Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 99/33/51. The contractual start date was in April 2003. The draft report began editorial review in August 2006 and was accepted for publication in October 2008. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None
Permissions
Copyright statement
© 2009 Queen’s Printer and Controller of HMSO. This monograph may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2009 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
This report describes a cluster randomised controlled trial and economic evaluation of two different psychological interventions delivered by health visitors (HVs) in their usual care setting, for women with depression soon after they had given birth. The aim of the trial was to reliably estimate any differences in outcomes for mother, child or family from training HVs in systematically detecting depressive symptoms and in delivering a psychological intervention based on either cognitive behavioural principles or person-centred principles in primary care at an individual level for women at risk of postnatal depression (PND). The secondary aim was to establish the relative cost-effectiveness of both psychological interventions from an NHS perspective relative to health visitor usual care.
The original NIHR Health Technology Assessment (HTA) programme call for proposals in 1999 proceeded from a widening recognition of the gravity of the condition and an increasing awareness of the potential impact of depression on a new mother’s infant and wider family.
The two experimental interventions built upon promising work on the potential for psychological interventions to help women recover from PND,1,2 as an alternative to pharmaceutical interventions. 3 There was also further indication of the potential role for HVs in this context. 4–7 The trial therefore aimed to build upon existing evidence and to address the limitations of previous research in the area of PND and to examine, in particular, the role of HVs in this context.
Health visitors in 103 clusters in 29 primary care trusts (PCTs), mainly from the former Trent region, and 4084 women consented to take part in the 3-year study, which began formally on 1 April 2003. There was a long pre-trial preparatory phase to surmount the research governance requirements; to enlist the support of interested HVs and GPs; and to arrange a comprehensive and detailed preparation of the HV intervention, which included an 8-day equivalent group training session.
The study also examined the use of the Edinburgh Postnatal Depression Scale (EPDS),8 which has been widely used in the UK to help detect women who are depressed after having their baby. It was designed to help indicate the top decile of women4 most likely to be suffering from depression and able to benefit from an intervention. As such, the outcome of greatest pragmatic interest for health visiting services was the proportion of women who had moved below the threshold for concern score. Also, because of the inefficiency of administering the EPDS to all postnatal women face-to-face at home,4 and the precedent of administering the self-reported assessment by post,9 the trial investigated the potential clinical and economic consequences of a postal 6-week EPDS administration.
Background
Depression
Mental health is considered to be ‘a state of well-being in which the individual realises his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community’. 10
Conversely, mental ill health covers mental health problems, strain, impaired functioning associated with distress, symptoms and diagnosable mental disorders such as schizophrenia and depression. 11 Each year, more than a quarter of European adults will experience mental ill health of one form or another,12 most commonly depression.
Postnatal mental health
Most women feel exhausted after the birth of their baby and will be tearful and feel low because of the exhaustion. There continues to be some debate about the classification of postnatal mental health conditions and whether PND exists as a unique diagnosis or whether depression occurring postnatally is just coincidental. 13 However, both of the internationally used classification systems no longer provide a separate category of PND. In effect, the presence of depression is determined by the same set of criteria, regardless of timing or context. When mood states were measured in a sample of pregnant women and a group of matched non-childbearing women,14 there were no differences between the two groups in rates of major or minor depression after the babies were born, but the postnatal women had more symptoms of depression. 14 Women do experience postnatal distress and less satisfaction in their relationships at this time, especially with their partners. 14,15 It has been proposed that the depressive symptoms or distress that some women experience are an appropriate response following childbirth and so should not be confused with clinical depression. 16 Any emphasis on depression might draw attention away from the social and cultural context of parenting and the changes and losses that accompany the birth of a baby and consequently the sharing of the responsibility for the distress that the women experience. 16
There is some evidence that women are more vulnerable to depression within the first 6 postnatal months, not just the first few postnatal weeks. 17 Because of issues of context and in particular the welfare of the infant, and other family members, health professionals need to be aware of the postnatal onset of depression, puerperal psychosis, post-traumatic stress disorder, panic disorder and relapse of other illnesses such as schizophrenia. 18
Within the first days after the birth of a baby, 39–85% of women feel more emotional than usual, weepy, irritable and anxious and have insomnia and a low mood because of what is called postnatal ‘blues’ or baby ‘blues’. 14 Women can be given information about symptoms and reassurance that postnatal blues resolve quickly within a few days, without treatment, and can be advised about self-help. However, there is no evidence for the effectiveness of these measures. 18
At the other extreme, puerperal psychosis is a severe mental illness affecting one or two per thousand women soon after delivery. 19 Women with a history of a postnatal mood disorder carry a very high risk of recurrence. The dramatic symptoms are severe depression with a risk of suicide or even infanticide. 20 Mania, hallucinations or delusions require urgent psychiatric treatment, often as an inpatient. This very small but important risk of suicide and infanticide in some severely depressed mothers manifests itself in violent methods, more often than in the population generally, sometimes before and sometimes after 6 weeks postnatally. 21 Although exceptionally serious, statistically suicide is rare and most HVs will never encounter maternal suicide.
In 1992 the International Classification of Diseases (ICD-10)22 first included an optional supplementary code for diseases that occur during and complicate pregnancy, childbirth or the puerperium (the O99 code can be applied to any form of mental disorder).
The American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)23 makes provision for a postpartum-onset specifier code that can be added to a diagnosis of manic depression, bipolar disorder or major depression among others, provided onset is within 4 weeks of childbirth. No reason for the 4-week timing is provided and the ICD does not suggest a time period for onset. The diagnosis of depression (irrespective of the gender of the sufferer or the timing of the episode) relies on the presence of at least five of the following symptoms for at least 2 continuous weeks:23
-
depressed mood
-
loss of interest or pleasure
-
significant increase or decrease in appetite
-
insomnia or hypersomnia
-
psychomotor agitation or retardation
-
fatigue or loss of energy
-
feelings of worthlessness or guilt
-
diminished concentration
-
recurrent thoughts of suicide.
Depression is far more common than psychosis at any time as well as in the context of pregnancy and childbirth. Depression can last for up to 1 year after delivery in about 4% of all mothers20 or a quarter of mothers who become depressed, and may last even longer. 24 But the relevance of this is not clear as not many studies have followed up women for long enough to determine the depression duration and no study has described in a standardised way the course of depression (in women) with respect to whether or not the episode occurred within the context of childbirth.
The proportion of postnatal women who might be depressed varies between 11%20 and 22%25,26 depending on the sample of women, the criteria used and the time of assessment postnatally. 14 Based on a meta-analysis of estimates from 59 studies internationally, the average prevalence of depression postnatally is 13%. 27 A later meta-analysis estimated that 14.5% of women may have a new episode of major or minor depression during the first 3 postnatal months, with 6.5% having a new episode of major depression. 28 The same review estimated a prevalence of 6.5–12.9% for major and minor depression at any time during the first postnatal year, and a 1–5.9% prevalence of major depression. 28
Consequences of depression
Depression is a public health problem with financial costs to the gross domestic product associated with sickness absence,29 mainly through lost productivity. There is a high risk of relapse. 30 The UK spends 12% of its total health expenditure on mental health,11 and the cost for antidepressant prescriptions is around £401 million. 31 The costs of the stigma and discrimination associated with mental ill health remain intangible.
Depression can lead to more deaths from suicide each year than there are deaths from road accidents. Suicide rates and mental health states vary across European countries, reflecting their diverse traditions, cultures, situations and religious variations in reporting suicide. 11 The number of deaths from psychiatric illness is underestimated as suicidal deaths may not be classified as such, to spare family feelings. 32 The sixth report of the confidential enquiries into maternal deaths in the UK, Why Mothers Die,21 reported suicide as the most common cause of maternal death for women in the first year after childbirth.
The natural history of PND varies among women, but around one-third develop a chronic problem with long-term adverse consequences. Although there is little evidence to date, there is a belief that women’s depression may affect their partners,33 who become depressed,34–36 thereby reducing their ability to cope with supporting the mother or caring for the new infant or other children.
There has been growing concern from the literature on the evidence of the effects that depression might have on the cognitive37 and emotional development of children38 and the attachment of infants to their mothers, particularly for boys, possibly well beyond infancy. 39 Boys whose mothers are depressed in the first year may have particular problems with reading. 40 Infants are highly sensitive to the quality of their interpersonal contacts, which are most often provided by the mother in the first few months of life. 39 This could be because the baby has a rapidly developing brain in the first 6 months of life and is heavily dependent on external stimulation and therefore particularly vulnerable during this sensitive period. 39,40 It is also possible that the association between PND and the development of infants represents a complex two-way interaction. 41 Also, mothers with depression are more likely to report parenting stress, negative perceptions of their infant’s behaviour and hostile feelings towards their infant. 42
Aware of the link, the European Union’s project on building mental health in infants, children and adolescents recognised the need to address PND. 11 Similarly, guidance from the National Institute for Health and Clinical Excellence (NICE) on treating depression in children and young people also referred to the need for parents’ own depression to be treated in parallel. 43
Causes of depression
The factors that can contribute to depression include an individual’s personal experiences, biological or inherited tendencies, social support factors, and economic and environmental factors. 11 For example, people with mental health problems are more likely than the general population to live in rented housing and to say they are dissatisfied with their accommodation. 44 Because of the growing concern over mental health, policy initiatives have been developed, recognising that health-care interventions alone are not the only solution.
There is no consensus about the cause of PND, but there is an association with risk in women who have a number of psychosocial risk factors. A meta-analysis of 59 studies27 used regression analyses to evaluate the relative contributions of several postnatal variables to the development of PND (Table 1). The strongest predictors are related to antenatal anxiety or depression, lack of social support and stressful life events. Weaker predictors are neuroticism, negative cognitive attributional style and obstetric variables. The suggestion that women having a traumatic delivery, by emergency Caesarean section, might be more likely to become depressed45 may be true only for women who have a previous history of a depressive disorder. 46 For the general population of women, complications such as forceps or emergency Caesarean section are not associated with depression. 46 A link between Caesarean section and PND was not established in a meta-analysis of suitable studies. 47
| Cohen’s da | |
|---|---|
| Depression antenatally | 0.75 |
| Anxiety antenatally | 0.68 |
| Social support | –0.63 |
| Stressful life events | 0.60 |
| Mother’s history of psychopathology | 0.57 |
| Self-esteem | |
| Childcare stress | |
| Neuroticism | 0.39 |
| Marital relationship | –0.13 |
| Infant temperament | |
| Maternity blues | |
| Obstetric variables | 0.26 |
| Marital status | |
| Negative cognitive attributional style | 0.24 |
| Socioeconomic status | |
| Unplanned/unwanted pregnancy |
Recognising that it is a simplification, O’Hara and Swain synthesised all of the risk factors that emerged from the meta-analysis27 to present a prototype of a pregnant women at risk of PND, as most likely to:
-
occupy a lower social stratum
-
have experienced stressors during pregnancy
-
have had a more difficult than normal pregnancy or delivery
-
be experiencing marital difficulties
-
experience her partner as providing little social support
-
perceive others in her social network as not supportive
-
have a history of psychopathology
-
show evidence of being at least mildly depressed, anxious and worried.
A prospective study48 of women recruited antenatally found that those who were depressed postnatally felt that the practical and emotional support provided by their partners was inadequate. The depressed women felt that they could not talk freely with their partners, they were not there for them when they needed them and they were not able to rely on them for childcare help as much as they would have liked. In general, they felt that their partners made their lives less easy. 48
Management of postnatal depression
Assessment and detection
There is a general problem with the detection of depression in primary care. 49 For many women with PND their problem will not have been fully recognised in routine clinical practice. 24,26,50 Because the onset of PND may be gradual, it is not easy to distinguish it from the fatigue and emotional liability that most mothers feel when adjusting to the demands of a new baby and recovering from childbirth. 50 It is also not easy to detect depression, partly because some women are not willing to disclose their true feelings. 51 Some women feel that they become depressed as a result of feeling exhausted, unwell, unsupported or isolated as mothers, with no time for themselves. 52 These women may not try to access professional or other support, either because they feel that their problem is not so bad or they ought to deal with it on their own or because they do not have anyone to ask for support. 52 Some women may feel that there is a stigma attached to being depressed and they may feel embarrassed or ashamed to seek help for what they might regard as a sign of personal inadequacy or an admission of failure on their part. 53 They may not regard professional intervention as relevant or may not want to be labelled as an unfit mother. 53
The EPDS is one of the mood assessment instruments most widely used in clinical practice. 54 It was not developed as a diagnostic test. 55 The EPDS is not adequate to confirm PND without a clinical interview to assess a mother’s mood, depressive symptoms and suicidal thoughts, and explore her relationship with the baby. 56
The National Screening Committee commissioned a review57 to evaluate the evidence of the validity of the EPDS as a screening tool; the most effective intervention for PND; and the size of the beneficial or adverse effects for interventions. The report stated that:
At present, it is not recommended to the National Screening Committee that screening for postnatal depression be introduced . . . the introduction of isolated screening programmes which are not part of a research project will not add to the evidence base which is agreed to be insufficient to justify the introduction of screening.
Until more research is conducted into its potential for routine use in screening for PND the NSC recommends that the EPDS should not be used as a screening tool.
It may, however, serve as a checklist as part of a mood assessment for postnatal mothers, when it should be used alongside professional judgement and a clinical interview. The professional administering it should have training in its appropriate use and should not use it as a pass/fail screening tool.
The difficulties of the EPDS have been openly discussed;58–61 many HVs do find the instrument valuable whereas others highlight the limitations. Some PCTs endorsed the systematic use of the EPDS by HVs and established a system of cascade HV training in its use. 62 Other PCTs were mindful of the criticism of the EPDS following the review commissioned by the National Screening Committee. This prompted some PCTs to restrict the use of the EPDS by HVs.
The guidance from the National Collaborating Centre for Primary Care18 on the postnatal care of women and their babies proposes that it is good practice to ask women who have had a baby how they are feeling emotionally, but cautions that the use of the EPDS is not acceptable to some women.
Pharmacological treatment for depression in primary care
There is not enough evidence from well-controlled and reported trials about the costs and benefits of different interventions for depression. Within the UK, depression in primary care is usually treated with either tricyclic antidepressants (TCAs) or, more recently, the newer non-tricyclic drugs or selective serotonin reuptake inhibitors (SSRIs). 29 The SSRIs are believed to be as effective as TCAs but less toxic in overdose. 29 Many people are uncertain about taking drugs for depression, believing that they are addictive or that drug treatment is not appropriate for what is seen as a reasonable reaction to adverse events. 29 There are certainly concerns about the risk of adverse neonatal outcomes following exposure to antidepressants during pregnancy. 63
Antidepressants are effective for postpartum depression. 64 However, it is not known which specific class of antidepressants or which individual antidepressant is most helpful; which is the best prevention for high-risk women; or what impact antenatal treatment or excretion of antidepressants via breast milk might have on the cognitive and emotional development of exposed infants. 64 Because there is insufficient information on the overall effectiveness of antidepressant drugs in PND, there are very little data upon which to base decisions about the safety of breastfeeding while taking these medications. 65 Women with PND prefer not to take antidepressants66 and so compliance is not good. Physicians either prescribe a reduced, potentially non-therapeutic dose, advise women not to breastfeed or delay offering treatment until the woman has finished breastfeeding. 67
An American expert panel68 reached a majority consensus on the appropriateness of including antidepressants (specifically SSRIs) and non-pharmacological treatments for women with severe depressive symptoms. For milder symptoms the panel gave equal endorsement to other treatment modalities or preferred psychotherapy over antidepressant medication. 68
Psychological interventions for mental health problems in primary care
Partly in response to concerns about antidepressants,29 over the past 25 years there has been a move towards increasing the availability of psychological interventions. 69
Psychological interventions include counselling and psychotherapy, and it can be difficult to distinguish between the two. Both cover a range of modalities, the most common being cognitive behavioural therapy (CBT) and psychoanalytic, psychodynamic, interpersonal and client-centred, non-directive approaches.
The British Association of Counselling (BAC)70 presents an ethical framework for good practice in counselling and psychotherapy, including values, principles and personal moral qualities. The BAC refers to counselling as:71
. . . the skilled and principled use of relationships which develop self-knowledge, emotional acceptance and growth, and personal resources.
. . . concerned with addressing and resolving specific problems, making decisions, coping with crises, working through feelings and inner conflict, or improving relationships with others.
Some patients with depression actively choose counselling over antidepressants. 72 The availability of counselling will depend upon the number of effectively trained practitioners.
In primary care a range of professionals can offer psychological interventions, including counsellors, community psychiatric nurses (CPNs), clinical psychologists, HVs and social workers. 69,73
In primary care, generic brief counselling74 or psychological interventions using non-directive psychotherapy are as effective as routine GP care, or perhaps more effective. 75–77 Generic counselling is as effective as antidepressants, although those taking antidepressants may recover more quickly. 72 In the short term psychological symptoms of patients who receive counselling may improve more than symptoms in those who have usual GP care. 69 Primary care patients may prefer brief psychotherapy to usual GP care75–77 and, given the choice, patients who choose counselling over antidepressants may improve more than those who have no strong preference. 72 Interventions using CBT also appear to be cost-effective in primary care78 and possibly helpful in preventing relapse. 30
Health visitors’ detection and treatment of postnatal depression
There is some evidence of the effectiveness of HVs in using psychological approaches to support women with PND. In a pioneering small randomised trial in Edinburgh and Livingston,1 HVs were asked to administer the EPDS to all women at around 6 weeks postnatally. Those who had a raised EPDS score were interviewed by psychiatric interview at 13 weeks postnatally, and those identified as depressed were allocated to an intervention group (IG) (n = 26) or a control group (CG) (n = 24). The IG were offered a postnatal one-to-one non-directive type counselling intervention of eight 1-hour weekly sessions by 17 HVs, whilst the CG received routine care. Outcomes included the Goldberg Standardised Psychiatric Interview and EPDS after 13 weeks. Although the HVs providing the intervention continued to visit the CG women, the statistically significant result was that 69% of the IG women (n = 18) recovered compared with 38% of the CG women (n = 9). In the absence of stronger evidence, the findings of this trial have been widely implemented throughout the UK.
The Lewisham primary prevention programme was one of the more important, small studies, which was not a randomised controlled trial. 6,79 The study compared outcomes for women screened antenatally as ‘vulnerable’ (using the Leverton questionnaire) in ‘Preparing for Parenthood’ (for first-time mothers) or ‘Surviving Parenthood’ (for second-time mothers) against routine primary care. The allocation to group was not random but by the baby’s date of birth and it was flawed because of the lack of concealment. HVs were asked to make contact with the women as soon as possible, in mid-pregnancy. There were five antenatal group sessions, beginning at 24 weeks, and six postnatal sessions, led by a clinical psychologist and a HV. At 3 months the women were interviewed, in part using the Present State Examination (PSE). Among the more vulnerable women, for those who had been offered the service, 19% (n = 48) were depressed compared with 40% of those who had not been offered the service. There was a significant reduction in EPDS for first-time mothers (n = 21) at 3 months compared with control subjects (n = 24), but no difference at 3 months for second-time mothers and no difference at 1 year for invited women. The authors concluded that some depression following childbirth can be prevented by brief psychological interventions, which can be incorporated within existing systems of antenatal classes and postnatal support groups, and pointed out that first-time mothers may be more likely to accept an invitation and attend meetings. 6
Following the Edinburgh trial1 Holden and Elliott wanted to give HVs the chance to take part in a training programme to adopt strategies for detecting PND and for early interventions. 4 To test whether the Edinburgh intervention, which appeared successful within a small trial, could be effective in routine HV practice they set up a three-centre study in Edinburgh, North Staffordshire and Lewisham, south-east London.
Health visitors were invited to a minimum of seven 2-hour training sessions and were asked to administer the EPDS to women, normally at the child health clinic, with a home visit for non-attenders. The preventive strategies included antenatal visits and education about PND, the realities of parenting and the potential benefit of support groups. 4 The study used an EPDS cut-off score of 12 so that each HV would counsel about three women on their caseload over the study period, using non-directive counselling (NDC). The HVs did not wish to be regarded as counsellors and preferred the term ‘listening visits’ to the term ‘non-directive counselling’. 4 In the North Staffordshire arm, the median EPDS score changed from 7 at baseline to 5 post training. 4 There were reported improvements in counselling skills and an increase in HVs’ mental health assessments, recording of symptoms and referrals to mental health services. Elliott et al. 7 suggested that the training and intervention should be evaluated using a rigorous research design. The study was not a randomised trial and the limited reporting suggests that it was probably subject to selection bias. It showed the potential role for HVs in using a structured approach for delivering an intervention following a brief training in psychological counselling for PND.
Another study with postnatal women, which was not a randomised controlled trial, explored the effect of care from HVs who were trained to detect PND using the EPDS and to manage PND using counselling and cognitive behavioural techniques, such as problem-solving. In total, there were 30 women who received routine primary care before the training and who became historical control subjects and 70 women who were seen after the HV training. 5 The study, which was not rigorously controlled, or reported, found a significant reduction in EPDS scores after the training. 5
Support for the role of health visitors in perinatal mental health
Health visitors have been working in multidisciplinary teams for some time in the area of prevention and the early identification of maternal depression and support for affected women. 80–88 A series of proposals and guidance has offered backing for the role of HVs in perinatal mental health. 79
NICE asked the National Collaborating Centre for Mental Health (NCCMH) to develop a clinical guideline on the treatment and management of mental health problems in the antenatal and postnatal period. 89 Before this, the National Service Framework (NSF) for Mental Health90 set priorities for the way that services were to be provided, four of which were relevant to the role of HVs. Standard one related to mental health promotion and emphasised the need to build capacity and capability in primary care by supporting staff through continuing professional development. Standards two and three referred to primary care and access to services. The NSF proposed protocols to be implemented for the management of PND, anxiety disorders and those needing referral to psychological therapies. The NSF recognised the role of HVs with training who could use routine contact with new mothers to identify PND and treat its milder forms. The NSF seventh standard90 related to actions to reduce suicides, by ensuring that staff would be competent to assess the risk of suicide among individuals at greatest risk. This standard was relevant to HVs, as maternal suicide was cited as the largest cause of maternal death in the first postnatal year. 21 The later review of the NSF prioritised investing more in mental health promotion. 91
The Scottish Intercollegiate Guidelines Network (SIGN) evidence-based guideline on PND and puerperal psychosis emphasised the role for HVs in the detection and management of PND. 92
The Department of Health published guidance in September 2003, Into the Mainstream, Implementation Plan: Mainstreaming Gender and Women’s Mental Health, for developing services for perinatal depression, which supported the role of HVs. 93
In the UK, the Sainsbury Centre for Mental Health, the Local Government Association, the NHS Confederation and the Association of Directors of Social Services produced a joint policy paper. 94 The report presented a vision for 2015, which minimised public fear, stigma and discrimination for people with mental health problems, shifted resources to primary care, invested in the mental health workforce and extended the availability of psychological therapies to people with a range of mental health problems.
Given the absence of a national policy on PND, HVs in many PCTs developed their own local policies,95 with differing strategies and integrated care pathways (ICPs) for the detection and management of the depression. 83 Some PCTs developed protocols for GPs for the management of PND, with information on treatment options and criteria for referral to the community mental health team. It is appropriate for HVs to refer some women to mental health services rather than offer support themselves. These circumstances include women who have obsessive compulsive disorder, eating disorders, post-traumatic stress disorder and panic disorder, as well those who have psychosis or suicidal plans, and other situations in which a HV feels very concerned. 7 This approach has been supported by Department of Health policy. 90,93
Health visitors’ professional support
Support for the role of HVs in perinatal mental health came from the HVs’ professional body. In 2000 the Community Practitioners’ and Health Visitors’ Association (CPHVA) established a Postnatal Depression and Maternal Mental Health (PDMMH) network for HVs to enhance perinatal services for women and their families. The PDMMH network facilitated the exchange of information on the development of ICPs, conferences, resources, publications and multicultural work. The CPHVA ran workshops about the use of the EPDS as part of a full mood assessment and advertised courses in identifying and managing perinatal depression.
An audit of the CPHVA membership was published in the network newsletter in June 2003. 96 The results suggested that 85% of PCTs had formal mechanisms for managing PND; 55% had a lead professional for perinatal mental health (72% of these being HVs); and 85% of PCTs were using the EPDS to some degree, but only 70% of these (sic) had received training in its proper use.
The generic role of health visitors
Health visiting relies on a sound interpersonal process and establishing a relationship with a client. The use of interpersonal skills and communication skills lie at the core of health visiting. 97 Whether regarded from a medical or psychosocial perspective, PND is acknowledged as an important health problem, and a key area of HVs’ work given their established role and unique personal contact with postnatal women. The following explains the historical, generic role of HVs and presents the context and rationale for their role in postnatal maternal health.
Health visiting has its origins in Salford, Manchester, where the Ladies’ Sanitary Reform Association first began home visiting to offer a universal service, with some focus on maternal and child welfare. 98,99 Since 1962 HVs have been qualified nurses, with special experience in child health, health promotion and health education, employed as part of the NHS community health service. They work with GPs and other primary health-care team workers (practice nurse, district nurse, midwife) and other community-based health and social care professionals, based within the GP surgery or practice premises or local health centre.
The Council for the Education and Training of Health Visitors100 identified the four main principles of health visiting as the philosophy underpinning practice:
-
the search for health needs
-
stimulation of the awareness of health needs
-
influencing policies that affect health
-
facilitating health-enhancing activities.
As policies within the NHS and in child health surveillance services have changed over time,101 so has the role of HVs. 99 In the 1990s HVs were encouraged to change the way that they worked, to offer a more targeted, needs-based service, rather than a universal service. The work of contemporary HVs is mainly around primary preventive activities on a broad range of health issues. However, recently there has been a strong drive for HVs to focus increasingly at the level of secondary prevention, targeting vulnerable children102 and using more community-based public health approaches. 103
The review of the British literature on health visiting104 indicated that HVs’ work can fall into the following categories:
-
individuals and groups with special needs
-
children with special needs
-
elderly
-
homeless families
-
mothers with PND
-
prevention of sudden infant death syndrome
-
traveller families, vulnerable families and families in poverty
-
child protection, domestic violence, childhood injury
-
child health services, child health surveillance.
Health visitors are concerned with all aspects of a woman’s health and the health and welfare of her child and family. HVs maintain a ‘caseload’ of individual clients and part of a HV’s role is to visit families with new babies, in their homes, as part of routine child health surveillance. Therefore, every family with a child under 5 years has a named HV who can advise parents on everyday infant and childcare difficulties and immunisation programmes, as well as signposting families to other sources of health support, for example housing, financial benefits or specialist services. Some HVs also work in corporate teams with HVs sharing the caseload and so families have access to different HVs.
The standard HV contact times for women with a baby are around 4 weeks antenatally, at a new birth visit and in well-baby clinics. Routine contacts for assessment of infants’ developmental progress are being phased out.
The effectiveness of health visiting
There has been wide discussion over the evidence of the effectiveness of the work of HVs. 97,104,105 One of the first systematic overviews of home visiting106 indicated that there were positive outcomes in children’s mental development, mental health and physical growth; reductions in mother’s anxiety, depression and tobacco use; and improvements in maternal employment and nutrition, among others. There are very few reports of UK-based research in health visiting. 107 The review of articles on the effectiveness of home visiting in relation to child and maternal outcomes107 found evidence to suggest that home visiting programmes for parents of young children can have an effect on improvements in:
-
various dimensions of parenting108
-
some child behaviour problems
-
cognitive development, especially for some groups of children
-
childhood accidental injury rates109
-
the detection and management of PND. 1
There was no evidence that home visiting increased the uptake of immunisations or hospital admissions. 107 As is often the case, the review indicated a need to address methodological limitations of trials in this area to provide, in particular,104 a clear theoretical framework; clear descriptions of the intervention content, intensity, timing and duration; process measures; long follow-up times; a client perspective and assessment of satisfaction.
The role of the health visitor in black and ethnic minority communities
There are specific mental health issues affecting Asian and other non-indigenous women bringing up children in the UK. For example, the suicide rate among women who are born in South Asia and live in England is higher than that in the general population. When they are providing supportive care, HVs need to consider cultural practices about childrearing.
English language is not an issue for some second-generation immigrant women who speak Punjabi and Urdu, and some HVs have used the EPDS with English-speaking women from Asian and other ethnic minority groups. Some women who have recently entered the UK from Pakistan are unable to speak English, and there are growing numbers of Arabic-speaking women as well as Kosovans, Kurdish people and asylum seekers from other mid-European countries and elsewhere. For Pakistani women, link workers are employed who speak Punjabi and can read Urdu. There are also interpreters and link workers who speak other relevant languages. Aside from any language difficulty, literacy for women from Pakistan is more likely to be an issue.
There are no effective, validated, culturally sensitive tools for many women who have English as a second language. As well as literacy and language difficulties, immigrant women may also be isolated, and so women who are vulnerable to PND may be missed. Some work is beginning to develop and validate linguistically and culturally competent tools for use in primary care, using link workers and health professionals to identify psychological distress and assist the early detection of women from South Asian communities who speak Bengali, Gujarati, Punjabi and Urdu, as well as those from other ethnic minority communities. This may be useful in instances in which it is not possible to detect PND in other ways.
A Punjabi Postnatal Depression Screening Questionnaire (PPDSQ) was developed by a consultant psychologist in Bradford City PCT and the University of Bradford. 110 Also, the CPHVA has supported the development of a pictorial method for women who have English as a second language, to detect those who may be depressed. This work is undergoing a pilot validation study.
Chapter 2 Literature review of the prevention and treatment of postnatal depression
Although the role of HVs has been promoted in perinatal mental health there is still not enough evidence upon which to base practice to prevent or treat PND. A literature search was performed in July 2005 to identify and synthesise published literature on trials of interventions to prevent or treat postnatal morbidity and the costs associated with these. This was not a systematic review.
The main method used to identify relevant articles was a search of electronic bibliographic databases from the first date that the databases would allow. The electronic databases searched to provide the best coverage of trials were:
-
health databases: MEDLINE, CINAHL, EMBASE – 1966 to July 2005
-
evidence-based databases: the Cochrane Library, covering the Cochrane Database of Systematic Reviews (CDSR) and the Cochrane Controlled Trials Register (CCTR)
-
PsycINFO – to date.
The search strategy used the key text words depression, postpartum, postnatal, review, trial, random, blind and systematic as follows:
exp Depression, Postpartum
(postnatal or post-natal or post natal or perinatal or peri-natal or peri natal).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
depress$.mp. [mp = title, original title, abstract, name of substance word, subject heading word]
exp psychological techniques/or exp psychotherapy
(post partum or postpartum or post-partum).mp. [mp = title, original title, abstract, name of substance word, subject heading word]
limit to “therapy (sensitivity)”
limit to (humans and English language and “therapy (sensitivity)”)
social.mp. [mp = title, original title, abstract, name of substance word, subject heading word]
(review$or trial$or random$or blind$or systematic$).mp. [mp = title, original title, abstract, name of substance word, subject heading word)
The articles were considered relevant if they included a population of antenatal or postnatal women; psychosocial or other interventions to offer additional support; maternal reports of health status, morbidity or PND measured using validated tools; reports of use of services; and a planned comparison group using a rigorous research design.
Of the 241 published articles identified through the search, 185 potentially relevant abstracts were scrutinised and assessed for eligibility criteria and methodological quality. In total, 64 papers were selected for review and 43 were regarded as suitable for inclusion in the review. Studies were included if they were randomised controlled trials in a population of antenatal or postnatal women and they examined any association between support or interventions, to prevent or treat PND. The articles were relevant if they included maternal reports of health status.
Studies that were not written in the English language were not included. In a systematic review, two reviewers independently assign a quality rating to each trial being reviewed. Criteria that contribute to the assessment of the methodological quality of a trial are a clear and accurate description of:
-
participant selection, inclusion and exclusion criteria, and recruitment response rates
-
statistical power and sample size determination
-
random allocation, concealment, blinding, control for potential bias
-
experimental and control interventions
-
length and completeness of follow-up, compliance and attrition
-
outcome measures and statistical analysis.
Poorly controlled trials are also likely to be poorly reported, but if a well-controlled trial is not well reported it will be assessed as poor quality and the results will not be incorporated into a systematic review.
In this particular review it was difficult to grade and rank the quality of each trial as many of the quality criteria were not reported in the articles. Few authors described a pre-trial sample size calculation and the number of participants required to achieve statistical power. In reporting results many authors reported only absolute numbers, without confidence intervals, or a mean value without a standard deviation.
The quality of each study was not graded but was judged according to whether the study included a clear and accurate description of the experimental design, a sample size determination, participants’ baseline characteristics and comparison of groups, randomisation, blinding, setting, intervention, control intervention, compliance and attrition.
Cochrane and other reviews111,112 were also examined for additional relevant trials. The following reviews from the CDSR (Cochrane Depression, Anxiety and Neurosis Group and Cochrane Pregnancy and Childbirth Group) were relevant:
-
Dennis CL, Creedy D. Psychosocial and psychological intervention for preventing postpartum depression. 113
-
Hodnett ED. Caregiver support for women during childbirth. 114
-
Barlow J, Coren E. Parent training programmes for improving maternal psychosocial health. 115
-
Ray KL, Hodnett ED. Caregiver support for postpartum depression. 116
All together there were 43 relevant trials identified from the literature search and the Cochrane and other reviews. These trials are summarised under the following six headings:
-
antenatal prevention of PND (9 trials)
-
perinatal support or treatment to prevent PND (10 trials)
-
postnatal support interventions (3 trials)
-
postnatal prevention of PND (5 trials)
-
postnatal treatment of PND (16 trials).
Trials of antenatal prevention of postnatal depression
Because the strongest predictors of PND are antenatal anxiety or depression, lack of social support and stressful life events, theoretically, addressing some of these features could prevent PND. The Cochrane review113 of psychosocial and psychological interventions for preventing postpartum depression included antenatal trials, and a qualitative review111 specifically examined antenatal group interventions to reduce PND. The antenatal trials that aimed to prevent PND are summarised in alphabetical order in Table 2.
| Authors, location | Method | Subjects | Intervention | Sample | Outcomes | Results and conclusions | Comments |
|---|---|---|---|---|---|---|---|
| Chabrol et al., 2002,118 Toulouse, Narbonne, France | Controlled randomised study | ‘At-risk women’ with EPDS scores > 8 on French version of EPDS | One antenatal session including an educational component, a supportive component and a CB component during hospitalisation | n = 22 IG; n = 38 CG | EPDS | Significant reductions in frequency of probable depression in IG: IG – 30.2%, mean EPDS = 5.0; CG – 48.2%, mean EPDS = 13.7 (p = 0.0067) | Poor quality. Many limitations. Not ITT. ‘This programme for prevention and treatment of postpartum depression is reasonably well accepted and efficacious’ |
| Gorman, 2002,119 Iowa and St Louis, USA | RCT | Pregnant women at risk of postpartum depression | Five individual antenatal sessions based on IPT by a mental health specialist, in late pregnancy, ending around 4 weeks postnatally | n = 24 IG; n = 21 CG | EPDS, SCID – at 4 and 24 weeks | Mean EPDS scores were 7.9 in the IG (n = 15) and 8.0 in the CG (n = 15) (NS) | Very small sample |
| Hayes et al., 2001,120 Queensland, Australia | RCT | Primiparous women | One-to-one education intervention by specially trained midwives conducted at 28–36 weeks in an interview room or in their own home, about mood changes and symptoms and help-seeking vs CG | n = 95 IG; n = 93 CG | POMS, NSSQ – at 8–12 weeks and 16–24 weeks |
There was a steady reduction in POMS scale scores over all subscales in both groups, with no difference between groups at any follow-up time Women in both groups were more depressed antenatally than postnatally |
Duration of IG and CG not described. Did not use a measure of PND |
| Logsden et al., 2005,121 Louisville, USA | Random assignment | Adolescent girls 32–36 weeks’ gestation | (1) Pamphlet, (2) video and (3) pamphlet and video vs (4) CG | n = 128 | CES-D – at 6 weeks | There were no significant differences in CES-D scores between groups at any follow-up time | The education intervention had no effect on women |
| Marks et al., 2003,122 London, UK | RCT with random permuted blocks of 8 and 16, stratified by 6 offices | Antenatal women with history of major depressive disorder | Continuous midwifery care vs standard maternity care | n = 51 IG; n = 47 CG | DIS DSM-III-R case of major or minor depression | No differences in rates of PND between treatment conditions | ‘Continuous midwifery care had no impact on psychiatric outcomes’ |
| Matthey et al., 2004,123 London, UK | RCT | Antenatal women and men | Preparation for parenthood programmes: (1) ‘Empathy’ (experimental, focusing on psychosocial issues related to becoming first-time parents) and (2) ‘Baby play’ (control) vs usual service ‘control’ | n = 51 IG; n = 47 CG | DIS DSM-III-R case of major or minor depression | Reduction in postpartum distress in some first-time mothers at 6 weeks postpartum. Women with low self-esteem who had received the intervention were significantly better adjusted on measures of mood and sense of competence | ‘This brief psychosocial intervention can be readily applied to antenatal classes and is suitable for those who attend preparation for parenthood classes’ |
| Stamp et al., 1995,124 Adelaide, Australia | RCT, women stratified by parity | English-speaking women with a single pregnancy identified as being more vulnerable to PND | Antenatal groups: two special classes – simple primary PND preventive intervention, focusing on access to information, practical and emotional preparation and support, and one postnatal group run by midwives vs CG | n = 64 IG; n = 65 CG | EPDS – at 6 weeks, 12 weeks and 6 months | 13%, 11% and 15% of the IG women scored over 12 on the EPDS at 6 weeks, 12 weeks and 6 months, respectively, compared with 17%, 15% and 10% of the CG women, respectively | Privately insured women not able to participate. Attendance 31% overall. Return rate 92%, 92% and 87% at 6 weeks, 12 weeks and 6 months, respectively |
| Zlotnick et al., 2001,125 Providence, USA | Pilot RCT | Pregnant women receiving public assistance with at least one risk factor for PND | Four antenatal group sessions ‘Survival skills for new moms’ – four sessions (1 hour) IPT-oriented intervention vs treatment as usual | n = 17 IG; n = 18 CG | BDI, SCID – at 3 months | Significant difference in BDI score changes between IG and CG (p = 0.001). Women in the IG were significantly less likely to develop postnatal major depression compared with CG women (p = 0.02) | ‘A 4-session IPT-oriented group intervention was successful in preventing major depression in the first 3 postpartum months.’ In total, 50% of eligible women declined; 77% of women were single; 88% attended three sessions. Very small sample |
The trials mainly included women variously assigned as vulnerable or high risk using a modified screening tool, or women having their first baby, or both. Among all trials several outcome measures were used, mainly at 3 months.
The trials of groups had poor attendance and were not successful in reducing PND. 117,124 In the two very small trials,118,125 one French and one American, with limited quality, there appeared to be some effect. It is unclear whether the comparatively good attendance rate and the outcomes would be reflected in a larger trial.
There was not enough evidence from antenatal-targeted interventions provided for ‘at-risk women’. 111 Overall, the women in the IG were just as likely to become depressed as those in the CG. These antenatal studies do not provide sufficient evidence upon which to base care.
Trials of perinatal support or treatment to prevent postnatal depression
The perinatal studies that aimed to prevent PND113,114 can be summarised as midwifery, ‘debriefing’ or counselling studies, massage, doulas (experienced lay women providing support to women in labour) or companionship in prevention of PND, and these are summarised in alphabetical order below (Table 3).
| Authors, location | Method | Subjects | Intervention | Sample | Outcomes | Results and conclusions | Comments |
|---|---|---|---|---|---|---|---|
| Field et al., 1997,126 Miami, USA | Random assignment | Middle socioeconomic status women recruited from prenatal class | Massage by partner every hour for a total of 4 hours and partner coaching in breathing during labour vs coaching from partners | n = 28 | CES-D, POMS |
There was less depressed mood on the POMS scale in the IG: IG 6.9; CG 14.9 Also on the CES-D: 15.4 vs 19.8 |
‘Data suggest that the massaged mothers had shorter labours, shorter hospital stay and less postpartum depression’ |
| Gamble et al., 2005,127 Brisbane, Australia | RCT | Postnatal women assessed in the immediate postpartum for risk of developing psychological trauma | One midwifery-led ‘debriefing’ within 72 hours of birth, then another 4–6 weeks postpartum by phone vs CG standard care | n = 50 IG; n = 53 CG | EPDS – at 12 weeks | 4/50 IG women EPDS score > 12 vs 15/53 of the CG women. Women in the IG reported decreased trauma and low relative risk of depression and stress | ‘A brief intervention for a distressing birth experience effective in reducing trauma symptoms, depression, stress and feelings of self-blame’ |
| Gordon et al., 1999,128 San Fransisco Bay, USA | Randomised study | Primiparous women aged ≥ 18 years, uncomplicated deliveries | Trained doulas in hospital-based labours and deliveries vs usual care | n = 149 IG; n = 165 CG | MHI from SF-36 – at 4–6 weeks postnatally | No difference in postpartum depression or self-esteem measures | ‘In general, women who had doulas were very enthusiastic about them’ |
| Hagan et al., 2004,129 Perth, Western Australia | Single blind randomised controlled study | English-speaking mothers of very preterm infants (< 33 weeks) | Six CBT sessions in programme by a research midwife, postnatal weeks 2–6, vs standard care | n = 101 IG; n = 98 CG | EPDS, BDI, GHQ, SADS – at 2 weeks, 2 months, 6 months and 12 months | 29% of IG diagnosed with major or minor depression vs 26% CG | ‘Intervention programme did not alter the prevention of depression’ |
| Lavender and Walkinshaw, 1998,130 Merseyside, UK | RCT | Postnatal primigravidous women with a single birth by normal delivery | Midwife ‘debriefing’, 30- to 120-minute sessions, on postnatal wards, vs CG | n = 56 IG; n = 58 CG | HAD scale – at 3 weeks | Women in the IG were less likely than women in the CG to have HAD scale anxiety and depression scores of more than 10 (p < 0.0001) | Sample size based on HAD scores > 7; reporting by HAD scores of 10. Follow-up time of 3 weeks is too early to evaluate morbidity after childbirth |
| Priest et al., 2003,131 Perth, Australia | RCT | Mothers under psychological care at the time of delivery | One midwife ‘debriefing’ after childbirth for 15 minutes to 1 hour | n = 875 IG; n = 870 CG | EPDS – at 8 weeks, 24 weeks, 52 weeks | 37/696 IG women scored > 12 on the EPDS compared with 42/705 CG women | 19% attrition at 1 year |
| Selkirk et al., 2006,132 Victoria, Australia | Random assignment | Women recruited in third trimester | Midwife ‘debriefing’ vs CG | n = 149 | DAS, STAI, EPDS, POMS, PSI | EPDS at 3 months postpartum: IG, 6.69 low intervention and 6.13 high intervention vs CG, 5.25 low intervention and 5.57 high intervention | ‘Debriefed women were no less likely to develop symptoms of postnatal depression (using EPDS) than women who did not receive debriefing’ |
| Small et al., 2000,133 Melbourne, Australia | RCT | Women who had given birth by Caesarean section, forceps or vacuum extraction | Midwife ‘debriefing’, at least 24 hours after the birth, up to 1 hour, in hospital vs standard care | n = 464 IG; n = 447 CG | EPDS, SF-36 subscales – at 6 months | 17% of women in debriefing scored ≥ 13 on EPDS vs 14% CG. Also poorer health on seven out of eight SF-36 subscales | CG women received a brief visit and a leaflet. Nearly all women found the debriefing helpful |
| Tam et al., 2003,134 China | RCT | Chinese women who had suffered suboptimal outcomes in pregnancy and labour | One to four ‘educational counselling’ sessions for high-risk women by a research nurse before discharge from hospital | n = 280 IG; n = 280 CG | HADS > 4 – at 6 weeks postpartum | 26/261 IG women depressed compared with 35/255 CG women. Mean depression scores 3.30 IG vs 3.50 CG | Short follow-up |
| Wolman et al., 1993,135 USA | RCT | 189 nulliparous labouring women | Additional companionship from community volunteer vs usual care | n = 92 IG; n = 97 CG | IG women attained higher self-esteem scores and lower postpartum depression and anxiety ratings at 6 weeks | ‘Companionship modifies factors that contribute to the development of postnatal depression’ |
The massage trial126 was not described sufficiently well and the sample size was too small, but the reported significant difference in the mean time in labour suggests that the intervention could be worthy of further investigation and longer follow-up.
Of the five midwifery debriefing studies, the two smaller studies, one in the UK130 and one in Australia,127 reported a short-term effect. The two larger trials,131,133 however, and the most recent132 did not report a positive outcome.
The trial of companionship135 suggested that self-esteem might be improved. The authors of the ‘doula’ trial128 indicated that participating women were very enthusiastic about the doulas and appreciated their knowledge, support and reassurance. Unlike other trials there were no differences demonstrated in perinatal outcomes.
The Cochrane review of caregiver support for women during childbirth concluded that there were a number of benefits for mothers and their babies, and there did not appear to be any harmful effects. 116
The trial of CBT for women with very preterm infants129 did not reduce the prevalence of major or minor depression at follow-up.
In the Chinese education sessions trial follow-up was only 6 weeks. 134
Trials of postnatal support
Three trials of postnatal interventions to support socially disadvantaged mothers examined maternal outcomes of feeling tired, feeling miserable and negative feelings. The studies included mothers in an eastern US city,136 262 mothers in Dublin137 and mothers in the eastern USA. 138 Mothers who received support were less likely to report being tired, unhappy, not wanting to go out and other negative feelings at 1 year postnatally. 137 In all three trials childhood immunisation was more likely to be complete in the IG. 138 Without valid and reliable methods of obtaining mothers’ evaluations, these trials were not large or rigorous enough to examine the impact of social support on maternal and child health outcomes.
The Hackney Daycare Study139 was a randomised controlled trial of 120 mothers with a child age from 6 months to 3½ years, allocated to receive a place at the Mapledene Early Years Centre, or not. Although not the main outcome, maternal psychological well-being was measured using the General Health Questionnaire (GHQ-12). Mothers in both groups had a mean GHQ-12 score of 10.8, indicating no apparent benefit as measured by the GHQ-12.
A Cochrane systematic review of parent-training programmes115 for improving maternal psychosocial health among population women or clinical groups of women included data from 20 studies. The meta-analysis showed that the intervention was associated with positive outcomes for depression, anxiety or stress, self-esteem and relationship with spouse or marital adjustment. The results suggested that parenting programmes could help promote positive mental health in the short term, but there was insufficient evidence regarding the long-term effectiveness of the programmes. 115
More recently there was a trial of two forms of postnatal social support offered to mothers living in disadvantaged inner-city areas of London. 140 Among the 367 IG women there was no evidence of an impact of either a programme of visits from HVs trained in supportive listening or the services of local community support organisations on maternal depression, child injury or maternal smoking, compared with the 364 women in the CG.
Postnatal trials to prevent postnatal depression
Because lack of social support and stressful life events have been correlated with the development of PND, many studies have aimed to ameliorate the potential impact of these by providing additional support or helping women develop coping techniques before depression develops. A Cochrane review of psychosocial and psychological interventions for preventing postpartum depression113 identified postnatal support trials that aimed to prevent PND by offering an intervention postnatally. These trials are summarised in alphabetical order in Table 4.
| Authors, location | Method | Subjects | Intervention | Sample | Outcomes | Results and conclusions | Comments |
|---|---|---|---|---|---|---|---|
| Armstrong et al., 1999,141 Armstrong et al., 2000,142 Fraser et al., 2000,143 Queensland, Australia | RCT double-blind | Women in the immediate postpartum with self-reported vulnerability factors (Brisbane Evaluation of Needs Questionnaire) | Nurse weekly home visiting structured programme of 20–60 minutes, minimum 18 per family (weekly for 6 weeks, fortnightly to 3 months, monthly to 12 months), supported by a social worker and paediatrician, vs standard community child health services | n = 90 IG; n = 91 CG | PSI, EPDS – at 6 weeks and 12 months |
Mean 6-week EPDS scores: IG 5.8 vs CG 20.7 (p = 0.003). Improved experience of the maternal role. No difference in breastfeeding or use of health services. Intervention was welcomed; 90 women were willing to accept the programme (one refused) No difference in mean EPDS scores at 4 months: IG 5.75 vs CG 6.64; 6.2% IG and 13.6% CG scored > 12 |
Targeted families in which child was at risk. Significant differences after randomisation. Focused on adjustment to parenting role 76% response to follow-up. Baseline EPDS, physical child abuse potential, PST all predicted level of PND at 12-month follow-up |
| Gunn et al., 1998,144 Melbourne, Australia | RCT with block randomisation stratified by recruiting centre | Postnatal women who gave birth at a rural and a metropolitan hospital, recruited on second or third day postnatally | GP appointment 1 week after discharge vs GP appointment 6 weeks after discharge | n = 232 IG; n = 243 CG | EPDS, SF-36 – at 3 months and 6 months |
3-month mean EPDS scores: IG 7.38 vs CG 7.48 (p = 0.85); 6-month mean EPDS scores: IG 5.87 vs CG 6.08 (p = 0.67) 3-month EPDS > 12: IG 16.6 vs CG 13.6 (p = 0.37); 6-month EPDS > 12: IG 11.6 vs CG 12.8 (p = 0.69) No difference in any SF-36 scores on any domain at 3 or 6 months 46.3% IG vs 51.4% CG breastfeeding at 6 months (p = 0.28) |
IG women were less likely to attend their appointment (p = 0.001). Many commented that the 1-week appointment was too early |
| MacArthur et al., 2002,145 West Midlands, UK | Cluster RCT | Postnatal women registered with 17 intervention practices and 19 control care practices. Recruitment time unclear | 42 midwives offering midwifery-led care, using symptom checklists, EPDS, no routine GP contact, last visits at 28 days, discharged at 10–12 weeks, vs 38 midwives trained in postnatal care and health and trial design offering control care | n = 101 IG; n = 98 CG | SF-36 physical component summary (PCS) and mental component summary (MCS) score, EPDS at 4 months |
Mean EPDS scores: IG 6.40 vs CG 8.06 (p < 0.0001). EPDS > 12: IG 14.39 vs CG 21.25 (p = 0.01) Mean PCS: IG 47.54 vs CG 50.50 (p = 0.002). Mean MCS: IG 46.68 vs CG 47.84 (p = 0.089). |
IG significantly more likely than CG to rate care as better than expected. Economic evaluation reported separately |
| Morrell et al., 2000,146 Sheffield, UK | RCT | Postnatal women who gave birth at an urban teaching hospital | Support workers offering up to 10 home visits of up to 3 hours in the first postnatal month vs usual postnatal care | n = 311 IG; n = 312 CG | SF-36, EPDS, DUFSS, breastfeeding – at 6 months | Mean EPDS: IG 7.4 vs CG 6.7 (p = 0.05) | ‘No evidence of any health benefit at the 6-week or 6-month follow-up.’ Cost per woman was £160 |
| Reid et al., 2002,147 Ayrshire and Grampian, Scotland | Pragmatic RCT | Primiparous women | 4 cells: (1) support pack, (2) support group, (3) support group and pack, (4) CG | (1) n = 250; (2) n = 250; (3) n = 253; (4) n = 251 | EPDS, SF-36, SSQ-6 – at 3 months and 6 months |
Mean EPDS scores: (1) 5.6, (2) 6.1, (3) 6.1, (4) 5.9 at 3 months Percentage scoring 12 or more on EPDS: (1) 12.0, (2) 16.8, (3) 15.2, (4) 11.7 at 3 months |
Low uptake of support groups (around six attenders, with 89 groups having no attenders). Cost per group was £21.31 per attendance, packs cost £1.75 |
There was some short-term benefit of the nurse home visiting programme in lower EPDS scores at 6 weeks,141 but there was no difference in maternal mood at 4 months. 142 The only other intervention that had an impact on mean EPDS scores at 4 months was the redesigned midwifery care trial. 145 There were some implementation problems with the early GP appointment trial144 and there were no significant differences in EPDS scores at 3 months.
In the support worker trial146 there were no differences in any of the instruments used, even though the women said that they felt that they had benefited from the intervention. The mean cost for the support worker service was £160 per woman.
The trial comparing social support groups and packs147 found that few women attended the groups, but more reported that they had read the pack at least once. The reasons given by those who did not attend were that the groups were too inconvenient or that they were too shy to attend alone. There was no difference in the mean EPDS scores between any of the groups or the percentage of women scoring 12 or more on the EPDS. The total cost for providing the packs was £439 and for running the postnatal support groups was £14,000. 147 The main outcomes indicated that intensive postpartum support showed promising results, and that identifying ‘at-risk’ mothers was helpful. 113 There was insufficient evidence that the diverse interventions reduced the number of postnatally depressed women.
Trials of postnatal treatment of postnatal depression
An early Cochrane review (withdrawn) to assess the effect of professional or social support interventions on postpartum depression was based on the theoretical premise that supportive relationships during the perinatal period could enhance a mother’s feeling of well-being. Two trials were included in the review,1,3 which concluded that professional and/or social support may help in the treatment of postpartum depression but that it was too early to draw conclusions for practice based on so little evidence. One of these trials3 was also included in a Cochrane review of antidepressant treatment for PND. 67 Since this early Cochrane review, further postnatal treatment studies of psychotherapy or psychological support have been published and reviewed13,112,148 and these are summarised below in alphabetical order (Table 5). The extensive range of approaches developed to treat PND reflects its broad aetiology. Among these trials are some in which the ‘therapist is not professionally prepared’. 149
| Authors, location | Method | Subjects | Intervention | Sample | Outcomes | Results and conclusions | Comments |
|---|---|---|---|---|---|---|---|
| Appleby et al., 1997,3 Manchester, UK | RCT, double-blind | Community postnatal women satisfying criteria for major depression at 6–8 weeks | (1) Fluoxetine 20 mg and one session CBC, (2) fluoxetine and six sessions CBC, (3) placebo and one session CBC, (4) placebo and six sessions CBC | n = 87 | EPDS, HRSD – at 1, 4 and 12 weeks | Fluoxetine more effective than placebo; six sessions of CBC more effective than one session of CBC; fluoxetine and CBC equally effective | 101/188 (54%) eligible women refused to participate (reluctance to take drug). Excluded breastfeeding. 61/87 completed (30% dropout) |
| Armstrong and Edwards, 2004,150 Queensland, Australia | RCT | Women with an EPDS score > 11 and infant 6 weeks–18 months, and medical certificate about physical activity | 12 pram-walking exercise sessions vs weekly social support meeting | n = 12 IG; n = 12 CG | EPDS and social support interview | There was a significant difference in mean (SD) EPDS scores between exercise group, 6.33 (3.67), and social support group, 13.33 (7.66) (p < 0.05) | Small sample. Exercise group had reduced feelings of depression and improved physical fitness; no change in perceived social support. Not ITT. Not generalisable |
| Chen et al., 2000,151 Kaohsiung, Taiwan | RCT | Postnatal women recruited on ward 2–3 days postnatally and scoring 9 or above on BDI at 3 weeks | Postnatal groups – four weekly meetings of 1.5–2 hours on transition to motherhood, postnatal stress, communication skills and life planning, vs CG. | n = 30 IG; n = 30 CG | BDI, PSS, ISEL, CSEI – at the end of the 4-week programme | 33% IG women depressed using BDI vs 60% CG women (p < 0.05). Attenders had significant positive changes in BDI, PSS and ISEL scores (p < 0.01) but no significant changes in any measure in the CG | Poor quality. 115 met the inclusion criteria; 60 enrolled; 44% returned screening questionnaire. The postnatal time of outcome measurement is not clear. 92% average attendance. |
| Cooper and Murray, 1997,152 Cooper et al., 2003,2 Cambridge, UK | RCT – the Cambridge treatment trial | Primiparous women screened to identify those who met DSM-III-R criteria for major depression | Home therapy 8–18 weeks. (1) NDC, (2) CBT, (3) dynamic psychotherapy (DPT) vs (4) routine care | (1) n = 49; (2) n = 42; (3) n = 48; (4) n = 52 | EPDS, SCID – at 18 weeks, 9 months and 18 months |
25–35% reduction in EPDS in three IGs vs 4% in the CG % women not depressed: (1) NDC 52%, (2) CBT 59%, (3) DPT 75%, (4) routine care 40% |
By 9 and 18 months’ follow-up differences between all four groups were not significant. Dropouts: (1) 14%, (2) 2%, (3) 17% |
| Dennis, 2003,153 British Columbia, Canada | RCT pilot study | Women with EPDS score > 9 at 8 weeks postpartum, defined as high risk for postpartum depression | Peer telephone support mother-to-mother using trained volunteers with a personal history of PND vs standard care | n = 34 IG; n = 27 CG | EPDS – at 4 months | Significant differences in EPDS scores >12 at 4 months: 15% IG vs 52% CG. Acceptance rate 67% | ‘Telephone-based peer support may effectively decrease depressive symptomatology among new mothers’ |
| Field et al., 1996,154 San Diego, US | Random assignment | Depressed adolescent mothers, identified using BDI | 10 massage therapy sessions for 30 minutes over 5 weeks vs 10 relaxation sessions for 30 minutes over 5 weeks | n = 32 | POMS 14-item depression scale, urinary cortisol | Massage therapy had a significant immediate effect on behavioural and stress hormone changes, including decreased anxious behaviour, pulse and salivary cortisol levels and urinary cortisol | Poor quality: small sample size, no true CG, randomisation unclear |
| Heh and Fu, 2003,155 Taipei, Taiwan | Random allocation | Women scoring over 10 on the EPDS (considered to be ‘at risk’ of PND) | Informational support about PND during the sixth week postpartum vs routine care | n = 35 IG; n = 35 CG | EPDS – at 3 months | 60% IG women scored below 10 on EPDS vs 31% CG women | ‘Informational support given postnatally may contribute to psychological well-being.’ No power calculation. Small sample |
| Holden et al., 1989,1 Edinburgh and Livingston, Scotland, UK | Controlled random order trial | Depressed women (psychiatric interview at 13 weeks postnatally) | One-to one ‘listening visits’ (eight 1-hour weekly sessions) by 17 HVs vs routine care | n = 26 IG; n = 24 CG | Goldberg, EPDS – after 13 weeks | 69% of IG women recovered vs 38% of CG women | The HVs providing the intervention continued to visit the CG women |
| Honey et al., 2002,156 Cardiff, UK | Block random allocation procedures | Women < 12 months postpartum scoring > 12 on EPDS | Eight HV 2-hour psychological–educational group (CBT and relaxation) vs routine primary care | n = 23 IG; n = 22 CG | EPDS, DUFSS, DAS |
Mean EPDS: 12.55 IG vs 15.63 CG 65% IG women scored below the cut-off for major probable PND (< 13) vs 36% CG women |
‘A brief psychological–educational group is an effective form of treatment for women with low postpartum mood’ |
| Milgrom et al., 2005,157 Melbourne, Australia | Cycled random allocation, by slips drawn from a bag. RCT | Community women with a diagnosis of depression confirmed by CIDI | 12 weeks × 90 minutes: (1) CBT, (2) group counselling, (3) one-to-one counselling vs (4) routine care | (1) n = 46; (2) n = 47; (3) n = 66; (4) n = 33 | BDI, Beck Anxiety Inventory, Social Provisions Scale | Proportions of post-intervention BDI scores below threshold for clinical depression were (1) 55%, (2) 64%, (3) 59% and (4) 29% | Psychological intervention per se was superior to routine care in reducing depression and anxiety |
| Misri et al., 2000, Vancouver, Canada. 158 | RCT | Women with major postpartum-onset depression | Six psychoeducational visits weekly, four with partners, vs six psychoeducational visits | n = 16 IG; n = 13 CG | EPDS, KSQ, DAS, PBI, MINI | Mean EPDS: 8.6 IG vs 14.7 CG (p = 0.013). Mean KSQ: IG 2.1 vs 6.6 CG (p = 0.021). Lower morbidity in partners who attended vs others (p = 0.01) | Poor quality: randomisation not described, small sample size, group differences in baseline characteristics |
| Misri et al., 2004,159 Vancouver, Canada | RCT | Women referred to tertiary care with DSM-IV criteria for major depression | Paroxetine plus 12 sessions of CBT vs paroxetine monotherapy | n = 16 IG; n = 19 CG | HRSD, EPDS – at 12 weeks | Both groups having antidepressant therapy and CBT showed improvement (p < 0.01) in mood and anxiety | No treatment as usual or CG |
| O’Hara et al., 2000,149 Iowa, USA | RCT | 120 postpartum women meeting DSM-IV criteria for major depression with modified SCID | 12 × 1-hour sessions of interpersonal psychotherapy (IPT) by 10 experienced psychotherapists vs waiting list control. Women with history of major depression separately randomised | n = 48 IG; n = 51 CG | IDD, amended HRSD, BDI, SAS, DAS, PPAQ, modified SCID – at 4, 8 and 12 weeks |
12-week HRSD scores: 8.3 IG vs 16.8 CG (p < 0.001). 12-week BDI scores: 10.6 IG vs 19.2 CG (p < 0.001). PPAQ and SAS scores improved in the IPT group No difference in DAS |
Most women were white and well educated 132 declined participation; 20% withdrew from IPT Women in the CG were phoned every 2 weeks Non-blinded raters |
| Onozawa et al., 2001,160 UK | RCT | Primiparous women 4 weeks postpartum, identified using EPDS | 12 × weekly 1-hour infant massage classes and 30-minute informal support group | n = 34 | EPDS | Significant differences between groups | Poor quality: small sample size, randomisation unclear, high drop-out rate from IG, analysis not ITT |
| Prendergast and Austin, 2001,161 Australia | RCT | Postnatal women with DSM-IV major or minor depression | Six modified CBC nurse-delivered home-based weekly 1-hour sessions vs standard care | n = 17 IG; n = 20 CG | EPDS, MADRS |
No significant difference post treatment; 70–80% recovered (EPDS < 10) in both groups 6-month postal follow-up |
‘Early childhood nurses could deliver modified CBT for PND.’ Perceived support from nurse appeared to be as effective as modified CBT |
| Wickberg and Hwang, 1996,162 Goteborg, Sweden | Controlled study | Women with EPDS ≥ 12 and major depression (MADRS) at 2 months and 3 months | Six × 1-hour counselling sessions by child health nurse vs routine care | n = 20 IG; n = 21 CG | MADRS – at about 19 weeks | 12/15 (80%) IG women showed no major depression after six sessions vs 4/16 (25%) CG women (p < 0.01) | Small sample, seriously ill excluded, randomisation not described. Nurses received 4 half-days of training |
Antidepressants to treat postnatal depression
The Cochrane review of antidepressant drug treatment for PND aimed to compare the effectiveness and safety of different antidepressants with other forms of treatment. 67 The Cochrane review included only one trial of fluoxetine,3 which was rated for methodological quality as category A. This was a community-based, randomised, double-blind controlled trial of 87 depressed postnatal women in Manchester that had four treatment groups:
-
fluoxetine 20 mg with one session of cognitive behavioural counselling (CBC) by a psychologist
-
fluoxetine with six sessions of CBC
-
placebo with one session of CBC
-
placebo with six sessions of CBC.
There was improvement in all groups and fluoxetine was more effective than placebo and six sessions of CBC were more effective than one session of CBC. Fluoxetine and CBC were equally effective for non-psychotic depression in postnatal women. However, 101/188 (54%) eligible women refused to take part, mainly due to reluctance to take the drug, and there was a 30% dropout rate with 61/87 women who agreed to participate, completing.
The review concluded that women with PND can be treated equally effectively with fluoxetine or a course of CBC in the short term and that there should be more, longer-term studies comparing different antidepressants and psychosocial interventions. 67
Psychosocial interventions
The withdrawn Cochrane review to assess the effect of caregiver support for postpartum depression included the Manchester trial3 of fluoxetine and cognitive behavioural-type counselling and the Edinburgh trial, which was a study of a HV one-to-one NDC intervention. 1 The review indicated that it would be premature to make practice recommendations based upon only two small trials. It indicated that future research should consider lay support; home visits, phone calls or group sessions; and the prevention and treatment of PND, including outcomes of symptoms, hospital admission rates and long-term maternal and infant and family well-being. Additionally, an economic evaluation would be necessary to determine the relative efficiency of the provision of care.
The Edinburgh trial tested one-to-one NDC visits,1 whilst the Manchester trial tested CBT3 and the Cambridge treatment trial2 tested CBT against person-centred therapy and psychodynamic psychotherapy. The Cambridge trial was the largest trial of psychological interventions for women with depression postnatally. Primiparous women were screened ‘in the early postpartum period’ to identify those who met DSM-III-R criteria for current major depressive disorder. Women were offered therapy in their homes from 8 to 18 weeks postpartum or routine care in four groups, as in Table 6. The EPDS and Structured Clinical Interview for DSM-IV Disorders (SCID) were administered at 18 weeks. In the short term there was a 25–35% reduction in EPDS in the IG compared with about 4% in the CG.
| Group | Intervention | Number in group | % no longer satisfying DSM-III-R criteria |
|---|---|---|---|
| Group 1 | Non-directive counselling | 49 | 52 |
| Group 2 | Cognitive behavioural therapy | 42 | 59 |
| Group 3 | Psychodynamic therapy | 48 | 75 |
| Group 4 | Routine primary care | 52 | 40 |
The trial found that there was a significant improvement following NDC, CBT or psychodynamic therapy immediately after treatment compared with routine care. 2 By 9 months there had been recovery in the CG so that there was little difference between the reduction in their EPDS scores and the reduction in the scores for the women who had received counselling or psychotherapy. 2 The improvements were well maintained in the CBT group up to 18 months and, using the percentages of women who dropped out of treatment early, the CBT appeared to be the most acceptable treatment.
The trial also found a significant benefit in mothers’ reports of relationship problems with their infants at 4 months postnatally. 163 Mothers’ reports also indicated evidence of a benefit from NDC at 18 months for emotional and behavioural problems.
On the basis that it works for major depression, the efficacy of interpersonal psychotherapy (IPT) was tested in a randomised controlled trial149 of 120 women in Iowa, USA, who met the DSM-IV criteria for major depression using a modified SCID. Most of the women were white and well educated. The IG women (n = 48) were offered 12 × 1-hour sessions of IPT, which were carried out by 10 experienced psychotherapists who were required to complete a 12-session course of IPT with a postpartum depressed woman ‘at a satisfactory level of competence’. The CG was a waiting list control (n = 51) who were phoned every 2 weeks. In total, 20% of women withdrew from IPT. After 12 weeks all scores except the Dyadic Adjustment Scale (DAS) were significantly better in the IG than the CG, as assessed by non-blinded raters.
The Australian study comparing CBT, group counselling and one-to-one counselling against routine primary care used an allocation method of drawing slips of paper from a bag and was therefore not free from bias. This study found improvements in all three groups compared with control, and the greatest benefit appeared to be associated with individual counselling. 157
In contrast, the very small Australian study of nurse-delivered CBC for women with depression found no significant difference immediately post treatment, but there may have been some effect at the 6-month follow-up. 161
A very small study156 in Cardiff, Wales, examined the effectiveness of a brief ‘psychoeducational group’ intervention for women who scored 12 or more on the EPDS. In total, 23 women were allocated to the intervention of eight 2-hour group meetings run by HVs. These covered education about childcare and accessing social support, cognitive behavioural techniques and relaxation techniques. Compared with the women in the CG who received routine primary care, the mean EPDS scores decreased significantly in the IG.
The very small controlled study162 in Goteborg, Sweden, included 20 IG women and 21 CG women who scored 12 or more on the EPDS at 2 months and again at 3 months interviewed with the Montgomery-Asberg Depression Rating Scale (MADRS) and diagnosed as having major depression. The IG women were offered 6-weekly 1-hour counselling sessions in the home or clinic by the child health nurse, who had received four half-day training sessions in NDC, whereas the CG received routine care. In total, 80% of women (12/15) in the IG showed no major depression after six sessions compared with 25% (4/16) of CG women (p < 0.01). Seriously ill women were excluded and the randomisation process was not described.
Other studies
Informational support
The small Taiwanese study155 of 70 women, offering information about PND, appeared to show some positive impact but it was not well reported.
Postnatal support groups
In the small Taiwanese study151 30 women who had a Beck Depression Inventory (BDI) score of 9 or more at 3 weeks attended a support group of five to six mothers with their infants. A total of 30 CG women completed two assessments. In the IG, 10 women (33.3%) remained depressed, compared with 18 women (60%) in the CG, as measured by a BDI score of less than 10, indicating a possible benefit from the intervention.
Psychoeducational visits with partners
The very small study158 of psychoeducational clinic visits for depressed women, with partner support in four of them, found lower EPDS scores in the women whose partners attended the support group, as well as less psychological morbidity in the partners themselves, compared with those who did not attend.
Pram-walking exercise programme
In a very small Australia study women who had an EPDS score of 12 or more at baseline were allocated at random to either an exercise group (n = 9), who were encouraged to attend two pram-walking sessions per week, or a social support group (n = 10), who met once per week. 150 The women were a well-educated group (who had a pram) and the analysis was not by intention to treat. The mean EPDS scores in the pram group were significantly lower than those in the social support group after 6 weeks, but there were no significant changes in social support in either group.
Telephone support
The pilot study153 of telephone-based peer support with 42 women found significant reduced EPDS scores in the IG at 4 months postnatally compared with the usual care group.
Summary of trials to treat postnatal depression
Most of these studies appeared to have positive benefits, at least in the short term. It seems that PND is amenable to treatment. However, the populations of women included were identified using different methods to assess depression, most often the EPDS, BDI or a psychiatric interview. The postnatal recruitment time varied from the first few postnatal days151 to 18 months in the pram-walking study. 150 The outcomes were measured using more than 23 different instruments. There were problems in recruiting and retaining women in the study. Half of the studies had a sample of 60 or fewer women, and most of the studies measured outcomes at 1 and 3 months postnatally. The exception was the Cambridge trial, which followed up women to 18 months postnatally. 152
Summary of the need for the PoNDER trial
The outcomes of health visiting studies and endorsements from official reports on the role of HVs in the context of PND indicate that HVs could have a clear role in the early detection of PND and in offering psychological interventions to women. There is not enough published evidence to determine the most effective and efficient intervention to be offered by HVs.
The PoNDER trial was commissioned, funded and initiated on the basis that there was growing demand for, and evidence of the effectiveness of, psychological interventions for the treatment of PND. Also, it was apparent that HVs were in an ideal position to detect women with depression, to establish a trusting relationship with postnatal women and to use their interpersonal skills and communication skills, which lie at the core of health visiting. HV skills in psychological approaches may depend on the training that they receive or their natural predisposition to offering a counselling intervention. 164 The PoNDER trial built upon the potential for HVs to develop appropriate skills, to adopt an effective role in the detection of depression and to offer effective support to eligible women.
The PoNDER trial was designed to be rigorously performed and reported165 and to address some of the methodological limitations of earlier work and, moreover, it was an economic evaluation.
Chapter 3 Rationale for the comparison of two psychological approaches
The two contrasting psychological approaches were investigated because, when the trial was commissioned, two promising trials of non-directive (person-centred) counselling and CBC for PND were included in an early Cochrane review. 1,3 In the first trial of ‘listening’ visits (based on Rogerian NDC), HVs in Edinburgh who had received a brief training in NDC were asked to visit depressed postnatal women for 1 hour each week for eight weeks. 1 The community-based, randomised, double-blind controlled trial of postnatal women3 in Manchester compared 20 mg of fluoxetine or placebo with one or six sessions of CBC. Other studies also reported promising findings of a positive effect from offering sessions with a person-centred (non-directive) approach1,2 and also from studies that had incorporated a cognitive behavioural component. 3,152,156,157,159
Person-centred counselling and CBC rely on different assumptions about the processes underpinning psychological change. The former is based on the idea that opportunities to explore difficulties with another, who listens non-judgementally and reflects empathically, allows a person to feel validated as a person and facilitates their abilities to manage their distress and find their own solutions. CBC assumes that events, thoughts and feelings are linked in a predictable way and that, by understanding these patterns, particularly where patterns of thinking lead to distress, there is the opportunity to make active change and test out new ways of thinking and behaving. There are therefore fundamental differences underpinning these two approaches, what they require of the person in the therapeutic role and of the client. It was therefore important to consider how each different approach impacted on outcomes.
The Cochrane review indicated that future research should consider the prevention and treatment of PND, including outcomes of symptoms, hospital admission rates and long-term maternal and infant and family well-being. The review concluded that an economic evaluation would be necessary to determine the relative efficiency of provision of care. Hence the trial was planned to compare the cost-effectiveness of the two contrasting psychological approaches for postnatal women.
Aims and objectives
Primary aim
The primary aim of the trial was to reliably estimate any differences in outcomes for postnatal women attributed to special training for HVs, delivered at GP practice (cluster) level, in systematically identifying depressive symptoms and delivering experimental psychological sessions, based on either cognitive behavioural principles166 or person-centred principles,167 compared with HV usual care (control).
Secondary aim
The secondary aim was to establish the relative cost-effectiveness of the HV training from an NHS perspective, relative to HV usual care.
Cluster level objective
The main objective at cluster level was to provide collaborating HVs in the intervention clusters with the skills to identify women with PND and to provide effective psychological sessions. It was not clinically appropriate to train HVs to provide this without developing their skills in assessing women and identifying depressive symptoms. In this trial HVs were trained to administer the EPDS8 and use clinical assessment skills to assess a mother’s mood, including depressive symptoms and suicidal thoughts, and to explore her feelings about the baby. 65
Individual level objectives
-
To identify women at risk of PND by the presence of depressive symptoms at 6 weeks postnatally. Eligible women were recruited to the study and the EPDS was administered postally to consented women at 6 weeks postnatally. Women who scored ≥ 12 on their 6-week postal EPDS were termed at-risk women. This pragmatically chosen threshold score recommended for clinical practice4 was used to identify women likely to benefit from psychological support and for whom a direct comparison would be made between the IGs and CG in the intention to treat analysis. The primary outcome was the proportion of at-risk women still scoring ≥ 12 on the EPDS at 6 months postnatally.
-
To identify IG women who were eligible for up to eight psychological sessions for 1 hour per week, based on either cognitive behavioural principles166 or person-centred principles. 167 To achieve this the IG HVs were asked to readminister the EPDS face-to-face at 8 weeks postnatally to at-risk women in the IG to identify those who scored ≥ 12 for a second time on the EPDS. It was inevitable that not all women with a 6-week EPDS ≥ 12 would be eligible for the psychologically informed sessions, as the study was designed to filter out women with transient depressive symptoms by the readministration of the EPDS at 8 weeks postnatally. The HVs also monitored uptake and compliance with the psychological sessions.
-
To identify any differences in costs for use of services for at-risk women in the IG versus use of services for at-risk women in the HV usual care (control) group.
Secondary objectives
The main aim of the trial was the clinically important question of the effectiveness of HV psychological sessions. A further set of objectives were:
-
To monitor any change in women’s health over time by following up and measuring outcomes for at-risk women at 6, 12 and 18 months postnatally.
-
To identify potential clinical or economic benefits of a postal administration of the 6-week EPDS versus face-to-face HV administration. Within the random allocation, each of the IG clusters had an equal chance of being allocated to one of four subgroups, and so there were two IGs using the face-to-face plus postal EPDS administration for comparison with two groups using postal-only EPDS administration.
-
To use the Schedule for Clinical Assessment in Neuropsychiatry (SCAN)168 to assess the severity of depression among at-risk women. SCAN interviews were also performed in at-risk women who had a range of 6-week postnatal EPDS scores, to investigate how well the EPDS administered in a primary care setting identified depressive symptoms in women who were truly depressed (according to the SCAN classification). It was also possible to assess the proportion of IG women who were classified as depressed but whose EPDS scores were below 12.
-
To examine outcomes in women’s partners to 18 months postnatally. When the women were followed up by postal questionnaire, a separate questionnaire was included for women’s partners to complete to monitor their health status over time.
-
To monitor infant development to 18 months postnatally. The 18-month women and partner questionnaires also included questions on infant development.
Objectives for all women who consented to take part in the trial
It is a recognised limitation of the EPDS that not all depressed women score 12 or more. In the first EPDS validation study8 using the threshold score of 12, the sensitivity for identifying depressed women was 86% and the specificity for detecting true negatives was 78%. A cut-off score of 10 reduced the failed detection rate to fewer than 10% but doubled the number of false positives to 10 women. Also, women may develop symptoms of depression before their baby is 6 months old, but not precisely at 6 weeks postnatally. Examining outcomes only for women who had a 6-week EPDS score ≥ 12 may have failed to identify the full effect of the cluster level intervention. Therefore, all consented women, not only the at-risk women, were followed up at 6, 12 and 18 months postnatally, to include all women who may have been depressed or who could have developed depression after 6 weeks postnatally. This allowed an examination of the broader impact of the HV training intervention beyond the at-risk women. The objectives for the cohort of all women who consented to take part in the study were the same as for the at-risk women, that is, to:
-
identify the proportion of all women in the intervention and control groups scoring ≥ 12 on the EPDS at 6 months postnatally
-
monitor the change in health of all women over time
-
monitor the change in health of all women’s partners over time
-
monitor infant development for all women to 18 months postnatally
-
identify any differences in costs for use of services for all women in the IGs versus women in the HV usual care group.
Design and methods
Overview of design
The study was a prospective pragmatic randomised cluster trial with clusters allocated at random to one of two experimental psychological approaches or HV usual care (control arm), stratified by number of expected births per year. It was a pragmatic trial of the effectiveness of an intervention offered under normal conditions, excluding as few women as possible and accommodating non-acceptance of the offered intervention and other co-interventions.
Pragmatic trials aim to establish the relative value of interventions, as they would be provided in routine care settings, to increase the external validity without adversely affecting the internal validity. Hence, the trial aimed to answer a real-life clinical question in a real-life clinical situation. 169 This means that the interventions reflected the clinical variation that exists in routine primary care contexts. 69 In the CG, routine care included all of the support that women would normally access, from HVs, GPs and elsewhere.
The clusters randomised in the trial were GP practices, and the HVs who worked with GPs, and held a caseload of families registered with the GP practice, were approached to take part. The intervention arm HVs were trained in delivering the psychological sessions to which their practice had been randomised.
Collaborating HVs approached pregnant eligible women aged over 17 years who were on their caseload to take part in the study. Women who consented and who had a live baby were sent a 6-week postal questionnaire. All women with a 6-week postal EPDS score ≥ 12 were regarded as at-risk women and were included in the main trial of the two psychological approaches, cognitive behavioural approach (CBA) and person-centred approach (PCA), compared with HV usual care. These two contrasting approaches were explored because earlier studies had found promising evidence of a positive effect from offering sessions with a person-centred (non-directive) approach1,2 and also from offering sessions that incorporated a cognitive behavioural component. 3,152,156,157,159
The IG at-risk women were invited for an interview using the SCAN. 168 Those who were found to be moderately or severely depressed were asked to state their preference for psychological sessions, an SSRI, or both. The EPDS does not provide sufficiently fine-tuned information to differentiate different levels of severity of clinical depression and does not assess depressive psychosis or mania, all of which are capable of being assessed in a standardised way using SCAN.
The IG at-risk women, all of whom had a postally administered EPDS score ≥ 12, were reassessed at 8 weeks postnatally by a face-to-face HV administration of the EPDS. Women were eligible for the psychological sessions to which their practice (cluster) had been randomised according to the HVs’ management protocol if they had an 8-week EPDS score ≥ 12. The intervention therefore comprised the package of HV training to develop skills in the assessment of postnatal women and the provision of psychological sessions, plus the option of an SSRI if a woman’s SCAN outcome indicated moderate or severe depression. In addition, there was a change to the original protocol so that HVs were able to provide the intervention to women irrespective of their EPDS score if the clinical assessment by the HV indicated that they might benefit from the intervention sessions.
All women were followed up at 6, 12 and 18 months postnatally, using postal questionnaires. The primary outcome was the proportion of at-risk women with a 6-month EPDS score ≥ 12. The trial is illustrated diagrammatically in Figure 1, and full details of the methods are explained below.
FIGURE 1.
Diagrammatic representation of overview of trial. CBA-F, cognitive behavioural approach face-to-face group; CBA-P, cognitive behavioural approach postal group; CG, control group; EPDS, Edinburgh Postnatal Depression Scale; PCA-F, person-centred approach face-to-face group; PCA-P, person-centred approach postal group; SCAN, Schedule for Clinical Assessment in Neuropsychiatry.
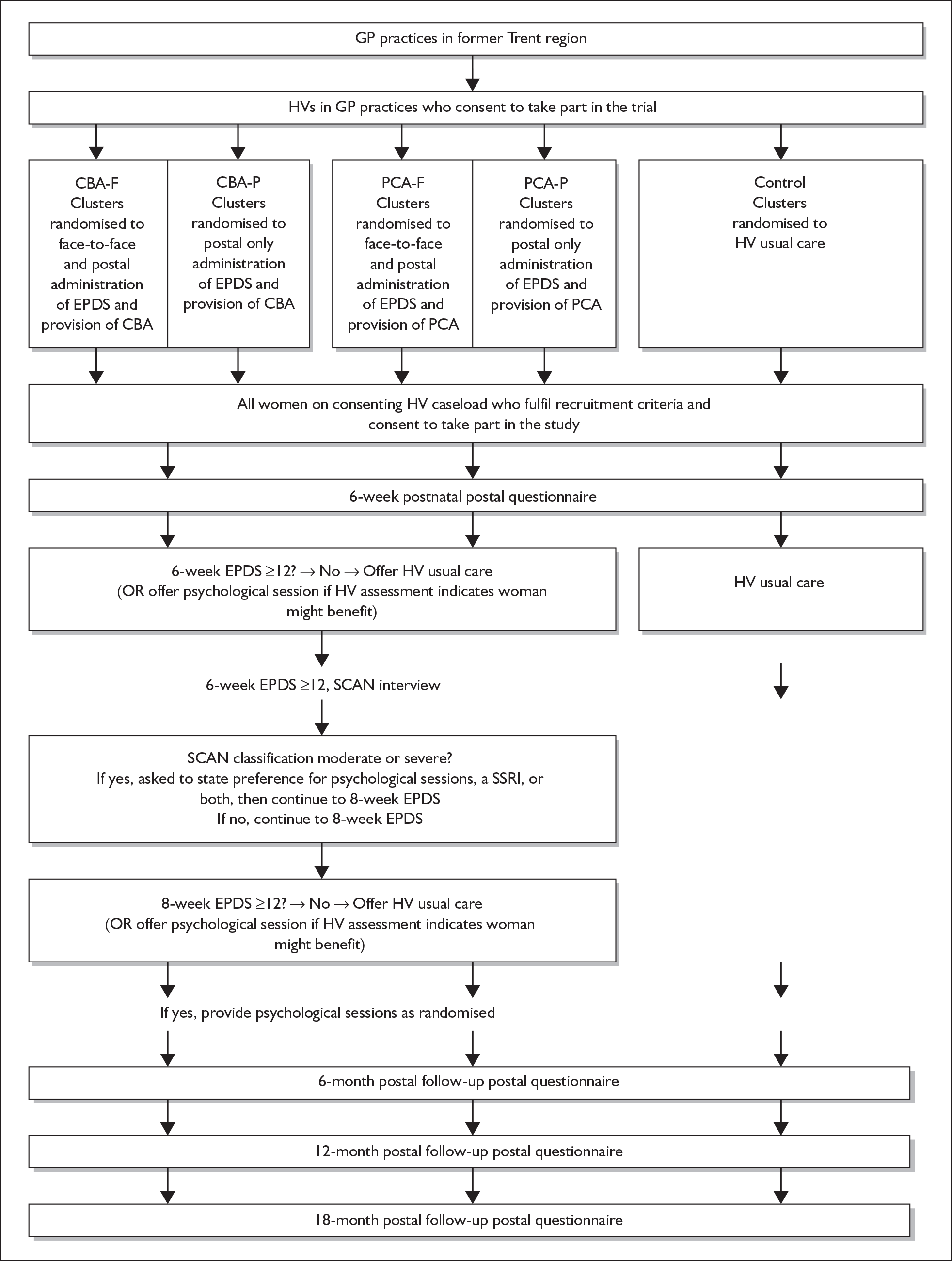
Pre-trial sample size calculation
The sample size calculation aimed to ensure that the trial had a large enough sample to identify any important effects and avoid the chance of producing a false-positive result (type I error) or of missing a clinically or practically important benefit, where one might exist (false-negative result, type II error).
The planned study population was pregnant women who were registered with participating practices and who proceeded to have a live birth during the recruitment phase. To take account of between-cluster variation when estimating the sample size (or performing the analysis) the sample size calculation has to be increased by a design effect based on the intracluster correlation coefficient (ICC).
Estimates of intracluster correlation coefficient
We used the ICC (ρ) estimate of 0.006 derived from 6-month EPDS scores by GP practice,146 which indicated little clustering by practice. 170 Among the interested practices, the annual rate of births ranged from 50 to 150 per practice, with an average of 78 births. To estimate the number of clusters required and the numbers of women to be recruited per group to have 90% power at the 5% two-sided level of significance, to detect a 15% absolute difference in the proportions of intervention and control women with a 6-month EPDS score ≥ 12 (35% versus 50%) we made the following assumptions. If 12–14% of all women would be eligible for the intervention,27 the average cluster size would be 6–8, 50% of at-risk women in the CG would have a 6-month EPDS score ≥ 12, and 50% of women would consent (Table 7). Within the IG there would consequently be 80% power to detect a 15% difference in the proportions of women with a 6-month EPDS score ≥ 12 (i.e. 42.5% versus 27.5%), between the two approaches (CBA versus PCA), as statistically significant at the 5% two-sided level.
| Significance (%) | Power (%) | ICC | Average cluster size | Total clusters | No. of women in intervention arm | No. of women in control arm |
|---|---|---|---|---|---|---|
| 5 | 90 | 0.006 | 6 | 87 | 346 | 173 |
| 5 | 90 | 0.006 | 7 | 75 | 348 | 174 |
| 5 | 90 | 0.006 | 8 | 66 | 350 | 175 |
We assumed an average cluster size of six women, which would require a total of 519 women recruited from 87 practices over 1 year. Assuming a 20% loss to follow-up at 6 months,33 we required 649 women in total and a recruitment phase of 15 months. The sample size calculation was based on a two-sided statistical test and assumed an allocation ratio of one PCA group to one CBA group to one CG. This was so that, first, the outcomes for all of the intervention clusters could be compared with the outcomes for all of the CG clusters and, second, that the outcomes for the two IGs could be compared.
Random allocation
Cluster not individual allocation
In general it is preferable to randomise at the individual participant level. However, an individual woman could not be the unit of randomisation because it was not possible to ask the HVs to provide the control usual care to one woman and then to provide an intervention to another without some contamination of the CG.
Thus, although cluster randomisation is less statistically efficient than individual randomisation,171 a cluster allocation was chosen to avoid major sources of bias and minimise contamination between groups, particularly as blinding was not possible. 170 The GP practice (cluster) was the unit of randomisation and intervention, because that is where the intervention was delivered, even though the effect was to be evaluated by measuring outcomes in individual women and analysing at the individual level, adjusting for clustering at the GP practice level. 165 To avoid any contamination between clusters, HVs for women in the control arm were not to be trained in the skills needed for the experimental intervention, which was not to be offered at any time in the control practices.
Cluster random allocation
To minimise any imbalance across the IGs, the details of practices were used to separate the clusters into three strata for random allocation. The three strata were based on the expected number of births per year, according to whether the HV caseload in the practice was small (less than 70), medium (70–100) or large (more than 100). Once stratified, the clusters were coded for allocation.
A computer-generated random list, using a program from the University of Southampton Medical Statistics and Computing Department, was prepared by Professor Mike Campbell, who was blind to the identity of the collaborating HVs and the GPs with whom they worked. This sequence was used to allocate clusters, stratified by the expected number of births per year, to one of the two main experimental groups, the CBA or the PCA, or to the CG. The two main experimental groups had an equal probability of face-to-face plus postal or postal-only EPDS administration, in a ratio of 1 CBA-F:1 CBA-P:1 PCA-F:1 PCA-P:2 control clusters. The random allocation took place in February and March 2003. To minimise selection bias the HVs were asked to consent to take part before allocation and were therefore blind to the allocation at the time of their consent. After the allocation some HVs expressed their strong disappointment about being in the CG but nevertheless continued to collaborate in the trial.
Participants
Inclusion and exclusion criteria
Cluster level inclusion and exclusion criteria
The setting for the trial was GP practices in the former Trent Regional Health Authority. The clusters were GP practices, and a cluster comprised the HVs and GPs working together in each GP practice. The HVs were the principal collaborators with support from the GPs. To be included in the trial the consenting HVs needed the support of their PCT, HV manager and at least one GP.
Individual level inclusion and exclusion criteria
There were few exclusion criteria to improve the external validity (generalisability) of the results by maximising the representativeness of the trial population. Women were eligible for the intervention if they were, first, at-risk women (who returned a 6-week EPDS score ≥ 12 on the postal questionnaire) and, second, had an 8-week EPDS score ≥ 12 when the EPDS was repeated face-to-face by the HV at 8 weeks postnatally. Women eligible for the intervention were therefore defined by two EPDS score ≥ 12. In addition, the HV was allowed to provide the intervention to those women whom the HV felt might benefit from the intervention, irrespective of their EPDS score.
To capture all women who might proceed to develop PND and become eligible for the HV psychological sessions, women were recruited if they were registered with participating GP practices, became 36 weeks pregnant during the recruitment phase of the trial, had a live baby and were on a collaborating HV’s caseload for 4 months postnatally. Women who did not or were unable to give informed consent were not included for ethical reasons. There was no upper age limit but HVs were asked not to invite women who were below 18 years of age or who had severe and enduring mental health problems, that is, who had been taking antipsychotic medication for a bipolar disorder or schizophrenia.
Women who were unable to understand, read or write English were not included in the trial. The trial was not designed to address the postnatal needs of non-English speaking women specifically. This is partly because of the difficulties involved in providing, for some, a culturally sensitive and appropriate assessment and intervention. There were numerous different first languages other than English among the women registered in the clusters, including a range of Asian, European, Middle Eastern, Scandinavian and Russian languages. Resources were available for the use of interpreters for women who spoke Punjabi and read Urdu, who would not have been able to read the trial literature and give their informed consent without the support of an interpreter. The cost and complications involved in using an interpreting service to provide an appropriate intervention for all women who were unable to understand English was prohibitive. The trial therefore focused on English-speaking women, including some women with different first languages.
Recruitment and consent
Cluster level recruitment
To facilitate recruitment trial information was disseminated before securing funding, aiming to capitalise on existing networks of GPs, HVs and primary care research and development leads interested in research in the region. There was notable support of Trent Focus personnel in the former Trent region, the acting research and development manager in Broxtowe and Hucknall PCT and the Barnsley research fellow in primary care.
Trent Focus Collaborative Research Network and GPs
The first recruitment method was via the Trent Focus Collaborative Research Network (CRN). To fulfil the normal requirements for this formal approach a practice briefing outlined the trial and explained the intervention and follow-up, what would be expected of participating practices, the covering of costs for involving HVs’ and practice time, and what practices should do if they were considering taking part. The CRN co-ordinator sent or gave information to 56 participating practices and forwarded to the principal investigator the details of those who were interested in the trial.
Trent Focus Collaborative Research Network and HVs
In January 2003 a letter was sent via the CRN to a further 53 HVs in Nottingham whose managers had been primed in 2001 about a different HTA PND study, which was approved but subsequently not funded. The letter included information for HVs explaining the special requirements for HVs in their potential role in the IG or CG, emphasising that they should avoid contamination and not discuss their allocation, training or protocol with HVs outside their practice.
Another letter was written to GPs in May 2003, with a practice briefing to pass on to interested HVs, to ask if there were changes in people’s circumstances. The Trent Focus CRN co-ordinators also provided information face-to-face when they had contact with GPs and HVs, and an article was placed in the Trent Focus newsletter in June 2003 to indicate that 15 further practices were required.
Other collaborative research networks in the region
A joint letter was sent in January 2003 to all of the GPs on the membership list for the networks BacReN (26 GPs), DocReN (8 GPs) and ShefReN (27 GPs), using the same approach as for the Trent Focus network, asking them to discuss the research with their HVs.
Academic departments of general practice
To make primary contact with other GPs a practice briefing was sent electronically within the academic departments to 19 GP practices in Nottingham and GPs in 16 practices in Sheffield. A request was made to the academic department in Leicester to ask if they would advertise the opportunity in the same way.
Community Practitioners’ and Health Visitors’ Association
Information about the trial was distributed at the CPHVA Harrogate conference in October 2002, where there was a special interest group meeting about PND. Also, short articles were sent to the CPHVA newsletter asking for expressions of interest in collaborating.
R&D offices in Trent
Alongside the application to PCTs for research governance approval, there was a request for information about the trial to be sent to HVs and HV managers via the internal PCT mailing system. Following this, several presentations were organised with the opportunity to give a presentation to HVs and their managers, to explain the rationale for the trial and the potential for collaborating in the trial. The greatest number of primary face-to-face contacts with HVs resulted from this direct approach to the Trent PCT research leads and the ensuing visits to PCTs. All interested HVs were asked to provide details of the number of expected births per year, the total practice population and contact details for the practice manager.
Primary care trust service managers
Directors of clinical services and managers for the health visiting services were approached directly and a series of meetings were arranged to further disseminate information about the trial. Personalised letters were sent to individual HVs who had expressed an interest in taking part.
Second approach to primary care trusts
When HVs in 72 clusters had consented, flyers were distributed via the PCT research leads, explaining that a further 18 clusters were required and highlighting confirmation from the Department of Health of NHS funds to cover the time that the HVs might spend in training, identifying or supporting women.
The letter presented the benefits for the HVs as an opportunity to:
-
experience the research process first hand
-
altruistically contribute to the evidence base of interventions for PND
-
generate data to contribute to the debate on the use of the EPDS8
-
take a two in three chance of being invited to attend training to develop skills in one of two different approaches to identify and support women with PND.
Presentations
There was an invitation to make a presentation to the Nottingham HVs Research Interest Group, the Lincolnshire Research Group and Nottinghamshire Healthcare, among others.
A co-applicant (EMcG), a PCT chief executive, acknowledging the major recruitment drive at the start and the possibility that saturation may have been reached at the time, suggested writing to all PCT chief executives to encourage them to support their HVs who might wish to take part in the trial.
Cluster level consent
Following approval from the Trent Multicentre Research Ethics Committee (MREC) in February 2003, at least one GP in each practice was asked to sign the consent form to indicate that they understood the HVs’ research role and that the GP practice would support their collaboration. The HVs and GPs then signed a consent form stating their duties before they volunteered the women in their practice as a cluster. 172,173
Once they had consented, the HVs were given details of the group allocation and, when relevant, the training cohorts, and a trial file with the HV protocol to guide the recruitment of women, administration of the EPDS and provision of information to the research office, according to allocation to group.
As not all of the clusters consented at the same time the randomisation process was repeated when there were sufficient clusters with enough HVs to comprise a training cohort for each psychological approach, plus the equivalent number of control HVs, to allow random allocation at one time. Because of this there were five successive training cohorts, to accommodate the training needs of the HVs who were recruited at different times.
Individual level recruitment
The protocol stated that IG women found to be at risk of PND would be offered an intervention as part of the trial. To avoid selection bias HVs were asked to invite all eligible women antenatally to consent to take part in the trial, before the development of any depression.
The HVs were asked to log the details of pregnant women and, to avoid disclosing personal details to the research office at a preconsent stage, they were asked to post the women a research information leaflet (RIL) and a consent form at 32–36 weeks antenatally. Women gave or sent their signed forms to the HVs, who were asked to send the originals and fax (or photocopy and post) the updated consented women’s log each week to the research office for monitoring the consent rate and preparing the 6-week questionnaire for posting.
Individual level consent
Normally consent to take part in a trial is obtained before randomisation, to reduce the possibility of selection bias. People in a randomised controlled trial would normally be asked to consent to be part of an experiment, having been informed of their chance of being allocated to the experimental intervention. Although the clusters consented before randomisation it was impossible to obtain women’s consent before the clusters were randomised.
There are ethical issues surrounding consent in cluster trials. 172,174 A balance was needed to retain women’s autonomy; to provide women with enough information to avoid increasing their concern, losing the good will of disappointed CG women and, because of lack of incentives, jeopardising the recruitment rate; and to avoid non-random selection bias and differential consent affecting the validity (SJL Edwards, 2002, personal communication). 173
It is recommended that consent should be sought at all possible levels, and for the trial these were the sponsor, the MREC, the PCTs, health-care professionals, as ‘guardians’, and individual women acting independently of the guardian.
The trial followed the Medical Research Council (MRC) guidance on cluster recruitment. 175 All women received explicit information about the trial and the same consent process was used for all women. The RIL explained that women were being asked to take part in a study in which one-third of HVs would continue to provide their usual care in up to 30 practices, whilst the other HVs would provide one of the two kinds of support being researched for women found to be at risk of PND. CG women were asked only to return their postal questionnaires, and they would still receive routine care. 171,173 Monitoring the rate of consent in each cluster assessed the scope for potential bias. The HVs were asked to document the women’s main reasons for choosing not to participate.
Baseline measurements
Baseline measurements at cluster level
The cluster level characteristics of PCT, number of GP partners, number of full-time equivalent HVs, practice population, expected births per year and Index of Multiple Deprivation (IMD)176 were collected and compared to establish the comparability of cluster characteristics, as well as the representativeness among other practices within the region and nationally.
Baseline measurements at individual level
The probability of an imbalance on important prognostic variables may be greater for a cluster randomised controlled trial than an individual randomised controlled trial. 171 The measurement of baseline individual level variables also allows an assessment of how the randomisation process has worked to produce directly comparable groups. Furthermore, this comparison can be used to indicate where any baseline adjustments, if any, should be made, depending upon how great the differences might be, as well as the predictive relationship of a characteristic with the primary outcome. We therefore measured sociodemographic baseline variables. The HVs collected details of women who were ineligible or who declined to take part in each cluster – whether a woman’s baby was her first, a girl or a multiple birth. They also collected information on whether a woman had had PND previously, had English as a first language, lived alone or lived in rented accommodation and on the type of housing. This information was compared with the details of consenting women and was used for describing the generalisability of the results. The MRC guidelines indicated that completely anonymised personal data could be used for such a purpose. 175
Six-week measurements
Six-week postal questionnaire
There was a change to the original protocol, replacing the BDI with the Clinical Outcomes in Routine Evaluation Outcome Measure (CORE-OM), as it was a more suitable instrument to measure the outcome of psychological therapy and because of cost considerations. The 6-week postal questionnaire included questions on demographics and feeding the baby and the following instruments:
-
the EPDS
-
the 36-item Short-Form Health Survey Questionnaire (SF-36v2)
-
CORE-OM
-
Measure of Social Relationships (MSR)
-
Life Events Questionnaire (LEQ)
The Edinburgh Postnatal Depression Scale
The EPDS8 is a self-report 10-item measure of depressive symptoms with a score ranging from 0 to 30 (the highest symptom level), which is widely used in research and clinical practice but which alone is inadequate for confirming depression without a clinical interview. The 10 questions ask women to indicate how they have been feeling over the previous 7 days, using a range of four options per question to indicate the frequency of the feeling, to provide a score of 0–4 per question. The tenth question asks about suicidal ideation.
The EPDS was originally developed as a screening tool because of the limitations in the number of available tools for screening for depression, many of which appeared to lack face validity for postnatal women. The tool was described as an acceptable, simple self-report scale, with satisfactory reliability and validity to minimise the chance of false-positive or false-negative results, as well as sensitivity to change over time. In addition, the tool was validated in a community setting. Originally, 13 items were selected from 21 as being most suitable, including seven newly constructed items and six adapted from other scales. The validity of this 13-item scale was established on 63 women and three items were removed to improve the specificity. The remaining 10 items were validated on 84 women at a mean of 12 weeks postnatally. A score of 13 identified all 21 women with a definite major depressive illness, but missed one probable major illness. There were 11 false positives at this threshold and four women with definite minor depression were missed, that is, they were false negatives. Using a threshold of 12 correctly included all people with probable and major definite depression and reduced the false negatives to three women, but increased the false positives to 14 women. At this threshold of 12, the sensitivity for identifying depressed women (true positives) was 86% and the specificity for identifying true negatives was 78%. The positive predictive value was 73%. A cut-off score of 10 reduced the failed identification rate to fewer than 10% but doubled the number of false positives to 10 women. A cut-off of 9 correctly identified all women with definite minor depression but it was judged that there would be an untenable workload for HVs if a lower threshold was used. 4
Sensitivity to change was calculated for an undisclosed number of women who repeated the score and who were interviewed for a second time, and mean scores were found to be reduced. The authors8 emphasised that the EPDS is not a substitute for a clinical assessment and that a score of 11 does not indicate the absence of depression. They suggested that a threshold score of 9 or 10 might be considered for use routinely in primary care. The tool has become widely used in the UK to identify the risk of PND at 6–8 weeks postnatally, using 12 as the threshold for concern.
In a study to assess the accuracy of the EPDS in identifying psychiatric problems in a representative community group of 702 postnatal women (aged 20–40 years)9 the return rate was 97% on a postally administered EPDS, completed when a woman’s baby was 6 weeks old. 39 All women who scored 13 or more, 142 of those who scored 10–12 and 45 of those who scored less than 10 on the EPDS were interviewed using a psychiatric interview using research diagnostic criteria for depression. Using a threshold EPDS score of 10.5 identified 90% of the women with major depression and 75% of the women with minor depression. The threshold of 12.5 identified 80% of women with major depression and 50% of those with minor depression. The sensitivity for identifying true positives was found to be 67.7%, rather than 86% as reported in the Cox validation study of 84 women. 8
A number of cautions have been raised about the EPDS. There is concern that women may not answer the questionnaire truthfully, because of fear of the stigma of depression, wanting to be a good mother and fear of having their baby taken away. 177 There is a general problem with the identification of depression in primary care,49 including PND 24,26,50 The EPDS is one of the mood assessment instruments most widely used in clinical practice, 54 but it was not developed as a diagnostic test55 and cannot be used to confirm PND without a clinical interview. It has advantages and disadvantages. 18,58–61 The EPDS was used in the trial to identify the women to be included because they were more likely to be at risk of PND (rather than as a screening instrument) and then as an outcome measure at 6 months.
In the trial a pragmatic threshold score of 12 was used, as recommended for clinical practice by its developers. 8,178 Women who scored ≥ 12 on their 6-week postal EPDS were termed at-risk women. The threshold score was used to identify the IG women more likely to benefit from psychological sessions and for whom a direct comparison would be made between the intervention and control groups. A cut-off score of 12 carries the risk of not including some depressed women who might score 10 or 11,8 but was used in the trial for consistency with previous work, which predicted ‘an untenable workload’ if a cut-off score of 9 or 10 was used. 4 The EPDS was therefore not used as a pass or fail tool.
It was recognised that women could simply be unhappy at the time of completion and it was recommended that women with a high score should complete another EPDS after 2 weeks to identify those who needed intervention, and this was the process we followed. 56 The lack of substantive evidence of potential benefit and therefore the likely inefficiency of working with women who were not truly depressed were also important considerations.
Administration of the 6-week EPDS
In the trial the EPDS was administered at 6 weeks postnatally to coincide with an existing HV contact. To identify potential clinical or economic benefits of a 6-week postal administration over a 6-week face-to-face HV administration, half of the IG HVs administered the EPDS face-to-face. Therefore there were two IGs using the face-to-face plus postal EPDS administration for comparison with two IGs using postal-only EPDS administration. All women received the EPDS as part of the large postal questionnaire, sent from the research office. Within the random allocation schedule, each of the IG clusters had an equal chance of being allocated to the face-to-face and postal administration or postal-only administration group (Table 8). The four IGs for comparison were (1) CBA: face-to-face and postal, (2) CBA: postal only, (3) PCA: face-to-face and postal and (4) PCA: postal only.
| Cognitive behavioural approach | Person-centred approach | |
|---|---|---|
| Face-to-face and postal administration of EPDS | CBA-F group | PCA-F group |
| Postal-only administration of EPDS | CBA-P group | PCA-P group |
Short-Form 36 (SF-36v2)
The SF-36179 was used to measure general health status among the women in the trial at 6 weeks postnatally. The SF-36 was originally developed to routinely monitor patient outcomes in medical practice, to survey health status in general population surveys and for health policy evaluations, research and clinical practice. The instrument was developed to measure a comprehensive range of health concepts and identify clinically and socially relevant differences in health status and changes over time. It can be completed individually by people aged 14 and over, by post or by a trained interviewer, either face-to-face or over the phone. The questionnaire consists of a 36-item scale covering eight health domains:
-
limitations in physical activities because of health problems: 10 items
-
limitations in social activities because of health or emotional problems: 2 items
-
limitations in usual role activities because of health problems: 4 items
-
bodily pain: 2 items
-
general mental health (psychological distress and well-being): 5 items
-
limitations in usual role activities because of emotional problems: 3 items
-
vitality (energy and fatigue): 4 items
-
general health perceptions: 5 items.
For the 10 questions on physical functioning, for example, the respondents indicate whether they are limited a lot, limited a little or not limited at all. Responses are scored and coded on a scale having from 3 to 5 points and are then summed and transformed for each domain onto a scale ranging from 0 (worst possible health) to 100 (best possible health).
The SF-36 was used in the trial as an appropriate measure of general health as it has been shown to be acceptable and easy to use, with good postal response rates, and to have good psychometric performance in terms of internal consistency using Cronbach’s alpha statistic, retest reliability and construct validity.
Clinical Outcomes in Routine Evaluation Outcome Measure
This instrument was developed to audit and measure the outcome of psychological therapy across a wide range of service types by measuring global distress, making it suitable for use as a self-report assessment tool as well as a self-report outcome, to distinguish clinical and general populations. 180 It is licensed for use without royalty charges, provided others do not change it or make financial profit from it. 181
There are 34 items, scored on a 5-point scale from 0 (not at all) to 4 (all or most of the time), with a higher score indicating worse health. Four of the items measure subjective well-being; 12 items measure problems or symptoms (anxiety, depression, physical or traumatic symptoms); 12 measure life functioning (general; with close and social relationships); and six measure risk of self-harm. Eight of the items are positively phrased. The tool is acceptable (overall omission rate 1.7%) with appropriate internal reliability (0.75–0.95 for all domains). Some questions are used to compare the intensity of a problem. The total mean score is calculated using the number of completed items as the denominator, to take into account missing data. The mean score for each of the four separate dimensions can be calculated separately, also using the number of completed items as the denominator.
Recently the scoring procedure for the CORE-OM has been changed and the new cut-off score is 1.0 and a clinical score is used, which is more consistent with other scoring systems. 182
Measure of Social Relationships
Lack of social support is one of the predictors of PND. The MSR questions were used to estimate the number of people to whom the woman felt close, including relatives, friends and acquaintances, distinguishing adults that the women lived with from others with whom the woman did not live. Inter-rater reliability is good and stability over time is moderate and statistically significant. 183 Adults with a total primary group size of three or fewer people have been shown to be at greatest risk of psychiatric morbidity.
Life Events Questionnaire
Brown and Harris184 indicated that a severe life event might act as a provoking agent and increase the risk of depression. One of the predictors of PND is stressful life events. 27 The LEQ was therefore used to investigate any relationship between brief depression and any recent stressful life event. The questionnaire consists of 12 questions, derived from the Life Events and Difficulties Scales interview by Brown and Harris on common life events that are likely to be threatening, such as bereavement, serious illness or financial crisis. Originally it was used as in a semistructured interview schedule. With only a yes or no response required it is regarded as being brief, convenient and acceptable to subjects. 185 Three or more threatening life events in the previous 6 months might predict a negative outcome.
Processing the 6-week questionnaires
Returned questionnaires for the IGs were opened and date stamped. The 6-week EPDS was manually scored and for consistency these EPDS scores (rather than the HV face-to-face scores) were used according to the research protocol to determine which women should have a repeat EPDS. For all IGs the HV was informed if the EPDS score on the postal questionnaire was 12 or more or the woman had replied positively to item 10 (the thought of self-harm). For the postal groups (CBA-P, PCA-P) the HV was informed of the complete EPDS score on the postal questionnaire. If the HV was unavailable the GP was informed about a positive score on item 10. The return date, the EPDS score and the date that the HV was informed of the score were recorded on the research office Excel spreadsheet.
The CG questionnaires were not opened, to avoid knowing what a woman’s EPDS score was in case, ethically, the research office was obliged to inform the HV of a raised score (or a positive response on item 10, indicating the thought of self-harm), which, in turn, may have affected the CG usual care. The questionnaires were therefore date stamped on the outside of the envelope and filed for 6 months before being opened. The return date was recorded on the research office Excel spreadsheet. Reminder telephone calls, reminder letters and duplicate questionnaires were used to gather missing responses.
The intervention
Cluster level intervention
The cluster level intervention comprised the package of HV training in assessing women and identifying depressive symptoms (using the EPDS and clinical assessment) and the delivery of either CBA166 or PCA167 psychological sessions to at-risk women.
The manualised HV training addressed therapy allegiance and prepared the HVs to provide an appropriate, pragmatic, distinctive, derivative approach, delivering critical elements from CBT or person-centred therapy, not psychotherapy.
The common areas for both training approaches were to enable HVs to acquire further generic skills in developing helpful relationships, such as positive regard and empathy. The cognitive behavioural training emphasised a normalising rationale and the identification of unhelpful patterns of behaviours, perceptions or thoughts in the woman’s life, in order to help the woman to change these herself. 166 The person-centred training used the three principles of the actualising tendency, a non-directive attitude and the necessary and sufficient conditions of change. 167 Further details of the HV training are provided in the section on training of the intervention group HVs.
Individual level intervention
The proportion of women with a 6-week EPDS score ≥ 12 was very important, as this was the group of at-risk women whose outcomes were compared across all IGs and the CG at 6 months postnatally. It was not possible to use the group of women eligible for the intervention with an EPDS score ≥ 12 on two occasions in the comparison as the HV 8-week EPDS scores were not available for the CG women.
At-risk women were interviewed at 7 weeks postnatally using the SCAN, which incorporates algorithms using ICD-10 criteria for depression to determine depression severity (none, mild, moderate or severe). 168 Those with an ICD-10 SCAN classification of moderate or severe depression were asked to state their preference for psychological sessions, an SSRI, or both.
The HV readministered the EPDS to at-risk women face-to-face at 8 weeks postnatally. Women with an 8-week EPDS score ≥ 12 were offered the psychological sessions as cluster randomised. These consisted of a 1-hour CBA or PCA session, focusing on the needs of the mother, once per week for up to 8 weeks, commencing around 8 weeks postnatally. Because of the limitations of the EPDS some HVs also offered the sessions to women, irrespective of their 6-week or 8-week EPDS scores, if their assessment indicated that they were likely to benefit.
Health visitor usual care
The system of health visiting in the UK provides unique routine contact with postnatal women, at a new birth visit and in well-baby clinics. HVs completed preallocation questionnaires to establish their usual care. This indicated that 67% of HVs had attended brief training in the previous 5 years on identifying or supporting women at risk of PND, and that they were more confident in identifying women with PND than supporting them. Practice varied with 47% of HVs using EPDS assessment at 6 weeks postnatally, according to PCT policy.
In both the control and intervention groups, HVs were typically not experienced in offering psychological sessions but would refer to a GP. After randomisation the control HVs continued to represent this variability, and women in the CG continued to receive the range of postnatal care as usually provided by these HVs. All HVs continued to fulfil other aspects of their role.
Outcome measurements
Primary outcome: at-risk women
The primary outcome was the difference between the proportion of at-risk women scoring ≥ 12 on the 6-week EPDS administered by postal questionnaire and the proportion scoring ≥ 12 at 6 months postnatally, to assess persisting risk of PND.
Four-month follow-up: at-risk women
A 4-month follow-up was proposed for IG women who received an intervention to compare outcomes immediately at the conclusion of the intervention sessions. However, the 4-month follow-up was not possible to achieve, mainly because it was impractical to send a further questionnaire, which may have imposed a further burden on already unwell women and may have served as a deterrent to returning the 6-month postal questionnaire (the primary outcome) 8 weeks later. For some women whose intervention did not begin exactly at 8 weeks postnatally, the outcome would have been assessed before the end of the intervention. It may also have led to a further degree of incomparability when only the women who had received an intervention were asked to complete a questionnaire at 4 months.
Secondary outcomes
A range of other outcomes was measured to capture the potential benefit from the intervention in different dimensions of health and use of services. The secondary outcomes were measured in at-risk women at 6, 12 and 18 months postnatally by postal questionnaires. Standard instruments were used as the main and secondary outcomes, with supplementary questions.
Six-month secondary outcomes: at-risk women
At-risk women’s 6-month follow-up questionnaire
A follow-up questionnaire was posted to the at-risk women just before their baby was 6 months old. Apart from the EPDS the other instruments were:
-
SF-12 Health Survey
-
CORE-OM
-
State–Trait Anxiety Inventory (STAI)
-
Parenting Stress Index (PSI) (Short Form)
-
Dyadic Adjustment Scale (DAS) (Short Form).
The SF-12 is a shorter instrument than the SF-36. 186 It contains the items that best represent the physical and mental health summary scores from the SF-36. 187 The SF-12 has two main dimensions, the physical component summary (PCS) and the mental component summary (MCS), with scores standardised to have a mean of 50 and a SD of 10, the same as for the reference population. As our trial had a large sample size and we monitored change in health over time, the SF-12 had advantages over the SF-36 in reducing some of the burden for the participants who were asked to complete several other measures in the follow-up questionnaires.
State–Trait Anxiety Inventory
Anxiety states are transitory, provoked by stimuli peculiar to certain individuals, with features of apprehension, feelings of tension, nervousness and worry, and arousal of the autonomic nervous system. Rather than a transitory state, trait anxiety refers to a relatively stable acquired predisposition to both perceive cues of certain situations as stressful and be activated to respond to the cues in a particular way, through past experience. The stronger the trait anxiety, the more likely that an individual will have a more elevated state anxiety in a particular stressful situation. It was important to assess women and their partners for anxiety disorders postnatally, to more accurately reflect adjustment to new parenthood. 188
The STAI189 is a self-administered questionnaire recommended for studying anxiety in research and clinical settings, to measure the level of intensity of an emotional state at a given point in time. It has been used in clinical practice and research to measure state and trait anxiety. Some items ask about the presence of anxiety symptoms and others ask about their absence. The 20 questions in the ‘State’ questionnaire ask respondents to report how they feel ‘right now, that is, at this moment’ and the ‘Trait’ questionnaire asks how they ‘generally (that is, how you usually) feel’. Each item is scored from 1 to 4 (with 4 indicating high anxiety), with a range from 20 to 80. A missing score for one or two items can be incorporated by calculating the mean score (1–4) for completed items and multiplying by 20. The normative state anxiety scores for 451 adult women were 35.2 (SD 10.4) and the trait anxiety scores were 34.8 (SD 9.19), with a trend for lower scores in older women.
Parenting Stress Index Short Form
The PSI Short Form190 is designed to measure any perceived stressful impact of having a young child. Respondents were asked to circle their responses on a 5-point scale to indicate their level of agreement with each statement, and were given a score of 1 for each ‘strongly agree’ response and a score of 5 for each ‘strongly disagree’ response. The first 12 items relate to the parenting distress subscale, which asks about feelings of parental competence, stresses associated with restrictions on lifestyle, conflicts with the child’s other parent, lack of social support and depression. The following 12 items relate to the parent–child dysfunctional interaction (PCDI) subscale, which asks about the parent’s perception that the child does not measure up to expectations and whether the interactions with the child are reinforcing. The final 12 questions relate to the difficult child subscale, which asks about the child’s behavioural characteristics that affect their management. The sum of the three subscales gives the total stress score. A separate defensive scoring total is derived from the responses to questions 1–3, 7–9 and 11. The mean total stress score is 224 (SD 38), the mean child domain is 98 (SD 20) and the mean parent domain is 127 (SD 26) for the parent of a 1-year old child.
Dyadic Adjustment Scale
This 32-item instrument191 was designed to measure components of the primary relationship between unrelated adult couples living together (whether married or not), as a snapshot at the time of data collection. The DAS is one of the tools most widely used to assess the severity of problems between couples. 192 The main components or subscales measured were dyadic consensus, satisfaction, cohesion and affectional expression. The 32-item scale can be incorporated into a self-completed questionnaire or used in an interview. Each of the subscales can also be used independently. Respondents indicate the extent of agreement between them and their partners on a Likert-type scale (always agree, almost always), and disagreement (occasionally disagree, frequently, almost always or always) with each of the items on the list of questions. The other items ask the respondent to indicate how often situations occur (all of the time, most of the time, more often than not, occasionally, rarely or never). The replies were all scored on a 6-point scale, where 0 is worst and the highest theoretical score 51 is best.
Twelve-month secondary outcomes: at-risk women
At-risk women’s 12-month follow-up questionnaire
The trial ended before the 12-month follow-up point was reached for many at-risk women. Therefore, a smaller number of postal questionnaires was administered at the 12-month postal follow-up. A 12-month follow-up questionnaire was posted to the at-risk women just before their babies were 1 year old. The questionnaire included the following instruments:
-
EPDS
-
SF-12
-
CORE-OM
-
STAI
-
PSI (Short Form)
-
DAS (Short Form).
Eighteen-month secondary outcomes: at-risk women.
At-risk women’s 18-month follow-up questionnaire
The trial ended before the 18-month follow-up point was reached for many at-risk women, therefore a smaller number of postal questionnaires was administered at this follow-up time. A follow-up questionnaire was posted to the women just before their babies were 18 months old. The questionnaire included the following instruments:
-
SF-12
-
CORE-OM
-
STAI
-
PSI (Short Form)
-
DAS (Short Form).
18-month SCAN interviews and monitoring remission and relapse
The 18-month follow-up assessed both the level of depression remaining at 18 months and the proportion of the time that women had felt well since their baby was born. During the 18-month follow-up visits, remission and relapse were assessed among women from all three groups, including the CG. The women were provided with an indication of their depression immediately after the SCAN interview, as a benchmark. The women were asked to remember how they felt over the previous 18 months using memorable dates, such as the baby’s and their own birthdays, Christmas, Easter and the summer holidays. They were asked to indicate on a user-friendly chart whether their health had previously been better or worse in comparison with the way that they felt over the most recent month. This kind of life charting is important in conditions that endure over time and where there might be great fluctuation over that time interval. 193
Six-, 12- and 18-month secondary outcomes: all women
All consented women, not only at-risk women, were followed-up at 6, 12 and 18 months postnatally, as some women with a postal 6-week EPDS score < 12 may have been depressed or may have developed depression after 6 weeks postnatally. At all time points postnatally the same postal questionnaire was sent to all consented women, including the same outcome measures as for the at-risk women.
Six-, 12- and 18-month secondary outcomes: partners
The self-perceived health status of the partners was measured by postal questionnaire at 6, 12 and 18 months after the baby was born.
A questionnaire for the women’s partners to complete was included in the same envelope as the questionnaire sent to the women, at the same three follow-up time points as the women. At 6 months this included demographic questions and the MSR, the LEQ, the SF-12, the PSI and the DAS. At 12 and 18 months it included the SF-12, the PSI and the DAS. At 18 months the partners’ postal follow-up questionnaire also included the CORE-OM.
Infant outcomes
To examine infant development outcomes from the perspective of both parents, on the 18-month questionnaire women and their partners completed questions on their toddler’s growth and development and on concerns about toddler development, the modified Behaviour Screening Questionnaire (BSQ) and the Checklist for Autism in Toddlers (CHAT). The scores on the infant outcomes were rescaled onto a 1–100 scale. The HVs extracted infant immunisation data from the GP records.
Behaviour Screening Questionnaire
The BSQ was developed to assess behavioural difficulties in 3-year-old children. It was modified for 18-month-old infants in a study to investigate the cognitive, social and emotional development of infants of mothers with PND, compared with infants of non-depressed mothers. 39 This modified questionnaire was administered at 18 months postnatally as part of the mother’s and partner’s questionnaires. It covers feeding and sleeping problems, temper tantrums, excessive dependency, miserable mood, relationships with peers and problems in management. All questions had a 3-point response rating to indicate no problem, a mild problem or a marked problem.
Checklist for Autism in Toddlers
The CHAT is a short questionnaire of nine items,194 which is completed by a parent to identify children aged 18 months who are at risk for a social–communication disorder. It looks at joint attention, pretend play, protodeclarative pointing and producing a point. It is quick and easy to complete with nine questions requiring a yes or no response. A negative response on five items indicates whether a child has a high or medium risk of developing autism.
Statistical analysis
All analyses were by intention to treat with a p-value of < 0.05 regarded as being statistically significant. The intention to treat primary statistical analysis included all women with both a 6-week and a 6-month EPDS score and there was no imputation of missing data. The trial was reported according to the CONSORT statement extension to cluster randomised trials. 195
Primary outcome
The primary outcome was the proportion of at-risk women with a 6-week EPDS score ≥ 12. The primary comparison was between those at-risk women in the combined clusters randomised to intervention and those women in practices randomised to provide HV usual care (control). The secondary comparison was to determine any differences between the proportions of women with a 6-week EPDS score ≥ 12 for the two main IGs.
A marginal generalised linear model, with coefficients estimated using generalised estimating equations,196 with robust standard errors and an exchangeable autocorrelation matrix in STATA v8197 was used to analyse the outcomes and allow for the clustered nature of the data. For binary outcomes, such as EPDS score < 12 or ≥ 12, a logit link with a binomial distribution for the outcome was used.
Secondary outcomes
For continuous outcomes, such as mean EPDS score, an identity link with a normal distribution for the outcome was used. Estimates for the group coefficients from these regression models were reported along with their associated 95% confidence intervals. In all of the analyses both a simple unadjusted model and a model to adjust the outcome comparisons for individual level covariates, for example lives alone, history of PND, life events and baseline (6-week) EPDS score, were fitted.
The exchangeable correlation structure corresponds to an equal correlation model, meaning that the correlations of outcomes with a cluster (GP practice) were constant.
For the other secondary maternal outcomes, that is, the CORE-OM, STAI, SF-12, PSI and DAS, the mean values were compared between the intervention and control groups at 6, 12 and 18 months using similar models.
The family outcomes collected from women’s partners at 6, 12 and 18 months were compared between the intervention and control groups. For the infants, outcomes at 18 months were compared between the intervention and control groups.
The primary analysis was for the at-risk women with an EPDS score ≥ 12 who had completed a 6-month EPDS score (n = 418). The analysis was also reported for the cohort of all women who consented and who completed a 6-week and a 6-month EPDS (n = 2659).
There is no general consensus on what procedure to adopt to allow for multiple comparisons198,199 Following this we have reported unadjusted p-values and confidence limits. However, because of multiple hypotheses testing, some caution should be applied in the interpretation of the p-values we have reported, particularly for the various secondary outcomes and end points.
Training the intervention group health visitors
Training Reference Group
The implementation of the psychotherapeutic HV training programmes and intervention was informed by the documented methodological prerequisites for comparative psychotherapy research. 200,201 The major requirement was to minimise any biasing effect of any of the researchers’ allegiances to either of the therapeutic approaches. To enhance the rigour and effectiveness of training for both psychotherapeutic approaches, to maximise the comparability of the programmes and to ensure that the trial would be considered by advocates of each method to have been a credible and fair test of that method, a Training Reference Group (TRG) was established before the trial, at the end of 2002. This comprised experienced academically based psychotherapy trainers from England and Scotland, including representatives of both the cognitive behavioural and person-centred approaches.
The TRG considered the potential for bias and distortion of results of comparative studies attributed to researchers’ loyalties to their preferred therapeutic method. 202 Two of the practical recommendations to try to minimise any potential impact of a researcher’s therapy allegiance unfairly influencing the effect size of the therapy compared were to include a mix of researchers who represent different therapy allegiances and to arrange for the people providing the therapy to be supervised by those representing the same intervention mode.
Training manuals
The two main psychotherapist trainers (TR and KT) were specialists with experience in practice as trainers and supervisors. They prepared a manual for each HV to keep throughout the trial, and a separate trainer’s manual. The manuals were to include the theoretical basis for the relevant psychological approach and the training plan so that, if necessary, the training could be replicated elsewhere. The manuals were drafted in January 2003 and final changes were made in February 2003.
Principles and standards for training for the intervention
The TRG held two verification meetings at the University of Sheffield in November 2002, chaired by Professor David Shapiro. The following summarises the main principles and standards for the HV training and manuals.
Recognising the training employed in previous trials in Edinburgh – ‘a brief training inthe principles of person-centred counselling’1 – and in Manchester, using CBT,3 the training in the planned trial was to prepare HVs to provide a brief, derivative intervention, not psychotherapy, mainly for pragmatic reasons. That is, the outcomes to be compared between the IG and CG would be associated with a brief training in delivering critical elements derived from one of the two therapies (cognitive behavioural therapy and person-centred therapy). The training had to be delivered at an appropriately pragmatic level to enthuse HVs and develop their skills, rather than to develop their theoretical knowledge, recognising the preference of HVs to support women with psychological difficulties rather than to become mental health workers. It was not intended that the HVs should regard themselves (or be regarded) as therapists, whose training takes much longer than 8 days. Therefore, the terms ‘person-centred approach’ and ‘cognitive behavioural approach’ were to be used consistently, to avoid the use of the term ‘therapy’, ‘counselling’ or ‘counsellors’.
Comparable training
The TRG was asked to verify that the training manuals for both intervention arms were comparable, with an appreciation of the differing ethos and styles of the two psychological approaches.
For the CBA the purpose of the training was to prepare HVs to provide a simple, easily communicated intervention related to the phenomenology of PND. The basis of the training was the worksheet approach, in which HVs learned to carry out a problem-focused assessment in five key areas of a woman’s experience and then select and use appropriate PND-specific worksheets for each woman.
For the PCA the purpose of the training was to prepare HVs using key principles and issues in such a way that they would be able to help the women to accept and ameliorate their depressive process.
The training preparations aimed to make the training experience equal, as far as possible, for all IG HVs. To enhance comparability it was agreed that all training cohorts should ideally be no larger than 12 (to allow for four small groups of three HVs working together during the training day) and no fewer than eight HVs. The training used the term ‘client’ or ‘woman’ rather than ‘patient’. Key qualities of the training environment were that they should be uninterrupted and secure and congruent with what would normally be expected of a training environment, with a pragmatic consideration of reproducibility and deliverability in the NHS.
Appropriate training
The TRG emphasised the avoidance of unfamiliar language and jargon, for example the term ‘negative automatic thoughts’, to avoid putting off HVs and to provide accessible, distinguishable, theoretically congruent and reproducible models with key skills. As well as being appropriate for the HVs, the intervention was planned to be appropriate for the women, with little time or energy to do too much homework.
Clinical supervision
The HVs also needed access to clinical supervision and support, for example when dealing with distressing information from a client, such as negative thoughts towards the baby. Regular formally structured reflective practice sessions using role-play were offered for HVs who may not have had the opportunity to work with affected women. HVs also attended peer-supervisory sessions.
Prior beliefs of health visitors
Because of the random allocation of clusters to the groups (control, CBA or PCA), the HVs would not be able to choose any preferred option. Therefore, there was the potential for incongruence between HVs’ personal predispositions or beliefs and one of the approaches. To be able to check the balance of the randomisation in terms of HVs’ prior beliefs, there was a prerandomisation measurement before random allocation of all of the HVs’ attitudes and levels of interest and motivation in counselling, using the Opinions on Psychological Problems (OPP)203 within a pre-trial questionnaire. The OPP is a self-report, two-part questionnaire developed to measure how people view the causes of and treatments for psychological problems. The first part measures how people view the causes of psychological problems. The second part, the treatment section, includes 47 questions about people’s views on what may help psychological problems. The questions are grouped under the following headings:
-
psychodynamic
-
humanistic/interpersonal
-
behavioural
-
cognitive
-
organic
-
social/economic
-
naïve.
Each question has six responses and is scored on a 6-point scale from –3 to + 3, where + 3 means agree strongly and –3 means disagree strongly. The HVs were asked to indicate their level of agreement with each of 37 statements. The OPP in the HV questionnaire included only 37 questions as the naïve questions were not included. The second part of the OPP was included in a post-trial questionnaire for intervention and control group HVs, when the intervention was complete, to assess any post-trial differences between the three main groups.
Pre-trial health visitor questionnaire
To gather personal views and experience within the pre-trial questionnaire, to establish baseline practice, HVs were asked to answer truthfully, without discussing any of their answers. Codes were used so that all answers could be treated completely confidentially. The questionnaire included questions about:
-
Skills – details, the title, length, year and location of training, qualifications achieved for training on identifying or supporting women at risk of postnatal depression.
-
Assessing and identifying women – at baseline, how much confidence they had in identifying and supporting women who may be at risk of postnatal depression and how, over the previous 6 months, they had assessed and identified women who might have been at risk of PND.
-
Use of the EPDS – personal use of the EPDS over the previous 6 months and whether used universally with every postnatal woman; at how many weeks, when administered; and whether used selectively and how they had decided to use it.
-
General experience – the number of years since they qualified and how many years they had worked as a HV.
-
Experience with PND – how they had supported women whom they felt were suffering from PND in the previous 6 months.
Introductory training day
The IG HVs were invited to attend an introductory day during the week before contact with the psychotherapist trainers, to introduce the features and problems that women report and the different ways of understanding PND and covering risk issues (Table 9). These were run by Jane Morrell (principal investigator, trained as a HV, with group work and presentation skills) and Jan Cubison (Sheffield Community Health Maternal and Mental Health Services). Before the introductory day was finalised, in January 2003, JM attended the 1-day training in London on Perinatal Depression: Detection in Primary Care, which was organised by the CPHVA to train HVs in the use of the EPDS.
| Introductory training day | Date | Location |
|---|---|---|
| 1 | 7 March 2003, 30 health visitors | East Retford, Lincolnshire |
| 2 | 24 March 2003, 19 health visitors | Nottingham |
| 3 | 29 April 2003, 16 health visitors | North Nottingham |
| 4 | 3 September 2003, 11 health visitors | Sheffield |
| 5 | 14 January 2004, 6 health visitors | Sheffield |
| 6 | 9 February 2004, 6 health visitors | Sheffield |
| 7 | 1 November 2004, 3 health visitors | Sheffield |
Each HV was provided with their own, named introductory training day manual, which they were asked not to share with anyone else, or copy, as one measure to reduce contamination when HVs may have come into contact with other HVs or their clients from another arm of the trial. They were also each given a copy of a scored EPDS, several copies of blank EPDS forms, laminated cards and sheets with questions to assist the clinical interview, and their own copy of the PowerPoint slides.
The day covered the use and meaning of the term ‘postnatal depression’, prevalence, factors associated with PND, consequences and a summary of the research about treatments for PND, including the pioneering work in Edinburgh on HV listening visits. 1 It also covered the limitations of research into PND and the need for the trial. The service perspective was presented, covering Why Mothers Die21 (confidential enquiry into maternal deaths) and the relevant standards within the NSF for mental health. 90
The clinical perspective covered core features of depression and core features of PND, distinguished from puerperal psychosis. The training on the clinical interview covered risk management and assessing risk to mothers, infants and children.
The practical skills development focused on how to recognise PND, describing the review commissioned by the National Screening Committee,57 the SIGN publication on PND. 92 The development and appropriate use of the EPDS were reviewed, covering its strength, limitations and recommended practice. The HVs were all asked to interview another HV, to gain experience in the practical use of the tool.
The HV protocol for the administration of the EPDS at 6 weeks postnatally within the trial was explained in detail, with a copy for each HV included within the introductory day manual. This indicated four main actions: first, when there was urgent concern about a woman (suicide risk, risk to the baby, risk to others and severe impairment); second, when there was a positive response to question 10 on the EPDS (indicating the risk of self-harm); third, the need to repeat the administration of the EPDS at 8 weeks postnatally if the score reached or exceeded the threshold of 12 when first administered at 6 weeks postnatally; and, finally, what to do if the EPDS score was below the threshold score of 12.
Five-day training
There were four CBA training cohorts and five PCA training cohorts (Table 10).
| Training cohort | Cognitive behavioural approach | Person-centred approach |
|---|---|---|
| 1 | 13 March 2003, 8 health visitors | 18 March 2003, 10 health visitors |
| 2 | 3 April 2003, 14 health visitors | 26 March 2003, 9 health visitors |
| 3 | 8 May 2003, 12 health visitors | 30 April 2003, 7 health visitors |
| 4 | 10 September 2003, 8 health visitors | 16 September 2003, 6 health visitors |
| 5 | 22 January 2004, 8 health visitors |
Evaluation of the health visitor training
Introductory day evaluation
The HVs were asked how they felt that the content of the day was pitched and about the background presentation, the presentations on the EPDS, the clinical interview, risk management, skills development and the time allocated to discussion. The final questions asked about their confidence in identifying and supporting women at risk of PND.
Five-day training evaluation
When each training cohort was completed, the HVs in both the CBA and PCA clusters were asked to complete a questionnaire to provide feedback on how the training was delivered and how helpful it was. They were asked to circle one answer on each line for each question, without discussing their answers with their colleagues. All of the questionnaires were coded so that answers could be treated completely confidentially. The HVs were told that the trainers would only receive a summary of the replies for the cohort of HVs, not individual replies. There were questions on the course content and methods (clarity of the course objectives, theoretical content, how the course was pitched, course structure, appropriateness of the educational methods) and the teaching (how motivating were the course leaders, effectiveness in relating to the group, competence, theoretical congruence of the course leaders’ teaching styles). The general questions asked about the relevance, appropriateness and acceptability of the course for HVs supporting women with PND, and how interesting it was. The skills questions asked about whether the course had improved the HVs’ understanding and skills in supporting women with PND, and how confident they felt in applying any skills that they had developed using the approach. The HVs were asked about how well the course had met their expectations, whether they would recommend this course to other HVs and, taking everything into account, how satisfied or dissatisfied they were with the five core training days they received as part of the research. They were asked to list the most important things that they had learned on the course and how, if at all, the content and delivery of the training could be different. They were then asked to list the three best and three worst things about their overall experience of the course, and to write any additional comments.
Intervention monitoring
When participants do not accept an intervention, the estimated treatment effects are diluted in an intention to treat analysis. The HVs in the IG were asked to complete a monthly intervention monitoring form to provide an update on which women had been offered and accepted intervention sessions, how many sessions had been audiotaped, and whether Agnew Relationship Measures (ARMs) had been completed.
Intervention process evaluation
Reviews of psychotherapy studies indicate that there is little evidence for the differential efficacy of therapies, partly because of the quality of the research evidence. 204 This is referred to within psychotherapy research as the equivalence paradox. It is assumed that, although different models may have specific effects, for example cognitive behavioural therapy operates by identifying and changing negative cognitions, all therapy models contain common factors or non-specific effects, such as warmth, reassurance, instillation of hope and feelings of support. To help understand how a therapy works, several process evaluation methods can be used, for example to look at a client’s change in mood, such as the Session Evaluation Questionnaire or the Session Impact Rating Scale. 205
Therapeutic alliance and Agnew Relationship Measure
One of the most frequently measured characteristics of the intervention in psychotherapy research is the quality of the therapeutic alliance between a client and therapist. This is characterised by, for example, the client–therapist bond and agreement about treatment goals and ways of achieving these. The quality of the therapeutic alliance or partnership has a significant positive contribution to the outcome. Among the tools considered for measuring the therapeutic alliance, some were firmly based in the context of therapeutic work with a client. In contrast, the ARM focuses on the relationship between the client and worker and is more easily transferable to the context of a HV and mother working together. An original validated 28-item ARM was shortened to a 12-item ARM, which has very high correlation with the longer version. 206,207 The short-form ARM was chosen as the least time-consuming, most easily completed and most comprehensive measure of alliance components with useful UK comparative data. These features were important in minimising the demands on the women in the PoNDER trial, as the HVs were asked to use the 12-item version of the ARM after each intervention session. This involved the woman completing one version and the HV completing a corresponding version of the brief questionnaire. The two forms both consist of 12 items and the instructions state, ‘Thinking about today’s meeting, please indicate how strongly you agree or disagree with each statement’, with responses given on a 7-point scale from strongly disagree to strongly agree. Four domains are covered:
-
bond, which concerns the friendliness, acceptance, understanding and support
-
partnership, concerning working jointly towards therapeutic goals
-
confidence, optimism and respect for the therapist’s professional competence
-
openness, the client’s feel freedom to disclose, without fear of embarrassment.
The responses were analysed at the dyad level, that is, the correlation of means across HV–client pairs, and at the session level. A total mean score was calculated, within a range from 1 to 7, with a higher score indicating a stronger alliance.
The PoNDER Adherence Rating Scale
To assess the level of adherence of HVs to the interventions that they had been trained to deliver, HVs were asked to tape record intervention sessions, so that sessions from both IGs could be rated.
Developing the PoNDER Adherence Rating Scale rating manual
A 26-item rating sheet and accompanying rating manual was designed and called the Ponder Adherence Rating Scale (PARS). The PARS was written by an experienced psychotherapy researcher blind to all details about the submitted tapes. Following discussion between the researcher and the HV trainers, the PARS was designed to rate the presence of three factors:
-
General facilitative conditions (GFC), which were assumed from the start to be equally present in both interventions. Seven of the 26 PARS items were intended to rate the presence of GFC, for example ‘Warmth: did the HV convey a sense of warmth towards the mother?’
-
CBA-specific factors (13 PARS items), for example ‘Problem solving: did the HV encourage the use of a problem-solving approach with the mother?’
-
PCA-specific factors (6 PARS items), for example ‘Self-concept: did the HV focus on valuing aspects of the mother’s self-concept?’
The women were given an RIL about the ARM and the audio recording of the sessions to explain that the purpose was to examine the effectiveness of the HV training, but that they could choose for the session not to be recorded or not to complete the ARM. The IG HVs were given a separate information sheet and checklist on completing the ARM and taping the intervention sessions.
Local co-ordinators and SCAN interviewers
The local co-ordinators (LCs) commenced in July 2003 and their main role was to liaise with, support and offer feedback to collaborating HVs. The LCs had weekly contact with the HVs, face-to-face or by telephone. Once the HV training modules were under way, support visits began at the end of July 2003 to prepare HVs for their varying collaborative roles in recruitment, follow-up and data collection. The research team acknowledged the HVs’ additional workload, particularly administrative, and possible stress as a result of taking part in the trial. The main elements of the LCs role were to ensure that the HVs were organised to follow the HV research protocol, to motivate them and to offer them practical support. The LCs’ face-to-face visits with the HVs allowed discussion to reinforce the protocol in relation to the women on their caseloads. The LCs had a list of things to discuss during a visit. Once recruitment was under way, in September 2003, the LCs began to collect information on the numbers of women invited to take part and the numbers consented or declined, to monitor the consent rate of eligible women in each practice. They discussed local tailored techniques that the HVs could use to maximise the consent rate per practice, for example using labels on records and computer prompts and putting up a display of the trial in the waiting area. The LCs offered feedback to HVs on progress individually, as well as collectively by way of a newsletter prepared and edited by one of the LCs (KR).
Preparation of local co-ordinators
To enhance their research role the LCs were able to attend training to develop their research skills and appreciation in critical appraisal, health economics, literature searching, qualitative research, research governance, statistics, use of NUD*Ist and NVivo qualitative software and use of the Statistical Package for Social Scientists (SPSS). The LCs also attended the Society for Reproductive and Infant Psychology conference in Sheffield in 2004. The LCs’ main training was in preparing them to undertake the SCAN interviews.
SCAN interview
The purpose of the SCAN168 interview was to establish the baseline severity of depression among those women with a 6-week EPDS score ≥ 12. A secondary aim of the SCAN interview was to examine the identification of depressive symptoms by the EPDS.
SCAN interviewers’ roles
In 1992 the ICD-10 first included a category for puerperal disorders, to be used when the other criteria for psychiatric diagnosis were not fulfilled. 22 The American Psychiatric Association DSM-IV classifies PND as major depression with postpartum onset, beginning within 4 weeks postpartum. 23
The SCAN was developed as a semistructured diagnostic interview, composed around the PSE, to be administered by a specially trained interviewer. Interviewers use suggested wording but can probe until they are satisfied with the information that they obtain. The respondents’ replies to the SCAN interview were recorded directly onto a laptop computer, to measure and classify psychiatric symptoms and behaviour. The SCAN is to be used by clinicians who know about psychopathology and who have taken a course at a training centre designated by the World Health Organization (WHO) and who are familiar with the glossary of differential definitions. The first part of the interview covers anxiety, depressive and bipolar disorders, physical functional health and use of alcohol and other substances. The second part covers abnormalities in speech, affect and behaviour and psychotic and cognitive disorders. For the trial, ICD-10 criteria were used to determine the severity of any depression (none, mild, moderate or severe), but data can be presented in different outputs according to both ICD-10 and DSM-IV definitions.
The first part of the interview is used to gain an overview of all possible physical and mental health problems, which are precisely rated later in the interview. The questions are categorised into unexplained physical symptoms, worrying, anxiety, obsessional symptoms, depressed mood, concentration, bodily functions, eating disorders, expansive mood, use of alcohol and use of other psychoactive substances.
Clinical severity is rated by taking account of the duration, frequency and intensity (interference with mental function) of symptoms. A zero rating indicates complete absence of a symptom. For an item to be rated, the symptom must be distressing, difficult to control and excessive – 1 indicates minor, not clinically significant; 2 indicates moderately severe for some of the time; and 3 indicates moderately severe for most of the time. Only ratings of 2 or 3 contribute to diagnostic categories; the mild rating is not regarded as being sufficiently clinically significant to meet specific diagnostic criteria.
SCAN training
The formal 2-week SCAN training for the SCAN interviewers (SIs) began in August 2003 in Leicester. The SIs had regular monthly meetings with Professor Pauline Slade for debriefing and to maintain quality control.
SCAN quality control
The SCAN trainer (Jane Smith) accompanied each of the SIs separately to SCAN interviews in women’s homes, to ensure that all of the SIs were working to the same standard and to prevent drift from the SCAN training protocol.
Identification of women for SCAN interview
The 6-week postal EPDS score determined which women were invited for a SCAN interview. All women with a 6-week EPDS score ≥ 12 were invited for interview, to determine the presence and severity of any depression (none, mild, moderate or severe). Further women who had borderline EPDS scores of 9–11, plus a random sample of those who scored between 0 and 8, were also invited for a SCAN interview, as part of the assessment of the performance of the EPDS (Figure 2).
FIGURE 2.
Procedure for SCAN interviews. CBA-F, cognitive behavioural approach face-to-face group; CBA-P, cognitive behavioural approach postal group; EPDS, Edinburgh Postnatal Depression Scale; PCA-F, person-centred approach face-to-face group; PCA-P, person-centred approach postal group; SCAN, Schedule for Clinical Assessment in Neuropsychiatry; SSRI, selective serotonin reuptake inhibitor.
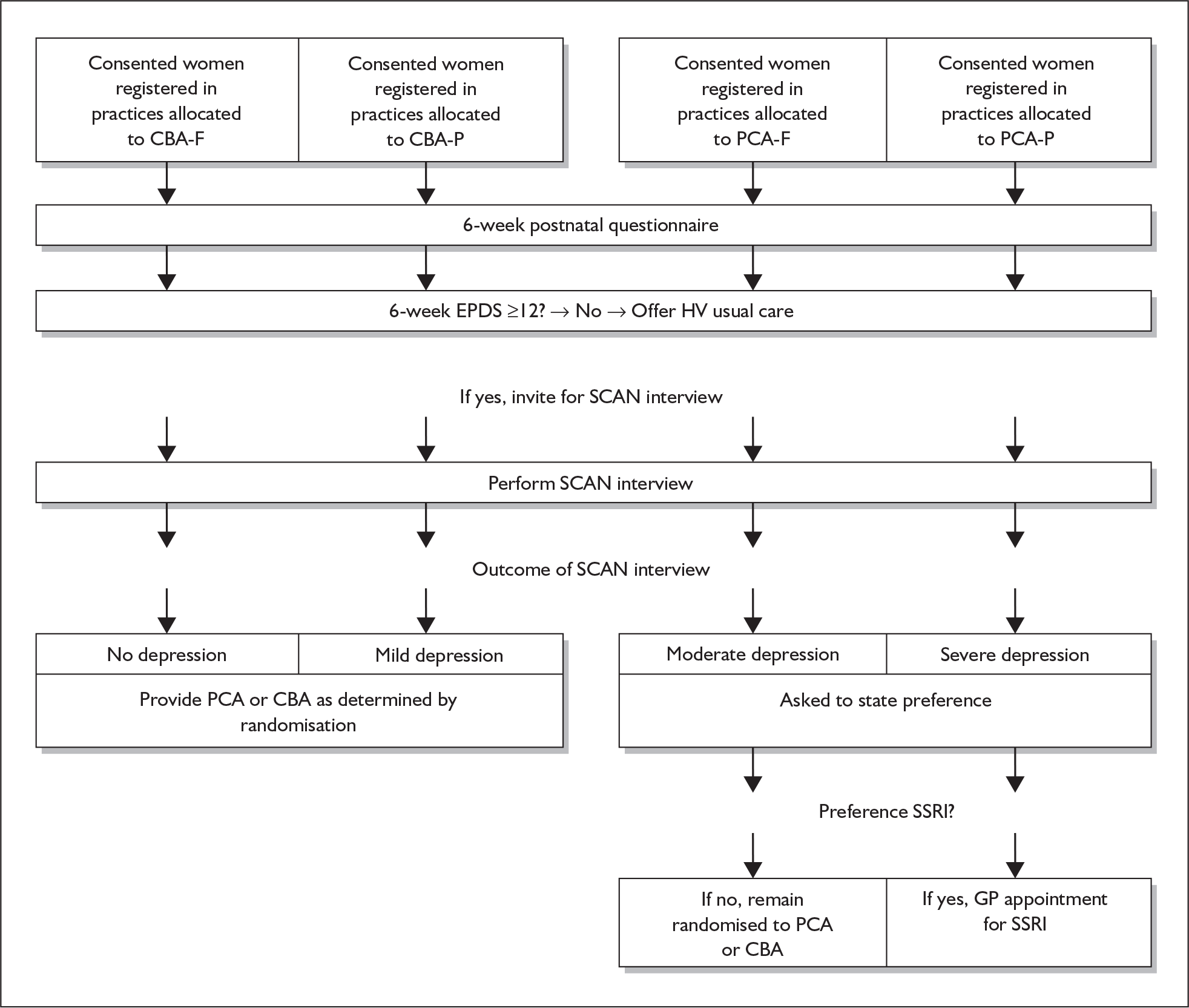
Each day, after all of the questionnaires of the IG women were scored manually in the research office, all women who scored 9 or more on the EPDS were identified for an interview, plus a selection of those who scored less than 9. The SIs were given each woman’s name (separately from her PCT, practice and id code to protect privacy), address and her baby’s date of birth. The SI contacted each woman to arrange the interview time, unless the woman’s HV stated a preference for contacting the woman first. For women for whom the SI could not get a reply on the phone, or for those who did not have a phone, the SI wrote invitation letters asking them to contact her. The replies from the women were grouped as consented, declined, missed or assumed declined, if the SI had unsuccessfully tried to make contact many times.
Before her SCAN interview, each woman was asked to sign a consent form. If the outcome was moderate or severe the woman was given an information sheet after the SCAN interview, which explained that the interview indicated that she might be feeling depressed. The sheet gave brief details about psychological therapies and antidepressants and indicated that the woman should discuss her planned care with the HV or an antidepressant could be prescribed by her GP.
Safety for SCAN interviewers and women
To prepare them for their role in visiting women’s homes unaccompanied, the LCs were made aware of the potential minimal risks of being invited into the home of a woman with a new baby. They were carefully prepared in personal safety by watching a video on lone working and by holding their own copy of a safety booklet, following lone working guidelines and reading about techniques in dealing with violence and aggression and defusion and de-escalation. The SIs also had a detailed plan about the sequence of contact when an SI did not inform her buddy that an interview was complete. 208 The HVs were asked to inform the research office of any circumstances in which there might be a safety risk in an SI going to visit a particular woman’s home alone. In cases in which a risk was anticipated, two SIs went to carry out the interview together. Conversely, the HVs had photographs of the SIs in their trial file, to show to the women who were invited for a SCAN interview.
Health visitor feedback and reward programme
To maintain the HVs’ enthusiasm, as well as the regular LC support visits, the principal investigator made a visit to the HV clusters, with some additional feedback presentations to the whole practice team. A HV reward system of vouchers was established in the autumn of 2004, based on the proportion of eligible women in a HV caseload who consented to take part and the proportion of women who were offered an intervention.
Approval for the trial
Application to the Multicentre Research Ethics Committee
In December 2002 the MREC application included a draft RIL, consent forms and questionnaires for the committee to consider. These drafts were to be further developed once the trial began, having been reviewed by the service users (consumer involvement) and the wording amended.
In January 2003 the MREC requested clarity on:
-
the CG HV continuing to provide care currently given
-
the use of the EPDS as part of the initial assessment and as an outcome
-
the recruitment of women
-
the protocol for women with severe depression
-
the recruitment of subjects for interview
-
infant outcomes
-
visits to women who scored ≥ 12 at 6 weeks postnatally
-
the Punjabi Postnatal Depression Screening Questionnaire (PPDSQ)110
-
safeguards, to avoid approaching women who had a stillbirth or perinatal death.
Adverse events
Around 6 months after recruitment began, a letter was sent to the GPs in the practices where the HVs worked to update them on recruitment and to reinforce the request about compliance with the practice flowchart. The letter also asked the GPs to inform the research office about all women in the trial who had attempted suicide, or who had died, or about other adverse events that had occurred.
Consumer involvement
In December 2002 a group of Asian women was invited to a focus group with a HV to talk about PND and to ask their views on the research proposal before the research began. Consultation with service users began in January 2003. HVs provided the names of women who had recently had a baby and had agreed to be interviewed, either individually or in a group situation, and a focus group was held on 13 August 2003. The women were asked to sign a consent form before any audiotaping of the discussion. The women were offered travelling expenses and were given tokens to recognise the value of their time. In light of the feedback from these women, the RIL was further developed to make the information easier to understand.
Administration
Application for indemnity
A non-clinical trial insurance certificate was issued by the University of Sheffield Department of Finance.
Application for research governance approval within primary care trusts
Whilst the trial was in progress, the research governance arrangements for health and social care, first published in 2001, were changed. 209 The second edition framework set out the principles, requirements and standards (including ethics) with an implementation plan for improving research and safeguarding the public.
Rather than complete a separate, local application form for each of the 39 PCTs in the region, a generic application form was sent to the research leads in the relevant PCTs and research alliances covering groups of PCTs. Because of the inconsistent approaches of the PCT research offices, on request, in different combinations, some PCTs were sent copies of, for example, the MREC application form, Annexe D, copies of the protocol and researchers’ CVs.
The communication below from one of the local research leads indicates some variation in the interpretation of the new rules:
I’ll let you know about how we can assist and on how the approval processes work locally. With the MREC approval, studies then have to pass to the LREC for local consideration. I’ll let you know how we fit in at this stage and how PCT support is indicated. The Alliance approval process (on behalf of PCTs) will start to operate when you need to apply for LREC consideration of your study after it has been to MREC. I’ll need a copy of all the MREC paperwork and correspondence. We’ll check PCT support as part of this process and forward on to our LREC. If ** is going to be the Local Investigator this submission would have to be in his name . . . . My main concern for you is the timescale as I noticed you wanted to randomise by early January. I note that you were going for MREC approval on 5 December . . . . LREC submission won’t be possible until MREC approval has been granted. I won’t get into detail here but the LREC deadline for January (and this affects the Alliance one) is quite early because of Christmas. There were sometimes special sub-groups of the LREC for consideration of MREC studies, although the schedule of these is normally set in months.
Financial costs of the collaboration of health visitors
In the past, health-care professionals’ time has been used in research usually without reward. The time of health-care professionals should be costed with reimbursement to ensure that participation in research is not at the expense of their normal roles. The document Attributing revenue costs of externally-funded non-commercial research in the NHS210 indicated which costs should be allocated as NHS service support and which should be allocated as NHS excess treatment costs. In the application for this funding, assumptions were made about the amount of time that it might take a HV to carry out each element of the research, and a cost was attributed to this. Key assumptions were that there would be, on average, 78 women per practice taking part in the study and that around 14% of these women (about 11 per practice) would be at risk of PND and eligible for the intervention. The cost per HV time was calculated as £17.50 per hour.
The CG HVs were asked to label and post prepared letters to eligible antenatal women (10 minutes) and then gain written consent from these women (10 minutes). HVs were asked to count the number of GP and HV contacts for 78 women, every 6 months, in the 18-month follow-up phase (30 minutes), amounting to 65 hours of time per practice or £14.50 per woman.
In the CBA and PCA postal-only groups, in addition to the role of HVs in the CG, HVs were asked to administer the EPDS at 8 weeks postnatally for women with a 6-week EPDS score ≥ 12 (30 minutes). For women eligible for the intervention, the HVs were asked to make a maximum of eight visits of 1 hour per week, amounting to a further 93.5 hours of HV time per practice or £20.98 per woman.
In the CBA and PCA face-to-face and postal administration groups, HVs were asked to administer the EPDS face-to-face to all consenting women at 6 weeks postnatally. This amounted to a further 39 hours of HV time per practice at £8.75 per woman.
In all intervention practices the HVs were also asked to attend the equivalent of 8 full days of training to prepare them to provide the intervention to at-risk women. Assuming two part-time HVs working per practice, the training was to involve 120 HVs, amounting to 64 hours (£1120) per HV, £2240 per practice and £134,400 for 120 HVs. The total request for service support costs and excess treatment costs in all 90 practices was £355,425 (£102,375 + £253,050).
The application for service support costs and excess treatment costs was tedious because, again, the rules were in the process of change. Funds for the reimbursement were all paid to Broxtowe and Hucknall PCT, which then sent the payments to individual PCTs.
This protracted process served as a disincentive to some PCTs, whose research leads wished the funding arrangements to be confirmed before allowing their HVs to participate in the trial.
Local Research Ethics Committees
Individual Local Research Ethics Committees (LRECs) also issued approval letters with differing requests to audit the research, and for annual reports, a final report and copies of materials sent for publication. An audit required an inspection of the final approved protocol, information sheets, consent forms, data collection tools, data storage arrangements, correspondence with the Research Ethics Committee, evidence of indemnity arrangements, sponsorship agreement, research governance approval letters, contractual agreements, research team CVs, consent documents, participant records, membership of the project advisory group and honorary contracts.
Application for honorary contracts
To ensure compliance with the changing requirements of the research governance framework for health and social care, towards the end of the recruitment phase, an honorary contract request form was completed for PCT R&D offices for the whole trial team, researchers and administrative staff. It was necessary for an individual who might have contact with ‘patients/staff or identifiable or sensitive data’, and such individuals had to attach a copy of their CV and give their home address and details of any Criminal Records Bureau Disclosures. Again, each PCT or cluster of PCT research offices stipulated differing requirements. The complexity of administrative arrangements created a further significant administrative burden for the trial.
Trial Advisory Group
The Trial Advisory Group (TAG), chaired by Professor Michael Barkham, met every 3 months throughout the duration of the trial. The purpose of the group was:
-
To provide overall supervision for the trial on behalf of the trial sponsor (the Department of Health by way of the HTA programme)
-
To ensure that the trial was conducted to the rigorous standards set out in the MRC guidelines for good clinical practice.
-
To concentrate on the progress of the trial against the project plan, adherence to the protocol, participant safety and the consideration of new information of relevance to the research question.
-
To provide advice, through its chair, to the principal investigator, the HTA programme and the host institution on all aspects of the trial.
In addition:
-
Membership should include an independent chair, at least two other independent members, one or two principal investigators and, when possible, a consumer representative. Involvement of independent members provides protection for both trial participants and the chief investigator.
-
Observers from the HTA programme and the host institution should be invited to all TSC meetings.
-
Responsibility for calling and organising TSC meetings lies with the principal investigator.
-
There may be occasions when the trial sponsor will wish to organise and administer these meetings for particular trials. In the HTA programme’s case this is unlikely, but they reserved the right to convene a meeting of the TSC in exceptional circumstances.
Chapter 4 Results and outcomes
Results
Cluster level recruitment and consent
Health visitors and GPs from 241 clusters expressed an interest in the trial, of whom 141 did not consent and participate in the study. There were 30 clusters allocated to CBA, 32 to PCA and 38 to control. Within the intervention clusters there were 13 allocated to CBA-F, 17 to CBA-P, 15 to PCA-F and 17 to PCA-P. Figure 3 illustrates the recruitment and allocation of clusters to each of the five groups, and the flow of the clusters up to 18 months’ follow-up, that is, the clusters in which women returned a questionnaire and contributed to overall data.
FIGURE 3.
Diagrammatic representation of cluster participation. CBA-F, cognitive behavioural approach face-to-face group; CBA-P, cognitive behavioural approach postal group; PCA-F, person-centred approach face-to-face group; PCA-P, person-centred approach postal group.
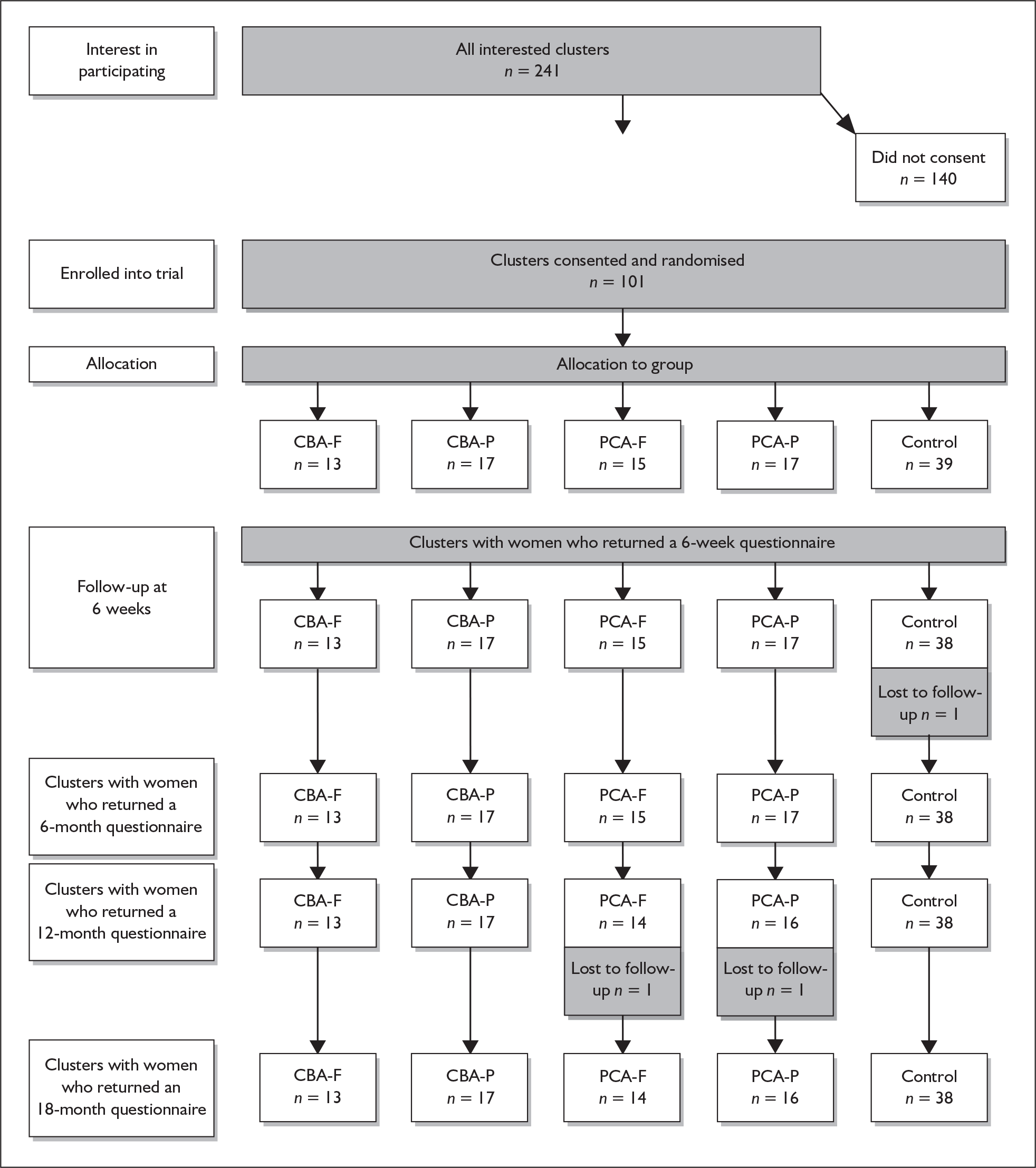
Baseline measurements at cluster level
The IMD 2004176 was used to compare the characteristics of the recruited GP clusters with those of the GP practices in the former Trent region and also with those of GP practices in England. The IMD measures deprivation for special census geographies called super output areas (SOAs). It combines indicators across seven domains into a single deprivation score and rank. The domains are income deprivation; employment deprivation; health deprivation and disability; education, skills and training deprivation; barriers to housing and services; living environment deprivation; and crime. Graphs were created using the functionality of geographical information systems (GIS) by coding IMD 2004 data to SOAs. These areas allow socially similar areas to be grouped together, allowing for more realistic patterns to emerge in the spatial data; it also allowed a GP practice to be tied to this measure. It is assumed that a practice placed in a SOA has the characteristics of that spatial unit rather than those of neighbouring ones. The source of the GP locations was an NHS website. 211 An automated extraction tool lifted and restructured the address and other information from the website before formatting and importing into a GIS.
IMD scores for GP practices in England, the former Trent Region and the PoNDER study
Across England, IMD scores vary considerably. A lower score signifies greater deprivation, indicating practices located in areas with multiple problems. The values for all GP practices in England, the former Trent Region and the PoNDER study are presented in Table 11.
| Number of GP practices | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|
| England, n = 32,533 | 0.72 | 86.36 | 21.7 | 15.7 |
| Former Trent region, n = 823 | 2.49 | 77.43 | 24.0 | 15.6 |
| PoNDER study GP clusters, n = 97 | 2.80 | 63.02 | 23.8 | 15.3 |
Description of the PoNDER study
The mean IMD for the 97 PoNDER study practices (23.8, SD 15.3) for which data were available was similar to the means for the 823 former Trent region practices (24.0, SD 15.6) and the 32,533 GP practices in England as a whole (21.7, SD 15.7). That is, the PoNDER study practices had similar levels of deprivation to GP practices in Trent and England.
Description of participating clusters
The clusters in which women contributed to the study are described below. The mean practice population was 7664 and the mean number of expected births per year was 79 (based on the actual number of births in the previous 2 years). The number of women in each cluster ranged from 1 to 140 (Table 12). Figures 4 and 5 indicate the distribution of registered practice populations and the total number of expected births per year in recruited clusters respectively. Figure 6 indicates the distribution of the number of women recruited per cluster.
| Descriptor | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|
| Total registered practice population | 2300 | 19,000 | 7664 | 3662 |
| Expected births per practice per yeara | 21 | 157 | 79 | 34 |
| Total number of women recruited to the study | 1 | 140 | 42 | 29 |
| IMD 2004 score for sample cases | 3 | 63 | 24 | 15 |
FIGURE 4.
Distribution of registered populations for GP practices in the study.
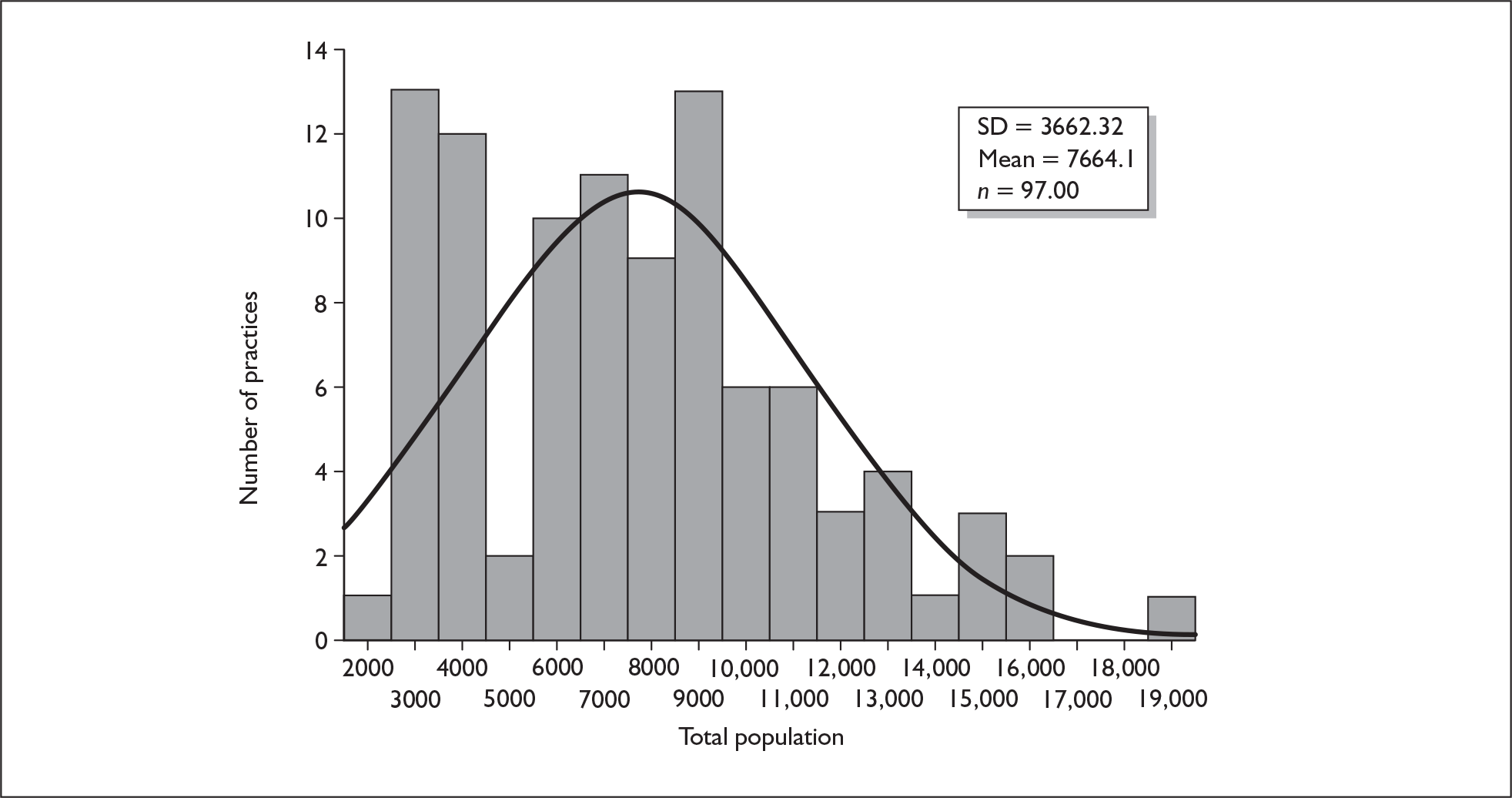
FIGURE 5.
Distribution of total expected births in GP practices in the study.
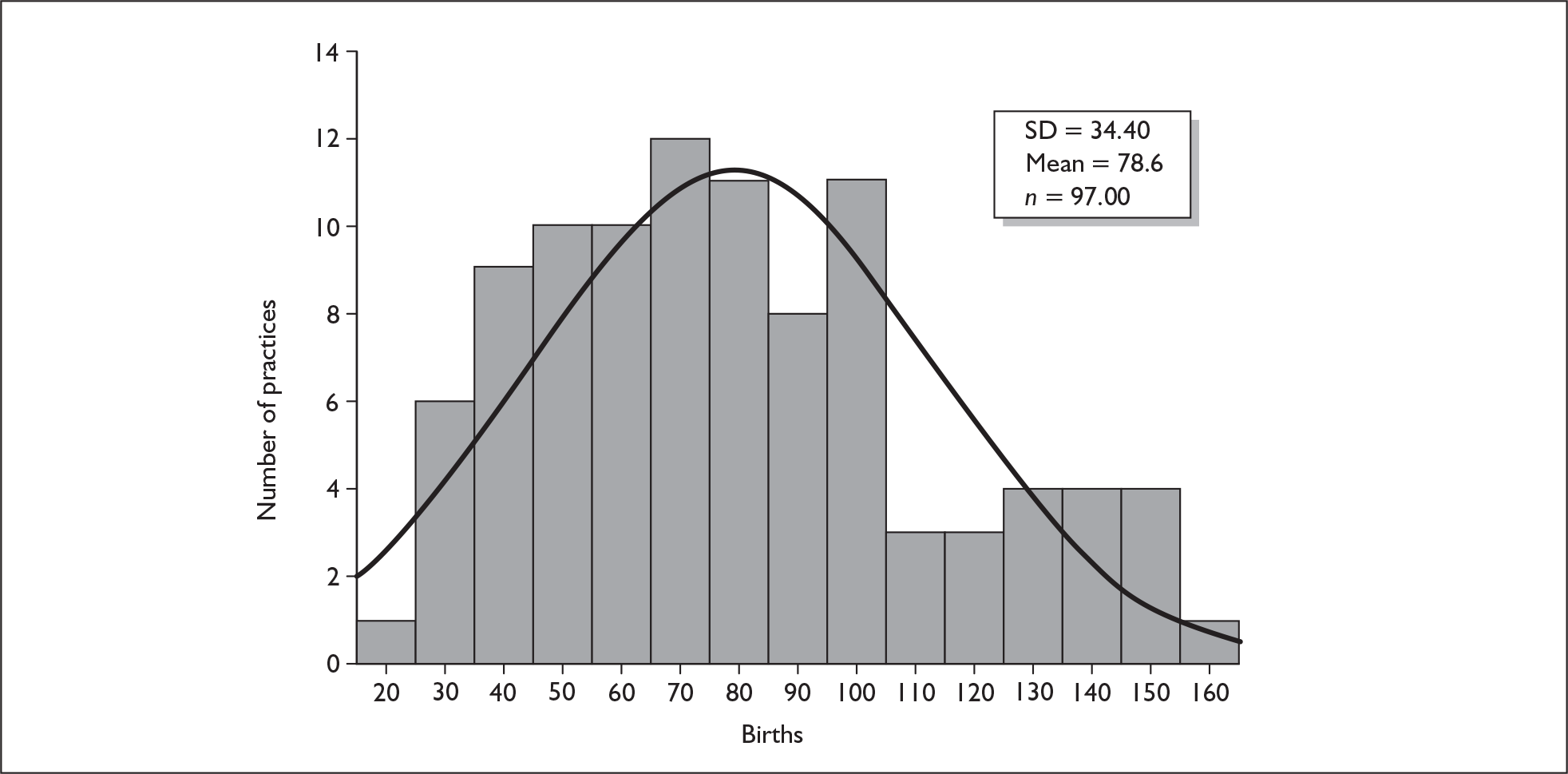
FIGURE 6.
Distribution of number of women consented per practice in the study.
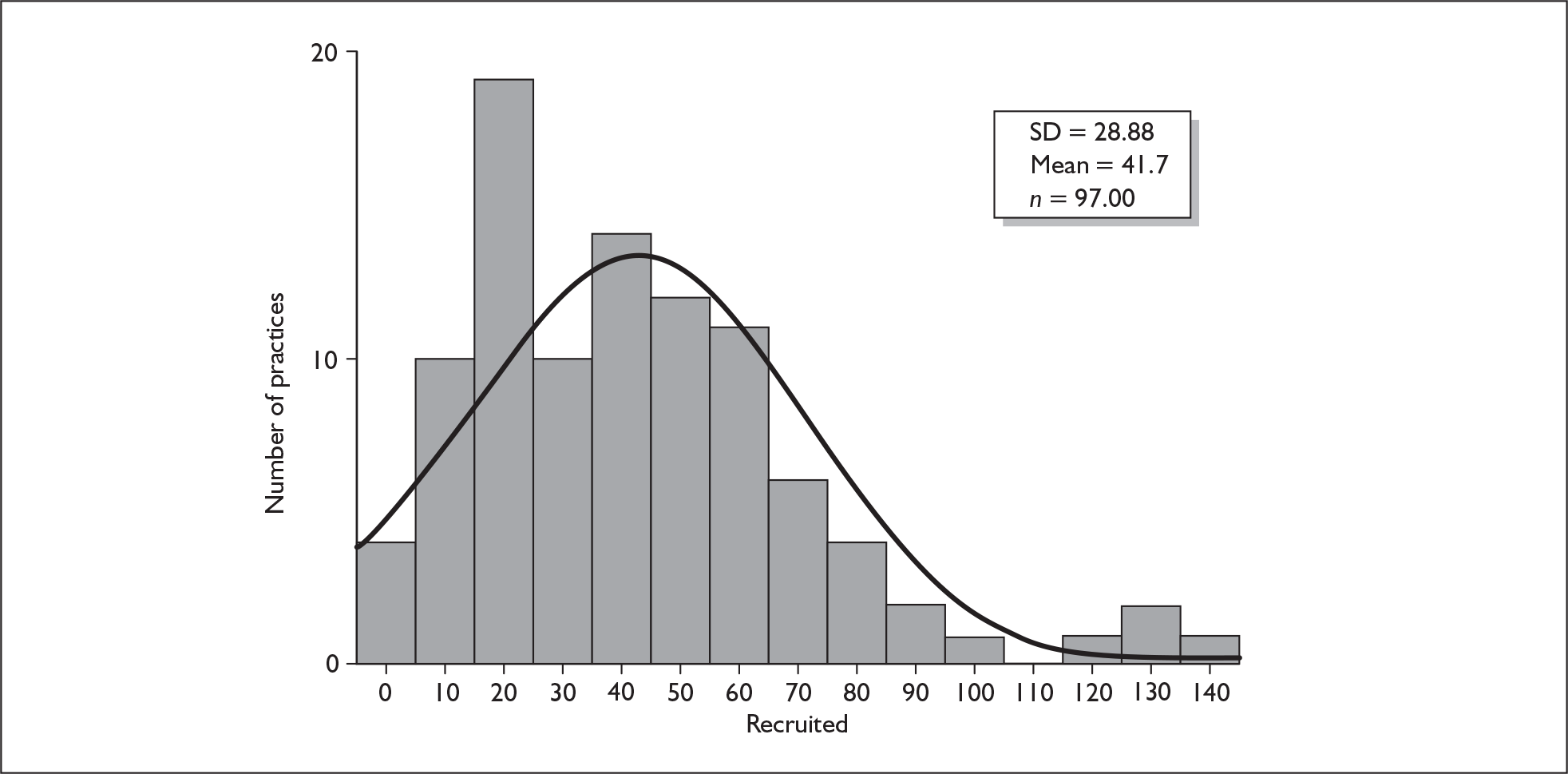
Individual level recruitment and consent to the trial
Baseline measurements at individual level: all recruited women
Among all of the 8716 women who were pregnant in the participating clusters during the recruitment phase for whom details were available, most of them spoke English as their first language and most were white British and living in a house with a husband or partner. Comparing the characteristics of the five groups there was some variation; however, all of the five groups were broadly similar (Table 13).
| Control (%) | CBA-F (%) | CBA-P (%) | PCA-F (%) | PCA-P (%) | Int (%) | All (%) | |
|---|---|---|---|---|---|---|---|
| Eligible | 92.0 | 90.9 | 84.1 | 87.5 | 90.0 | 87.8 | 89.3 |
| Consented | 51.4 | 64.1 | 52.2 | 59.1 | 47.0 | 56.2 | 53.3 |
| First baby | 45.4 | 31.9 | 43.0 | 42.8 | 37.0 | 39.0 | 41.3 |
| PND among all women | 8.5 | 7.0 | 7.8 | 7.2 | 9.8 | 8.1 | 8.3 |
| PND among women with a previous pregnancy | 15.7 | 10.3 | 13.7 | 12.6 | 15.6 | 15.3 | 14.1 |
| English first language | 99.7 | 99.4 | 94.6 | 99.6 | 99.0 | 97.8 | 98.5 |
| White British | 93.4 | 97.4 | 86.7 | 94.9 | 94.6 | 92.7 | 93.0 |
| Living with partner | 93.7 | 93.7 | 89.6 | 91.7 | 91.7 | 91.5 | 92.2 |
| Living alone | 3.2 | 2.5 | 5.6 | 3.8 | 3.2 | 3.9 | 3.7 |
| Living with others | 3.2 | 3.8 | 4.8 | 4.5 | 5.0 | 4.6 | 4.1 |
| Living in a house | 96.4 | 96.6 | 93.4 | 95.4 | 96.5 | 95.4 | 95.7 |
| Living in flat | 2.8 | 2.6 | 5.3 | 2.7 | 2.7 | 3.4 | 3.2 |
| Owner occupied | 76.4 | 74.6 | 57.9 | 74.4 | 74.9 | 69.6 | 71.8 |
| Rent council/HA | 13.6 | 17.1 | 29.3 | 15.4 | 17.0 | 20.4 | 18.2 |
| Rent privately | 7.0 | 5.4 | 8.5 | 5.3 | 4.3 | 6.0 | 6.3 |
| Twins/triplets | 1.1 | 1.9 | 0.9 | 1.4 | 1.8 | 1.6 | 1.4 |
In the 2001 national census data for England and Wales,212 91% of the population are recorded as white British, 69% lived in owner-occupied accommodation, 21% lived in council or housing association rented accommodation, and 7% rented privately. Therefore, the characteristics of all 8716 antenatal women in all consenting practices are broadly similar to those for the whole population.
Exclusion criteria applied
In total, 89.3% of all antenatal women were eligible to take part and 10.7% were ineligible. The main reasons that women were not eligible were that they were changing GP practice or address (4.8%), they were aged less than 18 years (1.4%) or they had mental health issues (1.1%), which meant severe and enduring mental health problems such as bipolar disorder or schizophrenia (Table 14).
| Control group | CBA-F | CBA-P | PCA-F | PCA-P | Int | All | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Age < 18 years | 26 | 0.9 | 10 | 0.9 | 39 | 2.2 | 15 | 1.3 | 27 | 1.7 | 91 | 1.8 | 117 | 1.4 |
| Baby died | 4 | 0.1 | 2 | 0.2 | 2 | 0.1 | 1 | 0.1 | 2 | 0.1 | 7 | 0.1 | 11 | 0.1 |
| Miscarriage/termination | 19 | 0.6 | 5 | 0.5 | 8 | 0.4 | 6 | 0.5 | 7 | 0.4 | 26 | 0.5 | 45 | 0.5 |
| Stillbirth | 6 | 0.2 | 1 | 0.1 | 4 | 0.2 | 5 | 0.4 | 2 | 0.1 | 12 | 0.2 | 18 | 0.2 |
| Moved away/temporary resident | 98 | 3.3 | 46 | 4.2 | 79 | 4.4 | 60 | 5.3 | 71 | 4.5 | 256 | 4.6 | 354 | 4.6 |
| Moved practice | 23 | 0.8 | 5 | 0.5 | 19 | 1.3 | 11 | 1.1 | 5 | 0.4 | 40 | 0.7 | 63 | 0.8 |
| Baby ill/premature | 9 | 0.3 | 6 | 0.5 | 7 | 0.4 | 7 | 0.6 | 5 | 0.3 | 25 | 0.4 | 34 | 0.4 |
| Child protection/social issues | 3 | 0.1 | 1 | 0.1 | 4 | 0.2 | 2 | 0.2 | 2 | 0.1 | 9 | 0.1 | 12 | 0.2 |
| Mental health issues | 16 | 0.6 | 8 | 0.8 | 19 | 1.3 | 16 | 1.6 | 8 | 0.6 | 51 | 0.9 | 67 | 0.9 |
Baseline measurements of consented women at individual level
Of all of the eligible pregnant women, 53.3% consented. Among those for whom details were available, the greatest proportion of women who did not consent said that they were not interested (76%), with others saying that they were too busy (7%) or not replying (11%). Table 15 presents the characteristics of the women who consented.
| Control (%) | CBA-F (%) | CBA-P (%) | PCA-F (%) | PCA-P (%) | Int (%) | All (%) | |
|---|---|---|---|---|---|---|---|
| First baby | 41.7 | 34.3 | 36.4 | 36.8 | 39.4 | 36.8 | 38.9 |
| PND among all women | 7.5 | 6.4 | 6.9 | 6.6 | 9.5 | 11.1 | 9.9 |
| PND among women with a previous pregnancy | 16.5 | 10.9 | 15.4 | 14.1 | 17.5 | 14.5 | 15.1 |
| English first language | 99.7 | 100.0 | 97.4 | 99.6 | 99.6 | 99.1 | 99.3 |
| White British | 94.5 | 98.6 | 91.6 | 97.7 | 96.2 | 95.7 | 95.3 |
| Living with partner | 94.5 | 95.1 | 90.8 | 94.4 | 94.3 | 93.5 | 93.8 |
| Living alone | 3.2 | 2.2 | 5.7 | 3.4 | 1.9 | 3.4 | 3.3 |
| Living with others | 2.3 | 2.7 | 3.5 | 2.2 | 3.8 | 3.1 | 2.8 |
| Living in a house | 97.1 | 97.5 | 94.8 | 96.8 | 97.3 | 96.5 | 96.7 |
| Living in flat | 2.4 | 2.2 | 4.3 | 1.6 | 2.0 | 2.6 | 2.5 |
| Owner occupied | 81.8 | 81.1 | 65.3 | 81.7 | 81.7 | 77.0 | 78.6 |
| Rent council/HA | 11.1 | 11.9 | 23.9 | 10.0 | 10.4 | 14.5 | 13.4 |
| Rent privately | 5.1 | 5.1 | 7.6 | 4.6 | 4.5 | 5.5 | 5.4 |
| Twins/triplets | 0.6 | 1.0 | 0.3 | 2.0 | 2.2 | 1.3 | 1.1 |
In total, 15.1% of women who consented to take part had had PND previously versus 14.1% of all antenatal women. Table 16 presents the characteristics of women who both consented and returned a 6-week questionnaire.
| Control | CBA-F | CBA-P | PCA-F | PCA-P | Int | All | |
|---|---|---|---|---|---|---|---|
| Maximum n | 1101 | 521 | 601 | 507 | 549 | 2116 | 3217 |
| First baby (%) | 46.4 | 37.4 | 40.6 | 39.4 | 43.5 | 40.3 | 42.4 |
| PND among all women (%) | 7.9 | 7.3 | 8.2 | 7.2 | 11.2 | 8.6 | 8.3 |
| PND among women with a previous pregnancy (%) | 14.8 | 10.8 | 14.0 | 12.9 | 17.7 | 13.9 | 14.2 |
| English first language (%) | 99.6 | 100 | 98.6 | 99.8 | 99.6 | 99.5 | 99.5 |
| White British (%) | 94.9 | 98.4 | 93.1 | 97.8 | 96.2 | 96.3 | 94.2 |
| Living with partner (%) | 95.2 | 96.1 | 91.2 | 95.2 | 94.8 | 94.4 | 94.6 |
| Living alone (%) | 2.7 | 1.8 | 5.0 | 2.5 | 1.2 | 2.7 | 2.7 |
| Living with others (%) | 2.1 | 2.1 | 3.4 | 2.3 | 4.0 | 3.0 | 2.7 |
| Living in a house (%) | 97.2 | 98.6 | 95.7 | 97.6 | 97.5 | 97.4 | 97.5 |
| Living in flat (%) | 2.3 | 1.2 | 3.1 | 1.6 | 1.8 | 1.9 | 2.0 |
| Owner occupied (%) | 85.8 | 83.9 | 70.2 | 85.1 | 82.8 | 80.4 | 82.2 |
| Rent council/HA (%) | 8.1 | 9.6 | 20.2 | 9.0 | 8.8 | 12.0 | 10.7 |
| Rent privately (%) | 4.5 | 4.9 | 6.8 | 3.3 | 4.9 | 5.0 | 4.9 |
| Twins/triplets (%) | 0.6 | 1.2 | 0.2 | 1.7 | 1.8 | 1.3 | 1.0 |
Individual level follow-up
The overall participant flow chart (Appendix 1, Figures 27 and 28) illustrate the number of women in the study at baseline and follow-up. Of the 7649 eligible women in all clusters, 4084 (53.4%) consented and 3449 returned a 6-week questionnaire (88% return rate). A total of 2875 women (72%) returned a 6-month questionnaire; 2029 women (61%) returned a 12-month questionnaire; and 1097 women (56%) returned an 18-month questionnaire (Appendix 1, Figure 27).
A total of 595 women returned a 6-week questionnaire and scored ≥ 12 on the EPDS to become the at-risk women. The follow-up of the at-risk women is illustrated in Figure 7 and Appendix 1, Figure 29.
FIGURE 7.
Flow chart for at-risk women by group (n = 595). CBA, cognitive behavioural approach; EPDS, Edinburgh Postnatal Depression Scale; PCA, person-centred approach.
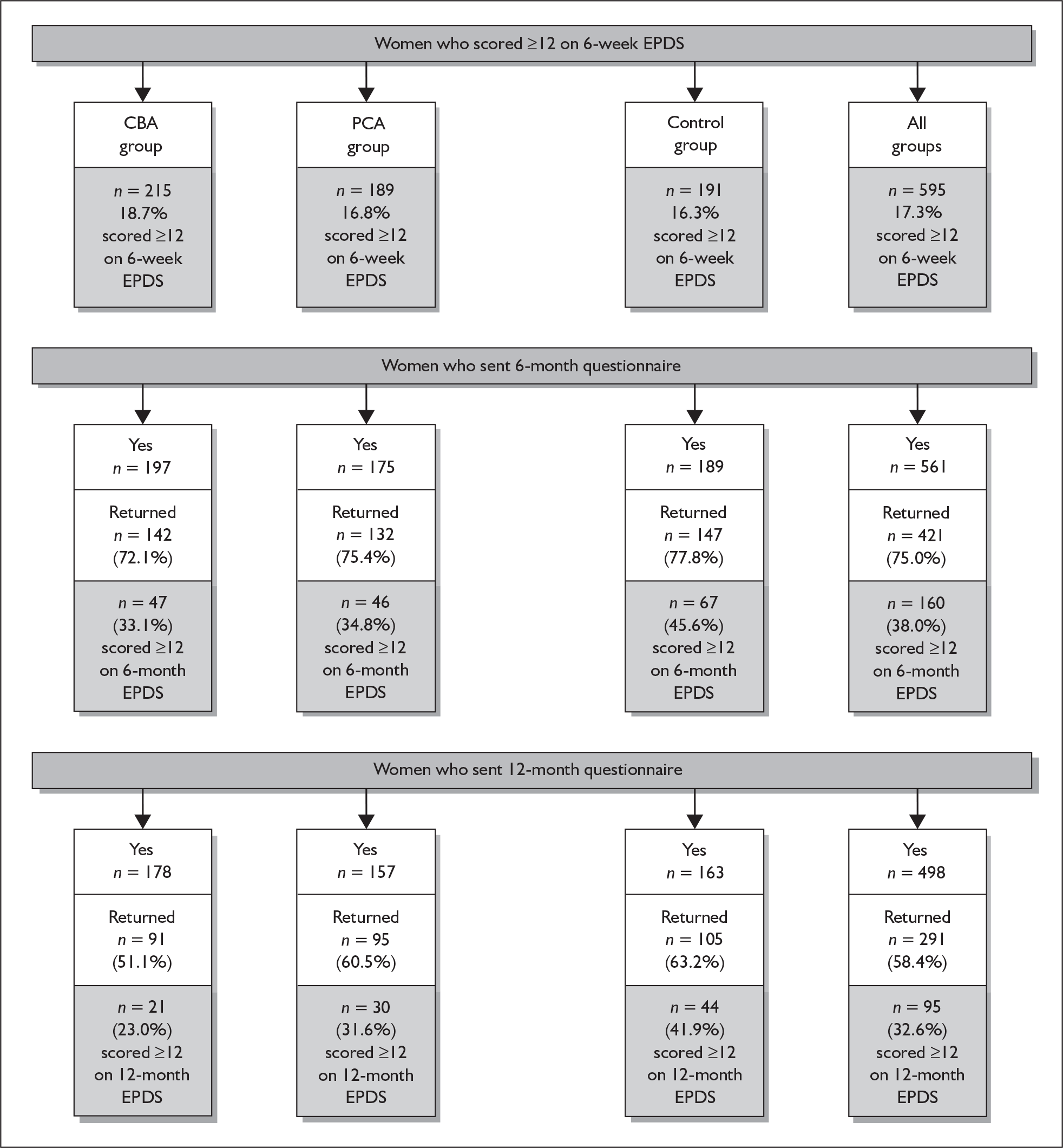
Individual level baseline measurements for at-risk women: intervention versus control
At 6 months 70.3% (418/595) of the at-risk women (those who had scored ≥ 12 on the 6-week EPDS) had a 6-month EPDS score available for the analysis. The characteristics of the at-risk women for whom a 6-month EPDS score was available (n = 418) are presented in Table 17. A slightly greater percentage of women in the IG had had PND before, lived alone and had experienced stressful life events in the previous 6 months.
| Control group | Intervention group | All | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| First baby | 73 | 49.7 | 124 | 45.8 | 197 | 47.1 | |||
| PND among all women | 13 | 9.4 | 44 | 17.5 | 57 | 14.6 | |||
| PND among women with a previous pregnancy | 13 | 18.1 | 44 | 30.6 | 57 | 26.4 | |||
| English first language | 136 | 92.5 | 266 | 98.2 | 402 | 96.2 | |||
| White British | 133 | 90.5 | 257 | 94.8 | 390 | 93.3 | |||
| Living alone | 7 | 4.8 | 19 | 7.1 | 26 | 6.3 | |||
| Living with others | 139 | 95.2 | 250 | 92.9 | 389 | 93.7 | |||
| Twins/triplets | 2 | 1.5 | 3 | 1.2 | 5 | 1.2 | |||
| Single girl | 60 | 43.8 | 140 | 52.4 | 200 | 49.5 | |||
| Single boy | 75 | 54.7 | 124 | 46.4 | 199 | 49.3 | |||
| Life events | 73 | 50.3 | 152 | 56.5 | 225 | 54.3 | |||
| n | Mean | SD | n | Mean | SD | n | Mean | SD | |
| Woman’s age when baby born (years) | 147 | 30.6 | 5.5 | 271 | 31.0 | 5.4 | 418 | 30.9 | 5.4 |
| Woman’s age when first child born (years) | 145 | 27.5 | 6.0 | 265 | 27.4 | 5.8 | 410 | 27.4 | 5.8 |
| No. of other children | 147 | 0.7 | 1.0 | 271 | 0.8 | 0.9 | 418 | 0.8 | 0.9 |
| EPDS 6 weeks | 147 | 15.4 | 3.2 | 271 | 15.1 | 2.9 | 418 | 15.2 | 3.0 |
| SF-12 PCS 6 weeks | 143 | 48.5 | 10.9 | 265 | 50.1 | 9.4 | 408 | 49.6 | 10.0 |
| SF-12 MCS 6 weeks | 143 | 29.4 | 9.2 | 265 | 29.1 | 8.0 | 408 | 29.2 | 8.4 |
| SF-6D 6 weeks | 142 | 0.59 | 0.08 | 268 | 0.60 | 0.07 | 410 | 0.60 | 0.07 |
| CORE-OM total score 6 weeks | 146 | 1.40 | 0.50 | 269 | 1.35 | 0.49 | 415 | 1.37 | 0.49 |
Individual level baseline measurements for women who returned a 6-month questionnaire
The characteristics of all of the women for whom a 6-week EPDS score was available and who returned a 6-month EPDS score (n = 2659) are presented in Table 18.
| Control group | Intervention group | All | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| First baby | 443 | 48.5 | 785 | 45.0 | 1228 | 46.2 | |||
| English first language | 877 | 96.0 | 1699 | 97.4 | 2576 | 96.9 | |||
| White British | 871 | 95.3 | 1686 | 96.6 | 2557 | 96.2 | |||
| Living alone | 31 | 3.4 | 58 | 3.3 | 89 | 3.4 | |||
| Living with others | 874 | 96.6 | 1680 | 96.7 | 2554 | 96.6 | |||
| Twins/triplets | 5 | 0.6 | 19 | 1.1 | 24 | 1.0 | |||
| Single girl | 406 | 48.0 | 819 | 48.3 | 1225 | 48.2 | |||
| Single boy | 434 | 51.4 | 859 | 50.6 | 1293 | 50.9 | |||
| Life events | 368 | 40.6 | 715 | 41.2 | 1083 | 41.0 | |||
| n | Mean | SD | n | Mean | SD | n | Mean | SD | |
| Woman’s age when baby born (years) | 913 | 32.0 | 5.1 | 1745 | 31.3 | 5.0 | 2658 | 31.5 | 5.1 |
| Age when first child born (years) | 889 | 29.0 | 5.3 | 1714 | 28.0 | 5.3 | 2603 | 28.4 | 5.3 |
| No. of other children | 914 | 0.7 | 0.8 | 1745 | 0.7 | 0.9 | 2659 | 0.7 | 0.9 |
| EPDS score 6 weeks | 914 | 6.8 | 5.0 | 1745 | 6.6 | 4.8 | 2659 | 6.7 | 4.8 |
| SF-12 PCS 6 weeks | 888 | 50.5 | 8.7 | 1719 | 51.4 | 8.0 | 2607 | 51.1 | 8.3 |
| SF-12 MCS 6 weeks | 888 | 42.7 | 9.5 | 1719 | 42.9 | 9.3 | 2607 | 42.9 | 9.4 |
| SF-6D 6 weeks | 885 | 0.66 | 0.09 | 1716 | 0.67 | 0.09 | 2601 | 0.67 | 0.09 |
| CORE-OM total score 6 weeks | 906 | 0.55 | 0.51 | 1735 | 0.51 | 0.49 | 2641 | 0.52 | 0.50 |
Outcomes
Primary outcome for at-risk women
Primary outcome: intervention group versus control group
Of the 418 at-risk women, 45.6% (67/147) in the CG versus 33.9% (93/271) in the IG scored ≥ 12 on the EPDS (Table 19). The absolute difference of 11.7% (95% CI 0.4 to 22.9%) was statistically significant (p = 0.028 adjusted for covariates). The adjusted odds ratio (0.6, 95% CI 0.38 to 0.995, p = 0.036) indicated that the at-risk women were 40% less likely then the CG women to have a 6-month EPDS score ≥ 12.
| 6-month EPDS | Int group | Control group | All | Absolute difference% | 95% CI | Odds ratio, int to control | 95% CI | p-value |
|---|---|---|---|---|---|---|---|---|
| Score < 12 | ||||||||
| n | 179 | 80 | 259 | |||||
| % | 66.1 | 54.4 | 62.0 | |||||
| Score ≥ 12 | ||||||||
| n | 92 | 67 | 159 | |||||
| % | 33.9 | 45.6 | 38.0 | 11.7 | 0.4 to 22.9 | 0.62 | 0.40 to 0.97 | 0.036 |
| 0.64a | 0.40 to 1.01a | 0.058a | ||||||
| 0.60b | 0.38 to 0.95b | 0.028b | ||||||
| 0.57c | 0.36 to 0.90c | 0.017c | ||||||
| Total n | 271 | 147 | 418 | |||||
The primary analysis was based on a complete case analysis with no substitution for missing data. The intention to treat analysis included all women with a 6-week EPDS score ≥ 12 and a valid 6-month EPDS score. After adjusting for covariates such as 6-week EPDS score, living alone, previous history of PND and any life events experienced, the point estimate of the odds ratio for the IG effect was relatively unchanged (at around 0.60) and this effect remained statistically significant or marginally significant.
Sensitivity analysis: imputation of missing 6-month EPDS data for at-risk women
In total, 595 at-risk women had a 6-week EPDS score ≥ 12 and 418 of these women also had 6-month follow-up EPDS scores. The results for these 418 women were therefore available for the primary statistical analysis. A sensitivity analysis was performed to impute the missing 6-month EPDS scores for the 177/595 (29.7%) at-risk women who were lost to follow-up. Two types of missing data imputation were performed:
-
last observation carried forward (LOCF)
-
regression imputation.
For most postnatal women symptoms of depression will naturally reduce over time, as seen in the CG at-risk women, among whom 54.4% (87/147) no longer had an EPDS score ≥ 12 at the 6-month follow-up. LOCF imputation represents the worst-case scenario, in which, for example, a 6-week EPDS score of 12 would be carried forward to be used as a woman’s missing 6-month EPDS score. This woman would therefore still be regarded as being in the above-threshold group of at-risk women.
Regression imputation is more logical for this group of postnatal women, as it better reflects the natural reduction in symptoms of depression over time. A regression imputation, based on 2659 women who returned both a 6-week and a 6-month EPDS, produced the following model (Figure 8):
FIGURE 8.
Scatter plot of the relationship between the 6-month and 6-week EPDS scores (n = 2659) with the regression imputation line of best fit.
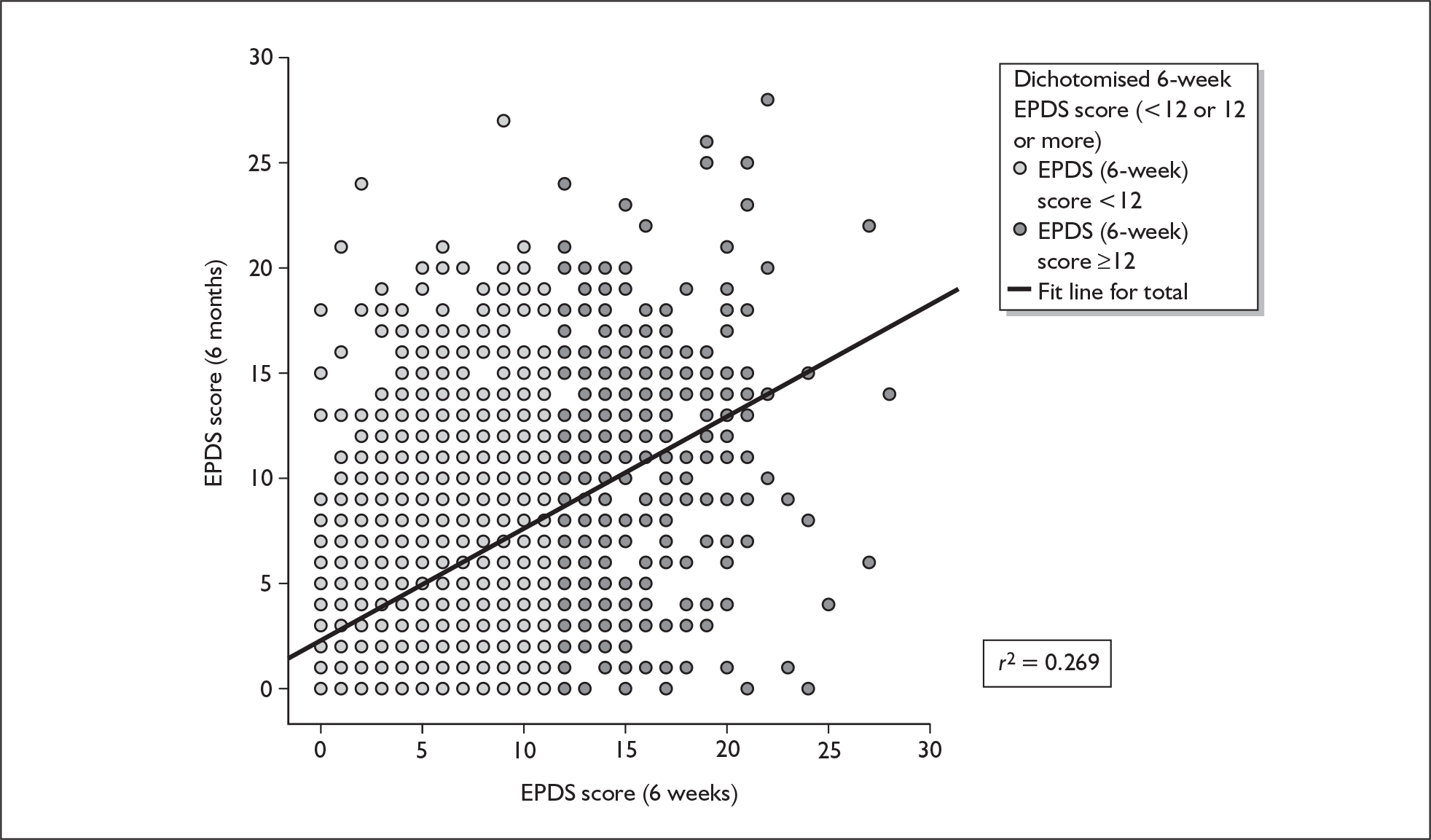
Using regression imputation, a woman with a 6-week EPDS score of 12 and a missing 6-month EPDS score would have a regression-imputed 6-month EPDS score of 8.6 [i.e. 2.287 + (12 × 0.526)]. Only women with a 6-week EPDS score ≥ 19 would have a 6-month EPDS score ≥ 12.
Table 20 shows the results of the sensitivity analysis for the imputation of missing data by LOCF and regression imputation compared with the primary statistical analysis. Using LOCF the results changed markedly and the observed treatment effect was smaller and not statistically significant. Using regression imputation the results were similar to those of the primary analysis although the treatment effect was smaller (odds ratio of 0.72 versus 0.62) and not statistically significant, with a p-value of 0.089 (compared with p = 0.036 for the observed data). The results for the regression-imputed model adjusted for covariates were statistically significant and very similar to the observed data (odds ratio of 0.62 versus 0.60).
| 6-month EPDS score ≥ 12 | Valid n | Difference (%) | 95% CI | Odds ratio, int to control | 95% CI | p-value | ||
|---|---|---|---|---|---|---|---|---|
| Control group | Int group | |||||||
| Primary analysis | ||||||||
| n | 67 | 92 | ||||||
| % | 45.6 | 33.9 | 11.7 | 0.4 to 22.9 | 0.62 | 0.40 to 0.97 | 0.036 | |
| 0.60a | 0.38 to 0.95a | 0.028 (n = 409)a | ||||||
| Total n | 147 | 271 | 418 | |||||
| LOCF | ||||||||
| n | 111 | 225 | ||||||
| % | 58.1 | 55.7 | 2.4 | –6.6 to 12.7 | 0.90 | 0.62 to 1.31 | 0.58 | |
| 0.87a | 0.59 to 1.27a | 0.47 (n = 582)a | ||||||
| Total n | 191 | 404 | 595 | |||||
| Regression | ||||||||
| n | 74 | 126 | ||||||
| % | 38.7 | 31.2 | 7.5 | –1.3 to 16.4 | 0.72 | 0.49 to 1.05 | 0.089 | |
| 0.62a | 0.41 to 0.96a | 0.032 (n = 582)a | ||||||
| Total n | 191 | 404 | 595 | |||||
Primary outcome: comparison of the CBA and PCA groups versus the control group
In total, 32.9% (46/140) of women in the CBA group versus 35.1% (46/131) in the PCA group had a 6-month EPDS score ≥ 12 (difference 2.2%, 95% CI –14.2% to 10.1%, p = 0.74) (Table 21). This suggests that the odds of having a 6-month EPDS score ≥ 12 in the PCA group is 1.09 (95% CI 0.64 to 1.88) times that of the odds in the CBA group. After adjusting for covariates (6-week EPDS score, living alone, history of PND, life events) the odds ratio for the PCA versus the CBA was 1.00 (95% CI 0.57 to 1.77, p = 0.99) and this effect was not statistically significant.
| 6-month EPDS | CBA group | PCA group | Control group | Odds ratio, CBA to control | 95% CI | p-value | Odds ratio, PCA to control | 95% CI | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Score < 12, n (%) | 94 (67.1) | 85 (64.9) | 80 (54.4) | ||||||
| Score ≥ 12, n (%) | 46 (32.9) | 46 (35.1) | 67 (45.6) | 0.59 | 0.35 to 0.99 | 0.046 | 0.65 | 0.38 to 1.10 | 0.108 |
| 0.62a | 0.36 to 1.06a | 0.080a | 0.66a | 0.39 to 1.14a | 0.137a | ||||
| 0.59b | 0.34 to 1.02b | 0.061b | 0.61b | 0.36 to 1.03b | 0.064b | ||||
| Total n | 140 | 131 | 147 |
Intracluster correlation coefficient for at-risk women
As recommended by the cluster CONSORT guidelines,197 Table 22 reports the observed ICC for the primary outcome.
| n | No. of clusters | Average cluster size | Min. to max. cluster size | ICC | 95% CI lower | 95% CI upper | |
|---|---|---|---|---|---|---|---|
| At-risk women | 418 | 86 | 4.9 | 1–15 | 0.037 | 0.000 | 0.114 |
Six-month secondary outcomes for at-risk women
Six-month secondary outcomes: intervention group versus control group
The mean EPDS was a secondary outcome. At 6 months, among the at-risk women who also had an EPDS score on their returned 6-month questionnaires, the mean EPDS score was 11.3 (SD 5.8) for women in the CG and 9.2 (SD 5.4) for women in the IG (Table 23). The mean difference was –2.1 (95% CI –3.4 to –0.8). This difference was statistically significant (p = 0.002) and remained statistically significant after adjusting for 6-week variables (p = 0.001).
| 6-month outcome | Control | Intervention | Unadjusted | Adjusteda | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Difference | 95% CI | p-value | Difference | 95% CI | p-value | |
| EPDS | 147 | 11.3 | 5.8 | 271 | 9.2 | 5.4 | –2.1 | –3.4 to –0.8 | 0.002 | –2.1 | –3.3 to –0.9 | 0.001 |
| SF-12 PCS | 142 | 54.3 | 9.0 | 263 | 53.0 | 7.6 | –1.4 | –3.5 to 0.7 | 0.204 | –1.7 | –3.6 to 0.1 | 0.069 |
| SF-12 MCS | 142 | 37.8 | 11.8 | 263 | 42.3 | 10.8 | 4.7 | 1.8 to 7.6 | 0.001 | 5.2 | 2.5 to 7.8 | 0.001 |
| SF-6D | 144 | 0.70 | 0.12 | 266 | 0.73 | 0.1 | 0.03 | 0.004–0.06 | 0.025 | 0.03 | 0.00 to 0.06 | 0.025 |
| CORE-OM well-being | 146 | 1.6 | 0.95 | 269 | 1.19 | 0.9 | –0.4 | –0.6 to –0.1 | 0.001 | –0.3 | –0.5 to –0.2 | 0.001 |
| CORE-OM risk | 145 | 0.2 | 0.37 | 269 | 0.10 | 0.2 | –0.1 | –0.1 to 0.0 | 0.135 | –0.0 | –0.1 to 0.0 | 0.149 |
| CORE-OM symptoms | 146 | 1.1 | 0.8 | 269 | 0.9 | 0.7 | –0.2 | –0.4 to –0.1 | 0.014 | –0.2 | –0.4 to –0.1 | 0.005 |
| CORE-OM functioning | 146 | 1.2 | 0.8 | 269 | 1.0 | 0.8 | –0.3 | –0.5 to –0.1 | 0.006 | –0.3 | –0.4 to –0.1 | 0.001 |
| CORE-OM total score | 146 | 1.1 | 0.7 | 269 | 0.8 | 0.6 | –0.2 | –0.4 to –0.1 | 0.006 | –0.2 | –0.4 to –0.1 | 0.001 |
| State anxiety (STAI) | 136 | 45.5 | 12.5 | 254 | 41.7 | 11.8 | –3.8 | –6.6 to 1.0 | 0.008 | –3.9 | –6.6 to –1.3 | 0.003 |
| Trait anxiety (STAI) | 130 | 45.0 | 10.9 | 257 | 41.6 | 10.4 | –3.4 | –5.9 to –0.9 | 0.008 | –3.7 | –6.1 to –1.4 | 0.002 |
| PSI parenting distress | 114 | 38.1 | 9.5 | 229 | 41.3 | 8.8 | 3.2 | 0.9 to 5.4 | 0.006 | 3.5 | 1.3 to 5.8 | 0.002 |
| PSI PCDI | 118 | 53.6 | 6.9 | 231 | 55.7 | 5.8 | 2.2 | 0.7 to 3.6 | 0.003 | 2.1 | 0.7 to 3.5 | 0.003 |
| PSI difficult child | 113 | 48.1 | 7.7 | 217 | 51.5 | 6.9 | 3.4 | 1.8 to 5.0 | 0.001 | 2.9 | 1.7 to 4.2 | 0.001 |
| PSI total stress | 106 | 139.6 | 20.4 | 211 | 148.9 | 17.0 | 9.2 | 4.8 to 13.7 | 0.001 | 9.3 | 137.3 to 13.4 | 0.001 |
In addition, there were also significant differences between the groups in the SF-12 MCS, the SF-6D, the CORE-OM total score, the STAI and the PSI, all in favour of the IG. The mean 6-month secondary outcome scores are presented in Table 23.
Six-month secondary outcomes: CBA-F, CBA-P, PCA-F and PCA-P versus control group
The mean 6-month EPDS score was 9.2 (SD 5.3) for the at-risk women in the CBA group and 9.2 (SD 5.5) in the PCA group (p = 0.99). There were no differences in the mean scores for any of the other secondary outcomes (Table 24). The mean 6-month EPDS score was 9.2 for each of the four IGs.
| 6-month outcome | Control | CBA | PCA | CBA | PCA | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | Difference (95% CI) | p-value | n | Mean (S.D) | Difference (95% CI) | p-value | Adjusteda difference (95% CI) | p-value | Adjusteda difference (95% CI) | p-value | |
| EPDS | 147 | 11.3 (5.8) | 140 | 9.2 (5.3) | –2.1 (–3.6 to –0.6) | 0.006 | 131 | 9.2 (5.5) | –2.1 (–3.5 to –0.6) | 0.005 | –2.1 (–3.5 to 0.6) | 0.004 | –2.1 (–3.4 to –0.8) | 0.002 |
| SF-12 PCS | 142 | 54.3 (9.0) | 134 | 53.8 (7.5) | –0.6 (–2.8 to 1.56) | 0.596 | 129 | 52.2 (7.7) | –2.1 (–4.4 to 0.3) | 0.081 | –0.9 (–2.9 to 1.2) | 0.354 | –2.5 (–4.6 to –0.4) | 0.018 |
| SF-12 MCS | 142 | 37.8 (11.8) | 134 | 42.0 (10.5) | 4.3 (1.0 to 7.6) | 0.010 | 129 | 42.7 (11.3) | 5.1 (1.9 to 8.3) | 0.002 | 4.6 (1.5 to 7.7) | 0.003 | 5.8 (2.8 to 8.7) | 0.001 |
| SF-6D | 144 | 0.70 (0.12) | 137 | 0.73 (0.13) | 0.03 (–0.0 to 0.63) | 0.051 | 129 | 0.73 (0.14) | 0.32 (–0.00 to 0.67) | 0.068 | 0.03 (0.00 to 0.06) | 0.025 | 0.32 (0.00 to 0.06) | 0.043 |
| CORE-OM well-being | 146 | 1.6 (1.0) | 138 | 1.2 (0.9) | –0.4 (–0.6 to –0.1) | 0.003 | 131 | 1.2 (0.9) | –0.3 (–0.6 to –0.1) | 0.006 | –0.4 (–0.6 to –0.1) | 0.001 | –0.3 (–0.5 to –0.1) | 0.003 |
| CORE-OM risk | 145 | 0.2 (0.4) | 138 | 0.1 (0.2) | –0.0 (–0.1 to –0.0) | 0.248 | 131 | 0.1 (0.2) | –0.1 (–0.1 to 0.0) | 0.101 | –0.0 (–0.1 to 0.0) | 0.206 | –0.0 (–0.1 to 0.0) | 0.155 |
| CORE-OM symptoms | 146 | 1.1 (0.8) | 138 | 0.9 (0.7) | –0.2 (–0.4 to –0.0) | 0.030 | 131 | 0.9 (0.7) | –0.2 (–0.4 to–0.0) | 0.023 | –0.2 (–0.4 to –0.0) | 0.014 | –0.2 (–0.4 to –0.1) | 0.012 |
| CORE-OM functioning | 146 | 1.3 (0.8) | 138 | 1.0 (0.7) | –0.3 (–0.5 to –0.1) | 0.008 | 131 | 1.0 (0.8) | –0.2 (–0.4 to –0.0) | 0.026 | –0.3 (–0.5 to –0.8) | 0.002 | –0.2 (–0.4 to –0.1) | 0.005 |
| CORE-OM total score | 146 | 1.1 (0.7) | 138 | 0.8 (0.6) | –0.2 (–0.4 to –0.1) | 0.011 | 131 | 0.8 (0.6) | –0.2 (–0.4 to –0.0) | 0.015 | –0.2 (–0.9 to –0.1) | 0.004 | –0.2 (–0.4 to –0.1) | 0.006 |
| State anxiety (STAI) | 136 | 45.5 (12.5) | 130 | 41.0 (11.7) | –4.4 (–7.7 to –1.1) | 0.009 | 124 | 42.0 (11.9) | –3.2 (–6.2 to –0.1) | 0.043 | –4.6 (–7.7 to –1.5) | 0.003 | –3.2 (–6.0 to 0.3) | 0.029 |
| Trait anxiety (STAI) | 130 | 45.0 (10.9) | 133 | 41.1 (9.6) | –3.9 (–6.8 to –1.1) | 0.007 | 124 | 42.1 (11.1) | –2.9 (–5.7 to –0.1) | 0.044 | –4.2 (–7.0 to –1.5) | 0.003 | –3.2 (–5.9 to –0.6) | 0.016 |
| PSI parenting distress | 114 | 38.1 (9.5) | 114 | 41.9 (8.6) | 3.8 (1.3 to 6.4) | 0.003 | 115 | 40.7 (9.0) | 2.6 (0.1 to 5.0) | 0.039 | 1.0 (0.0 to 2.0) | 0.039 | 1.2 (0.3 to 2.2) | 0.012 |
| PSI PCDI | 118 | 53.6 (6.9) | 116 | 55.3 (6.4) | 1.8 (–0.1 to 3.6) | 0.061 | 115 | 56.2 (5.1) | 2.6 (1.1 to 4.0) | 0.001 | 1.6 (–0.2 to 3.4) | 0.084 | 2.6 (1.2 to 4.0) | 0.001 |
| PSI difficult child | 113 | 48.1 (7.7) | 109 | 51.7 (7.1) | 3.5 (1.8 to 5.3) | 0.001 | 108 | 51.3 (6.6) | 3.3 (1.5 to 5.1) | 0.001 | 3.0 (1.5 to 4.5) | 0.001 | 2.9 (1.4 to 4.4) | 0.001 |
| PSI total stress | 106 | 139.6 (20.4) | 106 | 149.9 (18.1) | 10.3 (5.0 to 15.6) | 0.001 | 105 | 147.8 (15.7) | 8.2 (3.6 to 12.7) | 0.001 | 10.1 (5.1 to 15.1) | 0.001 | 8.4 (4.3 to 12.5) | 0.001 |
Twelve-month secondary outcomes for at-risk women
Of the 741 questionnaires not sent at 12 months, 597 (81%) were not sent because the women had not reached the 12-month postnatal follow-up time. Twelve-month outcomes were therefore available for 94 CG and 167 IG at-risk women.
Twelve-month EPDS scores for at-risk women: intervention versus control group
At 12 months, among the at-risk women who had an EPDS score on their returned 6-month questionnaires, the mean EPDS score was 10.6 (SD 6.2) for women in the CG and 8.1 (SD 5.6) for women in the IG (Table 25). This difference was statistically significant (p < 0.001). After adjusting for 6-week variables, the difference remained statistically significant (p = 0.005). Figure 9 shows the reduction in mean EPDS score over time in the intervention and control groups from 6 weeks to 12 months. Most of the benefit is gained at 6 months and is then maintained up to 12 months postnatally.
| 12-month outcome | Control | Intervention | Unadjusted | Adjusteda | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Difference | 95% CI | p-value | Difference | 95% CI | p-value | |
| EPDS | 94 | 10.6 | 6.2 | 167 | 8.1 | 5.6 | –2.6 | –4.3 to –0.9 | 0.003 | –2.4 | –4.1 to –0.7 | 0.005 |
| SF-12 PCS | 92 | 54.1 | 7.5 | 161 | 53.9 | 7.0 | –0.2 | –2.0 to 1.7 | 0.857 | –0.4 | –2.0 to 1.3 | 0.650 |
| SF-12 MCS | 92 | 40.8 | 10.9 | 161 | 44.9 | 10.9 | 4.1 | 1.3 to 6.9 | 0.004 | 3.8 | 1.0 to 6.6 | 0.008 |
| SF-6D | 93 | 0.7 | 0.1 | 165 | 0.8 | 0.1 | 0.0 | 0.0 to 0.1 | 0.007 | 0.0 | 0.0 to 0.1 | 0.013 |
| CORE-OM well-being | 94 | 1.4 | 0.9 | 167 | 1.1 | 0.9 | –0.3 | –0.5 to –0.1 | 0.013 | –0.3 | –0.5 to –0.1 | 0.013 |
| CORE-OM risk | 94 | 0.1 | 0.4 | 167 | 0.1 | 0.2 | –0.1 | –0.1 to 0.0 | 0.191 | –0.0 | –0.1 to 0.0 | 0.353 |
| CORE-OM symptoms | 94 | 1.1 | 0.8 | 167 | 0.8 | 0.7 | –0.2 | –0.5 to –0.1 | 0.010 | –0.2 | –0.4 to –0.0 | 0.021 |
| CORE-OM functioning | 94 | 1.2 | 0.8 | 167 | 0.9 | 0.8 | –0.3 | –0.5 to –0.1 | 0.005 | –0.3 | –0.5 to –0.1 | 0.011 |
| CORE-OM total score | 94 | 1.1 | 0.7 | 167 | 0.7 | 0.6 | –0.3 | –0.4 to –0.1 | 0.005 | –0.2 | –0.4 to –0.0 | 0.015 |
| State anxiety (STAI) | 93 | 45.0 | 13.2 | 162 | 40.7 | 12.6 | –0.4 | –8.1 to –0.7 | 0.019 | –4.2 | –7.8 to –0.5 | 0.025 |
| Trait anxiety (STAI) | 89 | 43.2 | 11.4 | 162 | 39.3 | 10.8 | –4.0 | –7.3 to –0.6 | 0.019 | –3.9 | –7.2 to –0.5 | 0.023 |
| DAS Likert | 89 | 3.3 | 1.4 | 158 | 3.8 | 1.4 | 0.5 | 0.1 to 0.8 | 0.011 | –0.2 | –0.6 to 0.1 | 0.217 |
| DAS | 89 | 19.2 | 3.2 | 154 | 18.2 | 3.0 | –0.9 | –1.8 to –0.1 | 0.027 | 0.0 | –0.7 to 0.8 | 0.965 |
| PSI parenting distress | 93 | 38.6 | 9.5 | 158 | 42.5 | 10.0 | 3.9 | 1.4 to 6.4 | 0.002 | 3.9 | 1.5 to 6.3 | 0.002 |
| PSI PCDI | 94 | 54.3 | 7.1 | 163 | 55.9 | 6.1 | 1.6 | –0.3 to 3.1 | 0.055 | 1.6 | 0.0 to 3.2 | 0.047 |
| PSI difficult child | 91 | 47.6 | 8.4 | 164 | 50.5 | 7.4 | 3.0 | 1.0 to 5.0 | 0.003 | 2.9 | 1.2 to 4.7 | 0.001 |
| PSI total stress | 90 | 140.7 | 21.4 | 156 | 148.7 | 19.2 | 8.1 | 3.1 to 13.0 | 0.001 | 8.1 | 3.6 to 12.6 | 0.000 |
FIGURE 9.
Mean EPDS scores for at-risk women at 6 weeks, 6 months and 12 months by intervention and control group.
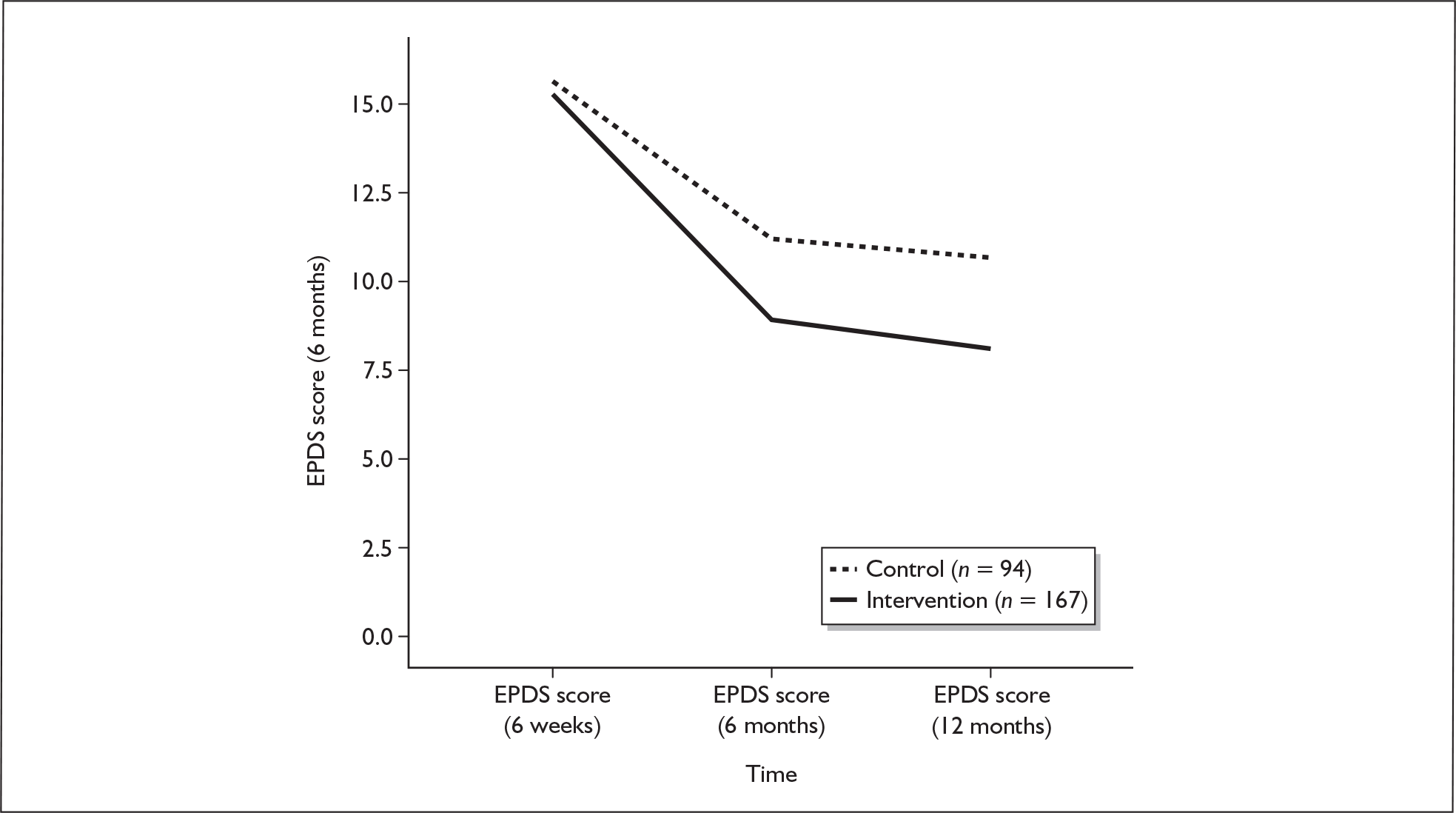
Twelve-month secondary outcomes for at-risk women: intervention versus control group
As well as a difference between the groups in mean EPDS score at 12 months there were also differences in the SF-12 MCS, the SF-6D, the CORE-OM total score, the STAI score and some of the PSI domains, all in favour of the IG (Table 25).
Twelve-month secondary outcomes for at-risk women: CBA and PCA versus control
Examining the two main IGs separately, the mean EPDS score was 8.0 (SD 5.4) for women in the CBA group and 8.3 (SD 5.9) for women in the PCA group.
Twelve-month secondary outcomes for at-risk women: CBA-F, CBA-P, PCA-F and PCA-P versus control
Examining all four IGs separately there were some differences between the 12-month mean EPDS scores for the women who returned a 12-month questionnaire, ranging from 7.4 (SD 5.0) for the CBA-P group to 9.0 (SD5.5) for the PCA-F group.
Eighteen-month secondary outcomes for at-risk women
Eighteen-month outcomes for at-risk women: intervention versus control
Of the 2113 questionnaires not sent at 18 months, 1879 (88.9%) were not sent because the women had not reached the 18-month postnatal follow-up time. The EPDS was not administered at 18 months as it is not validated for use beyond 12 months. There were some statistically significant differences between the CG and the IG at 18 months for some of the PSI subscales. These are presented in Table 26. Figures 10–13 illustrate the changes in mean scores for at-risk women from 6 weeks to 18 months for the secondary outcomes SF-12 MCS, SF-12 PCS, SF-6D and CORE-OM respectively.
| Outcome | Control | Intervention | Unadjusted | Adjusteda | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Difference | 95% CI | p | n | Difference | 95% CI | p | |
| SF-36 PCS 6W | 143 | 48.5 | 10.9 | 265 | 50.1 | 9.4 | |||||||
| SF-12 PCS 18M | 46 | 52.1 | 12.9 | 86 | 56.0 | 8.6 | 4.1 | 1.1 to 7.1 | 0.007 | 86 | 2.9 | –0.1 to 6.0 | 0.062 |
| SF–36 MCS 6W | 143 | 29.4 | 9.2 | 265 | 29.1 | 8.0 | |||||||
| SF-12 MCS 18M | 46 | 40.2 | 7.1 | 86 | 39.5 | 5.4 | –0.8 | –2.9 to 1.3 | 0.463 | 86 | –0.7 | –2.7 to 1.3 | 0.509 |
| SF-6D 6W | 142 | 0.59 | 0.08 | 268 | 0.60 | 0.1 | |||||||
| SF-6D 18M | 47 | 0.73 | 0.15 | 87 | 0.78 | 0.15 | 0.04 | –0.00 to 0.09 | 0.063 | 87 | 0.03 | –0.01 to 0.07 | 0.122 |
| CORE-OM well-being 6W | 146 | 2.1 | 0.74 | 269 | 2.0 | 0.7 | |||||||
| CORE-OM well-being 18M | 47 | 1.4 | 1.0 | 88 | 1.2 | 1.0 | –0.2 | –0.6 to 0.2 | 0.309 | 88 | –0.1 | –0.4 to 0.2 | 0.523 |
| CORE-OM risk 6W | 145 | 0.2 | 0.33 | 269 | 0.14 | 0.3 | |||||||
| CORE-OM risk 18M | 47 | 0.2 | 0.4 | 88 | 0.1 | 0.3 | –0.1 | –0.2 to 0.1 | 0.328 | 88 | –0.0 | –0.1 to.01 | 0.670 |
| CORE-OM symptoms 6W | 146 | 1.6 | 0.6 | 269 | 1.6 | 0.6 | |||||||
| CORE-OM symptoms 18M | 47 | 1.0 | 0.9 | 88 | 0.8 | 0.8 | –0.2 | –0.5 to 0.1 | 0.192 | 88 | –0.1 | –0.4 to 0.1 | 0.212 |
| CORE-OM functioning 6W | 146 | 1.6 | 0.6 | 269 | 1.5 | 0.6 | |||||||
| CORE-OM functioning 18M | 47 | 1.1 | 0.9 | 88 | 0.9 | 0.8 | –0.2 | –0.5 to 0.2 | 0.290 | 88 | –0.1 | –0.3 to 0.1 | 0.497 |
| CORE-OM total score 6W | 146 | 1.4 | 0.5 | 269 | 1.4 | 0.5 | |||||||
| CORE-OM total score 18M | 47 | 1.0 | 0.8 | 88 | 0.8 | 0.7 | –0.2 | –0.4 to 0.1 | 0.228 | 88 | –0.1 | –0.3 to 0.1 | 0.374 |
| State anxiety (STAI) 18M | 46 | 42.7 | 14.5 | 85 | 40.8 | 14.5 | –1.7 | –6.9 to 3.5 | 0.521 | 85 | –1.3 | –5.8 to 3.2 | 0.578 |
| PSI parenting distress 18M | 47 | 38.8 | 9.9 | 84 | 43.3 | 10.1 | 4.6 | 0.8 to 8.4 | 0.017 | 84 | 4.6 | 1.3 to 8.0 | 0.006 |
| PSI PCDI 18M | 46 | 53.5 | 7.6 | 87 | 55.2 | 6.3 | 1.4 | –1.0 to 3.8 | 0.243 | 87 | 1.2 | –0.9 to 3.4 | 0.263 |
| PSI difficult child 18M | 47 | 46.0 | 8.6 | 85 | 49.1 | 8.0 | 3.3 | 0.4 to 6.2 | 0.027 | 85 | 3.2 | 0.3 to 6.0 | 0.028 |
| PSI total stress 18M | 46 | 138.1 | 23.2 | 82 | 147.2 | 21.2 | 9.3 | 1.1 to 17.4 | 0.026 | 82 | 9.0 | 1.6 to 16.4 | 0.017 |
FIGURE 10.
Mean SF mental component summary (MCS) score for at-risk women from 6 weeks to 18 months, by intervention and control.
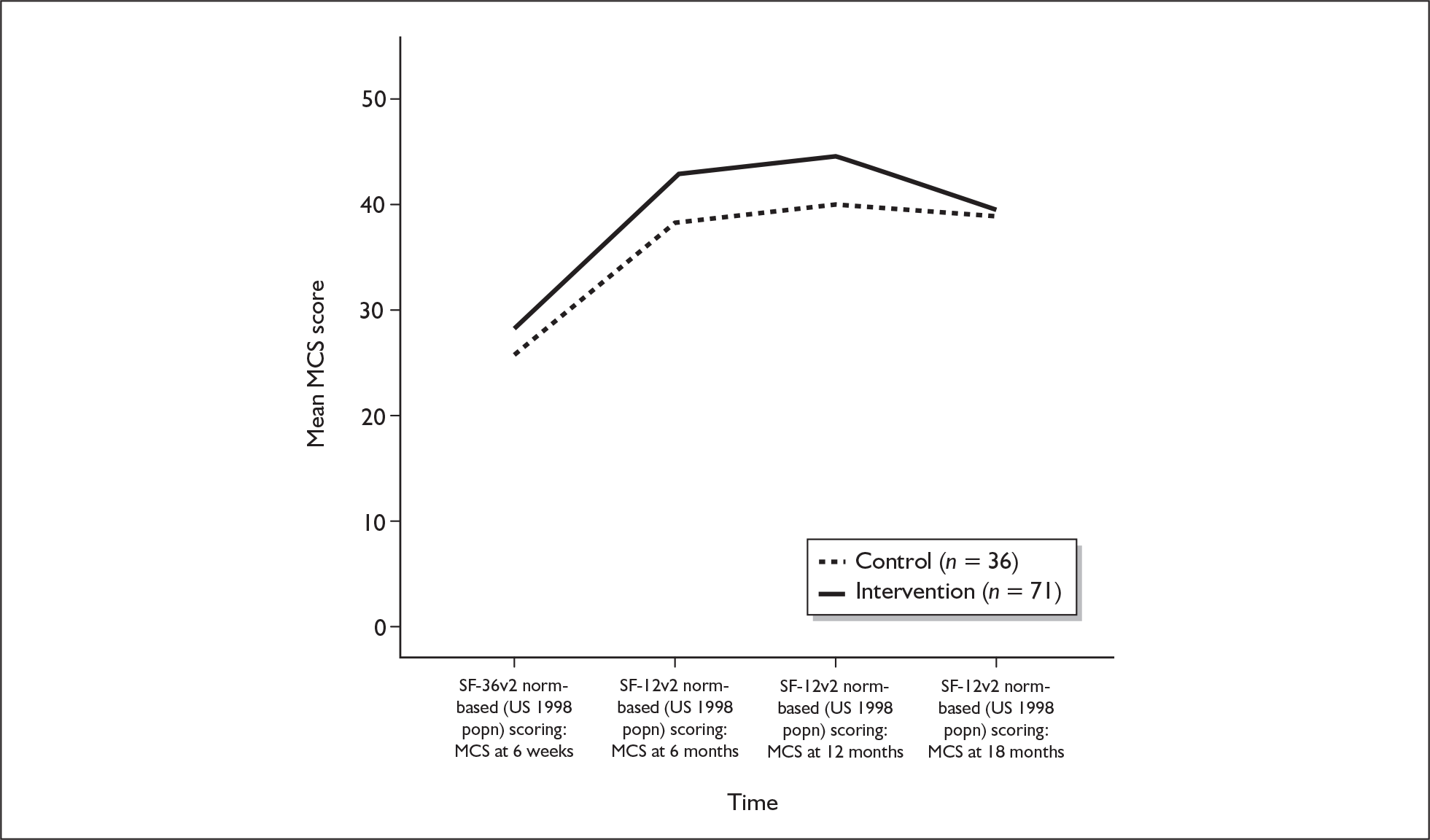
FIGURE 11.
Mean SF physical component summary (PCS) score for at-risk women from 6 weeks to 18 months, by intervention and control.
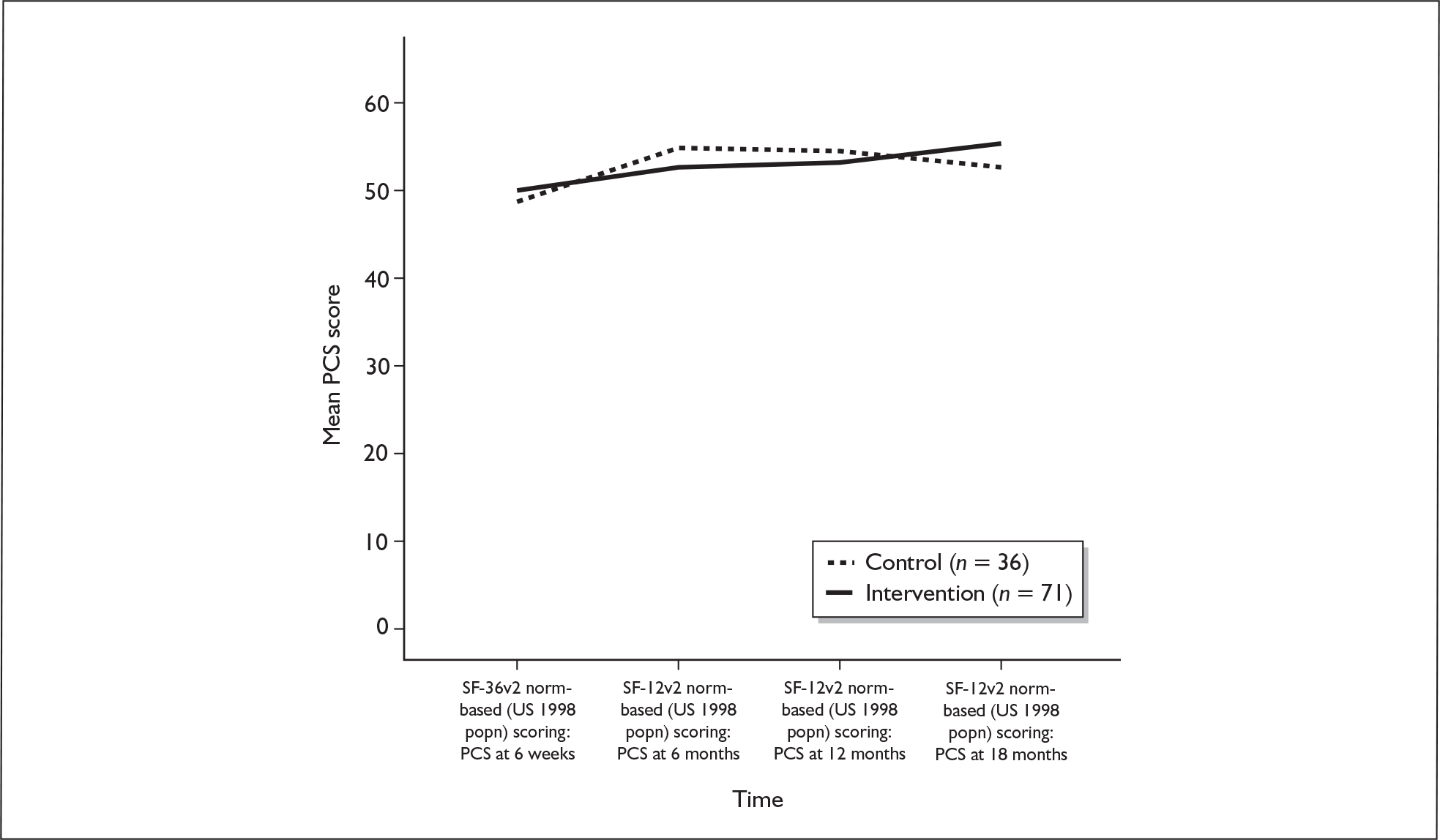
FIGURE 12.
Mean SF-6D scores for at-risk women from 6 weeks to 18 months, by intervention and control.
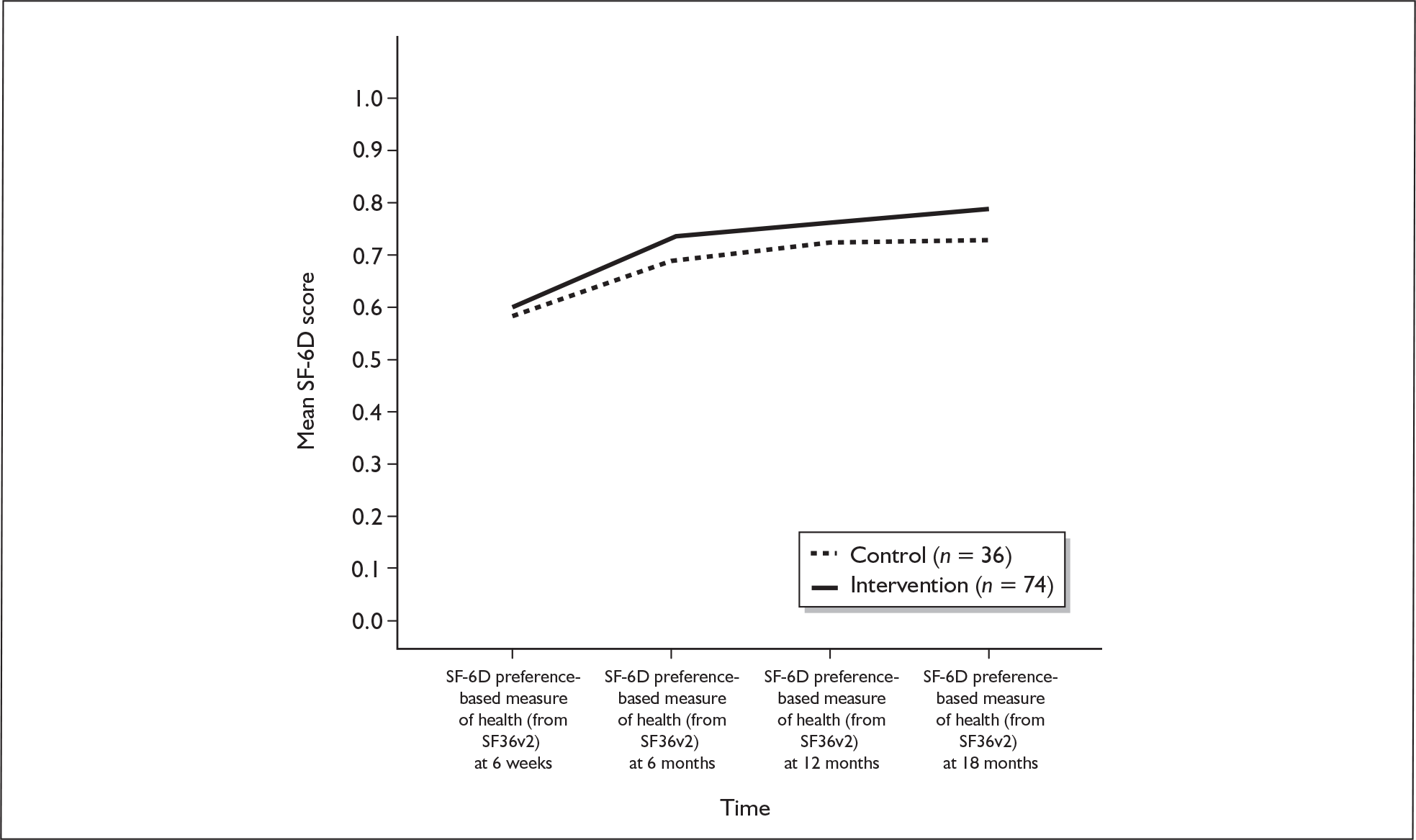
FIGURE 13.
Mean CORE-OM total score for at-risk women from 6 weeks to 18 months, by intervention and control.
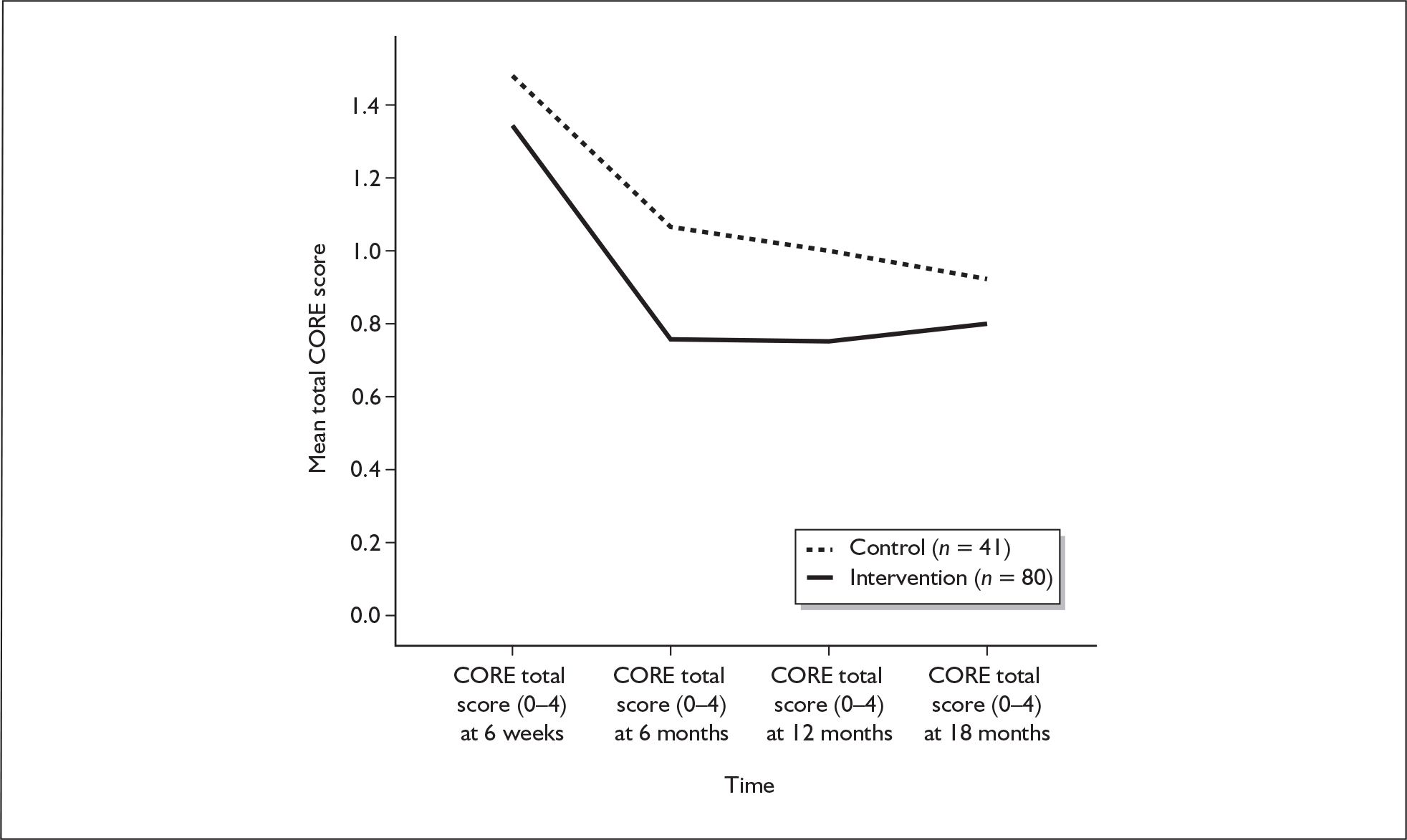
Figures 14 and 15 illustrate the changes in mean state anxiety and PSI scores for at-risk women from 6 months to 18 months.
FIGURE 14.
Mean state anxiety scores for at-risk women from 6 months to 18 months, by intervention and control.
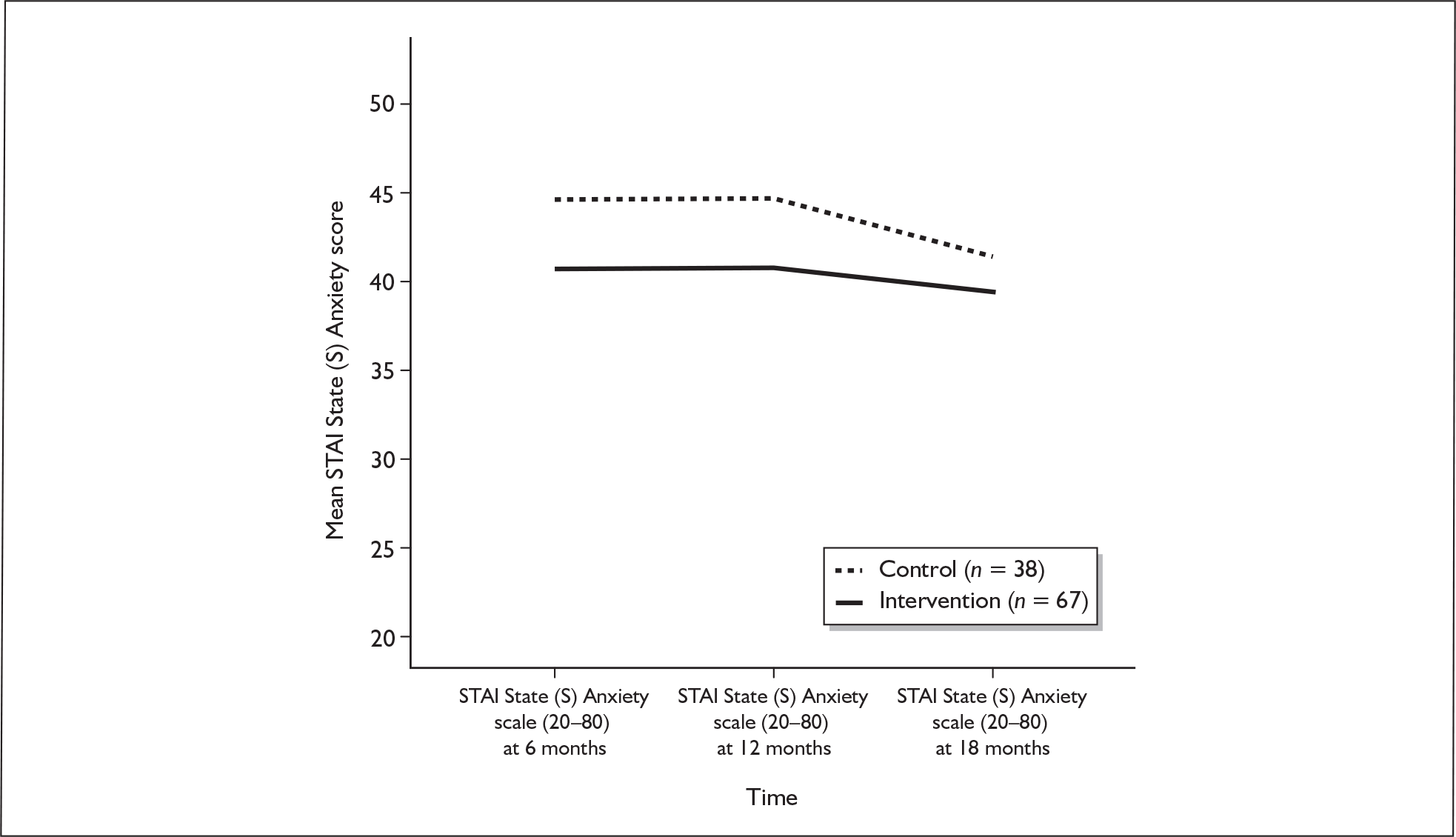
FIGURE 15.
Mean Parenting Stress Index total scores for at-risk women from 6 months to 18 months, by intervention and control.
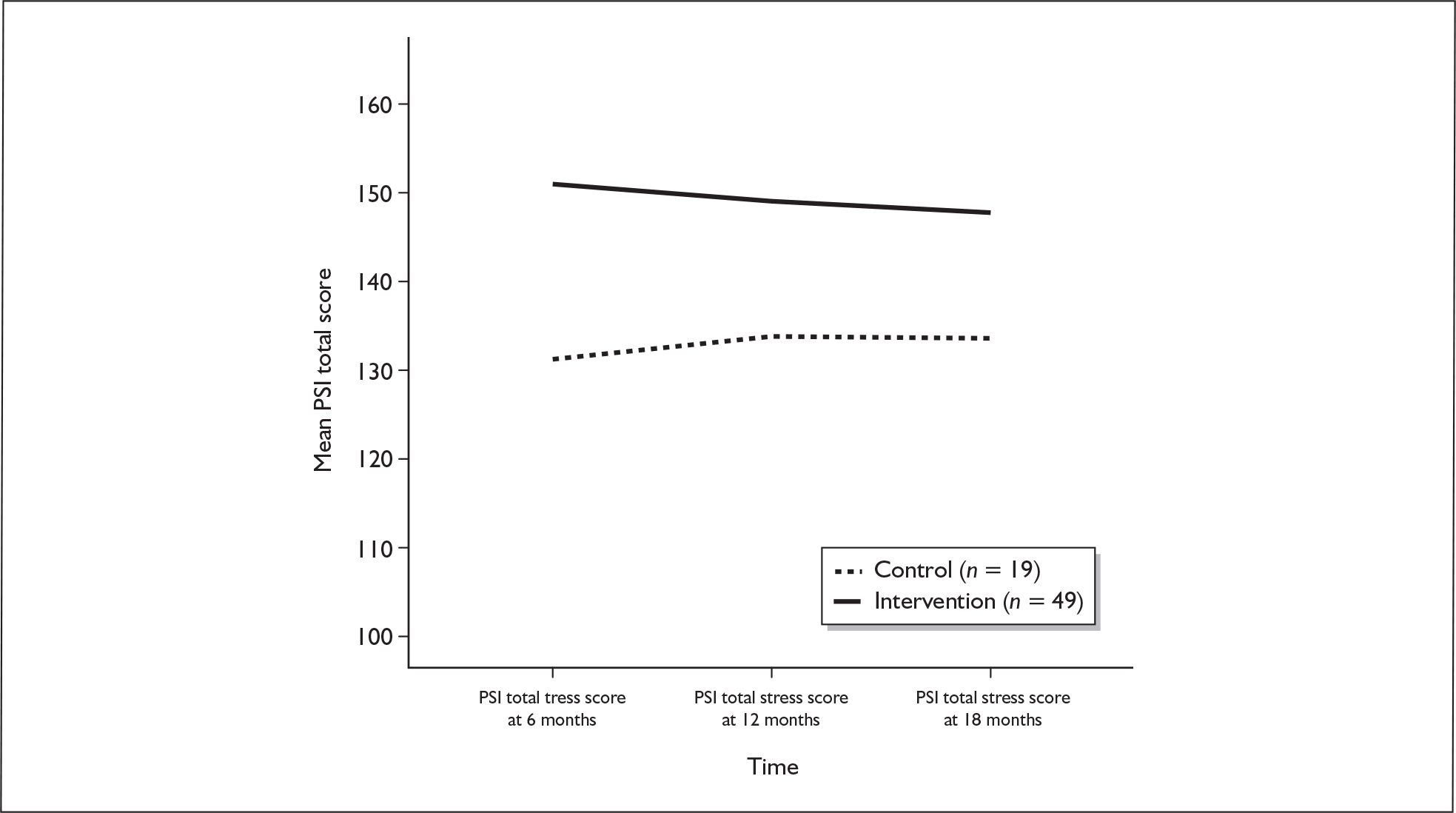
Remission and relapse to 18 months
The results from the unvalidated measure of at-risk women’s self-reported health for women who scored ≥ 18 on the 6-week EPDS are shown in Figure 16. This illustrates changes in symptoms of depression from the time of a baby’s birth to 18 months postnatally on a scale from 0 to 4, where 0 indicates no symptoms and 4 indicates severe symptoms of depression.
FIGURE 16.
Remission and relapse scores over 18 months for at-risk women, intervention vs control group.
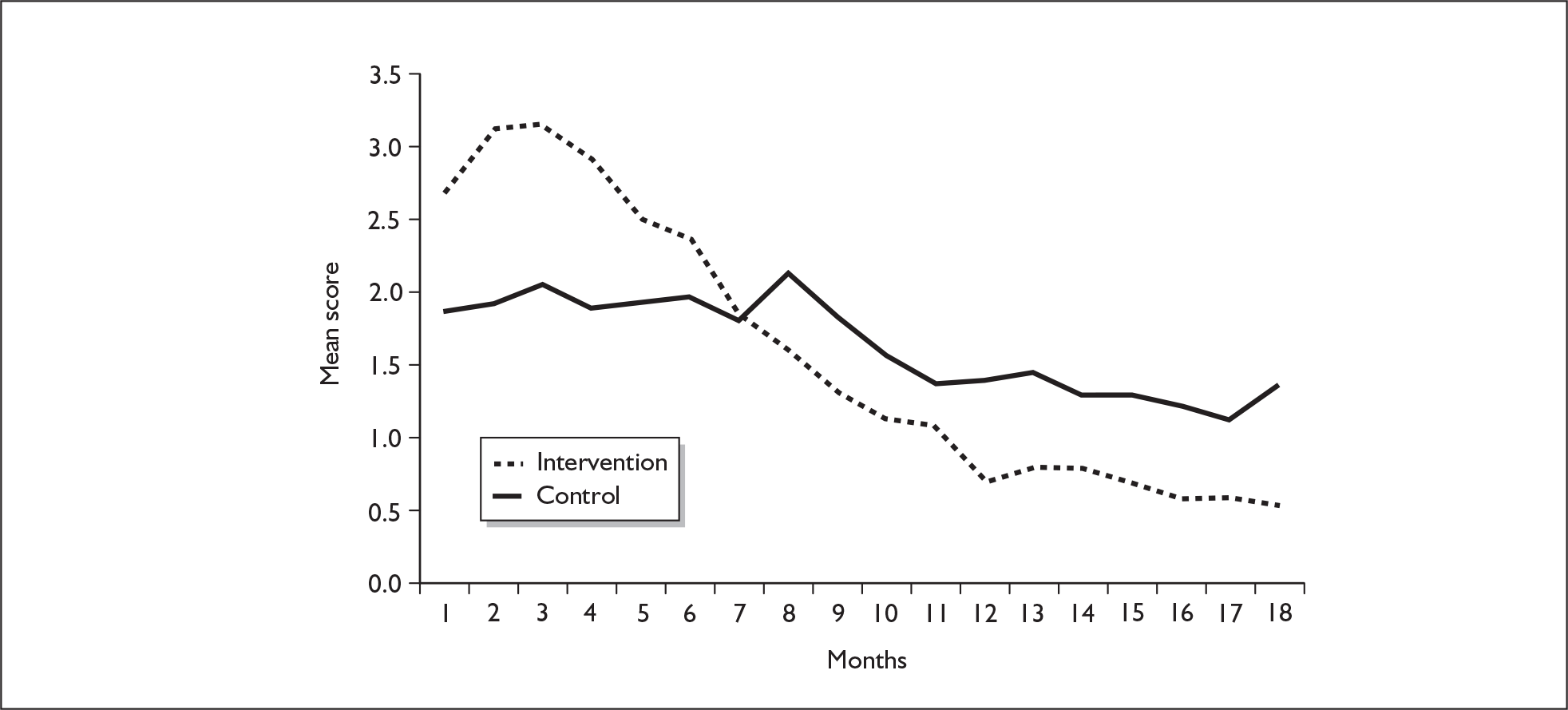
SCAN outcomes
Threshold score of 12
There were 860 SCAN interviews performed for the study, 355 with at-risk women. Of these 355 at-risk women the outcome for 18.6% (66/355) was mild depression and for 14.1% (50/355) was moderate or severe depression. That is, among all the at-risk women who had a SCAN interview, 32.7% (116/355) had an outcome of depression (Tables 27 and 28). Apart from depression, the SCAN indicated depersonalisation syndrome, generalised anxiety disorder, nightmares, non-organic insomnia or panic disorder in some women, some of these in conjunction with depression. In total, 38.3% (136/355) of at-risk women and 19.8% (170/860) of all women who were interviewed had some outcome on the SCAN (Table 29). The SCAN outcome was no depression for 219 women with a range of EPDS scores from 12 to 22. A total of 80 women with an outcome of mild depression had EPDS scores ranging from 5 to 25. Similarly, 52 women who had a SCAN outcome of moderate depression (either alone or with another outcome) had EPDS scores ranging from 7 to 27. Of the five women who had an outcome of severe depression, EPDS scores ranged from 7 to 25.
| None | Mild | Moderate | Severe | Total, n | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| EPDS < 12 | 487 | 96 | 14 | 2.8 | 3 | < 1 | 1 | < 1 | 505 |
| EPDS ≥ 12 | 239 | 67 | 66 | 19 | 46 | 13 | 4 | < 1 | 355 |
| Total | 726 | 84 | 80 | 9 | 49 | 6 | 5 | < 1 | 860 |
| Moderate or severe, n | Total, n | ||
|---|---|---|---|
| No | Yes | ||
| EPDS < 12 | 501 | 4 | 505 |
| EPDS ≥ 12 | 305 | 50 | 355 |
| Total | 806 | 54 | 860 |
| No outcome, n | Positive outcome, n | Total, n | |
|---|---|---|---|
| EPDS < 12 | 471 | 34 | 505 |
| EPDS ≥ 12 | 219 | 136 | 355 |
| Total | 690 | 170 | 860 |
Using a threshold of 12 (score ≥ 12), the sensitivity of the EPDS (the proportion of depressed women who scored ≥ 12 on the EPDS) was 0.866 (CI 0.808 to 0.923) and the specificity (the proportion of non-depressed women who scored ≤ 11 on the EPDS) was 0.671 (CI 0.637 to 0.705) (Table 30). The sensitivity for detecting moderate or severe depression using the threshold of 12 was 0.926 (CI 0.856 to 0.996), whereas the specificity was 0.622. The positive predictive value [proportion of women above the threshold of 12 on the EPDS (n = 355) who had an outcome of depression (n = 116)] was 32.7%.
| Detection of | Sensitivity | 95% CI | Specificity | 95% CI | Likelihood ratio + ve | 95% CI | Likelihood ratio –ve | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Mild, moderate or severe depression | 0.866 (116/134) | 0.808 to 0.923 | 0.671 (487/726) | 0.637 to 0.705 | 2.630 | 2.324 to 2.975 | 0.200 | 0.130 to 0.309 |
| Moderate or severe depression | 0.926 (50/54) | 0.856 to 0.996 | 0.622 (501/806) | 0.588 to 0.655 | 2.447 | 2.178 to 2.749 | 0.119 | 0.046 to 0.306 |
| Any SCAN outcome | 0.800 (136/170) | 0.740 to 0.860 | 0.682 (470/689) | 0.647 to 0.717 | 2.517 | 2.204 to 2.874 | 0.293 | 0.216 to 0.398 |
Threshold score of 13
Using a threshold of 13 (score ≥ 13) (Tables 31–34) the sensitivity of the EPDS was 0.791 and the specificity was 0.755 (Table 33). The sensitivity for detecting moderate or severe depression using the threshold of 13 was 0.852, whereas the specificity was 0.705 and the positive predictive value was 37.3% (106/284).
| None, n | Mild, n | Moderate, n | Severe, n | Total, n | |
|---|---|---|---|---|---|
| EPDS < 13 | 548 | 20 | 7 | 1 | 576 |
| EPDS ≥ 13 | 178 | 60 | 42 | 4 | 284 |
| Total | 726 | 80 | 49 | 5 | 860 |
| Moderate or severe, n | Total, n | ||
|---|---|---|---|
| No | Yes | ||
| EPDS < 13 | 568 | 8 | 576 |
| EPDS ≥ 13 | 238 | 46 | 284 |
| Total | 806 | 54 | 860 |
| No outcome, n | Positive outcome, n | Total, n | |
|---|---|---|---|
| EPDS < 13 | 548 | 28 | 576 |
| EPDS ≥ 13 | 178 | 106 | 284 |
| Total | 726 | 134 | 106 |
| Detection of | Sensitivity | 95% CI | Specificity | 95% CI | Likelihood ratio + ve | 95% CI | Likelihood ratio –ve | 95% CI |
|---|---|---|---|---|---|---|---|---|
| Mild, moderate or severe depression | 0.791 (106/134) | 0.722 to 0.860 | 0.755 (548/726) | 0.724 to 0.786 | 3.226 | 2.765 to 3.765 | 0.277 | 0.199 to 0.386 |
| Moderate or severe depression | 0.852 (46/54) | 0.757 to 0.947 | 0.705 (568/806) | 0.673 to 0.736 | 2.885 | 2.473 to 3.365 | 0.210 | 0.111 to 0.399 |
| Any SCAN outcome | 0.718 (122/170) | 0.650 to 0.785 | 0.765 (527/689) | 0.733 to 0.797 | 3.052 | 2.589 to 3.598 | 0.369 | 0.289 to 0.474 |
Intervention monitoring
At-risk women who returned a 6-month questionnaire
A total of 404 women who scored ≥ 12 on the 6-week postal EPDS were at-risk women, of whom 274 (67.8%) returned a 6-month questionnaire.
Health visitor administration of 8-week EPDS to at-risk women
The HV protocol stated that HVs should repeat the administration of the EPDS face-to-face at 8 weeks postnatally for all at-risk women to determine which women were eligible for the intervention. Of all of the 404 at-risk women, 70.8% (286/404) had an 8-week EPDS score and for 29.2% (118/404) the score was missing. Of those who had an 8-week EPDS score, for 60.5% of women (173/286) the score was < 12 and for 39.5% (173/286) the score was ≥ 12 (Table 35). Of the missing scores, 48% (57/118) were missing because the HV-administered face-to-face 6-week EPDS score was < 12. A further 27% (32/118) were missing for reasons to do with the women being absent or declining, and 20% (24/118) were absent for reasons to do with the HV being unavailable.
| All at-risk women (n = 404) | ||
|---|---|---|
| n | % | |
| 8-week EPDS: score < 12 | 173/296 | 60.5 |
| 8-week EPDS: score ≥ 12 | 113/286 | 39.5 |
| 8-week EPDS: score missing | 118/404 | 29.2 |
| HV offered sessions | 197/395 | 49.9 |
| Woman accepted sessions | 121/395 | 30.6 |
| Woman declined sessions | 76/197 | 38.6 |
| Prescribed antidepressants | 84/380 | 22.1 |
| Woman saw someone else | 148/374 | 39.6 |
Health visitor psychological intervention sessions offered to at-risk women
For the 395 at-risk women for whom data were available, 50% (197/395) were offered a psychological intervention session and therefore 50% (198/395) were not offered a session. In total, 31% of all at-risk women (121/395) received at least one psychological intervention session and, of those offered, 39% (76/197) declined (Table 35). There were 259 intervention sessions delivered in the CBA group and 242 intervention sessions delivered in the PCA group.
Figure 17 illustrates that, of the at-risk women who returned a 6-month EPDS, 46% (125/274) were offered intervention sessions and 29% (80/274) accepted the intervention sessions. Among the 32% (130/404) of women who did not return a 6-month EPDS score and therefore were no longer included in the trial, 55% (72/130) were offered sessions and 32% (41/130) received sessions. Figure 17 also illustrates that HVs offered sessions to women who had no 8-week EPDS score and who had an 8-week EPDS score < 12. Among all of the at-risk women, of whom according to the SCAN interviews most were not depressed, 197/404 (48.88) were offered sessions and 61% (121/197) accepted.
FIGURE 17.
Flow chart of at-risk women: 8-week EPDS assessment and intervention sessions offered.
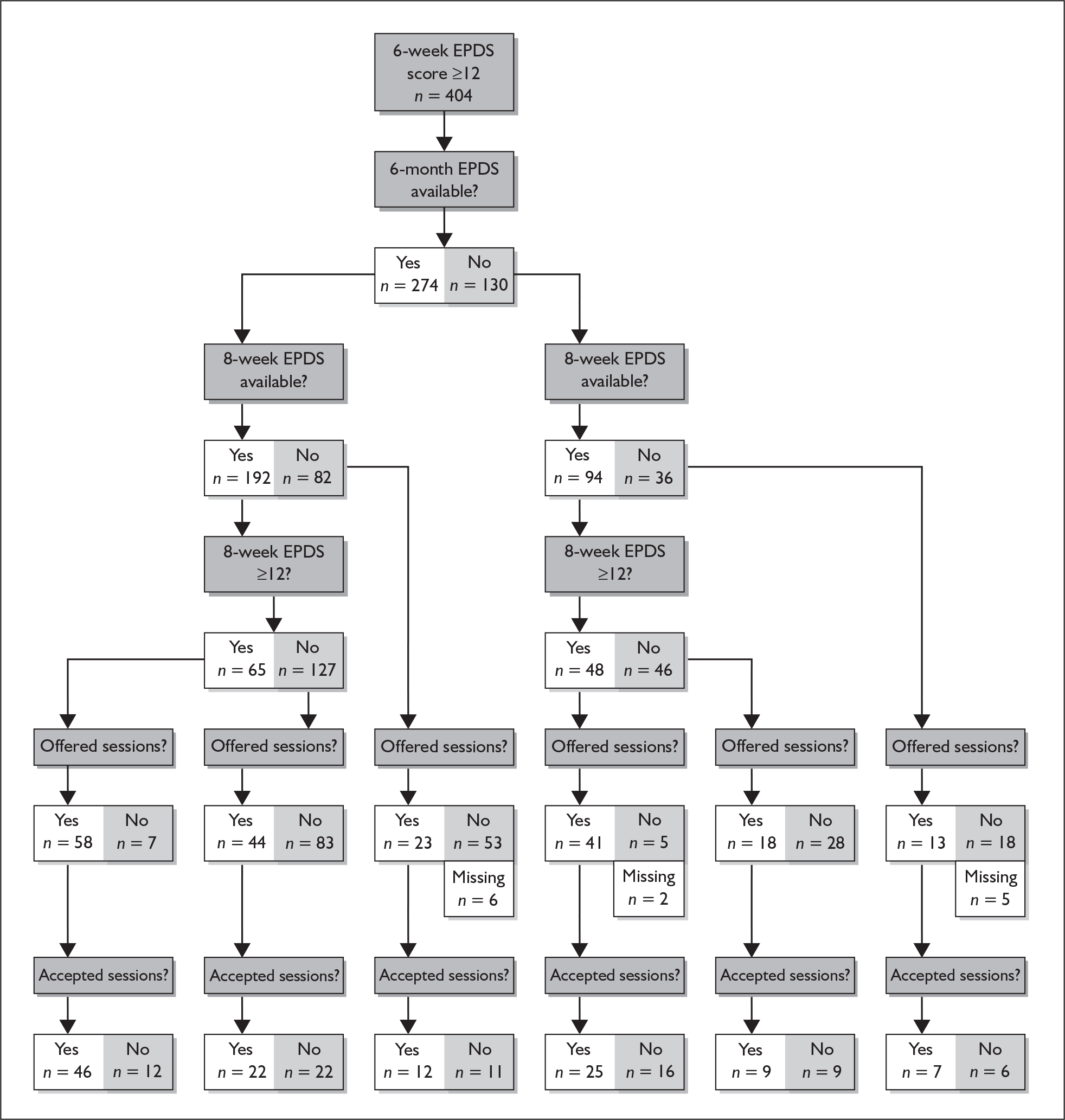
At-risk women receiving other support
About 22% (84/380) of the women had also been prescribed antidepressants, but not all of the women took these. Around 40% (148/374) were also receiving support apart from the HV. Most frequently (19.5%) the women received support from a GP (73/374); 8% of women were also in receipt of other mental health services and 6% attended a postnatal support group. Of possibly the greatest concern were the seven women who had an 8-week EPDS score ≥ 12 but who were not offered the psychological intervention sessions by the HV. Table 36 indicates that these seven women were supported by a GP, counsellor or mental health worker or were not classified as depressed.
| SCAN outcome | Health visitor description of support |
|---|---|
| Mild, n = 1 | Long-standing migraine problems causing low mood. Closely supported by GP. On low dose of amitriptyline |
| Moderate, n = 1 | Support from GP and counselling from surgery. Been taking antidepressants throughout pregnancy and postnatally, therefore not offered intervention sessions |
| No depression, n = 3 | 1. Attends clinic most weeks. Anxious. Own mother supportive |
| 2. GP prescribed fluoxetine | |
| 3. On fluoxetine at 1 month postnatally | |
| Other, n = 1 | Generalised anxiety disorder – seeing mental health worker, prescribed antidepressants |
| Missed, n = 1 | Health visitor said mother was coping well with children and commenced a 4-week baby massage course |
Preference for psychological intervention or antidepressants
There was no evidence that women preferred an antidepressant to the HV psychological intervention.
Six-month EPDS outcome for all women
Six-month EPDS outcome for all women: intervention versus control
At 6 months, among all of the women who had returned both a 6-week and a 6-month questionnaire, 16.4% in the CG scored ≥ 12 on the EPDS versus 11.7% in the IG. The absolute difference was 4.7% (95% CI 0.7 to 8.6). This effect was statistically significant (p = 0.003). After adjusting for covariates – 6-week EPDS score, living alone, previous history of PND and any life events – the point estimate of the odds ratio for the IG effect was relatively unchanged (at around 0.67) and this effect remained statistically significant (Table 37).
Figure 18 illustrates the change in EPDS score over time in the control and intervention groups for at-risk women and all women.
| 6-month EPDS score | Int group | Control group | All | Absolute difference (%) | 95% CI | Odds ratio, int to control | 95% CI | p-value |
|---|---|---|---|---|---|---|---|---|
| < 12, n (%) | 1540 (88.3) | 764 (83.6) | 2304 (86.6) | |||||
| ≥ 12, n (%) | 205 (11.7) | 150 (16.4) | 355 (13.4) | 4.7 | 0.7 to 8.6 | 0.67 | 0.51 to 0.87 | 0.003 |
| 0.68a | 0.52 to 0.88a | 0.004a | ||||||
| 0.67b | 0.52 to 0.86b | 0.002b | ||||||
| Total, n | 1745 | 914 | 2659 |
FIGURE 18.
Mean EPDS scores for at-risk women and all women from 6 weeks to 12 months by intervention and control group.
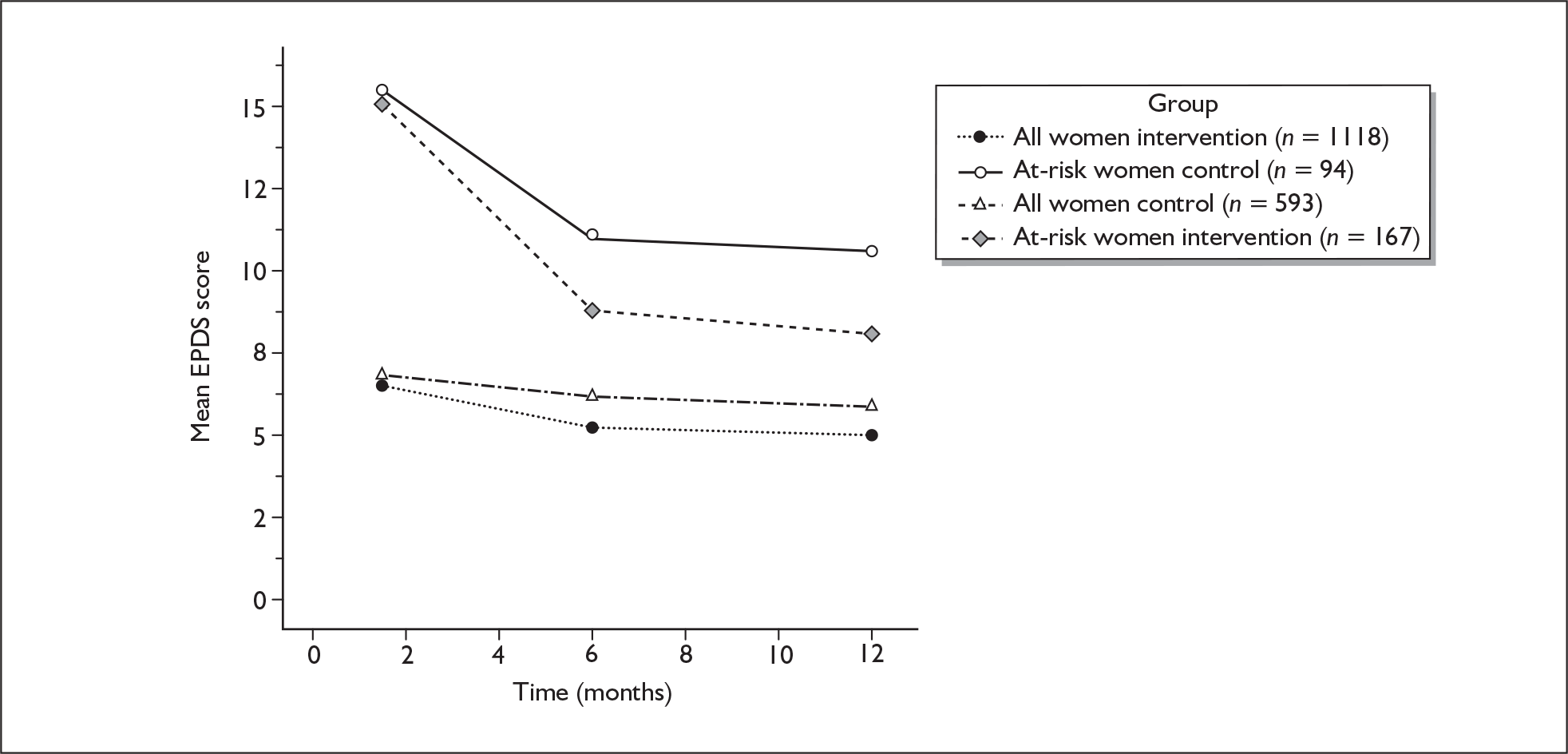
Intracluster correlation coefficient for all women
As recommended by the cluster CONSORT guidelines,197 Table 38 reports the observed ICC for the 6-month EPDS outcome.
| n | No. of clusters | Average cluster size | Min. to max. cluster size | ICC | 95% CI lower | 95% CI upper | |
|---|---|---|---|---|---|---|---|
| At-risk women | 418 | 86 | 4.9 | 1–15 | 0.037 | 0.000 | 0.114 |
| All women | 2659 | 100 | 26.6 | 1–101 | 0.009 | 0.000 | 0.022 |
Six-month EPDS outcomes: all women in the CBA and PCA groups versus the control group
Examining the two IGs separately for all women, 11.6% (98/848) of those in the CBA group and 11.9% (107/897) of those in the PCA group scored ≥ 12 on the 6-month EPDS (p = 0.80) (Table 39).
| 6-month EPDS score | CBA group | PCA group | Control group | OR, CBA to control | 95% CI | p-value | OR, PCA to control | 95% CI | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Score < 12, n (%) | 750 (88.4) | 790 (88.1) | 764 (83.6) | ||||||
| Score ≥ 12, n (%) | 98 (11.6) | 107 (11.9) | 150 (16.4) | 0.66 | 0.48 to 0.91 | 0.012 | 0.67 | 0.51 to 0.90 | 0.007 |
| 0.65a | 0.47 to 0.90a | 0.009a | 0.71a | 0.54 to 0.94a | 0.017a | ||||
| 0.64b | 0.46 to 0.89b | 0.0007b | 0.70b | 0.53 to 0.91b | 0.008b | ||||
| Total | 848 | 897 | 914 |
Six-month secondary outcomes for all women
Six-month secondary outcomes for all women: intervention versus control
The mean EPDS score was 6.4 (SD 5.2) in the CG and 5.5 (SD 4.7) in the IG (Table 40). This small difference was statistically significant (p = 0.001). As with the secondary outcomes for the at-risk women, most of the mean scores for all women were statistically significant in favour of the IG.
| 6-month outcome | Control | Intervention | Unadjusted | Adjusteda | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Difference | 95% CI | p-value | Difference | 95% CI | p-value | |
| EPDS | 914 | 6.4 | 5.2 | 1745 | 5.5 | 4.7 | –1.0 | –1.5 to –0.4 | 0.001 | –0.8 | –1.2 to –0.4 | 0.000 |
| SF-12 PCS | 885 | 54.5 | 6.8 | 1694 | 54.7 | 6.1 | 0.2 | –0.3 to 0.7 | 0.469 | 0.0 | –0.4 to 0.5 | 0.871 |
| SF-12 MCS | 885 | 47.6 | 10.5 | 1694 | 48.9 | 9.5 | 1.5 | 0.3 to 2.6 | 0.010 | 1.4 | 0.5 to 2.3 | 0.003 |
| SF-6D | 903 | 0.8 | 0.14 | 1712 | 0.8 | 0.13 | 0.0 | 0.0 to 0.0 | 0.001 | 0.0 | 0.0 to 0.0 | 0.000 |
| CORE-OM well-being | 907 | 0.8 | 0.82 | 1735 | 0.7 | 0.73 | –0.1 | –0.2 to –0.0 | 0.030 | –0.1 | –0.1 to –0.0 | 0.015 |
| CORE-OM risk | 906 | 0.1 | 0.20 | 1736 | 0.0 | 0.15 | –0.0 | –0.0 to 0.0 | 0.071 | –0.0 | –0.0 to 0.0 | 0.143 |
| CORE-OM symptoms | 907 | 0.6 | 0.61 | 1734 | 0.5 | 0.54 | –0.1 | –0.2 to –0.0 | 0.000 | –0.1 | –0.1 to –0.0 | 0.000 |
| CORE-OM functioning | 905 | 0.6 | 0.7 | 1735 | 0.5 | 0.6 | –0.0 | –0.2 to –0.0 | 0.002 | –0.1 | –0.1 to –0.0 | 0.001 |
| CORE-OM total score | 906 | 0.5 | 0.5 | 1736 | 0.5 | 0.5 | –0.1 | –0.1 to –0.0 | 0.001 | –0.1 | –0.1 to –0.0 | 0.000 |
| State anxiety (STAI) | 858 | 34.3 | 11.7 | 1634 | 33.2 | 10.9 | –1.3 | –2.7 to –0.1 | 0.042 | –1.3 | –2.5 to –0.1 | 0.033 |
| Trait anxiety (STAI) | 839 | 34.1 | 10.3 | 1635 | 33.1 | 9.6 | –1.1 | –2.3 to 0.0 | 0.059 | –1.1 | –2.1 to –0.1 | 0.032 |
| PSI parenting distress | 766 | 46.3 | 9.0 | 1422 | 47.4 | 8.6 | 1.1 | 0.2 to 2.0 | 0.014 | 1.2 | 0.4 to 2.0 | 0.003 |
| PSI PCDI | 776 | 56.9 | 4.8 | 1435 | 57.1 | 4.5 | 0.3 | –0.1 to 0.6 | 0.199 | 0.3 | –0.1 to 0.6 | 0.178 |
| PSI difficult child | 740 | 52.8 | 6.0 | 1365 | 53.3 | 5.6 | 0.5 | –0.1 to 1.1 | 0.078 | 0.5 | –0.0 to 1.1 | 0.054 |
| PSI total stress | 698 | 155.9 | 16.9 | 1310 | 157.9 | 15.3 | 2.1 | 0.3 to 3.9 | 0.021 | 2.3 | 0.6 to 3.9 | 0.007 |
Six-month secondary outcomes for all women: CBA and PCA versus control
The mean 6-month EPDS score was 5.5 (SD 4.7) for all women in both the CBA group and the PCA group (p = 0.94). There were no differences in the other secondary outcomes between the CBA group and the PCA group.
Six-month secondary outcomes for all women: CBA-F, CBA-P, PCA-F and PCA-P versus control
There were some differences between the unadjusted mean EPDS scores in the four IGs, which ranged from 4.9 in the CBA-F group to 6.0 in the CBA-P group (Table 41).
| 6-month outcome | Control | CBA-F | CBA-P | PCA-F | PCA-P | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | Difference (95% CI) | p-value | n | Mean (SD) | Difference (95% CI) | p-value | n | Mean (SD) | Difference (95% CI) | p-value | n | Mean (SD) | Difference (95% CI) | p-value | |
| EPDS | 914 | 6.4 (5.2) | 431 | 4.9 (4.6) | –1.9 (–3.6 to –0.3) | 0.024 | 417 | 6.0 (4.8) | –2.2 (–4.0 to –0.5) | 0.014 | 432 | 5.3 (4.8) | –1.8 (–3.1 to –0.5) | 0.007 | 465 | 5.7 (4.7) | –2.8 (–4.0 to –0.7) | 0.005 |
| SF-12 PCS | 885 | 54.5 (6.8) | 414 | 54.8 (5.6) | 0.31 (–0.4 to 1.0) | 0.396 | 401 | 54.2 (6.6) | –0.3 (–1.0 to 0.4) | 0.453 | 426 | 55.0 (6.0) | 0.5 (–0.3 to 1.3) | 0.193 | 453 | 54.6 (6.4) | 0.1 (–0.7 to 0.9) | 0.760 |
| SF-12 MCS | 885 | 47.6 (10.5) | 414 | 49.8 (9.2) | 2.2 (0.7 to 3.7) | 0.005 | 401 | 48.1 (9.8) | 0.6 (–0.7 to 1.9) | 0.366 | 426 | 49.3 (9.6) | 1.9 (0.2 to 3.5) | 0.025 | 453 | 48.6 (9.3) | 1.3 (–0.00 to 2.5) | 0.052 |
| SF-6D | 903 | 0.81 (0.14) | 419 | 0.84 (0.13) | 0.03 (0.12 to 0.51) | 0.001 | 408 | 0.81 (0.14) | 0.08 (–0.09 to 0.26) | 0.357 | 428 | 0.84 (0.13) | 0.03 (0.02 to 0.05) | 0.000 | 457 | 0.83 (0.13) | 0.22 (0.06 to 0.40) | 0.008 |
| CORE-OM well-being | 907 | 0.8 (0.8) | 429 | 0.6 (0.7) | –0.2 (–0.3 to –0.4) | 0.008 | 413 | 0.8 (0.8) | –0.0 (–0.1 to –0.1) | 0.597 | 428 | 0.7 (0.8) | –0.1 (–0.3 to –0.0) | 0.056 | 465 | 0.7 (0.7) | –0.1 (–0.2 to –0.0) | 0.056 |
| CORE-OM risk | 906 | 0.1 (0.2) | 429 | 0.0 (0.1) | –0.0 (–0.0 to 0.0) | 0.113 | 414 | 0.0 (0.1) | –0.0 (–0.0 to 0.0) | 0.417 | 428 | 0.7 (0.8) | –0.0 (–0.0 to 0.0) | 0.058 | 465 | 0.0 (0.2) | –0.0 (–0.0 to 0.0) | 0.086 |
| CORE-OM symptoms 6M | 907 | 0.6 (0.6) | 428 | 0.4 (0.5) | –0.1 (–0.2 to –0.1) | 0.000 | 413 | 0.5 (0.6) | –0.1 (–0.1 to –0.0) | 0.075 | 428 | 0.5 (0.5) | –0.1 (–0.2 to –0.1) | 0.000 | 465 | 0.5 (0.5) | –0.1 (–0.2 to –0.0) | 0.007 |
| CORE-OM functioning | 905 | 0.6 (0.7) | 429 | 0.5 (0.6) | –0.1 (–0.2 to –0.1) | 0.000 | 413 | 0.6 (0.6) | –0.1 (–0.1 to –0.0) | 0.095 | 428 | 0.5 (0.6) | –0.1 (–0.2 to –0.0) | 0.007 | 465 | 0.6 (0.6) | –0.1 (–0.2 to –0.0) | 0.016 |
| CORE-OM total score | 906 | 0.5 (0.5) | 429 | 0.4 (0.4) | –0.1 (–0.2 to –0.1) | 0.000 | 414 | 0.5 (0.5) | –0.1 (–0.1 to –0.0) | 0.119 | 431 | 0.5 (0.5) | –0.1 (–0.2 to –0.0) | 0.003 | 465 | 0.5 (0.5) | –0.1 (–0.2 to –0.0) | 0.010 |
| State anxiety (STAI) | 858 | 34.3 (11.7) | 407 | 31.9 (10.8) | –2.5 (–4.0 to –0.9) | 0.002 | 388 | 34.1 (11.0) | –0.4 (–1.8 to 1.0) | 0.596 | 399 | 32.9 (10.9) | –1.7 (–3.2 to –0.1) | 0.034 | 440 | 33.7 (10.7) | –0.9 (–2.3 to 0.6) | 0.242 |
| Trait anxiety (STAI) | 839 | 34.1 (10.3) | 396 | 32.1 (9.5) | –2.0 (–3.4 to –0.7) | 0.003 | 383 | 34.0 (9.6) | –0.2 (–1.5 to 1.0) | 0.702 | 410 | 32.8 (9.7) | –1.4 (–2.8 to –0.0) | 0.047 | 446 | 33.5 (9.6) | –0.7 (–2.1 to 0.6) | 0.288 |
| PSI parenting distress | 766 | 46.3 (9.0) | 342 | 48.0 (8.8) | 1.7 (0.7 to 2.7) | 0.001 | 319 | 46.6 (8.4) | 0.3 (–0.8 to 1.3) | 0.628 | 369 | 47.9 (8.4) | 1.6 (0.5 to 2.7) | 0.003 | 392 | 47.2 (8.6) | 0.8 (–0.2 to 1.9) | 0.125 |
| PSI PCDI | 776 | 56.9 (4.8) | 342 | 56.9 (4.6) | 0.0 (–0.4 to 0.4) | 0.970 | 322 | 56.8 (4.9) | –0.1 (–0.7 to 0.5) | 0.809 | 374 | (57.7) 3.8 | 0.9 (0.4 to 1.3) | 0.000 | 397 | 56.9 (4.8) | 0.0 (–0.5 to 0.6) | 0.862 |
| PSI difficult child | 740 | 52.8 (6.0) | 324 | 53.3 (5.9) | 0.5 (–0.4 to 1.5) | 0.237 | 302 | 53.2 (5.6) | 0.4 (–0.4 to 1.1) | 0.323 | 366 | (53.9) 4.9 | 1.1 (0.5 to 1.6) | 0.000 | 373 | 52.9 (5.9) | 0.1 (–0.8 to 0.9) | 0.846 |
| PSI total stress | 698 | 155.9 (16.9) | 313 | 158.5 (16.3) | 2.7 (0.6 to 4.7) | 0.011 | 288 | 156.7 (15.3) | 0.9 (–1.2 to 2.9) | 0.404 | 348 | (159.5) 13.6 | 3.6 (1.7 to 5.6) | 0.000 | 361 | 156.9 (15.8) | 1.1 (–1.2 to 3.4) | 0.368 |
Twelve-month secondary outcomes for all women
Of the 741 questionnaires not sent at 12 months, 597 (81%) were not sent because the women had not reached the 12-month postnatal follow-up time. Twelve-month outcomes were therefore available for 593 CG and 1118 IG women.
Twelve-month secondary outcomes for all women: intervention versus control
The mean EPDS score was 5.9 (SD 5.2) in the CG and 5.0 (SD 4.6) in the IG. This difference (–0.9) was statistically significant (p = 0.003). Most of the differences in mean CORE-OM and STAI scores were statistically significant, in favour of the IG (Table 42).
| 12-month outcome | Control | Intervention | Unadjusted | Adjusteda | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Difference | 95% CI | p-value | Difference | 95% CI | p-value | |
| EPDS | 593 | 5.9 | 5.2 | 1118 | 5.0 | 4.6 | –0.9 | –1.5 to –0.3 | 0.002 | –0.7 | –1.1 to –0.2 | 0.003 |
| SF-12 PCS | 579 | 55.0 | 6.4 | 1099 | 55.0 | 6.0 | 0.1 | –0.6 to 0.8 | 0.834 | –0.2 | –0.8 to 0.5 | 0.590 |
| SF-12 MCS | 579 | 48.7 | 9.8 | 1099 | 49.9 | 9.2 | 1.1 | 0.2 to 2.0 | 0.013 | 0.9 | 0.1 to 1.6 | 0.022 |
| SF-6D | 587 | 0.8 | 0.1 | 1110 | 0.8 | 0.1 | 0.0 | –0.0 to 0.0 | 0.087 | 0.0 | –0.0 to 0.0 | 0.521 |
| CORE-OM well-being | 593 | 0.7 | 0.8 | 1120 | 0.6 | 0.7 | –0.1 | –0.2 to –0.0 | 0.017 | –0.1 | –0.2 to –0.0 | 0.009 |
| CORE-OM risk | 593 | 0.1 | 0.2 | 1120 | 0.0 | 0.1 | –0.0 | –0.0 to 0.0 | 0.319 | –0.0 | –0.0 to 0.0 | 0.490 |
| CORE-OM symptoms | 593 | 0.6 | 0.6 | 1118 | 0.5 | 0.5 | –0.1 | –0.2 to –0.1 | 0.000 | –0.1 | –0.1 to –0.0 | 0.000 |
| CORE-OM functioning | 592 | 0.6 | 0.6 | 1119 | 0.5 | 0.6 | –0.1 | –0.2 to –0.0 | 0.001 | –0.1 | –0.1 to –0.0 | 0.001 |
| CORE-OM total score | 593 | 0.5 | 0.5 | 1120 | 0.4 | 0.5 | –0.1 | –0.2 to –0.0 | 0.001 | –0.1 | –0.1 to –0.2 | 0.001 |
| State anxiety (STAI) | 580 | 33.7 | 11.7 | 1097 | 32.4 | 10.7 | –1.5 | –2.7 to –0.2 | 0.019 | –1.4 | –2.5 to –0.2 | 0.020 |
| Trait anxiety (STAI) | 576 | 33.7 | 10.1 | 1091 | 35.4 | 9.5 | –1.4 | –2.5 to –0.3 | 0.014 | –1.4 | –2.4 to –0.3 | 0.009 |
| DAS Likert | 571 | 4.0 | 1.2 | 1077 | 4.1 | 1.2 | 0.01 | –0.0 to 0.2 | 0.098 | –0.0 | –0.1 to 0.1 | 0.670 |
| DAS | 561 | 18.2 | 3.3 | 1058 | 18.1 | 3.1 | –0.1 | –0.4 to 0.2 | 0.527 | –0.1 | –0.4 to 0.2 | 0.574 |
| PSI parenting distress | 581 | 46.5 | 8.8 | 1087 | 47.8 | 8.2 | 1.2 | 0.3 to 2.0 | 0.009 | –1.7 | –5.4 to 2.1 | 0.377 |
| PSI PCDI | 588 | 57.2 | 4.7 | 1102 | 57.1 | 4.8 | –0.1 | –0.5 to 0.4 | 0.741 | –0.1 | –0.5 to 0.4 | 0.741 |
| PSI difficult child | 572 | 51.8 | 6.5 | 1076 | 52.1 | 6.0 | 0.3 | –0.3 to 0.9 | 0.328 | 0.3 | –0.3 to 0.9 | 0.293 |
| PSI total stress | 558 | 155.6 | 17.1 | 1055 | 157.0 | 15.6 | 11.3 | –0.4 to 3.0 | 0.137 | 1.1 | –0.3 to 2.7 | 0.123 |
Twelve-month secondary outcomes for all women: CBA and PCA versus control
The mean EPDS score was 5.1 (SD 4.8) in the CBA group and 4.9 (SD 4.5) in the PCA group. There were no differences in the other secondary outcomes between the CBA group and the PCA group.
Twelve-month secondary outcomes for all women: CBA-F, CBA-P, PCA-F and PCA-P versus control
There were some differences between the unadjusted mean EPDS scores, which ranged from 4.9 (SD 4.4) in the CBA-F group to 5.3 (SD 4.8) in the CBA-P group.
Eighteen-month secondary outcomes for all women
Eighteen-month secondary outcomes for all women: intervention versus control
Of the 2113 questionnaires not sent at 18 months, 1879 (89%) were not sent because the women had not reached the 18-month postnatal follow-up time. Eighteen-month outcomes were therefore available for 318 CG and 706 IG women.
At the 18-month follow-up for all women who returned a questionnaire there were some statistically significant differences between the IG and CG on the SF-12 PCS, the SF-6D, some of the CORE-OM subscales and all domains on the PSI (Table 43).
| 18-month outcome | Control | Intervention | Unadjusted | Adjusteda | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | Difference | 95% CI | p-value | Difference | 95% CI | p-value | |
| SF-12 PCS | 286 | 57.2 | 10.1 | 634 | 59.1 | 7.2 | 1.8 | 0.6 to 3.1 | 0.005 | 1.4 | 0.2 to 2.6 | 0.022 |
| SF-12 MCS | 286 | 40.1 | 5.7 | 634 | 40.0 | 4.8 | –0.0 | –0.6 to 0.5 | 0.875 | –0.0 | –0.5 to 0.4 | 0.846 |
| SF-6D | 289 | 0.82 | 0.14 | 641 | 0.85 | 0.13 | 0.03 | 0.01–0.05 | 0.003 | –0.03 | 0.00 to 0.04 | 0.012 |
| CORE-OM well-being | 291 | 0.8 | 0.8 | 650 | 0.7 | 0.7 | –0.1 | –0.2 to 0.1 | 0.273 | –0.0 | –0.1 to 0.0 | 0.312 |
| CORE-OM risk | 291 | 0.1 | 0.2 | 650 | 0.0 | 0.2 | –0.0 | –0.0 to 0.0 | 0.440 | –0.0 | –0.0 to 0.0 | 0.996 |
| CORE-OM symptoms | 291 | 0.6 | 0.7 | 650 | 0.5 | 0.5 | –0.2 | –0.2 to –0.1 | 0.000 | –0.1 | –0.2 to –0.0 | 0.001 |
| CORE-OM functioning | 291 | 0.6 | 0.7 | 649 | 0.5 | 0.6 | –0.1 | –0.2 to –0.0 | 0.008 | 0.0 | –0.0 to 0.1 | 0.159 |
| CORE-OM total score | 291 | 0.5 | 0.6 | 650 | 0.4 | 0.5 | –0.1 | –0.2 to –0.0 | 0.005 | –0.1 | –0.1 to –0.0 | 0.011 |
| State anxiety (STAI) | 281 | 34.0 | 11.8 | 631 | 32.6 | 10.8 | –1.5 | –3.4 to 0.4 | 0.116 | –1.4 | –3.1 to 0.3 | 0.105 |
| PSI parenting distress | 288 | 46.8 | 9.2 | 636 | 48.4 | 8.1 | 1.5 | 0.3 to 2.8 | 0.013 | 1.6 | 0.5 to 2.7 | 0.004 |
| PSI PCDI | 289 | 55.8 | 6.1 | 650 | 56.8 | 5.0 | 0.9 | 0.3 to 1.6 | 0.004 | 0.9 | 0.3 to 1.5 | 0.005 |
| PSI difficult child | 281 | 50.2 | 7.2 | 642 | 51.2 | 6.4 | 1.0 | 0.1 to 2.0 | 0.028 | 1.0 | 0.1 to 1.9 | 0.036 |
| PSI total stress | 276 | 153.0 | 19.4 | 628 | 156.3 | 16.5 | 3.3 | 0.8 to 5.8 | 0.009 | 3.2 | 0.9 to 5.6 | 0.007 |
Secondary outcomes for women’s partners
Partner outcomes for at-risk women at 6, 12 and 18 months
There appeared to be little difference between the two main groups regarding the outcome scores for the at-risk women’s partners at 6 and 12 months. There was a pattern indicating some benefit in the IG partners versus the CG partners at the 18-month follow-up. There was a trend for the SF-12 PCS scores to be higher in the IG partners at all time points. The scores for the partners are presented in Table 44.
| 6 months | 12 months | 18 months | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| At-risk women | All women | At-risk women | All women | At-risk women | All women | |||||||||||||||||||
| Control | Intervention | Control | Intervention | Control | Intervention | Control | Intervention | Control | Intervention | Control | Intervention | |||||||||||||
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | |
| SF-12 PCS | 109 | 53.1 (7.8) | 191 | 54.0 (6.1) | 743 | 54.5 (6.1) | 1384 | 54.6 (5.6) | 50 | 53.4 (6.2) | 111 | 53.7 (5.8) | 417 | 54.5 (5.7) | 785 | 54.7 (5.4) | 24 | 51.8 (8.0) | 50 | 54.7 (6.9) | 178 | 54.2 (6.5) | 381 | 67.7 (6.4) |
| SF-12 MCS | 109 | 46.4 (10.8) | 191 | 46.4 (9.9) | 743 | 49.2 (8.7) | 1384 | 49.7 (8.8) | 50 | 48.9 (8.8) | 111 | 48.1 (10.3) | 417 | 50.1 (8.4) | 785 | 50.1 (8.9) | 24 | 48.9 (10.4) | 50 | 50.6 (10.0) | 178 | 50.4 (8.4) | 381 | 52.1 (8.3) |
| SF-6D | 110 | 0.80 (0.15) | 192 | 0.80 (0.13) | 747 | 0.84 (0.13) | 1391 | 0.85 (0.13) | 51 | 0.83 (0.14) | 113 | 0.82 (0.15) | 420 | 0.85 (0.13) | 787 | 0.85 (0.13) | 25 | 0.81 (0.16) | 50 | 0.84 (0.14) | 181 | 0.85 (0.13) | 384 | 0.87 (0.13) |
| DAS Likert | 22 | 4.3 (0.9) | 30 | 4.1 (1.4) | 150 | 4.3 (1.0) | 247 | 4.2 (1.2) | 53 | 4.0 (1.1) | 113 | 3.9 (1.3) | 429 | 4.2 (1.1) | 799 | 4.3 (1.1) | 25 | 3.8 (1.3) | 50 | 3.9 (1.3) | 179 | 4.2 (1.2) | 381 | 4.2 (1.2) |
| DAS | 22 | 17.4 (2.8) | 30 | 16.9 (3.1) | 150 | 16.6 (2.8) | 247 | 16.4 (2.7) | 53 | 17.4 (2.8) | 113 | 16.7 (2.7) | 425 | 17.1 (2.5) | 800 | 17.0 (2.7) | 25 | 16.0 (2.5) | 51 | 16.5 (3.1) | 179 | 16.4 (2.4) | 379 | 16.7 (2.7) |
| PSI parenting distress | 105 | 46.2 (7.4) | 175 | 45.0 (7.8) | 703 | 48.0 (7.5) | 1251 | 48.2 (7.8) | 52 | 46.8 (6.8) | 112 | 46.3 (9.4) | 424 | 48.3 (7.3) | 783 | 47.8 (8.2) | 24 | 44.3 (9.1) | 50 | 47.5 (10.0) | 177 | 48.0 (8.1) | 383 | 49.4 (8.0) |
| PSI PCDI | 104 | 54.7 (5.9) | 177 | 55.0 (5.5) | 701 | 56.2 (5.0) | 1262 | 56.2 (4.9) | 53 | 55.8 (5.2) | 112 | 56.3 (5.6) | 427 | 56.3 (4.9) | 792 | 56.2 (5.2) | 25 | 54.7 (5.2) | 51 | 55.2 (5.9) | 181 | 55.9 (5.4) | 385 | 56.5 (4.7) |
| PSI difficult child | 100 | 50.7 (5.7) | 171 |
50.3 (7.3) |
674 | 52.3 (5.5) | 1218 | 52.0 (6.1) | 53 | 51.1 (6.1) | 112 | 51.0 (6.9) | 421 | 51.6 (5.9) | 775 | 51.2 (6.2) | 25 | 48.2 (5.4) | 48 | 49.5 (8.0) | 1196 | 51.3 (6.1) | 367 | 51.1 (6.1) |
| PSI total stress | 99 | 151.4 (16.5) | 166 | 150.1 (17.7) | 660 | 156.2 (15.4) | 1180 | 156.3 (13.6) | 52 | 153.6 (15.3) | 112 | 153.7 (18.8) | 415 | 156.4 (15.3) | 765 | 155.0 (16.9) | 24 | 146.9 (16.9) | 48 | 151.7 (21.6) | 173 | 154.4 (17.5) | 366 | 156.9 (16.6) |
| CORE-OM well-being | 25 | 0.70.9) | 51 | 0.7 (0.8) | 180 | 0.6 (0.6) | 384 | 0.5 (0.7) | ||||||||||||||||
| CORE-OM risk | 25 | 0.1 (0.2) | 51 | 0.6 (0.4) | 180 | 0.0 (0.1) | 384 | 0.1 (0.3) | ||||||||||||||||
| CORE-OM symptoms | 25 | 0.7 (0.8) | 51 | 0.6 (0.7) | 180 | 0.5 (0.6) | 384 | 0.4 (0.5) | ||||||||||||||||
| CORE-OM functioning | 25 | 0.7 (0.7) | 50 | 0.6 (0.6) | 179 | 0.6 (0.6) | 383 | 0.5 (0.5) | ||||||||||||||||
| CORE-OM total score | 25 | 0.6 (0.6) | 51 | 0.5 (0.6) | 180 | 0.5 (0.4) | 384 | 0.4 (0.4) | ||||||||||||||||
| State anxiety (STAI) | 25 | 36.0 (13.1) | 49 | 32.9 (11.3) | 174 | 32.9 (10.4) | 374 | 31.1 (9.3) | ||||||||||||||||
Partner outcomes for all women at 6, 12 and 18 months
There appeared to be a little difference between the two main groups regarding the outcome scores for the partners of all women at 6 and 12 months. At 18 months postnatally there was a difference in the SF-12 PCS in favour of the IG partners. The mean SF-12 MCS, CORE-OM and DAS scores were also in favour of the IG partners at 18 months (Table 44).
Eighteen-month infant outcomes
Women’s replies to infant outcomes
There was some evidence of benefit associated with the intervention in infant outcomes according to at-risk women’s replies (Table 45). The IG at-risk women were more likely to say that they were not concerned about their child for 12 out of 15 questions. For the item ‘being slow to catch on’, 94.3% of IG at-risk women versus 76.6% of CG women said that they were not concerned (χ2 = 11.98, df = 3, p = 0.007). For the item ‘temper tantrums’, 59.8% of IG at-risk women versus 46.0% of CG women said that they were not concerned (χ2 = 6.6, df = 3, p = 0.086).
| Control group | Intervention group | Difference | p-value | |||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |||
| At-risk women | ||||||||
| Growth and development rescaled (0–100) | 43 | 34.17 | 12.92 | 84 | 32.12 | 12.61 | 2.05 | 0.396 |
| Behaviour Screening Questionnaire rescaled (0–100) | 42 | 28.10 | 10.02 | 78 | 26.23 | 9.68 | 1.86 | 0.328 |
| Concerns rescaled (0–100) | 46 | 10.29 | 12.11 | 85 | 6.43 | 7.80 | 3.86 | 0.055 |
| CHAT rescaled (0–100) | 47 | 4.96 | 5.58 | 87 | 2.94 | 6.22 | 2.03 | 0.057 |
| Infant outcomes rescaled total | 37 | 19.40 | 6.13 | 73 | 16.45 | 5.38 | 2.94 | 0.016 |
| All women | ||||||||
| Growth and development rescaled (0–100) | 318 | 33.44 | 13.07 | 706 | 32.16 | 12.49 | 1.28 | 0.143 |
| Behaviour Screening Questionnaire rescaled (0–100) | 303 | 25.42 | 10.41 | 658 | 24.04 | 10.30 | 1.38 | 0.056 |
| Concerns rescaled (0–100) | 340 | 6.17 | 7.52 | 739 | 5.03 | 5.68 | 1.14 | 0.013 |
| CHAT rescaled (0–100) | 340 | 2.84 | 6.41 | 742 | 2.29 | 5.62 | 0.55 | 0.172 |
| Infant outcomes rescaled total | 275 | 16.51 | 5.94 | 618 | 15.86 | 5.54 | 0.65 | 0.125 |
There was some evidence of benefit associated with the intervention in infant outcomes according to the replies of all women (Table 45). More IG women said that for 26 of the 29 behaviour questions their child had no problems. This was statistically significant for the management and discipline question and approaching significance for the temper tantrums question. The IG women were more likely to say that they had no concerns about 14 of the 15 aspects of their toddler’s development. For the item ‘paying attention’, 91.4% of IG women said that there was no problem versus 88.4% of CG women (χ2 = 8.086, df = 3, p = 0.044); the results approached significance for the item ‘being clumsy’ (p = 0.069) and the item ‘seeming unhappy’ (p = 0.053). For the at-risk women the mean aggregate infant outcome concern score was 19.4 (SD 6.1) for 37 women in the CG and 16.5 (SD 5.4) for the 73 women in the IG. The mean difference was –2.9 (95% CI –5.0 to –0.7, p = 0.008).
| ARM-SF scale | Women (n = 103) | Health visitors (n = 36) |
|---|---|---|
| Total mean ARM-SF score | 6.45 (0.49) | 5.73 (0.64) |
| Bond | 6.82 (0.36) | 6.47 (0.47) |
| Partnership | 6.58 (0.66) | 6.13 (0.79) |
| Confidence | 6.66 (0.54) | 5.24 (0.91) |
| Openness | 5.74 (1.18) | 5.08 (1.15) |
Partners’ replies to infant outcomes
Of the at-risk women for whom there was a full set of 6-week, 6-month, 12-month and 18-month data available, 87 IG partners and 47 CG partners replied to the 18-month questionnaire. There was no clear pattern in the responses from either group in the Toddler Growth and Development Questionnaire (TG&DQ) or the BSQ. For the concerns item ‘sleeping at night’, 80.6% of the IG women’s partners versus 58.6% of the CG women’s partners said that they were not concerned (χ2 = 13.28, df = 3, p = 0.004).
Of all women for whom there was a full set of 6-week, 6-month, 12-month and 18-month data available, 448 IG partners and 211 CG partners replied to the 18-month questionnaire. For the TG&DQ the IG partners were more likely to say that their child could do an activity for most of the questions. There was no pattern for partners’ responses to the BSQ or concerns questions. For the CHAT, the IG women’s partners were more likely to respond positively on most responses.
Immunisation data
Among the at-risk women for whom immunisation data were available, 54% (43/80) of infants in the IG versus 30% (9/30) of infants in the CG had received their measles, mumps and rubella (MMR) immunisation before 18 months (p = 0.03).
Among all women for whom immunisation data were available there were no differences observed between the groups in the number of infants who received immunisations up to 6 months. In total, 51% (277/540) of infants in the IG had received their MMR immunisation before 18 months versus 31% (59/190) of infants in the CG (p = 0.001).
Summary of infant outcomes
It appeared that, overall, for the women’s replies there was some indication that the IG women perceived fewer problems with their infants than CG woman at the at-risk women level. The pattern for the partners’ replies was more mixed.
Intervention process monitoring
PoNDER Adherence Rating Scale
Classification of audiotape recordings
The HVs were asked to audiotape intervention sessions to monitor adherence. A mean score ranging from 0 to 7 was calculated for the three PARS factors: GFC, PCA-specific items and CBA-specific items. Audiotapes for which the CBA-specific PARS scores were higher than the PCA-specific PARS scores were classified as being CBA. Tapes for which the PCA-specific PARS scores were higher than the CBA-specific PARS scores were classified as being PCA. In addition to completing a PARS for each tape, raters were also asked to use their professional judgement to indicate whether they believed that the tape that they had just rated belonged to a CBA or a PCA. This gave a second set of classifications based on expert judgement.
PARS rating procedure
The adherence assessment was limited because of the very small number of audiotapes that HVs submitted. HVs were asked to audiotape every intervention session so that a random sample of at least 10% of all sessions could be rated for adherence. In the event, only a very small number of audiotapes were submitted for rating, which limited the adherence assessment. In total, 46 session tapes were submitted for 46 sessions, which were delivered by just nine HVs. Additionally, 50% of the submitted tapes were inaudible and could not be rated. Therefore, tapes from 23 sessions were available for rating. Six of the 23 rated sessions were from the CBA intervention and 17 of the 23 tapes were from the PCA intervention. This was only 2.3% of the total number of CBA sessions delivered (n = 259) and 7.0% of the total number of PCA sessions delivered (n = 242). All 26 PARS items were randomly distributed throughout the rating scale. Raters were asked to rate each tape for the presence and extensiveness (but not the quality) of all 26 PARS items on a 7-point scale ranging from 1 ‘not at all present’ to 7 ‘extensively present’.
Steps were taken to ensure rater blindness to the original 46 tapes. All 46 sessions were rerecorded and randomly coded, resulting in 46 separate coded tapes. Each rater was given a randomly generated number sequence of the order in which they were to rate their tapes, to minimise rating multiple sessions submitted by the same HV in session sequence and thus avoid contaminating ratings.
PARS raters
The three raters were experienced psychotherapists who did not have an allegiance to either CBA or PCA approaches, but who had some awareness of both approaches from training and professional experience. Raters also read the trial training manuals prepared for both trial interventions. Rater A (the principal rater) was a 47-year-old man educated to PhD level in a psychotherapy-related topic and a United Kingdom Council for Psychotherapy (UKCP)-registered psychotherapist, working as a research fellow and psychotherapist in an NHS specialist psychotherapy service. He was originally trained in transactional analysis psychotherapy but was now practising, teaching, supervising and publishing, and had an allegiance to, psychodynamic–interpersonal psychotherapy.
Co-rater B was a 50-year-old man, educated to Masters level in psychotherapy-related topics and a UKCP-registered psychotherapist, currently working as a psychotherapist in an NHS specialist psychotherapy service as well as in an NHS specialist service for people given a diagnosis of personality disorder. He originally trained in both psychoanalytical psychotherapy and cross-cultural psychotherapy but was practising, teaching and supervising, and had an allegiance to, psychoanalytical psychotherapy.
Co-rater C was a 44-year-old woman educated to degree level and working as a university lecturer and visiting psychotherapist in an NHS specialist psychotherapy service. Originally trained in psychodynamic therapy she was now practising, teaching, supervising and publishing, and had an allegiance to, psychodynamic–interpersonal psychotherapy.
The aim was for rater A to rate all 46 tapes with raters B and C each co-rating half (expected to be 23 each). However, as 50% of the tapes were inaudible, rater A rated all 23 audible tapes and raters B and C co-rated 13 and 10 tapes respectively.
PARS results
There were no significant differences in group mean PARS scores for GFC between the two interventions. The number of tapes correctly classified by PARS score was:
-
rater A – 20/23 (87%) tapes (kappa = 0.64, p = 0.002)
-
rater B – 12/13 (92%) tapes (kappa = 0.81, p = 0.003)
-
rater C – 9/10 (90%) tapes (kappa = 0.74, p = 0.016)
The inter-rater levels of agreement on classification using PARS scores were:
-
raters A and B agreed on the classification of 11/13 (85%) tapes (kappa = 0.58, p = 0.021)
-
raters A and C agreed on the classification of 9/10 (90%) tapes.
PARS conclusion
The method used to measure the quality of adherence by the HVs to the two interventions they were trained to deliver had some limitations. Only a small number of HVs involved in the trial submitted any tapes at all for rating. It may be assumed that these tapes were only submitted by HVs who felt the most confident about their ability to deliver the intervention they had been trained to deliver. Half of the submitted tapes were inaudible and could not be rated, further reducing the generalisability of the adherence results. The rated tapes cannot therefore be considered to be, as originally intended, a random sample of all interventions delivered during the trial.
Given these limitations, the results show that most of the tapes were correctly classified by raters who had no allegiance to either of the two psychological interventions. The PARS scores for tapes from both interventions suggest that both interventions, as expected, contained a similar degree of GFC, as well as a satisfactory amount of the specific factors expected to be associated with each intervention to enable them to be identified as two separate interventions.
Agnew Relationship Measure Short Form (ARM-SF)
Data from the ARM-SF were collected from 36 HVs and 103 women for a total of 355 sessions. In total, 20 of these HVs had received training in CBA and 16 had received training in PCA. ARM-SF data, from either the women or the HVs, were provided by the CBA group for a total of 190 sessions delivered to 63 women. Similarly, ARM-SF data, from either the women or the HVs, were provided by the PCA group for a total of 165 sessions delivered to 40 women. This compares with a total of 501 sessions delivered in the whole trial, with 259 CBA sessions and 242 PCA sessions; that is, ARM data were available from 71% of all sessions, and 73% and 68% of CBA and PCA intervention sessions respectively.
There were large amounts of missing data. Many sessions had ARM-SF data from either the HV or the woman rather than from both. Data for a complete set of eight sessions were only available for seven (6.8%) woman–HV dyads; 31 (30.1%) woman–HV dyads had data for only one session. The mean number of sessions for both IGs for which data had been submitted was 3.45 (SD 2.31). The mean number of sessions from the CBA IG and the PCA IG for which data had been submitted was 3.02 (SD 2.05) and 4.13 (SD 2.54) respectively. The mean number of sessions that were delivered was 4.27 (SD 2.17) and 4.68 (SD 2.49) for the CBA and PCA IGs respectively.
ARM-SF data for all sessions
The mean ARM-SF scales across all sessions and for both IGs combined are presented in Table 46. Because of the amount of missing data, mean ARM-SF scores were computed across sessions.
There were no statistically significant between-group differences on any of the women or HV ARM-SF scales. The women’s scores were significantly higher than the scores of HVs for all ARM-SF scales (p ≤ 0.0001) apart from total mean ARM-SF score. The numerical differences between these scores are generally quite small ranging from 0.35 (bond) to 0.72 (mean ARM-SF). The largest difference of 1.42 for confidence suggests that women perceived the HVs as being more confident in delivering the interventions than the HVs did themselves.
ARM-SF scores for the CBA and PCA groups
Mean ARM-SF scores averaged across all sessions were also calculated separately for the two IGs (Table 47).
| ARM-SF scale | CBA intervention (n = 190 sessions) | PCA intervention (n = 190 sessions) | ||
|---|---|---|---|---|
| Women (n = 63) | Health visitors (n = 20) | Women (n = 40) | Health visitors (n = 16) | |
| Total mean ARM-SF score | 6.43 (0.50) | 5.65 (0.67) | 6.51 (0.49) | 5.84 (0.59) |
| Bond | 6.79 (0.36) | 6.42 (0.51) | 6.87 (0.36 | 6.55 (0.39) |
| Partnership | 6.56 (0.68) | 6.11 (0.77) | 6.61 (0.64) | 6.16 (0.82) |
| Confidence | 6.64 (0.53) | 5.12 (0.94) | 6.71 (0.56) | 5.41 (0.86) |
| Openness | 5.69 (1.24) | 4.95 (1.14) | 5.85 (1.06) | 5.25 (1.16) |
Within both IGs, as with the results for all sessions combined reported above, there were statistically significant differences between the women and the HVs, with women scoring all ARM-SF scales higher than the HVs (p = 0.002 for the CBA intervention; p = 0.025 for the PCA intervention).
There were no statistically significant differences in either women’s or HVs’ scores between the two IGs. However, both women and HVs in the PCA IG scored higher than women and HVs in the CBA group, albeit small differences on a 7-point scale. There is some evidence in the literature that the quality of alliance measured in the first few sessions of therapy is a major predictor of clinical outcome. 213,214 To rule out the possibility of a type II error, ARM-SF data for the first three sessions only were compared by IG. There were no significant differences between the women in the two IGs (t = < 1.8, df = 84, p = 0.100). There was a marginally significant difference on the ARM-SF confidence scale with PCA HVs scoring higher than CBA HVs [PCA confidence mean = 5.37 (SD 0.91); CBA confidence mean = 4.98 (SD 1.01); t = 1.91, df = 85, p = 0.059]. There were no other significant differences between HVs (t ≤ 1.64, df = 85, p = 0.09).
Comparative ARM-SF data
Having examined for differences between interventions and modes of delivery, the results were compared with other studies that have used the shortened version of the ARM-SF. 206,215,216 The Leeds Depression Project215 offered CBT to a clinically representative sample (clients n = 75; therapists n = 10; sessions n = 628). The Second Sheffield Psychotherapy Project216 compared CBT and psychodynamic–interpersonal psychotherapy (clients n = 95; therapists n = 5; sessions n = 1120). Comparative mean (SD) total ARM-SF scores from these studies are presented in Table 48 below.
| Study sample | Client total mean (SD) ARM-SF score | Therapist total mean (SD) ARM-SF score |
|---|---|---|
| PoNDER trial CBA intervention | 6.43 (0.50) | 5.65 (0.67) |
| PoNDER trial PCA intervention | 6.51 (0.49) | 5.84 (0.59) |
| PoNDER trial (all sessions) | 6.45 (0.49) | 5.73 (0.64) |
| Leeds Depression Project | 6.13 (0.70) | 5.47 (0.77) |
| Sheffield Psychotherapy Project | 5.75 (0.85) | 5.04 (0.89) |
These data show that the mean total ARM-SF scores from the PoNDER trial are comparable with those from previous psychotherapy studies in the UK.
ARM-SF summary results
The data show that women across all sessions and within both interventions returned high scores on all ARM-SF scales. Scores were above 6.0 on a 7-point scale for all ARM-SF scales, apart from for openness (range 5.69–5.85).
Scores for the HVs across all sessions and within both interventions were lower than the women’s scores on all ARM-SF scales. The scale with the largest differences between the women and the HVs was the ARM-SF confidence scale. The differences between women and HVs on confidence were 0.66 across all sessions, 1.52 in the CBA IG and 1.3 in the PCA IG. The openness scale was the lowest scoring scale for both women and HVs, across all sessions and within both interventions. The large SDs on this scale (1.06–1.24) for both women and HVs indicated substantial variation.
There were no significant differences in either HVs’ or women’s ARM-SF scores between the two interventions. There were significant differences across both interventions on HV scores only, depending on whether the EPDS was administered face-to-face or by post. HVs in both the CBA-F and the PCA-F groups who administered the EPDS face-to-face had significantly lower ARM-SF scores than HVs in both the CBA-P and the PCA-P groups in which the EPDS was administered by post. This difference was also significant when comparing the first three sessions with subsequent sessions. Total ARM-SF mean scores for both women and HVs were comparable with those of clients and therapists from the wider psychotherapy literature.
Health visitor pre-trial questionnaire
There were 128 pre-trial questionnaires returned by all of the HVs; 40 in each IG and 48 in the CG, before they were informed of their random allocation.
Most HVs (67%) who said that they had attended training about PND said that their training had taken place in the previous 5 years; three HVs said that they attended training in the 1980s. Most of this training (66%) lasted between half a day and 2 days. Most of the HVs who returned a questionnaire said that they already used the EPDS (79%), many with all postnatal women (47%). The EPDS was used by 60% of these HVs at 6 weeks postnatally. The HVs reported greater levels of confidence in identifying women with PND (85%) than in supporting women with PND (80%). Almost all of the HVs said that they had supported at least one woman in the previous 6 months who they felt was suffering from PND.
Pre-trial health visitor predispositions to psychological interventions and OPP
Table 49 indicates the mean OPP scores before the trial began of the HVs who completed a pre-trial questionnaire. The highest level of agreement among the pre-trial HV responses was with the humanistic group of questions. The lowest level of agreement among the pre-trial HV responses overall was with the organic and social economic group of questions. There appeared to be little difference between the three main groups, CBA, PCA and CG, in the pre-trial OPP scores, apart from the social economic scores for the PCA HVs and the CG HVs, which was of borderline statistical significance. Overall, the scores indicated a similarity between all of the HVs’ views on what they thought could help people with psychological problems. This indicated that there were no strong predispositions among the HVs regarding the usefulness of a CBA or PCA, which could have adversely affected their willingness to be trained in either approach or the training outcomes.
| Control group | CBA | PCA | p | ||||
|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | ||
| Psychodynamic | 46 | 0.58 (0.82) | 39 | 0.57 (0.95) | 37 | 0.44 (1.05) | 0.750 |
| Humanistic interpersonal | 46 | 2.34 (0.57) | 40 | 2.43 (0.42) | 41 | 2.37 (0.51) | 0.695 |
| Behavioural | 43 | 1.48 (0.84) | 40 | 1.60 (0.73) | 40 | 1.70 (0.90) | 0.507 |
| Cognitive | 46 | 1.37 (0.81) | 38 | 1.44 (0.79) | 37 | 1.45 (0.89) | 0.895 |
| Organic | 44 | 0.30 (1.02) | 37 | 0.31 (1.10) | 39 | 0.62 (1.10) | 0.330 |
| Social economic | 44 | 0.04 (1.24) | 40 | 0.37 (1.14) | 37 | 0.70 (1.15) | 0.046 |
Health visitor post-trial questionnaire
Post-trial training in identifying and supporting women
There were 135 post-trial questionnaires returned by all HVs, 42 in each IG and 51 in the CG. Most HVs (85%) said that they had attended training about identifying or supporting women at risk of PND, and 77% said that their training had taken place in the previous 5 years, with no HVs saying that they had attended training in the 1980s. Most of this training (80%) lasted between half a day and 5 days. Most of the HVs who returned a questionnaire said that they already used the EPDS (81%), many with all postnatal women (63%). The EPDS was used by all of these HVs at 6 weeks postnatally. The HVs reported slightly lower levels in confidence in identifying women with PND (71%) than in supporting women with PND (74%). All of the HVs said that they had supported at least one woman in the previous 6 months who they felt was suffering from PND.
Post-trial health visitor predispositions to psychological interventions and OPP
There were 60 OPP HV responses; 18 CBA, 24 PCA and 18 CG. Table 50 indicates the HVs mean post-trial OPP scores. The post-trial replies show that 78% of the CG versus 88% of the IG attended training to identify or support all women with PND. The length of training received ranged from half a day to 5 days for 100% of the CG HVs and 93% of the IG HVs, with 60% of the CG and 87% of the IG indicating that the training had taken place between 2000 and 2004. In total, 90% of the CG HVs had used the EPDS on 61% of all of their postnatal clients, with 95% of the IG HVs using it on theirs. The EPDS was used at 6 weeks postnatally by 67% of the CG and 88% of the IG. Levels of confidence in using the EPDS to identify women at risk of PND were 53% in the CG and 79% in the IG.
| Control group | Cognitive behavioural approach | Person-centred approach | p | ||||
|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | ||
| Psychodynamic | 17 | 0.29 (1.02) | 19 | 0.02 (1.07) | 23 | 0.03 (0.84) | 0.628 |
| Humanistic interpersonal | 17 | 2.26 (0.54) | 19 | 2.28 (0.75) | 23 | 2.47 (0.48) | 0.450 |
| Behavioural | 18 | 1.52 (0.99) | 18 | 1.80 (0.61) | 24 | 0.90 (1.02) | 0.007 |
| Cognitive | 17 | 1.19 (0.93) | 18 | 1.54 (0.59) | 23 | 0.84 (1.06) | 0.053 |
| Organic | 18 | 0.48 (1.25) | 17 | –0.47 (1.20) | 20 | 0.03 (1.03) | 0.062 |
| Social economic | 18 | –0.10 (1.20) | 20 | 0.08 (1.21) | 22 | 0.64 (0.99) | 0.101 |
Comparing the three groups, a post-trial difference emerged between the CBA group and the PCA group for replies to the behavioural, cognitive and organic groups of questions. This was statistically significant for the behavioural questions. The post-trial cognitive and behavioural scores were increased and highest in the CBA group and reduced and the lowest in the PCA group, with little change in the CG. The reduction in the PCA group could be interpreted as a development in these HVs’ beliefs in the value of the PCA following the training and interventions. Post trial there was little change from baseline in the humanistic interpersonal scores, with a small rise in the PCA group and a small reduction in the CBA group and CG. The psychodynamic scores were lower in all three groups post trial, with greater reductions in the IG HVs who had been trained. The post-trial organic scores were higher in the CG and much lower in both of the trained groups.
The post-trial social economic scores in the CBA group dropped considerably, with only a very small reduction in the PCA group. This could be consistent with CBA HVs believing that people could think about and work through their problems, despite social and economic difficulties. The post-trial scores both within groups and between groups indicate that the HVs who had access to the trial training changed their views about what might help people with psychological problems and this could be attributed to the training that they received.
Health visitor training evaluation
Health visitor evaluation of the introductory day
The HV questionnaires indicated a high level of satisfaction with the introductory training day. In total, 83–92% of the HVs felt that the presentations for the background, EPDS, clinical interview, risk management and skills development were good or very good. These levels of satisfaction are reflected in the rest of the responses. One person in the CBA group provided a poor response for four of the items. The CBA group were between 77% and 100% positive about all of the items. The PCA group indicated that they were between 91% and 100% positive across all of the items.
Health visitor evaluation of the 5 core training days
The replies of the IG HVs who returned a training evaluation questionnaire following the 5 core training days indicated a high level of satisfaction with the content and methods of the training. Most HVs in both of the IGs replied very or extremely/excellent to all of the questions, on a 5-point scale, relating to the training, course objectives, theoretical content, pitch, structure and appropriateness of models. The two groups were equally likely to say that they were very satisfied with the 5 core training days (59% CBA versus 59% PCA).
There were some differences between the two groups in favour of the PCA group HVs who seemed more likely to reply at the extremely positive end of the scale than the CBA HVs on questions relating to relevance, appropriateness, usefulness, acceptability and interest for HVs supporting women with PND. They were also more likely to reply definitely to the two questions on whether the core training days had improved their understanding and skills in supporting women with PND. The PCA HVs were also more likely than the CBA HVs to reply that they would definitely recommend the course to other HVs (67% compared with 29%).
Conversely, 55% of the CBA HVs said that they felt very confident in applying the skills that they had developed compared with 33% of the PCA HVs, and 39% of the CBA HVs said that they felt moderately confident in applying the skills that they had developed compared with 51% of the PCA HVs.
As well as the evaluation after the 5 core training days the HVs were asked to complete 16 questions on their post-training self-assessed level and knowledge and skill, on a 1–7 scale in which 1 was very poor and 7 was excellent. The scores for most HVs who replied to the questionnaire were at the upper end of the scale for most questions. In both IGs for some questions, two HVs’ replies were at the lower end of the scale. That is, they assessed their knowledge and skills as being poorer than those of other HVs in the same group.
Chapter 5 Economic analysis
Introduction
Psychological interventions for PND could have several important effects on costs and outcomes. The most obvious effects might be that HVs would be required to undertake more visits but that the prevalence of PND and its associated costs such as medication use would be reduced. Broader effects such as the impact on the baby, other children and the partner need also to be considered. An economic evaluation was undertaken alongside the study to capture any changes in resource use.
Economic evaluation methods
The economic evaluation followed the technology appraisal guidelines used by NICE217 and, as such, takes the NHS and social service perspective. One issue that was relevant to defining the perspective for this intervention was which family members should be included in the cost-effectiveness analysis. It is feasible that the intervention could have had an impact on the baby, other children and even the partner (for all women where there was one). The primary analysis presented was based on the costs of the mother at 6 months with a further analysis based on mother and baby costs at 12 months.
Costs
The following cost components were included in the economic evaluation:
-
HV contacts (including training if appropriate)
-
baby immunisations
-
GP contacts
-
prescriptions
-
social worker contacts
-
mother and baby or psychiatric unit admissions
-
other NHS contacts.
Resource use data from 6 weeks to 6 months were collected on a resource use log completed by HVs based on their own and GP records. For 6 months to 18 months, only HV and baby immunisation data were collected on the resource use log, with the remaining resources collected by way of the 12-month and 18-month questionnaires. Resource use was collected for the mother, baby, other children and the partner (if appropriate).
A set of unit costs (2003/4 prices) is given in Table 51. The main source of the unit cost data was Netten and Curtis,218 with additional information on training costs collected from the sessions instigated for the trial itself. Costs and quality-adjusted life-years (QALYs) were not discounted as analyses were only presented for costs and outcomes within 1 year.
| Resource | Unit cost (2003/4) | Source |
|---|---|---|
| HV hour of contact without CBA/PCA training | 77 | Netten and Curtis, 2004218 |
| HV hour of contact with CBA/PCA training | 79 | Table 53 |
| GP contacta | 30 | Netten and Curtis, 2004218 |
| Social work visitb | 108 | Netten and Curtis, 2004218 |
| Community mental health contactc | 29 | Netten and Curtis, 2004218 |
| Clinical mental health contactd,e | 129 | Department of Health, 2005219 |
| Mother and baby psychiatric unit dayd | 458 | Department of Health, 2005220 |
| Fluoxetine prescriptionf | 1.56 | BNF, 2005221 |
| Other prescriptiong | 2.79 | BNF, 2005221 |
| DTwP and Hib vaccination per dose | 20 | BNF, 2005221 |
| Men-C vaccination per dose | 18 | BNF, 2005221 |
| Inpatient admission (infant)d,h | 516 | Department of Health, 2005219 |
| A&E attendanced,i | 73 | Department of Health, 2005220 |
| NHS direct contactj | 25 | Hansard and Department of Health, 2005220 |
| Walk-in centre attendanced,k | 39 | Department of Health, 2005220 |
Training costs were gathered from the sessions undertaken as part of the trial and were primarily made up of trainer fees, travel and backfill health visiting (Table 52). Other sundries produce a cost of training of £1398 per HV. To use this within a unit cost of HV time it needed to be converted into an equivalent annual cost, based on a profile of training and supervision over the foreseeable future. Based on expert opinion (PS) we estimated that further training would be required 5-yearly, and 1 hour of clinical supervision would be required every month. This produced an annual equivalent cost of £988 per annum, assuming a 20-year working life and that annuity was charged at 3.5% and payable in advance (Table 53). This represented a 2.3% increase in the gross costs of a HV (£42,625 taken from Netten and Curtis218), which translated to a cost per hour of client time of £79 versus £77 in the CG.
| Item | Cost (2004/5) | Source |
|---|---|---|
| HV backfill for training | 63,832 | Study records |
| HV travel | 15,644 | Study records |
| Trainer costs | 42,089 | Study records |
| Manual development | 2000 | Study records |
| Room rental for training | 3072 | Study records |
| Refreshments | 940 | Study records |
| Introduction day | 3075 | Based on £41 per professional chargeable hour for clinical psychologist |
| Administration | 742 | Based on 8 days of clerical time |
| Total | 131,393 | |
| Cost per HV | 1398 |
| Year | Traininga | Supervisionb | Total | Discounted |
|---|---|---|---|---|
| 0 | 1398 | 816 | 2214 | 2214 |
| 1 | 816 | 816 | 788 | |
| 2 | 816 | 816 | 762 | |
| 3 | 816 | 816 | 736 | |
| 4 | 816 | 816 | 711 | |
| 5 | 524 | 816 | 1340 | 1128 |
| 6 | 816 | 816 | 664 | |
| 7 | 816 | 816 | 641 | |
| 8 | 816 | 816 | 620 | |
| 9 | 816 | 816 | 599 | |
| 10 | 524 | 816 | 1340 | 950 |
| 11 | 816 | 816 | 559 | |
| 12 | 816 | 816 | 540 | |
| 13 | 816 | 816 | 522 | |
| 14 | 816 | 816 | 504 | |
| 15 | 524 | 816 | 1340 | 800 |
| 16 | 816 | 816 | 471 | |
| 17 | 816 | 816 | 455 | |
| 18 | 816 | 816 | 439 | |
| 19 | 816 | 816 | 424 | |
| Net present value | 14,527 | |||
| Equivalent annual cost | 988 | |||
| Increase in PSSRU estimated health visitor gross cost (£42,625218) | 2.3% | |||
All GP contacts and prescriptions were included within the economic evaluation. However, because of the huge range of medications prescribed it was thought necessary to simplify the analysis. Prescriptions were split down into their nine main indications (which amounted to 83% of prescriptions), plus ‘other’. The most common prescription for each indication was then costed using the British National Formulary. 221 This was then combined to produce two unit costs, one for antidepressants and one for other prescriptions (Table 51).
‘Other NHS contacts’ also included a vast array of contacts, mostly unrelated to PND or any likely somatisation. Therefore, we identified all mental health-related contacts and classified these as ‘community mental health contacts’, that is, counsellor, CPN, community mental health team and mental health nurse contacts, or ‘clinical mental health contacts’, that is, crisis service, psychologist, psychotherapist, psychiatric outpatient and mother and baby psychiatric outpatient contacts.
One minor complication with respect to the costing was that the recommended vaccinations for children changed in 2005; vaccines containing whole cell pertussis and the live poliomyelitis vaccine are no longer used in the UK for the childhood immunisation programme. Consequently, the immunisations at 2, 3 and 4 months now consist of two immunisations rather than three. Immunisations were costed using the new schedule, excluding the resource use information for polio (which is now included in the injection with diphtheria).
Outcomes
The SF-6D, from a subset of SF-36 questions, was calculated for all women at 6 weeks and 6, 12 and 18 months. SF-6D scores were estimated using the UK tariff. 222 QALYs were estimated by calculating the area of the trapeziums beneath the SF-6D scores with respect to time. For a baseline (6-week) utility of 0.8 and a 6-month utility of 0.9, the QALYs over this period were [(0.8 + 0.9) × 0.5] × (20/52) years, or 0.33 QALYs. To adjust for different baseline scores, QALYs gained were then calculated by subtracting the rectangle formed with the baseline score from the QALY.
Analysis
The primary comparison for the economic analysis was based on the at-risk women and compared intervention and control groups at 6 months. This was termed the at-risk women analysis. Further analysis comparing at-risk women in the CBA and PCA groups was also undertaken. Also, a comparison of all women in the intervention and control groups at 6 and 12 months was undertaken. A further analysis comparing all women in the CBA and PCA groups was also undertaken.
The main economic analysis was based around costs and outcomes at 6 months postnatally for the mother. Further analyses also considered the costs for the baby and cost-effectiveness at 12 months. Allowance for the clustering was made by using the xtgee procedure in STATA196 for the women-level cost and QALY estimates. Covariate adjustment was not undertaken because of the negligible effect seen in the clinical analyses and the lack of a clear set of relevant variables for the adjustment of costs. Baseline costs were not collected within the study.
Cost and outcome data were to be combined to produce an incremental cost-effectiveness ratio, if appropriate. The main focus of the analysis was to plot data on the cost-effectiveness plane and their associated cost-effectiveness acceptability curves (CEACs). These plots were based on bootstrapped sample means, generated from cost–QALY pairs from the data. Interpretation of the CEACs was based around the probability of cost-effectiveness in the £20,000–30,000 per QALY range, to reflect the thresholds typically used by NICE to identify which interventions to fund.
For the estimation of CEACs the incorporation of clustering is more complex and is typically ignored within economic evaluations. CEACs were therefore based on crude means. Further subgroup analyses were also undertaken to identify differences between the different psychological therapies and the use of the postal versus face-to-face administration of the EPDS at 8 weeks.
The sensitivity analysis was based around the impact of different time frames and analytical perspectives on the cost-effectiveness results, in particular, changing the time frame from 6 months to 12 months, changing from the ‘at risk’ analysis to ‘all women as randomised’ analysis, and imputing missing data at 6 months.
Additionally, missing economic data were imputed to produce a data set that was comparable with that in the main clinical analyses (n = 418 at-risk women, n = 2659 all women). Multiple imputation using the ‘Norm’ software developed by Joseph Schafer was used. 223 Covariates used in the imputation were 6-week EPDS, age, receipt of state benefits, relationship with baby, health of baby, living alone, history of PND and life events. Given a missing data rate (γ) of around 30%, five data sets were generated in line with recommendations. 223 To allow the uncertainty associated with the multiple imputations to be fully incorporated into the analysis required standard errors across the five data sets. However, it was not clear how this could be achieved within STATA. Consequently, mean values across the data sets were used as a single imputed data set. Although losing the benefits of imputing multiple data sets, this still retained the properties of the Schafer imputation algorithm and was therefore considered a robust imputation method.
Results for at-risk women at 6 months (primary economic analysis)
Analysis of cost-effectiveness is bivariate in nature and, to capture the covariance between costs and effects, is best undertaken on paired data (i.e. using cases with both cost and effects data). This requirement, together with the use of multiple data sources, typically leads to attrition. Table 54 demonstrates that, of the analysable 418 at-risk women in the primary clinical analysis, 35% were lost at the time of the 6-month economic analysis. As not all women were followed up to 12 or 18 months, 71% and 86% of the data were missing for these analyses respectively. As it is prudent to give less emphasis to their associated results, we have placed the 12-month results, which also include costs associated with the baby, in Appendix 2 and an 18-month economic analysis was not reported.
| Costs estimate available | QALY estimate available | Paired cost and QALY available | Cumulative paired cost and QALY available | |
|---|---|---|---|---|
| 6-month analysis | 284 | 402 | 273 | 273 |
| 12-month analysis | 197 | 253 | 132 | 123 |
| 18-month analysis | 115 | 117 | 65 | 58 |
There were 63 clusters in the 6-month analysis, having from one to 12 cases (mean 4.3). The ICC for total cost at 6 months was 0.17 (95% CI 0.05 to 0.30) and for QALYs gained at 6 months it was 0.01 (95% CI 0.00 to 0.10). The distribution of costs showed the typical skew seen in most economic studies (Figure 19).
FIGURE 19.
Distribution of women’s costs at 6 months across all groups.
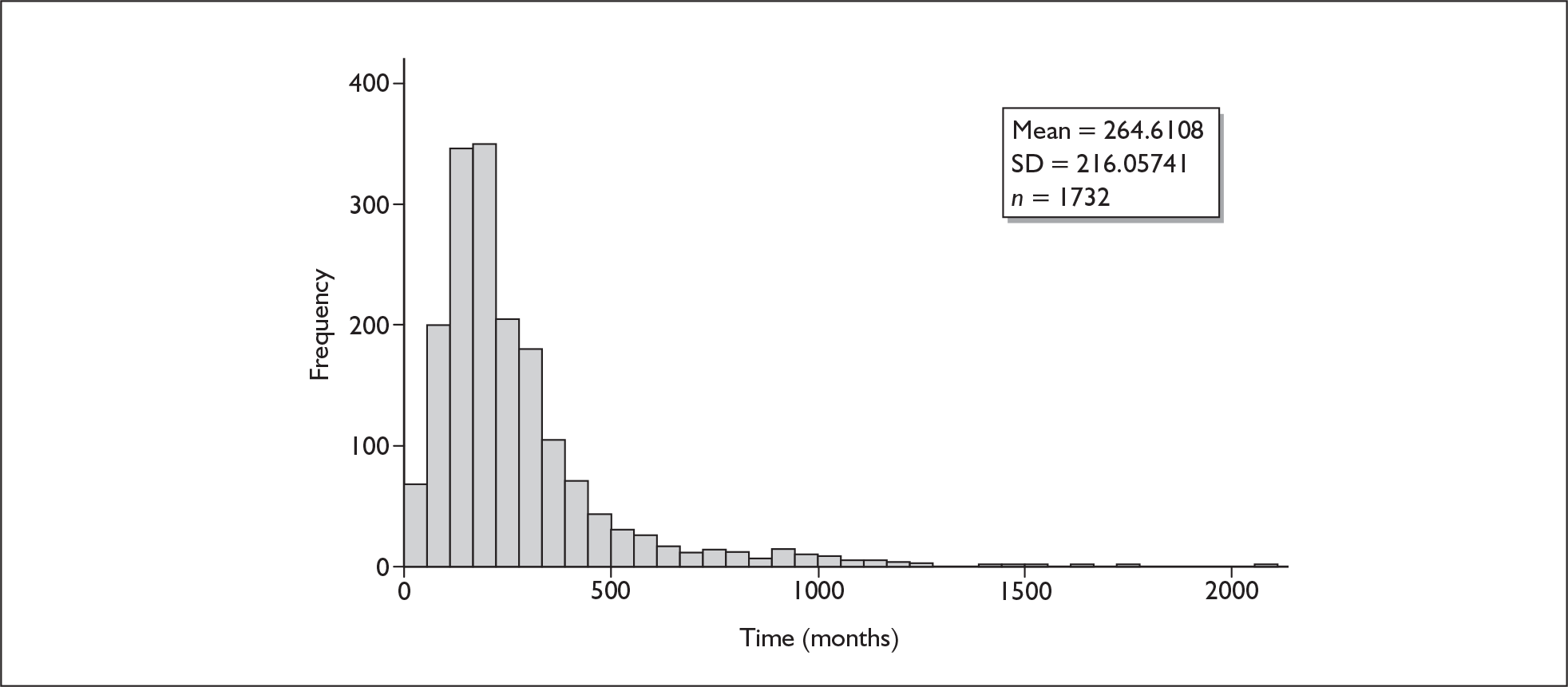
At 6 months there was no statistical difference in the total number of HV visits between the control and intervention groups (mean 8.5 versus 7.8, respectively) (Table 55). There was evidence that the content of the visits differed, with a reduction in the mean number of visits for the mothers in the IG (excluding those relating to PND); the IG women had a mean of 2.5 fewer visits. Also, the IG had double the number of visits for PND (mean 0.7 versus 1.4). Overall, the total mean time spent with the mother/baby by HVs was around 17 minutes lower in the IG, although this difference was not statistically significant.
| Item | Control mean (n = 78) | Intervention mean (n = 195) | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| HV total contactsa | 8.5 | 7.8 | –0.7 | –2.9 to 1.5 |
| HV contacts for babya | 6.8 | 6.1 | –0.7 | –2.3 to 1.0 |
| HV contacts for mothera | 5.3 | 2.8 | –2.5 | –4.0 to –1.1 |
| HV contacts for PNDa | 0.7 | 1.4 | 0.7 | 0.1 to 1.3 |
| Total HV minutes | 202.4 | 185.6 | –16.8 | –90.1 to 56.4 |
| GP contacts | 3.3 | 2.7 | –0.6 | –1.2 to 0.1 |
| Mother and baby unit days | 0.0 | 0.0 | 0.0 | |
| Community mental health contacts | 0.0 | 0.0 | 0.0 | –0.1 to 0.1 |
| Clinical mental health contacts | 0.0 | 0.0 | –0.0 | –0.0 to 0.0 |
| A&E attendances | 0.0 | 0.0 | 0.0 | |
| Social services contacts | 0.0 | 0.0 | –0.0 | –0.1 to 0.0 |
| Antidepressant prescriptions | 0.5 | 0.3 | –0.2 | –0.5 to 0.1 |
| Other prescriptions | 1.8 | 1.5 | –0.3 | –0.9 to 0.4 |
There were no A&E attendances or admissions to mother and baby psychiatric units within the sample, and other mental health contacts and social worker visits were rare. When combined with unit costs the overall cost of care for mothers at 6 months was £35 less in the IG although this difference was not statistically significant (Table 56). Mean costs in the CBA group were the lowest, followed by those in the PCA group, with the CG being the most costly (Table 57). The levels of significance of these differences were not tested statistically.
| Item | Control mean (n = 78) | Intervention mean (n = 195) | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| HV contacts | 260 | 245 | –15 | –110 to 79 |
| GP contacts | 100 | 83 | –17 | –36 to 3 |
| Mother and baby unit admissions | 0 | 0 | 0 | |
| Community mental health contacts | 1 | 1 | + 0 | –2 to 2 |
| Clinical mental health contacts | 2 | 1 | –1 | –4 to 3 |
| A&E attendances | 0 | 0 | 0 | |
| Social services contacts | 3 | 2 | –1 | –6 to 5 |
| Antidepressant prescriptions | 1 | 1 | –0 | –1 to 0 |
| Other prescriptions | 5 | 4 | –1 | –3 to 1 |
| Total cost | 374 | 339 | –35 | –137 to 67 |
| Item | Control mean (n = 78) | CBA mean difference from control (n = 116) | PCA mean difference from control (n = 79) |
|---|---|---|---|
| HV contacts | 259 | –27 | + 2 |
| GP contacts | 100 | –14 | –21 |
| Mother and baby unit admissions | 0 | 0 | 0 |
| Community mental health contacts | 1 | –0 | + 1 |
| Clinical mental health contacts | 2 | –1 | –0 |
| A&E attendances | 0 | 0 | 0 |
| Social services contacts | 3 | + 0 | –1 |
| Antidepressant prescriptions | 1 | –0 | –0 |
| Other prescriptions | 5 | –1 | –1 |
| Total cost | 374 | –45 | –21 |
The number of QALYs gained was greater in the IG (Table 58), although this was not statistically significant; comparing all groups the number of QALYS gained was greatest in the CBA group (Table 59). The position by which costs are lower and outcomes better in one group is often referred to as ‘dominance’. However, this does not take into account the sampling uncertainty associated with the cost and QALY pairs.
| Item | Control mean (n = 78) | Intervention mean (n = 195) | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| QALYs gained | 0.023 | 0.026 | + 0.003 | –0.004 to 0.010 |
| Total costs | 374.185 | 339.426 | –34.759 | –137.145 to 67.628 |
| Item | Control mean (n = 78) | CBA mean difference from control (n = 116) | PCA mean difference from control (n = 79) |
|---|---|---|---|
| QALYs gained | 0.023 | + 0.004 | + 0.002 |
| Total costs | 374 | –45 | –21 |
This uncertainty is best illustrated in the cost-effectiveness plane shown in Figure 20. At the centre of the cloud of points are the mean incremental cost and QALYs gained for the IG from Table 58 (–£35 and + 0.003). This shows that other combinations of costs and QALYs, which were consistent with the data, produced sample means in all four quadrants (i.e. positive and negative costs and QALYs in every combination). However, the preponderance of points were in the ‘south-east quadrant’ (i.e. lower costs and greater QALYs gained), and very few were in the ‘north-west quadrant’ (i.e. higher costs and fewer QALYs gained). For the other two quadrants the cost-effectiveness of the intervention is determined by how much we are willing to pay for a gain in QALYs.
FIGURE 20.
Plot of bootstrapped sample mean cost and quality-adjusted life-year (QALY) differences for at-risk women at 6 months. Note that positive values show the intervention group to be more costly or more effective in terms of QALYs.
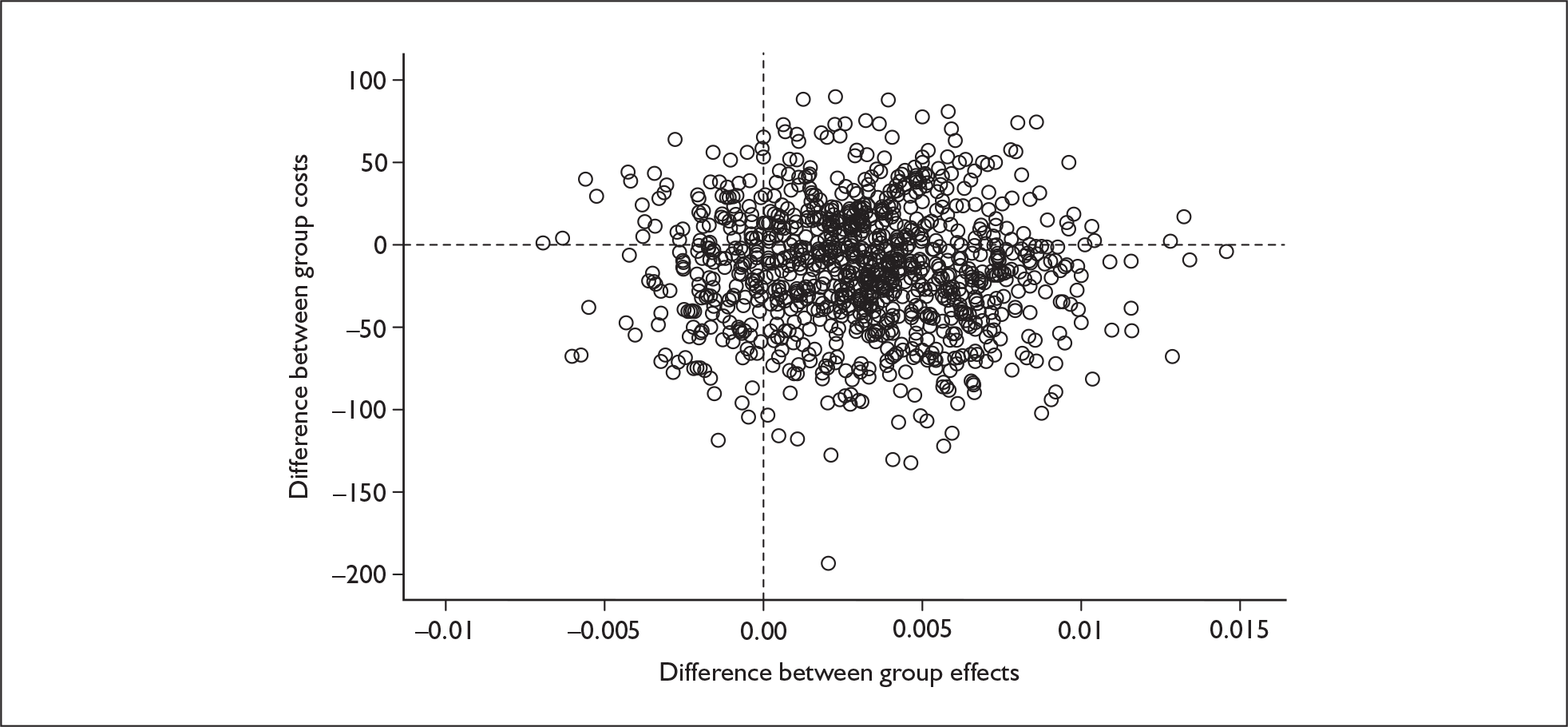
This information is summarised in a CEAC, shown in Figure 21. This shows the probability that the intervention was cost-effective at various ‘threshold values’ of a QALY. Even if we had placed no value on health gains, the intervention would have had a 65% chance of being cost-effective; this reflected the fact that 65% of observations in Figure 20 were in the southeast quadrant. In the range of QALY values between £20,000 and £30,000, the probability of the intervention being cost-effective was just over 80%.
FIGURE 21.
Cost-effectiveness acceptability curve for the intervention group at-risk women at 6 months. The y-axis shows the probability that the new treatment is cost-effective.
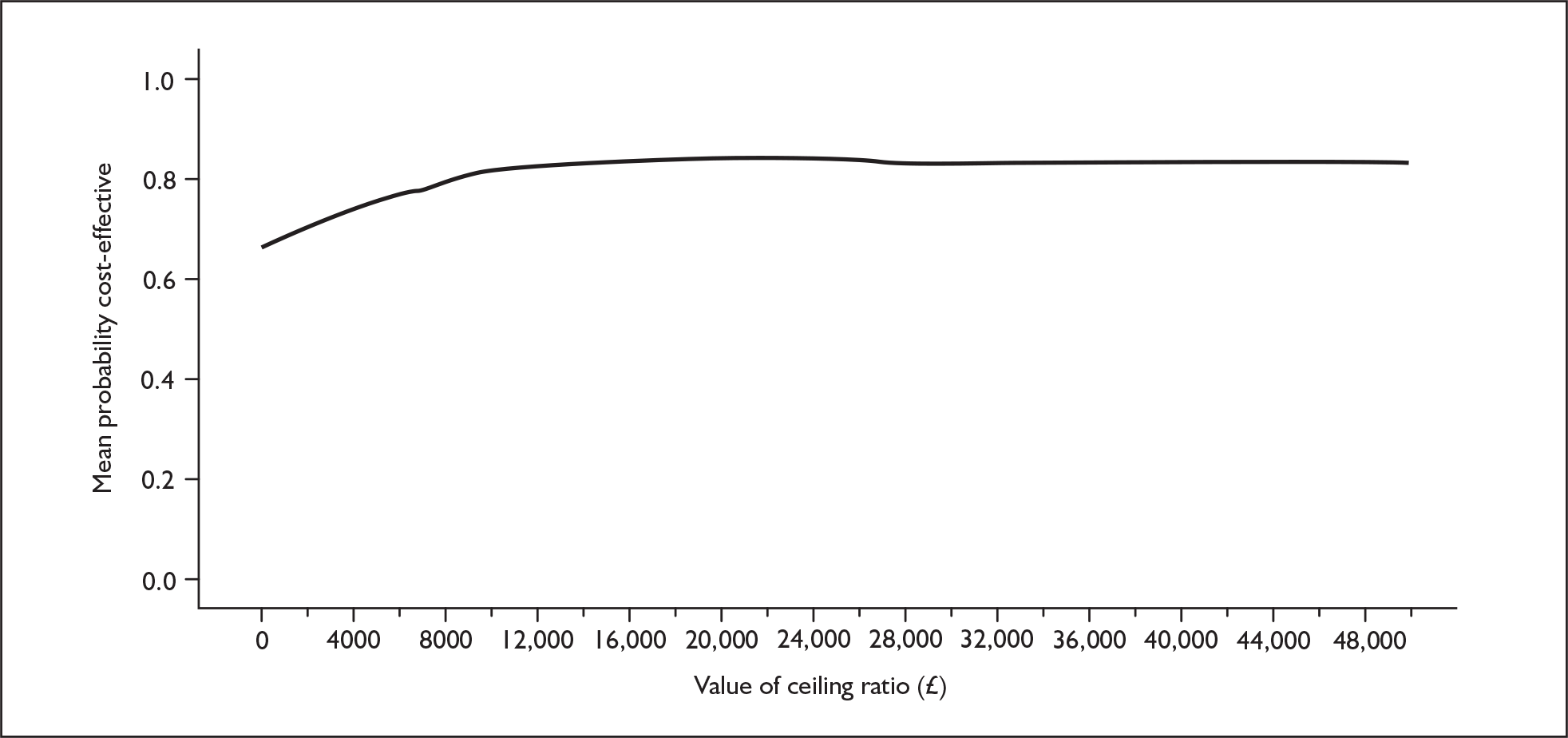
Comparing the CEACs for the control, CBA and PCA, the CBA had the highest probability of being cost-effective (Figure 22). In the range of QALY values between £20,000 and £30,000, the probability of CBA being cost-effective was just over 70%. Again, this reflected lower mean costs and higher mean QALYs gained. Figure 23 shows that the CBA-F group is the most likely to be cost-effective, although the difference between the curves is less prominent than before.
FIGURE 22.
Cost-effectiveness acceptability curves for at-risk women at 6 months: control vs CBA and PCA. The y-axis shows the proportion of simulations favouring each treatment. CBA, cognitive behavioural approach; PCA, person-centred approach.
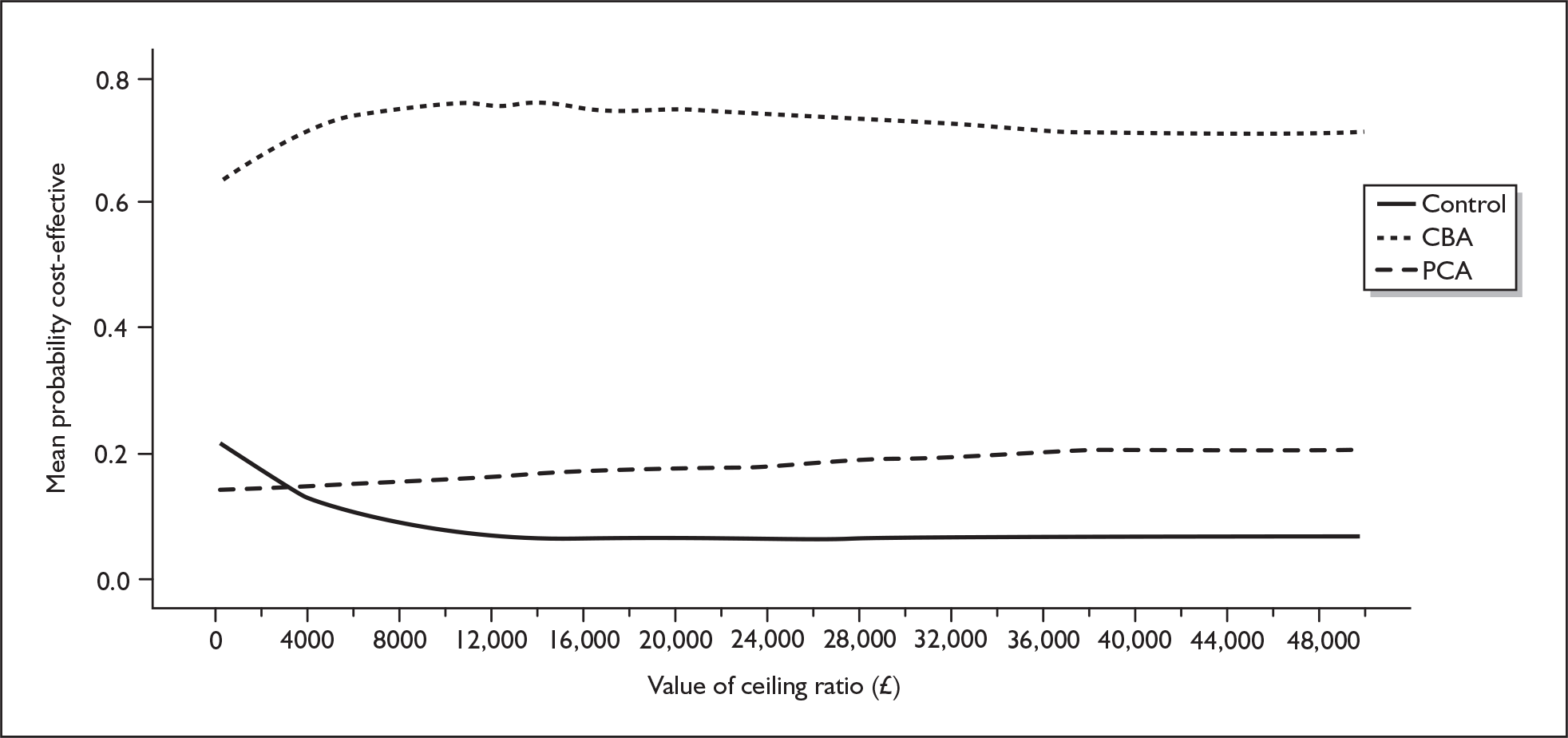
FIGURE 23.
Cost-effectiveness acceptability curves for intervention group at-risk women at 6 months: control vs CBA-F, CBA-P, PCA-F and PCA-P. The y-axis shows the proportion of simulations favouring each treatment. CBA-F, cognitive behavioural approach face-to-face group; CBA-P, cognitive behavioural approach postal group; PCA-F, person-centred approach face-to-face group; PCA-P, person-centred approach postal group.
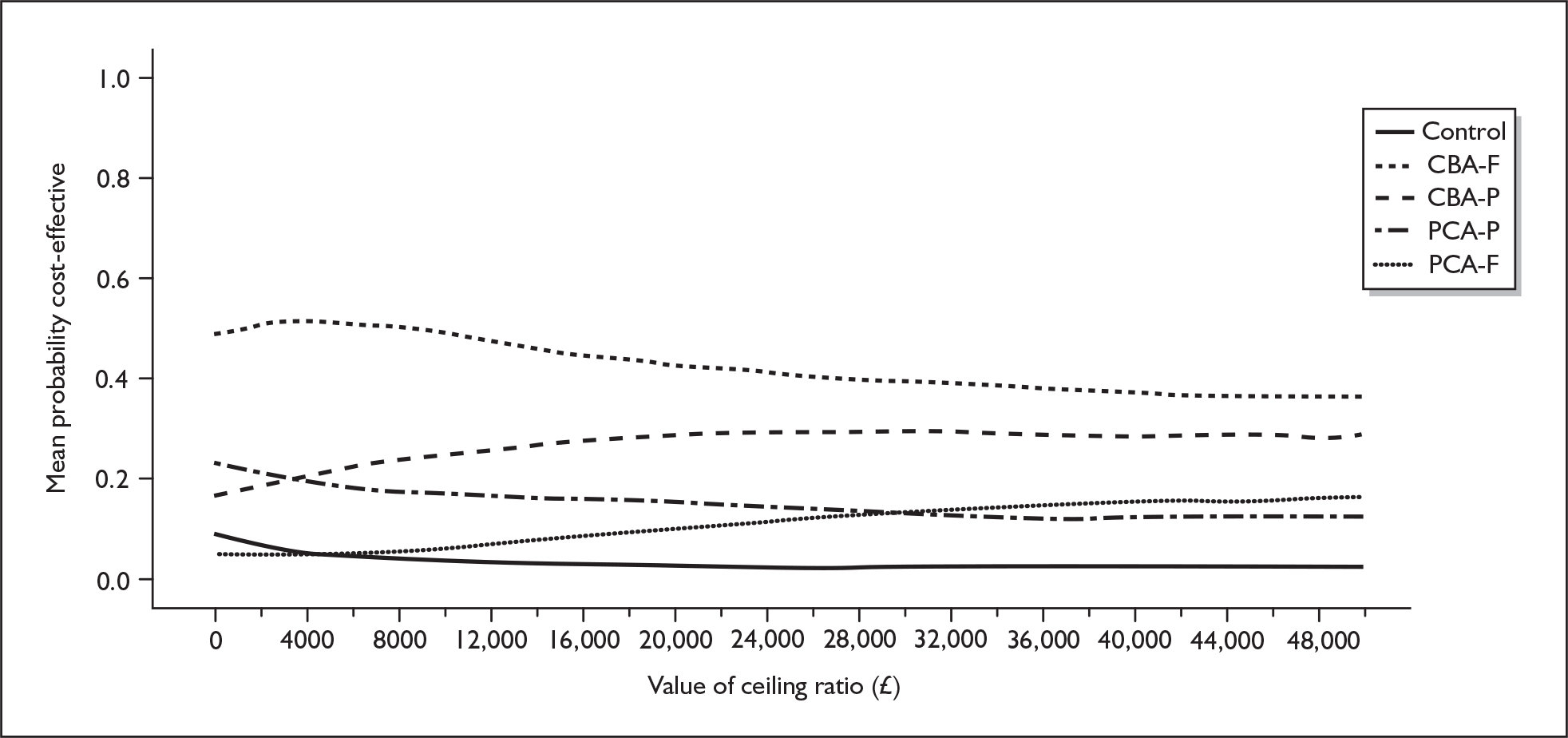
The imputation of missing data used a selection of covariates describing the baseline health of the mother and the baby and sociodemographic characteristics. Baseline EPDS scores were not different between at-risk women in the economic analysis subsample (n = 273) and those in the clinical analysis sample (n = 418) who had missing economic data (15.2 versus 15.2 respectively). Women in the economic analysis subsample were younger on average (30.4 years versus 31.7 years, p = 0.03) and there was also weak evidence of lower rates of previous PND (16.7% versus 24.5%, p = 0.07). Following imputation, the statistical analysis of total costs and QALY gains were repeated in STATA and the results are shown in Table 60.
| Item | Actual data, mean difference | 95% CI of the difference | Imputed data, mean difference | 95% CI of the difference |
|---|---|---|---|---|
| QALYs gained | + 0.003 | –0.004 to 0.010 | + 0.004 | –0.001 to 0.009 |
| Total costs | –34.759 | –137.145 to 67.628 | –40.088 | –99.300 to 19.124 |
All women at 6 months
A larger sample was available for the all-women economic analysis, although, again, many cases were lost to the analysis (Table 61). For the all-women analysis there were 70 clusters, having a range of 1–77 cases (mean 24.7). The ICC for total cost at 6 months was 0.20 (95% CI 0.13 to 0.28) and for QALYs gained at 6 months it was < 0.001 (95% CI 0.00 to 0.03).
| Costs estimate available | QALY estimate available | Paired cost and QALY available | Cumulative paired cost and QALY available | |
|---|---|---|---|---|
| 6-month analysis | 1797 | 2560 | 1732 | 1732 |
| 12-month analysis | 1279 | 1669 | 934 | 882 |
| 18-month analysis | 754 | 818 | 425 | 380 |
The IG had a lower mean number of HV contacts, although this was not statistically significant (Table 62). The IG women had a mean of 1.7 fewer visits per woman and, overall, the IG women used 10 minutes less HV time (95% CI –51 to 31). No significant differences were seen in the other cost components. Overall, the IG had lower mean costs and higher mean QALYs gained (Table 63), although neither was statistically significant. The CEAC showed a 99% chance of the intervention being cost-effective.
| Item | Control mean (n = 495) | Intervention mean (n = 1237) | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| HV total contactsa | 7.2 | 6.7 | –0.5 | –2.1 to 1.1 |
| HV contacts for babya | 6.6 | 6.2 | –0.4 | –1.8 to 1.0 |
| HV contacts for mothera | 4.0 | 2.3 | –1.7 | –2.9 to –0.6 |
| HV contacts for PNDa | 0.3 | 0.3 | + 0.0 | –0.2 to 0.2 |
| Total HV minutes | 143.9 | 133.9 | –10.0 | –51.3 to 31.4 |
| GP contacts | 2.7 | 2.4 | –0.3 | –0.8 to 0.1 |
| Mother and baby unit days | 0.0 | 0.0 | 0.0 | – |
| Community mental health contacts | 0.0 | 0.0 | + 0.0 | –0.0 to 0.0 |
| Clinical mental health contacts | 0.0 | 0.0 | + 0.0 | –0.0 to 0.0 |
| A&E attendances | 0.0 | 0.0 | 0.0 | – |
| Social services contacts | 0.0 | 0.0 | + 0.0 | –0.0 to 0.0 |
| Antidepressant prescriptions | 0.1 | 0.0 | –0.1 | –0.1 to 0.0 |
| Other prescriptions | 1.3 | 1.3 | + 0.0 | –0.3 to 0.3 |
| Item | Control mean (SD) | Intervention mean (SD) | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| QALYs gained | 0.028 | 0.030 | + 0.002 | –0.001 to 0.005 |
| Total costs | 271.868 | 251.900 | –19.968 | –75.729 to 35.792 |
When looking at the individual therapeutic approaches there appeared to be very little difference between the CBA and PCA groups in terms of costs and QALYs gained (Table 64). Figure 24 shows the CEAC at 6 months for all IG women, indicating that the cost-effectiveness of the intervention was close to ‘1’ for all reasonable QALY valuations. However, the CEAC in Figure 25 showed a marked difference. This result should be treated with caution as it is likely to be heavily influenced by clustering; this is accounted for in the univariate analysis of costs and QALYs shown in the tables but not in the bivariate analysis of cost-effectiveness shown in the figures.
| Item | Control mean | CBA mean difference from control | PCA mean difference from control |
|---|---|---|---|
| QALYs gained | 0.028 | + 0.002 | + 0.002 |
| Total costs | 271.856 | –18.450 | –21.830 |
FIGURE 24.
Cost-effectiveness acceptability curves for all intervention group women at 6 months. The y-axis shows the probability that the new treatment is cost-effective.
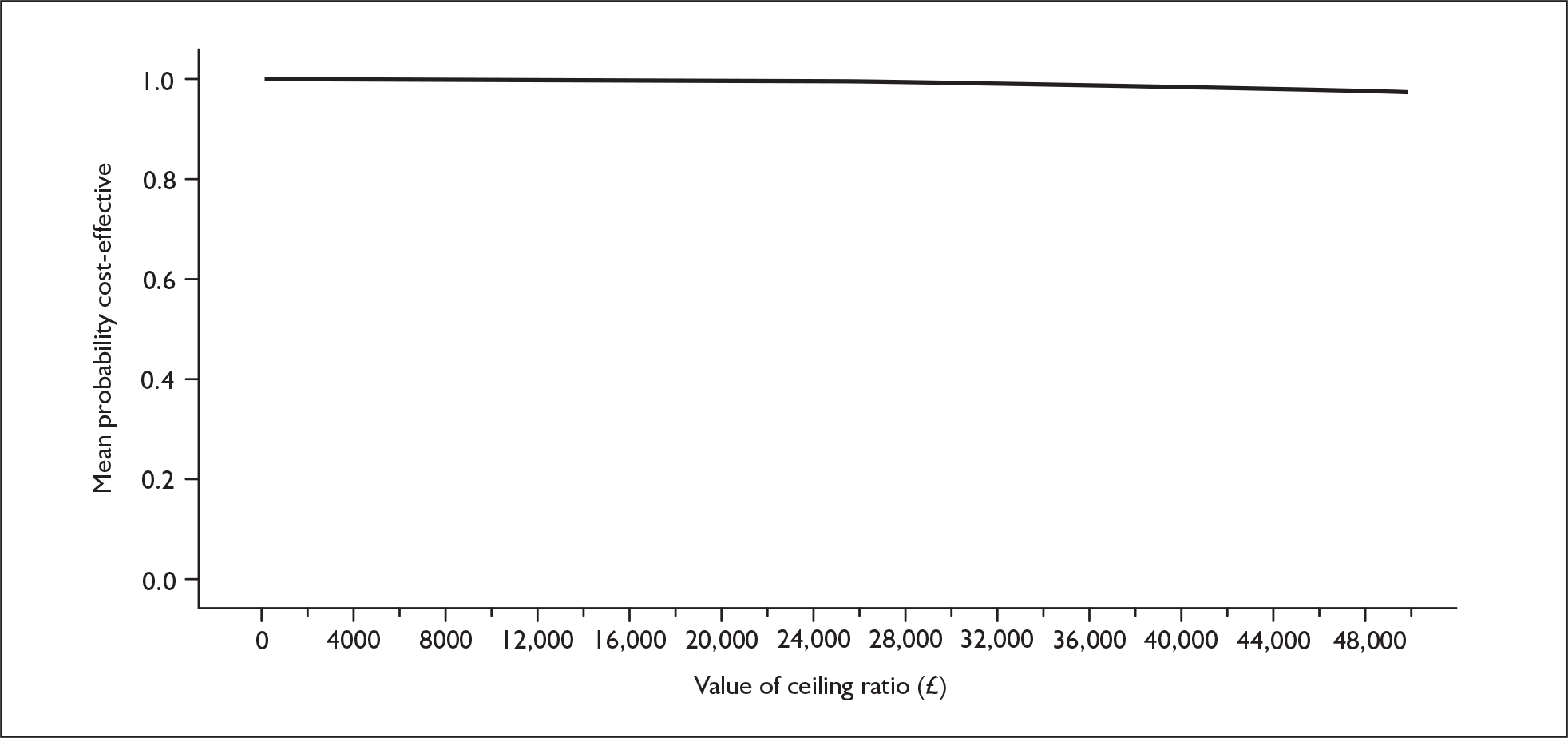
FIGURE 25.
Cost-effectiveness acceptability curves for all women at 6 months: control vs CBA and PCA. The y-axis shows the proportion of simulations favouring each treatment. CBA, cognitive behavioural approach; PCA, person-centred approach.
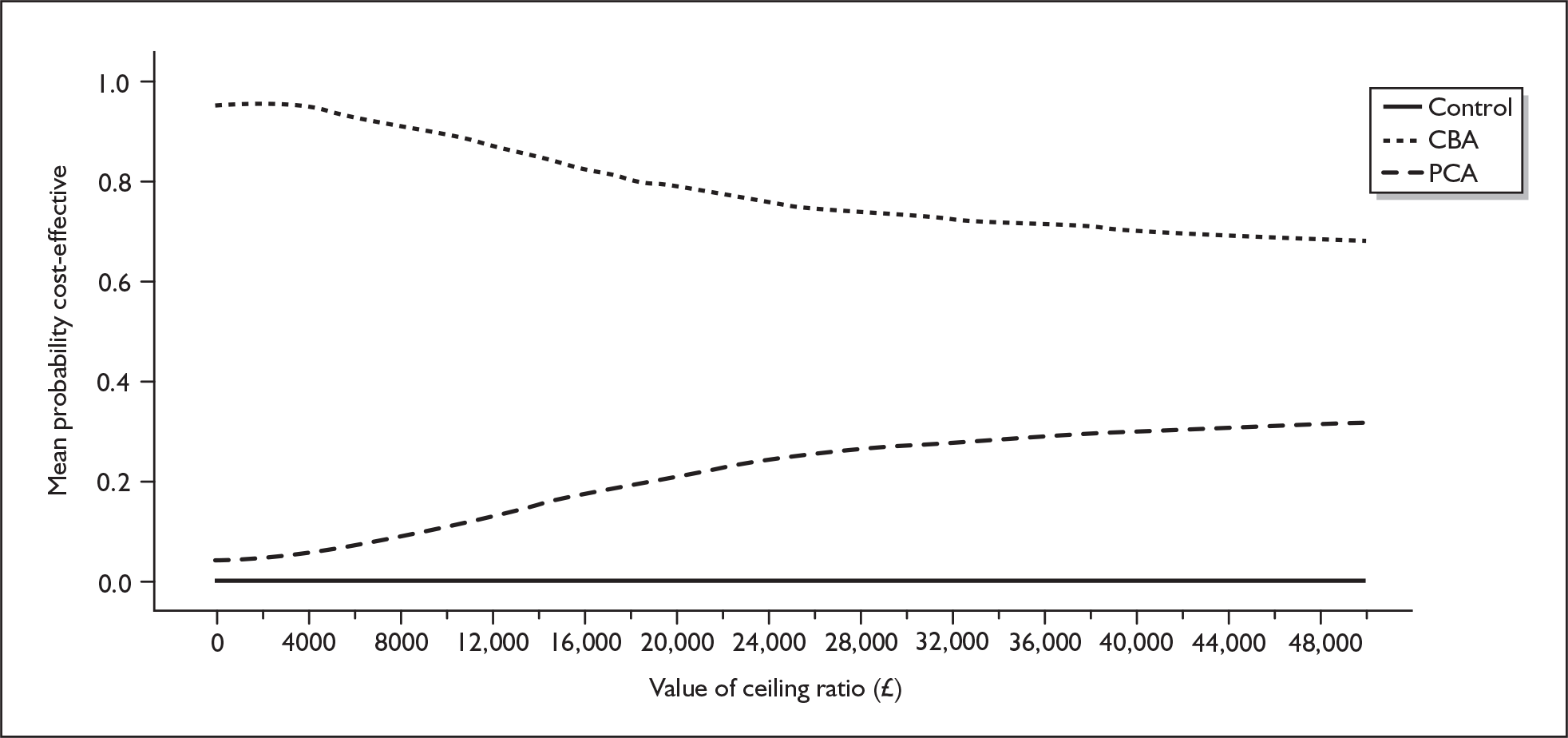
The imputation of missing data resulted in only slight differences in the costs and QALYs gained compared with the economic subsample (Table 65).
| Item | Actual data, mean difference | 95% CI of the difference | Imputed data, mean difference | 95% CI of the difference |
|---|---|---|---|---|
| QALYs gained | + 0.002 | –0.001 to 0.005 | + 0.003 | + 0.001 to 0.006 |
| Total costs | –19.968 | –75.729 to 35.792 | –36.035 | –68.423 to –3.646 |
The results of the cost-effectiveness analysis of the intervention at 12 months were severely weakened by the level of missing data, shown in Tables 54 and 61, and so they are shown in Appendix 2. No 18-month economic analyses are presented.
Discussion
The results show a consistent pattern of psychological approaches being cost-effective at funding levels used by NICE. This was achieved by lower mean costs and higher mean QALYs gained in the IG. Although these aggregate differences are not statistically significant in isolation, in combination they produce a high probability of the intervention being good value for money.
The findings were consistent across both the at-risk women and the all-women cohorts, and at the 12-month follow-up. CBA appeared to be the most cost-effective across all analyses when interpreting the CEACs, although these may be confounded by the clustering present within the trial (see Clustering, below).
To fully appreciate these results, however, we must consider the problems inherent in them. Three issues are of particular note: the impact of missing data, clustering and costing methods.
Missing data
There was a great deal of missing data as a result of several factors. First, the economic data collection depended on the HVs taking time away from work to manually abstract information from medical records. Second, to maximise the achievement of the required sample size for the 6-month primary analysis, the recruitment and 6-month follow-up phase was extended within the existing trial resources and time frame. Therefore, not all recruited women had reached their 12-month follow-up time and even fewer had reached their 18-month follow-up time before the trial closed and so they were not sent 12- and 18-month questionnaires. This effectively removed them from the complete-case cost-effectiveness analysis. Third, the economic data were produced from many individual observations; 6-month QALYs were produced from two utility estimates, 12-month QALYs were produced from three utility estimates, and 18-month QALYs were produced from four utility estimates. Cost data were even more susceptible, with total 6-month costs produced from nine cost components. In addition, cost-effectiveness estimates were calculated using pairs of cost and QALY data.
These problems have led economists to look at data imputation as a way of ameliorating such effects. Of these, multiple imputation appears to be the most promising approach, as it takes into account the uncertainty around the imputed data and can be adapted to incorporate the covariance between costs and QALYs. This approach was adopted in the PoNDER trial and applied to the 6-month data to generate results that were consistent with the main clinical analysis. These analyses showed few differences between those included and those excluded from the cost-effectiveness analysis and, in turn, did not change the economic results noticeably. This conferred greater confidence in the 6-month results as illustrated in the CEACs.
However, two issues remain. First, imputation was not undertaken for the 12- and 18-month analyses as it was considered that the higher rates of ‘missing data’ may have been more likely to reflect a non-random process. Given that imputation cannot account for systematic causes of missing data, it was thought that imputing data for the 12- and 18-month analyses would give undue credibility to these analyses. Second, imputation was used to generate data sets that were consistent with the main clinical analyses (at-risk women, n = 418, and all women, n = 2659). It would have been possible to impute a much larger data set based on all women randomised and for whom baseline data were available. This was not undertaken as it was thought that the interpretation of the results of the study as a whole was more robust when the basis of the economic and clinical analysis was consistent. It should be noted, however, that, as with the clinical analysis sample, those included in the economic sample had lower EPDS scores than those excluded (not shown).
Clustering
Within the economic analysis we took into account the inherent clustering of the data using cluster procedures available in STATA, and other economic evaluations based on cluster randomised controlled trials that have ignored this. 224 The high ICCs relating to costs in this study show that this is an important issue.
However, the cost-effectiveness analyses embodied within the CEACs presented do not take into account this clustering. No cluster randomised trial to our knowledge has carried this out, despite adjusting for clustering at the univariate level. 225,226 How this bivariate adjustment for cluster can be undertaken is not clear. Although it is possible to produce cost-effectiveness ratios for individual cases and estimate an ICC (which we have shown to be less than 0.001), this is of the average cost-effectiveness ratio and not the incremental cost-effectiveness ratio. Likewise, CEACs based on cluster means could be produced but they would need to be weighted and the basis of this weighting is open to debate.
Consequently, the CEACs may be biased by any cluster effect relating to cost-effectiveness. When considering this it is worth noting that the results shown in Table 58 and Figure 20 appear totally consistent in terms of the mean differences and the location of the sampled incremental cost-effectiveness ratio plots. This is also reflected in the shape of the CEAC, which reflects a ‘dominant’ intervention. Likewise, the results shown in Figure 22 appear to generally reflect the results shown in Table 59. It is only in the case of Table 64 and its associated CEAC in Figure 25 that large differences are noticeable between the cluster-adjusted results and the unadjusted cost-effectiveness analyses.
Finally, it should be noted that the mean estimates shown in the tables did take into account the clustering, and so the headline figures of (statistically insignificant) lower mean costs and higher mean QALYs gained in the IG remain unbiased.
Cost of training
The estimation of the cost of training in Table 52 is straightforward and, although there were assumptions regarding the intensity and frequency of retraining and clinical supervision, the estimate of equivalent annual cost in Table 53 was robust. The more uncertain aspect of training costs was how they were incorporated into the unit costs of the HVs.
The approach taken in this study was to allocate this cost in the same way as pre- and post-qualification training. This produced a cost per hour that was £2 higher for HVs trained in CBA versus PCA. This effectively allocated the cost across all women contacts, even those not related to PND.
An alternative approach would have been to allocate the cost of training only to visits related to PND. We did not adopt this approach, first, because the HV training also developed skills in systematically detecting depression, and so these were used outside the ‘therapeutic’ psychological intervention sessions. Second, there was some anecdotal evidence that the skills of HVs were used other than for women with PND. Table 62 shows that, among all women, an impact is identifiable on consultation numbers for problems relating to the mother, supporting our belief that the skills were being used in such a way that they had an impact on the broader HV caseload. This is consistent with our costing approach.
One important aspect of the HV training was that it appeared to have altered the pattern of health visiting contacts with the women in the IG. In particular, the overall level of visits reduced (although this was not statistically significant), with the greatest reduction in the visits relating to the mother that were not focused on PND. The level of visiting focused on PND was the same in both the intervention and control groups. This makes it difficult to identify an effect that is specific to the delivery of care relating to PND. Although the training seemed to have altered visiting patterns we can only speculate about why these changes occurred and their related therapeutic effects. So, although these changes were consistent with a hypothesis of training being associated with more targeted visiting and better quality of PND care, the study can not lend any evidence in support of this.
Other considerations
The economic analysis focused entirely on the differences in means, and consequently we used parametric tests. However, Figure 19 shows that the data were not normally distributed and so such parametric tests may have been prone to bias, especially in small samples. Alternative approaches, based on bootstrapping or non-linear transformations of the costs, are possible. However, the integration of these approaches with the cluster-adjusted analysis presented here is not straightforward and, also, with samples in excess of 200 (at-risk women) and 2000 (all women) the parametric tests should produce reasonably robust estimates. We felt that these sample sizes were such that a cluster-based analysis using parametric tests was the best approach to be adopted. Also, the CEACs were produced from (non-parametric) bootstrapped samples and therefore were not affected by the shape of the underlying distributions.
The focus on means may not help with other questions, which may be better tested using other methods, for example differences in the proportions of babies receiving full vaccinations or mothers receiving antidepressants. These issues were beyond the scope of the economic evaluation.
The tables of resource use show some interesting differences between the groups in terms of the nature of visits undertaken by HVs – more PND visits but fewer mother visits in at-risk women (see Table 55). Other analyses, not presented here, also show more specific differences between the CG and the IGs, and even between the CBA and PCA groups. The importance of these differences, and the reasons for them, are considered to be beyond the scope of this economic evaluation.
Although the main focus of the economic analysis was the costs and outcomes associated with the mother, with secondary analyses of costs associated with the baby, resource use and SF-12 data were collected for partners as well. It was envisaged that this would form a further sensitivity analysis around the analytical perspective of the study. However, incorporating these data into a ‘family-based’ analysis further compounded the missing data problems and so these analyses have not been presented.
Chapter 6 Qualitative interviews
Introduction
The purpose of the qualitative evaluation was to encourage women to discuss their experiences, attitudes and views in relation to the support that they received from their HV.
There has been a limited amount of research conducted to investigate how women perceive the support that they receive postnatally. 227 Having a baby changes a woman’s life and practical and social support from health professionals and family, friends and other mothers can reduce physical and emotional stress. Whether it is in the form of emotional, practical or simple reassurance, the way in which support is offered and delivered affects how it is perceived and experienced. 227
A woman may see her HV antenatally or they may meet for the first time around 11 days after the baby is born. Expectations about what the HV’s role will be and the characteristics of an ideal HV differ greatly. New mothers may have a broad range of expectations regarding the availability of advice on baby care, information about local services, help to deal with social problems, support for emotional problems and information about child protection or welfare issues.
The in-depth interviews
Semistructured interviews were carried out to supplement the quantitative data from the study by exploring in further detail women’s experiences of the care that they received during the postnatal period. An interview schedule was designed to elicit information about how the women were feeling and on how PND was assessed and discussed by health professionals and support was accessed and offered, and whether the women felt that the support that they received was beneficial or could be improved.
Method
Women who scored ≥ 12 on the EPDS were at risk of developing PND. As we had no systematic information on two successive administrations of the EPDS for the treatment as usual group, an inclusion score of ≥ 18 on the 6-week postal EPDS was selected to increase the equivalence of all groups. All women who scored ≥ 18 on the 6-week EPDS were sent a letter when their baby was 6 months old to invite them to take part in an interview at home. They were informed of the purpose of the interview and reassured about the confidentiality of the interview and that all transcripts were to be completely anonymised and no individual information was to be relayed back to the HVs, and then they were asked to sign a taping consent form. Transcriptions were imported into NVivo (QSR) software, which aids qualitative researchers to organise and examine large amounts of textual data.
Each woman was contacted at 6 months postnatally by a LC (AR, JS, KR, JF) to discuss the interviews and arrange a LC visit if the woman was interested in taking part. Women were reassured of confidentiality and advised that the interview would take about 30 minutes.
A total of 39 women were invited to participate, of whom six declined (too busy) and three could not be contacted as their address or phone number had changed. In total, 30 women agreed to take part; nine women from the CG and 10 and 11 from the CBA and PCA IGs respectively (Table 66). All women who agreed to participate were asked if they had a partner and, if so, if their partner would be willing to be interviewed. Sixteen partners agreed; five from the CG and four and six from the CBA and PCA IGs respectively. All participants were compensated for their time with a £15 voucher.
| PCA | CBA | Control | Total | |
|---|---|---|---|---|
| n | 11 | 10 | 9 | 30 |
| Age 18–25 years, n | 2 | 2 | 3 | 7 |
| Age 26–35 years, n | 6 | 5 | 4 | 15 |
| Age 36–45 years, n | 3 | 3 | 0 (missing n = 2) | 6 |
| Single parent | 1 | 1 | 1 | 3 |
| Partnered | 6 | 3 | 1 | 10 |
| First child | 7 | 8 | 6 | 21 |
| GP prescribed antidepressant | 6 | 5 | 7 | 18 |
Template analysis
A qualitative ‘template analysis’ approach was used228 in which themes are elicited from the data through an iterative process. This method was the most appropriate as it allows an a priori template of particularly important themes to be applied to a subsample of the data, to answer specific questions first and then to allow further, richer detail to emerge from the data. Templates are made up of hierarchically organised codes; the highest level codes are the broad themes whilst lower level codes are more narrowly focused aspects of the broader theme. The prespecified template focused on the original themes of women’s experiences of the EPDS and interventions (Figure 26 and Box 1).
Final template
-
Experience of depression
-
(a) Past history:
-
(i) previous depression (ii) previous postnatal depression
-
-
(b) Severity of current subjective depression:
-
(i) no low mood (ii) baby blues (iii) postnatal depression
-
-
(c) Assessment:
-
(i) EPDS (ii) other
-
-
(d) Life circumstances:
-
(i) feeling isolated
-
-
-
Experience of postnatal support
-
(e) Communication:
-
(i) inconsistent information from health visitors (ii) raising awareness of postnatal depression and what help is available
-
-
(f) Health visitor:
-
(i) practical
-
(ii) structured intervention:
-
(a) cognitive behavioural approach (b) person-centred approach
-
-
-
(g) GP – medication:
-
(i) time taken (ii) how helpful it was (iii) breastfeeding, reassurance
-
-
(h) Other:
-
(i) partner (ii) other family members (iii) friends (iv) Sure Start
-
-
(i) Help-seeking behaviour:
-
(i) contacting GP (ii) contacting health visitor (iii) reluctant to admit problems to health visitor
-
-
(j) Ideal support
-
FIGURE 26.
Initial analysis template for the PoNDER trial
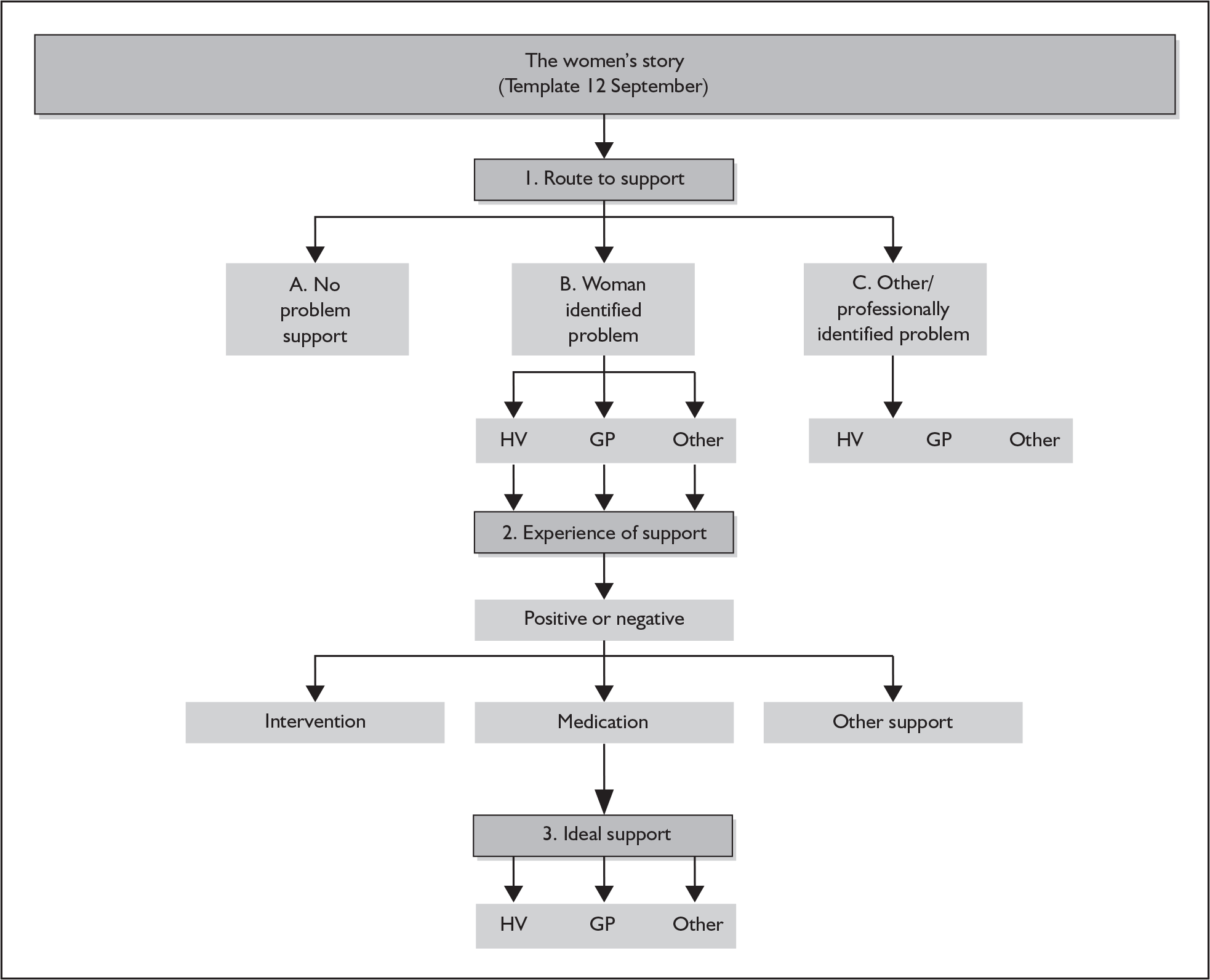
Three researchers developed the codes collectively and modified them after each successive reading of the interview transcripts. They then produced a final structured representation of themes, and the relationships between them, which adequately reflected the whole data set (Box 2).
-
Theme 1 – Women’s experiences of the postnatal period
-
1.1 Adapting to the new baby
-
1.2 Pressures of motherhood
-
1.3 Breastfeeding
-
-
Theme 2 – Help seeking
-
2.1 Help-seeking styles
-
2.2 Barriers to help
-
2.2.1 Presenting a coping image
-
2.2.2 Perception of the health visitor
-
2.2.3 Perceived role of the health professional
-
-
-
Theme 3 – Professional roles
-
3.1 Completing the EPDS
-
3.2 Information on postnatal depression
-
3.3 Relationship between the woman and the professional
-
3.4 Woman’s perception of the professional role
-
-
Theme 4 – Intervention or support
-
4.1 Person-centred approach
-
4.2 Cognitive behavioural approach
-
4.3 Treatment as usual intervention
-
4.4 Non-intervention support
-
4.5 Informal support
-
4.6 Ideal support
-
Results
The interviews were extremely successful in producing rich, complex and often lengthy accounts of women’s experiences of the postnatal period. The results concentrate on the key findings relating to the themes in the coding template. The ‘intervention or support’ theme addresses the central research question. All of the women have been given a unique identifying number (id) to protect their anonymity. As is clear from other sections of the report, typically the women who were not offered the intervention were in receipt of other services or support (Table 67).
| PCA (n = 11) | CBA (n = 10) | Total | |
|---|---|---|---|
| Offered intervention | 5 (4 antidepressants) | 5 (4 antidepressants) | 10 (48%) |
| Not offered intervention | 5 (3 antidepressants) | 3 (0 antidepressants) | 8 (38%) |
| Declined intervention | 1 (0 antidepressants) | 2 (1 antidepressant) | 3 (14%) |
The central focus of the interviews was the women’s reported accounts and views of the support that they had received from their HV during the 6-week to 6-month postnatal period. In the following sections the following abbreviations are used: I, received PCA/CBA intervention; NI, no PCA/CBA intervention offered; DI, declined PCA/CBA intervention; control, treatment as usual. The first theme emerged as a result of the interviewees discussing how they were feeling physically and emotionally.
Theme 1: Women’s experiences of the postnatal period
The theme describes how the women were feeling when their babies were 6 weeks to 6 months old, including reported signs that all was not well. Table 68 shows the nature of the reported negative feelings. Some women reported multiple symptoms. There were other factors affecting mood for some women, including physical illness, for example infected episiotomy and mastitis, the July 2005 bombings in London, illness of an elderly parent and a child’s ill health. Two of the women mentioned recent bereavements:
I lost my mum in the January and found I was having him in the June . . . . I think that is what it was.
PCA–NI, id 8
Yeah, deaths and that in t’ family.
Control, id 9
| Signs | Example |
|---|---|
| Crying | ‘There were days or a couple of weeks when I would be crying all the time’ (CBA–NI, id 1) |
| Feeling unable to ‘cope’ | ‘Not being able to cope if he was crying’ (PCA–NI, id 2) |
| Lack of sleep | ‘If you’re not getting any sleep everything gets on top of you and that’s how I felt’ (PCA–I, id 3) |
| Low mood | ‘I felt really, really depressed’ (CBA–NI, id 4) |
| Worrying | ‘Worrying about things that are totally irrelevant’ (PCA–I, id 5) |
| Anger/irritability | ‘You’re being angry and violent and this isn’t like you’ (CBA–I, id 6) |
| Feeling isolated | ‘I didn’t know anybody in the area, I did feel quite isolated I must say’ (PCA–I, id 3) |
| Feeling unsupported | ‘And I was really upset about that [partner referring to her hormones] and I thought “he doesn’t really understand at all” ’ (Control, id 7) |
Adapting to the new baby/loss of identity
Many women across all of the groups made comments about adapting to having a baby, commenting on their new role and new set of circumstances. This often emerged as a loss of role and identity. This was more frequent among first-time mothers. A sense of finality to the ‘change’ of becoming a mother also emerged from the data:
You suddenly turn into [baby’s names] mum instead of a human being.
CBA–I, id 10
That’s when I started crying for no reason . . . that I just couldn’t cope anymore and that life wasn’t fun and I wasn’t getting no enjoyment out of life at all and all it seemed to be is the chore of like housework, looking after the baby, sleepless nights, not getting to see friends anymore, not going out and just being a mother and a completely different life to what I’d had.
CBA–I, id 10
I did feel like I can’t cope . . . . You know you sort of feel like you might lose that part of you which is really you because suddenly you’re just changing nappies and just looking after this thing that you produced.
PCA–DI, id 11
I was a bit worried, I think all women think this, that it was a mistake in having a baby, because now my life is dramatically different, I couldn’t walk properly and I had this little thing to look after and I was thinking ‘Crumbs, what have I done?’, and there’s no way back.
PCA–I, id 13
Women, who already had a child, or children, also mentioned themselves and older siblings having to adapt to the newborn: ‘A few problems with me other child . . . she’s had a lot of attention and it was the backlash on that which I found hard to cope with’ (CBA–I, id 12).
Pressures of motherhood
Closely related to the above topic, many of the women felt that they had to conform to some sort of ‘ideal’ of motherhood and felt under pressure if they did not feel that they were achieving this ‘ideal’:
I wanted to be so perfect and I wanted to do everything well and I didn’t know how to do it or what to do.
PCA–DI, id 11
I suppose my anxiety sort of came out like that really . . . wanting to be perfect and not really being able to cope at times.
PCA–DI, id 11
Breastfeeding
Another frequently mentioned issue was breastfeeding. Many women reported that it affected their self-esteem and views of themselves as a mother:
I’ve got to be there to feed her all the time so I never get a break from her.
CBA–NI, id 15
I found that quite worrying that they wanted to keep an eye on her [the baby], I felt like it was my fault. I couldn’t feed her enough and it was my fault that she wasn’t putting on enough weight.
PCA–I, id 3
I was struggling with breastfeeding because I had mastitis twice and so feeding her was really very difficult and consequently she was quite unhappy . . . so she was feeding every 2 hours and 1 hour of that 2 hours she was feeding so I was physically absolutely exhausted, in pain and obviously that leads to being quite emotional.
CBA–I, id 16
You’re constantly in demand.
CBA–I, id 17
I really struggled, I was miserable, mainly to do with breastfeeding.
CBA–NI, id 18
For example, on the subject of breastfeeding, I never found [it] very easy . . . . And because I didn’t do it for as long as obviously is recommended . . . I did feel like I’d failed in lots of ways.
Control, id 14
Every feed was an actual nightmare so I don’t think that helped cos I wasn’t getting any sleep at all either so I just think of them as my very dark days.
Control, id 7
This woman also highlighted how having a difficult time breastfeeding affected her mood and her relationship with her son: ‘Sometimes I feel like I could just hate him and I just want to get away from him because just constantly so difficult to feed’.
Theme 2: Help seeking
Help-seeking styles
There appeared to be several processes underlying help-seeking behaviour for some women, in particular (1) self-recognition – women who were aware that they needed help and sought help, (2) those that responded to advice to seek help from others and (3) those that sought help for various other things, that is, their children’s illnesses, as a ‘way in’ to seeking help for themselves.
Because I was so desperate that I admitted that I needed help and I received it.
PCA–I, id 20 (this woman had had PND with a previous child)
I was starting to think, you know, hurt him rather than myself because you just want him to shut up and then you think about shaken baby syndrome and you think . . . oh, God that could be me. I can understand how people do that now. It’s not that they’re a bad parent. It’s just that they’re not coping and if I started to think badly of him then . . . I need help.
PCA–I, id 17
Driving on the M25 and I’ve actually had the thought as regards ‘Wouldn’t it be easier if I just drove off?’ and at that point I thought ‘No, something’s not quite right here, don’t be an idiot’.
Control, id 21
Women also accessed help via their children, indicating a difficulty in being explicit to health professionals and using other reasons to initiate contact.
I’d had a Caesarean section . . . so I couldn’t drive for 6 weeks . . . so I called him [GP] out . . . I called him for [baby’s name] but I did want to talk to him at the same time . . . but I used the excuse of him coming to see [baby].
CBA–NI, id 22
I had to take the children to the doctor . . . and she picked up that I wasn’t well or she said ‘How are you?’ and then of course it all came out.
CBA–NI, id 5
It was most frequently reported by women that other people’s prompting initiated the help-seeking behaviour:
It was sort of my partner saying to me ‘Right if you don’t go I’m basically making you an appointment, you are going, don’t sweep it under the carpet, you know you can’t just keep feeling like this’.
CBA–I, id 12
Only two women mentioned health professionals:
Oh yeah, I think if I hadn’t spoken to my health visitor when I did I perhaps wouldn’t have ended up going to the doctors and realising what was wrong.
Control, id 14
She [midwife) got me an appointment with the GP.
Control, id 25
Barriers to help
Presenting a coping image
One of the main barriers seems to be that the women wanted to present a ‘coping’ image, having a fear of seeming unable to look after their child and of what others might think:
You worry that you think that the health visitor might think you’re not coping.
CBA–I, id 10
I didn’t want anyone’s help to be honest after I had [previous child]. I was so frightened that people would think I couldn’t cope and take her off me.
PCA –I, id 20
I remember thinking ‘I don’t want her to think I’m not coping’, which is stupid really because I wasn’t.
CBA–I, id 17
This woman went on to say:
Especially . . . you’re stood in the middle of the surgery, with like six mums around you with six newborns and you just think well I’m hardly gonna turn round and go, you know, ‘I’m really not f***ing coping, help’.
I felt like terrible for the way I was feeling and I thought if I go tell somebody they must think, ‘She can’t look after her children’.
Control, id 24
Before when I was stressed out I didn’t want to speak to anybody about it because I didn’t want people to think, ‘I can’t do this’.
CBA–NI, id 1
Perception of the health visitor
Sometimes a major barrier to help was the woman’s perception of a particular health professional. This highlighted the importance of the professional’s openness to emotional issues:
So I think she wasn’t as person-centred and she didn’t really have the people skills to manage, you know, she could have, sort of offered advice and support in a much more supportive way instead of ‘Well, you haven’t done this, you haven’t done that’ and her tone was all wrong as well.
PCA–DI, id 11
One woman found that her particular HV was the barrier to support:
I did ask for support but I didn’t really get any. The HV responded, ‘Well you seem like you’re doing alright’, which kind of closes it off doesn’t it then.
Control, id 7
For some women their perception of their HV led them to decline the offer of a formal intervention: ‘I didn’t feel like talking to her. I didn’t really know her that well so . . . ’ (CBA–DI, id 4).
Perceived role of the health professional
Women commented on the perceived role of the health professional:
I didn’t feel it was something I wanted to discuss with the GP . . . I look at GPs as practical, physical health not, and I never used a GP in an emotional way . . . I just perceive them to be factual scientists.
CBA–I, id 16
Theme 3: Professional roles (experience of care from professionals)
Completing the EPDS
The interviewers asked the women about the ‘questionnaire’ (i.e. the EPDS) that the HVs used. However, there was no consensus and this seems to reflect a range of administrative styles:
I think it took us about an hour going through it, but I think the reason for that was because I was very low at that point and so she was making sure that she was understanding what was going on and how I was feeling.
CBA–I, id 16
She definitely came out and did a questionnaire but it was very informal . . . I don’t think I realised she was doing a questionnaire until I saw she was ticking boxes or whatever.
CBA–NI, id 22
It would appear that it is not always clear that a questionnaire is being administered, as no explanation had been given.
Only one woman was entirely negative about the scale: ‘I just felt it was stupid because . . . I just said sort of yes, no, yes, no, didn’t go into any detail, couldn’t be bothered’ (PCA–I, id 5).
Another woman commented on the same issue: ‘I think if they do pick you on the wrong day I think you do get a crazy score’ (PCA–NI, id 8). She went on to say:
I think it’s quite difficult to open up, to admit that you’re feeling that bad and at least when [HVs name] came with the Edinburgh scale, at least somebody knows that at that particular moment you feel dreadful.
This highlights the utility of the EPDS as a chance for the women to discuss their feelings if they choose to do so. Some women may not realise how low they are until they complete the questionnaire:
I started to do the questionnaire and that’s when I realised . . . . It told me that day when I sort of answered the questions as truthfully as I could that, you know, I just wasn’t feeling very good at all.
CBA–I, id 12
One woman from the CG did not do the EPDS and commented the following: ‘No nothing, I don’t think there were ever any real focus on how I were coping or not coping’ (Control, id 7).
These comments demonstrate that the interviewees also appreciated the EPDS because it shifted the focus onto their feelings rather than concentrating on the baby.
Information on postnatal depression
The women and their HVs were involved in a trial on PND and so the women were asked about the sort of information that they were given by their HVs and in some cases their GPs. Variations in how well informed women were about PND range from it being well defined to having no information at all:
At the antenatal classes that we had . . . she did mention it . . . she did say it was quite normal and it does happen and it happens generally to the most unlikely people, but she didn’t necessarily dwell on it but made us aware that it was something that people do naturally suffer from.
CBA–I, id 16
She [HV] did give me a leaflet which told me the signs to look out for if you were suffering from postnatal depression.
PCA–I, id 13
She [HV] did tell me exactly what it was all about [PND].
Control, id 24
Well she gave me leaflets on it, talked to me about how common it is and you mustn’t punish yourself for having this. You can’t help how you are, it’s just one of those things that unfortunately happens. And if you’ve got a predisposition to be depressed like I already have then you are a lot more likely to get it.
PCA–I, id 20
One of the women (id 12) had good information from both her GP and her HV. Other women had little or no information from health professionals and some professionals were reported as using the terminology ‘baby blues’:
I didn’t really know much about it to be honest . . . nothing from a . . . professional point of view.
PCA–I, id 3
No . . . I’m pretty sure they didn’t [explain about PND].
CBA–NI, id 22
This woman’s GP called it ‘baby blues’ even though she was prescribed antidepressants.
Erm, she [HV] didn’t say much really [about PND].
Control, id 9
She (GP) really didn’t explain much about it . . . I explained my feeling, and she says, ‘Right, well, sounds like you’ve got postnatal depression’ and put me on some medication. And really that was it. She didn’t explain or anything really.
PCA–I, id 26
One woman reported that she was told by her HV, ‘Oh, you’ve got baby blues. Pull yourself together. Get on with it’and the woman thought it was ‘Just disgraceful’ (PCA–DI, id 28). This may have contributed to the woman declining the intervention. However, this woman did get the support she needed from her GP.
Relationship between the woman and the professional
The perceived ‘personality characteristics’ of professionals were crucial in determining whether women had a positive or negative experience of the postnatal period.
Positive comments on the relationship
Those women who had received an intervention were extremely positive about their relationship with their HV and were encouraged to comment on how this relationship had changed over the time span of the intervention:
Very good, absolutely like a really good honest relationship and I feel very like I trust her [HV] and that, you know, that I can confide in her and talk to her really about everything that’s sort of like going on since I’ve had the baby.
CBA–I, id 10
So she [HV] was like supportive and kept in contact quite a lot, ringing me to see if I was ok and if I needed to talk, she was there sort of thing.
PCA–NI, id 30
This woman felt that continuity was important:
I always ask to speak to [HV] because I know her and it’s easier really if you know somebody.
PCA–NI, id 30
Before [intervention] I was really quiet and I owe so much to her [HV] and its really brought out of me to be open and everything.
PCA–I, id 31
A positive comment from a CG woman who was well supported by her HV: ‘I felt I could talk to her because I’d built a relationship with her when I’d had previous child’ (Control, id 24).
Negative comments on the relationship
All of the negative comments on the relationship with the HV were from women who had not been offered formal sessions of support or had declined and from women in the CG who perceived that they had received little or no support from their HV. All of these women were more positive about their relationships with their GP:
I don’t feel I had any support either as a new mum or emotionally or whatever else, I don’t think there was a relationship, to the point where both [partner’s name] and I would dread her coming out to weigh him . . . and as I say, at the point where we were told . . . that we’d had a new HV, thank God for that, hooray.
Control, id 21
If I had another problem I would go to the doctor rather than see the health visitor. I did find the doctor more sympathetic but then I did open up more to the doctor.
PCA–NI, id 8
At first I was using them [HVs] as I thought they were meant to be used, which was asking questions all the time and checking things out with them to make sure I was right, you know basic people to talk to as some kind of support. To at least make me feel as though I was doing things right, and if I wasn’t how to change it and do it slightly different. But then I soon realised that they weren’t giving me any help whatsoever.
PCA–DI, id 28
This woman went on to describe HVs as being ‘more like your Nanna telling you what to do’, and was very positive about the support from her GP.
Another woman also preferred the support of her GP: ‘She is alright to say she is a HV but she is not the best I’d say’ (CBA–NI, id 4).
Woman’s perception of the professional role
This section looks at how the role of the HV is perceived by women and it is particularly interesting to note the comments by the women who have had the intervention on how their preconceptions had changed.
One woman said:
I thought it was just snooping . . . that’s what I thought health visiting was. It’s trying to see if you’re doing anything wrong with your children for social services . . . I didn’t realise that it’s . . . not about that, it’s about keeping families together, not tearing them apart.
PCA–I, id 20
This view was echoed by another woman (CBA–I, id 10) who stated that before she would not have approached a HV for help because, ‘You worry . . . you think the HV might think you’re not coping’. She highlights the fact that going to her doctor felt more ‘comfortable . . . cos obviously I’ve been to him all my life’. However, following the intervention she goes on to say, ‘Had I known the support I would have got from the HV I know I would have done things differently’.
Another stated:
Oh I think before the visits you don’t really know them . . . if your baby’s alright and you’re alright . . . you only see them at assessments and things . . . I now know in the future if I’ve got any concerns, you know, I could just pick up the phone . . . yeah more confident towards them.
CBA–I, id 12
However, one woman would have liked more information about the role of the HV to facilitate appropriate access to the service.
There were comments on not knowing the function of the HV:
I don’t really know what their job is . . . . Nobody gave me like the parameters of this role of the HV and so, I think if that happened then you’d . . . know what the function was . . . and sort of be able to use them better.
PCA–DI, id 11
The reported comments suggest that perhaps women should be given clearer information on the role of the HV.
Theme 4: Intervention or support
The women who received one of the two psychological interventions reported very positive experiences overall, placing particular emphasis on the importance of having the opportunity for one-to-one discussions with the HV. It appears that from the women’s point of view the interventions have not only been ‘acceptable’ but also very successful.
Person-centred approach
Three of the five women made a comment on the nature of the approach. The HVs and the women tended to refer to them as ‘listening visits’. For one woman it was very appropriate for her:
Yeah . . . she did help me through; she made me understand why I was feeling like that . . . I don’t think I would be feeling like I am now if [HV] didn’t have come . . . because I have mainly talked I think it’s helped me in the fact that I can understand what I’m feeling rather than, er getting suggestions from other people . . . . It’s helped me work out what I should do to make myself feel better.
PCA–I, id 29
Other women commented on the benefits of the intervention:
I owe so much to her [HV] and it’s really brought out of me to be open and everything.
PCA–I, id 31
I think if my HV hadn’t been phoning me frequently and coming to visit me, I think it made the difference between tipping over into being depressed and just being a little bit miserable and eventually pulling myself together. So I did think it made a huge difference.
PCA–I, id 13
[I] was grateful for that one-to-one time . . . [it] was very valuable for me and [baby].
PCA–I, id 3
This woman went on to describe the one-to-one time as being: ‘For a purpose, specific, and an opportunity to talk about my issues’.
However, one woman found the approach more difficult:
She [HV] explained about listening visits . . . but I actually struggled to talk cos I’d rather be challenged. I’d rather be asked questions . . . so I did explain to [HV] after the seventh one [visit] that I’m struggling to talk so it’s not benefiting me . . . even though [HV] were ever so good.
PCA–I, id 26
This final comment perhaps shows the need for tailoring of any therapeutic approach to the needs of the individual.
The two women who were not offered the intervention had the same HV. One woman (PCA–NI, id 32) reported that she was told, ‘If you don’t feel any better, go and see your doctor’, whereas the other woman (PCA–NI, id 8) found the HV ‘helpful’ when it came to practical advice but didn’t see her as someone she would turn to for help with regards to ‘feeling low’.
Cognitive behavioural approach
The CBA group who received the intervention commented more on the specific components of the approach and how they interpreted the strategies being used, as well as making positive comments on the effect of the intervention:
But it was just talking about the relationship with my boyfriend and how I felt about baby and just talking through my week. What had helped. What hadn’t helped. What I could try and do to make myself feel better. Just looking on positives rather than negatives . . . . Find the thought patterns that led down the wrong way.
CBA–I, id 17
This woman went on to describe the sheets she had to fill in at home:
there was . . . thought pattern sheets, like three a week. When you go angry think what’s led you there, kind of thing, and work it backwards and then try and identify when it comes up again and try and intercept it before you get to the point of sitting and crying your eyes out.
CBA–I, id 17
Another woman commented that: ‘We’ve analysed all the reasons why I’ve been down and depressed, how to sort of, challenge negative thoughts’ (CBA–I, id 10). She also describes how the HV helped her:
The worst time . . . I couldn’t think about anything logically, whereas she sort of like focused me . . . it was also important that I don’t feel like I’m being judged at all.
CBA–I, id 10
One woman (CBA–I, id 17) reported that, ‘Just to have someone to sit and listen so you can just go “rah, rah, rah” and they go “right ok” ’. She described the sessions by saying ‘it was more of a talk with a friend than a counselling session . . . it was really informal’. She went on to comment that, ‘Every time she left the house I always felt that bit brighter and that bit better’.
Finally, another woman commented that, ‘It’s been absolutely brilliant’ (CBA–I, id 10).
Those women who were in the IG but who were not offered the intervention had very different experiences. This depended on whether they perceived themselves as being depressed. Overall they were positive about the support they received, which tended to be more practical in nature and focused more on the baby:
My HVs been really good for me . . . I used to go down to the baby clinic every 2 weeks to get [baby] weighed and whilst I was there I would say ‘He’s got a little bit of a cough, is that alright?’ . . . and she was very good.
CBA–NI, id 22
Another woman (CBA –NI, id 18) had a more negative experience as she reported saying to her HV: ‘We’ve coped with it fine, I needed your help then not now’. She also went on to say: ‘You know, you need the contact, somebody to talk to face to face, this is me, this is what’s happening to me now’.
One of the two women who declined the intervention stated: ‘I didn’t feel like talking to her. I didn’t really know her that well so . . . ’ (CBA–DI, id 4). She went to her GP for support. The second woman had an illness in the family and was too busy to have an intervention.
Treatment as usual – the control group
The CG experienced usual health visiting practice and their comments reflected the varied patterns of practice. Those women who had experienced support from the HV, for example home visits and encouragement from the HV to phone when they needed to, reported the most positive experiences:
I can talk to her. I’m not frightened to say anything in front of her. It’s not that she is going to judge me for how I’m feeling.
Control, id 24
She is very supportive and really it’s good having someone that you can talk to about how you really feel.
Control, id 14
This woman goes on to comment that, ‘She is not critical in anyway’ and ‘She always made another appointment with me so I always knew that I was going to be seeing her again fairly soon’. The HV also encouraged the woman to ‘just ring’ if she had any worries or concerns.
Another woman commented that, ‘And we just carried on talking and I were getting better as weeks went on’ (Control, id 19).
There were three women who received little or no support at all even though they reported that their HV was aware that they were having difficulties. It also seems that, for some, it depended on the personality and professional approach of the HV as one woman (Control, id 21) saw two HVs. The first she felt had dismissed her feelings and put it down to her ‘being a new mum’. The woman felt that she had a more positive experience with the second HV that she saw:
In fact she did what she said she was going to do. She said she’d get back to me and she did you know, she gave us alternatives . . . so for the three times I’ve seen her . . . she’s been consistently thorough and I think she’s done her best.
Control, id 21
Three women from this group reported that they had informed the HV that they were having difficulties but had little or no response.
One woman (Control, id 9) reported having very little contact even though she was on antidepressants and had told the HV about problems from her past. The woman seems to have been ‘let down’ after confiding in her HV. She commented: ‘They’re always having to rush off’ and felt that there was no time for her. She had told the HV:
How I were feeling and things like that, and I told her what had happened in t’past and erm, she said a few things and that were about it and I haven’t heard nowt from her since.
Control, id 9
One woman (Control, id 25) had burst into tears in front of the HV but felt she had little sympathy and commented, ‘And I went out feeling twice as bad as when I went in’. Another woman (Control, id 7) from the same practice stated, ‘I did ask for support but I didn’t really get any’, and goes on to say that she felt ‘closed off’ by her HV:
I didn’t really feel like the HV was very sympathetic really . . . and she didn’t really pick up on indicators I was trying to give her. Because I said to her at one time, ‘You know, I feel like I really can’t cope’ and she said, ‘Oh you’re doing alright’. I thought, ‘I’m not actually’, and that’s even quite difficult to admit to yourself isn’t it, that you’re not coping with your baby?
She also commented that she felt that the HV was ‘too judgmental’. This statement contrasts with some of the more positive comments from the group who received the intervention or who had a positive experience. It was important for them that the HV did not judge them and that they could feel free to say how they were feeling (see above).
Non-intervention support
Two women who had not been offered the intervention found support in new mums’ groups:
I found it better . . . to go to the support group for the mums and talk to other mums . . . I found that by helping other people [with depression] that I was actually helping myself figure it out as well.
PCA–NI, id 28
Just to be able to talk to other mums and say, ‘Yes I know what you mean’.
CBA–NI, id 1
Informal support
Often the informal support complimented the support that the women received from health professionals as it was more likely to be practical and often allowed the women time away from the baby/children.
My mum has been brilliant . . . she’s sort of like had the baby for a couple of hours and let me sort of like get some sleep, so my mum in particular has been . . . my rock kind of thing.
CBA–I, id 10
He [partner] just been there for me every step of the way.
CBA–I, id 12
This woman also goes on to say that her parents and in-laws have been very supportive by having the children.
Other women mentioned sisters and friends and this informal type of support was most important to the women who were receiving little or no support from health professionals: ‘She [HV] kept asking me how I were feeling, how I were coping but I just bottled all me feelings up’ (PCA–I, id 26).
Ideal support
All of the women in the IGs and those who received support in the CG thought that the support they had received was close to the ideal: ‘There is no fault with the support I’ve had at all’ (Control, id 14). This woman felt that she had good support from both her HV and her GP.
Another woman commented that:
I think the HV is one of the best resources by far, erm, I think any kind of, form of counselling because although the tablets have definitely helped me I think the counselling side and the talking things through with the HV has been as good without a doubt for me personally.
CBA–I, id 10
She goes on to say that:
Something sort of like to make people aware that you know you can go to your health visitor and you can ask for help if you need it and . . . you know, just get over that stigma thing.
Other comments included:
I just hope from this trial that health visitors will be able to visit as they did me and more if needed, cos I do think it’s important.
PCA–I, id 3
She was there from the first time she came round . . . I can’t say I would have changed it
PCA–I, id 31
I think the same as what I’ve had really. You know, got support from your health visitor, GP, if you want that but I think the one-to-one would work.
PCA–I, id 29
The support my health visitor gave me was excellent, it really was, it made an enormous difference.
PCA–I, id 13
Only one woman from the IG commented that she would like the option of counselling:
Counselling . . . I think that would be brilliant. That is what, when I went to my doctor, that is what I would have preferred rather than giving me pills. I would have rather gone and talked to somebody and been able to sit and try and work through it rather than ‘here, take a happy pill’. Because I didn’t want to go on the antidepressants, I really didn’t, but, it was a case of if I didn’t my son was gonna suffer. So it was the only option. If I’d have had the option of a non-drug way rather than a drug way I would have gone for counselling rather than going on pills.
CBA–I, id 6
This woman had a positive intervention but felt that it was not ‘proper’ counselling as the intervention sessions were so informal.
Another woman (PCA–I, id 20) made an important point about getting to know the HV antenatally: ‘I maybe think it would be a good idea if you met your HV more while you were pregnant to be honest.’ She goes on to explain:
10 days you’re discharged from your midwife and that’s the person you see in the community for 9 months and then suddenly it’s someone else and everything’s changed, everything’s completely changed.
PCA–I, id 20
For those women who were not offered the intervention it was suggested that a form of counselling could be offered:
It would have been better for me if someone had said, ‘I think we need to talk about this, do you want to speak to somebody?’, or maybe some counselling . . . or maybe to get it off my chest with [HV’s name], she’s pushed for time a lot, we do questionnaires and that but obviously didn’t have the time for me to sit there and say oh this has happened and that has happened, I think that would have helped, if I had just someone I could scream at.
CBA–NI, id 1
Health visitors who aren’t like your Nanna, they like have counselling training and . . . they’re able to listen to you . . . . All you want is someone to actually listen to what you’re saying, even if it’s complete crap and it’s all coming out wrong. You just want someone to say, ‘It’s alright, sit down and I’ll listen to what you’ve got to say’. That would do you the world of good and I think it would actually stop people from developing worse symptoms because people just won’t talk about it.
PCA–NI, id 28
This woman also suggested that evening visits would be helpful as this was often the worst time of day for her.
Another woman commented that:
I think what I would have liked is an opportunity to go and talk to some counsellor, probably. To go to somebody away from t’children . . . maybe gone to see somebody at the clinic or whatever, just not here, not with the kids and just have an opportunity to, say, ‘actually’ be honest about what I felt about ‘em without fear of it being, you know, a child protection thing because that also . . . it’s hard to admit to somebody that you hate your kids.
Control, id 7
Two women just wanted:
More support from my HV.
CBA–NI, id 4
If she’d [HV] just probably visited more often or was just more understanding and easier to talk to.
Control, id 25
One woman wanted to have more information about the HV role in advance and thought that women should be more informed about the service: ‘I didn’t know they can come to your house really’ (PCA–DI, id 11).
Two women did not mention the HV at all and wanted their support to come from the GP:
For them [GPs] to gi’ ya more advice and actually listen to ya. Talk about things, I mean, I know they’ve only got a short time erm, but just be a bit more supportive.
PCA–I, id 26
I would want what I got from my GP.
CBA–NI, id 22
Postnatal groups were mentioned frequently by women as an ‘ideal’: ‘I think more advice about groups, erm, postnatal groups or whatever’ (PCA–I, id 26). This woman also mentions family support.
One woman (PCA–I, id 3) would have liked to meet up with other mums and another was very enthusiastic about her experience in a group:
The absolutely fantastic thing about that surgery is they do a new mum group, which turned me around, it totally saved us, without a doubt, it was absolutely fantastic, I think it should be mandatory for all that they have to go to a group.
CBA–NI, id 18
Another woman commented that:
I think that something like the Sure Start PEEPS groups where you’re going as a play thing anyway to meet other mums and if that was . . . more accessible then I think that I perhaps would have admitted or realised that something wasn’t quite right earlier on.
Control, id 21
More specifically, several women stated that they would like to see groups for women with PND (CBA–I, id 12, and PCA–DI, id 11). One woman (PCA–NI, id 28) also suggested more support for those with existing mental health problems. Another thought: ‘Talking to other mums that have gone through it and come out of it at the other end’ would be most helpful (Control, id 19).
One woman reported: ‘I found it really good to listen to and to talk to other women’ (PCA–DI, id 11). This woman also suggested that perhaps antenatal classes should give women more time to discuss issues around PND so that they may feel more comfortable with them after the birth. In addition to this, one woman (PCA–NI, id 8) added that she would have liked there to be ‘someone who had been through it [PND] before’ in attendance at her postnatal group. This view was supported by another woman although she thought that the information should be given antenatally:
I think it needs to be brought up before you have the child . . . to get somebody to talk about it who had had it . . . I’d love to go somewhere and speak to a group of people and tell them how I feel and that it can happen to you . . . . If somebody had come and spoke to me when I was pregnant with her [baby] I’d still probably think, ‘I’m not going to get it’, but it’s nice to listen.
Control, id 24
One woman (CBA–NI, id 15) had previous episodes of depression and thought that there should be more information about the risk factors for PND. Other suggestions included having the baby taken off her hands once a week, ‘so you’ve got space to be yourself’, and she would have liked someone to ‘come and talk to me’ and not to be given repeat prescriptions.
One woman (PCA–NI, id 30) would have liked someone to phone her, perhaps once a week, to ask her how she was doing, as she herself would find it difficult to make a call and ask for help. Another woman (PCA–NI, id 32) wanted a 24-hour helpline for when she was feeling really low.
Another woman commented that:
Make it a bit more personal if possible . . . maybe bit more spontaneous phone calls [from HV] or yer know, ‘I’ve got half an hour free, can I just pop round?’ or something.
CBA–DI, id 5
In fact, a key aspect of ideal support was the availability of someone to talk to, and those women who had been offered very little had low expectations. Support could come from either the GP or the HV: ‘Just like, being on end of t’ phone if you need to talk to them’ (Control, id 9).
Discussion
The qualitative aspect of this trial was intended to illuminate and add texture to the women’s experiences of the HV support. The interviews produced rich data from a subsample of the overall data set representing the three main groups and the qualitative analyses were carried out without knowledge of the quantitative outcomes of the trial. Most of the interviewees reported some form of negative feelings and signs of distress. However, women experiencing depressive symptoms in the postnatal period appear reluctant to seek help as they have specific problems and fears and feel ‘pressure’ placed on them to cope. 229 This makes it intrinsically problematic for women to access help and for health professionals to identify when help is required.
Another barrier to help was women’s perceptions of the HV and their relationship with the HV. It is widely accepted that empathy, acceptance and a non-judgemental attitude are important in establishing good therapeutic relationships. 230 The women in this study commented that aspects of the ‘character’ of the HV and a good relationship with the HV were influential in whether they revealed their feelings. Therefore, the outcomes of the support or intervention offered could also be affected by the ‘personality’ of the HV and the relationship between the HV and the woman. The women from the treatment as usual group were more likely to be positive about their HV if they had positive perceptions of the HV and the HV’s role in supporting them.
The importance of the relationship with the HV was again apparent when HVs were using assessment measures such as the EPDS. The EPDS was generally well received by the women as it shifted the focus from the baby on to their own feelings. Women perceived the EPDS as an opportunity to talk about how they were feeling if they wanted to. It seems from these interviewees that the perception of the role of a HV and the relationship between the woman and her HV were key factors in whether they would open up. Many women felt that a HV was there for the baby and did not ‘trust’ their HV enough to open up to them. In fact, having an established relationship based on trust and a non-judgemental attitude seemed extremely important. This relationship could be with the HV, GP, partner or other mothers in postnatal groups. Understanding the role of the HV as someone who is there for them as well as their baby is therefore a key aspect.
For those women who had a good enough relationship with their HV to accept formal support, both the cognitive behavioural and person-centred approaches were very well received. A mother in the PCA arm did state in her interview that she would have preferred a more ‘directive’ approach but she completed seven sessions and appeared to have benefitted. There is no way of knowing if the improvements would have been greater if she had been offered a different approach. Despite opportunities for considerable HV input, and positive views of what they received, there was clearly a demand from some women for additional psychological input.
Conclusion
The interviews gave women the opportunity to tell their stories in their own words and generated valuable information about the acceptability of psychological interventions for PND. Those women who received the intervention felt that it was beneficial as a result of having time allocated specifically for them to talk about their feelings and experiences. Women who had not been offered any support identified ‘having someone to listen’ to them as their ideal. The results suggest that greater clarity around the role of the HV in relation to the well-being of new mothers and not just their babies would be helpful. HV training may need to emphasise how difficult it may be for new mothers to be open about their feelings and provide information around the nature of the fears that impede their expression. Actively acknowledging these sorts of difficulties and common fears in a proactive way may facilitate more open expression. It is also the case that women’s perceptions of the professional’s personal characteristics are crucial, and an emphasis on training in the development of empathy and a non-judgemental approach may be of great benefit.
Chapter 7 Discussion
This study was a pragmatic cluster randomised trial of a complex intervention. This study has generated evidence of the pragmatic effectiveness of a package of training for HVs in primary care to identify depressive symptoms and provide a psychologically informed intervention. 231 We found a reduction in depressive symptoms among IG at-risk women as measured by the EPDS and a difference in secondary outcomes at 6 and 12 months postnatally among at-risk women.
We also found a difference in depressive symptoms between intervention and control group women in the follow-up of all consented women at 6 months and 1 year postnatally.
In addition, there was some evidence of a benefit in favour of the IG women for some of the secondary outcomes at 18 months’ follow-up. Fewer women were followed up to 18 months, and the wide confidence intervals for the differences between the groups indicate that more uncertainty surrounds these outcomes.
Previous research
The trial has good internal and external validity and, considering all international publications on psychological interventions for women with PND,148,232 this trial provides the most robust evidence of benefit, which previous studies in the treatment of PND were unable to provide. Previous studies of postnatal psychological interventions performed in Edinburgh,1 Cambridge2 and Manchester3 showed positive short-term benefits for women but failed to provide good evidence to guide treatment recommendations. Small, non-representative sample size, attrition and brief follow-up limited these studies. The PoNDER trial has addressed these limitations and had more than twice as many participants as the previous largest study. 2 This is the only rigorously performed trial that followed up postnatal women to 18 months, as the final outcome in most previous studies of PND was measured at 1–3 months postnatally. 3 Furthermore, it is the only trial to incorporate an economic evaluation. As such, it is the first major investigation of this type.
Clusters
The trial achieved the required number of clusters as determined by the pre-trial sample size calculation. The IMD scores and other characteristics of recruited clusters showed that the collaborating GP practices were representative of those in the former Trent region and England as a whole, indicating good external validity.
The HVs who took part in the trial were interested in PND, research and accessing the training provided as part of the research. As such they were not all highly skilled in assessing women and offering effective support. The pre-trial HV questionnaire indicated a wide range of previous training in identifying and supporting women with PND, and a range of experience in administering the EPDS. This reflected varying activity among HVs and PCTs seeking to address the problem of PND. The HVs in the PoNDER trial had perhaps less access to training and other formal mechanisms for managing PND than the HVs who provided data for an audit of the wider CPHVA membership. 96 However, it is unclear how well the CPHVA or the PoNDER trial HVs’ responses represented HVs nationally. As we have no suitable comparison with the wider HV population to comment accurately on external validity for this aspect, a national survey of HVs to assess their knowledge and skills and beliefs concerning the causes of psychological problems203 would clarify the generalisability of the results. However, we believe the HVs represented a range of individual and professional characteristics, which were distributed equally among all groups.
Individual women
The pre-trial sample size calculation estimated that 50% of women might consent to take part. Over the recruitment phase 4084 (53.3%) eligible women did consent to take part and 3436 completed a 6-week postal questionnaire.
The women who did complete and return all of the instruments in the postal questionnaires at 6 weeks and 6, 12 and 18 months postnatally provide a possibly unique insight into the natural history of symptoms of depression and postnatal health over time in the CG. The return rates at all follow-up time points indicated that the participating women were highly committed to the research and willing to offer their time to support the trial.
Because the HVs collected demographic details of all pregnant women on their caseload, we could compare the features of the women who consented with those of the women who declined to participate and with those of women in England and Wales in 2001. 212 The characteristics of women in the study were broadly similar to those of women in England and Wales, where 91% of the population were recorded as white British versus 94.2% of respondents versus 93.0% of the 8716 who were eligible. In total, 69% of women in England and Wales lived in owner-occupied accommodation212 versus 71.8% of eligible women. Women from culturally diverse groups, those not fluent in English and women who had difficulty responding to a postal administration of EPDS or assessment of PND were not wholly represented.
Some HVs thought that women who had been previously affected by PND might not consent to take part in the trial, but this was not the case. A total of 17.3% (595/3449) of postnatal women in the PoNDER study compared with 18% (48/266) of CG postnatal women in an earlier trial of postnatal care146 had a 6-week EPDS score ≥ 12. We believe that the PoNDER study women were representative of women experiencing PND in real-world primary care. The similar characteristics of the at-risk women in the IG and CG indicated that the stratified randomisation process was very effective, imparting good internal validity.
Six-month primary outcome
The primary objective of the study was achieved by identifying a group of at-risk women with a 6-week EPDS score ≥ 12. The pre-trial sample size calculation was based on detecting an absolute difference of 15% (this is approximately equivalent to an odds ratio of 0.54) in the proportions of at-risk women with a 6-month EPDS score ≥ 12 [i.e. a minimum clinically important difference (MCID) of 15%]. We observed a statistically significant but smaller absolute difference (11.7%) than our anticipated MCID between the intervention and control group at-risk women in the proportions with a 6-month EPDS score ≥ 12 (the primary outcome). The 95% confidence interval suggests that the true treatment difference lies between 0.4% and 22.9%. Therefore, it is consistent with the data that the true treatment effect, although statistically significant, may be small and potentially not very clinically important. We are therefore unable to confirm or exclude our a priori clinically important effect of 15%.
Secondary outcomes
At 6 months the difference in the mean EPDS scores and other secondary outcomes, apart from the SF-12 PCS and the CORE-OM risk scores, reflected the results from the primary analysis. Most of the differences between the IG and CG at-risk women observed at 6 months postnatally were maintained over time, with some ‘plateauing’ towards 18 months postnatally. In addition to an enduring positive impact on the woman’s health, there appears to have been a positive impact on the woman’s interaction with her infant, as measured by the PSI.
Secondary outcomes were also measured in the follow-up of all women who consented to take part in the study at the same time points as those studied in the at-risk women. An interesting, unexpected finding was that the effect of the intervention was demonstrated not only in the at-risk women but also in the group of all women followed up as randomised, at 6 and 12 months postnatally, indicating some non-specific effect from the HV intervention extending beyond the at-risk women.
Contrasting benefits of the two psychological approaches
There was a 2.2% difference between the CBA (32.9%) and the PCA (35.1%) groups in the proportion of women who had a 6-month EPDS score ≥ 12 (95% CI –14.2% to 10.1%, p = 0.74). This type of finding is consistent with findings from the literature on psychological therapies, that different models of intervention result in broadly similar outcomes despite differences in theoretical bases and the style of intervention delivered. This is known as the equivalence paradox. 233 For example, a primary care trial for patients with depression comparing brief NDC and CBT7 found no significant difference in outcomes at 4 months leading to the conclusion that both interventions were equally effective in this setting to this follow-up point. Similar effects have been found in large data sets comparing person centred therapy and CBT in routine NHS primary care settings. 234
Economic analysis
The economic evaluation found that for the at-risk women the HV intervention was cost-effective over the HV usual care, and as such might be recommended by NICE. 217 The CBA had the highest probability of being cost-effective. In the range of QALY values between £20,000 and £30,000, the probability of CBA being cost-effective was just over 70%.
Administration of the EPDS face-to-face or postally
Just as no real difference was observed between the CBA group and the PCA group, there was no evidence to suggest that there was a benefit in outcome for any of the four separate CBA-F, CBA-P, PCA-F and PCA-F groups. Further disaggregations in the economic evaluation indicated that the face-to-face administration, in conjunction with the CBA intervention, might be more likely to be cost-effective.
Infant outcomes
With new mothers the earlier any benefit in postnatal health can be achieved, the sooner any potential negative impact on the infant can be ameliorated. We planned to use the Ainsworth235 and Bailey236 scales to monitor infant outcomes but were advised that the videotape analysis would be too costly and so this element of the trial was not funded.
From the women’s responses to the questions on infants, we observed some evidence that women in the IG had fewer concerns about the development of their infants than those in the CG at 18 months. For the at-risk women, the mean aggregate infant outcome concern score (where a higher score indicates greater concern) was 19.4 (SD 6.1) for 37 women in the CG and 16.5 (SD 5.4) for the 73 women in the IG. The mean difference was –2.9 (95% CI –5.0 to –0.7, p = 0.008).
It is important to note that the infant outcomes were based upon maternal self-report without any independent observations. Women with depression may perceive their infants differently, or an infant may interact differently with a mother who has been depressed. The infant behaviour may also indicate a two-way interaction. The instruments used to monitor infant outcomes were not well-validated tools, but the BSQ has been used in a previous study of infant outcomes,39 in which the greatest effect appeared to be in reducing the mother’s perception of her infant’s temper tantrums. The suggestion of a positive effect on the IG women’s perceptions of their infants at 18 months postnatally compared with the CG was not confirmed by the partners’ responses.
Partner outcomes
There appeared to be little difference in partner outcomes between the IG and the CG except in some domains at 18 months postnatally. This corresponds to the time when partners are more likely to take an active role in interacting with and caring for the infant. The partner outcomes were not straightforward but provided some evidence of a benefit. This may simply reflect the benefit we observed in the IG women.
p-Values
Some caution should be applied in the interpretation of the statistical p-values, particularly for the various secondary outcomes and end points because of the number of tests. As there is no general consensus on what procedure to adopt to allow for multiple comparisons198 we have reported unadjusted p-values and confidence limits.
Intracluster correlation coefficient
The ICC derived from the stratified clusters for the at-risk women in the trial (0.037), although higher than the estimate (0.006) used in the original sample size calculation, indicated little clustering. The number of at-risk women needed to treat, derived from the absolute risk, was moderately good in this context. 237
Potential sources of bias
The trial was designed specifically to minimise the effect of chance, contamination and bias. In a cluster randomised trial, in which there can be differential recruitment to clusters, it is vital to address the question of selection bias. In the trial the possibility of selection bias was minimised as the coded random allocation list was prepared by a statistician who was unaware of the identity of the HVs and the GPs, and the allocation to group was concealed from the participating HVs and GPs until they had signed their consent forms.
Blinding
Blinding of the intervention was not possible, but the statistician and the health economist were initially blinded to the women’s allocation to group for the data analysis. The SCAN interviewers were blinded to both the women’s EPDS scores and group.
Differential loss to follow-up
The 30% of women lost to follow-up were evenly distributed across the clusters and there was a limited dropout of the clusters. In total, 101 clusters were randomised and 86 clusters provided data for the primary analysis of 418 at-risk women. The average cluster size was 4.9 women, ranging from one to 15 at-risk women per cluster, and 85% (86/101) of clusters recruited to the trial were still included in the final primary analysis.
We explored the possibility that the higher reply rate among the CG at-risk women may have exerted a bias at the 6-month follow-up. A comparison of the 6-week EPDS scores of the women who did not return a 6-month EPDS with the 6-week EPDS scores of those who did showed that the mean EPDS was 16.2 (SD 3.6) in the IG and 15.1 (SD 2.9) in the CG, suggesting that the difference in non-reply rate may have biased the unadjusted results. However, we adjusted the 6-month comparisons for the 6-week EPDS scores.
Sensitivity analysis
Overall the sensitivity analysis and imputation of the missing 6-month EPDS scores for the 177/595 (29.7%) women who were lost to follow-up suggested that there may be a possibility of attrition bias, although the regression imputation method suggested that this bias on the estimated treatment effect may not be too large.
Potential effect of SCAN interviews
Unlike the IG at-risk women, none of the CG at-risk women were invited for a SCAN interview until 18 months postnatally. Although there is no reported evidence of a therapeutic benefit238 from SCAN interviews, we explored the possibility of potential bias introduced by a therapeutic effect of the SCAN interviews in the IG lasting 1 year. There were no differences in the mean scores of at-risk women who had or did not have a SCAN interview, making any SCAN therapeutic effect unlikely.
Potential effect of antidepressants
For the 31 IG at-risk women who had an outcome of moderate or severe depression on the SCAN interview, 26 accepted the psychological intervention sessions, one declined and 45% (14/31) also had a prescription for an SSRI. However, this was not exclusive to the IG, as the resource use logs indicated that CG women were also offered antidepressants. In total, 36.8% (46/125) of CG women said that they had been prescribed an antidepressant versus 28.5% (61/214) of IG women, suggesting that the greater improvement in the IG was not attributable to a higher rate of prescriptions for antidepressants.
Six-week EPDS scores and the SCAN
A secondary objective was to use the SCAN168 data to correctly classify IG at-risk women as having none, mild, moderate or severe depression. It was also possible to investigate how well the EPDS administered in a primary care setting identified depressive symptoms in women who were depressed according to the SCAN classification. In total, 3.6% (18/505) of lower-risk women with a 6-week EPDS score of < 12 were classified as depressed, indicating that a single administration of the EPDS did not identify all at-risk women. Unexpectedly, 67.7% (239/353) of at-risk women who had a SCAN interview were not classified as depressed, confirming the value of an 8-week second administration of the EPDS. We were aware before the trial began that the EPDS needed to be evaluated for routine use in primary care. 57 However, we were not aware of any other tool at the start of the trial that could confer advantages over the EPDS.
The identification of women with anxiety and depression, generalised anxiety disorder, depersonalisation syndrome, nightmares, non-organic insomnia, or panic disorder or other diagnostic outcomes highlighted that postnatal women experience other distressing mental health conditions postnatally and not just symptoms of depression.
The sensitivity of the EPDS in the PoNDER study, using the SCAN data, was lower than in the original validation study. 178 The positive predictive value was also lower than the positive predictive values in both of the other validation studies (Table 69). 8,9 The first study was based on a sample of women who were believed to be depressed. 8 The other larger study9 was on a community sample of 702 primiparous women in Cambridge and compared the EPDS scores with the outcomes of a Standardised Psychiatric Interview. The PoNDER study data are derived from a larger sample (n = 860) of women from a geographically and socioeconomically broader sample of not only primiparous women.
| Study and EPDS threshold | Sensitivity | Specificity | Positive predictive value |
|---|---|---|---|
| The PoNDER study, EPDS ≥ 12 | 0.791 | 0.755 | 32.7% |
| The PoNDER study, EPDS ≥ 13 | 0.866 | 0.671 | 37.3% |
| Validation study, EPDS ≥ 12.58 | 0.86 | 0.78 | 78% |
| Validation study, EPDS ≥ 129 | 0.677 | 0.925 | 66.7% |
At a threshold of 12 the EPDS at 6 weeks picked up symptoms that were self-reported as being present in the previous week and that were perhaps transient according to the SCAN interview at 7 weeks (which explores the previous 4 weeks in a clinical semistructured interview assessment of depressive symptoms). When the SCAN has been used in general population surveys, the prevalence of depression (mild, moderate or severe) is 2–3% (higher in women), whereas the threshold of 12 recommended for the EPDS typically classifies about 12% of women. Further evaluation using receiver operator characteristic (ROC) analysis is planned for the PoNDER study EPDS data and SCAN data to establish an optimal cut-off point.
Sensitivity and specificity are usually fixed properties of a test and do not change with the sample or population and the underlying prevalence of the disease. Positive predictive values and negative predictive values (predictive value of a negative test result) vary according to the prevalence of a disease in a population and therefore do change. In the trial, women with an EPDS score ≥ 12 had a 33% chance of being depressed (as indicated by the gold standard SCAN interview). In contrast, the negative predictive value was about 93%. Therefore, women who scored < 12 were highly likely to be not depressed. The EPDS is not an ideal outcome measure for comparing the incidence of true depression; however, the comparison between the groups was not affected by this, as the EPDS cut-off was the same for all groups.
Within the trial we needed to use the results from the first administration of the EPDS to identify a group of women with whom a direct comparison could be made in the intervention and control groups without contaminating the usual care provided in the CG. No pragmatic evidence was available on the proportions of women who would score < 12 on a second administration of the EPDS. What the results probably mean for everyday practice is that HVs should readminister the EPDS 2 weeks after the first administration, to select out those who are not depressed. Administering once only at 8 weeks postnatally would limit the possibility of early intervention for women who are moderately or severely depressed.
Health visitor training
The IG HVs were satisfied with the introductory day training and felt that the presentations for the background, EPDS, clinical interview, risk management and skills development were good. The IG HVs were also very positive about the 5 core training days, although the CBA HVs seemed to find the training more difficult than the PCA HVs. In anticipation of little difference in clinical outcomes between the two main IGs, we aimed to capture important differences where they existed to supplement the data. The changes in the OPP scores from baseline to post trial indicated that the CBA and PCA group HVs had assimilated the principles of their training.
The HVs reported marked differences in their approach following the training in providing psychological sessions; they said that they had become more confident and more perceptive within any setting. They believed that both the CBA and the PCA training had been excellent. It is not easy to determine which aspects of psychological sessions are effective, as when interventions from efficacy studies are transferred to a real-world situation other non-specific variables may modify the effect. There is, for example, variability in the practitioner offering a psychological intervention, the context and the natural course of the condition in each client receiving psychological sessions.
One important aspect of the HV training was that it appeared to have had an impact on the pattern of health visiting. In particular, the overall level of visits reduced (although this was not statistically significant), with the greatest reduction seen in the visits to the mother that were not related to PND. The level of visiting relating to PND was the same in both the intervention and control groups. This made it difficult to identify an effect specific to the delivery of care relating to PND. Although the training seemed to have altered visiting patterns we can only postulate as to why these changes occurred and their related therapeutic effects. Therefore, although these changes are consistent with a hypothesis of training being associated with more targeted health visiting and better quality PND care, the study can not lend any evidence in support of this.
Agnew Relationship Measure Short Form
The completed ARMs indicated that the women felt confident in their HVs and developed a facilitative relationship with them. Moreover, the high ARM scores, compared with those from other studies, indicated that following a brief training the HVs in both IGs were good at establishing a high-quality, warm, therapeutic relationship as rated by the women, with no significant differences between the two groups. This is despite evidence suggesting that CBT interventions are associated with a stronger alliance than psychodynamic–interpersonal interventions. 239 The ARM Short Form scores being lower for HVs than for women mirrors results from the wider psychotherapy literature showing divergence between client and therapist ratings using the ARM Short Form. 240 A meta-analysis of 79 studies214 showed a modest but consistent relationship between therapeutic alliance and clinical outcome (r = 0.22). Clients’ rather than therapists’ ratings seem to be the most predictive of outcome. 241
Adherence and audiotapes
Health visitor sessions were audiotaped to allow an independent assessment for treatment adherence. HVs providing intervention visits were generally reluctant to tape record their intervention visits because they felt uncomfortable doing so, were protective of their clients and also felt that the tape recording might adversely affect the nature of the intervention session. Some women chose not to consent to have their sessions tape recorded. We might assume that the HVs who submitted completed tapes were more confident than others who did not do so, but there were no differences between the CBA and PCA groups in this respect. We cannot extrapolate the results beyond those who submitted tapes. Despite the possibility of a bias towards the more confident HVs, it seems that HVs who submitted tapes did deliver two distinct identifiable interventions, in line with their original training. These results offer some indication that, following brief training, HVs delivered two distinct psychologically informed interventions and adhered to the intervention that they were trained to deliver. The failure to obtain enough tapes suggests that those providing psychological intervention sessions in a research context should be better prepared. There should be further work to explore the barriers to their use within psychological therapy trials more generally, such as perceived threats of exposure. This could be improved in future HTA trials by assessing implementation intentions.
Eight-week EPDS administration
The HVs failed to deliver the protocol as required, for many reasons. Despite the best efforts of the LCs and the principal investigator to implement the HV protocol, the HVs were not all obliging. The absence of 29% of the 8-week EPDS scores in the research context was clearly an undesirable consequence of a pragmatic trial.
This was not an explanatory trial and it is likely that in a real-world clinical context HVs would not always be able to administer a repeat EPDS for a range of practical reasons. Some of the at-risk women in the PoNDER trial chose not to complete it as they were feeling better or were unavailable, for example in hospital or staying away with their own mother. When a HV was absent on holiday or on sick leave, if they did not have a colleague trained in the use of the EPDS, the ideal follow-up assessment time was missed.
The aim of identifying depression at 6 weeks postnatally is to intervene as soon as possible for the benefit of the mother, infant and family. The SCAN data supported the finding that around 67% of at-risk women were not depressed. The HVs’ focus group feedback was that they felt that this was because at 6 weeks postnatally the EPDS picked up some transient symptoms. The HVs suggested that administering the EPDS for the first time at 8 weeks postnatally, once the women had begun to recover from some early postnatal exhaustion, then repeating it after 2 weeks, might more correctly indicate the women who were truly depressed. This time point would coincide with some improvement in postnatal physical health symptoms associated with depressive symptoms. 242 The association between physical postnatal disorders and depressive symptoms should be systematically evaluated in the context of identifying true depression postnatally.
Psychological intervention sessions
The SCAN outcomes and the proportion of at-risk women who had an 8-week EPDS < 12 indicated that, at 6–8 weeks postnatally, fewer at-risk women than expected were depressed. Overall, about half (197/404) of all of the IG at-risk women were offered sessions, and when there was a raised 8-week EPDS, 88% (99/113) of women were offered sessions.
Health visitors were able to use the combination of the women’s EPDS scores and their own assessment skills in their decisions to offer sessions to those IG women who, in their clinical judgement, were assessed as being likely to benefit from the sessions, as opposed to the requirements of the protocol for two EPDS scores ≥ 12. Rather than to increase the acceptability of the trial to HVs, this was because the HV training highlighted the limitations of the EPDS and that it was likely that some women with an EPDS score < 12 would be depressed. The study SCAN data confirmed this likelihood. It would have been unethical to withhold from a women a potentially effective intervention when a specially trained HV had identified clinical symptoms. When there was no 8-week EPDS, 31% (36/118) of women were offered sessions. That is, the absence of the 8-week EPDS score suggests that the HV 8-week face-to-face clinical assessment dominated the decision to offer the sessions. When the 8-week EPDS was < 12, 36% (62/173) of women were still offered sessions.
Of the women who had a SCAN interview, there were 6% (20/315) with an outcome of depression who were not offered sessions. Five of these women were prescribed an antidepressant, three attended a postnatal group and all of the others had a face-to-face administered 6-week or 8-week EPDS score < 12. This indicates some possible error due to a reliance on the face-to-face administered EPDS score.
Some women were not offered sessions as they were accessing other support. The HVs remained in close contact with the women and continued to see them when they attended well-baby clinics or accessed other supportive mothers via a baby massage or postnatal support group. This is perhaps a unique feature of the intervention, that the HVs could continue to observe the women’s progress, were generally aware of facilitating and impeding features and changes in the women’s lives, such as the departure of an abusive partner, and had an understanding of some factors affecting the women’s moods. That is, the HVs could still see the women as part of their usual care, rather than having to plan to see women in a formal session, as indicated in the protocol.
For those women who declined the sessions, the knowledge that the HV was aware of their problem and had offered sessions may in itself have been perceived as support. The HVs did explain to the women that they were able to return at any time to access further support when they felt that they required it, and many HVs reported that this happened 4–6 months postnatally, and sometimes later too.
The sessions offered to women may not have been acceptable for several reasons. Having a professional to talk to is regarded by women internationally as being important in helping them to recover from PND (for those who believe that professional help is appropriate). 243 However, reviews of women’s views on treatments for PND,244 and the impediments to women seeking help,245 provide consistent accounts that: women are reluctant to accept that they have a problem with depression; they avoid approaching health-care professionals for help; and they are reluctant to tell health-care professionals that they have a problem. Women remain concerned about stigma, and they perceive other social pressures and particularly a threat that their infant will be removed from them if they admit to being depressed. 245 An important influence on whether a woman accepts treatment is the nature of the relationship between the woman and the health professional. 245 The importance of a trusting relationship with the HV was identified during the qualitative interviews. In practical terms, postnatal women also find appointments inconvenient or they do not have time because of childcare responsibilities. 244
Qualitative interviews
These interviews indicated that, when they were received, the women valued the HV sessions. Although different models have specific effects, all models of therapy contain non-specific effects or common factors, such as warmth and feeling supported. The interviews indicated that the women were more likely to accept the intervention if they felt that they had a trusting relationship with the HV. The importance of the HV as a ‘known’ individual implies the desirability of antenatal contact. Future HV training should also include approaches to ensure that mothers perceive them as empathic and non-judgemental. HVs should also be trained to: present the role of the HV more clearly in relation to the well-being of mothers (not just the baby); discuss expectations of HVs by new mothers; and acknowledge the common fears of new mothers and how frequently mothers find it difficult to reveal their true feelings.
Interpretation
Six-month data were available for 395 IG at-risk women and, although it is likely that many of these women were not depressed, 50% (197/395) were offered psychological sessions. Of the 197 women who were offered sessions, 61.4% (121/197) accepted and 38.6% (76/197) declined. There were 259 intervention sessions delivered in the CBA group and 242 intervention sessions delivered in the PCA group.
The positive effect on the primary outcome arose in the IG despite the small number of psychological sessions accepted by the IG at-risk women and even fewer received by the lower-risk women. It is important to recognise that psychological interventions are not dichotomies in the context of continuing care. The positive effect overall may have been the result of a general improvement in HV care for women with PND.
The actions of some HVs in not uniformly following the protocol as required, that is, not administering the 8-week EPDS or not offering the sessions as indicated by the protocol, may have diluted some of the potential overall effect of the sessions and compromised the interpretation about the effectiveness, uptake and acceptability by the women (some qualitative data on this issue are provided). However, HVs, as with other clinicians, hold clinical autonomy and there is no degree of external control and, as a pragmatic trial, the HVs’ actions may have been representing what would happen in real-world primary care.
For the reasons stated below, one interpretation of this effect is that the IG HVs were operating differently overall to the CG HVs to produce the positive outcomes in the IG women and that the non-specific effect enhanced the effect of the small number of psychological sessions accepted by the at-risk women. Again, although the outcomes are consistent with the hypothesis of a non-specific effect we cannot provide direct evidence for this.
That is, the effect may have arisen in association with the package of IG HV training, comprising many components that are difficult to separate, any of which might affect the emotional status of pregnant women and new mothers. The HV intervention comprised all the newly acquired skills that the HVs developed as part of the pre-trial training in assessing women, identifying depressive symptoms and delivering the psychological intervention sessions.
The IG HVs also reported that they felt that PND had become destigmatised in their practices, generating a lot of discussion among the whole practice team. Taking part in the research included an antenatal contact for recruitment (which was common to the CG as well as the IG). The IG HVs felt that this established an early relationship for the 6-week postnatal assessment in the woman’s home and meant that women were more receptive. The HVs also felt that the professional–client role had been enhanced, as a better rapport developed with the women during the home visits to administer the EPDS at 6 and 8 weeks postnatally. The importance of this was echoed in the women’s replies in the qualitative analysis.
The HVs explained their role in PND so that the women would feel that attention was given to them rather than solely to the baby. The HVs said that the women felt that they were concerned about them as the focus had shifted from the baby to the mothers themselves. Also, the HVs felt that women were more able to ask for support and accessed more support than they may have done in the past.
The non-specific effect suggested by the results for the cohort of all women could be due to measurement bias or the delivery of a small number of psychological intervention sessions to a few women who were not at-risk women.
We believe that the training enhanced the IG HV role and it is also feasible that HVs in the CG were affected by participating in the trial. This may have been as a result of their additional reading or accessing additional training whilst collaborating in the trial, but we are unable to confirm this.
Summary of the strengths and weaknesses
The strengths of the study are related to the sample size achieved, the good internal validity and the precision of the results. The trial was conducted in a pragmatic setting and used a combination of quantitative and qualitative methods and an economic evaluation. There was support from participating HVs and an apparent measurable effect of the intervention on the primary outcome.
However, there are weaknesses, many beyond the control of the investigators. These include non-adherence to the protocol by HVs not administering the 8-week EPDS and loss to follow-up at 6, 12 and 18 months postnatally. This is distinct from the absence of 12- and 18-month follow-up data due to censoring by an end to the funding of the trial.
A further weakness was that, by not adhering to the protocol and offering the sessions as required, fewer women than expected were offered sessions, compounded by the number of women who declined the formal sessions. Furthermore, some HVs failed to complete the audiotapes of all of the sessions which took place.
Recommendations for further research
There are gaps remaining in the evidence about the assessment of postnatal women and the identification and management of depressive symptoms. The following areas should be investigated:
-
As a priority, further research should explore how to improve HVs’ accurate identification of symptoms of depression, anxiety and other mental health problems experienced by postnatal women. This might include further analysis of our existing data set, the revision of guidance on the use of the EPDS or the development of a new instrument, to be validated in a primary care setting and confirmed with a clinical interview.
-
Further analysis of our existing data set is needed to explore the features of women who declined HV psychological sessions, followed by qualitative work to understand what postnatal women perceive as being the requirements of HVs for the development of high-quality, warm, trusting and therapeutic relationships.
-
The trial was not designed to detect the unexpected non-specific effect of the HV intervention on all women as randomised. This observation should be tested in a trial focused on this issue to determine the mechanism of the effect by comparing the outcomes for all pregnant and postnatal women who receive usual HV care, with a brief intervention provided antenatally for all women in one group and a brief intervention provided postnatally for all women in another group, using a clinical interview at follow-up.
-
There should be a detailed study to find out whether women’s partners and their own mothers can help in the identification of depression and anxiety symptoms and whether non-professional support networks or other facilitating features can help minimise the development of postnatal mental health problems or help postnatal women with these problems recover more quickly. This could be a trial and economic evaluation of the provision of information and skills to the families of antenatal women compared with usual care.
-
The results presented here showed that the HV intervention was cost-effective with the main provisos relating to missing data and the treatment of clustering in the analysis. Our approach in the economic evaluation was consistent with the clinical analysis in this report and typical of most published economic evaluations. However, other viewpoints are possible and alternative approaches feasible. For example, adopting a Bayesian approach within WinBUGs could address the missing data and clustering issues. We propose that these analyses should be the subject of future research.
-
One further approach would be the reformulation of the economic evaluation into a cost-effectiveness model to allow a more structured approach to address policy questions, with the improved ability to look at longer-term costs within a modelling framework. This could form the basis of a value of information analysis that could identify systematically the areas of key importance to the policy decision and hence the priorities for future research.
Summary
The PoNDER study recruited the number of clusters and postnatal women required by the trial. The GP clusters and HVs were representative of those in England and Wales. A cohort of postnatal women representative of women experiencing postnatal depressive symptoms in real-world primary care was followed up from 6 to 18 months postnatally.
The HVs did not all adhere to the trial protocol requiring a repeat 8-week EPDS for all at-risk women and the provision of psychological sessions for all women with an 8-week EPDS score ≥ 12.
The SCAN data and the available 8-week EPDS scores indicated that more than half of the at-risk women were probably not depressed. This partly explains why HVs did not provide psychological sessions to all at-risk women. Using a threshold of 12 on the EPDS alone cannot be recommended for routine use at 6 weeks postnatally to determine which women might be offered psychological sessions.
At 6 months the trial observed a statistically significant difference between the proportions of CG women (45.6%) and IG women (33.9%) who had a 6-month EPDS score ≥ 12 (difference 11.7%, 95% CI 0.4 to 22.9%, p = 0.036). The point estimate is statistically not clinically significant, although the confidence interval includes a difference that would be clinically significant, and we are unable to confirm or exclude our a priori clinically important effect of 15%.
In total, 32.9% of CBA group women had a 6-month EPDS score ≥ 12, compared with 35.1% of PCA group women (difference 2.2%, 95% CI –14.2% to 10.1%, p = 0.74).
There were statistically significant differences between the intervention and control group at-risk women in mean secondary outcome scores.
In the cohort of all consented women followed up, 16.4% of CG women had a 6-month EPDS score ≥ 12, compared with 11.7% of women in the IG (difference 4.7%, 95% CI 0.7 to 8.6%, p = 0.003).
The unexpected non-specific effect of the HV intervention is suggested by the results for the cohort of all women who consented to take part in the study. Also, a non-specific effect is suggested by the results for the at-risk women, of whom less than one-third received the psychological sessions, and could indicate that the HVs offered enhanced postnatal care to the women in the study.
There was an indication of a benefit in the IG women’s perceptions of some of their infants’ behaviour at 18 months postnatally and some indication of a difference in the partners’ mean scores at 18 months postnatally.
Conclusion
This is the only large trial of a HV intervention for PND based in routine primary care. Brief training for HVs to both systematically identify women with symptoms of PND and deliver psychologically based sessions appeared to benefit postnatal women in their care.
Acknowledgements
We would like to sincerely thank the NIHR HTA programme for commissioning and funding the trial; all of the 4084 women who participated, generously giving their time and valuable input; and the local co-ordinators for all of their hard work, patience, professionalism and sense of humour: Marian Carey, Jane Elwood, Jane Fowlie, Karen Ricci, Anna Rigby, Diane Speier and Janet Spittlehouse.
We would also like to thank all of the health visitors (see below) and health visitor managers in the following PCTs for supporting the research, especially Broxtowe and Hucknall for administering the Department of Health funds for health visitor service support costs and excess treatment costs: Amber Valley, Barnsley, Broxtowe and Hucknall, Charnwood and North West Lincolnshire, Chesterfield, Derby Dales and South Derbyshire, East Lincolnshire, Erewash, Gedling, High Peak and Dales, Leicester City West, Lincolnshire South West Teaching, Mansfield, Melton, Rutland and Harborough, North Lincolnshire, North East Derbyshire, North East Lincolnshire, Newark and Sherwood, Northamptonshire Heartlands, Nottingham City, Rushcliffe, Sheffield South East, Sheffield South West, Sheffield West, South Leicestershire, West Lincolnshire.
We are extremely grateful to the Training Reference Group – David Shapiro, Honorary Professor, Universities of Leeds and Sheffield; Dr Chris Williams, Director GIPSI, University of Glasgow; Dr Ruth Williams, Institute of Psychiatry, Kings College, London; Professor Brian Thorne, The Norwich Centre; Mr Anthony Merry, School of Psychology, University of East London; Keith Tudor, Psychotherapist and Facilitator and Tom Ricketts, Course Director, Michael Carlisle Centre – and the Trial Advisory Group – Professor Michael Barkham, University of Leeds; Professor Jon Nichol, University of Sheffield; Dr Jane Morrell, University of Huddersfield; Dr Rachel Warner, Sheffield Health and Social Care NHS Foundation Trust; Professor Pauline Slade, University of Sheffield; Mr Simon Dixon, University of Sheffield; Dr Stephen Walters, University of Sheffield; Dr Graham Paley, Leeds Partnerships NHS Foundation Trust Psychological Therapies Services; Professor Terry Brugha, University of Leicester; Professor Nigel Mathers, University of Sheffield; Mrs Elizabeth McGuirk, Broxtowe and Hucknall PCT; Julie Alcock, Health Visitor East Lincolnshire PCT and Lynne Ramsden, Health Visitor Sheffield PCT.
We are also extremely grateful to Dr Cheryll Adams, Professional Officer for Research and Practice Development, CPHVA; Dr Robin S. Smith at the University of Sheffield for the geographical information systems analysis; Mind Garden for permission to use the STAI in the trial; and Psychological Assessment Resources for permission to use the PSI-SF.
We would like to express our sincere thanks to all of the participating health visitors for their collaboration:
Mary Abbott, Julie Alcock, Alison Addy, Ann Aljewicz, Doris Andrew, Maureen Appleby, Jane Askew, Julie Atkinson, Sue Baker, Ali Balderstone, Anne Bardgett, Paivi Barkaway, Brenda Bartle, Louise Bartlett, Barbara Beer, Ruth Bernard, Helen Bladen, Alison Bleby, Gill Booth, Debbie Boulton, Janine Bowes, Linda Bright, Susan Brighton, Pam Brojaka, Helen Brown, Wendy Bull, Liz Bunney, Janet Campbell, Judith Capper, Marian Carrick, Lesley Cassedy, Anne Chafer, Karen Clayton, Glynis Collier, Audrey Codman, Bronwen Curran, Jenny Cuthill, Sandra Davie, Ali Davy, Ann Dawson, Liz Day, Margaret Deehan, Marjorie Depeledge, Judy Derricott, Mary DeVille, Jane Dingley, Ruth Doggett, Francis Dooher, Beryl Douglas, Margaret Duffy, Chris Dunnington, Anne Early, Beryl Ecclestone, Helen Elleker, Wendy Faint, Cheryl Few, Mena Flewit, Stella Foster, Brigitte Fox, Sharon Frankland, Sharon Galvin, Zoe Garnett, Sarah Gec, Chris Gill, Sara Girling, Julia Glossop, Carmel Goodacre, Joy Green, Pat Gregson, Pauline Haggerty, Linda Handley, Beverly Harker, Liz Harris, Pippa Harwood, Jenny Hawkes, Catherine Holgarth, Jean Holliday, Fran Holmes, Margaret Hopkins, Lynne Iveson, Sue Jaye, Berny Johnson, Phillippa Johnson, Nuala Jones, Susan Jones, Dorothy Jones, Paula Kendall, Carole Keridge, Jane Kiernan, Pamela King, Angela Kirk, Caroline Krupa, Gillian Levick, Nicola Lilley, Hesta Litten, Lily Liu, Michele Lloyd, Joanne Longden, Barbara Lord, Linnette Lovelock, Liz Mair, Janet Mallett, Lorna Manistre, Cheryl Mayfield, Stephanie McHugh, Clare Mendelson, Karen Missen, Sandra Morrell, Helen Morris, Liz Moss, Ruth Nester, Jackie Noble, Joanne Oxby, Penny Pallister, Helen Pegg, Julie Pepper, Maggie Petty, Fiona Phipps, Neil Pilkington, Mary Poole, Judith Price, Charity Radnell, Lynne Ramsden, Catherine Richards, Sue Roberts, Sue Rushbrooke, Sue Russell, Angela Scarfe, Hazel Scott, Janet Shaw, Janet Short, Vicky Slinger, Janet Stables, Rachel Stanton, Linda Strong, Jennifer Sweeney, Jo Swift, Helen Surguy, Rosemary Symes, Helen Tacey, Clare Tagg, Margaret Thompson, Sue Thompson, Debbie Tompkins, Sue Twiddy, Jenny Walter, Olive Walker, Catherine Ward, Debra Ward, Angela Watson, Carol Whitham, Ann Wike, Linda Wilkinson, Rosalind Woodger, Julia Wroth, Mary Wykes.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Holden JM, Sagovsky R, Cox JL. Counselling in a general practice setting: controlled study of health visitor intervention in treatment of postnatal depression. Br Med J 1989;298:223-6.
- Cooper PJ, Murray L, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression. I. Impact on maternal mood. Br J Psychiatry 2003;182:412-9.
- Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive-behavioural counselling in the treatment of postnatal depression. Br Med J 1997;314:932-6.
- Gerrard J, Holden JM, Elliott SA, McKenzie P, McKenzie J, Cox JL. A trainer’s perspective of an innovative programme teaching health visitors about the detection, treatment and prevention of postnatal depression. J Adv Nurs 1993;18:1825-32.
- Seeley S, Murray L, Cooper PJ. The outcome for mothers and babies of health visitor intervention. Health Visitor 1996;69:135-8.
- Elliott SA, Leverton TJ, Sanjack M, Turner H, Cowmeadow P, Hopkins J. Promoting mental health after childbirth: a controlled trial of primary prevention of postnatal depression. Br J Clin Psychol 2000;39:223-41.
- Elliott SA, Gerrard J, Ashton C, Cox JL. Training health visitors to reduce levels of depression after childbirth: an evaluation. J Ment Health 2001;10:613-25.
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6.
- Murray L, Carothers AD. The validation of the Edinburgh Postnatal Depression Scale on a community sample. Br J Psychiatry 1990;157:288-90.
- World Health Organization . Strengthening Mental Health Promotion 2001.
- European Commission . Green Paper: Improving the Mental Health of the Population: Towards a Strategy on Mental Health for the European Union 2005.
- Wittchen HU, Jacobi F. Size and burden of mental health disorders in Europe: a critical review and appraisal of 27 studies. Eur Neurospsychopharmacol 2005;15:357-76.
- Boath E, Henshaw C. The treatment of postnatal depression: a comprehensive literature review. J Reprod Infant Psychol 2001;19:215-48.
- O’Hara MW, Zekoski EM, Philipps LH, Wright EJ. Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol 1990;99:3-15.
- Green J. Postnatal depression or perinatal dysphoria? Findings from a longitudinal community-based study using the Edinburgh Postnatal Depression Scale. J Reprod Infant Psychol 1998;16:143-55.
- Barclay LM, Lloyd B. The misery of motherhood: alternative approaches to maternal distress. Midwifery 1996;12:136-9.
- Hendrick V. Treatment of postnatal depression. Br Med J 2003;327:1003-4.
- National Collaborating Centre for Primary Care . Postnatal Care: Routine Postnatal Care of Women and Their Babies 2006.
- Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry 1987;150:662-73.
- Pitt B. ‘Atypical’ depression following childbirth. Br J Psychiatry 1968;114:1325-35.
- Lewis G. Why mothers die 2000–2002. London: CEMACH; 2004.
- World Health Organization . International Classification of Diseases 10 1992.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders-IV 1994.
- Kumar R, Robson KM. A prospective study of emotional disorders in childbearing women. Br J Psychiatry 1984;144:35-47.
- Paykel ES, Emms EM, Fletcher J, Rassaby ES. Life events and social support in puerperal depression. Br J Psychiatry 1980;136:339-46.
- Richards JP. Postnatal depression: a review of recent literature. Br J Gen Pract 1990;40:472-6.
- O’Hara MW, Swain AM. Rates and risk of postpartum depression – a meta-analysis. Int Rev Psychiatry 1996;8:37-54.
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner. Perinatal depression: prevalence, screening accuracy, and screening outcomes. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Hotopf M, Lewis G, Normand C. The treatment of depression: evaluation and cost-effectiveness. London: London School of Hygiene and Tropical Medicine; 2001.
- Scott J, Palmer S, Paykel E, Teasdale J, Hayhurst H. Use of cognitive therapy for relapse prevention in chronic depression. Br J Psychiatry 2003;182:221-7.
- Department of Health . Prescription Cost Analysis 2004.
- Drife J. Why mothers die. J R Coll Physicians Edinb 2005;35:332-6.
- Webster A. The forgotten father: the effect on men when partners have PND. Community Pract 2002;75:390-3.
- Ballard CG, Davis R, Cullen PC, Mohan RN, Dean C. Prevalence of postnatal psychiatric morbidity in mothers and fathers. Br J Psychiatry 1994;164:782-8.
- Boath EH, Pryce AJ, Cox JL. Postnatal depression: the impact on the family. J Reprod Infant Psychol 1998;16:199-203.
- Morgan M, Matthey S, Barnett B, Richardson C. A group programme for postnatally distressed women and their partners. J Adv Nurs 1997;26:913-20.
- Cogill SR, Caplan HL, Alexandra H, Robson KM, Kumar R. Impact of maternal postnatal depression on cognitive development of young children. Br Med J 1986;292:1165-7.
- Caplan HL, Cogill SR, Alexandra H, Robson KM, Katz R, Kumar R. Maternal depression and the emotional development of the child. Br J Psychiatry 1989;154:818-22.
- Murray L. The impact of postnatal depression on infant development. J Child Psychol Psychiatry 1992;33:543-61.
- Sharp D, Hay DF, Pawlby S, Schmucker G, Allen H, Kumar R. The impact of postnatal depression on boys’ intellectual development. J Child Psychol Psychiatry 1995;36:1315-36.
- Rutter M, Quinton D. Parental psychiatric disorder: effects on children. Psychol Med 1984;14:853-80.
- Cornish AM, McMahon CA, Ungerer JA, Barnett B, Kowalenko N, Tennant C. Maternal depression and the experience of parenting in the second postnatal year. J Reprod Infant Psychol 2006;24:121-32.
- National Institute for Health and Clinical Excellence . Latest NICE Guidance Sets New Standards for Treating Depression in Children and Young People 2005.
- Social Exclusion Unit . Social Exclusion and Mental Health 2004.
- Boyce PM, Todd AL. Increased risk of postnatal depression after emergency caesarean section. Med J Aust 1992;157:172-4.
- Murray L, Cartwright W. The role of obstetric factors in postpartum depression. J Reprod Infant Psychol 1993;11:215-9.
- Carter FA, Frampton CM, Mulder RT. Cesarean section and postpartum depression: a review of the evidence examining the link. Psychosom Med 2006;68:321-30.
- O’Hara MW. Social support, life events, and depression during pregnancy and the puerperium. Arch Gen Psychiatry 1986;43:569-73.
- Cooper JE. Detection and management of psychiatric disorders in primary care. Br J Psychiatry 2003;182:1-4.
- Holden JM. Postnatal depression: its nature, effects, and identification using the Edinburgh Postnatal Depression scale. Birth 1991;18:211-21.
- Riley D. Perinatal mental health. A sourcebook for mental health professionals. Oxford: Radcliffe Medical Press; 1995.
- Small R, Astbury J, Brown S, Lumley J. Depression after childbirth. Does social context matter?. Med J Aust 1994;161:473-7.
- McIntosh J. Postpartum depression: women’s help-seeking behaviour and perceptions of cause. J Adv Nurs 1993;18:178-84.
- Green JM, Henshaw C, Elliott S. Screening for perinatal depression. London: Jessica Kingsley; 2005.
- Leverton T, Henshaw C, Elliott S. Screening for perinatal depression. 1st edn. London: Jessica Kingsley; 2005.
- Holden J, Cox J, Holden J. Perinatal psychiatry: use and misuse of the Edinburgh Postnatal Depression Scale. London: Gaskell; 1994.
- Shakespeare J. An evaluation of screening for postnatal depression against the NSC handbook criteria. Oxford: National Screening Committee; 2001.
- Shakespeare J. Health visitor screening for PND using the EPDS: a process study. Community Pract 2002;75:381-4.
- Coyle B, Adams C. The EPDS: guidelines for its use as part of a maternal mood assessment. Community Pract 2002;75:394-5.
- Rowley C, Dixon L. The utility of the EPDS for health visiting practice. Community Pract 2002;75:385-9.
- Murray L, Woolgar M, Cooper P. Detection and treatment of postpartum depression. Community Pract 2004;77:13-7.
- Holden J, Elliott S, Gerrard J. The management of postnatal depression. Trainers resource. London: Sainsbury Centre for Mental Health; 1996.
- Cohen LS, Altshuler LL, Harlow BL, Nonacs R, Newport DJ, Viguera AC. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. JAMA 2006;295:499-507.
- Wisner KL, Parry BL, Piontek CM. Clinical practice. Postpartum depression. N Engl J Med 2002;347:194-9.
- Anonymous . The management of postnatal depression. Drug Ther Bull 2000;38:33-7.
- Whitton A, Warner R, Appleby L. The pathways to care in postnatal depression: women’s attitudes to postnatal depression and its treatment. Br J Gen Pract 1996;46:427-8.
- Hoffbrand S, Howard L, Crawley H. Antidepressant drug treatment for postnatal depression. Cochrane Database Syst Rev 2001;2.
- Altshuler LL, Cohen LS, Moline ML, Kahn DA, Carpenter D, Docherty JP. Treatment of depression in women: a summary of the expert consensus guidelines. J Psychiatr Pract 2001;7:185-208.
- Rowland N, Bower P, Mellor C, Heywood P, Godfrey C. Effectiveness and cost effectiveness of counselling in primary care. Cochrane Database Syst Rev 2001;3.
- British Association for Counselling and Psychotherapy . Ethical Framework for Good Practice in Counselling and Psychotherapy 2002.
- British Association for Counselling . Code of Ethics and Practice for Counsellors (revised Version of Earlier Editions in 1984 and 1990) 2006.
- Chilvers C, Dewey M, Fielding K, Gretton V, Miller P, Palmer B. Antidepressant drugs and generic counselling for treatment of major depression in primary care: randomised trial with patient preference arms. Br Med J 2001;31:772-5.
- Sibbald B, Addington-Hall J, Brenneman D, Freeling P. Counsellors in English and Welsh general practices: their nature and distribution. Br Med J 1993;2:29-33.
- Harvey I, Nelson SJ, Lyons RA, Unwin C, Monaghan S, Peters TJ. A randomized controlled trial and economic evaluation of counselling in primary care. Br J Gen Pract 1998;48:1043-8.
- Friedli K, King MB, Lloyd M, Horder J. Randomised controlled assessment of non-directive psychotherapy versus routine general-practitioner care. Lancet 1997;350:1662-5.
- Ward E, King M, Lloyd M, Bower P, Sibbald B, Farrelly S. Randomised controlled trial of non-directive counselling, cognitive-behaviour therapy, and usual general practitioner care for patients with depression. I: Clinical effectiveness. Br Med J 2003;2:1383-8.
- Hemmings A. Counselling in primary care: a randomised controlled trial. Patient Educ Couns 1997;32:219-30.
- Churchill R, Hunot V, Corney R. A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression. Health Technol Assess 2001;5:1-173.
- Elliott SA. Psychological strategies in the prevention and treatment of postnatal depression. Baillieres Clin Obstet Gynaecol 1989;3:879-903.
- Appleby L, Hirst E, Marshall S, Keeling F, Brind J, Butterworth T. The treatment of postnatal depression by health visitors: impact of brief training on skills and clinical practice. J Affect Disord 2003;77:261-6.
- Bostock J, Anderson S, Beck A, Parker A, Towers J. Health visiting outcome group: promoting mental health. Nottingham: Nottingham Community Health NHS Trust; 1994.
- Gutteridge K. Tamworth Postnatal Depression Support Group Portfolio. Tamworth: The Tamworth Postnatal Depression Support Group; 2001.
- Griffiths M. Edinburgh Postnatal Depression Scale. Hull: Hull and East Riding Community Health NHS Trust; 1999.
- Cullinan R. Health visitor intervention in postnatal depression. Health Visit 1991;64:412-4.
- Allen S. Early detection of postnatal depression. Nurs Stand 1993;8:25-8.
- Sheldrake D, Sillman C. Developing partnerships for practice: using the Edinburgh postnatal score. Br J Comm Health Nurs 1996;1:50-4.
- Tully C, Watson C, Abrams A. Postnatal depression: training health visitors to use the EPDS. Community Pract 1998;71:213-5.
- McConnell J, Baker M, Marks L. Experiencing a dilemma – accounts of working with PND. Community Pract 2005;78:251-4.
- National Collaborating Centre for Mental Health . Obtaining Views of Healthcare Professionals Who Have Cared for Women Who Have Experienced Mental Health Problems in the Antenatal and Postnatal Period to Inform the NICE Guideline on the Management of Mental Health in the Antenatal and Postnatal Period: Personal Testimonies 2004.
- Department of Health . National Service Framework for Mental Health. Modern Standards and Service Models 1999.
- Department of Health . The National Service Framework for Mental Health – Five Years on 2004.
- Scottish Intercollegiate Guidelines Network (SIGN) . Postnatal Depression and Puerperal Psychosis 2002.
- Department of Health . Women’s Mental Health. Into the Mainstream, Implementation Plan: Mainstreaming Gender and women’s Mental Health 2003.
- Sainsbury Centre for Mental Health . The Future of Mental Health: A Vision for 2015 2006.
- Armour M. Integrated care pathway for postnatal depression and other perinatal mental health problems. Dumfries: Dumfries and Galloway Primary Care NHS Trust; 2003.
- Coyle B, Adams C. Postnatal depression and maternal health network. London: Community Practioners’ and Health Visitors’ Association; 2003.
- Campbell F, Cowley S, Buttigieg M. Weights and measures: outcomes and evaluation in health visiting. London: Health Visitors’; 1995.
- Billingham K, Morrell J, Billingham C. Reflections on the history of health visiting. Br J Community Health Nurs 1996;1:386-92.
- Cowley S. Reflecting on the past; preparing for the next century. Health Visit 1996;69:313-6.
- Council for the Education and Training of Health Visitors . An Investigation into the Principles of Health Visiting 1977.
- Hall MB. Health for all children. Oxford: Oxford University Press; 1996.
- Boateng P. Every child matters. London: HM Treasury; 2003.
- Department of Health . The Chief Nursing Officer’s Review of the Nursing, Midwifery and Health Visiting Contribution to Vulnerable Children and Young People 2004.
- Elkan R, Kendrick D, Hewitt M, Robinson JJ, Tolley K, Blair M. The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature. Health Technol Assess 2000;4:1-339.
- Adams C. C linical effectiveness: a practical guide for the community nurse. London: CPHVA; 2003.
- Ciliska D. The effectiveness of home visiting as a delivery strategy for public health nursing interventions – a systematic overview. Toronto: McMaster University, Toronto; 1994.
- Bull J, McCormick G, Swann C, Mulvihill C. Ante- and postnatal home-visiting programmes: a review of reviews. London: Health Development Agency; 2004.
- Kendrick D, Elkan R, Hewitt M, Dewey M, Blair M, Robinson J. Does home visiting improve parenting and the quality of the home environment? A systematic review and meta-analysis. Arch Dis Child 2000;82:443-51.
- Roberts I, Kramer MS, Suissa S. Does home visiting prevent childhood injury? A systematic review of randomised controlled trials. Br Med J 1996;312:29-33.
- Bhatti-Ali R, Hussain A. The Development and Evaluation of a Punjabi Postnatal Screening Questionnaire 2000.
- Austin MP. Targeted group antenatal prevention of postnatal depression: a review. Acta Psychiatr Scand 2003;107:244-50.
- Lumley J, Austin MP, Mitchell C. Intervening to reduce depression after birth: a systematic review of the randomized trials. Int J Technol Assess Health Care 2004;20:128-44.
- Dennis CL, Creedy D. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev 2004;4.
- Hodnett ED. Caregiver support for women during childbirth. Cochrane Database Syst Rev 2002;1.
- Barlow J, Coren E. Parent-training programmes for improving maternal psychosocial health. Cochrane Database Syst Rev 2004;1.
- Ray KL, Hodnett ED. Caregiver support for postpartum depression. Cochrane Database Syst Rev 2001;3.
- Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T, Kirwan P. Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med 2000;30:1273-81.
- Chabrol H, Teissedre F, Saint-Jean M, Teisseyre N, Roge B, Mullet E. Prevention and treatment of post-partum depression: a controlled randomized study on women at risk. Psychol Med 2002;32:1039-47.
- Gorman L. Prevention of postpartum depression in a high risk sample. Iowa City. IA: University of Iowa; 2001.
- Hayes BA, Muller R, Bradley BS. Perinatal depression: a randomized controlled trial of an antenatal education intervention for primiparas. Birth 2001;28:28-35.
- Logsden MC, Birkimer JC, Simpson T, Looney S. Postpartum depression and social support in adolescents. J Obstet Gynecol Neonatal Nurs 2005;34:46-54.
- Marks MN, Siddle K, Warwick C. Can we prevent postnatal depression? A randomized controlled trial to assess the effect of continuity of midwifery care on rates of postnatal depression in high-risk women. J Matern Fetal Neonatal Med 2003;13:119-27.
- Matthey S, Kavanagh DJ, Howie P, Barnett B, Charles M. Prevention of postnatal distress or depression: an evaluation of an intervention at preparation for parenthood classes. J Affect Disord 2004;79:113-26.
- Stamp GE, Williams AS, Crowther CA. Evaluation of antenatal and postnatal support to overcome postnatal depression: a randomized, controlled trial. Birth 1995;22:138-43.
- Zlotnick C, Johnson SL, Miller IW, Pearlstein T, Howard M. Postpartum depression in women receiving public assistance: pilot study of an interpersonal-therapy-oriented group intervention. Am J Psychiatry 2001;158:638-40.
- Field T, Hernandez-Reif M, Taylor S, Quintino O, Burman I. Labor pain is reduced by massage therapy. J Psychosom Obstet Gynaecol 1997;18:286-91.
- Gamble J, Creedy D, Moyle W, Webster J, McAllister M, Dickson P. Effectiveness of a counseling intervention after a traumatic childbirth: a randomized controlled trial. Birth 2005;32:11-9.
- Gordon NP, Walton D, Macadam E, Derman J, Gallitero G, Garrett L. Effects of providing hospital-based doulas in health maintenance organization hospitals. Obstet Gynecol 1999;93:422-6.
- Hagan R, Evans SF, Pope S. Preventing postnatal depression in mothers of very preterm infants: a randomised controlled trial. Br J Obstet Gynaecol 2004;111:641-7.
- Lavender T, Walkinshaw SA. Can midwives reduce postpartum psychological morbidity? A randomized trial. Birth 1998;25:215-19.
- Priest SR, Henderson J, Evans SF, Hagan R. Stress debriefing after childbirth: a randomised controlled trial. Med J Aust 2003;178:542-5.
- Selkirk R, McLaren S, Ollerenshaw A, McLachlan AJ. The longitudinal effects of midwife-led postnatal debriefing on the psychological health of mothers. J Reprod Infant Psychol 2006;24:133-47.
- Small R, Lumley J, Donohue L, Potter A, Waldenstrom U. Randomised controlled trial of midwife-led debriefing to reduce maternal depression after operative childbirth. Br Med J 2000;321:1043-7.
- Tam WH, Lee DT, Chiu HF, Ma KC, Lee A, Chung TK. A randomised controlled trial of educational counselling on the management of women who have suffered suboptimal outcomes in pregnancy. Br J Obstet Gynaecol 2003;110:853-9.
- Wolman WL, Chalmers B, Hofmeyr GJ, Nikodem VC. Postpartum depression and companionship in the clinical birth environment: a randomized, controlled study. Am J Obstet Gynecol 1993;168:1388-93.
- Hardy JB, Street R. Family support and parenting education in the home: an effective extension of clinic-based preventive health care services for poor children. J Pediatr 1989;115:927-31.
- Johnson Z, Howell F, Molloy B. Community mothers’ programme: randomised controlled trial of non-professional intervention in parenting. Br Med J 1993;306:1449-52.
- O’Sullivan AL, Jacobsen BS. A randomized trial of a health care program for first-time adolescent mothers and their infants. Nurs Res 1992;41:210-15.
- Toroyan T, Roberts I, Oakley A, Laing G, Mugford M, Frost C. The Hackney Daycare Study – effectiveness and economic evaluation of out-of-home daycare for disadvantaged families: a randomised controlled trial. London: London School of Hygiene and Tropical Medicine; 2002.
- Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H. The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas. Health Technol Assess 2004;8.
- Armstrong KL, Fraser JA, Dadds MR, Morris J. A randomized, controlled trial of nurse home visiting to vulnerable families with newborns. J Paediatr Child Health 1999;35:237-44.
- Armstrong KL, Fraser JA, Dadds MR, Morris J. Promoting secure attachment, maternal mood and child health in a vulnerable population: a randomized controlled trial. J Paediatr Child Health 2000;36:555-62.
- Fraser JA, Armstrong KL, Morris JP, Dadds MR. Home visiting intervention for vulnerable families with newborns: follow-up results of a randomized controlled trial. Child Abuse Neglect 2000;24:1399-42.
- Gunn J, Lumley J, Chondros P, Young D. Does an early postnatal check-up improve maternal health: results from a randomised trial in Australian general practice. Br J Obstet Gynaecol 1998;105:991-7.
- MacArthur C, Winter HR, Bick DE, Knowles H, Lilford R, Henderson C. Effects of redesigned community postnatal care on womens’ health months after birth: a cluster randomised controlled trial. Lancet 2002;359:378-85.
- Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A. Costs and benefits of community postnatal support workers: a randomised controlled trial. Health Technol Assess 2000;4:1-100.
- Reid M, Glazener C, Murray GD, Taylor GS. A two-centred pragmatic randomised controlled trial of two interventions of postnatal support. Br J Obstet Gynaecol 2002;109:1164-70.
- Dennis CL. Treatment of postpartum depression, part 2: a critical review of nonbiological interventions. J Clin Psychiatry 2004;65:1252-65.
- O’Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiatry 2000;57:1039-45.
- Armstrong K, Edwards H. The effectiveness of a pram-walking exercise programme in reducing depressive symptomatology for postnatal women. Int J Nurs Pract 2004;10:177-94.
- Chen CH, Tseng YF, Chou FH, Wang SY. Effects of support group intervention in postnatally distressed women. A controlled study in Taiwan. J Psychosom Res 2000;49:395-9.
- Cooper PJ, Murray L, Murray L, Cooper PJ. Postpartum depression and child development. London: Guildford Press; 1997.
- Dennis CL. The effect of peer support on postpartum depression: a pilot randomized controlled trial. Can J Psychiatry 2003;48:115-24.
- Field T, Grizzle N, Scafidi F, Schanberg S. Massage and relaxation therapies’ effects on depressed adolescent mothers. Adolescence 1996;31:903-11.
- Heh SS, Fu YY. Effectiveness of informational support in reducing the severity of postnatal depression in Taiwan. J Adv Nurs 2003;42:30-6.
- Honey KL, Bennett P, Morgan M. A brief psycho-educational group intervention for postnatal depression. Br J Clin Psychol 2002;41:405-9.
- Milgrom J, Negri LM, Gemmill AW, McNeil M, Martin PR. A randomized controlled trial of psychological interventions for postnatal depression. Br J Clin Psychol 2005;44:529-42.
- Misri S, Kostaras X, Fox D, Kostaras D. The impact of partner support in the treatment of postpartum depression. Can J Psychiatry 2000;45:554-8.
- Misri S, Reebye P, Corral M, Milis L. The use of paroxetine and cognitive-behavioral therapy in postpartum depression and anxiety: a randomized controlled trial. J Clin Psychiatry 2004;65:1236-41.
- Onozawa K, Glover V, Adams D, Modi N, Kumar RC. Infant massage improves mother–infant interaction for mothers with postnatal depression. J Affect Disord 2001;63:201-7.
- Prendergast J, Austin MP. Early childhood nurse-delivered cognitive behavioural counselling for post-natal depression. Australas Psychiatry 2001;9:255-9.
- Wickberg B, Hwang CP. Counselling of postnatal depression: a controlled study on a population based Swedish sample. J Affect Disord 1996;39:209-16.
- Murray L, Cooper PJ, Wilson A, Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression: 2. Impact on the mother–child relationship and child outcome. Br J Psychiatry 2003;182:420-7.
- Shakespeare J, Blake F, Garcia J. How do women with postnatal depression experience listening visits in primary care? A qualitative interview study. J Reprod Infant Psychol 2006;24:149-62.
- Campbell MJ. Cluster randomized trials in general (family) practice research. Stat Methods Med Res 2000;9:81-94.
- Clark DM, Fairburn CG. Science and practice of cognitive behaviour therapy. Oxford: Oxford University Press; 1997.
- Sanders P. Mapping person-centred approaches to counselling and psychotherapy. Person-Centred Pract 2000;8:62-74.
- World Health Organization . Schedules for Assessment in Neuropsychiatry II 1999.
- Hotopf M, Churchill R, Lewis G. Pragmatic randomised controlled trials in psychiatry. Br J Psychiatry 1999;175:217-23.
- Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ. Methods for evaluating area-wide and organisational-based interventions in health and health-care: a systematic review. Health Technol Assess 1999;3.
- Donner A, Klar N, Donner A, Klar N. Design and analysis of cluster randomization trials in health research. London: Arnold Hodder Headline; 2000.
- Edwards SJ, Braunholtz DA, Lilford RJ, Stevens AJ. Ethical issues in the design and conduct of cluster randomised controlled trials. Br Med J 1999;318:1407-9.
- Hutton JL. Are distinctive ethical principles required for cluster randomized controlled trials?. Stat Med 2001;20:473-88.
- Edwards SJ, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J. Ethical issues in the design and conduct of randomised controlled trials. Health Technol Assess 1998;2.
- Medical Research Council . Cluster Randomised Trials: Methodological and Ethical Considerations 2002.
- Neal D. Index of Multiple Deprivation Item 5 (IMD). London: Economic Development Steering Group, Association of London Government; 2004.
- Shakespeare J, Blake F, Garcia J. How do women with postnatal depression experience listening visits in primary care? A qualitative interview study. J Reprod Infant Psychol 2003;24:149-62.
- Cox J, Cox J, Holden J. Perinatal psychiatry: use and misuse of the Edinburgh Postnatal Depression Scale. London: Gaskell; 1994.
- Ware JE, Sherbourne CD. The MOS 36-item Short Form Health Survey SF-36. Med Care 1992;30:473-83.
- Barkham M, Margison F, Leach C, Lucock M, Mellor-Clark J, Evans C. Service profiling and outcomes benchmarking using the CORE-OM: toward practice-based evidence in the psychological therapies. Clinical Outcomes in Routine Evaluation-Outcome Measures. J Consult Clin Psychol 2001;69:184-96.
- Evans C, Connell J, Barkham M, Margison F, McGrath G, Mellor-Clark J. Towards a standardised brief outcome measure: psychometric properties and utility of the CORE-OM. Br J Psychiatry 2002;180:51-60.
- Leach C, Lucock M, Barkham M, Noble R, Iveson S. Transforming between Beck Depression Inventory and CORE-OM scores in routine clinical practice. Br J Clin Psychol 2006;45:153-66.
- Brugha TS, Sturt E, Maccarthy B, Potter J, Wykes T, Bebbington PE. The Interview Measure of Social Relationships: the description and evaluation of a survey instrument for assessing personal social resources. Soc Psychiatry Psychiatr Epidemiol 1987;22:123-8.
- Brown GW, Harris T. Social origins of depression. London: Tavistock; 1978.
- Brugha TS, Cragg D. The List of Threatening Experiences: the reliability and validity of a brief life events questionnaire. Acta Psychiatr Scand 1990;82:77-81.
- Ware JE, Kosinski M, Gandek B. SF-12: how to score the SF-12 physical and mental health summary scales. Boston: Health Institute; 1995.
- Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: results from the IQOLA Project. J Clin Epidemiol 1998;51:1171-8.
- Matthey S, Barnett B, Howie P, Kavanagh DJ. Diagnosing postpartum depression in mothers and fathers: whatever happened to anxiety?. J Affect Disord 2003;74:139-47.
- Spielberger CD, Gorusch RL, Lushene R, Vagg PR, Jacobs GA. State-trait anxiety for adults, sampler set, manual, test, scoring key. Palo Alto, CA.: Mind Garden; 1983.
- Abidin RA. Parenting Stress Index. Lutz: Psychological Assessment Resources; 1995.
- Spanier GB. Dyadic Adjustment Scale. J Marriage Fam 1976;38:15-28.
- Sabourin S, Valois P, Lussier Y. Development and validation of a brief version of the Dyadic Adjustment Scale with a nonparametric item analysis model. Psychol Assess 2005;17:15-27.
- Osuch EA, Brotman MA, Podell D, Geraci M, Touaeau PL, Leverich GS, et al. Prospective and retrospective life-charting in posttraumatic stress disorder (the PTSD-LCM): a pilot study. J Trauma Stress 2001;14:229-39.
- Baron-Cohen S, Wheelwright S, Cox A, Baird T, Charman T, Swettenham J, et al. The early identification of autism: the Checklist for Autism in Toddlers (CHAT). J R Soc Med 2000;93:521-5.
- Campbell MK, Elbourne DR, Altman DG. CONSORT statement: extension to cluster randomised trials. Br Med J 2004;328:702-8.
- Diggle PJ, Heagerty P, Liang KY, Zeger SL. Analysis of longitudinal data. Oxford: Oxford University Press; 2002.
- Stata Statistical Software: release 8.0 [computer program]. Stata Corporation; 2003.
- Altman DG, Machin D, Bryant TN, Gardner MJ. Statistics with confidence. London: BMJ Books; 2000.
- Perneger TV. What’s wrong with Bonferroni adjustments. Br Med J 1998;316:1236-8.
- Kendall PC, Holmbck GVT, Lambert MJ. Bergin and Garfield’s handbook of psychotherapy and behaviour change. New York: Wiley; 2004.
- Hill CE, Lambert MJ, Lambert MJ. Bergin and Garfield’s handbook of psychotherapy and behaviour change. New York: Wiley; 2004.
- Luborsky L, Diguer L, Seligman DA, Rosenthal R, Krause ED, Johnson S. The researcher’s own therapy allegiances: a ‘wild card’ in comparisons of treatment efficacy. Clin Psychol 1999;6:95-106.
- Barker C, Pistrang N, Shapiro DA. Client’s beliefs about psychological problems using the Opinions about Psychological Problems. Couns Psychol Q 1992;5:325-36.
- Roth AD, Parry G. The implications of psychotherapy research for clinical practice and service development: lessons and limitations. J Ment Health 1997;6:367-80.
- Stiles WB, Reynolds SR, Hardy GE, Rees BL, Barkham M, Shapiro DA. Evaluation and description of psychotherapy sessions by clients using the session evaluation questionnaire and the session impacts scale. J Couns Psychol 1994;41:13-21.
- Stiles WB, Hardy GE, Cahill J, Barkham M, Agnew-Davies R. The Short ARM: A Short Form of the Agnew Relationship Measure n.d.
- Agnew-Davies R, Stiles WB, Hardy GE, Barkham M, Shapiro DA. Alliance structure assessed by the Agnew Relationship Measure (ARM). Br J Clin Psychol 1998;37:155-72.
- The Suzy Lamplugh Trust . Working Safely in Other people’s Homes 2002.
- Department of Health . Research Governance Framework for Health and Social Care 2005.
- Department of Health . Attributing Revenue Costs of Externally Funded Non-Commercial Research in the NHS (ARCO). 2005. www.dh.gov.uk/PublicationsAndStatistics/PublicationsPolicyAndGuidance/.
- National Health Service 2006. www.nhs.uk/England/Doctors/Default.aspx.
- Office for National Statistics . England Profiles 2001. www.statistics.gov.uk/census2001/profiles/64.asp.
- Horvath AO, Luborsky L. The role of the therapeutic alliance in psychotherapy. J Consult Clin Psychol 1993;61:561-73.
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. J Consult Clin Psychol 2000;68:438-50.
- Hardy GE, Cahill J, Shapiro DA, Barkham M, Rees A, Macaskill N. Client interpersonal and cognitive styles as predictors of response to time-limited cognitive therapy for depression. J Consult Clin Psychol 2001;69:841-5.
- Shapiro DA, Barkham M, Rees A, Hardy GE, Reynolds S, Startup M. Effects of treatment duration and severity of depression on the effectiveness of cognitive-behavioural therapy and psychodynamic-interpersonal therapy. J Consult Clin Psychol 1994;62:522-8.
- National Institute for Health and Clinical Excellence . Guide to the Methods of Technology Appraisal 2004.
- Netten A, Curtis L. Unit costs of health and social care. University of Kent, Canterbury: PSSRU; 2004.
- Department of Health . Trust Financial Returns 2004 2005.
- Department of Health . NHS Reference Costs 2004 2005.
- British Medical Association and Royal Pharmaceutical Society of Great Britain . British National Formulary (BNF). 2005.
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002;21:271-92.
- Schafer JL. Analysis of incomplete multivariate data. London: Chapman and Hall; 1997.
- Munro JF, Nichol JP, Brazier JE, Davey R, Cochrane T. Cost-effectiveness of a community based exercise programme in over 65 year olds: cluster randomised trial. J Epidemiol Community Health 2004;58:1004-10.
- Goodacre S, Nicholl J, Dixon S, Cross E, Angelini K, Arnold J. Cluster randomised controlled trial and economic evaluation of chest pain observation unit versus routine care. Br Med J 2004;328:254-60.
- Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M. Psychological treatment for insomnia in the management of long-term hypnotic drug use: a pragmatic randomised controlled trial. Br J Gen Pract 2003;53:923-8.
- Podkolinski J, Clement S. Psychological perspectives on pregnancy and childbirth. Edinburgh: Churchill Livingstone; 1998.
- King N, Symon G, Cassell C. Qualitative methods and analysis in organisational research: a practical guide. London: Sage; 1998.
- Reicher-Rossler A, Hofecker M. Postpartum depression: do we still need this diagnostic term?. Acta Psychiatr Scand 2003;108:51-6.
- Rogers CR. A way of being. Boston: Houghton Mifflin; 1980.
- National Institute for Health and Clinical Excellence . Antenatal and Postnatal Mental Health. Clinical Management and Service Guidance 2007.
- Morrell CJ. Review of interventions to prevent or treat postnatal depression. Clin Eff Nurs 2006:E135-61.
- Stiles WB, Shapiro DA, Elliott R. Are all psychotherapies equivalent?. Am Psychol 1986;41:165-80.
- Stiles WB, Barkham M, Twigg E, Mellor-Clark J, Cooper M. Effectiveness of cognitive-behavioural, person-centred, and psychodynamic therapies as practiced in UK National Health Service settings. Psychol Med 2006;36:555-66.
- Ainsworth MD, Blehar MC, Waters E, Wall S. Patterns of attachment: a psychological study of the strange situation. Hillside, NJ: Erlbaum; 1987.
- Bayley N. Bayley Scales of Infant Development. New York: Psychological Corporation; 1969.
- Bandolier . Number Needed to Treat (NNT) n.d. www.jr2.ox.ac.UK/bandolier/band59/NNT1.html.
- Jorm AF, Henderson AS, Scott R, MacKinnon AJ, Korten AE, Christensen H. Do mental health surveys disturb? Further evidence. Psychol Med 1994;1:233-7.
- Raue P, Goldfried M, Markham M. The therapeutic alliance in psychodynamic-interpersonal and cognitive behavioural therapy. J Consult Clin Psychol 2006;65:582-7.
- Stiles WB, Agnew-Davies R, Barkham M, Culverwell A, Goldfried MR, Halstead J. Convergent validity of the Agnew Relationship Measure and the Working Alliance Inventory. Psychol Assess 2006;14:209-20.
- Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: a meta-analysis. J Couns Psychol 1991;38.
- Brown S, Lumley J. Physical health problems after childbirth and maternal depression at six to seven months postpartum. Breast J Obstet Gynaecol 2000;107:1194-201.
- Oates MR, Cox JL, Neema P, Asten P, Glangeaud-Freudenthal N, Figueiredo B, et al. Postnatal depression across countries and cultures: a qualitative study. Br J Psychiatry 2004;184:s10-16.
- Henshaw CA. What do women think about treatments for postnatal depression?. Clin Eff Nurs 2004;8:170-5.
- Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth 2006;33:323-31.
Appendix 1 Participant flow charts
FIGURE 27.
Overall participant flow chart for 8716 pregnant women in all clusters.
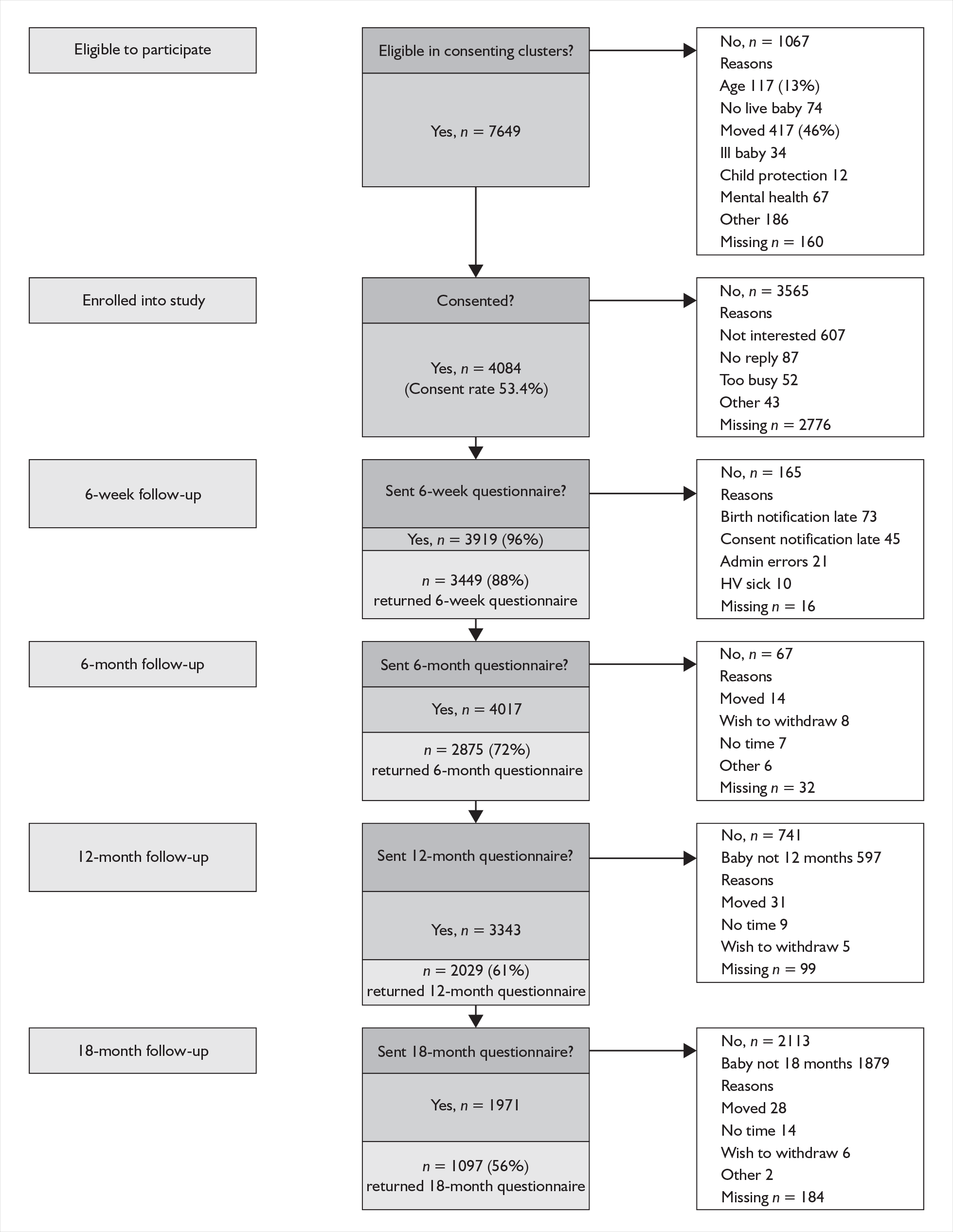
FIGURE 28.
Flow chart for the population of consented women who returned a 6-week questionnaire by group. CBA-F, cognitive behavioural approach face-to-face group; CBA-P, cognitive behavioural approach postal group; EPDS, Edinburgh Postnatal Depression Scale; PCA-F, person-centred approach face-to-face group; PCA-P, person-centred approach postal group.
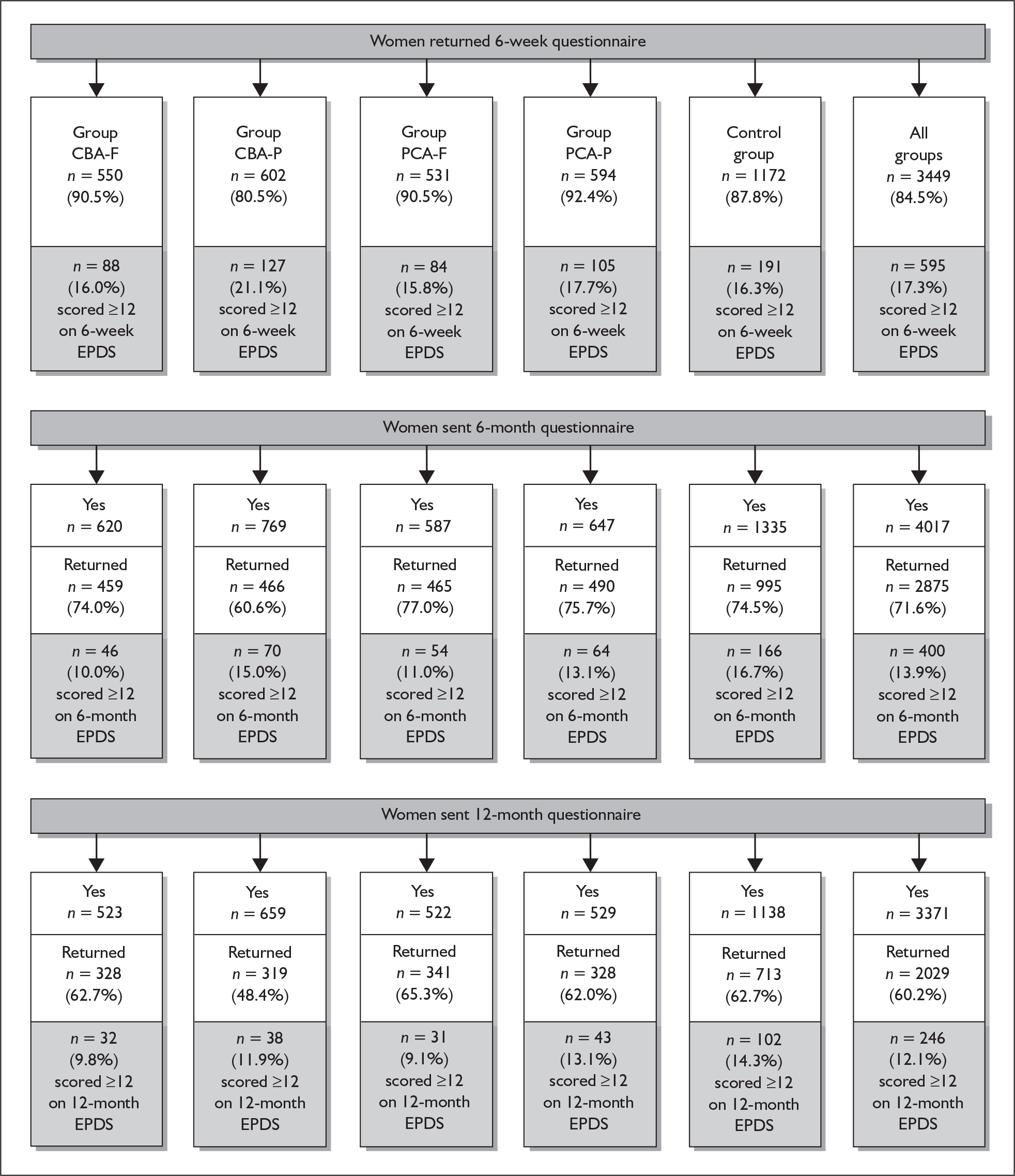
FIGURE 29.
Flow chart for at-risk women by group (n = 595). CBA-F, cognitive behavioural approach face-to-face group; CBA-P, cognitive behavioural approach postal group; EPDS, Edinburgh Postnatal Depression Scale; PCA-F, person-centred approach face-to-face group; PCA-P, person-centred approach postal group.
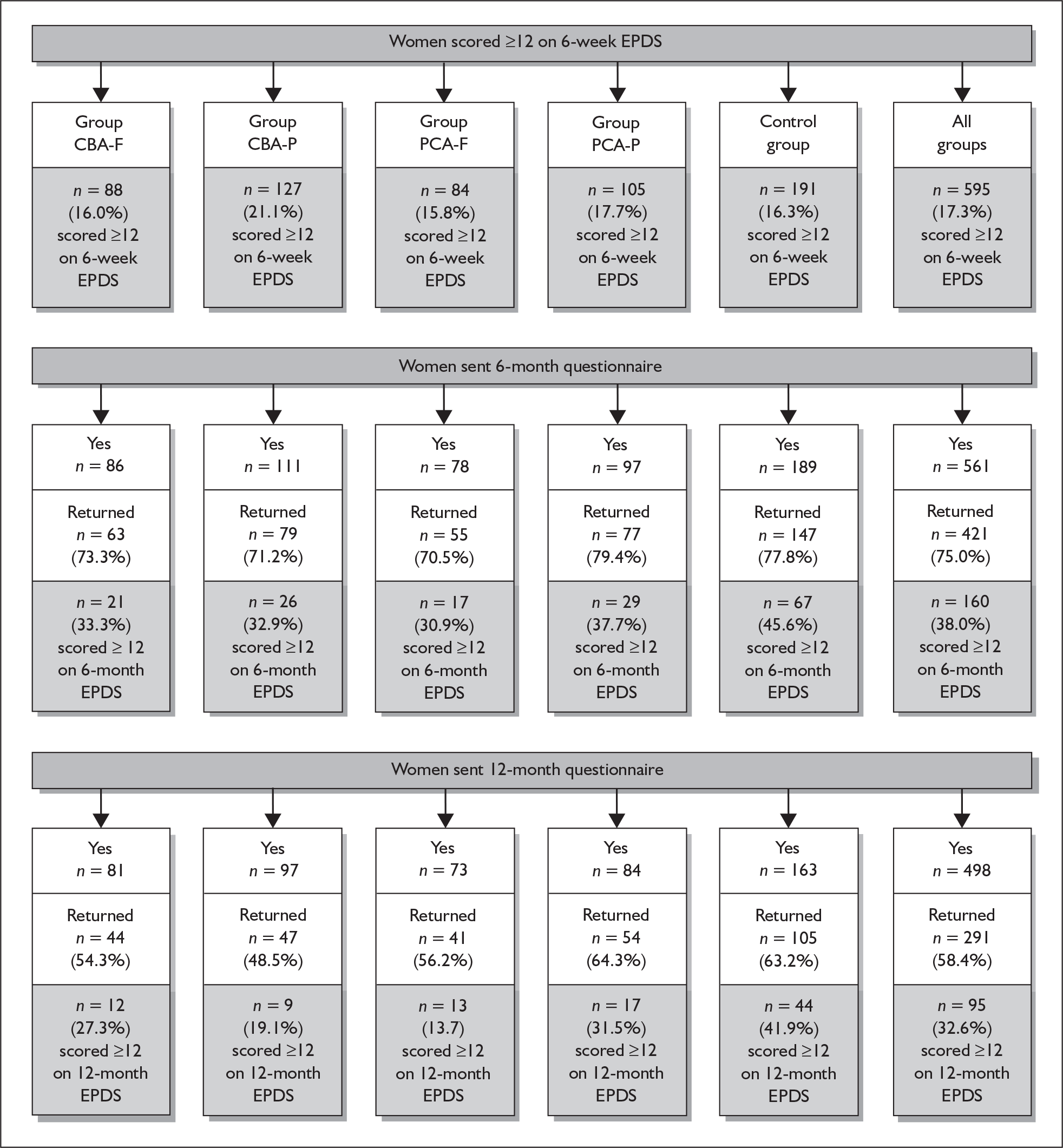
Appendix 2 Economic analysis
At-risk women at 12 months
When the perspective was shifted to mother and baby costs up to 12 months no statistically significant differences were seen in the main components of resource use or cost (Tables 70 and 71). There appeared to be some anomalous results with the CG using fewer health service resources for the care of the baby but generating higher costs. This was due to a greater proportion of the contacts being hospitalisations, which at £516 per day have a big influence on the mean. The inclusion of these costs was also responsible for the increase in the size of the 95% confidence intervals around total costs.
| Item | Control mean (n = 40) | Intervention mean (n = 83) | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| HV visits to 6 months | 8.6 | 8.3 | –0.3 | –3.7 to 3.2 |
| HV visits 6–12 months | 2.9 | 3.6 | + 0.7 | –0.4 to 1.8 |
| Number of vaccinations to 6 months | 8.4 | 8.2 | –0.2 | –1.0 to 0.7 |
| Health service contacts for baby to 6 months | 2.6 | 2.8 | + 0.2 | –0.9 to 1.2 |
| Health service contacts for baby 6–12 months | 2.2 | 2.5 | + 0.3 | –0.6 to 1.2 |
| Item | Control mean (n = 40) | Intervention mean (n = 83) | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| HV costs and other NHS costs for mother | 442 | 493 | + 51 | –142 to 243 |
| NHS costs for baby up 12 months | 486 | 352 | –134 | –408 to 140 |
| Total mother and baby costs at 12 months | 947 | 851 | –96 | –443 to 251 |
All of this information was summarised in the form of a CEAC (Figure 30). This showed the probability that the intervention was cost-effective at various threshold values of a QALY. Even with no value placed on health gains, the intervention had a 65% chance of being cost-effective; this reflected the fact that 65% of observations were in the southeast quadrant. In the range of QALY values between £20,000 and £30,000 the probability of the intervention being cost-effective was just over 80%.
FIGURE 30.
Cost-effectiveness acceptability curve for at-risk women at 12 months.
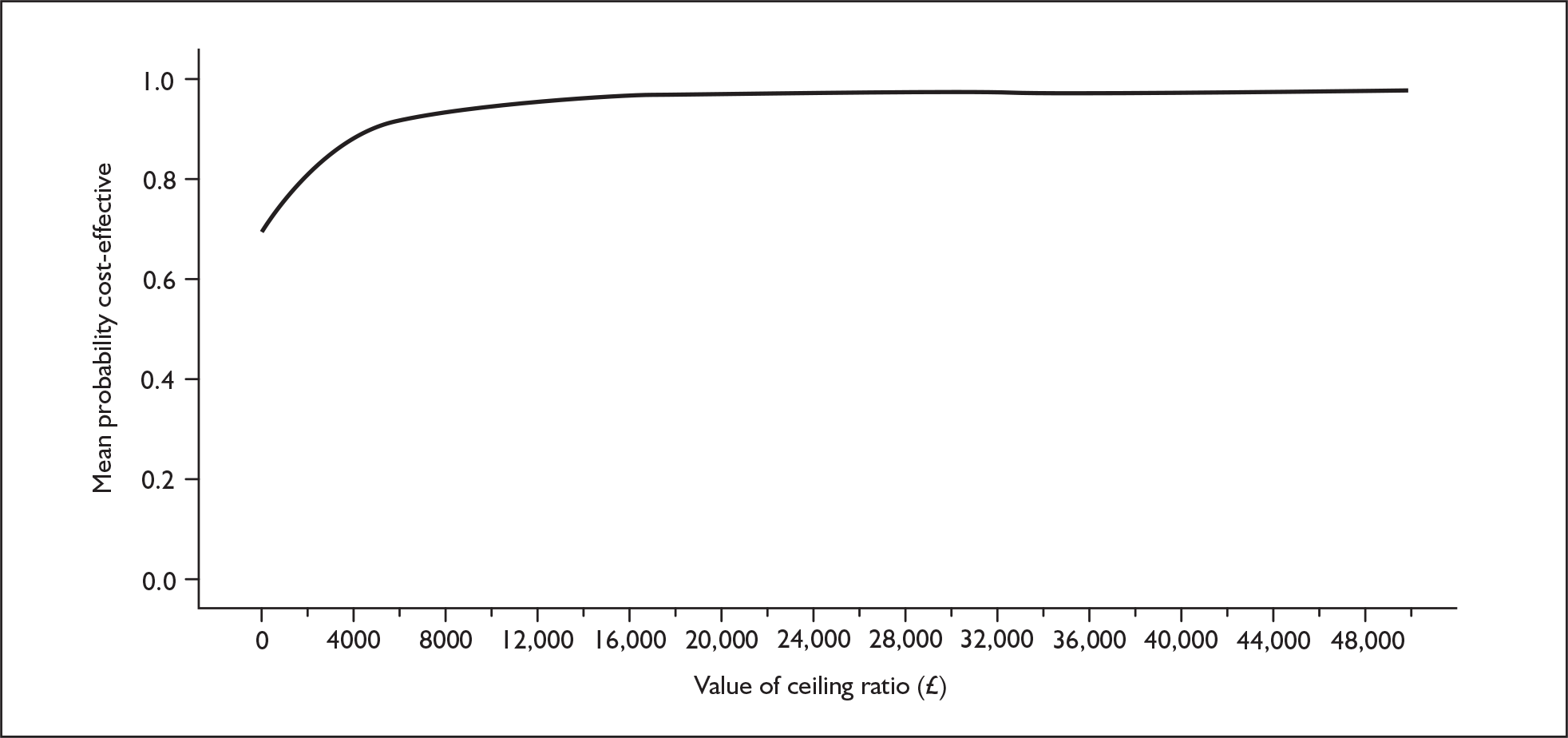
In summary, the 12-month analysis showed lower mean costs in the IG and higher mean QALYs gained (Table 72), and a greater than 90% chance of the intervention being cost-effective.
| Item | Control mean (n = 40) | Intervention mean (n = 83) | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| QALYs gained | 0.087 | 0.112 | + 0.025 | –0.008 to 0.059 |
| Total costs | 947 | 851 | –96 | –443 to 251 |
All women at 12 months
The 12-month data show a statistically significant increase in QALYs gained in the IG of 0.01 (95% CI 0.000 to 0.021) (Table 73). When combined with the almost identical costs in the two groups this produces a greater than 90% chance of the intervention being cost-effective in the £20,000–30,000 per QALY range (Figure 31).
| Item | Control mean (n = 20) | Intervention mean (n = 83) | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| QALYs gained | 0.107 | 0.117 | + 0.010 | 0.000 to 0.021 |
| Total costs | 772 | 763 | –9 | –177 to 159 |
FIGURE 31.
Cost-effectiveness acceptability curve for all women at 12 months.
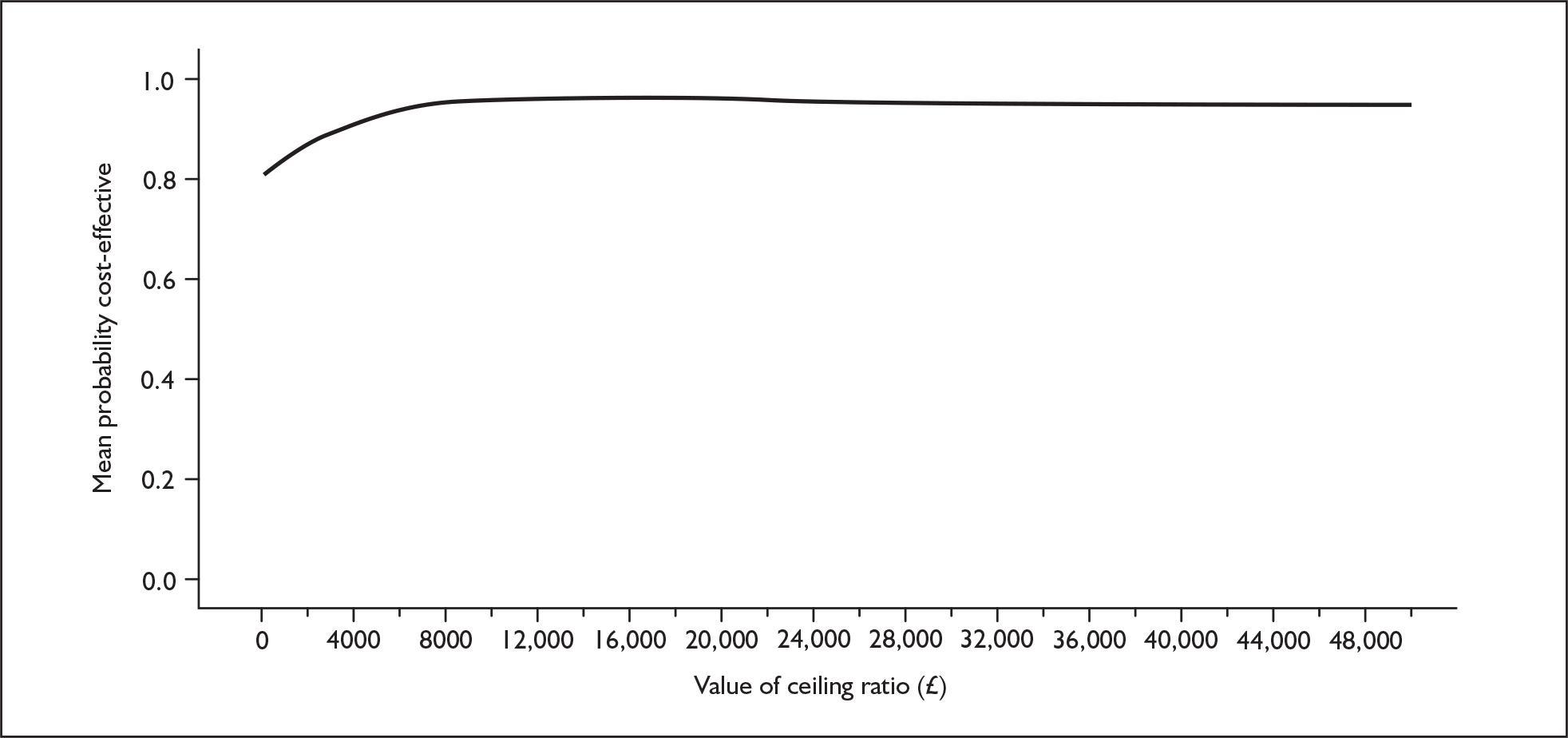
List of abbreviations
- ARM
- Agnew Relationship Measure
- BAC
- British Association of Counselling
- BacReN
- Barnsley Research Network
- BDI
- Beck Depression Inventory
- BSQ
- Behaviour Screening Questionnaire
- CBA
- cognitive behavioural approach
- CBA-F
- cognitive behavioural approach face-to-face group
- CBA-P
- cognitive behavioural approach postal group
- CBC
- cognitive behavioural counselling
- CBT
- cognitive behavioural therapy
- CCTR
- Cochrane Controlled Trials Register
- CDSR
- Cochrane Database of Systematic Reviews
- CG
- control group
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature (health database)
- CORE-OM
- Clinical Outcomes in Routine Evaluation Outcome Measure
- CPHVA
- Community Practitioners’ and Health Visitors’ Association
- CPN
- community psychiatric nurse
- CRN
- collaborative research network
- DAS
- Dyadic Adjustment Scale
- DocReN
- Doncaster Research Network
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders version IV
- DSM-III-R
- Diagnostic and Statistical Manual of Mental Disorders version III
- EPDS
- Edinburgh Postnatal Depression Scale
- GFC
- general facilitative conditions
- GHQ-12
- 12-item General Health Questionnaire
- GIS
- geographical information systems
- HADS
- Hospital Anxiety and Depression Scale
- HTA
- health technology assessment
- HV
- health visitor
- ICC
- intracluster correlation coefficient
- ICD-10
- International Classification of Diseases
- ICP
- integrated care pathway
- IG
- intervention group
- IMD
- Index of Multiple Deprivation
- IPT
- interpersonal psychotherapy
- ITT
- intention to treat
- LC
- local co-ordinator
- LEQ
- Life Events Questionnaire
- LOCF
- last observation carried forward
- LREC
- Local Research Ethics Committee
- MMR
- measles, mumps and rubella immunisation
- MRC
- Medical Research Council
- MREC
- Multicentre Research Ethics Committee
- MSR
- Measure of Social Relationships
- NDC
- non-directive counselling
- NICE
- National Institute for Health and Clinical Excellence
- NSF
- National Service Framework
- NUD*IST
- Non-numerical Unstructured Data by Indexing, Searching and Theorizing (software)
- NVivo
- qualitative software package capable of handling rich text records
- OPP
- Opinions on Psychological Problems
- PCA
- person-centred approach
- PCA-F
- person-centred approach face-to-face group
- PCA-P
- person-centred approach postal group
- PCDI
- parent–child dysfunctional interaction
- PCT
- primary care trust
- PND
- postnatal depression
- PPDSQ
- Punjabi Postnatal Depression Screening Questionnaire
- PSE
- Present State Examination
- PSI
- Parenting Stress Index
- PsycINFO
- database covering international literature in psychology and related fields
- RCT
- randomised controlled trial
- RIL
- research information leaflet
- SCAN
- Schedules for Clinical Assessment in Neuropsychiatry
- SCID
- Structured Clinical Interview for DSM-IV Disorders
- SD
- standard deviation
- SF-36
- 36-item Short-Form Health Survey Questionnaire
- SF-12
- 12-item Short-Form Health Survey Questionnaire
- SF-6D
- a classification for describing health, derived from a selection of SF-36 items
- SI
- SCAN interviewers
- SIGN
- Scottish Intercollegiate Guidelines Network
- ShefReN
- Sheffield Research Network
- SOAs
- super output areas
- SPSS
- Statistical Package for Social Scientists
- SSRI
- selective serotonin reuptake inhibitor
- STAI
- State–Trait Anxiety Inventory
- TAG
- Trial Advisory Group
- TCA
- tricyclic antidepressants
- TG&DQ
- Toddler Growth and Development Questionnaire
- TRG
- Training Reference Group
- QALY
- quality-adjusted life-year
- UKCP
- United Kingdom Council for Psychotherapy
- WHO
- World Health Organization
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Reimsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson, EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and costeffectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of Science Support, NETSCC, HTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington