Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 06/77/04. The contractual start date was in April 2008. The draft report began editorial review in April 2009 and was accepted for publication in October 2009. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None
Permissions
Copyright statement
© 2010 Queen’s Printer and Controller of HMSO. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2010 Queen’s Printer and Controller of HMSO
Chapter 1 Aim and background
Aim
The project will evaluate the clinical effectiveness and cost-effectiveness of the different methods for the removal earwax in adults and children. It will review systematically the evidence assessing the clinical effectiveness and cost-effectiveness of interventions that are currently available for softening and/or removing earwax, including the use of drops, irrigation, mechanical removal and other methods. The project will systematically search for, appraise and summarise evidence on the safety of the different methods, identifying any significant harms or adverse events (AEs). If the systematic review of cost-effectiveness shows that there are no appropriate good-quality economic evaluations, a new economic model relevant to the UK setting will be developed. Also, it will identify any research needs and use value-of-information approaches to help in prioritising them.
Description of the health problem
Earwax (cerumen) is a normal secretion in the external ear canal, produced by small glands in the ear. The purpose of earwax is generally thought to be to protect the ear by trapping any particles in the ear canal and preventing them from entering the deeper part of the ear. Particles may include dirt, dead skin or other fragments. Normally, earwax moves particles to the outer ear at a rate that prevents any significant build-up. When this process fails, there can be an excessive build-up of wax, which can block or occlude the auditory canal. 1,2 Although this can be a relatively minor problem, it can result in several other related problems, including hearing loss, discomfort, balance disorders, tinnitus and even infection. 3,4 It is often these symptomatic conditions that are the key concern for the person suffering from excessive earwax.
Although people with an excessive build-up of earwax can experience any of these conditions, hearing loss and the associated discomfort are probably the most frequent that occur. 5 The effects on hearing can be significant. Severity of hearing loss is measured by how well an individual can hear the frequencies or intensities of sound [measured by decibel (dB)] most often associated with speech. A person who can hear within the normal range can perceive sounds at a threshold intensity as low as 20 dB. Blockage of the ear from wax may elevate the hearing threshold to 40–45 dB. 6,7 In those presenting with age-related hearing loss, some will have earwax that, if removed, can reduce the hearing loss by around 10 dB. 8 The sense of blockage of the ear, the effects of hearing loss and the other comorbidities can cause discomfort and irritation to the person.
The occurrence of these related comorbidities provide evidence of the extent and severity of the build-up of earwax. Often people will present prior to the development of severe symptoms. In such instances, assessment of their condition is usually made based on the degree of occlusion of the auditory canal or tympanic membrane (TM), the extent of impaction of earwax, and the nature and characteristics of the earwax itself. These are often thought to be proportionally related to the severity of comorbidities. 7 Assessment of these symptoms is usually undertaken through direct visualisation of the ear canal with an otoscope. 9 There do not appear to be any documented standard criteria on which to base such judgements, meaning that they are open to variation in their measurement, reporting and interpretation. Such differences make judging the extent and severity of the earwax uncertain.
Aetiology
There are a number of possible causes of excess earwax or of the retention of earwax. 5,10–12 Small amounts of earwax are normal in the ear canal and excessive cleaning may interfere with the natural production of earwax. Other factors, such as the rate of earwax accumulation,10 use of hearing aids,11 small ear canals or skin conditions may also increase the risk of a build-up of earwax. In addition, different people appear to be at a higher risk of suffering from accumulation of earwax, with an increased risk for the elderly, men, people with intellectual impairment and secondary-care populations. 5,12
As people age, the cerumen glands atrophy (decline in effectiveness) and earwax becomes drier, making it a more extensive problem in the older age group. 1 Excessive earwax may also present as a problem in hearing assessments, blocking the view of the TM (or ear drum) during examination, and it can interfere with the fitting of hearing aids. Some 80% of patients attending a hearing aid repair department do so because of problems with earwax. 13 Recurrence of the problem does not seem uncommon and it is suggested that around 30% of elderly and mentally impaired individuals14 require regular treatment.
Pathology
Earwax is composed of the outer layers of the skin, which are discarded as part of a normal process of skin turnover and glandular secretions. 11 The skin is made up of three different layers, with the epidermis being the outermost layer. 15 The epidermis consists of different cells, the major cell type of which is keratinocytes. As part of the normal cycle of skin turnover, these cells push up through the epidermis and are eventually shed. 15 An over production of keratin or a failure in the separation of keratinocytes are thought to be possible factors leading to excessive earwax. For example, in a study of 20 patients with earwax, keratin was seen to account for up to 60% of the earwax plug. 16 Other research suggests that carotenoids (fat-soluble pigments) might contribute to the mechanism of the production of excessive earwax, but this requires further confirmation. 10,11
Earwax has two phenotypes. Wet wax is far more common in Caucasians17 and Africans,18 consisting of approximately 50% lipid (fat). 10 Dry wax is more frequent in East Asians,19 and only contains about 20% lipids. 20 There appear to be few other biochemical differences between the two types of wax. 10 Also, wax colour may vary from person to person.
Epidemiology
Although earwax and its associated problems are thought to be a common reason for attending primary care practices, data on its epidemiology in the general population are limited. Prevalence rates appear to vary widely, due in part to the different population groups under study, the likely variation in the interpretation of the degree of earwax present, and differences in the methods used to ascertain the data.
In an adult hearing screening study in Denmark, earwax was judged to be occluding in 2.1% of participants aged between 30 and 49 years. 21 This is similar to the rate of acoustically obstructing earwax (2.3%) identified in an earlier UK adult hearing screening study. 22 However, another estimate suggests that excessive or ‘impacted’ earwax is likely to be present in up to 5% of normal healthy adults, with higher rates in children, older people living in nursing homes and those with learning difficulties (approximately 10%, 57% and 36% of people in these three groups, respectively). 9,14 One of the limitations of the two screening studies is that the populations were those who agreed (from a random sample) to be screened for hearing loss and hence the estimates may not be representative of the general population. The latter study was a review of a number of different epidemiological studies but the estimates are also limited owing to differences in the methodologies, sample sizes and age of their included studies. This may explain the wide variation in ranges seen.
In a single-centre study of children aged 3–10 years in one region of the UK, the prevalence of partially occluding or totally occluding earwax was reported to be 43%. 23 The study suggested that the prevalence tends to decrease with age and that there is no difference in prevalence between gender. The authors of the study point out, however, that the sample was not a random one and the collection of data was undertaken during the winter months, which may explain the higher rates of earwax.
In older people who are admitted to an elderly care evaluation unit, 19% of those found to have a hearing impairment on assessment (55% of the total sample) had earwax occluding both ears. 24 The prevalence of bilateral earwax increased with age, from 9% in those aged 55–64 years and 65–74 years, to 13% in those aged 75–84, and to 27% in those over the age of 85 years. A UK survey of 300 consecutive general practice referrals of patients >60 years for hearing aids found a 29% prevalence of occluding wax. 25 However, it should be noted that these rates are from those with hearing impairment, rather than general population rates. It is also not clear whether the earwax was the cause of the hearing impairment. In another study of elderly participants (mean age 81 years) who had been identified as having hearing loss on screening, the occurrence of ‘impacted’ earwax was reported as 15.7% of ears. 26 One further study of hospitalised elderly patients in the USA reported that 35% of its sample suffered with ‘impacted’ earwax, 15% unilaterally and nearly 20% bilaterally. 5 Similar caveats apply to these latter two studies regarding the generalisability of their populations with that of the general population.
It is clear that these studies show a wide variation in their estimates of the prevalence of earwax and also their definition of the extent of the earwax. It is unclear, however, whether all of these people would have viewed their earwax as problematic or symptomatic, particularly in the studies that identified their estimates from a screened population. However, to generate an estimate of the numbers of people in the general population with earwax that potentially may be problematic (‘impacted’ or ‘occluding’), these estimates have been applied to the UK population size. An estimate of the prevalence in adults (aged 16–59 years) based on a figure of 2–5%9,21,22 and a UK adult population of 36,122,100 (taken from mid-2006 estimates27) suggests somewhere between 722,000 and 1,800,000 adults may have problematic earwax. Taking a range of 10–43%9,23 in children aged less than 16 years and a UK child population of 11,537,100,27 the range of the prevalence of potentially problematic earwax would be in the region of 1,154,000–4,961,000. In those older than 60 years there may be somewhere between 2,069,000 and 7,369,000 people with potentially problematic earwax (based on a range of 16–57%9,24,26 and a population of 12,928,10027). The wide ranges of these estimates, based on a number of different prevalence rates from different studies, each with their own particular limitations, illustrate the difficulty of pinpointing the extent of the earwax problem in the UK. Not all of these people will consult a health-care professional, but recent estimates suggest that health professionals perform up to 2 million ear irrigations in England and Wales per year. 11
Current service provision and description of interventions
Despite the problems associated with the accumulation of excessive earwax and the demands placed upon primary care within the UK National Health Service (NHS), it appears that there are no nationally agreed guidelines for its diagnosis and treatment. As a consequence, it is likely that services will vary with many based primarily on local custom and practice rather than a strong clinical evidence base. Some locally and internationally based guidelines have been developed28 and these, along with opinions from clinicians, including practice nurses, provide a basis for understanding the clinical pathway that may be followed by people who are suffering from the problems associated with excessive earwax. Problems that may lead a person to seek help include a feeling of a blockage, discomfort, hearing loss in one or both ears, tinnitus and/or dizziness.
In the UK, people requiring the removal of earwax have traditionally attended primary care practices for confirmation of the diagnosis and treatment. The method of treatment should take account of the severity of the condition, the possibility of any contraindications (e.g. perforations) or comorbidities (e.g. tinnitus), the skills of the practitioner and the setting for treatment. The majority of practitioners currently advise the use of some form of drops or softeners as a first stage. The British National Formulary (BNF) lists several preparations, including almond oil, olive oil, sodium bicarbonate drops, Cerumol®, Exterol®, Molcer®, Otex® and Waxsol®. Other softeners may also be used. A summary of different preparations is presented in Table 1, grouping them into water-based, oil-based or non-water-non-oil-based products, using the classification adopted by Hand and Harvey. 29 Not all of these preparations are currently available in the UK. Brand names will be used throughout the report unless those are unclear, when the generic name will be reported.
| Key ingredient | Preparation | Background information |
|---|---|---|
| Water-based preparations | ||
| Acetic acid (otic) | EarCalm |
Acetic acid (glacial) ear spray. Ph Eur 2% w/w, ethoxylated, stearyl alcohol, ethylparahydroxybenzoate (E218), propyl parahydroxybenzoate (E216), purified water. Supply 5 ml Dose: 1 metered dose (60 mg, 0.06 ml) sprayed into the affected ear at least 3 times daily, maximum 1 spray every 2–3 hours for 2 days after symptoms have disappeared but for no longer than 7 days (from age 12 years) Side effects/allergic reaction: Hives, difficulty breathing, swelling of face, lips, tongue or throat Contraindication: Hypersensitivity to acetic acid otic solution or perforated TM Internet price: Around £5.99 |
| Docusate sodium | Molcer® |
Docusate sodium 5%. Includes propylene glycol. Supply 15 ml Dose: Fill ear with solution and remain in position for a few minutes, repeat for 2 nights after which the wax can be removed (from age 12 years) Side effects/allergic reaction: Occasional skin irritations Contraindication: Perforated TM OTC cost: Around £1.90 |
| Waxsol® |
Docusate sodium 0.5%. Glycerine, water and phenonip (a preservative). Supply 10 ml Dose: 2 drops per night (from age 6 years) Side effects/allergic reaction: Occasional stinging or soreness Contraindication: Perforation of the TM or inflammation of the ear OTC cost: Around £1.26 |
|
| Colace® | Liquid docusate sodium stool softener (not available in the UK) | |
| Dioctyl-medo® or Diocytl | Liquid docusate sodium stool softener and maize oil (not available in the UK) | |
| Sodium bicarbonate | Care® (generic sodium bicarbonate may be used in practice) |
Sodium bicarbonate BP 5% w/v. Supply 10 ml Dose: 3–4 drops, 3–4 times per day, for 3–5 days (from age 5 years) Side effects/allergic reaction: Dryness inside the ear, mild stinging sensation Contraindication: Unknown OTC cost: Around £2.20 |
|
Triethanolamine polypeptide oleate condensate No longer available in the UK and discontinued in the USA |
Cerumenex® or Xerumenex® |
Triethanolamine polypeptide oleate condensate (10%). Inactive ingredients – chlorobutanol 0.5%, propylene glycol and water. Supplied in 6 ml and 12 ml Dose: 5 drops, 2–3 times daily, for up to 3 days; limit exposure to the ear canal to 15–30 minutes (age unknown) Side effects/allergic reaction: Temporary burning, skin rash, itching, pain in or around the ears, dizziness or hearing trouble Contraindication: Perforated TM, otitis media or hypersensitivity to triethanolamine polypeptide, seborrhoeic dermatitis and eczema affecting the external ear Only available over the internet Cost: Around £3.08 (not OTC) |
| Sodium chloride (saline) | Generic solutions available |
Sodium chloride 0.9%. Supply 20 × 0.5 ml Dose: 3–4 drops, 3–4 times per day, for 3–5 days (from age 6 months). Side effects/allergic reaction: None reported Contraindication: Unknown. OTC cost: Around £4.92 |
| Oil-based preparations | ||
| Chlorobutanol solution | Cerumol® |
Chlorobutanol 5%, paradichlorobenzene 2%, arachis (peanut) oil 57.3%. Supply 11 ml Dose: 5 drops twice per day for 3 days (adults and children) Side effects/allergic reaction: Uncommon – can experience tingling sensation or temporary mild deafness when applied Contraindication: Otitis externa, seborrhoeic dermatitis and eczema affecting the outer ear, perforated TM and allergy to peanuts OTC cost: Around £2.85 |
| Glycerine/glycerin | Earex (same as Otocerol) |
Almond oil BP 33.33%, Arachis (peanut) oil BP 33.33% and rectified camphor oil 33.33%. Supply 10 ml Dose: 4 drops twice daily for up to 4 days (from the of age 1 year) Side effects/allergic reaction: Temporarily stinging or burning when first applied Contraindication: Allergy to peanuts or soya, inflamed or infected ear OTC cost: Around £2.29 |
| Almond oil | Generic solutions available |
Almond oil. Supply 10 ml Dose: 3–4 drops, 3–4 times per day, for 3–5 days (from age of 6 months) Side effects/allergic reaction: None reported Contraindication: Allergy to almonds OTC cost: Around £2.07 |
| Olive oil | Earol (generic olive oil may be used in practice) |
Olive oil ear drops. Supply 92 ml with 10-ml dropper Dose: 3–4 drops, 3–4 times per day, for 3–5 days (from age of 6 months) Side effects/allergic reaction: None reported Contraindication: Unknown OTC cost: Around £2.25 |
| Non-water-non-oil-based preparations | ||
| Choline salicylate solution | Audax® |
Choline salicylate 21.61%, glycerol 12.62%. Supply 10 ml Discontinued from use |
| Earex Plus (same as Audax®) |
Choline salicylate 21.6% and glycerol 12.62%. Supply 10 ml Dose: Fill ear twice daily for up to 4 days (from age 1 year) Side effects/allergic reaction: None reported Contraindication: Perforated or bleeding TM OTC cost: Around £4.29 |
|
| Urea–hydrogen peroxide | Otex (UK brand name, same as Exterol®) |
Urea–hydrogen peroxide complex 5%, ear drops: 8-hydroxy-quinoline and glycerol. Supply 8 ml Dose: 5 drops twice daily for at least 3–4 days (from the age of 5 years) Side effects/allergic reaction: Unpleasant taste in mouth, temporary bubbling sensation, can aggravate the painful symptoms of excessive earwax, including some loss of hearing, dizziness and tinnitus Contraindication: Damaged TM, dizziness, pain, discharge, inflammation, infection and tinnitus within 2–3 days of irrigation or with history of ear problems OTC cost: Around £1.83 |
|
Carbamide peroxide Not available in the UK; available as OTC ear drops in the USA |
Debrox® |
Carbamide peroxide 6.5% (urea peroxide). Supply 15 ml Dose: 5–10 drops twice per day for up to 4 days (from the age of 12 years) Side effects/allergic reaction: rare or uncommon – burning, itching, redness, worsening ear pain, rash, abnormal sensation while putting the drops in the ear and temporary reduction in hearing Contraindication: Perforated TM any signs of infection or injury, pain or other irritation, drainage, discharge or bleeding from the ear Internet cost: Around US$7.89 (around £5.28) |
| Murine Ear® |
Carbamide peroxide 6.5% and otic solution. Supply 15 ml Dose: 5–10 drops twice daily for up to 4 days (from the age of 12 years) Side effects/allergic reaction: Temporary decrease in hearing, dizziness, ear pain or other irritation, decreased hearing for a prolonged period of time, or discharge or bleeding from the ear Contraindication: Perforated TM, ear drainage, discharge, pain, rash, irritation or dizziness Internet cost: Around US$6.49 (around £4.35) |
|
The intention of these remedies or drops is to either soften the wax prior to removal at the clinic or to help remove the wax on its own. Their specific action varies. For example, in vitro studies suggest that preparations including urea or glycerine increase water penetration of the earwax, while preparations including peroxide break up the earwax through the release of gas/bubbles, therefore aiding mechanical removal. 30 Limited data are available to guide people’s choice of drops in particular clinical situations. AEs differ for each intervention but are generally thought to be mild. It is usually suggested that people allow between 3 and 7 days for these remedies or drops to take effect, although for some it may take longer (i.e. 14 days of drops) or several cycles.
If the wax has not dissolved or dissipated using drops or remedies, people are recommended to attend the primary care practice to have the wax removed by mechanical removal, through either irrigation or curettage. 11 In irrigation, a pressurised flow of water is used to remove the earwax. Although flushing wax with metal piston syringes (e.g. Reiner-Alexander ear syringe) was common practice in primary care practices, these have largely been replaced with electronic irrigators, such as the oral jet irrigator, nebuliser or Propulse ear irrigator. 31,32 The use of metal piston syringes is no longer recommended. 33 Irrigation is contraindicated in people with perforated ear drums, history of ear surgery or chronic ear conditions. Reported harms of irrigation are pain, infection and injury to the ear, including TM perforation and tinnitus. 34,35 Curettage, which allows the removal of earwax under direct vision, using various implements, such as cerumen spoons, hooks, loops and probes, is rarely undertaken in primary care practices. Although it has the advantage of not using water to remove the earwax, and so perhaps lessening the risk of infection, it can be a difficult procedure, requiring specialist skill and time. 36
Increasingly the role of the general practitioner (GP) has been taken over by the practice nurse (or, for the house-bound, the district nurse), who can confirm the problem by examination of the ear, recommending/prescribing the use of the drops or remedies and then removing any wax by irrigation. 31 On most occasions irrigation will successfully remove earwax on the first attempt; however, for a limited proportion of people it may prove more difficult and these people may need to attend on several occasions. Rarely, when it proves impossible for the primary care practice to remove the earwax, the person will be referred to a hospital-based specialist.
With the availability of several different softeners and proprietary drops, some people decide to self treat. As with their use in primary care practices, drops provide the possibility of treating the wax to allow it to dissipate or dissolve without further treatment. While such preparations offer the opportunity for self-treatment, caution needs to be exercised when used in combination with cotton wool swabs, as inadvertent damage to the inner ear canal or TM can occur. People may make several attempts to clear the wax with drops before consulting their primary care practice. Having self-treated with drops, people subsequently consulting the primary care practice for treatment may be able to have their earwax removed without further delay. Although not currently recommended, and not widely available within the UK, some forms of syringes for self-treatment are available. Soft bulb irrigators can be used by people after drops to flush their own ears. These can be purchased from suppliers through the internet and over the counter (OTC) in some European countries and in the USA. Other syringes for self-treatment are available, including plastic piston syringes (e.g. The Real McCoy and Master Blaster).
A minority of people who are unable to have their ears cleared through self-care or at the primary care practice, or have particular clinical conditions (e.g. cholesteatoma), or contraindications to standard treatment (e.g. pre-existing perforations of the TM) may be referred to specialist care. Ear, nose and throat (ENT) or otolaryngology departments use techniques such as microsuction or curettage through direct microscopic or endoscopic vision to clear earwax. 33,37,38 These methods are used in combination with suction or the use of a Jobson-Horne probe and a St Bartholomew’s wax hook, or crocodile forceps. 38 This requires specialist equipment and considerable skill. 33,39 In very rare instances where clearance of earwax is prevented due to a narrowing of the external auditory canal, for example, surgery may be required. 11
In addition to the above technologies, complementary therapies can also be used (e.g. ear candling).
Chapter 2 Methods
Methods for reviewing effectiveness
The a priori methods for systematically reviewing the evidence of clinical effectiveness and cost-effectiveness are described in the research protocol (Appendix 1), which was sent to experts for comment. Although helpful comments were received relating to the general content of the research protocol, there was none that identified specific problems with the methods of the review. The methods outlined in the protocol are briefly summarised below. Methods for the economic evaluation are outlined in Chapter 5 (see Methods of the economic valuation).
Search strategy
A sensitive search strategy was developed, tested and refined by an experienced information specialist. Separate searches were conducted to identify studies of clinical effectiveness, cost-effectiveness, quality of life, AEs, resource use/costs and epidemiology/natural history. Sources of information and search terms are provided in Appendix 2. The most recent search was carried out in November 2008.
Searches for clinical effectiveness and cost-effectiveness were from database inception. Electronic databases searched included: The Cochrane Database of Systematic Reviews (CDSR); The Cochrane Central Register of Controlled Trials (CENTRAL); Centre for Reviews and Dissemination (CRD) (University of York) Database of Abstracts of Reviews of Effectiveness (DARE); Health Technology Assessment (HTA) database and the NHS Economic Evaluation Database (NHS EED); MEDLINE (OVID), PREMEDLINE In-Process & Other Non-Indexed Citations (OVID), EMBASE (OVID); CINAHL; BIOSIS; Web of Knowledge Science Citation Index (SCI); Web of Knowledge ISI Proceedings; Current Controlled Trials and the National Research Register (Historical).
Primary care conferences were searched for recent abstracts (from 2004). The searches had no language restrictions. Any non-English language articles were set to one side in a separate foreign language reference database (see Appendix 2). Bibliographies of related papers were screened for relevant studies, and experts were also contacted to identify any additional relevant published or unpublished studies that were not identified on searches.
Inclusion and data extraction process
Titles and abstracts of studies identified by the search strategy were assessed for potential eligibility by two independent reviewers. The full text of relevant papers was then obtained and inclusion criteria were applied by two independent reviewers. Any disagreements over eligibility were resolved by consensus or, if necessary, by arbitration to a third reviewer. Data were extracted by one reviewer using a standard data extraction form and checked by a second reviewer.
Inclusion criteria
Patients
Adults or children presenting with build-up of earwax requiring removal.
Interventions
All methods of earwax removal or softening, including:
-
drops
-
irrigation (e.g. syringing, electronic irrigators)
-
mechanical removal other than syringing (e.g. suction, probes and forceps)
-
other methods
-
combinations of above methods.
Outcomes
Studies were included if they reported one or more of the following outcome measures:
-
measures of hearing
-
adequacy of clearance of wax
-
quality of life
-
time to recurrence or further treatment
-
AEs
-
cost-effectiveness.
It was noted that measures assessing the extent or severity of earwax and the adequacy of clearance are often related to the degree of impaction. Although this term is frequently used, there is often no clear definition provided. It may or may not refer to wax that occludes the TM, to wax that is symptomatic to the individual and/or to a hardened plug of wax. As such, this systematic review will only use the term ‘impacted’ when there is either no definition or a lack of clarity in the definition provided in the study report. Also, where other outcomes are used with no clear definition this will be highlighted in the reporting of results.
Types of studies
Randomised controlled trials (RCTs) and controlled clinical trials (CCTs) (i.e. prospective non-randomised studies with a concurrent control group) were included for the assessment of the clinical effectiveness and, additionally, cohort studies were included for the assessment of AEs. Studies published only as abstracts or conference presentations were also considered for eligibility if sufficient information was presented to allow an appraisal of the methodology and assessment of results. Systematic reviews were used for background and as a source of references. For the review of cost-effectiveness any costing studies or cost-effectiveness evaluations (including modelling studies) were also eligible for inclusion.
Quality assessment
The quality of included RCTs and CCTs was assessed using criteria recommended by CRD. 40 Quality criteria were applied by one reviewer and checked by a second reviewer. At each stage, any differences in opinion were resolved through discussion or consultation with a third reviewer.
Data synthesis
Data were synthesised through a narrative review with tabulation of results of all included studies. Full data extraction forms are presented in Appendices 3–5. It was not considered appropriate to combine the included studies in a meta-analysis due to heterogeneity of the patient groups and comparator treatments (see Chapter 3, Quantity and quality of research available, for further details).
Chapter 3 Assessment of clinical effectiveness
Quantity and quality of research available
A total of 202 records of publications were identified through literature searching. Of these, 158 were excluded on title and abstract. Full reports for the remaining 45 were requested for more in-depth screening. Of these, 19 were excluded (see list of excluded studies in Appendix 6). An inclusion flow chart can be seen in Appendix 2.
Twenty-six published studies met the inclusion criteria – of these, 22 were RCTs and four were CCTs. These trials fell into three categories: studies undertaken in primary care (14 studies41–54), studies undertaken in secondary care (eight studies4,54–60), and studies of self-care or those undertaken in other care settings (four studies61–64). Where the setting was in emergency care this has been grouped under primary care in the present review because it was assumed that this was the first point of contact with a health professional. In some other cases the setting was not made explicit within the publication; where this was the case an assumed grouping was used based on the author(s) affiliation (e.g. if they worked in an outpatient clinic this was assumed to be a secondary care setting). Additionally, studies are also grouped by participant group (children, mixed adults and children, and adult groups). In some cases the study did not indicate who the target population was and these were classed under the mixed group as population ‘unknown’. In some of these studies a mean age of the study participants was given but no range or measure of variance was reported and so these were also classed under the mixed population group. The subsequent discussion of these studies (below) will follow these conventions (Table 2).
| Study | Settings | Population | Primary objective (SO or SI) | |
|---|---|---|---|---|
| Primary care | ||||
| Studies with immediate follow-up for softeners only | ||||
| Meehan, 200246 | Emergency care | Children | SO | |
| Whatley, 200347 | General paediatric clinic and children’s hospital emergency department | Children | SO | |
| Singer, 200049 | Emergency department in care centre | Adults and children | SO | |
| Studies with delayed follow-up for softeners only | ||||
| Dummer, 199244 | Primary care | Adults | SO | |
| Jaffe, 197850 | Primary care | Adults and children | SO | |
| Carr, 200152 | Primary care – self treatment | Adults and children | SO | |
| Fahmy, 198254 | Primary carea | Unknown | SO | |
| Studies with immediate follow-up for softeners plus irrigation | ||||
| General Practitioner Research Group, 196541 | Primary care | Adults | SI | |
| Pavlidis, 200542 | Primary care | Adults | SI | |
| General Practitioner Research Group, 196748 | Primary care | Adults and children | SI | |
| Amjad, 197551 | Primary care | Unknown | SI | |
| Studies with delayed follow-up for softeners plus irrigation | ||||
| Burgess, 196643 | Primary care | Adults | SI | |
| Lyndon, 199245 | Primary care | Adults | SI | |
| Eekhof, 200153 | Primary care (follow-up: oil delayed, water immediate) | Unclear | SI | |
| Secondary care | ||||
| Studies with delayed follow-up for softeners only | ||||
| Keane, 19954 | Secondary care | Unknown | SO | |
| Fahmy, 198254 | Secondary carea | Unknown | SO | |
| Studies with immediate follow-up for softeners plus irrigation | ||||
| Caballero, 200555 | Secondary care | Adult | SI | |
| Dubow, 195957 | Secondary care | Children | SI | |
| Chaput de Saintonge, 197359 | Secondary care | Unknown | SI | |
| Studies with delayed follow-up for softeners plus irrigation | ||||
| Fraser, 197060 | Secondary care | Unknown | SI | |
| Studies with delayed follow-up for other types of extraction | ||||
| Pothier, 200656 | Otolaryngology outpatient clinic (follow-up: immediate, but delayed if softeners used for endoscopic de-waxing) | Adult | N/A | |
| Saloranta, 200558 | Secondary care plus community home (preventative study) | Adults and children | N/A | |
| Other care | ||||
| Studies with immediate follow-up for softeners plus irrigation | ||||
| Hinchcliffe, 195561 | Military research | Adults | SI | |
| Roland, 200462 | Corporate research clinic | Adults | SI | |
| Studies with delayed follow-up for self-care | ||||
| Coppin, 200863 | Self-treatment/primary care (self-irrigation/nurse irrigation) | Adults | N/A | |
| Harris, 196864 | Self-treatment/primary care | Adults | N/A | |
There is very little consistency among the included studies, which makes it difficult to fully summarise the results and in many studies some basic data were not available. Across all of these studies there are variations in the characteristics of the participants recruited, in terms of age and, to some extent, gender, and in terms of the extent of the earwax problem. In many studies there is very limited discussion of baseline characteristics, which makes it difficult to establish the representativeness of the respective populations. Many of the included studies (eight studies4,42,43,46,51,55,57,61) were presented as either a short paper format (less than two sides), an abstract format or a conference proceeding, and, where this was the case, the available data were further limited.
Study sample sizes were typically small, varying from 36 participants45 to 237 participants,63 and only a few studies reported undertaking a sample size calculation (7 out of 24 studies45,47,49,52,53,56,63). In some studies the overall population sample size was not reported, rather the numbers of ears were presented. 42,43,60 Seventeen studies were two-arm comparisons,41–45,48–54,56,58,59,63,64 five were three-arm studies,46,47,55,57,62 and there was one study each with four,4 five61 and six60 intervention arms.
There were also a wide range of interventions used between the included studies and differences in the length of follow-up used. For ease of understanding the review that follows is also divided into studies of immediate follow-up and delayed follow-up (the exact length of follow-up will be discussed for each study individually) and into studies where the intention was to use a softening agent alone (even when subsequent irrigation was used, if this was after initial outcome assessment) and those where the intention was always to use a softening agent and an irrigation as the intervention. Owing to the wide variation in interventions and comparisons used in the included studies the review has not been split by the different comparisons. However, each comparison is reported in sequence, in line with the conventions discussed above (setting, population, follow-up, softening agent with or without irrigation).
The outcome measures used also varied across the included studies. Often information concerning the definitions of the outcome measures used was limited and in many cases it was not possible to assess how valid, objective or consistently applied these different measures were. In the instances where this was clear the review has made note of this; for all other studies it should be assumed that care is required in the interpretation of the outcomes. For the purpose of this review, the range of outcomes have been categorised as far as possible into those measuring the degree of occlusion; those measuring the ease of wax removal; those measuring participant satisfaction; those measuring recurrence of earwax; and AEs. Measures of the type and consistency of earwax removed were tabulated but not reported in the narrative synthesis. In many cases the baseline values were not presented for a particular outcome, which makes the interpretation of the evidence of the effectiveness of the interventions more difficult. Where pretreatment and post-treatment measurements of an outcome were reported this has been discussed (e.g. a study might report the varying degrees of occlusion before and after intervention). However, in many cases it is not clear how the final outcome is related to the finding at baseline (how many in the ‘no change category’ post intervention started in the fully occluded category pretreatment, how many were in the partially occluded and so on). Many of the studies also did not report measures of variance around the estimates presented.
A number of studies also did not report results of any statistical significance testing, and, of those that did, a number did not report the statistical analytical approach taken. As noted above, in some cases the allocation to interventions was undertaken on the basis of the number of ears rather than the number of participants. Also, in some studies where allocation was based on the number of participants, the analysis was undertaken on the number of ears. Where this is the case the present review has identified these studies. Care is recommended when interpreting the outcomes of these studies, as it is unclear whether valid statistical analyses (where reported) will have been undertaken (see Cochrane Handbookfor Systematic Reviewsof Interventions for discussion of appropriate analyses of these types of data65). Finally, there was a wide range in the publication dates of the included studies (1950–2007), and eleven studies were undertaken more than 20 years ago,41,43,48,50,51,54,57,59–61,64 which may affect the generalisability of the studies to current practice (and account for some of the other issues already raised above). It is likely in current practice that an irrigator rather than a metal syringe will be used for the removal of earwax; however, syringes were used for many of the included studies, although this may not always be clear because ‘syringing’ and ‘irrigation’ may sometimes be used interchangeably. The present report refers to ‘syringing’ only where this was the term reported by the included study. In the case of self-treatment, the present report uses the term ‘irrigation’ when a soft bulb was used, as these are not syringes, even if the study authors have referred to this as a self-syringe.
Studies in primary care settings
Characteristics of the primary care studies are shown in Table 3. Seven RCTs41,42,46–49,51 followed participants up immediately after interventions, and seven RCTs43–45,50,52–54 had a delay between intervention and follow-up.
| Study | Interventions | Participants | Outcomes |
|---|---|---|---|
| Immediate follow-up | |||
|
Author: Meehan and colleagues, 2002 46 Country: USA Number of centres: 1 Design: RCT Setting: Emergency care Follow-up: Immediate |
|
Target population: Cooperative patients, aged 1–18 years, presenting in a paediatric emergency department, with complete or partial TM occlusion Baseline characteristics: Age, mean years: 4.6 overall (no individual group details) Gender, M/F: 24 : 24 overall (no individual group details) |
Amount of TM visualised AEs |
|
Author: Whatley and colleagues, 2003 47 Country: USA Number of centres: 2 Design: RCT Setting: Children’s hospital emergency department or large general paediatric clinic in same town Follow-up: Immediate |
|
Target population: Children aged 6 months to 5 years with complete or partial cerumen obstruction of the TM Baseline characteristics: Age, mean (SD):Overall range: (16 months–5 years) Gender M/F (%): |
Proportion achieving complete visualisation of the TM AEs |
|
Author: Singer and colleagues, 2000 49 Country: USA Number of centres:1 Design: RCT Setting: Emergency department Follow-up: Immediate |
|
Target population: (e.g. inclusion criteria) ≥ 1 year with ear canal partially or totally occluded by cerumen, medically requiring visualisation of ear canal (i.e. earache, hearing loss, fever) and presenting in the emergency department Baseline characteristics: Age, mean years (SD):Gender M/F (%): |
Proportion of ears in which TM totally visible with or without irrigation or irrigation with 100 ml of irrigant Presence of AEs |
|
Author: General Practitioner Research Group, 1965 41 Country: UK Number of centres: 14 Design: RCT Setting: Primary care Follow-up: Immediate |
|
Target population: UK primary care practice patients, no details on severity of occlusions Baseline characteristics: Age, maximum incidence: Males: 31–50 years Females: 51–70 years 32% new patients, 53% without syringing for over 12 months Gender, all patients, M/F: 1.3 : 1 |
Volume of water for syringing and syringefuls used Ease of wax removal Character of syringed wax |
|
Author: Pavlidis and Pickering, 2005 42 Country: Australia Number of centres: 1 Design: RCT Setting: Primary care Follow-up: Immediate |
|
Target population: UK adult patients with earwax partially or totally occluding one or both ears, which would normally be syringed by their GP Baseline characteristics: Age, mean years (SD):Gender M/F (%): |
Mean number of syringing attempts Mean time to syringing (minutes) AEs |
|
Author: General Practitioner Research Group, 1967 48 Country: UK Number of centres: 10 Design: RCT Setting: Primary care Follow-up: Immediate |
|
Target population: UK primary care practice patients with all cases of earwax apart from minor degrees of wax easily removed without softening agent Baseline characteristics: Age groups, % of all patients: 10–30 years, 27 31–50 years, 34 51–70 years, 31 71 years and over, 8 Gender: Not reported |
Volume of water for syringing Ease of wax removal Character of wax AEs |
|
Author: Amjad and Scheer, 1975 51 Country: USA Number of centres: Not reported Design: RCT Setting: Primary care Follow-up: Immediate |
|
Target population: Patients with hard or impacted earwax Baseline characteristics: Age: Not reported Gender: Not reported |
Degrees of wax removal AEs (subjective and observations of objective side effects) |
| Delayed follow-up | |||
|
Author: Dummer and colleagues, 1992 44 Country: UK Number of centres: 1 Design: RCT Setting: Primary care Follow-up: Median number of days between visits 1 and 2 was 4 days (range 3–7 days) |
|
Target population: Adults between 19–90 years presenting in primary care practice with impacted or hardened earwax Baseline characteristics: Age, mean (years):Gender M/F: |
Amount, colour and consistency of wax Symptoms Hearing Global impression of treatment efficacy (patient and investigator) Tolerability of treatment |
|
Author: Jaffe and Grimshaw, 1978 50 Country: UK Number of centres: Up to 15 Design: RCT Setting: Primary care Follow-up: Patients asked to revisit GP after 3 instillations |
|
Target population: Patients presenting at primary care practice with earwax and who would normally be prescribed a cerumenolytic Baseline characteristics: Age distribution (years): group 1, group 2 0–9: 0, 1 10–19: 5, 1 20–29: 4, 9 30–39: 8, 6 40–49: 7, 5 50–59: 12, 15 60–69: 9, 6 70–79: 7, 7 80–89: 1, 3 Gender M/F: 1. 32 : 21 2. 25 : 28 |
Ease of syringing Doctors overall impression AEs |
|
Author: Fahmy and Whitefield, 1982 54 Country: UK Number of centres: Multicentre, but number of centres not reported Design: CCT Setting: Studies 1 and 2 in secondary care, study 3 in primary care Follow-up: 1 week |
Study 3:* n = 160 (286 ears)
|
Target population: Patients presenting with earwax problems in secondary care for studies 1 and 2 and primary care in study 3 Baseline characteristics: Age: Not reported Gender: Not reported |
Wax occlusion Wax consistency Ease of syringing |
|
Author: Carr and Smith, 2001 52 Country: USA and/or Canada Number of centres: Unclear Design: RCT Setting: Primary care – self-treatment Follow-up: 14 days |
|
Target population: Those suffering with occlusive cerumen in at least 1 ear (most presenting with other complaints and ceruminosis was noted incidentally) Baseline characteristics: Age, mean years for all (36 children and 33 adults):Age, mean years for children:Gender: Not reported |
Degree of cerumen |
|
Author: Lyndon and colleagues, 1992 45 Country: UK Number of centres: Unclear Design: RCT Setting: Primary care Follow-up: 5 days |
|
Target population: Patients aged 16 years or over presenting in general practice with symptoms of hardened earwax, in either or both ears, requiring cerumenolytic treatment Baseline characteristics: Age, mean years for all patients (range): 52 (19–86) Gender, M/F for all patients: 19 : 17 |
Degree of impaction Ease of syringing Global impression of efficacy Side effects/discomfort |
|
Author: Burgess 1966 43 Country: UK Number of centres:1 Design: CCT Setting: Primary care Follow-up: Between 2 and 7 days |
|
Target population: Patients in primary care with more than one-half of an ear occluded by wax Baseline characteristics: Age range for all patients, years: 18–75 Gender, M/F all patients: 32 : 18 |
Average total of water used Ease of removing wax Character of wax Side effects |
|
Author: Eekhof and colleagues, 2001 53 Country: The Netherlands Number of centres: 4 Design: RCT Setting: Primary care Follow-up: Immediate for water group but 3 days for oil group |
|
Target population: All patients with complaints resulting from earwax were offered syringing. After each attempt at syringing the auditory canal was checked with an auriscope and the extent of blocking was noted (obstruction levels of 0–25%, 25–49%, 50–74% and 75–100% were used). If earwax was persistent (> 75% after 5 attempts at syringing) patients were eligible to be included in the study Baseline characteristics: Age, mean years for all patients (SD): 51 (16) Gender, M/F for all patients: 20 : 22 |
Number of syringing attempts needed to remove wax |
Two RCTs46,47 compared docusate sodium (DS) versus triethanolamine polypeptide (TP) versus saline in children, while one RCT compared DS versus TP in a mixed population of adults and children. 49 Another trial51 compared TP versus carbamide peroxide in an unspecified population. All of these had immediate follow-up after treatment.
Of two RCTs44,50 comparing Cerumol, Dummer and colleagues44 compared Cerumol with Audax in an adult population. This RCT had a delayed follow-up, averaging 4 days between the first and second visit (range 3–7 days). The second study by Jaffe and Grimshaw50 compared Cerumol with Otocerol in a mixed population of adults and children. This study had a delayed follow-up, but the length was unspecified, with participants requested to revisit after three instillations. Cerumol was further compared with Waxsol in an RCT48 with a mixed population of adults and children. This RCT had an immediate follow-up after treatment. Another comparison, of Audax with Earex,45 was an RCT in a population of adults aged 16 years and above, and had a delayed follow-up of 5 days. A CCT by Fahmy and Whitefield54 compared Exterol with Cerumol in an unspecified population and had a delayed follow-up of 1 week. The trial consisted of three studies, but only study three was in a primary care setting (for study one and study two see Studies in secondary care settings, below).
One RCT52 compared aqueous sodium bicarbonate with aqueous acetic acid in a mixed population of children and adults. This trial had a delayed follow-up of 14 days. An RCT by the General Practitioner Research Group,41 as well as a CCT by Burgess,43 compared dioctyl-medo ear drops with oil in adults. These studies had an immediate follow-up and delayed follow-up of between 2 and 7 days after the intervention, respectively.
Eekhof and colleagues53 compared the instillation of water at body temperature with a group self-administering oil. The population for this RCT was unspecified, but had a mean age of 51 years for all participants. Follow-up was immediate after the water treatment, but delayed by 3 days for the oil arm of the study. There was only one RCT42 comparing either ‘wet’ (with prior instillation of warm tap water) syringing or ‘dry’ syringing (no prior instillation of water) in an adult population. Follow-up was immediately after treatment.
The methodology and quality of reporting of included studies was generally poor (Table 4). A number of studies pre-date RCT reporting guidelines, but this may also reflect set word limits for some of the publications. Only three RCTs47,49,52 were assessed as adequate for their randomisation procedure, with one assessed as partially meeting this criteria. 42 For several studies the method was judged inadequate,46,51,53 but for the majority41,44,45,48,50 it was not possible to judge due to a distinct lack of information. The same three studies47,49,52 that were judged adequate for their randomisation procedures were also judged as adequate in their concealment allocation. For the remaining RCTs, concealment of allocation was either inadequate42,53 or unknown,41,44–46,48,50,51 making it impossible to rule out selection bias.
| Study | Randomisation | Concealment of allocation | Baseline characteristics | Eligibility | Blinding of assessors | Care-provider blinding | Patient blinding | Reporting outcomes | ITT | Withdrawals explained |
|---|---|---|---|---|---|---|---|---|---|---|
| Meehan, 200246 | In | Un | Un | In | Un | Par | Par | In | In | In |
| Whatley, 200347 | Ad | Ad | Rep | Ad | Par | Par | Par | Ad | In | Ad |
| Singer, 200049 | Ad | Ad | Rep | Ad | Un | In | Par | In | In | Ad |
| General Practitioner Research Group, 196541 | Un | Un | Un | Un | Un | Par | Par | In | In | In |
| Pavlidis, 200542 | Par | In | Rep | Ad | In | In | In | In | In | In |
| General Practitioner Research Group, 196748 | Un | Un | Un | In | Un | Par | Par | In | In | In |
| Amjad, 197551 | In | Un | Un | In | Un | Par | Par | In | In | In |
| Dummer, 199244 | Un | Un | Un | Par | In | In | In | In | In | In |
| Jaffe, 197850 | Un | Un | Rep | Par | Un | Par | Par | In | In | In |
| Carr, 200152 | Ad | Ad | Un | Ad | Un | Par | Par | In | In | Ad |
| Lyndon, 199245 | Un | Un | Un | Ad | Un | Un | Un | In | In | Ad |
| Eekhof, 200153 | In | In | Un | Ad | Un | Un | Un | Ad | In | Un |
None of the studies were judged as adequate in their method for blinding caregivers or participants. While the difficulties in blinding for some of the interventions could have been addressed somewhat by blinding the assessor of the outcomes, none of the studies did so adequately. Measurement bias can therefore not be ruled out for the majority of included studies. With only 4 out of 14 studies reporting baseline characteristics,42,47,49,50 it is also not possible to judge the similarities between the treatment groups at baseline for the majority of the studies. Four studies were judged adequate for the description of missing values,45,47,49,52 but none of the studies reported an adequate intention-to-treat (ITT) analysis. Caution should be exercised in the interpretation of the results of these studies, as overall these appear to be at a high risk of bias, which may affect the direction of any effects shown.
Likewise, the CCTs (Table 5) appear at risk to bias and their results have to be interpreted with care. The two included studies43,54 were of low quality, with unreported baseline characteristics in both and blinding of outcome assessors adequate in only one study. 43 Neither study was judged to be adequate for eligibility criteria, primary outcome results, ITT analysis, missing values or representativeness of the populations.
| Study | Baseline characteristics | Eligibility | Blinding of assessors | Reporting outcomes | ITT | Withdrawals explained | Representativeness |
|---|---|---|---|---|---|---|---|
| Fahmy, 198254 | Un | Par | Un | Par | Un | Un | Un |
| Burgess, 196643 | Un | Par | Ad | In | In | In | Un |
Results of studies in primary care with immediate follow-up
The results of the studies in primary care are reported in Table 6.
| Immediate follow-up – children – softeners alone as primary objective | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Meehan and colleagues, 200246 | |||||||||||||||||||||||||||||
| DS | TP | Saline | p-value | ||||||||||||||||||||||||||
| TM occlusion | |||||||||||||||||||||||||||||
| n = 15 | n = 17 | n = 16 | |||||||||||||||||||||||||||
| Complete | 5 | 5 | 5 | Not reported | |||||||||||||||||||||||||
| Partial | 8 | 5 | 9 | ||||||||||||||||||||||||||
| Clear | 2 | 7 | 2 | ||||||||||||||||||||||||||
| TM occlusion after first irrigation | |||||||||||||||||||||||||||||
| n = 13 | n = 15 | n = 15 | |||||||||||||||||||||||||||
| Complete | 4 | 4 | 4 | Not reported | |||||||||||||||||||||||||
| Partial | 6 | 3 | 5 | ||||||||||||||||||||||||||
| Clear | 3 | 8 | 6 | ||||||||||||||||||||||||||
| TM occlusion after second irrigation | |||||||||||||||||||||||||||||
| n = 12 | n = 15 | n = 15 | |||||||||||||||||||||||||||
| Complete | 3 | 4 | 3 | Not reported | |||||||||||||||||||||||||
| Partial | 4 | 3 | 4 | ||||||||||||||||||||||||||
| Clear | 5 | 8 | 8 | ||||||||||||||||||||||||||
| Whatley and colleagues, 200347 | |||||||||||||||||||||||||||||
| DS | TP | Saline | p-value | ||||||||||||||||||||||||||
| n = 35 | n = 30 | n = 28 | |||||||||||||||||||||||||||
| Clear TM after agent, n (%) | 4 (12) | 4 (13) | 1 (4) | Not reported | |||||||||||||||||||||||||
| Clear TM after first irrigation, n (%) | 13 (38) | 12 (40) | 12 (43) | Not reported | |||||||||||||||||||||||||
| Clear TM after second irrigation, n (%) | 18 (53) | 13 (43) | 19 (68) | Not significant | |||||||||||||||||||||||||
| Immediate follow-up – mixed population – softeners alone as primary objective | |||||||||||||||||||||||||||||
| Singer and colleagues, 200049 | |||||||||||||||||||||||||||||
| DS (n = 27) | TP (n = 23) | Difference (95% CI) | |||||||||||||||||||||||||||
| Completely visualised ears after solvent only, n (%) | 5 (19) | 2 (9) | 9.8 (–8.8 to 28.5) | ||||||||||||||||||||||||||
| Completely visualised ears after solvent with or without irrigation, n (%) | 22 (82) | 8 (35) | 46.7 (22.3 to 71.1) | ||||||||||||||||||||||||||
| TM visualisation, n (%) | |||||||||||||||||||||||||||||
| Complete | Incomplete | Complete | Incomplete | Not reported | |||||||||||||||||||||||||
| After solvent only | 5 (19) | 22 (81) | 2 (9) | 21 (91) | |||||||||||||||||||||||||
| First 50-ml ear irrigation | 10 (45) | 12 (55) | 2 (10) | 19 (90) | |||||||||||||||||||||||||
| Second 50-ml ear irrigation | 7 (58) | 5 (42) | 4 (21) | 15 (79) | |||||||||||||||||||||||||
| Immediate follow-up – adult population – softeners and irrigation at primary objective | |||||||||||||||||||||||||||||
| General Practitioner Research Group, 196541 | |||||||||||||||||||||||||||||
| Dioctyl-medo (n = 77) | Oil-based control (n = 73) | p-value | |||||||||||||||||||||||||||
| No. of cases | Total quantity (ml) | Mean per case | No. of cases | Total quantity (ml) | Mean per case | ||||||||||||||||||||||||
| Number of syringefuls used | |||||||||||||||||||||||||||||
| 0.25–1 | 35 | 2123 | 60 | 26 | 1732 | 65 | Not tested | ||||||||||||||||||||||
| 1.25–2 | 13 | 1718 | 130.5 | 17 | 2329 | 136 | Not tested | ||||||||||||||||||||||
| 2.5–4 | 12 | 2243 | 187.5 | 17 | 3487 | 207 | Not tested | ||||||||||||||||||||||
| 5–15 | 6 | 2045 | 341 | 4 | 2613 | 653 | Not tested | ||||||||||||||||||||||
| Total | 66 | 8129 | 122 | 64 | 10,181 | 165.5 | Not tested | ||||||||||||||||||||||
| Ease of wax removal, N (%) | |||||||||||||||||||||||||||||
| Easy | 54 (70) | 42 (57) | |||||||||||||||||||||||||||
| Difficult | 17 (22) | 23 (32) | |||||||||||||||||||||||||||
| Partial | 3 (4) | 6 (8) | |||||||||||||||||||||||||||
| Failed | 2 (3) | 2 (3) | |||||||||||||||||||||||||||
| Character of syringed wax, N (%) | |||||||||||||||||||||||||||||
| Liquid | 14 (19) | 10 (14) | |||||||||||||||||||||||||||
| Shredded | 34 (46) | 28 (40) | |||||||||||||||||||||||||||
| Hard lumps | 26 (35) | 32 (46) | |||||||||||||||||||||||||||
| Failed | 3 | 2 | |||||||||||||||||||||||||||
| Not recorded | 0 | 1 | |||||||||||||||||||||||||||
| Pavlidis & Pickering, 200542 | |||||||||||||||||||||||||||||
| Wet syringing (n = 22) | Dry syringing (n = 17) | p-value | |||||||||||||||||||||||||||
| Mean number of syringing attempts (SD) | 7.5 (7.3) | 25.4 (39.4) | 0.043 | ||||||||||||||||||||||||||
| Mean time to syringing (minutes) | 6.5 | 15.4 | ns but p-value not reported | ||||||||||||||||||||||||||
| Immediate follow-up – mixed populations – softeners and irrigation as primary objective | |||||||||||||||||||||||||||||
| General Practitioner Research Group, 196748 | |||||||||||||||||||||||||||||
| Volume of water (fl oz) | Waxsol (n = 47) | Cerumol (n = 60) | p-value | ||||||||||||||||||||||||||
| No. of participants | Total volume | No. of participants | Total volume | ||||||||||||||||||||||||||
| 0.5 | 0 | 0 | 1 | 0.5 | Not reported | ||||||||||||||||||||||||
| 1 | 6 | 6.0 | 2 | 2.0 | |||||||||||||||||||||||||
| 2 | 13 | 26.0 | 4 | 8.0 | |||||||||||||||||||||||||
| 2.5 | 1 | 2.5 | 1 | 2.5 | |||||||||||||||||||||||||
| 3 | 3 | 9.0 | 5 | 15.0 | |||||||||||||||||||||||||
| 4 | 3 | 12.0 | 8 | 32.0 | |||||||||||||||||||||||||
| 5 | 0 | 0 | 1 | 5.0 | |||||||||||||||||||||||||
| 6 | 6 | 36.0 | 4 | 24.0 | |||||||||||||||||||||||||
| 7 | 2 | 14.0 | 2 | 14.0 | |||||||||||||||||||||||||
| 8 | 3 | 24.0 | 12 | 96.0 | |||||||||||||||||||||||||
| 9 | 0 | 0 | 2 | 18.0 | |||||||||||||||||||||||||
| 10 | 1 | 10.0 | 2 | 20.0 | |||||||||||||||||||||||||
| 12 | 6 | 72.0 | 8 | 96.0 | |||||||||||||||||||||||||
| 14 | 1 | 14.0 | 2 | 28.0 | |||||||||||||||||||||||||
| 16 | 2 | 32.0 | 2 | 32.0 | |||||||||||||||||||||||||
| 18 | 0 | 0 | 1 | 18.0 | |||||||||||||||||||||||||
| 24 | 0 | 0 | 1 | 24.0 | |||||||||||||||||||||||||
| 26 | 0 | 0 | 1 | 26.0 | |||||||||||||||||||||||||
| 40 | 0 | 0 | 1 | 40.0 | |||||||||||||||||||||||||
| Totals | 47 | 257.5 | 60 | 501.0 | |||||||||||||||||||||||||
| Mean volume per participant: | 5.5 fl oz (156 ml) | 8.4 fl oz (240 ml) | Not reported | ||||||||||||||||||||||||||
| No. of participants (%) | No. of participants (%) | p-value | |||||||||||||||||||||||||||
| ≤ 56 ml (2 fl oz) | 19 (40) | 7 (12) | p < 0.05 | ||||||||||||||||||||||||||
| > 56 ml | 28 (60) | 53 (88) | |||||||||||||||||||||||||||
| Proportion of participants needing: 14–112 ml: | 55% | 35% | p < 0.05 | ||||||||||||||||||||||||||
| Ease of removal, n (%) | |||||||||||||||||||||||||||||
| Easily removed | 39 (83) | 48 (80) | No p-values reported | ||||||||||||||||||||||||||
| Removed with difficulty | 6 (13) | 9 (15) | |||||||||||||||||||||||||||
| Partly removed | 1 (2) | 1 (2) | |||||||||||||||||||||||||||
| Failed | 1 (2) | 2 (3) | |||||||||||||||||||||||||||
| Character of wax (% of participants) | |||||||||||||||||||||||||||||
| Liquid | 17 | 17 | No p-values reported | ||||||||||||||||||||||||||
| Shredded | 46 | 35 | |||||||||||||||||||||||||||
| Hard lumps | 37 | 24 | |||||||||||||||||||||||||||
| Amjad and Scheer, 197551 | |||||||||||||||||||||||||||||
| Degree of wax removal, n (%) | |||||||||||||||||||||||||||||
| TP (n = 40) | Carbamide peroxide (n = 40) | p-value | |||||||||||||||||||||||||||
| Excellent (E) | 27 (68) | 2 (5) | Not reported | ||||||||||||||||||||||||||
| Good (G) | 8 (20) | 5 (12) | |||||||||||||||||||||||||||
| Fair (Fr) | 2 (5) | 4 (10) | |||||||||||||||||||||||||||
| Poor (Pr) | 3 (7) | 29 (73) | |||||||||||||||||||||||||||
| Effective (E + G: excellent + good) | 35 (88) | 7 (17) | |||||||||||||||||||||||||||
| Efficacy to pretreatment wax | |||||||||||||||||||||||||||||
| No. | E + G | Fr | Pr | E + G (%) | No. | E + G | Fr | Pr | E + G (%) | p-value | |||||||||||||||||||
| Impacted | 19 | 16 | 1 | 2 | 84 | 18 | 2 | 0 | 16 | 11 | Not reported | ||||||||||||||||||
| Hard | 16 | 14 | 1 | 1 | 88 | 16 | 3 | 2 | 11 | 19 | |||||||||||||||||||
| Loose | 1 | 1 | 0 | 0 | 100 | 3 | 1 | 0 | 2 | 33 | |||||||||||||||||||
| Soft | 4 | 4 | 0 | 0 | 100 | 3 | 1 | 2 | 0 | 33 | |||||||||||||||||||
| Complete obstruction | 36 | 31 | 2 | 3 | 86 | 32 | 4 | 3 | 25 | 13 | |||||||||||||||||||
| Partial obstruction | 4 | 4 | 0 | 0 | 100 | 8 | 3 | 1 | 4 | 38 | |||||||||||||||||||
| Delayed follow-up – adult population – softeners alone as primary objective | |||||||||||||||||||||||||||||
| Dummer and colleagues, 199244 | |||||||||||||||||||||||||||||
| Audax (n = 27, ears n = 54) | Cerumol (n = 23, ears n = 46) | p-value | |||||||||||||||||||||||||||
| Amount of wax (n, ears) | |||||||||||||||||||||||||||||
| Increased | 0 | 0 | Not reported across groups | ||||||||||||||||||||||||||
| No change | 24 (44%) | 22 (48%) | |||||||||||||||||||||||||||
| Decreased | 28 (52%) | 24 (52%) | |||||||||||||||||||||||||||
| Missing data | 2 (4%) | 0 | |||||||||||||||||||||||||||
| Colour of wax (n, ears) | |||||||||||||||||||||||||||||
| Darkened | 0 | 0 | States ns, but p-value not reported | ||||||||||||||||||||||||||
| No change | 10 | 9 | |||||||||||||||||||||||||||
| Lightened | 42 | 36 | |||||||||||||||||||||||||||
| Missing data | 2 | 1 | |||||||||||||||||||||||||||
| Consistency (n, ears) | |||||||||||||||||||||||||||||
| Hardened | 0 | 0 | States ns, but p-value not reported | ||||||||||||||||||||||||||
| No change | 6 | 5 | |||||||||||||||||||||||||||
| Softened | 46 | 40 | |||||||||||||||||||||||||||
| Missing data | 2 | 1 | |||||||||||||||||||||||||||
| Objective hearing (n, ears) | |||||||||||||||||||||||||||||
| Improved | 7 (13%) | 2 (4%) | States ns, but p-value not reported | ||||||||||||||||||||||||||
| No change | 45 (83%) | 44 (96%) | |||||||||||||||||||||||||||
| Worsened | 0 | 0 | |||||||||||||||||||||||||||
| Missing data | 2 (4%) | 0 | |||||||||||||||||||||||||||
| Overall assessment | |||||||||||||||||||||||||||||
| Investigator rated ‘effective’ (n, pts) | 36 | 22 | Unclear if tested | ||||||||||||||||||||||||||
| Overall assessment | |||||||||||||||||||||||||||||
| Participant rated ‘effective’ (n, pts) | 25 (93%) | 23 (100%) | States ns, but p-value not reported | ||||||||||||||||||||||||||
| Delayed follow-up – mixed populations – softeners alone as primary objective | |||||||||||||||||||||||||||||
| Jaffe and Grimshaw, 197850 | |||||||||||||||||||||||||||||
| Otocerol (n = 53) | Cerumol (n = 53) | p-value | |||||||||||||||||||||||||||
| Syringing needed | Yes: 39, no 14 | Yes: 47, no 6 | N requiring syringing p < 0.05 | ||||||||||||||||||||||||||
| Syringing needed by grade at entry | |||||||||||||||||||||||||||||
| Mild | Yes 6, no 7 | Yes 6, no 4 | Not reported | ||||||||||||||||||||||||||
| Moderate | Yes 19, no 7 | Yes 30, no 2 | |||||||||||||||||||||||||||
| Severe | Yes 14, no 0 | Yes 11, no 0 | |||||||||||||||||||||||||||
| Doctor reported ease of syringing | |||||||||||||||||||||||||||||
| 30/39 (76.9%) | 34/47 (72.3%) | χ2 = 0.25, ns | |||||||||||||||||||||||||||
| Ease of syringing by grade at entry | |||||||||||||||||||||||||||||
| Mild | Easy 5, not easy 1 | Easy 5, not easy 1 | Not reported | ||||||||||||||||||||||||||
| Moderate | Easy 14, not easy 5 | Easy 25, not easy 5 | |||||||||||||||||||||||||||
| Severe | Easy 11, not easy 3 | Easy 4, not easy 7 | |||||||||||||||||||||||||||
| Overall judgement effectiveness | |||||||||||||||||||||||||||||
| Success | 38 | 33 | ns | ||||||||||||||||||||||||||
| Failure | 10 | 13 | |||||||||||||||||||||||||||
| Partial | 5 | 7 | |||||||||||||||||||||||||||
| Fahmy and Whitefield, 198254 (see Table 10 for study 1 and 2 results in secondary care) | |||||||||||||||||||||||||||||
| Exterol (n = 157) | Cerumol (n = 129) | p-value | |||||||||||||||||||||||||||
| Initially hard | Initially soft | Initially hard | Initially soft | ||||||||||||||||||||||||||
| Wax dispersed without syringing | 45 | 19 | 12 | 15 | p < 0.001 | ||||||||||||||||||||||||
| Syringed easily | 60 | 22 | 52 | 14 | |||||||||||||||||||||||||
| Syringed with difficulty | 9 | 2 | 33 | 3 | |||||||||||||||||||||||||
| Carr and Smith, 200152 | |||||||||||||||||||||||||||||
| 10% sodium bicarbonate (n = 35) | 2.5% acetic acid (n = 34) | p-value | |||||||||||||||||||||||||||
| Mean change degree of cerumen | 0.66 | 0.78 | States ns but p-value not reported | ||||||||||||||||||||||||||
| Mean maximum change | 1.00 | 1.00 | |||||||||||||||||||||||||||
| Delayed follow-up – adult populations – softeners and irrigation as primary objective | |||||||||||||||||||||||||||||
| Lyndon and colleagues, 199245 | |||||||||||||||||||||||||||||
| Audax (n = 19, 38 ears) | Earex (n = 17, 34 ears) | p-value | |||||||||||||||||||||||||||
| Degree of impaction | |||||||||||||||||||||||||||||
| None | 10 | 6 | States ns but p-value not reported | ||||||||||||||||||||||||||
| Mild | 17 | 11 | |||||||||||||||||||||||||||
| Moderate (Mod) | 9 | 12 | |||||||||||||||||||||||||||
| Severe (Sev) | 2 | 3 | |||||||||||||||||||||||||||
| Missing data | 0 | 2 | |||||||||||||||||||||||||||
| Post-treatment | Post-treatment | p-value | |||||||||||||||||||||||||||
| None | Mild | Mod | Sev | None | Mild | Mod | Sev | ||||||||||||||||||||||
| Degree of impaction at end point by pretreatment score | |||||||||||||||||||||||||||||
| None | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | States ns but p-value not reported | ||||||||||||||||||||
| Mild | 3 | 4 | 0 | 0 | 2 | 4 | 0 | 0 | |||||||||||||||||||||
| Moderate | 6 | 12 | 8 | 0 | 3 | 7 | 11 | 1 | |||||||||||||||||||||
| Severe | 0 | 0 | 1 | 2 | 0 | 0 | 1 | 2 | |||||||||||||||||||||
| Audax (n = 38 ears) | Earex (n = 34 ears) | p-value | |||||||||||||||||||||||||||
| Ease of syringing, ears | |||||||||||||||||||||||||||||
| Not required | 15 | 7 | p < 0.005 for score of ‘not required’ or ‘easy’ | ||||||||||||||||||||||||||
| Easy | 22 | 12 | |||||||||||||||||||||||||||
| Difficult | 1 | 11 | |||||||||||||||||||||||||||
| Impossible | 0 | 0 | |||||||||||||||||||||||||||
| Missing data | 0 | 4 | |||||||||||||||||||||||||||
| Audax (n = 19) | Earex (n = 17) | ||||||||||||||||||||||||||||
| Global impression of efficacy, investigator* n = pts | |||||||||||||||||||||||||||||
| Completely effective | 8 | 5 | |||||||||||||||||||||||||||
| Very effective | 9 | 1 | |||||||||||||||||||||||||||
| Fairly effective | 2 | 7 | |||||||||||||||||||||||||||
| Not effective | 0 | 3 | |||||||||||||||||||||||||||
| Missing data | 0 | 1 | |||||||||||||||||||||||||||
| Total | 19 | 17 | |||||||||||||||||||||||||||
| Global impression of efficacy, participant* n = pts | |||||||||||||||||||||||||||||
| Completely effective | 8 | 5 | |||||||||||||||||||||||||||
| Very effective | 9 | 2 | |||||||||||||||||||||||||||
| Fairly effective | 2 | 7 | |||||||||||||||||||||||||||
| Not effective | 0 | 2 | |||||||||||||||||||||||||||
| Missing data | 0 | 1 | |||||||||||||||||||||||||||
| Total | 19 | 17 | |||||||||||||||||||||||||||
| *Investigators’ and participants’ own global impression of efficacy merged categories (not effective and fairly effective) were significantly in favour of Audax (p < 0.01). | |||||||||||||||||||||||||||||
| Burgess, 196643 | |||||||||||||||||||||||||||||
| Dioctyl-medo (n = 33 ears) | Maize oil (n = 41 ears) | p-value | |||||||||||||||||||||||||||
| Average water used | |||||||||||||||||||||||||||||
| 111 ml | 81 ml | Not reported | |||||||||||||||||||||||||||
| Ease of removal, N ears | |||||||||||||||||||||||||||||
| Easy | 19 | 33 | Not reported | ||||||||||||||||||||||||||
| Difficult | 11 | 5 | |||||||||||||||||||||||||||
| Partial | 3 | 3 | |||||||||||||||||||||||||||
| Failed | 1 | 0 | |||||||||||||||||||||||||||
| Character wax, N ears | |||||||||||||||||||||||||||||
| Liquid | 1 | 4 | Not reported | ||||||||||||||||||||||||||
| Shredded | 5 | 6 | |||||||||||||||||||||||||||
| Lumps | 27 | 31 | |||||||||||||||||||||||||||
| Delayed follow-up – mixed populations – softeners and irrigation as primary objective | |||||||||||||||||||||||||||||
| Eekhof and colleagues, 200153 | |||||||||||||||||||||||||||||
| Water (n = 22) | Control ‘oil’ (n = 20) | p-value | |||||||||||||||||||||||||||
| Mean number syringing attempts | |||||||||||||||||||||||||||||
| 3.0 (95% CI 2.4 to 3.6) | 2.4 (95% CI 1.7 to 3.1) | Difference 0.6 (95% CI –0.3 to 1.5); p = 0.18 | |||||||||||||||||||||||||||
| Mean number syringing attempts per participant by number earwax removed | |||||||||||||||||||||||||||||
| Number removed | Number removed | p-value | |||||||||||||||||||||||||||
| 1 | 4 | 6 | Not reported to be tested | ||||||||||||||||||||||||||
| 1.5 | 1 | 2 | |||||||||||||||||||||||||||
| 2 | 2 | 5 | |||||||||||||||||||||||||||
| 2.5 | 3 | 1 | |||||||||||||||||||||||||||
| 3 | 2 | 2 | |||||||||||||||||||||||||||
| 3.5 | 4 | 0 | |||||||||||||||||||||||||||
| 4 | 2 | 0 | |||||||||||||||||||||||||||
| 5 | 3 | 4 | |||||||||||||||||||||||||||
| 6 | 1 | 0 | |||||||||||||||||||||||||||
Softeners only studies
Adults
No studies were identified assessing an adult population comparing the use of softeners alone, with an immediate participant follow-up after treatment.
Children
Two studies46,47 with immediate follow-up in children aimed to assess the use of a softening agent alone and fall under the softener-only category. After initial assessment of the outcome from the use of the softening agent both of these studies subsequently used an irrigation technique and reassessed outcomes. Both studies compared DS, TP and saline.
Meehan and colleagues46 reported the number of children with complete, partial or no occlusion after DS, TP or saline alone in attendees at an emergency care department. Thirteen per cent of children were rated as clear in the DS treatment group; 41% were clear in the TP treatment group and 13% in the saline treatment group. The corresponding proportions with complete obstruction at baseline for the three groups, respectively, were 73%, 65% and 56%, with 27%, 35% and 44%, respectively, having partial obstruction of the TM. While it would appear that more children in the TP group had clear TMs after treatment, no statistical significance testing was reported of the difference between effects of the different softening agents. Thirty-three per cent, 29% and 31% of participants, respectively, for DS, TP and saline were still completely occluded, and 53%, 29% and 56% partially occluded for the three groups, respectively. Of these participants, irrigation was then used with varying results (Table 6). In around 50% of participants in all three groups the TM remained occluded or partially occluded after two irrigations.
Whatley and colleagues47 also reported the number and proportion of children with clear TM after use of the treatments. Twelve per cent of participants in the DS treatment group, 13% in the TP and 4% in the saline treatment group were reported as clear after softening treatment. The corresponding proportions of participants with complete occlusion of the TM at baseline for the three groups, respectively, were 91%, 80% and 79%. Similarly to the Meehan and colleagues study,46 some 32–57% of participants remained occluded after two irrigations. This study reported statistical testing only for the proportions clear after the second irrigation, which was not statistically significant.
Meehan and colleagues46 and Whatley and colleagues47 did not report this outcome.
Meehan and colleagues46 and Whatley and colleagues47 did not report this outcome.
Mixed or unknown populations
One study49 was identified assessing a mixed population with the a priori intention of comparing softeners alone, coupled with an immediate participant follow-up after treatment. This study compared DS with TP.
Singer and colleagues49 assessed the number of ears with complete visualisation after DS or TP in a mixed population of adults and children. The TM was completely visualised in 19% of DS and 9% of TP treated participants, respectively; however, the difference was not statistically significant [% difference DS–TP 9.8; 95% confidence interval (CI) –8.8 to 28.5]. At baseline 78% of participants in the DS arm and 78% of participants in the TP arm had completely obstructed TMs. Complete TM visualisation after treatment, with or without subsequent irrigation with normal saline solution, was statistically significantly greater for DS than TP [82% versus 35%, respectively; difference 46.7% (95% CI 22.3–71.1%)]. Results were also presented for numbers with a clear TM after a first and then second irrigation. This showed that a higher proportion of participants in the TP arm (79%) than the DS arm (42%) were still not completely clear after two irrigations. However, this was not tested for statistical significance between the two groups.
Singer and colleagues49 did not report this outcome.
Singer and colleagues49 did not report this outcome.
Singer and colleagues49 did not report this outcome.
Singer and colleagues49 found no cases of pain, vertigo, nausea or hearing loss.
Softeners and irrigation studies
Adults
There were two studies where the intention was to compare different softeners, which were then followed by syringing in an adult population, with an immediate participant follow-up after treatment. 41,42 The General Practitioner Research Group41 compared dioctyl-medo with an oil-based control, and Pavlidis and Pickering42 compared use of water prior to syringing (wet syringing) to no water prior to syringing (dry syringing). Neither of these studies reported on the baseline degree of occlusion in their populations.
Neither the General Practitioner Research Group41 or Pavlidis and Pickering42 reported on these outcomes.
The General Practitioner Research Group41 study reported on the number (or fractions) of syringefuls required to remove wax after using dioctyl-medo drops or an oil-based control. The mean amount of water required for the dioctyl-medo treatment group was 122 ml compared with 165.5 ml for the oil-based control group. The statistical significance of the difference between the two groups was, however, not tested. The study does report that there was an outlier for the control group and that removal of the outlier resulted in there being little difference between the treatment groups. Syringe capacity varied – 57, 85 and 112 ml – and the authors state that an exact analysis in relation to the number of syringefuls used, and in respect of each syringe size, was made. The study also categorised ease of wax removal (easy or difficult, partial or failed), with wax removal classed as easy for 70% of participants receiving dioctyl-medo and 57% of control participants receiving oil-based control treatment. The study did not report any statistical significance testing on these data. No baseline values of the degree of earwax were reported.
Pavlidis and Pickering42 reported on the mean number of syringing attempts for those in the ‘wet’ and ‘dry’ syringing groups. Wet syringing needed 7.5 attempts (mean), while dry syringing needed 25.4. This was seen to be statistically significantly different (p = 0.043). Pavlidis and Pickering42 suggest that the number of syringing attempts are unusually high due to the small volume of the syringe used (25 ml), which is smaller than syringes used by GPs (> 120 ml). No baseline values of the degree of earwax were reported
The General Practitioner Research Group41 reported that 92% of the dioctyl-medo group and 86% of the oil-based control group found the procedure tolerable. Pavlidis and Pickering42 did not report on this outcome.
Neither the General Practitioner Research Group41 nor Pavlidis and Pickering42 reported on these outcomes.
The General Practitioner Research Group41 found no AEs in 91% of the dioctyl-medo group and 89% of the oil-based control group. AEs were entirely related to the procedure of syringing, but no further details about the nature of these are reported. Pavlidis and Pickering42 reported transient dizziness for one participant only, after having both ears syringed, with all TM being intact at the end of syringing.
Children
No studies were identified assessing children and comparing softeners followed by syringing, with an immediate participant follow-up after treatment.
Mixed or unknown populations
Two studies48,51 were included that assessed the use of a softening agent and a syringing agent in mixed populations over a delayed period of follow-up. The General Practitioner Research Group48 study compared Waxsol with Cerumol, and the Amjad and Scheer51 study compared TP with carbamide peroxide.
Amjad and Scheer51 assessed degree of wax removal using TP and carbamide peroxide in an unspecified population. Excellent removal was reported for 68% of TP participants and 5% of carbamide peroxide participants, with good removal in 20% and 12% of participants, respectively. Effective removal (combining excellent and good) was reported for 88% of the TP-treated participants and 17% in the carbamide peroxide-treated participants. At baseline, 90% of participants in the TP group and 80% of participants in the carbamide peroxide group had complete obstruction of the TM, with 10% and 20% having partial obstruction for the two groups, respectively. The study also reports degree of wax removal as a function of pretreatment wax. This showed that in the TP group effective (rated as excellent or good) wax removal was achieved in 100% of participants with soft or loose pretreatment wax, whereas the corresponding value in the carbamide peroxide group was 33%. In those with hard or impacted wax at baseline some 88% and 84% (for the two categories respectively) in the TP group had ‘effective’ clearance. The corresponding rates in the carbamide peroxide group were 19% for those with hard wax pretreatment and 11% for those with impacted wax pretreatment. The study did not report any statistical significance testing of the data (Table 6).
The General Practitioner Research Group48 assessed the volume of water needed for syringing after the use of Waxsol and Cerumol in a population of adults and children. The mean volume per participant for the Waxsol treatment group was 156 ml [5.5 fluid ounces (fl oz)] per participant and for the Cerumol treatment group was 240 ml (8.4 fl oz). Ease of wax removal (easy or difficult removal, partly or failed removal) was also assessed by this study, with 83% of participants in the Waxsol treatment group and 80% in the Cerumol treatment group judged to have easily removed earwax. The study did not report if this outcome was tested for statistical significance. No baseline degree of occlusion were reported in the General Practitioner Research Group48 study. Amjad and Scheer51 did not report on this outcome.
Eighty-nine per cent of participants in the Waxsol treatment group and 95% in the Cerumol treatment group were reported to have found the treatment tolerable in the General Practitioner Research Group study. 48 No statistical analysis of the differences in this data was provided, however. Amjad and Scheer51 did not report on this outcome.
The General Practitioner Research Group48 and Amjad and Scheer51 did not report on this outcome.
Seven per cent of participants in the Waxsol and 5% in the Cerumol treatment group reported AEs in the General Practitioner Research Group study, but no details about the nature of these events or statistical testing of results are given. 48 There were no reported cases of AEs in the Amjad and Scheer study. 51
Results of studies in primary care with delayed follow-up
The results of the studies in primary care are reported in Table 6.
Softeners only studies
Adults
One study44 in adults, which had the initial objective to use softeners alone to clear the earwax, was included. Dummer and colleagues44 compared Audax and Cerumol and delayed participant follow-up for 4 days.
Dummer and colleagues44 measured the number of ears with post-treatment changes in the amount of wax present (increased, no change and decreased). Fifty-two per cent of ears for both treatments (Audax 28 ears, Cerumol 24 ears) were judged to have a reduced amount of wax. In both groups there were more than 40% with no change in the amount of wax present after treatment. No statistical analysis of the differences across the groups appeared to have been undertaken on these outcomes, however, and no baseline values of the degree of wax present were reported. Post-treatment performance-based hearing and change in performance-based hearing were assessed through a variety of tests. In the Audax group 13% of ears demonstrated improved hearing, whereas in the Cerumol group the figure was only 4%. There was no change in objective hearing in 83% of ears in the Audax group and 96% of ears in the Cerumol group. The paper states that there were no statistically significant differences between the groups; however a p-value was not reported. A global investigator impression of efficacy for the treatments was also undertaken; however, there appears to be a reporting error in terms of the number of participants in the groups and therefore care should be taken in the interpretation of this outcome. It is also unclear how this outcome was assessed.
Dummer and colleagues44 did not report on this outcome.
In a global impression assessment of the efficacy of the treatments, Dummer and colleagues44 found that 93% of participants rated the treatment as effective in the Audax treatment group and 100% rated it as effective in the Cerumol treatment group. The authors reported no statistically significant difference between the treatment groups, but no p-value was given. It was also unclear how this assessment was measured.
Dummer and colleagues44 did not report on this outcome.
In the study by Dummer and colleagues,44 a slight irritation to the ear was reported by two participants in the Audax treatment group, while in the Cerumol treatment group one participant experienced a slight itch and another a buzzing noise shortly after use. No further details of these events were reported.
Children
No studies were identified assessing children in a comparison of softeners alone, with a delayed participant follow-up.
Mixed or unknown populations
Three studies50,52,54 with mixed or unknown populations were included. All had a delayed follow-up and an intention to assess outcomes after softeners only. Carr and Smith52 compared a 10% solution of aqueous sodium bicarbonate with a 2.5% solution of acetic acid. The study had a 14-day follow-up. Fahmy and Whitefield54 compared Exterol and Cerumol, and participants were followed-up 1 week later. This study was one of three and, as previously mentioned, study one and two are covered under Studies in secondary care settings, below. Jaffe and Grimshaw50 assessed Otocerol and Cerumol with a revisit after three instillations of the interventions.
Carr and Smith52 measured the change in the degree of earwax, based on a scale of 1–4, where higher scores relate to higher degrees of occlusion. The mean change in the degree of cerumen was reported to be 0.66 in the 10% sodium bicarbonate group and 0.78 in the 2.5% acetic acid group. The study reports that the difference was not statistically significant, but no p-value was provided. No baseline values of the degree of occlusion were presented in the study.
Fahmy and Whitefield54 found the number of ears not requiring syringing was statistically significantly greater after treatment with Exterol (p < 0.001), with wax dispersal occurring in 41% of ears in the Exterol treatment group and 21% of ears in the Cerumol treatment group.
Jaffe and Grimshaw50 did not report on these outcomes.
After treatment, Fahmy and Whitefield54 found that ears were syringed easily in 52% of ears in the Exterol treatment group and 51% in the Cerumol treatment group. No data analysis of the differences between groups was presented. Exterol was statistically significantly superior to Cerumol, when the number of ears not requiring syringing (above) was combined with the number syringed easily (p < 0.001). Seven per cent of ears in the Exterol treatment group and 28% of ears in the Cerumol treatment group remained difficult to syringe after treatment. At baseline, 97 ears in the Exterol group and 86 ears in the Cerumol group were reported to be totally or subtotally occluded with earwax. The remaining ears (60 Exterol, 43 Cerumol) were rated as partially occluded at baseline. There are no data reporting post-treatment outcome in relation to pretreatment outcome, however.
Jaffe and Grimshaw50 wanted to establish if, after treatment with Otocerol or Cerumol, syringing was required. There was a statistically significant difference in favour of Otocerol, only 73% of Otocerol participants needed syringing compared with 89% of Cerumol participants (p < 0.05). At baseline the grade of impaction was assessed as mild, moderate or severe in 13, 26 and 14 participants in the Otocerol group, respectively, and in 10, 32 and 11 participants in the Cerumol group, respectively. Of the 26% of participants in the Otocerol group that did not require syringing after treatment, all of these were rated as mild or moderate at the start of the study. However, 11% of participants categorised as mild at baseline and 36% of participants categorised as moderate at baseline did require syringing after treatment with Otocerol. All of the participants in the Otocerol group with severe impaction at baseline (26%) required syringing post-treatment. In the Cerumol group a similar pattern emerged. Of the 11% of participants that did not require syringing after treatment, all had been rated as mild or moderate at the start of the study. However, 11% and 57% of participants rated as mild or moderate occlusion at baseline did require syringing after treatment. Finally, all of the 21% of participants with severe impaction at baseline required syringing post-treatment. No statistical analysis of this data was reported, however. Where syringing was required, the clinician’s rating of the ease of syringing was also reported (76.9% Otocerol versus 72.3% Cerumol were ‘easy to syringe’). This was not statistically significantly different between the treatment groups.
In the Jaffe and Grimshaw study,50 an overall judgement of effectiveness was categorised into success (defined as those in whom syringing was not required or where it was easy and no reports of side effects), failure (defined as those in whom syringing was difficult with or without side effects) and partial (defined as those who reported side effects, but in whom the doctor found it easy to syringe and had no reservations about using the product again). In the Otocerol group 72% were judged to be successes, 19% were judged to be failures and 9% were classed as partial successes. In the Cerumol group these figures were 62%, 25% and 13% for success, failure and partial categories, respectively. The overall judgement of effectiveness between the treatment groups was not statistically significant.
Carr and Smith52 did not report on this outcome.
These outcomes were not reported by Carr and Smith,52 Jaffe and Grimshaw50 or Fahmy and Whitefield. 54
These outcomes were not reported by Carr and Smith,52 Jaffe and Grimshaw50 or Fahmy and Whitefield. 54
Adverse events were divided into pain (0% Otocerol; 2% Cerumol) and irritation (6% Otocerol, 15% Cerumol) on application, and pain (2% Otocerol, 2% Cerumol) and irritation (8% Otocerol, 8% Cerumol) during use in the Jaffe and Grimshaw study. 50 There was one case (2%) of slight giddiness (no further details) in the Otocerol group. Thirteen per cent of participants suffered AEs in the Otocerol treatment group and 19% in the Cerumol treatment group, but one case included under Cerumol AEs was related to the unpleasant smell of the treatment. 50 The most common AEs were irritation on application, pain during use and irritation during use. The result was reported as statistically non-significant, but no p-value was given. Carr and Smith52 reported no cases of otitis externa or external auditory canal dermatitis for their treatments groups, while Fahmy and Whitefield54 did not report AEs.
Softeners and irrigation studies
Adults
There were two studies43,45 in which the intention was to compare different softeners, which were then followed by syringing in an adult population, with a delay in participant follow-up after treatment. Lyndon and colleagues study45 compared self-administered Audax and Earex followed by syringing, with a delayed follow-up of 5 days. Burgess43 compared dioctyl-medo and maize oil followed by syringing, with a delayed follow-up of 2–7 days.
Lyndon and colleagues’ study45 measured the degree of impaction from none to severe. After treatment, 26% of ears in the Audax treatment group and 18% of ears in the Earex treatment group had no wax impaction, but no p-value was reported. At baseline, 5% of ears in the Audax treatment group and 3% of ears in the Earex group had no impaction. Eighteen per cent, 68% and 8% of ears in the Audax group were rated as having mild, moderate and severe impaction at baseline, respectively. In the Earex group, these figures were 24%, 65% and 9%, respectively. Analysis of pre- and post-treatment impaction scores between the groups was reported as non-significant, with a trend towards less impaction for the Audax treatment; however, no p-value was given. Investigators also completed a global impression of efficacy rating (completely effective, very effective, fairly effective and not effective). This was statistically significant in favour of Audax (p < 0.01) for the merged categories of ‘not effective’ and ‘fairly effective’, but it was unclear whether this was for the investigator rating alone, participant rating alone (see below) or a combination of the two.
Burgess43 measured ease of removal and average water used. The diocytl-medo treatment group used on average 111 ml and the maize oil treatment group used 81 ml for syringing the wax. Ease of wax removal was measured for the number of ears, categorised as easy (58% dioctyl-medo, 80% maize oil) or difficult (33% dioctyl-medo, 12% maize oil), partial (9% diocytl-medo,7% maize oil) or failed. The only reported case of failure was for the dioctyl-medo group. This study did not report any statistical significance testing on the data. Burgess43 only reported baseline characteristics for all participants combined, where the study reports that 80% of ears were completely occluded at baseline. Consequently, there were no data reporting post-treatment outcome in relation to pretreatment outcome. Lyndon and colleagues45 also measured ease of syringing and found a statistically significant difference in favour of Audax, in that syringing was more frequently scored as ‘not required’ or ‘easy’ (97% ears in the Audax group, 56% ears in the Earex group, p < 0.005).
In the study by Lyndon and colleagues,45 participants completed a global impression of efficacy rating. Forty-two per cent of participants in the Audax treatment group and 29% of participants in the Earex treatment group rated the treatment as completely effective. The authors state that there was a statistically significant difference in favour of Audax (p < 0.01) for the ‘not effective’ and ‘fairly effective’ categories merged together, but it was unclear from the report whether this included the investigator rating alone (as above), participant rating alone or a combination. Burgess43 did not report on this outcome.
Children
There were no studies assessing children in a comparison of softeners followed by syringing, with a delayed participant follow-up.
Mixed or unknown populations
One study53 assessed an unspecified population (although reported a mean age of 51 years for all participants). Warm water as a softener was compared with oil, followed by syringing for both treatment groups. The study had an immediate follow-up for the warm water intervention, but a delayed follow-up of 3 days for the control group using oil.
Eekhof and colleagues53 did not report on this outcome.
Eekhof and colleagues53 reported the mean number of syringing attempts between the water and oil-control groups [water: 3.0 (95% CI 2.4 to 3.6), oil-control: 2.4 (95% CI 1.7 to 3.1)]. As the difference between means was not statistically significant (p = 0.18), warm water was reported to be as effective as oil as a softening agent. However, the study was not powered to test for statistical equivalence and so caution is required in interpreting this outcome. No baseline degree of earwax was reported.
Eekhof and colleagues53 did not report on this outcome.
Eekhof and colleagues53 did not report on this outcome.
Eekhof and colleagues53 did not report on this outcome.
Studies in secondary care settings
Eight studies undertaken in secondary care settings were identified (Table 7): seven were RCTs and one was a CCT. Three RCTs55,57,59 followed participants up immediately after interventions. One57 was a three-arm trial in children, of hydrogen peroxide, mineral oil or TP; one other55 was a three-arm trial in adults, of chlorobutanol, sodium carbonate and saline. The third study59 compared TP with olive oil; the participant group was not described in this study. Three included studies had a longer delay in their follow-up. Keane and colleagues’4 RCT, which appears to be in elderly adults, was a four-arm trial of Cerumol, sodium bicarbonate, sterile water and no treatment (control). The interventions were administered for 5 days, after which the participants were reassessed. Fraser60 assessed sodium bicarbonate, olive oil, Cerumol, Waxsol, TP and dioctyl to a within-participant control (one ear test, one ear control) in elderly participants over a period of 3 days follow-up. The third study, a CCT by Fahmy and Whitefield,54 included three separate studies, one of which was in participants from primary care and was discussed previously (Chapter 3, Studies in secondary care settings). Of the other two studies, one compared Exterol with glycerol and the other Exterol with Cerumol. The target population for these studies was not clear in the publication, but the ear drops were given over a one-week period before follow-up. In addition to the studies comparing the use of different softening agents, two other studies were included that either compared two de-waxing techniques56 or the application of a skin oil with no treatment. 58 In the first of these RCTs adults in an otolaryngology clinic requiring removal of earwax were randomised to endoscopic otoendoscopic de-waxing or microscopic de-waxing. In the second RCT, participants had their earwax removed and were then randomised to either Ceridal lipolotion skin oil or no treatment to assess the recurrence of cerumen. This study was undertaken in adults and children with learning difficulties and follow-up was for 12 months.
| Study | Interventions | Participants | Outcomes |
|---|---|---|---|
| Immediate follow-up | |||
|
Author: Caballero and colleagues, 2005 55 Country: Spain Number of centres: One Design: RCT Setting: Secondary care Follow-up: Immediate |
|
Target population: Adults with total cerumen obstruction Baseline characteristics: Age: 19–78 years Gender: Not reported |
Primary outcomes: Proportion of TM completely visualised |
|
Author: Dubow, 1959 57 Country: USA Number of centres: At least two Design: RCT Setting: Secondary care Follow-up: Immediate |
|
Target population: Children with at least one completely cerumen-occluded ear canal, disregarding other disorders, presenting in a paediatric clinic and in ‘office practice’ Baseline characteristics: Age range, years: 3–12 overall (no individual group details) Gender: Not reported |
Wax clearance |
|
Author: Chaput De Saintonge and Johnstone, 1973 59 Country: UK Number of centres: One Design: RCT Setting: Secondary care Follow-up: Immediate |
|
Target population: any patient with impacted wax attending outpatients Baseline characteristics: Age: Not reported Gender: Not reported |
Total volume of water Amount of wax removed |
| Delayed follow-up | |||
|
Author: Keane and colleagues, 1995 4 Country: Ireland Number of centres: One Design: RCT Setting: Secondary care Follow-up: 5-day trial |
|
Target population: Hospitalised patient with one or both ears impacted Baseline characteristics: Age: not reported Gender: not reported |
Primary outcomes: Percentage clearance and number of ears (clearance is explained by the ‘natural expulsion of earwax’) Secondary outcomes: AEs |
|
Author: Fahmy and Whitefield, 1982 54 Country: UK Number of centres: One Design: CCT Setting: Studies 1 and 2 in secondary care Follow-up: 1 week |
Study 1: n = 40 (80 ears)
|
Target population: patients presenting with earwax Baseline characteristics: Age: Not reported Gender: Not reported |
Wax occlusion Wax consistency Ease of syringing |
|
Author: Fraser, 1970 60 Country: UK Number of centres: Six hospitals Design: RCT Setting: Secondary care Follow-up: At least 3 days |
|
Target population: Geriatric attendees at hospitals, with bilateral hard earwax that occludes the external auditory meatus in both ears Baseline characteristics: Age: Not reported Gender: Not reported |
Ease of syringing Frequency of syringing Appearance of wax removed |
| De-waxing techniques | |||
|
Author: Pothier and colleagues, 2006 56 Country: UK Number of centres: One Design: RCT Setting: Otolaryngology outpatient clinic Follow-up: Treated and assessed on initial visit, unless cerumenolytics used and then unspecified delay |
|
Target population: Patients requiring removal of earwax from the ear canal to allow full view of TM, with a history of earwax Baseline characteristics: Age, mean years (SD, range):Gender M/F: |
Levels of pain and discomfort for patient Ease of de-waxing Time taken to de-wax |
| Prevention of recurrence after removal earwax | |||
|
Author: Saloranta and colleagues, 2005 58 Country: Finland Number of centres: Two Design: RCT Setting: Secondary care and community home for people with learning difficulties Follow-up: 12 months (visits also at 3 months and at a point of recurrence) |
|
Target population: Patients with learning difficulties. Had to have a history of impacted cerumen with symptoms like impaired hearing or sensation of blocked ear canal more often than once per year, and earwax completely obstructing the ear canal at the point of inclusion Baseline characteristics (learning difficulties):Age, mean years (range):Gender M/F: |
Recurrence of cerumen impaction AEs |
The quality of reporting and methodology of the included studies was generally poor (see Tables 8 and 9). Of the seven RCTs, none of the studies was assessed as having an adequate generation of the randomisation sequence. In one RCT the generation of the randomisation schedule was judged to be partially met,56 in three this was judged to be inadequate,57,58,60 and in the remainder it was not possible to judge due to a lack of information. 4,55,59 Only one RCT adequately met the criteria for concealment of allocation. 59 Therefore, most of these studies may be subject to selection bias, with the allocation sequence open to possible manipulation. Double-blinding (participant and caregiver) was assessed as being adequate only in one study. 59 While double-blinding may have been difficult for some interventions, blinding of the outcome assessors could have been undertaken; however, there were no studies that were assessed as adequately blinding the outcome assessors. This factor is particularly important when subjective outcome measures are used and therefore this may mean the studies are subject to measurement bias. Many studies did not present baseline characteristics of the participants within their intervention arms so it is unclear how similar the groups were at baseline. The description of withdrawals were assessed as being adequate in four studies,4,56–58 but only one of these studies also described an adequate ITT analysis. 56 Overall these studies are at a high risk of bias, which may affect the direction of any effects shown, and care should be taken in the interpretation of the results.
| Study | Randomisation | Concealment of allocation | Baseline characteristics | Eligibility | Blinding of assessors | Care-provider blinding | Patient blinding | Reporting outcomes | ITT | Withdrawals explained |
|---|---|---|---|---|---|---|---|---|---|---|
| Caballero, 200555 | Un | Un | Un | Par | Un | Un | Un | In | In | In |
| Dubow, 195957 | In | Un | Un | Ad | Un | Un | Un | In | In | Ad |
| Chaput de Saintonge, 197359 | Un | Ad | Un | In | Un | Ad | Ad | In | In | In |
| Keane, 19954 | Un | Un | Un | Un | Un | Un | Un | In | In | Ad |
| Fraser, 197060 | In | In | Un | Un | In | In | In | In | In | In |
| Pothier, 200656 | Par | In | Rep | Ad | In | In | In | In | Ad | Ad |
| Saloranta, 200558 | In | Un | Un | Ad | Un | Un | Un | In | In | Ad |
| Study | Baseline characteristics | Eligibility | Blinding of assessors | Reporting outcomes | ITT | Withdrawals explained | Representativeness |
|---|---|---|---|---|---|---|---|
| Fahmy, 198254 | Un | Par | Un | Par | Un | Un | Un |
The CCT54 was similarly judged to be only of low quality, the baseline characteristics between the study arms were unknown, the blinding of outcome assessors was unclear, and the report does not refer to withdrawals and dropouts or any ITT analysis. The results of this study should also be interpreted cautiously due to the high risk of bias.
Results of studies in secondary care with immediate follow-up
The results of studies in secondary care are reported in Table 10.
| Immediate follow-up – adult population – softeners and irrigation as primary objective | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Caballero and colleagues, 200555 | ||||||||||||||||
| Proportion of TM completely visualised | ||||||||||||||||
| Chlorobutanol (n = 32) | Sodium carbonate (n = 29) | Saline (n = 28) | p-value | |||||||||||||
| 21/32 (65.6%) | 16/29 (55.2%) | 12/28 (42.9%) | p = 0.209 | |||||||||||||
| Immediate follow-up – child population – softeners and irrigation as primary objective | ||||||||||||||||
| Dubow, 195957 | ||||||||||||||||
| Clearance: no. of cases (%) | ||||||||||||||||
| Hydrogen peroxide (n = 20) | Mineral oil (n = 19) | TP (n = 20) | p-value | |||||||||||||
| 7 (35%) | 8 (42%) | (14) 70% | Not reported | |||||||||||||
| Immediate follow-up – mixed populations – softeners and irrigation as primary objective | ||||||||||||||||
| Chaput de Saintonge and Johnstone, 197359 | ||||||||||||||||
| TP (n = 32) | Olive oil (n = 35) | p-value | ||||||||||||||
| Amount of wax removed (n) | ||||||||||||||||
| Complete | 20 | 21 | States ns, but p-value not reported | |||||||||||||
| Partial | 12 | 10 | ||||||||||||||
| Negligible | 0 | 4 | ||||||||||||||
| Volume of water used (n): (estimated by reviewer) | ||||||||||||||||
| 150 ml | 7 | 1 |
Overall p < 0.05 TP needed smaller volumes of water than olive oil |
|||||||||||||
| 300 ml | 14 | 14 | ||||||||||||||
| 450 ml | 4 | 6 | ||||||||||||||
| 600 ml | 2 | 2 | ||||||||||||||
| 750 ml | 0 | 2 | ||||||||||||||
| 900 ml | 1 | 7 | ||||||||||||||
| Delayed follow-up – adult population – softeners alone as primary objective | ||||||||||||||||
| Keane and colleagues, 19954 | ||||||||||||||||
| Cerumol (n = 24) | Sodium bicarbonate (n = 25) | Water (n = 24) | Control (n = 38) | p-value | ||||||||||||
| Impacted, % (n, ears) | 40.0 (16) | 53.8 (21) | 47.4 (18) | 68.4 (26) | ||||||||||||
| Moderately clear, % (n, ears) | 37.5 (15) | 25.6 (10) | 31.6 (12) | 26.3 (10) | p < 0.05, Cerumol vs control | |||||||||||
| Completely clear, % (n, ears) | 22.5 (9) | 20.6 (8) | 21.0 (8) | 5.3 (2) |
p < 0.05, Cerumol vs control p < 0.05, sodium bicarbonate vs control p < 0.05, water vs control |
|||||||||||
| Delayed follow-up – mixed populations – softeners alone as primary objective | ||||||||||||||||
| Fahmy and Whitefield, 198254 (see Table 6 for results of study in primary care) | ||||||||||||||||
| Study 1 | ||||||||||||||||
| Exterol (n = 20, ears n = 40) | Glycerol control (n = 20, ears n = 40) | p-value | ||||||||||||||
| Initially very hard wax | Initially hard wax | Initially very hard wax | Initially hard wax | |||||||||||||
| Wax dispersed without syringing, ears | – | 6 | – | – | Not stated | |||||||||||
| Syringed easily, ears | 15 | 14 | 2 | 18 | Not stated | |||||||||||
| Syringed with difficulty, ears | 5 | – | 14 | 6 | Not stated | |||||||||||
| Study 2 | ||||||||||||||||
| Exterol (n = 25, ears n = 50) | Cerumol (n = 25, ears n = 50) | p-value | ||||||||||||||
| Initially v hard | Initially hard | Initially soft | Initially v hard | Initially hard | Initially soft | |||||||||||
| Wax dispersed without syringing, ears | 4 | 14 | 2 | – | – | 5 | p < 0.001 | |||||||||
| Syringed easily, ears | 6 | 18 | 3 | – | 10 | 9 | ||||||||||
| Syringed with difficulty, ears | 2 | 1 | – | 8 | 17 | 1 | ||||||||||
| Delayed follow-up – mixed populations – softeners and irrigation as primary objective | ||||||||||||||||
| Fraser, 197060 (n = ears) | ||||||||||||||||
| Ease of syringing | ||||||||||||||||
| Sum scores | Difference (mean rank) | |||||||||||||||
| Test ears | Control ears | |||||||||||||||
| Cerumol (24 ears) | 92 | 122 | +30a (+11.9)b | |||||||||||||
| Olive oil (25 ears) | 116 | 140 | +24 (+3.4) | |||||||||||||
| Waxsol (26 ears) | 110 | 128 | +18 (+2.8) | |||||||||||||
| Sodium bicarbonate (124 ears) | Control | 0 (–3.5) | ||||||||||||||
| TP (24 ears) | 118 | 107 | –11 (–9.0) | |||||||||||||
| Dioctyl (25 ears) | 119 | 107 | –12 (–9.1) | |||||||||||||
| A positive difference indicates that the test were easier to syringe than the control ears. | ||||||||||||||||
| a Cerumol differed significantly from sodium bicarbonate (p < 0.05); all other comparisons were not significant. | ||||||||||||||||
| b When mean ranks were compared, Cerumol was significantly better than dioctyl and TP (p < 0.05). | ||||||||||||||||
| Frequency of syringing successes and failures | ||||||||||||||||
| Product better (n participants) | Scores equal (n participants) | Control better (n participants) | ||||||||||||||
| Cerumol (24 ears) | 15 | 5 | 4 | |||||||||||||
| Olive oil (25 ears) | 10 | 6 | 9 | |||||||||||||
| Waxsol (26 ears) | 11 | 6 | 9 | |||||||||||||
| TP (24 ears) | 7 | 7 | 10 | |||||||||||||
| Dioctyl (25 ears) | 8 | 5 | 12 | |||||||||||||
| No. of ears in which very forceful syringing failed | ||||||||||||||||
| Test ears | Control ears | |||||||||||||||
| Cerumol (24 ears) | 1 | 5 | ||||||||||||||
| Olive oil (25 ears) | 2 | 4 | ||||||||||||||
| Waxsol (26 ears) | 3 | 5 | ||||||||||||||
| TP (24 ears) | 5 | 3 | ||||||||||||||
| Dioctyl (25 ears) | 5 | 2 | ||||||||||||||
| Appearance of wax removed by syringing | ||||||||||||||||
| Percentage of lumps | Percentage partially broken up | Percentage completely broken up | ||||||||||||||
| Cerumol (24 ears) | 46 | 37 | 17 | |||||||||||||
| Olive oil (25 ears) | 40 | 44 | 16 | |||||||||||||
| Waxsol (26 ears) | 15 | 46 | 39 | |||||||||||||
| Sodium bicarbonate (124 ears) | 33 | 43 | 24 | |||||||||||||
| TP (24 ears) | 42 | 25 | 33 | |||||||||||||
| Dioctyl (25 ears) | 36 | 44 | 20 | |||||||||||||
| De-waxing techniques | ||||||||||||||||
| Pothier and colleagues, 200656 | ||||||||||||||||
| Endoscopic otoendoscope de-waxing (n = 50) | Microscopic de-waxing (n = 50) | p-value | ||||||||||||||
| Discomfort – median score on VAS (0–100) | 5 | 25 | p = 0.002 | |||||||||||||
| Pain – median score on VAS (0–100) | 3.5 | 10 | p = 0.075 | |||||||||||||
| Difficulty in de-waxing – median score on VAS (0–100) | 9 | 20 | p = 0.005 | |||||||||||||
| Time taken to perform de-waxing (minutes) | 1.8 | 3.3 | p = 0.001 | |||||||||||||
| Prevention of recurrence after removal of cerumen | ||||||||||||||||
| Saloranta and colleagues, 200558 | ||||||||||||||||
| Ceridal skin-oil (n = 13) | No treatment (n = 18) | p-value | ||||||||||||||
| Recurrence of cerumen impaction | 3 (23%) | 11 (61%) | p < 0.05 | |||||||||||||
| Recurrence in treated ears | 3/16 (19%) | 15/29 (52%) | p < 0.05 | |||||||||||||
Softeners only studies
There were no studies that assessed the use of softeners alone and followed participants up immediately.
Softeners and irrigation studies
Adults
One study55 was included that compared the use of chlorobutanol, sodium carbonate and saline (and subsequent irrigation) in an adult population and followed participants immediately afterwards.
Caballero and colleagues55 reported the proportion of participants in which the TM was completely visualised after treatment and irrigation. The study reports that there were no statistically significant differences among treatments with chlorobutanol, sodium carbonate or saline (66%, 55% and 43% for the three groups, respectively), although it was unclear from the study what the statistical analysis was testing. No baseline measures of the degree of occlusion were presented.
Caballero and colleagues55 did not report these outcomes.
Caballero and colleagues55 did not report these outcomes.
Caballero and colleagues55 did not report these outcomes.
Caballero and colleagues55 did not report AEs.
Children
One study57 comparing hydrogen peroxide, mineral oil or TP in children, with an immediate follow-up, was included.
Dubow57 reported the number of children with clearance of cerumen after treatment and syringing. The proportions of children rated as clear were 35% in the hydrogen peroxide group, 42% in the mineral oil group, and 70% in the TP group. The study did not report statistical significance testing on this data. No baseline measures of the degree of occlusion were presented.
Dubow57 did not report these outcomes.
Dubow57 did not report these outcomes.
Dubow57 did not report these outcomes.
One child in the Dubow57 study was reported to have an itching erythematous eruption of the external auditory meatus and surrounding area of the pinna of the ear. It was not clear to which group this child was allocated.
Mixed or unknown populations
One study59 in a mixed-population group immediately followed up participants having either TP or olive oil and subsequent syringing.
Comparing TP with olive oil, Chaput de Saintonge and Johnstone59 reported that 63% of participants in the TP group and 60% of participants in the olive oil group had complete removal of earwax at immediate follow-up. Rates of those with partial wax removal were 38% and 29% for the two groups, respectively. There were no participants in the TP group and 11% of participants in the olive oil group for whom the amount of wax removed was classified as negligible. The study reports that there were no statistically significant differences between the two intervention groups but the p-value was not presented. No baseline measures of the degree of occlusion were presented.
Chaput de Saintonge and Johnstone59 report that the volume of water used for syringing was statistically significantly less in the TP intervention arm than in the olive oil arm of their study; p < 0.05.
Chaput de Saintonge and Johnstone59 did not report these outcomes.
Chaput de Saintonge and Johnstone59 did not report these outcomes.
Chaput de Saintonge and Johnstone59 did not report AEs.
Results of studies in secondary care with delayed follow-up
The results of studies in secondary care are reported in Table 10.
Softeners only studies
Adults
One study4 was included that included adults and had the intention to assess outcomes after the use of only a softening agent, after a period of follow-up. The study compared Cerumol, sodium bicarbonate, water and no treatment, and follow-up was after 5 days.
Keane and colleagues’4 comparison of Cerumol, sodium bicarbonate, water and no treatment assessed the proportion of ears still impacted after treatments. The proportions appear to be similar between the groups (Cerumol 16%, sodium bicarbonate 21%, water 18%, no treatment 26%), except for a slightly higher proportion remaining impacted in the ‘no treatment’ group. No p-values or baseline measures of the degree of occlusion were reported. The proportion of ears assessed as moderately clear were statistically significantly different between the Cerumol (15%) and the ‘no treatment’ group (10%) only; p < 0.05. The proportion of ears assessed as completely clear was reported to be statistically significantly different between the Cerumol versus control group, the sodium bicarbonate versus control group and the water versus control group (Cerumol 9%, sodium bicarbonate 8%, water 8%, no treatment 2%) – all p < 0.05.
Keane and colleagues4 did not report these outcomes.
Keane and colleagues4 did not report these outcomes.
Keane and colleagues4 did not report these outcomes.
No participants were reported to have any irritation or contact sensitivity from any of the treatments in the Keane and colleagues4 study.
Children
There were no studies in children that assessed the use of softeners alone with a delayed follow-up.
Mixed or unknown populations
One study54 was included that assessed the use of a softening agent after a follow-up period of 1 week in an unknown population. Fahmy and Whitefield54 undertook two comparisons in secondary care (see Chapter 3, studies in secondary care settings, for primary care comparison). In one, a comparison of Exterol and glycerol was made and in the second a comparison of Exterol and Cerumol was made.
In the study comparing Exterol with glycerol, Fahmy and Whitefield54 found that in 15% of ears in the Exterol group the earwax had dispersed at follow-up; however, no ears in the glycerol group were identified where the earwax had dispersed after treatment. No statistical significance testing was reported. Participants with earwax remaining then went on to receive syringing (see below). In this study at baseline some 90% of participants in both the Exterol and the glycerol group had total occlusion of the TM. The remaining 10% in each group were rated as having partial occlusion at baseline. There were no data reporting post-treatment outcome in relation to pretreatment assessment in this study, however.
In the second study undertaken by Fahmy and Whitefield,54 comparing Exterol with Cerumol, the number of ears not requiring syringing was markedly greater (40%) with Exterol than with Cerumol (10%), p < 0.001. Participants with earwax remaining then went on to receive syringing (see below). In this study 46% of participants in the Exterol group were considered to have total or subtotal occlusion at baseline. The corresponding figure for the Cerumol group at baseline was 38%. The remaining 54% and 62% for each group, respectively, were rated as having partial occlusion at baseline. There were no data reporting post-treatment outcome in relation to the pretreatment outcome in this study.
In the first Fahmy and Whitefield54 study comparing Exterol with glycerol, the proportion of ears that were subsequently syringed easily were 85% in the Exterol group and 50% in the glycerol group. No statistical significance testing was reported. The number of ears that were syringed with difficulty was higher in the glycerol group (50%) than the Exterol group (15%), but no statistical significance testing was undertaken. The study reports that when the number of ears not requiring syringing (above) was added to the number syringed easily, Exterol was statistically significantly superior to the control group; p < 0.001.
In the Fahmy and Whitefield54 study comparing Exterol with Cerumol, the number of ears syringed easily were greater in the Exterol group (90%) than the Cerumol group (42%) (p-value not stated) and hence the number of ears syringed with difficulty was greatest in the Cerumol group (58% Cerumol versus 10% Exterol; p-value not stated). The authors report that when the number of ears not requiring syringing (see above) was added to the number syringed easily, Exterol was statistically significantly superior to Cerumol; p < 0.001.
Fahmy and Whitefield54 did not report these outcomes in either of their studies in secondary care.
Fahmy and Whitefield54 did not report these outcomes in either of their studies in secondary care.
Fahmy and Whitefield54 did not report AEs.
Softeners and irrigation studies
Adults
There were no studies in adult populations that assessed the use of softeners and irrigation with a delayed follow-up.
Children
There were no studies in children that assessed the use of softeners and irrigation with a delayed follow-up.
Mixed or unknown populations
One study,60 that assessed the use of a softening agent and irrigation over a delayed period of time in an unknown population, was included. This study compared sodium bicarbonate, olive oil, Cerumol, Waxsol, TP and dioctyl with a same participant control (of no treatment in one ear) over a 3-day period.
Fraser60 did not report these outcomes.
Ease of syringing was tested between each of the interventions and their corresponding same participant control in the Fraser60 study and then differences (between intervention and control) were tested across the interventions. No baseline values for the degree of earwax were presented in this study. Cerumol, olive oil and Waxsol showed a positive difference in ease of syringing rating than their respective controls, suggesting that the treatment ear was syringed more easily. TP and dioctyl showed a negative difference suggesting that the control ear was syringed more easily. Sodium bicarbonate was reported to be equivalent to the control. In addition, when the mean differences (between each intervention and same participant control) were compared across interventions, the study author reports that Cerumol differed statistically significantly from sodium bicarbonate (p < 0.05), but that all other comparisons were not statistically significant. When the mean rank of the differences (between each intervention and same participant control) were compared across interventions, Cerumol was statistically significantly better than dioctyl and TP (p < 0.05).
Similar patterns were seen in the frequency of syringing successes and failures with Cerumol, olive oil and Waxsol rated better than controls, and TP and dioctyl rated worse than controls. However, it should also be pointed out that a number of participants in each of these groups were scored equal to control on the frequency of syringing success and failure.
Fraser60 did not report these outcomes.
Fraser60 did not report these outcomes.
Frequency of otitis externa (inflammation of the external meatus) was reported by Fraser. 60 There were 12 ears (4%) that had otitis externa: in three ears it was reported to be bilateral and probably not due to the study; of the remaining six ears, three ears had received sodium bicarbonate, two Waxsol and one TP.
Additional studies
Along with the above studies in secondary care (Table 10), two additional studies were included which do not fit into the categories of softeners alone or softeners and syringing, owing to their interventions. The first (Pothier and colleagues56) compared two different de-waxing techniques: endoscopic otoendoscope de-waxing and microscopic de-waxing. The second (Saloranta and colleagues58) treated participants who had earwax removed by syringing at an initial evaluation with either a skin oil or no treatment, to evaluate recurrence over a 12-month period.
De-waxing techniques
Pothier and colleagues56 compared two different de-waxing techniques; endoscopic otoendoscope de-waxing and microscopic de-waxing. On a visual analogue scale (VAS) of 0–100 the difficulty of de-waxing was rated as less difficult in the endoscopic group (score 9) than in the microscopic group (score 20); p = 0.005. This corresponds to the difference in time taken to perform the de-waxing, which was also statistically significantly different between the two groups, where the endoscopic de-waxing took less time (1.8 versus 3.3 minutes; p = 0.001). Endoscopic de-waxing was also rated by participants (on a scale of 0–100) as causing less discomfort (score 5 versus 25) and less pain (score 3.5 versus 10) than the microscopic de-waxing procedure respectively (p-values for statistical significance = 0.002 and 0.075, respectively). At baseline 40% of participants in the endoscopic de-waxing arm and 52% of participants in the microscopic de-waxing arm had complete occlusion of the TM but this difference was not statistically significantly different; p = 0.69.
No complications were reported during de-waxing; however, one participant from each group sustained minor bleeding from ear canals. Five participants from the endoscopic group required conversion to microscopic de-waxing (three were successfully de-waxed, two were sent home with cerumenolytics) and two participants in the microscopic group were converted to endoscopic de-waxing (one was successfully de-waxed, one was sent home with cerumenolytics).
Prevention of recurrence
Saloranta and colleagues58 treated participants who had earwax removed by syringing at initial evaluation with either a skin oil (self-administered in those without learning difficulties) or no treatment, to evaluate recurrence over a 12-month period. Recurrence of impacted cerumen was seen in 23% of the Ceridal skin-oil-treated participants compared with 61% in those participants with no treatment (p < 0.05). The recurrence in treated ears was also statistically significantly less in the skin-oil-treated group (19%) than the non-treated group (52%); p < 0.005. The study also reports that there were no AEs observed in either group.
Studies of self-care
Two RCTs63,64 investigated the use of self-irrigation after participants had been assessed for earwax in primary care. One63 compared self-irrigation to nurse irrigation in adult participants who had been given sodium bicarbonate to use for at least 2 days. The follow-up was 1–2 weeks later for the comparison of interventions. A later follow-up (within 6 weeks) was undertaken to assess the need for further treatment and for the assessment of AEs and adherence to treatment. The other study64 randomised participants to either TP overnight and self-irrigation in the morning, or just self-irrigation in the morning. Both studies used soft bulb irrigators and followed up participants subsequent to the irrigation attempts. Table 11 shows the characteristics of the two self-care studies.
| Study | Interventions | Participants | Outcomes |
|---|---|---|---|
|
Author: Coppin and colleagues, 2008 63 Country: UK Number of centres: Seven primary care practices Design: RCT Setting: Self-care/primary care Follow-up: 1–2 weeks for comparison of interventions; within 6 weeks for assessment of further treatment AEs, rates and reasons for non-participation or non-compliance |
|
Target population: Adults consulting a GP or practice nurse with symptoms of occluding earwax (itching, sensation of blockage, reduced hearing) consenting to inclusion in study Baseline characteristics: Age, mean years (SD):Gender M/F: |
Primary outcomes: Reported symptoms and wax clearance Secondary outcomes: Further treatment required and acceptability of treatment |
|
Author: Harris 1968 64 Country: Ireland Design: RCT Number of centres: One Setting: Self-care/primary care Follow-up: 1 day |
|
Target population: All participants attending surgery and complaining of symptoms directly attributable to ceruminosis Baseline characteristics: Age and gender not reported |
Primary outcomes: (Not stated as primary or secondary) Wax clearance Meati clearance Colour cerumen Symptoms AEs |
The quality of the included RCT of self-irrigation63 (Table 12) compared with nurse irrigation was assessed as having reasonable quality. The method of generating the randomisation sequence and the concealment of allocation were rated as being adequate. These factors limit the risk from selection bias. Blinding of the participants and care-providers was not possible due to the nature of the intervention; however, the outcome assessors could have been blinded to the treatment allocation and this was therefore judged as inadequate. Withdrawals were reported but there appeared to be additional numbers missing in the analysis of many of the outcomes and there was no discussion of the application of an ITT principle to the analysis of data. The RCT of self-irrigation with or without a previous softener64 was assessed to be of low methodological quality. Details of the randomisation schedule and allocation were not adequately described and it is also unclear whether the outcome assessors were blinded to treatment allocation.
| Study | Randomisation | Concealment of allocation | Baseline characteristics | Eligibility | Blinding of assessors | Care-provider blinding | Patient blinding | Reporting outcomes | ITT | Withdrawals explained |
|---|---|---|---|---|---|---|---|---|---|---|
| Coppin, 200863 | Ad | Ad | Rep | Un | In | N/A | N/A | Ad | In | Par |
| Harris, 196864 | Un | Un | Un | Par | Un | Un | Un | In | In | Ad |
Results of studies in self-care settings
The results of studies in self-care are reported in Table 13.
| Coppin and colleagues, 2008:63 self-irrigation vs nurse irrigation | |||||
|---|---|---|---|---|---|
| Sodium bicarbonate + self-irrigation (n = 118) | Sodium bicarbonate + nurse irrigation (n = 119) | Difference groups (95% CI); p-value | |||
| Wax clearance (obstruction score 0 or 1), n (%) | 50/104 (48) | 64/102 (63) | 15% (1% to 28%); p = 0.03 | ||
| Requires no further clearance (based on normal clinical practice), n (%) | 51/100 (51) | 66/95 (69) | 18% (5% to 32%); p < 0.01 | ||
| Mean (SD) change in symptom score from baseline | –0.81 (1.44) | –1.26 (1.15) | –0.45 (–0.11 to –0.79); p = 0.01 | ||
| Satisfied with treatment, n (%) (agreed slightly or more) | 78/110 (71) | 105/106 (99) | 28% (19% to 29%); p < 0.001 | ||
| Use same treatment again, n (%) (agreed slightly or more) | 82/110 (75) | 106/106 (100) | 25% (17% to 25%); p < 0.001 | ||
| Treatment convenient, n (%) (agreed slightly or more) | 84/110 (76) | 95/105 (90) | 14% (4% to 24%); p < 0.01 | ||
| Harris, 1968:64 softeners and self-irrigation vs self-irrigation alone | |||||
| Clearance | |||||
| TP (n = 24) | Control (n = 21) | p-value | |||
| Completely cleared | 18 | 1 | p < 0.005 | ||
| Partially or not cleared | 6 | 20 | |||
| State of meati | Completely obscured | Partially obscured | Completely obscured | Partially obscured | |
| Before treatment | |||||
| 14 | 10 | 14 | 7 | ns | |
| After treatment | |||||
| Meati cleared | 8 | 10 | 0 | 1 | |
| Meati not cleared | 6 | 0 | 14 | 6 | |
Measures of occlusion
In the study by Coppin and colleagues,63 at baseline 63% of participants in the self-irrigation group had a completely occluded right ear and 67% a completely occluded left ear. In the nurse irrigation group these proportions were similar (62% with completely occluded right ear and 69% with a completely occluded left ear). After treatment the degree of obstruction was rated on a 4-point scale (0 = no or minimal wax with TM fully visible; 1 = minor amount of wax with TM essentially visible; 2 = moderate amount of wax with TM partially obscured; 3 = complete occlusion of TM) by a treatment nurse. Based on this nurse-evaluated score, wax ‘clearance’ (a combined score of 0 and 1) was seen in 48% of those in the self-irrigation group compared with 63% in the nurse-irrigation group; p = 0.03. There were no baseline data of the degree of obstruction using this particular scale hence no data on the post-treatment outcome in relation to the pretreatment outcome were presented. This score was reported to have been used in a pilot study by the report authors, and a reference is provided, although it is also not clear if this was a fully validated measure.
The proportion assessed as not requiring further clearance in the Coppin and colleagues63 study was higher in the nurse-irrigation group (69%) compared with those in the self-irrigation group (51%); p < 0.01. This assessment was undertaken by a GP or a nurse who may or may not have carried out the pretreatment assessment (28% were by the same nurse).
Harris64 reported the number of participants with complete clearance versus partial or incomplete clearance of earwax, with statistically significantly higher proportions of participants seen with completely cleared ears in the TP softened group (p < 0.005). Of those with completely obscured TM at baseline (n = 14 per treatment group) in the TP softening group, eight participants were completely cleared after treatment. In the self-irrigation only group no participants were completely cleared after treatment. Of those with partially obscured TM at baseline (n = 10) in the TP softening group, all 10 were reported to be cleared at follow-up. In the self-irrigation-alone group, seven participants had partially obscured TM at baseline and just one was cleared at follow-up (Table 13). Subsequent to follow-up, six TP participants had softened wax cleared in primary care with gentle syringing and 19 participants in the control group had wax cleared with normal syringing after examination at the surgery.
Measures of participant satisfaction
On a self-reported symptom score that ranged from 0 (no symptoms) to 6 (severe symptoms) which had previously shown high internal reliability in a pilot study, the mean change in score from baseline in the Coppin and colleagues63 study was better in those participants in the nurse-irrigation group than the self-irrigation group [difference –0.45 (95% CI –0.11 to –0.79; p = 0.01)].
In the Coppin and colleagues study,63 satisfaction with treatment was assessed on a 7-point scale that had previously been used in a pilot study. The proportion of participants who rated their satisfaction with treatment as satisfied slightly or more was higher in the nurse-irrigation group than the self-irrigation group, a difference of 28% (95% CI 19% to 29%); p < 0.001. It was unclear whether this scale was a fully validated measure of satisfaction with treatment.
Harris64 did not report satisfaction as an outcome.
Adverse events
There were no statistically significant differences between the two groups in the rating of treatment discomfort [difference of 7% (95% CI –6% to 19%)] in the Coppin and colleagues63 study (Table 14). There were also no statistically significant differences between rates of dizziness, infection, perforation or signs of trauma (differences between groups for each type = 0%). One participant in the nurse-irrigation group had bilateral otitis externa. Of the two participants that had perforations (one in each group), one had old scarring on the TM and one had pre-existing cholesteatoma (unclear which group each belonged to). In the Harris64 study, AEs were reported as one participant in the TP arm suffering erythema around the external auditory meatus. No other AEs were reported.
| Coppin and colleagues, 200863 | |||
|---|---|---|---|
| Sodium bicarbonate + self-irrigation (n = 118) | Sodium bicarbonate + nurse irrigation (n = 119) | Difference groups (95% CI); p-value | |
| Treatment discomfort (slight or more), n (%) | 43/100 (39) | 35/108 (32) | 7% (–6% to 19%); p = 0.30 |
| Treatment dizziness (slight or more), n (%) | 14/100 (13) | 14/108 (13) | 0% (–9% to 9%); p = 0.96 |
| Infection, n (%) | 1/97 (1) | 1/93 (1) | 0% (–3% to 3%); p = 1.00 |
| Perforation, n (%) | 1/97 (1) | 1/94 (1) | 0% (–3% to 3%); p = 1.00 |
| Signs of trauma, n (%) | 1/97 (1) | 1/94 (1) | 0% (–3% to 3%); p = 1.00 |
Studies in other care settings
One RCT62 was undertaken in a corporate research clinic in adult volunteers with excessive or impacted cerumen on examination (Table 15). The study compared TP, Murine and placebo with saline, and follow-up was immediate. One CCT61 was undertaken in a military research unit in a population of adult entrants to the Royal Air Force who had impacted cerumen (Table 15). The study compared sodium bicarbonate, Cerumol, hydrogen peroxide, olive oil and ‘no treatment’ control. Follow-up was also immediate. Both studies also followed the softening agents with an irrigation procedure before assessing the outcomes.
| Corporate research unit: adult population with immediate follow-up | |||
|---|---|---|---|
|
Author: Roland and colleagues, 200462 Country: USA Number of centres: One Design: RCT Setting: Corporate research clinic Follow-up: Immediate |
|
Target population: ≥ 18-year-old company employees, volunteering with excessive or impacted cerumen, required to have mild, moderate or complete cerumen occlusion Baseline characteristics: Age, mean years (range): 45 (22–66) overall (no individual group details) Gender M/F 51:23 (M/F ratio): (2.2:1) |
Main outcome: Post-treatment level of occlusion Other outcome: Otological signs and symptoms |
| Military research unit: adult population with immediate follow-up | |||
|
Author: Hinchcliffe, 195561 Country: UK Number of centres: One Design: CCT Setting: Military Follow-up: Immediate |
|
Target population: Adult entrants to the Royal Air Force in the 1950s, found to have hard wax obscuring the meatus in one or both ears on entrant examination Baseline characteristics: Age: Not reported Gender: Not reported |
No. of occasions wax meatus was not cleared within specified 5 minutes No. of cases with symptoms of discomfort |
The quality of reporting and methodology of the included studies was generally poor (Tables 16 and 17). In the RCT the randomisation schedule and the concealment of allocation were unknown, which may lead to an increased risk of selection bias. Blinding of outcome assessors and the participant were judged to be adequate, with blinding of the caregiver judged as partially met. The number of withdrawals was discussed, but there was no discussion on an analysis based on the ITT principle. The CCT was judged to meet the criteria only partially for blinding of outcome assessors, but the reporting of outcomes and any withdrawals values was inadequate. These studies are at a high risk of bias, which may affect the direction of any effects shown. Caution is therefore required when interpreting the results.
| Study | Randomisation | Concealment of allocation | Baseline characteristics | Eligibility | Blinding of assessors | Care-provider blinding | Patient blinding | Reporting outcomes | ITT | Withdrawals explained |
|---|---|---|---|---|---|---|---|---|---|---|
| Roland, 200462 | Un | Un | In | Ad | Ad | Par | Ad | Ad | In | Ad |
| Study | Baseline characteristics | Eligibility | Blinding of assessors | Reporting outcomes | ITT | Withdrawals explained | Representativeness |
|---|---|---|---|---|---|---|---|
| Hinchcliffe, 195561 | Un | Ad | Par | In | In | Un | Un |
Results of studies in other care settings
The results of studies in other care settings are reported in Table 18.
| Roland and colleagues, 200462 | ||||||
|---|---|---|---|---|---|---|
| Degree of occlusion | ||||||
| TP (n = 24) | Murine (n = 26) | Placebo (n = 24) | p-value | |||
| None, n (%) | 7 (29.2) | 4 (15.4) | 10 (41.7) | TP vs placebo p = 0.37 | ||
| Mild, moderate or complete occlusion | 17 (71) | 22 (85) | 14 (58) | Murine vs placebo p = 0.06 | ||
| Change from baseline in occlusion (estimated by reviewer) | ||||||
| Resolved: 30% | Resolved: 16% | Resolved: 42% | Not tested | |||
| Improved: 8% | Improved: 7% | Improved: 22% | ||||
| No change/worse: 62% | No change/worse: 77% | No change/worse: 38% | ||||
| Hinchcliffe, 195561 (n = ears) | ||||||
| Sodium bicarbonate (n = 37) | Cerumol (n = 37) | Hydrogen peroxide (n = 37) | Olive oil (n = 37) | Control (n = 37) | p-value | |
| No. of occasions wax meatus was not cleared within specified 5 minutes | 6 (16%) | 7 (19%) | 4 (11%) | 2 (5%) | 9 (24%) | |
Measures of occlusion
Participants in the RCT by Roland and colleagues62 were assessed for the degree of occlusion after treatment and syringing. The proportion of participants classified as having no occlusion was highest in the placebo group (41.7%). In the TP group the proportion with no occlusion was 29.2% and in the Murine group this was 15.4%. The proportion of participants classified as having mild, moderate or complete occlusion were subsequently lower in the placebo group and higher in the TP and Murine groups. While these data suggest that the placebo group had better outcomes than the TP and Murine groups, there were no statistically significant effects shown (p = 0.06). The change from baseline in the degree of occlusion was presented in a figure and estimated by a reviewer. This suggests that there was resolution of the earwax in 30% of the TP arm, 16% in the Murine arm and 42% in the placebo arm, but the differences were not tested statistically. The proportion rated as having an improvement in the amount the earwax was also higher in the placebo group (8% TP, 7% Murine, 22% placebo), and the proportion rated as having no change or a worsening of earwax was lower in the placebo group (62% TP, 77% Murine, 38% placebo), although again this was not tested for statistical significance. The degree of occlusion seen at baseline was not presented per intervention group, but the level of occlusion across all participants was presented.
Measures of ease of wax removal
In the Hinchcliffe CCT61 the outcome assessed was the number of occasions the wax meatus was not cleared within a prespecified 5 minutes. In all groups the proportions not cleared in the time frame were generally low (sodium bicarbonate 16%, Cerumol 19%, hydrogen peroxide 11%, olive oil 5% and control 24%), although the control arm appeared to have more participants ‘not cleared’ than the other comparisons. The study reports that olive oil was statistically significantly better than no treatment at all, but no p-value was reported to support this.
Measures of participant satisfaction
These outcome measures were not assessed by Roland and colleagues62 or Hinchcliffe and colleagues. 61
Measures of recurrence
These outcome measures were not assessed by Roland and colleagues62 or Hinchcliffe and colleagues. 61
Adverse events
In the Roland and colleagues62 RCT, rates of related AEs were low in all groups. One participant in the TP group and two in the Murine group had ear pruritis. One participant in the placebo group had ear discomfort and one participant in the TP group had contact dermatitis. There was only one AE classed as unrelated by the study authors, this was a case of vertigo seen in the TP group.
In the Hinchcliffe61 CCT AEs were only reported as numbers, no details of specific AEs were reported. All treatments except the control were associated with some AEs; these appeared to be higher in the Cerumol treatment arm (n = 22) than in the other treatments (sodium bicarbonate n = 4; hydrogen peroxide n = 6; olive oil n = 4), but no statistical significance testing was undertaken. The study author reports that symptoms of discomfort occurred significantly more often for Cerumol than for any other preparation, but no further data were reported to support this.
Outcomes of the above two studies are shown in Table 18.
Summary of results of the systematic review of clinical effectiveness
Quantity, quality and nature of evidence
-
Twenty-six clinical trials conducted in primary care (14 studies), secondary care (eight studies) or other care settings (four studies), met the inclusion criteria for the review. Of these studies, there were 22 RCTs and four CCTs.
-
The evidence on the clinical effectiveness of the different methods of earwax removal was diverse in terms of the people, interventions, comparators and outcomes assessed. Many of the studies suffered from limitations associated with the completeness of reporting of methods and results. For those where information was presented, they were generally considered to be of poor quality, with many studies providing only partial or inadequate consideration of potential biases. Many of the differences and inadequacies may reflect the long period during which the research findings have emerged (1950–2007), with changes to clinical practice and developments in the principles for the conduct of research evident.
-
A range of interventions have been used in the studies involving 16 different softeners with or without irrigation in various different comparisons. Most comparisons are of different oil-based softeners against water-based softeners. Doses are not always reported and timing of the intervention and follow-up assessment varies across the studies.
-
Participants in the trials also varied across the studies, in terms of age, sex and extent of earwax problem. In some cases few details of baseline characteristics are given in the study reports, so interpretation of results is difficult.
-
A range of outcome measures were reported across the studies often with limited information on the definition of these outcomes, making it difficult to assess their validity and objectivity, and how consistently they were applied. For example, measures of earwax removal might be reported in terms of clearance or visualisation of TM (described as complete, partial or negligible) or in terms of impaction or occlusion (described as none, mild, moderate or severe). Ease of earwax removal was reported in terms of number of attempts or the amount of liquid needed to achieve some degree of success. As a consequence, a pragmatic approach was taken to classify outcomes under these categories despite no evidence that these are directly comparable between studies.
-
Some studies reported measures of participant satisfaction, but these were not always assessed with valid measures. Measures of recurrence were rarely reported as most studies were of a short time frame. AEs were rarely reported.
-
Data analysis conducted in the trials was also variable with several studies not reporting the analytic approach used or results of statistical tests.
-
Due to these methodological issues, summarising the results of included studies was difficult and meta-analysis impossible. As such, care should be taken in interpreting the findings of the studies.
Results
-
Considering the studies that report statistical significant differences in outcomes measuring clearance of earwax (Tables 19 and 20) and ignoring any variations in methodological quality, results assessing the extent and ease of clearance of wax show that Cerumol, sodium bicarbonate, olive oil and water are all more effective than no treatment at removal of earwax; Cerumol is better than dioctyl, TP and sodium bicarbonate for ease of subsequent irrigation; TP is better than olive oil in the volume of water used in syringing; Audax is better than Earex for ease of removal by subsequent irrigation; Exterol and Otocerol are better than Cerumol in terms of the number of people requiring irrigation after treatment with softeners.
-
Other comparisons show that wet irrigation is better than dry irrigation for ease of removal; sodium bicarbonate drops followed by nurse irrigation is more effective than sodium bicarbonate drops followed by self-irrigation; softening with TP and self-irrigation is more effective than self-irrigation only; endoscopic de-waxing is better than microscopic de-waxing; recurrence of earwax and impacted earwax is less in ears that are treated with skin oil than those not treated.
-
Patient satisfaction was assessed in five studies through several different measures. Over 85% of people in two studies found the use of dioctyl-medo, oil-based softeners, Waxsol and Cerumol tolerable. In two other studies the effectiveness of softeners as judged by patients ranged from 29% for Earex to between 42% and 93% for Audax and 100% for Cerumol. In another study, people undergoing nurse irrigation were more satisfied than those self-irrigating their ears (difference 28%).
-
Adverse events appear to be minor, limited in extent and mainly related to irrigation. None of the studies reported perforation of the TM or serious infections. In the majority of studies fewer than 10% of people suffered any AE. Minor pain (0–21%) and irritation/itching of the ear (4–15%) were the main AEs.
Conclusion
Despite the relative benefits of certain softeners in aiding the extent and ease of earwax clearance, it is not possible to say that any one type of softener is superior in clearing earwax with or without subsequent irrigation on the evidence available. Separate studies have found significant benefits from wet syringing compared with dry syringing, from nurse irrigation rather than self-irrigation, and from endoscopic than microscopic de-waxing.
| Comparison | Study | Measure(s)a | Statistical significance |
|---|---|---|---|
| Audax | |||
|
|
Degree of impaction: None, mild, moderate or severe | Not statistically significant (no p-value reported) |
| Cerumol | |||
|
|
Wax dispersal without syringing | Statistically significant in favour of Exterol (p < 0.001) |
|
Wax dispersal without syringing | Statistically significant in favour of Exterol (p < 0.001) | |
|
|
Clearance: Impacted, moderately clear or completely clear | Statistically significant in favour of Cerumol for completely clear (p = 0.05) |
| Murine | |||
|
|
Occlusion: None or ‘mild-moderate-complete’ | Not statistically significant (p = 0.06) |
| TP | |||
|
|
TM visualisation: Complete or incomplete | Not statistically significant |
|
|
Amount of wax removed: Complete, partial or negligible | Not statistically significant (no p-value reported) |
|
|
Occlusion: None or ‘mild-moderate-complete’ | Not statistically significant (p = 0.37) |
| Sodium bicarbonate preparations | |||
|
|
Mean change in degree of cerumen | Not statistically significant (no p-value reported) |
|
|
Clearance: Impacted, moderately clear or completely clear | Statistically significant in favour of sodium bicarbonate for completely clear (p = 0.05) |
| Olive oil | |||
|
|
No of times wax meatus not cleared within 5 minutes | Statistically significant in favour of olive oil (no p-value reported) |
| Water | |||
|
|
Clearance: Impacted, moderately clear or completely clear | Statistically significant in favour of water for completely clear (p = 0.05) |
| Comparison | Study | Measure(s)a | Statistical significance |
|---|---|---|---|
| Audax | |||
|
|
Ease of syringing: not required, easy, difficult or impossible | Statistically significant in favour of Audax (p < 0.005) |
| Cerumol | |||
|
|
Ease of syringing | Mean ranks comparison statistically significant in favour of Cerumol (p < 0.05) |
|
|
Ease of syringing | Statistically significant in favour of Cerumol (p < 0.05) |
|
|
Ease of syringing | Mean ranks comparison statistically significant in favour of Cerumol (p < 0.05) |
|
|
Ease of syringing | Not statistically significant (no p-value reported) |
|
|
Number of people needing syringing | Statistically significant in favour of Otocerol (p = 0.05) |
| TP | |||
|
|
Ease of syringing: volume of water used for syringing | Statistically significant in favour of TP (p = 0.05) |
| Sodium bicarbonate preparations | |||
|
|
Ease of syringing | Not statistically significant (no p-value reported) |
| Water | |||
|
|
Mean number of syringing attempts | Not statistically significant (p = 0.18) |
| Olive oil | |||
|
|
No. of times wax meatus not cleared within 5 minutes | Statistically significant in favour of olive oil (no p-value reported) |
| Dioctyl-medo | |||
|
|
Ease of syringing | Not statistically significant (no p-value reported) |
Research in progress
We identified a total of five ongoing trials from our searches (Table 21). Schroeder and colleagues aimed to evaluate olive oil as a softening agent, comparing the usual care of self-administered olive oil for 5 days prior to irrigation versus 3 weeks. The primary outcome of the trial was ear canal clearance and the trial was set to finish in 2006.
| Contact name | Title | Funding body |
|---|---|---|
| Dr K Schroeder | Olive oil vs ear syringing for the removal of earwax in primary care: pragmatic randomised trial | Scientific Foundation Board, Royal College of GPs, UK |
| Mr S Gillett | Microsuction vs instruments for de-waxing: a randomised controlled trial | Royal United Hospital Bath NHS Trust, UK |
| Dr M Caballero | Chlorobutanol, potassium carbonate, and irrigation in cerumen removal | Hospital Clinic of Barcelona, Spain |
| Mr S MacKeith | The use of wax softeners (cerumenolytics) before de-waxing: a randomised clinical study | NHS R&D Support Funding, UK |
| Dr C Hand | The treatment of symptomatic earwax in primary care | None |
Gillett and colleagues aimed to investigate the differences in discomfort and/or complications between microsuction and the use of instruments. The trial was set to finish in July 2008, although no subsequent publication has been identified at the time of writing.
The third study by Caballero and colleagues was set in a hospital clinic in Spain and aimed to compare Otocerum® ear drops, Taponoto® ear drops and placebo. This is reported to be a phase IV trial, non-randomised, double-blind and parallel-assignment trial. The primary outcome was the proportion with a completely visualised TM, with either the treatments alone or with irrigation if needed. The study was expected to finish in October 2008 and no publication has so far been identified.
Two other controlled trials were identified from searches of the National Research Register. A study by MacKeith and colleagues was sited at the Bristol Royal Infirmary and aimed to evaluate wax softening agents used immediately prior to de-waxing by microsuction. The outcome was the impact of softening agents on the pain or discomfort of the procedure. The trial was anticipated to end in June 2007 and the trial status is shown as completed.
The second study, by Hand and the Suffolk and Norfolk Research and Development Consortium (SAND), aimed to compare preparations for the treatment of symptomatic earwax. No further details are provided and the trial was set to end in January 2007.
No publication of the trial data for any of the five studies has been found so far.
Chapter 4 Adverse events
A dverse outcomes that are reported to be associated with the removal of earwax, especially from ear irrigation, are well documented in the descriptive literature of the condition66–68 and also in studies reporting litigation and compensation claims that are related to earwax removal. 34,69,70 These include more serious adverse events (SAEs), which can be broadly grouped into ear infections (otitis externa, otitis media); damage to the ear (external auditory canal, perforation of TM), various levels of discomfort and noises (pain, vertigo, fullness of ear and tinnitus), and both temporary and permanent hearing impairment. 6,67,70 Some literature also suggests that people with diabetes may have an increased risk of suffering from malignant otitis externa as a result of irrigation. This is an infection of the external auditory canal and deep periauricular tissues, and may progress into skull base osteomyelitis with cranial nerve paralysis, and, in rare cases, may result in death. 71,72
However, despite the perception that there is a potential risk from earwax removal there were very few serious adverse outcomes reported in the RCTs that were identified in the systematic review of clinical effectiveness above (see Chapter 3). This may be due to factors relating to the study design, including small sample sizes and, in many cases, the short duration of follow-up. As such, a wider search of the literature was undertaken to identify any additional studies.
Searching
A targeted search of the literature was undertaken to identify additional studies reporting AEs associated with the removal of earwax, to assess the safety of earwax removal and to inform the economic modelling of the problem. The search was not restricted by study design. The following section complements the clinical effectiveness section, reporting overall results from both the RCTs identified, and any relevant observational studies. No systematic critique of the studies was undertaken; however, key methodological limitations of the studies are discussed in the relevant sections below. In addition, only AEs that the study authors attributed to the interventions were included. The studies were assessed on an ITT basis.
Adverse events from drops alone
Four RCTs4,44,50,52 were identified that included AEs from using drops alone with no irrigation. These RCTs are all critically assessed and data extracted in the clinical effectiveness section above (see Chapter 3). Two of these RCTs, by Carr and Smith52 and Keane and colleagues,4 did not find any AEs. The other two RCTs are shown in Table 22. One observational study by Midani and colleagues73 was identified and data is also summarised in Table 22. This was an open-label study of Sofenz cerumenolytic solution in 109 participants with excessive and impacted cerumen. A total of 58 AEs were reported, but only 16 were reported to be directly related to the treatment.
| Adverse outcome | Overall probability of AEs in study population (%) | Range of AEs across studies (%) | References |
|---|---|---|---|
| Defined AEs from studies | |||
| Giddiness | 0.94 | – | Jaffe and Grimshaw50 |
| Pain | 2.83 | – | Jaffe and Grimshaw50 |
| Itchiness/pruritus | 2.51 | 2.00–2.75 | Dummer and colleagues,44 Midani and colleagues73 |
| Skin irritation/erythema | 9.43 | 4.00–17.92 | Jaffe and Grimshaw,50 Midani and colleagues,73 Dummer and colleagues44 |
| Oedema | 3.67 | – | Midani and colleagues73 |
| Buzzing | 2.00 | – | Dummer and colleagues44 |
| Other ear disorders | 4.59 | – | Midani and colleagues73 |
| All studies that assessed AEs | |||
| 10.57 | 0–17.92% | Jaffe and Grimshaw,50 Carr and Smith,52 Keane and colleaguesa,4 Dummer and colleagues,44 Midani and colleagues73 | |
There were major differences in all of the studies in terms of population, drops used, care setting and methodologies used. Therefore, no formal meta-analysis of this data was attempted. However, an estimated probability for individually defined AEs from relevant studies was generated for illustration. An overall probability of an AE occurring was also calculated from the studies that included AEs as outcomes. Caution is required therefore in the interpretation of this data. The ranges of AEs reported for each condition and overall proportion for all AEs from the studies and the one observational study are reported in Table 22.
The overall number of AEs was 43 out of a total study population of 407 participants from the RCTs and observational study. The probability of minor AEs occurring was 10.57%. It is worth noting, however, that the probability of AEs may be variable depending on the type of drops used. The Cerumol arm of the Jaffe and colleagues RCT,74 for example, accounts for 13 AEs, whereas the arm using Otocerol accounts for a further eight AEs out of the total of 43. However, due to the heterogeneity of the studies it is not possible to draw any reliable conclusions about which drops are likely to cause more adverse outcomes than others. Based on data available it would seem that AEs from drops are relatively rare and tend to be of a mild nature.
Adverse events for drops and irrigation
An assumption was made that the reporting of AEs from drops and irrigation would be split into major AEs (those events that would be more likely to require additional treatment or resource use), and minor AEs (those that were likely to be transient and would not require additional treatment).
Major adverse events from drops and irrigation
Sixteen RCTs that included AEs as outcomes were identified. Three of these RCTs did not explicitly state what AEs had occurred and so it was not possible to assess whether the AEs were major or minor in nature, and so they are discussed separately, below. One other study, by Burgess43 was excluded because only the number of ears syringed were reported and it was not possible to tell how many participants were involved in the trial. Therefore, 12 RCTs were included.
In addition, two observational studies were identified. The first study was a retrospective analysis of 2400 patient records from a tinnitus clinic in the USA, who had experienced severe tinnitus. Eleven participants reported that their tinnitus started as a result of cerumen removal. However, it was not clear how many of the 2400 participants with severe tinnitus had actually received ear irrigation, and there was no clear association between the two events, and so the study was excluded. 75 The other study76 was a large prospective observational study (952 ears in 622 subjects) of people attending an ENT clinic in Nigeria, who were using drops to soften earwax and then undergoing irrigation of the ear with a Propulse II irrigation system. The only adverse outcomes reported were one participant with vertigo and another with a TM perforation. No minor AEs were reported. The study was undertaken in a different care setting to the UK, and the majority of participants were children, therefore this may limit the generalisability of the studies results. However, the equipment used and the ‘wet’ phenotype of cerumen is similar to both countries and populations and, as such, the study was included.
As described, the individual RCTs and the one observational study results were used to produce a probability for individually defined AEs. An overall probability of major AEs from drops and irrigation was also generated from all studies that included AEs as outcomes. Caution is recommended in the interpretation of these data. The RCTs were also heterogeneous, with reports from a variety of settings and using several different types of drops and irrigation techniques as active treatments and controls. Furthermore, the external validity of the Nigerian observational study to a UK context requires caution in its interpretation. The ranges of AEs reported for all major AE from the studies are reported in Table 23.
| Adverse outcome | Overall probability of AEs in study population (%) | Range of AEs across studies (%) | References |
|---|---|---|---|
| Defined AEs from studies | |||
| Tinnitus | 0 | – | No incidence in included studies |
| Vertigo | 0.16 | – | Ogunleye and Awobem76 |
| Perforated ear drum | 0.16 | – | Ogunleye and Awobem76 |
| Otitis media | 0 | – | No incidence in included studies |
| Otitis externa | 1.94 | 0.85–4.84 | Coppin and colleagues,63 Fraser60 |
| Permanent hearing loss | 0 | – | No incidence in included studies |
| Temporary hearing loss | 0 | – | No incidence in included studies |
| All studies that assessed AEs | |||
| 0.59 | 0–4.84 | Ogunleye and Awobem,76 Coppin and colleagues,63 Meehan and colleagues,46 Whatley and colleagues,47 Singer and colleagues,49 Pavlidis and Pickering,42 Amjad and Scheer,51 Lyndon and colleagues,45 Saloranta and colleaguesa,58 Roland and colleagues,62 Fraser,60 Dubow,57 Harris64 | |
There were nine occurrences of AEs in a total study population of 1515 participants. The overall probability of major adverse outcome was therefore 0.59%. Six of the nine AEs came from the Fraser and colleagues study60 (all otitis externa) involving 124 participants. If this study was excluded then the incidence of AEs would drop to 0.22%. This would be close to the Sharp and colleagues’6 estimation a 0.1% incidence of major complications based on their otolaryngological unit in Scotland. No incidence of tinnitus, otitis media and hearing loss were reported in any of the included studies. It would seem that major AEs occur relatively infrequently, but, given the heterogeneous nature of the studies included, this result should be interpreted with caution.
Minor adverse events from drops and irrigation
The same 12 RCTs that were identified for the major AEs section above were all included in this section. No observational studies were identified reporting rates of minor AEs from the literature search. As mentioned above an estimate of the probabilities of minor AEs from drops and ear irrigation were generated. These need to be treated as illustrative only. The ranges of AEs reported for each condition and overall proportion for all AEs from the studies are reported in Table 24.
| Adverse outcome | Overall probability of AEs in study population (%) | Range of AEs across studies (%) | References |
|---|---|---|---|
| Defined AEs from studies | |||
| Pain | 20.83 | 0 | Meehan and colleagues46 |
| Itchiness/pruritus | 3.01 | 1.69–4.05 | Roland and colleagues,62 Dubow57 |
| Skin irritation/dermatitis | 1.94 | 1.35–2.78 | Roland and colleagues,62 Lyndon and colleagues,45 Harris64 |
| Dizziness | 11.03 | 3.85–11.81 | Pavlidis and Pickering,42 Coppin and colleagues63 |
| Discomfort | 25.40 | 1.35–32.91 | Roland and colleagues,62 Coppin and colleagues63 |
| Ear bleed | 1.09 | – | Whatley and colleagues47 |
| Ear trauma | 0.84 | – | Coppin and colleagues63 |
| All studies that assessed AEs | |||
| 14.33 | 0–32.91 | Coppin and colleagues,63, Meehan and colleagues,46 Whatley and colleagues,47 Singer and colleagues,49 Pavlidis and Pickering,42 Amjad and Scheer,51 Lyndon and colleagues,45 Saloranta and colleaguesa,58 Roland and colleagues,62 Fraser,60 Dubow,57 Harris64 | |
There were 128 occurrences of AEs from a total study population of 893. Overall, the incidence of minor AEs was 14.33% from all the included studies. The Coppin and colleagues’ study reported 108 out of the 128 incidences of AEs. 63 The higher incidence of AEs in this study, especially for discomfort and dizziness suggest a more sensitive inclusion of AEs than the other studies. 63 One of the arms in the trial was a self-syringing group and this may also explain the higher number of AEs in the study. If this study was excluded then the probability of minor AEs would fall to 3.05% for the remaining included studies.
Three further RCTs41,48,61 reported an overall rate of AEs but did not define the adverse outcomes that had occurred therefore it was not possible to determine whether they were major or minor AEs. One of these studies, by Hinchcliffe and colleagues, reported only the number of ears treated and as it was not possible to determine how many participants there were in this trial it was excluded. There was a total 257 participants in the two remaining RCTs. 41,48 There were an estimated 21 AEs (the studies reported AEs only as a percentage of each arm with or without AE). This gave an overall probability of 8.17% for the occurrence of AEs. Another study76 in Nigeria using drops to soften earwax, and then irrigation of the ear, reported that there were no minor AEs.
The incidence of minor AEs is relatively common compared to the major AEs, but it is unclear how long many of these AEs last. It is likely, however, by their very nature, that they will be relatively transient and have little or no impact on resource use.
Conclusion
The evidence from the included RCTs and the two observational studies suggest that using both drops and ear irrigation are safe techniques for the removal earwax, with the number of SAEs being low. However, some studies may have been more sensitive at including AE data than others, and in many the length of follow-up was not suitable for capturing AEs. These factors and the methodological issues noted above (and in Chapter 3) suggest that care is required before interpreting earwax removal techniques as safe procedures. The probabilities of more SAEs obtained from this simple aggregation technique were not thought to be reliable enough to put into the economic model. The minor incidence rates were felt unlikely to have a major impact on either health-related quality of life (HRQoL) or resource use and so were also not used.
Chapter 5 Economic analysis
The aim of this section is to evaluate the cost-effectiveness of methods of earwax removal. A systematic review of the literature was conducted to identify economic evaluations on the use of softeners with or without irrigation and other methods of earwax removal. An economic model was then developed to compare different strategies to achieve earwax removal. This section will report the results of the systematic review, the rationale and the components of the economic evaluation, including the structure of the model, the sources of data on costs and benefits, assumptions underlying the model, and results of the analysis.
Systematic review
A systematic review of the literature was undertaken to identify economic evaluations considering the treatment of earwax. The methods for the systematic review are described in Chapter 2. The details of the inclusion and exclusion criteria are shown in Appendix 1 and the search strategies are shown in Appendix 2.
No cost-effectiveness studies were identified that met the inclusion criteria for the review.
Southampton Health Technology Assessments Centre (SHTAC) economic analysis
A modelled economic evaluation was undertaken to estimate the comparative cost-effectiveness of three alternative treatment strategies for earwax removal in adults, without any known contraindications to the use of softeners or irrigation.
Rationale for the model structure
With no nationally accepted guidelines for the management of symptomatic earwax in the UK (see Chapter 1, Current service provision and description of interventions), it was recognised that current practice would vary. Reflecting such variations in the economic model would be difficult, if not impossible. As a consequence a simplified model structure was developed using information from available practice guidelines, other published evidence and expert advice from clinicians and other health professionals. The model was developed from the NHS perspective, with each alternative treatment option involving primary care practitioners in diagnosing the condition and recommending subsequent treatment options.
Three options were considered in the economic model with the intention of reflecting current practice for the population under consideration and possible alternatives. The options considered in the model following presentation at primary care are (1) use of softening drops (softeners) for a week with return to the primary care practice for ear irrigation if no spontaneous earwax clearance occurs (current standard practice); (2) use of softeners for a week followed by self-irrigation and return to primary care if unsuccessful for professional irrigation; and (3) ‘no treatment’. The ‘no treatment’ or ‘do nothing’ option was included in the model as a universal comparator. It represents a hypothetical situation when no treatment is available or offered to the patient or the patient decides not to undergo treatment. Some anecdotal evidence suggests that some primary care practices no longer offer professional irrigation, with the suggestion that the condition will resolve itself. Details of the treatment strategies are provided in Chapter 5 (Model structure).
Population included in the model
The target population includes adults aged 35–44 years with earwax, who are eligible for any of the evaluated treatment alternatives. Patients who have a known contraindication for irrigation (such as current or pre-existing otitis media, vertigo, recurrent ear infection, history of ruptured TM, permanent hearing loss, acute illness or fever) are considered outside the scope of this economic evaluation. Although excessive earwax is more prevalent in older age groups, the 35–44 age group was selected as this was the group for whom evidence of effectiveness was available.
Perspective of the economic evaluation
As already stated, the perspective of the cost-effectiveness analysis is predominately that of the NHS; however, the out-of-pocket expenses on the OTC medications and equipment are also included. The out-of-pocket expenditures include softeners for all patients undergoing active treatments, bulb irrigators for patients choosing self-irrigation, and painkillers and antibiotics for those patients who had a SAE associated with irrigation. These cost items were added to the total cost of health-care resources associated with the treatment of earwax. However, out-of-pocket expenses are relatively small in comparison with the cost of resources used at primary and secondary care in the treatment of earwax.
Outcomes
Results of the model are reported as incremental costs and incremental benefits in terms of successful removal of earwax and additional quality-adjusted life-years (QALYs), and the incremental cost-effectiveness ratio (ICER) calculated with respect to ‘no treatment’.
Methods of the economic evaluation
Model structure
This section describes in detail the clinical pathways associated with each active treatment alternative introduced in Chapter 5 (SHTAC economic analysis) above. Figure 1 presents the structure of the model.
In the base-case scenario it was assumed that patients in each of the active treatments follow a GP’s advice to apply softeners for 1 week. The use of softeners has two advantages: first, the softeners assist any subsequent irrigation by softening earwax and, second, they facilitate a spontaneous earwax clearance in some patients, after which no irrigation is required. Use of softeners is considered to be the first line of treatment followed by irrigation as the second line of treatment. Finally, if the earwax is still not removed after three rounds of applying softeners and syringing, patients may be referred to secondary care for removal of earwax by a specialist otolaryngologist (OTL). In the first active treatment alternative (current or standard practice), patients presenting at primary care for earwax treatment are initially assessed by a GP (assumption used in the base-case analysis) or a nurse (a scenario analysis); they are advised to use olive oil or sodium bicarbonate for a week and if spontaneous earwax clearance does not occur then return to the practice for irrigation. The irrigation is administered by a practice nurse using an electric irrigator.
FIGURE 1.
The structure of the economic model of earwax treatment alternatives; OLT, otolaryngologist, a specialist doctor providing treatment at secondary care; SAE, serious adverse event.
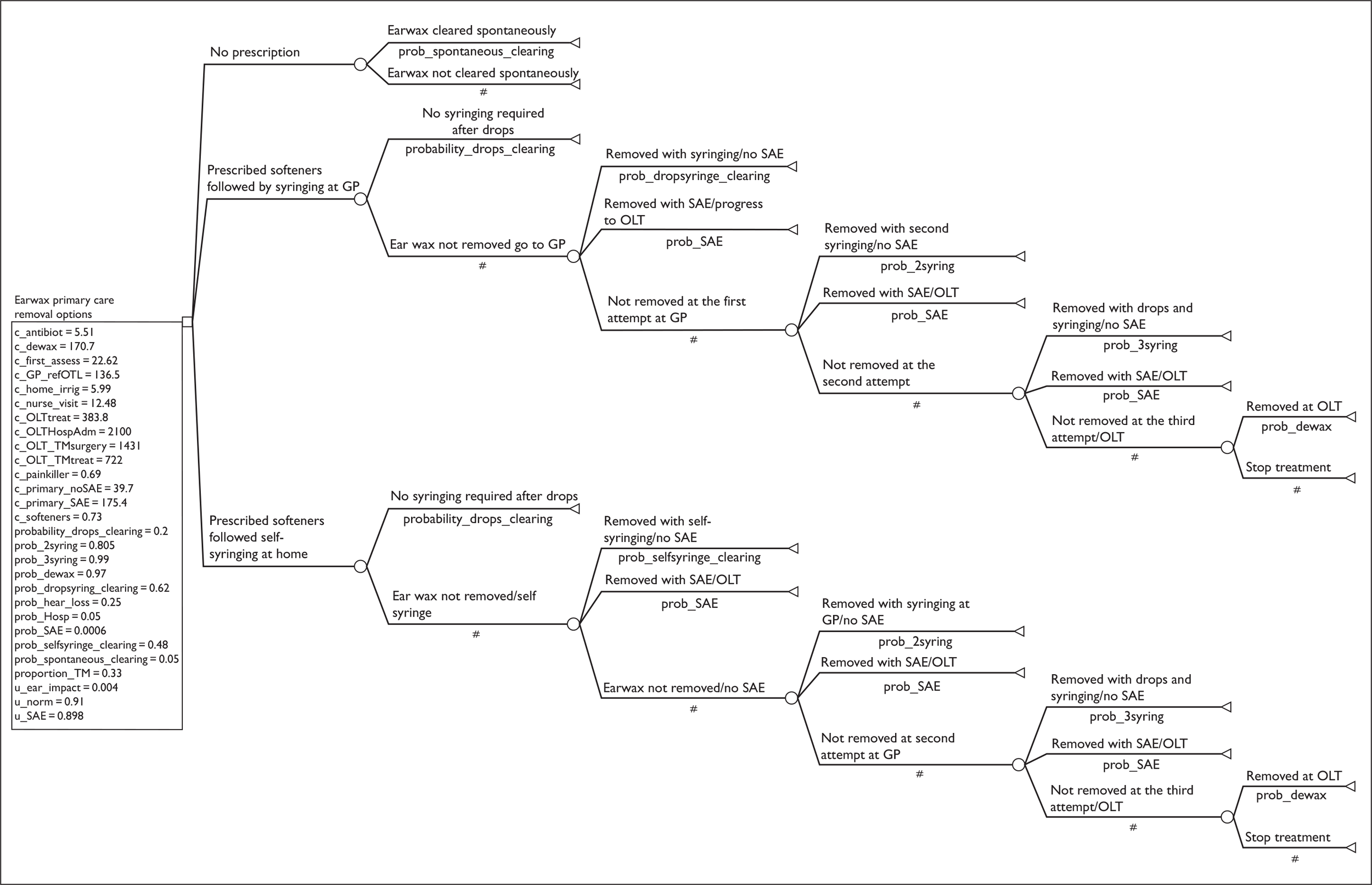
Alternatively, in the second active treatment option, patients may be advised to apply softeners for a week, and if spontaneous earwax clearance has not occurred they should proceed with self-irrigation using a bulb irrigator, which is available from chemists. Patients for whom self-irrigation does not result in earwax removal return to primary care for a second irrigation. Unlike the first irrigation, the second and third irrigations are administered professionally by a practice nurse using an electric irrigator. The second (and the third, if required) irrigation attempts do not require prior assessment by a GP.
The base-case scenario includes both active treatment alternatives, as well as a conventional ‘no treatment’ comparator.
There are no data to estimate the proportion of patients given each of the treatment options; therefore for the purpose of an economic evaluation the treatment strategies listed above represent the decision choices available for GPs and their patients.
Assumptions used in the model
The economic evaluation does not differentiate between patients who present with one or both ears occluded. Although this is a simplifying assumption, there were no reliable data that would allow differentiation of the outcomes with respect to unilateral or bilateral presentation of earwax.
While there is a non-zero probability of experiencing spontaneous earwax clearance associated with the first application of softeners, it is not the case for severely impacted and hardened earwax. In such instances, spontaneous earwax clearance assisted by softeners is unlikely to occur. Severely occluding and/or hardened earwax may not even be successfully removed at the first irrigation attempt at primary care and will require a second, and sometimes third, round of using softeners followed by irrigation in primary care. In such instances it is assumed that the use of drops merely facilitates the next professionally administered irrigation attempt, and is not associated with the probability of achieving a spontaneous earwax clearance.
If the first irrigation attempt was unsuccessful, the probability of a successful earwax removal at the second and the third irrigation attempt at primary care would not depend on whether the first irrigation was administered by a practice nurse or the patients themselves.
Most patients achieve the desired outcome (earwax removal) without a SAE associated with irrigation. It is assumed that the use of softeners alone as well as the ‘do nothing’ option are not associated with a SAE. In the base-case scenario the probability of a SAE is assumed to be the same regardless of the mode of irrigation (self-irrigation or administered by a practice nurse) and whether irrigation is undertaken for the first, second or the third time.
The published clinical evidence used to populate the model4,63 does not report an incidence of SAEs. However, the occurrence of a SAE was viewed as a clinically important factor, which can also affect the results of an economic evaluation. By including the likelihood of a SAE in the model we have effectively reduced the benefits that occur following successful removal of earwax. 4,63
As there are no published estimates of the incidence of SAEs associated with irrigation, an expert OTL’s opinion was obtained. The probability estimate of having a SAE as a result of irrigation was based on the observed rate of presentation to secondary care for treatment of a TM puncture/rupture or a serious ear infection. The corresponding assumption used in the model is that all the SAE patients are referred and treated at secondary care. However, it is possible that some patients with a TM puncture/rupture or a serious ear infection are monitored and treated by their GPs. If this is the case the estimate used in the model is an underestimate.
The patients who had a SAE associated with irrigation (typically a TM perforation or an infection) experience pain and discomfort. However, following the experts’ advice it was assumed that after 1 week the pain subsides and in 2 weeks most patients experience a spontaneous healing of a TM or resolution of a serious ear infection.
As discussed in Chapter 3, irrigation is a fairly safe procedure, with only a small proportion of patients experiencing minor complications such as superficial erythema and dizziness. Minor complications are assumed to be short-lasting and not significant enough to be associated with a measurable decrease in HRQoL or an additional use of health-care resources. Therefore, the minor complications are not included in the modelled economic evaluation. There is paucity of evidence on the incidence of more serious and possibly lasting complications such as tinnitus. These are not included in the modelled economic evaluation.
Apart from the temporary loss of hearing in the affected ear(s), there are a few other symptoms such as aural fullness, vertigo, itching and tinnitus that affect HRQoL of patients being treated for earwax problems. However, there are no published estimates of utility values associated with symptoms other than loss of hearing. Therefore, the estimated loss of utility for the model is limited to the loss of hearing that was applied to all patients until the earwax is cleared. In addition, utility decrements are applied to patients who experienced a SAE that involves both loss of hearing and pain.
Model type and characteristics
We developed an economic model of treatment alternatives for a single event of earwax removal. A deterministic decision tree (Figure 1) analysis was conducted, focusing on binary outcomes representing earwax that was removed or not removed, with results expressed as incremental cost per patient with earwax safely removed. Analysis also incorporated loss of utility associated with temporary loss of hearing due to occlusion, and for pain and loss of hearing due to a SAE, with results presented as incremental cost per QALY. The base-case analysis was conducted in a population aged 35–44 years, with the corresponding age-adjusted utility value of 0.91 (Kind and colleagues77).
Results of the deterministic decision-analytical model in terms of QALYs were extrapolated to a lifetime horizon (45 years) using an excel spreadsheet. The major assumption in these calculations was that, according to clinical experts, the recurrence rate of earwax is 0.35, which is close to one episode occurring every 3 years or 15 single presentations over the assumed time horizon. The age-specific utility values were used for the estimated effects (QALYs)77 as the cohort, aged 35 years at the baseline, was progressing through the different age categories. Both costs and outcomes were discounted using a 3.5% discounting rate. The calculations also take the UK age-adjusted annual mortality rate into account. Although the assumption of no treatment over this period of time is unlikely to be realistic, the no treatment alternative is included in the analysis for the purpose of maintaining consistency across all stages of an economic analysis. Table 25 presents characteristics of the decision-tree model and the lifetime extrapolation.
| Type of the model | Treatment alternatives/pathways | Outcome | Time horizon | Discounting |
|---|---|---|---|---|
| Deterministic decision tree |
No treatment Softeners followed by self-irrigation Softeners followed by irrigation administered by a practice nurse |
Binary outcome ‘earwax removed’ (yes/no) | 7 weeksa | Not applicable |
| Deterministic decision tree |
No treatment Softeners followed by self-irrigation Softeners followed by irrigation administered by a practice nurse |
QALY | 7 weeksa | Not applicable |
| excel model with interactive inputs from the deterministic decision treeb |
No treatment Softeners followed by self-irrigation Softeners followed by irrigation administered by a practice nurse |
QALY | Lifetime (until the baseline cohort of 35-year-olds reaches the age of 80) | 3.5% applied to both costs and outcomes |
Assessment of uncertainty (sensitivity analysis)
A deterministic sensitivity analysis was used to address particular areas of uncertainty in the model. We investigated the uncertainties around the probability estimates that were expected, a priori, to have a disproportionate impact on the study results.
Scenario analysis was used to address the uncertainty associated with some aspects of the chosen structure of the model.
Parameter uncertainty is addressed using probabilistic sensitivity analysis (PSA). Probability distributions are assigned to the point estimates used in the base-case analysis. The point estimates for treatment effects are reported in Tables 26 and 27.
| Treatment alternatives including ‘no treatment’ option | Probability of earwax removed (range used in the sensitivity analysis)a | Source | Comments |
|---|---|---|---|
| No treatment (spontaneous earwax removal) | 0.05 (0.035–0.065) | bKeane and colleagues, 19954 | The outcomes were assessed on an ordinal scale with three categories: ‘impacted’, ‘moderately clear’ and ‘completely clear’. The model outcome ‘earwax removed’ corresponds to the ‘completely clear’ (of wax) outcome in Keane and colleagues4 |
| Use of softeners preceding irrigation at primary care | 0.20 (0.14–0.26) | bKeane and colleagues, 19954 | |
| Softeners followed by self-irrigation | 0.48 (0.34–0.62) | Coppin and colleagues, 200763 | The outcomes were initially assessed on an ordinal 4-point scale assessing the degree of obstruction of the membrane (see Chapter 3, Research in progress). Coppin and colleagues63 reported a binary outcome of the degree of wax clearance. The model outcome ‘earwax removed’ corresponds to the combined scores of 0 (no or minimum wax with TM fully visible) and 1 (minor amount of wax with TM essentially visible) |
| Softeners followed by irrigation administered by nurse at primary care | 0.62c (0.43–0.81) | Coppin and colleagues, 200763 | |
| Second irrigation – at primary care | 0.805 (0.69–0.91) | Linear extrapolation | |
| Third irrigation – at primary care | 0.99 (0.95–1.0) | Expert advice | Remaining patients assumed to undergo de-waxing in secondary care |
| Successful de-waxing at secondary care without SAE | 0.97 (0.8–1.0) | Pothier and colleagues, 200656 |
| Event/treatment | Probability of event/treatment (range used in sensitivity analysis) | Source | Comments |
|---|---|---|---|
| SAE associated with irrigation administered by nurse at primary care | 0.0006 (0.0003–0.0009) | Expert advice |
The base-case estimate is based on 11 SAEs observed in secondary care, servicing the population of 300,000a The upper limit in the range is based on 18 SAEs observed annually in secondary care, servicing a population of 280,000a |
| SAE associated with self-irrigation | 0.0006 (0.0003–0.0009) | Expert advice | Assumed to be the same as the probability of SAE in primary care |
| Hospital admission for either myringoplasty or treatment of a serious infection | 0.05 (0.035–0.065) | Expert advice | |
| Probability of partial permanent hearing loss if myringoplasty is only partially successful | 0.25 (0.18–0.33) | Expert advice | |
| Proportion of patients with TM perforation in the total number of patients with SAE | 0.333 (0.23–0.43) | Expert advice | There are two types of SAE: a TM perforation and a serious ear infection. These SAEs differ with respect to treatment pathways and costs |
The purpose of this analysis was to test the robustness of the cost-effectiveness results to variation in structural assumptions and parameter inputs.
Data sources used in the model
This section of the report describes the inputs to the model, provides justification for their use, details their respective sources and explains their role in the model. The data used in the model have been collected from a variety of sources, chosen on the basis of appropriateness to the UK and the quality of the data as assessed by the reviewers and in consultation with clinical experts.
Clinical effectiveness data
As can be seen in Chapter 3, there is limited clinical effectiveness data available for the model. Two studies can be used: one study of the use of softeners alone by Keane and colleagues,4 which involved a ‘no treatment’ comparator, and one study by Coppin and colleagues,63 which compared self-irrigation with irrigation in primary care and estimated patient-relevant outcomes. Other estimates are from clinical evidence and experts’ advice, which suggests that earwax is eventually resolved in the majority of patients. Therefore, in the base-case analysis both active treatment arms are associated with a very high probability of successful earwax removal. Table 26 presents probability estimates of clinical effectiveness and Table 27 presents probabilities associated with a SAE used in the model.
Health states/utilities
A systematic literature search did not result in any published estimates of utility loss due to symptomatic earwax. As discussed in Chapter 5 (Assumptions used in the model), reduction in the quality of life associated with the range of symptoms caused by impacted earwax is limited to the loss of hearing and, for the small proportion of patients experiencing SAE, to the loss of hearing and pain. A targeted literature search identified some published utility decrements associated with the loss of hearing due to reasons other than symptomatic earwax. Table 28 presents the results.
| Source | Characteristics of the population | Method | Disutility value (standard error) | Degree of the hearing loss | Comments |
|---|---|---|---|---|---|
| Sullivan and Ghushchyan, 200678 |
N = 320; USA patients with the ICD-9-CM 389 conditiona |
SF-12 converted into EQ-5D | 0.006 (0.0001) | As defined by the ICD-9-CM diagnosis code 389 | The disutility estimate represents the marginal decrement in EQ-5D index scores after controlling for age, comorbidity, gender, race ethnicity income and education |
| Barton and colleagues, 200479 |
N = 609 UK patients with mean age of 68.4 who are eligible for a hearing aid |
HUI3, SF-6D and EQ-5D | 0.06,b 0.014,b 0.005,b respectively | Not reported |
One study78 reports utility decrement of 0.006 derived from patients with a range of conditions that result in mild to severe hearing loss [International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) diagnosis code 389], which can be used for an estimate of temporary hearing loss. The other study79 reports a utility gain associated with hearing improvement due to provision of a hearing aid. In this study the mean postintervention changes in European Quality of Life-5 Dimensions (EQ-5D) and Short Form-6 Dimensions (SF-6D) were similar, although the change in mean utility scores assessed by EQ-5D was not statistically different from zero. The mean utility score assessed by Health Utilities Index (HUI)3 demonstrated a significantly higher improvement of 0.06. As there is only a limited understanding of the degree of hearing loss associated with symptomatic earwax, it is not certain whether the estimates of utility gain due to the provision of hearing aid is comparable with the utility gain associated with earwax removal.
Table 29 shows the utility values used in the model for each health state in the cohort of 35- to 44-year-old patients presented at baseline with earwax. The age-specific population norm for the cohort of 35- to 44-year-old patients is 0.91. 77 In the base-case analysis the disutility value of 0.006 for the loss of hearing and the disutility value of 0.012 for the duration of SAE were used as, according to expert opinion, these estimates correspond to the loss of quality of life associated with symptomatic earwax. It should be noted that the experts were informed of the disutility value when asked to estimate the impact of a SAE on utility; therefore, this value was not obtained independent of the 0.006 disutility. The HUI3 value reported in the study of Barton and colleagues79 was used in the scenario analysis.
| Health state | Utility | Source | Time interval to which utility applies |
|---|---|---|---|
| Earwax causing temporary loss of hearing | 0.904 | Sullivan and Ghushchyan, 200678 | From the baseline and until earwax is removed and hearing restored |
| Earwax removed/hearing restored | 0.910 | Kind and colleagues, 199977 | Applies at the point of a successful earwax removal and until the exit from the model |
| SAE (serious infection and TM perforation) | 0.898 | Expert advice | Applies for 2 weeks from the SAE onset |
| Permanent slight loss of hearing as a result of TM perforation | 0.904 | Assumption | Applies for life to the 25% of patients for whom myringoplasty was not completely successful |
Assuming that the life expectancy of a person of 35 years of age is 45 years, the disutility value of 0.006,78 if assessed using the time trade-off method, would correspond to a half year of life traded for the symptomatic earwax being removed. By implication the disutility value of 0.0679 would correspond to 5 years of life traded for living without symptomatic earwax.
Resource use and cost data
As the analysis reflects an NHS perspective, UK specific resource use and costing data have been used where available. Cost data were obtained from a number of primary and secondary sources.
Table 30 shows categories of health-care resource use, the amount used, the unit prices and the associated cost of earwax presentation at primary care.
| Resource | Amount used | Unit cost (£) (2006–7 prices) | Source | Cost (£) |
|---|---|---|---|---|
| Pharmaceuticals (not NHS cost borne by patients) | ||||
| Softeners – olive oil | 10 ml | 0.73 | NHS electronic drug tariffa | 0.73 |
| Equipment and consumables | ||||
| Electric irrigator (Propulse III) used for irrigation at primary care | 1 item | 78.99 (excluding VAT) | www.medisave.co.uk/instruments-ear-syringe-c-240 241.html (price was valid until September 2008) | 2 × 78.99/2000 = 0.08a |
| Cleansing tablets for electric irrigator (assuming the machine is cleaned after each application) | 1 pack × 200 | 20 (including postage) | Expert advice (based on the actual primary care practice expenditures) | 20/200 = 0.1 |
| Cost of annual services of an irrigator | Annually | 60 | Expert advice | 2 × 60/2000 = 0.06a |
| Disposable jet tips for an electric irrigator | 1 pack 100 | 44.00 | www.medisave.co.uk/instruments-ear-syringe-c-240 241.html | 44/100 = 0.44 |
| Otoscope (including bulbs) | 1 item | 319.00 | Expert advice (assumed 4 years of use) | 319/4000 = 0.08a |
| Disposable tips for an otoscope | 1 pack × 850 | 47.00 (including postage) | Expert advice | 47/850 = 0.056 |
| Head torch (including bulbs) | 1 item | 60 | Expert advice (assumed to be replaced annually) | 60/1000 = 0.06 |
| Other disposable and non-disposable equipment (e.g. Noots Tank, Propulse reservoir, Jobson-Horne probe, capes) | Various | N/A | Uppal and colleagues80 (adjusted for 2006/07 prices) | 2.12 |
| (A) Subtotal: equipment and consumables | 3.00 | |||
| Staff cost | ||||
| GP consultation (primary assessment) | 5 minutes | 2.90 per minute | PSSRU,81 expert advice | 14.50 |
| (B) GP consultation + 20% clinical staff overhead 80 | 17.40 | |||
| GP SAE – related consultation (referral to secondary care) | 15 minutes | 2.90 per minute | PSSRU,81 expert advice | 43.50 |
| (C) GP SAE – related consultation + 20% clinical staff overhead 80 | 52.2 | |||
| Practice nurse consultation | 15 minutes | 0.383 per minute | PSSRU,81 expert advice | 8.00 |
| (D) Practice nurse consultation + 20% clinical staff overheads 80 | 9.6 | |||
| Subtotal | ||||
| Direct clinical cost of GP initial assessment | 17.40 | |||
| Direct clinical cost of GP referral and follow-up (used in self-irrigation with SAE) | 52.2 × 2 = 104.4 | |||
| Direct clinical cost of nurse session (used in the second and third irrigation episode) | 9.6 | |||
| Direct clinical cost of earwax treatment without SAE | 30.0 = [(A) + (B) + (D)] | |||
| Direct clinical cost of earwax treatment with SAE | 134.4 = [(A) + (B) + (D) + 2 × (C)] | |||
| Total costs (direct, indirect and private patient costs)a | ||||
| Cost of GP assessment | 22.62 | |||
| GP referral and follow-up only (used in self-irrigation-related SAE) | 136.45b | |||
| Nurse session (used in the second and third irrigation) | 12.48 | |||
| Earwax treatment without SAE | 39.70b | |||
| Earwax treatment with SAE (includes one GP referral one follow-up) | 175.40b | |||
The following assumptions were made in calculating the costs:
-
With respect to the cost of electric irrigator per patient (£0.08), the estimated annual number of patients presenting with earwax problems at the typical primary care practice was assumed to be about 1000. This was based on the mean number of three presentations per day. It was assumed that two electronic irrigators in use in the typical primary care practice (2 × £78.99) are replaced every 2 years during which time about 2000 patients are treated for earwax.
-
With respect to the cost of a nurse consultation (an ear irrigation session), the estimated average nurse time is an arithmetic mean between 10 minutes that are typically spent on irrigating one ear and 20 minutes spent on irrigating both ears. See Chapter 5 (Assumptions used in the model), which outlines assumptions of the model.
Different cost components are used in the model depending on the treatment option and the patients’ progression along the alternative treatment pathways as depicted in the decision tree (Figure 1). The ‘no prescription’ option is associated only with the cost of an initial assessment conducted either by a GP (base-case analysis) or a nurse (scenario analysis). Treatment of patients who applied softeners following consultation at the primary care practice and achieved a spontaneous earwax removal is associated with the cost of initial assessment and the cost of softeners (e.g. £22.62 + £0.73 = £23.35). Those patients who achieve clearance following a single professional irrigation at primary care incur the cost of the initial assessment, the softener cost and the cost of the irrigation administered by a practice nurse (£39.70 = earwax treatment without SAE in Table 30). Those patients suffering an AE incur, in addition to the above costs, a GP consultation in order to refer the patient to secondary care (OTL) and a follow-up consultation (£175.40 = earwax treatment with SAE in Table 30). Both consultations are assumed to take 15 minutes of GP time. The exact same costing process is followed for the second and third attempts at syringing in primary care, if required.
Table 31 shows the category of health-care resources associated with self-irrigation at home. Patients self-irrigating at home incur the cost of an initial consultation in primary care, the cost of softeners and a bulb irrigator. For those patients experiencing spontaneous clearing of earwax the costs include the cost of initial assessment and the cost of softeners only. Patients who are not successful at self-irrigation are assumed to present at primary care for the second and, if necessary, third irrigation that is administered by a practice nurse. Subsequent costs are incurred as per the option for attending primary care for syringing.
| Resource | Amount used | Unit cost (£) (2006–7 prices) | Source | Cost (£) |
|---|---|---|---|---|
| GP consultation (primary assessment) | ||||
| GP consultation including 20% staff overheads and 30% indirect cost | 5 minutes | 2.90 per minute | PSSRU, expert advice | 22.62 |
| Pharmaceuticals | ||||
| Softeners – olive oil | 10 ml | 0.73 | NHS electronic drug tariffa | 0.73 |
| Equipment | ||||
| Bulb irrigator (25 ml) | 1 itemb | 5.99 | Online costc | 5.99 |
| Total cost of earwax self-irrigation | 22.62 + 0.73 + 5.99 = 29.34 | |||
Table 32 shows the health-care resources used for dewaxing and treating SAE in secondary care.
Patients presenting at secondary care for treatment-related SAEs incur additional costs. As discussed above, two categories of SAE were included in the economic evaluation: TM perforation and serious infection. Following expert advice, all patients with SAEs experience pain and need to use painkillers for 1 week, incurring the associated cost. In addition, all patients with serious infection are prescribed antibiotics for 2 weeks, incurring the cost.
| Resource | Amount used | Unit cost (£) (2006–7 prices) | Source | Total cost (£) (comments) |
|---|---|---|---|---|
| Pharmaceuticals | ||||
| Analgesics, paracetamol 500 mg | 32 tablets | 0.69 | NHS electronic drug tariffa | 0.69 (applied to 100% of TM perforation patients assuming 1–2 tablets, 3 times per day, for 7 days) |
| Antibiotics, ofloxacin 200 mg | 10 | 5.51 | NHS electronic drug tariffa | 5.51 (applied to 100% of serious infection patients) |
| Antibiotic/steroid ear drops –clioquinol 1%/flumetasone 0.02% | 7.5 ml | 1.47 | NHS electronic drug tariffa | 1.47 (applied to 18% of SAE patients whom Hussain82 used in scenario analysis) |
| Investigations | ||||
| The total cost of investigations, such as audiometry, ear swabs for culture and sensitivity | N/A | N/A | Uppal and colleagues80 (adjusted for 2006–7 prices) | 42.40 (applied to 100% of SAE patients) |
| The total cost of a new and the follow-up appointments | Various | N/A | Uppal and colleagues80 (adjusted for 2006–7 prices) | 170.7b (applied to 100% of SAE patients) |
| Myringoplasty = minor ear procedure without CC (day case CZ08Y) | N/A | 705 | DHSc | 705 (applied to 5% of SAE patients in the model who were referred to OTL) |
| Hospital admission for a serious infection treatment = intermediate ear procedure without CC | 1377 | DHSc | 1377 (applied to 5% of SAE patients in the model patients who were referred to OTL) | |
| Total cost of OTL treatment | ||||
| De-waxing without a SAE | 170.7 | |||
| Treatment of serious infection without hospital admissiond | 42.4 + (2 × 170.7) + 5.51 + (0.18 × 1.47) = 389.57 | |||
| Treatment of serious infection with hospital admission | 42.4 + (2 × 170.7) + 1377 + 5.51 + (0.18 × 1.47) = 1766.57 | |||
| Treatment of TM perforation without surgeryd | 42.4 + (4 × 170.7) + 0.69 = 725.89 | |||
| Treatment of TM perforation with surgery | 42.4 + (4 × 170.7) + 705 + 0.69 = 1430.89 | |||
Treatment for SAEs by an OTL consists of initial and follow-up appointments, with a series of investigations (Table 32). Those treated on an outpatient basis require either two presentations for treatment of TM or four presentations for treatment of a serious infection. Those patients requiring hospital admission (5% of those referred to the OTL) for myringoplasty (surgical treatment of TM perforation) require on average either a day-case admission or an overnight admission, while a serious ear infection requires, on average, a 2-day hospital admission (expert opinion). The total secondary care cost of treating a TM perforation without admission is higher than that for a serious infection. In contrast, if a patient is admitted to hospital the cost of treatment of a serious infection becomes more expensive than for a TM perforation.
Base-case results of a single presentation model
Results of the base-case deterministic decision analysis of alternative approaches to earwax removal are presented in Table 33. The results are reported in terms of incremental costs and incremental gains: a gain in likelihood of earwax being successfully removed and additional QALYs. Table 33 shows results of the base-case analysis using a deterministic decision-analytic model with a 7-week time horizon. The ICER is calculated with respect to the conventional comparator ‘no treatment’.
| Treatment alternative | Cost (£) (2006–7 prices) | Probability of earwax being removed at the end of the seventh week | Incremental cost per successfully treated patienta | QALYs | Incremental cost per QALY (ICER)a |
|---|---|---|---|---|---|
| No treatment | 22.62 | 0.05 | – | 0.121727 | – |
| Softeners followed by self-irrigation | 37.28 | 0.999977 | 14.66 | 0.122327 | 24,433 |
| Softeners followed by irrigation at primary care | 42.38 | 0.999983 | 19.76 | 0.122342 | 32,130 |
In comparison with the ‘no treatment’ option, the additional cost of successful treatment of a patient with an earwax problem is £14.66 for the alternative beginning with the use of softeners and self-irrigation, and £19.76 for the alternative beginning with the use of softeners followed by irrigation at primary care. However, when two active treatment options are compared, the incremental cost of treating an additional patient with softeners followed by professional irrigation, as opposed to treating with a combination of softeners and self-irrigation, is about £850,000 per successful earwax removal. With the additional QALY gain of only 0.000015, this gives an ICER of £340,000 per QALY. This is because the additional gain associated with the option of softeners followed by irrigation at primary care is small, at 0.000006, or 6 additional patients in every 1,000,000 patients treated for earwax problems.
Both active treatment alternatives are associated with a very high probability of achieving an outcome (i.e. earwax removal), which, for all practical purposes, is not different from 1.0 (i.e. virtual certainty). Therefore, the above results can be interpreted within a cost-minimisation framework, which demonstrated that the same outcome can be achieved at a lesser cost if patients use softeners first, followed by self-irrigation, and present at primary care only if self-irrigation did not result in earwax removal. However, as further discussed in Chapter 7, the self-irrigation alternative may not be appropriate for every patient presenting at primary care with an earwax problem.
Although it was assumed in the base-case scenario that the probability of SAE in both active treatment alternatives is the same, there was no published clinical evidence to support this assumption. Neither was there consensus between the experts who provided feedback on the results of this study. Some clinical experts consider self-irrigation using a soft rubber bulb irrigator to be a completely safe alternative to the current practice involving professional irrigation. However, one expert advised that although a TM puncture is unlikely to occur when a soft rubber bulb irrigator is used, self-irrigation may not necessarily exclude the probability of having a SAE, such as displacing the ear drum and exerting traumatic pressure on the inner ear.
Two principal factors contributed to the base-case results: the difference in the estimated clinical effectiveness between the two active treatment options as reported by Coppin and colleagues63 (0.42 versus 0.68) and a small incremental gain in terms of QALYs. This was not surprising, given that in the base-case analysis the size of the disutility associated with hearing loss was only 0.006. 78 These and other parameter uncertainties are explored in the univariate and bivariate sensitivity analyses reported in Chapter 5 (Deterministic sensitivity analysis).
Lifetime extrapolation of results of a single presentation modelling
Table 34 shows the results of the lifetime extrapolation of the outcomes of the modelling of a single presentation with an earwax problem in 2006–7 prices.
| Treatment alternatives | No treatment | Softeners followed by self-irrigation | Softeners followed by irrigation at primary care |
|---|---|---|---|
| Total discounted cost (£)a | 178.85 | 294.84 | 335.17 |
| Total discounted QALYsa | 20.671636 | 20.676380 | 20.676500 |
| Incremental cost (£)b | – | 115.99 | 156.32 |
| Incremental effectb | – | 0.004744 | 0.004864 |
| ICER (£/QALY)b | £24,450 | £32,136 |
In comparison with no treatment, the difference in total discounted cost over 45 years is £116 for the treatment alternative involving self-irrigation and £156 for the treatment alternative involving professional irrigation. The corresponding discounted QALY gains are 0.004744 and 0.004864 for self-irrigation and the professional irrigation treatment alternatives, respectively. This translates into the estimated ICER of about £24,450 per QALY for the treatment alternative involving self-irrigation and £32,136 per QALY for the treatment alternative involving professional irrigation. The slight difference between base-case results and lifetime model results is due to rounding error in the very small effect differences between the three treatment pathways. When two active treatments are compared with each other the incremental cost of £40.30 and incremental QALY of 0.0001202 resulted in the ICER of more than £335,000.
Deterministic sensitivity analysis
Table 35 shows the variables that were included in the sensitivity analyses.
| Variable(s) | Base-case point estimate (range tested in the sensitivity analysis) | Type of analysis |
|---|---|---|
| 1. Probability of SAE associated with self-irrigation was varied | 0.0006 (0.0006–0.059) | Bivariate threshold analysis to identify the SAE value associated with softeners and self-irrigation being dominated by softeners and irrigation at primary care |
| 2.Clinical effectiveness of self-syringing | 0.48 (0.15–0.25) | Threshold analysis to identify the clinical effectiveness values associated with softeners and self-irrigation being dominated by softeners and irrigation at primary care |
| 3. Clinical effectiveness of irrigation at primary care | 0.62 (0.60–95) | Threshold analysis to identify the clinical effectiveness values associated with softeners and self-irrigation being dominated by softeners and irrigation at primary care |
| 4. Clinical effectiveness of softeners | 0.2 (0.01–0.5) | Univariate analysis |
| 5. Cost of self-irrigation (including softeners) | 6.72 (2.00–9.00) | Univariate analysis |
-
In the first sensitivity analysis the rate of AEs associated with irrigation administered by a practice nurse at primary care was kept at the same level as in the base-case analysis, while the rate of SAE associated with self-irrigation was increased until it reached the level at which the treatment alternative of softeners followed by irrigation at primary care became more cost-effective in terms of QALYs.
-
In the second sensitivity analysis both clinical effectiveness estimates associated with active treatments were altered, with the clinical effectiveness of self-irrigation decreasing and irrigation administered by a practice nurse increasing until the combination of the parameter values reached the level at which the alternative associated with self-irrigation was dominated by softeners followed by irrigation administered by a practice nurse at primary care.
-
In the remaining sensitivity analyses the model parameters were varied as indicated in Table 35.
Table 36 shows results of the sensitivity analyses.
| Parameter(s) tested | Parameter value(s) (base-case parameter-value) | Cost per successfully treated patient (£/successful earwax removal)a | QALYs gained per successfully treated patient | Incremental cost per QALY (ICER) (£/QALY)a | |||
|---|---|---|---|---|---|---|---|
| Softeners followed by self-irrigation | Softeners followed by irrigation at primary care | Softeners followed by self-irrigation | Softeners followed by irrigation at primary care | Softeners followed by self-irrigation | Softeners followed by irrigation at primary care | ||
| Base-case results | 14.66 | 19.76 | 0.122327 | 0.122342 | 24,433 | 32,130 | |
| 1. The threshold analysis of SAE associated with self-irrigationb |
0.00596 (0.0006) |
19.19 | 19.76 | 0.122324 | 0.122342 | 32,144 | 32,130 |
| 2.The threshold analysis of clinical effectiveness of self-irrigation | 0.25 (0.48) | 18.56 | 19.76 | 0.122301 | 0.122342 | 32,334 | 32,130 |
| 3. The threshold analysis of clinical effectiveness of irrigation at primary care | 0.92 (0.62) | 14.66 | 15.78 | 0.122327 | 0.122376 | 24,433 | 24,314 |
| 4. Clinical effectiveness of softeners | 0.01–0.5 (0.2) | 17.97–9.44 | 24.29–12.63 | 0.122313–0.122349 | 0.122332–0.122358 | 30,655–15,186 | 40,122–20,006 |
| 5. Cost of self-irrigation | £2.00– 9.00 (£5.99) | 11.47–17.07 | 19.76 | 0.122327–0.122327 | 0.122342–0.122342 | 19,119–28,455 | 32,130 |
The threshold analysis indicated that the results of a base-case scenario (a single event model) are robust to the small variations in the probability of SAE associated with self-irrigation. The probability of a SAE associated with self-irrigation needs to be increased approximately 10 times from the base-case value of 0.0006 to 0.00596 (while maintaining the probability of SAE associated with professional irrigation at the baseline level) before the treatment alternative associated with self-irrigation became dominated by the treatment alternative involving irrigation at primary care.
The threshold analysis indicated that the results are also robust with respect to the small variations in clinical effectiveness parameters (the probability of earwax removed). The cost of treatment involving self-irrigation remains less expensive, albeit fractionally less effective, until the probability of successful earwax removal using self-irrigation is decreased from 0.48 in the base case to 0.25 (ie. assumed to be two times less effective), while the probability of successful earwax removal using professional irrigation is increased from 0.62 to 0.92. When both extreme values are used in the base-case analysis, the treatment alternative involving self-irrigation is dominated by the treatment alternative involving irrigation at primary care.
Results of the one-way sensitivity analysis indicated that the outcomes are sensitive to the variation in the rate of successful earwax removal from the use of softeners. When the clinical effectiveness of the use of softeners increased from 0.01 to 0.5 the ICER decreased by about two times in both the active treatment arm in comparison to the ‘no treatment’ alternative. The ICER comparing softeners followed by irrigation at primary care remained unacceptably high when compared with treatment associated with self-irrigation (ICER = £329,098 per QALY at the value of clinical effectiveness of softeners equal to 0.5).
Results of the one-way sensitivity analysis indicated that the outcomes are not very sensitive to the variation in the cost of self-irrigation. When the cost was varied from £2.00 to £9.00 the ICER comparing treatment involving self-irrigation to no treatment changed from around £19,000 per QALY to almost £28,500 per QALY compared with the base-case estimate of ICER £24,433 per QALY. The ICER comparing softeners followed by irrigation at primary care remained unacceptably high when compared to treatment associated with self-irrigation (ICER = £534,933 per QALY at the cost of self-irrigation of £2; ICER = £173,819 per QALY at the cost of self-irrigation of £9.00).
Scenario analyses
Two scenario analyses were undertaken. In the first it was no longer assumed that a GP conducts the first assessment of patients presenting with an earwax problem; instead, the patients from all treatment arms were assessed by a nurse. In the second scenario analysis, as discussed in Chapter 5 (Health states/utilities) the estimate of a disutility value associated with the loss of hearing was taken from the study by Barton and colleagues,79 which used a HUI3 quality-of-life assessment tool.
By substituting a GP assessment cost with a nurse assessment cost, the total cost of earwax treatment without SAE at primary care decreased from £39.70 to £29.60. The latter estimate comprised the costs of softeners (£0.73) and initial assessment by a nurse (£12.48), followed by the cost of a professional irrigation session (£16.38). No changes in the GPs’ involvement in treating patients with SAE were assumed. Table 37 shows the results of this scenario analysis.
| Treatment alternative | Cost (£) (2006–7 prices) | Probability of earwax being removed at the end of the seventh week | Incremental cost per successfully treated patienta | QALYs | Incremental cost per QALY (ICER)a |
|---|---|---|---|---|---|
| No treatment | 12.48 | 0.05 | – | 0.121727 | – |
| Softeners followed by self-irrigation | 27.53 | 0.999977 | 15.05 | 0.122327 | 25,083 |
| Softeners followed by irrigation at primary care | 34.70 | 0.999983 | 22.22 | 0.122342 | 36,130 |
Reduction in the cost of assessment resulted in a reduction of the total cost of all treatment alternatives. However, the incremental costs in comparison with the ‘no treatment’ alternative have not changed significantly when translating into the ICER values, which are not substantially different from the base-case analysis results. When two active treatment options are compared, the estimated ICER is £462,670 per QALY, which is higher than the £340,000 per QALY in the base-case analysis. This is because the differences in cost between two active treatments increased from £5.10 in the base-case analysis to £7.17 in the scenario analysis, rendering the less expensive treatment strategy involving self-irrigation more cost-effective relative to strategy based solely on professional irrigation.
Table 38 shows the results of the second scenario analysis using the disutility values from Barton and colleagues. 79
| Treatment alternative | Cost (£) (2006–7 prices) | Probability of earwax being removed at the end of the seventh week | Incremental cost per successfully treated patienta | QALYs | Cost per QALY (ICER)a |
|---|---|---|---|---|---|
| No treatment | 22.62 | No change | – | 0.114769 | – |
| Softeners followed by self-irrigation | 37.28 | No change | No change | 0.120768 | 2444 |
| Softeners followed by irrigation at primary care | 42.38 | No change | No change | 0.120923 | 3211 |
When the disutility associated with the loss of hearing is assumed to be 0.06 (Barton and colleagues)79 or 10 times higher than the disutility estimate assumed in the base-case analysis, the ICER gained is substantially reduced for either of the active treatment alternatives when compared with no treatment. When these options are compared with each other the ICER is about £32,910 per QALY. The large difference between the ICER estimates in the base case and the scenario analysis is explained by the nature of the measurement instruments. Barton and colleagues79 commented that, unlike the EQ-5D, the HUI3 explicitly asks about a person’s capability to hear, and therefore it is not surprising that people with impaired hearing have lower levels of utility according to the HUI3 than according to the EQ-5D and SF-6D. Other studies on the clinical effectiveness and cost-effectiveness of digital hearing aids have identified similar differences. 83
Probabilistic sensitivity analysis
Table 39 reports the mean costs and outcomes from the PSA of results of a single presentation model. The PSA generated cost and QALY estimates for each active treatment alternative that were similar to those for the base-case analysis (see Table 33 for base-case analysis). Variables included in the PSA, distributions and parameters of distributions used can be seen in Appendix 7.
| Treatment alternative | Mean cost (£) | SD | Mean effects (QALY) | SD |
|---|---|---|---|---|
| No treatment | 22.62 | 2.3 | 0.121727 | 0.000014 |
| Softeners followed by self-irrigation | 37.20 | 2.6 | 0.122327 | 0.000011 |
| Softeners followed by irrigation at primary care | 42.30 | 3.6 | 0.122342 | 0.000009 |
Figure 2 shows the cost-effectiveness acceptability curves for all alternative treatments. The chart indicates the probability that a given treatment option is optimal compared with the alternatives. This suggests that a ‘no treatment’ option is a cost-effective option at lower threshold levels of willingness-to-pay for health outcomes (QALYs). At the threshold above £30,000 per QALY, the treatment involving self-irrigation becomes more likely an optimal option among the three alternative treatments. As the threshold is increased, softeners followed by irrigation at primary care is increasingly likely to be the optimal treatment alternative. At the threshold of about £330,000 per QALY both active treatment alternatives are equally likely to be optimal.
FIGURE 2.
Cost-effectiveness acceptability curves comparing no treatment, softeners followed by irrigation and softeners followed by self-irrigation.
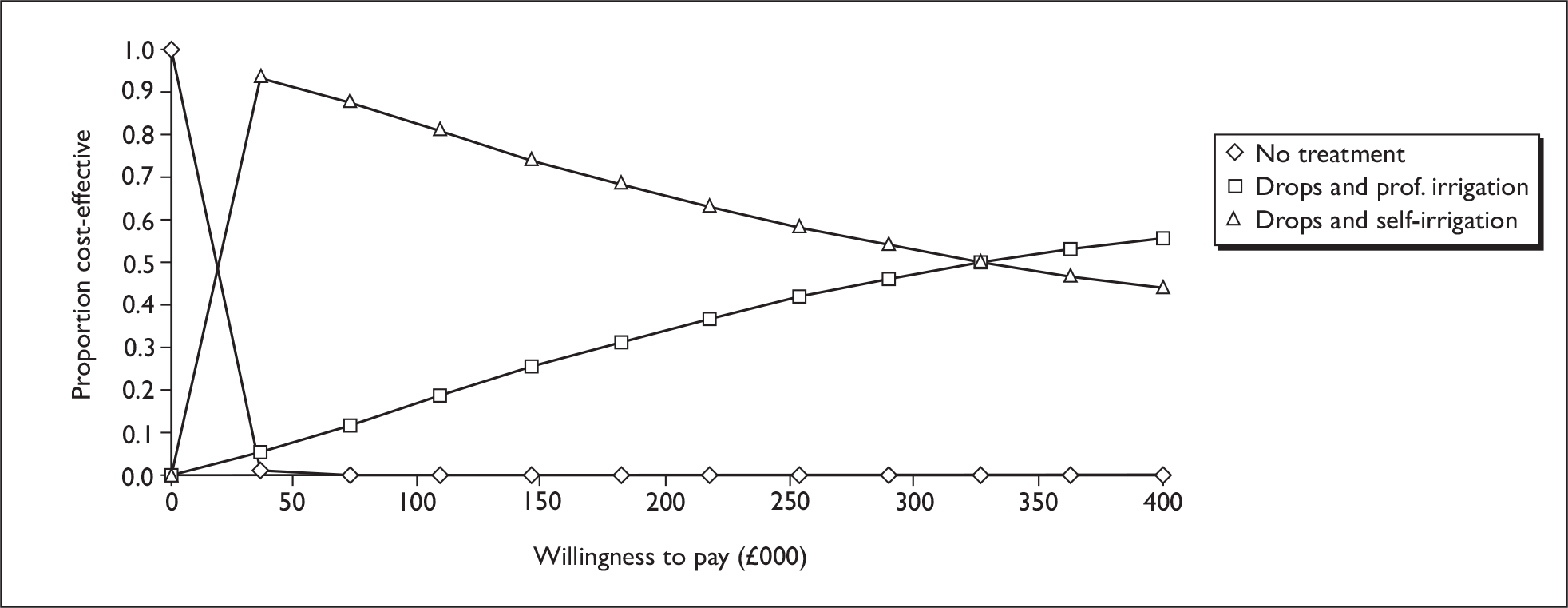
Summary of economic analysis
-
A systematic review of the literature found no existing economic evaluations that met the inclusion criteria of the review.
-
We developed a deterministic decision tree model from an NHS perspective to estimate comparative cost-effectiveness of treatment options for earwax following presentation at primary care. It focused on an adult population aged 35–44 years, with no contraindications to treatment options considered.
-
The decision tree model compares use of softeners for 1 week with return to the primary care practice for irrigation if no earwax clearance occurs (standard practice), use of softeners for 1 week followed by self-irrigation and return to primary care if unsuccessful for professional irrigation, and no treatment.
-
The structure and data inputs of the model were based on our systematic review of the literature on clinical effectiveness and cost-effectiveness of treatment, systematic searches on HRQoL and AEs associated with earwax and hearing loss, other published literature for costs, and consultation with clinical experts.
-
Results from the decision tree model were extrapolated over different time horizons to give an estimate of lifetime cost-effectiveness of treatment alternatives.
-
Base-case cost-effectiveness results suggest that the ICER for softeners followed by self-irrigation is about £24,400, and for softeners followed by irrigation at primary care it is about £32,100, compared with no treatment.
-
The ICER is over £340,000 when comparing the two active treatments as the additional gain associated with professional irrigation is very small, but at an additional cost.
-
The lifetime model ICERs are virtually the same as the base-case ICERs due to a constant recurrence rate of wax used in all three treatment pathways. The slight difference in base case and lifetime ICERs is due to rounding errors in the small effectiveness gains between treatment pathways. If there had been evidence that treatment reduced the frequency or likelihood of recurrence then the lifetime model would have been more informative.
-
Sensitivity analyses show results are mostly robust although outcomes are sensitive to variation in the rate of successful earwax removal from the use of softeners.
-
Scenario analyses show that results are not sensitive to reduced cost of irrigation in primary care, but are sensitive to changes in disutility value associated with loss of hearing.
-
Caution should be taken in interpreting the results of the economic evaluation. The paucity of evidence on the safety, benefits and costs of the different strategies necessitated the use of different assumptions developed from available evidence and expert advice. Uncertainty about the structure and inputs in the model brings into question the reliability of the results. With the focus on a selected population group (people aged 35–44 years with no contraindications) and the evaluation of an intervention which may only have relevance to a specific patient group, the findings may have limited applicability to the general population. As a consequence, the results of the economic evaluation should be regarded as exploratory and should not be used as a basis for changing policy and practice.
Chapter 6 Value of information analysis
Value of information analysis was used to help identify future research priorities. 84,85 Our first step was to calculate the population expected value of perfect information (PEVPI). This equates to the difference between the expected value of a decision based on perfect information and a decision based on currently available information. Calculating PEVPI provides a ‘preliminary screen’ with the purpose of eliminating research designs that have costs in excess of the PEVPI. In the event that no research designs were to pass this screening test further research investment would not be recommended.
For those research designs that do pass the initial screening test, the groups of parameters that may be investigated should be examined in terms of expected value of partial perfect information (EVPPI) for parameters. If the EVPPI exceeds the cost of the research design for a particular group of parameters, subsequent investment may be deemed worthwhile, whereas if the cost of a new study design exceeds the EVPPI then the additional research should not be undertaken. Both PEVPI and EVPPI are decision threshold specific, and will vary depending upon the health-care payer’s perspective of this threshold.
The analysis was conducted in the statistical package r. The decision tree model was replicated in r and code written to estimate the PEVPI and EVPPI. This acted as a technical validation of the original treeage model and facilitated reduced run times for the value of information analysis than could have been obtained with excel.
Figure 3 shows the PEVPI by decision threshold based on an annual population of 2 million67 and assuming that each patient is treated a mean of 1.25 times to achieve clearance. When the decision threshold is low the technology is not expected to be cost-effective and additional information is unlikely to change the decision. The PEVPI reaches a maximum when the threshold is equal to the ICER of the treatment options (the ICER for self-irrigation versus no treatment is £24k, whereas the ICER for GP irrigation versus self-irrigation is around £340k); that is where we are most uncertain about whether to adopt or reject the technology based on existing evidence. This analysis in Figure 3 assumes a 10-year lifespan of the technology.
FIGURE 3.
Population expected value of perfect information.
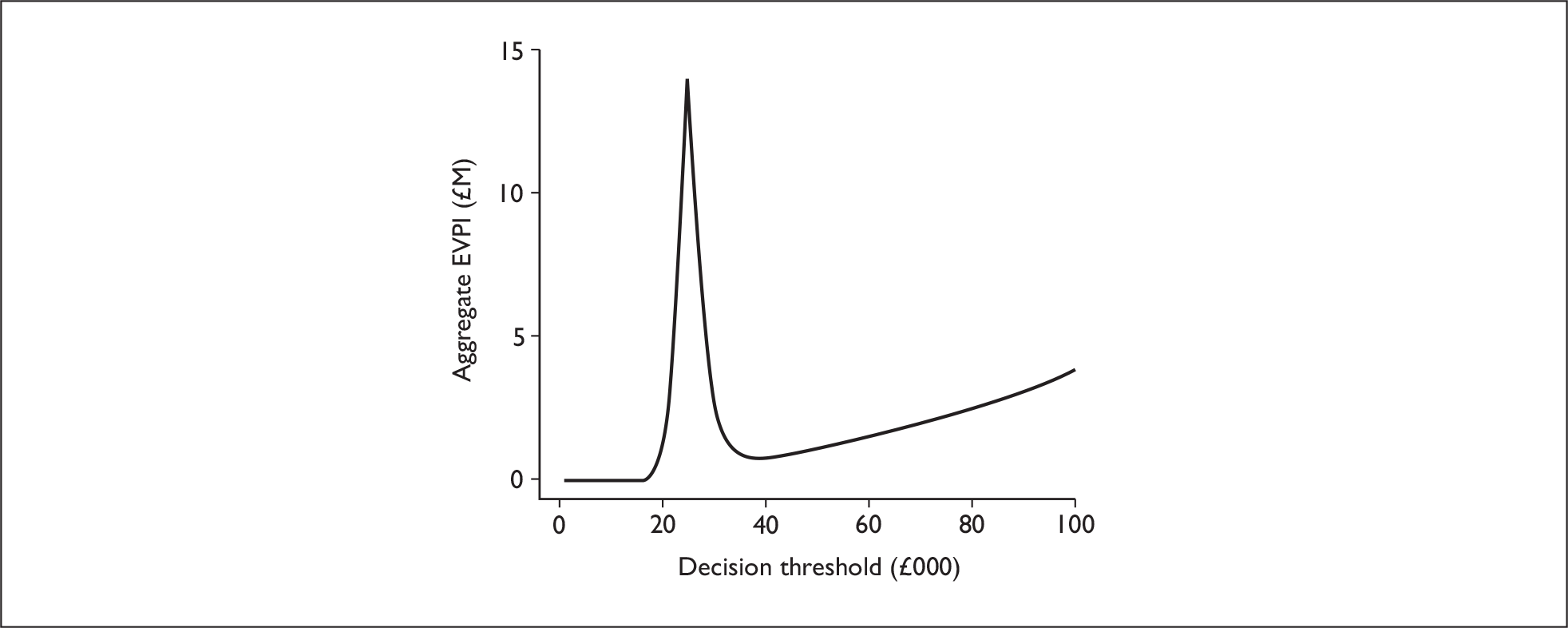
Figure 4 shows the PEVPI for a range of lifespan thresholds for the technology. These assume the technology will last for this period of time before a new technology comes along and replaces it. PEVPI is calculated as follows:
where T is the technology lifespan, r is the discount rate and I is the population incidence. The recent debate over the threshold to adopt for the lifespan of a technology is acknowledged,86 although a 10-year lifespan would seem a reasonable proxy for the estimation of uncertainty given the historical longevity of the technology revealed in the clinical effectiveness review. An alternative would have been to conduct an empirical exercise or solicit expert opinion perhaps through a Bayesian process, both of which Phillips and colleagues85 profess also have their weaknesses.
FIGURE 4.
Population expected value of perfect information for a range of lifespan thresholds.
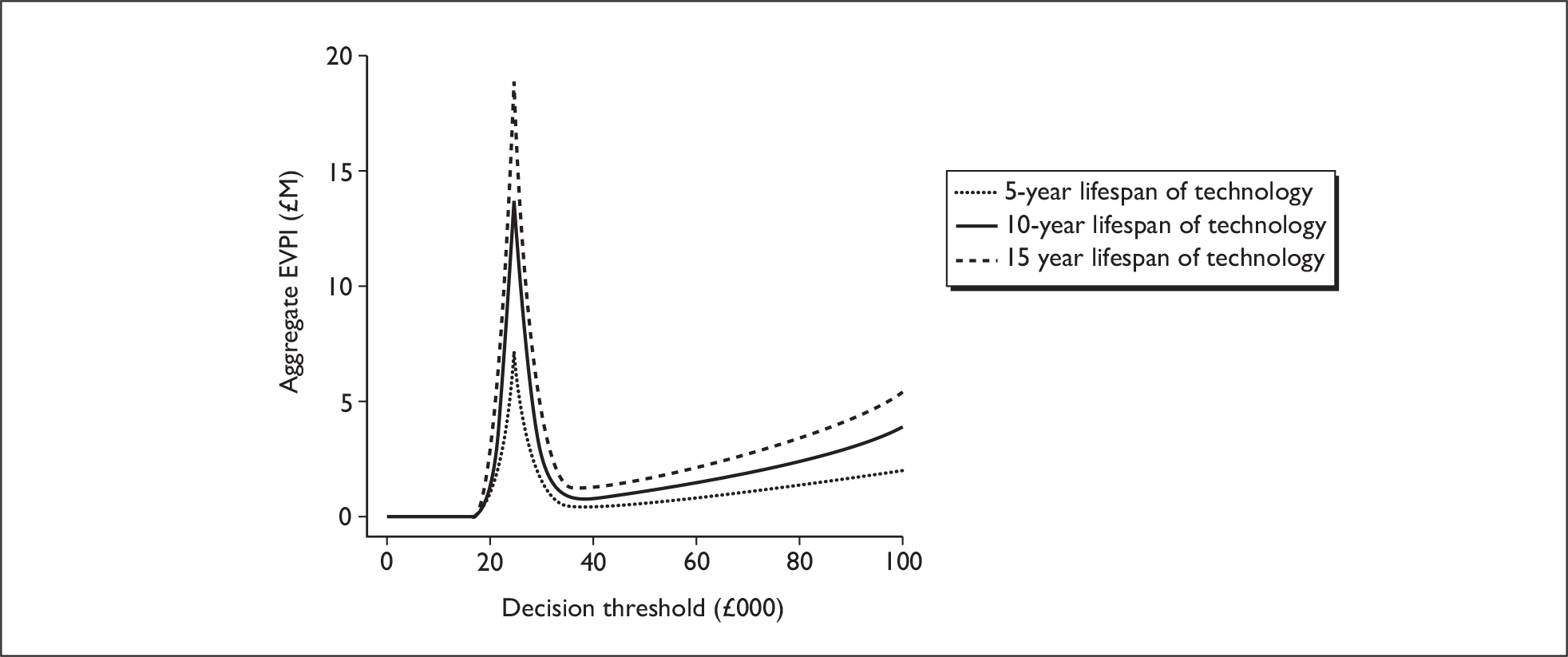
Figures 3 and 4 suggest that the decision problem passes the initial screening test for a common range of thresholds. Thus we proceed to calculate the EVPPI with the purpose of informing future research priorities and study designs.
Figure 5 shows the EVPPI conducted on selected groups of parameters. To reduce computational burden we followed the advice of Brennan and colleagues87 and used a higher number of runs in the inner loop (750) than the outer loop (500) for a total of 375,000 iterations per group of EVPPI parameters.
FIGURE 5.
Expected value of population perfect information for selected parameter groups.
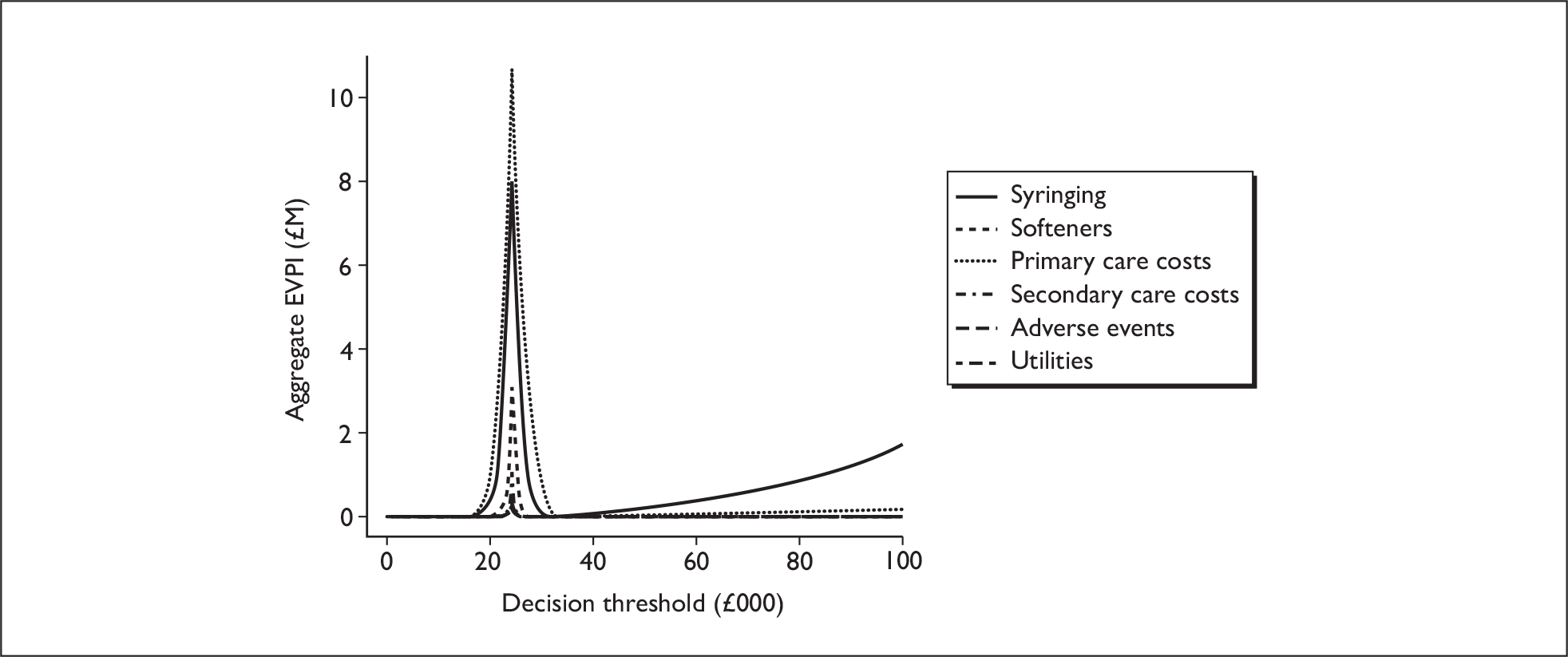
Choice of parameter groups was informed by potential study designs that could feasibly be conducted: utilities; primary care costs; secondary care costs; irrigation efficacy; softener efficacy; and frequency of AEs. The EVPPI is, again, a function of the choice of decision threshold.
Figure 6 shows the EVPPI in more detail around the generally accepted decision threshold adopted in the UK (i.e. between £20,000 and £30,000 per QALY). The figure illustrates that if future research is to be commissioned, it should prioritise improving the estimates of the costs of primary care and the efficacy of irrigation. These results are unsurprising as they are the principal drivers of the model. Secondary care costs are of far less importance as they are related to the management of AEs, which are deemed so rare as to have negligible impact on the analysis.
Whether this research should be undertaken depends upon the cost of the study into the groups of parameters and the exact threshold under which the decision is to be made. In this case it is likely that a prospective costing study or chart review for primary care costs and a clinical trial or observational study for irrigation efficacy would be required. If the threshold is £20,000 per QALY, it is unlikely that a clinical trial to inform irrigation efficacy could be undertaken, but a costing study could be performed within the EVPPI upper bound. However, if the adopted decision threshold is closer to the level of maximum uncertainty then investment in a clinical trial may be well founded. Investment in other groups of parameters is far less certain dependent upon the decision threshold.
FIGURE 6.
Expected value of population perfect information for selected parameter groups, highlighted for a decision threshold between £20,000 and £30,000.
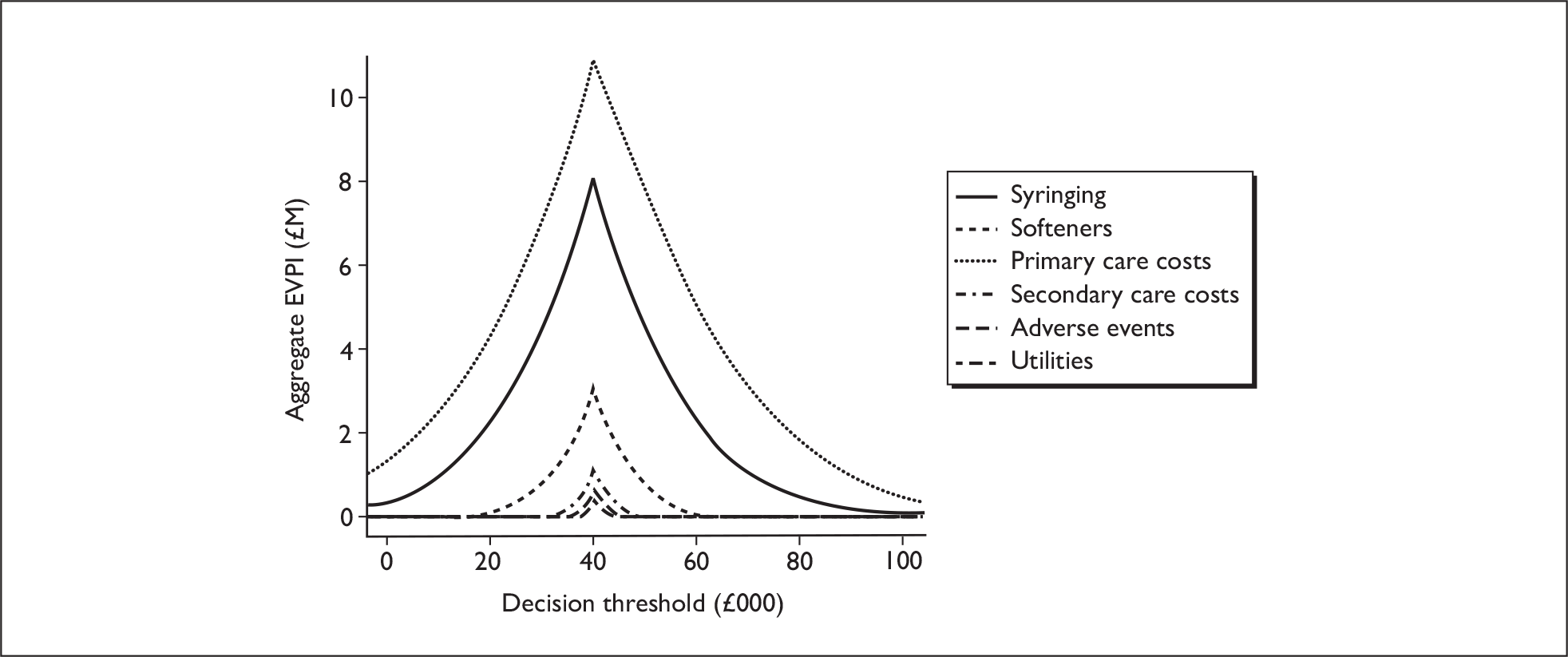
A caveat is that the CIs around many of the parameters included in the model have been estimated, rather than informed by published evidence, and it is these estimates which inform the analysis. Furthermore, the analysis does not strongly suggest further research on utilities would be warranted, as the published utility estimate used in the model is accompanied by a low variability. Perhaps, in retrospect, if there is doubt as to the validity of this estimate in the UK, as attested by expert advice, then a Bayesian model could have been used in which a prior probability was used to identify current expectations.
Chapter 7 Discussion
Statement of principal findings
Clinical effectiveness
Twenty-six clinical trials (22 RCTs and four CCTs) met the inclusion criteria of the review and were included for the assessment of the clinical effectiveness of methods for earwax removal. A range of interventions have been used in the studies, such as softeners with or without irrigation, in different populations and in different settings. Participants in the trials also varied across the studies in terms of age, sex and extent or severity of earwax. In some cases few details of baseline characteristics are given in the study reports, so interpretation of results was difficult. Outcomes also vary across studies often with limited information on the definitions used, making it difficult to assess their validity and objectivity, and how consistently they were applied. For example, measures of earwax removal might be reported in terms of clearance or visualisation of TM (described as complete, partial or negligible) or in terms of impaction or occlusion (described as none, mild, moderate or severe). Ease of earwax removal was reported in terms of number of attempts or the amount of liquid needed to achieve some degree of success. Methods of data analysis were also variable with several studies not reporting the analytic approach used or results of statistics tests. Due to these methodological issues, summarising the results of included studies was difficult and meta-analysis was judged inappropriate.
Considering the studies that report statistical significance, results from these studies suggest that Cerumol, sodium bicarbonate, olive oil and water are all more effective than no treatment for removal of earwax; Cerumol is better than dioctyl, TP and sodium bicarbonate for ease of subsequent irrigation; TP is better than olive oil in the volume of water used for syringing; Audax is better than Earex for ease of removal by subsequent irrigation; Exterol and Otocerol are better than Cerumol in terms of the number of people requiring irrigation after treatment with softeners; wet irrigation is better than dry irrigation for ease of removal; sodium bicarbonate drops followed by nurse irrigation is more effective than sodium bicarbonate drops followed by self-irrigation; endoscopic de-waxing is better than microscopic de-waxing; and recurrence of earwax and impacted earwax is less likely in ears treated with skin oil than those not treated.
Patient satisfaction with the different treatment options was rarely assessed. Comparisons of different softeners, including dioctyl-medo, oil-based softeners, Waxsol and Cerumol, showed that over 85% of people found them tolerable. When considering the effectiveness of different softeners, people’s responses ranged more widely, with 29% assessing Earex as effective compared with between 42% and 93% for Audax and 100% for Cerumol. Another comparison of nurse-versus-self-irrigation found that people were more satisfied with nurse irrigation (difference 28%). AEs were rare (usually < 10% of patients affected) and minor in nature. Most were limited to those associated with irrigation, such as minor pain (0–21%) and irritation/itching (4–15%). None of the studies reported perforation of the TM or infection. Although there was evidence assessing the comparative benefits of different interventions for removing earwax, it was of poor quality and equivocal. As a consequence it was not possible to identify a particular softener as being superior in clearing wax either with or without subsequent irrigation. Although separate studies have found benefits of wet syringing over dry syringing, from nurse-provided irrigation rather than self-irrigation and, endoscopic compared with microscopic de-waxing, the evidence was limited in nature and quality, so only tentative conclusions should be drawn.
Economic evaluation
Although we conducted a systematic review of the cost-effectiveness of the different methods for earwax removal, no economic evaluations were identified. As a consequence, a de novo economic model was developed to examine the cost-effectiveness of different alternative strategies, including softeners followed by irrigation in primary care (primary care option), softeners followed by self-irrigation (self-care option) and a ‘no treatment’ option. The results indicated that the self-care option (£24,433 per QALY) is likely to be more cost-effective than the primary care option (£32,130 per QALY) when compared with the ‘no treatment’ option over a 7-week time horizon. When the two active treatment options were directly compared, the incremental cost of treating an additional patient with the primary care option as opposed to self-care option was £340,000 per QALY. When assessed over a lifetime horizon (45 years) the cost per QALY compared to the ‘no treatment’ option was £24,450 for the self-care option to £32,136 for the primary care option. Similarly, when comparing the two active treatments over a lifetime horizon, the resultant incremental cost per QALY was over £335,000 for the primary care option. A constant recurrence rate of wax was assumed for all three treatment pathways due to a lack of data to model an alternative assumption. Therefore, the lifetime results are merely an extrapolation of costs and outcomes from the base-case model out to a 45-year period.
The results were fairly robust to a range of sensitivity and scenario analyses undertaken to explore parameter uncertainties of the modelled economic evaluation. Variations in measures of clinical effectiveness, rates of AE and costs resulted in cost per QALYs ranging between £15,000 and £40,000 for the two options compared to no treatment, and between £170,000 and £535,000 when the two active treatment options were compared. However, interpretation of these results should be undertaken with caution. Uncertainties as to current clinical practice and the paucity of clinical and economic evidence are considerable limitations to the economic evaluation. As a result the economic evaluation should be considered exploratory and not as a justification for any changes in practice.
Strengths and limitations of the assessment
The assessment has certain strengths:
-
It was independent of any vested interest.
-
The review brings together the evidence for the clinical effectiveness and cost-effectiveness of different methods of earwax removal using consistent methods of critical appraisal, presentation and transparency. In addition a de novo economic model has been developed, following recognised guidelines.
-
The evidence synthesis was guided by the principles for undertaking systematic reviews and economic evaluations. Prior to undertaking the assessment, the methods were set out in a research protocol (Appendix 1), and this was commented on by an advisory group. The protocol defined the research question, inclusion criteria, quality criteria, data extraction process and methods used to undertake the different stages of the assessment.
-
An advisory group has informed the review from its initiation, through the development of the research protocol and completion of the report.
-
Systematic searches were undertaken to identify data for the economic model, and main results were summarised and presented.
-
The quality of the clinical effectiveness studies was assessed using criteria recommended by the NHS CRD.
In contrast, the assessment was affected by certain limitations:
-
The studies identified by the systematic review of clinical effectiveness were published over a considerable period, from 1950 to 2007. Inevitably the nature of clinical trials in terms of their methods and their reporting in publications has changed significantly during this period. Of the trials included in this systematic review, those early published studies tended to provide very limited details of their methods and results. As a consequence, it was difficult to assess the quality of the studies and interpret their results appropriately. In addition, the technologies have continued to develop, with new softeners, methods of irrigation and changes in the nature of the service used to deliver the interventions. Again, this limits the comparability of the evidence.
-
Limited details are given in many of the studies of the participants involved in the studies, the dose and frequency of softeners used and the length of follow-up. All affect the generalisability of the findings.
-
The effectiveness of the different interventions for removing earwax was assessed through a range of different outcomes. While many of the outcomes assessed the extent and ease of clearance, the specific nature of the different outcomes varied considerably. The extent of clearance was assessed by outcomes such as amount of TM visualised, proportion achieving complete visualisation of the TM, degree of wax removal, hearing, wax clearance, wax occlusion, degree of impaction, amount of wax removed, recurrence of cerumen impaction and further treatment required. Ease of removal of earwax was assessed through outcomes such as volume of water for syringing and syringefuls used, mean number of syringing attempts, mean time to syringe, ease of wax removal, ease of syringing, frequency of syringing, and time taken to de-wax. In many of the studies there was no clear description or definition of these outcome measures. Many are open to subjective measurement and interpretation. As a consequence, it was difficult to directly compare and synthesise the outcomes from the different studies. No studies assessed benefits of the different interventions on quality of life. Although a limited proportion of studies did examine different measures of patient satisfaction, these were limited to whether patients were satisfied with the intervention and if they found them effective and tolerable. Again, these outcomes were not clearly defined or described and open to subjective interpretation.
-
Some studies used a different unit of allocation to that used for the analysis (e.g. participants compared with ears). Although there are methods for handling the analysis of such data, it was unclear whether these were followed by the primary studies.
-
Although recurrence of earwax is thought to be a common problem for sufferers, it was not considered in the studies included in the systematic review. Recurrence may be a consequence of differences in the anatomical structure of different people’s ears, a result of damage that has been caused to the mechanism that allows earwax to be removed or to the use of medical devices (e.g. hearing aids). Inevitably people within this group will use a disproportionate amount of services and research should focus on identifying methods for diagnosing, treating and, if possible, preventing further problems. The economic evaluation assumed a recurrence rate of one event every 3 years. Inevitably this was a simplification and some people will incur a higher recurrence rate.
-
Follow-up with authors to clarify details of their methods and results was not routinely undertaken. Given that the majority of studies that lacked such information were those published nearly 60 years ago, it was considered of limited value to do so as authors would be difficult to trace and further details of studies are unlikely to be available. As technologies have developed and practice has changed, these early studies may have been of more limited relevance to current practice. Where there were uncertainties in key aspects in more recent publications, contact was attempted and was beneficial in some cases.
-
Synthesis of the studies included in the systematic review of clinical effectiveness was through narrative review. Due to the limitations of the literature, meta-analysis was not possible.
-
The limitations evident in the systematic review of clinical effectiveness and cost-effectiveness and in the evidence on the epidemiology and aetiology of earwax have impacted upon the development of the de novo economic evaluation. With studies either lacking detail of study characteristics or being heterogeneous in nature, the evidence base was limited. As a consequence, assumptions were used to develop the structure of the clinical pathway and to populate the different elements of the model (see Chapter 5, Assumptions used in the model). This has rendered the economic evaluation as exploratory, from which definitive recommendations for changing clinical practice should not be drawn.
-
The economic evaluation was developed from a NHS perspective, with patients having to attend primary care for assessment prior to decisions about subsequent treatment. Inevitably, some people will not attend primary care for assessment and/or treatment and will either suffer from the problem untreated or decide to self treat. These people are not included within the evaluation. The rationale for excluding these people was that the intention of providing evidence to decision-makers as to possible future guidance to the NHS, and, as such, the research had to focus on aspects of current provision that could be affected by policy. This led to the exclusion of the evaluation of a service where advice from the NHS on self-syringing is provided without attendance at primary care practice (e.g. NHS Direct or through advice from pharmacists) or the effects of personal costs to the patient. Also, limited evidence was available as to the safety and effectiveness of self diagnosis and treatment.
-
With no definitive guidelines identified for the management of symptomatic earwax in the UK, the clinical pathway used to structure the economic evaluation was developed using assumptions based on available evidence and advice from clinical experts. As a consequence, it was uncertain if the clinical pathway used in the model was representative of current practice. For example, it was unclear who undertakes the first assessment within primary care, whether a practice nurse or a GP. Opinion appears to vary and it is likely that different primary care practices adopt different approaches. Also, the duration of the use of softeners was uncertain. Expert advice indicates that people use softeners for a week prior to self-based or primary-care-practice-based irrigation. Others have suggested that the effectiveness of softeners may not depend on the duration of their use49 with spontaneous clearance achieved in a short period (e.g. 20 minutes). Although alternatives have been examined through sensitivity and scenario analyses where possible, in some instances a pragmatic approach has been taken.
-
Similar concerns affect the parameter inputs used to populate the economic evaluation. No published evidence was found on the incidence of SAE associated with either professional irrigation or self-irrigation. As a consequence the base-case estimate was based on expert advice from an OTL. This may be an underestimate of the probability of SAE as it is based on the assumption that all patients are referred to secondary care. It is possible that some patients with SAE are first treated in primary care, and only those whose infection or TM perforation does not heal within the expected time are referred to secondary care. It was also assumed that the probability of SAE in both active treatment alternatives is the same regardless of the mode of irrigation (self-irrigation or administered by a primary care practice nurse) and whether irrigation is undertaken for the first, second or the third time, which may not correspond to actual clinical practice.
-
There were no published estimates of the loss of HRQoL associated with symptomatic earwax. The utility decrement of 0.006 (standard error = 0.0001) was obtained from Sullivan and Ghushchyan. 78 This was based on SF-12 quality-of-life estimates in the general US population, with the loss of hearing as defined by the ICD-9-CM diagnosis code 389. The original estimates were then converted into EQ-5D values. The estimates are not specific to patients presenting with earwax, although earwax is associated with temporary loss of hearing, as well as other symptoms. The utility decrement does not reflect minor complications, such as itching and tinnitus, and other minor symptoms, such as aural fullness and vertigo that affect HRQoL of patients with earwax problem. The direction of bias in the results of an economic evaluation associated with the use of utility decrement of 0.006 based on the ICD-9-CM diagnosis code 389 is unknown. An alternative utility estimate of 0.0679 obtained in the population eligible for a hearing aid was used in the scenario analysis. The results indicated that the ICER estimates are sensitive to the choice of value of the utility gain.
-
The economic evaluation was conducted for a general population of adults aged 35–44 years without any known contraindications to irrigation, reflecting the participants in the primary studies of efficacy used to develop the economic evaluation. Although limited epidemiological data were available, it was felt that this group may not represent those in which the condition is most prevalent. As such, the results may not necessarily apply to other population groups, such as the elderly, children and people with disabilities. This is particularly important when considering the use of new technologies, such as self-irrigation, which require care in their use and adherence to instruction. It is likely that self-irrigation will only be relevant to a subgroup of the general population and therefore it should not necessarily be considered as an option for all groups.
Comparison with previous reviews
The findings of our evidence synthesis are generally in line with those of other systematic reviews in the area. We identified four previous reviews,1,29,37,74 each with slightly different methodologies and therefore different number of included studies. One review74 included nine RCTs, as well as seven in vitro studies and centred on commercially available products obtainable to facilitate ear syringing. All included RCTs were quality assessed and date of last searching was 2002. Excluding the findings of the in vitro studies, the review found that no one product was superior to another.
A Cochrane Collaboration review updated in 2009, which included nine RCTs, centred on the effectiveness of ear drops only. 88 All included RCTs were quality assessed. Although most studies were judged not to be comparable and of poor quality, two46,47 of the nine included trials were meta-analysed. While the overall findings of the review were inconclusive, results from the meta analysis suggest TP is statistically superior to saline in preventing the need for syringing. A third review29 included 18 RCTs and concentrated on the effectiveness of topical preparations for the treatment of earwax. Trials were quality assessed and the date of last searching was January 2004. Preparations in this review were categorised into water-, oil- and non-water-based. Although the review undertook a meta-analysis, it also found that no one preparation was superior to another in either clearing earwax or facilitating syringing.
A more recent review37 included trials and systematic reviews,1,29 and considered treatments for both ear syringing and manual removal. The review carried out a grade evaluation of interventions for earwax on four of the included RCTs. 4,42,56,62 Date of last searching was June 2007. Similarly to our conclusion, the overall conclusion of the review was that there was not enough evidence showing softeners alone to be effective or that one type of softener is superior to another.
Our review differed from these previous reviews, in that we assessed studies by setting, intention to use softening agent alone or as part of the irrigation procedure, followed by population and subgrouped into immediate or delayed follow-up. We assessed all methods of treatment, including self-syringing, all available preparation comparisons and each study was assessed for methodological quality. We did not feel that quantitative pooling of the data was appropriate. In the Hand and Harvey study,29 data was combined. However, with such diverse outcomes and participant groups, we question whether this is appropriate. Furthermore, it is also questionable whether pooled data based on such poor quality studies provides reliable evidence about the effectiveness of these products.
Research recommendations
The systematic review of clinical effectiveness and cost-effectiveness and the development of the de novo economic evaluation have highlighted the paucity of good-quality evidence available to identify the most appropriate methods for the removal of earwax. This is a key concern given the prevalence of the condition, its implications for the use of health service resources and the apparent need to provide national guidance for practitioners. In addition, the potential for litigation has an influence on the provision of the service and unequivocal evidence is required to provide a safe, effective and efficient service. To provide clearer guidance, there will be a need for further research.
Much of the research identified in the systematic review has focused on the use of different drops to soften, dissipate or dissolve the wax, with limited attention being given to other facets, such as the method of mechanical removal, the role of the provider of the service, the effects of variations in practice and the importance of patient choice. Inevitably, it will be helpful to have clear evidence on the safety and effectiveness of the different drops and of the different methods for mechanical removal of earwax. However, a key concern that requires further research is how the different interventions are delivered and to which patient groups. Current practice, although thought to be variable nationally, tends to involve people attending primary care practices for diagnosis and treatment. Self-treatment with drops and then self-irrigation may offer a less costly alternative, with people only attending primary care practices if they are unable to clear the problem to their satisfaction. As a condition with a high recurrence rate, this would have the potential for reducing costs considerably. However, uncertainty remains as to whether self-irrigation is a safe and effective option that would be acceptable to patients and practitioners. By the nature of the process involved and concerns about litigation against the health service, it may be that the use of self-irrigation would be limited to a specific patient subgroup able to consent to its use and self treat. It would be helpful to identify this group and the safety, benefits and costs of the use of self-irrigation compared to current practice.
As such, it would be helpful to have an RCT to assess the clinical effectiveness and cost-effectiveness of self-treatment through the provision of drops and use of a soft bulb irrigator compared with standard practice. With the variation in current practice within the UK, the trial should focus on the role of the practice nurse in assessing the condition, recommending drops and irrigating the ears within the comparator. Where appropriate, it should consider the possibility of using different drops for softening the earwax, different durations of the use of softeners and the particular methods for irrigation. However, these should be considered secondary to the use of self-treatment and the provision of the service. The patient groups included in the trial should be representative of those currently attending primary care, with a predominance of more elderly patients. Recurrence is common among people with earwax and this aspect will need to be encompassed with any evaluation. The outcomes to be used in the RCT will be important and will need to be objective, clearly defined and assessed by validated outcome assessors to improve comparability. They should include relief from patient reported symptoms, measures of clearance, quality of life and patient satisfaction and AE.
An economic evaluation will be a key part of any subsequent research. It is evident that the data that would normally underpin an economic evaluation are very limited. Further evidence is required on the epidemiology of the condition in terms of the prevalence of the condition, levels of recurrence and its natural history. It will be important to measure the patient’s quality of life using an appropriate and validated measure (e.g. EQ-5D or HUI3) focusing on people with symptomatic earwax rather than surrogates associated with hearing loss. AEs are thought to be important factors in providing the service and it will be important to collect data from any RCT. Given their apparent rarity and limited length of follow-up of most RCTs, there will need to be additional research to collect data on SAEs from primary and specialist care databases (e.g. serious infections and perforations of the TM). Accurate data on the costs of the different treatment options will be important to the evaluation and should be collected prospectively as part of any study.
While an RCT incorporating an economic evaluation provides the most robust form of evidence, it is possible that investment in other forms of study design would provide appropriate data to help develop the current evaluation and allow decisions concerning policy to the NHS. A value of information analysis assessed the value of further research on utilities, primary care costs, secondary costs, irrigation efficacy, softener efficacy and frequency of AEs. At a decision threshold of between £20,000 and £30,000 the EVPPI identified improvements in estimates of costs associated with primary care and the efficacy of methods of irrigation as the key inputs for improved information. As such, a prospective costing study or chart review of primary care costs may provide useful data to improve the current economic evaluation within the bounds of acceptable research costs. Improving data on the efficacy of different methods of irrigation is likely to require a clinical trial which would be more costly, but could provide information for other parameters.
Chapter 8 Conclusions
The systematic review has shown limited good-quality evidence assessing the clinical effectiveness and cost-effectiveness of the different methods of earwax removal. As a consequence, it has proved difficult to differentiate between the different methods of earwax removal in terms of their effectiveness in clearing earwax, improving patient quality of life and satisfaction, or AEs. It appears that softeners do have some effect in helping to clear earwax in their own right or as a precursor to irrigation. However, which specific softeners are most effective remains unclear. There was limited consideration of the most effective method of irrigation or mechanical removal of earwax. Although irrigation was a key part of the treatment within many of the trials, the specific methods were not a focus of the analyses. Where the methods of irrigation or mechanical removal were assessed, the evidence was limited in quantity and/or methodological quality, so no clear guidance can be provided. The paucity of evidence on the benefits and costs of the different methods for the removal of earwax rendered the economic evaluation limited in its scope, and speculative, with many uncertainties remaining. Although it found self-treatment more cost-effective than primary care practice-based care, it focused on a limited population group (i.e. people 35–44 years with no contraindications) and was underpinned by several speculative assumptions (e.g. comparable clinical effectiveness). As such, the economic evaluation should be considered illustrative of the possible analysis that could be undertaken if a satisfactory evidence base were available. It does not provide evidence for recommendations that can be used to change clinical practice.
As a consequence, further research is required to identify the most effective method for the removal of earwax for different groups of people. The research should focus on those elements where uncertainty remains and that have the potential to impact on patients, the provision of the service and value for money. Although much of the research so far has looked at the role of softeners, perhaps the more important aspect for research is consideration of the method of mechanical removal and provision of the service. Traditionally, this has relied upon the patient attending the primary care practice for consultation, followed by the use of softeners and a further visit to have the earwax removed. Self-treatment may provide an alternative option for a specific group of people who find it acceptable and are able to undertake the procedure. It would provide the opportunity for those people to treat themselves when required, with the possibility of removing some of the burden from the health service. For many people professional care from the health service will continue to provide the most appropriate method for the removal of earwax and research should assess the role of the practice nurse and other members of the nursing team in the provision of care. In both instances research should assess the clinical effectiveness and cost-effectiveness of the different approaches, focusing on efficacy, acceptability to patients and practitioners, possible AEs and costs. While a RCT incorporating an economic evaluation would provide the most robust method for assessing several aspects of the removal of earwax, a prospective study of the costs of the provision of care within primary care may provide a less costly option in the first instance.
Acknowledgements
Contributions of authors
AJ Clegg: Developed the original research grant application, acted as principal investigator and project managed the research, developed the research protocol, assisted in the development of the search strategy, assessed studies for inclusion, extracted data from and quality assessed included studies, synthesised evidence, and drafted and edited the final report.
E Loveman: Developed the research protocol, led the systematic review of clinical effectiveness, assisted in the development of the search strategy, assessed studies for inclusion, extracted data from and quality assessed included studies, synthesised evidence, and drafted and edited the final report.
E Gospodarevskaya: Developed the research protocol, assisted in the development of the search strategy, assessed studies for inclusion and extracted data for the economic evaluation, led the development of the economic evaluation and drafted the final report.
P Harris: Developed the research protocol, assisted in the development of the search strategy, assessed studies for inclusion, extracted data from and quality assessed included studies, synthesised evidence and drafted the final report.
A Bird: Developed the research protocol, assisted in the development of the search strategy, assessed studies for inclusion and extracted data from included studies, synthesised evidence, developed the economic evaluation and drafted the final report.
J Bryant: Developed the original research grant application, developed the research protocol, and drafted and edited the final report.
DA Scott: Developed the original research grant application, acted as guarantor for the economic evaluation, developed the research protocol, developed the economic evaluation and drafted the final report.
P Davidson: Developed the original research grant application, developed the research protocol and assisted in the drafting of the final report.
P Little: Developed the original research grant application, developed the research protocol and assisted in the drafting of the final report.
R Coppin: Developed the original research grant application, developed the research protocol and assisted in the drafting of the final report.
We would like to thank members of our advisory group panel who provided expert advice and comments on the protocol and/or a draft of this report:
Professor George Browning, Emeritus Professor of Otorhinolaryngology, MRC Institute of Hearing Research, University of Glasgow, Glasgow Royal Infirmary, Glasgow, UK.
Deborah Williams, Bromley Primary Care Trust, Kent, UK.
Professor Mark E Lutman, Institute of Sound and Vibration Research, University of Southampton, Southampton, UK.
Steve Palmer, Senior Research Fellow, Deputy Director of the Team for Economic Evaluation and Health Technology Assessment and Head of NICE Programme, Centre for Health Economics, University of York, York, UK.
Desmond A Nunez, Director, Department of Otolaryngology Honorary Senior Lecturer, North Bristol NHS Trust and Bristol University, Bristol, UK.
We are also grateful to Karen Welch, Information Specialist (SHTAC, University of Southampton), for conducting the searches; Elizabeth Hodson, Information Assistant (Wessex Institute, University of Southampton), for retrieving references; Mr Jonathan Blanshard, Consultant ENT Surgeon (Basingstoke and North Hampshire NHS Foundation Trust, Basingstoke), Mr Paul Spraggs, Consultant ENT Surgeon (Basingstoke and North Hampshire NHS Foundation Trust, Basingstoke), Dorothy Wicke, Research Nurse (Oakley and Overton Partnership, Basingstoke), Joanne Nesbitt, Practice Nurse (Denton Park Medical Group, Newcastle PCT, Newcastle) and Julia Johns, Practice Nurse (Padnell Road Surgery, Hampshire PCT) for data for the economic model; and, Dr Jill Colquitt, Senior Research Fellow (SHTAC, University of Southampton), for reviewing a draft of this report.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Burton MJ, Doree CJ. Ear drops for the removal of ear wax. Cochrane Database Syst Rev 2003;3.
- Serafin J. Using colace (docusate sodium) to remove cerumen impactions. Geriatric Nurs 2008;29.
- Stone M, Fulghum RS. Bactericidal activity of wet cerumen. Ann Otol Rhinol Laryngol 1984;83:183-6.
- Keane EM, Wilson H, McGrane D, Coakley D, Walsh JB. Use of solvents to disperse ear wax. Br J Clin Pract 1995;49:71-2.
- Lewis-Cullinan C, Janken JK. Effect of cerumen removal on the hearing ability of geriatric patients. J Adv Nurs 1990;15:594-600.
- Sharp JF, Wilson JA, Ross L, Barr-Hamilton RM. Ear wax removal: a survey of current practice. BMJ 1990;301:1251-3.
- Crandell CC, Roeser RJ. Incidence of excessive/impacted cerumen in individuals with mental retardation: a longitudinal investigation. Am J Ment Retard 1993;97:568-74.
- Memel D, Langley C, Watkins C, Laue B, Birchall M, Bachmann M. Effectiveness of ear syringing in general practice: a randomised controlled trial and patients’ experiences. Br J Gen Pract 2002;52:906-11.
- McCarter DF, Courtney AU, Pollart SM. Cerumen impaction. Am Family Physician 2007;75:1523-8.
- Burkhart CN, Burkhart CG, Williams S, Andrews PC, Adappa V, Arbogast J. In pursuit of ceruminolytic agents: A study of earwax composition. Am J Otol 2000;21:157-60.
- Guest JF, Greener MJ, Robinson AC, Smith AF. Impacted cerumen: composition, production, epidemiology and management. QJM 2004;97:477-88.
- Brister F, Fullwood HL, Ripp T, Blodgett C. Incidence of occlusion due to impacted cerumen among mentally retarded adolescents. Am J Ment Defic 1990;15:594-600.
- Oliveira RJ. The active ear canal. J Am Acad Audiol 1997;8:401-10.
- Roeser RJ, Ballachanda BB. Physiology, pathophysiology, and anthropology/epidemiology of human ear canal secretions. J Am Acad Audiol 1997;8:391-400.
- Ryan TJ, Sinclair R, Warrell DA, Cox TM, Firth JD, Benz EJ. Oxford textbook of medicine. Oxford: Oxford University Press; 2003.
- Robinson AC, Hawke M, Naiberg J. Impacted cerumen: a disorder of keratinocyte separation in the superficial external ear canal?. J Otolaryngol 1990;19:86-90.
- Hanger HC, Mulley GP. Cerumen: its fascination and clinical importance: a review. J R Soc Med 1992;85:346-9.
- Stoeckelhuber M, Matthias C, Andratschke M, Stoeckelhuber BM, Koehler C, Herzmann S, et al. Human ceruminous gland: ultrastructure and histochemical analysis of antimicrobial and cytoskeletal components. Anat Rec A Discov Mol Cell Evol Biol 2008;228A.
- Omoto K. Polymorphic traits in peoples of eastern Asia and the Pacific. Isr J Med Sci 1973;9:1195-215.
- Hawke M. Update on cerumen and ceruminolytics. Ear Nose Throat J 2002;81:S1-4.
- Karlsmose B, Lauritzen T, Engberg M, Parving A. A randomised controlled trial of screening for adult hearing loss during preventive health checks. Br J Gen Pract 2001;51:351-5.
- Davis AC. The prevalence of hearing impairment and reported hearing disability among adults in Great Britain. Int J Epidemiol 1989;18:911-17.
- Fairey A, Freer CB, Machin D. Ear wax and otitis media in children. Br Med J 1985;291:387-8.
- Flugrath J, Lutz D, Hamdy RC. Hearing impairment and cerumen impaction in older patients. J Tenn Med Assoc 1993;86:301-2.
- Hawthorne MR, Nunez DA, Clarke GP, Robertshaw D. Direct referral hearing aid provision in the over sixties age group. J Laryngol Otol 1991;105:825-7.
- Lim JK, Yap KB. Screening for hearing impairment in hospitalised elderly. Ann Acad Med Singapore 2000;29:237-41.
- Office for National Statistics . Mid-2006 Population Estimates: Estimated Resident Population by Broad Age-Group n.d.
- Roland PS, Smith TL, Schwartz SR, Rosenfeld RM, Ballachanda B, Earll JM, et al. Clinical practice guideline: cerumen impaction. Otolaryngol Head Neck Surg 2008;139:S1-2.
- Hand C, Harvey I. The effectiveness of topical preparations for the treatment of earwax: a systematic review. Br J Gen Pract 2004;54:862-7.
- Allen S. Outer and middle ear problems. Pharm J 2006;276:83-6.
- Coppin R, Wicke D, Mehta R, Little P. Management of earwax in primary care: postal survey of UK GPs and practice nurses. Fam Pract 2004;21:413-14.
- Wilson PL, Roeser RJ. Cerumen management: professional issues and techniques. J Am Acad Audiol 1997;8:421-30.
- NHS Quality Improvement Scotland . Best Practice Statement: Ear Care 2006.
- Blake P, Matthews R, Hornibrook J. When not to syringe an ear. NZ Med J 1998;111:422-4.
- Sorensen VZ, Bonding P, Sorensen VZ, Bonding P. Can ear irrigation cause rupture of the normal tympanic membrane? An experimental study in man. J Laryngol Otol 1995;109:1036-40.
- Freeman RB. Impacted cerumen: how to safely remove earwax in an office visit. Geriatrics 1995;50:52-3.
- Browning G. Ear wax. Clin Evid 2008;15:504-13.
- Pothier DD. How we do it: Technical note: endoscopic removal of cerumen. Clin Otolaryngol 2006;31:153-5.
- Arulkumaran S, Skurr B, Tong H, Kek LP, Yeoh KH, Ratnam SS. No evidence of hearing loss due to fetal acoustic stimulation test. Obstet Gynecol 1991;78:283-5.
- NHS Centre for Reviews and Dissemination . Undertaking Systematic Reviews of Research on Effectiveness 2001.
- General Practitioner Research Group . A wetting agent to facilitate ear syringing. Practitioner 1965;195:810-12.
- Pavlidis C, Pickering JA. Water as a fast acting wax softening agent before ear syringing. Aust Fam Physician 2005;34:303-4.
- Burgess EH. A wetting agent to facilitate ear syringing. Practitioner 1966;197:811-12.
- Dummer DS, Sutherland IA, Murray JA. A single-blind, randomized study to compare the efficacy of two ear drop preparations (‘Audax’ and ‘Cerumol’) in the softening of ear wax. Curr Med Res Opin 1992;13:26-30.
- Lyndon S, Roy P, Grillage MG, Miller AJ. A comparison of the efficacy of two ear drop preparations (‘Audax’ and ‘Earex’) in the softening and removal of impacted ear wax. Curr Med Res Opin 1992;13:21-5.
- Meehan P, Isenhour JL, Reeves R, Wrenn K. Ceruminolysis in the pediatric patient: a prospective, double-blinded, randomized controlled trial. Acad Emerg Med 2002;9:521-2.
- Whatley VN, Dodds CL, Paul RI. Randomized clinical trial of docusate, triethanolamine polypeptide, and irrigation in cerumen removal in children. Arch Pediatr Adolesc Med 2003;157:1177-80.
- General Practitioner Research Group . Wax softening with a new preparation. Practitioner 1967;199:359-62.
- Singer AJ, Sauris E, Viccellio AW. Ceruminolytic effects of docusate sodium: a randomized, controlled trial. Ann Emerg Med 2000;36:228-32.
- Jaffe G, Grimshaw J. A multicentric clinical trial comparing Otocerol with Cerumol as cerumenolytics. J Int Med Res 1978;6:241-4.
- Amjad AH, Scheer AA. Clinical evaluation of ceruminolytic agents. Eye Ear Nose Throat Monthly 1975;54:76-7.
- Carr MM, Smith RL. Ceruminolytic efficacy in adults versus children. J Otolaryngol 2001;30:154-6.
- Eekhof JA, de Bock GH, Le CS, Springer MP. A quasi-randomised controlled trial of water as a quick softening agent of persistent earwax in general practice. Br J Gen Pract 2001;51:635-7.
- Fahmy S, Whitefield M. Multicentre clinical trial of Exterol as a cerumenolytic. Br J Clin Pract 1982;36:197-204.
- Caballero M, Navarrete P, Domenech J, Bernal-Sprekelsen M. Randomized Clinical Trial of Clorobutanol, Sodium Carbonate, and Irrigation in Cerumen Removal in Adults (abstract). XVIII IFOS World Congress 2005.
- Pothier DD, Hall C, Gillett S. A comparison of endoscopic and microscopic removal of wax: a randomised clinical trial. Clin Otolaryngol 2006;31:375-80.
- Dubow E. A simple method to assure proper pediatric ear examinations. Arch Pediatr 1959;76:360-3.
- Saloranta K, Westermarck T. Prevention of cerumen impaction by treatment of ear canal skin. A pilot randomized controlled study. Clin Otolaryngol 2005;30:112-14.
- Chaput de Saintonge DM, Johnstone CI. A clinical comparison of triethanolamine polypeptide oleate-condensate ear drops with olive oil for the removal of impacted wax. Br J Clin Pract 1973;27:454-5.
- Fraser JG. The efficacy of wax solvents: in vitro studies and a clinical trial. J Laryngol Otol 1970;84:1055-64.
- Hinchcliffe R. Effect of current cerumenolytics. Br Med J 1955;2.
- Roland PS, Eaton DA, Gross RD, Wall GM, Conroy PJ, Garadi R, et al. Randomized, placebo-controlled evaluation of Cerumenex and Murine earwax removal products. Arch Otolaryngol Head Neck Surg 2004;130:1175-7.
- Coppin R, Wicke D, Little P. Managing earwax in primary care: efficacy of self-treatment using a bulb syringe. Br J Gen Pract 2008;58:44-9.
- Harris PG. A controlled trial of a ceruminolytic in general practice. Clin Trial J 1968;5:1129-33.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons; 2008.
- Meyers AD, Meyers AD. Managing cerumen impaction. Postgrad Med 1977;62:207-9.
- Grossan M. Cerumen removal: current challenges. Ear Nose Throat J 1998;77:541-8.
- Meador JA, Meador JA. Cerumen impaction in the elderly. J Gerontol Nurs 1995;21:43-5.
- Morrison AW. Silence in court. J Laryngol Otol 1990;104:162-5.
- Price J. Problems of ear syringing. Practice Nurse 1997:14-8.
- Zivic RC, King S. Cerumen impaction management for clients of all ages. Nurse Pract 1993;18:29-36.
- Rubin JK. Aural irrigation with water: a potential pathogenic mechanism for inducing malignant external otitis?. Ann Otol Rhinol Laryngol 1990;99:117-19.
- Midani A, Carels I, Marks M, Wall M, Monoyer A, Michaux J-P, et al. Safety and efficacy of Sofenz ceruminolytic solution. Ear Nose Throat J 2006;85:87-92.
- Somerville G. The most effective products available to facilitate ear syringing. Br J Community Nurs 2002;7:94-101.
- Folmer RL, Shi BY. Chronic tinnitus resulting from cerumen removal procedures. Int Tinnitus J 2004;10:42-6.
- Ogunleye AO, Awobem AA. Trends of ear syringing at Ibadan, Nigeria. Afr J Med Sci 2004;33:35-7.
- Kind P, Hardman G, Macran S. UK population norms for EQ-5D. York: University of York, Centre for Health Economics; 1999.
- Sullivan P, Ghushchyan V. Mapping the EQ-5D index from the SF-12: US general population preferences in a nationally representative sample. Med Decis Making 2006;26:401-9.
- Barton GR, Bankart J, Davis AC, Summerfield AQ. Comparing utility scores before and after hearing-aid provision. Appl Health Econ Res Policy 2004;3:103-5.
- Uppal S, Jose J, Banks P, Mackay E, Coatesworth AP. Cost-effective analysis of conventional and nurse-led clinics for common otological procedures. J Laryngol Otol 2004;118:189-92.
- Netten A, Curtis L. Unit costs of health and social care. Canterbury, Kent: PSSRU, University of Kent; 2006.
- Hussain SSM. Hearing loss in the 4–8 kHz range following tympanic membrane perforation from minor trauma. Clin Otolaryngol 1995;20:211-12.
- Taylor RS, Paisley S, Davis A.C. Systematic review of the clinical and cost-effectiveness of digital hearing aids. Br J Audiol 2001;35:271-88.
- Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S. A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme. Health Technol Assess 2004;8.
- Girling AJ, Freeman G, Gordon J, Poole-Wilson P, Scott DA, Lilford R. Modelling payback from research into the efficacy of left-ventricular devices. Int J Technol Assess Health Care 2007;23:269-77.
- Philips Z, Claxton K, Palmer S. The half-life of truth: what are appropriate time horizons for research decisions? Medical Decision Making. Med Decis Making 2008;3:287-99.
- Brennan A, Kharroubi S, O’Hagan A, Chilcott J. Calculating partial expected value of information via Monte Carlo sampling algorithms. Med Decis Making 2007;2:7448-70.
- Burton MJ, Doree C. Ear drops for the removal of ear wax. Cochrane Database of Systematic Reviews 2009;1.
- Egger M, Smith GD, Altman DG. Systematic reviews in health care: meta analysis in context. London: BMJ; 2001.
- Drummond MF, O’Brien BJ, Torrance GW, Stoddart GL. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 1997.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess 2004;8.
- Eckermann S, Willan AR. Expected value of information and decision making in HTA. Health Econ 2007;16:195-209.
- Curtis L, Netten A. Unit costs of health and social care. Canterbury: PSSRU, University of Kent; 2006.
- Schwartz RH, Rodriguez WJ, Mc Aveney W, Grundfast KM. Cerumen removal: how necessary is it to diagnose acute otitis media. Am J Dis Child n.d.;137:1064-65.
Appendix 1 Protocol methods
Systematic review
A systematic review will be undertaken in accordance with the NHS Centre for Reviews and Dissemination (CRD) guidelines,40 published guidelines on meta-analysis,89 and criteria for appraising economic evaluations. 90,91
Literature searches
Literature will be identified from several sources including electronic databases, bibliographies of articles, grey literature and consultation with experts in the area. A comprehensive database of relevant published and unpublished articles will be constructed using the reference manager software package. The searches carried out will include:
-
General health and biomedical databases, including MEDLINE, EMBASE, Science Citation Index and BIOSIS.
-
Specialist electronic databases: DARE and The Cochrane Library.
-
Grey literature and conference proceedings.
-
Contact with individual experts and those with an interest in the field.
-
Checking of reference lists.
-
Research in progress: National Research Register (historical), UKCRN, Current Controlled Trials (CCT) and ClinicalTrials.gov.
All databases will be searched from their inception to the current date. In the first instance searches will be conducted in all languages, with non-English language articles set to one side in a separate foreign language reference database. Thereafter, an assessment of the volume of non-English language literature will be made and, translation and time restrictions permitting, these will be included in the review. Letters will be sent to experts to ask if they know of any relevant published or unpublished studies that we have not identified.
Study inclusion
Studies will be selected for inclusion in the review in a two-stage process using the predefined and explicit selection criteria outlined in Table 1 below. The full literature search results will be screened independently by two reviewers to identify all citations that may meet the inclusion criteria. Full manuscripts of all selected citations will be retrieved and assessed by two independent reviewers against the inclusion criteria. These criteria will be piloted on a sample of papers. Any disagreements over study inclusion will be resolved by consensus or if necessary by arbitration involving a third reviewer.
Planned inclusion/exclusion criteria
The planned inclusion/exclusion criteria for the systematic review are shown in Table 1.
| Interventions | All methods of earwax removal or softening, including:
|
| Population | Adults and children presenting with build-up of earwax requiring removal |
| Outcomes |
Measures of hearing Adequacy of clearance of wax (e.g. visualisation of tympanic membrane) Quality of life Time to recurrence or further treatment Adverse events (AEs) Measures of costs and cost-effectiveness (e.g. cost per quality-adjusted life-year) (Note: Studies must report summary statistics or present sufficient raw data to allow these to be calculated.) |
| Study design |
Randomised controlled trials Controlled clinical trials Cohort studies (AEs) Costing studies, cost-effectiveness evaluations (including modelling studies) (Note: Where there is evidence from different types of study design for a specific intervention, only those studies with the most rigorous designs will be included and data extracted.) |
Data extraction
The extraction of studies’ characteristics, methods and findings will be conducted by one reviewer and checked by a second reviewer using a predesigned and piloted data extraction form to avoid any errors. Any disagreements between reviewers will be resolved by consensus or, if necessary, by arbitration by a third reviewer.
Quality assessment
The methodological quality of all included studies will be appraised using a formal quality assessment criteria recommended by CRD40 (see below) and criteria for appraising economic evaluations. 90,91 Study quality will be assessed by one reviewer and checked by a second reviewer. Any disagreements between reviewers will be resolved by consensus or if necessary by arbitration involving a third reviewer.
Data synthesis
The results of included studies will be tabulated and summarised in a narrative review. The methods of data synthesis will be determined by the nature of the studies identified through searches and included in the review. Quantitative synthesis of results will be considered if there are several high-quality studies of the same design, but specific details are not possible until the data has been obtained. Sources of heterogeneity will be investigated using appropriate methods.
Economic evaluation
Cost-effectiveness will be assessed through a two-stage process. First, a systematic review of cost-effectiveness studies (full economic evaluations) will be undertaken to address the question of the cost-effectiveness of different methods for earwax removal in the different patient groups. The methods for the review will be analogous to those presented for the review of clinical effectiveness and results will be presented using a narrative synthesis. Quality assessment of cost-effectiveness studies will be conducted using a checklist adapted from those developed by Drummond and colleagues90 and Philips and colleagues. 91
Second, if no economic evaluation relevant to the UK setting is identified, construction of a de novo economic model will be considered where appropriate, with the aim of establishing the relative cost-effectiveness of the different interventions for removing earwax. The structure of the model will reflect current treatment pathways employed by clinicians and other health professionals for the removal of earwax. Any proposed alternatives to current practice identified in the literature or through consultation with practicing clinicians and other health professionals will also be considered. The structural validity of the model will be checked through consultation with clinicians and other health professionals in the UK who are experienced in earwax removal. The model will be either a decision tree or a Markov process model, although its design will be determined, in part, by the data available to populate it. Health states will likely comprise: occlusion, complete clearance and adverse events (AEs) (e.g. perforation leading to long-term hearing loss). It is expected that the model will be populated with the data from the systematic review of clinical effectiveness and cost-effectiveness, and from other routinely collected data sources [e.g. unit costs from the Personal Social Services Research Unit (PSSRU)]. If data are not identified from these sources, we will consider performing additional targeted searches and/or consultation with experts on all model inputs to provide appropriate data. The model will be from the perspective of the NHS and will include, where possible, all costs and consequences related to the NHS perspective and all patient-related benefits.
The base-case model will aim to focus on adults who are eligible for the entire range of treatment alternatives for earwax removal, although the model will aim to assess those interventions shown to be effective in the systematic review of clinical effectiveness. Subject to data availability, alternative versions of the model may be developed to examine subgroups that may respond differently to treatment. Possible subgroups will be identified through consultation with clinical advisors and through the evidence from the systematic review. Each alternative treatment pathway is likely to be quantified in terms of the success of treatment, symptom recurrence, serious AEs suffered, the resource cost of treatment and impact on patients’ quality of life. Costs will be presented in a base year and discounting of costs and benefits will be performed. Incremental costs and benefits will then be measured for alternative treatments. If possible, the outcome measure from the economic evaluation will be cost per quality-adjusted life-year (QALY).
The model’s underlying assumptions will be assessed through sensitivity analyses and threshold analysis for a range of parameters at which reasonable cost-effectiveness levels could be achieved. Probabilistic sensitivity analysis, whereby parameters are varied within reported ranges and distributions, will be undertaken to determine the impact of uncertainty upon the model.
Value of information analysis will be undertaken where possible to help identify future research priorities quantified by the value of reducing decision uncertainty (and its consequences in terms of the opportunity costs), which could be derived from additional research investment on earwax removal technologies. 84,85 It is intended that this approach will systematically appraise which future research would be most valuable and also assist in identifying appropriate research designs. 92
The model will be constructed in treeage pro 2007 or Microsoft excel and will be made as transparent as possible in order that it can be readily updated when new data emerge. The modelling work will follow guidelines for good practice as reported by Philips and colleagues. 91 Building a model is an iterative process and quality control checks will be included at several points during the process to ensure that appropriate structure and data are applied. This is necessary to ensure that the results can be relied upon to inform decision-makers regarding the cost-effectiveness of the intervention. There are several steps to this formal process:
-
A comparison of the model results with those from any other relevant models identified from our systematic review. Any differences between the results will be explored and, if necessary, appropriate modifications made to the model.
-
Model results will be analysed to ensure they accurately reflect the inputs used in the model. This ensures that the data used to populate the model are being applied at the correct times and locations. Extreme parameter values can be used to test whether the model behaves as expected.
-
The model will be critically appraised by a second health economist/modeller. This will allow the approach to be validated and permits any areas of disagreement to be resolved prior to generation of model results.
These three steps help ensure that all aspects of potential error in the model – a lack of internal validity, a lack of external validity and any omissions or biases from an individual health economist – are addressed.
Types and sources of information for economic evaluation
Information on the epidemiology of hearing impairment including the incidence, prevalence and prognosis of the condition will be identified from the literature and supplemented if necessary with clinical expertise.
Efficacy and safety data will be extracted from the clinical studies identified in our systematic review of clinical effectiveness. If there is a paucity of data on parameters, clinicians may need to be consulted in order to obtain estimates of, or variability around, the parameters included in the model. The outcomes are likely to be assessed in terms of symptom relief, AEs suffered and symptom recurrence.
In order to calculate cost per QALY the estimates of utility decrements for patients who suffer symptoms of hearing impairment and AEs typically associated with wax removal will be sought. Ideally utility weights for common adverse effects will be obtained from patient-based estimates (or, potentially, ‘guardian-based’ estimates in the case of children). These decrements may be reported in literature and preference will be given to the utility weights expressed in age- and sex-specific EQ-5D population norms for the UK. 77 Separate targeted searches will be undertaken to try and identify relevant data. If necessary, however, they will be obtained from alternative sources such as clinical opinion through contact with clinicians.
The pattern of resource use and their associated costs may be identified from published or official sources. If necessary these data will be supplemented by contact with clinicians and NHS trust finance departments. Major resource components will include treatment costs in terms of primary and/or secondary care visits (including staff costs, equipment and overheads), treatment of AEs and follow-up visits. All drug costs will be obtained from the British National Formulary (BNF) online. Inpatient days and outpatient visits costs will also be obtained from NHS reference costs. Unit costs for home visits by GPs or district nurses will be obtained from published data. 93
Quality assessment criteria
Quality criteria for assessment of experimental studies
|
Some instructions for using a checklist for RCTs
| Quality item | Coding | Explanation |
|---|---|---|
| 1. Was the assignment to the treatment groups really random? | ||
| Random sequence generation |
Adequate Partial Inadequate Unknown |
Adequate: Random numbers table or computer and central office or coded packages Partial: Envelopes (sealed) without further description or serially numbered opaque, sealed envelopes Inadequate: Alternation, case record number, birth date, or similar procedures Unknown: Just the term ‘randomised’ or ‘randomly allocated’, etc. |
| 2. Was the treatment allocation concealed? | ||
|
Concealment of randomisation The person(s) who decide on eligibility should not be able to know or be able to predict with reasonable accuracy to which treatment group a patient will be allocated. In trials that use good placebos this should normally be the case; however, different modes or timing of drug administration in combination with the use of small block sizes of known size may present opportunities for clinicians who are also involved in the inclusion procedure to make accurate guesses and selectively exclude eligible patients in the light of their most likely treatment allocation; in centres with very low inclusion frequencies combined with very brief follow-up times this my also present a potential problem because the outcome of the previous patient may serve as a predictor of the next likely allocation |
Adequate Inadequate Unknown |
Adequate: When a paper convinces you that allocation cannot be predicted (separate persons, placebo really indistinguishable, clever use of block sizes (large or variable). Adequate approaches might include centralised or pharmacy-controlled randomisation, serially numbered identical containers, on-site computer-based system with a randomisation sequence that is not readable until allocation, and other approaches with robust methods to prevent foreknowledge of the allocation sequence to clinicians and patients Inadequate: This option is often difficult. You have to visualise the procedure and think how people might be able to circumvent it. Inadequate approaches might include use of alternation, case record numbers, birth dates or week days, open random numbers lists, serially numbered envelopes (even sealed opaque envelopes can be subject to manipulation) and any other measures that cannot prevent foreknowledge of group allocation Unknown: No details in text; disagreements or lack of clarity should be discussed in the review team |
| 3. Were the groups similar at baseline regarding the prognostic factors? | ||
|
Baseline characteristics Main aim is to enable the reviewer to see which patients were actually recruited. It enables one to get a rough idea on prognostic comparability. A real check on comparability requires multivariable stratification (seldom shown) |
Reported Unknown |
Consult the list of prognostic factors or baseline characteristics (not included in this appendix). Reviewer decides |
| 4. Were the eligibility criteria specified? | ||
|
Prestratification Consult the list of prognostic factors or baseline characteristics (not included in this appendix) |
Adequate Partial Inadequate Unknown |
Single-centre study Adequate: Prestratification on at least one factor from the list or no prestratification if the number of patients exceeds a prespecified number Partial: Leave judgement to reviewer Inadequate: Stratification on a factor(s) not on our list or no stratification, whereas the number of patients is less than the prespecified number Unknown: No details in text and no way to deduce the procedure from the tables Multicentre study Adequate: Must prestratify on centre. Within each centre the criteria for single-centre studies also apply Partial: Impossible option Inadequate: No prestratification on centre or violating the criteria for single-centre studies (see above) Unknown: No details in text and no way to deduce the procedure from the tables |
| 5. Were outcome assessors blinded to the treatment allocation? | ||
|
Blinding of assessors The assessor may be the patient (self report), the clinician (clinical scale, blood pressure) or, ideally, a third person or a panel. Very important in judgement of cause of death but unimportant in judgement of death |
Adequate Inadequate Unknown |
Adequate: Independent person or panel or (self) assessments in watertight double-blind conditions Inadequate: Clinician is assessor in trial on drugs with clear side effects or a different influence on laboratory results, ECGs, etc. Unknown: No statements on procedures and not deducible |
| 6. Was the care-provider blinded? | ||
|
Blinding of caregivers Look out for good placebos (see, hear, taste, feel, smell), tricky unmasking side effects accounting for the subjectivity of the outcome measurements and the accessibility of co-interventions by the caregivers |
Adequate Partial Inadequate Unknown |
Adequate: Placebo described as ‘indistinguishable’ and procedures watertight (use your imagination with the ‘cheat’ in mind; e.g. statement that sensitive/unmasking laboratory results were kept separate from ward personnel) Partial: Just ‘double-blind’ in text and no further description of procedures or nature of the placebo Inadequate: Wrong placebo (e.g. fructose in trial on ascorbic acid) Unknown: No details in text |
|
Co-interventions Register when they may have an impact on any of the outcome phenomena. Consult the list of cointerventions (not included in this appendix). |
Adequate Partial Inadequate Unknown |
Adequate: Percentages of all relevant interventions in all groups Partial: One or more interventions omitted or omission of percentages in each group Inadequate: Not deducible Unknown: No statements |
| 7. Was the patient blinded? | ||
|
Blinding of patients This item is hard to define. Just the statement ‘double-blind’ in the paper is really insufficient if the procedure to accomplish this is not described or reasonably deducible by the reviewer. Good placebos (see, hear, taste, feel, smell), tricky unmasking side effects accounting for the subjectivity of the outcome measurements and the accessibility of co-interventions by the patient are required |
Adequate Partial Inadequate Unknown |
Adequate: Placebo described as ‘indistinguishable’ and procedures watertight Partial: Just ‘double-blind’ in text and no further description of procedures or nature of the placebo Inadequate: Wrong placebo Unknown: No details in text |
|
Compliance Dosing errors and timing errors |
Adequate Partial Inadequate Unknown |
Adequate: Medication Event Monitoring System (MEMS or eDEM) Partial: Blood samples, urine samples (use of indicator substances) Inadequate: Pill count or self report Unknown: Not mentioned |
|
Check on blinding Questionnaire for patients, caregivers, assessors and analysis of the results; the (early) timing is critical because the treatment effect may be the cause of unblinding, in which case it may be used as an outcome measure |
Reported Unknown |
Reviewer decides |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | ||
| Results for the primary outcome measure |
Adequate Partial Inadequate Unknown |
Adequate: Mean outcome in each group together with mean difference and its standard error (SE) or standard deviation (SD) or any CI around it or the possibility to calculate those from the paper. Survival curve with log-rank test and patient numbers at later time points Partial: Partially reported Inadequate: No SE or SD, or SD without N (SE = SD/N) Unknown: Very unlikely |
| 9. Did the analysis include an intention-to-treat (ITT) analysis? | ||
|
ITT Early dropout can make this very difficult. Strictest requirement is sensitivity analysis including early dropouts |
Adequate Inadequate |
Reviewers should not just look for the term ITT but assure themselves that the calculations were according to the ITT principle |
|
Dealing with missing values The percentage missing values on potential confounders and outcome measurements (seldom given) is a rough estimate of a trial’s quality. One can carry them forward, perform sensitivity analysis assuming the worst- and best-case scenarios, use statistical imputation techniques, etc. Note that the default option (deletion) assumes that the value is randomly missing, which seems seldom justified |
Adequate Partial Inadequate Unknown |
Adequate: Percentage of missing values and distribution over the groups and procedure of handling this stated Partial: Some statement on numbers or percentages Inadequate: Wrong procedure (a matter of great debate) Unknown: No mentioning at all of missing and not deducible from tables |
|
Loss to follow-up This item examines both numbers and reasons; typically an item that needs checking in the methods section and the marginal totals in the tables. Note that it may differ for different outcome phenomena or time points. Some reasons may be reasons given by the patient when asked and may not be the true reason. There is no satisfactory solution for this |
Adequate Partial Inadequate Unknown |
Adequate: Number randomised must be stated. Number(s) lost to follow-up (dropped out) stated or deducible (from tables) for each group and reasons summarised for each group Partial: Numbers, but not the reasons (or vice versa) Inadequate: Numbers randomised not stated or not specified for each group Unknown: No details in text |
Appendix 2 Literature searches and flow chart of included studies
The following databases were searched for published studies and recently completed and ongoing research. Searches were updated in December 2008.
-
General health and biomedical databases, including MEDLINE, EMBASE, Science Citation Index and BIOSIS.
-
Specialist electronic databases: DARE and the Cochrane library.
-
Grey literature and conference proceedings.
-
Contact with individual experts and those with an interest in the field.
-
Checking of reference lists.
-
Research in progress: National Research Register (historical), UK Clinical Research Network (CRN), Current Controlled Trials (CCT) and ClinicalTrials.gov.
Clinical effectiveness searches
The following strategies were used to search MEDLINE (OVID), 1966–2008. These were translated to search the other databases listed above.
-
cerumen/(578)
-
cerum*.tw. (531)
-
(ear* and wax*).tw. (581)
-
earwax*.tw. (60)
-
or/1–4 (1280)
-
randomized controlled trial.pt. (248764)
-
controlled clinical trial.pt. (76414)
-
randomized.ab. (160990)
-
placebo.ab. (103272)
-
clinical trials as topic.sh. (135286)
-
randomly.ab. (117274)
-
trial.ti. (71485)
-
exp Cohort Studies/(648803)
-
cohort.tw. (102947)
-
or/6–14 (1169187)
-
5 and 15 (114)
-
humans.sh. (10090140)
-
16 and 17 (105)
-
from 18 keep 1–105 (105)
Figure 7, shows the identification of studies for inclusion in the systematic review of clinical effectiveness.
FIGURE 7.
Flow chart of identification of studies for inclusion in the systematic review of clinical effectiveness. CCTs, controlled clinical trials; RCTs randomised controlled trials.
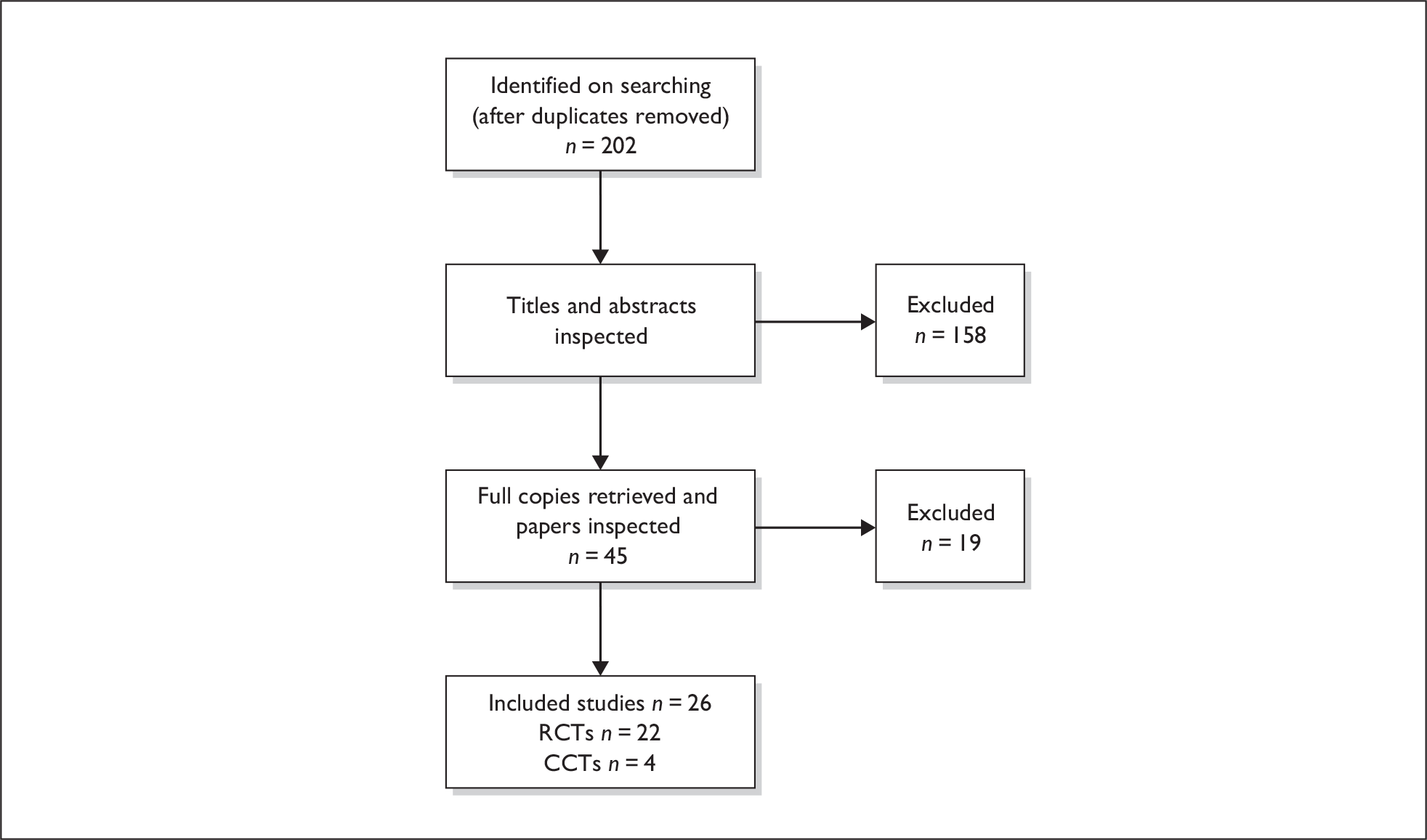
Foreign language publications
Two foreign language publications were identified on searches and are listed below. From their English language abstracts it would appear that neither of these had a comparator group, and would therefore not meet the inclusion criteria of our review. However, we were unable to fully screen these for inclusion.
-
Cassano P, Mora E, Damiani V, Passali FM, Passali D. Valutazione dell’efficacia cerumenolitica di Audispray. Otorinolaringol2002;52:131–5.
-
Cavallazzi GM, Bottero A. Impiego clinico di un nuovo ceruminolitico: considerazioni preliminary. Riv Orl Aud Fon 1988;8:197–200.
Appendix 3 Data extraction forms: primary care setting
Meehan and colleagues46
| Extracted by: PH | Checked by: EL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||||||
|
Author: Meehan and colleagues:46 Abstract Year: 2002 Country: USA Study design: Double-blind RCT Number of centres: One Setting: Emergency care Funding: None reported |
Duration of treatment: 15 minutes Other interventions used: Irrigation with 50 ml of saline if TM was still occluded after treatment, repeated once if needed |
Number of participants: 48 DS: n = 15 TP: n = 17 Saline: n = 16 Sample attrition/dropout: None reported, but numbers of participants in secondary outcomes are lower Inclusion criteria for study entry: Cooperative participants aged 1–18 presenting to a paediatric emergency department, with complete or partial TM occlusion Exclusion criteria for study entry: None reported |
Primary outcomes: Amount of TM visualised Secondary outcomes: AEs Method of assessing outcomes: Grades of TM occlusion – complete, partial or clear Length of follow-up: Immediate |
|||||||
| Baseline characteristics of participants | ||||||||||
| All | >DS (n = 15) | TP (n = 17) | Saline (n = 16) | p-value | ||||||
| Gender M/F | 24 : 24 | No p-values reported | ||||||||
| Mean age | 4.6 | |||||||||
| Median age | 3.5 | |||||||||
| TM occlusion – complete | 11 | 11 | 9 | |||||||
| TM occlusion – partial | 4 | 6 | 7 | |||||||
| Results | ||||||||||
| Primary outcomes | ||||||||||
| TM occlusion | DS (n = 15) | TP (n = 17) | Saline (n = 16) | p-value | ||||||
| Complete | 5 | 5 | 5 | No p-values reported | ||||||
| Partial | 8 | 5 | 9 | |||||||
| Clear | 2 | 7 | 2 | |||||||
| Comments: after solvent (intervention) only | ||||||||||
| Secondary outcomes | ||||||||||
| DS (n = 15) | TP (n = 17) | Saline (n = 16) | p-value | |||||||
| TM occlusion after one irrigation: | n = 13 | n = 15 | n = 15 | No p-values reported | ||||||
| Complete | 4 | 4 | 4 | |||||||
| Partial | 6 | 3 | 5 | |||||||
| Clear | 3 | 8 | 6 | |||||||
| TM occlusion after two irrigations: | n = 12 | n = 15 | n = 15 | No p-values reported | ||||||
| Complete | 3 | 4 | 3 | |||||||
| Partial | 4 | 3 | 4 | |||||||
| Clear | 5 | 8 | 8 | |||||||
| Comments: The most common AE was pain with irrigation overall (10/48) | ||||||||||
| Methodological comments | ||||||||||
|
Allocation to treatment groups: RCT – no other details reported Blinding: Study states double-blind evaluation, but no details reported Comparability of treatment groups: no details reported Method of data analysis: The abstract reports a trend for the efficacy of Cerumenex without irrigation and that adding irrigation improves the effectiveness of Colace, while a second irrigation does not improve outcomes. No data analysis or p-values are reported to support this Sample size/power calculation: None reported Attrition/dropout: None reported, but numbers of participants reported in secondary outcomes are lower |
||||||||||
| General comments | ||||||||||
|
Generalisability: No breakdown of baseline characteristics for the three groups is provided, population consists of American children attending a university paediatric emergency department Outcome measures: It is unclear how valid or objective the measure was, or how consistent the assessments were. Intercentre variability: N/A Conflict of interests: None reported |
||||||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
| 1. Was the assignment to the treatment groups really random? | Inadequate |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Inadequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Partial |
| 7. Was the patient blinded? | Partial |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Whatley and colleagues47
| Extracted by: EL | Checked by: PH | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||||||||
|
Author: Whatley and colleagues47 Year: 2003 Country: USA Study design: RCT Number of centres: Two Setting: Children’s hospital emergency department or large general paediatric clinic in same town Funding: Not stated |
Duration of treatment: Between 15 and 30 minutes depending on number of irrigations Other interventions used: In all groups, if, after 15-minutes, the TM was not completely visualised, the ear was irrigated with 50 ml of tepid tap water (85–95°F). If still not clear another irrigation was undertaken A 60-ml syringe with a 18-gauge angiocatheter precut to 1.5 cm in lengths was used for irrigation |
Number of participants: 96 assessed for eligibility, 3 refused to participate, 93 randomisedSample attrition/dropout: DS one discontinued study, one excluded from analysis (protocol violation). Inclusion criteria for study entry: Aged 6 months to 5 years with complete or partial cerumen obstruction of the TM (assessed by 1 of 4 investigators) Exclusion criteria for study entry: Otitis externa Myringotomy tubes presently or placed within the last 2 years Suspected perforation of TM Severe healing loss in 1 or both ears Known allergy to study agents Prior complication from irrigation |
Primary outcomes: Proportion achieving complete visualisation of the TM Secondary outcomes: Adverse events Method of assessing outcomes: Wax (based on colour and consistency) was characterised as soft, hard or mixed Complete obstruction defined as inability to visualise any of the TM, partial ability to visualise part of the TM but not all membrane landmarks, including light reflex, ossicles and mobility. To determine interobserver variability each investigator examined the same 26 ears prior to study initiation. A kappa value of 0.72 was obtained Length of follow-up: Immediate |
|||||||||
| Baseline characteristics of participants | ||||||||||||
| DS (n = 34) | TP (n = 30) | Saline (n = 28) | p-value | |||||||||
| Mean (SD) age, months | 36.4 (19.1) | 30.9 (15.2) | 36.7 (19.5) | p = 0.38 | ||||||||
| Gender, M/F (%) | 14:20 (41:59) | 13:17 (43:57) | 15:13 (54:46) | p = 0.59 | ||||||||
| Race, n (%) | ||||||||||||
| African American | 26 (76) | 15 (50) | 19 (68) | p = 0.16, between all groups | ||||||||
| 8 (24) | 14 (47) | 8 (29) | ||||||||||
| 0 | 1 (3) | 1 (3) | ||||||||||
| White | ||||||||||||
| Other | ||||||||||||
| Wax, n (%) | ||||||||||||
| Hard | 11 (32) | 12 (40) | 7 (25) | p = 0.57, between all groups | ||||||||
| Soft | 11 (32) | 12 (40) | 11 (39) | |||||||||
| Mixed | 12 (35) | 6 (20) | 10 (36) | |||||||||
| Complete obstruction at enrolment, n (%) | 31 (91) | 24 (80) | 22 (79) | p = 0.33 | ||||||||
| Results: Mean age (SD) in months for all participants 34.7 (18.1) gender for all (%) M 42 : F 50 (36 : 58) | ||||||||||||
| Primary outcomes | DS (n = 34) | TP (n = 30) | Saline (n = 28) | p-value | ||||||||
| Clear TM after agent, n (%) | 4 (12) | 4 (13) | 1 (4) | p-value not reported | ||||||||
| Clear TM after first irrigation, n (%) | 13 (38) | 12 (40) | 12 (43) | |||||||||
| Clear TM after second irrigation, n (%) | 18 (53) | 13 (43) | 19 (68) | Between the 3 groups, p = ns | ||||||||
| Comments: Potential confounders, including study site, different investigators and type of wax were analysed. The difference in the success rate between sites was not statistically significant (p = 0.64), nor was the difference between investigators (p = 0.58). The only trend was that the success rate for soft wax (68%) was higher than for mixed (50%) or hard (43%); p = 0.13. | ||||||||||||
| Secondary outcomes | DS (n = 34) | TP (n = 30) | Saline (n = 28) | p-value | ||||||||
| Comments: AEs – one patient had a small amount of ear canal bleeding after irrigation, but was able to complete the study (not reported which intervention group the participant was in). | ||||||||||||
| Methodological comments | ||||||||||||
|
Allocation to treatment groups: A computerised, random-number program was used. Syringes were placed in consecutively numbered envelopes by a hospital pharmacist. Each enrolled participants was then assigned the next numbered envelope Blinding: States double-blind, pharmacist loaded and sealed the syringes into envelopes, but not clear if any distinguishing factors between syringes or when the code was broken. Treatments were a different colour and any residues after drainage could enable investigators to determine which treatment a participant had received Comparability of treatment groups: No statistically significant differences in baseline characteristics. Compared with the paediatric clinic, a higher proportion of patients enrolled in the emergency department received TP (42% vs 15%) and fewer patients received saline (22% vs 45%). Visually race appears to be dissimilar; however, differences are shown as statistically not significant Method of data analysis: Categorical variables analysed using a chi-squared test or a Fisher’s exact test. Continuous variables analysed using ANOVA. p < 0.05 was considered statistically significant. sas statistical software version 8.02 (SAS Institute, Cary, NC) was used Sample size/power calculation: A sample size of 90 was estimated to achieve 80% power to detect a 40 percentage-point difference between the treatment groups ( = 0.05; χ2 with d = 2). A 40 percentage-point difference was considered to be significant, based on previous studies Attrition/dropout: In the docusate group 1 patient discontinued (due to the ear being irrigated before an agent was placed) and one was excluded |
||||||||||||
| General comments | ||||||||||||
|
Generalisability: Population was young children, predominantly of African American race (64%). Convenient sample, only assessed when an investigator was available Outcome measures: Inter-rater reliability assessed and reasonable Intercentre variability: No significant differences noted by investigators. There was an imbalance of the TP and normal saline treatment groups between the 2 sites, with a higher percentage of participants enrolled in the emergency department TP group (42% vs 15%) and fewer participants in the normal saline group (22% vs 45%). Participants in the DS treatment group at each site were evenly distributed (36% vs 39%). The differences in success rates between sites was not significant (p = 0.64) nor the differences between investigators (p = 0.58) Conflict of interests: None noted |
||||||||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
| 1. Was the assignment to the treatment groups really random? | Adequate |
| 2. Was the treatment allocation concealed? | Adequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Partial |
| 6. Was the care-provider blinded? | Partial |
| 7. Was the patient blinded? | Partial |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Singer and colleagues49
| Extracted by: PH | Checked by: EL | ||||||
|---|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | ||||
|
Author: Singer and colleagues, 49 Year: 2000 Country: USA Study design: Double-blind RCT Number of centres: One Setting: Emergency department Funding: None reported |
Duration of treatment: 10–15 minutes Other interventions used: If membrane was still obscured, ear irrigated with 50 ml of lukewarm normal saline solution. Repeated for a second time if TM was still obscured (50-ml syringe with 18-gauge angiocatheter at tip) |
Number of participants: 50 (1 ear only per patient)Sample attrition/dropout: None reported Inclusion criteria for study entry: ≥ 1 year, medially required visualisation of ear canal (i.e. earache, hearing loss, fever) and ear canal partially or totally occluded by cerumen Exclusion criteria for study entry: Known or suspected TM perforation, overt ear infection, uncooperative or allergy to solvent agents. |
Primary outcomes: Proportion of ears in which membrane totally visible with or without irrigation or irrigation with 100 ml irrigant. Secondary outcomes: Presence of AE Method of assessing outcomes: Partially or totally obscured TM not stated but an interobserver agreement on patients independent patient set was good, p = 0.79 (reference given) AE: Participants/parents were asked to indicate AEs during procedure Length of follow-up: Immediate |
||||
| Baseline characteristics of participants | |||||||
| DS (n = 27) | TP (n = 23) | p-value | |||||
| Mean age years (SD) | 38.7 (30.7) | 46.1 (29.1) | No p-values reported | ||||
| Gender M/F (%) | 16 (59), 11 (41) | 16 (70), 7 (30) | |||||
| Children ≤ 5 years (%) | 9 (33) | 4 (17) | |||||
| Completely occluded ears | 21 (78) | 18 (78) | |||||
| Results: 13% of participants ≤ 5 years old | |||||||
| Primary outcome: n (%) | DS (n = 27) | TP (n = 23) | Percentage difference, DS – TP (95% CI) | p-value | |||
| Completely visualised ears after solvent only | 5 (19) | 2 (9) | 9.8 (–8.8 to 28.5) |
No p-values reported |
|||
| Completely visualised ears after solvent with or without irrigation | 22 (82) | 8 (35) | 46.7 (22.3 to 71.1) | ||||
| TM visualisation, number (%)a | |||||||
| Complete | Incomplete | Complete | Incomplete | p-value | |||
| After solvent only | 5 (19) | 22 (81) | 2 (9) | 21 (91) | No p-values reported | ||
| First 50-ml ear irrigation | 10 (45) | 12 (55) | 2 (10) | 19 (90) | |||
| Second 50-ml ear irrigation | 7 (58) | 5 (42) | 4 (21) | 15 (79) | |||
| Comments: | |||||||
| a Subsets of same data as above. | |||||||
| Secondary outcomes | DS (n = 27) | TP (n = 23) | Percentage difference, DS – TP (95% CI) | p-value | |||
| AEs (i.e. pain, vertigo, nausea or hearing loss) | 0 (0) | 0 (0) | 0 (–7.8 to –7.8) | No p-values reported | |||
| Comments: | |||||||
| Methodological comments | |||||||
|
Allocation to treatment groups: Assignment was generated by computerised random numbers program. A series of opaque consecutively numbered syringes were prepared by hospital pharmacy, unconnected to the emergency department or enrolment process Blinding: States double-blind, but as solutions differ in colour (Colace = pink, Cerumenex = yellow) solvent likely to have become obvious when used Comparability of treatment groups: Groups are reported to be similar in age, sex and proportion of completely obscured TMs, but no r-values given. However, the mean age of the Colace group was lower, most likely because it included more than double the amount of children Method of data analysis: spss version 8.0 was used for statistical analysis and demographics were compared using chi-squared test, t-tests for continuous variables. No p- or r-values are reported. Outcomes are presented as point and interval estimates with the difference in proportions and 95% CI for the difference. Post hoc subgroup analysis based on participants’ age was performed. It is uncertain if the study was powered for a subgroup analysis and authors provide no data. Data not extracted Sample size/power calculation: 80% power to detect differences between groups in main outcome chi-squared test, α = 0.05), assuming after application of control solvent 40% of membranes completely visualised Attrition/dropout: No dropouts are reported and all 50 participants finished treatment |
|||||||
| General comments | |||||||
|
Generalisability: American cooperative paediatric and adult patients Outcome measures: Unclear how valid, objective or consistently applied the outcome measures were. Interobserver agreement was from an independent patient set Intercentre variability: N/A Conflict of interests: None reported |
|||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Adequate |
| 2. Was the treatment allocation concealed? | Adequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Inadequate |
| 7. Was the patient blinded? | Partial |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
General Practitioner Research Group41
| Extracted by: PH | Checked by: EL | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||||||||
|
Author: General Practitioner Research Group41 Year: 1965 Country: UK Study design: Double-blind RCT Number of centres: 14 Setting: Primary care Funding: None reported |
Duration of treatment: Half an hour before ear syringing Other interventions used: Syringing (standardised method of syringing, only metal type of ear syringe was used and size recorded) |
Number of participants: 150Sample attrition/dropout: None reported Inclusion criteria for study entry: None reported Exclusion criteria for study entry: None reported |
Primary outcomes: Volume of water for syringing and syringefuls used Secondary outcomes: Ease of wax removal Character of syringed wax Method of assessing outcomes: Removal: 1 = easy or difficult, 2 = partial or failed Earwax: 1 = liquid, 2 = shredded, 3 = hard lumps Length of follow-up: Immediate |
|||||||||
| Baseline characteristics of participants | ||||||||||||
| Age, maximum incidence | All (n = 150) | p-value | ||||||||||
| Males | 31–50 years | |||||||||||
| Females | 51–70 years | |||||||||||
| Gender M/F | 1.3 : 1 | |||||||||||
| Results: 32% of participants were new cases, 53% without syringing for over 12 months | ||||||||||||
| Primary outcomes | ||||||||||||
| Dioctyl (n = 77) | Control (n = 73) | p-value | ||||||||||
| No. of syringefuls used | No of cases | Total quantity (ml) | Mean per case | No of cases | Total quantity (ml) | Mean per case | No analysis conducted | |||||
| 0.25–1 | 35 | 2123 | 60 | 26 | 1732 | 65 | ||||||
| 1.25–2 | 13 | 1718 | 130.5 | 17 | 2329 | 136 | ||||||
| 2.5–4 | 12 | 2243 | 187.5 | 17 | 3487 | 207 | ||||||
| 5–15 | 6 | 2045 | 341 | 4 | 2613 | 653 | ||||||
| Totals | 66 | 8129 | 122 | 64 | 10,181 | 165.5 | ||||||
| Note: Difference in mean caused by one participant in control group requiring 15 syringefuls of water to remove the wax. After exclusion of this case virtually no differences between groups in respect of this factor. | ||||||||||||
| Comments: Maximum incidence for males in 31–51 year group, for females 51–70 year group. Syringes hold 2, 3 or 4 oz of water (57, 85 or 112 ml) and exact analyses was made in respect of each size syringe and number of syringefuls. | ||||||||||||
| Secondary outcomes | ||||||||||||
| Removal, n (%) | Dioctyl (n = 77) | Control (n = 73) | p-value | |||||||||
| Easy | 54 (70) | 42 (57) | ||||||||||
| Difficult | 17 (22) | 23 (32) | ||||||||||
| Partial | 3 (4) | 6 (8) | ||||||||||
| Failed | 2 (3) | 2 (3) | ||||||||||
| Comments: partial or failed removal combined was 8% for the dioctyl-medo group and 11% for the control group. Study reports differences, but no evidence of any statistical analysis. | ||||||||||||
| Character of wax, n (%) | Dioctyl (n = 77) | Control (n = 73) | p-value | |||||||||
| Liquid | 14 (19) | 10 (14) | ||||||||||
| Shredded | 34 (46) | 28 (40) | ||||||||||
| Hard lumps | 26 (35) | 32 (46) | ||||||||||
| Failed | 3 | 2 | ||||||||||
| Not recorded | 0 | 1 | ||||||||||
| Comments: AEs were negligible and mostly related to syringing. 91% of dioctyl participants vs 89% control had no side effects. 92% of dioctyl participants vs 86% control found procedure tolerable. | ||||||||||||
| Methodological comments | ||||||||||||
|
Allocation to treatment groups: Choice treatment by random selection. On ‘breaking the code’ it was found that 77 participants received dioctyl-medo and 73 participants were in the control group. No other details reported Blinding: Authors report double-blind trial. Doctor administers drops, assessments and syringing, but no other details reported Comparability of treatment groups: Distribution of participants between groups is reported to be ‘even’ in respect of age and sex, but only gender ration is reported Method of data analysis: Not reported Sample size/power calculation: Not reported Attrition/dropout: Not reported |
||||||||||||
| General comments | ||||||||||||
|
Generalisability: UK primary care practice patients, no details on severity of occlusions Outcome measures: Outcome measures open to subjective interpretation. Comparative results between the 2 preparations are reported to be unaffected by sex, age or duration of wax, but no description analysis given. Results slightly better in males, younger participants and cases of shortest duration. No statistical data to support this. Intercentre variability: Standardised syringing procedure reported, but no other details given. Conflict of interests: None reported |
||||||||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Unknown |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Partial |
| 7. Was the patient blinded? | Partial |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Pavlidis and Pickering42
| Extracted by: PH | Checked by: EL | ||||
|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | ||
|
Author: Pavlidis and Pickering42 Year: 2005 Country: Australia Study design: RCT Number of centres: One Setting: Primary care Funding: General Practice Education & Training, and General Registrars Association Registrar Scholarship & Research Fund funded consumables |
Duration of treatment:Other interventions used: Auroscopic ear canal inspection for all patients after each syringing attempt Patients with wax in both ears: a coin toss determined treatment for the left ear, with right ear receiving alternative |
Number of participants: 26, 39 earsSample attrition/dropout: None reported Inclusion criteria for study entry: ≥ 18 years old, with earwax partially or totally occluding one or both ears that GP would normally syringe Exclusion criteria for study entry: Actual or suspected TM perforation Previous ear surgery Current otitis media or otitis externa Swimming during previous 3 days Ear drops during previous 3 days Unable to lie down for 15 minutes Unable to consent |
Outcomes: Mean number of syringing attempts Mean time to syringing (minutes) AEs Method of assessing outcomes: Syringing – 25 ml of water for each syringing attempt until visibly clear Length of follow-up: Immediate |
||
| Baseline characteristics of participants | |||||
| Wet syringing (ears = 22) | Dry syringing (ears = 17) | p-value | |||
| Gender M/F (%) | 15 (68), 7 (32) | 11 (65), 6 (35) | |||
| Age, mean years (SD) | 63 (8) | 65 (20) | nsb | ||
| Mean duration of symptoms, days (SD) | 300 (421) | 249 (353) | nsb | ||
| Comments: Patients aged between 37 and 90 years. | |||||
| Results | |||||
| Outcomes | Wet syringing (ears = 22) | Dry syringing (ears = 17) | p-value | ||
| Mean no. of attempts (SD) | 7.5 (7.3) | 25.4 (39.4) | p = 0.043 (in favour of wet syringing) | ||
| Mean time to syringe ear, minutesa | 6.5 | 15.4 | nsb | ||
| Comments: 1 patient had both ears syringed and experienced dizziness (not vertigo). No other AEs were noted and all TMs were intact at end of syringing. | |||||
| a It is stated that the number of syringing attempts is unusually high due to the small volume of the syringe used (25 ml), with GP being reported as normally using larger metal ear syringes (> 120 ml). | |||||
| b For non-significant results no p-value is given. | |||||
| Methodological comments | |||||
|
Allocation to treatment groups: Patients were randomised by the toss of a coin, but for those with wax in both ears the coin toss always determined the treatment for the left ear. Authors acknowledged that randomisation procedure could have led to selection bias Blinding: Open, non-blinded trial Comparability of treatment groups: Differences between groups for age and mean duration of symptoms reported as non-significant Method of data analysis: Unpaired, two-tailed t-tests to compare group differences Sample size/power calculation: Not reported. It is stated that the study was not powered to detect major complications (approximately 1 in 1000 ears syringed) Attrition/dropout: Not reported |
|||||
| General comments | |||||
|
Generalisability: UK adult patients with earwax partially or totally occluding one or both ears, which would normally be syringed by their GP Outcome measures: Unknown how valid or objective the outcome measures were. All patients had their ears syringed by one of the research group to maintain technique consistency. It is stated that most patients preferred 15-minute water treatment to using softening preparation for some days at home prior to syringing, but no data are reported to support this Intercentre variability: N/A Conflict of interests: None reported. General Practice Education & Training, and General Registrars Association Registrar Scholarship & Research Fund funded consumables |
|||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Partial |
| 2. Was the treatment allocation concealed? | Inadequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Inadequate |
| 6. Was the care-provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
General Practitioner Research Group48
| Extracted by: PH | Checked by: EL | |||||||
|---|---|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||||
|
Author: General Practitioner Research Group48 Year: 1967 Country: UK Study design: Double-blind RCT Number of centres: 10 Setting: Primary care Funding: None reported |
Duration of treatment: 2 nights (10 minutes per treatment) Other interventions used: Syringing *Inserted with dropper by participants, following standardised instructions. If both ears are affected, procedure is repeated in the other ear |
Number of participants: 107Sample attrition/dropout: None reported Inclusion criteria for study entry: All cases of earwax Exclusion criteria for study entry: Minor degrees of wax easily removed without softening agent |
Outcomes: Volume of water for syringing Ease of wax removal Character of wax AEs Method of assessing outcomes: Water volumes calculated from the number or fraction of syringefuls required Removal of wax: easy, difficult, partial or failed Character of wax: liquid, shredded or hard lumps Length of follow-up: Immediate |
|||||
| Baseline characteristics of participants | ||||||||
| All (n = 107) | p-value | |||||||
| Age, % | ||||||||
|
10–30 years 31–50 years 51–70 years 71 years and over |
27 34 31 8 |
No p-values reported | ||||||
| Elapsed time since last syringing, % | ||||||||
|
≥ 12 months 10–12 months 7–9 months 4–6 months 1–3 months New cases Wax in left ear, % Wax in right ear, % Wax in both ears, % |
32 17 5 5 1 41 31 23 46 |
|||||||
| Results | ||||||||
| Outcomes: | Waxsol (n = 47) | Cerumol (n = 60) | p-value | |||||
| Volume of water, fl oz | No. of participants | Total volume | No. of particpants | Total volume | ||||
| 0.5 | 0 | 0 | 1 | 0.5 | No p-values reported | |||
| 1 | 6 | 6.0 | 2 | 2.0 | ||||
| 2 | 13 | 26.0 | 4 | 8.0 | ||||
| 2.5 | 1 | 2.5 | 1 | 2.5 | ||||
| 3 | 3 | 9.0 | 5 | 15.0 | ||||
| 4 | 3 | 12.0 | 8 | 32.0 | ||||
| 5 | 0 | 0 | 1 | 5.0 | ||||
| 6 | 6 | 36.0 | 4 | 24.0 | ||||
| 7 | 2 | 14.0 | 2 | 14.0 | ||||
| 8 | 3 | 24.0 | 12 | 96.0 | ||||
| 9 | 0 | 0 | 2 | 18.0 | ||||
| 10 | 1 | 10.0 | 2 | 20.0 | ||||
| 12 | 6 | 72.0 | 8 | 96.0 | ||||
| 14 | 1 | 14.0 | 2 | 28.0 | ||||
| 16 | 2 | 32.0 | 2 | 32.0 | ||||
| 18 | 0 | 0 | 1 | 18.0 | ||||
| 24 | 0 | 0 | 1 | 24.0 | ||||
| 26 | 0 | 0 | 1 | 26.0 | ||||
| 40 | 0 | 0 | 1 | 40.0 | ||||
| Totals | 47 | 257.5 | 60 | 501.0 | ||||
| Mean volume per participant | 5.5 fl oz (156 ml) | 8.4 fl oz (240 ml) | Not reported | |||||
| No. of participants (%) | No. of participants (%) | p-value | ||||||
| ≤ 56 ml (2 fl oz) | 19 (40) | 7 (12) | p < 0.05a | |||||
| > 56 ml | 28 (60) | 53 (88) | ||||||
| Proportion of participants needing 14–112 ml (%) | 55 | 35 | p < 0.05a | |||||
| Comments: | ||||||||
| a Reported to be significant at 5% level in favour of Waxsol for cases ≤ 2 fl oz (56 ml), remaining ‘in favour’ of Waxsol at 4 fl oz (112 ml). | ||||||||
| Ease of wax removal, no. of participants (%) | ||||||||
| Waxsol (n = 47) | Cerumol (n = 60) | p-value | ||||||
| Easily removed | 39 (83) | 48 (80) | No p-values reported | |||||
| Removed with difficulty | 6 (13) | 9 (15) | ||||||
| Partly removed | 1 (2) | 1 (2) | ||||||
| Failed | 1 (2) | 2 (3) | ||||||
| Character of wax, % of participants | ||||||||
| Liquid | 17 | 17 | No p-values reported | |||||
| Shredded | 46 | 35 | ||||||
| Hard lumps | 37 | 24 | ||||||
| Comments: Failed participant in Waxsol group – further syringing after a week cleared wax. Failed two participants in Cerumol group – one participant had wax removed after olive oil instillation and several attempts at syringing and instrumental means; the information for the other participant was not recorded. | ||||||||
| Waxsol (n = 47) | Cerumol (n = 60) | p-value | ||||||
| AEs, % of participants | 7 | 5 | No p-values reported | |||||
| Treatment found tolerable, % of participants | 89 | 95 | ||||||
| Comments: | ||||||||
| a No details reported. | ||||||||
| Methodological comments | ||||||||
|
Allocation to treatment groups: Choice treatment by random selection. On ‘breaking the code’ it was found that 47 participants received Waxsol and 60 participants received Cerumol. No other details reported Blinding: Authors report double-blind trial, but no details reported Comparability of treatment groups: No split for baseline characteristics of groups provided. Treatment groups are reported as reasonably matched, with the exception of a higher proportion of participants without prior treatment in the Cerumol group, but no data provided Method of data analysis: Some statistical significant differences commented on, but minimal details reported and analysis based on post hoc division based on volume water Sample size/power calculation: No details reported Attrition/dropout: No details reported |
||||||||
| General comments | ||||||||
|
Generalisability: UK Primary Care Practice patients, no details on severity of occlusions Outcome measures: Unclear how valid, objective and consistently applied the measures were Intercentre variability: Standardised instructions to patients reported, but no details given about possible variation in syringing procedure Conflict of interests: None reported |
||||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Inadequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Partial |
| 7. Was the patient blinded? | Partial |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Amjad and Scheer51
| Extracted by: PH | Checked by: EL | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||||||||
|
Author: Amjad and Scheer51 Year: 1975 Country: USA Study design: Double-blind RCT Number of centres: Not stated Setting: Primary care Funding: None reported |
Duration of treatment: Each affected ear was treated with 1 application of drops, which were left in the ear canal for 30 minutes Other interventions used: Irrigation with lukewarm water after treatment |
Number of participants: 80Sample attrition/dropout: None reported Inclusion criteria for study entry: Hard or impacted earwax Exclusion criteria for study entry: None reported |
Primary outcomes: Degrees of wax removal Secondary outcomes: AE (subjective and observations of objective side effects) Method of assessing outcomes: Excellent (removal of all wax), good (removal of most wax), fair (removal of some wax) and poor (removal of little or no wax) Degree of obstruction: complete or partial Length of follow-up: Immediate |
|||||||||
| Baseline characteristics of participants | ||||||||||||
| Pretreatment wax, number of ears | ||||||||||||
| TP (n = 40) | Carbamide peroxide (n = 40) | p-value | ||||||||||
| Impacted | 19 | 18 | No p-values reported | |||||||||
| Hard | 16 | 16 | ||||||||||
| Loose | 1 | 3 | ||||||||||
| Soft | 4 | 3 | ||||||||||
| Complete obstruction | 36 | 32 | ||||||||||
| Partial obstruction | 4 | 8 | ||||||||||
| Results | ||||||||||||
| Primary outcomes | ||||||||||||
| Efficacy of treatment, n (%) | TP (n = 40) | Carbamide peroxide (n = 40) | p-value | |||||||||
| Excellent | 27 (68) | 2 (5) | No p-value reported | |||||||||
| Good | 8 (20) | 5 (12) | ||||||||||
| Fair | 2 (5) | 4 (10) | ||||||||||
| Poor | 3 (7) | 29 (73) | ||||||||||
| Effective (‘excellent’ plus ‘good’) | 35 (88) | 7 (17) | ||||||||||
| Comments: | ||||||||||||
| Secondary outcomes | ||||||||||||
| TP (n = 40) | Carbamide peroxide n = 40 | p-value | ||||||||||
| AE | 0 | 0 | No p-value reported | |||||||||
| Efficacy to pretreatment wax | No. | E + G | F | P | E + G% | No. | E+G | F | P | E + G% | p-value | |
| Impacted | 19 | 16 | 1 | 2 | 84 | 18 | 2 | 0 | 16 | 11 | No p-value reported | |
| Hard | 16 | 14 | 1 | 1 | 88 | 16 | 3 | 2 | 11 | 19 | ||
| Loose | 1 | 1 | 0 | 0 | 100 | 3 | 1 | 0 | 2 | 33 | ||
| Soft | 4 | 4 | 0 | 0 | 100 | 3 | 1 | 2 | 0 | 33 | ||
| Complete obstruction | 36 | 31 | 2 | 3 | 86 | 32 | 4 | 3 | 25 | 13 | ||
| Partial obstruction | 4 | 4 | 0 | 0 | 100 | 8 | 3 | 1 | 4 | 38 | ||
| Comments: No., number of ears; E + G, effective (‘excellent’ plus ‘good’); F, Fair; P, Poor. | ||||||||||||
| Methodological comments | ||||||||||||
|
Allocation to treatment groups: 80 participants were randomly divided into equal intervention and control group Blinding: Study states double-blind evaluation, but no details reported Comparability of treatment groups: No details reported. Pretreatment wax appears similar Method of data analysis: None reported. Only descriptive/frequency data presented Sample size/power calculation: None reported Attrition/dropout: None reported |
||||||||||||
| General comments | ||||||||||||
|
Generalisability: No baseline characteristics provided, American population Outcome measures: It is unclear how valid or objective the measure was, or how consistent the assessments were; study states that no comparison between treatments was intended, as carbamide peroxide needs multiple instillations Intercentre variability: N/A – it appears to be a one-centre study Conflict of interests: Cerumenex distributed by Purdue Frederick Co., New York, NY |
||||||||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Inadequate |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Inadequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Partial |
| 7. Was the patient blinded? | Partial |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Dummer and colleagues44
| Extracted by: EL | Checked by: PH | |||||
|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||
|
Author: Dummer and colleagues44 Year: 1992 Country: UK Study design: RCT Number of centres: One Setting: Primary care Funding: Supported by Napp Laboratories Ltd |
Duration of treatment: 3 days Other interventions used: None reported *Drops for 3 days and assessed on 4th day in methods, drops for 4 days after which reassessment took place in summary |
Number of participants: 50 Audax: 27 Cerumol: 23 Sample attrition/dropout: None reported Inclusion criteria for study entry: Aged between 19 and 90 years, presenting with impacted or hardened earwax Exclusion criteria for study entry: Those with inflammation or the external auditory meatus, seborrhoeic dermatitis and eczema affecting the external ear, a perforated TM, a pre-existing ear infection requiring treatment with systemic antibiotics, known salicylate sensitivity, instrumentation of the ears (hearing aids), regular swimmers |
Primary outcomes: (Not defined as primary or secondary.) Outcomes included: amount, colour and consistency of wax, symptoms, hearing, global impression of treatment efficacy (patient and investigator) and tolerability Method of assessing outcomes: Amount of wax – considerable block to meatus, considerable but no blockage, medium, scanty Colour – black, brown, yellow, pale Consistency – concrete hard, firm, soft, runny Symptoms – none, deafness, blockage, pain, discharge, irritation Objective hearing – normal whispered voice test, abnormal whispered voice test, Rinne test abnormal, Weber test abnormal Length of follow-up: Median number of days between visits 1 and 2 was 4 days (range 3–7 days) |
|||
| Baseline characteristics of participants | ||||||
| Audax (n = 27) | Cerumol (n = 23) | p-value | ||||
| Mean age, years | 51 | 55 | ||||
| Gender, M/F, n | 18/9 | 14/9 | ||||
| Results: primary outcomes | ||||||
| Amount of wax | ||||||
| Audax (n = 27, ears = 54) | Cerumol (n = 23, ears = 46) | p-value | ||||
| Increased | 0 | 0 | Not reported across groups | |||
| No change | 24 (44%) | 22 (48%) | ||||
| Decreased | 28 (52%) | 24 (52%) | ||||
| Missing data | 2 (4%) | 0 | ||||
| Colour of wax | ||||||
| Darkened | 0 | 0 | States no significant differences, p-value not reported | |||
| No change | 10 | 9 | ||||
| Lightened | 42 | 36 | ||||
| Missing data | 2 | 1 | ||||
| Consistency of wax | ||||||
| Hardened | 0 | 0 | States no significant differences, p-value not reported | |||
| No change | 6 | 5 | ||||
| Softened | 46 | 40 | ||||
| Missing data | 2 | 1 | ||||
| Objective hearing | ||||||
| Improved | 7 (13%) | 2 (4%) | States no significant differences, p-value not reported | |||
| No change | 45 (83%) | 44 (96%) | ||||
| Worsened | 0 | 0 | ||||
| Missing data | 2 (4%) | 0 | ||||
| Overall assessment | ||||||
| Investigator rated ‘effective’ | 36 participantsa | 22 participants | Unclear if tested | |||
| Overall assessment | ||||||
| Participant rated ‘effective’ | 25 (93%) participants | 23 (100%) participants | States no significant differences, p-value not reported | |||
| Tolerability | 2 (both slight irritation to the ear) | 2 (1 slight itch, 1 buzzing noise after use) | ||||
| Subgroup data of 25 participants (12 Audax, 13 Cerumol) with abnormal hearing on entry. | ||||||
| a It is unclear if this is an error, as there only 27 participants in the group or if this should have said number of ears instead of patients as stated in the study. | ||||||
| Objective hearing | ||||||
| Improved | 7 | 2 | p < 0.05 (p-value not reported for other change variables) | |||
| No change | 4 | 11 | ||||
| Worsened | 0 | 0 | ||||
| Missing data | 1 | 0 | ||||
| Comments: No baseline scores reported for any of these measures. | ||||||
| Methodological comments | ||||||
|
Allocation to treatment groups: States ‘allocated at random’ but no further details of randomisation schedule or allocation concealment Blinding: States single-blind (investigator), but no details of how this was maintained Comparability of treatment groups: States treatment groups were well matched for age, sex and objective hearing Method of data analysis: Each ear was assessed separately (100 in total) and tests for differences between treatments were made between patients; p < 0.05 statistically significant. Mann–Whitney U-test for amount, colour, consistency, global efficacy. Fisher’s exact test for hearing test. Demographics chi-squared test Sample size/power calculation: Not reported Attrition/dropout: Missing data shown in tables, but reasons for missing data unclear |
||||||
| General comments | ||||||
|
Generalisability: Difficult to assess as minimal demographic characteristics presented Outcome measures: Unclear how valid, objective, or consistently applied the outcome measures used were Intercentre variability: Not applicable Conflict of interests: States supported by Napp Laboratories, who manufacture Audax |
||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Partial |
| 5. Were outcome assessors blinded to the treatment allocation? | Inadequate |
| 6. Was the care-provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Fahmy and Whitefield54
| Extracted by: EL | Checked by: AC | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | ||||||||||||
|
Author: Fahmy and Whitefield54 Year: 1982 Country: UK Study design: CCT Number of centres: One for study 1 and 2, multicentre for study 3, but number of centres not reported Setting: Studies 1 and 2 in secondary care, study 3 in primary care Funding: Not reported |
Study 1:Study 2:Study 3:Study 4:For all studies participants instilled 5–10 drops twice per day Duration of treatment: 1 week Other interventions used: |
Number of participants: Study 1: 40 participants (80 ears) completed the studyStudy 2: 50 patients (100 ears) completed the studyStudy 3: 160 patients (286 ears) completed the studySample attrition/dropout: Not reported but reports numbers as those ‘completing’ the study. Inclusion criteria for study entry: States as far as possible the protocol remained identical (for all studies); patients presenting with earwax problems Exclusion criteria for study entry: Patients with inflammation of the external meatus, middle ear pathology, e.g. mastoid cavities, or perforation of the TM; a scarred membrane did not constitute a contraindication |
Primary outcomes: (Not defined as primary or secondary.) Wax occlusion, wax consistency, ease of syringing Method of assessing outcomes: States each ear was assessed independently. No definitions of classification of outcomes noted Length of follow-up: 1 week |
||||||||||||
| Baseline characteristics of participants | |||||||||||||||
| Study 1, no. of ears | p-value | ||||||||||||||
| Exterol (n = 20, 40) | Glycerol control (n = 20, 40) | ||||||||||||||
| Degree of wax occlusion (ears) | |||||||||||||||
| Total | 36 | 36 | Not reported to be tested | ||||||||||||
| Partial | 4 | 4 | |||||||||||||
| Consistency of wax (ears) | |||||||||||||||
| Very hard | 20 | 16 | Not reported to be tested | ||||||||||||
| Hard | 20 | 24 | |||||||||||||
| Study 2, no. of ears | p-value | ||||||||||||||
| Exterol (n = 25, 50) | Cerumol (n = 25, 50) | ||||||||||||||
| Degree of wax occlusion (ears) | |||||||||||||||
| Total or subtotal | 23 | 19 | Not reported to be tested | ||||||||||||
| Partial | 27 | 31 | |||||||||||||
| Consistency of wax (ears) | |||||||||||||||
| Very hard | 12 | 8 | Not reported to be tested | ||||||||||||
| Hard | 33 | 27 | |||||||||||||
| Soft | 5 | 15 | |||||||||||||
| Study 3, no. of ears | p-value | ||||||||||||||
| Exterol (n = 157) | Cerumol (n = 129) | ||||||||||||||
| Degree of wax occlusion (ears) | |||||||||||||||
| Total or subtotal | 97 | 86 | Not reported to be tested | ||||||||||||
| Partial | 60 | 43 | |||||||||||||
| Consistency of wax (ears) | |||||||||||||||
| Hard | 114 | 97 | Not reported to be tested | ||||||||||||
| Soft | 43 | 32 | |||||||||||||
| Results | |||||||||||||||
| Study 1, no. of ears | p-value | ||||||||||||||
| Exterol (n = 20, 40 ears) | Glycerol control (n = 20, 40 ears) | ||||||||||||||
| Initially very hard wax | Initially hard wax | Initially very hard wax | Initially hard wax | ||||||||||||
| Wax dispersed without syringing | – | 6 | – | – | Not stated | ||||||||||
| Wax syringed easily | 15 | 14 | 2 | 18 | |||||||||||
| Wax syringed with difficulty | 5 | – | 14 | 6 | |||||||||||
| Comments: When the number of ears not requiring syringing is added to the number syringed easily, Exterol was statistically significantly superior to the control group; p < 0.001. After treatment with Exterol a significant number ears did not require syringing compared with glycerol. | |||||||||||||||
| Study 2, no. of ears: | p-value | ||||||||||||||
| Exterol (n = 25, 50 ears) | Cerumol (n = 25, 50 ears) | ||||||||||||||
| Initially very hard | Initially hard | Initially soft | Initially very hard | Initially hard | Initially soft | ||||||||||
| Wax dispersed without syringing | 4 | 14 | 2 | – | – | 5 | See comments | ||||||||
| Wax syringed easily | 6 | 18 | 3 | – | 10 | 9 | |||||||||
| Wax syringed with difficulty | 2 | 1 | – | 8 | 17 | 1 | |||||||||
| Comments: the number of ears not requiring syringing is markedly greater with Exterol than with Cerumol, p < 0.001. When the number of ears not requiring syringing is added to the number syringed easily, Exterol was statistically significantly superior to Cerumol; p < 0.001. | |||||||||||||||
| Study 3, no. of ears | p-value | ||||||||||||||
| Exterol (n = 157) | Cerumol (n = 129) | ||||||||||||||
| Initially hard wax | Initially soft wax | Initially hard wax | Initially soft wax | ||||||||||||
| Wax dispersed without syringing | 45 | 19 | 12 | 15 | See comments | ||||||||||
| Wax syringed easily | 60 | 22 | 52 | 14 | |||||||||||
| Wax syringed with difficulty | 9 | 2 | 33 | 3 | |||||||||||
| Comments: The number of ears not requiring syringing is markedly greater after treatment with Exterol than with Cerumol; p < 0.001. When the number of ears not requiring syringing is added to the number syringed easily, Exterol was statistically significantly superior to Cerumol; p < 0.001. | |||||||||||||||
| Methodological comments | |||||||||||||||
|
Allocation to treatment groups: Participants presenting with earwax were treated with alternate preparations on a sequential basis Blinding: Not reported Comparability of treatment groups: No baseline characteristics reported Method of data analysis: analysed by t-test and chi-squared test; appears to be selective statistical testing of differences Sample size/power calculation: Not reported Attrition/dropout: Text states numbers completing the study therefore unsure if any participants were potentially included, but not reported upon |
|||||||||||||||
| General comments | |||||||||||||||
|
Generalisability: No baseline demographic characteristics, UK population Outcome measures: Unclear how valid, objective or consistently applied the outcome measures were Intercentre variability: Not reported Conflict of interests: Dermal Laboratories supplied the Exterol and control preparations |
|||||||||||||||
Quality criteria for assessment of controlled clinical studies
| Item | Judgementa |
|---|---|
| Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| Were the eligibility criteria specified? | Partial |
| Were outcome assessors blinded to the treatment allocation? | Unknown |
| Were the point estimates and measure of variability presented for the primary outcome measure? | Partial |
| Did the analyses include an ITT analysis? | Unknown |
| Were withdrawals and dropouts completely described? | Unknown |
| Were participants likely to be representative of the intended population? | Unknown |
Jaffe and Grimshaw50
| Extracted by: EL | Checked by: AC | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||||||
|
Author: Jaffe and Grimshaw50 Year: 1978 Country: UK Study design: RCT Number of centres: Up to 15 Setting: Primary care Funding: None reported |
Duration of treatment: 3 nights Other interventions used: Patients were asked to gently cleanse the ear with cotton wool the following morning *No details of constitution of the treatment |
Number of participants: 106 Otocerol: 53 Cerumol: 53 Sample attrition/dropout: Not reported Inclusion criteria for study entry: Patients presenting with wax in their ears and who would normally be prescribed a cerumenolytic Exclusion criteria for study entry: Overt perforation of the drum or severe infection |
Primary outcomes: (Not defined as primary or secondary). Ease of syringing, doctors overall impression, adverse effects Secondary outcomes: See above Method of assessing outcomes: Not reported Length of follow-up: Patients asked to revisit GP after three instillations |
|||||||
| Baseline characteristics of participants | ||||||||||
| Otocerol (n = 53) | Cerumol (n = 53) | p-value | ||||||||
| Gender M/F | 32/21 | 25/28 | χ2 = 1.86, no p-value given | |||||||
| Age | Gender distribution | p-value | ||||||||
| Male | Female | Total | Male | Female | Total | |||||
| 0–9 years | 0 | 0 | 0 | 1 | 0 | 1 | Reports not statistically significant using the Kolmogorov–Smirnov test, but value itself not reported. | |||
| 10–19 years | 5 | 0 | 5 | 0 | 1 | 1 | ||||
| 20–29 years | 3 | 1 | 4 | 6 | 3 | 9 | ||||
| 30–39 years | 6 | 2 | 8 | 2 | 4 | 6 | ||||
| 40–49 years | 5 | 2 | 7 | 1 | 4 | 5 | ||||
| 50–59 years | 6 | 6 | 12 | 7 | 8 | 15 | ||||
| 60–69 years | 5 | 4 | 9 | 3 | 3 | 6 | ||||
| 70–79 years | 1 | 6 | 7 | 3 | 4 | 7 | ||||
| 80–89 years | 1 | 0 | 1 | 2 | 1 | 3 | ||||
| Grade of impaction | ||||||||||
| Mild | 13 | 10 | Not statistically significant, χ2 = 1.37, no p-value given | |||||||
| Moderate | 26 | 32 | ||||||||
| Severe | 14 | 11 | ||||||||
| Comments: Degree of impaction classified as mild (soft wax, which could be syringed at once if necessary), moderate (small plug of hard wax for which a cerumenolytic would usually be used before syringing) or severe (large plug of hard wax for which a cerumenolytic would be essential). Grades on presentation were more widely spread in the Otocerol group with more mild and severe cases but this was not statistically significant. | ||||||||||
| Duration of symptoms, median | 21 days | 14 days | ||||||||
| Results: primary outcomes | ||||||||||
| Syringing needed | ||||||||||
| Otocerol (n = 53) | Cerumol (n = 53) | p-value | ||||||||
| Yes 39, no 14 | Yes 47, no 6 | Difference in those requiring syringing χ2 = 3.94, p < 0.05 | ||||||||
| Syringing needed by grade at entry | ||||||||||
| Mild | Yes 6, no 7 | Yes 6, no 4 | ||||||||
| Moderate | Yes 19, no 7 | Yes 30, no 2 | ||||||||
| Severe | Yes 14, no 0 | Yes 11, no 0 | ||||||||
| Comments: | ||||||||||
| Results: secondary outcomes | ||||||||||
| Doctor reported ease of syringing, where required, n (%) | ||||||||||
| Otocerol (n decline from 53) | Cerumol (n declines from 53) | p-value | ||||||||
| Ease of syringing by grade at entry | ||||||||||
| 30/39 (76.9) | 34/47 (72.3) | χ2 = 0.25, not significant | ||||||||
| Mild | Easy 5, not easy 1 | Easy 5, not easy 1 | ||||||||
| Moderate | Easy 14, not easy 5 | Easy 25, not easy 5 | ||||||||
| Severe | Easy 11, not easy 3 | Easy 4, not easy 7 | ||||||||
| Adverse effects, total no, with side effects | 7 | 10 | Not statistically significantly different | |||||||
| Effects reported | ||||||||||
| Pain on application | 0 | 1 | ||||||||
| Irritation on application | 3 | 8 | ||||||||
| Pain during use | 1 | 1 | ||||||||
| Irritation during use | 4 | 4 | ||||||||
| Slight giddiness | 1 | 0 | ||||||||
| Unpleasant smell such that patient would not use again | 0 | 1 | ||||||||
| Doctor reported would not use product again, n patients | 8 | 9 | ||||||||
| Overall judgement effectiveness successa | 38 | 33 | Overall response better for Otocerol, but not statistically significantb | |||||||
| Failurec | 10 | 13 | ||||||||
| Partiald | 5 | 7 | ||||||||
| Comments: | ||||||||||
| a Defined as those in whom syringing was not required or where it was easy and no reports of side effects. | ||||||||||
| b The ratio of success–failure was highly significant in each group (p < 0.001 Otocerol, p < 0.01 Cerumol). | ||||||||||
| c Defined as those in whom syringing was difficult (with or without side effects). | ||||||||||
| d Defined as those who reported side effects but in whom the doctor found it easy to syringe and had no reservations about using the product again. | ||||||||||
| Methodological comments | ||||||||||
|
Allocation to treatment groups: States randomly allocated to either treatment according to a previously determined scheme (scheme not outlined) Blinding: States double-blind, but no other descriptions given Comparability of treatment groups: Slightly higher male–female ratio in the Otocerol group, but this was not statistically significant, neither was the age distribution between the two groups Method of data analysis: By chi-squared test, no other details reported Sample size/power calculation: Not reported Attrition/dropout: Not reported, from numbers assume none. Some outcomes reported subsets of patients |
||||||||||
| General comments | ||||||||||
|
Generalisability: Minimal detail of participant demographics, children and adults in sample Outcome measures: Unclear how valid, objective or consistently applied the outcome measures were Intercentre variability: 15 GPs took part in the trial, unclear if all from different centres, but the majority likely to be Conflict of interests: None reported |
||||||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Partial |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Partial |
| 7. Was the patient blinded? | Partial |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Carr and Smith52
| Extracted by: EL | Checked by: AC | ||||
|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | ||
|
Author: Carr and Smith52 Year: 2001 Country: USA and/or Canada Study design: RCT Number of centres: Unclear Setting: Primary care – self-treatment Funding: Not reported |
Duration of treatment: 4 drops daily for 14 days Other interventions used: No other ear drops during the duration of treatment |
Number of participants: 69 Sodium bicarbonate: 35 Acetic acid: 34 Sample attrition/dropout: Two participants out of the acetic acid group discontinued due to stinging in the ear canal Inclusion criteria for study entry: Those with occlusive cerumen in at least 1 ear; most presented with other complaints and ceruminosis was noted incidentally Exclusion criteria for study entry: History of TM perforation, present ventilation tubes, a mastoid cavity, otitis externa, or unwillingness to participate in the 2-week treatment regimen |
Primary outcomes: Degree of cerumen Secondary outcomes: Method of assessing outcomes: Degree of cerumen scored by 1 of the 2 examiners from 1–4 (1 = none, 2 = small amount on canal walls, 3 = TM visible but significant amount of cerumen present, 4 = occlusive cerumen). Reports based on scale used by Schwartz and colleagues94 (study looked at otitis media). Tested for reliability by 3 observers measuring 60 ears of people not in the study. Average change in score was averaged across both ears if both ears initially scored > 1. Maximum change was the best score in each participant Length of follow-up: 14 days |
||
| Baseline characteristics of participants | |||||
| Sodium bicarbonate (n = 35) | Acetic acid (n = 34) | p-value | |||
| Mean age, years | 27.0 | 25.3 | |||
| N, ears | 70 | 68 | |||
| Degree of cerumen | Not reported | Not reported | |||
| Results | |||||
| Primary outcomes | Sodium bicarbonate (n = 35) | Acetic acid (n = 34) | p-value | ||
| Mean change degree of cerumen | 0.66 | 0.78 | No difference, p-value not given | ||
| Mean maximum change | 1.00 | 1.00 | |||
| Comments: Multivariate analysis showed that differences in maximum scores were significantly related to age; children had higher average and maximum scores. | |||||
| Subgroup analyses, children onlya | Sodium bicarbonate (n = 16, 26 ears) | Acetic acid (n = 20, 29 ears) | p-value | ||
| Mean age, years | 8.7 | 7.26 | |||
| Mean change | 0.92 | 0.93 | |||
| Mean maximum change | 1.31 | 1.25 | |||
| Category change, n (ears) | |||||
| Change = 0 | 10 | 9 | |||
| Change = 1 | 10 | 15 | |||
| Change = 2 | 4 | 3 | |||
| Change = 3 | 2 | 2 | |||
| Comments: | |||||
| a For the child group the power to detect a difference was measured a priori and therefore subgroup reported here. Change scores between children and adults also presented, but not extracted here as no evidence it was an a priori decision. | |||||
| Adverse events: no cases of otitis externa or external auditory canal dermatitis. | |||||
| Methodological comments | |||||
|
Allocation to treatment groups: Each participant was given a dropper bottle of the study solution chosen randomly by the patient from a box where only the identical bottle caps were visible Blinding: Each bottle was marked as either A or B so that both patient and investigator were blinded to the solution used. Bottles were prepared by a hospital pharmacy, with unblinding occurring after completion of all data collection and analysis. Also states that although patients could detect the odour of acetic acid, in no case could the examiner detect it Comparability of treatment groups: No discussion from authors. Minimal demographic information reported, ages appear to be similar. No baseline scores of the primary end point Method of data analysis: Analysis done for average change in score and maximum change in score per patient using a Mann–Whitney U-test. Paediatric results were separated from the group and analysed independently. Interobserver difference in scoring cerumen was 0.76 Sample size/power calculation: The power to detect a difference of one category (paediatric group) (on the degree of cerumen) if it existed in the data was reported to be 85%. No other details of this calculation reported, nor any power calculation for the rest of the study Attrition/dropout: Two participants in the acetic acid group were withdrawn and reasons given, unclear whether an ITT analysis was undertaken |
|||||
| General comments | |||||
|
Generalisability: Unclear as minimal characteristics of participants given Outcome measures: Unclear how valid and objective the outcome measures were. Inter-rater reliability was assessed, however, and was good Intercentre variability: Unclear how many centres were involved Conflict of interests: None noted |
|||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Adequate |
| 2. Was the treatment allocation concealed? | Adequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Partial |
| 7. Was the patient blinded? | Partial |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Lyndon and colleagues45
| Extracted by: EL | Checked by: AC | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | ||||||||
|
Author: Lyndon and colleagues45 Year: 1992 Country: UK Study design: RCT Number of centres: Unclear Setting: Primary care Funding: Not reported |
Duration of treatment: 4 days (patients returned to clinic on fifth day for syringing) Other interventions used: States all centres used a standardised syringing procedure using tepid tap water *Choline salicylate (20%) and ethylene oxide-polyoxypropylene glycol (analgesics) combined with glycol and glycerol **Arachis oil, almond oil and rectified camphor oil |
Number of participants: 36 Audax: 38 ears (19 participants) Earex: 34 ears (17 participants) Sample attrition/dropout: 35 attended on both assessment days (1 Earex participant failed to return) Inclusion criteria for study entry: Patients presenting in general practice with symptoms of hardened earwax in either or both ears requiring cerumenolytic treatment; patients aged 16 years or over Exclusion criteria for study entry: Inflammation of the external auditory meatus, middle ear pathology or perforation of the TM, pre-existing ear infection requiring treatment with systemic antibiotics, known salicylate sensitivity |
Primary outcomes: (Not defined as primary or secondary.) Degree of impaction, ease of syringing, global impression of efficacy. Side effects/discomfort. Secondary outcomes: (see above) Method of assessing outcomes: Separate assessments were carried out at all times for the left and right ear. The degree of wax impaction was rated as non-existent (excluded the patient), mild (could be syringed once if necessary), moderate (small plug of hard wax) or severe (large plug of hard wax). Ease of syringing rated as not required, easy, difficult, impossible Length of follow-up: 5 days |
||||||||
| Baseline characteristics of participants | |||||||||||
| All participants | p-value | ||||||||||
| Male–female ratio | 19 : 17 | ||||||||||
| Mean age | 52 years (range 19 to 86 years) | ||||||||||
| Pretreatment degree of impaction | |||||||||||
| Audax, no. of ears = 38 | Earex, no. of ears = 34 | p-value | |||||||||
| None | 2 | 1 | |||||||||
| Mild | 7 | 8 | |||||||||
| Moderate | 26 | 22 | |||||||||
| Severe | 3 | 3 | |||||||||
| Results | |||||||||||
| Post-treatment score | |||||||||||
| Degree of impaction | Audax, no. of ears = 38 | Earex, no. of ears = 34 | p-value | ||||||||
|
None Mild Moderate (Mod) Severe (Sev) Missing data |
10 17 9 2 |
6 11 12 3 2 |
See below | ||||||||
| Degree of impaction at end point by pretreatment score | Post-treatment | Post-treatment | p-value | ||||||||
| None | Mild | Mod | Sev | None | Mild | Mod | Sev | ||||
| None | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | See below | ||
| Mild | 3 | 4 | 0 | 0 | 2 | 4 | 0 | 0 | |||
| Moderate | 6 | 12 | 8 | 0 | 3 | 7 | 11 | 1 | |||
| Severe | 0 | 0 | 1 | 2 | 0 | 0 | 1 | 2 | |||
| Comments: Although the difference between the two groups did not reach statistical significance, a trend was seen towards less impaction post-treatment in the Audax group than the Earex group. | |||||||||||
| Ease of syringing, ears | |||||||||||
| Not required | 15 | 7 | p < 0.005a | ||||||||
| Easy | 22 | 12 | |||||||||
| Difficult | 1 | 11 | |||||||||
| Impossible | 0 | 0 | |||||||||
| Missing data | 0 | 4 | |||||||||
| Comments: Paper states that six patients in the Audax group and three in the Earex group did not require syringing of either ear. This does not correspond with the number of ears reported as not requiring syringing in the table (and extracted above). | |||||||||||
| a Significant difference in favour of Audax in that syringing was more frequently scored as ‘not required’ or ‘easy’. | |||||||||||
| Investigator’s global impression efficacy (states no. ears, but n’s do not add up so assume no. patients) | |||||||||||
| Completely effective | 8 | 5 | |||||||||
| Very effective | 9 | 1 | |||||||||
| Fairly effective | 2 | 7 | |||||||||
| Not effective | 0 | 3 | |||||||||
| Missing data | 0 | 1 | |||||||||
| Total | 19 | 17 | |||||||||
| Participants’ global impression efficacy (states no. ears, but n’s do not add up so assume no. patients) | |||||||||||
| Completely effective | 8 | 5 | |||||||||
| Very effective | 9 | 2 | |||||||||
| Fairly effective | 2 | 7 | |||||||||
| Not effective | 0 | 2 | |||||||||
| Missing data | 0 | 1 | |||||||||
| Total | 19 | 17 | |||||||||
| Comments: States there was a statistically significant difference in favour of Audax (p < 0.01). ‘Not effective’ and ‘fairly effective’ categories were merged for the analysis. Unclear if this is investigator rating alone, participant rating alone or some combination. | |||||||||||
| AEs or discomfort | 0 | 1 (slight irritation), 1 (smell unacceptable) | |||||||||
| Methodological comments | |||||||||||
|
Allocation to treatment groups: States ‘according to a pre-determined randomisation allocation schedule’ Blinding: Not reported Comparability of treatment groups: No baseline characteristics reported between groups. Baseline degree of impaction appear to be similar Method of data analysis: Chi-squared test to compare reduction in impaction from pretreatment to post-treatment for each treatment, and the difficulty of syringing between treatments Sample size/power calculation: Study was designed to have 50 completing patients, although limited recruitment only generated complete data on 36 patients. This provided sufficient power, however, to differentiate between the two treatments. No details of sample size calculation to establish this is reported Attrition/dropout: One participant failed to return (no reason documented) |
|||||||||||
| General comments | |||||||||||
|
Generalisability: People over 16 years (19 years and over) Outcome measures: Unclear how valid, objective and consistently applied outcome measures were Intercentre variability: Uncertain how many centres Conflict of interests: None noted |
|||||||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Burgess43
| Extracted by: PH | Checked by: EL | ||
|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures |
|
Author: Burgess43 Year: 1966 Country: UK Study design: CCT Number of centres: One Setting: Primary care Funding: None reported |
Duration of treatment: 4 days Other interventions used: Syringing (Bacon syringe) *Participants were supplied with 1 box (10 capsules) and capsules were instilled 4–10 times |
Number of participants: 50 (74 ears)Sample attrition/dropout: Not reported Inclusion criteria for study entry: More than one-half of an ear occluded by wax Exclusion criteria for study entry: None reported |
Outcomes: Average total of water used, ease of removing wax and character of wax, side effects Method of assessing outcomes: Number or fraction of syringefuls required. Removal of wax: easy, difficult, partial and failed. Character of wax removed: liquid, shredded and lumps Length of follow-up: Between 2 and 7 days |
| Baseline characteristics of participants | |||
| All (n = 50, 74 ears) | p-value | ||
| Age | 18–75 years | No p-values reported | |
| Gender M/F | 32 : 18 | ||
| Ears completely occluded (%) | 59 (79.7) | ||
| Results | |||
| Outcomes | Dioctyl-medo (ears = 33) | Maize oil (ears = 41) | p-value |
| Average water volume | 111 ml | 81 ml | No p-values reported |
| Removal of wax, number of ears | |||
| Easy | 19 | 33 | |
| Difficult | 11 | 5 | |
| Partiala | 3 | 3 | |
| Faileda | 1 | 0 | |
| Character of removed wax, number of ears | |||
| Liquid | 1 | 4 | |
| Shredded | 5 | 6 | |
| Lumps | 27 | 31 | |
| Side effects | 0 | 0 | |
| Comments: | |||
| a All the partially successful removals and the one failed removal occurred in ears not completely occluded at baseline. | |||
| Methodological comments | |||
|
Allocation to treatment groups: Unknown – used coded capsules for treatment, with code unbroken until trial finished Blinding: Both GP and patient blinded to treatment Comparability of treatment groups: No details reported Method of data analysis: None reported Sample size/power calculation: None reported Attrition/dropout: None reported |
|||
| General comments | |||
|
Generalisability: No breakdown of baseline characteristics between groups provided, adult UK population. Outcome measures: It is unclear how valid or objective the measures are Intercentre variability: N/A Conflict of interests: Medo Chemicals Ltd supplied Dioctyl-medo ear drops |
|||
Quality criteria for assessment of controlled clinical studies
| Item | Judgementa |
|---|---|
| 1. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 2. Were the eligibility criteria specified? | Partial |
| 3. Were outcome assessors blinded to the treatment allocation? | Adequate |
| 4. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 5. Did the analyses include an ITT analysis? | Inadequate |
| 6. Were withdrawals and dropouts completely described? | Inadequate |
| 7. Were participants likely to be representative of the intended population? | Unknown |
Eekhof and colleagues53
| Extracted by: EL | Checked by: PH | |||||
|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||
|
Author: Eekhof and colleagues53 Year: 2001 Country: The Netherlands Study design: RCT Number of centres: Four Setting: Primary care Funding: Not reported |
Duration of treatment: 15 minutes Other interventions used: After 15 minutes a series of attempts at syringing was made (syringing methodology standardised, and method reported) for the intervention group, for the control group syringed after 3 days |
Number of participants: 130 participants (224 ears) initially syringed of which 42 had persistent earwax and randomised (59 ears) Intervention: 22 Control: 20 Sample attrition/dropout: None reported Inclusion criteria for study entry: All patients with complaints resulting from earwax offered syringing. After each attempt at syringing the auditory canal was checked with an auriscope and the extent of blocking noted (obstruction levels of 0–25%, 25–49%, 50–74% and 75–100%) were used. If earwax was persistent (> 75% after 5 attempts at syringing) then patient was eligible to be included in the study Exclusion criteria for study entry: TM perforation, middle ear operation, otitis externa, swimming within previous 72 hours, use of cerumenolytics in the previous 72 hours |
Primary outcomes: Number syringing attempts needed to remove wax Secondary outcomes: None Method of assessing outcomes: Unclear Length of follow-up: Immediate for water group, but 3 days for oil group |
|||
| Baseline characteristics of participants | ||||||
| All patients | p-value | |||||
| Gender: M/F | 20/22 | |||||
| Mean age | 51 years (SD 16) | |||||
| Results | ||||||
| Primary outcomes | Water (n = 22) | Oil (n = 20) | p-value | |||
| Mean number syringing attempts | 3.0 (95% CI 2.4, 3.6) | 2.4 (95% CI 1.7, 3.1) | Difference between means 0.6 (95% CI –0.3, 1.5), p = 0.18 | |||
| Number of syringing attempts needed per patient by intervention group | ||||||
| Mean no. attempts | Number of patients in which the earwax was removed after each attempt at syringing | p-value | ||||
| Water group | Oil group | |||||
| 1 | 4 | 6 | Not reported to be tested | |||
| 1.5 | 1 | 2 | ||||
| 2 | 2 | 5 | ||||
| 2.5 | 3 | 1 | ||||
| 3 | 2 | 2 | ||||
| 3.5 | 4 | 0 | ||||
| 4 | 2 | 0 | ||||
| 5 | 3 | 4 | ||||
| 6 | 1 | 0 | ||||
| Comments: Authors report, therefore, that water leads to comparable results; however, study not powered for equivalence but superiority. | ||||||
| Methodological comments | ||||||
|
Allocation to treatment groups: States ‘randomised’ study – allocation to groups by birth year, even or odd. In patients with both ears having persistent wax, both had the same strategy Blinding: None Comparability of treatment groups: Not reported Method of data analysis: Means compared with t-test. In patients with wax in both ears, the mean number of syringing attempts needed for both ears in one patient were used for the calculations. All ears still with persistent wax after 5 syringing attempts were given the value of 6 for the calculations Sample size/power calculation: A difference of 2 syringing attempts between the mean of the groups was found to be clinically significant, 13 people were therefore needed in each group. With groups of 20 and 22 patients a difference of 1.6 between means would be statistically significant Attrition/dropout: Not reported and n’s appear to add up |
||||||
| General comments | ||||||
|
Generalisability: Minimal details of population group reported; however, all included studies had five failed syringing attempts Outcome measures: Unclear how valid, objective and consistently applied the measures were. Number of attempts at syringing is a proxy for adequacy of clearance of wax Intercentre variability: No details reported, four centres included Conflict of interests: No funding source reported, reviewer assumes not funded directly (trainee GPs and no pharmaceutical agents used) |
||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Inadequate |
| 2. Was the treatment allocation concealed? | Inadequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Unknown |
Appendix 4 Data extraction forms: secondary care setting
Caballero and colleagues55
| Extracted by: EL | Checked by: PH | ||||
|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | ||
|
Author: Caballero and colleagues55 Year: 2005 Country: Spain Study design: RCT Number of centres: One Setting: Assume secondary care from author affiliation Funding: Not reported |
Duration of treatment: 15 minutes Other interventions used: after 15 minutes the ear was irrigated with 50ml of tepid water |
Number of participants: 90:Sample attrition/dropout: Not reported Inclusion criteria for study entry: Adults with total cerumen obstruction Exclusion criteria for study entry: Not reported |
Primary outcomes: Proportion of TM completely visualised Secondary outcomes: Not reported Method of assessing outcomes: Not reported Length of follow-up: Immediate |
||
| Baseline characteristics of participants (all participants aged 19–78 years) | |||||
| Results | |||||
| Primary outcomes | Chlorobutanol (n = 32) | Sodium carbonate (n = 29) | Saline (n = 28) | p-value | |
| Proportion of TM completely visualised | 21/32 (65.6%) | 16/29 (55.2%) | 12/28 (42.9%) | p = 0.209 | |
| Comments: unsure if p-value relates to comparison across all three groups | |||||
| Secondary outcomes | Chlorobutanol n = 32 | Sodium carbonate n = 29 | Saline n = 28 | p-value | |
| Comments: | |||||
| Note: If reviewer calculates a summary measure or confidence interval please indicate. | |||||
| Methodological comments | |||||
|
Allocation to treatment groups: States randomised, but no further details reported Blinding: Not reported Comparability of treatment groups: States groups were similar in age, race, sex, ear enrolled and wax consistency, but no data reported Method of data analysis: States variables were analysed with chi-squared test; p = 0.05 was statistically significant Sample size/power calculation: Not reported Attrition/dropout: None reported but numbers do not add up to 90 so assume one withdrew/dropped out |
|||||
| General comments | |||||
|
Generalisability: Unclear population Outcome measures: Unclear how valid the outcome measures were Intercentre variability: Not applicable Conflict of interests: Unknown |
|||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Partial |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Dubow57
| Extracted by: PH | Checked by: EL | ||||
|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | ||
|
Author: Dubow57 Year: 1959 Country: USA Study design: RCT Number of centres: At least two Setting: Assume secondary as paediatric clinic Funding: None reported |
Duration of treatment: Treatment administered by parents and left in ear overnight, followed by irrigation with warm water the following morning Other interventions used: Dropper bottle of liquid test material and a 2-oz Davol rubber ball and nozzle-type syringe |
Number of participants: 60Sample attrition/dropout:Inclusion criteria for study entry: children with at least 1 completely cerumen-occluded ear canal, without regard to other disorders, presenting in a paediatric clinic and in ‘office practice’ Exclusion criteria for study entry: acutely ill children, were the illness would prevent follow-up visit |
Primary outcomes: Wax clearance Secondary outcomes: None reported Method of assessing outcomes: Otological examination prior and after treatment Length of follow-up: Immediate |
||
| Baseline characteristics of participants: | |||||
| All (n = 60) | p-value | ||||
| Age | 3–12 years | No p-values reported | |||
| Race | All (including white, coloured and Chinese) | ||||
| Moderate – severe pain | 3 | ||||
| Results: | |||||
| Primary outcomes | Hydrogen peroxide (n = 20) | Mineral oil (n = 19) | Cerumenex (n = 20) | p-value | |
| Clearance: n (%) | 7 (35%) | 8 (42%) | (14) 70% | No p-values reported | |
| Comments: Number of patients calculated from percentages by reviewer. | |||||
| Secondary outcomes | Hydrogen peroxide (n = 20) | Mineral oil (n = 19) | Cerumenex (n = 20) | p-value | |
| Comments: AE – one itching erythematous eruption of the external auditory meatus and surrounding area of the pinna of the ear. | |||||
| Methodological comments | |||||
|
Allocation to treatment groups: Group was formed from children presenting themselves for paediatric examination. Children were randomly assigned to a group, unless there were language difficulties or other inability to achieve understanding by the parents, as procedure ‘would not be carried out properly’ Blinding: No details reported. Comparability of treatment groups: No details reported Method of data analysis: None reported Sample size/power calculation: None reported Attrition/dropout: One child in mineral oil group refused to be treated by parents |
|||||
| General comments | |||||
|
Generalisability: No baseline characteristics provided, population based on American children in late 1950s Outcome measures: It is unclear how the primary outcome was measured, how valid or objective the measure was or how many paediatricians took part in the examinations (consistency) Intercentre variability: N/A Conflict of interests: Cerumenex distributed by Purdue Frederick Co., New York, NY |
|||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Inadequate |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Chaput de Saintonge and Johnstone59
| Extracted by: PH | Checked by: EL | |||||
|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||
|
Author: Chaput de Saintonge and Johnstone59 Year: 1973 Country: UK Study design: Double-blind RCT Number of centres: One Setting: Secondary care Funding: None reported |
Duration of treatment: 20 minutes Other interventions used: Syringing by nursing staff with a hand syringe |
Number of ears: 67Sample attrition/dropout: Not reported Inclusion criteria for study entry: Any patient with impacted wax attending outpatients Exclusion criteria for study entry: None reported |
Outcomes: Total volume of water and amount of wax removed Method of assessing: Water used in syringing measured to nearest 50 ml Amount of wax removed: Complete, partial or negligible Length of follow-up: Immediate |
|||
| Baseline characteristics of participants: not reported | ||||||
| TP ears = 32 | Olive oil ears = 35 | p-value | ||||
| Results | ||||||
| Outcomes | ||||||
| TP ears (n = 32) | Olive oil ears (n = 35) | p-value | ||||
| Volume of water useda | ||||||
| 150 ml | 7 | 1 | p < 0.05 TP needs smaller volumes water than olive oil | |||
| 300 ml | 14 | 14 | ||||
| 450 ml | 4 | 6 | ||||
| 600 ml | 2 | 2 | ||||
| 750 ml | 0 | 2 | ||||
| 900 ml | 1 | 7 | ||||
| Amount of wax removed | ||||||
| Complete | 20 | 21 | States not significant, but no p-values reported | |||
| Partial | 12 | 10 | ||||
| Negligible | 0 | 4 | ||||
| Comments: | ||||||
| a Estimated from graph by reviewer, TP needed a significantly smaller volume of water for syringing than olive oil. | ||||||
| Methodological comments | ||||||
|
Allocation to treatment groups: Treatments were allocated in random order, no other details reported Blinding: Study states double-blind method was used and treatments were supplied in identical coded bottles, with codes not broken until trial completion Comparability of treatment groups: No details reported Method of data analysis: Mann–Whitney U-test used to test for differences in volume of water used Sample size/power calculation: None reported Attrition/dropout: None reported |
||||||
| General comments | ||||||
|
Generalisability: No baseline demographic characteristics, UK population Outcome measures: It is unclear how valid or objective the measures were Intercentre variability: N/A Conflict of interests: None reported. HR Napp Ltd supplied TP ear drops and assisted in setting up the trial |
||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Adequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Inadequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Adequate |
| 7. Was the patient blinded? | Adequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Keane and colleagues4
| Extracted by: PH | Checked by: EL | ||||
|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | ||
|
Author: Keane and colleagues4 Year: 1995 Country: Ireland Study design: Double-blind RCT Number of centres: One Setting: Secondary care Funding: None reported |
Duration of treatment: 5 days Other interventions used: aCerumol: Chlorbutol 5%, paradichlorobenzene 2%, arachis oil 57.3% bSodium bicarbonate: NaHCO3 5 g, glycerol and purified water |
Number of participants: n = 113, 97 randomised (155 ears) Cerumol: n = 24 (40 ears) Sodium bicarbonate: n = 25 (39 ears) Sterile water: n = 24 (38 ears) Control: n = 24 (38 ears) Sample attrition/dropout: 13 went home and 3 died, 97 completed study Inclusion criteria for study entry: One or both ears impacted Exclusion criteria for study entry: Known pathology of the ear canal and/or TM and those already on ear drops |
Primary outcomes: Percentage clearance and number of ears (clearance is explained by the ‘natural expulsion of earwax’) Secondary outcomes: AE Method of assessing outcomes: Auditory canal classification – 1. impacted wax in the external canal, 2. moderately clear external canal or 3. completely clear external canal. Examination and re-examination carried out by the same observer Length of follow-up: 5-day trial |
||
| Baseline characteristics of participants None reported Results |
|||||
| Primary outcomes: clearance % (no. of ears) | |||||
| Cerumol (n = 24) | NaHCO3 (n = 25) | Water (n = 24) | Control (n = 24) | p-value | |
| Impacted | 40.0 (16) | 53.8 (21) | 47.4 (18) | 68.4 (26) | |
| Moderately clear | 37.5 (15) | 25.6 (10) | 31.6 (12) | 26.3 (10) | p < 0.05 Cerumol vs control |
| Completely clear | 22.5 (9) | 20.6 (8) | 21.0 (8) | 5.3 (2) |
p < 0.05 Cerumol vs control p < 0.05 NaHCO3 vs control p < 0.05 water vs control |
| Comments: No significant differences between Cerumol, NaHCO3 or water. | |||||
| Secondary outcomes | |||||
| Cerumol (n = 24) | NaHCO3 (n = 25) | Water (n = 24) | Control (n = 24) | p-value | |
| Comments: AE – no cases of irritation or contact sensitivity. | |||||
| Methodological comments | |||||
|
Allocation to treatment groups: Participants were randomly divided into four groups. States treatment was allocated in random order and the ‘code was not broken until the trial was complete’. No other information provided. Unclear reporting over randomisation of participants in respect of number randomised Blinding: Authors state double-blind trial. The only information provided is that the drops were administered by nursing staff and that ears were examined and re-examined by same observer Comparability of treatment groups: Unknown, no baseline reported Method of data analysis: t-test, paired samples only; no adjustment for multiple comparisons made Sample size/power calculation: Not reported Attrition/dropout: No dropouts after randomisation. Poor reporting means it is unclear whether the 16 additional participants received any treatment |
|||||
| General comments | |||||
|
Generalisability: Possibly elderly hospitalised patients, but exact patient group unclear Outcome measures: Unclear how valid and objective the outcome classification was Intercentre variability: N/A Conflict of interests: None reported |
|||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Unknown |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Fraser60
| Extracted by: AC | Checked by: PH | ||||
|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | ||
|
Author: Fraser60 Year: 1970 Country: UK Study design: RCT Number of centres: Six hospitals Setting: Secondary care Funding: Not stated |
Duration of treatment: Ear drops were instilled once daily for 3 days prior to syringing for 15 minutes, except TP, which was used 15–30 minutes before syringing due to its claimed rapid action Other interventions used: None stated |
Number of participants: 248 ears from 124 people, with 1 ear per person providing a test and control ear Intervention: 124 ears Control: 124 ears Sample attrition/dropout: 18 patients failed to complete the trial due to errors in the procedure and 3 died Inclusion criteria for study entry: Participants had bilateral hard earwax that occludes the external auditory meatus in both ears; patients were from geriatric attendees at hospitals Exclusion criteria for study entry: None stated |
Primary outcomes: Ease of syringing, frequency of syringing, appearance of wax removed Secondary outcomes: see above Method of assessing outcomes: Not stated Length of follow-up: At least 3 days |
||
| Baseline characteristics of participants | |||||
| None reported | |||||
| Results | |||||
| Outcomes | |||||
| Ease of syringing | Sum scores | Difference (mean rank) | |||
| Test ears | Control ears | ||||
| Cerumol (24 ears) | 92 | 122 | +30a (+11.9)b | ||
| Olive oil (25 ears) | 116 | 140 | +24 (+3.4) | ||
| Waxsol (26 ears) | 110 | 128 | +18 (+2.8) | ||
| Sodium bicarbonate (124 ears) | Control | 0 (–3.5) | |||
| TP (24 ears) | 118 | 107 | –11 (–9.0) | ||
| Dioctyl capsules (25 ears) | 119 | 107 | –12 (–9.1) | ||
| Comments: The lower the score the easier the syringing. A positive difference indicates that the test were easier to syringe than the control ears. | |||||
| a Cerumol differed significantly from sodium bicarbonate (p < 0.05), all other comparisons were not significant. | |||||
| b When mean ranks were compared, Cerumol was significantly better than dioctyl and TP; p < 0.05. | |||||
| Frequency of syringing successes and failures | No. of patients in which: | Control better | |||
| Product better | Scores equal | ||||
| Cerumol (24 ears) | 15 | 5 | 4 | ||
| Olive oil (25 ears) | 10 | 6 | 9 | ||
| Waxsol (26 ears) | 11 | 6 | 9 | ||
| TP (24 ears) | 7 | 7 | 10 | ||
| Dioctyl capsules (25 ears) | 8 | 5 | 12 | ||
| No. of ears in which very forceful syringing failed | Test ears | Control ears | |||
| Cerumol (24 ears) | 1 | 5 | |||
| Olive oil (25 ears) | 2 | 4 | |||
| Waxsol (26 ears) | 3 | 5 | |||
| TP (24 ears) | 5 | 3 | |||
| Dioctyl capsules (25 ears) | 5 | 2 | |||
| Appearance of wax removed by syringing | Percentage of lumps | Percentage partially broken up | Percentage completely broken up | ||
| Oil-based solvents: | |||||
| Cerumol (24 ears) | 46 | 37 | 17 | ||
| Olive oil (25 ears) | 40 | 44 | 16 | ||
| TP (24 ears) | 42 | 25 | 33 | ||
| Dioctyl capsules (25 ears) | 36 | 44 | 20 | ||
| Water-based solvents: | |||||
| Waxsol (26 ears) | 15 | 46 | 39 | ||
| Sodium bicarbonate (124 ears) | 33 | 43 | 24 | ||
| Comments: Frequency of otitis externa (redness of the external meatus): total of 12 ears (4%); in 3 ears it was bilateral and probably not due to the study; of the remaining 6 ears, 3 ears had received sodium bicarbonate, 2 Waxsol and 1 TP. | |||||
| Methodological comments | |||||
|
Allocation to treatment groups: Sodium bicarbonate was used in one ear and another product in the other ear. Products were given code letters and were allocated at random to patients by an assistant. The ear in which the product was used was similarly randomised Blinding: Except for TP, the surgeon performing the syringing was neither aware of which drops a patient received, nor which was the test ear. For TP, the surgeon knew it had been used but not in which ear Comparability of treatment groups: No comparison made of participants baseline characteristics, although each patient had a test ear and a comparator ear to try and minimise differences Method of data analysis: Scores, difference in scores, mean rank and Wilcoxon one-sample ranking test used Sample size/power calculation: Not stated Attrition/dropout: Of 142 participants originally identified, 18 failed to complete the trial due to procedure errors and 3 died, leaving 124 participants |
|||||
| General comments | |||||
|
Generalisability: Unknown Outcome measures: Ease of syringing was compared for each preparation against sodium bicarbonate, with the difference between test and control ear calculated and tested for significance using the Wilcoxon one-sample ranking test. Differences in scores between test and control ears were ranked over all products. The sum of ranks and the mean rank for each product were compared with each other. Frequency of syringing and appearance of wax were other outcomes. Limited information is provided as concerns the definitions of outcome measures Intercentre variability: Syringing techniques were standardised and undertaken by one operator Conflict of interests: None stated |
|||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Inadequate |
| 2. Was the treatment allocation concealed? | Inadequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Unknown |
| 5. Were outcome assessors blinded to the treatment allocation? | Inadequate |
| 6. Was the care-provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Pothier and colleagues56
| Extracted by: AC | Checked by: PH | ||
|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures |
|
Author: Pothier and colleagues56 Year: 2006 Country: UK Study design: RCT (unblinded) Number of centres: One Setting: Otolaryngology outpatient clinic Funding: None reported |
Duration of treatment: Treated and assessed on initial visit, unless cerumenolytics used and then unspecified delay Other interventions used: Wax was removed with a Jobson–Horne probe or a wax hook (91%) or crocodile forceps or Zoellner Sucker (9%) |
Number of participants: n = 100 Intervention: n = 50 Control: n = 50 Sample attrition/dropout: No dropouts. Inclusion criteria for study entry: Patients requiring removal of earwax from the ear canal to allow full view of the TM with a history of earwax Exclusion criteria for study entry: People with active or previous external or middle ear pathology [i.e. mastoid cavities, active ear infections or any abnormality of TM (perforation or retraction)] |
Primary outcomes: Levels of pain and discomfort for patient, ease of de-waxing, time taken to de-wax Secondary outcomes: see above Method of assessing outcomes: Assessed by patient questionnaire (VAS) and through assessment by endoscopist Length of follow-up: Treated and assessed on initial visit, unless cerumenolytics used and then unspecified delay |
| Baseline characteristics of participants | |||
| Endoscopic (n = 50) | Microscopic (n = 50) | p-value | |
| Mean age (SD, range) years | 57.2 (16.86, 16–87) | 58.3 (17.3, 18–91) | Not stated |
| Male–female ratio (%) | 60:40 | 62:38 | Not stated |
| Mean % wax obscuring TM | 72.0 | 65.5 | Not stated |
| Number (%) of patients with TM completely obscured | 20 (40) | 26 (52) | 0.69 |
| Results | |||
| Primary outcomes | |||
| Endoscopic (n = 50) | Microscopic (n = 50) | p-value | |
| Discomfort – median score on VAS (0–100) | 5 | 25 | 0.002 |
| Pain – median score on VAS (0–100) | 3.5 | 10 | 0.075 |
| Difficulty in de-waxing – median score on VAS (0–100) | 9 | 20 | 0.005 |
| Time taken to perform de-waxing (minutes) | 1.8 | 3.3 | 0.001 |
| Comments: No complications were reported during de-waxing, however, one patient from each group sustained minor bleeding from ear canals. Five patients from the endoscope group required conversion to microscope (three successfully de-waxed, two sent home with cerumenolytics before finishing de-waxing) and two microscope patients converted to endoscope (one successfully de-waxed, one sent home with cerumenolytics). | |||
| Methodological comments | |||
|
Allocation to treatment groups: Opaque envelopes with single proforma with group marked Blinding: Blindly selected at random by patient. Endoscopist performing procedure informed patient of allocation Comparability of treatment groups: Study identified that patient groups were similar at baseline in terms of age, sex and proportion of TM obscured Method of data analysis: Data on discomfort, pain and difficulty were analysed using Mann–Whitney U-test and data on time taken used an unpaired t-test to compare means. ITT analysis was used Sample size/power calculation: Sample of 50 participants would provide power of 90% to detect a mean difference of 10 points assuming a standard deviation of 15, using a two-group test, at 5% significance Attrition/dropout: No patients dropped out |
|||
| General comments | |||
|
Generalisability: Patients from an otolaryngology outpatient clinic with a previous history of earwax, 60% male, mean age 57–58 years old Outcome measures: Levels of pain (0 = no pain; 100 = very painful) and discomfort (0 = no discomfort; 100 = very uncomfortable) were recorded by the patients using a visual analogue score sheet. Clinician assessed on a VAS the ease of de-waxing, the percentage of TM obscured by wax prior to randomisation and the time taken to de-wax. VASs have not been formally validated Intercentre variability: Not applicable Conflict of interests: None stated. Karl Storz loaned otoendoscopes and GVR Products loaned portable light sources |
|||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Partial |
| 2. Was the treatment allocation concealed? | Inadequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Inadequate |
| 6. Was the care-provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Adequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Saloranta and colleagues58
| Extracted by: EL | Checked by: AC | ||
|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures |
|
Author: Saloranta and colleagues58 Year: 2005 Country: Finland Study design: RCT Number of centres: Two Setting: Secondary care and community home for people with learning difficulties Funding: None reported |
Duration of treatment: Once a week for 12 months. Patients kept a diary of their treatment Other interventions used: Patients all had removal of the impacted earwax prior to randomisation, unclear by what method *Contains paraffinum liquidum, cyclomethicone and Buxus chinensis, Stiefel Laboratories (Ireland) Ltd |
Number of participants: 39 Ceridal: n = 20 (13 analysed, 16 ears) Control: n = 19 (18 analysed, 29 ears) Sample attrition/dropout: Numbers analysed were: Ceridal: 13 (1 death mother, 1 decrepitude, 2 lost to follow-up, 1 death, 2 excluded due to cholesteatoma) Control: 18 (1 death) Inclusion criteria for study entry: History of impacted cerumen, with symptoms like impaired hearing or sensation of blocked ear canal more often than once per year and earwax completely obstructing the ear canal at the point of inclusion Exclusion criteria for study entry: None noted |
Primary outcomes: (Not defined as primary or secondary.) Recurrence of cerumen impaction, AEs Secondary outcomes: see above Method of assessing outcomes: No details Length of follow-up: 12 months (visits also at 3 months and at a point of recurrence) |
| Baseline characteristics of participants (reported for those analysed not those recruited) | |||
| Ceridal (n = 13) | Control (n = 18) | p-value | |
| M/F | 7/6 | 8/10 | |
| Mean age (range), years | 34 (4–52) | 44 (1–74) | |
| Learning difficulties | 9 | 10 | |
| No treated ears | 16 | 29 | |
| Results | |||
| Primary outcomes | |||
| Ceridal (n = 13) | Control (n = 18) | p-value | |
| Recurrence | 3 (23%) | 11 (61%) | p < 0.05 |
| Recurrence in treated ears | 3/16 (19%) | 15/29 (52%) | p < 0.05 |
| Comments: There was also a trend in the timing of recurrent impaction; 73% of the control ears recurred within 3 months compared with 40% in the Ceridal group. | |||
| Secondary outcomes | |||
| Ceridal (n = 13) | Control (n = 18) | p-value | |
| AEs | 0 | 0 | |
| Comments: | |||
| Methodological comments | |||
|
Allocation to treatment groups: After removal of impacted cerumen, patients were randomised. Randomisation was undertaken for the whole study in advance by a co-worker. Forty envelopes were consecutively numbered – half of them randomly containing the treatment code and half of them the control code. This was carried out after extraction of the impacted earwax Blinding: No blinding evident, participants were seen and evaluated by one of the authors Comparability of treatment groups: No statistical analysis or comment from authors, mean age appears to be lower in the Ceridal group Method of data analysis: Differences between groups tested by Fisher’s exact test Sample size/power calculation: Not reported, however this is reported to be a pilot study Attrition/dropout: Numbers and reasons given |
|||
| General comments | |||
|
Generalisability: Large proportion of participants had learning difficulties Outcome measures: Unknown how valid or objective the outcome measures were Intercentre variability: None noted Conflict of interests: None noted |
|||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Inadequate |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Appendix 5 Data extraction forms: self-care and other care settings
Harris64
| Extracted by: PH | Checked by: EL | |||||||||
| Reference and design | Intervention | Participants | Outcome measures | |||||||
|
Author: Harris64 Year: 1968 Country: Ireland Study design: RCT Number of centres: One Setting: Primary care Funding: TP and bulb syringes supplied by HR Napp Ltd |
Duration of treatment: 12–24 hours Other interventions used: self-syringing with a maximum of 12 squirts of warm water using a 2 fl oz, soft rubber bulb, rat-tailed syringe the morning after the treatment, followed by auroscopic examination in the evening. If self-syringing was unsuccessful syringing was repeated at the surgery after the examination. |
Number of participants: 45 TP: 24 Control: 21 Sample attrition/dropout: No dropouts Inclusion criteria for study entry: All participants attending surgery and complaining of symptoms directly attributable to ceruminosis Exclusion criteria for study entry: Underlying systemic disease, perforated TM, chronic otitis externa or middle ear disease |
Outcomes: (Not stated as primary or secondary) Wax clearance Meati clearance Colour cerumen Symptoms AEs Method of assessing outcomes: auroscopic examination Length of follow-up: 1 day |
|||||||
| Baseline characteristics of participants | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Comments: majority of participants had earwax in both ears, but no breakdown provided. | ||||||||||
| Ceruminosis symptoms across both groups | Partially obscured TM (n = 17) | Completely obscured TM (n = 28) | ||||||||
| Impaired hearing | 8 | 28 | ||||||||
| Tinnitus | 9 | 10 | ||||||||
| Vertigo | 3 | 5 | ||||||||
| Irritation | 2 | 2 | ||||||||
| Pain | 2 | 1 | ||||||||
| Cerumen colour (n = 45) across both groups | ||||||||||
| Partial obstruction | Total obstruction | |||||||||
| Yellow, n = 6 | 3 | 3 | ||||||||
| Brown, n = 13 | 0 | 13 | ||||||||
| Black, n = 12 | 0 | 12 | ||||||||
| Comments: Baseline degree of obstruction reported (see results below). | ||||||||||
| Results | ||||||||||
| Outcomes | ||||||||||
| TP (n = 24) | Control (n = 21) | p-value | ||||||||
| Completely cleared | 18 | 1a | p < 0.005 (χ2 = 19.862) | |||||||
| Partially or not cleared | 6b | 20c | ||||||||
| Comments: | ||||||||||
| Six TP participants had softened wax cleared at surgery with gentle syringing after examination. Nineteen participants in the control group had wax cleared with normal syringing after examination at the surgery. | ||||||||||
| a Meatus cleared. | ||||||||||
| b Partial clearance. | ||||||||||
| c Not cleared. | ||||||||||
| TP (n = 24) | Control (n = 21) | p-value | ||||||||
| State of meati | ||||||||||
| Obscured completely | Obscured partially | Obscured completely | Obscured partially | |||||||
| Before treatment |
Within group comparison, before and after TP > 0.05 (not significant) (χ2 = 3.657) Control: not significant |
|||||||||
| 14 | 10 | 14 | 7 | |||||||
| After treatment | ||||||||||
| Meati cleared | 8 | 10 | 0 | 1 | ||||||
| Meati not cleared | 6 | 0 | 14 | 6 | ||||||
| Comments: The colour of wax had no effect on clearance or by treatment in either group (p-value not provided). | ||||||||||
| AEs | 1a | 0 | ||||||||
| Comments: | ||||||||||
| a Participant suffered erythema around the external auditory meatus, most likely due to TP. Resolved within 48 hours of treatment with topical corticosteroid cream. Some TP participants noted brownish liquid on pillow, presumed to be liquefied cerumen; no other details reported. | ||||||||||
| Methodological comments | ||||||||||
|
Allocation to treatment groups: States randomly assigned, no further details Blinding: Blinding not reported Comparability of treatment groups: Unknown, no details reported Method of data analysis: Chi-squared test for small numbers with Yates’ correction was calculated (fourfold table) Sample size/power calculation: None reported Attrition/dropout: None |
||||||||||
| General comments | ||||||||||
|
Generalisability: UK Primary Care practice population during 1968, suffering from ceruminosis predominantly in both ears Outcome measures: Unclear how valid, objective, or consistently applied the outcome measures used were Intercentre variability: N/A Conflict of interests: TP and bulb syringes supplied by HR Napp Ltd |
||||||||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Partial |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care-provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Coppin and colleagues63
| Extracted by: AC | Checked by: PH | ||
|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures |
|
Author: Coppin and colleagues63 Year: 2008 Country: UK Study design: RCT Number of centres: Seven primary care practices Setting: Primary care Funding: Royal College of General Practitioners Science Foundation Board and UK Department of Health Support for Science Fund |
Duration of treatment: 1–2 weeks Other interventions used: none stated |
Number of participants: n = 237 Intervention: n = 118 Control: n = 119 Sample attrition/dropout: Due to main outcome not documented. Intervention: n = 14 Control: n = 17 Inclusion criteria for study entry: Adults consulting a GP or practice nurse with symptoms of occluding earwax (itching, sensation of blockage, reduced hearing) consenting to inclusion in study Exclusion criteria for study entry: None stated |
Primary outcomes: Reported symptoms and wax clearance Secondary outcomes: Further treatment required and acceptability of treatment Method of assessing outcomes: Practice nurse (n = 230) or GP (n = 7) undertook initial assessment and practice nurses undertook all follow-up assessments. Other outcomes were assessed by patient questionnaire Length of follow-up: 1–2 weeks for comparison of interventions; within 6 weeks for assessment of further treatment, adverse effects, rates and reasons for non-participation or non-compliance |
| Baseline characteristics of participants | |||
| Bulb (n = 118) | Irrigation (n = 119) | p-value | |
| Mean symptom scorea at baseline (n = 205) | 2.37 (SD 1.44) | 2.41 (SD 0.90) | Not stated |
| Right ear completely obstructed with wax, n (%) | 73/116 (63) | 72/116 (62) | Not stated |
| Left ear completely obstructed with wax, n (%) | 78/116 (67) | 79/114 (69) | Not stated |
| Male–female ratio (%) | 66 : 34 | 63 : 37 | Not stated |
| Mean (SD) age, years | 57 (14) | 55 (16) | Not stated |
| Results | |||
| Primary outcomes | |||
| Bulb (n = 118) | Irrigation (n = 119) | Difference between groups (95% CI); p-value | |
| Mean (SD) change in symptom score from baseline | –0.81 (1.44) | –1.26 (1.15) | –0.45 (–0.11 to –0.79); p = 0.01 (0.02)b |
| Treatment discomfort (slight or more), n (%) | 43/110 (39) | 35/108 (32) | 7% (–6% to 19%); p = 0.30 |
| Treatment dizziness (slight or more), n (%) | 14/110 (13) | 14/108 (13) | 0% (–9% to 9%); p = 0.96 |
| Use same treatment again, n (%) (agreed slightly or more) | 82/110 (75) | 106/106 (100) | 25% (17% to 25%); p < 0.001 |
| Wax clearance (obstruction score 0 or 1), n (%) | 50/104 (48) | 64/102 (63) | 15% (1% to 28%); p = 0.03 |
| Comments: | |||
| a Symptoms score: 0 = no symptom to 6 = severe. | |||
| b Kruskal–Wallis test. | |||
| Secondary outcomes | |||
| Bulb (n = 118) | Irrigation (n = 119) | Difference between groups (95% CI); p-value | |
| Treatment convenient (agreed slightly or more), n (%) | 84/110 (76) | 95/105 (90) | 14% (4% to 24%); p < 0.01 |
| Satisfied with treatment, n (%) (agreed slightly or more) | 78/110 (71) | 105/106 (99) | 28% (19% to 29%); p < 0.001 |
| Requires no further clearance (based on normal clinical practice), n (%) | 51/100 (51) | 66/95 (69) | 18% (5% to 32%); p < 0.01 |
| Infection, n (%) | 1/97 (1) | 1/93 (1) | 0% (–3% to 3%); p = 1.00a |
| Perforation, n (%) | 1/97 (1) | 1/94 (1) | 0% (–3% to 3%); p = 1.00a |
| Signs of trauma, n (%) | 1/97 (1) | 1/94 (1) | 0% (–3% to 3%); p = 1.00a |
| Adverse events: 1 patient in the irrigation group had bilateral otitis externa and 2 patients had perforation (1 old scarring TM and 1 pre-existing cholesteatoma) | |||
| Comments: | |||
| a Fisher’s exact test used. | |||
| Methodological comments | |||
|
Allocation to treatment groups: Using sealed envelopes randomised using random number tables by person not involved data collection or recruitment Blinding: Patients received an envelope questionnaire and a box containing either ear drops, a bulb syringe and instructions or ear drops and a roll of card of similar weight to bulb and instructions on other treatment. Process was audited to assess whether recruitment was selective and confounded. Assessment of wax clearance could not be blinded Comparability of treatment groups: Baseline data on age, sex and ear obstruction were similar between groups Method of data analysis: States that ITT analysis using analysis of covariance and Kruskal-Wallis test for continuous outcomes and chi-squared test or Fisher’s exact test for dichotomous variables. Although it states ITT analysis was undertaken, denominators appear to vary with outcomes. Clustering was assessed and found not to affect outcomes Sample size/power calculation: Observed wax clearance was used for sample size calculation (α = 0.05 and power 80%) assuming clearance of wax by bulb of 75% and syringe 90% it was estimated that 100 patients per group and 236 in total if there was a loss to follow-up of 15% Attrition/dropout: Of the 434 patients invited, 69 declined/excluded, 237 randomised, a further 128 not randomised had notes searched. Of 237 randomised, 206 were followed up and 31 were lost to follow-up due to main outcome not documented (14 people from the intervention and 17 from the control group). Nurses monitored follow-up and noted all patients allocated to bulbs used them |
|||
| General comments | |||
|
Generalisability: Participants were from 7 primary care practices in Hampshire (UK), with over 60% male and a mean age between 55 and 57 years Outcome measures: Overall symptoms and acceptability of treatment were assessed using questions (7-point scale) validated in pilot study. Wax obstruction was measured by a practice nurse using previously described 4-point score (0 = no or minimal wax with TM fully visible; 1 = minor amount of wax with TM essentially visible; 2 = moderate amount of wax with TM partially obscured; 3 = complete occlusion of TM. (Note 0 and 1 were combined to form clinically clear) Intercentre variability: Not reported Conflict of interests: None stated |
|||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Adequate |
| 2. Was the treatment allocation concealed? | Adequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Unknown |
| 5. Were outcome assessors blinded to the treatment allocation? | Inadequate |
| 6. Was the care-provider blinded? | Not applicable |
| 7. Was the patient blinded? | Not applicable |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Partial |
Roland and colleagues62
| Extracted by: EL | PH | |||
|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |
|
Author: Roland and colleagues62 Year: 2004 Country: USA Study design: RCT Number of centres: One Setting: Corporate research clinic Funding: Funded by Alcon Research Ltd |
Duration of treatment: Each treatment consisted of up to two 15-minute applications of treatment/placebo Other interventions used: Ear drops were followed by a standardised irrigation procedure using a WaterPik Oral Jet Irrigator. Irrigation consisted of 50 ml of lukewarm water. If cerumen was cleared after a single application and irrigation, the second application was not conducted *10% triethanolamine polypeptide oleate condensate, Purdue Frederick Company **6.5% carbamide peroxide, Abbott Laboratories ***BBS sterile irrigating solution (saline containing 0.64% sodium chloride and physiological concentrations of multiple electrolytes), Alcon Laboratories |
Number of participants: 230 screened, 74 qualified for enrolment: 1, n = 24; 2, n = 26; 3, n = 24 Sample attrition/dropout: None reported Inclusion criteria for study entry: Volunteers from company employees who had excessive or impacted cerumen. Required to be ≥ 18 years with mild, moderate, or complete cerumen occlusion, as measured against a previously established 4-point scale (see outcomes for details) Exclusion criteria for study entry: Ear anomalies, diabetes, allergies to study medications, were pregnant or nursing or had instilled anything other than water in their ear in the previous 72 hours |
Primary outcomes: Post-treatment level of occlusion Secondary outcomes: Otological signs and symptoms Method of assessing outcomes: Assessed by ‘qualified specialist’ For degree of occlusion a scale of 0–3 used as follows:Unclear how valid and reliable this test is Adverse events Length of follow-up: Immediate |
|
| Baseline characteristics of participants | ||||
| All (n = 74) | p-value | |||
| Mean age, years (range) | 45 (22–66) | |||
| Mild occlusions | 10 | |||
| Moderate occlusions | 26 | |||
| Complete occlusions | 38 | |||
| Gender, M/F (M/F ratio) | 51 : 23 (2.2 : 1) | |||
| Results | ||||
| Primary outcomes | ||||
| Cerumenex (n = 24) | Murine (n = 26) | Placebo (n = 24) | p-value | |
| No occlusion | 7(29.2%) | 4 (15.4%) | 10 (41.7%) |
Cerumenex vs placebo; p = 0.37 Murine vs placebo; p = 0.06 |
| Mild, moderate or complete occlusion | 17 (71%) | 22 (85%) | 14 (58%) | |
| Comments: Statistical analysis of Cerumenex vs placebo was by chi-squared test, but analysis of Murine vs placebo was by Fisher’s exact test. | ||||
| Change from baseline in occlusion (estimated from figure) | Resolved: 30% | Resolved: 16% | Resolved: 42% | Not tested |
| Improved: 8% | Improved: 7% | Improved: 22% | ||
| No change/worse: 62% | No change/worse: 77% | No change/worse: 38% | ||
| Secondary outcomes | ||||
| Cerumenex (n = 24) | Murine (n = 26) | Placebo (n = 24) | p-value | |
| AEs related: | ||||
| Ear pruritis | 1 (4%) | 2 (8%) | 0 | |
| Ear discomfort | 0 | 0 | 1 (4%) | |
| Contact dermatitis | 1 (4%) | 0 | 0 | |
| AEs not related: | ||||
| Vertigo | 1 (4%) | 0 | 0 | |
| Comments: Number of applications – overall 90.5% required 2 applications, 9.5% had successful treatment outcome after 1 application and irrigation [Cerumenex: 2 (8%), Murine: 3 (12%), placebo: 2 (8%)]. Of those with a single application there were no differences between the interventions (p-value not reported). | ||||
| Methodological comments | ||||
|
Allocation to treatment groups: States randomly assigned, no further details Blinding: States observer- and participant-blind study. The outcome assessors and the participant were masked from treatment allocation by storing test articles out of view and administration was by clinic staff who did not perform the clinical assessments Comparability of treatment groups: States no statistically significant differences between demographic characteristics (age and gender) or between baseline degree of occlusion were observed between groups. No data reported, however, between groups Method of data analysis: Summary statistics (mean ± SD) calculated and either a chi-squared test or a t-test used Sample size/power calculation: No power calculations were undertaken as ‘planned as a descriptive study’ Attrition/dropout: None reported |
||||
| General comments | ||||
|
Generalisability: American volunteer participants between ages 22 and 66 years employed by the study sponsor (self-selection bias), so may not be representative of the total population in terms of being likely to have earwax problems Outcome measures: Unclear how valid or reliable the outcome measure is. Authors acknowledge that the distinction between mild and moderate occlusion is somewhat subjective Intercentre variability: Not applicable Conflict of interests: Funded by a private research company, unclear whether the company has any relation to the treatments compared. Drs Roland and Gross served as paid consultants for Alcon Research Ltd |
||||
Quality criteria for assessment of RCTs (NHS CRD)
| Item | Judgementa |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Inadequate |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Adequate |
| 6. Was the care-provider blinded? | Partial |
| 7. Was the patient blinded? | Adequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Hinchcliffe61
| Extracted by: PH | Checked by: EL | |||||
|---|---|---|---|---|---|---|
| Reference and design | Intervention | Participants | Outcome measures | |||
|
Author: Hinchcliffe61 Year: 1955 Country: UK Study design: CCT Number of centres: One Setting: Military Funding: Not reported |
Duration of treatment: half hour Other interventions used: Syringing with warm tap water |
Number of readings: n = 185, 37 ears per group Sample attrition/dropout: N/A Inclusion criteria for study entry: Air Force personnel with obscured TM, hard wax in the meatus in one or both ears Exclusion criteria for study entry: None reported |
Outcomes: No. of occasions wax meatus was not cleared within specified time (see below) No. of cases with symptoms of discomfort Method of assessing outcomes: The treatment was considered a failure if more than 5 minutes of syringing was needed to clear the wax AEs: Tingling or symptoms of irritation were noted before the ear/s was syringed Length of follow-up: Immediate |
|||
| Baseline characteristics of participants | ||||||
| Sodium bicarbonate (ears = 37) | Cerumol (ears = 37) | Hydrogen peroxide (ears = 37) | Olive oil (ears = 37) | Control (ears = 37) | p-value | |
| None reported | ||||||
| Results | ||||||
| Outcomes | ||||||
| Sodium bicarbonate (ears = 37) | Cerumol (ears = 37) | Hydrogen peroxide (ears = 37) | Olive oil (ears = 37) | Control (ears = 37) | p-value | |
| No. of occasions meatus not cleared | 6 | 7 | 4 | 2 | 9 | See comment field |
| No. of AEs | 4 | 22 | 6 | 4 | 0 | |
| Comments: It is stated that only olive oil was significantly better than no treatment at all, but no further data is reported to support this. It is also reported that symptoms of discomfort for Cerumol occurred significantly more often than any other preparation, but again no further data is reported to support this. | ||||||
| Methodological comments | ||||||
|
Allocation to treatment groups: The four treatment bottles were used in alphabetical order, with each fifth participant left untreated as a control Blinding: Treatments were contained in bottles labelled A, B, C and D, with no distinguishing marks. The doctor syringing the ears was not informed of which treatment if any had been used. Initial otoscopic examination carried out by a alternate doctor Comparability of treatment groups: Not reported Method of data analysis: Chi-squared test for small numbers was used Sample size/power calculation: None reported Attrition/dropout: None reported |
||||||
| General comments | ||||||
|
Generalisability: Adult entrants to the Royal Air Force in the 1950s, found to have hard wax obscuring the meatus on entrant examination Outcome measures: Unclear how valid, objective or consistently applied the outcome measure was Intercentre variability: N/A Conflict of interests: Not reported |
||||||
Quality criteria for assessment of controlled clinical studies
| Item | Judgementa |
|---|---|
| 1. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 2. Were the eligibility criteria specified? | Adequate |
| 3. Were outcome assessors blinded to the treatment allocation? | Partial |
| 4. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 5. Did the analyses include an ITT analysis? | Inadequate |
| 6. Were withdrawals and dropouts completely described? | Unknown |
| 7. Were participants likely to be representative of the intended population? | Unknown |
Appendix 6 Excluded studies
| Reasons for study exclusion | Number of studies |
|---|---|
| Intervention | 3 |
| Population | 0 |
| Outcomes | 0 |
| Study design | 16 |
| Total number of excluded studies | 19 |
Almeyda R, Babar-Craig H. A comparison of endoscopic and microscopic removal of wax: a randomised clinical trial. Clin Otolaryngol2007;32:73–4.
Baker BS. A clinical trial of a ceruminolytic agent. Trans Soc Occup Med 1969;19:62–3.
Burkhart CN, Burkhart CG, Williams S, Andrews PC, Adappa V, Arbogast J. In pursuit of ceruminolytic agents: a study of earwax composition. Am J Otol2000;21:157–60.
Burton MJ, Doree CJ. Ear drops for the removal of earwax. Cochrane Database Syst Rev2003;3: CD004400.
Cassano P, Mora E, Damiani V, Passali FM, Passali D. [Evaluation of cerumenolytic efficacy of Audispray.] Otorinolaringologia 2002;52:131–5.
Cavallazzi GM, Bottero A. [A new ceruminolytic agent in clinical use: Preliminary considerations.] Riv Ital Otorinolaringol Audiol Foniatr1988;8:197–200.
Ernst AA, Takakuwa KM, Letner C, Weiss SJ. Warmed versus room temperature saline solution for ear irrigation: a randomized clinical trial. Ann Emerg Med 1999;34:347–50.
Folmer RL, Shi BY. Chronic tinnitus resulting from cerumen removal procedures. Int Tinnitus J 2004;10:42–6.
Hand C, Harvey I. The effectiveness of topical preparations for the treatment of earwax: a systematic review. Br J Gen Pract 2004;54:862–7.
Leong AC, Aldren C. A non-randomized comparison of earwax removal with a ‘do-it-yourself’ ear vacuum kit and a Jobson-Horne probe. Clin Otolaryngol 2005;30:320–3.
Lewis-Cullinan C, Janken JK. Effect of cerumen removal on the hearing ability of geriatric patients. J Adv Nurs 1990;15:594–600.
Proudfoot J. Clinical trial of a ceruminolytic agent in general practice. Br J Clin Pract1968;22:69–70.
Masterson E, Seaton TL. How does liquid docusate sodium (Colace) compare with triethanolamine polypeptide as a ceruminolytic for acute earwax removal? J Fam Pract 2000;49:1076.
Robbins B. Randomized clinical trial of docusate, triethanolamine polypeptide, and irrigation in cerumen removal in children. J Pediatr2004;145:138–9.
Robinson, A. Docusate sodium with irrigation was better than triethanolamine polypeptide with irrigation for dissolving earwax. Evid Based Nurs 2001;4:48.
Somerville G. The most effective products available to facilitate ear syringing. Br J Community Nurs 2002;7:94–101.
Somerville G. Ear syringing improved hearing in general practice. Evid Based Nurs2003;6:85.
Spiro SR. A cost-effectiveness analysis of earwax softeners. Nurse Pract 1997;22:28–31, 166.
Williams D. Does irrigation of the ear to remove impacted wax improve hearing? Br J Community Nurs 2005;10:228–32.
Appendix 7 Variables included in the probabilistic sensitivity analyses
Table 40 lists variables included in probabilistic sensitivity analyses (PSA), distributions and parameters of distributions used.
| Variable | Distribution | Parameters |
|---|---|---|
| Probability of spontaneous earwax removal (no treatment) | Beta | Alpha = 40.5, beta = 769.5 |
| Probability of successful earwax removal with the use of softeners only | Beta | Alpha = 33.9, beta = 135.8 |
| Probability of successful earwax removal with self-syringing | Beta | Alpha = 21.7, beta = 23.5 |
| Probability of successful earwax removal with syringing administered by nurse at primary care | Beta | Alpha = 15.6, beta = 9.6 |
| Proportion of TM cases in the total number of SAEs | Beta | Alpha = 28.3, beta = 57.4 |
| Probability of SAE associated with both active treatments | Beta | Alpha = 15.4, beta = 25,578.9 |
| Hospital admission for either myringoplasty or treatment of a serious infection | Beta | Alpha = 40.5, beta = 769.5 |
| Probability of partial permanent hearing loss if myringoplasty is only partially successful | Beta | Alpha = 31.8, beta = 95.3 |
| Disutility associated with the loss of hearing | Gamma | Alpha = 3600, lambda = 600,000 |
| Cost of GP referral to OTL | Gamma | Alpha = 96.04, lambda = 0.703589744 |
| Cost of self-syringing | Gamma | Alpha = 96.04, lambda = 16.03338898 |
| Cost of nurse visit | Gamma | Alpha = 96.04, lambda =10.79101124 |
| Cost of earwax removal without SAE at primary care | Gamma | Alpha = 96.04, lambda = 2.653038674 |
| Cost of assessment and referral primary care associated with SAE | Gamma | Alpha = 96.04, lambda = 0.558696917 |
| Cost of secondary care treatment of serious infection | Gamma | Alpha = 96.04, lambda = 0.250234497 |
| Cost of secondary care treatment of TM | Gamma | Alpha = 96.04, lambda = 0.133019391 |
| Cost of hospital admission for serious infection treatment | Gamma | Alpha = 96.04, lambda = 0.045733333 |
| Cost of hospital admission for TM | Gamma | Alpha = 96.04, lambda = 0.067113906 |
| Cost of softeners | Gamma | Alpha = 96.04, lambda = 131.5616438 |
| Cost of de-waxing | Gamma | Alpha = 96.04, lambda = 0.562624487 |
List of abbreviations
- AE
- adverse event
- BNF
- British National Formulary
- CCT
- controlled clinical trial
- CDSR
- Cochrane Database of Systematic Reviews
- CI
- confidence interval
- CRD
- Centre for Reviews and Dissemination
- DARE
- Database of Abstracts of Reviews of Effectiveness
- dB
- decibel
- DS
- docusate sodium
- ENT
- ear, nose and throat
- EQ-5D
- European Quality of Life-5 Dimensions
- EVPI
- expected value of perfect information
- EVPPI
- expected value of partial perfect information
- GP
- general practitioner
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- HUI
- Health Utility Index
- ICD-9-CM
- International Classification of Diseases, Ninth Edition, Clinical Modification
- ICER
- incremental cost-effectiveness ratio
- ITT
- intention to treat
- N/A
- not applicable
- NHS
- National Health Service
- NHS EED
- National Health Service Economic Evaluation Database
- NS
- normal saline
- ns
- not significant
- OTC
- over the counter
- OTL
- otolaryngologist
- PEVPI
- population expected value of perfect information
- PSA
- probabilistic sensitivity analysis
- QALY
- quality-adjusted life-year
- r
- discount rate
- RCT
- randomised controlled trial
- SAE
- serious adverse event
- SAND
- Suffolk and Norfolk Research and Development Consortium
- SD
- standard deviation
- SF-6D
- Short Form-6 Dimensions
- SHTAC
- Southampton Technology Assessments Centre
- TM
- tympanic membrane
- TP
- triethanolamine polypeptide
- VAS
- visual analogue scale
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Riemsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson, EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost-effectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
-
Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial.
By Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al.
-
The effect of different treatment durations of clopidogrel in patients with non-ST-segment elevation acute coronary syndromes: a systematic review and value of information analysis.
By Rogowski R, Burch J, Palmer S, Craigs C, Golder S, Woolacott N.
-
Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care.
By Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al.
-
A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial.
By Gray AJ, Goodacre S, Newby DE, Masson MA, Sampson F, Dixon S, et al. , on behalf of the 3CPO study investigators.
-
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluation.
By Ara R, Pandor A, Stevens J, Rees A, Rafia R.
-
Adefovir dipivoxil and pegylated interferon alpha for the treatment of chronic hepatitis B: an updated systematic review and economic evaluation.
By Jones J, Shepherd J, Baxter L, Gospodarevskaya E, Hartwell D, Harris P, et al.
-
Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis.
By Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al.
-
A double-blind randomised placebo-controlled trial of topical intranasal corticosteroids in 4- to 11-year-old children with persistent bilateral otitis media with effusion in primary care.
By Williamson I, Benge S, Barton S, Petrou S, Letley L, Fasey N, et al.
-
The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model.
By Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R.
-
Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial.
By Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al.
-
Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis.
By Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
-
The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation.
By Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al.
-
Rapid testing for group B streptococcus during labour: a test accuracy study with evaluation of acceptability and cost-effectiveness.
By Daniels J, Gray J, Pattison H, Roberts T, Edwards E, Milner P, et al.
-
Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Honest H, Forbes CA, Durée KH, Norman G, Duffy SB, Tsourapas A, et al.
-
The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model.
By Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, et al.
-
Gemcitabine for the treatment of metastatic breast cancer.
By Jones J, Takeda A, Tan SC, Cooper K, Loveman E, Clegg A.
-
Varenicline in the management of smoking cessation: a single technology appraisal.
By Hind D, Tappenden P, Peters J, Kenjegalieva K.
-
Alteplase for the treatment of acute ischaemic stroke: a single technology appraisal.
By Lloyd Jones M, Holmes M.
-
Rituximab for the treatment of rheumatoid arthritis.
By Bagust A, Boland A, Hockenhull J, Fleeman N, Greenhalgh J, Dundar Y, et al.
-
Omalizumab for the treatment of severe persistent allergic asthma.
By Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al.
-
Rituximab for the treatment of relapsed or refractory stage III or IV follicular non-Hodgkin’s lymphoma.
By Boland A, Bagust A, Hockenhull J, Davis H, Chu P, Dickson R.
-
Adalimumab for the treatment of psoriasis.
By Turner D, Picot J, Cooper K, Loveman E.
-
Dabigatran etexilate for the prevention of venous thromboembolism in patients undergoing elective hip and knee surgery: a single technology appraisal.
By Holmes M, C Carroll C, Papaioannou D.
-
Romiplostim for the treatment of chronic immune or idiopathic thrombocytopenic purpura: a single technology appraisal.
By Mowatt G, Boachie C, Crowther M, Fraser C, Hernández R, Jia X, et al.
-
Sunitinib for the treatment of gastrointestinal stromal tumours: a critique of the submission from Pfizer.
By Bond M, Hoyle M, Moxham T, Napier M, Anderson R.
-
Vitamin K to prevent fractures in older women: systematic review and economic evaluation.
By Stevenson M, Lloyd-Jones M, Papaioannou D.
-
The effects of biofeedback for the treatment of essential hypertension: a systematic review.
By Greenhalgh J, Dickson R, Dundar Y.
-
A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: the BELLS study.
By Sullivan FM, Swan IRC, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al.
-
Lapatinib for the treatment of HER2-overexpressing breast cancer.
By Jones J, Takeda A, Picot J, von Keyserlingk C, Clegg A.
-
Infliximab for the treatment of ulcerative colitis.
By Hyde C, Bryan S, Juarez-Garcia A, Andronis L, Fry-Smith A.
-
Rimonabant for the treatment of overweight and obese people.
By Burch J, McKenna C, Palmer S, Norman G, Glanville J, Sculpher M, et al.
-
Telbivudine for the treatment of chronic hepatitis B infection.
By Hartwell D, Jones J, Harris P, Cooper K.
-
Entecavir for the treatment of chronic hepatitis B infection.
By Shepherd J, Gospodarevskaya E, Frampton G, Cooper, K.
-
Febuxostat for the treatment of hyperuricaemia in people with gout: a single technology appraisal.
By Stevenson M, Pandor A.
-
Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal.
By Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E.
-
Cetuximab for the treatment of recurrent and/or metastatic squamous cell carcinoma of the head and neck.
By Greenhalgh J, Bagust A, Boland A, Fleeman N, McLeod C, Dundar Y, et al.
-
Mifamurtide for the treatment of osteosarcoma: a single technology appraisal.
By Pandor A, Fitzgerald P, Stevenson M, Papaioannou D.
-
Ustekinumab for the treatment of moderate to severe psoriasis.
By Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A.
-
Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model.
By Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al.
-
Clinical and cost-effectiveness of epoprostenol, iloprost, bosentan, sitaxentan and sildenafil for pulmonary arterial hypertension within their licensed indications: a systematic review and economic evaluation.
By Chen Y-F, Jowett S, Barton P, Malottki K, Hyde C, Gibbs JSR, et al.
-
Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) – a pharmacoepidemiological and qualitative study.
By Wong ICK, Asherson P, Bilbow A, Clifford S, Coghill D, R DeSoysa R, et al.
-
ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening.
By Kitchener HC, Almonte M, Gilham C, Dowie R, Stoykova B, Sargent A, et al.
-
The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation.
By Black C, Clar C, Henderson R, MacEachern C, McNamee P, Quayyum Z, et al.
-
Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS).
By Robson SC, Kelly T, Howel D, Deverill M, Hewison J, Lie MLS, et al.
-
Randomised controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes.
By Jeffcoate WJ, Price PE, Phillips CJ, Game FL, Mudge E, Davies S, et al.
-
VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers.
By Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al.
-
A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: the VULCAN trial
By Michaels JA, Campbell WB, King BM, MacIntyre J, Palfreyman SJ, Shackley P, et al.
-
Communication of carrier status information following universal newborn screening for sickle cell disorders and cystic fibrosis: qualitative study of experience and practice.
By Kai J, Ulph F, Cullinan T, Qureshi N.
-
Antiviral drugs for the treatment of influenza: a systematic review and economic evaluation.
By Burch J, Paulden M, Conti S, Stock C, Corbett M, Welton NJ, et al.
-
Development of a toolkit and glossary to aid in the adaptation of health technology assessment (HTA) reports for use in different contexts.
By Chase D, Rosten C, Turner S, Hicks N, Milne R.
-
Colour vision testing for diabetic retinopathy: a systematic review of diagnostic accuracy and economic evaluation.
By Rodgers M, Hodges R, Hawkins J, Hollingworth W, Duffy S, McKibbin M, et al.
-
Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report.
By Bond M, Wyatt K, Lloyd J, Welch K, Taylor R.
-
Are adverse effects incorporated in economic models? An initial review of current practice.
By Craig D, McDaid C, Fonseca T, Stock C, Duffy S, Woolacott N.
-
Multicentre randomised controlled trial examining the cost-effectiveness of contrast-enhanced high field magnetic resonance imaging in women with primary breast cancer scheduled for wide local excision (COMICE).
By Turnbull LW, Brown SR, Olivier C, Harvey I, Brown J, Drew P, et al.
-
Bevacizumab, sorafenib tosylate, sunitinib and temsirolimus for renal cell carcinoma: a systematic review and economic evaluation.
By Thompson Coon J, Hoyle M, Green C, Liu Z, Welch K, Moxham T, et al.
-
The clinical effectiveness and cost-effectiveness of testing for cytochrome P450 polymorphisms in patients with schizophrenia treated with antipsychotics: a systematic review and economic evaluation.
By Fleeman N, McLeod C, Bagust A, Beale S, Boland A, Dundar Y, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of photodynamic diagnosis and urine biomarkers (FISH, ImmunoCyt, NMP22) and cytology for the detection and follow-up of bladder cancer.
By Mowatt G, Zhu S, Kilonzo M, Boachie C, Fraser C, Griffiths TRL, et al.
-
Effectiveness and cost-effectiveness of arthroscopic lavage in the treatment of osteoarthritis of the knee: a mixed methods study of the feasibility of conducting a surgical placebo-controlled trial (the KORAL study).
By Campbell MK, Skea ZC, Sutherland AG, Cuthbertson BH, Entwistle VA, McDonald AM, et al.
-
A randomised 2 × 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up.
By Waterhouse JC, Walters SJ, Oluboyede Y, Lawson RA.
-
The effectiveness and cost-effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13–19: a systematic review and economic evaluation.
By Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett-Page E, et al.
-
Dissemination and publication of research findings: an updated review of related biases.
By Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, et al.
-
The effectiveness and cost-effectiveness of biomarkers for the prioritisation of patients awaiting coronary revascularisation: a systematic review and decision model.
By Hemingway H, Henriksson M, Chen R, Damant J, Fitzpatrick N, Abrams K, et al.
-
Comparison of case note review methods for evaluating quality and safety in health care.
By Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al.
-
Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation.
By Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, et al.
-
Self-monitoring of blood glucose in type 2 diabetes: systematic review.
By Clar C, Barnard K, Cummins E, Royle P, Waugh N.
-
North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel non-randomised preference study.
By Lock C, Wilson J, Steen N, Eccles M, Mason H, Carrie S, et al.
-
Multicentre randomised controlled trial of the clinical and cost-effectiveness of a bypass-surgery-first versus a balloon-angioplasty-first revascularisation strategy for severe limb ischaemia due to infrainguinal disease. The Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial.
By Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FGR, Gillespie I, et al.
-
A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – the TOuCAN trial.
By Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al.
-
Randomised controlled trials for policy interventions: a review of reviews and meta-regression.
By Oliver S, Bagnall AM, Thomas J, Shepherd J, Sowden A, White I, et al.
-
Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs (NSAIDs) for the reduction of morphine-related side effects after major surgery: a systematic review.
By McDaid C, Maund E, Rice S, Wright K, Jenkins B, Woolacott N.
-
A systematic review of outcome measures used in forensic mental health research with consensus panel opinion.
By Fitzpatrick R, Chambers J, Burns T, Doll H, Fazel S, Jenkinson C, et al.
-
The clinical effectiveness and cost-effectiveness of topotecan for small cell lung cancer: a systematic review and economic evaluation.
By Loveman E, Jones J, Hartwell D, Bird A, Harris P, Welch K, et al.
-
Antenatal screening for haemoglobinopathies in primary care: a cohort study and cluster randomised trial to inform a simulation model. The Screening for Haemoglobinopathies in First Trimester (SHIFT) trial.
By Dormandy E, Bryan S, Gulliford MC, Roberts T, Ades T, Calnan M, et al.
-
Early referral strategies for management of people with markers of renal disease: a systematic review of the evidence of clinical effectiveness, cost-effectiveness and economic analysis.
By Black C, Sharma P, Scotland G, McCullough K, McGurn D, Robertson L, et al.
-
A randomised controlled trial of cognitive behaviour therapy and motivational interviewing for people with Type 1 diabetes mellitus with persistent sub-optimal glycaemic control: A Diabetes and Psychological Therapies (ADaPT) study.
By Ismail K, Maissi E, Thomas S, Chalder T, Schmidt U, Bartlett J, et al.
-
A randomised controlled equivalence trial to determine the effectiveness and cost–utility of manual chest physiotherapy techniques in the management of exacerbations of chronic obstructive pulmonary disease (MATREX).
By Cross J, Elender F, Barton G, Clark A, Shepstone L, Blyth A, et al.
-
A systematic review and economic evaluation of the clinical effectiveness and cost-effectiveness of aldosterone antagonists for postmyocardial infarction heart failure.
By McKenna C, Burch J, Suekarran S, Walker S, Bakhai A, Witte K, et al.
-
Avoiding and identifying errors in health technology assessment models: qualitative study and methodological review.
By Chilcott JB, Tappenden P, Rawdin A, Johnson M, Kaltenthaler E, Paisley S, et al.
-
BoTULS: a multicentre randomised controlled trial to evaluate the clinical effectiveness and cost-effectiveness of treating upper limb spasticity due to stroke with botulinum toxin type A.
By Shaw L, Rodgers H, Price C, van Wijck F, Shackley P, Steen N, et al. , on behalf of the BoTULS investigators.
-
Weighting and valuing quality-adjusted life-years using stated preference methods: preliminary results from the Social Value of a QALY Project.
By Baker R, Bateman I, Donaldson C, Jones-Lee M, Lancsar E, Loomes G, et al.
-
Cetuximab for the first-line treatment of metastatic colorectal cancer.
By Meads C, Round J, Tubeuf S, Moore D, Pennant M and Bayliss S.
-
Infliximab for the treatment of acute exacerbations of ulcerative colitis.
By Bryan S, Andronis L, Hyde C, Connock M, Fry-Smith A and Wang D.
-
Sorafenib for the treatment of advanced hepatocellular carcinoma.
By Connock M, Round J, Bayliss S, Tubeuf S, Greenheld W and Moore D.
-
Tenofovir disoproxil fumarate for the treatment of chronic hepatitis B infection.
By Jones J, Colquitt J, Shepherd J, Harris P and Cooper K.
-
Prasugrel for the treatment of acute coronary artery syndromes with percutaneous coronary intervention.
By Greenhalgh J, Bagust A, Boland A, Saborido CM, Fleeman N, McLeod C, et al.
-
Alitretinoin for the treatment of severe chronic hand eczema.
By Paulden M, Rodgers M, Griffin S, Slack R, Duffy S, Ingram JR, et al.
-
Pemetrexed for the first-line treatment of locally advanced or metastatic non-small cell lung cancer.
By Fleeman N, Bagust A, McLeod C, Greenhalgh J, Boland A, Dundar Y, et al.
-
Topotecan for the treatment of recurrent and stage IVB carcinoma of the cervix.
By Paton F, Paulden M, Saramago P, Manca A, Misso K, Palmer S, et al.
-
Trabectedin for the treatment of advanced metastatic soft tissue sarcoma.
By Simpson EL, Rafia R, Stevenson MD and Papaioannou D.
-
Azacitidine for the treatment of myelodysplastic syndrome, chronic myelomonocytic leukaemia and acute myeloid leukaemia.
By Edlin R, Connock M, Tubeuf S, Round J, Fry-Smith A, Hyde C, et al.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Consultant Adviser, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Dr Ruairidh Milne, Director of NETSCC External Relations
-
Ms Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Warwick Clinical Trials Unit
-
Director, Nottingham Clinical Trials Unit
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Ms Kay Pattison, NHS R&D Programme/DH, Leeds
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Mr A S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital
-
Dr Dianne Baralle, Consultant & Senior Lecturer in Clinical Genetics, Human Genetics Division & Wessex Clinical Genetics Service, Southampton, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Service User Representative
-
Professor Anthony Robert Kendrick, Professor of Primary Medical Care, University of Southampton
-
Dr Susanne M Ludgate, Director, Medical Devices Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr David Mathew Service User Representative
-
Dr Michael Millar, Lead Consultant in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, University College London
-
Mrs Una Rennard, Service User Representative
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr W Stuart A Smellie, Consultant, Bishop Auckland General Hospital
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Alan J Williams, Consultant in General Medicine, Department of Thoracic Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist Commissioning Advisory Group (NSCAG), Department of Health
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook Clinical Programmes Director, Bazian Ltd, London
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr Colin Greaves Senior Research Fellow, Peninsular Medical School (Primary Care)
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Miss Nicky Mullany, Service User Representative
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Mrs Jean Thurston, Service User Representative
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust, Bristol
-
Reader in Wound Healing and Director of Research, University of Leeds, Leeds
-
Professor Bipin Bhakta Charterhouse Professor in Rehabilitation Medicine, University of Leeds, Leeds
-
Mrs Penny Calder Service User Representative
-
Professor Paul Carding, Professor of Voice Pathology, Newcastle Hospital NHS Trust, Newcastle
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry, London
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol, Bristol
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and the London School of Medicine and Dentistry, London
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester, Manchester
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham, Nottingham
-
Dr Kate Radford, Division of Rehabilitation and Ageing, School of Community Health Sciences. University of Nottingham, Nottingham
-
Mr Jim Reece, Service User Representative
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton, Southampton
-
Dr Pippa Tyrrell, Stroke Medicine, Senior Lecturer/Consultant Stroke Physician, Salford Royal Foundation Hospitals’ Trust, Salford
-
Dr Sarah Tyson, Senior Research Fellow & Associate Head of School, University of Salford, Salford
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University, Cardiff
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health , London
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, MRC, London
-
Dr Ursula Wells PRP, DH, London
Interventional Procedures Panel
-
Consultant Surgeon & Honorary Clinical Lecturer, University of Sheffield
-
Mr David P Britt, Service User Representative, Cheshire
-
Mr Sankaran ChandraSekharan, Consultant Surgeon, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Mr Seamus Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor David Taggart, Consultant Cardiothoracic Surgeon, John Radcliffe Hospital
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Nadim Malik, Consultant Cardiologist/ Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Mr Michael Thomas, Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Mrs Isabel Boyer, Service User Representative, London
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Professor Robin Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Service User Representative, Gloucestershire
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician & Cardiologist, County Durham & Darlington Foundation Trust
-
Mr John Needham, Service User, Buckingmashire
-
Ms Mary Nettle, Mental Health User Consultant, Gloucestershire
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Howard Ring, Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry & Warwickshire Partnership Trust
-
Dr Alastair Sutcliffe, Senior Lecturer, University College London
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, MRC, London
-
Professor Tom Walley, HTA Programme Director, Liverpool
-
Dr Ursula Wells, Policy Research Programme, DH, London
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington