Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the HTA Programme on behalf of NICE as project number 07/17/01. The protocol was agreed in August 2007. The assessment report began editorial review in January 2008 and was accepted for publication in June 2008. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
K Stein is a member of the editorial board for Health Technology Assessment but was not involved in the editorial process for this report.
Permissions
Copyright statement
© 2009 Queen’s Printer and Controller of HMSO. This monograph may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NCCHTA, Alpha House, Enterprise Road, Southampton Science Park, Chilworth, Southampton SO16 7NS, UK.
2009 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Description of the problem
Snoring is the hallmark symptom of a spectrum of sleep-related breathing disorders collectively termed sleep-disordered breathing (SDB). Snoring is not a symptom of either sleep-related hypoventilation, as occurs in neuromuscular diseases or obesity, or the breathing patterns in Cheyne–Stokes respiration. The pathophysiological cause of SDB is sleep-induced intermittent airway obstruction. At one end of the spectrum is non-apnoeic or primary snoring without arousals, oxygen desaturations or significant changes in intrathoracic pressure. At the other end of the spectrum is severe obstructive sleep apnoea syndrome (OSAS) characterised by frequent apnoea/hypopnoea events, abnormally negative intrathoracic pressures, frequent arousals and disrupted sleep architecture, leading to excessive daytime sleepiness (EDS). Milder forms of OSAS and upper airway resistance syndrome (UARS) also form part of the spectrum. Patients with UARS have arousals during sleep related to abnormally increased work of breathing and increased upper airway resistance, but the respiratory disturbance index (RDI) may remain normal. These arousals commonly result in symptoms of EDS.
The frequency of apnoeas and hypopnoeas hourly measured by the apnoea/hypopnoea index (AHI) or the respiratory disturbance index (RDI) is used to differentiate non-apnoeic snoring from OSAS. An apnoea is defined in adults as a 10-second breathing pause, whereas a hypopnoea is categorised as a similar length event in which there is continued breathing but ventilation is reduced by at least 50% or a reduction of less than 50% from baseline is associated with either an oxyhaemoglobin desaturation of more than 3% or an arousal. 1 According to this definition non-apnoeic or primary snoring is classified by an AHI score of less than or equal to five. 1 However, it should be recognised that any cut-off in AHI score to classify different levels of airway obstruction is somewhat arbitrary. Severity can vary from night to night and symptoms from day to day in any one individual. Furthermore, AHI may rise with age in the population and therefore require age adjustment of any stratification system. 2 Stratification according to AHI should therefore be used to assign patients to an approximate level of severity when considering alternative treatment strategies.
Prevalence of snoring
Snoring is very common in the general population with around 35–45% of men and 15–28% of women reporting habitual snoring. 3,4 Risk factors for the development and worsening of snoring include increasing age, male gender, obesity (in part used as a proxy marker for neck circumference), alcohol ingestion, smoking, sedative use and nasal obstruction. Snoring is also more common in respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD). 5–8 Prevalence estimates of snoring have varied considerably from 16% to 89% depending on the populations studied, the definitions of snoring used, the investigations performed and the study design. 9 Conservative estimates for the prevalence of OSAS with EDS in middle-aged men (30–65 years) are in the range of 2.0% to 4.0%,10 whereas the prevalence of OSAS with EDS in women is probably about half that at around 1.0–2.0%. 10 Clearly, therefore, the majority of individuals who snore do not suffer from OSAS with EDS and would be classified as non-apnoeic or simple snorers. Obviously, however, a large proportion of this population would not be sufficiently disturbed by snoring to seek medical advice and, indeed, it is not clear from the current research what proportion of people would seek treatments if these were both successful and easily available.
Clinical significance of non-apnoeic snoring
It has been clearly demonstrated that systemic blood pressure fluctuates transiently with snoring. 11 However, the search for a potential association between heavy habitual snoring and hypertension, cerebrovascular disease and coronary artery disease has yielded conflicting results. 11–13 All of the studies showing associations between habitual snoring and cerebral infarction or myocardial infarction have been based on questionnaire data. 14–16 None of the studies linking non-apnoeic snoring and cardiovascular disease has used objective polysomnographic (PSG) measures of SDB, and studies that have excluded patients with diagnosed OSAS have found no such association. 13,17 There is also unresolved debate as to whether non-apnoeic snoring alone without OSAS can cause significant sleep fragmentation leading to EDS. EDS in patients with OSAS is a well-established correlate of the syndrome. However, attempts to assess this in non-apnoeic snoring have been confounded by studies of mixed patient populations, with OSAS, UARS and non-apnoeic snoring being assessed; sleep fragmentation as a result of a bed partner’s attempts to stop the snoring; and the high prevalence of moderate to severe sleepiness reported in the general population. 4,18
The clinical significance of non-apnoeic snoring is therefore somewhat equivocal, but its psychosocial impact is easily recognised. Loud intrusive snoring affects bed partners, family and even neighbours. Noise pollution and its resulting social disability, relationship disharmony and threatened marriage break-up19 is an important reason why an individual, often pressurised by a partner, will seek medical advice. In this respect, non-apnoeic snoring is an unusual ‘medical condition’ in that it is one commonly complained about not by the individual concerned but by their bed partner.
Snoring sound intensity and its frequency and duration are difficult to measure and accurately quantify. They are most usually assessed by means of a questionnaire directed at both the snorer and their bed partner. However, there is evidence that many patients are unable to accurately assess their own levels of snoring, with reports depending on factors such as perceived social stigma, health consciousness and the number of complaints from their bed partners. 20 Additionally, it has been found that agreement between patients’ and listeners’ perceptions of snoring is poor, and even two separate listeners do not always agree whether the emitted sound constitutes snoring or simply noisy breathing. 21,22 Snoring treatment assessment is further complicated by the fact that a subjective evaluation of snoring has seldom been confirmed when objective measurements of snoring sound intensity are performed. 22 Patients and/or their bed partners may report satisfaction with treatment and claim that snoring is diminished or disturbs the bed partner less. However, on objective post-treatment measurement there may be no significant difference observed in snoring duration, frequency or intensity. It has been posited that this difference between subjective and objective outcome measurements is due to a strong placebo effect and regression to the mean. Therefore, there is a clear need for randomised controlled trials (RCTs) in the assessment of different interventions for non-apnoeic snoring.
The World Health Organization recommends that an A-weighted equivalent continuous sound pressure level (SPL) at night of Laeq interior of 30 decibels (dB) and a maximum level of Lmax interior of 45 dB should not be exceeded. 23,24 Generally, calm breathing from the mouth at a 10-cm distance is barely audible and produces levels of 25 and 17 dB (A) SPL for inhalation and exhalation respectively. 25 Loud breathing measured at 1 m from the mouth can reach levels of 40 dB (A), with 40 dB (A) SPL generally considered as the transition point between breathing and snoring. 26,27 At 55 dB (A) SPL, noise can already be classified as acoustic pollution. Maximum snoring noise levels can reach even more than 90 dB (A) SPL. 26,28,29
Aetiology
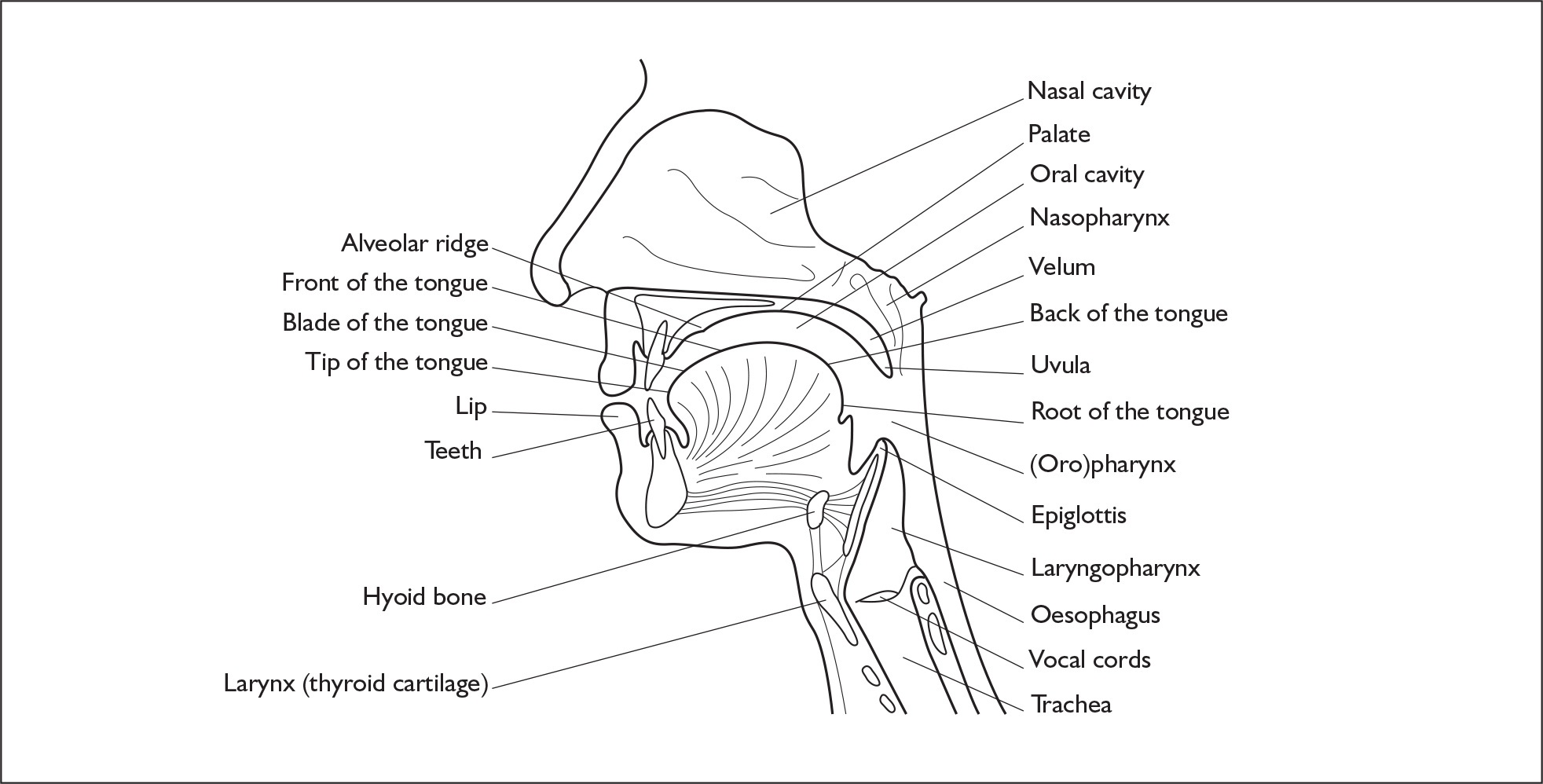
Snoring noise is generated because of the turbulent flow of air through the oropharyngeal segment of the upper airway. This area includes the soft palate, uvula, tonsils, tonsillar pillars, base of the tongue, and back and side walls of the throat. Figure 1 shows the anatomy of the upper airway structures implicated in the generation of snoring sound.
FIGURE 1.
Anatomy of the oropharyngeal segment of the upper airway tract.
Upper airway narrowing with sleep onset is a normal physiological process,30 but partial obstruction occurs because of a failure of the upper airway dilator muscles to stabilise the airway during sleep. Their innervation is complex and subject to reflex control. When a slight narrowing occurs, the speed of airflow through the narrowed segment increases (Venturi effect), which in turn provokes increased inspiratory negative pressure, further exacerbating the collapse (Bernoulli’s principle). Studies comparing snorers and non-snorers have confirmed that snorers generate more negative inspiratory pressures31 and have prolonged inspiration times31 and limitation of respiratory flow. 32 These changes lead to unstable turbulent airflow within the upper airway and tissue vibration, causing the production of a snoring sound. The loudness of snoring is determined by the force of the air being drawn in and the resistance that it meets. Pitch and tone of snoring are determined by the thickness and consistency of the vibrating tissue,33 as well as whether snoring is generated through the nose or mouth or both. 28 It has been consistently observed that snoring is worse during slow-wave sleep and during the early part of the night, whereas it is relatively rare during rapid eye movement (REM) sleep cycles. 34
Partial obstructions in the upper airway contribute to the problem of snoring. The abnormal narrowing found in patients with SBD may be due to mandibular changes, anatomical factors (e.g. obesity),35 a large soft palate,36 a large tongue,37 bimaxillary retrusion,37 or abnormal soft tissue function and increased collapsibility. 35 A supine sleeping posture is thought to further reduce the airway by allowing the effect of gravity on the soft tissues, encouraging the tongue and soft palate to fall back against the posterior pharyngeal wall.
The pattern of dynamic multilevel pharyngeal narrowing associated with snoring sound production occurs in different regions of the oropharynx to varying proportions in different individuals. In some patients it is predominantly palatal and nasopharyngeal, whereas in others it can be retroglossal or hypopharyngeal. The classification system most commonly used to categorise the site of airway obstruction is that developed by Fujita,38 in which type I is oropharyngeal obstruction only, type II is oropharyngeal and hypopharyngeal, and type III is hypopharyngeal obstruction alone. The correct identification and classification of the site(s) of airway narrowing are important in any workup as this will determine the most appropriate treatment strategies, especially those involving surgery.
Management
Diagnosis
The aim of investigating patients presenting with signs consistent with non-apnoeic snoring is to rule out more severe SDB disorders (i.e. UARS and OSAS) and other conditions. On initial screening, care is therefore taken to elicit evidence of any symptoms indicative of OSAS, for example EDS. This can be assessed using the Epworth Sleepiness Scale (ESS), which is a validated 24-point questionnaire that aims to assess the likelihood of falling asleep in a variety of situations. The score can be used to clinically subdivide patients into the normal range (ESS < 11), mild subjective daytime sleepiness (ESS 11–14), moderate subjective daytime sleepiness (ESS 15–18) or severe daytime sleepiness (ESS > 18). Depending on the history, in which care will be taken to assess patients presenting with ESS who snore for other underlying causes for the presenting symptoms, and examination findings, patients will be referred for one of several further procedures, including PSG or modified PSG, before formal treatment options are discussed. This is consistent with current guidelines from the Scottish Intercollegiate Guidelines Network on the management of obstructive sleep apnoea/hypopnoea syndrome in adults, which state that OSAS must be excluded before treatment is considered. 2
Sleep studies
The main purposes of sleep studies are to confirm or refute the diagnosis of OSAS or sleep-related problems and to assess their severity to guide management options. Sleep studies may therefore measure some aspects of ventilation either directly or indirectly to assess any possible compromise by upper airway obstruction and any consequences for sleep quality. Studies vary in their complexity from full PSG with recordings of 12–30 channels of various electrophysiological, breathing and movement signals to one-channel information studies such as oximetry. Recordings can be undertaken during part or all of a night’s sleep and may be performed in a sleep centre or at home, depending on the study complexity.
Polysomnography
PSG records sleep and breathing patterns simultaneously. A standard PSG typically consists of an electroencephalogram (EEG), an electrocardiogram (ECG), a segmental tibialis electromyogram, an electro-oculogram, and respiratory airflow, thoracoabdominal movement and oxygen saturation (oximetry) recordings. Body position and snoring levels are also frequently monitored.
Limited sleep studies
Limited sleep studies usually incorporate measurement of respiratory signals in combination with an indirect measure of arousal. The general combination of indices measured are airflow, thoracoabdominal movement, oximetry and heart rate measurement. Some studies additionally also assess snoring and indirect evidence of episodes of airflow obstruction. An advantage of limited sleep studies is that they can potentially be performed at home, thereby reducing the costs of accommodation in a sleep centre and attendant staffing costs. The cost of a typical home-based limited sleep study may be approximately only 20% of the cost of a hospital-based PSG. 2
Oximetry
Oximetry provides an assessment of the oxygen saturation of arterial blood arriving at the fingertip or earlobe with each pulse beat, giving a reading of the SpO2 level. The most commonly used methods to analyse oximetry results are to count the number of oxygen desaturations (dips) per hour greater than a certain value (often a 4% SpO2 dip rate of more than ten per hour) or the time spent during the study at less than an agreed SpO2 level (usually 90%). The readings also provide an indirect marker of transient arousals from sleep, with each arousal associated with an approximate rise in the heart rate of 6–10 beats per minute. Therefore, assessing oximeter tracings with the accompanying pulse rate recording can provide information about sleep fragmentation.
Assessment of the site of airway narrowing
Several techniques have been used to attempt to localise the level of the obstruction implicated in the generation of the snoring sound. Identification of the primary and secondary sites of obstruction may be used to determine the most appropriate treatment options and potentially provide some prediction of treatment outcome. The most commonly used techniques are:
-
visual inspection
-
fibreoptic endoscopy with or without Muller’s manoeuvre
-
sedation (sleep) nasendoscopy
-
upper airway pressure recordings during sleep
-
imaging and cephalometric radiography
-
acoustic analysis of the snoring sound.
Visual inspection
Visual inspection of the nose and pharynx is used to rule out gross anatomical obstructions or malignancies. Although inexpensive, available and easy to perform, it is carried out during wakefulness when the muscular tone and respiratory drive may be different from that during sleep. 39
Fibreoptic endoscopy with or without Muller’s manoeuvre
Fibreoptic endoscopy during wakefulness allows visualisation of the entire upper airway and the extent of airway collapse at different levels. Anatomic abnormalities can be assessed, including hypertrophy of the tongue, uvula and tonsils. Oedema of the soft palate and uvula may indicate snoring resulting in vibratory lesions. The extent of collapse at the velopharynx relative to collapse at the oropharyngeal level is used to predict surgical outcome. 32 Fibreoptic nasopharyngoscopy can additionally be combined with Muller’s manoeuvre. The manoeuvre consists of forced inspiratory effort against closed nasal and oral airways. The endoscope is inserted through the nostril while the patient is awake and supine, allowing examination of the retropalatal and retrolingual level of the pharynx. There are a number of limitations to the test. The patient is awake and therefore the pharyngeal muscular tone is much higher than in sleep, inspiratory effort may vary from patient to patient, thereby varying the degree of collapse, and there is a relatively large interobserver variation in determining the level of collapse.
Sedation (sleep) nasendoscopy
Sedation (sleep) nasendoscopy requires the sedation of the patient. Once snoring is achieved a fibreoptic nasendoscope is used to visualise the level of pharyngeal collapse and sound production. This technique is reasonably reliable at identifying the site of obstruction,34 and the cross-sectional area of the pharynx can be estimated to within 10% by this method when linked to a computer. 40 The technique, however, has three major limitations. First, the various levels of the upper airway cannot be studied simultaneously and therefore it is difficult to assess multilevel upper airway collapse. Second, it is unlikely that sedation-induced sleep correlates well with natural sleep; therefore, any observed snoring source and/or reduction in pharyngeal diameter under sedation may not also occur during natural sleep. Last, there is no currently standardised protocol for sedation. This results in wide variations from individual to individual, between sequential studies on the same individual and between centres. This is further compounded by evidence that most surgical failures for non-apnoeic snoring occur at the level of the palate. 41 Therefore, the poor predictive value of sleep nasendoscopy for the outcome of laser uvulopalatoplasty41 probably reflects a combination of limitations in both the test and the procedure.
Upper airway pressure recordings during sleep
Pressure measurements using several pressure transducers placed in the oesophagus and pharynx allow dynamic nocturnal investigation of the upper airway in patients. It has been shown that monitoring by use of pressure transducers within the oesophagus during sleep produces similar results to a full PSG but at significantly less cost. 42 However, one disadvantage of the pressure catheter method is that usually only the lowest limit of the obstructed airway segment is determined and the test may not adequately localise the level of tissue obstruction but rather the segment of airway collapse. In retrolingual obstructive events, therefore, it is difficult to assess whether or not the retropalatal airway is also collapsed. As the largest pressure gradient is retrolingual, this level is assumed to be the primary site of obstruction. However, as the largest pressure gradient is dissipated across the retrolingual area, little respiratory pressure remains to allow development of a large pressure gradient across the palate. 43 Further disadvantages of this method are that it does not allow for visualisation of the surrounding soft tissues and that the invasive nature of the test may influence the duration of sleep and the lowest stage of sleep attained.
Imaging and cephalometric radiography
Imaging techniques that have been used in attempts to identify structures involved in snoring sound generation include fluoroscopic techniques, computerised tomography (CT) scanning, magnetic resonance imaging (MRI) and cephalometric radiography (plain radiography of the airways). These techniques have had only limited success44–46 and may do little to guide therapeutic intervention. Furthermore, practicality, cost and excess radiation exposure have proved major limitations. Currently, therefore, cephalometric radiography is indicated only in patients with a retrolingual site of obstruction, with contributing skeletal abnormalities, in whom surgical procedures directed at this site are planned.
Acoustic analysis of the snoring sound
Acoustic analysis of the snoring sound has developed since the early 1990s. Acoustic techniques have been used in an effort to create theoretical mathematical models of snoring sound production to enable the level at which the sound is produced to be derived. Acoustic analysis has indicated that frequencies around 20 hertz (Hz) are associated with palatal fluttering, whereas obstruction at other sites gives a more diffuse frequency range. To date, acoustic analysis has been used to help diagnose OSAS,47 as an objective outcome measurement of snoring surgery,48–50 and in an attempt to differentiate the underlying mechanism of sound production. 51,52 Although these techniques seem to hold some promise as a diagnostic tool, they still require considerable further refinement.
Overall, given the present level of uncertainty of the tests outlined above in the accurate localisation of the airway obstruction and the prediction of the level of obstruction at which the snoring sound is generated, there is likely to be large variation in current practice as to which, if any, tests are performed. Coupled with patient preference and resource availability, decisions on alternative treatment strategies for the individual patient may still be based on history and clinical examination alone.
Interventions for non-apnoeic snoring
Deciding which of the various treatment options is most appropriate for the management of non-apnoeic snoring depends on the level of airway obstruction and therefore the source of the snoring sound generation; the intensity of the snoring sound and the amount of social disruption caused; and the characteristics of the individual patient.
There are a number of conservative treatment options by which a reduction in snoring may be achieved. These include weight reduction,14 the use of sleep positioning devices53 and a reduction in alcohol intake. 54 These are generally indicated either as a first-line treatment option or as an adjuvant intervention depending upon the patient’s lifestyle risk factors for snoring and the pathophysiological mechanism of snoring sound production. Additionally, non-prescription (over-the-counter) medications such as nasal dilators are also currently available on the market. The effects of non-prescription treatments for non-apnoeic snoring and OSAS have been reviewed by the American Academy of Sleep Medicine Clinical Practice Review Committee. 55
The findings of this review highlighted the paucity and low quality of the evidence currently available to support the use of external nasal dilator strips (ENDS), internal nasal dilators (INDS), lubricant nasal and oral products, oral dietary supplements and magnetic pillows and mattresses in the treatment of both non-apnoeic snoring and OSAS. 55 The Clinical Practice Review Committee concluded that there was insufficient information on these products to develop standards of practice recommendations.
As the current assessment is limited to a review of the clinical effects of surgical procedures and non-surgical devices for the management of primary snoring, a brief outline of the available devices and surgical techniques used as treatment options is given in the next section.
Non-surgical devices
Continuous positive airway pressure
CPAP functions as a pneumatic stent to maintain upper airway patency throughout all phases of sleep breathing. It operates by means of a flow generator that delivers pressure through air tubing to a nasal mask, nasal prongs or face mask worn overnight. Most patients require lifelong treatment and therefore long-term access to a CPAP machine. Major side effects of CPAP (e.g. significant epistaxis, paranasal sinusitis) are rare, but minor side effects (e.g. rhinitis, nasal bridge sores, claustrophobia, abdominal bloating) are common. Nasal symptoms are usually due to mouth leaks causing high flows of cool air through the nose, which can be minimised with the use of chin straps or a full face mask. Compliance rates, however, in patients with non-apnoeic snoring alone without OSAS tend to be low because of its airway drying effect, the discomfort of the device and to some extent the noise of the machine.
Mandibular advancement splints
Mandibular advancement splints (MAS) consist of an upper and lower dental bite plate connected by an angled strut. The device, which is inserted intraorally at night, produces anterior displacement of the mandible with the aim of enlarging the retroglossal space and increasing the upper airway diameter. 56 There are two main types of MAS: fixed and adjustable devices. Fixed devices are usually made using vacuum-formed blanks of polymer to construct gum shield-type trays that are joined together at an arbitrary or clinically recorded position. However, the disadvantage of this type of splint is that it is difficult to titrate to the individual patient accurately and cannot be adjusted once formed. Adjustable appliances come in a myriad of designs but are generally composed of those that use either an anterior locating device, which can be adjusted to protrude the lower component fixed to the jaw, or bilator connectors, which have either fixed or moveable telescopic arms. The advantage of the latter type of adjustable device is that it does not encroach on the anterior tongue space and does not protrude from the mouth. For both fixed and adjustable devices the maximal degree of mandible protrusion varies from device to device but is usually around 75% of the maximum possible. For use of all MAS devices patients must have an adequate number of teeth of sufficient strength and position for the device to be able to be worn. The adverse effects of MAS use include excess salivation, xerostomia, temporomandibular joint pain, dental pain, myofacial pain and bite change. One or more of these effects will occur in around 50–80% of patients. 57 The vast majority settle within 4 weeks and side effects abate with appliance withdrawal, but overall compliance is around 50–75%. 57,58
There are presently a large number of different MAS available on the market. Most appliances require dental impressions, bite registration and fabrication by a dental laboratory. 57 These custom-made appliances will then be fitted by a dentist. Taking the impression and fitting do not have a standard dental charge and there is marked variation in the UK in these charges. There are now also devices available in thermal labile material, such as Snore Guard® (Hays and Meade, Albuquerque, NM), which can be moulded to the patient’s teeth in the physician’s or dentist’s office,58 as well as devices such as the ‘boil-and-bite’ type mouthpieces, which are fitted by the user and purchased in pharmacies or via the internet. These types of devices are available at a cost of less than £50.
Tongue-retaining devices
These devices secure the tongue by negative pressure into a soft plastic bulb, thereby forcibly holding the tongue anteriorly while sleeping. 59 Tongue retaining devices (TRDs) affect genioglossus muscle activity but effects on other upper airway muscles have not been evaluated. 59,60 Unlike MAS, the tongue retainer can be used in edentulous patients.
Surgical procedures
The aim of palatal surgery is to limit the collapsibility of the oropharyngeal segment without interfering with normal function. A number of procedures have been developed that are based on the supposition that palatal flutter is one of the most important sound generator mechanisms in snore production. Therefore, reducing palatal flutter or vibration should theoretically reduce snoring. These procedures are based on one of two predominant themes: (1) reducing the length or volume of the palate and (2) stiffening the soft palate tissues.
Uvulopalatopharyngoplasty
Uvulopalatopharyngoplasty (UP3 or UPPP) was introduced by Ikematsu61 as the first surgical procedure for the treatment of snoring; it was later developed and introduced to the West by Fujita62 in 1981. Alongside tracheostomy and maxillary mandibular advancement (interventions outside the scope of the current appraisal) it is one of the most radical of the surgical procedures currently available. UP3 is designed to reduce excess tissue in the palate, uvula, and posterior and lateral pharyngeal walls. The procedure includes tonsillectomy, or de-epithelialisation of the tonsillar fossae if tonsillectomy has already been performed, followed by suture apposition of the denuded anterior and posterior faucial pillars and excision of 1–2 cm of the soft palate including the uvula. The exact amount of tissue excised varies, depending on individual palatal anatomy. The procedure is performed under general anaesthetic and therefore hospitalisation is necessary. A number of studies have indicated that UP3 is often complicated by severe postoperative pain. 63 Additionally, there may be some long-term complications with the procedure, such as nasopharyngeal regurgitation, persistent palatal dryness, long-term voice changes and a partial loss of taste. 57
Laser-assisted uvulopalatoplasty
In an attempt to overcome the limitations of UP3, in 1990 Kamami64 introduced the technique of laser-assisted uvulopalatoplasty (LAUP). The procedure involves laser excision of the uvula and a small portion of the soft palate, lateral to the base of the uvula, resulting in the formation of bilateral ‘Kamami trenches’. Unlike UP3, LAUP can be repeated to obtain the desired effect upon the airway. The number of procedures varies, with some patients requiring up to four sessions. The aim of staging treatment is to excise the minimal amount of palatal tissue needed to reduce snoring effectively while reducing the risk of venopharyngeal insufficiency. In the UK LAUP is generally performed under general anaesthetic as a day-case procedure and is argued to be a safer, more economical and more comfortable alternative to UP3. Although LAUP is generally associated with fewer complications than UP3, postoperative pain is reported to be similar for both procedures. 65,66 This may negatively affect patient compliance and is likely to be influential in patients abandoning treatment before the optimal amount of soft palate has been excised. 67
Uvulopalatal elevation palatoplasty
In this procedure a laser is used to excise a mucosal strip from the oral surface of the soft palate and uvula. Lateral palatal incisions are then formed to release the soft palate allowing the uvula flap to be reflected anteriorly onto the denuded oral surface of the soft palate. The uvula is then secured with Vicryl sutures. 68
Radiofrequency ablation (somnoplasty)
Radiofrequency ablation (RFA) is designed to shrink redundant tissue of the soft palate and improve the texture of the remaining palate so that it becomes more dynamically stable. 69 Radiofrequency energy (at a variety of frequencies and energy levels) is released into the palate tissue submucosally using an electrode delivery device. This creates a lesion within the palate. The body will then reabsorb this dead tissue, thus reducing the volume of the palate and shortening it. The area of the palate most commonly treated is the base of the uvula to the posterior nasal spine, with two additional lesions created laterally to the midline. The procedure may be performed on an outpatient basis with use of a topical local anaesthetic. As with LAUP the procedure can be repeated a number of times if the snoring symptoms persist. The most frequently reported complications with the procedure are mucosal erosion and ulceration. 70
RFA has also been used for the reduction of turbinates and tongue base ablation for the treatment of non-apnoeic snoring. 71,72 Current guidance on the use of RFA for snoring from the National Institute for Health and Clinical Excellence (NICE)73 highlights that there are no major safety concerns with the use of RFA, but evidence on the short-term efficacy is limited and long-term outcomes are uncertain.
Palatal stiffening procedures
There are a number of different palatal stiffening techniques used in the treatment of snoring. These include the cautery-assisted palatal stiffening operation (CASPO), injection snoreplasty, diathermy-assisted uvulopalatoplasty (DAUP), laser palatoplasty and Pillar implants.
CASPO uses cautery to burn the soft palate causing fibrosis and consequent stiffening upon healing. The procedure is performed during a single outpatient visit under local anaesthetic. As with RFA and LAUP the procedure can be repeated until the desired effect on snoring is gained. The procedure is less invasive than either UP3 or LAUP and there are generally fewer postoperative complications observed.
Injection snoreplasty is performed on an outpatient basis with use of a topical local anaesthetic. A sclerosing agent (such as 3% sodium tetradecyl sulphate, ethanol, and doxycycline or alcohol) is injected into the soft palate anterior to the uvula, which creates blistering, causing subsequent fibrosis and stiffening upon healing. As with CASPO the procedure may need to be repeated until the optimal treatment benefit is attained.
The Pillar implant system is theorised to stiffen and reduce the fluttering movement of the soft palate through the implantation of woven Dacron mesh inserts into pockets created in the soft palate. 74 As with CASPO and injection snoreplasty the subsequent stiffening of the palate that occurs is due to fibrosis of the palatal tissue upon healing. The technique is performed as a one-stage procedure, which may be combined with other upper airway procedures for snoring.
Tongue-base suspension procedure
The tongue-base suspension procedure involves the insertion of a titanium screw into the geniotubercle of the posterior aspect of the mandible in the floor of the mouth. A loop of suture is then passed through the tongue base and attached to the mandible bone screw. The resulting suspension or hammock of the tongue base by the device affects genioglossus muscle activity, preventing posterior tongue displacement and occlusion of the posterior pharyngeal wall. 75
Surgery for coincident nasal obstruction
Decreased nasal airflow has been implicated as a factor in snoring severity76 and as such any nasal obstruction may be treated before the consideration of any definitive snoring surgery. Previous studies estimate that 50–69% of non-apnoeic snorers with nasal symptoms have improved levels of snoring with nasal surgery alone. 77,78 This may include septoplasty, septorhinoplasty, turbinate reduction or sinus surgery.
Current service provision
There is currently no information available in the literature on current service provision for the treatment of non-apnoeic snoring or the costs associated with each type of intervention. Expert opinion provided to the Therapeutic Procedures Panel of the Health Technology Assessment (HTA) Programme during the development of the scope for this assessment indicated that significant variation exists across the UK in the provision of treatment. In some parts of the UK primary care trusts (PCTs) see surgery for primary snoring as cosmetic and therefore are reluctant to refer patients to an ear, nose, and throat (ENT) department for further assessment and surgery. In other parts of the UK there is a heavy clinical burden in ENT departments from patients with snoring. The Audit Commission report entitled Access to care for ear, nose, and throat and audiology services79 was undertaken as waiting times in this speciality have traditionally been amongst the longest and it is also less affected by emergency cases than other specialities. The report highlighted that there were major differences in waiting times for outpatient appointments and for surgery in various trusts. Waiting times were not directly linked to levels of demand and capacity. However, the NHS Modernisation Agency’s Demand Management Team cites evidence that, in many areas, waiting lists are managed with little agreement on clinical priority. 80 Interestingly, a small survey conducted in 2004 to assess levels of agreement on prioritisation of 11 different conditions commonly seen within ENT based on the perception of the relative importance of the condition found that there was strong agreement between different interest groups on the relative priority of both outpatient consultations and inpatient treatment for snoring. Across all interest groups (including members of the general public, non-ENT patients, NHS employees, PCTs and trust managers, general practitioners and ENT consultants) snoring that resulted in marital discord was ranked in the bottom three conditions for both outpatient consultation and inpatient treatment. 81
Further, expert opinion additionally indicated that when offered formal surgery many patients are reluctant to accept this, especially if warned about potential side effects. At the present time some dentists are offering MAS that patients can effectively try and ‘throw away’ if they do not receive any benefit. If this was promoted by general dental practitioners the potential uptake could be relatively large and would mean that patients miss out the step of seeing a general practitioner and onward referral when appropriate to ENT services. However, although this may be appropriate for patients with non-apnoeic snoring it would mean that patients at risk of OSAS may potentially miss out on the opportunity of having this diagnosis made and would therefore remain at risk of all of the concomitant problems associated with OSAS. Additionally, at the current time fitting of a MAS is not provided through NHS funding and there are marked variations in the costs associated with taking impressions and fitting the devices. These dental costs incurred by the patient may therefore presently limit the number of patients who are willing to try the use of a MAS. It is therefore unclear whether further promotion of the use of MAS in the management of non-apnoeic snoring would reduce the number of referrals to ENT for surgical procedures.
Chapter 2 Scope of the technology assessment
Aims and objectives
The purpose of this report is to assess the clinical effects and associated treatment costs of surgical procedures and non-surgical devices for the management of non-apnoeic snoring.
Interventions
The report assesses surgical procedures and non-surgical devices for which contact with a health-care professional (e.g. general practitioner, dentist or dental nurse), either in the NHS or private practice, is necessary to access the procedure or device. Contact in this context may be for initial onwards referral only. The scope of the report does not include the use of non-prescription (over-the-counter) treatments or devices for non-apnoeic snoring or studies that have assessed the effects of mandibular/maxillary advancement (Stanford stage 2) procedures.
The specific interventions included are:
-
non-surgical devices:
-
CPAP
-
MAS
-
TRD
-
-
surgical procedures:
-
surgery for coincident nasal obstruction (septoplasty, turbinate reduction, sinus surgery)
-
UP3 with or without tonsillectomy
-
LAUP
-
uvulopalatal elevation palatoplasty
-
uvulectomy alone
-
RFA of the soft palate or tongue base
-
palatal stiffening techniques (injection snoreplasty, CASPO, DAUP, Pillar implants)
-
tongue base suspension procedures.
-
Studies that assess adenoidectomy or tonsillectomy, either alone or in combination with each other, are not included. Additionally, studies that assess lifestyle modification interventions for the management of snoring, such as weight loss, sleep positioning devices, smoking or alcohol reduction programmes, are only included if directly compared with one of the eligible surgical procedures or non-surgical devices.
Population
The population consists of adults with non-apnoeic snoring defined by an AHI score of less than or equal to 5 who are eligible for surgical procedures or the use of non-surgical devices. In all patients a diagnosis of OSAS must have been excluded by sleep study. Additionally, studies that include groups of patients with a diagnosis of OSAS or UARS (AHI score > 5) as well as patients with diagnosed non-apnoeic snoring are included, provided that the outcomes are reported separately for each patient group.
Studies in which the patient group are snorers with a specific related co-morbidity such as chronic obstructive pulmonary disease (COPD), a neuromuscular disorder, asthma or heart failure are not included.
Relevant comparators
The interventions of interest will be compared with each other, placebo, lifestyle modification techniques or no intervention.
Outcomes
Studies reporting one or more of the objective or subjective outcome measures of snoring are included:
-
objective measures:
-
snoring recording and/or acoustic analysis of snoring sound
-
PSG, modified PSG or oximetry outcomes
-
cephalometric radiographs or MRI scans of palatal length or width
-
-
subjective measures:
-
ESS scores/symptoms of daytime sleepiness
-
patient and partner questionnaires and/or linear analogue scales related to snoring severity (it is recognised that patient-reported snoring outcomes are of dubious validity as patients will only be able to report on what they have been told by their bed partners)
-
patient and partner questionnaires and/or linear analogue scales related to quality of life
-
questionnaires and/or linear analogue scales related to sleep quality of bed partner
-
-
complications:
-
short- and long-term complications of treatment (e.g. nasal reflux on swallowing, temporal mandibular joint pain); when possible these were dichotomised into those that occurred in the immediate post-treatment period and longer-term complications and considered separately
-
need for further repeat procedures (other than those specified in the treatment protocol).
-
Study designs
RCTs, cross-over trials and controlled clinical trials (CCTs) will be included. Pre–post studies (with patients acting as their own controls) will also be included providing an objectively measured outcome is reported.
Pre–post studies reporting only subjectively measured outcomes will not be included.
Publication language and status
A full English-language text copy of the study has to be available for it to be included. Studies that are reported in abstract form only and for which no further information is available are excluded. Foreign-language papers are also excluded.
Overall aims and objectives of the assessment
This assessment reviews the evidence on the clinical effects (including both treatment benefits and harms) of surgical interventions and non-surgical devices for the management of non-apnoeic snoring. The report additionally provides an estimate of the range of the costs associated with each identified intervention based on current UK information. Drawing together the evidence on clinical effects and treatment costs, interventions for which future primary research would be of benefit will be identified.
Chapter 3 Assessment of clinical effects
Methods for reviewing clinical effects and treatment costs
Identification of studies
MEDLINE, EMBASE, CINAHL, the Cochrane Controlled Trials Register (CCTR) and NHS EED were searched for titles and abstracts of potentially relevant studies of clinical effects and treatment costs published between 1980 and 2007. No study design filters or language restrictions were applied to the search strategy.
The literature searches retrieved 1903 unique references after deduplication. All references were managed using Reference Manager software version 11. Full details of the search strategies are presented in Appendix 1.
Relevant studies were identified in two stages. Two reviewers screened titles and abstracts returned by the database searches independently. Full texts of any references that were considered relevant by either reviewer were obtained when available. The relevance of each paper was assessed according to the criteria set out in Chapter 2. Any discrepancies between the reviewers were resolved by recourse to the papers and, if necessary, a third reviewer was consulted. All duplicate papers were double-checked and excluded. The bibliographic details of excluded studies, along with the reason for their exclusion, are detailed in Appendix 2.
Review methods
Data extraction strategy
Data were extracted independently by one reviewer into a standardised form. When multiple publications of the same study were identified, these were linked together to form a ‘set’ of papers for each study. Data were then extracted and reported as a single study. A second reviewer then checked extracted data independently. Full details of the data extraction and quality assessment are reported in Appendix 3.
Quality assessment strategy
The quality of the individual studies was assessed by one reviewer and independently checked for agreement by a second. Study quality was assessed separately for RCTs/CCTs and pre–post studies according to criteria based on the Centre for Reviews and Dissemination (CRD) Report No. 4. 82 The main criteria assessed are outlined in the next two sections.
Internal validity
The assessment of internal validity examined the selection of study groups, the handling of potential confounders (baseline imbalance, co-intervention, treatment compliance), the blinding of assessors and data analysts, the validity and reliability of outcome measures, the rate of attrition and the appropriateness of data analyses.
External validity
External validity was assessed according to the ability of the reader to consider the applicability of the findings to a patient group in practice. Study findings can be effectively generalised only if they (1) describe a patient cohort that is representative of the affected patient population at large or (2) present sufficient details of their patient group baseline characteristics and outcome data to allow the reader to extrapolate findings to a patient group with different characteristics. Studies that presented adequate data on baseline participant characteristics, in which patients were representative of the patient group that would present in practice in the UK, were judged to be externally valid.
Data synthesis
Results were first broadly grouped according to the intervention (and comparator when applicable). Studies within each broad intervention group were then further subgrouped according to the specific intervention type, when necessary, and the study design.
Because of heterogeneity in the outcome measures assessed and the methods of measuring these between studies assessing the same type of intervention, it was not possible for studies to be further subgrouped by outcome measure. Results were therefore combined using a narrative synthesis82 with demographic data for each study and relevant quantitative results being tabulated.
Differences between studies assessing the same intervention were explored narratively by examining differences in the interventions, study duration and quality.
Treatment costs
The costs of the surgical procedures and non-surgical devices included initial treatment costs as well as the ongoing costs of care associated with the interventions. The costs of diagnostic tests (i.e. PSG or modified PSG to exclude a diagnosis of sleep apnoea) were not included in the treatment costs. These will depend on the staff levels in the centre where the sleep study is undertaken, the number and complexity of the studies performed and the cost of the equipment and premises. However, it should be noted that use of a MAS may not always be associated with patients requiring a sleep study (i.e. PSG or modified PSG) before use of the device, which is necessary before either surgery or use of CPAP is initiated, and this is likely to impact considerably on the overall treatment costs.
No studies were identified by the searches that had assessed any of the costs associated with providing the interventions of interest. Therefore, to fulfil the scope of the review, all costs were estimated based on data from the NHS reference costs (2006),84 data from device manufacturers and clinical opinion. It was not possible to estimate a cost associated with RFA of either the soft palate or the tongue base as the costs of both the somnoplasty generator and electrodes were considered to be ‘commercial in confidence’ by the manufacturers (Gyrus ENT) and were not available in the public domain through either NHS purchasing suppliers or the NHS Supply Chain.
To provide a limited analysis of the rough cost estimates for the other surgical procedures it was assumed that each procedure would entail an initial consultation with an ENT surgeon, the specific inpatient or day-case surgical procedure time and device costs (where relevant), and a follow-up consultation. For UP3 it was assumed that the procedure would entail an inpatient stay of 1 day, as this is the most common length of stay, although patients who experience significant haemorrhage or pain may have a more protracted stay, increasing the costs associated with the procedure. For LAUP, as this is potentially a multistage procedure that can be conducted in one, two or three stages, it was assumed that each additional procedure was associated with one additional follow-up visit. For CPAP, as there are numerous machines and face masks currently available on the market, the mean costs of the machines and masks available were used to provide the acquisition cost and the cost of an annual replacement of the face mask. In accordance with advice from one of the manufacturers (ResMed) it was assumed that the CPAP machine has a device life of 7 years and that the face mask will be replaced on an annual basis. In terms of the use of MAS there are currently no published NHS costs of dental devices for the management of snoring and therefore the cost was estimated based on clinical opinion. It was assumed that the dentist provided a Thornton Adjustable Positioner® (TAP), a device commonly used for the management of OSAS and snoring in the UK. Based on information provided in the Scottish Intercollegiate Guideline Network guideline on the management of obstructive sleep apnoea/hypopnoea syndrome in adults2 it was assumed that the device lasts for 2 years and that the patient would have one annual check-up. Under the new NHS dental contract a course of treatment is classified into a treatment band. Provision of a MAS was classified as band 3, as such treatment requires laboratory work (www.ic.nhs.uk), and 12 units of dental activity (UDA) were applied as appropriate to the band. 84 The national average reimbursement rate for a UDA is not known as this varies according to contract values negotiated locally by PCTs. Therefore, the value of a UDA was obtained from material published by Bath and North East Somerset Primary Care Trust (www.banes-pct.nhs.uk/documents/Board_Papers/2007/May/Agenda%20Item%2010%20Annex%201.pdf). This estimated the average reimbursement per UDA to be £20.91. Therefore, on the basis of provision of a MAS taking 12 UDA it was estimated that the cost of a MAS is approximately £250. The costs of both the CPAP machine and MAS were expressed as equivalent annual costs using the public sector discount rate of 3.5%.
Assessment of clinical effects
Because of the broad scope of the current review in terms of the number and different types of interventions, the review of clinical effects is presented as follows:
-
overview of the quantity and quality of included studies
-
review of the evidence for:
-
UP3 versus LAUP
-
UP3 alone
-
LAUP alone
-
RFA techniques including RFA and bipolar RFA of the soft palate and the tongue base
-
palatal stiffening techniques including Pillar implants and injection snoreplasty
-
CPAP
-
MAS
-
-
for each group of interventions, text and summary tables are presented on:
-
the quantity and quality of the studies
-
the study characteristics (summary table)
-
the study quality (summary table)
-
the study results
-
an overview of the clinical effects of the intervention(s).
-
Quantity and quality of research available
A total of 1903 titles and abstracts were screened for inclusion in the review of clinical effects and treatment costs. Of the titles and abstracts screened, 233 were ordered as full papers and assessed in detail. Six papers were unobtainable at the time of the assessment. The process of study selection is shown in Figure 2.
FIGURE 2.
Process of study selection.
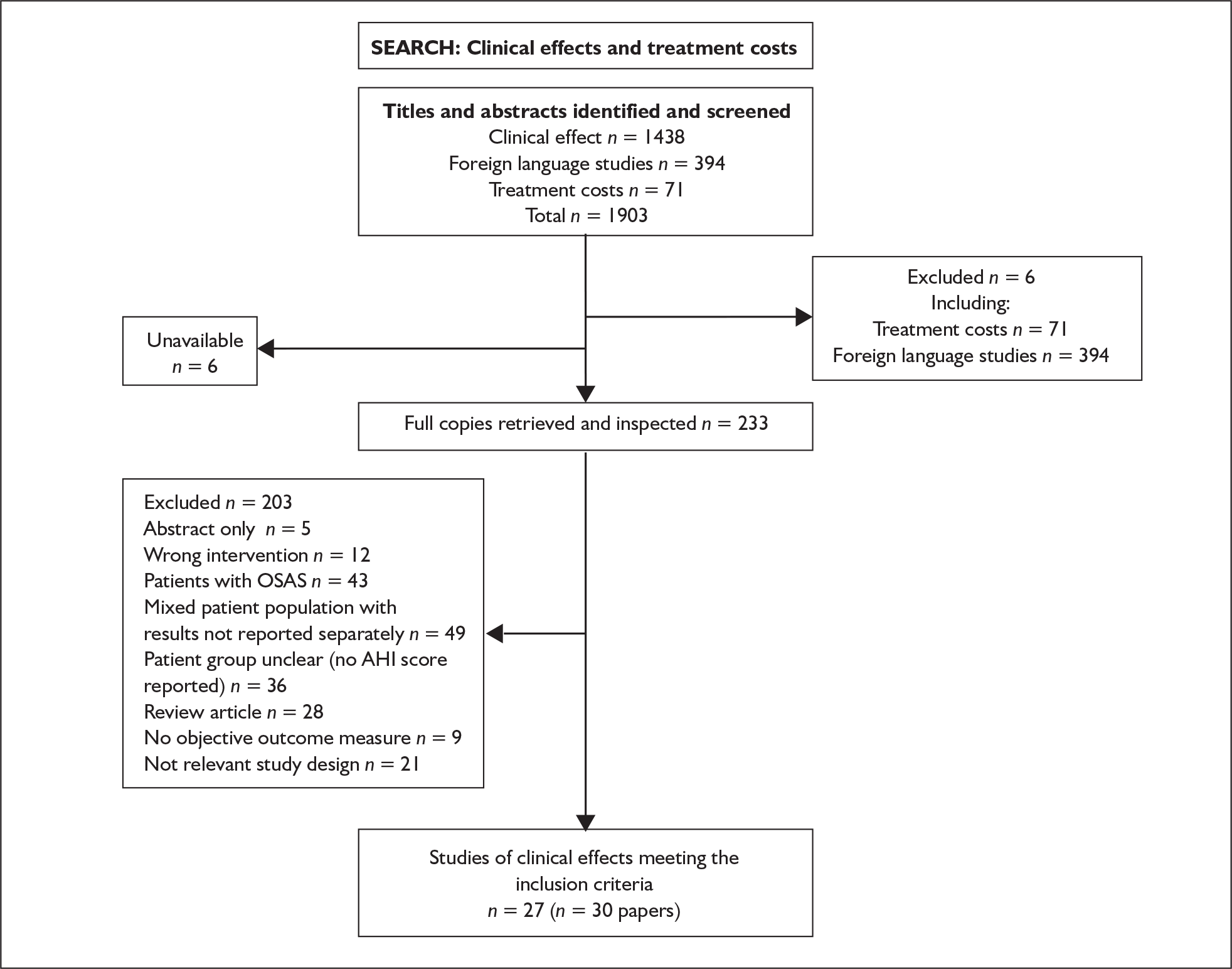
A total of 27 studies reported in 30 publications met the inclusion criteria. The identified studies assessed a broad range of interventions but the evidence base was predominantly weighted (89%) towards studies that had evaluated surgical procedures,49,86–109 with only three studies on either MAS or CPAP. 110–112 Of the studies on surgical procedures, these could broadly be grouped into assessments of UP3 versus LAUP (n = 2),86–88 UP3 alone (n = 7),49,89–94 LAUP alone (n = 3),93,95,96 RFA of the soft palate or tongue base (n = 6 and n = 1 respectively)103–109 and palatal stiffening techniques (Pillar implants and injection snoreplasty) (n = 4 and n = 1 respectively). 97–102 No studies were identified that had assessed surgery to improve coincidental nasal obstruction alone, uvulectomy alone, DAUP or tongue-based suspension procedures.
In terms of studies assessing non-surgical devices, only three studies were identified that met the inclusion criteria. Two of these had examined the use of a MAS,110,111,113 while one had assessed the effects of CPAP versus a no-intervention control. 112
Although studies could broadly be grouped into intervention categories, for both UP3 and LAUP, closer inspection of the interventions evaluated within the studies designated to both of these categories revealed that there was often variability between the interventions assessed. This was partly because the procedures were sometimes performed in a modified manner91,94,95 or in conjunction with a second procedure. 92,114 More frequently, however, it was because of a lack of clear reporting on the procedures conducted, which did not allow comparisons to easily be drawn,89,92 or the methods of study design and analysis. 89,90,94 Three studies evaluating UP3 alone89,90,94 assessed two or more different procedures but pooled the post-treatment results across the intervention groups and reported the results as a one-group pre–post study. In all of these studies there were potential differences (the degree to which varied across the studies) between the other interventional procedures assessed [LAUP, cautery-assisted uvulopalatoplasty (CAUP) and uvulopalatal elevation palatoplasty (UEP)] and the broad category grouping to which the studies were assigned. The interventions within the UP3 alone category were therefore more heterogeneous and the results liable to be more confounded than is readily apparent from the somewhat simplistic nomenclature adopted for study grouping. For all of the other intervention groups, although there were differences between the study interventions within some categories (e.g. RFA versus bipolar RFA), these were more clearly reported, and the results were reported by treatment group or as between-treatment group comparisons as appropriate. Table 1 provides a summary of the identified studies by intervention group and specific intervention evaluated, and Table 2 displays a summary of the interventions identified by the number of studies and design.
| Study ID | Intervention group | Specific intervention | Study design | n | Non-apnoeic snorers only |
|---|---|---|---|---|---|
| Osman 2000;86 200387 | UP3 versus LAUP | UP3 versus LAUP | RCT | 47 | + |
| Prasad 200388 | UP3 versus LAUP | UP3 versus LAUP | CCT | 60 | + |
| aOzmen 200689 | UP3 | UP3; LAUP; CAUP | Pre–post | 162 | + |
| bJanson 199490 | UP3 | UP3; conservative UP3 | Pre–post | 231 | + |
| Friberg 199591 | UP3 | UP3 | Pre–post | 56 | + |
| Prichard 199549 | UP3 | UP3 | Pre–post | 32 | + |
| Miljeteig 199492 | UP3 | UP3 | Pre–post | 38 | – |
| Neruntarat 200393 | UP3 | Uvulopalatal flap | Pre–post | 60 | + |
| cJones 200594 | UP3 | UP3; UEP | Pre–post | 54 | + |
| Neruntarat 200393 | LAUP | LAUP with septoplasty | Pre–post | 35 | + |
| Berger 200195 | LAUP | LAUP alone | Pre–post | 14 | + |
| Lauretano 199796 | LAUP | LAUP alone | Pre–post | 32 | – |
| Stuck 2005103 | RFA | Soft palate RFA; placebo | RCT | 26 | + |
| Cartwright 2000104 | RFA | Soft palate RFA; MAS | CCT | 20 | + |
| Hukins 2000105 | RFA | Soft palate RFA | Pre–post | 20 | + |
| Boudewyns 2000106 | RFA | Soft palate RFA | Pre–post | 45 | + |
| Haraldsson 2002107 | RFA | Soft palate RFA | Pre–post | 16 | + |
| Back 2002108 | RFA | Soft palate RFA | Pre–post | 20 | + |
| den Herder 2006109 | RFA | Tongue base RFA | Pre–post | 9 | – |
| Skjostad 200697 | Palatal stiffening | Pillar implants | RCT | 20 | + |
| Nordgard 200698 | Palatal stiffening | Pillar implants | Pre–post | 35 | + |
| Maurer 2005;99 2005100 | Palatal stiffening | Pillar implants | Pre–post | 40 | + |
| Ho 2004101 | Palatal stiffening | Pillar implants | Pre–post | 12 | + |
| Brietzke 2001102 | Palatal stiffening | Injection snoreplasty | Pre–post | 27 | + |
| Series 1994112 | CPAP | CPAP | Pre–post | 18 | + |
| Smith 2004113 | MAS | MAS | Pre–post | 35 | + |
| Fransson 2001;110 2003111 | MAS | MAS | Pre–post | 27 | – |
| Intervention group | Study designa | Total number of studies | Total n by intervention | ||
|---|---|---|---|---|---|
| RCT | CCT | Pre–post study | |||
| UP3 versus LAUP | 1 | 1 | 0 | 2 | 107 |
| UP3 alone | 0 | 0 | 7 | 7 | 633 |
| LAUP alone | 0 | 0 | 3 | 3 | 81 |
| Palatal stiffening | 1 | 0 | 4 | 5 | 134 |
| RFA | 1 | 1 | 5 | 7 | 156 |
| MAS | 0 | 0 | 2 | 2 | 62 |
| CPAP | 0 | 0 | 1 | 1 | 18 |
| Total | 3 | 2 | 22 | 27 | 1191 |
The identified evidence base, as well as covering a relatively broad number of interventions, also differed in terms of study design, sample sizes and duration of follow-up. As could be expected given the interventions examined, the studies were predominantly surgical case series that reported both pre- and post-treatment data. Across the 27 studies, three RCTs were identified (11%), two CCTs (7.5%) and 22 (81.5%) pre–post studies. In total, 23 (85%) of the studies included only patients with a diagnosis of non-apnoeic snoring, whereas the remaining four included patients with OSAS as well as those with primary snoring but reported results separately for both patient groups. 92,96,109–111 Sample sizes across the studies were small, ranging from 9 to 231, with a median of 32. Similarly, the duration of follow-up was highly variable and ranged from 10 days to 5 years. Across the studies there was a tendency for objective outcome measures, such as PSG parameter results or objective measures of snoring sound intensity, to be assessed for a shorter follow-up duration and subjective measures to be assessed at longer follow-up times.
Where sufficient baseline prognostic factors were adequately reported, the patient population included in the studies was relatively homogeneous. All patients, in accordance with the inclusion criteria, had undergone either full PSG, modified PSG, oximetry or a sleep study (unspecified) to rule out a diagnosis of OSAS at baseline. The mean age of patients in the majority of studies was between 40 and 50 years, although across the studies the range was from 19 to 83 years. All of the studies included a higher percentage of male than female patients, with the percentage of male participants ranging from 56% to 100%. Furthermore, nearly all studies recruited patients with a body mass index (BMI) classified in the range of ‘overweight’ but not ‘obese’, although there was some variation in BMI across the studies, with a range from 18.3 kg/m2 to 47.2 kg/m2 observed.
The included studies had mainly been conducted in an otolaryngology department (or equivalent) setting in a number of different countries. Of the identified studies, five had been conducted in North America (Canada or the USA),92,96,102,104,112 seven in Scandinavia (Norway, Sweden or Finland),90,91,97,98,107,108,110,111 five in the UK,49,86–88,94,113 and four in Europe (Germany, Netherlands and a European multicentre study). 99,100,103,106,109
Of the remaining studies two were conducted in Thailand2,114 and one each in Turkey,89 Israel,95 Hong Kong101 and Australia. 105 The year of study publication ranged from 1994 to 2006.
Outcome measures
The outcome measures assessed in the studies reflected the fact that non-apnoeic snoring is part of a spectrum of SDB, differentiated from mild OSAS only by the number of apnoeic and hypopnoeic events per hour of sleep. Across the studies PSG or oximetry results were therefore commonly reported. Additional outcomes reported were subjective and objective measures of snoring, EDS, patient or bed partner satisfaction with the procedure, changes in airway volume, T1 signal density changes on MRI and adverse events, with different methods of measurement and analysis being employed. The outcome measures could broadly be categorised as PSG parameter results; subjectively assessed snoring; daytime sleepiness; and objectively assessed snoring measures.
PSG parameter outcomes
These included measures of AHI (events/hour), apnoea index (AI; events/hour), duration of obstructive respiratory pattern (minutes), oxygen saturation of arterial blood (SaO2) nadir, sleep efficiency (percentage of time asleep compared with time spent in bed) and total sleep time. The outcomes were reported as mean and standard deviation or median and range. The common method of analysis for these outcomes was to compare the pre- and postintervention values and report the associated p-value for the change.
Subjectively assessed snoring and daytime sleepiness outcomes
These outcomes included measures of snoring, sleep disturbance and daytime sleepiness.
Subjective measures of snoring were either patient or partner reported and included measures of improvement in snoring, snoring severity and the number of patients who reported snoring. Outcomes were assessed by means of either categorical rating scales or continuous visual analogue scale (VAS). Sleep disturbance was partner or family assessed and included ratings of the need to sleep in another room because of partner’s snoring, difficulties in falling asleep and sleep disturbance because of snoring. Measurement was either by the number of partners reporting the outcome or the number of episodes per week. EDS was generally assessed using the standard ESS score,115 which is an eight-item scale with four response options per item. Items are scored from 0, ‘would never doze’, to 3, ‘high chance of dozing’, giving a total composite scale score between 0 and 24. Other methods of assessing daytime sleepiness were by use of a categorical rating scale and by counting the number of patients who reported falling asleep in the daytime. The other subjectively assessed outcome measures were quality of life and patient/bed partner satisfaction with the procedure.
Objective measures of snoring sound
The objectively assessed measures of snoring, by use of either snoring recordings or acoustic analysis of the snoring sound, included mean snoring volume (dB), snoring index (SI) (number of spikes in sound intensity exceeding 50 dB per hour of sleep), percentage of sleep time spent in loud snoring, maximal sound intensity (dB) and the snore energy ratio (Hz). Results were usually presented as the mean and standard deviation or the median and range. Pre- and postintervention results were compared, with the associated p-value for the difference reported.
Five studies also assessed other objectively measured outcomes. Neruntarat93,114 and Hukins and colleagues105 assessed changes in the soft palate length and width after treatment by means of measurements taken from a pre- and postoperative lateral cephalogram. Ozmen and colleagues89 examined changes in QTc by means of a pre- and postoperative standard ECG, whereas Back and colleagues108 assessed changes in T1 signal density of the soft palate using MRI. Postoperative changes in voice quality were examined by Haraldsson and colleagues107 using a nasal–oral ratio meter (NORAM).
Adverse events
The postoperative adverse events commonly assessed were pain, speech, swallowing difficulties and pharyngeal irritation. These were measured by means of either a continuous VAS or a categorical rating scale. The four studies97–101 that assessed the effects of palatal implants also reported the number of extrusions as a postoperative complication.
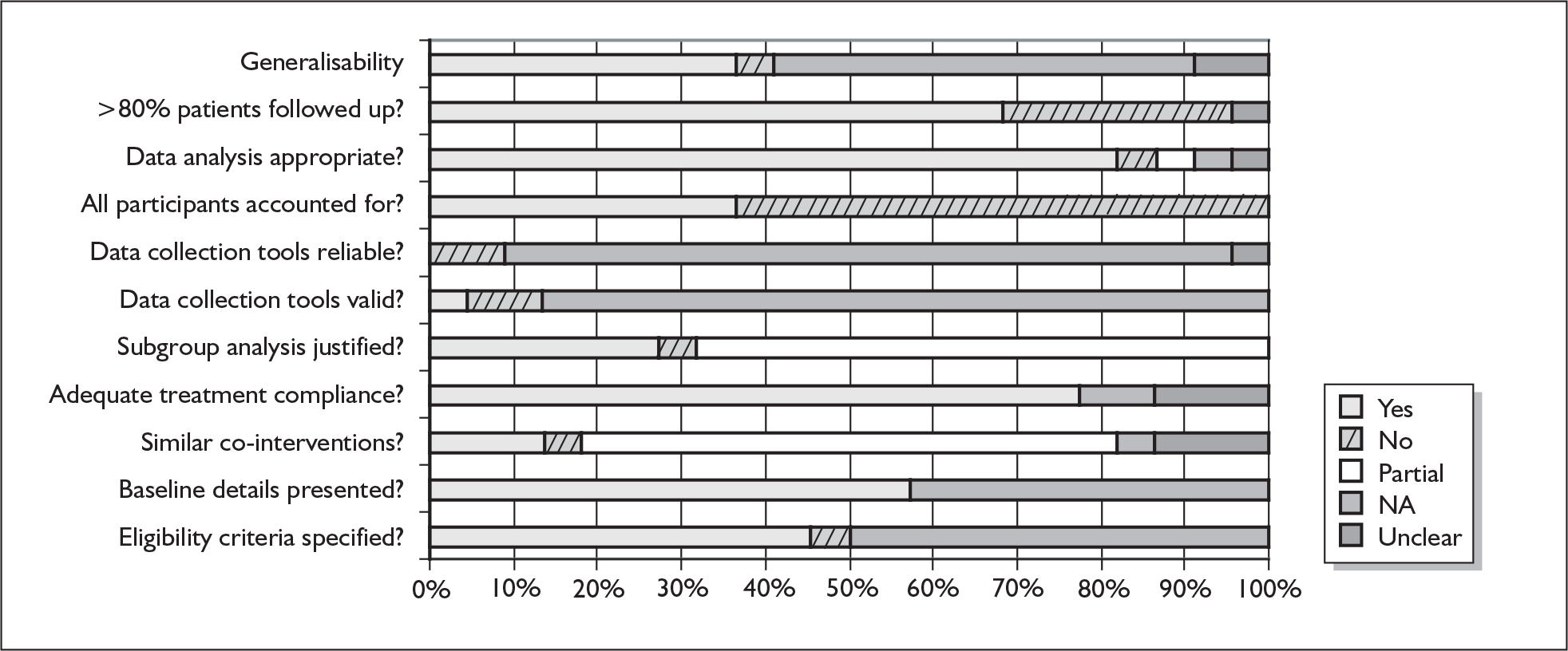
Study quality
The included studies were predominantly small and of low quality. An indication of study quality according to quality indicators, grouped by study design, is given in Figures 3–5. A further assessment of study quality is provided in each specific section of the report according to intervention group.
FIGURE 3.
Summary of study quality indicators for the three randomised controlled trials (RCTs).
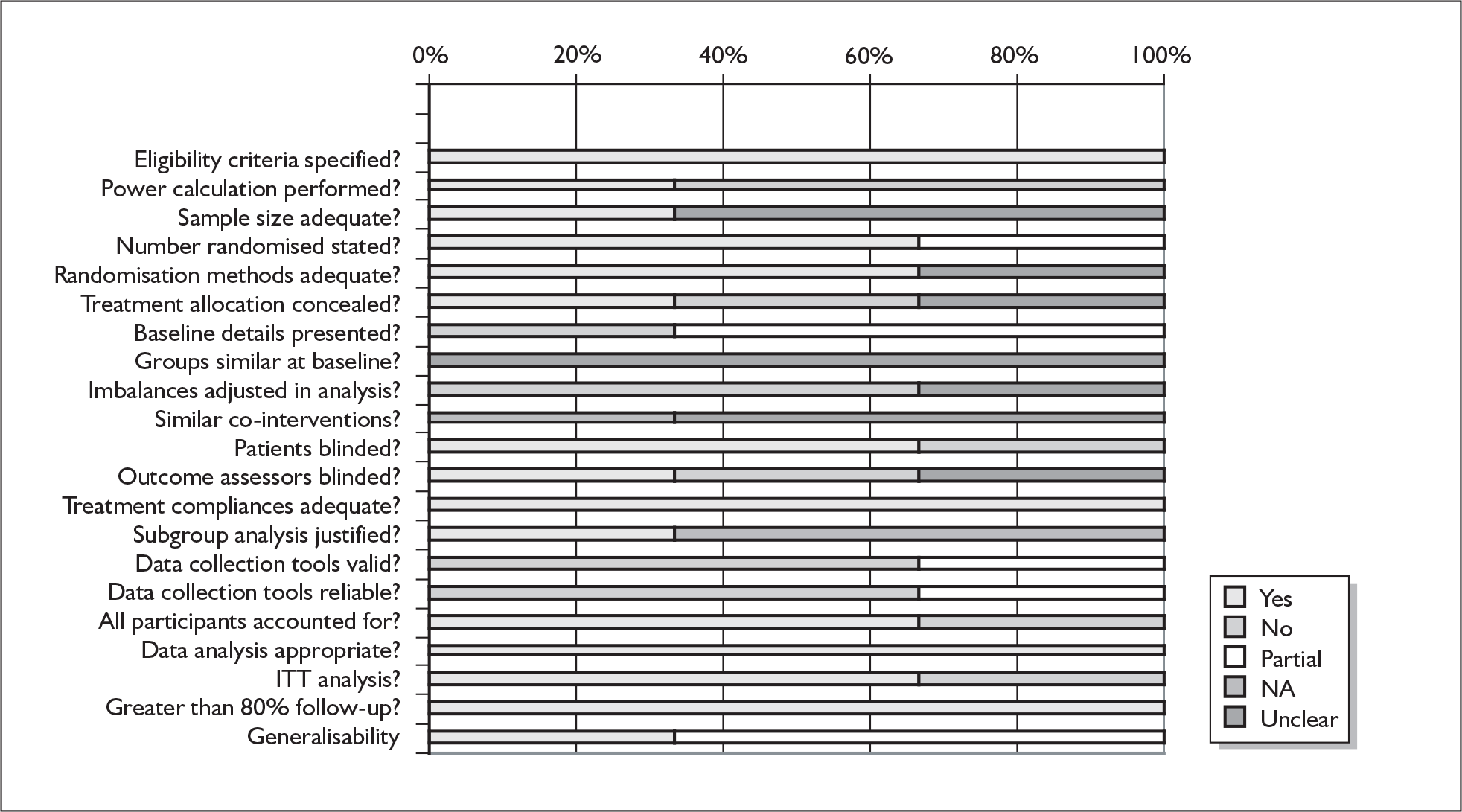
FIGURE 4.
Summary of study quality indicators for the two controlled clinical trials (CCTs).
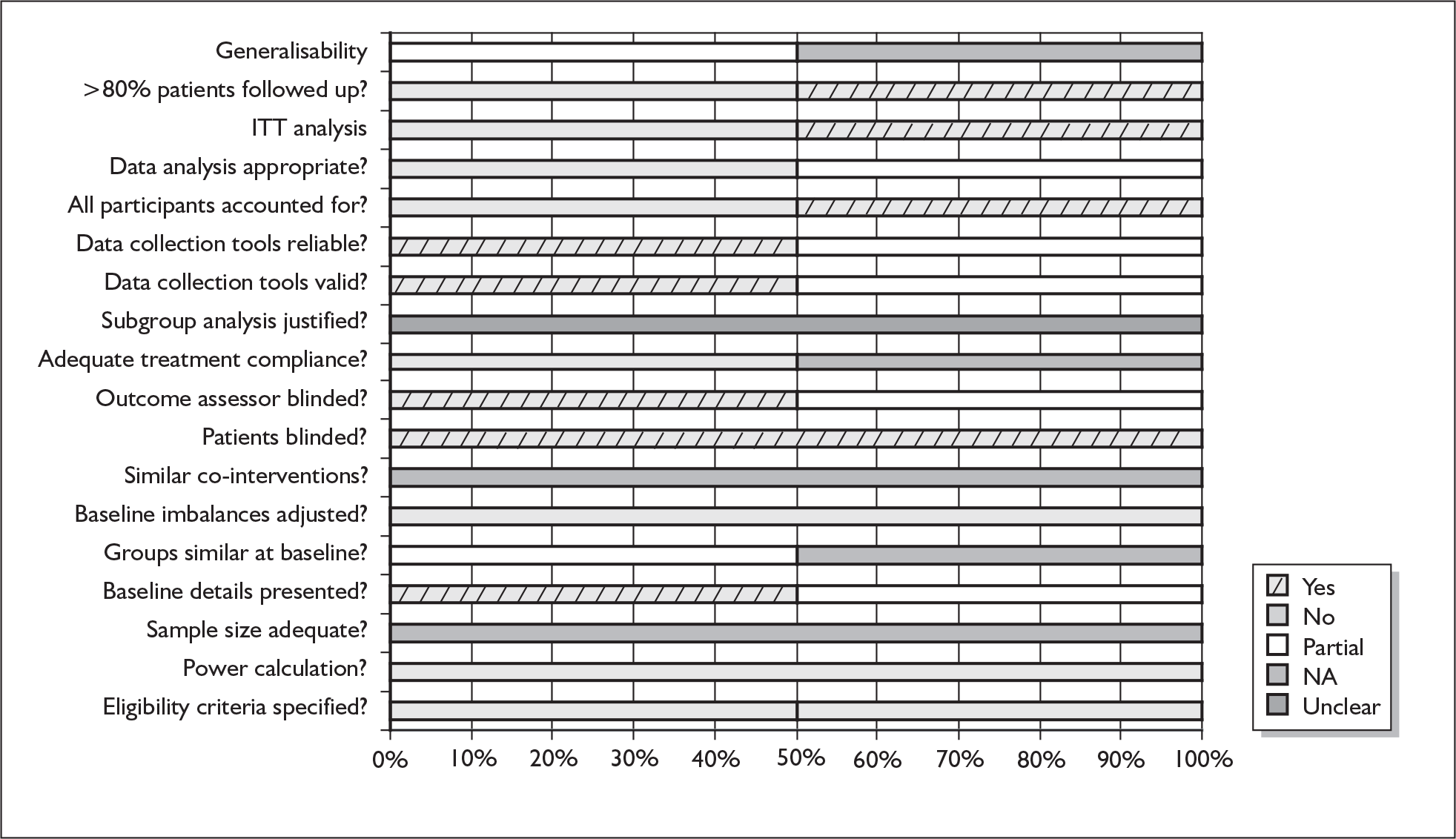
FIGURE 5.
Summary of study quality indicators for the 22 pre–post studies.
Excluded studies
Foreign language studies
A total of 394 foreign language studies were screened for inclusion as part of the review process. On the basis of title and abstract alone, none of them clearly met the inclusion criteria. However, 24 of these studies were marked as ‘unclear’ in that the full paper copy would merit retrieval for further assessment in any future review that does not exclude studies on the basis of the language of publication. The bibliographic details of these studies are provided in Appendix 4.
A total of 94 studies ‘narrowly’ missed the inclusion criteria. For the majority of these the reason for exclusion was that a ‘mixed’ population of patients with OSAS and patients with a diagnosis of non-apnoeic snoring had been assessed but the results had not been reported separately by patient subgroup. There were two other reasons for study exclusion. The first was because the patient group was unclear, as either PSG or oximetry had not been conducted at baseline to rule out OSAS or the results were reported as being less than one of the standard AHI cut-off scores that define non-apnoeic snoring or mild, moderate or severe OSAS (AHI ≤ 5; 5–15; 15–30 and > 30 respectively)1 but specific baseline AHI scores were not reported. In the case of papers in which it appeared that the population studied was made up of non-apnoeic snorers, authors were contacted for specific baseline AHI information or asked to confirm whether the AHI score for their study population was ≤ 5. At the time that data extraction was completed for this review, responses were still outstanding from five authors regarding their study populations: Johnston and colleagues,116 Gnuechtel and colleagues,117 Truy and colleagues,118 Mukai and colleagues119 and Clarke and colleagues. 120 The last reason for study exclusion in the case of pre–post studies was that no objective outcome measure had been reported. The bibliographic details of the 94 excluded studies with the reasons for exclusion are provided in Appendix 2.
Of relevance to the treatment of non-apnoeic snoring within a UK context, two RCTs121,122 were identified that had been conducted within the UK. Both of the trials were excluded from the review as neither, in line with current UK practice, had undertaken PSG or oximetry at baseline if patients presented with an ESS score of less than 10. Obstructive sleep apnoea had been ruled out in patients in both studies on the basis of the ESS score and clinical examination. The first of these trials, conducted by Belloso and colleagues,121 assessed differences in postoperative pain with LAUP compared with coblation uvulopalatoplasty in conjunction with tonsillectomy (CP). The impact of surgical technique in the reduction of subjectively assessed snoring loudness was also assessed at 1 year in the 30 patients completing treatment. Results indicated that there was a significant reduction in snoring loudness in both groups but no between-group differences were observed. However, significant reductions in postoperative pain were observed in the CP group after day 8 and were maintained until after day 15.
The second trial by Uppal and colleagues122 compared LAUP with punctate palatal diathermy in 83 patients. At a mean follow-up time of greater than 18 months there were no statistically significant differences between the treatment groups in measures of patient perception of benefit from surgery or subjective evaluations of snoring improvement. In the postoperative period, however, there were significant differences in the degree of pain in favour of treatment with punctuate palatal diathermy (mean difference = 22.14; 95% CI 7.98–36.31). The relative risk observed for treatment complications for LAUP relative to punctuate palatal diathermy was 1.42 (95% CI 0.93–2.17).
Uvulopalatopharyngoplasty versus laser-assisted uvulopalatoplasty
Quantity and quality of the studies
Two parallel group studies comparing UP3 with LAUP reported in three publications86–88 were included. The study by Osman and colleagues86,87 was a RCT. Participants were studied at both short-term and long-term follow-up times with results from the two time points reported separately in two papers published in 200086 and 200387 respectively. The other study by Prasad and colleagues88 was a non-randomised CCT. Across the two studies there were a total of 107 non-apnoeic snoring patients, of whom 45 underwent UP3 and 62 underwent LAUP. Table 3 summarises the characteristics of the two studies.
| Study ID | Study design | n | Follow-up duration | Participants | Outcomes | ||
|---|---|---|---|---|---|---|---|
| PSG test | Subjective | Objective | |||||
| Osman 2000;86 200387 | RCT | 47: UP3 = 18; LAUP = 29 |
Mean: 3.4 (2–11) months: n = 47, for subjective outcomes only Median: 45 (29–56) months: n = 23 for objective outcomes and long-term complications |
Baseline test: an overnight sleep study using a DENSA Compact Sleep Apnoea Screening System Participant demographics: age: 49.4 (27–71); male: n = 41 (87%); BMI: 28 (22–38); AHI: 4.4 ± 3.59; ESS: NR; smokers: n = 24 (48.9%) |
NR |
Number of patients reporting an improvement in their snoring Adverse events: postoperative pain in the first 24 hours after surgery. Assessed in a subgroup of 38 patients: long-term postoperative complications; occasional choking; dry throat; mild sore throat; food sticking in the throat |
Based on a subgroup of 38 patients: number of patients with SI change; SI; snoring loudness Adverse events: number of patients with postoperative complications; secondary bleeding; temporary velopalatal insufficiency; severe infection; need for repeat procedure (unscheduled) |
| Prasad 200388 | CCT | 60: UP3 = 27; LAUP = 33 | 1 year to > 4 years |
Baseline tests: unclear; authors contacted and it appears to be oximetry Participant demographics: age: LAUP: 49.45 ± 8.92 (31–56); UP3: 51.96 ± 12.07 (33–59); male: LAUP: n = 25 (76%); UP3: n = 23 (85%); BMI: NR; AHI: < 5; ESS: NR; smokers: NR |
NR | Partner’s snoring severity; difficulties falling asleep because of partner’s snoring; sleep disturbance because of partner’s snoring; need to sleep in a separate room because of partner’s snoring; quality of marital life | NR |
The baseline test to rule out OSAS in the Osman study86,87 was an overnight sleep study using a DENSA Compact Sleep Apnoea Screening System; in the Prasad study88 it appeared to be oximetry. Participant baseline demographics in both of the studies were not reported separately for the UP3 and LAUP groups except for age in the Prasad study. The mean age of the participants ranged from 49.40 to 51.96 years. The proportion of men was 87% and 76% in the two studies respectively. In the Osman study nearly half of the patients were smokers (48.9%), whereas the Prasad study did not report smoking status. Neither of the studies reported baseline ESS scores or alcohol consumption levels.
In the LAUP procedure in the Osman study86,87 two linear scars were created in the oral surface of the soft palate from the junction of the hard and soft palate to the uvula, followed by laser uvulectomy, whereas in the Prasad study88 the procedure consisted of approximating the soft palate against the velopharyngeal isthmus and excising any redundant portion along the uvula. The number of LAUP procedures per patient was not reported in either study. In the UP3 procedure in the Osman study86,87 1 cm of the soft palate was removed with the uvula, as well as the tonsils if present; the posterior pillar was then sutured to the anterior pillar followed by mucosa-to-mucosa closure of the palate using sutures. In the Prasad study88 the UP3 procedure consisted of excising the uvula and a rim of soft palate and removing both palatine tonsils and suturing of the mucosa. Follow-up duration in the two studies ranged from 2 months to 56 months (or > 4 years).
Outcomes
PSG parameter outcomes were not measured in either study. The objectively assessed outcomes were the number of patients with a SI change, SI and snoring loudness. They were measured only in the Osman study86,87 based on a subgroup of 38 patients. The subjectively assessed snoring outcomes reported were patient-reported improvement of snoring,86,87 partner-assessed snoring severity,88 difficulties falling asleep because of partner’s snoring,88 sleep disturbance because of partner’s snoring,88 need to sleep in a separate room because of partner’s snoring88 and quality of marital life. 88 Adverse events were reported only by Osman and colleagues. 86,87
In both the RCT and CCT, however, most of the outcomes reported were analysed pre- and postoperatively and few outcomes were analysed for between-group differences.
Study quality
Table 4 presents a summary of the key quality indicators for the two studies. Both of the studies were of poor quality with a lack of reporting of methods, in particular the CCT. The sample sizes were small and no power calculations were performed. Baseline details presented were not adequate and the data were not reported separately for the two comparison groups. Therefore, it cannot be judged how well the comparison groups were balanced in the RCT or how well the groups were matched in the CCT. The lack of blinding in the outcome assessment may introduce bias to the results in both studies. In the Prasad and colleagues study88 the response rate to the survey was 66% and no sensitivity analysis was conducted to assess the effect of response bias and how this could effect the results. In this study it is also unclear how the authors grouped the results for each of the treatment groups to perform the between-group comparisons.
| Quality criteria | Osman 2000;86 200387 | Prasad 200388 |
|---|---|---|
| Study design | RCT | CCT |
| Eligibility criteria specified? | + | – |
| Power calculation performed? | – | – |
| Sample size adequate? | ? | ? |
| Number randomised stated? | + | NA |
| Adequate methods of randomisation? | + | NA |
| Treatment allocation concealed? | – | NA |
| Adequate baseline details presented? | P | – |
| Groups similar at baseline? | ? | ? |
| Baseline imbalances adjusted for in analysis? | – | – |
| Similar co-interventions administered? | ? | ? |
| Patients blinded to treatment allocation? | – | – |
| Outcome assessors blinded to treatment? | – | – |
| Compliance with treatment adequate? | + | ? |
| Subgroup analysis justified? | + | NA |
| Data collection tools valid? | P | – |
| Data collection tools reliable? | P | – |
| All participants accounted for? | + | – |
| Data analyses appropriate? | + | P |
| Analysis conducted on ITT basis? | + | – |
| Greater than 80% of patients followed up? | + | – |
| Generalisability | Applicable for the same population | Unclear |
| Intercentre variability | NA | NA |
Results
Neither of these two studies measured PSG parameter outcomes.
Only the study by Osman and colleagues86,87 reported objective outcomes. The results are presented in Tables 5 and 6. The number of patients with a change in the SI was analysed based on a subgroup of 38 patients at short-term follow-up (mean 3.4 months, range 2–11 months after the surgery),86 and the results are reported separately for the UP3 and LAUP groups. SI was reported in the long-term follow-up study87 based on a subgroup of 23 patients pooled from both UP3 and LAUP groups at short-term and long-term follow-up (median 45 months, range 29–56 months after the surgery) respectively. Snoring was defined as a spike in breathing sound intensity starting from baseline and returning back to baseline whose amplitude was greater than 50 dB SPL.
| UP3a | LAUPb | Differences between groups | |
|---|---|---|---|
| Number of non-apnoeic snorers (in analysis) | 16 | 22 | NA |
| Percentage of patients who had a higher postoperative SI | 12.5% | 22.73%c | Not significant at the 5% level |
| Percentage of patients who had a lower postoperative SI | 87.5% | 77.27% | Not significant at the 5% level |
| SI (median value of snores/hour) | |
|---|---|
| Preoperative | 135.6 |
| Short-term follow-up (mean 3.4 months, range 2–11 months) | 38.2 |
| Long-term follow-up (median 45 months, range 29–56 months) | 21.7; significantly less than preoperative level, p < 0.01 |
| Long term vs short term | –0.9; p > 0.05 |
| Change in SI from baseline at long-term follow-up | |
| LAUP group (n = 12) | The reduction was significant, p < 0.01 |
| UP3 group (n = 11) | The reduction was significant, p < 0.05 |
| LAUP vs UP3 | Not significant, p > 0.05 |
In the short-term follow-up study,86 after the surgical procedure there was no significant difference found between the two groups in terms of the proportion of patients who had either a higher postoperative SI or a lower postoperative SI. The authors stated that the reduction in SI in both the UP3 and LAUP groups was significant. Also, the pooled mean SI for both groups combined reduced from 154 snores/hour at baseline to 75.84 snores/hour postoperatively (p < 0.0001). In the long-term follow-up study,87 SI measured in 23 patients dropped from 135.6 snores/hour at baseline to 38.2 snores/hour at short-term follow-up and 21.7 snores/hour at long-term follow-up. The authors stated that from baseline to long-term follow-up the reduction in SI in both the individual UP3 group (measured in 11 patients) and the individual LAUP group (measured in 12 patients) was statistically significant, but no significant differences were found between the UP3 and LAUP groups.
The authors of this study also indicated that, at short-term follow-up, reduction in pre-and postoperative median snore loudness was significant at the 0.1% level in UP3 patients and at the 10% level but not the 5% level in LAUP patients; UP3 was better than LAUP at reducing the median snore loudness (p < 0.05). At long-term follow-up the reduction in median snore loudness in pooled data from 38 patients was significant at the 1% level; however, the mean reduction was modest, being 191 ± 108 mV (or 3.8 dB, SD 2.2 dB) for 95% confidence limits. At long-term follow-up there was no significant difference between the UP3 and LAUP groups in the reduction in snoring loudness.
In the Osman study86,87 the number of patients reporting an improvement in their snoring at short-term follow-up was the only subjective result reported. It was assessed by a questionnaire with the following response options: absent, a lot better, slightly better, unchanged or worse. At short-term follow-up after the surgery 89% of the patients in the UP3 group and 83% in the LAUP group reported an improvement; at long-term follow-up the improvement declined to 83% and 76% respectively, as two patients in the UP3 group and one in the LAUP group were rereferred by their GP for late recurrence of snoring. The significance of the improvement and the differences between the two groups were not reported.
Adverse events were only reported by Osman and colleagues. 86,87 The results are shown in Table 7. Postoperative pain scores were assessed using a linear analogue scale with 0 indicating no pain and 4 indicating worst pain. In the first 24 hours following the LAUP treatment patients had significantly less pain (mean pain score 1.3) than following UP3 (mean pain score 1.7). One patient who underwent UP3 had severe postoperative infection. One patient in the UP3 group and two in the LAUP group at long-term follow-up needed an unscheduled repeat procedure. All other adverse events were minor and the differences between the two treatment groups were not statistically tested.
| UP3 | LAUP | p-value | |
|---|---|---|---|
| Number of non-apnoeic snorers analysed | 18 | 29 | NA |
| Postoperative pain score in the first 24 hours after surgerya | 1.7 | 1.3 | < 0.05 |
| Patients with complications (%) | 5.6b | 0 | NR |
| Patients with secondary bleeding (%) | 16.67 | 0 | NR |
| Patients with temporary velopalatal insufficiency (%) | 16.67 | 0 | NR |
| Patients with severe infection (%) | 5.56 | 0 | NR |
| Patients with long-term postoperative complications (%)c | 41.7 | 50 | NR |
| Patients with occasional choking (%)c | 16.7 | 16.7 | NR |
| Patients with dry throat(%)c | 25 | 0 | NR |
| Patients with mild sore throat(%)c | 8 | 25 | NR |
| Patients with food sticking in the throat(%)c | 8 | 8 | NR |
| Patients with unscheduled need for repeat procedure(%)c | 8.33 | 16.67 | NR |
In the Prasad study88 subjective snoring results were all partner assessed (see Table 8). None of these subjectively assessed outcomes was measured in the same way as in the Osman study.
| Comparison | Osman 2000;86 200387 | aPrasad 200388 | ||
|---|---|---|---|---|
| UP3 | LAUP | UP3 | LAUP | |
| Number of non-apnoeic snorers analysed | 18 | 29 | 27 | 33 |
| Patients reporting an improvement in their snoring | ||||
| Short-term follow-up | 89% | 83% | ||
| Long-term follow-up | 83% | 76% | ||
| Partners reporting snoringb | ||||
| Abolished | 19% | 15% | ||
| A lot better | 58% | 28% | ||
| Slightly better | 11% | 24% | ||
| Unchanged | 4% | 21% | ||
| Worse | 4% | 6% | ||
| Not recorded | 4% | 6% | ||
| Partners reporting difficulties falling asleep because of patient’s snoringc | ||||
| Always | 4% | 16% | ||
| Most often | 0% | 19% | ||
| Sometimes | 19% | 16% | ||
| Occasionally | 40% | 22% | ||
| Never | 33% | 24% | ||
| Not recorded | 4% | 3% | ||
| Partners reporting sleep disturbance because of patient’s snoringd | ||||
| No disturbed sleep | 59.26% | 39.40% | ||
| Reduced | 37.04% | 33.33% | ||
| Unchanged | 3.70% | 24.24% | ||
| Increased | 0% | 3.03% | ||
| Partners reporting need to sleep in a separate room because of partner’s snoring | ||||
| No longer need to sleep in a separate room | 81.48% | 65.63% | ||
| Need reduced | 11.11% | 15.63% | ||
| No change | 7.41% | 15.63% | ||
| Need increased | 0% | 3.11% | ||
| Partners reporting quality of marital lifee | ||||
| Improved | 40.74% | 30.3% | ||
| Unchanged | 33.33% | 57.58% | ||
| Undecided | 25.93% | 12.12% | ||
Improvement in snoring was measured as the percentage of patients with snoring ‘abolished’, ‘a lot better’, ‘slightly better’, ‘unchanged’ or ‘worse’. The authors stated that residual snoring was significantly more frequent following LAUP than following UP3, with snoring being abolished in 19% and 15% of the UP3 group and LAUP group respectively. Partners considered snoring as being a lot better in 58% of the UP3 group and 28% of the LAUP group, as being slightly better in 11% of the UP3 group and 24% of the LAUP group, and as unchanged in 4% after UP3 and 21% after LAUP.
Difficulties falling asleep because of partner’s snoring was assessed with the following response options: ‘no’, ‘occasionally’, ‘sometimes’, ‘most often’ and ‘always’. The authors stated that after UP3 partners were significantly less likely to have trouble falling asleep, with 33% of the partners in the UP3 group and 24% in the LAUP group never having difficulties falling asleep. Occasionally having difficulties falling asleep was reported by 40% of the partners in the UP3 group and 22% in the LAUP group, ‘always’ was reported by 4% of the UP3 group and 16% of the LAUP group, and ‘most often’ was reported by none of the UP3 group and 19% of the LAUP group.
Sleep disturbance because of partner’s snoring was assessed with response options of ‘no longer disturbed’, ‘reduced frequency’, ‘remains unchanged’ or ‘increased’. Disturbance of sleep and the need to wake up were reduced very significantly after both UP3 and LAUP, with 59.3% of partners in the UP3 group and 39.4% of partners in the LAUP reporting no disturbed sleep, and 37.0% in the UP3 group and 33.4% in the LAUP group reporting reduced sleep disturbance. The differences between the two groups were not statistically significant; however, there was a trend for LAUP to be less efficacious than UP3 (p = 0.064).
The need to sleep in a separate room because of partner’s snoring was assessed with response options of ‘no longer need to sleep in a separate room’, ‘frequency reduced’, ‘remains unchanged’ or ‘increased’. After surgery, 81.5% of the partners in the UP3 group and 65.6% of the partners in the LAUP group no longer needed to sleep in a separate room; 11.1% of the partners in the UP3 group and 15.6% of the partners in the LAUP group had the need reduced. The statistical significance for either the difference between the UP3 and LAUP groups or the change pre- and postoperatively was not reported.
Quality of marital life was also assessed but the response options were not reported. In total, 40.7% of the patients in the UP3 group and 30.3% in the LAUP group recorded an improvement in quality of marital life, whereas in 33.3% of the UP3 group and 57.6% of the LAUP group quality of marital life remained unchanged; 26.0% of the UP3 group and 12.1% of the LAUP group were undecided. Both groups also showed an improvement in quality of life but the results were not reported. The authors indicated that significantly more partners in the UP3 group reported an improvement in both quality of marital life and quality of life.
Summary of the results
Evidence on the clinical effects of UP3 versus LAUP was limited. The two identified studies86–88 were of poor quality and few between-group comparisons were made. Heterogeneity between the two studies precluded pooling of the evidence. Table 9 summarises the main results of the two studies.
| Osman 2000;86 200387 | Prasad 200388 | |||
|---|---|---|---|---|
| Study design | RCT | CCT | ||
| Comparison | UP3 | LAUP | UP3 | LAUP |
| Number of non-apnoeic snorers | 18 | 29 | 27 | 33 |
| Objective outcomes | ||||
| Reduction in SI: | ||||
| Pre- and post-treatment | + | + | ||
| Between groups | – | |||
| Reduction in median snore loudness: | ||||
| Pre and post-treatment | + | – | ||
| Between groups: short-term follow-up | +; favoured UP3 | |||
| Between groups: long-term follow-up | – | |||
| Subjective outcomes | ||||
| Patients reporting improvement in snoring | 89%a; 83%b | 83%a; 76%b | ||
| Partners reporting improvement in snoring | +; favoured UP3 | |||
| Partners reporting having trouble falling asleep | +; favoured UP3 | |||
| Partners reporting always having difficulties falling asleep | 4% | 16% | ||
| Partners reporting most often having difficult falling asleep | 0% | 19% | ||
| Partners reporting no disturbed sleep | 59.26% | 39.40% | ||
| Partners reporting reduced sleep disturbance | 37.04% | 33.33% | ||
| Partners reporting sleep disturbance unchanged | 3.7% | 24.24% | ||
| Partners no longer need to sleep in a separate room | 81.48% | 65.63% | ||
| Reduction in sleep disturbance: | ||||
| Pre- and post-treatment | + | + | ||
| Between groups | – | |||
| Partner-reported improvement in quality of marital life | +; favoured UP3 | |||
| Partner-reported improvement in quality of life | +; favoured UP3 | |||
| Adverse events | ||||
| 4-point VAS in the first 24 hours after surgery | +; favoured LAUP | |||
One RCT86,87 assessing the SI found that it was significantly reduced in both the UP3 and the LAUP groups (n = 18 and n = 29 respectively) at short-term follow-up after surgery (mean 3.4 months, range 2–11 months) but there was no significant difference between the two groups in the number of patients who had either a lower SI or a higher SI after the surgery. The UP3 (n = 11) and LAUP (n = 12) SI of 23 patients pooled from the two groups dropped from 135.6 snores/hour at baseline to 38.2 snores/hour at short-term follow-up and 21.7 snores/hour at long-term follow-up (median 45 months, range 29–56 months). The reduction from baseline to long-term follow-up was statistically significant. SI decreased from baseline to long-term follow-up in both the UP3 and LAUP groups; however, the reduction was not significantly different between the two groups.
In the RCT at short-term follow-up UP3 seemed significantly better than LAUP at reducing median snoring loudness; however, at long-term follow-up there was no significant difference between the two treatment groups.
In the CCT88 there was significantly more improvement following UP3 (n = 27) than following LAUP (n = 33) in subjectively measured snoring, difficulties falling asleep because of patient’s snoring, quality of marital life and quality of life. Also, UP3 tended to be more efficacious than LAUP in terms of the need to sleep in a separate room because of partner’s snoring, and sleep disturbance. However, patients in the LAUP group had significantly less pain than those in the UP3 group in the first 24 hours postoperatively.
Conclusions
Based on very limited evidence from two small poor-quality studies UP3 appears to be more efficacious than LAUP in improving some subjectively measured snoring outcomes and snoring-related problems. However, this effect was not consistently observed across all subjective outcome measures. Both UP3 and LAUP seemed to reduce the SI and snoring loudness; however, the effects did not differ between the two operations.
Uvulopalatopharyngoplasty alone
Quantity and quality of the studies
Seven pre–post studies49,89–94 that evaluated the effects of UP3 alone for non-apnoeic snoring met our inclusion criteria. One91 included both non-apnoeic snorers and patients with a diagnosis of OSAS but some outcomes were reported separately for non-apnoeic snorers. Study characteristics are summarised in Table 10.
| Study ID | n | Participants | Follow-up duration | Outcomes | ||
|---|---|---|---|---|---|---|
| PSG parameters | Subjective | Objective | ||||
| Friberg 199591 | 56 |
Baseline tests: oximetry Participant demographics: age: median 46 (26–74); male: n = 56 (100%); BMI: median 26.1 (18.3–35.4); AHI: NR; ODI: median 0 (0–6); ESS: NR; smokers: NR |
Median: 63 (37–83) months | ODI; nadir SaO2 (%) | Number of patients reporting excessive daytime sleepiness; number of patients reporting snoring; postoperative oesopharyngeal reflux; minor throat disturbances; change in voice quality | Duration of the obstructive respiratory pattern (percentage of total sleep time) |
| Janson 199490b;f | 231: UP3 = 155c; conservative = 76 |
Baseline tests: oximetry; PSG in 16 patients; clinical examination Participant demographics: age: UP3 45 (24–74), conservative 49 (18–79); male: UP3 n = 136 (87.7%), conservative n = 47 (62%); BMI: both groups: 25 ± 3; AHI: NR; ODI: < 5; ESS: NR; smokers: NR |
3 months: n = 105; 12 months: n = 50; 3 and 12 months: n = 54; 2 years: n = 49; 5 years: n = 9 | NR | Difficulty inducing sleep; difficulty maintaining sleep; excessive daytime sleepiness; excessive daytime tiredness; snoring occasional or moderate; snoring severe or frequent; morning headache; awakening because of trouble breathing; involuntarily falling asleep; falling asleep when relaxing; tendency to take a nap in the daytime; difficulty staying awake when driving | NR |
| Jones 200594 | 35: UEP = 19; TP = 16d |
Baseline test: PSG Participant demographics: age: UEP 47 (33–60), TP 46 (24–65); male: UEP n = 17/19 (89%), TP n = 13/16 (81%); BMI: UEP 31.4 (24.9–47.2), TP 29.6 (24.3–36.0); AHI (median): UEP 2.7 (0–12.8), TP 3.8 (1.0–10.9); ESS (median): UEP 7 (0–15), TP 9 (2–17); smokers: NR |
2–9 months for acoustic analysis: n = 35; 21 (11–26) months for questionnaire: n = 34 | NR | Postoperative improvement in snoring symptoms (assessed by patients) | Snore periodicity (%); snore energy ratio 0–200 Hz; snore energy ratio 0–250 Hz; snore energy ratio 0–400 Hz |
| Neruntarat 200593 | 60 |
Baseline tests: PSG; oximetry; nasopharyngoscopy and lateral cephalogram Participant demographics: age: 48.3 ± 10.2 (28–50); male: n = 50 (89.3%); BMI: 26.5 ± 2.4 (25.2–28.2); AHI: 3.2 ± 1.2; ESS: 8.1 ± 3.5; smokers: NR |
14.2 ± 3.2 (12–20) months | AHI; lowest SaO2 (%); mean SaO2 (%); sleep efficiency (%); snoring index; time spent in loud snoring (%) | Severity of snoring; ESS; postoperative pain VAS; swallowing problem VAS; speech problem VAS | Cephalometric parameters |
| Ozmen 200689 | 162e |
Baseline tests: PSG; otolaryngological examinations with additional paranasal sinus CT if needed Participant demographics: age: 35.2 ± 14.1 (21–51); male: n = 114 (70%); BMI: 28.1 ± 1.2; AHI: < 5; ESS: NR; smokers: n = 135 (83%) (mean one box of cigarettes/day) |
1 month | NR | Snoring score (partner assessed); surgical procedure success | Based on n = 153: QTc min; QTc max; QTc dispersion (milliseconds); postoperative adverse events |
| Prichard 199549 | 32 |
Baseline test: PSG Participant demographics: age: men 42.5 ± 10.6, women 39.9 ± 11.7; male: n = 18 (56%); BMI: men 28.2 ± 3.06, women 25.2 ± 3.06; AHI: 4.7 (0–15); ESS: NR; smokers: NR |
6 months | AHI | Snoring grade score | P50 snoring volume parameters; L1 snoring volume parameters; L5 snoring volume parameters |
| Miljeteig 199492 | 38 |
Baseline tests: PSG; nasopharynx, oropharynx and laryngopharynx examination by an otolaryngologist Participant demographics: age: NR; male: NR; BMI: NR; AHI: 5.1 ± 2.9; ESS: NR; smokers: NR |
Total length of follow-up 45 ± 20 months; objective outcomes assessed only at 13 ± 15 months | NR | NR | Snoring index; mean sound intensity; maximal sound intensity |
Five of the studies assessed UP3 alone. 49,89,91–93 In the other two studies, Jones and colleagues94 randomised patients into two parallel groups, one which underwent traditional palatoplasty with uvulectomy (TP) and the other which underwent UEP, and Janson and colleagues90 randomised patients to either UP3 or conservative treatment. However, in both of these studies pre- and post-treatment data were pooled across the two intervention groups and reported as the difference in pre- and post-treatment means. No between-group comparisons were conducted. Both studies were therefore classified as pre–post studies. The parallel group study by Janson and colleagues90 included a total of 231 patients, of whom 155 underwent UP3. The study by Ozmen and colleagues89 included 162 patients. All of the remaining studies were quite small, having less than 60 patients each. Across the studies a total of 538 patients underwent UP3. Patient baseline characteristics in the seven studies were not reported in detail. At baseline in five of the studies49,89,92–94 patients had a PSG and in the remaining two studies90,91 patients underwent oximetry to rule out OSAS. In the four studies that reported baseline examinations to assess the site of airway narrowing the tests included clinical examination alone,90 examination by an otolaryngologist including examination of the nasopharynx, oropharynx and laryngopharynx,92 thorough physical and otolaryngological examinations with the use of flexible nasopharyngoscopy with Muller’s manoeuvre and a lateral cephalogram,93 and otolaryngological examinations with additional paranasal sinus CT if needed. 89 The other three studies did not report baseline tests of upper airway narrowing. In the study by Miljeteig and colleagues92 that contained non-apnoeic snorers and OSAS patients, the baseline characteristics in terms of age, BMI, ESS, gender composition and smoking status were not reported by subgroup. In the remaining six studies that assessed non-apnoeic snorers only, of the patients who underwent UP3 treatment, mean age at baseline ranged from 35.2 to 48.3 years, except in the study by Friberg and colleagues91 in which it was reported as a median of 26.1 years (range 18.3–35.4 years). The majority of patients in these six studies were male, with the percentage ranging from 56% to 100%. BMI in these six studies ranged from 25.2 kg/m2 to 35.4 kg/m2. Only two studies reported baseline ESS scores,94,123 and smoking status was reported in only one study. Follow-up duration of the participants in the studies varied markedly from 1 to 83 months. The mean follow-up duration in the study by Miljeteig and colleagues92 was 45 months (SD 20 months), but only sleep data were recorded separately for the non-apnoeic snorers, these outcomes being measured at 13 months after surgery.
Treatment protocols
In all seven studies UP3 was performed according to the method described by Fujita,62 but the technique differed slightly between the studies and even within the same study, depending on the patient’s anatomy. In the study by Friberg and colleagues91 the technique was modified slightly to ensure velopharyngeal sphincter function postoperatively. In the study by Janson and colleagues90 three different UP3 techniques were used. In patients who had large tonsils and/or tonsils situated high up in a narrow angle to the uvula the classic UP3 technique including tonsillectomy was used (n = 55). Patients with a prolonged clumsy uvula but small tonsils and normal posterior pillars were treated with the CO2 laser technique (n = 31). In those with small tonsils, a prolonged uvula and/or pronounced posterior pillars the classical UP3 technique was used but without tonsillectomy (n = 70). In the study by Jones and colleagues94 patients received either TP or UEP. TP consisted of transoral excision using a CO2 laser of a central strip of the soft palate mucosa extending from the junction of the hard and soft palate to the soft palate free edge, with uvulectomy, whereas UEP involved removal of a central strip of soft palate mucosa as previously described, combined with suturing the oral surface of the uvula onto the oral surface of the soft palate. We consider these techniques as modified UP3 and therefore describe and synthesise this study together with the other UP3 studies. In the study by Miljeteig and colleagues92 some participants underwent additional or concurrent nasal surgery (e.g. turbinoplasty, septoplasty) for the purpose of improving upper airway patency. Neruntarat93 used the reversible uvulopalatal flap technique, introduced by Powell. 124 In this study the mucosa, submucosa with gland, and fat on the lingual surface of the uvula and soft palate were removed by cold knife dissection. The uvular tip was then amputated and the remaining uvula reflected back towards the soft palate and fixed with multiple sutures. Ozmen and colleagues89 assessed three different UP3 techniques, general UP3, LAUP and CAUP, in a total of 162 non-apnoeic snoring patients. Details of the techniques and the number of patients undergoing each procedure were not reported. In the study by Prichard and colleagues49 UP3 was performed with slight modification to ensure that the initial vertically orientated posterior pharyngeal folds were tightened to produce slight horizontal ridges.
Outcomes
Across the studies, PSG parameters,49,91,93 objective measures of snoring sound,49,92–94 patient- or partner-reported snoring levels,49,89,90,93,94 ESS90,93 and adverse events89–91,93 were reported. Additional outcomes assessed included changes in cephalometric parameters,93 corrected QT intervals89 and surgical procedure success. 89
Overall there was very little overlap between the studies in the outcomes assessed and little consistency in the way that they had been measured. This precluded grouping the studies according to outcome measure and limited the number of comparisons that could be drawn between the studies.
Study quality
The quality of the seven studies is summarised in Table 11. The studies were generally of low quality and, in particular, the level of reporting was inadequate. Most of the studies were relatively small. Patient selection criteria and baseline characteristics were generally only partially reported; there were often no data on baseline ESS, smoking status and level of alcohol consumption. In four of the studies49,89,91,92 details of the intervention were very limited. The data collection tools were not always valid and accurate for measuring the outcome of interest and there were few standardised instruments for measuring subjective outcomes across the studies. When reported treatment compliance across the studies was good but attrition rates were relatively high. Data analyses conducted were appropriate in all studies.
| Quality criteria | Friberg 199591 | Janson 199490 | Jones 200594 | Prichard 199549 | Miljeteig 199492 | Neruntarat 200593 | Ozmen 200689 |
|---|---|---|---|---|---|---|---|
| Eligibility criteria specified? | P | P | + | P | P | P | P |
| Adequate baseline details presented? | P | P | + | + | + | P | P |
| Are any co-interventions stated? | + | ? | NA | NA | ? | NA | – |
| Compliance with treatment adequate? | ? | + | + | + | + | + | ? |
| Subgroup analysis justified? | – | + | NA | NA | + | NA | NA |
| Data collection tools valid? | P | – | P | P | P | P | P |
| Data collection tools reliable? | P | – | P | P | P | P | P |
| All participants accounted for? | – | – | – | + | – | – | + |
| Data analyses appropriate? | + | + | + | + | – | + | + |
| Greater than 80% of patients followed up? | + | ? | – | + | + | + | + |
| Generalisability | P | P | + | + | + | P | P |
| Intercentre variability | NA | ? | NA | NA | NA | NA | NA |
Results
Friberg and colleagues91 undertook UP3 on 56 non-apnoeic snorers and reported both subjective results and objective sleep data measured at a median time of 63 months’ (range 37–83 months) follow-up. Postoperative sleep recording was performed in 53 patients. A significant worsening from baseline to follow-up was observed for the median oxygen desaturation index [ODI; increased from 0 (range 0–24) to 1 (range 0–24)]; the median duration of obstructive respiratory pattern [increased from 8% (range 0–43%) to 17% (range 0–74%)]; and the median nadir SaO2 level [decreased from 92% (97–84%) to 88% (95–73%). Consistent with these changes in oxygen saturation levels and obstructive respiratory pattern, the authors indicated that, according to the postoperative recording results, six patients developed mild to moderate OSAS after the surgery.
In the study median BMI also increased significantly after surgery (p = 0.0005). Changes in both ODI and obstructive respiratory pattern were significantly correlated with changes in BMI (p = 0.0003). Five of the six patients in whom OSAS developed postoperatively had gained weight.
Of 51 patients who preoperatively reported EDS, the number (%) of patients reporting no EDS, improvement in daytime sleepiness or no change in EDS after the operation was 29 (57%), 8 (16%) and 14 (27%) respectively. All of the 56 patients in the study preoperatively complained of having loud snoring. At follow-up 15 (27%) reported no snoring at all, 34 (60%) reported less snoring and seven (13%) reported persistent snoring. Overall, 87% of the patients with snoring were improved or cured. In none of the patients did snoring become worse. Of those who still snored, the majority reported that the snoring was much less loud but more high pitched. Changes in BMI correlated significantly with the degree of postoperative snoring (p = 0.04) but not with the degree of EDS (p = 0.13) and snoring.
No serious postoperative complications were observed. Of the 56 patients, seven reported minor throat disturbances such as dryness or increased mucous secretion, and one reported a change in voice quality.
Janson and colleagues90 assessed 231 patients: 155 underwent one of three UP3 procedures and 76 underwent conservative treatment. Subjective outcomes were reported in the 155 patients who underwent a UP3 procedure. All of the 155 patients classified their symptoms on a 5-point scale, multiple choice questionnaire. The questionnaire consisted of 16 symptom-related questions. Postoperative outcomes were assessed in 105 patients at 3 months and 50 patients at 12 months. Only a mixture of results for the two time points was reported. Subjective outcomes measured were the percentage of patients who reported either moderate or occasional problems, or severe or frequent problems, with snoring, involuntarily falling asleep, falling asleep when relaxing, difficulty staying awake when driving, daytime tendency to take a nap, difficulty maintaining sleep or inducing sleep, awakening because of trouble breathing, daytime tiredness and morning headache. All of the measured outcomes showed a statistically significant improvement after UP3. A summary of the percentage of patients reporting each problem pre-and postoperatively is displayed in Table 12 below.
| Problem | Moderate problem (%) | Severe problem (%) | ||
|---|---|---|---|---|
| Pretreatment | Post-treatment | Pretreatment | Post-treatment | |
| Snoring | 4 | 21 | 96 | 18 |
| Involuntarily falling asleep | 23 | 6 | 12 | 3 |
| Falling asleep when relaxing | 30 | 29 | 50 | 26 |
| Difficulty staying awake when driving | 21 | 6 | 8 | 1 |
| Daytime tendency to take a nap | 26 | 20 | 20 | 6 |
| Difficulty in maintaining sleep | 33 | 19 | 27 | 10 |
| Difficulty in inducing sleep | 14 | 11 | 7 | 4 |
| Trouble breathing causing awakening | 24 | 7 | 13 | 3 |
| Daytime tiredness | 31 | 30 | 54 | 7 |
| Morning headache | 29 | 10 | 15 | 2 |
Limited results at 1 year of follow-up after UP3 versus conservative treatment were reported by the authors in graphs and minimally in the text. It was unclear whether the p-values stated in the text were for the moderate/occasional problems, severe or frequent problems, or the total of both categories. The specific figures from the graphs were therefore not extracted. The authors indicated that after treatment the UP3 patients had significantly lower symptom scores than the conservatively treated patients for tendency to take a nap in the daytime (p < 0.05), EDS, morning headache (p < 0.01), difficulty in maintaining sleep, snoring, and waking because of trouble breathing (p < 0.001); significantly more patients in the UP3 group also felt rested on awakening in the morning (p < 0.01).
The side effects of UP3 observed in this study were minor, with a total of 42 patients experiencing events. In total, 35% of the 42 patients had undergone the classical (standard) UP3 treatment and 23% had undergone either the CO2 laser treatment or UP3 without tonsillectomy. The most frequent events were irritation in the throat (19 patients) followed by hypersecretion in the throat (four patients), nasal speech (three patients), nasal regurgitation (three patients) and tendency to vomit (one patient).
In the study by Jones and colleagues94 54 patients were randomised into two parallel groups to undergo either TP or UEP. Pre- and post-treatment data on 35 patients (16 in the TP group and 19 in the UEP group) were pooled across the two groups and reported as the difference between pre- and postoperative scores. At the first follow-up visit (mean 2.5 months) there was a significant decrease from baseline in the median (90th centile) measures of snore periodicity, from 87.5% (80–94%) to 84.0% (73–88%); however, this was not maintained at the second follow-up visit (mean 9.7 months), with a slight increase to 84.5% (73.5–91.5%). Acoustic parameters of the median (90th centile) snoring sound energy ratios for the frequency bands 0–200 Hz, 0–250 Hz and 0–400 Hz all demonstrated significant improvement from baseline at the first follow-up visit, being 74 (37–87), 83 (42–93), and 95 (56–97) at baseline, respectively, but reduced to 58.5 (18–83), 73 (18–86.5) and 85 (49.5–95.5) at the first visit respectively. Again, however, there was no significant difference from baseline values at follow-up visit two, with increases to 67 (14–89) in the 0- to 200-Hz band, 74 (27–93) in the 0- to 250-Hz band and 89 (50–97.5) in the 0- to 400-Hz band; of these, the snoring energy ratio of the 0- to 250-Hz band reached marginal significance. The authors indicated that a paired comparison of snore loudness between the early and late postoperative recordings showed a significant increase in snore loudness between recordings (p < 0.001).
The authors also reported that age, peak nasal inspiratory flow rate (measured as the best of three maximum rates), ESS and reported alcohol intake (units/week) were unrelated to either the early improvement or subsequent decline in the acoustic parameters after surgery.
At a median time of 21 months (range 11–26) after the surgery, based on 34 patients, 11.8% reported no improvement in snoring symptoms, 55.9% reported an improvement that was sustained for 1 year or less, and 32.3% reported an improvement that was sustained until the assessment time. The authors indicated that the objective acoustic outcomes were not correlated with the subjective outcomes on an individual patient level. Adverse events were not reported in this study.
In the study by Miljeteig and colleagues,92 which included both non-apnoeic snorers and patients with OSAS, only the objective outcomes of SI and sound intensity for 38 non-apnoeic snorers measured at a mean of 13 (SD 15) months’ follow-up were reported and compared with baseline values. The mean SI increased from 252 (SD 280) events/hour before surgery to 296 (SD 318) events/hour after surgery, but the change was not statistically significant. Changes in mean sound intensity from 64.8 dB (SD 7.2) at baseline to 65.4 dB (SD 7.0) post-treatment, and mean maximal sound intensity from 85.3 dB (SD 12.3) before surgery to 80.5 dB (SD 14.5) after surgery, were also not statistically significantly different. Adverse events were not reported in this study.
The study by Neruntarat93 assessed the effects of a reversible uvulopalatal flap. Data from 56 patients on subjectively assessed outcomes, cephalogram and PSG measured both at baseline and at a mean of 14.2 months (range 12–20) after the operation were analysed. Snoring sound was measured with a microphone placed at the trachea. Severity of snoring was graded by the patient’s bed partner or observer using a 10-cm VAS, with ‘no snoring’ and ‘severe snoring’ used as anchors. A 10-point VAS for postoperative pain, difficulty in swallowing and changes in speech was completed by the patients daily for 10 days postoperatively. Comparing the pre- and postoperative values, there were changes in the following variables: mean AHI score decreased from 3.2 (SD 1.2) to 3.0 (SD 1.8); sleep efficiency decreased from 88.6% (SD 8.6%) to 87.5% (SD 10.4%); mean lowest oxygen saturation increased from 86.4% (SD 9.6%) to 88.2% (SD 5.5%); and mean oxygen saturation increased from 95.2% (SD 1.8%) to 96.2% (SD 2.1%); however, none of these changes was significant. Significant changes were observed in the following variables: mean SI, from 245.8 (SD 40.8) events/hour to 42.5 (SD 20.7) events/hour; mean time spent in loud snoring, from 10.2% (SD 1.5%) to 3.8% (SD 2.8%); partner-assessed mean severity of snoring 10-point VAS score, from 8.2 (SD 3.4) to 2.6 (SD 1.4); and mean ESS, from 8.1 (SD 3.5) to 5.2 (SD 3.2). Snoring was considered to be cured if the bed partner-assessed VAS score was less than half of that at baseline. Based on this criterion the problem was eliminated in 88% (49/56) of patients. A positive and significant correlation was found between the changes in percentage of time spent in loud snoring and the changes in subjective severity of snoring VAS score (r = 0.42, p < 0.05), and between the changes in SI and the changes in subjective severity of snoring VAS score (r = 0.38, p < 0.05). Cephalometric data showed a significant decrease in two parameters: the length from posterior nasal spine to uvula (PNS-P) and the palatal width (PW). No significant changes were observed in the sella-nasion-point A angle (SNA), the sella-nasion-point B angle (SNB), the posterior airway space (PAS) or the length between mandibular plane and hyoid bone (MP-H). A summary of the pre- and post-treatment cephalometric data is displayed in Table 13.
| PNS-P (mm) | PW (mm) | SNA (°) | SNB (°) | PAS (mm) | MP-H (mm) | |
|---|---|---|---|---|---|---|
| Pretreatment | 45.7 ± 4.1 | 10.4 ± 2.1 | 80.5 ± 3.4 | 79.2 ± 2.9 | 10.2 ± 2.4 | 18.5 ± 3.2 |
| Post-treatment | 42.01 ± 2.8 | 8.4 ± 2.4 | 80.2 ± 4.5 | 79.5 ± 3.4 | 10.4 ± 3.2 | 18.2 ± 4.1 |
| p-value | < 0.001 | < 0.05 | NS | NS | NS | NS |
There was minimal morbidity associated with treatment. After the procedure the mean VAS scores for pain, swallowing problems and speech problems decreased from 6.9, 4.4 and 2.2, respectively, on day 1 to 1.1, 0.5 and 0.2, respectively, on day 10. Most patients (52/56) had mild to moderate pain (VAS score ≤ 7) for 5–7 days after the procedure. Two (4%) patients reported transient nasal regurgitation and one (2%) patient reported foreign body sensation. Bleeding, dysphagia, infection and nasopharyngeal stenosis were not observed.
In their study Ozmen and colleagues89 aimed to assess the association between snoring and excess risk for cardiac events by specifically assessing the effects of UP3 on QT dispersion. A total of 162 patients underwent one of three surgical procedures: general UP3, LAUP or CAUP. The number of patients in each of the procedure groups was not reported.
Surgical procedure success was assessed by the patient’s partner using a six-level snoring assessment table (from 0 indicating no snoring to 5 indicating snoring with hypopnoea or apnoea). At follow-up nine (6%) patients had a score of 2 and were considered to have mild or moderate snoring. They were therefore judged to have no improvement. Surgery was therefore classified as successful in 153 patients (94%). ECG data of corrected QT interval parameters QTc min, QTc max and QTc dispersion were analysed based on 153 patients who postoperatively had a 6-level snoring assessment score of < 2. Significant changes were found in all of the three variables. A summary of the mean pre- and post-treatment scores is displayed in Table 14.
| QTc min (milliseconds) | QTc max (milliseconds) | QTc dispersion (milliseconds) | |
|---|---|---|---|
| Pretreatment | 381.3 ± 7.8 | 449.6 ± 6.2 | 68.2 ± 8.4 |
| Post-treatment | 397.0 ± 5.9 | 440.0 ± 20.8 | 43.8 ± 6.2 |
| p-value | < 0.001 | < 0.001 | < 0.001 |
In this study no complications were observed.
Prichard and colleagues49 reported changes in objective measurements during sleep from baseline to 6 months post UP3 for 32 non-apnoeic snorers. No significant change in AHI was found after UP3. Snoring sound level was measured. The objective indices of snoring used were the proportion of sleep time during which the level exceeded 50 dB (P50) and the sound level (dB) above which 1% and 5% of the sound occurred (L1 and L5). A significant reduction in the snoring sound level was observed in the supine posture for all of the three indices, with the percentage of sleep time that exceeded 50 dB (median value) being 1.12 at baseline and 0.36 post treatment, the level above which 1% of the sound occurred (median value) being 50.6 dB preoperatively and 46.3 dB postoperatively, and the level above which 5% of the sound occurred (median value) being 43.6 dB preoperatively and 38.8 dB postoperatively.
Subjective snoring grade was assessed by the patient’s partner using the responses ‘nil’, ‘mild’, ‘moderate’ or ‘severe’, scoring 0, 1, 2 or 3 respectively. Decreases in snoring grades were observed. At baseline the percentage of partners reporting snoring being moderate and severe was 25% and 75% respectively; after surgery these values reduced to 18.8% and 12.5% respectively. Also, after surgery 15.6% reported no snoring and 53.1% reported mild snoring. The significance of the differences was not assessed statistically. No adverse events were reported.
A summary of the study results for PSG parameter outcomes, objectively assessed snoring sound outcomes, subjectively assessed snoring levels and adverse events are displayed in Tables 15–18 respectively. A further overall summary of the key study results is displayed in Table 19.
| Friberg 199591 | Janson 199490 | Jones 200594 | Miljeteig 199492 | Neruntarat 200593 | Ozmen 200689 | Prichard 199549 | ||
|---|---|---|---|---|---|---|---|---|
| Number of non-apnoeic snorers in study on UP3 | 56 | 155 | 35 | 38 | 60 | 162 | 32 | |
| Outcomes | ||||||||
| AHI (events/hour) | Pre | 3.2 ± 1.2 | 4.7 (0–15) | |||||
| Post | 3.0 ± 1.8 | 6.8 | ||||||
| p-value | NS | NS | ||||||
| ODI | Pre | 0 (0–24)b | ||||||
| Post | 1 (0–24)b | |||||||
| p-value | 0.0005 | |||||||
| Nadir SaO2 (%) | Pre | 92 (97–84)b | 86.4 ± 9.6 | |||||
| Post | 88 (95–73)b | 88.2 ± 5.5 | ||||||
| p-value | 0.0001 | NS | ||||||
| Mean SaO2(%) | Pre | 95.2 ± 1.8 | ||||||
| Post | 96.2 ± 2.1 | |||||||
| p-value | NS | |||||||
| Sleep efficiency (%) | Pre | 88.6 ± 8.6 | ||||||
| Post | 87.5 ± 10.4 | |||||||
| p-value | NS | |||||||
| Duration of obstructive respiratory pattern (%) | Pre | 8 (0–43)b | ||||||
| Post | 17 (0–74)b | |||||||
| p-value | 0.004 | |||||||
| Mild to moderate OSAS post-treatment | n = 6 (11%) | |||||||
| Friberg 199591 | Janson 199490 | bJones 200594 | Miljeteig 199492 | Neruntarat 200593 | Ozmen 200689 | Prichard 199549 | ||
|---|---|---|---|---|---|---|---|---|
| Number of non-apnoeic snorers in study on UP3 | 56 | 155 | 35 | 38 | 60 | 162 | 32 | |
| Outcomes | ||||||||
| Mean sound intensity (dB) | Pre | 64.8 ± 7.2 | ||||||
| Post | 65.4 ± 7.0 | |||||||
| p-value | 0.65 | |||||||
| Maximal sound intensity (dB) | Pre | 85.3 ± 12.3 | ||||||
| Post | 80.5 ± 14.5 | |||||||
| p-value | 0.84 | |||||||
| Snore energy ratio 0–200 Hz | Pre | 74 (37–87) | ||||||
| Post | T1: 58.5 (18–83); T2: 67 (14–89) | |||||||
| p-value | Pre vs T1: 0.02; pre vs T2: 0.077 | |||||||
| Snore energy ratio 0–250 Hz | Pre | 83 (42–93) | ||||||
| Post | T1: 73 (28–86.5); T2: 74 (27–93) | |||||||
| p-value | Pre vs T1: 0.002; pre vs T2: 0.039 | |||||||
| Snore energy ratio 0–400 Hz | Pre | 95 (56–97) | ||||||
| Post | T1: 85 (49.5–95.5); T2: 89 (50–97.5) | |||||||
| p-value | Pre vs T1: 0.047; pre vs T2: 0.162 | |||||||
| P50c | Pre | 1.49, 1.12, 0.4 | ||||||
| Post | 0.32, 0.36, 0.17 | |||||||
| p-value | 0.04, 0.01, 0.38 | |||||||
| L1c | Pre- | 51.6, 50.6, 45.6 | ||||||
| Post- | 45.3, 46.3, 42.8 | |||||||
| p-value | 0.01, 0.01, 0.21 | |||||||
| L5c | Pre | 41.0, 43.6, 39.9 | ||||||
| Post | 38.8, 38.8, 36.5 | |||||||
| p-value | 0.1, 0.01, 0.58 | |||||||
| SI (events/hour) | Pre | 252 ± 280d | 245.8 ± 40.8 | |||||
| Post | 296 ± 318d | 42.5 ± 20.7 | ||||||
| p-value | 0.70 | < 0.05 | ||||||
| Time spent in loud snoring (%) | Pre | 10.2 ± 1.5 | ||||||
| Post | 3.8 ± 2.8 | |||||||
| p-value | < 0.001 | |||||||
| Snore periodicity (%) | Pre | 87.5 (80–94) | ||||||
| Post | T1: 84.0 (73–88); T2: 84.5 (73.5–91.5) | |||||||
| p-value | Pre vs T1: < 0.001; pre vs T2: < 0.079 | |||||||
| Friberg 199591 | Janson 199490 | Jones 200594 | Miljeteig 199492 | Neruntarat 200593 | Ozmen 200689 | Prichard 199549 | |
|---|---|---|---|---|---|---|---|
| Number of non-apnoeic snorers on UP3 | 56 | 155 | 35 | 38 | 60 | 162 | 32 |
| Outcomes | |||||||
| Partner-assessed snoring: 10-cm VAS | Pre 8.2 ± 3.4, post 2.6 ± 1.4; p < 0.05 | ||||||
| Partner-assessed snoring: 6-point VAS | Pre: 100% of patients with a 6-point VAS of ≤ 4; post: 6% of patients with a 6-point VAS of 2 | ||||||
| Patients reporting snoring being a problem | MO: pre 4%, post 21%; SF: pre 96%, post 18% | ||||||
| Patients reporting no postoperative snoring | 27% | 15.6% | |||||
| Patients reporting postoperative decrease in snoring | 60% | ||||||
| Patients reporting postoperative loud persistent snoring | 13% | ||||||
| Patients reporting mild snoring | Pre 0%, post 53.1% | ||||||
| Patients reporting moderate snoring | Pre 25%, post 18.8% | ||||||
| Patients reporting severe snoring | Pre 75%, post 12.5% | ||||||
| Patients reporting postoperative snoring symptoms: | |||||||
| No improvement | 11.8% | ||||||
| An improvement sustained for ≤ 1 year | 55.9% | ||||||
| An improvement ‘until now’ | 32.3% | ||||||
| ESS | Pre 8.1 ± 3.5, post 5.2 ± 3.2; p < 0.001 | ||||||
| Patients reporting excessive daytime sleepiness: | |||||||
| No longer | 57% | ||||||
| Improved | 16% | ||||||
| No change | 27% | ||||||
| Patients reporting involuntarily falling asleep | MO: pre 23%, post 6%; SF: pre 12%, post 3% | ||||||
| Patients reporting falling asleep when relaxing | MO: pre 30%, post 29%; SF: pre 50%, post 26% | ||||||
| Patients reporting difficulty staying awake when driving | MO: pre 21%, post 6%; SF: pre 8%, post 1% | ||||||
| Patients reporting daytime tendency to take a nap | MO: pre 26%, post 20%; SF: pre 20%, post 6% | ||||||
| Patients reporting difficult in maintaining sleep | MO: pre 33%, post 19%; SF: pre 27%, post 10% | ||||||
| Patients reporting difficulty in inducing sleep | MO: pre 14%, post 11%, p < 0.05; SF: pre 7%, post 4%, p < 0.05 | ||||||
| Patients reporting trouble breathing causing awakening | MO: pre 24%, post 7%; SF: pre 13%, post 3% | ||||||
| Patients reporting daytime tiredness | MO: pre 31%, post 30%; SF: pre 54%, post 7% | ||||||
| Patients reporting morning headache | MO: pre 29%, post 10%; SF: pre 15%, post 2% | ||||||
| Study | Postoperative adverse events |
|---|---|
| Friberg 199591 | Serious complications: 0. Long-term adverse events (n/N): patients with minor throat disturbances such as dryness or increased mucous secretion: 7/56; patients reporting a change in voice quality: 1/56 |
| Janson 199490 |
Total number of patients with minor side effects: n = 42; irritation in the throat: 19; nasal speech: 3; hypersecretion in the throat: 4; nasal regurgitation: 3; tendency to vomit: 1 Patients who had standard technique and side effects: 35%; patients who had CO2 laser treatment and side effects: 23%; patients who had UP3 performed under local anaesthesia and side effects: 23% |
| Jones 200594 | NR |
| Miljeteig 199492 | NR |
| Neruntarat 200593 | Mean VAS (0 = none; 10 = excruciating or intense pain/extreme difficulty talking/unable to swallow without pain even after analgesic medication) for speech dropped from 2.2 in day 2 to 0.2 in day 10; for swallowing problem dropped from 4.4 in day 1 to 0.5 in day 10; for pain dropped from 6.9 in day 1 to 1.1 in day 10 |
| Ozmen 200689 | No complications |
| Prichard 199549 | NR |
| Study ID | n | Subjective outcomes | Objective snoring indices | PSG parameter outcomes | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Partner-assessed snoring severity (VAS) | Patients reporting no postoperative snoring | Patients reporting postoperative decrease/improvement in snoring | Patients reporting postoperative loud persistent snoring | Patients reporting either ‘moderate or occasional’ problems, or ‘severe or frequent’ problems, with snoring | Patients reporting either ‘moderate or occasional’ problems, or ‘severe or frequent’ problems, with sleeping difficulties | Patients reporting either ‘moderate or occasional’ problems, or ‘severe or frequent’ problems, with excessive daytime sleepiness | ESS | SI (events/hour) | Mean sound intensity (dB) | Maximal sound intensity (dB) | Snore energy ratio 0–200, 0–250 or 0–400 Hz (at short-term visit) | Snore energy ratio 0–200 or 0–400 Hz (at long-term visit) | Snore energy ratio 0–250 Hz (at long-term visit) | Snore periodicity (%) at short-term visit | Snore periodicity (%) at long-term visit | Time spent in loud snoring | Supine position with snoring sound level of P50, L1 or L5 | Lateral position with snoring sound level of P50, L1 or L5 | AHI | ODI | Nadir SaO2 (%) | Mean SaO2 (%) | Sleep efficiency (%) | Duration of obstructive respiratory pattern (%) | Patients with mild to moderate OSAS | ||
| Friberg 199591 | 56 | 27% | 60% | 13% | × | × | × | n = 6 (11%) | |||||||||||||||||||
| Janson 199490 | 155 | + | + | + | |||||||||||||||||||||||
| Jones 200594 | 35 | + | – | + | + | – | |||||||||||||||||||||
| Miljeteig 199492 | 38 | – | – | – | |||||||||||||||||||||||
| Neruntarat 200593 | 60 | + | + | + | + | – | – | – | – | ||||||||||||||||||
| Ozmen 200689 | 162 | 94% | |||||||||||||||||||||||||
| Prichard 199549 | 32 | 15.6% | + | – | – | ||||||||||||||||||||||
Summary of the results
The quality of the seven identified pre–post studies was generally poor, with small sample sizes ranging from 32 to 162. As there was little overlap between the studies with respect to the outcomes assessed it was difficult to aggregate the data and make useful comparisons between the studies.
Subjectively assessed snoring outcomes
Two studies, by Neruntarat93 and Janson and collegues,90 found a significant postoperative improvement in snoring outcomes. The study by Neruntarat93 (n = 56) assessed snoring with a 10-cm VAS and reported a mean (SD) reduction from 8.2 (3.4) at baseline to 2.6 (1.4) postoperatively. The study by Janson and colleagues90 (n = 155) detailed the percentage of patients reporting either ‘moderate or occasional’ or ‘severe or frequent’ problems with snoring; the percentage of patients reporting ‘moderate or occasional’ problems with snoring increased from 4% preoperatively to 21% postoperatively, whereas those reporting ‘severe or frequent’ problems with snoring decreased from 96% preoperatively to 18% postoperatively.
An overall improvement in snoring was reported by two studies. One study (n = 56) found that 27% of patients reported no postoperative snoring, 60% reported a decrease in snoring and 13% reported loud persistent snoring. In none of these patients had snoring become worse. Overall, 87% of the patients with snoring were improved or cured. The other study (n = 162) found that 94% of partners of patients reported an improvement in snoring.
One study (n = 32) reported different levels of snoring and found that, preoperatively, 75% of patients reported severe snoring and 25% reported moderate snoring, whereas, postoperatively, 12.5% reported severe snoring, 18.8% reported moderate snoring, 52.1% reported mild snoring and 15.6% reported no snoring.
Epworth Sleepiness Scale
One study (n = 60) assessed pre- and postoperative ESS and found a significant reduction from 8.1 (SD 3.5) to 5.2 (SD 3.2), respectively; however, with a preoperative mean ESS below 12, the reduction in the ESS may have little clinical relevance.
One study (n = 155) assessed the percentage of patients reporting either ‘moderate or occasional’ or ‘severe or frequent’ problems with EDS. A significant improvement in both of these outcomes was observed.
Another study91 (n = 56) reported postoperative EDS status and found that, of the 51 patients who preoperatively reported EDS, 57% no longer had EDS, 16% saw an improvement and 27% remained unchanged.
Other subjective outcomes
A range of measures of sleep problems were reported in one study (n = 56). The percentage of patients having each type of problem decreased significantly following UP3.
Objectively assessed snoring sound level
Relevant objective outcomes were reported in five of the seven identified studies.
Snoring sound intensity was reported in one study (n = 38); no significant pre–post changes in either the mean or maximal sound intensity were found. Pre- and postoperative snoring sound energy ratios were reported in one study (n = 35). Median (90th centile) snoring sound energy ratios for the frequency bands 0–200 Hz, 0–250 Hz and 0–400 Hz showed significant reductions from 74 (37–87), 83 (42–93) and 95 (56–97), respectively, at baseline to 58.5 (18–83), 73 (28–86.5) and 85 (49.5–95.5) at the short-term follow-up (mean 2.5 months). However, there were no significant differences from baseline values at the long-term follow-up (mean 9.7 months). Snoring volume parameters were reported in one study (n = 32). A significant reduction in the snoring sound level was observed in the supine position for all three indices: the percentage of sleep time during which the level exceeded 50 dB and the sound level above which 1% and 5% of the sound occurred. There was no significant reduction in snoring volume in the lateral sleeping posture. SI was reported in two studies. One study (n = 60) reported a significant reduction, whereas the other (n = 38) showed no significant change. The mean percentage of time spent in loud snoring was reported in one study (n = 60); there was a significant reduction from 10.2% (SD 1.5%) at baseline to 3.8% (2.8%) post-treatment. Snore periodicity was reported in one study (n = 35). The median (90th centile) percentage of snore periodicity decreased significantly from 87.5% (80–94%) at baseline to 84.0% (73–88%) at short-term follow-up (mean 2.5 months). This was not maintained at long-term follow-up (mean 9.7 months).
Other objective outcomes
QT intervals were reported in one study in 162 patients. Postoperative QTc max and QTc dispersion values were significantly shortened and postoperative QTc min values were significantly increased.
PSG parameter results
Three of the seven studies reported PSG parameter outcomes. AHI was reported in two studies (n = 60 and n = 32). No statistically significant changes were reported following the treatment.
Mean nadir SaO2, mean SaO2 and sleep efficiency were reported in one study (n = 60); these outcomes showed no significant pre- to postoperative changes. However, another study (n = 56) reported the median oxygen desaturation index, median duration of obstructive respiratory pattern and median nadir SaO2 in 53 patients and found significant worsening in these outcomes. In this study, according to the postoperative recording results, six patients were categorised as having mild to moderate OSAS postoperatively. In the study, median BMI also increased significantly after surgery. Changes in both ODI and obstructive respiratory pattern were significantly correlated with changes in BMI. Five of the six patients in whom OSAS developed postoperatively had gained weight.
Cephlometric measurement results
Cephalometric parameter results were reported in one study (n = 60). There were significant reductions in the mean distance between the posterior nasal spine and the soft palate, from 45.7 (SD 4.1) mm to 42.01 (SD 2.8) mm, and in the palatal width, from 10.4 (SD 2.1) mm to 8.4 (SD 2.4) mm. There were no changes in either the skeletal or the soft tissues measurements at the tongue base.
Adverse events
When reported, no or only minor morbidity was associated with the treatment, with postoperative pain, throat disturbances/irritation and speech and swallowing problems being the most common events. Most patients reported mild to moderate pain after the procedure that improved to minimal levels 10 days postoperatively. However, as only four studies reported adverse events it is difficult to draw any comparisons between the studies or make any firm generalisations.
Conclusions
Limited evidence from poor-quality studies showed that, for the treatment of non-apnoeic snorers, UP3 seemed to improve subjectively assessed snoring and reduce snoring-related problems, EDS and sleeping difficulties. On objectively assessed outcomes UP3 seemed to reduce snoring volume in the supine sleeping position and the percentage of sleeping time spent in loud snoring, and reduce snoring sound energy ratios and snore periodicity at short-term follow-up. UP3 also seemed to reduce the palatal width and the distance between the posterior nasal spine and soft palate. Evidence on SI and oxygen saturation levels is equivocal.
Based on the limited results, adverse events associated with UP3 appeared to be minor, with postoperative throat disturbances and pain being the most common.
Laser-assisted uvulopalatoplasty alone
Quantify and quality of the studies
Three pre–post studies were identified that evaluated the effects of LAUP alone for the treatment of non-apnoeic snoring. Of the three studies, one by Lauretano and colleagues96 completed LAUP on a sample of 52 patients, but the study only included 12 non-apnoeic snorers. The other two studies, by Berger and colleagues95 and Neuruntarat,114 only included 14 and 32 patients respectively. The total number of non-apnoeic snorers in the three studies was therefore 58. In the study by Lauretano and colleagues96 the objective outcomes analysed for non-apnoeic snorers were based on only three patients who underwent a postoperative PSG test. In this study baseline data for non-apnoeic snorers were based on a total of 32 patients who were recruited, not just the 12 non-apnoeic snorers who completed treatment. The mean age of patients in the three studies ranged from 35.2 to 51.2 years. The proportion of male patients ranged from 71% to 91%. Mean follow-up duration ranged from 2 months to 10.1 months. Patients in all three studies had a PSG test at baseline and mean AHI was reported. Mean BMI in these studies ranged from 26.2 kg/m to 28.08 kg/m2. None of the studies reported baseline ESS scores, smoking status or the level of alcohol consumption of patients. A summary of the study characteristics are displayed in Table 20.
| Study ID | Study design | n | Participants | Follow-up duration | Outcomes | ||
|---|---|---|---|---|---|---|---|
| PSG test | Subjective | Objective | |||||
| Berger 200195 | Pre–post | 14 |
Baseline tests: PSG; oximetry Participant demographics: age: 51.2 ± 7.5 (40–66); male: n = 10 (71%); BMI: 26.7 ± 3.7; AHI: 3.4 ± 2.1 (0–5.0); ESS: NR; smokers: NR |
10.1 ± 7.9 months | AHI; lowest SaO2 (%) | Snoring status (categorised); number of patients having five sleep-related symptoms at last follow-up visit; adverse events: pain duration; away from work because of severe pain; number with persistent throat dryness or itching; number exhibiting difficulty in nasal breathing | NR |
| bLauretano 199796 | Pre–post | 12 |
Baseline tests: PSG; oximetry Participant demographics: age: 47.13 ± 11.11 (19–83); male: n = 25 (78%); BMI: 28.08 ± 3.44 (22.4–35.4); AHI: 4.22 ± 3.24 (0–12.97); ESS: NR; smokers: NR |
2 months after last LAUP session | Based on n = 3: AHI; mean O2 desaturation (%); lowest O2 desaturation (%) | Based on n = 12: patients status of snoring (improved, no change or worse); patient satisfaction with LAUP (satisfied, neutral or unsatisfied) | NR |
| Neruntarat 2003114 | Pre–post | 35 |
Baseline tests: PSG Participant demographics: age: 35.2 ± 16.4 (22–54); male: n = 32 (91%); BMI: 26.2 ± 4.2 (20.5–28.2); AHI: < 5 for every patient; ESS: NR; smokers: NR |
5.2 ± 2.3 (4–6) months | NR | Severity of snoring VAS; nasal obstruction VAS; rhinorrhea; pruritus; sneezing; adverse event: postoperative pain | Nasal resistance |
Treatment protocols
The surgical mode of LAUP differed between the studies. In the study by Berger and colleagues95 two surgical techniques, type 1 and type 2 LAUP, were used, differing with respect to the mode of midline palatal vaporisation. Nine patients underwent type 1 LAUP, in which the uvular base was excised through the full palatal depth and then extended bilaterally to the anterior and posterior tonsillar pillars. Serial laser tonsillectomy was also performed, carried out in one to two sessions (mean 1.22). Five patients underwent type 2 LAUP, in which through-and-through full-thickness vertical trenches were created on the free edge of the soft palate, on either side of the uvula. The core of the uvula was removed from the bottom up in a ‘fishmouth’ manner, while the mucosa of the uvula was preserved. The uvula was shortened and thinned by up to 80–90% of the original size. Again, this was carried out in one to two sessions (mean 1.4). In the study by Lauretano and colleagues96 a hand-held CO2 laser was used to resect a wedge or crescent of soft palate on each side of the uvula and then ablate the uvula itself. Silver nitrate was applied in some cases for additional haemostasis. The palate was allowed to heal by secondary intention and the next LAUP session was performed 4–6 weeks later. The mean number of sessions was 2.5. In the study by Neruntarat114 laser-assisted septoplasty was performed in conjunction with LAUP and some patients also additionally underwent laser turbinectomy. The number of treatment sessions was not reported. Because of the use of a concomitant intervention the results of this study are more likely to be confounded than the results of the studies by Berger and colleagues95 and Lauretano and colleagues96 in terms of assessing the treatment effects of LAUP.
Outcomes
The objective outcomes assessed were PSG parameters95,96 and nasal resistance. 114 Subjective measures of patient- and partner-reported snoring levels included snoring severity scores114 and patient’s snoring status. 95,96 Snoring severity was partner assessed by Neruntarat114 using a 10-cm VAS with ‘no snoring’ and ‘severe snoring’ used as anchors. Snoring was considered to be cured in the study if follow-up scores were less than half those of baseline scores. Snoring status in the study by Berger and colleagues95 was measured using a scale with ratings of ‘improved’, ‘no change’ or ‘worse’, whereas Laurentano and colleagues96 assessed snoring status using a 7-point scale (1 = much worse, 4 = no change, 7 = much improved). Berger and colleagues additionally assessed levels of ESS and sleep-related symptoms. 95 The specific symptoms included: (1) night awakening, (2) morning fatigue, (3) daytime somnolence, (4) episodes of sleep apnoea and (5) involuntary body movements during sleep. These were categorised as ‘improved’, ‘no change’ or ‘worse’. The first three questions were addressed to the patients and the remaining two to their bed partners.
Nasal obstruction and nasal symptoms were additionally assessed by Neruntarat114 and adverse events were reported in two of the studies. 95,114
Study quality
The quality of the three studies (indicators summarised in Table 21) was generally low, with very small sample sizes. Inclusion and exclusion criteria were only well defined in one study. 114 None of the studies reported adequate baseline data on the participants. Compliance with treatment was adequate in all three studies; however, the data collection tools were not always valid and accurate in measuring the outcome of interest, i.e. all three studies assessed the level of snoring severity or status subjectively and therefore the results may be biased for this outcome. Two of the studies accounted for all of the participants in the analysis,95,114 but in the study by Lauretano and colleagues96 postoperative PSG results were only measured in three of the 12 patients. Data analyses conducted in two studies were appropriate95,114 and in one study96 the method was not reported.
| Quality criteria | Berger 200195 | Lauretano 199796 | Neruntarat 2003114 |
|---|---|---|---|
| Eligibility criteria specified? | – | P | + |
| Adequate baseline details presented? | P | P | P |
| Are any co-interventions stated? | NA | NA | + |
| Compliance with treatment adequate? | + | + | + |
| Subgroup analysis justified? | NA | + | NA |
| Data collection tools valid? | P | P | P |
| Data collection tools reliable? | P | P | p |
| All participants accounted for? | + | – | + |
| Data analyses appropriate? | + | ? | + |
| Greater than 80% of patients followed up? | + | – | + |
| Generalisability | + | + | P |
| Intercentre variability | NA | ? | NA |
Results
Berger and colleagues95 followed up patients at 4 weeks postoperatively and at a mean of 10.1 months (SD 7.9) after completion of LAUP treatment. At the short-term follow-up the snoring status in 79% of the patients was improved, in 14% it remained unchanged and in 7% it became worse. At the long-term follow-up the improvement declined, with 57% reporting improvement, 21% remaining unchanged and 21% becoming worse.
Assessment of sleep-related symptoms at long-term follow-up showed that 57% of the patients reported an improvement, whereas 36% reported no change and 7% felt worse. The changes were not tested for statistical significance. LAUP appeared to have no adverse effects on either AHI scores or the lowest SaO2 level, with no significant difference in changes in either parameter observed between baseline and follow-up. The specific point estimates for both outcomes and the associated variance are reported in Table 22.
| Berger 200195 | Lauretano 199796 | Neruntarat 2003114 | ||
|---|---|---|---|---|
| Number of non-apnoeic snorers | 14 | 3 | 35 | |
| Outcomes | ||||
| AHI (events/hour) | Pre | 3.4 ± 2.1 (0–5.0) | 4.22 ± 3.24 (0–12.97)b | |
| Post | 5.0 ± 4.4 (0–15.0) | 9.30 | ||
| p-value | NS | NS | ||
| Lowest SaO2 (%) | Pre | 92.3 ± 5.9 (82–100) | ||
| Post | 92.9 ± 5.4 (83–100) | |||
| p-value | NS | |||
| Mean O2 desaturation (%) | Pre | 94.4 ± 1.95 (91–98.5)b | ||
| Post | 94.9 | |||
| p-value | NS | |||
| Lowest O2 desaturation (%) | Pre | 89.68 ± 4.79 (83–95.9)b | ||
| Post | 90.3 | |||
| p-value | NS | |||
| Nasal resistance (Pa/ml/cm2) | Pre | 0.39 ± 0.8 | ||
| Post | 0.28 ± 0.5 | |||
| p-value | < 0.05 | |||
Postoperative pain was reported as lasting for a mean of 9.7 days (SD 3.5 days), with severe pain that precluded patients working lasting for 4.5 days (SD 3.1 days). Additionally, 36% of patients experienced persistent throat dryness or itching, and 17% had difficulty with nasal breathing.
In the study by Lauretano and colleagues,96 at 2-months’ follow-up the snoring status of the patients was improved in 75%, unchanged in 17% and worse in 8%. Patient satisfaction with LAUP was assessed on a 7-point scale, with 1 indicating very dissatisfied, 4 neutral and 7 very satisfied. Assessment indicated that 83% of the patients were satisfied with the results of the procedure and 17% were unsatisfied. On the basis of results from three patients, LAUP did not significantly affect either the mean or the lowest oxygen desaturation levels, with no significant differences in levels between baseline and follow-up. Adverse events were not reported in this study.
In the study by Neruntarat,114 at a mean follow-up duration of 5.2 months (range 4–6) partner-assessed snoring scores showed a significant decrease from 8.8 (SD 2.2) to 2.8 (SD 1.7) after surgery, and 91% of patients considered that their snoring was cured (i.e. the VAS score was less than half of that at baseline). Nasal obstruction as measured by a VAS decreased significantly from a mean of 6.2 (SD 3.2) Pa/ml/cm2 at baseline to 1.6 (SD 0.8) Pa/ml/cm2 after the surgery. The nasal symptoms of rhinorrhea, nasal pruritus and sneezing also showed similar decreases postoperatively, with changes from a mean of 5.8 (SD 1.4) to 2.1 (SD 1.8), 6.1 (SD 2.2) to 2.3 (SD 0.9) and 7.1 (SD 2.3) to 2.5 (SD 1.7) respectively. However, the significance of the changes was not tested. Postoperative pain assessed using a 10-point VAS was also mild to moderate, with a score of ≤ 4.
A summary of the PSG parameter and objective outcome results is displayed in Table 22. Additionally, Table 23 gives a summary of the subjective outcome results and Table 24 presents the adverse events associated with LAUP.
| Berger 200195 | Lauretano 199796 | Neruntarat 2003114 | |||
|---|---|---|---|---|---|
| Number of non-apnoeic snorers | 14 | 12 | 35 | ||
| Follow-up timeb | 1 | 2 | |||
| Outcomes | |||||
| Snoring severity (10-cm VAS) | Pre | 8.8 ± 2.2 | |||
| Post | 2.8 ± 1.7 | ||||
| p-value | < 0.05 | ||||
| Patients whose snoring severity (10-cm VAS) < half of that at baseline | 91% | ||||
| Patients whose snoring was: | |||||
| Improved | 79% | 57% | 75% | ||
| Unchanged | 14% | 21% | 17% | ||
| Worse | 7% | 21% | 8% | ||
| Patients whose five sleep-related-symptoms at last follow-up visit were: | |||||
| Improved | 57% | ||||
| Unchanged | 36% | ||||
| Worse | 7% | ||||
| Nasal obstruction (10-point VAS) | Pre | 6.2 ± 3.2 | |||
| Post | 1.6 ± 0.8 | ||||
| p-value | < 0.01 | ||||
| Rhinorrhea | Pre | 5.8 ± 1.4 | |||
| Post | 2.1 ± 1.8 | ||||
| p-value | NR | ||||
| Pruritus | Pre | 6.1 ± 2.2 | |||
| Post | 2.3 ± 0.9 | ||||
| p-value | NR | ||||
| Sneezing | Pre- | 7.1 ± 2.3 | |||
| Post- | 2.5 ± 1.7 | ||||
| p-value | |||||
| Patients who were: | |||||
| Satisfied with LAUP | 83% | ||||
| Neutral | 0% | ||||
| Dissatisfied with LAUP | 17% | ||||
| Study | Postoperative adverse events |
|---|---|
| Berger 200195 | No major complications, including postoperative haemorrhage |
| Most common complication was pain: pain duration, 9.7 ± 3.5 days; away from work because of severe pain, 4.5 ± 3.1 days | |
| Patients who had persistent throat dryness or itching, 36% | |
| Patients who exhibited difficulty in nasal breathing, 21% (one of whom had a pre-existing nasal obstruction) | |
| Lauretano 199796 | NR |
| Neruntarat 2003114 | Pain (VAS): ≤ 4, mild to moderate |
Summary of the results
The very limited evidence on the effects of LAUP came from three poor-quality pre–post studies with very small sample sizes. Heterogeneity between the three studies precluded pooling of the evidence. Following LAUP, based on a very small sample size of patients, no significant changes were observed in the objective PSG parameters of AHI (n = 17), lowest SaO2 (%) (n = 14), mean oxygen desaturation (%) (n = 3) and lowest oxygen desaturation (%) (n = 3).
LAUP significantly improved snoring, with snoring scores measured on a 10-cm VAS in 35 patients showing a significant decrease from 8.8 (SD 2.2) at baseline to 2.8 (SD 1.7) after surgery; also, 91% of these patients reported a postoperative snoring VAS that was less than half of the baseline value.
Subjectively assessed snoring status was reported in two studies. One study (n = 14) found that snoring tended to be improved at 4 weeks’ follow-up but that the improvement declined at long-term follow-up: snoring was improved in 79%, unchanged in 14% and worse in 7% of the patients at 4 weeks’ follow-up, and improved in 57%, unchanged in 21% and worse in 21% of the patients at long-term follow-up. In the other study (n = 12), snoring assessed at 2 months after the operation was improved in 75%, unchanged in 17% and worse in 8% of the patients.
After LAUP, nasal obstruction, as assessed using a VAS in 35 patients, decreased significantly from 6.2 (SD 3.2) Pa/ml/cm2 at baseline to 1.6 (SD 0.8) Pa/ml/cm2 after surgery. Nasal obstruction-associated symptoms assessed using a VAS also tended to be improved.
In one study (n = 14), sleep-related-symptoms at last follow-up (mean 10.1 months after surgery) were assessed. These were improved in 57%, unchanged in 36% and worse in 7% of patients.
Based on results from 12 patients, 83% reported satisfaction with LAUP and 17% reported that they were not satisfied with the procedure.
Adverse events were reported in two of the three studies. Postoperative pain was the most common complication of LAUP.
Table 25 gives an overall summary of the study results.
| Berger 200195 | aLauretano 199796 | Neruntarat 2003114 | ||
|---|---|---|---|---|
| Study design | Pre–post | Pre–post | Pre–post | |
| Follow-up timea | 1 | 2 | ||
| Subjective outcomes (%) | ||||
| Snoring severity (VAS) | + | |||
| Patients with snoring VAS < half of baseline value | 91 | |||
| Nasal obstruction VAS | + | |||
| Patients whose snoring was improved | 79 | 57 | 75 | |
| Patients whose snoring was unchanged | 14 | 21 | 17 | |
| Patients whose snoring was worse | 7 | 21 | 8 | |
| Patients whose five sleep-related-symptoms at last follow-up were improved | 57 | |||
| Patients whose five sleep-related-symptoms at last follow-up were unchanged | 36 | |||
| Patients whose five sleep-related-symptoms at last follow-up were worse | 7 | |||
| Nasal obstruction VAS | + | |||
| Patients who were satisfied with LAUP | 83 | |||
| Patients who were dissatisfied with LAUP | 17 | |||
| Objective outcomes | ||||
| Nasal resistance (Pa/ml/cm2) | + | |||
| PSG parameter outcomes | ||||
| AHI | – | – | ||
| Lowest SaO2 (%) | – | |||
| Mean O2 desaturation (%) | – | |||
| Lowest O2 desaturation (%) | – | |||
Conclusions
Based on poor quality pre–post studies with very small sample sizes, LAUP significantly reduced nasal resistance and improved subjective snoring scores. LAUP when used in conjunction with septoplasty and laser turbinectomy tended to improve nasal obstruction related symptoms. No major complications were reported with LAUP, except postoperative pain.
Radiofrequency ablation
Quantity and quality of the studies
A total of seven studies assessed the effects of RFA techniques. 103–109 In six of the studies surgery was to the soft palate103–108 and in the remaining study it was to the tongue base. 109 The available evidence consisted of one RCT by Stuck and colleagues,103 which compared soft palate RFA with placebo; one CCT conducted by Cartwright and colleagues,104 in which soft palate RFA was compared with the short-term use of a MAS; and five pre–post studies, four of which assessed RFA to the soft palate105–108 and one that evaluated bipolar RFA of the tongue base. 109
Study sample sizes were small ranging from 9 to 45 participants, with a median of 20. Overall there was a total of 151 participants across the studies. Duration of follow-up ranged from 10 weeks to 1 year.
In six of the studies patients had undergone a PSG at baseline to rule out OSAS103,105,106,108,109,124 and in the remaining study patients had undergone a sleep study (type unspecified). 107 Investigations at baseline to assess the site of airway narrowing included clinical examination alone;104 clinical examination in conjunction with endoscopy plus or minus cephalometric radiography;103,107,108 lateral cephalometry alone;105 and endoscopy alone. 109 In one study baseline tests were not reported. 106 The age range of participants included in the studies was from 26 to 67 years. When reported, the percentage of male participants ranged from 66% to 95%. 105–109 In the five studies reporting baseline BMI the mean BMI was 25.7–27.1 kg/m2, with a range from 22.0 to 34.6 kg/m2, indicating that patients were mainly overweight but not obese. Baseline ESS scores ranged from 4.5 to 11.4 across the studies. None of the studies reported the number of participants who smoked or the levels of alcohol consumption. Study characteristics are summarised in Table 26.
| Study ID | Study design | Intervention | n | Follow-up duration | Participantsa | Outcomes | ||
|---|---|---|---|---|---|---|---|---|
| PSG parameters | Subjective | Objective | ||||||
| Stuck 2005103 | RCT |
1. Soft palate RFA (two sessions; total energy delivery 3300 J) 2. Placebo |
26 | 10–14 weeks |
Baseline tests: PSG; clinical examination; nasendoscopy (awake) Participant demographics: age: 42.6 ± 0.6 (range 27–60); male: NR; BMI: NR; AHI: RFA: 5.4 ± 4.6, placebo: 5.2 ± 3.1; ESS: RFA: 5.4 ± 4.6, placebo: 5.2 ± 3.1; smokers: NR |
NR | Snoring scale score (partner reported); ESS; speech problems score; swallowing function score; taste score; pharyngeal irritation score | NR |
| Cartwright 2000104 | CCT |
1. Soft palate RFA (mean 1.5 sessions) 2. Oral appliance (Snore X) (worn at home for 2 weeks) |
20 |
RFA: 8.9 months (range 6–12 months) Snore X appliance: 2 weeks |
Baseline tests: PSG; clinical examination Participant demographics: age: RFA: 52.2 ± 10.18, oral appliance: 53.1 ± 11.61; male: NR; BMI: RFA: 28.20 ± 2.93, oral appliance: 30.20 ± 6.30; AHI: RFA: 5.91 ± 4.31, oral appliance: 4.87 ± 3.97; ESS: NR; smokers: NR |
AHI | Snoring scale score (partner reported); ESS | Percentage of sleep time with loud snoring (MESAM recording) |
| Hukins 2000105 | Pre–post | Soft palate RFA (3 sessions) | 20 | 2 months post final treatment session |
Baseline tests: PSG; lateral cephalometry. Participant demographics: age: 43.2 ± 11.1; male: 80%; BMI: 27.1 ± 2.80; AHI: 3.3 ± 3.1; ESS: 8.1 ± 4.0; smokers: NR |
AHI; AI; sleep efficiency; sleep arterial saturation; nadir sleep arterial saturation | ESS; sleepiness scale score (patient-reported VAS); snoring severity scale score (partner reported); postoperative pain; swallowing difficulties; speech changes; adverse events | Snoring intensity (dB); cephalometric parameters: angle between the sellar point to the nasion line and maxillary point; angle between the sellar point to the nasion line and mandibular point; posterior airspace; maximum soft palate width; distance between the posterior nasal spine and the tip of the uvula |
| Boudewyns 2000106 | Pre–post | Soft palate RFA (1–3 sessions with mean 692.3 ± 67.7 J per session) | 45 | 5 months |
Baseline tests: PSG Participant demographics: age: 43.7 ± 10.9; male: 86.4%; BMI: 26.6 ± 3.2; AHI: 5.1 ± 4.3; ESS: 8.0 ± 5.0; smokers: NR |
AHI; O2 min | Snoring score (partner reported); ESS; percentage treatment success; postoperative pain; adverse events | NR |
| Haraldsson 2002107 | Pre–post | Soft palate RFA (3 sessions; total energy delivery 3600 J) | 16 | 10 days post each procedure |
Baseline tests: Apnolog sleep study; clinical examination; endoscopy (awake) Participant demographics: age: 49.4 ± 10.4 (range 26–67); male: 68.6%; BMI: 26.2 ± 2.0 (range 22–30); AHI: NR; ESS: 11.4 ± 5.0; smokers: NR |
ODI | Snoring severity scale score (partner reported); ESS; postoperative pain; mean hypernasality score; mean nasal escape score; mean velopharyngeal snort score | Maximum snoring level sound (dB); hypernasality score (nasal–oral ratio meter; NORAM) |
| Back 2002108 | Pre–post | Soft palate RFA (bipolar) (2 sessions) | 20 | 3 months and 9.5 months |
Baseline tests: PSG; clinical examination; nasopharyngoscopy (awake); cephalometric radiographs; MRI Participant demographics: age: 43 (range 35–63)b; male: 95%; BMI: 25.7 (range 22.6–34.6)b; AHI: < 5; ESS: 4.5 (95% CI 1.0–16.7); smokers: NR |
NR | ESS score; snoring scale score (patient reported); snoring scale score (partner reported); percentage of patients with successful outcome, significant improvement or relapse on snoring scale score (patient reported); percentage of patients with successful outcome, significant improvement or relapse on snoring scale score (partner reported); ± postoperative pain; ± postoperative swelling sensation; ± postoperative speech difficulties; ± postoperative eating difficulties; adverse events | MRI oropharyngeal dimension measurements: length of the soft palate (mm); corrected length of the soft palate (mm); palatal width at 1 cm (mm); palatal width at the thickest part (mm); distance, tip of uvula to bottom of sella (mm); post-uvular space (mucosa) (mm); post-uvular space (CI–CII) (mm); area of the soft palate (cm2); number of patients with major, moderate and no/mild changes in T1 signal intensity |
| den Herder 2006109 | Pre–post | Tongue base RFA (bipolar) (mean number of sessions = 1.1, range 1–2) | 9 | 360 ± 132 days |
Baseline tests: PSG; endoscopy (sleep) Participant demographics: age: 45.4 ± 9.7; male: 66%; BMI: 26.5 ± 3.8; AHI: 2.5 ± 1.8; ESS: 6.6 ± 6.8; smokers: NR |
NR | ESSc | NR |
The studies differed slightly in their aims and objectives. Stuck and colleagues103 aimed to assess the efficacy of soft palate RFA compared with placebo sham surgery in their small RCT. In the CCT conducted by Cartwright and colleagues104 the objective was to evaluate the effectiveness of soft palate RFA and compare this with the effects of using a MAS (Snore X oral appliance; Snorex, Fremont, CA) for a 2-week treatment period. Consequently, four out of the five outcomes assessed were reported as pre-and postintervention scores for the RFA group alone, with only one outcome reported for both groups with a between-group comparison being made. The pre–post studies conducted by Hukins and colleagues,105 Boudewyns and van de Heyning106 and Back and colleagues108 all aimed to assess the clinical effectiveness and adverse events associated with RFA palatoplasty for the treatment of non-apnoeic snoring. The aim of the study conducted by Haraldsson and colleagues107 was to evaluate whether RFA tissue reduction is associated with voice changes as a result of velopharyngeal insufficiency in patients with heavy snoring, whereas den Herder and colleagues109 assessed the adverse events and complications associated with bipolar RFA of the tongue base.
Treatment protocols
There was some variation in treatment protocols between the studies. In the RCT by Stuck and colleagues103 patients underwent two consecutive treatment sessions of either RFA or placebo. In the first session three application sites were selected, with 600 J delivered to the midline and 2 × 450 J delivered approximately 1 cm lateral to the midline. In the second session four application sites were selected (not specified) with 1800 J delivered in total. The target temperature was 85°C, with a total of 3300 J delivered across both sessions. Placebo treatment followed the same protocol including local anaesthesia. In the placebo group the device needle was inserted into the soft palate but no RFA energy was delivered. Cartwright and colleagues104 in their CCT provided a mean number of 1.5 treatment sessions per patient with three treatment sites being selected. RFA energy was delivered to the midline and to two lateral sites at half of the energy level. The total energy level delivered per session was not reported. In their comparison group patients were fitted with a MAS for a 2-week treatment period. The group were then assessed using a counterbalanced split-night study, with and without the MAS.
The pre–post studies by Hukins and colleagues,105 Boudewyns and van de Heyning106 and Haraldsson and colleagues107 all assessed somnoplasty delivered in sequential treatment sessions, with a mean of 3, 2.7 and 3 sessions used respectively. Hukins and colleagues105 treated the middle, distal and proximal thirds of the midline palate sequentially over their treatment sessions with a mean of 650 J delivered per session. Across the sessions the total energy delivered was 1950 J. Boudewyn and van de Heyning106 also used a protocol of one lesion per treatment session, treating the caudal margin of the soft palate and the uvula in sequential sessions. The mean energy delivered per session was 692 J, with a mean total of 1877 J delivered across the sessions. The treatment protocol of Haraldsson and colleagues107 used a considerably higher total energy delivery with three lesions being created per session. The midline and each side of the soft palate 1 or 2 cm from the lower border were selected for treatment, with 600 J and 300 J delivered to each of the sites respectively. The mean total energy per treatment session was therefore 1200 J, with a total of 3600 J delivered across the three treatment sessions.
In contrast to the other identified studies Back and colleagues108 used bipolar RFA (coblation) in their treatment protocol. Three sites, including the midline and two lateral points on either side, were selected for treatment, with the procedure conducted in two sessions. The mean energy delivery per session, or total energy delivered, was not reported. Bipolar RFA of the tongue base was evaluated in the treatment protocol of den Herder and colleagues. 109 This study included both patients with a diagnosis of non-apnoeic snoring and patients with OSAS, with only pre- and postintervention ESS scores reported separately for the non-apnoeic snoring subgroup. Six application sites with an extension of 3 cm × 3 cm surrounding the papilla were selected for treatment. Energy was delivered with a probe through the dorsal surface of the tongue, with coagulations placed at a distance of 1.5–2 cm from each other. The mean number of treatment sessions per patient was 1.5 (range 1–3), with a total of 504 J delivered per treatment session. A summary of the study treatment protocols is shown in Table 27.
| Study ID | Study design | n | Device | No lesions | No sessions | Energy per session (J) | Total energy (J) |
|---|---|---|---|---|---|---|---|
| Stuck 2004103 | RCT | 23 | 1. Somnus; 2. Placebo | 7.0 | 2.0 | 1: 1500; 2: 1800 | 3300 |
| Cartwright 2000104 | CCT | 20 | 1. Somnus; 2. MAS | NR | 1.5 | NR | NR |
| Hukins 2000105 | Pre–post | 20 | Somnus | 1 | 3 | 650 | 1950 |
| Boudewyns 2000106 | Pre–post | 45 | Somnus | 1 | 2.7 | 692 | 1877 |
| Haraldsson 2002107 | Pre–post | 16 | Somnus | 3 | 3 | 1200 | 3600 |
| Back 2002108 | Pre–post | 18 | Coblation | NR | 3 | NR | NR |
| den Herder 2006109 | Pre–post | 9 | Coblation | 6 | 1.5 | 504 | 756 |
Outcomes
Across the studies PSG parameter outcomes,104–108 patient- or partner-reported snoring scale scores,103–108 objective measures of snoring sound,104,105,107 ESS103,105–107,109,124 and postoperative adverse events103,105–108 were reported. Additional outcomes included the nasal–oral hypernasality score107 and cephalometric parameters. 105 Each study had assessed a different subset of these outcomes, with only some overlap between the studies in the outcomes assessed. Moreover, the way in which the same outcome had been defined and measured was not always consistent between the studies for all measures. Further differences between the studies in terms of intervention, study design and the duration of follow-up meant that, even when outcomes had been defined and assessed in a similar way, such as for partner-reported snoring intensity and ESS, combining the studies in a meta-analysis was not appropriate.
Subjectively assessed snoring scale scores and ESS scores
Six of the studies had assessed bed partner-rated snoring levels using a 10-point VAS, with ‘no snoring’ and ‘excessive snoring, bed partner leaves the room’ or ‘loudest possible snoring’ as anchors. 103,105–107,124 In the CCT by Cartwright and colleagues104 treatment success at 8 weeks’ follow-up was defined as a VAS score of 3 or lower. Likewise, Boudewyns and van de Heyning106 defined a difference of 3 points at follow up as a significant improvement, and treatment success as a snoring scale score of 3 or less. Back and colleagues108 assessed both partner- and patient-reported snoring levels, with a successful treatment outcome being defined as a reduction in patient-reported snoring intensity from at least 7 to 0–3 points or a reduction in partner-reported snoring levels from at least 6 to 0–3 points. An improvement of 3 points in the scores was considered significant. Treatment relapse was defined as a change of more than 2 points in the scores between 3 and 9.5 months after treatment. None of the other three studies defined what constituted a clinically significant change in partner-assessed snoring level. 103,105,107 EDS was assessed in all seven of the studies using the ESS, with Hukins and colleagues105 also assessing this using a 10-point VAS with ‘no tendency to fall asleep’ and ‘constantly falling asleep’ as anchors. None of the studies defined what constituted a clinically meaningful change in levels of ESS.
Objective measures of snoring sound
Cartwright and colleagues104 assessed the percentage of time that snoring was loud, soft or absent using the MESAM-IV recording device; however, no definition of how loud and soft snoring were categorised was reported. In the studies by Hukins and colleagues105 and Haraldsson and colleagues107 objective snoring sound analysis was based on the maximum sound intensity; however, again, neither study reported what constituted a clinically meaningful reduction in snoring sound intensity.
Adverse events
Five of the studies examined the incidence of postoperative adverse events using either a 10-cm VAS, in which 0 = ‘no problems/not affected’ and 10 = ‘severe problems/severely affected’,103,105–107 or a 100-point scale. 108 Four of the studies assessed postoperative pain levels,105–108 three assessed both speech and swallowing difficulties,103,105,108 one examined swelling sensation108 and a further study also assessed both taste changes and pharyngeal irritation. 103
Nasal–oral hypernasality score
In the study by Harraldsson and colleagues107 hypernasality was assessed objectively by use of a nasal–oral ratio meter (NORAM), and subjectively by evaluation of the speech parameters of hypernasality, nasal escape and velopharyngeal snort (trained listener rated). These speech parameters were assessed on a 5-point scale in which 1 represented normal and 5 represented a severe deviation from normal.
Study quality
The methodological quality of the studies and the level of reporting was variable. All studies had reasonably well-defined inclusion criteria but none provided adequate baseline details on participants in terms of smoking status. Treatment compliance, when reported, was adequate and the rate of attrition low, with all studies achieving greater than 80% follow-up. Methods of statistical analysis were appropriate in all studies, but the reporting of significance levels was not consistent in two studies104,107 making it difficult to judge the relevance of the point estimates and standard deviations presented. The use of subjective patient- and partner-reported outcomes for levels of snoring intensity may mean that results are biased for this outcome, and only three studies104,105,107 provided an additional objective measure of snoring sound level. Sample sizes in all of the studies were small, and the length of follow-up generally inadequate to be able to judge the longer-term effectiveness of RFA techniques. The reporting of postoperative complications was variable making it difficult to draw comparisons between the studies concerning complication rates. Summaries of the study quality indicators are given in Table 28 for the controlled studies and in Table 29 for pre–post studies.
| Quality criteria | Stuck 2005103 | Cartwright 2000104 |
|---|---|---|
| Study design | RCT | CCT |
| Eligibility criteria specified? | + | + |
| Power calculation performed? | + | – |
| Sample size adequate? | + | ? |
| Number randomised stated? | P | NA |
| Adequate methods of randomisation? | + | NA |
| Treatment allocation concealed? | + | NA |
| Adequate baseline details presented? | – | P |
| Groups similar at baseline? | ? | P |
| Baseline imbalances adjusted for in analysis? | – | – |
| Similar co-interventions administered? | ? | ? |
| Patients blinded to treatment allocation? | + | – |
| Outcome assessors blinded to treatment? | + | ? |
| Compliance with treatment adequate? | + | + |
| Subgroup analysis justified? | NA | NA |
| Data collection tools valid? | – | P |
| Data collection tools reliable? | – | P |
| All participants accounted for? | – | + |
| Data analyses appropriate? | + | + |
| Analysis conducted on an ITT basis? | – | + |
| Greater than 80% of patients followed up? | + | + |
| Generalisability | P | P |
| Intercentre variability | NA | NA |
| Quality criteria | Hukins 2000105 | Boudewyns 2000106 | Haraldsson 2002107 | Back 2002108 | den Herder 2006109 |
|---|---|---|---|---|---|
| Study design | Pre–post | Pre–post | Pre–post | Pre–post | Pre–post |
| Eligibility criteria specified? | + | + | + | + | + |
| Adequate baseline details presented? | P | P | P | P | P |
| Are any co-interventions stated? | NA | NA | NA | NA | + |
| Compliance with treatment adequate? | + | + | + | + | + |
| Subgroup analysis justified? | NA | NA | NA | NA | + |
| Data collection tools valid? | P | P | P | P | P |
| Data collection tools reliable? | P | P | P | P | P |
| All participants accounted for? | + | – | + | – | + |
| Data analyses appropriate? | + | + | + | P | + |
| Greater than 80% of patients followed up? | + | + | + | + | + |
| Generalisability | P | P | P | P | – |
| Intercentre variability | NA | NA | NA | NA | NA |
Results
Soft palate radiofrequency ablation versus placebo
Stuck and colleagues103 assessed bed partner-rated snoring levels, ESS and postoperative adverse events in 23 patients (12 in the RFA group and 11 in the placebo group). At 10–14 weeks’ follow-up, mean bed partner-assessed snoring scores remained unchanged in the placebo group with a mean preoperative score of 8.4 (SD 1.6) and a mean postoperative score of 8.0 (SD 2.3). Conversely, scores decreased in the RFA group, from a mean preoperative score of 8.1 (SD 1.3) to a mean postoperative score of 5.2 (SD 2.4). There was a significant difference between the groups for the changes in snoring scale scores. EDS improved minimally in the placebo group, from 5.2 (SD 3.1) to 4.3 (SD 2.7), and to a slightly greater extent in the RFA group, from 5.4 (SD 4.6) to 3.9 (SD 3.3). The difference in postoperative ESS scores between the groups was not significant. Likewise, there were no significant differences within the two groups, or between the placebo and RFA groups, in VAS scores for the functional parameters of speech [1.0 (SD 1.4) versus 0.7 (SD 1.1); 0.4 (SD 0.8) versus 0.3 (SD 0.5)], swallowing [0.3 (SD 0.6) versus 0.3 (SD 0.5); 0.4 (SD 0.6) versus 0.4 (SD 0.5)], taste [0.4 (SD 0.5) versus 0.4 (SD 0.6); 0.3 (SD 0.7) versus 0.3 (SD 0.4)] or pharyngeal irritation [0.8 (SD 0.9) versus 0.6 (SD 1.4); 1.1 (SD 1.0) versus 1.5 (SD 1.8)] pre and post treatment respectively.
Soft palate radiofrequency ablation versus a mandibular advancement splint
Cartwright and colleagues104 assessed bed partner-rated snoring levels, the percentage of time that snoring was loud, soft or absent during sleep, AHI and EDS in 20 patients, 10 of whom underwent RFA and 10 of whom were fitted with a MAS. For the MAS group only data for the outcome of percentage of time that snoring was loud, soft or absent during sleep were reported. Consequently, for all other outcomes data for the RFA group were reported as pre- and postoperative means and the differences compared.
There was a significant decrease in partner-rated snoring levels in the RFA group, from a mean preoperative score of 7.5 (SD 2.5) to a mean postoperative score of 2.75 (SD 2.15). Seven of the ten patients had a partner-rated score of 3 or less at follow-up. Results were consistent between the group of patients who received one treatment only (n = 5) and those who underwent two procedures (n = 5), with a significant decrease in snoring levels from 6.4 (SD 2.7) to 1.8 (SD 1.3) and from 8.2 (SD 1.7) to 3.4 (SD 2.6) for the treatment groups respectively. Mean AHI scores increased from a baseline level of 7.0 (SD 5.8) to 13.5 (SD 21.8) in the five patients who underwent one procedure and from 4.8 (SD 1.9) to 6.3 (SD 5.7) in those undergoing two. Significance levels for the changes were not reported. ESS scores decreased in both the group of patients undergoing only one procedure and those undergoing two procedures, with changes from baseline of 13.4 (SD 4.7) to 4.2 (SD 2.4) and 6.6 (SD 2.2) to 3.8 (SD1.3) respectively. Again, significance levels for the changes were not reported.
In the MAS group the percentage of time that snoring was loud decreased from 10.62% (SD 9.83) without the device to 3.32% (SD 4.7) with the device. Comparison between the RFA treatment group and the MAS treatment group showed that there was no significant difference in the percentage of time spent in loud snoring between the groups, with 8.03% (SD 10.16) and 3.28% (SD 1.46) reported for the groups respectively. Comparison of subjective partner-assessed levels of snoring and the objective laboratory measure in the RFA group showed a non-significant positive association between the two measures (r = 0.49) indicating only a moderate correlation. No data on adverse events were reported.
Soft palate radiofrequency ablation alone
Hukins and colleagues105 assessed subjective and objective measures of snoring, levels of daytime sleepiness, PSG parameter results, palatal width and length, and adverse events. At 2 months’ follow-up there was a significant decrease in partner-reported snoring levels, from 7.5 (SD 1.5) preoperatively to 4.6 (SD 2.5) postoperatively. Although 18 of the 20 patients reported some improvement in subjective snoring, only eight patients reported an improvement of at least 50%. Improvements in snoring were observed after the first treatment to the middle third of the soft plate [6.2 (SD 2.0)] and the second treatment to the distal third [4.8 (SD 2.3)] but not after the last treatment to the proximal third [4.6 (SD 2.5)]. Objective measures of snoring sound intensity did not correlate with partner-reported snoring levels, with a small significant increase in snoring sound intensity observed postoperatively. Levels changed from 60.2 dB (SD 3.9) at baseline to 64.9 dB (SD 5.3) postoperatively. There was also a slight redistribution of snoring intensity, with a significant reduction in the proportion of time spent snoring in the range of 50–60 dB and an non-significant increase in snoring at 40–50 dB.
Levels of daytime sleepiness as measured by both the ESS and a 10-point VAS did not change significantly from pretreatment levels at post-treatment follow-up, with changes from 8.1 (SD 4.0) to 6.7 (SD 4.0) and 3.0 (SD 2.0) to 2.6 (SD 2.2) respectively. Likewise there were no significant differences between pre- and post-treatment scores for any of the PSG parameters assessed. AHI scores increased slightly from 3.3 (SD 3.1) to 6.6 (SD 8.1) post treatment, whereas AI scores remained constant with a pretreatment score of 19.4 (SD 7.9) and a post-treatment score of 19.2 (SD 9.6). Likewise percentage of sleep efficiency, percentage mean sleep SaO2 and percentage nadir sleep SaO2 remained constant with pretreatment scores of 82.6% (SD 9.6), 95.7% (SD 1.4) and 83% (SD 3.5), respectively, and postoperative scores of 82.5% (SD 11.8), 95.6% (SD 1.3) and 86.7% (SD 5.5) respectively.
There was no evidence of palatal shortening with no significant changes observed in cephalometric measures of palatal width and length across the treatment period. A summary of the results of the cephalometric measurements with the associated pre- and post-treatment point estimates is given in Table 30.
| Cephalometric parameters | Pre | Post | p-value |
|---|---|---|---|
| Angle between the sellar point to the nasion line and maxillary point (mean ± SD) (°) | 80.2 ± 4.5 | 79.5 ± 4.8 | NS |
| Angle between the sellar point to the nasion line and mandibular point (mean ± SD) (°) | 77.7 ± 5.3 | 77.4 ± 5.4 | NS |
| Posterior airspace (mean ± SD) (mm)a | 6.45 ± 2.41 | 4.80 ± 2.19 | NS |
| Maximum soft palate width (mean ± SD) (mm) | 10.11 ± 1.97 | 9.34 ± 2.19 | NS |
| Distance between the posterior nasal spine and the tip of the uvula (mean ± SD) (mm) | 38.17 ± 2.39 | 37.00 ± 2.77 | NS |
Levels of postoperative pain, swallowing difficulties and speech problems all remained low, although there was an non-significant trend for more prolonged symptoms after the second treatment. Pain scores ranged from 0.8 to 1.7 on day 3 postoperatively, and from 0.5 to 1.4 on day 7. Swallowing difficulty and speech problem scores ranged from 0.7 to 1.8 and 0.7 to 1.0 on day 3, and from 0.3 to 1.4 and 0.5 to 0.1 on day 7 respectively. Mucosal lesions developed in three patients but spontaneously healed by 3–5 weeks.
Boudewyns and van de Heyning106 included 45 patients in their European multicentre trial of sequential single-lesion RFA. The total length of follow-up was 20 weeks, with pain scores being assessed at days 1–3, weeks 1–2 and week 4 postoperatively. PSG parameters were recorded approximately 8 weeks after the last treatment session. One patient withdrew from the study.
At 20 weeks’ follow-up there was a small but significant reduction in partner-reported levels of snoring, with a mean decrease of 3.6 (SD 2.1) from baseline levels of 7.6 (SD 2.1) giving a mean postoperative snoring index score of 4.0. In total, 20 patients (44.4%) were categorised as a ‘treatment success’, attaining a score of 3 or less, with 38 (84.4%) categorised as ‘improved’, showing a decrease of 3 points on the scale from baseline. An improvement in daytime sleepiness was also observed. ESS scores decreased significantly from 8.0 (SD 5.0) at baseline to 6.0 (SD 4.3) postoperatively. Based on the 37 patients who underwent a second PSG at follow-up there were no significant changes in the AHI scores [5.1 (SD 4.3) at baseline versus 5.4 (SD 7.4) at follow-up] or in the lowest oxygen saturation during sleep [87.0% (SD 5.4) preoperatively versus 84.9% (SD 14.6) postoperatively]. Postoperative pain scores indicated that patients experienced only low levels of pain, with scores of 1.0 (SD 1.4), 0.4 (SD 1.0) and 1.0 (SD 1.4) recorded on postoperative days 1–3, weeks 1–2 and week 4 respectively. A total of 29 patients required non-narcotic analgesics, one patient required a narcotic analgesic and eight patients received steroids for post-treatment pain/oedema. The incidence of adverse events occurring during the 122 treatment sessions was generally low: the incidence rate of mucosal erosion was 15.6% (19 events); palatal fistula, uvula loss and excessive swelling all occurred with an incidence of 0.8% (one event each); and the rate of haemorrhage was 1.6% (two events).
Haraldsson and colleagues107 assessed 16 patients over a mean follow-up duration of 165 days. At this time point there was a significant decrease in partner-assessed snoring severity with a drop from a mean baseline score of 8.2 (SD 2.9) to 4.1 (SD 2.5) postoperatively. Objective snoring measurement showed that the maximum snoring level sound decreased by 7 dB from 53 dB at baseline to 45 dB at follow-up. The significance of the change was not reported. There was also a non-significant decrease in ESS scores, from a baseline mean of 11.4 (SD 5.0) to a postoperative mean of 8.2 (SD 4.4). There was no evidence of voice changes as a result of velopharyngeal insufficiency on either objective measures of NORAM analysis or subjective listener-rated scales. NORAM analysis scores were well below 10% in all patients, with a mean of 3.9 (95% CI 1.4–6.0) at baseline and 3.1 (95% CI 0.6–5.7) at follow-up. The listener-rated parameters of hypernasality, nasal escape and velopharyngeal snort did not change from baseline to follow-up, with all indices being scored as 1 (normal) at both time points. Visual analogue pain scores indicated that patients experienced a moderate amount of pain and discomfort, with a mean maximum pain score of 4.0 (SD 2.6) observed, which lasted for an average of 4.4 (SD 4.9) days. There was also an additional number of adverse events reported. Three patients sustained blanching at treatment 1, two patients developed ulcerations after the last treatment session, two patients complained of increased soft palate hyperreflexia and two patients sustained an otalgia.
Bipolar radiofrequency ablation alone
Back and colleagues108 assessed the effects of bipolar RFA (coblation) in 20 patients over a median follow-up period of 9.5 months (range 9–11.5 months). MRI oropharyngeal dimension measurements were assessed at 3 months’ follow-up, subjective snoring and daytime sleepiness were assessed at both 3 months’ and a median of 9.5 months’ follow-up, and adverse events were assessed for the first 2 weeks postoperatively. One patient failed to complete the assessments of subjective snoring severity and ESS, and a second failed to submit the partner-assessed questionnaire. Results were therefore based on a sample size of between 18 and 20 patients.
Patient-reported snoring severity decreased significantly from a median baseline level of 9.0 (95% CI 5–10) to a median level of 4.0 (95% CI 2–7) at 3 months’ follow-up and a median level of 5.0 (95% CI 2–10) at 9.5 months’ follow-up. Similar trends were observed for bed partner-reported snoring severity, with a decrease from a median baseline value of 6.5 (95% CI 5–8) to 4.0 (95% CI 1–8) and 5.0 (95% CI 1–7) at 3 and 9.5 months’ follow-up respectively. Patient- and bed partner-reported snoring severity questionnaire results from before treatment and at 3 and 9.5 months’ follow-up were significantly correlated (r = 0.79). When patient-reported snoring severity levels were assessed according to the criteria of significant improvement, successful outcome and relapse, 11 (58%) patients had a significant improvement and six (32%) had a successful treatment outcome at 3 months’ follow-up. At the 9.5-month follow-up 12 (63%) had achieved a significant improvement, seven (37%) had a successful outcome and four (21%) had relapsed. Assessment of bed partner snoring severity scores showed that, at the 3-month follow-up, seven (39%) patients had achieved a significant improvement and six (33%) had a successful treatment outcome. At the 9.5-month follow-up six (33%) were classified as having a significant improvement, five (28%) as having a successful outcome and one (6%) as having relapsed.
A significant decrease in ESS scores was observed, from a median value of 4.5 (95% CI 1.0–16.7) to median values of 2.0 (95% CI 0–8) at the 3-month follow-up and 3.5 (95% CI 0–8) at the 9.5-month follow-up. Changes in MRI oropharyngeal dimension measurements from baseline to 3 months showed a significant change in the distance between the tip of the uvula and the bottom of the stella, indicating a retraction of the uvula, from a median of 57.5 mm (95% CI 54–59) at baseline to a median of 55.5 mm (95% CI 51–57) at follow-up. There were no significant differences observed for any other MRI dimension measurements of the soft palate. Changes in T1 signal intensity, reflecting fibroid scar formation of the soft palate, were assessed, with major changes in nine patients, moderate changes in four patients and no/mild changes in six patients. The changes did not correlate significantly with the changes in the patient- and partner-assessed questionnaires over the first 3 months post treatment, with a correlation of r = –0.196 between patient-reported snoring intensity results and T1 signal changes and a correlation of r = –0.156 between bed partner-reported snoring intensity and T1 signal parameters. There was also no correlation between changes in ESS scores and T1 signal intensity changes (r = 0.064). A summary of the pre- and postoperative soft palate measurements and T1 signal intensity changes is shown in Table 31.
| Prea | Posta | p-value | |
|---|---|---|---|
| Length of the soft palate (mm) | 42 (39–44) | 42 (38–44) | NS |
| Corrected length of the soft palate (mm) | 44 (41–46) | 44 (42–47) | NS |
| Palatal width at 1 cm (mm) | 11 (10–11) | 10.5 (10–11) | NS |
| Palatal width at the thickest part (mm) | 11 (11–12) | 11 (11–12) | NS |
| Distance, tip of uvula to bottom of sella (mm) | 57.5 (54–59) | 55.5 (51–57) | NS |
| Postuvular space (mucosa) (mm) | 5 (4–6) | 5 (4–6) | NS |
| Postuvular space (CI–CII) (mm) | 14 (11–16) | 13 (11–14) | NS |
| Area of the soft palate (cm2) | 12.4 (11.4–13.5) | 12.55 (11.7–13.8) | NS |
| T1 signal intensity (n) | |||
| Major changes | 9 | ||
| Moderate changes | 4 | ||
| No/mild changes | 6 |
Postoperative pain scores in the study were highest immediately after treatment and gradually decreased during the 2-week follow-up period. Median pain scores of 46 (95% CI 13–92) at day 1 decreased to a median of 2 (95% CI 0–43) at the 7-day follow-up and then increased at day 11 (second procedure) to a median of 49 (95% CI 11.5–98) and decreased again to a median of 3 (95% CI 0–28) by day 17. Minor transient changes in speech, swallowing difficulties and problems eating also showed the same trend with a rapid decrease in scores by day 7 post treatment. The use of medication for pain was low, with a median of 2 (95% CI 1–7; range 0–27) doses during the 2-week postoperative period. One patient received corticosteroids for postoperative swelling and four required antibiotics for abscess caused by the insertion pointer. Additionally, mucosal blanchings of 5 mm and 10 mm in size were developed by six and two patients respectively. The blanchings correlated with the use of medication for pain (r = 0.88) but not with the use of antibiotics (r = 0.36). There was no sign left of the blanchings at the 3-month treatment follow-up. At the first follow-up four patients complained of a swelling sensation in the throat, and at 9.5 months’ follow-up two still retained the swelling sensation.
Tongue base radiofrequency ablation alone
den Herder and colleagues109 assessed bipolar RFA (coblation) of the tongue base in a mixed population of patients with a diagnosis of non-apnoeic snoring and patients with a diagnosis of OSAS. Only the outcome of daytime sleepiness assessed by means of the ESS was reported separately for the subgroup of non-apnoeic snorers. At a mean follow-up duration of 1 year, ESS scores had significantly decreased from a baseline mean of 6.6 (SD 6.8) to 2.4 (SD 3.4). No postoperative complications such as infections, abscess, haematoma or ulcerations of the tongue base occurred.
A summary of the study results for subjectively assessed snoring and ESS outcomes, objectively assessed snoring measurements and PSG parameter outcomes are displayed in Tables 32–34 respectively. A further summary table of the key study results is displayed in Table 35.
| Study ID | n | Intervention | Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Partner-assessed snoring severity (VAS) | Improvement of ≥ 50% | VAS score ≤ 3 | 3-point VAS decrease | ESS | |||||||
| Pre | Post | p-value | Pre | Post | p-value | ||||||
| Stuck 2004103 | 12 | RFA | 8.1 ± 1.3 | 5.2 ± 2.4 | 0.045b | 5.4 ± 4.6 | 3.9 ± 3.3 | 0.77b | |||
| 11 | Placebo | 8.4 ± 1.6 | 8.0 ± 2.3 | 5.2 ± 3.1 | 4.3 ± 2.7 | ||||||
| Cartwright 2000104 | 10 | RFA | 7.5 ± 2.5 | 2.75 ± 2.2 | < 0.001 | 70% | One procedure: 13.4 ± 4.7; two procedures: 6.6 ± 2.2 | One procedure: 4.2 ± 2.4; two procedures: 3.8 ± 1.3 | NR | ||
| 10 | MAS | ||||||||||
| Hukins 2000105 | 20 | RFA | 7.5 ± 1.5 | 4.6 ± 2.5 | < 0.001 | 40% | 8.1 ± 4.0 | 6.7 ± 4.0 | NS | ||
| Boudewyns 2000106 | 24 | RFA | 7.6 ± 2.1 | 4.0 | < 0.001 | 44.4% | 84.4% | 8.0 ± 5.0 | 6.0 ± 4.3 | 0.001 | |
| Haraldsson 2002107 | 16 | RFA | 8.2 ± 2.9 | 4.1 ± 2.5 | < 0.01 | 11.4 ± 5.0 | 8.2 ± 4.4 | NS | |||
| Back 2002108 | 18 | RFA | 6.5c (95% CI 5–8) | 5.0c (95% CI 1–7) | < 0.05 | 28% | 33% | 4.5 (95% CI 1–16.7) | 3.3 (95% CI 0–8) | < 0.05 | |
| den Herder 2006109 | 9 | Tongue base RFA | 6.6 ± 6.8 | 2.4 ± 3.4 | < 0.05 | ||||||
| Study ID | n | Intervention | Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Percentage of time in loud snoring | Snoring sound intensity (dB) | Maximum snoring sound level (dB) | |||||||||
| Pre | Post | p-value | Pre | Post | p-value | Pre | Post | p-value | |||
| Stuck 2004102 | 12 | RFA | |||||||||
| 11 | Placebo | ||||||||||
| Cartwright 2000103 | 10 | RFA | NR | 8.03 ± 10.16 | NSa; < 0.04b | ||||||
| 10 | MAS | 10.62 ± 9.83 | 3.28 ± 1.46 | ||||||||
| Hukins 2000104 | 20 | RFA | 60.2 ± 3.9 | 64.9 ± 5.3 | 0.03 | ||||||
| Boudewyns 2000105 | 24 | RFA | |||||||||
| Haraldsson 2002106 | 16 | RFA | 53 | 45 | NR | ||||||
| Back 2002107 | 18 | RFA | |||||||||
| den Herder 2006108 | 9 | Tongue base RFA | |||||||||
| Study ID | n | Intervention | Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | p-value | Pre | Post | p-value | Pre | Post | p-value | |||
| Apnoea/hypopnoea index | Apnoea index (n/h) | Sleep efficiency (%) | |||||||||
| Stuck 2004103 | 12 | RFA | 2.45 ± 1.51 | NR | |||||||
| 11 | Placebo | 2.68 ± 2.48 | NR | ||||||||
| Cartwright 2000104 | 10 | RFA | One procedure: 7.0 ± 5.8; two procedures: 4.8 ± .9 | One procedure: 13.5 ± 21.8; two procedures: 6.3 ± 5.7 | NR | ||||||
| 10 | MAS | ||||||||||
| Hukins 2000105 | 20 | RFA | 3.3 ± 3.1 | 6.6 ± 8.1 | NS | 19.4 ± 7.9 | 19.2 ± 9.6 | NS | 82.6 ± 9.6 | 82.5 ± 11.8 | NS |
| Boudewyns 2000106 | 24 | RFA | 5.1 ± 4.3 | 5.4 ± 7.4 | NS | ||||||
| Haraldsson 2002107 | 16 | RFA | |||||||||
| Back 2002108 | 18 | RFA | |||||||||
| den Herder 2006109 | 9 | Tongue base RFA | |||||||||
| Mean sleep arterial saturation (%) | Nadir sleep arterial saturation (%) | Oxygen desaturation index | |||||||||
| Stuck 2004103 | 12 | RFA | |||||||||
| 11 | Placebo | ||||||||||
| Cartwright 2000104 | 10 | RFA | |||||||||
| 10 | MAS | ||||||||||
| Hukins 2000105 | 20 | RFA | 95.7 ± 1.4 | 95.6 ± 1.3 | NS | 83.0 ± 3.5 | 86.7 ± 5.5 | NS | |||
| Boudewyns 2000106 | 24 | RFA | 87.0 ± 54 | 84.9 ± 14.6 | NS | ||||||
| Haraldsson 2002107 | 16 | RFA | 4.0 ± 3.4 | 3.3 ± 2.5 | NR | ||||||
| Back 2002108 | 18 | RFA | |||||||||
| den Herder 2006109 | 9 | Tongue base RFA | |||||||||
| Study ID | Study design | Group | Subjective outcomes | Objective snoring outcomes | PSG parameter outcomes | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Partner-assessed snoring severity (VAS) | Patient-assessed snoring severity (VAS) | Improvement of ≥ 50% | VAS score< 3 | 3-point VAS decrease | ESS | % of time in loud snoring | Snoring sound intensity (dB) | Maximum snoring sound level (dB) | AHI | AI | Sleep efficiency (%) | Mean sleep SaO2 (%) | Nadir sleep SaO2 (%) | ODI | |||
| Stuck 2004103 | RCT | RFAa | + | – | |||||||||||||
| Placebo | |||||||||||||||||
| Cartwright 2000104 | CCT | RFAa | + | 70% | –a | ||||||||||||
| MAS | + | ||||||||||||||||
| Hukins 2000105 | Pre–post | RFA | + | 40% | – | + | – | – | – | – | – | ||||||
| Boudewyns 2000106 | Pre–post | RFA | + | 44.4% | 84.4% | + | |||||||||||
| Haraldsson 2002107 | Pre–post | RFA | + | – | NR | NR | |||||||||||
| Back 2002108 | Pre–post | RFA | + | + | 28% | 33% | + | ||||||||||
| den Herder 2006109 | Pre–post | RFA | + | ||||||||||||||
Summary of results
Six studies assessed the effects of RFA of the soft palate (somnoplasty) and one the effects of RFA of the tongue base. The available evidence consisted of one RCT, one CCT and five pre–post studies. All of the studies were small with a median sample size of 20. In total, the available evidence for the effects of RFA is based on results from 151 participants. The duration of follow-up across the studies ranged from 10 weeks to 1 year and therefore there is limited evidence on the longer-term effectiveness of RFA for the treatment of snoring and no evidence for durations greater than 1 year. Results from one pre–post study with follow-up times of 3 and 9.5 months postoperatively showed a relapse rate of between 6% and 21% based on bed partner- and patient-reported snoring severity scores. 108 The potential for relapse and a less significant treatment benefit at longer postoperative times needs to be borne in mind when interpreting results on the effects of RFA from studies with a short follow-up duration.
Radiofrequency ablation of the soft palate
All six studies reported a significant post-treatment decrease in partner-rated snoring severity, with a decrease from a mean range of 6.5–8.4 preoperatively to a mean range of 2.75–5.2 post-treatment. 103–108 The unweighted mean change in pre- and post-treatment scores across the studies was 3.24. Only one study reported a mean VAS score of less than 3 for partner-reported snoring severity, but there was only a moderate correlation between partner-assessed snoring severity and objective measures of the percentage of time spent in loud snoring in this study. 104 The percentage of patients who achieved a decrease in VAS score of 3 points ranged from 28% to 70% in the three studies reporting this outcome. 104,106,108 When compared with placebo there was a significant treatment benefit of RFA for partner-reported snoring severity.
All studies reported a decrease in ESS scores from baseline. In two of the studies106,108 this was reported to be significant and in three103,105,107 it was not significant. One study did not report any significance value for the change. 104 However, as mean ESS scale scores were within the range considered normal at baseline in four of the six studies little change would be expected. 103,105,106,108 In two of the studies104,107 baseline scores were within the range of mild daytime sleepiness. In both studies post-treatment scores were within the range considered normal. 104,107
Snoring sound was measured objectively in three studies. 104,105,107 The results were not consistent between the studies for this outcome. In one study104 there was no significant difference between the percentage of time spent in loud snoring with RFA and the percentage of time spent in loud snoring with use of a MAS. The results for this study indicated only a moderate correlation between the percentage of time spent in loud snoring and partner-reported snoring severity levels. 104 In the second study105 there was a significant, but clinically irrelevant, increase in snoring sound intensity, and no correlation between objective measures of sound and partner-reported snoring levels. In the third study,107 although a decrease in the maximum snoring sound level was found, the significance level for the decrease of 7 dB was not reported.
There were no significant differences in pre-and postoperative PSG parameter outcomes when these were assessed. However, in one study104 AHI scores increased postoperatively to a level within the range of mild OSAS. No significance level for the increase in AHI scores was reported.
Based on the results from one study105 there was no evidence of any changes in palatal width or length postoperatively with RFA.
There was limited evidence from one study of a significant retraction of the uvula with RFA treatment, as measured by the distance between the tip of the uvula to the bottom of the sella. No further significant changes in palatal width, length or post-uvular space were found.
Based on results from one study107 including both objective and subjectively rated outcomes there was no evidence that RFA adversely affects the voice as a result of velopharyngeal insufficiency.
Postoperative pain was rated as low in three studies103,105,106 and moderate in two. 107,108 When RFA was compared with placebo there were no significant differences between the groups on measures of either pain, taste, speech or pharyngeal irritation. 103 Similar low levels of adverse effects on these outcomes were also reported in a second study. 105
Only three studies106–108 reported the rates of other adverse effects of treatment, limiting any comparisons that can be drawn between the studies. Furthermore, there was little consistency in the way that adverse events were defined, further limiting any comparisons that could be made. The percentage of mucosal blanchings and erosions ranged from 15.6% to 40% across three studies. 106–108 The rate of moderate adverse effects was generally low, with palatal fistula, uvula loss and excessive swelling all occurring in 0.8% of procedures106 and haemorrhage in 1.6%. 105 Rates of palate hyperreflexia and otalgia were both higher, occurring in 12.5% of all procedures. 107
Radiofrequency ablation of the tongue base
Based on the limited results reported in one study109 there was a significant decrease in ESS scores post treatment with bipolar RFA of the tongue base.
In one study109 no postoperative infections, abscess, haematoma or ulcerations of the tongue base were observed with bipolar RFA.
Conclusions
From the small number of studies available the evidence suggests that at 1 year of follow-up after RFA of the soft palate there is a significant decrease in partner-reported levels of snoring severity. However, any treatment benefit with RFA may only be moderate as an unweighted mean decrease of only 3.24 points was observed for partner-reported snoring levels. Additionally, relapse rates may be quite high at longer follow-up times. There is no strong evidence to suggest that subjectively assessed partner-reported snoring levels are correlated with objective measures of snoring sound intensity. In all studies treatment with RFA had a positive effect on levels of ESS but in only two studies did these reach statistical significance. However, this is likely to be a reflection of the fact that patients’ baseline levels of ESS were within the range considered normal, and therefore a floor effect would be in operation. The majority of the available evidence suggests that RFA has no detrimental or positive effects upon any PSG parameters, such as AHI or sleep oxygen saturation levels. Additionally, there was no evidence either from cephalometric or from MRI-assessed measurements of the palate that RFA has any overall significant effect on palatal width or length. No serious adverse events were reported and overall complication rates across the studies were low.
Palatal stiffening techniques
Quantity and quality of the studies
Five studies reported in six publications assessed the effects of palatal stiffening techniques for palatal flutter snoring. 97–102 Four studies assessed palatal implants and one assessed injection snoreplasty. The available evidence base consisted of one small RCT that evaluated the effects of increased rigidity in palatal implants97 and four pre–post studies, three of which assessed palatal implants98–101 and one that assessed injection snoreplasty. 102
Overall across the studies a total of 134 participants were included. Study sample size was small ranging from 12 to 40 with a median of 27. In the four studies that assessed palatal stiffening techniques97–101 the duration of follow-up ranged from 3 to 12 months. In the study by Brietzke and Mair102 that assessed injection snoreplasty follow-up was at 10 days post each treatment.
In all five studies patients had undergone either PSG or oximetry at baseline to rule out OSAS. 97–102 Additionally, clinical examination to assess the site of airway narrowing had been performed in all five studies. 97–102 Other tests used in conjunction with examination were awake endoscopy,99,100,102 fibreoptic nasopharyngolaryngoscopy,97 fibreoptic laryngoscopy in conjunction with indirect layngoscopy98 and measurement of the soft palate size and uvula width. 101 The mean age of the participants across the studies was 38–41.1 years, with a range of 24–72 years. In the four studies reporting the gender composition of their study sample the percentage of male participants ranged from 60% to 100%. 97,98,101,102 Mean baseline BMI in four studies ranged from 25.1 kg/m2 to 26.1 kg/m2 with a range of 20.2–29.7 kg/m2, indicating that the majority of patients were overweight but not obese. 97–101 Mean ESS scores were within general population norms ranging from 6.1 to 9.3 in the three studies reporting baseline sleepiness levels. 98–101 None of the studies reported the number of smokers or levels of alcohol consumption. A summary of the study characteristics of the five studies on palatal stiffening techniques is presented in Table 36.
Across the four studies assessing the effects of palatal implants the aims, objectives and treatment protocols were similar. 97–101 In the small RCT by Skjostad and colleagues97 the objective was to assess the safety and efficacy of the use of more rigid implants (rigidity 1.8) compared with standard implants (rigidity 1.0). The two effectiveness outcomes assessed were analysed as the difference between pre- and postoperative means for the two treatment groups separately, with comparisons between groups only being conducted for the number of extrusions. The aim of all three of the pre–post studies conducted by Nordgard and colleagues,98 Maurer and colleagues99 and Ho and colleagues101 was to assess the safety and effectiveness of Pillar implants for the treatment of primary snoring. The treatment protocol in all three studies consisted of three implants, with the first inserted in the midline at the trailing edge of the hard palate and the other two inserted approximately 5 mm laterally to the midline on each side. In all studies treatment was undertaken as one procedure under local anaesthesia. When reported (in two studies97,98) the mean operative time was approximately 8 minutes. Only one of the studies99,100 reported the need for a second procedure because of implant extrusion.
Brietzke and colleagues102 aimed to assess the effects of injection snoreplasty in their pre–post study. The treatment protocol consisted of a first injection to the soft palate midline of 2.0 ml of 1% sodium tetradecyl sulphate (10 mg/ml). For repeat procedures 3% Sotradecol™ (Bioniche Pharma; 30 mg/ml) was generally used and the site of injection modified to include the lateral areas of the soft palate as well as those not adequately stiffened by the previous procedure. Treatment sessions were performed 6–8 weeks apart, with a mean of 1.8 sessions per patient (range 1–4). Patients were followed up for 10 days post each procedure.
Outcomes
Across the studies PSG parameter outcomes,98–101 partner-reported snoring scale scores,97–101 patient and partner satisfaction ratings,97 the number of patients successfully treated,98,102 ESS scores98–101 and the effect of snoring on the sleep of family members101 had been reported. Additional outcome measures were objective measures of snoring sound,99,100,102 postoperative adverse events98–100,102 and the number of implant extrusions. 97–100 The studies had each assessed a subset of these outcomes, with a focus on subjectively assessed measures.
Subjectively assessed snoring outcomes and Epworth Sleepiness Scale scores
Three of the studies97–100 assessed partner-reported snoring scale scores measured on an 11-point or a 10-cm VAS, with the anchors of 0 (no snoring) and 10 (an intensity that causes bed partner to leave the room); in a further study a 100-point scale had been used. 101 Maurer and colleagues99,127 defined a decrease or increase of less than 1 cm on the VAS as unchanged, a decrease of more than 1 cm as a response, and any increase greater than 1 cm as a non-response. A decrease to less than 3 cm was defined as a success. Additionally, if there was an initial response to treatment at day 90, an increase of 3 cm after 1 year was considered as a relapse. None of the other three studies defined what constituted a clinically significant change in partner-assessed snoring level. 97,98,101
Skjostad and colleagues97 assessed patient and partner satisfaction with treatment using a categorical scale, with response options of ‘would recommend treatment‘, ‘undecided’ and ‘would not recommend treatment‘, and Norgard and colleagues98 assessed patient and partner satisfaction according to whether treatment would be recommended. Brietzke and Mair102 defined successful treatment of snoring as a rating of ‘snoring is gone’ or ‘snoring is no longer a problem’ by either the patient or their bed partner. Ho and colleagues101 additionally assessed the effect of snoring on family members using a categorical scale with the response options of ‘no snoring’, ‘mild snoring only’, ‘affects spouse only’, ‘affects whole family’ and ‘heard outside the house’, and the number of nights the bed partner had to leave the room because of loud snoring with the options of ‘0’, ‘1–2 nights’, ‘3–4 nights’, ‘5–6 nights’ and ‘7 nights’ in a week.
In the three studies97–100 that assessed EDS the ESS had been used.
Objective measures of snoring sound
Maurer and colleagues99,100 assessed the number of snores per hour and the maximum loudness of snoring, whereas Brietze and Mair102 assessed the fundamental frequency of involuntary palatal flutter snoring whilst awake by use of a stroboscope.
Adverse events
Three of the studies98–100,102 assessed the incidence of postoperative adverse events using a 10-cm VAS, in which 0 was ‘no problems/not affected’ and 10 was ‘severe problems/severely affected’. All three of the studies assessed postoperative pain levels, whereas two studies98–100 additionally examined speech problems and swallowing difficulties.
Study quality
Study quality was generally poor, with small sample sizes. All of the studies had reasonably well-defined inclusion criteria, but only two studies reported adequate baseline details on the participants. 99–101 Treatment compliance across the studies was good, with three studies97,98,101 additionally reporting the level of postoperative BMI for participants. The duration of follow-up was adequate in all studies, allowing for the process of fibrosis to be complete. However, the use of subjective patient- and partner-reported outcomes for levels of snoring severity may mean that results are biased for this outcome. Dropout rates were relatively high, particularly for the objectively assessed PSG parameter and snoring sound indices outcomes. In two studies99–101 the rate of follow-up achieved was less than 80% for some outcome measures. Data analyses, when conducted, were appropriate in all studies. A summary of study quality indicators is shown in Table 37 for the RCT and in Table 38 for the pre–post studies.
| Quality criteria | Skjostad 200697 |
|---|---|
| Study design | RCT |
| Eligibility criteria specified? | + |
| Power calculation performed? | – |
| Sample size adequate? | ? |
| Number randomised stated? | + |
| Adequate methods of randomisation? | ? |
| Treatment allocation concealed? | ? |
| Adequate baseline details presented? | P |
| Groups similar at baseline? | ? |
| Baseline imbalances adjusted for in analysis? | ? |
| Similar co-interventions administered? | NA |
| Patients blinded to treatment allocation? | + |
| Outcome assessors blinded to treatment? | ? |
| Compliance with treatment adequate? | + |
| Subgroup analysis justified? | NA |
| Data collection tools valid? | – |
| Data collection tools reliable? | – |
| All participants accounted for? | + |
| Data analyses appropriate? | + |
| Analysis conducted on an ITT basis? | + |
| Greater than 80% of patients followed up? | + |
| Generalisability | P |
| Intercentre variability | NA |
| Quality criteria | Nordgard 200698 | Maurer 200599,100 | Ho 2004101 | Brietzke 2001102 |
|---|---|---|---|---|
| Study design | Pre–post | Pre–post | Pre–post | Pre–post |
| Eligibility criteria specified? | + | + | P | P |
| Adequate baseline details presented? | P | + | + | P |
| Are any co-interventions stated? | NA | NA | NA | NA |
| Compliance with treatment adequate? | + | + | + | + |
| Subgroup analysis justified? | NA | NA | NA | NA |
| Data collection tools valid? | P | P | P | – |
| Data collection tools reliable? | P | P | P | – |
| All participants accounted for? | – | – | – | + |
| Data analyses appropriate? | + | + | + | NA |
| Greater than 80% of patients followed up? | + | – | – | + |
| Generalisability | + | + | P | P |
| Intercentre variability | NA | NA | NA | NA |
Results
Palatal implants
Rigid implants versus regular implants
Skjostad and colleagues97 assessed the effects of rigid implants versus regular implants in 20 patients. At 180 days’ follow-up there was a non-significant overall reduction in bed partner-rated snoring levels in the rigid implant group, from 8.1 to a postoperative mean of 6.1. In contrast, in the regular implant group there was a significant reduction from 7.7 to 4.7. No measure of variance was reported and no between-group comparison was conducted.
In the rigid implant patient group only two of the ten patients (20%) were satisfied and would recommend the procedure, six (60%) were undecided and two (20%) would not recommend the procedure. In the standard implant patient group eight of the ten patients (80%) were satisfied and would recommend the procedure and two (20%) were undecided. Of the bed partners, two of the ten partners (20%) in the rigid implant group would recommend the procedure, three (30%) were undecided and five (50%) would not recommend treatment. In the standard implant group five of the partners (50%) would recommend the procedure, four (40%) were undecided and one (10%) would not recommend it. No between-group comparisons were conducted.
Overall, four patients reported a total of five partial implant extrusions. All of the extrusions were laterally positioned and occurred in the group with rigid implants. No extrusions were observed in the standard implant group. The mean time of postoperative analgesic consumption was 0.95 days, with 11 (55%) patients not requiring any postoperative pain relief.
Regular implants alone
Nordgard and colleagues98 followed up 35 patients over a 1-year period, with assessments conducted at days 2, 14, 30, 80, 180 and 360 postoperatively. Postoperative adverse events were recorded for the first 30 days post treatment. One patient withdrew from the study because of tonsillectomy, and 30/34 underwent PSG at final follow-up.
At final follow-up there was a significant reduction in bed partner-reported snoring intensity scores, from a mean of 7.1 (SD 2.1) at baseline to 4.8 (SD 3.1). This corresponded to 17/34 (50%) patients having achieved a final VAS snoring score of less than or equal to 5. Eight of these patients (23.5%) had a final VAS score of less than 3. Mean ESS scores also decreased significantly from baseline levels of 9.3 (SD 4.1) to 5.6 (SD 3.8) at final follow-up. At 6-months’ follow-up 82.3% (28/34) of the partners and 91.2% (31/34) of the patients were satisfied with the treatment outcome. At final follow-up this had decreased to 70.6% (24/34) of partners and 79.7% (27/34) of patients being satisfied with postoperative snoring levels. This difference in levels of satisfaction between the 6- and 12-month follow-ups equated to a recurrence rate (patients no longer fulfilling the criteria for success) of 14.3% (4/28) for partners and 12.9% (4/31) for patients.
Based on 30 patients there was no significant change in the mean AHI, with the baseline score being 2.2 (SD 2.3) and the final follow-up score 3.3 (SD 3.8). Postoperative pain scores peaked on day 2 post treatment and declined by days 14 and 30, with mean scores of 2.0, 0.9 and 0.7 for each follow-up time respectively. The mean scores for both postoperative speech and postoperative swallowing difficulties followed a similar trend to that for postoperative pain scores. Mean scores for days 2, 14 and 30 were 3.0 and 0.9, 0.7 and 0.5, and 0.4 and 0.2 for swallowing and speech difficulties respectively. On average, patients took prescribed analgesics for 1.3 days after the procedure (range 0–6 days), with a mean total dose of 2.1 pills of diclofenac 50 mg (range 0–15 pills). The incidence of mild oedema at the base of the uvula was 2.8% (n = 1). No bleeding, haematoma or infection was observed either during the procedure or in the follow-up period. During follow-up 17.6% of patients had a partial implant extrusion of a total of eight implants (8.8%). All extrusions occurred laterally.
Maurer and colleagues99,127 assessed 40 patients over 1 year with follow-up times of 90, 180 and 360 days. PSG and SNAP (SNAP Laboratories, Glenview, IL) snoring sound recordings were performed at baseline and at day 90, whereas subjective snoring evaluation was additionally assessed at days 180 and 360. There was no pain evaluation before the procedure, with baseline pain scores being recorded at day 2 postoperatively. Attrition rates were 8/40 patients at all time points for the partner-assessed snoring level scores and 19/40 patients for both baseline and day 90 SNAP snoring sound recordings.
Based on results from 32 patients, partner-assessed snoring levels significantly decreased after treatment, from a mean of 7.1 (SD 2.1) at baseline to a mean of 4.2 (SD 2.7) at 3 months and 4.0 (SD 2.5) and 4.8 (SD 2.6) at 6 and 12 months respectively. The mean VAS reduction compared with baseline was 2.2 (SD 2.5) after 1 year. Successful treatment (a score of less than 3 cm) was achieved in 13 patients (41%) 90 days after the procedure, in 11 patients (34%) at day 180, and in seven patients (22%) after 1 year. A response (a decrease of 1 cm of more) was achieved in 23 patients (72%) at 90 days, in 20 patients (63%) at 6 months, and in 22 patients (69%) at final follow-up. An increase of more than 3 points after 1 year was observed in one patient. Comparison of the 1-year VAS scores with the 90-day scores indicated that 17 patients (53%) were unchanged, two patients (6%) had a further improvement of more than 3 points, and four patients (12.5%) had a relapse. ESS scores also decreased significantly from a baseline mean of 6.1 (SD 3.2) to a mean of 4.3 (SD 3.3) at day 90. They then increased slightly to a mean of 4.9 (SD 3.1) at 1 year but remained significantly different from baseline.
AHI scores increased significantly from a baseline mean of 3.7 (SD 2.3) to 5.5 (SD 5.4) at the 90-day follow-up. This was reflected by a significant increase in mean HI (hypopnoea index) score from 3.0 (SD 2.2) to 4.5 (SD 4.7) and an insignificant increase in mean AI score from 0.7 (SD 0.8) to 1.1 (SD 1.4). There were no significant changes in the ODI [3.4 (SD 2.9) versus 5.3 (SD 5.1)], mean oxygen saturation during recording [94.6 (SD 1.8) versus 94.3 (SD 1.7)] or sleep efficiency [88.2 (SD 8.1) versus 8.7 (SD 12.1)] from baseline to the 90-day follow-up. A significant decrease in minimal oxygen saturation during the recording from 89.8 (SD 4.1) at baseline to 87.1 (SD 5.8) at follow-up was observed.
None of the objectively assessed SNAP snoring sound parameters changed significantly from baseline to the 90-day follow-up based on the results of 21 patients. A summary of the SNAP snoring sound parameter results with associated mean pre- and post-treatment point estimates is given in Table 39.
| Parameter | Pre | Post | p-value |
|---|---|---|---|
| Snoring index (events/hour) | 273 ± 178 | 276 ± 172 | NS |
| Primary vibration frequency (Hz) | 107 ± 59 | 110 ± 59 | NS |
| Palatal vibration frequency (Hz) | 82 ± 19 | 80 ± 30 | NS |
| Velum-like snores types I and II (%) | 81 ± 25 | 85 ± 24 | NS |
| Resistance occurrence index (%) | 25 ± 16 | 23 ± 14 | < 0.05 |
| Maximum relative loudness (dB) | 15 ± 7 | 16 ± 6 | NS |
At the 90-day follow-up postoperative pain and speech difficulty scores both decreased significantly from mean baseline levels of 4.9 (SD 3.3) and 0.7 (SD 1.8) to 0.2 (SD 0.6) and 0.1 (SD 0.2) respectively. There was no significant change in swallowing difficulty scores, with a mean of 0.4 (SD 0.6) at baseline and a mean of 0.1 (SD 0.4) at follow-up. No surgical or postoperative complications were observed in the first 2 weeks post treatment. In ten patients a total of 13 implants (11%) partially extruded.
Ho and colleagues101 examined partner-reported snoring levels, the effect of snoring on the sleep of family members, the number of nights per week that the bed partner was required to leave the room because of snoring, AHI and daytime sleepiness levels in 13 patients. Objective SNAP snoring sound parameters were also assessed in five patients but no group mean data were reported. Two patients experienced extrusion of the implants and one patient was lost to follow-up. The results were therefore based on the nine male patients who completed the study.
At 3 months’ follow-up there was a significant decrease in partner-reported snoring levels, from a pretreatment mean of 79 (SD 17.2) to 48 (SD 20.4) postoperatively. There was also a trend towards fewer disturbances to family members’ sleep at follow-up compared with baseline. At baseline no partners reported that snoring was either absent or only mild, six partners reported that it affected only their sleep without disturbing other household members, and three reported that it was so loud it could be heard outside the house. At follow-up, five partners reported that snoring was now mild and four reported that it disturbed only their sleep without affecting other household members. Likewise, there was a trend towards a fewer number of nights per week that the bed partner needed to leave the room because of snoring. At baseline, three partners reported that they did not have to leave the room because of snoring, three reported that they needed to leave the room 1–2 nights per week and one each reported leaving on average 3–4 nights, 5–6 nights and 7 nights per week respectively. At follow-up, six partners reported that they did not now need to leave the room, one reported that they left 1–2 nights per week and two reported that they left 3–4 nights.
There was also a significant reduction in ESS scores from a baseline mean of 8.9 (SD 5.6) to 5.7 (SD 5.6) at 3 months. AHI scores increased slightly from 4.8 (SD 5.7) at baseline to 8.3 (SD 11.5) at follow-up, but the increase was not significant. Likewise, BMI did not change significantly across the follow-up period. There was no delayed postoperative bleeding or wound infection. Overall, extrusions occurred in 16.7% of 12 patients and in 8.8% of the 34 implants deployed.
Injection snoreplasty alone
In the pre–post study by Brietzke and Mair102 the duration of follow-up was 10 days post each procedure, but varied according to the number of treatment sessions, with a mean of 1.8 sessions per patient (range 1–4).
At follow-up 25 of the 27 patients (92%) reported a significant decrease in snoring. Based on the results from 13 patients there was an increase in voluntary awake palatal flutter snoring from 74.1 Hz at baseline to 105.4 Hz at follow-up, resulting in an average increase of 31.3 Hz. The significance of comparison of the means was not reported. Postoperative pain scores for days 1–5 showed that pain levels were generally low, with a score of 3 on day 1 that steadily decreased to a score of 1 on day 5.
A summary of the results for subjectively assessed snoring and ESS outcomes, objectively assessed snoring measurements and PSG parameter outcomes for studies assessing palatal stiffening techniques are displayed in Tables 40–42 respectively.
| Skjostad 200697 | Nordgard 200698 | Maurer 200599,100 | Ho 2004101 | Brietzke 2001102 | ||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Rigid implants | Regular implants | Regular implants | Regular implants | Regular implants | Injection snoreplasty | ||
| n | 10 | 10 | 30 | 32 | 9 | 27 | ||
| Outcome | ||||||||
| Partner-assessed snoring severity (VAS), mean ± SD | Pre | 8.1 | 7.7 | 7.1 ± 2 | 7.1 ± 2.1 | 79 ± 17.2 | ||
| Post | 6.1 | 4.7 | 4.8 ± 3.1 | 4.8 ± 2.6 | 48 ± 20.4 | |||
| p-value | 0.053 | <0.01 | < 0.001 | < 0.05 | 0.008 | |||
| VAS score ≤ 5 (%) | 50 | |||||||
| VAS score< 3 (%) | 23.5 | 22 | ||||||
| Response (VAS decrease of ≥ 1 cm) (%) | 69 | |||||||
| Patient satisfaction with treatment (%) | Satisfied | 20 | 80 | 79.7 | ||||
| Undecided | 60 | 20 | ||||||
| Unsatisfied | 20 | 0 | ||||||
| Partner satisfaction with treatment (%) | Satisfied | 20 | 50 | 70.6 | ||||
| Undecided | 30 | 40 | ||||||
| Unsatisfied | 50 | 10 | ||||||
| Snoring no longer a problem (%) | 92 | |||||||
| Effect of snoring on family members (pre- and post-treatment), n | No snoring | 0 | 0 | |||||
| Mild snoring | 0 | 5 | ||||||
| Affect spouse | 6 | 4 | ||||||
| Affect family | 0 | 0 | ||||||
| Heard outside house | 3 | 0 | ||||||
| Number of nights per week bed partner leaves the room because of snoring (pre-and post-treatment), n | 0 | 3 | 6 | |||||
| 1–2 | 3 | 1 | ||||||
| 3–4 | 1 | 2 | ||||||
| 5–6 | 1 | 0 | ||||||
| 7 | 1 | 0 | ||||||
| ESS score, mean ± SD | Pre | 9.3 ± 4.1 | 6.1 ± 3.2 | 8.9 ± 5.6 | ||||
| Post | 5.6 ± 3.8 | 4.9 ± 3.1 | 5.7 ± 5.6 | |||||
| p-value | < 0.001 | < 0.05 | 0.007 | |||||
| Skjostad 200697 | Nordgard 200698 | Maurer 200599,100 | Ho 2004101 | Brietzke 2001102 | |||
|---|---|---|---|---|---|---|---|
| Intervention | Rigid implants | Regular implants | Regular implants | Regular implants | Regular implants | Injection snoreplasty | |
| n | 10 | 10 | 21 | 21 | 9 | 13 | |
| Outcome | |||||||
| Snoring index (events/hour) | Pre | 273 ± 178 | |||||
| Post | 276 ± 172 | ||||||
| p-value | NS | ||||||
| Primary vibration frequency (Hz) | Pre | 107 ± 59 | |||||
| Post | 110 ± 59 | ||||||
| p-value | NS | ||||||
| Palatal vibration frequency (Hz) | Pre | 82 ± 19 | |||||
| Post | 80 ± 30 | ||||||
| p-value | NS | ||||||
| Percent velum-like snores (types I and II) | Pre | 81 ± 25 | |||||
| Post | 85 ± 24 | ||||||
| p-value | NS | ||||||
| Resistance occurrence index (%) | Pre | 25 ± 16 | |||||
| Post | 23 ± 14 | ||||||
| p-value | NS | ||||||
| Maximum relative loudness (dB) | Pre | 15 ± 7 | |||||
| Post | 16 ± 6 | ||||||
| p-value | NS | ||||||
| Voluntary awake palatal flutter snoring (Hz) | Pre | 74.1 | |||||
| Post | 105.4 | ||||||
| p-value | NR | ||||||
| Skjostad 200697 | Nordgard 200698 | Maurer 200599,100 | Ho 2004101 | Brietzke 2001102 | |||
|---|---|---|---|---|---|---|---|
| Intervention | Rigid implants | Regular implants | Regular implants | Regular implants | Regular implants | Injection snoreplasty | |
| n | 10 | 10 | 30 | 40 | 9 | 27 | |
| Outcome | |||||||
| AHI | Pre | 2.27 (0.2–5.3) | 2.2 ± 2.3 | 3.7 ± 2.3 | 4.8 ± 5.7 | ||
| Post | NR | 3.3 ± 3.8 | 5.5 ± 5.4 | 8.3 ± 11.5 | |||
| p-value | NS | < 0.05 | NS | ||||
| AI | Pre | 0.7 ± 0.8 | |||||
| Post | 1.1 ± 1.4 | ||||||
| p-value | NS | ||||||
| HI | Pre | 3.0 ± 2.2 | |||||
| Post | 4.5 ± 4.7 | ||||||
| p-value | < 0.05 | ||||||
| ODI | Pre | 3.4 ± 2.9 | |||||
| Post | 5.3 ± 5.1 | ||||||
| p-value | NS | ||||||
| O2 mean (%) | Pre | 94.6 ± 1.8 | |||||
| Post | 94.3 ± 1.7 | ||||||
| p-value | NS | ||||||
| O2 min (%) | Pre | 89.8 ± 4.1 | |||||
| Post | 87.1 ± 5.8 | ||||||
| p-value | < 0.05 | ||||||
| Sleep efficiency (%) | Pre | 88.2 ± 8.1 | |||||
| Post | 83.7 ± 12.1 | ||||||
| p-value | NS | ||||||
| Implant extrusions (%) | 8.3 | 0 | 8.8 | 11 | 8.8 | NA | |
Summary of results
Four studies assessed the effects of Pillar implants and one the effects of injection snoreplasty. The available evidence consisted of one RCT and four pre–post studies.
Study sample sizes were small with a median number of 27 patients per study. In total, therefore, evidence on the effects of palatal stiffening techniques for the management of non-apnoeic snoring is based on results from 134 patients. Duration of follow-up across the studies ranged from 3 to 12 months in the studies assessing Pillar implant techniques97–101 and was 10 days post each procedure for the study assessing injection snoreplasty. 102 Therefore there is only limited evidence on the effects of Pillar implants at post-treatment durations greater than 6 months (two studies) and no evidence on effects at a duration of greater than 1 year. Additionally, there is no evidence on the effects of injection snoreplasty other than in the 2-week post-treatment period. One pre–post study99,127 indicated that the relapse rate on a measure of partner-assessed snoring intensity was 12.5% between the follow-up times of 3 months and 1 year. Therefore, the possibility that studies with a shorter follow-up period will show a greater treatment benefit needs to be considered when extrapolating results from short-term studies into the longer term.
A summary of the key study results is displayed in Table 43.
| Study ID | Study design | Group | Subjective outcomes | Objective snoring indices | PSG parameter outcomes | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Partner-assessed snoring severity (VAS) | VAS score ≤ 5 (%) | VAS score< 3 (%) | Treatment success (VAS score< 3) (%) | Response (VAS decrease of ≥ 1 cm) (%) | ESS | Snoring index (events/hour) | Primary vibration frequency (Hz) | Palatal vibration frequency (Hz) | Percent velum-like snores (types I and II) | Resistance occurrence index (%) | Maximum relative loudness (dB) | Voluntary awake palatal flutter snoring (Hz) | AHI | AI | HI | ODI | O2 mean | O2 min | Sleep efficiency | |||
| Skjostad 200697 | RCT | Rigid implants | – | |||||||||||||||||||
| Regular implants | + | |||||||||||||||||||||
| Nordgard 200698 | PP | Rigid implants | + | 50 | 23.5 | + | – | |||||||||||||||
| Maurer 200599,100 | PP | Rigid implants | + | 22 | 69 | + | – | – | – | – | – | – | + | – | + | – | – | + | – | |||
| Ho 2004101 | PP | Rigid implants | + | + | – | |||||||||||||||||
| Brietzke 2001102 | PP | Injection snoreplasty | NR | |||||||||||||||||||
Pillar implants
There was no significant decrease in partner-rated snoring severity with the use of rigid implants in one study. 97 All four studies that assessed regular implants (one arm in the RCT)97 reported a significant post-treatment decrease in snoring levels from a mean range of 7.1–7.9 to a mean range of 4.7–4.8. The unweighted mean change in pre- and post-treatment scores across the studies was 2.68. 97–101 Two studies98–100 reported the percentage of patients achieving a VAS score of < 3 as 23.5% and 22% respectively. Patient satisfaction with treatment was 80% and partner satisfaction 50% and 70.6% in the two studies97,98 that assessed this outcome.
All three of the studies that assessed ESS reported a significant decrease in ESS scores post treatment. 98–101 Mean baseline ESS levels were within the range considered normal but a further reduction in scores was still attained at post-treatment follow-up, with a mean range of 4.9–5.7 across the studies. 98–101
Snoring sound was objectively measured in only one study. 99,100 There were no significant differences in any of the snoring sound indices assessed from baseline to follow-up. Therefore it would appear that there is little correlation in this study between the reduction in partner-assessed snoring severity from 7.1 (SD 2.1) to 4.8 (SD 2.6) and any objective measures of snoring sound.
There was no evidence of any consistent effects on any PSG parameters with the use of Pillar implants in three studies. 98–101 All three studies showed a slight increase in AHI scores from baseline but this was only significant in one study. 99,100
Data on postoperative pain and swallowing and speech difficulties were only reported in two studies. 98,99,127 Pain levels were reported as either mild or mild to moderate, with both swallowing and speech difficulties reported as mild. In all four of the studies postoperative pain was managed effectively with low levels of analgesics. No serious adverse events occurred.
Injection snoreplasty
In the one study that assessed injection snoreplasty, 92% of patients or their partners reported that snoring was no longer a problem at follow-up. 102
There was an increase in voluntary awake palatal flutter snoring of 31.3 Hz at post-treatment follow-up. No significance test for a comparison of the pre- and post-treatment means was reported.
Postoperative pain scores were all categorised as mild.
Conclusions
From the limited evidence available it appears that, in the year after treatment with Pillar implants, there is a significant decrease in partner- and patient-reported levels of snoring severity. However, this treatment benefit appears to be relatively modest, with an unweighted mean decrease of 2.68 points on a 10-point VAS scale. None of the studies attained a mean post-treatment score of less than 4 and, in the two studies in which it was reported, only 23.5% and 22% of patients achieved a VAS score of < 3. There is no evidence to suggest that partner-reported levels of snoring severity are corroborated by objective measures of snoring sound intensity, as no significant differences in any measure of objective snoring sound intensity were reported. In all studies Pillar implants had a significant positive benefit on ESS scores, but these were within the range considered normal at baseline. The limited available evidence also suggests that the use of Pillar implants does not have any significant positive or negative effects on any PSG-measured indices and, where any changes were reported, these may well be related to the ‘noise’ associated with the measurement of these parameters. Postoperative pain and swallowing and speech difficulties were all rated as mild or mild to moderate, and the use of the technology does not appear to be associated with any moderate or serious adverse events.
Given the limited very poor-quality evidence available on the effects of injection snoreplasty it is not possible to draw any conclusions regarding the safety and efficacy of this treatment without consideration of substantive further evidence on the use of this technology.
Continuous positive airway pressure
Quantity and quality of the studies
Only one study, conducted by Series and Marc,112 assessed the effects of CPAP in the treatment of non-apnoeic snoring. The aim of the study was to evaluate the effect of discontinuing nasal continuous positive airway pressure (NCPAP) treatment on the snoring characteristics of patients. The study included 18 non-apnoeic snorers who were allocated to either NCPAP or a no-treatment control group. The control group were studied twice, at baseline and at 30 days’ follow-up. The NCPAP group were studied at baseline and then underwent a second sleep study to determine the level of NCPAP required to abolish snoring. Patients remained on treatment at a level that banished their snoring for a 30-day period. A third sleep study was obtained on the first night without CPAP after the 30 days of treatment. Six patients from the intervention group were additionally followed up in a fourth sleep study 8–10 days after the end of the treatment period.
Although there was a no-treatment control group in the study, no between-group comparisons were undertaken and therefore the study was classified as a two-group parallel pre–post study. The total length of follow-up was 38–40 days.
All patients had undergone an overnight PSG with snoring measurement at baseline to rule out a possible diagnosis of OSAS. The patient group included in the study ranged in age from 25 to 64 years and was predominantly male (88.9%). The mean BMI was 29.1 kg/m2 and 22.2% were smokers. None of the patients had undergone previous treatment for snoring or were taking medication at the time of the study. Study characteristics are summarised in Table 44.
| ID | Study design | Intervention | n | Follow-up duration | Participantsa | Outcomes | ||
|---|---|---|---|---|---|---|---|---|
| PSG parameters | Subjective | Objective | ||||||
| Series 1994112 | Two-group parallel pre–post | CPAP versus no intervention | 18 | 38–40 days |
Baseline tests: PSG Participant demographics: age: range 25–64; male: 88.9%; BMI: 29.1 ± 4.24; AHI: CPAP: 2.9 ± 3.9, no intervention: 4.5 ± 3.9; ESS: NR; smokers: 22.2% |
AHI; AI | NR | Total sleep time; stages I–II (% TST); stages III–IV (% TST); stages REM (% TST); supine (% TST); snoring index (events/hour); % TST > 60 dB SPL; mean snoring level (dB SPL) |
Outcomes
The outcomes of interest were total sleep time, sleep architecture parameters and an objective measurement of snoring intensity. Snoring was defined as a spike in breathing sound intensity greater than 60 dB SPL. For each recording a computer interpretation of the sound recording gave the snoring index, the total sleep time (TST) spent at the different SPL values in 3-dB steps above 60 dB (60–72 dB) and the mean snoring level. Other outcomes assessed were AHI and AI.
Study quality
A summary of the quality of the study assessing NCPAP is displayed in Table 45 below. The study was a very small two-group parallel pre–post study with no-between group comparisons. Patient inclusion criteria were only partially specified and the reporting of baseline characteristics was limited. Treatment compliance was unclear, although it was reported that patients who were unable to tolerate treatment withdrew from the study and were replaced by further patients. The use of objectively assessed outcomes means that the results are likely to be valid for the outcomes assessed. However, because of the lack of reporting of clear inclusion criteria and limited baseline patient characteristics, it is difficult to assess to what extent the study results can be extrapolated to a wider patient population.
| Quality criteria | Series 1994112 |
|---|---|
| Study design | Two-group parallel pre–post |
| Eligibility criteria specified? | P |
| Adequate baseline details presented? | P |
| Are any co-interventions stated? | ? |
| Compliance with treatment adequate? | ? |
| Subgroup analysis justified? | NA |
| Data collection tools valid? | + |
| Data collection tools reliable? | ? |
| All participants accounted for? | – |
| Data analyses appropriate? | + |
| Greater than 80% of patients followed up? | + |
| Generalisability | ? |
| Intercentre variability | NA |
Results
In the NCPAP group the baseline snoring index score of 387 per hour (SD 150) was effectively abolished to a snoring index score of 15.1 per hour (SD 2.5), with a mean NCPAP level of 5.3 cmH2O (SD 0.5) (range 3–8 cmH2O). At post-treatment follow-up visit 1 (the first night without NCPAP) there was no significant difference between the baseline snoring index value [387 per hour (SD 150)] and the post-treatment value [320 per hour (SD 171)]. At post-treatment follow-up visit 2, no significant differences were observed in snoring index values from baseline, with snoring levels having returned to their pretreatment levels [387 per hour (SD 150) versus 374 per hour (SD 181.3)]. The percentage of TST spent with snoring levels > 60 dB SPL had significantly decreased from baseline at follow-up visit 1 [10.3% (SD 1.8) versus 7.4% (SD 1.5)]. This improvement was observed for sound pressure levels up to 69 dB SPL. However, by follow-up visit 2, post-treatment values were no longer significantly different from baseline values [10.3% (SD 1.8) versus 9.8% (SD 2.1)]. Likewise, at follow-up visit 1 the mean snoring level had significantly decreased from the baseline value of 66.4 dB SPL (SD 0.9) to 65.0 dB SPL (SD 0.9), but at follow-up visit 2 it was no longer significantly different from the baseline value, with a mean of 65.7 dB SPL (SD 0.98).
Both AHI and AI scores decreased significantly whilst patients were on therapy, from baseline values of 2.9 (SD 3.9) and 9.7 (SD 3.9), respectively, to 0.2 (SD 0.6) and 3.7 (SD 2.4) respectively. AHI scores, although increasing slightly from levels attained whilst on therapy, remained significantly lower than the baseline value at both follow-up visits 1 and 2, with values of 1.0 (SD1.5) and 1.1 (SD 1.5) respectively. AI values, in accordance with AHI scores, also increased from the levels attained whilst on therapy at both follow-up visits 1 and 2, with values of 8.2 (SD 4.2) and 6.9 (SD 4.8), respectively, no longer being significantly different from the baseline value. There were no significant differences in TST or sleep architecture parameters in the NCPAP treatment group compared with baseline values, across the treatment period and at follow-up visits 1 and 2. The mean values for TST and all sleep architecture parameters at baseline, on treatment and at follow-up visits 1 and 2 are presented in Table 46.
| Intervention | Skjostad 200697 | ||||||
|---|---|---|---|---|---|---|---|
| NCPAP | No-treatment control | ||||||
| Follow-up time | Baseline | NCPAP | 1 | 2 | Baseline | 1 | |
| n | 9 | 9 | 9 | 6 | 9 | 9 | |
| AHI | 2.9 ± 3.9 | 0.2 ± 0.6 | 1.0 ± 1.5 | 1.1 ± 1.5 | 4.5 ± 3.9 | 5.1 ± 3.6 | |
| p-valueb | < 0.05 | < 0.05 | < 0.05 | NS | |||
| AI | 9.7 ± 3.9 | 3.7 ± 2.4 | 8.2±4.2 | 6.9±4.8 | 8.6±4.8 | 9.9 ± 5.1 | |
| p-value | < 0.05 | NS | NS | NS | |||
| Total sleep time (TST) | 5.7 ± 0.9 | 5.7±0.9 | 6.0 ± 0.3 | 6.1 ± 1.5 | 6.2 ± 0.6 | 6.3 ± 0.9 | |
| p-value | NS | NS | NS | NS | |||
| Stages I–II (% TST) | 71.9 ± 3.6 | 71.1±4.2 | 72.3 ± 4.2 | 72.1 ± 3.0 | 72.0 ± 4.5 | 71.9 ± 3.6 | |
| p-value | NS | NS | NS | NS | |||
| Stages III–IV (% TST) | 13.8 ± 2.7 | 14.6±2 | 13.0 ± 3.3 | 13.7 ± 2.1 | 15.0 ± 4.8 | 14.4 ± 2.4 | |
| p-value | NS | NS | NS | NS | |||
| Stages REM (% TST) | 14.2 ± 1.5 | 14.3±3.0 | 14.6 ± 2.7 | 14.2 ± 3.0 | 13.0 ± 2.7 | 13.7 ± 3.3 | |
| p-value | NS | NS | NS | NS | |||
| Supine (% TST) | 40.1 ± 31.2 | 21.0±15.0 | 29.2 ± 20.1 | 16.0 ± 14.4 | 49.0 ± 27.0 | 42.3 ± 20.4 | |
| p-value | NS | NS | NS | NS | |||
| Snoring index (events/hour) | 387 ± 150 | 15.1±7.5 | 320 ± 171 | 374 ± 181 | 380 ± 108 | 388 ± 201 | |
| p-value | < 0.05 | NS | NS | NS | |||
| % TST> 60 dB SPL | 10.3 ± 5.4 | NR | 7.4 ± 1.5 | 9.8 ± 2.1 | 11.1 ± 6.0 | 10.5 ± 2.3 | |
| p-value | < 0.05 | NS | NS | ||||
| Mean snoring level (dB SPL) | 66.4 ± 0.9 | NR | 65.0 ± 0.9 | 65.7 ± 0.98 | 65.6 ± 0.9 | 65.1 ± 1.5 | |
| p-value | < 0.05 | NS | NS | ||||
Patients in the no-treatment control group showed similar levels of baseline snoring characteristics to those in the NCPAP group. In the control group the snoring index remained unchanged from baseline at follow-up, with values of 380 per hour (SD 108) and 388 per hour (SD 201) respectively. The percentage of TST > 60 dB SPL was similar at baseline and at follow-up: 11.1% (SD 6.0) versus 10.5% (SD 2.3). Likewise, the mean snoring level did not change significantly, from 65.6 dB (SD 0.9) at baseline to 65.1 dB (SD 1.5) at follow-up. As expected there were no significant differences between baseline and follow-up in the control group in AHI scores, TST or sleep architecture parameters. The mean baseline and follow-up values for all reported outcomes are displayed in Table 46.
Three patients in the NCPAP group discontinued treatment after a few nights because of the discomfort of the device. These patients were replaced at this point in the trial by a further three patients with similar baseline snoring indices. No adverse events were reported in either group.
Summary of the results
The very limited evidence available on the effects of NCPAP is only able to inform the effectiveness of NCPAP in the management of snoring indirectly, as the study was not designed to assess this outcome. There is therefore no direct evidence on the effects of CPAP in the management of snoring, and what evidence is available is based on the results of nine patients with a total follow-up time of 38–40 days. Given the paucity of this evidence it is not advisable to extrapolate the results of this study to a wider patient population who will need long-term treatment for the management of snoring. An overall summary of the study results is provided in Table 47.
| Intervention | Skjostad 200697 | |||
|---|---|---|---|---|
| NCPAP | No-treatment control | |||
| Follow-up time | NCPAP | 1 | 2 | 1 |
| n | 9 | 9 | 9 | |
| AHI | + | + | + | – |
| AI | + | – | – | – |
| Total sleep time (TST) | – | – | – | – |
| Stages I–II (% TST) | – | – | – | – |
| Stages III–IV (% TST) | – | – | – | – |
| Stages REM (% TST) | – | – | – | – |
| Supine (% TST) | – | – | – | – |
| Snoring index (events/hour) | + | – | – | – |
| % TST > 60 dB SPL | + | – | – | |
| Mean snoring level (dB SPL) | + | – | – | |
Objective measures of snoring sound
The use of CPAP at 5.3 cmH2O (SD 0.5) (range 3–8 cmH2O) effectively abolished snoring to a mean number of snores per hour of 15.1 (SD 2.5). However, relapse to a pretreatment level occurred rapidly without the use of CPAP.
Polysomnographic parameter outcomes
There was a significant decrease in both AHI and AI scores with the use of CPAP. There were no significant differences in TST or sleep architecture parameters with CPAP use compared with baseline values.
Conclusions
There is very little evidence available on the effects of CPAP for the management of non-apnoeic snoring. What evidence is available suggests that the use of CPAP may be effective in reducing levels of snoring, without having any adverse effects on PSG-measured parameters. However, given the poor-quality evidence available it is not possible to draw any definitive conclusions regarding the efficacy and safety of the use of CPAP for the management of non-apnoeic snoring.
Mandibular advancement splints
Quantity and quality of the studies
Two pre–post studies reported in three publications assessed the effects of MAS. 110,111,113 One further study104 (reported in the section on RFA) compared RFA to the soft palate with the short-term use of a MAS. The results of this study have already been presented in the section on RFA and therefore are not reported again. However, the results are included in the summary section as part of the overall evidence on the effects of MAS.
The aim of the studies by Smith and Battagel113 and Fransson and colleagues110,111 was to assess the effects of using a MAS with a minimum mandibular advancement of 5 mm. The study by Smith and Battagel113 used an adjustable Herbst splint, whereas Fransson and colleagues110,111 used a monobloc MAS. Smith and Battagel113 included 35 non-apnoeic snorers who were followed up before and 1 month after fitting the MAS. In total, 29 patients were followed up at 1 month and therefore included in the assessment of subjective questionnaire-assessed outcomes, with 11 completing a baseline and follow-up unsupervised overnight domiciliary sleep recording. Fransson and colleagues110,111 included both patients with a diagnosis of OSAS and those with non-apnoeic snoring. A total of 77 patients were included in the study: 50 with OSAS and 27 non-apnoeic snorers. Only limited results were reported separately for the non-apnoeic snoring subgroup, with 13 non-apnoeic snoring patients included in the 6-month follow-up of objectively measured snoring scores and 27 assessed for ODI scores at 2 years’ follow-up.
The study by Smith and Battagel113 included oximetry at baseline to rule out a diagnosis of OSAS, whereas the study by Fransson and colleagues110,111 included limited PSG assessment to categorise patients by diagnosis. No tests to assess the site of airway narrowing were reported by Smith and Battagel,113 whereas fibreoptic pharyngoscopic examination with Muller’s manoeuvre, in addition to subjective assessment of the degree of hypopharyngeal collapse and the presence or absence of tongue base hyperplasia, were employed by Fransson and colleagues. 110,111 Across the 62 non-apnoeic snorers included in the two studies, the mean age ranged from 44 to 52 years (range 28 to 70 years) and the percentage of male participants ranged from 57% to 66.7%. The mean BMI ranged from 26.8 kg/m2 to 28.4 kg/m2, indicating a patient population that was overweight but not obese. In the study by Smith and Battagel113 the mean baseline ESS score was 9.4 (SD 5.0). Neither of the studies reported the smoking status of patients nor levels of alcohol consumption. A summary of study characteristics is presented in Table 48.
| ID | Study design | Intervention | n | Follow-up duration | Participantsa | Outcomes | ||
|---|---|---|---|---|---|---|---|---|
| PSG parameters | Subjective | Objective | ||||||
| Smith 2004113 | Pre–post | Herbst MAS (advancement of at least 5 mm attempted) | 35 | 1 month |
Baseline tests: oximetry Participant demographics: age: 44 years (range 28–61); male: 57%; BMI: males: 28.4 ± 2.8, females: 26.8 ± 5.3; AHI: NR; ESS: 9.4 ± 5.0; smokers: NR |
Median O2; minimum O2; O2 dips > 4%/hour | ESS; adverse events (short term); adverse events (longer term) | Snoring noise levels (L5); snoring noises at L5–L95 (mV) |
| Fransson 2001;110 2003111 | Pre–post | MAS (advancement of 75% of the maximal protrusion range or a minimum of 5 mm) | 27 | 2 years |
Baseline tests: limited PSG; clinical examination; fibreoptic pharyngoscopic examination Participant demographics: age: 52 (range 37–70); male: 66.67%; BMI: 28 (range 23–35); AHI: NR; ESS: NR; smokers: NR |
ODI; SaO2 nadir | NR by subgroup | Snoring sound score (dB) |
Outcomes
Across the studies PSG parameter outcomes,110,111,113 objective measures of snoring sound intensity, ESS and adverse events were reported. In the study by Smith and Battagel113 respiratory noise levels were assessed at the 95th and 5th percentile levels, with the L5 level corresponding to the SPL exceeded 5% of the time in the test period and representing the highest noise level. The L95 level conversely corresponded to the noise level exceeded 95% of the time in the test period, representing background noise. EDS was assessed using the ESS and adverse events were categorised as short term (2–3 days) or long term (1 month). Fransson and colleagues110,111 measured snoring sound levels directly in decibels both pre- and post-treatment.
Study quality
A summary of the study quality indicators is shown in Table 49. The quality of both of the studies was relatively poor, with small sample sizes. Both studies had reasonably well-defined inclusion criteria but neither of them presented adequate baseline details on participants. For the study by Fransson and colleagues110,111 this was primarily because the study sample included patients with a diagnosis of OSAS and limited details were presented on the non-apnoeic snoring subgroup alone. Rates of treatment compliance, when reported, were adequate but were based on short-term follow-up data and therefore may be higher than would typically be seen in practice. Snoring sound levels were objectively assessed, limiting bias in the assessment of this outcome, but neither study also included a measure of patient- or partner-assessed snoring levels. It is therefore unclear whether any treatment benefit in terms of objective snoring sound reduction is perceived by the patient or their partner as an adequate reduction in snoring level. Sample sizes were small in both studies and only 31–48% of patients were included in the objective snoring sound evaluations. Data analysis in both studies was appropriate.
| Quality criteria | Smith 2004113 | Fransson 2001;110 2003111 |
|---|---|---|
| Study design | Pre–post | Pre–post |
| Eligibility criteria specified? | P | + |
| Adequate baseline details presented? | P | P |
| Are any co-interventions stated? | NA | P |
| Compliance with treatment adequate? | P | P |
| Subgroup analysis justified? | NA | + |
| Data collection tools valid? | P | P |
| Data collection tools reliable? | P | P |
| All participants accounted for? | – | + |
| Data analyses appropriate? | + | + |
| Greater than 80% of patients followed up? | – | – |
| Generalisability | + | ? |
| Intercentre variability | NA | NA |
Results
In the study by Smith and Battagel,113 at the 1-month follow-up there was a significant mean reduction of 2.5 (SD 2.5) points in the ESS score in the 29 patients assessed for this outcome [mean pretreatment score of 9.4 (SD 5.0) versus mean score of 6.9 (SD 4.8) at follow-up]. At this follow-up time subjective compliance rates were good, with 26 out of the 29 patients still using the MAS. Three patients were unhappy using the device, with two patients dissatisfied with the appliance aesthetics and one experiencing temporomandibular joint (TMJ) problems. A large percentage of patients complained of initial (2–3 days) muscular and TMJ discomfort (69% and 76% respectively); however, this had significantly decreased to 17% and 28%, respectively, at follow-up. The number of patients complaining of awakening with an abnormal bite, dry mouth or excessive salivation also decreased across the study period, although not significantly. In the short term 40% of patients complained of abnormal bite, 28% dry mouth and 21% excessive salivation. At the follow-up the figures were 28%, 17% and 3% respectively.
In total, 11 patients completed pre- and post-treatment sleep recordings. There was a significant reduction in snoring noise levels (L5), from a median of 449 (range 53–1212) pretreatment to 161 (range 9–442) with a MAS. The background noise level (L95) remained reasonably constant between recordings, with a median of 61 (range 0–322) pretreatment and a median of 12 (range 0–334) post-treatment. Correspondingly, the L5–L95 ratio decreased significantly with treatment, from a median baseline level of 240 (range 15–1015) to a median post-treatment level of 75 (range 9–417), indicating a significant reduction in noise level whilst wearing the MAS. None of the PSG-assessed parameters changed significantly with treatment as all were within normal limits at baseline.
In the study by Fransson and colleagues110,111 13 non-apnoeic snoring patients underwent a snoring sound recording at baseline and at 6 months’ follow-up. A significant reduction in snoring sound volume was observed with the use of a MAS, from a pretreatment volume of 63.5 dB to a post-treatment volume of 57.5 dB. No range or standard deviation was reported for either baseline or post-treatment snoring sound levels. A total of 27 patients additionally underwent limited PSG at 2 years’ follow-up. PSG parameter results were within the range of normal at baseline in all patients, with a mean ODI of 1.3 (range 0–3.8) and a mean SaO2 nadir of 91.5% (range 82.5–97.5%). At follow-up values had not changed significantly and remained within the normal range, with a mean ODI of 0.8 (range 0–7) and a mean SAO2 nadir of 92.6% (range 90.4–96.0%). No further outcomes were reported separately for the non-apnoeic snoring subgroup.
The results for ESS scores, objectively assessed snoring outcomes and PSG parameters are displayed in Tables 50–52 respectively.
| Smith 2004113 | Fransson 2001;110 2003111 | ||
|---|---|---|---|
| Intervention | MAS | MAS | |
| n | 29 | NA | |
| Outcome | |||
| ESS, mean ± SD | Pre | 9.4 ± 5.0 | |
| Post | 6.9 ± 4.8 | ||
| p-value | < 0.001 | ||
| Smith 2004113 | Fransson 2001;110 2003111 | ||
|---|---|---|---|
| Intervention | MAS | MAS | |
| n | 11 | 13 | |
| Outcome | |||
| L5 snoring sound level (mV)a | Pre | 449 (53–1212) | |
| Post | 161 (9–442) | ||
| p-value | < 0.05 | ||
| L95 background snoring level (mV)a | Pre | 61 (0–322) | |
| Post | 12 (0–334) | ||
| p-value | NS | ||
| L5–L95 snoring sound (mV)a | Pre | 240 (51–1015) | |
| Post | 75 (9–417) | ||
| p-value | < 0.01 | ||
| Mean snoring sound score (dB) | Pre | 63.5 | |
| Post | 57.5 | ||
| p-value | < 0.05 | ||
| Smith 2004113 | Fransson 2001;110 2003111 | ||
|---|---|---|---|
| Intervention | MAS | MAS | |
| n | 11 | 27 | |
| Outcome | |||
| % O2a | Pre | 95 (93–97) | |
| Post | 95 (93–96) | ||
| p-value | NS | ||
| Minimum % O2a | Pre | 89 (86–94) | |
| Post | 90 (86–94) | ||
| p-value | NS | ||
| O2 dips > 4%/houra | Pre | 2.8 (0.0–120.5) | |
| Post | 1.7 (0.0–37.8) | ||
| p-value | NS | ||
| ODIb | Pre | 1.3 (0–3.8) | |
| Post | 0.8 (0–7) | ||
| p-value | NS | ||
| SaO2 nadir (%)b | Pre | 91.5 (82.5–97.5) | |
| Post | 92.6 (90.4–96.0) | ||
| p-value | NS | ||
Summary of results
Two pre–post studies assessed the effects of use of a MAS,110,111,113 Additional very limited evidence on MAS use is also available from a small CCT104 in which the control group used a MAS for a 10-day treatment period. Patients in this study were then assessed using a counterbalanced split-night study, with and without the MAS. Study sample sizes were small, with a total of 72 patients included across the three studies. The objective snoring sound assessment, however, is based on only 34 patients and therefore the results should be interpreted with caution. The follow-up duration across the three studies ranged from 10 days to 2 years. However, once again objective snoring sound measures were all conducted within a follow-up period of 10 days to 6 months. Therefore, there is only very limited evidence available on the short-term effectiveness of MAS for snoring and no evidence on the longer-term effectiveness. An overall summary of the results is given in Table 53.
| Study ID | Study design | Subjective outcomes | Objective snoring outcomes | PSG parameter outcomes | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ESS score | L5 snoring sound level (mV) | L95 background snoring level (mV) | L5–L95 snoring sound (mV) | Mean snoring sound score (dB) | % O2 | Minimum % O2 | O2 dips > 4%/hour | ODI | SaO2 nadir (%) | ||
| Smith 2004113 | PP | + | + | – | + | – | – | – | |||
| Fransson 2001;110 2003111 | PP | + | – | – | |||||||
Epworth Sleepiness Scale
In one study113 there was a significant reduction in ESS scores in 29 patients with the use of a MAS at the 1-month follow-up, from 9.4 (SD 5.0) to 6.9 (SD 4.8) respectively. Neither of the other two studies either assessed ESS104 or reported ESS scores separately from the non-apnoeic snoring subgroup of patients. 110,111
Objective measures of snoring sound
In all three studies there was a significant reduction in the maximal snoring sound volume,113 mean snoring sound volume110,111 or the percentage of time spent in loud snoring104 with the use of a MAS. Maximal snoring sound volume decreased from a median of 449 (range 53–1212) at baseline to a median of 161 (range 9–442) with MAS use at the 1-month follow-up,113 mean snoring volume decreased from a pre-device use level of 63.5 dB to 57.5 dB with MAS use at 6 months,110,111 and the percentage of time spent in loud snoring decreased from 10.62% (SD 9.83%) to 3.32% (SD 4.7%) at 10 days’ follow-up. 104 A comparison of the percentage of time spent in loud snoring for patients who had undergone soft palate RFA with the percentage of time spent in loud snoring for those fitted with a MAS showed that the percentage point estimate favoured the MAS group; however, there was no significant difference between the groups for this outcome (10.62% versus 3.32% respectively).
Polysomnographic parameter outcomes
In two studies110,111,113 there were no significant changes in PSG-measured outcomes with the use of a MAS, at either 1 month or 2 years of follow-up post device use.
Adverse events
Only one of the three studies reported adverse events. 113 The percentage of minor side effects was relatively high, with 69% and 76% of patients experiencing muscular and TMJ discomfort respectively. The percentage of patients who experienced abnormal bite, dry mouth or excessive salivation was slightly lower although still common, ranging from 21% to 40%.
There was a significant reduction in the percentage of patients with muscular discomfort or TMJ pain at the 1-month follow-up although these remained common, with 17% and 28% of patients reporting the problem respectively. The percentage of patients with abnormal bite, dry mouth or excessive salivation also decreased from the initial short-term levels but not significantly. These side effects remained relatively common with 28%, 17% and 3% of patients reporting the problem respectively. 113
Conclusions
There is very limited evidence available on the effects of short-term MAS use on levels of snoring and no evidence on the effects of MAS use at treatment durations greater than 6 months. The limited evidence available suggests that use of a MAS may be effective in reducing levels of snoring sound intensity and the percentage of time spent in loud snoring in the short term. None of the studies examined the clinical significance of the reduction in time spent in loud snoring or the reduced volume levels. It is therefore unclear whether any objectively assessed reduction in snoring would translate into a treatment benefit that would be perceived as clinically relevant by the patient or their bed partner. In the short term, on evidence available from two studies,110,111,113 MAS use does not appear to have any detrimental or positive effects upon any PSG-measured parameters, such as oxygen desaturation levels. Adverse effects of treatment were assessed in only one study up to a treatment duration of 1 month. 113 Results from this study indicate that initial minor side effects of MAS use are very common but appear to reduce with longer-term wear. There is no evidence available on the adverse events associated with MAS use at treatment durations greater than 1 month.
Other related systematic reviews
One systematic review by Stuck and colleagues70 was identified that had assessed the effects of RFA surgery of the soft palate for the treatment of snoring. The review included 22 prospective and retrospective pre–post studies published before January 2003. The patient populations in the included studies were non-apnoeic snorers and patients with mild OSAS, with a maximum RDI of 10 or 15. A total of 19 of the included studies had used temperature-controlled RFA (somnoplasty), with the remaining three studies using the Ellman (monopolar),129 VidaMed130 or Coblation (bipolar)108 systems. Between one and four application sites per treatment session were selected. The review included four pre–post studies104–107 included in the present assessment of the effects of RFA for the treatment of non-apnoeic snoring. Eleven studies were included in the review analysis; seven that had measured partner-reported snoring levels using a VAS and four that had used snoring scores. The total number of patients included in the studies that had used a VAS for assessment was 231, and the total number of patients included in the studies using a snoring score was 114. Follow-up periods across the studies ranged from 6 to 12 weeks. In the studies that had used a VAS the weighted mean snoring score was significantly reduced from 8.1 (SD 1.8) at baseline to 3.5 (SD 2.2) postoperatively; the mean pooled treatment effect was 4.8 (SD 2.8). In the four studies that had used snoring scores the weighted mean snoring score was significantly reduced from 8.0 (SD 2.1) at baseline to 3.4 (SD 2.3) postoperatively; the mean pooled treatment effect was 4.7 (SD 3.1). Heterogeneity between the studies was not formally assessed. No serious adverse events were reported but there was significant variation in the overall complication rates reported, ranging from 0% to 50%. Four studies reported moderate complications in terms of severe palatal damage, including palatal fistula, uvula loss or sloughing. The authors concluded that RFA surgery of the soft palate leads to a significant reduction in subjective snoring, with snoring being reduced to a tolerable level. Nevertheless, CCTs and objective outcome assessment are still lacking and the findings need to be confirmed by RCTs.
Chapter 4 Associated treatment costs
The indicative costs and resource use associated with the surgical procedures or non-surgical devices identified in the review of clinical effects are displayed in Table 54.
| Parameters | Mean cost (£) | Number | Source | |
|---|---|---|---|---|
| UP3 costs (assuming one procedure) | ||||
| Initial consultation | Unit cost of outpatient initial (consultation) visit | 148.00 | 1 | NHS reference costs 200684 |
| Surgical procedurea | Unit cost of elective inpatient minor mouth or throat procedure | 992.00 | 1 | NHS reference costs 200684 |
| Follow-up consultation | Unit cost of outpatient follow-up (consultation) visit | 88.00 | 1 | NHS reference costs 200684 |
| Total | 1228.00 | |||
| Assumptions and range: total based on assumption of stay of 1 day | ||||
| Assuming extra day of hospital stay | 318.00 | NHS reference costs 200684 | ||
| Total | 1546.00 | |||
| LAUP costs (assuming between one and three procedures)b | ||||
| Initial consultation | Unit cost of outpatient initial (consultation) visit | 148.00 | 1 | NHS reference costs 200684 |
| Surgical procedure | Unit cost of elective day-case minor mouth or throat procedure | 551.00 | 1 | NHS reference costs 200684 |
| Follow-up consultation | Unit cost of outpatient follow-up (consultation) visit | 88.00 | 1 | NHS reference costs 200684 |
| Total | 787.00 | |||
| Assumptions and range: total based on assumption of one procedure and one follow-up visit | NHS reference costs 200684 | |||
| One additional procedure and follow-up visit | Unit cost of elective day-case minor surgery and out-patient follow-up visit | 639.00 | 2 | NHS reference costs 200684 |
| Total | 1426.00 | |||
| Two additional procedures and follow-up visits | Unit cost of elective day-case minor surgery and outpatient follow-up visit | 639.00 | 3 | NHS reference costs 200684 |
| Total | 2065.00 | |||
| Pillar implants (costs) (assuming one procedure) | ||||
| Initial consultation | Unit cost of outpatient initial (consultation) visit | 148.00 | 1 | NHS reference costs 200684 |
| Surgical procedure | Unit cost of elective day-case minor mouth or throat procedure | 551.00 | 1 | NHS reference costs 200684 |
| Pillar implants | Unit cost of three Pillar implants | 318.00–375.00 | 1 | Restore Medical (St Paul, MN) |
| Follow-up consultation | Unit cost of outpatient follow-up (consultation) visit | 88.00 | 1 | NHS reference costs 200684 |
| Total | 1105.00–1162.00 | |||
| CPAP | ||||
| Initial costs in first year | ||||
| Initial consultation | Unit cost of outpatient initial (consultation) visit | 148.00 | 1 | NHS reference costs 200684 |
| CPAP machine | 300.00 | 1 | ResMed (Abingdon, UK) | |
| CPAP mask | Annual cost of CPAP mask | 80.00 | ResMed | |
| Titration | Unit cost of 30-minute appointment with a specialist nurse | 57.00 | 1 | NHS reference costs 200684 |
| Total of initial CPAP costs (first year) | 585.00 | |||
| Assumptions: 7-year life span of CPAP machine, with an interest rate of 3.5% for initial cost | ResMed NICE methods guidance131 | |||
| Ongoing costs (yearly) | ||||
| CPAP device | Equivalent annual cost of CPAP device | 47.40 | 1 | |
| CPAP mask | Annual cost of CPAP mask | 80.00 | 1 | ResMed |
| Annual follow-up consultation | Unit cost of outpatient follow-up (consultation) visit | 88.00 | 1 | NHS reference costs 200684 |
| Total ongoing costs (yearly) | 215.40 | |||
| MAS (assuming device life of 2 years)c | ||||
| MAS device | NHS cost of dental device and its provision | 250.92 | 1 | 12 units of dental activity at £20.91 |
| MAS cost per year | 128.80 | 1 | ||
| MAS ongoing costs (yearly) | Unit cost of annual check-up | 19.47 | 1 | Cost of a consultant appointment, unpublished data |
It is difficult to compare the costs associated with the identified surgical procedures, which theoretically have a ‘one-off’ cost for the procedure(s), with those of the devices, which have an annual cost or cost per use. The cost for UP3 is approximately £1230 assuming that patients have a 1-day hospital stay but this rises to approximately £1550 if patients require an additional day of hospitalisation for postoperative recovery or complications. For LAUP the costs associated with one procedure are approximately £790 but rise to £1430 for a two-stage sequential procedure and £2070 for a three-stage procedure. Therefore, UP3 is more expensive than LAUP conducted as a one-stage procedure (with associated treatment costs of £1230 and £790 respectively) but cheaper than LAUP conducted as either a two- or three-stage procedure assuming that only 1 day of hospitalisation is required after UP3. If it is assumed that 2 days of hospitalisation are required post UP3 then LAUP conducted as either a one- or a two-stage procedure is cheaper than UP3; however, LAUP conducted as a three-stage procedure still remains more costly than UP3. When the use of Pillar implants is considered the approximate treatments costs range from £1110 to £1160 (depending on the manufacturer’s discount). Therefore, the cost of treatment with Pillar implants is similar to the cost incurred through undertaking UP3 with 1 day of hospitalisation but is considerably more than the cost of undertaking LAUP as a one-stage procedure; however, if LAUP is undertaken as a two- or three-stage procedure then the use of Pillar implants becomes the least-cost option.
The approximate annual treatment costs associated with the use of a CPAP machine and a MAS are £220 and £130 respectively. Therefore, use of a CPAP machine is on average more expensive than the use of a MAS. However, for both of these interventions there are a large number of different models currently available on the market, and use of a more expensive MAS and a cheaper CPAP machine may reverse this cost relationship.
Chapter 5 Discussion
Statement of principal findings
Uvulopalatopharyngoplasty versus laser-assisted uvulopalatoplasty
Evidence from one small RCT86,87 and one small CCT88 to support there being a difference in treatment effect between UP3 and LAUP on subjectively assessed snoring indices is equivocal. In the CCT88 significant differences between the two procedures were found on outcomes of partner-reported snoring status and difficulties falling asleep because of snoring, favouring treatment with UP3; however, no significant differences were observed on other measures, including partner-reported snoring status in the RCT. 86,87 Any treatment benefit for UP3 compared with LAUP is therefore likely to be of a relatively small magnitude. This contention is consistent with evidence from the RCT86,87 showing that at short-term follow-up both procedures were effective at significantly reducing the objectively measured snoring index from baseline, with no significant differences between the effects of the two procedures. Both UP3 and LAUP were effective at reducing snoring loudness but this reduction was modest (3.8 dB) and therefore may not be of great clinical consequence. Adverse events of the two procedures were comparable, except for levels of postoperative pain, which were significantly higher in the UP3 group. Relapse rates were consistent with those generally observed for the procedures in the short term at 11–17%, but longer-term relapse rates (14–18%) were smaller than those generally observed in both retrospective and prospective pre–post studies in the literature. 95,132
Uvulopalatopharyngoplasty alone
Evidence on the effects of UP3 from six of the seven pre–post studies49,89–91,93,94 showed that UP3 was effective in reducing a number of both patient- and bed partner-reported snoring outcomes; however, it would appear that approximately 12% of patients do not gain any treatment benefit in terms of a postoperative snoring reduction94 and relapse rates are approximately 24% 1 year postoperatively. 94 The overall results from four studies that assessed objective measures of snoring were mixed and equivocal. 49,92–94 Two of the studies indicated no significant differences in postoperative measures,92,94 one showed a significant reduction in the snoring index and percentage of time spent in loud snoring93 and a further study showed a significant reduction in one outcome but not another. 49 Evidence to support the generally observed significant reduction in subjectively assessed snoring indices with objective reductions in snoring sound is therefore limited. Postoperative pain reported in one study was moderate – 6.9 on a 10-point VAS – but decreased rapidly to 1.1 at 10 days post treatment. 93 Short- and medium-term (up to 1 year) morbidity associated with treatment was relatively minor, with throat disturbances reported in 12.5% of patients,90,91 nasal speech and nasal regurgitation in 1.9% of patients each90 and swallowing problems being reported as moderate in the immediate postoperative period – 4.4 on a 10-point VAS – but decreasing rapidly to 0.5 at 10 days’ follow-up. 93
Laser-assisted uvulopalatoplasty alone
The limited evidence from the three pre–post studies on LAUP95,96,114 with a total of 58 participants supports the fact that subjectively assessed snoring status or scores are significantly improved after the procedure. In two studies95,96 snoring status improved in 75–79% of patients 2 months postoperatively; however, in one of the studies96 this decreased to an improvement in 57% of patients at 10 months. This indicates that, like UP3, there may be a considerable relapse rate over longer postoperative follow-up times. None of the studies on LAUP assessed objectively evaluated snoring sound and therefore it is unclear whether any patient- or partner-reported benefit would be corroborated by objective sound measurements. Postoperative pain reported in two studies95,114 was mild to moderate (> 4 on a 10-point VAS) but decreased rapidly by day 10. Adverse events associated with the procedure were persistent throat dryness or itching (36%) and difficulties with nasal breathing (21%) but these were only reported in one study. 95
Radiofrequency ablation of the soft palate
Evidence on the effects of RFA of the soft palate was limited to six studies103–108 and RFA of the tongue base to one study. 109 The evidence base consisted of one RCT,103 one CCT104 and five pre–post studies. 106–110 Results from the RCT103 showed a significant treatment benefit on partner-assessed snoring levels compared with placebo over the 10- to 14-week follow-up period, with a postoperative score of 5.2 ± 2.4 versus 8.0 ± 2.3 for the treatment groups, respectively, on a 10-point VAS. Across six of the studies103–108 (including the RCT) RFA was associated with a postoperative reduction in partner-assessed snoring severity, with an unweighted mean decrease of 3.24 on a 10-point VAS; however, as the final mean postoperative scores were in the range of 2.8–5.2, any benefit of treatment may be moderate, as only one study achieved a final mean VAS score of less than 3. 104 Examination of the RFA treatment protocols across the studies showed no obvious relationship between the size of the reduction in partner-assessed snoring attained and whether treatment was conducted using a single-lesion or multiple-lesion protocol. Additionally, there appeared to be no relationship between the size of treatment benefit and the length of follow-up across the studies. Relapse rates were considerably lower than those observed with either UP3 or LAUP, ranging from 6% to 21% at 9.5 months’ follow-up.
Evidence from one CCT and two pre–post studies104,105,107 for an objective reduction in snoring sound levels with RFA is equivocal. Results from the CCT104 showed that there was no significant difference between the percentage of time spent in loud snoring after treatment with RFA and the percentage of time spent in loud snoring with use of a MAS. There was also no significant correlation between objective measures of snoring sound and partner-reported snoring severity levels. 104 Results from the two pre–post studies were mixed. One study105 showed a significant, but clinically irrelevant, increase in snoring sound intensity and no correlation between objective measures of snoring sound and partner-reported snoring levels, whereas the second study107 found a decrease of 7 dB in the maximal snoring sound level but did not report significance levels for the change.
Levels of postoperative pain and measures of swallowing, speech, taste and pharyngeal irritation were rated as low103,105,106 to moderate. 107,108 When RFA was compared with placebo there were no significant differences between the groups on measures of pain, taste, speech or pharyngeal irritation. 103 Rates of mucosal blanchings and erosions ranged from 15.6% to 40%. 106–108 Rates of all other reported moderate adverse events were low. 108
Results from the systematic review of RFA by Stuck and colleagues70 concur with the results of this present review. Their analysis included a total of 11 studies, seven of which assessed partner-reported snoring levels using a VAS and four that used snoring scores. In the Stuck and colleagues review70 studies were combined using a random-effects meta-analysis for each type of outcome measure to derive a pooled mean estimate of treatment effect; however, heterogeneity between the studies was not formally statistically assessed. In contrast, because of heterogeneity between the studies in terms of both study design and length of follow-up, the present review has relied on combining the six relevant studies using a narrative synthesis. The review by Stuck and colleagues70 found that the weighted mean snoring score was significantly reduced from 8.1 (SD 1.8) to 3.5 (SD 2.2) at a follow-up time of between 6 and 12 weeks postoperatively for studies that had assessed snoring using a VAS. Therefore, the mean pooled treatment effect was 4.8 (SD 2.8). These point estimates are within the range indicated within this assessment, which found that snoring scores were significantly reduced from a mean range of 6.5–8.4 preoperatively to a mean range of 2.75–5.2 post treatment. Our estimated unweighted change in mean pre- and post-treatment scores is slightly lower than that of Stuck and colleagues,70 which is likely to reflect differences in the review inclusion criteria, such as their inclusion of both retrospective and prospective pre–post studies and studies with a follow-up duration of between 6 and 12 weeks post treatment. This review includes three studies with a follow-up period of over 5 months,104,106,108 which are likely to give a more realistic indication of the slightly longer-term effects of RFA treatment.
Palatal stiffening techniques
Palatal stiffening techniques were assessed in five studies, four of which assessed Pillar implants97–101 and one that assessed injection snoreplasty. 102 The available evidence consisted of one small RCT comparing rigid implants with regular implants97 and four pre–post studies. 98–102 Four studies showed that regular Pillar implants were effective at reducing partner-rated snoring severity, with a decrease in snoring levels from a mean range of 7.1–7.9 to a mean range of 4.7–4.8 post treatment;97–101 however, any treatment benefit appears to be only moderate, with an unweighted mean decrease of 2.69 points on a 10-point VAS scale observed. In two studies98–100 the percentage of patients achieving a VAS score of less than 3, which is generally considered to be a clinically relevant reduction, ranged from 22% to 23.5%. Relapse rates reported in the two studies98–100 that followed up at 1 year ranged from 12.5% to 14.3% depending on how a relapse was defined. This indicates that any initial treatment benefit from implants may decrease in the longer term.
Evidence on the effects of Pillar implants on objectively measured snoring sound indices was limited to only one study. 99,100 This showed no significant differences in any snoring sound index (number of snores per hour and loudness).
Postoperative pain levels in two studies were reported as either mild (score of 2.0 on a 10-cm VAS)98 or moderate (score of 4.9 on a 10-cm VAS)99,100 and decreased rapidly post treatment. Likewise, speech difficulties were assessed as mild (VAS score of 0.7)99,100 or moderate (VAS score of 3.0). 98 All swallowing difficulties were classified as mild. 98–100 Rates of implant extrusion were reasonably low, ranging from 0% to 11%. 97–101
Continuous positive airway pressure
The only available evidence on the effects of CPAP for the treatment of non-apnoeic snoring came indirectly from a very small, low-quality, two-group parallel pre–post study that included nine patients in the treatment group. 112 Results indicated that the use of CPAP at 5.3 cmH2O (range 3–8 cmH2O) dramatically reduced the number of snores per hour from a mean of 387 (SD 150) to a mean of 15.1 (SD 2.5). No subjective snoring scores were evaluated. Given the very limited low-quality evidence available to support the use of CPAP it is not advisable to extrapolate the findings of this small study, which had a treatment duration of only 1 month, to a wider patient population in the longer term.
Mandibular advancement splints
Evidence on the effects of MAS from three studies104,110,111,113 was limited to objectively assessed snoring sound outcomes (i.e. no patient- or partner-evaluated outcomes were assessed). The evidence suggests that MAS improve objective outcomes, including the maximal snoring sound volume,113 the mean snoring sound volume110,111 and the percentage of time spent in loud snoring. 104 Comparison of the percentage of time spent in loud snoring between patients who had undergone soft palate RFA and those fitted with a MAS showed that the point estimates favoured use of a MAS, but this was not statistically significant. 104 Data on the adverse effects of MAS use were scarce and reported in only one study. 113 This study indicated that the incidence of minor side effects was relatively high, particularly for muscular and TMJ discomfort in the initial days of MAS use. Although minor side effects remained relatively common these had all decreased within the first month of use. 113
Associated treatment costs
The analysis of approximate treatment cost data was limited to the procedures of UP3, LAUP and Pillar implants and to CPAP devices and use of MAS. Because the costs identified for the surgical procedures are theoretically ‘one-off’ costs whereas those derived for the devices are annual costs or costs per use, few comparisons between the costs of surgical procedures and those of devices could be drawn. Additionally, as already highlighted, the costs of diagnostic tests (i.e. PSG or modified PSG) to exclude a diagnosis of sleep apnoea were not included in the treatment costs. However, use of a MAS may not always be associated with the requirement for a sleep study (i.e. PSG or modified PSG) before use of the device, which is necessary before either surgery or use of CPAP is initiated, and this is likely to impact considerably on the overall treatment costs.
In terms of the surgical procedures (i.e. UP3, LAUP and Pillar implants) there is no procedure that in all cases is the least-cost option. LAUP as a one-stage procedure is cheaper than both UP3 and Pillar implants but becomes more expensive than both UP3 and Pillar implants when performed as a two- or three-stage procedure. The use of Pillar implants is slightly cheaper than the use of UP3. Use of a MAS is on average cheaper than the use of a CPAP machine although there is considerable uncertainty regarding the costs of both of these devices because of the number of models on the market; use of a cheaper CPAP machine and a more expensive MAS than those used in the costings could therefore reverse this relationship.
Limitations of the evidence base
This assessment has highlighted that measuring snoring levels and impact are complex and therefore that accurate assessment of any intervention effects for non-apnoeic snoring is subject to a number of confounding factors. A general overview of these issues in relation to the current evidence base and their impact upon any conclusions that can be drawn regarding the effects of the technologies assessed is therefore outlined below.
This review included 27 primary studies on the effects of surgical procedures and non-surgical devices for the management of non-apnoeic snoring. In practice, however, the evidence base was heavily weighted towards studies that assessed surgical procedures (n = 24), with only one study on the effects of CPAP112 and two on the effects of MAS110,111,113 identified. This has clearly limited any conclusions that can be drawn regarding the effects of either of these devices, which are commonly used for the management of OSAS. 2 Additionally, despite identifying 24 studies on the effects of surgical procedures, the range of different procedures assessed was broad, which means that relatively few studies had assessed the same intervention. This was particularly pertinent for studies assessing the effects of UP3 in which different procedures (LAUP, CAUP and UEP) were performed as well as UP389,90,94 and in which the post-treatment results were pooled across the different intervention groups. In these studies any treatment effect is likely to be confounded and it is not possible to differentiate between the effects of the different procedures undertaken. Additionally, even for RFA procedures and Pillar implants, for which treatment protocols were reasonably similar, the strength of any conclusions that can be drawn is limited because of the small number of studies and the small sample sizes upon which the evidence is based.
The inclusion criteria for this review meant that it was restricted to studies in which patients had a diagnosis of OSAS ruled out at baseline; in addition, pre–post studies were included only if an objective measure of snoring sound indices, cephalometric radiographs or MRI scans of palatal length or width, or PSG parameter outcomes were reported. It is therefore acknowledged that a number of pre–post studies have been excluded. This is most likely to have impacted upon studies that have assessed the use of MAS, as a sleep study is indicated to rule out OSAS only before undertaking surgical procedures for primary snoring2 and not before the use of MAS. Furthermore, the definition of an AHI score of less than or equal to five to define primary snoring means that further studies have been excluded. Although employing stringent criteria to define the patient population means that the review is limited to only patients with non-apnoeic snoring, use of an AHI score to define the population is somewhat arbitrary and probably does not reflect the management of patients with non-apnoeic snoring and mild OSAS in practice.
Despite these limitations this review has included the best available evidence on the effects of both surgical procedures and non-surgical devices for simple snoring. However, even limiting the review to the most robust evidence has highlighted the paucity of the available evidence base and severely limited the conclusions that can be drawn. The majority of the included studies were of poor methodological quality with very small sample sizes. The total evidence available consisted of three RCTs, two CCTs and 22 pre–post studies, with a total of 1191 participants. Only five controlled studies were identified: one RCT86,87 and one CCT88 on the effects of UP3 versus LAUP; one RCT on RFA versus placebo;103 one CCT comparing RFA with MAS;104 and one RCT comparing the effects of regular versus rigid Pillar implants. 97 However, in almost all studies data were analysed as a change in the pre- and post-treatment mean in each group, with few between-group comparisons conducted. This basic failure to carry out an appropriate analysis prevents any direct comparison between interventions. Additionally, in these studies it was frequently unclear whether treatment groups were comparable at baseline,86–88,97,104 and the quality and level of reporting were generally poor. The remainder of the evidence base consisted of pre–post studies, with variations in treatment protocols, definition of outcome measures and length of follow-up.
Drawing any comparisons between the studies has been further hampered by the heterogeneity in the way that outcome measures were defined and assessed across studies. Subjective measures of snoring were both patient and bed partner reported. However, it is well recognised that there is often little agreement between partner and patient reporting of snoring134 and therefore potentially little comparability between these different outcomes. Additionally, there was a large diversity in the way that changes in snoring were measured across the studies. When categorical scales were used to assess changes in snoring status these were 2-point,104 3-point,86,87,91,96 4-point49 and 5-point scales,88,90 usually assessing snoring as being ‘mild, moderate or severe’ or ‘worse, unchanged, improved or absent’. When VAS were used these consisted of 6-point,135 10-point93,108,114 and 10-cm scales,104–107 with the post-treatment change reported as either mean and standard deviation or median and range. Additionally, very few studies actually defined what constituted a clinically significant reduction or a relapse in snoring levels, making it difficult to interpret whether any change in snoring was likely to be of clinical significance.
Only 12 studies had assessed snoring severity using an objective measure of snoring sound. One of these assessed the effects of UP3 versus LAUP,86,87 four assessed UP3 alone,49,92–94 three assessed soft palate RFA,104,105,107 two assessed use of MAS,110,111,113 and one each assessed Pillar implants99,100 and CPAP. 112 Even when snoring sound was assessed there was a disparity in the different parameters of the snoring noise evaluated. These included the number of snores per hour,86,87,92,93,99,100 the mean snoring sound intensity (dB),92,105 the maximum snoring noise intensity (dB),99,100,107 the percentage of time spent in loud snoring93,104 and the snoring energy ratio (Hz). 94 Again, there was little comparability across these studies in the outcomes assessed and how they were defined, and none of the studies indicated what could be considered a clinically significant reduction in snoring noise volume or frequency. An additional problem, confounding the interpretation of such different snoring sound parameters assessed, is that objective measures of snoring may be valid within one laboratory but are difficult to compare between different laboratories because of significant differences in measurement techniques. Furthermore, although all of the studies had assessed snoring sound as part of a sleep study, snoring may differ depending on whether it is measured at home or in the laboratory,136,137 and therefore it is difficult to interpret the clinical relevance of any objectively measured snoring sound reduction.
It is also generally recognised that there is a poor correlation between objectively assessed decreases in snoring and subjectively reported improvement. Only four of the twelve studies that assessed objective snoring sound parameters also reported the correlation between subjective and objective measures. Two of the studies had assessed the effects of UP393,94 and two the effects of soft palate RFA. 104,105 All four studies reported a significant decrease in patient- or bed partner-reported snoring severity but in only one of the studies on UP393 was this corroborated by significant decreases in objectively measured snoring sound parameters. In the remaining three studies there was no significant correlation between subjectively reported outcomes and objectively assessed measures of snoring, despite the subjective measures of effect showing a significant improvement in snoring status94 and partner-reported snoring levels. 104,105 Therefore, across the review there is little evidence to suggest that reductions in patient- or bed partner-assessed snoring levels are associated with a reduction in objectively measured snoring sound indices.
An additional issue highlighted by the studies is the disparity between patient- and bed partner-reported levels of snoring reduction in the short and longer term. Across the studies that reported both short- and long-term follow-up data the relapse rate varied from approximately 6% to 24% depending on the procedure and length of postoperative follow-up. Although it can be postulated that the decline in treatment benefit may represent long-term changes in the pharynx following surgery, this would appear unlikely as when measured objectively snoring volume does not seem to change significantly over time. 94,104,105 It would therefore appear to represent changes in self or partner reporting over time. To what degree this is due to the Hawthorne effect138,139 or to reporting bias is unclear, but this obviously confounds interpretation of study results, making it difficult to compare results from studies with different durations of follow-up.
The assessment of adverse events across the studies was also severely limited because of lack of reporting. It was frequently unclear whether no adverse events occurred or whether adverse events were just not reported. When adverse events were assessed, postoperative pain (n = 10),93,95,97–100,103,105,107,108,114 speech problems (n = 6),90,93,98–100,105,108 swallowing difficulties (n = 5)93,98,103,105,108 and throat disturbances (n = 6)90,91,95,103,106,108 were most frequently examined. Reporting of any further minor or moderate adverse events was highly variable and limited. Moreover, these tended to be limited to the immediate postoperative period with very few of the studies reporting any data on longer-term adverse events. This makes it impossible to compare the relative safety of the procedures and devices assessed.
Length of follow-up was also highly variable, ranging from 10 days to 5 years, which again, because of the confounding effect of a potential differential treatment effect size at short- and longer-term follow-up times, makes it difficult to draw any comparisons between the effects shown in the different studies. The majority of the included studies had a follow-up time of less than 1 year, and there was no evidence available on the effects of LAUP alone, RFA, palatal stiffening techniques, CPAP or MAS at follow-up durations greater than 1 year. Additionally, when studies had used an objective measure of snoring sound parameters these tended to be assessed at a shorter follow-up duration than subjectively assessed outcomes. Therefore, although there is evidence on the effects of UP3 versus LAUP and UP3 alone at treatment durations up to 4 and 5 years, respectively, this is based on subjectively assessed patient- or bed partner-reported snoring severity levels. There is no objectively measured evidence available on snoring sound levels for either UP3 versus LAUP or UP3 alone at follow-up durations greater than 4 months and 13 months respectively.
Overall, therefore, the main finding of this assessment is to highlight the paucity and poor quality of the evidence available on the effects of both surgical procedures and non-surgical devices for the management of primary snoring. Although the review has included the most robust evidence presently available, the results of the studies are likely to be subject to varying degrees of confounding, and differences between the studies have severely limited our ability to compare studies assessing the same interventions or to compare studies of different treatment options. These limitations should be strongly emphasised and used to temper the relative weight of the strength of the findings and conclusions presented.
Strengths and limitations of the assessment
Strengths and limitations of the clinical effects review
This assessment has used transparent and reproducible methods for conducting the review of clinical effects. However, there are a number of limitations that should be noted. The inclusion criteria, as stipulated in the project scope from the Health Technology Assessment Programme, meant that only those studies in which the patient population had a diagnosis of OSAS ruled out at baseline, through the use of either an overnight sleep study or oximetry, were included. Although this has clearly restricted the patient population included in this review to only those with a diagnosis of non-apnoeic snoring, it may also mean that other potentially relevant studies have not been included if a baseline AHI score was not reported. Additionally, the application of these criteria are likely to have severely restricted the included evidence on the use of MAS, as it is unlikely that, within a dental practice setting, patients would undergo a sleep study or oximetry before being fitted with a MAS.
Because of heterogeneity in the way that outcomes had been defined and measured in the included studies it was not possible to adequately synthesise the available evidence. This would have added strength to the findings and potentially provided a quantitative estimate of treatment effect. Additionally, evidence on adverse events associated with the procedures and devices was limited and therefore any conclusion that can be drawn regarding potential treatment harms is also severely restricted.
Associated treatment costs
It was not possible to derive a treatment cost for RFA of the soft palate or the tongue base because of the costs of the surgical device being classified as ‘commercial in confidence’ on approach to the device manufacturers. This has limited the comparison of the treatment costs to UP3, LAUP and Pillar implants for surgical procedures and to CPAP and MAS for non-surgical devices. Because of the number of different models currently available for both CPAP and MAS devices it was not possible to derive a cost for each model. Assumptions had to be made to derive a mean treatment cost for a CPAP machine. For MAS there is currently no information available on the range of costs associated with the manufacture of a splint and therefore costs were based upon clinical opinion and were limited to only one MAS model. Additionally, a number of simplifying assumptions had to be made regarding treatment to derive cost estimates and these are likely to be subject to uncertainty. The treatment costs provided should therefore be seen as indicative rather than as definitive.
Chapter 6 Conclusions
The available evidence on the effects of surgical procedures and non-surgical devices for the management of non-apnoeic snoring is predominantly of a low quality with small sample sizes. There are very few controlled studies available and, when these have been undertaken, few between-group comparisons have been conducted. This means that it is not possible to definitively compare the relative effectiveness of the different treatment options for the management of non-apnoeic snoring. The majority of evidence on the effects of surgical procedures and non-surgical devices comes from small pre–post studies. However, evidence synthesis has been severely limited because of heterogeneity in the way that outcomes have been defined and measured. Any conclusions regarding the effects of the assessed interventions are therefore somewhat tentative.
There was no evidence available that met the inclusion criteria on the effects of surgery to improve nasal obstruction alone, uvulectomy alone, DAUP or tongue-based suspension procedures in patients with non-apnoeic snoring.
With regard to snoring levels the evidence on the effects of UP3 compared with LAUP is equivocal; there appear to be no consistent and significant differences in terms of effectiveness between the two procedures. Across the other studies it is clear that UP3, LAUP, RFA of the soft palate and Pillar implants are all associated with a significant reduction in patient- or bed partner-reported snoring levels; however, the rate of relapse is variable, ranging from approximately 6% to 24% depending on the procedure and length of postoperative follow-up. Limited evidence on CPAP and use of MAS indicates that both of these devices are associated with a significant reduction in objectively assessed snoring sound parameters; however, it is unclear whether this reduction would translate into a treatment benefit that would be perceived as clinically relevant by patients or their bed partners.
Evidence of objective reductions in snoring sound parameters for UP3, LAUP, RFA and Pillar implants is limited and equivocal. There is therefore no strong evidence to suggest that reductions in patient- or bed partner-reported snoring levels are associated with a consistent reduction in objectively measured snoring sound indices.
The reporting of adverse events across the studies was limited, meaning that few comparisons between studies could be made. Overall across the studies, reported adverse events were mild to moderate, with postoperative pain and speech and swallowing difficulties reported most frequently.
Associated treatment costs
In terms of UP3, LAUP and Pillar implants there is no procedure that is clearly the least-cost option based on the limited analysis carried out. The use of LAUP as a one-stage procedure is cheaper than the use of both UP3 and Pillar implants; however, LAUP becomes more expensive than both UP3 and Pillar implants when performed as a two- or three-stage procedure. When comparing UP3 and Pillar implants the use of Pillar implants is slightly cheaper than the use of UP3. In terms of the use of either CPAP or MAS, use of a MAS appears cheaper than the use of a CPAP machine; however, there are a large number of models currently on the market for both devices and it was not possible to compare the costs associated with all of the models. Therefore, use of a more expensive MAS and a cheaper CPAP machine may reverse the cost relationship.
Other considerations
A number of interventions appear to be effective in the management of simple snoring. At present there are no comparative studies of all available treatments and so the relative effectiveness of all treatment options is not clear. Furthermore, different interventions appear to be associated with potentially different relapse rates, although this is somewhat confounded by differences in the length of postoperative follow-up times. In the management of primary snoring it should be highlighted that, given the absence of risk to health from snoring without apnoea or hypopnoea, and an absence of EDS, the patient is effectively being treated to decrease the social disturbance caused to their bed partner and family. It is therefore highly important that objective evidence on snoring is obtained before treatment and that treatment risks are minimised. The range of treatment options is presently large enough that a physician and patient can effectively choose from a number of options. It can therefore be suggested that, in the absence of evidence of any one treatment option being superior to the rest, patient choice is paramount. Additionally, the finding of differential relapse rates across the interventions suggests that the use of different interventions sequentially when necessary may be the optimal treatment strategy, which has the potential to increase treatment costs. Currently, however, this cannot be clarified. It should therefore be recognised that patients who have undergone either UP3 or LAUP would not be eligible to undergo subsequent treatment with either RFA or Pillar implants. On this basis it can be suggested that any sequential staging of treatment options should focus on trialling those interventions that are reversible or minimally invasive first.
Research recommendations
The evidence base assessed in the current review was highly heterogeneous both in terms of the way that outcome measures had been defined and measured and in terms of the level of reporting of study results.
Methods of measuring outcomes and of reporting in studies require standardisation. In particular, study authors need to be explicit regarding patient selection and provide details of methods used to assess the site of airway narrowing and patient baseline characteristics. Authors additionally need to define what constitutes a treatment success or failure a priori. When controlled studies are undertaken, to allow comparison between interventions, results must be analysed on the basis of between-group differences, not simply changes from baseline in each treatment group, as in many of the studies included in this review. Objective assessments of the number of snores per hour and the mean and maximum snoring volume should also be included, as should measures of bed partner quality of life. Adverse events should be clearly defined when necessary and all events reported.
There is very little controlled trial data currently available and, therefore, active controlled trials are warranted. In particular, there is currently only limited evidence available on CPAP and the use of MAS, and none of these studies has assessed partner-reported snoring levels as well as objectively assessed snoring sound indices. Trials of both of these devices with the use of both objective and subjectively assessed partner-reported outcomes are therefore needed.
There is currently no evidence available on either RFA of the soft palate or Pillar implants from studies that have included an objective outcome measure at durations of greater than 1 year post treatment. Evidence is therefore needed on the longer-term effects of both of these procedures.
Acknowledgements
We would like to thank Ms Alison Price and Ms Liz Hodson from the Wessex Institute for Health Research and Development for their help in document retrieval. We also grateful to Dr Rob Anderson from PenTAG for his comments on the protocol and advice on deriving cost data for the interventions.
Contribution of authors
Ms Caroline Main was responsible for project management, protocol development, inclusion screening, data extraction and checking, drafting of the clinical effects review, identification of costs and report preparation. Ms Zulian Liu provided project support and was responsible for data extraction and checking, drafting of the clinical effects review and report preparation. Mrs Karen Welch designed and executed the clinical effects review and cost literature search strategies. Mr Graeme Weiner commented on the protocol and final report and provided clinical input at all stages. Dr Simon Quentin Jones commented on the protocol and final report and provided clinical input at all stages. Professor Ken Stein commented on the protocol and final report and provided project direction at all stages.
About PenTAG
This report was commissioned by the HTA Programme on behalf of the Therapeutic Procedures Panel and was produced by the Peninsula Technology Assessment Group (PenTAG).
PenTAG is part of the Institute of Health Services Research at the Peninsula College of Medicine and Dentistry. PenTAG was established in 2000 and carries out independent health technology assessments for the UK HTA Programme and other local and national decision-makers. The group is multidisciplinary and draws on individuals’ backgrounds in public health, health services research, computing and decision analysis, systematic reviewing, statistics and health economics. The Peninsula College of Medicine and Dentistry is a school within the Universities of Plymouth and Exeter. The Institute of Health and Social Care Research is made up of discrete but methodologically related research groups, among which health technology assessment is a strong and recurring theme. Projects to date include:
Screening for hepatitis C among injecting drug users and in genitourinary medicine (GUM) clinics – systematic reviews of effectiveness, modelling study and national survey of current practice. Health Technol Assess 2002; 6(31).
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia – a systematic review. Health Technol Assess 2002; 6(33).
Systematic review of endoscopic sinus surgery for nasal polyps. Health Technol Assess 2003; 7(17).
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding – a systematic review and economic model. Health Technol Assess 2004; 8(3).
The effectiveness and cost-effectiveness of imatinib for first line treatment of chronic myeloid leukaemia in chronic phase. Health Technol Assess 2004; 8(28).
Do the findings of case series studies vary significantly according to methodological characteristics? Health Technol Assess 2005; 9(2).
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema – a systematic review and economic model. Health Technol Assess 2005; 9(29).
The effectiveness and cost-effectiveness of dual chamber pacemakers compared to single chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome – systematic review and economic evaluation. Health Technol Assess 2005; 9(43).
The effectiveness and cost-effectiveness of surveillance of Barrett’s oesophagus: exploring the uncertainty. Health Technol Assess 2005; 10(8).
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end stage renal disease patients on dialysis. Systematic review and economic evaluation. Health Technol Assess 2007; 11(18).
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly-diagnosed high grade glioma. Systematic review and economic evaluation. Health Technol Assess 2007; 11(45).
The effectiveness and cost-effectiveness of cardiac resynchronisation therapy for heart failure. Systematic review and economic evaluation. Health Technol Assess 2007; 11(47).
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA Programme or the Department of Health.
References
- The Report of an American Academy of Sleep Medicine Task Force . Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 1999;22:667-89.
- Scottish Intercollegiate Guidelines Network . Management of Obstructive Sleep Apnoea Hypopnoea Syndrome in Adults – a National Clinical Guideline 2003.
- Knuiman M, James A, Divitini M, Bartholomew H. Longitudinal study of risk factors for habitual snoring in a general adult population: the Bussselton Health Study. Chest 2006;130:1779-83.
- Honsberg AE, Dodge RR, Cline MG, Quan SF. Incidence and remission of habitual snoring over a 5- to 6-year period. Chest 1995;108:604-9.
- Peppard PE, Young T, Palta ME, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 2000;284:3015-21.
- Tishler PV, Larkin EK, Schluchter MD, Redline S. Incidence of sleep-diordered breathing in an urban adult population: the relative importance of risk factors in the development of sleep-disordered breathing. JAMA 2003;289:2230-7.
- Redline S, Schluchter MD, Larkin EK, Tishler PV. Predictors of longitudinal change in sleep-disordered breathing in a nonclinic population. Sleep 2003;26:703-9.
- Stoohs RA, Blum HC, Haselhorst M, Duchna HW, Guilleminault C, Dement WC. Normative data on snoring: a comparison between younger and older adults. Eur Respir J 1998;11:451-7.
- Schmidt-Nowara WW, Coultas DB, Wiggins CEA, Skipper BE, Samet JM. Snoring in a Hispanic-American population. Risk factors and association with hypertension and other morbidity. Arch Intern Med 1990;150:597-601.
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 1993;328:1230-5.
- Waller P, Bhopal R. Is snoring a cause of vascular disease: an epidemiological review. Lancet 1989;1:143-6.
- Duran J, Esnaola S, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 years. Am J Respir Crit Care Med 2001;163:685-9.
- Jones TM, Swift AC. Snoring: recent developments. Hosp Med 2000;61:330-5.
- Hoffstein V. Snoring. Chest 1996;109:201-22.
- Partinen M, Palomaki H. Snoring and cerebral infarction. Lancet 1985;2:1325-6.
- Hoffstein V. Blood pressure, snoring, obesity, and nocturnal hypoxemia. Lancet 1994;344:643-5.
- Schwab R, Ahmedd MM. Dynamic upper airway imaging during respiration in normal subjects and patients with sleep disordered breathing. Am Rev Resp Dis 1993;148:1385-400.
- Horner Rl, Shea SA, McIvor J, Guz A. Pharyngeal size and shape during wakefulness and sleep in patients with obstructive sleep apnoea. Q J Med 1989;72:719-35.
- Fleetham JA. Upper airway imaging in relation to obstructive sleep apnoea. Clin Chest Med 1992;13:399-416.
- Young T. Some methodologic and practical issues of reported snoring variability. Chest 1991;99:531-2.
- Hoffstein V, Mateika S, Anderson D. Snoring: is it in the ear of the beholder?. Sleep 1994;17:522-6.
- Hoffstein V, Mateika S, Nash S. Comparing perceptions and measurements of snoring. Sleep 1996;19:783-9.
- World Health Organization . Guidelines for Community Noise 2000.
- World Health Organization Regional Office for Europe . Noise and Health Home 2004.
- Schwartz AR, Thut DC, Russ B, Seelagy M, Yuan X, Brower RG, et al. Effect of electrical stimulation of the hypoglossal nerve on airflow mechanics in the isolated upper airway. Am Rev Resp Dis 1993;147:1144-50.
- Schafer J. Snoring, sleep apnea and upper airway. Stuttgart: Thieme; 1996.
- Wilson K, Stoohs RA, Mulrooney TF, Johnson LJ, Guilleminault C, Huang Z. The snoring spectrum: acoustic assessment of snoring sound intensity in 1,139 individuals undergoing polysomnography. Chest 1999;115:762-70.
- Dalmasso F, Prota R. Snoring: analysis, measurement, clinical implications and applications. Eur Respir J 1996;9.
- Pascualy RA, Soest SW. Snoring and sleep apnea: sleep well, feel better. New York: Demos Medical; 2000.
- Perez-Padilla J, West P, Kryger M. Snoring in normal young adults: prevalence in sleep stages and associated changes in oxygen saturation, heart rate and breathing pattern. Sleep 1987;10:249-53.
- Woodson BT, Garancis CJ, Toohill RJ. Histopathologic changes in snoring and OSA syndrome. Laryngoscope 1991;101:1318-22.
- Barthel SW, Strome M. Snoring, obstructive sleep apnea, and surgery. Med Clin North Am 1999;83:85-96.
- Scharf MB, Paparella MM, Shumrick DA, Gluckman JL, Meyerhoff WL. Otolaryngology: basic sciences and related principals. Philadelphia, PA: WB Saunders; 1991.
- Croft C, Pringle M. Sleep nasendoscopy: a technique for assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol 1991;16:504-9.
- Gleadhill IC, Schwartz AR, Schubert NM, Wise RA, Permutt S, Smith PL. Upper airway collapsibility in snorers and in patients with obstructive hypopnea and apnea. Am Rev Respir Dis 1991;143:1300-3.
- Maltais F, Carrier G, Cormier Y, Series F. Cephalometric measurements in snorers, non-snorers, and patients with sleep apnoea. Thorax 1991;46:419-23.
- de Berry-Borowiecki B, Kukwa A, Blanks RHI, Irvine CA. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope 1988;98:226-34.
- Fujita S, Fairbanks D, Fujita S, Ikematsu T. Snoring and obstructive sleep apnea. New York: Raven Press; 1987.
- Pepin JL, Levy P, Veale D, Ferretti G. Evaulation of the upper airway in sleep apnea syndrome. Sleep 1992;15:S50-5.
- Isono S, Morrison DL, Launois SH, Feroah TR, Whitelaw WA, Remmers JE. Static mechanics of the velopharynx of patients with obstructive sleep apnoea. J Appl Physiol 1993;75:148-54.
- El Badawey M, McKee G, Heggie N, Marshall H, Wilson JA. Predictive value of sleep nasendoscopy in the managment of habitual snorers. Ann Otol Rhinol Laryngol 2003;112:40-4.
- Tvinnereim M, Cole P, Haight JS, Hoffstein V. Diagnostic airway pressure recording in sleep apnoea syndrome. Acta Otolaryngol 1995;115:449-54.
- Hudgel DW. Variable site of airway narrowing among obstructive sleep apnea patients. J Appl Physiol 1986;61:1403-9.
- Jager L, Gunther E, Gauger J, Reiser M. Fluoroscopic MR of the pharynx in patient with obstructive sleep apnoea. Am J Neuroradiol 1998;19:1205-14.
- Ryan CF, Lowe AA, Li D, Fleetham JA. Three-dimensional upper airway computed tomography in obstructive sleep apnoea. Am Rev Respir Dis 1991;144:428-32.
- Shephard JW, Thawley SE. Evaluation of the upper airway by computerised tomography in patients undergoing uvulopalatopharyngoplasty for obstructive sleep apnoea. Am Rev Respir Dis 1989;140:711-16.
- Ariyasu L, Young G, Spinelli F. Uvulectomy in the office setting. Ear Nose Throat J 1995;74:721-2.
- Smithson AJ, White JE, Griffiths CJ, Prichard AJ, Close PR, Drinnan MJ, et al. Comparison of methods for assessing snoring. Clin Otolaryngol Allied Sci 1995;20:443-7.
- Prichard AJ, Smithson AJ, White JE, Close PR, Drinnan MJ, Griffiths CJ, et al. Objective measurement of the results of uvulopalatopharyngoplasty. Clin Otolaryngol Allied Sci 1995;20:495-8.
- Walker RP, Gatti WM, Poirier N, Davis JS. Objective assessment of snoring before and after laser-assisted uvulopalatoplasty [erratum appears in Laryngoscope 1997; 107: 148]. Laryngoscope 1996;106:1372-7.
- Weingarten CZ, Raviv G. Evaluation of criteria for uvulopalatoplasty (UPP) patient selection using acoustic analysis of oronasal respiration (SNAP testing). J Otolaryngol 1995;24:352-7.
- Quinn SJ, Daly N, Ellis PD. Observation of the mechanism of snoring using sleep nasendoscopy. Clin Otolaryngol Allied Sci 1995;20:360-4.
- Berry R, Block A. Effect of nasal spray, positinal therapy, and combination thereof in the asymptomatic snorer. Sleep 1994;17:5216-22.
- Stradling JR, Crosssy JH. Predictors and prevalence of obstructive sleep apnoea and snoring in 1001 middle-aged men. Thorax 1991;6:85-90.
- Meoli AL, Rosen CL, Kristo D, Kohrman M, Gooneratne N, Aguillard RN, et al. Nonpresciption treatments of snoring or obstructive apnea: an evaluation of products with limited scientific evidence. Sleep 2003;26:619-24.
- Bennett LS, Davies RJ, Stradling JR. Oral appliances for the management of snoring and obstructive sleep apnoea. Thorax 1998;53:S58-64.
- McGown AD, Makker HK, Battagel JM, L’Estrange PR, Grant HR, Spiro SG. Long-term use of mandibular advancement splint for snoring and obstructive sleep apnoea: a questionnaire survey. Eur Respir J 2001;17:462-6.
- Johnston CD, Gleadhill IC, Cinnamond MJ, Peden WM. Oral appliances for the management of severe snoring: a randomised controlled trial. Eur J Orthod 2001;23:127-34.
- Ono T, Lowe AA, Ferguson KA, Fleetham JA. A tongue retaining device and sleep-state genioglossus muscle activity in patients with obstructive sleep apnea. Angle Orthod 1996;66:273-80.
- Ono T, Lowe AA, Ferguson KA, Pae EK, Fleetham JA. The effect of the tongue retaining device on awake genioglossus muscle activity in patients with obstructive sleep apnea. Am J Orthod Dentofacial Orthop 1996;110:28-35.
- Ikematsu T. Study of snoring, 4th report: therapy. J Jpn Otol Rhinol Laryngol 1964;64:434-5.
- Fujita S, Conway W, Zorick F, Roth T. Surgical correction of anatomical abnormalities in obstructive sleep apnoea syndromes: UVPP. Otolaryngol Head Neck Surg 1981;89:923-93.
- Katsantonis GP, Friedman WH, Rosenblum BN, Walsh JK. The surgical treatment of snoring: a patient’s perspective. Laryngoscope 1990;100:138-40.
- Kamami YV. Laser CO2 for snoring. Preliminary results. Acta Otorhinolaryngol Belg 1990;44:451-6.
- Maw J, Marsan J. Uvulopalatopharyngoplasty versus laser-assisted uvulopalatopharyngoplasty in the treatment of snoring. J Otolaryngol 1997;26:232-5.
- Clarke RW, Yardley MP, Davies CM. Palatoplasty for snoring: a randomised controlled trial of three surgical methods. Otolaryngol Head Neck Surg 1998;119:288-92.
- Astor FC, Hanft KL, Benson C, Amaranath A. Analysis of short-term outcome after office-based laser-assisted uvulopalatoplasty. Otolaryngol Head Neck Surg 1998;118:478-80.
- Wilde AD, Swift AC. A day-case procedure for treating simple snoring. Clin Otolaryngol 1995;20.
- Coleman J, Rathfoot C. Oropharyngeal surgery in the management of upper airway obstruction during sleep. Otolaryngol Clin North Am 1999;32:263-76.
- Stuck BA, Maurer JT, Hein G, Hormann K, Verse T. Radiofrequency surgery of the soft palate in the treatment of snoring: a review of the literature. Sleep 2004;27:551-5.
- Li KK, Powell N, Riley RW, Troell RJ, Guilleminault C. Radiofrequency volumetric tissue reduction for treatment of turbinate hypertrophy: A pilot study. Otolaryngol Head Neck Surg 1998;119:569-73.
- Powell NB, Riley RW, Troell R. Radiofrequency volumetric reduction of the tongue: a porcine pilot study for the treatment of obstructive sleep apnoea syndrome. Chest 1997;111:1348-55.
- National Institute for Health and Clinical Excellence . Radiofrequency Ablation of the Soft Palate for Snoring 2005.
- Nordgard S, Stene BK, Skjostad KW. Soft palate implants for the treatment of mild to moderate obstructive sleep apnea. Otolaryngol Head Neck Surg 2006;134:565-70.
- Aragon S. Surgical management for snoring and sleep apnea. Dent Clin North Am 2001;45:867-79.
- Avidan AY. The development of central sleep apnea with an oral appliance. Sleep Med 2006;7:187-8.
- Low WK. Can snoring relief after nasal septal surgery be predicted?. Clin Otolaryngol Allied Sci 1994;19:142-4.
- Woodhead CJ, Allen MB. Nasal surgery for snoring. Clin Otolaryngol Allied Sci 1994;19:41-4.
- Audit Commission . Access to Care for Ear, Nose and Throat and Audilogy Services 2002.
- NHS Modernisation Agency Demand Management Team . Big Wizard 2002. www.natpact.nhs.uk/demand_management/wizards/big_wizard/index.php.
- Prasad KR, Kapoor PK, Kumar A, Reddy KT, Kumar BN. Waiting-list prioritization in the National Health Service. J Laryngol Otol 2004;118:39-45.
- Khan K, ter Riet G, Glanville J, Sowden A, Kleijnen J. Undertaking Systematic Reviews of Research on Effectiveness: CRD’s Guidance for Those Carrying Out or Comissoning Reviews 2001.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Roen K. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC Methods Programme. Swindon: ESRC; 2006.
- NHS Reference Costs 2005–2006 2006. www.dh.gov.uk/en/Publicationsandstatistics/%20Publications/PublicationsPolicyAndGuidance/DH_062884.
- The NHS Information Centre . NHS Dental Statistics for England Quarter 4: 31st March 2007 n.d. www.ic.nhs.uk/webfiles/publications/dentalq4/Quarterly%20publication%20Q4%202006–7.pdf (accessed 26 November 2007).
- Osman EZ, Osborne JE, Hill PD, Lee BW, Hammad Z. Uvulopalatopharyngoplasty versus laser assisted uvulopalatoplasty for the treatment of snoring: an objective randomised clinical trial. Clin Otolaryngol Allied Sci 2000;25:305-10.
- Osman EZ, bo-Khatwa MM, Hill PD, Lee BW, Osborne JE. Palatal surgery for snoring: objective long-term evaluation. Clin Otolaryngol Allied Sci 2003;28:257-61.
- Prasad KR, Premraj K, Kent SE, Reddy KT. Surgery for snoring: are partners satisfied in the long run?. Clin Otolaryngol Allied Sci 2003;28:497-502.
- Ozmen N, Cebeci BS, Kardesoglu E, Cincik H, Cekin E, Dincturk M, et al. QT dispersion in non-apneic simple snoring patients and the effect of surgical therapy on QT dispersion. Int J Cardiol 2006;113:82-5.
- Janson C, Hillerdal G, Larsson L, Hultcrantz E, Lindholm CE, Bengtsson H, et al. Excessive daytime sleepiness and fatigue in nonapnoeic snorers: improvement after UPPP. Eur Respir J 1994;7:845-9.
- Friberg D, Carlsson-Nordlander B, Larsson H, Svanborg E. UPPP for habitual snoring: a 5-year follow-up with respiratory sleep recordings. Laryngoscope 1995;105:519-22.
- Miljeteig H, Mateika S, Haight JS, Cole P, Hoffstein V. Subjective and objective assessment of uvulopalatopharyngoplasty for treatment of snoring and obstructive sleep apnea. Am J Respir Crit Care Med 1994;150:1286-90.
- Neruntarat C. Uvulopalatal flap for snoring on an outpatient basis. Otolaryngol Head Neck Surg 2003;129:353-9.
- Jones TM, Swift AC, Calverley PM, Ho MS, Earis JE. Acoustic analysis of snoring before and after palatal surgery. Eur Respir J 2005;25:1044-9.
- Berger G, Finkelstein Y, Stein G, Ophir D. Laser-assisted uvulopalatoplasty for snoring: medium- to long-term subjective and objective analysis [see comment]. Arch Otolaryngol Head Neck Surg 2001;127:412-17.
- Lauretano AM, Khosla RK, Richardson G, Matheson J, Weiss JW, Graham C, et al. Efficacy of laser-assisted uvulopalatoplasty. Lasers Surg Med 1997;21:109-16.
- Skjostad KW, Stene BK, Norgard S. Consequences of increased rigidity in palatal implants for snoring: a randomized controlled study. Otolaryngol Head Neck Surg 2006;134:63-6.
- Nordgard S, Stene BK, Skjostad KW, Bugten V, Wormdal K, Hansen NV, et al. Palatal implants for the treatment of snoring: long-term results. Otolaryngol Head Neck Surg 2006;134:558-64.
- Maurer JT, Hein G, Verse T, Hormann K, Stuck BA. Long-term results of palatal implants for primary snoring. Otolaryngol Head Neck Surg 2005;133:573-8.
- Maurer JT, Verse T, Stuck BA, Hormann K, Hein G. Palatal implants for primary snoring: short-term results of a new minimally invasive surgical technique. Otolaryngol Head Neck Surg 2005;132:125-31.
- Ho WK, Wei WI, Chung KF. Managing disturbing snoring with palatal implants: a pilot study. Arch Otolaryngol Head Neck Surg 2004;130:753-8.
- Brietzke SE, Mair EA. Injection snoreplasty: how to treat snoring without all the pain and expense [see comment]. Otolaryngol Head Neck Surg 2001;124:503-10.
- Stuck BA, Sauter A, Hormann K, Verse T, Maurer JT. Radiofrequency surgery of the soft palate in the treatment of snoring. A placebo-controlled trial [see comment]. Sleep 2005;28:847-50.
- Cartwright R, Venkatesan TK, Caldarelli D, Diaz F. Treatments for snoring: a comparison of somnoplasty and an oral appliance. Laryngoscope 2000;110:1680-3.
- Hukins CA, Mitchell IC, Hillman DR. Radiofrequency tissue volume reduction of the soft palate in simple snoring. Arch Otolaryngol Head Neck Surg 2000;126:602-6.
- Boudewyns A, van de Heyning P. Temperature-controlled radiofrequency tissue volume reduction of the soft palate (Somnoplasty®) in the treatment of habitual snoring: results of a European multicenter trial. Acta Otolaryngol 2000;120:981-5.
- Haraldsson PO, Karling J, Lysdahl M, Svanborg E. Voice quality after radiofrequency volumetric tissue reduction of the soft palate in habitual snorers. Laryngoscope 2002;112:1260-3.
- Back LJ, Tervahartiala PO, Piilonen AK, Partinen MM, Ylikoski JS. Bipolar radiofrequency thermal ablation of the soft palate in habitual snorers without significant desaturations assessed by magnetic resonance imaging. Am J Respir Crit Care Med 2002;166:865-71.
- den Herder C, Kox D, van Tinteren H, deVries N. Bipolar radiofrequency induced thermotherapy of the tongue base: its complications, acceptance and effectiveness under local anesthesia. Eur Arch Otorhinolaryngol 2006;263:1031-40.
- Fransson AM, Isacsson G, Leissner LC, Nasman AB, Alton MK. Treatment of snoring and obstructive sleep apnea with a mandibular protruding device: an open-label study. Sleep Breath 2001;5:23-3.
- Fransson AM, Tegelberg A, Leissner L, Wenneberg B, Isacsson G. Effects of a mandibular protruding device on the sleep of patients with obstructive sleep apnea and snoring problems: a 2-year follow-up. Sleep Breath 2003;7:131-41.
- Series F, Marc I. Changes in snoring characteristics after 30 days of nasal continuous positive airway pressure in patients with non-apnoeic snoring: a controlled trial. Thorax 1994;49:562-6.
- Smith AM, Battagel JM. Non-apneic snoring and the orthodontist: the effectiveness of mandibular advancement splints. J Orthod 2004;31:115-23.
- Neruntarat C. Laser-assisted outpatient septoplasty and laser-assisted uvulopalatoplasty for nasal obstruction and snoring. J Med Assoc Thai 2005;88:S66-72.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540-5.
- Johnston CD, Gleadhill IC, Cinnamond MJ, Peden WM. Oral appliances for the management of severe snoring: a randomized controlled trial. Eur J Orthod 2001;23:127-34.
- Gnuechtel MM, Keyser JS, Greinwald JH, Postma GN. Electrocautery versus carbon dioxide laser for uvulopalatoplasty in the treatment of snoring. Laryngoscope 1997;107:848-54.
- Truy E, Cote-Deplus I, Morgon A. Effectiveness of musculus palatopharyngeus resection in uvulopalatopharyngoplasty for snoring. J Otolaryngol 1995;24:79-83.
- Mukai S, Mukai C, Nitta M. Functions of the uvula and Z-pharyngoplasty. Psychiatry Clin Neurosci 2000;54:346-7.
- Clarke RW, Yardley MP, Davies CM, Panarese A, Clegg RT, Parker AJ. Palatoplasty for snoring: a randomized controlled trial of three surgical methods. Otolaryngol Head Neck Surg 1998;119:288-92.
- Belloso A, Morar P, Tahery J, Saravanan K, Nigam A, Timms MS. Randomized-controlled study comparing postoperative pain between coblation palatoplasty and laser palatoplasty. Clin Otolaryngol 2006;31:138-43.
- Uppal S, Nadig S, Jones C, Nicolaides AR, Coatesworth AP. A prospective single-blind randomized-controlled trial comparing two surgical techniques for the treatment of snoring: laser palatoplasty versus uvulectomy with punctate palatal diathermy. Clin Otolaryngol Allied Sci 2004;29:254-63.
- Banerjee A, Dempster JH. Laser palatoplasty: evaluation of patient benefit using the Glasgow benefit inventory. J Laryngol Otol 2000;114:601-4.
- Powell N, Riley R, Gulleminault C, Troell R. A reversible uvulopalatal flap for snoring and sleep apnea syndrome. Sleep 1996;19:593-9.
- Dierks E, Geller M, Roffwarg H, Johns D. Obstructive sleep apnea syndrome: correction by mandibular advancement. South Med J 1990;83:390-4.
- Anonymous . Restoring peace – and health – to troubled snorers. Johns Hopkins Med Lett, Health After 50 2002;14.
- Maurer JT, Huber K, Verse T, Hormann K, Stuck B. A mandibular advancement device for the ENT office to treat obstructive sleep apnea. Otolaryngol Head Neck Surg 2007;136:231-5.
- Gentil B, Lienhart A, Fleury B. Enhancement of postoperative desaturation in heavy snorers. Anesth Analg 1995;81:389-92.
- Taliaferro C. Submucosal radiosurgical uvulopalatoplasty for the treatment of snoring: is the monitoring of tissue impedance and temperature necessary?. Otolaryngol Head Neck Surg 2001;124:46-50.
- Back L, Palomaki M, Piilonen A, Ylikoski J. Sleep-disordered breathing: radiofrequency thermal ablation is a promising new treatment possibility. Laryngoscope 2001;111:464-71.
- National Institute for Health and Clinical Excellence . Guide to the Methods of Technology Appraisal 2004.
- Hicklin LA, Tostevin P, Dasan S. Retrospective survey of long-term results and patient satisfaction with uvulopalatopharyngoplasty for snoring. J Laryngol Otol 2000;114:675-81.
- Cahali MB. Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope 2003;113:1961-8.
- Wiggin C, Schmidt-Nowara WW, Coultas D, Samet JM. Comparison of self- and spouse reports on snoring and other symptoms associated with sleep apnea syndrome. Sleep 1990;13:245-52.
- Beran RG, Plunkett MJ, Holland GJ. Interface of epilepsy and sleep disorders. Seizure 1999;8:97-102.
- Series F, Marc I, Atton L. Comparison of snoring measured at home and during polysomnographic studies. Chest 1993;103:1769-73.
- Osman EZ, Osborne J, Hill PD, Lee BW. Snoring assessment: do home studies and hospital studies give different results?. Clin Otolaryngol Allied Sci 1998;23:524-7.
- Mayo E. The human problems of an industrial civilization. New York: Macmillan; 1933.
- Gillespie R. Manufacturing knowledge: a history of the Hawthorne experiments. Cambridge: Cambridge University Press; 1991.
- Anonymous . From LAUP to UPPP: a primer on procedures to treat snoring. Clin Laser Monthly 1994;12.
- Abbey NC, Block AJ, Green D, Hellard D, Mancuso A. A method for measuring pharyngeal volumes using magnetic resonance imaging in subjects who snore with and without nasal CPAP. Prog Clin Biol Res 1990;345:283-8.
- Antila J, Sipila J, Tshushima Y, Polo O, Laurikainen E, Suonpaa J. The effect of laser-uvulopalatopharyngoplasty on the nasal and nasopharyngeal volume measured with acoustic rhinometry. Acta Otolaryngol Suppl 1997;529:202-5.
- Berry RB, Block AJ. Positive nasal airway pressure eliminates snoring as well as obstructive sleep apnea. Chest 1984;85:15-20.
- Blythe WR, Henrich DE, Pillsbury HC. Outpatient uvuloplasty: an inexpensive, single-staged procedure for the relief of symptomatic snoring. Otolaryngol Head Neck Surg 1995;113:1-4.
- Brietzke SE, Mair EA. Injection snoreplasty: extended follow-up and new objective data. Otolaryngol Head Neck Surg 2003;128:605-15.
- Capper R, Gleadhill I, Cinnamond MJ. Uvulopalatopharyngoplasty for snoring: the Belfast experience. Ulster Med J 1994;63:8-11.
- Carenfelt C. Laser uvulopalatoplasty in treatment of habitual snoring. Ann Otol Rhinol Laryngol 1991;100:451-4.
- Casiano RR, Sheth S. Efficacy of cold-steel uvulopalatoplasty. Otolaryngol Head Neck Surg 1996;115:471-3.
- Chai F, Mitchell I. Snare palatoplasty. Aust J Otolaryngol 1998;3:149-50.
- Croft CB, Golding-Wood DG. Uses and complications of uvulopalatopharyngoplasty. J Laryngol Otol 1990;104:871-5.
- Cheng DS, Weng JC, Yang PW, Cheng LH. Carbon dioxide laser surgery for snoring: results in 192 patients. Otolaryngol Head Neck Surg 1998;118:486-9.
- Cooke ME, Battagel JM. A thermoplastic mandibular advancement device for the management of non-apnoeic snoring: a randomized controlled trial. Eur J Orthod 2006;28:327-38.
- Crestinu JM. Intrapalatine resection (IPR) in the treatment of sleep apnea and snoring. Plast Reconstr Surg 1991;87:467-9.
- den Herder C, van Tinteren H, de Vries N. Sleep endoscopy versus modified mallampati score in sleep apnea and snoring. Laryngoscope 2005;115:735-9.
- Drinnan MJ, Richardson HC, Close PR, Smithson AJ, White JE, Griffiths CJ, et al. Objective benefit of laser palatoplasty for non-apnoeic snoring. Clin Otolaryngol Allied Sci 1999;24:335-8.
- Ellis PD. Laser palatoplasty for snoring due to palatal flutter: a further report. Clin Otolaryngol Allied Sci 1994;19:350-1.
- Ellis PD, Williams JE, Shneerson JM. Surgical relief of snoring due to palatal flutter: a preliminary report. Ann R Coll Surg Engl 1993;75:286-90.
- Emery BE, Flexon PB. Radiofrequency volumetric tissue reduction of the soft palate: a new treatment for snoring. Laryngoscope 2000;110:1092-8.
- Ferguson M, Smith TL, Zanation AM, Yarbrough WG. Radiofrequency tissue volume reduction: multilesion vs single-lesion treatments for snoring. Arch Otolaryngol Head Neck Surg 2001;127:1113-18.
- Finkelstein Y, Talmi YP, Raveh E, Orlin J, Rudnicki C, Fried M, et al. Can obstructive sleep apnoea be a complication of uvulopalatopharyngoplasty?. J Laryngol Otol 1995;109:212-17.
- Fransson AM, Tegelberg A, Johansson A, Wenneberg B. Influence on the masticatory system in treatment of obstructive sleep apnea and snoring with a mandibular protruding device: a 2-year follow-up. Am J Orthod Dentofacial Orthop 2004;126:687-93.
- Fransson AM, Tegelberg A, Svenson BA, Lennartsson B, Isacsson G. Influence of mandibular protruding device on airway passages and dentofacial characteristics in obstructive sleep apnea and snoring. Am J Orthod Dentofacial Orthop 2002;12:371-9.
- Gordon AS, Giles ML, Harding DA, Morton RP. Surgery of snoring. J Laryngol Otol 1986;100:1263-7.
- Guilleminault C, Stoohs R, Clerk A, Simmons J, Labanowski M. Excessive daytime somnolence in women with abnormal respiratory efforts during sleep. Sleep 1993;16:S137-8.
- Hanada T, Furuta S, Tateyama T, Uchizono A, Seki D, Ohyama M. Laser-assisted uvulopalatoplasty with Nd:YAG laser for sleep disorders. Laryngoscope 1996;106:1531-3.
- Haraldsson PO, Bredbacka S. Laser-uvulopalatoplasty (LUPP) under local anesthesia: effective, safe and comfortable. J Otorhinolaryngol 1996;58:99-104.
- Hern JD, Hellier WP, Brasher PF. The treatment of snoring in the armed forces. J R Army Med Corps 1999;145:137-9.
- Hessel NS, de Vries N. Results of uvulopalatopharyngoplasty after diagnostic workup with polysomnography and sleep endoscopy: a report of 136 snoring patients. Eur Arch Otorhinolaryngol 2003;260:91-5.
- Hofmann T, Schwantzer G, Reckenzaun E, Koch H, Wolf G. Radiofrequency tissue volume reduction of the soft palate and UPPP in the treatment of snoring. Eur Arch Otorhinolaryngol 2006;263:164-70.
- Hultcrantz E, Johansson K, Bengtson H. The effect of uvulopalatopharyngoplasty without tonsillectomy using local anaesthesia: a prospective long-term follow-up. J Laryngol Otol 1999;113:542-7.
- Ingrams DR, Spraggs PD, Pringle MB, Croft CB. CO2 laser palatoplasty: early results. J Laryngol Otol 1996;110:754-6.
- Isberg A, Levring-Jaghagen E, Dahlstrom M, Dahlqvist A. Persistent dysphagia after laser uvulopalatoplasty: a videoradiographic study of pharyngeal function. Acta Otolaryngol 1998;118:870-4.
- Iseri M, Balcioglu O. Radiofrequency versus injection snoreplasty in simple snoring. Otolaryngol Head Neck Surg 2005;133:224-8.
- Issa FG, Sullivan CE. Upper airway closing pressures in snorers. J Appl Physiol 1984;57:528-35.
- Jones TM, Ho MS, Earis JE, Swift AC. Acoustic parameters of snoring sound to assess the effectiveness of the Muller manoeuvre in predicting surgical outcome. Auris Nasus Larynx 2006;33:409-16.
- Kamami YV. Outpatient treatment of snoring with CO2 laser: laser-assisted UPPP. J Otolaryngol 1994;23:391-4.
- Kezirian EJ, Powell NB, Riley RW, Hester JE. Incidence of complications in radiofrequency treatment of the upper airway. Laryngoscope 2005;115:1298-304.
- Koay CB, Freeland AP, Stradling JR. Short- and long-term outcomes of uvulopalatopharyngoplasty for snoring. Clin Otolaryngol Allied Sci 1995;20:45-8.
- den Herder C, van Tinteren H, de Vries N. Hyoidthyroidpexia: a surgical treatment for sleep apnea syndrome [reprint in Ned Tijdschr Geneeskd 2006; 150 (4):198–203]. Laryngoscope 2005;115:740-5.
- Krespi YP, Pearlman SJ, Keidar A. Laser-assisted uvula-palatoplasty for snoring. J Otolaryngol 1994;23:328-34.
- Kuhnel TS, Hein G, Hohenhorst W, Maurer JT. Soft palate implants: a new option for treating habitual snoring. Eur Arch Otorhinolaryngol 2005;262:277-80.
- Vinaya Kumar EC, Rao J, Chowdary S, Rao C. Management of tongue base obstruction in obstructive sleep apnoea syndrome. Indian J Otolaryngol 1999;52:58-62.
- Kyearmizakis DE, Chimona TS, Papadakis CE, Bizakis JG, Velegrakis GA, Schiza S, et al. Laser-assisted uvulopalatoplasty for the treatment of snoring and mild obstructive sleep apnea syndrome. J Otolaryngol 2003;32:174-9.
- Lamont J, Baldwin DR, Hay KD, Veale AG. Effect of two types of mandibular advancement splints on snoring and obstructive sleep apnoea. Eur J Orthod 1998;20:293-7.
- Laranne JE, Pukander JS, Laippala P. Uvulopalatopharyngoplasty with CO2, contact Nd-YAG or combined CO2 and Nd-YAG laser beams. Lasers Med Sci 1996;11:53-8.
- Larrosa F, Hernandez L, Morello A, Ballester E, Quinto L, Montserrat JM. Laser-assisted uvulopalatoplasty for snoring: does it meet the expectations?. Eur Respir J 2004;24:66-70.
- Liudahl JJ, Haydon RC, Rodman SM. Snoring and related problems: surgical correction. W V Med J 1986;82:127-30.
- Lysdahl M, Haraldsson PO. Uvulopalatopharyngoplasty versus laser uvulopalatoplasty: prospective long-term follow-up of self-reported symptoms. Acta Otolaryngol 2002;122:752-7.
- Macdonald A, Drinnan M, Johnston A, Reda M, Griffiths C, Wilson J, et al. Evaluation of potential predictors of outcome of laser-assisted uvulopalatoplasty for snoring. Otolaryngol Head Neck Surg 2006;134:197-203.
- Mair EA, Day RH. Cautery-assisted palatal stiffening operation. Otolaryngol Head Neck Surg 2000;122:547-56.
- Marklund M, Franklin KA. Dental appliances in the treatment of snoring. A comparison between an activator, a soft-palate lifter, and a mouth-shield. Swedish Dent J 1996;20:183-8.
- Miller S. CO2 laser uvulo-palato-pharyngoplasty. Aust J Otolaryngol 1996;2:287-9.
- Myatt HM, Mackay IS. Snoring – a simple surgical solution. Clin Otolaryngol Allied Sci 1996;21:419-24.
- Nordgard S, Wormdal K, Bugten V, Stene BK, Skjostad KW. Palatal implants: a new method for the treatment of snoring. Acta Otolaryngol 2004;124:970-5.
- O’Sullivan RA, Hillman DR, Mateljan R, Pantin C, Finucane KE. Mandibular advancement splint: an appliance to treat snoring and obstructive sleep apnea. Am J Respir Crit Care Med 1995;151:194-8.
- Powell NB, Riley RW, Troell RJ, Li K, Blumen MB, Guilleminault C. Radiofrequency volumetric tissue reduction of the palate in subjects with sleep-disordered breathing [see comment]. Chest 1998;113:1163-74.
- Prichard AJ, Marshall J, Ahmed A, Thomas RS, Hanning CD. Uvulopalatopharyngoplasty: the Leicester experience. J Laryngol Otol 1994;108:649-52.
- Reda M, Marshall HF, Gibson JG, Wilson JA. Objective assessment of soft palate morphology in habitual snoring and its modification by laser assisted uvulopalatoplasty. Clin Otolaryngol Allied Sci 1998;23:285-6.
- Reda M, Sims AJ, Collins MM, McKee GJ, Marshall H, Kelly PJ, et al. Morphological assessment of the soft palate in habitual snoring using image analysis. Laryngoscope 1999;109:1655-60.
- Remacle M, Jouzdani E, Lawson G, Jamart J. Laser-assisted surgery addressing snoring long-term outcome comparing CO2 laser vs CO2 laser combined with diode laser. Acta Otorhinolaryngol Belg 2002;56:177-82.
- Remacle M, Betsch C, Lawson G, Jamart J, Eloy P. A new technique for laser-assisted uvulopalatoplasty: decision-tree analysis and results. Laryngoscope 1999;109:763-8.
- Robertson C, Herbison P, Harkness M. Dental and occlusal changes during mandibular advancement splint therapy in sleep disordered patients. Eur J Orthod 2003;25:371-6.
- Robertson MS. A cure for snoring. N Z Med J 1985;98:103-4.
- Safaya A, Suri JC, Batra K. Uvulopalatopharyngoplasty – surgery for snoring. Indian J Otolaryngol 2002;54:204-7.
- Sandhu GS, Vatts A, Whinney D, Kotecha B, Croft CB. Somnoplasty for simple snoring – a pilot study. Clin Otolaryngol Allied Sci 2003;28:425-9.
- Sanner BM, Tepel M, Markmann A, Zidek W. Effect of continuous positive airway pressure therapy on 24-hour blood pressure in patients with obstructive sleep apnea syndrome. Am J Hypertens 2002;15:251-7.
- Simmons FB, Guilleminault C, Miles LE. The palatopharyngoplasty operation for snoring and sleep apnea: an interim report. Otolaryngol Head Neck Surg 1984;92:375-80.
- Skatvedt O. Laser-assisted uvulopalatoplasty: description of the technique and pre- and postoperative evaluation of subjective symptoms. J Otorhinolaryngol Rel Spec 1996;58:243-7.
- Stradling JR, Negus TW, Smith D, Langford B. Mandibular advancement devices for the control of snoring. Eur Respir J 1998;11:447-50.
- Tarabichi M. Microdebrider-assisted uvulopalatoplasty. Otolaryngol Head Neck Surg 1998;119:131-3.
- Tatla T, Sandhu G, Croft CB, Kotecha B. Celon radiofrequency thermo-ablative palatoplasty for snoring – a pilot study. J Laryngol Otol 2003;117:801-6.
- Troell RJ, Powell NB, Riley RW, Li KK, Guilleminault C. Comparison of postoperative pain between laser-assisted uvulopalatoplasty, uvulopalatopharyngoplasty, and radiofrequency volumetric tissue reduction of the palate. Otolaryngol Head Neck Surg 2000;122:402-9.
- Turnbull NR, Battagel JM. The effects of orthognathic surgery on pharyngeal airway dimensions and quality of sleep. J Orthod 2000;27:235-47.
- Tvinnereim M, Mitic S, Hansen RK. Plasma radiofrequency preceded by pressure recording enhances success for treating sleep-related breathing disorders. Laryngoscope 2007;117:731-6.
- Utley DS, Shin EJ, Clerk AA, Terris DJ. A cost-effective and rational surgical approach to patients with snoring, upper airway resistance syndrome, or obstructive sleep apnea syndrome. Laryngoscope 1997;107:726-34.
- Veres E. Clinical trial of an oral vestibular shield for the control of snoring. J Dent Assoc South Afr 1993;48:15-7.
- Verse T, Maurer JT, Pirsig W. Effect of nasal surgery on sleep-related breathing disorders. Laryngoscope 2002;112:64-8.
- Virkkula P, Bachour A, Hytonen M, Salmi T, Malmberg H, Hurmerinta K, et al. Snoring is not relieved by nasal surgery despite improvement in nasal resistance. Chest 2006;129:81-7.
- Vukovic L, Hutchings J. Patient evaluation of laser-assisted uvulopalatoplasty. J Otolaryngol 1996;25:404-7.
- Walker RP, Grigg-Damberger MM, Gopalsami C, Totten MC. Laser-assisted uvulopalatoplasty for snoring and obstructive sleep apnea: results in 170 patients. Laryngoscope 1995;105:938-43.
- Wareing MJ, Callanan VP, Mitchell DB. Laser-assisted uvulopalatoplasty: six and eighteen month results. J Laryngol Otol 1998;112:639-41.
- Wedman J, Miljeteig H. Treatment of simple snoring using radio waves for ablation of uvula and soft palate: a day-case surgery procedure. Laryngoscope 2002;112:1256-9.
- Weingarten C. Snare uvulopalatoplasty [see comment]. Laryngoscope 1995;105:1033-6.
- Welt S, Maurer JT, Hormann K, Stuck BA. Radiofrequency surgery of the tongue base in the treatment of snoring – a pilot study. Sleep Breath 2007;11:39-43.
- Whinney DJ, Williamson PA, Bicknell PG. Punctate diathermy of the soft palate: a new approach in the surgical management of snoring. J Laryngol Otol 1995;109:849-52.
- Wilson JA, Lester SE, Gibson GJ, Anari S, Steele JG, Steen IN, et al. Silencing the snorers: no gain without pain?. J Laryngol Otol 2006;120:570-4.
- Woodson BT. A tongue suspension suture for obstructive sleep apnea and snorers. Otolaryngol Head Neck Surg 2001;124:297-303.
- Wright S, Haight J, Zamel N, Hoffstein V. Changes in pharyngeal properties after uvulopalatopharyngoplasty. Laryngoscope 1989;99:62-5.
- Zinder DJ, Postma GN. Outpatient cautery-assisted uvulopalatoplasty. Laryngoscope 1995;105:1256-7.
Appendix 1 Search syntax and strategy
MEDLINE
Years searched 1980–2007
Searched 31 May 2007
-
exp snoring/(2128)
-
snoring.mp. (3231)
-
(snore or snores or snorers or snoring).tw. (2960)
-
or/1–3 (3365)
-
(appliance$1 or device$1 or implant$6 or splint$1 or intervention$2 or procedure$1 or surgery or surgical or suture$1 or injection$1 or mouthpiece$1 or operation$1 or cauter$).tw. (1905567)
-
continuous positive airway pressure/(936)
-
catheter ablation/(9727)
-
electrocoagulation/(8469)
-
electrosurgery/(2985)
-
laryngoscopy/(6236)
-
laser coagulation/(4407)
-
laser surgery/(16415)
-
mandible/su (8220)
-
mandibular advancement/mt (254)
-
mouth breathing/su (21)
-
nasal obstruction/su (627)
-
nasal septum/su (2176)
-
nose/su (2726)
-
occlusal splints/(944)
-
oral surgical procedures/(2444)
-
orthodontic appliances/(7510)
-
orthodontic appliances removable/(2279)
-
otorhinolaryngologic surgical procedures/(1607)
-
mandible/su (8220)
-
palate/su (1407)
-
palate soft/su (955)
-
palate hard/su (181)
-
pharynx/su (2113)
-
“prostheses and implants”/(28374)
-
rhinoplasty/(4594)
-
surgical procedures minimally invasive/(7760)
-
tongue/su (829)
-
turbinates/su (623)
-
uvula/su (700)
-
(CPAP or APRV or NCPAP or UPPP or UP3 or LAUP or CAUP or DAUP or MAS or MRA or TRD or RFA or CASPO).tw. (11514)
-
“continuous positive airway$1 pressure”.tw. (3228)
-
“airway$1 pressure release ventilation”.tw. (72)
-
(palatal implant$or palatal surgery).tw. (152)
-
(palatoplasty or somnoplasty or septoplasty or uvuloplasty or uvloplasty).tw. (860)
-
(uvulopalatoplasty or uvulopalatopharyngoplasty).tw. (641)
-
uvulectomy.tw. (60)
-
(“mandibular advancement” or “mandibular re?positioning” or “mandibular adjustment” or “mandibular re?adjustment”).tw. (571)
-
“transoral radiofrequency”.tw. (1)
-
tongue suture$1.tw. (1)
-
“tongue retaining device$1”.tw. (15)
-
“radiofrequency ablation”.tw. (3449)
-
stiffening.tw. (1226)
-
snoreplasty.mp. (7)
-
septorhinoplasty.tw. (192)
-
“turbinate reduction”.tw. (40)
-
(“sinus surgery” or “nasal surgery”).tw. (2763)
-
or/5–51 (1968010)
-
4 and 52 (1562)
-
limit 53 to year=“1980 – 2007” (1556)
-
limit 54 to (editorial or letter or “review”) (289)
-
54 not 55 (1267)
-
limit 56 to english language (1011)
-
56 not 57 (256)
Number of records retrieved: 1267 (1011 English language and 256 foreign language)
EMBASE
Years searched 1980–2007
Searched 24 May 2007
-
exp snoring/(2717)
-
snoring.mp. (3231)
-
(snore or snores or snorers or snoring).tw. (2652)
-
palatal flutter snoring/(2)
-
or/1–4 (3323)
-
(appliance$1 or device$1 or implant$6 or splint$1 or intervention$2 or procedure$1 or surgery or surgical or suture$1 or injection$1 or mouthpiece$1 or operation$1 or cauter$).tw. (1508234)
-
positive end expiratory pressure/(12025)
-
catheter ablation/(8120)
-
electrocoagulation/(1666)
-
electrosurgery/(1755)
-
laryngoscopy/(5836)
-
laser coagulation/(8899)
-
laser surgery/(12724)
-
mandible reconstruction/(1637)
-
mandibular resection/(722)
-
nose obstruction/su (453)
-
nose septum reconstruction/(789)
-
nose surgery/(2134)
-
nose reconstruction/(3198)
-
oral surgery/(2488)
-
exp orthodontic device/(366)
-
orthodontic appliances removable/(366)
-
ear nose throat surgery/(1074)
-
palatoplasty/(836)
-
pharynx reconstruction/(714)
-
rhinoplasty/(3198)
-
surgical technique/(165101)
-
palatal flutter snoring/su (2)
-
(CPAP or APRV or NCPAP or UPPP or UP3 or LAUP or CAUP or DAUP or MAS or MRA or TRD or RFA or CASPO).tw. (10823)
-
“continuous positive airway$1 pressure”.tw. (2970)
-
“airway$1 pressure release ventilation”.tw. (74)
-
(palatal implant$or palatal surgery).tw. (109)
-
(palatoplasty or somnoplasty or septoplasty or uvuloplasty or uvloplasty).tw. (795)
-
(uvulopalatoplasty or uvulopalatopharyngoplasty).tw. (591)
-
uvulectomy.tw. (43)
-
(“mandibular advancement” or “mandibular re?positioning” or “mandibular adjustment” or “mandibular re?adjustment”).tw. (263)
-
“transoral radiofrequency”.tw. (1)
-
tongue suture$1.tw. (2)
-
“tongue retaining device$1”.tw. (12)
-
“radiofrequency ablation”.tw. (3372)
-
stiffening.tw. (1115)
-
snoreplasty.mp. (6)
-
septorhinoplasty.tw. (157)
-
“turbinate$reduction”.tw. (34)
-
(“sinus surgery” or “nasal surgery”).tw. (2514)
-
or/6–45 (1600716)
-
5 and 46 (1592)
-
limit 47 to (editorial or letter or note or proceeding or “review”) (320)
-
47 not 48 (1272)
-
limit 49 to human (1240)
-
limit 50 to english language (1002)
-
from 51 keep 1–1000 (1000)
-
from 51 keep 1001–1002 (2)
-
from 53 keep 1–2 (2)
-
50 not 51 (238)
-
from 55 keep 1–238 (238)
Number of records retrieved: 1240 (1002 English language and 238 foreign language)
Cochrane Central Register of Controlled Trials
SNORING OR SNORES OR SNORER OR SNORERS
Number of records retrieved: 203
NHS EED
Searched 31 May 2007
-
exp snoring/ (2727)
-
(snore or snores or snoring or snorer$1).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] (3333)
-
or/1-2 (3333)
-
(cost adj2 effective$).ti,ab. (36840)
-
(cost adj benefit$).ti,ab. (4595)
-
cost effectiveness analysis/ (48752)
-
cost benefit analysis/ (26140)
-
budget$.ti,ab. (7856)
-
cost$.ti. (34871)
-
(cost$ adj2 (effective$ or utilit$ or benefit$ or minimi$)).ab. (40516)
-
(economic$ or pharmacoeconomic$ or pharmaco economic$).ti. (13584)
-
(price$ or pricing).ti,ab. (10102)
-
(financial or finance or finances or financed).ti,ab. (20844)
-
(fee or fees).ti,ab. (4758)
-
cost/ (19077)
-
cost minimization analysis/ (1136)
-
cost of illness/ (3837)
-
cost utility analysis/ (1920)
-
drug cost/ (29563)
-
health care cost/ (52658)
-
health economics/ (9223)
-
economic evaluation/ (3610)
-
economics/ (5151)
-
pharmacoeconomics/ (885)
-
budget/ (6964)
-
economic burden.ti,ab. (1426)
-
“resource use”.ti,ab. (1908)
-
or/4-27 (215353)
-
3 and 28 (87)
-
(editorial or letter or review).pt. (1253156)
-
29 not 30 (52)
-
from 31 keep 3,7,27 (3)
-
from 32 keep 1-3 (3)
Number of records retrieved: 394
Appendix 2 Excluded studies
| Study ID | Reason for exclusion |
|---|---|
| Anonymous 1994140 | Patient group unclear (appears mixed non-apnoeic snorers and OSAS); no objective outcome measure |
| Abbey 1990141 | Patients with OSAS |
| Antila 1997142 | Mixed patient population; no objective baseline assessment and results not reported separately |
| Back 2001130 | Mixed patient population; objectively assessed outcomes not reported separately by subgroup |
| Belloso 2006122 | No baseline PSG or oximetry performed (authors explicitly state OSAS was excluded by medical history, clinical examination and ESS index < 12) |
| Berry 1984143 | Mixed patient population; results not reported separately |
| Blythe 1995144 | Patient group unclear; no PSG or oximetry at baseline or follow-up |
| Brietzke 2003145 | Patients with mild OSAS (baseline RDI = 7.5) |
| Capper 1994146 | Mixed patient population; results not reported separately by definition used in current assessment of non-apnoeic snorers (AHI < 5). |
| Carenfelt 1991147 | Mixed patient population (non-apnoeic snorers and OSAS); results not reported separately by patient group |
| Casiano 1996148 | Mixed patient population; results not reported separately; no objective outcome measure |
| Chai 1998149 | Mixed patient population; results not reported separately; no objective baseline or outcome measurement |
| Charles 1990150 | Mixed patient population, results not reported for subgroups; PSG baseline results not reported; no objective outcome measure |
| Cheng 1998151 | No objective assessment at baseline or follow-up |
| Cooke 2006152 | Median AHI of ‘simple snorers’ = 5.5 (range 2.0–8.0) |
| Crestinu 1990153 | Patient group unclear, no baseline PSG or oximetry; no objective outcome measures |
| den Herder 2005154 | No intervention: study assesses correlation between sleep endoscopy results and modified mallampati score results |
| Drinnan 1999155 | Patients with mild OSAS; AHI > 5 |
| Ellis 1994156 | Mixed patient group; no objective outcome assessment |
| Ellis 1993157 | Patient group unclear, no objective baseline assessment (PSG or oximetry) reported |
| Emery 2000158 | Patients with mild OSAS (but AHI < 10) |
| Ferguson 2001159 | Mixed patient population (non-apnoeic snorers and OSAS); results not reported separately; PSG only undertaken in 12/47 patients at baseline; mean AHI = 6.0 (SD 4.3) |
| Finkelstein 1995160 | Mixed patient population; results not reported separately |
| Fransson 2004161 | Mixed patient population; results not reported separately |
| Fransson 2002162 | Mixed patient population; results not reported separately (paper on influence of mandibular protruding device on airway passage and dentofacial characteristics) |
| Gordon 1986163 | Mixed patient population; results not reported by subgroup; no objective outcome measure |
| Guilleminault 1993164 | Patient population unclear as baseline PSG results not reported |
| Hanada 1996165 | Mixed patient population (non-apnoeic snorers and OSAS); results not reported seperately [comment: arm A (type 1 LAUP) consists of primarily non-apnoeic snorers (34 non-apnoeic snorers and 8 OSAS patients) with mean baseline AI of 3.5; arm B consists of primarily OSAS patients (13 non-apnoeic snorers and 51 OSAS patients) with a mean AI of 14.0; if necessary we could use arm A as a pre–post study] |
| Haraldsson 1996166 | Mixed patient population (actual population unclear); no objective outcome measures |
| Hern 1999167 | Patient population unclear, no baseline PSG or oximetry; no objective outcome measures |
| Hessel 2003168 | Patients with OSAS; baseline AHI > 5 |
| Hofmann 2006169 | Mixed patient population; median baseline AHI is 8 in UP3 arm (range 1–29) and 5 or 6 (range 0–26) (reported differently in table and text) in RFA arm; results not reported separately for patients with AHI < 5 |
| Hultcrantz 1999170 | Mixed patient population; results not reported separately; no objective outcome measures |
| Ingrams 1996171 | Patient group unclear, results of baseline PSG not reported; no objective outcome measures |
| Isberg 1998172 | Mixed patient population (non-apnoeic snorers and OSAS); results not reported separately; no objective outcome assessment; study assesses persistent dysphagia after LAUP |
| Iseri 2005173 | Patients with mild OSAS; RDI > 5 |
| Issa 1984174 | No objective outcome assessment |
| Jones 2006175 | Study assessed effectiveness of Muller’s manoeuvre in predicting surgical outcomes; mixed patient population (baseline PSG not reported) and outcomes not reported by subgroup; outcomes of sensitivity and specificity reported |
| Kamami 1994176 | Mixed patient population; results not reported by subgroup; no baseline or outcome objective measurement |
| Kezirian 2005177 | Systematic review of complications of RFA treatment of the upper airway (not specific to snoring or OSAS) |
| Koay 1995178 | Patient group unclear (baseline PSG results not reported); no objective outcome measures |
| Kotecha 1998179 | Mixed patient population; results not reported separately |
| Krespi 1994180 | Patient population mixed (non-apnoeic snorers and OSAS); results not reported separately; no objective outcome measures |
| Kuhnel 2005181 | Patient group unclear (appears mixed non-apnoeic snorers and OSAS); no objective outcome measures |
| Kumar 2000182 | Patient group unclear, no baseline PSG or oximetry; no objective outcome measures |
| Kyearmizakis 2003183 | Mixed patient population (non-apnoeic snorers and OSAS); no objective outcome measure for outcomes assessed in non-apnoeic snorers |
| Lamont 1998184 | Mixed patient population; patients with AHI > 10 and AHI < 5; results not reported separately |
| Laranne 1996185 | Mixed patient population (non-apnoeic snorers and OSAS); results not reported separately |
| Larrosa 2004186 | Patient group non-apnoeic snorers and mild OSAS patients; mean AHI 15; results not reported separately by subgroup |
| Liudahl 1986187 | Mixed patient population; results not reported separately; baseline PSG results not reported; no objective outcome measure |
| Lysdahl 2002188 | Mixed patient population; results not reported separately; no objective outcome assessment |
| Macdonald 2006189 | Patients with mild OSAS; AHI > 5 |
| Mair 1996190 | Outcomes not assessed objectively |
| Marklund 1996191 | Patients unclear, no PSG or oximetry at baseline |
| Maw 199765 | Patients mixed; results not reported separately |
| Miller 1996192 | Mixed patient population; results not reported separately; PSG results at baseline not reported; no objective outcome measure |
| Myatt 1996193 | Mixed patient population; results no reported separately; no objective outcome assessment |
| Nordgard 2004194 | Outcomes not measured objectively |
| O’Sullivan 1995195 | Mixed patient population (non-apnoeic snorers and OSAS); results not reported separately |
| Powell 1998196 | Mixed patient population (non-apnoeic snorers, UARS, OSAS); results not reported separately |
| Prichard 1994197 | Patients unclear, no baseline PSG or oximetry; outcomes not assessed objectively |
| Reda 1998198 | Patient group unclear; unclear if PSG/oximetry undertaken at baseline |
| Reda 1999199 | Study assesses the morphological changes in the soft palate before and after LAUP. Patient population is unclear; results of objective baseline measurement (PSG) not reported |
| Remacle 2002200 | Patient population unclear, no objective baseline measurement (PSG or oximetry) |
| Remacle 1999201 | Mixed patient population; results not reported separately; baseline PSG results not reported |
| Robertson 2003202 | Mixed patient population; no assessment of snoring levels at baseline or outcome |
| Robertson 1985203 | Mixed patient population (non-apnoeic snorers and OSAS); results not reported separately; no objective outcome measure |
| Safaya 2002204 | Patient population unclear, no PSG or oximetry at baseline; no objective outcome assessment |
| Sandhu 2003205 | Patient group appears to be mixed (non-apnoeic snorers and OSAS); AHI or RDI not reported at baseline or follow-up |
| Sanner 2002206 | Only patients with OSAS given CPAP; non-apnoeic snorers no intervention |
| Simmons 1984207 | Mixed patient population; results not reported separately |
| Skatvedt 1996208 | Mixed patient population (unclear as baseline PSG was not conducted); no objective outcome measure |
| Stradling 1998209 | Patient group unclear (appears mixed); no baseline PSG or oximetry to exclude OSAS |
| Tarabichi 1998210 | Patient group unclear; outcomes not assessed objectively |
| Tatla 2003211 | Mixed patient population (non-apnoeic snorers and mild OSAS); results not reported separately |
| Troell 2000212 | Mixed patient population (non-apnoeic snorers, UARS, OSAS); results not reported separately |
| Turnbull 2000213 | Patient population not non-apnoeic snorers or OSAS patients |
| Tvinnereim 2007214 | Mixed patient population (non-apnoeic snorers and mild-moderate OSAS); results not reported separately |
| Uppal 2003122 | No objective baseline assessment (authors explicitly state that participants were screened by ESS score, with those < 10 eligible for inclusion; no nasendoscopy or oximetry was performed) |
| Utley 1997215 | Patient population with mild and moderate OSAS |
| Veres 1993216 | Patients group unclear, no baseline PSG or oximetry; no objective outcome measure |
| Verse 2002217 | Pre and post results reported for patients; four would meet inclusion criteria with AHI < 5 but the intervention in these patients is not reported separately and therefore the specific operation performed is not clear |
| Virkkula 2006218 | Patients with mild OSAS; AHI < 5 |
| Vukovic 1996219 | Patient population unclear; no baseline or objective outcome measure |
| Walker 1995220 | Mixed patient population (non-apnoeic snorers and OSAS); for the non-apnoeic snorers no objective baseline and outcome assessment was conducted |
| Wareing 1998221 | Patient population unclear; unclear if PSG or oximetry performed at baseline; no objective outcome measure |
| Wedman 2002222 | Baseline results of PSG not reported and so patient group not totally clear; outcomes not assessed objectively |
| Weingarten 1995223 | Mixed patient population (non-apnoeic snorers and OSAS); results not reported separately |
| Welt 2007224 | Outcomes not assessed objectively |
| Whinney 1995225 | Patient group unclear, no PSG or oximetry at baseline; no objective outcome assessment |
| Wilson 2006226 | No pre- or postoperative PSG or oximetry; patient group unclear |
| Woodson 2001227 | Mixed patient population; all AHI > 5 |
| Wright 1989228 | Mixed patient population; three patients with AI < 5, but AHI not reported. Assumed that when combined with HI score AHI > 5. Results also reported as IPD and not group means |
| Zinder 1995229 | Patient group unclear; no objective outcome assessment |
Appendix 3 Data extraction tables
The following abbreviations are used throughout Appendix 3: AI, apnoea index; AHI, apnoea/hypopnoea index; BMI, body mass index; CCT, controlled clinical trial; DIS, difficulty inducing sleep; EDS, excessive daytime sleepiness; ESS, Epworth Sleepiness Scale; HI, hypopnoea index; LAUP, laser-assisted uvulopalatoplasty; NA, not applicable; NR, not reported; ODI, oxygen desaturation index; OSAS, obstructive sleep apnoea/hypopnoea syndrome; PSG, polysomnography; RCT, randomised controlled trial; REM, rapid eye movement; RDI, respiratory disturbance index; SI, snoring index; SPL, sound pressure level; TST, total sleep time; UP3, uvulopalatopharyngoplasty; VAS, visual analogue scale.
Uvulopalatopharyngoplasty versus laser-assisted uvulopalatoplasty
| Osman 2000;86 200387 | |||||||
|---|---|---|---|---|---|---|---|
|
Titles: (1) Uvulopalatopharyngoplasty versus laser-assisted uvulopalatoplasty for the treatment of snoring: an objective randomised clinical trial; (2) Palatal surgery for snoring: objective long-term evaluation Country: UK Setting: Department of Ear, Nose and Throat (ENT) Surgery Study design: RCT |
|||||||
| Interventions | |||||||
|
Intervention 1: LAUP performed under general anaesthetic. In the procedure two linear scars were created in the oral surface of the soft palate from the junction of the hard and soft palate to the uvula, followed by laser uvulectomy with a KTP/532 potassium titanyl phosphate laser. A power setting of 12 W was used for the procedure with continuous exposure Intervention 2: UP3 performed under general anaesthetic. In the procedure 1 cm of the soft palate was removed with the uvula as well as the tonsils if present. The posterior pillar was then sutured to the anterior pillar followed by mucosa-to-mucosa closure of the palate using catgut sutures. Postoperative analgesia was standardised for a 10-day period in the form of regular oral or rectal diclofenac sodium. Concurrent treatment: NR Previous treatment(s): NR |
|||||||
| Participants | |||||||
|
Total n = 47 (n = 47 in short-term follow-up and n = 23 in long-term follow-up) Number of non-apnoeic snorers included: NA Tests to exclude OSAS: An overnight sleep study using a DENSA Compact Sleep Apnoea Screening System, which measures abdominal respiratory waveform, transcutaneous SaO2, pulse rate and oral/nasal airflow. Snoring was measured using the Snore Box recording device in the home Tests to assess the site of airway narrowing: Complete ear, nose and throat examination and sleep nasendoscopy to assess palatal flutter Inclusion criteria: Simple snores or patients with ‘mild OSA’ (AHI < 20); all had palatal flutter confirmed with sleep nasendoscopy Exclusion criteria: AHI > 20 Subgroups: Subgroup of 38 patients: LAUP, n = 22, UP3, n = 16; data from the study by Osman 200386 |
|||||||
| Participant baseline characteristics | |||||||
| Intervention | LAUP | UP3 | |||||
| n | 29 | 18 | |||||
| Age (years), mean (range) | 49.4 (27–71) | ||||||
| Male, n (%) | 41 (87) | ||||||
| BMI (kg/m2), mean (range) | 28 (22–38) | ||||||
| AHI score, mean (SD) | 4.4 (3.59) | ||||||
| ESS score, mean (range) | NR | ||||||
| Smokers, n (%) | 24 (48.9) | ||||||
| Outcome measures | |||||||
|
Outcome 1: Postoperative pain in the first 24 hours after surgery; linear analogue scale: 0 = no pain, 4 = worst pain. Definition of treatment success: NR Outcome 2: Postoperative complications (short-term follow-up results). Definition of treatment success: NR Outcome 3: Improvement in snoring (patient reported) (short-term follow-up results). Definition of treatment success: NR Outcome 4: Snoring index calculated as the number of snores per hour slept; snoring was defined as a spike in breathing sound intensity, starting from baseline and returning back to baseline, whose amplitude was greater than 50 dB SPL (short- and long-term follow-up results reported). Definition of treatment success: NR Outcome 5: Snoring loudness. Definition of treatment success: NA Outcome 6: Long-term postoperative complications (assessed in subgroup only). Definition of treatment success: NR Covariates: NR Total length of follow-up: Full study cohort (n = 47) assessed for subjective outcomes only: mean 3.4 months (range 2–11 months); subgroup of full study cohort assessed at long-term follow-up for objective outcomes and long-term complications: median 45 months (range 29–56 months) |
|||||||
|
Follow-up assessment times: Full study cohort (short-term follow-up): mean 3.4 months (range 2–11 months); long-term follow-up (subgroup): median 45 months (range 29–56 months) Rate of attrition at each follow-up time: First follow-up assessment: 0/47; second follow-up assessment: 24/47 Method of statistical analysis: The Wilcoxon-T non-parametric test for two independent groups |
|||||||
| Results | |||||||
| Outcome 1: Postoperative pain in the first 24 hours after surgery | |||||||
| Intervention | LAUP | UP3 | |||||
| n (in analysis) | 29 | 18 | |||||
| Pain score (mean) | 1.3 | 1.7 | |||||
| Outcome 2: Postoperative complications | |||||||
| Intervention | LAUP | UP3 | |||||
| n (in analysis) | 29 | 18 | |||||
| Patients with complications | 0/29 | 1/18. This patient was admitted to the intensive care unit for 24 hours following surgery because of an intraoperative anaesthetic problem | |||||
| Secondary bleeding (n) | 0 | 3/18 | |||||
| Temporary velopalatal insufficiency (n) | 0 | 3/18 | |||||
| Severe infection (n) | 0 | 1/18 | |||||
| Outcome 3: Improvement of snoring (patient reported) | |||||||
| Intervention | LAUP | UP3 | |||||
| n (in analysis) | 29 | 18 | |||||
| Patients reporting improvement in their snoring (n) | 24 (83%), then reduced to 22 (76%) as 2 patients referred by GP for late recurrence of snoring | 16 (89%), and then reduced to 15 (83%) as 1 patient was referred by GP for late recurrence of snoring | |||||
| Outcome 4: Snoring index (short-term follow-up results) | |||||||
| Intervention | LAUPa | UP3b | Difference between groups | ||||
| n (in analysis) | 22 | 16 | NA | ||||
| Patients with a higher postoperative snoring index, n | 5c | 2 | Not significant at the 5% level | ||||
| Patients with a lower postoperative snoring index, n | 17 | 14 | Not significant at the 5% level | ||||
| Outcome 4: Pre- and postoperative snoring index of the pooled 24 subjects (data from the study by Osman 200387) | |||||||
| Snoring index | Median value (snores/hour) | ||||||
| Preoperative | 135.6 | ||||||
| Postoperative: short term | 38.2 | ||||||
| Postoperative: long term | 21.7; significantly less than pre-operative, p < 0.01 | ||||||
| Long term verses short term | –0.9; p > 0.05 | ||||||
| Change in snoring index in LAUP group (n = 12) | Reduction significant; p < 0.01 | ||||||
| Change in snoring index in UP3 group (n = 11) | Reduction significant; p < 0.05 | ||||||
| LAUP vs UP3 at long-term follow-up | Not significant; p > 0.05 | ||||||
| Outcome 5: Median snoring loudness at short-term follow-up (check)d | |||||||
| Intervention | LAUP | UP3 | |||||
| n (in analysis) | 12 | 11 | |||||
| Reduction in pre-and postoperative median snore loudness | Significant at 10% level but not at 5% level | Significant at 0.1% level | |||||
| Outcome 5: Median snoring loudness at long-term follow-up (data from the study by Osman 200387) | |||||||
| Intervention | LAUP | UP3 | |||||
| n (in analysis) | 12 | 11 | |||||
| Reduction in pre- and long-term follow-up: pooled data of the 38 subjects | NA | NA | |||||
| Change in the 38 subjects: LAUP vs UP3 | NR | NR | |||||
| Outcome 6: Long-term postoperative complications (assessed in subgroup only) | |||||||
| Intervention | LAUP | UP3 | |||||
| n (in analysis) | 12 | 12 | |||||
| Long-term postoperative complications, n (%) | 6 (50) | 5 (41.7) | |||||
| Occasional choking, n (%) | 2 (16.7) | 2 (16.7) | |||||
| Dry throat, n (%) | 0 (0) | 3 (25) | |||||
| Mild sore throat, n (%) | 3 (25) | 1 (8) | |||||
| Food sticking in the throat, n (%) | 1(8) | 1 (8) | |||||
| Need for repeat procedure (unscheduled): two patients in the LAUP group and one patient in the UP3 group were re-referred by their GP for a late recurrence of snoring | |||||||
| Authors’ conclusions | |||||||
| LAUP and UP3 are effective treatments for snoring due to palatal flutter; however, because of complications, LAUP is preferable to UP3 unless sleep nasendoscopy demonstrates palatal flutter with vibration at the level of the tonsils | |||||||
| Methodological assessment criteria | |||||||
| 1. Study design | RCT | ||||||
| 2. Were the study eligibility criteria specified? | Yes | ||||||
| 3. Was a power calculation performed? | No | ||||||
| 4. Is the sample size adequate? | Unclear | ||||||
| 5. Is the number randomised stated? | Yes | ||||||
| 6. Is the study properly randomised?e | Yes | ||||||
| 7. Is allocation of treatment concealed?f | No | ||||||
| 8. Are adequate baseline details presented? | Partial, for the whole group only | ||||||
| 9. Are groups similar at baseline? | Unclear | ||||||
| 10. Are any baseline imbalances adequately adjusted for in the analysis? | No | ||||||
| 11. Are similar co-interventions administered? | Unclear | ||||||
| 12. Are patients blinded to treatment allocation? | No | ||||||
| 13. Are outcome assessors blinded? | No | ||||||
| 14. Is compliance with treatment adequate? | Yes | ||||||
| 15. Was any subgroup analysis justified? | Yes | ||||||
| 16. Were data collection tools shown or known to be valid for the outcome of interest?g | Partial (both objective and subjective outcomes assessed) | ||||||
| 17. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?h | Partial (both objective and subjective outcomes assessed) | ||||||
| 18. Were all study participants accounted for? | Yes (except for the subgroup analysis) | ||||||
| 19. Are data analyses appropriate? | Yes | ||||||
| 20. Is analysis conducted on an intention to treat basis? | Yes | ||||||
| 21. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||||||
| 22. Are the conclusions supported by the results? | Small group of subjects, unable to draw firm conclusions | ||||||
| 23. Generalisability | Applicable for the same population | ||||||
| 24. Intercentre variability | NA | ||||||
| 25. General comments | – | ||||||
| Prasad 200388 | |||
|---|---|---|---|
|
Title: Surgery for snoring: are partners satisfied in the long run? Country: UK Setting: Department of Otolaryngology, Head and Neck Surgery Study design: CCT |
|||
| Interventions | |||
|
Intervention 1: Laser-assisted uvulopalatoplasty (LAUP) performed using a KTP/532 potassium titanyl phosphate laser in a continuous mode at a setting of 8–10 W. Procedure consisted of approximating the soft palate against the velopharyngeal isthmus and excising any redundant portion along the uvula. Number of procedures per patient not reported. Anaesthesia protocol not reported Intervention 2. Uvulopalatopharyngoplasty (UP3) procedure consisted of excising the uvula and a rim of soft palate, removing both palatine tonsils and suturing of the mucosa. Anaesthesia protocol not reported Concurrent treatment: NR Previous treatment(s): NR |
|||
| Participants | |||
|
Total n = 91: LAUP, n = 50; UP3, n = 41. The study comprised a questionnaire-based survey of patients’ partners, with 60 respondents (response rate = 65.93%), 33 (66%) in the LAUP group and 27 (65.8%) in the UP3 group If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS (including test details): Unclear; the authors were contacted for further details and the test appears to be oximetry; authors confirmed baseline patient AHI < 5 (no further details provided) Tests to assess the site of airway narrowing (including test details): NR Inclusion criteria: NR Exclusion criteria: NR |
|||
| Patient baseline characteristics | |||
| Intervention | LAUP | UP3 | |
| n | 33 | 27 | |
| Age (years), mean (SD; range)a | 49.45 (8.92; 31–56) | 51.96 (12.07; 33–59) | |
| Male, n (%)a | 25 (76) | 23 (85) | |
| BMI (kg/m2), mean (range) | NR | NR | |
| AHI score, mean (SD)b | NR | NR | |
| Smokers, n (%) | NR | NR | |
| Outcome measures | |||
|
Outcome 1: Partner’s snoring severity. Assessed by a questionnaire with response options: absent; a lot better; slightly better; unchanged; worse. Definition of treatment success: NR Outcome 2: Difficulties falling asleep because of partner’s snoring. Assessed by a questionnaire with response options: no; occasionally; sometimes; most often; always. Definition of treatment success: NR Outcome 3: Sleep disturbance because of partner’s snoring. Assessed by a questionnaire with response options: no longer disturbed; reduced frequency; remains unchanged; increased. Definition of treatment success: NR Outcome 4: Need to sleep in a separate room because of partner’s snoring. Assessed by a questionnaire with response options: no longer need to sleep in a separate room; frequency reduced; frequency remains unchanged; frequency is increased. Definition of treatment success: NR Outcome 5: Quality of marital life. Assessed by means of a questionnaire, response options not reported. Definition of treatment success: NR Covariates: NR Total length of follow-up: 1 year to > 4 years Follow-up assessment times: One follow-up assessment survey between 1 year and > 4 years post procedure Rate of attrition: Response rate for survey = 66% Methods of statistical analysis: NR |
|||
| Results | |||
| Outcome 1: Partner’s improvement in snoringc | |||
| Intervention | LAUP | UP3 | Difference between groups |
| n (in analysis) | 33 | 27 | – |
| Snoring abolished (% | 15 | 19 | – |
| Snoring a lot better (%) | 28 | 58 | – |
| Snoring slightly better (%) | 24 | 11 | – |
| Snoring unchanged (%) | 21 | 4 | – |
| Snoring worse (%) | 6 | 4 | – |
| Not recorded (%) | 6 | 4 | – |
| Outcome 2: Difficulties falling asleep because of partner’s snoringd | |||
| Intervention | LAUP | UP3 | Difference between groups |
| n (in analysis) | 33 | 27 | – |
| Always (%) | 16 | 4 | – |
| Most often (%) | 19 | 0 | – |
| Sometimes (%) | 16 | 19 | – |
| Occasionally (%) | 22 | 40 | – |
| Never (%) | 24 | 33 | – |
| Not recorded (%) | 3 | 4 | – |
| Outcome 3: Sleep disturbance because of partner’s snoringe | |||
| Intervention | LAUP | UP3 | Difference between groups |
| n (in analysis) | 33 | 27 | – |
| No disturbed sleep, n (%) | 13/33 (39.40) | 16/27 (59.26) | – |
| Reduced, n (%) | 11/33 (33.33) | 10/27 (37.04) | – |
| Unchanged, n (%) | 8/33 (24.24) | 1/27 (3.70) | – |
| Increased, n (%) | 1/33 (3.03) | 0 (0) | – |
| Outcome 4: Need to sleep in a separate room because of partner’s snoring | |||
| Intervention | LAUP | UP3 | Difference between groups |
| n (in analysis) | 32 | 27 | – |
| No longer need to sleep in a separate room, n (%) | 21/32 (65.63) | 22/27 (81.48) | – |
| Need reduced, n (%) | 5/32 (15.63) | 3/27 (11.11) | – |
| No change, n (%) | 5/32 (15.63) | 2/27 (7.41) | – |
| Need increased, n (%) | 1/32 (3.11) | 0 (0) | – |
| Outcome 5: Quality of marital lifef | |||
| Intervention | LAUP | UP3 | Difference between groups |
| n (in analysis) | 33 | 27 | – |
| Improved, n (%) | 10/33 (30.3) | 11/27 (40.74) | – |
| Unchanged, n (%) | 19/33 (57.58) | 9/27 (33.33) | – |
| Undecided, n (%) | 4/33 (12.12) | 7/27 (25.93) | – |
|
Postoperative adverse events: NR Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||
| Authors’ conclusions | |||
| The long-term results show that partners are satisfied with the results of both LAUP and UP3. It would therefore be justified to continue to offer these procedures in the NHS, notwithstanding their relatively low priority | |||
| Reviewer’s comments | |||
| Very few details were presented on the intervention. No details were reported on the tests to rule out OSAS or assess the site of airway narrowing. Only details for the baseline prognostic factors of age and gender were reported; no details on BMI, smoking status or alcohol consumption were given for the groups. It is therefore unclear whether the groups were comparable at baseline. The response rate of 66% for the survey is moderate. It is unclear whether survey respondents may differ significantly in their treatment response from non-respondents. No sensitivity analysis was conducted to assess the effect of response bias and how this could affect the results. The numbers presented in the pie charts and the figures are not consistent in places and no consistent method appears to have been used in the rounding of numbers. It is also unclear how the authors grouped the results for each of the treatment groups to perform the between-group comparisons. Given the small sample size and the multiple comparisons performed, the authors’ conclusions may not be robust | |||
| Methodological assessment criteria | |||
| 1. Study design | Parallel two-group pre–post study with between-group comparisons | ||
| 2. Were the study eligibility criteria specified? | No | ||
| 3. Was a power calculation performed? | No | ||
| 4. Is the sample size adequate? | Unclear | ||
| 5. Is the number randomised stated? | NA | ||
| 6. Is the study properly randomised?g | NA | ||
| 7. Is allocation of treatment concealed?h | NA | ||
| 8. Are adequate baseline details presented? | No | ||
| 9. Are groups similar at baseline? | Unclear (prognostic variables not reported) | ||
| 10. Are any baseline imbalances adequately adjusted for in the analysis? | No | ||
| 11. Are similar co-interventions administered? | Unclear | ||
| 12. Are patients blinded to treatment allocation? | No | ||
| 13. Are outcome assessors blinded? | No | ||
| 14. Is compliance with treatment adequate? | Unclear | ||
| 15. Were any subgroup analyses justified? | NA | ||
| 16. Were data collection tools shown or known to be valid for the outcome of interest?i | No | ||
| 17. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest? j | No | ||
| 18. Were all study participants accounted for? | No | ||
| 19. Are data analyses appropriate? | Partial | ||
| 20. Is analysis conducted on an intention to treat basis? | No | ||
| 21. Are greater than 80% of patients included in the follow-up assessment? | No | ||
| 22. Are the conclusions supported by the results? | Partial | ||
| 23. Generalisability | Unclear | ||
| 24. Intercentre variability | One-centre study | ||
| 25. General comments | – | ||
Pre–post studies of uvulopalatopharyngoplasty alone
| Friberg 199591 | ||
|---|---|---|
|
Title: UPPP for habitual snoring: a 5-year follow-up with respiratory sleep recordings Country: Sweden Setting: Departments of Otorhinolaryngology and Clinical Neurophysiology Study design: Pre–post |
||
| Interventions | ||
|
Intervention (specific details): UP3 performed according to the method described by Fujita62 with slight modifications to ensure velopharyngeal sphincter function postoperatively. All patients were given preoperative and postoperative antibiotic treatment Concurrent treatment (specific details): NR Previous treatment(s) (specific details): NR |
||
| Participants | ||
|
Total n = 56 If this study includes a mixed patient population, number of non-apnoeic snorers included: not applicable Tests to exclude OSAS (including test details): Respiratory sleep recording that included measurements of respiratory and body movements by means of a sleep apnoea mattress [static charge-sensitive bed (SCSB)] and pulse oximetry. The duration of obstructive respiratory movement pattern, expressed as percentage of total sleep time, was calculated from the SCSB recordings. The average number of O2 desaturations that were ≥ 4% per sleep hour were calculated from the results of the pulse oximetry Tests to assess the site of airway narrowing (including test details): NR Inclusion criteria: Male with habitual snoring; complete preoperative respiratory sleep recording result negative for OSAS [the criteria for classifying OSAS are obstructive respiratory pattern > 45%, ODI > 6 and AI ≥ 5] Exclusion criteria: not reported Subgroups: not applicable |
||
| Participant baseline characteristics | ||
| n | 56 | |
| Age (years), median (range) | 46 (26–74) | |
| Male, n, (%) | 56 (100) | |
| BMI (kg/m2), median (range) | 26.1 (18.3–35.4) | |
| AHI score, median (range) | NR | |
| ODI score, median (range) | 0 (0–6) | |
| Duration (% of total sleep time) of obstructive respiratory pattern, median (range) | 8% (0–43%) | |
| Nadir SaO2, median (range) | 92% (97–84%) | |
| Number of patients reporting excessive daytime sleepiness (EDS), n | 51 | |
| Smoking status, n (%) | NR | |
| Outcome measures | ||
|
Outcome 1: Median ODI score (calculated from the results of pulse oximetry). Definition of treatment success: NR Outcome 2: Duration (percentage of total sleep time) of the obstructive respiratory pattern. Definition of treatment success: NR Outcome 3: Nadir SaO2. Definition of treatment success: NR Outcome 4: Number of patients reporting EDS scored on a three-grade scale from none to partial to complete recovery. Definition of treatment success: NR Outcome 5: Number of patients reporting snoring scored on a three-grade scale from none to partial to complete recovery. Definition of treatment success: NR Covariates: Association between changes in BMI and ODI, obstructive respiratory pattern and postoperative snoring were explored; association between postoperative recordings of sleep apnoea and postoperative snoring and EDS were also explored Total length of follow-up: Median 63 months (range 37–83) Follow-up assessment times: One follow-up assessment only Rate of attrition at each follow-up time: Only patients willing to undergo a follow-up sleep recording appear to have been included in the study: 53/56 patients underwent a follow-up sleep study Methods of statistical analysis: The Wilcoxon signed rank test was used to assess pre- and postoperative changes; Spearman’s rank correlation coefficient was used to study the correlation between variables |
||
| Results | ||
| Outcome 1: Median ODI score | ||
| n (in analysis) | 53 | |
| ODI score, median (range); p-value | 1 (0–24); p = 0.0005 | |
| Outcome 2: Duration (percentage of total sleep time) of the obstructive respiratory pattern | ||
| n (in analysis) | 53 | |
| Duration of obstructive respiratory pattern, median (range); p-value | 17% (0–74%); p = 0.004 | |
| Outcome 3: Nadir SaO2 | ||
| n (in analysis) | 53 | |
| Nadir SaO2, median (range); p-value | 88% (95–73%); p = 0.0001 | |
| Outcome 4: Number of patients reporting EDS | ||
| n (in analysis) | 51 (who preoperatively reported EDS) | |
| Excessive daytime sleepiness, n (%) | 29 (57) | |
| Improvement in daytime sleepiness, n (%) | 8 (16) | |
| No change in daytime sleepiness, n (%) | 14 (27) | |
| Outcome 5: Number of patients reporting snoringa | ||
| n (in analysis) | 56 (all complained of having loud snoring preoperatively) | |
| No snoring, n (%) | 15 (27) | |
| Decrease in snoring, n (%) | 34 (60) | |
| Loud persistent snoring, n (%) | 7 (13) | |
|
The postoperative recording results for six patients fulfilled the criteria for mild-moderate OSAS All patients stated that they would have this procedure repeated if necessary |
||
|
Association between BMI and changes in respiratory variables, snoring status and reports of EDS: Correlations between BMI and changes in both ODI and obstructive respiratory pattern postoperatively were significant (p = 0.003; Spearman’s rank correlation co-efficient). Changes in BMI also correlated significantly with reports of postoperative snoring (p = 0.04). There was no significant association between BMI and reports of EDS. Likewise, there was no significant association between results of postoperative recordings of sleep apnoea and patients’ subjective reports of EDS and snoring The correlation between nasal obstruction measures following the laser-assisted outpatient septoplasty (LAOS) procedure, the changes in total nasal resistance and the changes in subjective nasal obstruction was not statistically significant (p = 0.45; Pearson’s correlation) |
||
|
Postoperative adverse events: No serious preoperative or postoperative complications were reported Long-term adverse events: 7/56 patients reported minor throat disturbances such as dryness or increased mucous secretion; 1/56 patients reported a change in voice quality Need for repeat procedure (unscheduled): NR |
||
| Authors’ conclusions | ||
| UP3 is a safe and effective treatment for habitual snoring; however, it does not give complete protection against the development of OSAS, and postoperative weight gain implies a less satisfactory result of surgery for upper airway obstructions and snoring | ||
| Reviewer’s comments | ||
| Only very limited details on the intervention are provided. Likewise, limited inclusion criteria are stated. It appears that this may be a subgroup of a larger patient series (n = 125), in which the patients were willing to undergo a repeat sleep study at follow-up. The findings may therefore not be easily generalised to other patients undergoing UP3. The crude subjective assessment of snoring status limits the utility of the results | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | Partial | |
| 3. Are adequate baseline details presented? | Partial | |
| 4. Are any co-interventions clearly stated? | Unclear (5-year follow up); BMI had increased significantly | |
| 5. Is compliance with treatment adequate? | Yes | |
| 6. Were any subgroup analyses justified? | NA | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?b | Partial (mixture of objective and subjective outcome measures) | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?c | Partial (mixture of objective and subjective outcome measures) | |
| 9. Were all study participants accounted for? | No | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |
| 11. Are data analyses appropriate? | Yes | |
| 12. Are the conclusions supported by the results? | Partial | |
| 13. Generalisability | Only limited baseline information on participants is presented; however, ratio of male to female patients and BMI indicative of being overweight would appear representative of non-apnoeic snorers in general. Treatment of choice was mandibular advancement splints (MAS) rather than palatal surgery. No baseline information on smoking status or alcohol consumption presented | |
| 14. Intercentre variability | NA | |
| 15. General comments | – | |
| Janson 199490 | |||||
|---|---|---|---|---|---|
|
Title: Excessive daytime sleepiness and fatigue in nonapnoeic snorers: improvement after UPPP Country: Sweden Setting: Departments of Lung Medicine and Otorhinolaryngology Study design: Two-group parallel pre–post study |
|||||
| Interventions | |||||
|
Intervention 1: UP3. Three different techniques of UP3 were used depending on the anatomy of the subject: 55 patients who had large tonsils and/or tonsils situated high up in a narrow angle to the uvula were operated with classic UP3 (standard UP3), including tonsillectomy; 31 patients with a prolonged clumsy uvula but small tonsils and normal posterior pillars were treated with a CO2 laser technique; 70 patients with small tonsils, a prolonged uvula and/or pronounced posterior pillars (often web-like, attached far down onto the uvula) were operated under local anaesthesia with the same technique as for standard UP3, except for the tonsillectomy Intervention 2: Conservative treatment Concurrent treatment: NR Previous treatment(s): NR |
|||||
| Participants | |||||
|
Total n = 231 Number of non-apnoeic snorers included: NA Tests to exclude OSAS (including test details): Overnight oximetry (finger probe, Biox III) carried out in hospital under the supervision of a nurse, who also regularly noted whether or not the patient was asleep. A total of 16 patients had additional full-night PSG. Snoring was monitored with a microphone Tests to assess the site of airway narrowing (including test details): Clinical examination alone Inclusion criteria: Socially impairing snoring but without OSAS (AI < 5) Exclusion criteria: OSAS Subgroups: See outcomes |
|||||
| Participant baseline characteristics | |||||
| Intervention | UP3 | Conservative treatment | |||
| n | 155 | 76 | |||
| Age (years), mean (range) | 45 (24–74) | 49 (18–79) | |||
| Male, n (%) | 136 (87.7) | 47 (62) | |||
| Body mass (kg), mean ± SD | 80 ± 11 | 76 ± 13 | |||
| BMI (kg/m2), mean ± SD | 25 ± 3 | 25 ± 3 | |||
| ODI score, mean ± SD | 1.2 ± 1.4 | 1.1 ± 1.3 | |||
| Concurrent disease | |||||
| Ischaemic heart disease, n | 1 | 7 | |||
| Hypertension, n | 15 | 17 | |||
| Diabetes, n | 3 | – | |||
| Upper airway evaluation | |||||
| Possibly suitable for UP3 (%) | 51 | 37 | |||
| Clearly suitable for UP3 (%) | 29 | 11 | |||
| Proportion of patients with frequent loud snoring | Frequent problems: 96%; occasional problems: 4%; total: 100% | Frequent problems: 80%; occasional problems: 16%; total: 96% | |||
| Proportion of patients with awakenings because of nocturnal breathing problems | Frequent problems: 13%; occasional problems: 24%; total: 37% | Frequent problems: 7%; occasional problems: 25%; total: 32% | |||
| Proportion of patients with morning headache | Frequent problems: 15%; occasional problems: 29%; total: 44% | Frequent problems: 12%; occasional problems: 25%; total: 37% | |||
| Proportion of patients falling asleep in daytime | Frequent problems: 12%; occasional problems: 23%; total: 35% | Frequent problems: 9%; occasional problems: 11%; total: 20% | |||
| Proportion of patients with problems staying awake when driving | Frequent problems: 8%; occasional problems: 21%; total: 29% | Frequent problems: 2%; occasional problems: 13%; total: 15% | |||
| Outcome measures | |||||
|
All of the patients classified their symptoms on a 5-point scale, multiple-choice questionnaire. The questionnaire consisted of 16 symptom-related questions Outcome 1: Difficulty inducing sleep (DIS) measured on a 5-point scale with response options: (1) none/never; (2) small/seldom; (3) moderate/occasional; (4) severe/frequent; (5) very severe/very frequent. Definition of treatment success: NR Outcome 2: Difficulty maintaining sleep measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 3: Excessive daytime sleepiness (EDS) measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 4: Excessive daytime tiredness measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 5: Snoring measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 6: Morning headache measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 7: Awakening because of trouble breathing measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 8: Involuntarily falling asleep measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 9: Falling asleep when relaxing measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 10: Tendency to take a nap in the daytime measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 11: Difficulty staying awake when driving measured on a 5-point scale with response options as above. Definition of treatment success: NR Outcome 12: UP3 (1 year) vs conservative treatment. Definition of treatment success: NR Covariates: Association between BMI before the operation and symptomatic effect, and association between age, DIS or operation method and symptomatic outcome Total length of follow-up: 3 months after the operation in 105 subjects, 12 months after the operation in 50 subjects, both 3 and 12 months after the operation in 54 subjects, a further evaluation in 49 subjects 2 years after the operation, and an evaluation in 9 subjects after 5 years. The comparison was made between the 76 conservatively treated patients and the 104 UP3-treated patients who were evaluated after 1 year Follow-up assessment times: See above Rate of attrition at each follow-up time: Unclear Methods of statistical analysis: Analysis of variance (ANOVA) used for analysis for repeated measures within each group; factorial ANOVA used to analyse comparison between groups and the three operation methods; Spearman’s rank correlation used to assess association between variables and treatment outcome; a p-value of 0.05 (two-tailed) was considered significant |
|||||
| Results | |||||
| Outcomes 1–11: Change in reported symptoms before and 3 or 12 months after UP3 (n = 155; 3 months in 105 patients and 12 months in 50 patients) | |||||
| Method of measurement: NR | |||||
| Before | After | Before vs after | |||
| Moderate or occasional problems (%) | Severe or frequent problems (%) | Moderate or occasional problems (%) | Severe or frequent problems (%) | ||
| Difficulty inducing sleep | 14 | 7 | 11 | 4 | p < 0.05 |
| Difficulty maintaining sleep | 33 | 27 | 19 | 10 | p < 0.001 |
| Excessive daytime sleepiness | 36 | 41 | 21 | 7 | p < 0.001 |
| Excessive daytime tiredness | 31 | 54 | 30 | 7 | p < 0.001 |
| Snoring | 4 | 96 | 21 | 18 | p < 0.001 |
| Morning headache | 29 | 15 | 10 | 2 | p < 0.001 |
| Awakening because of trouble breathing | 24 | 13 | 7 | 3 | p < 0.001 |
| Involuntarily falling asleep | 23 | 12 | 6 | 3 | p < 0.001 |
| Falling asleep when relaxing | 30 | 50 | 29 | 26 | p < 0.001 |
| Tendency to take a nap in the daytime | 26 | 20 | 20 | 6 | p < 0.001 |
| Difficulty staying awake when driving | 21 | 8 | 6 | 1 | p < 0.001 |
|
Outcome: long-term effects of UP3 (for 49 patients after 2 years): compared with baseline a significant improvement in all outcomes was observed (p < 0.01), except for problems with falling asleep when relaxing and staying awake when driving (p < 0.05); compared with baseline there was also an increase in the number of patients with frequent snoring (10 vs 14; p < 0.05); otherwise, no significant differences in symptoms scores were found between the first- and second-year postoperative follow-up Outcome: long-term effects of UP3 (for nine patients after 5 years): compared with baseline (no patients) the number of patients who felt rested on wakening was seven and five, respectively, at the first- and fifth-year postoperative evaluation (p < 0.001); the number of patients with frequent snoring had decreased from nine to one and two, respectively, at the first- and fifth-year evaluation (p < 0.001) |
|||||
| Outcome 13: UP3 (1 year postoperative) vs conservative treatment | |||||
|
Note: Results are reported in graphs and minimally in the text. It is unclear whether the p-values stated in the text are for the moderate/occasional problems, severe or frequent problems, or the total of both categories. The specific figures from the graphs are therefore not extracted by us Authors report: After treatment the UP3 patients had significantly lower symptom scores for tendency to take a nap in the daytime (p < 0.05), EDS, morning headache (p < 0.01), difficulty maintaining sleep, snoring, and waking because of trouble breathing (p < 0.001) than the conservatively-treated patients. More patients in the UP3 group also felt rested when wakening in the morning (p < 0.01) Postoperative adverse events: Minor side effect after UP3 Method of measurement: NR |
|||||
| Total number of patients with minor side effects (n) | 42 | ||||
| Irritation in the throat (n) | 19 | ||||
| Nasal speech (n) | 3 | ||||
| Hypersecretion in the throat (n) | 4 | ||||
| Nasal regurgitation (n) | 3 | ||||
| Tendency to vomit (n) | 1 | ||||
| Patients who had standard technique and with side effects (%) | 35 | ||||
| Patients who had CO2 laser treatment and with side effects (%) | 23 | ||||
| Patients had UP3 performed under local anaesthesia and with side effects (%) | 23 | ||||
|
Long-term adverse events: NR Need for repeat procedure (unscheduled): NR No significant correlation was found between the result of treatment and change in body mass in the UP3-treated group |
|||||
| Authors’ conclusions | |||||
| UP3 is effective in relieving snoring and EDS in non-apnoeic snorers | |||||
| Methodological assessment criteria | |||||
| 1. Study design | Pre–post | ||||
| 2. Were the study eligibility criteria specified? | Partial | ||||
| 3. Are adequate baseline details presented? | Partial | ||||
| 4. Are similar co-interventions administered? | Unclear | ||||
| 5. Is compliance with treatment adequate? | Yes | ||||
| 6. Were any subgroup analyses justified? | Yes | ||||
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | No | ||||
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | No | ||||
| 9. Were all study participants accounted for? | No | ||||
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||||
| 11. Are data analyses appropriate? | Unclear | ||||
| 12. Are the conclusions supported by the results? | Yes | ||||
| 13. Generalisability | Unclear | ||||
| 14. Intercentre variability | One-centre study | ||||
| 15. General comments | – | ||||
| Jones 200594 | |||
|---|---|---|---|
|
Title: Acoustic analysis of snoring before and after palatal surgery Country: UK Setting: Department of Otolaryngology Head and Neck Surgery Study design: Parallel two-group pre–post study (patients were randomised into two treatment groups but only pre- and postoperative data were compared) |
|||
| Interventions | |||
|
Intervention 1: Traditional palatoplasty with uvulectomy (TP) performed transorally on an anaesthetised patient. Using a CO2 laser a central strip of soft palate mucosa extending from the junction of the hard and soft palate to the free edge of the soft palate was excised. The uvula was then amputated Intervention 2: Uvulopalatal elevation palatoplasty (UEP). Involved the removal of a central strip of soft palate mucosa as described previously. Using a CO2 laser a central strip of soft palate mucosa extending onto the oral surface of the uvula was performed. Instead of amputation of the uvula (as in TP) the raw surfaces of the soft palate and uvula were brought into apposition by reflecting, and then suturing, the oral surface of the uvula onto the oral surface of the soft palate Concurrent treatment: NR Previous treatment(s): NR |
|||
| Participants | |||
|
Total n = 54 (n = 35 in the analysis – those who underwent the operation, met the inclusion criteria and were adequately followed up) Number of non-apnoeic snorers included: 53 (after the operation one patient was subsequently found to have a presurgical AHI > 15 and therefore was excluded from the final analysis) Tests to exclude OSAS (including test details): Overnight PSG or limited respiratory sleep studies. Acoustic analysis of snoring sound and video measurements: snoring sounds were recorded onto a Sony digital audio tape (DAT) recorder using a microphone suspended from the boom arm of a microphone stand 60 cm above the mattress at the head end of the bed. An infrared camera, linked to a domestic video recorder, was directed at the patient’s head. The 4-hour DAT recordings were downloaded onto the computer hard disc and, using the video recordings and audio software package Cool Edit®, the recordings were searched for typical snoring sounds. Sound files comprising the first 100 inspiratory snores with the patient sleeping in a supine position were created and used for all analyses. The acoustic parameters assessed were: (1) snore duration (seconds): the average duration of each inspiratory snoring sound; (2) snore loudness (dB): the loudness calibration curve was used to calculate the loudness of the inspiratory snoring sounds included in the 100 snore files; the average loudness of the inspiratory snoring sounds included in the 100 snore files was also calculated; (3) snore periodicity (%): measured by segmenting the 100 snore files of each patient into 200-ms frames; each frame was classified as either periodic or non-periodic based on the autocorrelation function of the frame; snore periodicity was defined as the ratio of the number of periodic frames to the total number of frames; (4) energy ratio: the energy content of the frequency sub-bands 0–200 Hz, 0–250 Hz and 0–400 Hz was calculated on a frame-by-frame basis and the total energy of the 100 snore files was calculated; the frequency-band energy ratio for the 100 snore files was defined as the ratio of the sub-band energy to the total energy in all frames Tests to assess the site of airway narrowing (including test details): NR Inclusion criteria: Patients complaining of loud snoring every night causing social disruption and with an AHI < 15/hour Exclusion criteria: Patients with an AHI > 15/hour Subgroups: NA |
|||
| Participant baseline characteristics | |||
| Interventiona | UEP | TP | UEP vs TP |
| n randomised | 28 | 26 | No statistical differences demonstrable between the two groups for all parameters |
| n analysed | 19 | 16 | |
| Age (years), mean (range) | 47 (33–60) | 46 (24–65) | |
| Male, n (%) | 17/19 (89) | 13/16 (81) | |
| BMI (kg/m2), mean (range) | 31.4 (24.9–47.2) | 29.6 (24.3–36.0) | |
| AHI score, median (range) | 2.7 (0–12.8) | 3.8 (1.0–10.9) | |
| ESS score, median (range) | 7 (0–15) | 9 (2–17) | |
| Smokers, n (%) | NR | NR | |
| Median ethyl alcohol units/week (range) | 4 (1–6) | 3 (1–7) | |
| Mean peak nasal inspiratory flow rate, cmO2/min(range) | 148 (90–230) | 135 (80–190) | |
| Outcome measures | |||
|
Outcome 1: Snore periodicity (%) assessed as the ratio of the number of periodic frames to the total number of frames. Definition of treatment success: NR Outcome 2: Snore energy ratio 0–200 Hz. Definition of treatment success: NR Outcome 3: Snore energy ratio 0–250 Hz. Definition of treatment success: NR Outcome 4: Snore energy ratio 0–400 Hz. Definition of treatment success: NR Outcome 5: Postoperative improvement in snoring symptoms assessed by a questionnaire with response categories: no postoperative improvement; initial improvement not sustained for longer than 1 year; sustained improvement. Definition of treatment success: NR Covariates: Correlation between age, peak nasal inspiratory flow rate (measured as the best-of-three maximum rate), EES and alcohol intake and acoustic parameters; correlation between the objective acoustic and subjective questionnaire outcomes on an individual patient level. Age, peak nasal inspiratory flow rate, ESS score and reported alcohol intake (units/week) were unrelated to either the early improvement or the subsequent decline in the acoustic parameters after surgery; no relationship was found between the objective acoustic and subjective questionnaire outcomes on an individual patient level Total length of follow-up: 2–9 months for acoustic analysis in 35 patients; median of 21 (range 11–26) months for questionnaire in 34 patients Follow-up assessment times: The first postoperative recordings (T1) were made between 1.0 and 4.1 (mean 2.5) months; the second postoperative recording (T2) occurred between 5.9 and 17.5 (mean 9.7) months after surgery. The questionnaire was completed at a median of 21 months (range 11–26 months) after the surgery Rate of attrition at each follow-up time: Acoustic parameters second follow-up: 19/54; patient questionnaire: 20/54 Methods of statistical analysis: Repeated measures analysis of variance (ANOVA) performed for preoperative, early postoperative and late postoperative acoustic measurements; preoperative BMI (> 30 or < 30), type of palatoplasty and sex were incorporated as between-group variables; paired t-test analysis (with Bonferroni correction) was performed to compare the preoperative results with early and late postoperative results; multiple regressions used to assess contributions of age, peak nasal inspiratory flow rate, ESS score and alcohol intake to surgical outcome; questionnaire data was analysed using non-parametric methods; Spearman’s rank correlation used to assess association between subject questionnaire results and acoustic measures |
|||
| Results | |||
| Outcome 1: Snore periodicity (%) | |||
| n (in analysis) | 35 | ||
| Baseline, median (90th centile) | 87.5 (80–94) | ||
| First postoperative follow-up (T1), median (90th centile) | 84.0 (73–88) | Baseline vs T1: p < 0.001 | |
| Second postoperative follow-up (T2), median (90th centile) | 84.5 (73.5–91.5) | Baseline vs T2: p < 0.079 | |
| Outcome 2: Snore energy ratio 0–200 Hz | |||
| n (in analysis) | 35 | ||
| Baseline, median (90th centile) | 74 (37–87) | ||
| First postoperative follow-up (T1), median (90th centile) | 58.5 (18–83) | Baseline vs T1: p = 0.02 | |
| Second postoperative follow-up (T2), median (90th centile) | 67 (14–89) | Baseline vs T2: p = 0.077 | |
| Outcome 3: Snore energy ratio 0–250 Hz | |||
| n (in analysis) | 35 | ||
| Baseline, median (90th centile) | 83 (42–93) | ||
| First postoperative follow-up (T1), median (90th centile) | 73 (86.5–28) | Baseline vs T1: p = 0.002 | |
| Second postoperative follow-up (T2), median (90th centile) | 74 (27–93) | Baseline vs T2: p = 0.039 | |
| Outcome 4: Snore energy ratio 0–400 Hz | |||
| n (in analysis) | 35 | ||
| Baseline, median (90th centile) | 95 (97–56) | ||
| First postoperative follow-up (T1), median (90th centile) | 85 (95.5–49.5) | Baseline vs T1: p = 0.047 | |
| Second postoperative follow-up (T2), median (90th centile) | 89 (50–97.5) | Baseline vs T2: p = 0.126 | |
| Outcome 5: Postoperative improvement in snoring symptoms (assessed by 34 patients at a median of 21 (range 11–26) months after surgery) | |||
| n (in analysis) | 34 | ||
| No postoperative improvement, n (%) | 4 (11.8) | ||
| An initial improvement sustained for ≤ 1 year, n (%) | 19 (55.9) | ||
| An improvement ‘until now’b | 11 (32.3) | ||
|
The authors also stated that paired comparison of snore loudness between the early and late postoperative recordings showed a significant increase in snore loudness between recordings (p < 0.001) Postoperative adverse events: NR Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||
| Authors’ conclusions | |||
| Postoperative changes in the acoustic parameters of snoring sound following palatal surgery are demonstrable but short-lived. The subjective and objective results correlated poorly | |||
| Methodological assessment criteria | |||
| 1. Study design | Parallel two-group pre–post | ||
| 2. Were the study eligibility criteria specified? | Yes | ||
| 3. Are adequate baseline details presented? | Yes | ||
| 4. Are any co-interventions clearly stated? | NA | ||
| 5. Is compliance with treatment adequate? | Yes | ||
| 6. Were any subgroup analyses justified? | NA | ||
| 7. Were data collection tools shown or known to be valid for the outcome of interest?c | Partial (both objective and subjective outcome measures assessed) | ||
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?d | Partial (both objective and subjective outcome measures assessed) | ||
| 9. Were all study participants accounted for? | No | ||
| 10. Are greater than 80% of patients included in the follow-up assessment? | No | ||
| 11. Are data analyses appropriate? | Yes | ||
| 12. Are the conclusions supported by the results? | Yes | ||
| 13. Generalisability | Applicable to socially disrupted snorers with a AHI < 15/hour | ||
| 14. Intercentre variability | NA | ||
| 15. General comments | – | ||
| Miljeteig 199492 | ||
|---|---|---|
|
Title: Subjective and objective assessment of uvulopalatopharyngoplasty for treatment of snoring and obstructive sleep apnoea Country: Canada Setting: Department of Medicine and Otolaryngology Study design: Pre–post |
||
| Interventions | ||
|
Intervention (specific details): UP3, carried out as described by Fujita61 (no further details reported); in 29 patients additional surgery was performed at the time of UP3 (turbinoplasty, n = 20; septoplasty, n = 2; combined turbinoplasty and septoplasty, n = 7) Concurrent treatment (specific details): 18 non-apnoeics had nasal surgery in addition to UP3; details not reported Previous treatment(s): NR |
||
| Participants | ||
|
Total n = 100; patients were mailed postoperative questionnaires and 69 patients responded (response rate: 69%; 38 non-apnoeic snorers and 31 OSAS patients) If this study includes a mixed patient population, number of non-apnoeic snorers included: 38 Tests to exclude OSAS (including test details): PSG, carried out at a mean of 7 (SD 8) months before surgery, including measurements of snoring. Chest wall and abdominal movements were measured using inductance plethysmography, oronasal flow was detected using a pair of thermistors, and sound intensity was measured using a microphone placed on the forehead just above the level of the nasion. Normal breathing was registered at less than 50 dB. Snoring index (SI) was defined as the number of spikes in sound intensity exceeding 50 dB per hour of sleep. Mean (dB mean) and maximal (dB max) sound intensity were recorded Tests to assess the site of airway narrowing (including test details): Upper airway examination by an otolaryngologist including examination of the nasopharynx, oropharynx,and laryngopharynx Inclusion criteria: Patients who were originally referred to the sleep clinic because of snoring and who subsequently underwent UP3; they were unselected, consecutive patients taken from the surgical list Exclusion criteria: NR Subgroups: Non-apnoeic snorers = 58; OSAS = 42 (in analysis non-apnoeic snorers = 38; OSAS = 31) |
||
| Participant baseline characteristics | ||
| n a | 38 (non-apnoeic snorer subgroup) | |
| Age (years), mean ± SD (range) | Not reported by subgroup | |
| Male, n (%) | Not reported by subgroup | |
| BMI (kg/m2), mean ± SD (range) | Not reported by subgroup | |
| AHI score, mean ± SD | 5.1 ± 2.9 | |
| ESS score, mean (range) | Not reported by subgroup | |
| Smokers, n (%) | Not reported by subgroup | |
| SI (events/hour), mean ± SD | 252 ± 280 | |
| Mean sound intensity (dB), mean ± SD | 64.8 ± 7.2 | |
| Maximal sound intensity (dB), mean ± SD | 85.3 ± 12.3 | |
| Lowest O2 saturation (%), mean ± SD (range)] | Not reported by subgroup | |
| Outcome measures | ||
|
Outcome 1: SI assessed as the number of spikes in sound intensity exceeding 50 dB per hour of sleep. Definition of treatment success: NR Outcome 2: Mean sound intensity. Definition of treatment success: NR Outcome 3: Maximal sound intensity. Definition of treatment success: NR (Outcome data on snoring status, interference with bed partner’s sleep and satisfaction with surgery not reported separately by subgroup) Covariates: Correlation between preoperative characteristics (AHI, BMI, SI) and snoring was explored Total length of follow-up: 45 ± 20 months (PSG carried out at 13 ± 15months) |
||
|
Follow-up assessment times: After surgery, PSG was carried out at 13 ± 15 months and questionnaires were completed at 45 ± 20 months Rate of attrition at each follow-up time: 31/100 Methods of statistical analysis: Pre–post objective measures were compared using the Wilcoxon signed rank test and pre–post subjective measures were compared using chi-squared tests |
||
| Results | ||
| Outcomes 1–3: SI, mean sound intensity and maximal sound intensity | ||
| n (in analysis) | 38 | |
| SI (events/hour), mean ± SD | 296 ± 318; p = 0.70 | |
| Mean sound intensity (dB), mean ± SD | 65.4 ± 7.0, p = 0.65 | |
| Maximal sound intensity (dB), mean ± SD | 80.5 ± 14.5, p = 0.84 | |
| Outcome 4: Multiple linear regression analysis of AHI, BMI, preoperative SI with reduction in postoperative snoring | ||
|
Only preoperative SI correlated with postoperative SI (r2 = +0.49, p < 0.001) Postoperative adverse events: NR Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
||
| Authors’ conclusions | ||
| UP3 in unselected snoring patients has a poor success rate when assessed objectively but is quite successful if the assessment is based on the subjective impression of patients (and their bed partners) | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | Partial | |
| 3. Are adequate baseline details presented? | Yes (but not reported by subgroup) | |
| 4. Are any co-interventions clearly stated? | Unclear | |
| 5. Is compliance with treatment adequate? | Yes | |
| 6. Were any subgroup analyses justified? | Yes | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?b | Partial (both objective and subjective outcomes assessed) | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?c | Partial (both objective and subjective outcomes assessed) | |
| 9. Were all study participants accounted for? | No | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | No | |
| 11. Are data analyses appropriate? | Yes | |
| 12. Are the conclusions supported by the results? | Yes | |
| 13. Generalisability | Inclusive eligibility criteria | |
| 14. Intercentre variability | One-centre study | |
| 15. General comments | – | |
| Neruntarat 200393 | ||
|---|---|---|
|
Title: Uvulopalatal flap for snoring on an outpatient basis Country: Thailand Setting: Department of Otolaryngology Study design: Pre–post |
||
| Interventions | ||
|
Intervention (specific details): Reversible uvulopalatal flap (introduced by Powell). The procedure was performed under local anaesthesia on an outpatient basis instead of under general anaesthesia, with the patient sitting upright. The soft palate was anaesthetised with lidocaine 10% topical dispersion, and 5–10 ml lidocaine 10% topical dispersion and 5–10 ml lidocaine 1% with epinephrine solution was additionally injected at three points 1 cm from the lower rim of the palatal arch. The mucosa, submucosa with gland, and fat on the lingual surface of the uvula and soft palate were removed with cold knife dissection. The uvular tip was amputated and the uvula was reflected back toward the soft palate and fixated into its new position with multiple sutures of 3–0 polyglycolic acid. Mean operative time was 20.2 ± 7.4 (range 15–30) minutes Concurrent treatment (specific details): Postoperative medications included antibiotic suspension for 7 days and acetaminophen with codeine elixir and/or anaesthetic lozenges as needed for pain relief Previous treatment(s) (specific detai ls): NR |
||
| Participants | ||
|
Total n = 60 (n = 56 in the analysis) If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS (including test details): PSG if patients or bed partners reported any doubtful signs or symptoms of daytime sleepiness, restless disturbed sleep or observed apnoea. PSG included electroencephalogram, electro-oculogram, chin and leg electromyograms, electrocardiogram, airflow, thoracic and abdominal efforts, pulse oximetry and snoring sound (Alice 3 System; Healthdyne Technologies, Altanta, GA). Snoring sound was measured with a microphone placed at the trachea. The snoring events per hour (snoring index) and the percentage of sleep time in which snoring was loud, soft or absent were counted. Results were analysed according to the standards of the American Thoracic Society. OSAS was diagnosed when the sleep disturbance index (SDI) > 5 Tests to assess the site of airway narrowing (including test details): Thorough physical and otolaryngological examinations were performed. The nasopharynx, hypopharynx and larynx were visualised with the use of flexible nasopharyngoscopy with Muller’s manoeuvre performed at the levels of the nasopharynx and the base of the tongue. A lateral cephalogram was undertaken to assess bony and soft tissue measurements for baseline data and inclusion and exclusion purposes and for comparison of changes in the soft palate length and width after treatment. The traditional measurements to evaluate the airway included the angle between the sellar point to nasion line and maxillary point A (SNA) and mandibular point B (SNB), posterior airway space (PAS), distance between the posterior nasal spine and uvula (PNS-P), length between the mandibular plane and the hyoid bone (MP-H), and soft palate width (PW) Inclusion criteria: Patients who had a primary complaint of snoring and with an elongated uvula or thick soft palate Exclusion criteria: OSAS; patients with a primary complaint of apnoeic events; patients with severe nasal obstruction Subgroups: NA |
||
| Participant baseline characteristics | ||
| n | 56 | |
| Age (years), mean ± SD (range) | 48.3 ± 10.2 (28–50) | |
| Male, n (%) | 50 (89.3) | |
| BMI (kg/m2), mean ± SD (range) | 26.5 ± 2.4 (25.2–28.2) | |
| AHI score, mean ± SD | 3.2 ± 1.2 | |
| ESS score, mean ± SD | 8.1 ± 3.5 | |
| Smokers, n (%) | NR | |
| Sleep efficiency (%) | 88.6 ± 8.6 | |
| Nadir SaO2 (%) | 86.4 ± 9.6 | |
| Mean SaO2 (%) | 95.2 ± 1.8 | |
| Snoring index (events/hour) | 245.8 ± 40.8 | |
| Time spent in loud snoring (%) | 10.2 ± 1.5 | |
| Severity of snoring (partner assessed VAS), mean ± SD | 8.2 ± 3.4 | |
| Rapid eye movement (REM) sleep (%) | 14.1 ± 5.2 | |
| Cephalometric data: | ||
| SNA (°) | 80.5 ± 3.4 | |
| SNB (°) | 79.2 ± 2.9 | |
| PAS (mm) | 10.2 ± 2.4 | |
| PNS-P (mm) | 45.7 ± 4.1 | |
| PW (mm) | 10.4 ± 2.1 | |
| MP-H (mm) | 18.5 ± 3.2 | |
| Outcome measures | ||
|
Outcome 1: AHI score. Definition of treatment success: NA Outcome 2: Sleep efficiency (%). Definition of treatment success: NR Outcome 3: Nadir SaO2 (%). Definition of treatment success: NA Outcome 4: Mean SaO2 (%). Definition of treatment success: NR Outcome 5: Snoring index (events/hour). Definition of treatment success: NR Outcome 6: Time spent in loud snoring (%). Definition of treatment success: NR Outcome 7: Severity of snoring assessed by partner using a 10-cm VAS with ‘no snoring’ at the far left and ‘severe snoring’ at the far right. Definition of treatment success: snoring was considered to be cured if the VAS score after treatment was less than half of the baseline score Outcome 8: ESS score. Definition of treatment success: NR Outcome 9: Changes in cephalometric parameters. Definition of treatment success: NR Outcome 10: Mean VAS for pain, swallowing problems and speech problems after uvulopalatal flap procedure (10-cm VAS scale). Definition of treatment success: NR Covariates: Association between snoring measures, the changes in snoring index and changes in partner-reported snoring, and association between changes in percentage of time spent in loud snoring and changes in partner-reported snoring were explored Total length of follow-up: Mean 14.2 (SD 3.2; range 12–20) months Follow-up assessment times: Four (at follow-up at 1, 2 and 4 weeks and after a repeat PSG was completed at a mean of 14.2 months) Rate of attrition at each follow-up time: 0 Methods of statistical analysis: Pre–post data were analysed by Student’s t-test and Pearson’s correlation |
||
| Results | ||
| Outcomes 1–8 | ||
| n (in analysis) | 56 | |
| AHI score, mean ± SD | 3.0 ± 1.8; p = NS | |
| Sleep efficiency (%) | 87.5 ± 10.4; p = NS | |
| Lowest O2 saturation (%) | 88.2 ± 5.5; p = NS | |
| Mean O2 saturation (%) | 96.2 ± 2.1; p = NS | |
| Snoring index (events/hour) | 42.5 ± 20.7; p < 0.05 | |
| Time spent in loud snoring (%) | 3.8 ± 2.8; p < 0.001 | |
| Severity of snoring (partner, VAS), mean ± SDa | 2.6 ± 1.4; p < 0.05 | |
| ESS score, mean ± SD | 5.2 ± 3.2; p < 0.001 | |
| Outcome 9: Postoperative cephalometric parameters | ||
| n (in the analysis) | 56 | |
| SNA (°) | 80.2 ± 4.5; p = NS | |
| SNB (°) | 79.5 ± 3.4; p = NS | |
| PAS (mm) | 10.4 ± 3.2; p = NS | |
| PNS-P (mm) | 42.1 ± 2.8; p < 0.001 | |
| PW (mm) | 8.4 ± 2.4; p < 0.05 | |
| MP-H (mm) | 18.2 ± 4.1; p = NS | |
| Outcome 10: Mean VAS for pain, swallowing problems and speech problems after uvulopalatal flap procedure | ||
| Mean VAS (0 = none, 10 = excruciating or intense pain/extreme difficulty talking/unable to swallow without pain even after analgesic medication) for speech dropped from 2.2 in day 2 to 0.2 in day 10; for swallowing problems dropped from 4.4 in day 1 to 0.5 in day 10; for pain dropped from 6.9 in day 1 to 1.1 in day 10 | ||
|
Correlation: Positive and significant correlation was found between the changes in percentage of time spent in loud snoring and the changes in subjective severity of snoring VAS (r = 0.42; p < 0.05), and between the changes in snoring index and the subjective severity of snoring VAS (r = 0.38; p < 0.05) Postoperative adverse events: Transient nasal regurgitation: 2/56 (4%); foreign body sensation: 1/56 (2%); mild to moderate pain for 5–7 days (VAS ≤ 7): n = 52; bleeding, dysphagia, infection and nasopharyngeal stenosis were not observed Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
||
| Authors’ conclusions | ||
| Uvulopalatal flap decreases subjective and objective results of snoring. It appears to be a safe and effective procedure in carefully selected patients | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | Partial | |
| 3. Are adequate baseline details presented? | Partial | |
| 4. Are any co-interventions clearly stated? | NA | |
| 5. Is compliance with treatment adequate? | Yes | |
| 6. Were any subgroup analyses justified? | NA | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?b | Partial (both subjective and objective outcomes were assessed) | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?c | Partial (both subjective and objective outcomes were assessed) | |
| 9. Were all study participants accounted for? | No | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |
| 11. Are data analyses appropriate? | Yes | |
| 12. Are the conclusions supported by the results? | Yes | |
| 13. Generalisability | Applicable to primary snorers with an elongated uvula or a thick soft palate | |
| 14. Intercentre variability | One-centre study | |
| 15. General comments | – | |
| Ozmen 200689 | |||
|---|---|---|---|
|
Title: QT dispersion in non-apnoeic simple snoring patients and the effect of surgical therapy on QT dispersion Country: Turkey Setting: NR Study design: Pre–post |
|||
| Interventions | |||
|
Intervention: Three different techniques of UP3 were used: UP3 (uvulopalatopharyngoplasty), details NR; LAUP (laser-assisted uvulopalatoplasty), details NR; CAUP (cautery-assisted uvulopalatoplasty), details NR Concurrent treatment: NR Previous treatment(s): NR |
|||
| Participants | |||
|
Total n = 162 (after surgery 9/162 patients had mild or moderate snoring with a snoring assessment table score of 2; the ECG results of these patients were excluded) Number of non-apnoeic snorers included: 162 Tests to exclude OSAS (including test details): PSG in the preoperative first week, performed on each patient for a period of 8 hours at the sleep laboratory (Grass Model 78 polysomnography; Grass Technologies, West Warwick, RI). Patients were not allowed to use any medications in the 48 hours before PSG and to drink tea, coffee or alcohol on the day of testing. PSG was obtained at a paper speed of 10 mm/second and the monitor viewing rate was 30 seconds. 12-lead surface ECG for cardiac evaluation and standard echocardiogram were performed Tests to assess the site of airway narrowing (including test details): Ear, nose and throat examinations were performed as well as computerised tomography of the paranasal sinus if needed Inclusion criteria: Married patients who had simple snoring without apnoea, with a snoring score at or below level 4 on a 6-point scale Exclusion criteria: NR Subgroups: NR |
|||
| Participant baseline characteristics | |||
| n | 162 | ||
| Age (years), mean ± SD (range) | 35.2 ± 14.1 (21–51) | ||
| Male, n (%) | 114 (70) | ||
| BMI (kg/m2), mean ± SD | 28.1 ± 1.2 | ||
| AHI score, mean | < 5 | ||
| ESS score, mean | NR | ||
| Snoring score | ≤ 4 | ||
| Smokers, n (%) | 135 (83) (mean one box of cigarettes/day) | ||
| QTc min (milliseconds), mean ± SD | 381.3 ± 7.8 | ||
| QTc max (milliseconds), mean ± SD | 449.6 ± 6.2 | ||
| QTc dispersion (milliseconds), mean ± SD | 68.2 ± 8.4 | ||
| Outcome measures | |||
|
Outcome 1: Snoring assessed by partner on a 6-point scale (0 = no snoring, 1 = rarely soft snoring, 2 = continuous soft snoring without hypopnoea or apnoea, 3 = moderately loud snoring without hypopnoea or apnoea, 4 = loud snoring without hypopnoea or apnoea, 5 = snoring with hypopnoea or apnoea). Definition of treatment success: postoperative score of 0 or 1 Outcome 2: QTc min (milliseconds). Definition of treatment success: NR Outcome 3: QTc max (milliseconds). Definition of treatment success: NR Outcome 4: QTc dispersion (milliseconds). Definition of treatment success: NR Outcome 5: Surgical procedure success Covariates: NR |
|||
|
Total length of follow-up: 1 month Follow-up assessment times: 1 month Rate of attrition at each follow-up time: 0 Method of statistical analysis: Pre–post scores were compared using Student’s t-test; p-values of < 0.05 were considered significant |
|||
| Results | |||
| Outcome 1: Snoring score (partner) | |||
| n (in analysis) | 162 | ||
| Patients who had mild or moderate snoring after the operation, n (%) | 9 (6), with a snoring assessment score of 2 | ||
| Outcomes 2–4: QTc min, QTc max, QTc dispersion (milliseconds) | |||
| n (in analysis) | 153 | ||
| QTc min (milliseconds), mean ± SD | 397.0 ± 5.9; p < 0.001 | ||
| QTc max (milliseconds), mean ± SD | 440.0 ± 20.8; p < 0.001 | ||
| QTc dispersion (milliseconds), mean ± SD | 43.8 ± 6.2; p < 0.001 | ||
| Outcome 5: Surgical procedure success | |||
| n (in analysis) | 162 | ||
| Patients with surgical procedure success, n (%) | 153 (94) | ||
|
Postoperative adverse events: no complications Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||
| Authors’ conclusions | |||
| QT dispersion is increased in simple snoring patients without apnoea and it decreases after surgical intervention | |||
| Methodological assessment criteria | |||
| 1. Study design | Pre–post | ||
| 2. Were the study eligibility criteria specified? | Partial | ||
| 3. Are adequate baseline details presented? | Partial | ||
| 4. Are any co-interventions clearly stated? | No | ||
| 5. Is compliance with treatment adequate? | Unclear | ||
| 6. Were any subgroup analyses justified? | NA | ||
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial (both objective and subjective outcomes assessed) | ||
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial (both objective and subjective outcomes assessed) | ||
| 9. Were all study participants accounted for? | Yes | ||
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||
| 11. Are data analyses appropriate? | Yes | ||
| 12. Are the conclusions supported by the results? | Yes | ||
| 13. Generalisability | Relatively inclusive criteria | ||
| 14. Intercentre variability | One-centre study | ||
| 15. General comments | – | ||
| Prichard 199549 | |||
|---|---|---|---|
|
Title: Objective measurement of the results of uvulopalatopharyngoplasty Country: UK Setting: Department of Otolaryngology Study design: Pre–post |
|||
| Interventions | |||
|
Intervention (specific details): UP3 as described by Fujita,62 with slight modification to ensure that the initial vertically orientated posterior pharyngeal folds were tightened to just produce slight horizontal ridges. To ensure consistency of technique only two surgeons performed the operations Concurrent treatment (specific details): NR Previous treatment(s) (specific details): NR |
|||
| Participants | |||
|
Total n = 32 If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS (including test details): PSG. Recordings during sleep included electroencepholography (EEG) and electro-oculography (EOG) (for sleep staging), airflow and chest wall motion and O2 saturation. A continuous video recording was made from which the posture was assessed, and sound was recorded by a sound level meter placed 87 (SD 6) cm above the patient’s head. The sound signal was sampled at a frequency of 1 Hz and analysed by computer. Data were analysed for the whole sleep period and separately for the periods spent in the supine and lateral positions. The objective indices of snoring used were the proportion of sleep time during which the level exceeded 50 dBA and the sound level (dBA) above which 1% and 5% of the sound occurred. Tests to assess the site of airway narrowing: NR Inclusion criteria: Snoring subjects Exclusion criteria: AHI > 15 events/hour of sleep time Subgroups: NA |
|||
| Patient baseline characteristics | |||
| n | 32 | ||
| Age (years), mean (SD) | Men 42.5 (10.6), women 39.9 (11.7) | ||
| Duration of snoring (years), mean ± SD (range) | 13.4 ± 7.31 (1–20) | ||
| Male, n (%) | 18 (56) | ||
| BMI (kg/m2), mean (SD) | Men 28.2 (3.06), women 25.2 (3.06) | ||
| AHI score (events/hour), mean (range) | 4.7 (0–15) | ||
| ESS score, mean (range) | NR | ||
| Smokers, n (%) | NR | ||
| Snoring volume outcomes, median | |||
| P50 (% of sleep time that 50 dB exceeded) | |||
| All sleep positions | 1.49 | ||
| Supine position | 1.12 | ||
| Lateral position | 0.4 | ||
| L1 (level above which 1% of sound occurs, dBA) | |||
| All sleep positions | 51.6 | ||
| Supine position | 50.6 | ||
| Lateral position | 45.6 | ||
| L5 (level above which 5% of sound occurs, dBA) | |||
| All sleep positions | 41.0 | ||
| Supine position | 43.6 | ||
| Lateral position | 39.3 | ||
| Snoring severity grade (patient assessed) | |||
| No snoring | 0 | ||
| Mild snoring | 0 | ||
| Moderate snoring | 8 | ||
| Severe snoring | 24 | ||
| Outcome measures | |||
|
Outcome 1: AHI score. Definition of treatment success: NA Outcome 2: P50 snoring volume parameters (all sleep positions, supine position, lateral position). Definition of treatment success: NR Outcome 3: L1 snoring volume parameters (all sleep positions, supine position, lateral position). Definition of treatment success: NR Outcome 4: L5 snoring volume parameters (all sleep positions, supine position, lateral position. Definition of treatment success: NR Outcome 5: Subjective ‘snoring grade’ assessed by the responses ‘nil’, ‘mild’, ‘moderate’ and ‘severe’ and scored from 0 to 3. Definition of treatment success: NR Covariates: Correlations between changes in subjective and objective indices of snoring severity Total length of follow-up: 6 months Follow-up assessment times: 1 Rate of attrition at each follow-up time: 0 Methods of statistical analysis: Mean pre–post scores were analysed using the Wilcoxon signed rank test and Spearman’s correlation coefficient |
|||
| Results | |||
| Outcome 1: AHI score | |||
| Method of measurement: PSG | |||
| n (in analysis) | 32 | ||
| Postoperative AHI score | 6.8; p = NS | ||
| Outcomes 2–4: P50, L5 and L1 snoring volume parameters (all sleep positions, supine position, lateral position) | |||
| n (in analysis) | 32 | ||
| P50 (% of sleep time that 50 dB exceeded), median | |||
| All positions | 0.32; p = 0.04 | ||
| Supine | 0.36; p = 0.01 | ||
| Lateral | 0.17; p = 0.38 | ||
| L1 (level above which 1% of the sound occurs, dBA), median | |||
| All positions | 45.3; p = 0.01 | ||
| Supine | 46.3; p = 0.01 | ||
| Lateral | 42.8; p = 0.21 | ||
| L5 (level above which 5% of the sound occurs, dBA), median | |||
| All positions | 38.8; p = 0.1 | ||
| Supine | 38.8; p = 0.01 | ||
| Lateral | 36.5; p = 0.58 | ||
| Outcome 5: Subjective ‘snoring grade’ | |||
| n (in analysis) | 32 | ||
| No snoring, n | 5 | ||
| Mild, n | 17 | ||
| Moderate, n | 6 | ||
| Severe snoring, n | 4 | ||
| Outcome 6: Correlation between changes in subjective and objective indices of snoring severity (n = 32) | |||
| Change in L1 vs change in ‘snoring grade’ | |||
| All positions | r = 0.47 | p < 0.01 | |
| Supine | r = 0.2 | p = 0.29 | |
| Lateral | r = 0.52 | p < 0.01 | |
|
Postoperative adverse events: NR Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||
| Authors’ conclusions | |||
| There was evidence of both a subjective and objective small benefit of UP3 in the majority of patients; however, it is uncertain whether this improvement is long-lasting | |||
| Methodological assessment criteria | |||
| 1. Study design | Pre–post | ||
| 2. Were the study eligibility criteria specified? | Partial | ||
| 3. Are adequate baseline details presented? | Yes | ||
| 4. Are any co-interventions clearly stated? | NA | ||
| 5. Is compliance with treatment adequate? | Yes | ||
| 6. Were any subgroup analyses justified? | NA | ||
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial (both objective and subjective outcomes assessed) | ||
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial (both objective and subjective outcomes assessed) | ||
| 9. Were all study participants accounted for? | Yes | ||
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||
| 11. Are data analyses appropriate? | Yes | ||
| 12. Are the conclusions supported by the results? | Yes | ||
| 13. Generalisability | Applicable to primary snorers with AHI < 15 | ||
| 14. Intercentre variability | One-centre study | ||
| 15. General comments | – | ||
Pre–post studies of laser-assisted uvulopalatoplasty alone
| Berger 200195 | ||
|---|---|---|
|
Title: Laser-assisted uvulopalatoplasty for snoring: medium- to long-term subjective and objective analysis Country: Israel Setting: Department of Otolaryngology, Head and Neck Surgery Study design: Pre–post |
||
| Interventions | ||
|
Intervention (specific details): LAUP. Two surgical techniques (type 1 and type 2) of LAUP were used, differing with respect to the mode of midline palatal vaporisation. Nine patients underwent type 1 LAUP, in which a focused continuous beam of 15–20 W was used to excise the uvular base through the full palatal depth and then extended bilaterally to the anterior and posterior tonsillar pillars; serial laser tonsillectomy was also performed, carried out in one to two sessions (mean 1.22). Five patients underwent type 2 LAUP, in which through-and-through full-thickness vertical trenches were created on the free edge of the soft palate, on either side of the uvula, at a power setting of 15–20 W. With the use of a SwiftLase scanner attached to the carbon dioxide laser, the core of the uvula was removed from the bottom up in a ‘fishmouth’ manner, while the mucosa of the uvula was preserved. The uvula was shortened and thinned by up to 80–90% of the original size. This was carried out in one to two sessions (mean 1.4) Concurrent treatment: NR Previous treatment(s): NR |
||
| Participants | ||
|
Total n = 14 Tests to exclude OSAS: nocturnal PSG with simultaneous electrocardiography, electromyography and surface-electrode electro-oculography; air flow at the nose and mouth was monitored with thermistors, and respiratory effort was measured with inductive plethysmography; O2 saturation was measured with continuous pulse oximetry. OSA was established with an AHI of > 5 Tests to assess the site of airway narrowing: All patients underwent a complete otolaryngological examination, including flexible fibreoptic nasopharyngoscopic examination of the nose, pharynx and larynx Inclusion criteria: Patients who had bothersome snoring and who completed LAUP treatment Exclusion criteria: NR Subgroups: NA |
||
| Participant baseline characteristics (extract only non-apnoeic snorer subgroup details where applicable) | ||
| n | 14 | |
| Age (years), mean ± SD (range) | 51.2 ± 7.5 (40–66) | |
| Male, n (%) | 10 (71) | |
| BMI (kg/m2), mean ± SD (range) | 26.7 ± 3.7 (21.8–35.4) | |
| AHI score, mean ± SD (range) | 3.4 ± 2.1(0–5.0) | |
| ESS score, mean ± SD | NR | |
| Smokers, n (%) | NR | |
| Lowest O2 saturation (%), mean ± SD (range) | 92.3 ± 5.9 (82–100) | |
| Outcome measures | ||
|
Outcome 1: Snoring state categorised as ‘improved’, ‘no change’ or ‘worse’. Definition of treatment success: NR Outcome 2: Sleep-related symptoms, including (1) night awakening, (2) morning fatigue, (3) daytime somnolence, (4) episodes of sleep apnoea and (5) involuntary body movements during sleep, categorised as ‘improved’, ‘no change’ or ‘worse’. The first three questions were addressed to the patient and the remaining two to the bed partner. Definition of treatment success: NR Outcome 3: AHI score. Definition of treatment success: NA Outcome 4: Lowest O2 saturation (%). Definition of treatment success: NA Covariates: NR Total length of follow-up: 10.1 ± 7.9 months (mean ± SD) (range 3.5–36 months) after completion of the last laser treatment Follow-up assessment times: Twice for subjective analysis [4 weeks and 10.1 ± 7.9 months (mean ± SD) after completion of the last laser treatment] for the state of snoring; once postoperatively for objective analysis Rate of attrition at each follow-up time: 0 Methods of statistical analysis: Pre–post comparisons were analysed with paired t-tests and non-parametric data with the Mann–Whitney test; p-values of < 0.05 were considered significant |
||
| Results | ||
| Outcomes 1 and 2: Snoring state and five sleep-related symptoms | ||
| n (in analysis) | 14 | |
| First follow-up visit, n (%) | ||
| Improved | 11 (79) | |
| No change | 2 (14) | |
| Worsening | 1 (7) | |
| Last follow-up visit, n (%)a | ||
| Improved | 8 (57) | |
| No change | 3 (21) | |
| Worsening | 3 (21) | |
| Five sleep-related symptoms at last follow-up visit, n (%) | ||
| Improved | 8 (57) | |
| No change | 5 (36) | |
| Worsening | 1 (7) | |
| Outcomes 3 and 4: AHI score and lowest O2 saturation (%) | ||
| n (in analysis) | 14 | |
| RDI, mean ± SD (range) | 5.0 ± 4.4 (0–15.0); p = NS | |
| Lowest O2 saturation (%) mean ± SD (range) | 92.9 ± 5.4 (83–100); p = NS | |
|
Postoperative adverse events: No major complications, including postoperative haemorrhage. The most common adverse effect of LAUP was pain: pain duration: 9.7 ± 3.5 days (mean ± SD); pain severe enough to keep patients away from work: 4.5 ± 3.1 days (mean ± SD). Number (%) who complained of persistent throat dryness or itching: 5 (36); number (%) who exhibited difficulty in nasal breathing: 3 (21) (one of whom had a pre-existing nasal obstruction) Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
||
| Authors’ conclusions | ||
| The favourable subjective short-term results of LAUP deteriorated with time. In addition, PSG showed that the procedure caused mild OSAS in a number (3/14) of patients who formerly were non-apnoeic snorers | ||
| Reviewer’s comments | ||
| The number of subjects was too small to draw a firm conclusion | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | No | |
| 3. Are adequate baseline details presented? | Partial | |
| 4. Are any co-interventions clearly stated? | NA | |
| 5. Is compliance with treatment adequate? | Yes | |
| 6. Were any subgroup analyses justified? | NA | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?b | Partial (both subjective and objective outcomes assessed) | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?c | Partial (both subjective and objective outcomes assessed) | |
| 9. Were all study participants accounted for? | Yes | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |
| 11. Are data analyses appropriate? | Yes | |
| 12. Are the conclusions supported by the results? | The number of subjects too small (conclusions consistent with results but should be treated with caution because of small sample size?) | |
| 13. Generalisability | Applicable to non-apnoeic snorers | |
| 14. Intercentre variability | One-centre study | |
| 15. General comments | The number of subjects was too small to draw a firm conclusion | |
| Lauretano 199796 | ||
|---|---|---|
|
Title: Efficacy of laser-assisted uvulopalatoplasty Country: USA Setting: Private surgical group (outpatient setting) Study design: Pre–post |
||
| Interventions | ||
|
Intervention (specific details): LAUP, performed in an outpatient setting under local anaesthesia. A handheld CO2 laser was used to resect a wedge or crescent of soft palate on each side of the uvula and then to ablate the uvula itself. Laser settings 14–18 W, using the Sharplan Swiftlase™ system. Silver nitrate was applied in some cases for additional haemostasis. The palate was allowed to heal by secondary intention, and the next LAUP session was performed 4–6 weeks later. Typically LAUP was performed over several sessions, with the endpoint being the patient’s report of cessation of snoring or the patient’s inability to create a palatal ‘snort’ on office exam. Mean (SD) number of sessions 2.5 ± 0.67 Concurrent treatment (specific details): NR Previous treatment(s) (specific details): Surgical methods appear to have been offered after standard non-surgical methods (CPAP) and weight loss failed |
||
| Participants | ||
|
Total n = 90 non-apnoeic snorers and patients with OSAS were recruited (non-apnoeic snorers = 32). Of the 90 recruited, 52 completed LAUP, of whom 12 were non-apnoeic snorers. Patients were placed into the non-apnoeic snorers group based on a RDI ≤ 10 If this study includes a mixed patient population, number of non-apnoeic snorers included: 32 Tests to exclude OSAS (including test details): PSG, hospital-based, overnight studies conducted in and analysed by one of the sleep laboratories. Each patient’s sleep was analysed for the following variables: total apnoeas, total hypopnoeas, AI, HI, RDI, mean O2 desaturation, lowest O2 desaturation, mean duration of apnoea and longest duration of apnoea Tests to assess the site of airway narrowing (including test details): Otolaryngological evaluation (no details reported) Inclusion criteria: Snoring patients who underwent complete PSG and otolaryngological examination and who failed on standard non-surgical methods (not clearly presented) Exclusion criteria: NR Subgroups, based on RDI: Non-apnoeic snorers = 32; mild OSA = 20; moderate OSA = 16; severe OSA = 22 |
||
| Participant baseline characteristics (extract only non-apnoeic snorer subgroup details where applicable) | ||
| n | 32 snorers | |
| Age (years), mean ± SD (range) | 47.13 ± 11.11 (19–83) | |
| Male, n (%) | 25 (78) | |
| BMI (kg/m2), mean ± SD (range) | 28.08 ± 3.44 (22.4–35.4) | |
| AI, mean ± SD (range) | 0.83 ± 1.53 (0–6.4) | |
| HI, mean ± SD (range) | 3.33 ± 2.93 (0–19.2) | |
| AHI score, mean ± SD (range) | 4.22 ± 3.24 (0–12.97) | |
| ESS score, mean ± SD (range) | NR | |
| Smokers, n (%) | NR | |
| Mean O2 desaturation (%), mean ± SD (range) | 94.4 ± 1.95 (91–98.5) | |
| Lowest O2 desaturation (%), mean ± SD (range) | 89.68 ± 4.79 (83–95.9) | |
| Average duration of apnoeas (seconds), mean ± SD (range) | 9.10 ± 8.98 (0–25.8) | |
| Longest duration of apnoea (seconds), mean ± SD (range) | 13.42 ± 19.3 (0–85.2) | |
| Outcome measures | ||
|
Outcome 1: AI. Definition of treatment success: NR Outcome 2: HI. Definition of treatment success: NR Outcome 3: AHI score. Definition of treatment success: NR Outcome 4: Mean O2 desaturation (%). Definition of treatment success: NR Outcome 5: Lowest O2 desaturation (%). Definition of treatment success: NR Outcome 6: Patient’s snoring status assessed on a 7-point scale: 1 = much worse, 4 = no change, 7 = much improved. Definition of treatment success: NR Outcome 7: Patient satisfaction with LAUP assessed on a 7-point scale: 1 = very dissatisfied, 4 = neutral, 7 = very satisfied. Definition of treatment success: NR Covariates: NR Total length of follow-up: 2 months after completion of last LAUP session for follow-up examination Follow-up assessment times: A follow-up examination and a postoperative questionnaire Rate of attrition at each follow-up time: 0 Methods of statistical analysis: Mean change from pre to post; methods not reported |
||
| Results | ||
| Outcomes 1–5: PSG parameters | ||
| n (in analysis) | 3 | |
| AI | 1.00; p = NS | |
| HI | 8.30; p = NS | |
| AHI score | 9.30; p = NS | |
| Mean O2 desaturation (%) | 94.9; p = NS | |
| Lowest O2 desaturation (%) | 90.3; p = NS | |
| Outcome 6: Patient’s snoring status | ||
| n (in analysis) | 12 | |
| Improved, n (%) | 9 (75) | |
| No change, n (%) | 2 (17) | |
| Worse, n (%) | 1 (8) | |
| Outcome 7: Patient satisfaction with LAUP | ||
| n (in analysis) | 12 | |
| Satisfied, n (%) | 10 (83) | |
| Neutral, n (%) | 0 | |
| Dissatisfied, n (%) | 2 (17) | |
|
Postoperative adverse events: NR Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
||
| Authors’ conclusions | ||
| LAUP may be a reasonable treatment for patients with non-apnoeic snoring | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | Partial | |
| 3. Are adequate baseline details presented? | Partial | |
| 4. Are any co-interventions clearly stated? | NA | |
| 5. Is compliance with treatment adequate? | Yes | |
| 6. Were any subgroup analyses justified? | Yes | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial (both objective and subjective outcomes assessed) | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial (both objective and subjective outcomes assessed) | |
| 9. Were all study participants accounted for? | No (only n = 3 and n = 12 for objective and subjective outcomes respectively) | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | No (only 9% and 37.5% for objective and subjective outcomes respectively) | |
| 11. Are data analyses appropriate? | Unclear (not reported) | |
| 12. Are the conclusions supported by the results? | No (only based on n = 3) | |
| 13. Generalisability | OSAS and non-apnoeic snorers who failed on standard non-surgical methods | |
| 14. Intercentre variability | Unclear | |
| 15. General comments | – | |
| Neruntarat 2005114 | ||
|---|---|---|
|
Title: Laser-assisted outpatient septoplasty and laser-assisted uvulopalatoplasty for nasal obstruction and snoring Country: Thailand Setting: Department of Otolaryngology Study design: Pre–post |
||
| Interventions | ||
|
Intervention (specific details): Laser-assisted outpatient septoplasty (LAOS) performed in conjunction with LAUP; 14 (40%) patients additionally underwent laser turbinectomy. LAOS was performed with a CO2 laser (as originally performed by Kamami63) using the modification in which the procedure is performed by using a CO2 coupler (Sharplan Laser, Allendale, NJ) under local anaesthesia. Nasal mucosa were anaesthetised by insertion of a small piece of gauze containing 5% lidocaine with adrenaline into the nasal cavity. The surface of the deviated nasal septum was vaporised in an anterior-to-posterior direction within 2–3 mm of vertical height on its medial convex side using a power setting of 10 W; 14 (40%) patients also underwent laser turbinectomy in which two-thirds of the anterior end of the hypertrophic turbinate was vaporised. No nasal packing was required. Mean additional surgical time needed to perform the procedure = 10.4 (SD 3.4) minutes (range 10–15 minutes). LAUP was performed with a CO2 laser at 15–20 W. Vertical transpalatal incisions were made bilaterally through the soft palate lateral to the base of the uvula. This was followed by partial vaporisation of one-half to one-third of the uvula Concurrent treatment (specific details): Postoperative medication included an antibiotic and acetaminophen with codeine as needed for pain relief Previous treatment(s) (specific details): NR |
||
| Participants | ||
|
Total n = 35 Tests to exclude OSAS (including test details): PSG; RDI > 5 was diagnosed as OSA Tests to assess the site of airway narrowing (including test details): The nose, nasopharynx, hypopharynx and larynx were visualised with the use of a flexible endoscope, with Muller’s manoeuvre performed at the level of the nasopharynx and the base of tongue. A radiological sinus and cephalogram were taken routinely. Rhinomanometry was performed with Rhinoscreen (Erich Jaeger GmbH, Wuerzburg, Germany) with a total resistance at 150 Pa used for comparison Inclusion criteria: Patients with socially disruptive snoring with nasal obstruction who failed to respond to conservative treatments; occlusion by septal deviations less than two-thirds of the nasal lumen (mild to moderate degree); patients with an elongated uvula and thick soft palate were included for the treatment Exclusion criteria: OSAS (defined as patients who experienced daytime sleepiness or disturbed sleep and who had > five respiratory disturbances per hour of sleep); patients with a primary complaint of daytime sleepiness and or apnoeic events and patients with severe septal deviation (greater than two-thirds of the lumen) and evident maxillofacial abnormalities were excluded Subgroups: NA |
||
| Participant baseline characteristics | ||
| n | 35 | |
| Age (years), mean ± SD (range) | 35.2 ± 16.4 (22–54) | |
| Male, n (%) | 32 (91) | |
| BMI (kg/m2), mean ± SD (range) | 26.2 ± 4.2 (20.5–28.2) | |
| AHI score, mean | < 5; detailed score NR | |
| ESS score, mean (range) | NR | |
| Smokers, n (%) | NR | |
| Severity of snoring (partner, VAS), mean ± SD | 8.8 ± 2.2 | |
| Nasal obstruction VAS score, mean ± SD | 6.2 ± 3.2 | |
| Nasal resistance (Pa/ml/cm2), mean ± SD | 0.39 ± 0.8 | |
| Rhinorrhea (VAS), mean ± SD | 5.8 ± 1.4 | |
| Pruritis (VAS), mean ± SD | 6.1 ± 2.2 | |
| Sneezing (VAS), mean ± SD | 7.1 ± 2.3 | |
| Outcome measures | ||
|
Outcome 1: Severity of snoring assessed by partner on a 10-cm VAS in which ‘no snoring’ occupied the far left scale position and ‘severe snoring’ occupied the far right scale position. Definition of treatment success: snoring was considered to be cured by the bed partner or observer if the VAS score was less than half that at baseline Outcome 2: Nasal obstruction measured on a continuous VAS scale from 0 (none) to 10 (complete nasal obstruction). Definition of treatment success: NR Outcome 3: Nasal resistance measured by rhinomanometry. Definition of treatment success: NR Outcome 4: Postoperative pain measured on a continuous scale from 0 (none) to 10 (excruciating or intense pain) once daily for 10 days postoperatively. Definition of treatment success: NR Outcome 5: Rhinorrhea measured on a continuous scale from 0 (none) to 10 (severe/bothersome). Definition of treatment success: NR Outcome 6: Pruritus measured on a continuous scale from 0 (none) to 10 (very annoying). Definition of treatment success: NR Outcome 7: Sneezing measured on a continuous scale from 0 (none) to 10 (excruciating). Definition of treatment success: NR Covariates: the correlation between nasal obstruction measures following the LAOS procedure, the changes in total nasal resistance and the changes in subjective nasal obstruction Total length of follow-up: mean = 5.2 (SD 2.3) months (range 4–6 months) Follow-up assessment times: After the operation, every week in the first month and then every month for 4–6 months Rate of attrition at each follow-up time: 0 Methods of statistical analysis: Pre–post data compared using Student’s paired t-test; the correlation between nasal obstruction measures was analysed by Pearson’s correlation; p-values < 0.05 were considered to be significant |
||
| Results | ||
| Outcomes 1–3: Severity of snoring, nasal obstruction and nasal resistance | ||
| n (in analysis) | 35 | |
| Snoring severity VAS score, mean ± SD | 2.8 ± 1.7; p < 0.05 | |
| Nasal obstruction VAS score, mean ± SD | 1.6 ± 0.8; p < 0.01 | |
| Nasal resistance (Pa/ml/cm2), mean ± SD | 0.28 ± 0.5; p < 0.05 | |
| Patients with snoring cured, n (%) | 32 (91) | |
| Outcome 4: Postoperative pain | ||
| n (in analysis) | 35 | |
| Pain (VAS) | Minimal, ≤ 4 | |
| Outcomes 5–7: Nasal symptoms associated with nasal obstruction: rhinorrhea, pruritus and sneezing | ||
| n (in analysis) | 35a | |
| Rhinorrhea (VAS), mean ± SD | 2.1 ± 1.8 | |
| Nasal pruritus (VAS), mean ± SD | 2.3 ± 0.9 | |
| Sneezing (VAS), mean ± SD | 2.5 ± 1.7 | |
| The correlation between nasal obstruction measures following the LAOS procedure, the changes in total nasal resistance and the changes in subjective nasal obstruction was not statistically significant (p = 0.45; Pearson’s correlation) | ||
|
Postoperative adverse events: All patients tolerated the procedure well. One patient had pain during the LAOS procedure. There were two cases of minor bleeding, which was controlled with suction electrocautery. Nasal cavity oedema and crusting were observed at postoperative day 3 and week 1. There were no synechiae, no septal perforations and no emergent airway complications Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
||
| Author’s conclusions | ||
| LAOS is a simple and well-tolerated treatment for deviated nasal septum. It appears to be a safe and effective adjunct surgical procedure for snorers with nasal obstruction on an outpatient basis | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | Yes | |
| 3. Are adequate baseline details presented? | Partial | |
| 4. Are any co-interventions clearly stated? | Yes | |
| 5. Is compliance with treatment adequate? | Yes | |
| 6. Were any subgroup analyses justified? | NA | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?b | Partial (both objective and subjective outcomes assessed) | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?c | Partial (both objective and subjective outcomes assessed) | |
| 9. Were all study participants accounted for? | Yes | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |
| 11. Are data analyses appropriate? | Yes | |
| 12. Are the conclusions supported by the results? | Yes | |
| 13. Generalisability | Relatively inclusive eligibility criteria | |
| 14. Intercentre variability | One-centre study | |
| 15. General comments | – | |
Studies of radiofrequency ablation of the soft palate and tongue base
| Back 2002108 | ||||||
|---|---|---|---|---|---|---|
|
Title: Bipolar radiofrequency thermal ablation of the soft palate in habitual snorers without significant desaturations assessed by magnetic resonance imaging Country: Finland Setting: Departments of Otorhinolaryngology, Head and Neck Surgery Study design: Pre–post |
||||||
| Interventions | ||||||
|
Intervention: Bipolar radiofrequency thermal ablation (bRFTA) delivered as an outpatient procedure. The ENTec Coblator Plasma Surgery System with the ReFlex 55 wand (Arthrocare, Sunnyvale, CA) was used. The bipolar electrode was inserted into the mucosa in the midline of the soft palate, 1 cm below the junction of the hard and soft palate, and two additional entries were made laterally on both sides. A power level of 6 (216–234 voltage root-mean-square value) keeping the wand in position for 15 seconds was used. Patients were treated in two treatment sessions separated by 1 week Concurrent treatment: NR Previous treatment(s): Patients had not undergone any previous palatal surgery |
||||||
| Participants | ||||||
|
Total n = 20 (n = 18 or n = 19 in the analysis) If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS: PSG (no details reported) Tests to assess the site of airway narrowing: Clinical examination, cephalometric radiographs and fibreoptic nasopharyngoscopy with Muller’s manoeuvre. Magnetic resonance imaging (MRI) was also undertaken to assess palatal measurements before and after surgery Inclusion criteria: ODI 4% < 5; ODI 10% < 1; maximum O2 desaturation decrease of 85% Exclusion criteria: Patients with micrognathia; obstruction of the posterior airspace of the hypopharynx; BMI > 35 kg/m2; patients with coagulation, psychiatric/neurological disorders or implanted pacemakers; previous palatal surgery, speech or swallowing disorders, or ‘too sensitive throats’ Subgroups: NA |
||||||
| Patient baseline characteristics | ||||||
| n | 20 | |||||
| Age (years), median (range) | 43 (35–63) | |||||
| Male, n (%) | 19 (95) | |||||
| BMI (kg/m2), median (range) | 25.7 (22.6–34.6) | |||||
| AHI score, mean | < 5 | |||||
| ESS score, mean (95% CI) | 4.5 (1.0–16.7) | |||||
| Snoring score (patient, VAS), median (95% CI) | 9.0 (5–10) | |||||
| Snoring score (partner, VAS), median (95% CI) | 6.5 (5–8) | |||||
| MRI measurements, median (95% CI) | ||||||
| Length of the soft palate (mm) | 42 (39–44) | |||||
| Corrected length of the soft palate (mm) | 44 (41–46) | |||||
| Palatal width at 1 cm (mm) | 11 (10–11) | |||||
| Palatal width at the thickest part (mm) | 11 (11–12) | |||||
| Distance, tip of uvula to bottom of sella (mm) | 57.5 (54–59) | |||||
| Postuvular space (mucosa) (mm) | 5 (4–6) | |||||
| Postuvular space (CI–CII) (mm) | 14 (11–16) | |||||
| Area of the soft palate (cm2) | 12.4 (11.4–13.5) | |||||
| Outcome measures | ||||||
|
Outcome 1: ESS score (slightly modified Finnish version). Definition of treatment success: NR Outcome 2: Snoring scale score (answered by the patient; 0 = no snoring, 10 = heavy snoring, the partner leaves the room). Definition of treatment success: a reduction from at least 7 to 0–3 points on the VAS scale; additionally, an improvement of 3 points was considered significant; treatment relapse was defined as a change of more than 2 points in the scores between 3 and 9.5 (9–11.5) months after treatment Outcome 3: Snoring scale score (partner reported). Definition of treatment success: a reduction from at least 6 to 0–3 points; an improvement of 3 points was considered significant; treatment relapse was defined as a change of more than 2 points in the scores between 3 and 9.5 (9–11.5) months after treatment Outcome 4: Percentage of patients with successful outcome, significant improvement or relapse on the snoring scale score (patient reported). Definition of treatment success: a reduction from at least 7 to 0–3 points on the VAS scale; additionally, an improvement of 3 points was considered significant; treatment relapse was defined as a change of more than 2 points in the scores between 3 and 9.5 (9–11.5) months after treatment Outcome 5: Percentage of patients with successful outcome, significant improvement or relapse on the snoring scale score (partner reported). Definition of treatment success: a reduction from at least 6 to 0–3 points on the VAS scale; additionally, an improvement of 3 points was considered significant; treatment relapse was defined as a change of more than 2 points in the scores between 3 and 9.5 (9–11.5) months after treatment Outcome 6: MRI oropharyngeal dimension measurements (at 3-month follow-up). Definition of treatment success: NR Outcome 7: Postoperative pain, swelling sensation, speech problems and eating difficulties assessed on a 100-point VAS in which 0 = no difficulties and 100 = worst difficulties. Definition of treatment success: NR Covariates: linear regression analysis used to assess relationship between MRI dimension measurements and dependent snoring scale scores Total length of follow-up: median = 9.5 months (range 9–11.5 months) Follow-up assessment times: 3 months (MRI and subjective outcomes) and 9.5 months (range 9–11.5 months) (subjective outcomes only) Rate of attrition at each follow-up time: n = 1 [ESS score and snoring scale (patient assessed)]; n = 2 [snoring scale (partner assessed)] Methods of statistical analysis: Mean change (pre–post) assessed using the paired Wilcoxon signed rank test and analysis of variance (ANOVA); non-parametric Spearman’s correlation coefficients were used; linear regression analyses were used to study relationships between dependent and independent variables |
||||||
| Results | ||||||
| Outcomes 1 and 2: ESS score and snoring scale score (patient reported) | ||||||
| 3 months | 9.5 months | |||||
| n (in analysis) | 19 | 19 | ||||
| ESS score, median (95% CI) | 2.0 (0–8); p < 0.05 | 3.5 (0–8); p < 0.05 | ||||
| Snoring scale score (patient reported), median (95% CI) | 4.0 (2–7); p < 0.05 | 5.0 (2–10); p < 0.05 | ||||
| Outcome 3: Snoring scale score (partner reported) | ||||||
| 3 months | 9.5 months | |||||
| n (in analysis) | 18 | 18 | ||||
| Snoring scale score, median (95% CI) | 4.0 (1–8); p < 0.05 | 5.0 (1–7); p < 0.05 | ||||
| Outcome 4: Percentage of patients with successful outcome, significant improvement or relapse on snoring scale score (patient reported)a | ||||||
| 3 months | 9.5 months | |||||
| n (in analysis) | 19 | 19 | ||||
| Significant improvement, n (%) | 11 (58) | 12 (63) | ||||
| Successful outcome, n (%) | 6 (32) | 7 (37) | ||||
| Relapse, n (%) | – | 4 (21) | ||||
| Outcome 5: Percentage of patients with successful outcome, significant improvement or relapse on snoring scale score (partner reported)a | ||||||
| 3 months | 9.5 months | |||||
| n (in analysis) | 18 | 18 | ||||
| Significant improvement, n (%) | 7 (39) | 6 (33) | ||||
| Successful outcome, n (%) | 6 (33) | 5 (28) | ||||
| Relapse, n (%) | – | 1 (6) | ||||
| Outcome 6: MRI oropharyngeal dimension measurements (3-month follow-up)b | ||||||
| n (in analysis) | 20 | |||||
| Length of the soft palate (mm), median (95% CI) | 42 (38–44); p = 0.849 | |||||
| Corrected length of the soft palate (mm), median (95% CI) | 44 (42–47); p = 0.983 | |||||
| Palatal width at 1 cm (mm), median (95% CI) | 10.5 (10–11); p = 0.431 | |||||
| Palatal width at the thickest part (mm), median (95% CI) | 11 (11–12); p = 0.470 | |||||
| Distance, tip of uvula to bottom of sella (mm), median (95% CI) | 55.5 (51–57); p = 0.005 | |||||
| Postuvular space (mucosa) (mm), median (95% CI) | 5 (4–6); p = 0.327 | |||||
| Postuvular space (CI–CII) (mm), median (95% CI) | 13 (11–14); p = 0.259 | |||||
| Area of the soft palate (cm2), median (95% CI) | 12.55 (11.7–13.8); p = 0.420 | |||||
| T1 signal intensity: | ||||||
| Major changes, n | 9 | |||||
| Moderate changes, n | 4 | |||||
| No/mild changes, n | 6 | |||||
| Outcome 7: Postoperative pain, swelling sensation, speech problems and eating difficulties | ||||||
| Day 1 | Day 7 | Day 11 (second procedure) | Day 17 | |||
| n (in analysis) | NR | NR | NR | NR | ||
| Pain, median (95% CI) | 46 (13–92) | 2 (0–43) | 49 (11.5–98) | 3 (0–28) | ||
| Swelling sensation, median (95% CI) | 56 (9–100) | 4 (0–44.5) | 51 (16–81) | 3 (0–13) | ||
| Speaking, median (95% CI) | 58 (13–85) | 2 (0–31.5) | 46 (17.5–80) | 2 (0–5) | ||
| Eating, median (95% CI) | 56 (9–100) | 3 (0–44.5) | 50 (16–81) | 2 (0–13) | ||
|
Postoperative adverse events: n = 1 received corticosteroids for the postoperative swelling; n = 4 received antibiotics for abscess caused by the insertion pointer; n = 6 developed 5-mm mucosal blanching; n = 2 developed 10-mm mucosal blanching. The median dose of medication for pain = two during the 2-week operative period. At the 3-month follow-up there were no mucosal blanching signs; n = 4 complained of a swelling sensation in the throat. At the 9.5-month follow-up n = 2 complained of a swelling sensation in the throat Need for repeat procedure (unscheduled): NR |
||||||
| Authors’ conclusions | ||||||
| bRFTA of the soft palate on an outpatient basis in patients with sleep-disordered breathing seems to be an effective treatment for habitual snoring in patients without significant desaturations associated with excessive daytime sleepiness. MRI showed that the procedure was associated with changes in the dimensions of the soft palate and in the T1 signal intensity. The advantageous outcome in the questionnaires showed no association with the results of the MRI analyses | ||||||
| Methodological assessment criteria | ||||||
| 1. Study design | Pre–post study | |||||
| 2. Were the study eligibility criteria specified? | Yes | |||||
| 3. Are adequate baseline details presented? | Partial | |||||
| 4. Are outcome assessors blinded? | Partial (MRI radiologists blinded to intervention) | |||||
| 5. Is compliance with treatment adequate? | Yes | |||||
| 6. Were data collection tools shown or known to be valid for the outcome of interest?c | Partial (mixture of objective and subjective outcome measures) | |||||
| 7. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?d | Partial (mixture of objective and subjective outcome measures) | |||||
| 8. Were all study participants accounted for? | No | |||||
| 9. Are data analyses appropriate? | Partial (no adjustment made for multiple testing) | |||||
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |||||
| 11. Are the conclusions supported by the results? | Partial (only one change in soft palate dimension and snoring/daytime sleepiness outcomes only assessed objectively) | |||||
| 12. Generalisability | The patient group appears to be representative of those undergoing radiofrequency tissue volume reduction (RFTVR) for primary snoring | |||||
| 13. Intercentre variability | One-centre study | |||||
| Boudewyns 2000106 | ||
|---|---|---|
|
Title: Temperature-controlled radiofrequency tissue volume reduction of the soft palate (Somnoplasty®) in the treatment of habitual snoring: results of a European multicentre trial Country: European multicentre (Belgium, France, Spain, Germany, Netherlands, Sweden) Setting: Departments of Otorhinolaryngology, Head and Neck Surgery Study design: Pre–post |
||
| Interventions | ||
|
Intervention: Temperature-controlled radiofrequency tissue volume reduction of the soft palate (Somnoplasty®) performed on an outpatient basis under local anaesthesia. The needle was inserted in the midline of the soft palate and a mean of 692.3 ± 67.7 J delivered per treatment session. For these 45 patients a single midline lesion was utilised with a maximum of three treatment sessions. The first lesion was created about 1 cm above the caudal margin of the soft palate. Subsequent lesions were created in a caudal direction (at about one-third and two-thirds of the length of the uvula). Patients underwent one to a maximum of three treatment sessions, depending on the obtained improvement in snoring, separated by a treatment interval of 4–6 weeks: one treatment, n = 2; two treatments, n = 9; three treatments, n = 34 Concurrent treatment: NR Previous treatment(s): NR |
||
| Participants | ||
|
Total n = 45 (a single midline lesion was utilised with a maximum of three treatment sessions) If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS: Full-night PSG was performed before the first session Tests to assess the site of airway narrowing: NR Inclusion criteria: Patients seeking treatment for socially disturbing snoring with a RDI < 15 as documented by full-night PSG and a BMI < 30 kg/m2 Exclusion criteria: NR (for the purposes of analysis, patients were excluded if they underwent more than one lesion per treatment session, more than three treatment sessions, or lesions in areas of the palate other than the midline) Subgroups: NA |
||
| Patient baseline characteristics | ||
| n | 44 | |
| Age (years), mean ± SD | 43.7 ± 10.9 | |
| Male (%) | 86.4 | |
| BMI (kg/m2), mean ± SD | 26.6 ± 3.2 | |
| AHI score, mean ± SD | 5.1 ± 4.3 | |
| Lowest O2 saturation level, mean ± SD | 87.0 ± 5.4 | |
| ESS score, mean ± SD | 8.0 ± 5.0 | |
| Smokers, n (%) | NR | |
| Snoring index (VAS), mean ± SD | 7.6 ± 2.1 | |
| Outcome measures | ||
|
Outcome 1: Snoring index assessed using a VAS ranging from 0 ‘no snoring’ to 10 ‘very intense snoring causing the bed partner to leave the room’. Definition of treatment success: difference of 3 points on snoring index considered to be a significant improvement; snoring index of 3 or less points considered to be a treatment success Outcome 2: Treatment success. Definition of treatment success: a significant improvement in snoring: a difference of at least 3 points on snoring index; snoring must be reduced to a level that is no longer considered bothersome, i.e. a snoring index of 3 or less Outcome 3: ESS score of daytime sleepiness. Definition of treatment success: NA Outcome 4: AHI score. Definition of treatment success: NA Outcome 5: Lowest O2 saturation level. Definition of treatment success: NA Outcome 6: Pain score VAS (no details reported on the scale). Definition of treatment success: NA Covariates: correlation between the improvement in snoring index and the decrease in daytime sleepiness was explored Total length of follow-up: 20 weeks |
||
|
Follow-up assessment times: For pain score days 1–3, weeks 1–2 and week 4 after the treatment; for PSG about 8 weeks after the last treatment session Rate of attrition at each follow-up time: 1/45 Methods of statistical analysis: Student’s t-test used to assess changes in pre–post means; ordinal data (snoring index and ESS score ) were analysed using the Wilcoxon paired sample test; statistical significance was accepted at p < 0.05 |
||
| Results | ||
| Outcome 1: Snoring index | ||
| n (in analysis) | 44 | |
| Snoring index (VAS), mean ± SD | Postoperative: 4.0; difference preoperative vs postoperative: 3.6 ± 2.1; p < 0.001 | |
| Outcomes 2 and 3: Treatment success and ESS score | ||
| n (in analysis) | 44 | |
| Patients with successful treatment, n (%) | 20 (44.4) | |
| Patients with significant improvement, n (%) | 38 (84.4) | |
| ESS score of daytime sleepiness, mean ± SD | 6.0 ± 4.3; p = 0.001 | |
| Outcomes 4 and 5: AHI score and lowest O2 saturation level | ||
| n (in analysis) | 37 | |
| AHI score, mean ± SD | 5.4 ± 7.4; p = NS | |
| ODI (%), mean ± SD | 84.9 ± 14.6; p = NS | |
| Outcome 6: Pain score VAS (questionnaires were completed before the first procedure, at each interim visit and 8 weeks after the last procedure) | ||
| n (in analysis) | 44 | |
| Postoperative pain score VAS, mean ± SD | ||
| Days 1–3 | 1.0 ± 1.4 | |
| Weeks 1–2 | 0.4 ± 1.0 | |
| Week 4 | 0.1 ± 0.5 | |
|
Pain relief medication: 29/44 patients required non-narcotic analgesics, 1/44 patients required a narcotic analgesic and 8/44 patients received steroids for post-treatment pain/oedema Postoperative adverse events [number of events (incidence rate)]: Mucosal erosion: 19 (15.6%); palatal fistula: 1 (0.8%); uvula loss: 1 (0.8%); excessive swelling: 1 (0.8%); haemorrhage: 2 (1.6%) Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
||
| Authors’ conclusions | ||
| Temperature-controlled radiofrequency tissue volume reduction of the soft palate (Somnoplasty®) is a minimally invasive surgical procedure for snoring | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | Yes | |
| 3. Are adequate baseline details presented? | Partial | |
| 4. Are any co-interventions clearly stated? | NA | |
| 5. Is compliance with treatment adequate? | Yes | |
| 6. Were any subgroup analyses justified? | NA | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial (both objective and subjective outcomes assessed) | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial (both objective and subjective outcomes assessed) | |
| 9. Were all study participants accounted for? | No | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |
| 11. Are data analyses appropriate? | Yes | |
| 12. Are the conclusions supported by the results? | Yes | |
| 13. Generalisability | Relatively inclusive eligibility criteria | |
| 14. Intercentre variability | Not assessed | |
| 15. General comments | – | |
| Cartwright 2000104 | |||||
|---|---|---|---|---|---|
|
Title: Treatments for snoring: a comparison of somnoplasty and an oral appliance Country: USA Setting: Sleep Disorder Service and the Department of Otolaryngology and Bronchoesophagology Study design: Two-group parallel pre–post with between-group comparisons |
|||||
| Interventions | |||||
|
Intervention 1: Radiofrequency ablation (RFA) (somnoplasty) to reduce the tissue of the soft palate. The soft palate and uvula were first sprayed with a topical anaesthesia. Low-power radiofrequency energy was applied by a needle electrode to the soft tissue at the midline followed by two lateral injections at half of the energy level. The mean energy delivered was not reported. The entire procedure took approximately 20 minutes to complete. At the 8-week visit the snoring level was assessed by the partner and a second treatment was conducted if necessary; n = 5 underwent one procedure and n = 5 underwent two procedures Intervention 2: Snore X oral appliance (Snorex, Fremont, CA), a simple oral appliance of the tongue-retaining type worn for 2 weeks at home Concurrent treatment (specific details): NR Previous treatment(s) (specific details): Patients had not undergone previous pharyngeal surgery |
|||||
| Participants | |||||
|
Total n = 20 If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS: PSG using standard 12-channel recording. No further test details reported Tests to assess the site of airway narrowing: All patients were examined by an otolaryngologist Inclusion criteria: Age > 18 years; seeking treatment for the control of snoring; anaesthesia risk class I or II; not pregnant; RDI < 15; no other sleep disorder diagnosis Exclusion criteria: Anaesthesia risk class III or IV; RDI > 15 with the lowest O2 saturation < 80%; the presence of unstable psychiatric disorders, neurological disorders or swallowing disorders; previous pharyngeal surgery, upper respiratory tract cancer or radiation to upper airway tract; active upper respiratory tract infection; BMI > 32 kg/m2 Subgroups: NA |
|||||
| Patient baseline characteristics | |||||
| RFA | Oral appliance | Difference | |||
| n | 10 | 10 | |||
| Age (years), mean ± SD | 52.2 ± 10.18 | 53.1 ± 11.61 | NS | ||
| Male, n (%) | NR | NR | |||
| BMI (kg/m2), mean ± SD | 28.20 ± 2.93 | 30.20 ± 6.30 | NS | ||
| AHI score, mean ± SD | All 10 patients: 5.91 ± 4.31; 5 patients with one treatment: 7.0 ± 5.8; 5 patients with two treatments: 4.8 ± 1.9 | 4.87 ± 3.97 | NS | ||
| Lowest O2 saturation (%), mean ± SD | 89.30 ± 4.11 | 87.40 ± 5.66 | NS | ||
| ESS score, mean ± SD | All 10 patients: NR; 5 patients with one treatment: 13.4 ± 4.7; 5 patients with two treatments: 6.6 ± 2.2 | NR | NR | ||
| Smokers, n (%) | NR | NR | NR | ||
| Snoring loudness (partner, VAS), mean ± SD | 6.4 ± 2.7 and 8.2 ± 1.7 for the 5 patients with one treatment and the 5 patients with two treatments respectively. All 10 patients: 7.5 ± 2.50 | NR | NR | ||
| Outcome measures | |||||
|
Outcome 1: Snoring loudness assessed by partner using a 10-point VAS with a score of 10 representing the loudest snoring. Definition of treatment success: treatment successful if a score of 3 or lower at the 8-week visit Outcome 2: The MESAM recording device was used for both groups at the second sleep study to count the number of minutes of sleep during which snoring was loud, soft or absent. RFA group pre–post results. Definition of treatment success: NR Outcome 3: RDI. Other outcome measures: NA Outcome 4: ESS completed in the RFA group before and after the completion of the 8-week follow-up period. Definition of treatment success: NA Outcome 5: Percentage of sleep time with loud snoring in the RFA and Snore X groups. Definition of treatment success: NA Covariates: The relationship between the two snoring measures following treatment – the objective laboratory count and the partner’s home report – was explored Total length of follow-up: 8.9 months (range 6–12 months) Follow-up assessment times: RFA group: 3 days, 4 weeks and 8 weeks after treatment (i.e. patients who received two procedures were followed up at 16 weeks); Snore X group: 2 weeks Rate of attrition at each follow-up time: 0 Methods of statistical analysis: Student’s t-test used to assess pre–post differences in snoring loudness (VAS); t-test used to assess differences in the percentage of sleep time with loud snoring between the two treatment groups |
|||||
| Results | |||||
| Outcomes 1–4 | |||||
| RFA | Difference preoperative vs postoperative | ||||
| n (in analysis) | 10 (5 with one treatment and 5 with two treatments) | ||||
| Snoring loudness (partner, VAS), mean ± SDa | 5 patients with one treatment: 1.8 ± 1.3 | NR | |||
| 5 patients with two treatments: 3.4 ± 2.6 | NR | ||||
| All 10 patients: 2.75 ± 2.15 | p < 0.001 | ||||
| MESAM (% loud), mean ± SD |
5 patients with one treatment: 5.22 ± 4.47 5 patients with two treatments: 10.83 ± 13.9 |
NA | |||
| AHI score, mean ± SD | 5 patients with one treatment: 13.5 ± 21.8 | NR | |||
| 5 patients with two treatments: 6.3 ± 5.7 | NR | ||||
| All 10 patients: NR | NR | ||||
| ESS score, mean ± SD | 5 patients with one treatment: 4.2 ± 2.4 | NR | |||
| 5 patients with two treatments: 3.8 ± 1.3 | NR | ||||
| All 10 patients: NR | NR | ||||
| Outcome 5: Percentage of sleep time with loud snoring | |||||
| RFA | Snore X device | Difference between groups | |||
| n (in analysis) | 10 | 10 | |||
| Percentage of sleep time with loud snoring, mean ± SD | 8.03 ± 10.16 | 3.28 ± 1.46 (the half night with the Snore X: 3.32 ± 4.7; without: 10.62 ± 9.83;p > 0.046) | p > 0.24 | ||
|
Postoperative adverse events: NR Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||||
| Author’s conclusions | |||||
| RFA appears to be a viable alternative for the non-apnoeic snorer if an examination proves that there is little risk of obstructing the airway secondary to the usual oedema of the treated mucosa. There was no significant difference between the RFA group and the Snore X group in terms of the percentage of sleep time with loud snoring | |||||
| Methodological assessment criteria | |||||
| 1. Study design | Parallel two-group pre–post with between-group comparisons | ||||
| 2. Were the study eligibility criteria specified? | Yes | ||||
| 3. Was a power calculation performed? | No | ||||
| 4. Is the sample size adequate? | Unclear | ||||
| 5. Is the number randomised stated? | NA | ||||
| 6. Is the study properly randomised?b | NA | ||||
| 7. Is allocation of treatment concealed?c | NA | ||||
| 8. Are adequate baseline details presented? | Partial | ||||
| 9. Are groups similar at baseline? | Partial | ||||
| 10. Are any baseline imbalances adequately adjusted for in the analysis? | No | ||||
| 11. Are similar co-interventions administered? | Unclear | ||||
| 12. Are patients blinded to treatment allocation? | No | ||||
| 13. Are outcome assessors blinded? | Unclear | ||||
| 14. Is compliance with treatment adequate? | Yes | ||||
| 15. Were any subgroup analyses justified? | NA | ||||
| 16. Were data collection tools shown or known to be valid for the outcome of interest?d | Partial (both objective and subjective measures used) | ||||
| 17. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?e | Partial (both objective and subjective measures used) | ||||
| 18. Were all study participants accounted for? | Yes | ||||
| 19. Are data analyses appropriate? | Yes | ||||
| 20. Is analysis conducted on an intention to treat basis? | Yes | ||||
| 21. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||||
| 22. Are the conclusions supported by the results? | Yes | ||||
| 23. Generalisability | Relatively inclusive eligibility criteria | ||||
| 24. Intercentre variability | One-centre study | ||||
| 25. General comments | – | ||||
| den Herder 2006109 | ||
|---|---|---|
|
Title: Bipolar radiofrequency-induced thermotherapy of the tongue base: its complications, acceptance and effectiveness under local anaesthesia Country: Netherlands Setting: Departments of Otolaryngology/Head and Neck Surgery Study design: Pre–post |
||
| Interventions | ||
|
Intervention: RFA – bipolar radiofrequency-induced thermotherapy of the tongue base (RFTB) performed on an outpatient basis under local anaesthesia. A radiofrequency generator (CelonLab ENT power control unit; Olympus Medical Systems, Europa GmbH, Hamburg) was used for delivery of bipolar radiofrequency energy to six application sites for the first treatment with energy delivered with a disposable probe through the dorsal surface of the tongue. The area of the tongue had an extension of 3 cm × 3 cm and circumscribed the circumvallate papilla. The coagulations were placed at a distance of 1.5–2 cm from each other. The mean number of treatment sessions per patient was 1.5 (range 1–3). The total amount of energy delivered per treatment session was 504 J (7 W in 12 seconds = 84 J per lesion; diameter of lesion 4.9 mm) in less than 2 minutes. If required, a second treatment session was performed minimally 6 weeks after the primary session. Termination of the treatment or scheduling of an additional treatment depended on the results of the control PSG testing and subjective improvement of snoring or hypersomnolence. Preoperatively patients received 2500 mg amoxicillin with clavulanate potassium continued for 1 week postoperatively Concurrent treatment: RFTB was combined with other surgical treatment(s) in cases of retropalatal obstruction (large tonsils and long oedematous uvula) and severe multilevel obstruction as visualised during sleep endoscopy Previous treatment(s): Some patients had undergone previous unsuccessful pharyngeal surgery for OSAS (not reported by subgroup) |
||
| Participants | ||
|
Total n = 22 If this study includes a mixed patient population, number of non-apnoeic snorers included: 9 Tests to exclude OSAS (including test details): All patients had one night of standard PSG testing preoperatively to discriminate OSA (AHI > 5) from socially unacceptable snoring (SUS). PSG included sleep architecture (derived from an electroencephalogram, eye movements and a submental electromyogram), respiration (thoracic and abdominal measurements), O2 saturation, movements of limbs and intensity of snoring Tests to assess the site of airway narrowing (including test details): Sleep endoscopy with midazolam Inclusion criteria: Patients with SUS or OSAS; had at least narrowing or obstruction at tongue base level (Fujita type III), observed by sleep endoscopy with midazolam Exclusion criteria: NR Subgroups: Non-apnoeic snorers, n = 9; OSAS, n = 3 |
||
| Patient baseline characteristics | ||
| n | 9 (non-apnoeic snorers; n = 8 patients had one treatment session and n = 1 patient had two sessions) | |
| Age (years), mean ± SD | 45.4 ± 9.7 | |
| Male, n (%) | 6 (66) | |
| BMI (kg/m2), mean ± SD | 26.5 ± 3.8 | |
| AHI score, mean ± SD | 2.5 ± 1.8 | |
| ESS score, mean ± SD | 6.6 ± 6.8 | |
| Smokers, n (%) | NR | |
| Outcome measures | ||
|
Outcome 1: ESS score. Definition of treatment success: a cut point of ESS > 7 indicates disturbed or unrefreshing sleep Covariates: NR Total length of follow-up: 360 ± 132 days Follow-up assessment times: follow-up visits with clinical examination at 7 days and 6–8 weeks after surgery Rate of attrition at each follow-up time: 0 in this group Method of statistical analysis: Differences between pre- and post-treatment scores were analysed using the sign rank test |
||
| Results | ||
| Outcome 1: ESS score | ||
| n (in analysis) | 9 | |
| ESS score, mean ± SD | 2.4 ± 3.4; p < 0.05 | |
|
Postoperative adverse events: No postoperative complications such as infections, abscesses, haematomas or ulcerations of the tongue base occurred; no serious complications were seen in this group Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
||
| Authors’ conclusions | ||
| Bipolar RFTB in patients with obstruction at the tongue base only is a safe and simple procedure under local anaesthesia and can be effective in patients with SUS | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | Yes | |
| 3. Are adequate baseline details presented? | Partial | |
| 4. Are any co-interventions clearly stated? | Yes | |
| 5. Is compliance with treatment adequate? | Yes | |
| 6. Were any subgroup analyses justified? | Yes | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial (both objective and subjective outcomes assessed) | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial (both objective and subjective outcomes assessed) | |
| 9. Were all study participants accounted for? | Yes | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |
| 11. Are data analyses appropriate? | Yes | |
| 12. Are the conclusions supported by the results? | Yes (but the size of the subject group is too small) | |
| 13. Generalisability | Relatively inclusive eligibility criteria, applicable to patients with obstruction at the tongue base only (Fujita type III) | |
| 14. Intercentre variability | One-centre study | |
| 15. General comments | – | |
| Haraldsson 2002107 | |||
|---|---|---|---|
|
Title: Voice quality after radiofrequency volumetric tissue reduction of the soft palate in habitual snorers Country: Sweden Setting: Departments of Otorhinolaryngology and Neurophysiology Study design: Pre–post |
|||
| Interventions | |||
|
Intervention: Radiofrequency tissue volume reduction near or on the midline (600 J) and on each side of the soft palate (300 J), 1 or 2 cm from the lower border, with a maximum temperature of 85°C. The total energy per treatment session was 1200 J. A Somnus model 215 radiofrequency generator (Somnus Medical Technologies, Sunnyvale, CA) with disposable needles was used. Patients were given two tablets of 30 mg prednisolone, 500 mg paracetamol plus 30 mg codeine, and 50 mg diclofenac before surgery. Topical anaesthesia (lidocaine) was sprayed onto the velum and tongue before the velum was infiltrated with 4 ml lidocaine 10 mg/ml with adrenaline 5 µg/ml. Treatment was planned for a minimum of two and a maximum of four sessions with an interval of at least 1 month between treatments (mean number of treatments three) Concurrent treatment (specific details): NR Previous treatment(s): NR |
|||
| Participants | |||
|
Total n = 16 If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS (including test details): Apnolog sleep study (pulse oximetry, movements and breathing efforts on static charge-sensitive bed, sleep position and snoring microphone) Tests to assess the site of airway narrowing: Clinical examination of the upper airways including fibreoptic endoscopy with Muller’s manoeuvre Inclusion criteria: Age < 70 years; loud habitual snoring with or without excessive daytime sleepiness; palatal obstruction only (uvula length < 2.5 cm); BMI < 30 kg/m2; AHI < 15; nadir SaO2 > 85% Exclusion criteria: Speech or swallowing difficulties; excessive tongue base enlargement; neurological, endocrine, heart or lung disease Subgroups: NA |
|||
| Patient baseline characteristics | |||
| n | 16 | ||
| Age (years), mean (range) | 49.4 ± 10.4 (26–67) | ||
| Male, n (%) | 11 (68.6) | ||
| BMI (kg/m2), mean ± SD (range) | 26.2 ± 2.0 (22–30) | ||
| AHI score, mean ± SD (range) | NR | ||
| ODI, mean ± SD | 4.0 ± 3.4 | ||
| Maximum snoring sound level (dB), mean | 53 | ||
| ESS score, mean ± SD | 11.4 ± 5.0 | ||
| Snoring severity (partner, VAS), mean ± SD | 8.2 ± 2.9 | ||
| Speech analysis parameters: | |||
| Nasal–oral ratio meter (NORAM) analysis of hypernasality, mean (95% CI) | 3.9 (1.4–6.0) | ||
| Hypernasality (listener rated), mean | 1.0 | ||
| Nasal escape (listener rated), mean | 1.0 | ||
| Velopharyngeal snort (listener rated), mean | 1.0 | ||
| Outcome measures | |||
|
Outcome 1: ODI. Definition of treatment success: NR Outcome 2: Maximum snoring level sound (dB). Definition of treatment success: NR Outcome 3: Snoring severity scale score assessed on a 10-point VAS. Definition of treatment success: NR Outcome 4: ESS score. Definition of treatment success: NR Outcome 5: Maximum pain scale score assessed on a 10-point VAS. Definition of treatment success: NR Outcome 6: NORAM hypernasality score. Definition of treatment success: NR Outcome 7: Speech and language pathologist assessment of nasal escape and velopharyngeal snort assessed on a 5-point scale with 1 = normal and 5 = severe deviation from normal. Definition of treatment success: NR Covariates: NA Total length of follow-up: Mean 165 days Follow-up assessment times: One follow-up assessment at a minimum of 2 months postoperatively (mean 165 days) Rate of attrition at each follow-up time: NA Methods of statistical analysis: Student’s t-test was used to investigate changes between pretreatment and post-treatment values of the NORAM test; ordinal data such as speech evaluation, snoring index and ESS score were analysed using the Wilcoxon paired sample test |
|||
| Results | |||
| Outcomes 1–7 | |||
| n (in analysis) | 16 | ||
| ODI, mean ± SD | 3.3 ± 2.5; p = NR | ||
| Maximum snoring level sound (dB), mean | 45 | ||
| Snoring severity scale score, mean ± SD | 4.1 ± 2.5: p < 0.01 | ||
| ESS score, mean ± SD | 8.2 ± 4.4; p = NS | ||
| Maximum pain scale score, mean ± SD | 4.0 ± 2.6 | ||
| NORAM score, mean (95% CI) | 3.1 (0.6–5.7) | ||
| Hypernasality, mean | 1.0 | ||
| Nasal escape, mean | 1.0 | ||
| Velopharyngeal snort, mean | 1.0 | ||
|
Postoperative adverse events: Three patients sustained blanching at treatment one; two patients developed ulcerations after the last treatment session; two patients complained of increased soft palate hyper-reflexia; two patients sustained an otalgia Need for repeat procedure (unscheduled): NR |
|||
| Authors’ conclusions | |||
| Radiofrequency volumetric tissue reduction in the soft palate as a treatment for snoring did not have any significant adverse effects on velopharyngeal function and voice quality | |||
| Reviewer’s comments | |||
| Radiofrequency volumetric tissue reduction in the soft palate as a treatment for snoring did not have any significant adverse effects on velopharyngeal function and voice quality | |||
| Methodological assessment criteria | |||
| 1. Study design | Pre–post study | ||
| 2. Were the study eligibility criteria specified? | Yes | ||
| 3. Are adequate baseline details presented? | Partial | ||
| 4. Are outcome assessors blinded? | Unclear | ||
| 5. Is compliance with treatment adequate? | Yes | ||
| 6. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial (mixture of objective and subjective outcome measures) | ||
| 7. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial (mixture of objective and subjective outcome measures) | ||
| 8. Were all study participants accounted for? | Yes | ||
| 9. Are data analyses appropriate? | Yes | ||
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||
| 11. Are the conclusions supported by the results? | Yes | ||
| 12. Generalisability | The patient group appears to be representative of those undergoing radiofrequency volumetric tissue reduction for primary snoring | ||
| 13. Intercentre variability | One-centre study | ||
| Hukins 2000105 | ||||||
|---|---|---|---|---|---|---|
|
Title: Radiofrequency tissue volume reduction of the soft palate in simple snoring Country: Australia Setting: Departments of Pulmonary Physiology and Ear, Nose and Throat Surgery Study design: Pre–post |
||||||
| Interventions | ||||||
|
Intervention: Radiofrequency tissue volume reduction (RFTVR) to the middle, distal and proximal thirds of the midline of the palate successively at intervals of at least 2 weeks. Topical lidocaine (4%) followed by submucosal infiltration of 2% lidocaine with epinephrine was used as local anaesthetic. A radiofrequency generator (Somnus Medical Technologies, Sunnyvale, CA) and a hand-held electrode were used to deliver 650 ± 7.18 J (constant electrode temperature of 85°C) to the midline of the soft palate. The mean interval between treatments was 26.9 ± 12.1 days. Patients used the combination drug paracetamol/codeine (500 mg/30 mg) for up to 4 days after each treatment Concurrent treatment (specific details): NA Previous treatment(s) (specific details): Patients had not undergone previous surgical treatment other than tonsillectomy or adenoidectomy (when applicable) |
||||||
| Participants | ||||||
|
Total n = 20 If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS (including test details): PSG (sleep staging); oronasal flow (thermistor); chest and abdominal motion (inductance plethysmography; Respitrace, Ardsley, NY). Snoring sound intensity was measured using a sound intensity meter with the omnidirectional microphone set in a fixed position relative to the sound source 1 m above the patient’s head Tests to assess the site of airway narrowing (including test details): Lateral cephalometry Inclusion criteria: Age ≥ 18 years; habitual snoring; maximum snore intensity of 50 dB or greater; simple snoring or mild OSAS (AHI ≤ 15) Exclusion criteria: History of neurological, swallowing or unstable psychiatric disorder; BMI > 32 kg/m2; previous pharyngeal surgery (excluding tonsillectomy or adenoidectomy) Subgroups: NA |
||||||
| Patient baseline characteristics | ||||||
| n | 20 | |||||
| Age (years), mean ± SD | 43.2 ± 11.1 | |||||
| Male, n (%) | 16 (80) | |||||
| BMI (kg/m2), mean ± SD | 27.1 ± 2.8 | |||||
| AHI score, mean ± SD | 3.3 ± 3.1 | |||||
| Arousal index per hour of sleep, mean ± SD | 19.4 ± 7.9 | |||||
| Sleep efficiency (%), mean ± SD | 82.6 ± 9.6 | |||||
| Mean sleep SaO2 (%), mean ± SD | 95.7 ± 1.4 | |||||
| Nadir sleep SaO2 (%), mean ± SD | 88.3 ± 3.5 | |||||
| ESS score, mean ± SD | 8.1 ± 4.0 | |||||
| Sleepiness scale score (VAS), mean ± SD | 3.0 ± 2.0 | |||||
| Snoring severity (partner, VAS), mean ± SD | 7.5 ± 1.5 | |||||
| Snoring intensity (dB), mean ± SD | 60.2 ± 3.9 | |||||
| Cephalometric parameters: | ||||||
| Angle between the sellar point to the nasion line and maxillary point (°), mean ± SD | 80.2 ± 4.5 | |||||
| Angle between the sellar point to the nasion line and mandibular point (°), mean ± SD | 77.7 ± 5.3 | |||||
| Posterior airspace (mm), mean ± SD | 6.45 ± 2.41 | |||||
| Maximum soft palate width (mm), mean ± SD | 10.11 ± 1.97 | |||||
| Distance between the posterior nasal spine and the tip of the uvula (mm), mean ± SD | 38.17 ± 2.39 | |||||
| Outcome measures | ||||||
|
Outcome 1: ESS score. Definition of treatment success: NR Outcome 2: Sleepiness scale score assessed with a 10-point VAS ranging from ‘no tendency to sleep’ to ‘constantly falling asleep’. Definition of treatment success: NR Outcome 3: Snoring severity scale score assessed by partner with a 10-point VAS ranging from ‘no snoring’ to ‘very intense (partner leaves the bedroom)’. Definition of treatment success: NR Outcome 4: Snoring intensity (dB). Definition of treatment success: NR Outcome 5: Changes in polysomnographic variables. Definition of treatment success: NR Outcome 6: Changes in cephalometric parameters. Definition of treatment success: NR Outcome 7: Postoperative pain, swallowing difficulties and changes in speech measured on a 10-point VAS 3 and 7 days post each procedure. Definition of treatment success: NA Covariates: Relationship between baseline demographic variables, PSG results, cephalometric parameters, total energy delivered and time since first treatment and changes in subjective snoring outcomes were explored using forward stepwise linear regression (p < 0.5 was considered significant) Total length of follow-up: 2 months post final treatment session Follow-up assessment times: Patients were followed up post each treatment session and at 2 months after the final treatment session Rate of attrition at each follow-up time: NA Methods of statistical analysis: Clinical and cephalometric data were compared before and after treatment by a Mann–Whitney rank sum test; the relationships of baseline demographic, PSG and cephalometric data to improvements in subjective snoring were examined by forward stepwise linear regression |
||||||
| Results | ||||||
| Outcomes 1–4 | ||||||
| n (in analysis) | 20 | |||||
| ESS score, mean ± SD | 6.7 ± 4.0; p = NS | |||||
| Sleepiness scale score (VAS), mean ± SD | 2.6 ± 2.2: p = NS | |||||
| Snoring severity score (VAS), mean ± SDa | 4.6 ± 2.5: p < 0.001 | |||||
| Snoring intensity (dB), mean ± SDb | 64.9 ± 5.3; p = 0.03 | |||||
| Outcome 5: Changes in PSG variables | ||||||
| n (in analysis) | 20 | |||||
| AHI score, mean ± SD | 6.6 ± 8.1; p = NS | |||||
| Arousal index per hour of sleep, mean ± SD | 19.2 ± 9.6; p = NS | |||||
| Sleep efficiency (%), mean ± SD | 82.5 ± 11.8; p = NS | |||||
| Mean sleep SaO2 (%), mean ± SD | 95.6 ± 1.3; p = NS | |||||
| Nadir sleep SaO2 (%), mean ± SD | 86.7 ± 5.5; p = NS | |||||
| Outcome 6: Changes in cephalometric parameters | ||||||
| n (in analysis) | 20 | |||||
| Angle between the sellar point to the nasion line and maxillary point (°), mean ± SD | 79.5 ± 4.8; p = NS | |||||
| Angle between the sellar point to the nasion line and mandibular point (°), mean ± SD | 77.4 ± 5.4; p = NS | |||||
| Posterior airspace (mm), mean ± SD | 4.80 ± 2.19; p = NS | |||||
| Maximum soft palate width (mm), mean ± SD | 9.34 ± 2.19; p = NS | |||||
| Distance between the posterior nasal spine and the tip of the uvula (mm), mean ± SD | 37.00 ± 2.77; p = NS | |||||
| Outcome 7: Postoperative pain, swallowing difficulties and changes in speech 3 and 7 days after each procedure (rating on a 10-point VAS) | ||||||
| Treatment one (middle third) | Treatment two (distal third) | Treatment three (proximal third) | ||||
| Day 3 | Day 7 | Day 3 | Day 7 | Day 3 | Day 7 | |
| Pain, mean ± SD | 1.7 ± 1.2 | 0.5 ± 0.9 | 1.7 ± 1.7 | 1.4 ± 1.4 | 0.8 ± 1.4 | 0.5 ± 1.1 |
| Swallowing, mean ± SD | 1.7 ± 1.0 | 0.7 ± 0.7 | 1.8 ± 1.7 | 1.4 ± 1.4 | 0.7 ± 1.0 | 0.3 ± 0.8 |
| Speech, mean ± SD | 0.8 ± 1.0 | 0.1 ± 0.5 | 1.0 ± 1.4 | 0.5 ± 1.0 | 0.7 ± 1.5 | 0.1 ± 0.3 |
|
Postoperative adverse events: Three patients developed mucosal ulcers after treatment to the distal third of the palate; in one patient the lesion occurred following movement during treatment, which resulted in exposure of the mucosa to the active electrode Need for repeat procedure (unscheduled): NA |
||||||
| Authors’ conclusions | ||||||
| RFTVR palatoplasty is well tolerated with very low morbidity. It is associated with a subjective improvement in snoring; however, this improvement is accompanied by a marginal change in objective measures, suggesting either an acoustic change independent of sound intensity or a placebo effect. Placement of the lesions additionally appears to influence outcome | ||||||
| Reviewer’s comments | ||||||
| Adequate participant baseline details reported including somnographic data, cephalometric parameters and both objective and subject assessments of snoring intensity. Changes in the subjective assessment of snoring do not correlate with objective measures, both of sound intensity and of cephalometric parameters | ||||||
| Methodological assessment criteria | ||||||
| 1. Study design | Pre–post study | |||||
| 2. Were the study eligibility criteria specified? | Yes | |||||
| 3. Are adequate baseline details presented? | Partial | |||||
| 4. Are outcome assessors blinded? | NA | |||||
| 5. Is compliance with treatment adequate? | Yes | |||||
| 6. Were data collection tools shown or known to be valid for the outcome of interest?c | Partial (mixture of objective and subjective outcome measures) | |||||
| 7. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?d | Partial (mixture of objective and subjective outcome measures) | |||||
| 8. Were all study participants accounted for? | Yes | |||||
| 9. Are data analyses appropriate? | Yes | |||||
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |||||
| 11. Are the conclusions supported by the results? | Yes | |||||
| 12. Generalisability | The patient group appears to be representative of those undergoing RFTVR for primary snoring | |||||
| 13. Intercentre variability | One-centre study | |||||
| Stuck 2005103 | |||
|---|---|---|---|
|
Title: Radiofrequency surgery of the soft palate in the treatment of snoring: a placebo-controlled trial Country: Germany Setting: Outpatient Department, Department of Otorhinolaryngology Study design: Randomised placebo-controlled trial |
|||
| Interventions | |||
|
Intervention 1: Two consecutive sessions of radiofrequency (RF)-controlled surgery (Somnoplasty®) performed under local anaesthesia. The Somnus® radiofrequency generator Model S2 (Gyrus ENT, Bartlett, TN) was used for the generation of temperature-controlled RF energy. The surgical procedure was standardised. In session one, three application sites were selected (600 J in the midline and 2 × 450 J approximately 1 cm lateral to the midline). In session two, four application sites were chosen (4 × 450 J). In total, 3300 J were delivered in the RF group. The target temperature was set to 85°C. The procedure was performed by a single surgeon and the second session was performed 4–6 weeks after the first session. Patients did not receive any sedation, prophylactic antibiotics or corticosteroids Intervention 2. Placebo treatment given using the same standardised protocol, including local anaesthesia. The device needle was inserted but no RF energy was delivered. The second session was performed 4–6 weeks after the first session. Patients did not receive any sedation, prophylactic antibiotics or corticosteroids Concurrent treatment: NR Previous treatment(s): Patients had not undergone previous soft palate surgery |
|||
| Participants | |||
|
Total n = 26; 23 patients were included in the analysis (12 RF surgery and 11 placebo) If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS: PSG or ambulatory polygraphy were administered. No test details were reported Tests to assess the site of airway narrowing: Clinical assessment including rigid endoscopy (awake patient) to rule out retrolingual obstruction or significant tonsillar hypertrophy; the appearance of the epiglottic vallecular on laryngeal endoscopy was the main criterion used to evaluate retrolingual obstruction due to potential tongue-based hypertrophy Inclusion criteria: Patients with primary snoring; age ≥ 18 and ≤ 65; maximum BMI 35 kg/m2; no co-morbid disease and not professional voice user; no excessive daytime sleepiness; OSA ruled out by either PSG or ambulatory polygraphy Exclusion criteria: Significant retrolingual obstruction; tonsillar hypertrophy; previous soft palate surgery |
|||
| Patient baseline characteristics | |||
| RFA | Placebo | ||
| n | 12 | 11 | |
| Age (years), mean ± SD (range) | 42.6 ± 7.6 (27–60) | ||
| Male, n (%) | NR | NR | |
| BMI (kg/m2), mean (range) | NR | NR | |
| AHI score, mean ± SD (range)a | 2.45 ± 1.51 (0.7–5.3) | 2.68 ± 2.48 (0.2–9.2) | |
| ESS score, mean ± SD | 5.4 ± 4.6 | 5.2 ± 3.1 | |
| Smokers, n (%) | NR | NR | |
| Snoring scale score, mean ± SD | 8.1 ± 1.3 | 8.4 ± 1.6 | |
| Speech problems scale score, mean ± SD | 0.4 ± 0.8 | 1.0 ± 1.4 | |
| Swallowing function scale score, mean ± SD | 0.4 ± 0.6 | 0.3 ± 0.6 | |
| Taste problems scale score, mean ± SD | 0.3 ± 0.7 | 0.4 ± 0.5 | |
| Pharyngeal irritation scale score, mean ± SD | 1.1 ± 1.0 | 0.8 ± 0.9 | |
| Outcome measures | |||
|
Outcome 1: Mean snoring score assessed with a 10-cm VAS. ‘No snoring’ and ‘excessive snoring, bed partner leaves the room’ were used as anchors. Definition of treatment success: NR Outcome 2: Mean daytime sleepiness score assessed with the ESS. Definition of treatment success: NR Outcome 3: Mean speech problem score assessed with a 10-cm VAS. ‘No problems/not affected’ (0) and ‘severe problems/severely affected’ (10) were used as anchors. Definition of treatment success: NR Outcome 4: Mean swallowing function score assessed with a 10-cm VAS. ‘No problems/not affected’ (0) and ‘severe problems/severely affected’ (10) were used as anchors. Definition of treatment success: NR Outcome 5: Mean taste score assessed with a 10-cm VAS. ‘No problems/not affected’ (0) and ‘severe problems/severely affected’ (10) were used as anchors. Definition of treatment success: NR Outcome 6: Mean pharyngeal irritation score assessed with a 10-cm VAS. ‘No problems/not affected’ (0) and ‘severe problems/severely affected’ (10) were used as anchors. Definition of treatment success: NR Covariates: NR Total length of follow-up: 10–14 weeks from baseline Follow-up assessment times: Only one follow-up at 10–14 weeks Rate of attrition: n = 3; treatment group assignment and the reasons for withdrawal not reported |
|||
| Results | |||
| Outcomes 1–4 | |||
| RFA | Placebo | Differences between groups | |
| n (in analysis) | 12 | 11 | – |
| Mean snoring score, mean ± SD | 5.2 ± 2.4 | 8.0 ± 2.3 | p = 0.045 |
| Mean ESS score, mean ± SD | 3.9 ± 3.3 | 4.3 ± 2.7 | p = 0.77 |
| Mean speech problem scale score, mean ± SD | 0.3 ± 0.5 | 0.7 ± 1.1 | p > 0.05 |
| Mean swallowing function scale score, mean ± SD | 0.4 ± 0.5 | 0.3 ± 0.5 | p > 0.05 |
| Mean taste scale score, mean ± SD | 0.3 ± 0.4 | 0.4 ± 0.6 | p > 0.05 |
| Mean pharyngeal irritation scale score, mean ± SD | 1.5 ± 1.8 | 0.6 ± 1.4 | p > 0.05 |
|
Postoperative adverse events: NR Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||
| Authors’ conclusions | |||
| RF surgery was significantly better than placebo, although the reduction in snoring was only moderate in this group of patients | |||
| Reviewer’s comments | |||
| Methods of randomisation adequate. Original power calculation for 5% α error with 90% power based on 12 patients per group. There are n = 12 and n = 11 in RFA and placebo groups respectively. Appears on basis of power calculation that study should be adequately powered. Patient withdrawals per group and the reasons for withdrawal are not reported (supposition: n = 13 at baseline in each group, therefore n = 1 withdrawal in the RFA group and n = 2 in placebo group). Per protocol analysis conducted, not intention to treat. Non-parametric analysis appropriate given the skewed data. Postoperative adverse events not reported. Length of follow-up 10–14 weeks from baseline. Effect size for reduction in snoring scale scores only moderate (mean ± SD: 5.2 ± 2.4 on 10-point VAS; in current literature a reduction of snoring to a postoperative snoring score below 3 is regularly considered as a successful treatment). Longer-term implications of the moderate reduction in snoring levels are unclear, particularly given the subjective outcome measures used and the reduction in the efficacy of interventions at longer term follow-up | |||
| Methodological assessment criteria | |||
| 1. Study design | RCT | ||
| 2. Were the study eligibility criteria specified? | Yes | ||
| 3. Was a power calculation performed? | Yes | ||
| 4. Is the sample size adequate? | Yes | ||
| 5. Is the number randomised stated? | Partial (overall, but not by treatment group) | ||
| 6. Is the study properly randomised?b | Yes (computer generated) | ||
| 7. Is allocation of treatment concealed?c | Yes | ||
| 8. Are adequate baseline details presented? | No | ||
| 9. Are groups similar at baseline? | Unclear (prognostic variables not reported) | ||
| 10. Are any baseline imbalances adequately adjusted for in the analysis? | No | ||
| 11. Are similar co-interventions administered? | Unclear | ||
| 12. Are patients blinded to treatment allocation? | Yes | ||
| 13. Are outcome assessors blinded? | Yes | ||
| 14. Is compliance with treatment adequate? | Yes (all patients in analysis completed protocol) | ||
| 15. Were any subgroup analyses justified? | NA | ||
| 16. Were data collection tools shown or known to be valid for the outcome of interest?d | No | ||
| 17. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?e | No | ||
| 18. Were all study participants accounted for? | No | ||
| 19. Are data analyses appropriate? | Yes | ||
| 20. Is analysis conducted on an intention to treat basis? | No (per protocol) | ||
| 21. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||
| 22. Are the conclusions supported by the results? | Yes | ||
| 23. Generalisability | Unclear | ||
| 24. Intercentre variability | Only one treatment centre | ||
| 25. General comments | – | ||
Studies of palatal stiffening techniques
| Brietzke 2001102 | |||
|---|---|---|---|
|
Title: Injection snoreplasty: how to treat snoring without all the pain and expense Country: USA Setting: Otolaryngology Clinic at Walter Reed Army Medical Centre Study design: Pre–post |
|||
| Interventions | |||
|
Intervention: Palatal stiffening with injection snoreplasty performed as an outpatient procedure using topical anaesthesia (cetacaine oral spray followed by a benzocaine gel). Treatment one: 2.0 ml of 1% sodium tetradecyl sulphate (10 mg/ml) injected with a single needle penetration in to the midline soft palate. For repeat procedures: 3% sotradecol (30 mg/ml) was generally used and the site of injection modified to include the lateral areas of the soft palate as well as those areas not adequately stiffened by the previous procedure. Maximum procedure time 20 minutes. Follow-up appointments for possible reinjection were scheduled a minimum of 6 weeks after the previous procedure to allow for development of maximal palatal stiffening. The decision to proceed with further treatment was based on patient or sleeping partner dissatisfaction with the snoring response to the procedure. All procedures were performed by the same surgeons. Number of treatments: one, n = 10 (37%); two, n = 13 (48%); three, n = 4 (15%). Mean number of treatments 1.8. No antibiotics or steroids were prescribed Concurrent treatment: NR Previous treatment(s): Patients had not undergone previous surgical treatment for snoring |
|||
| Participants | |||
|
Total n = 27 If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS (including test details): All patients underwent an overnight sleep study with the diagnosis of primary snoring confirmed with a RDI of < 10 Tests to assess the site of airway narrowing (including test details): All patients underwent a thorough physical examination during the initial visit. The nasal cavity, nasopharynx, oropharynx and hypopharynx were evaluated using a flexible fibreoptic scope. The soft palate was observed for flutter and a videostrobe used to record the voluntary palatal flutter frequency Inclusion criteria: Primary snoring with a RDI of < 10 Exclusion criteria: Tonsillar hypertrophy on physical examination (defined as greater than 1+); a known history of co-morbid disease that could alter routine healing patterns (e.g. vascular disease, diabetes mellitus, significant periodontal disease, etc.); a history of previous surgical snoring treatment Subgroups: NA |
|||
| Patient baseline characteristics | |||
| n in analysis | 27 | ||
| Age, mean (range) | 42 (24–72) | ||
| Male, n (%) | 25 (92.5) | ||
| BMI, mean (range) | NR | ||
| AHI score, mean (range) | 1.7 (0–10) | ||
| ESS score, mean (range) | NR | ||
| Smokers, n (%) | NR | ||
| Other | NR | ||
| n in analysis | 26 | ||
| Palatal flutter snoring frequency (Hz), mean | 74.1 | ||
| ESS score, mean (range) | NR | ||
| Outcome measures | |||
|
Outcome 1: Successful treatment of snoring (patient or partner reported). Definition of treatment success: NR Outcome 2: Fundamental frequency of palatal flutter snoring. Definition of treatment success: NA Outcome 3: Pain score (0–10 VAS scale). Definition of treatment success: NA Covariates: NR Total length of follow-up: 10 days post each injection Follow-up assessment times: Days 1, 2, 3, 4, 5, 6, 7 and 10 Rate of attrition at each follow-up time: 0 Methods of statistical analysis: NR |
|||
| Results | |||
| Outcome 1: Successful treatment of snoring | |||
| n (in analysis) | 27 | ||
| ‘Snoring has gone’ or ‘snoring is no longer a problem’,n (%) | 25 (92%) | ||
| Snoring relapses in 1 year of follow-up | 0 | ||
| Outcome 2: Fundamental frequency of palatal flutter snoring | |||
| n (in analysis) | 13 | ||
| Fundamental frequency of palatal flutter snoring (Hz) | 105.4; difference: 31.3 | ||
| Outcome 3: Pain score VAS | |||
| n (in analysis) | 27 | ||
| Pain score VAS (postoperative), mean: | |||
| Day 1 | 3 | ||
| Day 2 | 2.4 | ||
| Day 3 | 2.2 | ||
| Day 4 | 1.4 | ||
| Day 5 | 1 | ||
|
Postoperative adverse events: No significant complications. There were no post-injection infections, palatal fistula or velopharyngeal insufficiency. Palatal mucosal breakdown was observed in six (22%) patients (healed with no sequelae) among a total of 48 (12.5%) total injection treatment sessions. Two of these six patients reported considerably more discomfort than the others over a longer period of time (5–10 days). The other four had minimal to no pain. All patients were treated supportively without antibiotics. There were no significant post-injection speech or swallowing difficulties Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||
| Authors’ conclusions | |||
| Injection snoreplasty is simple, safe and effective for primary snoring with advantages including simplicity, decreased expense, decreased post-treatment pain levels and minimal/no convalescence | |||
| Methodological assessment criteria | |||
| 1. Study design | Pre–post | ||
| 2. Were the study eligibility criteria specified? | Partial | ||
| 3. Are adequate baseline details presented? | Partial | ||
| 4. Are any co-interventions clearly stated? | NA | ||
| 5. Is compliance with treatment adequate? | Yes | ||
| 6. Were any subgroup analyses justified? | NA | ||
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | No | ||
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | No | ||
| 9. Were all study participants accounted for? | Yes | ||
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||
| 11. Are data analyses appropriate? | No analysis undertaken | ||
| 12. Are the conclusions supported by the results? | Measurement of successful treatment of snoring was subjective; insufficient information on how the success was defined; small group of subjects | ||
| 13. Generalisability | Applicable to primary snoring caused by palatal flutter | ||
| 14. Intercentre variability | One-centre study | ||
| 15. General comments | – | ||
| Ho 2004101 | |||
|---|---|---|---|
|
Title: Managing disturbing snoring with palatal implants: a pilot study Country: Hong Kong Setting: Departments of Otorhinolaryngology, Head and Neck Surgery Study design: Pre–post |
|||
| Interventions | |||
|
Intervention: Palatal stiffening performed under local anaesthesia through insertion of polyethylene terephthalate (PET) implants into the soft palate. The implants were 18 mm in length and 1.6 mm in diameter. Implants were placed at the median and paramedian positions of the soft palate at a distance of 5 mm apart in a sagittal plane. Two implants were placed in each of the first two patients, and three implants were used in the remaining 10 patients. Oral antibiotic treatment with cefuroxime 0.5 g/day and metronidazole 1.2 g/day was given for 1 week Concurrent treatment (specific details): NR Previous treatment(s): Patients had not undergone previous pharyngeal surgery |
|||
| Participants | |||
|
Total n = 12 (n = 9 in the analysis) If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS: Formal overnight PSG including electroencephalography, electro-oculography, oximetry, airflow monitoring with nasal thermister, chest and abdominal movement monitoring and leg movement monitoring was performed in all patients. Snoring was assessed with the SNAP sonographic system (SNAP Laboratories, Glenview, IL) in the last five patients recruited to the study. The snoring index was defined as the average number of snores per hour Tests to assess the site of airway narrowing: The size of the soft palate and the width of the uvula were measured before implantation. The length of the soft palate was measured from the soft–hard palatal junction to the base of the uvula at the midline. The width of the uvula was measured at the base at its junction with the soft palate proper Inclusion criteria: Disturbing snoring patients with an AHI < 15 and a BMI of ≤ 30 kg/m2 Exclusion criteria: Patients with known cardiovascular disease, a previous history of pharyngeal surgery or a history of swallowing or speech disorders were excluded Subgroups: NA |
|||
| Patient baseline characteristics | |||
| n | 9 | ||
| Age (years), mean (range) | 38 (29–53) | ||
| Male, n (%) | 9 (100) | ||
| BMI (kg/m2), mean ± SD (range) | 25.1 ± 2.9 (21–29.6) | ||
| AHI score, mean ± SD | 4.8 ± 5.7 | ||
| ESS score, mean ± SD | 8.9 ± 5.6 | ||
| Smokers, n (%) | NR | ||
| Loudness of snoring (partner, VAS 0–100), mean ± SD (range) | 79 ± 17.2 (50–100) | ||
| Outcome measures | |||
|
Outcome 1: Loudness of snoring assessed by partner on a VAS ranging from 0 ‘no snoring’ to 100 ‘snoring of maximal loudness, bed partner leaves the room’. Definition of treatment success: NR Outcome 2: AHI score. Definition of treatment success: NR Outcome 3: ESS score. Definition of treatment success: NR Outcome 4: Effect of the patient’s snoring on the sleep of family members assessed on a categorical scale with response options: ‘no snoring’, ‘mild snoring only’, ‘affects spouse only’, ‘affects whole family’, ‘heard outside house’. Definition of treatment success: NR Outcome 5: Number of nights per week that the bed partner has to leave the room because of the loud snoring of the patient assessed with response options: 0,1–2 nights, 3–4 nights, 5–6 nights, 7 nights in a week. Definition of treatment success: NR Outcome 6: Objective measure of loudness of snoring (SNAP). No group mean data reported. Definition of treatment success: NR Covariates: NR Total length of follow-up: 3 months Follow-up assessment times: 1 Rate of attrition at each follow-up time: 3/12 Method of statistical analysis: The Wilcoxon signed rank test was used to analyse paired data |
|||
| Results | |||
| Outcomes 1–3 | |||
| n (in analysis) | 9 | ||
| Loudness of snoring VAS, mean ± SD | 48 ± 20.4; p = 0.008 | ||
| AHI score, mean ± SD | 8.3 ± 11.5; p = 0.33 | ||
| ESS score, mean ± SD | 5.7 ± 5.6; p = 0.007 | ||
| Outcomes 4–6 | |||
| n (in analysis) | 9 | ||
| Preoperative | Postoperative (3 months) | ||
| Number of responses for: | |||
| No snoring | 0 | 0 | |
| Mild snoring | 0 | 5 | |
| Affects spouse only | 6 | 4 | |
| Affects whole family | 0 | 0 | |
| Heard outside house | 3 | 0 | |
| Number of responses for nights per week that the bed partner has to leave the room because of the loud snoring of the patient: | |||
| 0 night | 3 | 6 | |
| 1–2 nights | 3 | 1 | |
| 3–4 nights | 1 | 2 | |
| 5–6 nights | 1 | 0 | |
| 7 nights | 1 | 0 | |
| Outcome 7: Objective measure of loudness of snoring (SNAP) | |||
|
No group mean data reported Postoperative adverse events: Implant extruded: 2/12 (16.7%) patients and 2/34 (8.8%) implants Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||
| Authors’ conclusions | |||
| Palatal stiffening through insertion of PET implants in the soft palate is safe. Snoring decreased significantly at 3 months after surgery | |||
| Methodological assessment criteria | |||
| 1. Study design | Pre–post | ||
| 2. Were the study eligibility criteria specified? | Partial | ||
| 3. Are adequate baseline details presented? | Yes | ||
| 4. Are any co-interventions clearly stated? | Unclear | ||
| 5. Is compliance with treatment adequate? | Yes | ||
| 6. Were any subgroup analyses justified? | NA | ||
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial (both objective and subjective outcomes assessed) | ||
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial (both objective and subjective outcomes assessed) | ||
| 9. Were all study participants accounted for? | No | ||
| 10. Are greater than 80% of patients included in the follow-up assessment? | No | ||
| 11. Are data analyses appropriate? | Yes | ||
| 12. Are the conclusions supported by the results? | Too few subjects to draw firm conclusions | ||
| 13. Generalisability | Not applicable to patients with OSAS or with BMI > 30 kg/m2 or with known cardiovascular disease, previous history of pharyngeal surgery or history of swallowing or speech disorders | ||
| 14. Intercentre variability | One-centre study | ||
| 15. General comments | – | ||
| Maurer 2005;99 2005100 | |||
|---|---|---|---|
|
Titles: (1) Long-term results of palatal implants for primary snoring; (2) Palatal implants for primary snoring: short-term results of a minimally invasive surgical technique Country: Germany Setting: Sleep Disorders Centre, Departments of Otorhinolaryngology, Head and Neck Surgery Study design: Pre–post |
|||
| Interventions | |||
|
Intervention: Palatal stiffening under local anaesthesia. Three implants (18 mm in length and 1.5 mm in diameter) were placed in parallel into the soft palate near the junction of the soft and hard palate. Correct positioning was verified by palpation and transnasal pharyngoscopy post implantation. For the first 19 patients the anti-snoring device was used, with the Pillar Palatal Implant System (Restore Medical, St Paul, MN) used for subsequent patients Concurrent treatment: All patients were prescribed paracetamol and used it for 1–4 days maximally depending on their pain level. No patients needed narcotic analgesics or non-steroidal anti-inflammatory drugs. No patients were required to take time off work Previous treatment(s): Patients had not undergone previous pharyngeal surgery |
|||
| Participants | |||
|
Total n = 40 If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS (including test details): One night of fully attended PSG in the sleep disorders centre was performed according to standard criteria in every patient before the initiation of the therapy; the AI, HI, RDI, ODI, mean O2 saturation, lowest O2 saturation and the sleep efficiency (SE) were measured; those with RDI ≤ 15/hour were included. Patients underwent a second PSG 12 weeks after the procedure. Snoring was recording using the SNAP system with a microphone attached to an oronasal cannula. The snoring index (number of snores per hour), primary vibration frequency (Hz) (fundamental frequency of all snoring events), palatal vibration frequency (Hz) (frequency of all velum-like snoring events); percentage of velum-like snores (types I and II), resistance occurrence index (percentage of all respiratory events whose spectral profile suggests increased resistance to airflow) and maximum relative loudness (dB) (loudness of loudest 10% of all snores) were calculated Tests to assess the site of airway narrowing: Clinical examination including rigid and fibreoptic endoscopy during wakefulness Inclusion criteria: Age between 18 and 80 years; snoring due to palatal flutter; RDI ≤ 15/hour; BMI < 30 kg/m2; patient seeking treatment for snoring; provided informed consent; length of soft palate ≥ 25 mm; no simultaneous participation in another clinical study during the last 6 months Exclusion criteria: OSAS or upper airway resistance syndrome; pregnancy; breastfeeding women; drug abuse; acute infection of the respiratory tract; dysphagia or speech disorder; neurological or psychiatric disorder; nasal polyps or symptomatic septal deviation; previous history of pharyngeal surgery for snoring; previous history of radiation therapy to the upper respiratory tract Subgroups: NA |
|||
| Patient baseline characteristics | |||
| n | 40 | ||
| Age (years), mean ± SD (range) | 42.1 ± 9.0 (26–61) | ||
| Male, n (%) | Unclear | ||
| BMI (kg/m2), mean ± SD (range) | 25.2 ± 2.5 (20.2–29.7) | ||
| Neck circumference (cm), mean ± SD | 38.0 ± 3.4 | ||
| ESS score, mean ± SD | 6.1 ± 3.2 | ||
| Smokers, n (%) | NR | ||
| Snoring score (partner, VAS; n = 32), mean | 7.1 | ||
| History of chronic snoring (years), mean ± SD | 9.7 ± 7.9 | ||
| PSG parameters: | |||
| AI (events/hour), mean ± SD | 0.7 ± 0.8 | ||
| HI (events/hour), mean ± SD | 3.0 ± 2.2 | ||
| AHI (events/hour), mean ± SD | 3.7 ± 2.3 | ||
| ODI (events/hour), mean ± SD | 3.4 ± 2.9 | ||
| Mean O2 saturation during recording (%), mean ± SD | 94.6 ± 1.8 | ||
| Minimal O2 saturation during recording (%), mean ± SD | 89.8 ± 4.1 | ||
| Sleep efficiency (%), mean ± SD | 88.2 ± 8.1 | ||
| Snoring analysis (SNAP recording) (n = 21): | |||
| Snoring index (events/hour), mean ± SD | 273 ± 178 | ||
| Primary vibration frequency (Hz), mean ± SD | 107 ± 59 | ||
| Palatal vibration frequency (Hz), mean ± SD | 82 ± 19 | ||
| Velum-like snores (types I and II) (%), mean ± SD | 81 ± 25 | ||
| Resistance occurrence index (%), mean ± SD | 25 ± 16 | ||
| Maximum relative loudness (dB), mean ± SD | 15 ± 7 | ||
| Functional parameters: | |||
| Speech VAS, mean ± SD | 0.7 ± 1.8 | ||
| Swallowing VAS, mean ± SD | 0.4 ± 0.6 | ||
| Pain VAS, mean ± SD | 4.9 ± 3.3 | ||
| Outcome measures | |||
|
Outcome 1: PSG results (AI, HI, AHI, ODI, O2 mean, O2 min, sleep efficiency) recorded at day 90. Definition of treatment success: NR Outcome 2: Snoring index assessed with SNAP recording at day 90. Definition of treatment success: NR Outcome 3: Other snoring analysis results assessed with SNAP recording at day 90 (primary vibration frequency, palatal vibration frequency, velum-like snores types I and II, resistance occurrence index, maximum relative loudness). Definition of treatment success: NR Outcome 4: Snoring score assessed by the partner using a 10-cm VAS. Definition of treatment success: a decrease or increase of less than 1 cm on the 10-cm VAS after surgery was considered as unchanged; a decrease of 1 cm or more was considered as a response and any increase greater than 1 cm as a non-response; if the score decreased below 3 cm treatment was considered a success; if there was an initial response to treatment at day 90, an increase of 3 cm after 1 year was considered as a relapse Outcome 5: Treatment success. Definition of treatment success: as above Outcome 6: ESS score (daytime sleepiness and fatigue score). Definition of treatment success: NR Outcome 7: Functional parameters (postoperative pain, swallowing and speech difficulties) assessed by 10-cm VAS. Definition of treatment success: NR Covariates: The correlation of change in any of the SNAP parameters with change in the snoring score VAS was explored Total length of follow-up: 360 days Follow-up assessment times: Baseline, days 90, 180 and 360. PSG and SNAP recordings were performed at baseline and day 90 Rate of attrition at each follow-up time: 8/40 at all time points for VAS snoring score, 19/40 for baseline and 90-day SNAP recordings Methods of statistical analysis: Paired Student’s t-test for pre–post comparisons; for non-parametric data the Wilcoxon signed rank test |
|||
| Results | |||
| Outcome 1: PSG parameter results at day 90 | |||
| n (in analysis) | 40 | ||
| AI (events/hour), mean ± SD | 1.1 ± 1.4; p = NS | ||
| HI (events/hour), mean ± SD | 4.5 ± 4.7; p < 0.05 | ||
| AHI (events/hour), mean ± SD | 5.5 ± 5.4; p < 0.05 | ||
| ODI (events/hour), mean ± SD | 5.3 ± 5.1; p = NS | ||
| O2 mean (%), mean ± SD | 94.3 ± 1.7; p = NS | ||
| O2 min (%), mean ± SD | 87.1 ± 5.8; p < 0.05 | ||
| Sleep efficiency (%), mean ± SD | 83.7 ± 12.1; p = NS | ||
| Outcome 2: Snoring index at day 90 | |||
| n (in analysis) | 21 | ||
| Snoring index (events/hour), mean ± SD | 276 ± 172 | ||
| Outcome 3: Other SNAP recording results at day 90 (primary vibration frequency, palatal vibration frequency, velum-like snores type I and II, resistance occurrence index, maximum relative loudness). | |||
| n (in analysis) | 21 | ||
| Primary vibration frequency (Hz), mean ± SD | 110 ± 59; p = NS | ||
| Palatal vibration frequency (Hz), mean ± SD | 80 ± 30; p = NS | ||
| Velum-like snores (types I and II) (%) mean ± SD | 85 ± 24; p = NS | ||
| Resistance occurrence index (%), mean ± SD | 23 ± 14; p = NS | ||
| Maximum relative loudness (dB) mean ± SD | 16 ± 6; p = NS | ||
| Outcome 4: Snoring score | |||
| n (in analysis) | 32 | ||
| Snoring score VAS at: | |||
| Day 90, mean ± SD | 4.2 ± 2.7; p < 0.05 | ||
| Day 180, mean ± SD | 4.0 ± 2.5; p < 0.05 | ||
| Day 360, mean ± SD | 4.8 ± 2.6; p < 0.05 | ||
| Outcome 5: Treatment success (patient’s snoring evaluated by bed partner using a 10-cm VAS) | |||
| n (in analysis) | 32 | ||
| Patients with success at: | |||
| Day 90, n (%) | 13 (41) | ||
| Day 180, n (%) | 11 (34) | ||
| Day 360, n (%) | 7 (22) | ||
| Patients with a response achieved at: | |||
| Day 90, n (%) | 23 (72) | ||
| Day 180, n (%) | 20 (63) | ||
| Day 360, n (%) | 22 (69) | ||
| Reduction in VAS snoring score from baseline to day 360, mean ± SD | 2.2 ± 2.5 (for the 32 patients); 2.8 ± 1.5 (for the 10 patients who experienced a partial extrusion) | ||
| Outcome 6: ESS score | |||
| n (in analysis) | 32 | ||
| Day 90, mean ± SD | 4.3 ± 3.3; p < 0.05 | ||
| Day 360, mean ± SD | 4.9 ± 3.1; p < 0.05 | ||
| Outcome 7: Postoperative pain and swallowing and speech difficulties at day 90 | |||
| n (in analysis) | 32 | ||
| Speech, mean ± SD | 0.1 ± 0.2; p < 0.05 | ||
| Swallowing, mean ± SD | 0.1 ± 0.4; p = NS | ||
| Pain, mean ± SD | 0.2 ± 0.6; p < 0.05 | ||
|
Postoperative adverse events: All lesions healed without excessive scarring or other relevant sequelae. Implant extrusion: 10 patients; 13/120 (11%) implants Long-term adverse events: No severe adverse events were observed during the follow-up period Need for repeat procedure (unscheduled): Two patients who had two partial extrusions received two new implants |
|||
| Authors’ conclusion | |||
| The data indicate that there is a significant decrease in snoring and daytime sleepiness with the use of palatal stiffening over a period of 1 year | |||
| Methodological assessment criteria | |||
| 1. Study design | Pre–post | ||
| 2. Were the study eligibility criteria specified? | Yes | ||
| 3. Are adequate baseline details presented? | Yes | ||
| 4. Are any co-interventions clearly stated? | NA | ||
| 5. Is compliance with treatment adequate? | Yes | ||
| 6. Were any subgroup analyses justified? | NA | ||
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial (both subjective and objective outcomes assessed) | ||
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial (both subjective and objective outcomes assessed) | ||
| 9. Were all study participants accounted for? | No | ||
| 10. Are greater than 80% of patients included in the follow-up assessment? | No | ||
| 11. Are data analyses appropriate? | Yes | ||
| 12. Are the conclusions supported by the results? | Yes | ||
| 13. Generalisability | Relatively inclusive eligibility criteria | ||
| 14. Intercentre variability | One-centre study | ||
| 15. General comments | – | ||
| Nordgard 200698 | |||||
|---|---|---|---|---|---|
|
Title: Palatal implants for the treatment of snoring: long-term results Country: Norway Setting: Departments of Otolaryngology, Head and Neck Surgery Study design: Pre–post |
|||||
| Interventions | |||||
|
Intervention: Three palatal implants inserted under local anaesthesia. The implant is a braid of polyester filaments 18 mm long and 1.5 mm in diameter. The first implant was inserted in the midline about 5 mm distal to the trailing edge of the hard palate, and the further two implants were inserted 5 mm either side of the midline. Patients were given paracetamol 400 mg/codeine 40 mg and diclofenac 50 mg orally. Local anaesthesia was obtained by topical lidocaine spray and infiltration of the palate with lidocaine/adrenaline solution. No sedation was given. Mean operative time was 8 minutes (range 3–16 minutes) Concurrent treatment: The patients were given penicillin V orally 660 mg three times a day for 7 days as a prophylaxis against infection, and diclofenac 50 mg three times a day as an analgesic if necessary Previous treatment(s) (specific details): NR |
|||||
| Participants | |||||
|
Total n = 35 (34 in the analysis) If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS: PSG performed with a thin transnasal oesophageal catheter with pressure transducers combined with pulse oximetry and an actimeter (Reggie system; Camtech AS, Sandvika, Oslo, Norway). The airflow in the nose, oropharynx and hypopharynx was calculated from the differential pressures in the locations. Apnoeas were defined as an airflow of less than 10% of baseline and hypopnoea as a greater than 50% reduction in airflow, both for a duration of 10 seconds and a 3% drop in SaO2. The combined apnoea–hypopnoea index (AHI) was recorded and events registered as obstructive, central or mixed Tests to assess the site of airway narrowing: Transnasal fibreoptic laryngoscopy and indirect laryngoscopy. On transnasal fibreoptic laryngoscopy the physical dimensions of the upper airway assessed were: (1) the modified Mallampati index (MMP) grades I–IV; (2) tonsil size grades 0–IV according to the Friedman criteria; (3) tongue base volume related to the vallecula grades I–IV (grade I: open vallecula; grade II: vallecula filled; grades III and IV: epiglottis pushed posteriorly or against the posterior pharyngeal wall). On indirect laryngoscopy the visibility of the larynx was assessed according to (1) anterior commissure visible (2) posterior commissure visible and (3) not visible Inclusion criteria: Age > 18 years; AHI < 10; BMI < 30 kg/m2; soft palate length > 25 mm; tonsil size < 50% of airway; no significant nasal stenosis; bed partner present Exclusion criteria: NR Subgroups: NA |
|||||
| Patient baseline characteristics | |||||
| n | 34 | ||||
| Age (years), mean (range) | 43.7 (23–67) | ||||
| Male, n (%) | 26 (76) | ||||
| BMI (kg/m2), mean ± SD | 26.1 ± 2.3 | ||||
| AHI score, mean ± SD | 2.2 ± 2.3 | ||||
| ESS score, mean ± SD | 9.3 ± 4.1 | ||||
| Smokers, n (%) | NR | ||||
| Snoring intensity (partner, VAS), mean ± SD | 7.1 ± 2.1 | ||||
| Pain score (VAS), mean | 0.6 | ||||
| Swallowing difficulties (VAS), mean | 0.8 | ||||
| Speech difficulties (VAS), mean | 0.4 | ||||
| Outcome measures | |||||
|
Outcome 1: AHI score. Definition of treatment success: NR Outcome 2: Snoring intensity reported by bed partner measured on a VAS ranging from 0 ‘no snoring’ to 10 ‘intensity that causes the partner to leave the bedroom’. Definition of treatment success: NR Outcome 3: Treatment success according to criteria of partner satisfaction, patient satisfaction, VAS reduction > 50%, VAS < 5 and VAS < 3. Definition of treatment success: NR Outcome 4: ESS score. Definition of treatment success: NR |
|||||
|
Outcome 5: Postoperative pain scores measured on a VAS ranging from 0 to 10. Definition of treatment success: NR Outcome 6: Postoperative speech problems measured on a VAS ranging from 0 to 10. Definition of treatment success: NR Outcome 7: Postoperative swallowing problems measured on a VAS ranging from 0 to 10. Definition of treatment success: NR Covariates: The association of partner satisfaction with snoring reduction (VAS) and the physical parameters of soft palate length, MMP I–IV, larynx visibility I/II, tonsil grades I–IV, uvula grades I–IV and change in BMI was explored Total length of follow-up: 360 days Follow-up assessment times: 2–3 days, 14 days, 30 days, 90 days, 180 days and 360 days Rate of attrition at each follow-up time: For AHI: 1/35 at all of the visits except for the one at 360 days postoperatively at which it was 5/35 (30 patients completed the repeat PSG); for VAS scale of snoring intensity: 1/35 at each follow-up time; the patient was excluded from the study because of a tonsillectomy in the observation period Methods of statistical analysis: The Wilcoxon signed rank test was used for analysis of paired data (VAS scores and ESS scores) and a paired t-test when data had a normal distribution (AHI and BMI). Mann–Whitney U test was used to compare data from two independent samples (satisfaction of extrusion related to physical parameters and snoring-related symptoms). When these data had a normal distribution a t-test was used. Chi-squared test was used for analysis of categorical data in two groups. p-values ≤ of 0.05 were considered significant |
|||||
| Results | |||||
| Outcome 1: AHI score | |||||
| n (in analysis) | 30 | ||||
| AHI score, mean ± SD | 3.3 ± 3.8 (at day 360 after the surgery); p = NS | ||||
| Outcome 2: VAS score for snoring intensity, mean ± SD | |||||
| n (in analysis) | 34 | ||||
| 2–3 days postoperatively | 6.4 ± 2.7 | ||||
| 14 days postoperatively | 5.1 ± 2.5 | ||||
| 30 days postoperatively | 4.5 ± 2.5 | ||||
| 90 days postoperatively | 3.4 ± 2.1 | ||||
| 180 days postoperatively | 3.6 ± 2.1 | ||||
| 360 days postoperatively | 4.8 ± 3.1; change from baseline: p < 0.001 | ||||
| Outcome 3: Treatment success according to different criteria | |||||
| Time | Partner satisfaction, n (%) | Patient satisfaction, n (%) | VAS reduction > 50%, n (%) | VAS < 5 (VAS < 3 included), n (%) | VAS < 3, n (%) |
| 6 months | 28/34 (82.3) | 31/34 (91.2) | 17/34 (50) | 24/34 (70.6) | 8/34 (52.9) |
| 12 months | 24/34 (70.6) | 27/34 (79.7) | 13/34 (38.2) | 17/34 (50) | 8/34 (23.5) |
| Recurrence | 4/28 (14.3) | 4/31 (12.9) | 7/17 (41.2) | 8/24 (33.3) | 12/18 (66.7) |
| Outcomes 4–7 | |||||
| n (in analysis) | 34 | ||||
| ESS score, mean ± SD | 5.6 ± 3.8 (at 360 days); p < 0.001 | ||||
| Postoperative pain score (VAS), mean: | |||||
| Day 2 | 2.0 | ||||
| Day 14 | 0.9 | ||||
| Day 30 | 0.7 | ||||
| Postoperative swallowing difficulties (VAS), mean: | |||||
| Day 2 | 3.0 | ||||
| Day 14 | 0.7 | ||||
| Day 30 | 0.4 | ||||
| Postoperative speech difficulties (VAS), mean: | |||||
| Day 2 | 0.9 | ||||
| Day 14 | 0.5 | ||||
| Day 30 | 0.2 | ||||
|
Postoperative adverse events: Partial extrusion: 6/34 (17.6%) patients and 9/102 (8.8%) implants. One patient had a minor oedema at the base of the uvula. Two patients reported a mild transient metal taste Use of postoperative analgesics: Mean use of prescribed analgesics 1.3 days (range 0–6 days). Mean total dose of diclofenac 50 mg = 2.1 pills (range 0–15 pills). Eight of the patients (24%) did not take any analgesics at all Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||||
| Authors’ conclusions | |||||
| The palatal implant system is safe, is associated with very low patient morbidity and results in virtually no tissue damage. The effectiveness in treating snoring is comparable to other surgical methods | |||||
| Methodological assessment criteria | |||||
| 1. Study design | Pre–post | ||||
| 2. Were the study eligibility criteria specified? | Yes | ||||
| 3. Are adequate baseline details presented? | Partial | ||||
| 4. Are any co-interventions clearly stated? | Unclear | ||||
| 5. Is compliance with treatment adequate? | Yes | ||||
| 6. Were any subgroup analyses justified? | NA | ||||
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial (a mixture of both objective and subjective outcomes were assessed) | ||||
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial (a mixture of both objective and subjective outcomes were assessed) | ||||
| 9. Were all study participants accounted for? | No | ||||
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||||
| 11. Are data analyses appropriate? | Yes | ||||
| 12. Are the conclusions supported by the results? | Yes | ||||
| 13. Generalisability | Relatively inclusive eligibility criteria | ||||
| 14. Intercentre variability | One-centre centre | ||||
| 15. General comments | – | ||||
| Skjostad 200697 | |||||
|---|---|---|---|---|---|
|
Title: Consequences of increased rigidity in palatal implants for snoring: a randomized controlled study Country: Norway Setting: Departments of Otolaryngology/Head and Neck Surgery Study design: RCT |
|||||
| Interventions | |||||
|
Intervention 1: Palatal stiffening – regular implants (rigidity 1.0) with Pillar implant system. Three polyethylene terephthalate (PET) implants were placed sagittally in the muscular layer of the soft palate entering just below the posterior end of the hard palate with the patient under local anaesthesia. The first implant was inserted in the midline, followed by the other two approximately 5 mm laterally to the midline on each side Intervention 2: Palatal stiffening – stiffer implants (rigidity 1.8) with Pillar implant system. Three PET implants were placed in the soft palate with the patient under local anaesthesia. The first implant was inserted in the midline, followed by the other two approximately 5 mm laterally to the midline on each side All procedures were performed as a single one-stage procedure. Mean operating time was 7.4 minutes Concurrent treatment: All patients were given penicillin V 1 mg three times orally for 1 week to prevent infection Previous treatment(s): NR |
|||||
| Participants | |||||
|
Total n = 20 Number of non-apnoeic snorers included: 20 Tests to exclude OSAS: PSG; details of the test were not reported. Patients with AHI > 5 were excluded from the study Tests to assess the site of airway narrowing: All patients underwent a clinical examination including fibreoptic nasopharyngolaryngoscopy Inclusion criteria: Age > 18 years; AHI ≤ 5; BMI < 30 kg/m2; palatal length ≥ 25 mm; social snoring due to palatal flutter; tonsil hypertrophy < 50% of airway; no significant nasal obstruction; no previous history of pharyngeal surgery; bed partner present Exclusion criteria: NR Subgroups: NA |
|||||
| Patient baseline characteristics | |||||
| Regular implants | Stiffer implant | ||||
| On two different days | On each operating day | On two different days | On each operating day | ||
| n | 5 | 5 | 5 | 5 | |
| Age (years), mean (range) | 44.1 (29–61) | ||||
| Male, n (%) | 12 (60) | ||||
| BMI (kg/m2), mean (range) | 25.1 (21.4–28.9) | ||||
| AHI score, mean (range)a | 2.27 (0.2–5.3) | ||||
| ESS score, mean (range) | NR | ||||
| Smokers, n (%) | NR | ||||
| Snoring intensity (VAS), mean | 8.1 | ||||
| Outcome measures | |||||
|
Outcome 1: Snoring intensity (partner-assessed VAS). Definition of treatment success: the snoring intensity was evaluated on a scale from 0 ‘no snoring’ to 10 ‘an intensity that causes the partner to leave the bedroom’ Outcome 2: Patient satisfaction. Definition of treatment success: ‘patient would recommend treatment’, ‘undecided’ or ‘patient would not recommend treatment’ Outcome 3: Bed partner satisfaction. Definition of treatment success: ‘bed partner would recommend treatment’, ‘undecided’ or ‘bed partner would not recommend treatment’ Covariates: NR Total length of follow-up: 180 days Follow-up assessment times: 24 hours, 72 hours, 2 weeks, 30 days, 90 days and 180 days. PSG at 180 days after the treatment Rate of attrition at each follow-up time: 0 |
|||||
| Results | |||||
| Outcome 1: Snoring intensity (VAS)b | |||||
| Regular implants | Stiffer implants (rigid implants) | Difference between groups | |||
| n (in analysis) | 10 | 10 | |||
| Snoring intensity (VAS), mean | 4.7 (preoperative vs postoperative: p < 0.01) | 6.1 (preoperative vs postoperative: p = 0.053) | NR | ||
| Outcome 2: Patient satisfaction (the patients and their partners were asked if they would recommend the treatment to a friend or family member) | |||||
| Regular implants | Stiffer implants | Difference between groups | |||
| n (in analysis) | 10 | 10 | |||
| Patients who were satisfied and would recommend treatment, n (%) | 8 (80) | 2 (20) | NR | ||
| Patients who were undecided, n (%) | 2 (20) | 6 (60) | NR | ||
| Patients who would not recommend treatment, n (%) | 0 | 2 (20) | NR | ||
| Outcome 3: Bed partner satisfaction | |||||
| Regular implants | Stiffer implants | Difference between groups | |||
| n (in analysis) | 10 | 10 | |||
| Partners who were satisfied and would recommend treatment, n (%) | 5 (50) | 2 (20) | NR | ||
| Partners who were undecided, n (%) | 4 (40) | 3 (30) | NR | ||
| Outcome 4: Implant extrusions | |||||
| Regular implants | Stiffer implants | Difference between groups | |||
| n (in analysis) | 10 | 10 | |||
| Implant extrusions, n (%) | 0 | Patients 4 (40), extrusions 5 (17) | p < 0.05 | ||
|
Postoperative adverse events: Pain: the postoperative pain reported was mild, often compared with a mild infection of the throat that resolved in a couple of days; 11 (55%) patients did not take any pain medication at all; one patient reported tooth pain in a molar over a period of 5 days. Extrusions (see above table): four patients reported a total of five partial implant extrusions; all extrusions were observed in the group implanted with rigid implants (p < 0.05) Long-term adverse events: NR Need for repeat procedure (unscheduled): NR |
|||||
| Authors’ conclusions | |||||
| Rigid implants cause short time extrusions with loss of treatment effect. Regular implants reduce palatal snoring intensity with high patient and bed partner satisfaction | |||||
| Methodological assessment criteria | |||||
| 1. Study design | RCT | ||||
| 2. Were the study eligibility criteria specified? | Yes | ||||
| 3. Was a power calculation performed? | No | ||||
| 4. Is the sample size adequate? | Unclear | ||||
| 5. Is the number randomised stated? | Yes | ||||
| 6. Is the study properly randomised?c | Unclear | ||||
| 7. Is allocation of treatment concealed?d | Unclear | ||||
| 8. Are adequate baseline details presented? | Partial for the whole group only | ||||
| 9. Are groups similar at baseline? | Unknown | ||||
| 10. Are any baseline imbalances adequately adjusted for in the analysis? | Unclear | ||||
| 11. Are similar co-interventions administered? | Not reported | ||||
| 12. Are patients blinded to treatment allocation? | Yes | ||||
| 13. Are outcome assessors blinded? | Unclear | ||||
| 14. Is compliance with treatment adequate? | Yes | ||||
| 15. Were any subgroup analyses justified? | NA | ||||
| 16. Were data collection tools shown or known to be valid for the outcome of interest?e | Yes | ||||
| 17. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?f | Yes | ||||
| 18. Were all study participants accounted for? | Yes | ||||
| 19. Are data analyses appropriate? | Yes | ||||
| 20. Is analysis conducted on an intention to treat basis? | NA | ||||
| 21. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||||
| 22. Are the conclusions supported by the results? | Baseline heterogeneity unknown; small group of subjects | ||||
| 23. Generalisability | Inclusive eligibility criteria | ||||
| 24. Intercentre variability | One-centre study | ||||
| 25. General comments | – | ||||
Studies on continuous positive airway pressure
| Series 1994112 | |||||
|---|---|---|---|---|---|
|
Title: Changes in snoring characteristics after 30 days of nasal continuous positive airway pressure in patients with non-apnoeic snoring: a controlled trial Country: Canada Setting: Department of Pulmonology Study design: Two-group parallel pre–post study |
|||||
| Interventions | |||||
|
Intervention 1: Nasal continuous positive airway pressure (NCPAP). The positive pressure level was increased until snoring was abolished and treatment continued for 30 days. The mean effective NCPAP level was 5.3 (SD 0.5) cmH2O (range 3–8 cmH2O) Intervention 2: No intervention Concurrent treatment: NR Previous treatment(s): No previous treatment undergone; no patients were taking medication at the time of the study. Patients were told to avoid alcohol consumption for a minimum of 12 hours before each recording session |
|||||
| Participants | |||||
|
Total n = 18 (NCPAP, n = 9; no intervention, n = 9) If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS (including test details): Overnight PSG with snoring measurement, including determination of sleep stages (electroencephalogram C4A1, C3A2; electro-oculogram; submental electromyogram), nasal and mouth airflow with thermocouples, SaO2, electrocardiogram and thoracoabdominal movements by respiratory inductive plethysmography. The snoring sound pressure level (SPL) was displayed continuously. Sleep position was determined by visual monitor using an infrared camera. An arousal was defined as the simultaneous transition to a lighter sleep stage with eye movements and an increase in electromyographic activity of less than 15 seconds. Snoring was defined as a spike in breathing sound intensity greater than 60 dB SPL. For each recording a computer interpretation of the sound recording gave the snoring index (number of snoring episodes/hour of sleep), the total sleep time (TST) spent at the different SPL values in 3-dB steps above 60 dB (60–72 dB SPL), and the mean snoring level Tests to assess the site of airway narrowing: NR Inclusion criteria: History of regular snoring; free from upper airway infection throughout the study; PSG study to exclude OSAS Exclusion criteria: NR Subgroups: NA |
|||||
| Patient baseline characteristics | |||||
| NCPAP | No treatment | ||||
| n | 18 | ||||
| Age (years), range | 25–64 | ||||
| Male, n (%) | 16 (88.9) | ||||
| BMI (kg/m2), mean ± SD | 29.1 ± 4.24 | ||||
| Smokers, n (%) | 4 (22.2) | ||||
| Total sleep time (hours), mean ± SD | 5.7 ± 0.9 | 6.2 ± 0.6 | |||
| Stages I–II (% total sleep time), mean ± SD | 71.9 ± 3.6 | 72.0 ± 4.5 | |||
| Stages III–IV (% total sleep time), mean ± SD | 13.8 ± 2.7 | 15.0 ± 4.8 | |||
| Stages REM (% total sleep time), mean ± SD | 14.2 ± 1.5 | 13.0 ± 2.7 | |||
| AHI (events/hour), mean ± SD | 2.9 ± 3.9 | 4.5 ± 3.9 | |||
| Arousal index (events/hour), mean ± SD | 9.7 ± 3.9 | 8.6 ± 4.8 | |||
| Supine (% total sleep time), mean ± SD | 40.1 ± 31.2 | 49.0 ± 27.0 | |||
| Snoring index (events/hour), mean ± SD | 387 ± 150 | 380 ± 108 | |||
| % TST > 60 dB SPL, mean ± SD | 10.3 ± 5.4 | 11.1 ± 6.0% | |||
| Mean snoring level (dB SPL), mean ± SD | 66.4 ± 0.9 | 65.6 ± 0.9 | |||
| Outcome measures | |||||
|
Outcome 1: TST. Definition of treatment success: NR Outcome 2: Stages I–II (% TST). Definition of treatment success: NR Outcome 3: Stages III–IV (% TST). Other outcome measures: NR Outcome 4: Stages REM (% TST). Definition of treatment success: NR Outcome 5: AHI (events/hour). Definition of treatment success: NR Outcome 6: Arousal index (events/hour). Definition of treatment success: NR Outcome 7: Supine (% TST). Definition of treatment success: NR Outcome 8: Snoring index (events/hour). Definition of treatment success: NR Outcome 9:% TST > 60 dB SPL. Definition of treatment success: NR Outcome 10: Mean snoring level (dB SPL) Covariates: To determine whether the results could be explained by differences in body position between sleep studies the relation between snoring characteristics (snoring index, % TST > 60 dB SPL, mean snoring level) and the % TST supine were explored (no correlation between these variables at baseline and at the follow-up visits was found) Total length of follow-up: 38–40 days Follow-up assessment times: 30 days; subgroup (n = 6) also at 38–40 days Rate of attrition at each follow-up time: Three patients withdrew in the NCPAP group after a few days of treatment because of discomfort. They were replaced by patients with a similar snoring index Methods of statistical analysis: Baseline results of the two groups were compared using the unpaired t-test. In the control group baseline and follow-up results were compared with a paired t-test. The results obtained at the different follow-up visits in the NCPAP group were compared with baseline values by multivariate analysis of variance followed by Tukey’s test for multiple comparison for each variable. The individual values of the percentage TST spent at the different noise levels were dependent; the significance threshold was determined according to the Bonferroni criteria (p < 0.01) |
|||||
| Results | |||||
| Outcome 1: TST (intervention 1 and 2 results all insignificant compared with baseline) | |||||
| Intervention 1 (on NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Difference between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| TST, mean ± SD | 5.7 ± 0.9; p = NS | 6.0 ± 0.3; p = NS | 6.1 ± 1.5; p = NS | 6.3 ± 0.9; p = NS | NR |
| Outcome 2: Stages I–II (% TST) (intervention 1 and 2 results all insignificant compared with baseline) | |||||
| Intervention 1 (NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Difference between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| Stages I–II (% TST), mean ± SD | 71.1 ± 3.6; p = NS | 72.3 ± 4.2; p = NS | 72.1 ± 3.0; p = NS | 71.9 ± 3.6; p = NS | NR |
| Outcome 3: Stages III–IV (% TST) (intervention 1 and 2 results all insignificant compared with baseline) | |||||
| Intervention 1 (NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Difference between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| Stages III–IV (% TST), mean ± SD | 14.6 ± 2.7; p = NS | 13.0 ± 3.3; p = NS | 13.7 ± 2.1; p = NS | 14.4 ± 2.4 | NR |
| Outcome 4: Stages REM (% TST) (intervention 1 and 2 results all insignificant compared with baseline) | |||||
| Intervention 1 (NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Difference between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| Stages REM (% TST), mean ± SD | 14.3 ± 3.0; p = NS) | 14.6 ± 2.7; p = NS | 14.2 ± 3.0; p = NS | 13.7 ± 3.3; p = NS | NR |
| Outcome 5: AHI (intervention 1 and 2 results all insignificant compared with baseline) | |||||
| Intervention 1 (NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Difference between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| AHI (events/hour), mean ± SD | 0.2 ± 0.6 | 1.0 ± 1.5; p = NS | 1.1 ± 1.5; p = NS | 5.1 ± 3.6 | NR |
| Outcome 6: Arousal index (intervention 1 and 2 results all insignificant compared with baseline) | |||||
| Intervention 1 (NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Difference between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| Arousal index (events/hour), mean ± SD | 3.7 ± 2.40; p = NS | 8.2 ± 4.2; p = NS | 6.9 ± 4.8; p = NS | 9.9 ± 5.1 | NR |
| Outcome 7: Supine (% TST) (intervention 1 and 2 results all insignificant compared with baseline) | |||||
| Intervention 1 (NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Difference between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| Supine (% TST), mean ± SD | 21.0 ± 15.0 | 29.2 ± 20.1; p = NS | 16.0 ± 14.4 | 42.3 ± 20.4 | NR |
| Outcome 8: Snoring index | |||||
| Intervention 1 (NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Difference between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| Snoring Index (events/hour), mean ± SD | 15.1 ± 7.5; p = significant | 320 ± 171; p = NS | 374 ± 181.3; p = NS | 388 ± 201; p = NS | NR |
| Outcome 9: % TST > 60 dB SPL | |||||
| Intervention 1 (NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Difference between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| % TST > 60 dB SPL, mean ± SD | – | 7.4 ± 1.5; p = 0.02a | 9.8 ± 2.1; p = NS | 10.5 ± 2.3; p = NS | NR |
| Outcome 10: Mean snoring sound pressure level (dB) | |||||
| Intervention 1 (NCPAP) | Intervention 1 (first night post NCPAP) | Intervention 1 (8 days post NCPAP) | Intervention 2 (no intervention) | Differences between groups | |
| n (in analysis) | 9 | 9 | 6 | 9 | |
| Mean snoring sound pressure level (dB), mean ± SD | – | 65.0 ± 0.9; p = significant | 65.7 ± 0.98; p = NS | 65.1 ± 1.5; p = NS | |
|
Postoperative adverse events: Three patients withdrew from the NCPAP arm because of discomfort Long-term adverse events: NR Need for repeat procedure (unscheduled): NA |
|||||
| Authors’ conclusions | |||||
| NCPAP improves snoring but this effect is lost soon after stopping treatment | |||||
| Reviewer’s comments | |||||
| It is stated that the study is a controlled trial with random allocation but no between-group comparisons are made. Study design therefore appears to be a two-group parallel pre–post study. Limited study inclusion criteria are reported and only partial participant baseline characteristics are reported. It is therefore unclear how representative the study sample are of patients presenting with primary snoring that would be considered for treatment with CPAP. Three patients out of nine in the CPAP group withdrew because of treatment discomfort and were replaced. It is not clear whether the reported baseline characteristics for participants are from the original sample or from the sample that included the replacement participants. Multiple testing was corrected using Bonferroni criteria. Authors’ conclusions appear to be reasonable; however, it seems that snoring is only minimalised with use of CPAP and returns with CPAP withdrawal, although it does not immediately return to baseline levels | |||||
| Methodological assessment criteria | |||||
| 1. Study design | Two-group parallel pre–post | ||||
| 2. Were the study eligibility criteria specified? | Partial | ||||
| 3. Was a power calculation performed? | No | ||||
| 4. Is the sample size adequate? | No | ||||
| 5. Is the number randomised stated? | Yes | ||||
| 6. Is the study properly randomised?b | No | ||||
| 7. Is allocation of treatment concealed?c | No | ||||
| 8. Are adequate baseline details presented? | Partial | ||||
| 9. Are groups similar at baseline? | Partial | ||||
| 10. Are any baseline imbalances adequately adjusted for in the analysis? | Not applicable (within-group comparisons only) | ||||
| 11. Are similar co-interventions administered? | Unclear | ||||
| 12. Are patients blinded to treatment allocation? | No | ||||
| 13. Are outcome assessors blinded? | No | ||||
| 14. Is compliance with treatment adequate? | Unclear | ||||
| 15. Were any subgroup analyses justified? | Not applicable | ||||
| 16. Were data collection tools shown or known to be valid for the outcome of interest?d | Yes | ||||
| 17. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?e | Unclear | ||||
| 18. Were all study participants accounted for? | No | ||||
| 19. Are data analyses appropriate? | Yes | ||||
| 20. Is analysis conducted on an intention to treat basis? | Yes | ||||
| 21. Are greater than 80% of patients included in the follow-up assessment? | Yes | ||||
| 22. Are the conclusions supported by the results? | Yes | ||||
| 23. Generalisability | Only limited inclusion criteria and baseline characteristics reported –difficult to accurately assess how representative the patient group is of those considered eligible for a trial of CPAP | ||||
| 24. Intercentre variability | One-centre study | ||||
| 25. General comments | – | ||||
Studies on the use of a mandibular advancement splint
| Fransson 2001;110 2003111 | ||
|---|---|---|
|
Titles: (1) Treatment of snoring and obstructive sleep apnea with a mandibular protruding device: an open-label study; (2) Effects of a mandibular protruding device on the sleep of patients with obstructive sleep apnea and snoring problems: a 2-year follow-up Country: Sweden Setting: Department of Stomatognathic Physiology, Postgraduate Dental Education Centre Study design: Pre–post |
||
| Interventions | ||
|
Intervention: A monobloc mandibular advancement splint (MAS) (fabricated in heat-cured methylmetacrylate as two separate splints, which were glued together in a position indicated by an initial wax mould). An attempt was made to advance the mandible 75% of the maximal protrusion range or a minimum of 5 mm. The MAS covered the occlusal surfaces of the canines, premolars and molars and left the edges of the upper incisors free Concurrent treatment: NR Previous treatment(s): A total of 13 patients had undergone previous surgical procedures [UP3, laser uvulopalatoplasty (LUPP) or nasal surgery], 12 had been treated with NCPAP, 6 had lost weight and 30 had previously tried ‘other treatments like sewing a tennis ball on the back of pyjamas’ or a nasal dilator |
||
| Participants | ||
|
Total n at 2-year follow-up: 77 patients (27 non-apnoeic snorers and 50 patients with OSAS); in total, 65 were included in the analysis (21 non-apnoeic snorers and 44 patients with OSAS); 13 non-apnoeic snorers were included in the earlier 6-month follow-up study If this study includes a mixed patient population, number of non-apnoeic snorers included: n = 13 at 6-month follow-up and n = 27 at 2-year follow-up Tests to exclude OSAS: All patients underwent a one-night limited somnographic examination comprising recordings of pulse rate, arterial blood oxygen saturation (SaO2), respiratory movements, intensity and duration of snoring, and body position. Pulse rate and SaO2 were monitored continuously by a pulse oximeter ear probe (Pulsoxy Ohmeda Biox 3740; BOC Ohmeda, Göteborg, Sweden). Respiratory movements were registered using a mattress (Duorec PVDF mattress; C-A Tegner, Bromma, Sweden) that was placed under the bottom sheet in a conventional bed. A digital sound survey meter (Microphone CEL-231; Lucas CEL Instruments, Troy, MI) with a recording range of 30–135 dB recorded the snoring. The microphone was placed 50 cm above the patient’s head when in the prone position. The body position (side or supine) was registered with a body position amplifier (Vitalogs Respiration and Body Position Amplifier, Scan-Med A/S, Drammen, Norway). The same medical sleep specialist analysed all individual data in detail through all hours of sleep Tests to assess the site of airway narrowing: Fibreoptic pharyngoscopic examination including Muller’s manoeuvre. The degree of hypopharyngeal collapse was estimated subjectively and relative to the entire hypopharyngeal cross-sectional area as more or less than 50%. A subjective estimate on the presence or absence of tongue base hyperplasia was also made by visual inspection of the mouth Inclusion criteria: Complaints of snoring and/or a diagnosis of OSAS; sufficient teeth to enable the retention of the MAS Exclusion criteria: Maximal protrusion ability < 6 mm; indications for bi-level positive airway pressure (BIPAP) or tracheotomy; periodontally compromised dentition Subgroups: non-apnoeic snorers and OSAS |
||
| Patient baseline characteristics | ||
| n | 27 (total number of non-apnoeic snorers) | |
| Age, mean (range)a | 52 (37–70) | |
| Male, n (%)a | 14/21 (66.67) | |
| BMI (kg/m2), mean (range)a | 28 (range 23–35) | |
| Neck size (cm), mean (range)a | 39.9 (range 34–46) | |
| ODI score, mean (range) | 1.3 (0 – 3.8) | |
| SaO2 nadir (%), mean (range) | 91.5 (82.5–97.5) | |
| Snoring sound (dB) | 63.5 (no range or SD reported) | |
| Smokers, n (%) | NR | |
| Outcome measures | ||
|
The outcomes assessed for the overall patient population were: (1) degree of complaints of snoring and/or apnoea; (2) experience of MAS as a foreign object in the mouth; (3) assessment of treatment effect of MAS on snoring and/or apnoea; (4) awareness of loud and disruptive snoring; (5) night-time awakening; (6) excessive daytime sleepiness; (7) compliance Only results for the snoring sound score (6-month follow-up), ODI and SaO2 nadir (2-year follow-up) were reported separately for the non-apnoeic snorer subgroup Outcome 1: ODI (2-year follow-up results). Definition of treatment success: NR. Outcome 2: SaO2 nadir (2-year follow-up results). Definition of treatment success: NR Outcome 3: Snoring sound score (6-month follow-up results). Definition of treatment success: NR Covariates: NR Total length of follow-up: Follow-up was conducted at 6 months (snoring sound score) and 2 years Follow-up assessment times: 6 months and 2 years Rate of attrition at each follow-up time: Overall attrition at 2-year follow-up: 12 (six non-apnoeic snorers and six patients with OSAS); four patients had received CPAP, two had undergone surgery, three were lost to follow-up, one lost 35 kg in weight and two withdrew because of device intolerance Methods of statistical analysis: Two-tailed paired t-test with the null hypothesis of no difference between baseline (without MAS) and follow-up (with MAS) was performed on continuous measures; the McNemar test was used for dichotomous and dichotomised discrete variables; the Wilcoxon signed rank test was used to evaluate the long-term effects of the questionnaire outcome with and without MAS |
||
| Results | ||
| Outcomes 1 and 2: ODI and SaO2 (2-year follow-up) | ||
| n (in analysis) | 27 | |
| ODI, mean (range) | 0.8 (0–7) | |
| SaO2 nadir (%), mean (range) | 92.6 (90.4–96.0) | |
| Outcome 3: Snoring sound score (6-month follow-up) | ||
| n (in analysis) | 13 | |
| Snoring sound score (dB), mean | 57.5 (no range or SD reported) | |
|
Short-term adverse events: NR Long-term adverse events: NR Need for repeat procedure (unscheduled): NA |
||
| Authors’ conclusions | ||
| MAS treatment is associated with a significant reduction in subjective complaints such as disturbing snoring, apnoeas, daytime tiredness and poor quality of night sleep. In addition, favourable 6-month results were unchanged after 2 years | ||
| Reviewer’s comments | ||
| Only very limited baseline details are reported for the non-apnoeic snoring subgroup. Likewise, only the outcomes of ODI, SaO2 nadir and snoring sound score are reported by subgroup. The study uses both objective and subjective outcome measures | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | Yes | |
| 3. Are adequate baseline details presented? | Partial | |
| 4. Are any co-interventions clearly stated? | Unclear | |
| 5. Is compliance with treatment adequate? | Partial | |
| 6. Were any subgroup analyses justified? | Yes | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?b | Partial | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?c | Unclear | |
| 9. Were all study participants accounted for? | Yes | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |
| 11. Are data analyses appropriate? | Yes | |
| 12. Are the conclusions supported by the results? | Partly, but appear to be overly optimistic about the treatment effect in all patients. Only two-thirds of patients were treatment responders. BMI is higher in treatment non-responder group | |
| 13. Generalisability | Only limited baseline details are reported on the non-apnoeic snoring subgroup. Not possible to assess the generalisability of this patient group | |
| 14. Intercentre variability | NA | |
| 15. General comments | – | |
| Smith 2004113 | ||
|---|---|---|
|
Title: Non-apneic snoring and the orthodontist: the effectiveness of mandibular advancement splints Country: UK Setting: Orthodontic Department Study design: Pre–post |
||
| Interventions | ||
|
Intervention: Adjustable Herbst mandibular advancement splint (MAS). The appliance was designed to advance the mandible by the maximum comfortable amount of protrusion possible, with minimum vertical opening. An advancement of at least 5 mm was attempted Concurrent treatment: NA Previous treatment(s): NR |
||
| Participants | ||
|
Total n = 35 (11 were included in the pre and post overnight domiciliary sleep recordings) If this study includes a mixed patient population, number of non-apnoeic snorers included: NA Tests to exclude OSAS: Snoring noise levels, O2 saturation and pulse rate were recorded utilising a microphone connected to a noise level meter and a pulse oximeter (Ohmeda Biox 3740, Datex-Ohmeda, Hatfield, UK). The microphone, which recorded respiratory sound levels, was placed at the same vertical height and approximately 50 cm from the subject’s head. Participants were required to secure the pulse oximeter finger probe to their index finger, switch the microphone on and start the computer. An analogue to digital converter (ADC PL4.02) was used to transfer the data to a laptop computer, where up to 8 hours of sound profile and O2 saturation data were synchronised and stored using a specialist software program. Participants were asked to abstain from alcohol on the evenings of the recordings. Respiratory noise levels were assessed at the 95th and 5th percentile levels. The L5 level is the sound pressure level exceeded 5% of the time in the test period and represents the highest noise level. The L95 level is the noise level exceeded 95% of the time in the test period and represents background noise. These distinctions allow snoring sounds to be distinguished from background noise levels. The percentage mean and minimum O2 saturation levels, as well as 4% drops in the overnight O2 saturation, were calculated for each patient. A graphical display on the computer allowed visual assessment of the whole night and identification of artefactual sounds that were unrelated to other variables Tests to assess the site of airway narrowing: NR Inclusion criteria: Dentate adults; non-apnoeic snoring (confirmed by PSG) Exclusion criteria: NR Subgroups: NA |
||
| Patient baseline characteristics | ||
| n | 35 | |
| Age (years), mean (range) | 44 (28–61) | |
| Male, n (%) | 20 (57) | |
| BMI (kg/m2), mean ± SD | Males: 28.4 ± 2.8; females: 26.8 ± 5.3 | |
| ESS score, mean ± SD | 9.4 ± 5.0 | |
| Smokers, n (%) | NR | |
| Median oximetry and sound level results | ||
| n | 11 | |
| Age (years), median | 41.5 | |
| BMI (kg/m2), mean | 27.5 | |
| Mean O2 saturation level (%), median (range) | 95 (93–97) | |
| Minimum O2 saturation level (%), median (range) | 89 (86–94) | |
| O2 dips > 4%/hour, median (range) | 2.8 (0.0–129.5) | |
| L5 snoring (mV), median (range) | 449 (53–1212) | |
| L95 background (mV), median (range) | 61 (0–322) | |
| L5–L95 (mV), median (range) | 240 (51–1015) | |
| Outcome measures | ||
|
Outcome 1: ESS score. Measured on a range of 0–24. Definition of treatment success: NR Outcome 2: Short-term side effects associated with MAS wear (2–3 days). Side effects assessed were: (1) discomfort in the facial muscles; (2) discomfort in the jaw joint; (3) abnormal bite on awakening; (4) dry mouth during the night; (5) excessive night-time salivation. Definition of treatment success: NR Outcome 3: Longer-term side effects associated with MAS wear. Side effects assessed were: (1) discomfort in the facial muscles; (2) discomfort in the jaw joint; (3) abnormal bite on awakening; (4) dry mouth during the night; (5) excessive night-time salivation. Definition of treatment success: NR Outcome 4: Snoring noise levels (L5). Definition of treatment success: NR Outcome 5: Mean O2 saturation level (%). Definition of treatment success: NR Outcome 6: Minimum O2 saturation level (%). Definition of treatment success: NR Outcome 7: O2 dips > 4%/hour. Definition of treatment success: NR Outcome 8: L5–L95 (mV). Definition of treatment success: NR Covariates: NA Total length of follow-up: 1 month Follow-up assessment times: Only one follow-up assessment at 1 month Rate of attrition at each follow-up time: n = 6 for questionnaire survey; n = 0 for sleep study Methods of statistical analysis: Statistical evaluation was performed using the Wilcoxon matched-pairs signed rank test for differences in ESS scores, noise levels and O2 saturation; the McNemar test was used to identify differences in side effects in the short and longer term |
||
| Results | ||
| Outcome 1: ESS score | ||
| n (in analysis) | 29 | |
| ESS score, mean ± SD | 6.9 ± 4.8; p < 0.001 | |
| Outcome 2: Short-term side effects associated with MAS wear (2–3 days) | ||
| n (in analysis) | 29 | |
| Muscular discomfort, n (%) | 20 (69) | |
| Temporomandibular joint (TMJ) discomfort, n (%) | 22 (76) | |
| Wakes with abnormal bite, n (%) | 11 (40) | |
| Dry mouth, n (%) | 8 (28) | |
| Excessive salivation, n (%) | 6 (21) | |
| Outcome 3: Long-term side effects associated with MAS wear (1 month) (p-values are compared with short-term side effects) | ||
| n (in analysis) | 29 | |
| Muscular discomfort, n (%) | 5 (17); p < 0.001 | |
| TMJ discomfort, n (%) | 8 (28); p < 0.001 | |
| Wakes with abnormal bite, n (%) | 8 (28); p = NS | |
| Dry mouth, n (%) | 5 (17); p = NS | |
| Excessive salivation, n (%) | 1 (3); p = NS | |
| Outcomes 4–8 | ||
| n (in analysis) | 11 | |
| Snoring noise levels (L5), median (range) | 161 (9–442); p < 0.05 | |
| Median O2 saturation level (%), median (range) | 95 (93–96); p = NS | |
| Minimum O2 saturation level (%), median (range) | 90 (86–94); p = NS | |
| O2 dips > 4%/hour, median (range) | 1.7 (0.0–37.8); p = NS | |
| L5–L95 (mV), median (range) | 75 (9–417); p < 0.01 | |
|
Subjective compliance rates at 1 month: 26/29 patients were still using the appliance; three patients were unhappy wearing the Herbst splint because of appliance aesthetics (n = 2) and TMJ problems (n = 1) Need for repeat procedure (unscheduled): NA |
||
| Authors’ conclusions | ||
| The use of a MAS significantly improves snoring incidence and sleep quality in the majority of patients with non-apnoeic snoring. Additionally, the initial side effects of muscular and TMJ discomfort are mostly resolved after 1 month of appliance wear | ||
| Methodological assessment criteria | ||
| 1. Study design | Pre–post | |
| 2. Were the study eligibility criteria specified? | Partial | |
| 3. Are adequate baseline details presented? | Partial | |
| 4. Are any co-interventions clearly stated? | Not applicable | |
| 5. Is compliance with treatment adequate? | Partial | |
| 6. Were any subgroup analyses justified? | NA | |
| 7. Were data collection tools shown or known to be valid for the outcome of interest?a | Partial | |
| 8. Were the data collection tools known or shown to be consistent and accurate in measuring the outcome of interest?b | Partial | |
| 9. Were all study participants accounted for? | No | |
| 10. Are greater than 80% of patients included in the follow-up assessment? | Yes | |
| 11. Are data analyses appropriate? | Yes | |
| 12. Are the conclusions supported by the results? | Yes | |
| 13. Generalisability | Only limited baseline information on participants is presented; however, male–female ratio and BMI indicative of being overweight would appear representative of non-apnoeic snorers in general. Treatment of choice was MAS rather than palatal surgery. No baseline information on smoking status or alcohol consumption presented | |
| 14. Intercentre variability | NA | |
| 15. General comments | – | |
Appendix 4 Bibliographic details of foreign language studies marked as unclear
Barbieri M, Mora F, Passali FM, Barbieri A, Gaudini E, Cordone MP, et al. Surgical treatment of snoring with bipolar radiofrequencies. Rivista Italiana di Otorinolaringologia Audiologia e Foniatria 2003;23:34–8.
Bernecker F, Stasche N, Hormann K. [Snoring and sleep apnea syndrome: surgical treatment and MESAM-IV controlled, postoperative results]. [German]. Laryngorhinootologie 1993;72:398–401.
Bllassin R. Snoring treatment by velum curving with laser. Journal Francais D’Oto-Rhino-Laryngologie 1993;42:129–32.
Carenfelt C, Haraldsson PO. [Pharyngoplasty under local anesthesia against disabling snoring]. [Swedish]. Lakartidningen 1990;87:2420–1.
Chouard CH, Meyer B, Chabolle F, Fleury B. [Clinical results of the surgical treatment of 1222 cases of chronic snoring]. [French]. Annales d Oto-Laryngologie et de Chirurgie Cervico-Faciale 1990;107:154–8.
Cseh A, Hausler R. [Uvulo-palatopharyngioplasty: indication, technique and results in relation to ronchopathy and sleep apnea syndrome]. [German]. Schweizerische Rundschau fur Medizin Praxis 1996;85:684–8.
Cvetni V, Cvetni S, Kujundzi I, Batisti B, Sankovi F, Zdelar F. [Pathophysiologic mechanisms of functional disorders of the cardiorespiratory system in snoring]. [Croatian]. Plucne Bolesti 1990;42:208–12.
Fibbi A, Presta A, Fasciolo G. [A new mini-invasive technique for the treatment of sleep breathing disorders: preliminary results of a clinical experience]. [Italian]. Acta Otorhinolaryngologica Italica 1999;19:21–5.
Fleury B, Chabolle F, Laffont F, Schlegel H, Launois S, Ferrey-Hannin D, et al. The effect at three months of uvulopalatopharyngoplasty in the treatment of obstructive sleep apnoea syndrome in the adult. Revue des Maladies Respiratoires 1989;6:519–24.
Galindo Campillo AN, Garcia SM, Navarro CM, Toledano MA. [Somnoplasty: treatment of chronic snoring using radiofrequency irradiation of the palate]. [Spanish]. Acta Otorrinolaringologica Espanola 2003;54:686–92.
Gerek M, Akcam T, Durmaz A. [Radiofrequency thermal ablation of the soft palate in patients with snoring and mild sleep apnea]. [Turkish]. Kulak Burun Bogaz Ihtisas Dergisi 2005;14:67–78.
Grontved A, Jorgensen K, Petersen SV. [Surgical treatment of snoring and sleep apnea]. [Danish]. Ugeskrift for Laeger 1993;155:1279–80.
Hsueh JY, Hung CH. Long-term follow-up results of single staged laser-assisted uvulopalatoplasty (LAUP) for treatment of snoring. Tzu Chi Med J 1998;10:299–304.
Huet P, Sene JM, Rineau G, Mercier J, Legent F, Beauvillain C. [Evaluation of velopharyngeal function using an aerophonoscope before and after surgery for snoring]. [French]. Annales d Oto-Laryngologie et de Chirurgie Cervico-Faciale 1993;110:372–82.
Katahira H, Onda A, Ninomiya K, Teraoka Y, Kojima M, Kohno M. The clinical study and effect of oral appliance treatment at the patients with snore symptom. Ther Res 2005;26:283–92.
Losert-Bruggner B. [Determining the optimal position for snoring splints. Forced mandibular advance is not always required]. [German]. HNO 2000;48:955–9.
Makowski M, Koziej M, Cielicki J, Sliwiski P, Gorzelak K, Zieliski J. [Clinical picture and outcome of conservative treatment for obstructive sleep apnea]. [Polish]. Polskie Archiwum Medycyny Wewnetrznej 1995;93:234–41.
Manni JJ, Wouters HJ, Folgering HT. [Sleep apnea syndrome, snoring and uvulopalatopharyngoplasty]. [German]. Laryngologie, Rhinologie, Otologie 1986;65:566–9.
Meyer B, Chabolle F, Chouard CH. Uvulopalatopharyngoplasty for rhonchopathy without sleep apnea syndrome. Results and complications. Annales D’Oto-Laryngologie et de Chirurgie Cervico-Faciale 1988;105:291–7.
Mozota N, Jr, Mozota NM, Mozota NM, Abu SK, Mozota O, Jr. [Effectiveness of uvulopalatopharyngoplasty in snoring disorders and obstructive sleep apnea]. [Spanish]. Acta Otorrinolaringologica Espanola 1998;49:629–32.
Namyslowski G, Scierski W. [Laser assisted uvulopalatoplasty (LAUP) in the treatment of snoring and obstructive sleep apnea syndrome]. [Polish]. Otolaryngologia Polska 2001;55:363–8.
Pinto JA, Fomin DS. Snoring and obstructive sleep apnea: treatment with CO2 laser –preliminary results. Revista Brasileira de Otorrinolaringologia 1996;62:463–7.
Stenborg R, Yontchev E, Ejnell H, Hedner J. [A snoring plate – an individual preventive device against snoring is not very effective]. [Swedish]. Lakartidningen 1989;86:3891–2.
Vieira MBM, Leite SHP, Cunha FC. Zetapalatopharyngoplasty (ZPPP): new surgical technique for snoring and sleep apnea treatment. Revista Brasileira de Otorrinolaringologia 2001;67:56–60.
Glossary
- Apnoea
- An apnoea is defined in adults as a 10-second breathing pause. The frequency of apnoeas and hypopnoeas hourly measured by the apnoea/hypopnoea index (AHI) or the respiratory disturbance index (RDI) is used to differentiate non-apnoeic snoring from obstructive sleep apnoea/hypopnoea syndrome (OSAS). According to this definition non-apnoeic or primary snoring is classified by an AHI score of less than or equal to five.
- Applicability
- The extent to which the results of a study or review can be applied to the target population in practice.
- Appraisal of evidence
- Formal assessment of the quality of research evidence and its relevance to the clinical question according to predetermined criteria.
- Bias
- Systematic errors in the design and execution of a study that may lead to an over- or underestimation of the ‘true’ effect of a treatment or intervention.
- Blinding
- The practice of keeping the investigators or patients in a study ignorant of the group to which a participant has been assigned or of the population from which the participant has come. The purpose of ‘blinding’ is to protect against bias.
- Ceiling effects
- See floor and ceiling effects.
- Clinical effectiveness
- How well a drug, procedure, device or package of care works to produce a good outcome for a patient.
- Clinical trial
- Research study conducted with patients, usually to evaluate a new drug, device or procedure. Each trial is designed to answer scientific questions and to find better ways to treat individuals with a specific disease. See also randomised controlled trial.
- Cochrane Library
- The Cochrane Library consists of a regularly updated collection of evidence-based medicine databases including the Cochrane Database of Systematic Reviews. The Cochrane Library is available on CD-ROM and on the internet.
- Computerised tomography
- Computerised tomography (CT or CAT) is a medical imaging method that uses digital geometry processing to generate a three-dimensional image of the inside of internal body structures from a large series of two-dimensional radiography images taken around a single axis of rotation.
- Confidence interval
- This helps us assess the likely effect of an intervention by describing the range of possible effects that are consistent with the results of a study (or a combination of studies). A wide confidence interval indicates a lack of certainty or precision about the true size of the clinical effect and is seen in studies with too few patients. When confidence intervals are narrow they indicate more precise estimates of effects and a larger sample of patients studied. We usually interpret a 95% confidence interval as the range of effects within which we are 95% confident that the true effect lies.
- Confounding factor
- Something that introduces uncertainty and bias into an observed outcome, complicating interpretation of the result.
- Control group
- A group of patients recruited into a study that receives no treatment, a treatment of known effect or a placebo to provide a comparison for a group receiving an experimental treatment such as a new procedure.
- Controlled clinical trial
- A study that includes some form of control group that is not randomised.
- Correlation
- A measure of the strength of association between two or more variables. A positive correlation indicates that one variable has been observed to increase as the other increases; a negative correlation indicates that one decreases as the other increases.
- Diagnostic workup
- The process of making a diagnosis through tests, clinical history and clinical judgement.
- Effectiveness
- The extent to which a specific procedure or device, when used under usual or everyday conditions, does what it is intended to do.
- Efficacy
- The ability of a procedure, drug or device to control or cure an illness. Efficacy refers to the extent to which a specific intervention produces the intended (beneficial) effect under controlled conditions.
- Extrapolation
- The application of research evidence based on studies of a specific population to another population with similar characteristics.
- Floor and ceiling effects
- Problems encountered in some outcome measures when there are limits to how low or high a numerical value they can assume. These can make it difficult to assess the true effect of an intervention.
- Heterogeneity
- This term is used in meta-analysis and systematic reviews when the results or estimates of effects from separate studies seem to have different magnitudes or even different signs or directions. Differences in the patient populations, outcome measures, definition of variables and duration of follow-up of the studies included in the analysis create problems of non-compatibility. See also homogeneity.
- Homogeneity
- This means that the results of studies included in a systematic review are similar and there is no evidence of heterogeneity. Results are usually regarded as homogeneous when differences between studies could reasonably be expected to occur by chance.
- Hypopnoea
- A hypopnoea is categorised as a 10-second event in which there is continued breathing but ventilation is reduced by at least 50% or a reduction in ventilation of less than 50% from baseline is associated with either an oxyhaemoglobin desaturation of greater than 3% or an arousal.
- Incidence
- The rate of new occurrences of a condition or disease, often given as people per year or episodes per year.
- Inclusion criteria
- See selection criteria.
- Intention to treat analysis
- An analysis of a clinical trial in which patients are analysed according to the group to which they were initially randomly allocated, regardless of whether or not they dropped out, fully complied with the treatment or crossed over and received the alternative treatment.
- Magnetic resonance imaging
- A radiological technique designed to image internal structures of the body using magnetism, radio waves and a computer.
- Methodological quality
- The extent to which a study has conformed to recognised good practice in the design and execution of its research methods.
- Non-experimental study
- A study based on participants selected on the basis of their availability, with no attempt having been made to avoid problems of bias.
- Objective measure
- A measurement that follows a standardised procedure that is less open to subjective interpretation by potentially biased observers or study participants.
- Placebo
- A pill, medicine or procedure that has no physiological effect and is used as a dummy treatment.
- Placebo effect
- A beneficial (or adverse) effect produced by a placebo and not due to any property of the placebo itself.
- Pre–post study
- A study design that measures outcomes in one group of people, first before and then after an intervention is given or initiated.
- Prevalence
- The proportion of a population of people who are experiencing a condition or disease at a given time.
- Probability
- How likely an event is to occur, e.g. how likely a treatment or intervention will alleviate the symptom.
- Prognostic factor
- Patient or disease characteristics that influence the course of a particular condition. In a randomised trial to compare two treatments, chance imbalances in prognostic factors that influence patient outcomes are possible, especially if the size of the study is fairly small. In terms of analysis these prognostic factors become confounding factors.
- p-value
- If a study is carried out to compare two treatments the p-value is the probability of obtaining the results, or something more extreme, if there really was no difference between treatments. By convention, when the value of p is below 0.05 (i.e. less than 5%) the result is seen as statistically significant.
- Randomised controlled trial
- A trial in which people are randomly assigned to two (or more) groups, one (the experimental group) receiving the treatment that is being tested and the other (comparison or control group) receiving an alternative treatment, a placebo or no treatment. The two groups are followed up to compare differences in outcomes between them.
- Reliability
- The extent to which a method of measurement consistently gives the same results.
- Sample
- A part of the study’s target population from which the participants of the study will be recruited. If participants are drawn in an unbiased way from a particular population, the results can be generalised from the sample to the population as a whole.
- Selection criteria
- Explicit criteria used in systematic reviews to decide which studies should be included and excluded from consideration as potential sources of evidence.
- Self-report measure
- An outcome measure that uses the views and experience of the patient rather than clinical measurements.
- Standard deviation
- A measure of the spread, scatter or variability of a set of measurements.
- Validity
- Assessment of how well a tool or instrument measures what it is intended to measure.
List of abbreviations
- AHI
- apnoea/hypopnoea index
- AI
- apnoea index
- BMI
- body mass index
- CASPO
- cautery-assisted palatal stiffening operation
- CCT
- controlled clinical trial
- CT
- computerised tomography
- COPD
- chronic obstructive pulmonary disease
- CPAP
- continuous positive airway pressure
- ECG
- electrocardiogram
- EDS
- excessive daytime sleepiness
- EEG
- electroencephalogram
- ENT
- ear, nose and throat
- ESS
- Epworth Sleepiness Scale
- GP
- general practitioner
- Hz
- hertz
- LAUP
- laser-assisted uvulopalatoplasty
- MAS
- mandibular advancement splint
- MRI
- magnetic resonance imaging
- MSLT
- Multiple Sleep Latency Test
- ODI
- oxygen desaturation index
- OSAS
- obstructive sleep apnoea/hypopnoea syndrome
- PSG
- polysomnography
- RCT
- randomised controlled trial
- RDI
- respiratory disturbance index
- RFA
- radiofrequency ablation
- SDB
- sleep-disordered breathing
- SPL
- sound pressure level
- SaO2
- oxygen saturation of arterial blood
- SpO2
- oxygen saturation of arterial blood by pulse oximetry
- TMJ
- temporomandibular joint
- UARS
- upper airway resistance syndrome
- UP3
- uvulopalatopharyngoplasty
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Reimsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
Health Technology Assessment Programme
-
Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NCCHTA
-
Dr Andrew Cook, Consultant Advisor, NCCHTA
-
Dr Peter Davidson, Director of Science Support, NCCHTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NCCHTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NCCHTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NCCHTA
HTA Commissioning Board
-
Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programmes, Research and Development Directorate, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA Programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington