Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 06/75/02. The contractual start date was in February 2008. The draft report began editorial review in July 2009 and was accepted for publication in October 2009. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None
Permissions
Copyright statement
© 2010 Queen’s Printer and Controller of HMSO. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2010 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Introduction
Chronic kidney disease (CKD) is a long-term condition and has been described as the gradual, and usually permanent, loss of kidney function over time. 1 Early in the disease process, people with CKD often experience no symptoms and CKD has, for a long time, been an underdiagnosed condition. Even in the absence of symptoms, CKD appears to add significantly to the burden of cardiovascular disease (CVD) and death and, for an important minority, can progress to severe kidney function impairment and kidney failure (end-stage renal disease; ESRD). 2
In the last 10 years the focus on mild to moderate or ‘early’ CKD has grown. Its recognition as a major public health issue was highlighted by large population health surveys in the USA reporting an estimated 11% of the population as having evidence of renal impairment. 3 A number of authors have written of the ‘exploding’ CKD burden and have called for screening, early intervention and prevention as key steps in managing the individual and societal impact of the rising rates of disease.
End-stage renal disease
End-stage renal disease, severe renal function impairment or established renal failure is associated with high morbidity and mortality, poor quality of life, and high health service and societal costs. As the kidneys fail, the body becomes unable to excrete waste products, excess fluids and salts, or to control acidity. Haemoglobin production, blood pressure (BP) control and bone metabolism are also affected.
Since the first successful dialysis treatment in 1960, the nephrology community has focused much attention on the management of ESRD. 4 Data from 122 countries (representing 92% of the total world population) on treatment for ESRD identified that 1,783,000 people were receiving renal replacement therapy (RRT) by the end of 2004; 77% on dialysis and 23% with functioning renal transplants. Half of the dialysis patients, and more than 70% of transplant patients were from North America and Europe. 5 With an annual growth of approximately 6% compared with 2003, the number of people on RRT was rising globally. 5
In the UK in 2007, the UK Renal Registry reported an acceptance rate for new RRT patients of 109 patients per 1,000,000. 6 The point prevalence of RRT at the end of 2007 was 45,484, an annual population prevalence of 0.075% and a 5% increase on the previous year. The acceptance rate has been relatively stable over recent years, thus the rising prevalence is being driven largely by improvements in survival on RRT (Figure 1). The 1-year survival on RRT for patients starting RRT in 2006 was 94.8% [95% confidence interval (CI) 93.4 to 95.8] for all primary renal disease excluding diabetic nephropathy. Survival was reduced by age at onset of RRT. 7
FIGURE 1.
Change in Kaplan–Meier long-term survival by year of starting RRT; for incident patients aged 18–64 years. Reproduced from the UK Renal Registry Report (2008);7 UK Renal Registry, Bristol, UK; editors: David Ansell, Terry Feest, Andrew Williams and Chris Winearls. The data reported here have been supplied by the UK Renal Registry of the Renal Association. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the UK Renal Registry or the Renal Association.
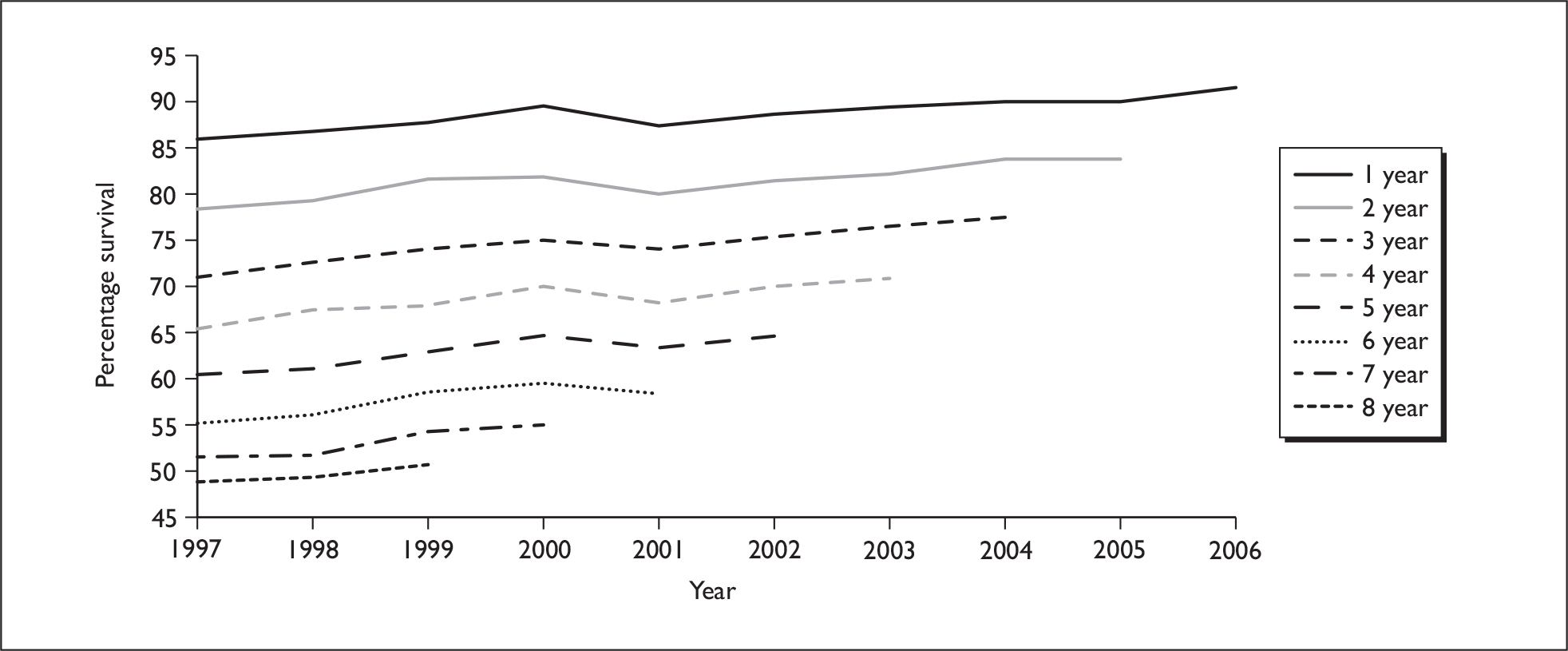
While survival on RRT has improved, more than 30% of 18–64 year olds die within 5 years of developing ESRD, and patients’ quality of life is impaired. 6,8,9
The number of people requiring RRT is expected to continue to increase as a result of population ageing, the increase in type 2 diabetes mellitus, improved technology facilitating access to RRT for patients with comorbidities and improved survival of people with ESRD. This has important resource implications for the NHS, which is estimated to spend 2% of the total annual NHS budget on delivering RRT, although this group comprises only 0.05% of the total population. 10 In 2002, the National Institute for Health and Clinical Excellence (NICE) estimated that the average annual cost of haemodialysis in a satellite renal unit was £21,000 per patient. 11
Definition of chronic kidney disease
Until recently, no agreed definition of CKD existed. Serum creatinine was commonly reported as a surrogate marker of filtration. The absolute upper limit of ‘normal’ serum creatinine value varied between laboratories and was vulnerable to patient characteristics such as age, sex, race, size, muscle bulk, diet, etc.,12,13 and various cut-off thresholds to define CKD had been reported. 14,15
The glomerular filtration rate (GFR) has become the most accepted test to assess filtration. 12 GFR defined as ‘the volume of plasma from which a given substance is completely cleared by glomerular filtration per unit time’, can be measured by assessing the clearance of exogenous or endogenous markers. 16 Commonly used exogenous markers include radioisotopic and non-radioisotopic substances such as inulin (gold standard), I-iothalamate, Cr-ethylenediaminetetraacetic acid (EDTA) and iohexol, but these are expensive and complex procedures for routine clinical use. 12,16
Creatinine is the principal endogenous marker that is used to measure GFR. Creatinine clearance measurement, calculated from timed urine collection (24-hour urine) and serum creatinine, can result in overestimation of GFR due to tubular secretion of creatinine and problems of accurate urine collection. 17,18 Estimating GFR based on serum creatinine and additionally correcting for variables such as age, gender, racial origin and body weight can be more reliable than 24-hour urinary creatinine clearance. 16 Two validated equations are commonly used to estimate GFR based on serum creatinine: the Modification of Diet in Renal Disease (MDRD) formula and the Cockcroft–Gault (CG) equation to estimate creatinine clearance. MDRD has been adopted by laboratories reporting estimated GFR (eGFR) in the UK, but modifications to the equation are being developed with an aim to improving accuracy. 19
Normal GFR in young adults is approximately 120–130 ml/min/1.73 m2, but varies with sex, ethnicity and body size, and declines with increasing age. In February 2002, with the aim of providing a uniform definition of CKD, the Kidney Disease Outcomes Quality Initiative (KDOQI) of the US National Kidney Foundation (NKF) introduced the following definition of CKD and stages of CKD:
Kidney damage (with or without decreased GFR) or decreased kidney function (GFR < 60 ml/min/1.73 m2) for 3 or more months where kidney damage is defined as pathological abnormalities or markers of damage including abnormalities in blood or urine tests or in imaging studies. 20
A threshold of GFR less than 60 ml/min/1.73 m2 was selected because it is less than half the level of normal adult GFR. 21 Additionally, this threshold (which is substantially above the level related to kidney failure) is detectable with current estimating equations for GFR based on serum creatinine, and there is evidence that GFR of 60 ml/min/1.73 m2 and lower is associated with an increased risk of complications of CKD and other adverse outcomes. 21
To avoid the misclassification of acute renal failure as CKD, the KDOQI required that reduced GFR and/or kidney damage must be present for at least 3 months. Further, the KDOQI classified CKD into five stages based on level of kidney function (Table 1). 20 The potential markers of kidney damage included proteinuria, haematuria, microalbuminuria in people with diabetes mellitus and abnormal imaging studies. Stage 3 CKD was regarded as the earliest stage of CKD for which GFR alone was a sufficient indicator of kidney disease.
| CKD stages | Definition |
|---|---|
| Stage 1 | Kidney damage with normal or raised GFR (≥ 90 ml/min/1.73 m2) |
| Stage 2 | Kidney damage with mildly impaired GFR (60–89 ml/min/1.73 m2) |
| Stage 3 | Moderately impaired GFR (30–59 ml/min/1.73 m2) |
| Stage 4 | Severely impaired GFR (15–29 ml/min/1.73 m2) |
| Stage 5 | End-stage renal failure or GFR (< 15 ml/min/1.73 m2) |
Prior to 2002, the lack of common definition and terminology made the study of CKD difficult; prevalence estimates varied widely and the translation of research findings into clinical practice or policy was challenging. The KDOQI classification of CKD has been adopted internationally and has raised the profile of CKD, facilitating research and identifying people with evidence of kidney function impairment that had previously gone undetected.
The UK Renal Association proposed modifications to stage 3, dividing it into 3A (eGFR 45–59 ml/min/ 1.73 m2) and 3B (30–44 ml/min/1.73 m2). 22 Recent NICE guidelines on the management of CKD proposed further modification of the staging system to include an indication of the presence of proteinuria. 23
Emerging ‘epidemic’: epidemiology of chronic kidney disease
With the introduction of the KDOQI definition for CKD, and analysis from large population-based US health surveys (Nutrition Health and Nutrition Examination Survey II; NHANES II) estimating that 11% of the over 20-year-old population may have evidence of CKD, a number of commentators described CKD as a major public health issue. 3,24–26 Analysis of repeated NHANES surveys suggested that the prevalence of CKD, as defined by the KDOQI (albeit reliant on a single measure of kidney function and therefore likely to over estimate the true prevalence of CKD), was increasing. 27,28 This is a finding in keeping with an ageing population and the rise in obesity, diabetes and hypertension. 29
Internationally, prevalence studies have been published from a wide range of countries across Europe, Asia, Central America and Australia. Methodologically they rely on two main approaches: population surveys or routine clinical laboratory data. In studies of stage 3–5 CKD, and therefore relying only on eGFR, estimates of prevalence have varied from 3.8%30 to 42.6%. 31 The reason for such heterogeneity may be contributed to by methodological differences (definition of chronicity, denominator used, sampling strategy, approach to minimisation of assay bias) as well as differences in the study population (age, sex, race, comorbidities). In Europe, Hallan and colleagues32 (2006) reported an adult population prevalence of 4.7% for CKD based on a single eGFR estimate, and a similar prevalence has been reported in Italy, Switzerland, Spain and Iceland. 33–36
In the UK, the only population-based survey estimate of CKD prevalence comes from a cohort of men aged 60–79 years and tested in 1998–2000. Wannamethee and colleagues37 estimated the prevalence of CKD to be 15.7%. In 2004–5, two studies, using routine laboratory data from the UK to estimate the prevalence of CKD based on eGFR, reported a prevalence of stage 3–5 CKD of 4.9%38 and 4.3% respectively. 39
Management of chronic kidney disease: a UK perspective
The international adoption of the KDOQI definition for CKD initiated the epidemiological recognition that a far greater proportion of the population than previously recognised had evidence of kidney function impairment.
In England, the National Service Framework for Renal Services set out a vision for renal services. In 2004, the first part of the framework focused on dialysis and transplantation, providing recommendations for a pathway of care and emphasising the place of planned identification and referral of patients who are progressing towards ESRD. 10 The second part delivered a framework for CKD as well as covering acute renal failure and end of life care. 2 The framework set out the expectation that people considered to be at risk of developing or having undetected CKD should be identified, assessed and managed proactively with a focus on interventions to preserve kidney function, and minimise disease progression and complications. It also acknowledged the cardiovascular burden in patients with CKD. The framework targeted, in particular, those with diabetes mellitus and hypertension, and supported the proactive monitoring for CKD in such high risk patient groups. 2
Chronic kidney disease guidelines first published by the UK Renal Association in 2005 sought to provide clarity on how people with CKD should be identified and optimally managed. 40 The National Service Framework set out the need for development of protocols around measuring kidney function and the estimation of eGFR. The UK Renal Association guidelines recommended the adoption of the simplified MDRD equation. 41
In 2006, the Quality and Outcomes Framework (QOF) incentive-based scheme supporting the General Medical Services contracts with primary care included a renal domain and set four renal criteria for primary care:
-
to establish a register of all patients with CKD (defined as an eGFR lower than 60 ml/min/1.73 m2)
-
for those on the register to have had a recorded BP in the previous 15 months
-
for the BP to be below 140/85 mmHg
-
for treatment with renin–angiotensin system blocking medicines.
The need, nationally, for access to consistent eGFR reporting was therefore critical to support the development of registers without introducing geographical inequalities. The UK National External Quality Assessment Scheme was charged with harmonising laboratory methodology in order to minimise variability between laboratories, and, in 2006, the routine laboratory reporting of eGFR was rolled out across the UK. 41
The introduction of eGFR reporting and in particular the decision to report values for eGFR only if lower than 60 ml/min/1.73 m2, treating all values higher than 60ml/min/1.73 m2 as ‘normal’, has made it very straightforward for clinicians to identify patients meeting the KDOQI definition of CKD.
Implications for health
Chronic kidney disease has the potential to affect a number of health areas:
-
progressive renal function loss and ultimately ESRD and the need for RRT
-
CKD-associated complications (anaemia, bone mineral metabolism disorders, hypertension)
-
CVD
-
survival
-
quality of life
-
anxiety.
These are considered in more depth in Chapter 3.
The treatment of CKD has focused the management of complications and preparation for ESRD and RRT. The introduction of medicines that inhibit the renin–angiotensin–aldosterone axis brought evidence of benefit in slowing the progression of kidney function decline and proteinuria. Recognition of the high cardiovascular morbidity and mortality among those with CKD of all stages suggests that there is also the potential to modify other risk factors for CVD.
Preventing progression and cardiovascular disease
In recent years there have been numerous trials of pharmacological interventions aimed at modifying the risk of renal disease progression and CVD. In 2008, NICE23 and the Scottish Intercollegiate Guidelines Network (SIGN)42 both published guidelines for the management of CKD. The management strategies for the prevention of progression of renal disease and reduction of cardiovascular risk have hinged largely on three areas:
-
BP control
-
lipid profile modification using statins
-
lifestyle risk factor modification.
Blood pressure control
NICE and SIGN guidelines note several systematic reviews and meta-analyses that support the important role of BP management in the prevention of progression of CKD. NICE recommended a target systolic BP below 140 mmHg and diastolic below 90 mmHg. SIGN recommended a target of below 130 mmHg for systolic BP. The guidelines also presented evidence for the role of reduction of proteinuria in reducing the risk of renal disease progression.
The role of two groups of antihypertensive agents, angiotensin converting enzyme inhibitors (ACE Is) and angiotensin receptor blockers (ARBs), has received particular attention in the management of CKD.
Angiotensin converting enzyme inhibitors
In people with non-diabetic CKD, ACE Is have little benefit over placebo or other antihypertensive treatments in reducing all-cause mortality (ACM). 43 A statistically significant reduction in the risk of developing ESRD alone, or doubling of serum creatinine and ESRD [relative risk (RR) reduction of 40% and 30% respectively] was observed from a meta-analysis of 11 trials and after adjustment for difference in study baseline characteristics. 43 The risk reduction was modified by, but independent of, change in BP and proteinuria. A benefit on renal outcomes from ACE Is was observed for those with proteinuria above 0.5 g/day. Below 0.5 g/day, a benefit could not be excluded but the findings were less robust.
Even in diabetics with CKD, ACE Is had no benefit on ACM44 unless patients were treated at maximum tolerable dose (RR 0.78, 95% CI 0.61 to 0.98),44 ACE Is reduced the risk of ESRD by 31% in diabetics when compared with placebo. 44 ACE Is can prevent the progression of micro- to macroalbuminuria (reported RR reduction of 55–65% versus placebo) in diabetic renal patients. 44,45 Regression from micro- to normoalbuminuria was also increased (RR 3.06, 95% CI 1.76 to 5.35). 44 When analysis was restricted to those with proteinuria, the findings were similar, with no evidence of benefit from ACE Is (as compared with placebo) on mortality, but a statistically significant effect on reduction of ESRD or doubling of serum creatinine (RR 0.60, 95% CI 0.49 to 0.73). 45
Angiotensin receptor blockers
Similar to ACE Is, ARBs have no significant impact on ACM in diabetics with CKD when compared with placebo or standard antihypertensive agents,44,46 or CVD morbidity and mortality. 46 However, there was evidence of a reduction in progression of CKD,44 with statistically significant risk reductions for ESRD (22%) and doubling of serum creatinine (21%). ARBs reduced progression from micro- to macroalbuminuria by more than 50% as well as significantly increasing the numbers returning from micro- to normoalbuminuria. Regarding adverse effects, the only significant increase observed was in hyperkalaemia.
Strippoli and colleagues44 identified three studies that compared ACE Is with ARBs. They found no evidence of a difference in effect on mortality or renal outcomes.
A systematic review by Casas and colleagues47 reported on effects of ACE Is or ARBs on renal outcomes, compared with placebo or other active interventions. Evidence of statistically significant risk reductions for ESRD was observed (RR 0.87, 95% CI 0.75 to 0.99). Small reductions in creatinine concentration (mean difference –7.07 µmol/l, 95% CI –13.26 to –0.88) and urinary albumin excretion (mean difference –15.7 mg/day, 95% CI –24.73 to –6.74) were reported, but significant heterogeneity among studies was noted. No significant difference was observed in change of GFR or on the composite end point of doubling of creatinine and ESRD. ACE Is/ARBs had no significant effects on GFR, ESRD or doubling of creatinine in diabetics. However, small reduction in urinary albumin excretion was observed in those with diabetic kidney disease (mean difference –12.21 mg/day, 95% CI –21.68 to –2.74). Casas and colleagues47 noted that larger studies were more likely to report smaller benefits, suggesting publication or other source of small study bias.
In people with CKD and diabetes with microalbuminuria, NICE and SIGN recommend treatment with ACE Is or ARBs regardless of BP. In non-diabetics with CKD, hypertension should be controlled using the range of available antihypertensives. However, both guidelines recommend that in the presence of proteinuria and CKD, hypertension should be managed first line with ACE Is/ARBs. 23,42
Anticholesteraemic agents
In a systematic review and meta-analysis of six trials, Strippoli and colleagues48 reported that statins had no significant benefits on mortality risk reduction in CKD when compared with placebo or other antilipaemic agents, although some benefit (19% reduction in ACM) in the predialysis group was observed. The same study reported a significant risk reduction in CVD morbidity (RR 0.75, 95% CI 0.66 to 0.85) and mortality (RR 0.81, 95% CI 0.73 to 0.90). The impact of statins on the rate of change in eGFR and proteinuria was variable between trials and between reviews. 48–50
NICE and SIGN guidelines recommend that statin therapy should be considered in all patients with stage 1–3 CKD with a predicted 10-year cardiovascular risk of at least 20%.
Lifestyle intervention
Both guidelines recommend that healthy lifestyle advice should be offered to people with CKD, supporting an active lifestyle, a healthy diet, maintenance of a healthy weight and stopping smoking. However, evidence to support how best to deliver these interventions to people with CKD was lacking, as were trials of intervention to estimate the potential effect size.
NICE and SIGN noted the place of protein restriction in certain clinical circumstances and the need for this to be carefully assessed and supported. Systematic review of protein restriction diets has reported evidence of reducing risk of ESRD and/or ACM by 31–77% (from only one study with 82 participants) as compared with usual protein diet. 51,52 Protein restricted diet in type 1 and type 2 diabetes mellitus had little impact on the decline of GFR. 52,53
The evidence base around treatments for CKD focuses on CKD as a single group and does not specifically identify the effectiveness of treatments for different stages of CKD. The benefits, and potential harms, to those with mild to moderate CKD have not been well reported.
When to refer to a specialist
Over the last two decades, commentators have noted the high proportion, 30–50% in some reports, of patients who are referred late to specialist nephrology care. 54–56 Late referral has been variously defined as the first referral to specialist nephrology care occurring between less than 1 month and 6 months prior to the patient requiring the initiation of RRT. Retrospective studies have demonstrated an association between late referral and poor outcomes on RRT when compared with those referred earlier. 57
In 2008, NICE and SIGN issued guidelines for the management of people with CKD. 23,42 Like the UK Renal Association guidelines, guidance was given about the clinical features that may make referral to a specialist appropriate. The guidelines aimed to strike a balance between early referral and service capacity, and identified uncertainties around the potential benefits (and harms) of early referral.
NICE recommended the following groups to be considered for referral to a specialist:
-
those with stage 4 and 5 CKD (with or without diabetes)
-
those with higher levels of proteinuria [albumin–creatinine ratio (ACR) of at least 70 mg/mmol] unless known to be due to diabetes and already appropriately treated proteinuria (ACR of at least 30 mg/mmol) together with haematuria and rapidly declining eGFR (more than 5 ml/min/1.73 m2 in 1 year, or more than 10 ml/min/1.73 m2 within 5 years)
-
those with hypertension that remains poorly controlled despite the use of at least four antihypertensive drugs at therapeutic doses
-
those with, or suspected of having, rare or genetic causes of CKD
-
those with suspected renal artery stenosis
-
those with CKD and renal outflow obstruction should normally be referred to urological services, unless urgent medical intervention is required.
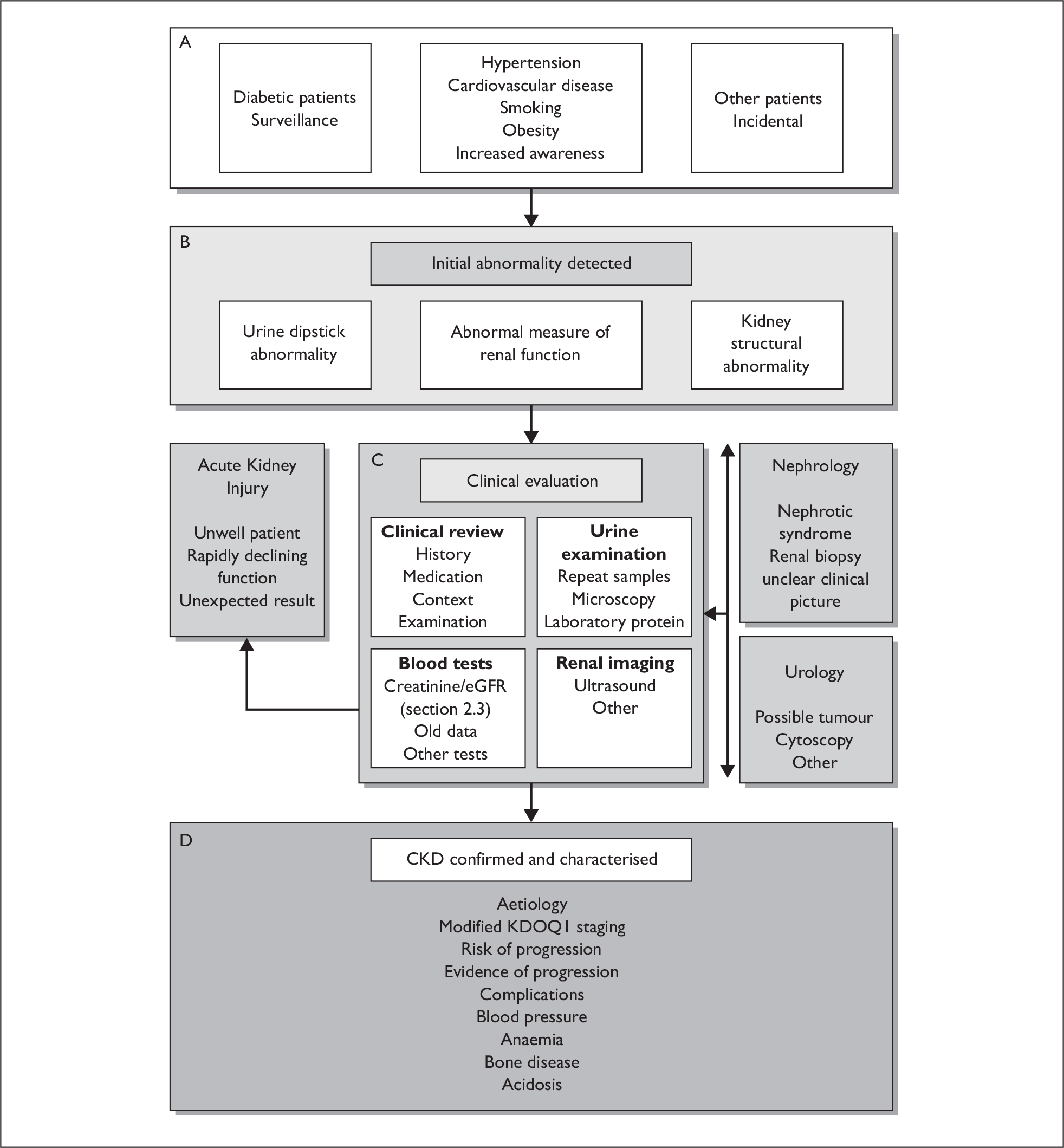
SIGN guidelines noted the lack of evidence about when to refer individuals to a specialist, and provided an algorithm (Figure 2) to aid decision-making which recognised that patients may seek medical attention for a number of different reasons.
FIGURE 2.
Algorithm to support decision-making for referral of patients with evidence of renal impairment. Reproduced with permission from SIGN guidelines 2008. 41
Attention has turned to earlier referral for CKD and the opportunity to intervene not only to delay progression of renal disease and treat its complications at this early stage, but also to prevent CVD. Early referral to specialist nephrology care might provide a patient with access to an array of investigations, preventative treatments, education, dietary advice, etc., with an aim of:
-
diagnosis of cause of renal disease – particularly to identify any causes that may be amenable to specific therapy
-
appropriate use of renoprotective interventions – diet, cessation of smoking and pharmacotherapy to delay/prevent the progression of the renal disease (antihypertensive and specific antiproteinuric agents)
-
appropriate use of cardioprotective interventions – pharmacotherapy to prevent/delay or minimise the impact of CVD (diet, exercise, smoking, lipid lowering therapy, smoking cessation and antiplatelet therapy)
-
control of other metabolic and endocrine complications such as anaemia and renal bone disease
-
preparation for a planned start to RRT – early intervention with all the above measures allows potential for a patient to reach RRT later and with fewer comorbidities, better nutrition and better psychological adjustment.
Aims and objectives
The aim of this report was to systematically review the evidence of the clinical effectiveness and cost-effectiveness of early referral strategies for management of people with markers of renal disease. There were three phases of research:
-
Systematic review of the evidence of clinical effectiveness – to assess and synthesise the evidence for early referral strategies. In addition, we sought to explore the natural progression of patients identified as having CKD and the characteristics for an effective early referral programme including:
-
– Which patient groups were likely to benefit most?
-
– What interventions were effective?
-
– How were those interventions delivered most effectively?
-
– At what stage in disease progression was the greatest benefit achieved?
-
– What were the barriers to early referral?
-
-
Systematic review of the evidence of cost-effectiveness – to assess and synthesise the evidence of cost-effectiveness of early referral strategies.
-
Economic analysis – informed by the findings of phases 1 and 2, to model the economic implications of different early referral strategies to assess the cost-effectiveness.
In Chapter 2 we set out the methods used for the literature reviews. The natural history of CKD is reported in Chapter 3. The impact of late referral is considered in Chapter 4. Chapter 5 reports the findings of the review of clinical effectiveness of early referral strategies, and Chapter 6 considers other models of care for people with CKD. Chapter 7 reports the findings from the review of evidence of cost-effectiveness and describes the economic modelling to assess the potential cost-effectiveness of different early referral strategies. Finally, Chapter 8 provides a discussion, implications for the health service and research recommendations.
Chapter 2 Methods
In this chapter we detail the methods used for the systematic review of the clinical effectiveness of early referral for CKD and for the review of the natural history of CKD. We also set out the methods for the supplementary chapter on models of care for CKD undertaken to support the development of the economics model and to supplement the limited evidence identified for clinical effectiveness. The methods for the economic modelling are described later, in Chapter 7.
Clinical effectiveness and cost-effectiveness literature reviews
Clinical effectiveness review method
Data sources and search strategy
Sensitive electronic searches were undertaken to identify studies comparing early referral to other care options for people with CKD. Initial searching was undertaken between January and April 2008, with the main search updated in February 2009. Electronic searches were restricted to reports published in the English language since 1990. We searched for meeting abstracts from January 2006 only. In addition, reference lists of all included studies were scanned to identify additional potentially relevant studies. The search strategy is summarised in Appendix 1 and included clinical and cost effectiveness studies. Search terms did not restrict based on timing of referral; studies of early or late referral were identified.
The following databases were searched:
-
Ovid MEDLINE, 1950 to 4 February 2009
-
Ovid MEDLINE In-Process and Non-Indexed Citations
-
EMBASE, 1988 to week 5 2008
-
Science Citation Index, 4 February 2008
-
ISI Proceedings, 4 February 2008
-
British Nursing Index, 1994 to January 2008
-
British Nursing Index Archive, 1985–96
-
Health Management Information Consortium, January 2008
-
Cumulative Index to Nursing & Allied Health Literature, 1982 to week 1 December 2007
-
Social Science Citation Index, 4 February 2008
-
Cochrane Central Register of Controlled Trials: Cochrane Library Issue 1 2008
-
Cochrane Database of Systematic Reviews: Cochrane Library Issue 1 2008
-
National Research Register Archive (up to October 2007), 19 March 2008
-
The UK Clinical Research Network, 19 March 2008
-
The European Dialysis and Transplant Nurses Association/European Renal Care Association 35th International Conference 2006 and 36th International Conference 2007 Final Programmes.
Additional searching was performed in NHS Economic Evaluation Database to support the cost-effectiveness literature review.
Study selection
Initial searching indicated that we would find very few randomised controlled trials (RCTs) of early referral strategies versus standard care. We therefore considered evidence from any study design that compared a strategy for early referral with a relevant comparator group. We included prospective and retrospective study designs. The research focused on adults with markers for early renal disease in either primary or secondary care. We included any intervention that aimed to achieve the early referral of people with markers of renal disease to specialist nephrology care. For retrospective studies, the definition of early referral was taken as referral at least 12 months before RRT. For prospective study designs, referral prior to reaching stage 5 CKD was required but other definitions of early referral were accepted (e.g. based on proteinuria thresholds in diabetic nephropathy). In the absence of a ‘gold standard’ for care, acceptable comparators included usual care, later referral (defined as less than 12 months prior to RRT for retrospective studies) or primary care. Outcomes of interest included:
-
renal function
-
onset of RRT
-
quality of life
-
ACM
-
CVD mortality
-
hospitalisations
-
emergency dialysis
-
survival on dialysis.
Details of the care package were also sought.
Titles, abstracts and keywords were reviewed by two systematic reviewers, independently, to identify studies that met the inclusion criteria outlined above. Full papers were then considered for inclusion. Discrepancies were resolved by discussion, with involvement of a third reviewer if necessary.
The search identified that there was a substantial evidence base on the effect of late referral (defined as less than 12 months prior to RRT) and, where studies included mortality as an outcome, this has been included in Appendix 5. A supplementary search for literature about potential barriers to early referral was conducted using MEDLINE (1996 to week 2 April 2008) and EMBASE (1996 to week 15 2008).
Quality assessment of included studies
Two systematic reviewers independently assessed the methodological quality of the included studies. The quality of included studies was assessed using the criteria outlined in the Centre for Reviews and Dissemination Report 4. 58 Checklists were adapted from those developed by NICE. 59
Data extraction
Data extraction from the included studies was carried out independently by two systematic reviewers. Study characteristics, outcome results and aspects of study quality were collected using a standardised form (see Appendix 2). Any discrepancies were resolved by discussion and, where necessary, by involvement of a third reviewer (two occasions relating to terminology).
Data synthesis
Study characteristics and results were tabulated; analysis was qualitative. It was not possible to pool results for quantitative analysis because of the heterogeneity of study characteristics and the diversity in reporting of outcomes.
Economics review methods
The literature searches focused on identifying studies that assessed the cost-effectiveness of nephrology referral strategies for individuals with stage 3 CKD. In addition to the databases mentioned above, the reference lists of relevant studies were hand-searched. All abstracts were reviewed and the full article was obtained for any studies that were potentially relevant. Articles cited by other relevant studies were also retrieved for review. The review focused primarily on studies relating to individuals without diabetes, as more formal care pathways were already in place for individuals with diabetes and diabetic nephropathy. 60
Study selection
Our inclusion criteria for formal appraisal were studies assessing the costs and consequences (long- or short-term) of early referral strategies for individuals with markers of renal disease. Early referral was defined as referral to a specialist prior to stage 4 CKD (i.e. eGFR higher than 30 ml/min/1.73 m2). We were not explicitly interested in extracting data from studies assessing the cost-effectiveness of population screening for proteinuria, but studies that looked at screening in non-diabetic populations were obtained to help inform the development of the economic model. Finally, studies assessing the cost-effectiveness of single interventions in individuals with CKD, such as the use of ACE Is to slow progression, were excluded from formal appraisal.
Quality assessment of included studies
Studies meeting our inclusion criteria were appraised using the British Medical Journal guidelines for reviewers of economic evaluations. 61 The quality of included decision models was also assessed against a published checklist for good practice in decision analytic modelling in health technology assessment. 62
Data extraction
Plans were made to formally extract data from studies directly assessing the cost-effectiveness of nephrology referral for individuals with stage 3 disease compared with referral at stage 4 or 5 (current practice).
Other literature reviews
Separate systematic reviews were undertaken to support the following areas of the report: natural history of CKD and models of care for CKD.
Search strategies
Natural history
A systematic literature review was conducted to identify relevant literature on the natural history of CKD. MEDLINE (1950 to March week 2 2008) and EMBASE (1996 to March week 4 2008) were searched. An internet search (Google scholar; http://scholar.google.co.uk/) was performed and potentially relevant studies were identified from clinical experts. Searches were restricted to the English language and were from 1998. Bibliographic searching of any included study was also undertaken (see Appendix 1 for the search strategy).
Systematic reviews, meta-analyses, observational cohorts and follow-up studies (prospective or retrospective) of adult populations with at least 2 years’ of follow-up were considered. RCTs were excluded owing to the highly selected nature of their participants. Those studies where the main study populations were defined as having CKD were included. However, studies with broader participant inclusion criteria (diabetes, CVD or hypertension) were considered for inclusion when participants with CKD accounted for a substantial number of the total study population. Studies with less than 100 subjects were excluded. While a definition of CKD based on the KDOQI classification was considered to be optimal, the definition of CKD used by the authors was accepted.
Included studies were quality assessed. Systematic reviews and meta-analyses were evaluated based on a methodology checklist outlined by NICE. 63 Other study designs were evaluated based on a quality assessment tool adapted from various methodological criteria. 39,64–67
Care model
Database searching was carried out in MEDLINE (1950 to present) and EMBASE (1996 to 2008 week 25) combining keywords and medical subject heading (see Appendix 1). Internet and bibliographic searches of included studies were performed. No relevant studies were identified from the Cochrane review database and Health Technology Assessment (HTA) journal database of published reports. Any full papers or abstracts published in English (evaluation, audit, description of care) that reported a model of care for the management of CKD patients were included. Care models of management of RRT patients were excluded.
Data extraction
Data extraction was undertaken by one author and checked by a second author. A specifically designed and piloted data extraction form was used for each component. Information about study design, participants, definition and measure of CKD and relevant outcomes of the study were extracted. The data were extracted for all participants and for relevant clinical subpopulation including stages of CKD, diabetes mellitus, CVD, high blood pressure (HBP), sex, age group and race.
In the review of reports of care models, additional data were extracted about: setting (primary, secondary or other); model of care or intervention provided or proposed; description of participants or staff involved; and relevant outcomes/outcomes foreseen including, primarily, clinical outcomes and attitudes of patient or health-care provider towards service and, secondarily, improvements or changes in care/service and barriers to implementation of services.
Data synthesis
For all reviews, the study characteristics and results were tabulated and analysed qualitatively. A thematic approach was adopted for analysis of the barriers to early referral and care models.
Chapter 3 Natural history
Introduction
Understanding the natural history of CKD is critical to understanding the effectiveness of interventions involving the ‘early’ referral of patients with CKD to specialists.
This review of the natural history of CKD focused on renal impairment defined by GFR. GFR was chosen because in the UK, since 2006, there has been universal reporting of eGFR from laboratories. In addition, general practitioners (GPs) in the UK have been asked to record all patients with an eGFR of less than 60 ml/min/1.73 m2 (stage 3 or higher) on a practice register. This cohort, therefore, makes up a critical and substantial component of the people increasingly labelled with CKD in the UK and for whom the appropriateness and timing of referral to a specialist is uncertain. The key outcomes of interest were ACM, cardiovascular mortality and morbidity, renal progression and ESRD, and quality of life.
Results
Description of included studies
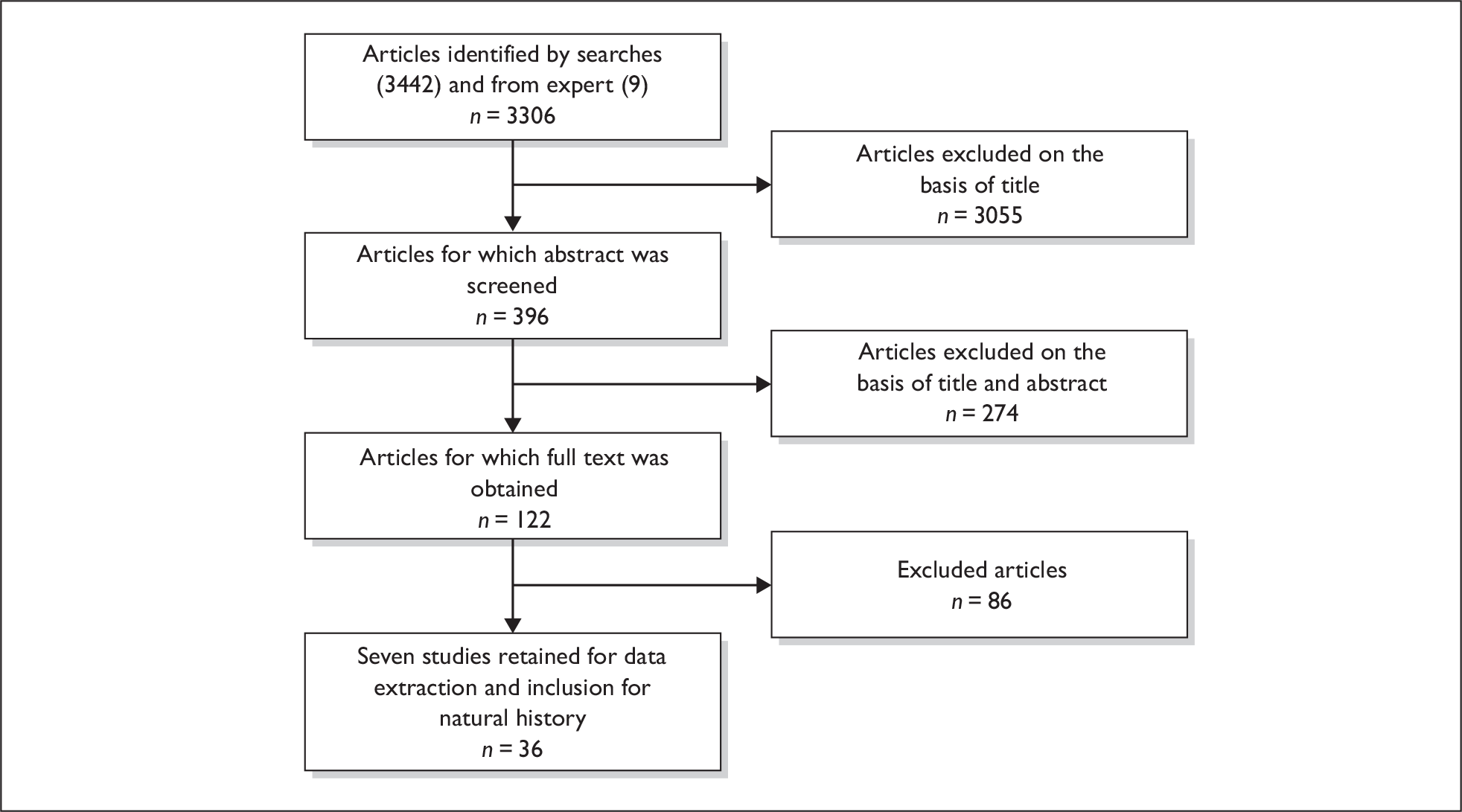
The process of study identification and the number of relevant published papers are given in Figure 3. Thirty-six studies were data extracted and appraised (42 published papers; five studies with more than one publication). Details of the excluded studies are given in Appendix 3.
FIGURE 3.
Representation of the flow of studies through the natural history review process.
A summary of the characteristics of the included studies is given in Table 2.
| Author/year/country | Study design | Total number of participants | % with CKD (of total participants) | DM | CVD | HBP | Median follow-up (years) | Mean age (years) | Definition of CKD used in the studya |
|---|---|---|---|---|---|---|---|---|---|
| (% of total participants unless specified) | |||||||||
| Astor 2008,85 USA | PC, Screened population, NHANES III | 14,586 | Stage 3 and 4: 5.8 | 4.8 | 7.6 | 47.1 | 8.7 | 44.2 | eGFR 15–59 and microA and macroA |
| Bruno 2007,79 Italy | PC, clinical population, (clinics, GP and clinical records) Casale Monferrato study | 1539 |
Stage 1: 7.3 Stage 2: 58.3 Stage 3a: 26.0 Stage 3b: 6.9 Stage 4: 1.4 |
All | – | – | 10b | – | eGFR < 60 and microA |
| Cvengros 2005,91 USA | PC, clinical population (hospital, renal clinic) | 207 | 100c | 47.8 | – | – | 1.3d | 59.77 | SCr ≥ 3 (unit not given) |
| Di 2007,69 Iceland (various) | SRe, includes PC, screened population | 2007, seven studies | Lowest quintile: 38.6c, varied by study | – | – | – | 3–20f | – | eGFR < 67.6 (lowest quintile) |
| Djamali 2003,83 USA | RC, clinical population (hospital, renal clinic) | CKD: 872; RRT: 890 |
Stage 1: 8 Stage 2: 28 Stage 3: 46 Stage 4: 16 Stage 5: 2 |
Stage 1: 10 Stage 2: 36 Stage 3: 43 Stage 4: 10 Stage 5: 1 |
– | – | 4.6f | 54 | SCr > 115 µmol/l |
| Drey 2003,95 UK | PC, clinical population. (laboratory database) | 1076 |
Stage 3: 52 Stage 4 and 5: 48 |
– | – | – | 5.5f | ≥ 70g: 74% | SCr ≥ 150 µmol/l |
| Eriksen 2006,96,97 Norway | PC, clinical population (laboratory database) | 3047 | Stage 3: 100 | – | – | – | 3.7 | 75 | eGFR 30–59 |
| Evans 2005,98 Sweden | PC, clinical population (68 medical laboratories across Sweden) | 920 | Stage 4 and 5: 100 | 31 | – | – | 5 | < 45g: 18.2%; 45–64: 40.9%; ≥ 65: 41.0% | M: SCr > 300 µmol/l; F: SCr > 250 µmol/l |
| Go 2004,75 USA | RC, clinical population (laboratory and clinical database) | 1,120,295 |
Stage 3a: 13.7 Stage 3b: 3.0 Stage 4: 0.6 Stage 5: 0.1 |
9.6 | 6.3 | 19.1 | 2.8 | 52.2 | eGFR < 60 |
| Gorodetskaya 2005,78 USA | PC, clinical population | 205 |
Stage 3: 24.9 Stage 4: 32.2 Stage 5: 13.6 |
Stage 3: 43 Stage 4: 44 Stage 5: 68 Dialysis: 40 GFR ≥ 60 ml/min/1.73 m2: 18 |
Stage 3: 12 Stage 4: 42 Stage 5: 36 Dialysis: 18 eGFR ≥ 60 ml/min/1.73 m2: 5 |
10 monthsd,f | 62.8 | eGFR < 70 (eGFR 60–70: 10.8%); dialysis: 18.5% | |
| Hallan 2006,32,99,100 Norway | PC, general population (community health screening), HUNT II | 65,604 | 4.7c | 3 | 7.9 | 11.1 | 8 | 49 | eGFR < 60 |
| Hemmelgarn 2006,101 Canada | RC, clinical population (laboratory service computerised database) | 10,184 |
Stage 3: 31.3 Stage 4 and worse: 4.1 |
Stage 2: 14.2 Stage 3: 19.8 Stage 4 and worse: 31 |
– | – | 2 | 75.1–77.8 | eGFR < 60 |
| Herzog 2004,92 USA | RC, clinical population (Medicare database) | 1,136,201 | 3.2c | 39.60h | 53.60h | 79.8h | 1.9 | 76.5g ≥ 80: 40% | CKD defined based on ICD-9 codes |
| Hovind 2001,93,102 Denmark | PC, clinical population (Steno Diabetes Center, diabetic nephropathy registry) | 301 | 100c | All | – | – | 6.7 | 36 | Diabetic nephropathy (persistent microalbuminuria > 200 mcg/min + retinopathy) |
| Hsu 2003,103 USA | RC, screened population (national data set on health and nutrition of the non-institutionalised US population), NHANES II & III, and USRDS |
B: 4112 W: 9238 |
B: 2.7c W: 3.1c |
B: 30h W: 71.81h |
– | – | 3–8 yearsb |
B: 61 W: 62 |
eGFR 15–59 |
| Imai 2008,82 Japan | PC, screened population (community health survey) | 120,727 |
Stage 3: 21.3 Stage 4 and worse: 0.01 |
– | – |
M: 17.8 F: 11.9 |
10b | Range 40–79 | eGFR < 60 |
| Irie 2006,81 Japan | PC, Screened population (community health survey) |
M: 30,764 F: 60,668 |
M: 3.0c F: 3.0c |
– | – | – | 10.1f | Range 40–79 | Data presented for eGFR < 60 and eGFR ≥ 60 |
| John 2004,104 UK | PC, clinical population (laboratory database) | 3822 (referred and unreferred) | 100c | – | – | – | 2.6 |
≥ 80: 66.4% |
M: SCr ≥ 180 µmol/l; F: SCr ≥ 135 µmol/l |
| Jones 2006,105 UK | RC, clinical population (renal unit database) | 726 |
Stage 3: 46 Stage 4: 35 Stage 5: 19 |
DN:17 | – | HN: 10 | 2.9 | 72 | eGFR < 15 to 59 |
| Keith 2004,106,107 USA | PC, clinical population (clinical database of HMO) | 27,998 |
Stage 2 (with proteinuria): 6.2 Stage 3: 40.3 Stage 4: 2.8 |
15.8 | 13.1 | 37.4 | 5.5 | 60.8 | eGFR < 90 (with proteinuria) |
| Khatami 2007,108 UK | RC, clinical population (hospital database) | 8160 | 24c | 5.5h | 1.6h | – | 4b |
M: 63.5i F: 67i |
GFR < 60 |
| Kollerits 2007,90 Austria | PC, clinical population (nephrology department in various countries) | 177 | 100c | None | – | – | 3.9f | 46.4 | CKD estimated based on SCr |
| Leehey 2005,109 USA | RC, clinical population (VA medical centre database) | 343 | 100b | All | – | – | 3a |
69g ≥ 65: 73% |
SCr > 124 µmol/l and microA |
| Levin 2001,84 Canada | PC, clinical population (seven Nephrology units) | 313 |
CrCl 10–49: 80.2 CrCl 50–75: 19.8 |
29.1 | 45.7 | 1.9 | 56.3 | CrCl 10–75 ml/min | |
| Maaravi 2007,86 Israel | PC, screened population (sampled from community) | 441 | 34.2c | 16.1 | 26.1 | 72.2 | 12b | All 70 years at initial examination | eGFR < 60 |
| Meisinger 2006,76 Germany | PC, screened population (community health survey), MONICA |
M: 3860 F: 3674 |
M: 12.4c F: 20.5c |
M: 9.4h F: 6.9h |
M: 11.5h F:4.1h |
M: 62.3h F:55.5h |
12.5 |
M: 62.4 F: 61.5 |
eGFR 15–59 |
| Mulec 1998,87 Sweden | RC, clinical population (database of type 1 DM patients) | 158 | 100c | All | – | – | 8f | 35.5 | Nephropathy (persistent macroA > 300 mg/24 hours) |
| O’Hare 2006,110 USA | RC, clinical population (VA Medicare database and USRDS) | 2,583,911 |
Stage 3: 18.4 Stage 4 and 5: 1.5 |
– | – | – | 3.17f | 63.6 | eGFR < 60 |
| Orlando 2007,111 USA | RC, clinical population (VA laboratory database) | 1553 | 100c | 52 | 49 | 92 | 3.6f | 70 | SCr ≥ 123.8 µmol/l |
| Patel 2005,80 USA | RC, clinical population (VA medical database) | 12,570 |
Stage 1 and 2: 18.0 Stage 3a: 18.0 Stage 3b: 8.0 Stage 4: 3.0 Stage 5: 1.0 |
All | 52 | 47 | 3b | 66 | eGFR < 60 (or proteinuria) |
| Rossing 2004,89 Denmark | PC, clinical population (registry of Steno Diabetes Center) | 227 | 100 c | All type 2 DM | 10 | – | 6.5 | 57 | Nephropathy (persistent macroA > 300 mg/24 hours) and retinopathy |
| Tarnow 2005,90 Denmark | PC, clinical population (sampled from Steno Diabetes Center) | 198 | 100c | All type 1 DM | 5.1 | 9b | 41 | Nephropathy (persistent macroA > 300 mg/24 hours) and retinopathy | |
| Tonelli 2006,68 Canada | SR, both general and clinical population | 1,371,990 from 39 studies | 100c | Range: 0–100 | Range: 0–100 | Range: 0–100 | 4.5 | 34–79 | Estimated CrCl or GFR: 60 ml/min (with or without standardisation to body surface area), SCr > 120 µmol/l |
| Tseng 2008,94 USA | RC, clinical population (national database of VHA diabetic patients) | 39,031 |
Stage 3: 92.4 Stage 4: 7.6 |
All | 67.1 | – | 1.6 | 70 | eGFR between 15 and 60 |
| Wannamethee 2006,37 UK | PC, general population (age and sex registers of GP) | 4029 | 15.6c | 15.5h | 27.1h | 38.8h | 6f | 67.7 | eGFR between 15 and < 60 |
| Weiner 2004,74 USA | PC, general population (community-based data sets) ARIC, CHS, FHS, FOS | 22,634 | 7.4c | 9.5 | – | 39.7 | 10b | 57.1 | eGFR 15 to < 60 ml/min/1.73 m2 |
We did not identify any systematic reviews of the natural history of CKD that considered all of the outcomes of interest, but we did identify three systematic reviews that presented information about some aspects of natural history.
One review compared the risk of ACM and cardiovascular mortality in those with CKD as compared with non-CKD populations where studies included a range of study participants from healthy adults to those with comorbidities. 68 We identified a second review comparing the risk of non-fatal myocardial infarction (MI) and cardiovascular mortality between those with evidence of CKD and no CKD in seven population studies of apparently healthy adults. 69 These two reviews overlapped in one study (NHANES II 2002),70 and Tonelli and colleagues68 reported data from three primary cohort studies [ARIC (Atherosclerosis Risk in Communities) 2003,71 CHS (Cardiovascular Heart Study) 2003,72 FHS (Framingham Heart Study) 199973] which were included by Di and colleagues69 as a single study that pooled individual patient data from the original studies. 74
These were good quality reviews (see Appendix 4) and we therefore focused our further searches on studies quantifying the extent of progression and mortality in CKD populations. We limited our included studies to only those defining their study populations as having CKD, rather than further comparing risk to the general population. We did include comparative studies if they had not been included in the above reviews or where additional information of interest in our review was available in the original study. One study75 from Tonelli and colleagues68 and two studies74,76 from Di and colleagues69 were identified in our searches and included as primary studies because they presented additional information pertinent to this review.
Finally, Dale and colleagues77 reviewed studies of health utility in people with CKD and ESRD. Only one study78 included this review met our inclusion criteria and was thus data extracted separately.
All other studies included were prospective (21) or retrospective cohorts (13). Two included studies, defining their study population based on the presence of diabetes only, were retained because participants with CKD accounted for a substantial number of the total study population. 79,80 Irie and colleagues81 reported on a subgroup of the participants included in the study by Imai and colleagues82 but reported on different outcomes and their work was, therefore, included as a separate study.
Definition of chronic kidney disease
Among the included studies, various definitions of renal impairment were reported. Definitions based on the KDOQI were the most widely used to describe CKD and classify stages, with an eGFR of less than 60 ml/min/1.73 m2 (stage 3 or worse) being the most commonly reported threshold (see Table 2). Others defined impaired renal function based on serum creatinine, creatinine clearance, microalbuminuria or some combination of measures. Several studies did not clearly define what they considered to be CKD, but they presented data for subgroups that met the inclusion criteria of our review and were therefore reported.
Where GFR was reported, most studies used the MDRD equation to estimate GFR; two studies used the CG equation. 83,84 The re-expressed, ID-MS (isotope dilution-mass spectrometry) traceable MDRD formula was used in two studies. 32,85 One compared the MDRD equation, the CG equation and the Mayo Clinic equations for estimating GFR. 86 Three studies used the Cr-EDTA injection87–89 while another study used the iohexol clearance technique90 to measure kidney function. Five studies did not specify which measure was used to assess renal function. 78,91–94 The systematic reviews included a variety of measures for assessing kidney function. 68,69
We were able to define two categories of study based on the populations they included:
-
Screened population – drawing from people in the community and using a population screening approach.
-
Clinical population – drawing from clinical record databases, laboratories, primary care or clinical settings and the blood sample taken for a clinical indication.
Methodological quality of included studies
The quality of cohort or follow-up studies was assessed based on the following four criteria:
-
sample selection
-
follow-up
-
determination of chronicity
-
measure of renal impairment.
A summary of the quality assessment is presented in Table 3. Only 13 studies adequately defined CKD to be chronic. Assay calibration for the measurement of serum creatinine is a major determinant of the accuracy of GFR,112 and differences between clinical laboratories in calibration of serum creatinine or assays could be a source of error. 113 Among the included studies, only 12 accounted for differences in assays over time or between labs. More than half of the studies had either complete follow-up or reported loss to follow-up of less than 10%. Most of the studies (27) fulfilled all or 85% of the criteria for study design and sample selection (see Appendix 4 for the quality assessment for systematic reviews).
| Study ID | Hypothesis/aim clearly described | Complete capture of study population | Clear inclusion and exclusion criteria | Clinical and demographic characteristics detailed | Information recorded prospectively (minimal recall bias) | Ascertainment of sample described | Assessment of outcome described | Number lost to follow-up reported | Loss to follow-up < 10% | Reason for loss to follow-up given | Characteristics of patients loss to follow-up described | Design specific sources of bias mentioned | Appropriate methods to deal with bias/confounding | Chronicity: adequately defineda | Accounted for differences in assays |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Astor 200885 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | Unclear | Yes |
| Bruno 200779 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Unclear | No | No |
| Cvengros 200591 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes | No | No |
| Djamali 200383 | Yes | Unclear | Yes | Yes | Yes | No | No | Yes | No | Yes | No | Yes | No | Yes | No |
| Drey 200395 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | No | No | Yes |
| Eriksen 200696 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | Yes | Unclear |
| Evans 200598 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | Yes | No |
| Go 200475 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes |
| Gorodetskaya 200578 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | No | No | No |
| Hallan 200632 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | No | Yes |
| Hemmelgarn 2006101 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | No | Yes |
| Herzog 200492 | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Complete | – | – | – | Yes | Yes | No | No |
| Hovind 200193 | Yes | Unclear | Yes | Yes | Yes | Yes | Unclear | No | – | – | – | Yes | Yes | Yes | No |
| Hsu 2003103 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | No | Yes |
| Imai 200882 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | No | Yes |
| Irie 200681 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes |
| John 2004104 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | No | No | Yes | Yes |
| Jones 2006105 | Yes | No | Unclear | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | Yes | Yes |
| Keith 2004106 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | Yes | Unclear |
| Khatami 2007108 | Yes | Unclear | Yes | Unclear | Yes | Yes | Yes | Complete | – | – | – | No | No | Unclear | Yes |
| Kollerits 200790 | Yes | Unclear | Yes | Yes | Yes | Unclear | No | Yes | No | Yes | Yes | Yes | Yes | Yes | No |
| Leehey 2005109 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | Yes | No |
| Levin 200184 | Yes | Unclear | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | No | No | Yes | No | No | No |
| Maaravi 200786 | Yes | Yes | Yes | Yes | Yes | Unclear | Unclear | Complete | – | – | – | Yes | Yes | Unclear | Unclear |
| Meisienger 200676 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Unclear |
| Mulec 199887 | Yes | Unclear | Yes | Yes | Yes | Yes | Unclear | Complete | – | – | – | No | No | Unclear | No |
| O’Hare 2006110 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | – | – | – | Yes | Yes | No | No |
| Orlando 2007111 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | No |
| Patel 200580 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Unclear | No |
| Rossing 200488 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Unclear | – | – | – | Yes | Yes | Yes | Unclear |
| Tarnow 200589 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No | Unclear |
| Tseng 200894 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Complete | – | – | – | Yes | Yes | Yes | No |
| Wannamethee 200637 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | No | No |
| Weiner 200474 | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | No | No | Yes | Yes | No | Yes |
Outcomes
The outcomes reported by included studies are summarised in Table 4. ACM was the most commonly reported outcome, with few studies reporting aspects of quality of life. Thirteen studies presented the outcomes by CKD stages as per the KDOQI. 32,75,78–80,82,83,85,94,101,106,110,111
| Study ID | ACM | CVD M&M | RRT | ESRD | CKDP | QoL |
|---|---|---|---|---|---|---|
| Astor 200885 | x | x | ||||
| Bruno 200779 | x | x | ||||
| Cvengros 200591 | x | |||||
| Di 200769 | x | |||||
| Djamali 200383 | x | x | ||||
| Drey 200395 | x | x | x | x | ||
| Eriksen 200696 | x | x | x | |||
| Evans 200598 | x | x | x | x | ||
| Go 200475 | x | x | x | |||
| Gorodetskaya 200578 | x | x | x | |||
| Hallan 200632 | x | x | ||||
| Hemmelgarn 2006101 | x | x | x | |||
| Herzog 200492 | x | |||||
| Hovind 200193 | x | |||||
| Hsu 2003103 | x | x | ||||
| Imai 200882 | x | |||||
| Irie 200681 | x | x | ||||
| John 2004104 | x | x | x | |||
| Jones 2006105 | x | x | x | |||
| Keith 2004106 | x | x | x | |||
| Khatami 2007108 | x | |||||
| Kollerits 200790 | x | x | ||||
| Leehey 2005109 | x | |||||
| Levin 200184 | x | x | x | x | ||
| Maaravi 200786 | x | |||||
| Meisienger 200676 | x | x | ||||
| Mulec 199887 | x | |||||
| O’Hare 2006110 | x | |||||
| Orlando 2007111 | x | x | ||||
| Patel 200580 | x | x | x | |||
| Rossing 200488 | x | x | x | x | ||
| Tarnow 200589 | x | x | ||||
| Tonelli 200668 | x | x | ||||
| Tseng 200894 | x | x | ||||
| Wannamethee 200637 | x | |||||
| Weiner 200474 | x | x |
In the following section, we present a summary of the results of studies of general CKD populations not restricted to specific subgroups. We then present data for the following pre-specified subgroups: diabetes mellitus, hypertension (HBP), CVD, gender, race and age.
All-cause mortality: general chronic kidney disease population
ACM risk in those with CKD compared with no CKD
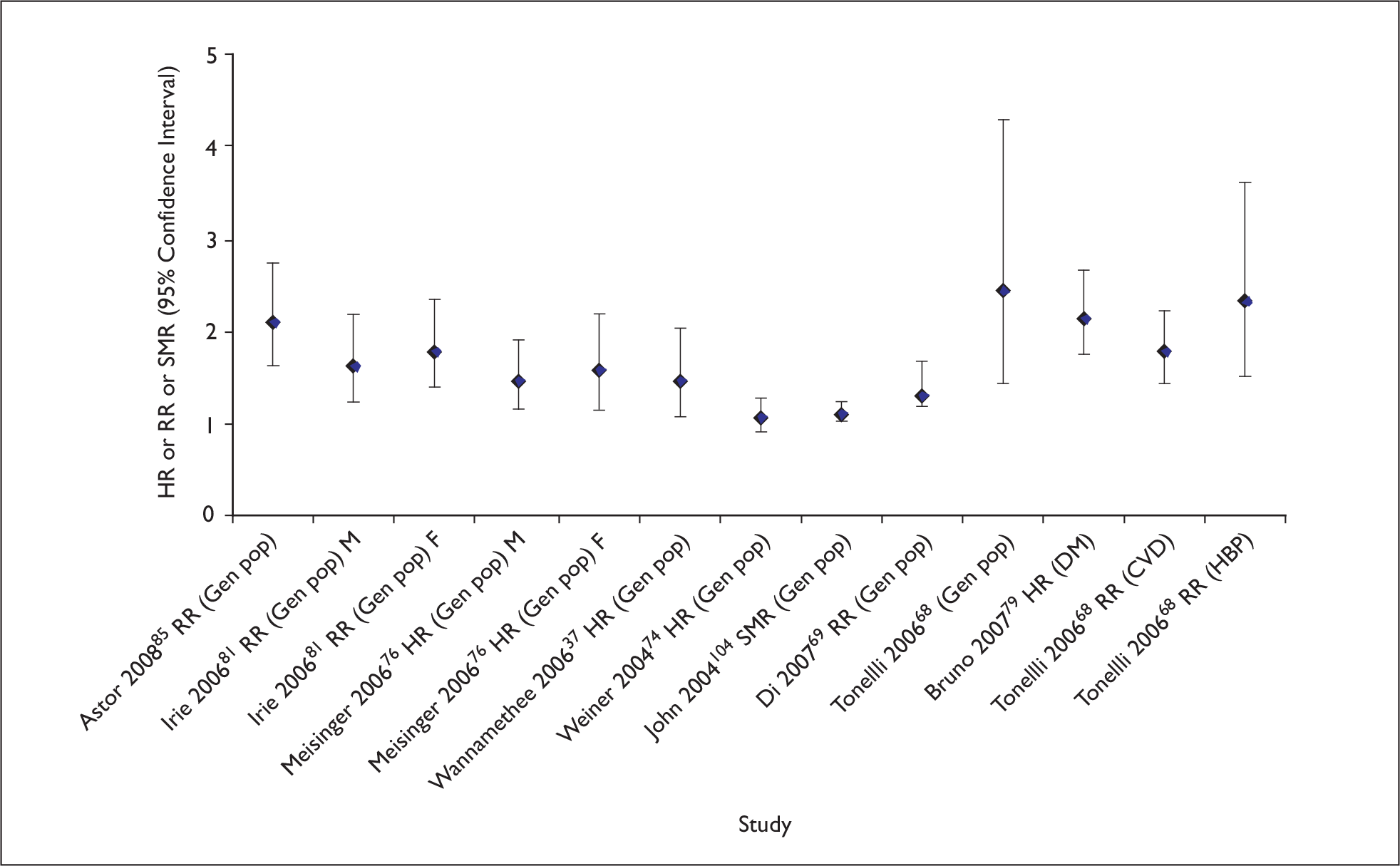
Eriksen and Ingebretsen96 reported a hazard ratio (HR) of 1.25 (95% CI 1.14 to 1.37) for each 10-ml/min/1.73 m2 decrease in eGFR. Five primary studies reported a small increased risk of mortality (risk ratios ranged from 1.12 to 1.78) for people with CKD as compared with those without CKD (Figure 4). 74,76,81,85,92 These studies were based on general populations undergoing health screening76,81,85 or clinical record database review,92 and all but one92 adjusted for comorbidities, age and sex. Herzog and colleagues92 adjusted for comorbidities only. A further two population health screening studies, comparing ACM in CKD cohorts with the population as standardised mortality rates (SMRs), noted higher risks of mortality with SMR 2.2 (95% CI 2.1 to 2.4)96 and SMR 8.3 (95% CI 7.5 to 9.2),98 but did not adjust for comorbidity (Figure 4). Evans and colleagues98 included a cohort of participants with marked renal impairment with a serum creatinine level of at least 250 µmol/l. John and colleagues104 reported age and sex-adjusted SMRs for a CKD cohort compared with the general population, based on laboratory data (SMR 1.53, 95% CI 1.44 to 1.62).
FIGURE 4.
Risk of all-cause mortality. Comparing those with CKD with those without CKD. aThree studies reported by Tonelli 200668 as ‘general populations’ with adjusted analysis; Sihvonen 2004115 included only people with rheumatoid arthritis so recoded as ‘clinical population’ in this review. Clin, clinical; CVD, cardiovascular diseases; DM, diabetes mellitus; F, female; FHS, Framingham Heart Study; Gen, general; HBP, high blood pressure; HR, hazard ratio; M, male; NHANES I, National Health and Nutritional Survey I; Pop, population; RR, relative risk; SMR, standardised mortality rate.
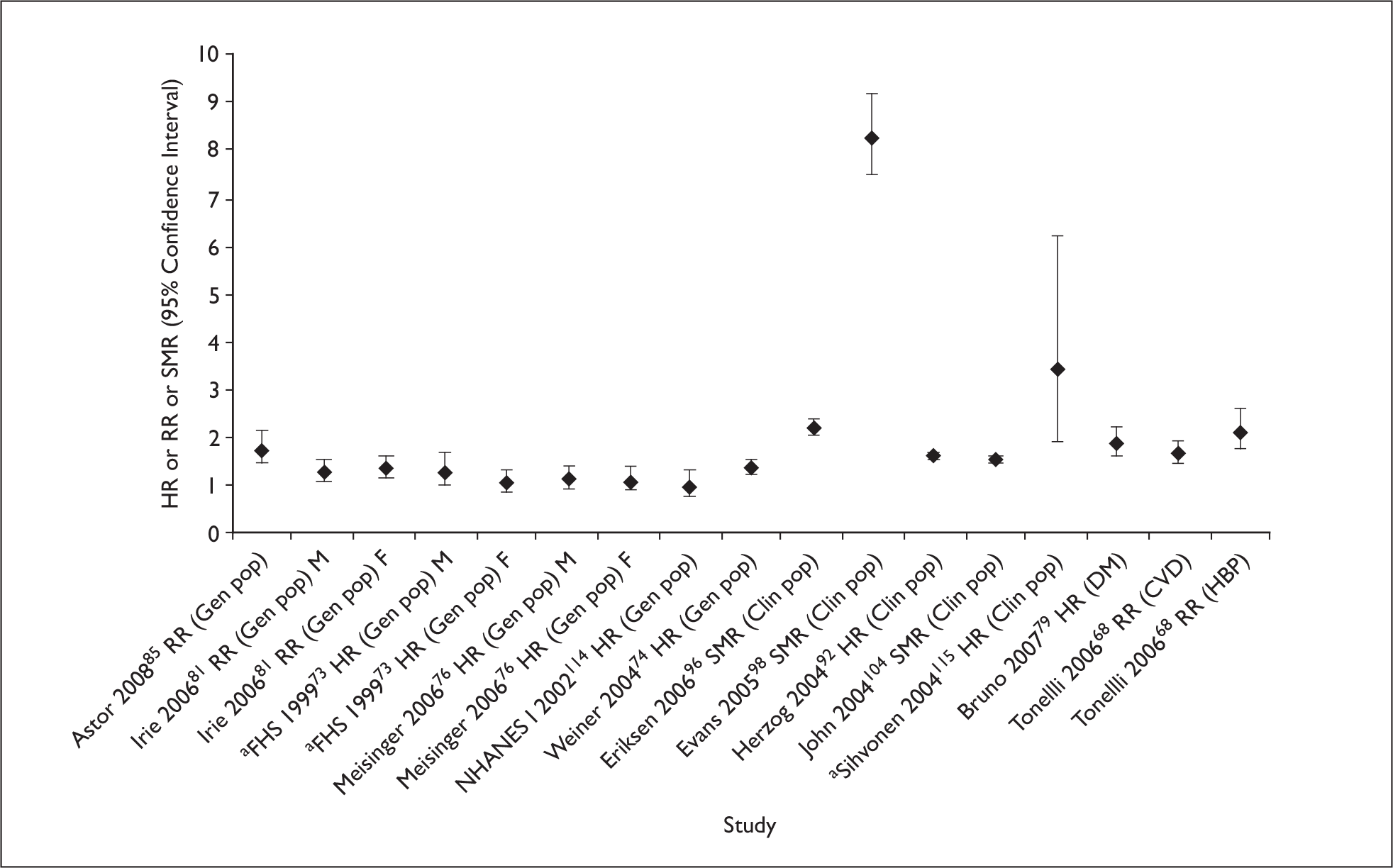
Tonelli and colleagues68 reported an unadjusted increased risk of death among those with CKD compared with no CKD in 93% of the 37 studies included in their meta-analysis (RR range 0.94–5.00); however, significant heterogeneity was noted. From a series of meta-regression analyses, authors reported that a greater risk associated with CKD was observed in younger patients, women and studies in ‘general populations’. In nine studies classed as including a ‘general population’, the risk for mortality in the CKD group was threefold higher (RR 3.0, 95% CI 2.18 to 4.11), but again substantial heterogeneity was observed. Studies based on population health survey data (NHANES I114 and II,70 FHS73) reported lower HR/RR of 1.38–2.26. One population-based heart risk factor study in North America (ARIC71) reported higher risk estimates (3.54); three studies included populations known to be at high risk of mortality and CKD (people over 65 years, aboriginal Australians, clinical records based cohort). Adjusted analysis for general population studies (possible for three studies) was also presented by Tonelli and colleagues68 and this reduced heterogeneity as well as reducing the risk estimate to close to 1 for all but one of the studies. Further details are given in Appendix 5.
Two studies reported adjusted risk of ACM by CKD stage (Table 5). 75,85 Go and colleagues,75 studying a clinical population, reported an increasing risk with stage from HR 1.2 for stage 3a to 5.9 for stage 5 (compared with no CKD). Astor and colleagues,85 studying a general population, also reported an increase in risk with stage.
| Study ID | Measures | Values (variance) | Reference group | Adjusted analysis |
|---|---|---|---|---|
| Astor 200884 | RR (95% CI) |
Stage 2: 1.05 (0.89 to 1.25) Stage 3–5: 1.77 (1.47 to 2.13) |
eGFR ≥ 90 ml/min/1.73 m2 | Age, sex, race/ethnicity, previous CVD, BP, use of antihypertensive medication, DM, smoking, BMI, physical activity, cholesterol and C-reactive protein |
| Go 200474 | HR (95% CI) |
Stage 3a: 1.2 (1.1 to 1.2) Stage 3b: 1.8 (1.7 to 1.9) Stage 4: 3.2 (3.1 to 3.4) Stage 5: 5.9 (5.4 to 6.5) |
eGFR ≥ 60 ml/min/1.73 m2 |
Age, sex, income, education, dialysis, prior CVD, DM, HBP, dyslipidaemia, cancer, serum albumin < 3.5g/dl, dementia, cirrhosis, chronic lung disease, proteinuria, prior hospitalisation |
ACM rate in populations with CKD
Four studies reported ACM per 10,000 person-years. 74–76,85 All reported death rates among those with CKD that were greater than for those with no CKD (definitions varied) (Table 6). Death rate varied substantially between studies; Wiener and colleagues74 reported the highest rate of 3080 deaths per 10,000 person-years, considerably more than any of the other studies. This study also reported a high death rate (980 per 10,000 person-years) in the population with no CKD. There was evidence that death rate increased with the degree of proteinuria85 and stage,75 and was higher in men than in women. 76
| Study ID | Measures | Values (variance) | Follow-up | Comparators/CKD other stages | Comments |
|---|---|---|---|---|---|
| Deaths per person-years | |||||
| Astor 200885 | Events/10,000 person-years (read from graph) |
Stage 3–5 no A: 290 Stage 3–5 microA: 510 Stage 3–5 macroA: 880 |
13 years | eGFR > 90 ml/min/1.73 m2 no A: 180 | |
| Go 200475 | Events/10,000 person-years |
Stage 3a: 108 Stage 3b: 476 Stage 4: 1136 Stage 5: 1414 |
Median 2.84 years | eGFR ≥ 60 ml/min/1.73 m2: 76 | |
| Meisinger 200676 | Events/10,000 person-years |
M: 329.3 F: 154.8 |
Median 12.5 years | eGFR ≥ 60 ml/min/1.73 m2: M: 194.7; F: 90 | |
| Weiner 200474 | Events/10,000 person-years | 3080 | Mean 8.3 years | eGFR ≥ 60 ml/min/1.73 m2: 980 | |
| Cumulative mortality within follow-up period | |||||
| Djamali 200383 | Deaths in 12.6 yearsa | 19.7% | 12.6 years | CKD defined as SCr > 115 µmol/l; presented as survival analysis in paper | |
| Eriksen 200696 | Deaths in 5 years (95% CI) | 32% (30 to 34) | 10 years | Presented as cumulative incidence of death in paper | |
| Deaths in 10 years (95% CI) | 52% (48 to 55) | ||||
| Evans 200598 | Deaths in 1 year | 3% | 5 years | Presented as survival rate in paper | |
| Deaths in 5 years | 39% | ||||
| Herzog 200492 | Deaths in 1 year CKD only | 8.2% | 1 year | CKD defined based on ICD-9-CM codes | |
| Deaths in 1 year CKD + CHF + anaemia | 22.9% | ||||
| Irie 200681 | Deaths in 10 years | 20.7% | 10 years | ||
| Jones 2006105 | Deaths in 1 year | 15% | 3 years | ||
| Deaths in 3 years | 25% | ||||
| Keith 2004106 | Deaths in 5 years |
Stage 3: 24.3% Stage 4: 45.7% |
5 years |
eGFR 60–89 ml/min/1.73 m2 no P: 10.2% Stage 2: 19.5% |
|
| Maaravi 200786 | Deaths in 12 years |
MDRD equation 36.4% CG equation 35.4% |
12 years | Presented as survival rate in paper | |
| Mortality (%) | |||||
| Drey 200395 | Deaths |
SCr > 1.7 mg/dl: 69% SCr 1.7–3.3 mg/dl: 69% SCr 3.4–5.7 mg/dl: 77% SCr > 5.7 mg/dl: 59% |
Mean 5.5 years | Median survival 35 months | |
| Go 200475 |
Stage 3a: 7.54% Stage 3b: 22.7% Stage 4: 62.2% |
Median 2.8 years | eGFR ≥ 60 ml/min/1.73 m2: 2.79% | ||
| Hemmelgarn 2006101 | Deaths | eGFR < 30 ml/min/1.73 m2: 6% | Median 2 years | ||
| John 2004104 | Deaths | 38.6% | Median 2.6 years |
Median survival 28.1 months CKD: SCr ≥ 135 µmol/l |
|
| Levin 200184 | Deaths | 2.6% | Median 1.9 years (462 patient years) |
Selected by physicians to be expected to be alive at 12 months CKD: CrCl 10–75 ml/min |
|
| Meisinger 200676 | Deaths | M: 30%; F: 17% | Median 12.5 years | eGFR ≥ 60 ml/min/1.73 m2: M: 22%; F: 10.7% | |
| Orlando 2007111 | Deaths |
Stage 3: 49% Stage 4: 52% Stage 5: 27% |
Mean 3.6 years |
Stage 1: 21% Stage 2: 31% |
|
| Tonelli 200668 | Deaths | 12.4% | Median 4.5 years | eGFR ≥ 60 ml/min/1.73 m2: 3.1% | |
Seven primary studies presented cumulative mortality for a specified time period. 81,83,86,92,96,98,105 At 1 year, mortality varied from only 3%98 to 15%. 105 At 5 years, 31–39% died. 96,98 For studies reporting 9.0–12.5 years’ follow-up, cumulative mortality ranged from 19.7% to 52.0%. 81,83,86,96 Five other studies presented the proportion of deaths in a given mean follow-up time and thus were not directly comparable. 68,76,84,101,104 Drey and colleagues95 reported an exceptionally high proportion of deaths (69%) in mean 5.5 years. The results of these are summarised in Table 6.
Four primary studies reported the proportion of deaths for different stages of CKD. 75,83,106,111 The proportion of people dying was observed to increase with declining eGFR.
Cardiovascular disease morbidity and mortality: chronic kidney disease population
Studies did not report a consistent definition of CVD morbidity and mortality, and reporting was often lacking in detail so caution should be used when drawing comparisons across studies.
CVD risk in those with CKD compared with no CKD
As for ACM, most studies observed a higher risk of CVD deaths or events in those with CKD as compared with people without CKD. As shown in Figure 5, the adjusted risk estimates for general population studies were reasonably consistent (RR 1.14–1.81) with the exception of studies by Astor and colleagues85 (RR 2.12, 95% CI 1.65 to 2.73), Weiner and colleagues74 (HR 1.09, 95% CI 0.91 to 1.29) (pooled analysis of four population-based health studies in the USA), and Tonelli and colleagues. 68 Across the 14 studies included in a review by Tonelli and colleagues68 that reported on CVD mortality and morbidity, the unadjusted RRs ranged from 1.43 to 3.73. The risk for CVD mortality was 2.47 (95% CI 1.42 to 4.30) in the CKD group as compared with the non-CKD population for three general population studies, but substantial heterogeneity was observed. 68 The authors described adjusted analysis for all 14 studies being particularly sensitive to age, with a greater risk associated with CKD in younger people (no details in paper). Di and colleagues69 also reported an increased risk of CVD morbidity and mortality (RR 1.41, 95% CI 1.19 to 1.68) from the meta-analysis of seven general population studies, with statistically significant heterogeneity observed (p = 0.045).
FIGURE 5.
Risk of cardiovascular morbidity and mortality. Comparing those with CKD with those without CKD. CVD, cardiovascular diseases; DM, diabetes mellitus; F, female; Gen, general; HBP, high blood pressure; HR, hazard ratio; M, male; Pop, population; RR, relative risk; SMR, standardised mortality rate.
Two studies, reporting the risk of CVD events associated with different stages of CKD, reported an increase with decreasing eGFR (Table 7).
| Study ID | Measures | Values (variance) | Reference group | Adjusted analysis |
|---|---|---|---|---|
| Astor 200885 | CVD deaths, RR (95% CI) |
Stage 2: 1.37 (1.07 to 1.75) Stage 3–5: 2.12 (1.65 to 2.73) |
eGFR ≥ 90 ml/min/1.73 m2 | Age, sex, race/ethnicity, previous CVD, BP, use of antihypertensive medication, DM, smoking, BMI, physical activity, cholesterol and C-reactive protein |
| Go 200475 | CVD events, HR (95% CI) |
Stage 3a: 1.4 (1.4 to 1.5) Stage 3b: 2.0 (1.9 to 2.1) Stage 4: 2.8 (2.6 to 2.9) Stage 5: 3.4 (3.1 to 3.8) |
eGFR ≥ 60 ml/min/1.73 m2 |
Age, sex, income, education, dialysis, prior CVD, DM, HBP, dyslipidaemia, cancer, serum albumin < 3.5g/dl; dementia, cirrhosis, chronic lung disease, proteinuria, prior hospitalisation |
CVD rate in populations with CKD
The rate of CVD deaths or events was reported in five studies and varied between studies by population, age, sex and CKD stage. 32,74–76,85 Rates of CVD events and deaths more than doubled from stage 3a to stage 3b.
Cardiovascular disease morbidity and mortality was reported for follow-up periods that ranged from a median of 23 months84 to 12.5 years. 76 Frequency of CVD death was low in the study by Levin and colleagues,84 where study participants were selected because they were thought to be clinically healthier. Proportions experiencing CVD death or a CVD event increased with CKD stage and were higher in men than in women. 32,75 Summarised results of the CVD rates and proportions experiencing CVD morbidity and mortality are presented in Table 8.
| Study ID | Measures | Values (variances) | Follow-up | Comparators/other CKD stages | Comments |
|---|---|---|---|---|---|
| Deaths per person-years | |||||
| Astor 200885 |
CVD deaths rate/10,000 person-years (read from graph) |
Stage 3–5 no A: 120 Stage 3–5 microA: 240 Stage 3–5 macroA: 410 |
13 years | eGFR ≥ 60 ml/min/1.73 m2: 50 | Adjusted to the incidence rates of a 60-year-old non-Hispanic white male |
| Go 200475 | CVD events rate/10,000 person-years |
Stage 3a: 365 Stage 3b: 1129 Stage 4: 2180 Stage 5: 3660 |
Median 2.8 years | eGFR ≥ 60 ml/min/1.73 m2: 211 | Rates standardised to age |
| Hallan 200632 | CVD deaths rate/10,000 person-years |
Stage 3a: 350 Stage 3b: 740 eGFR < 30 ml/min/1.73 m2: 1010 |
Median 8 years | eGFR ≥ 60 ml/min/1.73 m2: 40 | |
| Meisinger 200676 | CVD deaths rate/10,000 person-years |
M: 189.8 F: 87.1 |
Median 12.5 years | eGFR ≥ 60 ml/min/1.73 m2: M: 82.7; F: 33 | |
| Meisinger 200676 | Incident rates of MI/10,000 person-years |
M: 146.5 F: 48.2 |
Median 12.5 years | eGFR ≥ 60 ml/min/1.73 m2: M: 84.1; F: 22.9 | |
| Weiner 200474 | Incident rates of MI or fatal CHD/10,000 person-years | 1390 | Mean 8.3 years | eGFR ≥ 60 ml/min/1.73 m2: 650 | |
| Cumulative CVD mortality/morbidity | |||||
| Irie 200681 | Number of CVD deaths |
M: 82/824 (10.0%) F: 150/2073 (7.2%) |
10 fixed years | ||
| Keith 2004106 | Number of CHD | 3435/13,796 (24.9%) | 5.5 fixed years | ||
| Events (%) during follow-up | |||||
| Drey 200395 | Number of CVD deaths | 339/1071 (31.7%) | Mean 5.5 years | CKD: SCr ≥ 150.3 µmol/l | |
| Evans 200598 | Number of CVD deaths | 146/920 (15.9%) | Mean 4.4 years | CKD: stage 4 and 5 only | |
| Go 200475 | Number of CVD events |
Stage 3a: 34,690/153,426 (22.6%) Stage 3b: 18,580/34,275 (54.2%) Stage 4: 8809/7085 Stage 5: 3824/1373 |
Median 2.8 years | eGFR ≥ 60 ml/min/1.73 m2: 73,108/924,136 (7.9%) | An individual could experience more than one event –number of events presented |
| Hallan 200632 | Number of CVD deaths |
Total: 691/3057 (22.6%) Stage 3a: 456/2389 (19.1%) Stage 3b: 185/548 (33.8%) eGFR < 30 ml/min/1.73 m2: 50/120 (41.7%) |
Median 8 years | eGFR ≥ 60 ml/min/1.73 m2: 1913/62,099 (3.1%) | |
| John 2004104 | Number of CVD deaths or events | 497/3240 (15.3%) | Median 2.6 years |
CKD: M: SCr ≥ 180 µmol/l F: SCr ≥ 135 µmol/l |
|
| Levin 200184 | Number of CVD events | New or worsening symptoms: 48/244 (19.7%) | Median 23 months (462 patient years) | CKD: CrCl 10–75 ml/min | |
| Meisinger 200676 | Number of CVD events |
M: 83/480 (17.3%) F: 72/753 (9.6%) |
Median 12.5 years | eGFR ≥ 60 ml/min/1.73 m2: M: 317/3380 (9.4%); F: 115/2921 (3.9%) | |
| Meisinger 200676 | Number of incident MI |
M: 46/441 (10.4%) F: 31/737 (4.2%) |
Median 12.5 years | eGFR ≥ 60 ml/min/1.73 m2: M: 275/3221 (8.5%) F: 71/2894 (2.5%) | |
| Tonelli 200668 | Number of CVD events | 182/750 (24.3%) | Median 4.5 years | ||
| Weiner 200474 | Number of MI or fatal CHD events | 168/1664 (10.1%) | Mean 8.3 years | eGFR ≥ 60 ml/min/1.73 m2: 1111/20,970 (5.3%) | |
Renal outcome: chronic kidney disease population
Nineteen studies reported renal outcomes and included ESRD, RRT and/or CKD progression. The results are summarised in Table 9.
| Study ID | Measures | Values (variance) | Follow-up | Definitions of renal outcomes | Comments |
|---|---|---|---|---|---|
| ESRD | |||||
| Risk and rates | |||||
| Eriksen 200696 | HR (95% CI) of renal failure | 2.5 (1.89 to 3.31) | 10 years | Renal failure defined as irreversible stage 5 CKD or initiation of RRT | For each eGFR decrease of 10 ml/min/1.73 m2; adjusted for age and sex |
| Eriksen 200696 | Incidence rate ratio (95% CI) of renal failure | 5.3 (3.9 to 7.3) | 10 years | Renal failure defined as irreversible stage 5 CKD or initiation of RRT | Standardised to Tromsø general population |
| Hallan 200632 | HR (95% CI) of ESRD |
Stage 3a: 1.0 (reference) Stage 3b: 4.2 (1.5 to 11) eGFR < 30: 68.5 (30 to 156) |
Median 8 years | ESRD not defined | Adjusted for sex, age, diabetes, and hypertension (smoking, BMI and CVD at baseline were not significant) |
| Hallan 200632 | Incidence rate of ESRD/100 person-years |
Stage 3a: 0.04 Stage 3b: 0.2 eGFR < 30: 2.6 |
Median 8 years | ESRD not defined | |
| Cumulative ESRD and ESRD during follow-up duration | |||||
| Eriksen 200696 | Renal failure | 10 years | Renal failure defined as irreversible stage 5 CKD or initiation of RRT | ||
| 5 years cumulative incidence (95% CI) | 0.02 (0.01 to 0.02) | ||||
| 10 years cumulative incidence (95% CI) | 0.04 (0.03 to 0.06) | ||||
| Hallan 200632 | Number reaching ESRD |
Total: 38/3057 (1.2%) Stage 3a: 9/2389 (0.4%) Stage 3b: 7/548 (1.3%) eGFR < 30: 22/120 (18.3%) |
Median 8 years | ESRD not defined | eGFR ≥ 60 ml/min/1.73 m2: 13/62066 (0.02%) |
| Djamali 200383 | Kidney deaths (presented as kidney survival in the study) |
Stage 3: 13.5 years 12.9% Stage 4: 11.2 years 4.9% |
Mean 4.6 years | Kidney survival defined as time from first visit to time of last visit or incidence of ESRD or patient death with functional kidney |
Stage 1: 12.7 years 38.1% Stage 2: 12.1 years 26.8% Adjusted for age and sex |
| RRT | |||||
| Levin 200184 | Number reaching RRT |
Dialysis: 24/313 (7.7%) Transplant: 1/313 (0.3%) |
Median 1.9 years (462 patient years’ follow-up) | RRT was defined as need for either dialysis or transplantation | CKD: CrCl 10–75 ml/min |
| Incidence of RRT at 6 months | 10/268 (3.7%) | ||||
| Incidence of RRT at 12 months | 7/218 (3.2%) | ||||
| Incidence of RRT at 24 months | 18/94 (19.1%) | ||||
| Kollerits 200790 | Number reaching RRT | 29/177 (16.4%) | Mean 3.9 years | ||
| Drey 200395 | Number reaching RRT | 4% | Mean 5.5 years | RRT: either dialysis or transplantation | SCr ≥ 150.3 µmol/l |
| Hemmelgarn 2006101 | Number reaching dialysis | eGFR < 30: 81/87 dialysis (93.1%) | Median 2 years | eGFR < 90 ml/min/1.73 m2 | |
| Keith 2004106 | Number reaching RRT |
Stage 3: transplant 0.2%; dialysis 1.1% Stage 4: transplant 2.3%; dialysis 17.6% |
5.5 years | RRT defined as initiation of dialysis or renal transplantation |
Stage 2 no protein: transplant 0.01%; dialysis 0.06% Stage 2 + protein: transplant 0.2%; dialysis 0.9% |
| Evans 200598 | Number reaching dialysis | 739 (80.3%) | Median 4.4 years | Mean observation time in the RRT analysis was 2.0 (SD 1.8) years | |
| Number of transplantation | 248 (34%) | ||||
| Gorodetskaya 200578 | Number starting dialysis | Stage 4 +: 31/115 (27.0%) | Mean 10 (range 6–24) months | ||
| Jones 2006105 | Number starting RRT | 73 (10%) | Median 2.9 years | ||
| CKD progression | |||||
| Rate of CKD progression | |||||
| Djamali 200383 | Mean rate of CrCl decline (SD) ml/min/year |
Stage 3: 5.4 (7.4) Stage 4: 5.7 (5.6) Stage 5: 1.5 (8.5) |
Mean 4.6 years |
Stage 1: 11 (12) Stage 2: 8.4 (10) CKD: SCr > 115 µmol/l |
|
| Hemmelgarn 2006101 | Mean rate of eGFR decline (95% CI) ml/min/year |
Stage 3–5 Male: No DM: 3.5 (2.7 to 4.3) DM: 7.2 (5.9 to 8.6) Female: No DM: 2.0 (1.4 to 2.6) DM: 5.1 (3.8 to 6.3) |
Median 2 years | ||
| Gorodetskaya 200578 | Mean rate of decline in eGFR (IQR) ml/min/1.73 m2/year | Stage 4 +: 1.3 (2.4 to 0.4) | Mean 10 (range 6–24) months | ||
| Imai 200882 | Mean rate of decline in eGFR | Presented graphically only | |||
| Jones 2006105 | Mean rate of decline in eGFR (IQR) ml/min/1.73 m2/year |
Pre referral 5.4 (2 to 13) Post referral 0.34 (–3 to 3) |
Median 2.9 years | ||
| Proportion experiencing CKD progression during follow-up | |||||
| Kollerits 200790 | Proportion progressed to renal end point | 65/177 (36.7%) | Mean 3.9 years | Renal end point defined as RRT or doubling of baseline SCr | CKD estimated based on SCr |
| Doubling of baseline SCr without reaching ESRD | 36/177 (20.3%) | ||||
| John 2004104 | Proportion as per various rate of eGFR (ml/min/1.73 m2) decline per year |
eGFR decline: < 2: 79.3% 2–3.9: 8.7% ≥ 4: 12.4% |
Median 2.6 years |
CKD: M: SCr ≥ 180 µmol/l F: SCr ≥ 135 µmol/l |
|
| Jones 2006105 | Declining GFR (slopes more negative than 1 ml/min/1.73 m2) |
Post referral: Decline: 314/726 (43.3%) No decline: 412 (56.7%) Pre referral: Decline: 607 (83.6%) No decline: 119 (16%) |
Median 2.9 years | ||
| Khatami 2007108 | Proportion progressing to stages 4 and 5 | 22/520 (4.2%) | 4 years | eGFR < 60 ml/min/1.73 m2 at baseline | |
| Proportion regressed to stage 2 | ‘Approx 20%’ | ||||
| Proportion stable | ‘Approx 76%’ | ||||
| Orlando 2007111 | Proportion of progressors |
Stage 3: 70 (17%) Stage 4: 21 (24%) Stage 5: 6 (23%) |
Mean 3.6 years | Progression defined as from one stage to other |
Stage 1: 583 (48%) Stage 2: 276(31%) |
Eriksen and Ingebretsen96 reported a 2.5 times increase in the risk of developing ESRD for every 10-ml/min/1.73 m2/year decline in renal function, and the incidence of developing ESRD for those with an eGFR of less than 60 ml/min/1.73 m2/year was five times greater than for the general population. 96 Hallan and colleagues32 presented the adjusted risk of ESRD in different stages of CKD and noted a fourfold increase from stage 3a to stage 3b. From stage 4, the risk of ESRD was substantially increased (HR 68.5, 95% CI 30 to 156) and an incidence rate of 260 per 10,000 person-years was reported.
The rate of CKD progression was measured in terms of mean rate of decline of creatinine clearance by Djamali and colleagues,83 and they reported a mean 6.6-ml/min/year decline. Normal GFR decline was defined, by the KDOQI, as a reduction in eGFR by approximately 1 ml/min/1.73 m2/year from a normal level of 125 ml/min/1.73 m2. Jones and colleagues105 defined CKD progression as any slope more negative than a decline of 1 ml/min/1.73 m2/year. The study found that 84% of study participants had evidence of progression (slope decline of more than 1 ml/min/1.73 m2/year) with 52% of these experiencing fast progression (slope decline of at least 5 ml/min/1.73 m2/year). As they followed the cohort over time (and following referral to a specialist service) the mean rate of decline was noted to reduce. This may be the result of interventions, referral or stage of disease. John and colleagues104 also reported CKD progression according to rates of decline in GFR; 8.3% showed a decline of at least 5 ml/min/1.73 m2/year, 12.4% had decline rates between 2.0 and 4.9 ml/min/1.73 m2/year, with the remaining 79.3% having little evidence of renal function decline. Gorodetskaya and colleagues78 reported an estimated mean rate of decline in eGFR as 1.3 ml/min/1.73 m2/year [standard deviation (SD) 0.4–2.4] for those with an initial eGFR lower than 30 ml/min/1.73 m2. Djamali and colleagues83 reported that the absolute rate of CKD progression was fastest during stages 1 and 2. By contrast Hemmelgarn and colleagues101 reported the absolute rate of progression increased as eGFR declined.
Eriksen and Ingebretsen96 presented cumulative incidence of ESRD, reporting 2% and 4% at 5 and 10 years respectively. Another study reported incidence of RRT in 6 months (3.7%), 12 months (3.2%) and 24 months (19.1%). 84 The other studies presented the number starting dialysis or receiving a renal transplant as a proportion in a given follow-up time and, therefore, could not be compared directly. An exceptionally high proportion of RRT (80.3%) during 4.4 years’ follow-up was observed by Evans and colleagues. 98
One study presented the progression and regression of CKD (eGFR lower than 60 ml/min/1.73 m2) over 4 years of follow-up108 for a subset of 522 patients with a repeat creatinine. Around 4% progressed to stages 4 and 5, 20% improved to stage 2 or better, and most (76%) were stable during the 4 years of follow-up. Hemmelgarn and colleagues101 reported that 41% of study participants with stage 3 disease and approximately 25% (from graph) of those with eGFR lower than 30 ml/min/1.73 m2 had stable, or an increase in, eGFR during the 2-year study period. Orlando and colleagues111 reported that in stages 1 and 2, the highest proportion of people showed evidence of progression (48% and 31% respectively). In stage 3–5, 17–24% progressed. Of note, in each stage the proportion not progressing because of death increased (from 21% in stage 1 to 52% in stage 4). Nonetheless, 22–38% of the study population neither progressed nor died.
Quality of life
Two papers describe aspects of quality of life in patients with CKD. 78,91 One prospectively analysed the association between kidney function, health-related quality of life and estimates of utility in 205 people. 78 This was based on the data obtained from three measures of quality of life, i.e. Kidney Disease Quality of Life short form-36 (KDQOL-36™), Health Utilities Index (HUI) and time trade-off (TTO). KDQOL-36 is a specific measure of health-related quality of life for CKD that includes effects and burden of kidney disease and physical and mental health score while HUI-3 is a generic instrument that measures the population preference or utility function such as vision, pain, hearing or cognitive function. TTO measures the health preferences of patients. Health-related quality of life according to the KDQOL-36™ and HUI-3 was found to decrease significantly across the stages of CKD, but only once eGFR had fallen below 30 ml/min/1.73 m2 (with the exception of the mental health score which was unchanged with stage). For example, HUI-3 (ranges from 1 to –0.36 where 1 represents perfect health and 0 death, negative scores represent states considered worse than death) reported estimates of 0.67 (SD 0.31) for eGFR > 60 ml/min/1.73 m2, 0.67 (SD 0.31) at stage 3, 0.55 (SD 0.34) at stage 4 and 0.54 (SD 0.36) at stage 5. For TTO there was a small but statistically insignificant decline in quality of life from stage 3 to stage 5.
The other study prospectively investigated the effect of the internal health-specific locus of control (HLOC) on changes in depression state in patients with progressive CKD. 91 The study mostly described the psychological measure and predictors of chronic disease. Internal HLOC measures patients’ belief in personal control over their health outcomes. The study found that internal HLOC score change from baseline was a significant predictor for changes in depression from baseline to follow-up, with increased internal control on one’s health predicting lower depression. Further, Cvengros and colleagues91 identified that this association was restricted to those progressing to receive dialysis. The CKD patients who did not progress to end stage seemed to have no relation between changes in internal HLOC to follow-up depression.
Subgroup analysis
CKD with diabetes
The results from cohorts that included only people with diabetes mellitus are summarised in Appendix 6. In studies with at least 6–10 years’ follow-up, mortality was reported as ranging from 19.7%79 to 35.0%88 with cardiovascular deaths accounting for a substantial proportion of this. GFR declined at between 3.8 and 4.5 ml/min/1.73 m2/year and, after 6.5 years, 7% of the study population was reported to have ESRD. 88 Three studies presented data that compared diabetics with non-diabetics. 101,105,111 Jones and colleagues105 observed that diabetic nephropathy was a predictor for having ‘fast progressive’ disease (eGFR decline of > 5 ml/min/year). Hemmelgarn and colleagues101 showed that CKD progression increased as the stages increased, with higher progression in late stages (CKD stages 3 and 4). Relative to the non-diabetic population, Orlando and colleagues111 found a higher risk of progression among those with diabetes in stage 1–2 (RR versus no diabetes mellitus 1.32, 95% CI 1.13 to 1.55), but no difference in progression in higher stages.
CKD with cardiovascular disease and hypertension (HBP)
While many studies included people with CVD and hypertension (HBP), few presented data on outcomes stratified by these subgroups. One study compared the risk of CKD progression for different CKD stages for those with CVD at baseline with those without CVD. 111 Compared with no CVD at baseline, people with CVD in CKD stage 1–3 were at a 35–52% increased risk of progression; in stage 4–5 there was no difference in the risk of progression. 111 Others presented the number accepted onto RRT as a proportion in a given follow-up time (see Appendix 6). Tonelli and colleagues68 analysed ACM and CVD mortality for studies recruiting only patients with CVD or patients with HBP at baseline, comparing CKD with no CKD. For those with CVD and CKD at baseline, the RR of ACM compared with no CKD was 1.71 (95% CI 1.49 to 1.96), substantially lower than that reported in the studies in general populations summarised in the section All-cause mortality: general CKD population (RR 3.0), and possibly reflecting the nature of the ‘general population’ studies that included known high risk groups. The RR for CVD mortality was 1.8 (95% CI 1.45 to 2.24), again lower than the studies of general populations. For studies of populations with hypertension, Tonelli and colleagues68 reported an ACM RR of 2.15 (95% CI 1.17 to 2.61) and a CVD mortality RR of 2.35 (95% CI 1.52 to 3.64). See Appendix 6 for detailed results.
Gender, race and age in CKD
The age standardised risk of mortality was reported by Evans and colleagues98 to be higher in females with CKD (SMR 12.3, 95% CI 10.3 to 14.5) than in males (SMR 7.2, 95% CI 6.3 to 8.1), as compared with the general population. Males had higher cumulative mortality and cumulative incidence of ESRD after 10 years than females. 96 Drey and colleagues95 found a similar proportion of deaths in males (69.34%) as in females (67.76%) during 5.5 years of mean follow-up. Meisinger and colleagues76 and Irie and colleagues81 reported a higher risk of CVD mortality in females than in males (see Table 44, Appendix 6), while risk of ACM was similar in both genders. The rate of decline in GFR was found to be higher in males than in females. 82,101 See Appendix 6 for detailed results.
Chronic kidney disease seemed to have a greater impact on ACM risk (HR 1.83, 95% CI 1.33 to 2.52) for African-Americans than for white people (1.31, 95% CI 1.16 to 1.49) (ACM in those with CKD versus no CKD). 74 Similarly, risk of cardiovascular morbidity increased more in African-Americans with CKD (2.09, 95% CI 1.33 to 2.52) than in white people with CKD (1.01, 95% CI 0.84 to 1.21). 74 Additionally, Hsu and colleagues103 reported the 5-year incidence rate of ESRD cases was higher among African-Americans (5.4%) than among white people (1.1%).
The mortality and incidence rate ratios for ESRD were significantly higher in younger groups (less than 69 years old) than in older patients when comparing CKD with no CKD. 96 Hsu and colleagues103 also presented incident ESRD rates that were greater among younger patients (20–60 years old) than among older ones (61–74 years old). The mortality rate ranged from 0.4% per year for 18- to 44-year-old patients with an eGFR ≥ 60 ml/min/1.73 m2 to 36.0% per year for the most elderly patients (85–100 years old) with an eGFR ≤ 15 ml/min/1.73 m2. 110 The RR of mortality increased with decreasing eGFR, but the relative impact was less as age increased. 110 For example, risk of ACM for those with an eGFR of 40–49 ml/min/1.73 m2 decreased from HR 1.90 (95% CI 1.35 to 2.67) in 18–44 year olds to HR 1.35 (95% CI 1.32 to 1.39) in 65–74 year olds. Similarly, for those with eGFR of 30–39 ml/min/1.73 m2, the HR decreased from 3.58 (95% CI 2.54 to 5.05) in 18–44 year olds to HR 1.81 (95% CI 1.75 to 1.87) in 65–74 year olds. 110 Imai and colleagues82 reported that the mean rate of decline of GFR from an initial GFR of 30–39 ml/min/1.73 m2 was higher (3.28, SD 0.72 ml/min/year) in younger males (40–49 years old) than in those in older age groups, with mean rate of decline 0.91 (SD 3.28) in 50–59 year olds, 0.98 (SD 0.18) in 60–69 year olds and 1.24 (SD 0.25) in 70–79 year olds. No difference in progression rate across age groups in male participants with a starting GFR of 60–69 ml/min/1.73 m2 was observed, although the progression rate was much lower (0.31–0.36, SD 0.01–0.03 ml/min/year). 82 Among female participants, the mean rate of decline of GFR from an initial GFR of 60–69 ml/min/1.73 m2 was higher for ages 40–49 years (0.45, SD 0.01) ml/min/year than for 50–79 year olds (range 0.24–0.29, SD 0.01–0.02 ml/min/year). See Appendix 6 for detailed results.
Discussion
We identified 36 studies describing the natural history of CKD.
Studies could be broadly defined into two categories based on the types of study participants:
-
‘Screened population’ studies where researchers drew participants from the general population through some type of health survey process. This group included a mix of population surveys using robust methods to minimise participant selection bias and others relying on volunteers responding to calls to participate in health screening.
-
‘Clinical population’ studies where studies were based on the identification of people with evidence of CKD from clinical settings including laboratory data, hospital clinics and general practice registers. In common, these participants had all had a blood test for a clinical indication that identified them as having CKD. While some may have had blood tests as part of a general health check, the majority would have had a medical condition or symptoms that led to testing.
The significance of these differences in study design is that the age and comorbid profiles of the two groups differed, with those in clinical populations tending to be older and to have a greater burden of comorbidity.
While the studies were generally large, with adequate follow-up and minimal losses to follow-up, there were a number of limitations. The definition of CKD was not standard across all studies, and less than half were able to define chronicity (i.e. had more than one abnormal test result at least 3 months apart). This means that such studies will have overestimated the ‘CKD’ population and this may affect the associations observed between CKD and outcomes. In addition, the use of different definitions for clinical outcomes (and in some cases, the lack of clarity about the definition) made comparison between studies difficult. In particular, cardiovascular morbidity and mortality included a number of definitions and this is likely to account for at least some of the heterogeneity in results observed. Few studies reported their outcomes by race. While the studies covered a range of geographical areas, the heterogeneity in methods makes it difficult to determine if differences in outcomes were related to race. Finally, none of the studies described in any detail the health care available to their study populations. Differences in management between study populations may also be contributing to the heterogeneity in outcomes observed.
All-cause mortality rate was generally high in the studies included in this review; 24.3–39.0% at 5 years and 19.7–52% at 10–12.6 years. ACM rate was higher in males than females and increased with stage of CKD. Populations defined by having an eGFR < 60 ml/min/1.73 m2 were consistently found to have a higher mortality than comparator groups where there was no evidence of CKD.
In studies comparing risk in those with CKD with those without CKD, there was evidence that an eGFR <60 ml/min/1.73 m2 was a predictor of ACM in some but not all of the studies. Adjustment for comorbidities, age and sex reduced the RR. We observed that in studies constructed from the general population, the risk of ACM associated with CKD, after adjustment, was small. Many of the cohort studies included people with a range of comorbidities and often reported a higher risk of ACM. CKD commonly occurs in association with comorbidities known to increase the risk of cardiovascular mortality (HBP, diabetes mellitus, CVD, increased age), and adjustment for comorbidities consistently reduced ACM risk ratios. 76,79 We made a decision to exclude data from the control arms of RCTs. While such studies do provide a view of the natural history of the condition, the strict selection of patients to participate in RCTs means that their outcomes are very different. For example, Jafar and colleagues43 reported a meta-analysis of RCTs for ACE Is in non-diabetic renal disease. From pooled RCT data, they reported a low ACM (1.2% in a mean follow-up of 2.2 years) and a relatively high progression to ESRD (11.6%), reflecting the selection of trial participants and the difficulty in generalising such findings.
However, in studies constructed from populations with high levels of comorbidity (diabetes, hypertension, CVD), the risk of ACM associated with CKD, compared with no CKD, was somewhat higher. The reverse was observed in the review by Tonelli and colleagues,68 but for only the unadjusted analysis. This is an oversimplification of the true impact of CKD on mortality. Analyses by stage demonstrated a substantially increased risk associated with increasing stage. Indeed, stage 3b carried a markedly increased risk as compared with 3a.
Some of the variation in ACM between studies may have been as a result of methodological issues: definition of CKD, duration of follow-up and composition of the cohort. However, this does not appear to account for all the heterogeneity. For example, Eriksen and Ingebretsen96 and Djamali and colleagues83 both reported clinical cohorts defined based on more than one measure of eGFR < 60 ml/min/1.73 m2, one study was from the USA82 and one from Norway. 96 Despite both studies considering people with mild to moderate CKD, Djamali and colleagues83 reported a substantially lower death rate over the 12.6 years of follow-up than that reported by Eriksen and Ingebretsen96 (19.7% versus 52%).
With the exception of study by Weiner and colleagues,74 the risk of CVD morbidity and mortality was reported to be greater in those with CKD than those with no CKD, and again this risk increased as the CKD stage increased, even after adjustment for comorbidities. Reported rates of CVD morbidity and mortality varied between studies, reflecting definitions used for CVD and the other methodological issues outlined above.
Attention in the renal community has focused on early recognition of CKD with the aim of prevention of progression to ESRD. As for ACM, there was substantial heterogeneity in the reported proportion of patients progressing to ESRD and in the definitions used for renal progression. These differences related in part to methodological issues, but were substantially influenced by the study population characteristics and how the cohort was constructed. Clinical cohorts had higher progression rates even where patients were in ‘early’ stages of CKD at baseline, reflecting some selection bias when compared with the general population.
We found that frequency of ESRD as an outcome was variable and appeared to relate to patient characteristics. In studies of people identified as having a low eGFR as a result of population health screening, the risk of ESRD was low, even after 8 years of follow-up. Where patients were recruited from clinics into follow-up studies, the risk of ESRD was substantially greater, reflecting a selection bias that partly represents clinical practice. Those with lower eGFR, diabetes and HBP experienced a greater risk of progression to ESRD. While few studies reported the proportion of patients who did not show a change in renal function, where it was reported, stable or even improvements in eGFR were common place. Where progression in eGFR was observed, many participants had not progressed to ESRD during the course of follow-up (up to 8 years). For an individual with CKD, the most common outcome during study follow-up was death, not progression to ESRD. 32,95,104
CKD stage was associated with an increase in mortality and renal progression, with a substantially greater risk observed for those in stage 3b than those in stage 3a. The rate of renal progression also appeared to be variable and influenced by age, stage and comorbidities.
The impact of CKD on quality of life was rarely reported in the natural history literature. Cross-sectional analysis of the short form 36-item questionnaire results from a large population study in Australia116 which has noted significant impairment of quality of life for those with an eGFR < 60 ml/min/1.73 m2, even after adjustment for comorbidities. Mental health was affected the most in younger people and physical function in the older group.
In this chapter we focused on eGFR as a measure of renal function impairment, reflecting current clinical practice with the creation of CKD registers in primary care based on eGFR < 60 ml/min/1.73 m2. Proteinuria and, in diabetes, microalbuminuria have been widely accepted as independent markers of kidney damage. While all people with diabetes are screened for microalbuminuria, there is not yet a consensus on screening for microalbuminuria or proteinuria in adults without diabetes. Recent analysis of the Prevention of Renal and Vascular Endstage Disease cohort study in the Netherlands demonstrated the potential predictive value of testing for microalbuminuria in the general population. Microalbuminuria was associated with an increased risk of needing RRT over 9 years’ follow-up (20–100 mg/l, HR 3.0; 100–200 mg/l, HR 47). 117 However, a large number of people with microalbuminuria (and often no other renal risk factors) were identified from which only a small number required RRT. As with low eGFR, people with evidence of microalbuminuria or proteinuria were at increased risk of CVD. Intervention with ACE Is or statins in groups with microalbuminuria or proteinuria and other CVD risk factors has shown benefit in reducing progression, but it is unknown whether such benefits can be attained for those without other CVD risk factors, and at what cost. 118 Hallan and colleagues32 recently reported on the benefits of screening all people with reduced eGFR for microalbuminuria or proteinuria. This method improved the specificity of detecting people with significant kidney function impairment (1.4% of the population had both reduced eGFR and microalbuminuria or proteinuria as compared with 4.9% with reduced eGFR alone) without losing detection power for ESRD (identified 65.6% of people who developed ESRD versus 69.4% using eGFR alone). 100
Conclusion
Chronic kidney disease is an important marker of increased risk of ACM and ESRD. For many, other comorbidities, associated with CKD, contribute to this increased risk. However, there appears to be a substantial subgroup for whom an eGFR < 60 ml/min/1.73 m2 does not mark the start of declining kidney function. In the UK, there has been a change in approach to indentifying CKD in the population, utilising GPs to establish clinical registers of all patients with an eGFR < 60 ml/min/1.73 m2 from blood tests undertaken for a clinical indication. This opportunistic screening has identified large numbers of people with evidence of kidney function impairment that had previously gone unrecognised. The outcomes in people with CKD identified through such an approach remain uncertain, but as described here, there was evidence that the risk of renal progression and mortality were influenced by the approach adopted to identify people with CKD.
Chapter 4 Clinical effectiveness
Introduction
Late referral to specialist nephrology care is an important problem and numerous potential barriers have been identified. Evidence-based guidelines have recognised the need for earlier referral and, in particular, to allow for preparation for transplant or dialysis. In Appendix 7, the literature about the impact of ‘very’ late referral has been summarised. In these studies, very late referral was compared, in most cases, with referral that was 1–6 months before the initiation of dialysis or RRT. Thus patients included in these studies were in an advanced stage of CKD and might all now be considered to have been referred late to specialists.
In this chapter we consider whether there is evidence that early referral for CKD is clinically effective.
Definition
A definition for ‘early referral’ was not specified in the original commissioning brief. There are two elements to ‘early referral’: timing and the intervention. ‘Early’ can be defined in three ways:
-
Time in relation to another event such as starting RRT.
-
Severity or stage of disease.
-
Duration from the onset of the condition.
While duration from onset might be considered to be the gold standard definition, it is almost impossible to determine onset in the absence of regular population screening for a condition. For the purposes of our review, we accepted definitions of early based on time from dialysis (> 12 months) or severity (stage 3–4 disease).
‘Referral’ was defined as an appointment with a specialist in nephrology care (medical, nursing or other allied health-care professional).
Results
Study characteristics
The number of published papers identified at each stage of the systematic review is shown in Figure 6. There were 3306 articles identified by searches. The full text of 63 articles were retrieved for scrutiny against the inclusion and exclusion criteria. A total of 56 full text articles were excluded. Excluded studies, together with the reason for exclusion are listed in Appendix 3.
FIGURE 6.
Flowchart of identification of studies for inclusion in the systematic review of clinical effectiveness.
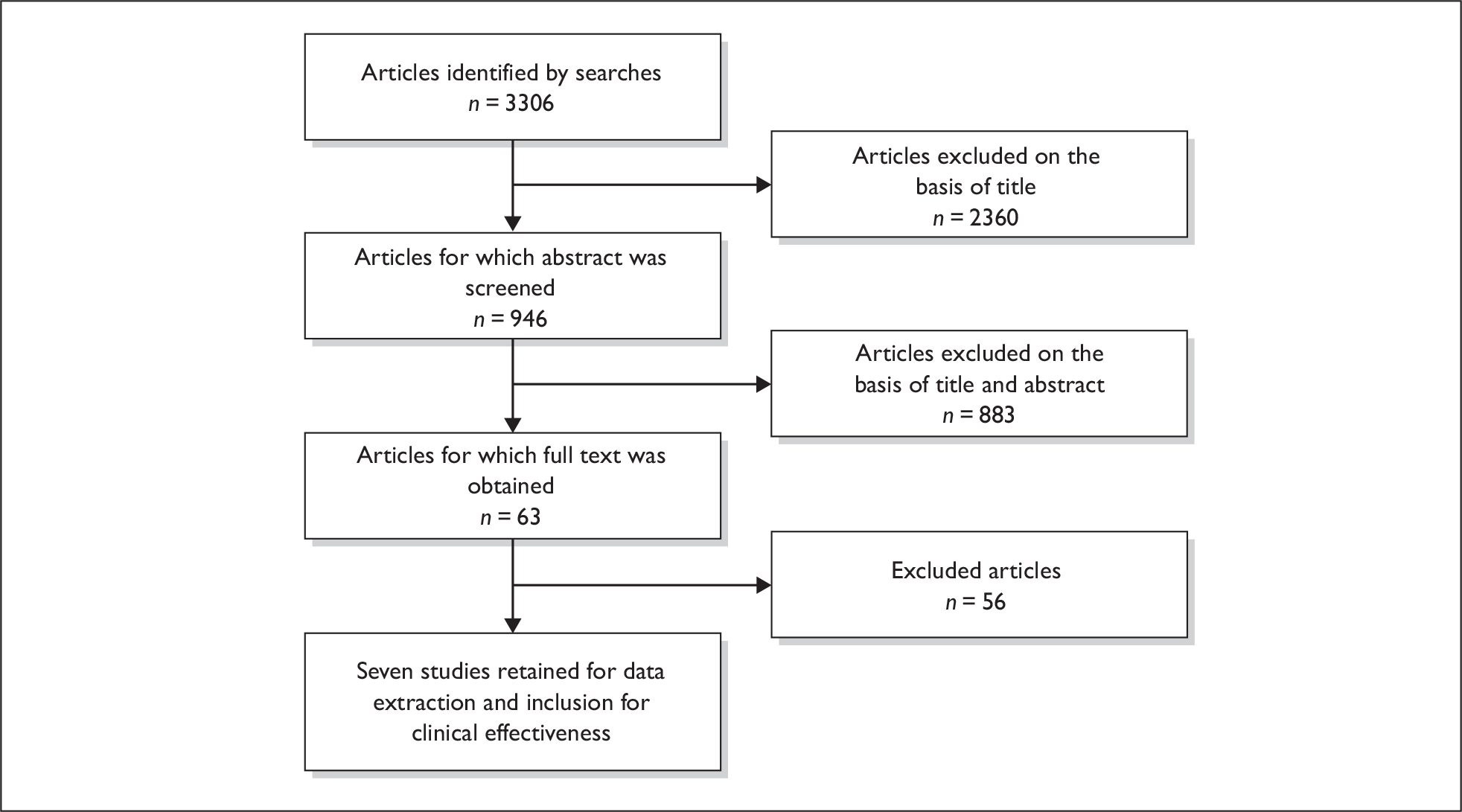
No systematic reviews were identified in the search. Seven studies56,111,119–123 met the inclusion and exclusion criteria, and were included in the review; their characteristics are summarised in Table 10. We did not find any randomised or controlled trials. All seven included studies were cohort designs. The key feature of these cohorts was how they were constructed in relation to the timing of the ‘intervention’ of interest to us – predialysis care. Five of the cohorts recruited people who were starting on dialysis for the first time and reviewed their records to define the timing of their first referral to nephrology care. 56,119,121–123 These cohorts, therefore, included only those people surviving and progressing to require dialysis and did not include people with CKD who died before reaching dialysis or who did not have a progressive deterioration in their renal function within the study period. We have called these ‘retrospective cohorts’ in terms of the timing of the cohort construction in relation to specialist referral. The remaining two cohorts identified people with CKD and followed them prospectively, comparing those who were referred to specialist care and those who were cared for only by a primary care physician. 111,120 We have called these ‘prospective cohorts’.
| Study | Jungers 2001121 | Kessler 2003119 | Khan 2005122 | Kinchen 2002123 | Martínez-Ramírez 2006120 | Orlando 2007111 | Roderick 200256 |
|---|---|---|---|---|---|---|---|
| Setting | |||||||
| Country | France | France | USA | USA | Mexico | USA | UK |
| Clinical Setting | Single hospital dialysis unit | 13 nephrology units (11 not for profit) in region (100%) | Centres for Medicare and Medicaid Services database | From 81 dialysis clinics in 19 states | Two diabetes clinics | North Caroline Veterans Administration laboratory database | Six nephrology units in one region of UK |
| Study design | |||||||
| Type of study | Cohort | Cohort | Cohort | Cohort | Cohort | Cohort | Cohort |
| Recruitment | Incident dialysis | Incident RRT (including pre-emptive transplant) | Incident dialysis | Incident dialysis | Randomly selected patients with type 2 diabetes and evaluated for nephropathy (proportion of total clinic not stated) | Selected all patients with two serum creatinine measurements at least 3 months ≥ 1.4mg/dl | Incident RRT |
| Recruitment period | 1989–98 | 1997–9 | 1995–8 | 1995–8 | Not stated | 1998–9 | 1996–7 |
| Retrospective or prospective | Retrospective in relation to ‘intervention’ of pre-dialysis care | Retrospective in relation to ‘intervention’ of pre-dialysis care | Retrospective in relation to ‘intervention’ of pre-dialysis care | Retrospective in relation to ‘intervention’ of pre-dialysis care | Prospective in relation to ‘intervention’ of pre-dialysis care | Prospective in relation to ‘intervention’ of pre-dialysis care | Retrospective in relation to ‘intervention’ of pre-dialysis care |
| Follow-up | Up to 5 years post RRT |
Up to 2 years post RRT Median follow-up for survival was 22.2 months (range, 1 day to 46.3 months) |
Up to 1 year post RRT | Post RRT follow-up median 2.2 years | 1 year | 3.5 years | 6 months post RRT |
| Participants | |||||||
| Total number | 1152 | 502 | 109,321 | 1041 | 117 | 1553 | 361 (only 353 reported in data tables) |
| Characteristics | |||||||
| Age | 53.8 (SD 17.2) years | 62.8 (SD 16) years | 75.5 (SD 5.8) years | Age < 65 years = 64.9% |
Study = 62.5 (SD 9.3) years Comparator = 62.8 (SD 9.9) years |
Median 70 (range 26–98) years | Median 64 (range 15–69) years |
| Sex % | 1.74 male/female ratio | 59.4% male; 40.6% female | 51% male; 49% female | 55.2% male; 44.8% female |
Study = 27 female (51%) Comparator = 25 female (38%) |
100% male | 60% male; 40% female |
| Diabetes % | 13.2% | 31.9% | 53% | 52.4% | 100% | 52% | Diabetic nephropathy 11–19% |
| CVD % | 15.1% | 57.2% | 59% | Not specified |
Study = 13% Comparator = 15% |
49% | Not specified |
| Hypertension % | Not specified | Not specified | 82% | 95.3% |
Study = 60% Control = 60% |
92% | Not specified |
| CKD stage % (at first referral/start of prospective study) | Not specified | Not specified | Not specified | Not specified |
Study: stage 1 = 42%; stage 2 = 37%; stage 3 = 21% Comparator: stage 1 = 39%; stage 2 = 34%; stage 3 = 27% |
NR | Not specified |
| Inclusion criteria | Consecutive patients with ESRD | Consecutive patients with ESRD |
≥ 67 years at initiation of dialysis Medicare as their primary payer with coverage for both institutional (part A) and physician/supplier (part B) services 24 months before initiation of dialysis |
Incident dialysis at one of the recruiting clinics No details of proportion agreeing to participate |
Diabetic nephropathy diagnosed by 24-hour urine protein/microalbuminuria | All patients with two creatinine values ≥ 1.4 mg/dl, at least 3 months apart | All patients with ESRD accepted onto the renal replacement programme of the six established units in the south and western region between 1 June 1996 and 31 May 1997 |
| Exclusion criteria | Patients with acute renal failure (n = 60) or advanced malignancy (n = 35) | Individuals with acute, reversible renal failure, those returning to dialysis following kidney graft failure | 26,769 were excluded because of the absence of Medicare part A claims or because Medicare was not the primary payer during the 24 months before initiation of dialysis | Patients were excluded if they were younger than 18 years of age or did not speak English or Spanish |
Transient cause of proteinuria < 18 years old |
Patients were excluded if: not followed in health-care organisation, primary care or nephrology clinics if RRT was initiated within 90 days of the abnormal creatinine measurement |
Patients with acute renal failure, those transferred in from other units already on dialysis and returns to dialysis from failed transplants were excluded |
| Comparator groups |
Duration of predialysis nephrological care: < 6 months = 258 6–35 months = 267 36–71 months = 225 ≥ 72 months = 307 |
Group 1 = 261 (patients referred to a nephrologist more than 12 months before initiation of RRT) Group 2 = 85 (patients referred 12 months or less but more than 4 months before first RRT) Group 3 = 42 (referred 4 months or less but more than 1 month before RRT) Group 4 (late referral) = 60 (CRF for more than 1 month but referred ≤ 1 month before RRT) Group 5 = 54 (‘acute disease’ with both CRF diagnosis and nephrology referral no more than 1 month before first RRT) |
Group 1 (no nephrology care in 24 months prior to dialysis) = 55,087 Group 2 (MNC during 24 months prior to dialysis but 0 visits in last 6 months) = 5820 Group 3 (MNC during 24 months prior to dialysis and 1–2 visits in last 6 months) = 24943 Group 4 (MNC during 24 months prior to dialysis and ≥ 3 visits in last 6 months) = 23,471 |
Group 1 = 399 (referral > 12months before dialysis) Group 2 = 184 (referral 4–12 months before dialysis) Group 3 = 245 (referral < 4 months before dialysis) |
Study (referred to nephrologists) = 52 Comparator (no access to nephrologists) = 65 |
Primary care physicians only = 1097 Nephrology (primary care physicians plus nephrology clinics) = 456 |
Time from referral to dialysis: Less than 1 month = 84 1–4 months = 40 (all less than 4 months = 124) 4–12 months = 52 > 12 months = 177 |
Three studies originated in the USA,111,122,123 two in France,119,121 one in Mexico120 and one in the UK. 56 A total of 114,073 people were reported in the included studies, but study size varied considerably, ranging from 117 to 109,321 people. One thousand six hundred and seventy participants had pre-ESRD at the time of inclusion in the cohort (i.e. participated in a ‘prospective cohort’ study).
One study was restricted to patients with diabetes mellitus and renal impairment. 120 The other six studies did not restrict their cohorts by the underlying cause of renal impairment; nonetheless, diabetes mellitus was commonly reported among participants, ranging from 13.2% to 52.4%. Males exceeded females in all of the studies, ranging from 51% to 100%.
Few of the studies reported information about the stage of CKD at key time points, i.e. first diagnosis or first referral to a specialist. Kessler and colleagues119 noted the time since first creatinine level > 177 µmol/l (2 mg/dl). Martínez-Ramírez and colleagues120 diagnosed renal impairment based on micro- (30–300 mg/dl) and macroalbuminuria (> 300 mg/dl). They reported that 40% had CKD stage 1, 35% stage 2 and 25% stage 3 at the start of their study period with a mean eGFR of 78.6–83.8 ml/min/1.73 m2. Orlando and colleagues111 defined CKD as a creatinine level ≥ 1.4 mg/dl and noted at baseline that 89% of study participants had evidence of proteinuria.
Quality of included studies
Each included study was quality assessed and the results are summarised in Table 11. While all the retrospective studies suffered from differences in the groups at baseline, attempts were made to adjust for these differences in the analysis. There were five main problems with the included studies in determining effectiveness of early referral:
-
None of the studies randomly allocated participants to the intervention groups. While attempts were made to adjust for differences in the analysis, unknown confounders could not be addressed. In particular, complex confounders such as confounding by indication could not be accounted for.
-
There were significant differences in the baseline characteristics of the comparison groups in all studies, with the exception of the study reported by Martínez-Ramírez and colleagues. 120
-
None of the studies adequately described the ‘intervention’ in terms of the type of care delivered to enable comparisons between studies.
-
Only two studies defined their cohorts prospectively in relation to the intervention. 111,120 Studies designed around cohorts of people starting dialysis miss all the people with CKD who have not yet progressed to end-stage disease or who die before they reach that point.
-
Only the two prospective studies reported the criteria they used to define CKD. 111,120 None of the studies defined the criteria for triggering referral to a specialist.
| Study | Jungers 2001121 | Kessler 2003119 | Khan 2005122 | Kinchen 2002123 | Martínez-Ramírez 2006120 | Orlando 2007111 | Roderick 200256 |
|---|---|---|---|---|---|---|---|
| Groups similar at baseline | No. Baseline characteristics significantly differed between the four quartiles in terms of gender and comorbidity (diabetic, vascular disease) | No. Baseline characteristics significantly differed between the referral groups in terms of age and comorbidity | No. Baseline characteristics significantly differed between the referral groups in terms of sex, cause of renal disease and visits to other health-care professionals | No. There were significant differences in baseline characteristics of patients between early, intermediate and late evaluation | Yes | No. Baseline characteristics significantly differed between the referral groups in terms of age, comorbidities, proteinuria, CKD stage | No. Baseline characteristics significantly differed between the referral groups in terms of age, comorbidities, cause of CKD and type of referring physician |
| Outcomes measured in a standard, valid and reliable way | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Dropouts/Withdrawals | 95 excluded (60 had acute or rapid progressive renal failure, 35 had advanced malignancy); 86 were lost to follow-up after moving out of the Paris area | Not stated | 26,769 were excluded because of the absence of Medicare part A claims or because Medicare was not the primary payer during the 24 months before initiation of dialysis | 213 did not have information about first referral to nephrologist | Seven (five withdrew; two lost to follow-up) | 133 (8%) lost to follow-up although no details provided | 50 (12%) had incomplete records and were excluded; 361 included but only 353 reported in analysis – not explained |
| Intention to treat analysis | Not applicable | Not applicable | Not applicable | Not applicable | Yes | Not applicable | Not applicable |
| Diagnosis based on more than one blood test | Criteria for referral not stated | Criteria for referral not stated | Criteria for referral not stated | Criteria for referral not stated | Diagnosis based on confirmed urinary protein | Yes (two creatinines, 3 months apart) | Criteria for referral not stated |
| Blinding | No | No | No | No | No | No | No |
| Did the study minimise the risk of bias | Adjusted for age, diabetes mellitus, hypertensive nephropathy and CVD | Statistically significant associated factors were adjusted for in final risk model | Statistically significant associated factors were adjusted for in final risk model | Statistically significant associated factors were adjusted for in final risk model | Statistically significant associated factors were adjusted for in final risk model | Range of factors considered to be of relevance were adjusted for in final risk model | Factors considered to be of relevance were adjusted for in risk model (no details given) |
Does early referral improve outcomes?
Renal function: progression and onset of RRT
Five studies reported creatinine clearance or eGFR at the start of RRT but did not report renal function at the time of referral, at first diagnosis or during follow-up. 56,119,121–123 Only two studies reported renal function over time as an outcome. 111,120
Renal function at the onset of RRT was not substantially or consistently altered by referral to the specialist team at least 12 months prior to requiring RRT. 56,119,121–123
Orlando and colleagues111 retrospectively compared those receiving care by primary care physicians alone with those receiving specialist nephrology input to assess progression (defined by change of stage or death). More progressed to a more advanced stage of CKD in the nephrology referral group at each stage of disease than the primary care only group, but fewer died. There was little difference in time spent in follow-up between groups in stages 1 and 2. For stage 3, 316 more days were spent in follow-up in the nephrology group than the primary care only group. The difference in deaths was particularly marked for those with stage 3 or worse CKD. Cox HRs for the risk of progression, adjusting for age, race, medication use, comorbidities and risk factors showed no statistically significant difference between nephrology referral and primary care only for those with stage 1 or 2 disease. For those with stage 3 or worse, nephrology care reduced progression or death (after adjustment) with an HR of 0.8 (95% CI 0.61 to 0.90) for stage 3 disease and 0.75 (95% CI 0.45 to 0.89) for stage 4. Of the 1553 participants, 26 progressed to ESRD during the 5-year follow-up with six (0.4%) in the primary care only group and 20 (1.29%) in the specialist care group. The higher progression in the referred group reflects, at least in part, that fewer people died during stages 3–5 and thus survived to require dialysis. 111
Martínez-Ramírez and colleagues120 reported that during the 1-year prospective follow-up of diabetic patients with evidence of early or overt nephropathy, only one patient deteriorated to requiring RRT (in the unreferred group). Among the group where no referral to a specialist service was available, mean (SD) eGFR deteriorated from 78.6 (28.1) ml/min/1.73 m2 to 66.6 (29.9) ml/min/1.73 m2, a statistically significant fall of 12.0 ml/min/1.73 m2 (p < 0.05). In the cohort referred early to specialist nephrology care, mean (SD) eGFR was 83.8 (26.1) ml/min/1.73 m2 at baseline and was not statistically significantly altered after 12 months [80.4 (35.5) ml/min/1.73 m2]. A similar pattern was observed regardless of whether the patient had early or overt diabetic nephropathy (defined by the presence of microalbuminuria with eGFR > 60 ml/min/1.73 m2 versus proteinuria or eGFR < 60 ml/min/1.73 m2). 120
Table 12 summarises the data from these studies.
| Study | Referral pattern | Change in kidney function | |||||
|---|---|---|---|---|---|---|---|
| Martínez-Ramírez 2006 120 | GFR baseline [mean (SD) ml/min/1.73 m 2 ] | GFR final [mean (SD)] | Change from baseline ( p -value) | Difference at final ( p -value) | |||
| Referral to specialist (SR) | 83.8 (26.1) | 80.4 (35.5) | –3.4 (NS) | 13.8 (p < 0.05) | |||
| No specialist referral (no SR) | 78.6 (28.1) | 66.6 (29.9) | –12.0 (p < 0.05) | ||||
| SR (early nephropathy) | 95.6 (20.9) | 98.8 (36.4) | 3.2 (NS) | 13.1 (NS) | |||
| No SR (early nephropathy) | 99.0 (21.6) | 85.7 (27.3) | –13.3 (p < 0.05) | ||||
| SR (overt nephropathy) | 71.1 (25.4) | 61.3 (22.2) | –9.8 (p < 0.05) | 10.5 (NS) | |||
| No SR (overt nephropathy) | 61.7 (24.6) | 50.8 (21.3) | –10.9 (p < 0.05) | ||||
| Orlando 2007 111 | Number transitioning through each stage and outcomes | ||||||
| Stage 1 | Stage 2 | Stage 3 | Stage 4 | Stage 5 | Pre-ACKD to ACKD | ||
| PCP-only | 995 | 624 | 209 | 28 | 6 | 1090 | |
| CKD progression | 445 (45%) | 156 (25%) | 14 (7%) | 4 (14%) | 1 (17%) | 27 (2%) | |
| Died | 231 (23%) | 217 (35%) | 131 (63%) | 20 (71%) | 2 (33%) | 509 (47%) | |
| Composite end pointa | 676 (68%) | 376 (60%) | 145 (69%) | 24 (86%) | 3 (50%) | 536 (49%) | |
| Median days spent in stage | 1168 | 1247 | 895 | 558 | 655 | 1936 | |
| Nephrology group | 222 | 263 | 207 | 58 | 20 | 440 | |
| CKD progression | 138 (62%) | 120 (46%) | 56 (27%) | 17 (29%) | 5 (25%) | 67 (15%) | |
| Died | 24 (11%) | 53 (20%) | 74 (36%) | 25 (43%) | 5 (25%) | 147 (33%) | |
| Composite end pointa | 162 (73%) | 173 (66%) | 130 (63%) | 42 (72%) | 10 (50%) | 214 (49%) | |
| Median days spent in stage | 1127 | 1100 | 1211 | 834 | 776 | 1991 | |
| aPCP-only vs nephrology p-value | 0.41 | 0.32 | < 0.001 | 0.03 | NA | < 0.001 | |
| bAdjusted HR (95% CI) | 1.08 (0.91 to 1.29) | 1.20 (0.99 to 1.45) | 0.80 (0.61 to 0.90) | 0.75 (0.45 to 0.89) | NA | 0.91 (0.76 to 0.99) | |
Mortality
All seven studies reported mortality as an outcome. 56,111,119–123 Roderick and colleagues,56 however, did not report it by the referral groups of interest here. Martínez-Ramírez and colleagues120 reported three deaths during the 1-year follow-up, all in the group who were not referred to specialist care, and all cardiovascular deaths. Orlando and colleagues111 reported higher numbers of deaths among those cared for in primary care than among those referred to a specialist. This pattern held at all stages of CKD.
In all of the retrospective studies, starting their cohorts from the initiation of dialysis, better dialysis survival was associated with early referral. This improvement was observed from 90 days119 to 5 years121 after initiation of dialysis. Jungers and colleagues121 reported survival was highest in the group referred more than 72 months prior to dialysis. The difference in survival could be observed from 3 months after starting dialysis and was marked by 5 years (77.3% in those referred > 72 months prior to dialysis versus 57.8% in those referred less than 6 months prior to dialysis; p < 0.001). CVD accounted for more than 50% of the deaths. The earlier referral groups (> 36 months and > 72 months) experienced fewer CVD deaths than those referred later. Adjusting for age, sex and comorbidities (diabetes mellitus, HBP, CVD), the RR of death for those with referral > 72 months prior to dialysis, as compared with < 6 months, was 0.24 (95% CI 0.10 to 0.59) at 1 year and 0.53 (95% CI 0.35 to 0.79) at 5 years. Kessler and colleagues119 reported an association between timing of referral and survival in the first 90 days after initiating dialysis, with an almost threefold increase in risk (HR 2.7, 95% CI 1.2 to 6.3) once referral was less than 12 months prior to dialysis, and as great as five times higher (HR 5.2, 95% CI 2.2 to 12.3) if referral was less than 1 month prior to dialysis after adjustment for age, sex and systolic BP. For survival over 3 months, the only independently associated factor relating to referral timing was for those referred between 1 and 4 months prior to dialysis, where a HR of 2.2 (95% CI 1.4 to 3.5) was observed compared with referral < 1 month. Khan and colleagues121 reported lower 1-year mortality on dialysis in those referred during the 24 months prior to dialysis (25–35%) as compared with those with no pre-dialysis referrals (51%) [HR 1.5 (95% CI 1.44 to 1.55) after adjustment for age, sex, race, erythropoietin injections, non-nephrology care and comorbidities]. There was evidence of a ‘dose-response’ gradient, with those receiving the most nephrology visits having the lowest mortality. Kinchen and colleagues123 reported lower mortality on dialysis in those referred more than 12 months, as compared to those referred less than 4 months, prior to dialysis. The differential in survival was observed to at least 3 years. An HR of 1.6 (95% CI 1.11 to 2.24) for later referral, as compared to referral > 12 months prior to dialysis, was observed after adjustment for type of dialysis, demographic characteristics, socioeconomic status, years of smoking, exercise status and Index of Coexistent Disease score. Table 13 provides a more detailed summary of the mortality data reported.
| All-cause mortality | |||||
|---|---|---|---|---|---|
| Predialysis nephrological care duration (months) | |||||
| Jungers 2001 121 | < 6 | 6–35 | 36–71 | ≥ 72 | |
| n | 86 | 67 | 40 | 54 | |
| 3 months’ mortality (SD) | 7.3% ± 1.7a | 4.2% ± 1.2 | 1.8% ± 0.9 | 0.7% ± 0.6 | |
| 1-year mortality (SD) | 13.6% ± 2.2b | 7.4% ± 1.6 | 7.2% ± 1.8 | 2.5% ± 0.9 | |
| 5 years’ mortality (SD) | 42.2% ± 4.2c | 34.7% ± 3.9 | 22.9% ± 3.7 | 22.8% ± 3.6 | |
| Cardiovascular mortality | |||||
| < 6 | 6–35 | 36–71 | ≥ 72 | ||
| At 5 years n (%) | 53 (62%) | 41 (61%) | 21 (52%) | 29 (52%) | |
| Duration of specialist care pre-dialysis (months) | |||||
| Kinchen 2002 123 | < 4 months | 4–12 months | > 12 months | ||
| n | 245 | 184 | 399 | ||
| 1-year mortality | 13.3% | 9.5% | 4.3% | ||
| 2 years’ mortality | 27.6% | 22.4% | 14.6% | ||
| 3 years’ mortality | 37.0% | 32.7% | 26.3% | ||
| Martínez-Ramírez 2006 120 | Primary care | Nephrology care | |||
| n | 65 | 52 | |||
| 1-year mortality | 3 (5%) | 0 | |||
| Khan 2005 122 | Frequency of specialist care pre-dialysis | ||||
| 0 MNC in 24 months before dialysis | 0 MNC in 6 months before dialysis | 1–2 MNC in 6 months before dialysis | ≥ 3 MNC in 6 months before dialysis | ||
| n | 55,087 | 5820 | 24,943 | 23,471 | |
| 1-year mortality | 51% | 35% | 33% | 25% | |
| Orlando 2007 111 | Primary care | Nephrology care | |||
| Proportion | Median days spent in each stage | Proportion | Median days spent in each stage | ||
| Stage 1 | 231 (23%) | 1168 | 24 (11%) | 1127 | |
| Stage 2 | 217 (35%) | 1247 | 53 (20%) | 1100 | |
| Stage 3 | 131 (63%) | 895 | 74 (36%) | 1211 | |
| Stage 4 | 20 (71%) | 558 | 25 (43%) | 834 | |
| Stage 5 | 2 (33%) | 655 | 5 (25%) | 776 | |
| Jungers 2001 121 | RR for death for PDNC ≥ 72 months | RR d | 95% CI | ||
| At 3 months | 0.13 | 0.03 to 0.58 | Adjusted for age, diabetes, hypertension, cardiovascular diseases and nephropathy. | ||
| At 1 year | 0.24 | 0.10 to 0.59 | |||
| At 2 years | 0.44 | 0.25 to 0.81 | |||
| At 3 years | 0.45 | 0.28 to 0.74 | |||
| At 5 years | 0.53 | 0.35 to 0.79 | |||
Hospitalisations
Three studies reported hospitalisations as an outcome. 56,111,121
Orlando and colleagues111 compared hospitalisations in the group referred to nephrology specialists with those with renal disease managed only in primary care. The number of hospitalisation days differed little between the two groups (mean 2.8 versus 2.5 days respectively; p = 0.03).
One study reported on the impact of early referral on hospitalisation in the first 6 months after dialysis was initiated. 56 Roderick and colleagues56 observed that those in the group with referral < 1 month prior to dialysis had more hospitalisation episodes within the first 6 months of dialysis than all others (1–4 months, 4–12 months and > 12 months) (mean 2.6 versus 1.7, p = 0.001). The median length of stay was shorter in those referred more than 1 month prior to dialysis (10 versus 18 days in the < 1-month group). Lengthening referral time to greater than 1 month prior to dialysis did not have any substantial effect on this outcome.
Jungers and colleagues121 reported the impact of referral on the duration of initial hospitalisation at the time of starting dialysis. They found a statistically significantly lower duration of initial hospitalisation in those referred at least 6 months prior to dialysis [mean 23.8 (SD 17.1) days] versus those referred 6 to 35 months prior to dialysis [mean of 7.5 (SD 8.9) days; p < 0.001] and some evidence of a dose response with improvements out to referral > 72 months prior to dialysis.
Emergency dialysis
Kessler and colleagues119 reported statistically significantly higher emergency dialysis among those referred late than those referred more than 12 months prior to dialysis (83.3% versus 29.1%; p < 0.001).
Quality of life
None of the included studies reported quality of life as an outcome.
Barriers to early referral
None of these studies reported barriers as an outcome. In discussion, Khan and colleagues122 noted the challenge of identifying patients with CKD early enough so that early referral intervention could be undertaken. Kinchen and colleagues123 noted that the reasons for late referral were numerous and included a lack of symptoms, non-compliance, lack of access to care, and primary care physicians’ attitudes and knowledge. Orlando and colleagues111 acknowledges that specialist nephrology referral for all patients with CKD, even if restricted to all with stage 3 disease or worse, was beyond the capacity of existing nephrology services.
What elements of early referral design and delivery are important?
Because of the nature of the studies identified (largely retrospective with regards to the ‘intervention’ of early referral), the characteristics of the intervention were poorly reported. In the study by Martínez-Ramírez and colleagues,120 the referred cohort received a total of three visits in 12 months to see a single nephrologist along with standard care of monthly visits to a primary care physician who was instructed not to modify the prescriptions of the nephrologist.
A number of studies did, however, describe aspects of management and how they differed between early referral to a specialist as compared with remaining in generalist care.
Blood pressure control
In the two prospective studies of early referral for CKD, improvements in BP control were observed. Martínez-Ramírez and colleagues120 reported statistically significant improvements in systolic BP in the referred cohort [140 (SD 30) mmHg to 130 (SD 21) mmHg] while BP control deteriorated in the unreferred group [140 (SD 19) mmHg to 145 (SD 23) mmHg] (p < 0.05). Orlando and colleagues111 reported that a higher proportion of patients in the nephrology care group had good BP control (41% versus 36%; p = 0.06).
At the initiation of dialysis, Jungers and colleagues121 reported BP was lower in all the group referred more than 6 months prior to dialysis and lowest in the group referred more than 72 months prior to dialysis [systolic BP mean 171 (SD 23) mmHg in the < 6-month group versus 148 (SD 17) mmHg in the 6- to 35-month group and 141 (SD 12) mmHg in the ≥ 72 months group; p < 0.001]. However, Kessler and colleagues119 and Kinchen and colleagues123 did not observe statistically significant differences in BP control at the start of dialysis. Khan and colleagues122 and Roderick and colleagues56 did not report BP control.
Other clinical markers
Four studies56,111,121,123 reported serum albumin was statistically significantly higher if referred early, but none presented information about the underlying diagnoses. Those with nephrotic syndrome may have presented earlier, but have relatively preserved renal function despite their apparently poor clinical markers, e.g. low albumin as a result of heavy proteinuria. Kinchen and colleagues123 described statistically significant differences in serum albumin < 36 g/l at the time of initiation of dialysis (60.5% versus 77.9%; p < 0.001), when comparing early and late referral. Orlando and colleagues111 reported albumin levels < 40 g/l in 59% versus 49% (p < 0.001) (early versus late respectively). Roderick and colleagues56 noted albumin was lower in those referred less than 1 month prior to dialysis [mean 32 g/l (SD 0.83)] than for those with referral > 12 months [mean 37 g/l (SD 0.56)] (p < 0.001). Khan and colleagues122 found no statistically significant difference in albumin. Kinchen and colleagues123 also described statistically significant differences in haematocrit < 0.3% (56% versus 68.1%; p < 0.001). Khan and colleagues,122 Roderick and colleagues56 and Orlando and colleagues111 did not observe substantial differences in haematocrit between early and late referral groups.
Treatments
Martínez-Ramírez and colleagues120 reported statistically significant improvements in systolic BP in the referred cohort. In terms of treatments, the use of ACE Is increased more in the referred group and there was substantially higher use of ARBs and statins. Non-steroidal anti-inflammatory drug use fell in the referred group, but increased in the unreferred group (Table 14). Orlando and colleagues,111 however, reported no statistically significant differences between the groups for lipid lowering agent or ACE I use.
| Comparisons of baseline and final treatments between cohorts, number (%) | ||||||
|---|---|---|---|---|---|---|
| Treatment | Referred | Unreferred | ||||
| Baseline | Final | Change | Baseline | Final | Change | |
| ACE I | 25 (48) | 44 (90)a,b | 19 (42) | 35 (53) | 37 (70)b | 2 (17) |
| ARBs | 1 (2) | 22 (45)a,b | 21 (43) | 0 (0) | 2 (4) | 2 (4) |
| Statins | 2 (4) | 21 (43)a,b | 19 (39) | 10 (16) | 5 (9) | –5 (–7) |
| Aspirin | 11 (21) | 12 (24) | 1 (3) | 8 (15) | 4 (7) | –4 (–8) |
| Other NSAID | 6 (11) | 0 (0)a,b | –6 (–11) | 3 (5) | 17 (32)b | 14 (27) |
Roderick and colleagues56 reported that vitamin D supplementation (late 20% versus early 40%), phosphate binders (late 29% versus early 44%), sodium bicarbonate (late 10% versus early 28%), lipid lowering agents (late 6% versus early 11%) and erythropoietin (late 5% versus early 23%) were all prescribed more frequently in those referred more than 12 months before starting dialysis.
Kinchen and colleagues123 described statistically significant differences in the following factors when comparing early and late referral: exercise one or more times per week (26.3% versus 14.9% respectively; p < 0.001); and erythropoietin treatment (25.3% versus 12.7%; p < 0.001).
Which patient groups benefit the most from referral and at what stage of disease?
Kinchen and colleagues122 reported that late referral was associated with a greater hazard of death on dialysis in diabetic subgroups (HR 2.4, 95% CI 1.28 to 4.47); in black ethnic subgroups (HR 6.9, 95% CI 1.07 to 44.71); and if the cause of the ESRD is attributed to diabetes or hypertension (HR 2.0, 95% CI 1.14 to 3.46) (Table 15). Martínez-Ramírez and colleagues120 noted a more marked effect of nephrology referral on those with early diabetic nephropathy (microalbuminuria) compared with those with overt proteinuria (Table 15).
| Martínez-Ramírez 2006 120 | Progression | GFR baseline [mean (SD)] | GFR final [mean (SD)] | Change from baseline ( p -value) | Difference between groups ( p -value) |
| Referral to specialist | 83.8 (26.1) | 80.4 (35.5) | –3.4 (NS) | 13.8 (p < 0.05) | |
| No referral to specialist | 78.6 (28.1) | 66.6 (29.9) | –12.0 (p < 0.05) | ||
| ER (early diabetic nephropathy) | 95.6 (20.9) | 98.8 (36.4) | 3.2 (NS) | 13.1 (NS) | |
| LR (early diabetic nephropathy) | 99.0 (21.6) | 85.7 (27.3) | –13.3 (p < 0.05) | ||
| ER (overt diabetic nephropathy) | 71.1 (25.4) | 61.3 (22.2) | –9.8 (p < 0.05) | 10.5 (NS) | |
| LR (overt diabetic nephropathy) | 61.7 (24.6) | 50.8 (21.3) | –10.9 (p < 0.05) | ||
| Kinchen 2002 123 | Mortality [HR (95% CI)] for different durations of specialist care pre-dialysis | ||||
| > 12 months | 4–12 months | < 4 months | |||
| All patients | 1.0 (reference group) | 1.4 (0.92 to 1.99) | 1.6 (1.11 to 2.24) | Adjusted for type of dialysis, demographic characteristics, socioeconomic status, years of smoking, exercise status and Index of Coexistent Disease score. Sensitivity analyses: redefinition of late referral, time of evaluation missing | |
| DM – yes | 1.0 | 1.6 (0.84 to 2.94) | 2.4 (1.28 to 4.47) | ||
| DM – no | 1.0 | 0.6 (0.23 to 1.61) | 0.9 (0.42 to 1.97) | ||
| Ethnicity – white | 1.0 | 1.0 (0.60 to 1.73) | 1.5 (0.92 to 2.37) | ||
| Ethnicity – black | 1.0 | 1.8 (0.26 to 12.30) | 6.9 (1.07 to 44.71) | ||
| Attributed cause of ESRD – hypertension or DM | 1.0 | 1.1 (0.59 to 1.93) | 1.99 (1.14 to 3.46) | ||
| Attributed cause of ESRD – glomerulonephritis or other | 1.0 | 1.0 (0.35 to 2.63) | 0.6 (0.22 to 1.51) | ||
| Age < 65 years | 1.0 | 1.4 (0.68 to 2.91) | 1.5 (0.82 to 2.87) | ||
| Age ≥ 65 years | 1.0 | 1.0 (0.46 to 1.99) | 1.7 (0.86 to 3.22) | ||
Orlando and colleagues111 observed that the impact of nephrology care on the composite end point of renal progression and death was only observed for stages 3–5. In stages 1–2 there was no statistically significant difference between nephrology care and primary care alone and, if anything, survival/renal progression were better in the primary care alone group.
Discussion
In comparison to the considerable literature base about the effect of late referral (see Appendix 7), we identified only seven studies that considered the impact of early referral on outcomes in people with evidence of renal impairment. 56,111,119–123 This was despite adopting a wide definition of ‘early’ and ‘referral’.
Five of the studies were retrospective, based on cohorts established at the time of starting RRT and then looking back to identify the timing and format of care in the months and years prior to RRT. 56,119,121–123 Two studies compared management solely by primary care physicians to referral to specialist nephrology services for patients with evidence of CKD. 111,120
No clinical trials were identified. No studies randomised patients to specialist care versus primary care or current practice. Few studies reported the stage of CKD, or other markers of renal impairment, at the time of referral to specialist services.
As a result it is difficult to draw conclusions about the clinical effectiveness of early referral strategies or indeed, what aspects of the strategies are driving the effect on outcomes.
Referral strategies
The limitations of the studies are discussed below, but one of the major difficulties was reporting of what the referral strategy encompassed. The limited details have been summarised in Table 16. Most studies based referral on ‘clinical indication’ that was not further specified. One screened all patients with diabetes mellitus as a high-risk group for renal disease. Management appeared to focus on pharmacotherapy for management of complications of CKD or for modification of cardiovascular risk and renal progression. None of the studies considered whether cardiovascular risk reduction could be delivered through optimisation of the management of the other comorbidities. eGFR, proteinuria, albuminuria and serum creatinine were all described as screening tests.
| Population selection | ||||
|---|---|---|---|---|
| Screening | High risk groups | Opportunistic | Clinical indication | |
| Testing | ||||
| Albuminuria | Martínez-Ramírez 2006120 | Martínez-Ramírez 2006120 | ||
| Creatinine | Orlando 2007111 | |||
| eGFR | ||||
| Not described | Jungers 2001;121 Kessler 2003;119 Khan 2005;122 Kinchen 2002;123 Roderick 200256 | |||
| Testing | ||||
|---|---|---|---|---|
| Albuminuria | Creatinine | eGFR | Not described | |
| Sampling | ||||
| Single sample | ||||
| Two samples, 3 months apart | Orlando 2007111 | |||
| Repeat sampling and exclusion of reversible causes | Martínez-Ramírez 2006120 | |||
| Not described | Jungers 2001;121 Kessler 2003;119 Khan 2005;122 Kinchen 2002;123 Roderick 200256 | |||
| Cut-off level to define referral |
Martínez-Ramírez 2006120 Albumin > 30 mg/dl |
Orlando 2007111 Creatinine > 140 mg/dl |
||
| Not described | Jungers 2001;121 Kessler 2003;119 Khan 2005;122 Kinchen 2002;123 Roderick 200256 | |||
| Management | |||||
|---|---|---|---|---|---|
| Management of reversible causes of impaired renal function | Medicine interventions | Lifestyle modification | Preparation for RRT | Not described | |
| Management of complications of CKD | Cardio-protection | ||||
| Population selection | |||||
| Screening | Martínez-Ramírez 2006120 | Martínez-Ramírez 2006120 | |||
| High risk groups | Martínez-Ramírez 2006120 | Martínez-Ramírez 2006120 | Orlando 2007111 | ||
| Opportunistic | |||||
| Clinical indication | Roderick 200256 | Roderick 200256 | Roderick 200256 | Jungers 2001;121 Kessler 2003;119 Khan 2005;122 Kinchen 2002123 | |
Evidence of clinical effectiveness of early referral
Despite the difficulties around the definition of CKD and referral, we sought to report what evidence was available about the effect of early referral on clinical outcomes.
Progression
One of the key aims of referral to specialist nephrology services is to initiate interventions to stop or slow progression towards ESRD. Many studies have demonstrated the effectiveness of ACE Is and ARBs in reducing the progressive decline in eGFR in trials. 42–46 BP control is also important. 42 The comparison of nephrology referral for all those with diabetic nephropathy versus those with no access to nephrologists in Mexico120 demonstrated better preservation in function in those referred to a specialist. The comparator group, with no access to specialist services, experienced a mean decline in renal function of 12 ml/min/1.73 m2, which is approximately three times higher than we found described in the natural history review. 88 This pattern was observed regardless of degree of baseline microalbuminuria. There was a high proportion of stage 1 and 2 CKD patients in this study and, as described by Djamali and colleagues,83 the absolute rate of decline may be at its fastest during these stages. Orlando and colleagues111 reported a higher risk (RR 1.32, 95% CI 1.13 to 1.55) of progression in stage 1–2, but not stage 3–5 for people with diabetes than those with no diabetes. The high rate of decline in function in the primary care only group may, therefore, be generalisable to a wider clinical setting.
Similarly, Orlando and colleagues111 reported better outcomes for a composite end point of death or progression in those referred to specialists with stage 3 disease or worse. However, looking at renal progression alone, the crude data suggest more people in specialist care experienced progression. This may be as a result of differences in case-mix, survival and referral bias (where the sick or low risks are not referred by GPs) rather than due to differences in care. Predialysis survival was noted to be better in the group referred to specialists. 111 This finding may reflect a selection bias where people considered to have other serious comorbidities were less likely to be referred. However, a composite end point of death and renal progression was found to be significantly reduced by referral to a specialist for people with stage 3–5 CKD, even after adjustment for comorbidities and age.
Mortality
If patients progress to ESRD and survive to dialysis then there was evidence that post-dialysis survival was improved by early referral, even for referral more than 72 months prior to dialysis. Improved survival was sustained beyond that relating to initial establishment on RRT. This suggests that the survival advantage was not simply explained by technical preparation for dialysis and nutritional status. The differential effect of early referral to a specialist (> 72 months) on survival post dialysis lasted for at least 5 years.
The clinical difference at initiation of dialysis may reflect differences in care that are markers for overall care, or may in part reflect an improvement in clinical status of the patient at the time he or she starts dialysis that is causally linked to survival. Some hypothesise that they are markers for improved cardiovascular risk modification that then manifest in improved survival long after the early dialysis phase. 121 However, in the types of studies presented, the differences in clinical markers may also reflect selection bias, where clinical staffs are selecting the healthiest and fittest to refer for dialysis. 123,124
Kessler and colleagues119 noted those referred late had low contact with primary care compared with those referred early. If CKD was diagnosed only within 1 month of requiring dialysis, then 43.4% of patients received no regular primary care input.
There was little evidence that hospitalisations were affected in the pre- or post-dialysis phase by early specialist referral beyond 1 month prior to starting dialysis.
Other measures of effectiveness
Given the chronic nature of this condition and the important potential to effect quality of life it was perhaps surprising that no studies reported aspects of quality of life.
The nature of what early referral meant in terms of clinical care was essentially not described. The limited detail available has been summarised above. Looking at the impact of different care on aspects of management (of risk factors) and prescribing identified inconsistencies between studies. However, BP control and/or ACE I/ARB prescribing were the most consistently identified differences between referral and standard non-specialist care. The use of CVD risk modifiers such as statins was also reported to be higher in specialist care by some authors. 111,120
Which groups likely to benefit most
There was very limited information about subgroups that may have the most to benefit. Referral less than 12 months prior to starting dialysis was associated with poorer outcomes in certain groups: African-Americans, those with diabetes and those with hypertension;123 a finding consistent with other studies of late referral (see Appendix 7). The authors did not report whether certain groups benefited more from early referral. Orlando and colleagues111 reported that the benefit of referral to a specialist was not observed until stage 3 or worse. In contrast, in patients with diabetes, the greatest gains were reported when referral was made at the earliest stage (microalbuminuria). 120 It is important to note that studies defined their cohorts based on meeting criteria for chronic CKD. In clinical practice, when a patient first presents with a reduced eGFR or evidence of renal damage, it is often not immediately possible to determine the chronicity or otherwise of their condition. A proportion of patients presenting with apparently ‘early’ features of CKD will in fact have an acute renal problem that requires rapid referral to a nephrologist or, in some cases, urologist. 23,41
Limitations of the evidence base
The major limitations of the evidence base have been alluded to already. The lack of studies and in particular RCTs made assessment of effectiveness of strategies for early referral difficult. The Cochrane Renal Group noted, in 2002, that there was a paucity of RCT data for interventions in renal disease, lower than all other internal medicine specialties. Furthermore, patients with renal disease are under-represented in many large intervention trials. For example, an analysis of 86 intervention trials for CVD between 1998 and 2005 noted that 80% excluded ESRD and 75% excluded patients with known CKD. 125 Indeed much of the evidence base around the management of patients with renal disease has relied on observational studies, extrapolation of RCT findings from other clinical groups and expert opinion.
Our review included all study designs, and has found evidence that there are some differences in the outcomes experienced after referral to a specialist compared with remaining in primary care. Some of those differences may be explained by the complex decision-making process around selecting which patients to refer. Adjustment for confounding in the analysis corrects for some of the differences in case-mix but not all. There are, however, differences in the care received by people in specialist care when compared with primary care. Differences in the medicines prescribed and markers of their general clinical condition support the hypothesis that care differs.
The evidence base reviewed here was not helpful in unpacking which components of a model of care are important. Orlando and colleagues111 provided the only estimate of the RR of ACM and progression comparing referral to a nephrologist with primary care alone. This study relied on routine health-care data and the two groups were significantly different at baseline. Observed differences were adjusted for in the analysis, but this adjustment could not account for unmeasured differences between the two groups. The generalisability of this study was also limited; the data were based on a veterans’ health-care organisation (participants were all male) and the study took place in the USA, where non-specialist health care is very different from the primary care provision in the UK.
Conclusions
The studies identified provide some evidence to support the role of ‘early’ referral for CKD, identifying benefits in terms of BP control and renal progression among those referred earlier to specialist services. Very early referral benefits may be greater for certain clinical groups (those with diabetes) while others may show little gain until at least stage 3 disease. The evidence reviewed in this chapter does support the need for further good quality RCTs of methods of care delivery and timing of intervention. While referral to a specialist might be one approach to achieving optimal care, other care models exist. Given the large proportion of the population with stage 1–3 CKD and, from the review of natural history, the low progression to ESRD but significant cardiovascular morbidity and mortality once population screening is adopted, there may be appropriate and alternative ways of delivering care to such patients. The next chapter considers the other models of care delivery for CKD and the evidence of effectiveness.
Chapter 5 Models of care
Introduction
Two decades of rapid expansion in services for people with kidney disease have focused largely on delivery of care for people with severe impairment of kidney function and those requiring RRT. In 2002, the UK Renal Association126 supported the early detection and referral of people with evidence of CKD to enable early treatment with the aim of halting disease progression in those with CKD and preventing kidney function impairment in those who were at high risk of developing CKD. The need for involvement of primary care in early identification was highlighted along with the need for access to expert nephrology assessment in order to reduce complications, including ESRD. 126
The shift in focus to active early recognition and management of chronic conditions has been a growing focus for health services in recent years. Along with growing demand and changing population demographics, important drivers for change included the recognition that people with chronic diseases frequently did not receive advice about modifying risk factors and did not feel included in the treatment decision-making process. 127 Various chronic care models have been proposed but the essence is consistent, with a focus on self-care and including recognition of the importance of community services, informal support networks, multidisciplinary support and primary care in delivering care alongside specialist services. Chronic care models have now been adopted within the World Health Organization in recognition of the global nature of the challenge to support and manage people with chronic illnesses. 128
In the management of diabetes mellitus, the chronic care model has been widely adopted and well studied. Care often includes a combination of self-management using various interventions along with management in partnership with primary and secondary care; a model with demonstrable clinical effectiveness and cost-effectiveness. Improvements in health outcomes including glycosylated haemoglobin, fasting blood glucose levels and diabetes knowledge were observed when patients were provided with group-based diabetes education programmes. 129 There was evidence to support disease management (an organised, practical, integrated and population-based approach of management to health-care services that focused on particular disease and aspects of delivery services) and case management (an intervention to manage patients at high risk of poor outcomes and includes identification of an individual, assessment, development of a care plan, implementation and monitoring of outcomes). 130 Similarly, multifaceted, professional intervention and enhancing the role of nurses in diabetes care have shown improvements in patients’ health outcomes and process of care. 131
A similar kind of care including educational interventions, involvement of multiskilled professionals and enhancing the role of professionals may prove advantageous in CKD management. Here we report evidence about the types of care models that have been adopted for the management of CKD patients. The methods used to identify these studies were outlined in Chapter 2.
Result
Initially, 40 studies were identified, of which three were excluded as they described only the components of care that should be considered132,133 or evaluated the care received before and after a clinical trial [RENAAL: The Reduction in Endpoint Study in NIDDM (non-insulin dependent diabetes mellitus) with the Angiotensin II Antagonist Losartan Study]. 134 They did not describe or evaluate a model of care. Thus a total of 37 studies were included and categorised into four groups:
-
surveys/audits (n = 4) surveys/audits of current care provision135–138
-
evaluation studies (n = 13) evaluating single services or comparing different services139–151
-
descriptive studies (n = 7) describing single services, groups of services, individual specialties within services or an intervention for care152–158
-
aspirational studies (n = 14) reporting proposals for how the services/model of care for CKD management could be in future. 159–172
The findings from these papers are presented below. Firstly, using the survey data, we provide an overview of the types of models of care delivery in the UK. We then present details of the types of models of care described in the literature, picking out commonality in the facets of the care programmes. The evidence of effectiveness for the models of care is summarised and, finally, the substantial literature describing aspirations for renal services is considered with regards to potential key components of care models.
Overview of existing models of care delivery
Chronic kidney disease management in the UK has been reported in the two surveys. 135,136 A questionnaire by Ahmad and colleagues135 surveyed all 72 renal units in the UK and focused on the management of CKD patients with stages 4 and 5. Similarly, Jones and colleagues136 surveyed all 71 renal units and 11 district general hospital nephrology units, asking about systems of care for stable uncomplicated CKD patients that did not rely on direct contact with nephrologists. Five basic types of management pattern for CKD patients were reported: multidisciplinary renal teams, low clearance clinics, predialysis education,135 nurse-led clinics and shared care scheme (SCS)136 (Table 17).
| Type of care | Number of units providing care | Detail of care | ||
|---|---|---|---|---|
| Multidisciplinary renal team services (MSRT)135 | 70/72 units (97%) |
Multidisciplinary teams consisted of dietician, dialysis education provider, anaemia co-ordinator, pharmacist, social worker, access co-ordinator, counsellor, diabetic nurse, occupational therapist, psychologist, physiotherapist and blood pressure nurse Regular multidisciplinary teams meetings held as a part of this service |
Regular MSRT meeting | 47/70 units (67%) |
| Monthly meeting | 36% | |||
| Weekly meeting | 49% | |||
| Shared care (SC) scheme136 | 2/76 units (3%) | Stable uncomplicated CKD patients referred to SC where they are under the care of a GP but supervised by nephrologists based on clinical information and regular review. Patients attended the clinic every 6–12 months (as per the letter and blood form sent to them) and GP gathered clinical information (BP, urinanalysis, etc.) according to the SC form. Most of the time the practice nurse completed these forms. The patients examination result was reviewed by nephrologists and referred to hospital clinic or retained in SC as needed | Developing SC | 6/76 (8%) units |
| Planning nurse management | 2/76(3%) units | |||
| Developing initial assessment by nurse for new referrals | 1/76 units (1%) | |||
| Low clearance clinics135 | 50/70 units (71%) | These clinics were run for managing patients approaching RRT. Services carried out by renal nurse included delivery of CKD education, counselling, transplant education, prescribing and altering prescription under medical supervision, and communication with other personnel involved in the CKD patient care. Nephrologists and renal nurse reviewed patient on alternate basis | Renal nurse involvement in 84% of units | |
| Predialysis education135 | 13/76 units (17%) | The education was about types of dialysis, dietary restrictions, fluid balance, CKD-related anaemia, and renal bone disease, which were all well covered. Less commonly included were aspects of cardiovascular risk factors, sexual health and psychological support. Education materials were available in audio and Braille or translated in other languages. Specific dialysis education provider, dialysis nurses, transplant co-ordinators, dieticians and pharmacists were involved | ||
Multidisciplinary renal teams were reported by 97% of the renal units and comprised different skilled professionals who, along with nephrologists, managed CKD patients. Regular meetings brought the team together. 135 Dieticians and dialysis education providers were common, attending CKD clinics in more than 95% of the renal units. 135 Additionally, 70% of units ran satellite clinics for CKD patients in a general district hospital from where patients could access the full team services. 135 Only two units reported to have shared primary and secondary care schemes. 136 A further six centres were developing SCSs; three were developing nurse-led services where nurse specialists would manage stable patients and/or the initial assessment of new referrals. 136 Low clearance clinics were run by 71% of units to manage patients approaching RRT, while 10 units were planning to set up such clinics. Most of the low clearance clinics were run by specialist renal nurses who had various roles including communicating with the staff involved in CKD management, patient education, counselling, transplant assessments, prescribing under medical supervision and reviewing patients. 135 Pre-dialysis education was noted in 16% of the units136 where dialysis nurses, transplant co-ordinators, dieticians and pharmacists provided dialysis education to CKD patients. 135
A survey of the organisation of care provided to CKD stage 3–5 patients by nephrology clinics in Italy139 highlighted important and frequent deviations from guidelines in the centres’ policies for caring for CKD patients including: the definition of low eGFR, management of anaemia and bone mineral metabolism, and preparation for dialysis. A report of a local CKD network established in the UK (membership included: local GPs, consultant nephrologists, consultant nurses, commissioners, a patient representative and representatives from the primary care trusts) described a network approach with supporting referral guidelines and an education programme that had been introduced to support increasing local demand on nephrology services. 140
Models of care observed (from evaluative/descriptive studies)
From the 19 evaluation and descriptive papers, three broad models of care were identified: multidisciplinary care (MDC), structured care by an individual specialty, and educational interventions. Among the MDCs, two were SCSs. Structured care by an individual specialty included studies reporting on a single clinical specialty (e.g. nurses, pharmacists) operating a service in isolation or as part of a multidisciplinary group (Table 18). The models of care are described in more detail below. Some of the papers described more than one model of care. 153,154,157,158
| Study ID | Description of care | MDC | SCIS | EI |
|---|---|---|---|---|
| Bending 2007152 | Joint diabetes and renal clinic at Eastbourne, UK | ✗ | ||
| Compton 2002153 | The Healthy Start Program at Ochsner Clinic in New Orleans, LA, USA | ✗ | ||
| A renal disease management programme within a managed care setting – Boston, MA, USA | ||||
| CKD programme at Western New England Renal and Transplant Associates | ✗ | |||
| The division of Nephrology at Virginia Commonwealth University/Medical College of Virginia, VA, USA | ✗ | |||
| Cortes-Sanabria 2008141 | Primary care led by family physician with educative intervention [IMSS Primary Health-Care Units (Unidad de%%Medicina Familiar)] in Guadalajara City, Mexico | ✗ | ||
| Curtis 2005142 | Multidisciplinary clinic of hospitals in Canada and Italy | ✗ | ||
| Ghossein 2002154 | Comprehensive renal care clinic called Healthy Living at Northwestern Memorial Hospital in Chicago, IL, USA | ✗ | ✗ | |
| Hardy 2007143 | Redesigned service for the management of diabetic nephropathy and diabetics with microalbuminuria at Whiston Diabetes Centre, Mersyside, UK (SCS) | ✗ | ||
| Harnett 2008144 | Primary care service and virtual care service | ✗ | ||
| Harris 1998145 | Multidisciplinary case management clinic (general practice medicine of Regenstrief Health Center, IN, USA, affiliated with multispecialty outpatient facility) | ✗ | ||
| Hemmelgarn 2007146 | Multidisciplinary clinic of Canada (Southern Alberta Renal program) | ✗ | ||
| Hostetter 2003155 | National Kidney Disease Education Program, MD, USA | ✗ | ||
| Jones 2006147 | SIMON programme of Southampton, UK, that includes intensive hospital nephrology clinic (HC) and shared primary and nephrology care scheme (SCS) | ✗ | ||
| Joy 2005156 | Physicians–pharmacist collaborative practice model | ✗ | ||
| Kelly 2008148 | Pharmacist-led structured care (a protocol driven clinic) | ✗ | ||
| Leung 2005149 | Pharmacist and diabetes specialist-led structured care at hospital | ✗ | ||
| Minutolo 2005137 | Physician-led primary care service and nephrologist-led secondary care service | ✗ | ||
| Minutolo 2006138 | Physician-led primary care service and specialist (nephrologists or diabetologists)-led secondary care service | ✗ | ||
| Richards 2008150 | Disease management programme of West Lincolnshire Primary Care Trust, UK | ✗ | ||
| Thanamayooran 2005151 | Multidisciplinary nephrology clinic of Halifax, Canada (tertiary care hospital) | ✗ | ||
| Thomas 2004157 | Patient-centred management and education at South-west Thames, UK (Primary care) | ✗ | ✗ | |
| Thomas 2005158 | A patient-centred education programme at local family doctor surgeries (primary care) | ✗ | ✗ |
Multidisciplinary care
Multidisciplinary care was the most commonly described approach to the management of CKD populations. Table 19 details the services and settings. MDC models were described in primary care150 and hospital-based clinics. 142,143,145,146,151,152,154 The MDC disease management programmes based in primary care involved community-based teams of nurses, dieticians, social workers and GPs with a wide scope including a named nurse available to each patient. 150 Hospital care-based MDC nephrology clinics comprised nurses, nurse-educators, social workers, dieticians, nephrologists and academics. Joint diabetics and renal clinics included MDC teams with specialists from clinical specialties. 152 Some described a case management approach with a named team for individual patients. 145
| Reference | Study type | Type of CKD patients | Multidisciplinary clinic | Facets of MDC programme | Staff delivering the programme | Comparator group |
|---|---|---|---|---|---|---|
| Bending 2007152 | Descriptive | Established diabetes kidney disease | Joint diabetes and renal clinic at Eastbourne, UK | Referral through diabetes specialist service for initial diagnosis and then for follow-up depending upon the level of SCr in order to provide renal support therapy. The service includes a prior routine structured screening for microalbuminuria and clinical proteinuria and early intervention (ACE I/ARB) to control BP and glycaemia in all patients to halt the development of incipient diabetic nephropathy | NA | |
| Compton 2002153 | Descriptive review paper | CKD at early stages | The Healthy Start program at Ochsner Clinic in New Orleans | Multidisciplinary programme, aimed to intervene in CKD at early stage, thus slowing progression of the disease and improving patient outcomes | NR | NA |
| Compton 2002153 | Descriptive review paper | CKD patients, stage not specified | A renal disease management programme within a managed care setting, Boston, MA, USA | Multidisciplinary programme promoting early referral where interventions to slow the progression of the disease could have impact on the morbidity and mortality associated with CKD. Educational opportunities provided to patients and family members | Primary care physicians, nephrologists, nephrology nurses, nutritionists | NA |
| Curtis 2005142 | Cohort study, those exposed to MDC vs standard nephrology care | Incident dialysis patients | Multidisciplinary clinic of hospitals in Canada and Italy | MDC included educational programmes as well as regular, protocolised clinic and laboratory follow-up of patients with CKD. The frequency of both visits and laboratory tests was predetermined, based on the level of kidney function with reminder system to facilitate follow-up. Regularly scheduled blood work and clinical examination and pre-specified educational topics were reviewed with each patient |
Canada – nurse, educator, physician, social worker, nutritionist, and pharmacist Italy – programme dedicated nephrologists and multidisciplinary nurses who took responsibility for implementing recommended diagnostic and intervention strategies |
Standard nephrology care Nephrologists with access to facilities and staff of multidisciplinary clinic for their patients. Care was standardised and managed according to standard unit practices |
| Ghossein 2002154 | Evaluation of comprehensive renal care | CKD stage 3–5 | Comprehensive renal care clinic called ‘Healthy Living’ at Northwestern Memorial Hospital, Chicago, IL, USA | Main aspects of programme were treating the complications of CKD (anaemia, renal osteodystrophy), providing nutritional support, identifying and managing comorbidities, preparing for transplantation and dialysis. The main aim of the service was to slow or stabilise the progression of CKD. The referring primary care physicians were given educational sessions including lectures and discussions (one-to-one or small group). Clinical parameters and medication of the patients were monitored and were screened to check for comorbid conditions. Education on dialysis provided to patients | Nephrologists, physician assistant, nurses, nutritionist, having an access to renal social workers, patient educator, renal dietician, separate transplant team | NA |
| Hardy 2007143 | Evaluation of redesigned service | Type 2 diabetic patients with microalbuminuria and diabetic nephropathy | Redesigned service for the management of diabetic nephropathy and diabetics with microalbuminuria at a single diabetes clinic | Uncomplicated patients were discharged to primary care, while complicated problems were followed in dedicated hospital-based clinics. A specialist nephropathy clinic was established to focus on multifactorial interventions. Patients with diabetic kidney disease referred from primary care (or within hospital) were sent to ‘new patient clinic’ for assessment, consultation, education and optimisation of treatment with subsequent visits at one of the other dedicated ‘nephropathy’ clinics. 6–8 patients visited each clinic for approximately 35 minutes per patient. Following each of these nephropathy clinics, all patients were discussed in detail in a multidisciplinary team meeting | Diabetologists, diabetes nurse, consultant and a senior clinical fellow having access to nephrologists. Three nephropathy clinics: one led by consultant, two led by diabetes nurse specialist | Before redesigning of the service, patients with diabetic kidney disease were cared for within a ‘general’ diabetic outpatient clinic in secondary care which included new referrals, follow-ups and patients with a wide range of complications |
| Harris 1998145 | Randomised controlled clinical trial of an intensive multidisciplinary case management programme | Chronic renal insufficiency (SCr > 1.4 mg/dl) | Multidisciplinary case management clinic (general practice medicine of Regenstrief Health Center, affiliated with multispecialty outpatient facility) | The frequency of this case management clinic was every 6 months, 4 months or 3 months depending on SCr level. Intervention patient received a comprehensive programme that included medication review, compliance assessment, education, surveillance of patients, dietary counselling, social service interview and communication with primary care provider where appropriate. The use of ACE I was increased, BP control improved; use of nephrotoxic drugs and protein intake decreased, barriers to care decreased | Nephrologists, nephrology fellow, a renal nurse, a renal dietician and a social worker |
Usual care Patients got usual primary care from physicians with access to nephrologists if referred to the standard renal service |
| Hemmelgarn 2007146 | Retrospective cohort study, compared MDC with non-MDC | CKD stage 3 and greater | Multidisciplinary clinic in Canada (hospital based) | Programme included patient education, laboratory and clinical examinations (every 1–3 months and every 3–6 months respectively). Education session included discussion about CKD, fluid and dietary restrictions, monitoring BP, medicine management, and lifestyle modification to reduce CVD risk and delay CKD progression. Patients were provided with a booklet produced by the Kidney Foundation | Primary nephrologists (referred their patients to MDC), specialised clinic nurse, registered dietician and social worker |
Non-MDC Description not reported |
| Jones 2006147 | Retrospective review of SIMON programme | CKD stage 3–5 | SIMON programme of Southampton, UK, that includes intensive hospital nephrology clinic (HC) and shared primary and nephrology care scheme | Initially all patients were reviewed in hospital renal clinic. Those requiring continued care were retained in HC. Stable and uncomplicated patients were enrolled in shared primary and nephrology care scheme by nephrologists, and monitored by using clinical and laboratory reviews recorded in primary care without attending renal unit. Blood and urine tests and clinical examination (BP, weight, medications, etc.) carried out every 6–12 months if necessary. Data recorded in SIMON database which was reviewed by nephrologists electronically. Nephrologists and primary care physicians communicated between each other regarding patients recall to the HC or any changes in medication. SIMON programme used a computerised graphing system that allowed visual analysis of changes in GFR and other blood test | Nephrologists, primary care physicians, nurses | NA |
| Richards 2008150 | Evaluation of disease management programme | CKD stages 4 and 5, and those at borderline of CKD 3/4 | Disease management program of West Lincolnshire Primary Care Trust, UK | Patient education (encouraged to engage in their own care and to raise awareness of cardiovascular risk factors), medicine management, dietetic advice and optimisation of clinical management to achieve clinical targets. The programme had same the fundamentals as the multidisciplinary renal clinic but had wider scope and was proactive. There was a named nurse for each patient who could be accessed directly by telephone or face-to-face without needing an appointment. Patients received proactive intervention from the clinical team at a frequency dictated by the patient’s risk assessment and/or by the patients themselves | Delivered by a community-based team of nurses, dietician and social worker | NA |
| Thanamayooran 2005151 | Review of a prospective cohort | CKD patients with CrCl < 60 ml/min | Multidisciplinary nephrology clinic of Halifax, Canada (tertiary care hospital) |
Patients were seen annually, every 6 months or every 3 months according to the level of GFR. The service was free of charge to the patient including medical, surgical and ancillary cost. Although there was no protocol for care, consensus was set for some of the clinical parameters like BP control, using ACE Is and ARBs, metabolic control of calcium, phosphate, parathyroid hormone and control of anaemia A large peritoneal dialysis and haemodialysis programme was maintained at this centre |
Nurses, nurse-educators, social workers, dieticians and full time academic nephrologists | NA |
Shared care scheme
The Southampton Integrated Monitoring of Nephrology (SIMON) programme was the only structured SCS reported in detail in the literature that formally spanned secondary and primary care. 147 It included an intensive hospital nephrology clinic and shared primary and nephrology care scheme. All patients were initially seen at the hospital nephrology clinic and while patients with stable CKD were monitored regularly through the shared primary and nephrology care scheme, complicated patients and those requiring continued care were retained in the hospital nephrology clinic.
The other described MDC involved referral from primary care to hospital care, or between two specialist clinics, in the usual way. 143,145,146,151,152,154
Structured care by an individual specialty
Apart from nephrologists, CKD management has been influenced by the involvement of other health-care professionals. Pharmacy programmes included structured clinics solely led by pharmacists using protocols to manage the medication of patients with microalbuminuria and nephropathy. 148 Pharmacists also operated within structured disease management programmes implemented by pharmacists and diabetes specialists managing diabetic nephropathy patients together. 149 Joy and colleagues156 described the support of pharmacists as part of a multidisciplinary team for the management of CKD patients. Some care programmes were run by renal specialist nurses, or renal specialists working closely with general nurses. 157,158 Two studies compared the care given in primary care with that of specialists (nephrology and diabetology) in Italy. 137,138 Care by GPs was also compared with virtual clinic management (Table 20). 144
| Reference | Study type | Type of CKD patients | SCIS | Detail of care | Comparator group |
|---|---|---|---|---|---|
| Harnett 2008144 | Evaluation study of patients monitored in primary care compared with virtual clinic | CKD patients, all stages | Virtual care as per CKD management guidelines | Virtual care: CKD patients were monitored remotely by regular blood tests followed by sending regular reports based on their blood and urine tests (haemoglobin, urine protein:creatinine ratio, cholesterol and estimated GFR) | GPs led primary care |
| Joy 2005156 | Descriptive, editorial | CKD patients, stage not specified | Physician–pharmacist collaborative practice model | Pharmacists as a part of multidisciplinary health-care team involved in CKD management. Those with specialised training in nephrology were members of national nephrology organisations (USA) and involved in following activities:
|
NA |
| Kelly 2008148 | Evaluation study of a structured care programme to manage patients with microalbuminuria and nephropathy | Patients with microalbuminuria and nephropathy | Pharmacist-led structured care (clinic) | Patients were referred to this clinic by a physician based on referral and diagnostic criteria. Patients attended the clinic four to six weekly until optimisation of their treatment (using pharmacists prescribing recommendations and clinic standards), allocated appointment time being 30 minutes. Clinical examination included checking BP, pulse, weight, lipids, renal function, liver function, HbA1c and early morning ACR. FBC, calcium and phosphate were also measured. A medical history and full drug history using two or more sources were completed. Knowledge of their drug treatments and smoking status were ascertained with patients. Smoking cessation services provided | NA |
| Leung 2005149 | Prospective cohort study of a diabetes management programme | Type 2 diabetic nephropathy | Pharmacist and diabetes specialist-led structured care at hospital | Pharmacist, diabetes specialist implemented this disease management programme that included periodic laboratory assessments, patient adherence, risk factors control, and use of renin–angiotensin system inhibitor |
Usual care Description not reported |
| Minutolo 2005137 | Evaluation study of primary care compared with nephrology care | Hypertensive CKD patients (excluding patients with eGFR < 15 ml/min/1.73 m2) | Primary care: led by physician | Laboratory tests within 1 week after enrolment, and clinical examination of renal disease of patient were carried out followed by a medical visit (height, weight and BP measured and recorded). Preliminary laboratory tests record and structured anonymous form provided by co-ordinator centre to physician. Physicians aware of BP targets in CKD patients | Nephrology care: nephrologists led |
| Minutolo 2006138 | Cross-sectional study comparing primary care with nephrology care and diabetology care | Diabetic CKD (eGFR between 15 and 60 ml/min/1.73 m2) | Primary care: led by physician | Medical history (including cardiovascular events), demographic data, laboratory data and current therapy data recorded at each medical visit of patient as per structured anonymous form provided by the co-ordinating centre. Physicians were aware of BP, HbA1c and LDL targets in CKD patients |
Nephrology care: led by nephrologists Diabetology care: led by diabetologists |
| Thomas 2004157 | 4-year evaluation study (ongoing study); result presented for first phase of the study | Diabetic renal disease | Nurses led management in collaboration with GP | Patient-centred management and education at south-west Thames (primary care). Diabetes care and education during GP visit and practice nurse consultations in each practice | NA |
| Thomas 2005158 | A 4-year prospective study; only first year findings presented | Diabetic renal disease | Renal specialist nurse working closely with local community nurses and doctors | A patient-centred education programme at local family doctor surgeries (primary care). A renal specialist nurse working closely with local community nurses and doctors. Education provided to patient | NA |
Educational intervention
Educational interventions for care in CKD were described by some of the studies. Generally, two types of educational programme were observed: education of general staff and patient education. 141,142,146,150,153–158 The education programmes varied in content and delivery style and are detailed further in Table 21.
| Reference | Study type | Type of CKD patients | Setting | Detail of care | Staff involved | Comparator |
|---|---|---|---|---|---|---|
| Compton 2002153 | Descriptive paper | CKD patients, stage not specified | CKD programme at Western New England Renal and Transplant Associates | Guidelines, a charting format and a self-care manual were developed. Education classes for patients and family members held twice a month. Clinical parameters (bone disease, anaemia, blood pressure, hypercholesterolemia, nutrition, acidosis and palliative care issues) addressed. CKD patients followed by nephrology team | Nephrologists and nurse practitioners | NA |
| Compton 2002153 | Descriptive paper | CKD patients, stage not specified | Division of Nephrology at Virginia Commonwealth University/Medical College of Virginia, VA, USA | Development of a CKD patient education. Performance-based programme was designed that included 1-hour class every week prior to clinic for patient and family member | Nephrologists, a nurse practitioner, transplant co-ordinator, clinical social worker, nutritionist and a pharmacist. An instructional designer (pursuing her doctorate in education) | NA |
| Cortes-Sanabria 2008141 | A pilot study for cluster-randomised trial | Patients with diabetes mellitus and CKD | Primary care led by family physician with educative intervention IMSS Primary Health-Care Units (Unidad de%%Medicina Familiar, UMF) in Guadalajara City, Mexico | An educative intervention included theory course, analytical literature review and discussion of real clinical cases led by two investigators. Clinical and biochemical examination performed at baseline, at the end of educative intervention and 6 months after intervention. All patients had routine monthly visits and management according to their primary care physician’s clinical criteria | Physicians | Family physician without educative intervention |
| Hostetter 2003155 | Descriptive | CKD patients, all stages | US national kidney disease education programme | Resource for patients, carers and primary care physicians. Provides information about testing, treatment and risk factors via a website. Supporting work to ensure clear targets are embedded in health-care system to support the management of CKD | Health-care professionals representing organisations involved in CKD under the umbrella of the National Institute for Health | NA |
Description of the key facets of the care programmes
Various facets of programmes for CKD management have been reported within the three types of care model identified. See Table 22 for a summary of the different elements of the programmes.
| References | Patient education | Health-care professional education | Medicine management | Nutritional advice | Patients surveillance | Social care service | Managing/preventing complication | Dialysis and transplant management | Structured screening programme |
|---|---|---|---|---|---|---|---|---|---|
| Bending 2007152 | ✗ | ✗ | ✗ | ||||||
| aCompton 2002153 | ✗ | ✗ | ✗ | ✗ | |||||
| Cortes-Sanabria 2008141 | ✗ | ✗ | |||||||
| Curtis 2005142 | ✗ | ✗ | ✗ | ✗ | |||||
| Ghossein 2002154 | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Hardy 2007143 | ✗ | ✗ | ✗ | ||||||
| Harnett 2008144 | ✗ | ||||||||
| Harris 1998145 | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Hemmelgarn 2007146 | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Jones 2006147 | ✗ | ✗ | |||||||
| Joy 2005156 | ✗ | ✗ | ✗ | ||||||
| Kelly 2008148 | ✗ | ✗ | |||||||
| Leung 2005149 | ✗ | ✗ | ✗ | ||||||
| Minutolo 2005137 | ✗ | ✗ | |||||||
| Minutolo 2006138 | ✗ | ✗ | |||||||
| Richards 20081150 | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Thanamayooran 2005151 | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Thomas 2004157 | ✗ | ||||||||
| Thomas 2005158 | ✗ |
Patients surveillance
Patient surveillance, including regular clinical and laboratory examinations (e.g. BP, weight, haemoglobin, calcium, phosphate, other metabolic parameters) along with medical review, was the most commonly reported element of care within all models of care. Patient clinic visits or follow-up varied from monthly to annually depending on the level of kidney function and clinical need. 142,146,147,151,152 Appointments lasted for 30–35 minutes143,148 and some included discussion of a patient in a multidisciplinary team meeting. Harnett and colleagues144 reported so-called ‘virtual methods’ to conduct this surveillance with a patient attending a practice nurse for examinations and the results being logged for a remote specialist team to review them in the context of that patient’s clinical record. 147 None of the studies described in any detail how patients were selected for inclusion in the CKD care model. Most appeared to rely on measures of eGFR (or creatinine thresholds), but there was rarely a description of why patients were originally tested (i.e. clinical need versus screening) or whether other factors were used to influence selection for further management.
Patient education
Patient education included reviewing pre-specified educational topics with patients,142 discussion about CKD, dietary restriction, monitoring BP, medicine management, lifestyle modification,146,150 education on dialysis154 and discussion about clinical parameters. 153 Some CKD management programmes developed a guideline, self-care manual or performance-based programme for patient education with education classes held prior to clinics. 153 A patient-centred education and management approach was reported where renal nurses were working along with other specialists and primary care teams. 157,158
Health-care professional education
Only three papers reported education provided to health-care professionals. 141,154,156 In two studies, primary family physicians were provided with educational sessions. 141,154 The educational intervention to physicians included lectures based on interactive theory–practice models and discussions (one-to-one or small group discussion of real cases led by investigators). Lectures included a theory course covering various aspects such as basic anatomy and physiology of kidney, epidemiology and clinical measures and advanced topics such as associated comorbidities, prevention and management.
Medicine management
With the aim of optimisation of treatment, most of the CKD programmes considered medicine management; in particular the use of ACE Is and ARBs. 145,149 Pharmacist-led structured care models included medicine management and optimisation of treatment which were based on prescribing recommendations and clinical standards. 148 Medicine management included a full drug history and ascertaining patients’ knowledge of their medicine treatments. 148
Managing/preventing complications
Some of the MDC clinics focused on the management and prevention of complications associated with CKD. 146,149,150,152,154 Education on lifestyle and cardiovascular risk factors was provided to reduce CVD risk and to delay CKD progression. 146,149,150 To prevent the development of diabetic nephropathy, some care focused on screening for microalbuminuria and clinical proteinuria. 152 Ghossein and colleagues154 mentioned that a comprehensive renal care programme included screening for, and treating, the complications of CKD such as anaemia and renal osteodystrophy. Additionally, some MDCs endeavoured to run structured screening programmes (screening for comorbid conditions, microalbuminuria or proteinuria, or to identify those to prepare for dialysis and transplant). 152,154 The separation of ‘new referral’ assessment from follow-up was reported to enable more focused clinics and to identify patients where no follow-up was required. 143
Nutritional advice
Nutritional advice was provided as a part of education programmes146,153 or as a separate element of more comprehensive care models. 145,150,154
Social care
A few models of care included a component related to social care services. 142,145,146,151 Social care workers were involved to decrease barriers to care by interviewing patients and by direct intervention if needed. 145 Others stated that social workers were also involved in providing education to patients. 146
Assessment of effectiveness
Clinical markers
Patients under the care of a MDC were consistently reported to have improved clinical surrogates such as BP, glycosylated haemoglobin and cholesterol when compared with before the start of treatment in the MDC (Table 23). Patients under the care of the SIMON programme had a significant reduction in mean BP after referral. 147 Likewise BP was improved when patients attended multidisciplinary nephrology clinics and redesigned services. 143,151 It was observed that in the redesigned service for diabetic nephropathy patients, the mean fall in BP was –11/7 mmHg (148/80 mmHg at baseline to 137/73 mmHg at follow-up, p < 0.001) and 33% achieved a BP target of 125/75 mmHg. 143 Moreover, patients’ glycosylated haemoglobin and low density lipoprotein cholesterol improved and there was minimal progression of microalbuminuria to diabetic nephropathy, and the proportion of patients with proteinuria fell. Similarly, in a multidisciplinary nephrology clinic, mean BP fell from 151 ± 27/80 ± 13 mmHg at the initial visit to 135 ± 18/75 ± 11 mmHg at follow-up of 4 years. 151
| Reference | Clinical parameters | Outcomes/values [mean (SD)] | Duration of follow-up | Type of care | |||
|---|---|---|---|---|---|---|---|
| Cortes-Sanabria 2008141 | BP [(systolic/diastolic) mmHg] | Physician with educative intervention: –22.0 (20.2)/–9.8 (11.3) | Physician without educative intervention: 10.8 (24.3)/2.7 (11.6) | p < 0.05 | 1 year | Primary care with physician getting educative intervention | |
| Curtis 2005142 | Haemoglobin (g/l) | At dialysis start | After 12 months post dialysis | p < 0.0001 | 1 year | MDC as an addition to standard nephrology care | |
| Standard nephrologists’ care: 90 (14) | Standard nephrologists’ care: 110 (17) | ||||||
| MDC and nephrologists’ care: 102 (18) | MDC and nephrologists’ care: 120 (16) | ||||||
| Hardy 2007143 | BP [(systolic/diastolic) mmHg] | At baseline: 148/80 | After follow-up: 137/73 | Mean fall in BP –11/7 mmHg, 33% achieved BP target of 125/75 mmHg | p < 0.001 | Mean 26 (SD 10) months | Redesigned diabetic nephropathy clinic |
| HbA1c% | At baseline: 7.7(1.7%) | After follow-up: 7.4 (1.3%) | 44% (56/127) achieved the 7% HbA1c target | p = 0.03 | |||
| LDL-C (mmol/l) | At baseline: 2.8 (1) | After follow-up: 2.1 (0.8) | 81% (103/127) achieved the LDL-C target of < 2.6 mmol/l | p < 0.001 | |||
| Harris 1998145 | BP [(systolic/diastolic) mmHg] |
At enrolment MDC: 143 (23)/83 (13) Usual care: 145 (26)/82 (12) |
3rd through 5th year after enrolment MDC: 142 (17)/79 (8) Usual care: 145 (17)/78 (9) |
Non-significant both at baseline and after 5 years | 5 years | MDC vs usual care | |
| Jones 2006147 | BP [(systolic/diastolic) mmHg] | Before referral | After referral | p < 0.001 | 3 years from the first referral | MDC, shared care scheme (SIMON programme) | |
| SC: 152/82 (read from graph) | SC: 148/80 (read from graph) | ||||||
| HC: mean 156 (29)/84 (14) | HC: 150 (21)/81 (11) | ||||||
| Kelly 2008148 | BP [(systolic/diastolic) mmHg] | At entry to the clinic: 150.5 (19.3)/79.7 (10.2) | At exit: 132.6 (15.2)/67.8 (10.5) | p < 0.001 | 18 months from the entry | Pharmacist-led structured care | |
| Cholesterol (mmol/l) | At entry: 4.56 (1.06) | At exit: 4.03 (1.07) | p < 0.001 | 18 months from the entry | |||
| HbA1c (%) | At entry: 8.5 (1.7) | At exit: 8.2 (1.7) | p < 0.05 | 18 months from the entry | |||
| Leung 2005149 | Greater reductions in BP and LDL-C reported | Values not reported in abstract | 2 years | Pharmacist and diabetes specialist led structured care | |||
| Minutolo 2005137 | BP [% (95% CI)] | Nephrology care: 21.5 (15.6 to 27.4) | Primary care: 5.8 (2.9 to 8.6) | p < 0.0001 | 1 year | Nephrology care vs primary care | |
| Minutolo 2006138 | BP | Nephrology care assessment 100%, patients at goal 14.2% | Primary care assessment 100%, patients at goal 10.3% | Diabetology care assessment 100%, patients at goal 13.4% | p = 0.421 | 6 months | Nephrology care vs primary care vs diabetology care |
| HbA1c | Assessment 87.6%, patients at goal 60.5% | Assessment 45.6%, patients at goal 46.4% | Assessment 98.4%, patients at goal 31.8% | p < 0.0001 | 6 months | ||
| Haemoglobin | Assessment 98.1%, patients at goal 70.9% | Assessment 81%, patients at goal 72.8% | Assessment 94.7%, patients at goal 89.3% | p < 0.0001 | 6 months | ||
| Richards 2008150 | BP (median, IQR) [(systolic/diastolic) mmHg] | Before enrolment: 139 (124–154)/76 (69–84) | After enrolment: 130 (125–145)/71 (65–79) | Target < 130/< 80 mmHg |
Systolic: p = 0.05 Diastolic: p = 0.002 |
9 months from the enrolment | Primary care-based disease management programme |
| Cholesterol (median, IQR) mmol/l | Before enrolment: 4.6 (3.9–5.4) | After enrolment: 4.2 (3.5–5.0) | Target < 5 mmol | 9 months from the enrolment | |||
| Thanamayooran 2005151 | BPa [(systolic/diastolic) mmHg] | Initial visit: 151 (27)/80 (13) | After 4 years of follow-up: 135 (18)/75 (11) | Initial visit p < 0.0001 vs all subsequent years | 4 years of follow-up from initial visit | Multidisciplinary nephrology clinic | |
| Haemoglobin (g/l) | Initial visit | Follow-up visits | 4 years of follow-up from initial visit | ||||
| Stage 3, 124 (17) | Stage 3, 123 (16) | ||||||
| Stage 4, 117 (18) | Stage 4, 116 (18) | ||||||
| Stage 5, 100 (18) | Stage 5, 107 (13) | ||||||
Structured care programmes run by pharmacists resulted in clinically and statistically significant improvements in mean BP (from 150.5 ± 19.3/79.7 ± 10.2 mmHg to 132.6 ± 15.2/67.8 ± 10.5 mmHg, p < 0.001). Similar trends of significant results were observed for cholesterol and glycosylated haemoglobin in CKD patients. 148 Likewise, CKD management by collaborative approach between pharmacists and diabetes specialists proved to be beneficial with improvements in clinical surrogates (BP and low density lipoprotein cholesterol) and risk reduction of end points compared with those receiving usual care. 149 Those using educative intervention among family physicians have shown clinical improvements in BP and kidney function. 141
Where comparator groups of patients were available, the findings were less consistent.
Curtis and colleagues142 reported patients exposed to MDC had clinical benefits including higher levels of haemoglobin, albumin and calcium at dialysis start than those receiving standard care. Minutolo and colleagues137 reported that hypertensive patients with CKD under nephrology care seemed to have improved BP (21.5% patients reached BP target of 130/80 mmHg, 95% CI 15.6 to 27.4, p < 0.0001) compared with primary care (5.8%, 95% CI 2.9 to 8.6). Patients were 2.6 times less likely to have reached their target BP in primary care versus nephrology care (after adjustment for age, diabetes and eGFR). However, in patients with diabetic renal disease, there was little difference in the proportions achieving target BP (10–14%), with similarly low levels in nephrology, diabetology and primary care. 137
Harris and colleagues,145 reporting the only RCT, showed no difference in weight, BP or creatinine clearance when they compared people managed in an intensive MDC management programme with those receiving standard care.
Prescription changes
Statistically significantly higher prescriptions of renin–angiotensin aldosterone system (RAAS) inhibitor agents were noted. 143,147 Prescription rates were found to be significantly higher in specialist care than in primary care, and the choice of medicines differed. 137,138 Nephrologists were more likely to use dual blockade of RAAS using ACE Is and ARBs and were more likely to prescribe loop diuretics than either primary care physicians or diabeteologists. 138 These differences existed after accounting for clear differences in case-mix. Use of antihypertensives (including RAAS inhibitor agents) and cholesterol reducing drugs (statins) appeared to increase with the involvement of pharmacists and diabetes specialists in CKD care. 148,149 Prescription of ACE I, in those without contradictions, increased from 66% to 100%, while that of ARBs (single or in combination) increased by 29%. 148 Prescriptions for antihypertensive agents by physicians who underwent an educative intervention were higher than those by physicians without educative intervention. 141 Harris and colleagues,145 however, reported little difference in prescribing behaviour between those cared for in intensive multidisciplinary case management and those receiving standard care.
Long-term outcomes
Long-term outcomes have been reported only for MDC models. See Table 24 for outcomes reflecting mortality and CKD progression.
| Survival/mortality | |||||||
|---|---|---|---|---|---|---|---|
| Reference | Outcomes/measure | Values | p-value | Comparator | Duration of follow-up | Type of care | |
| Curtis 2005142 | Survival advantage (Kaplan–Meier survival) |
MDC Statistically significant survival |
p = 0.01 | Compared with standard nephrology care | Mean 41 (SD = 34) months | MDC vs standard nephrology care | |
| Hardy 2007143 | Mortality rate | 2.2/100 py | REENAL trial 6.8/100 py; IDNT trial 5.8/100 py | Mean 26 (SD = 10) months | Redesigned diabetic nephropathy clinic | ||
| Harris 1998145 | Cumulative mortality after 5 years | Intervention group: 59 (29%) | p = 0.29 | Control group: 77 (33%) | 5 years | Multidisciplinary case management clinic | |
| Survival advantage | HRa 0.90, 95% CI 0.71 to 1.14 | p = 0.36 | Compared with control group | ||||
| Hemmelgarn 2007146 | Death | MDC: 61 (32.6%) | Non-MDC: 77 (41.2%) | 3 years | MDC compared with non-MDC | ||
| Reduction in the risk of death | HRb 0.50, 95% CI 0.35 to 0.71 | Compared with non-MDC | 3 years | ||||
| Hospitalisation | 123 (65.8%) at least one hospitalisation | 131(70.1%) at least one hospitalisation | 3 years | ||||
| Reduction in the risk of hospitalisation | HRb 0.83, 95% CI 0.64 to 1.06 | p = 0.18 | Compared with non-MDC | 3 years | |||
| CKD progression | |||||||
| Ghossein 2002154 | GFR decline | CKD stage 3: calculated GFR decreased during the first 7.5 months and then continued to decrease albeit at a reduced rate. CKD stages 4 and 5: stabilised throughout the 15 months of follow-up. Presented in a graph. No values given | Comprehensive renal care clinic called Healthy Living | ||||
| Hardy 2007143 | Rate of doubling of serum creatinine | 1.4/100 py | REENAL trial 7.9/100 py; IDNT trial 3.9/100 py | Mean 26 (SD = 10) months | Redesigned diabetic nephropathy clinic | ||
| Rate of ESRD | 1.1/100 py | REENAL trial 6.8/100 py; IDNT trial 5.4/100 py | Mean 26 (SD = 10) months | ||||
| Jones 2006147 | Decline in eGFR, ml/min/1.73 m2 (median, IQR) | Before referral: –5.2 (–12.8 to –1.9) | After referral: –0.5 (–3.3 to 2.5) | p < 0.001 | 5 years | MDC, shared care scheme (SIMON programme) | |
| SCS < 6 months: –2.7 (–9.4 to –1.3) | SCS < 6 months: –0.3 (–2.7 to 1.4) | ||||||
| SCS > 6 months: – 4.1 (–11.3 to –1.4) | SCS > 6 months: 0.1 (–1.2 to 1.7) | ||||||
| HC: –6.2 (–13.9 to –2.4) | HC: –0.9 (–5.2 to 3.4) | ||||||
| Richards 2008150 | Decline in eGFR, ml/min/1.73 m2 (median, IQR) |
Before enrolment (preceding 9 months) –3.69 (–7.46 to –1.49) |
After enrolment (subsequent 12 months) 0.32 (–2.61 to 3.12) |
p < 0.001 | 12 months from the enrolment | Primary care based disease management programme | |
|
Patients with decline of eGFR ≥ 5 ml/min/1.73 m2 (median, IQR) |
Before enrolment –9.90 (–12.36 to –6.55) |
After enrolment –1.70 (–6.41 to 1.64) |
p < 0.001 | 12 months from the enrolment | |||
| Preservation of renal function (as per CKD stages) | Stage 3 to stage 2 = 3 patients; stage 3 to stage 4 = 15 patients; stage 4 to stage 3 = 103 patients; stage 4 to stage 5 = 1 patient; stage 5 to stage 4 = 4 patients; stage 5 to dialysis = 8 patients | 12 months from the enrolment | |||||
Survival or mortality
Hemmelgarn and colleagues146 and Curtis and colleagues142 compared MDC with standard care, reporting a significant survival advantage for those CKD patients attending MDC clinics. A significant reduction in the risk of death (adjusted) (HR 0.50, 95% CI 0.35 to 0.71) was observed in MDC patients compared with non-MDC patients by Hemmelgarn and colleagues,146 but no difference in hospitalisation rates were reported. Similarly, Leung and colleagues149 reported on adjusted risk reduction for mortality and ESRD (HR 0.40, 95% CI 0.23 to 0.68) for MDC compared with usual care.
Curtis and colleagues142 noted that incident dialysis patients who had received MDC had better survival on dialysis than those in standard care. In addition, the redesigned nephropathy clinic reported lower rates of mortality than two major renal studies: RENAAL (Reduction in End points in NIDDM with the Angiotensin II Antagonist Losartan) trial and IDNT (Irbesartan in Diabetic Nephropathy Trial) trial (2.2/100 person-years versus 6.8/100 person-years and 5.8/100 person-years respectively). 143 However, an RCT of MDC management found no significant survival advantage of CKD patients within MDC compared with usual care, despite heavy costs for various aspects of the MDC intervention group. 145
CKD progression
Most authors reported that MDC had a positive impact on slowing CKD progression (see Table 24). In an MDC clinic with an SCS, the median decline in GFR slowed significantly from –5.2 (–12.8 to –1.9) ml/min/1.73 m2/year before referral to –0.5 (–3.3 to 2.5) ml/min/1.73 m2/year after referral (p < 0.001). 147 Others reported that in patients with CKD stage 3, GFR decreased at a slower rate and those with CKD stages 4 and 5 had stable eGFR throughout the 15-month follow-up while receiving care within a comprehensive renal clinic involving a multidisciplinary team. 154 The diabetes clinic taking care of diabetic nephropathy patients reported lower event rates such as doubling of serum creatinine (1.4/100 person-years) and ESRD (1.1/100 person-years) after the service was redesigned compared with previous trials on management of diabetic nephropathy: REENAL trial and IDNT trial. 143 Leung and colleagues,149 reported that the rate of renal decline slowed in patients with diabetic nephropathy where pharmacist and diabetes specialist worked together.
Attitudes of patients/health-care providers
The service delivered by joint diabetes and renal clinics for the patients with established diabetic kidney disease at Eastbourne, UK, has been appreciated by patients and was considered to be a level of care expected by GPs. 152 Joint clinics have also been supported by NICE. 173
The perception of Canadian nephrologists towards MDC-based CKD clinics has been presented in one survey. 159 More than 90% of nephrologists reported that MDC-based CKD clinics were easily accessible to them. Regarding decision-making on referral to MDC clinics, most (more than 80%) of the nephrologists found calculated creatinine clearance the most useful method rather than depending on estimated months before ESRD. Fifty-seven per cent of nephrologists reported that they referred patients with a creatinine clearance of 20–29 ml/min, while around 30% reported earlier referral with creatinine clearance between 30 and 59 ml/min as the best time for referral. Others referred at lower creatinine clearance (10–19 ml/min). The survey also presented information about perceptions of the availability of multidisciplinary staff. More than 90% of nephrologists reported that they had excellent access to nurses, dieticians and social workers. Around 64% believed that pharmacists were comparatively less commonly available. According to nephrologists’ opinion, nurses provided more information about dialysis to patients than about palliative care, prognosis or pre-emptive transplant.
Overall, nephrologists (94.5%) believed that MDC-based clinics were superior to conventional clinics. Most of them (83%) also thought that this kind of clinic could be managed by nurses using algorithms, thus helping to reduce the burden on nephrologists. They were supportive of the value of MDC clinics for those with stable and slowly progressing CKD but reported that the clinics were not sufficiently funded.
Aspirational model of care
Fourteen papers describing aspirations for the care of patients with CKD were reviewed. 159–172
Two broad categories of aspirations for care were described:
-
optimal management of CKD patients
-
integrated approach for CKD management.
Optimal management
Four papers proposed similar ranges of strategies of care for the management of early CKD patients that they hoped would lead to improved outcomes. 160–163 The emphasis was on early detection of CKD and associated comorbid conditions. The proposals focused mainly on the need for delaying CKD progression, and preventing or treating complications by using timely intervention. Importantly, these papers identified the need for precise measures to stratify CKD patients into groups that may help to predict future risks. Patient education, to increase awareness of CKD and risk of comorbidities in CKD, was recommended as a part of optimal management. Moreover, two papers highlighted the importance of having co-ordinated care for the management of early CKD. 162,164
Authors proposed that implementing the strategy of optimal management and early detection of the disease may help reduce hospitalisation, morbidity and mortality, and eventually help to reduce cost. For example, identifying comorbid conditions like anaemia and CVD at earlier states, and treating them, may reduce the risk of future morbidity and mortality. Controlling BP, proteinuria and other metabolic parameters may reduce the risk of CKD-related comorbidities. Authors were proponents of the use of ACE Is and ARBs, identifying CKD at earlier stages and referring patients to the nephrologists to slow CKD progression. The use of existing data from patient database systems to develop an intervention programme to optimally managed CKD patients was suggested. 160
Integrated approach for management
Seven papers proposed the advantages of collaborative approaches in CKD management. 164,165,167–172 Involvement of multidisciplinary staff (GPs with specialist interest, specialist nurses, pharmacists, nutritionists, etc.) and co-operation between these staff may aid early referral and management. The key role of nurses was highlighted as: patient educators, care managers communicating between care providers and support staff, and following up patients to monitor their progression. 166–168 Four of the papers suggested that patients should be managed and evaluated in primary care by skilled support staff, with only complex or severe cases referred to specialists or nephrologists in secondary care. 166,168,171,172 Furthermore, they noted the importance of care plans being developed based on evidence-based practice guidelines. Recognition that CKD was a chronic and complex condition was found to be useful in supporting collaboration and education needs. 164 The proponents of an integrated approach for management also hoped that it would contribute to reducing mortality and hospitalisation and delaying progression. Moreover, this co-operative care potentially provided a mechanism to deliver optimal management of CKD at early stages and thus increase quality of care and improve quality of life of patients while reducing cost.
Similar to the above proposals, A vision for the future of renal services, 2002126 also focused on prioritising early diagnosis and treatment of those with CKD and those who were at risk of developing CKD. The authors recommended the need for clinical networks as a model of future services provision. Details of the network focused on preparation for end-stage disease and those with progressive renal disease, but did note the need to integrate services across disciplines and to deliver a flexible and appropriate care for the individual patient’s needs. They also noted the need to tackle inequalities, giving attention to the elderly, children, socially disadvantaged, ethnic minorities and those with comorbidity. 126
Key themes from aspirational proposals
Thematic review of the aspiration studies identified the following key elements to care:
Strategy for early detection
Early identification of CKD and those who are at risk of CKD was seen as critical. Screening was discussed in the context of using eGFR and albuminuria in diabetes. Screening of higher risk group patients (> 65 years of age, any form of CVD, diabetes, a family history of CKD, hypertension) was noted and development of new screening strategies focused on the link between CKD and CVD.
Measures for defining at risk groups
Although CKD could be defined in terms of serum creatinine or urinary albumin levels, GFR estimation was proposed as the most precise measure to stratify CKD risk. High risk patients such as those with CVD, hypertension and diabetes were recognised. Urinary albumin was noted to be an important, and independent, risk factor.
Strategies for delaying progression
There was a focus of attention on development and implementation of strategies to delay progression. The need to determine individualised information about a patient’s probability of progression to renal end points was a priority. Identifying comorbid conditions, with timely intervention to prevent and manage these complications, was also considered crucial. Authors cited various examples of ‘effective drug therapy’: some antihypertensives agents (ACE Is or ARBs), antilipaemic agents (statins) to halt disease progression, and treating anaemia.
Co-ordinated care
The need for co-ordinated care tailored to the patients needs was recognised. Delivery was dichotomised between the need for nephrology specialist input versus primary care. Vision of shared care models utilising multidisciplinary skill sets needed high levels of co-ordination, but offered a potential way to reduce the burden on secondary care while ensuring high-quality patient care.
Patient education
It was highlighted that patient participation in his or her own care was essential for optimal management of chronic diseases. Increasing patient awareness of CKD and associated risk factors may help reduce the development of irreversible renal damages and other complications.
Discussion
Currently, specialist renal care is widely delivered through multidisciplinary teams in secondary care, and while attention is shifting towards how to care for the many people with evidence of CKD, the focus remains on the more intensive care needs of those with advanced CKD. Integration of specialist renal care with primary care was not a major feature in the UK, beyond that of referral; although at the time of the surveys there was evidence that some shared care practices were being developed. Since the last survey, CKD was introduced into primary care QOF targets and CKD care in the UK has been undergoing a period of substantial change. In this chapter we sought to explore the literature for evidence of other models for delivering care to people with CKD who did not rely solely on early referral to a specialist nephrologist. While a number of models of care were described in the literature, disappointingly, only one RCT evaluating the effectiveness of different care models was identified. 145
Three principal models of care were reported:
-
Multidisciplinary clinics – very much developed along the lines of those for dialysis patients, but generally restricted to secondary care. Only two studies reported a primary care-based MDC where specialists and primary care practitioners worked together to deliver care to people with CKD. 147,150 These adopted a secondary care-led approach, using primary care only as a vehicle to obtain routine monitoring and referral but with most decision-making driven by specialists. In some, the wider determinants of health were addressed through support from social workers facilitating access to care and financial services, and from a range of professionals providing health lifestyle advice.
-
Structured care delivered by individual specialties – a number of papers reported the often protocol driven utilisation of particular clinical specialists to deliver components of care for people with CKD. The roles of pharmacists, nurses, nutritionalists and other medical specialists (diabetologists) were all described.
-
Educational initiatives – either directed at health-care professionals or for the patients and carers. Education was recognised as being key in underpinning the delivery of a service, although some of the MDCs reported little about the value of working together across specialties as a method for education of health-care practitioners.
However, the division, while assisting in classification and description of the types of intervention, was somewhat artificial in practice with an overlap in approaches reported for the more comprehensive care packages. Nonetheless, a substantial number of the reports described services that appeared to adopt a single model operating in isolation.
Many of the MDC reports described the separation of CKD clinics from other renal services including, in some cases, from new referrals. Where reported, clinics offered high intensity of care but with low throughput of patients; a challenge when trying to deliver care for large numbers of patients.
While information technology (IT) systems would undoubtedly have supported many of the clinics described, the innovative use of IT and virtual follow-up through the review of clinical data by a specialist, remote from the patient, was also reported. The time taken to review these ‘virtual’ records was not described and, in the absence of an RCT and long-term follow-up, the potential safety and effectiveness of this approach could not be assessed. Others utilised multidisciplinary meetings to discuss patients’ care and management, remote from the patient. Again, the time taken to undertake this work was not described.
Regardless of the care model adopted or the attributes of the model, there was evidence of positive effects with regard to clinical markers and long-term outcomes from observational studies reliant on ‘before and after’ study designs. One cohort study comparing MDC to standard care did report benefit142 but the only RCT145 found no evidence of improvements in clinical parameters, long-term survival or renal progression; a lack of benefit despite substantial additional cost. In other clinical settings, however, intensive and aggressive risk factor management has been demonstrated to be of clinical benefit in RCTs. The Steno-2 study,174 in people with diabetes and microalbuminuria, randomised people to intensive management of their diabetes and cardiovascular risk factors versus standard best practice. The clinical setting was the same, only the interventions differed between groups. Here, patients receiving intensive diabetes management had better cardiovascular (HR 0.47 for CVD, 95% CI 0.24 to 0.73) and renal outcomes (HR 0.39 for nephropathy, 95% CI 0.17 to 0.87) after follow-up of 7.8 years.
So, despite universally promising results from observational data and evaluations, the only clinical trial has failed to demonstrate clinical benefit.
All of the models that provided some level of evaluation had methodological issues. Many of the studies were descriptive, relying on individual patient clinical findings at referral versus after care for a given period. If referral reflected the first recognition and proactive management of the person’s CKD, then improvements in various clinical parameters might be expected regardless of where or how that care was given. Where evaluations of a new service were conducted, most relied on evidence of change in care or clinical parameters compared with before entry into the care programme. Without a comparator group, it is difficult to interpret the changes observed in both these study designs. Regression to the mean may account for some of the changes observed. The effect of the model of care on health outcomes is difficult to assess.
Evaluations against a control group provided this comparison but, where made retrospectively, were vulnerable to bias and gave little detail of the care received by patients. Harris and colleagues145 reported the only RCT of a nephrology case management intervention compared with standard care (general practice plus referral to specialist standard renal care as per normal) and, unlike the positive findings of other studies, they found no difference in the outcomes of patients receiving MDC care versus standard care. Despite being a reasonable quality RCT, with very similar groups at baseline, the two care models ran in the same hospital outpatient unit. Staff were independent but the opportunity for ‘contamination’ between the two groups was high. Indeed, the number of visits to the unit was similar in the intervention and standard care arms.
The review of aspirational literature identified a dichotomy in thinking about CKD management perhaps not truly reflected in the evaluation studies to date. Like the evaluation literature, there was a strong sense from many authors describing a vision for future services of the need for specialist nephrology input at the earliest opportunity in order to minimise the risk of renal disease progression. Others, however, described an approach more consistent with chronic disease management and the recognition of the need for a collaborative approach across disciplines; utilising the skills to deliver enhanced care to large numbers of people with the intensity and skill mix tailored to suit the individual patient’s clinical requirements. Notably, this literature rarely identified the uncertainty regarding what interventions work, or the lack of good quality evaluations or trials. The authors consistently reiterated beliefs and assumptions.
In this chapter we have drawn together a body of literature describing a range of potential models of care for people with CKD, beyond that of early referral to nephrologists. We have noted a number of limitations. The diversity makes this literature difficult to identify when searching both in finding search terms sufficiently broad as to find the range of care models but also when seeking publications. We have restricted searches to published literature. Additional descriptive literature is likely to exist in grey literature sources and this will have been omitted here. We are, however, confident that any trials would have appeared in published form. Data extraction was undertaken by a single reviewer using a piloted template and checked by a second reviewer. The themes reported here were developed iteratively by one reviewer as the data were analysed and checked by a second reviewer.
Conclusions
A range of different models or components of care were reported in the literature and there was some evidence of an impact on surrogate end points such as BP control and renal progression. Authors reported aspects of care that fitted well within the chronic disease care model: the need for multidisciplinary teams; good communication between clinical staff involved in care and with patients; the role of self-care and education; and the utilisation of other allied health-care professionals to deliver aspects of care. However, the literature also identified the challenge of polarisation of attitudes towards care: specialist care delivered by early referral to specialists in kidney disease versus a shared care and collaboration approach based on increasing the skills of a wider pool of health-care professionals. While tackling CKD in the context of diabetes and diabetes services was discussed, we did not identify literature reporting on approaches to tackle CKD as part of a group of conditions that increase the risk of CVD. There was once again a striking lack of high-quality trials of effectiveness. The components of the models of care reported here provide a useful source of information about the feasibility of delivering aspects of care; pilots of potential models. The only controlled trial reported compared an MDC clinic with standard case management care and found little evidence of improvements in patient care. 145 This perhaps reflects the fact that only a minority of patients have highly complex needs that gain substantial benefits from the very structured input of formal case management from an MDC (Figure 7). For many, a more straightforward care package may be optimal and, for most, education and supported self-care may be all that is required. Indeed, much of this care and education would be generic to a number of chronic conditions (diabetes, CVD and hypertension), and a combined approach that acknowledges this overlap could be trialled. Such an approach could then dovetail with screening programmes that seek to identify people at increased cardiovascular risk. 175,176 The challenge, then, is to be able to identify who requires which level of care and to ensure that people can move between levels to access the most appropriate care for them at the appropriate time. The identification of the relatively small, but important, group of people with rapidly worsening kidney function, acute kidney injury and specific renal diagnoses that are both treatable and reversible will also be critical to the success of any intervention.
FIGURE 7.
Pyramid model of population health management for long-term conditions. [Adapted from Department of Health (2004) Improving Chronic Disease Management.]177
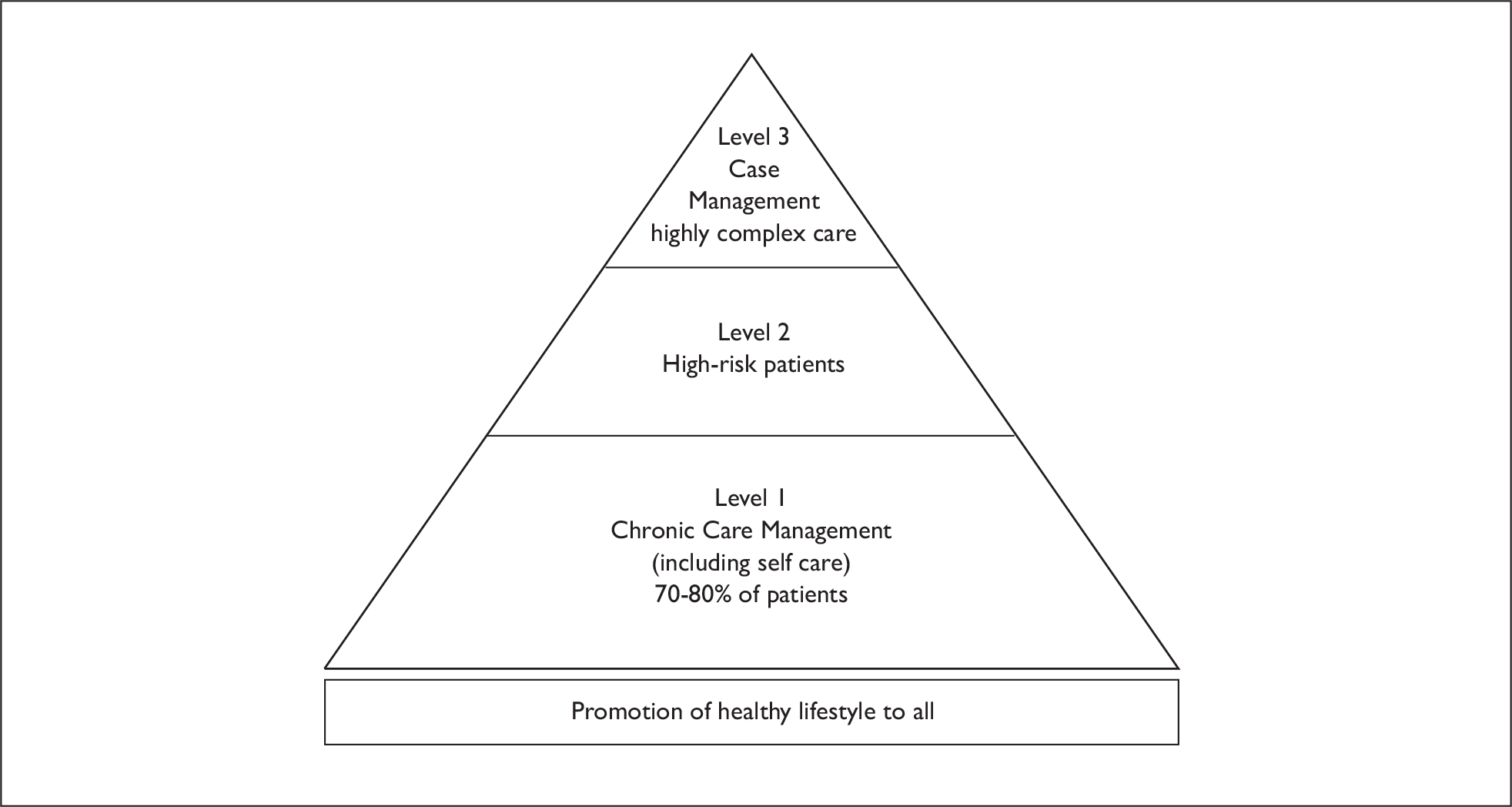
The literature described here could be viewed as feasibility studies, and any future trial of models for the management of CKD should draw on these approaches. It seems likely that a successful model of care will draw on a range of health-care skills and disciplines. High-quality RCTs are needed to assess the effectiveness of any such intervention.
Chapter 6 Cost-effectiveness and economic modelling
The aim of this chapter is to assess the existing evidence relating to the long-term cost-effectiveness of early referral strategies for patients with markers of renal disease, and to develop a new economic model to assess the cost-effectiveness of early referral strategies from the perspective of the NHS. The chapter focuses on the cost-effectiveness of interventions in individuals with non-diabetic CKD, as formal care pathways are already established for individuals with diabetes and diabetic nephropathy.
Review cost-effectiveness studies
Systematic searches of the literature revealed no studies that directly matched our inclusion criteria. Two studies were identified that assessed the cost-effectiveness of screening for proteinuria178,179 and one study assessed the cost-effectiveness of nephrology referral for patients with late stage 4 CKD. 180 The findings of these studies are summarised briefly below.
McLaughlin and colleagues180 developed a Markov model assessing the cost per life-year of nephrology referral for patients with a creatinine clearance rate of 20 ml/min (equivalent to late stage 4 CKD) compared with nephrology referral upon development of uraemia. The analysis was conducted from the perspective of the Canadian health-care provider, over a 5-year time horizon. Applying rates of renal function decline of 5.6 ml/min/year and 7.7 ml/min/year in the referral and control arms respectively (using data obtained from Canadian cohort studies), the model predicted that earlier referral would increase survival and life-years free of dialysis, and be cost saving from a health service provider’s perspective. This was based on an effect estimate obtained from a prospective study that showed education could increase dialysis free survival by an average of 4.6 months in patients with deteriorating renal function. 181 The model took into consideration ACM and total costs of care, but it is unclear whether the model captured potential differences in costs associated with cardiovascular morbidity between the two groups.
Boulware and colleagues179 conducted a modelling study to assess the cost-effectiveness of screening for proteinuria using dipstick urinalysis in adults with neither hypertension nor diabetes, and in adults with hypertension. The authors developed a Markov model that tracked renal function decline in individuals with proteinuria identified through screening, compared with renal function decline in individuals with undetected proteinuria. Those identified through screening were assumed to be treated with ACE Is which slowed progression of renal insufficiency by 30% and reduced ACM by 23%; the RR reductions were taken from a systematic review of RCTs. The study concluded that screening for proteinuria would not be cost-effective in individuals with neither hypertension nor diabetes, but would be cost-effective in individuals with hypertension [incremental cost-effectiveness ratio (ICER): US$18,621 per quality-adjusted life-year (QALY) (£11,232/QALY)]. However, the model did not appear to consider cost savings or utility gains associated with the prevention of cardiovascular morbidity.
Atthobari and colleagues178 subsequently conducted a cost-effectiveness analysis of screening for albuminuria that did take into consideration the effects of ACE Is on cardiovascular events. The economic evaluation was based on data from the Prevention of Renal and Vascular Endstage Disease Intervention Trial (PREVEND IT); a study that assessed the effect of fosinopril (an ACE I) on the incidence of cardiovascular events in individuals with albuminuria (> 15 mg/day), normal BP (< 160/100 mmHg) and normal cholesterol. 182 The study considered the costs of screening for albuminuria and treating identified cases with fosinopril, and the hospital costs associated with CVD events over a follow-up period of 46 months. Based on a non-significant risk reduction for CVD events associated with fosinopril (HR 0.87, 95% CI 0.49 to 1.57), the authors estimated that screening for albuminuria would cost €16,700 (£14,671) per life-year gained. Using bootstrap resampling to assess uncertainty, the authors estimated a 59% chance of the ICER falling below a willingness-to-pay threshold of €20,000 (£17,570) per life-year gained.
In addition to the above studies assessing cost-effectiveness of screening for proteinuria, a number of studies have assessed the cost-effectiveness of using ACE Is and ARBs in individuals with renal insufficiency. Most of these studies have been carried out for individuals with diabetes, and have found the use of these medications to be cost saving or highly cost-effective. 183–187 However, a few studies have also looked at the cost-effectiveness of ACE Is in individuals with non-diabetic nephropathies and have reported similar findings. 188,189 These studies demonstrate the potential for non-diabetic CKD management to be improved.
A report to Kidney Health Australia, identified through searches of grey literature, also suggests that improved treatment for individuals with hypertension, proteinuria, and or diabetes may offer a cost-effective option for preventing the incidence of CKD and ESRD. 190 This study made use of Markov models to assess the cost-effectiveness of various improved treatment and screening strategies for hypertension, proteinuria and diabetes. The authors concluded that intensive treatment for individuals with hypertension (without diabetes) would cost ∼A$15,589 (£8247) per QALY gained, compared with standard management. They also suggest that screening for hypertension, proteinuria and diabetes would offer a cost-effective approach to reducing morbidity and mortality associated with CKD. These cost-effectiveness estimates were modelled using data from trials of individual clinical interventions (addition of ACE Is for diabetics, intensive glycaemic control for diabetics, intensive management for individuals with hypertension, and ACE Is for those with proteinuria) and do not explicitly imply the involvement of early referral to a nephrologist.
In addition to the above economic evaluations, a number of costs of illness studies were identified through our literature searches. These studies have been reviewed by Khan and Amedia. 191 Most were based on the retrospective analysis of insurance claims of individuals with CKD in the USA. A consistent finding was that health-care expenditures increase markedly through the stages of CKD to ESRD – mainly as a result of higher rates of hospitalisations due to comorbidities. The costs peak upon transition to ESRD requiring the initiation of RRT. This pattern of expenditure demonstrates the potential for early interventions that slow CKD progression and reduce the incidence of cardiovascular events.
Economic modelling
Model structure
A Markov cohort model was developed to represent the natural history of CKD using treeage pro 2008 (Figure 8). Direct health service costs under current practice were then incorporated into the model. Following this, alternative early referral strategies were superimposed on top of the baseline model, and relative costs and consequences were assessed.
FIGURE 8.
Representation of the Markov model structure. As well as transiting down through the CKD stages, individuals can transit across the comorbidity states as they develop microalbuminuria, proteinuria and CVD. Individuals in all states can die from CVD or other causes in any cycle of the model. Not all of the possible transitions are marked on the diagram (individuals with stage 3b and stage 4 CKD can also transit to microalbuminuria, proteinuria and CVD states).
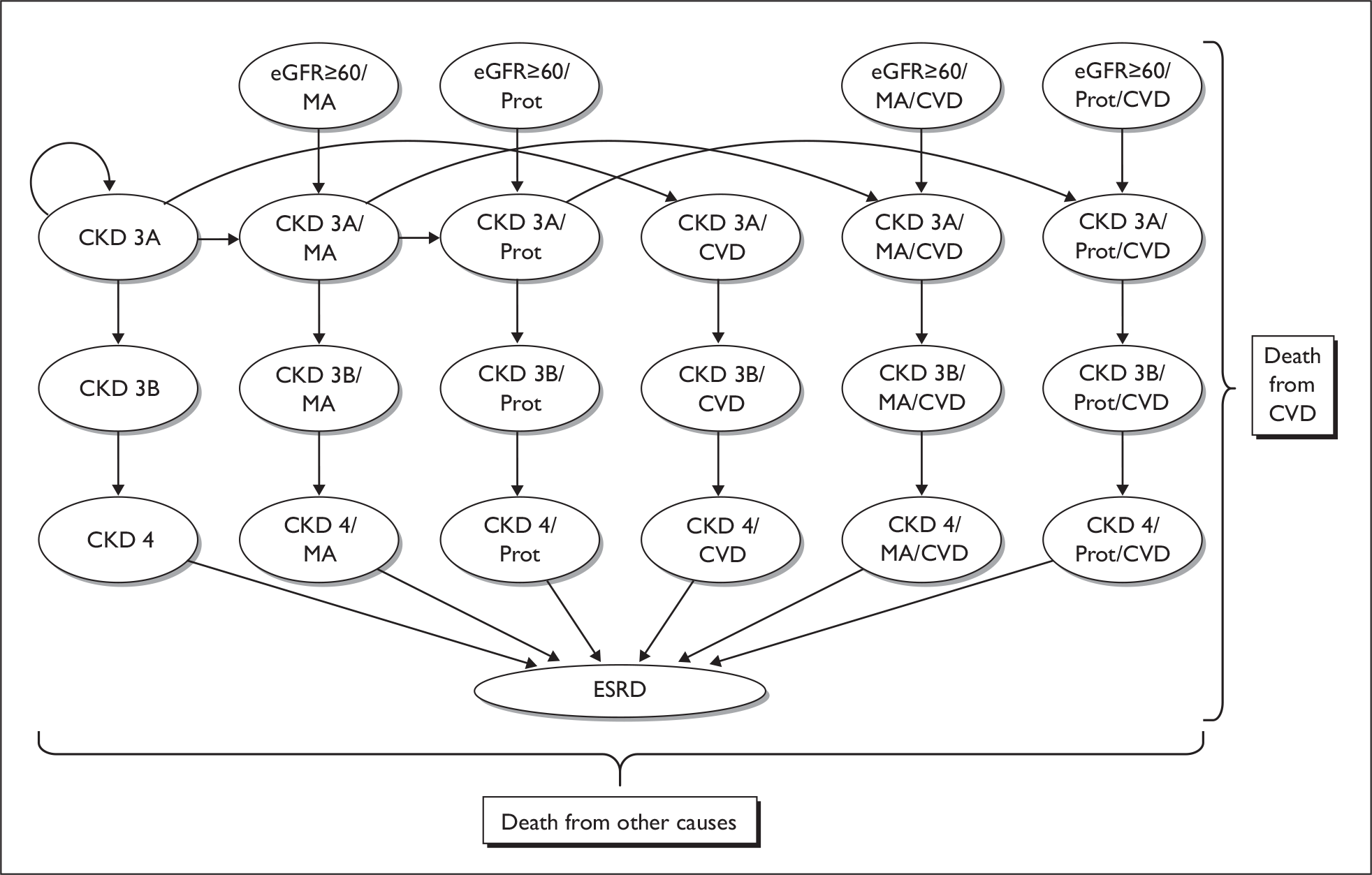
The states of the model are based on the stages of CKD as defined by the KDOQI,20 although stages 1 and 2 were combined to form a single state (eGFR ≥ 60 ml/min/1.73 m2) with microalbuminuria or overt proteinuria used as the defining marker of kidney damage, and stage 3 was separated into two states: CKD 3a (eGFR 45–59 ml/min/1.73 m2) and CKD 3b (eGFR 30–44 ml/min/1.73 m2).
In addition to the core CKD states described above, further states were defined to keep track of comorbidities known to influence CKD progression and/or the incidence of cardiovascular events; ACR 30–299 mg/g, ACR ≥ 300 mg/g and prevalent CVD. States were also defined to keep track of cardiovascular mortality and mortality from other causes.
Cohort simulation was used to analyse the model, based on annual transition and event probabilities estimated from the literature. Within each cycle of the model, proportions could die from other causes, experience fatal cardiovascular events, experience non-fatal cardiovascular events and develop ACR 30–299 mg/g and ACR ≥ 300 mg/g. A representation of the model structure is presented in Figure 8. Details of the model cohort, transition probabilities, and incorporated costs are described below. In developing the natural history model we selected the most appropriate studies from the natural history review (see Chapter 3), where quality was deemed to be adequate and reporting allowed the relevant variables to be extracted.
Cohort details
The starting point for the analysis was taken as a cohort of individuals identified as having CKD in a primary care setting, but as yet unknown to nephrology services. People with diabetes were excluded from the analysis, as in the UK they already receive annual checks for kidney disease, have a structured care programme and are more likely to be on appropriate treatments than individuals with CKD without diabetes.
As we wanted to model cardiovascular events and CKD progression according to patient history, i.e. levels of urine albumin/protein and CVD status, we attempted to identify demographic and CVD risk profile data for cohorts stratified by these variables.
In order to build up a picture of the demographic/risk characteristics for the cohort strata of interest, we used a UK study reporting demographic information and cardiovascular risk factors for 11,731 individuals with reduced eGFR, collected as part of routine practice from 17 primary care practices across Kent, Surrey and Greater Manchester (Table 25) in the UK. 192 This study also reported proportions with diabetes and pre-existing CVD. In addition we assumed that 32% of the cohort would have an ACR ≥ 30 mg/g, as reported for a US cohort identified through population screening,193 and that the mean cholesterol–high-density lipoprotein ratio would be 5.1. 194
| n = 11,731 | Proportion | |
|---|---|---|
| Demographics | ||
| Male | 3949 | 0.337 |
| Female | 7782 | 0.663 |
| Characteristics | ||
| Age (mean) years | 72 | |
| BMI (mean) kg/m2 | 27.48 | |
| SBP (mean) mmHg | 139.71 | |
| Comorbidities | ||
| Diabetes | 1568 | 0.134 |
| Hypertension | 8839 | 0.753 |
| Treated hypertension | 5739 | 0.649 |
| All CVD (IHD, PVD, HF, cerebrovascular disease) | 3691 | 0.315 |
We then stratified the original cohort by ACR level (< 30 mg/g; ≥ 30 mg/g), pre-existing CVD (yes; no) and diabetes status (yes; no) using adjustment factors estimated from a number of studies where individuals with CKD had been cross-classified by these variables (Table 26). For example, when stratifying the cohort by ACR level, the proportion of people with hypertension was calibrated to be 1.34 times higher in the 31.8% with an ACR ≥ 30 mg/g than in the 68.2% with an ACR < 30 mg/g.
| Comorbidity | With comorbidity | Without comorbidity | RR ratio | Source |
|---|---|---|---|---|
| ACR ≥ 30 mg/g | ||||
| Hypertension (%) | 78.3 | 58.3 | 1.343 | Foster 2007195 |
| Diabetes (%) | 34.9 | 9.9 | 3.525 | Foster 2007195 |
| CVD (%) | 38.6 | 16 | 2.413 | Foster 2007195 |
| % male | 63.9 | 47.2 | 1.354 | Foster 2007195 |
| Prevalent CVD | ||||
| Hypertension (%) | 84.3 | 62.1 | 1.357 | Weiner 2006196 |
| Diabetes | 24.2 | 13.9 | 1.741 | Weiner 2006196 |
| % male | 49.9 | 33 | 1.512 | Weiner 2006196 |
| Diabetes | ||||
| Mean systolic BP (mmHg) | 146 | 144 | 1.014 | Gerstein 2000198 |
| Hypertension (%) | 91.5 | 89.3 | 1.025 | Lorber 2006197 |
| Mean BMI | 31.2 | 27.6 | 1.130 | Lorber 2006197 |
Further to the adjustments outlined in Table 26, it was assumed that systolic BP would be 5 mmHg higher, and the total cholesterol/high density lipoprotein ratio 0.2 units higher in individuals with an ACR ≥ 30 mg/g, CVD or both. 195,196 Finally, in removing people with diabetes from each of the strata, adjustments were made to reflect the fact that BMI tends to be higher in these individuals. 197 The estimated cohort profiles for the four strata of interest are presented in Table 27.
| eGFR 15–59 ml/min/1.73 m2 | ||||
|---|---|---|---|---|
| ACR < 30 mg/g with no CVD | ACR < 30 mg/g with CVD | ACR ≥ 30 mg/g with no CVD | ACR ≥ 30 mg/g with CVD | |
| Demographics | ||||
| Male (%) | 0.272 | 0.412 | 0.323 | 0.489 |
| Female (%) | 0.728 | 0.588 | 0.677 | 0.511 |
| Age (mean) years | 72 | 72 | 72 | 72 |
| Risk characteristics | ||||
| BMI (mean) kg/m2 | 27.0 | 27.0 | 27.0 | 27.0 |
| SBP (mean) mmHg | 137.4 | 142.4 | 142.4 | 142.4 |
| Cholesterol–HDL ratio | 5.0 | 5.2 | 5.2 | 5.2 |
| Comorbidities (%) | ||||
| Hypertension | 62.9 | 85.5 | 81.5 | 100. |
| Treated hypertension | 40.8 | 55.5 | 52.9 | 64.9 |
| Annual CVD event risk from QRISK2 | 3.0 | 3.5 | 3.3 | 3.6 |
Transition probabilities
CVD risk estimation
Annual cardiovascular event risks for the different disease states were built up through a staged approach. Annual base risks were first estimated for each cohort stratum using the demographic/risk profiles in Table 27 and the QRISK2 (ClinRisk Ltd, University of Nottingham, UK) web-based risk calculator. 199 This is based on a CVD risk algorithm which has been developed and validated for the general population of England and Wales. 200 Adjustments were made for gender and the proportion of people with hypertension within each stratum. These risk estimates reflect the average annual probabilities of cardiovascular events in cohorts with these risk profiles, without CKD or pre-existing CVD. Included in the definition of CVD events are coronary heart disease (angina and myocardial infarction), stroke and transient ischaemic attacks. Although there is likely to be a tendency for those with an ACR ≥ 30 mg/g or with CVD to be older than those with CKD alone, we assumed a constant age of 72 years across the strata when calculating base risks for incorporation in the model. This is because Markov models have to be analysed for cohorts of a single age. In addition, the effect of increasing age on cardiovascular events was incorporated in the model using an HR for increasing age (see below).
Following estimation of the base risks, we estimated annual probabilities of CVD events for each disease state by multiplying the base risks by RRs and/or HRs for CVD events associated with reduced eGFR, ACR 30–299 mg/g, ACR ≥ 300 mg/g and pre-existing CVD (Table 28). The RRs associated with reduced eGFR, ACR 30–299 mg/g and ACR ≥ 300 mg/g were obtained from a study based on data from NHANES III. 84 This study reported RRs for cardiovascular mortality by eGFR category (15–59 ml/min/1.73 m2, 60–89 ml/min/1.73 m2 and ≥ 90 ml/min/1.73 m2) and ACR levels (< 30 mg/g, 30–299 mg/g and ≥ 300 mg/g). We assume that the RRs for any CVD event (fatal and non-fatal) would be similar. The RRs were adjusted for all the factors in Table 27 used to generate the base risks.
| Morbidity/comorbidity | HR or RR | 95% CI | Source |
|---|---|---|---|
| CKD 1 and 2 (ACR 30–299 mg/g) | 2.19 | 1.45 to 3.29 | Astor 200884 |
| CKD 1 and 2 (ACR ≥ 300 mg/g) | 3.40 | 0.99 to 8.28 | Astor 200884 |
| CKD 3–4 (ACR < 30 mg/g) | 2.36 | 1.67 to 3.34 | Astor 200884 |
| CKD 3–4 (ACR 30–299 mg/g) | 3.01 | 2.04 to 4.42 | Astor 200884 |
| CKD 3–4 (ACR ≥ 300 mg/g) | 4.35 | 2.39 to 7.90 | Astor 200884 |
| Pre-existing CVD (HR) | 1.38 | Parikh 2008194 | |
| HR for 10-year increase in age | 1.57 | 1.46 to 1.69 | Weiner 2006196 |
To estimate the increased risk of cardiovascular events in people with pre-existing CVD, we used an adjusted HR associated with prevalent CVD based on data reported by Parikh and colleagues. 194 We estimated the HR inferred by existing CVD in people with CKD by dividing the HR associated with having CKD and CVD by the HR associated with having CKD without CVD.
In order to incorporate the increased probability of cardiovascular events with increasing age, we incorporated an HR for CVD events associated with a 10-year increase in age. 196 The HR was adjusted for pre-existing CVD and CKD and other classical risk factors.
When using HRs to estimate annual event probabilities, base risks were converted to average rates before being multiplied by HRs, and then converted back into risks (probabilities). The resultant annual CVD event risks for each disease state in the model are reported in Table 29.
| CKD stage | Annual CVD event risks | |||||
|---|---|---|---|---|---|---|
| CKD | CKD with ACR 30–299 mg/g | CKD with ACR ≥ 300 mg/g | CKD with CVD | CKD with ACR 30–299 mg/g and CVD | CKD with ACR ≥ 300 mg/g and CVD | |
| Stage 1 and 2 | 0.073 | 0.113 | 0.109 | 0.169 | ||
| Stage 3a | 0.071 | 0.100 | 0.145 | 0.112 | 0.150 | 0.216 |
| Stage 3b | 0.071 | 0.100 | 0.145 | 0.112 | 0.150 | 0.216 |
| Stage 4 | 0.071 | 0.100 | 0.145 | 0.112 | 0.150 | 0.216 |
The risk estimates reported in Table 29 represent approximations of the annual risk of experiencing any CVD event (fatal and non-fatal myocardial infarction, angina, fatal and non-fatal stroke, and transient ischaemic attacks). We assume that fixed proportions of people experiencing CVD events would die as a result within the year of the event. Proportions of 25% and 50% were selected for CVD events occurring in those with CKD stage 3a, and CKD stages 3b and 4 respectively in order that the model predicted cumulative cardiovascular mortality in line with the different CVD mortality rates observed for these subgroups in similar cohorts32,194,196 (see Model validation). Given the great uncertainty surrounding these assumptions, we subjected them to extensive sensitivity analysis. For purposes of costing, 33.5% of non-fatal events were assumed to be major (myocardial infarction or stroke) and 66.5% of non-fatal events were assumed to be non-major (angina, transient ischaemic attacks) – based loosely on numbers of non-fatal major and other CVD events reported in the Heart Protection Study. 201 Again, these assumptions were subjected to sensitivity analysis.
Chronic kidney disease progression
In order to generate annual transition probabilities for CKD stage progression, we used a data set of all individuals with a recorded eGFR (calculated from recorded serum creatinine results) extracted from the Primary Care Clinical Informatics Unit (PCCIU) research database for another study. 39 The PCCIU research database comprises patient data from 320 Scottish primary care practices (∼1.8 million patients). This represents 38% of Scottish practices and has been shown to be representative of the Scottish population. We simulated CKD progression over a 5-year period using reported rates of eGFR decline by level of urine albumin/protein at baseline, and calculated the average proportion of individuals that would be expected to transit annually from each CKD state to the next state. In the first instance we applied annual rates of eGFR decline of –2.5 ml/min/year for people with a normal ACR, –3.5 ml/min/year for people with microalbuminuria and –5.5 ml/min/year for people with proteinuria as reported in the MDRD study. 202 However, application of the resultant CKD transition probabilities resulted in estimates of cumulative ESRD incidence significantly higher than the rates reported for general CKD cohorts in the literature. We therefore proportionally reduced these rates until they gave estimates of ESRD close to the cumulative 10-year incidence of ESRD observed in the study by Eriksen and Ingebretsen. 96 This study consisted mainly of individuals with early stage 3 disease (eGFR 45–59 ml/min/1.73 m2) and so probably underestimated the incidence of CKD in our cohort. The resultant transition probabilities are displayed in Table 30. We assumed that individuals in the cohort had established CKD and so, by definition, could not regress to less severe CKD states. It was also assumed that individuals could progress a maximum of one CKD stage per year.
| Reduced eGFR alone | |||||
| CKD 1 and 2 | CKD 3a | CKD 3b | CKD 4 | CKD 5 | |
| CKD 1 and 2 | |||||
| CKD 3a | 0 | 0.927 | 0.073 | 0 | 0 |
| CKD 3b | 0 | 0 | 0.952 | 0.048 | 0 |
| CKD 4 | 0 | 0 | 0 | 0.966 | 0.034 |
| Reduced eGFR with ACR 30–299 mg/g | |||||
| CKD 1 and 2 | CKD 3a | CKD 3b | CKD 4 | CKD 5 | |
| CKD 1 and 2 | 0.930 | 0.070 | 0 | 0 | 0 |
| CKD 3a | 0 | 0.895 | 0.105 | 0 | 0 |
| CKD 3b | 0 | 0 | 0.931 | 0.069 | |
| CKD 4 | 0 | 0 | 0 | 0.950 | 0.050 |
| Reduced eGFR with ACR ≥ 300 mg/g | |||||
| CKD 1 and 2 | CKD 3a | CKD 3b | CKD 4 | CKD 5 | |
| CKD 1 and 2 | 0.880 | 0.120 | 0 | 0 | 0 |
| CKD 3a | 0 | 0.833 | 0.167 | 0 | 0 |
| CKD 3b | 0 | 0 | 0.882 | 0.118 | 0 |
| CKD 4 | 0 | 0 | 0 | 0.911 | 0.089 |
Albumin–creatinine ratio
Individuals in the cohort were allowed to develop ACR 30–299 mg/g or ACR ≥ 300 mg/g over the course of the simulation. As we could find no evidence on the rate at which people with a low eGFR develop these complications, we used the rates reported for people with diabetes in the base-case analysis; 2% (95% CI 1.9 to 2.2) per year for development of ACR 30–299 mg/g, and 2.8% (95% CI 2.5 to 3.2) per year for development of ACR ≥ 300 mg/g from ACR 30–299 mg/g. 203
Mortality from other cause
In each cycle of the model, individuals experience an age- and sex-adjusted probability of dying from causes other than CVD or ESRD. These probabilities were estimated by removing deaths due to CVD and renal disease from the data used to derive the interim life-tables published by the UK Office for National Statistics. 204,205
Utilities
A recent review of the literature77 identified only one study reporting utility values (based on community preferences) for the full range of CKD states (stages 1 and 2 through to ESRD pre and post dialysis). This US study used HUI-3 to assign utility scores to 269 patients spread across the CKD stages. 78 Unfortunately this study did not report utility scores by cohort strata (microalbuminuria, proteinuria and CVD), so we had to apply the same utility scores to CKD stages regardless of complication/comorbidity status. As a result our model may underestimate QALY gains attributable to the prevention of non-fatal CVD events.
Resource use and costs
Prior to assessing the incremental cost of early referral strategies, it was first important to establish the level of care that people with reduced eGFR, identifiable through primary care registers, currently receive in primary care. Following the development of standard resource use profiles, we estimated the incremental cost of implementing formal referral strategies, at various eGFR and ACR cut-offs, to an SCS described by Jones and colleagues147 and described in Models of care.
Patients referred to a specialist either received care from nephrology outpatient clinics, or if considered stable, were referred back to primary care where they received regular clinical reviews from their GP, which were then appraised remotely by nephrologists. This intervention was selected for the model as it was the best described intervention identified in Models of care which incorporates some element of ‘early referral’. There was also some evidence that can deliver a change in outcomes.
The baseline scenario against which all referral strategies are assessed is formal referral to, and hospital-based care under, a nephrologist upon transit to stage 5 CKD (referred to as standard practice from here on). All unit costs used in the analysis are presented in Table 31. Table 32 presents estimated resource use and total costs by CKD stage and comorbidity status, pre referral.
| Average | Lower | Upper | Source of uncertainty | Source | |
|---|---|---|---|---|---|
| Clinical inputs | |||||
| Consultant-led face-to-face outpatient (first visit) | £200.00 | £101.00 | £243.00 | Quartiles | NHS reference costs (2006–7)208 |
| Consultant-led face-to-face outpatient (follow-up visits) | £114.68 | £59.24 | £129.73 | Quartiles | NHS reference costs (2006–7)208 |
| GP consultation | £30.00 | £24.00 | £34.00 | With and without qualification and direct care staff costs | Unit costs of health and social care (2007)209 |
| Practice nurse consultation | £8.00 | Unit costs of health and social care (2007)209 | |||
| Consultant result reviews (assume 10 minutes per review) | £12.17 | £5.17 | £19.17 | Lower limit assumes a registrar, upper assumes consultant carrying out reviews | Unit costs of health and social care (2007)209 |
| Drug costs (per year on treatment) | |||||
| ACE I or ARB | £98.04 | £49.59 | £146.49 | Lower limit (generic); upper limit (non-generic) | British National Formulary (2008)210 |
| Other antihypertensive drug | £103.12 | £58.32 | £96.36 | Lower limit (generic); upper limit (non-generic) | British National Formulary (2008)210 |
| Statins | £100.08 | £17.04 | £183.12 | Lower limit (generic); upper limit (non-generic) | British National Formulary (2008)210 |
| Antiplatelet agents (aspirin) | £3.36 | British National Formulary (2008)210 | |||
| Blood and urinalysis | |||||
| ACR test | £2.16 | £1.04 | £5.93 | Range from survey of providers | NICE clinical guideline (2008)211 |
| Blood tests (plasma/serum creatinine) | £3.00 | No uncertainty reported | NHS reference costs (2007)208 | ||
| Annual hospitalisation costs associated with CVD events | |||||
| CVD death | £3012.67 | £2751.30 | £3270.30 | 2.5th and 97.5th percentile of gamma distribution fitted using reported mean and standard error | Heart Protection Study Collaborative (2006)201 |
| Major non-fatal CVD event (MI or stroke) | £8044.84 | £7806.70 | £8294.10 | 2.5th and 97.5th percentile of gamma distribution fitted using reported mean and standard error | Heart Protection Study Collaborative (2006)201 |
| Other CVD event (angina or transient ischaemic attack) | £3944.85 | £3810.00 | £4091.50 | 2.5th and 97.5th percentile of gamma distribution fitted using reported mean and standard error | Heart Protection Study Collaborative (2006)201 |
| History of CVD event (but no event current year) | £247.96 | £211.40 | £291.20 | 2.5th and 97.5th percentile of gamma distribution fitted using reported mean and standard error | Heart Protection Study Collaborative (2006)201 |
| Co-morbidity status CKD stage |
CKD only | CKD with ACR > 30mg | CKD with CVD | CKD with ACR > 30mg & CVD | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3a | 3b | 4 | 3a | 3b | 4 | 3a | 3b | 4 | 3a | 3b | 4 | |
| Proportion with hypertension | 0.629 | 0.629 | 0.629 | 0.815 | 0.815 | 0.815 | 0.855 | 0.855 | 0.855 | 1.000 | 1.000 | 1.000 |
| Proportion of those with hypertension on hypertensive medication | 0.622 | 0.721 | 0.746 | 0.622 | 0.721 | 0.746 | 0.722 | 0.821 | 0.846 | 0.722 | 0.821 | 0.846 |
| Mean number of hypertensive medications per treated individual | 1.66 | 1.76 | 1.84 | 1.66 | 1.76 | 1.84 | 1.66 | 1.76 | 1.84 | 1.66 | 1.76 | 1.84 |
| Proportion of those on hypertensive medication on ACE I/ARB | 0.43 | 0.375 | 0.325 | 0.43 | 0.375 | 0.325 | ||||||
| Proportion of all those with CVD on ACE I/ARB | ||||||||||||
| Proportion of total cohort on ACE I/ARB | 0.168 | 0.170 | 0.153 | 0.218 | 0.220 | 0.198 | 0.411 | 0.411 | 0.411 | 0.411 | 0.411 | 0.411 |
| Proportion of total cohort on a statin | 0.196 | 0.227 | 0.235 | 0.253 | 0.294 | 0.304 | 0.507 | 0.507 | 0.507 | 0.507 | 0.507 | 0.507 |
| Proportion of total cohort on antiplatelet agents (aspirin) | 0.196 | 0.227 | 0.235 | 0.253 | 0.294 | 0.304 | 0.514 | 0.514 | 0.514 | 0.514 | 0.514 | 0.514 |
| Consultations | ||||||||||||
| Primary care consultations in those with treated hypertension | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| Primary care consultations in those without treated hypertension | 1 | 1 | 1 | 1 | 1 | 1 | 4 | 4 | 4 | 4 | 4 | 4 |
| Costs (£) | ||||||||||||
| Average annual cost of consultations | 65.21 | 70.82 | 72.23 | 75.62 | 82.89 | 84.72 | 120.00 | 120.00 | 120.00 | 120.00 | 120.00 | 120.00 |
| Average annual medication costs | 86.35 | 104.90 | 112.53 | 111.89 | 135.92 | 145.80 | 198.43 | 220.16 | 230.01 | 216.35 | 241.77 | 253.28 |
| Average annual health service costs for CKD and CVD management | 151.56 | 175.72 | 184.76 | 187.51 | 218.80 | 230.52 | 318.43 | 340.16 | 350.01 | 336.35 | 361.77 | 373.28 |
Table 33 shows estimated resource use and costs by CKD stage and comorbidity status, after implementation of the referral intervention. All costs are presented in 2006–7 prices.
| CKD alone | ACR > 30 mg/g | ACR > 300 mg/g | CKD with CVD | CKD with ACR > 30 mg/g and CVD | CKD with ACR > 300 mg/g and CVD | |
|---|---|---|---|---|---|---|
| CKD stages 1 and 2 | £376.56 | £780.60 | £583.96 | £839.70 | ||
| CKD stage 3a | £344.37 | £376.56 | £780.60 | £572.07 | £583.96 | £839.70 |
| CKD stage 3b | £475.15 | £532.86 | £796.10 | £584.95 | £599.02 | £850.02 |
| CKD stage 4 | £492.00 | £542.34 | £804.61 | £593.03 | £608.48 | £858.27 |
Standard practice
In order to come up with estimates of annual resource use and costs of referral by stage of CKD and level of comorbidity (CVD and ACR > 30 mg/g), we used a combination of published data and assumptions based on expert opinion.
One of the main sources of current resource use data for unreferred CKD was the study by Stevens and colleagues,192 which reported hypertension rates and antihypertensive medication use by stage of CKD for a retrospective sample of 11,731 patients with an eGFR below 60 ml/min/1.73 m2. The cohort was identified, using computerised records, from patients across 17 primary practices in England, who had a valid serum creatinine test between 1998 and 2003. The cohort was largely unknown to nephrology services.
Primary care resource use and medication costs were estimated by CKD stage for the four cohort strata described in Table 27. We based our costing, as far as possible, on resource use data reported by Stevens and colleagues. 192 However, as this study relied on data collected between 1998 and 2003, we also attempted to update the initial costing to reflect possible increases in the use of resources for these individuals in recent years. The initial estimates were used in the base-case analysis.
Consultation costs
Stevens and colleagues192 reported the proportion of people by reduced eGFR categories (stage 3a, stage 3b and stage 4 ml/min/1.73 m2) on hypertensive medication. We assumed all people on hypertensive medication192 would undergo on average four primary care consultations per year – the mean number of primary care visits reported for people with hypertension enrolled in an RCT of hypertension self-monitoring. 206 Three of these visits were costed as consultations with a practice nurse, and one was costed as a consultation with a GP. For those people without hypertension, or with untreated hypertension, we assumed one routine visit to the GP per year, unless they had comorbid CVD, in which case we assumed four GP visits per year.
Medication costs
The following data, reported by Stevens and colleagues,192 were used to build up a picture of annual medication consumption and costs by CKD stage and comorbidity status: the proportion of people with hypertension receiving any hypertensive medication; the proportion of people on hypertensive medication receiving ACE Is or ARBs; the mean number of hypertensive medications prescribed per patient with treated hypertension; and the proportion of patients with comorbid CVD receiving ACE Is or ARBs, antiplatelet agents, and lipid lowering agents. We also assumed that the level of hypertensive medication use would be 10 percentage points higher in those with comorbid CVD. As Stevens and colleagues192 did not report the proportion of people without CVD on statins and antiplatelet agents, we assumed that 50% of people without CVD receiving hypertensive treatment would also receive these medications (based on expert opinion of individuals within the research team).
For medication use under nephrology care, we assumed that 90% of all people with hypertension, an ACR > 30 mg/g or comorbid CVD would receive an ACE I.
The annual cost of being on different types of medication was estimated using unit prices from the British National Formulary, for a range of generic and non-generic drugs in each drug category (ACE Is/ARBs, other antihypertensive medications, statins, antiplatelet agents). The unit costs presented in Table 7 represent the average annual costs of being on any drug within each of the specific categories.
Total health service costs
The unit cost information in Table 31 was applied to the resource use information in Table 32 (proportions using medications and mean numbers of consultation for the different subgroups) to derive total health service costs by CKD stage and comorbidity status (see Table 32). For CKD stages 1 and 2, we assumed the same level of resource use as for people with stage 3 CKD with an ACR > 30 mg/g. We assumed that upon transit to stage 5 CKD, prior to initiation of dialysis, individuals incur the average cost of those with stage 4 CKD under hospital nephrology care. For those with stage 5 CKD on dialysis, we applied published UK estimates of the annual cost of different modes of dialysis,207 weighted according to the proportions of people on these different modes as detailed in the Renal Registry Report (2008). 7 Data from the Aberdeen nephrology clinic suggest that 40% of surviving patients will commence dialysis within a year of transiting to stage 5. For subsequent years, we assumed the percentage of surviving patients on dialysis increased to 80%, with the remaining 20% managed conservatively. Costs associated with transplantation were not factored in as it was assumed that transplant rates would be low in the aging cohort considered in the model.
In attempting to update the health service costs under current practice, to reflect possible increases in certain types of recourse use, we increased the proportion of individuals on hypertensive medications, ACE Is and statins by 10%.
Early referral strategy
In estimating the costs of a formal referral strategy for people with reduced eGFR on GP registers, we followed the description of the SIMON programme, as reported by Jones and colleagues. 147
In this shared primary and secondary care nephrology scheme, people with reduced eGFR were first referred to nephrologist for assessment. Those considered to be stable and uncomplicated were then managed under an SCS where they were monitored by nephrologists through clinical and biochemical reviews recorded in primary care. Those considered to be unstable and/or complicated were managed under hospital outpatient care, but could be referred to shared care at a later date should their condition stabilise.
The scheme required an administrative system where patient records and reviews were stored on a central database. For those under shared care, administrators sent out blood and urine test forms every 6–12 months, depending on clinical condition, and asked that the patient attend their primary care practice to have the tests performed. The patient’s BP, weight, medications and urinalysis (ACR) results were recorded by practice nurses and then sent back to the administrative staff. Results were entered into the database and nephrologists reviewed the results via an electronic system, which used specialist software to chart trends in eGFR and other blood tests. If a patient’s renal function deteriorates significantly, or there is concern about BP control, the patient can be recalled for hospital care. Through this system, nephrologists can also advise on medication use.
We used the above description along with available unit cost data and several assumptions to estimate the average annual cost of implementing this system for cohorts of patients with varying levels of renal insufficiency and comorbidity.
Consultation costs
Upon referral to nephrology services, all patients incur the cost of an initial face-to-face consultation with a nephrologist (see Table 31). Then, by CKD stage and level of comorbidity, we assume that certain proportions of patients will be considered stable enough to be managed under shared care (see below). For these people, we assume an average time to enrolment in shared care of 3.6 months, as reported by Jones and colleagues,147 and assume that on average two follow-up nephrology outpatient visits are required during this period. Once patients are enrolled in the SCS, we assume that they incur the cost of one primary care review within the year.
Those who remain under hospital care from initial referral onward incur the cost of the initial consultation followed by the cost of three follow-up outpatient visits within the year of referral.
For consultation costs in subsequent years we assume a mean number of 1.5 primary care reviews per year for those managed under shared care, and four outpatient follow-up visits per year for those managed under hospital care. Those under hospital care are assumed to also require four visits to their GP each year. The cost of a shared care review was taken as the cost of a practice nurse consultation, the cost of an ACR and serum creatinine test, plus the cost for 10 minutes of a nephrologist’s time (consultant or registrar) to review results.
Unit costs for nephrology outpatient visits were taken from the Department of Health’s NHS reference costs (2006–7)208 and the unit cost for consultations with nurse practitioners and GPs were taken from the Unit costs of health and social care 2007. 209
In addition, we applied an annual cost per patient of £5.22 to cover administrative costs for the formal referral strategy, maintenance of the database, operation of the call–recall system, and purchasing and updating of any software required for reviewing results. This is based on a previous estimation carried out by the authors (GS and PM) of the administrative costs per patient of operating a systematic screening programme for diabetic retinopathy (unpublished data). It includes the cost of running a call–recall system, of storing and maintaining patient’s data electronically on a central server, and of purchasing specialist software to aid the grading process.
Proportions under shared care and hospital care
Assumptions were made regarding the proportions of people who would be managed under shared care and hospital care by CKD stage and level of comorbidity. We assumed that 50% of those with stage 3b or stage 4 CKD (ACR < 300 mg/g) would be managed under shared care, and that 100% of patients with an ACR > 300 mg/g would be retained for management under hospital care. For those with stage 3a CKD, we assumed that 75% of those with an ACR < 300 mg/g would be managed under shared care, and that 100% of patients with an ACR > 300 mg/g would be managed under hospital care.
Medication costs
We assumed that under the formal referral strategy, the proportion of people with hypertension on any hypertensive medication would increase by 10 percentage points compared with standard practice (lower resource use scenario).
For those under hospital care after initial referral, we assumed that 90% of all people with hypertension, an ACR > 30 mg/g or comorbid CVD would receive an ACE I or ARB. For those under shared care, we inflated the proportions of individuals on ACE Is or ARBs in primary care (under current practice) using multipliers estimated from the study by Jones and colleagues;148 the proportion using ACE Is or ARBs increased by 58% for those managed under shared care after referral to the SIMON programme. We also applied proportional increases in the use of lipid lowering agents and aspirin, as reported for all patients enrolled in the SIMON programme, to estimate the levels of use of these medications under the formal referral strategy.
Total health service costs
Using the above assumptions, we estimated average annual costs of care by CKD stage and level of comorbidity, under a formal early referral programme (see Table 35). In addition, we assumed that people with stages 1 and 2 CKD would incur the same costs as those with stage 3a CKD with an ACR > 30 mg/g. For those with stage 5 CKD, prior to initiation of dialysis, we assumed the average annual cost across comorbidity groups in those with stage 4 CKD. The same assumptions were applied, as described above, for individuals on dialysis.
Additional hospital costs associated with CVD events
Costs associated with CVD events were taken from a published cost-effectiveness study which assessed patient level hospitalisation costs associated with major cardiovascular events (myocardial infarction, stroke), other CVD events (angina, transient ischaemic attacks, etc.) and CVD deaths. 201 This study also reported hospitalisation costs in the years following CVD events, when no other CVD events occurred (see Table 7). These costs were applied in the model as transition costs. Given the high CVD mortality risk in people with ESRD (∼0.125 per year), we assumed that 50% of these people would experience a CVD event each year; with a CVD event fatality rate of 25%, this results in an annual risk of CVD mortality of 0.125. Those experiencing non-fatal CVD events incur the associated hospitalisation costs.
Effectiveness
In the absence of robust effectiveness evidence for the shared care strategy reported by Jones and colleagues,148 we applied a relative effect estimate obtained from a cohort study assessing the impact of nephrology referral on CKD progression and ACM, assuming that the shared care strategy might have a similar effect on CKD progression and CVD. Orlando and colleagues111 reported HRs associated with early referral for a composite end point of progression to the next stage of CKD or death. These HRs were reported for each CKD stage and were similar for CKD stages 3 and 4 (0.80, 95% CI 0.61 to 0.90 and 0.75, 95% CI 0.45 to 0.89 respectively). Given the lack of statistically significant difference between these estimates we assumed a constant HR of 0.8 associated with early referral across stages 3 and 4. Although Orlando and colleagues111 did not report the impact of early referral on CVD events separately, many of the deaths occurring in the cohort were due to CVD causes. We therefore applied the HR directly to the CKD transition probabilities and CVD event risks used in the natural history model. Given the large uncertainty surrounding the relative effectiveness of early referral, we varied this parameter substantially in the sensitivity analysis.
Cost-effectiveness analysis
In the first instance we assessed the incremental cost-effectiveness of early referral for everyone with an eGFR below 60 ml/min/1.73 m2 (CKD 3a) compared with referral upon transit to stage 5 CKD (from here on referred to as standard practice). Although this may no longer represent current practice in the UK, we decided to use this as the base comparator as it provides a useful reference point against which to compare all referral cut-offs incrementally. We then assessed the incremental cost-effectiveness of scenarios where referral occurs only for those with an eGFR below 45 ml/min/1.73 m2 (CKD 3b), or below 30 ml/min/1.73 m2 (CKD 4). Under these scenarios we assumed that those above the thresholds would experience the same CVD event risks and transition probabilities as those under standard care, but that they would incur an eGFR and ACR monitoring cost; these individuals would have to be monitored in primary care in order to be picked up and appropriately referred upon falling below the thresholds. The cost of monitoring was taken as the cost of two consultations per year with a practice nurse for urinalysis and a plasma creatinine test. We also assumed that monitoring in primary care, under this referral strategy, would incur the same administrative costs as referral to the nephrology SCS (£5.22).
We then assessed the cost-effectiveness of referring only those people with ACRs over 30 mg/g or 300 mg/g (microalbuminuria or proteinuria respectively). Finally, we assessed the cost-effectiveness of referring anyone with stage 3b CKD and an ACR > 30 mg/g, and anyone with stage 3b or an ACR > 300 mg/g. The latter strategy is similar to referral criteria recommended in recent clinical guidelines on the management of CKD. 212 The model was run over a 35-year time horizon using a discount rate of 3.5% for future costs and consequences. Discounting was applied to adjust for positive time preference: the observation that society prefers to receive benefits in the present and incur costs in the future. The discount rate currently recommended by the UK Treasury (http://www.hm-treasury.gov.uk/) is 3.5%.
The cohort was initially distributed across the CKD and comorbidity states (Table 34) according to proportions reported by Stevens and colleagues. 192 Within each CKD category we applied proportions with microalbuminuria and proteinuria as reported for the NHANES III cohort. 193 Given that CVD prevalence is higher in those with microalbuminuria and proteinuria, we adjusted the proportions with CVD in the microalbuminuria/proteinuria states accordingly.
| CKD alone | ACR > 30 mg/g | ACR > 300 mg/g | CKD with CVD | CKD with ACR > 30 mg/g and CVD | CKD with ACR > 300 mg/g and CVD | |
|---|---|---|---|---|---|---|
| Stage 3a | 0.447 | 0.070 | 0.023 | 0.112 | 0.066 | 0.022 |
| Stage 3b | 0.108 | 0.009 | 0.003 | 0.051 | 0.030 | 0.010 |
| Stage 4 | 0.012 | 0.004 | 0.008 | 0.004 | 0.008 | 0.013 |
Sensitivity analysis
Following the base-case analysis we explored the impact of varying uncertain model parameters and assumptions. The model was rerun for the following scenarios, most of which are biased against early referral:
-
Annual rates of eGFR decline were doubled.
-
The risk of ACR > 30 mg/g development was set to zero.
-
CVD event risks were halved.
-
The effect of nephrology referral on CVD events was set to zero.
-
The effect of nephrology referral on eGFR decline (CKD progression) was set to zero.
-
The effect of nephrology referral on CVD events and eGFR decline was simultaneously halved.
-
The effects of nephrology referral on CVD events and eGFR decline were halved and constrained to last 5 years (the median length of follow-up in the study by Orlando and colleagues). 111
-
Costs for standard care were set at their upper limit.
-
Costs of care under early nephrology referral were doubled.
-
Costs associated with fatal and non-fatal CVD events were varied within the 95% confidence limits of their assigned distributions (see Probabilistic sensitivity analysis).
The cost of caring for people with ESRD was also subjected to sensitivity analysis. For the lower limit we applied the lowest dialysis cost estimates reported by Baboolal and colleagues207 and also assumed that only 70% of patients with ESRD would end up on dialysis, i.e. 30% would be managed conservatively. For the upper limit we applied high dialysis cost estimates207 and assumed that 60% of patients would commence dialysis within a year of transiting to ESRD, and that the proportion on dialysis would subsequently increase to 90%. In addition, we explored the impact of allowing for increasing cardiovascular event rates by CKD stage, and assessed the potential impact of allowing for non-linear rates of eGFR decline (by applying higher rates of eGFR decline for people with stage 4 CKD). Finally, we considered a scenario where individuals with an ACR ≥ 30 mg/g were considered separately from the main cohort.
Probabilistic sensitivity analysis
The impact of joint uncertainty across all model parameters was assessed using probabilistic sensitivity analysis. Monte Carlo simulation was employed whereby values were simultaneously selected for each parameter from an assigned distribution and the results recorded. The process was repeated 1000 times to give an estimate of the sampling distribution of cost and effect differences between the referral strategies. These results were then used to generate cost-effectiveness acceptability curves.
Gamma distributions were fitted to all cost parameters. As we had no information on the statistical precision of our CKD cost estimates (under standard practice), base-case costs were treated as means for these parameters and variances were selected so that our feasible high cost estimates fell below the 97.5th percentiles of the resultant distributions. For CKD costs under nephrology referral, distributions were centred on our base-case estimates and assigned variances so that feasible high estimates fell within the 95% CIs of resultant distributions. The same principals were followed when assigning distributions to costs associated with ESRD. For costs associated with cardiovascular events, we applied gamma distributions using means and reported standard errors. 201
For probabilities of CKD stage progression we assigned beta distributions. We centred these distributions on the base-case estimates and selected variances so that high estimates fell within the 97.5th percentiles of the resultant distributions. For probabilities of developing microalbuminuria and proteinuria, we assigned beta distributions using point estimates and CIs reported for individuals with diabetes. 203 For RRs of CVD events conveyed by CKD, ACR > 30 mg/g, and ACR > 300 mg/g, we assigned log normal distributions using reported point estimates and CIs. 84 The same approach was used to assign a log normal distribution to the HR associated with nephrology referral. 111 For CVD event fatality rates, and the ratio of major to minor CVD events (used in the cost calculation), we reduced and increased point estimates by 50% and assigned uniform distributions.
Given the uncertainty underlying our effectiveness estimate, we also ran a probabilistic sensitivity analysis where the distribution for this parameter was centred on a 10% risk reduction (as opposed to a 20% risk reduction).
Model validation
The predicted survival curve for the CKD cohort (without early referral) was compared with the survival curve for an age- and sex-matched cohort of the UK general population (Figure 9). As anticipated, predicted life expectancy was lower for the CKD cohort than for the age- and sex-matched general population. Our model predicts a reduction in life expectancy of 2.5 years, from 13.45 years to 10.93 years.
FIGURE 9.
Predicted survival curve compared with the sex- and age-matched survival curve for the UK general population. CKD, chronic kidney disease.
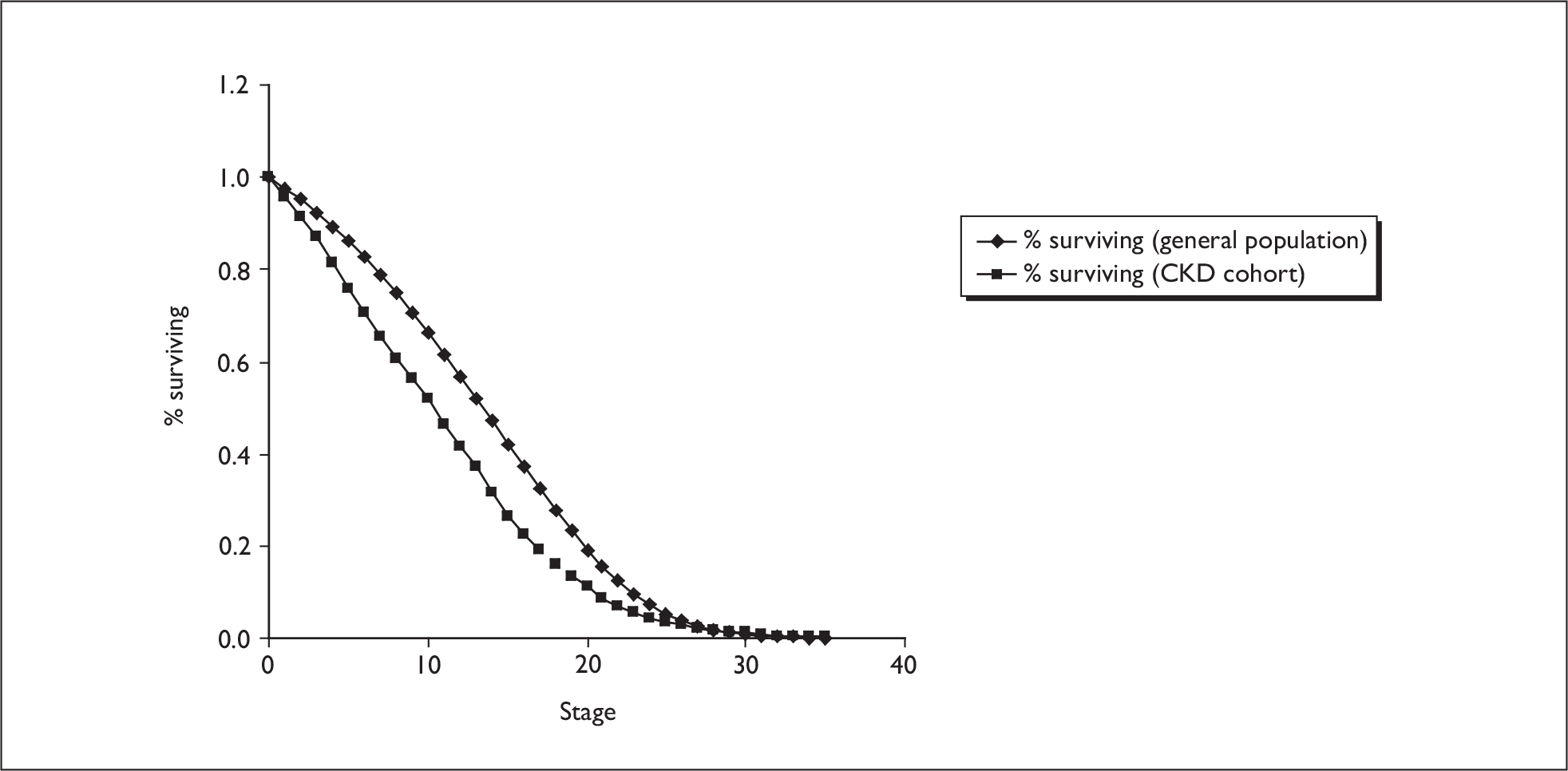
Figure 10 shows the cumulative incidence of ESRD, cardiovascular mortality and other cause mortality predicted by the model using the base-case parameter estimates and assumptions. Values reported in the literature for these outcomes in CKD cohorts vary widely. To give some examples, Menon and colleagues213 reported a 10-year cumulative incidence for ESRD of around 50% for those with a baseline eGFR between 24.5 and 55.5 ml/min/1.73 m2 enrolled in the MDRD study. However, about 50% of individuals in this cohort had either polycystic or glomerular disease. Wakai and colleagues214 reported a 7-year cumulative incidence for ESRD of 23.3% in a Japanese cohort with immunoglobulin A nephropathy. On the other hand, Eriksen and Ingebretsen96 reported a cumulative 10-year incidence for ESRD of only 4% in a cohort of individuals with stage 3 CKD (identified through routine clinical measurements).
FIGURE 10.
Predicted cumulative incidence of end-stage renal disease (ESRD), cardiovascular mortality and mortality from other causes. CVD, cardiovascular disease.
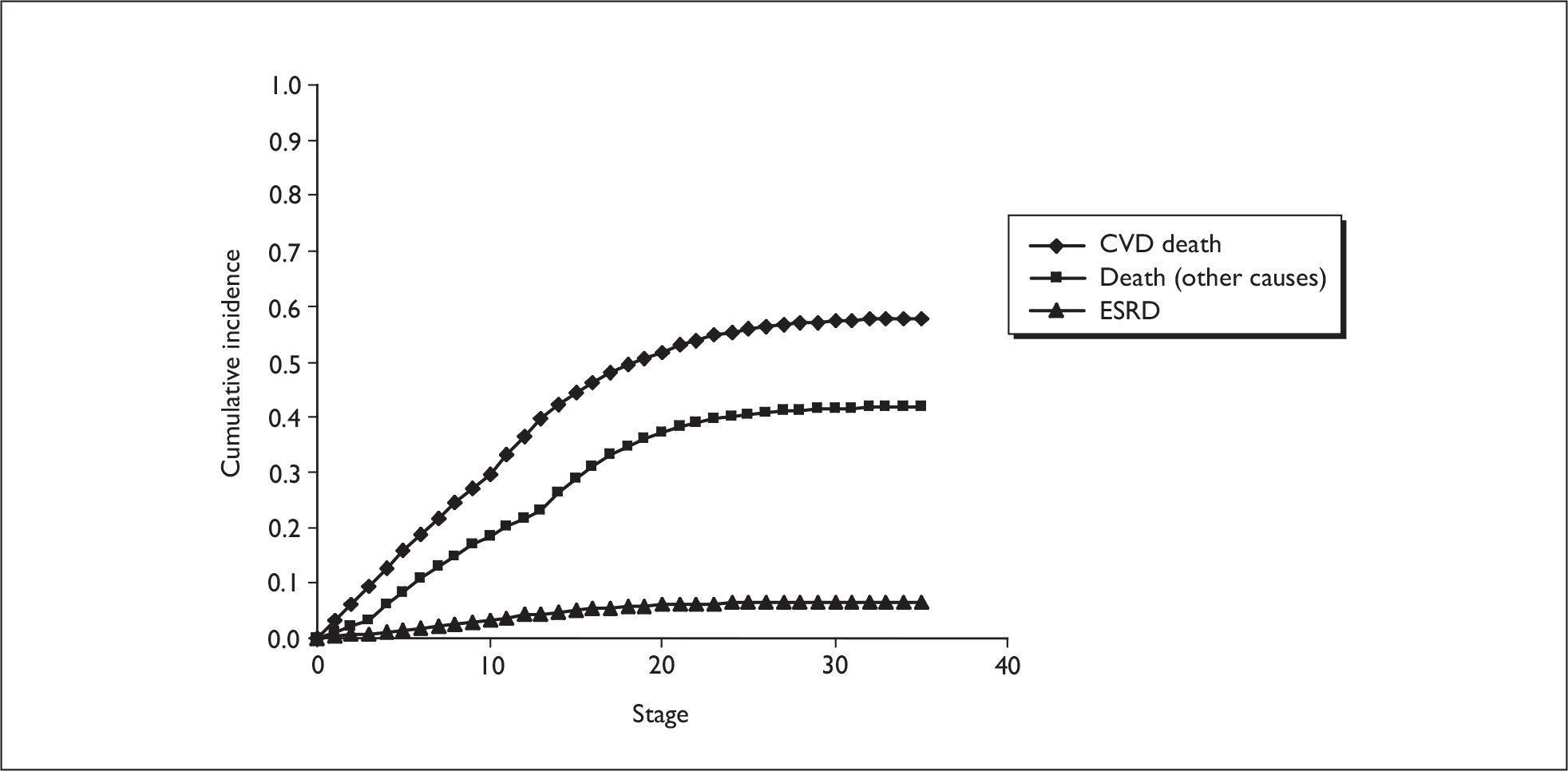
The corresponding 10-year cumulative incidence of ESRD predicted for the cohort modelled in the current analysis is 3.5%, indicating that our estimates are on the conservative side. We assessed the impact of increasing CKD progression rates through sensitivity analysis.
The 10-year cumulative incidence of cardiovascular mortality predicted by the model is 30% (Figure 10). Comparisons with estimates from published cohort studies are complicated by the fact that few studies have looked at long-term cardiovascular outcomes in CKD cohorts identified through case finding in general practice. Parikh and colleagues194 report a 10-year cumulative incidence for cardiovascular mortality of 16% and 21% for groups with stage 3a and 3b CKD respectively with no pre-existing CVD. Hallan and colleagues,32 on the other hand, report higher 8-year cumulative incidence rates of approximately 20% and 40% for cohorts with stage 3a and 3b CKD respectively (including individuals with pre-existing CVD and diabetes). However, Weiner and colleagues196 report a lower 10-year cumulative incidence of ∼35% for a composite outcome of myocardial infarction, fatal coronary heart disease, ACM and non-fatal stroke. Although the cohort in this latter study consisted of individuals identified through screening, rather than individuals picked up as part of routine clinical practice, it raises the possibility that our model may be overestimating fatal and non-fatal CVD events. Given the variation in reported estimates, we subjected the CVD event risks and event fatality rates to extensive sensitivity analysis.
Results
The base-case results are presented in Table 35 and Figure 11. The axis of Figure 11 indicates that under baseline parameter estimates and assumptions, all strategies generate more QALYs than the practice of referral upon transit to CKD stage 5 (standard practice). Referral for everyone with an eGFR below 30 ml/min/1.73 m2 (CKD 4) had an ICER of £5923 compared with standard practice.
| Strategya | Total cost | Incremental cost | Effectiveness (QALYs) | Incremental effectiveness | ICER |
|---|---|---|---|---|---|
| Standard practice | £11,796 | 5.579 | |||
| Refer at CKD 3a | £13,487 | £1691 | 5.992 | 0.413 | £4091 |
| Refer at CKD 3b | £12,808 | £1012 | 5.811 | 0.232 | £4352 |
| Refer at CKD 4 | £12,129 | £332 | 5.635 | 0.056 | £5923 |
| Refer ACR 30–299 mg/g | £12,596 | £800 | 5.733 | 0.154 | £5194 |
| Refer ACR ≥ 300 mg/g | £12,308 | £512 | 5.628 | 0.049 | Dominated |
| Refer at CKD 3b or ACR ≥ 30 mg/g | £13,051 | £1255 | 5.870 | 0.291 | £4313 |
| Refer at CKD 3b or ACR ≥ 300 mg/g | £12,915 | £1118 | 5.827 | 0.248 | £4508 |
FIGURE 11.
Base-case cost-effectiveness results. ACR, albumin–creatinine ratio; CKD, chronic kidney disease; QALYs, quality-adjusted life-years.
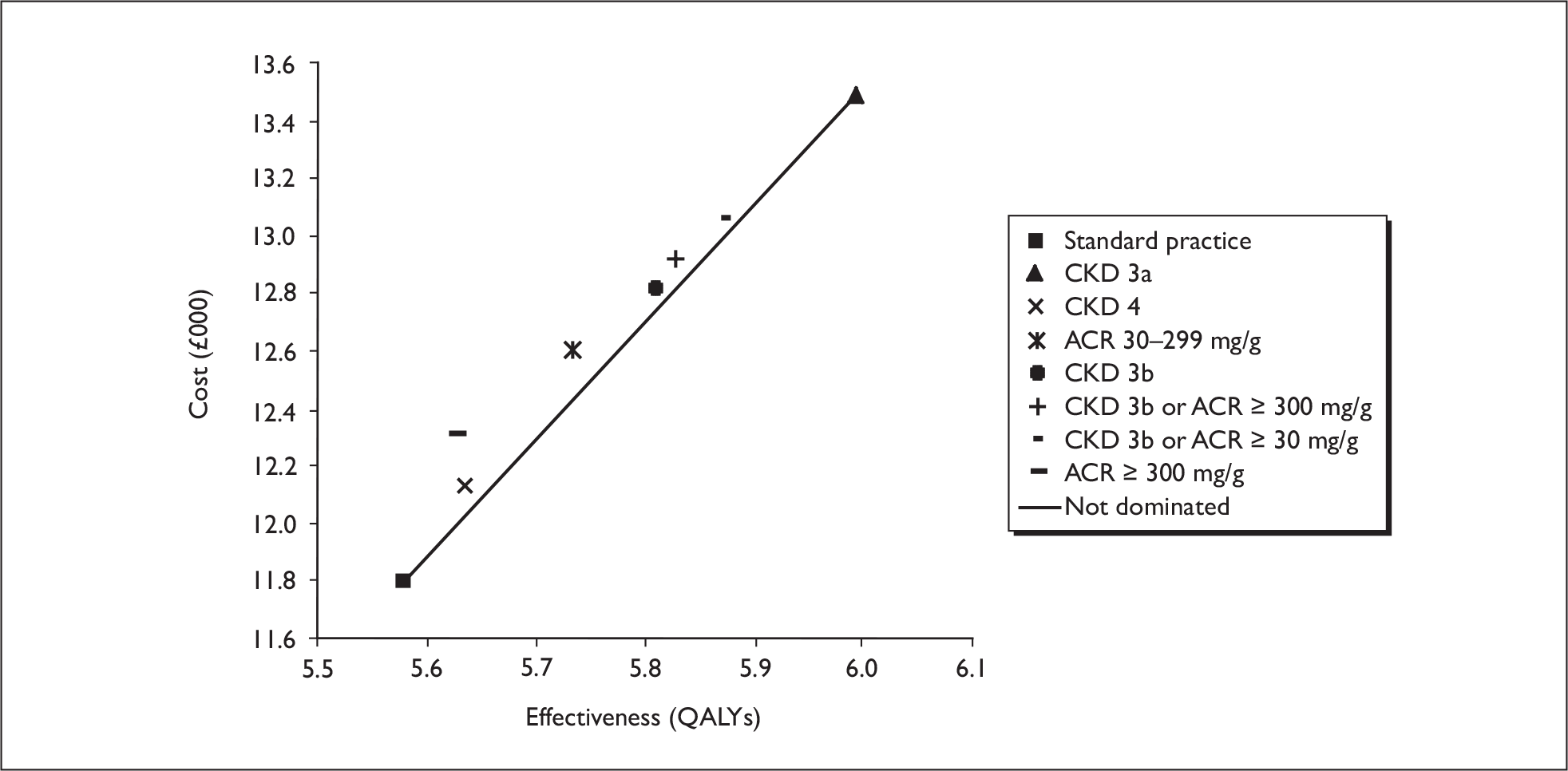
Referral for everyone with an eGFR below 60 ml/min/1.73 m2 (CKD 3a) generated the most QALYs and, compared with referral for everyone at CKD 4, had an ICER of ∼£3806 per QALY. Compared with referral for everyone at CKD 3b, referral at CKD 3a had an ICER of £3751 per QALY. The referral strategy based purely on the presence of proteinuria was dominated by the strategy of referral at stage 4. Compared with strategies of referral for those with ACR > 30 mg/g only, those with CKD 3b or ACR > 30 mg/g, or those with CKD 3b or ACR > 300 mg/g, referral at stage 3a had an ICER of ∼£3440 per QALY, £3573 per QALY and ∼£3473 per QALY respectively. Thus CKD 3a is the preferred strategy from the base-case analysis.
The QALY gains associated with early referral are attributable to survival improvements (Figure 12) and a reduction progression, and in the cumulative incidence of ESRD (Figure 13). Compared with referral upon transit to stage 5 CKD, referral at CKD 3a is associated with an increase of 0.605 discounted life-years (0.97 undiscounted life-years) and an 18% reduction in the cumulative incidence of ESRD.
FIGURE 12.
Survival curves with and without early referral to nephrology services (referral for everyone with eGFR < 60 ml/min/1.73 m2). CKD, chronic kidney disease.
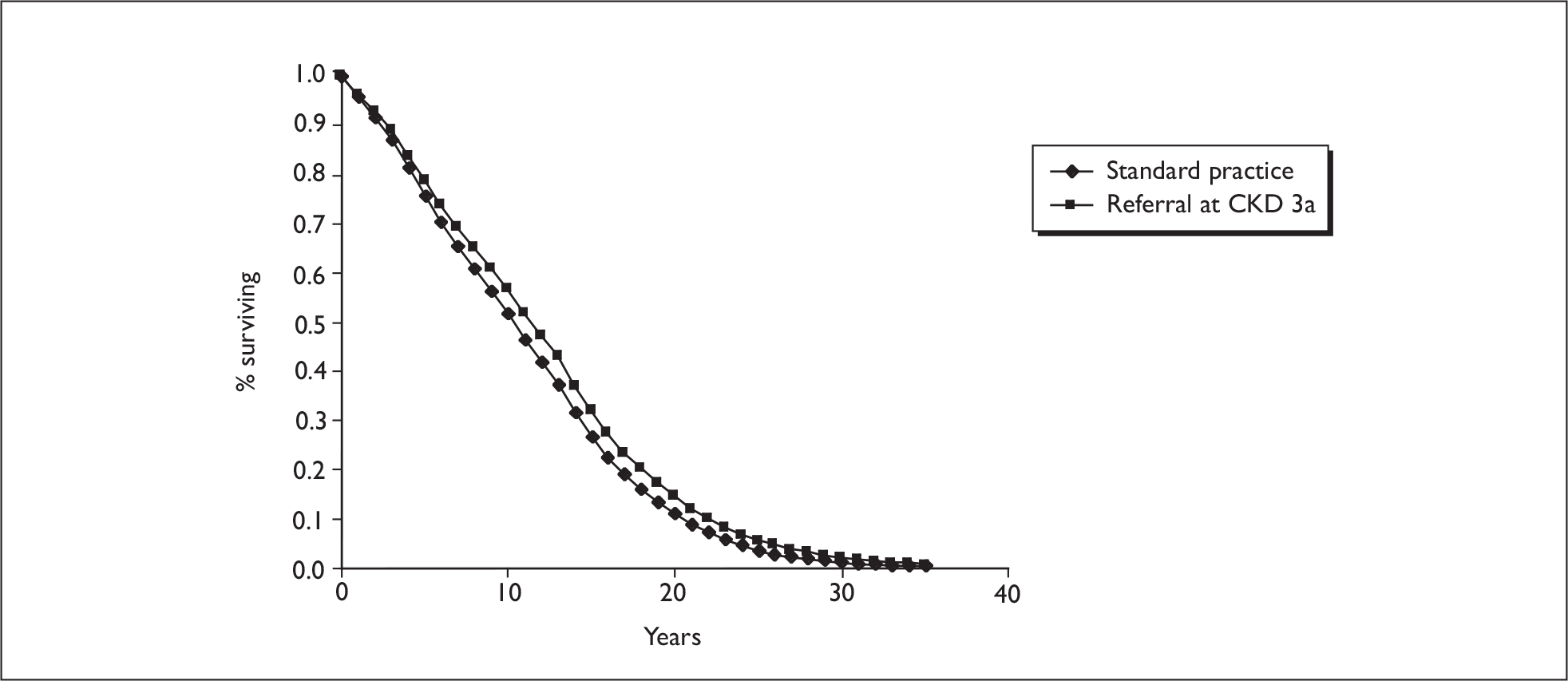
FIGURE 13.
Cumulative incidence of ESRD with and without early referral to nephrology services (referral for everyone with eGFR < 60 ml/min/1.73 m2). CKD, chronic kidney disease.
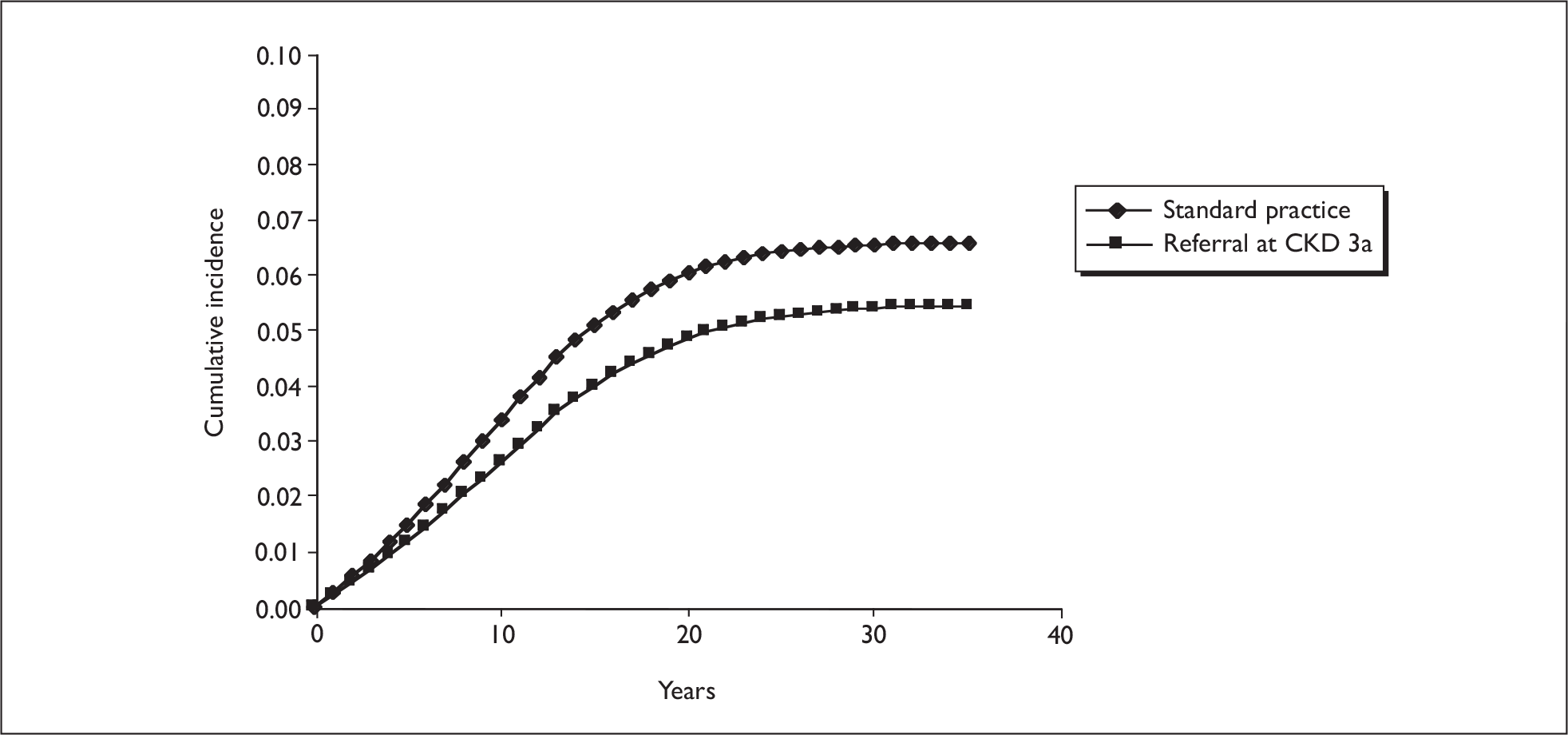
Deterministic sensitivity analysis
The findings of various deterministic sensitivity analyses are presented in Table 36.
| Scenarios | Incremental cost | Incremental effectiveness (QALYs) | ICER |
|---|---|---|---|
| Refer CKD stage 3 (base case) | £1691 | 0.413 | £4091 |
| Annual rates of eGFR decline doubled | £388 | 0.437 | £888 |
| Risks for ACR > 30 mg/g development are zero | £2031 | 0.322 | £6314 |
| CVD event risks halved | £1659 | 0.337 | £4923 |
| No direct effect of referral on CVD events | £1730 | 0.087 | £19,885 |
| Zero effect of referral on CKD progression | £2631 | 0.230 | £8218 |
| Effect of referral on CKD progression and CVD events halved | £2118 | 0.199 | £10,662 |
| Effect of referral on CKD progression and CVD events halved and constrained to last 5 years | £2360 | 0.095 | £24,908 |
| High costs for standard practice | £1430 | 0.413 | £3460 |
| Costs of care under nephrology referral doubled | £6624 | 0.413 | £16,027 |
| Lower limit for CVD event costs | £1708 | 0.413 | £4132 |
| Lower limits for ESRD costs | £1830 | 0.413 | £4428 |
| Discount rate 6% | £1449 | 0.308 | £4704 |
| 10-year time horizon | £1257 | 0.154 | £8158 |
| Costs under early nephrology referral doubled, effect sizes halved, base risk for ACR > 30 mg/g development halved | £6856 | 0.200 | £34,323 |
The model results were most sensitive to underlying rates of eGFR decline, the underlying risk of developing ACR > 30 mg/g, the effect of referral on eGFR decline (CKD progression) and the costs of care under formal early nephrology referral. When we halved the rates of eGFR decline, the model predicted a cumulative 10-year incidence of ESRD below that reported by Eriksen and Ingebretsen. 96 However, early referral remained cost-effective under this specification, as it did under all other one-way sensitivity analyses presented in Table 36.
In addition to the scenarios presented in Table 36, halving and doubling CVD event fatality rates did not alter the overall findings, with referral at CKD 3a (< 60 ml/min/1.73 m2) remaining the preferred strategy across all values.
When several parameters were simultaneously weighted against early nephrology referral, the ICER for referral at CKD 3a approached a value unlikely to be considered cost-effective (final row of Table 36).
In order to assess the potential implications of a non-linear pattern of eGFR decline, we modelled a scenario where the rate of eGFR decline increases at stage 4 compared with stages 3a and 3b. For this analysis we used the rates of decline reported in the MDRD study202 for individuals with stage 4 CKD, while maintaining the lower rates of decline for those with 3a and 3b. This improved the cost-effectiveness of all referral options. Compared with referral at stage 5, the ICERs for referral at stages 4, 3b and 3a decreased to £3103, £2817 and £2954 per QALY respectively. Compared with referral at stage 4, the ICER for referral at stage 3b was £2729 per QALY, and compared with referral at stage 3b, the ICER for referral at stage 3a dropped to £3132 per QALY.
Adjustment of cardiovascular events rates by CKD stage, to give a pattern of increasing cardiovascular mortality consistent with data reported by Go and colleagues,75 was found to have little impact on cost-effectiveness. Referral at stage 3a remained the most cost-effective strategy under this scenario, with an ICER of £4360 per QALY versus standard practice, and an ICER of £4011 and £4133 per QALY versus referral at stage 4 and stage 3b respectively.
Finally, we explored a scenario where individuals with an ACR ≥ 30 mg/g were considered separately. Although early referral in this group saves more QALYs on average, compared with the CKD cohort as a whole, average costs are also higher owing to the higher costs of managing this group under the early referral scheme. Under this scenario the ICERs for referral at stage 3a were £4009, £3951 and £4074 compared with standard practice, referral at stage 4 and referral at stage 3b respectively.
Probabilistic sensitivity analysis
Figure 14 plots the probability of each strategy being considered the most cost-effective option for different values of societal willingness to pay for an additional QALY, using optimistic assumptions about effectiveness of early referral.
FIGURE 14.
Cost-effectiveness acceptability curves for alternative referral strategies. ACR, albumin–creatinine ratio; CKD, chronic kidney disease.
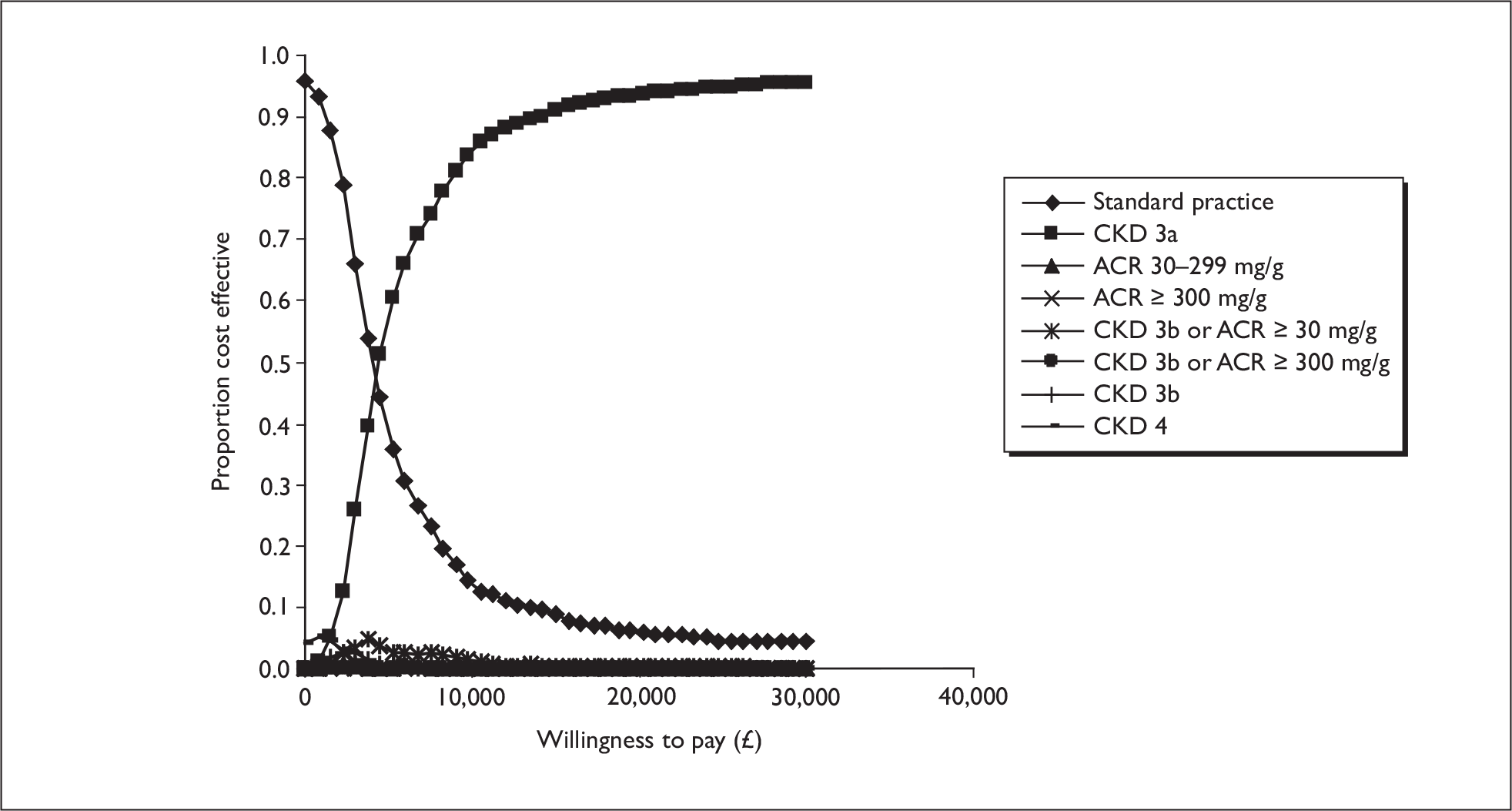
Above a willingness-to-pay threshold of ∼£4100, referral for everyone with an eGFR < 60 ml/min/1.73 m2 (referral at CKD 3a) has the highest probability of being the most cost-effective option.
However, when the distribution for the effectiveness of early referral is centred on a 10% risk reduction (for CKD progression and cardiovascular events) and constrained to last 5 years, the acceptability curve indicates only a 55% chance of early referral (at stage 3a) being cost-effective at a willingness-to-pay threshold of £30,000 per QALY (Figure 15).
FIGURE 15.
Cost-effectiveness acceptability curves for alternative referral strategies when baseline CKD progression rates are centred on feasible low estimates. ACR, albumin–creatinine ratio; CKD, chronic kidney disease.
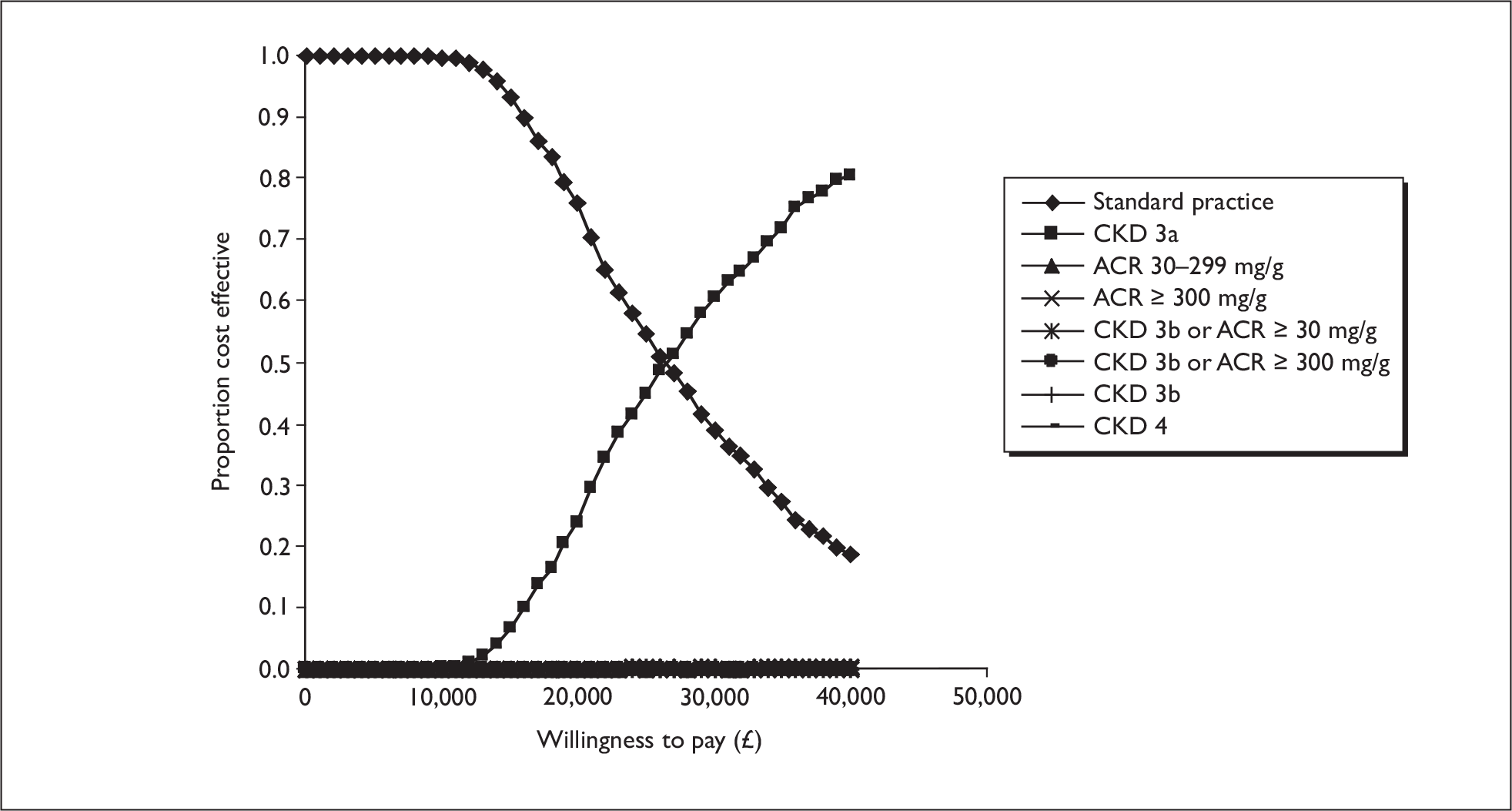
Discussion
This modelling exercise has attempted to assess the cost-effectiveness of referring individuals with markers of renal disease (based on various eGFR and ACR cut-offs) to a shared care nephrology programme. The baseline strategy against which the early referral strategies are compared is referral to nephrology upon transit to stage 5 CKD. Although this may not reflect current practice, it provides a useful baseline against which to compare the alternative referral cut-offs incrementally.
Results of the base-case analysis suggest early referral may offer an efficient use of scarce health service resources. All strategies produced more QALYs than standard practice (referral upon transit to stage 5 CKD). Referral for everyone with an eGFR below 30 ml/min/1.73 m2 (stage 4 CKD) produced 0.056 additional QALYs per patient at an additional cost to the NHS of £332 per patient (ICER: £5923 per QALY). Compared with referral upon transit to stage 4 CKD, referral at stage 3b increases the number of QALYs gained (0.176) for a increase in cost of £679 (ICER: ∼£3857 per QALY). Referral at stage 3a again increases the number of QALYs gained (0.181) compared with referral at stage 3b, with an ICER of £3751 per QALY. Thus, under the base-case parameter values and assumptions, referral at stage 3a is the preferred option on grounds of cost-effectiveness.
Referral for everyone with stage 3b CKD, or ACR > 30 mg/g, is more effective and more costly than referral based on an eGFR < 45 ml/min alone, as these strategies reach individuals at stage 3a who have evidence of kidney damage. Compared with referral at CKD 3b, they have higher ICERs than referral for everyone with stage 3a CKD (£4119 and £6625 per QALY versus £3751 per QALY respectively), due to the fact that they result in no reduction in progression or cardiovascular event rates for the large portion of the cohort with stage 3a CKD alone. However, when the group with microalbuminuria or proteinuria is considered separately, the ICER for referral at stage 3a is slightly more favourable than the ICER for referral at stage 3a for the cohort as a whole (£4009 versus £4091 relative to standard practice respectively).
The superiority of earlier referral observed in the model is due to the fact that as patients progress to more severe disease states, they experience higher costs associated with CKD management and experience a higher risk of cardiovascular events and death. The costs incurred in preventing progression to more severe disease states are offset by the costs and life-years saved as a result. In particular, the earlier referral occurs, the lower the cumulative incidence of ESRD, which is associated with very high annual costs and mortality (∼£27,000 per patient per year). Deterministic sensitivity analysis confirms this in revealing that the ICER is highly sensitive to changes in the baseline risk of CKD progression and the effect of referral on the risk of CKD progression and cardiovascular events. When we applied more conservative CKD progression rates, and reduced the effect of early referral on CKD progression and cardiovascular events, the ICER for early referral rose above £30,000 per QALY, the threshold applied by NICE to guide decisions on cost-effectiveness.
A factor that was not formally considered in the current analysis is the possibility that CKD cohorts have a higher background risk of mortality from other causes. This was because no published data were identified indicating that CKD confers an increased risk for this outcome. However, unpublished data from a cohort study in Aberdeen, UK suggest that this may be the case (Dr Keith McCullough, University of Aberdeen, personal communication, 2009). To investigate the potential impact of such an effect, we multiplied other cause mortality by 2.36; the HR for CVD mortality associated with CKD. Under this scenario, the cost-effectiveness of early referral decreased only slightly, with the ICER for referral at stage 3a increasing to £5167 compared with standard practice.
Affordability and feasibility
Although, our analysis suggests that early referral and improved management of individuals with CKD may represent a cost-effective use of health service resources, the affordability and feasibility of the intervention is questionable. To give an indication of the potential impact of moving from a strategy of referral to shared care at stage 4 to referral at stage 3a, recent QOF data suggest that there are ∼1.74 million adults registered in England and Scotland as having stage 3a CKD or worse under the QOF. Assuming 74% have stage 3a CKD and 21% have stage 3b CKD,202 the net incremental cost of moving to a shared care strategy at stage 3a would be in the region of £1.02B over 3 years (discounted at 3.5%). The corresponding cost of moving to a strategy of shared care at stage 3b would be ∼£375M. These estimates are based on the modelled net incremental cost per patient of referral at stage 3a or stage 3b versus referral at stage 4 (over a 3-year time horizon) multiplied by 1.74 million. The unit costs for referral, upon which these estimates are based, may not reflect the true cost of scaling up nephrology services to the level required to meet the extra demand (increased numbers of nephrologists, increased clinic space and increased administrative costs). Assuming that referral at stage 4 is the current practice, and that existing nephrologists are working at capacity, movement to early referral at stage 3a might require somewhere in the region of 1300 additional nephrologists, while movement to referral at stage 3b would require ∼500 additional nephrologists across England and Scotland. These estimates are based on further assumptions that an individual nephrologist could manage ∼1250 stage 3a patients per year under an SCS (assuming 25% would require outpatient hospital treatment while the rest could be managed in primary care) or 800 stage 3b patients per year (assuming 50% would require outpatient hospital treatment). As these numbers are unlikely to prove feasible, it is likely that alternative approaches to the management of individuals with CKD will have to be found.
Comparison with other studies
As outlined in the review section of this chapter, we were unable to identify any published studies specifically assessing the cost-effectiveness of early referral strategies (referral during stage 3a) for patients with markers of renal disease. However, our finding that referral at stage 4 CKD is highly cost-effective compared with referral upon transit to stage 5 CKD is consistent with the previously published modelling study by McLaughlin and colleagues. 180 Our findings are also generally consistent with studies showing the use of ACE Is to be cost-effective in individuals with non-diabetic nephropathies. 188,189 Improved uptake and appropriate use of ACE Is is one of the mechanisms by which early referral may reduce progression and prevent cardiovascular mortality. Our findings are also consistent with the substantial body of evidence that shows early treatment of diabetic nephropathies with ACE Is or ARBs to be highly cost-effective, owing to their preventive effect on progression to ESRD. 215,216
Strengths and weakness of the study
Owing to a lack of data on the natural history of CKD in individuals without diabetes, and a lack of evidence on the costs and effects of early referral, our model should be seen as an exploratory piece of research. Many assumptions had to be made regarding the transition of individuals through the CKD stages, the risk of cardiovascular events by stage, and the costs and effectiveness of early referral. In particular, more research is required to assess eGFR decline rates in individuals with early stage 3 CKD. In our base-case analysis, we estimated CKD transition rates by applying average rates of eGFR decline in line with rates reported in the literature for individuals with clinically established CKD to a cohort of individuals with an eGFR < 60 ml/min/1.73 m2 identified in primary care. Although these progression rates gave a predicted cumulative incidence of ESRD in line with that observed for a similar cohort,96 there is emerging evidence to suggest that a subset of patients identified with a low eGFR in primary care are relatively stable and do not in fact progress. Some may even regress to less severe stages of disease. Our analysis makes the assumption that everyone in the cohort has progressive renal insufficiency, and as a result may overestimate cost-effectiveness of early referral individuals with stable eGFR who do not progress, and underestimate cost-effectiveness for individuals who have more progressive disease. More detailed investigation in primary care to identify those individuals who are progressive could potentially improve cost-effectiveness and affordability of early referral strategies.
Another weakness of the study is that, due to lack of evidence, the modelling relies on an effectiveness estimate for early referral taken from the only prospective study looking at the impact of early referral on a cohort that included individuals without diabetes. Although this was one of the highest quality studies identified by the clinical effectiveness review (see Chapter 5), controlling for various patient characteristics and treatment factors expected to influence outcome (diabetes, proteinuria and hypertension), it may still be subject to bias. Moreover, the cohort was entirely male, 50% had diabetes and the vast majority had proteinuria (89%). Therefore, there is a question over whether the 20% reduction in CKD progression and cardiovascular mortality observed for early referral in this cohort can be achieved in mixed gender CKD cohorts without diabetes. Another factor that may limit the generalisability of the Orlando study111 is that the primary care arm may not reflect current primary care standards in the UK. Primary care management for people with CKD in the UK may have substantially improved as a result of the introduction of the QOF. Thus, the relative effect achievable through early referral may be diminished. Sensitivity analysis demonstrates that cost-effectiveness is highly sensitive to the relative effect of early referral on CKD progression and/or cardiovascular event risks (see Table 36).
Potential for future research and further modelling
Although we attempted to use the best available evidence on the natural history of early CKD progression and the effectiveness of early referral, data in these areas are incomplete. There is clear need for prospective cohort studies to assess CKD progression and the incidence of cardiovascular events in individuals who have been identified as having an eGFR < 60 ml/min, with and without other complications/comorbidities such as microalbuminuria, proteinuria, diabetes and pre-existing CVD. This is particularly pertinent for those with mild CKD who have been detected through opportunistic testing and who, in the past, would not have come to the attention of a renal physician. Once these data are available they will allow more accurate modelling of the cost-effectiveness of referral based on different eGFR cut-offs and other comorbidities.
In addition, there is a clear need for prospective randomised studies to assess the effect of early referral or improved management strategies on the progression of CKD and the incidence of CVD events in the different subgroups of interest. The cost-effectiveness results reported here assume that early referral is associated with a 20% reduction in the risk of progression to the next stage or CVD mortality, regardless of CKD stage or level comorbidity. This was based on a reported HR associated with referral for individuals with CKD, which was adjusted for various comorbidities known to influence outcomes; but a question remains over the generalisability of these findings, particularly to cohorts with early stage 3 CKD.
No cardiovascular risk estimating equations were available at the time of writing, which incorporated eGFR, microalbuminuria or proteinuria as risk factors for cardiovascular events. As a result, we had to apply adjusted RR estimates for CVD events (associated with specific renal disease markers) to baseline risks for the cohort based on classical CVD risk factors. This staged approach will result in imprecision in the overall estimate of CVD event risk within each stage of the model. If in the future risk estimating equations that incorporate markers of renal disease become available, we will be able to update the model accordingly.
Reducing the risk of CKD progression and CVD in primary care also presents a feasible option for improving the management of individuals with markers of renal disease. This modelling study has focused on the potential cost-effectiveness of early referral to a specialist, but it is not the act of referral itself that reduces the risk of progression. A combination of factors such as obtaining better BP control, increasing appropriate use of ACE Is and other medications, and encouraging positive lifestyle changes are the likely mechanisms by which referral to a specialist affects the progression of disease. Appropriate use of these interventions may already be improving in primary care under the QOF, and it may be the case that further improvements can be achieved in a primary care setting without the need for referral. Furthermore, if the relative benefits of nephrology care were to be limited to improving the quality of life of patients within stage (through better management of anaemia for example), rather than preventing progression and prolonging life, then this would favour referral at later stages. Given the potentially prohibitive costs of implementing the SCS we have modelled here, it is pertinent that further research explores ways of improving management and outcomes for individuals with CKD in primary care.
Conclusions
Strategies to improve the management of people with CKD may offer an efficient use of health service resources. However, given the great uncertainty surrounding many parameter estimates, the effectiveness and cost-effectiveness of early referral needs to be demonstrated in prospective randomised studies. In addition, research is required to assess whether improved outcomes can be achieved for people with early stage renal disease through improved management in the primary care setting.
Chapter 7 Discussion
Overview of findings
In the previous chapters we have presented the findings of a series of systematic reviews and the development of an economic model assessing aspects of the clinical effectiveness and cost-effectiveness of early referral for CKD.
The review of the natural history of CKD identified evidence that reduced eGFR was a predictor for mortality, CVD, renal disease progression and ESRD. In cohorts of people with CKD, death was a common outcome regardless of whether the cohort was population or clinically based. The association between CKD and these outcomes was attenuated by taking into account comorbidities and age. Increasing stage of CKD was associated with higher levels of ACM, CVD and renal outcomes. A substantial increase in the risk of ACM and renal outcomes was noted when stage 3a was compared to stage 3b.
While RR estimates for ACM and renal outcomes increased with stage, the number of people in the affected category reduced. This should be borne in mind when considering where to target care. It may be possible to identify subgroups at higher risk of poor health outcomes but, because the prevalence of CKD falls steeply with eGFR, the absolute numbers of people experiencing a negative outcome will also fall.
The concept of ‘early referral’ implies a stage in an inevitable pathway. Though limited, there was some evidence that there may be a subgroup of people for whom the label of CKD does not result in progressive deterioration in kidney function or an increased risk of CVD. This subgroup was rarely considered in the literature and poorly characterised, but may account for more than 50% of those with CKD defined by KDOQI. This group will have little to gain from referral and the potential for harm from investigation, anxiety and unnecessary treatment. At the current time, there is no good way to identify such individuals. Any models of care for CKD should, therefore, be evaluated in the context of an RCT to ensure the benefits sufficiently outweigh the harms for people with different stages of CKD. Indeed, even the evidence base around the effectiveness of pharmacological treatments (ACE I/ARB, statins) have largely considered CKD as a single group and have not considered the effect size for different stages of CKD.
Literature considering the effectiveness of early referral for CKD was limited and again there was heavy reliance on a study design that recruits people at the time of initiating RRT, with retrospective consideration of the care they have received. We found evidence that referral to a nephrology specialist more than 12 months prior to starting RRT (and even as early as more than 72 months before RRT) may improve outcomes including long-term survival on RRT. This also supports the survival benefits being related to not only planning and preparation for RRT but also risk factor modification for causes of mortality (in particular CVD).
Only two studies provided information about the impact of referral on the pre-RRT phase of care (and thus also included people who did not survive to dialysis). 111,120 Here there was some evidence that early referral (defined by degree of renal impairment) could be beneficial in terms of slowing progression and reducing mortality. A conclusion that must be treated with some caution for the following reasons: patients were not randomly allocated to the treatment groups; one study included only patients with diabetes and described a care setting likely to be substantially different from that in the UK; and very little information was available about what care was received. While little information was available about the care given, those in the early referral groups were more likely to be on ACE Is or ARBs. BP control was generally tighter in the referred group and some authors reported higher prescribing of statins.
The review of models of care for people with CKD found a dichotomy in the literature between early referral to specialist teams and approaches to shared care across a range of disciplines but including the primary care team. Three models of care were described: multidisciplinary clinics (including shared care across specialties and with primary care); structured care packages led by an individual clinical specialty (such as renal nurses or pharmacists); and educative approaches to develop skills in both patients and professionals. Where evaluations were reported, there was evidence of the potential for well-designed services to provide benefit, with improvements in markers of disease and care. However, the reliance on self-reporting and descriptive or before-and-after designs by many authors did not allow robust assessment of effectiveness. Indeed, the only RCT (of MDC delivered as a case management programme versus standard care that combined primary care plus referral to a nephrologist in the usual way) found no statistically significant benefit but substantially higher cost.
We did not find any cost-effectiveness studies of early referral for CKD. One cost-effectiveness study of referral of patients with creatinine clearance rate of 20 ml/min (equivalent to advanced stage 4 CKD) versus referral on the development of clinically significant uraemia (e.g. established ESRD) reported potential cost savings with the earlier referral approach. The model derived effect estimates of potential benefits from a prospective study of an education intervention that had demonstrated improvements in dialysis free survival. The model focused on renal outcomes. 180
In the absence of high-quality RCT evidence of clinical effectiveness of early referral, we undertook an economic modelling exercise to assess the potential cost-effectiveness of referring individuals with markers for renal disease. This allowed us to determine what factors were driving the economic model and where uncertainty was having the greatest impact. We constructed a Markov model utilising the evidence from the review of the natural history of CKD and clinical effectiveness of early referral. Using individual patient creatinines from primary care to estimate GFR for our cohort, we applied reported eGFR decline rates to simulate how people with CKD might progress through CKD stages and the outcomes they might encounter. In order to consider the potential cost impact of an early referral strategy, we used the best described referral programme reported in the models of care review (a shared care programme described by Jones and colleagues)147 as an example of how a service might operate. We compared this to referral to a nephrology service in stage 5 as a base case. We recognise that this may no longer reflect current practice in the UK but, as the review of models of care noted, UK practice was evolving rapidly and was not uniform across the country. We therefore felt that this provided a simple and transparent model against which to compare our hypothetical referral strategies. Moreover, this approach still allowed us to assess the incremental costs and consequences of sequentially increasing the eGFR referral cut-off up through the disease stages. The estimates of potential health benefits from such an intervention were obtained from a study using routine health-care data to retrospectively compare early referral to a nephrology service with primary care only. All the referral strategies considered produced more QALYs than our standard care package. Referral at stage 3a was considered to be the best option with an ICER of £973 per QALY. Thus the base-case modelling suggested that a package of early referral has the potential to offer a cost-effective use of resources. The model was found to be most sensitive to changes in the baseline risk of CKD progression (including the assumption that all patients have progressive diseases) and the effect of referral on risk of CKD progression.
Implications for health-care delivery
We have reported evidence of the potential for improvements in the care of people with CKD. While an early referral model, combining some form of shared care between primary and secondary care, has the potential to be cost-effective, it is unlikely that such a model is affordable or feasible. Key areas of uncertainty were identified around the natural history of people with CKD, in particular stage 1–3 CKD identified by the current ‘opportunistic screening’ approach, and whether subgroups can be identified where the risk of progression is low.
Indeed, the approaches already adopted in the UK to identify people with CKD have brought to the attention of the health-care system many people who would have previously gone unrecognised. 217,218 The majority of these people have stage 3 CKD. Such people are not those previously cared for by renal services. They would also not have made up a large component of people in clinical trials for treatments for CKD. As a result, the evidence for the optimal care of such people is unclear and this review further identifies the importance of well-designed clinical trials of interventions that will address the care of people with CKD.
CVD was observed to be high among those with an eGFR < 60 ml/min/1.73 m2. At the current time CKD is not included as a high risk group in the cardiovascular risk calculators widely used to determine a person’s need for CVD prevention. The National Screening Committee has been considering the place of vascular risk factor screening (including screening for CKD) for a number of years, and in England progress continues towards the introduction of an ‘NHS health check’ screening programme. 175 All 40–74 year olds not already known to have diabetes mellitus, CVD or CKD will be invited for a 5 yearly risk factor check. Anyone with a BP ≥ 140/90 mmHg will be assessed for CKD with a blood test to estimate GFR. This wider population screening will further identify people who would not previously have come to the attention of services. The potential health benefits and harms from early identification and intervention in such a group remain poorly understood. Population screening studies have been conducted to determine if people with previously unknown CKD can be identified effectively. Various combinations of age, comorbidity, microalbuminuria and eGFR criteria have been used. To date, we have found no evidence of evaluation of these screening approaches in combination with an intervention to assess the effectiveness in reducing morbidity and mortality in the screened population. 175,219,220
The focus of this review was to consider the evidence of clinical effectiveness and cost-effectiveness of ‘early referral’ to specialist services. The model of CKD services considered in the economics analysis relied heavily on specialist referral to secondary care but recognised that it was not feasible to do this in isolation from primary care. To implement a referral programme such as the SIMON model for all patients with CKD stage 3 or worse, even if it was possible to define a subgroup for whom progression was unlikely and referral therefore unnecessary, would require nephrology specialist capacity that is currently unavailable and unlikely to be affordable or feasible. Chapter 5 identified other options, all capable of delivering changes in clinical markers of improved control of risk factors that should be considered and evaluated in RCTs to identify the most clinically effective and cost-effective way forward.
The care of people with CKD in the UK is in a state of change. In recent years, attention has become more focused on the care of people with CKD, including the ‘early’ recognition and management of people with mild and moderate disease. The introduction of CKD to QOF has placed primary care at the centre of this process. The evidence from this review supports the adoption of approaches that seek to develop shared care between primary and secondary care, rather than focusing on early specialist referral. The economic modelling undertaken here suggests that interventions that can achieve the sort of health gains in reduction of progression, ESRD, CVD and mortality reported in the clinical effectiveness review have a good chance of being cost-effective and are, therefore, worthy of further evaluation.
Future research
A number of critical areas of uncertainty were highlighted in this review and economic analysis. Further research is, therefore required and the research priorities in order of need are summarised below.
-
Cohort study of the natural history of CKD stage 1–3. A number of cohort studies are underway in the UK focusing on different populations (the elderly; black and Indian-Asians; laboratory detected CKD). The current natural history literature has identified that how a population was detected has important implications in terms of comorbidities and outcomes. The challenge, therefore, has been in applying the findings from the literature to what the natural history will be for people encountered in clinical practice.
In order to better understand the impact of the changing approaches to CKD detection we need to understand the natural history of CKD in relevant populations. People included in cohort studies should reflect the different approach being adopted to identify CKD in clinical practice: population screening; screening of high risk groups; laboratory-detected CKD; and opportunistic detection as part of routine clinical care (e.g. addition to the QOF CKD register).
Cohorts might be constructed from existing clinical data (laboratory or QOF registers) and involve record linkage to provide long-term follow-up or will require recruitment and follow-up of people with CKD. The introduction of screening programmes that include CKD should include an element of follow-up, particularly for those who were found to have evidence of kidney impairment.
Where possible such cohort studies should include measure of eGFR, creatinine, microalbuminuria and proteinuria as well as emerging prognostic markers. Details of current care should be collected to allow a better understanding about where the opportunities are to optimise care. Measures of quality of life and the impact of diagnosis should be included along with the traditional outcomes of CVD morbidity and mortality, renal progression and ESRD.
Based on the event rates reported in the natural history literature, a cohort constructed from patients identified with CKD through opportunistic screening might anticipate observing 500 deaths for every 1000 patients followed up for 10 years with 40 people progressing to ESRD. General population screening will identify a ‘healthier’ population and mortality could be expected to be lower; 250 per 1000 followed for 10 years with 10 people progressing to ESRD.
-
Review of the clinical effectiveness and cost-effectiveness of the main pharmacological interventions in people with CKD stage 1–3. Secondary research reviewing published studies of ACE Is/ARBs and statins reporting for this subgroup of CKD may be sufficient. A protocol has been published on Cochrane to this end but it is likely that most trials have not reported for these subgroups of CKD. 221 Individual patient data meta-analysis from the key trials may provide sufficient data, but outcomes among such trial participants have been substantially different from population studies suggesting they are highly selected. RCTs of such interventions in patients with CKD stage 1–3 may be required.
-
An RCT of models of care for people with CKD. Management of CKD is complex and the approach needs to be tailored to fit a patient’s needs. A population-based model of chronic disease management with intensive case management for those with complex needs, disease management for those with more straightforward CKD, and supported self-care for those with stable and mild CKD with few other risk factors for CVD could draw on aspects of many of the reports in Chapters 4 and 5. An intervention should consider skill mix, education and support, communication, barriers to referral, sustainability and feasibility. RCTs will need to break down such a model to evaluate aspects of care, comparing how different levels of care are delivered and who delivers them: MDC teams, specialist nephrologist, specialist nurse, GP with special interest, GPs and practice nurses, etc. As a priority, shared care (with proactive involvement of primary care with delivery of more than simply a phlebotomy service) should be compared to standard specialist nephrology and primary care. Any trials should include prospective economic evaluations.
Conclusions
Despite substantial focus on the early identification and proactive management of CKD in the last few years, we have identified significant evidence gaps about how best to manage people with CKD. There was some evidence to suggest that the care of people with CKD could be improved and, because these people are at risk from both renal and cardiovascular outcomes, strategies to improve the management of people with CKD have the potential to offer an efficient use of health service resources. However, given the great uncertainty surrounding many parameter estimates, the effectiveness and cost-effectiveness of care strategies need to be demonstrated in prospective randomised studies prior to implementation. Given the numbers of people now being recognised as having markers of kidney impairment, there is an urgent need for further research to support service change. The natural history of CKD in this new population of people identified as having kidney impairment needs to be better understood. For many, CKD occurs as part of a complex comorbidity cluster, with hypertension, diabetes mellitus and CVD. In focusing on developing and evaluating approaches to provide care for people with CKD, it will be important to keep sight of opportunities to avoid developing silos of care and to balance with the need to identify those who have the most to gain from early specialist intervention.
Acknowledgements
We would like to thank Professor P. Hannaford, Director of Division of Applied Health Science, University of Aberdeen, and GP for comments on the near final draft and providing advice around the primary care assumptions for the economics model; and Ms E. Fairley and Dr E. Okpo for their contribution to the systematic reviewing and data extraction of papers for Chapters 2 and 4.
Contributions of authors
Dr C. Black (Senior Clinical Lecturer, Public Health) led the review and drafted the final report; she also led the review of clinical effectiveness. Ms P. Sharma (Research Assistant, Public Health) drafted sections of the background and led the review of natural history and care models. Ms D. McGurn (Systematic reviewer) data extracted and drafted the chapter on late referral. Mr G. Scotland (Research Fellow, Health Economics) and Dr P. McNamee (Senior Research Fellow, Health Economics) undertook the cost-effectiveness analysis and drafted this section. Ms L. Robertson (Research Assistant, Public Health) and Ms P. Sharma developed the search strategy and undertook all searching. Dr N. Fluck (Consultant Nephrologist) and Dr K. McCullouch (Nephrologist) provide clinical expertise. Professors W. Cairns Smith (Professor of Public Health) and A. MacLeod (Professor of Medicine and Therapeutics) provide research methods expertise. All authors contributed to the design, the interpretation of findings and populating the economics model, and read and commented on the final draft.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Department of Health . Second Progress Report on the Renal NSF 2007. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_074811 (accessed May 2009).
- Department of Health . National Service Framework for Renal Services – Part Two: Chronic Kidney Disease, Acute Renal Failure and End of Life Care 2005. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4101902 (accessed June 2009).
- Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis 2003;41:1-12.
- McGregor SM. How common is early chronic kidney disease? A background paper prepared for the UK Consensus Conference on Early Chronic Kidney Disease. Nephrol Dial Transplant 2007;22:ix8-ix18.
- Grassmann A, Gioberge S, Moeller S, Brown G. ESRD patients in 2004: global overview of patient numbers, treatment modalities and associated trends. Nephrol Dial Transplant 2005;20:2587-93.
- Ansell D, Feehally J, Fogarty D, Ford D, Hodsman A, Tomson C, et al. UK Renal Registry: The Eleventh Annual Report 2008. www.renalreg.com/Reports/2008.html (accessed May 2009).
- Ansell D, Roderick P, Hodsman A, Ford D, Stennkamp R, Tomson C. Survival and Causes of Death of UK Adult Patients on Renal Replacement Therapy in 2007: National and Centre-Specific Analyses. The UK Renal Registry: The Eleventh Annual Report 2008. www.renalreg.com/reports/renal-registry-reports/2008/ (accessed May 2009).
- Merkus MP, Jager KJ, Dekker FW, Boeschoten EW, Stevens P, Krediet RT. Quality of life in patients on chronic dialysis: self-assessment 3 months after the start of treatment. The Necosad Study Group. Am J Kidney Dis 1997;29:584-92.
- Evans RW, Manninen DL, Garrison LP, Hart LG, Blagg CR, Gutman RA, et al. The quality of life of patients with end-stage renal disease. N Engl J Med 1985;312:553-9.
- Department of Health . National Service Framework for Renal Services: Part One – Dialysis and Transplantation 2004. www.dh.gov.uk/en/Publicationsandstatistics/PublicationsPolicyAndGuidance/DH_4070359 (accessed June 2009).
- National Institute for Health and Clinical Excellence . Guidance on Home Compared With Hospital Haemodialysis for Patients With End-Stage Renal Failure 2002. http://guidance.nice.org.uk/TA48 (accessed May 2009).
- Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function – Measured and estimated glomerular filtration rate. N Engl J Med 2006;354:2473-83.
- Jones CA, McQuillan GM, Kusek JW, Eberhardt MS, Herman WH, Coresh J, et al. Serum creatinine levels in the US population: third National Health and Nutrition Examination Survey. Am J Kidney Dis 1998;32:992-9.
- Wesson LG. Physiology of the human kidney. New York, NY: Grune & Straton; 1969.
- Couchoud C, Pozet N, Labeeuw M, Pouteil-Noble C. Screening early renal failure: Cut-off values for serum creatinine as an indicator of renal impairment. Kidney Int 1999;55:1878-84.
- Lamb EJ, Tomson CRV, Roderick PJ. Estimating kidney function in adults using formulae. Ann Clin Biochem 2005;42:321-45.
- Snyder S, Pendergraph B. Detection and evaluation of chronic kidney disease. Am Fam Physician 2005;72:1723-32.
- Traynor J, Mactier R, Geddes CC, Fox JG. How to measure renal function in clinical practice. BMJ 2006;333:733-7.
- Levey AS, Schoolwerth AC, Burrows NR, Williams DE, Stith KR, McClennan W. Comprehensive public health strategies for preventing the development, progression, and complication of CKD: Report of an Expert Panel Convened by Centers for Disease Control and Prevention. Am J Kidney Dis 2009;53:522-35.
- Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Int Med 2003;139:137-47.
- Levey AS, Eckardt K-U, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: A position statement from Kidney Disease Improving Global Outcomes (KDIGO). Kidney Int 2005;67:2089-100.
- The Renal Association . Consensus Statement on Management of Early CKD, February 2007 2007. www.renal.org/CKDguide/consensus.html (accessed April 2009).
- National Institute for Health and Clinical Excellence . Early Identification and Management of Chronic Kidney Disease in Adults in Primary and Secondary Care 2008. http://guidance.nice.org.uk/CG73 (accessed March 2009).
- Levey AS, Atkins R, Coresh J, Cohen EP, Collins AJ, Eckardt KU, et al. Chronic kidney disease as a global public health problem: approaches and initiatives – a position statement from Kidney Disease Improving Global Outcomes. Kidney Int 2007;72:247-59.
- Levin A. The advantage of a uniform terminology and staging system for chronic kidney disease (CKD). Nephrol Dial Transplant 2003;18:1446-51.
- Schoolwerth AC, Engelgau MM, Hostetter TH, Rufo KH, Chianchiano D, McClellan WM, et al. Chronic kidney disease: a public health problem that needs a public health action plan. Prev Chronic Dis 2006;3.
- Saydah S, Eberhardt M, Rios-Burrows N, Williams D, Geiss L, Dorsey R. Prevalence of chronic kidney disease and associated risk factors – United States, 1999–2004. JAMA 2007;297:1767-8.
- Castro AF, Coresh J. CKD surveillance using laboratory data from the population-based National Health and Nutrition Examination Survey (NHANES). Am J Kidney Dis 2009;53:S46-S55.
- Coresh J, Stevens AL, Levey AS. Chronic kidney disease is common: What do we do next?. Nephrol Dial Transplant 2008;23:1122-5.
- Coresh J, Byrd-Holt D, Astor BC, Briggs JP, Eggers PW, Lacher DA. Chronic kidney disease awareness, prevalence, and trends among U.S. adults, 1999 to 2000. J Am Soc Nephrol 2005;16:180-8.
- Iseki K, Kinjo K, Iseki C, Takishita S. Relationship between predicted creatinine clearance and proteinuria and the risk of developing ESRD in Okinawa, Japan. Am J Kidney Dis 2004;44:806-14.
- Hallan SI, Dahl K, Oien CM, Grootendorst DC, Aasberg A, Holmen J, et al. Screening strategies for chronic kidney disease in the general population: Follow-up of cross sectional health survey. BMJ 2006;333:1047-50.
- Cirillo M, Laurenzi M, Mancini M, Zanchetti A, Lombardi C, De Santo NG. Low glomerular filtration in the population: Prevalence, associated disorders, and awareness. Kidney Int 2006;70:800-6.
- Nitsch D, Dietrich DF, von Eckardstein A, Gaspoz JM, Downs SH, Leuenberger P. Prevalence of renal impairment and its association with cardiovascular risk factors in a general population: results of the Swiss SAPALDIA study. Nephrol Dial Transplant 2006;21:935-44.
- Otero A, Gayoso P, Garcia F, de Francisco AL. on behalf of the EPIRCE study group . Epidemiology of chronic renal disease in the Galician population: results of the pilot Spanish EPIRCE study. Kidney Int Suppl 2005;99:S16-19.
- Viktorsdottir O, Palsson R, Andresdottir MB, Aspelund T, Gudnason V, Indridason OS. Prevalence of chronic kidney disease based on estimated glomerular filtration rate and proteinuria in Icelandic adults. Nephrol Dial Transplant 2005;20:1799-807.
- Wannamethee SG, Shaper AG, Lowe GD, Lennon L, Rumley A, Whincup PH. Renal function and cardiovascular mortality in elderly men: the role of inflammatory, procoagulant, and endothelial biomarkers. Eur Heart J 2006;27:2975-81.
- de LS, Chan T, Stevens P, O’Donoghue D, Hague N, Dzregah B, et al. Identifying patients with chronic kidney disease from general practice computer records. Fam Pract 2005;22:234-41.
- Ali T, Black C, Prescott G, MacLeod A, Simpson C, Khan I, et al. Preventing End Stage Renal Disease: Informing the Development of a Public Health Strategy. Chief Scientist Office – Research in Focus 2007. www.sehd.scot.nhs.uk/cso/Publications/ExecSumms/OctNov07/Ali.pdf (accessed July 2008).
- The Renal Association . The UK CKD Guidelines (2005) 2005. www.renal.org/CKDguide/ckd2005.html (accessed May 2009).
- Lamb EJ. United Kingdom guidelines for chronic kidney disease. Scand J Clin Lab Invest Suppl 2008;241:16-22.
- Scottish Intercollegiate Guidelines Network . Diagnosis and Management of Chronic Kidney Disease 2008. www.sign.ac.uk/guidelines/fulltext/103/index.html (accessed December 2008).
- Jafar TH, Schmid CH, Landa M, Giatras I, Toto R, Remuzzi G, et al. Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann Int Med 2001;135:73-87.
- Strippoli GF, Bonifati C, Craig M, Navaneethan SD, Craig JC. Angiotensin converting enzyme inhibitors and angiotensin II receptor antagonists for preventing the progression of diabetic kidney disease. Cochrane Database Syst Rev 2006;4.
- Kshirsagar AV, Joy MS, Hogan SL, Falk RJ, Colindres RE. Effect of ACE inhibitors in diabetic and nondiabetic chronic renal disease: a systematic overview of randomized placebo-controlled trials. Am J Kidney Dis 2000;35:695-707.
- Siebenhofer A, Plank J, Horvath K, Berghold A, Sutton AJ, Sommer R, et al. Angiotensin receptor blockers as anti-hypertensive treatment for patients with diabetes mellitus: meta-analysis of controlled double-blind randomized trials. Diabet Med 2004;21:18-25.
- Casas JP, Chua W, Loukogeorgakis S, Vallance P, Smeeth L, Hingorani AD, et al. Effect of inhibitors of the renin-angiotensin system and other antihypertensive drugs on renal outcomes: systematic review and meta-analysis. Lancet 2005;366:2026-33.
- Strippoli GF, Navaneethan SD, Johnson DW, Perkovic V, Pellegrini F, Nicolucci A, et al. Effects of statins in patients with chronic kidney disease: meta-analysis and meta-regression of randomised controlled trials. BMJ 2008;336:645-51.
- Sandhu S, Wiebe N, Fried LF, Tonelli M. Statins for improving renal outcomes: a meta-analysis. J Am Soc Nephrol 2006;17:2006-16.
- Fried LF, Orchard TJ, Kasiske BL. Effect of lipid reduction on the progression of renal disease: A meta-analysis. Kidney Int 2001;59:260-9.
- Fouque D, Laville M, Boissel JP. Low protein diets for chronic kidney disease in non diabetic adults. Cochrane Database Syst Rev 2006;2.
- Robertson L, Waugh N, Robertson A. Protein restriction for diabetic renal disease. Cochrane Database Syst Rev 2007;4.
- Zarazaga A, Garcia-De-Lorenzo L, Garcia-Luna PP, Garcia-Peris P, Lopez-Martinez J, Lorenzo V, et al. Nutritional support in chronic renal failure: systematic review. Clinical Nutrition 2001;20:291-9.
- Lameire N, Van BW. The pattern of referral of patients with end-stage renal disease to the nephrologist--a European survey. Nephrol Dial Transplant 1999;14:16-23.
- Nakamura S. N. Effect of early nephrology referral on the initiation of hemodialysis and survival in patients with chronic kidney disease and cardiovascular diseases. Circ J 2007;71:511-16.
- Roderick P, Jones C, Drey N, Blakeley S, Webster P, Goddard J, et al. Late referral for end-stage renal disease: a region-wide survey in the south west of England. Nephrol Dial Transplant 2002;17:1252-9.
- Chan MR, Dall AT, Fletcher KE, Lu N, Trivedi H. Outcomes in patients with chronic kidney disease referred late to nephrologists: a meta-analysis. Am J Med 2007;120:1063-70.
- Centre for Reviews and Dissemination . Undertaking Systematic Reviews of Research on Effectiveness: CRD’s Guidance for Those Carrying Out or Commissioning Reviews 2001. www.york.ac.uk/inst/crd/report4.htm (accessed March 2008).
- National Institute for Health and Clinical Excellence . The Guidelines Manual 2007 – All Chapters 2007. www.nice.org.uk/aboutnice/howwework/developingniceclinicalguidelines/clinicalguidelinedevelopmentmethods/theguidelinesmanual2007/the_guidelines_manual_2007.jsp (accessed March 2008).
- National Institute for Health and Clinical Excellence . Type 2 Diabetes: The Management of Type 2 Diabetes 2008. www.nice.org.uk/Guidance/CG66 (accessed May 2008).
- Drummond FM, Jefferson OT. Guidelines for authors and peer reviewers of economic submissions to the BMJ. BMJ 1996;313:275-83.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess 2004;8.
- National Institute of Clinical Excellence . The Guidelines Manual-Appendix B: Methodology Checklist: Systematic Reviews and Meta- Analyses 2007. www.nice.org.uk/niceMedia/pdf/GuidelinesmanualAppendixB.pdf (accessed 30 March 2008).
- Critical Appraisal Skills Pragramme . 12 Questions to Help You Make a Sense of Cohort Study. Public Health Resource Unit 2004. www.phru.nhs.uk/Pages/PHD/resources.htm (accessed 26 March 2008).
- Sanderson S, Tatt ID, Higgins J. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol 2007;36.
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377-84.
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses 2008. www.ohri.ca/programs/clinical_epidemiology/oxford.htm (accessed March 2008).
- Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, et al. Chronic kidney disease and mortality risk: A systematic review. J Am Soc Nephrol 2006;17:2034-47.
- Di AE, Danesh J, Eiriksdottir G, Gudnason V. Renal function and risk of coronary heart disease in general populations: new prospective study and systematic review. PLoS Med 2007;4.
- Muntner P, He J, Hamm L, Loria C, Whelton P. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol 2002;13:745-53.
- Manjunath G, Tighiouart H, Ibrahim H, MacLeod B, Salem D, Griffith J, et al. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol 2003;41:48-55.
- Manjunath G, Tighiouart H, Coresh J, MacLeod B, Salem D, Griffith J, et al. Level of kidney function as a risk factor for cardiovascular outcomes in the elderly. Kidney Int 2003;63:1121-9.
- Culleton BF, Larson MG, Wilson PWF, Evan JC, Parfrey PS, Levy D. Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int 1999;56:2214-19.
- Weiner DE, Tighiouart H, Amin MG, Stark PC, MacLeod B, Griffith JL, et al. Chronic kidney disease as a risk factor for cardiovascular disease and all-cause mortality: a pooled analysis of community-based studies. J Am Soc Nephrol 2004;15:1307-15.
- Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351.
- Meisinger C, Doring A, Lowel H. Chronic kidney disease and risk of incident myocardial infarction and all-cause and cardiovascular disease mortality in middle-aged men and women from the general population. Eur Heart J 2006;27:1245-50.
- Dale PL, Hutton J, Elgazzar H. Utility of health states in chronic kidney disease: a structured review of the literature. Curr Med Res Opin 2008;24:193-205.
- Gorodetskaya I, Zenios S, McCulloch CE, Bostrom A, Hsu CY, Bindman AB, et al. Health-related quality of life and estimates of utility in chronic kidney disease. Kidney Int 2005;68:2801-8.
- Bruno G, Merletti F, Bargero G, Novelli G, Melis D, Soddu A, et al. Estimated glomerular filtration rate, albuminuria and mortality in type 2 diabetes: the Casale Monferrato study. Diabetologia 2007;50:941-8.
- Patel UD, Young EW, Ojo AO, Hayward RA. CKD progression and mortality among older patients with diabetes. Am J Kidney Dis 2005;46:406-14.
- Irie F, Iso H, Sairenchi T, Fukasawa N, Yamagishi K, Ikehara S, et al. The relationships of proteinuria, serum creatinine, glomerular filtration rate with cardiovascular disease mortality in Japanese general population. Kidney Int 2006;69:1264-71.
- Imai E, Horio M, Yamagata K, Iseki K, Hara S, Ura N, et al. Slower decline of glomerular filtration rate in the Japanese general population: A longitudinal 10-year follow-up study. Hypertens Res 2008;31:433-41.
- Djamali A, Kendziorski C, Brazy PC, Becker BN. Disease progression and outcomes in chronic kidney disease and renal transplantation. Kidney Int 2003;64:1800-7.
- Levin A, Djurdjev O, Barrett B, Burgess E, Carlisle E, Ethier J, et al. Cardiovascular disease in patients with chronic kidney disease: Getting to the heart of the matter. Am J Kidney Dis 2001;38:1398-407.
- Astor BC, Hallan SI, Miller ER, Yeung E, Coresh J. Glomerular filtration rate, albuminuria, and risk of cardiovascular and all-cause mortality in the US population. Am J Epidemiol 2008;167:1226-34.
- Maaravi Y, Bursztyn M, Hammerman-Rozenberg R, Stessman J. Glomerular filtration rate estimation and mortality in an elderly population. QJM 2007;100:441-9.
- Mulec H, Blohme G, Grande B, Bjorck S. The effect of metabolic control on rate of decline in renal function in insulin-dependent diabetes mellitus with overt diabetic nephropathy. Nephrol Dial Transplant 1998;13:651-5.
- Rossing K, Christensen PK, Hovind P, Tarnow L, Rossing P, Parving HH. Progression of nephropathy in type 2 diabetic patients. Kidney Int 2004;66:1596-605.
- Tarnow L, Hildebrandt P, Hansen BV, Borch-Johnsen K, Parving H-H. Plasma N-terminal pro-brain natriuretic peptide as an independent predictor of mortality in diabetic nephropathy. Diabetologia 2005;48:149-55.
- Kollerits B, Fliser D, Heid IM, Ritz E, Kronenberg F. MMKD Study G . Gender–specific association of adiponectin as a predictor of progression of chronic kidney disease: the Mild to Moderate Kidney Disease Study. Kidney Int 2007;71:1279-86.
- Cvengros JA, Christensen AJ, Lawton WJ. Health locus of control and depression in chronic kidney disease: a dynamic perspective. J Health Psychol 2005;10:677-86.
- Herzog CA, Muster HA, Li S, Collins AJ. Impact of congestive heart failure, chronic kidney disease, and anemia on survival in the Medicare population. J Card Fail 2004;10:467-72.
- Hovind P, Rossing P, Tarnow L, Smidt UM, Parving HH. Progression of diabetic nephropathy. Kidney Int 2001;59:702-9.
- Tseng C-L, Kern EFO, Miller DR, Tiwari A, Maney M, Rajan M, et al. Survival benefit of nephrologic care in patients with diabetes mellitus and chronic kidney disease. Arch Intern Med 2008;168:55-62.
- Drey N, Roderick P, Mullee M, Rogerson M. A population-based study of the incidence and outcomes of diagnosed chronic kidney disease. Am J Kidney Dis 2003;42:677-84.
- Eriksen BO, Ingebretsen OC. The progression of chronic kidney disease: a 10-year population-based study of the effects of gender and age. Kidney Int 2006;69:375-82.
- Eriksen BO, Ingebretsen OC. In chronic kidney disease staging the use of the chronicity criterion affects prognosis and the rate of progression. Kidney Int 2007;72:1242-8.
- Evans M, Fryzek JP, Elinder CG, Cohen SS, McLaughlin JK, Nyren O, et al. The natural history of chronic renal failure: results from an unselected, population-based, inception cohort in Sweden. Am J Kidney Dis 2005;46:863-70.
- Hallan S, Astor B, Romundstad S, Aasarod K, Kvenild K, Coresh J. Association of kidney function and albuminuria with cardiovascular mortality in older vs younger individuals. Arch Intern Med 2007;167:2490-6.
- Hallan SI, Ritz E, Lydersen S, Romundstad S, Kvenild K, Orth SR. Combining GFR and albuminuria to classify CKD improves prediction of ESRD. J Am Soc Nephrol 2009;20:1069-77.
- Hemmelgarn BR, Zhang J, Manns BJ, Tonelli M, Larsen E, Ghali WA, et al. Progression of kidney dysfunction in the community-dwelling elderly. Kidney Int 2006;69:2155-61.
- Hovind P, Tarnow L, Rossing P, Teerlink T, Stehouwer CD, Emeis JJ, et al. Progression of diabetic nephropathy: role of plasma homocysteine and plasminogen activator inhibitor-1. Am J Kidney Dis 2001;38:1376-80.
- Hsu CY, Lin F, Vittinghoff E, Shlipak MG. Racial differences in the progression from chronic renal insufficiency to end-stage renal disease in the United States. J Am Soc Nephrol 2003;14:2902-7.
- John R, Webb M, Young A, Stevens PE. Unreferred chronic kidney disease: a longitudinal study. Am J Kidney Dis 2004;43:825-35.
- Jones C, Roderick P, Harris S, Rogerson M. Decline in kidney function before and after nephrology referral and the effect on survival in moderate to advanced chronic kidney disease. Nephrol Dial Transplant 2006;21:2133-43.
- Keith DS, Nichols GA, Gullion CM, Brown JB, Smith DH. Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med 2004;164:659-63.
- Gullion CM, Keith DS, Nichols GA, Smith DH. Impact of comorbidities on mortality in managed care patients with CKD. Am J Kidney Dis 2006;48:212-20.
- Khatami Z, Handley G, Narayanan K, Weaver JU. Applicability of estimated glomerular filtration rate in stratifying chronic kidney disease. Scand J Clin Lab Invest 2007;67:297-305.
- Leehey DJ, Kramer HJ, Daoud TM, Chatha MP, Isreb MA. Progression of kidney disease in type 2 diabetes – Beyond blood pressure control: An observational study. BMC Nephrol 2005;6.
- O’Hare AM, Bertenthal D, Covinsky KE, Landefeld CS, Sen S, Mehta K, et al. Mortality risk stratification in chronic kidney disease: One size for all ages?. J Am Soc Nephrol 2006;17:846-53.
- Orlando LA, Owen WF, Matchar DB. Relationship between nephrologist care and progression of chronic kidney disease. N C Med J 2007;68:9-16.
- Coresh J, Astor BC, McQuillan G, Kusek J, Greene T, Van Lente F, et al. Calibration and random variation of the serum creatinine assay as critical elements of using equations to estimate glomerular filtration rate. Am J Kidney Dis 2002;39:920-9.
- Murthy K, Stevens LA, Stark PC, Levey AS. Variation in the serum creatinine assay calibration: A practical application to glomerular filtration rate estimation. Kidney Int 2005;68.
- Garg AX, Clark WF, Haynes B, House AA. Moderate renal insufficiency and the risk of cardiovascular mortality: Results from the NHANES I. Kidney Int 2002;61:1486-94.
- Sihvonen S, Korepelaa M, Mustonen J, Laippala P, Pasternack A. Renal disease as a predictor of increased mortality among patients with rheumatoid arthritis. Nephron 2004;96:107-14.
- Chow FYF, Briganti EM, Kerr PG, Chadban SJ, Zimmet PZ, Atkins RC. Health-related quality of life in Australian adults with renal insufficiency: a population-based study. Am J Kidney Dis 2003;41:596-604.
- van der Velde M, Halbesma N, de Charro FT, Bakker SJL, de Zeuw D, de Jong PE, et al. Screening for albuminuria identifies individuals at increased renal risk. J Am Soc Nephrol 2009;20:852-62.
- Fried L. Are we ready to screen the general population for microalbuminuria?. J Am Soc Nephrol 2009;20:686-8.
- Kessler M, Frimat L, Panescu V, Briancon S. Impact of nephrology referral on early and midterm outcomes in ESRD: EPidemiologie de l’Insuffisance REnale chronique terminale en Lorraine (EPIREL): results of a 2-year, prospective, community-based study. Am J Kidney Dis 2003;42:474-85.
- Martínez-Ramírez HR, Jalomo-Martinez B, Cortes-Sanabria L, Rojas-Campos E, Barragan G, Alfaro G, et al. Renal function preservation in type 2 diabetes mellitus patients with early nephropathy: a comparative prospective cohort study between primary health care doctors and a nephrologist. Am J Kidney Dis 2006;47:78-87.
- Jungers P, Massy ZA, Nguyen-Khoa T, Choukroun G, Robino C, Fakhouri F, et al. Longer duration of predialysis nephrological care is associated with improved long-term survival of dialysis patients. Nephrol Dial Transplant 2001;16:2357-64.
- Khan SS, Xue JL, Kazmi WH, Gilbertson DT, Obrador GT, Pereira BJG, et al. Does predialysis nephrology care influence patient survival after initiation of dialysis?. Kidney Int 2005;67:1038-46.
- Kinchen KS, Sadler J, Fink N, Brookmeyer R, Klag MJ, Levey AS, et al. The timing of specialist evaluation in chronic kidney disease and mortality. Ann Int Med 2002;137.
- Khan IH, Catto GR, Edward N, MacLeod AM. Chronic renal failure: factors influencing nephrology referral. QJM 1994;87:559-64.
- Himmelfarb J. Chronic kidney disease and the public health: gaps in evidence from interventional trials. JAMA 2007;297:2630-3.
- The Renal Association . A Vision for the Future of Renal Services 2002. www.renal.org/Statements/NSFsub.html (accessed October 2008).
- Blendon RJ, Schoen C, DesRoches C, Osborn R, Zapert K. Common concerns amid diverse systems: health care experiences in five countries. Health Aff 2003;22:106-21.
- Epping-Jordan JE, Pruitt SD, Bengoa R, Wagner EH. Improving the quality of health care for chronic conditions. Qual Saf Health Care 2004;13:299-305.
- Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Evid Based Nurs 2005;8.
- Norris SL, Nichols PJ, Caspersen CJ, Glasgow RE, Engelgau MM, Jack L, et al. The effectiveness of disease and case management for people with diabetes. A systematic review. Am J Prev Med 2002;22.
- Renders CM, Valk GD, Griffin SJ, Wagner EH, Eijk Van JT, Assendelft WJ. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care 2001;24:1821-33.
- Goeddeke-Merickel CM. The goals of comprehensive and integrated disease state management for diabetic kidney disease patients. Adv Chronic Kidney Dis 2005;12:236-42.
- Ifudu O, Friedman EA. Managing chronic renal insufficiency--intertwined roles of non-nephrologist and nephrologist. J Natl Med Assoc 2003;95:43-54.
- Leung WY, So WY, Tong PC, Lo MK, Lee KF, Ko GT, et al. The renoprotective effects of structured care in a clinical trial setting in type 2 diabetic patients with nephropathy. Nephrol Dial Transplant 2004;19:2519-25.
- Ahmad A, Roderick P, Ward M, Steenkamp R, Burden R, O’Donoghue D, et al. Current chronic kidney disease practice patterns in the UK: a national survey. QJM 2006;99:245-51.
- Jones C, Roderick P, Rogerson M. A national survey of shared care schemes for managing chronic kidney disease. BRS Conference Programme; 2004.
- Minutolo R, De NL, Zamboli P, Chiodini P, Signoriello G, Toderico C, et al. Management of hypertension in patients with CKD: differences between primary and tertiary care settings. Am J Kidney Dis 2005;46:18-25.
- Minutolo R, Sasso FC, Chiodini P, Cianciaruso B, Carbonara O, Zamboli P, et al. Management of cardiovascular risk factors in advanced type 2 diabetic nephropathy: a comparative analysis in nephrology, diabetology and primary care settings. J Hypertens 2006;24:1655-61.
- Locatelli F, Zoccali C, SIR SIN. Study Investigators. Clinical policies on the management of chronic kidney disease patients in Italy. Nephrol Dial Transplant 2008;23:621-6.
- Hobbs H, Irving J, Farmer C, Jenkins K, John I. The Impact of EGFR Implementation on Clinical Practice: Finding Solutions through a CKD Network n.d.
- Cortes-Sanabria L, Cabrera-Pivaral CE, Cueto-Manzano AM, Rojas-Campos E, Barragan G, Hernandez-Anaya M, et al. Improving care of patients with diabetes and CKD: a pilot study for a cluster-randomized trial. Am J Kidney Dis 2008;51:777-88.
- Curtis BM, Ravani P, Malberti F, Kennett F, Taylor PA, Djurdjev O, et al. The short- and long-term impact of multi-disciplinary clinics in addition to standard nephrology care on patient outcomes. Nephrol Dial Transplant 2005;20:147-54.
- Hardy KJ, Furlong NJ, Hulme SA, O’Brien SV. Delivering improved management and outcomes in diabetic kidney disease in routine clinical care. Br J Diabetes Vasc Dis 2007;7:172-8.
- Harnett P, Grigoriou A, Mapplebeck S, Almond M. Virtual CKD Clinic Provides Equivalent Surveillance When Compared to Primary Care n.d.
- Harris LE, Luft FC, Rudy DW, Kesterson JG, Tierney WM. Effects of multidisciplinary case management in patients with chronic renal insufficiency. Am J Med 1998;105:464-71.
- Hemmelgarn BR, Manns BJ, Zhang J, Tonelli M, Klarenbach S, Walsh M, et al. Association between multidisciplinary care and survival for elderly patients with chronic kidney disease. J Am Soc Nephrol 2007;18:993-9.
- Jones C, Roderick P, Harris S, Rogerson M. An evaluation of a shared primary and secondary care nephrology service for managing patients with moderate to advanced CKD. Am J Kidney Dis 2006;47:103-14.
- Kelly CJG, Booth G. Pharmacist-led structured care for patients with diabetic nephropathy. Br J Diabetes Vasc Dis 2008;8:86-8.
- Leung WY, So WY, Tong PC, Chan NN, Chan JC. Effects of structured care by a pharmacist-diabetes specialist team in patients with type 2 diabetic nephropathy. Am J Med 2005;118.
- Richards N, Harris K, Whitfield M, O’Donoghue D, Lewis R, Mansell M, et al. Primary care-based disease management of chronic kidney disease (CKD), based on estimated glomerular filtration rate (eGFR) reporting, improves patient outcomes. Nephrol Dial Transplant 2008;23:549-55.
- Thanamayooran S. R. Effectiveness of a multidisciplinary kidney disease clinic in achieving treatment guideline targets. Nephrol Dial Transplant 2005;20:2385-93.
- Bending J, Kingswood C. Joint diabetes renal clinics are ‘best practice’. Br J Diabetes Vasc Dis 2007;7.
- Compton A, Provenzano R, Johnson CA. The nephrology nurse’s role in improved care of patients with chronic kidney disease. Nephrol Nurs J 2002;29:331-6.
- Ghossein C, Serrano A, Rammohan M, Batlle D. The role of comprehensive renal clinic in chronic kidney disease stabilization and management: The Northwestern experience. Semin Nephrol 2002;22:526-32.
- Hostetter TH, Lising M. National kidney disease education program. J Am Soc Nephrol 2003;14:S114-S116.
- Joy MS, DeHart RM, Gilmartin C, Hachey DM, Hudson JQ, Pruchnicki M, et al. Clinical pharmacists as multidisciplinary health care providers in the management of CKD: A joint opinion by the nephrology and ambulatory care practice and research networks of the American College of Clinical Pharmacy. Am J Kidney Dis 2005;45:1105-18.
- Thomas N. Collaboration between hospital and primary care can improve the management of diabetic nephropathy. Br J Diabetes Vasc Dis 2004;4:202-4.
- Thomas N. Can we delay the progression of chronic kidney disease (CKD) by improving collaboration between renal units and primary care teams?. EDTNA ERCA J 2005;31:178-81.
- Mendelssohn DC, Toffelmire EB, Levin A. Attitudes of Canadian nephrologists toward multidisciplinary team-based CKD clinic care. Am J Kidney Dis 2006;47:277-84.
- Anon . Combating chronic kidney disease: A managed care perspective. Am J Manag Care 2002;8:S112-S113.
- Anon . PCPs need to step up their care of patients with CKD. Dis Manag Advis 2007;13:13-5.
- Levin A. The need for optimal and coordinated management of CKD. Kidney Int Suppl 2005:S7-10.
- St Peter WL, Schoolwerth AC, McGowan T, McClellan WM. Chronic kidney disease: issues and establishing programs and clinics for improved patient outcomes. Am J Kidney Dis 2003;41:903-24.
- Curtin RB, Becker B, Kimmel PL, Schatell D. An integrated approach to care for patients with chronic kidney disease. Seminars in Dialysis 2003;16:399-402.
- Mendelssohn DC. Coping with the CKD epidemic: the promise of multidisciplinary team-based care. Nephrol Dial Transplant 2005;20:10-2.
- Chen RA, Scott S, Mattern WD, Mohini R, Nissenson AR. The case for disease management in chronic kidney disease. Dis Manag 2006;9:86-92.
- Kirby R. Multidisciplinary care for kidney disease patients. Nat Clin Pract Nephrol 2006;2.
- Tomlinson J. How do we re-design the treatment? A background paper prepared for the UK Consensus Conference on early chronic kidney disease. Nephrol Dial Transplant 2007;22:ix39-44.
- Komenda P, Levin A. Analysis of cardiovascular disease and kidney outcomes in multidisciplinary chronic kidney disease clinics: complex disease requires complex care models. Curr Opin Nephrol Hypertens 2006;15:61-6.
- Spry L. Building the chronic kidney disease management team. Adv Chron Kidney Dis 2008;15:29-36.
- Frankel A, Brown E, Wingfield D. Management of chronic kidney disease. BMJ 2005;330:1039-40.
- Rutecki GW. Putting guidelines for chronic kidney disease into practice. Consultant 2006;46.
- National Institute for Health and Clinical Excellence . Type 2 Diabetes: The Management of Type 2 Diabetes (update) 2008. www.nice.org.uk/guidance/index.jsp?action=byID%26o=11983 (accessed December 2008).
- Gaede P, Vedel P, Larsen N, Jensen GVH, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003;348:383-93.
- Heffernan C. Screening for Chronic Kidney Disease: An Evidence Based Review for the National Screening Committe 2008. www.screening.nhs.uk/ckd (accessed June 2009).
- NHS Scotland . Keep Well Scotland 2009. www.keepwellscotland.com/ (accessed 24 September 2009).
- Department of Health . Improving Chronic Disease Management 2004. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4075214 (accessed May 2009).
- Atthobari J, Asselbergs FW, Boersma C, de VR, Hillege HL, van Gilst WH, et al. Cost-effectiveness of screening for albuminuria with subsequent fosinopril treatment to prevent cardiovascular events: A pharmacoeconomic analysis linked to the prevention of renal and vascular endstage disease (PREVEND) study and the prevention of renal and vascular endstage disease intervention trial (PREVEND IT). Clin Ther 2006;28:432-44.
- Boulware LE, Jaar BG, Brancati FL, Powe NR. Screening for proteinuria in US adults: a cost-effectiveness analysis. J Am Med Assoc 2003;290:3101-14.
- McLaughlin K, Manns B, Culleton B, Donaldson C, Taub K. An economic evaluation of early versus late referral of patients with progressive renal insufficiency. Am J Kidney Dis 2001;38:1122-8.
- Binik YM, Devins GM, Barre PE, Guttmann RD, Hollomby DJ, Mandin H, et al. Live and learn: patient education delays the need to initiate renal replacement therapy in end-stage renal disease. J Nerv Ment Dis 1993;181:371-6.
- Asselbergs FW, Diercks GF, Hillege HL, Van Boven AJ, Janssen WM, Voors AA, et al. Prevention of Renal and Vascular Endstage Disease Intervention Trial (PREVENT IT) Investigators. Effects of fosinopril and pravastatin on cardiovascular events in subjects with microalbuminuria. Circulation 2004;110:2809-16.
- Clark WF, Churchill DN, Forwell L, Macdonald G, Foster S. To pay or not to pay? A decision and cost-utility analysis of angiotensin-converting-enzyme inhibitor therapy for diabetic nephropathy. CMAJ 2000;162:195-8.
- Stafylas PC, Sarafidis PA, Grekas DM, Lasaridis AN. A cost-effectiveness analysis of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in diabetic nephropathy. J Clin Hypertens 2007;9:751-9.
- Rosen AB, Hamel MB, Weinstein MC, Cutler DM, Fendrick A, Vijan S. Cost-effectiveness of full Medicare coverage of angiotensin-converting enzyme inhibitors for beneficiaries with diabetes. Ann Int Med 2005;143:89-9.
- Palmer AJ, Annemans L, Roze S, Lamotte M, Rodby RA, Cordinnier DJ. An economic evaluation of irbesartan in the treatment of patients with type 2 diabetes, hypertension and nephropathy; cost-effectiveness of Irbesartan in Diabetic Nephropathy Trial (IDNT) in the Belgian and French settings. Nephrol Dial Transplant 2003;18:2059-66.
- Palmer AJ, Tucker D.M., Valentine WJ, Roze S, Gabriel S, Cordonnier DJ. Cost-effectiveness of irbesartan in diabetic nephropathy: a systematic review of published studies. Nephrol Dial Transplant 2005;20:1103-9.
- Ruggenenti P, Schieppati A, Remuzzi G. Progression, remission, regression of chronic renal diseases. Lancet 2001;357:1601-8.
- van Hout BA, Simeon GP, McDonnell J, Mann JF. Economic evaluation of benazepril in chronic renal insufficiency. Kidney Int Suppl 1997;63:59-62.
- Howard K, Salkeld G, White S, Chadban S, Craig J, McDonald S, et al. The Cost-Effectiveness of Early Detection and Intervention to Prevent the Progression of Chronic Kidney Disease in Australia 2006. www.kidney.org.au/ (accessed 2009).
- Khan S, Amedia CA. Economic burden of chronic kidney disease. J Eval Clin Pract 2008;14:422-34.
- Stevens PE, O’Donoghue DJ, de LS, Van VJ, Klebe B, Middleton R, et al. Chronic kidney disease management in the United Kingdom: NEOERICA project results. Kidney Int 2007;72:92-9.
- Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. J Am Med Assoc 2007;298:2038-47.
- Parikh NI, Hwang SJ, Larson MG, Levy D, Fox CS. Chronic kidney disease as a predictor of cardiovascular disease (from the Framingham Heart Study). Am J Cardiol 2008;102:47-53.
- Foster MC, Hwang SJ, Larson MG, Parikh NI, Meigs J.B., Vasan RS, et al. Cross-classification of microalbuminuria and reduced glomerular filtration rate: associations between cardiovascular disease risk factors and clinical outcomes. Arch Intern Med 2007;167:1386-92.
- Weiner DE, Tabatabai S, Elsayed E, Bansal N, Griffith J, Salem DN, et al. Cardiovascular outcomes and all cause mortality: Exploring the interaction between CKD and cardiovascular disease. Am J Kidney Dis 2006;48:392-401.
- Lorber D, Reddan D. Clinical characteristics of chronic kidney disease patients with and without diabetes: a subanalysis of the PAERI study. Clin Nephrol 2006;66:11-6.
- Gerstein HC, Mann JF, Pogue J, Dinneen SF, Halle JP, Hoogwerf B, et al. Prevalence and determinants of microalbuminuria in high-risk diabetic and nondiabetic patients in the Heart Outcomes Prevention Evaluation Study. The HOPE Study Investigators. Diabetes Care 2000;23:B35-B39.
- Welcome to the QRISK® 2 Cardiovascular Disease Risk Calculator 2009. http://qr2.dyndns.org/ (accessed April 2009).
- Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:1475-82.
- Heart Protection Study Collaborative . Lifetime cost-effectiveness of simvastatin in a range of risk groups and age groups derived from a randomised trial of 20,536 people. BMJ 2006;333:1145-9.
- Hunsicker LG, Adler S, Caggiula A, England BK, Greene T, Kusek JW, et al. Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney Int 1997;51:1908-19.
- Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR, et al. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int 2003;63:225-32.
- Office of National Statistics . Mid-2005 Population Estimates: England and Wales; Estimated Resident Population by Single Year of Age and Sex 2006. www.statistics.gov.uk/statbase/ssdataset.asp?vlnk=9389%26More=Y (accessed February 2009).
- Office of National Statistics . Death by Age, Sex and Underlying Cause, 2005 Registrations: Health Statistics Quarterly 30 2006. www.statistics.gov.uk/StatBase/ssdataset.asp?vlnk=9346%26Pos=%26ColRank=272 (accessed February 2009).
- McManus RJ, Mant J, Roalfe A, Oakes RA, Bryan S, Pattison HM, et al. Targets and self monitoring in hypertension: randomised controlled trial and cost effectiveness analysis. Br Med J 2005;331.
- Baboolal K, McEwan P, Sondhi S, Spiewanowski P, Wechowski J, Wilson K. The cost of renal dialysis in a UK setting – a multicentre study. Nephrol Dial Transplant 2008;23:1982-9.
- Department of Health . NHS Reference Costs 2006–07 2008. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_082571 (accessed February 2009).
- Curtis L. Unit Costs of Health and Social Care 2007. Personal Social Service Research Unit (PSSRU) 2008. www.pssru.ac.uk/uc/uc2007contents.htm (accessed February 2009).
- British Medical Association and Royal Pharmaceutical Society of Great Britain . British National Formulary 2008.
- National Institute for Health and Clinical Excellence . Chronic Kidney Disease Costing Report: Implementing NICE Guidance 2008. www.nice.org.uk/nicemedia/pdf/CG73CostingReport.PDF (accessed September 2009).
- Burden R, Tomson C. Identification, management and referral of adults with chronic kidney disease: Concise guidelines. Clin Med 2005;5:635-42.
- Menon V, Wang X, Sarnak MJ, Hunsicker LH, Madero M, Beck GJ, et al. Long-term outcomes in nondiabetic chronic kidney disease. Kidney Int 2008;73:1310-15.
- Wakai K, Kawamura T, Endoh M, Kojima M, Tomino Y, Tamakoshi A, et al. A scoring system to predict renal outcome in IgA nephropathy: from a nationwide prospective study. Nephrol Dial Transplant 2006;21:2800-8.
- Burnier M, Zanchi A. Blockage of the renin-angiotensin-aldosterone system: a key therapeutic strategy to reduce renal and cardiovascular events in patients with diabetes. J Hypertens 2006;24:11-25.
- Palmer AJ, Annemans L, Roze S, Lapuerta P, Chen R, Gabriel S, et al. Irbesartan is projected to be cost and life saving in a Spanish setting for treatment of patients with type 2 diabetes, hypertension, and microalbuminuria. Kidney Int Suppl 2005;67:S52-S54.
- Hobbs H, Stevens P, Klebe B, Irving J, Cooley R, O’Donoghue D, et al. Referral patterns to renal services: what has changed in the past 4 years?. Nephrol Dial Transplant 2009:1-8.
- Philips LA, Donovan KL, Philips AO. Renal quality outcomes framework and eGFR: impact on secondary care. QJM 2009;102:415-23.
- Krol E, Rutkowski B, Czarniak P, Kraszewska E, Lizakowski S, Szubert R, et al. Early detection of chronic kidney disease: Results of the PolNef Study. Am J Nephrol 2009;29:264-73.
- Vassalotti JA, Gracz-Weinstein L, Gannon MR, Brown WW. Targeted screening and treatment of chronic kidney disease. Lessons learned from the Kidney Early Evaluation Program. Dis Manag Health Outcomes 2006;14:341-52.
- Blackburn RC, Parke CL, Sharma P, McCullough K, Black C. Angiotensin converting enzyme inhibitors and angiotensin receptor blockers for adults with early (stage 1–3) non-diabetic chronic kidney disease (Protocol). The Cochrane Database of Systematic Reviews 2009.
- Anees M, Mumtaz A, Nazir M, Ibrahim M, Rizwan SM, Kausar T. Referral pattern fof hemodialysis patients to nephrologists. J Coll Physicians Surg Pak 2007;17:671-4.
- Arora P, Obrador GT, Ruthazer R, Kausz AT, Meyer KB, Jenuleson CS, et al. Prevalence, predictors, and consequences of late nephrology referral at a tertiary care center. J Am Soc Nephrol 1999;10:1281-6.
- Avorn J, Bohn RL, Levy E, Levin R, Owen WF, Winkelmayer WC, et al. Nephrologist care and mortality in patients with chronic renal insufficiency. Arch Intern Med 2002;162:2002-6.
- Baker A, McMahon A, Cockfield SM. Delayed referral of patients with chronic kidney disease is an independent risk factor for mortality. J Am Soc Nephrol 2003;14.
- Barril G, Sanz P, Bardon E, Andrino T, Cigarran S, Selgas R. Earliest referral to advanced chronic kidney disease unit (ACKDU) could prevent renal osteodystrophy (ROD). J Am Soc Nephrol 2002;13:672A-3A.
- Brown WW, Collins A, Chen SC, King K, Molony D, Gannon MR, et al. Identification of persons at high risk for kidney disease via targeted screening: the NKF Kidney Early Evaluation Program. Kidney Int Suppl 2003;63:S50-S55.
- Burton CJ, Feest TG. Does referral to a renal clinic slow the progression of diabetic nephropathy? An audit of 100 consecutive referrals. Kidney Int 1999;55.
- Caskey FJ, Wordsworth S, Ben T, de Charro FT, Delcroix C, Dobronravov V, et al. Early referral and planned initiation of dialysis: what impact on quality of life?. Nephrol Dial Transplant 2003;18:1330-8.
- Cass A, Cunningham J, Arnold PC, Snelling P, Wang Z, Hoy W. Delayed referral to a nephrologist: outcomes among patients who survive at least one year on dialysis. Med J Aust 2002;177:135-8.
- Chan MR, Dall AT, Fletcher KE, Lu N, Trivedi H. Outcomes in patients with chronic kidney disease referred late to nephrologists: A meta-analysis. Am J Med 2007;120:1063-70.
- Chandna SM, Schulz J, Lawrence C, Greenwood RN, Farrington K. Is there a rationale for rationing chronic dialysis? A hospital based cohort study of factors affecting survival and morbidity. BMJ 1999;318:217-23.
- Curtis BM, Barrett BJ, Djurdjev O, Singer J, Levin A. Evaluation and treatment of CKD patients before and at their first nephrologist encounter in Canada. Am J Kidney Dis 2007;50:733-42.
- Dautlich J, Worth D, Strang J. Chronic renal insufficiency: unmet need for referral to a renal physician. Kidney Int 1999;55.
- Dogan E, Erkoc R, Sayarlioglu H, Durmus A, Topal C. Effects of late referral to a nephrologist in patients with chronic renal failure. Nephrology 2005;10:516-19.
- Ellis PA, Reddy V, Bari N, Cairns HS. Late referral of end-stage renal failure. QJM 1998;91:727-32.
- Fan SL, Marsh FP, Raftery MJ, Yaqoob MM. Do patients referred late for peritoneal dialysis do badly?. Perit Dial Int 2002;22:630-2.
- Fox CH, Brooks A, Zayas LE, McClellan W, Murray B. Primary care physicians’ knowledge and practice patterns in the treatment of chronic kidney disease: An Upstate New York Practice-based Research Network (UNYNET) study. J Am Board Fam Med 2006;19:54-61.
- Goransson LG, Bergrem H. Consequences of late referral of patients with end-stage renal disease. J Int Med 2001;250:154-9.
- Harris SAC, Brown EA, Lamping DL, Constantinovici N, Henderson L, Roderick P, et al. Effect of late referral to a nephrologist on quality of life of elderly dialysis patients. Kidney Int 1999;55.
- Hyder M, Manchester G, Fan PY. Referral patterns for renal insufficiency. J Gen Intern Med 2000;15.
- Innes A, Rowe PA, Burden RP, Morgan AG. Early deaths on renal replacement therapy: the need for early nephrological referral. Nephrol Dial Transplant 1992;7:467-71.
- Iseki K. Analysis of referral pattern and survival in chronic dialysis patients in Okinawa, Japan (1993–1997). Clin Exp Nephrol 2002;6:43-8.
- Ismail N, Neyra R, Hakim R. The medical and economical advantages of early referral of chronic renal failure patients to renal specialists. Nephrol Dial Transplant 1998;13:246-50.
- Jungers P, Zingraff J, Page B, Albouze G, Hannedouche T, Man NK. Detrimental effects of late referral in patients with chronic renal failure: a case-control study. Kidney Int Suppl 1993;41:S170-S173.
- Jungers P, Zingraff J, Albouze G, Chauveau P, Page B, Hannedouche T, et al. Late referral to maintenance dialysis: detrimental consequences. Nephrol Dial Transplant 1993;8:1089-93.
- Jungers P, Skhiri H, Giatras I, Muller S, Fumeron C, Touam M, et al. Beneficial effects of early nephrological referral of chronic renal failure patients. J Am Soc Nephrol 1997;8.
- Kazmi W, Khan SS. Late referral and it’s association with probability or being wait-listed for cadaveric kidney transplant. Am J Kidney Dis 2002;39.
- Kazmi WH, Obrador GT, Khan SS, Pereira BJ, Kausz AT. Late nephrology referral and mortality among patients with end-stage renal disease: a propensity score analysis. Nephrol Dial Transplant 2004;19:1808-14.
- Klebe B, Irving J, Stevens PE, O’Donoghue DJ, de LS, Cooley R, et al. The cost of implementing UK guidelines for the management of chronic kidney disease. Nephrol Dial Transplant 2007;22:2504-12.
- Lhotta K, Zoebl M, Mayer G, Kronenberg F. Late referral defined by renal function: association with morbidity and mortality. J Nephrol 2003;16:855-61.
- Lin CL, Wu MS, Hsu PY, Huang CC. Improvement of clinical outcome by early nephrology referral in type II diabetics on hemodialysis. Ren Fail 2003;25:455-64.
- Lin CL, Chuang FR, Wu CF, Yang CT. Early referral as an independent predictor of clinical outcome in end-stage renal disease on hemodialysis and continuous ambulatory peritoneal dialysis. Ren Fail 2004;26:531-7.
- Locatelli F, Vecchio LD, Pozzoni P. The importance of early detection of chronic kidney disease. Nephrol Dial Transplant 2002;17:2-7.
- London R, Solis A, Goldberg GA, Wade S, Chan WW. Examination of resource use and clinical interventions associated with chronic kidney disease in a managed care population. J Manag Care Pharm 2003;9:248-55.
- Lusenti T, Rustichelli R, Cardarelli F, Gregorini M, Borgatti P, Giacometti P, et al. The early referral to nephrologist preserves renal function in patients with chronic renal failure associated to renal artery stenosis. Nephrol Dial Transplant 2006;21.
- Mendelssohn DC, Barrett BJ, Brownscombe LM, Ethier J, Greenberg DE, Kanani SD, et al. Elevated levels of serum creatinine: recommendations for management and referral. CMAJ 1999;161:413-17.
- Ohmit SE, Flack JM, Peters RM, Brown WW, Grimm R. Longitudinal Study of the National Kidney Foundation’s (NKF) Kidney Early Evaluation Program (KEEP). J Am Soc Nephrol 2003;14:S117-S121.
- Paris V, Ballerini L. Patient flow analysis and referrals: how 1,137 ESRD patients started dialysis during 1998–1999. EDTNA ERCA J 2002;169:160-63.
- Rao M, Lindberg J, Port FK, Lin F, Kausz AT, Pereira BJG, et al. Patterns of referral to the nephrologist for chronic kidney disease care – Results from the STRIDE registry. J Am Soc Nephrol 2002;13.
- Rasgon SA, Yeoh HH, Kujubu D, Bhalotra S, Tompkins CP. Importance of early referral to the nephrologist. J Am Soc Nephrol 2003;14.
- Ratcliffe PJ, Phillips RE, Oliver DO. Late referral for maintenance dialysis. Br Med J (Clin Res Ed) 1984;288:441-3.
- Ravani P, Marinangeli G, Stacchiotti L, Malberti F. Structured pre-dialysis programs: more than just timely referral?. J Nephrol 2003;16:862-9.
- Roderick P, Drey N, Webster P, Blakely S, Mason J, Tomson C. Late referral for renal replacement therapy in the South West Region – how common is it and what are its determinants and sequelae?. Kidney Int 1999;55:2588-9.
- Roderick P, Jones C, Tomson C, Mason J. Late referral for dialysis: improving the management of chronic renal disease. QJM 2002;95:363-70.
- Roubicek C, Brunet P, Huiart L, Thirion X, Leonetti F, Dussol B, et al. Timing of nephrology referral: influence on mortality and morbidity. Am J Kidney Dis 2000;36:35-41.
- Rutherford PA, Rutherford S, Drew PJT. Adverse effects of late referral for nephrological opinion. Kidney Int 1997;52.
- Schmidt RJ, Domico JR, Sorkin MI, Hobbs G. Early referral and its impact on emergent first dialyses, health care costs, and outcome. Am J Kidney Dis 1998;32:278-83.
- Schwenger V, Morath C, Hofmann A, Hoffmann O, Zeier M, Ritz E. Late referral – a major cause of poor outcome in the very elderly dialysis patient. Nephrol Dial Transplant 2006;21:962-7.
- Sesso R, Belasco AG. Late diagnosis of chronic renal failure and mortality on maintenance dialysis. Nephrol Dial Transplant 1996;11:2417-20.
- Shin SJ, Kim HW, Chung S, Chung HW, Lee SJ, Kim YS, et al. Late referral to a nephrologist increases the risk of uremia-related cardiac hypertrophy in patients on hemodialysis. Nephron 2007;107:c139-c146.
- Stack AG. Impact of timing of nephrology referral and pre-ESRD care on mortality risk among new ESRD patients in the United States. Am J Kidney Dis 2003;41:310-18.
- Stoves J, Bartlett CN, Newstead CG. Specialist follow up of patients before end stage renal failure and its relationship to survival on dialysis. Postgrad Med J 2001;77:586-8.
- Thomas MC. Early referral of patients with pre-end-stage kidney disease. Nephrology 2007;12:S41-S43.
- Wavamunno MD, Harris DC. The need for early nephrology referral. Kidney Int Suppl 2005;94:S128-S132.
- White CA, Pilkey RM, Lam M, Holland DC. Pre-dialysis clinic attendance improves quality of life among hemodialysis patients. BMC Nephrol 2002;3.
- Winkelmayer WC, Owen WF, Levin R, Avorn J. A propensity analysis of late versus early nephrologist referral and mortality on dialysis. J Am Soc Nephrol 2003;14:486-92.
- Wu M-S. Improvement in clinical outcome by early nephrology referral in type II diabetics on maintenance peritoneal dialysis. Perit Dial Int 2003;23:39-45.
- Agency for Healthcare Research and Quality . Late referral to specialty care contributes to poor outcomes among patients with kidney failure. Res Activities 2002:4-5.
- Agency for Healthcare Research and Quality . Early referral of patients with chronic kidney disease reduces complications and mortality. Res Activities 2005.
- Agency for Healthcare Research and Quality . Studies show that early nephrologist referral and frequent visits improve survival among ESRD patients. Res Activities 2002:17-8.
- Altman JJ, Elian N, Grun S, Gerard HG, Feldman S. The outcome of advanced chronic nephropathy in type 1 and type 2 diabetic and non-diabetic patients: a prospective study. Diabetes Metab 1999;25:144-9.
- Boes E, Fliser D, Ritz E, Konig P, Lhotta K, Mann JF, et al. Apolipoprotein A-IV predicts progression of chronic kidney disease: the mild to moderate kidney disease study. J Am Soc Nephrol 2006;17:528-36.
- Bruno G, Biggeri A, Merletti F. Apolipoprotein A-IV predicts progression of chronic kidney disease: the mild to moderate kidney disease study. Diabetes Care 2003;26:2353-8.
- Busch M, Franke S, Wolf G, Brandstadt A, Ott U, Gerth J, et al. The advanced glycation end product N(epsilon)-carboxymethyllysine is not a predictor of cardiovascular events and renal outcomes in patients with type 2 diabetic kidney disease and hypertension. Am J Kidney Dis 2006;48:571-9.
- Chandie Shaw PK, Baboe F, van Es LA, van der Vijver JC, van de Ree MA, de Jonge N, et al. South-Asian type 2 diabetic patients have higher incidence and faster progression of renal disease compared with Dutch-European diabetic patients. Diabetes Care 2006;29:1383-5.
- Chauveau P, Combe C, Rigalleau V, Vendrely B, Aparicio M. Restricted protein diet is associated with decrease in proteinuria: consequences on the progression of renal failure. J Ren Nutr 2007;17:250-7.
- Chonchol M, Shlipak MG, Katz R, Sarnak MJ, Newman AB, Siscovick DS, et al. Relationship of uric acid with progression of kidney disease. Am J Kidney Dis 2007;50:239-47.
- Christensen PK, Rossing P, Nielsen FS, Parving HH. Natural course of kidney function in Type 2 diabetic patients with diabetic nephropathy. Diabetic Med 1999;16:388-94.
- Costacou T, Ellis D, Fried L, Orchard TJ. Sequence of progression of albuminuria and decreased GFR in persons with type 1 diabetes: a cohort study. Am J Kidney Dis 2007;50:721-32.
- Damman K, Navis G, Voors AA, Asselbergs FW, Smilde TD, Cleland JG, et al. Worsening renal function and prognosis in heart failure: systematic review and meta-analysis. J Card Fail 2007;13:599-608.
- Dean BB, Dylan M, Gano A, Knight K, Ofman JJ, Levine BS. Erythropoiesis-stimulating protein therapy and the decline of renal function: a retrospective analysis of patients with chronic kidney disease. Curr Med Res Opin 2005;21:981-7.
- Drummond K, Mauer M. International Diabetic Nephropathy Study G . The early natural history of nephropathy in type 1 diabetes: II. Early renal structural changes in type 1 diabetes. Diabetes 2002;51:1580-7.
- Earle KK, Porter KA, Ostberg J, Yudkin JS. Variation in the progression of diabetic nephropathy according to racial origin. Nephrol Dial Transplant 2001;16:286-90.
- Edwards MS, Wilson DB, Craven TE, Stafford J, Fried LF, Wong TY, et al. Associations between retinal microvascular abnormalities and declining renal function in the elderly population: the Cardiovascular Health Study. Am J Kidney Dis 2005;46:214-24.
- El Kossi MM, Ibrahim A, Lock TJ, el Nahas AM. Impact of cardiac transplantation on kidney function: a single- center experience. Transplant Proc 2003;35:1527-31.
- Fliser D, Kronenberg F, Kielstein JT, Morath C, Bode-Boger SM, Haller H, et al. Asymmetric dimethylarginine and progression of chronic kidney disease: the mild to moderate kidney disease study. J Am Soc Nephrol 2005;16:2456-61.
- Fliser D, Kollerits B, Neyer U, Ankerst DP, Lhotta K, Lingenhel A, et al. Fibroblast growth factor 23 (FGF23) predicts progression of chronic kidney disease: the Mild to Moderate Kidney Disease (MMKD) Study. J Am Soc Nephrol 2007;18:2600-8.
- Fried L, Solomon C, Shlipak M. Inflammatory and prothrombotic markers and the progression of renal disease in elderly individuals. J Am Soc Nephrol 2004;15:3184-91.
- Hadjadj S, Duly-Bouhanick B, Bekherraz A, Bridoux F, Gallois Y, Mauco G, et al. Serum triglycerides are a predictive factor for the development and the progression of renal and retinal complications in patients with type 1 diabetes. Diabetes Metab 2004;30:43-51.
- Hebert LA, Greene T, Levey A, Falkenhain ME, Klahr S. High urine volume and low urine osmolality are risk factors for faster progression of renal disease. Am J Kidney Dis 2003;41:962-71.
- Henry RMA, Kostense PJ, Bos G. Mild renal insufficiency is associated with increased cardiovascular mortality: The Hoorn study. Kidney Int 2002;62:1402-7.
- Hovind P, Rossing P, Tarnow L, Parving HH. Smoking and progression of diabetic nephropathy in type 1 diabetes. Diabetes Care 2003;26:911-16.
- Hovind P, Rossing P, Tarnow L, Smidt UM, Parving HH. Remission and regression in the nephropathy of type 1 diabetes when blood pressure is controlled aggressively. Kidney Int 2001;60:277-83.
- Hoy WE, Kondalsamy-Chennakesavan S, McDonald S, Wang Z. Renal disease, the metabolic syndrome, and cardiovascular disease. Ethn Dis 2006;16:46-51.
- Hsu CCC, Bray MS, Kao WHL, Pankow JS, Boerwinkle E, Coresh J. Genetic variation of the renin-angiotensin system and chronic kidney disease progression in black individuals in the atherosclerosis risk in communities study. J Am Soc Nephrol 2006;17:504-12.
- Imbasciati E, Gregorini G, Cabiddu G, Gammaro L, Ambroso G, Del Giudice A, et al. Pregnancy in CKD stages 3 to 5: fetal and maternal outcomes. Am J Kidney Dis 2007;49:753-62.
- Iseki K, Ikemiya Y, Iseki C, Takishita S. Prevalence of high fasting plasma glucose and risk of developing end-stage renal disease in screened subjects in Okinawa, Japan. Clin Exp Nephrol 2004;8:250-6.
- Jacobsen P, Rossing K, Tarnow L, Rossing P, Mallet C, Poirier O, et al. Progression of diabetic nephropathy in normotensive type 1 diabetic patients. Kidney Int Suppl 1999;71:S101-S105.
- Jacobsen P, Rossing P, Tarnow L, Hovind P, Parving HH. Birth weight--a risk factor for progression in diabetic nephropathy?. Journal of Internal Medicine 2003;253:343-50.
- Jafar TH, Stark PC, Schmid CH, Landa M, Maschio G, Marcantoni C, et al. Proteinuria as a modifiable risk factor for the progression of non-diabetic renal disease. Kidney Int 2001;60:1131-40.
- Jafar TH, Schmid CH, Stark PC, Toto R, Remuzzi G, Ruggenenti P, et al. The rate of progression of renal disease may not be slower in women compared with men: a patient-level meta-analysis. Nephrol Dial Transplant 2003;18:2047-53.
- Jafar TH, Stark PC, Schmid CH, Landa M, Maschio G, de Jong PE, et al. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition. A patient-level meta-analysis. Ann Int Med 2003;139:244-52.
- Jovanovic DB, Djukanovic L. Analysis of factors influencing chronic renal failure progression. Ren Fail 1999;21:177-87.
- Jude EB, Anderson SG, Cruickshank JK. Natural history and prognostic factors of diabetic nephropathy in type 2 diabetes. J Assoc Physicians 2002;95:371-7.
- Kasiske BL, Lakatua JD, Ma JZ, Louis TA. A meta-analysis of the effects of dietary protein restriction on the rate of decline in renal function. Am J Kidney Dis 1998;31:954-61.
- Kim SB, Kwon S, Lee SK, Park JS. Association of atherosclerotic coronary artery disease and pulse pressure with renal disease progression. Ren Fail 2003;25:1019-27.
- Kohli HS, Bhat A, Aravindan, Sud K, Jha V, Gupta KL, . Spectrum of renal failure in elderly patients. Int Urol Nephrol 2006;38:759-65.
- Kristjansson K, Ljungman S, Bengtsson C, Bjorkelund C, Sigurdsson JA. Microproteinuria and long-term prognosis with respect to renal function and survival in normotensive and hypertensive women: A 24-year follow-up of a representative population sample of women in Gothenburg, Sweden. Scand J Urol Nephrol 2001;35:63-70.
- Kronborg J, Solbu M, Njolstad I, Toft I, Eriksen BO. Predictors of change in estimated GFR: a population-based 7-year follow-up from the Tromso study. Nephrol Dial Transplant 2008;23:2818-26.
- Larsson A, Helmersson J, Hansson L-O, Basu S. Increased serum cystatin C is associated with increased mortality in elderly men. Scand J Clin Lab Invest 2005;65:301-5.
- Leeder SR, Mitchell P, Liew G, Rochtchina E, Smith W, Wang JJ. Low hemoglobin, chronic kidney disease, and risk for coronary heart disease-related death: The Blue Mountains Eye Study. J Am Soc Nephrol 2006;17:279-84.
- Lerma EV. ACE inhibitors, but not angiotensin II receptor antagonists, reduce all cause mortality in diabetic nephropathy. Evid Based Med 2005;10.
- Locatelli F, Del Vecchio L, Andrulli S, Marai P, Tentori F. The role of underlying nephropathy in the progression of renal disease. Kidney Int Suppl 2000;75:S49-S55.
- Mann JF, Gerstein HC, Yi QL, Franke J, Lonn EM, Hoogwerf BJ, et al. Progression of renal insufficiency in type 2 diabetes with and without microalbuminuria: results of the Heart Outcomes and Prevention Evaluation (HOPE) randomized study. Am J Kidney Dis 2003;42:936-42.
- Marcotte L, Godwin M. Natural history of elevated creatinine levels. Can Fam Physician 2006;52:1264-5.
- Massy ZA, Nguyen Khoa T, Lacour B, scamps-Latscha B, Man NK, Jungers P. Dyslipidaemia and the progression of renal disease in chronic renal failure patients. Nephrol Dial Transplant 1999;14:2392-7.
- McClellan WM, Langston RD, Presley R. Medicare patients with cardiovascular disease have a high prevalence of chronic kidney disease and a high rate of progression to end-stage renal disease. J Am Soc Nephrol 2004;15:1912-9.
- Menon MK, Naimark DM, Bargman JM, Vas SI, Oreopoulos DG. Long-term blood pressure control in a cohort of peritoneal dialysis patients and its association with residual renal function. Nephrol Dial Transplant 2001;16:2207-13.
- Merkin SS, Coresh J, ez Roux AV, Taylor HA, Powe NR. Area socioeconomic status and progressive CKD: The atherosclerosis risk in communities (ARIC) study. Am J Kidney Dis 2005;46:203-13.
- Middleton RJ, Foley RN, Hegarty J, Cheung CM, McElduff P, Gibson JM, et al. The unrecognized prevalence of chronic kidney disease in diabetes. Nephrol Dial Transplant 2006;21:88-92.
- Morita S, Fukuhara S, Akizawa T, Asano Y, Koshikawa S, Koide K, et al. Prognostic factors for a composite end-point of renal outcomes in patients with chronic kidney disease. Ther Apher Dial 2006;10:72-7.
- Muhlhauser I, Sawicki PT, Blank M, Overmann H, Bender R, Berger M. Prognosis of persons with type 1 diabetes on intensified insulin therapy in relation to nephropathy. J Int Med 2000;248:333-41.
- Neild GH, Thomson G, Nitsch D, Woolfson RG, Connolly JO, Woodhouse CR. Renal outcome in adults with renal insufficiency and irregular asymmetric kidneys. BMC Nephrol 2004;5.
- Orth SR, Hallan SI. Smoking: a risk factor for progression of chronic kidney disease and for cardiovascular morbidity and mortality in renal patients--absence of evidence or evidence of absence?. Clin J Am Soc Nephrol 2008;3:226-36.
- Perlman RL, Kiser M, Finkelstein F, Eisele G, Roys E, Liu L, et al. The longitudinal chronic kidney disease study: a prospective cohort study of predialysis renal failure. Semin Dial 2003;16:418-23.
- Ruggenenti P, Perna A, Mosconi L, Pisoni R, Remuzzi G. Urinary protein excretion rate is the best independent predictor of ESRF in non-diabetic proteinuric chronic nephropathies. Kidney Int 1998;53:1209-16.
- Rigalleau V, Lasseur C, Raffaitin C, Perlemoine C, Barthe N, Chauveau P, et al. Prediction of glomerular filtration rate decline in diabetic subjects with impaired renal function. Nephrol Dial Transplant 2007;22:959-60.
- Rottey S, Vanholder R, De Schoenmakere G, Lameire N. Progression of renal failure in patients with compromised renal function is not always present: evaluation of underlying disease. Clin Nephrol 2000;54:1-10.
- Samuelsson O, Attman PO. Is smoking a risk factor for progression of chronic renal failure?. Kidney Int 2000;58.
- Sesso R, Prado F, Vicioso B, Ramos LR. Prospective study of progression of kidney dysfunction in community-dwelling older adults. Nephrology 2008;13:99-103.
- Song KH, Ko SH, Kim HW, Ahn YB, Lee JM, Son HS, et al. Prospective study of lipoprotein(a) as a risk factor for deteriorating renal function in type 2 diabetic patients with overt proteinuria. Diabetes Care 2005;28:1718-23.
- Stam F, Van GC, Decker A. Endothelial dysfunction contributes to renal function-associated cardiovascular mortality in a population with mild renal insufficiency: The Hoorn study. J Am Soc Nephrol 2006;17:537-45.
- Stojceva-Taneva O, Polenakovic M, Grozdanovski R, Sikole A. Lipids, protein intake, and progression of diabetic nephropathy. Nephrol Dial Transplant 2001;16:90-1.
- Thomas MC, Rosengard-Barlund M, Mills V, Ronnback M, Thomas S, Forsblom C, et al. Serum lipids and the progression of nephropathy in type 1 diabetes. Diabetes Care 2006;29:317-22.
- Ueda H, Ishimura E, Shoji T, Emoto M, Morioka T, Matsumoto N, et al. Factors affecting progression of renal failure in patients with type 2 diabetes. Diabetes Care 2003;26:1530-4.
- Wang MC, Tsai WC, Chen JY, Huang JJ. Stepwise increase in arterial stiffness corresponding with the stages of chronic kidney disease. Am J Kidney Dis 2005;45:494-501.
- Wasse H, McClellan W. Risk for progression to ESRD: Further evidence from population-based studies. J Am Soc Nephrol 2006;17:2092-3.
- Wright JR, Shurrab AE, Cheung C, Waldek S, O’Donoghue DJ, Foley RN, et al. A prospective study of the determinants of renal functional outcome and mortality in atherosclerotic renovascular disease. Am J Kidney Dis 2002;39:1153-61.
- Levin A. Consequences of late referral on patient outcomes. Nephrol Dial Transplant 2000;15:8-13.
- Obrador GT, Pereira BJ. Early referral to the nephrologist and timely initiation of renal replacement therapy: a paradigm shift in the management of patients with chronic renal failure. Am J Kidney Dis 1998;31:398-417.
- Avorn J, Winkelmayer WC, Bohn RL, Levin R, Glynn RJ, Levy E, et al. Delayed nephrologist referral and inadequate vascular access in patients with advanced chronic kidney failure. J Clin Epidemiol 2002;55:711-16.
- Navaneethan SD, Aloudat S, Singh S. A systematic review of patient and health system characteristics associated with late referral in chronic kidney disease. BMC Nephrol 2008;9.
- Wauters JP, Lameire N, Davison A, Ritz E. Why patients with progressing kidney disease are referred late to the nephrologist: on causes and proposals for improvement. Nephrol Dial Transplant 2005;20:490-6.
- Winkelmayer WC, Glynn RJ, Levin R, Owen WF, Avorn J. Determinants of delayed nephrologist referral in patients with chronic kidney disease. Am J Kidney Dis 2001;38:1178-84.
- Ifudu O, Dawood M, Iofel Y, Valcourt JS, Friedman EA. Delayed referral of black, Hispanic, and older patients with chronic renal failure. Am J Kidney Dis 1999;33:728-33.
- Navaneethan SD, Nigwekar S, Sengodan M, Anand E, Kadam S, Jeevanantham V, et al. Referral to nephrologists for chronic kidney disease care: is non-diabetic kidney disease ignored?. Nephron 2007;106:c113-c118.
- Mendelssohn DC, Kua BT, Singer PA. Referral for dialysis in Ontario. Arch Intern Med 1995;155:2473-8.
- Wauters JP, Bosson JL, Forneris G, Turc-Baron C, Golshayan D, Paternoster G, et al. Patient referral is influenced by dialysis centre structure in the Diamant Alpin Dialysis cohort study. Nephrol Dial Transplant 2004;19:2341-6.
- Steel J, Ellis P. Do demographic variables affect the timing of referral to the nephrologist?. EDTNA ERCA J 2002;28:185-7.
- Montgomery AJ, McGee HM, Shannon W, Donohoe J. Factors influencing general practitioner referral of patients developing end-stage renal failure: a standardised case-analysis study. BMC Health Serv Res 2006;6.
- Cass A, Cunningham J, Snelling P, Ayanian JZ. Late referral to a nephrologist reduces access to renal transplantation. Am J Kidney Dis 2003;42:1043-9.
- Obialo CI, Ofili EO, Quarshie A, Martin PC. Ultralate referral and presentation for renal replacement therapy socioeconomic implications. Am J Kidney Dis 2005;46:881-6.
- Kee F, Reaney E, Savage G, O’Reilly D, Patterson C, Maxwell P, et al. Are gatekeepers to renal services referring patients equitably?. J Health Serv Res Pol 2007;12:36-41.
- Sprangers B, Evenepoel P, Vanrenterghem Y. Late referral of patients with chronic kidney disease: no time to waste. Mayo Clin Proc 2006;81:1487-94.
- Cass A, Cunningham J, Snelling P, Wang Z, Hoy W. Urban disadvantage and delayed nephrology referral in Australia. Health Place 2003;9:175-82.
- Boulware LE, Troll MU, Jaar BG, Myers DI, Powe NR. Identification and Referral of Patients With Progressive CKD: A National Study. Am J Kidney Dis 2006;48:192-204.
- Parry RG, Crowe A, Stevens JM, Mason JC, Roderick P. Referral of elderly patients with severe renal failure: questionnaire survey of physicians. BMJ 1996;313.
- Campbell JD. The timing of referral of patients with end-stage renal disease. Dial Transplant 1989;18:660-86.
Appendix 1 Search strategy summary
Searches for clinical effectiveness
Databases searched
MEDLINE (Ovid)
MEDLINE® In-Process & Other Non-Indexed Citations and Ovid MEDLINE® 1950 to present
-
Kidney Failure, Chronic/
-
exp “Referral and Consultation”/
-
1 and 2
-
(renal or kidney or nephropath$or nephrolog$).tw.
-
referr$.tw.
-
(timing or timely or time or early or earlier or late or later).tw.
-
(referr$and (kidney or renal or nephrolog$)).m_titl.
-
4 and 5 and 6
-
3 or 7 or 8
-
limit 9 to (nglish language and yr=“1990 – 2008”)
EMBASE (Ovid) 1988 to 2008 Week 05
-
Kidney Failure, Chronic/
-
(renal or kidney or nephropath$or nephrolog$).tw.
-
referr$.tw.
-
(timing or timely or time or early or earlier or late or later).tw.
-
(referr$and (kidney or renal or nephropath$or nephrolog$)).m_titl.
-
2 and 3 and 4
-
exp patient referral/
-
1 and 7
-
2 and 3 and 4
-
5 or 8 or 9
-
limit 10 to (English language and yr= “1990 – 2008”)
SCIENCE CITATION INDEX (SCI) searched on 4 February 2008
-
Topic=((renal or kidney or nephropath* or nephrolog*) and referr*)
-
Databases = SCI-EXPANDED; timespan = 1990–2008
-
#1 AND Language=(English) AND Document Type=(Meeting Abstract OR Meeting Summary OR Meeting-Abstract)
-
Databases = SCI-EXPANDED; timespan = 1990–2008
ISI Proceedings
-
Topic=((renal or kidney or nephropath* or nephrolog*) and referr*)
-
Timespan = All Years. Databases = STP
-
Refined by: Document Type=(PROCEEDINGS PAPER OR MEETING ABSTRACT) > Document Type=(PROCEEDINGS PAPER OR MEETING ABSTRACT)
British Nursing Index, British Nursing Index Archive, HMIC, CINAHL
-
(kidney or renal or nephrolog$or nephropath$).mp. and referr$.tw. [mp=ti, ab, hw, it, ot]
The National Research Register (NRR) archive up to October 2007
The UK Clinical Research Network
COCHRANE LIBRARY
CDSR and CENTRAL
-
(referral to the paediatric):ti
-
(renal or kidney or nephropath* or nephrolog*) and (refer or referral):ti and (renal or kidney or nephropath* or nephrolog*) and (refer or referral):ab, from 1990 to 2008 in Cochrane Reviews and Clinical Trials
Additional searches for cost-effectiveness
NHS EED searched on 26 March 2008
-
MeSH Diabetic Nephropathies EXPLODE 1 2
-
MeSH Kidney Diseases EXPLODE 1
-
MeSH Kidney Failure, Chronic EXPLODE 1 2
-
#1 or #2 or #3
-
MeSH Referral and Consultation EXPLODE 1
-
#4 and #5
-
renal OR kidney OR Nephrolog*:tw
-
refer*
-
timing OR timely OR time OR early OR earlier OR late OR later
-
#7 and #8 and #9
-
refer*:ti
-
kidney OR ren
-
kidney OR renal OR Nephrolog*:ti
-
#11 and #12
-
#6 or #10 or #13
Searches for natural history
Databases searched
MEDLINE (Ovid) 1996 to March 2008
-
Exp *Kidney Failure, Chronic/
-
Exp *Natural History/
-
Exp Disease Progression/
-
renal or kidney or nephropath$or nephrolog$).tw.
-
CKD.tw.
-
Natural course.tw.
-
Disease course.tw.
-
(Cohort or follow up or follow-up or longitudinal or prospective or screening or cross sectional or cross-sectional).tw.
-
(renal or kidney or nephropath$or nephrolog$).ti.
-
Exp Mass Screening/
-
Exp cohort studies/or exp cross-sectional studies/
-
Exp “review”/
-
Mass screen$.tw.
-
Review.ti.
-
Population-based stud$.tw.
-
1 or 4 or 5 or 9
-
2 or 3 or 6 or 7
-
8 or 10 or 11 or 12 or 13 or 14 or 15
-
(Cohort or follow up or follow-up or longitudinal or prospective or screening or cross sectional or cross-sectional).ti.
-
Population-based stud$.ti.
-
18 or 19 or 20
-
disease course or natural course).ti.
-
17 or 22
-
16 and 21 and 23
-
Limit 24 to (English language and humans and yr= “1998–2008”)
EMBASE (Ovid) 1996 to March 2008
Similar keywords as outlined in MEDLINE search were used with slight modification.
Searches for care model
Databases searched
MEDLINE (Ovid) 1950 to June 2008
-
exp *Kidney Failure, Chronic/
-
exp *Patient Care Management/
-
(renal or kidney or nephro$or ckd).ti
-
(manag$or service or care or practice or pathway).ti.
-
1 and 2
-
3 and 4
-
5 or 6
-
limit 7 to (English language and yr=“2002 – 2008”)
-
Animals/
-
8 not 9
EMBASE (Ovid) 1996 to June 2008
Similar keywords as outlined in MEDLINE search were used with slight modification.
Appendix 2 Data extraction form
Clinical effectiveness
DATA EXTRACTION FORM (NICE guidelines manual)
Person extracting data:
Date:
Bibliographic reference:
| Ref ID | |
| Authors | |
| Title | |
| Journal | |
| Volume (issue) | |
| Year | |
| Pages | |
| Reference type | Abstract Full publication |
| Country | |
| Stated aim of study | |
| Source of funding |
Study type:
| Study type | |
| Prospective/retrospective |
Number of patients:
| Patient selection | |
| How were patients identified | |
| Inclusion criteria | |
| Exclusion criteria | |
|
Number of patients started/completed Give numbers and reasons (if reported) and indication if withdrawals were similar to those who completed study |
|
|
Classification of CKD (e.g. KDOQI) Number of patients at different stages of CKD |
Patient characteristics at baseline
| Data and indication if there were any significant differences observed |
| Definition of early/late referral (months) | |
| Other definitions |
Intervention
| Initiation of referral | |
|
Intervention studied Give as much detail as possible: setting, care, treatments, staffing, number and duration of visits, education |
Comparison
| Alternative treatment |
Length of follow-up
Outcome measures
| Primary outcomes | |
| Secondary outcomes | |
| Safety | |
| Adverse effects |
Results
| Renal Function | |
| All-cause mortality | |
| CVD mortality | |
| Onset of RRT | |
| Quality of life | |
| Barriers to early referral | |
| Hospitalisation | |
| Emergency dialysis | |
| Survival on dialysis | |
| Costs | |
| Treatments | |
| Subgroups | |
|
Integrity/Fidelity of Intervention Was the intervention implemented as planned? Adherence Exposure Quality of delivery Participant responsiveness Programme differentiation Subgroup variation |
Additional comments:
Appendix 3 Excluded studies
Clinical effectiveness
| Study | Reason for exclusion |
|---|---|
| Anees 2007222 | Cross-sectional survey |
| Arora 1999223 | ER defined as < 12 months |
| Avorn 2002224 | ER defined as < 12 months |
| Baker 2003225 | Late referral |
| Barril 2002226 | Not early CKD |
| Brown 2003227 | Screening |
| Burton 1999228 | Too little detail |
| Caskey 2003229 | ER defined as < 12 months |
| Cass 2002230 | ER defined as < 12 months |
| Chan 2007231 | Review; ER defined as < 12 months |
| Chandna 1999232 | Timing of referral not assessed |
| Curtis 2007233 | Timing of referral not assessed |
| Dautlich 1999234 | Referral patterns |
| Department of Health 20052 | Not relevant to area |
| Dogan 2005235 | ER defined as < 12 months |
| Ellis 1998236 | ER defined as < 12 months |
| Fan 2002237 | ER defined as < 12 months |
| Fox 2006238 | Qualitative study of primary care practices and knowledge regarding CKD |
| Goransson 2001239 | ER defined as < 12 months |
| Harris 1999240 | ER defined as < 12 months |
| Hyder 2000241 | Referral patterns |
| Innes 1992242 | Not comparing ER with LR |
| Iseki 2002243 | ER defined as < 12 months |
| Ismail 1998244 | Review; non-systematic |
| Jones 2006147 | Evaluating the effectiveness of a shared care scheme |
| Jones, 2006105 | Natural history of CKD before and after first referral to nephrologist |
| Jungers 1993245 | ER defined as < 12 months |
| Jungers 1993246 | ER defined as < 12 months |
| Jungers 1997247 | Abstract 1997 |
| Jungers 2001121 | ER defined as < 12 months |
| Kazmi 2002248 | ER defined as < 12 months |
| Kazmi 2004249 | ER defined as < 12 months |
| Klebe 2007250 |
Economics Cost of implementing CKD guidelines |
| Komenda 2006169 | Non-systematic review |
| Lhotta 2003251 | ER defined as < 12 months |
| Lin 2003252 | ER defined as < 12 months |
| Lin 2004253 | ER defined as < 12 months |
| Locatelli 2002254 | Non-systematic review |
| London 2003255 | Predictors of suboptimum care |
| Lusenti 2006256 | Specific RAS intervention |
| McLaughlin 2001180 | Economic evaluation |
| Mendelssohn 1999257 | Guidelines |
| Nakamura 200755 | ER defined as < 12 months |
| Ohmit 2003258 | Screening |
| Paris 2002259 | Does not report mortality |
| Rao 2002260 | Patterns of referral |
| Rasgon 2003261 | Insufficient detail |
| Ratcliffe 1984262 | 1984 |
| Ravani 2003263 | ER defined as < 12 months |
| Roderick 1999264 |
Abstract 1999 Published in full reference ID 15 |
| Roderick 2002265 | Avoid ability of late referral |
| Roubicek 2000266 | ER defined as < 12 months |
| Rutherford 1997267 | ER defined as < 12 months |
| Schmidt 1998268 | Economic evaluation |
| Schwenger 2006269 | ER defined as < 12 months |
| Sesso 1996270 | ER defined as < 12 months |
| Shin 2007271 | ER defined as < 12 months |
| Stack 2003272 | ER defined as < 12 months |
| Stoves 2001273 | ER defined as < 12 months |
| Thanamayooran 2005151 | Evaluation of a multidisciplinary clinic |
| Thomas 2007274 | Guidelines |
| Tseng 200894 | Not comparing early with late referral |
| Wavamunno 2005275 | Non-systematic review |
| White 2002276 | Evaluation of pre-dialysis clinic |
| Winkelmayer 2003277 | ER defined as < 12 months |
| Wu 2003278 | ER defined as < 12 months |
| AHRQ 2002279 | Summary of research findings |
| AHRQ 2005280 | Summary of research findings |
| AHRQ 2002281 | Summary of research findings |
Natural history
| Study | Reason for exclusion |
|---|---|
| Adler 2003203 | RCT, do not give outcomes by CKD group |
| Altman 1999282 | Less than 100 patients |
| Boes 2006283 | Mainly prediction study |
| Bruno 2003284 | Study of incidence |
| Busch 2006285 | RCT |
| Chandie 2006286 | Does not include the cohort of CKD |
| Chauveau 2007287 | Less than 100 patients |
| Chonchol 2007288 | Does not separate out people with CKD from people without CKD |
| Chow 2003115 | Cross-sectional study |
| Christensen 1999289 | Less than 100 patients |
| Costacou 2007290 | Less than 100 patients |
| Dale 200877 | Reviews most of the studies including patients with ESRD |
| Damman 2007291 | Cohort of patient with heart failure |
| Dean 2005292 | Less than 2 years’ follow-up |
| Drummond 2002293 | Does not separate out people with CKD from people without CKD |
| Earle 2001294 | Less than 100 patients |
| Edwards 2005295 | Does not identify those with or without CKD |
| El Kossi 2003296 | Cohort of transplant not CKD |
| Fliser 2005297 | Study of prediction only |
| Fliser 2007298 | Duplicate cohort as above so only use one with relevant information |
| Fouque 200651 | RCT |
| Fried 200150 | Does not mention the difference of declining GFR |
| Fried 2004299 | Presents the data by changing eGFR not by CKD |
| Hadjadj 2004300 | Less than 100 patients |
| Hebert 2003301 | Does not report the progression of CKD for whole cohort or relevant subgroup |
| Henry 2002302 | Does not present data by CKD group |
| Hovind 2003303 | Does not separate out people with or without CKD |
| Hovind 2001304 | Does not split data by CKD |
| Hoy 2006305 | Includes Australian Aborigines only |
| Hsu 2006306 | Includes black people only |
| Imbasciati 2007307 | Less than 100 patients |
| Iseki 2004308 | Does not separate patients with or without CKD |
| Jacobsen 1999309 | Does not separate patients with or without CKD |
| Jacobsen 2003310 | Does not separate patient with or without CKD |
| Jafar 2001311 | RCT and cohort defined only by protein |
| Jafar 200143 | Duplicate of above study |
| Jafar 2003312 | RCT and cohort defined by sex only |
| Jafar 2003313 | Cohort defined by protein and blood pressure |
| Jovanovic 1999314 | Less than 100 patients |
| Jude 2002315 | Cohort presented by protein only, not by eGFR |
| Kasiske 1998316 | Does not present change in renal function |
| Kim 2003317 | Less than 100 patients |
| Kohli 2006318 | Less than 100 patients |
| Kristjansson 2001319 | Does not define by CKD group |
| Kronborg 2008320 | Do not report data for CKD subgroup |
| Kshirsagar 200045 | Study predicting risk not giving a rate of decline in GFR |
| Larsson 2005321 | Does not define by CKD group |
| Leeder 2006322 | Presented by haemoglobin subgroup |
| Lerma 2005323 | Editorial |
| Locatelli 2000324 | Comparison of two RCTs |
| Mann 2003325 | Does not identify subgroups of CKD |
| Marcotte 2006326 | Less than 100 patients |
| Massy 1999327 | No relevant subgroups |
| McClellan 2004328 | Cohort of patients with acute myocardial infarction |
| Menon 2008329 | Includes patients who were initially restricted to protein diet in RCTs |
| Merkin 2005330 | Cohort defined by socioeconomic status only |
| Middleton 2006331 | Testing the value of different screening criteria |
| Morita 2006332 | Follow-up < 2 years |
| Muhlhauser 2000333 | Does not separate based on creatinine values |
| Neild 2004334 | Cohort of people with reflux, specific renal diagnosis |
| Orth 2008335 | Not a systematic review |
| Perlman 2003336 | Does not include the cohort of CKD but those with ESRD |
| Ruggenenti 1998337 | Cohort analysis of RCT |
| Rigalleau 2007338 | Comment |
| Rottey 2000339 | Less than 100 patients |
| Samuelsson 2000340 | Letter |
| Sesso 2008341 | Does not separate out by CKD group |
| Song 2005342 | Less than 100 patients |
| Stam 2006343 | Does not separate out by CKD group |
| Stojceva-Taneva 2001344 | Less than 100 patients |
| Thomas 2006345 | Less than 100 patients |
| Ueda 2003346 | Less than 100 patients |
| Wang 2005347 | Cross-sectional study |
| Wasse 2006348 | Editorial |
| Wright 2002349 | Less than 100 patients |
Appendix 4 Quality assessment
| Di 200768 | Tonelli 200667 | |
|---|---|---|
| Internal validitya | ||
| The study addresses an appropriate and clearly focused question | Well covered | Well covered |
| A description of the methodology used is included | Well covered | Well covered |
| The literature search is sufficiently rigorous to identify all the relevant studies | Well covered | Well covered |
| Study quality is assessed and taken into account | Not addressed | Well covered |
| There are enough similarities between the studies selected to make combining them reasonable | Adequately addressed | Adequately addressed |
| Overall assessment of the study | ||
| How well was the study done to minimise bias? Code ++, + or – | ++ | ++ |
| If coded as + or – what is the likely direction in which bias might affect the study results? | NA | NA |
| Description of the study | ||
| What types of study are included in the review?b | Cohort | Cohort |
|
How does this review help to answer your key question? Summarise the main conclusion of the review and how it relates to the relevant key question. Comment on any particular strengths or weaknesses of the review |
Study found that there is a moderate association between lower than average eGFR and CHD risk in general healthy population. Inclusion of participants from community with high response and follow-up rates were the main strength of this study. Study found less evidence for heterogeneity among studies and publication bias. Measurement bias was minimised by checking for serum creatinine assay within included studies; however, study failed to check for chronicity of CKD increasing the risk of inclusion of participants with acute renal failure | This study concluded that CKD (non-dialysis dependent) is associated with an increased risk for all-cause mortality or cardiovascular death and supports intervention in patients with CKD to prevent adverse outcomes. Overall, the study was of good quality. The study did not account for the chronicity (> 3 months) of CKD which may have reduced classification bias by reducing cases with acute renal failure |
Appendix 5 Summarised result of Chapter 3
| Study ID | Measures | Values (variance) | Adjusted for what | Comparator/reference group |
|---|---|---|---|---|
| ACM | ||||
| HR or RR | ||||
| Astor 200885 | RR (95% CI) | 1.77 (1.47 to 2.13) | Age, sex, race/ethnicity, previous cardiovascular diseases, blood pressure, use of antihypertensive medication, diabetes, smoking, body mass index, physical activity, cholesterol and C-reactive protein | eGFR ≥ 90 ml/min/1.73 m2 |
| Eriksen 200696,97 | HR (95% CI) (stage 3 only) | 1.25 (1.14 to 1.37) | Sex and age | For each eGFR decrease of 10 ml/min/1.73 m2 |
| Herzog 200492 | HR CKD only (95% CI) | 1.64 (1.58 to 1.70) | Associated comorbidity | Compared to those without CKD, CHF or anaemia |
| HR CKD + CHF + anaemia (95% CI) | 3.63 (3.52 to 3.75) | CKD defined based on ICD-9-CM and CPT codes | ||
| Irie 200681 | RR (95% CI) |
M: 1.31 (1.12 to 1.52) F: 1.39 (1.20 to 1.62) |
Age, high blood pressure, smoking, alcohol, diabetes, cholesterol, body mass index, urinary protein | eGFR > 100 ml/min/1.73 m2 |
| Meisinger 200676 | HR (95% CI) |
M: 1.17 (0.97 to 1.41) F: 1.12 (0.90 to 1.39) |
Age and survey, history of diabetes, smoking, body mass index, alcohol, high blood pressure, physical activity, dyslipidaemia | eGFR ≥ 60 ml/min/1.73 m2 |
| Tonelli 200668 | RR (95% CI) | 3.0 (2.18 to 4.11) (NB heterogeneity reported) | Pooled estimate therefore variable with each included study (range 0.94–5.00) | eGFR ≥ 60 ml/min/1.73 m2 |
| FHS 1999a | HR (95% CI) |
M: 1.31 (1.02 to 1.68 F: 1.08 (0.87 to 1.34) |
Adjusted | eGFR ≥ 60 ml/min/1.73 m2 |
| NHANES I 2002a | HR (95% CI) | 1.00 (0.76 to 1.32) | Adjusted | eGFR ≥ 60 ml/min/1.73 m2 |
| Shivonen 2004a | HR (95% CI) | 3.48 (1.95 to 6.21) | Adjusted | eGFR ≥60 ml/min/1.73 m2 |
| Weiner 200474 | HR (95% CI) | 1.36 (1.21 to 1.53) | Age, sex, high blood pressure, diabetes, systolic blood pressure, body mass index, cholesterol, smoking, alcohol, left ventricular hypertrophy, high school graduation and race | eGFR ≥60 ml/min/1.73 m2 |
| SMR | ||||
| Eriksen 200696,97 | Mortality rate ratio (95% CI) | 2.2 (2.1 to 2.4) | Standardised for age and sex | Tromsø general population |
| Evans 200598 | SMR (95% CI) | 8.3 (7.5 to 9.2) | Standardised for age and sex | Swedish population |
| John 2004104 | SMR (95% CI) | 1.53 (1.44 to 1.62) | Standardised for age and sex | Population of south-east England |
| Cardiovascular morbidity and mortality | ||||
| HR or RR | ||||
| Astor 200885 | RR of CVD deaths (95% CI) | 2.12 (1.65 to 2.73) | Age, sex, race/ethnicity, previous cardiovascular diseases, blood pressure, use of antihypertensive medication, diabetes, smoking, body mass index, physical activity, cholesterol and C-reactive protein | eGFR ≥ 90 ml/min/1.73m2 |
| Irie 200681 | RR of CVD deaths (95% CI) |
M: 1.65 (1.25 to 2.18) F: 1.81 (1.39 to 2.36) |
Adjusted for age, high blood pressure, smoking, alcohol, diabetes, cholesterol, body mass index, urinary protein | eGFR>100 ml/min/1.73 m2 |
| Meisinger 200676 | HR for CVD deaths (95% CI) |
M: 1.48 (1.15 to 1.92) F: 1.60 (1.17 to 2.18) |
Adjusted for age and survey, history of diabetes, smoking, body mass index, alcohol, high blood pressure, physical activity, dyslipidaemia | Without CKD |
| Meisinger 200676 | HR for incident MI (95% CI) |
M: 1.51 (1.09 to 2.10) F: 1.67 (1.07 to 2.61) |
Adjusted for age and survey, history of diabetes, smoking, body mass index, alcohol, high blood pressure, physical activity, dyslipidaemia | Without CKD |
| Tonelli 200668 | RR of CVD mortality (95% CI) |
2.47 (1.42 to 4.30) (heterogeneity reported) |
Adjustment varies between the included studies | eGFR ≥ 60 ml/min/1.73 m2 |
| Wannamethee 200637 | HR for CVD death (95% CI) |
eGFR < 60 ml/min/1.73 m2: 1.49 (1.10 to 2.03) eGFR 60–69 ml/min/1.73 m2: 1.27 (0.95 to 1.68) |
Adjusted for age, smoking, activity, alcohol, body mass index, cardiovascular diseases, diabetes, forced expiratory volume 1, albumin, systolic blood pressure, left ventricular hypertrophy, high blood pressure, high-density lipoprotein-cholesterol | eGFR > 70 ml/min/1.73 m2 |
| Weiner 200474 | HR of MI/fatal CHD (95% CI) | 1.09 (0.91 to 1.29) | Age, sex, high blood pressure, diabetes, systolic blood pressure, body mass index, cholesterol, smoking, alcohol, left ventricular hypertrophy, high school graduation and race | eGFR ≥ 60 ml/min/1.73 m2 |
| Di 200769 | RR for CHD (95% CI) | 1.32 (1.19 to 1.68) | Adjusted varies between the included studies | eGFR ≥ 60 ml/min/1.73 m2 |
| John 2004104 | SMR for CVD mortality (95% CI) | 1.14 (1.03 to 1.25) | Standardised for age and sex | Population of south-east England |
Appendix 6 Summarised result (subgroups) of Chapter 3
| Study ID | Measures | Value (variance) | Notes | |
|---|---|---|---|---|
| Total CKD | CKD stages | |||
| ACM | ||||
| Bruno 200779 | HR of mortality (95% CI) | 1.92 (1.64 to 2.23) |
Stage 1: reference Stage 2: 0.83 (0.58 to 1.17) Stage 3a: 1.02 (0.70 to 1.49) Stage 3b: 1.10 (0.72 to 1.68) Stage 4: 4.12 (2.36 to 7.18) |
HR adjusted for age and sex. Compared with eGFR ≥ 60 ml/min/1.73 m2 |
| Bruno 200779 | Mortality rate per 10,000 person-years | 953 |
Stage 1: 42.5 Stage 2: 49.5 Stage 3a: 85.8 Stage 3b: 108.8 Stage 4: 377.1 |
Compared to 487 with eGFR ≥ 60 ml/min/1.73 m2 |
| Patel 200580 | Mortality rate per 10,000 person-years |
eGFR > 60 no proteinuria: 470 eGFR > 60 + proteinuria: 580 Stage 3a: 810 Stage 3b: 1500 Stage 4: 2010 Stage 5: 2980 |
||
| Cumulative mortality within follow-up period | ||||
| Bruno 200779 | Number of deaths | 304/1539 (19.75%) |
Stage 1: 37/113 (32.7%) Stage 2: 329/898 (36.6%) Stage 3a: 217/400 (54.3%) Stage 3b: 66/106 (62.3%) Stage 4: 21/21 (100%) |
10 years’ follow-up |
| Tarnow 200489 | Number of deaths | 51 (26%) | 9 years’ follow-up | |
| Rossing 200488 | Number of deaths | 79 (35%) | Median follow-up 6.5 years | |
| Tseng 200894 | Number of deaths | 6934 (17.8%) |
Stage 3a: 3984/27,312 (14.6%) Stage 3b: 1963/8760 (22.4%) Stage 4: 987/2959(33.4%) |
Median follow-up 19.3 (range < 0.01 to 24) months |
| Tseng 200894 | Number of dialysis-free deaths | 6454 (16.5%) |
Stage 3a: 3854/27,312 (14.1%) Stage 3b: 1810/8760 (20.7%) Stage 4: 790/2959 (26.7%) |
|
| CVD morbidity/mortality | ||||
| Bruno 200779 | HR of CVD deaths (95% CI) | 2.16 (1.74 to 2.68) |
Stage 1: reference Stage 2: 0.77 (0.46 to 1.29) Stage 3a: 0.96 (0.55 to 1.67) Stage 3b: 1.19 (0.65 to 2.17) Stage 4: 4.64 (2.15 to 10.01) |
Adjusted for age and sex, compared with GFR ≥ 60: 1 |
| Bruno 200779 | CVD deaths rate per 10,000 person-years | 507 |
Stage 1: 19.5 Stage 2: 22.9 Stage 3a: 43.8 Stage 3b: 64.3 Stage 4: 213.6 |
Compared to 225 with GFR≥60 |
| Cumulative cardiovascular mortality/events during follow-up | ||||
| Bruno 200779 | Number of CVD deaths | 162/1539 (10.5%) |
Stage 1: 17/113 (15%) Stage 2: 152/898 (16.9%) Stage 3a: 111/400 (27.8%) Stage 3b: 39/106 (36.8%) Stage 4: 12/21 (57.1%) |
Mean follow-up 10 years |
| Tarnow 200489 | CVD events (95% CI) | 11% (8 to 14) | 9 years’ follow-up | |
| Rossing 200488 | Number of deaths | 55/227 (24.2%) | Median follow-up 6.5 years | |
| Rossing 200488 | Number of new CVD events | Range: 7–38 (3–17%) | Median follow-up 6.5 years | |
| Renal outcomes | ||||
| Leehey 2005109 | Mean rate of decline of GFR (range) ml/min/1.73 m2/year | 4.5 (–14 to 32) | ||
| Mulec 199887 | Rate of decline in GFR (SD) ml/min/1.73 m2/year | 3.8 (3.7) | ||
| Hovind 200193 | Mean rate of GFR decline (SD) ml/min/1.73 m2/year | 4.0 (0.2) | Median follow-up 6.7 (range 3–14) years | |
| Rossing 200488 | Mean rate of decline of GFR (SD) ml/min/year | 5.2 (4.1) | Not standardised to body surface area | |
| Hemmelgarn 2006101 | Rate of decline in eGFR (95% CI) ml/min/1.73 m2/year |
Stage 2: F: 1.6 (1.0 to 2.1); M: 2.1 (1.6 to 2.6) Stage 3: F: 2.8 (2.3 to 3.3); M: 3.6 (3.1 to 4.2) Stage 4: F: 2.9 (2.2 to 3.7); M: 3.2 (2.3 to 4.0) |
Adjusted for age | |
| Patel 200580 | Rate of progression to ESRD as events per 100 person-years |
eGFR > 60 no proteinuria: 0.0 eGFR > 60 + proteinuria: 0.2 Stage 3a: 0.3 Stage 3b: 1.7 Stage 4: 14.2 Stage 5: 0 |
Progression to ESRD is defined as a change to an estimated GFR less than 15 ml/min/1.73 m2 | |
| Rate of any progression as events per 100 person-years |
eGFR > 60 no proteinuria: 3.2 eGFR > 60 + proteinuria: 7.8 Stage 3a: 10.5 Stage 3b: 11.8 Stage 4: 15.1 Stage 5: 0 |
Any progression of CKD is defined as a change to any disease group category with a lower GFR and/or presence of proteinuria with at least a 20 % decrease in estimated GFR (to avoid trivial changes in CKD classifications) | ||
| Orlando 2007111 | HR of progression (95% CI) |
Stage 1 to 2: 1.32 (1.13 to 1.55) Stage 2 to 3: 1.18 (0.97 to 1.43) Stage 3 to 4: 1.13 (0.86 to 1.50) |
Compared to non-diabetics CKD | |
| Rossing 200488 | Proportion of doubling of baseline serum creatinine | 63/227 (28%) | Median follow-up 6.5 years | |
| Khatami 2007108 | Proportion progressed to CKD stages 4 and 5 | 8.6% | 4 years’ follow-up, eGFR < 60 ml/min/1.73 m2 at baseline | |
| Jones 2006105 | Proportion of progressors | 64/314 (20.4%) |
≤ –5 ml/min/year: 32/145 (22%) > –5 to ≤ –1 ml/min/year: 32/169 (19%) |
Non-progressors 60/412 (15%). Progression defined as ≤ –1 ml/min/year Median follow-up 2.9 years |
| Rossing 200488 | Number reaching ESRD within follow-up | 15 (7%) | Median follow-up 6.5 years (range 3–17) | |
| Tseng 200894 | Number of dialysis during follow-up | 841 (2.2%) |
Stage 3a: 203/27,312 (0.7%) Stage 3b: 251/8760 (2.9%) Stage 4: 387/2959 (13.1%) |
Median 19.3 months (1.6 years) |
| Study ID | Measures | Values (variances) | Comparator | Comments | |
|---|---|---|---|---|---|
| Total CKD | CKD stages | ||||
| CKD with CVD | |||||
| Levin 200184 | Proportion of RRT |
At 6 months: 4/118 (3.4%) At 12 months: 6/92 (6.5%) At 24 months: 6/31 (19.4%) |
No CVD At 6 months: 10/268 (3.7%) At 12 months: 7/218 (3.2%) At 24 months: 18/94 (19.1%) |
Median follow-up 23 months | |
| Orlando 2007111 | HR for progression (95% CI) |
Stage 1 to 2: 1.35 (1.14 to 1.61) Stage 2 to 3: 1.52 (1.23 to 1.93) Stage 3 to 4: 0.86 (0.64 to 1.17) |
Compared with no CVD | ||
| Tonelli 200668 | RR for ACM (95% CI) | 1.71 (1.49 to 1.96) | Compared with no CVD | Pooled from nine studies | |
| Tonelli 200668 | RR for CVD mortality | 1.8 (1.45 to 2.24) | Compared with no CVD | Pooled from seven studies | |
| Tseng 200894 (diabetic population at baseline) | HR for dialysis (95% CI) | 1.25 (1.17 to 1.33) | Adjusted for nephrology referrals, age, sex, race, poverty, index eGFR, life threatening disease, physical comorbid, mental morbidity, no of visits | ||
| HR for dialysis free death (95% CI) | 1.30 (1.27 to 1.32) | ||||
| HR for ACM (95% CI) | 1.29 (1.27 to 1.32) | ||||
| CKD with HBP | |||||
| Orlando 2007111 | HR of CKD progression (95% CI) |
Stage 1 to 2: 0.8 (0.66 to 1.35) Stage 2 to 3: 0.93 (0.72 to 1.57) Stage 3 to 4: 0.91 (0.77 to 1.53) |
Compared with no HBP | ||
| Tonelli 200668 | HR of ACM (95% CI) | 2.15 (1.77 to 2.61) | Compared with no HBP | Pooled from eight studies | |
| Tonelli 200668 | HR of CVD mortality (95% CI) | 2.35 (1.52 to 3.64) | Compared with no HBP | Pooled from three studies | |
| Study ID | Measure | Age groups | Value (variance) | Comments |
|---|---|---|---|---|
| ACM | ||||
| Bruno 200779 | HR of ACM (95% CI) | < 70 years | 1.51 (1.07 to 2.13) | eGFR < 60 vs ≥ 60, adjusted for age and sex (diabetics at baseline) |
| ≥ 70 years | 1.09 (0.89 to 1.35) | |||
| Evans 200598 | SMR for ACM (95% CI) | < 69 years | 20.6 (11 to 35.3) | All population CKD stages 4 and 5 |
| Eriksen 200696,97 | Cumulative mortality of 10 years (95% CI) | < 69 years | 0.17 (0.14 to 0.21) | All population CKD stage 3 |
| 70–79 years | 0.49 (0.45 to 0.54) | |||
| > 79 years | 0.84 (0.80 to 0.89) | |||
| Drey 200395 | Number of deaths in median follow-up of 5.5 years | < 50 years | 17/70 (24.3%) |
Median survival time: 50–59 years: 55 months > 80 years: 26 months |
| 50–59 years | 27/52 (51.9%) | |||
| 60–69 years | 92/159 (57.9%) | |||
| 70–79 years | 246/379 (64.9%) | |||
| > 80 years | 354/410 (86.3%) | |||
| Eriksen 200696,97 | Mortality rate ratios (95% CI) | < 69 years | 3.1 (2.5 to 3.9) | All population CKD stage 3 |
| 70–79 years | 2.0 (1.8 to 2.3) | |||
| > 79 years | 2.2 (2.0 to 2.3) | |||
| Cardiovascular morbidity and mortality | ||||
| Bruno 200779 | HR of CVD mortality (95% CI) | < 70 years | 1.46 (0.85 to 2.51) | eGFR < 60 vs ≥ 60, adjusted for age and sex (diabetics at baseline) |
| ≥ 70 years | 1.07 (0.80 to 1.42) | |||
| John 2004104 | SMR for CVD mortality (95% CI) | < 60 years | 10.8 (1.28 to 20.32) | Compared to population of south-east England; standardised for age and sex |
| ≥ 80 years | 0.96 (0.86 to 1.06) | |||
| ESRD | ||||
| Eriksen 200696,97 | 10 years’ cumulative incidence of ESRD (95% CI) | < 69 years | 0.07 (0.05 to 0.11) | All population CKD stage 3 |
| 70–79 years | 0.04 (0.02 to 0.07) | |||
| > 79 years | 0.03 (0.01 to 0.05) | |||
| Cumulative incidence | ||||
| Hsu 2003103 | Incident of ESRD (4 years and 6 years) | Age 20–60 years | Black people: 14,593; white people: 20,323 | Fixed 1991–6 and 1994–9 |
| Age 61–74 years | Black people: 6714; white people: 18,693 | |||
| Drey 200395 | Incident of ESRD in follow-up | < 60 years | 28 (21%) | Mean 5.5 years |
| ≥ 60 years | 11 (1.5%) | |||
| Eriksen 200696,97 | Incidence rate ratios of ESRD (95% CI) | < 69 years | 36.6 (21.2 to 63.2) | All population CKD stage 3 |
| 70–79 years | 3.1 (2.3 to 7.0) | |||
| > 79 years | 3.7 (2.2 to 6.2) | |||
| Hsu 2003103 | New ESRD cases (1996)/CRI prevalence (1991) | Age 20–60 years | Black people: 0.099; white people: 0.017 | |
| Age 61–74 years | Black people: 0.027; white people: 0.008 | |||
| Study ID | Measures | Value (variances) | Comments | |
|---|---|---|---|---|
| Male | Female | |||
| ACM | ||||
| Evans 200598 | SMR of mortality (95% CI) | 7.2 (6.3 to 8.1) | 12.3 (10.3 to 14.5) | Compared to general Swedish population |
| Eriksen 200696,97 | 10 years’ cumulative mortality (95% CI) | 0.61 (0.56 to 0.67) | 0.47 (0.43 to 0.50) | |
| Eriksen 200696,97 | Number of deaths during follow-up | 383 (41%) | 576 (27%) | Median follow-up 3.6 years |
| Drey 200395 | Number of deaths during follow-up | 448/646 (69.35%) | 288/425 (67.76%) | Mean 5.5 years |
| Eriksen 200696,97 | Mortality rate ratios (95% CI) | 2.4 (2.2 to 2.7) | 2.1 (1.9 to 2.3) | |
| Renal outcomes | ||||
| Eriksen 200696,97 | 10 years’ cumulative incidence of ESRD (95% CI) | 0.08 (0.05 to 0.11) | 0.03 (0.02 to 0.04) | |
| Eriksen 200696,97 | ESRD during follow-up |
Stage 5: 33 (4%) RRT: 2 (0.2%) |
Stage 5: 25 (1%) RRT: 2 (0.1%) |
Median follow-up 3.6 years |
| Hsu 2003103 | Incidence of ESRD (4 and 6 years) |
Black people: 10,555 White people: 22,001 |
Black people: 10,752 White people: 17,015 |
1991–6 and 1994–9 |
| Eriksen 200696,97 | ESRD incidence rate ratios | 6.5 (4.3 to 9.9) | 4.3 (2.7 to 6.9) | |
| Hsu 2003103 | New ESRD cases(1996)/CRI prevalence (1991) |
Black people: 0.069 White people: 0.015 |
Black people: 0.044 White people: 0.008 |
|
| Hovind 200193 | Mean rate of GFR decline (SD) ml/min/1.73 m2/year | 4.1 (0.3) | 4.0 (0.4) | Median follow-up 6.7 years |
Appendix 7 Late referral for CKD: evidence of the impact on health outcomes
Background
As CKD progresses towards ESRD, the patient and clinical team need to prepare. Decisions about RRT modality, preparation for transplant if appropriate, establishment of vascular access for haemodialysis, nutritional preparation, management of anaemia, and fluid and electrolyte balance are all important aspects of preparations. During this time, patients and their carers need support and also the time to plan and prepare. The 12 months prior to dialysis have been described by some as a critical time, and yet very late referral to specialist renal services remains common place. Between 20% and 50% of referrals reportedly occur within 4 months of the need to start dialysis. 54–56,350,351
In searching for literature about the effectiveness of early referral for CKD, we identified a substantial literature evidencing the implications of late referral and this is summarised here.
Chan and colleagues57 recently published a meta-analysis which compared the differences in mortality and duration of hospitalisation in CKD patients who were referred early to a nephrologist versus those who were referred late. They concluded that late referral of CKD patients significantly increased the risk of death (RR 1.99, 95% CI 1.66 to 2.39).
Chan and colleagues’57 review focused on ACM and hospitalisation in dialysis patients in relation to the timing of referral to specialist nephrology care. In this appendix, we considered other outcomes, including cardiovascular mortality and morbidity and quality of life, and sought information about what criteria or factors triggered referral. We focused on studies reporting, as a minimum, mortality as an outcome and comparing referral less than 12 months before the initiation of RRT to earlier referral.
Results
Twenty-seven studies were identified from the literature search. Of these, 10 studies were excluded because they did not measure mortality, leaving 17 studies.
The studies reported findings from a wide range of countries: three studies from the UK,236,237,273 a further four from Europe,239,251,266,269 three from the USA,249,277,352 five from Asia,243,252,253,271,278 one from Australia/New Zealand230 and one from Brazil. 270 All 17 studies were available in full publication.
All 17 of the studies were retrospective, based on recruiting participants at the initiation of RRT.
The time interval used to define ‘late referral’ differed among the studies. Three studies237,243,270 considered ‘late referral’ as being less than 1 month between first contact with renal specialty and the commencement of dialysis. Seven studies230,236,239,271,273,277,352 defined ‘late referral’ as being less than 3 months between referral and starting dialysis. A definition of less than 16 weeks/4 months was used in two studies,249,266 while one study251 determined ‘late referral’ in relation to GFR. Patients with a GFR < 20 ml/min/1.73 m2 at first referral were grouped as ‘late referral’. The remaining four studies252,253,269,278 considered late referral as being referred less than 6 months prior to commencing RRT.
Six of the 17 studies included in excess of 1000 participants. 230,243,249,273,277,352 The majority of the studies included smaller patient groups, where participant numbers ranged from 52 to 270. The number of study participants across all studies totalled 16,600. Only one study reported a measure of renal function at the time of referral. 251 Four of the studies specified in their methods that people with acute renal failure were excluded. 230,239,249,266 Table 45 summarises the included studies.
| Study ID | Country | Definition of late referral | Total number starting dialysis | Inclusion criteria | Total number of study participants | % late referrals |
|---|---|---|---|---|---|---|
| Avorn 2002352 | USA | ≤ 90 days | 17,884 | Adequate records; ‘insured’ patients; first diagnosis of renal disease > 1 year prior to dialysis; > 30 days dialysis (exclusion: second dialysis not received but survived > 1 month or > 2 months between dialysis) | 3014 | 34 |
| Cass 2002230 | Australia and New Zealand | < 3 months | 5590 | Patients with ESRD; started RRT in Australia (exclusion: ARF, death or transplantation within first year of dialysis) | 4243 | 26.9 |
| Ellis 1998236 | UK | < 12 weeks | 198 | Commencing RRT due to ESRD | 198 | 32.3 |
| Fan 2002237 | UK | < 30 days | 211 | Started HD for first time (exclusion: established on HD for > 30 days) | 98 | 28 |
| Goransson 2001239 | Norway | < 3 months | 242 | Patients with renal failure/serum creatinine > normal for > 1 year (exclusion: ARF and entering RRT due to failing kidney graft) | 242 | 81.7 |
| Iseki 2002243 | Japan | < 28 days | 1551 | Exclusion: patients who died within first month of RRT; difficulty in confirming the first start day or serum creatinine level at first visit | 1162 | 21.4 |
| Kazmi 2004249 | USA | ≥ 4 months | 4024 | ≥ 18 years old; completed questionnaire; survived first 60 days dialysis (exclusion: ARF, pre-emptive or kidney transplant recipients, AIDS or cancer patients, returning to dialysis) | 2195 | 34 |
| Lhotta 2003251 | Austria | GFR < 20 ml/min/1.73 m2 | NR | Starting RRT | 75 | 56 |
| Lin 2003252 | Taiwan | < 6 months | NR | Type 2 diabetic receiving HD for at least 6 months (exclusion: switching between modalities) | 115 | 54 |
| Lin 2004253 | Taiwan | < 6 months | NR | RRT for at least 3 months (exclusion: switching modalities) | 105 | 57 |
| Roubicek 2000266 | France | < 16 weeks | 309 | Dialysis for the first time, available medical records (exclusion: acute irreversible or rapidly progressing renal failure) | 270 | 34 |
| Schwenger 2006269 | Germany | < 8 weeks | 280 | Initiating HD | 254 | 47 |
| Sesso 1996270 | Brazil | < 1 month | 252 | Exclusion: diabetic ESRD; diagnosis made > 1 and < 3 months before dialysis | 184 | 57.6 |
| Shin 2007271 | Korea | < 90 days | 119 | Receiving HD for 4-hour session three times/week (exclusion: those transferred from another dialysis programme, hypersensitivity to membrane, current infection, malignancy, liver disease, autoimmune disease, receiving drugs that affect immunity) | 119 | 43.7 |
| Stoves 2008273 | UK | < 90 days | 1260 | (Exclusion: in receipt of transplant, transfer away from the unit) | 1260 | 37.1 |
| Winkelmayer 2003277 | USA | < 90 days | NR | Diagnosis of renal disease > 1 year before first dialysis (exclusion: patients on single dialysis and survived > 1 month or limited dialysis treatment and survived > 2 months) | 3014 | 34 |
| Wu 2003278 | Taiwan | < 6 months | NR | Type 2 diabetic nephropathy, new onset ESRD, on PD for more than 3 months | 52 | 69 |
Mortality
1-year mortality
Five studies reported the 1-year mortality rate after initiating RRT. 236,237,243,271,277 Three studies reported the RR of death at 1 year, comparing late to early referral249,277,352 (Table 46). Two further studies reported mortality at 3 and 6 months and were included in the table for completeness. 266,270
| Study ID | ER | LR | Risk ratioa late vs early (95% CI) unadjusted | Risk ratioa late vs early (95% CI) adjusted | Adjusted for | ||
|---|---|---|---|---|---|---|---|
| % deaths | % of ER deaths due to CVD | % deaths | % of LR deaths due to CVD | ||||
| Avorn 2002352 | NR | NR | NR | NR | NR | RR 1.37 (1.22 to 1.52) | Age, race, socioeconomic status, presence of any renal diagnosis in year before dialysis |
| Ellis 1998236 | 27.5 | NR | 39.5 | NR | NR | NR | |
| Fan 2002237 | 2.8 | NR | 7.4 | NR | NR | NR | ‘No significant difference between ER and LR groups’ |
| Iseki 2002243 | 10.9 | NR | 15.1 | NR | NR | NR | |
| Kazmi 2004249 | NR | NR | NR | NR | HR 1.44 (1.15 to 1.80) | HR 1.42 (1.12 to 1.80) | Social demographics, insurance cover, comorbidities, cause of kidney disease |
| Roubicek 2000266 | 4.2 (3 months) | 50 | 4.2 | 67 | |||
| Sesso 1996270 | 12.9 (6 months) | 40 | 29.2 | 35 | HR 2.77 (1.36 to 5.55) | HR 2.05 (0.93 to 4.54) | Adjustment NR |
| Stoves 2008273 | 13.0 | NR | 26.0 | NR | NR | NR | |
| Winkelmayer 2003277 | 25.2 | NR | 32.2 | NR | HR 1.36 (1.22 to 1.51) | Age, gender, race, socioeconomic status, comorbidities | |
The 1-year ACM after initiation of RRT varied substantially between studies, ranging from 2.8%237 to 27.5%236 in the early referral group. In late referral groups, 1-year mortality ranged from 7.4%237 to 39.5%. 236 Studies consistently reported higher mortality in the late referral group than in the early group at 1 year. This was also found at 6 months,270 but at 3 months a small study266 reported no difference. The statistical significance of the differences was not reported by most authors.
Two studies provided data on the percentage of death attributable to CVD. At 3 months, CVD mortality accounted for 50% of deaths in the early referral group and 67% in the late referral group. 266 At 6 months, 40% of deaths and 35% respectively were reported. 270
Three studies reported risk of death associated with late as compared to early referral at 1 year. 249,277,352 Avorn and colleagues352 and Kazmi and colleagues249 found a statistically significant increase in risk among those referred late (37–42% greater risk than early referral) after adjustment for social demographics, insurance cover, comorbidity and aetiology of kidney disease. Winkelmayer and colleagues277 reported a non-significant difference [odds ratio (OR) 1.03, 95% CI 0.84 to 1.25] between the groups at 1 year after adjusting for social demographics and comorbidity.
5-year mortality
Mortality rates at 5 years after initial referral were reported in five studies. 239,243,252,266,273 In the early referral groups, mortality ranged from 27.6%252 to 51.5%239 at 5 years, and in the late referral groups this ranged from 36.1%266 to 83.3%. 278 The 5-year mortality rate was higher in the late referral group in all but two studies where there was little difference. 243,266
Iseki243 reported no difference in risk of mortality with referral timing after adjustment (factors adjusted for were not reported) (HR 1.02, 95% CI 0.77 to 1.35). Roubicek and colleagues266 did not report details, but also found no statistically significant difference after adjustment. Lin and colleagues252 reported a lower RR of death in those referred early as compared to late (RR 0.45, 95% CI 0.25 to 0.81).
A further six studies reported follow-up for greater than 1 year (summarised in Table 47). The longest follow-up was reported by Shin and colleagues271 at 6.7 years and 23% (early referral) versus 42% (late referral) died. Of the five studies where RR was estimated, only one reported no statistically significant difference in mortality comparing early and late referral. 251 Schwenger and colleagues269 calculated the RR of death in the late referral group at 1.7 years after initiation of dialysis. The RR of late referral for patients under the age of 75 years was 2.32 (95% CI 1.48 to 3.64). For patients over 75 years, the RR was 1.8 (95% CI 0.97 to 3.34). Lin and colleagues252 reported risk of death for patients receiving haemodialysis and peritoneal dialysis separately. The greatest impact from early referral on survival after dialysis was observed in the peritoneal dialysis group (RR 0.29, 95% CI 0.07 to 0.48).
| Study ID | Follow-up | ER | LR | Risk ratio (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|
| Deaths (% unless otherwise stated) | % of ER deaths due to CVD | Deaths (% unless otherwise stated) | % of LR deaths due to CVD | Late vs early unadjusted | Late vs early adjusted | Adjusted for | ||
| Cass 2002230 | 5 years | 15 deaths/100 patient-years | NR | 20 deaths/100 patient-years | NR | HR 1.3 (1.14 to 1.48) | HR 1.19 (1.05 to 1.35) | Age, sex, number of comorbidities, presence of primary renal disease and indigenous status |
| Goransson 2001239 | 5 years | 51.5 | NR | 73.2; p = 0.018 | NR | NR | NR | |
| Iseki 2002243 | 5 years | 33.8 | NR | 35.1 | NR | NR | HR 1.02 (0.77 to 1.35) | Age, sex, comorbidities, diabetes |
| Kazmi 2004249 | Mean 2 years | NR | NR | NR | NR | NR | HR 1.21 (1.02 to 1.43) | Insurance status, angina, education level, employment, treatment modality, ESRD network |
| Lhotta 2003251 | 4 years | 24.2 | NR | 45.2 | NR | HR 2.12 (0.92 to 4.85) | Referral NS | Only higher comorbidity score was associated with mortality and retained in the model |
| Lin 2003252 | 5 years | 27.6 | 42 | 64.8 | 47 | RR for ER 0.42 (0.25 to 0.87) | RR for ER 0.45 (0.25 to 0.81) | Glycaemic control, age, haemoglobin, albumin, cholesterol, residual renal function |
| Lin 2004253 | 5 years | NR | NR | NR | NR | NR |
HR for ER (haemodialysis) 0.45 (0.25 to 0.81) HR for ER (peritoneal dialysis) 0.29 (0.07 to 0.48) |
Age, haemoglobin, albumin, cholesterol |
| Roubicek 2000266 | 5 years | 48 | 61.4 | 44 | 60.9 | NR | NR | |
| Schwenger 2006269 | 1.7 years | NR | NR | NR | NR | NR |
RR < 75 years 2.32 (1.48 to 3.64) RR ≥ 75 years 1.8 (0.97 to 3.34) |
Factors not reported |
| Shin 2007271 | 6.7 years | 23 | 37.5 | 42 | 69.6 (p < 0.05) | NR | NR | |
| Stoves 2008273 | 5 years | 45 | 39 | 69 | 30 | NR | HR 1.43 (0.115); p < 0.001 | Age, diabetes, albumin, ‘transplantability’ |
| Wu 2003278 | Mean 3.3 years | 43.8 | 43 | 83.3 (p < 0.05) | 47 | RR for ER 0.42 (0.15 to 0.67) | RR for ER 0.41 (0.19 to 0.90) | Glycaemic control, creatinine clearance, age |
Death due to CVD was reported in four studies. 252,266,271,273 CVD accounted for similar proportions of deaths in the early and late referral groups, with the exception of Shin and colleagues271 who reported substantially lower proportion of deaths due to CVD in the early versus late referral groups (9% versus 30.8%; p = 0.04).
Specialist visits
Two studies provided a breakdown on the number of visits to a nephrology specialist by the early and late referral group. 277,352 Avorn and colleagues352 reported 67.9% of the early referral group receive more than five specialist visits compared to 14.5% in the late referral group and also reported an increased RR of death at 1 year in those receiving fewer than five specialist visits prior to initiation on dialysis (RR 1.15, 95% CI 1.03 to 1.28). Again, a greater percentage of specialists visits was recorded in the early than in the late referral group in the study by Winkelmayer and colleagues. 277 In the early group, 17.6% of participants received more than 10 specialist visits versus 11.2% in the late group.
The remainder of the studies failed to comment on specialist visits. Fan and colleagues237 was the only study that described pre-dialysis education by a nurse team. Both referral groups were noted to have had pre-dialysis education. None of the studies reported details of dietician input.
Preparing for dialysis
The choice of peritoneal dialysis was reported in two studies. 237,253 Both reported that choice was available of both early and late referral, although Fan and colleagues237 noted that in the late referral group some participants were initiated on haemodialysis initially as an emergency. Final modality decisions were made at a later date.
The percentage of haemodialysis patients with functioning permanent vascular access at the initiation of dialysis was reported in three studies. 239,266,270 Goransson and Bergrem239 reported 43% of the early referral group versus 0% in the late referral group had functioning permanent vascular access. Sesso and Belasco270 and Roubicek and colleagues266 reported similarly low proportions with permanent access in the late referral group (53.1% versus 0%, early versus late and 70.7% versus 26.9%, early versus late, respectively).
Hospitalisation
There were more days spent in hospital, around the time of commencing RRT, in the late referral group than in the early group. 236,239,251,266 Ellis and colleagues236 reported a median of 9.7 days of hospitalisation in the early group and a median of 25 days in the late group (no p-value given). Lhotta and colleagues251 observed a mean initial hospital duration of 13 ± 12.5 days for early referral patients and 19.5 ± 14.1 days for late referral patients (p = 0.04). Length of initial hospitalisation reported by Roubicek and colleagues266 was 20 ± 21.5 days for the early referral group compared to 33.3 ± 21.8 days for late referral patients (p < 0.001). Lastly, Goransson and Bergrem238 showed the duration of hospital stay around the commencement of dialysis to be more than four times longer for late referral patients than early referral patients – median of 31 (7–73) versus 7 (1–59) days (late versus early respectively). Again the difference between the groups was found to be statistically significant with p < 0.0001.
Treatments
Three studies reported on antihypertensive medication use among those referred late as compared to early. 239,251,271 Goransson and Bergrem239 reported a median of two antihypertensive medications per person in both the late and early referral groups. Lhotta and colleagues251 also noticed no significant difference in ACE I use between referral groups (early 90.9% versus late 88.1%; p = 0.92). Shin and colleagues,271 however, found substantial differences in antihypertensive medication use with higher prescribing in the early referral group (early versus late: ACE I 81% versus 11%; ARB 43% versus 6%; β-blocker: 72% versus 15%; calcium channel blockers 42% versus 8%).
Goransson and Bergrem239 reported oral calcitrol was more likely to be prescribed to those referred early than late (89% versus 8%), but other authors found little difference.
Predialysis erythropoietin was prescribed more in those who were referred early. 239,251
Quality of life
Quality of life was not reported by any of the studies.
Triggers for referral
None of the studies reported the triggers or criteria used to determine when to refer. None reported on the characteristics of the patients at the time of referral.
Barriers to early referral
None of our included studies of late referral reported data on barriers to referral. A supplementary search was undertaken to identify barriers to referral. The findings are summarised thematically below.
A recent systematic review by Navaneethan and colleagues353 reviewed the evidence on patient and health system characteristics associated with late referral. The review included prospective and retrospective observational studies, and physician surveys in which adult patients were referred within 6 months before initiation of dialysis, or referred to nephrologists in stage 5 CKD. The authors concluded that a combination of patient and health system characteristics were associated with late referral of patients with CKD. Overall, being older, belonging to a minority group, being uninsured, suffering from multiple comorbidities, and the lack of communication between primary care physicians and nephrologists contributed to late referral of patients with CKD. Factors associated with late referral identified from this review and from other studies are discussed below, categorised as follows: disease related, patient related, health-care system related and physician related.
Disease related
In some cases, late referral may be inevitable owing to the pathogenesis and mode of onset of the kidney disease, such as irreversible acute renal failure. De novo acute diseases may lead to referral that is unavoidably late and at the stage of irreversible kidney damage. On the other hand, some kidney diseases may progress so slowly that the development of symptoms goes almost unnoticed. Overall, such disease-related causes do not account for more than 15–20% of the presently observed late referral cases. 354
Patient related
Age
The increasing age of patients was associated with late referral in several studies conducted in North America. Winkelmayer and colleagues355 showed that patients aged between 75 and 84 years were 73% more likely to be referred late than 65- to 74-year-olds (OR 1.73, 95% CI 1.44 to 2.08; p < 0.001). This association was more significant in patients over 85 years (OR 2.66, 95% CI 1.87 to 3.79; p < 0.001). Ifudu and colleagues356 concluded that even patients aged > 55 years were referred late (OR 4.7, 95% CI 1.37 to 16.0) when compared to patients aged < 55 years. Navaneethan and colleagues357 found that age > 75 years was significantly associated with late referral among patients in a community in New York in comparison to patients aged < 75 years (p = 0.03). A physician survey conducted in Canada concluded that primary care physicians are less likely to refer older patients to nephrologists than younger patients. 358
In contrast, studies from France,246 Europe,359 the UK360 and Ireland361 did not find any age differences in patients with CKD who were referred early compared to those who were referred late.
Gender
Winkelmayer and colleagues355 found that sex was not associated with late referral (OR 1.16, 95% CI 0.99, 1.37; p = 0.068). Several other studies reported no gender differences in the referral of patients with CKD including one from France246 and one European. 359
Race
Winkelmayer and colleagues355 identified a significant association between race other than black or white and late referral (OR 1.68, 95% CI 1.21 to 2.32). Kinchen and colleagues123 and Ifudu and colleagues356 showed that black and Hispanic patients were referred late. In contrast, Steel and Ellis,360 from the UK, concluded that white people might be referred later to nephrologists than black people, although the results were non-significant (p = 0.08). Two studies from the USA223,357 and one from France246 did not identify any association between race and late referral of patients with CKD.
Social disadvantage
In an Australian study, the proportion of patients referred late varied between areas and was higher in areas of greater social disadvantage. Patients from densely populated areas with a predominantly indigenous population experienced more late referrals to nephrologists than other populations. 362
A study from the USA363 reported that the homeless and unemployed were more likely to present as ultra late referral (< 1 month) (OR 6.0, p = 0.004) and concluded that poor socioeconomic status was a major contributor to delayed referral. There was no significant association, however, between education and referral pattern. 363
In contrast, a study from Northern Ireland showed that less affluent populations are generally referred earlier to specialists than the more affluent. 364
Comorbidity
The presence of comorbid illness was associated with late referral in most studies. Kinchen and colleagues123 found that patients with higher index of coexistent disease score (combination of index of physical impairment and index of disease severity) were nearly twice as likely to be referred late than their counterparts with lower scores (OR 1.8, 95% CI 1.16 to 2.84). Similar results were seen in two European studies. 124,358 Wauters and colleagues359 concluded that the presence of an active cancer would delay the referral of patients with CKD to nephrologists. In a Scottish study, Khan and colleagues124 allocated CKD patients to low, intermediate, and high risk groups based on their age and the presence of other comorbidities (heart disease, diabetes and pulmonary disease). The presence of these coexisting illness resulted in late referral. A physician survey by Mendelssohn and colleagues358 identified that the presence of comorbidity would result in late or non-referral by physicians. Navaneethan and colleagues357 determined that patients referred late had a higher Charlson Comorbidity Index (calculated with 17 comorbidities) than patients referred earlier (OR 1.17, 95% CI 1.04 to 1.32, p = 0.009).
In contrast, Winkelmayer and colleagues355 determined that the presence of hypertension (OR 0.47, 95% CI 0.40 to 0.56), malignancy (OR 0.73, 95% CI 0.59 to 0.91), coronary artery disease (OR 0.69, 95% CI 0.58 to 0.82) and diabetes (OR 0.82, 95% CI 0.69 to 0.97) resulted in earlier referral to nephrologists than for patients with no comorbidities. Patients with CKD and other coexisting illness may have their renal function monitored more frequently as part of routine chemistry panels. Early referral may reflect enhanced physician awareness of the relationship between these diseases and CKD progression, or increased physician attentiveness to management of patients with CKD, because of an increased frequency of patient–physician interaction. These seemingly contradictory results could be attributed to geographic variations, type of patients included and provider misconceptions about the outcome of patients with multiple comorbidities on dialysis. 353
Other studies have not demonstrated an association between the presence of comorbidity and late referral. 223,361
Aetiology of renal disease
Patients with non-diabetic kidney disease were 1.4 times (95% CI 1.15 to 5.26) more likely to be referred later to nephrologists than patients with diabetic kidney disease. 357 Patients with congenital kidney disease were referred earlier than patients with hypertensive renal disease. Patients with rapidly progressing kidney disease were referred earlier than patients who had gradual worsening of renal function (OR 7.1, 95% CI 2.9 to 16.7). 246
Patient non-compliance
Patient compliance with appointments was identified as a major issue in two studies and accounted for ∼40% of late referrals. Jungers and colleagues246 and Sprangers and colleagues365 reported that 42% of late referrals could be attributed to patient non-compliance. Patients may be reluctant to visit a nephrologist because of lack of disease awareness and/or understanding, denial, fear of the unknown, fear of loss of independence and economic difficulties. 365
Health-care system related
Type and location of referral and dialysis centre
In a survey of a cohort of incident dialysis patients in three European regions, Wauters and colleagues359 identified that late referral was more frequent in large city centres than in the private or regional structures (OR 7.3, 95% CI 1.8 to 30).
The distance to the centre might also be a reason for late referral, but in one study concerning a rural population in the USA,268 the distance to the dialysis centre was not a determining factor. In contrast, for patients of lower socioeconomic classes, an Australian study showed a correlation between higher rates of late referrals and the distance to dialysis centres. 366 In Northern Ireland, Kee and colleagues364 also reported that increasing distance to the nearest renal centre was associated with later referral.
Physician factors
Winkelmayer and colleagues355 found that hospital physicians (not renal specialists), rather than GPs, were more likely to refer patients with CKD later to nephrologists. A finding repeated in several studies. 54,359
In a study by Boulware and colleagues,367 hypothetical clinical vignettes were used to assess physician evaluation of the severity of CKD, recommendations for referral, and awareness of current guideline recommendations. The participants were randomly selected from a nationally representative sample of physicians (family medicine and internal medicine physicians) and nephrologists. Compared to the nephrologists, both physician groups were worse at identifying patients with stage 3 (GFR 30–59 ml/min/1.73 m2) or stage 4 (GFR 15–29 ml/min/1.73 m2) CKD. Physicians were less likely to recommend referral for the patient scenarios and requested input from the referring nephrologist at a less frequent rate than recommended. Physicians were less likely than nephrologists to be aware of existing practice guidelines, and awareness of the guidelines did increase the likelihood of referral by the primary care physician. 367
In a study from Ireland,361 which also used clinical scenarios to evaluate referral behaviour, it was demonstrated that fewer than half of the patients were referred after the first encounter, whereas nearly all patients were referred as the renal function worsened and the patients became symptomatic. As the scenarios increased in complexity, the likelihood of referral decreased. 361
Mendelssohn and colleagues358 concluded that ‘rationing by physicians about the need for dialysis’ was a major factor in late referral. This non-referral was influenced by age and coexisting disease, and physicians evaluated the distance of dialysis centres and overcrowding of the nearest dialysis centres before referring a patient with CKD. 358 Similar rationing by physicians was not, however, demonstrated in a survey conducted in England. 368 Specialists (other than nephrologists) were likely to recommend referral for patients with CKD later than primary care physicians. 368
In a survey of referring physicians, Campbell369 documented the reasons for late referral. These included perception by the referring physicians of being evaluated negatively by nephrologists in 43% of cases, lack of communication or faulty communication between primary care physicians and nephrologists (37%), and lack of specific referral criteria for patients with ESRD (31%). It was also reported that more than 90% of referring primary care physicians felt that they had inadequate training regarding timing or indications for referral of patients with CKD. 369
Discussion
We identified a substantial number of reports about the impact of late referral on outcomes after the initiation of dialysis. All studies recruited patients to their study at the time of initiation of dialysis. Thus all these studies focus on reporting outcomes among those who survive to dialysis. Those dying prior to dialysis were excluded. Notably, ACM on dialysis was high, though variable across studies. Variability between studies may be explained by differences in baseline characteristics, the health care received and the small size of some of the studies.
At 1 year, mortality was consistently higher in the late versus early referral group regardless of the definition of early referral. At longer follow-up, the majority of studies reported higher mortality in the late referral group but Iseki (Japan)243 and Roubicek and colleagues (France)266 found little difference. While absolute differences in mortality were observed, the relative difference, once adjusted for comorbidities, was less. In those reaching dialysis, CVD accounted for a substantial proportion of deaths. Other outcomes were less well reported but there was evidence that late referral impacted on the number of clinic appointments with specialists, access to choice about dialysis modality and preparation for dialysis with permanent vascular access established before dialysis started. In addition, there was evidence of an increased requirement for hospitalisation around the start of dialysis in those referred late to specialist services.
None of the studies reported eGFR at the time of referral, so the definition relied on a retrospective consideration of time prior to dialysis. One study defined ‘late referral’ as referral once the eGFR was < 20 ml/min. Here, authors reported mortality to be higher in the late referral group in the first year of dialysis. The difference was, however, accounted for by difference in comorbidity and age. The difference in care received was also poorly described. It was, therefore, difficult to determine whether timing of referral was mainly a surrogate for severity at the time referred, degree of comorbidity or the care delivered. The triggers for referral were not reported and data on barriers to early referral were not collected. Very late presentation to nephrology services can occur as a result of an acute and aggressive deterioration in renal function. The studies were generally poor at explicitly excluding people with an acute renal event from their analysis.
A review of additional literature seeking to identify potential barriers to early referral found a range of potential patient, health-care system and physician related factors described. Reporting of the variability of the importance of different factors suggested that individual health-care systems would have to consider local issues when designing or modifying services to optimise referral timing. Good communication between primary care and hospital physicians, and nephrology specialists was important in ensuring timely and appropriate referral.
Conclusions
The impact of late referral on predialysis survival and outcomes has not been studied. There was evidence that late referral impacts negatively on survival on dialysis particularly in the first year. The implications for care delivery and preparation for RRT were significant but the impact on patient quality of life was not reported. Many potential barriers to earlier referral have been described in the literature and by health-care system and local setting as well as by patient- and physician-related factors. Communication between aspects of the health-care system was important to ensure appropriate referral.
List of abbreviations
- ACE I
- angiotensin converting enzyme inhibitor
- ACM
- all-cause mortality
- ACR
- albumin–creatinine ratio
- ARB
- angiotensin receptor blocker
- ARIC
- Atherosclerosis Risk in Communities
- BMJ
- British Medical Journal
- BP
- blood pressure
- CG
- Cockcroft–Gault
- CHS
- Cardiovascular Heart Study
- CI
- confidence interval
- CKD
- chronic kidney disease
- CVD
- cardiovascular disease
- EDTA
- ethylenediaminetetraacetic acid
- eGFR
- estimated glomerular filtration rate
- ESRD
- end-stage renal disease
- FHS
- Framingham Heart Study
- GFR
- glomerular filtration rate
- GP
- general practitioner
- HBP
- high blood pressure
- HR
- hazard ratio
- HUI
- Health Utilities Index
- HLOC
- health-specific locus of control
- ICER
- incremental cost-effectiveness ratio
- IT
- information technology
- KDOQI
- Kidney Disease Outcomes Quality Initiative
- KDQOL-36
- Kidney Disease Quality of Life short form-36
- MDC
- multidisciplinary care
- MDRD
- Modification of Diet in Renal Disease
- MI
- myocardial infarction
- NHANES
- National Health and Nutritional Examination Survey
- NICE
- National Institute for Health and Clinical Excellence
- NKF
- National Kidney Foundation
- OR
- odds ratio
- QALY
- quality-adjusted life-year
- QOF
- Quality and Outcomes Framework
- RAAS
- renin–angiotensin aldosterone system
- RCT
- randomised controlled trial
- RR
- relative risk
- RRT
- renal replacement therapy
- SCS
- shared care scheme
- SD
- standard deviation
- SIGN
- Scottish Intercollegiate Guidelines Network
- SIMON
- Southampton Integrated Monitoring of Nephrology
- SMR
- standardised mortality rate
- TTO
- time trade-off
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Riemsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson, EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost-effectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
-
Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial.
By Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al.
-
The effect of different treatment durations of clopidogrel in patients with non-ST-segment elevation acute coronary syndromes: a systematic review and value of information analysis.
By Rogowski R, Burch J, Palmer S, Craigs C, Golder S, Woolacott N.
-
Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care.
By Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al.
-
A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial.
By Gray AJ, Goodacre S, Newby DE, Masson MA, Sampson F, Dixon S, et al. , on behalf of the 3CPO study investigators.
-
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluation.
By Ara R, Pandor A, Stevens J, Rees A, Rafia R.
-
Adefovir dipivoxil and pegylated interferon alpha for the treatment of chronic hepatitis B: an updated systematic review and economic evaluation.
By Jones J, Shepherd J, Baxter L, Gospodarevskaya E, Hartwell D, Harris P, et al.
-
Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis.
By Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al.
-
A double-blind randomised placebo-controlled trial of topical intranasal corticosteroids in 4- to 11-year-old children with persistent bilateral otitis media with effusion in primary care.
By Williamson I, Benge S, Barton S, Petrou S, Letley L, Fasey N, et al.
-
The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model.
By Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R.
-
Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial.
By Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al.
-
Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis.
By Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
-
The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation.
By Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al.
-
Rapid testing for group B streptococcus during labour: a test accuracy study with evaluation of acceptability and cost-effectiveness.
By Daniels J, Gray J, Pattison H, Roberts T, Edwards E, Milner P, et al.
-
Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Honest H, Forbes CA, Durée KH, Norman G, Duffy SB, Tsourapas A, et al.
-
The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model.
By Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, et al.
-
Gemcitabine for the treatment of metastatic breast cancer.
By Jones J, Takeda A, Tan SC, Cooper K, Loveman E, Clegg A.
-
Varenicline in the management of smoking cessation: a single technology appraisal.
By Hind D, Tappenden P, Peters J, Kenjegalieva K.
-
Alteplase for the treatment of acute ischaemic stroke: a single technology appraisal.
By Lloyd Jones M, Holmes M.
-
Rituximab for the treatment of rheumatoid arthritis.
By Bagust A, Boland A, Hockenhull J, Fleeman N, Greenhalgh J, Dundar Y, et al.
-
Omalizumab for the treatment of severe persistent allergic asthma.
By Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al.
-
Rituximab for the treatment of relapsed or refractory stage III or IV follicular non-Hodgkin’s lymphoma.
By Boland A, Bagust A, Hockenhull J, Davis H, Chu P, Dickson R.
-
Adalimumab for the treatment of psoriasis.
By Turner D, Picot J, Cooper K, Loveman E.
-
Dabigatran etexilate for the prevention of venous thromboembolism in patients undergoing elective hip and knee surgery: a single technology appraisal.
By Holmes M, C Carroll C, Papaioannou D.
-
Romiplostim for the treatment of chronic immune or idiopathic thrombocytopenic purpura: a single technology appraisal.
By Mowatt G, Boachie C, Crowther M, Fraser C, Hernández R, Jia X, et al.
-
Sunitinib for the treatment of gastrointestinal stromal tumours: a critique of the submission from Pfizer.
By Bond M, Hoyle M, Moxham T, Napier M, Anderson R.
-
Vitamin K to prevent fractures in older women: systematic review and economic evaluation.
By Stevenson M, Lloyd-Jones M, Papaioannou D.
-
The effects of biofeedback for the treatment of essential hypertension: a systematic review.
By Greenhalgh J, Dickson R, Dundar Y.
-
A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: the BELLS study.
By Sullivan FM, Swan IRC, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al.
-
Lapatinib for the treatment of HER2-overexpressing breast cancer.
By Jones J, Takeda A, Picot J, von Keyserlingk C, Clegg A.
-
Infliximab for the treatment of ulcerative colitis.
By Hyde C, Bryan S, Juarez-Garcia A, Andronis L, Fry-Smith A.
-
Rimonabant for the treatment of overweight and obese people.
By Burch J, McKenna C, Palmer S, Norman G, Glanville J, Sculpher M, et al.
-
Telbivudine for the treatment of chronic hepatitis B infection.
By Hartwell D, Jones J, Harris P, Cooper K.
-
Entecavir for the treatment of chronic hepatitis B infection.
By Shepherd J, Gospodarevskaya E, Frampton G, Cooper, K.
-
Febuxostat for the treatment of hyperuricaemia in people with gout: a single technology appraisal.
By Stevenson M, Pandor A.
-
Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal.
By Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E.
-
Cetuximab for the treatment of recurrent and/or metastatic squamous cell carcinoma of the head and neck.
By Greenhalgh J, Bagust A, Boland A, Fleeman N, McLeod C, Dundar Y, et al.
-
Mifamurtide for the treatment of osteosarcoma: a single technology appraisal.
By Pandor A, Fitzgerald P, Stevenson M, Papaioannou D.
-
Ustekinumab for the treatment of moderate to severe psoriasis.
By Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A.
-
Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model.
By Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al.
-
Clinical and cost-effectiveness of epoprostenol, iloprost, bosentan, sitaxentan and sildenafil for pulmonary arterial hypertension within their licensed indications: a systematic review and economic evaluation.
By Chen Y-F, Jowett S, Barton P, Malottki K, Hyde C, Gibbs JSR, et al.
-
Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) – a pharmacoepidemiological and qualitative study.
By Wong ICK, Asherson P, Bilbow A, Clifford S, Coghill D, R DeSoysa R, et al.
-
ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening.
By Kitchener HC, Almonte M, Gilham C, Dowie R, Stoykova B, Sargent A, et al.
-
The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation.
By Black C, Clar C, Henderson R, MacEachern C, McNamee P, Quayyum Z, et al.
-
Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS).
By Robson SC, Kelly T, Howel D, Deverill M, Hewison J, Lie MLS, et al.
-
Randomised controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes.
By Jeffcoate WJ, Price PE, Phillips CJ, Game FL, Mudge E, Davies S, et al.
-
VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers.
By Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al.
-
A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: the VULCAN trial
By Michaels JA, Campbell WB, King BM, MacIntyre J, Palfreyman SJ, Shackley P, et al.
-
Communication of carrier status information following universal newborn screening for sickle cell disorders and cystic fibrosis: qualitative study of experience and practice.
By Kai J, Ulph F, Cullinan T, Qureshi N.
-
Antiviral drugs for the treatment of influenza: a systematic review and economic evaluation.
By Burch J, Paulden M, Conti S, Stock C, Corbett M, Welton NJ, et al.
-
Development of a toolkit and glossary to aid in the adaptation of health technology assessment (HTA) reports for use in different contexts.
By Chase D, Rosten C, Turner S, Hicks N, Milne R.
-
Colour vision testing for diabetic retinopathy: a systematic review of diagnostic accuracy and economic evaluation.
By Rodgers M, Hodges R, Hawkins J, Hollingworth W, Duffy S, McKibbin M, et al.
-
Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report.
By Bond M, Wyatt K, Lloyd J, Welch K, Taylor R.
-
Are adverse effects incorporated in economic models? An initial review of current practice.
By Craig D, McDaid C, Fonseca T, Stock C, Duffy S, Woolacott N.
-
Multicentre randomised controlled trial examining the cost-effectiveness of contrast-enhanced high field magnetic resonance imaging in women with primary breast cancer scheduled for wide local excision (COMICE).
By Turnbull LW, Brown SR, Olivier C, Harvey I, Brown J, Drew P, et al.
-
Bevacizumab, sorafenib tosylate, sunitinib and temsirolimus for renal cell carcinoma: a systematic review and economic evaluation.
By Thompson Coon J, Hoyle M, Green C, Liu Z, Welch K, Moxham T, et al.
-
The clinical effectiveness and cost-effectiveness of testing for cytochrome P450 polymorphisms in patients with schizophrenia treated with antipsychotics: a systematic review and economic evaluation.
By Fleeman N, McLeod C, Bagust A, Beale S, Boland A, Dundar Y, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of photodynamic diagnosis and urine biomarkers (FISH, ImmunoCyt, NMP22) and cytology for the detection and follow-up of bladder cancer.
By Mowatt G, Zhu S, Kilonzo M, Boachie C, Fraser C, Griffiths TRL, et al.
-
Effectiveness and cost-effectiveness of arthroscopic lavage in the treatment of osteoarthritis of the knee: a mixed methods study of the feasibility of conducting a surgical placebo-controlled trial (the KORAL study).
By Campbell MK, Skea ZC, Sutherland AG, Cuthbertson BH, Entwistle VA, McDonald AM, et al.
-
A randomised 2 × 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up.
By Waterhouse JC, Walters SJ, Oluboyede Y, Lawson RA.
-
The effectiveness and cost-effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13–19: a systematic review and economic evaluation.
By Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett-Page E, et al.
-
Dissemination and publication of research findings: an updated review of related biases.
By Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, et al.
-
The effectiveness and cost-effectiveness of biomarkers for the prioritisation of patients awaiting coronary revascularisation: a systematic review and decision model.
By Hemingway H, Henriksson M, Chen R, Damant J, Fitzpatrick N, Abrams K, et al.
-
Comparison of case note review methods for evaluating quality and safety in health care.
By Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al.
-
Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation.
By Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, et al.
-
Self-monitoring of blood glucose in type 2 diabetes: systematic review.
By Clar C, Barnard K, Cummins E, Royle P, Waugh N.
-
North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel non-randomised preference study.
By Lock C, Wilson J, Steen N, Eccles M, Mason H, Carrie S, et al.
-
Multicentre randomised controlled trial of the clinical and cost-effectiveness of a bypass-surgery-first versus a balloon-angioplasty-first revascularisation strategy for severe limb ischaemia due to infrainguinal disease. The Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial.
By Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FGR, Gillespie I, et al.
-
A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – the TOuCAN trial.
By Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al.
-
Randomised controlled trials for policy interventions: a review of reviews and meta-regression.
By Oliver S, Bagnall AM, Thomas J, Shepherd J, Sowden A, White I, et al.
-
Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs (NSAIDs) for the reduction of morphine-related side effects after major surgery: a systematic review.
By McDaid C, Maund E, Rice S, Wright K, Jenkins B, Woolacott N.
-
A systematic review of outcome measures used in forensic mental health research with consensus panel opinion.
By Fitzpatrick R, Chambers J, Burns T, Doll H, Fazel S, Jenkinson C, et al.
-
The clinical effectiveness and cost-effectiveness of topotecan for small cell lung cancer: a systematic review and economic evaluation.
By Loveman E, Jones J, Hartwell D, Bird A, Harris P, Welch K, et al.
-
Antenatal screening for haemoglobinopathies in primary care: a cohort study and cluster randomised trial to inform a simulation model. The Screening for Haemoglobinopathies in First Trimester (SHIFT) trial.
By Dormandy E, Bryan S, Gulliford MC, Roberts T, Ades T, Calnan M, et al.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of Science Support, NETSCC, HTA
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Director of NHS Support, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Dr Ruairidh Milne, Director of Strategy and Development, NETSCC
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, Univeristy of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Professor Hywel Williams, Professor of Dermato-Epidemiology, University of Nottingham
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies & Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Ms Jane Bates, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Professor Glyn Elwyn, Primary Medical Care Research Group, Swansea Clinical School, University of Wales
-
Dr Ron Gray, Consultant Clinical Epidemiologist, Department of Public Health, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, University of Sheffield
-
Dr Jennifer J Kurinczuk, Consultant Clinical Epidemiologist, National Perinatal Epidemiology Unit, Oxford
-
Dr Susanne M Ludgate, Medical Director, Medicines & Healthcare Products Regulatory Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, Joint Director, National Collaborating Centre for Mental Health, University College London
-
Mrs Una Rennard, Service User Representative
-
Dr Phil Shackley, Senior Lecturer in Health Economics, School of Population and Health Sciences, University of Newcastle upon Tyne
-
Dr W Stuart A Smellie, Consultant in Chemical Pathology, Bishop Auckland General Hospital
-
Dr Nicholas Summerton, Consultant Clinical and Public Health Advisor, NICE
-
Ms Dawn Talbot, Service User Representative
-
Dr Graham Taylor, Scientific Advisor, Regional DNA Laboratory, St James’s University Hospital, Leeds
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Pharmaceuticals Panel
-
Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor in Child Health, University of Nottingham
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Mrs Barbara Greggains, Service User Representative
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Professor Jonathan Ledermann, Professor of Medical Oncology and Director of the Cancer Research UK and University College London Cancer Trials Centre
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Dr Lesley Wise, Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Therapeutic Procedures Panel
-
Consultant Physician, North Bristol NHS Trust
-
Professor of Psychiatry, Division of Health in the Community, University of Warwick, Coventry
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School, Coventry
-
Ms Maree Barnett, Acting Branch Head of Vascular Programme, Department of Health
-
Mrs Val Carlill, Service User Representative
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Mr Mark Emberton, Senior Lecturer in Oncological Urology, Institute of Urology, University College Hospital, London
-
Professor Steve Goodacre, Professor of Emergency Medicine, University of Sheffield
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and The London School of Medicine and Dentistry
-
Mr Paul Hilton, Consultant Gynaecologist and Urogynaecologist, Royal Victoria Infirmary, Newcastle upon Tyne
-
Professor Nicholas James, Professor of Clinical Oncology, University of Birmingham, and Consultant in Clinical Oncology, Queen Elizabeth Hospital
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Kate Radford, Senior Lecturer (Research), Clinical Practice Research Unit, University of Central Lancashire, Preston
-
Mr Jim Reece Service User Representative
-
Dr Karen Roberts, Nurse Consultant, Dunston Hill Hospital Cottages
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health
-
Ms Kay Pattison, Section Head, NHS R&D Programme, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
-
Professor Tom Walley, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist, National Commissioning Group (NCG), London
-
Director, NHS Sustainable Development Unit, Cambridge
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Professor Mike Kelly, Director, Centre for Public Health Excellence, NICE, London
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Ms Jeanett Martin, Director of Nursing, BarnDoc Limited, Lewisham Primary Care Trust
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Miss Nicky Mullany, Service User Representative
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Ken Stein, Senior Clinical Lecturer in Public Health, University of Exeter
-
Dr Kieran Sweeney, Honorary Clinical Senior Lecturer, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Professor Margaret Thorogood, Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington