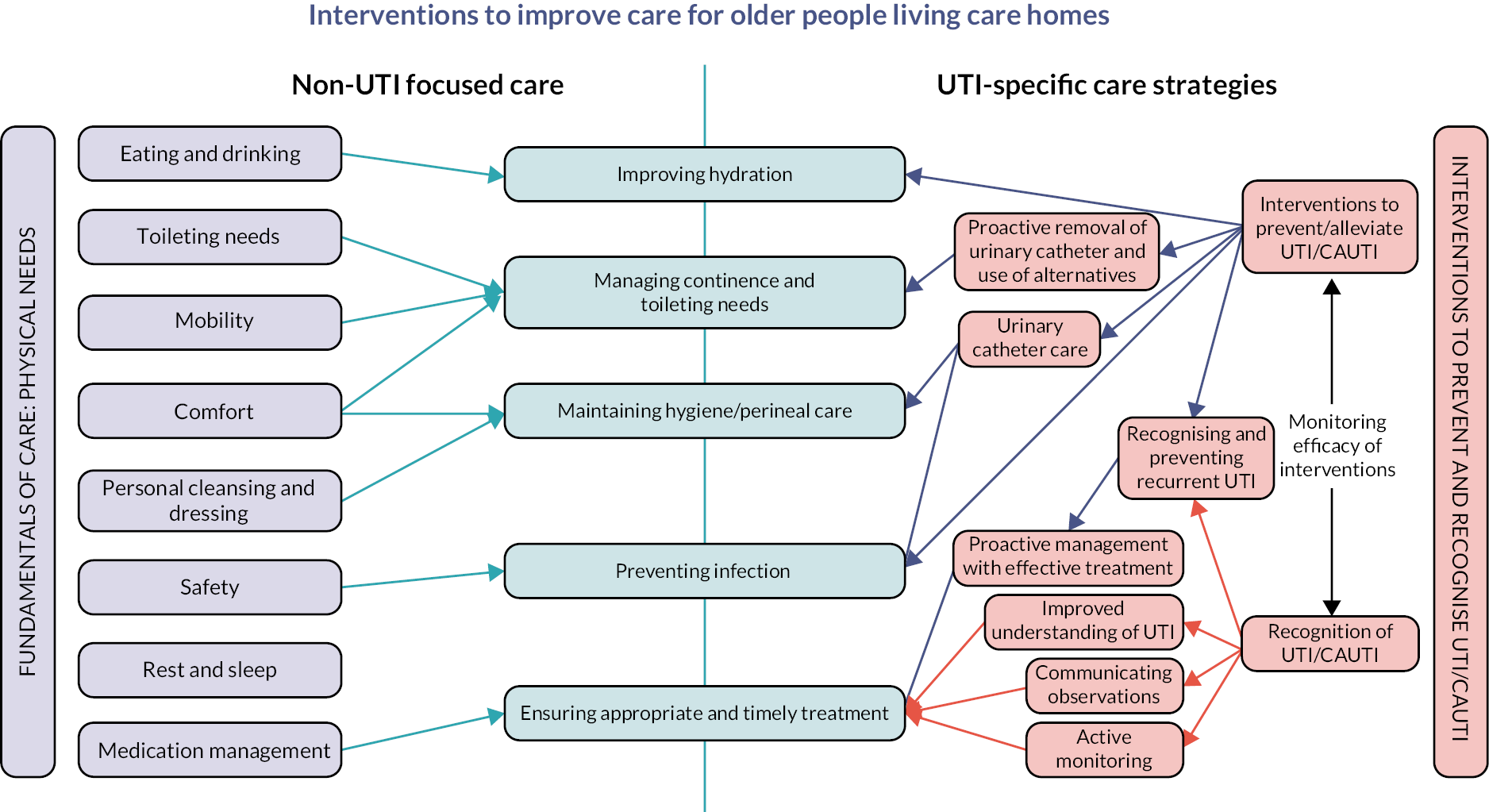
Conceptualising what happens
The research team met to consider feedback from the stakeholder interviews and workshops, scoping literature and PAG input. Discussions highlighted that many of the activities and interventions that had been highlighted could be labelled as ‘core’ or fundamental care. The concept of fundamental care49 was further explored as a potential overarching theory, since the prevention of UTI and CAUTI in older people living in care homes requires attention to key aspects of fundamental physical and psychosocial needs of individuals within the context of supported living. Figure 4 conceptualises how physical care needs are focused around eight aspects of fundamental care49 and how these align with specific strategies to prevent and recognise UTI/CAUTI in older people. As the delivery of care within care homes was described by stakeholders as being focused on fundamental care needs rather than infection prevention specifically, linking the two may highlight to staff the importance of their role in UTI/CAUTI prevention rather than this being viewed as something outside of their influence. Moreover, this may enable care home managers to align UTI/CAUTI prevention strategies to their wider organisational goals in supporting a culture of safety and person-centredness and promoting the implementation of changes and knowledge mobilisation relating to UTI/CAUTI prevention.
FIGURE 4.
How fundamental care interventions to meet the physical care needs of older people are aligned with strategies to prevent and recognise UTI/CAUTI.
If … then tentative hypotheses
A series of if … then statements were developed (see Appendix 2) using the information gathered from our stakeholder workshops and interviews, PAG members and scoping searches. These statements made a tentative link between activities or interventions (as described by stakeholders and reported in the literature) and outcomes. They suggested contexts within which staff resources and responses (mechanisms) may operate. The statements covered seven broad theme areas:
-
meeting hydration needs
-
preventing RUTI
-
preventing CAUTI
-
understanding how a UTI presents in a resident
-
recognising UTI and communicating concerns
-
active monitoring and watchful waiting
-
involving the resident and family.
The statements were tested against the evidence that was found in stage 2 and later refined into CMOc.
Stage 2: searching process
The purpose of this stage of the project was to determine whether the initial programme theories were supported by evidence within the literature and to ensure all relevant literature had been identified. The research team began stage 2 by using the publications identified in stage 1 to further develop and test the seven broad theme areas postulated and to identify gaps in the evidence retrieved. The stage 1 searches provided a large number of articles identified to be within scope for the review (n = 1141), each requiring an assessment of the full text to determine their potential to inform theory building. Therefore, we adopted a more targeted approach to the additional searches undertaken in stage 2 to address gaps in evidence and inform the realist synthesis. 46 These purposive, supplementary searches focused specifically on continence care and UTI, hydration and UTI, non-antimicrobial strategies for RUTI, the recognition of soft signs and family involvement in older peoples’ care in care homes.
Search strategy
Details of the search strategy for each of the supplementary searches can be found in Appendix 3. These searches took place between July and December 2021. Articles were stored in EndNoteTM database software and then transferred to CovidenceTM online software for deduplication, screening, selection and appraisal. Additional papers were identified by members of the research team and the PAG. The results of the supplementary searches are reported in Chapter 3 with a summary of searches and retrieval in Appendix 4.
Selection and appraisal of documents
The screening and full-text review of manuscripts were conducted using CovidenceTM software with each article being assessed by two members of the research team independent of each other. All core project team members were involved in the full-text review process, which was undertaken to determine relevance and rigour. The review of each manuscript was cross-checked by a second team member and any conflicts were resolved by the cochief investigators. The existing list of tags was applied to articles identified as relevant.
Inclusion
The test of inclusion for studies informing a realist review is based on relevance and rigour. 40 Relevance is defined as the extent to which evidence can contribute to theory building, testing and refinement, and rigour as the extent to which the methods used to generate that piece of data are credible and trustworthy. As Pawson50 asserts, in a realist synthesis, the strategy is to provide a comprehensive explanation of the subjects, circumstances and respects in which a programme theory works (or not) and so there is potential for a study to offer credible explanatory evidence, even when the quality of the study may be poor. The quality (rigour) and relevance of the evidence were assessed during the research synthesis,50 and its contribution to the development of the explanatory account and to the review questions and aims highlighted. 51
Included studies were organised into three broad evidence areas and data extracted:
-
UTI symptom presentation and the effectiveness of strategies to prevent UTI/CAUTI and its recurrence
-
implementation of interventions and knowledge mobilisation in care homes to recognise and prevent UTI/CAUTI
-
organisational culture and approaches in care homes in the promotion of UTI/CAUTI prevention strategies.
To focus the review on strategies of efficacy in the prevention of UTI and its recurrence, the project team further assessed the identified studies according to the degree of certainty about the potential for effectiveness in older people. This reduced the number of papers for data extraction by excluding articles reporting insufficient evidence of efficacy for UTI prevention strategies. Strategies found to be lacking in evidence included continence care and management of incontinence, hygiene and non-pharmacological treatments (e.g. cranberry formulations, chokeberry juice, Chinese teas).
Articles in the second and third categories were subjected to a further assessment, with articles excluded at this point if they offered insufficient detail to support development or testing of the programme theories.
Data extraction
Realist synthesis takes an iterative approach to the development, refinement and testing of theories. This is facilitated by the data extraction process. We used an approach developed previously by Williams et al. 51 for the test of relevance and rigour, adapting a ‘relevant and good enough’ flowchart for use as the first step in the data extraction process for considering the relevance and trustworthiness of the evidence within the appraised articles (see Appendix 5). This was checked by at least two members of the team. Discrepancies were resolved through discussion among the research team, with deliberation focusing on whether the inference drawn from the research by the reviewers was sound. 50
The data extraction process was undertaken by a single researcher (distributed across six team members), with a 50% proportion of those identified for inclusion being peer reviewed and checked by a second researcher. A bespoke data extraction form (see Appendix 6) was used to structure the relevant information, document insights and chart data so that the theory areas are populated with evidence on what appears to work, for whom, how and in what contexts. 41 A summary table was included to record the study characteristics, including methods, settings, approach to analysis, outcomes and limitations.
Stage 3: analysis, synthesis and hypothesis testing
Analysis and synthesis processes
Realist synthesis uses triangulation to bring the different sources of evidence together in the development of theory. Abductive and retroductive analysis52 facilitates a theory-driven approach to understanding the CMOc by stimulating the consideration of how something might or might not fit a particular phenomenon (abduction) and what conditions need to exist for a concept to exist (retroduction). This process creates an iterative and critical revisiting of evidence and stakeholder input to identify patterns and contingencies and move from ‘if … then’ statements to CMOc.
A set of potential CMOcs were produced that best reflected the programme theory as refined in stage 2 of the research. For each of the included studies, the implications of its findings were explored to discern the requirements of successful programmes. 50 Evidence sources were examined in respect of explanations given about the mechanisms by which interventions were considered to work (or not). The data were organised into evidence tables to enable comparison of the findings and identification of patterns across studies that offered insight about the necessary ingredients of successful interventions. The process of analysis and synthesis was undertaken by five members of the research team with input from the wider project team and PAG, including our patient and public representatives.
Programme theory testing
To test and refine the programme theory, we conducted nine ‘teacher–learner’ interviews with a range of participants (see Report Supplementary Material 1). A mixture of purposive and convenience sampling was used to gain perspectives from individuals reflective of the different audiences likely to be interested in acting on the findings from this review. Semistructured interview schedules, guided by the content of the CMOc, were used to ensure the interviews focused on participants’ perspectives of the theories as relevant to their role and expertise (see example in Report Supplementary Material 2). The theories of relevance to each participant were introduced to them by the researcher to enable them to comment on them from their own experience and using their own examples. Participants were invited to question the theories and reflect on their relevance from their perspectives of the realities of practice. All interviews were conducted online by a member of the research team and lasted between 30 and 65 minutes. Interviews were audio-recorded and fully transcribed.
Analysis of teacher–learner interviews
The recordings of teacher–learner interviews in stages 3 were transcribed and organised thematically using the topic guide areas and a modified qualitative descriptive process. This involved familiarisation, constructing themes and defining and naming themes aligned with the topic areas. These were triangulated with the CMOc to form part of the abductive and retroductive processes undertaken by the research team.
Resource gap analysis
Our consideration of the literature and engagement with stakeholders helped us to identify a wide range of resources in use in care homes to support the prevention and recognition of UTI and CAUTI. All resources identified were read multiple times and classified thematically according to the group of interest (i.e. older adults or long-term care residents), the intended end users of the resource (e.g. care home staff, prescribers, GPs), the clinical action within the care pathway (e.g. prevention, diagnosing, managing or prescribing), the domain influenced by the resource to support the user (e.g. knowledge or behaviour) and the tool type (e.g. leaflet, checklist, toolkit, algorithm). Information on publication year and publisher or developer of the resource was also collated. A summary of each tool was created, with all information cross-tabulated using Notion software (%www.notion.so) to identify any themes.
Stage 4: consultation
Stakeholder conference
Stakeholders from residential care providers, IPC services, general practice, quality improvement, integrated care systems, NHS England (NHSE) and regulators were approached to participate in a consultation event in June 2022. The aim of the event was to ensure that our theories resonated with their experience and insights of the field and to gain their advice on tailoring the research outputs for different audiences and targeting the dissemination of findings appropriately. Although we had planned a face-to-face event, it was not possible to bring the participants together for more than 2 hours due to participants’ clinical and work pressures. Among those who expressed an interest in participating, there was a preference to meet virtually. The event was therefore held via Microsoft Teams and the breakout discussions recorded and transcribed.
The evidence-informed programme theories were presented and shared with stakeholders to test clarity and fit with current strategies and quality initiatives for recognising and preventing UTI in older people in care homes. In addition, our gap analysis of the existing types of resources in use in care homes, including physical deterioration and escalation tools, decision aids, toolkits and guidelines, was discussed with stakeholders and an example of how digital tools might work in the care home setting was also shared. Report Supplementary Material 3 lists the representatives who attended the stakeholder conference and Report Supplementary Material 4 includes the presentation and breakout room topic guides.
Analysis of feedback from stakeholder event
The approach used for the analysis of scoping workshops and interviews in stages 1 and 3 was also used for the recordings of the stakeholder event, which were transcribed and organised thematically using the topic guide areas and a modified qualitative descriptive. As before, this involved familiarisation, constructing themes and defining and naming themes aligned with the topic areas. These were triangulated with the CMOc forming part of the abductive and retroductive processes undertaken by the research team.
Chapter 3 Findings
Stage 1: scoping, concept mining and initial theory development
Scoping interviews
We held a series of theory-building workshops in which a total of 39 stakeholders contributed to the identification of common approaches used and issues that arise in relation to recognising and preventing UTI for older people living in care homes. Four workshops were held online, two of which were in residential care homes and involved people in the role of care home director or manager, senior carer and continence champion, activities co-ordinator, healthcare support worker and cook. We had originally planned to involve care home residents and family carers within the care home workshops, but this was not possible to arrange in the context of the COVID-19 pandemic. However, an individual online discussion took place with one care home resident together with the care home manager and with a family carer. Details of the participants in the scoping interviews are shown in Table 1.
| WS | No | Description of participants |
|---|---|---|
| WS1 and WS3 – residential care home | 9 | Care home director/managers (3) Deputy manager (1) Head of care (1) Senior care assistant (1) Care assistant (1) Activities co-ordinator (1) Cook (1) |
| WS2 – IPS SIG | 20 | Nurses from across acute and community healthcare trusts, CCG and a private provider |
| WS4 – CCG | 7 | GP (1) Nurse leads (6) in enhanced care home support/nurse facilitator roles. |
| Individual interviews | ||
| Interview 1 | 1 | Care home resident |
| Interview 2 | 1 | Relative/carer of resident in a care home |
| Interview 3 | 1 | Lay/public representative |
Many of the participants in the scoping interviews indicated that the prevention of UTI and CAUTI was an aspect of care that had been the subject of considerable focus over the past 2–3 years. The driver for this focus was primarily driven by the need to reduce admissions to hospital and the association with Gram-negative bacteraemia.
Keeping people out of hospital. Our local acute trust is 'under the cosh’. … Care homes are fairly risk averse, due to CQC coming around, they feel they need to take them (residents) to hospital. … Antibiotic guardianship is important, but there are also cases where people are dying whilst in ambulances.
GP, CCG
For UTIs and CAUTIs, one driver was increased UTIs leading to increased falls and increased effects of dementia, therefore addressed as challenging.
IPC Nurse, CCG, IPS SIG
Care home staff and IPC specialists identified that preventative approaches were primarily focused on improving the hydration of residents.
Prior to COVID, we were doing a lot on UTIs, promoting hydration, Gram-negative work, educating staff on fluid input – the I Hydrate resources were being implemented, including drinks trolleys.
IPC Nurse, Community NHS Trust, IPS SIG
We also have a ‘hydration station’ now, following interaction with the CQC and their initiative. It does get used, and drinks are continually being offered and they can help themselves.
Care Home Manager
Another home described how residents were encouraged to drink at least 2 litres of fluid every day and how this was supported by the electronic system, including staff hand-held devices, for recording and monitoring resident fluid intakes.
We use an electronic system. It has a chart you can click and refine down to today’s date and check how much they have had today, and it breaks down what they’ve been offered and what they’ve drunk so we can keep a really close eye on it.
Care Home Manager
Initiatives to improve the recognition of UTI and CAUTI had concentrated on discouraging the use of dip sticks to ‘diagnose’ infection and the consequent prescription of antibiotics.
… a lot of the time the GP will ask for a dipstick of the urine and if showing anything, will lead straight to antibiotics and do not provide an alternative such as more hydration in the next 24 hours. The alternatives are not proposed before going down the prescription route.
Lead Nurse, CCG
‘To dip or not to dip’ used with care homes and GPs and links also made with acute trusts to promote system-wide approach. This is important to avoid conflicting expectations.
IPC practitioner, IPS SIG
A checklist tool ‘Don’t be a Dipstick’ was used by home staff to communicate any concerns about a resident to the GP.
Care home staff spoke about the importance of knowing residents and how this helped them to recognise the changes that might be an indication of a UTI or CAUTI. This was highlighted as being particularly important where residents had cognitive deficits. One relative felt that enabling relatives to visit the resident at any time was important as they can help with understanding the resident’s needs.
Normal signs that come to us are change of behaviour. The only way to detect change in behaviour for residents that suffer from dementia is to understand their care records and past history of how they behave generally in the care home and can sometimes be a very small change. … As our staff work closely with the residents and spend a lot of time with them. They therefore recognise that this is a small change of behaviour for a particular resident at their stage of dementia. I believe this is the key thing, where carers can assist with the detection of a UTI.
Care Home Director
They can be more sleepy, aggressive, or angry. I have noticed in the past that some ladies will not drink at all after a certain time because they are worried about getting up too many times to use the toilet in the night. There will be an increase of falls.
Care home cook and carer
Important to ask, ‘What is it about ‘normal self’ that isn’t right?’ An example of a resident with dementia who always talks clearly and articulately when she is getting a UTI, which is different from her usual self.
IPC practitioner, IPS SIG
Early signs such as an increase in the resident’s temperature, falling over, disorientation and, most importantly, changes in a resident’s behaviour were highlighted as key in recognising a UTI/CAUTI.
They haven’t got a temperature, not this, not that, but we know something is not right. And that is really hard to get through to a GP.
Care Home Manager
However, participants also commented that this knowledge of residents was not always listened to by GPs and other HCPs and that communication and shared language were important to getting messages across.
GPs and paramedics need a clear message to have trust in what care staff are telling them.
IPC practitioner, IPS SIG
It’s really hard to get through to the GP – response is – ‘if there’s nothing really medical, there’s nothing we can do.’ ‘Well, you’re the GP, come out’.
Care Home Manager
Several tools were mentioned by lead nurse in CCGs and the IPC SIG, but this was not evident in the responses of care home staff, who focused on discussion and monitoring the resident over time.
RESTORE2 is used, aiming to get the homes to look at the person holistically. We try to get them to use the new score and encourage fluids and do the bits before they get a doctor to prescribe antibiotics. For people showing soft signs of UTI, we try to encourage the new score to be used.
Lead Nurse, CCG
It (RESTORE2) has been incredible and we have used it for 2 years. It has changed the way we deliver care. It is very important as externals look at their baseline of what Restore2 looks like for a residence.
Care Home Manager
SBAR is a communication tool that helps staff know exactly what to communicate without getting flustered (can be difficult to be precise under pressure).
IPC practitioner, IPS SIG
We have literature – ‘don’t be a dipstick’ – using this for about 6 months which includes a checklist to go through. This is then faxed to the GP. The staff are however aware that dipsticks cannot tell much so they merely carry out for their benefit.
Care Home Manager
We would discuss as a team if somebody has noticed someone acting out of character, is more sleepy or is not getting up as many times in the night. We would come together as a team to bring the next thing in place, and encourage fluids, and encourage foods with more fluid in it. The following day, they will regroup again to see how the resident is.
Care home cook and carer
Stakeholders discussed how active monitoring was used where there was diagnostic uncertainty around a suspected UTI. They described how the whole team would come together to undertake activities such as encouraging fluids and extra monitoring.
The line often used is TLC, and doctors have said that. Keep a close eye on them, so that could be increasing checks to half hourly, ensuring that you are pushing fluids more, making sure they are using the bathroom frequently. Going through the little things that you would do to prevent infections or further decline.
Care home workshop
The experience of residents and family members was discussed with care home staff and some of the IPC practitioners in the IPS SIG workshop also commented on how the involvement of families sometimes created challenges for care home staff trying to follow best practice, including active monitoring.
Relatives of residents with a history of frequent UTI who have had antibiotics regularly can put pressure on for antibiotic treatment and don’t always accept explanations of the reasons for not treating.
IPC practitioner, IPS SIG
Our initial discussions with stakeholders in relation to the management RUTI suggested that low-dose antibiotics were the primary prophylactic treatment strategy. Most stakeholders were unaware of other non-antibiotic treatment options such as D-mannose or methenamine hippurate. One stakeholder mentioned an alternative that was used for a period until it ran out of stock.
Our urologists are very keen on rolling out a prophylaxis for UTI (which is a type of non-antibiotic antibiotic), which became popular until they ran out of stock.
GP, CCG
Access to specialist continence advice was also mentioned as a barrier to support in managing or treating residents with RUTIs.
Continence providers can be expensive also. For us there are two continence providers, and the difficulty is the fact that some homes fall between [the two] and can get caught in the politics of neither side taking responsibility and providing for them continence support.
RN, CCG
From a continence advisor (CA) perspective, while they currently did not offer a service to support care homes in managing residents with RUTI it was recognised that this was an important gap in care provision for this population. The demands on the continence service from acute care are considerable and their service to care homes is focused on managing incontinence and generally delivered by continence care assistants. They indicated that support for managing residents with RUTI would require input from more senior, experienced CAs but that these resources are limited.
What stakeholders said about making best practice happen
Stakeholders mentioned the use of champions to support the promotion of hydration in care homes. The use of a ‘hydration champions’ network was described as an effective way for peer sharing of what strategies have worked well in practice and where others have been harder to implement. The value of face-to-face interactions was also mentioned.
Stakeholders highlighted the importance of training and developing the skillset of staff working in care homes. It was also acknowledged that care staff and health professionals supporting care homes do not always have sufficient knowledge and the need for sourcing more specialist training was identified.
Face-to-face training is also so important. The human touch cannot really be substituted. The webinars are great, and I would support them but you need to have the face to face training as well. Agreed that interactive training is good.
Care Home Manager
Care home managers and staff identified that fostering good communication across the team was at the heart of the leadership and culture of the home.
The key to the whole thing is communication. We communicate on a daily basis, specifically we have a huddle in the daytime, a huddle in the afternoon also. You can have a huddle at any time, even in between. This is how we feel we are all aware of how a resident is doing, or if there is a concern with that resident, if we have learnt something new about a resident.
Care Home Manager
Having a more flattened team structure whereby everyone, regardless of their role, was involved in worked to provide person-centred care was also mentioned.
We keep trying, so we also discussed the fact that we tried something, and it doesn’t work, and then ask what shall we try again? This is what has led us to work as a team .... We as directors also join the huddles as we also need to be educated as to how the residents are doing.
Care Home Director
These stakeholder insights were discussed by the research team and were used to inform the screening of the results from the scoping search and to shape our development of initial theory if … then statements.
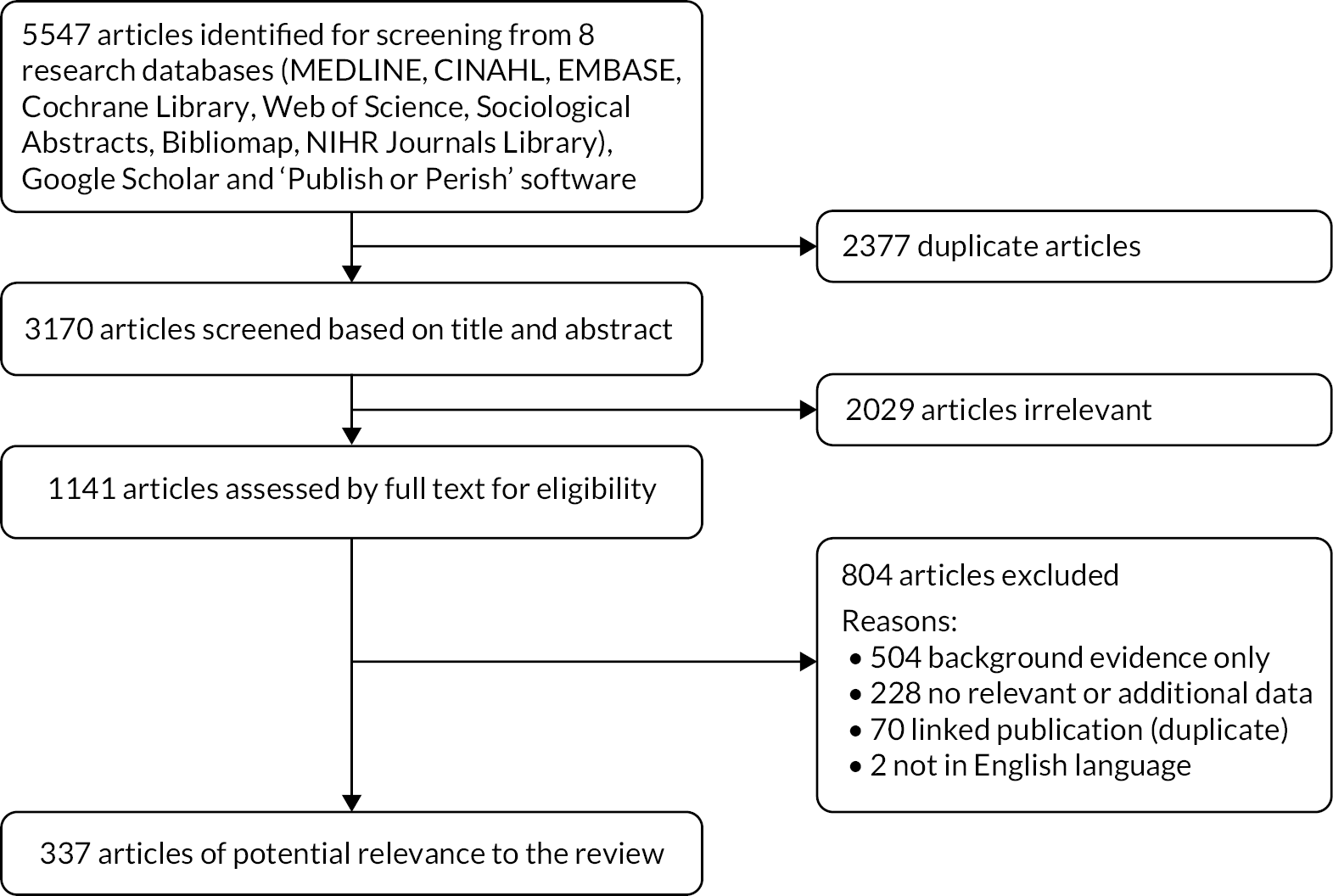
Scoping search
The scoping search identified 5547 results, with 3170 after deduplication. Following screening and full-text review against the inclusion criteria 337 articles were retained as having the potential to inform theory development (Figure 5). From these papers, the research team used a series of questions (Box 2) to identify key terms, concepts and potential explanations about UTI/CAUTI prevention and recognition among older people living in care homes.
FIGURE 5.
Flow diagram illustrating scoping search process in stage 1. Reproduced from Prieto et al. 45 Published by the BMJ Publishing Group Limited. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/.
Identification of tentative theory areas conceptualising what happens to prevent and recognise urinary tract infection/catheter-associated urinary tract infection
Our consultation with the PAG, stakeholder interviews and workshops, together with evidence from the literature, was discussed in depth by the research team. We remained mindful of the need to avoid silo thinking that would lead us to overlook other potentially important ideas and sources of evidence that could be useful for theory building. To inform our further review and data extraction from the literature, we developed a set of early narrative propositions, which were also informed by our conceptualisation of how fundamental care49 aligns with the strategies that could be useful in the prevention and recognition of UTI/CAUTI:
-
Care home staff are best placed to recognise early signs and symptoms of UTI and their active involvement in assessment, with clear roles and responsibilities, provides opportunities to instigate preventative measures.
-
Care home staff require support to understand the signs and symptoms of UTI and to communicate with confidence key clinical observations within their team and to primary care staff.
-
With training on evidence-based UTI/CAUTI interventions, incontinence planning and hydration care home staff are empowered to focus on UTI prevention strategies and to challenge requests to catheterise and order urine cultures.
-
Use of a multifaceted intervention, including education, skilled facilitation and feedback, is more likely to be successful in improving use of UTI-prevention strategies.
-
Multidisciplinary working, with shared goals and common language, is important for involving care home staff in the recognition, prevention and diagnosis of UTI.
-
Care home residents and their families may be more supportive of efforts to reduce use of antibiotics if they are informed about the topic of antimicrobial resistance and involved in decisions about use of alternative preventative strategies to minimise risk of UTI.
-
Effective leadership and an embedded culture of safety and improvement are needed to support care home staff in recognising UTI as preventable and not inevitable.
-
Interventions that are a good fit with actual situations in practice and align with external programmes and services are more likely to be effective.
-
Involving care staff in the design of interventions that are tailored to address contextual factors means they are more likely to be used and useful in overcoming challenges for implementation.
The results of the scoping search and stakeholder interviews were then organised into four topic areas for further exploration:
-
developing interventions to optimise good practice
-
delivering and sustaining good practice
-
care home context and culture
-
co-design and multiagency working.
If … then tentative hypotheses
Further interrogation of the literature by the research team enabled the expansion of the narrative propositions into preliminary hypotheses in the form of ‘if–then’ statements. 53 These were developed iteratively and refined over several virtual meetings. Table 2 provides an indicative sample of these hypotheses with the full list in Appendix 2. This offered initial explanations of how different types of interventions for preventing and recognising UTI/CAUTI in care home settings might work.
| IF | THEN |
|---|---|
| If care home staff are more aware of the importance of hydration, need to increase opportunities and choice of drinks | …then residents will be supported to drink more fluids |
| If care home staff are trained to implement evidence-based CAUTI interventions, incontinence planning and hydration activity | …they are empowered to challenge requests to catheterise and order urine cultures |
| If there is a common understanding of signs and symptoms of UTI (through education and use of language that is appropriate for the level of clinical knowledge) | …then it is likely that appropriate information will be communicated accurately across the care home and healthcare team |
Stage 2: retrieval and review of the evidence
Initial programme theory
Having screened the literature from the initial scoping search and identified four broad topic areas to guide further screening and selection of studies the research team developed a concept diagram. This situated the resident at the centre of the effort to prevent and recognise UTI/CAUTI. Our deliberations led us to propose that care home context and culture, including the resources available, and the perspective taken on safety and quality were central to the design, delivery and sustainability of interventions described in the literature we had identified. Figure 6 illustrates the relationship between these five aspects.
FIGURE 6.
Conceptual diagram of initial programme theory. Reproduced from Prieto et al. 45 Published by the BMJ Publishing Group Limited. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/.
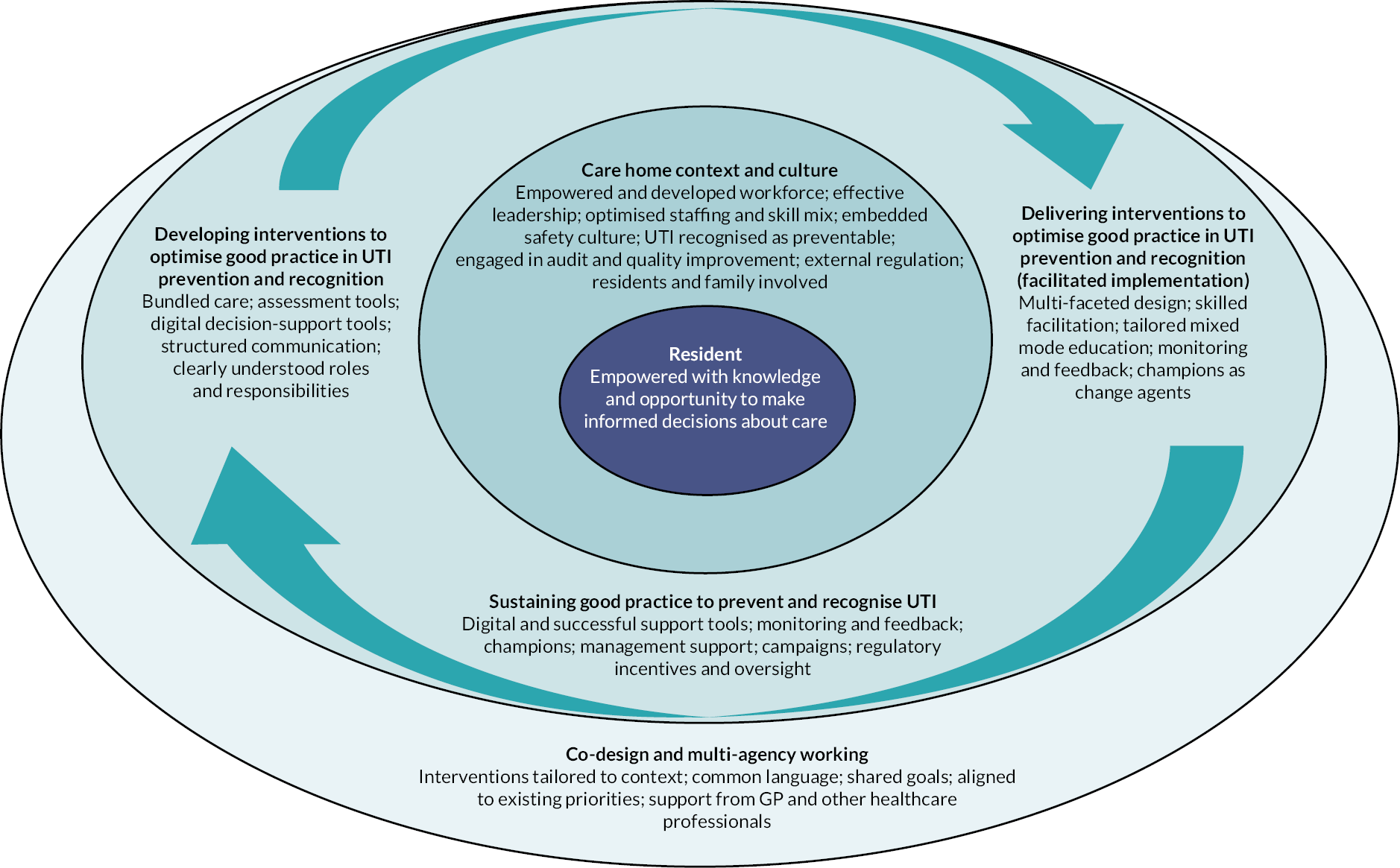
This refinement guided the search strategy in stage 2 and informed the design of the data extraction tool (see Appendix 6).
Supplementary searches
Supplementary searches were undertaken to identify additional studies that took account of the concepts and issues identified by stakeholders and members of the PAG. These supplementary searches yielded 1029 articles in total, with 897 after deduplication (see Appendix 4). Following screening, 865 articles were excluded as not relevant and two further articles were excluded as they were not in English language.
Soft signs
Approaches to observing ‘soft signs’ of deterioration in older people in care homes were identified, including use of early warning tools to support care home staff and family carers to recognise physical deterioration and take the appropriate actions. The search was carried out in June 2021 and entailed an iterative approach starting with a website page on ‘RESTORE2’, an early warning tool, then following links and references. A search on Google Scholar was also undertaken, along with database searches using MEDLINE, CINAHL and OpenGrey.
Non-antimicrobial therapeutic interventions for recurrent urinary tract infection
Low-dose antimicrobial prophylaxis for the management of patients with RUTI is established practice and covered by a recent National Institute for Health and Care Excellence (NICE) guideline on antimicrobial prescribing for RUTI. 54 A further highly focused search was carried out by the research team in September 2021 to identify relevant studies relating to the management of RUTI using non-antimicrobial treatments. It involved citation searching of key review publications, including the NICE guideline54 and two further review papers. 55,27 The output of this search comprised primary evidence underpinning these reviews of relevance to the realist synthesis. This evidence was reviewed by a member of the PAG with expertise as a consultant urogynaecologist to ensure other relevant evidence had not been missed, and an experienced CA for contextual information about the potential challenges in the use of non-antimicrobial treatments for RUTI in care home settings. They identified two further articles. One of these,56 a recently published European Urology Association guideline, was cross-checked for further primary research but no additional studies was identified.
Hydration and urinary tract infection
A search for studies on hydration as a preventative measure for UTI and interventions to increase fluid intake in older people in care homes was undertaken in November 2021, using key papers to identify search terms and carry out reference and citation searching. A search of bibliographic databases (MEDLINE, CINAHL, SCIE Social Care Online) followed, along with a search for grey literature.
Family involvement
The purpose of this search was to locate evidence on family involvement in the diagnosis and management of UTI/CAUTI in older people living in care homes. Using five papers found during the scoping search, a citation search was undertaken in December 2021 using key words and index terms around family involvement. A search of bibliographic databases (MEDLINE, CINAHL, SCIE Social Care Online, NICE Evidence) followed, along with a search for grey literature.
Continence care and urinary tract infection
This search was undertaken in December 2021. It sought to identify evidence linking UTI prevention to continence care and bladder management, including avoidance of IUCs. It also encompassed a search of literature on the role of CAs and other specialists in the prevention of UTI in older people in care homes. A search of bibliographic databases (MEDLINE, CINAHL, SCIE Social Care Online) followed, along with a search for grey literature.
Selection and appraisal of documents
Of the articles screened, 30 were identified as requiring a review of the full text to determine their relevance to the emergent programme theory, of which 10 were added to the review.
The final number of studies included to support the programme theories was 56 (see Appendix 8, Table 6), comprising evidence from the scoping and supplementary searches of bibliographic databases and articles identified by members of the project team and the PAG (see Appendix 4). Evidence from grey literature was used to inform and contextualise the findings, although none was utilised in the final analysis of data. Evidence tables were constructed to organise the data and enable comparison of the findings.
Stage 3: analysis, synthesis and hypothesis testing
Theory development and testing
The evidence from the studies included in the review was discussed by the research team during virtual meetings, together with the perspectives of the stakeholders gathered in stage 1. The background literature that provided the underlying rationale for the inclusion of theories was considered alongside the included studies and provided the research team with a comprehensive overview of the findings. The team worked together to develop a set of CMOcs that were aligned with the literature and what had been learnt from stakeholders. These were arranged under three theory areas (Table 3) and suggested how interventions might be made to work in the care home setting.
| CMOc | Theory areas |
|---|---|
| Theory area 1 – strategies to support accurate recognition of UTI | |
| 1 | Recognition of UTI is informed by skills in clinical reasoning |
| 2 | Decision-support tools enable a whole care team approach to communication |
| 3 | Active monitoring is recognised as a legitimate care routine |
| Theory area 2 – care strategies for residents to prevent UTI/CAUTI | |
| 4 | Hydration is recognised as a care priority for all residents |
| 5 | Systems are in place to drive action that helps residents to drink more |
| 6 | Good infection prevention practice is applied to IUCs |
| 7 | Proactive strategies are in place to prevent RUTI |
| Theory area 3 – making best practice happen | |
| 8 | Care home leadership and culture foster safe fundamental care |
| 9 | Developing knowledgeable care teams |
The following sections present the rationale for each theory area, together with the related CMOc and underpinning evidence. The refinements made in light of the teacher–learner interviews in stage 3 and the stakeholder event in stage 4 are described. In CMOc 7, which relates to the prevention of RUTI, the lack of studies that focused on older people in care homes meant that the research team relied on national and international guidance along with the input of expert stakeholders to provide the care home perspective.
Teacher–learner interviews
We conducted nine teacher–learner interviews to test how the theories resonated with the experience of those involved in organising and delivering care and if there were further insights that would help us to refine the CMOC that had been produced. The participants are summarised in Table 4 (see Report Supplementary Material 1 for additional details).
| Participant role | Healthcare setting |
|---|---|
| Registered nurse | Care home |
| Care assistant | Care home |
| Consultant urologist | Acute care |
| Continence specialist | Community |
| GP | Primary care |
| Quality improvement lead | Acute care |
| Community matron | Community |
| Geriatrician | Acute care |
| Bladder and bowel specialist | Acute care |
Theory area 1 – strategies to support accurate recognition of urinary tract infection
Stakeholder feedback – stage 1
Stakeholders in stage 1 identified that the accurate recognition of UTI was an aspect of care that required care home staff to understand the ways in which infection could be recognised and know how to communicate this to colleagues and GPs. The capacity of the workforce to discriminate between some of the ‘soft signs’ that they assumed were related to a UTI and other conditions was important. Stakeholders in care homes indicated that they were using some of the tools, for example, RESTORE2 to assist with making some of these decisions.
Context–mechanism–outcome configuration 1: recognition of urinary tract infection is informed by skills in clinical reasoning
Figure 7 depicts CMOc 1, which is described below followed by a discussion of the underpinning evidence.
FIGURE 7.
Context–mechanism–outcome configuration 1: recognition of UTI is informed by skills in clinical reasoning.
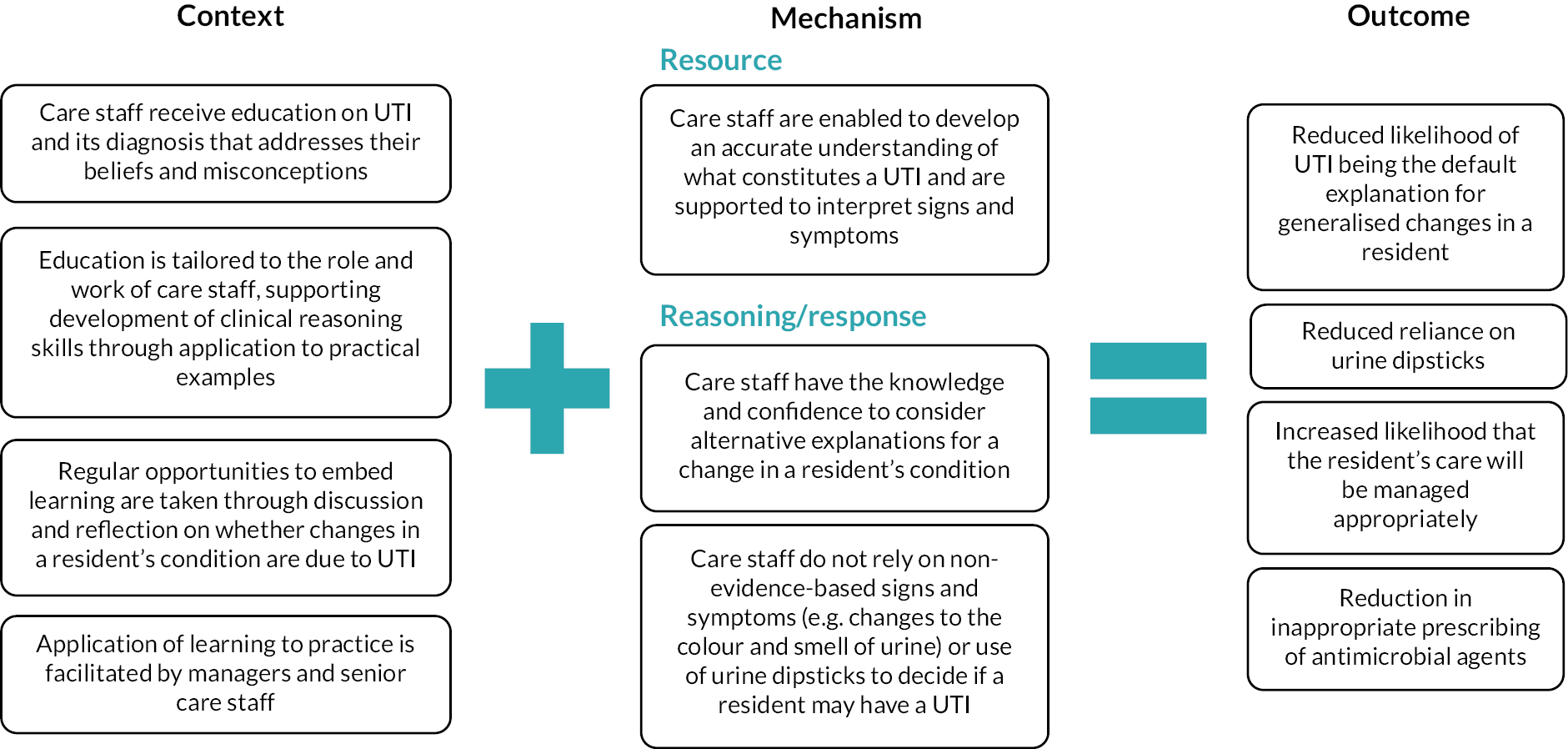
Context
It can be difficult for care home staff to change their intuitive understanding of UTI. Creating opportunities for staff to engage in learning and reflection around their beliefs about UTI and their experiences in the workplace is important in order to challenge their thinking and support improvements in knowledge and practice. Educational interventions on UTI that are tailored to the role and work of care home staff are effective in care homes where there is a commitment to supporting shared learning, reflection and application to practice.
Mechanism
When managers and senior care staff create opportunities to embed learning through application in practice (e.g. huddles to review suspected UTI), care staff are enabled to improve their understanding of what constitutes a UTI. Being supported to interpret signs and symptoms can improve knowledge, ability and confidence to differentiate between UTI and other diagnoses while considering reasons for changes based on their knowledge of the resident and family members’ familiarity with what is normal for them. This process of more deliberative reasoning can reduce reliance on non-evidence-based signs and symptoms (e.g. changes to the colour and smell of urine) and the use of urine dipsticks to decide if a resident may have a UTI.
Outcome
Alternative explanations for a change in condition rather than UTI being the default explanation are explored, which may reduce antibiotic prescriptions and improve the management of infection.
Rationale – the role of care home staff in recognising urinary tract infection
Despite receiving the least clinical training, care home support workers contact with residents means they notice changes in their condition that may be signs or symptoms of UTI or another illness. 57,58 These include changes in behaviour,57,59 reduced mobility and falls,58–60 increased confusion,57–61 delirium,58,60,61 irritability, restlessness and aggressive behaviours,57,58,60 discomfort,57,58 poor appetite,57,58,60 lethargy,57,58,60 changes to fluid intake and output,60 changes in the smell and colour of urine58–60 or just ‘not being right’. 57,60
While care home staff can feel confident in their ability to identify changes in a resident’s behaviour that may indicate illness,57,62 they have some difficulty distinguishing UTI from other illnesses with similar presentations, especially in residents with dementia. 62 This is not surprising given that evaluating symptoms in care home residents is known to be highly complex. 61 The ability of care home staff to interpret their initial observations is influenced by their beliefs and understanding of UTI signs and symptoms,60,61 together with their knowledge of the resident over a period,63 including previous infections. 55 Fear of missing a UTI diagnosis has been identified as a driver for attributing non-specific signs and symptoms to UTI without considering other possibilities,58,60,61,64 particularly in residents with a history of infection.
These issues can lead care home staff to assume that non-specific signs and symptoms are caused by a UTI. 59–61 This is reinforced through misplaced emphasis among GPs and care home staff on objective measures, such as urine dipstick results to confirm their suspicions of a UTI, without the addition of localising symptoms, or placing greater importance on symptoms such as changes in the smell or colour of urine and dehydrated skin, leading to overtreatment. 58,61,62
It can be difficult for care home staff to change their intuitive understandings of what constitutes a UTI. 61 A realist synthesis of workforce development interventions for improving the skills and care standards of support workers in older people’s care, authors proposed that interventions that were tailored to the support worker’s own practice were considered to make learning more real by prompting resonance. Well-designed educational programmes that account for how care home staff conceptualise UTI58,60,61,64 help improve the accuracy of their knowledge, increase their ability to recognise evidence-based signs and symptoms of UTI and consider alternative explanations for changes in a resident’s condition.
Summary of evidence underpinning context–mechanism–outcome configuration 1
Evidence for strategies that are successful in improving knowledge and understanding about signs and symptoms of urinary tract infection
Three intervention studies designed to reduce inappropriate prescribing for UTI in care home residents through a combination of tailored education and assessment/communication tools to assist care home staff in managing residents with suspected infection are used to inform this CMOc. 60,65,66
The effectiveness of a tailored complex intervention to reduce antibiotic prescribing for UTI in nursing homes in Denmark was reported by Arnold and colleagues. 65 The intervention incorporated an assessment tool and a communication tool informed by previous studies67–69 and an interactive case-based education session. It was co-designed with stakeholders and informed by prior qualitative research involving observations of care and interviews with key health and care staff.
The intervention was evaluated in a 6-month unblinded parallel group cluster RCT (CRCT) of 22 nursing homes. Primary outcome analysis demonstrated that the number of antibiotic prescriptions for UTI per resident was 134 per 84,035 days at risk in the intervention group and 228 per 77,817 days at risk in the control group. The antibiotic prescription rate for UTI was reduced by half in the intervention group [rate ratio 0.51 (95% CI 0.37 to 0.71) in the unadjusted model and 0.42 (0.31 to 0.57) in the adjusted model] without substantial increases in all-cause hospitalisations or all-cause mortality compared with the control group. The appropriateness of prescribing decisions was reported to have increased, although assessment relied on a UTI diary, which was completed by nursing home staff on less than half of occasions.
The educational session was delivered by the lead researcher on two to five occasions within each of 11 nursing homes in the intervention arm. In addition to technical evidence-based content, this drew on participants’ experience and understanding of UTI in order to challenge their thinking, improve their clinical reasoning and prompt them to consider alternative explanations for generalised changes in a resident’s condition. The assessment tool incorporated a reflection component designed to support this process, comprising four questions to discuss with a colleague prior to determining next steps. The emphasis was on encouraging a more deliberative approach to assessment to avoid UTI being the default explanation for non-specific symptoms.
The success of the intervention was attributed to tailoring of the intervention to increase effect, usability and ease of implementation. 61 While it was not possible to distinguish the impact of each component of the intervention, a qualitative study undertaken in parallel with 12 participants in six of the intervention nursing homes suggested that gaining new knowledge and developing a systematic approach to assessment through observation and reflection were the most important aspects of the intervention. 70 The extent of direct involvement of managers varied between nursing homes. At those where managers regularly reminded staff to use the intervention, participants reported this to have strengthened implementation. Each home also identified one to two nurses to be project champions, to support its implementation. Strategies used by the champions included using the tool during daily triage meetings between team leaders and care assistants, supporting one-to-one discussions with staff and raising awareness of the tools as part of their regular visits to wards. Good alignment with their professional values to support quality improvement and educational activities was identified as a factor that motivated them to drive the intervention.
The researchers reported how the most important challenge was the need to create a solid understanding of the reflection tool among staff. 70 Some participants identified that the clinical content of the intervention was difficult to understand and how there was a need to unlearn and de-implement existing beliefs and practices relating to UTI. This led to some staff collaborating with a colleague to use the tool. Competing work priorities also impacted on its use, participants reporting difficulty remembering to use it when busy. These findings have implications for the delivery of a labour-intensive educational intervention, including provision of support for staff designated as project champions, in order to facilitate use of the tool and ongoing learning and reflection in practice.
The feasibility and acceptability of a multifaceted intervention to reduce antibiotic prescribing for infections (Reducing Antimicrobials in Care Homes or ‘REACH’) were tested in six nursing and residential care homes in the UK. 60 The intervention was designed to assist care home staff to manage residents with suspected infection (UTI, respiratory tract infection, skin and soft-tissue infection) in order to reduce antibiotic prescribing. It was adapted from an intervention originally designed and developed in Canada67 and comprised a decision-support tool (algorithm), a small group interactive training programme, infection-specific care pathways and a structured communication tool based on situation, background, assessment, recommendation (SBAR).
A 6-month non-randomised feasibility study using a mixed-methods approach with an embedded process evaluation was undertaken. Small group interactive case-based training sessions of 1–2 hours were delivered by the research team, with different versions for junior and senior staff. Care home staff indicated their preference for face-to-face training over provision of a training digital versatile disc (DVD) and handbook. Champions were appointed in each home to deliver training to new staff and those who were unable to attend the original session, and to assist the research team with data collection. They promoted the engagement of staff in the intervention by addressing misconceptions at opportune moments in care, and discussing the algorithm and documentation in handover, staff meetings and in casual break-time conversations. The process evaluation included ethnographic observations, pre- and post-implementation interviews and focus groups, and an analysis guided by normalisation process theory. The researchers reported some proof-of-concept evidence that the intervention reduced antibiotic prescribing, with engagement and commitment to the study among care home managers and staff regarded as high. There was variation in the extent of engagement within and between participating care homes, which was potentially influenced by factors, including the provision of support by care home managers, the effectiveness of the project champions and the existence of social and organisational structures within homes, including clarity about roles and responsibilities, which enabled empowerment among staff at all levels to be involved. Provision of support with communicating observations and concerns about a resident’s condition was seen as a facilitator. Some managers reported challenges in appointing a champion.
A CRCT to measure the impact of interprofessional education and a decision-support tool on the rate of urine culture testing and antimicrobial prescribing for UTI was conducted in 42 nursing homes in Canada. 66 Authors reported a significant reduction in the rate of urine testing and antibiotic prescribing for UTI without an increase in mortality or admissions to hospital or emergency department visits. This initial reduction was not maintained over time, with outcome rates returning towards the baseline. The researchers considered that the degree to which educational themes resonated with care home staff, physicians and family carers may have explained the relative difference in urine culture rates and prescription rates between the intervention and control groups. They concluded that regular feedback cycles, clinical decision reminders and educational efforts were needed to sustain changes in practice, which has important implications for ongoing provision of education and support to facilitate application of learning to practice.
Context–mechanism–outcome configuration 2: decision-support tools enable a whole care team approach to communication
Figure 8 depicts CMOc 2, which is described below followed by a discussion of the underpinning evidence.
FIGURE 8.
Context–mechanism–outcome configuration 2: decision-support tools enable a whole care team approach to communication.
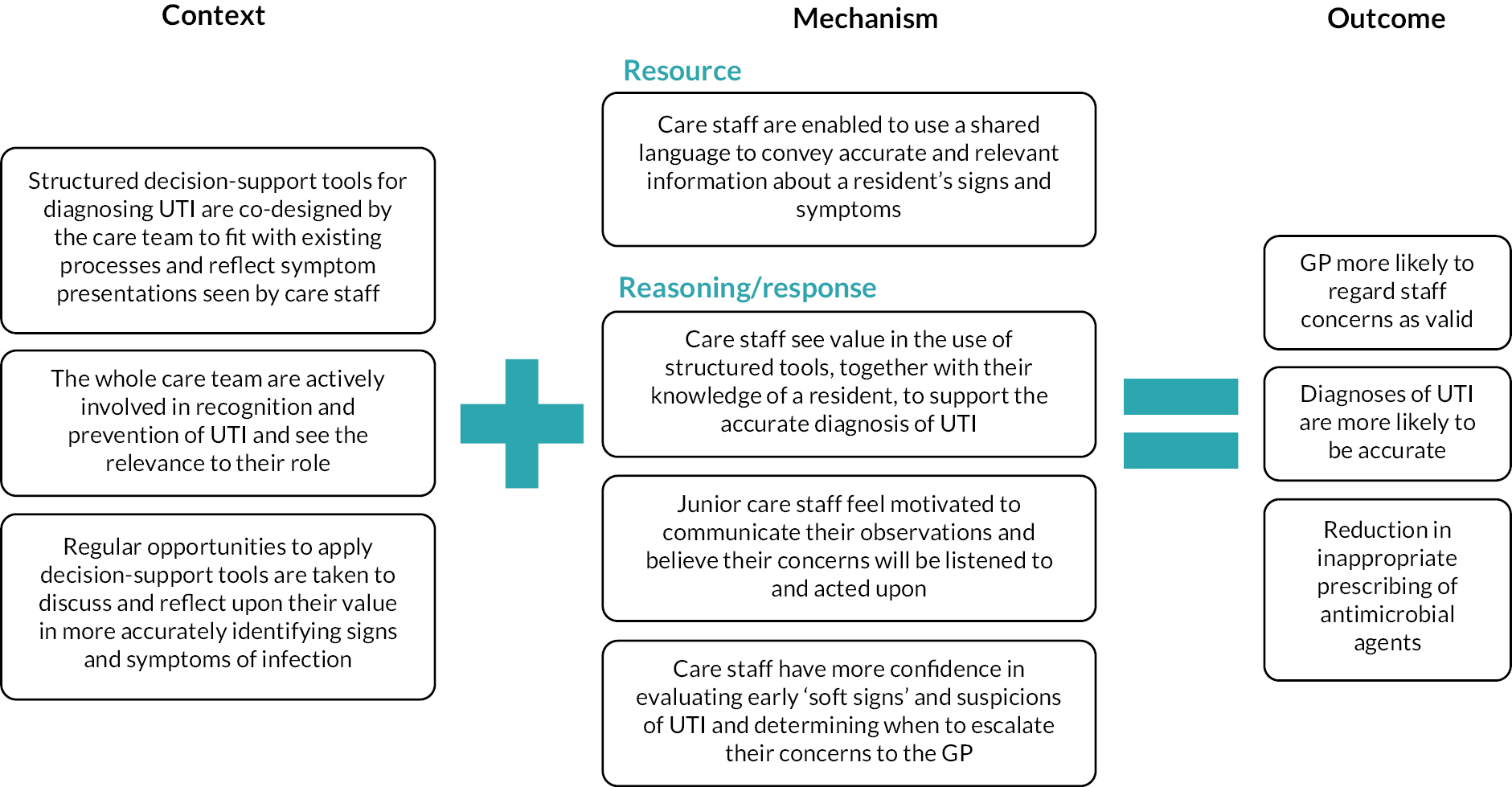
Context
Decision-support tools that are designed to assist care home staff in determining whether changes in a resident’s condition or behaviour could be due to UTI or another cause may be successful in reducing unnecessary antibiotic prescribing and prompting preventative actions when they involve the whole care team and are coproduced to meet the needs of the care home. The degree of fit of a decision-support tool to the resident’s presentation can determine its perceived usefulness to support assessment and decision-making. Tools that are coproduced to align with existing processes and reflect the range of symptom presentations observed in care home residents are more likely to be used. This is facilitated where care home staff at all levels see the relevance to their role of being actively involved in UTI prevention and recognition and where there are opportunities to discuss and reflect upon observations when using a tool, thereby seeing its value in more accurately identifying signs and symptoms of infection.
Mechanism
Decision-support tools enable staff to gather and convey accurate and relevant information about a resident’s signs and symptoms using a shared language and terms they understand that accurately represent the resident’s condition. When care staff see the value in using structured tools, they can contribute objectively to assessment through their knowledge of the resident and ability to observe early changes. Care staff are motivated to convey their concerns when clinicians value and trust their input, as they believe these will be acted upon. Early soft signs and suspicions of UTI can be evaluated, enabling care staff to have more confidence in deciding when to escalate their concerns to the GP.
Outcome
Structured evaluation processes increase the likelihood of GPs regarding the concerns of care home staff as valid, supporting the accurate diagnosis of UTI and appropriate antimicrobial prescribing.
Rationale – the role of care home staff in communicating and acting upon changes in a resident that may indicate urinary tract infection
Care staff have a key role in the recognition of UTI, especially when residents have a limited ability to communicate concerns or feelings. 57 However, staff may not share their concerns through a lack of confidence in their interpretation of the resident’s condition, their ability to communicate their concerns using the correct technical language or professional barriers keeping them from expressing their opinion. 63 Experiences of not being listened to resulted in feelings of powerlessness and uncertainty when deciding what to do. Feedback from nurses and physicians was found to be the most important influence on the care assistant’s choice of action. When their views were considered, they felt included in the decision-making process.
In a prospective descriptive study of written documentation by nursing assistants, nurses and GPs when infection was suspected in older people living in nursing homes, researchers reported that nursing assistant-initiated investigation was undertaken in almost half of the episodes evaluated as possible infection or infection. 71 Nursing assistants were also the main initiators in episodes evaluated as non-infection. It was unclear how nursing assistants conveyed information about changes in a resident to registered nurses or how this information was used. Researchers suggested that nursing assistants do not necessarily use the same language as registered nurses and do not always feel secure in conveying their suspicions about infection to senior colleagues.
In a study describing how physicians in the Netherlands depend on registered nursing staff for information to make an assessment,72 authors described that the poorer the quality or conveyance of information, the more difficult it can be for physicians to make a treatment decision. While some physicians considered nursing staff to be capable of recognising signs of infection and judging when the physician should see a resident, others indicated that the experience and level of education of the nurse could affect the quality of the information provided. Similarly, researchers Chaaban et al. 73 described that physician’s decision to prescribe antibiotics was influenced by their perception of registered nurses’ competence, knowledge levels and ability to communicate their clinical observations.
These studies highlight the importance of addressing both professional and communication barriers in the design of complex interventions to improve communication in relation to suspected infection and ensuring appropriate treatment.
Summary of evidence underpinning context–mechanism–outcome configuration 2
Evidence for strategies that are successful in improving accurate identification of urinary tract infection signs and symptoms
The evidence included in this review draws on four studies. 60,65,66,74 Three studies suggest that care home staff place more importance on their own knowledge of a resident than information provided in decision-support tools and do not necessarily use them as intended; when there is misalignment between the two, they are inclined to follow their own reasoning and ignore the tool. 60,65,66 The degree of fit of a decision-support tool to the resident’s presentation may determine its perceived usefulness, acting as a reference for symptoms of infection and actions to take when there is good alignment, but being less useful when symptoms do not fit with a resident’s presentation, particularly in those with dementia. This creates a disconnect between guidance and the realities of practice, which may be avoided where coproduction is used to design the decision-support tools ensuring they alignment with practice and existing processes in care homes.
Two intervention studies60,65 engaged care home staff in the pre-intervention stage of the research to inform the design of a decision-support tool. This enabled the tools to be tailored to the needs of staff and reflect experience in practice in addition to empirical evidence. Researchers incorporated a list of non-specific signs and symptoms, including change in behaviour in the resident, at the beginning of an algorithm before listing specific evidence-based signs of symptoms of infection. 60 Care home staff described how the algorithm reflected usual practice but found it more challenging to assess for UTI than for respiratory or skin and soft-tissue infection. A reason given for this was that the evidence-based symptoms of UTI were difficult to observe in residents, particularly those with incontinence or dementia, and did not reflect the symptoms staff usually looked for.
Nurses reported how respiratory infections were easier to manage than UTI because they perceived there to be more actions to take, including using nebulisers, encouraging fluids, simple linctus and monitoring observations. This suggests that the actions taken to prevent and manage UTI were less well understood or considered insufficient to fulfil the need to be ‘doing something’.
The algorithm was found to be of value in situations where care home staff lacked prior knowledge of a resident. 60 Researchers observed that it appeared to work as a checklist, helping staff to justify their decision to contact the GP. When care staff were familiar with a resident, fear of missing a UTI was an important driver in some staff considering their own knowledge of the person to be more important than use of the algorithm, particularly for those residents with a history of previous infection. The SBAR communication tool was perceived to be more useful when the GP was unfamiliar with the resident, helping senior staff to convey information in a logical way by providing more vocabulary and structure. 60
Difficulties inherent in delivering changes in practice when existing beliefs and practices about UTI override the intervention was evident in this study. Staff were more likely to ignore the algorithm when the listed symptoms were not a good fit with the resident’s presentation or were deemed irrelevant. Some staff placed greater importance on symptoms such as blood in the urine, change in smell or colour of urine and dehydrated skin, which were not included in the algorithm because of lack of supporting evidence. 60 However, others reported that they were more alert to the symptoms indicated on the algorithm and were therefore less likely to rely on non-evidence-based observations as indicators of infection and used it as a cue to contact the GP.
In a RCT previously described,65 the intervention included an assessment tool and a communication tool, which were co-designed during the pre-intervention phase of the study. The communication tool was based on SBAR to provide a means to structure communication with the GP. However, compared to the assessment tool, which formed part of the educational intervention, staff found the communication tool less useful and relevant, particularly when observations had already been recorded on the assessment tool. 70 Participants were familiar with the principles of SBAR and perceived they were already applying this to their practice and initially felt that the communication tool was too complex and difficult to understand. They expressed difficulty using it with residents with dementia, who could not describe their symptoms as well as other residents which resulted in it being used less often than the assessment tool. The few participants who did use it with the GP reported that it did not make any difference in their communication.
Similarly, participants in the ‘BHiRCH-NH’ study74 found limited use for a structured communication tool based on SBAR, together with condition-specific care pathways and a ‘Stop and Watch’ early warning tool as staff perceived they were ‘already doing something similar’. The study developed and tested a complex intervention with implementation support designed to reduce avoidable admissions in nursing homes by early detection and assessment of UTI, dehydration, respiratory infection and exacerbation of chronic heart failure. It was based on an intervention developed and tested in the USA,75 which was further developed in collaboration with ‘BHiRCH-NH’ stakeholders. Implementation support was informed by the PARiHS framework76 and evaluated in a 10-month pilot CRCT of 14 nursing homes in the UK with an embedded process evaluation.
Individual-level data on nursing home residents, their family carers and staff and system level data using resident records were used to measure reduction in hospital admissions and ‘avoidability’ of admissions. Implementation was evaluated using process-level data, including recruitment rates, completeness of outcome measures, data collection and return rate of questionnaires. Individual semistructured interviews were conducted with nursing home managers, nurses, care assistants and family carers that delivered the intervention.
Outcome analysis demonstrated no reduction in hospitalisations, although the low number of hospitalisations for the four conditions suggested that this was an unsuitable primary outcome measure. There was also no effect on the use of the assessment tools with only limited evidence that the Stop and Watch tool or care pathways were used. Few nursing homes in the trial reported having used the interventions before, although staff who were already aware of the need for early detection frequently reported they were ‘already doing it’. One practice development champion reported how the structured approach to communication made it more likely that their concerns were regarded by the GP as valid.
The care pathways devised for assessment of UTI and dehydration in the study74 were of interest given how early, non-specific changes such as confusion, changes in the characteristics of urine (colour, smell) and dehydrated skin can be falsely attributed to a UTI. 60,61 The primary assessment for dehydration was to check blood pressure and weight, whereas for UTI, increased frequency or urgency, discomfort on passing urine and lower abdominal discomfort/pain was assessed. For residents with positive indicators for UTI a second assessment was prompted, including a urine dipstick test for UTI and an assessment of fluid intake, urine concentration, urine output, skin turgor and blood pressure for dehydration. Since the assessment tools were not used as intended and their approach to the assessment of residents with non-specific changes was not elaborated by the researchers, it is unclear how early changes in a resident’s condition were interpreted and acted upon.
The researchers suggested that the implementation of the intervention may have been more acceptable and effective if developed collaboratively with each nursing home, thereby addressing any specific issues they were facing. 74 They also identified limited engagement among care staff despite their key role in early detection, suggesting that the intervention may be beneficial in residential care homes rather than nursing homes, given they are not required to employ nurses. It was unclear from the study findings how the work of nurses and care assistants was organised in the nursing homes studied or the extent to which care assistants were actively involved in early detection of deterioration and assessment for UTI.
Evidence for a whole care team approach
To promote a whole care team approach to the prevention and recognition of UTI in care homes, staff working at all levels need to see the relevance to their role of being actively involved. In the study by Hughes et al.,60 there was evidence of the algorithm being used by some staff but not others. Provision of the decision-support tool empowered some junior (unregistered) staff to go to a senior member of staff with clearer information on a resident who was unwell, whereas others felt it was not their role to do this. There was apparent confusion regarding who could use the algorithm with uncertainty about whether it was for use by any member of staff or only senior staff. Moreover, not all staff considered it was appropriate to the role of more junior staff, some of whom considered there was no need as they already reported everything to the nurse. Similarly, there were mixed views about including junior staff in training sessions. This reveals the importance of clarifying roles within care teams when a new practice or way of working is introduced to address both the value placed in it by staff working in different roles and the potential for professional hierarchy to create barriers to knowledge brokering. 77
In the studies by Arnold et al.,62,70 nurses with a role in facilitating the intervention acted in a supervisory capacity. This meant they were not involved at the time when care staff first suspected a UTI in a resident, but instead offered support in reflecting on their assessment and use of the tool. The researchers reported how it became apparent, early in the implementation phase of the study, that there were problems with understanding the tool, leading them to conclude that it was important for healthcare support workers to use the tool with a colleague rather than alone.
Evidence for the role of project champions
Intervention studies that enlisted champions within studies reported on their effectiveness. Champions played a key role in facilitating implementation of the interventions, often instigating opportunities for ongoing learning through application tools in practice. 60,74 This included creating learning moments at critical points in care, for example, considering if it was necessary to contact the GP immediately, discussing the algorithm and corresponding documentation in situations such as handover times, regular staff meetings and in casual break-time conversations and provision of ‘friendly reminders’ to utilise the algorithm and complete documentation. 60 Such opportunities were important in addressing barriers to implementation, which included lack of time, skills and competence.
Champions reported how support from care managers to allow dedicated time for them to enact their role was helpful, along with frequent and regular visits by the researcher, which served to encourage them in their role and emphasise the importance of the study. 60 External support was a feature of the BHiRCH-NH study74 and was provided through monthly coaching calls, a 1-day training and preparation workshop delivered to champions by the research team, handbooks and web-based resources. Practice development champions reported how staff saw value in the Stop and Watch tool, particularly for care assistants and domestic staff who had not previously received any training about early signs of residents’ deteriorating health. Some noted that the tools had provided a formal structure and emphasis on this aspect of care. However, champions considered use of a Stop and Watch form to document observations was unnecessary, as they already had a place in the resident’s care record to note any changes in their condition. This is important because if the ‘champions’ of an intervention are unconvinced about its use this is likely to impact on the motivation and engagement of other staff.
In the BHiRCH-NH, one of the intervention homes withdrew from the study following the training workshop owing to a lack of knowledge, skills and expertise on the part of the champions and a lack of management support. In another home, the champion reported having trouble engaging staff in the project. Most champions engaged in information sharing and training about the project and in one home the champions had integrated elements of the intervention into the electronic care record and their regular morning meetings to review residents. The monthly coaching calls helped to motivate them to continue facilitating the intervention, although the uptake of these calls was variable. Several champions suggested it would have been helpful if the study team had communicated more directly with staff about the project and delivered staff training. This highlights the issue that care homes may not have staff with the skills and expertise to deliver staff training in a way that supports innovation and change.
Champions pointed to the critical role of the manager in providing authority and support for the project, including giving time for the champions to implement the intervention. Managerial endorsement was recognised by champions to be important in motivating staff to engage in training and use of the tools given this was not part of mandatory training or organisational policy. 60,74
Context–mechanism–outcome configuration 3: active monitoring is recognised as a legitimate care routine
Figure 9 depicts CMOc 3, which is described below followed by a discussion of the underpinning evidence.
FIGURE 9.
Context–mechanism–outcome configuration 3: active monitoring is recognised as a legitimate care routine.
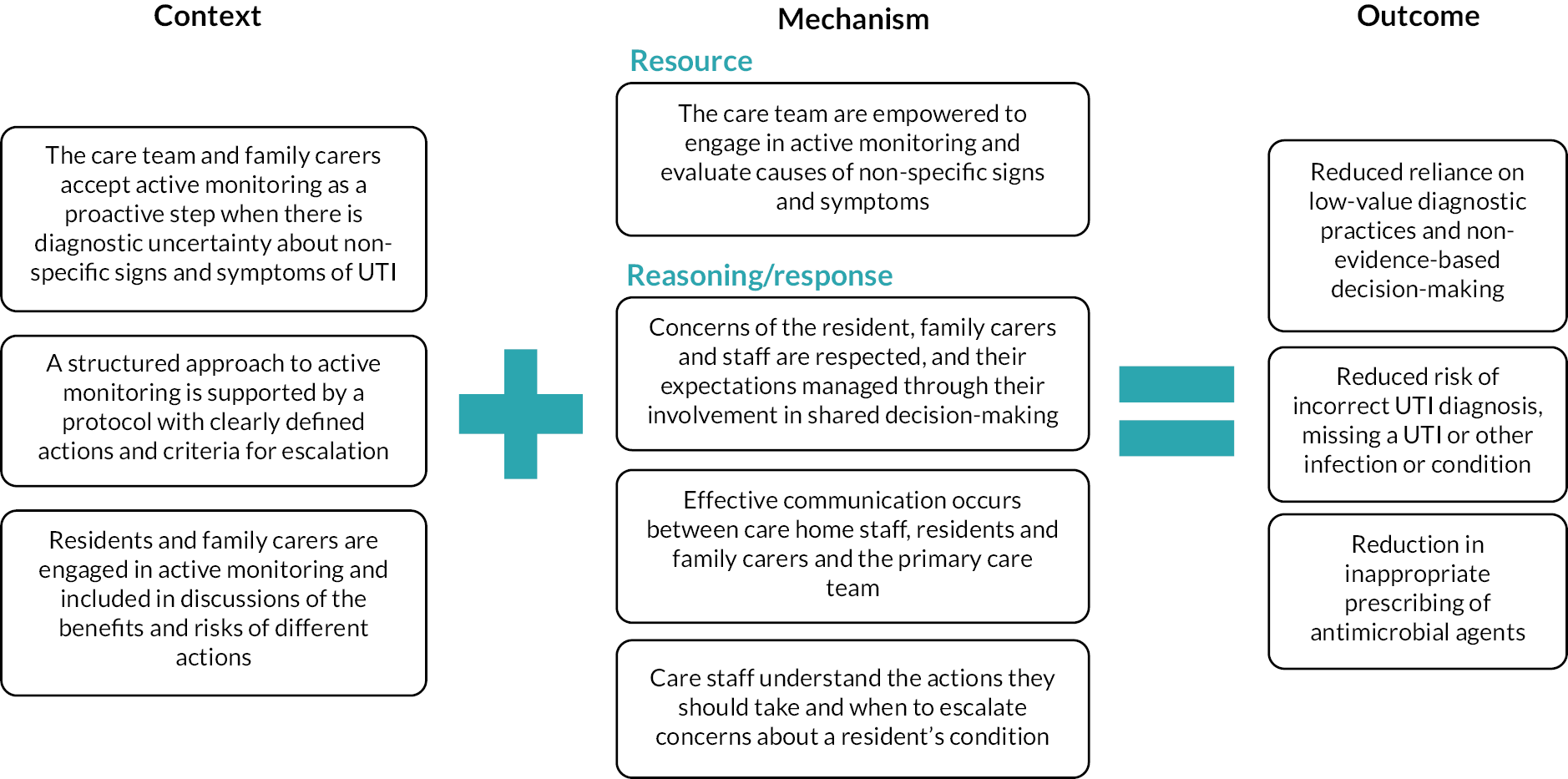
Context
When there is diagnostic uncertainty about UTI in a resident with early, non-specific signs, GPs are reliant on the observations and actions of care home staff to inform their decision-making. In care homes where the care team and family carers accept active monitoring as a proactive step in response to diagnostic uncertainty, the use of a protocol provides a structured approach to monitoring of the resident’s condition and a framework for shared decision-making (SDM).
Mechanism
Active monitoring can be initiated by care home staff using a protocol for monitoring and escalating concerns about a resident’s condition to a clinician or by a clinician in collaboration with care home staff and family carers. Care home staff are enabled to monitor and investigate causes of early, non-specific signs and symptoms without resorting to low-value diagnostic practices and non-evidence-based decision-making. Direct engagement with the resident and family carers provides opportunities to discuss the benefits and risks to different actions and strategies, enabling them to ask questions, feel listened to and respected. Involvement of staff and a resident’s family in SDM promotes acceptance of active monitoring as a proactive step when there is diagnostic uncertainty and helps to manage the concerns and expectations of the resident, family carer and care staff. Staff who understand the actions they should take and when to escalate their concerns about a resident’s condition can incorporate this more deliberative approach into the care routine allowing time to check for other underlying causes of early changes.
Outcome
A slower, more reflective approach increases the likelihood of a correct UTI diagnosis, not missing another infection or condition and reducing the potential for overuse of antibiotics.
Rationale – identifying urinary tract infection in older adults
Processes that support recognition of UTI by care home staff, nurse practitioners and GPs are critical to driving improvements in UTI prevention as they enable informed assessment of individual residents and monitoring of the effectiveness of prevention strategies. Identifying UTI in older adults is known to be complex as symptom presentation is often atypical. 78 Early signs and symptoms of a UTI can sometimes be indistinguishable from other infections or medical conditions. 13,79,80
In older adult women, especially those living in care homes, UTI symptoms can be less pronounced and more generalised than in younger age groups, making diagnosis more difficult. 13,74 Non-specific symptoms, such as new onset or worsening of confusion, are assumed to be caused by a UTI in older adults despite there being many other potential causes. 81 For example, symptoms linked to dehydration, including fatigue83 and changes in cognitive function,83 can be mistaken for a UTI. Diagnosis is even more difficult in those with dementia when individuals are unable to effectively communicate how they are feeling. 84,85
These complexities pose challenges when assessing for UTI, particularly in those with dementia and can lead to overdiagnosis. 58,60,62 Asymptomatic bacteriuria (bacteria in the urine without urinary tract symptoms) is common in older adults, particularly among those living in care homes, with increased frequency in residents with confusion or dementia, or incontinence of bladder and bowel. 31 The presence of an IUC further increases the prevalence of ASB in both men and women. 13 Distinguishing UTI/CAUTI from ASB is therefore problematic in older adults, given its often atypical symptom presentation and the increased prevalence of ASB.
National and international diagnostic guidance discourages screening or treatment for ASB in older adult women, including the use of urine dipsticks in care homes as a test for UTI, relying instead on a combination of observed signs and symptoms to diagnose a UTI in this population. 31,86,87 However, changing behaviours specific to use of urine dipsticks can be difficult as care home staff can lack knowledge about ASB, and they may rely on the dipstick as a simple way to identify a reason for an increase in a resident’s delirium/confusion, which can be otherwise difficult to determine. 58 Moreover, a positive result serves to validate a care worker’s suspicion of UTI and may be requested by the GP as an objective measure or to ‘rule out’ a UTI. 58 Urine dipsticks are still used in some cases and can influence the UTI decision-making process in a way that could lead to overdiagnosis.
Summary of evidence underpinning context–mechanism–outcome configuration 3
Evidence for managing expectations and involvement of care home staff and family members
General practitioners recognise that concern from care home staff and family about a UTI/CAUTI being missed can result in pressure to prescribe antibiotics, even if diagnostic criteria are unclear. 58,64,88,89 Care staff depend on their previous knowledge of a resident’s condition and their experience to make decisions about the early changes they observe and may have an expectation that antibiotics are an appropriate treatment. This rapid, intuitive decision-making can lead to inappropriate or premature suspicion of UTI60,61 and may also reinforce family carers’ concerns about the need to act.
One study suggested that some care home staff were unable to identify the signs and symptoms of deterioration indicative of a serious infection in their residents. 58 A metasynthesis of qualitative research on antibiotic prescribing practices in long-term care facilities found that doctors reported how nurse pressure could sometimes lead to increased use of antibiotics. 88 Family pressure on nurses and doctors to prescribe was a theme reported in seven of the eight studies included in the review, with increased expectation to have a prescriber assess the resident or to prescribe an antibiotic. The fear of poor outcomes for the resident or litigation from the family was reported as something that affected decision-making. Research to clarify the UTI communication pathway in nursing homes61 showed that care assistants are usually involved in providing a clinical history for GPs. The study highlighted the issue of one-way communication with the GP, which could cause a delay in management when more information was needed. Some primary care staff also reported that nursing home staff contacted the GP too early in an illness, when there were actions, they could have taken to understand and address non-specific symptoms. 61
Involving family carers is key to detection and early action as they can often identify subtle changes in a resident’s condition. However, they may need support to communicate their concerns to care staff. A qualitative study in the UK90 explored family carers’ perspectives on their involvement in the timely detection of changes in their relative’s health in 13 UK nursing homes. Findings revealed that families felt they could be involved in identifying subtle changes in a resident’s condition in three ways: noticing signs of changes in health, informing care staff about what they noticed and providing history and educating care staff about their family member’s changes in health. While family carers noticed timely signs of changes in health, they did not always communicate this information to care staff for various reasons. Families suggested they could be supported to detect timely changes in health by developing effective working practices with care staff, but involvement needs to be negotiated, better supported and given more legitimacy and structure within the care home.
Evidence for use of active monitoring and shared decision-making when there is diagnostic uncertainty
In a realist synthesis of evidence examined effective de-implementation of practices, described as a process of changing or stopping low-value practices across health and care services. 91 One CMOc focused specifically on the recognition that patients’ expectations influence consultations. Authors reported that when low-value practices are relied upon for diagnosis or management of infection, improving the HCP’s ability to communicate with patients and implement alterative active intervention strategies such as ‘watchful waiting’ can validate concerns, increase the patient’s sense of autonomy and improve the patient–clinician relationship. Evidence for watchful waiting in this context covered a wide range of conditions using protocols that proposed ‘doing nothing’ strategies, various types of monitoring and actions and/or delayed prescribing.
Watchful waiting was considered as a mechanism to use if there is diagnostic uncertainty or pressure for low-value investigations. 91 The synthesis drew on evidence from various healthcare settings to explain how forms of this strategy could reduce reliance and use of low-value practices. A key finding was that diagnostic worry was one of the main reasons associated with the use of low-value tests. 92,93 One of the included studies examined low-value diagnostic tests in primary care and five specific communication behaviours that providers employed. 93 The study found that tests were ordered less when watchful waiting or discussing how risks outweigh benefits were employed. Evidence showing how watchful waiting was useful in reducing low-value or ineffective prescribing practice was also reviewed. Two studies undertaken in children with acute otitis media94,95 highlighted that giving parents information on monitoring the condition of the child and safety netting by delaying antibiotics and/or follow-up visits played the key role in success. The realist review findings underlined the influence of patients’ expectations on the outcome of consultations and highlighted the importance of SDM as part of the context for watchful waiting. 91
Shared decision-making in clinical management can be improved with enhanced communication between healthcare providers, trusting relationships and shared mutual knowledge. A realist synthesis explored how SDM could be facilitated for older people with multiple health and care needs. 96 The need for enhanced communication skills among healthcare providers was a common theme across research studies, including the ability to address with people the uncertainty involved in many medical and care decisions. Longer consultations were linked to greater patient satisfaction and improved SDM, which is likely to be related to the opportunity for people to ask questions and feel listened to and respected. The quality of individual clinicians’ communication skills and their ability to fosters trusting relationships with older people and their families is fundamental to SDM. Partnership working between different health and care professionals was seen as key to decision-making for older adults with complex needs.
Evidence for active monitoring as a strategy to reduce overdiagnosis of urinary tract infection
Multiple guidelines reference a period of monitoring when there are initial signs and symptoms of infection that are unclear or do not meet diagnostic thresholds in older adults. 33,86,97,98 Active monitoring and other forms of early monitoring for infection have been identified as a key part of the UTI care pathway. In 2020, the American Medical and Dental Association produced a consensus statement that addresses the management and prevention of UTI in post-acute and long-term care settings. 97 The guidelines are directed at primary care providers and state that where there is diagnostic uncertainty in the presentation of UTI signs and symptoms, a period of ‘active monitoring’ (previously referred to as watchful waiting or careful observation) should be put in place. This includes frequent monitoring of vital signs, paying attention to hydration status (recording fluid intake/stimulating intake) and repeated physical assessments by nursing home staff. They reported that supportive care, including increased fluid intake, may help resolve the issue and reduce the need for antibiotics. When discussing with those who work with care home staff in the UK and researchers, the term ‘active monitoring’ was preferred to that of ‘watchful waiting’ or ‘wait and see’ as it more clearly defined the period and intention when targeting UTI in care homes. However, in the following section of this report, the terms can be used interchangeably.
The active monitoring process can be triggered at the care home level or initiated by healthcare providers (Figure 10). When initiated by care home staff, it is commonly at the outset of any perceived deterioration in the resident’s condition or concerns about possible signs and symptoms of a UTI. It guides staff as to what steps to take before alerting the clinician. 60,61,98 This includes monitoring the resident over a defined period, ruling out other causes of the change in condition and actions such as monitoring fluid intake. 60,61,98 In these situations, the protocol for active monitoring may be embedded as part of a reflection and monitoring tool that care home staff have been trained to use and aligned with communication tools that may be used to relay information to the HCP. 61 In other studies, active monitoring is initiated by the clinician in collaboration with care home staff and often targets residents that do not meet the threshold for diagnostic criteria for UTI outlined in guidance36,97 and/or for a specified period if symptoms are mild and patient at minimal risk for deterioration. 66,103
FIGURE 10.
Active monitoring in the UTI prevention and management pathway.
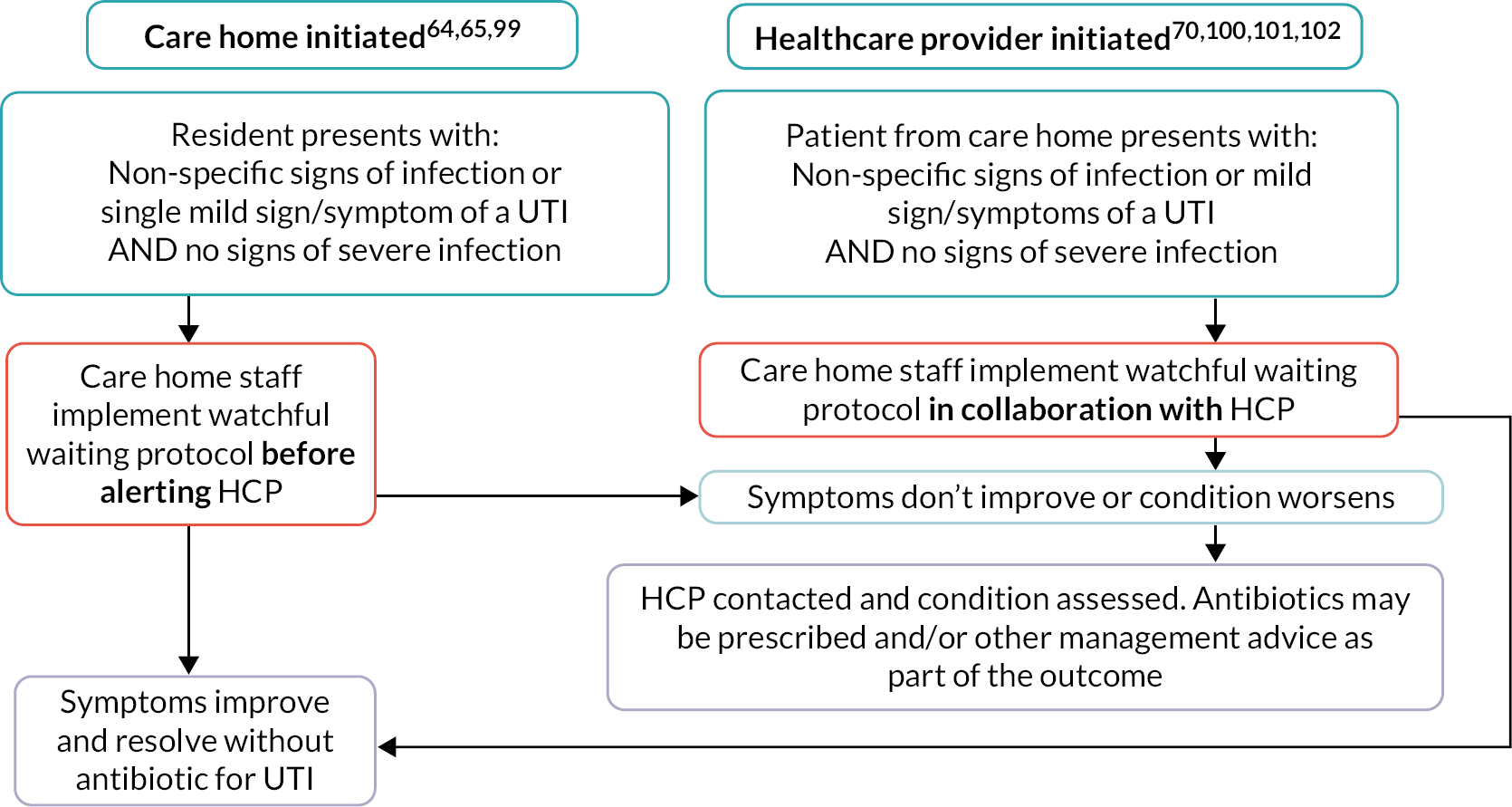
Evidence for the use of active monitoring as a strategy to prevent and manage urinary tract infection in care homes
Active monitoring periods, within a well-defined UTI management protocol, offer the opportunity for staff to reflect on decisions before responding intuitively. In a study in the USA,59 nurses working in care homes were randomly allocated to a self-paced group, or a forced deliberation group, and were given a questionnaire with UTI scenarios. Participants indicated what actions they would take in each situation. In the forced deliberation group, nurses were required to consider each scenario for at least 30 seconds before responding in order to discourage fast, intuitive decision-making. The team assessed what signs and symptoms were attached to outcomes specific to seeking care from the clinician. The findings revealed that when nurses made slower decisions, they were more likely to rely on guidance-informed signs and symptoms of infection for UTI before contacting the clinician. The authors discussed how this deliberation could also benefit the resident if it allows for the initiation of symptom management strategies when criteria are not met (e.g. increasing fluid intake, improving personal hygiene).
Active monitoring as part of the care decision pathway is usually evaluated as part of a larger, multifaceted intervention and it is difficult to distinguish its impact on outcomes. Studies identified in this review indicate that active monitoring embedded as part of a decision-making tool or process can contribute to increased use of this strategy103 and decreased antibiotic use for UTI without adversely affecting UTI-related hospital admissions or other adverse outcomes. 65,66,103,104
In a UK feasibility study with a qualitative component, researchers aimed to refine an algorithm to assist care home staff to manage residents with suspected UTI. 60 The team collaborated with staff across care homes to develop the management algorithm and provided training targeted at nursing staff and senior carers (responsible for contacting the GP) and the other care staff (not responsible for contacting the GP, but responsible for observations and patient care). Where a resident had two or more symptoms of a UTI or dysuria alone, the algorithm recommended contacting the clinician. If not, they were required to ‘wait and see’ and monitor the resident’s temperature every 6 hours and contacting the GP if there was no improvement after 12 hours. In addition, monitoring symptoms, offering analgesia, encouraging fluids and providing supportive care were recommended. In the qualitative component of the study, staff discussed barriers to using the ‘wait and see’ approach. These included the reliance of staff on their experience to guide action; for example, if a resident had a history of septicaemia, they were less likely to follow the algorithm. Some care staff felt that the algorithm helped them to liaise with family members about the management of infection but commented that more training on how to communicate with relatives would be useful as they found it difficult to suggest the ‘wait and see’ process when they were not registered nurses. They also highlighted that written information for relatives would be helpful, so they were aware of when this might be employed.
In Sweden, researchers103 conducted a CRCT trial of a multifaceted educational intervention for nurses and physicians to change prescribing of antibiotics in 58 nursing homes. The intervention included small educational group sessions with nurses and physicians, feedback on prescribing, presentation of guidelines and written materials. Findings showed that the intervention had a modest effect on prescribing with a significantly higher proportion of infections being handled by physicians using ‘wait and see’ as part of the intervention when comparing the intervention group with the control. This did not correlate with any adverse effects or difference in hospital admissions.
Other studies that include active monitoring have demonstrated improved prescribing for UTI and AMS outcomes in care homes, with no indication of increased mortality or hospitalisations. In a CRCT in Canada,66 researchers measured the impact of an interprofessional education package and a decision tool on the rate of urine culture testing and antimicrobial prescribing for UTI, showed a significant decrease in prescribing for UTI when comparing intervention and control groups, with no difference in hospital admissions and a significant decrease in mortality in the intervention group compared to the control. If the resident had clear symptoms of a UTI, the decision tool included a period of monitoring and encouraging fluids for 24 hours unless the resident’s condition was deteriorating rapidly.
In a multimodal quality improvement study, 25 nursing homes were randomly assigned to intervention or control groups to use a simplified diagnostic algorithm for UTI in care home residents. 104 The use of the algorithm was supported by a 1-hour webinar on national guidance and the role of nursing home staff in AMS in care homes, posters and other educational materials for staff, an active monitoring sheet designed to improve the identification and documentation of signs and symptoms of a UTI, audit materials and coaching sessions. Findings showed a reduction in antibiotic use for unlikely cystitis by 27% [adjusted incident rate ratio (AIRR) 0.73 (95% CI 0.59 to 0.91); p = 0.004] and overall antibiotic use by 17% [AIRR 0.83 (95% CI 0.70 to 0.99); p = 0.04]. There was no difference in rates of all-cause hospitalisation or mortality between the two groups.
Active monitoring prescribed before treatment may be a way to reduce the influence of some of the drivers of overprescribing for UTI, especially if used as a way to monitor a resident when their status changes. However, the safety of delayed prescribing when an individual has evident signs and symptoms of a UTI is less well understood for older age groups. According to national guidance in the UK: ‘When there is clinical uncertainty about whether a condition is self-limiting or is likely to deteriorate, backup prescribing (also known as delayed prescribing) offers healthcare professionals an alternative to immediate antimicrobial prescribing. It encourages self-management as a first step but allows a person to access antimicrobials without another appointment if their condition gets worse’. 54 It has become part of the recommended management regime for women with uncomplicated lower UTI within national guidance within the UK. 54,86
Although other evidence supports the safety of a delayed prescribing approach for women with a UTI,105 work undertaken by Shallcross et al. 100 looked at English electronic patient records from 2007 to 2015 and the relationship between using ‘no antibiotic’ or ‘deferred antibiotics’ for UTI in adults over 65 years, BSI and mortality. The study found the odds of BSI were equivalent in patients who were not treated with antibiotics at once and those who were treated on the date of their UTI consultation [adjusted odds ratio (aOR) 1.13, 95% CI 0.97 to 1.32; p = 0.105]. Delaying or withholding antibiotics was associated with increased odds of death in the subsequent 60 days (aOR 1.17, 95% CI 1.09– to 1.26; p = < 0.001). However, the authors state that there was limited evidence that increased deaths were attributable to urinary-source BSI and that there were significant challenges with the data used. This large-scale study and earlier concerns discussed about deterioration of residents highlight the need to ensure that any active monitoring protocol has clear criteria for monitoring and escalating concerns to a clinician (see Figure 10).
Urinary tract infection decision tools for care home staff evaluated in this review were developed for staff with varying levels of ability to detect signs and symptoms of deterioration in a resident. To provide additional support in detecting signs of deterioration or serious infection, UTI decision tools targeting care home staff in the UK reference known national resources developed for this purpose. 19,54,99 In the development of a UTI leaflet for care home staff, family and residents, authors identified that care home staff had limited confidence and ability to identify signs and symptoms of serious infection or deterioration. 58 The tool targeting care staff and residents was designed with pictorial safety-netting information specific to signs and symptoms of serious infection, which aligned with a decisional algorithm for nurses and healthcare providers to use. 33,58,101 Using the supplementary materials from these studies, Figure 11 summarises the specific components and considerations in decision-support tools to support active monitoring.
Teacher–learner interviews
In stage 3, the teacher–learner interviews supported the content and synthesis underpinning CMOc 1, 2 and 3 and reflect the findings from the literature. They articulated that identifying UTIs in care home residents was complex and there was recognition that the use of urine dipsticks for this population was not an objective measure that could be used to diagnose a UTI. Healthcare support workers’ knowledge of their residents, having the confidence to voice their concerns and having other members of staff valuing their opinions was highlighted and concurs with the evidence we found (CMOc 1, CMOc 2).
… valuing the person who’s closest to the resident, and it might be the most junior person there if they know the person well, then they’re opinion is worth more than anyone else’s I think and giving people the confidence to express their concerns.
GP
However, it was also recognised that there was not always a shared language for communicating or describing signs and symptoms to enable an accurate diagnosis (CMOc 2).
A lot of the time the nursing staff would say – ‘she’s confused’ and that would be a word for saying she’s going into delirium and so she has a UTI. But when you ask them to define what they mean by confused there was a range between – a little bit cranky to full-blown delirium.
GP
A general physician explained how watchful waiting offered a mechanism of action that was not focused on antibiotic use:
… there is a very strong case for doing something, which is also the attraction for getting the nursing home resident onto antibiotic treatment because then you are doing something, then everyone can relax because we are doing something ... Watchful waiting is also action – it’s not passive.
Academic trainee General Physician
Stakeholder workshop
Stakeholders from a wide range of settings and professions agreed with the context and reasoning of the CMOc in this theory area and echoed the issues raised by stakeholders in stage one and in the teacher–learner interviews in stage 3. Referring to the use of soft signs where residents were not quite their usual selves with often subtle changes in their routines or behaviours.
They have no temperature, there’s no issues, is just the confusion and some behaviour issues, that’s what we notice, and we don’t do dipstick all the time automatically, we try to resolve as much as we can, but if it is not then we contact the GP and let them know. Yeah, mainly communication.
Care Home Manager
Stakeholders described several different tools designed to be used in care homes for the early recognition of illness to streamline observations and communications between care staff and the GP or acute care. Most cited were RESTORE and NEWS2 tools for recognising deterioration in a resident and the SBAR tool for aiding communication of their findings.
Several stakeholders described some of the difficulties with care homes adopting the tools despite them having been simplified for the care environment. This resonates with the research-based evidence that underpins CMOc 2 and CMOc 3.
Stakeholders acknowledged the importance of active monitoring (watchful waiting) when seeing a resident with non-specific symptoms of UTI (CMOc 3).
I do like the idea of the active monitoring because I think there are situations in the care home setting where we probably do want to see what’s happening to someone. What does the trajectory, or the trend in their illness – is this just a fluctuation within their normal fluctuations, within their normal behaviour or is there something that suggests that things are getting worse?
GP
Others recognised that while this might be the right approach, there are often pressures from care home residents’ family members to do something which resonated with the response we had elicited in stage 1 and the teacher–learner interviews.
Some families, if they’ve had numerous courses or side effects from antibiotics, may be more willing to accept kind of an active watch and wait process whereas others have maybe had negative effects of a UTI being diagnosed later and ended up in hospital will be more keen for active …
GP
Other perceived pressures to act may be because of a concern that a UTI could be missed and might progress to something more serious. This includes perceived pressure from regulators, as described by one stakeholder:
... I understand that often the care homes are carrying responsibility for something, if something goes wrong, you know then it is tricky, you know and CQC can be quite heavy handed sometimes if things don’t go right on a few occasions. So, there’s a tendency perhaps to over diagnose in some situations especially if something has gone wrong before.
GP
Perceived pressure from family members and concern about a UTI being missed were also concerns identified in the findings of research studies included in this review. It is possible that recent initiatives across care homes to implement use of tools for the early recognition of illness and physical deterioration and the rapid initiation of treatment have added to this sense of pressure to act early to circumvent deterioration, hospital admission and more complex treatment.
Theory area 2 – care strategies for residents to prevent urinary tract infection and catheter-associated urinary tract infection
Stakeholder feedback – stage 1
Stakeholders in stage 1 identified a range of barriers that existed to optimising hydration of care home residents. These were reflected in the evidence that we reviewed and synthesised and included a lack of education and training for staff leading to missed opportunities to increase fluid consumption of residents, pressures on staff time, residents’ attention and preferences, the range of equipment and choice of fluids to meet resident preferences and minimal attention to monitoring or measuring what residents consume in reality.
In relation to CAUTI, participants commented that the number of IUCs inserted in care homes was relatively few. However, when residents were admitted to hospital, they sometimes returned with an IUC and when the reason for its insertion was unclear, this may mean that IUC remained in situ without a clinical indication. Care home staff were aware of the risks associated with the use of IUC and managers identified that there was a focus on IPC principles in training and education.
Stakeholders indicated that RUTI in care home residents was a major issue, particularly related to the potential for the inappropriate prescription of antimicrobials. They highlighted that access to specialist advice, particularly CAs, was scarce and that the awareness of potential interventions among care home staff was limited. This is reflected in the evidence available to the research team to explore this area of care.
Context–mechanism–outcome configuration 4: hydration is recognised as a care priority for all residents
Figure 12 depicts CMOc 4, which is described below followed by a discussion of the underpinning evidence.
FIGURE 12.
Context–mechanism–outcome configuration 4: hydration is recognised as a care priority for all residents. a, Refer to CMOc 9 on well-designed education.
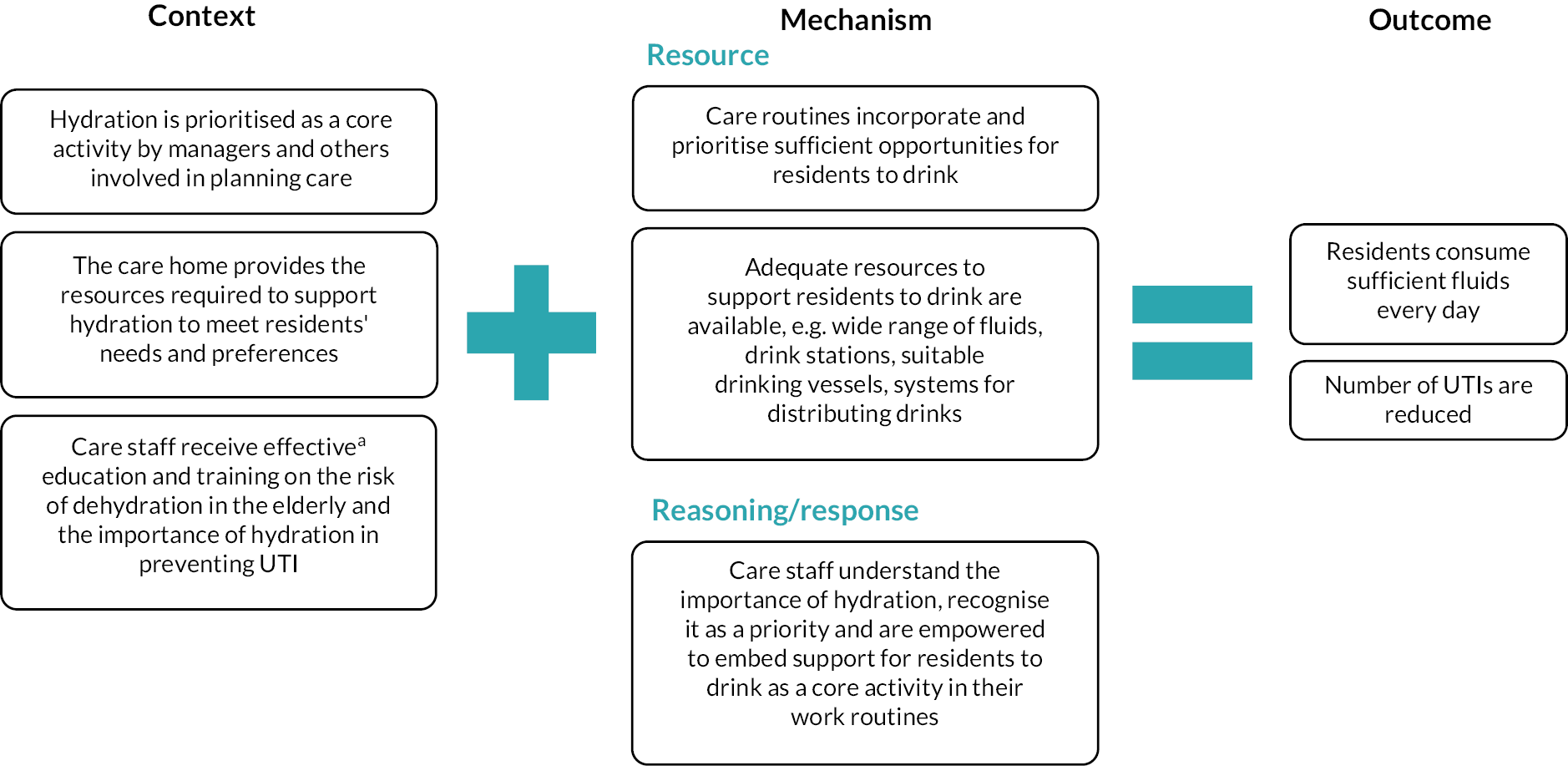
Context
Supporting residents to drink is one of many competing care priorities and its importance for preventing UTI and other health conditions is not always recognised by care home staff. Care home managers and unit/team leaders who determine care routines and allocate staff to tasks need to recognise resident hydration as a priority and identify the required resources to support this, including staff time, range of fluids and equipment. Focused education and training help care home staff to understand the importance of hydration in reducing the risk of UTI, appreciate age-related changes that affect residents’ experiences of thirst and taste, and dispel myths about hydration.
Mechanism
Increased knowledge and support from unit/team leaders will enable care staff to understand the need to plan sufficient structured drinking opportunities into care routines, extend the range of fluids offered to increase choice and recognise the importance of encouraging and supporting residents to drink more. When care staff know that hydration is a priority, they will feel able to include enough drinking opportunities for all residents into their care routines. Staff will also have increased awareness of the importance of hydration and more confidence to devote resources, including their time, to providing residents’ preferred drinks and supporting them to consume the drinks they are offered according to their capability and support needs.
Outcome
Increasing the number of drinking opportunities for all residents and allocating staff time to supporting them to drink will result in residents consuming sufficient fluids every day to prevent them becoming underhydrated and reduce their risk of developing UTI.
Rationale – the link between adequate hydration and urinary tract infection
Adequate hydration is recognised as a fundamental care need,107 but ensuring that the frail older people residing in care homes consume enough fluids during their waking hours can be challenging. The risk of dehydration is increased in the elderly because of reduced thirst reflect, cognitive and physical impairments and reduced renal function. 108,109
Minimum fluid intake of 2 l/day for adult women and 2.5 l/day for men has been recommended, including from solid food moisture,110 although 1500 ml/day is the absolute minimum for maintaining health. 111 In the UK, people aged 75 years or over have a significant risk of developing BSI secondary to UTI, and the pattern of marked increases in cases of E. coli BSI during summer months suggests that dehydration may be a contributory factor. 11,112
The link between dehydration and UTI is difficult to demonstrate, especially in a care home population where data are difficult to collect and controlled study designs are unfeasible and unethical. In a RCT of pre-menopausal women with fluid intake of less than 1.5 l/day, the group assigned to increasing their fluid intake had a significant reduction in episodes of cystitis (1.7, 95% CI 1.5 to 1.8 vs. 3.2 95% CI 3.0 to 3.3; p < 0.01) and antimicrobial treatment (p < 0.001). 113
Summary of evidence underpinning context–mechanism–outcome configuration 4
Evidence for strategies that are successful in increasing hydration and reducing urinary tract infection
We identified seven reports of five studies, which informed CMOc 4 and 5. They described multimodal interventions aimed at increasing hydration and preventing UTI in care home residents. 5,6,114–118 All were pragmatic in design, which reflects the challenges of conducting research in a care home setting. Three studies6,115,117 used improvement science methods to test the effect of hydration initiatives on fluid intake and measured adverse outcomes including UTI. 114,117 Two studies used a pre–post evaluation design to test a hydration intervention116 and education programme. 5 The effect of the intervention on the occurrence of UTI, falls and hospital admissions was measured by Booth116 and included an exploration of care staff perspectives on resident and contextual barriers to hydration. One study was a descriptive report of a hydration intervention. 118
Increasing drinking opportunities and residents’ choice of drinks was a core component of all these studies. This required a focus on reviewing and changing care routines to ensure that hydration was prioritised by staff, both opportunistically and as part of mealtimes and other organised activities. Drinks menus were devised based on residents’ expressed, rather than assumed, preferences. This often resulted in a wider range of drinks being made available than care homes had previously provided. Ensuring that residents were provided with their preferred drinking vessels that could be used easily supported them to drink independently and consume more fluid. 115 The involvement of the whole care team including chefs, housekeepers and activity co-ordinators in addition to the care staff enabled the co-design of changes, which were built around the feedback of observations of practice. 6,114,116,118 Engaging with the whole team ensured ownership of the changes and helped to embed these in everyday practice.
The long-term impact of the interventions was evaluated differently in these studies. In one study, researchers measured daily laxative and antibiotic consumption, weekly incidence of adverse health events and average fluid intake of a random sample of six residents collected by direct observation. 114 The interventions were associated with an increase in the amount and range of fluids consumed, with evidence that mean fluid intakes were increased above 1500 ml for a sustained period within one of the two care homes involved in the study. However, the number of participants was insufficient to demonstrate a reduction in incidence of UTI. The interventions were also associated with a significant decrease in laxative use, which suggests that the observed increase in fluids offered and consumed was real and extended across the resident population.
In a similar study, the safety cross (a simple visual tool containing 31 boxes where each box counts as a day in the month) was used to capture data on the occurrence of UTIs requiring antibiotics and/or admissions to hospital. 117 The implementation of seven daily structured drinks rounds was associated with a 58% reduction in UTI requiring antibiotics and 36% reduction in admissions due to UTI. Similarly, the DRInK-Up initiative116 was associated with a reduction in the number of UTIs from 51 pre to 37 post intervention, and a significant reduction in recorded falls (t = 3.148, df 19, p = 0.005) and an increase in the fluid intake of 13 residents by an average of 147 ml over the 24 weeks of the project, but for the remaining 11 it either decreased or did not change. 116
Care home managers are key to prioritising the time available to staff to undertake drinks rounds and support residents who require assistance to drink. Care homes with strong leadership and management support for meeting the hydration needs of residents were more likely to demonstrate success through incorporating hydration into the routine of care and endorsing it as a critical care activity. 6,114,116,117 Identification of specific staff to undertake specialist roles such as creating a hydration team, hydration aide or nominated champions creates a shared understanding that enables care staff to devote sufficient time offering drinks between meals, sitting with and encouraging residents to consume fluids, documenting how much they drank and reporting problems. 117,118
Four of the studies included staff education as part of a multimodal approach to increase understanding of the importance of hydration in reducing the risk of UTI and enable staff to recognise how normal patterns of care delivery can limit the number and type of drinks that residents are offered. 5,114,116,117 In one study, interactive training that included an emotional mapping exercise where participants considered their own fluid and drinking vessel preferences and how these related to those of their residents, decision-making using case studies and making and tasting thickened fluids resulted in a significant increase in self-reported knowledge across all six facets of hydration care. 5 Training can also highlight that alterations in the thirst reflex and taste may occur as part of the ageing process and therefore many elderly people prefer strongly flavoured drinks, and their preferences can change over their time in the home. 6,118 Challenging pre-existing beliefs about fluids and fluid provision and dispelling those that are unfounded; for example, believing water is better than other fluids, also assist staff to recognise the need for more person-centred approaches to hydration.
The I-Hydrate study5 found that the level of knowledge self-reported by care staff was not always reflected in the actual care observed and staff also struggled to relate their own drinking preferences to those of their residents. This suggests that more skills in self-assessment and opportunities for reflection among care staff may be needed to enable ‘unlearning’ to occur and new knowledge to be applied. Training alone is unlikely to effect changes in practice, as care staff may not feel sufficiently empowered to influence their colleagues or initiate the type of system changes that might be required to embed a greater focus on hydration. 5 Methods of training need to account for the care home environment where resource pressures make it difficult to release staff for training and ensure that a shared understanding is achieved by all care staff. Additional opportunities to embed learning, for example, during unit-based ‘huddles’ and use of mixed media to communicate key messages are important to reinforce education messages. 6,117
Context–mechanism–outcome configuration 5: systems are in place to drive action that helps residents to drink more
Figure 13 depicts CMOc 5, which is described below followed by a discussion of the underpinning evidence.
FIGURE 13.
Context–mechanism–outcome configuration 5: systems are in place to drive action that helps residents to drink more.
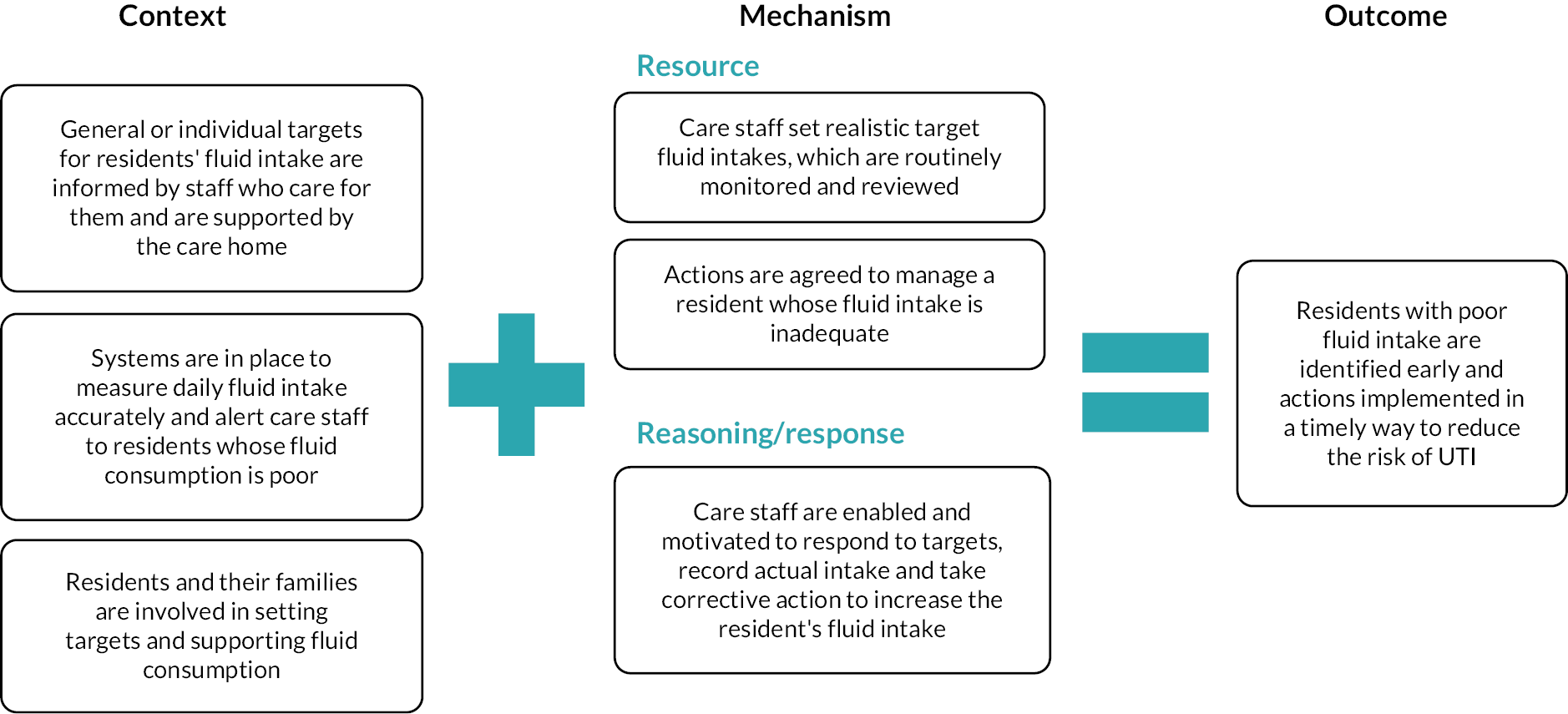
Context
Setting daily fluid intake targets for individual residents or other more general care targets, such as completion of a specified number of drinks rounds during the day, focuses attention on the importance of hydration and the actual amount consumed by residents. Organisational support and positive reinforcement by managers are important to ensure this activity is prioritised alongside systems to measure fluid intake and identify residents whose fluid consumption is poor. Targets are more likely to be enacted when they are informed by the staff who spend most time with residents and are linked to wider staff education on the importance of hydration and how to support residents to drink. Involvement of residents and family members in setting targets supports fluid consumption in some residents.
Mechanism
When realistic targets are set, care staff can agree and enact strategies to manage individual residents whose intake is poor. Systems that measure accurate daily intake and initiate action in response to the consumption of insufficient fluids by individual residents encourage staff to recognise the importance of identifying poor intake and reporting consumption accurately so that intervention can be initiated promptly when indicated. Feedback of data on completion of drinks rounds and number of UTIs is an important impetus for action as it enables both successes and areas for improvement to be highlighted.
Outcome
Residents at risk of dehydration are identified and timely intervention increases the fluid consumption of all residents, preventing them from becoming underhydrated and reducing their risk of developing UTI.
Rationale
Refer to CMOc 4.
Summary of evidence underpinning CMOc 5
Evidence for strategies that are successful in addressing poor fluid intake to reduce urinary tract infection
In addition to the evidence provided in CMOc 4, we identified studies that investigated use of fluid intake targets in care homes to address poor fluid intake. Two studies116,118 calculated individual targets for each resident based on a standardised formula or those identified by professional staff as at risk of dehydration. The rationale for this was to increase awareness of the importance of drinking among staff, families and residents. They found that while it is feasible to increase fluid intake in older residents, it can be challenging to achieve optimal intakes for all. 6,116 Fluid intake targets can create a tension for staff between responsibility for ensuring fluid intake targets are met while not forcing residents to drink. One study highlighted how encouraging residents to drink was seen as important but considered unacceptable if this stepped over to ‘forcing’ a resident to drink. 116
These studies also highlighted that documentation and monitoring of all residents’ fluid consumption are frequently inconsistent and inaccurate. 114,116 Problems with the reliability of fluid balance charts, which may be completed by several staff over different shifts and record the amount offered rather than the amount consumed, was reported. 114,116 In the DRInK-Up study, fluid charts were often completed by night staff who used standardised volumes and drink times to document that the resident had met their daily fluid intake target, regardless of whether this had happened.
Knowing how much a fluid a resident has consumed is important because it ensures that poor intakes do not go unnoticed and unaddressed by staff. 114 Defined systems or processes for both accurately monitoring intakes and acting in response to residents with poor fluid consumption are required and can be facilitated by approaches such as drinks diaries117 as an alternative to traditional fluid balance charts. Digital solutions linked to a resident’s electronic care record may also assist, but these approaches must fit with the care homes systems and electronic infrastructure for them to be used effectively. In care homes where hydration is prioritised and supported by managers and nurse leaders, recording fluid consumption can drive action to prevent dehydration.
Where managers and senior staff regularly review data on drinks rounds and provide feedback, the impetus for staff to keep going is reinforced. 117,118 The importance of support from the organisation and managers in signposting hydration as a priority in the allocation of staff duties and offering praise and positive reinforcement is also highlighted. 116 The use of nominated champions from within the homes to disseminate information and collate data on the implementation of hydration rounds and occurrence of UTI was also important in the project by Lean et al. 117 Expert support from professional staff external to the home, such as speech therapist, occupational therapist and dietician118 and from care commissioners was also a key success factor. 117
Stage 3: teacher–learner interviews
Teacher–learner interviews supported the content and synthesis underpinning CMOc 4 and 5. Participants pointed to some of the current work that they were involved in and were cognisant of some of the barriers that existed to getting traction and sustainability in this setting, particularly post COVID-19. The delivery of training on hydration was often described as being part of a specific hydration initiative, frequently delivered by quality improvement leads external to the homes. The training was usually held in short 1- to 2-hour sessions. One community matron highlighted a project that was providing hydration training as part of an initiative to identify UTI.
We work closely with our care homes using the ‘stop and watch’ and we are doing a massive hydration project at the moment with them. Getting carers to understand signs of UTI and about promoting hydration. Giving out information on ‘stop and watch’ and hydration booklets made simplified and for all staff.
Quality Improvement Lead
Stage 4: stakeholder workshop feedback
Stakeholders agreed with the content of CMOc 4 and 5 reiterating that fluid intake overall is very poor in older people in care homes while recognising how challenging this aspect of care is, particularly in residents with dementia. There was agreement that hydration needed to be prioritised and incorporated into everyday practice.
… making every contact count. I think with hydration, there’s so much or so many moments that we could use in a care setting where we could incorporate the hydration into it, whether it’s having that time when you’re having one to one with the patient, you could use those moments, whether it’s family time, when they’re visited by their families.
Local Government Lead
… making it part of everyday activities so you’re not stopping something to do it, you’re just doing it as well.
IPC Nurse Specialist
The use of a range of training materials and/or quality improvement initiatives happening in care homes were discussed. These were largely driven by NHSE/Integrated Care Systems and aimed at supporting the reduction of antimicrobial prescribing for UTI/CAUTI. It was felt that, if presented appropriately, the work accomplished in the StOP UTI project was supportive of these and would help facilitators to consider the contextual and staff response aspects of implementation.
… there’s going to be one (hydration) pilot in each NHSE region, they’re all on very similar themes in terms of encouraging, motivating, residents to drink more. The hydration pilots will take forward some of these recommendations in terms of work routines, education and training, and systems and documentation to alert staff to residents with poor intake.
CCG IPC Lead
… we’re making very short videos […] on hydration, specifically for care home staff and carers in their own homes…and urinary incontinence to really bring up that broader sort of issue, also all the positive benefits of good hydration even though people are worried about incontinence.
Pharmacist, NHSE
Support from care home managers and senior staff was also acknowledged to be an important contextual factor and that introducing any form of training/education on hydration needed organisational buy-in to be successful.
Context–mechanism–outcome configuration 6: good infection prevention practice is applied to indwelling urinary catheters
Figure 14 depicts CMOc 6, which is described below followed by a discussion of the underpinning evidence.
FIGURE 14.
Context–mechanism–outcome configuration 6: good infection prevention practice is applied to IUCs. a, Refer to CMOc 9 on well-designed education.
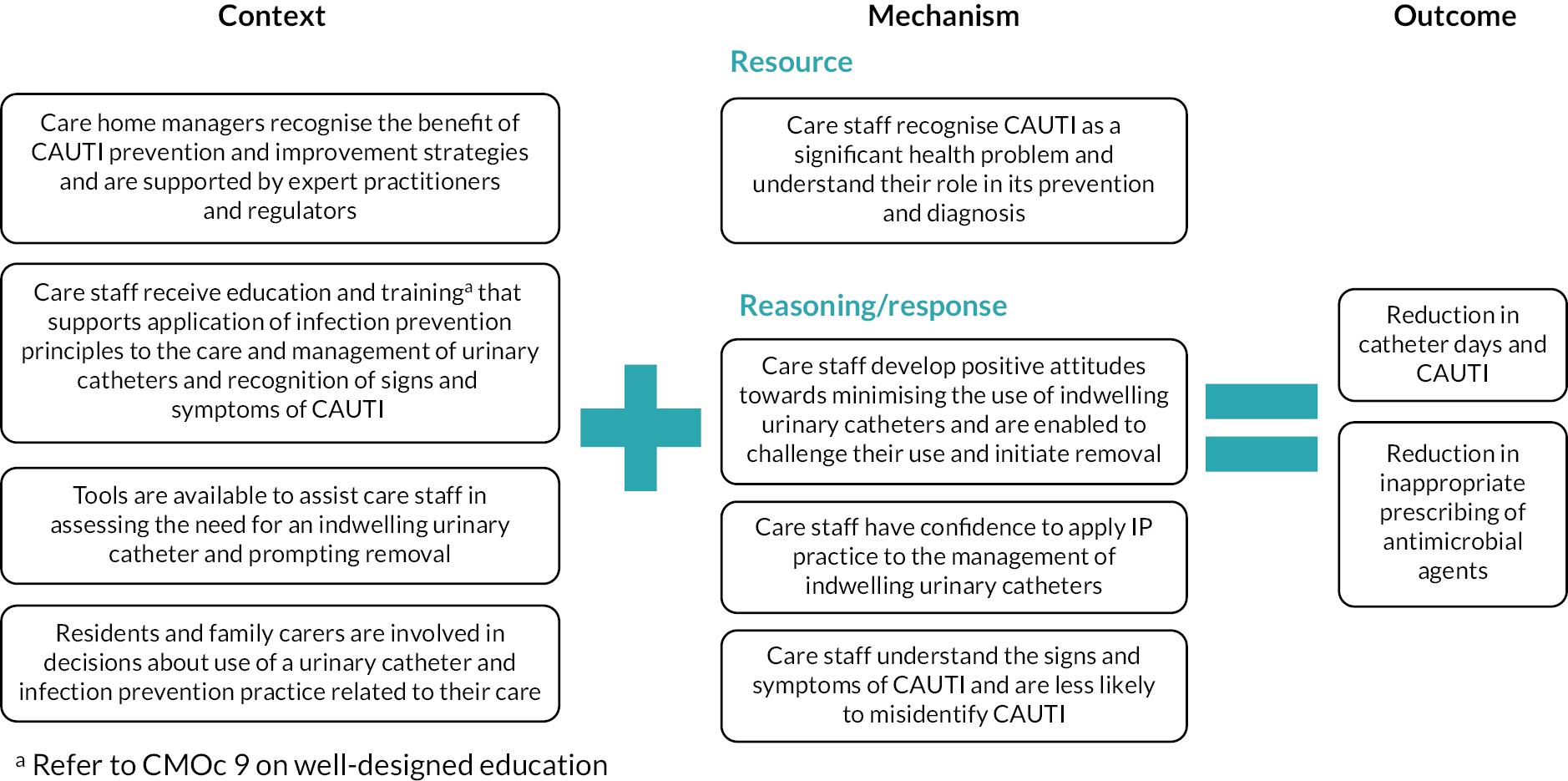
Context
Successful application of strategies to prevent CAUTI is underpinned by education targeting both the technical aspects of catheter care and management and the socioadaptive aspects of implementing quality improvement, such as leadership and engagement. Judicious use of IUCs is more likely to occur in care homes that are supported by IPC and quality improvement specialists and when regulators and commissioners attend to this aspect of care. This is more likely in care homes where the resident and family carer are involved in decisions about catheter use and tools are used to support assessment and prompt removal.
Mechanism
Well-designed education and training enable care staff to recognise that CAUTI is an important health problem and that they have a key role in its prevention. Care staff who become less accepting of the use of catheters are able to challenge their use and initiate removal. Being supported to improve their knowledge, ability and confidence equips care staff to apply principles of infection prevention to the care and management of urinary catheters. By understanding the signs and symptoms of CAUTI, they are less likely to misidentify infection.
Outcome
The continuing need for a catheter is assessed and prompt removal of catheters without a clear indication reduces the prevalence of catheter use in care home residents and therefore the risk of CAUTI and the inappropriate use of antimicrobial agents.
Rationale – the risk of urinary tract infection associated with urinary catheters
Residents who have an IUC are at increased risk of UTI because the catheter bypasses the normal defences of the body. The drainage system becomes colonised by micro-organisms derived from the perineum and when the closed system is handled. Micro-organisms then have direct access to the bladder and if able to invade the bladder tissue will cause CAUTI. There are a small number of indications for long-term catheterisation (e.g. chronic urinary retention due to obstruction or neurogenic bladder) where no treatment options are available, but they may also be inserted for inappropriate reasons such as incontinence or acute retention.
The duration of catheterisation is the dominant risk factor for CAUTI. The presence of micro-organisms in urine without symptoms of UTI is called ‘bacteriuria’, and virtually all catheterised patients develop bacteriuria within 1 month. Approximately 50% of catheterised residents develop symptomatic CAUTI and experience repeat episodes for the duration of catheterisation. 16,119
Approximately 10% of nursing home residents will have an IUC, although this proportion can vary significantly. 120 The most effective interventions to prevent CAUTI are focused on removing the catheter if there is no good indication for its use. A key factor influencing the prevalence is the number of patients discharged from hospital with a urinary catheter where there is no clear reason for its insertion and the reason for continuing need. This can make it difficult for the care home to make decisions about the appropriateness of the catheter and plan for its removal. 25
Systematic reviews of IUC inserted in acute care settings, Meddings et al. 119,121 found a significant reduction in catheter use and CAUTI associated with reminder and stop order systems. These approaches used regular assessment of the need for the catheter and consideration of alternatives to drive proactive removal of catheters. In the care home setting, chronic retention and incontinence are more common drivers of long-term catheter use. General principles for preventing the contamination of urine drainage systems have been described in evidence-based guidelines, although few studies have explored their implementation in care homes settings. 16,19
Since long-term catheters will always be colonised by micro-organisms, the ability to assess relevant clinical signs of infection, rather than relying on positive urine cultures or non-specific signs such as cloudy or odorous urine, is essential to ensure that CAUTI are identified and treated appropriately.
Summary of evidence underpinning context–mechanism–outcome configuration 6
Evidence for strategies that are successful in preventing catheter-associated urinary tract infection
Three systematic reviews relevant to care home25,122,123 and a programme of work funded by AHRQ in the USA consisting of two linked studies informed this CMOc. 124,125 A systematic review of strategies to reduce UTI in care home residents focused on interventional studies with a comparison group which reported UTI as an outcome. 25 Thirteen studies evaluated interventions to target catheter use and care, including prompting removal of unnecessary catheters, comparing alternatives such as intermittent catheterisation, catheter maintenance, securement and catheter change at regular intervals, and improving continence care and other aspects of IPC practice. Authors concluded that CAUTI can be reduced in care homes by applying a trial without catheter, where patients are admitted with an IUC that has no clear indication of an appropriate need and using protocols to avoid the insertion of IUC for managing urinary retention and incontinence. They also highlighted the need to discuss alternatives to IUC with residents, families and care staff. Other strategies should target the management of the catheter and knowledge of staff about aseptic insertion and appropriate care of catheters. 25
A systematic review of barriers relevant to CAUTI prevention and the use of the Theoretical Domains Framework (TDF) to suggest appropriate behaviour change strategies122 identified 25 studies, only one of which was conducted in a care home. Authors identified barriers related to environmental context and resources such as lack of documentation, and lack of time and equipment to support alternative strategies; knowledge and motivation barriers related to the risk of catheters and benefits of interventions targeting CAUTI; and social influences on the need for catheters from patients/relatives, responsibility for decision-making and lack of peer support. Suggested interventions to reduce CAUTI included evidence-based guidelines, education and enablement.
A similar rapid review of interventions for CAUTI prevention in primary, secondary and care home settings informed by the TDF123 prioritised the suggested behavioural interventions through a stakeholder consultation. This process indicated that strategies focused on improved communication at the crucial point of patient transfer between different healthcare settings was a key intervention that also required standardised nationwide computer-based documentation and checklists for when patients were discharged or admitted to care settings. Stakeholders also proposed information for patients and relatives about the advantages and disadvantages of IUC and specific guidance to promote catheter alternatives.
A large AHRQ-funded multimodal programme in 404 nursing homes in the USA implemented an intervention bundle that comprised a technical bundle and a socioadaptive bundle. 124 The technical bundle included education related to the indications for IUC use, regular assessment, incontinence care planning, hydration and aseptic catheter insertion and maintenance and the socioadaptive bundle, supported understanding and implementation of the technical components through developing positive attitudes and behaviour towards IPC, empowering the care teams, promoting leadership and a resident safety culture, effective communication and resident and family engagement. This study was well resourced by AHRQ, and each group of participating homes was led by a local organisational lead with expertise in quality improvement and supported by a coach from the overarching research body, and clinical experts from IPC, general medicine, health service research in the national project team.
The outcome measures were the incidence of CAUTI based on a definition combining objective clinical findings with urine cultures, and the percentage of total resident days with a catheter (utilisation). Homes collected data daily on the number of CAUTI, catheter and resident days using practical data collection tools. These were reviewed monthly with the national project team to identify data trends, identify barriers, learn by sharing and provide feedback to national team about resources required for implementation.
In the 404 care homes that participated in the project, the adjusted rate of CAUTI decreased from 6.42 to 3.33 [incidence rate ratio (IRR) 0.46, 95% CI 0.36 to 0.58; p < 0.001], despite no change in the catheter utilisation rate (4.5% vs. 4.9%). The adjusted rate of urine culture/1000 resident days also decreased from 3.52 to 3.09 (IRR 0.85, 95% CI 0.77 to 0.94; p = 0.001). These findings suggest a low prevalence of catheters at the beginning of the study and the primary driver of CAUTI reduction was improvement in infection prevention associated with catheter management rather than strategies to reduce catheter days.
National reporting systems in the USA require care homes to report residents with catheters and this prompted assessment and removal on admission. A survey of nursing home leaders in the USA concluded that IUC were not perceived to be an important safety priority. Leaders considered prevalence was low and strategies were in place to restrict their use. Other problems such as falls, overuse of antimicrobials and pressure ulcers were given greater priority with key influences over prioritisation being state surveillance requirements, concerns of family members and the requirements of the organisation. 126 This may partially explain the findings as remaining catheters were likely to be in place for appropriate reasons and the emphasis on IPC practice and hydration was effective in preventing CAUTI, even in those with long-term IUC. Improving the diagnosis of CAUTI was demonstrated by the reduction in urine cultures and the potential for the bundles to reduce overdiagnosis of CAUTI. This suggests that national directives or quality indicators might play an important role in increasing preventative activity and reducing IUC use.
The extensive support from a professional team and a suite of educational tools available in a range of formats was key to the success of this intervention. 125 In an exploration of the experience of organisation and care home level leads in the programme suggested that, from their experience, the programme increased the evaluation of early catheter removal and use of alternatives to catheterisation. They considered that staff had a greater awareness of CAUTI prevention practice, and a willingness to modify practice and to educate other team members. This was helped by the collection and review of relevant data, and identification of barriers to implementation and opportunities for improvement. Improved staff knowledge and practical tools for identifying CAUTI symptoms were identified as critical in facilitating staff to discuss with physicians about when catheters, urine cultures and antibiotics were warranted. However, a high turnover of staff was a major barrier to sustainability as it required repeated education, and some homes experienced challenges in obtaining support from physicians and clinical staff with a perception that it would be too burdensome and of no benefit. Gaining buy-in was influenced by strong, trusting relationships between staff which created greater enthusiasm for the project and its benefits.
Stage 3: teacher–learner interviews
Teacher–learner interviews reflected that removal of IUC was the best outcome for residents, but where an IUC was indicated, good catheter care was paramount. They highlighted that registered nurses in nursing care home settings are trained to undertake catheter care and bladder washout and that care assistants are taught about catheter care during their induction, but that this training may not be reinforced or repeated.
It was also highlighted by interviewees that residents admitted to hospital for an episode of acute care were sometimes discharged with an IUC, but with no indication as to when the catheter was inserted nor its indication.
Most of the residents who are discharged from hospital, they come with catheter, but there is no indication why they are catheterized.
Care Home Manager
Catheters and hospitals – we rarely get information about when the last catheter was introduced, when its due to be changed, they don’t provide spare catheters on discharge and sometimes when we can’t get the information it’s a pity because we don’t want to take the risk of leaving a catheter in longer than it should, we would take the catheter out and put a new one in. But that’s not good for the person, we know that it increases the risk of infection but we don’t want to be in the situation where things drag for weeks and weeks just because we can’t get the information.
RN, Care Home
A registered nurse described a model of liaison between the care home and the acute services, which helped in relaying information between the care home and the hospital, particularly in relation to any prescribed items, such as bladder washouts. He indicated sometimes residents would be discharged without the necessary equipment and the home would then have to have the items prescribed by the GP.
We always have a contact with hospital, whether they are admitted or discharged from hospital following an emergency stay, and we do ask for two weeks of any prescribed substances, whether that’s medication, wound care products and bladder washouts but because it looks like we speak different languages in that respect they don’t see a bladder washout or wound care products as something that is prescribed again. But we also have our frailty matron based at the hospital and does that role of liaison and we often ask her to just pop in the ward and check. She speaks our language, and she speaks hospital language. She can relay to hospitals what we need in a way they understand and vice versa. But she is not on call 24 hours a day or 7 days a week.
RN, Care Home
Stage 4: stakeholder workshop
Stakeholders agreed with the content of CMOc 6. The issue of residents returning from hospital with a catheter, but with no indication as to why, was raised by a care home manager and the representative from the National Care Association reinforcing the comments in the teacher–learner interviews. This suggests that a more joined-up approach across care systems is required. Despite national guidance recommendations about the information that needs to accompany a person leaving hospital with an IUC, this is not always available to care home staff.
… I was just going to mention about the catheter, most of the residents who are discharged from hospital, they come with catheter, but there is no indication why they are catheterized. So, we have to go back to the hospital, we don’t get anything, so we speak to the GP we decide to TWOC, and most of the time TWOC is successful. You know there is no need of catheter, and we then start to encourage them with fluids, and which helps a lot. We have seen that many, many times, residents coming from hospital.
Care Home Manager
The potential for what may have been a short-term solution to an issue while a resident was in hospital becoming a long-term indwelling device was commented on by one of the stakeholders and has implications for resident safety and health outcomes.
… some of our residents have a catheter put in when they’re in hospital and then we’re unaware why they will have a TWOC (trial without catheter) when they come out, but normally by that point nothing passes, so they end up having it in all the time.
National Care Association representative
Context–mechanism–outcome configuration 7: proactive strategies are in place to prevent recurrent urinary tract infection
Figure 15 depicts CMOc 7, which is described below followed by a discussion of the underpinning evidence.
FIGURE 15.
Context–mechanism–outcome configuration 7: proactive strategies are in place to prevent RUTI.
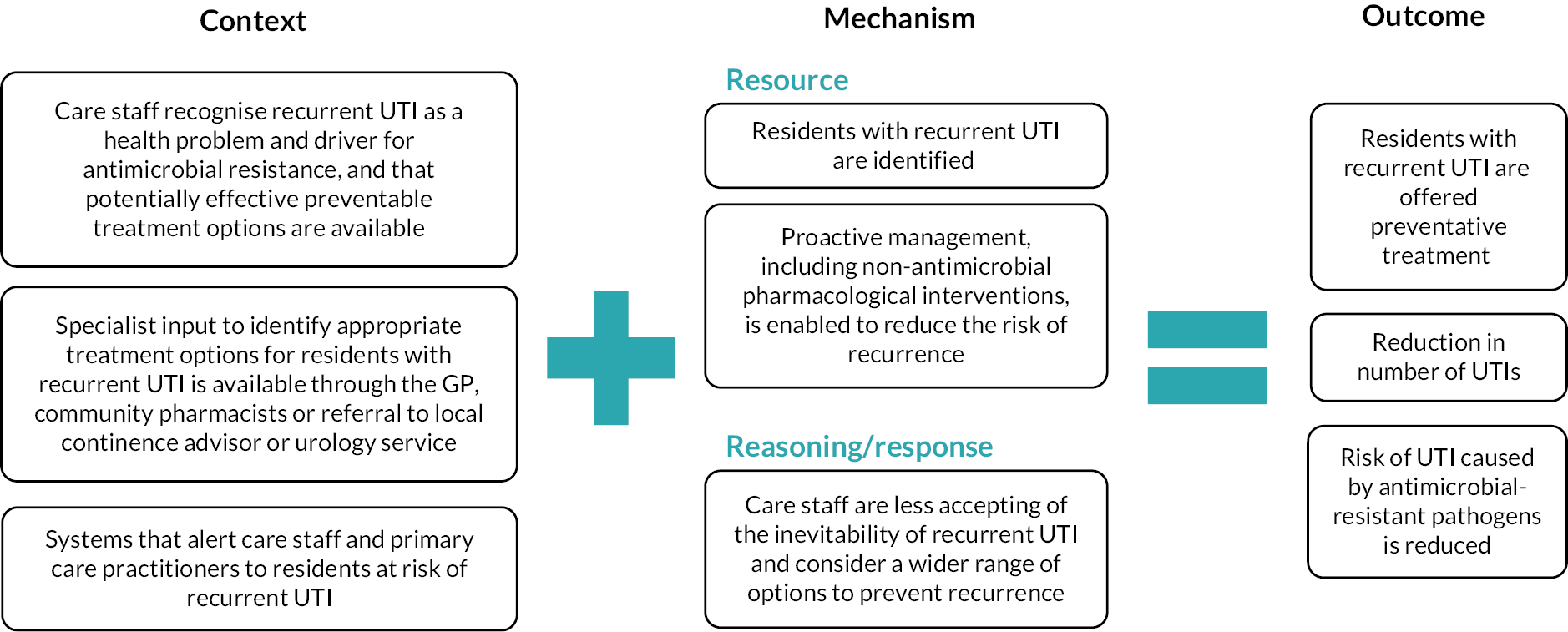
Context
It is important for care home staff to recognise RUTI as a health problem that impacts on the safety of residents and to have greater awareness of potential treatment options. Having processes to alert staff to residents at risk of RUTI and access to expert advice for making treatment decisions that are acceptable to the resident are essential prerequisites for the prevention of RUTI.
Mechanism
When care staff know which residents are at risk of RUTI, they can be proactive in considering non-pharmacological and pharmacological options for its prevention. This makes it less likely that staff will accept RUTI as inevitable.
Outcome
Preventative strategies are initiated to reduce the risk of RUTI and admission to hospital, thereby preventing residents from being exposed to the development of antibiotic-resistant infection.
Rationale – focusing on pharmacological approaches to prevention recurrent urinary tract infection
Older people are at greater risk of developing UTI and if three or more UTIs occur within 12 months the person is considered to have RUTI. Identifying residents as having RUTIs can be perceived as encouraging the use of antimicrobial agents to treat ASB and there is limited awareness among care home staff of well-evidenced pharmacological strategies for preventing RUTI. In addition to managing underlying physical problems such as high post-void volume, there are clinical guidelines which support the use of a range of pharmacological therapies to reduce the risk of RUTI, including low-dose antimicrobial therapy, topical oestrogen, D-mannose and methenamine hippurate.
The options for managing patients with RUTI are complex and require a careful evaluation of the individual to identify and address underlying risk factors and select the best approach to treatment. Urology and continence advisory services have a significant role in preventing RUTI in primary care and care home settings. Although care home staff and GPs may recognise that some residents experience RUTI, they may lack systems to clearly identify them and trigger an assessment and initiate prophylactic treatment.
Factors contributing to the risk of recurrent urinary tract infection
Women have a greater lifetime risk of UTI than men. In older women, risk factors for RUTI include previous history of UTI before menopause, urinary incontinence, atrophic vaginitis due to oestrogen deficiency, increased post-void urine volume and functional status deterioration. 56 Oestrogen plays a key role in controlling the natural defences of the lower urinary tract against UTI. In premenopausal women, both circulating and vaginal oestrogens facilitate vaginal colonisation with lactobacilli which maintains an acidic vaginal pH and inhibits the growth of uropathogens. Post menopause, the reduction in circulating and vaginal oestrogens results in a decline in lactobacilli and increase in colonisation of the vagina by gut organisms such as E. coli, which are then able to invade the urinary tract. 27 In older men, risk factors include abnormalities of urinary tract function or structure, incomplete bladder emptying and immunosuppression. 56 E. coli. accounts for between 70% and 95% of UTI and repeated antimicrobial treatment for recurrent RUTI is associated with increased risk of developing infections caused by antimicrobial resistant pathogens. 11,27,54,127
Antibiotic or other non-pharmacological agents may be considered as an option for prophylaxis in people with RUTI, to reduce the risk of recurrent infections and their associated morbidity. 56
Summary of evidence underpinning context–mechanism–outcome configuration 7
This CMOc was informed by national and international guidelines54,56 and one comprehensive narrative review. 27 The guidelines do not specifically consider the application of recommendations in care home residents. However, a consultant urogynaecologist who was a member of the PAG member provided information on other relevant evidence and advice on strategies that might be feasible to apply in a care home setting. Contextual information about the potential challenges in the use of treatments for RUTI in care home settings were also discussed with an experienced CA.
The European Association of Urology (EAU) Guidelines56 on urological infections recommend that risk factors for RUTI should be identified and where possible addressed, including the use of clean intermittent catheterisation to treat significant residual urine. Low-dose antimicrobial prophylactic (LDAP) is considered the current standard treatment for RUTI. 54 However, to minimise the risk of developing infections caused by resistant pathogens, clinical guidelines recommend trying non-antimicrobial measures first where possible. 56 An overview of the evidence for the efficacy of pharmacological interventions that would be feasible to consider for preventing RUTI in care home residents is described in Appendix 9.
Most of the evidence for prevention of RUTI has been derived from studies conducted in secondary care and outpatient settings. Although treatment of RUTI is accepted as required for adults presenting to primary care or urological services, the extent to which residents in care homes with RUTI are identified and managed to prevent further infections is unknown and evidence for the application of prevention strategies in care home is missing.
Awareness among care home staff of pharmacological strategies for preventing UTI are limited, although hydration and cranberry juice are perceived as important. 58,62 There are also concerns that labelling residents as having RUTIs would encourage treatment of ASB. 64
The options for managing patients with RUTI are complex and require a careful evaluation of the individual to identify and address underlying risk factors and select the best approach to treatment. Urology and continence advisory services therefore have an important role in preventing RUTI. In a study by Klay et al.,128 27 care home residents with incontinence or overactive bladder were assessed by a CA who developed an individualised treatment plan, which was implemented during the following 12 months. In addition to bladder diaries, pelvic floor exercises and anticholinergic agents, preventative strategies also included topical oestrogen and increasing fluid and fibre intake. The intervention was associated with an 80% reduction (31 to 6) in UTIs. This study highlights the value of input from a specialist CA in preventing UTI.
If care home staff were aware of the treatments available to prevent UTI, had documentation systems that enabled both the care staff and GPs to recognise a resident who has RUTIs and improved access to advice and support from community continence or secondary elderly medicine/frailty services on management strategies, then action could be taken to initiate appropriate pharmacological or non-pharmacological interventions to reduce the risk of subsequent UTI. The teacher–learner interviews in stage 3 were essential in helping the research team to refine the content of the CMOc.
Stage 3: teacher–learner interviews
Recurrent UTIs in older people in care homes was recognised as an issue across different stakeholders. Interviews with stakeholders in care homes suggested that the potential to prevent RUTI was not something that they had considered, although they felt they did have residents who would benefit from this. One stakeholder flagged the difficulty of confirming RUTIs is due to many of the residents being incontinent and the resulting difficulty of obtaining uncontaminated samples to confirm UTI. Stakeholders also cautioned about labelling a resident as having RUTIs. While this may be accurate in some cases/for some residents, some UTI diagnoses may be based on intuitive rather than definitive diagnoses, for example, on a positive dipstick and an increase in confusion.
I guess it is the number of prescriptions, the problem with that is that some of the diagnoses in primary care are presumptive – if its anything like the hospital is and an old person comes in confused, they probably suspect it’s a UTI until proven otherwise. That’s not correct but that is the thinking.
Geriatrician
I think once they have been put into the box [of recurrent UTI] it’s very hard to get out of. So, for recurrent UTI, see if you can see again with fresh eyes. There are of course some people who do have recurrent UTIs. You have to look retrospectively into the diagnosis, decide, has this person been hospitalised with urosepsis or is it just because we were thinking wrongly about UTIs before.
Geriatrician
The standard treatment in care homes for RUTI appears to be low-dose prophylactic antibiotics and that the threshold for anybody being managed any differently is due to a secondary care intervention either by an elderly care or urology clinic where, for example, D-mannose may be recommended. A resident admitted to a care home with a history of RUTIs may already be prescribed low-dose antibiotics, but stakeholders confirmed that there was not a standardised system for identifying residents at risk of RUTIs. While homes do record UTIs and antibiotic prescriptions, these data are not routinely reviewed to identify residents who have RUTI, and this would require staff to know what to look for and check retrospectively in the notes.
Well, I don’t think we have a standard procedure. We have a couple of residents who have a history of recurrent UTIs. None of our residents are on prophylaxis of antimicrobial or any kind of pharmacological intervention. So not sure really what to say. Just this preliminary conversation has made me think that we should have probably more guidelines, or some things in a procedure rather than knowing our residents well.
RN, Care Home
Likewise, our primary care stakeholder mentioned that GP practices will record antibiotic prescriptions for care home residents, but current IT systems do not have an automatic flag to alert to residents who have had RUTI.
… the easiest way would be through coding. So, if it was coded each time as ‘suspected UTI’ or ‘confirmed UTI’ then that code is searchable but the system won’t automatically be searching it unless we ask it to and it’s the kind of search – you would have to run it live at certain points in time to be able to monitor it.
GP
Continence specialists recognise that services provided by bladder bowel/urology clinics are not usually accessible for residents in care homes. Care homes likewise recognise that access to specialist services is patchy and referral into urology from the home would be unusual.
It’s rare to imagine a scenario where we would be looking at referring to urology. I think because of the lack of clarity – to refer somebody where we think they might be having some UTIs but we are not sure, we can’t really say how many and we don’t have culture evidence … that would be quite a woolly referral to urology … I’m not sure they’d even accept that.
GP
More often, the culture, particularly by nursing staff, is to use specialist services for incontinence pads as opposed to more proactive approaches or holistic assessments for detecting/preventing UTIs. Homes with a model where they have access to an elderly care physician or frailty matron who would undertake comprehensive review of a resident may identify a resident with RUTIs.
So, if they are aware that someone is going repeatedly to A&E and being treated for UTIs that would trigger a review from [the elderly care consultant] to look at what we can do within this person’s care plan to avoid this happening.
GP
There are also some differences between nursing and residential care home access to specialist care. One stakeholder explained that residential homes rely on the community nursing team for support who may not be able to deliver specialist interventions such as topical oestrogens.
I think nursing homes, it would be much easier [to use topical oestrogens] because they’ve got registered carers there 24/7. Some residential homes may not be so easy and that I know that a lot of residential homes rely on community nursing to do a lot of basic care and community nursing would not be in a position to be able to deliver topical oestrogen treatments to residents.
Bladder and bowel specialist
Stakeholders highlighted several key interventions that could be done – some with support from specialist services – such as increasing fluids, oestrogen replacement, bladder scanning to check and manage any problems with retention, reviewing residents’ general dexterity and their ability to maintain hygiene, sit on the toilet, etc.
In the ideal world it would be really good for all these patients to be bladder scanned. And probably more should have a vaginal examination or certainly a perineal examination. But in reality, it’s not possible we just haven’t got the work force to be able to do that.
Bladder and bowel specialist
There are instances, particularly for residents who have capacity to consent to treatment, where vaginal oestrogen might be prescribed but no stakeholders reported using D-mannose or other non-antimicrobial approaches.
We have had residents where it’s been tried – I think particularly where there’s been recurrent cystitis symptoms, maybe not confirmed UTIs but just more generic symptoms. I think there is a big issue with residents with dementia and giving anything vaginally, examination etc. can be quite limited if they don’t have capacity and they don’t understand … it’s not something we can do without somebody agreeing to it. The sorts of people I’m thinking about are people who have capacity, who can describe their symptoms, perhaps can give a sample so we have more evidence that they’re getting infections or not. And sometimes if they’re not, but getting lots of symptoms, we can try vaginal oestrogen.
GP
Stage 4: stakeholder workshop
Stakeholders agreed with the content of CMOc 3 and there was considerable discussion about the need for RUTI prevention to have a greater prominence in the current initiatives. Specialist antimicrobial pharmacists were identified as having a role in helping care home staff and GPs to consider non-antimicrobial pharmacological options. One stakeholder mentioned a recent NHSE initiative whereby a pharmacist or pharmacist technician, linked to a GP practice or primary care network, undertakes structured medication reviews, working with the care homes to upskill them in recognising residents at risk of RUTI and on types of interventions to support them in preventing RUTIs.
GP practice or primary care network has received funding to appoint a clinical pharmacist or pharmacy technician, and they are encouraged to do something called a structured medication review on patients who are high risk for one reason or another, sometimes because of polypharmacy or patients on high dose opioids but one group of patients that’s also relevant is patients with recurrent infection getting repeated courses of antibiotics, and so we’re now working with UKHSA colleagues to develop toolkits to support those pharmacists to review patients with recurrent infection and look at strategies like avoidance, vaccination, infection prevention but also non antibiotic alternatives.
Pharmacist, NHSE
When considering the resources available to care home staff that would help them to more easily identify residents who were at risk of RUTI, it was suggested that an assessment tool might be helpful.
Is there an assessment tool you know similar to MUST or body mapping and that sort of thing which is updated really to identify residents that are increased risk of recurrent urinary tract infections or CAUTIs, but definitely for the recurrent urinary tract infections. So, when you get to a certain amount of urinary tract infections they’ve had, is there a point where they have – where they trigger on a risk assessment, on a risk matrix and then you implement additional mitigations.
IPC practitioner, CCG
Education and training of staff to help them know what actions to take to prevent RUTIs was also recognised as key.
I think there are a lot of care homes who would be more than happy to look at recurrent UTI’s in a more structured way, but they just haven’t got the skills and knowledge and training to be able to do that.
Clinical specialist
Theory area 3: making best practice happen
Stakeholder feedback – stage 1
Stakeholders in stage 1 spoke about the culture of the care home indirectly through the discussion. It was clear that having flat organisational structures that were inclusive of all members of the care home team was considered important. Communication across the team was highlighted and the willingness to try to improve was evident in the responses from one of the care homes that participated. There was a widespread recognition that education of care staff was crucial to enabling staff to accept and participate in change, deliver high-quality care and feel confident in the information they communicated to colleagues and GPs.
Context–mechanism–outcome configuration 8: care home leadership and culture fosters safe fundamental care
Figure 16 depicts CMOc 8, which is described below followed by a discussion of the underpinning evidence.
FIGURE 16.
Context–mechanism–outcome configuration 8: care home leadership and culture fosters safe fundamental care.
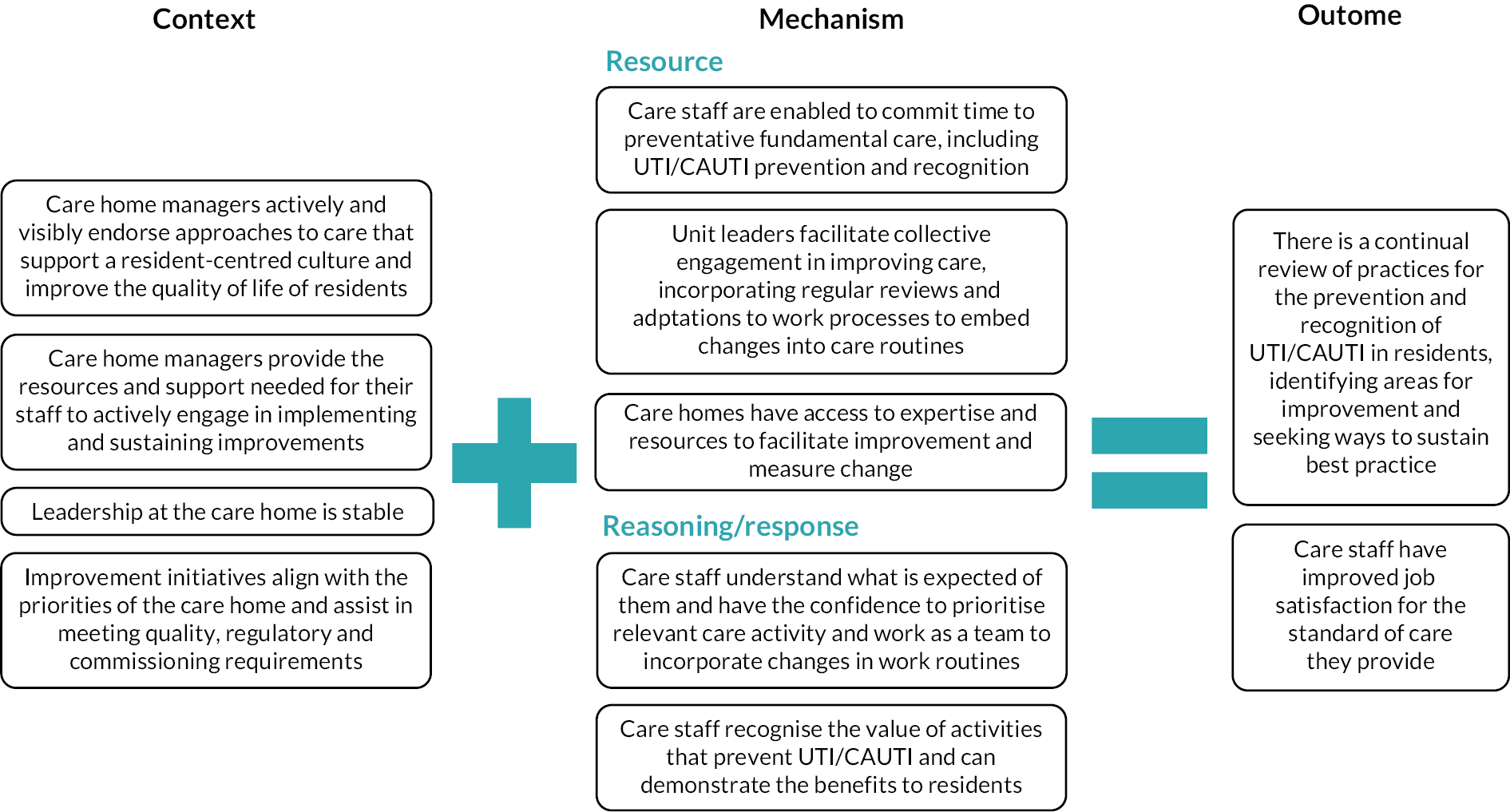
Context
For best practice to be used and sustained within a care home, it is vital for care home managers to endorse changes in practice and provide the necessary support and resources for their staff to implement them. Care home leadership needs to be stable and the care home manager’s understanding of an intervention is crucial to ensure that structural and operational factors that can hamper implementation efforts are addressed. Priorities identified by regulators and commissioners of care can influence the attention care home managers give to an intervention and impacts what work staff understand as important and how care home resources are deployed.
Mechanism
When care home managers enable their staff to commit time to preventative fundamental care, staff are permitted to be more actively involved with change efforts and have the confidence to prioritise care activity towards preventing UTI/CAUTI. The extent of fit of intervention requirements with the daily work of the care home, including how these requirements impact workload, practices and routines, and the degree of influence managers and staff have over implementation, is key to their engagement. Unit leaders who facilitate regular reviews and adaptations to work processes enable collective engagement in embedding changes into care routines. Access to expertise and resources facilitates improvement efforts and sustained change is more likely when there are demonstrable benefits to residents and staff.
Outcomes
The level of engagement with interventions from care home managers influences the uptake and sustainability of changes to care practices and drives a culture of continuous improvement. This helps to improve job satisfaction among staff for the care they deliver.
Rationale – engaged leadership facilitates the uptake and sustainability of practice change
Leadership is described in the general literature as a key factor in improving care and managing challenges in health and social care. Leadership can be defined as ‘a process whereby an individual influences a group of people in order to achieve a common goal’. 129 Its contribution is considered equally important in enhancing the quality of care in care homes as in other safety critical environments. In a review of the impact of work culture on the quality of care in care homes,130 authors reported that 9 of the 10 articles included in the review highlighted the importance of leadership and management to support quality of care. Safety culture in care homes is driven by the values, attitudes and actions of the organisation, managers and staff and resident’s families, care commissioners and regulators also have an influence on resident safety. Quality of care, effective communication and teamwork are all influenced by the leadership displayed by care home managers and nurse leaders within this setting. In the studies included in our review, there was a thread that focused on the importance of leadership in bringing about the change that interventions intended.
Summary of underpinning evidence
Leadership and prioritisation by care home managers
Care home managers have a pivotal role in the prioritisation and delivery of best practice within care homes. As highlighted within theory areas 1 and 2, the extent of a care home manager’s engagement and commitment to delivering an intervention relating to UTI prevention or recognition impacts on its success. 6,60,70,125 This is also reported across the wider literature on implementing changes in care homes. 131–133 In the included studies, care home managers’ commitment was demonstrated through their understanding of an intervention and through visible actions that supported it.
Committed and stable leadership from care home managers
Care home managers who understood the purpose of an intervention and the potential benefits of embedding strategies to prevent and recognise UTI/CAUTI as everyday practice can convey their expectations of their staff for implementation efforts. 132 Managers’ commitment was demonstrated through visible actions that supported interventions, such as providing opportunities for staff to acquire the skills needed to use the intervention in their work and endorsing any changes necessary for implementation, such as agreeing changes to routines and allocation of staffing resources. 60,74,89,131–135 These practical actions were necessary for staff to believe they had the authority to incorporate and prioritise changes in their work6,60,74,89,131–133 and were vital in managing workload pressure, which was highlighted as an issue in several studies. 60,70,125
When care home managers are not sufficiently visible in their endorsement of new ways of working, the intervention often fails. 74 In their pilot trial of an intervention to reduce avoidable admissions in nursing homes, the researchers recognised how managers who signed up to participate in the study may have regarded this as something requiring their co-operation rather than their sustained and visible leadership. This meant they may not have provided the leadership and pragmatic support required to enable staff to engage in the intervention, such as their release from normal duties.
Across the wider literature, the extent of buy-in and engagement by care home managers was reported as crucial in the implementation of changes to practice in care homes. 121,131,133 In a study to improve urinary continence care in care homes, researchers found that early managerial buy-in and engagement was a prerequisite to supporting what was required to implement the intervention over a sustained period Rycroft-Malone et al. 131 This CRCT involved 24 care homes across four European countries, including England, Netherlands, Ireland and Sweden. Successful implementation was dependent on whether sites prioritised their involvement in the study and the facilitation programme. Authors explained how the active and visible participation of managers was important for the allocation of resources and provision of support. In care homes where the study was prioritised and where manager and staff support were sustained, this resulted in collective engagement in the intervention. Engagement was also impacted by the fit and alignment of the project to the priorities of the care home and the potential to tailor the approach to meet the ongoing needs of both the home and the internal project facilitator.
Similarly, researchers reported how care home managers who understood the purpose of an intervention and the potential benefits of embedding it as everyday practice conveyed their expectations of staff for implementation efforts. In their process evaluation of a RCT of dementia care mapping (DCM) in care homes in the UK, the researchers undertook qualitative semistructured interviews with care home managers and intervention leads participating in the intervention arm of the trial. 132 They found that managerial support and leadership approaches towards implementing DCM were highly variable and that implementation was easily destabilised by management changes or competing managerial priorities. Care home managers explained that when deciding whether to participate in research, they considered whether the intervention would fit into the care home workload, practices and routines and the degree of control they would retain over implementation. 134 This underlines the importance of fit and alignment of a project with the needs of the home,131 the need for it to explicitly address care home specific patterns of working135 and the value of co-design as an approach to developing complex interventions. 61,74
Stable care home leadership was identified as central to optimal implementation in the studies included in the synthesis. Implementation efforts were easily undermined by management changes or constant staff turnover. 75,124,135,131–133,136 For care homes in a time of instability, expectations that complex interventions could be implemented may not have been realistic. 132 One study of hydration found changes in leadership meant care home staff were unclear on the expectations of their role, meaning interventions were not embedded into routine practice. 6
Structural and operational factors that can hamper implementation effort include the size of the care home could limit the number of staff available for attending training or to champion changes. 89,132 Where there was insufficient support for the intervention, either through structural challenges or motivations of the managers, this would lead to incomplete or poorly implemented interventions. 125,132,133
The potential role of commissioners and regulators of care
Regulatory priorities and judgements from inspection reports can impact the priority care home managers afford an intervention, which in turn influences what work staff understand as important and how care home resources are deployed.
A realist process evaluation for a RCT of facilitation to implement urinary continence care recommendations found that where interventions aligned with regulatory imperatives, care home managers were more likely to consider the intervention useful, prioritise continence care and engage and support the implementation process. 131 Equally, where regulatory requirements focused on other areas of care, care home managers were less committed to the intervention, impacting involvement with the intervention from the care home as a whole. 131 Studies reporting resources provided by regulatory bodies for improvement efforts, such as trainers and facilitators, found that care home managers and staff valued the assistance. 124,125,133 However, this did not necessarily mean all care homes would participate. For example, even with external facilitation, 28 out of 118 care homes taking part in a qualitative evaluation of a safety improvement programme withdrew during the start of the intervention and a third of those remaining considered that involvement was too time consuming. 133 Similarly, in a large AHRQ-funded implementation programme that included a Technical Bundle and Socioadaptive Bundle which included sustained support from external organisational leads and coaches, several nursing homes did not complete the study due to time constraints, competing priorities and staff turnover and shortages, suggesting challenges in implementing and sustaining the approach over time. 124
Initial decisions to implement interventions might be mediated by motivations to respond to regulatory imperatives. However, continued participation could lead care home managers to value the benefits to their staff and residents, such as recognising that changes improved residents’ quality of life. 133 This could transform their reason for supporting changes from one influenced by external pressures to one where there was alignment with person-centred approaches. Potentially, this change in motivation could encourage a cyclical review of improvement efforts that embedded changes in practices. 135
The ability of staff to incorporate regular reviews and adaptations to processes as part of their daily work dictated how well an intervention was implemented. 6,125,131,132 Interventions with more complex components that fell outside current routines and roles were less likely to be supported by the care home workforce and therefore unlikely become part of the everyday work. As such, it was important that modifications to current ways of working were considered and endorsed by care home leaders. The I-Hydrate project demonstrated the importance of this for increasing drinking opportunities for residents by building in more drinks rounds into the care home routine. 6 In this way, staff understood what was expected of them and that there was a collective effort to improve this area of resident care.
However, making accommodations for complex interventions could be perceived to be beyond the capacity of the care home. A process evaluation of a RCT of implementing DCM in care homes found that even with external support, for many homes, completing intervention requirements was too intensive and difficult for care home managers to support. 136 Where the time and effort required to implement complex interventions on top of their usual work was perceived as burdensome and overwhelming, care home manager support for embedding practices decreased or was withdrawn125,132 In addition, at times, alignment of an intervention with care home routines might not always be enough, care home managers also needed to understand that this would enhance current processes and practices. An example from Rycroft-Malone et al. 131 demonstrated that if care home managers perceived similar work was already being carried out within their care home, then care home managers could disengage or withdraw their support for implementation efforts.
Staff time
Enabling staff to commit time to fundamental care is a key feature of studies. 6,125,131 Care home managers and unit leaders were key to who was involved in team discussions of residents. When care home staff who worked closest with residents were included, they could bring insights from their knowledge of residents and observations of subtle changes that inform actions for care. 125 However, short staffing, management changes and daily demands for running the care home could impact care home managers commitment to interventions and how they expected staff to use their time. 89,131,132 In addition, if care home managers had weak relationships with their staff, for example, by being new to the role, this could affect the engagement of care home staff for making change happen. 131
Celebrating progress
Care home managers and care home organisations helped to embed these changes by developing policies and processes that reinforced best practices and ensuring the work remained a priority. 6,124,125 Wilson et al. 6 described how improvement work for hydration was made visible by displaying progress in communal areas; this not only reinforced to staff the benefit of the changes, but also highlighted to visitors, such as family members, that this fundamental work was a priority for the care home.
In care homes where there had been good engagement for prevention and recognition of UTI/CAUTI or related interventions, care home practices were reviewed, adapted and sustained at time of follow-up. 6,75,89,131,133 Amongst the care home staff, there was increased awareness of their role in prevention and recognition of CAUTI/UTI, their ability to identify symptoms and improved technical skills for prevention and assessments. 6,124,125,131 In some cases, there was evidence that care home staff were empowered to challenge the advice of HCPs when it conflicted with the knowledge they had acquired. Krein et al. 125 provide examples where physician orders for indwelling catheters, the use of antibiotics and ordering urine cultures were questioned by care home staff. Staff empowerment and recognition of the benefits changes had within the care home were linked to increased job satisfaction. 89,125,131
Measuring and acting on change
Public health surveillance is recognised as an effective strategy for preventing and controlling disease by systematically collecting and analysing data and feeding back results to those who can change practice to prevent infections occurring. 137 Its purpose is to empower decision- makers to lead and manage more effectively by providing timely, useful evidence about the quality of care and it is useful for measuring both the need for interventions and the effects of interventions. This was demonstrated by Scanlon et al. 138 who identified a high and increasing rate of CAUTI among patients receiving home care from a home healthcare agency in routine surveillance data which was benchmarked against the CAUTI rate in other similar patient populations. Such comparisons require the application of consistent case definitions for infection and standard methods of data collection. The home care surveillance alerted the agency to problems with the management of urinary catheters and triggered an internal review of urinary catheter policies, standards of care and patient-teaching tools. Evidence-based polices were developed and incorporated into a bladder bundle adapted for home care which included ongoing assessment of the need for indwelling catheterisation, consideration of alternative management options and practice related to insertion and ongoing maintenance. These changes were associated with a reduction in CAUTI that could be demonstrated in the surveillance data and feedback to care staff.
There are considerable challenges for care homes in collecting the necessary data to support surveillance of both CAUTI and UTI. Defining these infections is challenging, especially in the frail elderly who may not present or be able to express relevant symptoms. Studies that have reported the use of surveillance in a residential care setting are predominantly conducted in the USA where large long-term care facilities are more likely to have access to both the technological and expert support that is required to enable data capture. 124 In a multimodal programme, focused on implementing CAUTI prevention practices and improving safety culture, simplified instructions and practical hands-on tools were used to support care staff to gather monthly outcome data and apply surveillance criteria. However, since care homes may lack the required clinical and technical expertise to design surveillance the system was supported by external experts who worked with each facility to coach them on data collection at the onset of the project. 124
In a UK study117 on the effect of improving hydration of rates on UTI, a simple, paper-based tool to enable staff to capture data on rates of UTI was used. Wilson et al. 114 found care homes participating in their improvement project had limited access to computers. Homes were required to report rates of UTI to the regulatory body (CCG), but cases were based on antimicrobial treatment and strongly biased by the relationships between GPs and care staff and their attitudes to diagnosis and treatment of UTI. Indeed, improvement in the precision of UTI diagnosis is difficult to distinguish from true reduction in UTI due to the implementation of prevention strategies. 117
Although benchmarking by regulators of rates of UTI may play a key role in highlighting the importance of the problem and prioritising activity focused on its prevention, systems need to address the need for standard case definitions and data collection methods, simple tools to support care homes collect data and mechanisms to facilitate care home staff to act on the results. 124 Quality indicators for nursing homes have been proposed as a quality improvement initiative, for example, hospitalisation rates. 139 However, adjusting for variations in case mix and identifying realistic outliers is challenging and the use of financial penalties may encourage under-reporting.
Leadership by project champions and unit leaders
Among the intervention studies included in this review, several utilised internal care home staff as practice development champions to facilitate implementation and deliver training and information to colleagues. 60,65,74,117,131 They were often assigned to the role by their care home manager, although some managers reported challenges in appointing a champion. 60,74 While there is evidence to suggest that project champions can play an important role in delivering an intervention,60,65,74,117,131 both champions and managers have reported issues with enactment of the role. 60,74,131 These include difficulties engaging colleagues in changing practice and in securing dedicated time for the role.
Downs et al. 74 highlighted how champions need support to develop the knowledge and skills of facilitation and questioned whether it is reasonable to expect staff in care homes to bring about complex change. Rycroft-Malone et al. 131 reported how internal project facilitators working in care homes need to learn over time to develop the confidence and personal growth required to enact their role and support changes in practice. In their evaluation of two types of facilitation for implementing changes in continence care in care homes, they found potential for learning over time to happen where there was greater fit and alignment of the interventions to expectations, prioritisation and engagement within the care home. This was triggered by internal facilitators’ personal characteristics and abilities, including personal and formal authority, in combination with a supportive environment prompted by managers.
In the I-Hydrate study6 unit leaders who role-modelled good practice, assigned staff responsibility for relevant tasks and provided supervision and monitoring were better able to embed changes that promoted choice and regular drinking opportunities than care homes where senior support was absent. The researchers concluded that the role of the unit leader is critical to embed and sustain practice that supports resident hydration. Briefing staff and allocating each of them to a specific role (e.g. serving or assisting) were important to making protected drinks time work and encouraged a greater sense of teamwork. This exemplifies how staff in more senior positions who have formal authority are well placed to lead change within care homes. This is supported by the findings of a realist review of staff behaviours that promote quality in care homes,140 which illustrated how unit-level supervisors can promote better team working through minimising conflict and role-modelling behaviours that promote team relationships.
Coaching support by external organisational leads
Krein et al. 125 described ways in which organisational leads enacted their roles as external facilitators, including acting as intermediaries, translating instructions for programme implementation, conveying information between the national team and the participating facilities and acting as coaches providing feedback, encouragement and support. They reported how these leads helped facilities understand their infection data in relation to local and national benchmarks, including provision of targeted feedback to enhance evidence-based practices, hence making their surveillance data actionable. These external partners helped to identify opportunities for improvement that then empowered facility teams to lead and sustain local efforts. However, it was found that the resources needed at the level of the organisational leads was not always adequate to meet programme demands and facility needs.
Improving safety culture in care homes
The leadership provided by care home managers is instrumental in setting the agenda, focusing priorities within the home and making those priorities visible. 133 One study suggested that wide variation in urinary catheterisation rates in care homes in England may be due to differences in care home culture. 141 The study involved interviews with care home managers, nurses and care assistants to explore how decisions were reached about catheter use and removal. Participants in homes with a lower prevalence of catheterisation demonstrated a proactive and person-centred approach to care, prioritising toileting, mobility and comfort as fundamentals of care. Conversely, those in care homes with higher rates of catheter use had a more task-oriented focus, reporting how staff shortages and time pressures prevented them from supporting residents’ toileting needs, with catheters reducing their workload when caring for residents with incontinence and poor mobility. The researchers noted how a care home manager’s attitude to catheters was usually reflected by other staff, signifying their impact as leaders. Staff in homes with higher catheter use viewed them to preserve dignity by reducing urine smells and preventing wetting of pads, clothing and bedding, whereas those in homes with lower use considered catheters to undermine a person’s dignity.
In a study of nursing homes in Connecticut, care home leaders were interviewed to explore views of their top priority safety and quality concerns and decision-making around the use of urinary catheters. 126 None identified CAUTI as a high-priority concern and factors which appeared to influence leaders’ priorities fell into four major categories: resident-related (i.e. the event frequently occurred in the population), organisational (i.e. the corporation had identified it as a priority), external (i.e. focus of state regulators) and the concern of family members. 126 The majority of those interviewed believed they had effective measures in place to address catheter use and the risk of infection, with extremely low rates of catheter use in eight of the facilities, which contributed to de-prioritisation of this issue.
The AHRQ study aimed to improve safety culture, teamwork and communication the use of a socioadaptive bundle, which promoted internal leadership, resident and family engagement and effective communication. Emphasis was placed on creating safety teams; engaging leadership, front-line staff, residents and family members; enhancing communication strategies pertinent to residents’ safety; and sustained progress towards goals. 124 In an associated study,142 authors reported small improvements in several safety culture measures as a result of participating in study. There was no relationship between individual care home safety culture ratings and CAUTI rates, or improvements in CAUTI during the study.
A study investigating the relationship between safety culture and adverse events in care home in the USA identified that ‘supervisor expectations and actions promoting resident safety’ were the second highest scoring dimension. 143 Leadership style is a key influence on organisational quality, empowering care home staff and supporting a safety culture to improve resident experience and care outcomes.
Encouraging a culture of relational working
Two studies6,60 identified how clarity of roles and responsibilities is needed to facilitate intervention implementation. Wilson et al. 6 demonstrated the importance of this for increasing drinking opportunities for residents. Incorporating more drinks rounds into the care home routine and ensuring clarity about who was responsible for topping up supplies of drinks enabled staff to understand what was expected of them, resulting in a collective effort to improve this area of resident care. Hughes et al. 60 highlighted the need to encourage a culture of relational working. They noted how some participants in their study did not realise that any member of staff could be involved in recognising when a resident was unwell. Moreover, there were mixed views among staff about whether or not junior staff should be involved in training sessions. This reveals how misunderstandings and ambiguities about roles and responsibilities can impact on care delivery. 144
Teacher–learner interviews
A key thread from the stakeholders which highlighted some of the challenges to making best practice happen included the complexity of residents being cared for in the care home setting, particularly the added difficulties presented by residents with cognitive impairment and the high turnover of care staff which can affect continuity of care.
Stakeholders also described that making best practice happen requires leaders who involve all of the team, where individual talents are recognised and the junior staff who are often closest to the resident are valued and given the confidence to express their concerns.
You have to be open to get everybody involved, and everybody can make a difference, and if you, if you celebrate individual talents and their expertise and recognise them and people feel valued, they’re going to be much more likely to run with something.
IPC Nurse specialist
Stakeholder workshop
Stakeholders discussed local approaches such as brief mid-morning meetings (huddles) or different handover styles between the different staff groups.
… a quick unit meeting at maybe 10:00 o’clock – any problems, anything you notice, anything you know the nurse needs to pass on to the GP or something and that works quite well, because that gives a voice.
Clinical Lead, County Council
A walking handover in the morning is a good thing where the carer hands over to the carer. Because a lot of what the nurse hands over to the next nurse is not of interest to the care staff. It’s different information.
Clinical Lead, County Council
System-wide approaches were also raised; one stakeholder mentioned how they could use network meetings to ensure learning is shared across providers.
I want to go back to that relationship within the ICS where we join hands together with all our providers to make sure that we make these standing agenda items in our network meetings, to keep discussing them over and over again, and sharing of learning as to how we can keep them going across the ICS learning from each other.
Head of IPC, ICS
Others cited national initiatives designed to support care homes with best practice. The work from these initiatives aims to include reviewing work routines, education and training and systems and documentation. Two specifically cited initiatives were: hydration pilots, which will report on measures including UTIs, and structured medication reviews which will include upskilling staff in recognising and intervening for residents with RUTI. One stakeholder also described using a ‘bundle’ for promoting hydration which focuses more on actions that care homes can take and tailoring the care plan for the individual resident.
The role of champions was felt to be widespread. Often champions had a topic-specific role such as IPC, others had a wider name which enables the champion to focus on other aspects of care and prevention activities.
I think champions have been rather overused. we need to be a bit more sort of thoughtful about, and think, well, you know, maybe not have a hydration champion, but- it’s getting people to lead the way and come up with the ideas because the ideas will come from the grassroots.
IPC nurse specialist
Context–mechanism–outcome configuration 9: developing knowledgeable care teams
Figure 17 depicts CMOc 9, which is described below followed by a discussion of the underpinning evidence.
FIGURE 17.
Context–mechanism–outcome configuration 9: developing knowledgeable care teams.
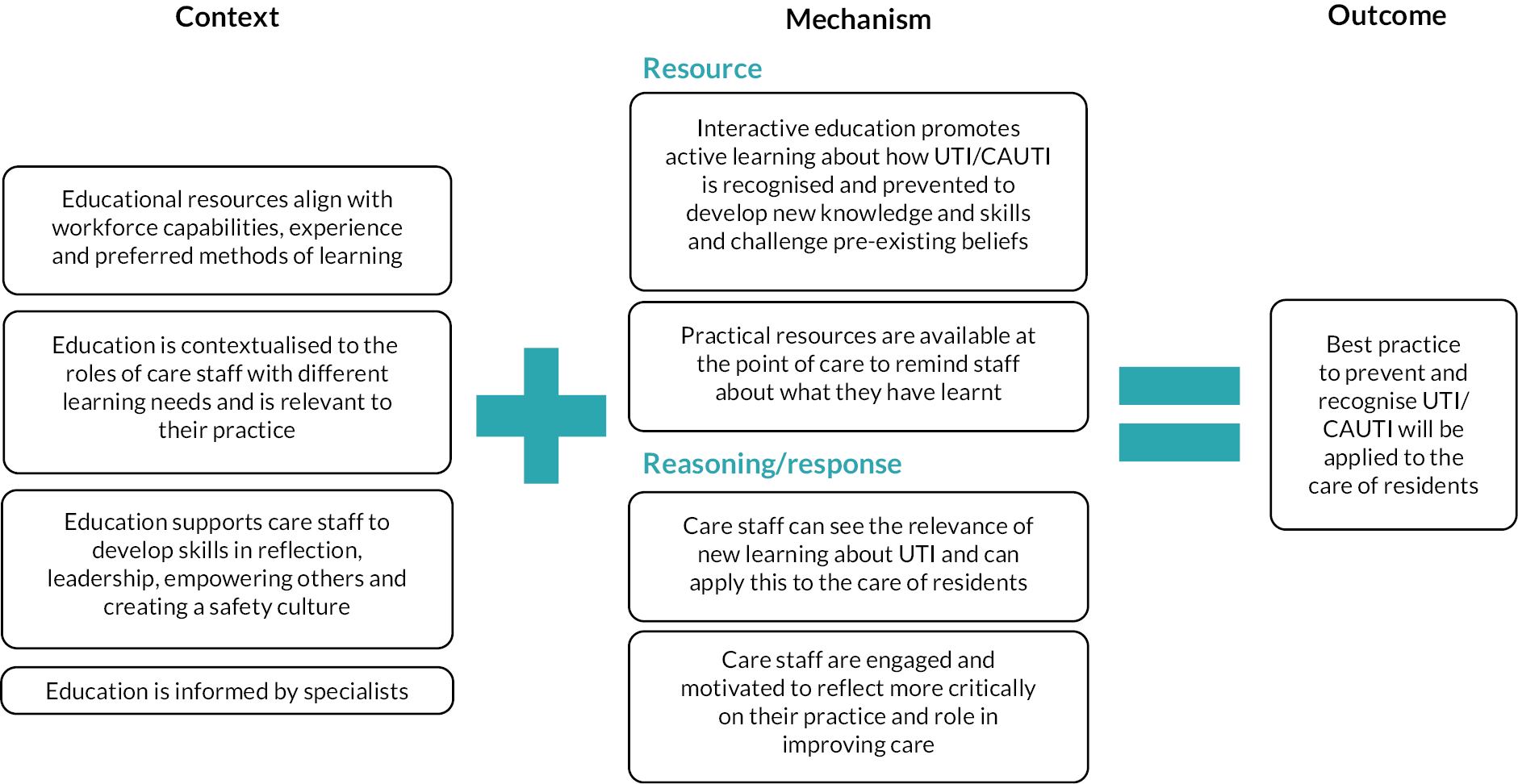
Context
Education and training that is flexible, uses a range of delivery modes, is informed by specialists and is planned to meet the learning needs of the whole workforce is more likely to be effective in improving knowledge and skills in the prevention and recognition of UTI/CAUTI. When education is contextualised to the roles of care staff at different levels, this ensures it is relevant to their practice. Education strategies that enable staff to develop skills in reflection, leadership, empowering others, addressing implementation challenges and creating a resident safety culture are likely to be more effective in supporting change than education focused purely on technical skills.
Mechanism
Education that resonates with the work of care staff enables them to see the relevance of new learning to their practice. Interactive approaches that promote active learning enables care staff to unlearn their assumptions about UTI/CAUTI prevention and recognition and apply their knowledge and understanding to how they deliver care. Experiential learning generates greater motivation and interest and helps participants to reflect more critically on their practice and role in improving care. Where education is aligned to practical resources at the point of care, these can remind staff to apply the learning to their practice.
Outcome
A knowledgeable care team assists in the acceptance and sustainability of improvements in practice to prevent and recognise UTI/CAUTI.
Rationale – the importance of well-designed education for care home staff
In the UK, most direct care of residents is delivered by care assistants with a limited formal training. In England, care assistants are required to undertake the Care Certificate during their induction to the role. 145 This comprises 15 standards that define the expected knowledge, skills and behaviours of care staff and includes training on nutrition (including fluids) and IPC (focused on standard precautions), but not on UTI and its prevention and recognition.
Qualified nursing staff in care homes are mostly in leadership roles and will also have responsibility for care planning, medications and other clinical tasks. They may have experience of UTI but specific training on strategies to support the prevention and management will be variable. Residential care homes employ few registered nurses and therefore non-professional staff have a wider responsibility for decision-making about the care of the residents. The education needs of these groups of staff needs to be considered carefully. Although care assistants provide care under the supervision of a registered nurse, in practice, most care may be delivered without supervision or monitoring. 146 It is therefore difficult for senior staff to gauge whether care staff are applying what is learnt in training to their everyday practice.
Education and training of care home staff has challenges, including a lack of access to specialist expertise to design and deliver it, poor infrastructure and resources to deliver education, difficulty in creating time for staff to receive education, integrating training into shift patterns and managing the continuous demand due to a high turnover of staff. 5,60,125 Although online or digital solutions can help, staff report a lack of time to watch videos and prefer to learn face to face. 70,125
Summary of evidence underpinning context–mechanism–outcome configuration 9
Education was a key component of many of the interventions in care homes discussed in the preceding theory areas and was important in changing perceptions about UTI and encouraging staff to recognise that a different approach was necessary. 61,70,74,114 This means that educational approaches must consider developing flexible materials, a variety of delivery modes and sufficient sessions. 60,124,125 It also needs to be designed to account for the perspectives and learning needs of a multiskilled, multicultural workforce. 5 However, education alone is not a ‘magic bullet’ to change staff care practices to improve resident outcomes.
Education should be framed to reflect staff experience and learning needs
The most effective education for care home staff is contextualised so that it resonates with their experience, and they can see the relevance to their practice. 5,51,60,70 Education that is interactive, provides practical experience and promotes active learning which emphasises the development of skills rather than just knowledge is key. 5,124,147 Using experiential learning or workshops generates greater motivation and interest and helps participants to reflect more critically on the delivery of care and their role in improving care, for example, role play, problem solving, sharing individual experiences. 5 In addition to condition-specific education, relational and communication skills can be developed so that care staff feel better equipped to discuss care with relatives. Staff in residential homes suggested that it would be useful to have training on how to deal with relatives’ concerns or to include relatives in the training, especially relatives of residents prone to infection. 60 They discussed their discomfiture, not being nurses, in attempting to persuade relatives to ‘wait and see’ when they demanded antibiotics as soon as the resident showed any sign of being unwell.
Transferring learning across the workforce
Some studies have used ‘train-the-trainer’ approaches to support the transfer knowledge from experts to care staff, although this required the creation of simple training resources to support the trainers. 60,124 Support staff have been found to feel they lack the authority to implement change, often due to hierarchical structures within the workplace. 148 Ensuring equitable education opportunities across the workforce is difficult when workloads are high, and time is at a premium. Relying on a small number of staff undergo training and cascade knowledge is unlikely to have the necessary effect as staff have little authority to translate the knowledge into the required system changes in their work areas. 5
Support to implement change is therefore required from senior staff and managers combined with organisational values which reflect a willingness to improve. This type of culture needs to be supported by staff at all levels who are empowered and motivated to enact change. 149 Education strategies that include socioadaptive elements focused on enhancing attitudes and behaviours and emphasising topics/areas such as leadership, empowering staff, addressing implementation challenges and creating a resident safety culture are likely to be more effective than education focused purely on technical skills. 124
Translating education into change in practice also requires resources at the point of care delivery to remind staff about what they have learnt. Examples include pocket cards and infographics124 that may help to overcome some of the language and individual capacity to take in new concepts. Short, informal briefings or explanation, for example, huddles, has been found to be of value in supporting the whole team to adopt change,5,60,117 although it is suggested that these lose impact without the case-based exercises that are more likely to encourage reflection. 70 Supported hands-on practice, supervision and access to experts to model practice may help to develop skills and confidence. 70,134
Technical language is also a key consideration as terminology that is understood by registered nurses may be too complex for care assistants who may also lack the necessary underpinning knowledge of the human body and how it works. 70 Nurses need to create opportunities to continue explaining and discussing the intervention to reinforce the learning and embed change into routine practice, and they also need to be able to explain the rationale for it to other external professional staff. 70 Specific guidance and decision-support tools may be particularly useful in giving staff step-by-step instructions to guide staff practice. 60,70 The role that unconscious incompetence can play in the recognition of training needs was described by researchers in a study that tested participants perception of their knowledge before and after and interactional education session and found their high self-rated knowledge was not reflected in observed practice. 5
Reflection, unlearning and reframing knowledge
Reflection is a key element of effective education as it enables participants to recognise any gaps in their understanding and apply their knowledge and experience to different situations. Emotional mapping activity designed to encourage staff to reflect upon their own hydration needs and preferences in relation to those of their residents was used by Greene et al. 5 However, participants found it difficult to relate their experience to that of the residents they cared for and did not recognise how the lack of opportunity or choice of drinks that care routines offered their residents impacted on meeting resident’s individual hydration needs.
While registered nurses and midwives are required by their professional code to reflect on their practice,150,151 this is not the case for care assistants some of whom will have trained outside the UK and may be less familiar with this concept. Education for care staff needs to build skills in developing reflective practice to help increase staff empowerment, and create a reflective culture open to change, where staff can be helped to challenge their assumptions, ‘unlearn’ previous approaches and confidently identify gaps in their practice. 152,153
Implementing changes in practice requires some ‘unlearning’ and this was a finding in the study by Arnold et al65,74, where some participants identified there was a need to unlearn and de-implement existing beliefs and practices relating to UTI in order to develop a more accurate understanding. Similarly, the study by Greene et al. 5 found that care staff attitudes were strongly influenced by their pre-existing beliefs about fluid provision and societal discourse about fluids such as recommending water over other fluids. 5 Eliciting beliefs is important as unfounded or incorrect assumptions will adversely affect the care staff provide to residents. Greene et al. 5 found that staff made drink choices for residents because they deemed some drinks, for example, coffee, as unhealthy even though the residents preferred it. Key to ‘unlearning’ is the process of reflecting on existing knowledge and practice.
Stakeholder workshop
Education as a way of improving care was also described with different initiatives, including educational videos being created specifically for care home staff or quality improvement training sessions. Stakeholders mentioned some of the barriers to training which included the openness of the managers/leadership to champion the training, the difficulty in getting junior staff to training and delivering training to staff who are not necessarily interested or who do not have the confidence to share what they have learnt.
… you do get a lot of care home managers that come to this training rather than the frontline staff which could implement the change and then when we do get frontline staff because the situation is so fluid in the care homes, they could, you know, just not be able to attend like last minute.
IPC Nurse, CCG
… there is literally no point in sending a care staff to training if they have no passion or interest in it, because they’re not then going to pay attention or come back and feed that out to the rest of the staff. They may be interested in it but not have the confidence to then go and share and lead a training.
National Care Association representative
The delivery of training was often described as being in 1- to 2-hour sessions. Stakeholders mentioned the need for support from managers to deliver the training and one mentioned starting with senior carers who can cascade to more junior staff. The educational level and literacy of the unqualified healthcare assistant staff was also mentioned as a consideration when designing training.
You have a wide variety of educational standards – you have some that are pretty on the ball and can run with it, you have some that can barely read and write, you have a lot of language barriers, English not being first language.
Quality Improvement lead
Stakeholders also recognised that education alone was not likely to sustain any changes in practice without reinforcement.
Resource gap analysis
The resources available for the prevention, diagnosis and management of UTI including optimal antimicrobial use include a range of materials intended for wide audiences, that is, leaflets for patients and users, algorithms for HCPs, antimicrobial prescribing guidelines for prescribers, e-learning modules, etc. were mapped. The resources evaluated are presented in Appendix 7, Table 5. The following content summarises the resources available according to the thematic categories, making recommendations to address the gaps identified.
Clinical action within the care pathway
The resources available can be mapped along the pathway of UTI prevention, diagnosis and management. Most of the resources reviewed, however, focused on diagnosis and management of UTI or CAUTI, with a much smaller proportion concerned about the prevention of infection.
Few of the resources presented a holistic overview of the inter-relation between hydration and elimination or embedding prevention of UTI/CAUTI among activities of daily living and autonomy, leaving a fragmented landscape of clinical tools interested primarily on a portion of such landscape, therefore demanding that clinicians and other users of the tools spend time considering how best integrate recommendations from different resources.
Such specific focus may be appropriate in some cases but, overall, tools would appear to be written with limited relation to other existing or complementary documents, and as there are tools produced by national agencies. An example of this apparent disconnection can be seen between the recommendations and guidance towards antimicrobial prescribing, and different diagnostic algorithms and flowcharts, where users are, for example, not forewarned about the unintended consequences of requesting urine samples.
Some resources including the ‘Toolkit to reduce CAUTI and other HCAIs in long-term care facilities’ from the AHRQ in the USA, as well as the I-Hydrate range from the University of West London, do provide the comprehensive overview of the different, interlocked components of UTI prevention, diagnosis and management.
Supporting knowledge or behaviours
Most resources aim to improve clinical decision-making among professionals, and, to an extent, carers. The educational component, for example, offering information about the mechanisms that lead to UTI, is infrequent. While the tools are developed to support professionals, who are expected to already have education in this area, it may be beneficial for future resources to be recognised as valuable sources of information for carers and relatives, with help from professionals.
Interestingly, while the resources focus on improving professional behaviours, most interventions do not consider some of the behavioural drivers which may be preventing patients from following the guidance. For example, behaviours such as regular drinking of fluids are promoted, appropriately, as cornerstones of prevention of dehydration. However, professionals are not really given indications about the behaviours implemented by some patients out of fear or anxiety (i.e. to avoid needing to use the toilet late in the evening or at night) or anticipating difficulties to be supported to go to the toilet due to lacking staffing levels.
Intended end user
Most of the resources are developed with a wide range of health and care professionals in mind, from GPs and other primary care professionals, to nursing home carers and staff at long-term care facilities. Besides antimicrobial prescribing, limited to specific professional cadres, the clinical decision-making illustrated in the tools and resources regarding the diagnosis and management of dehydration and UTI seems well matched to the knowledge, skills and competences available among the intended end users of the tools. On the other hand, some of the resources (for instance, Reliance On Carer Guidelines) are complicated by many necessary steps with limited information about what to do whenever any intervention is applied but fails to improve the target factors associated to UTI.
Patients and, to an extent, relatives and families are users yet to be adequately supported by the resources available. Both content and format of the tools suggest that these resources are not intended to be used by patients and users. This does not necessarily mean that patients may not be using them, but to do so, they would have to address issues about health literacy, with hardly any content presented in a suitable format following health information principles, and with clear instructions about what they should do with underpinning evidence or reasons. However, as resources tailored to patients are scarce, it is difficult to be conclusive about gaps related to patients’ skills and self-care behaviours.
Proposed solutions and future resources
The gaps identified could be addressed, following discussion and consensus with clinicians, patients and relatives, researchers and decision-makers.
Implementation and knowledge mobilisation of interventions
The resources available are, perhaps naturally, aimed at a selected group of clinicians, patients and service users together with professional and informal carers. The wide range of stakeholders identified together with the emphasis on clinical interventions leaves, on the other hand, gaps regarding the implementation of these interventions. It is difficult to identify whether the stakeholders targeted by the tools are also responsible for implementing the behavioural or structural factors and resources which are required to warrant the success of the improvement interventions.
This unclear attribution of responsibilities is crucial considering that clinicians and care workers typically involved in care homes and long-term care facilities may be unlikely to have received any prior education or training on implementation of interventions. The development of implementation models and resources would be welcomed and useful, particularly for interventions interested in promoting self-care behaviours and preventing UTI, which require the use of resources like reminder mats, or assets like healthcare staff and staff time.
The resources evaluated may be accompanied by other complementary documents which may focus on the implementation of interventions rather than the interventions to be implemented. It is also possible that the developers of resources to improve UTI care consider these interventions in the same range as many other clinical interventions routinely applied in clinical practice, therefore not requiring additional support towards knowledge mobilisation. Unfortunately, the documents evaluated do not mention if these accompanying implementation guides do exist.
Evaluating success and return on investment of interventions
In addition to resources focused on implementation of interventions, it would be beneficial for future tools to offer evidence about the improvements seen in the literature for the interventions advocated, both in isolation and as part of multimodal or bundled strategies. Although it is likely that once implemented, the interventions may perform less well than as reported in the literature, data about the expected return on investment of resources would allow decision-makers, clinicians and users to consider their existing context and assets before deciding on which interventions may be optimal for their situation.
Shared decision-making
Few of the resources seem to adopt a SDM approach to prevention of UTI/CAUTIs. The limited patient-directed materials, and lacking content in the tools for professionals, focused on fostering SDM between patients, relatives and professionals offer an opportunity to develop materials, underpinned by appropriate evidence, about preferences and patient-reported outcomes and interventions. This SDM would be beneficial considering the recurrences of hydration issues and challenges among patients, and to maximise their autonomy.
In the next chapter, we discuss the key issues raised by our synthesis and the implications that they have for care home leaders and staff, care systems and regulators.
Chapter 4 Discussion and conclusions
Introduction
Our review has provided an explanatory account of how the design and delivery of interventions can work to improve the prevention and recognition of UTI in older people living in care homes. The reason for using a realist approach was the recognition that the evidence about UTI prevention in care homes is varied, with few RCTs or other evidence on the effectiveness of interventions. In addition, as some of the relevant research has been conducted outside the UK, there is a need to consider the practicality of implementing strategies to support UTI identification and prevention in UK care homes. In this chapter, we consider the implications of our findings for the organisation and delivery of care for older people living in care homes, comment on the limitations and challenges associated with the review and provide recommendations for future research.
Fundamental care
The prevention of UTI and CAUTI in older people living in care homes requires attention to their fundamental care needs (Figure 18), with clear communication across the whole care team that is trusted and valued by residents and their family or significant others. 49 This necessitates a context of person-centred care and a culture of quality and safety, promoted by commissioners, regulators and providers, where leadership and resources are committed to supporting preventative action by knowledgeable care staff.
FIGURE 18.
Fundamental Care Framework. Image obtained from %https://ilccare.org/the-framework/; Content within image derived from Feo et al. (2017). 49
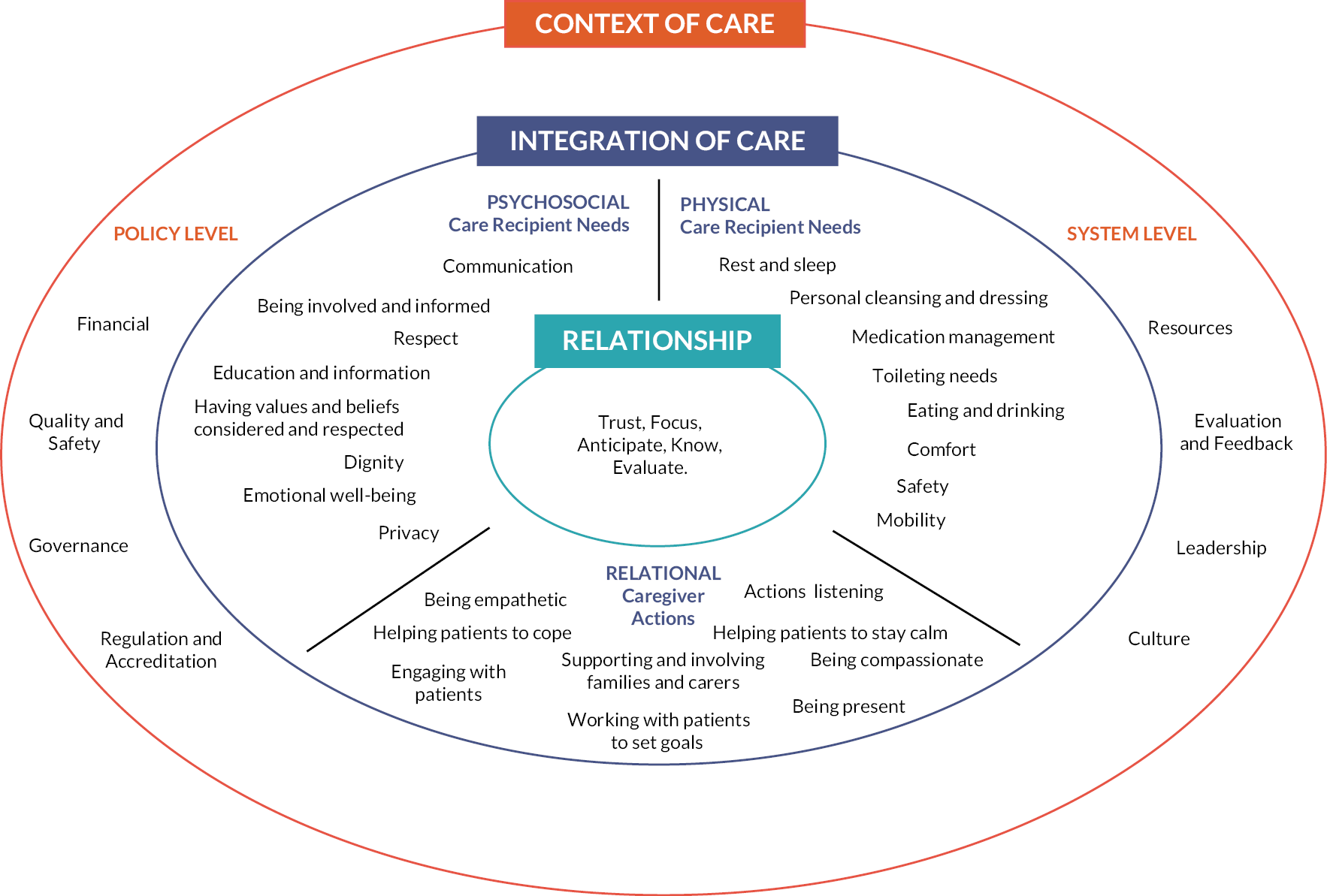
Our synthesis suggests that ownership and empowerment among direct care staff for the prevention and recognition of UTI and CAUTI can be improved through its integration into care home systems and routines designed to meet residents’ needs and through its proper alignment with AMS goals. Linking fundamental care as a means of preventing UTI and CAUTI helps care staff to recognise how their role is important. Education and training that challenges assumptions and low-value practices assists in building confidence to communicate observations and arrive at informed decisions.
Integrating urinary tract infection prevention and recognition as part of person-centred care of older people
In the conception of this review, our reasoning for exploring both the prevention and recognition of UTI was that the latter was critical to developing effective prevention strategies. However, the evidence we have found has highlighted other hidden synergies between these two concepts, which emphasise the value of integrating them into the design and delivery of person-centred care.
Preventing and recognising UTI in older people is complex. Not only do underlying risk factors in older people increase their susceptibility to UTI, but they commonly present with atypical symptoms. The prevalence of UTI among care home residents can lead staff to assume non-specific symptoms are most likely due to UTI and that acquiring UTI is an inevitability for some residents. They may not appreciate the extent to which inappropriate treatment of UTI makes infections more difficult to treat and impacts on resident health and well-being in addition to driving the emergence of antimicrobial-resistant infection. If care staff are not aware that it is possible to prevent UTI and lack knowledge and training in how to do so, they are likely to see their role as exclusively about supporting its diagnosis and treatment.
Decisions about a UTI diagnosis are often based on observations of non-specific signs such as changes in the characteristics of urine or alertness of the resident combined with a urine dipstick test, which is perceived by some as being an objective test that provides a definitive indication that a UTI is present. Resources that aim to improve the reliability of UTI recognition can help care staff to distinguish and communicate evidence-based signs and symptoms of UTI. 32,60,61 However, given the overlap between some non-specific symptoms, which are common to both UTI and dehydration, existing decision-support tools may be missing an important opportunity to address hydration as a fundamental care need. Figure 19 illustrates the signs and symptoms of dehydration and UTI. The sets in the Venn diagram illustrate those signs and symptoms for which there is evidence of association with dehydration or UTI, while the intersection shows the signs and symptoms common to both. Signs that are often used as indicators, but are less reliable on their own, are listed outside of the circles. If attention was directed at improving a resident’s hydration, this might alleviate their symptoms and reduce the risk of them developing UTI, as indicated by the arrows in Figure 19.
The importance of recognising the synergy between UTI diagnosis and prevention is illustrated by the work of Lean et al. 117 They demonstrated a reduction in UTI-related hospital admissions associated with a strategy that combined increasing residents’ fluid intake with reducing the reliance on urine dipsticks to diagnose UTI. Decision-support tools targeting the appropriate diagnosis of UTI by care home staff should also incorporate decision-making about increasing fluid intake to exclude or manage dehydration as a potential cause of the symptoms and emphasise the role hydration plays in preventing UTI.
Our realist synthesis has identified proactive management of residents with urinary catheters together with informed decision-making about signs and symptoms of CAUTI as critical to preventing CAUTI and reducing inappropriate use of antimicrobials. However, this also necessitates support at a system level, including education that empowers staff to remove catheters and influence appropriate antibiotic prescribing decisions.
In relation to the proactive management of residents with RUTI, we found a single improvement study in a care home setting. 128 However, we used evidence from our stakeholders and relevant clinical guidelines to inform CMOc 7. The actions that care home staff take are often informed by their knowledge that a resident has had a prior UTI or has a history of septicaemia, which can result in heightened concern about the risk of deterioration and an early decision to contact the GP. 60 Conversely, ‘labelling’ a resident as having RUTI raises concerns about encouraging the treatment of ASB. 64
However, this overlooks the value of strategies aimed at the preventing RUTI, which would be available to older people outside a care home setting. 27,54,56 A combination of factors is a barrier to the proactive management of RUTI in care home residents. These include a lack of awareness about pharmacological options and guidelines on their use, lack of access to specialist staff such as CAs or urologists who could advise on investigation and treatment, and an absence of systems which could support the identification of repeat episodes of UTI and trigger action to offer treatment to affected residents. This further illustrates the need to integrate recognition with the prevention of UTI.
These findings highlight a need to unify the content of education and decision-support resources so that they align to the goals of fundamental care49 and highlight the intersection between the prevention and recognition of UTI.
Aligning urinary tract infection prevention with sepsis prevention and diagnostic stewardship
The recent emphasis on sepsis prevention and the development of tools for use in care homes to detect early ‘soft signs’ of deterioration and sepsis has focused efforts on early recognition and escalation of concerns using structured communication tools. This creates a sense of the imperative to act and a fear of missing infection/sepsis, rather than a broader approach, which considers UTI as a possible cause and recognises the prevention of UTI as a goal and safety priority.
In addition, early warning tools aim to streamline observations and communicate changes in a resident to the GP to support the early identification of rapid deterioration/sepsis (e.g. RESTORE2, NEWS2, Stop and Watch). These tools are different to those designed to improve decision-making and communication about suspected UTI. 60,65 However, because both tend to be structured around SBAR communication tools, these differences may not be apparent to care staff. 60,70 It is therefore conceivable that these tools create conflicting messages about (1) the need to act rapidly to avoid deterioration and (2) considering alternative explanations for a change in a resident’s condition and avoiding unnecessary antibiotic prescribing. The focus on structured communication in these tools may divert from a more holistic assessment which recognises dehydration as a driver of deterioration and the need to support a resident to drink.
Delivering education that works
Non-clinical staff deliver most of the resident care and may not have the underpinning clinical knowledge to help them make sense of the complex concepts involved in the identification and prevention of UTI. Residential homes have less access than nursing homes to registered nurses who understand pathophysiology and fundamentals of nursing care and across the care home sector there are significant difficulties in recruiting and retaining nurses to work in care home settings because of recent changes in UK policy and the impact of COVID-19. 3
Education needs to resonate with the experience of care staff if it is to change thinking and embed learning131 and care home leaders need to create the time and opportunity for education to occur and fosters a culture where staff are supported to share their knowledge and observations. 61 Although the use of virtual approaches to education provides flexibility and extends the reach across the workforce, it is not always preferred by care staff and does not easily support discussion and reflection. 61 Interactive approaches to education that draw on real cases enable care staff to articulate their thoughts and experience and encourage them to reflect on the resident’s needs are key to the learning process and critical to building a solid understanding to underpin effective and appropriate decision-making. 5,70 However, interactive education is resource intensive and needs to be sustainable, especially in the context of a high staff turnover. 61,124,125 Our synthesis identified that reflective conversations, huddles and ‘stop and think’ strategies allow time for staff to discuss and pay attention to how a resident’s condition is developing. This also provides brief, but protected time, for education messages to be reinforced. 6,61,117,70
Even where care homes employ registered nurses, ensuring education is appropriate, evidence-based and supports the ‘unlearning’ of existing beliefs requires input from specialists and expert facilitation. 5,124 Routine care may be informed by misconceptions and myths, with staff placing emphasis on practices that have little evidence of efficacy or relevance (e.g. cranberry juice), or a lack of knowledge about what strategies are effective in preventing UTI. Stopping ineffective or harmful practices which are embedded as a routine will not happen without a de-implementation strategy that focuses on system changes rather than education alone. Interventional studies aimed at improving diagnostic stewardship in care homes illustrate how difficult it can be for care staff to change their intuitive understanding of UTI and differentiate between UTI and other diagnoses. De-implementation strategies also need to consider the relationship between the care staff, resident and their relatives to ensure that it is managed in a clear and supportive way. 91
Facilitating improvement in practice in care homes
Alignment and fit of improvement strategies with care home systems and routines of care is key to making best practice happen. 124,131 Co-design of interventions, education and monitoring processes is important to achieve this so that those with knowledge of the setting and those with relevant clinical expertise can inform the creation of resources that work in the context of the knowledge and skills of staff, and residents who have limited ability to communicate their symptoms. The facilitation available to long-term care settings is also a crucial component of getting buy-in from staff to make improvements sustainable and this is not always available within care homes outside the research programme. External and internal facilitation are required, and Mody et al. 124 demonstrated that this can work but requires considerable resource and access to a range of different specialist expertise to support local facilitators. Working in a network that provides peer support enables learning across the system. 125
Our research suggests that the access to specialist support for care home staff is not uniform and where expertise could be available, this is not always recognised or utilised appropriately. For example, where care staff mentioned specialists such as CAs, this was most likely in relation to accessing incontinence pads, rather than advise on preventing UTI. Our stakeholders identified that different models of support were currently in existence, some of which had grown out of the historical set up of services and others where acute hospital staff supported homes with a specialist frailty service or through community matrons. Understanding the local context in which a care home or group of care homes operates is vital to understanding how support is accessed and how preventative fundamental care can be optimised. In the UK, specialist pharmacists and community matrons are untapped potential sources of expertise and advice that could be used to support the identification and prevention of UTI, for example, by undertaking a clinical review of residents who have been frequently prescribed antibiotics for UTI. Specialist practitioners could play a role in:
-
developing systems to collect, analyse and interpret data to support improving the quality of care
-
designing and facilitating education programmes
-
adapting evidence-based guidance to inform care homes policies and procedures
-
advising on the investigation and treatment of residents who have RUTI
-
co-creating systems to support decision-making by care staff, for example, catheter removal, recognition of UTI/CAUTI.
‘Champions’ were used in several studies, often as part of a wider intervention programme and as an internal resource and facilitator. There was some evidence that champions could be helpful in facilitating change or improving care. 60,74 However, they need to be endorsed and supported by managers, enabled to develop the right knowledge and skills and have dedicated time and sufficient authority to enable them to deliver the role. 60,74,131
Involving the resident and family carers
This review has highlighted the important role that family members can play in the prevention and early detection of UTI in residents. Although relatives often feel powerless, they can also overrule staff decisions about the need to contact a GP. 89 Stakeholders in this research described the value of the knowledge that families have about the resident, how they can recognise subtle signs or changes in behaviour which are unusual for their relative and can alert staff to intervene early with strategies that may avert a UTI. Care staff described the importance of involving family members in decisions about care, including the rational for active monitoring as opposed to prescribing and in preventative strategies such as promoting hydration. However, care staff also reported that dealing with relatives’ demands for action to be taken could be challenging. Training for staff on how to handle discussions with relatives was proposed by participants in the study by Potter. 89 Furthermore, Powell et al. 90 suggest that legitimising family involvement is a possible solution to supporting those who do wish to contribute.
Leadership in care homes
The importance of leadership by care home managers in the implementation of interventions in care homes was apparent in the evidence included in this review. This is not surprising given their crucial role in instigating changes to how care is delivered in care homes. Researchers have noted a difference between managers who see their participation in an intervention study as something requiring their co-operation and those who are actively and visibly engaged in delivering and sustaining changes to practice. 60,74
Amidst the many other competing priorities and demands placed on care homes, emphasis on UTI prevention can be lost. The prominence given to UTI prevention and recognition as a safety priority and regulatory imperative will impact on the attention it receives by care home managers and the value and resource directed towards it by their staff. 131
Taking a system-level approach
Care homes in England are predominantly privately owned, with some not-for-profit providers. They range from stand-alone small homes to large care home groups. Care home residents reflect a mixture of both private and local authority funded places. The limited resource available to fund care, the variability in size of care homes, the low number of registered clinical staff employed in the sector and a lack of information technology infrastructure make it challenging for some care homes to harness the skills and resources required to drive best practice. Regulatory and inspection frameworks aligned to evidence on the prevention and recognition of UTI and person-centred approaches can help to prioritise the focus for improvement and mobilise the resources needed as demonstrated by the AHRQ study in the USA. 124
The formation of Integrated Care Services (ICS) in England that are now responsible for developing integrated care strategies across health and social care will offer new opportunities to address the challenges of recognising and preventing UTI in care homes. They have a role in creating a better co-ordinated system-wide approach to framing priorities for UTI prevention, distilling programmes with actionable interventions based on easily collected data that align and fit with the priorities of care homes. 124,131 There is also an opportunity to increase the specialist practitioner resource to provide the required access to expertise, which supports the co-design and implementation of improvement initiatives in care homes.
Strengths and limitations of the review
Strengths
The realist approach used in this review enabled us to bring together multiple types of evidence to inform our theory-driven explanation of how interventions to improve the prevention and recognition of UTI might work in care homes for older people. The evidence we drew upon helped us to build explanations based on detailed accounts of processes underlying the implementation of complex interventions. Many of the studies we used would not have been included in a systematic review of evidence but were relevant to our review. Consequently, our programme theory, comprising nine CMOc, offers new insight into the requirements for current and future local or national initiatives aimed at preventing UTI/CAUTI in care homes which can be used by care commissioners, regulators, care providers and care home leaders and staff to put evidence into action.
The high degree of stakeholder engagement throughout the lifetime of the project has enabled us to sense-check our programme theory and take account of multiple perspectives, including those of people living in, working with and visiting care homes in England.
We intended to produce materials to support the prevention and recognition of UTI in care home settings but questioned the value of adding further tools to the existing range of resources we identified. Instead, we conducted a gap analysis to establish where additional resources might be useful, thereby informing where the development of future tools will add value and meet the needs of care homes.
Limitations
The COVID-19 pandemic required us to adapt our approach and work mainly online both in our interactions with stakeholders and as a research team. Care home staff were quite rightly focused on the imperatives of safeguarding residents and securing access to staff was challenging. We also wanted to have greater input from residents and their families, but this was not possible in the circumstances. While it is hard to tell what consequences the move to online workshops had on theory formulation in stage 1, we were satisfied that the level of engagement achieved through virtual meetings with care home staff facilitated contributions that were important in shaping the review. Moreover, the shift to online working made it possible to expand on the workshops planned in stage 1 by holding two additional meetings with healthcare practitioners. We were disappointed that our ability to consult with care home residents and family carers was severely hampered as this would have added valuable insights to inform the review. The move to virtual meetings also had an impact on our intention to bring a wide range of stakeholders together, including representatives of care home residents, at a face-to-face event towards the end of the project with many preferring to meet virtually. We acknowledge that these adaptations may have limited the generation of insights and discussion to inform both the review and our strategies for development and dissemination of outputs. For this reason, we recognise the importance of continuing to engage with stakeholders as part of our ongoing work, reporting this process and any outcomes.
Studies focusing on the prevention of UTI and CAUTI in care home settings were predominantly from the USA and Europe where the regulatory and funding systems for the long-term care of the elderly has some differences, particularly in the USA where national reporting plays a significant role in driving improvements in care. Furthermore, care homes (also known as nursing homes) in the USA provide a range of medical services including post-acute care, rehabilitation, palliative and hospice care, as well as long-term care. Medicare is the federal health insurance programme for people who are 65 years or older, certain younger adults with disabilities and those with end-stage renal disease. It covers short nursing home stays for older adults. Long-term care in nursing homes is covered by either private pay or Medicaid. Medicaid provides health coverage, which includes eligible low-income older adults and those with disabilities. The studies undertaken in the UK and Europe were focused primarily on interventions to reduce antimicrobial resistance through stewardship but had significant learning that was transferable to the prevention and recognition of UTI.
Our synthesis tried to take account of these differences, but we are aware that we will not have reflected all realities. This is particularly true of the limited evidence that we were able to identify in relation to family involvement, which as a research team we felt was a potentially important theory area. Although we conducted a supplementary search, we found insufficient evidence to develop a stand-alone theory but included it as a thread through our final theories.
Similarly, our supplementary search on continence care and UTI found there was a lack of evidence demonstrating that urinary incontinence was a cause of UTI, although UTI could be a contributory factor to urinary incontinence. There was also a paucity of evidence on the effect of using incontinence pads or alternative approaches to toileting on the risk of UTI. Therefore, while programmes aimed at improving the management of urinary incontinence may include proactive management of patients at risk of RUTI,128 there is insufficient evidence to include continence care and support with toileting as a potential strategy for preventing UTI. This perhaps reflects the lack of prioritisation of research on problems that are considered inevitable for the frail elderly and may therefore be an important area for further research.
Through the review, we identified several tools and resources that were being used by staff in care homes in addition to those reflected in the literature. It became clear that adding another set of tools was not going to be helpful and that any resource we developed needed to follow the principles of co-design and fit discussed earlier and address some of the challenges faced by care home leaders. The difficulty in bringing stakeholders together to achieve this was insurmountable within the period for this review. However, we will continue this element of the project over the next 12 months with the funding that was made available in the grant.
Equality, diversity and inclusion
Participant representation
As a realist synthesis, this study included stakeholders representative of the community of interest, which in this case was people residing in care homes, their families and individuals working in and with care homes. We had originally planned to host our stakeholder discussions at care homes across three geographical locations, but this was not feasible because of the pandemic. We instead ran online workshops and individual interviews that sought to ensure we included in these the views of staff working within the home, across the primary care and secondary care interface. We also sought views from a resident in the home who was supported in taking part and from relatives of residents. We recognise that having to alter our approach meant it was harder for residents and their families to participate in the stakeholder discussions and we may have had greater representation from these groups had we been able to conduct the stakeholder interviews face to face as originally planned.
Reflections on the research team
Our research team was predominantly female and included researchers from different geographies and at different career stages and with a range of experience and expertise in health and social care research and in realist synthesis. This was the first opportunity for JP to lead a major study and she was supported in this role by the co-chief investigator HL with mentoring from JRM, who oversaw the methodological approach to the realist review. Our most junior member of staff was provided with a development opportunity as this was their first role as a research assistant. They were given support and training to develop in their role.
We sought to include several patient and public representatives in this research, all with experience of the care home sector as carers. One of our PPI members was themselves physically disabled and because of this, had significant experience of UTI. We had a PPI co-applicant with considerable experience in health and social care research to chair our PAG and, finally, we purposely sought a male PPI representative as our other representatives were female.
While the benefits for people that participated in the research, either as stakeholders or lay representatives, may not be immediately obvious, this research has highlighted how strategies for the detection and prevention of UTI can be implemented as part of routine care across care homes, which serve a diverse population of older people.
Implications and recommendations
Implications for practice
The review findings point towards actionable recommendations for UTI prevention and recognition in the care of older people living in care homes, which we describe in relation to organisational and system level actions. These centre on the need to align UTI prevention and recognition to the goals of person-centred, fundamental care and prioritise this in routine daily care to improve quality and safety. For example, understanding and targeting personal barriers to drinking more fluids, such as fears about incontinence and getting to the toilet, may assist in addressing poor fluid intake. This in turn can help to reduce falls, confusion and drowsiness, as well as UTI.
Care home providers
Best practice to prevent and recognise UTI in care home residents requires focusing on a set of evidence-informed actions as part of routine daily care with the involvement of the whole care team, including individual residents, their family carers and care home staff.
Preventative actions include:
-
supporting each resident’s hydration preferences and needs
-
using fluid intake monitoring systems that enable realistic targets and actions to be agreed for residents with poor fluid consumption
-
accessing specialists who can support the care of residents with RUTI
-
applying infection prevention practice to the care and management of IUCs.
Accurate recognition of UTI requires:
-
knowledge of the individual resident and what is normal for them
-
understanding of evidence-based signs and symptoms of UTI
-
use of structured tools that align with existing care processes and a shared language to convey accurate and relevant information to HCPs.
Care home staff need opportunities to:
-
develop knowledge and skills so they can interpret a resident’s signs and symptoms and consider possible explanations for generalised changes in their condition
-
reflect on practice and learn from each other about how to recognise a UTI and support preventative actions.
System level
A system-wide approach with regulatory and inspection frameworks aligned to evidence on prevention and recognition of UTI is vital to ensure that resources and infrastructure are available to enable care home managers and their staff to prioritise this as part of person-centred care.
There is a need to:
-
integrate the prevention of UTI with diagnostic and AMS in the care of older people living in care homes
-
harmonise the prevention and recognition of UTI decision and communication tools with those focused on recognising deterioration to facilitate adoption and integration in care homes
-
use co-creative approaches to develop and implement resources and improvement initiatives that involve the whole care team, residents and family carers
-
build a knowledgeable workforce of care home support workers and registered nurses who can deliver evidence-informed care and communicate their observations in a way that enables care to be reviewed before escalation
-
improve access to expert practitioners and services to support the provision of personalised, multidisciplinary assessment and treatment plans for residents with RUTI who have the greatest potential to benefit from effective treatment.
Research recommendations
Well-designed research to improve the prevention and recognition of UTI in older people living in care homes should address the following:
-
perspectives and beliefs of residents and family carers relating to the prevention and recognition of UTI and the concept of active monitoring to avoid unnecessary treatment
-
the effectiveness of specialist practitioners in supporting initiatives to recognise and prevent UTI, including expertise in facilitating improvement
-
the effectiveness of preventative pharmacological and non-pharmacological interventions to manage RUTI in care homes
-
the effectiveness of non-traditional education interventions such as huddles or structured reflection to facilitate decision-making in care homes
-
in co-creating interventions research should be explicit about the elements of an intervention that can be tailored to individual care homes and those which are important to deliver as intended.
Conclusion
At the outset of this review, we identified that the coherence and detail of what works for providers to prevent UTI and CAUTI in older people living in UK care homes was lacking. What we now know is that care home staff have a vital role in the prevention and recognition of UTI, which can be enabled through integration and prioritisation within the systems and routines of care homes and delivery of person-centred care. Promoting fundamental care as a means of facilitating a holistic approach to prevention and recognition of UTI helps staff to recognise how they can contribute to AMS and recognition of sepsis as part of good care. Challenging assumptions made by care home staff about the presentation of UTI is complex and requires education that facilitates ‘unlearning’ and questioning of low-value practices. Programmes to prevent UTI need to be co-designed and supported through active and visible leadership by care home managers. Involvement of specialist practitioners, such as community matrons, pharmacists, CAs and infection prevention specialists, may help to create a network of practitioners that provide peer support for change.
Additional information
Contributions of authors
Jacqui Prieto (https://orcid.org/0000-0002-5524-6775) (Associate Clinical Professor) was the co-chief investigator, led the design of the study, was involved in all aspects of the review process and theory development, including stakeholder consultation. As joint lead author of this report, she drafted and commented on all aspects of the report.
Jennie Wilson (https://orcid.org/0000-0002-4713-9662) (Professor) was a co-investigator and was involved in the design of the review and contributed to all stages of the review process and conducting teacher–learner interviews. She contributed to drafting and commenting on the content of this report.
Alison Tingle (https://orcid.org/0000-0002-5557-8120) was a co-investigator, contributed to the stakeholder engagement and undertaken interviews and workshops with key stakeholders, supported the PPI co-applicant and PPI PAG members and led the resource review. She contributed to theory development and drafting and commenting on the content of this report.
Emily Cooper (https://orcid.org/0000-0002-5043-4187) was a co-investigator, contributing to scoping of data, data analysis, extraction and synthesis and theory development and drafting and commenting on the content of this report.
Melanie Handley (https://orcid.org/0000-0002-8037-5042) was a co-investigator, contributing to scoping of data, data analysis, extraction and synthesis and theory development.
Jo Rycroft-Malone (https://orcid.org/0000-0003-3858-5625) (Professor) was a co-investigator, oversaw the methodological approach to realist synthesis and commented on the methods chapter of this report.
Jennifer Bostock (https://orcid.org/0000-0001-9261-9350) was a lay co-investigator and chaired the PAG, contributed to stakeholder involvement and advised on the content of resident and carer interviews. She commented on theory development throughout the project.
Lynne Williams was a co-investigator and contributed to the stakeholder scoping workshop component of the study.
Heather Loveday (https://orcid.org/0000-0003-2259-8149) (Professor) was the co-chief investigator, led the design of the study, was involved in all aspects of the review process and theory development, including stakeholder consultation. As joint lead author of this report, she drafted and commented on all aspects of the report.
Acknowledgements
We would like to thank all the PAG members who gave their valuable time and expertise to inform this review: Anita Astle, Susan Bennett, Jennifer Bostock (Chair), Leah Jones, James McMahon, Lona Mody, Annabelle Stigwood, and Mark Stott. Thanks to Lois Woods and Simon Briscoe for their expertise and support in undertaking scoping and supplementary bibliographic and database searches and to Jemima Kakpa and Christine Logan for their administrative support through the project.
Our thanks to the individuals and organisations who contributed through participation in our scoping workshops, teacher–learner interviews and final stakeholder event. Organisations included: Alzheimer’s Society, Buttercup House Care Home, Chiswick Nursing Centre, Care Quality Commission, NHS Fareham & Gosport CCG, Hampshire County Council, Infection Prevention Society Care Home Special Interest Group, National Care Forum, NHS England and Improvement, NHS Hampshire, Southampton and Isle of Wight CCG, NHS London South West CCG, NHS North Hampshire CCG, NHS West Hampshire CCG, Oxford AHSN, The Oaks Care Home, and Wessex AHSN.
This project was supported by the National Institute for Health and Care Research ARC Wessex.
Dedication
Lead author Jacqui Prieto would like to dedicate this report to her late father, Mr George Kilner, who at the time of the research was living in a residential care home. George’s courage in facing the many challenges of living with dementia was testament to the steadfastness he showed throughout his life.
Ethics statement
On 5 October 2020, the study was identified as a service evaluation/service development following submission to the UK Health Research Authority. We sought ethics approval from the University of Southampton Faculty Ethics Committee to engage with and interview stakeholders. Ethics approval was given on 15 October 2020 (reference number ERGO ii 53942.A1).
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available anonymised data may be granted following review.
Information governance statement
The study did not handle any personal information.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/DADT3410.
Primary conflicts of interest: The following Committee Memberships were active during the lifetime of the project:
Jo Rycroft-Malone: HSDR Programme Director 2015–22, NIHR Strategy Board 2015–22, NIHR Journals Library Editorial Board 2016–8.
Jennifer Bostock: HSDR Funding Committee Member 2018–20, HTA Clinical Evaluation and Trials Committee Member 2020.
Publication
Prieto J, Wilson J, Tingle A, Cooper E, Handley M, Rycroft Malone J, et al. Preventing urinary tract infection in older people living in care homes: the ‘StOP UTI’ realist synthesis [published online ahead of print August 8 2024]. BMJ Qual Saf 2024. https://doi.org/10.1136/bmjqs-2023-016967
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Munson S. Care Home Stats: Number of Settings, Population &Amp; Workforce 2022. www.carehome.co.uk/advice/care-home-stats-number-of-settings-population-workforce (accessed 29 October 2022).
- Office for National Statistics . Care Homes and Estimating the Self-Funding Population, England: 2021 to 2022 n.d. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/socialcare/articles/carehomesandestimatingtheselffundingpopulationengland/2021to2022 (accessed 29 October 2022).
- Skills for Care . The State of the Adult Social Care Sector and Workforce in England 2022. www.skillsforcare.org.uk/Adult-Social-Care-Workforce-Data/Workforce-intelligence/documents/State-of-the-adult-social-care-sector/The-state-of-the-adult-social-care-sector-and-workforce-2022.pdf (accessed 29 October 2022).
- Kojima G. Prevalence of frailty in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc 2015;16:940-5.
- Greene C, Canning D, Wilson J, Bak A, Tingle A, Tsiami A, et al. I-Hydrate training intervention for staff working in a care home setting: an observational study. Nurse Educ Today 2018;68:61-5.
- Wilson J, Bak A, Tingle T, . Improving hydration of care home residents by increasing choice and opportunity to drink: a quality improvement study. Clin Nutr 2019;38:1820-7.
- Gharbi M, Drysdale JH, Lishman H, Goudie R, Molokhia M, Johnson AP, et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all-cause mortality: population-based cohort study. BMJ 2019;364.
- Caljouw MAA, den Elzen WPJ, Cools HJM, Gussekloo J. Predictive factors of urinary tract infections among the oldest old in the general population. A population-based prospective follow-up study. BMC Med 2011;9.
- Public Health England . English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR). Annual Report 2017 2017.
- Vihta KD, Stoesser N, Llewelyn MJ, Quan TP, Davies T, Fawcett NJ, et al. Trends over time in Escherichia coli bloodstream infections, urinary tract infections, and antibiotic susceptibilities in Oxfordshire, UK, 1998–2016: a study of electronic health records. Lancet Infect Dis 2018;18:1138-49.
- Abernethy J, Guy R, Sheridan EA, Hopkins S, Kiernan M, Wilcox MH, et al. E. coli Bacteraemia Sentinel Surveillance Group . Epidemiology of Escherichia coli bacteraemia in England: results of an enhanced sentinel surveillance programme. J Hosp Infect 2017;95:365-75.
- Biggel M, Heytens S, Latour K, Bruyndonckx R, Goossens H, Moons P. Asymptomatic bacteriuria in older adults: the most fragile women are prone to long-term colonization. BMC Geriatr 2019;19.
- Rowe TA, Juthani-Mehta M. Diagnosis and management of urinary tract infection in older adults. Infect Clin North Am 2014;28:75-89.
- Eriksen HM, Koch AM, Elstrøm P, Nilsen RM, Harthug S, Aavitsland P. Healthcare-associated infection among residents of long-term care facilities: a cohort and nested case-control study. J Hosp Infect 2007;65:334-40.
- Genao L, Buhr GT. Urinary tract infections in older adults residing in long-term care facilities. Ann Long-Term Care 2012;20:33-8.
- Loveday HP, Wilson JA, Pratt RJ, . epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2014;86:S1-70.
- McNulty C, Verlander NQ, Turner K, Fry C. Point prevalence survey of urinary catheterisation in care homes and where they were inserted, 2012. J Infect Prev 2014;15:122-6.
- Marwick C, Santiago VH, McCowan C, . Community acquired infections in older patients admitted to hospital from care homes versus the community: cohort study of microbiology and outcomes. BMC Geriatr 2013;13.
- NICE Clinical Guideline 139 . Healthcare-Associated Infections: Prevention and Control in Primary and Community Care 2012.
- NICE Guideline 109 . Urinary Tract Infection (Lower): Antimicrobial Prescribing 2019.
- Gould D, Gaze S, Drey N, Cooper T. Implementing clinical guidelines to prevent catheter-associated urinary tract infections and improve catheter care in nursing homes: systematic review. Am J Infect Control 2017;45:471-6.
- Spilsbury K, Hanratty B, McCaughan D. Supporting Nurses in Care Homes. York: University of York Project Report; 2015.
- Dudman J, Meyer J, Holman C, Moyle W. Recognition of the complexity facing residential care homes: a practitioner inquiry. Prim Health Care Res Dev 2018;19:584-90.
- Lee MH, Lee GA, Lee SH, Park YH. Effectiveness and core components of infection prevention and control programmes in long-term care facilities: a systematic review. J Hosp Infect 2019;102:377-93.
- Meddings J, Saint SL, Krein S, . Systematic review of interventions to reduce urinary tract infection in nursing home residents. J Hosp Med 2017;12:365-8.
- Prieto J, Wilson J, Bak A, Denton A, Flores A, Lusardi G, et al. A prevalence survey of patients with indwelling urinary catheters on district nursing caseloads in the United Kingdom: the Community Urinary Catheter Management (CCaMa) Study. J Infect Prev. 2020;21:129-35.
- Sihra N, Goodman A, Zakri R, Sahai A, Malde S. Nonantibiotic prevention and management of recurrent urinary tract infection. Nat Rev Urol 2018;15:750-76.
- O’Kelly K, Phelps K, Regen EL, Carvalho F, Kondova D, Mitchell V, et al. Why are we misdiagnosing urinary tract infection in older patients? A qualitative inquiry and roadmap for staff behaviour change in the emergency department. Eur Geriatr Med 2019;10:585-93.
- Phillips CD, Adepoju O, Stone N, Moudouni DKM, Nwaiwu O, Zhao H, et al. Asymptomatic bacteriuria, antibiotic use, and suspected urinary tract infections in four nursing homes. BMC Geriatr 2012;12.
- Beech E. To Dip or Not To Dip – A Patient Centred Approach to Improve the Management of UTI in the Care Home Environment 2017. https://federationinfectionsocieties.com/wp-content/uploads/2017/03/FISDay01-H10-1315-ElizabethBeech.pdf (accessed 29 October 2022).
- Nicolle LE, Gupta K, Bradley SF, Colgan R, DeMuri GP, Drekonja D, et al. Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin Infect Dis 2019;68:e83-110.
- Public Health England . Diagnosis of Urinary Tract Infections Quick Reference Tool for Primary Care for Consultation and Local Adaption 2019. www.gov.uk/government/publications/urinary-tract-infection-diagnosis (accessed 29 October 2022).
- Public Health England . English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) 2018. www.gov.uk/government/publications/english-surveillance-programme-antimicrobial-utilisation-and-resistance-espaur-report (accessed 29 October 2022).
- Bardsley M, Blunt I, Davies S, Dixon J. Is secondary preventive care improving? Observational study of 10-year trends in emergency admissions for conditions amenable to ambulatory care. BMJ Open 2013;3.
- Thornley T, Ashiru-Oredope D, Beech E, Howard P, Kirkdale CL, Elliott H, et al. Antimicrobial use in UK long-term care facilities: results of a point prevalence survey. J Antimicrob Chemother 2019;74:2083-90.
- Nace DA, Drinka PJ, Crnich CJ. Clinical uncertainties in the approach to long term care residents with possible urinary tract infection. J Am Med Dir Assoc 2014;15:133-9.
- Public Health England . Annual Epidemiological Commentary: Gram-Negative Bacteraemia, MRSA Bacteraemia, MSSA Bacteraemia and C. Difficile Infections, up to and Including Financial Year April 2018 to March 2019 2019.
- NHS Improvement/Public Health England . Preventing Healthcare Associated Gram-Negative Bloodstream Infections: An Improvement Resource 2017. www.england.nhs.uk/wp-content/uploads/2020/08/Gram-negative_IPCresource_pack.pdf (accessed 29 October 2022).
- Fasugba O, Mitchell BG, McInnes E, Koerner J, Cheng AC, Cheng H, et al. Increased fluid intake for the prevention of urinary tract infection in adults and children in all settings: a systematic review. J Hosp Infect 2020;104:68-77.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34.
- Rycroft-Malone J, McCormack B, Hutchinson AM, DeCorby K, Bucknall TK, Kent B, et al. Realist synthesis: illustrating the method for implementation research. Implement Sci 2012;7.
- Rycroft-Malone J, Burton C, Hall B, McCormack B, Nutley S, Seddon D, et al. Improving skills and care standards in the support workforce for older people: a realist review. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005356.
- Booth A. EVIDENT Guidance for Reviewing the Evidence: A Compendium of Methodological Literature and Websites n.d. https://doi.org/10.13140/RG.2.1.1562.9842.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11.
- Prieto J, Wilson J, Tingle A, Cooper E, Handley M, Rycroft Malone J, et al. Preventing urinary tract infection in older people living in care homes: the ‘StOP UTI’ realist synthesis [published online ahead of print August 8 2024]. BMJ Qual Saf 2024. https://doi.org/10.1136/bmjqs-2023-016967.
- Booth A, Briscoe S, Wright JM. The ‘realist search’: a systematic scoping review of current practice and reporting. Res Syn Meth 2020;11:14-35.
- Harzing AW. Publish or Perish 2007. https://harzing.com/resources/publish-or-perish (accessed 29 October 2022).
- Dalkin SM, Greenhalgh J, Jones D, Cunningham B, Lhussier M. What’s in a mechanism? Development of a key concept in realist evaluation. Implement Sci 2015;10.
- Feo R, Rasmussen P, Wiechula R, Conroy T, Kitson A. Developing effective and caring nurse-patient relationships. Nurs Stand 2017;31:54-63. https://doi.org/10.7748/ns.2017.e10735.
- Pawson R. Digging for nuggets: how ‘bad’ research can yield ‘good’ evidence. Int J Soc Res Methodol 2006;9:127-42.
- Williams L, Rycroft-Malone J, Burton CR, Edwards S, Fisher, Hall B, et al. Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions. BMJ Open 2016;6.
- Meyer SB, Lunnay B. The application of abductive and retroductive inference for the design and analysis of theory-driven sociological research. Sociol Res Online 2013;18:86-9.
- Gollwitzer PM. Implementation intentions: strong effects of simple plans. Am Psychol 1999;54:493-50.
- NICE Guideline 112 . Urinary Tract Infection (Recurrent): Antimicrobial Prescribing 2018.
- Perrotta C, Aznar M, Mejia R, Albert X, Ng CW. Oestrogens for preventing recurrent urinary tract infection in postmenopausal women. Cochrane Database of Syst Rev 2008;2. https://doi.org/10.1002/14651858.CD005131.pub2.
- Bonkat G, Bartoletti R, Bruyèreet F, Cai T, Geerlings SE, Köves B, et al. EAU Guidelines n.d. https://uroweb.org/guidelines/urological-infections (accessed 29 October 2022).
- Tingstrom P, Milberg A, Sund-Levander M. Early nonspecific signs and symptoms of infection in institutionalized elderly persons: perceptions of nursing assistants. Scand J Caring Sci 2010;24:24-31.
- Jones LF, Cooper E, Joseph A, Allison R, Gold N, Donald I, et al. Development of an information leaflet and diagnostic flow chart to improve the management of urinary tract infections in older adults: a qualitative study using the Theoretical Domains Framework. BJGP Open 2020;4. https://doi.org/10.3399/bjgpopen20X101044.
- Beeber AS, Kistler CE, Zimmerman S, Dictus C, Ward K, Farel C, et al. Nurse decision-making for suspected UTI infections in nursing homes: potential targets to reduce antibiotic overuse. J Am Med Dir Assoc 2021;22:156-63. https://doi.org/10.1016/j.jamda.2020.06.053.
- Hughes C, Ellard D, Campbell A, Potter R, Shaw C, Gardner E, et al. A multifaceted intervention to reduce antimicrobial prescribing in care homes: a non-randomised feasibility study and process evaluation. Health Serv Deliv Res 2020;8:1-150.
- Arnold SH, Olesen JA, Jensen JN, Bjerrum L, Holm A, Kousgaard MB. Development of a tailored, complex intervention for clinical reflection and communication about suspected urinary tract infections in nursing home residents. Antibiotics 2020;9. https://doi.org/10.3390/antibiotics9060360.
- Jones LF, Williamson H, Downing P, Lecky DM, Harcourt D, McNulty C. A qualitative investigation of the acceptability and feasibility of a urinary tract infection patient information leaflet for older adults and their carers. Antibiotics 2021;10. https://doi.org/10.3390/antibiotics10010083.
- Sund-Levander M, Tingström P. Clinical decision-making process for early nonspecific signs of infection in institutionalised elderly persons: experience of nursing assistants. Scand J Caring Sci 2013;27:27-35.
- Chambers A, MacFarlane S, Zvonar R, Evans G, Moore JE, Langford BJ, et al. A recipe for antimicrobial stewardship success: using intervention mapping to develop a program to reduce antibiotic overuse in long-term care. Infect Control Hosp Epidemiol 2019;40:24-31.
- Arnold SH, Jensen JN, Bjerrum L, Siersma V, Bang CW, Kousgaard MB, et al. Effectiveness of a tailored intervention to reduce antibiotics for urinary tract infections in nursing home residents: a cluster, randomised controlled trial. Lancet Infect Dis 2021;21:1549-56.
- Pasay DK, Guirguis MS, Shkrobot RC, Slobodan JP, Wagg AS, Sadowski CA, et al. Antimicrobial stewardship in rural nursing homes: impact of interprofessional education and clinical decision tool implementation on urinary tract infection treatment in a cluster randomized trial. Infect Control Hosp Epidemiol 2019;40:432-7.
- Loeb M, Brazil K, Lohfeld L, McGeer A, Simor A, Stevenson K, et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomised controlled trial. BMJ 2005;331.
- McMaughan DK, Nwaiwu O, Zhao H, Frentzel E, Mehr D, Imanpour S, et al. Impact of a decision-making aid for suspected urinary tract infection on antibiotic overuse in nursing homes. BMC Geriatr 2016;16. https://doi.org/10.1186/s12877-016-0255-9.
- Ydemann M. Communication in a hospital by means of a standardised method. Ugeskr Laeger 2012;174:1798-801.
- Kousgaard MB, Olesen JA, Arnold SH. Implementing an intervention to reduce use of antibiotics for suspected urinary tract infection in nursing homes: a qualitative study of barriers and enablers based on Normalization Process Theory. BMC Geriatr 2022;22. https://doi.org/10.1186/s12877-022-02977-w.
- Allemann H, Sund-Levander M. Nurses’ actions in response to nursing assistants’ observations of signs and symptoms of infections among nursing home residents. Nurs Open 2015;2:97-104.
- van Buul LW, van der Steen JT, Doncker SM, Achterberg WP, Schellevis FG, Veenhuizen RB, et al. Factors influencing antibiotic prescribing in long-term care facilities: a qualitative in-depth study. BMC Geriatr 2014;14:1-36.
- Chaaban T, Alouah M, Lombrail P, Febvre HL, Mourad A, Morvillers JM, et al. Decisional issues in antibiotic prescribing in French nursing homes: an ethnographic study. J Public Health Res 2019;8.
- Downs M, Blighe A, Carpenter R, Feast A, Froggatt K, Gordon S, et al. A Complex Intervention to Reduce Avoidable Hospital Admissions in Nursing Homes: A Research Programme Including the BHiRCH-NH Pilot Cluster RCT. Programme Grants Appl Res 2021;9. https://doi.org/10.3310/pgfar09020.
- Ouslander JG, Lamb G, Tappen R, Herndon L, Diaz S, Roos BA, et al. Interventions to reduce hospitalisations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc 2011;59:745-53.
- Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care 1998;7:149-58. https://doi.org/10.1136/qshc.7.3.149.
- Currie G, White L. Inter-professional barriers and knowledge brokering in an organizational context: the case of healthcare. Organ Stud 2012;33:1333-61.
- Gbinigie OA, Ordonez-Mena JM, Fanshawe TR, Plüddemann A, Heneghan C. Diagnostic value of symptoms and signs for identifying urinary tract infection in older adult outpatients: systematic review and meta-analysis. J Infect 2018;77:379-90. https://doi.org/10.1016/j.jinf.2018.06.012.
- Chu CM, Lowder JL. Diagnosis and treatment of urinary tract infections across age groups. Am J Obstet Gynecol 2018;219:40-51.
- Berman P, Hogan DB, Fox RA. The atypical presentation of infection in old age. Age Ageing 1987;16:201-7. https://doi.org/10.1093/ageing/16.4.201.
- Mayne S, Bowden A, Sundvall PD, Gunnarsson R. The scientific evidence for a potential link between confusion and urinary tract infection in the elderly is still confusing-a systematic literature review. BMC Geriatr 2019;19:1-5.
- Hooper L, Abdelhamid A, Attreed NJ, Campbell WW, Channell AM, Chassagne P, et al. Clinical symptoms, signs and tests for identification of impending and current water-loss dehydration in older people. Cochrane Database Syst Rev 2015;4.
- Benton D. Dehydration influences mood and cognition: a plausible hypothesis?. Nutrients 2011;3:555-73. https://doi.org/10.3390/nu3050555.
- Balogun SA, Philbrick JT. Delirium, a symptom of UTI in the elderly: fact or fable? A systematic review. Can Geriatr J 2014;17.
- Pryor C, Clarke A. Nursing care for people with delirium superimposed on dementia. Nurs Older People 2017;29:18-21.
- Scottish Intercollegiate Guidelines Network (SIGN) . Management of Suspected Bacterial Lower Urinary Tract Infection in Adult Women 2020. www.sign.ac.uk (accessed 29 October 2022).
- NICE Quality Standards (SQ90) . Urinary Tract Infections in Adults 2015. www.nice.org.uk/guidance/qs90 (accessed 5 December 2023).
- Fleming A, Bradley C, Cullinan S, Byrne S. Antibiotic prescribing in long-term care facilities: a meta-synthesis of qualitative research. Drugs Aging 2015;32:295-303.
- Potter R, Campbell A, Ellard DR, Shaw C, Gardner E, Agus A, et al. Multifaceted intervention to reduce antimicrobial prescribing in care homes: a process evaluation of a UK-based non-randomised feasibility study. BMJ Open 2019;9.
- Powell C, Blighe A, Froggatt K, McCormack B, Woodward-Carlton B, Young J, et al. Family involvement in timely detection of changes in health of nursing homes residents: a qualitative exploratory study. J Clin Nurs 2018;27:317-27.
- Burton CR, Williams L, Bucknall T, Fisher D, Hall B, Harris G, et al. Theory and practical guidance for effective de-implementation of practices across health and care services: a realist synthesis. Health Serv Deliv Res 2021;9:1-102.
- Fenton JJ, Kravitz RL, Jerant A, Paterniti DA, Bang H, Williams D, et al. Promoting patient centered counseling to reduce use of low-value diagnostic tests: a randomized clinical trial. JAMA Intern Med 2016;176:191-7.
- May L, Franks P, Jerant A, Fenton J. Watchful waiting strategy may reduce low-value diagnostic testing. J Am Board Fam Med 2016;29:710-7. https://doi.org/10.3122/jabfm.2016.06.160056.
- Little P, Gould C, Williamson I, Moore M, Warner G, Dunleavey J. Pragmatic randomised controlled trial of two prescribing strategies for childhood acute otitis media. BMJ 2001;322:336-42. https://doi.org/10.1136/bmj.322.7282.336.
- MacGeorge EL, Caldes EP, Smith RA, Hackman NM, San Jose A. Reducing unwarranted antibiotic use for pediatric acute otitis media: the influence of physicians’ explanation and instruction on parent compliance with ‘watchful waiting’. J Appl Commun Res 2017;45:333-45. https://doi.org/10.1080/00909882.2017.1320575.
- Bunn F, Lynch J, Goodman C, Sharpe R, Walshe C, Preston N, et al. Improving living and dying for people with advanced dementia living in care homes: a realist review of Namaste Care and other multisensory interventions. BMC Geriatr 2018;18:1-5.
- Ashraf MS, Gaur S, Bushen OY, Chopra T, Chung P, Clifford K, et al. Infection Advisory SubCommittee for AMDA—The Society of Post-Acute and Long-Term Care Medicine . Diagnosis, treatment, and prevention of urinary tract infections in post-acute and long-term care settings: a consensus statement from AMDA’s Infection Advisory Subcommittee. J Am Med Dir Assoc 2020;21:12-24.e2. https://doi.org/10.1016/j.jamda.2019.11.004.
- Scottish Antimicrobial Prescribing Group (SAPG), Health Improvement Scotland, NHS Scotland . Decision Aid for Diagnosis and Management of Suspected Urinary Tract Infection (UTI) in People Aged 65 Years and Over 2021. www.sapg.scot/media/5844/decision-aid-for-diagnosis-and-management-of-suspected-uti-in-people-over-65-years.pdf (accessed 29 October 2022).
- Royal College of Physicians (RCP) . National Early Warning Score (NEWS) 2: Standardising the Assessment of Acute-Illness Severity in the NHS 2017. www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2.
- Shallcross L, Rockenschaub P, Blackburn R, Nazareth I, Freemantle N, Hayward A. Antibiotic prescribing for lower UTI in elderly patients in primary care and risk of bloodstream infection: a cohort study using electronic health records in England. PLOS Med 2020;17.
- TARGET . Treating Your Infection UTI Leaflet, for Older Adults and Those Who Care for Them. Version 2.4. 2018. https://elearning.rcgp.org.uk/mod/book/view.php?id=12647&chapterid=442.
- AMDA – The Society for Post-Acute and Long-Term Care Medicine . The IOU Study: Improving Outcomes of UTI Toolkit n.d. https://paltc.org/content/iou-toolkit.
- Pettersson E, Vernby A, Mölstad S, Lundborg CS. Can a multifaceted educational intervention targeting both nurses and physicians change the prescribing of antibiotics to nursing home residents? A cluster randomized controlled trial. J Antimicrob Chemother 2011;66:2659-66.
- Nace DA, Hanlon JT, Crnich CJ, Drinka PJ, Schweon SJ, Anderson G, et al. A multifaceted antimicrobial stewardship program for the treatment of uncomplicated cystitis in nursing home residents. JAMA Intern Med 2020;180:944-51. https://doi.org/10.1001/jamainternmed.2020.1256.
- Little P, Moore MV, Turner S, Rumsby K, Warner G, Lowes JA, et al. Effectiveness of five different approaches in management of urinary tract infection: randomised controlled trial. BMJ 2010;340.
- Toward Optimized Practice (TOP) Working Group for Urinary Tract Infections in Long Term Care Facilities . Diagnosis and Management of Urinary Tract Infections in Long Term Care Facilities: Clinical Practice Guideline n.d. www.albertahealthservices.ca/assets/info/asm/if-asm-cpg-diagnosis-management-urinary-tract-infection-ltcf.pdf (accessed 29 October 2022).
- Care Quality Commission (CQC) . Dignity and Nutrition for Older People: Review of Compliance 2011. www.cqc.org.uk/sites/default/files/documents/20111007_dignity_and_nutrition_inspection_report_final_update.pdf (accessed 29 October 2022).
- El-Sharkawy AM, Sahota O, Maughan RJ, Lobo DN. The pathophysiology of fluid and electrolyte balance in the older adult surgical patient. Clin Nutr 2014;33:6-13. https://doi.org/10.1016/j.clnu.2013.11.010.
- Hooper L, Bunn D, Jimoh FO, Fairweather-Tait SJ. Water-loss dehydration and aging. Mech Ageing Dev 2014;136–137:50-8. https://doi.org/10.1016/j.mad.2013.11.009.
- European Food Safety Authority (EFSA) Panel on Dietetic Products . Scientific opinion on dietary reference values for water. EFSA J 2010;8. https://doi.org/10.2903/j.efsa.2010.1459.
- Ferry M. Strategies for ensuring good hydration in the elderly. Nutr Rev 2005;63:S22-9. https://doi.org/10.1111/j.1753-4887.2005.tb00151.x.
- Wilson J, Elgohari S, Livermore DM, Cookson B, Johnson A, Lamagni T, et al. Trends among pathogens reported as causing bacteraemia in England, 2004–2008. Clin Microbiol Infect 2011;17:451-8.
- Hooton TM, Vecchio M, Iroz A, Tack I, Dornic Q, Seksek I, et al. Effect of increased daily water intake in premenopausal women with recurrent urinary tract infections: a randomized clinical trial. JAMA Intern Med 2018;178:1509-15. https://doi.org/10.1001/jamainternmed.2018.4204.
- Wilson J, Tingle A, Bak A, Greene C, Tsiami A, Loveday H. Improving fluid consumption in older people in care homes: an exploration of the factors contributing to under-hydration. Nurs Resid Care 2020;22:139-46. https://doi.org/10.12968/nrec.2020.22.3.139.
- Bak A, Wilson J, Tsiami A, Loveday H. Drinking vessel preferences in older nursing home residents: optimal design and potential for increasing fluid intake. Br J Nurs 2018;27:1298-304.
- Booth J, Agnew R. Evaluating a hydration intervention (DRInK Up) to prevent urinary tract infection in care home residents: a mixed methods exploratory study. J Frailty Sarcopenia Falls 2019;4:36-44.
- Lean K, Nawaz RF, Jawad S, Vincent C. Reducing urinary tract infections in care homes by improving hydration. BMJ Open Qual 2019;8. https://doi.org/10.1136/bmjoq-2018-000563.
- Long EM, Rickenbrode A, Thibodeaux T. Practice brief: a hydration initiative in a long-term care facility. Geriatr Nurs 2013;34:340-2.
- Meddings J, Rogers MAM, Krein SL, Fakih MG, Olmsted RN, Saint S. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf 2014;23:277-89.
- McNulty CA, Bowen J, Foy C, Gunn K, Freeman E, Tompkins D, et al. Is there an opportunity to reduce urinary catheter-related infections? Exploring variation in catheterisation rates in care homes. Br J Infect Control 2006;7:22-8.
- Meddings J, Rogers MAM, Macy M, Saint S. Systematic review and meta-analysis: reminder systems to reduce catheter-associated urinary tract infections and urinary catheter use in hospitalized patients. Clin Infect Dis 2010;51:550-60.
- Atkins L, Sallis A, Chadborn T, Shaw K, Schneider A, Hopkins S, et al. Reducing catheter-associated urinary tract infections: a systematic review of barriers and facilitators and strategic behavioural analysis of interventions. Implement Sci 2020;15. https://doi.org/10.1186/s13012-020-01001-2.
- Wanat M, Borek AJ, Atkins L, Sallis A, Ashiru-Oredope D, Beech E, et al. Optimising interventions for catheter-associated urinary tract infections (CAUTI) in primary, secondary and care home settings. Antibiotics 2020;9:1-13. https://doi.org/10.3390/antibiotics9070419.
- Mody L, Greene TM, Meddings J, . A national implementation project to prevent catheter-associated urinary tract infection in nursing home residents. JAMA Intern Med 2017;177:1154-62.
- Krein SL, Harrod M, Collier S, Davis KK, Rolle AJ, Fowler KE, et al. A national collaborative approach to reduce catheter-associated urinary tract infections in nursing homes: a qualitative assessment. Am J Infect Control 2017;45:1342-8. https://doi.org/10.1016/j.ajic.2017.07.006.
- Sreedhara M, Mazor KM, DuBeau C, Field TS, Ela JM, Gurwitz JH. Nursing home leaders’ views on catheter use and CAUTI as a quality and safety concern. J Am Geriatr Soc 2015;63:S213-4.
- Bell BG, Schellevis F, Stobberingh E, Goossens H, Pringle M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis 2014;14:1-3.
- Klay M, Marfyak K. Use of a continence nurse specialist in an extended care facility. Urol Nurs 2005;25.
- Northouse PG. Leadership: Theory & Practice. Sage Publications; 2021.
- André B, Sjøvold E, Rannestad T, Ringdal GI. The impact of work culture on quality of care in nursing homes: a review study. Scand J Caring Sci 2014;28:449-57.
- Rycroft-Malone J, Seers K, Eldh AC, Cox K, Crichton N, Harvey G, et al. A realist process evaluation within the Facilitating Implementation of Research Evidence (FIRE) cluster randomised controlled international trial: an exemplar. Implement Sci 2018;13.
- Kelley R, Griffiths AW, Shoesmith E, McDermid J, Couch E, Robinson O, et al. The influence of care home managers on the implementation of a complex intervention: findings from the process evaluation of a randomised controlled trial of dementia care mapping. BMC Geriatr 2020;20.
- Marshall M, Pfeifer N, de Silva D, Wei L, Anderson J, Cruickshank L, et al. An evaluation of a safety improvement intervention in care homes in England: a participatory qualitative study. J R Soc Med 2018;111:414-21. https://doi.org/10.1177/0141076818803457.
- Surr CA, Shoesmith E, Griffiths AW, Kelley R, McDermid J, Fossey J. Exploring the role of external experts in supporting staff to implement psychosocial interventions in care home settings: results from the process evaluation of a randomized controlled trial. BMC Health Serv Res 2019;19.
- Buswell M, Goodman C, Roe B, Russell B, Norton C, Harwood R, et al. What works to improve and manage fecal incontinence in care home residents living with dementia? A realist synthesis of the evidence. J Am Med Dir Assoc 2017;18:752-60.
- Low LF, Fletcher J, Goodenough B, Jeon YH, Etherton-Beer C, MacAndrew M, et al. A systematic review of interventions to change staff care practices in order to improve resident outcomes in nursing homes. PLOS One 2015;10. https://doi.org/10.1371/journal.pone.0140711.
- Thacker SB, Berkelman RL. Public Health Surveillance in the United States. Epidemiol Rev 1988;10:164-90.
- Scanlon KA, Wells CM, Woolforde L, Khameraj A, Baumgarten J, . Saving lives and reducing harm. A CAUTI reduction program. Nurs Econ 2017;35:134-41.
- Xu D, Kane R, Arling G. Relationship between nursing home quality indicators and potentially preventable hospitalisation. BMJ Qual Saf 2019;28:524-33.
- Haunch K, Thompson C, Arthur A, Edwards P, Goodman C, Hanratty B, et al. Understanding the staff behaviours that promote quality for older people living in long term care facilities: a realist review. Int J Nurs Stud 2021;117.
- McNulty C, Bowen J, Howell-Jones R, Walker M, Freeman E. Exploring reasons for variation in urinary catheterisation prevalence in care homes: a qualitative study. Age Ageing 2008;37:706-10.
- Smith SN, Greene MT, Mody L, Banaszak-Holl J, Petersen LD, Meddings J. Evaluation of the association between Nursing Home Survey on Patient Safety culture (NHSOPS) measures and catheter-associated urinary tract infections: results of a national collaborative. BMJ Qual Saf 2018;27:464-73.
- Abusalem S, Polivka B, Coty MB, Crawford TN, Furman CD, Alaradi M. The relationship between culture of safety and rate of adverse events in long-term care facilities. J Patient Saf 2019;17:299-304.
- Robbins I, Gordon A, Dyas J, Logan P, Gladman J. Explaining the barriers to and tensions in delivering effective healthcare in UK care homes: a qualitative study. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003178.
- Skills for Care . Care Certificate Workbook 2022. www.skillsforcare.org.uk/Developing-your-workforce/Care-Certificate/Care-Certificate-workbook.aspx (accessed 29 October 2022).
- Spilsbury K, Meyer J. Making claims on nursing work: exploring the work of healthcare assistants and the implications for registered nurses' roles. J Res Nurs 2005;10:65-83. https://doi.org/10.1177/136140960501000104.
- Mody L, Meddings J, Edson BS, McNamara SE, Trautner BW, Stone ND, et al. Enhancing resident safety by preventing healthcare-associated infection: a national initiative to reduce catheter-associated urinary tract infections in nursing homes. Clin Infect Dis 2015;61:86-94.
- Lindeman MA, Black K, Smith R, Gough J, Bryce A, Gilsenan B, et al. Changing practice in residential aged care using participatory methods. Educ Health (Abingdon) 2003;16:22-31.
- Lopez SH. Emotional labor and organized emotional care: conceptualizing nursing home care work. Work Occup 2006;33:133-60.
- Nicol JS, Dosser I. Understanding reflective practice. Nurs Stand 2016;30:34-42. https://doi.org/10.7748/ns.30.36.34.s44.
- Nursing & Midwifery Council . The Code Professional Standards of Practice and Behaviour for Nurses, Midwives and Nursing Associates 2015. www.nmc.org.uk/globalassets/sitedocuments/nmc-publications/nmc-code.pdf (accessed 29 October 2022).
- Page S, Meerabeau L. Achieving change through reflective practice: closing the loop. Nurse Educ Today 2000;20:365-72. https://doi.org/10.1054/nedt.2000.0430.
- Yeatts DE, Shen Y, Yeatts PE, Solakoglu O, Seckin G. Shared decision-making in nursing homes: factors associated with the empowerment of direct care workers. J Aging Health 2016;28:621-43.
- NICE Guideline . Urinary Tract Infection (Recurrent): Antimicrobial Prescribing n.d. www.nice.org.uk/guidance/ng112 (accessed 29 October 2022).
- Ahmed H, Farewell D, Jones HM, Francis NA, Paranjothy S, Butler CC. Antibiotic prophylaxis and clinical outcomes among older adults with recurrent urinary tract infection: cohort study. Age Ageing 2019;48:228-34. https://doi.org/10.1093/ageing/afy146.
- Albert X, Huertas I, Pereiro II, Sanfelix J, Gosalbes V, Perrota C. Antibiotics for preventing recurrent urinary tract infection in non-pregnant women. Cochrane Database Syst Rev 2004.
- Price JR, Guran LA, Gregory WT, McDonagh MS. Nitrofurantoin vs other prophylactic agents in reducing recurrent urinary tract infections in adult women: a systematic review and meta-analysis. Am J Obstet Gynecol 2016;215:548-60.
- Schwenger EM, Tejani AM, Loewen PS. Probiotics for preventing urinary tract infections in adults and children. Cochrane Database Syst Rev 2015. https://doi.org/10.1002/14651858.CD008772.pub2.
- Hidalgo G, Chan M, Tufenkji N. Inhibition of Escherichia coli CFT073 fliC expression and motility by cranberry materials. Appl Environ Microbiol 2011;77:6852-7.
- Juthani-Mehta M, Perley L, Chen S, Dziura J, Gupta K. Feasibility of cranberry capsule administration and clean-catch urine collection in long-term care residents. J Am Geriatr Soc 2010;58:2028-30. https://doi.org/10.1111/j.1532-5415.2010.03080.x.
- Jepson RG, Williams G, Craig JC. Cranberries for preventing urinary tract infections. Cochrane Database Syst Rev 2012. https://doi.org/10.1002/14651858.CD001321.pub5.
- Kranjčec B, Papeš D, Altarac S. D-mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial. World J Urol 2014;32:79-84. https://doi.org/10.1007/s00345-013-1091-6.
- Lenger SM, Bradley MS, Thomas DA, Bertolet MH, Lowder JL, Sutcliffe S. D-mannose vs other agents for recurrent urinary tract infection prevention in adult women: a systematic review and meta-analysis. Am J Obstet Gynecol 2020;223:265.e1-13. https://doi.org/10.1016/j.ajog.2020.05.048.
- Nalliah S, Fong JSH, Thor AYY, Lim OH. The use of chemotherapeutic agents as prophylaxis for recurrent urinary tract infection in healthy nonpregnant women: a network meta-analysis. Indian J Urol 2019;35:147-55. https://doi.org/10.4103/iju.IJU_378_18.
- Bakhit M, Krzyzaniak N, Hilder J, Clark J, Scott AM, Mar CD. Use of methenamine hippurate to prevent urinary tract infections in community adult women: a systematic review and meta-analysis. Br J Gen Pract 2021;71:e528-37. https://doi.org/10.3399/BJGP.2020.0833.
- Harding C, Mossop H, Homer T, Chadwick T, King W, Carnell S, et al. Alternative to prophylactic antibiotics for the treatment of recurrent urinary tract infections in women. BMJ 2022;376. https://doi.org/10.1136/bmj-2021-0068229.
- Eriksen B. A randomized, open, parallel-group study on the preventive effect of an estradiol-releasing vaginal ring (Estring) on recurrent urinary tract infections in postmenopausal women. Am J Obstet Gynecol 1999;180:1072-9. https://doi.org/10.1016/s0002-9378(99)70597-1.
- Ferrante KL, Wasenda EJ, Jung CE, Adams-Piper ER, Lukacz ES. Vaginal estrogen for the prevention of recurrent urinary tract infection in postmenopausal women: a randomized clinical trial. Female Pelvic Med Reconstr Surg 2021;27:112-7.
- Raz R, Stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med 1993;329:753-6. https://doi.org/10.1056/NEJM199309093291102.
- Raz R, Colodner R, Rohana Y, Battino S, Rottensterich E, Wasser I, et al. Effectiveness of estriol-containing vaginal pessaries and nitrofurantoin macrocrystal therapy in the prevention of recurrent urinary tract infection in postmenopausal women. Clin Infect Dis 2003;36:1362-8. https://doi.org/10.1086/374341.
Appendix 1 Search strategy for stage 1 scoping search, September 2020
Some material reproduced from Prieto et al. 45 Published by the BMJ Publishing Group Limited. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/.
Overview of databases and numbers of results
| Database | Date run | Results | Notes |
|---|---|---|---|
| CINAHL Plus with full text (EBSCOhost) | 26 September 2020 | 619 | |
| Ovid MEDLINE | 26 September 2020 | 669 | |
| Ovid EMBASE | 26 September 2020 | 1870 | |
| Cochrane Library | 26 September 2020 | 295 | 5 Cochrane Reviews 290 trials |
| ASSIA | N/A | N/A | Not available at Southampton |
| Bibliomap | 26 September 2020 | 0 | |
| Sociological Abstracts (ProQuest) | 1 October 2020 | 4 | |
| Scopus | N/A | N/A | Used Web of Science instead |
| Web of Science – Core Collection | 1 October 2020 | 865 | Core Collection includes the Social Sciences Citation Index. |
| NIHR Journals Library | 1 October 2020 | 2 | StOP UTI and PRINCESS. The PRINCESS papers are already retrieved from the other databases. |
| TOTAL | 4322 | ||
| TOTAL after deduplication | 2648 |
Main search
| Source/database, host, date searched | Search strategy | Number of results |
|---|---|---|
| CINAHL Plus with full text (EBSCOhost)
26 September 2020 |
|
619 |
Limiters – Published Date: 1 January 2010–31 December 2020
Limiters – Published Date: 1 January 2010–31 December 2020 Narrow by Language: – English |
||
| Ovid MEDLINE(R) and Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Daily and Versions(R) 1946–25 September 2020 Date searched: 26 September 2020 |
|
669 |
|
||
| Ovid EMBASE 1996–2020 Week 39
Date searched: 26 September 2020 |
|
1870 |
|
||
|
||
| Cochrane Library
%Cochranelibrary.com Date run: 26 September 2020 |
|
295 |
|
||
|
||
| Bibliomap %https://eppi.ioe.ac.uk/webdatabases/SearchIntro.aspx
Date searched: 26 September 2020 |
|
0 |
| Sociological Abstracts (via ProQuest)
Date searched: 1 October 2020 |
((ti((urinary NEAR/3 infection*) OR ‘urinary tract infection*’) OR ab((urinary NEAR/3 infection*) OR ‘urinary tract infection*’)) OR (ti(uti OR CAUTI OR utis OR CAUTIs) OR ab(uti OR CAUTI OR utis OR CAUTIs)) OR (ti(cystitis OR pyelonephritis OR bacteriuria) OR ab(cystitis OR pyelonephritis OR bacteriuria)) OR (ti(kidney NEAR/3 infection*) OR ab(kidney NEAR/3 infection*))) AND (MAINSUBJECT.EXACT(‘Nursing Homes’) OR MAINSUBJECT.EXACT(‘Long Term Care’) OR (ti((care OR residential OR nursing OR ‘aged care’ OR geriatric) NEAR/3 (home* OR facilit*)) OR ab((care OR residential OR nursing OR ‘aged care’ OR geriatric) NEAR/3 (home* OR facilit*))) OR (ti((‘long term’ OR long-term OR longterm) NEAR/3 (care OR facilit* OR centre OR center OR institution*)) OR ab((‘long term’ OR long-term OR longterm) NEAR/3 (care OR facilit* OR centre OR center OR institution*))) OR (ti(‘residential care’ OR ‘institutional care’ OR ‘aged care facilities’ OR ‘old* people* home*’ OR ‘rest home*’) OR ab(‘residential care’ OR ‘institutional care’ OR ‘aged care facilities’ OR ‘old* people* home*’ OR ‘rest home*’)) OR (ti((care OR centre OR center) NEAR/3 day) OR ab((care OR centre OR center) NEAR/3 day)))Limits applied | |
| Databases: Sociological Abstracts Narrowed by year: 2014; 2016; 2017; Language: English |
||
| Web of Science Core Collection
Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan = All years Date searched: 1 October 2020 |
OR AB = (urinary NEAR/3 infection* OR ‘urinary tract infection’)
|
865 |
|
||
Indexes = SCI-EXPANDED, SSCI, A&HCI, CPCI-S, CPCI-SSH, BKCI-S, BKCI-SSH, ESCI, CCR-EXPANDED, IC Timespan = 2010–20 |
||
| NIHR Journals Library %www.journalslibrary.nihr.ac.uk/
Date searched: 1 October 2020 |
(‘urinary tract infection*’ or uti or cauti or cystitis or pyelonephritis or bacteriuria or ‘kidney infection*’) AND (‘nursing home*’ or ‘care home*’ or ‘residential home*’ or ‘geriatric home*’ or ‘rest home*’ or ‘old* people’ or ‘elder* care’) 0 results ‘urinary tract infection’ AND ‘care home’ 0 results ‘urinary tract infection’ 17 results |
2 |
Two relevant studies:
|
||
| Both of the PRINCESS study papers were retrieved in the other database searches. ‘urinary tract infection’ or ‘urinary tract infections’ 4014 results 2011–20: 1569 results 2021–30: 290 results ‘urinary tract infection’ or ‘urinary tract infections’ AND ‘older people’ |
||
| 0 results ‘urinary tract infection’ AND care home = 0 results ‘urinary tract infection’ AND old = 0 results ‘urinary tract infection’ AND elderly = 0 results ‘urinary tract infection’ AND geriatric = 0 results ‘old people’ or ‘older people’ or elderly or ‘care home’ 4067 results Limited to HRCS health category: Renal and Urogenital 107 results – not finding UTIs |
||
Exploratory AHRQ safety program search
| Source/database, host, date searched | Search strategy | Number of results | |||
|---|---|---|---|---|---|
| Collated publications of the AHRQ Safety Program for Long-Term Care | |||||
| Scopus %Scopus.com
Date searched: October 2020 |
|
2 | |||
| Google Scholar
Date searched: October 2020 |
|
4 | |||
| Program final report | %www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/quality-resources/tools/cauti-ltc/modules/final-report.pdf
References |
5 | |||
| Program website
%www.ahrq.gov/hai/quality/tools/cauti-ltc/about-toolkit.html Date searched: October 2020 |
References on webpage = 6 – not program related publications
|
6 | |||
| Citation searching of eight key papers | |||||
| Scopus %Scopus.com
And Google Scholar Date searched: October 2020 |
Paper | Forward citations Scopus (Scholar)
(cited by) |
Backward citations
Scopus (of which papers published within the last 10 years) (references) |
Notes | 391 |
| Adkins J. Participating in a national project, Pennsylvania nursing homes reduce CAUTI. Patient Saf Advis 2016;13(4):149–53. | 0 (0) | 0 (0) | Not indexed in Scopus. Carried out a Reference field search for both title and the URL. |
||
| Bradley S. Evaluating the effect of infection control practices on reduction of CAUTIs in Pennsylvania long-term care facilities. Patient Saf Advis 2016;13(4):154–9. | 0 (0) | 0 (0) | Not indexed in Scopus. Carried out a Reference field search for both title and the URL. |
||
| Hutton DW, Krein SL, Saint S, Graves N, Kolli A, Lynem R, Mody L, et al. Economic evaluation of a catheter-associated urinary tract infection prevention program in nursing homes. J Am Ger Soc 2018;66(4):742–7. | 5 (13) | 29 (20) | |||
| Krein SL, Harrod M, Collier S, Davis KK, Rolle AJ, Fowler KE, Mody L. A national collaborative approach to reduce catheter-associated urinary tract infections in nursing homes: a qualitative assessment. Am J Infect Control 2017;45(12):1342–8. | 4 (9) | 26 (22) | |||
| Krein SL, Greene M, King B, Welsh D, Fowler KE, Trautner BW, et al. Assessing a National Collaborative Program to prevent catheter-associated urinary tract infection in a veterans health administration nursing home cohort. Infect Control Hosp Epidemiol 2018;39(7):820–5. | 4 (4) | 24 (20) | |||
| Meddings J, Saint S, Krein S, Gaies E, Reichert H, Hickner A, et al. Systematic review of interventions to reduce urinary tract infection in nursing home residents. J Hosp Med 2017;12(5):365–8. | 18 (23) | 115 (50) | |||
| Mody L, Meddings J, Edson BS, McNamara SE, Trautner BW, Stone ND, et al. Enhancing resident safety by preventing healthcare-associated infection: a national initiative to reduce catheter-associated urinary tract infections in nursing homes. Clin Infect Dis 2015;61(1):86–94. | 25 (48) | 53 (21) | |||
| Mody L, Greene TM, Meddings J, Krein SL, McNamara SE, Trautner BW, et al. A national implementation project to prevent catheter-associated urinary tract infection in nursing home residents. JAMA Intern Med 2017;177(8):1154–62. | 44 (57) | 41 (28) | |||
| Publish or Perish | Adkins 2016 0 Bradley 2016 0 Hutton 2018 10 Krein 2017 7 Krein 2018 4 Meddings 2017 22 Mody 2015 37 Mody 2017 54 |
134 | |||
| Key authors’ publications | |||||
| Author institution web page and Scopus | Krein = total 153 Meddings = total 77 Mody = total 211 Saint = total 240 |
681 | |||
Appendix 2 ‘If … then’ statements
Some material reproduced from Prieto et al. 45 Published by the BMJ Publishing Group Limited. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/.
Hydration
-
If staff are encouraged to focus on resident hydration, then they will be more confident that they can support them to drink (Booth, Lean, Wilson).
-
If staff are more aware of the importance of hydration, need to increase opportunities and choice of drinks, then residents will be supported to drink more fluids (Booth, Lean, Wilson).
-
If more drinking opportunities are incorporated into daily activities, then staff can devote more time to supporting residents to drink and the frequency of UTI among residents decreases (Booth, Lean, Wilson).
-
If fluid intake targets are set, then the residents will be supported to drink more fluids (Booth, Lean, Wilson).
-
If drinking rounds are monitored by Drinks Champion, then they will be delivered … (Booth, Lean, Wilson).
Preventing recurrent urinary tract infection
-
If care home residents are identified (using assessments, through review of care and medical notes, from recurrent UTI, from other conditions/characteristics known to increase risk of UTI, from catheter use) as potentially benefiting from the use of non-antibacterial prophylaxis (cranberry capsules, herbal teas, oestrogen treatment) and use of the prophylaxis is seen as a routine and important part of their care (correct dosage, timing of administration, recording/reporting of administration), then it is likely there will be a reduction in UTI/CAUTI.
Preventing catheter-associated urinary tract infection
-
If educational material is available in a range of formats and delivered by knowledgeable practitioners in a way that fits workforce abilities, then practice is improved.
-
If an improvement programme addresses not only knowledge barriers, but also a broad range of behavioural constructs to support change (e.g. beliefs, emotions, reinforcement, environmental context and resources) and aligns with external programmes and services, then it is more likely to be effective.
-
If care home staff are trained to implement evidence-based CAUTI interventions, incontinence planning and hydration activity they are empowered to challenge requests to catheterise and order urine cultures (Mody 2017).
-
If care home staff (nurses and healthcare support workers) are trained to implement evidence-based CAUTI interventions, incontinence planning and hydration activity, then rates of CAUTI will be minimised (practice will be enhanced; Mody 2017).
-
If care home staff have access to skilled facilitation (coaching) implementation of evidence-based CAUTI interventions, incontinence planning and hydration activity then improvement is more likely to succeed.
-
If a collaborative approach is used with feedback to care home staff, then they are motivated to adhere to best practice.
Understanding what constitutes a urinary tract infection
-
If care home staff understand the signs and symptoms of UTI in their residents and can communicate key clinical observations within their team and to primary care staff (common language and common understanding of what needs to be communicated), then the accuracy of UTI diagnosis will be improved (Arnold 2020).
-
If there is a common understanding of signs and symptoms of UTI (through education and use of language that is appropriate for the level of clinical knowledge), then it is likely appropriate information will be communicated accurately across the care home and healthcare team (Arnold 2020).
-
If an improvement programme addresses not only knowledge barriers, but also a broad range of behavioural constructs to support change (e.g. beliefs, emotions, reinforcement, environmental context and resources) and aligns with external programmes and services, then it is more likely to be effective (Chambers 2018; Pasay 2019).
Recognising urinary tract infection and communicating concerns
-
If the responsibilities of the care home staff in the recognition and diagnosis process of UTI for their residents are understood and they feel confident in raising and communicating concerns with colleagues, then potential UTIs are likely to be investigated and treated (Arnold 2020).
-
If care home staff (nurses and healthcare support workers) are actively involved in assessing and recognising early signs and symptoms suggestive of UTI and physicians have confidence in the information they provide, then opportunities to instigate preventative measures (e.g. increased oral hydration, support with hygiene, support with toileting) and avoid unnecessary antibiotic treatment are more likely to be applied.
-
If there is a common understanding of signs and symptoms of UTI (through education and use of language that is appropriate for the level of clinical knowledge), then it is likely appropriate information will be communicated accurately across the care home and healthcare team.
-
If an algorithm is a good fit with actual situations in practice and supports communication by care staff with clear roles and responsibilities, then it may promote use of preventative measures (e.g. encouraging fluid intake) before contacting the doctor for a suspected infection (Potter 2019; Hughes 2020; Pasay 2019).
-
If interventions for improving UTI recognition and diagnosis are designed with those involved (care home staff and primary care staff), then interventions are more likely to be used and be useful because they identify and overcome the challenges for implementation.
-
If assessment/decision tools allow for systematic gathering and structuring of relevant information (signs and symptoms that may or may not relate to UTI) that can be used to assess and communicate the likelihood someone has a UTI (through evidence-based algorithms) and are considered easy to use and useful to those using them, then they can improve recognition/diagnosis of UTI (Arnold 2020).
-
Digital support tools could help care assistants make good decisions or re-enforce good decision making. Tools need to provide rapid responsive information and be appropriate for existing technology.
Active monitoring
-
If residents and family members are engaged on the topic of AMR, better informed about alternative preventative strategies to minimise risk of UTI and involved in decisions, then they may be more supportive of efforts to reduce use of antibiotics (Potter 2019 – REACH study; Chambers 2018; Pasay 2019).
-
If care home staff (nurses and healthcare support workers) are actively involved in assessing and recognising early signs and symptoms suggestive of UTI and physicians have confidence in the information they provide, then opportunities to instigate preventative measures (e.g. increased oral hydration, support with hygiene, support with toileting) and avoid unnecessary antibiotic treatment are more likely to be applied (Chaaban 2019; Tingstrom 2010).
Involving the resident and family
-
If interventions for improving UTI recognition and diagnosis are designed with those involved (care home staff and primary care staff), then interventions are more likely to be used and be useful because they identify and overcome the challenges for implementation (Arnold 2020).
-
If an intervention is multidisciplinary (addressing the nurse–physician–family triad), incorporates audit and feedback and is integrated into existing quality, safety and IPC programmes, then this may be more influential in reducing unnecessary antibiotic prescribing in care home settings.
-
If residents and families are better informed about alternative preventative strategies to minimise risk of UTI, they may be more supportive of efforts to reduce use of antibiotics.
-
If family members are engaged on the topic of AMR and involved in decisions about ill residents, then this may build confidence and trust, promoting partnership working.
-
If care home staff have access to skilled facilitation (coaching) implementation of evidence-based CAUTI interventions, incontinence planning and hydration activity, then improvement is more likely to succeed (Mody 2017).
-
If educational material is available in a range of formats and delivered by knowledgeable practitioners in a way that fits workforce abilities, then practice is improved (Mody 2017).
-
If a collaborative approach is used with feedback to care home staff, then they are motivated to adhere to best practice (Mody 2017).
Appendix 3 Stage 2 supplementary and purposive searches to support programme theory development
Some material reproduced from Prieto et al. 45 Published by the BMJ Publishing Group Limited. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/.
Soft signs and patient deterioration
Highly focused searches to identify relevant results only. Ignored results to do with recognising soft signs in hospitals, and results to do with the NEWS tool for measurable signs, that is not soft signs.
| Source/database, host, date searched | Search strategy | Number of results |
|---|---|---|
| RESTORE2 web pages on AHSN website and Google searches
Date searched: June 2021 |
Iterative searching, by following links from the RESTORE2 webpages, and Google searches including the following keywords: patient and deteriorat*, care home, evaluation. Searching for specific tools as they were identified (e.g. Significant Care, Significant 7, Stop and Watch, Is my resident unwell?), ‘soft sign*’ | 31 |
| CINAHL (EBSCOhost)
Date searched: 5 July 2021 |
10 results, 0 relevant. |
0 |
| Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R) 1946–2 July 2021 Date searched: 5 July 2021 |
38 results, 0 relevant to UTI or infections in care homes |
0 |
| Open Grey
Date searched: 5 July 2021 |
‘soft sign’ = 0 results ‘soft signs’ = 1 result, 0 relevant (dyslexia) |
0 |
Non-antimicrobial therapeutic interventions for recurrent urinary tract infection, including oestrogen therapy
Highly focused searches carried out by the research team to identify relevant results only.
| Source/database, host, date searched | Search strategy | Number of results |
|---|---|---|
| Reference checking of the following key review publications. Date searched: September 2021 |
|
13 |
| Added after consultation with experts | Bonkat et al., 2022 – EAU guidelines Harding – Hippurate trial results (2022) |
2 |
Hydration to prevent urinary tract infection
The research team set a date limit of the most recent 5 years to retrieve only the most recent publications.
| Source/database, host, date searched | Search strategy | Number of results |
|---|---|---|
| Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R) 1946–29 November 2021 Date searched: 30 November 2021 |
|
56 |
| CINAHL (EBSCOhost)
30 November 2021 Date searched: 30 November 2021 |
|
49 |
| SCIE Social Care Online | Subject term ‘hydration’ include this term only AND all fields ‘urinary tract infection’ = 0 results Subject term ‘hydration’ include this term only AND all fields ‘infection’ = 2 results, 2015-current = 0 results. Subject term: ‘older people’ include narrower terms AND subject term: ‘hydration’ = 29 results, 2016-current = 7 results |
7 |
| Citation searching of key papers using Scopus | ||
|
Scopus
Date searched: 30 November 2021 |
Citation search of Wilson 2019 | 8 |
| Reference search of Wilson 2019 (only include 2016 onwards) | 4 | |
| Citation search of Scott 2020 | 5 | |
| Reference search of Scott 2020 (only include 2016 onwards) | 8 | |
| Other grey literature | ||
| SCIE website
Date searched: 30 November 2021 |
www.scie.org.uk/search?sq=hydration+AND+urinary+tract+infection
4 results, 3 relevant (2 are the same resource) |
2 |
| NHS Improvement website: %England.nhs.uk
Date searched: 30 November 2021 |
0 results for both urinary tract infection AND hydration | 0 |
| AHSN Network: %ahsnnetwork.com
Date searched: 30 November 2021 |
1 result for hydration or hydrate (Good Hydration! project) | 1 |
| Open Grey
Date searched: 2 December 2021 |
Hydrat* AND ‘urinary tract infection*’ = 0 results; hydrat* AND infection* = 0 results; ‘urinary tract infection*’ = 8 results, none on prevention or older people = 0. | 0 |
| Google searches
Date searched: 1–2 December 2021 |
(hydrate OR hydration) AND ‘urinary tract infection’ AND site: %.nhs.uk
About 3860 results, first 10 pages browsed = 11 results (hydrate OR hydration) AND ‘urinary tract infection’ AND site: %.gov.uk About 537 results, first 5 pages browsed = 4 results (hydrate OR hydration) AND ‘urinary tract infection’ AND site: %.org.uk About 1440 results, first 5 pages browsed = 4 results (hydrate OR hydration) AND ‘urinary tract infection’ AND site: %.ac.uk About 2990 results, first 5 pages browsed = 1 result |
|
| RCN %rcn.org.uk
Date searched: 2 December 2021 |
search box: urinary tract infection 3 results, none relevant Search box: hydration 22 results, none relevant |
0 |
| AGE UK %ageuk.org.uk
Date searched: 2 December 2021 |
search box: urinary tract infections 0 results linking hydration and UTIs |
0 |
| CQC %cqc.org.uk
Date searched: 2 December 2021 |
Search themed publications (n = 47), 0 relevant results | 0 |
Family involvement
A date limit of 10 years was applied in line with the main search.
| Source/database, host, date searched | Search strategy | Number of results |
|---|---|---|
| Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R) 1946–2 December 2021 Date searched: 3 December 2021 |
|
303 |
|
||
| CINAHL (EBSCOhost)
3 December 2021 |
|
63 |
|
||
| SCIE Social Care Online
Date searched: 3 December 2021 |
Subject term ‘families’ AND subject term ‘care homes’ NOT title ‘visit*’: 172 records limited to 2012 onwards: 56 records Subject term ‘families’ AND subject term ‘infectious diseases’ NOT title ‘visit*’ – 10 results, none relevant All fields: ‘urinary tract infection*’ AND subject term ‘families’ = 0 results. |
56 |
| NICE Evidence
Date searched: 3 December 2021 |
Various iterations of the following search terms: family, families, care homes, family participation, family engagement, family involvement, family influence 1 potentially relevant result – also identified in Social Care Online (Honoured guests. 2017) Other results were to do with the impact of visiting restrictions during the recent pandemic and not to do with involvement in care of the resident. |
0 |
| Citation searching of key papers using Scopus | ||
|
Scopus
Date searched: 3 December 2021 |
Mangal 2021 citations Mangal S, Pho A, Arcia A, Carter E. Patient and family engagement in catheter-associated urinary tract infection (CAUTI) prevention: a systematic review. Jt Comm J Qual Patient Saf 2021;47(9):591–603. |
1 |
| Mangal 2021 references (within 10-year date limit) | 31 | |
| Powell 2018 citations Powell C, Blighe A, Froggatt K, McCormack B, Woodward-Carlton B, Young J, et al. Family involvement in timely detection of changes in health of nursing home residents: a qualitative exploratory study. J Clin Nurse 2018;27(1–2):317–27. |
15 | |
| Powell 2018 references (within 10-year date limit) | 21 | |
| Other grey literature | ||
| SCIE (Social Care Institute for Excellence)
Date searched: 3 December 2021 |
%scie.org.uk > subject topic ‘Care homes’ – 69 resources browsed, 1 relevant result | 1 |
| Open Grey
Date searched: 3 December 2021 |
Various combinations of keywords family, families, engagement, involvement, participation, care home* or urinary tract infection* or infection* = 0 results | 0 |
| NHS Improvement
%England.nhs.uk Date searched: 3 December 2021 |
Various combinations of keywords family, families, engagement, involvement, participation, care home* or urinary tract infection* or infection* = 0 results | 0 |
| Age UK
Date searched: 3 December 2021 |
Hand-searched Reports and briefings, Consultation responses, and Evaluation reports = 0 results for family involvement in decision-making for UTIs, infection or in care homes | 0 |
| CQC %cqc.org.uk Date searched: 3 December 2021 | Hand search of publications section – 1 results | 1 |
| Google searches
Date searched: 3 December 2021 |
(family engagement) AND (‘care home*’) AND ‘care decisions’ AND (site: %.org.uk OR site: %.nhs.uk OR site: %.gov.uk) About 2360 results, first 5 pages browsed – 0 relevant results (family involvement) AND (‘care home*’) AND ‘care decisions’ AND (site: %.org.uk OR site: %.nhs.uk OR site: %.gov.uk) About 2250 results, first 5 pages browsed – 2 potentially relevant results. (family OR families) AND (‘care home*’) AND (decision* OR involvement) AND (site: %.org.uk OR site: %.nhs.uk OR site: %.gov.uk) About 219,000 results, first 5 pages browsed – 0 relevant results |
2 |
Continence and urinary tract infection
| Source/database, host, date searched | Search strategy | Numṭṭber of results |
|---|---|---|
| Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R) 1946–8 December 2021 Date searched: 9 December 2021 |
|
170 |
|
||
|
||
| CINAHL Plus with full text (EBSCOhost)
Date searched: 9 December 2021 |
|
142 |
|
||
|
||
|
||
| SCIE Social Care Online
Date searched: 9 December 2021 |
Subject term: ‘incontinence’ AND All fields: ‘urinary tract infections*’ AND Subject term: ‘care homes’ = 0 results All fields: ‘continence’ AND All fields: ‘urinary tract infections*’ AND Subject term: ‘care homes’ = 1 result (public reporting of quality indicators) Subject term: ‘incontinence’ AND All fields: ‘urinary tract infections*’ AND Subject term: ‘older people’ = 0 results |
2 |
| All fields: ‘continence’ AND All fields: ‘urinary tract infections*’ AND Subject term: ‘older people’ = 0 results All fields: ‘continence advisor*’ OR All fields: ‘continence specialist*’ = 0 results Subject term: ‘incontinence’ AND All fields: ‘nurse specialist*’ = 0 results Subject term: ‘incontinence’ AND All fields: ‘nurse practitioner*’ = 1 result (continence care for people with dementia at home) |
||
| Other grey literature | ||
| SCIE website
%www.scie.org.uk Date searched: 8 December 2021 |
45 results for continence, 2 relevant 89 results for incontinence, 0 relevant 4 results for continence advisor, 1 relevant |
3 |
| NHS Improvement website: %England.nhs.uk
Date searched: 8 December 2021 |
33 publication results for continence, 0 relevant 0 publication results for incontinence 0 results for continence advisor |
0 |
| AHSN Network: %ahsnnetwork.com
Date searched: 8 December 2021 |
0 results continence, incontinence, advisor | 0 |
| Open Grey (DANS Easy Archive)
Date searched: 8 December 2021 |
3 results for continence, 0 relevant | 0 |
| RCN
%rcn.org.uk Date searched: 8 December 2021 |
Search box: continence 15 results, 1 relevant Search box: incontinence 14 results, 0 relevant Search box: continence advisor – 0 results Search box: continence specialist – 0 results |
1 |
| AGE UK
%ageuk.org.uk Date searched: 8 December 2021 |
Search box: continence 37 results, 1 relevant Search box: incontinence 58 results, 0 relevant |
1 |
| CQC
%cqc.org.uk Date searched: 8 December 2021 |
22 results for continence, 0 relevant 14 results for incontinence, 0 relevant |
0 |
| Google searches
Date searched: 9 December 2021 |
‘continence care’ AND ‘urinary tract infection*’ AND ‘care home*’ AND (site: %.org.uk OR site: %.nhs.uk OR site: %.gov.uk) About 337 results, first 5 pages screened, 4 results (‘continence advisor’ or ‘continence specialist’) AND (‘care home*’) About 214 results, first 5 pages screened, 4 results |
8 |
Appendix 4 Summary of stage 2 searches and retrieval
Some material reproduced from Prieto et al. 45 Published by the BMJ Publishing Group Limited. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/.
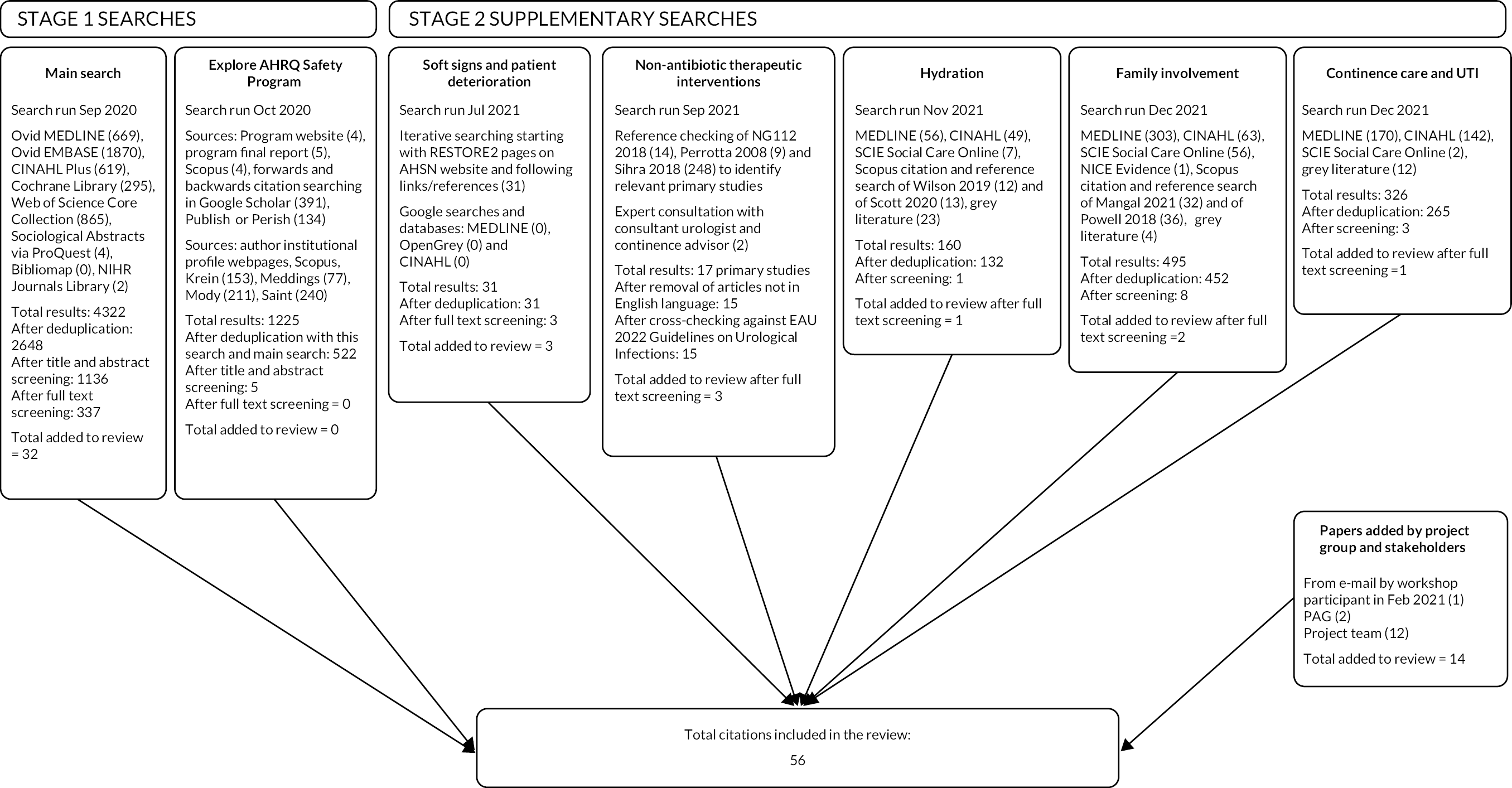
Appendix 5 Relevant and good enough flowchart
Some material reproduced from Prieto et al. 45 Published by the BMJ Publishing Group Limited. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/.
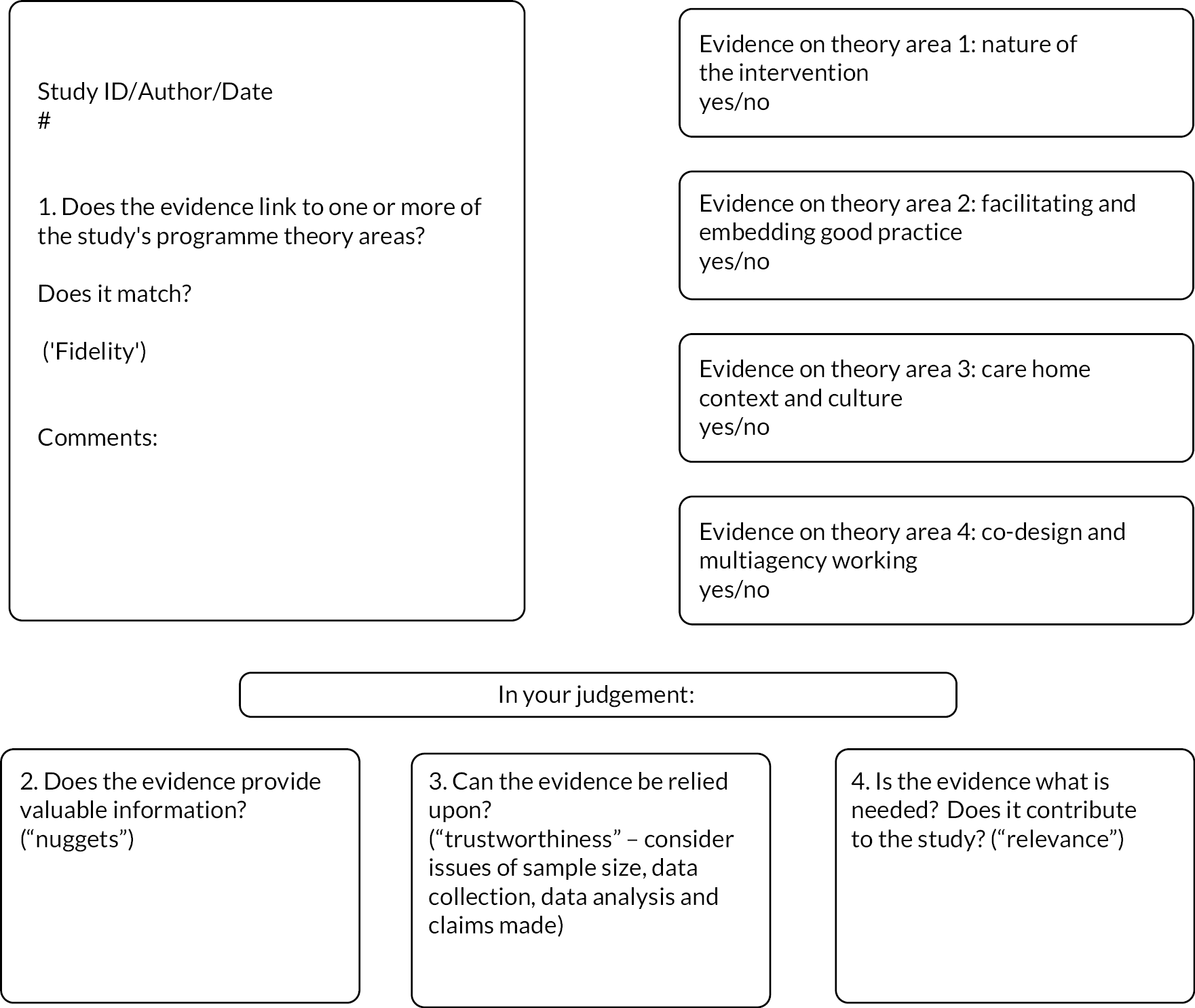
Appendix 6 Data extraction form – completed example
Some material reproduced from Prieto et al. 45 Published by the BMJ Publishing Group Limited. This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See http://creativecommons.org/licenses/by/4.0/.
| Study ID and full reference | |
|---|---|
| # | 3964 |
| Document type | Journal article |
| What is the study’s aim/purpose? | Paper describes the development of a tailored, complex intervention for a cluster-randomised trial that targets the knowledge of UTI and communication skills in nursing home staff to reduce antibiotic prescriptions. |
| What is the intervention (if applicable)? | Pre-intervention – development of a reflection tool (decision aid) and a communication tool (ISBAR), collectively referred to as a ‘dialogue tool’, together with a case-based education session to support nursing home staff to convey relevant information to the GP on their observations of residents whom they consider may have a UTI to reduce misdiagnosis and unnecessary prescribing of antibiotics. |
| Design/method and its appropriateness for the aims/purpose of the study | Mixed methods including participatory observations in nursing homes, interviews with stakeholders and survey of GPs to inform the design of a tailored complex intervention and identify and address barriers to implementation. Design/method appropriate for the aims/purpose of the study. |
| Sample type and size | Observations in nursing home; focus group with three healthcare helpers and two healthcare assistants; ‘double’ interview with one GP and one medical secretary; ‘double’ interview with two senior citizens; individual interviews with two registered nurses; two single interviews and then four short telephone interviews with a head nurse and nurse involved in the pilot study. Purposive sampling. |
| Population and setting | Healthcare helpers and assistants working in nursing homes in Denmark, other key stakeholders including registered nurses, a GP, a medical secretary and two senior citizens. |
| Data collection method | Participatory observations in nursing homes; interviews; focus group |
| Approach to analysis | Qualitative |
| Effect of intervention on UTI vs. comparator (if applicable) | N/A |
| Side effects of treatment (if applicable) | N/A |
| Evidence of adherence to treatment (if applicable) | N/A |
| Conclusions | Need to change the beliefs of nursing home staff about UTIs and their management to deliver sustainable change in antibiotic prescribing behaviour. |
| Limitations | Small sample – one nursing home. Authors note that patient perspective may be under-represented as the two senior citizens who participated as stakeholders were a retired GP and a retired nurse. Nursing home residents were not included. The only nursing home informants in the pilot study were registered nurses (n = 2) as other staff were absent (due to holiday or illness). Approach to and use of participatory observations not described in the paper other than stating these were done in five nursing homes by the primary investigator. |
| Companion papers | Protocol for the RCT (Arnold et al., 2020) gives additional background and care home context relating to UTI. |
| Topic 1: Developing interventions to optimise good practice | |||||
|---|---|---|---|---|---|
| Prompts: | |||||
| Bundled care | Tools for
assessing soft signs, decision support, structured communication |
Roles, responsibilities and skills of staff | Aligned to existing priorities | Support from GP and other health professionals | Other |
| Actions before contacting the GP added to the tool, including increased observation of the resident and preventative hygienic measures (e.g. improved intimate hygiene). Tool adapted to accommodate a checkbox to record non-specific symptoms, together with a definition of delirium to avoid confusion between the two. Space to record changes in urine (smelly, unclear) added even though the researchers recognised this is not a diagnostic sign as nursing home staff searched for a space to put this and leaving it out could become a barrier to using the dialogue tool. Final intervention contains a dialogue tool comprising a reflection (to prompt discussion with colleagues and embed UTI learning) and a communication component (to structure clinical history collection, communication of clinical history and decision-making around if UTI and treatment required) and a case-based educational session (to address UTI knowledge gaps and introduce the dialogue tool). | |||||
| Healthcare helpers communicate their observations to the healthcare assistant or registered nurse, who are the only ones permitted to contact the GP directly. When the GP is not available to discuss directly with nursing home staff (found to be the most common situation) a message is conveyed to the GP by the medical secretary. Nursing home staff work with a spectrum of non-specific behavioural symptoms ranging from delirium to slight change. They understand that delirium requires immediate medical attention and a slight change requires observation and preventative measures such as ensuring fluid intake. ‘Sound knowledge of UTIs and good communication skills are central to providing sufficient and correct information for physicians to make an appropriate treatment decision.’ Care home staff first noticing/evaluating possible symptoms of UTI in complex residents were the least clinically trained for this. Communication of UTI passed through a number of professionals (healthcare assistants, nurses, GPs, medical secretaries). History taking and reporting unstructured and could focus on known and insignificant details. Not recognising UTI as diagnosis of exclusion, expectation that non-specific symptoms indicated UTI. Reliance on intuitive reasoning leading to suspicion of UTI. | |||||
| How is care relating to UTI prevention and recognition integrated into daily care and prioritised? | |||||
| Healthcare helpers and assistants are the first to notice if a nursing home resident appears different than usual. Healthcare assistants and nurses equated mild confusion with delirium and saw this as a symptom of UTI. Fear of missing a UTI diagnosis appeared to underpin this, which also explained why they found it hard to disregard a positive urine (dipstick) test. All healthcare staff involved in the tailoring of the tool equated a positive urine tests smelly and unclear urine with UTI. They uncritically suspected UTI when they observed a nonspecific symptom. Responsibility for UTI prevention and recognition is with healthcare helpers and healthcare assistants who recognise subtle changes that may indicate UTI. | |||||
| Other findings of relevance (not relating to prompts) | |||||
| Objective, measurable results of urine tests prioritised by GP over subjective assessments of signs and symptoms (‘soft signs’) when making a diagnosis. Interviews with nursing home staff found that when using the decision flowchart with a clinical case of a resident with non-specific behavioural changes and smelly urine, their intuitive reasoning led to inappropriate suspicion of UTIs even though they recognised urinary symptoms were absent. Nursing assistant said she ignored the other possible paths in the flowchart when the resident had light confusion, seeing this (incorrectly) as ‘one or more constitutional symptoms’ of UTI. Findings revealed it can be difficult for nursing home staff to change their intuitive understandings of what constitutes a UTI. The tool incorporated a reflective discussion section for staff to check their understanding and learn from each other. Education session included content designed to shift thinking towards UTI as a diagnosis of exclusion (ruling out alternative causes of symptoms before deciding on UTI). Researchers explained findings according to the dual process theory of cognition (intuitive and analytical system – thinking fast and slow) and also cognitive dissonance to explain the reaction of staff when their knowledge and practice were misaligned with the definition of UTI used in the reflection tool. | |||||
| Is the evidence provided in this theory area good and relevant enough to be included in the synthesis (consider issues of sample size, data collection, data analysis, claims made and any limitations)? | |||||
| Yes | |||||
| Topic 2: Delivering and sustaining good practice | ||||
|---|---|---|---|---|
| Prompts: | ||||
| Multifaceted design | Skilled facilitation | Tailored mixed mode education, huddles | Monitoring and feedback | Champions as change agents |
| Successful support tools | Management support | Campaigns | Regulatory incentives and oversight | Other |
| How is the intervention delivered and what impact does this have on implementation of practices to recognise and prevent UTI? | ||||
| The plan for the intervention is to introduce the tool through a case-based education session that addressed UTI knowledge gaps and demonstrated the use of the tool. The tool would be used as part of the clinical history gathering and reporting and as reflection within the care home team for what the preventative measures and diagnosis were. The intervention aims to address knowledge gaps, address commonly held misunderstandings of UTI to develop and embed more evidence-based understanding across all care home staff through discussion/reflection with colleagues to check observations, thinking and actions. To improve clinical history gathering and reporting within the care home and when communicating with GPs. | ||||
| Other findings of relevance (not relating to prompts) | ||||
| Is the evidence provided in this theory area good and relevant enough to be included in the synthesis (consider issues of sample size, data collection, data analysis, claims made and any limitations)? | ||||
| No | ||||
| Topic 3: Care home context and culture | ||||
|---|---|---|---|---|
| Prompts: | ||||
| Empowered and developed workforce | Effective leadership | Optimised staffing and skill mix | Safety culture embedded | Engaged in audit and Quality Improvement |
| UTI recognised as preventable | External regulation | Involves resident and family | Engaged and empowered residents | Other |
| How do individuals/teams and residents/families become empowered to engage in UTI prevention and recognition? By recognising the roles each staff member has in recognition of UTI, the intervention was developed to be appropriate to their expected level of clinical/resident knowledge (e.g. working with their knowledge about how a resident is when well, their understanding of the signs of UTI, the language they are familiar with for UTI). The tool allows for structured information gathering and communication with colleagues and GPs. |
||||
| Other findings of relevance (not relating to prompts) | ||||
| Knowledge of UTI – consider the ‘reverse triangle’ that UTI is a diagnosis of exclusion rather than the default diagnosis. | ||||
| Is the evidence provided in this theory area good and relevant enough to be included in the synthesis (consider issues of sample size, data collection, data analysis, claims made and any limitations)? | ||||
| Yes | ||||
| Topic 4: Co-design and multiagency working | |||||
|---|---|---|---|---|---|
| Prompts: | |||||
| Tailored to context | Common language | Shared goals | Aligned to existing priorities | Support from GP and other HCPs | Other |
| Tool tailored to needs of staff across five cycles. This included: including a space to record intuitive and non-evidence based but commonly held beliefs of the signs of UTI (e.g. look and smell of UTI). Space to record dipstick results (as this was an expected test by GPs). Simplifying language. Focus on gathering and communicating clinically relevant information. | |||||
| Adapted Loeb diagnostic algorithm originally developed for physicians and nurses for use by healthcare helpers, assistants and nurses using vocabulary understandable to them. GPs reported that they thought the nursing home staff sometimes contacted general practice too early in the illness. |
|||||
| What is the nature of relationships between care home staff and the HCPs/agencies they work with and how do relationships impact on involvement in UTI prevention and recognition? | |||||
| ‘The workflow in the nursing homes and the communication pathway from the bedside of the resident to the GP mean that the task of evaluating highly complex patients falls on the healthcare staff least trained for it.’ ‘The information about the condition of the residents passes through many actors before reaching the GP.’ |
|||||
| ‘Nursing home staff’s reports to the GP about the conditions of the residents often included insignificant deviations from the norm, and descriptions were often vague.’ Paper highlights some issues of trust that GPs have with care home staff. This appears to be through missing information, concerns that some contact is unnecessary and communication that is not focused. Communication for UTI is usually conducted via telephone and GPs rarely visit for UTI, prescribing based on the information they are provided by the care home. | |||||
| How does the work of UTI prevention and recognition align with/relate to other priorities? | |||||
| Seems to be a disconnect between prevention (not really discussed) and preventative or non-ABs measures not considered (according to GPs) and recognition in that many non-specific symptoms considered to be linked to UTI. Shows high awareness of possibility of UTI, concerns around not spotting UTI – but suggests limited understanding of prevention and alternative methods. | |||||
| Other findings of relevance (not relating to prompts) | |||||
| Protocol for the RCT gives additional background and care home context relating to UTI. | |||||
| Is the evidence provided in this theory area good and relevant enough to be included in the synthesis (consider issues of sample size, data collection, data analysis, claims made and any limitations)? | |||||
| Yes | |||||
Appendix 7 Resources to support prevention and recognition of UTI and CAUTI in the care home setting
| Name | Year | Producer | Target group | Intended end user | Clinical action | Action type | Tool type | Website | Location |
|---|---|---|---|---|---|---|---|---|---|
| UTI Checklist | 2021 | HCAI Steering Group, Care Home Steering Group, NHS | 65 and over, long-term care residents, older people | Care home staff | Diagnosis, management, prevention, UTI | Decision- making | Checklist | www.knowledgeanglia.nhs.uk/LinkClick.aspx?fileticket=cBFku0NQWkU%3D&tabid=824&portalid=1&mid=981 | UK |
| Urinary tract infections – a leaflet for older adults and carers | 2021 | TARGET, UK Health Security Agency, Jun (2021) | Older people | Carers, older adults | UTI | Decision-making, educational | Leaflet | %www.rcgp.org.uk/clinical-and-research/resources/toolkits/amr/target-antibiotics-toolkit/-/media/22C7A1B941F54956A58532E90E8F24A5.ashx | UK |
| Urinary tract infection (recurrent): antimicrobial prescribing guideline | 2018 | NICE | Children, young people | Carers, patients, prescribers | Prescribing, UTI | Decision-making | Guide | %www.nice.org.uk/guidance/ng112 | UK |
| Toolkit to reduce CAUTI and other HAIs in long-term care facilities | 2021 | Agency for Healthcare Research and Quality AHRQ | Long-term care residents | Care home staff, prescribers, nurse practitioners | CAUTI, HAIs, UTI | Decision-making, educational | Toolkit | %www.ahrq.gov/hai/quality/tools/cauti-ltc/index.html | US |
| Recurrent uncomplicated urinary tract infections in women: AUA/CUA/SUFU Guideline, 2019 | 2019 | American Urological Association, (AUA), Canadian Urological Association (CUA), Society of Urodynamics, Female Pelvic Medicine & Urological Reconstruction (SUFU). | Women | GPs, prescribers | Diagnosis, management, prescribing, UTI | Decision-making | Algorithm, guideline | %www.auanet.org/guidelines/guidelines/recurrent-uti | US |
| Professional UTI Prevention Checklist | 2019 | NHS, South Norfolk CCG | 65 and over, long-term care residents, older people | Care home staff, community nurses, GPs, nurse practitioners | Diagnosis, management, prevention, UTI | Decision-making | Checklist, guide | www.knowledgeanglia.nhs.uk/LinkClick.aspx?fileticket=afgf-1BpS-k=&tabid=1849&portalid=1&mid=1233 | UK |
| ‘Guidance on urinary tract infections (UTI) for care home staff’ | 2018 | Infection Prevention Control, NHS, adapted by NHS Hartlepool and Stockton-on-Tees CCG, Sep 2018 | Long-term care residents | Care home staff | Diagnosis, UTI | Decision-making | Guide, quick reference tool | %www.infectionpreventioncontrol.co.uk/content/uploads/2018/12/Guidance-on-UTIs-for-care-home-staff.pdf | UK |
| ‘Flowchart for suspected UTI in catheterised adults or those over 65 years’ | 2020 | Target, UK Health Security Agency | 65 and over, adults with a catheter | Care home staff, community nurses, GPs, nurse practitioners, prescribers | Diagnosis, UTI | Decision-making | Flowchart, quick reference tool | %https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/927195/UTI_diagnostic_flowchart_NICE-October_2020-FINAL.pdf | UK |
| ROC-Guidelines-Holistic-Hydration-Care-Assessment-Tool | 2018 | Hydration nurse specialist | Older people | Care home staff, carers, nurse practitioners | Hydration | Decision- making, educational | Guide, guideline | N/A | UK |
| RESTORE2 – Recognise Early Soft Signs, Take Observations, Respond, Escalate | 2020 | NHS West Hampshire CCG | 65 and over, older people | Care home staff, carers | Deterioration, management, UTI | Decision-making | Decision aid, guide, poster, quick reference tool | UK | |
| Indwelling urinary catheter maintenance-checklist | 2017 | AHRQ | Adults with a catheter, long-term care residents | Care home staff | CAUTI, management | Decision-making | Checklist | US | |
| Hydration at Home Toolkit, including ‘Hydration at home’ e-learning modules, Hydration at home toolkit: |
2020 | Wessex AHSN, Hampshire County Council | 65 and over, long-term care residents, older people | Care home staff, carers, residents, prescribers | Hydration, management | Educational | e-learning resource, leaflet, poster, toolkit | %https://wessexahsn.org.uk/projects/354/hydration-at-home-toolkit | UK |
| Decision aid for diagnosis and management of suspected urinary tract infection (UTI) in people aged 65 years and over | 2021 | Healthcare Improve-ment Scotland, NHS Scotland | 65 and over, long-term care residents | Care home staff | Diagnosis, management, prescribing, prevention, UTI | Decision-making | Decision aid, flowchart | Scotland, UK | |
| Decision aid for diagnosis and management of suspected urinary tract infection (UTI) in older people. Actions for ‘Care Home and Prescriber | 2017 | Public Health Agency | Long-term care residents, older people | Care home staff, nurse practitioners, prescribers | Diagnosis, management, UTI | Decision-making | Checklist, decision aid, flowchart | %https://nhslguidelines.scot.nhs.uk/media/1755/decision-aid-for-urinary-tract-infection-uti-in-older-people.pdf | UK |
| Catheter-associated urinary tract infection (CAUTI) toolkit |
2015 | AHRQ | Adults with a catheter | Nursing home staff, community nurses, GPs, nurse practitioners, prescribers | CAUTI, prevention | Decision-making | Toolkit | US |
Appendix 8 List of included studies
| Authors and date | Title | Source | Country | Practice setting | CMOc |
|---|---|---|---|---|---|
| Abusalem et al. (2019)143 | The relationship between culture of safety and rate of adverse events in long-term care facilities | Journal of Patient Safety | USA | Long-term care facilities | 8 |
| Allemann and Sund-Levander (2015)71 | Nurses’ actions in response to nursing assistants’ observations of signs and symptoms of infections among nursing home residents | Nursing Open | Sweden | Nursing homes | 2 |
| Arnold et al. (2021)65 | Effectiveness of a tailored intervention to reduce antibiotics for urinary tract infections in nursing home residents: a cluster, randomised controlled trial | The Lancet Infectious Diseases | Denmark | Nursing homes | 1, 2, 3, 8 |
| Arnold et al. (2020)61 | Development of a tailored, complex intervention for clinical reflection and communication about suspected urinary tract infections in nursing home residents | Antibiotics | Denmark | Nursing homes | 1, 2, 3, 9 |
| Ashraf et al. (2020)97 | Diagnosis, treatment, and prevention of urinary tract infections in post-acute and long-term care settings: a consensus statement from AMDA’s Infection Advisory Subcommittee | The Journal of Post-Acute and Long-Term Care Medicine | USA | Post-acute and long-term care settings | 3 |
| Atkins et al. (2020)122 | Reducing catheter-associated urinary tract infections: a systematic review of barriers and facilitators and strategic behavioural analysis of interventions | Implementation Science | N/A | N/A | 6 |
| Bak et al. (2018)115 | Drinking vessel preferences in older nursing home residents: optimal design and potential for increasing fluid intake | British Journal of Nursing | UK | Care homes | 4 |
| Beeber et al. (2021)59 | Nurse decision-making for suspected urinary tract infections in nursing homes: potential targets to reduce antibiotic overuse. | Journal of the American Medical Director’s Association. | USA | Nursing homes | 1, 3 |
| Bonkat et al. (2022)56 | European Association of Urology Guidelines on urological infections | https://uroweb.org/guidelines/urological-infections | Europe | N/A | 7 |
| Booth et al. (2019)116 | Evaluating a hydration intervention (DRInK Up) to prevent urinary tract infection in care home residents: a mixed methods exploratory study | Journal of Frailty, Sarcopenia and Falls | UK | Care homes | 4, 5 |
| Bunn et al. (2018)96 | Supporting shared decision making for older people with multiple health and social care needs: a realist synthesis | BMC Geriatrics | UK | Care homes | 3 |
| Burton et al. (2021)91 | Theory and practical guidance on de-implementation of practices across health and care services: a realist synthesis | Health Services and Delivery Research Journals Library | UK | NHS | 3 |
| Buswell et al. (2017)135 | What works to improve and manage faecal incontinence in care home residents living with dementia? A realist synthesis of the evidence (FINCH) | The Journal of Post-Acute and Long-Term Care Medicine | UK | Care homes | 8 |
| Chaaban et al. (2019)73 | Decisional issues in antibiotic prescribing in French nursing homes: an ethnographic study | Journal of Public Health Research | France | Nursing homes | 2 |
| Chambers et al. (2018)64 | A recipe for antimicrobial stewardship success: using intervention mapping to develop a program to reduce antibiotic overuse in long-term care | Infection Control and Hospital Epidemiology | Canada | Long-term care | 1, 3, 7 |
| Xu et al. (2019)139 | Relationship between nursing home quality indicators and potentially preventable hospitalisation | BMJ Quality and Safety | USA | Nursing homes | 8 |
| Downs et al. (2021)74 | A complex intervention to reduce avoidable hospital admissions in nursing homes: a research programme including the BHiRCH-NH pilot cluster RCT 2021 | NIHR Journals Library | UK | Nursing homes | 2, 8, 9 |
| Fleming et al. (2015)88 | Antibiotic prescribing in long-term care facilities: a meta-synthesis of qualitative research | Drugs and Aging | Long-term care facilities | 3 | |
| Greene et al. (2018)5 | I-Hydrate training intervention for staff working in a care home setting: an observational study | Nurse Education Today | UK | Care homes | 4, 8, 9 |
| Haunch et al. (2021)140 | Understanding the staff behaviours that promote quality for older people living in long term care facilities: a realist review | International Journal of Nursing Studies | UK | Long-term residential care facilities | 8 |
| Hughes et al. (2020)60 | A multifaceted intervention to reduce antimicrobial prescribing in care homes: a non-randomised feasibility study and process evaluation | HS&DR Report,NIHR Journal Library | UK | Care homes | 1, 2, 3, 8, 9 |
| Jones et al. (2020)58 | Development of an information leaflet and diagnostic flow chart to improve the management of urinary tract infections in older adults: a qualitative study using the Theoretical Domains Framework | BJGP Open | UK | Care homes | 1, 3, 7 |
| Jones et al. (2021)62 | A qualitative investigation of the acceptability and feasibility of a urinary tract infection patient information leaflet for older adults and their carers | Antibiotics | UK | Care homes and primary care | 1, 3, 7 |
| Kelley et al. (2020)132 | The influence of care home managers on the implementation of a complex intervention: findings from the process evaluation of a randomised controlled trial of dementia care mapping | BMC Geriatrics | UK | Care homes | 8 |
| Klay and Marfyak (2005)128 | Use of continence nurse specialist in extended care facility | Urologic Nursing | USA | Long-term care facilities | 7 |
| Kousgaard et al. (2022)70 | Implementing an intervention to reduce use of antibiotics for suspected urinary tract infection in nursing homes – a qualitative study of barriers and enablers based on Normalization Process Theory |
BMC Geriatrics | Denmark | Nursing homes | 1, 8, 9 |
| Krein et al. (2017)125 | A national collaborative approach to reduce catheter-associated urinary tract infections in nursing homes: a qualitative assessment | American Journal of Infection Control | USA | Nursing homes | 6, 8, 9 |
| Lean et al. (2019)117 | Reducing urinary tract infections in care homes by improving hydration | BMJ Open Quality | UK | Care homes | 4, 5, 8 |
| Long et al. (2013)118 | Practice brief: a hydration initiative in a long-term care facility | Geriatric Nursing | USA | Long-term care | 4, 5 |
| Low et al. (2015)137 | A systematic review of interventions to change staff care practices in order to improve resident outcomes in nursing homes | PLOS One | Australia | Nursing homes | 8 |
| Marshall et al. (2018)133 | An evaluation of a safety improvement intervention in care homes in England: a participatory qualitative study | Journal of the Royal Society of Medicine | UK | Care homes | 8 |
| McNulty et al. (2008)141 | Exploring reasons for variation in urinary catheterisation prevalence in care homes: a qualitative study | Age and Aging | UK | Care homes | 8 |
| Meddings et al. (2017)25 | Systematic review of interventions to reduce urinary tract infection in nursing home residents | Journal of Hospital Medicine | USA | Nursing homes | 6 |
| Mody et al. (2015)147 | A targeted infection prevention intervention in nursing home residents with indwelling devices: a randomized clinical trial | Clin Infect Dis | USA | Nursing homes | 9 |
| Mody et al. 2017124 | A national implementation project to prevent catheter-associated urinary tract infection in nursing home residents | JAMA Internal Medicine | USA | Nursing homes | 6, 8, 9 |
| Nace et al. (2020)104 | A multifaceted antimicrobial stewardship program for the treatment of uncomplicated cystitis in nursing home residents | Journal of the American Medical Association Internal Medicine | USA | Nursing homes | 3 |
| NICE (2018)54 | NICE Guideline 112. Urinary tract infection (recurrent): antimicrobial prescribing. | National Institute for Health and Care Excellence | England, UK | N/A | 7 |
| Ouslander et al. (2011)75 | Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II Collaborative Quality Improvement Project | Journal of the American Geriatrics Society | USA | Nursing homes | 8 |
| Pasay et al. (2019)66 | Antimicrobial stewardship in rural nursing homes: impact of interprofessional education and clinical decision tool implementation on urinary tract infection treatment in a cluster randomized trial | Infection Control and Hospital Epidemiology | Canada | Nursing homes | 1, 2, 3 |
| Petterson et al. (2011)103 | Can a multifaceted educational intervention targeting both nurses and physicians change the prescribing of antibiotics to nursing home residents? A cluster randomized controlled trial | Journal of Antimicrobial Chemotherapy | Sweden | Nursing homes | 3 |
| Potter et al. (2019)89 | Multifaceted intervention to reduce antimicrobial prescribing in care homes: a process evaluation of a UK-based non-randomised feasibility study (REACH study) | BMJ Open | UK | Care homes (nursing and residential) | 3, 8 |
| Powell et al. (2018)90 |
Family involvement in timely detection of changes in health of nursing homes residents: a qualitative exploratory study | Journal of Clinical Nursing | UK | Nursing homes | 3 |
| Rycroft-Malone et al. (2018)131 | A realist process evaluation within the Facilitating Implementation of Research Evidence (FIRE) cluster randomised controlled international trial: an exemplar | Implementation Science | England, Netherlands, Republic of Ireland and Sweden | Care homes | 8 |
| Scanlon et al. (2012)138 | Reducing catheter-associated urinary tract infections in home care: a performance improvement project | Nursing Economics | USA | Home care | 8 |
| Shallcross et al. (2021)100 | Antibiotic prescribing for lower UTI in elderly patients in primary care and risk of bloodstream infection: a cohort study using electronic health records in England | PLOS Medicine | England, UK | Adults aged 65 years and older in primary care | 3 |
| Sihra et al. (2018)27 | Nonantibiotic prevention and management of recurrent urinary tract infection | Nature Reviews Urology | N/A | 7 | |
| Smith et al. (2018)142 | Evaluation of the association between Nursing Home Survey on Patient Safety culture (NHSOPS) measures and catheter-associated urinary tract infections: results of a national collaborative | BMJ Quality and Safety | USA | Nursing homes | 8 |
| Sreedhara et al. (2015)126 | Nursing home leaders’ views on catheter use and CAUTI as a quality and safety concern | Journal of the American Geriatrics Society | USA | Nursing homes | 8 |
| Sund-Levander and Tingstrom (2013)63 | Clinical decision-making process for early nonspecific signs of infection in institutionalised elderly persons: experience of nursing assistants | Scandinavian Journal of Caring Sciences | Sweden | Nursing homes and home care | 1, 2 |
| Surr et al. (2019)134 | Exploring the role of external experts in supporting staff to implement psychosocial interventions in care home settings: results from the process evaluation of a randomized controlled trial | BMC Health Services Research | UK | Care homes | 8, 9 |
| Tingstrom et al. (2010)57 |
Early nonspecific signs and symptoms of infection in institutionalized elderly persons: perceptions of nursing assistants | Scandinavian Journal of Caring Sciences | Sweden | Nursing homes | 1, 2 |
| van Buul et al. (2014)72 | Factors influencing antibiotic prescribing in long-term care facilities: a qualitative in-depth study | BMC Geriatrics | Netherlands | Nursing homes | 2 |
| Williams et al. (2016)51 | Improving skills and care standards in the support workforce for older people: a realist synthesis of workforce development interventions | BMJ Open | UK | Health and social care services for older people | 5 |
| Wilson et al. (2019)6 | Improving hydration of care home residents by increasing choice and opportunity to drink: a quality improvement study | Clinical Nutrition | UK | Care homes | 4, 5, 8 |
| Wilson et al. (2020)114 | Improving fluid consumption of older people in care homes: an exploration of the factors contributing to under-hydration | Nursing and Residential Care | UK | Care homes | 4, 5, 9 |
| Wanat et al. (2020)123 | Optimising interventions for catheter-associated urinary tract infections (CAUTI) in primary, secondary and care home settings | Antibiotics | Multicountry; mostly USA | Primary, secondary and care home settings | 6 |
Appendix 9 Summary of evidence for pharmacological interventions to prevent recurrent urinary tract infection
This overview of the evidence underpinning the management of RUTI has been drawn from a recent NICE guideline on antimicrobial prescribing for RUTI (NG112),154 the European Association of Urology Guidelines,56 which developed recommendations based on GRADE methodology, and a comprehensive narrative review. 27 There is a lack of evidence for the use of pharmacological interventions for RUTI in care homes and the guidelines do not specifically consider the application of recommendations in care home residents. A consultant urogynaecologist who was a member of the PAG provided information on other relevant evidence and advice on strategies that might be feasible to apply in a care home setting. Contextual information about the potential challenges in the use of treatments for RUTI in care home settings were also discussed with an experienced continence advisor. The following summarises the evidence for the efficacy of common agents to manage RUTI, which might be feasible to use in care home residents.
Low-dose antimicrobial prophylaxis
Low-dose antimicrobial prophylaxis using a daily dose of trimethoprim, nitrofurantoin, amoxicillin or cefalexin is considered the current standard treatment for RUTI. 154 However, because of the risk of developing infections caused by resistant pathogens, behavioural modifications and non-antimicrobial measures should be tried first where possible. 56 The EAU search identified four meta-analyses, which all concluded that antibiotic prophylaxis is the most effective approach against RUTI.
While most studies were not focused specifically on older people, a recent retrospective cohort study linked GP and hospital records for 19,969 adults (15,653 female and 4043 male) aged > 65 with a history of RUTI to compare the risk of UTI reoccurrence in those who were prescribed low dose antimicrobial prophylaxis for at least 3 consecutive months. Of male patients, 12.6% were on low dose antimicrobial prophylaxis and it was associated with a significantly lower risk of clinical recurrence [adjusted hazard ratio (HR) 0.49, 95% CI 0.45 to 0.54] and UTI-related hospitalisation (adjusted HR 0.78, 95% CI 0.64 to 0.94). Of female patients, 14.2% were on low dose antimicrobial prophylaxis and it was associated with a significantly lower risk of clinical recurrence (adjusted HR 0.57, 95% CI 0.55 to 0.59), but the risk of hospitalisation could not be assessed due to unmeasured confounding with underlying illness. 155
Potential side effects of low dose antimicrobial prophylaxis need to be considered. A Cochrane review of the efficacy of low dose antimicrobial prophylaxis in preventing RUTI included 19 studies and concluded that although it was more effective in preventing UTI than non-antimicrobial pharmaceutical interventions, it was associated with more side effects, particularly vaginal candidiasis. 156 Gastrointestinal disturbance has also been reported as a significant side effect of low dose antimicrobial prophylaxis with nitrofurantoin. 157 There is no consensus about the optimal duration of low dose antimicrobial prophylaxis, with studies reporting treatment duration of 3–12 months, and once discontinued UTIs tend to re-occur. 56
Probiotics
Probiotics are products containing viable, defined micro-organisms, which are intended to exert health benefits by altering the normal microflora in a body compartment. In the case of RUTI Lactobacillus spp. given orally or via pessary have been proposed as a probiotic treatment. However, a systematic review of the effect of probiotics on rates of RUTI found no significant difference between probiotics and placebo or antibiotics. The nine included studies had a high risk of bias and could not be used to draw firm conclusions about the efficacy of probiotics as a treatment for RUTI. There are also no firm data on the most appropriate route of administration, optimal dosage or duration of treatment. 158
Cranberries
Cranberries contain proanthocyanins, which are thought to prevent adherence of E. coli with P fimbriae and also inhibit motility of Pseudomonas aeruginosa, E. coli and Proteus mirabilis. 159 A number of randomised controlled trials have assessed the efficacy of cranberries in preventing UTI recurrence but have used different formulations of cranberry (e.g. juice, tablets, capsules, syrup or fruit powder). Most studies are small scale with a high risk of bias and the attrition rate is also frequently high. One study conducted in a care home found it challenging to maintain consumption of the required volume of cranberry juice and many residents disliked the acrid flavour. 160 In the absence of large, well-designed RCTs, there is insufficient evidence for the most effective dose of proanthocyanins and formulation that is well tolerated to support the use of cranberry preparations for preventing RUTI. 161
D-mannose
D-mannose is a monosaccharide isomer of glucose, which, if taken orally, is rapidly absorbed and excreted in the urinary tract. It has a similar structure to urothelial glycoprotein receptors and by binding to the type 1 fimbriae adhesins on enteric bacteria it prevents them from attaching to uroepithelial cells. In a randomised trial of D-mannose, nitrofurantoin and no prophylaxis162 in 308 women with history of RUTI, the recurrence rate did not differ significantly between patients who took standard nitrofurantoin prophylaxis (50 mg daily) and those taking D-mannose (2 g in 200 ml water daily) with UTI occurring in 14.6% and 20.4%, respectively. Both treatment groups had a significantly lower risk of a recurrent cystitis episode compared to patients in the no prophylaxis group (Risk Ratio (RR) 0.239, 95% CI 0.146 to 0.392; p < 0.0001 and RR 0.335, 95% CI 0.222 to 0.506; p < 0.0001). Side effects were reported by 17.9%, but these were mild and did not require the prophylaxis to be stopped. Patients in the D-mannose group had a significantly lower risk of side effects compared to patients in the nitrofurantoin group (RR 0.276, 95% CI 0.132 to 0.574; p < 0.0001).
In a systematic review and meta-analysis of eight studies conducted in outpatient settings, D-mannose appeared to be protective for RUTI versus placebo (pooled RR 0.23; 95% CI 0.14 to 0.37) with possibly similar effectiveness to antibiotics (Pooled RR 0.39; 95% CI 0.12 to 1.25). D-mannose was well tolerated with minimal side effects. 163
A systematic review and network meta-analysis of chemotherapeutic agents as prophylaxis for RUTI in healthy nonpregnant women evaluated the efficacy, tolerability, adverse effects and cost of D-mannose and two antibiotics. 164 The network metanalysis included six RCTs and found that D-mannose had the highest efficacy, with fosfomycin second and nitrofurantoin third (although this was based on only one fosfomycin study). Nitrofurantoin was associated with the least adverse effects and fosfomycin the most adverse effects, although these did not cause participants to drop out from the trial. D-mannose is available to purchase as a powder or tablets but is not classified as a medicine; therefore, while it was found to have a superior efficacy to nitrofurantoin, it was less cost-effective.
Methenamine hippurate
Methenamine hippurate has been proposed as a treatment to prevent RUTI as it is hydrolysed to the bactericidal agent formaldehyde in acidic environments such as the distal tubules of the kidney. It has been evaluated in a systematic review, but the evidence has been considered inconclusive and large, well-conducted randomised trials are required to demonstrate efficacy. 27,56,165 A recent pragmatic randomised non-inferiority trial, which compared clinical effectiveness of low-dose antibiotic prophylaxis with methenamine hippurate (1 g oral dose twice daily) in 205 women recruited from secondary care,166 found the efficacy was similar for both treatments. This suggests that methenamine hippurate might be appropriate for women with a history of RUTI.
Topical oestrogen
Oral oestrogens that have been studied in the prevention of RUTI reduced vaginal pH but did not reduce the frequency of RUTI or increase the number of Lactobacilli in the urinary tract of women and were associated with increased adverse effects such as breast tenderness and mild vaginal bleeding. Thus, topical oestrogens are recommended for the prophylaxis of RUTI rather than systemic administration. 56
A number of small-scale RCTs on the use of vaginal oestrogen for the prevention of RUTI in postmenopausal women have been conducted. 55 Three studies compared topical oestrogen with placebo. One study randomly assigned postmenopausal patients with a history of RUTI to receive either an estradiol-releasing vaginal ring (53 women) or no oestrogen treatment (55 women) for 36 weeks or until the first recurrence of UTI for the control group. 167 After 36 weeks, the cumulative likelihood of being UTI free was 45% in estradiol ring group compared to 20% in control group. The estradiol treatment lowered vaginal pH and increased maturity of vaginal and urethral mucosal cells. Ferrante et al. 168 conducted a randomised, placebo-controlled trial of vaginal oestrogen (ring or cream) in 35 postmenopausal women with history of RUTI. Treatment with vaginal oestrogen reduced UTI versus placebo (11/18 vs. 16/17 p = 0.041) with more than 90% of women on placebo experiencing a UTI compared with only 50% of those assigned to oestrogen. Adherence to treatment was greater with the ring than the cream.
In an early RCT by Raz et al.,169 postmenopausal women with a history of RUTI were assigned to intervention (0.5 mg estriol vaginal cream applied nightly for 2 weeks then twice weekly for 8 months) or placebo (same cream applied in same way without estriol) and followed up monthly at outpatient visits for evidence of UTI. The loss to follow-up was high with only 36/93 estriol and 24/43 placebo completing 8 months of treatment. Patients discontinued due to side effects (mild irritation, burning, itching), lack of compliance and RUTI (especially in the placebo group). The cumulative proportion remaining free of UTI was significantly higher in estriol group (p < 0.00) and the annualised median incidence of UTI significantly lower in estriol group (0.5 vs. 5.9 per patient year, p < 0.001). The estriol treatment was associated with significant decrease in vaginal pH versus placebo (p < 0.001) and increase in vaginal lactobacilli.
A subsequent RCT by the same research group170 compared the use of topical estriol with nitrofurantoin in postmenopausal women with history of RUTI. Participants were randomly assigned to estriol pessary (daily for 2 weeks and then once every 2 weeks for 9) or daily nitrofurantoin capsule. Occurrence of UTI was assessed at monthly outpatient visit over a 9-month period. In the analysis, 79/86 of estriol and 71/85 of control group were included. Twenty-seven and 23 respectively dropped out due to adverse effects (9 vs. 14) or lack of compliance (13 vs. 6). Seventy-nine women in the estriol group had 1.6 UTI/women (two episodes per woman per year) compared to a rate of 0.6 (0.8/woman/year) in the 71 included in the control group (p < 0.001). Side effects were similar in both groups.
Vaginal topical oestrogen seems to reduce the risk of RUTI; creams may be more effective than rings or pessaries, although the optimal dosage for prophylaxis or appropriate duration is unclear. More large-scale RCTs are required to understand its efficacy and potential side effects compared to low-dose antibiotics. The practicality of using topical oestrogen in the frail elderly population of care homes has not been evaluated.
Glossary
Abduction is an analytical process where something new is seen in evidence or observation and an inference about the cause is made and explained.
Active monitoring commences when a decision is made (and agreed with the resident/resident’s family) that it is clinically appropriate to start a period of monitoring, possibly while the resident receives symptomatic support, but without any specific or significant clinical intervention at this stage.
Antimicrobial stewardship is a systematic approach to improving antimicrobial use, with a view to improving clinical outcomes and minimising adverse events relating to their use, including the development of antimicrobial resistance.
Asymptomatic bacteriuria refers to bacteria in the urine without urinary tract symptoms.
Bloodstream infection/Bacteraemia is when a bacterial infection enters the bloodstream from elsewhere in the body, such as the skin, lungs, kidneys or bladder.
Care home includes both residential homes and care homes with on-site nursing (international terms include long-term care facility, residential care facility and skilled nursing facility).
Care home with nursing is a care home where, in addition to personal care and accommodation, qualified nursing care is provided to ensure that the full needs of the person are met.
Care Quality Commission is the regulator for healthcare and socialcare services in England.
Catheter-associated urinary tract infection is a urinary tract infection associated with a urinary catheter, which is a tube inserted into the bladder through the urethra to drain urine.
Clinical Commissioning Group is an NHS organisation with responsibility for a local population that plans, arranges and funds health services. Individual general practitioners are also members of these organisations.
Context means the conditions that facilitate or constrain the operation of different interventions(s) or programme(s).
Context–mechanism–outcome configuration is a statement, diagram or drawing that illustrates the relationship between particular features of contexts, mechanisms and outcomes.
Mechanism is the generative force that leads to outcomes. It often denotes the reasoning (cognitive or emotional) of the various ‘actors’, that is, care home staff, residents, relatives and visiting healthcare professionals. Identifying the mechanisms goes beyond describing ‘what happened’ to theorising ‘why it happened, for whom and under what circumstances’.
Outcome is the impact or behaviours that result from the interaction of mechanisms and context.
Patient and public involvement is the involvement of patients and the public in the design, management and conduct of research or the design of health services.
Programme theory is a set of theoretical explanations or assumptions about how a programme, process or intervention is expected to work. Programme theory specifies what mechanisms are associated with which outcomes and what features of the context will affect whether or not those mechanisms operate.
Retroduction is an analytical process used in realist synthesis to understand the cause of an event. SBAR is a structured communication tool based on situation, background, assessment, recommendation.
Urinary tract infection is an infection involving any part of the urinary system, including urethra, bladder, ureters and kidney.
List of abbreviations
- AHRQ
- Agency for Healthcare Research and Quality
- AMR
- antimicrobial resistance
- AMS
- antimicrobial stewardship
- ASB
- asymptomatic bacteriuria
- CAUTI
- catheter-associated urinary tract infection
- CMO
- context–mechanism–outcome
- CMOc
- context–mechanism–outcome configuration
- CRCT
- cluster randomised controlled trial
- DCM
- dementia care mapping
- GP
- general practitioner
- HCP
- healthcare professional
- HR
- hazard ratio
- ICS
- Integrated Care Services
- IPC
- infection prevention and control
- IUC
- indwelling urinary catheter
- LDAP
- low-dose antimicrobial prophylactic
- NHSE
- National Health Service England
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- PAG
- Project Advisory Group
- PPI
- patient and public involvement
- RN
- registered nurse
- RUTI
- recurrent urinary tract infection
- SBAR
- situation, background, assessment, recommendation
- SDM
- shared decision-making
- UTI
- urinary tract infection
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/DADT3410).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.