Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 16/101/02. The contractual start date was in March 2018. The draft report began editorial review in May 2022 and was accepted for publication in March 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2024 Price et al. This work was produced by Price et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Price et al.
Chapter 1 Literature review
Literature reviews underpinning EDITION’s intervention development had the following objectives:
-
Investigate the effectiveness and acceptability of de-escalation training interventions.
-
Understand barriers and facilitators to adult acute and adult forensic mental health inpatient staff’s engagement in de-escalation of conflict.
Consequently, the following chapter is divided into two sections, the first meeting objective (1) and the second objective (2).
Review A: the effectiveness and acceptability of de-escalation training programmes for healthcare staff working in adult acute and forensic mental health inpatient settings
Rationale
The authors’ original systematic review of de-escalation training effectiveness and acceptability identified 38 eligible studies. 1 A lack of high-quality evidence limited conclusions as to the effectiveness of de-escalation training on clinical safety outcomes. This was an update of our previous review1 and was not registered with Prospero, but the review protocol can be accessed here: https://fundingawards.nihr.ac.uk/award/16/101/02.
Objective
To provide a rigorous and up-to-date synthesis of the evidence for the acceptability and effectiveness of de-escalation training for mental health staff.
Methods
Eligibility criteria
Inclusion criteria
Studies were included that met the following criteria:
Population: healthcare staff (qualified and unqualified) working with adult populations (18–65 years) with mental health difficulties.
Intervention: training with a de-escalation techniques component.
Comparison: all controlled studies meeting eligibility criteria, irrespective of their control condition. Comparisons of two or more active interventions or of an active treatment with a ‘no treatment’ comparator will be included.
Outcomes (effectiveness): changes in rates of conflict (e.g. violence, verbal and physical aggression) and use of restrictive interventions (e.g. seclusion and physical restraint) post training. Secondary outcomes were cognitive (e.g. knowledge), affective (e.g. confidence) and skills-based (e.g. de-escalation performance) changes in trainee performance.
Outcomes (acceptability): Defined, for the purpose of the review, as intervention uptake, adherence and participant satisfaction and views.
Design: randomised controlled trials (RCTs), nRCTs, controlled before-and-after (CBA) and interrupted time series (ITS) designs. All studies that (1) asked trainees or trainers for their views of interventions using qualitative or quantitative methods, and/or (2) studies that quantitatively assessed non-participation, withdrawal, or adherence rates.
Information sources
Searches were undertaken on the following electronic databases: Allied and Complementary Medicine Database (AMED), Applied Social Sciences Index and Abstracts (ASSIA), Social Services Abstracts, British Nursing Index (and archive), Excerpta Medica database (EMBASE), Medical Literature Analysis and Retrieval System Online (MEDLINE), PsycINFO, Cochrane Library (all sources), Social Sciences Citation Index (SSCI) + SCIEXPANDED, Cumulative Index to Nursing and Allied Health Literature (CINAHL), the metaRegister of Controlled Trials. Grey literature including user-led projects, service evaluations, policy documents and third sector reports was sought from government and charity websites, the British National Bibliography for Report Literature and Google Scholar. All databases were searched from 1 month prior to the date of the searches conducted in the original review (August 2014) to the date of the new search date (12–16 October 2017).
Search strategy
The search strategy was developed using search terms relevant to the review objectives using the key concepts of mental health, staff attitudes, de-escalation, training and violence (full strategy available upon request). Searches were limited to English-language publications only. No other search restrictions were applied.
Selection process
All potentially eligible records were imported into Endnote version 9, where duplicate references were identified and deleted. The records were then uploaded to ‘Covidence’ (Melbourne, VIC, Australia), which is a systematic review-management software programme. Using Covidence, two reviewers independently screened titles and abstracts for eligibility against the inclusion/exclusion criteria. Full texts were retrieved when both reviewers agreed on inclusion or where there was a disagreement, the full-text article. Two reviewers independently assessed the full texts against the eligibility criteria and disagreements were resolved through discussion with the wider project team.
Data-collection process and data items
Data extraction from eligible studies by one reviewer then independently verified by another reviewer. Discrepancies were resolved by discussion between the two reviewers with reference to the relevant paper and, where necessary, discussion with the wider project team. Data extraction was informed by a pre-specified data-extraction sheet detailing:
-
study information (author, date, country, study design, single/multisite)
-
recruitment (setting, method, inclusion/exclusion criteria)
-
intervention (intervention components and development, duration, frequency, facilitators, delivery methods, control/comparator)
-
participant characteristics (service users: age, gender, ethnicity; staff: professional status, experience, age, gender)
-
primary outcome (changes in the rate of conflict and restrictive interventions)
-
secondary outcomes (cognitive, affective and skill-based outcomes)
-
acceptability outcomes [quantitative: % drop-out, number of staff approached, number consented, response rate, adherence (number of sessions attended); qualitative: participant satisfaction, views of intervention, any other qualitative comments].
Risk of bias assessment
Evidence of clinical effectiveness was quality assessed by two independent researchers using the Risk Of Bias In Non-randomised Studies of Interventions (ROBINS-I) tool. 2 Qualitative acceptability evidence was assessed by two independent researchers using the consolidated criteria for reporting qualitative research (COREQ) criteria for qualitative research. 3
Effect measures and synthesis methods
Because of the heterogeneity of study designs and outcome measures in the included studies, and because of the small number of studies providing data for the primary and secondary outcomes, meaningful pooling of quantitative data was not possible. Narrative syntheses of clinical effectiveness and acceptability were, therefore, conducted in parallel. Quantitative effectiveness data were tabulated by review outcome (changes in rates of conflict, changes in rates of containment, cognitive, affective and skills-based) and Cohen’s d Standardised Effect Sizes were calculated for all studies except those not reporting means and standard deviations (SDs) or those that omitted the outcome of a statistical test. Quantitative and qualitative acceptability were analysed separately. Quantitative acceptability data were tabulated and synthesised within the following theoretically important outcomes: percentage drop-out, number of staff approached, number consented, response rate, adherence (number of sessions attended). Due to the sparsity of qualitative acceptability data available, no formal qualitative analysis was possible. As such the limited qualitative comments on participant views on training were organised into related themes and synthesised into brief narratives for each theme.
Results
Search results
All eligible results (n = 3309) were imported into Endnote version 9 where duplicate references were identified and removed, resulting in 2774 papers to be screened for eligibility. Twenty-nine results were eligible for retrieval of full texts. Of these, 21 were excluded (8 wrong intervention, 5 wrong population, 4 wrong study design, 2 wrong setting, 2 wrong language) leaving 8 new papers eligible for inclusion in the updated review. These eight papers were combined with the 38 studies from our original and 46 studies were included in the synthesis.
Study characteristics
Characteristics of the 46 included studies are presented in Table 1. Of the included studies, 12 used non-randomised controlled studies, two used retrospective cohort study designs, 27 used uncontrolled pre and post designs and 10 reported qualitative findings (five of which reported only qualitative findings). No RCTs were identified in the search.
| Author (date) | Country | Study design | Single vs. multisite | Setting | Sample size | Outcome measures | Statistical analyses |
|---|---|---|---|---|---|---|---|
| Azuela and Robertson (2016)4 | New Zealand | Uncontrolled pre and post (repeated measures) | Single | Non-specified psychiatric inpatient wards (n = not reported) | 23 mental health professionals Baseline: n = 23 Follow-up: n = 23 |
Primary outcome Study-specific measure of knowledge, skills and attitudes |
Multivariate analysis of variance |
| Beech and Leather (2003)5; Beech (2008)6 | UK | Uncontrolled pre and post | Single | University setting | 243 undergraduate nursing students (numbers at baseline and follow-up points not reported) | Primary outcome Study-specific measure of attitudes, beliefs and confidence |
Paired sample t-tests |
| Beech (2001)7 | UK | Uncontrolled pre and post | Single | University setting | 53 undergraduate nursing students (numbers at baseline and follow-up points not reported) |
Primary outcome Study-specific measure of attitudes |
Wilcoxon matched-pairs signed-rank |
| Biondo (2017)8 | USA | Mixed methods (qualitative study and post training survey) | Single | University setting | 73 postgraduate mental health nursing students | Primary outcome Study-specific measure of empathy, skills and self-efficacy |
Descriptive statistics |
| Bjorkdahl et al. (2013)9 | Sweden | Uncontrolled pre and post (time series) | Multi | Non-specified psychiatric inpatient wards (n = 41) | Baseline: 854 ward staff Follow-up: 260 ward staff |
Primary outcome Study-specific measure of emotion regulation |
Mann–Whitney U-test |
| Bowers et al. (2006)10 | UK | Uncontrolled pre and post | Multi | Acute admission psychiatric wards (n = 2) | Baseline: 254 shift reports Follow-up: 1315 shift reports Baseline: (n = 28 staff) Follow-up: (n = 30 staff) Baseline: (n = 31 staff) Follow-up: (n = 26 staff) Baseline: (n = 39 staff) Follow-up: (n = 32 staff) |
Primary outcome PCC-SR11 Secondary outcomes APPQ12 MBI13 WAS14 |
One-tailed Mann–Whitney U-tests Independent samples t-tests |
| Bowers et al. (2008)15 | UK | Non-RCT | Multi | 8 acute psychiatric wards (3 experimental, 5 control wards) | 2074 shift reports (experimental wards) 3242 shift reports (control wards) |
Primary outcome PCC-SR11 |
Ordinal logistic regression |
| Calabro et al. (2002)16 | USA | Uncontrolled pre and post (repeated measures) | Single | Non-specified psychiatric inpatient wards (n = 12) | 118 ward staff Baseline: n = 118 ward staff Follow-up: n = 118 |
Primary outcome Study-specific measure of knowledge, attitude, self-efficacy and behavioural intention |
Paired t-tests |
| Carmel and Hunter (1990)17 | USA | Retrospective cohort study | Single | Non-specified psychiatric inpatient wards (n = 27) | 9 trained wards 18 untrained wards |
Primary outcome Staff injuries |
Not reported |
| Chigbundu (2015)18 | USA | Qualitative study | Single | Acute mental health inpatient setting | 16 mental health nurses | N/A | N/A |
| Collins et al. (1994)19 | Scotland | Uncontrolled pre and post (repeated measures) | Single | University setting | Mixed sample of 26 undergraduate student nurses and ward staff. Baseline n = 26 Follow-up: n = 23 |
Primary outcome Attitude to aggressive behaviour questionnaire19 |
Descriptive statistics |
| Collins (2014)20 | USA | Qualitative study | Single | Non-specified psychiatric hospital | 7 ward staff | N/A | N/A |
| Cowin et al. (2003)21 | Australia | Uncontrolled pre and post (time series) | Single | Non-specified psychiatric unit | 40 mental health nurses Baseline: 21 mental health nurses Follow-up: 19 mental health nurses |
Primary outcome Study-specific measure of knowledge and attitudes |
Analysis of variance |
| Davies et al. (2016)22 | UK | Uncontrolled pre and post (time series) | Single | Medium secure psychiatric forensic unit | Baseline: 79 ward staff Follow-up: 67 ward staff |
Primary outcome Confidence in Coping with Patient Aggression Instrument23 |
Paired t-tests |
| Geoffrion et al. (2017)24 | Canada | Uncontrolled pre and post | Single | Psychiatric intensive care and psychiatric emergency | 2 units (routinely collected data in both units) | Primary outcome Seclusion and restraint incidence |
Regression (no further information provided) |
| Gertz (1980)25 | UK | Mixed methods (qualitative study and uncontrolled pre and post) | Single | Non-specified psychiatric setting | 1 unit (routinely collected data) | Primary outcome Assaults |
Descriptive statistics |
| Goodykoontz and Herrick (1990)26 | USA | Mixed methods (qualitative study and uncontrolled pre and post) | Single | Non-specified psychiatric setting | Not reported | Primary outcome Burnout Scale27 |
Descriptive statistics |
| Grenyer et al. (2003)28 | Australia | Uncontrolled pre and post (repeated measures) | Single | Non-specified psychiatric setting | 34 ward staff Baseline: 34 Follow-up: 34 |
Confidence in Coping with Patient Aggression Instrument23 Attitude to aggressive behaviour questionnaire19 (No primary outcome specified) |
Paired t-tests |
| Hahn et al. (2006)29 | Switzerland | Non-RCT | Multi | Acute psychiatric wards (n = 6) | Experimental group: 29 mental health nurses Control group: 34 mental health nurses |
Primary outcome Management of Aggression and Violence Attitude Scale30 |
Wilcoxon signed rank test for matched pairs |
| Ilkiw-Lavalle et al. (2002)31 | Australia | Mixed methods (qualitative study and uncontrolled pre and post) | Multi | Acute psychiatric units (n = 3) | 103 mental health staff (mixed sample of professionals and ward staff) Baseline: n = 103 Follow-up: n = 103 |
Primary outcome Study-specific measure of knowledge |
Paired t-tests |
| Infantino and Musingo (1985)32 | USA | Non-RCT | Single | Non-specified psychiatric inpatient setting | Experimental group: 31 ward staff Control group: 65 ward staff |
Primary outcome Injuries and assault frequency (No primary outcome specified) |
Not reported |
| Jonikas et al. (2004)33 | USA | Uncontrolled pre and post | Single | Non-specified psychiatric inpatient units (n = 3) | Routinely collected incidence data from 3 units 6 months pre and post training | Primary outcome Physical restraint |
Two-way analysis of variance |
| Laker et al. (2010)34 | UK | Uncontrolled pre and post | Single | Psychiatric intensive unit (n = 1) | Routinely collected incidence data from one unit 12 months pre and post training | Primary outcome Incidents requiring de-escalation or restraints |
Poisson regression |
| Lee et al. (2012)35 | UK | Retrospective cohort study | Multi | PICU (n = 5) | n = 3 ‘SCIP’ trained units n = 2 control and restraint trained wards |
Primary outcome Incidence of ‘disturbed behaviour’ |
Poisson regression |
| Martin (1995)36 | USA | Uncontrolled pre and post | Single | Non-specified psychiatric inpatient setting | Routinely collected incidence data in one psychiatric unit 12 months pre and post training | Aggression frequency Aggression severity (No primary outcome specified) |
Descriptive statistics |
| Martinez (2017)37 | USA | Mixed methods (qualitative study and uncontrolled pre and post) | Single | University setting | 15 undergraduate mental health nursing students | Study-specific measure of knowledge Mental health nurse clinician confidence scale38 (No primary outcome specified) |
Paired t-tests |
| McIntosh et al. (2003)39 | USA | Non-RCT | Multi | Non-specified psychiatric inpatient setting (n = 2) | Experimental group: 56 mental health professionals Control group: 34 mental health professionals |
Primary outcome Self-efficacy scale40 |
One-tailed t-test |
| McLaughlin et al. (2010)41 | UK | Mixed methods (qualitative study and uncontrolled pre and post) | Single | Acute psychiatric wards (n = 1) | 18 ward staff | Primary outcome Verbal aggression measure41 |
Descriptive statistics |
| Moore (2010)42 | USA | Uncontrolled pre and post | Single | Non-specified psychiatric inpatient setting (n = 2) | Incident data collected 12 months pre and post training | Primary outcome Moore Safety Code Team Analysis Tool42 |
Descriptive statistics |
| Nau et al. (2009)43 | Germany | Mixed methods (qualitative study and uncontrolled pre and post) | Single | School of nursing | 68 students (unclear proportion retained at follow-up) | Primary outcome Confidence in Coping with Patient Aggression Instrument23 |
Wilcoxon |
| Nau et al. (2010)44 | Germany | Non-RCT | Single | University setting | Experimental group: 52 undergraduate nursing students Control group: 52 undergraduate nursing students |
Primary outcome DABS45 |
Wilcoxon signed-rank test (differences within groups) and Mann–Whitney test (differences between groups) |
| Nau et al. (2011)46 | Germany | Non-RCT | Single | University setting | Experimental group: 52 undergraduate nursing students Control group: 52 undergraduate nursing students |
Primary outcome Confidence in Coping with Patient Aggression Instrument23 |
Wilcoxon signed-rank test (differences within groups) and Mann–Whitney test (differences between groups) |
| Needham et al. (2004)47 | Switzerland | Uncontrolled pre and post | Multi | Acute psychiatric wards (n = 2) | 273 aggressive incidents | The Staff Observation Aggression Scale–Revised (SOAS-R)48 | Chi-squared tests were employed to compare incidence rates of events, using hospitalisation days as the unit of analysis. The severity of aggression was compared across periods by the Student’s t-test |
| Needham et al. (2005)49 | Switzerland | Non-RCT | Multi | University setting | Experimental group: 57 Control group: 60 |
Confidence in Coping with Patient Aggression Instrument23 The SOAS-R48 (No primary outcome specified) |
Univariate analysis of variance across three time points |
| Nijman et al. (1997)50 | Netherlands | Non-RCT | Single | Non-specified psychiatric inpatient wards (n = 3) | Experimental group: n = 2 wards Control group: n = 1 ward |
Primary outcome SOAS-R48 |
Not reported |
| Paterson et al. (1992)51 | UK | Uncontrolled pre and post | Single | Not reported | 25 mental health nurses (how many completed pre and post measures was not clearly reported) | Study-specific measure of knowledge Study-specific measures of de-escalation performance and job satisfaction. General Health Questionnaire52 (No primary outcome specified) |
t-test Wilcoxon test Wilcoxon test |
| Rice et al. (1985)53 | Canada | Non-RCT | Single | One maximum security forensic psychiatric hospital | Experimental group: 62 ward staff Control group: 37 ward staff |
Primary outcome Study-specific measures of knowledge, confidence and performance Secondary outcomes Assault frequency Use of PRN (extra) medicines |
Simplified time series analysis designed for studies with relatively few observations 2 × 2 repeated measures analyses of variance in which the factors were Group (experimental and control), and Time (pre and post course) |
| Robinson et al. (2011)54 | Australia | Mixed methods (qualitative study and uncontrolled pre and post) | Single | One mental health service | Baseline: 24 participants Follow-up: 24 participants |
Perceived self-efficacy scale55 (No primary outcome specified) |
Paired t-tests |
| Sjostrom et al. (2001)56 | Sweden | Uncontrolled pre and post | Single | Non-specified psychiatric inpatient setting | 386 aggressive incidents | Social Dysfunction Aggression Scale57 SOAS-R48 (No primary outcome specified) |
Cox proportional hazards models |
| Smoot and Gonzales (1995)58 | USA | Non-RCT | Multi | Non-specified psychiatric inpatient wards (n = 2) | Routinely collected incidence data 6 months pre and post training | Primary outcome Assault frequency |
Descriptive statistics |
| Taylor and Sambrook (2012)59 | UK | Uncontrolled pre and post (time series) | Single | Non-specified psychiatric inpatient wards (n = 1) | Routinely collected incidence data 8 months pre and post training. MBI sample size not reported |
Frequency of ‘challenging behaviour’ MBI13 (No primary outcome specified) |
Two-tailed Fisher’s exact p = 0.011 MBI scores descriptive only |
| Thackrey et al. (1987)23 | USA | Non-RCT | Multi | Mixed settings: general psychiatric hospitals (n = 2) and one forensic hospital (n = 1) | Experimental group: 68 health professionals and paraprofessionals Control group: 57 health professionals and paraprofessionals |
Primary outcome Confidence in Coping with Patient Aggression Instrument23 |
Not reported |
| Whittington and Wykes (1996)60 | UK | Non-RCT | Multi | General psychiatric hospitals (n = 2) | Experimental group: 47 members of nursing staff (89% registered nurses) Control group: 108 members of nursing staff (71% registered nurses) |
Primary outcome Assaults directly reported to researchers via daily telephone contacts with ward staff |
Comparisons between groups were evaluated using chi-squared tests of association and changes within groups using the McNemar change test |
| Wondrak and Dolan (1992)61 | UK | Non-RCT | Single | University setting | Experimental group: 14 undergraduate nursing students Control group: 15 undergraduate nursing students |
Primary outcome Study-specific measure of de-escalation performance |
Repeated measures t-tests |
| Yang et al. (2014)62 | USA | Uncontrolled pre and post | Single | Acute psychiatric inpatient unit | Routinely collected incidence data 6 months pre and post training | Primary outcome Seclusion and restraint frequency |
Hierarchical logistic regression |
Risk of bias assessment
According to (ROBINS-I), 18 studies were assessed to be at moderate risk of bias and 21 presented a serious risk (Table 2). The 10 qualitative studies met between 6 and 24 COREQ items (Table 3).
| Study | Selection bias | Intervention classification | Adherence | Missing data | Measurement of outcomes | Selective reporting | Global |
|---|---|---|---|---|---|---|---|
| Azuela et al. (2016)4 | Moderate | Moderate | Not reported | Low | Moderate | Low | Moderate |
| Beech et al. (2003; 2008)5,6 | Serious | Low | Serious | Moderate | Serious | Moderate | Serious |
| Beech (2001)7 | Serious | Moderate | Moderate | Moderate | Serious | Moderate | Serious |
| Bjorkdahl et al. (2013)9 | Moderate | Low | Moderate | Moderate | Moderate | Moderate | Moderate |
| Bowers et al. (2006)10 | Moderate | Low | Moderate | Moderate | Moderate | Low | Moderate |
| Bowers et al. (2008)15 | Serious | Moderate | Serious | Moderate | Serious | Moderate | Serious |
| Calabro et al. (2002)16 | Moderate | Moderate | Low | Moderate | Moderate | Moderate | Moderate |
| Carmel et al. (1990)17 | Low | Low | Low | Not reported | Not reported | Low | Low |
| Collins et al. (1994)19 | Low | Serious | Low | Moderate | Serious | Serious | Serious |
| Cowin et al. (2003)21 | Moderate | Serious | Moderate | Moderate | Serious | Serious | Serious |
| Davies et al. (2016)22 | Low | Low | Low | Moderate | Serious | Low | Serious |
| Geoffrion et al. (2017)24 | Serious | Moderate | Not reported | Not reported | Moderate | Serious | Serious |
| Gertz (1980)25 | Critical | Critical | Critical | Critical | Critical | Critical | Critical |
| Goodykoontz et al. (1990)26 | Moderate | Low | Low | Moderate | Serious | Serious | Serious |
| Grenyer et al. (2003)28 | Moderate | Low | Moderate | Not reported | Moderate | Moderate | Moderate |
| Hahn et al. (2006)29 | Moderate | Low | Moderate | Moderate | Moderate | Moderate | Moderate |
| Ilkiw-Lavalle et al. (2002)31 | Low | Moderate | Moderate | Low | Moderate | Moderate | Moderate |
| Infantino et al. (1985)32 | Serious | Low | Low | Low | Low | Low | Serious |
| Jonikas et al. (2004)33 | Moderate | Moderate | Serious | Low | Low | Low | Moderate |
| Laker et al. (2010)34 | Moderate | Serious | Moderate | Moderate | Serious | Moderate | Serious |
| Lee et al. (2012)35 | Moderate | Serious | Moderate | Moderate | Moderate | Moderate | Moderate |
| Martin (1995)36 | Moderate | Moderate | Moderate | Serious | Moderate | Moderate | Serious |
| Martinez (2017)37 | Serious | Moderate | Moderate | Low | Moderate | Moderate | Serious |
| McIntosh et al. (2003)39 | Moderate | Low | Moderate | Moderate | Moderate | Low | Moderate |
| McLaughlin et al. (2010)41 | Moderate | Low | Not reported | Not reported | Moderate | Serious | Serious |
| Moore (2010)42 | Moderate | Moderate | Serious | Low | Serious | Serious | Serious |
| Nau et al. (2009)43 | Moderate | Moderate | Moderate | Low | Moderate | Moderate | Moderate |
| Nau et al. (2010)44 | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Nau et al. (2011)46 | Moderate | Moderate | Moderate | Moderate | Moderate | Serious | Moderate |
| Needham et al. (2004)47 | Moderate | Moderate | Serious | Moderate | Serious | Low | Serious |
| Needham et al. (2005)49 | Moderate | Moderate | Moderate | Not reported | Serious | Moderate | Moderate |
| Nijman et al. (1997)50 | Serious | Moderate | Moderate | Moderate | Serious | Moderate | Serious |
| Paterson et al. (1992)51 | Moderate | Moderate | Low | Not reported | Not reported | Serious | Moderate |
| Rice et al. (1985)53 | Moderate | Moderate | Moderate | Moderate | Serious | Moderate | Moderate |
| Robinson et al. (2011)54 | Moderate | Moderate | Moderate | Serious | Serious | Moderate | Serious |
| Sjostrom et al. (2001)56 | Serious | Serious | Moderate | Moderate | Moderate | Moderate | Serious |
| Smoot et al. (1995)58 | Moderate | Moderate | Low | Moderate | Moderate | Moderate | Moderate |
| Taylor et al. (2012)59 | Serious | Serious | Serious | Moderate | Moderate | Moderate | Serious |
| Thackrey et al. (1987)23 | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate | Moderate |
| Whittington et al. (1996)60 | Moderate | Serious | Moderate | Moderate | Serious | Serious | Serious |
| Wondrak et al. (1992)61 | Moderate | Moderate | Moderate | Moderate | Serious | Serious | Serious |
| Yang et al. (2014)62 | Moderate | Serious | Not reported | Moderate | Serious | Moderate | Serious |
| Study | Research team and reflexivity | Study design | Analysis and findings | Global |
|---|---|---|---|---|
| Biondo (2017)8 | 4 | 4 | 5 | 13 |
| Chigbundu (2015)18 | 4 | 13 | 7 | 24 |
| Collins (2014)20 | 7 | 9 | 5 | 21 |
| Gertz (1980)25 | 3 | 2 | 5 | 10 |
| Goodykoontz and Herrick (1990)26 | 0 | 6 | 0 | 6 |
| Ilkiw-Lavalle et al. (2002)31 | 3 | 5 | 2 | 10 |
| Martinez (2017)37 | 6 | 5 | 2 | 13 |
| McLaughlin et al. (2010)41 | 0 | 5 | 3 | 8 |
| Nau et al. (2009)43 | 3 | 7 | 3 | 13 |
| Robinson et al. (2011)54 | 0 | 8 | 5 | 13 |
Intervention intensity and content
The included studies considered interventions that varied widely in terms of content and the setting in which they were delivered. Of the 45 studies, seven studies did not provide enough detail to accurately categorise the content of training (see Report Supplementary Material 1, SM1.1). Training duration ranged from 1.5 hours to 6 weeks.
Primary outcome
Rates of conflict
In total six studies of moderate quality provided outcome data related to rates of conflict. One study measured impact of training on conflict broadly (including aggression, self-harm, absconding, rule-breaking, medication refusal, drug and alcohol use) and found a significant effect (effect size (ES) 0.13) in reducing conflict. 10 This finding represented a 44% decrease in verbal aggression, a 53% decrease in physical aggression, a 72% decrease in self-harm and a 43% reduction in absconding attempts. 10 However, when this study was repeated using a controlled design, no effects on conflict outcomes were detected. 15
Another study reported reductions in patient assaults post training but did not test significance. 58 Two studies measured patient assault-related injuries. One found a reduction but did not test significance16 and the other found a statistically significant reduction in rate of injuries, although the effect size was not calculable. 17 Two studies found negative effects of training in relation to assaults on staff. One study measured impact of training on what they referred to as ‘disturbed behaviour’ (defined as any untoward incident involving patient behaviour that met the threshold for incident reporting) and found a non-significant negative effect of training between intervention and control wards. 35 The hazard ratio for staff assaults in the de-escalation training arm of the study was 48% higher than for staff in the usual care arm (control and restraint training). 35 One study found a significant, medium-sized effect (0.64) increasing rates of assaults post training, attributed to increased patient acuity in the follow-up period. 53
In total, 12 weak-quality studies provided outcome data related to rates of conflict. One study, again, measured conflict broadly and found no statistically significant difference in rates between trained and untrained wards. 15 One study found a significant overall reduction in conflict59 but the omission of SD prevented calculation of effect size. One study only referred to the measurement of ‘incidents’ but did not define what this meant or test the significance of a reported reduction in frequency post training. 26 Two studies found statistically significant reductions in assaults compared with control conditions, one study measuring rates at ward level47 and one following up individual trainees. 32 Neither study reported the required statistics to calculate effect sizes. Two studies found reductions in patient assaults compared with control conditions but neither reached statistical significance. 34,60 One study found a reduction in assaults comparing 12 months pre and post training but did not test significance. 25
Two studies measured aggression, incorporating verbal and physical aggression and, again, both found reductions compared with control conditions that did not reach statistical significance. 50,56 One study measured actual and threatened physical aggression separately and found a negligible reduction in actual aggression and an increase in threatened aggression although the statistical significance of neither finding was reported. 36 One study measured verbal aggression alone and reported a reduction without evaluating statistical significance. 41
Rates of containment
In total, four studies of moderate quality provided outcome data on rates of containment. One uncontrolled pre and post study measured impact of training on rates of ‘restraint’ (definition limited to ‘physical restraint’ interpreted as ‘manual restraint’ excluding seclusion or mechanical or chemical restraint). They found a significant reduction in frequency of restraint usage at 3 months (representing an 85% decrease) and 6 months (99% decrease) follow-up which was maintained at 9 and 12 months. 33 Two studies found no effect on containment use. One study measured containment broadly including manual restraint, seclusion, rapid tranquilisation, time out, PRN (extra psychotropic medicines), transfer to psychiatric intensive care, special observations (intermittent or continuous) and show-of-force and found no reduction associated with training. 10 The other moderate-quality study reporting no effect measured impact on PRN only. 53
In total, five studies of weak methodological quality provided outcome data on rates of containment. One uncontrolled pre and post study in two wards measured impact of training on frequency and duration of ‘restraint’ (definition included manual and mechanical restraint) and ‘seclusion’ (defined as confinement of a patient in a ward area from which they cannot freely leave). Both the number and duration of restraint and seclusion episodes in the training period (10 months) and in the post-training period (21 months) were significantly reduced compared with the pre-training period (21 months). 24 Because of the omission of SDs in their reporting, calculations of effect sizes were not possible. One study, which again used the broad definition of ‘containment’, measured rates pre and post training using a controlled design (three training wards and five control (no intervention) wards). 15 On the intervention wards there was a significant, medium-sized (0.33) pre and post reduction in containment. There was no overall difference in containment detected between intervention and control wards but there were two significant effects detected at individual containment item level (‘PRN’ and ‘Transfer to PICU’). No SDs were reported for the comparisons with control wards for these two items, so we were unable to calculate effect sizes.
An uncontrolled pre and post study in two wards measured the effect of training on ‘coercive measures’ but did not provide further definition. 47 They found a significant reduction in rates of coercive measures between the pre-training period (3 months) and the post-training period (3 months). However, because of the lack of reported means and SDs, no effect size calculation was possible. An additional, uncontrolled pre and post study measured rates of manual restraint and rapid tranquilisation associated with training. 34 They found a significant reduction in both manual restraint (0.4) and rapid tranquilisation (0.52) after training, once differences in patient demographics between pre and post periods (6 months pre, 6 months post training) were adjusted for. However, the confidence intervals (CIs) for these effects were wide (manual restraint CI 0.17 to 0.94; rapid tranquilisation CI 0.23 to 1.21). The final study, rated as methodologically weak, was an uncontrolled pre and post study in a single ward, which measured rates of ‘restraint’ and ‘seclusion’ (no more specific definition provided for either) associated with training. 62 They found a small (self-reported, the necessary statistics for calculation were omitted) non-significant effect of training in reduced rates of both seclusion and restraint.
Secondary outcomes
Cognitive outcomes
Knowledge outcomes: In total, five studies of moderate methodological quality provided outcome data on changes in trainee knowledge following training. Four of these studies found significant improvements post training. 16,31,51,53 Two of these studies provided sufficient statistical information to calculate effect sizes: one reported a medium-sized effect (0.73)16 and one reported large effects (effect sizes ranged from 1.13 to 2.2 between different staff subgroups). 31 One study did not assess the significance of reported improvements in trainee knowledge. 28 Although these studies rated as moderate methodological strength according to the ROBINS-I, there were some specific problems with measurement that should be considered in the interpretation of training impact on this outcome. All five studies developed study-specific scales to measure knowledge outcomes and only one study provided any robust evidence of internal consistency and reliability [Ilkiw-Lavelle31 (Cronbach’s alpha 0.86)].
In total, six studies of weak methodological quality provided outcome data on changes in trainee knowledge. 5,19,21,36,37,41 Only two studies measured the significance of changes: one found a significant effect of training, but effect size calculation was not possible owing to the omission of a SD. 5 The other found a non-significant improvement in knowledge. 21 No weak study tested the internal consistency of their measure of de-escalation knowledge.
Affective outcomes: In total, 15 studies of moderate methodological quality and 11 studies of weak methodological quality reported on changes associated with trainee affective outcomes associated with training. These studies measured a range of relevant outcomes relating to emotion regulation, confidence and self-efficacy, fear and anxiety, attitudes, stress and burnout and empathy.
Emotion regulation: One moderate-quality study measured ‘emotion regulation’ which they defined as ‘awareness and control of feelings, especially fear and anger’ (p. 398)9 and found a significant, large effect (2.24) of training in enhancing this outcome (follow-up measurements were conducted between 3 and 6 months post training). Two weak studies measured emotion regulation outcomes. One weak study61 used a non-randomised controlled design and measured emotion regulation immediately pre and post training in role-play scenarios. They used an observer rated scale [including the following subscales: ‘calm’, ‘upset’, ‘angry’, ‘relaxed’, ‘defensive’ (p. 111)] and a self-report scale [including the following subscales: ‘anger’, ‘upset’, ‘anxiety’, ‘in control’ (p. 109)]. They found significant and large (0.76–5.24) pre-and-post effects of training on observer-rated items including ‘relaxed’, ‘defensive’, ‘upset’ and ‘calm’ but no significant change on ‘angry’. However, there were significant, medium to large (0.69–2.81) effects observed in the control group on ‘relaxed’ and ‘upset’, indicating a significant impact of practice effects on emotion regulation. No between-group analysis was conducted. In terms of self-report outcomes, they found significant, large effects in the trained group (0.79–1.5) on ‘anger’ and ‘in control’. There were no significant self-rated changes in the control group.
The other weak study measuring emotion regulation7 used an uncontrolled pre and post design and measured the following item related to emotion regulation (of a 20-item questionnaire measuring attitudes to aggression in student nurses): ‘When a patient gets aggressive, I get so nervous I can hardly think straight’ (p. 208). They found no effect of training on this item. Of the three studies measuring emotion regulation outcomes, only Bjorkdahl et al. 9 provided any evidence of internal consistency (Cronbach’s alpha 0.83).
Confidence and self-efficacy: Nine moderate-quality studies measured either trainee confidence16,23,28,43,46,49,51,53 or self-efficacy. 39 Five of these were non-randomised controlled studies23,39,46,49,53 and four uncontrolled pre and post studies. 16,28,43,51 Five studies measured these outcomes only immediately pre and post training. 16,28,46,51,53 Four studies included an additional longer-term follow-up, one at 2 weeks post training,43 one at 8 months,49 one at 6 months post training39 and one at 18 months. 23 All nine studies reported improvements in these outcomes associated with training at follow-up, eight found statistically significant improvements and one study53 failed to assess the significance of the improvement. Four studies provided the necessary statistical information to calculate effect sizes and, of these, three produced small effects (range 0.19–0.34)16,28,39 and one a large effect (0.87). 46 Improvements in confidence were retained in all studies that included a longer-term follow-up. 23,39,43,49
Nine studies of weak methodological quality provided outcome data related to confidence or self-efficacy. Eight measured confidence6,7,19,22,26,36,37,41 and one measured self-efficacy. 54 All nine studies used uncontrolled pre and post designs. Six studies measured these outcomes immediately pre and post training7,22,26,37,41,54 and three studies included longer-term follow-up time points. One study had an additional follow-up at 6 months,19 one study had four time points across 8 months (two pre, two post training, no more specific detail provided)6 and the final study measured confidence 12 months pre and post training. 36 All nine weak studies found improvements in confidence or self-efficacy but only five assessed significance6,7,22,37,54 and the statistical reporting in these five studies did not allow for effect size calculation. All three weak studies including longer-term post-training follow-ups found that improved confidence had been retained. 6,19,36 Of the 18 studies measuring confidence or self-efficacy outcomes, nine used validated measures,16,22,28,37,39,43,49,53,54 with Cronbach’s alphas ranging between 0.7153 and 0.97. 39
Fear and anxiety: Two moderate-quality studies measured outcomes related to staff fear or anxiety. 39,44 Both were non-randomised, controlled studies. One study measured these outcomes immediately pre and post training44 and the other measured pre and post and included an additional 6-month follow-up time point. 39 McIntosh39 measured ‘anxiety arousal’, which was defined as the level of concern about patient-perpetrated violence experienced by staff at work, and found no effect of training on this outcome post training or at 6 months follow-up. Nau et al. measured ‘fear’ (no further description provided) as a subscale of the observer-rated DABS. 44 They found significantly reduced fear from pre and post within trained subjects as well as between trained and untrained groups. The statistical reporting did not permit calculations of the sizes of these effects.
One weak-quality study measured outcomes related to staff fear. This study adopted a non-randomised uncontrolled design36 and measured ‘Fear when managing aggressive or potentially aggressive patients’ (p. 212) 12 months pre and post training. They found reduced fear at 12 months but failed to assess the significance of this reported effect. Two out of three studies measuring fear or anxiety outcomes provided evidence of the internal consistency of scales used. Nau et al. 44 reported a Cronbach’s alpha of 0.87 for the DABS scale and McIntosh (2003) reported a Cronbach’s alpha or between 0.88 and 0.97 for the Self-efficacy scale. 39
Attitudes: Six moderate-quality studies measured outcomes related to trainee attitudes. 4,10,16,28,29,49 Two of these were non-RCTs29,49 and four adopted uncontrolled pre and post designs. 4,10,16,28 Five studies measured attitudes immediately pre and post training, with only one study including an additional 3-month follow-up. 49 Three studies measured trainee attitudes to patient aggression,28,29,49 two studies measured attitudes to using de-escalation4,16 and one study measured trainee attitudes to personality disorder. 10
Two moderate-quality studies reported significant effects of training in improving trainee attitudes to aggression. 28,49 Grenyer et al. 28 found significant effects of training on four of eight subscales of the ‘Attitudes to Aggressive Behaviour Questionnaire’, with effect sizes ranging between 0.33 and 0.97. Needham et al. 49 found a significant effect (sample size calculation was not possible due to statistical reporting) of training on a visual analogue scale which measured positive and negative attitudes towards patient aggression, but no effect of training on the ‘Perception of Aggression Scale’. One study found no effect of training on trainee attitudes. 29 Both studies measuring attitudes to using de-escalation found significant effects of training;4,16 a medium effect size of 0.39 was calculable for one of these studies. 16 The only study measuring attitudes to personality disorder found no effect of training. 10
Three weak-quality studies measured outcomes related to trainee attitudes. 19,41,47 All three studies used uncontrolled pre and post designs and all measured attitudes to patient aggression immediately pre and post training, except Collins,19 who included an additional 6-month follow-up time point. Only Needham et al. 47 found a significant effect of training on ‘Subjective perceptions of the severity of aggressive incidents’ (effect size calculation was not possible). Only three of nine studies measuring trainee attitudes provided a rigorous test of internal consistency. 16,29,49
Cronbach’s alphas for the Management of Aggression and Violence Scale (MAVAS) ranged from 0.25 (situational factors), 0.41 (external factors), 0.54 (internal factors) to 0.71 (management approach) on its four subscales. 29 Needham et al. 49 reported Cronbach’s alphas of 0.69 (factor 1) and 0.67 (factor 2) for the two subscales of the Perception of Aggression Scale (POAS). The final study, Calabro et al.,16 reported a Cronbach’s alpha of 0.68 of their study-specific measure of attitudes, knowledge, self-efficacy and behavioural intention in respect of training.
Stress and burnout: Two studies rated as moderate methodological quality measured stress and burnout as training outcomes. 10,51 Both studies used uncontrolled pre and post designs and both measured stress and burnout at a single time point immediately pre and post training. Bowers et al. 10 used the Maslach Burnout Inventory (MBI)13 (Cronbach’s alpha of 0.86) and Paterson et al. 51 used the General Health Questionnaire52 to measure stress and burnout (Cronbach’s alpha 0.82–0.86). Paterson et al. 51 found significantly reduced stress and burnout associated with training (effect size not calculable due to statistical reporting) and Bowers et al. 10 found no significant effect of training on burnout.
Two studies rated as weak in methodological quality measured burnout as a training outcome. 26,59 Both studies used uncontrolled pre and post designs and measured stress and burnout at a single time point immediately pre and post training. Goodykoontz and Herrick 26 used The Burnout Scale27 and Taylor and Sambrook59 used the MBI. 13 Both studies reported reduced burnout in trainees in the post-training period, but both failed to test the significance of these changes.
Skills-based outcomes: Seven moderate-quality studies provided outcome data related to trainee de-escalation skills. Two used a non-randomised controlled design29,44 and five used an uncontrolled pre and post design. 4,10,16,51,53 Six measured skills outcomes at a single time point immediately pre and post training4,10,16,29,44,51 and one study included an additional 15-month follow-up time point. 53 Six of the seven studies providing data on this outcome found a significant effect of training. 4,10,16,44,51,53 Effect sizes were calculable for two of these studies. In one study, medium effect sizes were reported for two skills outcomes relevant to de-escalation, measured with the support (staff supportiveness of patients) (0.6) and autonomy (degree of autonomy and independence granted to patients) (0.68) subscales of the Ward Atmosphere Scale (WAS). 10 The remaining study reported a small effect (0.16) of training on ‘behavioural intention’ (intention to use de-escalation). 16 Only three of seven moderate-quality studies measured skills outcomes using validated scales. These reported Cronbach’s alphas ranging between 0.69 and 0.79 (subscales of the WAS),10 0.87 (DABS)44 and between 0.25 and 0.71 (subscales of the MAVAS). 29
One weak study provided outcome data related to trainee de-escalation skills. They used a non-randomised controlled design61 and measured skills at a single time point immediately pre and post training. The authors found significant improvements associated with training on the following subscales of their observer-rated measure to assess skills changes: ‘ability to defuse the situation’, ‘ability to deal with the situation’, ‘ability to control the situation’, ‘ability to be supportive’, ‘ability to deal with criticism’ and ‘effective use of confrontation’ (p. 111). They found no significant effect of training on ‘eye contact’, ‘posture’ or ‘empathy’ (p. 111). Effect sizes for the subscales with significant effects ranged between 0.8 and 2.0. No Cronbach’s alphas were reported for these scales.
Intervention acceptability
Participant drop-out rate was reported in 23 studies and ranged from 0% to 58.0% (M = 17.0%). 5–7,10,15–17,19,21,23,26,28,31,37,39,41,43,44,54,56,59,60 Explanations for dropouts or data removal were offered in eight of these studies and included missing data points,17,39,44 possible conflicts,10,15 insufficient completion of content23,39,59 and removal after data collection due to invalid responses. 16,44,59 Response rates were reported in 15 studies and ranged from 14% to 100% with a mean average of 74%. 5,7,10,15,16,23,28,31,32,37,41,44,58–60
Participant satisfaction
A total of 12 studies provided some qualitative evaluation of participant’s views on and experiences of the interventions. In one study, many participants perceived the training to have no positive impacts but no further information on these views was discussed. 43 One study reported a mix of positive and negative perceptions of the training intervention. 19 The remaining 10 studies reported positive views of the training from the majority of, if not all, participants. Suggested improvements to the training by participants are described in the following four themes.
Duration, frequency and availability: Participants discussed the importance of offering regular refresher courses to increase the frequency of training and maintain learning. 26,31,41,58 Conflicting views on duration were reported; some felt training was too long and others requested that increased content and time to process learning be included. 26 Participants reported a need for more opportunities to complete de-escalation, and related, training courses in general. 20
Delivery methods: Participants felt training should be tailored to the clinical context in which they were employed31 and more specific clinical examples provided from these contexts. They felt it was important to include role plays and opportunities to practise real de-escalation interventions using a diverse array of case examples. 8,20,26,31 Live demonstrations were reported as preferable to video-recorded examples26 and there were requests for trainer observation and feedback on real staff–patient interactions. 31,58 Some participants requested smaller training groups,8 while others felt training ward teams together was preferable to support whole-team approaches. 25,41 It was felt that all members of the multidisciplinary team (MDT) should be trained in de-escalation techniques. 25,41 Access to a de-escalation manual on wards was also suggested. 58
Intervention content: In multiple studies participants felt it was important to include a more in-depth coverage of the components of de-escalation. 8,20 There was a perceived need for focus on early detection of aggression20 and consideration of ‘illness and non-illness related aggression’. 31 Participants felt it was important to cover theoretical models of de-escalation8 and also that training should be tailored to individuals and cultures. 20
Facilitator attributes: Participants felt trainers with current ward experience to be more credible facilitators and emphasised the importance of trainers linking training content with personal experiences working on the wards. 31
Review B: a Theoretical Domains Framework-informed, qualitative evidence synthesis of barriers and facilitators to the de-escalation of conflict in adult acute and adult forensic mental health inpatient settings
Rationale
There has been no prior review which has adopted implementation science and behaviour change theory to identify factors that influence de-escalation behaviours in adult acute and adult forensic mental health inpatient settings.
Objective
To identify barriers and enablers to effective staff engagement in the de-escalation of conflict behaviours in adult acute and adult forensic inpatient mental health settings.
Methods
The protocol for this review was registered with PROSPERO: CRD42018089753.
Eligibility criteria
Qualitative studies and qualitative components of mixed-methods studies that considered the engagement of healthcare staff in the de-escalation of conflict behaviours in adult acute and forensic mental health inpatient settings. English-language papers. No date restrictions were imposed. Studies conducted in learning disability, child/adolescent or geriatric settings were excluded, as were papers concerned with only the prevention of conflict, rather than de-escalation.
Search strategy
Electronic database searches were conducted in January 2018, using AMED, British Nursing Index (and archive), EMBASE, MEDLINE, PsycINFO and CINAHL. Free-text searches relating to key concepts such as ‘de-escalation’, ‘mental health’ and ‘conflict’ were combined with relevant medical subject heading (MeSH) terms/subject headings.
Eligibility screening
Search returns were uploaded to Covidence, a review-management programme. Two reviewers independently screened titles and abstracts. Data extraction was conducted by PM and another member of the co-applicant team verified 10% of extractions. Discrepancies were resolved through discussion and, where necessary, third-party arbitration.
Data extraction and synthesis
Article characteristics, such as country of origin and language and setting, study characteristics, including aims, methods, participants, data collection and data analysis procedures, and key findings were recorded using a bespoke extraction form.
Data were synthesised in three stages.
Stage 1: All included studies were uploaded to NVivo10 (QSR International, Warrington, UK). Six frameworks (one per conflict behaviour) were developed using the Framework function of NVivo10, with columns representing the 14 Theoretical Domains Framework (TDF) domains and rows representing each included study. Line-by-line analysis of the results sections of each included study was then conducted. Barriers and enablers were summarised, labelled and assigned to the relevant cell. A permanent link between the summaries and the original data was created using the Create Summary Link function of NVivo10.
Stage 2: Labelled summaries within each framework column were grouped by similarity, integrated and relabelled as themes, allowing a visual overview of the common and divergent issues emerging across included studies within each framework.
Stage 3: Findings across frameworks were analysed and integrated into a single framework describing barriers to and enablers of staff engagement in de-escalation of conflict. The integration of findings across frameworks was conducted by two researchers (PM and OP) and the process was reviewed by the wider research team in a series of meetings, to resolve any disagreements and ensure rigour.
Quality/risk of bias assessment
All eligible studies were assessed using the COREQ criteria for qualitative research. All eligible qualitative studies were assessed for quality, but no study was excluded on the grounds of quality.
Results
The frequency of extracted data varied according to domains (see Report Supplementary Material 1, SM1.2). To present an applicable and theoretically rich synthesis, we only report findings related to domains with high rates of extracted data. The domains Reinforcement, Goals, Behavioural Regulation and Social Influences were underrepresented, with each identified in fewer than six papers (see Report Supplementary Material 1, SM1.2); as such, data relating to these domains are not reported here, due to limited relevance. A summary of all findings, however, is provided in Report Supplementary Material 1, SM1.3. The following provides analysis of barriers and facilitators in the 10 most prominent theoretical domains. These were: Knowledge; Skills; Memory, attention and decision processes; Environmental context and resources; Social/professional role and identity; Beliefs about capabilities; Optimism; Beliefs about consequences; Intention; Emotion.
Knowledge
To effectively apply de-escalation strategies, staff must possess specific Knowledge. Articles highlighted the importance of formal, procedural and patient-related knowledge.
Formal knowledge
Unsurprisingly, knowledge of de-escalation, and alternatives to control and restraint, is important. 63,64 When combined with knowledge of the patient, being aware of a range of de-escalation strategies allows staff to select and adapt specific interventions, tailored to the individual, to avoid use of containment. 63,65–72 Conversely, a lack of knowledge can lead to staff ‘defaulting’ to an authoritarian approach. This may be particularly relevant to staff responses to absconding behaviour, where staff feel that there are few alternatives to disciplining approaches (warnings, deterrents) available. 73
Knowledge regarding psychopathology also appears to be important. An awareness of symptoms and psychiatric/behavioural indicators can assist staff in predicting the occurrence of an incident, its trajectory and the level of risk present. 64,65,74 Psychiatric knowledge may improve attitudes, beliefs and attributions regarding ‘problematic’ behaviour, all of which directly affect de-escalation behaviour. 68,71,75–79 Unfortunately, inaccurate beliefs and attributions are common; for example, aggression or agitation as ‘acting out’,71 staff ‘attention’ reinforces self-harm,80 engaging with suicidal patients is ‘inappropriate’,81 punitive techniques, such as denying access to therapy, lead to improvements in behavioural and emotional self-regulation. 79 Such beliefs can lead to authoritarian and emotional staff responses to conflict behaviours. 82
Knowledge of the patient
Patient knowledge allows staff to predict incidents,66,73,83,84 identify early warning signs of potential conflict behaviours,67 select and apply individually tailored de-escalation interventions63,68,70,72,83,85,86 and improves therapeutic relationships. 86,87 Diffusion of relevant information, to all stakeholders, to enhance this knowledge is important to de-escalation. 75 Data suggest that an awareness of patients’ typical presentation can be helpful in prediction of conflict. 66,67,73,83–86,88 Changes in presentation can serve as an ‘early warning’ for escalating behaviour, thus allowing staff to intervene early. 65,67,84 Staff should also be aware of individuals’ history, significant life events, and relationships with other patients, triggers and typical trajectory of distress. This knowledge facilitates the selection of appropriate de-escalation interventions. 67,69–71,86 Knowledge of the patient can also promote empathy among staff and provide a sense of predictability and safety during incidents. 71 Some evidence suggests that patients respond better to staff who know them. 88
Understanding the meaning of behaviour is also important. For example, conflict behaviour often has a communicative value;89 improved understanding of patient motivation improves staff attitudes towards patients,90 increases a desire to help and assists staff in moving from coercive to alliance-based responses to conflict behaviour. 77,82 Limited knowledge regarding the meaning or function of behaviour leads to a blanket response to escalation, without personalisation. 76
Skills
Psychological skills are a major factor influencing the effective use of de-escalation. The importance of empathic communication and interpersonal skills, the development of the therapeutic relationship, and the role of psychological skills in optimising assessments and formal interventions are emphasised.
Empathic communication and interpersonal skills
Authentic engagement and empathic communication are perceived as sufficient, in and of themselves, to defuse unsafe situations without containment. Non-medicalised, authentic91,92 engagement with patients can create a sense of safety. 67,72 Rapport,73 active listening, and direct acknowledgement and validation of patient behaviour,85,90,93–96 experiences97 and concerns71,82,97 can be helpful to de-escalate a potentially dangerous incident. Calm, non-provocative language should be used,67,72,88 and any directions should be accompanied by an explanation and communicated with respect and care. 88 Limit-setting is generally acceptable to patients if delivered with empathy and an explanation. 88 Compassion and support should be maintained, even in the wake of a serious incident. 98
Data suggest that, while essential in managing all conflict behaviour, communication and interpersonal skills may be most important in the de-escalation of self-harming or suicidal behaviour. Engagement is described as ‘the difference between life and death’ (p. 309). 81 Both staff and patients identify the following qualities as useful when engaging in de-escalation of self-harm/suicide: empathy, respect, a willingness to help, respecting space, expertise and autonomy, negotiation, communicating hope and avoiding overreaction and judgement. 76–79,81,83,85,89,90,93–96,99–103
Therapeutic relationship
A strong, pre-established therapeutic relationship can optimise and enhance de-escalation,81 promote help-seeking before de-escalation is required,76,101,102 facilitate compliance82,97,98,104,105 and motivate patients to avoid dangerous behaviours. 73,75,90,94 The data indicate that developing the relationships for de-escalation can be difficult with involuntarily detained patients. 77 Patients may perceive trusting relationships with staff to be ‘risky’, citing concerns about reliability and consistency. 98 Staff must also be aware of the tension between casual, informal interactions, which serve to develop strong therapeutic relationships, and the need to maintain ‘professionalism’, something that is also valued by patients. 72 Use of containment interventions further damages patient trust in staff and results in a cycle of conflict followed by containment. 86
Assessment and flexible intervention
Assessments to inform individualised de-escalation approaches should be made at admission, including clinical history, current presentation, symptoms, suicidality and mental state. 73 Assessment, however, is considered an ongoing process, whereby staff are attentive to the full range of environmental, patient, milieu and relational factors66,67,72,106,107 that may precipitate conflict behaviours. Staff should be aware of person-specific triggers that may cause an escalation, and behavioural cues that indicate the likely onset of unsafe behaviour. 67,69,83,85,108 When conflict is active, staff must determine how and when to intervene,66,67 considering the success of past methods of intervention. 68 Even when containment is being used, stuff must repeatedly assess whether there is a necessity to continue. 104
Any assessment of conflict behaviour will inevitably incorporate, either implicitly or explicitly, an attribution of the cause of the behaviour. Data indicate that attribution directly impacts the nature of de-escalation intervention;71 for example, staff are less likely to use control and restraint if the behaviour is attributed to illness, rather than the person. 67
Intervention approaches are clearly articulated for aggression and self-harm/suicide; limited data are provided for the other conflict behaviours. Basic approaches, including emotional support, reassurance, comforting, focusing on the future, grounding, and distraction techniques,83,85,87,93,101 problem-solving, negotiation, collaboratively identifying solutions67,82,97,104,105 and limit-setting,86 can be used to effectively deescalate conflict situations. Passive intervention should be considered; giving an individual time and space, disengaging, or delaying intervention can allow patients to self-regulate. 63,66,67,69 Whatever intervention approach is taken, patient autonomy must be prioritised; punitive, or corrective, interventions generally lead to increased patient distress. 101
Data emphasise the need for individualised intervention, based on patient need. 76,89,91,95,107 Staff must be flexible in the selection and application of intervention, considering both the individual and the context. 68,71 The personalised adjustments are dependent on knowledge of the individual, highlighting earlier emphases on strong therapeutic relationships and assessment. Indeed, early discussions regarding personal triggers, behavioural indicators and preferences about how and when staff should engage can guide the selection and application of intervention strategies. 83,108
Memory, attention and decision processes
Data relevant to this domain included awareness of antecedents to conflict, and how and when to intervene.
Awareness of antecedents
Good practice, in relation to de-escalation, appears to be contingent upon staff awareness of patient behaviours, interactions and milieu ‘flow’. 64–67,74 By maintaining an awareness of subtle changes in the environment, staff can identify the antecedents of conflict, informing decisions about intervention. As indicated previously, staff must have a good knowledge of the patients they are supporting to identify likely triggers, early warning signs, changes in emotional states and person-specific cues of aggression. 67,73,99 Similarly, characteristics of the milieu, such as noise levels, movement, pacing and agitation, can offer an early indication of the likelihood of conflict. Combined, this form of fluid assessment allows staff to effectively predict and neutralise conflict episodes without containment. However, some early warning signs are difficult to identify73 or are ignored by staff. 109 This may contribute to the advent or escalation of conflict behaviours or, importantly, avoid unnecessary intervention.
How and when to intervene
Staff must be able to, firstly, identify situations that are becoming unsafe, and, secondly, predict the likely outcome; the outcome of each of these decision processes will dictate if, how and when they intervene. 66 Ultimately, staff must differentiate between behaviours that can be tolerated (benign), and those that require control. 67 If the decision is made to intervene, the nature of the intervention is often informed by ethical principles of respect, dignity, self-determination and safety, and an assessment of the patient’s historical responses to intervention. 72
Environmental context and resources
The inpatient environment directly influences use of de-escalation. Relevant impacts across three sub-themes were derived from the analysis: Organisational culture, Resources and Ward Environment.
Organisational culture
Ethos: The underlying beliefs, assumptions and values of an organisation directly influence the use of de-escalation procedures. The ethos of an organisation will manifest itself in the behaviours of its staff; principles such as respect for individuals and safety as a human right, and the expectation that staff will prioritise therapeutic engagement, remain calm when dealing with conflict, and focus on helping, rather than correcting, are linked to the use of de-escalation. 67,81,91 Unfortunately, coercive practices are often justified at the organisational level. For example, forced medication is typically justified by existing legal frameworks and the view that treatment is ‘necessary’. 104
Procedures: Formal clinical systems can prevent conflict behaviours and facilitate the use of de-escalation. Emergency systems and procedures must be reliable and effective if staff are to engage in de-escalation safely and confidently. 110 Additionally, risk assessment protocols and procedures for updating risk assessments should be clear, consistent and communicated among staff teams, to optimise intervention. 84 Co-produced care plans and ‘Positive Behaviour Support’ (PBS) plans also appear to enhance de-escalation; these documents are typically developed by psychologists and are designed to reinforce positive behaviours by enhancing staff and patient awareness of behavioural sequences. As such, they typically identify triggers, behaviour functions, early warning signs and patient preferences for reactive and proactive means of calming distress. 72,108
Staff support: Formal methods of staff support, such as debriefing and clinical supervision, have been found to promote active learning69 and can enhance de-escalation. 64,72,106 Staff express general dissatisfaction with a lack of post-incident debriefing and support. 73 Staff also value less-formal support processes to enhance de-escalation practices, such as emotional sharing and mutual support between colleagues. 80
Resources
Staff: Low staffing can be a barrier to the implementation of planned de-escalation strategies, such as PBS plans. 108 Low staff numbers also are implicated in de-escalation in medication refusal; when limited staff are available, or if there is a high load of acutely unwell patients, negotiation only occurs with patients who are deemed to be dangerous, or a positive outcome is predicted. 104 Some findings suggest, however, that staff mix is more important than absolute staff numbers. 71 Balanced staffing, ensuring a mix of skill and experience, can facilitate de-escalation, while a poor staff mix contributes to ineffective teamwork and poor communication. 69,71,72,106,109 Experienced staff are perceived better at deciding when to intervene, and are more likely to use de-escalation, in response to aggressive behaviour. 69
The type of staff also influences patient behaviour and the use of de-escalation. The presence of ‘authority figures’, such doctors and male nurses, can defuse conflictual situations, and having male nurses present makes staff more comfortable and confident engaging in de-escalation. 72 Well-trained nurses are seen to be most effective in managing self-harm, without containment. 80 Conversely, bank/agency staff may lack the skills and experience to identify escalating behaviours and can miss early opportunities to intervene. 99 Bank/agency staff are also often experienced by patients as aggressive in response to escalations. 109 Poorly or inadequately trained staff, and those who are unfamiliar with the ward and patients, find it difficult to predict escalating conflict behaviour. 71
Time: Often related to overall staffing levels, time, or lack thereof, represents a significant factor in the use of de-escalation on inpatient psychiatric units. The effectiveness of de-escalation is widely reported as being dependent on a strong, pre-existing therapeutic relationship; these relationships can only be developed over time. 97 Data indicate that a lack of resources, including time, has a direct impact on the quality of relationships, interventions such as sensory rooms,111 negotiation,104 observation93 and listening to patient concerns. 89
Activities: A lack of ward activities prevents these being used as de-escalation strategy. 72,112
Ward environment
Physical environment, social environment and rule application: Though difficult to manipulate, the physical environment of inpatient wards can contribute to the incidence of conflict and influence staff responses. The availability of a sensory room offers another de-escalation approach, and an alternative to containment. 113 Staff indicate that the availability of a sensory room allows agitated or aggressive patients a space to engage in self-soothing behaviours in private, thus regaining a sense of control. 111 If available, the use of sensory rooms should be incorporated into care plans. 113 When a ward has a high load of acutely unwell patients, staff may use de-escalation techniques, such as negotiation, less. 82 Patients value flexibility in the application of normal rules, where it can be facilitated safely, as a de-escalation strategy. 92,114,115
Social/professional role and identity
Aspects of professionals’ role perception was a consistent impact on de-escalation behaviour in the evidence reviewed. How staff perceive that their professional role influences the nature of their response to conflict. The conceptualisation of nursing as a supportive, ‘helping profession’,75 and the pursuit of professionalism, characterised by calmness, emotional control64 and the prioritisation of staff and patient safety,96 facilitate effective responses. 86 How staff view their role can also lead to negative outcomes; for example, when the nursing role is viewed as that of a gatekeeper or educator, this can lead to corrective approaches that escalate conflict. 86 Demanding respect (from patients), strictness and a need for authority and control appear to be most problematic aspects of typical responses. 116,117
Staff peer support
Having a strong staff team, where staff feel they can rely on each other, enhances de-escalation. 70 Good communication and a sense of ‘community’ among staff allows for transfer of de-escalation knowledge. 63 When seeking support after an incident, staff prefer to receive this from peers who have shared similar experiences; this assists in processing emotions and may help staff to maintain therapeutic relationships with patients in advance of future de-escalation events. 75
Beliefs about capabilities
Confidence is perceived as having an important impact on de-escalation and is influenced by team factors, patient factors and training. The perception of colleagues being supportive increases staff confidence, while the perception of peer support, length of time working together and clinical supervision increases the use of de-escalation. 67,72 Knowledge of patients increases staff confidence when responding to conflict. 67 Training is perceived as improving confidence to de-escalate conflict. Conversely, a lack of or inadequate training is perceived as contributing to anxious and avoidant behaviour100 that prevents the development of relationships that would facilitate de-escalation when conflict occurs. 109
Optimism
Much of the extracted Optimism data highlighted a pervasive perception among staff that de-escalation is ineffective and is of limited value in many circumstances. 64,69,73,96,97,101,113 Staff indicate that some conflict situations cannot be resolved through de-escalation64,97,101,104,113 and, in particular circumstances, containment is inevitable:69 for example, when de-escalation has previously been unsuccessful,66 there are high levels of risk73,77 and when patients are seen as being unable to make ‘reasonable decisions’. 97
Beliefs about consequences
Staff beliefs around de-escalation and outcome expectancies influence the nature of intervention. When attempting to manage patient aggression, staff are guided by an ‘on-the-spot’ risk assessment. The intensity of the situation, how the incident has progressed and the potential impact on others (milieu) dictate the nature of the intervention,66 and, when perceived as necessary, containment is used to prevent harm. 69,72 Similarly, when addressing rule-breaking, staff will assess the level of ‘disruptiveness’, use limit-setting when necessary to maintain control and the safety of the ward,88 and progress to containment if the desired response is not attained. 86 In some scenarios, non-intervention is preferred. Staff acknowledge that not all behaviour needs to be controlled; non-intervention can protect the milieu, does not disrupt the ward atmosphere and, in some cases, can lead to better outcomes than intervention. 67,89
When managing medication refusal, staff justifications for coercive measures are nuanced, incorporating both risk and ethical considerations. Untreated psychosis is seen as requiring ‘care’ and may be dangerous to both the individual and others, and therefore must be addressed through medication, using force if necessary. 82,104,117,118 Despite an awareness of the tension between impaired capacity and patient autonomy and acknowledging that forced medication may be humiliating for the individual, staff often perceive an ethical responsibility to the person to forcibly administer medication. 82,117 Primarily, medication is seen as being ‘in the best interest’ of the patient; untreated psychosis is viewed as degrading, and medication refusal as a function of pathology, therefore forced treatment is conceptualised as ‘humane’. 104 Staff believe that patients will later reflect, acknowledge they were unwell and unable to make rational decisions, and therefore accept that forced medication was necessary and be ‘grateful’. 97
When staff view themselves as in danger, self-preservation motivates the containment. However, behaviour modification principles also heavily influence decisions not to use de-escalation. Some staff report containment (in this context, interchangeable with punishment) as necessary to moderate conflict behaviours and reduce future incidents. 69,74,100 Some staff view basic de-escalation techniques, such as advice, instruction and directing to ward rules, as ‘too weak’ to change target behaviours and, as such, will typically opt for containment to enforce compliance. 86 When managing absconding attempts, ‘soft’ techniques, such as emotional support and family involvement, are only used until more ‘appropriate’ (i.e. restrictive) measures can be put in place. 73 Ultimately, staff see few alternatives to containment in response to attempts to abscond.
The use of sensory rooms in inpatient facilities has become more common; these settings provide sensory stimulation, in a ‘demand-free’ environment, that is largely controlled by the patient. Data suggest that these rooms have several benefits, including reduction in aggression, stress relief, the promotion of self-management and emotional regulation, and improved control over maladaptive behaviours, and may represent a meaningful alternative to medication and control and restraint interventions. 111,113,119 Despite the stated benefits, some staff indicated that the sensory room may lead to an increased intensity of distressing emotions for some patients and were sceptical about the long-term effect of the intervention.
Intention
Staff will use de-escalation strategies, initially, when they believe that a situation is becoming unsafe, either for the patient or for others. Conversely, in explosive situations, where there are no clear precipitants and escalation occurs almost immediately, containment is used. Staff perceive these escalations as being more unpredictable and unsafe, thus containment is required. 66 In medication refusal, the evidence is less clear; some data suggest that staff use extensive engagement, discussion, and negotiation to prevent forced medication104 while other data suggest these approaches are either not used, or used minimally, even when patient concerns are communicated clearly and calmly. 117,118 Rather threat, supported by legal justifications, is used and, if ineffective, force is used. 104
Data suggest that an intention to remain calm, when confronted by a conflict situation, facilitates the use of de-escalation. 67 Similarly, when managing self-harm, staff intention to respond with empathy, explore with the patient the reasons for the behaviour and discuss methods for managing urges in the future, predicts these behaviours. 77 Staff intentions, however, are influenced by organisational intentions; for example, in settings where mild-moderate self-harm is tolerated, de-escalation approaches are commonly used, whereas in settings where this is not the case, control and restraint are used both in response to self-harm and when self-harm is anticipated. 77,83
Emotion
Patient conflict behaviours can lead to a range of emotional responses in staff. Aggression, stress and fear appear to be the most common staff responses to aggression and violence. 70,74 Other factors contributing to fear responses include patient complexity and staff experience, and the size and gender of the patient, which can influence decision-making, with regard to intervention strategy. 72,106
Attributions play a significant role in staff emotional responses. When aggression is attributed to illness, staff may experience neutral or ‘positive’ emotions, such as warmth, empathy and compassion; however, when the same behaviour is attributed to the individual, staff may respond with irritation and resentment. 64,74,120 Similarly, when self-harm and suicidal behaviour are perceived as a purposeful act, directed at others, staff can feel manipulated and disrespected, and experience frustration and anger. 80,100 These responses largely come down to the perception of choice; if the patient is seen to have control over the problematic behaviour, staff emotional responses are generally negative.
Staff emotions have behavioural consequences. Staff feeling ‘safe’ when confronted with an aggressive situation facilitates de-escalation. 68 Conversely, extreme negativity, fear, and a sense of powerlessness can lead to use of containment instead of de-escalation. 70,74,106,110 These emotions can also lead to avoidance, withdrawal and poor general care practices. 64,74 Self-harm behaviours, on the other hand, lead to fear, uncertainty and a sense of rejection and powerlessness among staff, which result in reduced engagement and therapeutic nihilism. 81,100,103,121 Such emotions can also result in hypervigilance, with staff anxiety about self-harm driving the use of more invasive interventions. 80 Similar behavioural responses to difficult emotions are seen in absconding, where feelings of guilt, anxiety and concern lead to a greater reliance on containment. 73 In medication refusal, frustration and desperation can lead to staff using threats against patients,97 while frustration with continued drug and alcohol misuse can lead to ‘unprofessional behaviour’ and an overzealous focus on ‘catching’ patients. 115
Due to the emotional intensity of the work, staff working with patients who self-harm must balance the demands of care provision with effective self-care. 78 Poor therapeutic response and repeated exposure to self-harm can trigger strong emotions in staff, and staff report often feeling overwhelmed by emotion;80,99,103 excessive ‘feeling’, described as sadness, sorrow and discomfort, is associated with over-involvement and compromises professional boundaries. 96 Attempts to actively supress, rather than manage, difficult emotions are ineffective and may lead to staff becoming ‘distant’ and withdrawing from patients. 80,99
Beyond self-management strategies, staff utilise external supports to manage emotions. 76 Acknowledging difficult emotions, such as fear and anxiety, can improve de-escalation practice,103 and staff pursue both formal support, such as debriefing,99,106 and informal support, such as ‘letting off steam’ and communicating difficult emotions with colleagues, to manage their emotional state. When managing aggressive patients, these strategies allow staff to ‘calm down’ and re-engage with patients. 64
Chapter 2 Qualitative studies
Aim
To identify barriers to and enablers of implementing or engaging in de-escalation in practice, at individual, team and organisational levels.
Methods
Focus groups (FGs) and individual interviews were conducted with patients, ward staff, carers and MDT professionals purposively sampled from adult acute mental health inpatient wards, psychiatric intensive care units (PICUs) and low-, medium- and high-secure mental health inpatient wards. All current inpatients at the study sites who had capacity to consent to participate were eligible. Eligible carers self-identified as close friends or family members of the study sites’ inpatients. Topic guides were structured around the 14 domains of the TDF: knowledge; skills; identity; beliefs about capabilities; optimism; beliefs about consequences; reinforcement; intentions; goals; memory, attention and decision processes; environmental context and resources; social influences; emotions; and behavioural regulation. Consequently, participants were asked about the influence of each domain on mental health staff’s ability to use de-escalation. Concepts were explained in simple language and the interview schedule was reviewed and piloted with the study’s patient and public involvement (PPI) advisory panel.
Price (a mental health nurse) and McPherson (a clinical psychologist) conducted FGs in adult acute, PICU and low and medium secure adult forensic settings. McPherson conducted individual interviews. Barley (a health psychologist) and Goodman (a Master’s psychology graduate who also worked as a healthcare assistant in the high secure setting) conducted FGs in the high-secure adult forensic settings. Goodman conducted individual interviews. All FGs and interviews were digitally recorded (with consent) and transcribed verbatim. Transcribed data were combined and analysed using Framework analysis. 122 Deductive coding was informed by the TDF domains with emerging barriers and enablers coded inductively within each domain.
A service user researcher (Grundy), a carer researcher (Cree) and members of the project team (Papastavrou Brooks, Johnston, Price, Goodman) undertook data analysis. Coders met regularly to discuss emergent codes, develop a provisional coding framework, discuss alternative interpretations of data, and ensure that codes remained grounded in the data. The coding framework was developed iteratively over the course of these meetings until agreement across coders was reached. At this point, the coding frameworks were reviewed with the study’s PPI advisory panel. Data handling and analysis were supported with NVivo software.
Study 1: a Theoretical Domains Framework-informed qualitative investigation of barriers and facilitators to the de-escalation of conflict in adult acute mental health inpatient and psychiatric intensive care settings
Sample description
The sample consisted of 26 individual interviews with inpatients (data collected in 2014) from seven adult acute and PICU wards across four hospitals in three UK mental health trusts in northern England. These included three female, two mixed and one male acute ward and one PICU. The demographic characteristics of the inpatient participants are provided in Table 4. A further 20 individual interviews were conducted with ward staff (including qualified and unqualified nurses) (data collected in 2014) including three male PICUs, one female acute ward and one male acute ward in three UK mental health trusts. The demographic characteristics of the ward staff participants is provided in Table 5. Two FGs were conducted with MDT professionals. MDT focus group (FG) 1 had six participants and FG 2 had two participants. There was a single individual interview with one occupational therapist. MDT data were collected in 2018. MDT participants (n = 9) were recruited from four adult acute and PICU wards across two hospitals in a single UK mental health trust in northern England. These included one female, one mixed and one male acute ward and one PICU. The demographic characteristics of MDT professional participants is provided in Table 6. One FG with three carers and three individual carer interviews were conducted with carers recruited from one UK mental health trust in northern England. Carer data were collected in 2018. The demographic characteristics of the carer participants is provided in Table 7. The total sample size for study 1 was 61.
| Age | Gender | Ethnicity | Containment interventions experienced in response to escalating aggression | Diagnoses | Used illicit substances in past 12 months | MHA status | Time spent as inpatient (in past 12 months) | Previous admissions |
|---|---|---|---|---|---|---|---|---|
| 18–30: n = 8 (30.77%) |
Female: n = 18 (69%) |
Black British Caribbean: n = 1 (3.85%) |
Physical restraint: n = 17 (65.38%) |
Psychotic disorders: n = 12 (46.15%) |
Yes: n = 13 (50%) |
Detained: n = 21 (80.77%) |
0–4 months: n = 17 (65.38%) |
0: n = 2 (7.69%) |
| 31–43: n = 11 (42.31%) |
Male: n = 8 (31%) |
Black British African: n = 1 (3.85%%) |
Compulsory IM medicines: n = 11 (42.31%) |
Mood disorders: n = 8 (30.77%) |
5–8 months: n = 4 (15.38%) |
1: n = 3 (11.54%) |
||
| 44–60: n = 6 (23.08%) |
Chinese: n = 1 (3.85%) |
Seclusion: n = 9 (34.62%) |
Anxiety disorders: n = 6 (23.08%) |
9–12 months: n = 4 (15.38%) |
2–5: n = 12 (46.15%) |
|||
| 61+: n = 1 (3.85%) |
Other Asian background: n = 1 (3.85%) |
PRN medicines: n = 19 (73.08%) |
Personality disorders: n = 7 (26.92%) |
Missing n = 1 (3.85%) |
> 6: n = 8 (30.77%) |
|||
| White Irish: n = 2 (7.69%) |
Increased observations: n = 17 (65.38%) |
Dissociative disorder: n = 2 (7.69%) |
||||||
| Other white background: n = 2 (7.69%) |
Time out: n = 17 (65.38%) |
|||||||
| White British: n = 18 (69.23%) |
None: n = 2 (7.69%) |
| Age | Gender | Clinical role | Clinical experience |
|---|---|---|---|
| 18–30: n = 6 (30%) |
Female: n = 10 (50%) |
Ward manager: n = 1 (5%) |
< 2 years: n = 4 (20%) |
| 31–43: n = 9 (45%) |
Male: n = 10 (50%) |
Team leader: n = 3 (15%) |
2–5 years: n = 8 (40%) |
| 44–60: n = 4 (20%) |
Staff nurse: n = 6 (30%) |
> 5–15 years: n = 8 (40%) |
|
| Missing: n = 1 (declined to disclose) (5%) |
Nursing assistant: n = 10 (50%) |
| Age | Gender | Clinical role | Clinical experience |
|---|---|---|---|
| 18–30: n = 3 (33.33%) |
Male: n = 3 (33.33%) |
Occupational therapist: n = 2 (22.22%) |
< 2 years: n = 1 (11.11%) |
| 31–43: n = 5 (55.55%) |
Female: n = 6 (66.66%) |
Staff nurse: n = 1 (11.11%) |
2–5 years: n = 2 (11.11%) |
| 44–60: n = 1 (11.11%) |
Senior nurse manager: n = 1 (11.11%) |
> 5–15 years: n = 4 (44.44%) |
|
| Ward manager: n = 2 (22.22%) |
> 15 years: n = 2 (22.22%) |
||
| Senior clinical nurse: n = 1 (11.11%) |
|||
| Psychiatric registrar: n = 1 (11.11%) |
|||
| Clinical psychologist: n = 1 (11.11%) |
| Age | Gender | Ethnicity | Age of person cared for | Gender of person cared for | Ethnicity of person cared for | Interventions person care for experienced | Diagnosis person cared for | Person cared for detained MHA past year | Person cared for behaviours directed at carer | Person cared for behaviours directed at MH staff | Person cared for use of illicit substances in past year | Person cared for previous admissions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 31–43: n = 1 (16.67%) |
Female: n = 5 (83.33%) |
White British: n = 6 (100%) |
18–29: n = 2 (33.33%) |
Male: n = 3 (50%) |
White British: n = 6 (100%) |
Physical restraint: n = 3 (50%) |
Psychotic disorders: n = 4 (66.66%) |
Yes: n = 2 (33.33%) |
Verbal aggression: n = 3 (50%) |
Verbal aggression: n = 2 (33.33%) |
Yes: n = 1 (16.67%) |
1: n = 4 (66.66%) |
| 44–60: n = 2 (33.33%) |
Male: n = 1 (16.67%) |
30–39: n = 2 (33.33%) |
Female: n = 3 (50%) |
Coerced IM: n = 2 (33.33%) |
Mood disorders: n = 1 (16.67%) |
No: n = 4 (66.66%) |
Physical aggression: n = 3 (50%) |
Physical aggression: n = 2 (33.33%) |
No: n = 5 (83.33%) |
2–5: n = 2 (33.33%) |
||
| > 60: n = 3 (50%) |
40+: n = 2 (33.33%) |
Seclusion: n = 1 (16.67%) |
Anxiety disorders: n = 1 (16.67%) |
Physical Violence: n = 1 (16.67%) |
None: n = 4 (66.66%) |
|||||||
| PRN medication: n = 4 (66.66%) |
Personality disorders: n = 3 (50%) |
None: n = 3 (50%) |
||||||||||
| Enhanced observation: n = 2 (33.33%) |
||||||||||||
| Time out: n = 1 (16.67%) |
||||||||||||
| None: n = 1 (16.67%) |
Results
Longer direct quotes (Q) supporting the following interpretations are provided in Report Supplementary Material 2, SM2.1.
Participant accounts indicated that de-escalation involves a social encounter between a staff member or, multiple staff members, and, generally, a lone patient. These encounters were characterised by intense reciprocal attention to the physical and emotional behaviour of the other. They typically involved fluctuating changes in the cognition, affect and arousal of both parties that resulted from perception (e.g. perceived intention and perceived attitude). These states of cognition, affect and arousal were labelled as ‘internal states’ in the analysis. Safety during de-escalation encounters was maintained by actions intended to regulate both their own and the other’s internal states (Figure 1); for example, through explanation, stimulation of positive emotions or creating a more soothing and private environment for the encounter. Importantly, this process was a reciprocal, rather than a unidirectional, ‘staff de-escalates patient’ process. On the contrary, there were many examples of patients de-escalating dysregulated staff behaviour (e.g. Q1).
FIGURE 1.
De-escalation encounter.
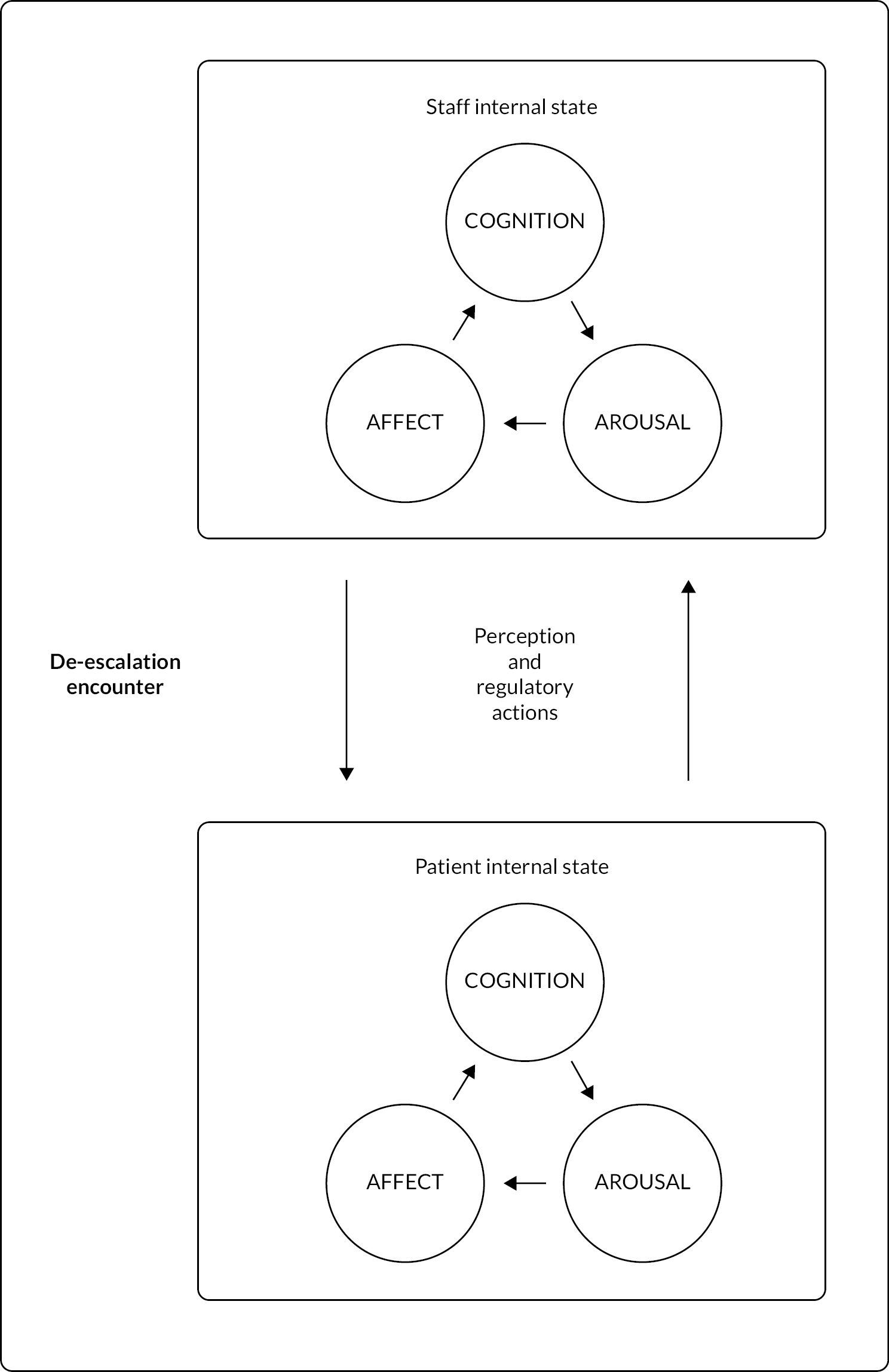
As such, patients, carers and professionals tended to discuss de-escalation in terms of a broad range of factors that impacted on staff and patient internal states and their capacity for self-regulation during de-escalation encounters. These factors were subsumed under six prominent Theoretical Domains. Four related to capability and motivational factors including skills, knowledge, emotion and social/professional role and identity and two related to opportunity factors including social influences, and environmental context and resources.
Skills
Psychological skills
Six core psychological skill domains for de-escalation were identified from synthesis of stakeholder perspectives. These were divided into connecting domains, regulating domains and an additional domain, labelled as ‘pliability’. ‘Connecting domains’ related to staff members’ ability to engage in behaviours that confirm and validate patient distress and to their ability to reduce social distance, that is, to engage with patients in authentic, reciprocal human interactions on equal terms. ‘Regulating domains’ related, firstly, to staff’s ability to remain calm and assess and understand the threat level present, and the causes and function of the behaviour requiring de-escalation. They, secondly, related to staff’s ability to create the cognitive, emotional, and physical conditions needed for de-escalation, either through autonomy-confirming techniques (e.g. offering choices, providing time and space, collaborative problem-solving) or limit-setting techniques (e.g. instructions and deterrents).
The ‘pliability domain’ cut across connecting and regulating domains and referred to staff ability to mould their de-escalation behaviours according to individual patient preferences and the changing dynamics of critical incidents as they unfolded. For example, many staff participants pointed to wide variations in the levels of intimacy and informality they would adopt in de-escalation events depending on the patient involved. Female patients valued staff who were able to combine empathy and understanding with a firmness and discipline that enabled them to contain difficult emotions, for example Q2.
The core de-escalation skill domains were, broadly, presented as prerequisites for effective engagement in a series of ‘de-escalation processes’ which staff participants reported as occurring in a loosely linear pattern. These processes were noticing a relevant change in the patient’s behaviour then either engaging in a process of ‘watchful waiting’ or deciding to intervene. If intervention was deemed necessary, there was broad agreement that the first step should be to manipulate the environment, for example, by inviting the patient into a private space or encouraging other patients to leave. The second step was to ground and reassure, for example, by providing safety statements such as ‘you’re safe’, ‘we are nurses’, ‘you’re in hospital’, ‘we will not harm you’ (male ward manager 1, acute ward). The remaining steps related to a logical process of clarifying then helping to address the problem by distracting, resolving, or reframing. The importance of post-event support was widely emphasised irrespective of whether a process of ‘watchful waiting’ or intervention had been adopted.
The richest data in terms of specific de-escalation processes related to reframing techniques. Both staff and patients pointed to the importance of stimulating memory to de-escalation. For example, PICU staff described routinely asking the patient to recount events preceding admission and felt this helped to promote insight and re-contextualise the patient’s current circumstances. Patients often described staff who would point to their shared history with staff, or a time when they had done something well, as a means of stimulating positive memories and emotions that would reduce anger. Both staff and patients agreed that de-escalation was unlikely to occur where staff had failed to create positive short-term memory of their conduct through attentive engagement with patient emotions and demonstration of trustworthiness and care, for example Q3.
Physical skills
The physical de-escalation skills participants described, perhaps, counterintuitively, aimed to communicate vulnerability (not fear). This was to communicate a non-violent intention and to render violent actions less socially congruent. For example, many staff participants described initiating sitting down, even when this was unreciprocated by the patient, for this reason. Importantly, some patients described experiences where staff would remain seated when confronted from a standing position and experienced this as belittling. This demonstrated how, at a surface level, similar behaviours could communicate importantly different messages to patients. Initiating sitting communicates vulnerability by relinquishing an optimal physical stance for self-defence, whereas remaining seated communicates a lack of concern for the physical threat posed by the patient and is, thus, experienced as emasculating. Other physical behaviours staff described as useful in communicating vulnerability and trust included ensuring a minimal staff presence necessary to maintain safety and adopting open body language with arms placed by sides. There were exceptions. Some staff participants reported that keeping arms by sides interfered with their ability to conceal visible tremor in situations involving heightened aggression. There was broad agreement among staff that visible anxiety could cause feelings of stigma in patients during incidents, but patients did not always share in this agreement (e.g. Q4).
The main divergence between staff, patient and carer views related to the use of physical touch as a de-escalation skill. Female patients and carers identified a central role for use of touch. For example, carers discussed its importance when the level of distress was so high that the individual found it difficult to respond to verbal communication. The most frequently mentioned form of touch was holding patients’ hands, or even just for staff to be ‘within enough distance to put out their hand and comfort’ (female carer, Carer FG 1) (i.e. simply sharing the patient’s space in a more intimate way could be calming in and of itself). Carers talked a lot about the value of hugs as a way of responding to patient distress. Only ‘old-school’ (female carer, carer FG 1) staff were viewed as being willing to give hugs to patients. This indicated either that more experienced staff were more flexible in their implementation of interpersonal boundaries (i.e. able to consider individual and situational differences) or differing practice norms between generations of nurses. There was a consensus among carers that patients were so deprived of physical contact on inpatient wards that they would seek it through physical restraint (e.g. Q5).
Knowledge
Understanding people
Trauma and behavioural scripts: Both patients and staff accounts indicated the importance of staff understanding how aggressive behavioural scripts could be activated through behaviour that mimics patients’ past trauma. One patient drew comparisons between staff de-escalation approaches in different hospitals which underscored the importance of this understanding (Q6). Relatedly, many staff participants described de-escalation of anger that was, ostensibly, related to unmet needs but, they felt, was implicitly motivated by antagonism to authority. They described situations where attempts to meet needs and provide explanations were met with newly generated grievances, counterarguments, and escalating confrontation. They emphasised the importance of understanding the significance of authority representations in the context of both coercive psychiatry and childhood abuse and neglect, and to respond to the behaviour in unexpected and surprising ways that moved out of the anticipated dialogue, reframing authority representations and humanising staff. These responses typically involved humour, swearing or blunt acknowledgement of the dynamic, as it was unfolding, for example Q7.
Patient-specific knowledge: There was agreement across stakeholder groups on the importance of gathering and effectively utilising patient-centred information to inform de-escalation; for example, triggers of traumatic memories in staff behaviour or the environment, the social and cultural norms of the patient and known strategies for de-escalation that worked in the past. However, there were contrasts in carer and MDT professional perspectives on how this ‘patient knowledge’ was constructed. Staff tended to value one-directional processes such as MDT discussions, reading patient notes or handover sheets as useful sources of this information but also recognised that these processes could diffuse, through nursing teams, unhelpful and inaccurate preconceptions about patients. Carers, by contrast, felt that patient knowledge with utility to de-escalation could only be derived from authentic ‘knowing’ of patients, built up through consistently reciprocal interactions over time. In this sense, they prioritised knowing patients over knowledge of or about patients (e.g. Q8)
Moral formulations: Carers and patients felt that moral formulations constructed by staff as a way of understanding patient behaviour represented a key barrier to de-escalation. They provided numerous examples of evaluatively loaded expressions they had experienced in typical staff language, for example ‘bad’, ‘nasty’, ‘difficult’ (Female Carer 1). Carers felt that the moral judgements that were communicated through these expressions betrayed a superficial understanding of patients and that de-escalation required, instead, deep understanding and connection with the feelings and needs underlying patient behaviour. By contrast, staff tended to identify deficits in understanding in terms of specific illness knowledge. Most commonly, they reported a lack of knowledge of how to reduce distress in aggression they linked with auditory hallucinations (e.g. Q9).
Conceptualisations of de-escalation
Despite the breadth and extent of skills described by participants, there was a substantial cohort of participants, represented across all stakeholder groups, who rejected the concept of de-escalation as consisting of a discrete set of skills. Rather, these participants conceptualised de-escalation as a ‘process’ that occurred within the context of a mutually trusting relationship. The centrality of relationship quality to de-escalation was, most clearly, illuminated in the context of medication refusal. Multiple staff provided accounts of patients who would only accept medication from specific staff. They described how these preferences could be accommodated by waiting until the preferred staff member was next on shift to avoid the need to enforce medication. In one extreme example, the patient’s carer would come into the inpatient environment each evening to administer the patient’s medication. This relationship-focused, flexible conceptualisation of de-escalation contrasted sharply with other commonly held understandings. For example, some participants appeared to conceptualise de-escalation as efforts to enforce patient compliance without using restrictive interventions. These participants found it difficult to engage with the potential for meaningful negotiation or conceding ground to meet patient needs, and often viewed de-escalation as part of a sequence of events that inevitably ended in restraint. So enmeshed, at times, were participant conceptualisations of de-escalation and restraint that they did not always meaningfully distinguish between the two interventions. For example, participants often observed that multidisciplinary professionals did not get involved in ‘de-escalation’ because ‘de-escalation’ would damage their relationships with patients, for example Q10.
Emotion
Professionals emphasised the importance of ‘nursing intuition’ to de-escalation, especially when engaging in the process of de-escalation with an unknown patient. This referred to the need to be consciously attuned to the emotions of the patient and professionals’ own instinctual emotional responses, as a way of understanding and therefore de-escalating conflict situations. Participants emphasised that, unlike other nursing procedures that, with practice and repetition, could become automatic or semiautomatic, de-escalation required genuine emotional engagement with the unique emotional contours of each conflict situation. However, staff’s use of instinctual responses to guide de-escalation relied on a high level of emotional self-knowledge and management. Staff often demonstrated a lack of awareness of their own emotions and how they were expressed in behaviour, finding it difficult to ‘step back’ (MDT FG 1) from a situation instead being subconsciously led by their instant emotional reaction.
Deficits in this emotional awareness were perceived as having several key consequences for de-escalation. Staff who were unreflective about their own emotions were more likely to utilise restrictive practices as a way of reducing their own anxiety. Secondly, unidentified anxiety was felt to cause staff to respond to aggression by ‘squaring up to’ (MDT FG 1) patients or mirroring an aggressive tone of voice without consciously realising they were doing it. Frustration that was not acknowledged and dealt with was seen as causing staff to ‘take it out’ (MDT FG 1) on patients or other staff, and act abusively. However, emotional management was not seen by either staff or carers as involving staff masking their emotions in front of patients, but instead being aware of them and their impact, and therefore being able to use them productively to engage patients. Emotional masking was felt to be impossible in a psychiatric context, since staff were also human, and in high-intensity situations could not fully hide their emotions. Carers believed that patients often had enhanced abilities at reading body language and tone, and therefore could pick up on and be affected negatively by staff’s emotions, if staff did not acknowledge or articulate them. This underscored the importance of congruence between thoughts, feelings and verbal and physical behaviour and, more broadly, of honesty and emotional openness, to de-escalation (e.g. Q11).
Staff in general felt that they were not given the appropriate structures (such as formal debriefs) to be able to process the impact of incidents such as restraint and self-harm on staff members. They felt they were left with no alternative but to individually suppress difficult emotions to function at work. The lack of an outlet for collective processing of emotions, combined with a perceived lack of knowledge and skills relating to working with patients with severe trauma histories, contributed to a process staff referred to as ‘burnout’. They characterised burnout as diminished emotional capacity to relate to patients in a therapeutic way. The lack of debriefing was also felt to (1) reduce their ability to understand and mitigate the traumatic impact of incidents on team members and (2) reduce their sensitivity to the harm done to patients by restrictive interventions (e.g. Q12).
Social influences
Ward team culture
Regime: Patient, ward staff and carer accounts focused extensively on ward team cultures that they felt worked in opposition to de-escalation practice. These accounts reflected a cycle of violence, in which staff would use maladaptive coping strategies (e.g. excessive rules, stringent boundary maintenance) to manage their fear of patient violence. Patients would then respond to these coping strategies with violence, thereby reinforcing staff fear and furthering the perceived need for more boundaries and rules. In addition to aggravating rules, patients also described, as a feature of dysfunctional teams, attempts to control patient narratives of their experiences as inpatients, as a way of maintaining safety. For example, patients observed a marked intolerance among staff of dissent and criticism of practice. During the limited occasions when patient views on practice were consulted, for example, in ward community meetings, they described feeling steered towards accepting explanations for poor practice or shortfalls in provision that, they felt, were unduly apologetic to staff and services. An additional manifestation of fear cultures was demands for unconditional patient respect of staff, irrespective of whether this was reciprocated in staff treatment of patients. The sense of injustice resulting from these practices was compounded by the presence of what they called ‘propaganda materials’ (female patient 4, acute ward) in the environment (e.g. Q13). The propaganda materials that this patient was referring to were posters in ward environments demanding patient respect of staff (without concomitant demands for staff to respect patients) or expressing zero tolerance of patient violence. Patients reported that these cultural practices had such an aggravating impact on patient’s general affect and level of arousal that attempts at de-escalation, where attempted, were unlikely to be successful.
Vulnerability: The consequences of fear cultures within ward teams were not limited to staff treatment of patients, but also affected their treatment of each other. Descriptive accounts of these teams indicated that they displayed a marked contempt for vulnerable colleagues (e.g. new starters, newly qualified nurses, students and non-regular staff) and a suspicious disdain for outsiders (e.g. MDT professionals, senior nurses). Both groups were perceived as representing a threat to established risk-management practices (the former group through unfamiliarity, and the latter group through unwelcome change initiatives). Participants described a culture in which the practices of new starters would be closely monitored, by established staff, to assess and, if necessary, modify their inclination towards assimilation to the existing culture. This generated pressure in vulnerable staff to demonstrate ‘competence’ through practices that conflicted with de-escalation (e.g. premature use of restrictive interventions and inflexible application of ward rules). These social dynamics therefore encouraged sadomasochistic ways of relating to others, where avoidable conflict was initiated to gain social approval, inviting violence from patients, for example Q14.
Ideology
Deserving and undeserving patients: A universal feature of teams, described by all stakeholder groups, was shared ideologies related to patient deservingness of care. Staff often used the term ‘behavioural’ to signal to each other whether an observed behaviour or patient was worthy or unworthy of de-escalating responses. This was based on a subjective clinical judgement as to whether the person’s behaviour could be linked to mental illness. There was, rarely, reflection on how, given the complexity of psychopathologies and trauma characterising inpatient populations, these judgements could ever be made with any degree of accuracy. Carers linked these ideologies with a desire to make patients ‘take responsibility’ (Carer FG) and that this desire manifested itself at the point of de-escalation through unhelpful behaviours, for example Q15.
Beliefs about behaviour change: The perceived need to encourage patients in distress to ‘take responsibility’ at the point of de-escalation was, again, linked by carers with what were labelled as ‘behaviourist beliefs’ within the analysis. Commonly shared in ward teams, these included beliefs that empathetic responses to distress ‘reward’ or ‘reinforce’ negative behaviours and coping strategies, and the belief that making hospital ‘too nice’ (MDT FG 1) for patients lengthens inpatient stays. They also related to more fundamental staff beliefs on the value of punishment and reward in eliciting desired behaviours from patients. Patient and carer views often sharply contrasted with ward staff views in this respect. The former tended towards the view that undesirable behaviours could be reduced through addressing underlying sources of distress and were sceptical about the value of punishment and reward in long-term behaviour change, for example Q16.
Multidisciplinary team participants emphasised that behaviourist beliefs functioned, in practice, in contradiction to their intended aims, in that patients would ‘progress the pathway in a different way’ (MDT FG 1) (i.e. become so unwell or so aggressive that they required transfer to PICU or forensic services). Although not exclusively, behaviourist beliefs and assessments of deservingness appeared more commonly in discussions of patients labelled with personality disorder and directly informed differential treatment, for example Q17.
Attitudes to personality disorder: There was evidence that National Institute for Health and Care Excellence (NICE) guidelines recommending alternatives to inpatient admissions for people with borderline personality disorder had exacerbated already pernicious attitudes to patients within this group. Many staff expressed nihilistic views of working with these ‘untreatable’ (Male Staff Nurse 2, PICU) people, often held the view that hospital is not the right place for them and bemoaned the lack of available specialist services. It was unclear whether this viewpoint reflected a genuine need for an alternative setting or a desire among staff to limit the time they had to interact with a patient group they found difficult. This uncertainty was reflected in the diversity of explanations provided for why patients with diagnoses of personality disorder should not be on acute wards. For example, the same participant expressed the contradictory positions that it was not helpful for patients with this diagnosis to be in hospital at all, and that it was simply that acute staff lacked the skills to manage this patient group, necessitating a specialist service, for example Q18. Overall, it was clear that these attitudes prevented staff from connecting with the distress underlying behaviour in this group, perceived as so fundamental to de-escalation by carer participants.
Environmental context and resources
Organisational structure and culture
Hierarchical barriers to information availability and utility: There were extensive data from all stakeholder groups describing how hierarchical professional structures and group interests limit the availability of accurate information about patients to enhance de-escalation. Participants described marginalisation of perspectives at every layer of inpatient organisational structures: between medical and nursing staff, between senior nursing management and ward teams, between multidisciplinary teams and unqualified nurses, between nursing teams and patients, and between inpatient services, broadly, and carers, for example Q19. There was a strong perception among many participants, cutting across stakeholder groups, that these structural problems ensured that those who knew least about the patient had most influence on de-escalation strategies.
Senior nurses consistently expressed the view that psychiatrists tended to be invested in traditional medical hierarchies and disregarded the views of nurses. They drew on strategies for de-escalation of medication refusal as examples of this, where, they felt, nurses were often required to enforce medication when de-escalation strategies were available. For example, these nurses reported that nursing proposals to delay forced treatment, to identify and resolve psychosocial stressors were often overruled by psychiatrists. They made the broader observation that the paternalism inherent to the medical model undermined the confidence of nurses to make common-sense decisions in relation to de-escalation. For example, MDT professionals reported a common belief among nursing staff that depot dates determined categorically when the medication should be administered, and that this resulted in the avoidable use of force to administer medication. This was perceived as partially driven by anxiety about asking doctors to rewrite depot prescriptions and partially by mistaken beliefs about the authority of these systems (professionals noted a lack of specific policy guidelines on the issue). In contrast, MDT professionals felt that a ‘three-day grace period’ in which to negotiate with the patient was unlikely to result in any significant deterioration in mental state or increases in other risks. Carers broadly and some staff, for example Q20, felt there was a lack of information provided to patients about antipsychotic medication and side effects, which they felt was rooted in the, they felt mistaken, belief that increased transparency would create more, rather than fewer, problems with adherence.
Other structural barriers precluding relevant staff input on de-escalation included the exclusion of unqualified staff from ward rounds. This had the effect of marginalising, from key de-escalation decisions, the staff group who spent most time with the patient, and prevented unqualified staff from developing the knowledge required to de-escalate typical patient concerns, for example Q21.
Power and alienation: Senior nursing leadership was perceived as failing to foster the quality of relationship with ward staff that would make accurate information about sources of conflict and de-escalation strategies available. A culture of distance and alienation between front-line ward staff and nursing management was attributed to a lack of meaningful clinical input and blame-based contact. This had evidently engendered a siege mentality among staff, and a sense that those outside the direct care team lacked a credible understanding of the context in which decisions and expectations were implemented. Participants indicated this created a culture of back-covering and secrecy that rendered critical events involving de-escalation invisible to senior leaders. Thus, there was an identified need for closer working relationships that fostered open dialogue around de-escalation practice and supported learning rather than blame, for example Q22.
Exclusion of patient and carer perspectives: Power imbalances between different groups also affected the quality of information gathered after de-escalation had occurred. The exclusion of patient perspectives from written communications was perceived as having a significant impact on the availability of accurate information for de-escalation. For example, the lack of direct patient contribution to nursing notes was felt to limit reliable communication of what had worked in terms of de-escalation. Nursing notes were, more broadly, identified as a major source of patient distrust in qualified nurses, who were perceived as documenting incidents from a biased and self-exculpatory perspective that was then taken as authoritative by others reading their accounts. Conversely, increased attempts to embed patient perspectives in systems (e.g. through co-produced de-escalation plans) were reported positively across stakeholder groups, for example Q23.
Overall, carers described similar experience to patients in terms of marginalisation from discussions and decisions relevant to de-escalation. Where their perspectives were sought, they were given the impression that staff ‘didn’t actually believe anything [they] said’ (Male Carer 1). MDT professional discussion of how they involved carers in decision-making confirmed these perspectives, as they exclusively framed carer involvement in terms of how to get carers to ‘see the benefits’ (MDT FG 2) of a plan they might be resistant to, to get them ‘on board’ (MDT FG 2). Conflicting perspectives with carers were perceived by MDT professionals as stemming fundamentally from a lack of knowledge on the part of carers.
Positive risk-taking: Staff were very much aware of the potential value in adopting less restrictive approaches to self-harm but felt that broader organisational support for positive risk-taking was currently lacking. Consequently, nursing staff were perceived as feeling the need to intervene aggressively at every incident of self-harm and that clinical management was almost exclusively based upon removal of means. MDT professionals felt that this only escalated patient desire to self-harm and tended to increase severity when the opportunity eventually arose, for example Q24.
Environmental stressors
Staff and patients described sources of environmental stress that had a persistently aggravating impact on patients’ level of arousal and affect. They emphasised that any attempt to enhance de-escalation must first address these sources of distress. Environmental stressors were subsumed under four categories: environmental signifiers of coercion and disrespect; ward procedures; patient community conflict; sensory input.
Environmental signifiers of coercion and disrespect: Patients described a range of visual cues and design features of inpatient wards that were either fear-inducing or alienating, or both. They identified as particularly unhelpful posters within the environment that instructed or threatened patients about their behaviour. Patients also found visual evidence of coercion within the environment (e.g. seclusion-room doors and pinpoint alarms) distressing and felt that staff used these as visual cues to intimidate patients into compliant behaviour. Staff accounts, to some extent, corroborated these perceptions, for example Q25.
The door to the nursing office remaining closed was a consistent and significant source of alienation for patients. They described feeling intimidated approaching this ‘staff-only’ space and difficulty in rousing staff from within to meet their needs. This resulted in many examples of escalating frustration and distress occurring immediately outside the staff office, for example Q26. Notably, multiple patients identified being invited into staff-only areas (e.g. nursing offices or medication clinics) as an effective de-escalation strategy. This highlighted the significance of segregated staff spaces both as a potent source of conflict and as a symbol of disrespect for patients.
Clinical processes: Both patients and staff provided extensive accounts of ward processes that, they felt, in their current format were incompatible with de-escalation. These processes generated feelings of dependence, exclusion or isolation, humiliation and loss of control, in patients. These were, consistently: ward rounds, nursing shift handovers, prescribing consultations, waiting times, medication rounds, mealtimes and admission. In respect of admissions, specifically, patient participants emphasised that experiencing trauma (use-of-force and/or social isolation) at admission can make it impossible to recover the trust in staff necessary for de-escalation to work. Staff and patients identified the need for improvements to provide a greater sense of power and control over these experiences. These included: greater involvement of patients in handover and prescribing; smaller ward rounds with fewer attending staff; measures to avoid social isolation or use of force on admission; more efficient management of patient requests; elimination of institutionalised practices around medication rounds (inflexible timing, queuing, use of the ‘stable-door’); and creating a less dehumanising experience of mealtimes (i.e. being observed, plastic cutlery, being required to remain in the dining area until patients have finished eating), for example Q27.
Patient community conflict: Patients prioritised patient community conflict as a source of environmental stress. There were widespread reports of insufficient and, often, no staff present in communal areas to detect and intervene in patient-to-patient conflict. Patients felt that rules mandating patient assembly and blocking patient access to bedrooms impeded their ability to escape victimising behaviour and wanted these practices eliminated or minimised, for example Q28. The patient community dynamic that was most focused on by staff participants was what they perceived as ‘prison cultures’ on male wards. This referred to perceived patterns of behaviour in which patients (typically young, frightened, with prior experience of the criminal justice system) would attempt to establish a hierarchy within the patient community by initiating conflict with patients and/or staff. This required careful attention in relationships: for example, by providing subtle reassurance (that does not undermine masculine self-confidence), orienting the patient to the differences between hospital and prison and avoiding escalating confrontation in the presence of other patients (furthering the perceived need to secure dominance). There was some limited support among patients and staff for training patients in de-escalation, for example Q29.
Sensory input: Patients acknowledged the contribution environmental noise made to escalations, by impairing their ability to monitor the source of auditory stimulation and increasing fear of other patients. However, many felt this problem was currently managed through the joyless suppression of all noise without reference to meaning and context. Patients were broadly critical of the absence of calming spaces equipped with sensory equipment that would enable their escape from distress caused by other patients and environmental noise, for example Q30. Several patients and nurses made specific reference to the value of having objects to safely kick and punch, for example, beanbags, mattresses and pillows, as a de-escalation strategy. This activity was perceived as useful in providing distraction from urges to self-harm or be violent, reducing anger and coping with distressing auditory hallucinations, for example Q31.
Social/professional role and identity
Professional boundaries
Staff conceptualisation of appropriate professional boundaries has an important motivating impact on de-escalation engagement. Descriptions of boundary maintenance ranged from staff who identified self-disclosure and reciprocity as their primary protection against assault, to staff who concealed their name badge from patients to maintain anonymity. The maintenance of narrow boundaries was felt to be underpinned by beliefs relating to how personal safety is maintained, that is, by displaying no emotional vulnerability, disclosing no personal information, and controlling narratives by accepting no patient criticism. Beliefs about appropriate professional boundaries also restricted staff ability to use physical touch as a de-escalation strategy, identified as important by both patients and carers. Broadly, participants felt that narrow professional boundaries precluded authentic connections with patients and thereby de-escalation capability, for example Q32.
Role perception
Correctional, health-educator and task-oriented role perceptions were identified as problematic in terms of de-escalation engagement. Helpful role perceptions had the following features: a conceptualisation of working with ‘people not patients’, an appreciation of reciprocal and authentic relationships (characterised as ‘professional friendships’) and humility, for example Q33.
Social identity
There was evidence gender, seniority and age have an important influence on the range of strategies available to de-escalating staff. Staff recognised that female patients who had experienced sexual trauma would often respond better to a female than to a male at times of distress (due to perpetrators of sexual abuse being overwhelmingly male). However, staff failed to recognise that the same was likely to be true of male patients under their care and did not explicitly recognise or discuss how they would manage a situation where male patients were triggered by the presence of male staff if they were distressed or dissociating. This was exacerbated by staff beliefs that ‘self-harm is more on the female side than the male side’ (female occupational therapist 1, acute ward), meaning that staff on male wards didn’t feel there was a value to attending training on self-harm and suicide, making it unlikely that staff would be able to recognise and respond appropriately to male self-harming behaviours. Overall, staff seemed better applying knowledge of trauma to female patients, understanding the impact of this on how they might need to be de-escalated, and being able to recognise and respond to self-harming behaviour, and had difficulties seeing male patients as vulnerable in a similar way.
Counterproductive beliefs about gender also extended to the staff team, with staff reporting that male staff members felt they needed to take the lead in conflict situations, pushing female staff out of the way to be at the front, since they felt they ‘should be the protector’ (MDT FG 1) of female staff, to ‘not let a woman get hit’ (MDT FG 1). This was seen as unhelpful for de-escalation for numerous reasons. As discussed above, it neglected the impact of male staff re-triggering a patient who had experienced trauma from a male perpetrator. The presence of men (particularly in a group) was also felt to increase male aggressiveness as it could be threatening to their masculinity, as well as not making use of the fact that similar ideologies within the patient group meant they were less likely to hit a female member of staff or even ‘present as aggressive’ (MDT FG 1) in front of them. This set of beliefs about men needing to take the leading role in de-escalation and restraint was not endorsed by MDT participants and was felt by them to increase the number of patient assaults on staff and aggravate conflict situations.
Male patients had a strong view that women possessed feminine qualities that were naturally more suited to de-escalation. It was also felt easier for female nurses to stimulate empathy and remorse in male patients because of the commonality of moral commitments against violence to women. Conversely, female gender could be a disadvantage in the case of men from cultures in which accepting guidance/instruction from females is uncustomary. There was broadly an indication that de-escalation between opposite genders was uncomplicated by gender competition. A minority felt more senior staff could employ authoritative approaches that would not be accepted from junior staff. There was agreement across participants that young staff de-escalating older patients created an abnormal and potentially undignified social dynamic, which required skill and resilience to navigate, for example Q34.
Study 2: a Theoretical Domains Framework-informed qualitative investigation of barriers and facilitators to the de-escalation of conflict in adult forensic mental health inpatient settings
Sample description
The sample consisted of two FGs (FG 1 n = 7; FG 2 n = 4) and nine individual interviews with 20 inpatients (data collected in 2018) from six wards across three hospitals in two UK NHS mental health trusts (one in northern England and one in southern England). These included one low secure ward (male), two medium secure wards (one male, one female) and three high secure wards (all male). The characteristics of the inpatient participants are provided in Table 8. Three FGs (FG 1: n = 8; FG 2: n = 6; FG 4: n = 5) were conducted with 19 members of ward staff (unqualified and qualified nurses) (data collected 2018). Ward staff were recruited from seven wards across two hospitals in two UK NHS mental health trusts. These included one low secure ward (male), two medium secure wards (one male, one female) and four high secure wards (all male). The characteristics of the ward staff participants are provided in Table 9. Three FGs (FG 1: n = 4; FG 2: n = 11; FG 3: n = 9) were conducted with 24 MDT professionals (data collected 2018). MDT professionals were recruited from six wards across two hospitals in two UK mental health trusts (one in northern England and one in southern England). These included two medium secure wards (one male, one female) and four high secure wards (all male). The characteristics of MDT professionals are provided in Table 10. Four individual interviews were conducted in 2018 with carers recruited from one UK NHS mental health trust in southern England. The characteristics of carer participants are provided in Table 11. The total sample size for study 2 was 67.
| Age | Gender | Ethnicity | Containment interventions experienced | Diagnoses | Used illicit substances in past 12 months | MHA status | Time spent as inpatient (in past 12 months) | Previous admissions |
|---|---|---|---|---|---|---|---|---|
| 18–30: n = 8 (40%) |
Female: n = 4 (20%) |
White British: n = 13 (65%) |
Physical restraint: n = 15 (75%) |
Psychotic disorders: n = 13 (65%) |
Yes: n = 3 (15%) |
Detained: n = 20 (100%) |
0–4 months: n = 1 (5%) |
0: n = 5 (25%) |
| 31–43: n = 9 (45%) |
Male: n = 16 (80%) |
Black British: n = 3 (15%) |
Compulsory medication given by injection: n = 6 (30%) |
Mood disorders: n = 8 (40%) |
5–8 months: n = 3 (15%) |
1: n = 1 (5%) |
||
| 44–60: n = 2 (10%) |
Mixed white and black African: n = 1 (5%) |
Seclusion: n = 15 (75%) |
Anxiety disorders: n = 7 (35%) |
9–12 months: n = 9 (45%) |
2–5: n = 4 (20%) |
|||
| Not reported: n = 1 (5%) |
Asian or Asian British Pakistani: n = 1 (5%) |
PRN medication: n = 13 (65%) |
Personality disorders: n = 11 (55%) |
> 1 year: n = 7 (35%) |
> 6: n = 2 (10%) |
|||
| Other: n = 1 (5%) |
Increased observation: n = 14 (70%) |
Other: n = 2 (10%) |
Not reported: n = 8 (40%) |
|||||
| Not reported: n = 1 (5%) |
Time out: n = 8 (40%) |
| Age | Gender | Clinical role | Clinical experience |
|---|---|---|---|
| 18–30: n = 3 (15.79%) |
Female: n = 14 (73.68%) |
Ward manager: n = 4 (21.05%) |
< 2 years: n = 4 (21.05%) |
| 31–43: n = 9 (47.37%) |
Male: n = 5 (26.32%) |
Staff nurse: n = 7 (36.84%) |
2–5 years: n = 2 (10.53%) |
| 44–60: n = 7 (36.84%) |
Nursing assistant: n = 8 (42.11%) |
> 5–15 years: n = 7 (36.84%) |
|
| > 15 years: n = 6 (31.58%) |
| Age | Gender | Clinical role | Clinical experience |
|---|---|---|---|
| 18–30: n = 3 (12.5%) |
Female: n = 15 (62.5%) |
Senior nurse manager: n = 1 (4.17%) |
< 2 years: n = 1 (4.17%) |
| 31–43: n = 6 (25%) |
Male: n = 9 (37.5%) |
Senior clinical nurse: n = 2 (8.33%) |
2–5 years: n = 3 (12.5%) |
| 44–60: n = 15 (62.5%) |
Social worker: n = 1 (4.17%) |
> 5–15 years: n = 7 (29.17%) |
|
| Psychiatrist: n = 4 (16.67%) |
> 15 years: n = 13 (54.17%) |
||
| Clinical psychologists: n = 5 (20.83%) |
|||
| Occupational therapists: n = 2 (8.33%) |
|||
| RRPIs: 9 (37.5%) |
| Age | Gender | Ethnicity | Age of person cared for | Gender of person cared for | Ethnicity of person cared for | Interventions person care for experienced | Diagnosis of person cared for | Person cared for detained MHA past year |
|---|---|---|---|---|---|---|---|---|
| 44–60: n = 4 |
Female: n = 4 |
White British: n = 2 (50%) |
18–29: n = 1 (25%) | Male: 4 | White British: n = 2 (50%) | Physical restraint: n = 3 (75%) |
Psychotic disorders: n = 2 (50%) |
n = 4 |
| Black British: n = 1 (25%) |
30–39: n = 1 (25%) |
Black British: n = 1 (25%) |
Coerced IM: n = 2 (50%) |
Personality disorders: 2 (50%) |
||||
| Mixed white and black African: n = 1 (25%) |
40+: n = 2 (50%) |
Mixed white and black African: n = 1 (25%) |
Seclusion: n = 3 (75%) |
|||||
| PRN medication: n = 1 (25%) |
Results
Key results of this study are summarised, rather than presented in full as the data have been published here. 124,125 Analysis of professional, paraprofessional, and patient perspectives in low, medium and high-secure adult inpatient services revealed nine prominent theoretical domains relevant to engaging in de-escalation. Seven domains related to capability and motivation factors, including Knowledge, Psychological skills, Behavioural regulation, Social/professional role and identity, Reinforcement, Emotion, and Beliefs about consequences. Two domains related to opportunity factors, including Social influences and Environmental context. Prominent theoretical domains are therefore presented in the following analysis under two overarching categories: ‘Capability and motivation domains’ and ‘Opportunity domains’.
Capability and motivation domains
Participant perspectives consistently indicated that de-escalation is dependent on key staff capabilities in creating the relational context for de-escalation to work. Key psychological Skills included authenticity (display of outward behaviours consistent with internal thoughts and emotions) and vulnerability (the ability to share and to trust patients with information about the self). Key Knowledge requirements related to knowing and understanding the person involved. Relevant Emotion factors related to the need for staff to be attuned to both the emotions of the patient and their own emotions to understand and respond effectively to incidents requiring de-escalation. The need for staff to be emotionally present and available in the broader context of their general relationships with patients was also emphasised (this facilitated patient trust, seen as the most instrumental relational component of successful de-escalation). Analysis revealed a consistent, mutually reinforcing relationship between Knowledge, Emotion and Skill domains (see Figure 1). For example, expressions of vulnerability and authentic connections with patients enhanced staff knowledge and understanding of the person. Knowing and understanding the person reduced negative emotion in staff and enabled them to remain attuned and emotionally present during de-escalation events. Attunement to the emotional states of self and others facilitated authentic behaviours and so on.
Desired Behavioural regulation strategies identified by professional participants included advanced de-escalation planning and post-event debriefing. These interventions were both enhanced by and helped to develop knowledge and understanding of patients (Figure 2). Debriefing and planning also helped to modify staff Beliefs about consequences of engaging in de-escalation where perceptions of danger were disproportionate and/or based on faulty assumptions (see Figure 2). The Social/professional role and identity of nursing staff had an important impact on de-escalation engagement. Beliefs about professional boundaries restricted staff willingness to engage in authentic behaviour and expression of vulnerability. Finally, there was an indication that greater recognition and formal thanks of staff might help in terms of Reinforcement of de-escalation practice and the suggestion that this might have additional benefits in terms of staff’s emotional preparedness (see Figure 2).
FIGURE 2.
Capability and motivation domains.
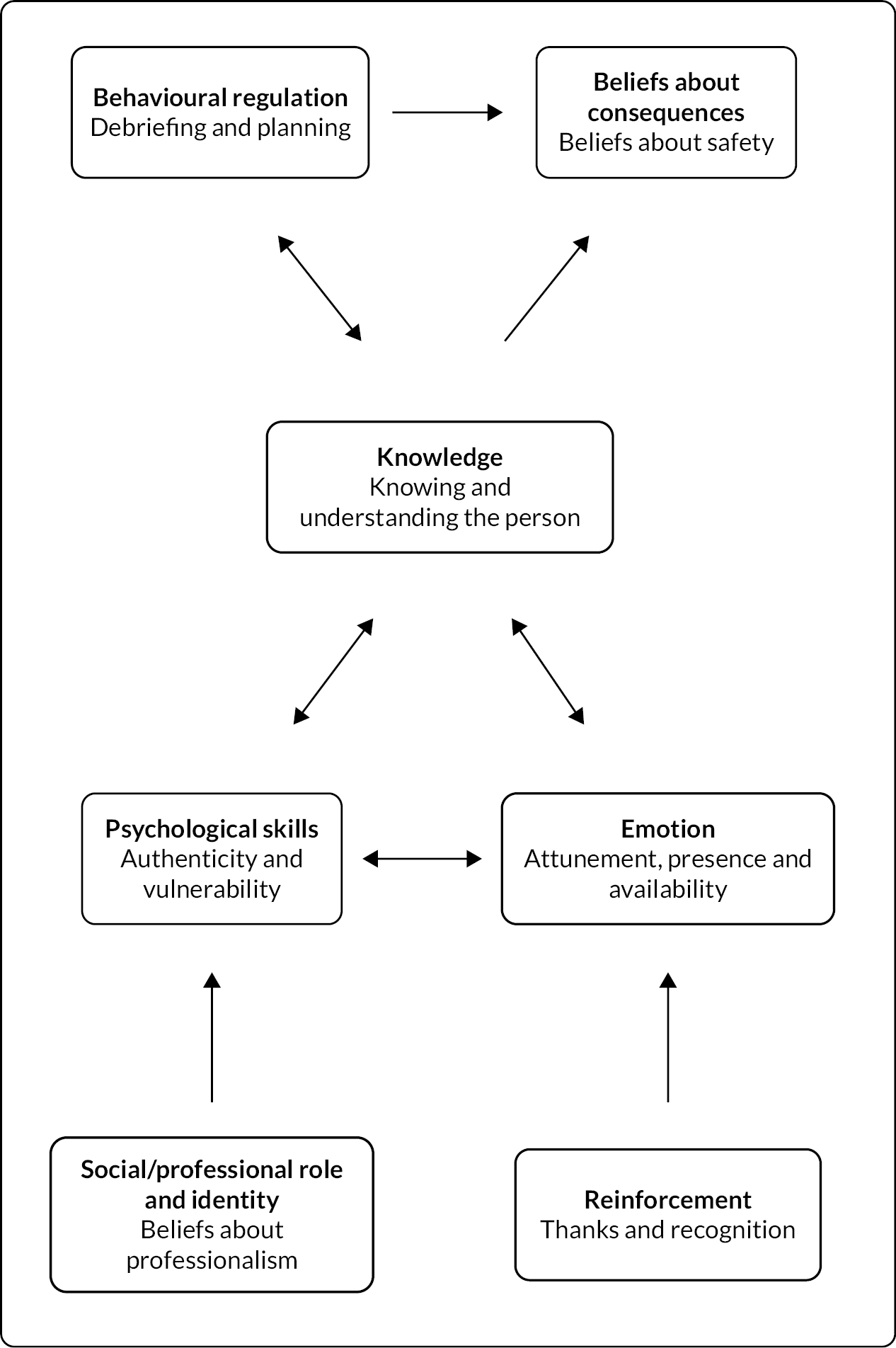
Opportunities
Participant accounts indicated that opportunities for de-escalation could be created through collaborative prescribing (Figure 3). This was an aspect of care forensic patients described having no input into and was a major source of alienation for patients. There was a perception among staff and patients that medication refusal often served as means of reclaiming lost power. There was indication that enhancing patient knowledge of medicines prescribed, as well as increasing involvement in decision-making, may help to improve relationships between prescribers, ward staff and patients and facilitate safer resolution of medication-related conflict. Patients and staff both felt that the systematic exclusion of unqualified staff from MDT decision-making had two key impacts on de-escalation. Firstly, excluding the staff group that often had the most knowledge about the patient impacted the quality of decision-making and planning in relation to de-escalation. Secondly, it prevented unqualified nursing staff from developing the clinical knowledge (e.g. around medicines) that helped to de-escalate anger or distress associated with a lack of understanding/information provision.
FIGURE 3.
Opportunity domains.
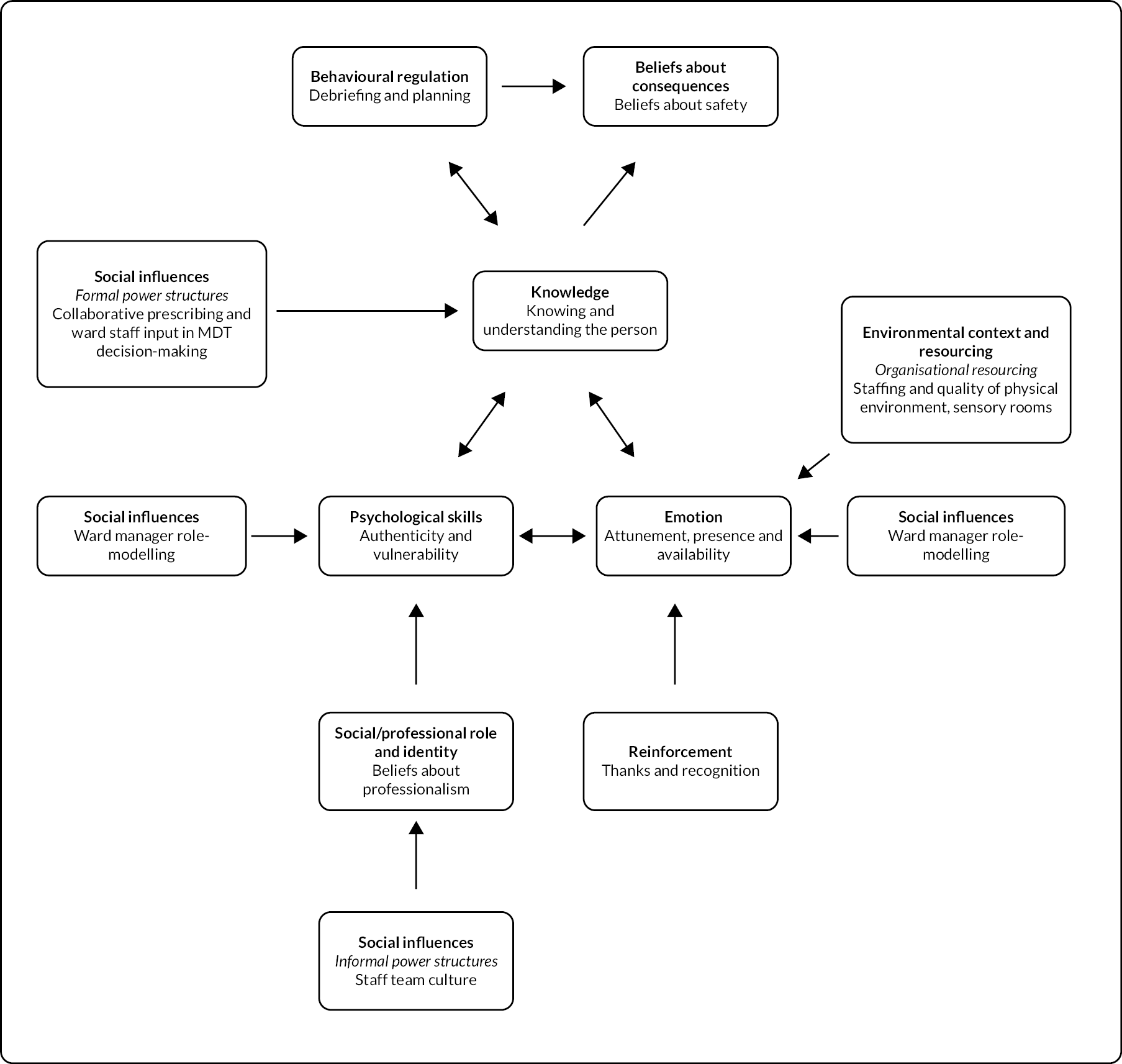
Informal power structures in staff teams also restricted opportunity for de-escalation (see Figure 3). Team cultures often stigmatised emotional vulnerability in staff and what was labelled in the analysis ‘therapeutic intimacy’ (openness and reciprocity) in staff–patient relationships. These shared beliefs had two consequences for de-escalation. Firstly, they reduced the quality of staff–patient relationships and, secondly, they rendered staff dependent on dysfunctional emotion regulation strategies (suppression) to function at work. Participants identified a range of consequences to the latter problem including psychological distress, resentment and subtle retaliation behaviours (e.g. refusing patient requests). Improvements to the physical environment including the creation of sensory rooms and greater staffing resources were also perceived as likely to create more opportunities for de-escalation (see Figure 3).
Chapter 3 Intervention development
Aim
To develop a feasible, acceptable, contextually sensitive training intervention to enhance effective de-escalation in practice.
Methods
The approach to intervention development was guided by the Behaviour Change Wheel126 and followed the principles of Experience-based Co-design. 127 The process consisted of five phases: (1) charting and synthesis of behaviour change targets; (2) stakeholder events to prioritise and organise behaviour change targets and generate intervention ideas; (3) intensive working with smaller co-design teams to develop an intervention draft; (4) stakeholder event to refine and finalise the intervention; and (5) reporting of the final intervention according to the Template for Intervention Description and Replication (TIDieR) guidelines for intervention description and replication. 128
Charting and synthesis of behaviour change targets
The chief investigator and a senior co-I (Lovell) conducted the synthesis of work package 1 (WP1) data. A chart was developed with columns as theoretical domains and rows as WP1 studies then key findings from each study were inputted into relevant cells. OP and KL then reviewed the charts independently to identify discrete behaviour change targets for the intervention emerging within theoretical domains and across WP1 studies. This process was conducted using the operational assumption that all behaviour change targets would be included, at this initial stage, irrespective of whether they were represented across one or all WP1 data contexts (adult acute, adult forensic). Decisions in relation to contextual applicability were delegated to the expert stakeholder groups. Differences in perspectives on either the importance or the articulation of behaviour change targets were resolved through discussion and third-party arbitration was not required.
Stakeholder events to organise and prioritise behaviour change targets and generate intervention ideas
Three groups of expert stakeholders were established consisting of service users and carers (n = 11), violence-reduction training specialists and academics (n = 10) and current clinical staff (n = 10). Participants were selected, using key informant sampling,129 from the clinical and academic networks of the investigation team and from consultation with the study PPI panel. Three separate full-day workshops were convened at the University of Manchester. Keeping the groups separate was intended to maximise input of each group into intervention development. Feedback from the PPI panel indicated that power imbalances between the groups could not be adequately addressed without initially separating the groups. However, it was felt that the final event should include mixed groups to ensure overall acceptability to all stakeholder groups. Full-day sessions (9–4 p.m.) were, therefore, convened with each of the three groups.
For each group an identical process was followed. Participants were provided with detailed summaries of WP1 findings in advance of the meetings. In the morning sessions, participants were provided with a set of numbered cards. Each numbered card displayed a single behaviour change target. The cards were numbered so they could be linked with summaries of the WP1 data to which they pertained, and, thereby, be evaluated by delegates in the context of their original sources. The data summaries were provided in a manual to each delegate at the start of each day. Participants were then invited to group behaviour change targets according to how they should be addressed by the intervention. This had several intended functions. The first was pragmatic in terms of the need to reduce the longlist of behaviour change targets down to a feasibly deliverable set of intervention components. The second was to enhance the acceptability and feasibility of the intervention through genuine involvement of stakeholders from the configuration of the intervention through to determining format, delivery methods and content. The third was that stakeholder configuration of behaviour change targets could generate new understanding of important connections between behaviour change targets and interactions cutting across theoretical domains that had not emerged from our development work.
Facilitating researchers documented group discussions to ensure an accurate record of delegates’ decision-making and reasoning was maintained. Once participants had completed the grouping exercise, they were asked to name each group of behaviour change targets before moving on to the prioritisation exercise. In the prioritisation exercise, participants were, simply, asked to distinguish behaviour change targets as high or low priority for inclusion in the intervention. Where any group labelled a behaviour change target as ‘low priority’ the reason was documented, and the target flagged for exclusion. Targets were excluded either where there was consensus across groups that the target was low priority or where specific feedback was given over safety and/or paradoxical impacts on staff behaviour or feasibility. Finally, in the afternoon session, delegates were invited to review their groups of behaviour change targets and make recommendations as to how (1) capabilities should be enhanced, (2) opportunities should be created and (3) motivation should be increased by the intervention. They were further invited to make recommendations as to the content, format and delivery methods of the intervention.
Intensive working with smaller co-design teams to develop an intervention draft
This process involved intensive working between the chief investigator (Price), the research associate based at the host institution (Papastavrou Brooks), the implementation scientist (Brooks), the behaviour change psychologist (Armitage) and the study’s PPI advisory panel. Literature reviews were conducted to identify evidence for the stakeholder-generated intervention ideas. Evidence sought included evidence for safety, effectiveness and implementation. Formal behaviour change techniques were then applied using the Behaviour Change Techniques taxonomy version 1130 and draft training materials and protocols for each of the intervention components were developed then reviewed with the PPI panel. Multiple events at the University of Manchester were held to develop and record video case studies for de-escalation training (with volunteer service users, clinicians and professional actors). The three novel models of reflective practice were also piloted with local clinician volunteers and the PPI panel, and their feedback was documented.
Stakeholder event to refine and finalise the intervention
The final stakeholder event, bringing together the three expert stakeholder groups, was held at the University of Manchester in May 2020. Participants were provided with the protocols and materials associated with each of the 16 intervention components prior to the meeting. At the meeting, participants were placed in groups according to the stakeholder group they belonged to (again, this was based on the recommendation of the PPI advisory panel). The format of the event involved presentations of each of the 16 intervention components, including the rationale, underpinning evidence and intervention materials and procedures. After each component was presented, the groups were asked to discuss and consider its suitability according to the APPEASE criteria. 131 The APPEASE criteria are affordability, practicability, effectiveness and cost-effectiveness, acceptability, side effects/safety and equity considerations. The criteria are designed to make contextually relevant decisions on intervention content and delivery. 131 Once these discussions were concluded, each group was invited to feed back their views to the whole group. Each component was then subject to a show-of-hands vote, with components winning a majority vote from the whole group being incorporated into the final intervention.
Reporting of the EDITION intervention according to the Template for Intervention Description and Replication guidelines for intervention description and replication
The intervention description provided in the results section conforms to the TIDieR checklist for intervention description and replication. 128 As such, the rationale, materials, procedures, delivery methods, persons responsible for delivery, relevant locations, dose and frequency and methods for measuring adherence are described. Tailoring and modification are not addressed as both these items will be actioned, necessarily, based on our mixed-methods process evaluation in WP3.
Results
Results of the charting and synthesis of behaviour change targets exercise
The process of charting and synthesising WP1 learning generated 44 discrete behaviour change targets for review by the expert stakeholder groups (Table 12).
| Theoretical domain | Study 1: updating the evidence (Review B) | Study 2: extending the evidence to forensic settings | Study 3: enhancing the evidence in acute/PICU settings | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Ward staff | Carers | Patients | MDT | Ward staff | Carers | Patients | MDT | ||
| Knowledge | |||||||||
| (1) Trauma education | x | x | x | x | x | x | x | x | x |
| (2) Personality disorder | x | x | x | x | x | x | x | ||
| Behavioural regulation | |||||||||
| (3) Debriefing | x | x | x | x | x | x | x | x | |
| (4) Advance de-escalation planning | x | x | x | x | x | x | x | x | |
| Skills | |||||||||
| (5) Therapeutic engagement with voices | x | ||||||||
| (6) Relationship and engagement skills | x | x | x | x | x | x | x | x | x |
| (7) De-escalation skills | x | x | x | x | x | x | x | x | x |
| Emotion | |||||||||
| (8) Enhanced emotion regulation (staff) | x | x | x | x | x | x | x | x | x |
| Social influences | |||||||||
| (9) Behaviourist principles in the context of trauma (use of punishment) | x | x | x | x | x | x | |||
| (10) Mutual support in staff team | x | x | x | x | x | x | x | x | |
| (11) Attitudes to vulnerability in staff team | |||||||||
| (12) Attributions and moral judgements (and reflection in language) | x | x | x | x | x | x | x | x | x |
| (13) Role-modelling de-escalation and attendant values (vulnerability, authenticity) | x | x | x | x | x | ||||
| (14) Tolerance of patient dissent/criticism | x | ||||||||
| (15) Tolerant and flexible regimes | x | x | x | x | x | x | x | x | x |
| (16) Collaborative antipsychotic prescribing | |||||||||
| Environmental context and resources | |||||||||
| (17) Environmental signifiers of coercion and disrespect | x | x | x | x | x | x | |||
| (18) Quality and objectivity of nursing notes describing patient experiences and behaviour | x | x | x | x | |||||
| (19) Admission experience (social isolation and use of force) | x | x | x | x | x | x | x | ||
| (20) Closer working relationship between nursing leadership and ward staff | x | x | x | x | x | x | x | ||
| (21) Feedback mechanisms that increase the visibility of critical events | |||||||||
| (22) Reduced blame, increased accountability | |||||||||
| (23) Open dialogue (culture of critical discussion of practice) | |||||||||
| (24) Recovery-focused management of self-harm (self-harm tolerance/safe self-harm) | x | x | x | x | x | x | x | ||
| (25) Positive risk-taking strategy | x | x | x | x | x | x | |||
| (26) Policy changes for de-escalating medication refusal (cooling-off periods) | x | x | x | x | x | x | |||
| (27) Management of patient requests | x | x | x | x | x | ||||
| (28) Stimulating, age-appropriate and voluntary structure of activities | x | x | x | x | x | x | x | ||
| (29) Skill and social mix in staff teams | x | x | x | x | x | x | |||
| (30) Brief, on-ward training of non-regular staff | x | x | x | x | |||||
| (31) Administrative burden | x | x | x | x | x | x | x | x | |
| (32) Staff presence in communal areas | x | x | x | x | |||||
| (33) Training patients in de-escalation | x | x | |||||||
| (34) Implementation of sensory modulation | x | x | x | x | |||||
| (35) Modify patient perceptions of environments as prisons | x | x | x | x | |||||
| (36) Patient community conflict (noise, distressing behaviour, vicarious trauma) | x | x | x | x | x | x | x | x | |
| (37) Task-shifting between qualified and unqualified nursing staff | x | x | x | ||||||
| (38) Interdisciplinary cohesion | x | x | x | ||||||
| (39) Service user involvement in handover | |||||||||
| (40) Reducing ward-round related anxiety | |||||||||
| Social/professional role and identity | |||||||||
| (41) Reflection on professional boundaries and role perceptions | x | x | x | x | x | x | x | x | |
| Reinforcement | |||||||||
| (42) Formalisation of thanks and appreciation of de-escalation practice | x | x | |||||||
| (43) Enhance patient knowledge, skills and confidence in challenging poor practice | x | ||||||||
| Goals | |||||||||
| (44) ‘Zero’ targets for restraint and seclusion | x | ||||||||
Results of behaviour change target grouping exercises
Synthesising outcomes of grouping exercises across the three expert stakeholder groups indicated that the intervention should seek to enhance de-escalation through the following five mechanisms:
-
enhancing de-escalation skills and modifying attitudes, knowledge and understanding of patients
-
changing power dynamics (service user involvement, enhanced democratisation of inpatient services)
-
changing the environment (sensory modulation, reducing visible evidence of coercion)
-
changing clinical systems and organisational context (systems to ensure a culture of de-escalation, i.e. reducing blame, increasing accountability)
-
changing attitudes to vulnerability within staff teams.
Results of prioritisation exercises
Outcomes of the prioritisation exercises flagged the following behaviour change targets for exclusion.
24. Recovery-focused management of self-harm (safe self-harm/self-harm tolerance)
There was agreement across expert stakeholder groups that the WP1 data did not sufficiently support this as a target for intervention. Delegates felt that: (1) there were insufficient data to indicate how this would be operationalised in a manner that would be acceptable to service users and staff; (2) that it may conflict with other aims of the intervention, for example, to enhance staff’s understanding of the communicative function of self-harm and reduce supportiveness; (3) that tolerance of self-harm was already incorporated in existing psychological approaches. Based on this feedback, this target was excluded from the intervention.
26. Policy changes for de-escalating medication refusal (cooling off periods)
Clinical delegates indicated that this target was already reflected in current policy. It was, therefore, excluded from the intervention.
29. Skill and social mix in staff teams
Clinical delegates agreed that while they supported this as a salient factor to enhancing de-escalation, an intervention targeting skill mix was unlikely to be feasible under currently prevailing operational conditions. This target was, therefore, excluded from the intervention.
31. Administrative burden
Clinical and academic delegates did not perceive this as a feasible target for intervention within existing frameworks of professional accountability. They further observed that this target may conflict with other indicated changes needed, for example, advance de-escalation planning and debriefing.
33. Training patients in de-escalation
Service user delegates flagged this target for exclusion. They felt that this target communicated the wrong message in terms of with whom the responsibility for enhanced de-escalation rested. They felt that an intervention addressing this target could be alienating for service users and that it would be unlikely to be accepted or achieve its intended safety outcome.
37. Task-shifting between qualified and unqualified nursing staff
While clinical delegates acknowledged the potential benefit for de-escalation, they felt that the time frames of the project were not realistic in terms of the level of training that would be required to upskill unqualified staff in the relevant activities (e.g. ward rounds).
44. ‘Zero targets’ for restraint and seclusion
Given the nature of the clinical environments involved in the project, neither clinical nor academic delegates considered this a feasible target for the intervention. It was excluded from the intervention.
Results of the ‘generating preliminary ideas for intervention exercise’
Synthesis of discussion across stakeholder groups generated proposals for 16 distinct intervention components across the 5 intervention mechanisms recommended by expert stakeholders. These included: de-escalation training; three novel reflective groups (two targeted at staff, one targeted at patients); an intervention to involve patients in shift handovers; an intervention to reduce service distress in ward rounds; an intervention to reduce social isolation and use of force at admission; a collaborative prescribing intervention; a sensory modulation and support-planning intervention; a boxing intervention; a patient-reported environmental audit tool; post-incident debriefing; an intervention to enhance patient and staff feedback; a website detailing policy commitments to a ‘Just and learning’ rather than a blame culture; ‘Safety huddles’ (regular on-shift meetings to discuss de-escalation); an intervention to change attitudes to vulnerability within staff teams. Detailed summaries of the intervention ideas and stakeholder recommendations for intervention format, content and delivery methods are provided in Report Supplementary Material 3, SM3.1–SM3.5.
Results of stakeholder event to refine and finalise the intervention
The expert stakeholder group elected to incorporate 11 of the 16 provisional intervention components into the final intervention (Table 13). Two of the three novel reflective practice models (‘Conflict formulation’ and ‘Negotiated boundaries’) were incorporated. However, the ‘Reclaiming narratives’ reflective group for patients was excluded following feedback from the PPI advisory panel. The panel felt strongly that this intervention had high potential to cause distress to service users and that the model placed too much demand on service users to discuss feelings and needs in the presence of other service users whom they may not know well and trust sufficiently.
| Intervention component | Affordable | Practical | Effective | Cost-effective | Acceptable | Safety | Equity | Incorporated | |
|---|---|---|---|---|---|---|---|---|---|
| Service user/carer researcher + RRPI-delivered components | (1) De-escalation training: Four modules: ‘Introduction to trauma’, ‘Creating trauma-sensitive clinical environments’, ‘Verbal de-escalation’, ‘Sensory-based de-escalation and compassionate engagement with voices’. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES |
| Psychology-delivered components (novel reflective practice models) | (2) Conflict formulation: Formulation sessions with staff teams. Model analyses feelings, needs and contextual factors (historical, environmental and societal) of staff and patient inputs into conflict situations. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES |
| (3) Reclaiming narratives: A similar model to conflict formulation (feelings, needs, context) but adapted for delivery with groups of patients. Designed to help patients collectivise and resolve conflicts with staff. | ✔ | ✔ | ✘ | ✘ | ✘ | ✘ | ✔ | NO | |
| (4) Negotiated boundaries: A model for reflection on interpersonal boundaries, limit-setting and vulnerability in staff. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES | |
| Senior nurse-delivered components | (5) Debriefing: Post-incident debriefing using a similar model to conflict formulation. Implemented after every incident of seclusion and/or restraint. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES |
| (6) Symmetrical feedback: An intervention to enhance the quality, extent and impact of staff and patient feedback on conflict, de-escalation and safety. Anonymous feedback boxes in staff and patient areas. Monthly feedback sessions between senior nurses and ward teams. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES | |
| (7) Just and Learning website: Dedicated website providing resources to develop a ‘just and learning culture’ that increases accountability and reduces blame. | ✔ | ✔ | ✘ | ✘ | ✔ | ✔ | ✔ | NO | |
| Ward team and patient-delivered components | (8) Patient handover: An intervention to involve patients in handover. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES |
| (9) Insiders’ guide and welcoming committee: An intervention to reduce use-of-force and social isolation on admission by establishing a welcoming committee comprised of service users and staff and patient-led ward orientation materials. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES | |
| (10) Patient-reported environmental audit tool: An 18-item tool completed by patients to audit the environment for factors relevant to de-escalation. Feeds into ward community meeting and negotiation and action over unmet items. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES | |
| (11) Safety huddles: On shift meetings to discuss de-escalation, including triggers, early warning signs and de-escalation strategies as well and to provide mutual support. | ✔ | ✔ | ✘ | ✘ | ✘ | ✘ | ✘ | NO | |
| (12) Protection of non-regular staff: Orientation materials to ward philosophy and expectations of staff behaviour and de-escalation. Brief on ward training of non-regular staff. | ✔ | ✔ | ✘ | ✘ | ✔ | ✔ | ✔ | NO | |
| Occupational therapy and physio-delivered components | (13) Sensory modulation and support planning: Sensory equipment targeting key mechanisms of emotion regulation: proprioception, vestibular input and deep pressure on the skin. Support-planning document assessing: (1) triggers, (2) ‘signs I need support or space’, (3) preventive calming strategies, (4) reactive calming strategies and (5) sensory equipment. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES |
| (14) Boxing intervention: An intervention to reduce feelings of shame and humiliation and promote safe use of touch between staff and patients. Boxing is a target-based activity which may reduce intrusive memories and flashbacks. Pad-work drills and punch-bags made available to patients. | ✔ | ✔ | ✘ | ✘ | ✘ | ✘ | ✔ | NO | |
| Psychiatrist-delivered components | (15) Manchester Collaborative Prescribing Approach: An intervention allowing prescriber and patient to share decision-making when starting or swapping antipsychotic medication using decision aids. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES |
| (16) Ward round standards: Ten standards for ward rounds designed to reduce patient anxiety. | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | ✔ | YES |
Two of the three senior nurse-delivered components (‘Post-incident debriefing’ and ‘Symmetrical feedback’) were incorporated. However, the group were not sufficiently persuaded that ward staff would engage with the ‘Just and learning website’. As such, they did not think that the finance and other resources that would be invested in the website’s development would translate into improved outcomes related to de-escalation. The ‘Just and learning website’ was, therefore, excluded from the final intervention.
Three of five proposed ward team and patient-delivered interventions (‘Patient handover’, ‘Insiders’ guide and welcoming committee’ and ‘Patient-reported environmental audit tool’) were incorporated. However, ‘Safety huddles’ and ‘Protection of non-regular staff’ were both recommended for exclusion. ‘Safety huddles’ were felt to be philosophically inconsistent with other aspects of the proposed intervention, which aim to reduce social distance between staff and patients, increase collaboration and improve relationships. It was highlighted that the ‘Patient handover’ had been proposed on the basis that handovers, in their current format, involve on-ward meetings in which patients are talked about but excluded from. Introducing another such meeting was, therefore, felt unlikely to be effective. ‘Safety huddles’ were excluded from the final intervention on this basis. The group were also sceptical about the potential for impact of the ‘Protection of non-regular staff’ intervention and felt it unlikely that nursing staff would engage with this process. ‘Protection of Non-regular staff’ was excluded for this reason. This meant that both interventions from the expert stakeholder-conceived intervention mechanism ‘Changing attitudes to vulnerability within staff teams’ were excluded. However, one of the proposed reflective practice models ‘Negotiated boundaries’ aims to change attitudes to vulnerability in staff and this mechanism, therefore, remains present in the intervention.
One of two proposed occupational therapy and physiotherapy-delivered interventions (‘Sensory Modulation and Support Planning’) was incorporated. The evidence supporting the boxing intervention, which was limited, conflicting and derived from non-clinical samples, did not persuade the group. There were concerns over unintended effects including the potential for hyperarousal caused by exercise and reinforcing violent actions for the purpose of emotion regulation. However, there were important differences in perspectives between delegates from adult acute and delegates from adult forensic inpatient settings, with the former keen to adopt and the latter unequivocally against adoption. The boxing intervention was, ultimately, not adopted. Both psychiatry-delivered interventions ‘Manchester Collaborative Prescribing Approach’ and ‘Ward Round Standards’ were incorporated as was the service user and carer researcher and RRPI-delivered ‘De-escalation Training’. A summary of the final intervention components mapped to theoretical domains, behaviour change targets and behaviour change techniques is provided in Report Supplementary Material 3, SM.3.6–SM3.11.
Reporting of the EDITION intervention according to the Template for Intervention Description and Replication guidelines for intervention description and replication
Rationale for the EDITION intervention
The EDITION study’s development work, consisting of a systematic review of qualitative evidence and large-scale (all sectors of adult acute and forensic inpatient services) qualitative inquiry, used the Behaviour Change Wheel126 to identify the spectrum of factors that influence staff capability, opportunity and motivation to use de-escalation. Participants, in the qualitative elements, tended to conceptualise de-escalation as an intersubjective ‘process’, occurring in the context of social encounters between staff and patients. Safe resolution of these encounters, therefore, depended as much on staff and patient collaboration as on the application of a discrete set of staff skills (i.e. ‘doing with’ rather than ‘doing to’).
Both staff and patient participants described paying intense attention to behaviour of those involved in de-escalation encounters, taking actions to regulate their own internal state (cognition, affect, arousal) and taking actions to regulate the internal states of others involved (e.g. explaining, stimulating positive memories, manipulating the environment to create feelings of safety). Participants emphasised that there are a wide range of complex, interacting factors that affect staff and patient capacity to engage optimally in the regulation processes they recommended. For staff, factors restricting their capacity for behaviour regulation during de-escalation encounters included:
-
their individual skill levels
-
their knowledge of the patient(s) involved in the encounter
-
cultures of contempt for vulnerability within staff teams
-
common, ideological representations of mental health problems (especially personality disorder) constructed in teams and organisations
-
punitive organisational cultures where blame and sanction deter staff willingness to take positive risks.
Factors restricting patient capacity for behaviour regulation during de-escalation encounters included:
-
illiberal ward regimes (myriad rules, enforced inflexibly)
-
environmental signifiers of threat and disrespect (visible evidence of coercion, organisational messaging demanding unconditional patient respect for staff)
-
alienating conduct of key clinical and ward processes (ward rounds, handovers, prescribing, waiting times, medication rounds, mealtimes, admission)
-
patient community conflict [lack of staff in communal areas to influence/intervene, lack of opportunity to escape distressing behaviour, prison cultures (men only)].
The overriding perspective was, therefore, that de-escalation was unlikely to be impacted by interventions that do not address the key sources of interpersonal and environmental stress that inhibit staff and patient regulation capability when de-escalation encounters occur. This perspective has intuitive validity and is supported by the most widely cited models of aggression,132 which propose that de-escalation can only occur when an individual has the resources available to reappraise an aggravating stimulus (e.g. consider alternative interpretations of the behaviour of others), assess its importance and weigh the costs and benefits of different behavioural responses. Others can shape the re-appraisal process by, for example, engaging in behaviours that modify the person’s initial assessment of their intentions and attitude (regulatory actions). However, where an individual’s capacity to engage in a reappraisal process is overwhelmed by their state of cognition, affect and/or arousal, an immediate impulsive action occurs. The problem that this presents for de-escalation is exacerbated by the observation that aggravating stimuli are not always primarily interpersonal. 111 For example, a person’s mood and level of arousal may be so affected by aversive light, temperature, or noise that the behaviour of others may have little to no impact on their capacity for self-regulation. This might further provide an explanation as to why existing evaluations of de-escalation training, which have predominantly focused on knowledge and skills development, have provided limited evidence of impact on conflict and containment outcomes. 1
The EDITION intervention aims to optimise the safety outcomes of de-escalation encounters through interventions targeted at key sources of environmental and interpersonal stress for staff and patients. The sources identified in our development work are consistent with the best available evidence on conflict and containment in adult and forensic mental health inpatient settings,133,134 and they indicate a need for behaviour change at every layer of inpatient organisational structures and across all key stakeholders (psychiatry, occupational therapy, patients and ward staff, clinical psychology, nursing leadership and RRPI teams). The following provides detailed descriptions of 11 distinct intervention components designed for these purposes.
Intervention component descriptions (aims, materials, procedures, delivery methods, persons responsible for delivery, relevant locations, dose and frequency)
-
De-escalation training
The de-escalation training package aims to:
-
modify staff’s knowledge and attitudes of conflict behaviours through trauma education
-
demonstrate best-available evidenced techniques for de-escalation in the context of trauma
-
demonstrate skills to reduce distress associated with voice hearing.
The training consists of four modules to meet its aims: ‘Module 1 Introduction to trauma’; ‘Module 2 Creating trauma-sensitive clinical environments’; ‘Module 3 Verbal de-escalation’; ‘Module 4 Sensory-based de-escalation and compassionate engagement with voices’ (more detailed content Table 14). In summary, Module 1 provides a general introduction to traumatic development and experience, for example definitions, prevalence, neurobiological and psychological consequences, and uses a combination of didactic teaching and video presentations. Module 2 introduces a suite of bespoke interventions designed to minimise patient exposure to traumatic reminders and the re-enactment of abuse and neglect dynamics in clinical relationships, in ward routines, in clinical processes and procedures, and clinical interventions. The EDITION interventions are described in detail throughout the remainder of this chapter. Module 2 also provides opportunity for implementation discussion and practice. Module 3 focuses on verbal de-escalation in the context of traumatic development and experience. Specific foci included de-escalation techniques to avoid activation of aggressive behavioural scripts,132 the aetiology of hostile-dominant interpersonal styles135 and effective intervention and, finally, de-escalation mapped to typical aggression functions (e.g. fear/protection, accessing tangibles). 136 Each area of focus is highlighted by bespoke video case studies developed for the EDITION programme. Module 4 first explores the use of sensory modulation in the prevention and management of aggression. Then, a concluding session, led by service user researcher Andrew Grundy, explores how to reduce distress, shame and isolation in the experience of voice-hearing in inpatient settings by adopting principles of compassionate engagement (similar to principles underpinning the Maastricht approach to accepting and working with voices137).
Module 1: Introduction to trauma
|
Module 2: Creating trauma sensitive clinical environments
|
Module 3: Verbal de-escalation
|
Module 4: Sensory-based de-escalation, and compassionate engagement with voices
|
Service users, carers and RRPIs received 1 day’s ‘train-the-trainer’ training and were provided with a manual that detailed the rationale, aims and slide-by-slide facilitator guidance for each element of the training. Teaching methods included didactic teaching, written and video bespoke case studies and group activities. Training was service user (Grundy) and carer (Cree) delivered with support from an RRPI and a co-investigator (Price or Callaghan). Training took place in a booked room, away from the ward areas at each participating clinical site. The training duration was a single day (7 hours) and was undertaken in the first week of the 8-week intervention-embedding phase on each of the 10 participating wards. The number of days training conducted was at the ward manager’s discretion, but the EDITION team emphasised we would train as many days in the first week as it would take to reach a critical mass of ward staff. This tended to be 3 days of training with approximately 10 attending staff per day.
-
2. ‘Conflict formulation’
The conflict formulation model aims to:
-
deconstruct moral judgements about conflict by:
-
providing a model of formulation that does not pathologise the patient or see conflict originating only from them
-
encouraging staff to imaginatively engage with patient perspectives (needs and feelings) and to be open and honest about how their own feelings and needs contribute to conflict situations
-
think critically about the social, institutional and historical context in which these interactions occur
-
-
provide a forum for mutual support in staff teams.
Each session requires bespoke materials developed for the EDITION study. These included, firstly, a feelings card pack (n = 90) and a needs card pack (n = 72). These were developed in partnership with the study’s PPI advisory panel. Secondly, they included a laminated PowerPoint slide titled ‘Understanding feelings and needs in context’ detailing relevant contextual factors to conflict situations at the level of individuals, the environment/institution and social injustice (Figure 4). These were derived from our development work and supplementary evidence review.
FIGURE 4.
Understanding feelings and needs in context.

Each session followed the stepwise process outlined in Figure 5. The first step is to identify, from an individual volunteer or a staff team, a conflict with a patient that is provoking negative emotion and/or causing difficulties that need resolving. This will be the focus of the session. Then step 2 is to enable the team to describe the conflict, ventilate emotions and express intuitive understandings of patient behaviour. The facilitator should not attempt to modify the group’s understandings, biases or self-protective mechanisms. Step 3 is a group exercise to identify feelings and needs of staff and patient in relation to the conflict. Identifying feelings is used for the purpose of identifying and articulating unmet needs. Needs-based analysis is useful to progressing beyond moral formulations of behaviour. 138 While it is possible to formulate moral judgements about the strategies people use to get their needs met, it is difficult to morally evaluate the presence or absence of a need. Identifying needs also provides a useful basis for resolutions to reduce conflict. Step 4 aims to enhance group members’ understanding of, and empathy for, factors outside staff and patient control that might explain why feelings and needs sequences are expressed the way they are in this unique care context/working environment. The purpose of this is to re-locate individual, trait-based explanations for conflict to richer, historically, environmentally and situationally informed explanations. Again, analysis of care or work context factors can provide further practical indications of how the context can be changed to reduce conflict. In stage 5, the group is asked to summarise and integrate the discussions and perspectives of the group to develop a shared functional understanding (feelings, needs, context) of staff and patient inputs into the relevant conflict; then, to plan around meeting needs and changing the work or care context to reduce negative emotion and conflict.
FIGURE 5.
Conflict formulation model.

-
3. ‘Negotiated boundaries’
The ‘Negotiated boundaries’ groups aimed to:
-
minimise unnecessary boundary setting and enhance de-escalation skills
-
create team cultures that are protective of vulnerability and receptive to new/marginal ideas and perspectives on clinical practice
-
enhance the quality of staff–patient relationships through critical reflection on professional boundaries and role perceptions
-
provide a forum for mutual support in staff teams.
Each session requires bespoke materials developed for the EDITION study. Three separate magnet packs were developed based on three session topics. The first pack (n = 42) had a single patient behaviour labelled on it, for example ‘spitting on the floor’. These were derived from literature review of boundary and limit-setting evidence in mental health inpatient settings. Every patient behaviour reported as preceding a boundary-setting response from staff was extracted from the literature. The magnets consisted of behaviours falling under the categories of sexual expression; structure, rules and routine; aggression and exploitation; relationships and trust; emotional expression; self-harm and suicide. The second pack (n = 88) had a single interpersonal boundary labelled on it, for example ‘hiding your surname from patients or concealing or modifying ID badges’. These were derived from review of evidence related to interpersonal boundaries in mental health inpatient settings. Interpersonal boundaries fell under the following categories: equity and expediency; intimacy; distance; exploitation and abuse; disclosure; generosity and kindness; values; dress; emotional expression. The third pack (n = 23) had a staff behaviour, attitude or attribute labelled on it, for example ‘staff displaying visible self-harm scars’. The magnets fell under the following categories: attitudes to vulnerability; attitudes to divergent opinions, practices and approaches to care; social pressure and courage; victimisation and bullying; team responses to stress and trauma; secrecy. Facilitators were provided with a magnetic whiteboard to facilitate the session, which was installed in a private room in the clinical settings.
Each of the three, distinct, sessions followed the same process:
-
Participants will then be asked to review each boundary and organise the magnets into ‘negotiable’ and ‘non-negotiable’ groups.
-
For each boundary, participants will be asked to:
-
identify whose need the boundary serves (i.e. staff’s, patients’ or both)
-
identify the specific need the boundary protects (e.g. safety, respect, equality, cohesion, convenience)
-
explore ways of negotiating this boundary, including:
-
alternative ways the same need can be met without setting blanket boundaries on patient behaviour
-
skills in implementing the boundary safely.
-
-
Clinical psychology staff (clinical psychologists and assistant psychologists) were trained in both ‘Conflict formulation’ and ‘Negotiated boundaries’ in one training session (duration 2–3 hours). Invitations were sent to all members of clinical psychology at each of the study sites. Training took place in a booked room, away from the ward areas at each participating clinical site, and was undertaken in the first week of the 8-week intervention embedding phase on each of the 10 participating wards. The training consisted of presenting the rationale for both groups, then practising both groups as they would be delivered in practice. All psychologists trained in the intervention were provided with a detailed facilitator manual. Piloting of the groups indicated that both groups had a duration of approximately 1 hour. Feedback from the expert stakeholders and PPI advisory panel indicated that the conflict formulation model should be used at a frequency of twice per month and the boundaries sessions once per month. The sessions with ward staff were held in a private room away from ward area.
-
4. Debriefing
The debriefing model aims to:
-
create a culture of accountability where ward staff can learn from critical events without fear of recrimination;
-
create closer working relationships between nursing leadership and ward staff that foster shared responsibility for safety;
-
improve staff’s ability to develop a functional understanding (feelings, needs, context) of incidents where seclusion and restraint have been used, including both staff and patient inputs into conflict.
The debriefing model (Figure 6) was similar to the ‘Conflict formulation’ model but with additional emphasis on data-gathering, diffusion of learning, and shorter-term changes to staff behaviour, the routine or the environment, that could rapidly avoid recurrence of the need for seclusion or restraint. After each episode of restraint and seclusion staff ward staff were asked to complete a proforma with the following sections: incident facts (description of relevant behaviours without causal explanations or subjective descriptions, e.g. ‘aggressive’); your feelings prior to initiation of seclusion or restraint; your needs prior to initiation of seclusion or restraint; context questions (resourcing, location, time, impact of others present, environment) and actions needed to prevent recurrence.
FIGURE 6.
Debriefing model.

An interview proforma for patients to complete, at their preference, with or without either a senior nurse (external to the ward team, a modern matron, operational manager or nurse consultant) or a member of the clinical psychology team, was also developed. This should be completed, voluntarily, and as soon as the patient was well enough to engage with the process. The patient proforma included the following sections: incident description; your feelings before restraint/seclusion; your needs before restraint/seclusion; context questions [behaviour of others, memories, bad news, waiting, staff communication (asked to stop, asked to do, request denial), environment, physical health, time]. Senior nurses and/or psychologists were provided with the EDITION study’s feelings and needs cards packs to facilitate this activity with patients.
The patient proforma was developed with the study’s PPI advisory panel to increase acceptability. This co-production exercise raised the important question of whether the engagement of patients in post-incident debriefing, and the sensitive questions implicated in this (e.g. memories triggering the event), might require patients to re-live traumatic experiences and cause harm. The advisory group were emphatic that the primary trauma in this context is the seclusion and restraint itself, and that gathering of pertinent information from patients is essential to limiting patient exposure to further trauma. The group did recommend that there should be emphasis on the voluntariness of patient involvement in the process.
Once the data-gathering process was complete, senior nurses were asked to populate charts with the feelings, needs, context and resolution data they had gathered from staff and patient proformas. An example populated chart is provided in Report Supplementary Material 3, SM3.12 (not a real scenario). They were then asked to organise a meeting (1 hour duration) with ward staff involved in the incident. During these meetings, staff teams were asked to inspect the chart for its validity and refine, as needed, based on group discussion, and/or populate cells where no data had been collected, then agree on courses of action to prevent recurrence. Once these meetings were concluded, the senior nurse would e-mail ward staff to ensure diffusion of learning to all relevant persons. The debriefing sessions were planned to take place, ideally, after every incident in which seclusion or restraint was used. In environments where restraints and seclusion happened at such high frequency this would be unfeasible, senior nurses were asked to select the event occurring that week that they felt represented the most valuable learning opportunity for teams.
-
5. ‘Symmetrical feedback’
The symmetrical feedback intervention aims to:
-
enhance the impact of staff and patient feedback on clinical practice and improve safety
-
provide staff and patients with opportunity to feedback anonymously and without recrimination
-
strengthen lines of accountability between clinical leadership and ward staff
-
improve de-escalation practice by creating a culture of open and constructive criticism of practice.
Two metal feedback boxes per ward were installed in patient and staff areas. Ward managers were advised to install them in discreet areas so that anonymous feedback could be provided. This was easily facilitated for staff but presented more of a problem for patient areas owing to potential ligature risk. The feedback boxes were advertised with posters (developed with the PPI advisory panel) displayed on the walls, explaining the purpose, emphasising the option to give feedback anonymously and encouraging feedback. Two-sided feedback proformas were provided alongside the boxes. Proformas were identical for staff and patients and asked respondents to provide: a description of the issue (positive or negative); impact of the issue on staff and/or patients; suggestions to resolve the issue raised; tick boxes to indicate if the respondent would like public, private or no feedback to their concern.
Feedback boxes were emptied once weekly by senior nurses (operational managers, modern matrons or nurse consultants) and checked for urgent safeguarding information. They then collated feedback for once-monthly feedback sessions with ward teams. The structure of these sessions was developed from a review of evidence relating to the impact of feedback on performance. If a shame response is triggered by negative feedback, learning is inhibited, and performance deteriorates rather than improves. 139 A process was, therefore, designed explicitly to avoid triggering shame responses in staff attending the monthly feedback sessions. Accordingly, the structure of each session was designed to frame the process of responding to critical feedback as an intellectual, skills-based (rather than emotional) exercise to make improvements to practice.
To achieve these objectives, the hour-long feedback sessions (held in private rooms away from the ward) were divided into three 20-minute sections. In the first section, attendees were asked to review with the senior nurse and ward manager examples of genuine patient feedback unrelated to their ward, hospital or trust (example feedback forms were developed using genuine patient feedback extracted from publicly available Care Quality Commission reports) and were asked to respond to them as if they were a complaint that had been made about their ward. In the second 20-minute section, the senior nurse and ward manager reviewed feedback from the staff box, inviting suggestions, discussion and reflection from staff on how leadership could make appropriate changes. A key function of this was to role-model open and reflective responses to critical feedback. In the final 20 minutes of the session, the group reviewed the actual patient feedback from their ward to identify actions needed to improve practice and the environment for patients. Sessions were, therefore, structured to ensure that attendees were not exposed to the content most likely to be threatening to self-perceptions until they had been habituated to the process of responding to critical feedback.
Senior nurses were trained in both ‘Debriefing’ and ‘Symmetrical feedback’ models in one training session (duration 3 hours). The training involved presentation of evidence and the rationale underpinning the two models and opportunities to practise facilitation. Invitations were sent to senior nurses (modern matrons, nurse consultants and operational managers) at each hospital. Training took place in private rooms at the clinical sites. All senior nurses trained in the interventions were provided with detailed facilitator manuals.
-
6. ‘Patient handover’
The patient handover aimed to:
-
consistently incorporate the patient voice in handover and in nursing notes and thereby to reduce bias in the understandings and representations of patients that are constructed through these processes;
-
reduce feelings of alienation, disempowerment and suspicion generated by nursing shift handovers;
-
increase the frequency of nurse–patient interactions.
The patient handover required a named nurse on each shift to collect a direct quote from each patient using a proforma developed for the EDITION study. The verbatim quotes are then read out in each handover and transcribed into the patient’s notes.
-
7. Patient-reported environmental audit tool
The patient-reported environmental audit tool aimed to:
-
increase feelings of safety by giving patients the power to influence the safety of the ward’s social and physical environment;
-
modify aspects of the environment that function in opposition to de-escalation and reduced conflict;
-
empower patients to challenge unsafe practices.
A patient who was willing and had capacity to engage with the process was asked to complete a 17-item audit tool (see Report Supplementary Material 3, SM 3.13) assessing aspects of the social and physical environment relevant to de-escalation and reduced conflict. Items were generated from our WP1 development work and wider evidence review. The volunteer patient was supervised and supported in this activity by an allocated member of nursing staff. The audit tool was added as a permanent item to participating wards’ community meetings. At the community meeting, the audit’s outcome and a discussion and negotiation about unmet items took place. Training took place at the study sites in a booked room that was away from the ward areas in the first week of the 8-week, intervention-embedding phase.
-
8. Insiders’ guide and welcoming committee
The ‘Insiders’ guide’ and Welcoming committee’ aimed to reduce the use-of-force and social isolation on admission by reassuring patients about the nature and philosophy of the environment on admission.
Service user-led development of ward information materials, ensuring content matches service user needs and priorities, has been demonstrated to result in large reductions in complaints. 140 Rates of satisfaction and complaints correlate strongly with violence in in-patient settings. 141 Our own research indicates that necessary trust in staff required for effective de-escalation cannot be easily recovered where patients have a traumatic experience of admission. The ‘Insiders’ guide’ aimed to give patients as much control as could be achieved safely over the content of ward information/orientation materials provided to new patients. This assumed that patients have access to unique knowledge and perspectives on ward environments that may be reassuring to new patients, and secondly, because fear of other patients is known to be a major source of distress for patients, especially early in their admission. 142 Messages from the patient community are therefore likely to help reduce anxiety.
Meetings were organised between the EDITION research associates/service user researchers and the patients on each of the participating wards. Patients were asked about what they would have liked to have known about the ward on admission. The research associates did not influence the content of the discussion except, if necessary, to provide examples of information known to be important to patients (derived from literature review). Patients were additionally asked to comment on their preferred design for the booklets and select a picture for the front cover. Once the meetings were concluded, a prototype was developed by a Service User Researcher (Motala). Notes from the meetings and their subsequent translation into the booklets were consciously maintained to remain as faithful as possible to both the language and the ideas that the patients shared. The prototype was then shared with the ward managers, who were asked to review the content of each booklet to ensure it included no confidential information or discriminatory language. They were asked to avoid making any other editorial decisions outside these two criteria.
Welcoming committees consisting of two members of nursing staff, two members of house-keeping staff and two patient-welcomers were established (where patients had capacity) in each of the participating wards. The committees met fortnightly to explore thoughts and emotions that had arisen when interacting with new patients and to discuss how the ward environment could be made more welcoming to new admissions. Within 24 hours after admission to the ward, two members of the welcoming committee (one staff member, and one patient) formally welcomed each new patient. They were asked to introduce themselves, present the admission with a copy of the ‘Insiders’ guide’ and give them a brief tour of the ward. A clinical psychologist supervised patient-welcomers in these activities.
Ward managers were trained in the ‘Patient handover’, ‘Patient-reported environmental audit tool’, ‘Insiders’ guides’ and ‘Welcoming committees’ in one training session (duration 2–3 hours). The ward manager and deputy ward managers of each participating ward, the chief investigator and a research associate typically attended these meetings. Training took place in a booked room at each of the study sites and there was one training session per ward. The training took place in the first week of the 8-week ‘intervention embedding’ data-collection phase. The training consisted of presentations of the rationale, underpinning evidence and recommended procedure, and group discussion on optimal approaches to implementation. Intervention manuals were provided for each of the interventions. Research associates assisted the ward teams in the implementation of the interventions at each of the study sites. The research associates supported and encouraged ward staff and patient engagement with each of the three ward team and patient-delivered intervention components.
-
9. Sensory modulation and support planning
The primacy of cognitive triggers for aggression is implicit in traditional models of de-escalation132 and may neglect the influence of neurological, biological and environmental stressors. These stressors may exacerbate arousal and affect to such an extent that cognitive scripts are not accessible to negotiation or influence via verbal de-escalation. 111 ‘Bottom-up’ interventions are needed to modify arousal and affect that do not depend solely on cognitive approaches. The sensory modulation and support-planning intervention aimed to address this problem by increasing the availability of sensory modulation equipment on mental health inpatient wards. There is evidence that individualised safety planning combined with sensory modulation resources helps to reduce use of containment interventions through earlier and more effective calming interventions. 143,144 Service user researcher-developed support plans were developed to enhance staff and patient knowledge and skills in the use of sensory modulation and increase staff sensitivity to triggers, early warning signs and patients’ preferred de-escalation strategies.
The process of identifying sensory equipment with the highest probable impact was informed by review of the sensory modulation literature. Communicating a safe environment depends on the manipulation of external sensory input (e.g. visual, gustatory, olfactory, auditory and tactile). A sense of internal safety can be created by manipulating somatic senses, that is, awareness of firm pressure on the skin (deep touch), a sense of where one’s limbs are in space (proprioception), and balance and awareness of spatial orientation (vestibular), to provide a grounding orientation. 111 A recommended equipment list was developed by extracting, from the published literature, all equipment targeting external and somatic sensory inputs. The list was then disseminated to operational managers in each of the study sites, who were asked to (1) review the equipment for its safety (infection control, ligature risk and potential for use as weapons) and affordability before purchasing and (2) identify a private space within the ward environments to use as a sensory room.
The ‘sensory and support plan’ booklets were developed by a service user researcher (Motala) to enhance acceptability to patients. These assessment documents had five sections: ‘Assessment of triggers’, ‘Signs I need support or space’, ‘Calming strategies’ (divided into ‘preventive’ and ‘reactive’), ‘Sensory equipment’, ‘Easy access plan’. The structure and content of the documents were informed by review of the conflict and containment literature and evidence on support/safety planning in inpatient mental health settings. Triggers assessed for included: pain and side effects; staff or patient behaviours that trigger traumatic memories; outside hospital stressors (e.g. relationships with family members/friends, finances/benefit payments, looking after homes/pets); times (times of day, significant dates/times of year); the ward environment (noise, light, temperature); the ward routine (waiting, mealtimes, medication rounds, sleep disturbances caused by observations, being woken up, boredom, bad news). ‘Signs I need support or space’ required patients to review a list of behaviours extracted from the ‘Forensic Early Signs of Aggression Inventory’145 and identify whether each behaviour represented a signal to staff that they needed increased support or increased time and space from staff (see Report Supplementary Material 3, SM 3.14). The option for patients to identify a behaviour as a sign they needed increased space was based on the emphasis patients, in our qualitative data, placed on the value of limited or no intervention in response to escalations (behaviour that might be loud or restless or involving aggression that was directed at property rather than people). Patients were encouraged to add behaviours that were not included in the Forensic Early Signs of Aggression Inventory.
Patients were then asked to identify, from a list of ‘preventive calming strategies’, staff actions that they find helpful in preventing escalations of distress. This list was developed from WP1 data, from wider evidence review and from working with the PPI advisory panel. Again, patients were able to identify prevention actions that were not present on our list. In the ‘reactive calming strategies’ section, patients were given a free-text space to describe ideal staff responses to escalations of distress. A page with pictorial representations of the sensory equipment available followed this, and patients were asked, simply, to identify which items they found calming. The final page of the document consists of an A4-sized ‘easy access plan’ which provides a composite overview of all relevant data derived from the assessment. The occupational therapists were asked to laminate two copies of these, provide the patient with a copy to keep and place the other copy in a visible and accessible location in the nursing office (we recommended a large, pocket wall-hanger, with an individual pocket for each patient’s support plan). Consequently, the support-planning system proposed was paper-based. This was intended to maximise patient and staff access to the plans and their utility.
Occupational therapists were trained in the sensory modulation and support-planning approach in a single training session (duration 2–3 hours). Invitations were sent to all occupational therapists attached to the participating wards. Training took place in a booked room at the study sites, away from the ward areas. Training content included: sensory processing in severe mental illness; communicating a safe environment (external and internal sensory inputs); sensory assessment; sensory equipment; support-planning procedure; implementation approach. All occupational therapists attending were provided with an intervention manual, the list of recommended sensory equipment and a bulk supply of the support-planning booklets.
-
10. ‘Manchester Collaborative Antipsychotic Prescribing Approach (M-CAP)’
The Manchester Collaborative Antipsychotic Prescribing approach aimed to create the relational conditions for de-escalation by allowing prescribers and patients to share decision-making when starting or swapping antipsychotic medication. The M-CAP was developed by Dr Richard Drake based on qualitative inquiry146 conducted at the University of Manchester. The approach was identified as a potential solution to the need to increase service user involvement in antipsychotic prescribing at the EDITION expert stakeholder events. A supplementary review of available tools by the EDITION team identified no suitable alternatives. The decision to adopt the M-CAP was, therefore, based on the endorsement of the three expert stakeholder groups.
The M-CAP uses bespoke decision aids to support the following, stepwise prescribing procedure. In step 1, the patient is provided with a list of adverse effects (see Report Supplementary Material 3, SM 3.15) derived from The Liverpool University Neuroleptic Side Effect Rating Scale (LUNSERS). 147 The list instructs the patient to select the five most troublesome effects and to rank their importance. In step 2, the prescriber uses the Table of Antipsychotic Adverse Effects (see Report Supplementary Material 3, SM 3.16) to identify four antipsychotics to be presented to the patient in step 3. Two principles should guide selection of these drugs: firstly, that they should minimise the adverse effects ranked by the patient as far as possible, especially those ranked as most severe; and given that this is unlikely to be completely achievable, the four drugs should contrast the ranked adverse effects, so the patient has a meaningful choice between adverse effect profiles; secondly, that the prescriber should view all as appropriate treatments and be willing to prescribe any one of them. For example, all might need to be long-acting injectable medications, or the prescriber might avoid drugs unavailable from their trust. In step 3, the patient is presented with four cards (one per each antipsychotic selected). These are selected from a pack of 32 cards, each containing the name of the antipsychotic on one side and an abbreviated version of the adverse effect profile on the other (see Report Supplementary Material 3, SM 3.17). The cards are presented name-down so that only the side effect profiles are visible (this is so that preconceptions do not influence the patient’s decision). The patient is asked to review the alternatives and identify which one they most prefer, then that is the medicine that is prescribed.
-
11. Ward round standards
The ward rounds standards intervention aimed to:
-
reduce patient anxiety and distress from ward rounds
-
ensure patient perspectives are represented and that decisions are made collaboratively.
A list of ward round standards was developed from review of evidence describing patient experiences of ward rounds and through work with the study’s PPI advisory panel. This process generated 10 standards to modify factors contributing to ward round-related distress and anxiety (see Report Supplementary Material 3, SM 3.18).
Psychiatrists were trained in ‘Ward round standards’ and the ‘Manchester Collaborative Prescribing Approach’ in a single training session (2 hours duration) delivered by Dr Richard Drake, the chief investigator, and a research associate. Invitations were sent to all medics (consultants, staff grades, registrars and senior house officers) attached to the participating wards. Training took place in a booked room, away from the ward areas at each participating clinical site, and was undertaken in the first week of the 8-week intervention embedding phase. The training content included the rationale and procedures for both interventions and a discussion about optimal implementation approaches. Trainees were provided with intervention manuals for both interventions as well as intervention materials (antipsychotic decision aids and a large ward round standards poster to be displayed in the room in which ward rounds are conducted).
Methods for measuring adherence to the EDITION intervention
A 30-item checklist for assessing staff adherence to the 11 components of the EDITION intervention was developed and piloted in the WP3 feasibility evaluation.
Chapter 4 Feasibility evaluation
Aim
The feasibility evaluation aimed to deliver and evaluate the feasibility, acceptability and potential impact of an evidence-based, de-escalation intervention for adult acute and forensic mental health inpatient settings and had the following objectives:
-
Establish the feasibility of embedding our intervention into secondary care mental health inpatient services by monitoring training uptake and engagement rates, and exploring, from multiple stakeholder perspectives, potential barriers to and enablers of its implementation.
-
Establish the feasibility of conducting a RCT to determine the clinical and cost-effectiveness of our intervention, by quantifying participant recruitment and retention, and identifying the optimal strategies to overcome any difficulties experienced.
-
Examine the applicability (content validity) and acceptability (full and partial completion rates, sensitivity-to-change) of trial outcome measures.
-
Collect outcome data to help inform the parameters of a fully powered trial, including identification and SD of the proposed primary outcome measure for sample size.
Methods
Design
Mixed-method, uncontrolled, feasibility evaluation. An uncontrolled design permitted the inclusion of a diverse range of clinical settings and an in-depth examination of contextual variation in training effects. Projects evaluating similar interventions have used uncontrolled designs at the feasibility/pilot stage, successfully progressing to full RCTs. 148 Clinical outcome data were collected over a 24-week period in 10 wards. Each ward had an 8-week pre-intervention, baseline data-collection phase, an 8-week intervention embedding data-collection phase and an 8-week post-intervention data-collection phase.
Sampling
Site, ward, participant selection and sample size
Two NHS mental health trusts participated in the study. These sites were engaged from the funding application stage. The two trusts were selected partially because, together, they provide the full spectrum of mental health inpatient services including high-secure adult forensic services (only three English trusts provide this service). They were, additionally, selected because of contrasts in populations served. One of the trusts serves a large, inner-city population where all the boroughs served have an even mix of White British and ethnic minority populations. The other trust serves smaller towns and cities where the populations are overwhelmingly White British. This was important in determining contextual variation in the acceptability, feasibility and potential impact of the intervention. Wards were selected from trusts according to the study’s need for a diverse range of care contexts. We aimed to recruit adult acute inpatient wards, psychiatric intensive care wards; low-, medium- and high-secure adult forensic wards; and male, female and mixed-gender wards. The process of selecting wards was purposive. The research team met with the clinical directors (nursing and medicine) at each of the four participating hospitals (two in each participating trust) and communicated their needs in terms of ward function and gender. Then, expressions of interest were distributed to ward managers whose wards met the specified criteria. Those expressing an interest and who confirmed capacity and capability to participate were recruited into the study. Eligible participants for qualitative and quantitative elements were all patients with capacity to provide consent in the target settings and carers, mental health nurses, nursing assistants, occupational therapists, occupational therapy assistants, psychiatrists, clinical psychologists, assistant psychologists, service managers and RRPIs.
The sample size of 10 wards was proposed based on two factors. Firstly, we required a large enough sample to incorporate the contextual diversity required by the commissioning brief. Our sample included two general adult acute psychiatric wards, two psychiatric intensive care wards, two low-secure, two medium- and two high-secure adult forensic wards. And, secondly, we needed to recruit a sample that was large enough to understand barriers and enablers of intervention implementation and data collection in the intervention arm of a definitive trial (powered trials of similar interventions using the same148 or similar149 outcomes have approximately 15 wards in the intervention and control arms). Consistent with the changing nature of the patient populations in these settings, retention was assessed at ward rather than patient level. Recruitment targets of 50 staff and 50 patients at each time point were based on feasibility estimates from our previous studies. 150,151
Data collection
Feasibility outcomes
The primary outcomes for the study were feasibility outcomes. Recruitment and retention rates, intervention uptake and engagement rates, full and partial completion rates for our proposed outcome measures and variability and potential floor and ceiling effects in these outcomes, were quantitatively assessed. We monitored adverse events and serious adverse events and reported these to our steering committee. Our preferred primary outcome for a full trial is the Patient and Staff Conflict Checklist (PCC-SR), a validated measure of conflict and containment rates. The nurse-in-charge at the end of every shift therefore completed the PCC-SR at each participating site throughout the 24-week data-collection period. The PCC-SR logs the frequency of 22 conflict (e.g. verbal aggression, physical aggression) and eight containment (e.g. seclusion, restraint) events that have occurred on the shift. Conflict and containment scores are obtained by summing the total number of events for each category. The tool has demonstrated reliability (inter-rater reliability 0.69 kappa coefficient152) and validity. 11,152 Owing to problems with missing data associated with the PCC-SR in previous, large trials,148 we tested a range of different strategies to enhance staff completion of this measure including: embedding research associates in clinical areas; e-mail/telephone reminders by the CI; ward-level incentives (vouchers to buy items for the ward); stimulation of between-ward competition.
Training outcomes
Consenting participants were video-recorded pre and post training completing a standardised role-play. The system proposed was that recordings would be sent to independent external raters who were blind to pre or post training designation and rated de-escalation performance using the English-Modified De-escalating Aggressive Behaviour Scale (EM-DABS), a validated observer-rated measure. The viability of this process has been demonstrated and the tool demonstrates good inter-rater reliability intraclass correlation (ICC) (3,1) = 0.752. 44,153 Acceptability of EDITION’s de-escalation training was assessed using the Training Acceptability Rating Scale (TARS), which measures knowledge, confidence, applicability, quality and satisfaction of training. 154 The TARS was completed by all consenting trainees immediately after each de-escalation training session.
Clinical outcomes
Clinical outcomes were selected in partnership with the study’s PPI advisory panel, assisted by a logic model derived from WP1 learning (AP1). Outcomes and the time points at which they were completed by staff and patient participants are presented in Table 15.
| Time point 1 (week 1/24) | Time point 2 (week 4/24) | Time point 3 (week 8/24) | Time point 4 (week 12/24) | Time point 5 (week 17/24) | Time point 6 (week 20/24) | Time point 7 (week 24/24) | |
|---|---|---|---|---|---|---|---|
| Study phase | Pre intervention | Embedding | Post intervention | ||||
| Clinical staff participants | COM-B | COM-B | COM-B | COM-B | |||
| APDQ | APDQ | APDQ | APDQ | ||||
| ACMQ | ACMQ | ACMQ | ACMQ | ||||
| VPC | VPC | VPC | VPC | ||||
| EQ-5D-5L | EQ-5D-5L | EQ-5D-5L | EQ-5D-5L | ||||
| Patient participants | CES | CES | CES | CES | CES | CES | CES |
| PEESS | PEESS | PEESS | PEESS | PEESS | PEESS | PEESS | |
| VPC | VPC | VPC | VPC | VPC | VPC | VPC | |
| EQ-5D-5L | EQ-5D-5L | EQ-5D-5L | EQ-5D-5L | EQ-5D-5L | EQ-5D-5L | EQ-5D-5L | |
Staff-reported clinical outcomes
Staff-reported clinical outcomes were collected at four time points at weeks 1 and 8 (start and end of the pre-training period) and weeks 16 and 24 (start and end of the post-training period). At each time point, staff completed the following three questionnaires:
-
(1) Capabilities, opportunities and motivation to use de-escalation (COM-B questionnaire).
The COM-B is a six-item questionnaire that assesses physical capability, psychological capability, physical opportunity, social opportunity, conscious motivation and automatic motivation to engage in a given task. Capabilities, opportunities and motivations are measured on 11-point Likert-type scales. The scale demonstrates reliability (ICCs 0.554 to 0.833) and validity (pairwise correlations rs < 1.0).
-
(2) Attitudes to Containment Measures Questionnaire (ACMQ)
The ACMQ (staff version) is an 11-item questionnaire that measures staff perceptions of the acceptability of restrictive practices on 5-point Likert scales (strongly agree to strongly disagree). The scale demonstrates good construct validity and high internal consistency (α = 0.97). 155
-
(3) Attitudes to Personality Disorder Questionnaire (APDQ)
The APDQ is a 37-item, valid and reliable (Cronbach’s alpha 0.9412) measure of mental health staff attitudes to people diagnosed with a ‘personality disorder’. Items are rated on 6-point Likert scales between ‘never’ and ‘always’.
-
(4) Violence Prevention Climate (VPC)
The VPC is a 14-item questionnaire that measures the VPC on inpatient mental health wards. It has two subscales, ‘staff actions’ and ‘patient actions’, which demonstrate good internal consistency (Cronbach’s alpha 0.89 and 0.76156). Items are rated on 5-point Likert scales (strongly agree to strongly disagree).
Patient-reported clinical outcomes
Patient-reported outcomes were collected at seven time points: three in the pre-training phase, one in the embedding phase and three in the post-training phase. The increased time points for patients were planned to enable the detection of potentially important impacts of training for patients who would already be discharged/transferred at later time points. At each time point, patients completed the following three questionnaires.
-
(1) Perceived Expressed Emotion in Staff Scale (PEESS)
The PEESS is a 20-item measure with three subscales (criticism, intrusiveness and supportiveness). It has demonstrated validity and reliability (subscale alphas 0.72 for criticism, 0.68 for intrusiveness, 0.87 for supportiveness157).
-
(2) Coercion Experience Scale (CES)
The CES is a 44-item valid and reliable (Cronbach’s alpha 0.67–0.93158) measure of the psychological impact of restrictive interventions on patients. It has six sub-scales: ‘humiliation’, ‘physical adverse effects’, ‘interpersonal separation’, ‘negative environmental influences’, ‘fear’ and ‘coercion’. Items are rated on a 5-point Likert scale from ‘not stressful’ to ‘extreme stress’.
-
(3) VPC
As above. The VPC can be administered to staff and patients.
Data analysis
Consistent with the feasibility design, data analysis was mostly descriptive. Intervention uptake and engagement rates were quantitatively assessed. We used descriptive statistics, including frequency distributions and measures of central tendency and dispersion, to assess the completeness and variability of our proposed outcome measures at each data-collection point. Changes on the participant and staff outcome measures between the pre- and post-intervention periods were examined using the following analyses. To assess the effect of training phase (baseline, embedding and follow-up) on conflict and containment, separate two-level random-intercept negative binomial models with shift (level 1) nested within wards (level 2) were fitted using the MENBREG command. Given the desire to compare counts across study phases rather than shift, the fixed part of each model included study phase as a categorical variable as the ‘time’ component. The fixed part of the model also included number of staff per shift.
For the staff secondary outcomes, data were analysed using two-level linear mixed models with a random intercept for staff ID. Again, as the interest was in comparing pre- and post-intervention phases rather than the difference in scores between assessment points, the fixed part of the model included study phase as a binary pre-intervention/post-intervention indicator. For the patient secondary outcomes, two-level linear mixed models with a random intercept for participant ID were used to account for the repeated measurements per person. The fixed effects included study phase, in this case a categorical variable measuring pre-intervention (time points 1, 2 and 3), embedding (time point 4) and post-intervention (time points 5, 6 and 7) phases. The staff, service use, cost and EuroQol-5 Dimensions five-level version (EQ-5D-5L) data were analysed descriptively (mean, 95% CI: frequency, per cent, 95% CI). In addition, exploratory ordinary least-squares regression (OLS) analyses were used to explore possible covariates of the costs of staff on wards (collected using the PCC-SR measure) and the costs of managing conflict and containment events.
Results
Feasibility outcomes
Recruitment and retention
Ten wards were recruited into the study. These consisted of:
-
two male, high-secure adult forensic mental health admission wards (one ward was in the personality disorder clinical pathway, the other in the mental illness clinical pathway);
-
one female, medium-secure adult forensic acute admission ward and one female adult forensic low secure treatment ward;
-
two mixed-sex, psychiatric intensive care wards (both mixed-sex);
-
one male medium-secure adult forensic assessment wards and one male adult forensic low-secure treatment ward;
-
one female adult acute inpatient ward and one male adult acute inpatient ward.
All wards except one completed the full 24 weeks of data collection. The ward that withdrew [at week 13 of data collection (5 weeks post training)] had sustained and severe staffing shortages due to the COVID pandemic and was unable to support intervention or data-collection activities. Recruitment of staff and patients to collect clinical outcome data was very good. For patients, 81% of the total recruitment target was achieved (283/350 data collections across seven time points). This increased to 88% (283/320) when wards that were closed to in-person data collection (due to COVID) in the follow-up time periods were excluded. We collected no clinical outcome data where remote data collection was required, despite efforts to facilitate this from both the research team and clinicians. For staff, 68% of the total recruitment target was achieved (135/200 data collections across four time points). This increased to 75% (135/180) when wards that were closed to in-person data collection (due to COVID) in the follow-up time periods were excluded. An overview of these data is provided in Table 16.
| Overall | Exclusion of periods where wards were closed to researchers due to COVID-19 | ||||
|---|---|---|---|---|---|
| Target | Total completed | % of data collection target met | Target (excluding) | Total completed | % of data collection target achieved |
| PCC-SR (proposed primary outcome) | |||||
| 3780 shift reports | 2360 shift reports | 62 | 3444 shift reports | 2343 shift reports | 68 |
| Secondary outcomes (patients) | |||||
| 350 [50 completions per time point (n = 4) seven time points] | 283 | 81 | 320 | 283 | 88 |
| Secondary outcomes (ward staff) | |||||
| 200 [50 completions per time point (n = 4)] | 135 | 68 | 180 | 135 | 75 |
Intervention uptake, engagement and adherence
Two hundred and seventy-six mental health staff in total were trained in the EDITION intervention. Two hundred and fourteen ward staff attended the de-escalation training (mean per ward 21.4, median 26, mode 28, range 16–40). All 10 wards engaged with and completed training. Sixteen clinical psychology staff (14 clinical psychologists, 2 assistant psychologists) were trained in Conflict Formulation and Negotiated Boundaries (mean per ward 1.6, median 1, mode 1, range 1–3). Clinical psychology staff from all 10 wards completed training. Seven occupational therapists (one per ward) were trained in the sensory modulation and support-planning intervention. Seven of 10 wards’ occupational therapists completed training. Two of three wards that did not engage cited insufficient expertise and one ward a lack of capacity. Fourteen senior nurses (five modern matrons, six operational managers, one nurse consultant and two advanced practitioners) were trained in the Debriefing and Symmetrical Feedback interventions (mean per ward 1.4, median 1, mode 1, range 1–2). Senior nurses from all 10 wards completed training.
Eight psychiatrists (one senior house officer, one staff grade and six consultants) from six wards were trained in the Collaborative Prescribing and Ward Rounds interventions (mean per ward 1.3*, median 2, mode 2, range 1–2). The four wards where psychiatrists did not engage with the training cited insufficient capacity (n = 1) or did not respond to invitation. It is notable that no ward serving male patients at medium-secure forensic level or higher engaged with the psychiatry-delivered interventions. Fifteen ward managers (n = 10) and deputy ward managers (n = 5) attended training in the ward staff and patient-delivered interventions. Ward managers/deputy ward managers from all 10 wards completed training.
The 30-item adherence tool was piloted in each of the 10 wards across the four study sites. There were several difficulties associated with collecting these data, some of which were access-related because of COVID restrictions on non-clinical staff, and some were due to the nature of intervention. The preliminary data derived from this process were promising in terms of intervention engagement. Only one ward’s psychology staff did not implement any of the reflective practice groups, citing insufficient capacity. Seven of 10 wards implemented both groups in the follow-up periods and one ward implemented only Conflict Formulation (the reasons for this were not elucidated).
The senior nurse interventions were implemented in 80% of the wards (one ward withdrew due to COVID-19 disruption, the other ward was closed to non-clinical staff due to COVID, so non-implementation was assumed). Seven of 10 wards ran face-to-face debriefing sessions following physical restraint/seclusion (one ward withdrew, one ward was non-responsive to data requests and one ward, a low-secure ward, reported no incidents of seclusion or restraint in the follow-up periods). At least 9/10 wards (9/10 includes the ward who withdrew but excludes the closed ward that did not respond to remote data requests) installed the feedback boxes and distributed the relevant materials (posters and feedback forms) soliciting staff and patient feedback. However, only 2/10 wards ran face-to-face Symmetrical Feedback sessions, indicating potentially lower acceptability or other feasibility issue. In the low secure male ward, the ward manager and modern matron made strenuous efforts to engage patients and staff in providing feedback, but none was provided. This was the same ward that reported no incidents of seclusion and restraint, and it is possible that this intervention may be more suited to environments with higher levels of staff–patient conflict.
All wards except the ward that withdrew and the closed ward that did not respond to data requests (8/10) implemented the Patient Handover and Patient-Reported Environmental Audit tool, and this implementation was maintained throughout the post-intervention follow-up period. Seven of 10 wards implemented the Insiders’ guides and Welcoming committee intervention. One psychiatric intensive care ward initially engaged but declined to use the guide when it was developed, as its content contained critical content related to the staff team. This ward also had very high acuity and there were not considered to be any patients with capacity to engage with the welcoming process.
Only 2/10 ward’s psychiatrists used the collaborative prescribing intervention in the follow-up periods. Common reasons cited for non-use included lack of capacity, concerns over risk and lack of opportunity (prescribing events occurring at insufficient frequency). Due to COVID-19 restrictions, ward rounds were only observable in 3/10 study wards and a range of 4–7/10 standards were met in ward rounds that were observed. Similarly, only 2/10 wards implemented the sensory modulation and support-planning intervention. The reasons for this were largely due to difficulties purchasing the equipment within the project’s required time periods, concerns over cross-infection risk in the context of COVID-19, capacity issues in the context of the COVID-19 pandemic and concerns among occupational therapists that they lacked the required expertise.
Full and partial completion rates of outcome measures
PCC-SR Overall completion rate of the PCC-SR was 62% (2360/3780) of possible completions. However, when wards that required remote data collection (due to COVID) were excluded the completion rate increased to 68% (2343/3444). The completion rate was only 5% (17/336) where remote data collection was required, emphasising the importance of researcher–staff team relationships in maximising engagement with this measure. Importantly, the completion rate increased in the post-intervention period. Excluding the wards where remote data collection was required, completions increased from 65% (876/1344) in the pre-intervention period to 76% (855/1120) in the post-intervention period (an overview of these data is provided in Table 16). This finding should be considered in the context of 70% of participating wards completing follow-up data collection in the COVID-19 pandemic, where unprecedented demands were placed on inpatient staff. 159 This strongly indicated that the strategies to increase completion the research team tested throughout data collection were becoming optimised in the follow-up data-collection period. The most effective strategies for increasing completion rates were ward-level incentives (a voucher each week for the ward with the highest completion rate at the participating hospital), stimulating inter-ward competition (weekly e-mails announcing results and encouraging competition) and, perhaps most importantly, the engagement of staff teams by researchers attending the wards in person.
Clinical outcomes Completion rates for the staff-reported clinical outcomes were good (Table 17), ranging between 80% full completion (ACMQ) and 100% full completion (COM-B). Completion rates for the patient-reported clinical outcomes were also acceptable (Table 18), ranging between 68% for the ‘Coercion’ factor of the CES and 92% for the ‘Intrusiveness’ factor of the PEESS and the ‘Staff Behaviours’ factor of the VPC.
| Outcome | Pre | Post | Subscale | Pre | Post | Overall % |
|---|---|---|---|---|---|---|
| Invited | Completed | |||||
| APDQ | 83 | 52 | Enjoyment | 74 | 46 | 88 |
| Security | 78 | 46 | 88 | |||
| Acceptance | 77 | 46 | 88 | |||
| Purpose | 77 | 47 | 90 | |||
| Enthusiasm | 83 | 49 | 94 | |||
| ACMQ | 83 | 51 | 62 | 41 | 80 | |
| VPC | 53 | 47 | Staff behaviours | 50 | 41 | 87 |
| Patient behaviours | 50 | 45 | 96 | |||
| COM-B | 83 | 52 | 83 | 52 | 100 | |
| Outcome | Pre | Embedding | Post | Subscale | Pre | Embedding | Post | Overall % |
|---|---|---|---|---|---|---|---|---|
| Invited | Completed | |||||||
| PEEES | 137 | 44 | 102 | Support | 112 | 34 | 87 | 82 |
| Intrusiveness | 124 | 38 | 97 | 92 | ||||
| Criticism | 109 | 36 | 91 | 83 | ||||
| VPC | 137 | 45 | 103 | Staff behaviours | 131 | 38 | 94 | 92 |
| Patient behaviours | 123 | 38 | 93 | 89 | ||||
| CES | 137 | 44 | 102 | Total | 74 | 19 | 57 | 53 |
| Humiliation | 91 | 22 | 67 | 64 | ||||
| Physical adverse effects | 104 | 29 | 77 | 74 | ||||
| Separation | 106 | 27 | 76 | 74 | ||||
| Negative environment | 107 | 28 | 76 | 75 | ||||
| Fear | 114 | 28 | 76 | 77 | ||||
| Coercion | 98 | 26 | 69 | 68 | ||||
Training outcomes
English-Modified De-escalating Aggressive Behaviour Scale
In the pre-intervention period, only seven participants, in total, were recruited and video-recorded completing the standardised role plays. This was despite significant energy invested by researchers engaging staff with this activity. In response, the research term determined that this activity was not feasible or acceptable to staff and this research activity was, therefore, discontinued.
Training Acceptability Rating Scale
Quantitative ratings The following findings are presented in a manner consistent with our previous studies evaluating training using the TARS outcome measure. 160 Of the 214 TARS submitted, three were removed due to random answering. For individual questions one, two, five and six on the acceptability subscale, there was a median score of 6, with questions three and four presenting a median score of 5 (out of a possible range of 1–6). Most participants ‘strongly agreed’ that the training was generally acceptable (57.8%), effective/beneficial (55.0%) and consistent with good practice (46.5%). Approximately half of participants ‘strongly agreed’ that it had high social validity (50.2%), that it was appropriate (49.8%) and the training was unlikely to harm patients (48.6%). The questions on the perceived impact subscale had a possible score range of 0–3. Most participants answered ‘a great deal’ to questions 11–15 related to: how competent the course leaders were (77.6%); their satisfaction with the training (62.6%); how well the training covered the course topics intended (64.9%); how the leaders related to the training group (76.3%); how motivating the leaders were (66.4%). However, the most frequent response to questions 7–10 was ‘quite a lot’. These questions asked whether the training: improved understanding (47.4%); helped them to develop skills (51.7%); increased confidence (49.3%); would be used by them in future (46.9%). An overview of these findings is provided in Table 19.
| Question/domain (possible score range) | n | Median | IQR | Range |
|---|---|---|---|---|
| (1) General acceptability (1–6) | 211 | 6 | 5–6 | 1–6 |
| (2) Perceived effectiveness (1–6) | 211 | 6 | 5–6 | 1–6 |
| (3) Negative side effects (1–6) | 208 | 5 | 5–6 | 0–6 |
| (4) Inappropriateness (1–6) | 211 | 5 | 5–6 | 2–6 |
| (5) Consistency (1–6) | 211 | 6 | 5–6 | 2–6 |
| (6) Social validity (1–6) | 211 | 6 | 5–6 | 0–6 |
| (7) Did the training improve your understanding? (0–3) | 211 | 2 | 2–3 | 0–3 |
| (8) Did the training help you to develop skills? (0–3) | 211 | 2 | 2–3 | 0–3 |
| (9) Has the training made you more confident? (0–3) | 211 | 2 | 1–2 | 0–3 |
| (10) Do you expect to make use of what you learnt in the training? (0–3) | 211 | 2 | 2–3 | 0–3 |
| (11) How competent were those who led the training? (0–3) | 210 | 3 | 3–3 | 1–3 |
| (12) In an overall, general sense, how satisfied are you with the training? (0–3) | 211 | 3 | 2–3 | 1–3 |
| (13) Did the training cover the topics it set out to cover? (0–3) | 211 | 3 | 2–3 | 1–3 |
| (14) Did those who led the training sessions relate to the group effectively? (0–3) | 211 | 3 | 3–3 | 1–3 |
| (15) Were the leaders motivating? (0–3) | 211 | 3 | 2–3 | 1–3 |
| Total ‘acceptability’ Q1–6 (1–36) | 208 | 33 | 30–35 | 11–36 |
| Total ‘perceived impact’ Q7–15 (0–27) | 210 | 23 | 20–25 | 5–27 |
| Total TARS Q1–15 (6–63) | 206 | 55 | 50–59 | 21–63 |
Within-group changes on staff- and patient-reported outcome measures
Within group changes on staff-reported outcome measures
Patient and staff conflict checklist To assess the effect of training phase (baseline, embedding and follow-up) on conflict and containment, separate mixed-effects models were fit in Stata Version 14. Poisson and negative binomial distributions were compared using likelihood ratio tests, and in both cases models accounting for overdispersion were favoured (conflict χ12 = 3371.88, p < 0.001; confinement χ12 = 1200.26, p < 0.001). Two-level random-intercept negative binomial models with shift (level 1) nested within wards (level 2) were fitted using the MENBREG command. The fixed part of each model included study phase to compare incidence rate between pre-intervention, embedding and post-intervention phases of the study, and number of staff per shift (Table 20).
| IRR | SE | p | 95% CI | ||
|---|---|---|---|---|---|
| Conflict | Embedding | 0.55 | 0.04 | <0.001 | 0.48 to 0.62 |
| Follow-up | 0.45 | 0.03 | <0.001 | 0.39 to 0.50 | |
| N staff | 1.11 | 0.01 | <0.001 | 1.08 to 1.14 | |
| Containment | Embedding | 1.03 | 0.06 | 0.644 | 0.92 to 1.15 |
| Follow-up | 0.80 | 0.04 | <0.001 | 0.72 to 0.89 | |
| N staff | 1.08 | 0.01 | <0.001 | 1.06 to 1.11 |
The embedding and follow-up phases of the study were associated with a reduction in conflict incidents: the embedding phase had a 45% reduction in incidents and the follow-up phase saw a 55% reduction in incidents compared with baseline (Figure 7). The number of staff on ward was associated with an increase in number of conflicts; for each additional staff member, there was an 11% increase in number of incidents.
FIGURE 7.
Number of incidents of conflict per shift for the baseline, embedding and follow-up periods of study.
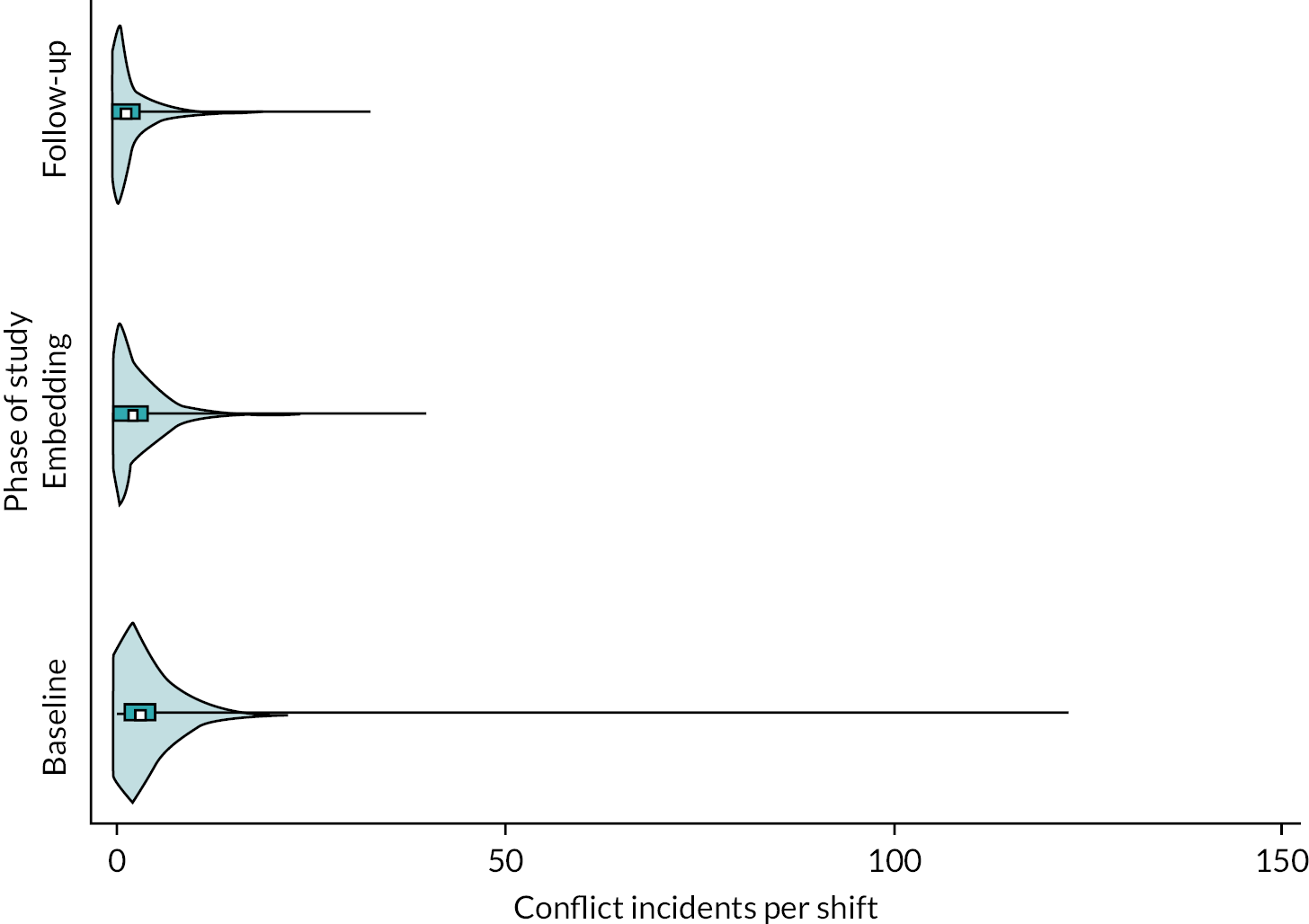
Compared with baseline, the follow-up phase also saw a 20% reduction in number of containments (Figure 8). The number of staff on ward was also associated with the number of containments, with an additional staff member associated with an 8% increase in the number of containments.
FIGURE 8.
Number of incidents of containment per shift for the baseline, embedding and follow-up periods of study.

Staff-reported clinical outcomes The change in staff-reported outcomes was analysed using linear mixed models with a random intercept for staff ID to account for the repeated measures. As no measurements were taken during the embedding phase for staff, scores are compared pre and post implementation of the intervention. Examination of Table 21 suggests that there was no detectable, statistically significant change in staff outcomes between the pre- and post-intervention phases of the study.
| Outcome | Subscale | Pre | Post | Mean diff. | p | 95% CI |
|---|---|---|---|---|---|---|
| APDQ | Security | 2.05 (0.85) | 1.98 (0.79) | 0.07 | 0.625 | −0.20 to 0.33 |
| Acceptance | 2.45 (0.58) | 2.45 (0.58) | 0.02 | 0.804 | −0.17 to 0.22 | |
| Purpose | 2.40 (1.10) | 2.3 (1.05) | −0.05 | 0.815 | −0.43 to 0.34 | |
| Enthusiasm | 3.15 (1.18) | 3.19 (1.38) | 0.22 | 0.267 | −0.17 to 0.62 | |
| ACMQ | 2.12 (0.54) | 2.03 (0.47) | −0.08 | 0.393 | −0.27 to 0.11 | |
| VCP | Staff behaviours | 4.26 (0.47) | 4.28 (0.50) | −0.01 | 0.938 | −0.20 to 0.19 |
| Patient behaviours | 2.90 (0.49) | 2.93 (0.58) | 0.02 | 0.818 | −0.19 to 0.24 | |
| COM-B | 49.39 (7.51) | 50.52 (7.29) | 0.79 | 0.495 | −1.49 to 3.07 |
Patient-reported clinical outcomes The effect of the study phase (pre, embedding and post) on patient outcome measures was established using a linear mixed model with a random intercept for participant ID to account for the repeated measures per person. Examination of Table 22 suggests that there were very few changes in these measures, with only the Support subscale of Perceived Expressed Emotion in Staff (PEES) and the Staff behaviours subscale of the VPC showing small increases in the embedding phase; however, these effects were not sustained into the follow-up period.
| Outcome | Subscale | Pre | Embedding | Post | Study phase | Mean diff. | p | 95% CI |
|---|---|---|---|---|---|---|---|---|
| PEES | Support | 26.88 (6.71) | 29.71 (6.25) | 28.31 (6.43) | Embedding | 2.13 | 0.026 | 0.26 to 4.00 |
| Follow-up | 1.49 | 0.066 | −0.10 to 3.07 | |||||
| Intrusiveness | 9.39 (2.15) | 9.26 (2.47) | 9.40 (1.67) | Embedding | −0.05 | 0.883 | −0.66 to 0.57 | |
| Follow-up | 0.05 | 0.846 | −0.47 to 0.57 | |||||
| Criticism | 17.24 (5.20) | 15.72 (5.78) | 17.71 (4.88) | Embedding | −1.21 | 0.093 | −2.63 to 0.20 | |
| Follow-up | −0.44 | 0.474 | −1.64 to 0.76 | |||||
| VPC | Staff behaviours | 3.64 (0.86) | 3.88 (.74) | 3.66 (0.81) | Embedding | 0.21 | 0.025 | 0.03 to 0.39 |
| Follow-up | 0.12 | 0.189 | −0.06 to 0.29 | |||||
| Patient behaviours | 3.16 (0.68) | 3.16 (.65) | 3.05 (0.71) | Embedding | 0.04 | 0.721 | −0.16 to 0.23 | |
| Follow-up | −0.09 | 0.321 | −0.26 to 0.08 | |||||
| CES | Total | 2.05 (1.07) | 2.18 (1.00) | 1.98 (1.23) | Embedding | 0.12 | 0.587 | −0.32 to 0.56 |
| Humiliation | 2.19 (1.06) | 2.22 (1.02) | 2.05 (1.22) | Follow-up | 0.13 | 0.474 | −0.23 to 0.49 | |
| Physical adverse effects | 1.43 (1.19) | 1.53 (1.21) | 1.69 (1.21) | |||||
| Separation | 1.67 (1.25) | 1.72 (1.38) | 1.78 (1.14) | |||||
| Negative environment | 1.60 (1.16) | 1.52 (0.97) | 1.82 (1.18) | |||||
| Fear | 1.18 (1.43) | 0.96 (1.23) | 1.43 (1.54) | |||||
| Coercion | 2.16 (1.32) | 1.92 (1.16) | 2.04 (1.31) |
Chapter 5 Economic analysis
Aims
The key aim of the economic component was to provide information about the range of data needed and the data collection and costing methods of the economic component for a future integrated clinical and economic trial. Key objectives were to estimate:
-
the staff time required to provide and implement current and new training package;
-
the staff time required to implement conflict and containment strategies to manage episodes of conflict;
-
the overall time costs of staff on shift in the wards, including NHS, bank and agency, to provide a context for the costs of training and managing conflict and containment as well as indicate the level of variance between trusts;
-
the costs of inpatient stay and EQ-5D-5L utility values.
Methods
Service use and costs
Staff and service use data were collected for the wards in each trust using a range of sources and methods, which are detailed below for each cost category. Service use data were costed in UK £s at 2020–21 prices, using published national unit costs for England. 161 The unit cost per hour of NHS staff time, for Agenda for Change (AfC) Bands 3–8b, were based on those estimated in the Unit Costs of Health and Social Care published by the Personal Social Services Research Unit. 161 Staff costs for AfC Bands 1–3 were estimated using the same methodology. 161–164 The costs of bank and agency ward staff were estimated using national guidance, price caps and a toolkit for effective use of staff banks. 165 The cost per hour of NHS staff incorporates employer on costs, overheads, sick leave, training days and annual leave. The cost per hour to the NHS for bank and agency staff incorporates employer on costs plus agency and bank fees or costs. Where necessary costs were inflated to 2020–21 prices using the Hospital and Community Health Services (HCHS)/NHS Cost Inflation indices. 161
The costs of the training intervention were estimated from two sources. Firstly, ward-level data reported the number of staff attending training, by AfC band, at the start of the embedding period. The duration of training was not recorded. For costing, it was assumed that each training session would take staff away from ward duties for a full daytime shift. The second source of data was the intervention diaries, covering the embedding period. The intervention diaries provided information about the different components of the intervention in terms of staff time to deliver and attend training and staff time spent on associated activities such as feedback, debriefing and auditing. The intervention diaries were completed by the champions leading each component of the intervention. The data collected included the time of the champions preparing for each training activity, and the time spent by champions and ward staff attending training and/or participating in activities associated with the training. The AfC band for each member of staff was recorded, allowing costs to be estimated according to the grade of staff. The two sets of data were costed and analysed separately.
The rates of conflict and containment episodes were collected using the PCC-SR measure. The unit costs of these events in England were developed by Bowers et al. in the City 128 study. 166 These unit costs align with PCC-SR tool and were inflated to 2020–21 prices for this component of the study. 161 Additionally, detailed discussions with staff from wards were used to explore possible variation in the staff resources used to manage episodes of conflict.
The PCC-SR measure was used to collect daily data on the numbers of qualified and unqualified NHS staff as well as bank and agency staff, by shift (a.m., p.m. or night shift). Qualified staff were defined as AfC band 5 and above and costed as band 5. Unqualified staff were defined as AfC band 4 and below and costed as band 3. Daytime shifts (a.m., p.m.) were assumed to be 8 hours. Night-time shifts were assumed to be 12.67 hours and the whole shift costed at the daytime rate plus the unsocial hours allowance for the AfC band (time plus 35% for unqualified staff and time plus 30% for qualified staff). Data on the use of bank and agency staff were also collected from the wards, for the pre- and post-intervention periods of the study. These data were costed and used to assess whether there were differences between the data collected at ward level and the data collected using the shift report PCC-SR measure. The staff time (NHS and bank/agency staff) and costs were also used to assess variation in the costs of staff on shift between trusts. This was based on the number of observations from each source and whether the 95% CIs on the number and costs of staff overlapped.
Discussions within the study team and initial scoping work with the trusts involved indicated it would be useful to add discharge length of stay data to the economic component. This was to give an initial indication of the level of variability in these measures within and between wards. As this was an addition to the funded study, it was outside the scope and resources of the feasibility study to collect and analyse individual patient-level data. Trusts were asked to provide information about number of discharges, average length of stay and discharge destination data at the ward (rather than individual patient) level from the standardised, routine data sets, for the pre- and post-implementation periods. These data were costed as length of stay multiplied by the average cost per day of a secure mental health unit. 161 The inpatient stay data were analysed descriptively to give an indication of variation in average length of stay and costs on the ward by place of discharge. Accordingly, the costs of patients whose stay on the ward was ongoing and costs post discharge were excluded.
Health status, utility and quality-adjusted life-years
The data were used to provide preliminary estimates of utility and quality-adjusted life-years (QALYs) and assess the feasibility of using the measure in a full trial. The latter included a comparison of the patient-completed and staff-completed versions to explore whether the estimated QALYs differ.
The EQ-5D is a generic measure of health status with three (original version) or five (current version) levels of severity that can be used across different population groups between or within studies. 129 It is the measure preferred by the NICE for economic evaluations in healthcare. Coping with conflict can be physically and psychologically harmful to staff. Accordingly, staff were asked to complete the EQ-5D-5L to assess if it is sufficiently sensitive to identify staff health issues and whether de-escalation training has the potential to improve health. As the QALY is a key measure of health benefit recommended by NICE, this will help to inform the design of future economic evaluations about the relative cost-effectiveness of training. However, there are concerns that the measure may not be suitable for evaluations of interventions for people with severe mental health problems. 167–169 Nevertheless, the measure has been used in economic evaluations of interventions for people with severe mental health problems. 170–175
The EQ-5D-5L was used in this feasibility study and has five items (mobility, self-care, usual activities, pain/discomfort, anxiety/depression) rated on five levels of severity, between no problems and severe problems. The data were collected at four time points for staff (start and end of pre-intervention period, start and end of post-intervention period) and at seven time points for patients (weeks 1, 4, 8 pre interventions; week 12 intervention embedding phase; weeks 16, 20 and 24 post intervention). Published population tariffs were applied to the EQ-5D-5L data, using the crosswalk algorithm,176,177 to calculate utility values. The actual number of follow-up points for participants was dependent on the staff and patients both available and able to complete the EQ-5D-5L at the assessment point. This meant that completion varied in the number of assessment points (1–7) and the assessment period when the EQ-5D-5L was first completed. Accordingly, QALYs were estimated as the average (mean) utility of the first and last completed EQ-5D-5L; the average utility was multiplied by the time between completion of the first and last assessments.
Results
NHS staff time and costs of training and embedding intervention
Table 23 summarises the number of staff training days and staff costs associated with the initial training element of the intervention. Report Supplementary Material 4, SM4.1 reports the unit cost per hour of NHS and bank/agency staff time by AfC band. Although Trust A has a higher total number of staff attending training and staff costs, the average (mean) number of staff and cost per training day is similar between the two trusts. Staff attended training across AfC bands 2–7 in each trust.
| Measure | Trust A, six wards | Trust B, three wards |
|---|---|---|
| Number of training days | 23 | 9 |
| Total number staff attending training | 128 | 38 |
| Total cost staff attending training | £36,944 | £10,888 |
| Mean staff per training day (95% CI) | 6 (4 to 7) | 4 (3 to 5) |
| Minimum–maximum | 2–11 | 1–9 |
| Mean staff cost per training day (95% CI) | £1030 (£720 to £1339) | £1210 (£900 to £1520) |
| Minimum–maximum | £396–3177 | £206–2716 |
Table 24 summarises the NHS staff time and costs to deliver training and embed the intervention from the intervention diaries. The number of wards included in the diary reports varied within and between trusts over the different components of training and activity. Overall, the time and costs of the different training components varied between the two trusts, reflecting differences in the number and types of ward and staff training needs. However, several items across both trusts were left blank and treated as not reported in the summary presented in Table 24.
| Trainor/lead role preparation and delivery | Trainee attendance and post-training activities | |||||
|---|---|---|---|---|---|---|
| Training item | AfC band | Total hours | Total cost | AfC band | Total hours | Total cost |
| Conflict formulation | ||||||
| Trust A, 1 ward, 2 training sessions | 7–8a | 13.80 | £851 | 2–6 | 12.00 | £362 |
| Trust B, 2 wards, 1 training session | 8a and 4 | 5.17 | £426 | 3 and 5 | 5.00 | £144 |
| Sensory support plans | ||||||
| Trust A | N.R. | N.R. | N.R. | N.R. | N.R. | N.R. |
| Trust B, 3 wards, 7 days activity | 5–7 | 54.12 | £2525 | N.A. | N.A. | N.A. |
| Debriefing | ||||||
| Trust A, 2 wards, 9 days activity | N.R. | 18.67 | £1310 | 5–7 | 9.50 | £508 |
| Trust B, 3 wards, 16 days activity | 8a | 36.83 | £2585 | 3–7 | 29.50 | £1037 |
| Negotiated boundaries | ||||||
| Trust A, 3 wards, 4 training sessions | 8a and 4 | 6.50 | £504 | 3 and 5 | 26.25 | £682 |
| Trust B T, 2 wards, 1 training session | 8b and 4 | 1.00 | £92 | 3–7 | 1.67 | £60 |
| Collaborative prescribing | ||||||
| Trust A, 1 ward, 1 day activity | N.A. | N.A. | N.A. | N.R. | 0.17a | £6.86a |
| Trust B | N.R. | N.R. | N.R. | N.R. | N.R. | N.R. |
| Patient-reported audit tool | ||||||
| Trust A, 4 wards, 17 days activity | 2–7 | N.R. | N.R. | 2–7 | 45.75 | £1535 |
| Trust B, 2 wards, 7 days activity | 3–7 | N.R. | N.R. | 3–7 | 25.17 | £630 |
| Patient handover | ||||||
| Trust A, 3 wards, 20 days activity | 2–7b | N.R. | N.R. | 2–7 | 40.62 | £1435 |
| Trust B, 1 ward, 2 days activity | N.R. | N.R. | N.R. | N.R.c | 9.16 | £236c |
| Insider’s guide | ||||||
| Trust A, 3 wards, 16 days activity | 3b | N.R. | N.R. | 2–7 | 62.00 | £1499 |
| Trust B, 1 ward, 2 days activity | N.R. | N.R. | N.R. | 2–6 | 5.50 | £71 |
| Symmetrical feedback | ||||||
| Trust A | 7 | 8.25 | £508 | N.R. | N.R. | N.R. |
| Trust B | 8a | 9.00 | £632 | N.R. | N.R. | N.R. |
Number and cost of ward staff and conflict/containment episodes
Table 25 reports the overall number and costs of staff on the ward and conflict/containment episodes per shift. The number and costs of conflict/containment episodes by type of event are shown in the Report Supplementary Material 4, SM 4.3. Comparing the 95% CIs, there appeared to be differences in the number of staff and the number of episodes between the two trusts, although no differences in the costs of conflict and containment episodes.
| Item | Mean number (95% CI) | Mean cost (95% CI) | n |
|---|---|---|---|
| Number and costs of staff per shift | |||
| Trust A | 7 (6.8 to 7.1) | £2453 (£2385 to £2521) | 1044 |
| Trust B | 5 (5.2 to 5.4) | £1646 (£1613 to £1679) | 1308 |
| Number and costs of conflict/containment episodes per shift | |||
| Trust A | 8 (7.1 to 8.2) | £406 (£361 to £450) | 1076 |
| Trust B | 4 (3.7 to 4.1) | £415 (£390 to £440) | 1327 |
Report Supplementary Material 4, SM4.2 and SM4.3 report the detailed results of the exploratory regression analyses to identify potential covariates of the cost of ward staff and the cost of conflict and containment episodes. Table 26 summarises these potential covariates in terms of whether they are statistically significant at the 5% significance level. The results in Table 26 suggest that shift, ward and follow-up period may be important factors to consider in the design of a full trial, in terms of data collection and analysis methods. However, it is important to note that regression analyses reported here could only consider variables collected within the PCC-SSR; accordingly additional factors may be important moderators or mediators of costs. These regression analyses should also be treated with caution given the relatively small sample size and uncontrolled nature of the data collected. The nature of the feasibility study means the detailed regression results are unlikely to be sufficient to determine differences over time or setting.
| Covariate | Cost of ward staff, p | Cost of conflict and containment episodes, p |
|---|---|---|
| Total cost of conflict and containment episodes | Not assessed | |
| Total cost of staff | <0.001 | |
| Night shift (vs. day shift) | <0.001 | <0.001 |
| Ward number (vs. ward 1) | ||
| 2 | <0.001 | <0.001 |
| 3 | <0.001 | 0.355a |
| 5 | <0.001 | <0.001 |
| 7 | <0.001 | 0.103a |
| 8 | <0.001 | <0.001 |
| 9 | <0.001 | 0.001 |
| 10 | <0.001 | <0.001 |
| Post lockdown (vs. pre lockdown) | 0.009 | 0.197a |
| Study period (vs. pre intervention) | ||
| Embedding period | 0.924a | 0.156a |
| Post intervention | 0.373a | <0.001 |
| Constant | <0.001 | <0.001 |
Inpatient stay
Ward-level data from case notes on number of discharges by discharge destination were reported by both trusts. These are shown in Table 27 for the pre- and post-intervention periods. There were differences in the number of discharges reported by the two trusts. One trust (WLM) reported 8/100 (8%) of discharges. The length of stay was not reported for this trust. The number of wards for which data were reported was higher in the pre-implementation period (n = 10/10; 100%) than the post-intervention period (n = 5/10; 50%). This may reflect the different timings of the implementation phase and subsequent post-intervention period.
| Discharge destination | Pre implementation, 10 wards | Post implementation, 5 wards | ||
|---|---|---|---|---|
| Number | Per cent | Number | Per cent | |
| Usual place of residence | 64 | 64 | 55 | 67 |
| Temporary place of residence | 11 | 11 | 16 | 20 |
| Repatriation | 0 | 0 | 0 | 0 |
| Penal establishment or police station | 0 | 0 | 1 | 1 |
| NHS other hospital provider – ward for general patients | 1 | 1 | 1 | 1 |
| NHS other hospital – ward for mentally ill patients or those with learning disability | 3 | 3 | 0 | 0 |
| Not applicable – patient died or stillbirth | 1 | 1 | 0 | 0 |
| Non-NHS (other than local authority) run care home | 3 | 3 | 4 | 5 |
| High-dependency ward within same NHS Hospital | 1 | 1 | 0 | 0 |
| Rehab ward within same NHS Hospital | 4 | 4 | 0 | 0 |
| Supported living accommodation | 1 | 1 | 0 | 0 |
| Discharge destination not reported | 3 | 3 | 1 | 1 |
| Total discharges | 100 | 82 | ||
The average length of stay per discharge destination was reported using ward-level data in one trust (Trust A). The length of stay was costed as £834 per day, the average cost per day of a secure mental health unit. 161 Table 28 summarises the average length of stay and cost by discharge destination. Measures of variance for the average length of stay were not available in the data collected and are not reported here.
| Discharge destination | Pre implementation, 10 wards | Post implementation, 5 wards | ||
|---|---|---|---|---|
| Average length of stay | Average cost (£) | Average length of stay | Average cost (£) | |
| Usual place of residence | 50 | 41,793 | 40 | 33,678 |
| Temporary place of residence | 32 | 26,385 | 43 | 36,227 |
| Repatriation | 0 | 0 | 0 | 0 |
| Penal establishment or police station | 0 | 0 | 0 | 0 |
| NHS other hospital provider – ward for general patients | 5 | 4170 | 109 | 90,906 |
| NHS other hospital – ward for mentally ill patients or those with learning disability | 159 | 132,606 | 0 | 0 |
| Not applicable – patient died or stillbirth | 94 | 78,396 | 0 | 0 |
| Non-NHS (other than local authority) run care home | 455 | 379,053 | 80 | 66,720 |
| High-dependency ward within same NHS Hospital | 0 | 0 | 0 | 0 |
| Rehab ward within same NHS Hospital | 0 | 0 | 0 | 0 |
| Supported living accommodation | 0 | 0 | 0 | 0 |
| Non-NHS-run hospital | 80 | 66,720 | 30 | 25,020 |
| Discharge destination not reported | 99 | 82,566 | 5 | 4170 |
Health status, utility and quality-adjusted life-years
Overall, 104/200 (52%) staff fully or partially completed the EQ-5D-5L at one or more time points; 76/104 (73%) of the staff fully or partially completed the measure at only one time point and 28/104 (27%) completed the measure at two or more time points. In comparison, 137/350 (39%) patients fully or partially completed the EQ-5D-5L at least once. Of these, 63/137 (46%) patients completed the EQ-5D-5L at only one time point and 74/137 (54%) at two or more time points. The number and timing of assessments points for participants were dependent on the staff and patients being both available and able to complete the EQ-5D-5L at the study-defined assessment point. This meant that completion varied in the number of assessment points (1–7) and the assessment period when the EQ-5D-5L was first completed. Accordingly, Table 29 reports the proportions of participants reporting no problems for each of the five domains at the participants first and last assessment point. The full results of the EQ-5D-5L by domain and level of severity are reported in Report Supplementary Material 4. The aim of data analysis was to explore the level and variation of health status, utility and QALYs to inform the design of a subsequent integrated clinical and economic trial, rather than assess the impact of the intervention on these measures. The results indicate that, as might be expected, there appear to be differences in the health status of staff and patients at the participants’ first assessment. Fewer patients reported no problems on each of the five domains, compared to staff ratings of their health. Additionally, the 95% CIs of the per cent of patients with no problems do not overlap with those of staff. However, this does not hold at the participants’ last follow-up assessment. However, the low completion rates and possible differences in the timing and length of time between assessments mean that it is not possible to draw any conclusions from this.
| EQ-5D-5L domain | Participant’s first assessment | Participant’s last follow-up | ||
|---|---|---|---|---|
| Staff | Patient | Staff | Patient | |
| Mobility | ||||
| n/N | 98/104 | 87/129 | 25/27 | 46/70 |
| % | 94 | 67 | 93 | 66 |
| 95% CI | 88 to 97 | 59 to 75 | 73 to 98 | 54 to 76 |
| Self-care | ||||
| n/N | 104/104 | 100/132 | 26/27 | 59/70 |
| % | 100 | 76 | 96 | 84 |
| 95% CI | – | 68 to 82 | 76 to 99 | 74 to 91 |
| Usual activity | ||||
| n/N | 100/104 | 75/129 | 26/27 | 44/71 |
| % | 96 | 58 | 96 | 62 |
| 95% CI | 90 to 99 | 49 to 66 | 78 to 99 | 50 to 73 |
| Pain | ||||
| n/N | 80/104 | 60/131 | 20/27 | 37/71 |
| % | 77 | 46 | 78 | 52 |
| 95% CI | 68 to 84 | 37 to 54 | 58 to 90 | 41 to 63 |
| Anxiety/depression | ||||
| n/N | 74/103 | 37/132 | 21/27 | 25/70 |
| % | 72 | 28 | 78 | 36 |
| 95% CI | 62 to 80 | 21 to 36 | 58 to 90 | 25 to 48 |
Table 30 reports the utility scores estimated from the EQ-5D-5L, as well as the days follow-up between participants’ first and last assessment and QALYs. The data indicate some differences between staff and patients in utility scores at the first and last assessment (based on no overlap between the 95% CIs). The design of the feasibility study and aim of this analysis mean that it is not appropriate to draw conclusions about the effect of the intervention on participants’ health status or QALYs. A table reporting the EQ-5D-5L by domain scores is provided in Report Supplementary Material 4, SM 4.4.
| Participant’s first utility score | Participant’s last follow-up utility score | |||||||
|---|---|---|---|---|---|---|---|---|
| Measure | n | Mean | Standard error | 95% CI | n | Mean | Standard error | 95% CI |
| EQ-5D-5L utility scores, available data | ||||||||
| Staff | 103 | 0.92 | 0.01 | 0.89 to 0.94 | 27 | 0.91 | 0.04 | 0.84 to 0.98 |
| Patient | 126 | 0.62 | 0.03 | 0.57 to 0.67 | 68 | 0.70 | 0.03 | 0.64 to 0.77 |
| Days follow-up, participant’s first and final assessment | ||||||||
| Staff | 28 | 154 | 29 | 94 to 214 | ||||
| Patient | 74 | 96 | 15 | 67 to 126 | ||||
| QALYs, estimated from participant’s first and final assessment, complete case data | ||||||||
| Staff | 27 | 0.40 | 0.07 | 0.25 to 0.55 | ||||
| Patient | 63 | 0.20 | 0.04 | 0.12 to 0.28 | ||||
Chapter 6 Process evaluation
Methods
Data collection
A process evaluation of the EDITION intervention was conducted across the four study sites and 10 participating wards. This explored the contextual feasibility, acceptability and perceived effects of the interventions. The process evaluation adopted an ethnographic approach. Structured observational methods were used focusing on professional and service user interaction with the intervention. Each of the research associates in the four sites (Papastavrou Brooks, Goodman, Robinson) conducted participant observation. Planned observation duration was 15 hours per ward in the 8-week pre-implementation phase and 15 hours per ward in the post-implementation phase (300 hours total across 10 participating wards). Observations were guided by a schedule structured around the mechanisms generated in the intervention development stage of the study. Individual interviews were conducted in parallel with observations to ensure that all groups and perspectives of those who engaged with the intervention were captured. Interview schedules explored the contextual feasibility, acceptability and perceived impact of the trained techniques and interventions. Qualitative data collected were digitally recorded and transcribed verbatim.
Data analysis
Analysis of interview and observational data was conducted according to the constant comparative method where analysis was conducted concurrently with data collection so that emerging issues could be explored iteratively. Anonymised verbatim transcripts of audio recordings and typed observation notes were imported into the software package NVivo for data management and analysis. Analysis used Framework methodology,122 facilitating a combination of inductive and deductive coding. The project team met regularly to develop the coding framework, to discuss alternative interpretations and ensure the coding framework remained grounded in the data. All coded data were summarised in a series of frameworks using the Framework function of NVivo10. Framework columns represented the perceived effects (Observations) and the contextual acceptability (Interviews) of the intervention. Deductive coding of acceptability data was informed by the Theoretical Framework of Acceptability (TFA), which enables examination of intervention acceptability according to the following theoretically important domains: affective attitude, burden, perceived effectiveness, ethicality, intervention coherence, opportunity costs and self-efficacy. 178 We examined differences in perspectives between respondent subgroups by ordering frameworks using the ‘order by sample characteristic’ function of NVivo 10. Data trustworthiness was ensured through multiple analysts (including service users) involved in the coding of data.
Results
Observational data
Our ability to collect observational data was significantly limited by restrictions on researcher access to the wards because of the COVID pandemic. We were able to collect 80% of pre-intervention observational data (120 hours in eight participating wards) and 50% (75 hours in five of 10 participating wards) of post-intervention data. Another problem was that restricted room capacities and changes to the normal delivery of key ward processes often restricted ability to observe activities that were the target of the intervention. Acknowledging the limitations of these data, the following presents researchers’ (Papastavrou Brooks, Goodman, Robinson, Rita Hira and Josie Broyd) perspectives on staff and patient interactions with intervention and its perceived effects.
Pre-intervention observations
Knowledge and attitudes
On multiple wards staff were observed to lack a trauma-informed approach to care. This presented in the form of dismissive responses to patient distress, callous humour when discussing a patient’s traumatic experiences with colleagues and patients indicating that they did not feel comfortable approaching members of staff for support. There was potential evidence of compassion fatigue evidenced by trivialising responses to patient expressions of anxiety, for example ‘You’re definitely not dying’, avoidance of distressed service users and conversations between colleagues mocking patients. In contrast, there was evidence of staff awareness of the negative effects of stigmatising language, particularly about personality disorders. Gaps in staff knowledge in relation to the ward environment and risk were inferred from failures to monitor trigger points and make efforts to modify what appeared to be an environment that was too chaotic for anxious patients to tolerate.
Skills
Deficits in interpersonal skills in staff were observed, for example, in social and self-awareness (staff were observed whispering and laughing to each other in communal areas in a manner that appeared intended to exclude patients). Researchers noticed a style of nursing communication which they attributed to the desire, among staff, to avoid reinforcing behaviour that they found difficult to manage (e.g. patient criticism of the ward regime, other concern or reassurance-seeking). This style of communication involved withholding facial or verbal empathy when cues of distress were expressed and in situations where it appeared socially congruent to respond with empathy. This behaviour was perceived as intentional and underpinned by an understanding of psychological behaviourism that informed them that these responses would be most likely to make the problem (and the person) ‘go away’. Because of these interactions, patients were often left without interventions to reduce distress.
Emotional expression and attitudes to vulnerability
Two wards in particular presented evidence of staff valuing emotional authenticity in interactions with patients and interactions between colleagues. This was evident in displays of empathy and sincerity when interacting with patients and discussion of the emotional impact of their work with colleagues. Staff openness with patients in terms of their emotions was observed in younger staff or new starters. On the other wards observed, there was no evidence of discussion of emotions between colleagues and no expressions of vulnerability in staff interactions with patients, indicating that an outward appearance of emotional resilience was a valued aspect of maintaining safety. Evidence of attitudes towards vulnerability was also observed in interactions between ward staff and the observing researchers. On three of the participating wards, researchers described feeling ‘taken care of’, ‘supported’ and ‘included’. This might have suggested a more protective attitude to more vulnerable colleagues, but researchers did note that these actions did not appear to correspond with treatment of bank and agency staff.
Social distance and the social environment
Researchers observed marked social distance between ward staff and patients, exemplified at the most fundamental level by ward staff’s apparent preference for congregating in the ward office rather than sharing the social spaces of patients. The ward office door was continuously noted as a source of division and conflict between staff and patients. Nursing offices doors were, typically, kept shut. Service users were often observed knocking on the office door in attempts to seek staff support or make requests, which were commonly ignored by staff in the office. Some patients would make attempts to enter the office, or knock profusely, or become irate due to being forced to wait for a response from staff. In these instances, staff would typically leave the office to provide support, to reprimand or re-direct patients away from the office.
On most wards, conscious attempts to reduce social distance between staff and patients were observed, at least superficially. In some instances, researchers characterised these attempts as ‘performative’: for example, engaging warmly with patients when staff needed information or a bureaucratic task completing, and routinely sitting with patients at mealtimes but only interacting with other staff. In one of the female forensic wards, there was signage displayed to enforce social distance between staff and patients. For example, extending beyond the ubiquitous ‘please knock’ signs, this ward had a poster that instructed patients not to come within 6 feet of the nursing office door. This had been installed as a solution to the disturbances patients were causing attempting to rouse staff from inside. Other signage included ‘Zero Tolerance’ and ‘Respect Us’ posters. These posters typically presented kindly and receptive-looking people dressed in nurses’ uniforms, and appeared to communicate a message proximal to ‘please don’t hit me, I’m only trying to do my job’. The image these posters conveyed of professionals often seemed at odds with the attitudes and behaviours staff displayed towards and around patients.
Notably, social distance was much less marked between patients and non-regular staff, indicating either that unfamiliarity with the staff team increases motivation to engage therapeutically with patients or that the desire for social distance in permanent staff increases due to burnout and/or exposure to toxic culture. Despite these negative observations, researchers noted ‘exceptions to the rule’ in staff teams, where individual staff members would engage with patients in a warm, approachable and authentic manner. Again, they did observe that these individuals tended to be either non-regular staff or staff who were relatively new to the team. Researchers noted that patients approached these staff to get their needs met, repeatedly, and when alternative staff appeared to be available.
Organisational context
Insufficient staff numbers were commonly observed across all wards. There was an important difference in organisational context observed. On the two adult forensic female wards, researchers observed a near-total absence of more senior clinical managers and clinicians. Importantly, these two wards were observed as having the most hierarchical behaviours and relationships between staff groups and between staff and patients. For example, they observed that ward managers had a separate office, off the ward, and that qualified nurses often spoke to support workers and housekeepers in a condescending manner. These observations might indicate that the modelling of social relationships at more senior layers of the hierarchical structure permeates to ward-level relationships, including those between staff and patients.
Post-intervention observations
Knowledge and attitudes
Evidence of staff practice changes because of increased trauma awareness was observed on one of the wards in the post-intervention period. Ward staff displayed an increased awareness of patient triggers and the importance of not undermining patients. The negative attitudes to patients expressed in conversations between staff in the pre-intervention period persisted. There was evidence of changes in knowledge and behaviour in relation to sensory modulation.
Skills
Researchers observed changes in staff skills after training. Field notes reflect adjustments of tone and body language to being calm, open and less threatening. On one ward, multiple instances of staff giving patients space and time (e.g. being willing to tolerate escalations without use of containment) were observed, which was emphasised in the de-escalation training. Honesty and clarity about the timeliness of completing patient requests were observed across most wards, with staff providing clear explanations of when requests would be met, or why they couldn’t be. Although some instances of staff not keeping promises and taking excessive time to follow through with requests were noted, these were in the minority. Staff communication and social skills were generally observed as having improved. The researchers observed evidence of patients appearing increasingly comfortable approaching staff because of these changes.
Emotional expression and attitudes to vulnerability
Researchers observed changes in the respect in the post-intervention period: for example, greater active inclusion of student nurses in conversations, more welcoming receptions to visitors to the ward and increased mutual support in the staff teams.
Social distance and the social environment
Significant physical and social segregation between staff and patients remained present on wards but active attempts by staff to reduce this were observed. For example, staff were seen actively joining groups of patients in activities, sitting with patients. Although the office door often remained a physical barrier between staff and patients and a source of conflict, staff congregation appeared less commonly. Researchers noted increases in staff emphasis on patient choices and autonomy. On one of the female adult forensic wards, a psychiatrist was observed extensively engaging patients with the intervention and encouraging patients to engage with the environmental audit tool and attend community meetings to discuss outcomes.
Systems and organisational context
There were no changes in the staff resourcing problems observed in the pre intervention but, as alluded to in previous themes, there was some evidence observed of senior clinicians on the wards engaging patients in the intervention.
Interview and focus group data
Sample description
Individual interviews (n = 11) and FGs (n = 10) were conducted with 11 ward staff (seven qualified and four unqualified nurses), inpatients (n = 10), psychiatrists (n = 5), senior nurses (n = 4), clinical psychologists (n = 6), occupational therapists (n = 5), RRPIs (n = 6): a total sample size of 47. Longer direct quotes (Q) supporting the following interpretations are provided in Report Supplementary Material 5, SM5.1.
Results
Psychiatrists (ward rounds and collaborative prescribing)
Affective attitude Most psychiatrists in PICU and forensic settings felt that the collaborative prescribing intervention was not feasible in these settings. PICU patients were perceived as lacking capacity when prescribing decisions were made (i.e. close to admission). By the time they were well enough to engage they were ready to be transferred to a less-restrictive setting or be discharged. Psychiatrists in forensic settings pointed to a lack of opportunity to use the intervention, within the study time frames, as patients were often on stable medication and changes were needed infrequently (Q1).
Burden Psychiatrists found some of the ward round standards burdensome. The requirements to escort patients to and from the ward round room and facilitate patient access to ward round records generated additional workload and increased the duration of ward round (Q2).
Confidence There was evidence of a lack of confidence among some psychiatrists in giving patients meaningful choices. Two PICU psychiatrists gave examples of choices they would be willing to grant, such as between oral or intramuscular medicines, but did not feel confident in allowing patients to choose a specific medicine. This was grounded in scepticism of patient skills and knowledge to make informed choices and concern over accountability if unsafe events occurred after a patient had chosen their own medicine (Q3). Confidence issues also affected psychiatrist engagement with the ward round standards. Some felt insufficiently confident escorting patients from ward rounds because they are not trained in physical restraint techniques.
Opportunity costs A minority felt that existing collaboration in prescribing (this was limited to information provision on side effects) was adequate. From this perspective, any novel intervention targeting collaborative prescribing represented opportunity costs without benefit. Others were concerned that increasing patient involvement would result in changes to patient expectations that could not be met. They were concerned that patients might learn to demand changes to their medicines every time they encountered a distressing side effect (Q4). They felt that increasing patient sensitivity to side effects and involvement in their minimisation might reduce adherence and increase medication-related conflict with staff. They emphasised that none of the currently available antipsychotics are without distressing side effects. Psychiatrists also pointed to opportunity costs associated with ward round standards. For example, PICU psychiatrists stated that while they understood the rationale for not asking patients about symptoms in ward rounds, they observed that they did not always have time to see patients in any other context except ward round. As such, the ward round was the only setting in which vital clinical and risk information could be gleaned from patients.
Ethicality Some PICU psychiatrists, while recognising, in principle, the value of increasing patient choice in prescribing decisions, felt that the need to manage risk outweighed the benefits of increased autonomy (Q5). They provided examples of patients choosing medicines that they were happy with but would not adequately reduce their risk to others (this perspective missed that the intervention allowed prescribers to limit choices to medicines they were willing to prescribe). Ideals in relation to doctor–patient relationships also influenced how acceptable they found the intervention. Two psychiatrists appeared to characterise the ideal doctor–patient relationship as the sharing of knowledge and advice by a responsible expert with a naïve and passive recipient of medical intervention. They felt, fundamentally, that patients relied on them to make important decisions on their behalf.
Intervention coherence Important issues related to understanding were raised but these often related to broader concepts (e.g. shared decision-making and collaborative working) rather than the specific interventions. Psychiatrists often claimed to work collaboratively with patients but rarely provided examples that extended beyond information provision (Q6).
Perceived effectiveness The consensus of PICU and forensic psychiatrists was that the intervention may be effective in reducing medication-related conflict in general adult acute mental health settings, that is, where patients have the capacity and present lower risk. Multiple psychiatrists felt some of the ward round standards may cause paradoxical increases in conflict: for example, that offering patients the option of using first names might reduce patient respect for psychiatrists or generate alienation by failing to recognise the power imbalances between patients and psychiatrists (Q7).
Psychologists (conflict formulation and negotiated boundaries)
Affective attitude Psychologists uniformly reported staff enjoyment of the sessions, that the formats of the groups were stimulating, novel, safe and, occasionally, humorous. They often commented that the groups stimulated alternative perspectives on patients and boundaries that would not have been elicited without the groups. They did report that the conflict formulation group placed demands on staff to be vulnerable in that it required them to label and articulate feelings in in the presence of colleagues. The format required participation from all present, so there was no opportunity to avoid this entirely. Psychologists commonly observed initial discomfort and reticence in staff and there was conflicting evidence on whether this problem was resolved through repeated exposure. Some felt that staff’s willingness to be vulnerable increased through repeat attendance and others felt less emotionally open staff did not increase engagement over multiple sessions.
Some psychologists reported anxiety that the conflict formulation group would lead to disclosures of historical trauma by staff participants that they would be unable to contain. Although they observed no evidence of psychological distress, they did highlight that the groups tended to be ran with groups of staff that they knew quite well. There was a view that the psychological competency of facilitators and their relationship dynamic with the participant group need careful consideration to reduce the risk of adverse effects. A minority of psychologists reported unwanted emotions during the groups. One reported that the groups revealed punitive attitudes among attending staff that made her feel angry and that they found it difficult to suppress this emotion when providing alternative perspectives (Q8).
Burden Burden was reported in terms of time required to prepare for and facilitate sessions. There was uniform agreement that the time required was worth the investment given the value they attached to the groups. Participants reported that preparation time reduced with familiarity (Q9).
Confidence Two psychologists reported their confidence was affected by awareness that the groups were part of a research trial and that, because of this, they wanted to deliver them well. Another described feeling a lack of confidence managing discussions where there was marked imbalance of opinions in the group. They expressed a lack of confidence in reducing distress in staff holding marginal perspectives (Q10).
Ethicality Psychologists felt that the values of the groups aligned with the values of the participating wards and their own. They did discuss value clashes between group participants but felt these were positive and an intended function of the groups (Q11).
Intervention coherence All psychologists demonstrated understanding of the intended functions of the groups and indicated that attending staff shared this understanding. However, some psychologists reported that the card exercises involved in the Conflict Formulation model were not immediately intuitive to attending staff, especially when it came to identifying their own feelings (Q12). There was evidence that the distinction between EDITION’s novel reflective practice groups and existing reflective practice had not always been made clear in the promotion of the groups to staff and that, in a minority of wards, this might have reduced attendance.
Perceived effectiveness Psychologists felt that the groups were effective in increasing staff’s awareness and flexibility in boundary application with patients. A secondary outcome perceived was greater team cohesion and enhanced empathy between colleagues. There were caveats to this, in that these were perceived from observations of groups rather than actual observations of changes in practice on the wards. Some were uncertain of how long these changes would be sustained (Q13). They reported changes in staff’s functional understanding of patient behaviour, especially in relation to perceived motives.
Occupational therapists (sensory modulation and support plans)
Affective attitude Occupational therapists were positive about the sensory modulation and support-planning intervention but were concerned about safety (Q14). They felt they lacked the in-depth knowledge of sensory assessment to deliver the intervention safely. They were concerned about adverse reactions to sensory intervention. These concerns were found in one participating trust but not in the other.
Burden Burden associated with the intervention included identifying COVID secure spaces for the room and disinfecting the equipment before and after use. Some of the equipment was quite expensive and there were concerns that opportunity costs would mount as equipment would be damaged by patients and require replacement (Q15).
Opportunity costs Participants identified the potential for damaged relationships if a patient with sensory impairment has an adverse reaction to a piece of equipment (this did not happen during the study). They observed that time spent engaging patients in sensory interventions comes at the expense of alternative interventions. Because the intervention was occupational therapist (OT)-led, and OTs were external to the ward team, it was felt that that it could cause alienation in nursing staff who might perceive the intervention as another ‘top-down’ innovation imposed without adequate support (Q16). OTs recommended that the training and implementation approach should be more joined-up between OTs and nursing staff in future evaluations.
Ethicality OTs broadly endorsed the values underpinning the intervention, which they felt were consistent with OT ‘models of practice’ and that sensory modulation was an important gap in current provision (Q17). However, in one of the trusts, OTs felt that the infrastructure to upskill the workforce and deliver the intervention was lacking. Consequently, they felt they had a duty of care to patients not to implement an intervention that may cause harm. OTs at the other trust, who held the view that a simple assessment of sensory items patients found alerting and calming was sufficient to maintain safety, raised no concerns.
Intervention coherence OTs demonstrated an accurate understanding of the aims of the intervention, that is, to increase patient access to sensory intervention through the upskilling of nursing staff, to manage patient distress proactively rather than reactively (Q18) and to modify adverse environmental impacts on patient arousal and affect.
Perceived effectiveness OTs felt the intervention had the potential to be effective (Q19), with caveats. They were concerned that the intervention could be overstimulating for acutely ill patients. Simplifying and making the plans more accessible to patients was felt to enhance effectiveness.
Senior nurses (debriefing and symmetrical feedback)
Affective attitude Senior nurses presented positive attitudes towards the two senior nurse-led components and the EDITION intervention overall but described a perception that some ward staff members were overwhelmed with the breadth of changes demanded by the project (Q20). One senior nurse expressed frustration at the lack of engagement from ward staff and patients on their allocated ward. Again, this was the low secure male ward reporting low levels of conflict and containment, suggesting that the EDITION intervention may be more suited to acute settings.
Burden Senior nurses described substantial time commitment invested in the two intervention components and identified engaging staff in completing the debriefing and feedback forms as the most time-consuming elements (Q21). They reported ward busyness as a major constraint to nursing staff’s engagement. There was an overall view that the EDITION interventions had real value but would be optimised by implementation support provided by a seconded band 6 nurse (it was felt 0.4FTE would be sufficient time).
Confidence Some limitations were identified in the training provided to senior nurses. One participant felt that the training was too brief and that providing training inclusively of ward staff would have enhanced implementation and confidence. Confidence was further reduced by COVID-19 delays, which lengthened the time from training to implementation (Q22). Confidence was perceived as increasing through the process of delivering the interventions and engagement with the research team. The senior nurses recommended refresher training and regular supervision with the research team and intervention leads at other study sites, to enhance confidence.
Opportunity costs Senior nurses reported that they prioritised the EDITION over existing interventions. As such, this resulted in already embedded interventions not being utilised (Q23).
Ethicality Senior nurses recognised the value in the debriefing intervention and the importance of providing opportunities for ward staff and patients to raise issues with management directly. Most felt the intervention aligned with ward staff values and participating trusts (Q24). They did observe different attitudes towards the interventions between established and junior/inexperienced staff. They felt more experienced individuals often held core restrictive beliefs that were resistant to change and misaligned with the philosophical orientation of the interventions.
Intervention coherence The feedback in terms of understanding of the intervention, again, related to the large number of intervention components and the resultant confusion this caused among ward staff. They reported that this confusion resolved through staff engagement with the interventions over time. Some described patient written content on debriefing and feedback forms that indicated they had not understood the purposes of the interventions.
Perceived effectiveness Senior nurses deemed the recommended debriefing process was effective but that running debriefing sessions with staff from busy acute wards was not always feasible. One senior nurse felt that, while recognising the need for closer working relationships between senior clinicians and ward staff, the existing hierarchical disconnection may have reduced staff’s willingness to be open and honest during debriefing sessions within the trial period. Senior nurses in forensic settings reported much fewer problems with contextual feasibility and felt that both interventions were highly relevant to their clinical environments (Q25). These nurses planned to continue implementation after the study had finished, including wider roll-out to other forensic settings in the trust.
RRPIs (de-escalation training)
Affective attitude Positive views of the EDITION de-escalation training were expressed by RRPIs at all study sites. They valued the content on trauma, the group activities and the service user and carer researcher facilitation (Q26). All RRPIs were extremely positive and enthused by the wider project and happy to have been involved in its implementation.
Burden Because a lot of the training content was perceived as ‘out of the comfort zone’ for RRPIs there was a significant burden identified in terms of reading and re-reading the facilitator manuals outside of the 1-day ‘train-the-trainer’ training (Q27). There were practical burdens associated with delivering the training in the context of the COVID-19 pandemic, in terms of new restrictions on room capacity. One of the video case studies involved a patient spitting at a member of staff and one of the RRPIs had experienced this in their clinical practice. They reported that this resulted in the re-living of this experience and mild distress. However, they had used this experience as an education tool to explain, to trainees, the neurobiological processes involved in re-experiencing traumatic events in response to interpersonal/environmental stimuli.
Confidence RRPIs commonly reported a lack of confidence, especially in the delivery of the neurobiological aspects of the trauma module (Q27). They expressed anxiety about being asked questions that they could not answer while delivering the training. Confidence improved through delivery of the training but, like the senior nurses, they wanted more supervision meeting with members of the research team and suggested a forum for RRPIs to discuss the material and problem-solve in any future evaluation of the training.
Opportunity costs RRPI involvement in the delivery of the de-escalation training required delegation of normal training to colleagues. Other than mild guilt associated with this RRPIs reported no opportunity costs associated with the delivery of training.
Ethicality Broadly, trainers felt the values and ethics behind the training package aligned with their own personal and professional beliefs in terms of increasing the ‘patient-centredness’ of inpatient mental healthcare. There was less certainty in views as to whether the training content aligned with ward staff’s views. Like the clinical psychologist who reported experiencing anger at the punitive attitudes the Negotiated Boundaries exercise elicited, one RRPI described feeling ‘angry and ashamed’ by the cynical attitudes to increasing patient control over their experiences of inpatient care. The discussions this RRPI referred to related to the Creating Trauma-Sensitive Clinical Environments (module 2), which introduces a range of measures (Patient Handover, Patient-Reported Environmental Audit Tool, Collaborative Prescribing) designed to reduce patient experiences of powerlessness. Encouragingly, the RRPIs reported that many of the participating wards are continuing to use the EDITION interventions and that the RRPI teams continue to use the de-escalation training content.
Intervention coherence Prevention and management of violence and aggression (PMVA) trainers presented a coherent understanding of the training package and the project. Their main observation in response to interviewer questions about ward’s staff’s understanding was that they felt some staff had the ‘misconception’ that the training attempted to excuse intolerable patient behaviours. However, this may have represented values differences between the RRPIs and the research team, on one hand, and ward staff, on the other, rather than differences in understanding.
Perceived effectiveness RRPIs felt that the training had improved attitudes in staff who had attended. There were different perspectives on how the impact on service user and carer facilitation could be maximised. The research team consciously avoided the use of lived experience ‘testimonies’ on the advice of our PPI advisory panel. Rather we wanted the service users and carers to be educators and facilitators of the training content. Some RRPIs felt that this resulted in the servicer user researcher facilitator’s (Grundy) lived experience not being properly contextualised until the final module of the day (focused on nursing interventions to reduce isolation and shame associated with voice-hearing). Other RRPIs disagreed with this perspective and felt that having the voice-hearing content towards the end of the training allowed relationships between the ward staff and the service user and carer researchers to develop throughout the day without preconceptions about diagnoses influencing this process. On the contrary, they felt this enhanced rather than diminished the emotional and educational impact of the content on voice hearing.
Ward staff (Patient Handover, Patient-Reported Environmental Audit tool, Insiders’ Guide and Welcoming Committee)
Affective attitude In general, ward staff and ward managers identified value in the interventions and benefit from attending de-escalation training. Most participants described the training as novel and informative and appreciated the group activities and the service user and carer facilitation. There was an exception. On one of the wards, a ward manager reported that her staff had found some of the content condescending and more in keeping with environments that had not already done significant work to reduce the use of restrictive interventions (Q28). This participant drew attention to a video case study in which PRN was used without consideration of alternatives when, in fact, none of EDITION’s video case studies included a scenario of this nature (there was one video case study in which a patient is refused PRN due to there being no ‘objective signs of distress’). The observation that this feedback came only from a ward with a particularly strong identity in terms of reducing use of containment interventions raised some interesting possibilities. Either the ward was already functioning at a level too advanced for the EDITION training or receptiveness to evidence-based practice is reduced in wards where a strong sense of positive identity has been developed through engagement with practice-based evidence and innovation.
The non-training-based interventions were particularly valued by ward staff participants. They were evidently pleased with the reflective practice models, which were experienced as useful and interesting. There was one important exception. One member of ward staff felt the Conflict Formulation model had the potential to raise difficult memories for staff and cause distress. Ward staff felt generally that the interventions to involve patients more in care and the maintenance of safety (Patient Handover, Patient-Reported Environmental Audit tool, Insiders’ Guide and Welcoming Committee) were needed and, perhaps, most encouragingly, that they were valued by patients who were keen to engage with them. One ward manager held the view that ward staff were not sufficiently qualified to engage patients with sensory modulation equipment and that this should be the preserve of OTs alone. Overall, ward staff expressed some of the most positive views of the EDITION interventions among all professional groups. This is, perhaps, surprising given that they assumed much of the burden of intervention. It is possible that attendance at de-escalation training with the whole team protected nursing staff from the ‘silo effect’ that other professionals identified as a limitation of the project, or that it was a consequence of selection bias in the ward staff who were interviewed.
Burden Substantial burden was associated with implementing the interventions. Some of the recommended sensory equipment was expensive and all of it required a financial investment by the wards. There was additional burden associated with the sensory equipment in the context of the COVID-19 pandemic, as a raft of new requirements for infection control were introduced. Burdens associated with the ward interventions were exacerbated by staff reports of heavy workloads (Q29), high acuity and the introduction of other new initiatives by the trust that coincided with the EDITION project. One staff member drew particular attention to burden associated with the patient handover intervention and felt that the time this intervention demanded was likely to outweigh any potential benefit.
Confidence The interventions delivered by ward staff were generally felt to be within their remit and abilities. With regard to the training, one member of nursing staff reported that the de-escalation training had significantly increased their confidence as it had validated their existing practices (potentially indicating that their existing practice contrasted with other team members’).
Opportunity costs The main opportunity costs of the interventions, from ward staff’s perspective, was that they had to be completed either in addition to essential routine activities or instead of additional activities that could have been completed.
Ethicality Nursing staff and ward managers, broadly, felt the training and interventions were aligned to their organisation’s values. These participants emphasised the importance of ‘collaborative working’, ‘least restrictive practice’ and ‘patient-centred interventions’. One staff member highlighted the importance of ensuring those staff assigned to lead intervention components shared the values of the project (implying they did not always feel that had been the case during the study).
Intervention coherence Ward staff demonstrated a clear understanding of the aims of the project in terms of enhancing de-escalation and reducing conflict and containment. However, they reported that patients’ understanding of the interventions was not always apparent (Q30). There were multiple reports of patients misunderstanding the purpose of interventions, attributed partially to a lack of capacity on the part of patients and partially to lack of adequate explanation by the ward and the research teams.
Perceived effectiveness Most commonly, staff felt the training was valuable and interventions provided a simple but effective way with which to improve care. Some staff felt the overall project had created a safer working environment, offered valuable opportunities for reflection and important dialogue, and offered a fresh perspective. Others felt the interventions had made little-to-no difference to the overall ward environment and staff–patient interactions. Again, participants expressing this view worked on the ward that had a strong, pre-existing identity centred on the reduction of containment interventions.
The sensory modulation and support-planning intervention was perceived as effective in enhancing staff’s understanding of patients and providing a safe space for patients to escape distressing sensory input/interpersonal conflict (Q31). Ward staff felt the Insiders’ guides helped in both managing patient expectations and providing reassurance on admission. Participants reported that the guides remained in use after the study, which provided an important indicator of acceptability and perceived clinical value. The Patient-Reported Environmental Audit tool was reported as providing a ‘helpful, fresh perspective’ on environmental safety by involving patients in decision-making.
Patients (Patient Handover, Patient-Reported Environmental Audit tool, Insiders’ Guide and Welcoming Committee)
Affective attitude Patients from forensic inpatient settings presented overwhelmingly positive and some negative sentiments to the interventions they experienced. They felt the Symmetrical Feedback and Debriefing interventions were good initiatives and provided positive feedback on the layout of My Handover, debriefing and feedback forms. Multiple patients felt that the interventions addressed important shortfalls in existing practice. One patient felt strongly that the involvement of patients in completing debriefing forms was an important positive change in practice as it allowed patients an opportunity to express their version of events following use of restraint and or seclusion.
However, some patients stated they were happy with current practice and so felt the suggested changes were unnecessary. Some patients expressed discomfort with the idea of addressing psychiatrists by their given names and others stated they didn’t feel escorting patients back from ward round to the ward was an appropriate job for consultant psychiatrists. Patients also expressed negative feelings related to the tedium of completing paperwork as a part of the interventions. Some reported a perception that interventions were not completed properly, or with care, by staff, specifically the patient handover, debriefing and feedback forms.
Patients provided varied feedback on sensory and support plans. Some felt they were a good initiative and could increase staff understanding and were impressed by the idea of introducing sensory activities and personalised plans (Q32). Others felt that sensory interventions were childish and condescending for use with adult patients. Collaborative prescribing was felt to be a positive intervention, but patients were sceptical as to whether doctors would adopt the intervention. The Insider’s guide also brought mixed feelings from different patients in forensic settings. Some reported feeling proud of their involvement in the guides and others that they were inappropriate for these setting as they suggest the ward was like a hotel not a hospital.
Burden Few burdens were identified by patients. Interestingly, they presented conflicting perspectives of the effect of the interventions on staff workload. Some felt that interventions increased workload and strain on staff, with particular emphasis on the patient handover, which patients felt was completed too regularly, and added significant unnecessary work as only important information needed to be handed over. In contrast, other patients felt the patient handover increased efficiency by making staff more proactive in addressing patient needs. Patients recognised that staffing resource was lacking and as a result engaging in additional activities increased burden for an already strained workforce (Q33).
Confidence Of the few comments provided by patients with regard to their confidence in engaging in interventions, only the feedback intervention was discussed. Multiple patients felt concerned about giving feedback due to fears of negative consequences, or due to generally feeling too timid to provide feedback on the ward (Q34). They noted how giving feedback directly through their primary nurse might increase confidence to engage in the intervention. These findings rather undermined the assumption implicit in the intervention that providing opportunities to give feedback anonymously would provide patients with the confidence to provide honest feedback on practice.
Ethicality Some patients perceived that staff were not taking some interventions seriously, specifically the debriefing and feedback interventions. One felt that the values of staff should be questioned if they did not want to engage with interventions that they felt were clearly designed to protect patients and improve quality of care (Q35).
Intervention coherence Some patients reported inadequate explanation of the interventions, and some felt that the language used in the sensory and support-planning documents was too complex and needed to be simplified (Q36).
Perceived effectiveness Patients perceived a potential overall benefit to the project and, in the environments where it was implemented, an observable positive effect of the sensory modulation and support-planning intervention. Staff support for and buy-in to interventions was felt to be pivotal for their success. On some of the wards, patients reported than the patient handover and debriefing interventions had reduced staff–patient conflict and improved staff response to patient expressions of distress. Again, patients observed that the patient handover had continued to be implemented after the end of the trial phase of the EDITION project, indicating perceived value and acceptability.
Patients felt that adjustments to the time frames of certain interventions would have improved effectiveness. Many patients highlighted that debrief forms needed to be provided to patients with temporal proximity to when the incident had happened after seclusion had been terminated, but with a delay of no more than 2 weeks after this. They suggested forms were often provided after a significant delay following the incident, which they felt limited effectiveness.
Differing feedback was provided about when was best to provide the Insiders’ guides to new admissions. Multiple patients felt the guide should be provided early in the admission process, with as early as the first 24 hours being suggested by one patient, while another argued they should only be provided after the first week to allow time to process the admission experience. A further suggestion was made to give patients time to consider all the information in the guide before being introduced to the welcoming committee.
Discussion
The EDITION study co-designed a training intervention to enhance de-escalation in adult acute and adult forensic mental health inpatient settings. The EDITION intervention represents the first study to co-design an intervention to enhance de-escalation using behaviour change methodology. The intervention was informed by evidence synthesis of 108 primary research studies and qualitative interviews and focus groups with 128 participants including current inpatients, ward staff, MDT staff (including RRPIs) and carers and relatives. Our qualitative work indicated that an intervention to enhance de-escalation, as well as imparting knowledge and skills to trainees, should address key sources of interpersonal and environmental stress that influence staff and patient capacity for self-regulation when de-escalation encounters occur. Qualitative findings indicated that for staff, these were: by their individual skill levels; their knowledge of the patient/s involved in the encounter; cultures of contempt for vulnerability within staff teams; common, ideological representations of mental health problems (especially personality disorder) constructed in teams and organisations; punitive organisational cultures where blame and sanction deter staff willingness to take positive risks. For patients, capacity for self-regulation was influenced by: illiberal ward regimes (myriad rules, enforced inflexibly); environmental signifiers of threat and disrespect (visible evidence of coercion, organisational messaging demanding unconditional patient respect for staff); alienating conduct of key clinical and ward processes (ward rounds, handovers, prescribing, waiting times, medication rounds, mealtimes, admission); patient community conflict (lack of staff in communal areas to influence/intervene, lack of opportunity to escape distressing behaviour).
A co-designed intervention targeting sources of environmental and interpersonal stress was developed. Because of the multiplicity of key sources of stress affecting staff and patient self-regulation capacity, the intervention was necessarily complex and included 11 behaviour change components targeted at key stakeholders at every layer of the inpatient organisational structure. A single-day de-escalation training package was developed. Service user and carer researchers led delivery of the package. Every element of training was oriented towards increasing staff knowledge of the impact of traumatic experience on behaviour and re-traumatising aspects of the inpatient experience. Ward staff and inpatients were asked to deliver three distinct intervention components designed to reduce patients’ experience of powerlessness during their inpatient admission. The Patient Handover aimed to consistently incorporate the patient voice in handover and in nursing notes and thereby attempted to reduce bias in the understandings and representations of patients that are constructed through these processes. The Patient-Reported Environmental Audit aimed to increase feelings of safety by giving patients the power to influence the safety of the ward’s social and physical environment. The Insiders’ Guide and Welcoming Committee aimed to reduce the use of force and social isolation on admission by reassuring patients about the nature and philosophy of the environment on admission.
Psychiatrists were asked to adopt a collaborative prescribing intervention to involve patients in selecting their own antipsychotic medicine using decision aids based on antipsychotic side-effect profiles. They were further asked to implement 10 ward round standards designed to reduce patient anxiety and distress in ward rounds. Both interventions targeted the extreme asymmetry of power inherent in these clinical processes (inadvertently mimicking the dynamics of abusive and/or neglectful relationships). Occupational therapists were asked to increase patient access to sensory modulation interventions and implement a novel support-planning process. This targeted adverse environmental impacts on patients’ capacity for self-regulation and staff’s awareness and sensitivity to typical escalation trajectories and ability to personalise de-escalation interventions.
Clinical psychologists were asked to implement two novel models of reflective practice. The first ‘Conflict Formulation’ aimed to deconstruct moral formulations of patient behaviour, firstly, by adopting a systematic approach to analysis of staff and patient emotional and needs-based inputs into conflict with patients, and, secondly, through systematic analysis of historical, environment/institutional and social justice impacts on staff and patient conflict inputs. It was hypothesised that this more egalitarian model of formulation would enhance de-escalation behaviours by deepening understandings of conflict and enhancing empathy. The second model of reflective practice, Negotiated Boundaries, aimed to increase reflection on the necessity of ‘limit-setting’ responses to conflict and enhancing de-escalation skills, therapeutic over and under-involvement in relationships with patients and attitudes to vulnerability in colleagues. Senior nurses were asked to implement two interventions designed to narrow the space between leadership and ward staff that abuse and poor practice can persist in. The Debriefing intervention aimed to improve staff’s functional understanding of events involving restraint and seclusion and the Symmetrical Feedback intervention aimed to enhance staff and patient’s feelings of security and control by offering opportunity to give feedback anonymously on clinical practice.
Feasibility of conducting a definitive randomised controlled trial
Feasibility studies prior to a RCT should demonstrate the feasibility of recruitment and data collection, acceptability and engagement with the intervention, feasibility of randomisation and sample size estimates for a full trial, assessment of potential harms and preliminary effects. 179
Feasibility of recruitment and data collection
Nine of the 10 wards completed all 24 weeks of data collection (one ward withdrew at 13 weeks (after training) owing to staff shortages caused by the COVID-19 pandemic). One of EDITION’s primary objectives in terms of establishing the feasibility of a full RCT was to identify effective methods to increase completion rates of the proposed primary outcome, the PCC-SR. The PCC-SR has demonstrated reliability10 and validity152 and has a range of benefits as a primary outcome for a full trial. For example, the PCC-SR standardises the collection of conflict containment data across service providers that often use varying definitions for conflict behaviours and differing thresholds for reporting. As a composite measure of conflict and containment, the PCC-SR also controls for substituting effects between different conflict or containment events: for example, staff compensating for restrictions on the use of seclusion or physical restraint by increasing their use of PRN (as required) medicines or changes in restrictions on patient behaviour modifying the way conflict is expressed (e.g. a locked-door policy may reduce absconding attempts but increase violence or self-harm).
A major problem with the PCC-SR measure in previous RCTs has been large amounts of missing data. For example, the ‘Safewards’ RCT had > 45% PCC-SR data missing, hence the need to understand what helps to increase staff completion rates. The EDITION study team tested a range of strategies to enhance staff completion. We established that the most effective strategies for increasing completion rates are researcher face-to-face access to the ward areas, ward-level incentives (vouchers to buy items for the ward) and stimulating inter-ward competition.
When wards that were closed to researcher access because of COVID were excluded (this represented 336/3780 or 8.9% of possible completions) the overall completion rate in the EDITION study was 2343/3444 or 68%. However, importantly, completion rates increased between the baseline and follow-up phases. In the pre-intervention phase, 876/1344 or 65% of shift reports were completed. In the post-intervention phase completions increased to 855/1120 or 76%, strongly indicating that the strategies for enhancing staff completion were becoming optimised in latter stages of the study. This finding should be considered in the context of seven out of 10 participating wards completing post-intervention data collection during the COVID-19 pandemic. This introduced unprecedented pressures placed on mental health inpatient staff. 159 The fact that we achieved increased completion rates in this context indicates that applying our strategies in a post-pandemic context should increase completion rates still further.
Recruitment of staff and patients for completion of secondary outcomes was also good. For patient clinical outcomes, 81% (283/350) of the recruitment target was met across the seven time points [excluding remote data collection due to COVID-19, this rose to 88% (283/320)]. For staff-reported clinical outcomes, 68% of the total recruitment target was achieved [excluding remote data collection due to COVID-19, this increased to 75% (135/180)] across the four time points. Secondary outcomes were also largely acceptable, with full completion rates between 80% (ACMQ) and 100% (COM-B) for staff respondents. The patient-reported clinical outcome measures also had good full completion rates, except the CES, which was just 53%. The other patient measures (VPC and PEESS) had full completion rates of > 80%. The CES should be considered for exclusion prior to a full RCT.
Acceptability and engagement with the intervention
The intervention was broadly well engaged, with 275 professionals and paraprofessionals across 10 wards being trained in the EDITION intervention. The TARS outcomes (n = 214) indicate that the de-escalation training was acceptable, with most participating ‘strongly agreeing’ that the training was generally acceptable. Most of the interventions were in use in the study’s follow-up periods, with two important exceptions. Only 2/10 wards were using the sensory modulation and support-planning intervention in the post-intervention data-collection period. One trust’s occupational therapists felt that they lacked the required expertise to implement sensory modulation. A rapid review of literature conducted by the EDITION team during the intervention development phase of the study indicated that patient reports of increased arousal/agitation following access to sensory rooms/equipment on mental health inpatient wards occurs infrequently (between 2% and 6% of pre and post measurements). The addition of an occupational therapist to the co-investigation team in any future evaluation is likely to be important to enhancing engagement with this intervention. There were also problems with purchasing equipment and COVID-19 infection risk, indicating advanced preparation to mitigate these problems may be required in a full trial. The other intervention with poor engagement was the Collaborative Prescribing intervention, which was only used by 2/10 wards’ psychiatrists in the follow-up data-collection period. Our process evaluation indicated that there were values clashes between psychiatrists and the intervention which limited engagement, as well as concerns about risk and accountability. Modifications or exclusion of the intervention should be considered prior to further evaluation.
Feasibility of randomisation and sample size estimates for a full trial
The commissioning brief required that we evaluate the intervention in a broad range of settings. As such the need to explore contextual diversity was prioritised over what would have been our ideal design for a feasibility trial and we used an uncontrolled design. However, randomisation is feasible in these settings as evidenced both in recent trials of similar interventions148 and in the study team’s (Price, Lovell, Drake) recent trial of increased access to psychological therapies in acute psychiatric wards. 149 The Safewards RCT148 demonstrated that masking of ward staff in terms of experimental versus control conditions is feasible (74% of control-group staff believed they were in the experimental group) but an appropriate active control for the EDITION intervention will need to be identified in advance of a definitive RCT. We have identified the SD of the proposed primary outcome measure for sample size calculation.
Assessment of potential harms and preliminary effects
We collected adverse event data fortnightly from each of the 10 wards’ ward managers. Ward managers were asked to provide a summary of reported incidents to researchers and state (1) whether the rate of incidents was within expected norms for the ward and if not (2) whether the reported change was, in their view, attributable to the intervention. There were no reports that indicated a relationship between the intervention and increases in unsafe events. There was one serious adverse event during the study, which was assessed by an independent assessor as unrelated to the EDITION intervention. As such, there were no obvious safety signals associated with the EDITION intervention.
There was a signal of a potential effect on the proposed primary outcome (PCC-SR). The incidence rate of conflict events reduced by 45% in the embedding phase and 55% in the follow-up phase, compared to the pre-intervention phase. The incidence of containment events also reduced over the course of the study, with a 20% reduction in the follow-up phase compared to the pre-intervention phase. The uncontrolled design does not allow for inferences to be drawn about what caused these effects. Overall, only small changes were observed on the secondary outcome measures for staff and patients, with a lot of uncertainty in these estimates. There were only two statistically significant effects on patient outcomes that were detected in this non-powered analysis. Further limitations include the purposively selected sample of wards. A purposive sample was necessary to ensure contextual diversity in the ward functions that were specified by the funders’ commissioning brief. However, all wards in each of the participating sites that met the eligibility criteria were invited to submit expressions of interests. Wards were included in the study on a first come first served basis. It is possible, therefore, that the wards that participated in this study were, perhaps unrepresentatively, open to changing their practice.
Economic outcomes
The costs of the training intervention were estimated from two sources. Firstly, ward-level data reported the number of staff attending training, by AfC band, at the start of the embedding period. Secondly, intervention diaries were completed by champions leading the components of the intervention during the embedding period. Overall, the average (mean) number of staff and cost per day for the initial training was similar between the two trusts, with training attended by staff across AfC bands 2–7 in each trust. Overall, the time and costs of staff to embed the different components of the intervention varied between the two trusts. However, the number of wards included in the diary reports varied within and between trusts over the different components of activity. This may reflect differences in the timing of embedding periods and the number and types of ward and staff training needs as well as the feasibility design of this study. Several items across both trusts were left blank and treated as not reported. It is not clear from the diaries whether these were missing data or the training/activity was not undertaken at the trust. In terms of a full trial, further work is needed to refine ways of collecting these data consistently.
The overall number and costs of staff on the ward and conflict/containment episodes per shift were estimated from the PC-SSR measure. There appeared to be differences in the number and costs of staff on the ward for each shift, which may reflect variation in the number and needs of patients. However, there were insufficient data to assess this. The economic study did not include an assessment of the possible impact of the intervention on overall staff time and costs on shift. Training interventions may have the potential to reduce staff absence and/or turnover, which may also impact on the need for and cost of bank and agency staff on wards. 180
The number of conflict and containment episodes also varied between the two trusts, although there were no apparent differences in the costs of these episodes. Exploratory regression analyses suggest that shift, ward and follow-up period may be important factors to consider in the design of an integrated clinical and economic effectiveness trial, in terms of data collection and analysis methods. However, it is important to note that the regression analyses only considered variables collected within the PC-SSR. Further exploratory work with healthcare professionals would be useful to identify if there are additional factors that may be important moderators or mediators of costs. Note these regression analyses should also be treated with caution given the relatively small sample size and uncontrolled nature of the data collected. The nature of the feasibility study means the detailed regression results are unlikely to be sufficient to determine differences over time or setting. Several assumptions were required to cost staff time, due to limitations in the data collected. Further work to refine the sources and methods of data collection is needed. Published unit costs of conflict/containment episodes from a single source were used to estimate the costs of these events. However, the unit costs were published in 2007. Although they were inflated to 2020–21 prices, changes in the organisation and staffing of wards as well as approaches to dealing with conflict may have changed. Discussions with staff in the two trusts indicated that the number, AfC band and time of staff to manage conflict and containment episodes varied considerably and that staff found it difficult to assess these factors. It was outside the resources and scope of this study to identify service use and unit costs of these events. This suggests further work, using qualitative methods, audit and diaries is needed to validate or update the unit costs of conflict and containment episodes.
The average length of stay and costs of inpatient care varied widely according to discharge destination. The most frequently reported discharge destinations were usual residence and temporary residence. Data about discharges and inpatient length of stay were limited to patients discharged and were collected from the trusts for the pre- and post-intervention periods. The number of wards for which data were reported was higher in the pre-implementation period (n = 10/10; 100%) than in the post-intervention period (n = 5/10; 50%). This may reflect the different timings of the implementation and embedding phase and subsequent post-intervention period. The data on inpatient stay were reported as an average over all the discharges for each destination. Given the feasibility design and resources of the study, it was not possible to collect individual-level data for each discharge for analysis. Accordingly, measures of variance for the average length of stay were not available in the data collected and are not reported here.
Despite the limitations, the data give a preliminary indication that it is feasible to collect information about inpatient stay from trust routine data sets. However, further work is needed to inform the design of an integrated clinical and economic effectiveness trial. This includes work to (1) explore the extent to which it is possible to provide anonymised, individual-level data about ongoing and completed inpatient episodes and spells from trusts within the prevailing UK and NHS ethical, governance and data protection framework at the time of designing a future trial and (2) assess the reliability, costs and value of other data-collection methods.
An average unit cost for high-dependency secure provision for people with severe mental health problems was used to cost the inpatient stay. This average unit cost does not differentiate between the costs of care on the different wards included in the inpatient stay analysis. NHS reference costs are available for secure mental health inpatient stay according to combinations of diagnosis/symptoms/risk (categorised as low/medium risk or medium/high risk). However, this requires individual patient-level data, rather than average inpatient by ward type. Data-collection methods for inpatient stay in future trials need to be consistent with the available national unit cost data. The cost associated with the discharge destination is also an area to be considered in the design of integrated clinical and economic effectiveness trial.
A further limitation of the costing analyses was the exclusion of prescribing costs. As noted earlier, there were limited resources for the feasibility study. Accordingly, the focus of the economic component was to assess staff time and costs associated with the training and with managing cost and containment events, which are areas that would be most likely to be directly affected by the intervention. Prescribing and costs can vary widely between participants, for a range of sociodemographic, clinical and organisational reasons. Further work prior to a full integrated clinical and economic trial would be useful to assess the level of variance in prescribing and prescribing costs and assess how best to capture the data as well as identify and control for key baseline covariates (e.g. participant sociodemographic and clinical characteristics, prescribing protocols, clinician characteristics, ward and trust characteristics).
Health status data were collected from staff and patients using the EQ-5D-5L129 to inform the full trial data-collection and analysis methods. The actual number of follow-up points for participants was dependent on the staff and patients both available and able to complete the EQ-5D-5L at the assessment point. This meant that completion varied in the number of assessment points (1–4 for staff; 1–7 for patients) and the assessment period when the EQ-5D-5L was first and last completed.
Overall, 76/104 (73%) of staff fully or partially completed the EQ-5D-5L at only one time point and 28/104 (27%) completed the measure at two or more time points. In comparison, 63/137 (46%) patients fully or partially completed the EQ-5D-5L at only one time point and 74/137 (54%) at two or more time points. The results indicate that, as might be expected, there appear to be differences in the health status of staff and patients at the participants’ first assessment but not at their last follow-up assessment. Additionally, there is an indication that the measure differentiates between type of participant. However, it is not possible to draw any conclusions from this, since it may reflect differences in the timing and length of time between assessments as well as lower numbers having a final assessment. Overall, the results from the EQ-5D-5L indicate that while it is feasible to collect the data from some staff and patients, the number of participants who fully or partially completed the measure is low. The low level of completion may reflect a variety of factors, including whether participants were on the ward and available to complete the EQ-5D-5L at the study-defined assessment point. A full trial would need to ensure that data can be captured consistently from the same participants over time to assess whether any changes at follow-up can be attributed to the intervention. Accordingly, further work is needed to use the EQ-5D-5L in a full clinical trial. This could include further work to understand why the completion rates were low as well as how to embed the measure in the outcome data-collection process.
The resource use and health status data were collected as part of a feasibility study. The aim, scope and resources available for the study limit the extent to which any conclusions can be reached about the actual cost implications and health consequences of the training intervention. However, the work demonstrates that some resource use and health status data can be collected and indicates key areas for further development and refinement of the data-collection methods, to help ensure reliable and consistent data are collected for any economic evaluation.
Equality, diversity and inclusion
A strength of the EDITION study, in this respect, is the involvement of people with serious mental health problems as co-applicants on the project, as members of the study’s PPI advisory panel, as expert stakeholders contributing to the design of the intervention, as research participants and as training delivery leads. Weaknesses included an all-white British co-applicant team. An additional important weakness was that although clinical and academic experts who contributed to intervention co-design had excellent representation of people from black and ethnic minority backgrounds, this was not the case for the group with lived experience of mental health services. Although invitations to black and ethnic minority experts were made, there was no uptake. Future work should consider strategies for engaging stakeholders from black and ethnic minority backgrounds with lived experience of mental health services.
Patient and public involvement
There were important strengths and weaknesses in this respect. The patient and public advisory panel was engaged throughout and influenced all aspects of the research. PPI methods in relation to the co-design of the intervention were weaker. On the first stakeholder day, there was insufficient time allowed to complete all activities. There was also important critical feedback about inaccessible language used in the exercise materials and managing group dynamics (ensuring all had equal opportunity to speak). Consequently, the initial ideas for intervention were much more strongly influenced by clinical and academic experts. This was to some extent mitigated by the engagement of service user and carer researchers, the PPI panel, and expert stakeholders with lived experience in latter stages of intervention development but was, nevertheless, an important weakness. The service user and carer researchers were long-standing collaborators of the study team. It is, therefore, a possibility that less experienced PPI researchers would require greater preparation to deliver the training roles in practice.
Conclusions
The EDITION study developed an evidence-based and co-designed training intervention to enhance de-escalation in adult acute and adult forensic mental health inpatient settings. The intervention was informed by evidence synthesis of 108 primary research studies and qualitative inquiry with 128 participants. Co-design of the intervention resulted in a complex intervention with 11 behaviour change components delivered by service user and carer researchers, Reducing Restrictive Practices Instructors, ward staff and patients, psychiatrists, clinical psychologists, nursing leadership and occupational therapists. The training was very well engaged with 275 professionals and paraprofessionals from 10 participating wards completing training. Conducting a RCT of the EDITION intervention is likely to be feasible. The strategies to enhance completion rates of the PCC-SR (proposed primary outcome) were successful (rising from 65% in the pre-intervention to 76% in the post-intervention phase). Recruitment rates for secondary outcomes were also good: 81% of the target for patients was met and 68% for staff. The secondary outcome measures had excellent full completion rates except for the CES (patient-reported), which may need to be removed in a full trial. It was feasible to collect resource use and health status data to inform an economic analysis of the intervention in a full trial.
Acknowledgements
The research team would like to acknowledge all service users, clinical staff and violence-reduction experts for their contributions to the development of the intervention, as well as all the staff and patients who participated as research participants. We also acknowledge the major contribution of the two participating trust’s Research and Innovation departments and their clinical studies officers, without whom we would not have achieved the level of engagement and research activity that we did.
Contributions of authors
Owen Price (https://orcid.org/0000-0002-4601-3363) was responsible for overall co-ordination of the project.
Cat Papastavrou Brooks (https://orcid.org/0000-0002-3055-5301) analysed and wrote up WP1 qualitative data in adult acute settings, co-led WP2 intervention design and co-ordinated WP3 data collection.
Isobel Johnston (https://orcid.org/0000-0001-5891-9472) led WP1 qualitative inquiry in low and medium secure forensic settings and the WP3 process evaluation.
Peter McPherson (https://orcid.org/0000-0003-0998-9137) led the qualitative evidence synthesis and collected WP1 qualitative data.
Helena Goodman (https://orcid.org/0000-0002-4644-258X) led WP1 qualitative inquiry in high-secure forensic settings and collected WP3 data.
Andrew Grundy (https://orcid.org/0000-0002-6562-6894) co-led training delivery with Lindsey Cree and analysed TARS data.
Lindsey Cree (https://orcid.org/0000-0002-7460-0266) co-led training delivery with Andrew Grundy and analysed TARS data.
Zahra Motala (https://orcid.org/0000-0003-0858-2837) was service user lead for the development of intervention materials.
Jade Robinson (https://orcid.org/0000-0001-9478-2274) collected and analysed WP3 data.
Michael Doyle (https://orcid.org/0000-0002-3560-3966) was site lead for Trust A.
Nicholas Stokes (https://orcid.org/0000-0002-1906-8545) analysed WP3 data.
Christopher J Armitage (https://orcid.org/0000-0003-2365-1765) (behaviour change scientist) designed and oversaw WP2 intervention development.
Elizabeth Barley (https://orcid.org/0000-0001-9955-0384) was site lead for Trust B and analysed and wrote up data from WP1 and WP3.
Helen Brooks (https://orcid.org/0000-0002-2157-0200) (implementation scientist) designed and oversaw WP2 intervention development.
Patrick Callaghan (https://orcid.org/0000-0003-3175-5361) led training delivery and supervised the service user (Andrew Grundy) and carer (Lindsey Cree) training leads.
Lesley-Anne Carter (https://orcid.org/0000-0002-1193-8681) led the statistical analysis.
Linda M Davies (https://orcid.org/0000-0001-8801-3559) led the economic analysis.
Richard J Drake (https://orcid.org/0000-0003-0220-4835) led the training of psychiatrists.
Karina Lovell (https://orcid.org/0000-0001-8821-895X) was WP3 lead and mentored the CI.
Penny Bee (https://orcid.org/0000-0002-5600-0400) was qualitative research lead.
Ethics statement
Both work packages requiring ethical approval (WP1 and WP3) received HRA approval. Work package 1 received ethical approval from Yorkshire and The Humber, South Yorkshire Ethics Committee on 5 March 2018 (ref: 18/YH/0035). Work Package 3 received ethical approval from West of Scotland Research Ethics Service on 17 December 2019 (ref: 19/WS/0098).
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to available data will be granted following exclusive use period until 1 September 2024.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Price O, Baker J, Bee P, Lovell K. Learning and performance outcomes of mental health staff training in de-escalation techniques for the management of violence and aggression. Br J Psychiatry 2015;206:447-55.
- Sterne J, Hernán M, Reeves B, Savović J, Berkman N, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;12.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57.
- Azuela G, Robertson L. The effectiveness of a sensory modulation workshop on health professional learning. J Ment Health Train Educ Pract 2016;11:317-31.
- Beech B, Leather P. Evaluating a management of aggression unit for student nurses. J Adv Nurs 2003;44:603-12.
- Beech B. Aggression prevention training for student nurses: differential responses to training and the interaction between theory and practice. Nurse Educ Pract 2008;8:94-102.
- Beech B. Sign of the times or the shape of things to come? A 3-day unit of instruction on ‘aggression and violence in health settings for all students during pre-registration nurse training’. Accid Emerg Nurs 2001;9:204-11.
- Biondo J. De-escalation with dance/movement therapy: a program evaluation. Am J Dance Ther 2017;39:209-25.
- Bjorkdahl A, Hansebo G, Palmstierna T. The influence of staff training on the violence prevention and management climate in psychiatric inpatient units. J Psychiatr Ment Health Nurs 2013;20:396-404.
- Bowers L, Brennan G, Flood C, Lipang M, Oladapo P. Preliminary outcomes of a trial to reduce conflict and containment on acute psychiatric wards: City Nurses. J Psychiatr Ment Health Nurs 2006;13:165-72.
- Bowers L. TAWS Paper 3: The Validity of the Patient-Staff Conflict Checklist (PCC-SR) Evaluated (Internet) 2008. www.kcl.ac.uk/ioppn/depts/hspr/research/ciemh/mhn/projects/taws/TAWS-IP03.pdf (accessed 3 January 2023).
- Bowers L, Allan T. The attitude to personality disorder questionnaire: psychometric properties and results. J Personal Disord 2006;20:281-93.
- Maslach C, Jackson S, Leiter M. MBI: Maslach burnout inventory. Sunnyvale, CA: CPP Incorporated; 1996.
- Moos R. Evaluating Treatment Environments. A Social Ecological Approach. London: John Wiley & Sons; 1974.
- Bowers L, Flood C, Brennan G, Allan T. A replication study of the city nurse intervention: reducing conflict and containment on three acute psychiatric wards. J Psychiatr Ment Health Nurs 2008;15:737-42.
- Calabro K, Mackey TA, Williams S. Evaluation of training designed to prevent and manage patient violence. Issues Ment Health Nurs 2002;23:3-15.
- Carmel H, Hunter M. Compliance with training in managing assaultive behavior and injuries from inpatient violence. Hosp Community Psychiatry 1990;41:558-60.
- Chigbundu N. Lived Experiences of Mental Health Nurses With Verbal De-Escalation Techniques and Multisensory Room Strategies. PhD Thesis 2015.
- Collins J. Nurses attitudes toward aggressive behavior following attendance at the prevention and management of aggressive behavior program. J Adv Nurs 1994;20:117-31.
- Collins M. Attitudes Concerning a Program for Managing Violence at the Colorado Mental Health Institute. Doctoral Dissertation 2014.
- Cowin L, Davies R, Estall G, Berlin T, Fitzgerald M, Hoot S. De-escalating aggression and violence in the mental health setting. Int J Ment Health Nurs 2003;12:64-73.
- Davies B, Griffiths J, Liddiard K, Lowe K, Stead L. Changes in staff confidence and attributions for challenging behaviour after training in positive behavioural support within a forensic medium secure service. J Forens Psychiatry Psycho 2016;26:847-61.
- Thackrey M. Clinician confidence in coping with patient aggression: assessment and enhancement. Prof Psychol Res Pr 1987;18:57-60.
- Geoffrion S, Goncalves J, Giguère C, Guay S. Impact of a program for the management of aggressive behaviors on seclusion and restraint use in two high-risk units of a mental health institute. Psychiatr Q 2018;89:95-102.
- Gertz B. Training for prevention of assaultive behavior in a psychiatric setting. Hosp Community Psychiatry 1980;31:628-30.
- Goodykoontz L, Herrick CA. Evaluation of an inservice education program regarding aggressive behavior on a psychiatric unit. J Contin Educ Nurs 1990;21:129-33.
- Pines A, Aronson E. Burnout: From Tedium to Personal Growth. New York: Free Press; 1981.
- Grenyer BFS, Ilkiw-Lavalle O, Biro P, Middleby-Clements J, Comninos A, Coleman M. Safer at work: development and evaluation of an aggression and violence minimization program. Aust N Z J Psychiatry 2004;38:804-10.
- Hahn S, Needham I, Abderhalden C, Duxbury JAD, Halfens RJG. The effect of a training course on mental health nurses’ attitudes on the reasons of patient aggression and its management. J Psychiatr Ment Health Nurs 2006;13:197-204.
- Duxbury J. Testing a new tool: the Management of Aggression and Violence Attitude Scale (MAVAS). Nurse Res 2003;10:39-52.
- Ilkiw-Lavalle O, Grenyer B, Graham L. Does prior training and staff occupation influence knowledge acquisition from an aggression management training program?. Int J Ment Health Nurs 2002;11:233-9.
- Infantino JA, Musingo S-Y. Assaults and injuries among staff with and without training in aggression control techniques. Hosp Community Psychiatry 1985;36:1312-4.
- Jonikas J, Cook J, Rosen C, Laris A, Kim J. A program to reduce use of physical restraint in psychiatric inpatient facilities. Psychiatr Serv 2004;55:818-20.
- Laker C, Gray R, Flach C. Case study evaluating the impact of de-escalation and physical intervention training. J Psychiatr Ment Health Nurs 2010;17:222-8.
- Lee S, Gray R, Gournay K. Comparing the outcomes of the application of C&R (general service) and SCIP in the management of disturbed behaviour in mental health care. J Ment Health 2012;21:307-17.
- Martin KH. Improving staff safety through an aggression management program. Arch Psychiatr Nurs 1995;9:211-5.
- Martinez A. Implementing a workplace violence simulation for undergraduate nursing students: a pilot study. J Psychosoc Nurs Ment Health Serv 2017;55:39-44.
- Bell A, Horsfall J, Goodin W. The Mental Health Nursing Clinical Confidence Scale: a tool for measuring undergraduate learning on mental health clinical placements. Aust N Zeal J Ment Health Nurs 1998;7:184-90.
- McIntosh D. Testing an intervention to increase self-efficacy of staff in managing clients perceived as violent. PhD. Cincinnati: University of Cincinnati; 2003.
- Ozer E, Bandura A. Mechanisms governing empowerment effects: a self-efficacy analysis. J Pers Soc Psychol 1990;58:472-86.
- McLaughlin S, Bonner G, Mboche C, Fairlie T. A pilot study to test an intervention for dealing with verbal aggression. Br J Nurs 2010;19:489-94.
- Moore D. The least restrictive continuum. Inst Nurs News 2010;6:5-6.
- Nau J, Dassen T, Needham I, Halfens R. The development and testing of a training course in aggression for nursing students: a pre and post-test study. Nurse Educ Today 2009;29:196-207.
- Nau J, Halfens R, Needham I, Dassen T. Student nurses’ de-escalation of patient aggression: a pretest-posttest intervention study. Int J Nurs Stud 2010;47:699-708.
- Nau J, Halfens R, Needham I, Dassen T. The de-escalating aggressive behaviour scale: development and psychometric testing. J Adv Nurs 2009;65:1956-64.
- Nau J, Dassen T, Needham I, Halfens R. Sensitivity, specificity and predictive value of Confidence in Managing Patient Aggression Scale on de-escalating behaviour. J Clin Nurs 2011;20:2584-6.
- Needham I, Abderhalden C, Meer R, Dassen T, Haug H, Halfens R, et al. The effectiveness of two interventions in the management of patient violence in acute mental inpatient settings: report on a pilot study. J Psychiatr Ment Health Nurs 2004;11:595-601.
- Nijman H, Muris P, Merckelbach H, Palmstierna T, Wistedt B, Vos A, et al. The staff observation aggression scale-revised (SOAS-R). Aggress Behav 1999;25:197-209.
- Needham I, Abderhalden C, Zeller A, Dassen T, Haug H, Fischer JE, et al. The effect of a training course on nursing students’ attitudes toward, perceptions of, and confidence in managing patient aggression. J Nurs Educ 2005;44:415-20.
- Nijman HL, Merckelbach HL, Allertz WF, a Campo JM. Prevention of aggressive incidents on a closed psychiatric ward. Psychiatr Serv 1997;48:694-8.
- Paterson B, Turnbull J, Aitken I. An evaluation of a training course in the short-term management of violence. Nurse Educ Today 1992;12:368-75.
- Goldberg D. The Detection of Psychiatric Illness by Questionnaire. London: Oxford University Press; 1972.
- Rice M, Helzel M, Varney G, Quinsey V. Crisis prevention and intervention training for psychiatric hospital staff. Am J Community Psychol 1985;13:289-304.
- Robinson T, Hills D, Kelly B. The evaluation of an online orientation to rural mental health practice in Australia. J Psychiatr Ment Health Nurs 2011;18:629-36.
- Lee C, Witta E. Online students’ perceived self-efficacy: does it change? 2001;1 and 2.
- Sjostrom N, Eder DN, Malm U, Beskow J. Violence and its prediction at a psychiatric hospital. Eur Psychiatry 2001;16:459-65.
- Wistedt B, Rasmussen A, Pedersen L, Malm U, Träskman-Bendz L, Wakelin J, et al. The development of an observer-scale for measuring social dysfunction and aggression. Pharmacopsychiatry 1990;23:249-52.
- Smoot S, Gonzales J. Cost-effective communication skills training for state hospital employees. Psychiatr Serv 1995;46:819-22.
- Taylor KN, Sambrook S. CBT for culture change: formulating teams to improve patient care. Behav Cogn Psychother 2012;40:496-503.
- Whittington R, Wykes T. An evaluation of staff training in psychological techniques for the management of patient aggression. J Clin Nurs 1996;5:257-61.
- Wondrak RF, Dolan BM. Dealing with verbal abuse: evaluation of the efficacy of a workshop for student nurses. Nurse Educ Today 1992;12:108-15.
- Yang C, Hargreaves W, Bostrom A. Association of empathy of nursing staff with reduction of seclusion and restraint in psychiatric inpatient care. Psychiatr Serv 2014;65:251-4.
- Berring L, Hummelvoll J, Pederson L, Buus N. A co-operative inquiry into generating, describing, and transforming knowledge about de-escalation practices in mental health settings. Issues Ment Health Nurs 2016;37:451-63.
- Heckemann B, Breimaier H, Halfens R, Schols J, Hahn S. The participant’s perspective: learning from an aggression management training course for nurses. Insights from a qualitative interview study. Scand J Caring Sci 2016;30:574-85.
- Johnson M, Hauser P. The practices of expert psychiatric nurses: accompanying the patient to a calmer personal space. Issues Ment Health Nurs 2001;22:651-68.
- Johnson ME, Delaney KR. Keeping the unit safe: the anatomy of escalation. J Am Psychiatr Nurses Assoc 2007;13:42-5.
- Delaney KR, Johnson ME. Keeping the unit safe: mapping psychiatric nursing skills. J Am Psychiatr Nurses Assoc 2006;12:198-207.
- Berring L, Pedersen L, Buus N. Coping with violence in mental health care settings: patient and staff member perspectives on de-escalation practices. Arch Psychiatr Nurs 2016;30:499-507.
- Chambers M, Kantaris X, Guise V, Välimäki M. Managing and caring for distressed and disturbed service users: The thoughts and feelings experienced by a sample of English mental health nurses. J Psychiatr Ment Health Nurs 2015;22:289-97.
- Camuccio C, Chambers M. Managing distressed and disturbed patients: the thoughts and feelings experienced by Italian nurses. J Psychiatr Ment Health Nurs 2012;19:807-15.
- Johnson M, Delaney K. Keeping the unit safe: a grounded theory study. J Am Psychiatr Nurses Assoc 2006;12:13-21.
- Kontio R, Välimäki M, Putkonen H, Kuosmanen L, Scott A, Joffe G. Patient restrictions: are there ethical alternatives to seclusion and restraint?. Nurs Ethics 2010;17:65-76.
- Grotto J, Gerace A, O’Kane D, Simpson A, Oster C, Muir-Cochrane E. Risk assessment and absconding: perceptions, understandings and responses of mental health nurses. J Clin Nurs 2015;24:855-65.
- Drach-Zahavy A, Goldblatt H, Granot M, Hirschmann S, Kostintski HC. Patients’ aggression in psychiatric settings. Qual Health Res 2012;22:43-5.
- Hargate R, Howden S, Tarpey E, Walker T. The PARALLEL Study (imPAct of expeRiencing Another’s seLf harm and suicidaL bEhaviour in hospitaL). J Forensic Pract 2017;19:258-68.
- Shaw D, Sandy P. Mental health nurses’ attitudes toward self-harm: curricular implications. Heal SA Gesondheid 2016;21:406-14.
- Mattson A, Binder P. A qualitative exploration of how health care workers in an inpatient setting in Norway experience working with patients who self-injure. Nord Psychol 2012;64:272-90.
- Hagen J, Hjelmeland H, Knizek B. Relational principles in the care of suicidal inpatients: experiences of therapists and mental health nurses. Issues Ment Health Nurs 2017;38:99-106.
- Karman P, Kool N, Gamel C, van Meijel B. From judgment to understanding. Mental health nurses’ perceptions of changed professional behaviors following positively changed attitudes toward self-harm. Arch Psychiatr Nurs 2015;29:401-6.
- Wilstrand C, Lindgren B, Gilje F, Olofsson B. Being burdened and balancing boundaries: a qualitative study of nurses’ experiences caring for patients who self-harm. J Psychiatr Ment Health Nurs 2007;14:72-8.
- Lees D, Procter N, Fassett D. Therapeutic engagement between consumers in suicidal crisis and mental health nurses. Int J Ment Health Nurs 2014;23:306-15.
- Vuckovich P. Strategies nurses use to overcome medication refusal by involuntary psychiatric patients. Issues Ment Health Nurs 2009;30:181-7.
- Tofthagen R, Talseth A-G, Fagerström L. Mental health nurses’ experiences of caring for patients suffering from self-harm. Nurs Res Pract 2014;2014:1-10.
- Hunt I, Clements C, Saini P, Rahman M, Shaw J, Appleby L, et al. Suicide after absconding from inpatient care in England: an exploration of mental health professionals’ experiences. J Ment Health 2016;25:245-53.
- Weber M. Triggers for self-abuse: a qualitative study. Arch Psychiatr Nurs 2002;16:118-24.
- Vatne S, Fagermoen M. To correct and to acknowledge: two simultaneous and conflicting perspectives of limit-setting in mental health nursing. J Psychiatr Ment Health Nurs 2007;14:41-8.
- O’Donovan A. Pragmatism rules: the intervention and prevention strategies used by psychiatric nurses working with non-suicidal self-harming individuals. J Psychiatr Ment Health Nurs 2007;14:64-71.
- Maguire T, Daffern M, Martin T. Exploring nurses’ and patients’ perspectives of limit setting in a forensic mental health setting. Int J Ment Health Nurs 2014;23:153-60.
- Looi G, Engström A, Sävenstedt S. A self-destructive care: self-reports of people who experienced coercive measures and their suggestions for alternatives. Issues Ment Health Nurs 2015;36:96-103.
- Lindgren B, Wilstrand C, Gilje F, Olofsson B. Struggling for hopefulness: a qualitative study of Swedish women who self-harm. J Psychiatr Ment Health Nurs 2004;11:284-91.
- Wiklander M, Samuelsson M, Åsberg M. Shame reactions after suicide attempt. Scand J Caring Sci 2003;17:293-300.
- Lindgren B, Aminoff C, Graneheim U. Features of everyday life in psychiatric inpatient care for self-harming: an observational study of six women. Issues Ment Health Nurs 2015;36:82-8.
- Cardell R, Pitula C. Suicidal inpatients’ perceptions of therapeutic and nontherapeutic aspects of constant observation. Psychiatr Serv 1999;50:1066-70.
- Vatne M, Naden D. Crucial resources to strengthen the desire to live: experiences of suicidal patients. Nurs Ethics 2016;23:294-307.
- Kool N, van Meijel B, Bosman M. Behavioral change in patients with severe self-injurious behavior: a patient’s perspective. Arch Psychiatr Nurs 2009;23:25-31.
- Gerace A, Oster C, O’Kane D, Hayman C, Muir-Cochrane E. Empathic processes during nurse–consumer conflict situations in psychiatric inpatient units: a qualitative study. Int J Ment Health Nurs 2018;27:92-105.
- Wijnveld A, Crowe M. Walking a fine line: managing the tensions associated with medication non-adherence in an acute inpatient psychiatric setting. J Clin Nurs 2010;19:1378-86.
- Chorlton E, Smith I, Jones S. Understanding how people who use illicit drugs and alcohol experience relationships with psychiatric inpatient staff. Soc Psychiatry Psychiatr Epidemiol 2015;50:51-8.
- Hagen J, Knizek B, Hjelmeland H. Mental health nurses’ experiences of caring for suicidal patients in psychiatric wards: an emotional endeavor. Arch Psychiatr Nurs 2017;31:31-7.
- Tzeng W, Yang C, Tzeng N, Ma H, Chen L. The inner door: toward an understanding of suicidal patients. J Clin Nurs 2010;19:1396-404.
- Thomas J, Haslam C. How people who self-harm negotiate the inpatient environment: the mental healthcare workers perspective. J Psychiatr Ment Health Nurs 2017;24:480-90.
- Shopman S, Schrock R, Schnepp W, Buscher A. ‘Then I just showed her my arms…’. Bodily sensations in moments related to self-injurious behaviour. A hermeneutic phenomenological study. J Psychiatr Ment Health Nurs 2007;14:587-97.
- Talseth A, Jacobsson L, Norberg A. Physicians’ stories about suicidal psychiatric inpatients. Scand J Caring Sci 2000;14:275-83.
- Vuckovich P, Artinian B. Justifying coercion. Nurs Ethics 2005;12:370-80.
- Haglund K, Von Knorring L, Von Essen L. Forced medication in psychiatric care: patient experiences and nurse perceptions. J Psychiatr Ment Health Nurs 2003;10:65-72.
- Ward L. Ready, aim Fire! Mental health nurses under siege in acute inpatient facilities. Issues Ment Health Nurs 2013;34:281-7.
- Reade C, Nourse R. Intervening to prevent violence in psychiatric units. J Psychiatr Ment Health Nurs 2012;42:14-7.
- Davies B, Mallows L, Hoare T. ‘Supporting me through emotional times, all different kinds of behaviour.’ Forensic mental health service users understanding of positive behavioural support. J Forens Psychiatry Psycho 2016;27:530-50.
- Kumar S, Guite H, Thornicroft G. Service users’ experience of violence within a mental health system: a study using grounded theory approach. J Ment Health 2001;10:597-611.
- Oyelade O, Smith A, Jarvis M. Dismissing de-escalation techniques as an intervention to manage verbal aggression within mental health care settings: attitudes of psychiatric hospital-based Nigerian mental health nurses. Afr J Nurs Midwifery 2017;19:1-18.
- Sutton D, Wilson M, Van Kessel K, Vanderpyl J. Optimizing arousal to manage aggression: a pilot study of sensory modulation. Int J Ment Health Nurs 2013;22:500-11.
- Kontio R, Anttila M, Lantta T, Kauppi K, Joffe G, Välimäki M. Toward a safer working environment on psychiatric wards: service users’ delayed perspectives of aggression and violence-related situations and development ideas. Perspect Psychiatr Care 2014;50:271-9.
- Smith S, Jones J. Use of a sensory room on an intensive care unit. J Psychosoc Nurs Ment Health Serv 2014;52:22-30.
- Alexander J. Patients’ feelings about ward nursing regimes and involvement in rule construction. J Psychiatr Ment Health Nurs 2006;13:543-53.
- Price O, Wibberley C. An exploratory study investigating the impact of the procedures used to manage patient substance misuse on nurse-patient relationships in a medium secure forensic unit. J Psychiatr Ment Health Nurs 2012;19:672-80.
- Salzmann-Erikson M, Söderqvist C. Being subject to restrictions, limitations and disciplining: a thematic analysis of individuals’ experiences in psychiatric intensive care. Issues Ment Health Nurs 2017;38:540-8.
- McKeown M, Chandley M, Jones F, Wright K, Duxbury J, Foy P. Explorations of cooperation and recalcitrance in secure mental health hospitals. Eur Psychiatry 2016;33.
- Crabtree S. Medication, healing and resistance in East Malaysia. Ment Health Relig Cult 2005;8:17-25.
- Björkdahl A, Perseius K, Samuelsson M, Lindberg M. Sensory rooms in psychiatric inpatient care: staff experiences. Int J Ment Health Nurs 2016;25:472-9.
- Higgins A, Barker P, Begley C. Clients with mental health problems who sexualize the nurse-client encounter: the nursing discourse. J Adv Nurs 2009;65:616-24.
- Byford S, Sharac J, Lloyd-Evans B, Gilburt H, Osborn D, Leese M, et al. Alternatives to standard acute in-patient care in England: readmissions, service use and cost after discharge. Br J Psychiatry 2010;197:s20-5.
- Ritchie J, Spencer L. Analyzing Qualitative Data. London: Routledge; 1994.
- Price O, Baker J, Bee P, Grundy A, Scott A, Butler D, et al. Patient perspectives on barriers and enablers to the use and effectiveness of de-escalation techniques for the management of violence and aggression in mental health settings. J Adv Nurs 2018;74:614-25.
- Johnston I, Price O, McPherson P, Armitage C, Brooks H, Bee P, et al. De-escalation of conflict in forensic mental health inpatient settings: a Theoretical Domains Framework-informed qualitative investigation of staff and patient perspectives. BMC Psychol 2022;10:1-7.
- Goodman H, Papastavrou Brooks C, Price O, Barley E. Barriers and facilitators to the effective de-escalation of conflict behaviours in forensic high-secure settings: a qualitative study. Int J Ment Health Syst 2020;14:1-6.
- Michie S, van Stralen M, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6.
- Donetto S, Pierri P, Tsianakas V, Robert G. Experience-based Co-design and healthcare improvement: realizing participatory design in the public sector. Des J 2015;18:227-48.
- Hoffman T, Glasziou P, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: Template for Intervention Description and Replication (TIDieR) checklist and guide. BMJ 2014;348.
- Marshall MN. Sampling for qualitative research. Family Practice 1996;13:522-6.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95.
- Curtis K, Van BPharm C, Lam M, Asha S, Unsworth A, Clements A, et al. Implementation evaluation and refinement of an intervention to improve blunt chest injury management: a mixed-methods study. J Clin Nurs 2017;26:4506-18.
- Allen J, Anderson C, Bushman B. The general aggression model. Curr Opin Psychiatry 2018;19:75-80.
- Bowers L. Safewards: a new model of conflict and containment on psychiatric wards. J Psychiatr Ment Health Nurs 2014;21:499-508.
- Bowers L, Alexander J, Bilgin H, Botha M, Dack C, James K, et al. Safewards: the empirical basis of the model and a critical appraisal. J Psychiatr Ment Health Nurs 2014;21:354-64.
- Daffern M, Day A, Cookson A. Implications for the prevention of aggressive behavior within psychiatric hospitals drawn from interpersonal communication theory. Int J Offender Ther Comp Criminol 2012;56:401-19.
- Daffern M, Howells K. Antecedents for aggression and the function analytic approach to the assessment of aggression and violence in personality disordered patients within secure settings. Personal Ment Health 2007;2007:126-37.
- Corstens D, Escher S, Romme M, Longden E. Psychosis, Trauma and Dissociation: Evolving perspectives on severe psychopathology. Hoboken, NJ: Wiley-Blackwell; 2018.
- Rosenberg M. Nonviolent Communication. A Language of Life: Life-Changing Tools for Healthy Relationships (Nonviolent Communication Guides). Encinitas, CA: Puddle Dancer Press; 2015.
- Wang W, Song S, Wang J, Liu Q, Huang L, Chen X. Shame on you! When and why failure-induced shame impedes employees’ learning from failure in the Chinese context. Front Psychol 2021;12.
- Springham N, Robert G. Experience based co-design reduces formal complaints on an acute mental health ward. BMJ Open Qual 2015;4.
- El Malky M, El Wahab S, El-Amrosy S, El Fiky E. Patients’ satisfaction about quality of care and aggressive behavior in psychiatric hospitals. Int J Nurs Sci 2016;6:25-34.
- Quirk A, Lelliott P, Seale C. Risk management by patients on psychiatric wards in London: an ethnogrpahic study. Health Risk Soc 2005;7:85-91.
- Putkonen A, Kuivalainen S, Louheranta O, Repo-Tiihonen E, Rynnanen O, Kautiainen H, et al. Cluster-randomized controlled trial of reducing seclusion and restraint in secured care of men with schizophrenia. Psychiatr Serv 2013;64:850-5.
- Lee S, Cox A, Whitecross F, Williams P, Hollander Y. Sensory assessment and therapy to help reduce seclusion use with service users needing psychiatric intensive care. J Psychiatr Intensive Care 2010;6:83-90.
- Fluttert F, Van Meijel B, Bjorkly S, Van Leeuwen M, Grypdonck M. The investigation of the early warning signs of aggression in forensic patients by means of the ‘Forensic Early Signs of Aggression Inventory’. J Clin Nurs 2012;22:1550-8.
- Brooks H, Harris K, Bee P, Lovell K, Rogers A, Drake R. Exploring the potential implementation of a tool to enhance shared decision making (SDM) in mental health services in the United Kingdom: a qualitative exploration of the views of service users, carers and professionals. Int J Ment Health Syst 2017;11.
- Day J, Wood G, Dewey M, Bentall R. A self-rating scale for measuring neuroleptic side-effects: validation in a group of schizophrenic patients. Br J Psychiatry 1995;166:650-3.
- Bowers L, James K, Quirk A, Simpson A, Stewart D, Hodsoll J. SUGAR . Reducing conflict and containment rates on acute psychiatric wards: the Safewards cluster randomised controlled trial. Int J Nurs Stud 2015;52:1412-22.
- Berry K, Raphael J, Wilson H, Bucci S, Drake R, Edge D, et al. A cluster randomised controlled trial of a ward-based intervention to improve access to psychologically-informed care and psychological therapy for mental health in-patients. BMC Psychiatry 2022;22:1-15.
- Duxbury J. Implementing the Six Core Strategies (REsTRAIN YOURSELF): Working in partnership to minimise harm to patients and staff by reducing the use of physical restraint. London: Health Foundation; 2016.
- Duxbury J, Baker J, Downe S, Jones F, Greenwood P, Thygesen H, et al. Minimising the use of physical restraint in acute mental health services: the outcome of a restraint reduction programme (‘REsTRAIN YOURSELF’). Int J Nurs Stud 2019;95:40-8.
- Bowers L, Douzenis A, Galeazzi G, Forghieri M, Tsopelas C, Simpson A, et al. Disruptive and dangerous behaviour by patients on acute psychiatric wards in three European centres. Soc Psychiatry Psychiatr Epidemiol 2005;40:822-8.
- Mavandadi V, Bieling P, Madsen V. Effective ingredients of verbal de-escalation: validating an English modified version of the ‘de-escalating aggressive behaviour scale’. J Psychiatr Ment Health Nurs 2016;23:357-68.
- Davis J, Rawana E, Copponi D. Acceptability of behavioural staff management techniques. Behav Resid Treat 1989;4:23-44.
- Dack C, Ross J, Bowers L. The relationship between attitudes towards different containment measures and their usage in a national sample of psychiatric inpatients. J Psychiatr Ment Health Nurs 2012;19:577-86.
- Hallett N, Huber J, Sixsmith J, Dickens G. Measuring the violence prevention climate: development and evaluation of the VPC-14. Int J Nurs Stud 2018;88:97-103.
- Forster J, Finlayson S, Bentall R, Day J, Randall F, Wood P, et al. The perceived expressed emotion in staff scale. J Psychiatr Ment Health Nurs 2003;10:109-17.
- Bergk J, Flammer E, Steinert T. ‘Coercion Experience Scale’ (CES): validation of a questionnaire on coercive measures. BMC Psychiatry 2010;10.
- Foye U, Dalton-Locke C, Harju-Seppänen J, Lane R, Beames L, Vera San Juan N, et al. How has COVID-19 affected mental health nurses and the delivery of mental health nursing care in the UK? Results of a mixed-methods study. J Psychiatr Ment Health Nurs 2021;28:126-37.
- Grundy A, Walker L, Meade O, Fraser C, Cree L, Bee P, et al. Evaluation of a co-delivered training package for community mental health professionals on service user- and carer-involved care planning. J Psychiatr Ment Health Nurs 2017;24:358-66.
- Jones K, Burns A. Unit Costs of Health and Social Care. Kent: Personal Social Services Research Unit; 2021.
- HM Revenue and Customs . Rates and Thresholds for Employers 2020 to 2021 n.d. www.gov.uk/guidance/rates-and-thresholds-for-employers-2020-to-2021#class-1-national-insurance-rates (accessed 3 January 2023).
- The NHS Staff Council . NHS Terms and Conditions of Service Handbook 2021. www.nhsemployers.org/publications/tchandbook (accessed 3 January 2023).
- NHSBSA . Employer Contribution Rate Arrangements to Remain for 2020 21 n.d. www.nhsbsa.nhs.uk/employer-contribution-rate-arrangements-remain-202021 (accessed 3 January 2023).
- NHS . Reducing Expenditure on NHS Agency Staff: Rules and Price Caps [Updated 12 February 2021] n.d. www.england.nhs.uk/reducing-expenditure-on-nhs-agency-staff-rules-and-price-caps/#rules-and-price-caps (accessed 3 January 2023).
- Bowers L, Whittington R, Nolan P, Parkin D, Curtis S, Bhui K, et al. The City 128 Study of Observation and Outcomes on Acute Psychiatric Wards: Research Report Produced for the National Co-ordinating Centre for the NIHR Service Delivery and Organisation Programme (NCCSDO). London: HMSO; 2006.
- Brazier J. Is the EQ-5D fit for purpose in mental health?. Br J Psychiatry 2010;197:348-9.
- Mulhern B, Mukuria C, Barkham M, Knapp M, Byford S, Soeteman D, et al. Using generic preference-based measures in mental health: psychometric validity of the EQ-5D and SF-6D. Br J Psychiatry 2014;205:236-43.
- Barton G, Hodgekins J, Mugford M, Jones P, Croudace T, Fowler D. Measuring the benefits of treatment for psychosis: validity and responsiveness of the EQ–5D. Br J Psychiatry 2009;195:170-7.
- Shields G, Buck D, Elvidge J, Hayhurst K, Davies L. Cost-effectiveness evaluations of psychological therapies for schizophrenia and bipolar disorder: a systematic review. Int J Technol Assess Health Care 2019;35:317-26.
- Jones S, Riste L, Barrowclough C, Bartlett P, Clements C, Davies L, et al. Reducing relapse and suicide in bipolar disorder: practical clinical approaches to identifying risk, reducing harm and engaging service users in planning and delivery of care the PARADES (Psychoeducation, Anxiety, Relapse, Advance Directive Evaluation and Suicidality) programme. Program Grants Appl Res 2018;6:1-296.
- Lovell K, Bee P, Bower P, Brooks H, Cahoon P, Callaghan P, et al. Training to enhance user and carer involvement in mental health-care planning: the EQUIP research programme including a cluster RCT. Program Grants Appl Res 2019;7:1-140.
- Morrison A, Pyle M, Gumley A, Schwannauer M, Turkington D, MacLennan G, et al. Cognitive–behavioural therapy for clozapine-resistant schizophrenia: the FOCUS RCT. Health Technol Assess 2019;23.
- Haddock G, Pratt D, Gooding P, Peters S, Emsley R, Kelly J, et al. Randomised controlled trial of feasibility and acceptability of suicide prevention therapy in acute psychiatric wards. BJ Psych Open 2019;5.
- Plappert H, Hobson-Merrett C, Gibbons B, Baker E, Bevan S, Clark M, et al. Evaluation of a primary care-based collaborative care model (PARTNERS2) for people with diagnoses of schizophrenia, bipolar, or other psychoses: study protocol for a cluster randomised controlled trial. Br J Gen Pract 2021;5.
- NICE . Position Statement on Use of the EQ-5D-5L Value Set for England (Updated October 2019) 2019. www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l (accessed 3 January 2023).
- van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012;15:708-15.
- Sekhon M, Cartwright M, Francis J. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017;17.
- Pearson N, Naylor PJ, Ashe MC, Fernandez M, Yoong S, Wolfenden L. Guidance for conducting feasibility and pilot studies for implementation trials. Pilot Feasibility Stud 2020;6:1-12.
- NICE . Costing Statement: Violence and Aggression. Implementing the NICE Guideline on Violence and Aggression 2015.
List of abbreviations
- ACE
- adverse childhood experience
- ACMQ
- Attitudes to Containment Measures Questionnaire
- AfC
- agenda for change
- APDQ
- attitudes to personality disorder questionnaire
- CBA
- controlled before-and-after
- CES
- Coercion Experience Scale
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EM-DABS
- English-Modified De-escalating Aggressive Behaviour Scale
- ES
- effect size
- FG
- focus group
- ICC
- intraclass correlation
- ITS
- interrupted time series
- MAVAS
- Management of Aggression and Violence Scale
- MBI
- Maslach Burnout Inventory
- M-CAP
- Manchester Collaborative Antipsychotic Prescribing Approach
- MDT
- multidisciplinary team
- MH
- mental health
- MHA
- Mental Health Act
- NICE
- National Institute for Health and Care Excellence
- NHS
- National Health Service
- OT
- occupational therapist
- PBS
- positive behaviour support
- PEES
- Perceived Expressed Emotion in Staff
- PEESS
- Perceived Expressed Emotion in Staff Scale
- PICU
- psychiatric intensive care unit
- PMVA
- prevention and management of violence and aggression
- POAS
- Perception of Aggression Scale
- PPI
- patient and public involvement
- PRN
- pro re nata
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trials
- ROBINS-I
- Risk Of Bias in Non-Randomised Studies of Interventions
- SCIP
- Strategies for Crisis Intervention and Prevention
- SD
- standard deviation
- SOAS-R
- Staff Observation Aggression Scale–Revised
- TARS
- Training Acceptability Rating Scale
- TDF
- Theoretical Domains Framework
- TIDieR
- Template for Intervention Description and Replication
- VPC
- Violence Prevention Climate
- WAS
- Ward Atmosphere Scale
- WP
- work package
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/FGGW6874).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
