Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the HTA programme on behalf of NICE as project number 08/51/01. The protocol was agreed in September 2008. The assessment report began editorial review in August 2009 and was accepted for publication in February 2010. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
None
Permissions
Copyright statement
© 2010 Queen’s Printer and Controller of HMSO. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2010 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Description of health problem
The first part of the chapter (see sections Growth hormone deficiency to Small for gestational age) describes the health problem individually for the different conditions covered in this review, in terms of their aetiology and epidemiology. The second part of the chapter (see sections Impact of health problem to Current usage in the NHS) covers the impact of the health problems and measurement of disease for all the conditions combined.
Growth hormone deficiency
Growth hormone deficiency (GHD) occurs when the pituitary gland fails to produce sufficient levels of growth hormone (GH).
There is some debate about the diagnostic criteria for GHD: the diagnosis of GHD includes short stature, growth velocity (GV) below the 25th percentile for at least 1 year, and delayed bone age. 1 Rosenfeld2 suggests other criteria: height > 3 standard deviations (SDs) below the mean, < –2 SD to –3 SD for age and deceleration in growth (such as GV < 25th percentile for age), GV < 5th percentile where there is no other explanation, a predisposing condition along with growth deceleration or other signs of pituitary dysfunction. Juul and colleagues3 found ‘large heterogeneity in the current practice of diagnosis and treatment of childhood GHD’. Their survey of European paediatricians found that the cut-off points of GH peak response used for diagnosis of deficiency clustered around 10 ng/ml or 20 mU/l.
The primary goals of recombinant human growth hormone (rhGH) treatment for children with GHD are to normalise height during childhood, for the treated child to reach a ‘normal’ adult height (AH) as defined by the parental target and for mature somatic development to be reached around age 25. 4 The British Society for Paediatric Endocrinology and Diabetes (BSPED) recommends 3- or 6-monthly growth monitoring, annual insulin-like growth factor-1 (IGF-1)/ insulin-like growth factor building protein-3 (IGFBP-3) monitoring, and compliance assessment at each appointment. 5
Aetiology, pathology and prognosis
Growth hormone deficiency can be caused by a variety of factors, but in many cases the cause is unknown. In some children, failure or reduction in GH secretion is congenital, and may be accompanied by other pituitary hormone deficiencies. In others, GHD is acquired as a result of trauma (either at birth or later in childhood), histiocytic infiltration (build up of tissue cells), lymphoma or leukaemia, tumours involving the pituitary gland or hypothalamus or following radiotherapy. 6 Untreated patients have a final height (FH) of 134–146 cm in males and 128–134 cm in females. 1
Incidence and prevalence
The UK Child Growth Foundation estimates that GHD of unknown origin occurs in about one in every 3800 births,7 but reliable figures are difficult to obtain for GHD that is associated with radiotherapy and other causes. Figures from a study in Belgium8 indicate an overall prevalence of GHD of 1 in 5600. The origin of GHD was stated to be unknown in 41% of the patients in this Belgian study, congenital in 20% and acquired in 35%. 8 While the authors of this study state that these yearly numbers have remained similar across the 16 years of the study, these were not collected as part of a formal screening study, and, as a result, the study authors believe that this figure is an underestimation. 8
A Danish study calculated incidence rates of childhood-onset growth hormone deficiency (CO-GHD), based on 1823 patients incident during 1980–99. The average incidences per 100,000 population were calculated to be 2.58 [95% confidence interval (CI) 2.3 to 2.88] for males, and 1.70 (95% CI 1.48 to 196) for females. The differences between the sexes was statistically significant (p < 0.001). 9 Other sources suggest that the disorder is two to three times more common in boys than in girls. 7 A hereditary factor may be identified in some children; about 3% of children with GHD also have an affected sibling. 7
Turner syndrome
Aetiology, pathology and prognosis
Turner syndrome (TS) is caused by the complete or partial absence of the second sex chromosome in girls, with or without cell line mosaicism (the presence of two populations of cells with different genotypes in one individual), leading to the presence of characteristic physical features including, but not limited to, short stature. 10,11 Other features of TS can include skeletal abnormalities, higher risk of scoliosis, cardiovascular abnormalities, lymphoedema, and higher rates of hearing problems and ear malformations. 11
While short stature is the most common clinical feature of TS,11 in the majority of girls with TS the missing or abnormal second chromosome causes ovarian failure, leading to lack of pubertal progression and sexual maturation. TS girls therefore receive estrogen replacement therapy as part of their treatment.
Untreated, the average AH deficit in women with TS is 20 cm, with the average height being 143 cm (4 ft 8 in.). 12 Cases of reduced stature are thought to be predominantly due to haploinsufficiency of the short stature homebox-containing (SHOX) gene. 13 Not all girls with TS will require rhGH treatment and the condition does not necessarily involve a deficiency in natural GH secretion, although there may be a relative lack of sensitivity to GH, and, in some cases, diminished secretion. 6,14
Incidence and prevalence
The European Surveillance of Congenital Abnormalities (EUROCAT) reported in 2003 that TS occurred in 2.08 per 10,000 births in the UK in 2002,15 which equates to approximately one in 2500 live-born females. 11 A Belgian study analysed age at diagnosis of 242 TS girls who were treated with rhGH between 1991 and 2002. 16 The median age at diagnosis was 6.6 (range 0–18.3) years. Although the survey found that 22% of girls were diagnosed after the age of 12 years, there was a general increase in earlier diagnosis in infancy and childhood compared with a previous survey.
A study in Denmark17 identified a standardised mortality rate (SMR) of 2.89 in their TS population, which was increased compared with the general population. However, this significantly decreased over the 3 years of the study. It is unclear if this is due to a real decrease in mortality, better care of individuals with TS, or an increase in karyotypes with lower mortality. 17
Prader–Willi syndrome
Prader–Willi syndrome (PWS) is a genetic disorder characterised by short stature, abnormal body composition, hypogonadism, obesity, dysmorphic features, hyperphagia (compulsive overeating), hypotonia (diminished muscle tone), and specific learning and behavioural issues. 18
Aetiology, pathology and prognosis
The genetic basis of the syndrome is a deletion on the long arm of the paternally derived chromosome 15 (15q11-q13), which is found in approximately 70% of affected individuals. 19 Other abnormalities have been identified, including maternal uniparental disomy (two maternal copies of chromosome 15 and no paternal chromosome 15), imprinting mutations and translocations. Abnormalities to chromosome 15 lead to disruption of the hypothalamus, which controls appetite. The combination of impaired growth, abnormal body composition and hypothalamic dysfunction (hyperphagia, hypogonadism) is suggestive of GHD.
Birth length and weight are normal or just below normal in PWS, but growth is slow due to poor feeding. The child is noticeably short from around the first year of life and remains short throughout childhood [mean height standard deviation score (HtSDS) –2] despite normal growth rate. 20 Hypotonia at birth improves towards the end of the first year of life, and developmental milestones are achieved although delayed. By 2 or 3 years of age the hyperphagic phase of the condition begins, and, unless eating is controlled, the child will become obese. 18
Behavioural features include food seeking, temper tantrums, obsessive–compulsive disorders, high pain threshold, sleep disturbances, and skin picking. Learning disabilities are always present to some degree. 20 Hypogonadism causes delayed but complete puberty in females, although menses are infrequent or absent. Males have cryptorchidism (undescended testis) at birth and usually require androgen replacement therapy from mid-puberty, even after successful orchidopexy. 18
During adolescence, the growth rate declines as a result of the absence of pubertal growth spurt. Reported mean FHs in the UK are 155 cm (–3.2 SD) for males and 147 cm (–2.8 SD) for females. 21 Body composition shows increased fat mass (FM) and reduced fat-free mass, resulting in a high fat–lean body mass (LBM) ratio, even in children with normal weight–height ratios. In addition, bone mineral density is reduced. The reduced bone density is multifactorial; in older patients this is due to sex steroid deficiency (hypogonadism), whereas in younger patients this is due to hypotonia, which responds to rhGH therapy. 22
The prognosis of the condition in adulthood can be reasonable if the person can find occupation and can live in an environment where access to food can be controlled. However, many adults with the disorder develop morbid obesity, often accompanied by type 2 diabetes, resulting in premature death from cardiorespiratory failure. 18
Incidence and prevalence
One UK study estimated a birth incidence for PWS of 1 : 20,000, with a lower bound of 1 : 29,000. 23 The study gave a population prevalence of 1 : 52,000, considered the lower bound, with county rates varying from 1 : 42,000 to 1 : 67,000. 23 The overall death rate for the PWS population aged 3.4–56 years was found to be around 3% in one UK study compared with the standard death rate of about 0.3% each year for people in England and Wales up to the age of 55 years. 23
Chronic renal insufficiency
Chronic renal insufficiency (CRI) is defined as a persistent elevation of serum creatinine and/or urea level. It can be caused by a variety of conditions, including congenital disorders, glomerular disorders and infections. Growth failure associated with CRI can be caused by acidosis, rickets, GH resistance, inadequate nutrition and anorexia. 24 Children with CRI experience impaired growth once their glomerular filtration rate (GFR) falls to 50% of normal, with increasing problems once the GFR falls below 25%. 25 Following kidney transplantation, chronic graft rejection and treatment with steroids can restrict growth and development. 26 Patients undergoing haemodialysis or peritoneal dialysis can be considered for rhGH treatment, as well as those who have received kidney transplantations.
Aetiology, pathology and prognosis
Chronic renal insufficiency is characterised by a GFR of < 75 ml/min per 1.73 m2 of body surface area (BSA). 27 The term chronic kidney disease (CKD) is also sometimes used,27 following guidelines developed by the National Kidney Foundation (NKF) Kidney Disease Outcomes Quality Initiative (KDOQI). 28
The aetiology of growth failure in children with CRI includes abnormalities in the GH-IGF-1 axis, together with nutritional and metabolic problems. 27 Nutritional supplementation in malnourished children with CRI can improve growth. 29–31 The NKF KDOQI guidelines recommend that patients’ existing nutritional deficiencies and metabolic abnormalities should be corrected before considering treatment with rhGH. 32 However, it is estimated that growth remains suboptimal, even with energy intake above 80% of the recommended daily allowance. 33
Not all patients with CRI will be shorter than average, but figures from the UK Renal Registry indicate that 29% of transplant patients and 41% of dialysis patients are below the second percentile for height. 34 Children with congenital disorders (approximately 60% of children with CRI)26 are usually of normal length at birth, but are below the 3rd percentile for height within their first year and remain parallel to normal percentiles throughout childhood. 26 A cohort study of CRI patients who grew up before rhGH treatment was available reported that more than two-thirds remained shorter than the average population. 35 One study reported a mean height from birth to age 10, which was –2.37 SD ± 1.6 below the mean. 26 Similarly, FH is reported to be reduced to below the 3rd percentile in patients who developed end-stage renal failure (ESRF) in childhood. 26 Adult FH was more than 2 SDs below the mean for approximately 60% of boys and 41% of girls who started renal replacement therapy before they were 15 years old. 36
Incidence and prevalence
It is difficult to find accurate figures for CRI, and these do not appear to be available nationally. The UK Renal Registry reports an incidence of established renal failure (ERF) of 8.0 per million of the population who are under the age of 15 years. 37 However, ERF is more severe than CRI, so can really serve only as a guide to the minimum number of patients for whom rhGH might be appropriate.
The UK Renal Registry reported that in 2005 there were 748 patients under the age of 18 years who were on renal replacement therapy in the UK’s 13 paediatric renal centres,34 corresponding to a prevalence of 47.7 per million. 37 However, the number of patients with CRI will be higher than this, as not all will require renal replacement therapy. ERF is reported to be more common in males than in females (ratio 1.54 : 1), due to the prevalence of males with renal dysplasia and obstructive uropathy causing ERF. 37
Small for gestational age
There are various thresholds for defining a child as being born ‘small for gestational age’ (SGA), the most commonly used being where the birth height or weight is ≤ 2 SDs below the population average, or is below the 10th centile for birthweight. 38 However, this group is heterogeneous in composition. Between 50% and 70% of these babies are ‘constitutionally small’ but otherwise healthy. The other babies in the group are those who have not reached their height or weight potential, having possibly experienced fetal growth restriction (FGR). 38 For this reason, the terms intrauterine growth restriction/retardation (IUGR) and SGA are not synonymous: a child born SGA has not necessarily undergone IUGR or FGR, and a child who has IUGR or FGR may not necessarily be born SGA.
Aetiology, pathology and prognosis
There are several possible causes for children being born SGA. These include maternal factors (such as age, ethnicity, weight, height, parity, medical conditions, smoking, malnutrition and alcohol abuse), placental factors, and fetal factors (such as chromosomal abnormalities and genetic defects). 39 Children classified as SGA may have concurrent diagnoses, such as familial short stature, TS, GHD or skeletal dysplasia. 39
More than 80% of babies born SGA will achieve catch-up growth (GV greater than the median for chronological age and gender39) during their first 6 months,40 with catch-up growth completed within 2 years for most SGA infants. 41,42 However, babies born prematurely who are SGA may take around 4 years to achieve catch-up growth. 43 Around 50% of the children who do not experience catch-up growth at this stage will go on to achieve their target height. It has been estimated that approximately 10% of SGA children remain at a height below –2 SD throughout their childhood. 44,45 Children who are born SGA with low birth weight and who do not achieve catch-up growth by the age of 2 years face a relative risk of short stature (< –2 SDs) of 5.2 at the age of 18 years.
Incidence and prevalence
A study of US births estimated an annual incidence of 91,000 infants born SGA, using a definition of SGA as –2 SDs, or equivalent to the 2.3 percentile. 39 A Swedish study of full-term births in 1973–5 found that 5.4% of neonates were SGA, defined as being < –2 SD for birth length and/or height. 46 However, other studies have cited an incidence of around 3% of babies being born SGA. 47,48
SHOX deficiency
Aetiology, pathology and prognosis
The SHOX gene is located on the distal ends of the X and Y chromosomes. This gene plays a significant role in long bone growth, and normal growth requires two functional copies. 49,50 Growth impairment can result from having a haploinsufficiency of SHOX, or from mutations. 49 Clinical features associated with short stature homeobox-containing gene deficiency (SHOX-D) include disproportionate shortening of the middle sections of the limbs (mesomelia), bowing of the forearms and lower legs, cubitus valgus (increased carrying angle of elbow) and Madelung deformity of the wrist. 49 However, not all people with SHOX-D will have these physical characteristics. Langer syndrome is a rare homozygous (or compound heterozygous) form of SHOX-D. It is characterised by extreme dwarfism, profound mesomelia and severe limb deformity. 49,51,52
Incidence and prevalence
Short stature homeobox-containing gene deficiency could be the underlying cause of restricted height in some children whose short stature cannot be explained by an underlying pathology. Estimates of the prevalence of SHOX haploinsufficiency in children with short stature of unknown origin range from 1% to 12.5%. 13,53–59 Rappold and colleagues56 studied 900 short children and found SHOX mutations in 2.4% of the patients with short stature of unknown origin, implying a prevalence of at least 1 in 2000 children. Binder and colleagues57 reported a lower prevalence of SHOX haploinsufficiency, estimating it to be 1 : 4000.
Short stature homeobox-containing gene deficiency also causes short stature in people with concurrent diagnoses. Huber and colleagues59 reported that 68% of 56 children with dyschondrosteosis (a rare form of dwarfism) had SHOX anomalies. Other screening studies have reported it as the cause of short stature in approximately 70% of patients with Léri–Weill syndrome (LWS). 60 Girls with TS have only one copy of the SHOX gene, and this haploinsufficiency causes short stature in some girls and women with the condition. 49
A small study61 that compared 26 SHOX-haploinsufficient people with 45 of their relatives and general population standards found that the SHOX haploinsufficient cohort was 2.14 SDs (3.8 cm) shorter at birth and 2.1 SDs shorter throughout childhood. Females were more severely affected than males, with women’s FH being 2.4 SDs (14.4 cm) shorter than unaffected siblings, and men’s FH being 0.8 SDs (5.3 cm) shorter. SHOX haploinsufficiency led to short stature in 54% of the cohort, short arms in 92% and Madelung deformity in 73%. It is not clear whether the SHOX haploinsufficient cohort in this study had concurrent diagnoses. 61
Impact of health problem
Severe short stature may be physically debilitating in untreated children,62 with children being at greater risk of bullying at school and social isolation. 63 Some children with short stature may also have difficulties with emotionally immature behaviour, anxiety and poor school performance. 64 However, not all children who are shorter than their peers will experience problems. For example, the Royal College of Obstetricians and Gynaecologists states that the majority of children born SGA do not have any appreciable morbidity or mortality. 38 However, others indicate that children born SGA who remain short may suffer from alienation, low self-esteem, impaired social dynamics, behavioural problems, lower educational achievement and professional success. 39,43
Children with short stature can also be at increased risk of morbidity and mortality in later life. For example, the risk of cardiovascular morbidity is increased in patients with GHD,65 TS,66 and PWS,67 while some patients with growth disorders may also be at increased risk of type 2 diabetes and metabolic syndrome. 67,68 Low birth weight is also associated with future increased risk of coronary heart rate and stroke. 69
Outcome measures
The main parameter used to measure the efficacy of rhGH treatment is growth. This reflects the main goals of therapy, which are physiological catch-up growth if possible, achievement of normal height during childhood, timely and normal growth during puberty and normal height in adulthood. In children with PWS, treatment with rhGH aims to improve body composition as well as boosting growth.
Measures of growth include:
-
Final height (FH) or adult height (AH) Measured either in centimetres or expressed as a standard deviation score (SDS), this is the best measure of how rhGH treatment affects growth. FH has been achieved when the growth rate has slowed to less than some specified amount (e.g. 1–2 cm/year), and radiographs of the wrist and hand show that the epiphyses have closed (often expressed as a bone age of more than 14–15 years). 6 Ideally, FH would be calculated in comparison with an untreated control group in a randomised controlled trial (RCT). Some non-RCT designs use historical controls, which may overestimate the effects of rhGH treatment. Similarly, database studies may not include all relevant factors or be representative samples of treated patients. 6
-
Near-final height (NFH) Sometimes reported where it is assumed that FH has been reached using the above criteria, but it is acknowledged that growth may not yet be quite complete. 6
-
Height Usually measured standing, using a wall-mounted Harpenden stadiometer or a similar device. For very young children, supine length is measured.
-
Height standard deviation score (HtSDS) This expresses height relative to norms for children of the same age, allowing comparisons that are independent of age or gender. The normal population mean is zero and a normal SD score will lie between –2 and +2 SDs. Increase over time in SDS or upward centile crossing implies catch-up growth and a decrease implies growth failure. Calculation of SDS depends on the reference data used, i.e. normal height for children in the same country.
-
Growth velocity (GV) Also referred to as height velocity, this is the change in height over a specified period, e.g. cm/year. Although the overall effectiveness of rhGH in treating short stature is to be found in measures of FH, velocity may be a better interim growth measure than height attained at a particular age, as it is independent of growth in previous years.
-
Growth velocity standard deviation score (GVSDS) This is the GV relative to norms for children of the same age.
-
Bone age (BA) A measure of skeletal maturity, usually determined by examining the relative positions of the bones in the left hand and wrist from a radiograph. The measurement of BA relative to chronological age is important in height-prediction models. In addition, BA assessments are used to evaluate when the epiphyses have closed and growth is complete. The interim assessment of BA is important in determining whether treatment is advancing bone maturity, such that short-term GV might come at the expense of early closure of the epiphyses. Clinical trials often measure BA to monitor whether this is accelerating undesirably fast in rhGH-treated patients compared with control patients. Height for BA can also be used as an estimate of improved height potential in response to rhGH therapy, especially in short-term studies.
Measures of body composition assess obesity and the amount of fat relative to other body tissues. Body mass index (BMI) calculates the ratio of body mass to the square of body height, expressed as kg/m2. The National Institute for Health and Clinical Excellence (NICE) recommends BMI as providing a practical estimate of overweight in children, although mentions that it needs to be interpreted with caution as it is not a direct measure of adiposity. 70 Dual-energy X-ray absorptiometry (DEXA) can be used to measure lean mass (fat-free mass) and percentage body fat, which can be used to indicate body composition.
Physiological outcomes reported in studies of rhGH may include assessments of the concentrations of hormones, glucose, cholesterol, and markers of bone and general metabolism. Such measures are important for assessing the biochemical, metabolic and adverse effects of rhGH, and can have implications for long-term health. IGF-1 is an endocrine hormone that is produced by the liver, and its production is stimulated by GH. Lower than normal levels are therefore seen in people with growth disorders. The insulin-like growth factor building proteins (IGFBPs) act as carrier proteins for IGF-1. There are six IGFBPs, with IGFBP-3 being the most abundant. 71 IGF-1 is monitored during rhGH therapy as there is a theoretical concern that persistently elevated levels may predispose the patient to other diseases later in life. Monitoring levels also helps to tailor the dose to the individual. As IGFBP-3 binds IGF-1, monitoring this gives an indication of the levels of ‘free’ IGF-1 in circulation. High levels of IGF-1 with low levels of IGFBP-3 may be linked with breast, colorectal and prostate cancer. 72,73
Current service provision
Management of rhGH therapy
Children who receive rhGH therapy require regular review by consultant paediatric endocrinologists. Older children and adolescents in need of continued rhGH therapy may enter transitional care arrangements that involve consultations with both paediatric and adult growth specialists. 74 A system of shared care is sometimes used for rhGH therapy in the UK,1 with diagnosis and assessment of growth being carried out in hospital outpatient consultations and some GPs writing prescriptions and possibly monitoring adverse events (AEs). In other areas, all care including prescriptions and monitoring of compliance and side effects takes place in secondary care.
Administration of rhGH is usually carried out at home by the patient or a family member, after training, by subcutaneous injection, using either needled or needle-free devices, usually pharmaceutical companies’ devices rather than syringe and needle. Termination of rhGH therapy is indicated if there is a poor response (< 50% increment in GV within the first year) or when FH is achieved. In children with CRI, therapy with rhGH is stopped at the time of a transplant. Therapy would not resume until at least 1 year post transplant, and is dependent upon the absence of catch-up growth. 1
Relevant guidance
Current guidance from NICE on the use of rhGH in England and Wales for children with growth failure due to GHD, TS, PWS or CRI was published in 2002. 75 This is discussed further later in the chapter (see Place of the intervention in the treatment pathway). Since 2002, a range of guidance on the use of rhGH in children with short stature has been published by various national health agencies and clinical expert groups for GHD, TS, CRI, PWS and SGA, but guidance for children with SHOX-D is lacking.
Guidelines on the use of rhGH for the treatment of girls and women with TS (published in 2007, relevant to US practice) recommended that treatment with rhGH should be considered as soon as growth failure has been identified, and its potential risks and benefits have been discussed with the family. It also provided rhGH dosing information and a comprehensive set of recommendations for the diagnosis, evaluation, monitoring and ongoing care of children with TS. 11
Summary guidelines76 and detailed recommendations27 on the use of rhGH for short stature in children with CRI (published in 2005–6, relevant to US practice) recommended that therapy should not commence unless patients exhibit clearly defined CRI and attain appropriate phosphorus and parathyroid hormone status. 76 The detailed recommendations included rhGH dosing information and a treatment algorithm outlining appropriate steps to improve growth and overall health outcomes. 27
Consensus statements on using rhGH therapy in children and adults born SGA (published in 200339 and 2007,77 relevant to European and US practice) emphasised the need for accurate diagnosis of SGA and recommended that rhGH therapy should be considered in children who are SGA and older than 2 years of age. However, this reflects differences in licensing in Europe and America. The Food and Drug Administration (FDA) authorisation is for children aged 2 years and over with no catch-up growth (no criteria specified), and no specified HtSDS at start of treatment or reference to mid-parental height. 78 By contrast, the European Medicines Agency (EMEA) authorisation is for children aged 4 years and over, with a HtSDS of –2.5 at start of treatment, with a GV < 0 SDs and HtSDS > 1 SD below mid-parental height. 79 In addition, the licensed dose is 70 µg/kg/day in the USA and 35 µg/kg/day in Europe.
For UK populations, guidelines on rhGH therapy for children with GHD, TS, CRI, PWS and SGA was published in 2006 by BSPED. 1 This guidance provided recommendations for shared care between GPs and specialists, together with dosing information and treatment entry and exit criteria.
Description of technology under assessment
Somatropin (rhGH) has been available since 1985, following the withdrawal of cadaveric human pituitary GH due to possible transmission of Creutzfeldt–Jakob disease. 6 rhGH is a synthetic form of human GH, produced by recombinant deoxyribonucleic acid (DNA) technology, having a sequence identical to that of pituitary-derived human GH. Licensed dosages vary for the different indications (Table 1), depending on whether the treatment is aiming to replace GH to normal levels (for children with GHD) or being used in supraphysiological doses where there is no hormone deficiency but some lack of sensitivity to the hormone. It is given as a subcutaneous injection, usually at night (to mimic the child’s natural fluctuations in GH). 6
| Indication | Dosea | Licensed drugs (manufacturers) |
|---|---|---|
| GHD | 23–39 mcg/kg daily, or 0.7–1.0 mg/m2 daily |
Humatrope (Eli Lilly & Co. Ltd) Zomacton (Ferring Pharmaceuticals UK) NutropinAq (Ipsen Ltd) Norditropin Simple Xx (Novo Nordisk Ltd) Genotropin (Pfizer Ltd) Omnitrope (Sandoz Ltd) Saizen (Merck Serono) |
| TS | 45–50 mcg/kg daily or 1.4 mg/m2 daily |
Humatrope (Eli Lilly & Co. Ltd) Zomacton (Ferring Pharmaceuticals UK) NutropinAq (Ipsen Ltd) Norditropin Simple Xx (Novo Nordisk Ltd) Genotropin (Pfizer Ltd) Omnitrope (Sandoz Ltd) Saizen (Merck Serono) |
| PWS, with GV > 1 cm/year (in combination with energy-restricted diet) | 35 mcg/kg daily or 1.0 mg/m2 daily; max. 2.7 mg daily |
Genotropin (Pfizer Ltd) Omnitrope (Sandoz Ltd) |
| CRI in children | 45–50 mcg/kg daily or 1.4 mg/m2 daily |
Humatrope (Eli Lilly & Co. Ltd) NutropinAq (Ipsen Ltd) Norditropin Simple Xx (Novo Nordisk Ltd) Genotropin (Pfizer Ltd) Omnitrope (Sandoz Ltd) Saizen (Merck Serono) |
| SHOX-D | 45–50 mcg/kg daily | Humatrope (Eli Lilly & Co. Ltd) |
| Growth disturbance (current HtSDS –2.5 and parental adjusted HtSDS, –1) in short children born SGA, with a birth weight and/or length below –2 SDs, who failed to show catch-up growth (HV SDS < 0 during the last year) by 4 years of age or later | 35 mcg/kg daily or 1.0 mg/m2 daily |
Humatrope (Eli Lilly & Co. Ltd) Norditropin Simple Xx (Novo Nordisk Ltd) Genotropin (Pfizer Ltd) Omnitrope (Sandoz Ltd) Saizen (Merck Serono) |
Seven pharmaceutical companies have UK marketing authorisations for various indications, as shown in Table 1.
Adverse events (AEs) have been reported in patients using rhGH. For example, sleep apnoea and sudden death among patients with PWS who have one or more of the following risk factors: severe obesity, history of upper airway obstruction or sleep apnoea, or untreated respiratory infection. 80,81 There are potential risks of acromegaly, hyperglycaemia and glucosuria if the recommended dosage is exceeded. 81 Patients receiving rhGH should be monitored for glucose intolerance, as the drug may induce a state of insulin resistance. 81 It is also recommended that thyroid function should be monitored. 81 Possible side effects mentioned for 1–10% of patients include hypersensitivity to solvent, hypothyroidism, injection site pain (reaction) and oedema. 81 Treatment should be discontinued in the event of intracranial hypertension,81 although it may be possible to restart treatment at a lower dose for patients who develop benign intracranial hypertension. Treatment with rhGH leads to increasing sensitivity to GH, expressed as an increase in serum IGF-1. 81
Omnitrope, marketed by Sandoz, is a biosimilar product. This means that it is an active substance that is similar, but not identical, to the other drugs considered in this review. The issue of rhGH therapy and biosimilars in clinical practice was the subject of a recent Parliamentary Summit. 30 The current review assesses the clinical effectiveness and cost-effectiveness of rhGH, without reference to the brand product or manufacturer. Discussion of the comparative safety and efficacy of biosimilars compared with reference products is therefore beyond the scope of this review.
Place of the intervention in the treatment pathway
The place of rhGH in the treatment pathway depends on the child’s particular condition or syndrome, and age at diagnosis. Appropriate timing of treatment with rhGH will depend on the underlying pathology. rhGH therapy is contraindicated in cases of progressive tumour activity and should not be used for growth promotion in children with closed epiphyses.
GHD
Treatment with rhGH is currently recommended by NICE to help increase the growth of children with GHD. 75 For children with congenital GHD, rhGH therapy is not generally started before the child is 4 years old. 6 However, if there is profound growth failure or evidence of recurrent hypoglycaemia, which may occur in infants under the age of 1, treatment may be started earlier. For children who acquire GHD at an older age, treatment can start at a time that is appropriate to their condition and stage of growth. Treatment is discontinued after the first year if there is a poor response, i.e. < 50% increase in growth rate, or if compliance or growth rate remains poor thereafter. Otherwise treatment can continue until GV is < 2 cm/year, assessed over 6–12 months, when FH is achieved. Other clinical advice suggests that treatment is necessary for the patient to attain peak bone mass, which may not be until the age of 25 or 26 in some people. A recent survey of paediatric endocrinologists (56 responses out of 72 questionnaires) found that 56% of clinics provide transfer clinics for patients ending paediatric treatment and transferring to the care of an adult endocrinologist. Of the 56 respondents, 80% retest for GHD prior to transfer, 55% transfer all rhGH-treated patients and the remainder transfer only those who are still GH deficient on retesting. 74
Transition phase
The transition phase in GHD is defined as the period from near FH, usually around the mid to late teens, until about 25 years of age, or when final adult height has been reached. At the stage of near FH, it is important to re-evaluate whether the patient is still GH deficient, and if they need to continue with treatment and monitoring. Some cases, such as isolated GHD with a genetically identified mutation or multiple pituitary hormone deficiency (MPHD), severe GHD due to genetic causes, pituitary abnormalities, congenital hypopituitarism or acquired GHD from tumours or cranial irradiation, are likely to require a continuation of therapy. However, cases of unknown origin and isolated cases of GHD carry a lower likelihood of requiring continuing treatment. 4 The BSPED consensus document suggests testing IGF-1 levels: if these are lower than –2 SD then these patients require GH stimulation retests. A peak GHD level of < 5 µg/l during the transition phase is indicative of severe GHD. 5
During the transition phase the authors of the consensus paper recommend that monitoring of patients should include weight and BMI at least 6-monthly, IGF-1, quality of life (QoL), waist circumference and fasting glucose annually, and body composition and total and low-density lipoprotein (LDL) cholesterol every 2–5 years. 5
Turner syndrome
Current NICE guidance recommends that rhGH treatment for girls with TS should begin at the earliest age possible, to boost growth. 75 Some patients with profound growth retardation and failure to thrive may commence treatment earlier than those who are diagnosed later. A Belgian study16 found that median age at diagnosis of 242 girls was 6.6 (range 0–18.3) years, although the survey found that 22% of girls were diagnosed after the age of 12 years. Some clinical expert advice suggests that the mean age for starting treatment is 8–9 years of age as many girls are not diagnosed until later in childhood, although there has been a recent trend towards earlier diagnosis.
Prader–Willi syndrome
NICE guidance currently recommends the use of rhGH for children with PWS to improve height, body composition and bone mineral density. For children with PWS, treatment with rhGH is intended to improve body composition and metabolism as well as increase FH. Its place in the treatment pathway depends on age at diagnosis. Children with PWS are assessed for obesity, potential for obstructive sleep apnoea and ongoing respiratory illness before treatment is considered. Low muscle tone and its impact on the child’s development are also considered.
Chronic renal insufficiency
Treatment with rhGH is currently recommended by NICE to help increase the growth of prepubertal children with CRI. 75 The guidance recommends that treatment should be stopped after a renal transplantation, and re-established after only 1 year if it has been ascertained that catch-up growth has not occurred. 75 The place of rhGH in the treatment pathway for children with CRI depends on age at diagnosis, and on clinical factors related to management of the child’s condition. rhGH treatment can take place either before or after renal transplant, although allograft rejection can be a concern if rhGH treatment is given post transplant.
Small for gestational age
Previous NICE guidelines did not consider children born SGA, as rhGH was not licensed for this indication at the time. 82 Children born SGA but with no comorbidities may not be diagnosed until they fail to achieve catch-up height by the age of 2–4 years,39 or when they start school. The International SGA Advisory Board indicated that SGA children aged 2–4 years who show no evidence of catch-up with a height of –2.5 SD should be eligible for rhGH treatment. They also recommended that treatment should be considered in children older than four years who show no catch up at a height –2 SD or less. 39 The European licence for rhGH is for children aged 4 years and over.
SHOX deficiency
Currently, there is no NICE guidance available for the use of rhGH in children with SHOX-D. Initiation of rhGH treatment for children with SHOX-D depends on age at diagnosis. Clinical evaluation is used to assess growth failure, but GH provocation tests are not required once SHOX-D has been established via a positive SHOX DNA blood test.
Current usage in the NHS
According to a survey of endocrine clinics published in 2006 by BSPED,74 4758 patients have been receiving rhGH in the UK, of which 4168 were in England and Wales. Responses to the survey gave a breakdown of rhGH use by diagnosis for 3951 of the 4758 patients, indicating that 57.4% of the patients on rhGH were treated for GHD, 18.7% for TS, 4.6% for PWS, 5.2% for SGA, 2.5% for CRI, and 11.6% for other diagnoses. If we assume that these 3951 patients are a representative sample of the total population of rhGH-treated patients in the UK, the total numbers of rhGH-treated patients with each diagnosis would be around 2731 with GHD, 890 with TS, 219 with PWS, 247 with SGA, 119 with CRI, and 552 with other diagnoses. It is possible that the number of children with CRI who received rhGH in this survey was underestimated, as some patients with CRI are managed in nephrology clinics, rather than paediatric endocrine clinics. 74 The number of patients treated with rhGH for SHOX-D was not reported in the survey and published figures are not available. Expert advice indicates that very few SHOX-deficient patients are currently receiving rhGH, for example only two of between 350 and 400 patients in one unit receiving rhGH are being treated for this. The level of service provision for SHOX-deficient patients would be similar to that required for a patient with TS.
Anticipated costs associated with intervention
The costs associated with rhGH therapy interventions comprise:
-
the drug (dose adjusted for body weight)
-
self-therapy training of the patients and their parents (involving home visits by specialist and community nurses)
-
monitoring of treatment effectiveness (involving paediatric endocrinology outpatient visits for blood tests, a test of pituitary function, and an assessment of BA by hand radiograph).
The costs of training patients and their parents are limited to the first year of treatment. During each year of treatment, until they stop growing, patients would typically attend two outpatient consultations. Estimates of the current costs of these components of the rhGH interventions for patients with GHD, TS, PWS, CRI and SGA are provided in Chapter 4 (see Estimation of costs).
Chapter 2 Definition of the decision problem
Decision problem
Recombinant human growth hormone is currently recommended by NICE75 for children with a proven clinical diagnosis of GHD, TS or PWS, and for prepubertal children with CRI. Since the last review, rhGH has received marketing authorisation for the treatment of children born SGA and for children with growth failure associated with SHOX-D. The scope of the current project is broader than that for the previous systematic review6 in that it covers body composition as an outcome measure for all disease areas, and also includes biochemical and metabolic markers. In addition, evidence for the use of rhGH for children born SGA, or with SHOX-D (conditions not considered in the original review) are included in this report. For these reasons, the current systematic review was undertaken as a complete review not an update. The aim of this health technology assessment (HTA) is to assess the clinical effectiveness and cost-effectiveness of rhGH for children with GHD, TS, PWS, CRI, SHOX-D and those born SGA.
Interventions
The intervention is rhGH, also known as somatropin. It is marketed as the following products: Humatrope (Eli Lilly & Co.); Zomacton (Ferring Pharmaceuticals); NutropinAq (Ipsen); Norditropin SimpleXx (Novo Nordisk); Genotropin (Pfizer); Omnitrope (Sandoz) and Saizen (Merck Serono).
Population, including subgroups
The population consists of children with one of the following conditions: GHD, TS, PWS, CRI, SHOX-D, being born SGA. No age-specific definition of a child was given during the scoping process for this review. Possible subgroups could be children with different causes of GHD, and children with CRI who are either pretransplant or post transplant. However, analysis of the effectiveness of rhGH treatment for any of these subgroups of patients is limited by the available data and the statistical power of the identified trials.
Transition of care from paediatric to adult endocrine services of young people requires patients to have repeat testing of their GH axis to be sure that they need to continue treatment. This transition period is only considered within this review where evidence from the identified studies allows for patients whose linear growth is not complete.
Relevant comparators
The standard comparator for this review is management strategies without rhGH. This includes placebo injections and no treatment.
Outcomes
Clinical outcomes of interest include: FH gained, HtSDS, GV, GVSDS, body composition, biochemical/metabolic markers, AEs of treatment; health-related quality of life (HRQoL). Direct costs include estimates of all health-care resources consumed in the provision of the intervention, including diagnostic tests, administration and monitoring costs – as well as consequences of those interventions, such as treatment of adverse effects.
Overall aims and objectives of assessment
The aim of this report is to assess the clinical effectiveness and cost-effectiveness of rhGH treatment for children with GHD, TS, PWS, CRI, SHOX-D and those born SGA.
The objectives are to:
-
summarise the evidence of clinical effectiveness and cost-effectiveness of rhGH when compared with management strategies without rhGH
-
develop, where appropriate, an economic model adapting an existing cost-effectiveness model6 or constructing a new model using best available evidence to determine cost-effectiveness in the UK
-
identify priorities for future research.
Chapter 3 Assessment of clinical effectiveness
Methodology
The methods for the systematic review of clinical effectiveness were described a priori in the research protocol (Appendix 1), which was sent to experts for comment. We received helpful comments relating to the general content of the research protocol, but there was none that identified specific problems with the methods of the review. The methods are summarised below.
Search strategy
An experienced information specialist developed and tested search strategies for this review. Separate searches were carried out to identify studies reporting clinical effectiveness, cost-effectiveness, HRQoL, resource use and costs, and epidemiology/natural history of the conditions. The search strategy for MEDLINE, shown in Appendix 2, was adapted as appropriate for a number of other electronic databases. We searched: The Cochrane Database of Systematic Reviews (CDSR); The Cochrane Central Register of Controlled Trials; NHS Centre for Reviews and Dissemination (NHS CRD, University of York) Database of Abstracts of Reviews of Effectiveness (DARE) and the NHS Economic Evaluation Database (NHS EED); MEDLINE (OVID); EMBASE (OVID); National Research Register (NRR); Current Controlled Trials; ISI Proceedings; Web of Science; and BIOSIS. For all disease areas we searched the databases from their inception to June 2009. This meant there was some duplication of earlier work for the previous review, but this was necessary as the present review required searches for additional outcomes, such as biochemical and metabolic markers. Searches were limited to the English language.
Relevant conferences (European Society for Paediatric Endocrinology, The Endocrine Society, American Association of Endocrinologists, Paediatric Academic Societies) were searched for recent abstracts (up to June 2009) to assess against the inclusion criteria. Bibliographies of related papers were screened for relevant studies, and we contacted experts to identify any additional published or unpublished references. We also assessed the MSs to NICE for any additional studies that met the inclusion criteria.
Inclusion and data extraction process
Titles and abstracts of studies identified by the search strategy were assessed for potential eligibility by two reviewers. The full text of relevant papers was then obtained, and inclusion criteria were applied by two independent reviewers. At both stages of the screening process, any differences in opinion on inclusion of a particular study were resolved through discussion. Data from included studies were extracted by one reviewer using a standard data extraction form and checked by a second reviewer. Any discrepancies were identified and resolved through discussion.
Quality assessment
The quality of included studies was assessed using NHS CRD (University of York) criteria. 83 Quality criteria were applied by one reviewer and checked by a second reviewer, with differences in opinion resolved by discussion. The criteria used are shown in Appendix 3. Publication bias was not assessed.
Inclusion criteria
Patients
The inclusion criteria required the patient group to be children with growth disturbance due to one of the following licensed conditions:
-
insufficient secretion of GH (GHD)
-
Turner syndrome, confirmed by chromosome analysis
-
Prader–Willi syndrome, confirmed by genetic testing
-
chronic renal insufficiency (prepubertal children only)
-
short stature homeobox-containing gene deficiency, confirmed by DNA analysis
-
small for gestational age (see below).
The licensed indication81 for SGA is for growth disturbance (current HtSDS –2.5 and parental adjusted HtSDS –1) in short children born SGA, with a birth weight and/or length below –2 SD, who failed to show catch-up growth [height velocity (HV) SDS < 0 during the last year] by 4 years of age or later. However, the review group could not find any RCTs whose inclusion criteria matched these criteria exactly. Following discussions with NICE, the team amended the criteria to be: ‘growth disturbance (current HtSDS < –2.5, but with no reference to parental height) in short children born SGA with a birth weight and/or length below –2 SD, who failed to show catch-up growth (with no particular criteria specified) by 3 years of age or later.’
Studies that included adolescents and young adults who have completed linear growth were excluded from the systematic review of effectiveness.
Interventions
Recombinant human growth hormone (somatropin).
Comparators
Management strategies without somatropin.
Outcomes
The following outcomes were included in the review, where data were available:
-
final height gained
-
height standard deviation score (height relative to the distribution of height in children of the same chronological age)
-
growth velocity
-
growth velocity standard deviation score (GV relative to the distribution of growth in children of the same chronological age or bone age)
-
body composition
-
biochemical and metabolic markers
-
adverse effects of treatment
-
HRQoL.
Types of studies
-
Fully published RCTs were included in the review, and systematic reviews of RCTs were included as sources of information. Indicators of a systematic review include: explicit search strategy, inclusion criteria, data extraction and assessment of quality. While important information on FH and long-term AEs will only be available in longer, observational studies, there was a practical limit on the number of studies that could be included for this review. A pragmatic decision was therefore taken to limit study type to RCTs, in an attempt to capture the most methodologically robust data for all six of the disease areas included in this review.
-
Studies published only as abstracts or conference presentations were included in the primary analysis of clinical effectiveness and cost-effectiveness if sufficient details were presented to allow an appraisal of the methodology and assessment of results.
-
Non-English language studies were excluded.
-
In an effort to capture all randomised evidence, all identified RCTs were included with no restriction on length of treatment, size of study population, or design (parallel group or crossover design). Crossover studies could potentially be problematic as children’s growth continues without treatment, making comparisons between the different arms less straightforward than in a parallel-group trial. However, we have attempted to include discussion of this in the quality assessment of studies.
Data synthesis
-
Clinical effectiveness studies were synthesised through a narrative review with tabulation of results of included studies. Key outcome measures are reported in tables in the text, and other outcomes are shown in the full data extraction forms in Appendix 4. For conciseness, where a study reported outcome measures after 1 and 2 years, only the final year’s outcomes are included in the table, as these show the longest duration of treatment effect.
-
Where data were of sufficient quality and homogeneity, a meta-analysis of the clinical effectiveness studies was considered using review manager 5.0 software.
-
Quality-of-life studies were synthesised using the same methods as above, i.e. narrative review and meta-analysis only if feasible.
Results
A brief overview of the results of the searches is presented below. Owing to the extensive nature of this multiple technology appraisal (MTA), the clinical effectiveness results for the six different disease areas are presented separately (see sections Growth hormone deficiency to SHOX-D). For all disease areas throughout the screening and data extraction process, differences in opinion were generally minor and easily resolved without the involvement of a third reviewer.
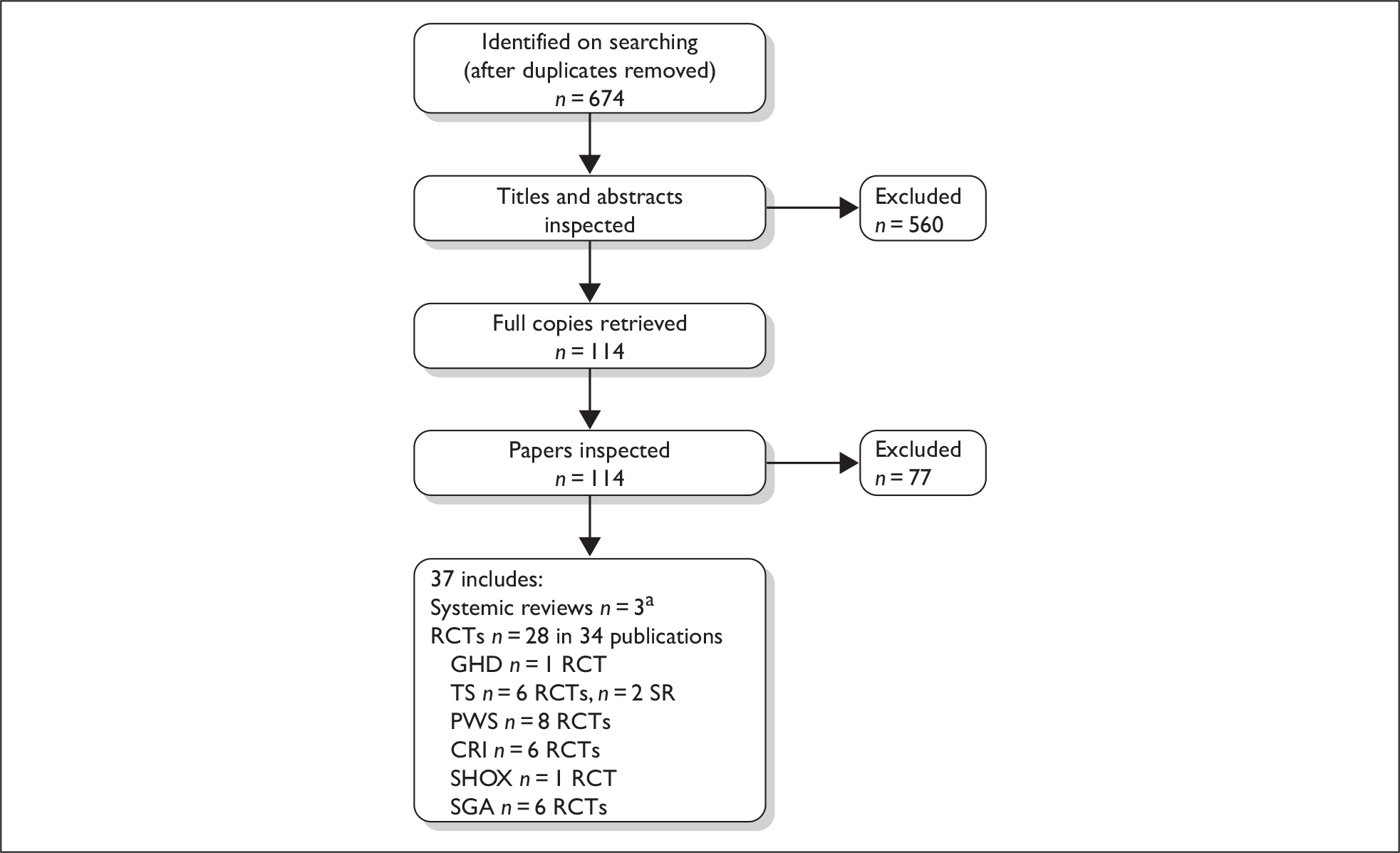
Quantity and quality of research available
The number of references considered at each stage of the review is shown in Figure 1. Of the 674 references identified, 560 were excluded on inspection of their titles and abstracts. The full papers of 114 references were retrieved and assessed against the inclusion criteria. A total of 77 of the retrieved full papers were rejected at this stage, mostly due to the patient group not meeting the inclusion criteria (n = 40) or due to a non-RCT study design (n = 27). A list of papers excluded at this stage is included in Appendix 5, together with reasons for exclusion. A total of 28 RCTs in 34 publications were included in the systematic review of clinical effectiveness. Appendix 6 lists conference abstracts that were identified as being of interest, but which contained insufficient information to be included in the review of clinical effectiveness.
FIGURE 1.
Flow chart of identification of published studies for inclusion in the systematic review of clinical effectiveness. aOne of the systematic reviews was the previous Health Technology Assessment report written for the National Institute for Health and Clinical Excellence, so this was not data extracted. It is discussed briefly (in Summary of previous systematic reviews).
An overview of the included studies is given in Table 2. Only one SGA paper and one TS paper reported FH; none of the other conditions’ studies reported FH as an outcome measure. None of the papers reported specific QoL measures. All disease areas included at least one paper which reported outcomes on height gained, body composition, biochemical markers and AE. The characteristics and quality assessment of the included studies are discussed in each of the relevant disease-specific results chapters.
| Author and date | Total (n) | Outcomes included in the systematic review | ||||||
|---|---|---|---|---|---|---|---|---|
| FH | Height gained/HtSDS | GV/growth SDS | Body composition | Biochemical/metabolic markers | QoL | AE | ||
| GHD | ||||||||
| Soliman84 | 19 | ✓ | ✓ | ✓ | ||||
| TS | ||||||||
| Davenport 200785 | 89 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Stephure 200586 and Rovet 199387 | 154 | ✓ | ✓ | ✓ | ✓ | |||
| Quigley 200212 | 232 | ✓ | ✓ | |||||
| Gravholt 200288 | 12 | ✓ | ✓ | |||||
| Gravholt 200589 | 9 | ✓ | ✓ | |||||
| Johnston 200190 | 58 | ✓ | ||||||
| PWS | ||||||||
| Festen 200791 | 20 | ✓ | ✓ | ✓ | ||||
| Festen 200792 | 29 | ✓ | ✓ | ✓ | ✓ | |||
| de Lind van Wijngaarden 200993 and Festen 200894 | 42 infants, 49 children | ✓ | ✓ | ✓ | ||||
| Carrel 199995 and Myers96 | 54 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Carrel 200422 and Myers97 and Whitman98 | 32 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Hauffa 199799 | 19 | ✓ | ✓ | ✓ | ✓ | |||
| Lindgren100,101 | 29 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Haqq 2003102 | 14 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| CRI | ||||||||
| Sanchez 2002103 | 23 | ✓ | ✓ | ✓ | ✓ | |||
| Hokken-Koelega 1991104 | 20 | ✓ | ✓ | ✓ | ||||
| Hokken-Koelega 1996105 | 11 | ✓ | ✓ | ✓ | ||||
| Powell 1997106 | 69 | ✓ | ✓ | ✓ | ||||
| The Pharmacia and Upjohn Study Group 1996107 | 203 | ✓ | ✓ | |||||
| Fine 1994108 | 125 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| SHOX-D | ||||||||
| Blum 200749 | 52 | ✓ | ✓ | ✓ | ✓ | |||
| SGA | ||||||||
| De Schepper 2007109 | 40 | ✓ | ✓ | ✓ | ||||
| Lagrou 2008110 | 40 | ✓ | ✓ | ✓ | ||||
| Carel 2003111 | 168 | ✓ | ✓ | ✓ | ||||
| de Zegher 1996112 | 54 | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| de Zegher 2002113 | 13 | ✓ | ✓ | ✓ | ||||
| Philip 2009114 | 151 | ✓ | ✓ | |||||
Comparison with previous review
The previous review by Bryant and colleagues6 included a number of studies that were excluded from the present review. As described above (see Inclusion and data extraction process) and in the research protocol, the present review included only RCTs as these form the highest level of evidence in the hierarchy of clinical trial designs. 83 The previous review included two non-RCT studies for GHD,115,116 four for TS,117–120 two for CRI121,122 and one for PWS. 123 In addition, the previous review included two RCTs for TS, which have been excluded from the present review. The first of these, by Rosenfeld and colleagues,124,125 was excluded from the present review as it used methionyl growth hormone (met-GH) rather than rhGH. The second TS RCT was by Ross and colleagues,126 which reported cognitive function. This was not one of the outcome measures listed in the inclusion criteria for the present review, so this RCT was excluded. The previous review also included a PWS RCT by Whitman and colleagues,127 which was considered for the current review. However, the study reported psychological outcomes rather than a measure of HRQoL, so this study did not meet our inclusion criteria.
Growth hormone deficiency
Quantity and quality of research available
One study met the inclusion criteria for this review, and the key characteristics are presented in Table 3. The full data extraction form in Appendix 4 has further details.
| Reference | Intervention | Control group | Total randomised and withdrawals | Duration of randomised treatment |
|---|---|---|---|---|
| Soliman et al. 199684 |
GH 15 U/m2/week n = 9 Overall mean age ± SD: 6.8 ± 2.1 |
No treatment n = 10 Overall mean age ± SD: 6.8 ± 2.1 |
Total n = 19 No withdrawals reported |
1 year |
Soliman and Abdul Khadir84 recruited two groups of GH-deficient children and one group of children who were not GH deficient. These groups were then subdivided into treatment groups: group 1a received 30 units (U)/m2/week of rhGH and group 1b received 15 U/m2/week. Group 2a received 15 U/m2/week and group 2b received no treatment. Group 3 (non-GHD short children) was subdivided in the same way as group 2. Group 2 was the only group in this study with GHD and with children randomised to either rhGH or no treatment, and, as such, is the only group considered in this report. The treatment groups’ baseline characteristics were similar. The study used a dose of 15 U/m2/week, and it is not clear how this corresponds to the licensed dose as neither milligrams (mg) nor international units (IUs) are used.
Overall the quality of the reporting of the included study was mixed (Table 4). No details were given on randomisation or allocation to treatment groups. For example, Soliman and Abdul Khadir84 recruited children into specified groups according to peak GH response to provocation, and these groups were then divided at random into two subgroups. No further details were given. The low patient numbers will affect interpretation of results from this trial.
| Soliman84 | |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Inadequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Adequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
The comparator group did not receive placebo: this could mean that both care providers and patients would have been aware of whether they were receiving treatment, which, in turn, can affect reporting of some outcomes. Soliman and Abdul Khadir84 appear to have carried out an intention-to-treat analysis (ITT), which can protect against attrition bias.
Growth outcomes
The Soliman84 study reported GV and HtSDS, and these are presented in Table 5. The data extraction forms in Appendix 4 list further outcome measures, such as BA.
| Study | Mean (SD) | GH | No treatment | p-value |
|---|---|---|---|---|
| Soliman 84 | HtSDS | –2.3 ± 0.45 | –2.8 ± 0.45 | < 0.05 |
| GH 15 U/m2/week (n = 9) vs no treatment (n = 10); 12 months | 8.4 ± 1.4 | 5.7 ± 1.8 | < 0.05 |
Children in the treated group in the Soliman study grew an average of 2.7 cm/year faster than those receiving no treatment in the 12 months of the study, and the difference between groups was statistically significant (p < 0.05). Similarly, children in the treated group had a statistically significantly higher HtSDS: –2.3 ± 0.45 versus –2.8 ± 0.45 in the untreated group (p < 0.05).
Body composition outcomes
Soliman and Abdul Khadir84 did not report body composition outcomes.
Biochemical markers
The results reported for IGF-1 levels in the Soliman study84 are shown in Table 6. Further biochemical markers, such as insulin, are included in the data extraction tables in Appendix 4.
| Study | Outcomes | GH | Control | p-value |
|---|---|---|---|---|
|
Soliman 84 GH 15 U/m2/week (n = 9) vs no treatment (n = 10); 12 months |
IGF-1 (ng/ml) | 91.2 ± 30.4 | 49.4 ± 19 | < 0.05 |
The IGF-1 levels at 12 months are statistically significantly higher in the treated than in the untreated group: 91.2 ± 30.4 versus 49.4 ± 19.
Quality of life
Soliman and Abdul Khadir84 did not report QoL results.
Adverse events
Adverse events were not reported by Soliman and Abdul Khadir. 84
Summary
One trial examining the effectiveness of rhGH for GHD met the inclusion criteria for the review.
-
The quality of the included study was mixed. It was an unblinded study, which can have an impact on outcome reporting but did report an ITT analysis.
-
Children in the rhGH group grew 2.7 cm/year faster than children in the untreated group during the 1-year study, and had a statistically significantly higher HtSDS: –2.3 ± 0.45 versus –2.8 ± 0.45.
-
The IGF-1 levels were statistically significantly higher in the treated group than in the untreated group.
-
The included study did not report QoL or AE.
Turner syndrome
Quantity and quality of research available
Six studies assessing the effectiveness of GH for growth restriction in TS met the inclusion criteria for the review. 12,85,86,88–90 The key characteristics of these studies are presented in Tables 7–12. Appendix 4 has further details.
| Reference | Intervention | Control group | Total randomised and withdrawals | Duration of randomised treatment |
|---|---|---|---|---|
| Stephure and CGHAC 200586 and Rovet et al., 1993 87 |
rhGH 0.30 mg/kg/week (n = 76) Mean age (± SD): 10.3 ± 1.8 |
No rhGH treatment (n = 78) Mean age (± SD): 10.9 ± 1.7 |
Total n = 154 Sample attrition: rhGH, n = 15; control, n = 35 |
Until HV < 2 cm/year and BA ≥ 14 year |
| Davenport et al. 200785 |
rhGH 50 µg/kg/day (n = 45) Mean age (± SD): 1.98 ± 1.01 |
No treatment (n = 44) Mean age (± SD): 1.97 ± 1.01 |
Total n = 89 Sample attrition: rhGH, n = 4; control, n = 6 |
2 years |
| Gravholt et al. 200288 |
rhGH 0.1 IU/kg/day Overall age range: 9.5–14.8 years (median 12.9) |
Placebo Overall age range: 9.5–14.8 years (median 12.9) |
Total n = 12 Withdrawals not reported |
Crossover RCT, 2 months in each arm |
| Gravholt et al. 200589 |
rhGH (1.3 ± 0.3) mg/day Overall mean age (± SD): 15.9 ± 1.8 |
Placebo Overall mean age (± SD): 15.9 ± 1.8 |
Total n = 9 Sample attrition: n = 1 |
Crossover RCT, 2 months in each arm |
| Johnston et al. 200190 |
rhGH 28–30 IU/m2/week (n = 22) Mean age (range): 9.0 (5.2–15.4) |
Ethinyloestradiola 50–75 ng/kg/day (n = 13) Mean age (range): 9.1 (6.0–13.7) |
Total n = 58b Sample attrition: n = 12 |
1 year |
| Quigley et al. 200212 |
rhGH 0.27 mg/kg/week (n = 45) Mean age (± SD): 9.7 ± 2.7 rhGH 0.36 mg/kg/week (n = 49) Mean age (± SD): 9.8 ± 2.9 |
Placebo (n = 41) Mean age (± SD): 9.4 ± 2.7 |
Total n = 232b Sample attrition: n = 8 |
18 months |
| Stephure and CGHAC86 | Davenport et al.85 | Gravholt et al. 200288 | Gravholt et al. 200589 | Johnston et al.90 | Quigley et al.12 | |
|---|---|---|---|---|---|---|
| 1. Was the assignment to the treatment groups really random? | Un | Ad | Un | Un | In | Un |
| 2. Was the treatment allocation concealed? | Un | Ad | Un | Un | Un | Un |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Rep | Rep | Not rep | Not rep | Rep | Rep |
| 4. Were the eligibility criteria specified? | Ad | Ad | In | In | In | Ad |
| 5. Were outcome assessors blinded to the treatment allocation? | Un | Un | Un | Un | Un | Un |
| 6. Was the care provider blinded? | In | In | Un | Un | Un | Un |
| 7. Was the patient blinded? | In | In | Un | Ad | Un | Par |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Ad | Ad | Ad | Ad | Ad | In |
| 9. Did the analyses include an ITT analysis? | In | In | In | In | In | In |
| 10. Were withdrawals and dropouts completely described? | Ad | Ad | In | Ad | Ad | Ad |
| Study | Outcomes (mean ± SD) | GH | Control | p-value |
|---|---|---|---|---|
|
Stephure and CGHAC 86 Protocol completion, rhGH 0.30 mg/kg/week (n = 61) vs no treatment (n = 43) |
Height (cm) | 147.5 ± 6.1 | 141.0 ± 5.4 | < 0.001 |
| Change in height (cm) | 28.3 ± 8.9 | 19.0 ± 6.1 | < 0.001 | |
| HtSDS (age-specific turner) | 1.4 ± 1.0 | 0.2 ± 0.9 | < 0.001 | |
| HtSDS (adult Turner) | 0.7 ± 0.9 | –0.3 ± 0.8 | < 0.001 | |
| Change in HtSDS (age-specific Turner) | 1.6 ± 0.6 | 0.3 ± 0.4 | < 0.001 | |
|
Stephure and CGHAC 86 Addendum follow-up, rhGH 0.30 mg/kg/week (n = 40) vs no treatment (n = 19) |
Height (cm) | 149.0 ± 6.4 | 142.2 ± 6.6 | < 0.001 |
| Change in height (cm) | 30.3 ± 8.3 | 21.6 ± 6.2 | < 0.001 | |
| HtSDS (age-specific Turner) | 0.9 ± 0.9 | –0.1 ± 1.0 | < 0.001 | |
| HtSDS (adult Turner) | 0.9 ± 0.9 | –0.1 ± 1.0 | < 0.001 | |
| Change in HtSDS (age-specific Turner) | 1.1 ± 0.5 | 0.0 ± 0.5 | < 0.001 | |
|
Davenport et al. 85 GH (n = 41) vs no treatment (n = 37); 2 years |
Height (cm) | 99.5 ± 7.6 | 91.9 ± 7.2 | < 0.0001 |
| HtSDS | –0.34 ± 1.10 | –2.16 ± 1.22 | < 0.0001 | |
| GV (cm/year) | 8.4 ± 1.6 | 5.5 ± 1.8 | < 0.0001 | |
| GV SDS | 0.70 ± 1.11 | –1.63 ± 1.29 | < 0.001 | |
|
Johnston et al. 90 |
Change in HSDS in first year | +0.7 (0.7) | +0.4 (0.9) | < 0.05 |
|
Quigley et al. 12 GH 1, rhGH 0.27 (n = 45); GH 2, rhGH 0.36 (n = 49) vs placebo (n = 41); 1 year |
GV 0–18 months (cm/year) | 1: 6.6 ± 1.12 2: 6.8 ± 1.1 | 4.2 ± 1.1 | < 0.001 |
| Study | Outcomes (mean ± SD) | GH | Control | p-value |
|---|---|---|---|---|
|
Davenport et al. 85 GH (n = 41) vs no treatment (n = 37); 2 years |
Weight (kg) | 16.62 ± 2.86 | 13.81 ± 2.50 | < 0.0001 |
| WtSDS | 0.20 ± 1.06 | –1.37 ± 1.36 | < 0.0001 | |
| BMI (kg/m2) | 16.72 ± 1.70 | 16.24 ± 1.29 | 0.1724 | |
|
Gravholt et al. 88 GH 0.1 IU/kg/day vs placebo; 2 monthsa |
FM total (g/kg) | 231.0 ± 49.5 | 247.8 ± 58.1 | 0.04 |
| LBM total (g/kg) | 725.4 ± 44.8 | 710.5 ± 54.6 | 0.05 | |
|
Gravholt et al. 89 GH 1.3 mg/day vs placebo; 2 monthsb |
FM total (g/kg) | 274.5 ± 55.5 | 312.9 ± 74.7 | nr |
| LBM total (g/kg) | 692.8 ± 55.5 | 655.2 ± 73.7 | nr |
| Study | Outcomes (mean ± SD) | GH | Control | p-value |
|---|---|---|---|---|
|
GH (n = 41) vs no treatment (n = 37); 2 years |
IGF-1 SDS | 1.26 ± 0.72 | –0.69 ± 0.84 | < 0.0001 |
| IGFBP-3 SDS | 0.97 ± 0.94 | –1.12 ± 1.13 | < 0.0001 | |
| ∆IGF-1 SDS | 1.53 ± 0.93 | –0.09 ± 0.87 | nr | |
|
Gravholt et al. 88 GH 0.1 IU/kg/day vs placebo; 2 monthsa |
IGF-1 (µg/l) | 380.5 ± 116.3 | 179.8 ± 79.4 | < 0.0005 |
| IGFBP-3 (µg/l) | 5982 ± 1557 | 4344 ± 787 | 0.002 | |
|
Gravholt et al. 89 GH 1.3 mg/day vs placebo; 2 months |
IGF-1 (µg/l) | 661 ± 192 | 288 ± 69 | nr |
| IGFBP-3 (µg/l) | 5157 ± 741 | 4146 ± 573 | Unclear |
| Study | AE (n) | GH | Control | p-value |
|---|---|---|---|---|
|
Stephure and CGHAC 86 GH (n = 74) vs no treatment (n = 64) |
Surgical procedures | 37 | 17 | 0.005 |
| Otitis media | 35 | 17 | 0.014 | |
| Ear disorder | 15 | 4 | 0.024 | |
| Joint disorder | 10 | 2 | 0.036 | |
| Respiratory disorder | 8 | 1 | 0.037 | |
| Sinusitis | 14 | 4 | 0.041 | |
| Goitre | 0 | 4 | 0.004 | |
| Death (ruptured aortic aneurysm) | 0 | 1 | nr | |
| Elevated transamine levels | 1 | 0 | nr | |
| Intracranial hypertension | 1 | 0 | nr | |
|
Davenport et al. 85 GH (n = 45) vs no treatment (n = 44), 2 years |
Serious AEs, n (%) | 4 (9) | 4 (9) | nr |
| Treatment-emergent AEs, n (%) | 42 (93) | 43 (98) | nr | |
| Quigley et al. 12 | Otitis media (occurrence/worsening), n (%) | 54/186 (29%) | 6/46 (13%) | 0.037 |
Two of the included studies were of a crossover design,88,89 and these compared doses of 0.1 IU/kg/day88 and a mean of 1.3 ± 0.3 mg/day (alone or in combination with oestradiol)89 with placebo. The group receiving oestradiol is not discussed further here. Of the remaining studies, two compared rhGH with no treatment,85,86 one with low-dose estrogen,90 and one with placebo. 12 Stephure and colleagues86 administered a rhGH dose of 0.30 mg/kg/week, with a maximum weekly dose of 15 mg. The dose of 50 µg in the Davenport study85 is comparable with that of Stephure and colleagues. Those in the Quigley study12 were slightly different: group 1 received 0.27 mg/kg/week and group 2 received 0.36 mg/kg/week. Johnston and colleagues90 gave a dose of 28–30 IU/m2/week. All studies included at least one treatment arm with a dose that was broadly comparable with the licensed dose of 45–50 µg/kg/day or 1.4 mg/m2/day.
Four of the six included studies reported growth outcomes, including height gain and change in HtSDS. 12,85,86,90 The remaining two studies reported body composition and biochemical marker outcomes. 88,89
The trials varied considerably in size. The two crossover trials were small, with 1288 and nine89 participants. The Stephure86 and Quigley12 studies were larger, with 154 and 232 participants, respectively. Johnston and colleagues90 recruited 58 patients, and Davenport and colleagues recruited 89. 85 The included trials also ranged in length. The groups in Quigley and colleagues12 remained randomised for 18 months, the Davenport study85 for 2 years and the Johnston study lasted for 1 year. 90 Protocol completion in the Stephure86 study was defined as annualised GV less than 2 cm/year and BA of 14 years or greater, which we have interpreted to mean FH. In contrast, the two Gravholt studies88,89 were short crossover trials, with rhGH treatment for 2 months.
Five12,86,88–90 of the six trials recruited broadly similar age groups, whilst the sixth by Davenport and colleagues85 specifically targeted very young girls with TS. As a result their girls have much younger mean ages of 1.98 ± 1.01 and 1.97 ± 1.01 for treatment and control groups, respectively.
Four of the included studies reported baseline characteristics that were similar between groups. 12,85,86,90 However, none reported p-values for between-group differences, so there may have been small differences at baseline. For example, in the study by Stephure and the Canadian Growth Hormone Advisory Committee (CGHAC) 2005,86 girls in the rhGH group were on average 3 cm shorter than those in the control group. The SD values indicate overlapping CI, suggesting there is no statistically significant difference between the two groups. However, the 3-cm difference could have an impact on end of study height. The other two studies, reported by Gravholt and colleagues, were of crossover design. One reported baseline characteristics for the whole study group89 and the other did not appear to report any baseline conditions. 88
The six included trials were generally of poor methodological quality, and poorly reported (Table 8). Only one reported adequate methods of randomisation to treatment groups. 85 Davenport and colleagues85 stratified their participants by age and then randomised them using a blinded phone-in process. Four of the six trials did not describe randomisation techniques. 12,86,88,89 Johnston and colleagues90 reported that five participants were reallocated from the oestrogen group to receive rhGH: it is unclear when this occurred and therefore method of randomisation was judged inadequate.
Concealment of treatment allocation was also judged to be adequate in the Davenport trial, and ‘unknown’ in the remaining five. In the Gravholt89 study it is unclear how allocation to treatment groups had taken place. The study had only nine participants, and these were simply reported to have been given the treatment regimen sequentially and in random order.
Blinding of participants, those who provide care and those who assess outcomes can protect against the reporting of some outcomes being affected by the knowledge of which treatment is being received. Blinding of outcome assessors, care providers and patients was judged ‘unknown’, ‘inadequate’ or ‘partial’ in five out of the six trials; Gravholt and colleagues89 adequately blinded their patients by administering placebo in place of both rhGH and the oestradiol.
None of the six studies included here used an ITT analysis. This kind of analysis can protect the study from attrition bias, where, for example, participants withdrawing from the treatment arm could represent AE or treatment failure.
Growth outcomes
Four out of the six included studies reported growth outcomes, and key measures are shown in Table 9. Please see Appendix 4 for additional outcomes. Neither of the studies by Gravholt and colleagues88,89 reported growth outcomes.
Two studies reported height at the end of the study: both found a statistically significant difference between the treated and untreated groups (p < 0.0001). 85,86
Children in the treated group in the Stephure study86 were 6.5 cm taller on average than the untreated group at protocol completion. However, there was a 3-cm difference between the groups’ mean heights at baseline. Mean change from baseline was therefore 9.3 cm more in the rhGH than in the untreated group at the end of protocol completion (28.3 ± 8.9 vs 19.0 ± 6.1).
The Stephure study86 also reported an addendum follow-up (approximately 10 years since randomisation), which included 66% of rhGH patients and 44% of the control group. The treated group’s mean FH was 149.0 ± 6.4 cm compared with 142.2 ± 6.6 cm in the untreated group (p < 0.001), i.e. a difference of 6.8 cm. Mean change from baseline to FH was 8.7 cm more in the rhGH than in the untreated group.
In the Davenport study85 the mean difference was 7.6 cm (height at study end was 99.5 ± 7.6 cm in the treated group vs 91.9 ± 7.2 cm in the untreated group, p < 0.0001).
Height standard deviation score is also reported by Davenport and colleagues85 and Stephure and CGHAC. 86 Both authors report statistically significant differences between groups for this outcome, with the treated groups both achieving higher HtSDS. In the Stephure study86 the HtSDS is reported for the age-specific Turner population and for the adult Turner population.
The difference in change in height was statistically significant between groups in the two studies that reported it. Stephure and colleagues86 report a change in height at protocol completion of 28.3 ± 8.9 cm versus 19 ± 6.1 in the untreated group, p < 0.001. Davenport and colleagues85 reported a 2-year height gain of 20.4 ± 3.3 cm (treated group) versus 13.6 ± 3.5 cm (untreated group), p < 0.001 (not shown in table). Change in HtSDS in both the Stephure86 and Johnston90 studies was higher in the treated than untreated group: 1.6 ± 0.6 (treated) versus 0.3 ± 0.4 (untreated), p < 0.001, at protocol completion in the Stephure study; 0.7 (0.7) versus 0.4 (0.9), p < 0.05, in the Johnston study90 after 1 year.
Growth velocity was statistically significantly greater in the treated groups in the Stephure,86 Davenport85 and Quigley12 studies. Davenport and colleagues85 reported GV at the end of the first and second year. Although this was greater in the treated groups at both times, GV fell in the second year in both groups: 8.4 ± 1.6 cm/year (treated group) versus 5.5 ± 1.8 (untreated). Additionally, Davenport and colleagues85 measured GV SDS at the end of the first and second years. Again, this was greater in the treated group at the end of the first year: 1.75 ± 1.25 versus 0.8 ± 0.95, p < 0.001, but was reduced by the end of the second year in both groups: 0.70 ± 1.11 (treated) versus –1.63 ± 1.29 (untreated), p < 0.001. Quigley and colleagues reported GV after 18 months. This was broadly similar in both the lower- and higher-rhGH-dose groups: both were significantly higher than that in the placebo (Pla) group: 6.6 ± 1.1 (GH 0.27/Pla group) versus 6.8 ± 1.1 (GH 0.36/Pla group) versus 4.2 ± 1.1 (Pla/Pla group), p < 0.001 compared with placebo.
Bone age differences for the younger participants in the Davenport study were statistically significant:85 the GH-treated group at 2 years had a mean BA of 4.24 ± 1.35 versus 3.38 ± 1.11 in the untreated group, p = 0.0033. Davenport and colleagues85 also reported BA/chronological age; this is lower in the treated group, and the difference was statistically significant: 0.64 ± 0.80 versus 0.21 ± 0.96, p < 0.001.
Body composition outcomes
Three of the TS studies reported body composition outcomes, and these are presented in Table 10. One of the studies reported weight, weight standard deviation score (WtSDS) and BMI,85 whereas the remaining two reported FM, bone mineral content (BMC) and LBM for arms, legs, trunk and head, and as a total. 88,89 Please see Appendix 4 for BMC results.
Weight and WtSDS were significantly greater in the group receiving rhGH than in the untreated group in the Davenport study,85 reported as 16.62 kg ± 2.86 versus 13.81 kg ± 2.50, and 0.20 ± 1.06 versus –1.37 ± 1.36, respectively (p < 0.0001 for both comparisons).
Two studies considered FM, BMC and LBM. 88,89 In both studies the total FM was greater in the untreated group than in the treated group, and LBM was slightly higher in treated than in untreated patients (Table 10). The differences between groups were of borderline statistical significance in one study88 but no p-values were presented in the other study. 89
Biochemical markers
Three of the studies85,88,89 reported biochemical outcomes. Key results are shown in Table 11 – other outcomes are in Appendix 4.
Two studies reported mean levels of IGF-1 at end of treatment. In both studies IGF-1 levels were statistically significantly higher in the group receiving rhGH. One study88 reported values of 380.5 ± 116.3 versus 179.8 ± 79.4 in the treated and untreated groups, respectively (p < 0.0005). The other89 reported 661 ± 192 versus 288 ± 69 (p-value not reported) for treated and untreated patients, respectively.
Davenport and colleagues85 reported that IGF-1 SDS was significantly greater in the treated group (1.26 ± 0.72 vs –0.69 ± 0.84, p < 0.0001). Change in IGF-1 SDS from baseline to year 2 was 1.53 ± 0.93 versus –0.09 ± 0.87 in the treated and untreated groups, respectively.
One Gravholt study88 reported that IGFBP-3 levels were statistically significantly higher in the treated group than in the untreated group (5982 ± 1557 vs 4344 ± 787, respectively, p = 0.002). The other study by Gravholt and colleagues89 reported higher IGFBP-3 SDS values in treated patients, but no clear p-value was reported. 89 Davenport and colleagues85 found that IGFBP-3 SDS was higher in their treated group (0.97 ± 0.94 vs –1.12 ± 1.13, p < 0.0001).
Fasting glucose and fasting insulin were reported in the two studies by Gravholt and colleagues,88,89 both of which were raised in the groups receiving GH in each study. Mean glucose (nmol/l) was 4.28 ± 0.5988 and 4.46 ± 0.4089 in the treated groups, versus 4.02 ± 0.4488 and 4.04 ± 0.4789 in the untreated groups. This difference reached statistical significance in the first study,88 p = 0.046. Mean fasting insulin levels in the first Gravholt study88 were 17.17 ± 8.30 versus 8.58 ± 4.27, p = 0.007.
Quality of life
None of the TS studies reported QoL as an outcome.
Adverse events
Adverse events were reported by only four of the studies. 12,85,86,90 Details presented by three of the studies are shown in Table 12 (the fourth study did not present figures90).
The group receiving GH in the Stephure study86 experienced a statistically significantly greater level of all AEs (where statistical significance was reported), with the exception of goitre, and one instance of death from ruptured aortic aneurysm, which occurred in the untreated group. The one case of elevated transamine levels in the treated group led to withdrawal from the study.
Davenport and colleagues85 report the same level of serious adverse events (SAEs) for both the treated and untreated groups. For treatment-emergent AEs, defined as ‘events or conditions that began or worsened after study entry’, the results were similar. There were 42 (93%) in the treated group and 43 (98%) in the untreated group. Most treatment-emergent AEs were ear disorders.
Quigley and colleagues12 found a significant difference in levels of occurrence or worsening of otitis media between the treated group (29%) and the control group (13%), p = 0.037. Ear pain and ear disorder were reported as not differing between groups. Three girls discontinued rhGH due to hypertension, ulcerative colitis and brain tumour. The authors stated that these were not directly related to GH. Overall, AEs were not presented separately for the groups; however, five were reported to have accidentally overdosed on the study drug. Five further events described as possibly related to the study drug were hypertension (two), surgical procedures (two) and scoliosis (one).
Five participants were reallocated from the group receiving estrogen to rhGH after concerns over early breast development in the study by Johnston and colleagues. 90 Seven patients developed ‘coincidental disorders’ not severe enough to warrant treatment discontinuation. The authors reported that compliance problems led to the withdrawal of four patients, but no details were given. It is unclear which treatment groups these latter events occurred in.
Summary
Six trials examining the effectiveness of GH for growth disturbance in patients with TS met the inclusion criteria for the review.
The reporting and methodological quality of the studies was poor. Of the six included studies, one reported adequate randomisation to treatment groups,85 one study described adequate concealment of treatment allocation85 and one adequately blinded the patient to treatment by administering placebo. 89 None of the included trials used an ITT analysis.
Children in the rhGH group in the Stephure86 study grew an average of 9.3 cm more from baseline than those in the untreated group. In a study of younger children85 the difference was 7.6 cm. Both of these were statistically significant results. In the same two studies85,86 the groups receiving rhGH achieved a significantly higher HtSDS.
Change in height and change in HtSDS were statistically significantly greater in the groups treated with rhGH. 85,86,90
Growth velocity was greater in the treated groups in three studies that reported this outcome,12,85,86 although this was greater in the first year and fell in the second year in both treatment groups where this was reported separately. 85
One study86 found a significant difference in BA between groups, being higher in the treated patients.
Fat mass and LBM were reported in two studies. 88,89 In both, the total FM was at a lower level in the treated groups, compared with those untreated, and LBM was higher in the treated groups compared with untreated. There was no statistically significant difference in BMI between treated and untreated girls in one study. 85
The IGF-1 levels were substantially higher in the treated groups in the studies reporting this outcome. 88,89 IGF-1 SDS was also significantly higher in the group receiving GH. 85 Levels of IGFBP-3 and IGFBP-3 SDS were also found to be higher in children treated with GH. 85,88,89
Levels of fasting glucose and fasting insulin were both raised in the treated groups in two studies. 88,89
There were variable levels of detail in the reporting of AEs across the six studies. Two studies did not discuss these. 88,89 In those studies that did, no clear picture emerges. One found greater levels of AEs in the treated group,86 one found similar levels across groups,85 one found significantly higher levels of or worsening of otitis media, and one reported seven patients with ‘coincidental disorders’ and four withdrawals due to compliance problems, but gave no further details.
Prader–Willi syndrome
Quantity and quality of research available
Eight RCTs in 13 publications of the clinical effectiveness of rhGH in patients with PWS met the inclusion criteria for this review. 22,91–102 Their key characteristics are shown in Table 13 – see Appendix 4 for further details.
| Reference | Intervention | Control group | Total randomised and withdrawals | Duration of randomised treatment |
|---|---|---|---|---|
| Carrel et al. 2004,22 Myers et al. 2007,97 and Whitman et al. 200498 |
rhGH 1 mg/m2/day n = 15 Mean age ± SD (months): 13 ± 8 |
No treatment n = 14 Mean age ± SD (months):15 ± 0 |
n = 32 Sample attrition: n = 3a |
1 year |
| Carrel et al. 199995 and Myers et al. 199996 |
GH 1 mg/m2/day n = 35 Mean age (years): 9.8 |
No treatment n = 19 Mean age (y): 10.0 |
n = 54 No withdrawals |
1 year |
| de Lind van Wijngaarden et al. 200993 and Festen et al. 200894 |
1 mg/m2/day Infants (< 3.5 years): n = 19 Children (> 3.5 years): n = 23 Median (IQR) age: infants 2.0 (1.6–3.1), children 6.8 (5.4–8.8) |
No treatment Infants (< 3.5 years): n = 19 Children (> 3.5 years): n = 21 Median (IQR) age: infants 1.3 (1.0–2.8); children 5.9 (4.7–7.4) |
n = 104 enrolled Sample attrition: 4 infants and 5 children |
1 year for infants, 2 years for children |
| Festen et al. 200791 |
GH 1 mg/m2/day n = 10 Median age (IQR) (years): 6.2 (5.1–71) |
No treatment n = 10 Median age (IQR) (years): 5.8 (4.9–7.8) |
n = 20 Withdrawals: none |
2 years |
| Festen et al. 200792 |
GH 1 mg/m2/day n = 15 Median (IQR) age, yr: 2.3 (1.7–3.0) |
No treatment n = 14 Median (IQR) age, year: 1.5 (1.2–2.7) |
n = 43 Sample attrition: n = 14 |
12 months |
| Haqq et al. 2003102 |
GH 0.043 mg/kg/day n = 6 Overall mean age ± SD (years): 9.7 ± 3.3 |
Placebo n = 6 Overall mean age ± SD (years): 9.7 ± 3.3 |
14 randomised Sample attrition: n = 2 |
Crossover RCT, 6 months in each arm |
| Hauffa 199799 |
GH: 0.15 IU/kg/day n = 8 Mean age ± SD (years): 8.25 ± 2.4 |
No treatment n = 9 Mean age ± SD (years): 7.56 ± 2.0 |
N = 19 Sample attrition: n = 3 |
1 year |
| Lindgren et al. 1998101 and 1997100 |
GH 0.1 IU/kg/day n = 15 Mean age (range) (years): 6.8 (3.6–11.9) |
No treatment n = 14 Mean age (range) (years): 6.4 (3.3–11.7) |
Total n = 29 Sample attrition: n = 2 |
1 year |
It was not possible to perform any meta-analysis of outcomes from the PWS studies due to variation in the trials’ participants’ ages, dosing calculations, and methods of presenting results. The included studies had well-matched patient groups, whose baseline characteristics were generally similar in the treated and untreated groups. Median baseline HtSDS was lower in the rhGH group than in the untreated group in the study reported by both Festen and colleagues94 and by de Lind van Wijngaarden and colleagues,93 although the interquartile ranges (IQRs) were similar [–2.0 (–3.1 to –1.7) versus –2.5 (–3.3 to –1.9), respectively]. Other exceptions were the crossover study by Haqq and colleagues,102 which presented baseline characteristics for the study population as a whole, and the study by Lindgren and colleagues,100,101 which reported slightly lower baseline GV SDS in the rhGH group [–1.9 ± 2.0, range –6.4 to –0.9, vs –0.1 (SD not reported) range –1.7 to –2.71].
Five of the studies were RCTs, which compared 1 mg/m2/day rhGH with no treatment for 122,92–98 or 291,93,94 years. The study by Haqq and colleagues102 was a crossover RCT, which compared 0.043 mg/kg/day of rhGH with placebo injections, with patients spending 6 months in each treatment arm. There does not appear to have been a washout phase between the two treatment phases, which could affect the generalisability of results.
The doses used in the included studies reflect the various marketing authorisations for this drug (0.035 mg/kg body weight or 1.0 mg/m2 BSA), with 1 IU of rhGH being equivalent to approximately 0.33 mg/kg. The study reported by both de Lind van Wijngaarden and colleagues93 and Festen and colleagues94 reported results separately for infants and children. Two RCTs reported results for infants and toddlers aged between 1 and 2.5 years. 22,92,97,98 The five remaining trials were in children aged between approximately 6 and 10 years old. The studies were generally small, randomising between 14102 and 5495,96 children. The study reported by both de Lind van Wijngaarden and colleagues93 and Festen and colleagues94 had a total of 91 participants, but as children and infants were randomised separately, the randomised comparisons were of rhGH versus no treatment within two smaller groups (42 infants and 49 children). This was the only study to report a sample size/power calculation,93,94 and it is not clear whether the other studies were adequately powered to detect a difference between treatment groups.
With the exception of the two RCTs by Festen and colleagues,91,92 the studies did not clearly state which of their reported outcomes were primary or secondary measures of effect. Seven of the eight trials reported measures of body composition. The two RCTs by Festen and colleagues91,92 focused on body composition and biochemical markers, and did not report any measure of change in height. The other six studies all reported GV SDS or an indicator of linear GV. 102 IGF-1 and other biochemical markers were reported by five RCTs. 22,92–99
One RCT was reported in three papers, by Carrel and colleagues,22 Myers and colleagues97 and Whitman and colleagues. 98 The most complete data were reported by Carrel and colleagues,22 and these data are included in the tables in this section.
The included studies were generally poorly reported (Table 14) and lacked information on method of randomisation or concealment of allocation. It is possible that selection bias could have affected the trials if they were not properly randomised, but there is insufficient information provided on which to make such a judgement. The trial by Haqq and colleagues102 was a crossover study, and did not report baseline characteristics separately for the two groups. The other studies reported baseline characteristics, which indicated that patients in the two treatment groups were comparable at the start of the study. With the exception of the crossover trial by Haqq and colleagues,102 which had a placebo-injection group, the studies were open label, with the comparator groups receiving no treatment. Although this could have allowed a degree of bias in reporting and assessing results, measurement of objective outcomes, such as height gained, is less likely to be open to bias. Only two of the studies reported results on an ITT basis,91,96 so attrition bias could have affected the remaining studies.
| Carrel et al.,22 Myers et al.,97 Whitman et al.98 | Carrel et al.,95 Myers et al.96 | de Lind van%%Wijngaarden et al.,93 Festen et al.94 | Festen et al.91 | Festen et al.92 | Haqq et al.102 | Hauffa et al.99 | Lindgren et al.,101 Lindgren et al.100 | |
|---|---|---|---|---|---|---|---|---|
| 1. Was the assignment to the treatment groups really random? | Un | Un | Un | Un | Un | Un | Un | Un |
| 2. Was the treatment allocation concealed? | Un | Un | Un | Un | Un | Un | Un | Un |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Rep | Rep | Rep | Rep | Rep | Not rep | Rep | Rep |
| 4. Were the eligibility criteria specified? | Ad | Ad | Ad | Ad | Ad | Ad | Ad | Ad |
| 5. Were outcome assessors blinded to the treatment allocation? | Un | Un | Un | Un | Un | Un | Un | Un |
| 6. Was the care provider blinded? | In | In | In | In | In | Un | In | In |
| 7. Was the patient blinded? | In | In | In | In | In | Ad | In | In |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Ad | Ad | Ad | Ad | Ad | Ad | In | Ad |
| 9. Did the analyses include an ITT analysis? | In | Ad | In | Ad | In | In | In | In |
| 10. Were withdrawals and dropouts completely described? | In | Ad | Ad | Ad | In | In | In | Ad |
The outcome measures for the included studies are shown in Tables 15–17. The p-values in the tables refer to between-group differences, as this is the comparison of interest for this report. Some of the studies reported statistical significance in change from baseline for each of the treatment groups individually, but not for between-group comparisons. To avoid confusion with the between-group comparison p-values, such results have not been included in the tables below and are not discussed in the text. The full data extraction tables in Appendix 4 include any statistical significance for change from baseline for individual treatment groups without between-group comparisons.
| Study | Outcomes (mean ± SD) | GH | Control | p-value |
|---|---|---|---|---|
|
Carrel et al. 22 rhGH 1 mg/m2/day (n = 15) vs. no treatment (n = 14); 1 year |
Change in height (cm) | 15.4 ± 2.3 | 9.2 ± 3.2 | < 0.001 |
| Height SDS | –0.2 ± 1.5 | –1.5 ± 0.7 | nr | |
| GV SDS | 5.0 ± 1.8 | 1.2 ± 1.4 | nr | |
|
Carrel et al. 95 and Myers et al. 96 GH 1 mg/m2/day (n = 35), vs. no treatment (n = 19); 1 year |
Height SDS | –0.6 ± 1.2 | –1.6 ± 1.2 | < 0.01 |
| Mean GV (cm/year) | 10.1 ± 2.5 | 5.0 ± 1.8 | < 0.01 | |
| Mean GV SDS | 4.6 ± 2.9 | –0.7 ± 1.9 | < 0.01 | |
|
de Lind van Wijngaarden et al. ,93 Festen et al. 94 (infants) rhGH 1 mg/m2 (n = 19) vs. no treatment (n = 19); 1 year |
HtSDS median (IQR) | –0.9 (–1.6 to –0.1) | –1.8 (–3.5 to –1.4) | 0.003 |
| ΔHtSDS median (IQR) | 1.2 (1.0 to 1.6) | –0.2 (–0.6 to 0.3) | < 0.0001 | |
|
de Lind van Wijngaarden et al. ,93 Festen et al. 94 (children) rhGH 1 mg/m2 (n = 23) vs. no treatment (n = 21); 2 years |
HtSDS median (IQR) | –0.5 (–0.8 to 0.0) | –2.6 (–3.4 to –2.3) | < 0.0001 |
| ΔHtSDS median (IQR) | 1.4 (1.3 to 1.8) | –0.1 (–0.4 to 0.1) | < 0.0001 | |
|
Festen et al. 91 rhGH 1 mg/m2/day (n = 10) vs. no treatment (n = 10); 2 years |
Height SDS median (IQR) | –0.6 (–0.9 to –0.3) | –3.0 (–3.5 to –1.8) | nr |
|
Festen et al. 92 rhGH 1 mg/m2/day (n = 15) vs. no treatment (n = 14); 1 year |
Height SDS median (IQR) | –1.6 (–2.1 to –0.8) | –2.3 (–3.9 to –1.5) | nr |
|
Haqq et al. 102 rhGH 0.043 mg/kg/day (n = 12) vs. placebo (n = 12); 6 months |
HtSDS | –1.2 ± 1.1 | –1.3 ± 1.3 | nr |
| GV (cm/year) | 7.5 ± 3.5 | 4.5 ± 2.7 | < 0.05 | |
|
Hauffa 99 rhGH 0.15 IU/kg/day (n = 7) vs. no treatment (n = 9); 1 year |
Height SDS | 1.07 | –0.25 | nr |
| HV SDS | 5.5 | –2.3 | 0.0012 | |
|
Lindgren et al. 101 and Lindgren et al. 100 rhGH 0.1 IU/kg/day (n = 15) vs. no treatment (n = 12); 1 year |
HtSDS mean (range) | –0.4 (–2.7 –1.9) | –1.8 (–5.1 –0.2) | nr |
| GV (SDS) mean ± SD (range) | 6.0 ± 3.2 (1.4–11.9) | –1.4 (–3.2 –0.3) | nr |
| Study | Outcomes (mean ± SD) | GH | Control | p-value |
|---|---|---|---|---|
|
Carrel et al. 22 rhGH 1 mg/m2/day (n = 15) vs no treatment (n = 14); 1 year |
Mean % body fat | 23.2 ± 8.9 | 32.7 ± 8.8 | 0.03 |
| Change in body fat (%) | –4.8 ± 5.7 | +4.1 ± 4.6 | 0.001 | |
| Change in LBM (kg) | 3.6 ± 0.5 | 1.8 ± 0.7 | < 0.001 | |
|
Carrel et al. ,95 Myers et al. 96 GH 1 mg/m2/day (n = 35), vs no treatment (n = 19); 1 year |
Body fat (%) | 38.4 ± 10.7 | 45.8 ± 8.8 | < 0.01 |
| Lean mass (kg) | 25.6 ± 4.3 | 21.7 ± 5.0 | < 0.01 | |
| BMI (kg/m2) | 23.7 ± 6.3 | 25.2 ± 8.9 | n/s | |
|
de Lind van Wijngaarden et al. ,93 Festen et al. 94 (infants) rhGH 1 mg/m2 (n = 19) vs no treatment (n = 19); 1 year median (IQR) |
BMI (kg/m2) | 16.3 (15.7 to 18.2) | 16.4 (15.4 to 19.8) | nr |
| BMI (SDS) | 0.3 (–0.1 to 1.6) | 0.3 (–0.6 to 1.6) | 0.72 | |
|
de Lind van Wijngaarden et al. ,93 Festen et al. 94 (children)a rhGH 1 mg/m2 vs no treatment; 2 years median (IQR) |
BMI (kg/m2) | 17.5 (16.1 to 21.1) | 19.1 (17.8 to 20.8) | |
| BMI (SDS) | 1.1 (–0.2 to 1.7) | 1.4 (1.1 to 1.6) | 0.19 | |
| Fat % (SDS) | 1.9 (0.7 to 2.3) | 2.4 (2.1 to 2.7) | < 0.001 | |
| Fat (SDS) | 1.1 (0.6 to 2.0) | 4.5 (0.9 to 2.0) | < 0.01 | |
| LBMage (SDS) | –0.1 (–1.3 to 0.6) | –2.5 (–3.8 to –1.4) | < 0.001 | |
| LBMHtSDS | –1.9 (–2.4 to –1.4) | –2.3 (–2.7 to –1.3) | < 0.05 | |
|
Festen et al. 91 rhGH 1 mg/m2/day (n = 10) vs no treatment (n = 10); 2 years median (IQR) |
BMI (kg/m2) | 16.3 (15.8 to 19.0) | 18.5 (17.5 to 20.6) | < 0.05 |
| BMI SDS | 0.4 (–0.3 to 1.1) | 1.2 (0.9 to 1.5) | < 0.05 | |
| LBM SDS | –1.2 (–1.7 to –1.1) | –2.8 (–3. to 1.9) | nr | |
| Fat % SDS | 1.7 (0.9 to 1.9) | 2.1 (1.9 to 2.4) | nr | |
|
Festen et al. 92 rhGH 1 mg/m2/day (n = 15) vs no treatment (n = 14); 1 year median (IQR) |
BMI (kg/m2) | 16.4 (15.2 to 18.5) | 15.5 (14.9 to 17.6) | nr |
| BMI SDS | 0.3 (–0.9 to 1.8) | –0.4 (–0.8 to 1.3) | nr | |
| Body fat (%) | 22.5 (11.3 to 33.2) | 22.8 (19.5 to 32.9) | nr | |
| LBM (%) | 74.8 (63.7 to 82.3) | 73.6 (61.6 to 75.9) | nr | |
|
Haqq et al. 102 rhGH 0.043 mg/kg/day (n = 12) vs placebo (n = 12); 6 months |
BMI (kg/m2) | 31.2 ± 8.9 | 32.8 ± 9.7 | < 0.05 |
| BMI (SDS) | 2.4 ± 0.5 | 2.5 ± 0.6 | nr | |
| Body fat (%) | 49.7 ± 5.8 | 54.1 ± 5.6 | < 0.05 | |
| FM (kg) | 26.1 ± 12.8 | 29.1 ± 14.1 | < 0.05 | |
| Lean mass (kg) | 24.1 ± 8.8 | 22.4 ± 8.5 | < 0.05 | |
|
Lindgren et al. ,101 Lindgren et al. 100 rhGH 0.1 IU/kg/day (n = 15) vs. no treatment (n = 12) |
BMI (SDS) | 2.0 (–2.4 to 6.7) | 2.5 (0.1 to 6.1) | nr |
| Body fat (%) | 30.9 ± 11.4 | 38.2 ± 9.1 | nr |
| Study | Outcomes (mean ± SD) | GH | Control | p-value |
|---|---|---|---|---|
|
Carrel et al. 22 rhGH 1 mg/m2/day (n = 15) vs no treatment (n = 14); 1 year |
IGF-1 (ng/ml) | 231 ± 98 | 51 ± 28 | < 0.001 |
|
Carrel et al. 95 and Myers et al. 96 GH 1 mg/m2/day (n = 35), vs no treatment (n = 19); 1 year |
IGF-1 (ng/ml) | 522 ± 127 | 121 ± 52 | < 0.01 |
| IGFBP-3 (mg/l) | 3.5 ± 0.73 | 2.07 ± 0.45 | < 0.01 | |
|
de Lind van Wijngaarden et al. 93 and Festen et al. 94 (infants) rhGH 1 mg/m2 (n = 19) vs no treatment (n = 19); 1-year median (IQR) |
IGF-1 (ng/ml) | 179.0 (119.5 to 241.0) (n = 12) | 33.0 (22.5 to 47.8) (n = 15) | nr |
| IGF-1 SDS | 2.5 (1.4 to 2.9) | –2.6 (–4.1 to –0.7) | < 0.0001 | |
| IGFBP-3 (ng/ml) | 2.2 (1.6 to 2.4) (n = 12) | 0.9 (0.7 to 1.3) (n = 12) | nr | |
| IGFBP-3 SDS | 0.5 (0.0 to 1.2) (n = 12) | –2.4 (–3.5 to –1.2) (n = 12) | nr | |
|
de Lind van Wijngaarden et al. 93 and Festen et al. 94 (children)a rhGH 1 mg/m2 vs no treatment; 2-year median (IQR) |
IGF-1 (ng/ml) | 424.0 (313.0 to 570.0) (n = 20) | 92.0 (61.8 to 130.0) (n = 16) | nr |
| IGF-1 SDS | 2.4 (2.1 to 2.8) | –1.6 (–2.5 to –1.0) | < 0.0001 | |
| IGFBP-3 (ng/ml) | 2.8 (2.6 to 3.2) (n = 20) | 1.5 (1.2 to 1.8) (n = 16) | nr | |
| IGFBP-3 SDS | 0.6 (0.3 to 1.1) (n = 20) | –1.7 (–2.3 to –1.2) (n = 16) | < 0.001 | |
|
Festen et al. 91 rhGH 1 mg/m2/day (n = 10) vs no treatment (n = 10); 2-year median (IQR) |
IGF-1 SDS year 2 | 2.3 (2.1 to 2.9) | –2.0 (–2.7 to 1.0) | < 0.001 |
| IGFBP-3 SDS year 2 | 0.6 (0.4 to 1.1) | –1.8 (–2.7 to –1.5) | < 0.001 | |
|
Festen et al. 92 rhGH 1 mg/m2/day (n = 15) vs no treatment (n = 14); 1-year median (IQR) |
IGF-1 SDS | 1.7 (0.1 to 2.5) | –2.6 (–4.1 to –0.4) | < 0.001 |
| IGFBP-3 SDS | 0.4 (–0.3 to 1.1) | –3.1 (–4.0 to –2.2) | < 0.05 | |
|
Haqq et al. 102 rhGH 0.043 mg/kg/day (n = 12) vs placebo (n = 12); 6 months |
IGF-1 (ng/ml) | 720 ± 379 | 232 ± 182 | < 0.001 |
| IGFBP-3 (ng/ml) | 6029 ± 1311 | 4247 ± 1209 | < 0.01 | |
|
Lindgren et al. 101 and Lindgren et al. 100 rhGH 0.1 IU/kg/day (n = 15) vs no treatment (n = 12); 1 year |
IGF-1 SDS | 1.8 (–0.1 to 4.1) | –1.4 (–2.9 to –0.3) | nr |
Growth outcomes
Changes in height and other growth outcome measures are shown in Table 15. The infants in the study by Carrel and colleagues22 who received rhGH for a year grew an average of 6.2 cm more than those in the untreated group (p < 0.001). None of the other studies reported change in height as an outcome measure.
Two studies reported a statistically significant difference in HtSDS at end of treatment between treated and untreated patients. 93–96 Treated patients in the study reported by both Carrel and colleagues95 and Myers and colleagues96 had a mean HtSDS of –0.6 ± 1.2 compared with –1.6 ± 1.2 in the untreated group (p < 0.01). The studies reported by de Lind van Wijngaarden and colleagues93 and by Festen and colleagues94 also reported statistically significant improvements in height for rhGH-treated infants and children compared with unmatched controls. The rhGH-treated infants in their study had a median HtSDS of –0.9 compared with –1.8 in the untreated patients (p = 0.003). This reflected a change from baseline HtSDS of +1.2 for treated infants and –0.2 for untreated infants (p < 0.0001). After 2 years of treatment with rhGH, children had a median HtSDS of –0.5 compared with –2.6 in untreated children (p < 0.001). 93
Festen and colleagues91 reported that the difference between the two groups was statistically significant at year 1 (year 1 HtSDS –1.3 vs –2.8, p < 0.01). At year 2, the difference between the two groups was even greater (–0.6 compared with –3.0 in the treated and untreated groups, respectively), but no p-value was reported. 91 The other five studies all reported that HtSDS values were higher in treated than in untreated children, but did not report whether or not differences between groups were statistically significant.
The five studies that used GV as an outcome measure all reported faster growth in the treated group than in the untreated group, although statistical significance for differences between groups was only reported for three of these. The mean GV in the studies reported by Carrel and colleagues95 and by Myers and colleagues96 was twice as fast in the treated children as in the untreated children (10.1 vs 5.0, p < 0.01). The corresponding mean GV SDS values were 4.6 in the treated children and –0.7 in the untreated children (p < 0.01), indicating faster than average growth in the treated group and slower than average growth in the untreated patients. Similarly, Hauffa and colleagues99 reported a positive GV SDS for treated children and a negative one for untreated children (5.5 vs –2.3, p = 0.0012). Haqq and colleagues102 calculated GV that was 3 cm/year faster in patients receiving rhGH than in patients in the placebo arm (7.5 vs 4.5, p < 0.05).
Two of the included studies reported BA as an outcome measure. There was no statistically significant difference in BA at follow-up between patients in the treated and untreated groups in the study reported by both Carrel and colleagues95 and by Myers and colleagues. 96 Lindgren and colleagues100,101 reported similar change from baseline in both groups (1.4 in the treated group, 1.5 in the untreated group), but did not report whether or not there was any statistical significance to their results.
Body composition
Seven of the trials reported changes in body composition, as shown in Table 16. 22,91–94,100–102 The trial by Hauffa and colleagues99 did not report any results but stated that there were no significant within- or between-group changes for BMI, skinfold thickness, waist or hip circumference.
Four of the trials reported a statistically significantly lower percentage of body fat in patients treated with rhGH than in those with no treatment or placebo. In the trial reported by Carrel and colleagues22 mean percentage body fat was 10% lower for treated patients than for untreated patients (p = 0.03). On average, treated patients in this trial experienced an approximately 5% reduction in body fat, compared with an average 4% increase in the untreated patients’ body fat (p = 0.001). The other two trials that found a statistically significant difference reported that treated patients had approximately 4% (Haqq and colleagues102) or 7% (Carrel95 and Myers96) less body fat than those in the comparator group. De Lind van Wijngaarden and colleagues93 did not report percentage body fat for infants, but did report this outcome for the children in their study who were over 4 years of age (n = unclear). Children who received rhGH for 1 year had a median percentage body fat SDS of 1.5, compared with 2.3 in the control group (p < 0.001). After 2 years of treatment, the SDS values were 1.9 versus 2.4 for the treated and untreated groups. respectively (p < 0.001).
Four trials reported that patients treated with rhGH had statistically significantly higher LBM93,95,96,102 or a larger improvement in LBM than untreated patients. 22 In the trial reported by Carrel and colleagues,22 treated patients’ LBM increased by 1.8 kg more than the improvement seen in the untreated group (3.6 vs 1.8 kg, p < 0.001). Treated patients in the other two studies had approximately 2 kg102 or 4 kg95,96 more LBM than their untreated counterparts (p < 0.05 and p < 0.01, respectively). De Lind van Wijngaarden and colleagues93 reported that change in trunk LBM was statistically significantly better for treated than for untreated infants (1.7 vs 0.7, respectively). For children, they reported SDS for LBM adjusted for age and height, as well as change in trunk LBM. All of these outcomes were statistically significantly better for treated children than for untreated children after both 1 and 2 years of treatment.
Six of the studies reported BMI, with mixed results. Festen and colleagues91 reported a BMI of 16.1 at year 1 for treated patients and 18.5 for untreated patients (p < 0.05), with similar results at year 2. Haqq and colleagues102 also reported a statistically significant difference of 1.6 in BMI (31.2 vs 32.8 for treatment phase vs placebo phase in a small crossover RCT, p < 0.05). By contrast, the RCTs reported by Carrel95 and Myers96 and by de Lind van Wijngaarden93 found no statistically significant difference between treated and untreated patients. Neither of the other RCTs that reported BMI gave a value for between-group statistical significance, and both treated and untreated patients had similar values. 92,100,101
There was no statistically significant difference in bone mineral density between treated and untreated patients in the study reported by Carrel and colleagues. 22 No statistically significant differences in progression of scoliosis or onset of scoliosis in either infants or children were reported by de Lind van Wijngaarden. 93
Biochemical and metabolic markers
The included studies reported a range of biochemical and metabolic markers, and key results are included in Table 17 – see Appendix 4 for further outcomes. For conciseness, only the key outcomes of IGF-1, IGFBP-3, insulin and glucose are discussed in the narrative summary below.
All of the RCTs reported IGF-1 values or IGF-1 SDS as an outcome measure, and found that levels were higher in rhGH-treated patients than in untreated children. Three studies reported that IGF-1 values were statistically significantly higher in rhGH-treated patients than in untreated patients. 22,95,96,102 Three studies reported that IGF-1 SDS values were statistically significantly higher in treated than in untreated patients. 91–94
The included studies had well-matched patient groups, whose baseline characteristics were similar in the treated and untreated groups. The only exception was the crossover study by Haqq and colleagues,102 which presented baseline characteristics for the study population as a whole, and the study by Lindgren and colleagues,100,101 which reported slightly lower baseline GV SDS in the rhGH group [–1.9 ± 2.0, range –6.4 to –0.9, vs –0.1 (SD not reported) range –1.7 to –2.71].
Three of the RCTs reported IGFBP-3 values,93,95,96 and these were higher in treated patients than in untreated patients. In the trial reported by Carrel95 and Myers,96 patients treated with rhGH had a mean level of 3.5 mg/ml compared with 2.07 in the untreated patients (p < 0.01). Haqq and colleagues reported mean values of 6029 ng/ml in the treated patients and 4247 ng/ml in the untreated patients (p < 0.01). 102 Treated children and infants in the study reported by de Lind van Wijngaarden and colleagues93 had higher IGFBP-33 values than untreated children, although no p-values were reported for between-group comparisons.
The three studies that reported IGFBP-3 SDS found positive values in the treated children, with SDS of 0.492,93 and 0.5 (year 1) or 0.6 (year 2). 91,93 In comparison, untreated patients’ median scores were between –2.491,93 and –3.192 in year 1 and between –1.793 to –1.891 in year 2. Differences between treated and untreated patients were statistically significant in all three studies (p < 0.05,92 p < 0.001,93 p < 0.00191).
The RCT reported by Carrel and colleagues22 reported that there was no statistically significant difference in fasting insulin levels between the treated and untreated infants in their study (5.6 vs 5.7 μIU/ml, respectively). Two other studies91,95,96 reported slightly higher insulin levels in treated patients, but did not report p-values. The study by Haqq and colleagues102 reported very similar levels in both treated and untreated patients. Glucose levels appeared to be similar in both treated and untreated patients in the two studies that presented this as an outcome, but neither study reported any p-values. 91,102
Quality of life
None of the included studies reported a measure of HRQoL.
Adverse events
None of the studies reported AEs in any detail. Neither of the studies reported by de Lind van Wijngaarden and colleagues93 and by Festen and colleagues94 nor the one reported by Festen and colleagues91 reported on AEs at all. In the other study by Festen and colleagues,92 the paper stated that rhGH treatment did not induce disadvantageous effects on carbohydrate metabolism, sleep-related breathing disorders or thyroid hormone levels. Hauffa and colleagues99 reported that one patient in the rhGH group developed pseudotumour cerebri after increasing the starting dose to the final dose, but their symptoms resolved on discontinuation. No abnormalities of glucose regulation were observed in either group. None of the patients in the study reported by Carrel and others95,96 experienced pseudotumour cerebri. Two of their patients who received rhGH experienced headaches within the first 3 weeks, but these resolved with temporary stoppage and gradual reinstitution of treatment.
Carrel and colleagues22 commented that there was no evidence of changes in the prevalence of scoliosis with rhGH treatment, although another paper reporting the same study reported that there was progression of scoliosis in one patient. 97 Lindgren and colleagues100,101 and Haqq and colleagues102 reported that there was no severe progression of scoliosis (angle ≥ 20°) during their RCTs.
Lindgren and colleagues100,101 noted that one child in their study developed low levels of thyroxine without any change in TSH levels. He received substitution with l-thyroxine during the rhGH treatment. Carrel and colleagues22 commented that no child in their RCT required thyroid hormone therapy. Haqq and colleagues102 reported that only one patient required thyroid hormone replacement while receiving rhGH treatment.
Summary
The evidence for the clinical effectiveness of HGH as a treatment for PWS comes from eight small RCTs (one crossover trial and seven parallel group trials), reported in 13 publications. The included studies were generally poorly reported and only two91,96 presented results on an ITT basis.
Only one of the studies reported changes in height. Infants who received rhGH for 1 year grew an average of 6.2 cm more than those in the untreated group (p < 0.001). 22 Two studies reported a statistically significant difference in HtSDS between treated and untreated patients. The difference was 1 SDS (favouring rhGH treatment) in one study,95,96 and > 2 (year 2) in the other. 93
Treated patients grew 3 cm/year faster than untreated patients in one RCT102 and 5 cm/year faster in another. 95,96 Another study reported a positive GV SDS for treated patients and a negative one for untreated children (5.5 vs –2.3). 99 The differences between groups were statistically significant in all three studies.
Two of the included studies reported BA as an outcome measure, and this was similar in both treatment groups. 95,96,100,101
Four trials reported a statistically significantly lower percentage of body fat (between 1%93 and 10%22 lower) in patients treated with rhGH than in those with no treatment or who were given placebo.
Three trials reported that patients treated with rhGH had statistically significantly higher LBM,95,96,102 or a larger improvement in LBM, than untreated patients. 22 One study reported that LBM SDS was significantly better in treated than in untreated children. 93
Two studies found that BMI was statistically significantly lower in treated patients than in untreated patients. 91,102 However, another RCT95,96 found no statistically significant difference between the two groups, and three more studies did not report a p-value for between-group statistical significance. 92,93,100,101
Insulin-like growth factor-1 values were statistically significantly higher in patients treated with rhGH than in untreated patients in three studies.
Two RCTs reported IGFBP-3 values that were statistically significantly higher in treated patients than in untreated patients. 95,96,102 Three studies91–93 reported positive IGFBP-3 SDS values in treated patients and negative values in untreated children; differences between the groups were statistically significant.
Four of the studies reported insulin levels, with varying results. One study22 reported that there was no statistically significant difference between treated and untreated infants. Insulin levels in another study95,96 appeared to be considerably higher in treated patients than in untreated patients. Another study91 reported higher insulin levels in treated patients at year 1 but lower levels than in untreated patients at year 2. Similar values in both groups were also reported. 102
None of the included studies reported a measure of HRQoL.
None of the studies reported AEs in any detail.
Chronic renal insufficiency
Quantity and quality of research available
Six RCTs of patients with CRI met the inclusion criteria for this review,103–108 and their key characteristics are shown in Table 18 – further details are shown in Appendix 4. The inclusion criteria for this systematic review specified that children should be prepubertal. Five of the studies stated in their inclusion criteria that patients should be prepubertal/Tanner stage 1, but one study included both prepubertal and pubertal patients. 107 However, we have included outcome measures from this study where data were presented separately for prepubertal children and pubertal children.
| Reference | Intervention | Control group | Total randomised and withdrawals | Duration of randomised treatment |
|---|---|---|---|---|
| The Pharmacia and Upjohn Study Group 1996107 |
rhGH 1 IU/kg/week n = 106 Mean ± SD age (years): 12.6 ± 3.4 |
No treatment n = 97 Mean ± SD age (years): 12.1 ± 3.1 |
Total n = 203 Sample attrition: n = 49 |
1 year |
| Fine et al. 2004108 |
rhGH 0.05 mg/kg/day n = 82 Mean ± SD age (years): 6.0 ± 3.9 |
Placebo n = 43 Mean ± SD age (years): 5.7 ± 3.6 |
Total n = 125 Sample attrition: rhGH 26, placebo 15 |
2 years |
| Hokken-Koelega et al. 1991104 |
rhGH 4 IU/m2/day then placebo n = 8 Median (range) age (years): 8.7 (4.4 to 11.3) |
Placebo, then 4 IU/m2/day rhGH n = 8 Median (range) age (years): 8.6 (4.4 to 16.0) |
Total n = 20 Sample attrition: n = 4 |
6 months in each arm |
| Hokken-Koelega et al. 1996105 |
rhGH/placebo 4 IU/m2 daily s.c.i. n = 6 Median (range) age (years): 12.1 (9.1 to 18.7) |
Placebo/4 IU/m2 rhGH daily s.c.i. n = 5 Median (range) age (years): 11.1 (8.3 to 14.9) |
Total n = 11 No withdrawals |
6 months in each arm |
| Powell et al. 1997106 |
rhGH 0.05 mg/kg/day n = 30 Mean age (years) ± SD: 5.6 ± 2.0 |
No treatment n = 14 Mean age (years) ± SD: 5.7 ± 2.6 |
Total: n = 69 Sample attrition: 20 withdrew; 4 rhGH patients and 1 control patient excluded from analyses |
1 year |
| Sanchez et al. 2002103 |
rhGH 0.05 mg/kg/day n = 12 Mean age (± SD) 9.7 ± 4.5 |
No treatment n = 11 Mean age (± SD) 11 ± 1.8 |
Total: n = 23 Sample attrition: rhGH, n = 1; control, n = 1 |
12 months |
The included RCTs were of different designs (two crossover and four parallel group). Three of the parallel-group RCTs were open label, with the comparator groups receiving no treatment,103,106,107 and one was placebo controlled. 108 The two crossover studies104,105 had placebo and treatment phases. There does not appear to have been a washout phase in either of the crossover trials, so a carry-over effect could have affected results. The doses all appeared to correspond to those specified in the marketing authorisation, but dosages were reported differently, with some using IUs and others using mgs, and some using doses based on weight, whereas others used surface area. Randomised treatment duration was 6 months in the two crossover trials,104,105 2 years in one study108 and 12 months in the other studies.
Three of the studies investigated rhGH treatment in children who had received a kidney transplant at least 1 year before starting the study103,105,107 and the other three studied children who had CRI. 104,106,108 There was considerable variation in the age of children in the included studies, ranging from 5.6106 to 12.6107 years old. Two of the studies were relatively large (n = 203107 and n = 125108), one was of medium size (n = 69106), and the remaining three were rather small (n = 23,103 n = 20104 and n = 11105).
Only one study107 specified a primary outcome. The Pharmacia and Upjohn Study Group107 designed their study to test GFR, with GV and HtSDS being used as secondary outcomes. The other studies reported various outcomes relating to growth, body composition and biochemical/metabolic markers, but did not specify which were primary outcomes. Only Sanchez and colleagues103 mentioned a power calculation, and this appears to have been based on bone formation rates in a previous study, so it is not clear what the primary outcome was for the included study. The lack of clarity around primary outcomes and power calculations, together with the small size of three of the studies,103–105 suggests that the trials may have been underpowered to detect differences in outcomes relating to growth and body composition.
The included studies had well-matched patient groups, whose baseline characteristics were similar in the treated and untreated groups.
None of the included RCTs provided clear information on method of randomisation or concealment of allocation (Table 19), so it is not possible to say whether or not selection bias may have affected these studies. The studies all reported eligibility criteria, and presented baseline characteristics that indicated that groups (within trials) were similar at the start of the studies.
| The Pharmacia and Upjohn Study Group107 | Fine et al.108 | Hokken-Koelega et al.104 | Hokken-Koelega et al.105 | Powell et al.106 | Sanchez et al.103 | |
|---|---|---|---|---|---|---|
| 1. Was the assignment to the treatment groups really random? | Un | Un | Un | Un | Un | Un |
| 2. Was the treatment allocation concealed? | Un | Un | Un | Un | Un | Un |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Rep | Rep | Rep | Rep | Rep | Rep |
| 4. Were the eligibility criteria specified? | Ad | Ad | Ad | Ad | Ad | Ad |
| 5. Were outcome assessors blinded to the treatment allocation? | Un | Un | Un | Un | Un | Par |
| 6. Was the care provider blinded? | In | Un | Un | Un | In | In |
| 7. Was the patient blinded? | In | Ad | Ad | Ad | In | In |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Ad | Ad | Ad | Ad | Ad | Ad |
| 9. Did the analyses include an ITT analysis? | In | In | In | Ad | In | In |
| 10. Were withdrawals and dropouts completely described? | Ad | Ad | Ad | Ad | Ad | Ad |
The studies gave little information on whether or not outcome assessors were blinded to patients’ treatment groups, although Sanchez and colleagues103 did comment that skeletal radiographs were reviewed by a single observer who had no information about patients’ clinical condition or treatment status. In addition, three of the trials gave patients in the comparator group no treatment, so it would have been clear to patients and their care providers whether or not they were receiving rhGH. In three trials, patients in the comparator group had placebo injections. It is not clear whether or not their care providers were also blinded to treatment group. Lack of blinding could have led to performance bias in measuring treatment effect, but the objective nature of outcomes such as height change and GV would have protected against bias to a certain degree.
All the studies presented results as mean values with SDs or standard errors to give a measure of variability. The studies all provided adequate details of any patients who withdrew from the study, but only one study105 presented results on an ITT basis (no patients withdrew from this study). Attrition bias could therefore have affected the results of the non-ITT studies, i.e. if there had been unbalanced and selective withdrawal from different treatment groups within a study, or if particular patients were more likely to withdraw or be excluded from the analysis.
There was a statistically significant difference between treated and untreated children’s birth length SDS in one study,111 but baseline height was the same in both groups. The very small study by de Zegher and colleagues113 reported slightly lower baseline GV in treated compared with untreated children [5.1 (range 4.0–6.8) vs 6.4 (range 5.3–7.5) cm/year, respectively]. Otherwise, the studies’ treatment groups were generally comparable at baseline, with no discernible differences between treated and untreated patients.
The outcome measures for the included studies are shown in Tables 20–22 below. The p-values in the tables refer to between-group differences.
| Study | Outcomes (mean ± SD) | rhGH (SD) | Control (SD) | p-value |
|---|---|---|---|---|
|
The Pharmacia and Upjohn Study Group 107 rhGH 1 IU/kg/week (n = 30) vs no treatment (n = 28); 1 year |
Change in HtSDS | +0.6 0.3 | +0.1 ± 0.3 | < 0.0001 |
| Change in GV (cm/year) | 3.7 ± 1.6 | 0.3 ± 1.6 | < 0.0001 | |
|
Fine et al. 108 rhGH 0.05 mg/kg/day (n = 82) vs placebo (n = 43); 2 years |
HtSDS | –1.6 | –2.9 | nr |
| GV (cm/year) | 7.8 ± 2.1 (n = 55) | 5.5 ± 1.9 (n = 27) | < 0.00005 | |
|
Powell et al. 106 rhGH 0.05 mg/kg/day (n = 30) vs no treatment (n = 14); 1 year |
Height gain (cm) | 9.1 ± 2.8 | 5.5 ± 1.9 | < 0.0001 |
| HtSDS change from baseline | 0.8 ± 0.5 | 0.0 ± 0.3 | < 0.0001 | |
|
Sanchez et al. 103 rhGH 0.05 mg/kg (n = 12) vs no treatment (n = 11); 1 year |
HtSDS | –1.1 ± 1.0 | nr | nr |
| Annual GV (cm/year) | 8.0 ± 2.1 | 4.8 ± 1.7 | < 0.01 | |
|
Hokken-Koelega et al. 104 1: 4 IU/m2 rhGH then placebo (n = 8) 2: Placebo then 4 IU/m2 rhGH (n = 8); 6 months each arm |
GV (cm/6 months) | 1: 5.2 (1.2) | 1: 1.5 (0.4) | < 0.0001 |
| 2: 4.4 (1.6) | 2: 2.4 (1.0) | |||
| HV SDS | 1: 6.9 (2.4) | 1: –3.0 (1.6) | < 0.0001 | |
| 2: 5.0 (4.5) | 2: –0.5 (3.2) | |||
|
Hokken-Koelega et al. 105 1: 4 IU/m2 rhGH then placebo (n = 6) 2: Placebo then 4 IU/m2 rhGH (n = 5); 6 months each arm |
GV (cm/6 months) | 1: 5.3 (1.0) | 1: 1.5 (0.9) | < 0.0001 |
| 2: 3.9 (1.3) | 2: 1.9 (0.7) | |||
| HV SDS | 1: 9.1 (2.9) | 1: –1.3 (2.9) | < 0.0001 | |
| 2: 5.3 (4.0) | 2: –0.4 (1.7) |
| Study | Outcomes (mean ± SD) | GH | Control | p-value |
|---|---|---|---|---|
|
Fine et al. 108 rhGH 0.05 mg/kg/day (n = 82) vs placebo (n = 43) |
Weight gain after 2 years (kg) | 6.7 ± 2.2 | 4.6 ± 2.7 | 0.0004 |
|
Powell et al. 106 rhGH 0.05 mg/kg/day (n = 30) vs no treatment (n = 14) |
Weight gain (kg) | 3.5 ± 1.5 | 2.2 ± 1.0 | 0.007 |
| Change in weight for HtSDS | 0.4 ± 0.7 | 0.4 ± 0.5 | 0.8703 | |
|
Sanchez et al. 103 rhGH 0.05 mg/kg (n = 12) vs no treatment (n = 11) |
Change in SDS for weight | 0.2 ± 0.3 | –0.3 ± 0.3 | < 0.01 |
| Study | Outcomes (mean ± SD) | GH | Control | p-value |
|---|---|---|---|---|
|
Fine et al. 108 rhGH 0.05 mg/kg/day (n = 82) vs placebo (n = 43) |
IGF-1 (μg/l) | 244 ± 128 (n = 47) | 135 ± 80 (n = 20) | 0.0001 |
|
Powell et al. 106 rhGH 0.05 mg/kg/day (n = 30) vs no treatment (n = 14) |
IGF-1 SDS change from baseline | 0.2 ± 1.0 | nr | 0.006 |
| IGFBP-3 SDS change from baseline | 4.0 ± 3.2 | nr | 0.011 | |
|
Hokken-Koelega et al. 104 1: 4 IU/m2 rhGH then placebo (n = 8) 2: Placebo then 4 IU/m2 rhGH (n = 8) |
IGF-1 ng/ml | 1: 264 ± 168 | 1: 160 (104) | nr |
| 2: 268 ± 120 | 2: 160 (95) | |||
| IGF-1 SDS for BA | 1: 2.6 ± 2.0 | 1: –0.2 ± 1.5 | < 0.0001 | |
| 2: 2.9 ± 2.0 | 2: 0.3 ± 1.6 | |||
| IGFBP-3 ng/ml | 1: 7708 ± 2323 | 1: 6102 ± 1892 | nr | |
| 2: 8706 ± 2275 | 2: 6501 ± 1988 | |||
| IGFBP-3 SDS for BA | 1: 5.0 ± 1.3 | 1: 3.7 ± 1.3 | < 0.0001 | |
| 2: 5.2 ± 1.4 | 2: 3.9 ± 1.4 | |||
|
Hokken-Koelega et al. 105 1: 4 IU/m2 rhGH then placebo (n = 6) 2: Placebo then 4 IU/m2 rhGH (n = 5) |
IGF-1 ng/ml | 1: 594 ± 180 | 1: 240 ± 143 | nr |
| 2: 488 ± 237 | 2: 321 ± 94 | |||
| IGF-1 SDS for BA | 1: 5.4 ± 2.8 | 1: 1.0 ± 2.5 | < 0.0001 | |
| 2: 3.4 ± 0.5 | 2: 6.4 ± 1.9 | |||
| IGFBP-3 ng/ml | 1: 7457 ± 2088 | 1: 5681 ± 1588 | nr | |
| 2: 8495 ± 2921 | 2: 6228 ± 2193 | |||
| IGFBP-3 SDS for BA | 1: 4.5 ± 1.5 | 1: 3.7 ± 2.9 | nr | |
| 2: 3.9 ± 1.5 | 2: 5.3 ± 1.5 |
Growth outcomes
Key growth outcome measures are shown in Table 20 – see Appendix 4 for other outcome measures. Only one of the included studies reported height gain. Powell and colleagues106 found that treated children grew an average of 3.6 cm more than their untreated counterparts after 1 year of treatment (9.1 cm vs 5.5 cm, p < 0.0001). All children in the study by The Pharmacia and Upjohn Study Group107 experienced an improvement in HtSDS, but this was statistically significantly higher in the children treated with rhGH than in the untreated children (0.6 vs 0.1, p < 0.0001). RhGH-treated children in the study by Powell and colleagues106 had a statistically significantly higher HtSDS at end of 12 months than untreated children (0.8 vs 0.0, p < 0.0001).
One of the six studies reported change in GV, and this was statistically significantly faster in treated than in untreated children. 107 Four studies reported GV at end of treatment, all reporting statistically significantly faster growth in children who received rhGH treatment than in untreated children. 103–105,107,108 The 2-year study by Fine and colleagues108 reported that rhGH-treated patients’ GV in the first year was 4.2 cm/year faster than the untreated patients’ (p < 0.00005). The difference between the two groups was less in the second year (2.3 cm/year faster in rhGH-treated children) but the difference between groups was still statistically significant (p < 0.00005) when comparing the difference in change from baseline in those patients who completed 2 years of the study. A statistically significant difference in GV between groups of just over 3 cm/year was reported by both The Pharmacia and Upjohn Study Group107 (3.4 cm/year difference, p < 0.0001) and by Sanchez and colleagues103 (3.2 cm/year difference, p < 0.01).
The two crossover studies by Hokken-Koelega and colleagues104,105 also reported statistically significantly faster growth velocities in patients during the rhGH phase compared with the placebo phase, with an average of 2.9 cm/6 months difference in velocity. In the study of children with CRI, patients who received rhGH followed by placebo grew at an average velocity of 5.2 cm/6 months during treatment compared with 1.5 cm/6 months in the placebo phase. Patients who received placebo followed by rhGH grew 2.4 cm/6 months during the placebo phase compared with 4.4 cm/6 months in the treatment phase. The overall mean effect of rhGH was statistically significant (p < 0.0001). Statistical tests showed that there was no significant carry-over effect (–0.04 cm/6 months, p = 0.94). The crossover study in children who had received a renal transplant had similar results. Patients grew, on average, 3.8 cm/6 months faster during the active treatment phase in the group who received rhGH followed by placebo, and 2 cm/6 months faster in the active treatment phase for patients who received placebo followed by rhGH (p < 0.0001 for overall effect of rhGH vs placebo). 105 Hokken-Koelega and colleagues reported that there was no significant carry-over effect (0.5 cm/6 months, p = 0.30). 104,105
The two crossover trials,104,105 but none of the parallel-group RCTs, reported GVSDS. Both trials reported positive SDS values during the active treatment phases and negative scores during the placebo phases. The reported difference in scores between active treatment and placebo phases in the trial of children with chronic renal failure (CRF) was 7.7 (p < 0.0001),104 and in the trial of children who had received a renal transplant the difference was 8.0 (p < 0.0001). 105
Bone age was reported by five of the six studies. The studies by Powell and colleagues106 and Sanchez and colleagues103 reported that there was no statistically significant difference in BA between the treated and untreated patients. The two crossover studies by Hokken-Koelega and colleagues reported small differences with slightly lower mean ages for rhGH overall compared with placebo (mean differences –0.01 years104 and –0.5 years105) but did not present any p-values for these comparisons. Fine and colleagues108 reported that the change in BA between baseline and 2 years was greater in patients treated with rhGH than in untreated patients for those who completed both years of the study (2.3 vs 1.6 years, p = 0.0001).
Body composition
Measures of body composition were reported by three of the studies, and selected outcomes are shown in Table 21. 103,106,108 Other outcomes are tabulated in the data extraction forms in Appendix 4. Children treated with rhGH gained statistically significantly more weight than those in the control groups in the studies reported by Fine and colleagues108 (2.1 kg more in 2 years, p = 0.0004) and by Powell and colleagues106 (1.3 kg more in 1 year, p = 0.007). However, there was no statistically significant difference between groups in change in weight for HtSDS. Sanchez and colleagues103 did not report actual weight gain, but reported a statistically significant difference in change in SDS for weight that favoured treatment with rhGH (0.2 vs –0.3, p < 0.01). Although Powell and colleagues106 reported a statistically significantly greater weight gain in treated patients, the weight for HtSDS was the same for both groups (0.4, p = 0.8703).
Biochemical markers
The included studies reported a range of biochemical and metabolic markers, and these are included in Table 22. For conciseness, only the key outcomes of IGF-1, IGFBP-3, insulin and glucose are discussed in the narrative summary below. In addition, the studies reported a range of markers related to liver function. These are not reported in Table 22 or discussed in the narrative summary below, but are included in the data extraction forms in Appendix 4. No data from Sanchez and colleagues are included in Table 22 as their results focussed on liver function and did not report IGF, insulin or glucose.
Four studies reported IGF-1 as an outcome measure,104–106,108 and levels were higher in treated patients than in untreated patients. IGF-1 values were statistically significantly higher in treated patients at both years 1 and 2 in the study by Fine and colleagues108 (p = 0.0004 and p = 0.0001, respectively), but only approximately one-half of the randomised patients were included in this analysis. Powell and colleagues106 also reported that IGF-1 and IGF-1 SDS values were statistically significantly higher for treated patients than untreated patients (p < 0.006). 106 The two crossover studies by Hokken-Koelega and colleagues104,105 reported that IGF-1 SDS for BA was statistically significantly higher for treated than for untreated patients (2.7 higher in treated children with CRF104 and 3.7 higher in treated children who were post transplant,105 p < 0.0001 for both).
Three studies reported IGFBP values,104–106 and in all three the IGFBP-3 values were higher in the treated patients. Powell and colleagues106 reported that IGFBP-3 and corresponding SDS values were statistically significantly higher in treated patients than in untreated patients (p < 0.011). Hokken-Koelega and colleagues104 reported that the IGFBP-3 SDS for bone age was statistically significantly higher for treated patients (p < 0.0001).
Fine and colleagues108 reported that fasting insulin levels were statistically significantly higher in rhGH patients than in untreated patients after 2 years (p = 0.03). Similarly, Hokken-Koelega and colleagues105 reported slightly higher insulin values in treated children, but did not present p-values.
Quality of life
Five of the included studies did not report QoL as an outcome measure. One study107 reported QoL but did not present data for prepubertal patients (the licensed patients) separately from pubertal patients, so it is not discussed here.
Adverse events
Hokken-Koelega and colleagues105 reported that no patients in their study had an acute rejection episode, and that there were no SAEs. Sanchez and colleagues103 reported that two patients with normal rates of bone formation experienced acute rejection episodes after 3 and 12 months of rhGH therapy. One of these episodes was associated with non-compliance to immunosuppressive medications and both reversed after treatment with methylprednisolone. There were no rejection episodes in untreated patients.
Fine and colleagues108 reported that there were no differences between groups in year 1. In the second year, eight of 55 rhGH patients experienced asthma or wheezing, but all episodes were preceded by upper respiratory tract infections. Fine and colleagues108 reported that there were no clinically significant side effects associated with rhGH treatment. Hokken-Koelega and colleagues104 reported that serum alkaline phosphate was significantly increased during rhGH treatment, but returned to pretreatment levels when rhGH therapy was replaced by placebo (p < 0.0001). There was no significant change in parathyroid hormone concentration during either treatment schedule, and thyroid function was reported to have been normal. The Pharmacia and Upjohn Study Group107 did not present AEs separately for prepubertal and pubertal children, so no data are reported here. Powell and colleagues106 did not report AEs from their study. 106
Summary
The evidence for the clinical effectiveness of rhGH as a treatment for short stature owing to CRI comes from six RCTs, two of which were crossover trials. The trials were generally poorly reported, and only one105 presented ITT results. Three of the studies had fewer than 25 participants, which suggests that the trials may have been underpowered to detect differences in outcomes relating to growth and body composition.
One study reported that rhGH-treated patients grew an average of 3.6 cm more than their untreated counterparts after 1 year of treatment. Two studies reported that HtSDS was statistically significantly better in treated children than in untreated children.
Five studies reported that change in GV or GV SDS was statistically significantly faster for children who received rhGH treatment than for untreated children, with between-group differences in velocity ranging from 3.2 cm/year103 to 4.2 cm/year108 in the parallel-group trials.
Two studies reported that there was no statistically different difference in BA between the treated and untreated patients. Two reported small differences with slightly lower mean ages for rhGH overall compared with placebo, but did not present any p-values for these comparisons. One study reported that the change in BA between baseline and 2 years was greater in patients treated with rhGH than in untreated patients for those who completed both years of the study.
IGF-1 levels were statistically significantly higher in treated patients than in untreated patients in two of the four studies that reported this outcome.
Three studies reported that IGFBP-3 values were higher in the treated patients. Only one of these reported that differences between groups were statistically significant.
Insulin levels were statistically significantly higher in children receiving rhGH than in those receiving placebo injections or no treatment.
Four studies presented data on AEs. Two rhGH-treated patients in one study experienced acute rejection episodes (one associated with non-compliance to immunosuppressive medications) but both reversed after treatment with methylprednisolone. There were no SAEs reported.
Children born SGA
Quantity and quality of research available
In the UK, rhGH is licensed for use in children born SGA who are over 4 years of age, have a current HtSDS of < 2.5, with a parental adjusted HtSDS of –1, had a birth weight and/or length SDS of < –2, and have failed to show catch-up growth during the previous year (HV SDS < 0). No RCTs meeting these criteria were identified. Following discussion with NICE, the criteria were amended in order to include evidence from RCTs on rhGH. As discussed above (see Inclusion criteria), the following amended criteria were agreed: growth disturbance (current height < –2.5, no reference to parental height), birth weight and/or length < –2 SD and failure to show catch-up growth (no stated criteria) by the age of 3 years.
Six studies109–114 met the amended inclusion criteria for this review, and their key characteristics are shown in Table 23 – see Appendix 4 for further details. In the UK, the licensed dose of rhGH for SGA children is 0.035 mg/kg/day, which equates to 0.105 IU/kg/day. Only the study by Phillip and colleagues114 included a treatment arm with the licensed dose; the other studies all used approximately two or three times the UK licensed dose.
| Reference | Intervention | Control group | Total randomised and withdrawals | Duration of randomised treatment |
|---|---|---|---|---|
| Phillip et al. 2009114 |
1: rhGH 0.033 mg/kg/day (n = 51), mean age (± SD): 5.5 ± 1.5 2: rhGH 0.1 mg/kg/day (n = 51), mean age (± SD): 5.5 ± 1.4 |
No treatment, (n = 47) Mean age (± SD): 5.6 ± 1.4 |
Total n = 151 Sample attrition: 2 |
1 year |
| Carel et al. 2003111 |
rhGH: 0.2 IU/kg/day, n = 112 Mean age (± SD):12.7 ± 1.4 |
No treatment, n = 56 Mean age (± SD): 12.8 ± 1.6 |
Total n = 168 Sample attrition: For treatment: rhGH, n = 21; control, n = 23 For analysis: rhGH, n = 10; control, n = 9 |
Until AH reached (mean = 2.7 ± 0.6 years) |
| De Schepper et al. 2007 109 |
High-dose rhGH: 66 ± 3 µg/kg/day, n = 11 Mean age (± SD): 5.1 ± 1.6 |
No treatment, n = 14 Mean age (± SD): 5.1 ± 1.4 |
Total n = 40 Sample attrition: n = 15 |
2 years |
| de Zegher et al. 1996112 |
1: rhGH 0.2 IU/kg/day, n = 20 2: rhGH 0.3 IU/kg/day, n = 21 Mean age (± SD): 1: 5.4 ± 0.5 2: 5.1 ± 0.4 |
No treatment, n = 13 Mean age (± SD): 4.9 ± 0.5 |
Total: n = 54 Sample attrition: rhGH 1: n = 2 rhGH 2: n = 1 Control: n = 1 |
2 years |
| de Zegher et al. 2002113 |
High-dose rhGH 100 µg/kg/day, n = 9 Mean age (range): 6.3 (4.0–8.0) |
No treatment, n = 4 Mean age (range): 4.7 (2.3–6.3) |
Total n = 13 Sample attrition: not reported |
2 years |
| Lagrou et al. 2008110 |
rhGH 0.066 mg/kg/day, n = 20 Mean age (± SD): 5.5 ± 1.6 |
No treatment, n = 20 Mean age (± SD): 5.1 ± 1.3 |
Total n = 40 Sample attrition: 1 |
2 years |
Treatment duration was comparable across five of the six included studies. Four of the trials stated a treatment duration of 2 years. 109,110,112,113 Carel and colleagues111 administered GH for an average of 2.7 ± 0.6 years, until the participants reached AH. The children in the study by Phillip and colleagues114 received treatment for 2 years, but only the first year allowed a randomised comparison between GH and no treatment.
The mean age of participants was similar both across groups within studies and across five of the six trials included. 109,110,112–114 The mean ages of groups in these trials ranged from 4.7 (2.3–6.3)113 to 6.3 (4.0–8.0) years. The Carel study111 included older children with mean ages of 12.7 ± 1.4 in the rhGH group and 12.8 ± 1.6 in the control group.
The six included trials were generally of poor methodological quality (Table 24).
| Carel et al.111 | De Schepper et al.109 | de Zegher et al.112 | de Zegher et al.113 | Lagrou et al.110 | Phillip et al.114 | |
|---|---|---|---|---|---|---|
| 1. Was the assignment to the treatment groups really random? | Un | Un | Un | Un | Un | Ad |
| 2. Was the treatment allocation concealed? | In | Un | Un | Un | Un | Un |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Rep | Rep | Rep | Rep | Rep | Rep |
| 4. Were the eligibility criteria specified? | Ad | Ad | Ad | Ad | Ad | Ad |
| 5. Were outcome assessors blinded to the treatment allocation? | Un | Un | Par | Un | Un | Par |
| 6. Was the care provider blinded? | In | Un | Un | Un | Un | In |
| 7. Was the patient blinded? | In | In | In | In | In | In |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Ad | Ad | Ad | Ad | Ad | Ad |
| 9. Did the analyses include an ITT analysis? | In | In | In | Ad | In | In |
| 10. Were withdrawals and dropouts completely described? | Ad | Ad | Ad | Ad | In | In |
Phillip and colleagues114 reported that a centralised computer-controlled system was used to randomly assign children to groups. In the other five trials it was unclear whether the assignment to treatment groups was really random. This was reflected in the assessment of whether treatment allocation was concealed, with one exception being the study by Carel and colleagues,111 which reported that group assignment was not masked and this was therefore judged to be inadequate.
The blinding of outcome assessors can defend against bias affecting the measurement of some outcomes. In two trials112,114 outcome assessors for BA were blinded to chronological age and treatment allocation. It was not stated whether this extended to assessors of other outcomes. In the remaining four trials it was not stated whether the outcome assessors were blinded.
Performance bias, where knowledge of treatment can potentially lead to differences in care provided can be protected against by blinding care givers and patients. The care provider was not blinded to treatment in the studies by Carel and colleagues111 or Phillip and colleagues,114 and in the four remaining trials this was unknown. In each of the six trials blinding of the patient was inadequate as no placebo was used. Only one of the trials conducted an ITT analysis. 113 This guards against bias arising where for example only the results of patients who did not experience AE or compliance issues are included in the analysis.
Growth outcomes
All six studies109–114 reported growth outcomes, and these are presented in Table 25.
| Study | Outcomes (mean ± SD) | rhGH | Control | p-value |
|---|---|---|---|---|
|
Phillip et al. 114 1: rhGH 0.033 mg/kg/day (n = 51) 2: rhGH 0.1 mg/kg/day (n = 51) vs untreated (n = 47); 1 year |
HtSDS | 1: –2.3 ± 0.6 | –3.0 ± 0.6 | nr |
| 2. –1.8 ± 0.8 | ||||
| Change in HtSDS | 1: 0.8 ± 0.3 | 0.1 ± 0.3 | nr | |
| 2: 1.4 ± 0.4 | ||||
| Additional height gained (cm)a | 1: 3.3 ± 0.2, 95% CI 2.9 to 3.7 | n/a | nr | |
| 2: 6.5 ± 0.2, 95% CI 6.0 to 6.9 | ||||
|
Carel et al. 111 0.2 IU/kg/day (n = 91) vs untreated (n = 33) |
AH total height gain (cm) | 26 ± 7 | 22 ± 6 | 0.005 |
| End of treatment: HtSDS | –2.1 ± 1.0 | nr | nr | |
| AH HtSDS | –2.1 ± 1.0 | –2.7 ± 1.0 | 0.005 | |
| AH total height gain SDS | 1.1 ± 0.9 | 0.5 ± 0.8 | nr | |
| AH difference from target HtSDS | –0.9 ± 1.2 | –1.7 ± 1.2 | 0.005 | |
|
De Schepper et al. 109 High-dose rhGH (n = 11) vs untreated (n = 14); 2 years |
HtSDS year 2 | –1.7 ± 0.7 | –3 ± 1 | < 0.0001 |
|
de Zegher et al. 112 1: rhGH 0.2 IU/kg/day (n = 20) 2: rhGH 0.3 IU/kg/day (n = 19) vs untreated (n = 13); 2 years |
Gain in HtSDS | 1: 2.1 ± 0.1 | 0.2 ± 0.1 | < 0.001b |
| 2: 2.5 ± 0.1 | ||||
| Gain in HtSDS for BA | 1: 1.0 ± 0.2 | 0.0 ± 0.3 | < 0.05b | |
| 2: 1.2 ± 0.4 | ||||
| GV (cm/year) | 1: 10.2 ± 0.2 | 5.7 ± 0.3 | < 0.001 | |
| 2: 11.0 ± 0.4 | ||||
| GV SDS | 1: 4.3 ± 0.3 | –0.9 ± 0.3 | < 0.001b | |
| 2: 5.2 ± 0.4 | ||||
|
de Zegher et al. 113 High-dose rhGH (100 µg/kg/day) (n = 9) vs no treatment (n = 4); 2 years |
HtSDS | –1.8 (–3.9 to –0.5) | –3.0 (–3.3 to –2.5) | nr |
| GV (cm/year) | 8.5 (6.3 to 10.2) | 5.6 (4.4 to 6.8) | nr | |
|
Lagrou et al. 110 rhGH 0.066 mg/kg/day (n = 20) vs untreated (n = 19) |
HtSDS | –1.9 ± 0.7 | –3.1 ± 0.9 | < 0.001 |
Carel and colleagues111 reported AH for the 70% of control patients and 89% of treated patients for whom these data were available. They reported a mean gain in AH of 26 ± 7 cm in the treated group compared with 22 ± 6 cm in their untreated group (p = 0.005). They also reported AH SDS, which was statistically significantly higher in the rhGH treated group (–2.1 ± 1.0) compared with the untreated group (–2.7 ± 1.0), p = 0.005. Similarly, the SDS for AH total gain was statistically significantly higher in treated patients than with untreated patients (1.1 ± 0.9 vs 0.5 ± 0.8, p = 0.002). Carel and colleagues111 also reported the difference from target HtSDS. This was statistically significantly lower in the group receiving GH, compared with the control group (–0.9 ± 1.2 vs –1.7 ± 1.2, p = 0.005).
Children who received the licensed dose of 0.033 mg/kg/day for 1 year in the study by Phillips and colleagues114 gained an average of 3.3 ± 0.2 cm in height compared with children in the untreated control group. Those receiving the higher dose of 0.1 mg/kg/day rhGH gained an average of 6.5 ± 0.2 cm compared with untreated children. No p-values were presented for between-group comparisons, although the CIs suggest a statistically significant difference.
de Zegher and colleagues112 found that gain in HtSDS at the end of the study was higher in the group receiving a higher dose [2.1 ± 0.1 (0.2 IU/kg/day) vs 2.5 ± 0.1 1 (0.3 IU/kg/day) vs 0.2 ± 0.1 (untreated), p < 0.001 treated vs untreated groups]. The other study by de Zegher and colleagues113 reported higher HtSDS in treated patients, but did not present p-values. However, there were only four patients in the no-treatment group, so between-group comparisons are difficult.
Phillips and colleagues114 found that HtSDS was higher in the two rhGH-treated groups than in the untreated groups (–2.3 ± 0.6, –1.8 ± 0.8 and –3.0 ± 0.6 for the 0.033 mg/kg/day (licensed dose), 0.1 mg/kg/day and untreated groups, respectively). These scores reflected changes of 0.8 and 1.4 in SDS for the licensed- and high-dose groups, respectively, compared with a change of only 0.1 in the untreated patients’ mean SDS value.
Three109,110,113 of the included studies that used higher doses of rhGH reported that HtSDS was higher in the treated groups than in the untreated groups. De Schepper and colleagues109 and de Zegher and colleagues113 reported HtSDS at the end of the first and second years of treatment. In each of these studies, at both time points, the SDS was higher in the treated group, and this difference between groups increased in the second year. In De Schepper and colleagues’109 study at the end of year 1, HtSDS in the treated group was –2.1 ± 0.7 versus –3.1 ± 1 in the untreated group (p < 0.0001). In year 2, HtSDS in the treated group was –1.7 ± 0.7 compared with 3.1 ± 1 in the untreated group (p < 0.0001). At the end of 2 years’ treatment, the treated group in the Lagrou110 study had a statistically significantly higher mean HtSDS (–1.9 ± 0.7) than the untreated group (–3.1 ± 0.9), p < 0.001.
Two studies109,110 were suitable for meta-analysis of the HtSDS outcome because they were sufficiently homogeneous in terms of dose, duration of treatment, and the children’s mean age at start of treatment. However, both trials were small (≤ 20 girls in each treatment group), which affects the validity of tests for heterogeneity, and both used twice the licensed dose, so a meta-analysis of these was considered unlikely to add to the evidence base.
Growth velocity (cm/year) was greater at the end of year 2 in the groups receiving rhGH in the two studies that presented results for this outcome. 112,113 de Zegher and colleagues 1996112 found an increased GV in their group receiving a higher dose of GH, and a greater GV for their treated participants overall: 10.2 ± 0.2 (0.2 IU/kg/day) versus 11.0 ± 0.4 (0.3 IU/kg/day) versus 5.7 ± 0.3 (untreated), p < 0.001 untreated versus treated. The de Zegher 1996 study112 also found that GV SDS was statistically significantly higher at the end of treatment in the treated groups [4.3 ± 0.3 (0.2 IU/kg/day) and. 5.2 ± 0.4 (0.3 IU/kg/day)] compared with –0.9 ± 0.3 in the untreated group (p < 0.001 for untreated vs treated groups).
de Zegher and colleagues 1996112 reported BA. The gain in BA (years) was statistically significantly greater in the groups receiving GH than in those who were untreated. The 0.2 IU/kg/day rhGH group had a mean gain of 1.35 ± 0.16, compared with 1.33 ± 0.24 in the 0.3 IU/kg/day rhGH group and 0.84 ± 0.07 in the untreated group (p < 0.001 treated vs untreated groups). This is reflected in the gain in HtSDS for BA: 1.0 ± 0.2 (0.2 IU/kg/day) versus 1.2 ± 0.4 (0.3 IU/kg/day) versus 0.0 ± 0.3, p < 0.05, treated versus untreated groups.
Body composition outcomes
Four of the included studies reported body composition outcomes. 109,110,112,113 These results are shown in Table 26. It should be noted that all of these studies used higher doses of rhGH than the UK licensed dose.
| Study | Outcomes (mean ± SD) | rhGH | Control | p-value |
|---|---|---|---|---|
|
De Schepper et al. 109 High-dose rhGH (n = 11)a vs untreated (n = 14); 2 years |
WtSDS | –1.8 ± 1 | –3.4 ± 1.6 | < 0.0001 |
| Lean mass (kg) | 15.5 ± 3.4 | 12.2 ± 2.5 | < 0.0001 | |
| FM (kg) | 2.9 ± 1 | 3.1 ± 1.1 | n/s | |
| Lean mass (%) | 82 ± 3 | 77 ± 5 | < 0.05 | |
| FM (%) | 15 ± 2 | 20 ± 5 | < 0.05 | |
|
de Zegher et al. 112 1: rhGH 0.2 IU/kg/day (n = 20) 2: rhGH 0.3 IU/kg/day (n = 19) vs untreated (n = 13); 2 years |
Weight gain (kg) |
1: 6.9 ± 0.6 2: 7.8 ± 0.5 |
3.6 ± 0.4 | < 0.001a |
| Gain in WtSDS |
1: 1.3 ± 0.1 2: 1.8 ± 0.1 |
0.4 ± 0.1 | < 0.001a | |
|
de Zegher et al. 113 High-dose rhGH (100 µg/kg/day) (n = 9) vs no treatment (n = 4); 2 years |
WtSDS (mean and range) | –2.1 (–3.6 to –0.9) | –3.8 (–4.8 to –3.2) | nr |
| BMI SDS(mean and range) | –1.2 (–3.4 to –0.4) | –2.1 (–2.9 to –1.4) | nr | |
|
Lagrou et al. 110 rhGH 0.066 mg/kg/day (n = 20) vs untreated (n = 19) |
WtSDS | –2.3 ± 1.2 | –3.7 ± 1.5 | < 0.01 |
| BMI (SDS) | –1.5 ± 1.1 | –2.0 ± 1.5 | ns |
De Schepper and colleagues reported a WtSDS for treated patients that was almost half that for untreated patients (–1.8 vs –3.4; p < 0.0001). Lagrou and colleagues110 found that WtSDS at the end of year 2 was statistically significantly higher in their treated group (–2.3 ± 1.2) than in their untreated group (–3.7 ± 1.5; p < 0.01). Similar values were reported by de Zegher and colleagues,113 although no p-values were given.
de Zegher and colleagues 1996112 also reported gain in WtSDS and weight gain (kg). For both of these outcomes the difference was statistically significant and higher in the groups treated with GH. Mean weight gain (kg) was 6.9 ± 0.6 (0.2 IU/kg/day) versus 7.8 ± 0.5 (0.3 IU/kg/day) versus 3.6 ± 0.4 in the untreated group (p < 0.001 treated vs untreated groups). This pattern was reflected in the gain in WtSDS, which was 1.3 ± 0.1 in the 0.2 IU/kg/day group, 1.8 ± 0.1 in the 0.3 IU/kg/day group and 0.4 ± 0.1 in the untreated group (p < 0.001 untreated vs treated groups).
Lean mass and FM were reported in kilograms and as a percentage by De Schepper and colleagues. 109 Lean mass (kg) increased from year 1 to year 2 in both groups, and was greater in the group receiving GH at both times (13.2 ± 3.4 vs 10.9 ± 2.4 and 15.5 ± 3.4 vs 12.2 ± 2.5 for years 1 and 2, respectively). The p-value was reported as p < 0.0001, but it is unclear at which time point this p-value refers to. Lean mass (%) remained virtually unchanged from year 1 to year 2, but was higher in the rhGH group (82 ± 3 vs 77 ± 5 at year 2). The difference between treated and untreated groups was statistically significant (p < 0.05), but it is unclear whether this refers to the year 1 or year 2 data.
The difference in FM (%) between the two groups was statistically significant: 15 ± 2 versus 20 ± 5, p < 0.05.
Two studies reported BMI SDS. 110,113 One of these reported that there was no statistically significant difference between treated and untreated children,110 and the other reported similar values but gave no p-value. 113
Biochemical markers
Two of the included studies, both of which used higher doses than the UK licensed dose, reported biochemical markers. 112,114 These results are shown in Table 27.
| Study | Outcomes (mean ± SD) | rhGH | Control | p-value |
|---|---|---|---|---|
|
de Zegher et al. 112 1: rhGH 0.2 IU/kg/day (n = 20) 2: rhGH 0.3 IU/kg/day (n = 19) vs untreated (n = 13) 2 years |
Serum IGF-1 (µg/l) |
1: 332 ± 29 2: 655 ± 69 |
168 ± 46 | < 0.01 untreated vs group 1 |
| Serum IGFBP-3 (mg/l) |
1: 6.10 ± 0.35 2: 6.50 ± 0.52 |
4.00 ± 0.58 | < 0.001 untreated vs group 1 | |
|
Phillip et al. 114 1: rhGH 0.033 mg/kg/day (n = 51) 2: rhGH 0.1 mg/kg/day (n = 51) vs untreated (n = 47) 1 year |
IGF-1 (ng/ml) |
1: 345.6 ± 177 2. 594.3 ± 221 |
176 ± 107 | nr |
| IGF-1 SDS |
1: 0.9 ± 1.9 2. 3.3 ± 2.1 |
–0.9 ± 1.2 | nr | |
| IGFBP-3 (µg/l) |
1: 4.8 ± 1.1 2: 6.1 ± 1.4 |
3.9 ± 1.1 | nr |
Serum IGF-1 levels were statistically significantly higher in rhGH treated groups at the end of treatment. In one study,112 children receiving 0.2 IU/kg/day rhGH had values of 332 ± 29, compared with 655 ± 69 in the 0.3 IU/kg/day group and 168 ± 46 in the untreated group (p < 0.01, 0.2 IU/kg/day vs untreated group) after 2 years’ treatment. Phillip and colleagues114 reported similar IGF-1 values as de Zegher and colleagues112 after 1 year’s treatment, and, in addition, reported that IGF-1 SDS was higher in rhGH treated patients than in untreated patients. Values were 0.9 ± 1.9 and 3.3 ± 2.1 in the low- and high-dose groups, respectively, and 0.9 ± 1.2 in the untreated group.
Serum IGFBP-3 levels were also greater in the groups receiving rhGH. In the 1-year study,114 values were lowest in untreated patients (3.9 ± 1.1 µg/l) and higher in the two rhGH groups (4.8 ± 1.1 and 6.1 ± 1.4 for the low- and high-dose groups, respectively). No p-values were reported. At the end of year 2 in the second study, mean values were 6.10 ± 0.35 in the 0.2 IU/kg/day rhGH group, 6.50 ± 0.52 in the 0.3 IU/kg/day rhGH group and 4.00 ± 0.58 in the untreated group (p < 0.001, untreated vs 0.2 IU/kg/day rhGH group). 112
Quality of life
None of the included studies reported QoL outcomes.
Adverse events
Four of the included studies discussed AEs in varying detail. 109,111,112,114
Carel and colleagues111 found that 44% of patients reported AE, with 10% of these reporting four or more. It was not stated whether these patients were from the treated or untreated group. The authors described two AEs that they believed to be causally related to treatment; one slipped capital epiphysis after 1.5 years of treatment and one simple seizure episode 10 minutes after first injection. The authors do not state if these led to withdrawal. Sixteen severe AEs in 14 patients were reported. These were not thought by the authors to be related to treatment, and included trauma, psychiatric symptoms, abdominal symptoms, otitis, asthma, variocele, striae and migraine. De Schepper and colleagues109 stated only that no participants ‘had a noteworthy adverse event during the two years of study’. No further details were given.
de Zegher and colleagues 1996112 reported four SAEs. The authors suggested that these might not be linked to GH, but gave no further details. The authors described two treated children versus one untreated child hospitalised as a result of viral disease (group/dose not reported). There was one case of aggravated cutaneous eczema reported in group 1 (0.2 IU/kg/day). Three treated children (group/dose not given) reported possible increase in size or number of pigmented naevi. Treatment was not interrupted in any of these cases.
Phillip and colleagues114 reported AEs only for the 2-year study overall, so it was not possible to compare the treated and untreated children. The majority (349/358) of AEs in the study were of mild to moderate severity, the most common events (57%) being childhood infections. Of 16 SAEs reported, three were described as likely to be related to rhGH. Two of these (convulsions and papilloedema) resolved on discontinuation of treatment, and the third (epilepsy) stabilised when treatment was withdrawn.
Summary
Six109–113 trials examining the effectiveness of GH in children born SGA met the inclusion criteria for the review. The quality of the included studies was generally poor, and only one undertook an ITT analysis. 113 All but one114 of the trials used higher than licensed doses of rhGH.
One trial reported total gain in AH, and found this was approximately 4 cm higher in people who had received rhGH. The difference between groups was statistically significant (p < 0.005). 111 AH gain SDS was also statistically significantly higher in people who had received rhGH. 111 However, the study used a dose which was approximately twice the licensed dose, and it was carried out in children with a mean age of 12.7 years at start of treatment. This may limit the generalisability of the trial.
One study114 reported that patients who received 0.033 mg/kg/day of rhGH (the licensed dose) gained an additional 3.3 cm height compared with untreated children, and those who received 0.1 mg/kg/day gained 6.5 cm of additional height after 1 year’s treatment.
Height SDS was found to be statistically significantly higher in children treated with GH in two studies,109,110 and higher, but with no reported p-value, in two others. 113,114
Growth velocity (cm/year) was greater in the treated groups at the end of year 2 in the two studies that reported this outcome,112,113 but the difference was reported to be statistically significant in only one. 112
Weight standard deviation score was statistically significantly higher in children treated with rhGH in one110 of the three studies reporting this outcome.
Lean mass was reported in one study,109 and was statistically significantly greater in the treated group. Two studies reported BMI SDS. 110,113 One of these reported that there was no statistically significant difference between treated and untreated children,110 and the other reported similar values but gave no p-value. 113
One study112 reported that serum IGF-1 and IGFBP-3 levels were statistically significantly higher in patients treated with rhGH, and another114 reported similar results but did not present p-values.
Reporting of AEs was limited in detail, and only reported by four of the trials. 109,111,112 One trial111 reported two events in treated children that may have been linked to GH. They did not discuss if these led to discontinuation of the drug. A second trial109 reported only that there were ‘no noteworthy’ AEs recorded. A third trial112 reported four SAEs, which were not linked to the study drug. Three of 16 SAE in another trial114 were linked with rhGH, and these resolved/stabilised once treatment was discontinued.
SHOX deficiency
Quantity and quality of research available
Only one study of patients with SHOX met the inclusion criteria for this review,49 and its key characteristics are shown in Table 28. The 2-year multicentre RCT by Blum and colleagues49 compared a daily injection of 50 µg of rhGH with no treatment in 52 prepubertal children with confirmed SHOX-D. The manufacturer’s recommended dose is 45–50 µg/kg body weight,81 but as the study did not report mean baseline weight of participants it is not possible to comment on whether or not the study reflects the licensed dose. The study also included a non-randomised rhGH-treated group of patients with TS, but this group will not be discussed further in this report.
| Reference | Intervention | Control group | Total randomised and withdrawals | Duration of randomised treatment |
|---|---|---|---|---|
| Blum et al. 200749 |
rhGH 50 µg/day, n = 27 Mean age ± SD (years): 7.5 ± 2.7 |
No treatment, n = 25 Mean age ± SD (years): 7.3 ± 2.1 |
Total n = 52 Sample attrition: 1 |
2 years |
The included study was generally poorly reported (Table 29), with little information on method of randomisation or concealment of allocation. Patients in the comparator arm received no treatment, so the patients themselves and their care providers would have been aware of whether or not they were receiving the study drug. The patients in the two groups had similar baseline characteristics, although target HtSDS was statistically significantly lower for the rhGH group (–1.3 ± 1.0 vs –1.5 ± 0.9, p = 0.013). Baseline IGFBP-3 SDS was slightly higher for the rhGH group (0.6 ± 1.3 vs 0.1 ± 1.1), although the difference was not statistically significant. The analysis was not reported on an ITT basis as one discontinuing patient was excluded from the analysis. The study did not include discussion of sample size or a power calculation, so it is not possible to determine whether or not it was adequately powered to detect a difference in the primary outcome (first-year GV).
| 1. Was the assignment to the treatment groups really random? | Un |
| 2. Was the treatment allocation concealed? | Un |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Rep |
| 4. Were the eligibility criteria specified? | Ad |
| 5. Were outcome assessors blinded to the treatment allocation? | Para |
| 6. Was the care provider blinded? | In |
| 7. Was the patient blinded? | In |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Ad |
| 9. Did the analyses include an ITT analysis? | In |
| 10. Were withdrawals and dropouts completely described? | In |
Growth outcomes
Table 30 shows growth outcomes at the end of 2 years’ treatment. Children treated with rhGH gained approximately 6 cm more height than those in the control group (p < 0.001). Although all children remained below average height, the HtSDS was statistically significantly lower in the untreated group (–3.0 ± 0.2 vs –2.1 ± 0.2, p < 0.001). Blum and colleagues49 also commented that 41% of rhGH-treated patients reached a height within the normal range for age and gender (> –2.0 SDS), compared with only one patient in the untreated group. There was no statistically significant difference between the groups in catch-up of BA.
| Study | Outcomes (mean ± SD) | rhGH | Control | p-value |
|---|---|---|---|---|
|
Blum et al. 49 rhGH 50 µg (n = 27) vs no treatment (n = 24); 2 years |
Height gain (cm) | 16.4 ± 0.4 | 10.5 ± 0.4 | < 0.001 |
| Ht SDS | –2.1 ± 0.2 | –3.0 ± 0.2 | < 0.001 | |
| HV (cm/year) | 7.3 ± 0.2 | 5.4 ± 0.2 | < 0.001 | |
| HV SDS | 2.3 ± 0.3 | –0.4 ± 0.1 (n = 22) | < 0.001 |
The difference in GV (1.9 cm/year) between the two groups during the second year of the study was statistically significant (p < 0.001). Children in the rhGH group had a positive HV SDS, i.e. their GV was above average for their age group. By comparison, those in the untreated group had a negative score, indicating slower growth than normal for their age group. Again, the difference between the groups was statistically significant (p < 0.001).
Body composition
The included study did not report body composition as an outcome measure.
Biochemical markers
Blum and colleagues49 did not report biochemical outcomes in any detail. However, they did state that IGF-1 SDS values were in the low-normal range for both groups at baseline, but increased to the upper-normal range in the rhGH-treated group. In 10 (37%) of the rhGH-treated children, IGF-1 concentrations exceeded +2 SDS at least once during treatment, whereas none of the untreated patients experienced this. Similarly, IGFBP-3 SDS values were close to the normal mean in both groups at baseline, but increased to the upper-normal range in the treated group.
Quality of life
The included study did not report QoL as an outcome measure.
Adverse events
The rate of treatment-emergent AE was higher in the rhGH group than in the no-treatment arm (Table 31), but these were reported to have mostly been common childhood illnesses.
| Study | Outcomes (mean ± SD) | rhGH | Control | p-value |
|---|---|---|---|---|
|
Blum et al. 49 rhGH 50 µg (n = 27) vs no treatment (n = 24); 2 years |
At least 1 treatment-emergent AE (%) | 85 | 68 | nr |
| Arthralgia | 3 | 2 | nr | |
| Increased number of cutaneous naevi | 2 | 0 | nr | |
| Recurrent otitis media | 1 | 1 | nr | |
| Scoliosis | 1 | 0 | nr |
There were no significant changes in thyroid function reported during the study, and no SAEs occurred in the patients with SHOX-D.
Summary
The evidence for the clinical effectiveness of rhGH as a treatment for short stature owing to SHOX-D comes from the single RCT that met the inclusion criteria for this review. The study was unblinded and did not report an ITT analysis.
By the end of the second year, children treated with rhGH had gained statistically significantly more height than those in the control group (approximately 6 cm more), with no statistically significant difference in catch-up of BA. HtSDS was statistically significantly higher in treated than in untreated patients.
Treatment with rhGH led to a statistically significantly greater GV in both years 1 and 2 (3.5 cm/year greater than untreated patients in year 1, and 1.9 cm/year greater in year 2). The HV SDS was positive, i.e. above the average for chronological age, during both years of rhGH treatment whereas untreated children had negative HV SDS.
Treatment with rhGH raised IGF-1 and IGFBP-3 levels to the upper normal range.
Treatment of the children with SHOX-D in this RCT was not associated with any SAE.
Transition phase in GHD
The scope for this review requested that, if evidence allows, the assessment report should consider the transition of care from paediatric to adult endocrine services of young people whose linear growth is not complete. Although a number of ‘transition phase’ studies were assessed for inclusion in the review of clinical effectiveness, these included patients who had completed linear growth. Therefore, they did not meet the inclusion criteria for this review.
Once a patient’s linear growth has ceased, he or she may still not have reached peak bone mass, which would increase the risk of osteoporosis later in life. Continued rhGH treatment in these patients beyond completion of linear growth can be beneficial for improving bone mass. For example, Conway and colleagues128 randomised 160 18- to 25-year-olds with severe GHD who had received rhGH during childhood to continued treatment (n = 109) or no treatment (n = 51). They reported that 2 years of continued treatment was associated with approximately 3.5% greater increase in bone mineral density of the lumbar spine than in those who had discontinued treatment. 128
Continued rhGH treatment can also improve body composition in young adults whose linear growth is complete. Five papers129–133 were identified that reported changes in body composition, biochemical markers, QoL or AE for this patient group. However, as the patients had completed linear growth they did not meet the inclusion criteria for this review and are therefore beyond the scope of this review.
Summary of previous systematic reviews
The searches for this systematic review identified three systematic reviews. One of these was the previous HTA report,6 discussed above (see Comparison with previous review), and another was a Cochrane review related to that work. 134 The third reference was a new systematic review of GH in TS,135 and this is discussed below.
The new systematic review was conducted in Canada in 2007 by the Canadian Agency for Drugs and Technologies in Health (CADTH). 135 The quality of the systematic review was good. Inclusion and exclusion criteria relating to the primary studies were reported. The review included RCTs or comparative observational studies that compared rhGH with placebo or no treatment, included females with TS, measured growth (FH, interim height, GV), AE and QoL. Those studies that included fewer than 20 patients, or administered rhGH for less than 1 year, were excluded. The Jadad scale and the Hailey scale were used in quality assessment, but no further details were reported.
The CADTH included 19 studies, 10 of which reported data from six RCTs. 135 Three of the six RCTs included in the CADTH review were excluded from the present systematic review. One was excluded as it was a conference abstract from 1991, another was excluded because its outcome measures did not match our inclusion criteria, and the third was excluded because it did not compare rhGH with a treatment arm that did not contain somatropin.
The CADTH authors judged the RCTs to be of good quality, and the observational studies of fair quality, using the Jadad scale. However, they do not describe this in detail in their report. The present systematic review used the CRD quality assessment criteria83 rather than the Jadad scale. This, along with the difference in included studies, may explain this discrepancy in judgement of quality between the two reports.
The CADTH systematic review found that growth was accelerated and height increased in girls taking rhGH for TS. There were no SAEs reported in the included studies. The cost-effectiveness and cost–utility analyses (CUA) in the CADTH study are discussed in Chapter 4 (see Description of the identified studies). The CADTH study135 concluded that the evidence suggested that rhGH is effective in improving growth and FH in girls with TS, but found no evidence available to suggest that rhGH improves QoL.
Chapter 4 Assessment of cost-effectiveness
Introduction
The aim of this section is to assess the cost-effectiveness of GH treatment in children with GHD, TS, PWS, CRI, SGA and SHOX-D compared with no treatment. The economic analysis comprises the following:
-
a systematic review of the literature on the cost-effectiveness of GH treatment (see first section: Systematic review of existing cost-effectiveness evidence)
-
a review of the HRQoL of people with GHD, TS, PWS, CRI, SGA, SHOX-D (see second section: Review of research on QoL)
-
a review of the MSs to NICE (see third section: Review of manufacturers’ submissions)
-
a de novo Southampton Health Technology Assessments Centres (SHTAC) economic model and cost-effectiveness evaluation (see fourth section: SHTAC independent economic evaluation).
A previous HTA report has estimated the cost-effectiveness of GH treatment. 6 In that report, a cost-effectiveness model, which estimated lifetime treatment costs and benefits in terms of cost per centimetre gained, was constructed. Those analyses are extended in the present report by including QoL factors in the economic modelling.
Systematic review of existing cost-effectiveness evidence
Methods for the systematic review of cost-effectiveness
A systematic literature search was undertaken to identify economic evaluations for rhGH in children. The details of the search strategy for the cost-effectiveness studies are in Appendix 2. The MSs were reviewed for any additional studies. Titles and abstracts of studies identified by the search strategy were assessed for potential eligibility by two health economists. Full text versions of relevant papers were retrieved and checked by two health economists. Any differences in judgement were resolved through discussion. The quality of the cost-effectiveness studies was assessed using a critical appraisal checklist based on that by Drummond and Jefferson,136 the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) checklist137 and the NICE reference case. 138
Results of the systematic review of cost-effectiveness
A total of 220 potentially relevant studies were identified in the cost-effectiveness searches and one in the QoL searches. Five full papers were retrieved with only two economic evaluations meeting the inclusion criteria. For all disease areas throughout the screening and data extraction process, differences in opinion were generally minor and easily resolved without the involvement of a third reviewer. The characteristics and results of the evaluations are discussed below.
Description of the identified studies
The literature search did not identify any economic evaluations conducted across the entire range of conditions of interest or any for the population of England and Wales. Table 32 provides a summary of the characteristics and base-case findings for the two published North American economic evaluations for human GH for children with TS135 and GHD. 139
| Study/Details | CADTH135 | Joshi et al.139 |
|---|---|---|
| Publication year | 2007 | 2006 |
| Organisation | Canadian agency for drugs and technologies in health | Novo Nordisk |
| Country | Canada | USA |
| Study type | CEA and CUA | CEA and CUA |
| Study perspective | Canadian health-care system | The US health-care payers’ perspective |
| Study population | Female population aged 10 years at baseline with TS, receiving treatment for 5 years until 15 years old |
|
| Intervention | rhGH | rhGH (Norditropin) |
| Model type | Deterministic decision-analytical model | Deterministic decision-analytical model |
| Time horizon | Lifetime (assumed to be until age of 81 years) | Lifetime (assumed to be the age of 78 years for males and age 80 for females)a |
| Discounting | 5% applied to both costs and benefits (QALYs) | 3% applied to both costs and benefits (QALYs) |
| The primary clinical treatment effects modelled/assessed | 147.5 cm was the FH in the intervention group, 141 cm was the FH in the control group | The ‘success’ of treatment is defined as achieving ‘normal height’, i.e. FH within two SDs of the gender-specific population mean |
| Source of clinical evidence for the primary effect | Stephure and colleagues86 | Not indicated. Appears to be an assumption. The probability of ‘success’ was assumed to be 90% if treatment started at age 3 and continued until age 18. The probability of ‘success’ was assumed to be 75% if treatment started at the age of 5 and continued until the age of 16 |
| Health-benefit outcome | QALY | QALY |
| QoL gain, per year | 0.042 | 0.189 |
| Results | Individuals with rhGH treatment had an additional discounted cost of C$153,593 and an additional discounted benefit of 0.63 QALY. The cost-effectiveness was estimated as C$243,078 per QALY gained | For the cohort of 5–16 years, individuals with rhGH had an additional discounted cost of US$155,005 and an additional discounted benefit of 4.2 QALY. The cost-effectiveness was US$36,995 per QALY gained. For the cohort of 3–18 years, cost per QALY was US$42,556 |
The cost-effectiveness studies were assessed against the critical appraisal checklist (Table 33). Generally, the CADTH study135 was of a higher quality; the effectiveness of the treatment had been established through a systematic review, and the estimates for parameter values are more appropriate than the study by Joshi and colleagues. 139
| Item | CADTH135 | Joshi et al.139 | |
|---|---|---|---|
| 1 | Is there a well-defined question? | Yes | Yes |
| 2 | Is the patient group in the study similar to those of interest in UK NHS? | Yes | Yes |
| 3 | Is the correct comparator used that is routinely used in the UK NHS? | Yes | Yes |
| 4 | Is the study type and modelling methodology reasonable? | Yes | Yes |
| 5 | Is an appropriate perspective used for the analysis? | ? | ? |
| 6 | Is the health-care system or setting comparable to UK? | ? | ? |
| 7 | Is the effectiveness of the intervention established based on a systematic review? | Yes | No |
| 8 | Is the model structure appropriate and does it fit with the clinical theory of the disease process? | Yes | Yes |
| 9 | Are assumptions reasonable and appropriate? | Yes | No |
| 10 | Are health benefits measured in QALYs using a standardised and validated generic instrument from a representative sample of the public? | ? | No |
| 11 | Are the resource costs used reasonable and appropriate for the UK NHS? | Yes | Yes |
| 12 | Are the health states and parameters used in the model described clearly and are they reasonable and appropriate for the UK NHS? | Yes | No |
| 13 | Is an appropriate discount rate used? | Yes | Yes |
| 14 | Has the model been validated appropriately? | ? | ? |
| 15 | Is sensitivity analysis undertaken and presented clearly? | ? | ? |
Modelling approach
Both economic evaluations presented cost-effectiveness analyses using simple deterministic decision-analytical models. Both assumed that the clinical benefit achieved as a result of the rhGH treatment in the patients’ early years will last through their lifetime. Joshi and colleagues139 assumed that age-adjusted normal height was achieved after the first year of treatment. Subsequently, the benefits in terms of ‘normal height years’ and associated utility gain were assigned from the second year of treatment. Conversely, the CADTH study135 did not assume that patients experienced any improvement in HRQoL during the treatment. The utility gain is associated with the completion of treatment rather than with achieving normal height, as normal height was not achieved in the review of clinical effectiveness.
The cohorts differed with respect to age at baseline, duration of treatment and probability of achieving normal height at the end of treatment (see Table 32 above). The CADTH study135 used the characteristics and clinical effectiveness data from the TS RCT,86 whereas Joshi and colleagues139 did not provide any clinical evidence for either the baseline characteristics of the two cohorts of patients with GHD or the assumed clinical effectiveness estimates.
Joshi and colleagues139 assumed a 20% dropout rate after 12 months of treatment and related it to the slight pain experienced by patients, although no clinical evidence was presented to support this assumption. The CADTH study135 did not adjust the final outcomes for the dropout rate, effectively assuming it to be zero. As none of the TS patients achieved normal height, the CADTH study135 did not differentiate between partial and complete success of rhGH treatment. In contrast, Joshi and colleagues139 assumed that those patients who completed treatment but did not achieve normal height still acquire a partial utility gain. However, no justification for this assumption is provided.
Discounting was appropriately applied to costs and benefits in both studies, although the discounting rates were different from the 3.5% recommended by NICE138 (3% in the study by Joshi and colleagues139 and 5% in the CADTH study135).
Estimation of final outcomes (QALYs)
Both studies highlighted the difficulty of translating intermediate (clinical) outcomes to final outcomes (QALYs). There is an apparent paucity of utility-based estimates of HRQoL in rhGH patients and an absence of such estimates obtained from children eligible for rhGH treatment (see below, Review of research on quality of life). Therefore, the authors chose alternative utility estimates that, despite acknowledged shortcomings, were judged to meet the requirements of their economic models. The utility increment associated with rhGH treatment reported in the two studies ranged from 0.04135 to 0.189. 139
Joshi and colleagues139 adapted the QoL indexes presented in the Wessex Development and Evaluation Committee (DEC) report. 140 The indexes estimated in the report were not derived using one of the methodologically rigorous techniques for obtaining utility estimates, such as time trade-off (TTO) or standard gamble (SG)141 and cannot therefore be interpreted as ‘utilities’. Furthermore, the utility element of that report was a set of scenarios not based on primary or secondary data sources and thus could not be considered reliable or valid. 6 Joshi and colleagues139 used utility estimates of 0.781 for the pretreatment and no treatment groups, although this is different to the value 0.884, reported in the DEC report. Those patients who achieved success, i.e. normal height, had a utility of 0.97 applied from the start of the second year of treatment. Patients with partial success were assumed to acquire a partial utility gain defined as 35% less than the full utility gain associated with achieving normal height. The value was stated to be between 0.884 and 0.940.
The CADTH study135 did not use absolute utility values associated with each health state but applied an incremental utility value of 0.04 for patients receiving treatment with rhGH. The utility increment was estimated from a TTO survey in a small sample of adults with TS142 (see below, Review of research on qulity of life). The patients in the QoL study were asked how many years they would be willing to lose from their life to attain an average stature. The answers were translated into the incremental utility estimate of 0.04. The CADTH study135 stated that TS patients do not attain an average stature, and so this estimate is likely to be an overestimate and bias the result of economic evaluation in favour of rhGH treatment.
Estimation of costs
Joshi and colleagues139 included costs for paediatric consultations and rhGH treatment. The CADTH study135 also included costs for X-ray examination. The unit costs reported in the economic evaluations reflect the difference in clinical practices in Canada and the USA, the price difference of the unit of resources expressed in Canadian and US dollars, and the difference in methodological approach adopted in the two studies. For example, the CADTH study135 excluded the specialist visits as these do not differ between the intervention and the control groups. The total incremental cost reported varies according to the length of treatment but is consistent between the two studies.
Model results
The cost-effectiveness analysis in the CADTH study135 used an incremental difference of 6.5 cm in FH between the intervention and control groups, based on their clinical review. They calculated the undiscounted cost-effectiveness as C$26,529 per centimetre of improved FH and the discounted incremental cost-effectiveness ratio (ICER) was C$23,630 per centimetre of improved FH. They estimated an ICER of C$243,078 per QALY gained. The authors concluded that for an average patient with TS, rhGH treatment is unlikely to be cost-effective unless the payer is willing to pay more than C$200,000 to obtain a QALY.
Joshi and colleagues139 calculated the difference in ‘normal height years’ between the intervention and the control groups to estimate the incremental cost per normal height year. It was assumed that normal height was achieved by patients in the intervention group, but not in the control group. The incremental gain in ‘normal height years’ in the cohort of 5- to 16-year-olds was 17.4 (discounted). The corresponding value in the cohort of 3- to 18-year-olds was 21.1 (discounted), which translated into an incremental cost per additional year of normal height of $8900 (discounted) in the cohort of 5- to 16-year-olds and an incremental cost per additional year of normal height of $9300 (discounted) in the cohort of 3- to 18-year-olds. They estimated an ICER of about $37,000 per QALY gained for treating children with GHD from ages 5 to 16 years and an ICER of about $42,600 per QALY gained for treating children with GHD from ages 3 to 18 years. The authors concluded that the cost-effectiveness of rhGH compares favourably to accepted threshold values and represents reasonable value for money.
In both studies the deterministic one-way analyses indicated that the results were sensitive to variations in the utility estimate, the starting age of treatment, the duration of treatment and the daily dosage. The results were also sensitive to assumptions about clinical effectiveness139 and to variations in the price of rhGH. 135
The two economic evaluations arrived at opposite conclusions about the value for money of the rhGH treatment in children. The economic evaluation conducted for the CADTH study135 may provide a more reliable estimate of the cost-effectiveness as it has used clinical data from a reasonable quality RCT and TTO utility estimates. In contrast, the assumptions about clinical effectiveness of rhGH treatment by Joshi and colleagues139 did not seem to be supported by clinical evidence. Furthermore they also used indexes, interpreted as utility weights, which do not appear to be reliable or valid.
Summary and conclusion of the systematic review of cost-effectiveness studies
We undertook a systematic review of the literature in order to identify existing models in this area. The systematic review of published economic evaluations identified two North American studies relevant to the target population and no studies conducted in the UK. The results of the two identified studies produced two very different estimates of cost-effectiveness. This difference is largely due to the choice of utility estimates and assumptions on the effectiveness. As discussed below (see next section, below, Review of research on QoL), there is a paucity of reliable estimates of utility gains associated with GH treatment. Therefore, the results of both studies should be treated with caution. In particular, Joshi and colleagues139 adapted QoL indexes that were not derived according to the NICE reference case and could not be considered reliable or valid. 6 The literature study did not identify studies that we could use for this review and so a de novo independent economic model was required.
Review of research on QoL
Systematic review of HRQoL studies
A systematic review was undertaken to identify HRQoL studies for rhGH for children. The HRQoL searches were undertaken to populate a lifetime economic model with utilities to calculate QALYs, so studies with adults and children were eligible for inclusion. Titles and abstracts of studies identified by the search strategy were assessed for potential eligibility by two health economists. Full text versions of relevant papers were retrieved and checked by two health economists. Any differences in judgement were resolved through discussion. The details of the search strategy for QoL are in Appendix 2.
The titles and abstract of the studies identified by the search strategy were assessed on the basis of the following criteria:
-
disease condition as defined in Table 1 (Chapter 1) of this report
-
primary research using a preference/utility based measure for the conditions interest
-
primary research using a generic measure [i.e. Short Form questionnaire-36 items (SF-36)] that can be translated into a utility-based estimate
-
primary research using a condition-/disease-specific QoL measure and an algorithm that allowed disease-specific QoL to be converted into utility values.
Exclusion criteria for the systematic literature search were:
-
primary research reporting QoL that could not be converted into utility values using a validated mapping algorithm
-
background or discussion papers that did not report a QoL measure for the conditions of interest
-
papers reported in language other than English.
The search strategy identified 391 articles that were potentially relevant. After the abstracts had been screened, 24 articles were identified and full papers were retrieved for these articles. After checking the retrieved studies, six papers met the inclusion criteria. These are summarised in Table 34. A further targeted search linking height to HRQoL is reported below (see Height and health-related QoL).
| Study/Details | Bannink et al.143 | Bertella et al.144 | Busschbach et al.145 | Carel et al.146 | Koltowska-Haggstrom et al.147 | Sandberg et al.148 |
|---|---|---|---|---|---|---|
| Publication year | 2006 | 2007 | 1998 | 2005 | 2008 | 1998 |
| Country | The Netherlands | Italy | The Netherlands | France | England and Wales | USA |
| Study type | QoL observational cohort study matched to normal population | QoL observational cohort study | QoL observational case–control study | QoL observational cohort study matched to normal population | Estimated utilities from a survey of general population in England and Wales, and mapped to an observational cohort study | QoL observational case–control study |
| Study population | 49 participants with TS | 13 participants with PWS |
17 participants with CO renal failure 25 with TS 25 with GHD |
568 participants with TS |
894 participants with CO and AO GHD CO-onset GHD occurred in 21.6% |
140 participants with GHD 53 participants with GHD who had siblings |
| Study population age | 19.6 ± 3.0 years (14.8–25.8 years) | 27.08 ± 4.55 years (20–33 years) | Between 24 years ± 4.1 (ISS) and 28 years ± 4.9 (TS) | 22.6 ± 2.6 years | 40 ± 16.5 years | 26.1 ± 6.5 years (18.8–46.9 years) |
| Comparator population | Dutch general population | No comparator | 44 normal short participants (not diagnosed with ISS) | French general population | England and Wales general population | 53 controls (unaffected siblings) |
| Intervention (s) | GH treatment was for 7.1 ± 2.7 years | GH treatment in 5 participants, but had ceased treatment 1–4 years before being enrolled in the study | GHD treated with rhGH during childhood |
GH treatment for 4.8 ± 2.2 years 72% received estrogen treatment |
GH treatment |
Pituitary-derived rhGH and recombinant GH. GHD treatment was for 4.5 ± 3.1 years (0.9 to 14.3) |
| Included QoL instrument used | SF-36 | SF-36 | TTO | SF-36 | QoL-AGHDA with utility weights from EQ-5D | SF-36 |
| Time period when HRQoL instruments administered | HRQoL evaluation occurred 2.8 (1.6) years after rhGH discontinuation | HRQoL evaluation at the beginning, during and after rhGH discontinuation | HRQoL evaluation in adulthood after rhGH discontinuation if applicable | HRQoL evaluation occurred 6 years after rhGH discontinuation | HRQoL evaluation at baseline and last reported visit follow up for 1–6 years | After rhGH discontinuation |
| Methodology of collecting QoL data | The SF-36 was administered after rhGH treatment had been discontinued for at least 6 months and FH had been reached | The SF-36 was administered at the beginning of the treatment and then again at intervals of 6, 12 and 24 months to patients and parents | TTO asked the participants the maximum number of years they were willing to give up in order to obtain average stature | A postal survey including the SF-36 and GHQ-12 sent to participants |
Both the EQ-5D and QoL-AGHDA were completed by general population A regression model was used to estimate utility weights for QoL-AGHDA items in an observational study |
Eligible GHD subjects completed SF-36 questionnaire over the telephone, in addition to same-sex siblings |
| Results |
Women with TS treated with rhGH reported significantly better HRQoL in social functioning, role limitations, and emotional and bodily pain domains compared with normal population Other domains were roughly equal to normal population |
PWS showed significant improvement during rhGH therapy on SF-36 in vitality, physical functioning, general health, social functioning, role limitation because of emotional problems, general mental health and total scale |
The patients with GHD were hardly prepared to make a trade-off Participants with TS or renal failure had an estimated reduction in QoL of 2–4% Women with TS made an average TTO for their infertility of 9% |
HRQoL was not statistically different from the reference values obtained for young French women from the general population |
QoL-AGHDAUTILITY scores were higher in patients with CO than with AO, both at baseline 0.75 (SD 0.173) vs 0.64 and at the last reported visit) 0.82 (SD 0.167) vs 0.76. Patients with CO-GHD gained less than AO patients with regard to the total gain 0.18 (SD 0.488) vs 0.35 |
The GHD sample had only a significantly lower score from the sibling control group on general health scale (p < 0.05) The rest of the QoL domains showed not significant difference |
Growth hormone deficiency
Three relevant studies were identified that met the inclusion criteria. 145,147,148 Sandberg and colleagues148 used the SF-36 in participants with GHD. The study reported no baseline data, and reported SF-36 only after rhGH treatment had finished compared with non-GHD siblings and the general population. Therefore, the study was of no value in investigating the gain in HRQoL from rhGH treatment.
The second study, by Busschbach and colleagues,145 used the TTO method, a preference-based approach that asks people to quantify the numbers of years of life they would be willing to give up to overcome a particular state of health. The participants were asked the number of years they were willing to trade off at the end of their life in order to obtain average stature. The TTO was completed by people with GHD, TS and CRI (see below for TS and CRI). There were 25 adults with isolated GHD included in the study. The sample of GHD men made only a negligible trade off (less than 2%), whereas the sample of GHD women were willing to make a slightly larger trade off of around 2% of their expected length of life to reach average height. The major drawbacks with this study were the small sample of between 17 and 25 people with each condition of interest, the retrospective design and the lack of a control group. Also it is unlikely that gaining average stature is a realistic possibility for most people with the conditions of interest. Furthermore, for one of the conditions of interest (GHD) the patients had received rhGH treatment, and for another condition (CRI) it was unclear whether they had or had not received rhGH treatment as children. It is likely that any rhGH treatment will underestimate the TTO made to gain average stature, as these participants have already benefited from an increase in extra height. It was decided that this study did not provide a robust enough estimate of preference of health states to be used in the model.
The third study, by Koltowska-Haggstrom and colleagues,147 mapped European Quality of Life-5 Dimensions quality of life measure (EQ-5D) values to a disease-specific QoL assessment of GHD (QoL-AGHDA) instrument from a survey. This was then used to transform QoL-AGHDA scores from a cohort of patients from the Kabi International Metabolic Database (now Pfizer) (KIMS) database into utility-weighted QoL-AGHDA scores (QoL-AGHDAUTILITY). A good response rate of 84% was achieved, and 921 individuals from the general population of England and Wales responded to the survey. A regression model was used to estimate utility weights for QoL-AGHDA (R2 = 0.42). The EQ-5D responses were used as the dependent variable and the QoL-AGHDA responses were used as independent dummy variables with age as a covariate.
The patient cohort from the KIMS database consisted of 894 patients from England and Wales. However, only 21.6% had childhood-onset (CO)-GHD (applicable to the scope). The study was carried out in adults and it is unclear whether the CO-GHD group had had prior rhGH treatment. This may undervalue gain in HRQoL if this is the case. An inclusion criterion for the study was no treatment for rhGH for a minimum of 6 months prior to entry. The mean age for the whole cohort was 40 years old (SD16.5) at diagnosis and 45 years old (SD 14.3) at entry into KIMS. The study reported that patients with CO-GHD had a QoL-AGHDAUTILITY value of 0.75 (SD 0.173) at baseline compared to the last reported visit score of 0.82 (SD 0.166). The study reports mean gain in QoL-AGHDAUTILITY per year of 0.05 (SD 0.117). They also reported a total gain of 0.18 (SD 0.488), and it is assumed that this is the QALY gain over the study duration worked out using trapezoid formula compared to the baseline QoL-AGHDAUTILITY values. A last observation carried forward (LOCF) method was used. The average length of follow-up in the study for the CO-GHD was not reported and so is not possible to verify the QALY gain or gain per year.
In the combined cohort of adult-onset GHD (AO-GHD) (78%) and CO-GHD (22%) the greatest improvement in utility occurred within the first year of rhGH treatment. Subsequently, the QoL improvement is maintained when compared with the general population over a 6-year follow-up. It is unclear whether this benefit from rhGH treatment is maintained after treatment has stopped.
The limitations of this study were that it was observational with no control, and that the EQ-5D had not been conducted amongst the participants of the KIMS database. Furthermore, the regression model used to translate EQ-5D scores to disease specific measure explained less than one-half of the sample variation of the EQ-5D values. Nevertheless, the study provided an estimate of utility at baseline and at the last reported visit in one of the conditions of interest. The study’s generalisability to the other conditions of interest is unclear and it was felt that any attempt to link utilities in this study to the other conditions of interest was difficult due to the difference in height outcomes.
Turner’s syndrome
There were three studies that met the inclusion criteria for people with TS. 143,145,146 Two143,146 of these were not useful as they reported SF-36 only scores after rhGH treatment had been completed compared to a cohort of women from the general population. Therefore, they could not be used to investigate the gain in HRQoL from rhGH treatment. Busschbach and colleagues142 used a TTO method (described above) with 25 women with TS who had not received rhGH treatment as children. Their average TTO was small in the region of 4% of their life-years to reach an average height for the general population.
Prader–Willi syndrome
One study met the inclusion criteria. 144 This was potentially useful as it shows the gain in HRQoL from rhGH treatment over a 24-month period. However, the study had several limitations that make its results highly uncertain. It was a small study with only 13 Italian adult participants with PWS, of whom five had previously undergone rhGH treatment. There was no control group. At the last recorded observation (24 months) there were only nine participants left in the study. A new study mapping from SF-36 to a UK based EQ-5D preference-based utility index has recently been published, which provides an algorithm for this to be done. 149
However, the PWS QoL study is for adults who have received rhGH and it is unclear how this relates to the QoL gain for a group of children, and whether this QoL benefit would be maintained throughout their lifetime.
CRI
One study was identified that met the inclusion criteria. 142 Busschbach and colleagues used a TTO approach for 17 adults who had childhood-onset renal failure. It is unclear whether the participants received any rhGH treatment prior to the TTO assessment. The participants were asked what percentage of the years of their expected life they were willing to trade to reach normal height and to not experience health states involving a kidney transplant and dialysis. The resulting TTO associated with renal failure was 4% to reach normal height.
SGA
No relevant HRQoL studies that were identified met the inclusion criteria.
SHOX-D
No relevant HRQoL studies that were identified met the inclusion criteria.
Height and health-related QoL
The NICE reference case clearly states that the measure of health outcome used in the cost-effectiveness analysis should be QALYs calculated with utilities derived from a validated, generic, preference-based measure of HRQoL. 138 The clinical effectiveness review in Chapter 3 found no RCTs that reported HRQoL measures as an outcome and the additional search for HRQoL studies (above) located only one relevant study by Koltowska-Haggstrom147 in one of the conditions of interest (GHD) that was strictly applicable to the NICE reference case. 138
Therefore, a targeted search was conducted to identify publications that reported gains and losses in utility in relation to variation in height, as height is one of the primary outcome measures of GH treatment. Details of the search are in Appendix 2. One full paper by Christensen and colleagues150 was identified.
The study used the 2003 Health Survey for England, with 14,416 observations for adults (aged > 18 years). 151 HRQoL was measured using the EQ-5D with the UK tariff. Height was converted from centimetres to HtSDS using a UK population algorithm. Inter-relationships between variables were assessed using ordinary least squares (OLS) linear regressions, controlling for age, weight and gender. All OLS analyses were controlled for multicollinearity (close interaction between explanatory variables). Where there were any highly correlated variables (weight and BMI) then one variable was omitted from the regression. The regression analyses included two-level categorical variables (‘sex’, ‘limiting longstanding illness’ and ‘social class’) to explore the relationship between height and HRQoL while controlling for these confounding factors. 150
There was a positive correlation between an increase in height and a participant’s EQ-5D score. The mean EQ-5D scores were lower in the shorter compared with taller subjects, as well as lower than the overall population mean. The authors’ report an analysis of variance (ANOVA) combined with post hoc Tukey’s Honestly Significant Difference (HSD) test for homogeneous subgroups, which showed that the sample could be split into three meaningful subgroups, each significantly different (p < 0.05) from each other in terms of their EQ-5D scores. The first subgroup ‘HtSDS ≤ –2.0’ had significantly lower EQ-5D scores than the second group ‘–2.0 > HtSDS ≤ 0’ and the third group ‘HtSDS > 0’. The second subgroup had significant lower scores than the third group. A multivariate linear analysis using the previously identified subgroups was undertaken to predict the variation in HRQoL. The full model predicted only one-third of the sample variation in EQ-5D (R2 = 0.318, 0.343 and 0.290) based on 11,946 observations. 150
The model predicted that for those people shorter than –2.0 HtSDS, an improvement of 1 HtSDS will result in a change in EQ-5D score of 0.061. However, for the subgroup between –2.0 and 0 HtSDS the gain in EQ-5D is much reduced (a 1-HtSDS improvement increases EQ-5D score by only 0.010). One drawback to the Christensen study150 is that the population used to elicit QoL values are not from the conditions of interest but from the general population.
Summary and conclusions of the QoL review
The systematic review of QoL identified six studies that met the inclusion criteria. None of the studies was in a childhood population. This is to be expected, given the difficulties in conducting preference-based QoL studies in children. 152 Three studies reported the SF-36 in adults but were not useful on further examination, as they reported SF-36 scores only after rhGH treatment. One poor-quality study reported SF-36 at baseline, 6 months, 12 months and 24 months for a small cohort of adult participants with PWS, and the scores from this study were mapped to a UK-based EQ-5D preference-based utility index by a subsequent study.
There were only two studies that reported change in QoL using preference-based measures in the conditions of interest. 145,147 The first study145 used TTO methodology for people with GHD, TS and CRI. The number of years that the participants were willing to trade to reach average height was in the range of 0–4%. However, there were several limitations to this study and it was felt that it did not generally provide a robust estimate of utility gain from rhGH treatment. The second study147 used a regression model to give utility weights (based on the EQ-5D from a UK population) to the disease-specific QoL-AGHDA. The KIMS database was then used to transform patients QoL-AGHDA values into QoL-AGHDAUTILITY values. However, it was in an adult population and it is unclear whether they had previously had rhGH treatment as children. This study was specific to patients with GHD and is unlikely to be generalisable to the other conditions of interest.
An additional targeted search was undertaken for QoL in relation to height. One study was identified by Christensen and colleagues,150 which provided utility estimates based on the EQ-5D for different HtSDS from the Health Survey for England for an adult general population. The study provides a common utility gain that could be compared across all of the conditions of interest that could be used with the clinical effectiveness outcomes from the RCTs.
Based on the review of the QoL literature, there is likely to be a small gain in utility for individuals receiving GH treatment. However, this is based on a proxy measure of gain in height from shorter people in the general population. This excludes many relevant potential benefits and disadvantages of rhGH treatment that it is not possible to capture without good-quality evidence from the conditions of interest. This is especially true for PWS as additional HRQoL gain from improved body composition is unlikely to be captured with this method. Furthermore, there is also uncertainty over the impact of extrapolating back into childhood with adult utility data.
Review of the manufacturers’ submissions
Six of the seven manufacturers submitted evidence to be considered for this review. Five out of the six MSs consisted of a written report and an electronic model supporting the cost-effectiveness analyses. The sixth MS by Sandoz did not comply with the NICE template for the MTA and presented a description of the product (Omnitrope) and what appears to be a cost-minimisation analysis using Genotropin as a comparator (defined as a reference product). The collaborative submission is appraised below and a critique of the Sandoz submission is presented below (see Sandoz submission to NICE).
A de novo economic model has been used by the five collaborating manufacturers involved in the submission to the MTA of rhGH. Under Pfizer’s leadership, a common modelling framework was developed and used in the cost-effectiveness analysis of treatment in children with GHD, TS, PWS, CRI and SGA. Each of the collaborating manufacturers presented essentially the same model with some minor modifications, for example changes in the unit price of rhGH. The model developed was based upon the previous HTA report6 but has been extended to consider longer-term outcomes in order to estimate cost-effectiveness in terms of QALYs. One manufacturer, Merck Serono, produced its own version of the model and so the health benefits differ slightly to the other models.
The MSs also included a rapid review on QoL that was undertaken by Eli Lilly on behalf of the collaboration of manufacturers. The aim of the main review was to provide a rapid search to identify the key papers that explored the impact of short stature in childhood, and the impact of short stature in transition to adulthood and as adults. The overall conclusion from this review highlighted the inconsistent findings relating to the role of short stature in QoL and psychosocial functioning in both childhood and adulthood.
Modelling approach
In the MSs, the base-case analyses estimated the incremental cost of rhGH per centimetre of height gained relative to no treatment (in order to compare with previous HTA report6) and the incremental cost of rhGH per QALY gained relative to no treatment. The utility scores used in the model in children with GHD, TS, CRI and children who were SGA were based upon the study by Christensen and colleagues,150 discussed above (see Description of the identified studies). A gain in height was assumed to be associated with QoL improvements, which was assessed using the EQ-5D utility scale. In patients with PWS the QoL gain was based upon a small study of adult patients with PWS, together with an estimation of the benefits associated with a reduced risk of diabetes. The assumptions used to derive QoL utility improvements are discussed above (see Review of research on QoL).
The economic evaluation of rhGH treatment in conditions such as GHD, TS, SGA and CRI is based on a single clinical effect of additional height gained as a result of treatment. This clinical effect and many of the other parameters used in the model are estimated from the Kabi International Growth Study (KIGS) database,153 which is a large-scale collaborative database developed by Pfizer for the safety and efficacy of treatment with rhGH. It includes data from more than 60,000 treated patients in over 50 countries for all licensed indications, i.e. GHD, TS, PWS, SGA and CRI. Table 35 shows the input parameters used in the manufacturers’ model that have been derived from the KIGS database. The costs used in the manufacturers’ model were based upon those used in the previous HTA report, and inflated to current prices where appropriate. 6
| Parameter | GHD | TS | PWS | CRI | SGA |
|---|---|---|---|---|---|
| No. of patients | |||||
| Start of treatment | 7036 | 2749 | 485 | 806 | 990 |
| Near adult height | 2547 | 1349 | 75 | 157 | 127 |
| Age | |||||
| Start | 9.14 | 9.3 | 7.42 | 9 | 8.18 |
| End | 16.37 | 16.45 | 15.21 | 13.95 | 14.18 |
| Dropout rate | |||||
| Percentage at 1 year | 0.04 | 0.0273 | 0.02 | 0.117 | 0.03 |
| Dose | |||||
| 0–17 years of age (mg/kg/day) | 0.03 | 0.04 | 0.03 | 0.04 | 0.04 |
| Utility | |||||
| Treated | 0.83 | 0.8 | 0.76 | 0.8 | 0.81 |
| Untreated | 0.69 | 0.69 | 0.67 | 0.69 | 0.69 |
| HtSDS | |||||
| Treated | –1.17 | –2.24 | –1.36 | –2.17 | –2.01 |
| Untreated | –2.99 | –3.18 | –2.22 | –2.99 | –3.23 |
The cost-effectiveness analysis of rhGH treatment in PWS is based on an alternative structure of the model that estimates the utility gain based on a small study of 13 adult patients with PWS144 (see Review of research on QoL, above) who received rhGH for 2 years and a further utility gain for reduced diabetes risk. However, the PWS QoL study is for adults who have received rhGH and it is unclear how this relates to the QoL gain for a group of children, and whether this QoL benefit would be maintained throughout their lifetime. Furthermore, the two methods154,155 used by the Pfizer submission to translate SF-36 scores into utilities were not based on choice-based methods like TTO or SG, which produce utilities more rigorously. 141 The model assumes that individuals with PWS and diabetes would have a 10% lower QoL than those without. Based on Pfizer’s submission to the Pharmaceutical Benefits Advisory Committee in Australia, it was assumed that the prevalence of diabetes in patients with PWS would reduce from 8% to 2%, although it was not possible to verify these assumptions in the reference provided.
An alternative model structure that allowed for the second clinical effect (a reduction in the risk of osteoporosis) was also presented in a scenario analysis for GHD. In this model it was assumed that a proportion of GHD children continue treatment until they reach the age of 25 years.
The manufacturers’ model makes the following assumptions:
-
Patients with conditions of interest have the same life expectancy as the general population of England and Wales in the treated and untreated groups.
-
Patients can continue rhGH treatment or discontinue treatment at the end of 1 year.
-
Untreated children do not gain any utility benefit throughout the course of the lifetime of the model.
-
Treatment costs and monitoring costs are applied over the treatment years. Health benefits, as measured by QoL associated with particular attained heights, are maintained over patients’ lifetimes. The full utility value is applied after 2 years of treatment.
-
Compliance is assumed to be 90% in the base-case analysis and this was assumed to not impact efficacy.
-
Adverse events are not considered in the model for both the treated and non-treated patients.
-
In the base case, for all conditions except PWS, rhGH treatment affects only FH and does not affect the risk of morbidities, such as osteoporosis fracture or diabetes.
-
The MS estimated the average height at the end of treatment for the control group from the previous HTA report.
Appraisal of the manufacturer cost-effectiveness analysis
A summary of the MS compared with the NICE reference case requirements138 is given in Table 36 and indicates that the submission meets most of the requirements. See Appendix 9 for a tabulation of the critical appraisal of the submission against the Drummond and colleagues’ checklist. 136
| NICE reference case requirements | Included in submission |
|---|---|
| Decision problem: as per the scope developed by NICE | ✓ |
| Comparator: no treatment alternative | ✓ |
| Perspective on costs: NHS and PSS | ✓ |
| Perspective on outcomes: all health effects on individuals | ✓ |
| Type of economic evaluation: cost-effectiveness analysis | ✓ |
| Synthesis of evidence on outcomes: based on a systematic review | No evidence synthesis |
| Measure of health benefits: QALYs | ✓ |
| Description of health states for QALY calculations: use of a standardised and validated generic instrument | ✓ |
| Method of preference elicitation for health-state values: choice-based method (e.g. TTO, SG, not rating scale) | ✓ |
| Source of preference data: representative sample of the public | ✓ |
| Discount rate: 3.5% p.a. for costs and health effects | ✓ |
Cost-effectiveness results
The mean daily per-patient cost for each of the manufacturer’s GH treatments was based upon the unit cost shown in Table 37. Merck Serono stated that there will be a reduced cost of £20.87 through the use of the Merck Serono Easypod™, which they report will reduce vial wastage and increase compliance.
| Manufacturer/product | Unit cost (£/mg) |
|---|---|
| Genotropin (Pfizer) | 23.19 |
| Humatrope (Eli Lilly) | 18.00 |
| NutropinAq (Ipsen) | 20.70 |
| Saizen (Merck Serono) | 23.19 |
| Norditropin SimpleXx (Novo Nordisk) | 21.39 |
The base-case analyses for Pfizer, Eli Lilly, Ipsen and Merck Serono are shown in Table 38. Merck Serono produced their own version of the model and so the health benefits differ slightly from the other models.
| Manufacturer | GHD continueda | GHD | TS | PWS | CRI | SGA | |
|---|---|---|---|---|---|---|---|
| Incremental QALY | 3.48 | 3.48 | 2.83 | 2.30 | 2.53 | 2.98 | |
| Height gain (cm) | 32.24 | 32.24 | 7.95 | 25.59 | 4.48 | 21.92 | |
| Pfizer | Incremental cost (£) | 72,003 | 61,124 | 84,078 | 74,849 | 40,325 | 54,088 |
| ICER (£/QALY) | 20,673 | 17,552 | 29,757 | 32,540 | 15,962 | 18,167 | |
| Cost per cm gain (£) | 2233 | 1896 | 10,576 | 2925 | 9001 | 2467 | |
| Eli Lilly | Incremental cost (£) | 57,043 | 65,654 | 31,574 | 42,340 | ||
| ICER (£/QALY) | 16,176 | 36,237 | 12,498 | 14,221 | |||
| Cost per cm gain (£) | 1747 | 8258 | 7048 | 1932 | |||
| Ipsen | Incremental cost (£) | 65,198 | 54,779 | 75,243 | 36,129 | ||
| ICER (£/QALY) | 18,721 | 15,730 | 26,630 | 14,301 | |||
| Cost per cm gain (£) | 2022 | 1699 | 9464 | 8065 | |||
| Merck Seronob | Incremental cost (£) | 72,719 | 84,077 | 40,325 | 54,087 | ||
| 65,711 | 75,847 | 36,416 | 48,839 | ||||
| ICER (£/QALY) | 20,881 | 29,757 | 15,962 | 18,167 | |||
| 18,869 | 26,844 | 14,414 | 16,404 | ||||
| Cost per cm gain (£) | 2256 | 10,576 | 9001 | 2467 | |||
| 2038 | 9540 | 8129 | 2228 |
The base-case results for the Novo Nordisk model using KIGS data are shown in Table 39. They also reported alternative ICERs using patient level data.
| GHD continueda | GHD | TS | CRI | SGA | |
|---|---|---|---|---|---|
| Incremental QALY | 3.70 | 3.70 | 2.89 | 2.90 | 2.77 |
| Height gain (cm) | 27.45 | 27.45 | 7.95 | 3.65 | 5.67 |
| Incremental cost (£) | 71,264 | 58,637 | 79,976 | 41,388 | 51,745 |
| Cost per QALY (£) | 19,276 | 15,861 | 27,720 | 14,254 | 18,655 |
| Cost per cm gain (£) | 2596 | 2136 | 10,060 | 11,345 | 9123 |
Manufacturers’ conclusions
The authors suggested that many of the health benefits associated with rhGH treatment are not quantifiable and cannot be modelled easily. Many of these benefits would improve overall patient QoL and, possibly, duration of life. These benefits include self-esteem, improvements in sleep and concentration, and increased appetite as well as increases in LBM, total bone mass and muscle strength. These benefits may lead to reduced risk of diabetes, obesity and cardiovascular diseases.
The manufacturers concluded that their economic analyses demonstrated that rhGH is cost-effective for the treatment of short children with GHD, CRI and those born SGA, and borders on cost-effectiveness for the treatment of TS and PWS. They stated that the values for cost/centimetre compared favourably to those reported in the previous NICE assessment6 and supported the recommendation of rhGH for children with GHD, TS and CRI, plus its extension to include SGA children.
Summary of general concerns
-
Clinical effectiveness estimates for height gain were taken from an observational cohort rather than an RCT. It is not clear whether the subset of the KIGS database chosen was representative of the UK patient population or, for example, whether the subset chosen may be more severe.
-
For three of the conditions (GHD, PWS and SGA) the estimates of height gain, in centimetres, were considerably higher than those shown in the trials due to the estimates used for end height in the control group.
-
All conditions, except PWS, used mortality rates from the general population. It is likely that individuals with these conditions, in particular CRI, will have increased mortality compared with the general population.
-
The manufacturers have used the Christensen study150 for their HRQoL utility values but have not taken these from the regression analysis from this study. Instead, they have used the relationship between EQ-5D and height without controlling for other factors. Utility gain attributed to height is likely to be capturing the combined effects of other (unobserved) variables, such as age, longstanding illness and gender. For example, older generations generally have lower QoL because of their age. Not controlling for other factors, in particular age, results in the overestimation of the utility values. Furthermore, the group with the lowest height and QoL (< –3 SDS) had few observations and individuals in this group were generally elderly (mean age > 70 years).
-
Treatment cost is calculated by rounding up to the nearest whole year of treatment.
-
There is high uncertainty associated with the assumptions and sources used to estimate QoL gain in the PWS model. These were based on a small study of adult patients with PWS and it is unclear how this relates to the QoL gain for a group of children, and whether this QoL benefit would be maintained throughout their lifetime. The methods used to derive values from the SF-36 for utilities were based on rating scales and therefore did not use choice-based methods, such as the SG and TTO. QoL gain also estimated utility gain from reduced diabetes prevalence but this evidence could not be verified. There are considerable difficulties extrapolating the benefit from treating children with rhGH to their health benefits as adults.
Sandoz submission to NICE
Sandoz presented an analysis comparing Omnitrope with Genotropin. The MS contained a comparison of the annual cost of treatment with Omnitrope and with Genotropin in patients with GHD and TS. However, the MS did not comply with NICE guidance for a MTA,138 as QALYs were not estimated and a cost-effectiveness analysis was not presented. The MS attempted a cost-minimisation analysis, implicitly suggesting that treatment with Omnitrope is equally effective as treatment with Genotropin (in terms of additional height in children with GHD and TS) but is associated with less cost to the UK NHS. A critical appraisal of the Sandoz MS is given in Appendix 10.
SHTAC independent economic evaluation
Overview
A comparison of the costs and benefits of rhGH compared with no treatment in cohorts of children with GHD, TS, PWS, CRI and SHOX-D and children who are SGA was made using decision-analytical models. Models were constructed in Microsoft excel according to standard modelling methods. 138 To identify data to populate the model, systematic searches were conducted to locate studies on the natural history and epidemiology of the indicated conditions, HRQoL and costs.
Costs were derived from published studies (where available), and from national and local NHS unit costs. The model was from the perspective of the NHS and PSS, as only these direct costs were included. The model estimates the lifelong costs and benefits from rhGH treatment. The costs and benefits were discounted at 3.5%, as recommended by NICE. 138 The base year for the costs was 2008. The intervention effect in terms of improvement in HtSDS was derived from the systematic review of effectiveness reported in Chapter 3. The outcome of the economic evaluation is reported as cost per QALY gained and cost per centimetre gained.
Description of the model
A decision-analytical model was designed for the economic evaluation of rhGH for treatment of GHD, TS, PWS, CRI, SGA and SHOX-D, and was based upon one developed in the previous HTA report. 6 The current model compares a cohort of patients receiving rhGH during their childhood with a cohort of patients who were not treated with rhGH. The state transition Markov model has a cycle length of 1 year and a lifetime horizon. A Markov model was used as these are suitable for lifetime analyses with few health states. 156 The base-case decision-analytical model includes health states for alive and dead. The England and Wales population mortality rates are applied in each cycle for patients, with an adjustment using the SMRs for each of the conditions.
The model assumes that a daily subcutaneous injection of rhGH is administered for the duration of treatment, unless a patient from the treatment cohort drops out of treatment or dies. The parameters of the model that determine the age at the start of treatment, the duration of treatment and the annual dropout rates are estimated from the KIGS database described in the MS or based upon advice from our clinical advisory group, and vary between conditions. A daily dose is calculated according to the child’s weight. The dose regimen corresponds to the licensed indication of rhGH in children (and adults, in a scenario analysis of the GHD cohort).
Health-care resources included for the cost of patient monitoring apply to both the treatment and no treatment cohorts. The cost categories and unit costs are consistent with the costs used in the previous HTA report for rhGH. 6 The discount rate of 3.5% is applied to both costs and final outcomes.
Patients from the treatment cohort who stay in treatment receive a benefit of an additional height gain relative to patients in the no treatment cohort. Patients who drop out of treatment stop accumulating height gain, so their growth progression is no different from the height gain in the no treatment cohort. In each yearly cycle, individual HRQoL is estimated based upon their height gain. Individuals are assumed to maintain the same HRQoL after treatment has stopped for the rest of their lifetime. In each cycle, the total costs and QALYs are calculated by multiplying the individual costs and HRQoL by the number of people in the cohort still alive for the treatment and no treatment cohorts. The total lifetime costs and QALYs are calculated for the treated and non-treated groups by aggregating the costs and QALYs in each cycle. The total discounted QALY gain, and cost of treatment for the treatment and no treatment cohorts are calculated. Thus, the cost-effectiveness of rhGH is calculated:
Parameters used in the model and the data sources used to derive them are described in more detail below (see Model validation).
A list of the model assumptions is given below. Assumptions are applied to all conditions unless explicitly stated otherwise. All assumptions were tested in sensitivity analyses.
-
The diagnostic costs were not included in the analysis as they were assumed to be the same for both rhGH-treated and no-treatment patients.
-
The base case assumes no dropout or discontinuation of treatment. This was based upon advice from our clinical advisory group that this was likely to be a relatively rare occurrence. The base-case model therefore evaluates just rhGH treatment versus no treatment.
-
There are two health states for alive or dead in the model, and the transition between them is based on age-related mortality data.
-
The mortality rates were assumed to be higher than for the England and Wales general population estimates for untreated and treated cohorts for all conditions.
-
It was assumed that there would be no reduction in mortality as a result of rhGH treatment. There is a lack of data to assume otherwise.
-
The model time horizon is 100 years and all individuals are assumed to die by this age.
-
Effectiveness estimates for the conditions were based on selection of the best-quality evidence from the clinical effectiveness review in Chapter 3. RCTs were only selected if the follow up length was at least 2 years after the start of treatment. Where there were no appropriate RCTs, long-term observational studies were considered. In the case of SGA, the most appropriate RCT was for only 1 year.
-
Compliance was assumed to be 85% in the base case, with no loss of efficacy for rhGH treatment. 157
-
An additional scenario was undertaken for the GHD condition where treatment continued for a transition phase into adulthood to age 25. This was only applicable for 34% of the GHD population. 158 No additional benefit, in terms of height gained, was assumed from this additional treatment.
-
In the treatment and no-treatment cohorts, all children are monitored until they reach adulthood, assumed to be the age of 17 years.
Evaluation of uncertainty
The evaluation of the cost-effectiveness of GH treatment is based on uncertain information about variables, such as clinical effect, HRQoL and resource use. This uncertainty was evaluated using deterministic and probabilistic sensitivity analyses. One-way deterministic sensitivity analyses were conducted to evaluate the influence of individual parameters on the model results and to test the robustness of the cost-effectiveness results to variations in the structural assumptions and parameter inputs (see Sensitivity analyses, below).
Multiparameter uncertainty in the model was addressed using probabilistic sensitivity analysis (PSA) (see below). 159 In PSA, probability distributions are assigned to the point estimates used in the base-case analysis. The model is run for 1000 iterations, with a different set of parameter values for each iteration, by sampling parameter values at random from their probability distributions. The uncertainty surrounding the cost-effectiveness of the GH treatment is represented on a cost-effectiveness acceptability curve (CEAC) according to the probability that the intervention will be cost-effective at a particular willingness-to-pay threshold. Appendix 12 reports the parameters included in the PSA, the form of distribution used for sampling each parameter, and the upper and lower limits assumed for each variable.
Model validation
The Southampton Health Technology Assessments Centre (SHTAC) model was validated by checking the model structure, calculations and data inputs for technical correctness. The completed cost-effectiveness model was verified by another health economist. The SHTAC model was checked for internal consistency against the MS economic models by running the SHTAC model with the inputs used in MS models to ensure similar results. The robustness of the model to changes in input values was tested using sensitivity analyses to ensure that any changes to the input values produced changes to the results of the expected direction and magnitude. Finally, the model results were compared with those from previous studies including the previous HTA report and this is discussed in more detail in Chapter 6.
Data sources
Life expectancy
Several studies have attempted to assess the mortality rate of adults with the conditions of interest. Nielsen and colleagues160 conducted a meta-analysis to assess overall SMR for men and women with benign pituitary disease. Six studies were included in the meta-analysis of sex-specific mortality. Studies (total 5412 patients) reported SMR for men of 2.06 (CI 1.94 to 2.2) and women 2.8 (CI 2.59 to 3.02). However, these analyses were for hypopituitarism rather than GHD.
Shoemaker and colleagues161 followed up 3439 women in the UK, who were diagnosed with TS between 1959 and 2002, to the end of 2006. Mortality in women with TS is three times higher than in the general population, is raised for almost all major causes of death, and is raised at all ages. SMR was 3.9 in women aged 15–44 years old and 2.6 in women aged 45–84 years.
Population-based morbidity and mortality data for PWS are not available, except from regional cross-sectional surveys. 162 A recent regional survey in England indicates high morbidity and mortality rates. Lifetime mortality rates were roughly three times higher than the general population. Within these studies the data are insufficient to construct survival curves.
Mortality and causes of death in treatment for children with end-stage renal disease was estimated in a Dutch cohort study between 1972 and 1992. 163 Of all 381 patients, 85 had died. The SMR was 31.0 over this period and 21.0 in the last cohort between 1992 and 2002.
Kajantie and colleagues164 studied the relationship between small size at birth and all-cause and non-cardiovascular mortality in 13,830 individuals born between 1924 and 1944 in Helsinki, Finland. They found that small size at birth is associated with increased all-cause mortality at all ages among adult women but only with premature death in adult men.
We were unable to find any information on mortality rates for SHOX-D.
Using UK life tables, we estimated the life expectancy of adults with these conditions using the SMRs described above. Normal adult life expectancy was estimated to be 75 years for men and 79 years for women. Life expectancy for patients with hypopituitarism was reduced to 68 years for men and 70 years for females. Life expectancy with TS was reduced to 70 years for females. We estimated the life expectancy with CRI to be reduced to 35 years for men and 42 years for females, using the end-stage renal disease mortality rates as a proxy in the absence of any available data for CRI. This may underestimate life expectancy, as not all patients with CRI will go on to develop end-stage renal disease.
In the base-case model, we assume that for all conditions the life expectancy is lower than that of the general UK population, and investigate general population life expectancy in sensitivity analyses.
Effectiveness data
The start and end age of treatment, and the duration of treatment, are shown in Table 40. For GHD, CRI, PWS and SGA there are no RCTs with a duration of more than 3 years, so we used data from the KIGS database. 153 SHOX-D was not included in the KIGS database and so we assumed that these children start treatment at the same age as those in the Blum RCT49 and continue treatment for the same duration as for children with TS in the KIGS database. For the purposes of the model we rounded the start age and treatment duration.
| GHD | TS | PWS | CRI | SGA | SHOX-D | |
|---|---|---|---|---|---|---|
| Source | KIGS153 | CGHAC86 | KIGS153 | KIGS153 | KIGS153 | Blum49 |
| Starting age (years) | 9 | 10 | 7 | 9 | 8 | 7 |
| Age at end of treatment (years) | 16 | 16 | 15 | 14 | 14 | 14 |
| Treatment duration (years) | 7 | 6 | 8 | 5 | 6 | 7 |
| Sex (males, %) | 70 | 0 | 50 | 71 | 60 | 48 |
For GHD, some children continue to receive rhGH treatment into adulthood. This is shown as an additional scenario for GHD, for which it is assumed that 34% of GHD patients continue treatment158 until age 25 years with a dose of 0.4 mg/day. 6 These individuals do not receive any additional benefit associated with height gain from this treatment in the model.
The clinical effect of rhGH was taken from the systematic review in Chapter 3. Where possible the clinical effect was taken from the best-quality RCT, for which children had treatment for a sufficiently long time to capture HtSDS height gain, which we assumed would be at least 2 years. For GHD, these data were not available, as the only available RCT was for only 1 year, and so we have used observational data (KIGS database)153 to estimate the clinical effect (Table 41). For SGA, there were no RCTs available for the licensed dose and so we used a study with 1-year treatment. 114 For TS, height gain was reported in terms of age-specific TS HtSDS, but the mean age-specific value was not reported. We assumed that the age-specific TS HtSDS was that reported in the KIGS database. 153 Several studies have not reported the height gain in centimetres, and for these studies we converted HtSDS values to centimetres, using the height table from the Health Survey for England (HSE) 2003. 151
| Parameter | GHD | TS | PWS | CRI | SGA | SHOX-D |
|---|---|---|---|---|---|---|
| Source | KIGS153 | CGHAC86 | ade Lind van Wijngaarden et al.93 | Fine et al.108 | Philip et al.114 | Blum et al.49 |
| Treatment cohort | ||||||
| Starting HtSDS | –2.99 | –3.4b | –2.0 | –2.9 | –3.1 | –3.3 |
| Final HtSDS | –1.17 | –1.8b | –0.5 | –1.6 | –2.3 | –2.1 |
| Control cohort | ||||||
| Starting HtSDS | –2.99 | –3.3b | –2.5 | –2.9 | –3.1 | –3.3 |
| Final HtSDS | –2.99 | –3.0b | –2.6 | –2.9 | –3.0 | –3 |
| Treatment effect | ||||||
| Treatment height gain (SDS) | 1.82 | 1.3 | 1.6 | 1.3 | 0.7 | 0.9 |
| Treatment height gain (cm) | 12.8c | 9.3 | 11.1c | 9.2c | 3.3 | 5.9 |
| QoL gain | 0.069 | 0.069 | 0.021 | 0.059 | 0.043 | 0.055 |
A review of compliance with rhGH was conducted by Merck Serono as part of the MSs. It found that estimates for compliance ranged from 69% to 95% for the studies identified. One study estimated concordance in 75 children by using data on GP prescriptions over 12 months. 157 Between one and two injections/week were missed by 16% of the children, and 23% missed more than two injections/week. Based on this study, we assumed a compliance of 85%.
Health-related quality of life
There was a lack of good-quality HRQoL data expressed in terms of utility in the RCTs and other QoL studies for most of the conditions of interest (see Review of research on QoL, above). Only one study was found that was appropriate to the conditions of interest and this was for GHD. 147 However, it was in an adult population and it was uncertain whether the participants had already benefited from GH as children; the QoL utility gain from this study was similar to that from the Christensen and colleagues study150 for GHD. For the other studies the most appropriate utility measurement was from the study by Christensen and colleagues,150 which measured QoL using the EQ-5D in a large sample of the general UK population (HSE). The utility values are not from the conditions of interest; nevertheless it does provide a common utility gain that could be compared across all the conditions of interest and that could be used with the clinical effectiveness outcomes from the RCTs. It was assumed for children that the adult gain in utility from increased height derived from the Christensen and colleagues study would be the same as a utility gain in children.
This study assessed HRQoL estimates through the use of ordinary least squares (OLS) linear regression, which controlled for age, weight and gender. More details on the study are reported above (see Height and health-related QoL, above). We assumed that individuals in the treated and untreated cohorts would have no difference in terms of age, gender, social class, weight and longstanding illness. The differences in HRQoL utility estimates between the treated and untreated cohorts are therefore derived from their differences in height. According to the regression, for those people shorter than –2.0 HtSDS an improvement of 1 HtSDS will result in a change in HRQoL utility of 0.061; for the subgroup between –2.0 and 0 HtSDS, a 1 HtSDS improvement increases utility by 0.01. These values were used in the SHTAC estimation of cost-effectiveness.
For patients with PWS there may be an additional health benefit associated with improved body composition. Any improvements in body composition may lead to reduced risk of diabetes and cardiovascular disease. However, there is considerable difficulty estimating the magnitude of this effect and extrapolating short-term treatment in childhood to lifelong benefit. There was one study of poor quality in adults with PWS but this was not considered to be a robust estimate of QoL benefit (see Review of research on QoL). The MS estimated a QoL benefit from reduced diabetes risk but it was not possible to verify this evidence. Due to the high uncertainty around the estimates of QoL benefit, we assumed no benefit due to body composition in the base case and then conducted sensitivity analyses using the studies mentioned above.
Estimation of costs
The costs used in the SHTAC model were based upon those used in the previous HTA report. 6 The annual cost of monitoring associated with each condition was calculated for each arm of the model using treatment pathways described in that report. Treatment costs are calculated on the basis of mean dose of rhGH. Unit costs for drugs were taken from the British National Formulary (BNF)165 and, for consultations, outpatient visits and procedures, from NHS Reference Costs. 166 The base year used for the analysis was 2008; where necessary, costs were inflated to that year.
Based on advice from our clinical advisory group, the resource use was the same as for the previous HTA report except for nurse visit time was assumed to be the same for all conditions and patients would have two outpatient visits per year. Furthermore, patients would no longer have a hand X-ray at the end of treatment. The resource use is similar for all conditions, except GHD where 20% of treated children have a pituitary test each year. The unit costs applied to the resource use estimates for monitoring tests were provided by the finance department at Southampton University Hospital Trust [personal communication, Southampton University Hospitals Trust: unit costs (unpublished database), 2008]. The hourly cost of community nursing is taken from the Unit Costs of Health and Social Care. 167 All children are monitored until they reach adulthood, assumed to be at the age of 17 years old. The unit costs and resource use are shown in Tables 42 and 43, respectively.
| Costs component | Cost (£) | Source |
|---|---|---|
| Cost per outpatient attendance first contact face-to-face paediatric endocrinology (HRG code 302F) | 206.28 | NHS ref costs 2007/8166 |
| Cost per outpatient attendance subsequent contact face-to-face paediatric endocrinology (HRG code 302F) | 127.97 | NHS ref costs 2007/8166 |
| Specialist community nurse per patient contact (1 hour) | 73 | PSSRU 2008167 |
| Community nurse per patient visit (1 hour) | 64 | PSSRU 2008167 |
| Blood tests (for full blood count, chemical profile, thyroid and IGF) | 51 | SUHT 2008 |
| X-ray, hand (BA test) | 28.64a | NHS ref costs 2006/7166 |
| Pituitary function test (glucagon, insulin stress test), includes 2 hours’ nurse time | 207.50 | SUHT 2008 |
| GHD | TS, PWS, CRI, SGA, SHOX-D | |
|---|---|---|
| No treatment monitoring | ||
| Outpatient visit | 2 | 2 |
| Blood test | 1 | 1 |
| Treatment 1st year | ||
| Specialist nurse home visit (hours) | 1 | 1 |
| Community nurse home visits (hours) | 4 | 4 |
| Outpatient visit | 2 | 2 |
| Blood test | 1 | 1 |
| Pituitary function test | 0.2 | 0 |
| GH treatment subsequent year | ||
| Outpatient visit | 2 | 2 |
| Blood test | 1 | 1 |
| Hand X-ray | 1 | 1 |
| Pituitary function test | 0.2 | 0 |
| End of treatment | ||
| Outpatient visit | 1 | 1 |
The unit cost of the drug used in the manufacturers’ models varies between £18.00 and £23.19 per milligram. As this review is for the cost-effectiveness of somatropin, rather than being dependent on manufacturers’ different device costs, we have assumed an rhGH cost in the base case that is the average of the six manufacturers’ unit cost of rhGH given in the BNF 58 (Table 44). This gives an average price of £21.06. This was done for consistency between the different conditions, despite the average cost of rhGH for each condition actually varying depending on which and how many manufacturers have a licence for the condition of interest. The maximum and minimum price of rhGH will be used in a sensitivity analysis. Drug costs are calculated according to the dosage used (Table 45) and the weight of the child. 165 The weight of children at different ages was taken from a long-term observational database (Appendix 13). 153
| rhGH | BNF 58 price (£) (per mg) |
|---|---|
| Genotropin | 23.19 |
| Humatrope | 18.00 |
| Norditropin | 21.39 |
| Saizen | 23.18 |
| Nutropin | 20.70 |
| Zomacton | 19.92 |
| Average cost | 21.06 |
| Condition | ||||||
|---|---|---|---|---|---|---|
| GHD | TS | PWS | CRI | SGA | SHOX-D | |
| Drug dosage (mg/kg/day) | 0.025 | 0.045 | 0.035 | 0.045 | 0.035 | 0.045 |
Estimation of cost-effectiveness
This section reports the cost-effectiveness results for a cohort of children for each of the conditions of interest who received rhGH treatment. Results for costs and QALYs are presented for children in the cohort for a treated and untreated cohort, with costs and benefits discounted at 3.5%. The cost-effectiveness of rhGH compared to no treatment is presented as incremental cost per QALY and incremental cost per centimetre gained. The results are shown in Table 46 for each condition. In the base-case analysis, all conditions, except GHD, used the clinical benefit seen in the best-quality RCT for each condition (see Chapter 3). The cost-effectiveness of rhGH versus no treatment varied from £23,196 for GHD to £135,311 for PWS per QALY gained.
| Condition | Treatment | Costs (£) | QALYs | Inc. costs (£) | Inc. QALYs | ICER (£/QALY) | Gain (cm) | ICER (£/cm) |
|---|---|---|---|---|---|---|---|---|
| GHD | No rhGH | 2211 | 16.8 | |||||
| rhGH | 38,031 | 18.4 | 35,820 | 1.54 | 23,196 | 12.80 | 2798 | |
| TS | No rhGH | 1965 | 15.9 | |||||
| rhGH | 62,752 | 17.4 | 60,787 | 1.54 | 39,460 | 9.30 | 6536 | |
| PWS | No rhGH | 2646 | 17.6 | |||||
| rhGH | 67,794 | 18.1 | 65,148 | 0.48 | 135,311 | 11.10 | 5869 | |
| CRI | No rhGH | 1876 | 11.6 | |||||
| rhGH | 35,877 | 12.4 | 34,001 | 0.87 | 39,273 | 9.20 | 3696 | |
| SGA | No rhGH | 2432 | 17.1 | |||||
| rhGH | 34,431 | 18.1 | 31,999 | 0.97 | 33,079 | 3.30 | 9697 | |
| SHOX-D | No rhGH | 2646 | 16.8 | |||||
| rhGH | 53,434 | 18.1 | 50,788 | 1.25 | 40,531 | 5.90 | 8608 |
The incremental cost per QALY gained for PWS is very high despite a similar or greater height gain compared with the other conditions as a result of rhGH treatment. This is due to the PWS cohort having a starting HtSDS that is much closer to population norms with most of the gain in height occurring between –2.0 and 0 HtSDS. Therefore, using the Christensen regression estimates, this is associated with a lower utility gain (see Health-related quality of life, above) and a smaller QALY gain when compared with the other conditions. With the exception of PWS, all conditions have an ICER lower than £41,000 per QALY gained.
A further analysis was undertaken to see the effect of continuation of rhGH treatment into adulthood for 34% of the original cohort until the age of 25 years. The incremental cost per QALY was £28,244 (Table 47).
| Condition | Treatment | Costs (£) | QALYs | Inc. costs (£) | Inc. QALYs | ICER (£/QALY) | Gain (cm) | ICER (£/cm) |
|---|---|---|---|---|---|---|---|---|
| GHD continuers | No rhGH | 2211 | 16.8 | |||||
| rhGH | 45,826 | 18.4 | 43,615 | 1.54 | 28,244 | 12.80 | 3407 |
Sensitivity analyses
Cost-effectiveness of rhGH treatment – deterministic sensitivity analysis
One-way deterministic sensitivity analyses were performed, in which model parameters were systematically and independently varied, using a realistic minimum and maximum value. The sensitivity analysis investigated the effect of uncertainty around the model structure and for variation in parameters on the cost-effectiveness results, in order to highlight the most influential parameters. The effects of uncertainty in multiple parameters were addressed using PSA, which is reported later in this section. Where possible, the parameters were varied according to the ranges of the CIs of these parameters, based on the published estimate. Where these data were not available an alternative suitable range was chosen. The same ranges were used in the deterministic and probabilistic sensitivity analyses and these are described in Appendix 12.
Table 48 shows the results for each of the conditions using the KIGS database153 for estimate of the clinical benefit. The KIGS database, a large observational study of children treated with rhGH, was used for the effectiveness of GHD in the base case reported above. According to these results, an ICER of rhGH versus no treatment varied from an ICER of £18,980 per QALY gained for SGA to £144,050 per QALY gained for PWS. Results are of a similar magnitude to the base case with the exception of the SGA analyses. The ICER for SGA is much lower in this analysis because the incremental clinical height gain is lower in the RCT effectiveness data than in the KIGS effectiveness data.
| Condition | Treatment | Height (HtSDS) | Costs (£) | QALYs | Incremental costs (£) | Incremental QALYs | ICER(£/QALY) |
|---|---|---|---|---|---|---|---|
| TS | No rhGH | –3.18 | 1965 | 15.8 | |||
| rhGH | –2.24 | 62,752 | 17.1 | 60,787 | 1.28 | 47,553 | |
| PWS | No rhGH | –2.22 | 2646 | 17.4 | |||
| rhGH | –1.36 | 67,794 | 17.9 | 65,148 | 0.45 | 144,050 | |
| CRI | No rhGH | –2.99 | 1876 | 11.5 | |||
| rhGH | –2.17 | 35,877 | 12.2 | 34,001 | 0.74 | 46,245 | |
| SGA | No rhGH | –3.23 | 2432 | 16.8 | |||
| rhGH | –2.01 | 34,431 | 18.4 | 31,999 | 1.69 | 18,980 | |
| SHOX-D | No rhGH | –3.18 | 2646 | 16.6 | |||
| rhGH | –2.24 | 53,434 | 17.9 | 50,788 | 1.31 | 40,531 |
The discount rates used for the analyses have a large effect on the results, due to the upfront costs and the health outcomes stretching over the life time of the model. Table 49 shows the results using the discount rates used in the previous HTA report, i.e. costs 6% and benefits 1.5%. Using these discount rates, rhGH treatment is more cost-effective. For all conditions, except PWS, the ICER reduces to less than £30,000 per QALY.
| Condition | Incremental costs (£) | Incremental QALYs | ICER (£/QALY) | Gain (cm) | ICER (£/cm) |
|---|---|---|---|---|---|
| GHD | 32,407 | 2.49 | 12,999 | 12.80 | 2532 |
| TS | 55,753 | 2.49 | 22,358 | 9.30 | 5995 |
| PWS | 58,075 | 0.79 | 73,836 | 11.10 | 5232 |
| CRI | 31,609 | 1.22 | 25,804 | 9.20 | 3436 |
| SGA | 29,362 | 1.57 | 18,690 | 3.30 | 8898 |
| SHOX-D | 45,937 | 2.05 | 22,436 | 5.90 | 7786 |
Tables 50–55 report the results of the deterministic sensitivity analyses for the conditions for the most influential parameters. Other variables were varied in sensitivity analyses but were found to only have a negligible effect on the results. The cost-effectiveness results are fairly sensitive to the variation in parameters included in the deterministic sensitivity analysis. For all of the conditions the model results are most sensitive to treatment start age and length, compliance and utility gain.
| Parameter | Baseline | Upper value | Lower value | ICER (£/QALY) | ||
|---|---|---|---|---|---|---|
| Upper value | Lower value | Range | ||||
| Dosage (mg/kg) | 0.025 | 0.039 | 0.023 | 35,917 | 21,379 | 14,538 |
| Utility gain per HtSDS | 0.061 | 0.073 | 0.049 | 19,776 | 28,047 | 8271 |
| Compliance (%) | 85 | 100 | 70 | 27,205 | 19,187 | 8018 |
| Treatment age (years) | 9–16 | 11–16 | 7–16 | 19,279 | 25,659 | 6380 |
| Cost of rhGH treatment (£/mg) | 21.06 | 23.19 | 18.00 | 25,493 | 19,895 | 5598 |
| Utility benefit spread over | 2 years | 1 year | 7 years | 22,732 | 25,638 | 2906 |
| SMR | 2.4 | 2.4 | 1 | 23,196 | 22,184 | 1012 |
| Parameter | Baseline | Upper value | Lower value | ICER (£/QALY) | ||
|---|---|---|---|---|---|---|
| Upper value | Lower value | Range | ||||
| Utility gain per HtSDS | 0.061 | 0.073 | 0.049 | 33,131 | 48,778 | 15,647 |
| Treatment age (years) | 10–16 | 12–16 | 8–16 | 30,505 | 45,105 | 14,600 |
| Compliance | 85% | 100% | 70% | 46,376 | 32,544 | 13,832 |
| Cost of rhGH treatment (£/mg) | 21.06 | 23.19 | 18.00 | 43,424 | 33,766 | 9658 |
| Dosage (mg/kg) | 0.045 | 0.05 | 0.4 | 43,815 | 35,106 | 8709 |
| Utility benefit spread over | 2 years | 1 year | 6 years | 38,672 | 42,753 | 4081 |
| SMR | 2.4 | 2.4 | 1 | 39,460 | 37,308 | 2152 |
| Parameter | Baseline | Upper value | Lower value | ICER (£/QALY) | ||
|---|---|---|---|---|---|---|
| Upper value | Lower value | Range | ||||
| Compliance (%) | 85 | 100 | 70 | 159,062 | 111,560 | 47,502 |
| Cost of rhGH treatment (£/mg) | 21.06 | 23.19 | 18.00 | 148,924 | 115,755 | 33,169 |
| Treatment age (years) | 7–15 | 9–15 | 5–15 | 119,036 | 144,159 | 25,123 |
| Utility benefit spread over (years) | 2 | 1 | 8 | 132,645 | 152,275 | 19,630 |
| Dosage (mg/kg) | 0.035 | 0.035 | 0.03 | 135,311 | 116,084 | 19,227 |
| Utility gain per HtSDS | 0.061 | 0.073 | 0.049 | 128,030 | 143,471 | 15,441 |
| SMR | 2.4 | 2.4 | 1 | 135,311 | 129,640 | 5671 |
| Parameter | Baseline | Upper value | Lower value | ICER (£/QALY) | ||
|---|---|---|---|---|---|---|
| Upper value | Lower value | Range | ||||
| Treatment age (years) | 9–14 | 11–14 | 7–14 | 28,080 | 46,477 | 18,397 |
| Utility benefit spread over | 2 years | 1 year | 5 years | 38,253 | 54,105 | 15,852 |
| Utility gain per HtSDS | 0.061 | 0.073 | 0.049 | 33,188 | 48,091 | 14,903 |
| Compliance (%) | 85 | 100 | 70 | 46,181 | 32,365 | 13,816 |
| SMR | 21 | 21 | 1 | 39,273 | 28,820 | 10,453 |
| Cost of rhGH treatment (£/mg) | 21.06 | 23.19 | 18.00 | 43,232 | 33,585 | 9647 |
| Dosage (mg/kg) | 0.045 | 0.05 | 0.04 | 43,623 | 34,923 | 8700 |
| Parameter | Baseline | Upper value | Lower value | ICER (£/QALY) | ||
|---|---|---|---|---|---|---|
| Upper value | Lower value | Range | ||||
| Utility gain per HtSDS | 0.061 | 0.073 | 0.049 | 27,641 | 41,180 | 13,539 |
| Treatment age (years) | 8–14 | 10–14 | 6–14 | 25,675 | 37,921 | 12,246 |
| Compliance (%) | 85 | 100 | 70 | 38,888 | 27,270 | 11,618 |
| Cost of rhGH treatment (£/mg) | 21.06 | 23.19 | 18.00 | 36,408 | 28,296 | 8112 |
| Dosage (mg/kg) | 0.035 | 0.04 | 0.035 | 37,781 | 33,079 | 4702 |
| Utility benefit spread over | 2 years | 1 year | 6 years | 32,422 | 35,818 | 3396 |
| SMR | 2.4 | 2.4 | 1 | 33,079 | 31,657 | 1422 |
| Parameter | Baseline | Upper value | Lower value | ICER (£/QALY) | ||
|---|---|---|---|---|---|---|
| Upper value | Lower value | Range | ||||
| Utility gain per HtSDS | 0.061 | 0.073 | 0.049 | 33,868 | 50,457 | 16,589 |
| Compliance (%) | 85 | 100 | 70 | 47,657 | 33,406 | 14,251 |
| Treatment age (years) | 7–14 | 9–14 | 5–14 | 33,787 | 44,666 | 10,879 |
| Cost of rhGH treatment (£/mg) | 21.06 | 23.19 | 18.00 | 44,615 | 34,664 | 9951 |
| Dosage (mg/kg) | 0.045 | 0.05 | 0.04 | 45,018 | 36,045 | 8973 |
| Utility benefit spread over | 2 years | 1 year | 7 years | 39,733 | 44,729 | 4996 |
| SMR | 2.4 | 2.4 | 1 | 40,531 | 38,822 | 1709 |
The deterministic sensitivity results for GHD are shown in Table 50. The results varied between £19,187 and £35,917 per QALY gained and were most sensitive to dosage.
The deterministic sensitivity results for TS are shown in Table 51. The results varied between 30,505 and £48,778 per QALY gained and were most sensitive to utility gain.
The deterministic sensitivity results for PWS are shown in Table 52. The results varied between £111,560 and £159,062 per QALY gained and were most sensitive to compliance.
The deterministic sensitivity results for CRI are shown in Table 53. The results varied between £28,080 and £54,105 per QALY gained and were most sensitive to the treatment start age and length of treatment.
The deterministic sensitivity results for SGA are shown in Table 54. The deterministic sensitivity results varied between £25,675 and £41,180 per QALY gained and were most sensitive to utility gain.
The deterministic sensitivity results for SHOX-D are shown in Table 55. The deterministic sensitivity results varied between £33,406 and £50,457 per QALY gained and were most sensitive to utility gain.
For patients with PWS there may be an additional health benefit associated with improved body composition, which may reduce the risk of diabetes and other morbidities. In addition, there is considerable difficulty estimating the magnitude of this effect and extrapolating short-term treatment in childhood to lifelong benefit. In the base case we have assumed that there is no HRQoL benefit associated with changes in body composition. In this section we present a scenario analysis for additional changes in body composition. However, there is a difficulty linking changes in lean FM to changes in utility, as there are no utility studies for lean FM. For this reason we have focused on changes in BMI.
Picot and colleagues168 conducted a targeted search to identify published utility estimates for the BMI values relevant to an adult obese population. The search aimed to identify estimates of the change in utility scores based on the unit change in BMI values. Utility estimates were considered only where they used a validated, multiattribute utility scale (e.g. EQ-5D) or appropriate methodology (e.g. SG or TTO techniques) and provided a clear definition of utility scores. They suggest the values reported by Hakim and colleagues169 represent the most methodologically sound estimates derived from subjects across a wide range of obesity levels. Hakim and colleagues169 found that a one-unit decrease in BMI, over a period of 1 year, was associated with a gain of 0.017, which was independent of age or gender.
In Chapter 3 (see Body composition), RCTs for PWS reported mixed results for changes in BMI with a maximum BMI difference of 1.8 kg/m2 between treated and untreated groups after 2 years’ treatment. Assuming this change in BMI is maintained lifelong, and therefore there is an additional utility of 0.031, the cost-effectiveness of PWS would be £54,800 per QALY gained.
Probabilistic sensitivity analyses
In the probabilistic sensitivity analyses (PSAs) the main parameters were sampled probabilistically from an appropriate distribution using similar ranges as used in the deterministic sensitivity analyses. The parameters sampled were: starting age, length of treatment, dose, HtSDS at the start and end of treatment for both the rhGH and no treatment cohorts, utility increment for gains in height and all costs used in the base case excluding the cost of rhGH.
The distribution assigned to each variable included in the PSA and the parameters of the distribution are reported in Appendix 12. One thousand simulations were run for each condition of interest in this analysis. Table 56 reports the mean costs and outcomes from the PSA and the ICER for rhGH compared with no treatment, based on the mean values generated in the PSA. Table 57 shows the 2.5% and 97.5% percentiles for the PSA.
| Condition | Treatment | QALYs | Costs (£) | Inc. QALYs | Inc. costs (£) | ICER (£/QALY) |
|---|---|---|---|---|---|---|
| GHD | No rhGH | 16.81 | 2277 | |||
| rhGH | 18.36 | 37,719 | 1.543 | 35,517 | 23,019 | |
| TS | No rhGH | 15.89 | 1952 | |||
| rhGH | 17.43 | 62,128 | 1.546 | 60,176 | 38,931 | |
| PWS | No rhGH | 17.61 | 2639 | |||
| rhGH | 18.19 | 67,716 | 0.576 | 65,076 | 113,075 | |
| CRI | No rhGH | 11.57 | 1874 | |||
| rhGH | 12.44 | 35,702 | 0.868 | 33,828 | 38,951 | |
| SGA | No rhGH | 17.09 | 2429 | |||
| rhGH | 18.06 | 34,283 | 0.966 | 31,854 | 32,963 | |
| SHOX-D | No rhGH | 16.80 | 2633 | |||
| rhGH | 18.07 | 53,027 | 1.267 | 50,394 | 39,781 |
| Condition | Incremental QALYs | Incremental costs (£) | ICERs | |||
|---|---|---|---|---|---|---|
| Min. | Max. | Min. | Max. | Min. | Max. | |
| GHD | 1.27 | 1.83 | 25,306 | 46,043 | 15,752 | 31,309 |
| TS | 0.77 | 2.35 | 43,478 | 77,707 | 21,758 | 81,026 |
| PWS | –0.33 | 1.43 | 49,419 | 78,677 | –838,603 | 1,055,815 |
| CRI | 0.43 | 1.30 | 21,580 | 44,294 | 21,553 | 77,929 |
| SGA | 0.52 | 1.48 | 23,179 | 40,773 | 19,945 | 64,614 |
| SHOX-D | 0.53 | 2.12 | 37,854 | 62,023 | 21,524 | 95,600 |
The cost-effectiveness results from the PSA are slightly lower than those from the deterministic analyses for GHD, TS, CRI, SGA and SHOX-D (which were £23,196, £39,460, £39,273, £33,079 and £40,531, respectively). The cost-effectiveness results from the PSA for PWS, however, are much lower than the deterministic estimates. This is due to non-linearity in the PWS model as a result of the baseline starting HtSDS for the treated group being at –2.0 HtSDS. This is also the height at which the utility gain per unit HtSDS changes and thus an individual with a starting height slightly lower than –2.0 HtSDS will have much higher utility gain than one with a starting height slightly higher than –2.0 HtSDS. This non-linearity results in a higher incremental QALY in the PSA results, therefore decreasing the ICER in the PSA.
Scatter plots are shown for the incremental cost and incremental QALYs for each of the conditions in Figures 2–7. The difference in the dispersion of costs and QALY data points between the six conditions reflects the different levels of uncertainty in each condition. The spread of costs and to a greater extent QALYs is more compact in GHD than for the other conditions. This is because the standard errors are much smaller due to the effectiveness data coming from the KIGS database, which has a large number of observations. This creates a tighter probability distribution around the mean value.
FIGURE 2.
Cost-effectiveness plane – incremental cost and incremental QALYs for rhGH treatment and no treatment in growth hormone deficiency.
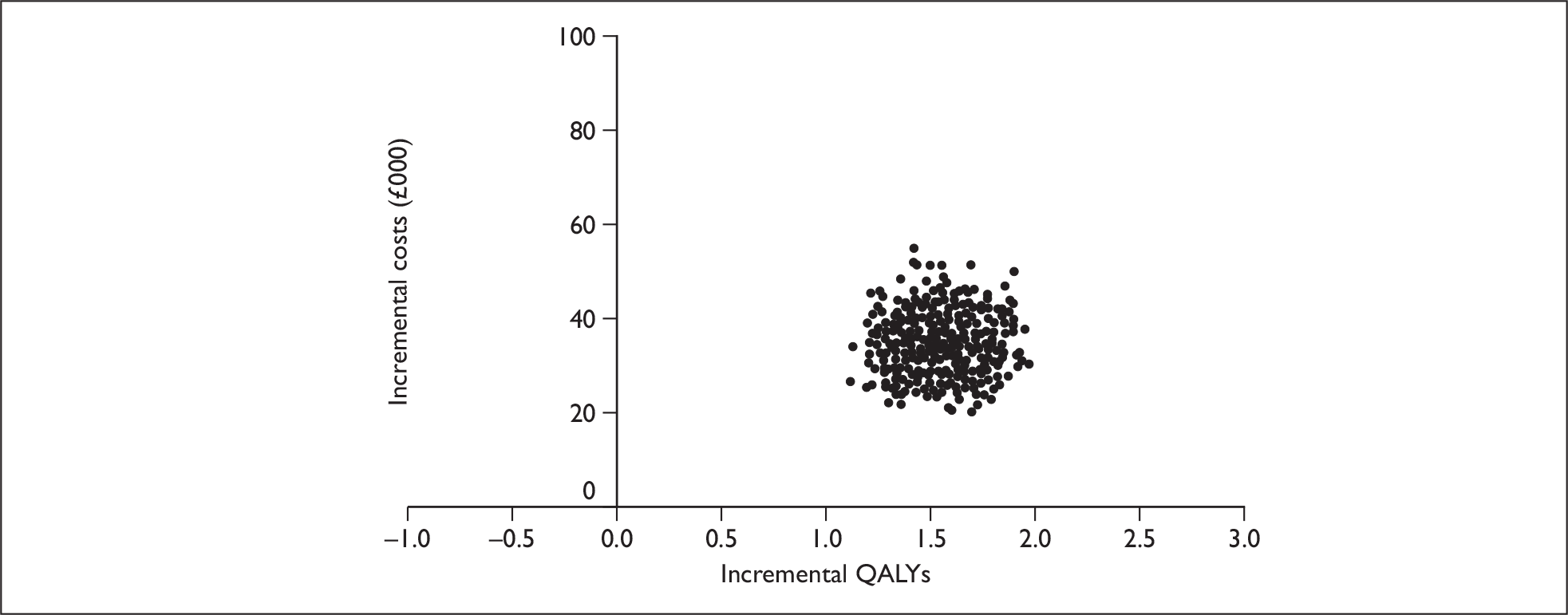
FIGURE 3.
Cost-effectiveness plane – incremental cost and incremental QALYs for rhGH treatment and no treatment in Turner syndrome.
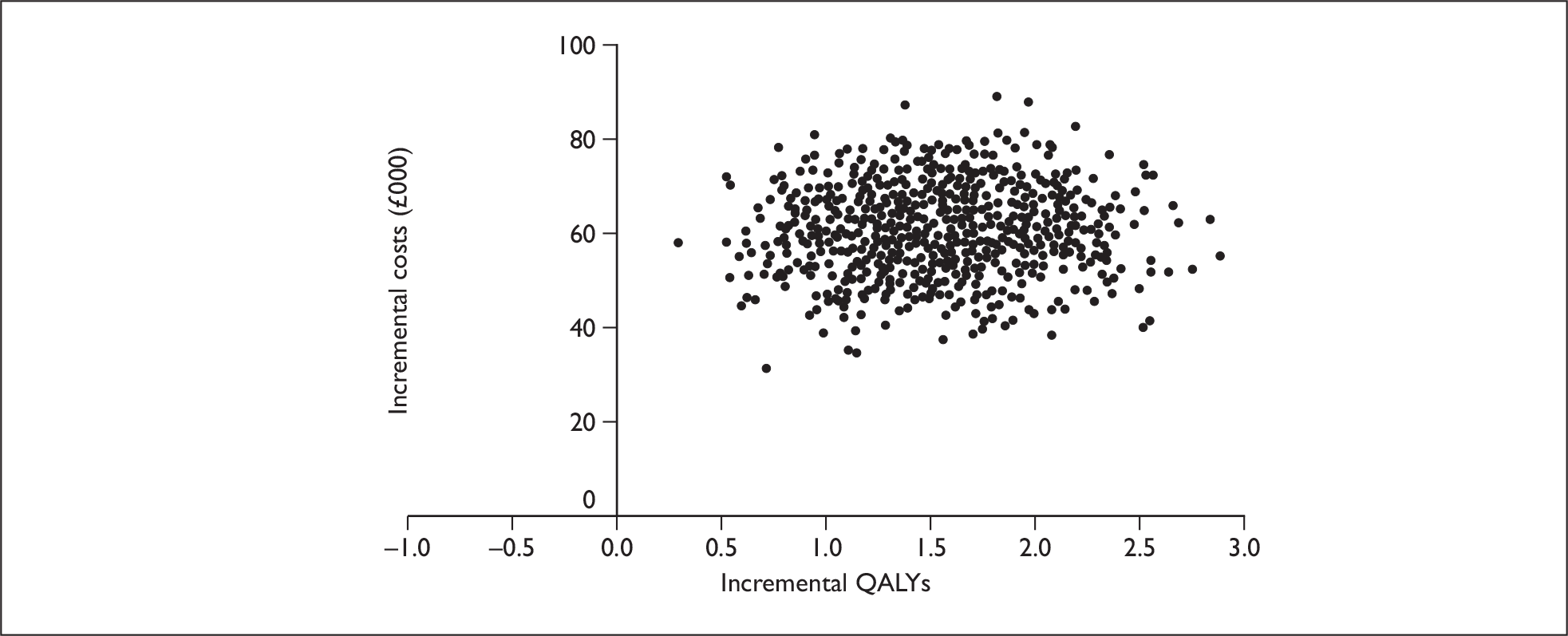
FIGURE 4.
Cost-effectiveness plane – incremental cost and incremental QALYs for rhGH treatment and no treatment in Prader–Willi syndrome.
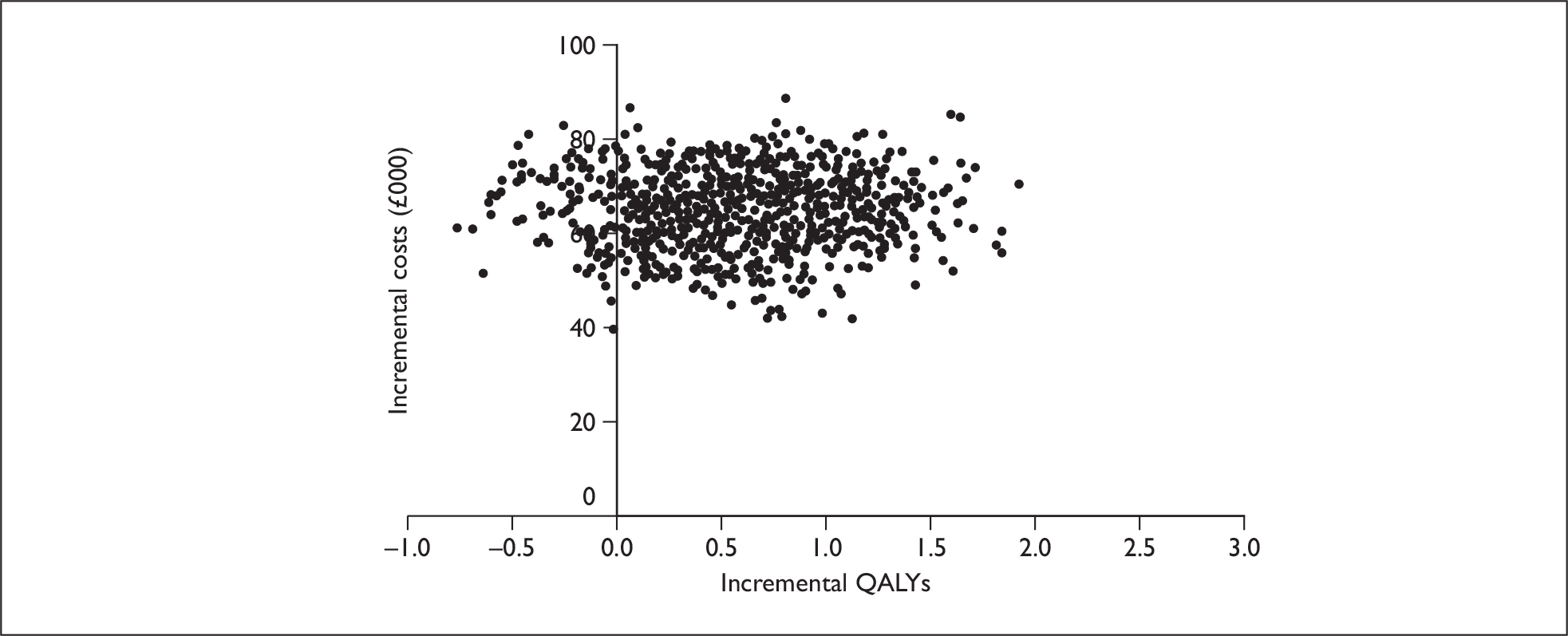
FIGURE 5.
Cost-effectiveness plane – incremental cost and incremental QALYs for rhGH treatment and no treatment in chronic renal insufficiency.
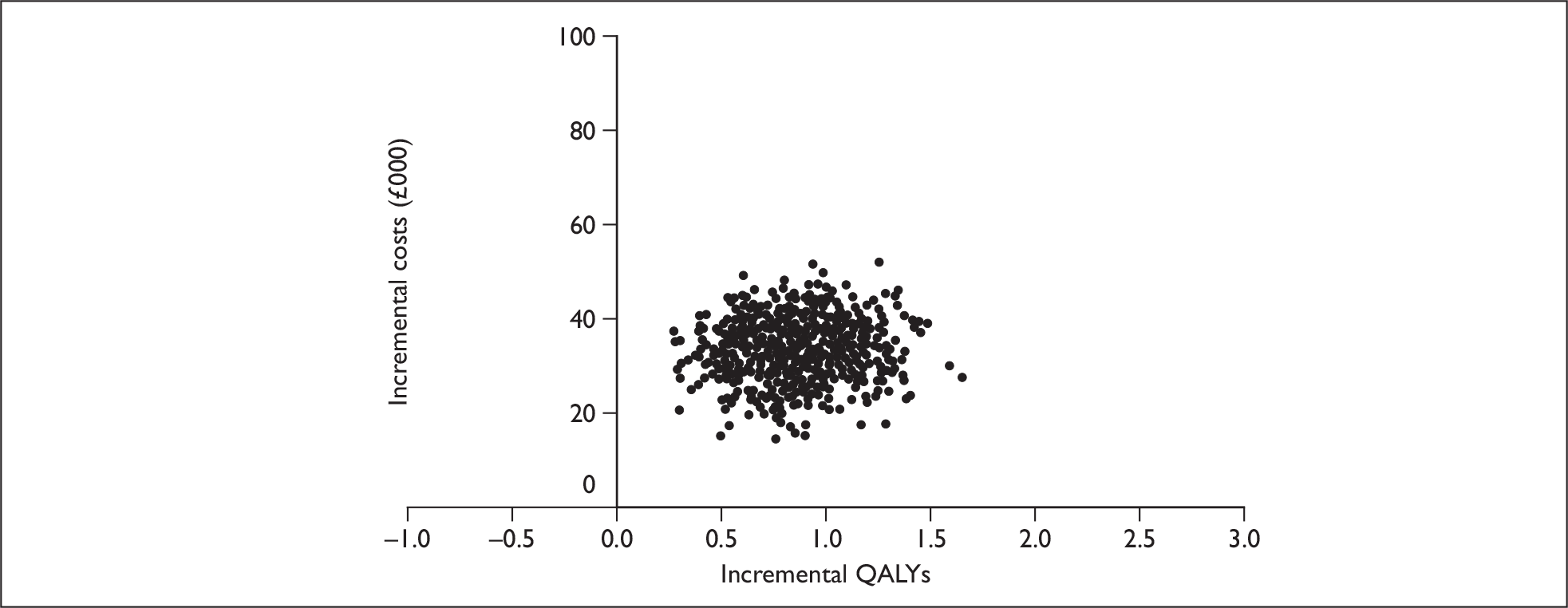
FIGURE 6.
Cost-effectiveness plane – incremental cost and incremental QALYs for rhGH treatment and no treatment for the condition ‘small for gestational age’.
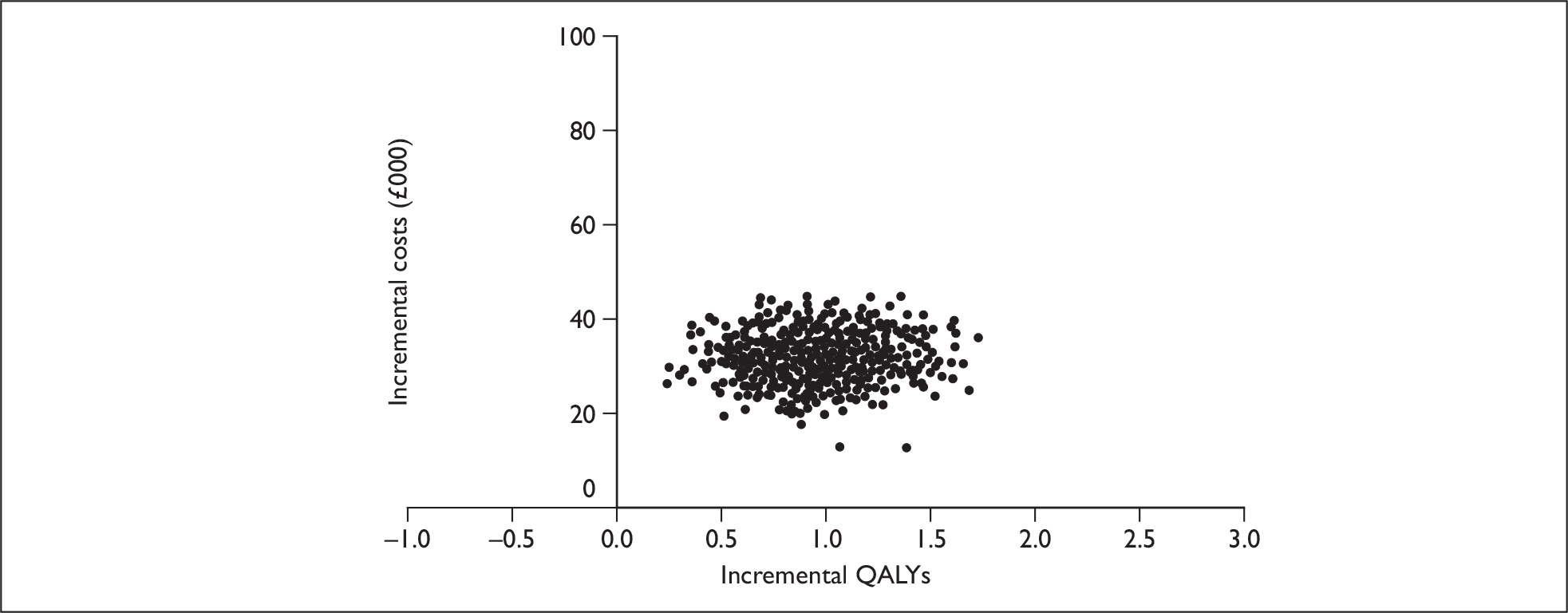
FIGURE 7.
Cost-effectiveness plane – incremental cost and incremental QALYs for rhGH treatment and no treatment in short stature homeobox-containing gene deficiency.
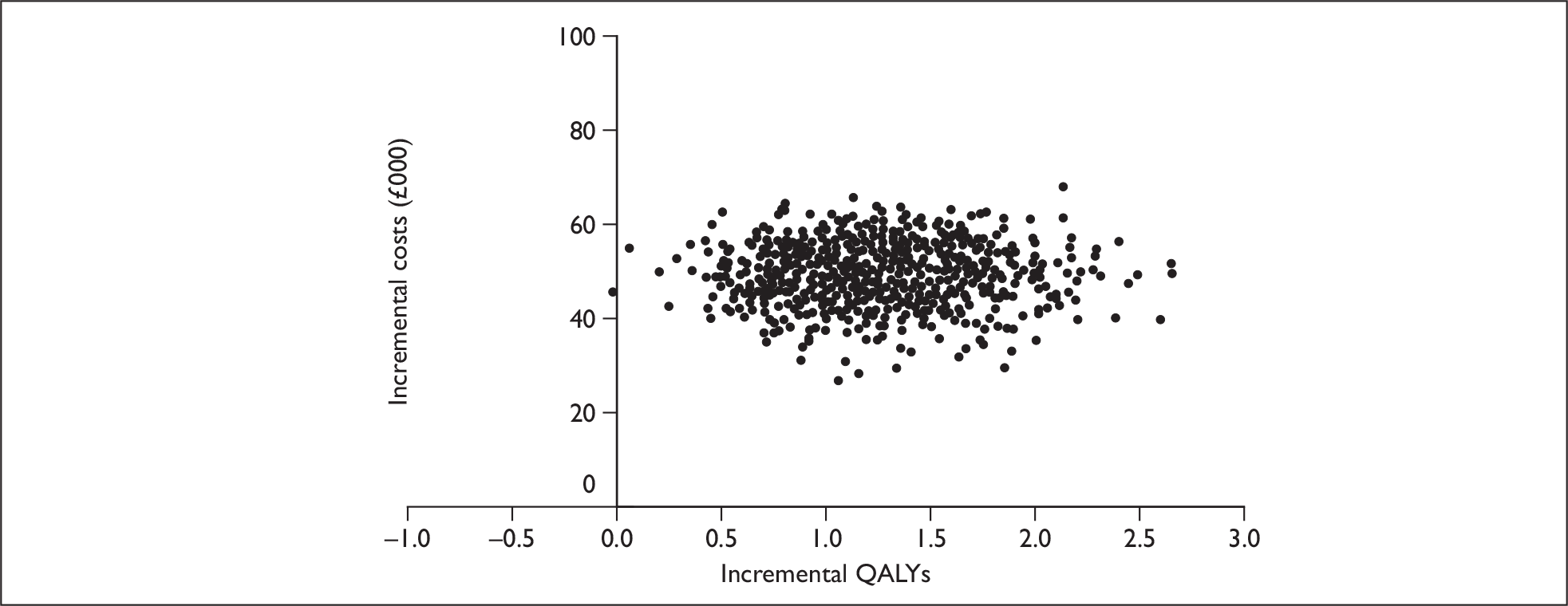
In addition, a CEAC was also derived, representing the proportion of simulations when GH treatment is cost-effective for a range of willingness-to-pay thresholds, up to £100,000, see Figure 8.
FIGURE 8.
Cost-effectiveness acceptability curve for rhGH treatment and no treatment for all the conditions.
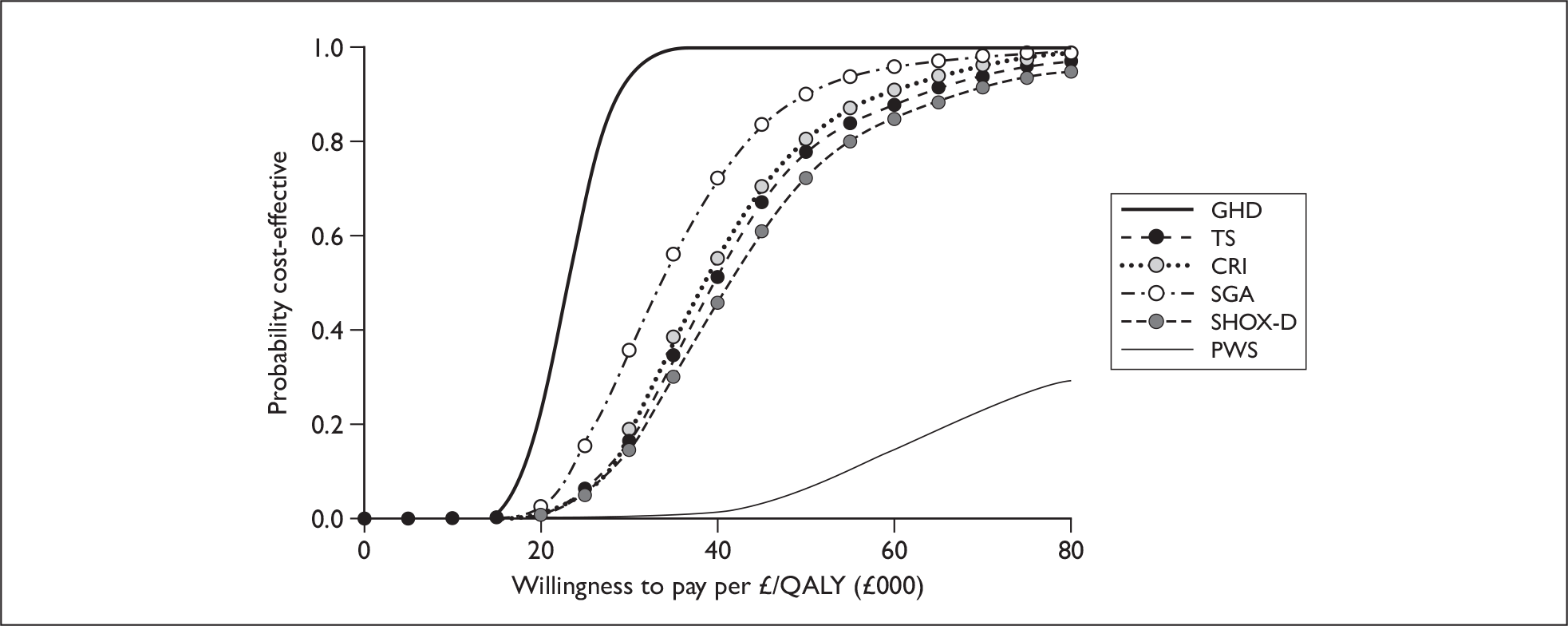
In this analysis, rhGH treatment had the probability of being cost-effective at willingness-to-pay thresholds of £20,000, £30,000 and £50,000 per QALY as: 22%, 95% and 100% for GHD, 2%, 19% and 78% for TS, 0%, 1% and 8% for PWS, 2%, 16% and 80% for CRI, 4%, 38% and 90% for SGA, and 1%, 15% and 74% for SHOX-D, respectively.
Summary of cost-effectiveness
-
A systematic search of the literature found two fully published economic evaluations of rhGH treatment for TS and GHD. The results from the studies varied due to the choice of utility estimates and assumptions on the effectiveness.
-
A systematic search for published studies of QoL for patients with individuals with the conditions of interest who had rhGH identified six studies, although none of these was in children. These were generally small studies of poor quality. One study was considered of reasonable quality. 147 This study estimated HRQoL for adults with GHD.
-
An additional targeted search was undertaken for QoL in relation to height, which identified one study150 that provided utility estimates based on the EQ-5D for different HtSDS from HSE.
-
Six of the seven manufacturers submitted evidence to be considered for this review. One MS by Sandoz did not comply with the NICE template for MTA and presented a description of the product (Omnitrope) and what appears to be a cost-minimisation analysis using Genotropin as a comparator (defined as a reference product). The other five out of the six MSs consisted of a written report and an electronic model supporting the cost-effectiveness analyses. This model was used by the five collaborating manufacturers involved in the submission to the MTA of rhGH in the cost-effectiveness analysis of treatment in children with GHD, TS, PWS, CRI and SGA.
-
Each of the collaborating manufacturers presented essentially the same model with some minor modifications. The model developed was based upon the previous HTA report6 but has been extended to consider longer term outcomes in order to estimate cost-effectiveness in terms of QALYs.
-
The utility scores used in the MS model in children with GHD, TS, CRI and SGA were based upon the study by Christensen and colleagues,150 which estimates QoL associated with height for a general population survey. However, they used the utility point estimates, based only on height, instead of the regression analysis from the study, which controlled for other key variables.
-
In the manufacturers’ base case, the cost-effectiveness results for all conditions were less than £30,000 per QALY gained. They estimated ICERs of: £17,552 for GHD, £29,757 for TS, £32,540 for PWS, £15,962 for CRI, and £18,167 for SGA per QALY gained.
-
The authors of this report developed an independent model, based upon the previous HTA report, and extended to consider longer term outcomes in order to estimate cost-effectiveness in terms of QALYs.
-
From this independent model, the incremental cost per QALY estimates of rhGH compared to no treatment were: £23,196 for GHD, £39,460 for TS, £135,311 for PWS, £39,273 for CRI, £33,079 for SGA and £40,531 for SHOX-D. A further analysis was run for PWS, which included a lifelong improvement of body composition of 1.8 kg/m2 BMI and an associated additional utility of 0.031. Under these assumptions there was a more favourable ICER of £54,800 per QALY gained.
-
The effect of a range of parameter values in the economic model were evaluated in sensitivity analyses. The model results were found to be most sensitive to the discount rate used. When the previous NICE discount rate of 6% for costs and 1.5% for benefits was used, all conditions were cost-effective for a willingness-to-pay threshold of £30,000 per QALY. The model results are also sensitive to treatment start age and length, compliance and utility gain.
-
The PSA estimated the probability of each of the conditions to be cost-effective at £30,000 to be: 95% for GHD, 19% for TS, 1% for PWS, 16% for CRI, 38% for SGA and 15% for SHOX-D.
Chapter 5 Assessment of factors relevant to the NHS and other parties
Guidance from NICE already recommends treatment with rhGH for children who have short stature that is associated with GHD, TS, PWS and CRI. Prescriptions associated with these conditions are therefore already part of primary care trusts’ (PCTs’) budgets, and are unlikely to increase significantly. However, advice from our clinical advisory group indicates that many families of children with PWS are now seeking treatment in infancy rather than in mid-childhood, and there may also be some increase in the number of prescriptions for GHD associated with oncology, as greater numbers of children are surviving childhood cancers. The newly licensed conditions SHOX-D and SGA are not covered by NICE guidance at the time of writing. Of the estimated 4758 UK patients currently receiving rhGH,74 a breakdown by diagnosis for 3951 of them found that only 5.2% (205 patients) were receiving treatment for short stature that was associated with being born SGA. Advice from our clinical advisory group indicates that there is unlikely to be a large increase in prescriptions for children who were SGA.
The BSPED survey74 did not include patients with SHOX-D, and it is not clear how many children with this condition are currently receiving treatment. Children with short stature due to unknown causes, or with other conditions, such as LWS, not currently covered by NICE guidance, might have an underlying SHOX-D. The availability of prescriptions to these new groups of patients could therefore have a budgetary impact. However, these conditions are very rare, so there is unlikely to be a large increase in people requiring treatment.
Chapter 6 Discussion
Statement of principal findings
Growth hormone deficiency
The use of rhGH as replacement therapy is well established in children who have a deficiency of the natural hormone. Therefore, most clinicians would consider it unethical to withhold treatment and there is a corresponding lack of RCT evidence in the literature. Only one trial84 met the inclusion criteria for the review of rhGH in children with GHD, and this did not report FH. No details were reported on randomisation or allocation to treatment groups or blinding. The included patients (n = 19) were part of a larger study, which was generally poorly reported. After a year’s treatment, HtSDS was statistically significantly higher in treated than in untreated children, although actual height was not reported. Children who received rhGH for 1 year had grown at a mean velocity of 2.7 cm/year faster than untreated children, which was statistically significantly faster. The low patient numbers mean that the evidence base for GHD is weak. Thus, there is very limited evidence of a slight increase in growth for children with GHD treated with GH, based on one study of mixed quality. Estimates of height gain in the previous HTA report6 suggested FH gains of approximately 1.3–1.6 SDS (i.e. within 2 SDs of the normal mean) with rhGH treatment. However, these figures were from retrospective single-cohort studies that were not included in the present review.
The cost-effectiveness estimate of rhGH treatment in GHD is about £23,200 per QALY gained or £2,800 per centimetre gained. As there were no appropriate RCTs, the KIGS database was used for the estimate of height gain from rhGH. 153 This estimate for height gain was higher than for the other conditions. The previous HTA report6 estimated a cost per centimetre gained of £6000 using 8 years’ treatment compared to the 7 years used in our analysis and a slightly lower height gain from the KIGS database. 153 The cost-effectiveness estimate for the cohort of GHD who continue rhGH treatment into adulthood was £28,200 per QALY gained and £3400 per centimetre gained.
Turner syndrome
Six trials met the inclusion criteria for the review of GH for growth disturbance in patients with TS. 12,85,86,88–90 There is some evidence of effectiveness across all reported growth outcomes for girls with TS. However, these results are reported in studies of poor reporting and methodological quality, and in some cases of short duration. Of the six included studies, none of the included trials used an ITT analysis, one reported adequate randomisation to treatment groups,85 one study described adequate concealment of treatment allocation,85 and one adequately blinded the patient to treatment by administering placebo. 89
In a large RCT that followed girls until FH, children in the rhGH group grew an average of 9.3 cm more from baseline than those in the untreated group. 86 In a study of younger children over 2 years, the difference was 7.6 cm. 85 Both of these were statistically significant results. Weight and WtSDS were found to be significantly greater in the treated group in one study of younger girls with TS. 85
The searches for this study identified a new systematic review, conducted in Canada in 2007. 135 The review concluded that rhGH is effective in improving growth and FH in girls with TS, but found no evidence available in the clinical trials to suggest that rhGH improves QoL. The evidence discussed in the present review reflects this, as we found some evidence for increased height but no RCT evidence for improvements in QoL.
In summary, there is some evidence of effectiveness across all reported growth outcomes for girls with growth disturbance as a result of TS. There is also evidence of improved body composition. These results are reported in studies of poor reporting and methodological quality, and, in some cases, short duration, issues that may affect the validity of these findings. The previous HTA report6 found that treated girls’ FH was approximately 5 cm taller than untreated controls. The full publication of the large Canadian RCT86 since the earlier HTA report6 has shown a slightly larger difference in FH of 9.3 cm, as reported in the present review.
The cost-effectiveness estimate of rhGH treatment in TS is about £39,500 per QALY gained, or £6500 per centimetre gained. The estimate of cost-effectiveness compares with the estimate of about £130,000 per QALY (at current exchange rates) from CADTH,135 which used a lower QoL benefit for rhGH of 0.042 than used in our analysis. The previous HTA report estimated a less favourable cost per centimetre gained of £16,000 as a lower estimate for height gain of 3.9 cm (compared with 9.3 cm) was used.
PWS
Eight small, rather poorly reported RCTs were included for PWS. 22,91–102 Participants’ average ages ranged from 13 months to 10 years. Only the crossover study102 used a placebo injection; the parallel-group RCTs had no treatment as the comparison arm.
Treated patients grew an average of 3–5 cm/year faster than untreated patients. Only one22 of the studies reported actual change in height, with infants treated with rhGH growing an average of 6.1 cm more than untreated patients during 1 year. HtSDS was statistically significantly greater in treated patients than in untreated patients after 1 year (1–1.5 SDS higher) or 2 years of rhGH treatment (> 2 SDSs).
Four22,95,96,102 trials reported a statistically significantly lower percentage of body fat (between 1% and 10% lower) in patients treated with rhGH than in those receiving placebo or no treatment. Three93,95,96,102 trials reported that patients treated with rhGH had statistically significantly higher LBM or a larger improvement in LBM than untreated patients. Clinical advice indicates that rhGH characteristically increases LBM and reduces FM, although weight and BMI do not always change. This is reflected in the RCTs’ findings, where changes in BMI were statistically significant in two studies,91,102 there were no statistical differences in two other studies,93,95,96 and results were similar between groups in the other two studies. 92,100,101
In summary, patients treated with rhGH grew faster than untreated patients, and tended to have lower body fat percentages. Measurements in treated patients were reported to be statistically significantly better than in untreated patients in several studies, but the included studies were rather small and did not report power calculations or specify a primary outcome, so it is not clear whether they were adequately powered. These findings were comparable with growth and body composition outcomes reported in the previous HTA review. 6 However, the previous review also reported an uncontrolled, single-cohort study of 16 children, which suggested that rhGH treatment normalised FH.
The cost-effectiveness estimate of rhGH treatment in PWS is about £135,300 per QALY gained or £5,900 per centimetre gained. The ICER values for PWS were higher due to the majority of the height gain occurring within –2 HtSDS of average height where a lower utility gain is experienced. The previous HTA report6 presented a cost per HtSDS gained of £40,815 and this compares with the current report’s estimate of £44,718.
For PWS patients, there may be an additional health benefit associated with improved body composition, which may reduce the risk of diabetes and other morbidities. There is considerable difficulty with extrapolating between childhood treatment and adult morbidity and QoL.
In the clinical effectiveness review, RCTs for PWS reported mixed results for changes in BMI, with a maximum BMI difference of 1.8 between treated and untreated groups after 2 years’ treatment. Assuming this change in BMI is maintained lifelong, and therefore there is an additional utility of 0.031, the cost-effectiveness of PWS would be £54,800 per QALY gained.
Chronic renal insufficiency
The evidence for rhGH in children with CRI came from six RCTs,103–108 three of which had fewer than 25 participants,103–105 and these might not have been sufficiently powered to test for a real difference between groups. Three103,105,107 of the studies included children who had received renal transplants, and three104,106,108 were for children with CRI who had not had a transplant.
One study106 reported that treated children grew an average of 3.6 cm more than untreated children in 1 year, with HtSDS being statistically significantly better in treated children than in untreated children in two studies. Growth was statistically significantly faster in treated children than in untreated children, with between-group differences in velocity ranging from 3.2 cm/year to 4.2 cm/year in the parallel-group trials. 103,106–108 Children treated with rhGH showed statistically significant improvements in weight gain or WtSDS compared with untreated children in three studies. 103,106,108 No QoL data were reported for prepubertal children with CRI. Two rhGH-treated patients in one study91,102 experienced acute rejection episodes but both reversed after treatment with methylprednisolone. There were no SAEs reported.
In summary, treatment with rhGH led to small but statistically significant improvements in growth in children with CRI in two trials,106,107 one of which included post-transport patients and the other included children with CRI who had not received a transplant. The previous HTA review6 reported differences in HtSDS of approximately 0.8 SD and 1.3 SD for 1 and 2 years of treatment, respectively. The present review found slightly greater differences, favouring rhGH, of approximately 1 SDS for 1 year and just over 2 SDSs for 2 years’ treatment.
The cost-effectiveness estimate of rhGH treatment in CRI is about £39,300 per QALY gained or £3,700 per centimetre gained. The previous HTA report estimated a cost per centimetre gained of £7,403 and this was based upon treatment for only 3 years compared with 5 years in this analysis. CRI has a lower QALY gain than the other conditions as we assumed that children with CRI would have a much shorter life expectancy than the general population due to their renal failure.
SGA
The licensing criteria for rhGH in children born SGA with growth disturbance state that eligible children need to have a current HtSDS ≤ –2.5, a parental-adjusted HtSDS ≤ –1, a birth weight/length SDS ≤ –2 SDS, and have failed to show catch-up growth, defined as GV SDS < 0 during the previous year, by 4 years of age or later. None of the RCTs screened for this review met the inclusion criteria; these were therefore modified, retaining the current height and birth weight/length SDS criteria. Studies’ inclusion criteria were required to state that no catch-up growth had taken place by 3 years of age but no specific criteria were used for this. The amended inclusion criteria did not require any definition of parental height.
This could affect the generalisability of the results as it is possible that the trials included children with a genetic factor for short stature. However, such children would presumably have a shorter target height than children whose parents are closer to the population mean. So children who meet the marketing authorisation may actually have a greater possibility for increased growth than those in the clinical trials. The other difference between the marketing authorisation criteria and the adapted inclusion criteria used in this review was that the included trials had children as young as 3 years of age, whereas the licensed population in the UK is children over the age of 4 years. It is possible that an early start for treatment could lead to better results than would be generalisable to the licensed population. However, in practice, the mean age of the children in the included studies was over 4 years of age for all the trials, so results should be generalisable to the licensed population.
Six trials met the modified inclusion criteria for this review of growth disturbance in children born SGA. 109–114 However, only one of the studies used the licensed dose for rhGH;26 the others all used two or three times the licensed dose. Several trials did not meet the inclusion criteria for this review as they included patients with heights of < –2 SDS rather than < –2.5 SDS as stated in the marketing authorisation. These are listed in Appendix 5, with reason for exclusion given as ‘wrong patient group’.
One trial reported AH,111 and patients who had received rhGH gained an extra 4 cm of height compared with the control group. The difference between treated and untreated patients was statistically significant, as was the difference in adult HtSDS. Another study114 reported that patients who received 0.033 mg/kg/day rhGH (the licensed dose) gained an additional 3.3 cm height compared with untreated children, and those who received 0.1 mg/kg/day gained 6.5 cm of additional height after 1 year’s treatment. HtSDS was found to be greater in children treated with GH in the four studies that reported this outcome. 110,111,113,114
Weight standard deviation score was higher in treated than in untreated groups after both 1 and 2 years of treatment in three studies reporting this outcome. 109,110,113 Lean mass was reported in one study, being greater in the treated group.
There is very limited evidence of a slight increase in AH gained in centimetres and SDS, and some evidence of an increase in HtSDS in children receiving rhGH in these studies. There is also limited evidence of improved body composition outcomes, including a statistically significant mean difference in WtSDS between treated and untreated children. This evidence is from trials that did not meet the licensed inclusion criteria exactly, used higher than the licensed dose in all but one study, and were generally of poor quality, with few participants in many cases.
The cost-effectiveness estimate of rhGH treatment in SGA is about £33,000 per QALY gained or £9700 per centimetre gained. The height gain from the clinical review indicated that the gain for SGA was smaller than for the other conditions.
SHOX deficiency
Only one study49 reported the use of rhGH in children with SHOX-D, and this was open label and generally poorly reported. Treated children grew approximately 2 cm/year faster than their untreated counterparts after 2 years of treatment, with a rate of 3.5 cm/year quicker than untreated children during the first year. After 2 years of treatment, children were approximately 6 cm taller than the control group and HtSDS was statistically significantly higher in treated than in untreated patients. Treatment with rhGH raised IGF-1 and IGFBP-3 levels to the upper-normal range, but there were no SAEs reported during the study.
The ICER estimate of rhGH treatment in SHOX-D is about £40,500 per QALY gained or £8000 per centimetre gained.
General discussion
This review updates a previous assessment report. 6 The criteria for this extended review were broadened to include children with SHOX-D or who were born SGA, as well as those with GHD, TS, PWS or CRI. In addition, we actively searched for all outcome measures including growth, body composition, biochemical markers and QoL.
The review focuses on increase in height as ‘centimetres gained’ and also as HtSDS, i.e. a comparison with average heights for the child’s peer group. One goal of treatment is to prevent future loss of height, i.e. a child may remain short compared with their peers, but still be taller than they would have been without treatment. This is an important outcome, especially where attainment of average AH is sometimes an unrealistic possibility. Unrealistic expectations of height gain have been shown to affect QoL. For example, a French survey of young women with TS found that higher expectations from treatment were associated with lower QoL scores. 146 This review identified a paucity of evidence for QoL data in children receiving rhGH, and as such it is difficult to quantify the way in which a child’s life can be changed by treatment other than in terms of centimetres of height gained.
In the previous HTA report,6 a cost-effectiveness model was constructed that estimated lifetime treatment costs and benefits in terms of cost per centimetre gained. Those analyses are extended in the present report by including QoL factors in the economic modelling. The cost-effectiveness of rhGH has been evaluated by decision-analytical models using clinical trial data for the gain in height, apart from GHD, which used KIGS data. 153 The analysis presented both cost-per-QALY outcomes and cost per centimetre height gained for comparison with the previous HTA report, as shown in Tables 58–60.
| GHD | TS | PWS | CRI | SGA | SHOX-D | |
|---|---|---|---|---|---|---|
| Incremental QALYs | 1.54 | 1.54 | 0.48 | 0.87 | 0.97 | 1.25 |
| Incremental costs (£) | 35,820 | 60,787 | 65,148 | 34,001 | 31,999 | 50,788 |
| ICER (£/QALY) | 23,196 | 39,460 | 135,311 | 39,273 | 33,079 | 40,531 |
| Height gain (cm) | 12.8 | 9.3 | 11.1 | 9.2 | 3.3 | 6.3 |
| Cost per cm gain (£) | 2798 | 6536 | 5869 | 3696 | 9697 | 8062 |
| GHD | TS | PWS | CRI | SGA | |
|---|---|---|---|---|---|
| Incremental QALYs | 3.48 | 2.83 | 2.3 | 2.53 | 2.98 |
| Incremental costs (£) | 61,124 | 84,078 | 74,849 | 40,325 | 54,088 |
| ICER (£/QALY) | 17,552 | 29,757 | 32,540 | 15,962 | 18,167 |
| Height gain (cm) | 32.24 | 7.95 | 25.59 | 4.48 | 21.92 |
| Cost per cm gain (£) | 1896 | 10,576 | 2925 | 9001 | 2467 |
| GHD | TS | PWSa | CRI | |
|---|---|---|---|---|
| Incremental costs (£) | 53,373 | 61,770 | 56,663 | 54,009 |
| Height gain (cm)b | 8.85 | 3.9 | 1.36 | 7.29 |
| Cost per cm gain (£) | 6029 | 15,997 | 40,815 | 7403 |
The cost-effectiveness results from the SHTAC model for rhGH treatment vary widely between conditions, from about £23,000 for GHD to £135,000 for PWS per QALY gained. The ICERs for TS, CRI and SGA and SHOX-D were between about £33,000 and £40,500 per QALY gained. This indicates that rhGH is unlikely to be cost-effective for TS, PWS, CRI, SGA and SHOX-D at a willingness-to-pay threshold of £20,000 to £30,000. However, the results were sensitive to the discount rate used. All conditions, except PWS, would be cost-effective at a £30,000 willingness-to-pay threshold using the previous NICE discount rate of 6% for costs and 1.5% for benefits. For all the conditions, the model results are most sensitive to treatment start age and length, compliance and utility gain.
The cost-effectiveness results in the current report varied from those in the MS and the previous HTA report. 6 The incremental costs reported are generally consistent between the three models, with slight variations due to different dose, cost, and treatment start age and duration. In general, the results, presented in terms of centimetres gained, are more favourable in the current analyses than in the previous HTA report. 6 This is due to higher estimates in height gain and lower incremental costs in the current report. The height gains in the MS for GHD, PWS and SGA appear extremely high and inconsistent with those found in the review of clinical effectiveness. The ICERs in the MS are considerably more favourable than the current analysis, due to higher estimates of utility gain. The current analyses and the MS have chosen utility estimates from the same study. 150 However, the manufacturers have not taken these values from the regression analysis from this study. Instead they have used the relationship between EQ-5D and height without controlling for other factors.
In general, the incremental costs consist primarily of the rhGH drug costs, while other costs have little effect on model results. For the cost-effectiveness results, the key issue is the choice of utility values. The utility gain from rhGH is assumed to last over the patients’ lifetimes and hence most of the QALY gain is in adulthood.
The results were sensitive to the length of treatment, for example by treating children from an earlier age. Current best practice is usually regarded as treating children as early as possible and this is likely to mean a longer treatment duration, which increases the cost of treatment and thus the ICER. It is unclear whether there will be an associated extra increase in height as most of the RCTs followed up children for a short time period, for less than 3 years. The previous HTA report suggested that height gains were greatest in the first year or two of treatment but stopping treatment before achieving FH generally leads to loss of growth gains, and so should not be advised.
The results were sensitive to the clinical effect. The treatment effect has been obtained, where possible, from the best-quality RCT available. However, as indicated in Chapter 3 (see Results), these trials were generally of poor quality and were not long-term trials. We also used the clinical treatment effect from the KIGS observational study but the results were largely similar to those reported from the RCTs.
There are limitations to the QoL estimates used in the model. There was a lack of good QoL studies conducted in the conditions of interest. Therefore, evidence based on these studies was not used in the main analysis. The utility estimates were based upon a study that estimated utility in the general adult population according to height. The study provides a common utility gain that could be compared across all the conditions of interest. Furthermore, it also provided the possibility the outcomes from the RCTs identified in the clinical effectiveness could be used. However, this still remains a major source of uncertainty in the model.
The QoL gains were highest for individuals with lower starting height; for those with starting height < –2 HtSDS the QoL gain was minimal. For example, those with PWS had a starting height of –2 HtSDS, and so for this group of patients the health gain is small and therefore rhGH has high ICER values compared with no treatment. Patients with PWS may experience an improvement in body composition due to rhGH but this was difficult to quantify, especially in the long term, due to lack of long-term data.
The current analysis assumes in the base case that all children with the conditions of interest will have reduced life expectancy. This was based upon some evidence to suggest that these children would have a lower life expectancy due to increased risk of cardiovascular disease, due to abdominal obesity and raised blood pressure. Furthermore, those children with CRI have a much reduced life expectancy. We have used the end-stage renal disease mortality rates as a proxy in the absence of any available data for CRI. This may underestimate life expectancy and overestimate ICER values, as not all patients with CRI will go on to develop end-stage renal disease. Bengtsson170 suggests that rhGH can rectify most of the cardiovascular abnormalities associated with GHD, although there appear to be few long-term observational studies that confirm this claim. Therefore, we assumed that rhGH will not increase life expectancy.
Apart from as a scenario analysis for PWS, the current analysis has not considered other benefits in addition to height gain within the model. The base case does not include possible benefits from changes in body composition, such as reduced risk of diabetes or cardiovascular disease, which may even result in increases in life expectancy. At this stage, these health gains would be purely speculative and it is not possible to verify if they exist or quantify them. It is also possible that there may be additional psychological benefits such as improved self-esteem.
Strengths and limitations of the assessment
Strengths
-
The systematic review and economic evaluation were carried out independently, with no vested interest, and results are presented in a consistent and transparent manner.
-
Evidence for clinical effectiveness came from RCT data, considered to be the highest level of evidence.
-
The project followed established methodology and principles for conducting a systematic review. The methods used were defined a priori in a research protocol (see Appendix 1), and this was circulated to clinical experts and agreed with NICE before the project started.
-
A clinical advisory group reviewed and commented on drafts of the protocol and the final report.
-
A de novo economic model was developed following recognised guidelines.
Limitations and uncertainties
As specified in the protocol, the systematic review was restricted to RCTs, because these provide the highest level of evidence for clinical effectiveness. The majority of the studies included in this review lasted for between 6 months and 2 years, with very few continuing long term or to AH. Many of the trials excluded patients from analyses due to incomplete follow-up data or patient withdrawal. The short duration of the RCTs means it is difficult to assess effectiveness of rhGH in the context in which it would be prescribed in real life, i.e. for many years in some cases.
None of the RCTs included in this review reported any assessment of QoL issues, and the literature has conflicting conclusions regarding the effect of short stature on QoL. It is therefore difficult to make any judgement about the impact of rhGH on the quality of a person’s daily life. Many of the children with the health conditions covered in this review will have a variety of other physical problems. While rhGH treatment can help to improve growth, height and body composition to some extent, QoL issues associated with underlying health problems will continue to affect some children.
Given the lack of QoL data for this patient group, it is possible that QALYs do not capture all the benefits of treatment for these children.
We did not identify any RCTs that met the original inclusion criteria for children born SGA. Following discussion with NICE, we therefore amended the criteria as detailed in Chapter 3 (Inclusion and data extraction process). The main difference was that we included studies of children who failed to show catch-up growth by 3 years of age (rather than 4 years) but did not specify exact criteria for this. Although this will have allowed slightly younger children to be included, the evidence presented in this report is still relevant to the UK SGA population. We also removed the reference to parental height, so it is possible that children in the included trials were naturally shorter than those in the general population. Only one of the included trials used the licensed dose, so results from the other five could overstate the effectiveness of rhGH treatment for this patient group.
We found only one RCT of rhGH in children with GHD,84 so the evidence base for this condition is rather weak. However, the previous HTA report6 also included observational studies for GHD, TS, PWS and CRI. Non-randomised evidence for this condition has therefore been summarised previously in the literature and is publicly available.
The included trials were generally poorly reported, and often had low numbers of participants. Primary outcomes were not clearly specified, and few studies reported power calculations. It is therefore possible that some trials were underpowered to detect ‘real’ differences between the treatment groups, even where such differences were reported to be statistically significant.
The included studies were heterogeneous in terms of participants, dosages and study duration. The results are therefore presented as a narrative summary, and it was not appropriate to meta-analyse the data.
The review did not assess publication bias or selective reporting of outcomes, so it is not possible to comment on the degree to which these affect the evidence base.
The economic model used the suggested doses given in the BNF. 165 However, the RCTs used doses that were sometimes outside the licensed doses.
Chapter 7 Conclusions
Implications for service provision
Guidance from NICE already recommends treatment with rhGH for children who have short stature that is associated with GHD, TS, PWS and CRI, so prescriptions associated with these conditions are already in place. Advice from our clinical advisory group indicates that there may be a trend towards earlier prescribing for PWS, and many families are now seeking treatment in infancy rather than in mid-childhood. There may also be an increase in treatment associated with acquired GHD as the proportion of children surviving cancers and associated treatment increases.
The newly licensed conditions SHOX-D and SGA are not covered by NICE guidance at the time of writing. Of the estimated 4758 UK patients currently receiving rhGH, only approximately 5% were receiving treatment for short stature associated with being born SGA. A recent survey by BSPED found that there had been little change in the number of prescriptions in recent years. 74
It is not clear how many children with SHOX-D are currently receiving treatment. The availability of prescriptions to these new groups of patients could theoretically have a budgetary impact. However, the number of children with this condition is small so there is unlikely to be a large increase in prescriptions.
Suggested research priorities
-
There is a lack of RCT evidence for the effects of rhGH treatment on FH, as it is impractical to run such long studies. However, longer studies beyond 2 years would be helpful in improving the evidence base for long-term treatment, even if near-FH rather than final AH were reported.
-
None of the included RCTs reported measures of HRQoL. There is a need to develop and validate a standardised QoL assessment that is specifically designed for children and adults. Future RCTs should include this as an outcome measure in order to assess the impact of small increases in height on daily QoL. This would also be helpful for developing utilities for cost-effectiveness analysis of rhGH treatment for these conditions.
-
Good-quality trials of continuation/discontinuation of rhGH in children who have finished growing are required, which report consistent and clinically relevant outcomes, and which are standardised in terms of dose.
-
Good-quality trials are needed of GH in children born SGA, where the children included and the dose administered match the licensing criteria.
-
It was difficult to establish when treatment is initiated for the different disease areas, as this depends on age at diagnosis. Further work to survey national practices or policies would be helpful in terms of providing information for future updates of this review and economic evaluation.
-
Although figures for the use of renal replacement therapy are available, there is little epidemiological data available on the incidence and prevalence of CRI. Epidemiological studies would therefore be useful.
-
Good-quality observational studies are needed, which show the long-term effects of rhGH, particularly the effect of treatment on body composition, psychological benefits (such as improved self-esteem), long-term morbidities (such as diabetes or cardiovascular disease) and life expectancy, particularly for PWS.
-
Further research is also necessary to establish the QoL benefits associated with rhGH in adults and children with these conditions. Well-conducted qualitative studies could provide data to inform future developments in this area.
-
Monitoring of AEs associated with long-term rhGH treatment is required, with a central register to record the effects of long-term elevations in IGF-1 levels.
-
More research is needed to assess the long-term effect on QoL for individuals who had rhGH as children.
Acknowledgements
We would like to thank members of our advisory group who provided expert advice and comments on the protocol and/or a draft of this report: Dr Justin Davies, Consultant in Paediatric Endocrinology, Southampton University Hospital Trust; Dr Justin Warner, Consultant in Paediatric Endocrinology and Diabetes, University Hospital of Wales; Ms Pauline Musson, Paediatric Endocrine Nurse Specialist, Southampton University Hospital Trust, and two anonymous clinical experts (one paediatric endocrinologist and one adult endocrinologist). We are also grateful to: David Turner, WIHRD (Health Economist) for work on the protocol; Liz Hodson, Library Assistant, WIHRD, University of Southampton; and Jill Colquitt, Senior Research Fellow, SHTAC, University of Southampton, for retrieving references and reviewing a draft of this report, respectively.
Contribution of authors
Development of protocol Andrea Takeda, Jackie Bryant, Louise Baxter, Keith Cooper.
Epidemiology/background Andrea Takeda, Louise Baxter, Jackie Bryant, Geoff Frampton.
Literature searching Karen Welch.
Inclusion screening Louise Baxter, Andrea Takeda.
Data extraction/critical appraisal Louise Baxter, Andrea Takeda.
Health economics Keith Cooper, Alex Bird, Elena Gospodarevskaya.
Drafting of report Andrea Takeda, Louise Baxter, Keith Cooper, Alex Bird, Jackie Bryant, Geoff Frampton, Elena Gospodarevskaya.
Project co-ordinator Andrea Takeda.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Kirk J, Butler G. Treatment of children with recombinant human growth hormone (r-hGH). Shared Care Guidelines; 2006.
- Rosenfeld RG. Editorial: Is growth hormone deficiency a viable diagnosis?. J Clin Endocrinol Metab 1997;82:349-51.
- Juul A, Bernasconi S, Clayton PE, Kiess W, DeMuink-Keizer Schrama S. and Drugs and Therapeutics Committee of the European Society for Paediatric Endocrinology (ESPE) . European audit of current practice in diagnosis and treatment of childhood growth hormone deficiency. Horm Res 2002;58:233-41.
- Warner J. and British Society for Paediatric Endocrinology and Diabetes . Submission of Evidence for the National Institute of Clinical Excellence Health Technology Appraisal: The Use of Human Growth Hormone in Children (review) 2008.
- Growth Hormone Research Society . Consensus guidelines for the diagnosis and treatment of growth hormone (GH) deficiency in childhood and adolescence: summary statement of the GH research society. J Clin Endocrinol Metab 2000;85:3990-3.
- Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al. Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation. Health Technol Assess 2002;6.
- UK Child Growth Foundation . Growth Hormone Deficiency n.d. www.childgrowthfoundation.org/ghd.htm (accessed 12 May 2008).
- Thomas M, Massa G, Craen M, de Zegher F, Bourguignon JP, Heinrichs C, et al. Prevalence and demographic features of childhood growth hormone deficiency in Belgium during the period 1986–2001. Eur J Endocrinol 2004;151:67-72.
- Stochholm K, Gravholt CH, Laursen T, Jorgensen JO, Laurberg P, Andersen M, et al. Incidence of GH deficiency: a nationwide study. Eur J Endocrinol 2006;155:61-7.
- Turner H. A syndrome of infantilism, congenital webbed neck, and cubitus valgus. Endocrinology 1938;23:566-74.
- Bondy CA. Clinical practice guideline: care of girls and women with Turner syndrome: a guideline of the Turner Syndrome Study Group. J Clin Endocrinol Metab 2007;92:10-25.
- Quigley CA, Crowe BJ, Anglin DG, Chipman JJ. Growth hormone and low dose estrogen in Turner syndrome: results of a United States multi-center trial to near-final height. J Clin Endocrinol Metab 2002;87:2033-41.
- Rao E, Weiss B, Fukami M, Rump A, Niesler B, Mertz A, et al. Pseudoautosomal deletions encompassing a novel homeobox gene cause growth failure in idiopathic short stature and Turner syndrome. Nat Genet 1997;16:54-63.
- Gravholt CH. Epidemiological, endocrine and metabolic features in Turner syndrome. Eur J Endocrinol 2004;151:657-87.
- WHO Collaborating Centre for the Epidemiological Surveillance of Congenital Anomalies n.d. www.eurocat.ulster.ac.uk/pdf/EUROCAT-Annual-Report-2005-for-WHO.pdf (accessed 22 April 2009).
- Massa G, Verlinde F, De SJ, Thomas M, Bourguignon JP, Craen M, et al. Trends in age at diagnosis of Turner syndrome. Arch Dis Child 2005;90:267-8.
- Stochholm K, Juul S, Juel K, Naeraa RW, Gravholt CH. Prevalence, incidence, diagnostic delay, and mortality in Turner syndrome. J Clin Endocrinol Metab 2006;91:3897-902.
- Paterson WF, Donaldson MD. Growth hormone therapy in the Prader–Willi syndrome. Arch Dis Child 2003;88:283-5.
- Cassidy SB. Prader–Willi syndrome. Characteristics, management, and etiology. Alabama J Med Sci 1987;24:169-75.
- Chen C, Visootsak J, Dills S, Graham JM. Prader–Willi syndrome: an update and review for the primary pediatrician. Clin Pediatr 2007;46:580-91.
- Butler M. Prader–Willi syndrome: current understanding of cause and diagnosis. Am J Med Genet 1990;35:319-32.
- Carrel AL, Moerchen V, Myers SE, Bekx MT, Whitman BY, Allen DB. Growth hormone improves mobility and body composition in infants and toddlers with Prader-Willi syndrome. J Pediatr 2004;145:744-9.
- Whittington JE, Holland AJ, Webb T, Butler J, Clarke D, Boer H. Population prevalence and estimated birth incidence and mortality rate for people with Prader-Willi syndrome in one UK Health Region. J Med Genet 2001;38:792-8.
- Sarborio P, Hahn S, Hisano S, Latta K, Scheinman J, Chan J. Chronic renal failure: and overview from a pediatric perspective. Nephron 1998;80:134-48.
- Tönshoff B, Mehls O. Growth retardation in children with chronic renal insufficiency: current aspects of pathophysiology and treatment. J Nephrol 1995;8:133-42.
- Schaefer F, Wingen AM, Hennicke M, Rigden S, Mehls O. Growth charts for prepubertal children with chronic renal failure due to congenital renal disorders. European Study Group for Nutritional Treatment of Chronic Renal Failure in Childhood. Pediatr Nephrol 1996;10:288-93.
- Mahan JD, Warady BA, Fielder P, Gipson DS, Greenbaum L, Juarez-Congelosi MD, et al. Assessment and treatment of short stature in pediatric patients with chronic kidney disease: a consensus statement. Pediatr Nephrol 2006;21:917-30.
- National Kidney Foundation Kidney Disease Outcomes Quality Initiative . K/DOQI/Clinical/Practice/Guidelines/for/Chronic/Kidney/Disease:/Evaluation,/Classification,/and/Stratification./Part/4./Definition/and/Classification/of/Stages/of/Chronic/Kidney/Disease n.d. www.kidney.org/PROFESSIONALS/kdoqi/guidelines_ckd/toc.htm (accessed 23 February 2009).
- Kari J, Gonzalez C, Ledermann S, Shaw V, Rees L. Outcome and growth of infants with severe chronic renal failure. Kidney Int 2000;57:1681-7.
- Parekh R, Flynn J, Smoyer W, Milne J, Kershaw D, Bunchman T, et al. Improved growth in young children with severe chronic renal insufficiency who use specified nutritional therapy. J Am Soc Nephrol 2001;12:2418-26.
- Wingen AM, Mehls O. Nutrition in children with preterminal chronic renal failure. Myth or important therapeutic aid?. Pediatr Nephrol 2002;17:111-20.
- National Kidney Foundation Kidney Disease Outcomes Quality Initiative . Clinical Practice Guidelines for Nutrition in Chronic Renal Failure n.d. www.kidney.org/PROFESSIONALS/kdoqi/guidelines_updates/doqi_nut.html (accessed 23 February 2009).
- Furth SL. Growth and nutrition in children with chronic kidney disease. Adv Chronic Kidney Dis 2005;12:366-71.
- Lewis M, Shaw J, Reid C, Evans J, Webb N, Verrier-Jones K, et al. UK Renal Registry Report 2006 Bristol, UK: UK Renal Registry; 2006.
- Groothof J, Offringa M, Van Eck-Smit B, Gruppen M, Van der Kar N, Wolff ED, et al. Severe bone disease and low bone mineral density after juvenile renal failure. Kidney Int 2003;63:266-75.
- Rizzoni G, Broyer M, Brunner F, Brynger H, Challah S, Kramer P, et al. Combined report on regular dialysis and transplantation of children in Europe, XIII, 1983. Proc Eur Dial Trans Assoc 1985;21.
- Lewis M, Shaw J, Reid C, Evans J, Webb N, Verrier-Jones K, et al. UK Renal Registry Report 2006 2006:227-41.
- Royal College of Obstetricians and Gynaecologists . The Investigation and Management of the Small-for-Gestational-Age Fetus 2002.
- Lee PA, Chernausek SD, Hokken-Koelega ACS, Czernichow P. International small for gestational age advisory board consensus development conference statement: management of short children born small for gestational age, April 24–October 1, 2001. Pediatrics 2003;111:1253-61.
- Karlberg J, Albertsson-Wikland K, Kwan EY, Lam B, Low LC. The timing of early postnatal catch-up growth in normal, full-term infants born short for gestational age. Horm Res 1997;48:17-24.
- Ong K, Ahmed M, Emmett P, Preece M, Dunger DB. for the Avon Longitudinal Study of Pregnancy and Childhood Study Team . Association between post-natal catch-up growth and obesity in childhood: prospective cohort study. BMJ 2000;320:967-71.
- Albertsson-Wikland K, Karlberg J. Postnatal growth of children born small for gestational age. Acta Paediatr 1997:193-5.
- Huiming Y, Meng M, Chaomin W, Fan Y. Growth Hormone Treatment for short stature in children with intrauterine growth retardation (protocol). Cochrane Database Syst Rev 2006.
- Karlberg J, Albertsson-Wikland K. Growth in full term small-for-gestational-age infants: from birth to final height. Pediatr Res 1995;38:733-9.
- Tuvemo T, Cnattingius S, Jonsson B. Prediction of male adult stature using anthropometric data at birth: a nationwide population-based study. Pediatr Res 1999;46:491-5.
- Albertsson-Wikland K, Karlberg J. Natural growth in children born small for gestational age with and without catch-up growth. Acta Paediatr 1994;399:64-70.
- Karlberg J, Albertsson-Wikland K. Growth in full term small-for-gestational-age infants: from birth to final height. Pediatr Res 1995;38:733-9.
- Hokken-Koelega A, De Ridder M, Lemmen R, Den Hartog H, De Muinck Keizer-Schrama S, Drop S. Children born small for gestational age: do they catch up?. Pediatr Res 1995;38:267-71.
- Blum WF, Crowe BJ, Quigley CA, Jung H, Cau D, Ross JL, et al. Growth hormone is effective in treatment of short stature associated with short stature homeobox-containing gene deficiency: two year results of a randomized, controlled, multicenter trial. J Clin Endocrinol Metab 2007;92:219-28.
- Eli Lilly . Lilly and Humatrope: A Lasting Commitment 2006.
- Langer L. Mesomelic dwarfism of the hypoplastic ulna, fibula, mandible type. Radiology 1967;89.
- Zinn AR, Wei F, Zhang L, Elder FF, Scott CI, Marttila P, et al. Complete SHOX deficiency causes Langer mesomelic dysplasia. Am J Med Genet 2002;110:158-63.
- Binder G, Schwarze CP, Ranke MB. Identification of short stature caused by SHOX defects and therapeutic effect of recombinant human growth hormone. J Clin Endocrinol Metab 2000;85:245-9.
- Ezquieta B, Cueva E, Oliver A, Gracia R. SHOX intragenic microsatellite analysis in patients with short stature. J Pediatr Endocrinol Metab 2002;15:139-48.
- Ogata T, Muroya K, Sasaki G, Nishimura G, Kitoh H, Hattori T. SHOX nullizygosity and haploinsufficiency in a Japanese family: implication for the development of Turner skeletal features. J Clin Endocrinol Metab 2002;87:1390-4.
- Rappold GA, Fukami M, Niesler B, Schiller S, Zumkeller W, Bettendorf M, et al. Deletions of the homeobox gene SHOX (short stature homeobox) are an important cause of growth failure in children with short stature. J Clin Endocrinol Metab 2002;87:1402-6.
- Binder G, Ranke MB, Martin DD. Auxology is a valuable instrument for the clinical diagnosis of SHOX haploinsufficiency in school-age children with unexplained short stature. J Clin Endocrinol Metab 2003;88:4891-6.
- Stuppia L, Calabrese G, Gatta V, Pintor S, Morizio E, Fantasia D, et al. SHOX mutations detected by FISH and direct sequencing in patients with short stature. J Med Genet 2003;40.
- Huber C, Rosilio M, Munnich A, Cormier-Daire V. High incidence of SHOX anomalies in individuals with short stature. J Med Genet 2006;43:735-9.
- Binder G, Renz A, Martinez A, Keselman A, Hesse V, Riedl SW, et al. SHOX haploinsufficiency and Leri-Weill dyschondrosteosis: Prevalence and growth failure in relation to mutation, sex, and degree of wrist deformity. J Clin Endocrinol Metab 2004;89:4403-8.
- Allen DB. Growth hormone therapy for short stature: is the benefit worth the burden?. Pediatrics 2006;118:343-8.
- Munns C, Glass I, Flanagan S, Hayes M, Williams B, Berry M, et al. Familial growth and skeletal features associated with SHOX haploinsufficiency. J Pediatr Endocrinol Metab 2003;16:987-96.
- Voss LD, Mulligan J. Bullying at school: are short pupils at risk? Questionnaire study in a cohort. BMJ 2000;320:612-13.
- Tanaka T, Cohen P, Clayton PE, Laron Z, Hintz RL, Sizonenko PC. Diagnosis and management of growth hormone deficiency in childhood and adolescence: Part 2: Growth hormone treatment in growth hormone deficient children. Growth Horm IGF Res 2002;12:323-41.
- Rosén T, Wilhelmsen L, Bengtsson BA. Altered lipid pattern explains increased cardiovascular mortality in hypopituitary patients with growth hormone deficiency. Clin Endocrinol 1998;48:525-6.
- Elsheikh M, Dunger DB, Conway GS, Wass JAH. Turner’s Syndrome in adulthood. Endocrine Reviews 2002;23:120-40.
- Höybe C, Hilding A, Jacobsson H, Thorén M. Metabolic profile and body composition in adults with Prader-Willi syndrome and severe obesity. J Clin Endocrinol Metab 2002;87:3590-7.
- Reinehr T, Kleber M, Toschke A. Small for gestational age (SGA) status is associated with metabolic syndrome in overweight children. Eur J Endocrinol 2009;160:579-84.
- Barker D. Mothers, babies, and disease in later life. London: British Medical Journal Publishing Group; 1998.
- National Institute for Health and Clinical Excellence National Collaborating Centre for Primary Care . Obesity: The Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children 2006.
- Rajaram S, Baylink D, Mohan S. Insulin-like growth factor-binding proteins in serum and other biological fluids: regulation and functions. Endocrine Reviews 1997;18:801-31.
- Cohen P, Peehl D, Lamson G, Rosenfeld R. Insulin-like growth factors (IGFs), IGF receptors, and IGF-binding proteins in primary cultures of prostate epithelial cells. J Clin Endocrinol Metab 1991;73:401-7.
- Lippman M. The development of biological therapies for breast cancer. Science 1993;259:631-2.
- Ezquieta B, Cueva E, Oliver A, Gracia R. SHOX intragenic microsatellite analysis in patients with short stature. J Pediatr Endocrinol Metab 2002;15:139-48.
- National Institute of Health and Clinical Evidence . Guidance on the Use of Human Growth Hormone (somatropin) in Children With Growth Failure 2002.
- National Kidney Foundation . KDOQI Clinical Practice Guidelines for Bone Metabolism and Disease in Children With Chronic Kidney Disease n.d. www.kidney.org/professionals/KDOQI/guidelines_pedbone/guide11.htm (accessed 23 February 2009).
- Clayton PE, Cianfarani S, Czernichow P, Johannsson G, Rapaport R, Rogol A. Consensus statement: management of the child born small for gestational age through to adulthood: A consensus statement of the International Societies of Pediatric Endocrinology and the Growth Hormone Research Society. J Clin Endocrinol Metab 2007;92:804-10.
- Pfizer . Genotropin Full Prescribing Information n.d. www.accessdata.fda.gov/drugsatfda_docs/label/2008/020280s060lbl.pdf (accessed 29 July 2009).
- Eli Lilly . Humatrope 6mg, 12mg, or 24mg Powder and Solvent for Solution for Injection n.d. http://emc.medicines.org.uk/medicine/601/SPC/Humatrope%206mg,%2012mg,%20or%2024mg%20powder%20and%20solvent%20for%20solution%20for%20injection (accessed 2 June 2009).
- Sandoz . Omnitrope Summary of Product Characteristics n.d. www.emea.europa.eu/humandocs/PDFs/EPAR/Omnitrope/H-607-PI-en.pdf (accessed 2 June 2009).
- Eli Lilly and Company Ltd . Humatrope 6mg, 12mg, or 24mg Powder and Solvent for Solution for Injection n.d. http://emc.medicines.org.uk (accessed 23 December 2008).
- Grunfeld C, Thompson M, Brown SJ, Richmond G, Lee D, Muurahainen N, et al. Recombinant human growth hormone to treat HIV-associated adipose redistribution syndrome: 12-week induction and 24-week maintenance therapy. JAIDS 2007;45:286-97.
- NHS Centre for Reviews and Dissemination . Undertaking Systematic Reviews of Research on Effectiveness 2001.
- Soliman AT, Abdul Khadir MM. Growth parameters and predictors of growth in short children with and without growth hormone (GH) deficiency treated with human GH: a randomized controlled study. J Trop Pediatr 1996;42:281-6.
- Davenport ML, Crowe BJ, Travers SH, Rubin K, Ross JL, Fechner PY, et al. Growth hormone treatment of early growth failure in toddlers with Turner syndrome: a randomized, controlled, multicenter trial. J Clin Endocrinol Metab 2007;92:3406-16.
- Stephure DK. Canadian Growth Hormone Advisory Committee . Impact of growth hormone supplementation on adult height in turner syndrome: results of the Canadian randomized controlled trial. J Clin Endocrinol Metab 2005;90:3360-6.
- Rovet J, Holland J. Psychological aspects of the Canadian randomized controlled trial of human growth hormone and low-dose ethinyl oestradiol in children with Turner syndrome. The Canadian Growth Hormone Advisory Group. Horm Res 1993;39:60-4.
- Gravholt CH, Naeraa RW, Brixen K, Kastrup KW, Mosekilde L, Jorgensen JO, et al. Short-term growth hormone treatment in girls with Turner syndrome decreases fat mass and insulin sensitivity: a randomized, double-blind, placebo-controlled, crossover study. Pediatrics 2002;110:889-96.
- Gravholt CH, Hjerrild BE, Naeraa RW, Engbaek F, Mosekilde L, Christiansen JS. Effect of growth hormone and 17beta-oestradiol treatment on metabolism and body composition in girls with Turner syndrome. Clin Endocrinol 2005;62:616-22.
- Johnston DI, Betts P, Dunger D, Barnes N, Swift PG, Buckler JM, et al. A multicentre trial of recombinant growth hormone and low dose oestrogen in Turner syndrome: near final height analysis. Arch Dis Child 2001;84:76-81.
- Festen DA, van TA, Duivenvoorden HJ, Hokken-Koelega AC. Adiponectin levels in prepubertal children with Prader–Willi syndrome before and during growth hormone therapy. J Clin Endocrinol Metab 2007;92:1549-54.
- Festen DAM, Wevers M, Lindgren AC, Bohm B, Otten BJ, Wit JM, et al. Mental and motor development before and during growth hormone treatment in infants and toddlers with Prader–Willi syndrome. Clin Endocrinol 2008;68:919-25.
- de Lind van Wijngaarden Roderick FA, de Klerk L, Festen D, Duivenvoorden HJ, Otten B, Hokken-Koelega ACS. Randomized controlled trial to investigate the effects of growth hormone treatment on scoliosis in children with Prader-Willi syndrome. J Clin Endocrinol Metab 2009;94:1274-80.
- Festen DAM, de Lind van Wijngaarden R, van Eekelen M, Otten BJ, Wit JM, Duivenvoorden HJ, et al. Randomized controlled GH trial: effects on anthropometry, body composition and body proportions in a large group of children with Prader–Willi syndrome. Clin Endocrinol 2008;69:443-51.
- Carrel AL, Myers SE, Whitman BY, Allen DB. Growth hormone improves body composition, fat utilization, physical strength and agility, and growth in Prader–Willi syndrome: a controlled study. J Pediatr 1999;134:215-21.
- Myers SE, Carrel AL, Whitman BY, Allen DB. Physical effects of growth hormone treatment in children with Prader–Willi syndrome. Acta Paediatr 1999;88:112-14.
- Myers SE, Whitman BY, Carrel AL, Moerchen V, Bekx MT, Allen DB. Two years of growth hormone therapy in young children with Prader–Willi syndrome: Physical and neurodevelopmental benefits. Am J Med Genet 2007;143A:443-8.
- Whitman B, Carrel A, Bekx T, Weber C, Allen D, Myers S. Growth hormone improves body composition and motor development in infants with Prader–Willi syndrome after six months. J Pediatr Endocrinol 2004;17:591-600.
- Hauffa BP. One-year results of growth hormone treatment of short stature in Prader–Willi syndrome. Acta Paediatr 1997;423:63-5.
- Lindgren AC, Hagenas L, Muller J, Blichfeldt S, Rosenborg M, Brismar T, et al. Effects of growth hormone treatment on growth and body composition in Prader–Willi syndrome: a preliminary report. The Swedish National Growth Hormone Advisory Group. Acta Paediatr 1997;423:60-2.
- Lindgren AC, Hagenas L, Muller J, Blichfeldt S, Rosenborg M, Brismar T, et al. Growth hormone treatment of children with Prader–Willi syndrome affects linear growth and body composition favourably. Acta Paediatr 1998;87:28-31.
- Haqq AM, Stadler DD, Jackson RH, Rosenfeld RG, Purnell JQ, LaFranchi SH. Effects of growth hormone on pulmonary function, sleep quality, behavior, cognition, growth velocity, body composition, and resting energy expenditure in Prader–Willi syndrome. J Clin Endocrinol Metab 2003;88:2206-12.
- Sanchez CP, Kuizon BD, Goodman WG, Gales B, Ettenger RB, Boechat MI, et al. Growth hormone and the skeleton in pediatric renal allograft recipients. Pediatr Nephrol 2002;17:322-8.
- Hokken-Koelega ACS, Stijnen T, De Muinck Keizer-Schrama SMPF, Wit JM, Wolff ED, De Jong MCJW, et al. Placebo-controlled, double-blind, crossover trial of growth hormone treatment in prepubertal children with chronic renal failure. Lancet 1991;338:585-90.
- Hokken-Koelega AC, Stijnen T, de Jong RC, Donckerwolcke RA, Groothoff JW, Wolff ED, et al. A placebo-controlled, double-blind trial of growth hormone treatment in prepubertal children after renal transplant. Kidney Int 1996;53:128-34.
- Powell DR, Liu F, Baker BK, Hintz RL, Lee PD, Durham SK, et al. Modulation of growth factors by growth hormone in children with chronic renal failure. The Southwest Pediatric Nephrology Study Group. Kidney Int 1997;51:1970-9.
- Broyer M, Jureidini KF, Proesmans W, Janssen F, van Acker K, Du Caju M, et al. Pharmacia & Upjohn Study Group. Results and side-effects of treating children with growth hormone after kidney transplantation – a preliminary report. Acta Paediatrica 1996;417:76-9.
- Fine RN, Kohaut MEC, Brown MD, Perlman AJ. Growth after recombinant human growth hormone treatment in children with chronic renal failure: Report of a multicenter randomized double-blind placebo-controlled study. J Pediatr 1994;124:374-82.
- De Schepper J, Thomas M, Beckers D, Craen M, Maes M, de Zegher F. Growth hormone treatment and fat redistribution in children born small for gestational age. J Pediatr 2008;152:327-30.
- Lagrou K, Froidecoeur C, Thomas M, Massa G, Beckers D, Craen M, et al. Concerns, expectations and perception regarding stature, physical appearance and psychosocial functioning before and during high-dose growth hormone treatment of short pre-pubertal children born small for gestational age. Horm Res 2008;69:334-42.
- Carel JC, Chatelain P, Rochiccioli P, Chaussain JL. Improvement in adult height after growth hormone treatment in adolescents with short stature born small for gestational age: results of a randomized controlled study. J Clin Endocrinol Metab 2003;88:1587-93.
- de Zegher F, Maes M, Gargosky SE, Heinrichs C, Du Caju MVL, Thiry G, et al. High-dose growth hormone treatment of short children born small for gestational age. J Clin Endocrinol Metab 1996;81:1887-92.
- de Zegher F, Ong K, van HM, Mohn A, Woods K, Dunger D. High-dose growth hormone (GH) treatment in non-GH-deficient children born small for gestational age induces growth responses related to pretreatment GH secretion and associated with a reversible decrease in insulin sensitivity. J Clin Endocrinol Metab 2002;87:148-51.
- Phillip M, Lebenthal Y, Lebl J, Zuckerman-Levin N, Korpal-Szczyrska M, Marques JS, et al. European multicentre study in children born small for gestational age with persistent short stature: comparison of continuous and discontinuous growth hormone treatment regimens. Horm Res 2009;71:52-9.
- Cutfield W, Lindberg A, Chatelain P, Ranke M, Wilton P. Final height in idiopathic growth hormone deficiency: the KIGS experience. Acta Paediatr 1999;88:72-5.
- August G, Julius J, Blethen S. Adult height in children with growth hormone deficiency. Paediatrics 1998;102.
- Dacou-Voutetakis C, Karavanaki-Karanassiou K, Petrou V, Georgopoulos N, Maniati-Christidi M, Mavrou A. The growth pattern and final height of girls with Turner syndrome with and without human growth hormone treatment. Paediatrics 1998;101:663-8.
- Hochberg Z, Zadik Z. Final height in young women with Turner syndrome after GH therapy: an open controlled study. Eur J Endocrinol 1999;141:218-24.
- Pasquino AM, Passeri F, Municchi G, Segni M, Pucarelli I, Larizza D, et al. Final height in Turner syndrome patients treated with growth hormone. Horm Res 1996;46.
- Taback SP, Collu R, Deal CL, Guyda HJ, Salisbury S, Dean HJ, et al. Does growth-hormone supplementation affect adult height in Turner’s syndrome?. Lancet 1996;348:25-7.
- Haffner D, Schaefer F, Nissel R, Wuhl E, Tonshoff B, Mehls O. Effect of growth hormone treatment on the adult height of children with chronic renal failure. German Study Group for Growth Hormone Treatment in Chronic Renal Failure. N Engl J Med 2000;343:923-30.
- Janssen F, Van Damme L, Van Dyck M, Hall M, Schurmans T, Herman J, et al. Impact of growth hormone treatment on a Belgian population of short children with renal allografts. Pediatr Transplant 1997;1.
- Angulo M, Castro-Magana M, Canas J, Arguello R, Lamerson M, Tapiador C, et al. Final height in Prader-Willi syndrome (PWS) children treated with recombinant growth hormone (rhGH). Pediatr Res 2000;47.
- Rosenfeld RG. Acceleration of growth in Turner syndrome patients treated with growth hormone: summary of three-year results. J Endocrinol Invest 1989;12:49-51.
- Rosenfeld RG. Non-conventional growth hormone therapy in Turner syndrome: the United States experience. Horm Res 1990;33:137-43.
- Ross JL, Feuillan P, Kushner H, Roeltgen D, Cutler GB. Absence of growth hormone effects on cognitive function in girls with Turner syndrome. J Clin Endocrinol Metab 1997;82:1814-17.
- Whitman BY, Myers S, Carrel A, Allen DA. treatment/control group study of growth hormone treatment: Impact on behavior – A preliminary look. Endocrinologist 2000;10:31-7.
- Conway GS, Szarras-Czapnik M, Racz K, Keller A, Chanson P, Tauber M, et al. Treatment for 24 months with recombinant human GH has a beneficial effect on bone mineral density in young adults with childhood-onset GH deficiency. Eur J Endocrinol 2009;160:899-907.
- Mauras N, Pescovitz OH, Allada V, Messig M, Wajnrajch MP, Lippe B, et al. Limited efficacy of growth hormone (GH) during transition of GH-deficient patients from adolescence to adulthood: a phase III multicenter, double-blind, randomized two-year trial. J Clin Endocrinol Metab 2005;90:3946-55.
- Attanasio AF, Shavrikova E, Blum WF, Cromer M, Child CJ, Paskova M, et al. Continued growth hormone (GH) treatment after final height is necessary to complete somatic development in childhood-onset GH-deficient patients. J Clin Endocrinol Metab 2004;89:4857-62.
- Norrelund H, Vahl N, Juul A, Moller N, Alberti KG, Skakkebaek NE, et al. Continuation of growth hormone (GH) therapy in GH-deficient patients during transition from childhood to adulthood: impact on insulin sensitivity and substrate metabolism. J Clin Endocrinol Metab 2000;85:1912-17.
- Underwood LE, Attie KM, Baptista J. Genentech Collaborative Study Group . Growth hormone (GH) dose–response in young adults with childhood-onset GH deficiency: a two-year, multicenter, multiple-dose, placebo-controlled study. J Clin Endocrinol Metab 2003;88:5273-80.
- Drake WM, Carroll PV, Maher KT, Metcalfe KA, Camacho-Hubner C, Shaw NJ, et al. The effect of cessation of growth hormone (GH) therapy on bone mineral accretion in GH-deficient adolescents at the completion of linear growth. J Clin Endocrinol Metab 2003;88:1658-63.
- Baxter L, Bryant J, Cave CB, Milne R. Recombinant growth hormone for children and adolescents with Turner syndrome. Cochrane Database Syst Rev 2007;1.
- Li H, Banerjee S, Dunfield L, Kirby J, Jones M, Hamilton J, et al. Recombinant human growth hormone for treatment of Turner Syndrome: systematic review and economic evaluation. Canadian Agency for Drugs and Technologies in Health (CADTH); 2007.
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 1996;313:275-83.
- Weinstein MC, O’Brien B, Hornberger J, Jackson J, Johannesson M, McCabe C, et al. Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR Task Force on Good Research Practices: Modeling Studies. Value Health 2003;6:9-17.
- National Institute for Health and Clinical Excellence . Guide to the Methods of Technology Appraisal 2008.
- Joshi AV, Munro V, Russell MW. Cost-utility of somatropin (rDNA origin) in the treatment of growth hormone deficiency in children. Curr Med Res Opin 2006;22:351-7.
- Anthony D, Stevens A. Growth Hormone in Children (for Growth Hormone Deficiency, Turner’s Syndrome, Chronic Renal Failure and Idiopathic Short Stature) 1996.
- Drummond MF, O’Brien B, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005.
- Wit J-M, Boersma B, De Muinck Keizer-Schrama SMPF, Nienhuis HE, Oostdijk W, Otten BJ, et al. Long-term results of growth hormone therapy in children with short stature, subnormal growth rate and normal growth hormone response to secretagogues. Clin Endocrinol 1995;42:365-72.
- Bannink EM, Raat H, Mulder PG, Keizer-Schrama SM. Quality of life after growth hormone therapy and induced puberty in women with Turner syndrome. J Pediatr 2006;148:95-101.
- Bertella L, Mori I, Grugni G, Pignatti R, Ceriani F, Molinari E, et al. Quality of life and psychological well-being in GH-treated, adult PWS patients: a longitudinal study. J Intellect Disabil Res 2007;51:302-11.
- Busschbach JJ, Rikken B, Grobbee DE, De Charro FT, Wit JM. Quality of life in short adults. Horm Res 1998;49:32-8.
- Carel JC, Ecosse E, Bastie-Sigeac I, Cabrol S, Tauber M, Leger J, et al. Quality of life determinants in young women with turner’s syndrome after growth hormone treatment: results of the StaTur population-based cohort study. J Clin Endocrinol Metab 2005;90:1992-7.
- Koltowska-Haggstrom MK. Growth hormone (GH) replacement in hypopituitary adults with GH deficiency evaluated by a utility-weighted quality of life index: A precursor to cost-utility analysis. Clin Endocrinol 2008;68:122-9.
- Sandberg DE, MacGillivray MH, Clopper RR, Fung C, LeRoux L, Alliger DE. Quality of life among formerly treated childhood-onset growth hormone-deficient adults: a comparison with unaffected siblings. J Clin Endocrinol Metab 1998;83:1134-42.
- Ara R, Brazier J. Deriving an Algorithm to Convert the Eight Mean SF-36 Dimension Scores into a Mean EQ-5D Preference-Based Score from Published Studies (Where Patient Level Data Are Not Available). Value Health 2008.
- Christensen TL, Djurhuus CB, Clayton P, Christiansen JS. An evaluation of the relationship between adult height and health-related quality of life in the general UK population. Clin Endocrinol 2007;67:407-12.
- Sproston K, Primatesta P. Health Survey for England 2003. Volume 1: Cardiovascular disease. London: HMSO; 2004.
- Petrou S, McIntosh E. Measuring the benefits of growth hormone therapy in children: a role for preference-based approaches?. Arch Dis Child 2008;93:95-7.
- Pfizer UK . KIGS (Pfizer International growth study) database for Western Europe. The Clinical and Cost-Effectiveness of Growth Hormone (Genotropin®) in Children 2008.
- Fryback DG, Lawrence WF, Martin PA, Klein R, Klein BE. Predicting Quality of well-being scores from the SF-36: results from the Beaver Dam Health Outcomes Study. Med Decis Making 1997;17:1-9.
- Shmueli A. The SF-36 profile and health-related quality of life: an interpretative analysis. Qual Life Res 1998;7:187-95.
- Cooper K, Brailsford SC, Davies R, Raftery J. Modelling health care interventions. J Oper Res Soc 2007;58:168-76.
- Kapoor RR, Burke SA, Sparrow SE, Hughes IA, Dunger DB, Ong KK, et al. Monitoring of concordance in growth hormone therapy. Arch Dis Child 2008;93:147-8.
- Bonfig W, Bechtold S, Bachmann S, Putzker S, Fuchs O, Pagel P, et al. Reassessment of the optimal growth hormone cut-off level in insulin tolerance testing for growth hormone secretion in patients with childhood-onset growth hormone deficiency during transition to adulthood. J Pediatr Endocrinol Metab 2008;21:1049-56.
- Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. Oxford: Oxford University Press; 2006.
- Nielsen EH, Lindholm J, Laurberg P. Excess mortality in women with pituitary disease: a meta-analysis. Clin Endocrinol 2007;67:693-7.
- Shoemaker MJ, Swerdlow AJ, Higgins CD, Wright AF, Jacobs PA. Mortality in women with turner syndrome in Great Britain: a national cohort study. J Clin Endocrinol Metab 2008;93:4735-42.
- Lee PDK. Growth hormone and mortality in Prader–Willi syndrome. Growth Genetics &Amp; Hormones 2006;22:17-23.
- Groothoff JW. Long-term outcomes of children with end-stage renal disease. Pediatr Nephrol 2005;20:849-53.
- Kajantie E, Osmond C, Barker DJ, Forsen T, Phillips DI, Eriksson JG. Size at birth as a predictor of mortality in adulthood: a follow-up of 350 000 person-years. Int J Epidemiol 2005;34:655-63.
- British Medical Association and Royal Pharmaceutical Society of Great Britain . British National Formulary 2009.
- Department of Health . NHS Reference Costs 2006.
- Curtis L. Unit costs of health and social care. University of Kent, Canterbury: Personal Social Services Research Unit; 2008.
- Picot J, Jones J, Colquitt J, Gospodaresvskaya E, Loveman E, Baxter L, et al. The clinical-effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess 2009;13.
- Hakim Z, Wolf A, Garrison L.P. Estimating the effect of changes in body mass index on health state preferences. Pharmacoeconomics 2008;20:393-404.
- Bengtsson BA. Untreated growth hormone deficiency explains premature mortality in patients with hypopituitarism. Growth Horm IGF Res 1998;8:77-80.
- Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care 2005;21:240-5.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess 2004;8.
Appendix 1 Protocol methods
A review of the evidence for the clinical effectiveness and cost-effectiveness of somatropin will be undertaken systematically following standard guidelines from the NHS Centre for Reviews and Dissemination (CRD). 83 An expert advisory group of clinical experts and service users where appropriate will support the review team at key stages of the project.
Search strategy
A search strategy will be developed and tested by an experienced information scientist. The strategy will be designed to identify studies reporting clinical effectiveness, cost-effectiveness, HRQoL, resource use and costs, epidemiology and natural history.
The draft clinical effectiveness search strategy for MEDLINE is shown in Appendix 2. This will be adapted for other databases.
A number of electronic databases will be searched including: The Cochrane Database of Systematic Reviews (CDSR); The Cochrane Central Register of Controlled Trials; NHS CRD (University of York) Database of Abstracts of Reviews of Effectiveness (DARE) and the NHS Economic Evaluation Database (NHS EED); MEDLINE (Ovid); EMBASE (Ovid); National Research Register; Current Controlled Trials; ISI Proceedings; Web of Science; and BIOSIS. Bibliographies of related papers will be assessed for relevant studies where possible.
The MSs to NICE will be assessed for any additional studies that meet the inclusion criteria.
Experts will be contacted to identify additional published and unpublished references.
Searches will be carried out from the inception date of the database. Although this will involve duplication of searches carried out for the previous review, it will be necessary to identify trials reporting body composition as an outcome measure, as these may not have been identified for all conditions in the previous review. For databases of abstracts and conference presentations searches will only be carried out for the past 2 years to capture any research that has not yet been fully published. All searches will be limited to the English language, and will be updated around February 2009.
Inclusion and exclusion criteria
Patients
Children with growth disturbance, as per licensed indication for each preparation available.
Interventions
Recombinant human growth hormone (somatropin).
Comparators
Management strategies without somatropin.
Outcomes
The following outcomes will be included, where data are available:
-
final height gained
-
height standard deviation score
-
growth velocity
-
growth velocity standard deviation score
-
body composition, and biochemical/metabolic markers as appropriate
-
adverse effects of treatment
-
HRQoL.
Types of studies
-
Fully published RCTs or systematic reviews of RCTs will be included. Indicators of a systematic review include: explicit search strategy, inclusion criteria, data extraction and assessment of quality. Where we judge it necessary and appropriate, we will consider the inclusion of evidence from other non-randomised studies. Full economic evaluations (cost-effectiveness studies, cost–utility studies, cost–benefit studies) and reviews of economic evaluations will be included in the review of cost-effectiveness.
-
Studies published only as abstracts or conference presentations will be included only in the primary analysis of clinical effectiveness and cost-effectiveness if sufficient details are presented to allow an appraisal of the methodology and assessment of results.
-
Non-English language studies will be excluded.
Inclusion and data extraction process
-
Two reviewers will assess the titles and abstracts of studies identified by the search strategy for potential eligibility.
-
The full text of relevant papers will be requested for further assessment, and these will be screened independently by two reviewers.
-
Data will be extracted by one reviewer using a standard data extraction form and checked by a second reviewer.
-
At each stage, any discrepancy will be resolved by discussion, with involvement of a third reviewer where necessary.
Quality assessment
The quality of included clinical effectiveness studies will be assessed using NHS CRD (University of York) criteria. 83 The methodological quality of the economic evaluations will be assessed using accepted frameworks such as the international consensus-developed list of criteria developed by Evers and colleagues171 and Drummond and colleagues. 141 For any studies based on decision models we will also make use of the checklist for assessing good practice in decision-analytical modelling (Philips and colleagues). 172
Quality criteria will be applied by one reviewer and checked by a second reviewer, with differences in opinion resolved by discussion and involvement of a third reviewer where necessary.
Methods of analysis/synthesis
-
Clinical effectiveness and cost-effectiveness studies will be synthesised through a narrative review with tabulation of results of included studies.
-
Where data are of sufficient quality and homogeneity, a meta-analysis of the clinical effectiveness studies will be performed using appropriate software.
-
Quality-of-life studies will be synthesised using the same methods as above, i.e. narrative review and meta-analysis as appropriate.
Appendix 2 Literature search strategies
Search strategies for MEDLINE are shown below. Strategies for other databases are available from the authors.
rhGH clinical effectiveness
MEDLINE: all years 1950–2008, search date: 23 June 2009.
-
growth disorders/
-
growth failure.ti,ab.
-
growth deficien*.ti,ab.
-
Prader-Willi Syndrome/
-
prader-willi.ti,ab.
-
turner syndrome/
-
(Turner*2 adj syndrome).ti,ab.
-
growth hormone deficien*.ti,ab.
-
GH deficien*.ti,ab.
-
GHD.ti,ab.
-
exp renal insufficiency chronic/
-
(chronic adj2 (renal or kidney*) adj2 (failure or insufficien*)).ti,ab.
-
(CRI or CRF).ti,ab.
-
“small for gestational age”.ti,ab.
-
“short for gestational age”.ti,ab.
-
infant small for gestational age/
-
“short stature homeobox-containing gene”.ti,ab.
-
“short stature homeobox”.ti,ab.
-
SGA.ti,ab.
-
SHOX.ti,ab.
-
PHOG.ti,ab.
-
“Pseudoautosomal homeobox-containing osteogenic gene”.ti,ab.
-
or/1-22
-
human growth hormone/or growth hormone/
-
(somatropin* or somatotropin* or somatotrophin* or genotropin* or saizen* or zomacton* or nutropin* or norditropin* or omnitrope* or humatrope*).ti,ab.
-
24 or 25
-
exp child/or exp adolescent/or exp infant/
-
child preschool/
-
(child* or infant* or adolescen* or girl* or boy* or prepubert* or pre-pubert*).ti,ab.
-
or/27-29
-
23 and 26 and 30
-
randomized controlled trial.pt.
-
controlled clinical trial.pt.
-
exp Randomized Controlled Trial/
-
exp Randomized Controlled Trials as Topic/
-
exp random allocation/
-
Double-Blind Method/
-
Single-Blind Method/
-
((singl* or doubl* or trebl*) adj9 (blind* or mask*)).ti,ab.
-
placebo*.ti,ab,sh.
-
random*.ti,ab.
-
(medline or medlars or embase or scisearch or cinahl).ti,ab,sh.
-
(systematic* adj5 review*).mp.
-
(systematic adj5 overview*).mp.
-
(methodolog* adj5 review).mp.
-
(methodolog* adj5 overview).mp.
-
(methodolog* adj5 research*).mp.
-
meta analysis.pt.
-
meta-analysis.sh.
-
(meta-analys* or meta analys* or metaanalys*).mp.
-
((hand adj5 search*) or (manual* adj5 search)).mp.
-
(electronic* database* or bibliographic* database* or computer* database* or online database*).mp.
-
(Health Technology Assessment* or Medical Technology Assessment*).ti,ab,in.
-
or/32-53
-
31 and 54
-
limit 55 to (english language and humans)
-
kidney transplantation/
-
(renal or kidney*).ti,ab.
-
57 or 58
-
26 and 30 and 54 and 59
-
60 not 56
-
growth hormone/or human growth hormone/
-
30 and 54 and 59 and 62
-
63 not 56
-
61 or 63
-
limit 65 to (english language and humans)
-
55 or 66
-
(editorial or letter or comment).pt.
-
67 not 68
-
from 69 keep 1-13,21-22
Cost-effectiveness
MEDLINE: all years 1950 to current, search date 24 June 2009.
-
exp economics/
-
exp economics hospital/
-
exp economics pharmaceutical/
-
exp economics nursing/
-
exp economics medical/
-
exp “Costs and Cost Analysis”/
-
Cost Benefit Analysis/
-
value of life/
-
exp models economic/
-
exp fees/and charges/
-
exp budgets/
-
(value adj2 (money or monetary)).tw.
-
(economic adj2 burden).tw.
-
(expenditure* not energy).tw.
-
budget*.tw.
-
(economic* or price* or pricing or financ* or “fee” or “fees” or pharmacoeconomic* or pharma economic* or pharmaco-economic*).tw.
-
(decision adj1 (tree* or analys* or model*)).tw.
-
Resource Allocation/
-
(unit cost or unit-cost or unit-costs or unit costs or drug cost or drug costs or hospital costs or health-care costs or health care cost or medical cost or medical costs).tw.
-
((value or values or valuation) adj2 (money or monetary or life or lives or costs or cost)).tw.
-
(cost adj2 (util* or effective* or efficac* or benefit* or consequence* or analys* or minimi* or saving* or breakdown* or lowering or estimate* or variable* or allocation* or control* or illness* or affordable* or instrument* or technolog* or fee* or charge* or charges)).tw.
-
Markov Chains/
-
Monte Carlo Method/
-
exp Decision Support Techniques/
-
(resource adj2 (use* or utili* or allocat*)).tw.
-
or/1-25
-
growth disorders/
-
growth failure.ti,ab.
-
growth deficien*.ti,ab.
-
Prader-Willi Syndrome/
-
prader-willi.ti,ab.
-
turner syndrome/
-
(Turner*2 adj syndrome).ti,ab.
-
growth hormone deficien*.ti,ab.
-
GH deficien*.ti,ab.
-
GHD.ti,ab.
-
exp renal insufficiency chronic/
-
(chronic adj2 (renal or kidney*) adj2 (failure or insufficien*)).ti,ab.
-
(CRI or CRF).ti,ab.
-
“small for gestational age”.ti,ab.
-
“short for gestational age”.ti,ab.
-
infant small for gestational age/
-
“short stature homeobox-containing gene”.ti,ab.
-
“short stature homeobox”.ti,ab.
-
SGA.ti,ab.
-
(SHOX or PHOG).ti,ab.
-
“idiopathic short stature”.ti,ab.
-
“Pseudoautosomal homeobox-containing osteogenic gene”.ti,ab.
-
or/27-48
-
human growth hormone/
-
(somatropin* or somatotropin* or somatotrophin* or genotropin* or saizen* or zomacton* or nutropin* or norditropin* or omnitrope* or humatrope*).ti,ab.
-
or/50–51
-
26 and 49 and 52
-
growth disorders/ec or growth hormone/ec
-
53 or 54
-
limit 55 to (human and english language)
-
(editorial or letter).pt.
-
56 not 57
-
“growth hormone”.ti,ab.
-
26 and 49 and 59
-
58 or 60
-
limit 61 to (english language and humans)
Quality-of-life searches
Searched 30 September 2008.
-
“Quality of Life”/
-
(hql or hqol or “h qol” or hrqol or “hr qol”).ti,ab.
-
(“hye” or “hyes”).ti,ab.
-
(euroqol or “euro qol” or “eq5d” or “eq 5d”).ti,ab.
-
Quality-Adjusted Life Year/
-
“quality adjusted life”.ti,ab.
-
(qaly$or qald$or qale$or qtime$).ti,ab.
-
“disability adjusted life”.ti,ab.
-
“quality of wellbeing”.ti,ab.
-
“quality of well being”.ti,ab.
-
daly$.ti,ab.
-
(SF-36 or SF-36 or short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirtysix or shortform thirty six or short form thirty six or short form thirtysix or short form thirty six).ti,ab.
-
health$year$equivalent$.tw.
-
disutil*.ti,ab.
-
“Value of Life”/
-
rosser.ti,ab.
-
willingness to pay.tw.
-
standard gamble$.tw.
-
time trade off.tw.
-
time tradeoff.tw.
-
health utilit*.ab.
-
exp Health Status/
-
exp Health Status Indicators/
-
“Activities of Daily Living”/
-
“Patient Acceptance of Health Care”/
-
“health-related quality of living”.ti,ab.
-
“health-related quality of life”.ti,ab.
-
(patient* adj2 (preference* or satisfaction or acceptance)).ti,ab.
-
(health adj (“state” or “status” or “states”)).ti,ab.
-
or/1-29
-
growth disorders/
-
growth failure.ti,ab.
-
growth deficien*.ti,ab.
-
Prader-Willi Syndrome/
-
prader-willi.ti,ab.
-
turner syndrome/
-
(Turner*2 adj syndrome).ti,ab.
-
growth hormone deficien*.ti,ab.
-
GH deficien*.ti,ab.
-
GHD.ti,ab.
-
exp renal insufficiency chronic/
-
(chronic adj2 (renal or kidney*) adj2 (failure or insufficien*)).ti,ab.
-
(CRI or CRF).ti,ab.
-
“small for gestational age”.ti,ab.
-
“short for gestational age”.ti,ab.
-
infant small for gestational age/
-
“short stature homeobox-containing gene”.ti,ab.
-
“short stature homeobox”.ti,ab.
-
SGA.ti,ab.
-
SHOX.ti,ab.
-
PHOG.ti,ab.
-
“Pseudoautosomal homeobox-containing osteogenic gene”.ti,ab.
-
or/31-52
-
human growth hormone/
-
(somatropin* or somatotropin* or somatotrophin* or genotropin* or saizen* or zomacton* or nutropin* or norditropin* or omnitrope* or humatrope*).ti,ab.
-
54 or 55
-
30 and 53 and 56
-
limit 57 to (english language and humans)
-
(edtorial or letter or comment).pt.
-
58 not 59
-
HIV.ti,ab.
-
60 not 61
Appendix 3 Quality assessment
| Criteria | Judgement |
|---|---|
| 1. Was the assignment to the treatment groups really random? | Adequate/partial/inadequate/unknown |
| 2. Was the treatment allocation concealed? | Adequate/inadequate/unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported/unknown |
| 4. Were the eligibility criteria specified? | Adequate/partial/inadequate/unknown |
| 5. Were outcome assessors blinded to the treatment allocation? | Adequate/inadequate/unknown |
| 6. Was the care provider blinded? | Adequate/partial/inadequate/unknown |
| 7. Was the patient blinded? | Adequate/partial/inadequate/unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate/partial/inadequate/unknown |
| 9. Did the analyses include an ITT analysis? | Adequate/inadequate |
Appendix 4 Data extraction tables
GHD data extraction forms
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Soliman et al. 1996 84 Country: Egypt Study design: RCT Number of centres: not stated Funding: not reported |
(Group 1 not data extracted as dose–response arm) 1a. GH 30 U/m2/week as a daily s.c. dose 1b. GH 15 U/m2/week as a daily s.c. dose 2a. GH 15 U/m2/week as a daily s.c. dose 2b. No treatment (Group 3 not data extracted as not GHD) 3a. GH 15 U/m2/week as a daily s.c. dose 3b. No treatment Duration of treatment: 1 year |
Target population: prepubertal children with GHD Number of participants: total 77 (19 in group 2) 1. Group I: 34 children with peak GH response to provocation < 7 µg (not data extracted as dose–response arm) 2. Group 2: 19 children with peak GH response to provocation between 7 and 10 µg/l (2a: 9, 2b: 10) 3. Group 3: 24 children with normal peak GH response (not data extracted as not GHD) Sample attrition/dropout: none reported for group 2 Inclusion criteria for study entry: Inclusion criteria not clearly stated Subjects were prepubertal, and BA was < 10 years at initiation of therapy, and < 3rd percentile height for chronological age None of the children had haemoglobinopathy, hepatic or renal impairment. No child had a reduced weight relative to height, other systemic disease, history of head trauma or cranial irradiation, malnutrition, psychosocial dwarfism or hypothyroidism |
Primary outcomes: not stated Secondary outcomes: GV, HtSDS, BA delay, IGF-1, glucose, FT4, TSH, GH Method of assessing outcomes: height measured on a stadiometer, normal population data were according to Tanner, skeletal age examined yearly according to Greulich and Pyle, height determined at 3-month intervals, and height GV calculated from height at beginning and end of therapy. HtSDS calculated using age-matched population mean height and SD |
| BA, bone age; FT4, free thyroxine; TSH, thyroid-stimulating hormone; s.c., subcutaneous; U, unit. | |||
| Characteristics of participants: growth parameters and hormonal data | |||
| Characteristic | GH 15 U/m2/week (n = 9) | No treatment (n = 10) | Overall |
| Age (years) | 7.1 ± 1.9 | 6.6 ± 1.6 | 6.8 ± 2.1 |
| GV (cm/years) | 3.65 ± 1.1 | 4.3 ± 1 | 3.9 ± 1.1 |
| HtSDS (–) | 3.4 ± 0.8 | 3.1 ± 0.6 | 2.8 ± 1 |
| BA delay | 2.1 ± 0.8 | 1.8 ± 0.65 | 1.9 ± 1 |
| GH peak after clonidine (µg/l) | 8.4 ± 1.3 | ||
| GH peak after insulin (µg/l) | 8.1 ± 1.6 | ||
| IGF-1 (ng/ml) | 58.5 ± 42.5 | 52.4 ± 21.3 | 59 ± 33 |
| Glucose (mmol/l) 0 min | 3.6 ± 0.6 | 4.1 ± 0.5 | |
| Glucose (mmol/l) 120 min | 5.4 ± 0.5 | 4.9 ± 0.45 | |
| FT4 (pmol/l) | 16.5 ± 2.1 | 14.6 ± 1.4 | |
| TSH (µIU/ml) | 1.4 ± 0.4 | 1.6 ± 0.3 | |
| Results | |||
| Outcomes | GH 15 U/m2/week (n = 9) | No treatment (n = 10) | p-value |
| GV (cm/years) | 8.4 ± 1.4a,b | 5.7 ± 1.8 | |
| HtSDS (–) | 2.3 ± 0.45a,b | 2.8 ± 0.45 | |
| BA delay | 2.25 ± 0.8 | 1.93 ± 0.75 | |
| GH peak after clonidine (µg/l) | 8.6 ± 1.1 | 8.2 ± 1 | |
| GH peak after insulin (µg/l) | 8.5 ± 1.4 | 8.3 ± 1.2 | |
| IGF-1 (ng/ml) | 91.2 ± 30.4a,b | 49.4 ± 19 | |
| Glucose (mmol/l) 0 min | 4.3 ± 0.6 | 4.5 ± 0.8 | |
| Glucose (mmol/l) 120 min | 5.1 ± 0.4 | 4.4 ± 0.6 | |
| FT4 (pmol/l) | 17.4 ± 2.2 | 15.6 ± 1.4 | |
| TSH (µIU/ml) | 2.4 ± 0.5 | 2.2 ± 0.5 | |
|
a p < 0.05 before vs after 1 year. b p < 0.05 ‘a’ vs ‘b’ subgroups. |
|||
|
Methodological comments Allocation to treatment groups: Three groups of children were identified and recruited according to their peak GH response to provocation then subsequently allocated ‘at random’ to two subgroups within that group. No further details on randomisation were provided. Blinding: Blinding is not reported. Comparability of treatment groups: Treatment groups appear comparable, but no p-value is reported. Method of data analysis: Data are presented as mean ± SD. Sample size/power calculation: None reported. Attrition/dropout: None reported for group 2, although n = 4 excluded from group 1b due to lack of compliance. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Inadequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Adequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
TS data extraction forms
| Reference and design | Intervention | Participants | Outcome measures | |
|---|---|---|---|---|
|
Quigley et al. 2002 12 Country: USA Study design: RCT, dose response Number of centres: 50 Funding: author/group appear to be employed by Eli Lilly & Co. |
1. Growth hormone (GH) (Humatrope) 0.27 mg/kg/week, with oral placebo (GH 0.27/Pla) 2. GH 0.27 mg/kg/week with LDE (GH 0.27/LDE)(not data extracted) 3. GH 0.36 mg/kg/week with oral placebo (GH 0.36/Pla) 4. GH 0.36 mg/kg/week with LDE (GH 0.36/LDE) (not data extracted) 5. Placebo injection with oral placebo (Pla/Pla) GH/placebo injections: s.c., in equally divided doses, initially 3 times per week; oral placebo given daily Duration of treatment: Placebo group for first 18 months of the study; subjects completed the full study when HV was less than 2 cm/year and BA ≥ 15 year Other interventions used: Ethinyl E2 daily, 25–200 ng/kg/day depending on age |
Target population: prepubertal girls with TS (first 18 months of the study data extracted, as placebo group joined group 3 after this time) Number of participants: total = 232, stratified by age and randomised. 224 completed 180 days’ active therapy and have baseline data reported 1. 45 2. 47 3. 49 4. 42 5. 41 Sample attrition/dropout: No further details on withdrawals are given (n = 8) Inclusion criteria for study entry: Karyotypically proven TS ≥ 5 years old BA ≤ 12 years Prepubertal < 10th percentile for height on NCHS standard HV < 6 cm/year Exclusion criteria for study entry: Presence of any Y chromosomal component in karyotype Concurrent treatment with agent that might influence growth Clinically significant systemic illness |
Primary outcomes: NFH (cm) (no placebo group), changes in HtSDS from baseline to end point (no placebo group) Secondary outcomes: changes in: BA, height (cm), impact of GH dose, effect of LDE Method of assessing outcomes: subjects were assessed every 3 months for first 6 years then 6 months until study completion: height using stadiometer, weight and pubertal status. Blood chemistry and thyroid function tests at every visit. Glucose and insulin every 6 months. IGF-1 every 3 months for first 18 months, at 24 months then annually. X-ray of the left wrist and hand for BA performed every 6 months for 24 months then annually. HtSDS calculated with reference to general population and to Lyon TS growth data Length of follow-up: 18 months for placebo-controlled study |
|
| BA, bone age; LDE, low-dose estrogen; NCHS, National Center for Health Statistics; Pla, placebo. | ||||
| Characteristics of participants | ||||
| Baseline (mean ± SD) | GH 0.27/Pla (n = 45) | GH 0.36/Pla (n = 49) | Pla/Pla (n = 41) | |
| Age (years) | 9.7 ± 2.7 | 9.8 ± 2.9 | 9.4 ± 2.7 | |
| BA (years) | 7.9 ± 2.3 | 7.9 ± 2.3 | 7.9 ± 2.4 | |
| Height (cm) | 119.2 ± 13.6 | 118.6 ± 12.5 | 117.6 ± 13.6 | |
| HtSDS (NCHS) | –2.7 ± 0.9 | –2.9 ± 0.9 | –2.9 ± 0.9 | |
| HtSDS (NCHS) | 0.3 ± 1.0 | 0.2 ± 0.8 | 0.2 ± 0.9 | |
| Mid-parental height (cm) | 164.6 ± 6.1 | 162.9 ± 5.9 | 162.4 ± 5.0 | |
| Mid-parental height SD score | 0.27 ± 0.93 | 0.00 ± 0.91 | –0.08 ± 0.77 | |
| Prestudy GV | 4.1 ± 1.2 | 4.0 ± 1.2 | 4.1 ± 1.2 | |
| Results | ||||
| Outcomes | GH 0.27/Pla (n = 45) | GH 0.36/Pla (n = 49) | Pla/Pla (n = 41) | p-value |
| GV 0–18 months (cm/year) | 6.6 ± 1.1 | 6.8 ± 1.1 | 4.2 ± 1.1 | < 0.001a |
|
a Compared with placebo. The 6-monthly GV results are presented on a difficult-to-read graph – could not data extract. Authors state that HV declined slightly in all GH groups after the initial peak but was significantly greater than that of the placebo group. |
||||
| Adverse effects | GH | Placebo | p-value | |
| Otitis media (occurrence/worsening) | 54/186 (29%) | 6/46 (13%) | 0.037 | |
|
Comments Ear pain and ear disorder were not different in frequency between groups. Otitis media was reported in 41% of subjects overall, ear pain in 27% and hypothyroidism in 16% and oedema in 3%. There were no disorders that occurred significantly more frequently in subjects receiving the higher dose. Serious AEs (defined as death, life-threatening cancer, hospitalisation, permanently disabling, drug overdose or resulting in congenital anomaly in an offspring) were reported for 47 out of 232 subjects; 31/47 of these were hospitalised for surgical procedures, either for elective management of conditions associated with TS or related to accidental injury; 11 were hospitalised for other reasons: infectious illness/dehydration n = 5, psychosis n = 1, abnormal liver function tests n = 1, vaginal bleeding n = 1, haematuria n = 1, cardiac failure n = 1, hypertension n = 1; and the remaining five were reported to have accidentally overdosed on the study drug. AEs that were considered unexpected and possibly related to the study drug were reported for 5/232 subjects (2%): hypertension n = 2 (in 1 subject this had been present for 11 years), surgical procedures n = 2, scoliosis n = 1. There were no reports of deaths, cancer or neoplasia. |
||||
|
Methodological comments Allocation to treatment groups: Authors state that subjects were randomised in a double blind fashion, but no further details are given. Blinding: States double blind. Placebo is given by injection. BA radiographs were read by a single observer who was blinded to treatment status. Comparability of treatment groups: Treatment groups appear similar at baseline. Method of data analysis: Data obtained during the initial 18-month placebo-controlled phase are reported for each of the five original randomisation groups. ITT performed for all subjects who received 180 days of active treatment. Sample size/power calculation: Not reported. Attrition/dropout: Withdrawals not discussed; eight patients were randomised but did not complete treatment. |
||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Partial |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
| Reference and design | Intervention | Participants | Outcome measures | |
|---|---|---|---|---|
|
Stephure and The Canadian Growth Hormone Advisory Committee86 and Rovet et al. 199387 (no extractable data, so no further information extracted here) Year: 2005 Country: Canada Study design: RCT Number of centres: multicentre Funding: Eli Lilly Canada Inc. |
Intervention: (GH group) rhGH (Humatrope, Eli Lilly Canada) by daily s.c.i. 6 times weekly (0.30 mg/kg/week, maximum weekly dose 15 mg) Control: no GH treatment Other interventions used: girls with primary ovarian failure received standardised sex steroid replacement: ethinyloestradiol 2.5 µg/day at age 13, 5.0 µg/day at age 14, and 2.0 µg on days 1–24 with medroxyprogesterone acetate 10 mg on days 15–24 of each month at age 15 and thereafter |
Target population: prepubertal girls, aged 7–13 years, with a diagnosis of TS documented by peripheral blood karyotype Number of participants: 154 (95 in Rovet) prepubertal girls Intervention: 76 (51 in Rovet) Control: 78 (44 in Rovet) Sample attrition/dropout: Overall, 15 withdrew from GH; 35 from control: addendum follow-up 8 from GH; 9 from control 1997 follow-up only, 5 from GH; 13 from control core protocol data only, 2 from GH; 13 from control Sample crossovers: N/A Inclusion criteria for study entry: Height less than the 10th percentile for chronological age on the growth charts of the NCHS of the USA An annualised GV less than 6.0 cm/year during a 6-month prerandomisation period Diagnosis of TS documented by peripheral blood karyotype. Phenotypic females with identifiable Y chromosome eligible to participate if had undergone prior gonadectomy Exclusion criteria for study entry: Clinically significant chronic systemic illness, prior treatment with GH, anabolic steroids, estrogens, craniospinal radiation or inadequate thyroxine replacement for hypothyroidism were excluded A spontaneous or stimulated serum GH level was 8.0 µg/l or greater in all subjects |
Primary outcomes: BA (years), height (cm), HtSDS (age specific/adult Turner), change in height (cm), change in HtSDS (age-specific Turner) Secondary outcomes: Method of assessing outcomes: routine haematology, biochemistry and thyroid function studies were monitored every 3 months (every 6 in control after first year), BA interpreted by central reader using Greulich and Pyle annually. Age-specific and AH SD scores (SDS, height SD score) and the change in height SD scores at protocol completion and follow-up relative to baseline were calculated according to published standards for girls with TS Length of follow-up: subjects returned for follow-up every 3 months until study completion, protocol completion criteria required annualised GV less than 2 cm/year and BA 14 years or greater Addendum follow-up = height and safety follow-up at least 1 year following latest core protocol visit |
|
| Characteristics of participants (mean ± SD) | ||||
| Baseline characteristics | GH (n = 61) | No treatment (n = 43) | p-value | |
| Age | 10.3 ± 1.8 | 10.9 ± 1.7 | ||
| Baseline BA (years) | 8.8 ± 1.4 | 8.9 ± 1.3 | ||
| Baseline height (cm) | 119.1 ± 8.5 | 122.0 ± 7.8 | ||
| Baseline HtSDS (age-specific Turner) | –0.2 ± 0.9 | –0.1 ± 0.8 | ||
| Adjusted mid-parental height (cm)a | 160.7 ± 6.2 | 159.3 ± 5.8 | ||
| 45,X karyotype (%) | 62.3 | 58.1 | ||
|
Comments a Adjusted mid-parental height = [(father height – 13 cm) + mother height]/2. Baseline results for patients who completed the protocol. Baseline data for patients who also had follow-up are very similar. No baseline characteristics differed at p < 0.05. |
||||
| Results: protocol completion characteristics (mean ± SD) | ||||
| Primary outcomes | GH (n = 61) | No treatment (n = 43) | GH effect:b mean (95% CI) | p-value |
| Age (years) | 16.0 ± 0.8 | 16.5 ± 0.9 | c | 0.002 |
| Time since randomisation (years) | 5.7 ± 1.6 | 5.7 ± 1.6 | ||
| BA (years) | 14.4 ± 0.8 | 14.5 ± 0.9 | –0.1 (0.5 to 0.3) | ns |
| Height (cm) | 147.5 ± 6.1 | 141.0 ± 5.4 | 7.2 (6.0 to 8.4) | < 0.001 |
| HtSDS (age-specific Turner) | 1.4 ± 1.0 | 0.2 ± 0.9 | 1.2 (1.0 to 1.5) | < 0.001 |
| HtSDS (adult Turner) | 0.7 ± 0.9 | –0.3 ± 0.8 | 1.1 (0.8 to 1.3) | < 0.001 |
| Change in height (cm) | 28.3 ± 8.9 | 19.0 ± 6.1 | 7.2 (6.0 to 8.3) | < 0.001 |
| Change in HtSDS (age-specific Turner) | 1.6 ± 0.6 | 0.3 ± 0.4 | 1.3 (1.1 to 1.5) | < 0.001 |
|
ns, not significant. b ANCOVA model with treatment, baseline HtSDS, baseline HtSDS by treatment interaction, baseline age, and baseline age by treatment interaction. Explanatory variables were removed from the model when not significant. GH effect is estimated by differences of least-squares means for treatment. c Age at protocol completion was significantly different between control and GH, p = 0.002, this reflects the similar numerical difference at baseline and completion, and the lower SD at completion due to the narrower age range. Protocol completion criteria required an annualised GV of less than 2 cm/year and a BA of 14 years or greater. |
||||
| Results: addendum follow-up characteristics (mean ± SD) | ||||
| Primary outcomes | GH (n = 40) | No treatment (n = 19) | GH effect:b mean (95% CI) | p-value |
| Age (years) | 20.7 ± 2.5 | 21.2 ± 2.0 | ||
| Time since randomisation (years) | 10.6 ± 1.7 | 10.7 ± 1.4 | ||
| BA (years) | 15.1 ± 1.0 | 15.2 ± 1.0 | 0.0 (–0.6 to 0.6) | ns |
| Height (cm) | 149.0 ± 6.4 | 142.2 ± 6.6 | 73. (5.4 to 9.2) | < 0.001 |
| HtSDS (age-specific Turner) | 0.9 ± 0.9 | –0.1 ± 1.0 | 1.1 (0.8 to1.4) | < 0.001 |
| HtSDS (adult Turner) | 0.9 ± 0.9 | –0.1 ± 1.0 | 1.1 (0.8 to 1.4) | < 0.001 |
| Change in height (cm) | 30.3 ± 8.3 | 21.6 ± 6.2 | 7.3 (5.4 to 9.1) | < 0.001 |
| Change in HtSDS (age-specific Turner) | 1.1 ± 0.5 | 0.0 ± 0.5 | 1.1 (0.8 to 1.4) | < 0.001 |
|
Comments As for completion characteristics. |
||||
| Adverse event | GH (n = 74) | No treatment (n = 64) | p-value | |
| Surgical procedures | 37 | 17 | 0.005 | |
| Otitis media | 35 | 17 | 0.014 | |
| Ear disorder | 15 | 4 | 0.024 | |
| Joint disorder | 10 | 2 | 0.036 | |
| Respiratory disorder | 8 | 1 | 0.037 | |
| Sinusitis | 14 | 4 | 0.041 | |
| Goitre | 0 | 4 | 0.004 | |
| Death (ruptured aortic aneurysm) | 0 | 1 | nr | |
| Elevated transamine levelsd | 1 | 0 | nr | |
| Intracranial hypertension | 1 | 0 | nr | |
|
Comments d Leading to withdrawal from study. After protocol completion there was no significant difference in auditory acuity (conductive or neurosensory) between groups (data not shown). There were no significant between group differences in change from baseline to end point in fasting blood glucose, glycated haemoglobin (HbA1c), serum T4 or TSH (data not shown). |
||||
|
Methodological comments Allocation to treatment groups: Eligible subjects were stratified for height relative to chronological age at entry and randomly assigned. Blinding: Unblinded – control received no treatment. No mention of blinding of assessors. Comparability of treatment groups: No statistically significant differences between groups at baseline (stated, p-values not given). Method of data analysis: Data are reported as mean ± 1 SD unless stated otherwise. Differences between groups at baseline and end point for characteristics such as age and duration of therapy were assessed by one-way ANOVA or Fisher’s exact test, as appropriate. No ITT analysis. Sample size/power calculation: Not calculated. Attrition/dropout: Dropout is discussed: 15 withdrew from the GH group; 35 from the control. Addendum follow-up: eight from GH, nine from control; 1997 follow up only: five from GH, 13 from control; core protocol data only: two from GH, 13 from control. |
||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate (no treatment) |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Davenport et al. 2007 85 Country: USA Study design: RCT, open label Number of centres: 11 Setting: US paediatric endocrine centres Funding: Supported by Eli Lilly (EL) & Co., along with grants from universities; four of the authors are employed by EL, most of the authors have received grant support from EL, as well as consulting and lectureship fees from EL and other pharmaceutical companies in the past |
1. Recombinant growth hormone (Humatrope) daily s.c.i. of 50 µg/kg/day 2. No treatment Duration of treatment: 2 years Other interventions used: none |
Target population: girls with TS, aged 9 months to 4 years Number of participants: total: 89 (The efficacy data exclude 1 subject who was found after study entry to have a 46,XX karyotype) 1. 45 2. 44 Sample attrition/dropout: Overall dropouts 10, GH group 4, no treatment 6 Reasons for discontinuation: Control: Parents’ decision n = 2 Scheduling problems n = 1 Request for GH n = 2 Lost to follow-up n = 1 GH: Relocation n = 1 Lost to follow-up n = 3 Compliance rated as excellent by authors: 95% of subjects received 80% of scheduled injections Inclusion criteria for study entry: Aged 9 months to 4 years Karyotype proven TS Normal urinalysis, haemoglobin and thyroid stimulating hormone Adequate thyroid hormone replacement for at least 6 months in those with hypothyroidism Written informed consent from legal guardians Exclusion criteria for study entry: Presence of Y-chromosomal component in the karyotype in subjects with gonads in situ Autosomal abnormality Concurrent treatment that might influence growth Clinically relevant systemic illness No specific eligibility criteria based on height or GV |
Primary outcomes: change in SDS for length or height (depending on age) from baseline to 2 years. A height gain of at least 0.5 was considered clinically significant Secondary outcomes: serum IGF-I, IGFBP-3, bone tumour markers, identify factors associated with treatment response, determine whether outcome could be predicted by regression model using these factors, assess safety of GH treatment in young cohort Method of assessing outcomes: Age-appropriate measures were obtained at each visit for length using infant measuring box (children < 2 years or older, children for whom accurate standing measurements could not be obtained) Standard wall-mounted stadiometer (children older than 2 years) Both length and height measured for girls between 2 and 3 years old; length measurements in these cases were used for the analyses Length/HtSDS were calculated on the basis of data for aged matched girls from the US Centers for Disease Control Mid-parental height calculated as follows: (father’s height – 13 cm + mother’s height)/2 and converted to SDS using normative height data for women at 20 years of age Serum IGF-1, IGFBP-3 and bone turnover markers were measured at baseline, 4 months, 1 year and 2 years SDSs were calculated using Esoterix’s data for healthy controls BA radiographs obtained at baseline, 1 year, and 2 year and read by blinded independent assessors Safety was assessed on each visit based on reported AE, detailed history and physical examinations Length of follow-up: 4-monthly intervals for the 2 years of treatment |
| Baseline characteristics of participants (mean ± SD) | |||
| Variable | GH (n = 45) | No treatment (n = 43) | p-value |
| Chronological age (years) | 1.98 ± 1.01 | 1.97 ± 1.01 | nr |
| BA (years)a | 1.95 ± 0.89 | 1.88 ± 0.96 | nr |
| BA–CA | –0.06 ± 0.56 | –0.14 ± 0.42 | nr |
| Length/height (cm) | 78.9 ± 8.6 | 77.6 ± 8.7 | nr |
| Length/HtSDS | –1.42 ± 1.00 | –1.76 ± 1.07 | nr |
| MPH (cm)b | 164.4 ± 5.0 | 164.4 ± 4.7 | nr |
| MPH SDSb | 0.17 ± 0.77 | 0.16 ± 0.73 | nr |
| Weight (kg) | 10.35 ± 2.28 | 9.92 ± 2.47 | nr |
| WtSDS | –1.31 ± 1.18 | –1.77 ± 1.46 | nr |
| BMI (kg/m2) | 16.48 ± 1.37 | 16.24 ± 1.29 | nr |
| Head circumference (cm)c | 47.2 ± 2.4 | 46.7 ± 2.1 | nr |
| Head circumference SDSc | 0.09 ± 1.05 | –0.14 ± 1.19 | nr |
| Karyotype distribution: 45,X | 27/45 (60%) | 29/43 (67%) | |
| Karyotype distribution: 45,X/46,XX | 7/45 (16%) | 7/43 (16%) | |
| Karyotype distribution: other | 11/45 (24%) | 7/43 (16%) | |
| IGF-1 SDSd | –0.25 ± 0.85 | –0.39 ± 0.95 | nr |
| IGFBP-3d | –0.66 ± 1.08 | –0.83 ± 1.05 | nr |
|
CA, chronological age. a Baseline BA missing for two subjects in each group. b Father’s height missing for one GH subject at both baseline and end point. c Baseline data missing for one subject in each group; one control subject had an erroneous value at baseline, so the value was not used; end point data missing for two control subjects. d Baseline data missing for eight control subjects and three GH-treated subjects; end point data missing for four control subjects and seven GH subjects. |
|||
| Results (mean ± SD) | |||
| Outcomes | GH (n = 41) | No treatment (n = 37) | p-value |
| Chronological age (years) | 4.03 ± 1.05 | 4.03 ± 1.03 | 0.9944 |
| BA (years)a | 4.24 ± 1.35 | 3.38 ± 1.11 | 0.0033 |
| BA–CA | –0.64 ± 0.80 | 0.21 ± 0.96 | < 0.0001 |
| Length/height (cm) | 99.5 ± 7.6 | 91.9 ± 7.2 | < 0.0001 |
| Length/HtSDS | –0.34 ± 1.10 | –2.16 ± 1.22 | < 0.0001 |
| MPH (cm)b | 164.7 ± 4.9 | 164.1 ± 4.9 | 0.5608 |
| MPH SDSb | 0.22 ± 0.76 | 0.12 ± 0.76 | 0.5607 |
| Weight (kg) | 16.62 ± 2.86 | 13.81 ± 2.50 | < 0.0001 |
| WtSDS | 0.20 ± 1.06 | –1.37 ± 1.36 | < 0.0001 |
| BMI (kg/m2) | 16.72 ± 1.70 | 16.24 ± 1.29 | 0.1724 |
| Head circumference (cm)4>c | 51.1 ± 1.5 | 49.9 ± 1.4 | 0.0004 |
| Head circumference SDSc | 1.17 ± 1.03 | 0.30 ± 0.99 | 0.0004 |
| IGF-1 SDSd | 1.26 ± 0.72 | –0.69 ± 0.84 | < 0.0001 |
| IGFBP-3d | 0.97 ± 0.94 | –1.12 ± 1.13 | < 0.0001 |
|
Comments For table footnotes, see corresponding notes above, under Baseline characteristics of participants. The between group difference for change in HtSDS after 2 years was 1.6 ± 0.6, p < 0.001 – this analysis was performed on data from the 78 subjects with karyotype proven TS who completed the 2-year study. The between-group difference was significant by 4 months and increased progressively. Total 2-year height gain was 13.6 ± 3.5 cm for the control group, vs 20.4 ± 3.3 cm for the GH group (p < 0.001). Data are reported as mean ± SD unless noted otherwise. |
|||
| No treatment (n = 37) | GH (n = 41) | p-value | |
| First-year GVe (cm/year) | 8.0 ± 2.4 | 11.7 ± 2.4 | < 0.0001 |
| Second-year GV (cm/year) | 5.5 ± 1.8 | 8.4 ± 1.6 | < 0.0001 |
| First-year GV SDS | –0.83 ± 0.95 | 1.75 ± 1.25 | < 0.0001 |
| Second-year GV SDS | –1.63 ± 1.29 | 0.70 ± 1.11 | < 0.001 |
| e Numbers in groups not known for first-year results; data are reported as mean ± SD unless noted otherwise. At the 2-year time point (when heights of both groups were compared with US standards), only 7% of GH-treated subjects remained below –2.0 SDS (~2.3 percentile); in contrast, 57% of the control subjects were below –2.0 SDS at 2 years (p < 0.0001). | |||
| Outcome | GH (n = 41) | No treatment (n = 37) | p-value |
| Baseline to 2-year change: IGF-I SDS | 1.53 ± 0.93 | –0.09 ± 0.87 | nr |
| Adverse effects | |||
| Adverse effects | GH (n = 45) | No treatment (n = 44) | |
| Serious AE, n (%)f | 4 (9) | 4 (9) | |
| Treatment-emergent AEg | 42 (93) | 43 (98) | |
|
f Control group: one subject each was hospitalised for surgical repair of an atrial septal defect, croup/bronchiolitis, gastroenteritis and dehydration. GH: one subject each was hospitalised for gastroenteritis/dehydration, bacterial pneumonia, persistent bleeding after tonsillectomy and hypoxaemia after adenoidectomy. g Events or conditions that began or worsened after study entry: many of these events were related to ear disorders. There was no detrimental effect of GH treatment on frequency of episodes of otitis media, rates of ear tube insertion, middle ear function or hearing. Most other events reported with a high frequency were typical childhood illnesses that were considered unlikely to have been related to GH treatment. There were no significant changes or between-group differences in serum TSH. AEs have been reported for the full group numbers. |
|||
|
Methodological comments Allocation to treatment groups: Children were stratified by age (9 months to 2.5 years and > 2.5–4 years) and then randomised using a blinded phone in process, in a 1 : 1 ratio. Blinding: Assessors of BA radiographs were blinded; it is not reported if assessors of other outcomes were blinded. Control group did not receive placebo injections. Comparability of treatment groups: The two groups appear broadly similar at baseline. BA–chronological age, length/HtSDS, IGF-1 SDS and IGFBP-3 SDS were slightly lower in the GH group at baseline. Weight measures were slightly higher in this group. No p-value, so unknown if these differences are minimal. Method of data analysis: The primary efficacy analysis was conducted on the baseline–2-year change in HtSDS for all subjects who had measurements at both time points (not ITT) using an ANOVA model with treatment group and baseline age group as explanatory variables. For analyses of changes in HtSDS, 1-sided tests were used, with the significance level set at 0.05. All other analyses of efficacy variables were conducted using 2-sided tests, with the significance level set at 0.05. Serious AEs, treatment-emergent AEs and laboratory data were summarised for all subjects who entered the study. Data are reported as mean ± SD unless noted otherwise. Sample size/power calculation: No calculation. Attrition/dropout: Overall dropouts 10, GH group 4, no treatment 6. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Adequate |
| 2. Was the treatment allocation concealed? | Adequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Gravholt et al. 2005 88 Country: Denmark Study design: Randomised, placebo-controlled crossover study Number of centres: not reported Funding: Government grant to Novo Nordisk Centre for Research in Growth and Regeneration. One author recipient of honoraria from Pharmacia and Novo Nordisk, and a second author is recipient of a research grant from Eli Lilly, Novo Nordisk and Roche |
1. GH 0.1 IU/kg/day s.c. 2. Placebo Age-matched control group studied once (not data extracted) Duration of treatment: 2 months in each arm. No washout period between the two study periods Other interventions used: At least 6 months before inclusion in the study all girls had received GH (0.1 IU/kg/day) |
Target population: girls with TS Number of participants: total 12; numbers allocated to each group not given Sample attrition/dropout: not reported Inclusion/exclusion criteria for study entry: not stated |
Primary outcomes: not stated Secondary outcomes: body composition, insulin sensitivity, other biochemical/metabolic markers, markers of ovarian function (not data extracted) Method of assessing outcomes: Participants studied at the end of every 2-month period, IGF-1, IGFBP-3 and IGFBP-1 and other biochemical markers tested at the end of every study period. Body composition measured by whole body DEXA Length of follow-up: 4 months |
| DEXA, dual-energy X-ray absorptiometry. | |||
| Characteristics of participants: 12 girls with TS, aged 9.5–14.8 years (median 12.9) – not reported | |||
| Outcomes | GH 0.1 IU/kg/day s.c. | Placebo | p-value |
| FM arms (g/kg total body weight) | 32.9 ± 8.2 | 36.0 ± 8.6 | 0.12 |
| FM legs (g/kg total body weight) | 98.7 ± 18.7 | 104.9 ± 17.8 | 0.340 |
| FM trunk (g/kg total body weight) | 80.7 ± 27.4 | 88.1 ± 35.4 | 0.1 |
| FM head (g/kg total body weight) | 18.7 ± 3.3 | 18.7 ± 3.1 | 0.5 |
| FM total (g/kg total body weight) | 231.0 ± 49.5 | 247.8 ± 58.1 | 0.04 |
| BMC arms (g/kg total body weight) | 3.6 ± 0.8 | 3.5 ± 0.7 | 0.6 |
| BMC legs (g/kg total body weight) | 10.5 ± 1.7 | 10.6 ± 1.8 | 0.3 |
| BMC trunk (g/kg total body weight) | 7.9 ± 1.5 | 8.0 ± 1.4 | 0.4 |
| BMC head (g/kg total body weight) | 7.9 ± 1.1 | 8.0 ± 1.2 | 0.9 |
| BMC total (g/kg total body weight) | 29.6 ± 3.6 | 30.1 ± 3.6 | 0.1 |
| LBM arms (g/kg total body weight) | 62.9 ± 6.4 | 60.5 ± 6.6 | 0.1 |
| LBM legs (g/kg total body weight) | 205.7 ± 23.7 | 202.0 ± 25.9 | 0.2 |
| LBM trunk (g/kg total body weight) | 378.8 ± 17.4 | 369.3 ± 29.6 | 0.046 |
| LBM head (g/kg total body weight) | 78.0 ± 15.2 | 78.8 ± 13.6 | 0.5 |
| LBM total (g/kg total body weight) | 725.4 ± 44.8 | 710.5 ± 54.6 | 0.05 |
| IGF-1 (µg/l) | 380.5 ± 116.3 | 179.8 ± 79.4 | < 0.0005 |
| IGFBP-1 (µg/l) | 3.1 ± 2.4 | 7.3 ± 4.7 | 0.002 |
| IGFBP-3 (µg/l) | 5982 ± 1557 | 4344 ± 787 | 0.002 |
| IGF-1/IGFBP-3 ratio | 0.065 ± 0.014 | 0.041 ± 0.013 | < 0.0005 |
| Fasting glucose (mmol/l) | 4.28 ± 0.59 | 4.02 ± 0.44 | 0.046 |
| Fasting insulin (pmol/l) | 17.17 ± 8.30 | 8.58 ± 4.27 | 0.007a |
| Fasting glucagon (ng/l) | 97.8 ± 43.4 | 79.2 ± 23.3 | 0.08 |
| ISIcomp | 10.3 ± 9.8 | 20.9 ± 16.0 | 0.003 |
| RHOMA | 3.34 ± 1.70 | 1.56 ± 0.87 | 0.001 |
| AUC insulin (pmol/l/24 h) | 61 344 ± 28 547 | 40 868 ± 16 112 | 0.006 |
| AUC glucose | 6922 ± 570 | 6707 ± 464 | 0.3 |
| AUC lactate (mmol/l/540 min) | 5255 ± 1224 | 4589 ± 1165 | 0.2 |
| AUC alanine (µmol/l/540 min) | 2230 ± 548 | 2081 ± 368 | 0.4 |
| AUC glycerol (µmol/l/540 min) | 648 ± 208 | 527 ± 104 | 0.1 |
| AUC BOH (µmol/l/540 min) | 1215 ± 1486 | 589 ± 385 | 0.2 |
| AUC lactate OGTT (mmol/l/120 min) | 11569 ± 2438 | 10239 ± 1674 | 0.09 |
| AUC alanine OGTT (µmol/l/120 min) | 2848 ± 730 | 2665 ± 459 | 0.3 |
| AUC glycerol OGTT (µmol/l/120 min) | 444 ± 83 | 408 ± 96 | 0.2 |
| AUC BOH OGTT (µmol/l/120 min) | 564 ± 812 | 319 ± 268 | 0.3 |
| AUC FFA OGTT (µmol/l/120 min) | 2.43 ± 0.77 | 2.06 ± 0.91 | 0.1 |
|
Comments AUC, area under the curve; BOH, 3-hydroxybutyrate; FFA, free fatty acids; HOMA, homeostasis model assessment index; ISIcomp, composite whole-body insulin sensitivity index; OGTT, oral glucose tolerance test; R, fasting insulin (22.5 × e–ln fasting glucose). a Wilcoxon two-tailed test. Numbers entered into each group unclear. |
|||
|
Adverse effects Not reported. |
|||
|
Methodological comments Allocation to treatment groups: States randomised, but no other details. No details of numbers allocated to groups. Blinding: States placebo used, no other details given. Comparability of treatment groups: Appear comparable, but unclear if the details are from baseline. Method of data analysis: Groups were compared using Student’s two-tailed paired t-test, independent t-test, Mann–Whitney U-test or Wilcoxon test as appropriate. States that all data were tested for period as well as carry-over effects: authors state this did not affect significance. Results expressed as mean ± SD. Statistical significance was assumed for p < 5%. Sample size/power calculation: Not reported. Attrition/dropout: Not reported/discussed, no numbers allocated to groups specified. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Unknown |
| 4. Were the eligibility criteria specified? | Inadequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Gravholt et al. 2005 89 Country: Denmark Study design: randomised, placebo-controlled, crossover trial Number of centres: not reported Funding: Government grant to Novo Nordisk Centre for Research in Growth and Regeneration |
All girls were treated with placebo + placebo, GH + placebo or GH + 17β oestradiol (this latter group’s results are not data extracted) for a 2-month period each completed by a 24-h blood sampling period. The treatment regimen was given sequentially and in random order Doses: 1. GH [1.3 ± 0.3 (0.7–1.8)] mg/day [mean ± SD (range)] 2. 17β oestradiol [0.39 ± 0.16 (0.25–0.6)] mg/day A pubertal stage-matched healthy control group (n = 10) was studied once (not data extracted) Duration of treatment: 6 months Other interventions used: At least 5 months before inclusion in the study all TS girls received GH [1.3 ± 0.3 (0.7–1.8)] mg/day [mean ± SD (range)] and 17β oestradiol [0.39 ± 0.16 (0.25–0.6)] mg/day |
Target population: girls with TS Number of participants: total 9; no numbers given for treatment groups Sample attrition/dropout: One girl was excluded for non-compliance with study protocol Inclusion/exclusion criteria for study entry: all girls with TS previously verified by chromosomal karyotyping. No other criteria stated |
Primary outcomes: not stated Secondary outcomes: insulin sensitivity, glucose tolerance, body composition Method of assessing outcomes: participants were studied at the end of every 2-month period. IGF-1, IGFBP-3 and IGFBP-1 tested at each study visit. Body composition measured by DEXA Length of follow-up: 8 months (including initial observation period of 2 months) |
| Characteristics of participants: baseline data given for Turner participants as 1 group; did not extract data for healthy controls | |||
| TS | p-value | ||
| Age (years) | 15.9 ± 1.8 | ||
| Weight (kg) | 49.1 ± 11.0 | ||
| Height (cm) | 148.3 ± 4.0 | ||
| BMI (kg/m2) | 22.2 ± 4.0 | ||
| Results | |||
| Outcomes | GH | Placebo | p-value |
| FM arms | 41.2 ± 10.2 | 46.3 ± 12.9 | Unclear which groups the p-values in the paper are referring to: not data extracted here |
| FM legs | 122.4 ± 22.2 | 135.1 ± 30.2 | |
| FM trunk | 96.2 ± 27.9 | 116.6 ± 38.7 | |
| FM head | 14.7 ± 2.1 | 14.8 ± 2.5 | |
| FM total | 274.5 ± 55.5 | 312.9 ± 74.7 | |
| BMC arms | 4.5 ± 0.4 | 4.2 ± 0.3 | |
| BMC legs | 11.7 ± 0.8 | 11.9 ± 0.9 | |
| BMC trunk | 9.0 ± 1.1 | 8.9 ± 0.7 | |
| BMC head | 7.3 ± 1.2 | 7.2 ± 1.2 | |
| BMC total | 32.5 ± 2.6 | 32.1 ± 2.0 | |
| LBM arms | 61.2 ± 6.5 | 56.5 ± 10.4 | |
| LBM legs | 213.2 ± 24.1 | 197.2 ± 29.0 | |
| LBM trunk | 356.8 ± 20.9 | 339.9 ± 30.4 | |
| LBM head | 61.6 ± 10.7 | 61.3 ± 10.4 | |
| LBM total | 692.8 ± 55.5 | 655.2 ± 73.7 | |
| IGF-1 (µg/l) | 661 ± 192 | 288 ± 69 | |
| IGFBP-1 (µg/l) | 1.8 ± 1.2 | 4.2 ± 2.8 | |
| IGFBP-3 (µg/l) | 5157 ± 741 | 4146 ± 573 | |
| Fasting glucose (mmol/l) | 4.46 ± 0.40 | 4.04 ± 0.47 | |
| Fasting insulin (pmol/l) | 147.1 ± 54.0 | 86.1 ± 41.0 | |
| Fasting glucagon (ng/l) | 37.4 ± 12.6 | 43.0 ± 26.1 | |
| ISIcomp | 7.0 ± 3.7 | 14.7 ± 8.7 | |
| RHOMA | 4.12 ± 1.60 | 2.24 ± 1.31 | |
| AUC insulin (pmol/l/24 h) | 8710 ± 4728 | 5848 ± 4312 | |
| AUC glucose | 119 ± 10 | 111 ± 13 | |
| AUC lactate (nmol/l/480 min) | 4853 ± 1520 | 5532 ± 2120 | |
| AUC alanine (µmol/l/480 min) | 1864 ± 627 | 2230 ± 543 | |
| AUC glycerol (µmol/l/480 min) | 516 ± 245 | 491 ± 220 | |
| AUC BOH (µmol/l/480 min) | 947 ± 1372 | 338 ± 437 | |
| AUC lactate OGTT (mmol/l/120 min) | 3614 ± 976 | 3718 ± 948 | |
| AUC alanine OGTT (µmol/l/120 min) | 855 ± 190 | 840 ± 159 | |
| AUC glycerol OGTT (µmol/l/120 min) | 117 ± 56 | 99 ± 42 | |
| AUC BOH OGTT (µmol/l/120 min) | 96 ± 96 | 57 ± 68 | |
| AUC FFA OGTT (µmol/l/120 min) | 0.83 ± 0.18 | 0.75 ± 0.27 | |
| AUC, area under the curve; BOH, 3-hydroxybutyrate; FFA, free fatty acids; HOMA, homeostasis model assessment index; ISIcomp, composite whole-body insulin sensitivity index; OGTT, oral glucose tolerance test; R, fasting insulin (22.5 × e–ln fasting glucose). | |||
|
Adverse effects Not reported/discussed. |
|||
|
Methodological comments Allocation to treatment groups: Unclear whether allocation to treatment groups has taken place, or whether participants all took the same combination of drugs in the same time period. Blinding: No details given, although is stated that placebo + placebo given and GH + placebo in those groups. Comparability of treatment groups: Not reported – baseline information given for TS participants as a whole. Method of data analysis: Groups were compared using Student’s two-tailed paired t-test and an independent t-test when normally distributed, Mann–Whitney and Wilcoxon used for non-parametric data. Results expressed as mean ± SD. Statistical significance was assumed for p < 5%. Sample size/power calculation: Not reported. Attrition/dropout: One patient excluded for non-compliance with study protocol. No further details given. No washout period. Unclear on whether is randomised or treatment simply given ‘in a random order’ (p. 617). |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | nr |
| 4. Were the eligibility criteria specified? | Inadequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Adequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Johnston et al. 2001 90 Country: UK Study design: RCT Number of centres: six Funding: Pharmacia & Upjohn |
1. GH 28–30 IU/m2 surface area/week daily s.c.i. 2. Low-dose estrogen: ethinyloestradiol 1.0 µg/day for < 10 years and 2.0 µg/day for > 10 years (approx 50–75 ng/kg body weight daily) 3. Combined ethinyloestradiol and GH (not data extracted) Duration of treatment: 1 year in these groups (group 2 changed to group 3 after the first year, not data extracted, and treatment continued until height increases had fallen below 1 cm/year) Other interventions used: not stated for year 1 |
Target population: girls with TS Number of participants: total 58 1. 22 2. 13 3. 23 Sample attrition/dropout: 7 withdrawals, 5 girls reallocated from estrogen to GH: it is unclear at what point this occurred Inclusion criteria for study entry: not stated Exclusion criteria for study entry: other growth-limiting disorders, prior hormone therapy |
Primary outcomes: height gain at AH Secondary outcomes: growth-enhancing effect of LDE (not data extracted), change in HSDS Method of assessing outcomes: standing height, sitting height, and weight were measured at 3-month intervals; HtSDSs were derived from published Turner height standards, BA was initially determined at yearly intervals and calculated using the Tanner–Whitehouse RUS method applicable to normal female population. Various biochemical measures performed at study entry and annually, including triglycerides, cholesterol and TSH Length of follow-up: 1 year |
| RUS, radius, ulna and finger (or short) bones. | |||
| Characteristics of participants | |||
| Characteristic | GH 28–30 IU/m2 surface area/week (n = 22) | Low-dose estrogen: ethinyloestradiol (n = 13) | p-valuea |
| Age (years) | 9.0 (5.2 to 15.4) | 9.1 (6.0 to 13.7) | |
| BA (years) | 8.0 (3.3 to 13.5) | 7.9 (3.0 to 13.7) | |
| Height (cm) | 113.2 (93.2 to 135.1) | 114.0 (94.6 to 140) | |
| HSDS for CA | –0.3 (–2.1 to 1.2) | –0.1 (–1.5 to 1.8) | |
| HSDS for BA | 0.6 (–0.8 to 3.3) | 1.0 (–0.6 to 2.4) | |
| Mid parental HSDS | –0.2 (0.8) | –0.3 (1.1) | |
|
a Not extracted, as unclear which groups of the three to which this refers. Results are expressed as mean (range) or (SD). |
|||
| Results | |||
| Outcomes | GH 28–30 IU/m2 surface area/week (n = unclear) | Low-dose estrogen: ethinyloestradiol (n = unclear) | p-value |
| Change in HSDS in first year | +0.7 (0.7) | +0.4 (0.9) | < 0.05 |
|
Adverse effects Three of 58 girls ceased GH early because of serious health events not directly related to GH or LDE: one each with hypertension, ulcerative colitis and brain tumour. One patient in group 3 died from aortic dissection shortly after treatment cessation. Compliance problems led to the withdrawal of four patients. Seven others developed coincidental disorders but these were not considered sufficient to invalidate continued participation in the study. Five girls from group 2 were allocated to LDE were re-allocated to GH due to concerns over early breast development at age range 6.2–8.9 years. |
|||
|
Methodological comments Allocation to treatment groups: States randomised, no other details given. Five girls reallocated from estrogen to GH; it is unclear at what point this occurred. Blinding: Unknown, no details given. Comparability of treatment groups: Authors state that the groups were similar for the main monitoring parameters. Method of data analysis: Within-group results were compared using the paired Student’s t-test. Between-group results were compared using analysis of variance. Parental HtSDS values were calculated using normal population data. Sample size/power calculation: Not reported. Attrition/dropout: Seven withdrawals: three out of 58 girls ceased GH early because of serious health events not directly related to GH or LDE. Compliance problems led to the withdrawal of four patients. Treatment centres had the option of stopping ethinyloestradiol therapy if girls showed unacceptable premature breast development or excessive bone maturation: this occurred in five cases. Group numbers for FH data are lower; for the 1-year data they are unclear. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Inadequate |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Inadequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
PWS data extraction forms
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Lindgren et al. 1997,100 1998,101 Countries: Sweden and Denmark Study design: RCT Number of centres: multicentre Funding: Pharmacia & Upjohn |
1. 0.1 IU/kg/day GH by s.c.i. 2. No treatment Duration of treatment: 2 years (only year 1 data extracted, as no control arm in year 2) Other interventions used: special dietary instructions more than 1 year before start of treatment and throughout the study period to ensure constant energy intake per kilogram of body weight |
Target population: prepubertal children aged 3–12 years with PWS Number of participants: total n = 29 1. n = 15 2. n = 14 An additional group of non-PWS obese children was also studied, but data from this group were not data extracted Sample attrition/dropout: Two control group patients excluded from analysis Inclusion criteria for study entry: fulfilled diagnostic criteria for PWS and had either a paternal deletion or maternal disomy of chromosome region 15q11-13; projected FH < 165 cm (boys) and 154 cm (girls) |
Primary outcomes: not stated Secondary outcomes: HtSDS; GV SDS, BMI SDS, lean mass, % body fat Method of assessing outcomes: height and WtSDS calculated with reference to the standard for healthy Swedish children; BA was assessed according to Tanner–Whitehouse 2/RUS; % body fat estimated by DEXA QoL questionnaires completed (but no extractable data reported) Length of follow-up: 1 year |
| Characteristics of participants | |||
| Mean (range) | 0.1 IU/kg/day GH (n = 15) | No treatment (n = 12) | p-value |
| Age (years) | 6.8 (3.6 to 11.9) | 6.4 (3.3 to 11.7) | |
| BA (years) | 6.6 (3.3 to 13.0) | 5.4 (3.3 to 10.2) | |
| Sex (f/m) | 7/8 | 5/7 | |
| Target HtSDS | 0.4 (–1.3 to 1.8) | –0.1 (–1.5 to 1.0) | |
| HtSDS | –1.6 (–4.0 to 0.5) | –1.7 (–5.3 to 0.4) | |
| BMI (SDS) | 3.0 (–0.7 to 7.6) | 2.1 (–1.3 to 5.1) | |
| GV (SDS) mean ± SD (range) | –1.9 ± 2.0 (–6.4 to 0.9) | –0.1 (–1.7 to 2.71) | |
| IGF-1 (SDS) | –1.6 (–3.0 to –0.6) | –1.4 (–2.4 to –0.1) | |
| Fat-free mass (kg) by DEXA: mean ± SD | 14.9 ± 4.1 | 14.1 ± 3.0 | |
| Fat-free mass (kg) by BIA: mean ± SD | 14.6 ± 3.9 | 13.6 ± 3.3 | |
| Body fat (%) by DEXA: mean ± SD | 40.0 ± 10.5 | 34.8 ± 7.9 | |
| Body fat (%) by BIA: mean ± SD | 44.6 ± 9.2 | 41.3 ± 10.7 | |
|
Comments BIA, bioelectrical impedance analyser; DEXA, dual-energy X-ray absorptiometry. GV SDS was during 12 months before treatment commenced. |
|||
| Results | |||
| Mean (range) | 0.1 IU/kg/day GH (n = 15) | No treatment (n = 12) | p-value |
| BA (years) | 8.0 (5.5 to 13.9)a | 6.9 (3.9 to 11.4) | |
| BA (years) change from baseline | 1.4 (0.0 to 2.8) | 1.5 (0.4 to 2.6) | |
| HtSDS | –0.4 (–2.7 to 1.9)a | –1.8 (–5.1 to –0.2) | |
| BMI (SDS) | 2.0 (–2.4 to 6.7)a | 2.5 (0.1 to 6.1) | |
| GV (SDS) mean ± SD (range) | 6.0 ± 3.2 (1.4 to 11.9)a | –1.4 (–3.2 to –0.3) | |
| IGF-1 (SDS) | 1.8 (–0.1 to 4.1)a | –1.4 (–2.9 to –0.3) | |
| Fat-free mass (kg) by DEXA: mean ± SD | 19.8 ± 5.2b | 15.2 ± 2.9 | |
| Fat-free mass (kg) by BIA: mean ± SD | 21.7 ± 8.9b | 14.8 ± 3.5 | |
| Body fat (%) by DEXA: mean ± SD | 30.9 ± 11.4b | 38.2 ± 9.1 | |
| Body fat (%) by BIA: mean ± SD | 30.3 ± 10.5b | 43.3 ± 12.9 | |
|
a Change from baseline p < 0.05. b Change from baseline p < 0.001. |
|||
|
Adverse effects Intravenous glucose tolerance test was normal and unchanged in all children. Basal fasting insulin levels were significantly increased throughout the group in the GH group (from 10.4 mU/I ± 2.7 SD to 19.2 mU/I ± 10.5 SD, p < 0.001). No severe progression of scoliosis (angle ≥ 20°) in either group. Bone mineral density did not differ between groups. One child developed low levels of thyroxine without any change in TSH levels. He received substitution with l-thyroxine during the GH treatment. The increased levels of fasting insulin during the treatment may be regarded as laboratory AE. However, both levels of fasting glucose and HbA1c were unchanged and, although increased compared with pretreatment, insulin levels were still within the normal range. |
|||
|
Methodological comments Allocation to treatment groups: States children were randomised, but no further details given. Blinding: Open label. Comparability of treatment groups: Baseline age, height, BMI and HVs stated to be similar in both PWS groups. Method of data analysis: Student’s two-tailed paired and unpaired t-tests were used for normally distributed values, and non-parametric tests were used otherwise. Single regression analysis used for statistical comparisons. Not ITT. Data were analysed as change from baseline rather than between-group differences. Sample size/power calculation: Not reported. Attrition/dropout: One patient excluded at baseline evaluation because she had a severe scoliosis that required surgical intervention; one patient was excluded after 6 months in the control arm because she developed central precocious puberty. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Carrel et al. 2004,22 Myers et al. 2007,97 Whitman et al. 200498 Country: USA Study design: RCT Number of centres: two Funding: supported by Pharmacia Inc. (Pfizer) |
1. 1 mg/m2/day GH 2. No treatment Duration of treatment: 1 year Other interventions used: 0.1 g/kg of deuterium-labelled water was given on day 1 and 0.15 g/kg of oxygen-18 water |
Target population: infants and toddlers with PWS Number of participants: Total: n = 32 (Whitman et al. ); n = 29 (Carrel et al. ); n = 25 (Myers et al. ) 1. n = 15 2. n = 14 In Whitman paper – 30 patients completed first 6 months: n = 18, n = 12 Sample attrition/dropout: none in difference in n between Whitman paper and others suggests seven patients dropped out Inclusion criteria for study entry: confirmed diagnosis of PWS; age 4–37 months |
Primary outcomes: not stated Secondary outcomes: % body fat, LBM, bone mineral density, GV SDS, change in height, IGF-1; mobility (not data extracted as not per protocol) Method of assessing outcomes: Harpenden stadiometer used for length/height for children > 2, otherwise an infantometer was used; body composition measured by DEXA Length of follow-up: 1 year |
| Characteristics of participants | |||
| Mean ± SD | 1 mg/m2/day GH (n = 15) | No treatment (n = 14) | p-value |
| Age (months) | 13 ± 8 | 15 ± 0 | ns |
| Per cent female | 50 | 42 | ns |
| Length/HtSDSa | –1.6 ± 1.2 | –1.3 ± 1.1 | |
| GV SDS | 1.4 ± 1.8 | 1.2 ± 1.4 | |
| Body fat (%)a | 28 ± 7 | 29 ± 12 | |
| Lean mass (kg)a | 5.8 ± 1.9 | 6.9 ± 2.0 | |
| BMD (g/cm2)a | 0.60 ± 0.08 | 0.64 ± 0.09 | |
| Total cholesterol (mg/dl) | 163 ± 34 | 170 ± 30 | |
| IGF-1 (ng/dl)a | 34 ± 21 | nr | |
| Fasting insulin (μIU/ml) | 4.8 ± 3.7 | ||
|
Comments a From Myers paper, which had unclear patient numbers. Baseline data are also given by Whitman et al. These have not been data extracted as they differ slightly from the group presented here. Whitman’s results were for 6 months, so it is assumed that the Carrel data supersede these. |
|||
| Results | |||
| Mean ± SD | 1 mg/m2/day GH (n = 15) | No treatment (n = 14) | p-value |
| Mean % body fat | 23.2 ± 8.9 | 32.7 ± 8.8 | 0.03 |
| Change in body fat | –4.8% ± 5.7% | 4.1% ± 4.6% | 0.001 |
| Change in LBM (kg) | 3.6 ± 0.5 | 1.8 ± 0.7 | < 0.001 |
| Change in height (cm) | +15.4 ± 2.3 | 9.2 ± 3.2 | < 0.001 |
| GV SDS | 5.0 ± 1.8 | 1.2 ± 1.4 | |
| IGF-1 (ng/ml) | 231 ± 98 | 51 ± 28 | < 0.001 |
| Fasting insulin (μIU/ml) | 5.6 ± 7.1 | 5.7 ± 7.1 | ns |
| Bone mineral density (%) | 14.1 ± 10.4 | 9.0 ± 6.9 | ns |
| Total cholesterol (mg/dl) | 159 ± 40 | 183 ± 43 | |
| Length/HtSDSb | –0.2 ± 1.5 | –1.5 ± 0.7 | |
|
Comments b From Myers paper, which had unclear patient numbers. GVSDS in GH patients, p < 0.001 compared with baseline. Length/HtSDS change from baseline in GH group, p < 0.005. |
|||
|
Adverse effects No changes in the prevalence of scoliosis were seen between the treatment and control groups (Carrel et al. ) although Myers et al. comment on progression of scoliosis in one patient. No other adverse effects were noted during this study, and no subject required thyroid hormone therapy. After the first 6 months, two children showed a 3.5 SD increase in head circumference. This was monitored, but the later papers do not mention it. |
|||
|
Methodological comments Allocation to treatment groups: Randomisation following stratification by age (4–18 months and 19–37 months) and sex. No further details given. Myers and Whitman papers state that a 60 : 40 ratio was used, but this does not reflect numbers in the Carrel study, suggesting that attrition bias may have affected the results. Blinding: None. Comparability of treatment groups: Similar at baseline. Method of data analysis: The t-test for between-group comparisons. Does not appear to be ITT. Data reported by Whitman et al. was for 25 patients who completed the first 6 months. All three papers appear to report data for a slightly different version of the patient group. Sample size/power calculation: Not reported. Attrition/dropout: Difference in n between Whitman paper and others suggests that seven patients dropped out. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Carrel et al. 1999,95 Myers et al. 199996 Country: USA Study design: open RCT Number of centres: not reported Funding: Genentech Foundation for Growth and Development |
1. GH 1 mg/m2/day 2. No treatment Duration of treatment: 1 year Other interventions used: standardised caloric intake |
Target population: children with PWS without prior GH therapy Number of participants: Total: n = 54 1. n = 35 2. n = 19 Sample attrition/dropout: none Inclusion criteria for study entry: genetically confirmed patients with PWS were aged 4–16, with skeletal maturation < 13 for girls and < 15 for boys Exclusion criteria for study entry: prior GH therapy |
Primary outcomes: not clearly stated Secondary outcomes: HtSDS; GV; GVSDS; body fat; lean mass; BM; IGF-1; IGFBP-3; insulin; cholesterol; HDL-C; strength and agility (not data extracted as not per protocol) Method of assessing outcomes: height measured by Harpenden stadiometer; Greulich and Pyle method of determining BA; body composition assessed using DEXA Length of follow-up: 1 year |
| HDL-C, high-density lipoprotein cholesterol. | |||
| Characteristics of participants | |||
| Mean ± SD | GH 1 mg/m2/day (n = 35) | No treatment (n = 19) | p-value |
| Sex (% female) | 42 | 58 | |
| Mean age (years) | 9.8 | 10.0 | |
| Prepubertal (n) | 34 (97%) | 17 (90%) | |
| HtSDS | –1.1 ± 1.3 | –1.5 ± 0.8 | |
| Mean GV (cm/year) | 4.72 ± 2.2 | 5.18 ± 1.5 | |
| Mean GV SDS | –1.0 ± 2.5 | –0.9 ± 1.7 | |
| BA | 9.1 ± 3.6 | 8.4 ± 3.1 | |
| Body fat (%) | 46.3 ± 8.4 | 42.6 ± 8.1 | |
| Lean mass (kg) | 20.5 ± 6.3 | 20.5 ± 5.0 | |
| BMI (kg/m2) | 25.0 ± 6.7 | 24.2 ± 6.5 | |
| IGF-1 (ng/ml) | 127 ± 67 | 139 ± 64 | |
| IGFBP-3 (ng/ml) | 1.73 ± 0.49 | 1.84 ± 0.64 | |
| Insulin-0 hour (mIU/l) | 11.2 ± 9.9 | 9.3 ± 6.2 | |
| Insulin-2 hour (mIU/l) | 49.5 ± 40.7 | 41.6 ± 42.5 | |
| Total cholesterol (mg/dl) | 184 ± 36 | 190 ± 36 | |
| HDL-C (mg/dl) | 42 ± 8 | 44 ± 9 | |
| Femoral neck BMD (g/cm3) | 0.656 ± 0.19 | 0.636 ± 0.9 | |
| Spine BMD (g/cm3) | 0.744 ± 0.14 | 0.753 ± 0.12 | |
| Scoliosis (°) | 9.1 ± 6.0 | 14.7 ± 11.0 | |
| Free fatty acids (mmol/I) | 0.6 ± 0.4 | 0.6 ± 0.3 | |
| Triglycerides (mg/dl) | 91.6 ± 57.9 | 84.3 ± 39.6 | |
| Results | |||
| Mean ± SD | GH 1 mg/m2/day (n = 35) | No treatment (n = 19) | p-value |
| HtSDS | –0.6 ± 1.2 | –1.6 ± 1.2 | < 0.01 |
| Mean GV (cm/year) | 10.1 ± 2.5 | 5.0 ± 1.8 | < 0.01 |
| Mean GV SDS | 4.6 ± 2.9 | –0.7 ± 1.9 | < 0.01 |
| BA | 10.6 ± 3.5 | 9.8 ± 3.0 | ns |
| Body fat (%) | 38.4 ± 10.7 | 45.8 ± 8.8 | < 0.01 |
| Lean mass (kg) | 25.6 ± 4.3 | 21.7 ± 5.0 | < 0.01 |
| BMI (kg/m2) | 23.7 ± 6.3 | 25.2 ± 8.9 | ns |
| IGF-1 (ng/ml) | 522 ± 127 | 121 ± 52 | < 0.01 |
| IGFBP-3 (ng/ml) | 3.5 ± 0.73 | 2.07 ± 0.45 | < 0.01 |
| Insulin-0 hour (mIU/l) | 18.6 ± 14.6 | 8.8 ± 5.4 | |
| Insulin-2 hour (mIU/l) | 70.2 ± 44.2 | 47.1 ± 34.1 | |
| Total cholesterol (mg/dl) | 166 ± 34 | 193 ± 34 | < 0.01 |
| HDL-C (mg/dl) | 50 ± 10 | 44 ± 8 | < 0.01 |
| Femoral neck BMD (g/cm3) | 0.797 ± 0.09 | 0.707 ± 0.09 | < 0.05 |
| Spine BMD (g/cm3) | 0.834 ± 0.15 | 0.793 ± 0.13 | |
| Scoliosis (°) | 12.1 ± 7.0 | 16.6 ± 10.0 | |
| Free fatty acids (mmol/I) | 0.72 ± 0.40 | 0.64 ± 0.30 | < 0.01 |
| Triglycerides (mg/dl) | 86.0 ± 62.0 | 94.2 ± 49.0 | |
|
Comments The p-values are for paired t-test before and after GH therapy, compared with either baseline values of treated patients or 12-month values of non-treated patients. |
|||
|
Adverse effects Headaches in two patients treated with GH within first 3 weeks. Symptoms resolved with temporary cessation and gradual re-institution of GH. No pseudotumour cerebri. |
|||
|
Methodological comments Allocation to treatment groups: reported as randomised 60 : 40. Method not stated. Blinding: None. Comparability of treatment groups: Similar at baseline. Method of data analysis: ITT. Data were analysed using a Student’s t-test for paired samples or two related samples. Sample size/power calculation: Not reported. Attrition/dropout: None. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Adequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
de Lind van Wijngaarden et al. 2009,93 Festen et al. 200894 Country: The Netherlands Study design: RCT Number of centres: 18 Funding: not stated |
1. 1 mg/m2 s.c. daily 2. No treatment Duration of treatment: 1 year for infants and 2 years for children After 1st year, infants were all offered a second year of GH treatment. Not discussed here as no control group Other interventions used: caloric intake and activity level standardised and monitored |
Target population: infants and prepubertal children with PWS, who were not severely overweight, naive to GH treatment Number of participants: total n = 104 enrolled, n = 91 were available for follow-up: 42 infants (< 3.5 years) and 49 children over 3.5 years. Randomised groups not clear The following are the groups analysed at year 1: Infants:1. n = 19, 2. n = 19 Children:1. n = 23, 2. n = 21 Sample attrition/dropout: four infants and five children excluded from analysis Inclusion criteria: genetically confirmed diagnosis of PWS; age 6 months –14 years; BA < 14 (girls) or 16 (boys); prepubertal – Tanner breast stage ≤ 2 for girls and testicular volume < 4ml for boys Exclusion criteria: non-cooperative behaviour; on medication to reduce fat |
Primary outcomes: not stated in Festen paper, scoliosis in Lind van Wijngaarden paper Secondary outcomes: HtSDS, BMI, BMI SDS, head circumference SDS, IGF-1, IGF-1 SDS, IGFBP-3, IGFBP-3 SDS, IGF-1/BP3 (SDS), LBM and scoliosis Method of assessing outcomes: Harpenden stadiometer used to measure height, using a mean of three values. Anthropometric measurements taken at baseline and every 3 months; DEXA used for fat measurements. FM, fat % and LBM were transformed into SDS, adjusting for age and sex. LBM is related to height, so LBM HtSDS were computed by comparing LBM of PWS with LBM of healthy children with the same height and sex. IGF-1 and IGFBP-3 were transformed to SDS using sex- and age-matched Dutch references Length of follow-up: 1 year (infants), 2 years (children) |
| Characteristics of participants from Festen et al. 200894 (other than scoliosis and trunk LBM/BSA), as this is the most complete | |||
| Baseline characteristics of infants (6 months to 3 years) | |||
| Median (IQR) | 1 mg/m2 s.c. daily rhGH (n = 20) | No treatment (n = 22) | p-value |
| Sex (m/f) | 12/8 | 16/6 | |
| Age (years) | 2.0 (1.6 to 3.1) | 1.3 (1.0 to 2.8) | |
| HtSDS | –2.3 (–2.8 to –0.7) | –2.1 (–3.2 to –1.0) | |
| BMI (kg/m2) | 16.4 (15.1 to 18.6) | 16.1 (14.7 to 18.2) | |
| BMI (SDS) | 0.5 (–0.9 to 1.9) | –0.8 (–1.7 to 1.6) | |
| Head circumference (SDS) | –0.8 (–1.6 to –0.3) | –1.1 (–1.8 to –0.5) | |
| IGF-1 (ng/ml) | 27.0 (22.0 to 35.0) (n = 11) | 47.0 (17.0 to 52.0) | |
| IGF-1 (SDS) | –1.9 (–2.8 to –1.3) (n = 11) | –1.6 (–2.6 to –0.4) (n = 11) | |
| IGFBP-3 (ng/ml) | 0.8 (0.7 to 1.1) (n = 11) | 1.1 (0.8 to 1.3) (n = 11) | |
| IGFBP-3 (SDS) | –2.6 (–3.3 to –2.0) (n = 11) | –1.5 (–2.6 to –0.7) (n = 11) | |
| IGF-1/BP3 (SDS) | –0.9 (–2.0 to –0.4) (n = 11) | –0.3 (–1.7 to 0.6) (n = 11) | |
| Scoliosis (%) | 7 (37) (n = 19) | 4 (21) (n = 19) | |
| Trunk LBM/BSA | 7.4 (6.9 to 8.0) (n = 19) | 7.3 (7.0 to 7.7)(n = 19) | |
| Baseline characteristics of children (3–14 years) | |||
| Median (IQR) | 1 mg/m2 s.c. daily rhGH (n = 25) | No treatment (n = 22) | p-value |
| Sex (m/f) | 13/12 | 8/14 | |
| Age (years) | 6.8 (5.4 to 8.8) | 5.9 (4.7 to 7.4) | |
| HtSDS | –2.0 (–3.1 to –1.7) | –2.5 (–3.3 to –1.9) | |
| BMI (kg/m2) | 17.7 (16.0 to 22.3) | 18.1 (17.2 to 19.9) | |
| BMI (SDS) | 1.2 (0.1 to 2.2) | 1.3 (1.1 to 1.6) | |
| Head circumference (SDS) | –0.8 (–1.5 to –0.2) | –0.6 (–1.2 to –0.1) | |
| IGF-1 (ng/ml) | 60.0 (46.5 to 96.5) (n = 21) | 56.0 (42.0 to 88.0) (n = 18) | |
| IGF-1 (SDS) | –1.7 (–2.3 to –1.2) (n = 21) | –1.9 (–2.6 to –1.2) (n = 18) | |
| IGFBP-3 (ng/ml) | 1.3 (0.9 to 1.5) (n = 21) | 1.2 (0.9 to 1.5) (n = 18) | |
| IGFBP-3 (SDS) | –1.9 (–2.8 to –1.2) (n = 21) | –2.2 (–3.1 to –1.4) (n = 18) | |
| IGF-1/BP3 (SDS) | –0.5 (–1.0 to 0.5) (n = 21) | –0.6 (–1.6 to 0.3) (n = 18) | |
| Fat% (SDS) | 2.1 (1.7 to 2.7) (n = ?) | 2.3 (1.9 to 2.6) (n = ?) | |
| Fat (SDS) | 1.2 (0.8 to 2.0) (n = ?) | 1.2 (0.7 to 1.6) (n = ?) | |
| LBM age (SDS) | –1.7 (–3.0 to –1.0) (n = ?) | –1.9 (–3.4 to –1.2) (n = ?) | |
| LBM HtSDS | –1.7 (–3.8 to –0.6) (n = ?) | –1.4 (–2.9 to 0.9) (n = ?) | |
| Trunk fat (%) | 36.0 (24.8 to 46.2) (n = ?) | 36.0 (29.2 to 41.2) (n = ?) | |
| Scoliosis (%) | 7 (30) (n = 23) | 9 (43) (n = 21) | |
| Trunk LBM/BSA | 8.0 (7.5 to 8.4)(n = 23) | 7.6 (7.1 to 8.1) (n = 21) | |
|
Comments n is unclear for body composition measures, as these were only available for children over the age of 4 at the start of the study. The p-values are for change in GH group vs control group. |
|||
| Results: infants (6 months to 3 years), mostly from de Lind van Wijngaarden 2009 et al.93 as this is the most complete data | |||
| Median (IQR) | 1 mg/m2 s.c. daily rhGH 1 year (n = 19) | No treatment (n = 19) | p-value |
| HtSDS | –0.9 (–1.6 to –0.1) | –1.8 (–3.5 to –1.4) | 0.003 |
| ΔHtSDS | 1.2 (1.0 to 1.6) | –0.2 (–0.6 to 0.3) | < 0.0001 |
| BMI (kg/m2) | 16.3 (15.7 to 18.2) | 16.4 (15.4 to 19.8) (n = 15) | |
| BMI (SDS) | 0.3 (–0.1 to 1.6) | 0.3 (–0.6 to 1.6) | 0.72 |
| ΔTrunk LBM | 1.7 (1.3 to 2.1) | 0.7 (0.4 to 0.9) | < 0.0001 |
| ΔTrunk LBM/BSA | 1.2 (0.7 to 1.8) | 0.3 (–0.3 to 0.6) | 0.002 |
| Head circumference (SDS) | 0.0 (–0.9 to 0.7) (n = 16) | –0.8 (–1.6 to –0.3) (n = 15) | < 0.001 |
| IGF-1 (ng/ml) | 179.0 (119.5 to 241.0) (n = 12) | 33.0 (22.5 to 47.8) (n = 15) | |
| IGF-1 (SDS) | 2.5 (1.4 to 2.9) | –2.6 (–4.1 to –0.7) | < 0.0001 |
| IGFBP-3 (ng/ml) | 2.2 (1.6 to 2.4) (n = 12) | 0.9 (0.7 to 1.3) (n = 12) | |
| IGFBP-3 (SDS) | 0.5 (0.0 to 1.2) (n = 12) | –2.4 (–3.5 to –1.2) (n = 12) | |
| IGF-1/BP3 (SDS) | 2.3 (1.7 to 3.4) (n = 12) | –1.1 (–2.1 to 0.0) (n = 12) | < 0.001 |
| Onset scoliosis (%) | 4 (21) (n = 19) | 2 (11) (n = 19) | 0.71 |
| Progression of scoliosis | –6.0 (–12.5 to 12.8) (n = 19) | –7.5 (–7.5 to –5.0) (n = 19) | 0.48 |
| Results for children (3–14 years), mostly from de Lind van Wijngaarden 2009 et al.,93 as this is the most complete data | |||
| Median (IQR) | 1 mg/m2 s.c. daily rhGH | No treatment | p-value |
| Year 1 results | |||
| N = 23 | N = 21 | ||
| HtSDS | –1.0 (–1.5 to –0.3) | –2.5 (–3.4 to –2.3) | < 0.0001 |
| ΔHtSDS | 0.9 (0.7 to 1.3) | –0.1 (–0.2 to 0.1) | < 0.0001 |
| BMI (kg/m2) | 17.5 (15.3 to 19.8) (n = 21) | 18.6 (17.6 to 19.7) (n = 21) | |
| BMI (SDS) | 0.8 (–0.1 to 2.1) | 1.4 (1.0 to 1.6) | 0.05 |
| ΔTrunk LBM | 1.8 (1.4 to 2.3) | 0.7 (0.1 to 0.8) | < 0.0001 |
| ΔTrunk LBM/BSA | 1.3 (0.7 to 1.7) | 0.0 (–0.4 to 0.3) | < 0.0001 |
| Head circumference (SDS) | –0.2 (–1.2 to 0.2) (n = 21) | –0.6 (–0.9 to 0.3) (n = 21) | |
| IGF-1 (ng/ml) | 337.0 (274.3 to 474.3) (n = 21) | 55.0 (42.5 to 94.8) (n = 12) | |
| IGF-1 (SDS) | 2.3 (1.5 to 2.8) | –2.5 (–3.1 to –1.5) | < 0.0001 |
| IGFBP-3 (ng/ml) | 2.5 (2.2 to 2.9) (n = 21) | 1.3 (0.8 to 1.5) (n = 12) | |
| IGFBP-3 (SDS) | 0.4 (–0.1 to 0.8) (n = 21) | –2.4 (–3.5 to –1.8) (n = 12) | < 0.001 |
| IGF-1/BP3 (SDS) | 2.5 (2.0 to 3.0) (n = 21) | –0.8 (–1.4 to –0.2) (n = 12) | < 0.001 |
| Fat % (SDS) | 1.5 (0.7 to 2.1) (n = ?) | 2.3 (2.0 to 2.6) (n = ?) | < 0.001 |
| Fat (SDS) | 0.9 (0.2 to 1.4) (n = ?) | 1.3 (0.7 to 1.9) (n = ?) | < 0.001 |
| LBM age (SDS) | –0.5 (–1.3 to 0.7) (n = ?) | –2.1 (–4.1 to –1.3) (n = ?) | < 0.001 |
| LBM HtSDS | –1.5 (–2.3 to –0.7) (n = ?) | –1.9 (–2.9 to 0.0) (n = ?) | < 0.05 |
| Trunk fat (%) | 28.0 (16.9 to 36.7) (n = ?) | 37.2 (32.0 to 42.5) (n = ?) | < 0.001 |
| Onset scoliosis (%) | 5 (22) (n = 23) | 6 (29) (n = 21) | 0.52 |
| Progression of scoliosis | –3.5 (–7.3 to 1.8) (n = 23) | 0.0 (–1.0 to 1.0) (n = 21) | 0.60 |
| Year 2 results | |||
| N = 23 | N = 21 | ||
| HtSDS | –0.5 (–0.8 to 0.0) | –2.6 (–3.4 to –2.3) | < 0.0001 |
| ΔHtSDS | 1.4 (1.3 to 1.8) | –0.1 (–0.4 to 0.1) | < 0.0001 |
| BMI (kg/m2) | 17.5 (16.1 to 21.1) (n = 20) | 19.1 (17.8 to 20.8) (n = 20) | |
| BMI (SDS) | 1.1 (–0.2 to 1.7) | 1.4 (1.1 to 1.6) | 0.19 |
| ΔTrunk LBM | 2.8 (2.6 to 3.5) | 0.8 (0.4 to 1.0) | < 0.0001 |
| ΔTrunk LBM/BSA | 1.4 (0.5 to 1.7) | –0.2 (–0.5 to –0.1) | < 0.0001 |
| Head circumference (SDS) | –0.1 (–1.1 to 0.5) (n = 20) | –0.6 (–1.1 to 0.3) (n = 20) | < 0.05 |
| IGF-1 (ng/ml) | 424.0 (313.0 to 570.0) (n = 20) | 92.0 (61.8 to 130.0) (n = 16) | |
| IGF-1 (SDS) | 2.4 (2.1 to 2.8) | –1.6 (–2.5 to –1.0) | < 0.0001 |
| IGFBP-3 (ng/ml) | 2.8 (2.6 to 3.2) (n = 20) | 1.5 (1.2 to 1.8) (n = 16) | |
| IGFBP-3 (SDS) | 0.6 (0.3 to 1.1) (n = 20) | –1.7 (–2.3 to –1.2) (n = 16) | < 0.001 |
| IGF-1/BP3 (SDS) | 2.5 (1.8 to 2.9) (n = 20) | –0.6 (–1.2 to –0.1) (n = 16) | < 0.001 |
| Fat % (SDS) | 1.9 (0.7 to 2.3) (n = ?) | 2.4 (2.1 to 2.7) (n = ?) | < 0.001 |
| Fat (SDS) | 1.1 (0.6 to 2.0) (n = ?) | 4.5 (0.9 to 2.0) (n = ?) | < 0.01 |
| LBM age (SDS) | –0.1 (–1.3 to 0.6) (n = ?) | –2.5 (–3.8 to –1.4) (n = ?) | < 0.001 |
| LBM HtSDS | –1.9 (–2.4 to –1.4) (n = ?) | –2.3 (–2.7 to –1.3) (n = ?) | < 0.05 |
| Trunk fat (%) | 33.3 (17.3 to 40.9) (n = ?) | 37.9 (35.0 to 45.7) (n = ?) | < 0.001 |
| Onset scoliosis (%) | 5 (22) (n = 23) | 7 (33) (n = 21) | 0.14 |
| Progression of scoliosis | 3.3 (–4.3 to 11.9) (n = 23) | –5.0 (–9.0 to –2.0) (n = 21) | 0.27 |
|
Comments n is unclear for body composition measures, as these were only available for children over the age of 4 at the start of the study. The p-values are for change in GH group vs control group. Progression of scoliosis is change in Cobb angle during study |
|||
|
Adverse effects Not reported – the reader is referred to three other papers by the same author, but two of these appear to be other smaller studies. |
|||
|
Methodological comments Allocation to treatment groups: Prior to randomisation, infants were stratified for age and children (> 3.5 years) for BMI. All participants were randomised to GH treatment or no GH treatment. Blinding: A double-blind placebo-controlled study was considered unethical. Comparability of treatment groups: Anthropometric parameters were similar in the two groups, although no p-values are presented. Method of data analysis: Reference data for the DEXA were not available for children under the age of 4, so only those > 4 years were included in the analysis. Data were expressed as median (IQR) as most were not Gaussian distributed. Differences from baseline between groups were calculated using Mann–Whitney U-tests. The p-values are for change in GH group vs control group. Sample size/power calculation: De Lind van Wijngaarden reports that the power calculation estimated a total number of 40 patients (infants and prepubertal children) to yield a power of 0.80. Attrition/dropout: Two excluded before treatment (one had a dose reduction due to high IGF-1 levels, another had spinal surgery for scoliosis and two other medical problems). In total, four infants and five children excluded from analysis – presumably due to incomplete study period for the other patients. Infants with repeated measures were older (p = 0.025), possibly reflecting early diagnosis of PWS during recent years. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures | ||
|---|---|---|---|---|---|
|
Festen et al. 2007 91 Country: The Netherlands Study design: RCT Number of centres: not stated Funding: supported by Pfizer |
1. 1 mg/m2/day somatropin by s.c.i. (restricted to 0.5mg/m2/day in the first 4 weeks to avoid fluid retention). 2. No treatment Duration of treatment: 2 years Other interventions used: caloric intake and activity levels standardised 3 months before study |
Target population: prepubertal, generally not overweight children with PWS Number of participants: Total n = 20 1. n = 10 2. n = 10 Sample attrition/dropout: none Inclusion criteria for study entry: genetically confirmed diagnosis of PWS, age 4–9 years, prepubertal |
Primary outcomes: adiponectin levels, body composition, carbohydrate metabolism and triglyceride levels Secondary outcomes: associations between adiponectin and body composition, carbohydrate metabolism and triglyceride levels; effect of GH on these parameters Method of assessing outcomes: anthropometric measurements at baseline, year 1 and year 2 (standing height, weight, BMI); body composition assessed using DEXA; biochemical marker assays performed in the same laboratory. HtSDS and BMI SDS calculated from age- and sex-specific Dutch reference data Length of follow-up: 2 years |
||
| Characteristics of participants: median (IQR) | |||||
| Characteristic | 1 mg/m2/day GH (n = 10) | No treatment (n = 10) | p-value | ||
| N (male/female) | 10 (5/5) | 10 (3/7) | |||
| Age (years) | 6.2 (5.1 to 7.1) | 5.8 (4.9 to 7.8) | |||
| HtSDS | –2.2 (–3.1 to –1.8) | –2.8 (–3.4 to –2.0) | |||
| BMI (kg/m2) | 16.9 (15.8 to 17.7) | 17.3 (16.4 to 19.3) | |||
| BMI SDS | 0.8 (0.1 to 1.2) | 1.1 (0.6 to 1.5) | |||
| Adiponectin (mg/l) | 15.9 (13.3 to 23.9) | 17.1 (13.1 to 23.1) | |||
| Glucose (mmol/l) | 4.8 (4.6 to 5.0) | 4.4 (4.3 to 4.7) | |||
| Insulin (mU/l) | 6.0 (3.8 to 10.0) | 5.5 (4.8 to 7.3) | |||
| Insulin–glucose ratio | 1.3 (0.8 to 2.1) | 1.3 (1.0 to 1.6) | |||
| HOMA index | 0.8 (0.5 to1.3) | 0.7 (0.6 to 0.9) | |||
| Triglycerides (mmol/l) | 0.9 (0.7 to 1.7) | 0.7 (0.6 to 1.0) | |||
| IGF-1 SDS | –1.7 (–2.2 to –1.2) | –1.7 (–2.9 to –1.0) | |||
| IGFBP-3 SDS | –2.0 (–3.0 to –1.3) | –2.5 (–3.2 to –1.5) | |||
| LBM SDS | –2.2 (–2.7 to –2.0) | –2.3 (–2.8 to –1.8) | |||
| FM SDS | 0.8 (0.6 to 1.0) | 0.8 (0.6 to 1.2) | |||
| Per cent fat SDS | 1.7 (1.6 to 2.0) | 1.8 (1.5 to 2.4) | |||
| Trunk fat/total fat | 0.44 (0.34 to 0.47) | 0.4 (0.35 to 0.46) | |||
|
Comments HOMA, Homeostasis Model Assessment index. Adiponectin levels were compared with healthy matched controls |
|||||
| Results (median, IQR) | |||||
| Outcomes | 1 mg/m2/day GH (n = 10) | No treatment (n = 10) | p-value change from baseline group 1 vs group 2 | ||
| Year 1 | Year 2 | Year 1 | Year 2 | ||
| HtSDS | –1.3a (–1.7 to –0.8) | –0.6a (–0.9 to –0.3) | –2.8 (–3.5 to –2.0) | –3.0 (–3.5 to –1.8) | < 0.01b |
| BMI (kg/m2) | 16.1c (15.2 to 17.6) | 16.3 (15.8 to 19.0) | 18.5 (17.6 to 19.3) | 18.5 (17.5 to 20.6) | < 0.05c |
| BMI SDS | 0.2c (–0.2 to 0.8) | 0.4 (–0.3 to 1.1) | 1.3 (1.0 to 1.6) | 1.2 (0.9 to 1.5) | < 0.05c |
| Adiponectin (mg/l) | 24.7 (15.0 to 25.9)a,b | 24.6 (15.4 to 28.2)a,b | 13.4 (11.6 to 21.4) | 15.8 (12.5 to 19.2) | < 0.05b |
| Glucose (mmol/l) | 4.4 (4.2 to 5.0) | 4.6 (4.2 to 5.0) | 4.6 (4.3 to 4.8) | 4.7 (4.3 to 4.9) | |
| Insulin (mU/l) | 9.0 (6.5 to 13.5)a | 7.5 (6.0 to 11.5) | 6.0 (3.3 to 8.3) | 11.0 (6.0 to 24.0)a | |
| Insulin–glucose ratio | 2.1 (1.5 to 2.6)a | 1.6 (1.5 to 2.2) | 1.3 (0.8 to 1.9) | 2.3 (1.4 to 2.2)a | |
| HOMA index | 1.2 (0.8 to 1.8) | 1.0 (0.7 to 1.5) | 0.8 (0.4 to 1.0) | 1.4 (0.8 to 3.0)a | |
| Triglycerides (mmol/l) | 0.8 (0.6 to 1.3) | 0.7 (0.6 to 0.8) | 0.6 (0.5 to 1.0) | 1.0 (0.6 to 1.0) | |
| IGF-1 SDS | 2.3 (1.6 to 3.0)a,c | 2.3 (2.1 to 2.9)a,c | –2.5 (–3.2 to –0.8) | –2.0 (–2.7 to 1.0) | < 0.001c |
| IGFBP-3 SDS | 0.5 (–0.1 to 1.0)a,c | 0.6 (0.4 to 1.1)a,c | –2.4 (–3.8 to –1.9) | –1.8 (–2.7 to –1.5) | < 0.001c |
| LBM SDS | –1.6 (–1.9 to –1.4)a | –1.2 (–1.7 to –1.1)a | –2.5 (–3.0 to –1.8) | –2.8 (–3. to 1.9)a | |
| FM SDS | 0.5 (0.2 to 1.0) | 0.9 (0.4 to 1.4) | 1.1 (0.9 to 1.2)a | 1.2 (0.9 to 1.4)a | |
| Per cent fat SDS | 1.4 (0.9 to 1.7)a | 1.7 (0.9 to 1.9)a | 2.1 (1.8 to 2.2) | 2.1 (1.9 to 2.4)a | |
| Trunk fat/total fat | 0.4 (0.33 to 0.42) | 0.41 (0.34 to 0.46) | 0.41 (0.40 to 0.44) | 0.41 (0.38 to 0.45) | |
|
Comments Adiponectin levels were compared with healthy matched controls. a p < 0.05 compared with baseline corrected for multiple testing. b p < 0.05 change compared with baseline in GH group vs control group corrected for multiple testing. c p < 0.001 change compared with baseline in GH group vs control group corrected for multiple testing. |
|||||
|
Adverse effects Not reported. |
|||||
|
Methodological comments Allocation to treatment groups: Stratified by age and BMI prior to randomisation. No further details given. Blinding: Open-label trial. Comparability of treatment groups: Similar at baseline. Note: adeponectin levels were compared against healthy controls, not the untreated PWS group. Method of data analysis: Most data not Gaussian distributed, so data expressed as median (IQR) and non-parametric tests were used. Mann–Whitney U-tests used for differences between groups. Adiponectin levels of PWS children were compared with reference data of healthy sex- and age-matched controls (n = 40) with Wilcoxon signed-rank test. Sample size/power calculation: Not reported. Attrition/dropout: None. |
|||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Adequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Festen et al. 2007 92 Countries: The Netherlands and Sweden Study design: RCT Number of centres: multicentre Funding: Pfizer |
1. GH 1 mg/m2/day 2. No treatment Duration of treatment: 12 months Other interventions used: dietary advice given and compliance evaluated every 3 months |
Target population: PWS infants and toddlers Number of participants: Total: 43 evaluated at baseline, then 29 entered treatment 1. n = 15 2. n = 14 Sample attrition/dropout: 14 were excluded from the study, and this appears to have taken place post-randomisation Inclusion criteria for study entry: Genetically confirmed diagnosis of PWS; aged 6 months to 3 years at start of protocol Exclusion criteria for study entry: severe scoliosis (> 20°); extremely low dietary intake |
Primary outcomes: psychomotor development (BSID-II) (not data extracted as not per protocol) Secondary outcomes: body composition; IGF-1 and IGFBP-3 Method of assessing outcomes: height measured with a Harpenden stadiometer; Dutch references used to calculate age- and sex- specific SDS for median height, BMI and head circumference; body composition in Dutch participants measured using DEXA; IGF in Dutch children measured using an immunometric technique, and in Swedish infants using a semi-illuminescent technique Length of follow-up: 12 months |
| BSID-II, Bayley Scales of Infant Development II. | |||
| Characteristics of participants | |||
| Median (IQR) | GH 1 mg/m2/day (n = 15) | No treatment (n = 14) | p-value |
| Sex (m/f) | 7/8 | 8/6 | |
| Age (years) | 2.3 (1.7 to 3.0) | 1.5 (1.2 to 2.7) | |
| HtSDS | –2.6 (–3.3 to –1.8) | –2.3 (–3.3 to –1.1) | |
| BMI (kg/m2) | 16.3 (14.5 to 17.8) | 15.9 (14.7 to 16.8) | |
| BMI SDS | –0.3 (–1.1 to 1.3) | –0.9 (–1.8 to –0.8) | |
| Head circumference SDS | –1.0 (–1.7 to –0.3) | –1.1 (–1.8 to –0.9) | |
| Body fat (%) | 26.2 (22.2 to 28.9) | 25.8 (23.1 to 27.7) | |
| LBM (%) | 72.1 (69.8 to 75.7) | 73.3 (70.9 to 75.2) | |
| IGF-SDS | –2.1 (–2.7 to –1.7) | –2.0 (–2.6 to –0.3) | |
| IGFBP-3 SDS | –2.8 (–3.5 to –2.4) | –1.8 (–3.4 to –0.9) | |
| Results | |||
| Median (IQR) | GH 1 mg/m2/day (n = 15) | No treatment (n = 14) | p-value |
| Age (years) | 3.3 (2.7 to 4.0) | 2.6 (2.3 to 3.8) | |
| HtSDS | –1.6b (–2.1 to –0.8) | –2.3 (–3.9 to –1.5) | |
| BMI (kg/m2) | 16.4 (15.2 to 18.5) | 15.5 (14.9 to 17.6) | |
| BMI SDS | 0.3 (–0.9 to 1.8) | –0.4a (–0.8 to 1.3) | |
| Head circumference SDS | –0.2b,c (–1.2 to 0.6) | –1.1c (–1.6 to –0.6) | |
| Body fat (%) | 22.5 (11.3–33.2) | 22.8 (19.5 to 32.9) | |
| LBM (%) | 74.8 (63.7 to 82.3) | 73.6 (61.6 to 75.9) | |
| IGF-SDS | 1.7b,d (0.1 to 2.5) | –2.6d (–4.1 to –0.4) | |
| IGFBP-3SDS | 0.4a,c (–0.3 to 1.1) | –3.1c (–4.0 to –2.2) | |
|
a p < 0.05. b p < 0.005: 12 vs 0 months. c p < 0.05. d p < 0.001: GH vs control. |
|||
|
Adverse effects No results presented. Paper states that compared to randomised controls, GH did not induce disadvantageous effects on carbohydrate metabolism, sleep-related breathing disorders, and thyroid hormone levels. |
|||
| Comments | |||
|
Methodological comments Allocation to treatment groups: Children were stratified for age before randomisation. No further details given. Blinding: Open label. Comparability of treatment groups: Similar at baseline, although GH group had slightly older median age. Method of data analysis: For repeated measurement analysis, only children with 2 BSID-II scores were included. BSID-II can only be used if developmental age is maximally 3–5 years. Non-parametric statistics used as data not Gaussian distributed. Mann–Whitney U-tests used for two-tail differences at baseline, one-tailed ANCOVA used for data analysis. Sample size/power calculation: Not reported. Attrition/dropout: 14 of the original 43 were excluded from repeated BSID-II analysis, and therefore do not appear to have been randomised. However, the paper later states that results of 14 patients were excluded from analysis – not clear if this is the same 14, but assumed to be so, i.e. they were excluded post randomisation. Reasons for exclusion: Five children had not reached 1 year of study, one infant was excluded due to thyroid hormone deficiency, eight had already passed the upper limit of BSID-II after 1 year of follow-up (divided equally between the GH group and the control group). |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Haqq et al. 2003 102 Country: USA Study design: Double blind placebo-controlled crossover Number of centres: one Funding: grants from the General Clinical Research Center and Pharmacia Corp. |
1. GH 0.043 mg/kg/day plus inactive ingredients, by daily s.c.i. 2. Placebo injection of inactive ingredients, by daily s.c.i. Duration of treatment: 6 months in each treatment arm, 12 months overall Other interventions used: none |
Target population: children with PWS Number of participants: total n = 14 randomised, but data only given for n = 12 1. n = 6 2. n = 6 Sample attrition/dropout: n = 2 Inclusion criteria for study entry: PWS; naive to GH treatment Exclusion criteria for study entry: other chronic illnesses, taking medications that impact on long-term bone mineralisation or body composition |
Primary outcomes: not stated Secondary outcomes: linear GV, body composition, pulmonary function, sleep, behaviour, cognition, resting energy expenditure (last five not data extracted as not per protocol) Method of assessing outcomes: assessed at 0.6 and 12 months; anthropometric measurements, side effects and compliance measured at 3 and 9 months; BA determined at 0 and 12 months using Greulich and Pyle analysis of wrist radiographs; height measured at 0.6 and 12 months using wall-mounted stadiometer; body composition measured using DEXA Length of follow-up: 6 months for outcomes, 12 months overall |
| Characteristics of participants | |||
| Mean ± SD | All patients (n = 12) | p-value | |
| Age (years) | 9.7 ± 3.3 | ||
| Sex (m/f) | 6/6 | ||
| BA (years) | 10.0 ± 4.2 | ||
| BMI SDS | 2.5 ± 0.7 | ||
| IGF-1 (ng/ml) | 169.3 ± 155.7 | ||
| IGF-1 SDS | –1.10 ± 1.15 | ||
| IGFBP-3 (ng/ml) | 2169 ± 1010 | ||
| IGFBP-3 SDS | –1.67 ± 1.10 | ||
| Mean height (cm) | 128.9 ± 19.7 | ||
| BMI (kg/m2) | 30.8 ± 8.3 | ||
| BMI (SDS) | 2.5 ± 0.7 | ||
| HtSDS | –1.3 ± 1.2 | ||
| GV (cm/year) | 4.2 ± 2.3 | ||
| Body fat (%) | 54 ± 5.3 | ||
| FM (kg) | 29.6 ± 16.7 | ||
| Lean mass (kg) | 22.5 ± 10.9 | ||
| Lumbar spine BMD (SDS) | –0.51 ± 0.30 | ||
| Total BMC (g) | 1263 ± 451 | ||
|
Comments Mean BA also reported as 10.2 ± 4.1 years later in the paper. |
|||
| Results | |||
| Outcomes | GH 0.043 mg/kg/day (n = 12) | Placebo (n = 12) | p-value |
| BMI (kg/m2) | 31.2 ± 8.9 | 32.8 ± 9.7 | < 0.05 |
| BMI (SDS) | 2.4 ± 0.5 | 2.5 ± 0.6 | |
| HtSDS | –1.2 ± 1.1 | –1.3 ± 1.3 | |
| GV (cm/year) | 7.5 ± 3.5 | 4.5 ± 2.7 | < 0.05 |
| Body fat (%) | 49.7 ± 5.8 | 54.1 ± 5.6 | < 0.05 |
| FM (kg) | 26.1 ± 12.8 | 29.1 ± 14.1 | < 0.05 |
| Lean mass (kg) | 24.1 ± 8.8 | 22.4 ± 8.5 | < 0.05 |
| Lumbar spine BMD (SDS) | –0.33 ± 1.4 | –0.4 ± 1.4 | |
| Total BMC (g) | 1337 ± 453 | 1342 ± 453 | |
| IGF-1 (ng/ml) | 720 ± 379 | 232 ± 182 | < 0.001 |
| IGFBP-3 (ng/ml) | 6029 ± 1311 | 4247 ± 1209 | < 0.01 |
| Leptin (ng/ml) | 49.7 ± 39.3 | 54.3 ± 46.2 | 0.06 |
| Ghrelin (pmol/l) | 272 ± 204 | 361 ± 309 | 0.11 |
| FT4 (pmol/l) | 12.9 ± 1.5 | 14.8 ± 1.4 | < 0.05 |
| TSH (mU/l) | 1.81 ± 0.79 | 2.04 ± 1.13 | |
| Insulin (pmol/l) | 64.2 ± 42.6 | 64.2 ± 39 | |
| Glucose (mmol/l) | 5.0 ± 0.7 | 4.8 ± 0.5 | |
| Osteocalcin (nmol/l) | 10.5 ± 5.7 | 7.8 ± 5.9 | 0.06 |
| Triglycerides (mmol/l) | 0.80 ± 0.52 | 0.92 ± 0.42 | |
| Total cholesterol (mmol/l) | 4.7 ± 0.9 | 4.5 ± 1.7 | |
|
Comments Mean BA (in all patients) increased to 11.3 ± 3.7 by the end of 12 months, compared with a chronological age of 9.7 ± 3.3 years. Mean height increased to 134.6 ± 19.3 cm. Only one patient required thyroid hormone replacement while receiving GH treatment. |
|||
|
Adverse effects No patient developed a significant degree of scoliosis (> 20°). No evidence of impaired fasting glucose concentrations. GH treatment resulted in supranormal IGH-I and normal IGFBP-3 concentrations, but the consequences of this are unknown. |
|||
|
Methodological comments Allocation to treatment groups: Reported to be randomised, but no further details given. Blinding: Both GH and placebo injections were given using a Genotropin pen. Comparability of treatment groups: Data only presented for whole group – crossover study design. Method of data analysis: Not ITT. Differences between groups calculated using paired t-tests. For data not distributed normally, Wilcoxon signed-rank tests were used. p < 0.05 considered statistically significant. Weight, height and BMI SDS obtained using Epi Info 2000 (www.cdc.gov/epiinfo/). Sample size/power calculation: Not reported. Attrition/dropout: Two patients withdrew – one due to relocation, one due to non-compliance with daily injections. Not clear which group they belonged to. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | nr |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Adequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Hauffa 1997 99 Country: Germany Study design: Open RCT Number of centres: one Funding: Pharmacia & Upjohn, Germany |
1. GH 0.075 IU/kg/day for first month, then continued at dose of 0.15 IU/kg/day to a maximum of 8 IU/day 2. No treatment Duration of treatment: 2-year study with control arm during 1st year Other interventions used: not stated |
Target population: children aged 3–12 with PWS Number of participants: total n = 19 randomised, n = 17 included in study, n = 16 analysed 1. n = 8 2. n = 9 Sample attrition/dropout: two not entered following randomisation, one excluded from analysis due to AE-related dose reduction Inclusion/exclusion criteria for study entry: prepubertal, 3–12 years old, PWS (confirmed by molecular genetics), projected FH < 3rd centile for German population |
Primary outcomes: not stated Secondary outcomes: changes in HtSDS, GV SDS, IGF-1, IGFBP-3 Method of assessing outcomes: nr Length of follow-up: 1 year |
| Characteristics of participants | |||
| Mean ± SD | GH 0.15 IU/kg/day (n = 7) | No treatment (n = 9) | p-value |
| Age (years) | 8.25 ± 2.4 | 7.56 ± 2.0 | |
| Sex f/m | 3/4 | 4/5 | |
| BA (years) | 7.91 ± 4.3 | 6.76 ± 2.4 | |
| Height (cm) | 120.9 ± 16.3 | 120.5 ± 11.2 | |
| Weight (kg) | 35.9 ± 18.2 | 32.5 ± 8.7 | |
| Hip circumference (cm) | 78.8 ± 19.6 | 77.6 ± 11.5 | |
| Target height (cm) | 172.9 ± 8.5 | 174.8 ± 8.2 | |
| Results | |||
| HV SDS | 5.5 | –2.3 | 0.0012 |
| HtSDS | 1.07 | –0.25 | |
| IGF-1 | Increased significantly (p < 0.008), sometimes to above the upper limit of the reference range | ‘At or slightly below lower limit of reference range’ | |
| IGFBP-3 | Increased significantly (p < 0.008), mostly to above the upper limit of the reference range | ‘Within normal range’ | |
|
Comments Height gain (1.02 SD) remained unchanged when analysed in relation to BA. No significant within- or between-group changes were detected for sitting height, BMI, skinfold thickness, waist or hip circumference or serum lipids. |
|||
|
Adverse effects One patient in GH group developed pseudotumour cerebri after increasing the starting dose to the final dose. Symptoms resolved on discontinuation. No abnormalities of glucose regulation observed in either group. |
|||
|
Methodological comments Allocation to treatment groups: Randomised (method not stated). Blinding: open label. Comparability of treatment groups: similar at baseline. Method of data analysis: No details given. Sample size/power calculation: Not reported. Attrition/dropout: 19 randomised, two not entered (reasons not stated), one not included in analysis (discontinued after an AE then resumed at half of the dose). |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Inadequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
CRI data extraction forms
| Reference and design | Intervention | Participants | Outcome measures | ||
|---|---|---|---|---|---|
|
Sanchez et al. 2002 103 Country: USA Study design: RCT Number of centres: one Funding: partly funded by Genentech Foundation for Growth and Development, and the Casey Lee Ball Foundation |
1. 0.05 mg/kg rhGH, daily s.c.i 2. No treatment Duration of treatment: 12 months Other interventions used: All patients received either monoclonal or polyclonal anti-T cell therapy and were maintained on a 3-drug immunosuppressive regimen. None was given vitamin D sterols, oral calcium supplements or anticonvulsant medications |
Target population: prepubertal paediatric kidney allograft recipients Number of participants: total 23 1. 12 2. 11 Sample attrition/dropout: group 1, one; group 2, one Inclusion criteria for study entry: pre-pubertal children, stable renal function for at least 1 year post operation, normal bone formation rates, patients with adynamic lesions who had not previously been treated with rhGH were also included Exclusion criteria for study entry: secondary hyperparathyroidism |
Primary outcomes: appears to be skeletal changes, but not stated clearly Secondary outcomes: HtSDS, WtSDS, GV Method of assessing outcomes: height and weight measured at 3-month intervals; height measured using fixed wall-mounted stadiometer; bone biopsy and histomorphometry bone mass measured by DEXA; blood samples every 3 months; BA determined by Greulich and Pyle method from radiographs of left hand and wrist. WSDS and HSDS calculated using values for 50th percentile for children of same CA and sex Length of follow-up: 12 months |
||
| Characteristics of participants | |||||
| Characteristic | 0.05 mg/kg rhGH (n = 12) | No treatment (n = 11) | p-value | ||
| Mean age ± SD (years) | 9.7 ± 4.5 | 11 ± 1.8 | ns | ||
| Sex | 18 boys, 5 girls | (Groups combined) | |||
| Mean interval since transplantation (years) | 3.4 ± 2.5 | (Groups combined) | |||
| HtSDS | –2.0 ± 1.1 | Not given, but ‘did not differ’ stated | |||
| Mean HtSDS 12 months before study | –2.2 ± 0.8 | –2.6 ± 1.0 | ns | ||
| Annual GV 12 months before study (cm/year) | 5 ± 2.0 | 4 ± 2.0 | ns | ||
| BA (years) | 7.1 ± 3.6 | 8.8 ± 2.4 | ns | ||
| Tanner score | 1.9 ± 0.8 | 2.1 ± 1.1 | ns | ||
| GFR (ml/min) | 58 ± 15 | 58 ± 14 | |||
| Results (mean ± SE) | |||||
| Outcomes | 0.05 mg/kg rhGH (n = 12) | No treatment (n = 11) | p-value | ||
| HtSDS for height at end of study | –1.1 ± 1.0 (p < 0.02 compared with baseline) | No change from baseline | |||
| Annual GV (cm/year) | 8.0 ± 2.1 | 4.8 ± 1.7 | < 0.01 | ||
| Change in WtSDS | 0.2 ± 0.3 | –0.3 ± 0.3 | < 0.01 | ||
| BA (years) | 8.5 ± 3.4 | 9.5 ± 2.8 | ns | ||
| Tanner score | 1.9 ± 0.7 | 2.2 ± 1.0 | ns | ||
| GFR (ml/min) | 61 ± 13 (change from baseline p = ns) | 67 ± 19 (change from baseline p = ns) | |||
| Biochemical markers | Baseline | Final | Baseline | Final | |
| Serum calcium (mg/dl) | 9.8 ± 0.7 | 10 ± 0.6 | 9.4 ± 0.5 | 9.6 ± 0.7 | |
| Serum phosphorous (mg/dl) | 4.8 ± 0.8 | 4.8 ± 0.7 | 4.5 ± 0.8 | 4.2 ± 0.7 | |
| Serum osteocalcin (ng/ml) | 24 ± 2.7 | 24 ± 0.3 | 20 ± 2.3 | 17 ± 1.7 | |
| Serum parathyroid hormone (pg/ml) | 55 ± 5.0 | 55 ± 5.3 | 38 ± 4.0 | 34 ± 2.5 | |
| Serum alkaline phosphate (IU/I) | 239 ± 9.0 | 255 ± 9.0 | 225 ± 9.0 | 198 ± 6.4 | |
| Serum 1,25-dihydroxyvitamin D (pg/ml) | 43 ± 4.3 | 52 ± 4.7 | 39 ± 3.3 | 50 ± 3.1 | |
| Bone histomorphology | Baseline | Final | Baseline | Final | |
| Bone area (%) | 20 ± 2.6 | 21 ± 4.0 | 20 ± 4.8 | 22 ± 6.4 | |
| Osteoid area (%) | 8.8 ± 4.0 | 7.9 ± 1.8 | 6.1 ± 2.5 | 8.2 ± 2.3 | |
| Eroded perimeter (%) | 5.4 ± 4.8 | 4.0 ± 2.2 | 2.2 ± 1.7 | 3.0 ± 1.5 | |
| Bone formation rate (μm2/mm2/day) | 266 ± 212 | 348 ± 304 | 262 ± 180 | 390 ± 232 | |
| SDS for bone mass at lumbar spine, based on CA | –0.1 ± 1.6 | –0.1 ± 1.3 (p = ns) | –1.7 ± 0.9 | –2.1 ± 1.0 (p < 0.5) | |
| SDS for bone mass corrected for height age | 1.1 ± 1.3 | 0.7 ± 0.8 (change from baseline p = ns) | 0.01 ± 1.0 | –0.3 ± 1.2 (p < 0.05 change from baseline) | |
|
Comments Baseline serum levels of calcium, phosphorous, parathyroid hormone, alkaline phosphate, osteocalcin, and 1,25-dihydroxyvitamin D did not differ between patients given rhGH and untreated controls. Values remained unchanged after 12 months’ follow-up in both groups. IGF-1 baseline values were similar between groups (actual values not given), and did not change from baseline in the untreated group. Change from baseline was significant for the treated group (p < 0.001), although subgroup analysis indicated that this was only in the subgroup of patients with normal rates of bone formation, who experienced an increase in serum IGF-1 levels of 54 ± 25% after 3 months and 98 ± 35% after 12 months of rhGH (p < 0.05). Serum IGF-1 levels remained unchanged in patients with adynamic bone, and values did not differ from those obtained in the untreated group. Cumulative dose of prednisone did not differ between groups. Two patients with normal rates of bone formation experienced acute rejection episodes after 3 and 12 months of rhGH therapy. One was associated with non-compliance to immunosuppressive medications. Both episodes reversed after treatment with methylprednisolone. No rejection episodes in untreated patients. |
|||||
|
Methodological comments Allocation to treatment groups: Statistician who had no information about patients’ clinical or biochemical characteristics randomised to treatment groups depending on their initial bone histological finding. Details of randomization procedure not given. Not stratified by height, etc. Blinding: Control group did not receive placebo injections. Comparability of treatment groups: p = ns for difference in age at baseline. Method of data analysis: Not ITT as two patients who withdrew were excluded from analysis. Unpaired t-tests were used to compare changes from baseline. Sample size/power calculation: Sample size estimated with 80% power to detect differences in group means and a two group comparison that required 20 patients per group. Appears to have been based on bone formation rates in a previous study, and it is not clear what the primary outcome for the present study is. Attrition/dropout: Two withdrawals: one in group 1 due to glucose intolerance after 3 months (which resolved in stopping treatment); one in group 2 due to being assigned to control group. Two group 1 patients also failed to undergo second bone biopsy. |
|||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Adequate |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Partial |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
The Pharmacia and Upjohn Study Group 1996 107 Country: international Study design: open-label RCT Number of centres: multicentre Funding: Pharmacia & Upjohn |
1. Daily s.c.i. of GH (1 IU/kg/week) 2. No treatment Duration of treatment:1 year of randomised treatment, followed by 1 year of GH treatment for both groups (only year 1 randomised data included here) Other interventions used: not reported |
Target population: children who had received a kidney transplant Number of participants: Total: n = 203 1. n = 106 2. n = 97 Sample attrition/dropout: 23 excluded from analysis of renal function; 49 excluded from analysis of growth Inclusion criteria for study entry: ≥ 12 months since transplantation; 2 height measurements over last 6 months; height SDS < –2 or GV below the 25th centile; GFR ≥ 20ml/min/1.73m2; normal serum thyroid hormone levels; testicular volume < 8 ml or breast development < B2 Exclusion criteria for study entry: HV ≥ 75th centile, dialysis therapy, any form of malignancy or treatment with GH during past 12 months |
Primary outcomes: GFR Secondary outcomes: transplant rejections; GV; HtSDS Note: data extracted only where reported separately for prepubertal children Method of assessing outcomes: auxological and biochemical assessments every 3 months. GFR measured by insulin clearance, or creatinine clearance (Morris method) Length of follow-up: 1 year (later follow-up not data extracted as not randomised) |
| Characteristics of participants | |||
| Mean ± SD | 1 IU/kg/week GH | No treatment | p-value |
| Boys/girls | 71/35 | 72/25 | |
| Age (years) | 12.6 ± 3.4 | 12.1 ± 3.1 | |
| Proportion prepubertal (%) | 53 | 63 | |
| Years since transplantation | 3.6 ± 2.3 | 3.2 ± 2.4 | |
| Proportion cadaver donors (%) | 81 | 86 | |
| HtSDS | –3.2 ± 1.4 | –3.1 ± 1.1 | |
| GV before treatment (cm/year) | 3.6 ± 2.2 | 4.0 ± 2.1 | |
| GFR (insulin)(ml/min/1.73 m2) | 48 ± 27 | 48 ± 26 | |
| GF (Morris) (ml/min/1.73 m2) | 51 ± 21 | 51 ± 2.1 | |
| Rejection episodes prior to study (n) | |||
| 0–1 episode | 69 | 63 | |
| 2–4 episodes | 30 | 32 | |
| 5–8 episodes | 7 | 1 | |
|
Comments N not clear for patient groups at baseline. |
|||
| Results | |||
| Mean ± SD change from baseline | 1 IU/kg/week GH (n = 28) | No treatment (n = 30) | p-value |
| Change in GV (cm/year) | 3.7 ± 1.6 | 0.3 ± 1.6 | < 0.0001 |
| Change in HtSDS | +0.6 ± 0.3 | +0.1 ± 0.3 | < 0.0001 |
|
Comments Primary outcome (GFR) and other outcomes not data extracted as not reportedly separately for prepubertal children. |
|||
|
Methodological comments Allocation to treatment groups: Randomised centrally, but no further details given. Blinding: Open label. Comparability of treatment groups: No p-values given. Appear to be similar, although control group contained 10% more prepubertal patients than treatment group and no. of patients with a high no. of acute rejections was higher in the GH-treated patients (seven vs one). Method of data analysis: No information given. Sample size/power calculation: Not stated. Attrition/dropout: 23 excluded from analysis of renal function (treatment occurred without randomisation, GFR < 20 ml/min/1.73 m2; transplantation < 12 months before study entry; non-compliance); 49 excluded from analysis of growth [abnormal thyroid function, growing too well (or not being short enough) before the study, previous growth not documented]. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Fine et al. 1994 108 Country: USA Study design: RCT Number of centres: 17 Funding: Genentech |
1. GH 0.05 mg/kg/day s.c. 2. Placebo in equivalent volume. Dose adjusted every 3 months for change in weight Duration of treatment: 2 years’ treatment was discontinued at renal transplantation, significant adverse event, or when BA > 15 years for boys and > 14 years for girls and growth rate was < 2 cm/year. Treatment was paused if a patient’s height percentile exceeded the Tanner target percentile for mid-parental height (4/82 group 1, 11/42 group 2) Other interventions used: dialysis was permitted as required; multivitamins, vitamin D analogue and various other therapies were permitted as required |
Target population: prepubertal growth-retarded children with CRF Number of participants: Total: n = 125 1. n = 82 2. n = 43 Sample attrition/dropout: group 1 – 13 in year 1, 13 in year 2; group 2 – 12 in year 1, 3 in year Inclusion criteria for study entry: irreversible renal insufficiency, creatinine clearance > 5 and < 75 ml/min/1.73 m2, height < 3rd percentile for CA, BA < 10 years for girls and < 11 years for boys, prepubertal status (Tanner stage 1) Exclusion criteria for study entry: evidence of a specific cause for growth failure other than CRF inability to obtain accurate height measurements, use of corticosteroids or other medications that influence growth, diabetes mellitus, active malignant disease or treatment of a malignant disease within past year, use of any other investigational drug therapy within 2 months of randomisation |
Primary outcomes: not stated Secondary outcomes: GV, HtSDS height age, BA, Cumulative ΔHA – ΔBA, weight gain, triceps skinfold thickness, mid-arm muscle circumference Method of assessing outcomes: anthropometric measurements made by same observer every 3 months; radiological evaluation of BA every 6 months. HSDS calculated using age- and sex-specific norms from the NCHS Length of follow-up: 2 years |
| Characteristics of participants | |||
| Mean ± SD | GH 0.05 mg/kg/day (n = 82) | Placebo (n = 43) | p-value |
| Age (years) | 6.0 ± 3.9 | 5.7 ± 3.6 | |
| Sex (f/m) | 21/61 | 14/28 | |
| Height age | 4.0 ± 2.9 | 3.8 ± 2.8 | |
| BA | 4.2 ± 3.0 | 4.2 ± 2.9 | |
| HtSDS | –2.9 ± 0.9 | –2.9 ± 1.0 | |
| Standardised height | –2.94 ± 0.86 (n = 55) | –2.82 ± 0.97 (n = 27) | |
| IGF-1 (µg/ml) | 121 ± 73 (n = 55) | 141 ± 94 (n = 20) | |
| Fasting insulin (pmol/l) | 70.3 ± 43.6 (n = 40) | 87.8 ± 71.1 (n = 21) | |
| Postprandial insulin (pmol/l) | 25.8 ± 26.8 (n = 43) | 30.1 ± 14.6 (n = 19) | |
| Fasting glucose (mmol/l) | 5.1 ± 1.1 (n = 49) | 5.0 ± 0.7 (n = 24) | |
| Postprandial glucose (mmol/l) | 5.3 ± 1.8 (n = 37) | 6.0 ± 1.7 (n = 21) | |
| HbA1c (%) | 5.1 ± 0.9 (n = 48) | 5.4 ± 1.0 (n = 24) | |
| Creatinine (μmol/l) | 174 ± 111 (n = 48) | 173 ± 97 (n = 24) | |
| Creatinine (mg/dl) | 2.3 ± 1.5 (n = 48) | 2.3 ± 1.3 (n = 24) | |
| Creatinine clearance (ml/sec/1.73 m2) | 0.55 ± 0.33 (n = 48) | 0.52 ± 0.31 (n = 24) | |
| Creatinine clearance (ml/min/1.73 m2) | 32.8 ± 19.5 (n = 48) | 31.1 ± 18.3 (n = 24) | |
| Blood urea nitrogen (mmol/l) | 15.6 ± 6.6 (n = 48) | 16.0 ± 7.3 (n = 24) | |
| Blood urea nitrogen (mg/dl) | 43.6 ± 18.5 (n = 48) | 44.9 ± 20.5 (n = 24) | |
| Results | |||
| Mean ± SD | GH 0.05 mg/kg/day (n = 82) | Placebo (n = 43) | p-value |
| GV year 1 (cm/year) | 10.7 ± 3.1 (n = 55) | 6.5 ± 2.6 (n = 27) | < 0.00005 |
| GV year 2 (cm/year) | 7.8 ± 2.1 (n = 55) | 5.5 ± 1.9 (n = 27) | < 0.00005 |
| HtSDS at year 2 | –1.6, p < 0.00005 compared with baseline | –2.9, p = 0.52 compared with baseline | |
| Roche–Wainer–Thissen predicted AH at 2 years (cm) | 5.4 | –0.4 | < 0.00005 |
| Weight gain after 2 years (kg) | 6.7 ± 2.2 | 4.6 ± 2.7 | 0.0004 |
| Triceps skinfold thickness (mm) | –1.6 ± 2.6 | 0.6 ± 3.8 | 0.006 |
| Mid-arm muscle circumference (cm) | 2.1 ± 1.1 | 1.3 ± 1.2 | 0.007 |
| Change in BA at 2 years (years) | 2.3 ± 0.7 | 1.6 ± 0.5 | 0.0001 |
| Standardised height (1 year) | –1.93 ± 1.01 (n = 55) | –2.90 ± 0.95 (n = 27) | |
| Cumulative change in HA – change in BA, year 1 | 0.28 ± 0.45 (n = 43) | –0.04 ± 0.36 (n = 21) | |
| Cumulative change in HA – change in BA, year 2) | 0.15 ± 0.62 (n = 43) | –0.12 ± 0.43 (n = 21) | 0.08 |
| Standardised height (2 year) | –1.55 ± 1.16 (n = 55) | –2.91 ± 1.04 (n = 27) | < 0.00005 |
| Height age (1 year) | 4.5 ± 2.7 (n = 43) | 5.0 ± 3.2 (n = 21) | |
| Height age (2 year) | 5.6 ± 2.9 (n = 43) | 5.7 ± 3.3 (n = 21) | < 0.00005 |
| BA (1 year) | 4.6 ± 2.6 (n = 43) | 5.2 ± 3.1 (n = 21) | |
| BA (2 year) | 5.8 ± 2.8 (n = 43) | 6.0 ± 3.2 (n = 21) | 0.0001 |
| IGF-1 (μg/l), year 1 | 286 ± 158 (n = 47) | 167 ± 97 (n = 20) | 0.0004 |
| IGF-1 (μg/l), year 2 | 244 ± 128 (n = 47) | 135 ± 80 (n = 20) | 0.0001 |
| Fasting insulin (pmol/l) year 1 | 104.9 ± 54.5 (n = 40) | 76.9 ± 28.4 (n = 21) | |
| Fasting insulin (pmol/l) year 2 | 80.9 ± 42.8 (n = 40) | 59.1 ± 34.6 (n = 21) | 0.03 |
| Postprandial insulin (pmol/l), year 1 | 36.6 ± 29.0 (n = 43) | 27.7 ± 17.2 (n = 19) | |
| Postprandial insulin (pmol/l), year 2 | 29.0 ± 20.7 (n = 43) | 27.2 ± 16.9 (n = 19) | 0.32 |
| Fasting glucose (mmol/l), year 1 | 5.2 ± 0.6 (n = 49) | 5.2 ± 1.0 (n = 24) | |
| Fasting glucose (mmol/l), year 2 | 5.0 ± 0.6 (n = 49) | 5.1 ± 0.7 (n = 24) | 0.70 |
| Postprandial glucose (mmol/l), year 1 | 5.4 ± 1.1 (n = 37) | 5.1 ± 1.2 (n = 21) | |
| Postprandial glucose (mmol/l), year 2 | 5.4 ± 1.1 (n = 37) | 5.5 ± 1.1 (n = 21) | 0.28 |
| HbA1c (%), year 1 | 5.0 ± 0.8 (n = 48) | 5.0 ± 0.8 (n = 24) | |
| HbA1c (%), year 2 | 4.9 ± 0.7 (n = 48) | 5.0 ± 0.8 (n = 24) | 0.33 |
| Creatinine (μmol/l), year 1 | 218 ± 163 (n = 48) | 192 ± 96 (n = 24) | |
| Creatinine (μmol/l), year 2 | 269 ± 205 (n = 48) | 219 ± 114 (n = 24) | 0.08 |
| Creatinine (mg/dl), year 1 | 2.9 ± 2.1 (n = 48) | 2.5 ± 1.3 (n = 24) | |
| Creatinine (mg/dl), year 2 | 3.5 ± 2.7 (n = 48) | 2.9 ± 1.5 (n = 24) | 0.08 |
| Creatinine clearance (ml/sec/1.73 m2), year 1 | 0.55 ± 0.42 (n = 48) | 0.51 ± 0.33 (n = 24) | |
| Creatinine clearance (ml/sec/1.73 m2), year 2 | 0.49 ± 0.35 (n = 48) | 0.48 ± 0.34 (n = 24) | 0.63 |
| Creatinine clearance (ml/min/1.73 m2), year 1 | 32.8 ± 25.2 (n = 48) | 30.7 ± 19.9 (n = 24) | |
| Creatinine clearance (ml/min/1.73 m2), year 2 | 29.3 ± 21.3 (n = 48) | 28.9 ± 20.4 (n = 24) | 0.63 |
| Blood urea nitrogen (mmol/l), year 1 | 16.1 ± 8.8 (n = 48) | 17.7 ± 8.7 (n = 24) | |
| Blood urea nitrogen (mmol/l), year 2 | 17.2 ± 8.7 (n = 48) | 15.9 ± 7.1 (n = 24) | 0.26 |
| Blood urea nitrogen (mg/dl), year 1 | 45.0 ± 24.5 (n = 48) | 49.7 ± 24.4 (n = 24) | |
| Blood urea nitrogen (mg/dl), year 2 | 48.2 ± 24.5 (n = 48) | 44.5 ± 20.0 (n = 24) | 0.26 |
| Serum alkaline phosphatase level change from baseline (IU/l), year 1 | 120.1 ± 130.1 (n = 48) | 45.6 ± 90.0 (n = 24) | 0.014 |
| Serum alkaline phosphatase level change from baseline (IU/l), year 2 | nr | ns | |
|
Comments Mean fasting insulin levels changed significantly in patients with GH between baseline and 12 months (p = 0.0005) but not between baseline and 24 months. Changes in placebo group were not significant. Postprandial insulin levels also significant for GH group between baseline and year 1 (p = 0.0089) but not significant between baseline and 24 months. Changes from baseline in placebo group were not significant. No significant change in HbA1c or thyroxine or TSH in either group at either time period. Biochemical measurements: There was no significant difference in the variation in the serum calcium, phosphorous, triglyceride or cholesterol levels between the two groups during the first 2 years of treatment. |
|||
|
Adverse effects No differences between groups in year 1. Year 2 asthma or wheezing in 8 out f 55 GH patients and none of placebo. All episodes preceded by upper respiratory tract infections. ‘No clinically significant side effects were associated with rhGH treatment.’ During the 1st 12 months, 19 out of 82 patients had low titre GH antibodies (i.e. anti-GH antibody serum binding by radioimmunoassay at least twice background values after 10-fold dilution), but over 2 years there was no significant difference in growth rate between patients who acquired anti-GH antibodies and those who did not. |
|||
|
Methodological comments Allocation to treatment groups: No information on randomisation except performed to place 2/3 in treatment and 1/3 in placebo and to maintain balance in age, sex, standardised height, degree of renal function and primary renal disease. Blinding: Placebo used in equivalent volume, but no further detail given. Comparability of treatment groups: IGF-1 and fasting insulin levels were higher in the placebo group, but were not reported to have been significantly different. Method of data analysis: Between- and within-group comparisons were made with two-tailed t-tests; p < 0.05 was considered statistically significant. Many outcome measures are only presented for patients who completed both years of the study. Not ITT. Sample size/power calculation: Not reported. Attrition/dropout: GH: 13 in year 1, 13 in year 2; placebo: 12 in year 1, 3 in year 2. 41% of total withdrawals were due to renal transplant, 24% requested removal, 15% non-compliance. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Adequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures | ||
|---|---|---|---|---|---|
|
Hokken-Koelega et al. 1991 104 Country: international Study design: crossover RCT Number of centres: multicentre Funding: Novo Nordisk A/S Denmark |
1. 4 IU/m2 biosynthetic human GH daily s.c.i., followed by crossover to placebo 2. Placebo followed by crossover to biosynthetic human GH daily s.c.i. Duration of treatment: 6 months in each arm of the study Other interventions used: phosphate-binding medication, calcium supplements and 1,25-dihydroxy vitamin D |
Target population: prepubertal children with CRF and severe growth retardation Number of participants: total 20 1. 8 2. 8 Original assignment not stated Sample attrition/dropout: Four left due to kidney transplantation Inclusion/exclusion criteria for study entry: CRF ≥ 1 year, creatinine clearance below 20 ml/min/1.73 m2, HtSDS for age < –1.88 and HV for age < 25th percentile, prepubertal (Tanner stage I), BA < 10 years for girls and 12 years for boys, no evidence of growth retardation cause other than CRF, normal thyroid function, no osteodystrophy, no previous treatment with anabolic steroids, sex steroids or recombinant human erythropoietin |
Primary outcomes: not stated Secondary outcomes: GV, GV SDS, BA (years), IGF-1 and IFG-II plasma concentrations Method of assessing outcomes: height measured with a Harpenden stadiometer; BA calculated from radiographs at start of study and every 6 months. Baseline height expressed as SDS for CA compared with Dutch reference data. GV expressed as SDS for CA compared with references derived from Infant–Childhood–Puberty Model. Length of follow-up:12 months |
||
| Characteristics of participants (median, range) | |||||
| Characteristic | 4 IU/m2 hGH/placebo (n = 8) | Placebo/4 IU/m2 hGH (n = 8) | p-value | ||
| Age (years) | 8.7 (4.4 to 11.3) | 8.6 (4.4 to 16.0) | |||
| Sex (m/f) | 6/2 | 4/4 | |||
| BA (years) | 7.4 (3.7 to 10.2) | 7.5 (3.7 to 10.6) | |||
| HtSDS | –2.3 (–3.9 to –1.8) | –2.7 (–5.6 to –2.0) | |||
| GV (cm/6 months) | 1.6 (0 to 3.0) | 1.4 (0.2 to 2.6) | |||
| Weight for height (%) | 98.2 (86.7 to 113.5) | 101.5 (90.3 to 116.5) | |||
| Mean (SD) GV (cm/6 months) 6 months pre-study | 1.5 (0.7) | 1.5 (0.5) | |||
| Mean (SD) HV SDS 6 months prestudy | –3.2 (1.4) | –2.9 (2.0) | |||
| Mean (SD) BA (years) 6 months prestudy | 6.9 (2.3) | 7.7 (2.6) | |||
| Mean (SD) IGF-1 (ng/ml) SDS for BA | 173 (135) | 197 (94) | |||
| 0.8 (2.7) | 1.4 (1.6) | ||||
| Mean (SD) IGF-II (ng/ml) SDS for BA | 1160 (485) | 1178 (483) | |||
| 2.5 (3.0) | 3.4 (4.0) | ||||
|
Mean (SD) IGFBP-3 (ng/ml) SDS for BA |
5429 (1352) | 6559 (2552) | |||
| 3.2 (1.1) | 4.2 (2.1) | ||||
|
Mean (SD) IGFBP-1 (ng/ml) SDS for BA |
195 (126) | 190 (115) | |||
| 30 (20) | 29 (17) | ||||
| Results | |||||
| Outcomes | 4 IU/m2 hGH/placebo (n = 8) | Placebo/4 IU/m2 hGH (n = 8) | Overall mean effect of GH minus effect of placebo | ||
| After 6 months’ GH | After 6 months’ placebo | After 6 months’ placebo | After 6 months’ GH | ||
| Mean (SD) GV (cm/6 months) | 5.2 (1.2) | 1.5 (0.4) | 2.4 (1.0) | 4.4 (1.6) |
2.9 (95% CI 2.3 to 3.5) (p < 0.0001) |
| Mean (SD) HV SDS | 6.9 (2.4) | –3.0 (1.6) | –0.5 (3.2) | 5.0 (4.5) | 7.7 (p < 0.0001) |
| Mean (SD) BA (years) | 7.0 (1.9) | 7.6 (1.7) | 8.0 (2.6) | 8.4 (2.8) | –0.01 |
| Mean (SD) IGF-1 (ng/ml) SDS for BA |
264 (168) 2.6 (2.0) |
160 (104) –0.2 (1.5) |
160 (95) 0.3 (1.6) |
268 (120) 2.9 (2.0) |
106 2.7 (p < 0.0001) |
| Mean (SD) IGF-2 (ng/ml) SDS for BA |
1174 (361) 2.8 (2.8) |
983 (336) 0.9 (2.2) |
1192 (340) 3.4 (2.4) |
1346 (492) 4.6 (3.4) |
172 1.6 |
|
Mean (SD) IGFBP-3 (ng/ml) SDS for BA |
7708 (2323) 5.0 (1.3) |
6102 (1892) 3.7 (1.3) |
6501 (1988) 3.9 (1.4) |
8706 (2275) 5.2 (1.4) |
1906 1.3 (p < 0.0001) |
|
Mean (SD) IGFBP-1 (ng/ml) SDS for BA |
119 (95) 16.4 (16.8) |
185 (119) 27.1 (22.4) |
215 (106) 32 (19.5) |
140 (90) 20 (16.6) |
–70 (p < 0.0001) –11.2 (p < 0.0001) |
|
Comments For GV, there was no significant carry-over effect (–0.04 cm/6 months, p = 0.94). Period check was –0.9 cm/6 months (p < 0.06). |
|||||
|
Adverse effects Serum alkaline phosphate was significantly increased during GH treatment, but returned to pretreatment levels when GH therapy was replaced by placebo (p < 0.0001). There was no significant change in parathyroid hormone concentration during either treatment schedule. Thyroid function was normal. |
|||||
|
Methodological comments Allocation to treatment groups: States randomly and blindly assigned, but no further details given. Blinding: Stated to be double blind. Comparability of treatment groups: Similar at baseline, although IGF-1 and IGFBP-3 were higher in group 2 at baseline. Method of data analysis: Not ITT. Paper states that statistical methods appropriate for crossover trials were used but no further details were given. Treatment effects were calculated and tested after taking into account any period effect. Sample size/power calculation: No information in paper. Attrition/dropout: Four children left the study to have kidney transplants; 3 at 6 months and 1 at 7 months. |
|||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Unknown |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures | ||||
|---|---|---|---|---|---|---|---|
|
Hokken-Koelega et al. 1996 105 Country: international Study design: crossover RCT Number of centres: multicentre Funding: Novo Nordisk A/S |
1. 4 IU/m2 GH/placebo daily s.c.i. 2. Placebo/4 IU/m2 GH daily s.c.i. Duration of treatment: 6 months in each arm Other interventions used: immunosuppressive therapy |
Target population: prepubertal children after renal transplant Number of participants: total n = 11 1. n = 6 2. n = 5 Sample attrition/dropout: none Inclusion criteria for study entry: postrenal transplant (≥ 12 months), stable condition without rejection episodes (≥ 12 months), HtSDS for age < –1.88 and HV for age < 50th percentile OR HtSDS above –1.88 with HV < 25th percentile, prepubertal (Tanner stage I), BA < 10 years for girls and 12 years for boys, prednisone dose ≤ 0.25 mg/kg/day ≥ 6 months, no evidence of growth retardation cause other than following renal transplant, normal thyroid function and acid–base balance, no previous treatment with sex steroids |
Primary outcomes: not stated Secondary outcomes: HV, GVSDS, BA, GFR, ERPF, IGF-1 measures, insulin and other biochemical markers Method of assessing outcomes: same investigator examined children at enrolment and every 3 months; height measured with a Harpenden stadiometer until three consecutive readings within 0.2 cm; GV references derived from Infant–Childhood–Puberty Model; Dutch reference data used for baseline HtSDS; BA determined from wrist radiographs Length of follow-up: 12 months |
||||
| Characteristics of participants | |||||||
| Median, range | 4 IU/m2 GH/placebo (n = 6) | Placebo/4 IU/m2 GH (n = 5) | p-value | ||||
| Age (years) | 12.1 (9.1 to 18.7) | 11.1 (8.3 to 14.9) | |||||
| Sex (m/f) | 5/1 | 4/1 | |||||
| HtSDS | –3.0 (–7.6 to –1.2) | –2.6 (–3.6 to –2.1) | |||||
| GV (6 months) | 1.4 (0.5 to 2.6) | 0.8 (0.6 to 1.8) | |||||
| BMI SDS | 3.1 (–1.1 to 4.2) | 1.3 (–0.2 to 3.7) | |||||
| GFR (ml/min/1.73 m2) | 62 (56 to 81) | 38 (19 to 74) | |||||
| BA (years) | 9.5 (7.9 to 11.5) | 7.5 (5.2 to 10.5) | |||||
| Results (mean, SD) | |||||||
| Outcomes | 4 IU/m2 GH/placebo (n = 6) | Placebo/4 IU/m2 GH (n = 5) | Overall mean effect of GH minus effect of placebo | ||||
| Prestudy | After 6 months’ GH | After 6 months’ placebo | Prestudy | After 6 months’ placebo | After 6 months’ GH | ||
| HV (cm/6 months) | 1.5 (0.7) | 5.3 (1.0) | 1.5 (0.9) | 1.0 (0.5) | 1.9 (0.7) | 3.9 (1.3) | 2.9 (95% CI 1.9 to 3.9) (p < 0.0001) |
| GVSDS | –1.7 (1.8) | 9.1 (2.9) | –1.3 (2.9) | –3.3 (0.9) | –0.4 (1.7) | 5.3 (4.0) | 8.0 (p < 0.0001) |
| BA (years) | 9.5 (1.7) | 9.7 (1.4) | 10.5 (2.2) | 7.7 (2.2) | 8.0 (2.1) | 8.1 (1.2) | –0.5 |
| GFR (ml/min/1.73 m2) | 66 (13) | 80 (30) | 64 (1) | 44 (22) | 49 (22) | 47 (38) | 5.5 |
| ERPF (ml/min/1.73 m2) | 261 (75) | 254 (87) | 264 (77) | 173 (79) | 191 (62) | 184 (86) | –15.6 |
|
IGF-1 (ng/ml) SDSBA |
280 (121) 0.9 (1.6) |
594 (180) 5.4 (2.8) |
240 (143) 1.0 (2.5) |
274 (89) 2.8 (1.8) |
321 (94) 3.4 (0.5) |
488 (237) 6.4 (1.9) |
228 3.7 (p < 0.0001) |
|
IGF-2 (ng/ml) SDSBA |
759 (114) 0.5 (0.9) |
799 (186) 1.1 (1.7) |
689 (31) 0.0 (0.4) |
728 (349) 0.9 (3.2) |
898 (56) 2.2 (1.2) |
900 (63) 2.3 (1.0) |
73 0.5 |
|
IGFBP-3 (ng/ml) SDSBA |
4902 (1099) 2.8 (1.8) |
7457 (2088) 4.5 (1.5) |
5681 (1588) 3.7 (2.9) |
5787 (1037) 3.8 (0.7) |
6228 (2193) 3.9 (1.5) |
8495 (2921) 5.3 (1.5) |
1698 0.9 |
|
IGFBP-1 (ng/ml) SDSBA |
52 (32) 4.7 (4.6) |
52 (23) 4.6 (3.5) |
71 (43) 7.5 (6.3) |
83 (40) 9.7 (6.8) |
62 (28) 6.7 (4.9) |
43 (35) 5.1 (5.2) |
–19 –2.1 |
| Cholesterol (mM/l) | 6.4 (1.1)a | 6.0 (1.0)a | 6.5 (1.8)a | 6.3 (0.7)a | 6.5 (0.7)a | 6.2 (0.6)a | –0.3 |
| LDL mM/l | 4.0 (1.4) | 3.2 (0.6) | 4.0 (2.3) | 3.7 (1.0) | 4.1 (0.9) | 3.7 (0.7) | –0.5 |
| Apolipoprotein A1 (mg/dl) | 155 (22) | 163 (29) | 130 (45) | 171 (52) | 151 (18) | 141 (25) | 10 |
| Apolipoprotein B (mg/dl) | 110 (33) | 91 (18) | 113 (40) | 111 (28) | 112 (20) | 115 (27) | –9 |
| Fructosamine (mM/l) | 282 (40) | 296 (16) | 277 (36) | 338 (59) | 313 (62) | 312 (37) | 8 |
| OGTT – glucose (mM/l) | |||||||
| Fasting | 4.7 (1.2) | 5.3 (0.9) | 5.1 (1.1) | 5.2 (0.3) | 4.5 (0.5) | 4.8 (0.3) | 0.3 |
| Integrated | 738 (163) | 784 (165) | 691 (79) | 943 (249) | 846 (143) | 854 (168) | 55 |
| OGTT – insulin (μU/ml) | |||||||
| Fasting | 20 (14) | 38 (12) | 22 (14) | 12 (5) | 19 (15) | 17 (8) | 7 |
| Integrated | 2481 (1006) | 4582 (3042) | 3648 (1643) | 2319 (1019) |
2349 (444) |
4267 (1092) | 1532 (p < 0.05 GH vs placebo) |
|
Comments ERPF, effective renal plasma flow; GVSDS, chronological age; SDSBA, SDS for BA. a p < 0.05 GH vs placebo. For HV, there was no significant carry-over effect (0.5 cm/6 months, (p = 0.30). Period effect was 0.9 cm/6 months (p = 0.06). Cholesterol and other outcomes above were compared against controls. Not data extracted as not part of randomised study. |
|||||||
|
Adverse effects None of the patients had an acute rejection episode during the study. No SAEs. |
|||||||
|
Methodological comments Allocation to treatment groups: States randomly and blindly assigned to groups, but no further details given. Blinding: No details provided. Comparability of treatment groups: Similar at baseline (although BA 2 years higher in group 1). Method of data analysis: Paper states that statistical methods appropriate for crossover trials were used. Reference cited, but no further details given. Treatment effects were calculated and tested after taking into account any period effect. ANOVA used to test influence of baseline variables. Correlations were tested by Spearman non-parametric test. ITT analysis performed. Sample size/power calculation: Not stated. Attrition/dropout: All children completed the study. |
|||||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Adequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Adequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures | |
|---|---|---|---|---|
|
Powell et al. 1997 106 Country: USA Study design: multicentre, open-label RCT Number of centres: 26 Funding: Genentech Inc.; government grants |
1. 0.05 mg/kg/day s.c. rhGH 2. No treatment Duration of treatment: 1 year Other interventions used: |
Target population: prepubertal children with chronic renal failure Number of participants: total 69 entered, 44 analysed 1. n = 30 2. n = 14 Sample attrition/dropout: 20 left (12 ESRF, six entered puberty, one allergic to rhGH, one drowned); four group 1 and one group 2 completed study but were excluded as they had insufficient serum for the 0- and 12-month protein assays Inclusion criteria for study entry: irreversible renal insufficiency (GFR > 10 and < 40 ml/min/1.73 m2), height < fifth percentile for age, age > 2.5 years, ability to stand for height measurement, BA < 10 for girls and 11 for boys, Tanner stage I Exclusion criteria for study entry: serum albumin < 2.5 g/dl, receiving medications that influence growth, presence of illness affecting growth, diabetes mellitus, presence or past history of malignancy |
Primary outcomes: not specified Secondary outcomes: height gain; HtSDS; BA; mid-arm muscle circumference; triceps skinfold thickness; weight gain; various IGF measures; insulin; ALS; GHBP Method of assessing outcomes: anthropometric measurements taken at 0, 3 and 12 months; height measured using wall-mounted stadiometer; BA determined by a left hand and wrist radiograph at 0 and 12 months Length of follow-up: 1 year |
|
| Characteristics of participants (mean ± SD) | ||||
| Characteristic | 0.05 mg/kg/day rhGH (n = 30) | No treatment (n = 14) | p-value | |
| Sex (% male) | 83 | 86 | ||
| GFR (ml/min/1.73 m2) | 27.5 ± 8.9 | 27.6 ± 8.8 | ||
| Age (years) | 5.6 ± 2.0 | 5.7 ± 2.6 | ||
| BA (years) | 4.0 ± 1.5 (n = 27) | 4.2 ± 1.8 | ||
| HtSDS | –2.7 ± 0.7 | –2.7 ± 0.8 | ||
| Weight for HtSDS | 0.0 ± 1.3 | –0.2 ± 1.5 | ||
| MAMC (cm) | 14.1 ± 1.6 (n = 29) | 14.4 ± 2.8 | ||
| TSF (mm) | 7.9 ± 3.2 (n = 29) | 8.5 ± 3.2 | ||
| IGF-1 (nM) | 15 ± 10 | 10 ± 5 | ||
| IGF-1 SDS | –0.7 ± 1.3 | –1.2 ± 1.0 | ||
| Free IGF-1 (pM) | 71 ± 41 (n = 17) | 141 ± 94 (n = 9) | 0.029 | |
| IGF-2 (nM) | 100 ± 29 | 101 ± 41 | ||
| IGF-2 SDS | 1.2 ± 1.2 | 1.1 ± 1.3 | ||
| Insulin pM b | 19 ± 14 | 52 ± 66 | 0.021 | |
| Total IGF (nM) | 115 ± 34 | 111 ± 45 | ||
| IGFBP-1 (nM) | 18 ± 9 | 17 ± 21 | ||
| IGFBP-1 SDS | 2.4 ± 0.6 | 2.1 ± 1.4 | ||
| IGFBP-2 (nM)a | 50 ± 17 | 51 ± 26 | ||
| IGFBP-3 (nM)b | 130 ± 50 | 109 ± 25 | ||
| IGFBP-3 SDSc | 1.7 ± 2.0 | 0.7 ± 1.1 | ||
| ALS (nM) | 207 ± 81 | 179 ± 40 | ||
| GHBP (pM) | 183 ± 104 | 144 ± 104 (n = 12) | ||
| GHBP SDS | 0.4 ± 1.7 | 0.0 ± 1.3 (n = 12) | ||
|
a Values > normal range (22 ± 11), p < 0.001. b Values not different from normal range (98 ± 17). c Values > normal range (–0.2 ± 0.7), p = 0.013. |
||||
| Results (mean ± SD change from 0–12 months) | ||||
| Outcome | 0.05 mg/kg/day rhGH (n = 30) | No treatment (n = 14) | p-value | |
| BA (years) | 1.0 ± 0.3 (n = 27) | 0.9 ± 0.4 (n = 13) | 0.5282 | |
| Height gain (cm) | 9.1 ± 2.8 | 5.5 ± 1.9 | < .0001 | |
| Weight gain (kg) | 3.5 ± 1.5 | 2.2 ± 1.0 | 0.007 | |
| HtSDS | 0.8 ± 0.5 | 0.0 ± 0.3 | < 0.0001 | |
| Weight for HtSDS | 0.4 ± 0.7 | 0.4 ± 0.5 | 0.8703 | |
| MAMC (cm) | 1.2 ± 0.9 (n = 29) | –0.2 ± 1.7 (n = 13) | 0.0015 | |
| TSF (mm) | –1.9 ± 2.5 (n = 29) | 0.9 ± 1.2 (n = 13) | 0.0003 | |
| IGF-1 (nM) | No actual values presented – only small diagram, which is hard to read accurately. Not data extracted | < 0.006 | ||
| IGF-1 (SDS) | 0.2 ± 1.0 | No change from baseline – no values reported | < 0.006 | |
| Free IGF-1 (pM) | } | No actual values presented – only small diagram, which is hard to read accurately. Not data extracted | < 0.0464 | |
| IGF-2 (nM) | < 0.006 | |||
| IGF-2 SDS | 2.1 ± 1.3 | No change from baseline – no values reported | < 0.006 | |
| Insulin (pM) | } | No actual values presented – only small diagram which is hard to read accurately. Not data extracted | < 0.017 | |
| Total IGF (nM) | < 0.011 | |||
| IGFBP-1 (nM) | < 0.017 | |||
| IGFBP-1 SDS | < 0.017 | |||
| IGFBP-2 (nM) | ns | |||
| IGFBP-3 (nM) | < 0.011 | |||
| IGFBP-3 SDS | 4.0 ± 3.2 | No change from baseline – no values reported | < 0.011 | |
| ALS (nM) | } | No actual values presented – only small diagram, which is hard to read accurately. Not data extracted | < 0.011 | |
| GHBP (pM) | ns | |||
| GHBP SDS | ns | |||
|
Comments 10 healthy children (80% male; mean age 7.4 ± 2.7 years) provided serum samples for control values for IGFBP-2 and IGFBP-3 measurements. |
||||
|
Adverse effects Not reported. |
||||
|
Methodological comments Allocation to treatment groups: Randomised 1 : 2, no information on method of randomisation. Groups balanced for age, gender, height, GFR at baseline and nature of primary renal disease Blinding: Open label. Comparability of treatment groups: Free IGF-1 and insulin were statistically significantly higher in control group, otherwise groups were similar. 10 healthy children (80% male; mean age 7.4 ± 2.7 years) provided serum samples for control values for IGFBP-2 and IGFBP-3 measurements. Mean age for control children was approximately 2 years older than for the randomised children. Method of data analysis: Not ITT. Data presented as mean ± SD but converted to log10 values for statistical analysis. ANCOVA used to test differences between groups; p ≤ 0.05 considered significant. Multiple regression analysis used to analyse effect of multiple variables on change in HtSDS, but not data extracted here. Sample size/power calculation: Not reported, and primary outcome not clearly defined. Attrition/dropout: 20 left (12 ESRF; six entered puberty; one allergic to rhGH; one drowned); four group 1 and one group 2 completed study but were excluded as they had insufficient serum for the 0- and 12-month protein assays. |
||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
SGA data extraction forms
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Lagrou et al. 2008 110 Countries: Belgium and Luxembourg Study design: RCT Number of centres: 11 Funding: Belgian Study Group for Paediatric Endocrinology/GH provided by Pfizer |
1. GH 0.066 mg/kg/day 2. Untreated (did not receive placebo injections) Duration of treatment: 2 years Other interventions used: none stated |
Target population: prepubertal children born SGA Number of participants: total: 40 1. 20 2. 20 Sample attrition/dropout: One treated patient dropped out due to family problems Inclusion/exclusion criteria for study entry: birth weight and or length below –2 SD for gestational age, CA between 3 and 8 years, current height below –2.5 SD, GV SDS below +1.0 SD during the last 6–18 months Exclusion criteria for study entry: gestational age < 34 weeks; endocrine disease, including GH deficiency; severe chronic disease; Turner, Noonan or Down Syndrome or other genetically confirmed syndromes; chromosomal abnormalities, bone disease, current or previous irradiation therapy, current or previous (up to 18 months before inclusion) treatment with glucocorticoids, severe mental retardation (IQ ≤ 50) |
Primary outcomes: GV Secondary outcomes: HtSDS, WtSDS, BMI SDS, head circumference SDS, perception of short stature (not data extracted), perception of changes in height and physical appearance (not data extracted), perceptions of changes in psychosocial functioning (not data extracted) Method of assessing outcomes: standard auxological assessment of height, weight and head circumference measurements every 6 months, SDS calculated using British references, psychological assessments performed at start of study and after 2 years of follow-up (not data extracted) Length of follow-up: 2 years |
| Characteristics of participants | |||
| Characteristic | GH 0.066 mg/kg/day (n = 20) | Untreated (n = 20) | p-value |
| Birth WtSDS | –2.7 ± 0.9 | –2.6 ± 0.8 | ns |
| Gestational age | 37.3 ± 2.1 | 38.2 ± 1.6 | ns |
| Age (years) | 5.5 ± 1.6 | 5.1 ± 1.3 | ns |
| HtSDS | –3.3 ± 0.6 | –3.2 ± 0.9 | ns |
| WtSDS | –3.8 ± 1.3 | –3.9 ± 1.4 | ns |
| BMI (SDS) | –1.7 ± 1.1 | –2.0 ± 1.5 | ns |
| Head circumference (SDS) | –2.7 ± 1.4 | –2.8 ± 1.6 | ns |
| Results (mean ± SD) | |||
| Outcomes | GH 0.066 mg/kg/day (n = 20) | Untreated (n = 19) | p-value |
| HtSDS | –1.9 ± 0.7 | –3.1 ± 0.9 | < 0.001 |
| WtSDS | –2.3 ± 1.2 | –3.7 ± 1.5 | < 0.01 |
| BMI (SDS) | –1.5 ± 1.1 | –2.0 ± 1.5 | ns |
| Head circumference (SDS) | –2.0 ± 1.4 | –2.8 ± 1.5 | < 0.05 |
|
Adverse effects Tolerance only discussed in terms of perceptions of the injection by parents and children. No AEs reported or discussed. |
|||
|
Methodological comments Allocation to treatment groups: States randomised taking into account: gender, chronological age, WtSDS and study centre, no further details. Blinding: No details given, untreated participants not given placebo injections. Comparability of treatment groups: Authors report no differences in the auxological parameters between groups at baseline. Method of data analysis: Differences of continuous variables between subgroups were evaluated by Students unpaired t-test or by the Mann–Whitney U-test as appropriate. The level of significance of difference was set at p < 0.05. Sample size/power calculation: Based on 0.8 power to detect a significant difference (p = 0.05). 20 subjects in each group were required, assuming a difference of 2 cm/year in GV and a SD of 2.2 cm/year. Attrition/dropout: One treated patient dropped out due to family problems. Data for untreated group is for 19 after 2 years, no explanation of this. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Carel et al. 2003 111 Country: France Study design: RCT Number of centres: not stated Funding: Sanofi–Synthélabo |
1. Daily GH injections: 0.2 IU/kg/day (0.067 mg/kg/day) 2. No treatment Duration of treatment: Until reached AH. The mean duration of treatment was 2.7 ± 0.6 years Other interventions used: none stated |
Target population: children born SGA Number of participants: total 168 1. 112 2. 56 Sample attrition/dropout: For treatment: group 1, n = 21; group 2, n = 23 For analysis: group 1, n = 10; group 2, n = 9 Inclusion criteria for study entry: birth length < –2 SDS for gestational age and term > 30 weeks; at study inclusion, height ≤ –2.5 for age or less; CA > 10.5 years for girls and > 12.5 years for boys; BA ≥ 9 years for girls and ≥ 10 years for boys; peak plasma GH concentration after pharmacological stimulation at least 10 µg/l to exclude GH deficiency; Tanner stage I or II, with testicular volume < 8 ml or uterus length < 50 mm Exclusion criteria for study entry: chromosomal abnormalities in girls; constitutional bone diseases, any chronic disease interfering with growth; steroid or sex steroid treatment; dysmorphic syndromes other than Russell–Silver; no catch-up growth criteria were specified |
Primary outcomes: AH SDS Secondary outcomes: gain in SD units between height at inclusion and AH Method of assessing outcomes: follow-up visits were every 3 months for the treated group, and every 6 months for the control group and the following data recorded: height, weight, CA, pubertal stage, dose and tolerance. BA analysed yearly. SDS calculation appears to be based on French registry study Length of follow-up: criteria for stopping treatment/follow-up were < 1 cm growth over the last 6 months, and a BA of ≥ 15 years for girls, and ≥ 16 years for boys. Only 4% of patients met this criteria when treatment was stopped, so authors considered treatments to be almost complete for analytical purposes if GV was 2 cm or less over the last 6 months, or BA was ≥ 13 years for girls, and ≥ 15 years for boys. Patients who had discontinued follow-up before reaching AH were contacted later for a final AH measurement. Those who had not reached AH were maintained in the analysis without correction |
| Characteristics of participants | |||
| Characteristic | Daily GH injections: 0.2 IU/kg/day (0.067 mg/kg/day) (n = 102) | Untreated (n = 47) | p-value |
| Target height | –1.2 ± 0.9 | –0.9 ± 1.0 | |
| Duration of pregnancy (weeks) | 39 ± 2 | 39 ± 2 | |
| Birth length (SDS) | –2.8 ± 0.8 | –3.1 ± 1.0 | < 0.05 |
| Birth WtSDS | –1.8 ± 0.8 | –1.9 ± 0.8 | |
| Age (years) | 12.7 ± 1.4 | 12.8 ± 1.6 | |
| Height (cm) | |||
| HtSDS | –3.2 ± 0.7 | –3.2 ± 0.6 | |
| WtSDS | –1.9 ± 0.7 | –2.2 ± 0.6 | |
| GV (cm/year) | |||
| BA (years) | 10.6 ± 1.4 | 10.8 ± 1.6 | |
| Pubertal (Tanner stage II) (%) | 22 | 21 | |
|
Comments Four patients had Russell–Silver syndrome. GV and height (cm) were not detailed for the groups as a whole, but for boys and girls within the group separately. |
|||
| Results | |||
| Outcomes | Daily GH injections: 0.2 IU/kg/day (0.067 mg/kg/day) (n = 91) | Untreated (n = 33) | p-value |
| At inclusion: age (years) | 12.6 ± 1.5 | 12.9 ± 1.4 | |
| At inclusion: HtSDS | –3.2 ± 0.6 | –3.2 ± 0.6 | |
| At inclusion: height (cm) | nr for whole group | nr for whole group | |
| At end of treatment: age (years) | 15.7 ± 1.5 | nr | |
| At end of treatment: HtSDS | –2.1 ± 1.0 | nr | |
| At end of treatment: height (cm) | nr for whole group | nr | |
| At AH measurement: age (years) | nr | nr | |
| At AH measurement: HtSDS | –2.1 ± 1.0 | –2.7 ± 1.0 | 0.005 |
| At AH measurement: height (cm) | nr for whole group | nr for whole group | |
| At AH measurement: total height gain (cm) | 26 ± 7 | 22 ± 6 | 0.005 |
| At AH measurement: total height gain (SDS) | 1.1 ± 0.9 | 0.5 ± 0.8 | 0.002 |
| At AH measurement: difference from target HtSDS | –0.9 ± 1.2 | –1.7 ± 1.2 | 0.005 |
|
Comments A difference of 0.6 SDS was observed in FH between the control and treated groups (95% CI 0.2 to 0.9). (A difference of 0.4 was observed at baseline, unclear if this is accounted for in finding the 0.6 result significant.) The measurements above that have not been reported for the whole group are reported in the paper separately for boys and girls. |
|||
|
Adverse effects Overall, 44% of treated patients reported AEs, 10% having 4 or more events. The most frequently reported events involved the respiratory system (19%), osteomuscular system (14%), central nervous system (9%), and digestive tract (8%). Authors state that all of these were mild, reversible, benign conditions that were unlikely to be related to GH treatment. 16 AEs recorded in 14 treated patients were considered severe: trauma, psychiatric symptoms, abdominal symptoms, otitis, asthma, varicocele, striae, and migraine. Again, authors state that these are unlikely to be related to GH treatment – two were causally related to treatment: one slipped capital epiphysis after 1.5 years of treatment and had one single seizure episode 10 minutes after first injection. |
|||
|
Methodological comments Allocation to treatment groups: Allocation sequence generated centrally and faxed to participants. Blinding: Group assignment was not masked, and the treated group was twice as large as the control group. Comparability of treatment groups: There is a significant difference in birth length between the treated and untreated groups, with the treated group being longer than the untreated group (p = 0.04). On other characteristics the groups appear to be broadly similar. Method of data analysis: Means and SD values are presented. Mann–Whitney U-test to compare groups. An α risk of 5% was set as the significance threshold. Not ITT. Sample size/power calculation: Not reported. Attrition/dropout: Four patients in the treatment group were excluded from analysis due to severe diseases interfering with growth (sickle cell anaemia, pulmonary hypertension, type 1 neurofibromatosis and severe prematurity). Five patients assigned to the treatment group refused GH treatment but remained in the study and were analysed as part of the control group; 15 patients left the study early (14 in control and one in the treated group). Treatment was completed in 4/102 patients and almost complete in 64/102. The reasons for interrupting treatment early were: growth rates considered insufficient by patient/physician (n = 12), weariness with the treatment (n = 10), loss to follow-up (n = 5), satisfaction with height (n = 2), local intolerance (n = 1), and striae attributed to the treatment by the patient (n = 1). In addition, some of the investigators wrongly considered that the treatment duration was limited to 3 years and stopped the treatment early (n = unclear). 102 treated and 47 control patients are included in the analysis. Authors state that group reassignments or protocol deviations concerned 12 and 5 patients followed to AH in the treated and control groups respectively. Appear to have been significant problems with attrition for various reasons, appears to be fully described. Group assignment was not blinded and, despite the study being randomised and centrally allocated, the treatment group is twice as large as the control: either this was 2 : 1 randomisation (this is not reported) or large numbers of the control group dropped out after randomisation, or possibly swapped to the treatment group: this is unclear. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Inadequate |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures | ||
|---|---|---|---|---|---|
|
De Schepper et al. 2007 109 Country: Belgium Study design: RCT Number of centres: eight Funding: Belgian Study Group for Paediatric Endocrinology/Pfizer |
1. High-dose GH: 66 ± 3 µg/kg s.c. once daily, adjusted every 6 months to body weight 2. Untreated (did not receive placebo injections) Duration of treatment: 2 years Other interventions used: none stated |
Target population: children born SGA Number of participants: total: 40 (25) 1. 11 2. 14 Sample attrition/dropout: The trial cohort was reduced from 40 to 25 based on the availability of the same absorptiometry apparatus to assess body composition in a homogeneous fashion across eight centres. No anthropometric differences were detectable between the study population and the non-included subcohort (authors state, no data reported) Inclusion criteria for study entry: birth weight, length or both < –2 SD for gestational age, current height < –2.5 SDGV < +1 SD in the last 6–18 months, age between 3 and 8 years at study start Exclusion criteria for study entry: premature birth (gestational age < 34 weeks); evidence for endocrine or bone disease; severe chronic disease; Turner, Noonan, Down or other genetic syndrome; irradiation treatment; current or previous glucocorticoid treatment; severe cognitive dysfunction (est. IQ < 50) |
Primary outcomes: none clearly stated Secondary outcomes: HtSDS and WtSDS, anthropometric and absorptiometric characteristics Method of assessing outcomes: study participants seen every 3 months, height measured with Harpenden stadiometer, and weight with electronic scale. Mid-upper arm circumference and four skinfolds were measured at study start and after 1 and 2 years Length of follow-up: 2 years |
||
| Characteristics of participants | |||||
| Characteristic | High-dose GH (GH) (n = 11)a | Untreated (n = 14) | p-value | ||
| Age (years) | 5.1 ± 1.6 | 5.1 ± 1.4 | |||
| Gestational age (weeks) | 37 ± 3 | 38 ± 2 | |||
| Birth WtSDS | –2.4 ± 0.8 | –2.5 ± 0.8 | |||
| Birth length (SDS) | –3.1 ± 0.6 | –2.9 ± 0.7 | |||
| Mid-parental heightb | –0.9 ± 0.8 | –0.8 ± 0.7 | |||
| HtSDS | –3.3 ± 0.7 | –3.2 ± 1 | |||
| WtSDS | –3.5 ± 1.2 | –3.6 ± 1.5 | |||
| Subscapular skinfold (mm) | 5.4 ± 1.1 | 6.4 ± 2.1 | |||
| Triceps skinfold (mm) | 7.9 ± 1.4 | 8.3 ± 2.1 | |||
| Subscapular/triceps | 0.7 ± 0.2 | 0.8 ± 0.2 | |||
| Sum skinfolds (mm) | 22.1 ± 3 | 24.3 ± 6 | |||
| Body fat fraction (%) | 12.9 ± 2.1 | 14.1 ± 3.6 | |||
| MUAMA (cm) | 12.8 ± 2.5 | 14.1 ± 3.5 | |||
| MUAFA (cm) | 5.5 ± 1.1 | 5.7 ± 1.7 | |||
| Lean mass (kg) | 10 ± 3 | 9.9 ± 2.2 | |||
| FM (kg) | 2.3 ± 0.5 | 2.5 ± 0.9 | |||
| Lean mass (%) | 78 ± 4 | 77 ± 5 | |||
| FM (%) | 15 ± 3 | 20 ± 5 | |||
| Trunk fat (kg) | 0.7 ± 0.3 | 0.8 ± 0.4 | |||
| Limb fat (kg) | 1.1 ± 0.3 | 1.2 ± 0.5 | |||
| Trunk fat/limb fat | 0.6 ± 0.2 | 0.6 ± 0.2 | |||
| Trunk fat/leg fat | 0.8 ± 0.3 | 0.8 ± 0.3 | |||
|
MUAFA, mid upper arm fat area; MUAMA, mid upper arm muscle area. a Not significant for baseline comparisons between groups. b [Father’s HtSDS + mother’s HtSDS]/2. |
|||||
| Results | |||||
| Outcomes | High-dose GH (GH) (n = 11)a | Untreated (n = 14) | p-valuea | ||
| 1 year | 2 years | 1 year | 2 years | ||
| HtSDS | –2.1 ± 0.7b | –1.7 ± 0.7b,e | –3.1 ± 1c | –3 ± 1c | < 0.0001 |
| WtSDS | –2.4 ± 1.3b | –1.8 ± 1b,e | –3.5 ± 1.4 | –3.4 ± 1.6c | < 0.0001 |
| Subscapular skinfold (mm) | 4.7 ± 0.8c | 5.1 ± 1 | 5.7 ± 1.8c | 6 ± 2.1 | ns |
| Triceps skinfold (mm) | 4.9 ± 1.5b | 5.5 ± 2.1b | 8.2 ± 2.3 | 7.9 ± 2.4 | < 0.001 |
| Subscapular/triceps | 1 ± 0.3d | 1 ± 0.3b,f | 0.7 ± 0.2 | 0.8 ± 0.2i | 0.001 |
| Sum skinfolds (mm) | 16.6 ± 3.4b | 18.1 ± 5d | 22.4 ± 5.8c | 22.9 ± 6.8 | < 0.005 |
| Body fat fraction (%) | 9.1 ± 2.1b | 10.1 ± 3d | 13.3 ± 3.5 | 13.4 ± 3.5 | < 0.005 |
| MUAMA (cm) | 15.2 ± 2.9b | 17 ± 2.7b,g | 13.3 ± 2.3d | 14.1 ± 2.9b,h | < 0.005 |
| MUAFA (cm) | 3.6 ± 1.2b | 4.3 ± 1.9d,h | 5.8 ± 2 | 5.7 ± 1.9 | 0.001 |
| Lean mass (kg) | 13.2 ± 3.4b | 15.5 ± 3.4b,e | 10.9 ± 2.4b | 12.2 ± 2.5b,e | < 0.0001 |
| FM (kg) | 2.4 ± 0.7 | 2.9 ± 1c,g | 2.8 ± 1.1c | 3.1 ± 1.1b,h | ns |
| Lean mass (%) | 82 ± 3d | 82 ± 3c | 77 ± 6 | 77 ± 5 | < 0.05 |
| FM (%) | 15 ± 3d | 15 ± 2c | 20 ± 6 | 20 ± 5 | < 0.05 |
| Trunk fat (kg) | 0.9 ± 0.3 | 1 ± 0.3c | 0.9 ± 0.5 | 1 ± 0.6b | ns |
| Limb fat (kg) | 0.9 ± 0.5 | 1.3 ± 0.7g | 1.4 ± 0.6c | 1.5 ± 0.6 | < 0.05 |
| Trunk fat/limb fat | 1 ± 0.5d | 0.9 ± 0.3d,f | 0.6 ± 0.2 | 0.7 ± 0.2i | < 0.0001 |
| Trunk fat/leg fat | 1.5 ± 0.7d | 1.3 ± 0.4d,f | 0.8 ± 0.3 | 0.9 ± 0.3i | < 0.0001 |
|
Comments a Difference between untreated and treated group (analysis of variance) unclear if this is totals over the 2 years of the study, including baseline measurements. b p < 0.0005 paired t-test or Wilcoxon rank test@ baseline – year 1, baseline – year 2. c p < 0.05. d p < 0.005. e p < 0.0005 paired t-test or Wilcoxon rank test: year 1 – year 2. f Elevated for age. g p < 0.005. h p < 0.5. i Normal for age. GH treatment was accompanied by a gain of lean mass (p < 0.0001) and by a centripetal redistribution of FM (p < 0.0001) but not by an overall gain or loss of FM. The effects of high dose GH on adiposity are not readily detectable in the trunk and are essentially limited to the limbs. |
|||||
|
Adverse effects Authors state that ‘none had a noteworthy adverse event during the 2 years of study’. |
|||||
|
Methodological comments Allocation to treatment groups: States randomised, no information reported on allocation to groups. Original trial cohort was 40, this was reduced to 25 due to availability of equipment. Blinding: No information on blinding reported, untreated group did not receive placebo injections. Comparability of treatment groups: Groups appear comparable at baseline – authors state there were no detectable baseline differences in the subgroups. Method of data analysis: Results are expressed as mean ± SD. Repeated measures analysis of variance was used to test for differences between subgroups. The level of statistical significance was set at p < 0.05. Sample size/power calculation: None reported. Attrition/dropout: 15 children from the original cohort were withdrawn due to issues with availability of measuring equipment – unclear at what stage this happened. No dropouts are reported from the 25 included in the study, apart from this. |
|||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
de Zegher et al. 2002 113 Countries: UK and Belgium Study design: RCT Number of centres: two Funding: Pharmacia Ltd |
1. High-dose GH (100 µg/kg/day) 2. No treatment Duration of treatment: 2 years Other interventions used: None stated |
Target population: short children born SGA Number of participants: total 13 1. 9 2. 4 Sample attrition/dropout: nr Inclusion criteria for study entry: birth weight/length < –2 SD for gestational age, current height < –3.0 SD, GV below 0.0 SD, age between 2 and 8 years Exclusion criteria for study entry: identified syndrome other than Silver–Russell |
Primary outcomes: not clearly stated Secondary outcomes: growth response and its relationship to pretreatment GH secretion (not data extracted) HtSDS, WtSDS, BMI SDS, GV (cm/year) Method of assessing outcomes: Overnight GH profiles and GH stimulation tests at baseline (not data extracted), intravenous glucose tolerance tests were performed at baseline, yearly on GH treatment and 3 months post GH treatment. Height, weights and BMI converted to age- and sex- adjusted SDS using current UK reference data Length of follow-up: 2 years |
| Characteristics of participants | |||
| Characteristic | High-dose GH (100 µg/kg/day) (n = 9) | No treatment (n = 4) | p-value |
| Age (years) | 6.3 (4.0 to 8.0) | 4.7 (2.3 to 6.3) | |
| HtSDS | –3.6 (–5.5 to –2.8) | –3.1 (–3.4 to –2.8) | |
| WtSDS | –4.5 (–7.2 to –2.6) | –3.8 (–5.5 to –2.7) | |
| BMI SDS | –2.3 (–5.0 to –0.7) | –2.0 (–4.2 to –0.1) | |
| GV (cm/year) | 5.1 (4.0 to 6.8) | 6.4 (5.3 to 7.5) | |
| Results (means and ranges) | |||
| Outcomes | High-dose GH (100 µg/kg/day) (n = 9) | No treatment (n = 4) | p-value |
| Age (years) (year 1) | 7.2 (5.0 to 8.8) | 5.7 (3.3 to 7.3) | |
| Age (years) (year 2) | 8.2 (6.0 to 9.9) | 6.5 (4.3 to 8.3) | |
| HtSDS (year 1) | –2.4 (–4.6 to –1.4)a | –3.0 (–3.3 to –2.7) | |
| HtSDS (year 2) | –1.8 (–3.9 to –0.5)a | –3.0 (–3.3 to –2.5) | |
| WtSDS (year 1) | –2.9 (–4.7 to –1.7)a | –4.0 (–5.4 to –3.2) | |
| WtSDS (year 2) | –2.1 (–3.6 to –0.9)a | –3.8 (–4.8 to –3.2) | |
| BMI SDS (year 1) | –1.6 (–3.8 to –0.8)a | –2.3 (–3.9 to –1.3) | |
| BMI SDS (year 2) | –1.2 (–3.4 to –0.4)a | –2.1 (–2.9 to –1.4) | |
| GV (cm/year) (year 1) | 11.0 (7.4 to 13.3) | nr | |
| GV (cm/year) (year 2) | 8.5 (6.3 to 10.2) | 5.6 (4.4 to 6.8) | |
|
Comments a p < 0.0001 from baseline. Authors state that GH-treated children showed significant increments in HtSDS, WtSDS and BMI SDS over 2 years (all p < 0.0001). Untreated SGA children remained on their height, weight and BMI SD levels. Glucose and insulin metabolism markers not data extracted as reported for the treated group, no results reported for controls. Authors state that compared to baseline levels, children in the treated group showed significant increases in fasting levels of insulin (year 1, p = 0.003; year 2, p = 0.0002) and decreases in insulin sensitivity (year 1, p = 0.003; year 2, p = 0.0002). |
|||
|
Adverse effects Not reported/discussed. No child showed impaired glucose tolerance. |
|||
|
Methodological comments Allocation to treatment groups: Randomised on a 2 : 1 basis, no further details. Blinding: No details given. No placebo used. Comparability of treatment groups: Groups appear similar. Method of data analysis: Means and ranges are presented. Changes in height/weight, glucose and insulin parameters analysed using paired t-tests. ITT. Sample size/power calculation: Not reported. Attrition/dropout: Not reported. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Unknown |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Adequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
| Reference and design | Intervention | Participants | Outcome measures | |
|---|---|---|---|---|
|
de Zegher et al. 1996 112 Country: Belgium Study design: open-label RCT Number of centres: multicentre Funding: support from Pharmacia Peptide Hormones |
1. GH 0.2 IU/kg/day s.c. 2. GH 0.3 IU/kg/day s.c. 3. Untreated Duration of treatment: 2 years Other interventions used: None stated |
Target population: children born SGA Number of participants: total 54 1. 20 2. 21 3. 13 Sample attrition/dropout: group 1, n = 2; group 2, n = 1; group 3, n = 1 Inclusion/exclusion criteria for study entry: birth weight/length < –2 SD for gestational age, HtSDS for age < –2.5, GV SDS for age < +1, CA between 2 and 8 years, serum GH concentration > 10 µg/l after exercise, glucagon or insulin tolerance test, available growth data concerning the period preceding the start of the study Exclusion criteria for study entry: endocrine disorders, Turner or Downs syndrome, previous or concomitant irradiation or anabolic steroid therapy, severe chronic disease, severe mental retardation |
Primary outcomes: not clearly stated Secondary outcomes: height, HtSDS, GV, GV SDS, WtSDS, weight gain, BMI and BMI SDS, serum IGF-1, IGF-II, IGFBP-3, osteocalcin Method of assessing outcomes: study visits including history, auxological evaluation, BA determination, and dose adjustment were scheduled every 6 months. Biochemical examinations were performed yearly. All BAs were read according to Tanner–Whitehouse II method, HtSDS for BA was used as an index of FH prognosis Length of follow-up: 2 years |
|
| Characteristics of participants | ||||
| Characteristic | GH 0.2 IU/kg/day (n = 20) | GH 0.3 IU/kg/day (n = 19) | Untreated (n = 13) | p-value |
| Birth weight (g) | 2082.0 ± 139.0 | 1842.0 ± 115.0 | 1996.0 ± 136.0 | ns |
| Birth length (cm) | 42.3 ± 1.1 | 42.5 ± 0.9 | 42.1 ± 1.1 | ns |
| Chronological age (years) | 5.4 ± 0.5 | 5.1 ± 0.4 | 4.9 ± 0.5 | ns |
| BA (years) | 4.5 ± 0.5 | 3.7 ± 0.5 | 3.7 ± 0.5 | ns |
| HtSDS | –3.5 ± 0.2 | –3.7 ± 0.2 | –3.4 ± 0.3 | ns |
| GV (cm/year) | 6.6 ± 0.4 | 7.0 ± 0.5 | 6.7 ± 0.7 | ns |
| GV SDS | –0.9 ± 0.2 | –0.7 ± 0.3 | –0.6 ± 0.3 | ns |
| Weight (kg) | 13.2 ± 0.9 | 12.3 ± 0.7 | 12.0 ± 0.8 | ns |
| WtSDS | –2.5 ± 0.2 | –2.9 ± 0.2 | –2.8 ± 0.2 | ns |
| BMI | 14.0 ± 0.4 | 13.8 ± 0.4 | 13.5 ± 0.4 | ns |
| BMI SDS | –1.8 ± 0.4 | –1.8 ± 0.3 | –2.0 ± 0.4 | ns |
| Serum IGF-1 (µg/l) | 107.0 ± 15.0 | 108.0 ± 14.0 | 108.0 ± 21.0 | ns |
| Serum IGF-2 (µg/l) | 557.0 ± 44.0 | 748.0 ± 60.0 | 699.0 ± 103.0 | ns |
| Serum IGFBP-3 (mg/l) | 3.34 ± 0.33 | 3.36 ± 0.38 | 3.35 ± 0.38 | ns |
| Serum osteocalcin (µg/l) | 69.0 ± 3.0 | 69.0 ± 2.0 | 63.0 ± 3.0 | ns |
| Results are mean ± SEM. The 52 participating children were considered to have no specific syndrome (n = 33), Silver–Russell syndrome (n = 10), fetal alcohol syndrome (n = 4), Dubowitz syndrome (n = 3), 4p- syndrome (n = 1) or lacrimo-auriculo-dento-digital syndrome (n = 1). | ||||
| Results | ||||
| Outcomes at 2 years, unless otherwise stated | GH 0.2 IU/kg/day (n = 20) | GH 0.3 IU/kg/day (n = 19) | Untreated (n = 13) | p-value |
| Gain in BA (years) | 1.35 ± 0.16 | 1.33 ± 0.24 | 0.84 ± 0.07 | < 0.001 treated vs untreated |
| GV (cm/year) (year 1) | 11.5 ± 0.4 | 12.0 ± 0.4 | nr | |
| GV (cm/year) | 10.2 ± 0.2 | 11.0 ± 0.4 | 5.7 ± 0.3 | < 0.001 untreated vs treated; < 0.05 group 1 vs group 2 |
| GV SDS (year 1) | 5.3 ± 0.3 | 5.8 ± 0.4. | nr | |
| GV SDS | 4.3 ± 0.3 | 5.2 ± 0.4 | –0.9 ± 0.3 | < 0.001 untreated vs treated |
| Gain in HtSDS | 2.1 ± 0.1 | 2.5 ± 0.1 | 0.2 ± 0.1 | < 0.001 untreated vs treated |
| Gain in HtSDS for BA | 1.0 ± 0.2 | 1.2 ± 0.4 | 0.0 ± 0.3 | < 0.05 untreated vs treated |
| Weight gain (kg) | 6.9 ± 0.6 | 7.8 ± 0.5 | 3.6 ± 0.4 | < 0.001 untreated vs treated |
| Gain in WtSDS | 1.3 ± 0.1 | 1.8 ± 0.1 | 0.4 ± 0.1 | < 0.001 untreated vs group 1; < 0.01 group 1 vs group 2 |
| Serum IGF-1 (µg/l) (year 1) | 274 ± 30 | 392 ± 43 | 145 ± 23 | < 0.01 group 1 vs untreated; < 0.05 group 1 vs group 2 |
| Serum IGF-1 (µg/l) | 332 ± 29 | 655 ± 69 | 168 ± 46 | < 0.0001 group 1 vs group 2; < 0.01 group 1 vs untreated |
| Serum IGF-II (µg/l) (year 1) | 745 ± 72 | 944 ± 101 | 756 ± 108 | |
| Serum IGF-II (µg/l) | 834 ± 53 | 966 ± 56 | 881 ± 125 | ns |
| Serum IGFBP-3 (mg/l) (year 1) | 5.37 ± 0.42 | 6.35 ± 0.44 | 3.88 ± 0.48 | |
| Serum IGFBP-3 (mg/l) | 6.10 ± 0.35 | 6.50 ± 0.52 | 4.00 ± 0.58 | ns for group 1 vs 2; < 0.001 untreated vs group 1 |
| Serum osteocalcin (µg/l) (year 1) | 89.4 ± 5.9 | 93.6 ± 9.9 | 59.9 ± 1.9 | |
| Serum osteocalcin (µg/l) | 100.0 ± 8.6 | 102.7 ± 9.8 | 72.5 ± 7.3 | < 0.05 untreated vs group 1, ns group 1 vs group 2 |
|
Comments Results are mean ± SEM. Compliance: Over 2 years less than 10 injections were said to be missed in 36/38 children. In two children, respectively, 3% and 8% of the injections were reportedly omitted. Children with and without specified syndromes appeared to present similar growth responses. The GV during the first year was higher than during the second year, both in group 1 (11.5 ± 0.4 vs 8.8 ± 0.2 cm/year) and group 2 (12.0 ± 0.4 vs 10.0 ± 0.3 cm/year). After 2 years all untreated children still had a HtSDS < –2.2, whereas this was no longer the case for 35/38 treated children. BMI and BMI SDS remained similar in the three groups after 1 and 2 years. BMI of the study population is reported, not separately for the groups, or treated vs untreated. Fasting serum insulin concentrations were twice as high (p = 0.01) in treated children compared with untreated children both after 1 year (20.3 ± 2.2 mU/l vs 10.6 ± 2.4 mU/l) and 2 years (18.9 ± 3.0 mU/l vs 9.4 ± 1.3 mU/l) with no difference between the treated groups. |
||||
|
Adverse effects Four SAEs, which authors state conceivably not related to GH. One treated child received antibiotics for possible osteomyelitis of the distal tibia. Three children hospitalised in relation to viral diseases: one untreated and two treated. Treatment was not interrupted. Cutaneous eczema was aggravated in one child in group 1, no treatment interruption. Three treated children reported a possible increase in size or number of pigmented naevi, treatment was not interrupted. After 2 years, all HbA1c values were normal. |
||||
|
Methodological comments Allocation to treatment groups: Stated to be weighted randomisation, no further details. Blinding: Open label. Assessor for BA blinded to chronological age and treatment randomisation. Comparability of treatment groups: No significant differences at baseline. Method of data analysis: Wilcoxon rank-sum test used for differences between groups for growth variables, and Student’s t-test for biochemical markers. Statistically significant differences were considered to be obtained at p < 0.05. Results are mean ± SEM. Not ITT. Paper does not mention if there were any adjustments for multiple comparisons. Sample size/power calculation: None reported. Attrition/dropout: Two children allocated to 0.3 IU/kg did not start. Two children dropped out of the study for psychosocial reasons, one control after the start visit and one child from group 1 after 19 months. |
||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Partial |
| 6. Was the care provider blinded? | Unknown |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Adequate |
Data extraction form for primary studies
| Reference and design | Intervention | Participants | Outcome measures | |
|---|---|---|---|---|
|
Phillip et al. 2009 114 Country: multinational Study design: RCT Number of centres: multicentre Funding: Novo Nordisk |
1. rhGH 0.033 mg/kg/day 2. rhGH 0.1 mg/kg/day 3. Untreated Duration of treatment: 2 years, but data only extracted for year 1 as control group received rhGH in year 2 Other interventions used: none |
Target population: 3- to 8-year-olds with persistent short stature, born SGA Number of participants: total n = 15 1. n = 51 2. n = 51 3. n = 47 Sample attrition/dropout: n = 2 Inclusion/exclusion criteria for study entry: birth weight/length ≤ –2 SDS; HtSDS ≤ –2.5 SDS; GV SDS ≤ 0 during last 3 months; parental height ≥ –2 SDS; normal response to GH test |
Primary outcomes: measurement of height during 2 years. Treatment effect was additional height gain compared with untreated children Secondary outcomes: HtSDS, IGF-1, IGFBP-3, glucose, insulin Method of assessing outcomes: Harpenden stadiometer; sex-adjusted target height calculated based on national references; BA assessed using radiograph; HtSDS calculated using appropriate population references by country Length of follow-up: 1 year |
|
| Characteristics of participants | ||||
| Mean ± SD | rhGH 0.033 mg/kg/day (n = 51) | rhGH 0.1 mg/kg/day (n = 51) | No treatment (n = 47) | p-value |
| Sex (m/f) (%) | 55/45 | 47/53 | 51/49 | nr |
| Birth length (cm) | 44.3 ± 5.3 | 44.6 ± 4.3 | 43.9 ± 5.0 | nr |
| Birth weight (kg) | 1.9 ± 0.6 | 2.0 ± 0.6 | 2.0 ± 0.6 | nr |
| Gestational age (weeks) | 36.9 ± 3.6 | 37.6 ± 3.3 | 37.5 ± 3.2 | nr |
| Target HtSDS | –0.9 ± 0.6 | –0.8 ± 0.6 | –0.9 ± 0.8 | nr |
| Height (cm) | 99.0 ± 9.3 | 98.9 ± 9.0 | 99.2 ± 7.9 | nr |
| HtSDS | –3.1 ± 0.5 | –3.2 ± 0.7 | –3.1 ± 0.5 | nr |
| Age (years) | 5.5 ± 1.5 | 5.5 ± 1.4 | 5.6 ± 1.4 | nr |
| BA (years) | 4.7 ± 1.8 | 4.9 ± 1.8 | 5.0 ± 1.9 | nr |
| BA–CA | 0.8 ± 0.2 | 0.8 ± 0.2 | 0.8 ± 0.2 | nr |
| IGF-1 (ng/ml) | 116.7 ± 59.4 | 145.9 ± 92.3 | 130.0 ± 84.1 | nr |
| IGFBP-3 (μg/l) | 3.2 ± 0.9 | 3.5 ± 0.9 | 3.4 ± 1.1 | nr |
| IGF-1 SDS | –1.4 ± 0.6 | –1.1 ± 0.9 | –1.2 ± 1.0 | nr |
| Fasting glucose (mmol/l) | 4.6 ± 0.6 | 4.7 ± 0.6 | 4.6 ± 0.4 | nr |
| Fasting insulin (μIU/ml) | 3.1 ± 2.8 | 2.7 ± 1.9 | 2.8 ± 3.3 | nr |
| HbA1c (%) | 5.2 ± 0.4 | 5.2 ± 0.3 | 5.1 ± 0.4 | nr |
| Results at year 1 (mean ± SD) | ||||
| rhGH 0.033 mg/kg/day (n = 51) | rhGH 0.1 mg/kg/day (n = 51) | No treatment (n = 45) | p-value | |
| HtSDS | –2.3 ± 0.6 | –1.8 ± 0.8 | –3.0 ± 0.6 | nr |
| Change in HtSDS | 0.8 ± 0.3 | 1.4 ± 0.4 | 0.1 ± 0.3 | nr |
| Additional height gain (cm) | 3.3 ± 0.2 (95% CI 2.9 to 3.7) | 6.5 ± 0.2 (95% CI 6.0 to 6.9) | n/a | nr |
| IGF-1 (ng/ml) | 345.6 ± 177 | 594.3 ± 221 | 176.3 ± 107 | nr |
| IGFBP-3 (μg/l) | 4.8 ± 1.1 | 6.1 ± 1.4 | 3.9 ± 1.1 | nr |
| IGF-1 SDS | 0.9 ± 1.9 | 3.3 ± 2.1 | –0.9 ± 1.2 | nr |
| Fasting glucose (mmol/l) | 4.8 ± 0.5 | 5.0 ± 0.5 | 4.8 ± 0.6 | nr |
| Fasting insulin (μ IU/ml) | 5.3 ± 3.5 | 8.9 ± 5.0 | 4.1 ± 6.3 | nr |
| HbA1c (%) | 5.3 ± 0.4 | 5.3 ± 0.2 | 5.2 ± 0.4 | nr |
|
Adverse events Only reported for overall 2-year study, so treatment arms are different (no control arm). The majority (349/358, 73.5%) of AEs were mild to moderate in severity, and the most common events (57%) were childhood infections. 16 SAEs were reported, three of which were likely to be related to rhGH (convulsions, epilepsy, papilloedema – all stabilised/resolved after rhGH discontinued). |
||||
|
Methodological comments Allocation to treatment groups: Randomised 1 : 1 to double-blind treatment in the two rhGH groups or to a control group that was untreated in the first year and received rhGH in the second. A computer-controlled, centralised system was used to assign treatment. Blinding: BA assessed centrally by clinicians blinded to subject’s characteristics (other than gender) and treatment. Comparability of treatment groups: Similar at baseline, but no p-values reported. Method of data analysis: Mixed-effects model (ANCOVA) used where effects of age, sex and treatment duration were included. Tests were two-sided F-tests, performed at the 5% significance level. Sample size/power calculation: At least 50 patients per group were required to detect a difference in height gain of 0.75 cm between the two rhGH groups with a power of 90% and a significance level of 0.05. To allow for comparison with the third group, and allowing for a dropout rate of 20%, 180 patients were required to be enrolled. Attrition/dropout: Two randomised patients missing from analysis. Reasons not given. |
||||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Adequate |
| 2. Was the treatment allocation concealed? | Unclear |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Partial |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
SHOX deficiency data extraction forms
| Reference and design | Intervention | Participants | Outcome measures |
|---|---|---|---|
|
Blum et al. 2007 49 Countries: international (14) Study design: RCT Number of centres: 33 Funding: Eli Lilly & Co. |
1. Daily s.c.i. of 50 µg GH 2. No treatment 3. Daily s.c.i. of 50 µg GH Duration of treatment: 2 years Other interventions used: |
Target population: prepubertal children with SHOX-D Number of participants: total 68 patients had SHOX gene deletions or mutations, of which 52 with SHOX-D enrolled. A further 26 (group 3) with TS were enrolled as an additional GH arm 1. n = 27 2. n = 25 3. n = 26 (not data extracted as not per protocol) Sample attrition/dropout: one Inclusion criteria for study entry: confirmed SHOX-D; age ≥ 3 years; prepubertal (Tanner stage 1); height < 3rd percentile or < 10th percentile with HV < 25th percentile; BA < 10 years (boys) or < 8 years (girls); < 9 years (TS girls); no GH deficiency or resistance; no chronic disease; no growth-influencing medications |
Primary outcomes: First year GV Secondary outcomes: comparison between treatment effects in SHOX-D and patients with TS (not data extracted as not per protocol); AEs Method of assessing outcomes: height, IGF-1 and IGFBP-3 measured at baseline, 3 months, 6 months, then at 6-month intervals for remainder of the 2 years; left hand and wrist radiographs for BA performed at baseline, 1 year and 2 year – assessed centrally using Greulich and Pyle method; glucose and routine blood analysis at baseline and first year. HtSDS calculated using a central European reference Length of follow-up: 2 years |
| Characteristics of participants (mean ± SD, unless otherwise stated) | |||
| Characteristic | SHOX-D | p-value, group 1 vs group 2 | |
| Group 1: 50 µg GH (n = 27) | Group 2: no treatment (n = 25) | ||
| Complete deletion of SHOX gene (n) | 18 | 16 | |
| Partial gene deletions (n) | 2 | 2 | |
| Point mutations (n) | 7 | 7 | |
| Female/male (%) | 52/48 | 56/44 | |
| LWS/ISS phenotype (%) | 56/40 | 44/56 | 0.689 |
| Chronological age (years) | 7.5 ± 2.7 | 7.3 ± 2.1 | 0.914 |
| BA (years) | 6.6 ± 2.8 | 6.5 ± 2.0 | 0.928 |
| BA–CA | –1.0 ± 0.9 | –0.8 ± 0.8 | 0.809 |
| BA SDS | –1.2 ± 1.1 | –1.0 ± 1.0 | 0.641 |
| HtSDS | –3.3 ± 1.0 | –3.3 ± 0.8 | 0.111 |
| Target HtSDS | –1.3 ± 1.0 | –1.5 ± 0.9 | 0.013 |
| BMI SDS | 0.2 ± 0.9 | 0.6 ± 0.9 | 0.147 |
| IGF-1 SDS | –0.8 ± 1.0 | –0.9 ± 1.0 | 0.521 |
| IGFBP-3 SDS | 0.6 ± 1.3 | 0.1 ± 1.1 | 0.058 |
| ISS, idiopathic short stature; LWS, Léri–Weill syndrome. | |||
| Results (mean ± SD, unless otherwise stated) | |||
| Outcome | SHOX-D | p-value group 1 vs group 2 | |
| Group 1: 50 µg GH | Group 2: no treatment | ||
| Baseline HV (cm/year) | 4.8 ± 0.3 (n = 18) | 5.0 ± 0.5 (n = 14) | 0.721 |
| Baseline HV SDS | –1.2 ± 0.3 (n = 12) | –1.0 ± 0.6 (n = 10) | 0.605 |
| Baseline HtSDS | –3.3 ± 0.2 (n = 27) | –3.2 ± 0.2 (n = 24) | 0.822 |
| 1st-year HV (cm/year) | 8.7 ± 0.3 (n = 27) | 5.2 ± 0.2 (n = 24) | < 0.001 |
| 1st-year HV SDS | 3.0 ± 0.3 (n = 25) | –0.7 ± 0.2 (n = 22) | < 0.001 |
| 1st-year HtSDS | –2.6 ± 0.2 (n = 27) | –3.1 ± 0.2 (n = 24) | < 0.001 |
| 2nd-year HV (cm/year) | 7.3 ± 0.2 (n = 27) | 5.4 ± 0.2 (n = 24) | < 0.001 |
| 2nd-year HV SDS | 2.3 ± 0.3 (n = 27) | –0.4 ± 0.1 (n = 22) | < 0.001 |
| 2nd-year HtSDS | –2.1 ± 0.2 (n = 27) | –3.0 ± 0.2 (n = 24) | < 0.001 |
| 2nd-year height gain (cm) | 16.4 ± 0.4 (n = 27) | 10.5 ± 0.4 (n = 24) | < 0.001 |
| Catch-up of BA | 1.34 ± 0.07 | 1.1 ± 0.09 | 0.161 |
| AEs | |||
| SHOX-D | p-value group 1 vs group 2 | ||
| Group 1: 50 µg GH (n = 27) | Group 2: no treatment (n = 25) | ||
| At least 1 treatment-emergent AE (mostly common childhood illnesses) (%) | 85 | 68 | |
| Arthralgia | 3 | 2 | |
| Gynecomastia (males) | 1 (n = 12 males) | 0 (n = 12 males) | |
| Increased number of cutaneous naevi | 2 | 0 | |
| Recurrent otitis media | 1 | 1 | |
| Scoliosis | 1 | 0 | |
| Diabetes | 0 | 0 | |
|
Comments Overall, 41% of GH-treated patients with SHOX-D reached a height within the normal range for age and gender (> –2.0 SDS), compared with only one patient in the control group. For the GH-treated patients with SHOX-D, 1st year GV was somewhat greater for males (9.3 ± 0.5 cm/year) than for females (8.4 ± 0.5 cm/year), the baseline to second-year change in GV was very similar. Subgroup analysis for ISS phenotype vs LWS phenotype presented but not data extracted as not per protocol. IGF-1 SDS were in the low-normal range in each of the study groups at baseline and remained there for the untreated group. In the GH-treated group, values increased to the upper-normal range. IGF-1 concentrations exceeded two SDS at least once during GH treatment in 10 (37%) of patients and no untreated patients. IGFBP-3 SDS at baseline were closer to the normal mean than the corresponding IGF-1 SDS in both study groups and increased to the upper-normal range in the treated group. There was a strong relationship between IGF-1 SDS and IGFBP-3 SDS values during GH treatment, such that no subject had an IGF-1 SDS in the upper tertile with an IGFBP-3 SDS in the lower tertile. No significant changes in thyroid function. No SAEs were reported for subjects with SHOX-D. |
|||
|
Methodological comments Allocation to treatment groups: After stratification by sex and according to presence or absence of LWS, patients were randomised on a 1 : 1 basis. No further details given. Blinding: Blood analyses were carried out in a central facility. Open label. Comparability of treatment groups: Similar at baseline, although target HtSDS is statistically significantly lower in the rhGH group. Method of data analysis: HtSDS calculated using a central European reference. Sample size/power calculation: Not reported. Attrition/dropout: One subject who discontinued with no postbaseline height data was excluded from the efficacy analyses; all patients were included in the safety analyses. ANOVA used for between-group differences. |
|||
Quality criteria for assessment of experimental studies
| 1. Was the assignment to the treatment groups really random? | Unknown |
| 2. Was the treatment allocation concealed? | Unknown |
| 3. Were the groups similar at baseline in terms of prognostic factors? | Reported |
| 4. Were the eligibility criteria specified? | Adequate |
| 5. Were outcome assessors blinded to the treatment allocation? | Partial |
| 6. Was the care provider blinded? | Inadequate |
| 7. Was the patient blinded? | Inadequate |
| 8. Were the point estimates and measure of variability presented for the primary outcome measure? | Adequate |
| 9. Did the analyses include an ITT analysis? | Inadequate |
| 10. Were withdrawals and dropouts completely described? | Inadequate |
Appendix 5 List of excluded studies
Excluded due to wrong patient group (n = 40)
Arends NJ, Boonstra VH, Mulder PG, Odink RJ, Stokvis-Brantsma WH, Rongen-Westerlaken C, et al. GH treatment and its effect on bone mineral density, bone maturation and growth in short children born small for gestational age: 3-year results of a randomised, controlled GH trial. Clin Endocrinol 2003;59:779–87.
Arends NJ, Boonstra VH, Hokken-Koelega AC. Head circumference and body proportions before and during growth hormone treatment in short children who were born small for gestational age. Pediatrics 2004;114:683–90.
Argente J, Gracia R, Ibanez L, Oliver A, Borrajo E, Vela A, et al. Improvement in growth after two years of growth hormone therapy in very young children born small for gestational age and without spontaneous catch-up growth: results of a multicenter, controlled, randomized, open clinical trial. J Clin Endocrinol Metab 2007;92:3095–101.
Arwert LI, Deijen JB, Witlox J, Drent ML. The influence of growth hormone (GH) substitution on patient-reported outcomes and cognitive functions in GH-deficient patients: a meta-analysis. Growth Horm IGF Res 2005;15:47–54.
Attanasio AF, Shavrikova E, Blum WF, Cromer M, Child CJ, Paskova M, et al. Continued growth hormone (GH) treatment after final height is necessary to complete somatic development in childhood-onset GH-deficient patients. J Clin Endocrinol Metab 2004;89:4857–62.
Attanasio AF, Shavrikova EP, Blum WF, Shalet SM. Quality of life in childhood onset growth hormone-deficient patients in the transition phase from childhood to adulthood. J Clin Endocrinol Metab 2005;90:4525–9.
Barton JS, Hindmarsh PC, Preece MA, Brook CGD. Blood-pressure and the renin-angiotensin aldosterone system in children receiving recombinant human growth-hormone. Clin Endocrinol 1993;38:245–51.
Boguszewski M, Bertsson-Wikland K, Aronsson S, Gustafsson J, Hagenas L, Westgren U, et al. Growth hormone treatment of short children born small-for-gestational-age: the Nordic Multicentre Trial. Acta Paediatr 1998;87:257–63.
Boonstra VH, Arends NJ, Stijnen T, Blum WF, Akkerman O, Hokken-Koelega AC. Food intake of children with short stature born small for gestational age before and during a randomized GH trial. Horm Res 2006;65:23–30.
Bundak R, Darendeliler F, GüNöZ H, Baş F, Saka N, Neyzi O. Growth hormone treatment in short children with intrauterine growth retardation. J Pediatr Endocrinol Metab 2001;14(3):313–18.
Butenandt O, Lang G. Recombinant human growth hormone in short children born small for gestational age. German Study Group. J Pediatr Endocrinol 1997;10:275–82.
Carrascosa A, Esteban C, Espadero R, Fernandez-Cancio M, Andaluz P, Clemente M, et al. The d3/fl-growth hormone (GH) receptor polymorphism does not influence the effect of GH treatment (66 microg/kg per day) or the spontaneous growth in short non-GH-deficient small-for-gestational-age children: results from a two-year controlled prospective study in 170 Spanish patients. J Clin Endocrinol Metab 2006;91:3281–6.
Carroll PV, Littlewood R, Weissberger AJ, Bogalho P, McGauley G, Sonksen PH, et al. The effects of two doses of replacement growth hormone on the biochemical, body composition and psychological profiles of growth hormone-deficient adults. Eur J Endocrinol 1997;137:146–53.
Chatelain P, Job JC, Blanchard J, Ducret JP, Olivier M, Sagnard L, et al. Dose-dependent catch-up growth after 2 years of growth hormone treatment in intrauterine growth-retarded children. J Clin Endocrinol Metab 1994;78:1454–60.
Christiansen JS, Vahl N, Norrelund H, Jorgensen JO. Effects of GH replacement in young patients with childhood onset GH deficiency. Int J Clin Pract 2002;126(Suppl.):S32–6.
Conway GS, Szarras-Czapnik M, Racz K, Keller A, Chanson P, Tauber M, et al. Treatment for 24 months with recombinant human GH has a beneficial effect on bone mineral density in young adults with childhood-onset GH deficiency. Eur J Endocrinol 2009;160:899–907.
Crabbe R, von HM, Engrand P, Chatelain P. Recombinant human growth hormone for children born small for gestational age: Meta-analysis confirms the consistent dose–effect relationship on catch-up growth. J Endocrinol Invest 2008;31:346–51.
Czernichow P, Fjellestad-Paulsen A. Growth hormone in the treatment of short stature in young children with intrauterine growth retardation. Horm Res 1998;49(Suppl.2):23–7.
de Zegher F. Growth hormone treatment of short children born small for gestational age. Clin Pediatr Endocrinol 1997;6(Suppl. 10):129–33.
de Zegher F, Bertsson-Wikland K, Wilton P, Chatelain P, Jonsson B, Lofstrom A, et al. Growth hormone treatment of short children born small for gestational age: metanalysis of four independent, randomized, controlled, multicentre studies. Acta Paediatr 1996;85(Suppl. 417):27–31.
de Zegher F, Butenandt O, Chatelain P, bertsson-Wikland K, Jonsson B, Lofstrom A, et al. Growth hormone treatment of short children born small for gestational age: reappraisal of the rate of bone maturation over 2 years and metanalysis of height gain over 4 years. Acta Paediatr 1997;423(Suppl.):207–12.
Fine RN, Stablein D, Cohen AH, Tejani A, Kohaut E. Recombinant human growth hormone post-renal transplantation in children: a randomized controlled study of the NAPRTCS. Kidney Int 2002;62:688–96.
Fjellestad-Paulsen A, Czernichow P, Brauner R, Bost M, Colle M, Lebouc JY, et al. Three-year data from a comparative study with recombinant human growth hormone in the treatment of short stature in young children with intrauterine growth retardation. Acta Paediatr 1998;87:511–17.
Gram J, Hansen TB, Jensen PB, Christensen JH, Ladefoged S, Pedersen FB. The effect of recombinant human growth hormone treatment on bone and mineral metabolism in haemodialysis patients. Nephrol Dial Transplant 1998;13:1529–34.
Guest G, Berard E, Crosnier H, Chevallier T, Rappaport R, Broyer M. Effects of growth hormone in short children after renal transplantation. French Society of Pediatric Nephrology. Pediatr Nephrol 1998;12:437–46.
Hokken-Koelega AC, Sas T, van PY. Effects of long-term growth hormone treatment on body composition, carbohydrate metabolism, blood pressure and lipids in short children born small for gestational age. Horm Res 2003;59(Suppl.1):138.
Ibanez L, Fucci A, Valls C, Ong K, Dunger D, de ZF. Neutrophil count in small-for-gestational age children: contrasting effects of metformin and growth hormone therapy. J Clin Endocrinol Metab 2005;90:3435–9.
Ingulli E, Tejani A. An analytical review of growth-hormone studies in children after renal-transplantation. Pediatr Nephrol 1995;9:S61–5.
Jorgensen JO, Norrelund H, Vahl N, Juul A, Skakkebaek NE, Christiansen JS. Continuation of growth hormone therapy versus placebo in transition-phase patients with growth hormone deficiency: impact on body composition, insulin sensitivity, and thyroid function. J Pediatr Endocrinol 2002;15(Suppl. 5):1355–60.
Juul A, Andersson AM, Pedersen SA, Jorgensen JO, Christiansen JS, Groome NP, et al. Effects of growth hormone replacement therapy on IGF-related parameters and on the pituitary–gonadal axis in GH-deficient males. A double-blind, placebo-controlled crossover study. Horm Res 1998;49:269–78.
Mauras N, Pescovitz OH, Allada V, Messig M, Wajnrajch MP, Lippe B, et al. Limited efficacy of growth hormone (GH) during transition of GH-deficient patients from adolescence to adulthood: a phase III multicenter, double-blind, randomized two-year trial. J Clin Endocrinol Metab 2005;90:3946–55.
Nguyen VT, Misra M. Transitioning of children with GH deficiency to adult dosing: changes in body composition. Pituitary 2009;12:125–35.
Norrelund H, Vahl N, Juul A, Moller N, Alberti KG, Skakkebaek NE, et al. Continuation of growth hormone (GH) therapy in GH-deficient patients during transition from childhood to adulthood: impact on insulin sensitivity and substrate metabolism. J Clin Endocrinol Metab 2000;85:1912–17.
Underwood LE, Attie KM, Baptista J, Genentech Collaborative Study Group. Growth hormone (GH) dose–response in young adults with childhood-onset GH deficiency: a two-year, multicenter, multiple-dose, placebo-controlled study. J Clin Endocrinol Metab 2003;88:5273–80.
Vahl N, Juul A, Jorgensen JO, Orskov H, Skakkebaek NE, Christiansen JS. Continuation of growth hormone (GH) replacement in GH-deficient patients during transition from childhood to adulthood: a two-year placebo-controlled study. J Clin Endocrinol Metab 2000;85:1874–81.
Vimalachandra D, Hodson EM, Willis NS, Craig JC, Cowell C, Knight JF. Growth hormone for children with chronic kidney disease. Cochrane Database Syst Rev 2006;Issue 3:CD003264.
Vimalachandra D, Craig JC, Cowell CT, Knight JF. Growth hormone treatment in children with chronic renal failure: a meta-analysis of randomized controlled trials. J Pediatr 2001;139:560–7.
Whitman BY, Myers S, Carrel A, Allen D. A treatment/control group study of growth hormone treatment: Impact on behavior: a preliminary look. Endocrinologist 2000;10(4 Suppl.1):31–7.
Willemsen RH, Arends NJ, Bakker-van Waarde WM, Jansen M, van Mil EG, Mulder J, et al. Long-term effects of growth hormone (GH) treatment on body composition and bone mineral density in short children born small-for-gestational-age: six-year follow-up of a randomized controlled GH trial. Clin Endocrinol 2007;67:485–92.
Wilton P, bertsson-Wikland K, Butenandt O, Chaussain JL, de ZF, Jonsson B, et al. Growth hormone treatment induces a dose-dependent catch-up growth in short children born small for gestational age: a summary of four clinical trials. Horm Res 1997;48 (Suppl. 1):67–71.
Excluded due to study design (n = 27)
Bannink EM, van Pareren YK, Theunissen NC, Raat H, Mulder PG, Hokken-Koelega AC. Quality of life in adolescents born small for gestational age: does growth hormone make a difference? Horm Res 2005;64:166–74.
Boguszewski MC, de ZF, bertsson-Wikland K, Nordic Study Group for Growth Hormone Treatment in SGA Children and the Belgian Study Group for Pediatric Endocrinology. Serum leptin in short children born small for gestational age: dose-dependent effect of growth hormone treatment. Horm Res 2000;54:120–5.
Carroll PV, Drake WM, Maher KT, Metcalfe K, Shaw NJ, Dunger DB, et al. Comparison of continuation or cessation of growth hormone (GH) therapy on body composition and metabolic status in adolescents with severe GH deficiency at completion of linear growth. J Clin Endocrinol Metab 2004;89:3890–5.
Coutant R, Carel JC, Letrait M, Bouvattier C, Chatelain P, Coste J, et al. Short stature associated with intrauterine growth retardation: final height of untreated and growth hormone-treated children. J Clin Endocrinol Metab 1998;83:1070–4.
Crompton C. Recombinant human growth hormone (r-hGH) treatment in children. Nephrology 2005;10(Suppl. 5):224–30.
de Zegher F, Hokken-Koelega A. Growth hormone therapy for children born small for gestational age: height gain is less dose dependent over the long term than over the short term. Pediatrics 2005;115:e458–62.
de Zegher F, Du Caju MV, Heinrichs C, Maes M, De SJ, Craen M, et al. Early, discontinuous, high dose growth hormone treatment to normalize height and weight of short children born small for gestational age: results over 6 years. J Clin Endocrinol Metab 1999;84:1558–61.
de Zegher F, bertsson-Wikland K, Wollmann HA, Chatelain P, Chaussain JL, Lofstrom A, et al. Growth hormone treatment of short children born small for gestational age: growth responses with continuous and discontinuous regimens over 6 years. J Clin Endocrinol Metab 2000;85:2816–21.
Donaldson MDC. Growth hormone therapy in Turner syndrome: current uncertainties and future strategies. Horm Res 1997;48(Suppl. 5):35–44.
Festen DA, Vissert TJ, Otten BJ, Wit JM, Duivenvoorden HJ, Hokken-Koelega AC. Thyroid levels in children with Prader-Willi syndrome before and during growth hormone treatment. Clin Endocrinol 2007;67:449–56.
Fine RN. Long-term use of recombinant human growth hormone (r-hGH) in children with chronic renal insufficiency (CRI). Clin Pediatr Endocrinol 1997;6(Suppl.10):81–4.
Fine RN, Attie KM, Kuntze J, Brown DF, Kohaut EC. Recombinant human growth hormone in infants and young children with chronic renal insufficiency. Genentech Collaborative Study Group. Pediatr Nephrol 1995;9:451–7.
Fine RN, Brown DF, Kuntze J, Wooster P, Kohaut EE. Growth after discontinuation of recombinant human growth hormone therapy in children with chronic renal insufficiency. The Genentech Cooperative Study Group. J Pediatr 1996;129:883–91.
Fine RN, Kohaut E, Brown D, Kuntze J, Attie KM. Long-term treatment of growth retarded children with chronic renal insufficiency, with recombinant human growth hormone. Kidney Int 1996;49:781–5.
Hokken-Koelega ACS. Growth hormone treatment in children before and after renal transplantation. J Pediatr Endocrinol Metab 1996;9:359–64.
Hokken-Koelega A, Mulder P, De JR, Lilien M, Donckerwolcke R, Groothof J. Long-term effects of growth hormone treatment on growth and puberty in patients with chronic renal insufficiency. Pediatr Nephrol 2000;14:701–6.
Juul A, Vahl N, Jorgensen JO, Christiansen JS, Sneppen SB, Feldt-Rasmussen U, et al. Consequences of stopping growth hormone (GH) therapy in young GH deficient patients with childhood onset disease. Growth Horm IGF Res 1998;8(Suppl.A):15–19.
Mahan JD, Warady BA, Fielder P, Gipson DS, Greenbaum L, Juarez-Congelosi MD, et al. Assessment and treatment of short stature in pediatric patients with chronic kidney disease: a consensus statement. Pediatr Nephrol 2006;21:917–30.
Mauras N, Attie KM, Reiter EO, Saenger P, Baptista J. High dose recombinant human growth hormone (GH) treatment of GH-deficient patients in puberty increases near-final height: a randomized, multicenter trial. Genentech, Inc., Cooperative Study Group. J Clin Endocrinol Metab 2000;85:3653–60.
Maxwell H, Rees L. Randomised controlled trial of recombinant human growth hormone in prepubertal and pubertal renal transplant recipients. British Association for Pediatric Nephrology 1998;79:481–7.
Mehls O, Broyer M, bertsson-Wikland K, Allen B, Baur L, Beetz R, et al. Growth response to recombinant human growth hormone in short prepubertal children with chronic renal failure with or without dialysis. Acta Paediatr 1994;83(Suppl. 399):81–7.
Monson JP. Indications for GH replacement in adolescents and young adults. J Endocrinol Invest 2005;28(Suppl. 5):52–5.
Nissel R, Ucur E, Mehls O, Haffner D. Final height after long-term treatment with recombinant human growth hormone (R-HGH) in children with uremic growth failure. Nephrol Dial Transplant 2006;21:367–8.
Querfeld U, Haffner D, Wuhl E, Wingen AM, Wolter K, Friedrich B, et al. Treatment with growth hormone increases lipoprotein(a) serum levels in children with chronic renal insufficiency. Eur J Pediatr 1996;155:913.
Rosenfeld RG, Attie KM, Frane J, Brasel JA, Burstein S, Cara JF, et al. Growth hormone of Turner’s syndrome: beneficial effect on adult height. J Pediatr 1998;132:319–24.
Simon D, Leger J, Fjellestad-Paulsen A, Crabbe R, Czernichow P. Intermittent recombinant growth hormone treatment in short children born small for gestational age: Four-year results of a randomized trial of two different treatment regimens. Horm Res 2006;66:118–23.
Wilton P, Gunnarsson R. Clinical experience with Genotropin in growth hormone deficient children. Acta Paediatr Scand 1988;343(Suppl.):95–101.
Excluded due to wrong intervention (n = 4)
Rosenfeld RG. Acceleration of growth in Turner syndrome patients treated with growth hormone: summary of three-year results. J Endocrinol Invest 1989;12(8 Suppl.3):49–51.
Rosenfeld RG, Hintz RL, Johanson AJ, Sherman B. Results from the first 2 years of a clinical trial with recombinant DNA-derived human growth hormone (somatrem) in Turner’s syndrome. Acta Paediatr Scand 1987;331(Suppl.):59–69.
Rosenfeld RG, Frane J, Attie KM, Brasel JA, Burstein S, Cara JF, et al. Six-year results of a randomized, prospective trial of human growth hormone and oxandrolone in Turner syndrome. J Pediatr 1992;121:49–55.
Wilson DM, Frane JW, Sherman B, Johanson AJ, Hintz RL, Rosenfeld RG. Carbohydrate and lipid metabolism in Turner syndrome: effect of therapy with growth hormone, oxandrolone, and a combination of both. J Pediatr 1988;112:210–17.
Excluded due to wrong outcomes (n = 4)
Gravholt CH, Leth-Larsen R, Lauridsen AL, Thiel S, Hansen TK, Holmskov U, et al. The effects of GH and hormone replacement therapy on serum concentrations of mannan-binding lectin, surfactant protein D and vitamin D binding protein in Turner syndrome. Eur J Endocrinol 2004;150:355–62.
Lagrou K, Vanderfaeillie J, Froidecoeur C, Thomas M, Massa G, Tenoutasse S, et al. Effect of 2 years of high-dose growth hormone therapy on cognitive and psychosocial development in short children born small for gestational age. Eur J Endocrinol 2007;156:195–201.
Ross JL, Feuillan P, Kushner H, Roeltgen D, Cutler GB, Jr. Absence of growth hormone effects on cognitive function in girls with Turner syndrome. J Clin Endocrinol Metab 1997;82:1814–17.
Whitman BY, Myers S, Carrel A, Allen D. The behavioral impact of growth hormone treatment for children and adolescents with Prader–Willi syndrome: a 2-year, controlled study. Pediatrics 2002;109:E35.
Reason for exclusion – repeat publication with no new randomised data
Lindgren AC, Ritzen EM. Five years of growth hormone treatment in children with Prader-Willi syndrome. Swedish National Growth Hormone Advisory Group. Acta Paediatr 1999;88(Suppl. 433):109–11.
Reason for exclusion – conference paper pre-2006
Fine RN, Kohaut EC, Frane JW, Perlman AJ. Multicenter randomized double-blind placebo-controlled study of recombinant human growth-hormone (r-hGH) in children with chronic-renal-failure (CRF). Clin Res 1993;41:A283.
Reason for exclusion – previous HTA report
Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al. Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation. Health Technol Assess 2002;6(18).
Reason for exclusion – conference paper abstract
Christensen T, Buckland AG, Bentley A, Djuurhus C, Wing C. Economic evaluation of somatropin (Norditropin) for the treatment of short children born small for gestational age (SGA). Value Health 2008;11:A223.
Reason for exclusion – children of short stature, not part of scope
Lee JM, Davis MM, Clark SJ, Hofer TP, Kemper AR. Estimated cost-effectiveness of growth hormone therapy for idiopathic short stature. Arch Pediatr Adolesc Med 2006;160:263–9.
Reason for exclusion – disease-specific QoL measure used
Abs R, Mattsson AF, Bengtsson BA, Feldt-Rasmussen U, Goth MI, Koltowska-Haggstrom M, et al. Isolated growth hormone (GH) deficiency in adult patients: baseline clinical characteristics and responses to GH replacement in comparison with hypopituitary patients. A sub-analysis of the KIMS database. Growth Horm IGF Res 2005;15:349–59.
Bannink EM, van Pareren YK, Theunissen NC, Raat H, Mulder PG, Hokken-Koelega AC. Quality of life in adolescents born small for gestational age: does growth hormone make a difference? Horm Res 2005;64:166–74.
Bulow B, Erfurth EM. A low individualized GH dose in young patients with childhood onset GH deficiency normalized serum IGF-1 without significant deterioration in glucose tolerance. Clin Endocrinol 1999;50:45–55.
Deijen JB, Arwert LI, Witlox J, Drent ML. Differential effect sizes of growth hormone replacement on quality of life, well-being and health status in growth hormone deficient patients: a meta-analysis. Health Qual Life Outcomes 2005;3:63.
Dixon S, McEwan P, Currie CJ. Estimating the health utility of treatment in adults with growth hormone deficiency. Journal of Outcomes Research 2003;7:1–12.
Koltowska-Haggstrom M, Hennessy S, Mattsson AF, Monson JP, Kind P. Quality of life assessment of growth hormone deficiency in adults (QoL-AGHDA): comparison of normative reference data for the general population of England and Wales with results for adult hypopituitary patients with growth hormone deficiency. Horm Res 2005;64:46–54.
Koltowska-Haggstrom M, Mattsson AF, Monson JP, Kind P, Badia X, Casanueva FF, et al. Does long-term GH replacement therapy in hypopituitary adults with GH deficiency normalise quality of life? Eur J Endocrinol 2006;155:109–19.
Lagrou K, Xhrouet-Heinrichs D, Massa G, Vandeweghe M, Bourguignon JP, De SJ, et al. Quality of life and retrospective perception of the effect of growth hormone treatment in adult patients with childhood growth hormone deficiency. J Pediatr Endocrinol 2001;14(Suppl. 5):1249–60.
McKenna SP, Doward LC, Alonso J, Kohlmann T, Niero M, Prieto L, et al. The QoL-AGHDA: an instrument for the assessment of quality of life in adults with growth hormone deficiency. Qual Life Res 1999;8:373–83.
Mcmillan CV, Bradley C, Gibneyt J, Russell-Jones DL, Sonksent PH. Evaluation of two health status measures in adults with growth hormone deficiency. Clin Endocrinol 2003;58:436–45.
Malik IA, Foy P, Wallymahmed M, Wilding JPH, MacFarlane IA. Assessment of quality of life in adults receiving long-term growth hormone replacement compared to control subjects. Clin Endocrinol 2003;59:75–81.
Murray RD, Skillicorn CJ, Howell SJ, Lissett CA, Rahim A, Smethurst LE, et al. Influences on quality of life in GH deficient adults and their effect on response to treatment. Clin Endocrinol 1999;51:565–73.
Saller B, Mattsson AF, Kann PH, Koppeschaar HP, Svensson J, Pompen M, et al. Healthcare utilization, quality of life and patient-reported outcomes during two years of GH replacement therapy in GH-deficient adults: comparison between Sweden, The Netherlands and Germany. Eur J Endocrinol 2006;154:843–50.
Sandberg DE, MacGillivray MH, Clopper RR, Fung C, LeRoux L, Alliger DE. Quality of life among formerly treated childhood-onset growth hormone-deficient adults: a comparison with unaffected siblings. J Clin Endocrinol Metab 1998;83:1134–42.
Sheppard L, Eiser C, Davies HA, Carney S, Clarke SA, Urquhart T, et al. The effects of growth hormone treatment on health-related quality of life in children. Horm Res 2006;65:243–9.
Reason for exclusion – mixed patient group of adults and children
Mcmillan CV, Bradley C, Gibney J, Healy ML, Russell-Jones DL, Sonksen PH. Psychological effects of withdrawal of growth hormone therapy from adults with growth hormone deficiency. Clin Endocrinol 2003;59:467–75.
Reason for exclusion – review article
Petrou S, McIntosh E. Measuring the benefits of growth hormone therapy in children: a role for preference-based approaches? Arch Dis Child 2008;93:95–7.
Reason for exclusion – unclear whether adult or child onset
Suzukamo Y, Noguchi H, Takahashi N, Shimatsu A, Chihara K, Green J, et al. Validation of the Japanese version of the Quality of Life-Assessment of Growth Hormone Deficiency in Adults (QoL-AGHDA). Growth Horm IGF Res 2006;16:340–7.
Appendix 6 List of eligible abstracts
The following conference abstracts were identified in searches and were of relevance to the review, but did not contain sufficient information to be included.
Gardner M, Boshart M, Carron L, Sandberg D. Effects of growth hormone in childhood on quality of life end points: a systematic review. Paediatric Acadamic Societies’ (PES) Conference, Baltimore, May 2009.
Phillip M, Lebl J, Steensberg A, Kappelgaard A-M, Ibanez L. Metabolic parameters during growth hormone treatment in short children born small for gestational age. Hormone Research 2008;70(Suppl.1);100.
Salgin B. Effect of growth hormone treatment on insulin secretion and sensitivity in relation to growth of children born small for gestational age. Hormone Research 2008;70(Suppl.1);76.
Appendix 7 List of ongoing studies
Searches identified two relevant RCTs, which are ongoing
Study NCT00190658 aims to compare the mean first-year GV of somatropin-treated prepubertal patients with SHOX-D with the GV of a control group of untreated prepubertal patients with SHOX-D. Both groups will be compared to a somatropin-treated group of girls with TS.
-
Sponsor: Eli Lilly & Co.
-
Estimated end date: December 2010.
Study NCT00625872 focuses on the effect of a 1-year somatropin treatment (0.035 mg/kg/day or 0.067 mg/kg/day) on neuromuscular function and cognitive performance in short children born SGA. Height gain and GV are included as secondary outcome measures. Inclusion criteria are birth length- and/or birth weight-SDS adjusted to gestational age < –2.0, current HtSDS < –2.5 and parental adjusted HtSDS below –1, GV SDS < 0 during the last year before inclusion.
-
Sponsor: Pfizer.
-
End date: not reported.
Appendix 8 Critique of industry submissions (clinical effectiveness)
Six of the seven manufacturers submitted reports to NICE, and these are briefly appraised below. Please see Chapter 4 (Review of the manufacturers’ submissions) for a discussion of the economic models and results included in the MSs.
SHTAC review of clinical effectiveness in Eli Lilly’s submission
Comprehensiveness of ascertainment of published studies
-
The MS uses the Novo Nordisk systematic review, which did not include SHOX. The MS states (p. 13) that the evidence for SHOX came from Lilly’s databases, i.e. there was no systematic review for this. The conditions listed as inclusion criteria for SGA include IUGR, which was not in the NICE scope. The comparator was clearly stated to be ‘no treatment’. However, the inclusion criteria also state that active-controlled RCTs were included. This is then contradicted by the exclusion criteria, which state that studies comparing somatropin with other treatments known or presumed to affect growth would be excluded.
-
The MS clearly reports search dates, search strategies and databases searched.
-
Enough detail was provided for the searches to be reproducible.
-
The MS does not present information on searches for ongoing studies.
-
Conference proceedings were excluded from the review.
-
The MS includes a separate search for QoL data in adolescents and adults.
Searches identified
The MS contains a summary of the included trials, but there is no tabulation of details such as study type, treatment arms, etc. The review included the following RCTs:
-
GHD Five placebo/no treatment-controlled RCTs (mostly during transition phase): Jorgensen 2002 (excluded by SHTAC as mean age = 20), Underwood 2003 (excluded by SHTAC as mean age = 23.8), Drake 2003, Shalet 2003 and Mauras 2005 (all excluded by SHTAC as patients had completed linear growth). The manufacturer included six other studies that were either dosing studies or compared two different versions of somatropin.
-
TS Nine RCTs (three placebo controlled: Gravholt 2002, 2005; Quigley 2002; all included by SHTAC) and six other studies [Bannick 2006, van Pareren 2003, Sas 2001 (all excluded by SHTAC as dose studies), Davenport 2007, Johnston 2001, CGHAC 2005 (all included by SHTAC)].
-
CRI Four CTs: de Graaf 2003 (SHTAC excluded as this is analysis of body proportions in an RCT that we have already included for height and body composition outcomes – Hokken Koelega 1991), Hertel 2002 (SHTAC excluded as compares two doses, no placebo arm), Sanchez 2002 (included by SHTAC), Fine 2002 (SHTAC excluded as includes pubertal children, with no separate data analysis).
-
SGA Twenty RCTs identified, of which six had placebo or no treatment as control arm [Boguszweski 1998, Butenadt 1997, Arends 2003 2004, Boonstra 2006 (SHTAC excluded these as patient group did not meet our criteria), van Pareren 2003 (SHTAC excluded as this is a follow-up of a dose–response study)].
-
PWS not relevant for this drug.
-
SHOX not included in systematic review. Reported data comes from the GDFN study (n = 78), Blum et al. 2007 (SHTAC included this).
-
None of the additional studies met SHTAC’s inclusion criteria.
Clinical analysis
-
The MS also reports observational studies, in particular data from the KIGS database.
-
Given that the manufacturer included a range of studies that did not meet SHTAC’s inclusion criteria, it is not possible to compare their conclusions with those of SHTAC.
-
The MS did not include a meta-analysis or indirect comparison.
-
The MS includes a short narrative summary of the included trials for each disease, but there is no overall tabulation of the included studies’ characteristics or results and no quality assessment of the trials.
-
The MS uses the same outcome measures as the SHTAC review.
-
The MS reports more detail on AEs from observational studies in addition to the limited information available in the RCTs.
Interpretation
-
The MS does not present any tabulated data from the studies included in the systematic review; there is simply a short narrative summary of each disease. It is therefore not possible to assess whether or not the manufacturer’s analysis is supported by data in the included trials.
Key issues
-
The manufacturer’s systematic review included a broad range of studies, for example dosage studies, which did not meet their own inclusion criteria.
-
Very little detail is presented for the included studies (e.g. patient characteristics, treatment arms, length of study) and there is no tabulation of data. The manufacturer’s conclusions seem to be based on both trials that met their inclusion criteria and those that clearly did not (e.g. dosage studies).
SHTAC review of clinical effectiveness in Novo Nordisk’s submission
Comprehensiveness of ascertainment of published studies
-
Databases searched and the dates of searches are specified. Searches were conducted from the date of the original NICE appraisal – w/c 28 August 2008, and from 1996 to w/c 28 August 2008 for SGA (not included in the last review).
-
Search strategies are supplied in the appendices.
-
Search strategies are detailed and appear reproducible.
-
Novo Nordisk does not appear to have searched for other ongoing studies, but do report on two ongoing studies, specifically of Norditropin – NESGAS and NordiNet IOS.
-
Conference proceedings were not searched for and are listed in the exclusion criteria.
Clinical analysis
-
Novo Nordisk did not include PWS or SHOX. Uncontrolled trials were included. For long-term effects of rhGH treatment, i.e. FH/AH/near adult height, open-label extension studies were ‘deemed to be appropriate as the length of the RCTs was likely to be too short to capture the long term treatment effect’. Dose–response trials have been included. In the case of SGA, these form the majority of the submission.
-
SGA Novo Nordisk have included 21 studies. None of these was included in SHTAC’s MTA. Exclusions in the SHTAC MTA were on the basis of patient group not meeting the inclusion criteria or on design, as 14 of the 21 were dose–response studies. The five studies included in our MTA were not included in the Novo Nordisk submission. Novo Nordisk also included open-label extension studies.
-
GHD Novo Nordisk have included 13 studies. One of these is the GHD study included in SHTAC’s MTA. Eight are transition-phase studies – these are not included in SHTAC’s systematic review. Four are dose–response studies and therefore are excluded from the MTA. Two are biosimilars compared with their reference product.
-
TS Novo Nordisk discuss the Turner Cochrane Review. A total of 23 studies were included, including the six included in SHTAC’s MTA. The remaining studies were dose response, with the exception of one, which compared once-daily versus twice-daily injections.
-
CRI Novo Nordisk have included nine studies, five of which were included in SHTAC’s MTA. Of the four excluded from the MTA, two were dose–response studies, one was excluded on patient group.
-
Nothing in the excluded reasons indicates why all of SHTAC’s included SGA papers are excluded.
Conclusions
-
SGA It is not possible to compare the conclusions as the studies included in the two reviews are so different.
-
GHD Again the conclusions are difficult to compare as Novo Nordisk include transition phase studies, which SHTAC excluded from the main systematic review as patients had completed linear growth; dose–response studies; and studies comparing biosimilars to their reference drug. Novo Nordisk’s conclusions tend to be based on dose–response studies, and how far an outcome/result is dose dependent.
-
TS Novo Nordisk concludes that height is improved in a ‘dose-dependent’ manner: The SHTAC MTA does not include dose–response studies or consider dose issues. SHTAC has concluded that there is evidence of improved body composition and height outcomes in girls with TS; this needs to be weighed against issues of quality of reporting and size of trials.
-
CRI Height conclusions are dose related, and body composition ‘does not appear to be negatively influenced by rhGH therapy’.
-
Outcome measures are broadly similar.
-
Additional AE rates from KIGS and NCGS databases are included in an appendix.
Interpretation
-
SGA Conclusions do not appear to fully reflect Novo Nordisk’s analyses, although the analysis contains few results and is a broad summary in itself. Very few of the points discussed in the analyses compare treated and untreated groups, predominantly focusing on dose–response or differences in the treated group from baseline.
-
TS Apart from height outcomes, few results are reported and, again, the focus is often on dose-related effects. The summary somewhat overstates the evidence presented.
-
CRI Conclusions do appear to match analyses, although again few detailed results are presented. Novo Nordisk does not comment on the quantity/quality of research available to support their conclusions.
-
GHD Novo Nordisk considered transition-phase studies alongside non-transition phase studies for height and other outcomes, but separately for biochemical/body composition markers. The authors then summarise that the transition phase studies may lead to an underestimation of growth in children with GHD. Other conclusions appear to match the analyses.
-
Quality is discussed to a degree in the results sections – it is mentioned, for example, if trials are short, or low in patient numbers. However, this, or its possible effects on conclusions/findings, is not referred to in the summary.
Key issues
-
The submission does not include the SGA papers included in SHTAC’s review, but does include studies whose patients do not meet the birth length/WtSDS criteria and/or current HtSDS criteria included.
-
Dose–response studies are included for all conditions.
SHTAC review of clinical effectiveness in Pfizer’s submission
Comprehensiveness of ascertainment of published studies
-
The manufacturer supplied full details of the systematic review, specifying dates and databases searched.
-
Search strategies were supplied.
-
Enough detail was provided for the searches to be reproducible.
-
Inclusion criteria differed from that used by SHTAC in that cohort, observational, and retrospective studies were included. The manufacturer’s inclusion criteria defined children as being < 16 years old, whereas SHTAC included those up to 18 since they may still be growing and thus able to benefit from rhGH treatment. The manufacturer did not specify what the comparator should be (NICE’s final scope indicates that this should be treatment without somatropin).
-
The manufacturer restricted the review to only those studies which used Genotropin, or were sponsored by Pfizer. They excluded studies which used a competitor’s brand of somatropin. However, they also report the results of the Novo Nordisk full systematic review – see SHTAC assessment of the Novo Nordisk MS for more details.
-
The MS does not report ongoing studies.
-
The MS does not state whether or not they searched for conference proceedings.
Searches identified (studies for Genotropin)
-
GHD Three RCTs and 17 observational studies. None of the three RCTs met our inclusion criteria. Coelho et al. (2008) compared two doses of Genotropin; Romer et al. (2007) compared omnitrope with Genotropin; Dorr et al. (2003) compared Genotropin delivered via two different devices.
-
TS One RCT and eight observational studies: the single RCT by Johnston (2001) was also included in the SHTAC review.
-
PWS Twelve RCTs (three from previous appraisal) and six observational studies. One of these (Festen 2007) is not included in our review as it is not a fully randomised study (children were stratified by age, and only the under-12s were randomized – older children were all given rhGH, but results were not reported separately for the randomised patients). Two of the studies included by the manufacturer have been combined by SHTAC, as they report data from the same RCT [Festen et al. 2008 and de Lind van Wijngaarden 2009 (cited as Roderick et al. 2009 in the MS)].
-
CRI No new RCTs, three observational studies. The submission discusses only the Broyer study from the previous review, and not the others that SHTAC included as these were not observing Genotropin.
-
SGA Thirteen RCTs, 10 observational studies. Of the 13 RCTs, only five reported treatment versus no treatment/placebo. SHTAC excluded the review by Lagrou (2007) as its outcomes did not meet our inclusion criteria. We also excluded the reviews by Bundak (2001) and Carracosa (2006) as their patient groups did not match our criteria. We included the De Schepper (2008) study and the de Zegher (2002) studies.
-
None of the manufacturer’s included studies reported QoL as an outcome measure.
-
The MS also includes a summary of the Novo Nordisk systematic review. Please see SHTAC’s appraisal of that submission for further details.
Clinical analysis
-
The manufacturer has only included RCTs of its own brand of somatropin, so it is not possible to compare their findings directly with those of SHTAC.
-
GH and SGA RCTs The MS and SHTAC reviews included different RCTs, so it is not possible to compare the evidence reported. The RCTs included for GHD were not placebo/no treatment controlled.
-
PWS The MS includes two studies (Roderick et al. 2009 and Festen et al. 2008), which appear to be the same RCT – SHTAC has treated these as one RCT to avoid double-counting.
-
Given that the manufacturer included a range of studies that did not meet SHTAC’s inclusion criteria, and focused only on studies of their own product, it is not possible to compare their conclusions directly with those of SHTAC.
-
The MS did not include a meta-analysis or indirect comparison. Results are presented in tables and there is a narrative synthesis for each disease area.
-
The MS uses the same outcome measures as the SHTAC review.
-
The MS includes data from the KIGS database, which is not included in the SHTAC review of clinical effectiveness as it is observational data. Additional adverse event data from the KIGS database is presented on p. 97 of the MS.
Interpretation
-
The manufacturer’s interpretation of the clinical data in the RCTs matches their analyses.
-
There are separate sections discussing the results of RCTs and of observational studies.
-
Data from observational studies have not been checked by SHTAC.
Key issues
-
The manufacturer’s systematic review included dose comparison studies for GHD, which SHTAC excluded.
-
Many of the studies included for the manufacturer’s review of SGA studies were excluded by SHTAC, as their patients did not meet our inclusion criteria.
SHTAC review of clinical effectiveness in Merck Serono’s submission
Comprehensiveness of ascertainment of published studies
-
The MS uses the SHTAC review conducted in 20026 and the systematic review conducted by Novo Nordisk for studies published since then (see Novo Nordisk critique) for the licensed indications for Saizen (GHD, TS, CRI and SGA).
Searches identified
-
Studies identified and reported are all those from the previous SHTAC report (RCTs and non-RCTs reporting FH) plus RCTs published since then identified by the Novo Nordisk review.
-
GHD No additional RCTs were reported for GHD although an additional one is included in the SHTAC MTA (Mauras 2005).
-
TS 4 RCTs (Johnston 2001; CGHAC 2005; Quigley 2002; Davenport 2007). However, the MS did not identify two RCTs included in the SHTAC MTA (both Gravholt 2005).
-
CRI Three RCTs (de Graaf 2003; Fine 2002; Sanchez 2002). Two of these (de Graaf and Fine) are not included in the SHTAC MTA review because they do not meet our inclusion criteria. One RCT (Fine 2004) is not included in the MS but meets the SHTAC MTA inclusion criteria and is therefore included in that.
-
SGA Four RCTs (Buttenandt 1997; Boguszewski 1998; Arends 2004; Van Pareren 2003). These do not match the studies identified in the SHTAC MTA (from which they are excluded on the basis of patient group and study design).
-
The MS does not identify any RCTs that meet the inclusion criteria of the SHTAC MTA that are not already included.
Clinical analysis
-
Evidence reported is broadly similar to the SHTAC MTA in that it uses RCTs in the original SHTAC report; there are some discrepancies on RCTs since that time and on the extra indication SGA.
-
Narrative synthesis is somewhat selective. All included studies are tabulated, but only height results are reported.
-
Manufacturer’s submission also includes some non-systematic review data on psychological outcomes and body composition, and long-term data from the KIGS observational database.
-
Conclusions are generally similar to the SHTAC MTA.
-
GHD The MS has used the previous SHTAC review so conclusions on growth are similar but no data on LBM/biochemical markers.
-
TS Conclusions are broadly similar to the SHTAC MTA in terms of growth and LBM.
-
CRI Conclusions broadly similar to the SHTAC MTA in terms of growth; no statement on other outcomes.
-
SGA Conclusions broadly similar to the SHTAC MTA in terms of growth; no statement on other outcomes.
-
Growth outcomes measures are same as the SHTAC MTA.
Interpretation
-
Overall MS interpretation of the clinical data matches the MS analyses, although the MS relies heavily on the previous SHTAC report. The new evidence is not really synthesised except for SGA, which includes studies that are not in the SHTAC MTA. Conclusions are based on selective statements and focus on height outcomes.
-
Manufacturer’s submission states that new data has ‘not materially changed the understanding of the efficacy of GH in children’.
Questions
-
The major areas of discrepancy compared with the SHTAC MTA relate to studies omitted from the MS (GHD 1, TS 2, CRI 1 and SGA 5).
SHTAC review of clinical effectiveness in Ipsen Ltd’s submission
Comprehensiveness of ascertainment of published studies
-
The databases and dates searched are specified.
-
Search strategies were supplied and appear comprehensive enough to be reproducible.
-
Ongoing studies were not searched for or reported in this submission.
-
Conference proceedings were excluded.
-
This review includes CRI, GHD and TS, and ‘somatropin’ as intervention, including products from other manufacturers, and published and available in full studies in the English language. Exclusion criteria given but reasons for individual studies’ exclusions not stated.
-
Assessment of article quality looks at allocation concealment, patient blinding, investigator blinding, baseline differences of the experimental groups and ‘completeness of follow-up’. The MS did not appear to assess if there was an ITT analysis, or care-provider blinding.
Clinical analysis
-
For the results of the systematic review, we are referred to the submission prepared by Novo Nordisk. Studies are not referenced in the text. No conclusions in this submission, apart from on the limitations of RCTs for FH data, and the subsequent need to rely on observational studies (i.e. KIGS database) for this. The number of studies for each condition reporting certain outcomes is given, but the results are in the Novo Nordisk submission and not detailed in the Ipsen submission.
-
Manufacturer has included 11 GHD studies; most appear to be transition-phase studies.
-
MS states that nine TS studies were found.
-
MS states that four CRI studies were found.
-
Limited new data on FH from RCTs, so appear to have included observational studies for this outcome. However, no references are given in the text so cannot check.
-
The MS states that ‘there are limited data available on the effect of GH on height in RCTs [therefore] use of observational data from … KIGS was appropriate.’ This appears to have been used to inform the economic model.
-
A ‘rapid appraisal of the literature’ was undertaken by Eli Lilly for QoL ‘impact of short stature in adults’ due to lack of data on children and QoL.
-
No conclusions stated here: referred to Novo Nordisk submission.
-
There are no indirect comparisons included here.
-
No outcome results are reported here, but those outcomes reported in the included studies reflect those in the SHTAC review.
-
GHD Four out of eight studies reporting AE ‘found that a higher dose was associated with a greater incidence of AEs and/or serious AEs’. The remaining studies reported no differences between groups. Only one study in the SHTAC review reported AEs, with a slightly higher percentage in the GH group experiencing these. Only one event in each group was thought to be study drug related: oedema in GH and sluggishness in placebo. MS reports AEs that are thought to be related to study drug.
-
CRI Three studies in the MS report AEs: one study reported a higher number of SAEs related to GH therapy compared with no treatment; another study reported SAEs that were ‘therapy-related’. SAEs related to therapy reported here include diabetes mellitus, hypertension and injection pain. This is not reflected in the studies included in SHTAC review. Difficulty with comparisons as there are no references in the text.
-
TS A greater incidence of AE in the GH group was reported in two out of four studies reporting AEs in the SHTAC review. In the MS, one study showed GH to be associated with ‘greater incidence of treatment emergent AEs’. No major differences between the groups were found in the other studies in the MS.
-
No references are given for these studies and AEs, and no proportions/means are reported – just these general results.
Interpretation
-
No interpretation included here – referred to the Novo Nordisk submission.
Key issues
-
Inclusion of observational data to inform FH differs from SHTAC review.
-
Studies not referenced here – cannot cross-check with SHTAC review. See Novo Nordisk submission for further details.
SHTAC review of clinical effectiveness in Sandoz’s submission
Comprehensiveness of ascertainment of published studies
-
The submission did not include a systematic review, so there were no details of search strategies, databases or dates searched.
Searches identified
-
The MS includes details of two phase III studies: AQ-study and LYO-study. Neither meets SHTAC’s inclusion criteria; AQ-study compares different doses of omnitrope with a reference product and LYO-study is a non-comparative trial.
Clinical analysis
-
The evidence reported in the Sandoz submission is from trials specific to their biosimilar product. The submission does not include any trials of rhGH versus no treatment. It is therefore not possible to compare their submission with the evidence presented in the SHTAC systematic review.
-
The submission uses the same outcome measures as the SHTAC review.
-
The submission includes a summary of AEs from the AQ-study and the LYO-study, neither of which was included in the SHTAC review. The manufacturer stated that the safety profiles of omnitrope and Genotropin were comparable.
Interpretation
-
The manufacturer’s interpretation of the clinical data matches their analyses.
Key issues
-
The manufacturer presents evidence for the use of omnitrope compared with other somatropin formulations, but does not present any information for its effectiveness compared with no treatment. The included studies did not meet SHTAC’s inclusion criteria.
Appendix 9 Critical appraisal of manufacturers’ economic evaluation
| Item | MSa | |
|---|---|---|
| 1 | Is there a well-defined question? | Yes |
| 2 | Is the patient group in the study similar to those of interest in UK NHS? | Yes |
| 3 | Is the correct comparator used that is routinely used in NHS? | Yes |
| 4 | Is the study type and modelling methodology reasonable? | Yes |
| 5 | Is an appropriate perspective used for the analysis? | Yes |
| 6 | Is the health-care system or setting comparable to UK? | Yes |
| 7 | Is the effectiveness of the intervention established based on a systematic review? | No |
| 8 | Is the model structure appropriate and does it fit with the clinical theory of the disease process? | Yes |
| 9 | Are assumptions reasonable and appropriate? | Yes |
| 10 | Are health benefits measured in QALYs using a standardised and validated generic instrument from a representative sample of the public? | Yes |
| 11 | Are the resource costs used reasonable and appropriate for the NHS? | Yes |
| 12 | Are the health states and parameters used in the model described clearly and are they reasonable and appropriate for the NHS? | ? |
| 13 | Is an appropriate discount rate used? | Yes |
| 14 | Has the model been validated appropriately? | ? |
| 15 | Is sensitivity analysis undertaken and presented clearly? | Yes |
Appendix 10 Critical appraisal of Sandoz MS (cost-effectiveness)
This appendix describes a critical appraisal of the cost-effectiveness section of the Sandoz MS. The submission attempts a cost-minimisation analysis comparing omnitrope with Genotropin (which was defined as the reference product) in patients with GHD and TS, rather than a cost-effectiveness analysis. There is no indication that a systematic review of clinical evidence has been undertaken. The cost-effectiveness analysis according to NICE guidance138 was not presented.
Appraisal of the manufacturer cost-effectiveness analysis
A summary of the MS compared with the NICE reference case requirements is given in Table 62.
| NICE reference case requirements | Included in submission |
|---|---|
| Decision problem: as per the scope developed by NICE | ✗a |
| Comparator: no treatment alternative | ✗a |
| Perspective on costs: NHS and PSS | ✓b |
| Perspective on outcomes: all health effects on individuals | ✗c |
| Type of economic evaluation: cost-effectiveness analysis | ✗ |
| Synthesis of evidence on outcomes: based on a systematic review | No evidence synthesis |
| Measure of health benefits: QALYs | ✗ |
| Description of health states for QALY calculations: use of a standardised and validated generic instrument | ✗ |
| Method of preference elicitation for health state values: choice based method (e.g. TTO, SG, not rating scale) | ✗ |
| Source of preference data: representative sample of the public | ✗ |
| Discount rate: 3.5% p.a. for costs and health effects | ✗ |
Summary of general concerns
The MS did not comply with NICE’s recommended structure138 and did not estimate QALYs or present cost-effectiveness analysis. The MS attempted a cost-minimisation analysis, implicitly suggesting that treatment with omnitrope is equally effective as treatment with Genotropin (in terms of additional height in children with GHD and TS), but is associated with less cost to the NHS. Due to the number of uncertainties it is not clear whether this assertion is justified. In particular, there was limited clinical efficacy data to support the non-inferiority of omnitrope compared with Genotropin. The only head-to-head RCT comparing omnitrope with Genotropin was of insufficient duration and might not have been designed as a non-inferiority trial. The MS did not include any clinical evidence in relation to licensed indications other than GHD. Without clinical evidence that unequivocally demonstrated the non-inferiority of omnitrope in comparison with Genotropin, the results of a cost-minimisation analysis cannot be confirmed.
The results of the cost comparison reported in the MS were not comparable with the results of cost-effectiveness analysis reported in the submissions by Pfizer, Eli Lilly, Ipsen, Novo Nordisk and Merck Serono because Sandoz have not presented results either as an estimated incremental cost per QALY or as an incremental cost per extra centimetre gained, and the reported cost was neither a lifetime cost nor the cost per duration of treatment (until near-adult height is achieved).
Appendix 11 Quality of life from HSE 2003
The Health Survey for England database was reanalysed in a similar way to Christensen and colleagues for adults aged older than 18 years. The HSE 2003 contains variables for height (estht) and EQ-5D (eqmean). Incomplete records were omitted. For those with complete records (n = 13,321), the HSE 2003 data had mean AH for males of 175 cm (SD 7.2) and mean AH for females of 161 cm (6.8). There were 50 observations less than –3 SDS or greater than 3 SDS (i.e. 0.4%) and 617 observations less than –2 SDS or greater than 2 SDS (4.6%).
An analysis was completed to see the effect of different ages on QoL scores using a subset of people of age 18–49 years and over 50 years old. QoL score for all ages was 0.86; age 18–49 years QoL had mean 0.91 (SD = 0.18); and age 50+ years QoL had mean 0.8 (SD = 0.26). The QoL in the younger category was significantly better than for the older category and so it is logical to estimate the EQ-5D for each of these age groups.
There were few individuals in the SDS < –3 group and the estimates are highly variable. In addition, the majority of these individuals are in the older age group (mean age 72 years). It is therefore more logical to fit the distribution to all data and use this in the model.
| SDS | Age 18–49 years | Age 50+ years | ||
|---|---|---|---|---|
| n | Eqmean | n | Eqmean | |
| < –3.0 | 5 | 0.85 | 24 | 0.63 |
| –3 to < –2.5 | 6 | 0.75 | 62 | 0.70 |
| –2.5 to < –2.0 | 42 | 0.88 | 161 | 0.73 |
| –2 to < –1.5 | 140 | 0.85 | 397 | 0.78 |
| –1.5 to < –1.0 | 475 | 0.91 | 798 | 0.79 |
| –1.0 to <–0.5 | 845 | 0.90 | 1133 | 0.78 |
| –0.5 to < 0 | 1331 | 0.90 | 1288 | 0.82 |
| 0 to < 0.5 | 1485 | 0.91 | 1029 | 0.81 |
| 0.5 to < 1.0 | 1288 | 0.91 | 707 | 0.83 |
| 1.0 to < 1.5 | 837 | 0.91 | 368 | 0.84 |
| 1.5 to < 2.0 | 431 | 0.91 | 152 | 0.85 |
| 2.0 to < 2.5 | 201 | 0.92 | 41 | 0.84 |
| 2.5 to < 3.0 | 42 | 0.89 | 12 | 0.83 |
| > 3.0 | 20 | 0.98 | 1 | 0.90 |
| Age | Fitted QoL score |
|---|---|
| 18–49 years | –0.0024x2 + 0.0177x + 0.9017 |
| > 50 years | –0.0054x2 + 0.0297x + 0.817 |
FIGURE 9.
Relationship between height (HtSDS) and EQ-5D score for adults aged 18 –50 years in HSE 2003.
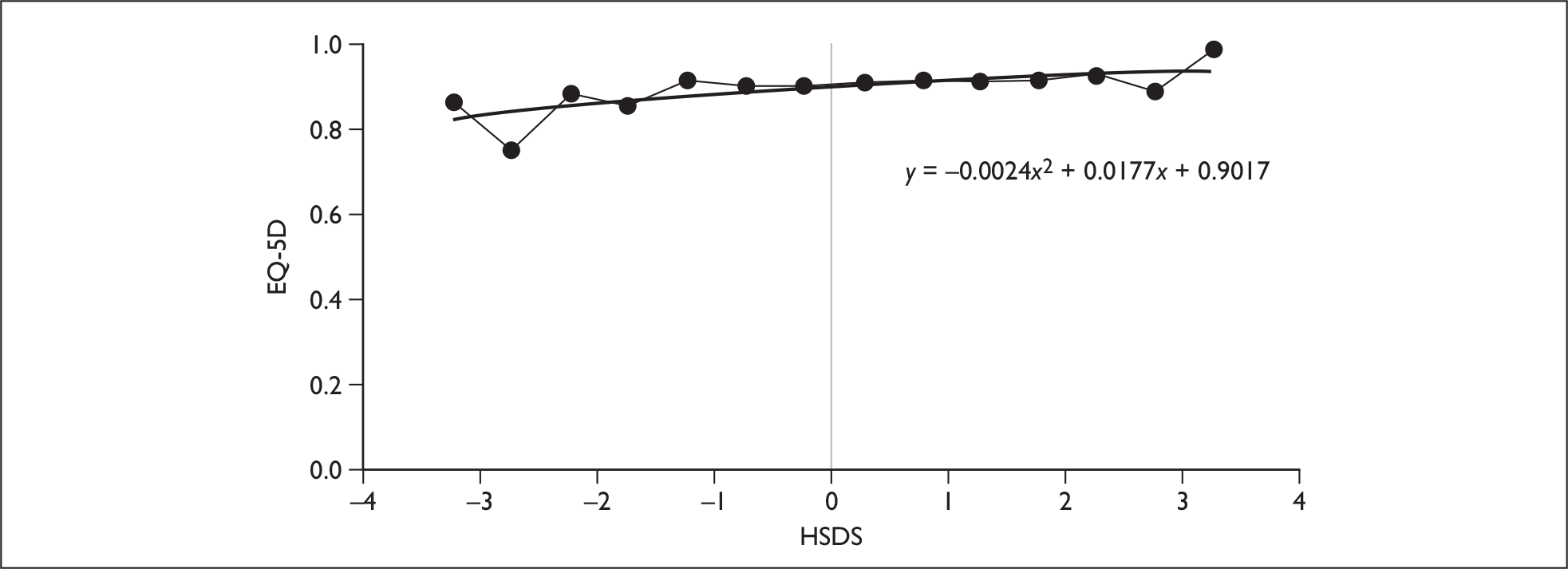
FIGURE 10.
Relationship between height (HtSDS) and EQ-5D score for adults aged older than 50 years in HSE 2003.
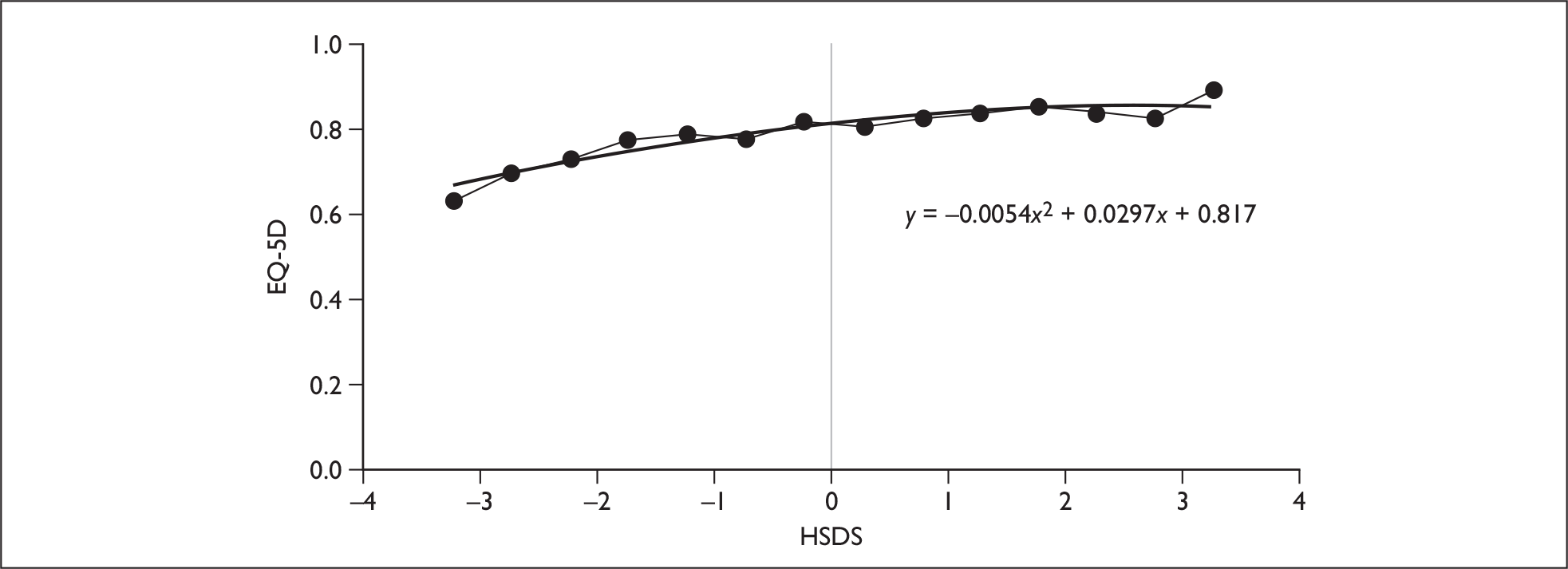
Appendix 12 Input parameters for probabilistic sensitivity analysis
The distribution assigned to each variable included in the PSA and the parameters of the distribution are reported in this appendix.
Health-state utility
The utility increments for HtSDS below –2.0, between –2.0 and 0, and above 0 were sampled using estimated standard errors. These were derived from an assumption that a variation of plus or minus 20% was an appropriate CI for the average utility gain. No other summary statistic was available. These were sampled using a normal distribution.
Compliance
The compliance of the model was based on the range of 69% to 95% compliance estimated in the compliance review conducted by Merck Serono. The estimated ‘standard errors’ for compliance was derived from this range, as this was thought to provide the best estimate of variability due to lack of other summary data.
Height standard deviations
The reported mean HtSDSs were taken from the applicable RCTs and KIGS data for both the treated and untreated groups consistent with the base-case analysis. The standard errors were calculated for each mean HtSDS, except for PWS, for which there was no mean reported; in this case a median value was assumed to adequately represent the mean. A SD of 1 was used to estimate the standard error for PWS. This is consistent with the level of dispersion reported for the other conditions. The HtSDS were simulated using the normal distributions. See Table 67 for mean and standard errors for each condition:
| Health-state utility | Mean | ‘Standard error’ | 95% CI | Distribution | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Below –2 HtSDS | 0.061 | 0.0061 | 0.049 | 0.730 | Normal |
| Between –2 and 0 HtSDS | 0.010 | 0.0010 | 0.008 | 0.120 | |
| Above 0 HtSDS | 0.002 | 0.0002 | 0.0016 | 0.0024 | |
| Mean | ‘Standard error’ | Alpha | Beta | Distribution | |
|---|---|---|---|---|---|
| Compliance | 0.85 | 0.085 | 14.150 | 2.497 | Beta |
| Condition | HtSDS | Mean | Standard error | Distribution |
|---|---|---|---|---|
| GHD | Treated baseline | –2.99 | 0.0134 | Normal |
| Treated end | –1.17 | 0.0216 | ||
| Untreated baseline | –2.99 | 0.0134 | ||
| Untreated end | –2.99 | 0.0216 | ||
| TS | Treated baseline | –3.40 | 0.1152 | |
| Treated end | –1.80 | 0.0206 | ||
| Untreated baseline | –3.40 | 0.1220 | ||
| Untreated end | –3.10 | 0.2294 | ||
| PWS | Treated baseline | –2.00 | 0.2000 | |
| Treated end | –0.50 | 0.2085 | ||
| Untreated baseline | –2.50 | 0.2132 | ||
| Untreated end | –2.60 | 0.2182 | ||
| CRI | Treated baseline | –2.90 | 0.1214 | |
| Treated end | –1.60 | 0.1925 | ||
| Untreated baseline | –2.90 | 0.0994 | ||
| Untreated end | –2.90 | 0.1525 | ||
| SGA | Treated baseline | –3.10 | 0.0700 | |
| Treated end | –2.30 | 0.0840 | ||
| Untreated baseline | –3.10 | 0.0729 | ||
| Untreated end | –3.00 | 0.0894 | ||
| SHOX-D | Treated baseline | –3.30 | 0.1925 | |
| Treated end | –2.10 | 0.0385 | ||
| Untreated baseline | –3.30 | 0.1600 | ||
| Untreated end | –3.00 | 0.0408 |
| Mean | ‘Standard error’ | 95% CI | Distribution | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Starting age | |||||
| GHD | 9.0 | 1.020 | 7.0 | 11.0 | Normal |
| TS | 10.0 | 1.020 | 8.0 | 12.0 | |
| PWS | 7.0 | 1.020 | 5.0 | 9.0 | |
| CRI | 9.0 | 1.020 | 7.0 | 11.0 | |
| SGA | 8.0 | 1.020 | 6.0 | 10.0 | |
| SHOX-D | 8.0 | 1.020 | 6.0 | 10.0 | |
| Treatment length | |||||
| GHD | 7.0 | 1.0200 | 5.0 | 9.0 | Normal |
| TS | 6.0 | 1.0200 | 4.0 | 8.0 | |
| PWS | 8.0 | 1.0200 | 6.0 | 10.0 | |
| CRI | 5.0 | 1.0200 | 3.0 | 7.0 | |
| SGA | 6.0 | 1.0200 | 4.0 | 8.0 | |
| SHOX-D | 7.0 | 1.0200 | 5.0 | 9.0 | |
| Childhood dose | Mean | ‘Standard error’ | 95% CI | Distribution | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| GHD | 0.025 | 0.00255 | 0.020 | 0.030 | Normal |
| TS | 0.045 | 0.00255 | 0.040 | 0.050 | |
| PWS | 0.035 | 0.00255 | 0.030 | 0.040 | |
| CRI | 0.045 | 0.00255 | 0.040 | 0.050 | |
| SGA | 0.035 | 0.00255 | 0.030 | 0.040 | |
| SHOX-D | 0.040 | 0.00255 | 0.040 | 0.050 | |
Starting age and treatment length
The starting age and treatment length were sampled using estimated ‘standard errors’. These were derived from CIs placed 2 years either side of the mean starting age and treatment length. This method was used instead of calculating the standard errors from the KIGS database. It was felt that the very small standard errors from KIGS did not reflect the possible variability in starting age and treatment length. These were sampled using normal distributions.
Childhood drug dose
The means for the childhood drug dose for all the conditions were the same as used in the base-case analysis. The estimated ‘standard errors’ attempted to express the appropriate variability of doses used in the KIGS database and also the maximum doses suggested in the BNF. These were sampled using normal distributions.
Proportion of males
The reported mean proportion of males for each condition was taken from the KIGS database for both the treated and untreated groups. This was consistent with the base-case analysis. The standard errors were calculated for each mean proportion of males and sampled using a normal distribution.
Costs
Costs included in the PSA were those related to outpatient visits, nurse visits and monitoring tests. Drug costs were not varied in the PSA, but were included at values quoted in the BNF. Costs derived from NHS Reference Costs were sampled using estimated ‘standard errors’. These assumed that a variation of plus or minus 25% was an appropriate CI for the average reference costs. The estimated standard errors are shown in column 3 of the Table 71. Parameters for gamma distributions (shown in columns 4 and 5) were derived using the means and estimated ‘standard errors’. The simulated values were inflated to 2008–9 prices using appropriate inflation indices, as for the base-case and deterministic sensitivity analyses.
| Proportion of males | Mean | Standard error | Distribution |
|---|---|---|---|
| GHD | 0.70 | 0.0100 | Normal |
| TS | 0.00 | 0.0000 | |
| PWS | 0.50 | 0.0045 | |
| CRI | 0.71 | 0.0040 | |
| SGA | 0.596 | 0.0032 | |
| SHOX-D | 0.48 | 0.0019 |
| Item | Mean | ‘Standard error’ | Alpha | Beta | Distribution |
|---|---|---|---|---|---|
| Outpatient (first) | 206.28 | 24.57 | 126.07 | 1.64 | Gamma |
| Outpatient (subsequent) | 127.97 | 11.40 | 126.07 | 1.02 | |
| Specialist nurse | 73.00 | 6.50 | 126.07 | 0.58 | |
| District nurse | 64.00 | 5.70 | 126.07 | 0.51 | |
| Blood test | 51.00 | 4.54 | 126.07 | 0.40 | |
| X-ray | 28.64 | 2.55 | 126.07 | 0.23 | |
| Pituitary function test | 246.50 | 21.95 | 126.07 | 1.96 |
Appendix 13 Weight tables for males and females by age (Western Europe KIGS)
| Age (years) | Weight (kg) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| SGA | GHD | PWS | CRI | TS | |||||
| Male | Female | Male | Female | Male | Female | Male | Female | Female | |
| 0 | 4.00 | 3.0 | 6.01 | 5.63 | 4.00 | 3.00 | 4.00 | 3.00 | 3.00 |
| 1 | 6.00 | 5.7 | 8.40 | 7.96 | 9.41 | 8.37 | 8.14 | 6.60 | 7.03 |
| 2 | 8.07 | 8.48 | 10.18 | 9.81 | 10.96 | 10.15 | 10.42 | 9.60 | 10.19 |
| 3 | 10.10 | 10.04 | 12.18 | 11.98 | 14.48 | 12.08 | 12.39 | 11.77 | 11.91 |
| 4 | 11.13 | 11.39 | 13.97 | 13.63 | 17.67 | 15.92 | 14.26 | 13.13 | 13.80 |
| 5 | 13.63 | 13.62 | 15.72 | 15.41 | 20.55 | 20.00 | 16.24 | 15.22 | 15.56 |
| 6 | 15.58 | 15.79 | 17.79 | 17.49 | 23.37 | 23.18 | 17.98 | 18.15 | 17.67 |
| 7 | 17.96 | 17.86 | 20.15 | 19.76 | 26.96 | 26.64 | 20.14 | 19.33 | 20.20 |
| 8 | 20.06 | 19.86 | 22.76 | 22.41 | 31.48 | 29.42 | 22.42 | 21.47 | 23.14 |
| 9 | 22.27 | 22.45 | 25.4 | 25.42 | 35.82 | 33.94 | 24.92 | 23.41 | 26.57 |
| 10 | 24.93 | 24.83 | 28.5 | 28.79 | 40.95 | 41.24 | 27.49 | 26.42 | 30.04 |
| 11 | 27.73 | 28.52 | 31.74 | 32.02 | 44.46 | 44.29 | 30.49 | 30.17 | 34.05 |
| 12 | 31.08 | 31.71 | 35.00 | 35.99 | 51.70 | 47.49 | 34.08 | 34.78 | 38.47 |
| 13 | 34.53 | 35.36 | 39.28 | 40.26 | 57.96 | 52.80 | 37.43 | 37.27 | 42.33 |
| 14 | 38.89 | 38.22 | 44.40 | 44.19 | 63.80 | 56.84 | 41.15 | 39.80 | 46.00 |
| 15 | 44.33 | 40.27 | 49.91 | 47.72 | 69.02 | 59.07 | 44.84 | 41.03 | 49.05 |
| 16 | 49.04 | 43.05 | 54.47 | 49.97 | 74.43 | 56.32 | 48.70 | 41.15 | 51.47 |
| 17 | 53.50 | 47.03 | 58.5 | 53.38 | 74.14 | 61.15 | 50.4 | 42.66 | 52.53 |
List of abbreviations
- AE
- adverse event
- AH
- adult height
- AUC
- area under the curve
- AO-GHD
- adult-onset growth hormone deficiency
- BA
- bone age – a measure of skeletal maturity evaluated on the basis of the relative positions of the bones generally in the left hand and wrist
- BMC
- bone mineral content
- BMI
- body mass index (kg/m2)
- BNF
- British National Formulary
- BSA
- body surface area
- BSPED
- British Society for Paediatric Endocrinology and Diabetes
- CA
- chronological age
- CADTH
- Canadian Agency for Drugs and Technologies in Health
- CDSR
- Cochrane Database of Systematic Reviews
- CEA
- cost-effectiveness analysis
- CEAC
- cost-effectiveness acceptability curve
- CGHAC
- Canadian Growth Hormone Advisory Committee
- CI
- confidence interval
- CKD
- chronic kidney disease
- CO-GHD
- childhood-onset growth hormone deficiency
- CRF
- chronic renal failure
- CRI
- chronic renal insufficiency
- CUA
- cost–utility analysis
- DARE
- Database of Abstracts of Reviews of Effectiveness
- DEC
- Development and Evaluation Committee
- DEXA
- dual-energy X-ray absorptiometry
- DNA
- deoxyribonucleic acid
- EMEA
- European Medicines Agency
- EQ-5D
- European Quality of Life-5 Dimensions
- ERF
- established renal failure
- ESRF
- end-stage renal failure
- EUROCAT
- European Surveillance of Congenital Abnormalities
- FDA
- Food and Drug Administration
- FGR
- fetal growth restriction
- FH
- final height
- FM
- fat mass
- FT4
- free thyroxine
- GFR
- glomerular filtration rate
- GH
- growth hormone
- GHD
- growth hormone deficiency
- GV
- growth velocity (generally cm/year)
- GVSDS
- growth velocity standard deviation score – growth velocity relative to distribution of growth in children of the same chronological age (or bone age if specified)
- HDL-C
- high-density lipoprotein cholesterol
- HRG
- Healthcare Resource Group
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- HtSDS
- height standard deviation score – height relative to distribution of height in children of the same chronological age (or bone age if specified)
- HV
- height velocity
- HVSDS
- Height Velocity Standard Deviation Score
- ICER
- incremental cost-effectiveness ratio
- IGF
- insulin-like growth factor
- IGFBP
- insulin-like growth factor building proteins
- IQR
- interquartile range
- ISPOR
- International Society for Pharmacoeconomics and Outcomes Research
- ISS
- idiopathic short stature
- ITT
- intention to treat
- IU
- international unit (3 IU = 1 mg)
- IUGR
- intrauterine growth restriction/retardation
- KDOQI
- Kidney Disease Outcomes Quality Initiative
- KIGS
- Kabi International Growth Study Database (now Pfizer)
- KIMS
- Kabi International Metabolic Study Database (now Pfizer)
- LBM
- lean body mass
- LDL
- low-density lipoprotein
- LWS
- Léri–Weill syndrome
- m2
- square metres (in this context referring to body surface area)
- met-GH
- methionyl growth hormone
- mg
- milligram
- MPHD
- multiple pituitary hormone deficiency
- MS
- manufacturer’s submission
- MTA
- multiple technology appraisal
- NCHS
- National Centre for Health Statistics
- NFH
- near-final height – height measured when growth is assumed to be near completion
- NHS CRD
- National Health Service Centre for Reviews and Dissemination
- NHS EED
- National Health Service Economic Evaluation Database
- NICE
- National Institute for Health and Clinical Excellence
- NKF
- National Kidney Foundation
- nr
- not reported
- ns
- not statistically significant
- OLS
- ordinary least squares
- PAH
- predicted adult height – extrapolating adult height from childhood height
- Pla
- placebo
- PSA
- probabilistic sensitivity analysis
- PSS
- Personal Social Services
- PWS
- Prader–Willi syndrome
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- QoL-AGHDA
- quality of life assessment of growth hormone deficiency in adults
- QoL-AGHDAUTILITY
- utility-weighted score
- RCT
- randomised controlled trial
- rhGH
- recombinant human growth hormone
- SAE
- serious adverse event
- SAR-SR
- Social Adjustment Scale-self rating
- s.c.
- subcutaneous
- s.c.i.
- subcutaneous injection
- SD
- standard deviation
- SDS
- standard deviation score
- SF-36
- Short Form questionnaire-36 items
- SG
- standard gamble
- SGA
- small for gestational age
- SHOX
- short stature homeobox-containing gene
- SHOX-D
- short stature homeobox-containing gene deficiency
- SHTAC
- Southampton Health Technology Assessments Centre
- SMR
- standardised mortality rate
- TS
- Turner syndrome
- TTO
- time trade-off
- U
- unit
- WtSDS
- weight standard deviation score
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Riemsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA, Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant LD, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost-effectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
-
Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial.
By Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al.
-
The effect of different treatment durations of clopidogrel in patients with non-ST-segment elevation acute coronary syndromes: a systematic review and value of information analysis.
By Rogowski R, Burch J, Palmer S, Craigs C, Golder S, Woolacott N.
-
Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care.
By Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al.
-
A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial.
By Gray AJ, Goodacre S, Newby DE, Masson MA, Sampson F, Dixon S, et al. , on behalf of the 3CPO study investigators.
-
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluation.
By Ara R, Pandor A, Stevens J, Rees A, Rafia R.
-
Adefovir dipivoxil and pegylated interferon alpha for the treatment of chronic hepatitis B: an updated systematic review and economic evaluation.
By Jones J, Shepherd J, Baxter L, Gospodarevskaya E, Hartwell D, Harris P, et al.
-
Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis.
By Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al.
-
A double-blind randomised placebo-controlled trial of topical intranasal corticosteroids in 4- to 11-year-old children with persistent bilateral otitis media with effusion in primary care.
By Williamson I, Benge S, Barton S, Petrou S, Letley L, Fasey N, et al.
-
The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model.
By Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R.
-
Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial.
By Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al.
-
Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis.
By Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
-
The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation.
By Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al.
-
Rapid testing for group B streptococcus during labour: a test accuracy study with evaluation of acceptability and cost-effectiveness.
By Daniels J, Gray J, Pattison H, Roberts T, Edwards E, Milner P, et al.
-
Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Honest H, Forbes CA, Durée KH, Norman G, Duffy SB, Tsourapas A, et al.
-
The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model.
By Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, et al.
-
Gemcitabine for the treatment of metastatic breast cancer.
By Jones J, Takeda A, Tan SC, Cooper K, Loveman E, Clegg A.
-
Varenicline in the management of smoking cessation: a single technology appraisal.
By Hind D, Tappenden P, Peters J, Kenjegalieva K.
-
Alteplase for the treatment of acute ischaemic stroke: a single technology appraisal.
By Lloyd Jones M, Holmes M.
-
Rituximab for the treatment of rheumatoid arthritis.
By Bagust A, Boland A, Hockenhull J, Fleeman N, Greenhalgh J, Dundar Y, et al.
-
Omalizumab for the treatment of severe persistent allergic asthma.
By Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al.
-
Rituximab for the treatment of relapsed or refractory stage III or IV follicular non-Hodgkin’s lymphoma.
By Boland A, Bagust A, Hockenhull J, Davis H, Chu P, Dickson R.
-
Adalimumab for the treatment of psoriasis.
By Turner D, Picot J, Cooper K, Loveman E.
-
Dabigatran etexilate for the prevention of venous thromboembolism in patients undergoing elective hip and knee surgery: a single technology appraisal.
By Holmes M, C Carroll C, Papaioannou D.
-
Romiplostim for the treatment of chronic immune or idiopathic thrombocytopenic purpura: a single technology appraisal.
By Mowatt G, Boachie C, Crowther M, Fraser C, Hernández R, Jia X, et al.
-
Sunitinib for the treatment of gastrointestinal stromal tumours: a critique of the submission from Pfizer.
By Bond M, Hoyle M, Moxham T, Napier M, Anderson R.
-
Vitamin K to prevent fractures in older women: systematic review and economic evaluation.
By Stevenson M, Lloyd-Jones M, Papaioannou D.
-
The effects of biofeedback for the treatment of essential hypertension: a systematic review.
By Greenhalgh J, Dickson R, Dundar Y.
-
A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: the BELLS study.
By Sullivan FM, Swan IRC, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al.
-
Lapatinib for the treatment of HER2-overexpressing breast cancer.
By Jones J, Takeda A, Picot J, von Keyserlingk C, Clegg A.
-
Infliximab for the treatment of ulcerative colitis.
By Hyde C, Bryan S, Juarez-Garcia A, Andronis L, Fry-Smith A.
-
Rimonabant for the treatment of overweight and obese people.
By Burch J, McKenna C, Palmer S, Norman G, Glanville J, Sculpher M, et al.
-
Telbivudine for the treatment of chronic hepatitis B infection.
By Hartwell D, Jones J, Harris P, Cooper K.
-
Entecavir for the treatment of chronic hepatitis B infection.
By Shepherd J, Gospodarevskaya E, Frampton G, Cooper K.
-
Febuxostat for the treatment of hyperuricaemia in people with gout: a single technology appraisal.
By Stevenson M, Pandor A.
-
Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal.
By Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E.
-
Cetuximab for the treatment of recurrent and/or metastatic squamous cell carcinoma of the head and neck.
By Greenhalgh J, Bagust A, Boland A, Fleeman N, McLeod C, Dundar Y, et al.
-
Mifamurtide for the treatment of osteosarcoma: a single technology appraisal.
By Pandor A, Fitzgerald P, Stevenson M, Papaioannou D.
-
Ustekinumab for the treatment of moderate to severe psoriasis.
By Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A.
-
Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model.
By Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al.
-
Clinical and cost-effectiveness of epoprostenol, iloprost, bosentan, sitaxentan and sildenafil for pulmonary arterial hypertension within their licensed indications: a systematic review and economic evaluation.
By Chen Y-F, Jowett S, Barton P, Malottki K, Hyde C, Gibbs JSR, et al.
-
Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) – a pharmacoepidemiological and qualitative study.
By Wong ICK, Asherson P, Bilbow A, Clifford S, Coghill D, R DeSoysa R, et al.
-
ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening.
By Kitchener HC, Almonte M, Gilham C, Dowie R, Stoykova B, Sargent A, et al.
-
The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation.
By Black C, Clar C, Henderson R, MacEachern C, McNamee P, Quayyum Z, et al.
-
Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS).
By Robson SC, Kelly T, Howel D, Deverill M, Hewison J, Lie MLS, et al.
-
Randomised controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes.
By Jeffcoate WJ, Price PE, Phillips CJ, Game FL, Mudge E, Davies S, et al.
-
VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers.
By Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al.
-
A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: the VULCAN trial.
By Michaels JA, Campbell WB, King BM, MacIntyre J, Palfreyman SJ, Shackley P, et al.
-
Communication of carrier status information following universal newborn screening for sickle cell disorders and cystic fibrosis: qualitative study of experience and practice.
By Kai J, Ulph F, Cullinan T, Qureshi N.
-
Antiviral drugs for the treatment of influenza: a systematic review and economic evaluation.
By Burch J, Paulden M, Conti S, Stock C, Corbett M, Welton NJ, et al.
-
Development of a toolkit and glossary to aid in the adaptation of health technology assessment (HTA) reports for use in different contexts.
By Chase D, Rosten C, Turner S, Hicks N, Milne R.
-
Colour vision testing for diabetic retinopathy: a systematic review of diagnostic accuracy and economic evaluation.
By Rodgers M, Hodges R, Hawkins J, Hollingworth W, Duffy S, McKibbin M, et al.
-
Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report.
By Bond M, Wyatt K, Lloyd J, Welch K, Taylor R.
-
Are adverse effects incorporated in economic models? An initial review of current practice.
By Craig D, McDaid C, Fonseca T, Stock C, Duffy S, Woolacott N.
-
Multicentre randomised controlled trial examining the cost-effectiveness of contrast-enhanced high field magnetic resonance imaging in women with primary breast cancer scheduled for wide local excision (COMICE).
By Turnbull LW, Brown SR, Olivier C, Harvey I, Brown J, Drew P, et al.
-
Bevacizumab, sorafenib tosylate, sunitinib and temsirolimus for renal cell carcinoma: a systematic review and economic evaluation.
By Thompson Coon J, Hoyle M, Green C, Liu Z, Welch K, Moxham T, et al.
-
The clinical effectiveness and cost-effectiveness of testing for cytochrome P450 polymorphisms in patients with schizophrenia treated with antipsychotics: a systematic review and economic evaluation.
By Fleeman N, McLeod C, Bagust A, Beale S, Boland A, Dundar Y, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of photodynamic diagnosis and urine biomarkers (FISH, ImmunoCyt, NMP22) and cytology for the detection and follow-up of bladder cancer.
By Mowatt G, Zhu S, Kilonzo M, Boachie C, Fraser C, Griffiths TRL, et al.
-
Effectiveness and cost-effectiveness of arthroscopic lavage in the treatment of osteoarthritis of the knee: a mixed methods study of the feasibility of conducting a surgical placebo-controlled trial (the KORAL study).
By Campbell MK, Skea ZC, Sutherland AG, Cuthbertson BH, Entwistle VA, McDonald AM, et al.
-
A randomised 2 × 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up.
By Waterhouse JC, Walters SJ, Oluboyede Y, Lawson RA.
-
The effectiveness and cost-effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13–19: a systematic review and economic evaluation.
By Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett-Page E, et al.
-
Dissemination and publication of research findings: an updated review of related biases.
By Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, et al.
-
The effectiveness and cost-effectiveness of biomarkers for the prioritisation of patients awaiting coronary revascularisation: a systematic review and decision model.
By Hemingway H, Henriksson M, Chen R, Damant J, Fitzpatrick N, Abrams K, et al.
-
Comparison of case note review methods for evaluating quality and safety in health care.
By Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al.
-
Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation.
By Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, et al.
-
Self-monitoring of blood glucose in type 2 diabetes: systematic review.
By Clar C, Barnard K, Cummins E, Royle P, Waugh N.
-
North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel non-randomised preference study.
By Lock C, Wilson J, Steen N, Eccles M, Mason H, Carrie S, et al.
-
Multicentre randomised controlled trial of the clinical and cost-effectiveness of a bypass-surgery-first versus a balloon-angioplasty-first revascularisation strategy for severe limb ischaemia due to infrainguinal disease. The Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial.
By Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FGR, Gillespie I, et al.
-
A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – the TOuCAN trial.
By Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al.
-
Randomised controlled trials for policy interventions: a review of reviews and meta-regression.
By Oliver S, Bagnall AM, Thomas J, Shepherd J, Sowden A, White I, et al.
-
Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs (NSAIDs) for the reduction of morphine-related side effects after major surgery: a systematic review.
By McDaid C, Maund E, Rice S, Wright K, Jenkins B, Woolacott N.
-
A systematic review of outcome measures used in forensic mental health research with consensus panel opinion.
By Fitzpatrick R, Chambers J, Burns T, Doll H, Fazel S, Jenkinson C, et al.
-
The clinical effectiveness and cost-effectiveness of topotecan for small cell lung cancer: a systematic review and economic evaluation.
By Loveman E, Jones J, Hartwell D, Bird A, Harris P, Welch K, et al.
-
Antenatal screening for haemoglobinopathies in primary care: a cohort study and cluster randomised trial to inform a simulation model. The Screening for Haemoglobinopathies in First Trimester (SHIFT) trial.
By Dormandy E, Bryan S, Gulliford MC, Roberts T, Ades T, Calnan M, et al.
-
Early referral strategies for management of people with markers of renal disease: a systematic review of the evidence of clinical effectiveness, cost-effectiveness and economic analysis.
By Black C, Sharma P, Scotland G, McCullough K, McGurn D, Robertson L, et al.
-
A randomised controlled trial of cognitive behaviour therapy and motivational interviewing for people with Type 1 diabetes mellitus with persistent sub-optimal glycaemic control: A Diabetes and Psychological Therapies (ADaPT) study.
By Ismail K, Maissi E, Thomas S, Chalder T, Schmidt U, Bartlett J, et al.
-
A randomised controlled equivalence trial to determine the effectiveness and cost–utility of manual chest physiotherapy techniques in the management of exacerbations of chronic obstructive pulmonary disease (MATREX).
By Cross J, Elender F, Barton G, Clark A, Shepstone L, Blyth A, et al.
-
A systematic review and economic evaluation of the clinical effectiveness and cost-effectiveness of aldosterone antagonists for postmyocardial infarction heart failure.
By McKenna C, Burch J, Suekarran S, Walker S, Bakhai A, Witte K, et al.
-
Avoiding and identifying errors in health technology assessment models: qualitative study and methodological review.
By Chilcott JB, Tappenden P, Rawdin A, Johnson M, Kaltenthaler E, Paisley S, et al.
-
BoTULS: a multicentre randomised controlled trial to evaluate the clinical effectiveness and cost-effectiveness of treating upper limb spasticity due to stroke with botulinum toxin type A.
By Shaw L, Rodgers H, Price C, van Wijck F, Shackley P, Steen N, et al. , on behalf of the BoTULS investigators.
-
Weighting and valuing quality-adjusted life-years using stated preference methods: preliminary results from the Social Value of a QALY Project.
By Baker R, Bateman I, Donaldson C, Jones-Lee M, Lancsar E, Loomes G, et al.
-
Cetuximab for the first-line treatment of metastatic colorectal cancer.
By Meads C, Round J, Tubeuf S, Moore D, Pennant M, Bayliss S.
-
Infliximab for the treatment of acute exacerbations of ulcerative colitis.
By Bryan S, Andronis L, Hyde C, Connock M, Fry-Smith A, Wang D.
-
Sorafenib for the treatment of advanced hepatocellular carcinoma.
By Connock M, Round J, Bayliss S, Tubeuf S, Greenheld W, Moore D.
-
Tenofovir disoproxil fumarate for the treatment of chronic hepatitis B infection.
By Jones J, Colquitt J, Shepherd J, Harris P, Cooper K.
-
Prasugrel for the treatment of acute coronary artery syndromes with percutaneous coronary intervention.
By Greenhalgh J, Bagust A, Boland A, Saborido CM, Fleeman N, McLeod C, et al.
-
Alitretinoin for the treatment of severe chronic hand eczema.
By Paulden M, Rodgers M, Griffin S, Slack R, Duffy S, Ingram JR, et al.
-
Pemetrexed for the first-line treatment of locally advanced or metastatic non-small cell lung cancer.
By Fleeman N, Bagust A, McLeod C, Greenhalgh J, Boland A, Dundar Y, et al.
-
Topotecan for the treatment of recurrent and stage IVB carcinoma of the cervix.
By Paton F, Paulden M, Saramago P, Manca A, Misso K, Palmer S, et al.
-
Trabectedin for the treatment of advanced metastatic soft tissue sarcoma.
By Simpson EL, Rafia R, Stevenson MD, Papaioannou D.
-
Azacitidine for the treatment of myelodysplastic syndrome, chronic myelomonocytic leukaemia and acute myeloid leukaemia.
By Edlin R, Connock M, Tubeuf S, Round J, Fry-Smith A, Hyde C, et al.
-
The safety and effectiveness of different methods of earwax removal: a systematic review and economic evaluation.
By Clegg AJ, Loveman E, Gospodarevskaya E, Harris P, Bird A, Bryant J, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of rapid point-of-care tests for the detection of genital chlamydia infection in women and men.
By Hislop J, Quayyum Z, Flett G, Boachie C, Fraser C, Mowatt G.
-
School-linked sexual health services for young people (SSHYP): a survey and systematic review concerning current models, effectiveness, cost-effectiveness and research opportunities.
By Owen J, Carroll C, Cooke J, Formby E, Hayter M, Hirst J, et al.
-
Systematic review and cost-effectiveness evaluation of ‘pill-in-the-pocket’ strategy for paroxysmal atrial fibrillation compared to episodic in-hospital treatment or continuous antiarrhythmic drug therapy.
By Martin Saborido C, Hockenhull J, Bagust A, Boland A, Dickson R, Todd D.
-
Chemoprevention of colorectal cancer: systematic review and economic evaluation.
By Cooper K, Squires H, Carroll C, Papaioannou D, Booth A, Logan RF, et al.
-
Cross-trimester repeated measures testing for Down’s syndrome screening: an assessment.
By Wright D, Bradbury I, Malone F, D’Alton M, Summers A, Huang T, et al.
-
Exploring the needs, concerns and behaviours of people with existing respiratory conditions in relation to the H1N1 ‘swine influenza’ pandemic: a multicentre survey and qualitative study.
By Caress A-L, Duxbury P, Woodcock A, Luker KA, Ward D, Campbell M, et al.
-
Influenza A/H1N1v in pregnancy: an investigation of the characteristics and management of affected women and the relationship to pregnancy outcomes for mother and infant.
By Yates L, Pierce M, Stephens S, Mill AC, Spark P, Kurinczuk JJ, et al.
-
The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: results from 36 national telephone surveys in the UK.
By Rubin GJ, Potts HWW, Michie S.
-
The impact of illness and the impact of school closure on social contact patterns.
By Eames KTD, Tilston NL, White PJ, Adams E, Edmunds WJ.
-
Vaccine effectiveness in pandemic influenza – primary care reporting (VIPER): an observational study to assess the effectiveness of the pandemic influenza A (H1N1)v vaccine.
By Simpson CR, Ritchie LD, Robertson C, Sheikh A, McMenamin J.
-
Physical interventions to interrupt or reduce the spread of respiratory viruses: a Cochrane review.
By Jefferson T, Del Mar C, Dooley L, Ferroni E, Al-Ansary LA, Bawazeer GA, et al.
-
Randomised controlled trial and parallel economic evaluation of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR).
By Peek GJ, Elbourne D, Mugford M, Tiruvoipati R, Wilson A, Allen E, et al.
-
Newer agents for blood glucose control in type 2 diabetes: systematic review and economic evaluation.
By Waugh N, Cummins E, Royle P, Clar C, Marien M, Richter B, et al.
-
Barrett’s oesophagus and cancers of the biliary tract, brain, head and neck, lung, oesophagus and skin.
By Fayter D, Corbett M, Heirs M, Fox D, Eastwood A.
-
Towards single embryo transfer? Modelling clinical outcomes of potential treatment choices using multiple data sources: predictive models and patient perspectives.
By Roberts SA, McGowan L, Hirst WM, Brison DR, Vail A, Lieberman BA.
-
Sugammadex for the reversal of muscle relaxation in general anaesthesia: a systematic review and economic assessment.
By Chambers D, Paulden M, Paton F, Heirs M, Duffy S, Craig D, et al.
-
Systematic review and economic modelling of the effectiveness and cost-effectiveness of non-surgical treatments for women with stress urinary incontinence.
By Imamura M, Abrams P, Bain C, Buckley B, Cardozo L, Cody J, et al.
-
A multicentred randomised controlled trial of a primary care-based cognitive behavioural programme for low back pain. The Back Skills Training (BeST) trial.
By Lamb SE, Lall R, Hansen Z, Castelnuovo E, Withers EJ, Nichols V, et al.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Consultant Adviser, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Professor Ruairidh Milne, Director of NETSCC External Relations
-
Ms Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Warwick Clinical Trials Unit
-
Director, Nottingham Clinical Trials Unit
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Ms Kay Pattison, NHS R&D Programme/DH, Leeds
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Mr A S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital
-
Dr Dianne Baralle, Consultant & Senior Lecturer in Clinical Genetics, Human Genetics Division & Wessex Clinical Genetics Service, Southampton, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Service User Representative
-
Professor Anthony Robert Kendrick, Professor of Primary Medical Care, University of Southampton
-
Dr Susanne M Ludgate, Director, Medical Devices Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr David Mathew Service User Representative
-
Dr Michael Millar, Lead Consultant in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, University College London
-
Mrs Una Rennard, Service User Representative
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr W Stuart A Smellie, Consultant, Bishop Auckland General Hospital
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Alan J Williams, Consultant in General Medicine, Department of Thoracic Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist Commissioning Advisory Group (NSCAG), Department of Health
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook Clinical Programmes Director, Bazian Ltd, London
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr Colin Greaves Senior Research Fellow, Peninsular Medical School (Primary Care)
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Miss Nicky Mullany, Service User Representative
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Mrs Jean Thurston, Service User Representative
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust, Bristol
-
Reader in Wound Healing and Director of Research, University of Leeds, Leeds
-
Professor Bipin Bhakta Charterhouse Professor in Rehabilitation Medicine, University of Leeds, Leeds
-
Mrs Penny Calder Service User Representative
-
Professor Paul Carding, Professor of Voice Pathology, Newcastle Hospital NHS Trust, Newcastle
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry, London
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol, Bristol
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and the London School of Medicine and Dentistry, London
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester, Manchester
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham, Nottingham
-
Dr Kate Radford, Division of Rehabilitation and Ageing, School of Community Health Sciences. University of Nottingham, Nottingham
-
Mr Jim Reece, Service User Representative
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton, Southampton
-
Dr Pippa Tyrrell, Stroke Medicine, Senior Lecturer/Consultant Stroke Physician, Salford Royal Foundation Hospitals’ Trust, Salford
-
Dr Sarah Tyson, Senior Research Fellow & Associate Head of School, University of Salford, Salford
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University, Cardiff
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health , London
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, MRC, London
-
Dr Ursula Wells PRP, DH, London
Interventional Procedures Panel
-
Consultant Surgeon & Honorary Clinical Lecturer, University of Sheffield
-
Mr David P Britt, Service User Representative, Cheshire
-
Mr Sankaran ChandraSekharan, Consultant Surgeon, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Mr Seamus Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor David Taggart, Consultant Cardiothoracic Surgeon, John Radcliffe Hospital
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Nadim Malik, Consultant Cardiologist/ Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Mr Michael Thomas, Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Mrs Isabel Boyer, Service User Representative, London
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Professor Robin Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Service User Representative, Gloucestershire
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician & Cardiologist, County Durham & Darlington Foundation Trust
-
Mr John Needham, Service User, Buckingmashire
-
Ms Mary Nettle, Mental Health User Consultant, Gloucestershire
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Howard Ring, Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry & Warwickshire Partnership Trust
-
Dr Alastair Sutcliffe, Senior Lecturer, University College London
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, MRC, London
-
Professor Tom Walley, HTA Programme Director, Liverpool
-
Dr Ursula Wells, Policy Research Programme, DH, London
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington