Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 06/32/01. The contractual start date was in June 2007. The draft report began editorial review in February 2010 and was accepted for publication in May 2010. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Within the last 5 years Tim Coleman has undertaken consultancy work for Pierre Fabre Laboratories, France and also Johnson & Johnson. Both companies produce nicotine replacement therapy. Matthew Taylor has recently received funding from a company called Synergenz, which produces a diagnostic test for assessing patients’ genetic risks of developing lung cancer. He evaluated the test’s potential cost-effectiveness, based on its impact on stopping people smoking. Andy McEwan receives a personal income from Cancer Research UK via the University College London. He has received travel funding, honoraria and consultancy payments from manufacturers of smoking cessation products (Pfizer Ltd, Novartis UK and GSK Consumer Healthcare Ltd). He also receives payments for providing training to smoking cessation specialists and receives royalties from books on smoking cessation.
Permissions
Copyright statement
© 2010 Queen’s Printer and Controller of HMSO. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2010 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Introduction
Smoking remains a major, international cause of morbidity and mortality, and killed approximately 80,000 people in England in 2007. 1 Reducing smoking is therefore a major priority for governments and health systems like the UK National Health Service (NHS). Following the publication of the Government’s White Paper, Smoking Kills,2 in 1998, a comprehensive tobacco control strategy has been implemented, aimed at reducing uptake of smoking and increasing quitting among existing smokers. The strategy has involved a combination of population tobacco control interventions (such as price rises, an advertising ban and smoke-free legislation) combined with treatment for dependent smokers through the NHS. Treatment is provided principally through a national network of NHS Stop Smoking Services (NHS SSS), first implemented in 2000 after piloting in a number of deprived areas. 3 Similar services have been set up in the other UK countries. The NHS SSS provide evidence-based smoking cessation treatment, which is highly cost-effective,4 and over 4 million people have set a quit date through the services since their inception, with over 2 million stopping smoking at 4 weeks5 and a substantial proportion remaining permanently abstinent. Nevertheless, it is estimated that approximately 75% of these 4-week quitters subsequently relapse back to smoking (‘relapsers’) within 6 months of their quit date. 6 This project aimed to investigate whether and how the NHS SSS could reduce this proportion of relapsers.
Background
Smoking as a drug dependence
There is strong evidence of pharmacological, as well as psychological, dependence on cigarettes. 1 Nicotine obtained from cigarettes meets all the standard criteria used to define a drug of addiction or dependence and most smokers continue to smoke because they are addicted to nicotine. Smoking is therefore a difficult behaviour to change, often taking several attempts over a period of years before permanent cessation is successfully achieved and as such, can be seen as a chronically relapsing behaviour. This is similar to other drug taking behaviour that persists in the face of serious negative health consequences. 7 Hence, although the majority of smokers report wanting to stop, each year only around a third make a quit attempt and only 2% succeed. 1
The process of relapse
Attempts to stop smoking are characterised by a period of initial abstinence followed by an extended period when the abstainer is at a high risk of relapse, but this risk reduces over time. 8 The risk of relapse is greatest in the first few weeks after quitting when withdrawal effects peak, hence relapse to smoking occurs quickly, with many smokers not even managing to stay abstinent for 1 day. 9 Lapses (defined as isolated events or slips followed by a renewal of abstinence) predict subsequent relapse (defined as fully going back to smoking), and those who maintain abstinence for the first 2 weeks are more likely to be abstinent 6 months later. 10 After the first few weeks of abstinence, withdrawal symptoms reduce and confidence in remaining abstinent increases. 9 However, abstainers continue to relapse for months, even years, after the quit attempt, although a recent study of natural relapse patterns in different populations indicated that relapse dropped to around 5% after more than 2 years. 11
The process of relapse is not yet fully understood, and theoretical models focus on specific mechanisms of drug motivational processes (e.g. Herd),12 which increasingly recognise relapse to smoking as a dynamic process difficult to predict and prevent, and likely to involve a complex interaction of factors. 13 Individual factors, such as more dependent smoking, craving, self-efficacy, perceived benefits of smoking, and cues, such as the presence of smokers, situations or behaviours associated with previous smoking, as well as negative effects (e.g. stress), have been shown to trigger lapses and relapse. 14–16
Little is known about how to prevent relapse. Early theorists12 believed that abstainers should try to recognise the high-risk situations in which they are likely to relapse and then learn to use cognitive and behavioural strategies to cope with these situations. Over time, the use of effective medications has also been added to these strategies. Shiffman13 recently summarised current thinking suggesting that treatment needed to ‘imbue the person with the ability to respond more effectively to a wide range of situational challenges’. However, very few interventions have been shown to be effective for relapse prevention, an issue we discuss further below. 17
The need for support with quitting and the NHS SSS
In contrast to the evidence base for relapse prevention treatments, evidence for the use of acute cessation treatments has grown rapidly over recent decades and a variety of effective treatments now exist which can increase the success of stopping smoking up to fourfold18 compared with no support. In the UK, NHS SSS were set up to offer evidence-based treatment to smokers wanting to stop, in recognition of the fact that many smokers needed such support and although these services are cost-effective, relapse is still the most common outcome for those using them. 6
The English Department of Health (DoH) publishes guidance for the NHS SSS to ensure they target their efforts at those most in need, in particular routine and manual smokers, and deliver the most effective treatment,19 referring to guidance on efficacy. 20 The NHS SSS aim to reach as many smokers as possible through health professionals’ brief interventions, their onward referral to the NHS SSS of those who need more support and also with smokers’ self-referrals. 19 In general, the NHS SSS offer flexible treatment, which usually involves the most effective combination of individual or group behavioural therapy, backed-up by the offer of smoking cessation medications, such as nicotine replacement therapy (NRT), bupropion and, more recently, varenicline. 19
Historically, the success of NHS SSS has been measured by monitoring the numbers of smokers who access services and set dates for quitting smoking, and, of these, the numbers who are not smoking 4 weeks after their quit dates; challenging primary care trust (PCT) targets have been set for delivery against these measures. 21 Recent guidance indicates an aspiration that, in time, at least 5% of smokers from areas served by NHS SSS should set quit dates with services’ help annually but, currently, monitoring of ‘4-week quitters’ is still required. Although services are encouraged to offer, for at least 4 weeks after smokers’ quit dates, the most effective cessation treatments (including behavioural support), there is little contemporary information on the treatments actually offered. Also concerns have been expressed that the focus on 4-week quit rates militates against the provision of support beyond this initial period, despite the possibility that treatments like relapse prevention interventions might sustain successful quit attempts in the longer term. 3 In addition, although the services are encouraged to monitor longer-term success at 1 year,19 their funding is not dependant on this and many services find such monitoring difficult in practice. For these reasons the focus on NHS SSS delivering short-term quitters is likely to deter services from offering relapse prevention treatments.
Given the addictive nature of smoking, this focus on short-term therapy is at odds with the extended duration of therapy and follow-up recognised for other drugs of dependence. 22 Understanding relapse, methods to reduce relapse and the feasibility and effectiveness of introducing these in NHS SSS are therefore important issues to explore.
Rationale for current research
At the time this project was commissioned, a Cochrane review23 (and summary journal article with searching until August 2004)24 had found no evidence for the effectiveness of any specific type of relapse prevention intervention (RPI) but also noted that there was only a small evidence base from which this conclusion was drawn. The review included trials delivered to smokers with varied characteristics both before and after their quit attempts had started. However, subgroup analysis of smokers who had completed smoking cessation programmes, which provided data most relevant to the UK context, found some evidence for the effectiveness of NRT and bupropion in relapse prevention. It was possible that the methods used to combine outcome data, interventions and population groups in the Cochrane review, may have obscured real effects and, therefore, there was a need to update this using refined methodology to ensure any effective RPIs, particularly those of relevance to the NHS SSS, were identified.
Clearly, if an updated review demonstrated one or more RPIs to be effective for preventing relapse to smoking, determining whether or not the use of such therapies could represent good value to the NHS would be important. Although we were aware of no trials conducted in the UK, using a modelling-based approach and incorporating all available efficacy evidence could determine the likely cost-effectiveness of any effective interventions that might be introduced into the UK context. This would provide useful information to inform policy decisions about the need for further research into RPIs; the utility of their introduction of into routine NHS SSS clinical care or even whether or not it would be in the best interests of the NHS not to pursue further use or evaluations of RPIs at this time. For this modelled, health economic evaluation, estimates for the effectiveness of RPIs derived from an updated efficacy review would be appropriate.
Another important issue was the need to clarify the ‘natural history’ of relapse among smokers attempting cessation with help from effective, evidence-based cessation treatments, such as those delivered by the NHS SSS. Previously, an attempt to derive relapse curves describing the experiences of smokers who try to stop smoking unsupported found that most are smoking again within 8 days and only 3–5% are still abstinent at 6–12 months. 8 However, as supported quit attempts are more successful than unsupported ones, relapse curves for smokers who attempt to stop smoking while using evidence-based support are likely to be very different. Although relapse curves for smokers trying to quit with the use of NRT had been produced, these incorporated insufficient data to predict confidently relapse in the very early stages of smokers’ quit attempts when the highest rate of relapse might be expected. 25 Consequently, we undertook a systematic review to derive ‘relapse curves’ reflecting the experiences of smokers, such as those treated by NHS SSS, who use evidence-based cessation therapies to help them stop smoking. We aimed to determine the proportions of treated smokers still abstinent at set times after starting quit attempts to help inform future decisions about when, in relation to the initiation of quit attempts, future experimental relapse prevention treatments might be tested or, indeed, when effective ones might be introduced into clinical practice.
Finally, we wanted to determine that, should any RPIs be found to be effective or promising for further evaluation, how feasible it could be to either test or introduce these into routine NHS SSS clinical practice. To achieve this aim we undertook qualitative work and a survey of NHS SSS managers to ascertain current practice and any barriers to introducing effective RPIs.
Objectives
-
To survey NHS SSS managers in order to:
-
Describe and categorise RPIs that are currently used in UK NHS SSS.
-
Describe the current treatment provided by UK NHS SSS for smokers who are trying to stop.
-
Ascertain barriers to the trialling or introduction of RPIs within current clinical practice.
-
-
To update estimates of effectiveness in the Cochrane review on interventions for preventing relapse to smoking, altering analysis methods, as appropriate, to enhance interpretation of findings.
-
To assess which studies, included in 1 above, provide findings that are generalisable to NHS SSS and which test interventions that might be acceptable to introduce within the UK.
-
To determine the cost-effectiveness of those RPIs, identified in 3 above, which could potentially be delivered by the NHS SSS.
-
To derive ‘relapse to smoking’ curves for smoking cessation attempts made with the support of evidence-based cessation treatments, such as those delivered by NHS SSS, using (1) prolonged and (2) point abstinence from smoking as outcome measures.
-
To identify deficiencies in the evidence base concerning the use of RPIs for smoking cessation and to identify priorities for future research.
Research methods
The project was divided into four distinct phases with very different methodologies: qualitative research with a convenience sample of NHS SSS managers to inform the development of a subsequent survey of all UK NHS SSS managers; a systematic review investigating the efficacy of RPIs; a cost-effectiveness analysis; and a further systematic review to derive the relapse curves for smokers receiving evidence-based treatment of the type delivered by the NHS SSS. These four phases of the research are described in detail in the following four chapters and the methods used in each phase of the project are described at the outset of each. Perhaps because so little is known about the relapse process, researchers testing out interventions aimed at preventing relapse, have tended to develop their own criteria as to what RPIs should encompass. There is no internationally accepted definition for RPIs, the components parts of RPIs, how these are used and who they are targeted at are generally defined by the investigators themselves such that in some studies it can be difficult to tell the difference between smoking cessation and RPIs.
Consequently, for our survey of NHS SSS managers we derived a definition for RPIs which was informed by our qualitative research and so, relevant to their context; for our ‘efficacy’ systematic review, we used investigators’ (i.e. trialists’) definitions for RPIs and in our ‘relapse curve’ review we defined relapse as any return to smoking after a quit date set within trials.
Chapter 2 Provision of relapse prevention interventions in NHS SSS
Background
As stated in Chapter 1, the effectiveness and cost-effectiveness of NHS SSS are well established, with more than half of English services’ clients achieving self-reported abstinence from smoking for at least 4 weeks. 6 However, rates of relapse to smoking are high, with around 75% of those abstinent 4 weeks after their quit date restarting smoking by 1 year. 6 The use of effective RPIs could therefore greatly improve long-term cessation rates for the NHS SSS, but little is known about the current provision of RPIs in the services and the feasibility of adding these to existing treatment provision, should effective RPIs be identified.
We therefore carried out two complementary studies to explore these factors. The first was a qualitative study with a convenience sample of 16 health professionals working in the UK NHS SSS that aimed to explore managers’ understanding of the term RPIs, their attitudes towards, and experiences of, providing RPIs in clinical practice and factors that they thought could hinder or encourage the efficient provision of RPIs in the services. Building on the findings of this study, we then carried out a UK-wide survey of NHS SSS managers to describe and quantify the current provision of RPIs in services in the UK and ascertain barriers to the trialling, or introduction, of RPIs within clinical practice.
Methods
Qualitative research
Design
Health professionals attending a UK-wide smoking cessation conference in 2007 were asked to indicate their willingness to be interviewed at a later date on relapse prevention provision with NHS SSS and 23 professionals provided contact details. All 23 professionals were e-mailed 7 months after the conference, invited to reconfirm their willingness to take part and agree a convenient time to be interviewed. Non-respondents to the e-mail were contacted via telephone 2 weeks later. We identified issues of potential importance to RPIs from the literature and, using these, a semi-structured interview schedule, with prompts was developed (see Appendix 1). Throughout interviews, open-ended questions were used to encourage participants to give their views and these were conducted by one author (SA) via telephone in January and February 2008. Interviews covered the following subjects: knowledge and understanding of relapse prevention, types and duration of RPI provided, and barriers and challenges encountered. Each interview lasted 20–25 minutes and all were audio-taped and transcribed verbatim.
Analysis
Box 1 summarises the process of data analysis, which involved using the Framework Method. 26 The first stage of analysis involved one author identifying initial themes or concepts which were derived from the data, rather than being imposed by the researchers. 27 The definition of emergent themes and categories were checked against the data, and subsequently refined in an iterative process. 28 Themes and subthemes were given unique codes and a manageable index was constructed. The index was subsequently applied to the raw data, and the references were noted in the margins of the transcripts. The next stage involved constructing charts with rows and columns for each of the main themes and subthemes that emerged. This process of ‘charting’ allows allocation of the main themes to each column on the chart, and each interview transcript is assigned to a particular row; it ensures that enough data and context are included in the charts such that the analyst is not required to go back to the transcribed data to understand the point being made. 26 After charting all the interviews, interview text relating to the research aims and objectives was collated from the themes and subthemes. Finally, two additional authors read a sample of 10 randomly selected transcripts and confirmed that the transcripts were coded consistently and they contained data that supported the key findings of the study, with any disagreements being resolved by discussion.
SA reads all transcripts in an iterative process to identify themes and subthemes
SA designs a framework (index) with themes and subthemes and their working definitions
TC and AMcN agree working definitions for the emerging themes and subthemes
SA codes the transcripts for the themes. Data relating to each theme is assembled. TC and AMcN independently read 10 randomly selected transcripts to see if they are being coded consistently
Working definitions for themes and subthemes are refined. The framework (index) is restructured to reflect the changes
SA recodes the transcripts using the refined definitions
TC and AMcN check reliability of the data and interpretation of the findings at each stage of the process
Survey
Using emergent findings from our systematic review (see Chapter 3, Results) and the qualitative research detailed below, issues of potential importance to the provision of RPIs in the NHS SSS were identified and, from these, a structured questionnaire was developed (see Appendix 2) which was made available online at a temporary website address (www.smokingcessationmanagers.org). The questionnaire was designed to obtain information pertaining to current provision of treatment for smoking cessation as well as current and future RPI provision and then the feasibility of providing the most promising RPIs in routine clinical practice. A clear definition of RPIs was provided at the outset of the questionnaire, (building on that discussed in the introductory chapter), namely ‘Relapse Prevention Interventions (or Relapse Prevention Treatments) are behavioural or drug therapies delivered after acute smoking cessation treatment has ended and resulted in abstinence from smoking. Relapse Prevention Interventions therefore seek to reduce relapse to smoking among abstinent smokers’. We also distinguished RPIs from interventions delivered to smokers within quit attempts who had recently lapsed and were smoking again and which aimed to prevent brief lapses from becoming full relapses. Our qualitative work suggested that such interventions were frequently deployed (see below) and so respondents were, asked to indicate provision of such treatments.
The Smoking Cessation Service Co-ordinator (SCSC) database of England, Scotland, Wales and Northern Ireland (a database held by organisers of a national conference held annually for health professionals working in the NHS SSS across the UK and for whom membership was updated annually) was used in December 2008 to identify 185 managers of the UK NHS SSS. Managers were e-mailed a flyer advertising the survey with a link to the survey homepage and asked to complete the questionnaire hosted there. Non-respondents were followed up via a reminder e-mail and telephone call inviting them to visit the survey homepage and complete the survey. Responses were anonymous and data were summarised descriptively using spss, version 16.0, for Microsoft Windows®. No hypotheses generating statistical analyses were originally planned, but some comparisons are presented for descriptive purposes.
Results
Qualitative research
Of the 23 individuals who had indicated their willingness to participate in the study, four could not be contacted and three potential participants indicated that they no longer wished to participate, leaving a total of 16 individuals with whom interviews were conducted (12 with females). Fifteen interviewees were smoking cessation professionals who were also responsible for overseeing the day-to-day activities of their respective services or actively involved in managing one aspect of the service in which they worked and one was a regional tobacco control lead.
Three broad themes emerged from interview data: beliefs, knowledge and understanding of relapse prevention; RPIs for abstinent/lapsed and relapsed smokers, and barriers and challenges (Box 2).
Prevention of lapses
Treatment of lapses
Treatment of relapsed smokers
Relapse prevention support for abstinent/lapsed and relapsed smokers Support for abstinent/lapsed smokersContent:
Behavioural counselling and pharmacotherapy
Telephone follow-up
Social activities
Uptake
Support for relapsed smokersContent:
Rolling groups
Recycling – fresh quit attempt
Uptake
Barriers and challengesFunding
Government targets
Paucity of information about effective relapse prevention interventions
The following sections describe these themes in more detail. Quotes are reported in Boxes 3–6 and are attributable to individual interviewees by code numbers.
‘Relapse prevention is making sure that, to try and stop people lapsing back to smoking, that’s what I understand relapse prevention would mean’. Interviewee no 8
‘It is some action, some clinical action that the practitioner takes in order to prevent the patient from in the first place lapsing that automatically implies that it would help prevent relapse’. Interviewee no 12
‘Relapse prevention to me is, we have an open clinic, we see them initially for at least 7 weeks, but it doesn’t finish at either at 6 or 7 weeks, they can come for as long as they like’. Interviewee no 13
Treatment of lapses‘Well it’s for people who have tried to stop smoking and have lapsed, and they don’t want to go back through the whole system again, they just need something to get them back on track again’. Interviewee no 10
‘I’ve always felt that it’s enabling clients to remain quit in the long-term...so that at the point where they’ve had one lapse, they actually get support to prevent them from turning into one great big relapse’. Interviewee no 2
Treatment of relapsed smokers‘It’s really about people who have relapsed to smoking, regularly, and have gone into full-blown relapse, where they are now smoking regularly, and they need help to actually stop’. Interviewee no 1
‘We run a group, so they can come in for a series of sessions which cover general healthy lifestyle, like healthy eating, getting advice, and stress reduction’. Interviewee no 6
‘Well everything that is involved in behavioural support, going through every situation they may encounter, preparing themselves for that, looking at tactics to cope with situations...if they’ve got anything in particular they’re worried about, we will approach it in a practical but relaxed manner’. Interviewee no 2
‘We work with people, whatever their issues/triggers are, we would deal with, it doesn’t matter what it is, if its debt management, crisis resolution, if in quitting smoking they’ve got problems that need dealing with, we would deal with it’. Interviewee no 5
‘I would strongly recommend that (pharmacotherapy) because as I said, a lot of patients reported that they actually relapsed right after they are not provided with medications’. Interviewee no 3
‘I think it (pharmacotherapy) would be fantastic’. Interviewee no 5
Telephone follow-up‘We do telephone follow-ups, say between 6 and 12 months, just to ask them how they are getting on, and to let them know they can access the service again and again, at any point they need’. Interviewee no 18
‘The problem you have there is if you are going to phone everybody, you have to have the manpower, the resources to do that, from a resource point of view, I wouldn’t have time to phone everybody at the moment’. Interviewee no 13
‘It would be very hard for us to that, to phone everyone up would be ideal but impossible at the moment’. Interviewee no 15
Social activities‘We do use interventions such as diversion therapy, by getting people into community groups and community support...we don’t send them home to continue sorting out themselves, we get them out in the community, get them busy and get them involved in things, they need to be busy and out there and feeling useful…we get them to go to care homes and just you know, do peoples’ hair and make them cups of tea, its just engaging them with whatever involves them’. Interviewee no 5
Uptake‘I think the picture is actually, people poorly attend relapse prevention. Because they feel once they’ve actually reached the quit, they don’t need any help...a lot of smokers don’t want you chasing them up, a lot of them are fed up if you do contact them’. Interviewee no 6
‘We used to, a couple of times a year, we’d put on like an open session, and invite everybody who’d been to the group in the last year, we’d put on a bit of food and make it a social event, and do some stuff about staying quit, but very few people attended, so it tended to be a waste of our time, so we didn’t continue it’. Interviewee no 16
‘We don’t have any formal relapse groups, but there are no barriers to re-entry of the service, for example in my 12-week group, drop-in group, people can come along who have relapsed and rejoin the group again’. Interviewee no 12
‘We have a rolling group that is open for anybody who wants to come back in at any time’. Interviewee no 14
Recycling‘Yes, it’s a new quit attempt isn’t it? (For relapsed smokers). You would go over the reasons for relapse and then you need to go through the whole process of another quit attempt’. Interviewee no16
Uptake‘A lot of people would rather, even though you’ve built up a rapport, struggle than bother you, so they think, oh no, I’ve failed now, they may have had one, two cigarettes, they don’t contact you, so that tends to be a problem’. Interviewee no 8
‘I think, when you, from my experience as an ex-smoker, if you’re trying to give up, and you’ve slipped up, and then somebody is ringing you, you think Oh God no, it’s that woman again, and feel really bad’. Interviewee no 13
‘The trouble is when people do relapse there’s sort of, they’re embarrassed to come back’. Interviewee no 15
‘We used to have a relapse prevention session, wherein we invite everyone that came to our service to attend these clinics, but we don’t do that anymore because of financial pressures’. Interviewee no 3
‘I think most primary care trusts would be prepared to pay for a course of treatment, but not an extended course of treatment, that’s why they cut down to stop methods unlikely to be funded locally’. Interviewee no 4
Government targets‘If you’ve got very busy clinics and you have Department of Health Targets to meet, you know, there’s always a bit of a squeeze, in terms of how much time you’ve got for people to see you beyond their successful 4 week quit’. Interviewee no 7
‘I think you know, the fact that we are so target driven, and the fact that reporting successes is at a month rather than if it was 3 months or something like that, you know the whole drive would be to see patients longer … although I think targets are probably a good thing overall, because it does focus you on hitting the three pots and all the rest of it, but I think it can be a bit counter productive’. Interviewee no 14
Paucity of Information‘I don’t think we’ve got anything in black and white, to be honest’. Interviewee no 1
Knowledge and understanding of relapse prevention
Interviewees had diverse perceptions of relapse prevention as a concept and shared no common definition of what this should entail (Box 3). Their definitions of relapse prevention mostly appeared to be informed by the ways in which the cessation services for which they worked currently attempted to help abstinent smokers to remain stopped and achieve long-term abstinence. Interviewees believed that relapse prevention should be mainly provided for abstinent smokers to help them remain smoke-free and prevent lapses by extending their acute treatment. Some health professionals also believed that RPIs could be used for the treatment of lapsed (i.e. people who had smoked one or two cigarettes) or relapsed smokers (i.e. people who were now smoking regularly again).
Prevention of lapses
Most participants understood/thought that relapse prevention involved preventing lapses by providing treatment for longer than a ‘usual’ 7- to 8-week period, believing that, irrespective of the type of intervention used, offering acute cessation treatment for longer periods would ensure that more smokers remained abstinent. Almost all participants stated that relapse to smoking was most frequent when smokers ran out of medication, which perhaps explains the strong belief that extending treatment would prevent lapses. Treatments described were often group or individual behavioural support, extended beyond the usual time frame for which acute cessation treatment was provided.
Treatment of lapses
A small number of interviewees described relapse prevention as providing support for smokers who have already had a minor ‘lapse’ (i.e. smoked a few cigarettes during an otherwise abstinent period) to prevent subsequent complete relapse. Interviewees believed that a single lapse could be sufficient to precipitate a later, complete relapse and that managing these would substantially reduce the risk of smokers returning to regular smoking. Interviewees, again, provided a content-centred definition for relapse prevention as being the treatment of lapses citing the provision of behavioural support and pharmacotherapy as potentially effective for those who had smoked a few cigarettes during an otherwise abstinent period.
Treatment of relapsed smokers
Interviewees also described relapse prevention as providing treatment for smokers who have fully relapsed to smoking. They defined this, again, in terms of the content of the relapse prevention intervention and revealed that this usually involved encouraging the client to begin a fresh quit attempt and begin acute cessation treatment again, or attend ‘rolling groups’ (defined below).
Relapse prevention interventions for abstinent/lapsed and relapsed smokers
Interviewees described RPIs for abstinent/lapsed and relapsed smokers in terms of the types of support which could be provided and this differed for the two groups. Behavioural treatments, telephone follow-up calls and social activities represented the bulk of interventions provided for abstinent smokers and those who had experienced brief lapses, whereas rolling groups and recycling (in which relapsed smokers are treated as fresh quit attempts) were treatment modalities that interviewees described as being accessed by relapsed smokers. Interviewees also reflected on the uptake of such support when offered within their services (Boxes 4 and 5).
Support for abstinent/lapsed smokers: content
Interviewees revealed that behavioural counselling was one of the most favoured forms of treatment for smokers who remained abstinent or who despite one or two brief lapses remained smoke-free. This was described as being provided either individually or to groups in which clients are helped to identify situations and triggers that might lead to smoking lapses or relapse and taught strategies to help overcome cigarette urges and prevent lapses or full-blown relapse to smoking. Clients are also helped to understand that relapse is a spontaneous, unplanned thought process or phenomenon which is often triggered by external factors such as holidays, bereavement, and unexpected personal or financial difficulties, and are equipped with strategies to deal with these. Few individuals spontaneously mentioned the use of pharmacotherapy to prevent relapse, but all were asked to comment on the feasibility of using pharmacotherapies for relapse prevention (given emerging evidence on its effectiveness, see Chapter 3, Pharmacotherapy interventions) and most interviewees were positive about this.
Some interviewees reported that their services provide telephone follow-up calls or text messaging to support abstinent clients who had completed acute cessation treatment. Advisors kept in touch with abstinent smokers via telephone to provide motivation and support, when needed, and to help them remain smoke-free with relatively short calls (< 10 minutes) made at convenient times for clients. During the call, the advisor reiterated the advantages of remaining smoke-free and reminded clients to contact the service once he/she experiences the urge to smoke a cigarette. Interviewees were quick, however, to point out that this proactive telephone counselling was logistically difficult and, as many clients found the calls intrusive, not a favoured intervention. They believed calls could be an unwelcome reminder for smokers that abstinence could be difficult to maintain.
Interviewees talked about using ‘diversion therapy’ as a RPI for abstinent smokers. This was often reported to involve engaging clients in activities designed to take their minds off smoking, and provide them with feelings of well-being and importance, Activities were specially organised and could be conducted by the smoking cessation service or in community or leisure centres. Regular group activities could be led by an abstinent smoker and those described included baking/cooking, community services and visiting hospices or nursing homes to lend support to residents.
Interviewees revealed that where RPIs had been offered, most clients did not access them, making it difficult to sustain their provision; clients generally used services for help with cessation and interviewees’ perceived that their services might not be viewed as providers of support to prevent relapse.
Support for relapsed smokers: content
In some services, smokers who had already been treated but had relapsed to smoking were able to access ‘rolling groups’. Health professionals described this as an ‘open door’ policy, with relapsed clients always free to return to the service and rejoin cessation-orientated support groups. ‘Rolling groups’ would not have fixed start or completion dates, so clients wishing to re-enter the service for help would be able to do so. Groups were perceived as able to provide clients the opportunity to mix with individuals who had received acute cessation treatment, relapsed, but had been able to become abstinent again. The groups are often led by a trained advisor, focusing on helping smokers deal with circumstances that might lead to relapse.
In other services smokers who have suffered a full-blown relapse were encouraged to re-enter complete cessation treatment programmes. Interviewees reporting this believed that, after complete relapse to smoking, support aimed at relapse prevention is no longer appropriate and the individuals need to restart the quitting process.
It was perceived that this process of ‘re-cycling’ was often hampered by smokers’ unwillingness to admit relapses and re-engage with smoking cessation advisors due to profound feelings of failure and embarrassment. Health professionals believed an important focus in the management of smoking relapse should be to help the smoker overcome such emotions and suggested that making clients aware of the possibility of relapse, early in their quit attempts, might prepare smokers for relapse to diminish such negative emotions arising.
Barriers and challenges to using relapse prevention interventions
Funding and pressure to meet Government targets (which are focused on short-term cessation) and paucity of information on the effectiveness of RPIs were repeatedly identified as challenges to their provision (Box 6).
Funding
Nearly all health professionals stated that drug budgets and funding constituted major obstacles to the introduction of RPIs. A number of interviewees revealed that they had stopped providing RPIs due to a lack of funds for additional support beyond that provided during cessation treatment. Interviewees were positive about providing these interventions for motivated smokers, if health authorities allocated adequate funding.
Government targets focused on short-term cessation
Interviewees’ accounts suggested that the need to meet Government targets for NHS SSS exerts considerable pressure on them. Even for health professionals who were interested in and willing to provide RPIs, the pressure to achieve short-term cessation for smokers (i.e. 4-week quits) often reduced the amount of time and resources that could be devoted to RPIs. Interviewees recognised this conflict and repeatedly identified this as a substantial barrier to the provision of RPIs within their services.
Paucity of information about effective relapse prevention interventions
A lack of available evidence on the effectiveness of RPIs was also perceived as a barrier to their use by some participants. It was believed that it would be easier to provide these interventions for motivated smokers if there was a readily available and accessible evidence base detailing the relative effectiveness of different RPIs. Many indicated that they would be able to integrate RPIs into their mainstream service, but only if there was sufficient evidence regarding the effectiveness of these interventions.
Survey
A total of 96 managers completed the survey (52% response rate): 54 responded to the first e-mail and completed the questionnaire, with a further 42 respondents completing the survey after e-mail and telephone reminders.
Current provision of smoking cessation treatments
Table 1 shows the provision of cessation treatments reported by managers as being used in services they ran; reported treatments for relapse prevention are also shown. Nearly all, 99%, reported that their services provided individual behavioural interventions, with NRT the next most popular treatment provided, by 98% (Table 1). A high proportion of managers (92.7%, n = 85) also reported that their services recommended NRT combinations (this question was not asked in relation to relapse prevention provision).
| Type of treatment% of those providing cessation or RPI (n) | ||||||
|---|---|---|---|---|---|---|
| Individual behavioural counselling | Group behavioural counselling | Telephone counselling | NRT | Bupropion | Varenicline | |
|
Cessation (n = 96) |
99% (95) | 87.5% (84) | 81.2% (78) | 97.9% (94) | 86.5% (83) | 92.7% (89) |
|
Relapse prevention (n = 56) |
73.2% (41) | 53.6% (30) | 76.8% (43) | 48.2% (27) | 21.4% (12) | 19.6% (11) |
Current provision of RPIs
More than half of respondents, 58.3% (n = 56) reported that their services currently provided RPIs and Table 1 shows managers’ reported provision of the different types. The most popular form of RPI was telephone follow-up counselling, reported to be provided by just over three-quarters of the managers providing RPIs, followed by individual counselling (54%). Pharmacotherapy support was reported to be provided by under half of those providing RPIs, with NRT being the most frequently used.
Of those services reporting provision of RPIs, 60.7% (n = 34) stated that these were offered to abstinent smokers for as long as these clients perceived they required them, 25.0% (n = 14) for 3–6 months and one service (1.8%) did so for ≤ 3 months. Of the 40 services reporting that they did not currently provide RPIs, 42.5% (n = 17) had provided such interventions in the past and cited the following reasons for no longer offering this kind of support: pressure to meet government targets (64.7%, n = 11) services; poor client attendance (70.6%, n = 12); inadequate funding (29.4%, n = 5); and a belief that RPIs are ineffective (17.6%, n = 3).
Managers that responded to the first survey e-mail were compared to those that completed the survey after a reminder. There was no association between timing of responses and reported provision of RPI [odds ratio (OR) 0.77, 95% confidence interval (CI) 0.34 to 1.75].
Current provision of treatment for brief lapses
A large percentage of managers of NHS SSS, 77.1% (n = 74), also reported providing treatment for clients who had suffered a brief lapse to smoking. Of these, 72.9% of services (n = 70) indicated the types of support provided: one-to-one sessions (32.8%, n = 23); rolling groups and drop-in sessions (7.1%, n = 5); telephone support of services (8.5%; n = 6); combinations of pharmacotherapy, telephone support, and one-to-one behavioural counselling (15.7%, n = 11); while 35.7% (n = 25) services continued acute cessation treatment. Although managers who provided RPIs were more likely to provide treatment for brief lapses than those not providing RPIs, this was not statistically significant (OR 1.55, 95% CI 0. 59 to 4.04, p = 0.37).
There was no association between timing of responses to the survey and reported provision of treatment of brief lapses (OR 1.92, 95% CI 0.70 to 5.26).
Feasibility of relapse prevention interventions
Respondents were asked to indicate the likelihood of future RPI provision within their NHS SSS. Managers who had indicated that RPIs were not currently provided were asked to indicate the likelihood of providing RPIs in the future and those already providing RPIs were asked about the likelihood of continuing this provision. Nearly two-thirds, 65.6% (n = 63) managers, thought it very likely or likely that they would continue to provide, or start to provide, RPIs in their services, with the remainder not sure or thinking it unlikely that they would provide RPIs in the future. Among the latter group, the reasons cited for this were: cessation orientated targets focused on 4-week quit rates (66.7%, n = 22); inadequate funding (42.9%, n = 14); and the fact that clients had usually relapsed before they recontacted the cessation service (24%, n = 8).
The 33 respondents who indicated that they were not sure or thought it unlikely that their services would provide RPIs in the future, were then asked to assume that barriers to provision of RPIs were removed, and to hypothesise, in this instance, which RPIs they might encourage their NHS SSS to offer to abstinent quitters after smoking cessation treatment. Of these, around three-quarters thought it very likely or likely that they would provide individual or group behavioural counselling without the hindrance of barriers [(78.8%, n = 26) and (72.7%, n = 24) respectively], followed by NRT (57.6%, n = 19), NRT combinations (54.5%, n = 18), varenicline (24.2%, n = 8) and bupropion (21.2%, n = 7).
There was no association between timing of responses to the survey and the reported likelihood of future relapse prevention provision (OR 1.05, 95% CI 0.45 to 2.46).
Discussion
Summary of findings
Qualitative research
The sample of health professionals interviewed did not have a shared definition or understanding of RPIs. Instead, interviewees used their experiences to conceptualise relapse prevention, often basing this on the kinds of RPIs that the services in which they worked offered to clients. Interviewees believed that introducing RPIs into NHS SSS would be hindered by lack of funding, current performance targets focused on achieving short-term abstinence from smoking and the lack of an evidence base. They reported low uptake of RPIs in services providing them and interviewees were negative about introducing additional, proactive telephone support counselling as an RPI, but were much more positive about the possibility of using pharmacotherapy for this purpose.
Survey
Just over half of the managers responding to the survey reported providing RPIs based on the definition we provided and used throughout this report, despite at the time the survey was carried out, a weak evidence base (for pharmacological RPIs)23 and an absence of guidance on the provision of RPIs within NHS SSS. The most frequently provided RPIs were telephone and individual behavioural counselling, RPIs for which there was no evidence of effectiveness; which has not changed as a consequence of reviews conducted within this report. Around three-quarters of the managers also reported treating lapses among smokers trying to stop, but as this is not the main focus of this report and there is only a very small evidence base to support this kind of intervention, such provision is not discussed further. Most managers of NHS SSS were favourably inclined towards continuing or introducing RPIs but were most positively orientated towards providing those for which there was very little evidence of effectiveness. Similar to the findings from the qualitative research, the most commonly cited reasons for not providing RPIs were the NHS SSS short-term abstinence targets and inadequate funding for RPI delivery.
Strengths and limitations
To our knowledge, these are the first studies to explore smoking cessation professionals’ experiences of, beliefs about, and current provision of RPIs within the NHS SSS or indeed in any other health system and the findings have highlighted relevant issues that could hinder or facilitate the introduction of RPIs into the NHS. Our qualitative research sample was small and it is possible that by interviewing a larger, more diverse group, we would have found other important factors relating to the use of RPIs, however, similarities inherent in the accounts we obtained, suggest that we have identified most of the major issues. Also, as our sample comprised volunteers from those attending a smoking cessation conference, one might expect their views on RPIs to be better informed than those of others working in the field. Our survey results are based on smoking cessation managers’ self reports and may have overestimated the rates of RPI provision; for example, managers may have been unwilling to reveal that they do not provide some form of RPI in their services. However, we believe that biases in the reporting among this sample are an unlikely explanation for our findings, given the lack of current evidence on the effectiveness of RPIs at the time the survey was carried out. The survey is also limited by the response rate as just over half of managers completed the online questionnaire. A greater response rate may have produced more varied results; non-responders to the survey may have different experiences of providing RPIs in their services, although a comparison of the two waves of responses to the survey showed that there were no differences in variables relevant to the focus of this report.
Important emergent issues
The varied descriptions of RPIs in the qualitative research indicated that health professionals working in the NHS SSS did not share a common definition of what these interventions should involve. While some believed relapse prevention should be aimed at lapsed smokers, more commonly it was perceived appropriate for preventing relapse among smokers who were still abstinent and attempting to quit, in concordance with the definition we use in this report. However, often no distinction was made between RPIs and routine cessation treatment. It is, perhaps, unsurprising to find differences of opinion about RPIs among health professionals, because the scientific literature on the subject at the time the research was carried out described studies which conceptualised relapse prevention in different ways too23 (as discussed in the next chapter).
When provided with a definition of RPIs, over half the managers in the survey reporting providing them, despite the then weak evidence base,23 and two-thirds reported being likely to provide them in the future. This enthusiasm may have reflected a desire to improve support provided to smokers, who have a high relapse rate from acute cessation treatment, or their anecdotal experience of the effectiveness of RPI, or a perception that smokers appreciate being provided with RPIs. While this wasn’t explored in our research, there was little support for the latter explanation as participants in the qualitative research expressed concern about the low uptake of RPIs, which had often led to these being withdrawn, and was perceived as a major potential barrier to their successful introduction. They also thought that relapsed smokers were embarrassed about their ‘failure’ and hence did not return for treatment. This view is consistent with the literature; lapsed smokers often feel guilty12 and experience negative affect and decreased confidence in their ability to quit. 29
Managers favoured behavioural intervention over drug treatments and, at the time of the survey, there was insufficient evidence to say whether either was, indeed, effective. However, our subsequent systematic review (see Chapter 3), found drug treatments and not behavioural ones effective for smokers who achieve abstinence after receiving support, as those using NHS SSS do. This suggests that overall findings from this report could help the NHS SSS clinical practice to become more evidence based. Survey respondents preferred telephone follow-up of clients for behavioural RPIs, though there is no evidence that this is effective and, conversely, the qualitative interviewees found little or no enthusiasm for this, citing that few abstinent smokers welcomed this type of contact that was also logistically challenging to undertake.
We examined whether the preference for the provision of behavioural treatments reflected provision of acute cessation treatment. While this could explain the use of telephone support (81% of services provided telephone support as acute cessation treatment), this explanation does not clarify the disparity between the high percentage of services offering bupropion and varenicline for acute cessation treatment and the low percentage offering these pharmacotherapies for relapse prevention, despite at the time some, albeit weak, evidence for their effectiveness. 23 In the absence of any barriers, individual and group counselling were also favoured for relapse prevention, while the pharmacotherapies were the least favoured. However, when provision of RPIs was explored in the qualitative research, interviewees believed that pharmacotherapy used as extended treatment for relapse prevention could be easily integrated into current routine practice, as long as costs were addressed.
In addition to cost, the other substantive perceived barrier to any form of RPI provision were the current performance management targets for the NHS SSS. For example in October 2002, the English DoH stated an aim that 800,000 smokers would successfully quit following help from smoking cessation services by 200621 and this was subsequently translated into an aspiration that services should treat at least 5% of their local population of smokers in the course of a year, with an expected validated success range of 35% to 70% at 4 weeks. 1 For these targets, success involves smokers achieving a 4-week period of abstinence, so there is considerable pressure on services to achieve a high throughput of smokers who manage to stop smoking for at least 1 month. Interviewees’ comments reflected this perceived pressure and indicated that the provision of RPIs, which, if effective, could be expected to improve longer term but not short-term quit rates, could not be a priority for services without a change in the targets against which they are measured.
The survey data indicated that current provision of acute cessation treatment largely reflects UK guidance,30,31 and our survey suggests that similar evidence-based guidance is needed to support managers wishing to provide RPIs in order to ensure that, in the future, the most promising and effective RPIs can be introduced into routine care, assuming that any perceived barriers are removed.
Chapter 3 Systematic review investigating effectiveness of relapse prevention interventions
Background
A 2005 Cochrane review found no convincing evidence for the effectiveness of either behavioural or pharmacological RPIs. 23 However, trials investigating drug treatments provided relatively weak evidence that extended courses of NRT might reduce relapse among abstinent quitters. 23 An update of the 2005 review again found behavioural RPIs ineffective, but findings for drug interventions were less straightforward; bupropion was not found to work for relapse prevention, whereas the one trial of varenicline found this effective and the length of smokers’ abstinence periods prior to starting RPIs appeared to influence their effectiveness. 17 Two large trials, in which participants were abstinent for only 24 and 48 hours before commencing NRT as a relapse prevention treatment found NRT effective for this, but two smaller ones with much longer abstinence periods did not. 17 Methods of combining outcomes in Cochrane reviews may have obscured real effects of RPIs; both pooled smoking status at final follow-up,17,23 resulting in data collected at different times after randomisation and hence at varying periods into participants’ quit attempts, being aggregated. For example, abstinence rates at 5 and 12 months after participants started RPI treatments could be combined, potentially yielding clinically heterogeneous comparisons.
The research question
In this chapter, we address the research question, ‘Are smoking relapse prevention interventions effective in reducing rates of relapse to smoking?’ by conducting a systematic review with an identical search strategy to that used in the Cochrane reviews, but in which only data collected at similar follow-up time points are synthesised. We investigate the impact of RPIs delivered to both recently-abstinent and non-abstinent smokers, but our primary analyses determine the effects of RPIs delivered to smokers who are recently-abstinent (referred to as abstinent smokers or abstainers), because this is the way relapse prevention treatments would probably be used in routine clinical practice in the UK. We also assess the impact of using RPIs alongside traditional smoking cessation treatments by analysing trials which randomise (non-abstinent) smokers and which deliver RPIs and cessation therapies simultaneously. In summary this review investigates whether or not pharmacological or behavioural RPIs increase long-term abstinence from smoking when delivered to smokers or to smokers who have managed to stop and remain abstinent for a period.
Methods
Search strategy
The search strategies undertaken were identical to those used in the 2005 Cochrane review23 and intended to update this and so were conducted between 2004 (when searches for this review concluded) and July 2008. In addition to searching the Cochrane Tobacco Addiction Group register of trials, we also searched MEDLINE, the Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, PsycINFO, the Science Citation Index and Social Science Citation Index. To identify grey literature we also searched the abstracts of the annual meeting of the Society for Research on Nicotine and Tobacco, contacting authors for further information about their research, where relevant. The bibliographies of retrieved references were also scanned for further relevant publications and studies in all languages/from all countries were considered. Full details of search strategies used are documented in Appendix 3.
The titles and abstracts identified from searches were assessed independently by two authors (TC and AMcN). Studies were excluded if it was clear that the study did not refer to a randomised controlled trial (RCT) of an intervention used for relapse prevention. Two authors then independently assessed each study to determine whether it met the pre-specified selection criteria, with any difference being resolved through discussion with remaining authors.
Inclusion and exclusion criteria
Type of studies
Randomised control trials with a minimum of 6 months’ follow-up after randomisation, including studies that randomised smokers and also people who had recently smoked and were now abstinent. Trials of behavioural interventions that randomised smokers were included only if study titles and abstracts explicitly mentioned a focus on relapse prevention or maintenance or if the study tested the effect of extended telephone contact after an initial intervention had been delivered, irrespective of whether or not a specific focus on relapse prevention or maintenance was mentioned.
Types of participants
Individuals who had quit smoking on their own, individuals undergoing enforced abstinence and smokers participating in treatment programmes.
Types of interventions
Interventions which investigators in individual studies state are intended to prevent relapse to smoking compared to either:
-
No intervention.
-
A shorter or less intensive intervention.
-
An intervention not oriented towards relapse prevention.
These were either behavioural interventions:
-
Group meetings.
-
Face-to-face sessions.
-
Written or other materials.
-
Proactive or reactive telephone support.
Or:
-
Pharmacological interventions.
Main outcome measure
The primary outcome for this review was abstinence from smoking, ascertained preferably as continuous abstinence, with point prevalence abstinence used if this was not recorded.
Data extraction strategy
All authors participated in data extraction with two authors working independently on each paper, using a specially designed data extraction form and differences being resolved through discussion. The data extracted included:
-
Description of study (design, duration of trial, unit of randomisation, unit of analysis).
-
Description of treatments (type, dose, duration).
-
Participants (inclusion and exclusion criteria, demographic data, number lost to follow-up).
-
Outcome measure (primary and secondary).
-
Results (abstinence at 1–3 months, 6–9 months and 12–18 months).
Attempts to obtain missing data from the authors of the manuscripts were made, where possible. Data were checked and entered into review manager, version 5, by one author (SA).
Quality assessment
The methodological quality of the included studies was assessed using the Cochrane Collaboration’s recommended tool for assessing the risk of bias which evaluated aspects of trial design: methods of randomisation sequence generation and allocation concealment; blinding; adequate assessment of incomplete data; comparability of groups at baseline; and whether treatments were adequately described.
Data analysis
For studies with similar types of intervention, a meta-analysis was performed to calculate a weighted intervention effect across trials using a random effect (DerSimonian and Laird) model and results are expressed as pooled ORs with 95% CIs. Numbers needed to treat (NNT) for additional beneficial outcomes were calculated using pooled baseline event rates, where significant comparisons were seen. Statistical heterogeneity was assessed using I2 and where heterogeneity levels were detected (I2 > 80%), studies were summarised individually. 32 Follow-up time points were defined as follows: (1) short term, 1 month (permitted range 1–3 months), (2) medium term, 6 months (range 6–9 months) and (3) long term, 12 months (range 12–18 months), with the long-term follow-up point considered as the primary end point time. In trials of pregnant/postpartum women, abstinence was also reported at delivery or the last follow-up prior to this. Where there were multiple intervention groups within a trial, pair-wise comparisons were made for each active intervention versus control, with the results in the non-control being divided by the number of pair-wise comparisons, so participants in the control group were not double counted. Funnel plots were used to assess publication bias.
Results
Number of studies identified
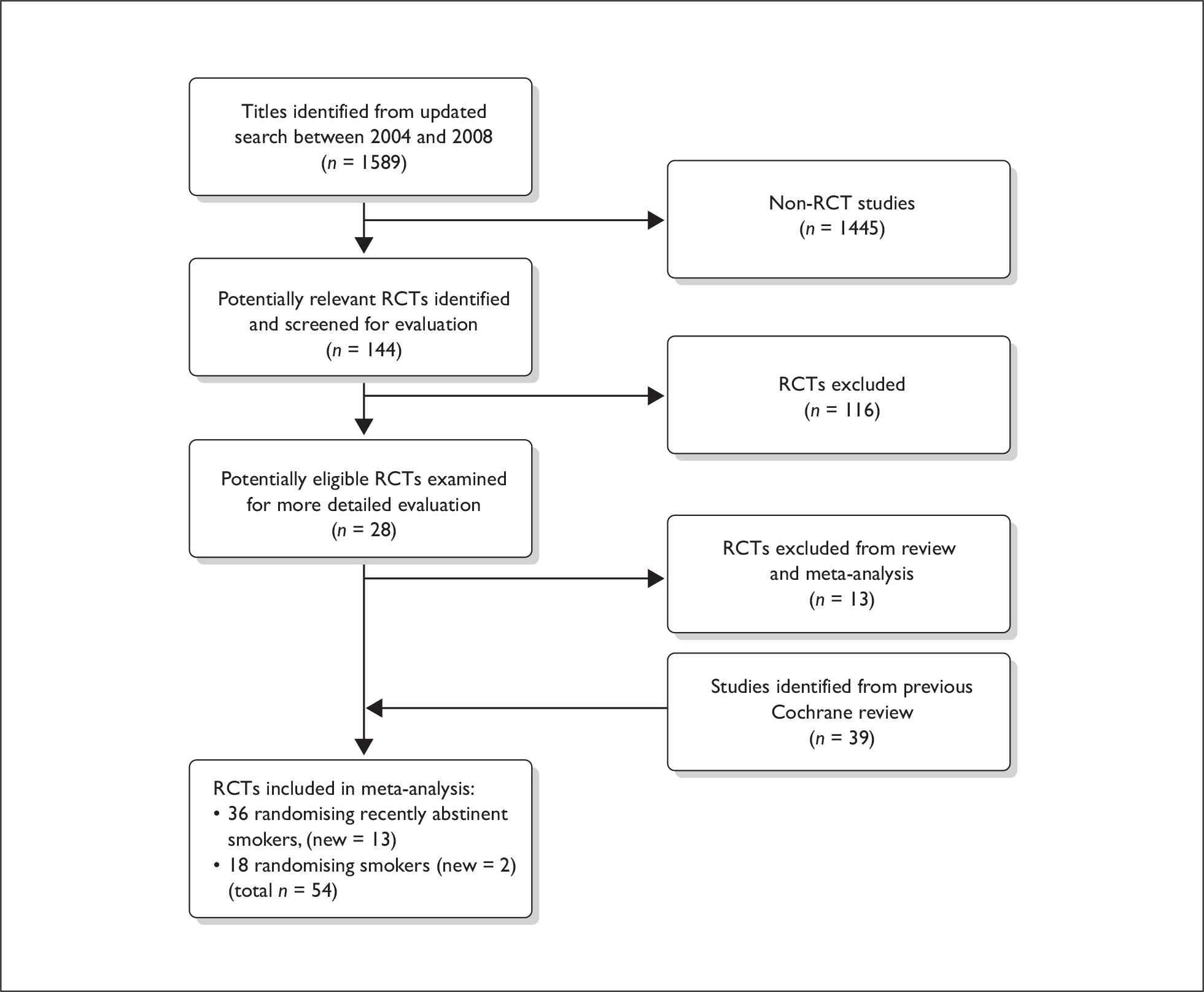
The search strategy generated 1598 potentially relevant references and after title/abstract assessment 144 papers were retrieved and examined; results of this process are summarised in Figure 1.
FIGURE 1.
Flow chart of study retrieval process.
Included studies
Fifteen studies met our inclusion criteria, and these were added to the 39 studies from the earlier Cochrane review,23 giving 54 studies in total that are summarised in Tables 4–10; 18 randomised smokers and 36 abstinent smokers.
Studies randomising abstinent smokers
Of the 36 studies33–39,40,41,63–89 randomising abstinent smokers, 2840,41,63–88 investigated the effectiveness of behavioural interventions for relapse prevention (14 in pregnant or postpartum women) and eight investigated pharmacotherapies. 33–39,89 Of these 36 studies, 1336,63,64,66,69,73,76,78–80,86,88,89 measured continuous abstinence, 2833–39,40,41,64,65,67,68,70–77,79,81–85,87 point prevalence abstinence (defined as not smoking within either the previous 7 or 30 days) and five36,64,73,76,79 used both. Twenty-seven33–40,63,65,67–72,75–81,83,84,86–89 trials verified self-reported smoking status using either expired air carbon monoxide (20 trials),31,34–39,63,67,69,72,78–80,84,86–89 urinary or saliva cotinine (six trials),65,68,70,71,75,81 or saliva thiocyanate (one trial)40 and nine trials41,64,66,73,74,76,77,82,85 presented self-reported abstinence only. All studies used a parallel group design except one which was cluster randomised;41 however, any dependency in the data due to clustering was found to be negligible and, therefore, this study was analysed with the others.
The methodological quality of all included studies is summarised in Table 2.
| Study | Method of sequence generation described | Allocation concealment | Blinding | Incomplete outcome data adequately addressed | Groups comparable at baseline | Treatments adequately described |
|---|---|---|---|---|---|---|
| Becona and Vazquez (1997)42 | No | Unclear | No information | Not reported | Yes | Yes |
| Borland et al. (2004)76 | Yes | Not used | Participants blinded | Yes | Yes | Yes |
| Brandon et al. (1987)52 | No | Unclear | No information | Not reported | Yes | Yes |
| Brandon et al. (2000)77 | No | Not used | No information | Yes | Yes | Yes |
| Brandon et al. (2004)78 | No | Not used | No information | Yes | Yes | Yes |
| Buchkremer et al. (1991)43 | No | Unclear | No information | Yes | Not reported | Yes |
| Conway et al. (2004)41 | Yes | Unclear | No information | Not reported | Not reported | Yes |
| Copeland et al. (2006)79 | Yes | Unclear | Therapists blinded | Yes | Yes | Yes |
| Covey et al. (2007)33 | Yes | Adequate | Participants and clinicians | Yes | Yes | Yes |
| Croghan et al. (2007)34 | Yes | Adequate | Participants and clinicians | Yes | Yes | Yes |
| Curry et al. (1988)44 | Yes | Unclear | No information | Yes | Yes | Yes |
| Davis and Glaros (1986)45 | No | Unclear | No information | Not reported | Yes | Yes |
| Emmons et al. (1988)46 | No | Unclear | Therapists blinded | Yes | Yes | Yes |
| Ershoff et al. (1995)75 | No | Unclear | Clinicians blinded | Yes | Yes | Yes |
| Fortmann and Killen (1995)35 | Yes | Unclear | No information | Yes | Yes | Yes |
| Hall et al. (1984)48 | No | Unclear | No information | Yes | Yes | Yes |
| Hall and Killen (1985)53 | No | Unclear | No information | Not reported | Yes | Yes |
| Hall et al. (1987)54 | No | Unclear | Therapists blinded | Yes | Yes | Yes |
| Hajek et al. (2001)63 | No | Adequate | No information | Yes | Yes | Yes |
| Hajek et al. (2002)80 | Yes | Adequate | No information | Yes | Yes | Yes |
| Hannover et al. (2009)64 | Yes | Unclear | No blinding | Yes | Yes | Yes |
| Hasuo et al. (2004)81 | Yes | Not used | No blinding | Yes | Yes | Yes |
| Hays et al. (2001)36 | Yes | Adequate | Investigators and participant blinded | Yes | Yes | Yes |
| Hurt et al. (2003)37 | No | Unclear | Investigators and participant blinded | Yes | Yes | Yes |
| Japuntich et al. (2006)58 | No | Unclear | No information | Yes | Yes | Yes |
| Killen et al. (1984)55 | Yes | Unclear | No information | Yes | Yes | Yes |
| Killen et al. (1990)38 | Yes | Adequate | Participants and therapists blinded | Yes | Yes | Yes |
| Lando et al. (1996)59 | No | Unclear | No information | Yes | Yes | Yes |
| Killen et al. (2006)60 | Yes | Unclear | No information | Yes | Yes | Yes |
| Klesges et al. (1999)82 | No | Unclear | No information | Yes | Yes | Yes |
| Lifrak et al. (1996)56 | Yes | Unclear | No information | Yes | Yes | Yes |
| Lowe et al. (1997)40 | No | Unclear | No information | Yes | Not reported | Yes |
| Mayer et al. (2006)83 | No | Unclear | Investigators blinded | Yes | Yes | Yes |
| McBride et al. (1999)65 | Yes | Unclear | No information | Yes | Yes | Yes |
| McBride et al. (2004)66 | No | Unclear | No information | Not reported | Not reported | Yes |
| Mermelstein et al. (2003)84 | No | Unclear | Investigators blinded | Yes | Yes | Yes |
| Morasco et al. (2006)67 | No | Unclear | No information | Yes | Yes | Yes |
| Niaura et al. (1999)49 | No | Unclear | Counselors blinded | Yes | Yes | Yes |
| Niaura (2005)39 | No | Unclear | Participants blinding | Not reported | Yes | Yes |
| Pbert et al. (2004)68 | No | Unclear | No information | Yes | Yes | Yes |
| Powell and McCann (1981)85 | No | Unclear | No information | Yes | Yes | Yes |
| Ratner et al. (2000)69 | No | Unclear | Data collectors blinded | Not reported | Not reported | Yes |
| Razavi et al. (1999)86 | Yes | Adequate | No blinding | Yes | Yes | Yes |
| Ruger et al. (2008)70 | No | Unclear | No information | Not reported | Yes | Yes |
| Schmitz et al. (1999)50 | No | Unclear | Raters blinded | Yes | Yes | Yes |
| Schroter et al. (2006)51 | No | Unclear | No information | Yes | Yes | Yes |
| Secker-Walker et al. (1995)71 | No | Unclear | No information | Yes | Yes | Yes |
| Secker-Walker et al. (1998)72 | No | Unclear | No information | Yes | Yes | Yes |
| Severson et al. (1997)73 | Yes | Unclear | No information | Yes | Yes | Yes |
| Shoptaw et al. (2002)57 | Yes | Unclear | No information | Yes | Yes | Yes |
| Smith et al. (2001)87 | Yes | Unclear | No blinding | Yes | Yes | Yes |
| Stevens and Hollis (1989)88 | Yes | Unclear | No information | Yes | Yes | Yes |
| Tonstad et al. (2006)89 | Yes | Unclear | Participants and investigators blinded | Yes | Yes | Yes |
| Van’t Hof et al. (2000)74 | No | Unclear | No information | Not reported | Yes | Yes |
Studies randomising smokers
Of the 18 studies42–46,48–60 that randomised smokers, nine investigated the effectiveness of interventions matched for programme length,42–46,48–51 six compared interventions of varying programme lengths52–57 and two trials examined the effectiveness of RPI adjuncts to cessation programmes. 58,59 Thirteen of these trials verified self-reported smoking abstinence with carbon monoxide measurements,42,45,46,48–50,52–55,57,58,60 one used saliva thiocyanate,44 another saliva cotinine,59 two verified abstinence with urine cotinine43,56 and one used self-reported abstinence only. 51 We categorised one study which randomised 362 cigarette smokers prior to their receiving open-label treatment with bupropion and NRT60 with the ‘randomising smokers’ group, but the 2009 Cochrane review17 judged this to have randomised abstinent smokers.
Excluded studies
Details of excluded studies are summarised in Table 3; these were retrieved and examined, but failed to meet one or more of the inclusion criteria in terms of study participants, type of interventions and type of outcome measures. The 2009 Cochrane review17 excluded one study which we have included;39 this randomised abstinent smokers to receive 5-mg or 20-mg rimonabant or placebo for 42 weeks after 10 weeks of open-label treatment with rimonabant. We excluded two studies which are included in the Cochrane review:17 one randomised abstinent smokers who had lapsed, rather than smokers or abstinent smokers61 and the other included many participants who were not smokers and analysed their outcomes with smokers. 62
| Study | Reason for exclusion |
|---|---|
| Boyle et al. (2007)90 | The study did not test the effect of extended telephone contact after an initial intervention was delivered. It randomised participants into a no contact control group and a telephone counselling group |
| Chirikos et al. (2004)91 | A cost-effectiveness analysis of secondary data |
| Cox et al. (2004)92 | Examined the efficacy of bupropion in smokers with a past history of depressive disorder |
| Fang et al. (2004)93 | A literature review of postpartum relapse prevention strategies |
| George et al.(2000)94 | Mainly a smoking cessation study that compared the American Lung Association’s behavioural programme to a manualised smoking cessation treatment programme designed for patients with schizophrenia |
| Hoving et al. (2006)95 | Examined predictors of smoking relapse, did not compare two or more interventions |
| Japuntich et al. (2006)58 | Examined the efficacy of internet interventions for smoking cessation only |
| Juliano et al. (2006)61 | The study investigated the effect of rapid smoking on lapses, not relapse |
| Ma et al. (2005)96 | Examined predictors of smoking cessation and maintenance in pregnancy. It did not compare two or more interventions |
| Partin et al. (2006)97 | Examined the effectiveness of an intervention for increasing repeat treatment for tobacco dependence |
| Rigotti et al. (2006)98 | Telephone counselling was not delivered after an initial intervention |
| Suplee (2005)99 | Randomised individuals from a non-probability convenience sample |
| Sutton and Gilbert (2007)100 | Telephone counselling was not delivered after an initial intervention, not focused on relapse prevention |
Comparison categories
To enable interpretation of findings and avoid heterogenic comparisons, we have divided trials into nine categories according to their participants (i.e. smokers or abstinent smokers) and the types of intervention delivered (i.e. pharmacological or behavioural and subcategories within each). Within each category, details of included studies, characteristics of interventions and outcome assessments are provided and the effectiveness of interventions is investigated, where appropriate, by meta-analysis. The 10 comparison categories are as follows:
Studies randomising abstinent smokers
-
Behavioural interventions in pregnant and postpartum women.
-
Behavioural interventions in other population groups (including aided, unaided and enforced abstinent smokers).
Pharmacotherapy interventions:
-
Bupropion.
-
NRT.
-
Varenicline.
-
Rimonabant.
Studies randomising smokers
-
Behavioural programmes with interventions and control groups matched for contact time and duration.
-
Behavioural programmes with interventions of different intensity.
-
Relapse prevention adjuncts to cessation programmes.
-
Pharmacotherapy interventions – bupropion.
Studies randomising abstinent smokers
Behavioural interventions in pregnant and postpartum women
Details of included studies
Table 4 gives details of studies in this category. Of the 14 studies,40,63–75 13 were carried out within hospitals, clinics or health centres40,63–74 and one study was conducted within paediatric practices. 73 All provided information on age of participants, smoking history, educational and employment status and eight studies information on race or ethnicity of participants. 40,65–68,70,74,75 Two studies were conducted in low-income women67,70 and four studies randomised postpartum women only. 64,69,73,74 All 14 studies40,63–75 provided details of smoking status at different follow-up points in pregnant women who had stopped smoking prior to randomisation or in postpartum women who were still abstinent after delivery.
| Study | Setting/ randomisation | Participants | Interventions | Outcome measure/follow-up points | Verification |
|---|---|---|---|---|---|
| Ershoff et al. (1995)75 | USA, randomisation occurred prior to patient contact | 171 pregnant recent quitters, average length of prior abstinence 31 days |
Two groups: Four booklets given at baseline visit, four relapse prevention booklets mailed weekly A 1-page tip sheet on behavioural techniques for avoiding relapse |
Point prevalence abstinence at the end of pregnancy | Urinary cotinine verified abstinence |
| Hajek et al. (2001)63 | UK, cluster randomisation | 249 pregnant recent quitters |
Advice from midwife Usual care |
Continuous abstinence at the end of pregnancy and in the medium term | Carbon monoxide verified abstinence |
| Hannover et al. (2009)64 | Germany, simple randomisation based on alternation | 304 women who were abstinent at baseline |
Telephone booster sessions 4 and 12 weeks after counselling and motivational interviewing Usual care |
Continuous abstinence at medium and long term | Self-reported abstinence only |
| Lowe et al. (1997)40 | USA, method of randomisation not stated | 78 pregnant women who had quit within the past 3 months |
Relapse prevention materials, counselling, reinforcement at routine visits by clinic staff Usual care |
Point prevalence abstinence at the end of pregnancy | Saliva thiocyanate verified abstinence |
| McBride et al. (1999)65 | USA, randomisation method not stated | 897 pregnant smokers and recent quitters |
Three groups: Pre/postpartum group: self-help booklet, personalised letter, relapse prevention kit, prepartum telephone counselling, postpartum telephone counselling and three postpartum newsletters at 2, 6 and 12 weeks postpartum Prepartum group: all of the above except postpartum telephone counselling and postpartum newsletters Booklet only group |
Point prevalence abstinence at short, medium and long term | Salivary cotinine verified |
| McBride et al. (2004)66 | USA, randomisation method not stated | 625 pregnant women, 54% already quit |
Usual care: provider advice to quit smoking at first prenatal visit and mailed self-help guide Woman-only: usual care components, late pregnancy relapse prevention kit, six counselling calls (three in pregnancy and three postpartum) by health advisor Partner assisted: woman-only intervention and partner assistance |
Continuous abstinence at the end of pregnancy and at short, medium and long term | Self-reported abstinence |
| Morasco et al. (2006)67 | USA, randomisation method not stated | 33 women who had spontaneously quit smoking |
A 90-minute psychotherapy session, followed by bimonthly prenatal telephone calls during pregnancy, and monthly calls after delivery, in addition to usual care Usual care: smoking cessation booklet |
Point prevalence abstinence at the end of pregnancy and at medium term | Carbon monoxide verified |
| Pbert et al. (2004)68 | USA, randomisation by centre | 158 pregnant women who had quit spontaneously at baseline |
Special intervention, included provider training, office practice management system to screen for smoking status and programme boards to co-ordinate transfer of documentation among clinics Usual care: interventions were brief and delivered during prenatal and postnatal clinic visits |
Point prevalence abstinence at the end of pregnancy, short and medium term | Saliva cotinine verified abstinence |
| Ratner et al. (2000)69 | Canada, computer-generated randomisation | 251 pregnant women, abstinent for 6 weeks prior to delivery |
Brief hospital intervention after birth, written materials and eight telephone follow-up calls postpartum Usual care without any tobacco reduction counselling |
Continuous abstinence at medium and long term | Carbon monoxide verified abstinence |
| Ruger et al. (2008)70 | USA, randomisation method not stated | 49 abstinent smokers at baseline |
Motivational intervention at three home visits Usual care |
Point prevalence abstinence at medium and long term | Salivary cotinine verified abstinence |
| Secker-Walker et al. (1995)71 | USA, randomisation method not stated | 165 women who had quit smoking during pregnancy |
Individual counselling at first, second and third prenatal visits and at 36 weeks’ gestation and 6 weeks post partum Usual care |
Point prevalence abstinence at the end of pregnancy and at long term | Urine cotinine/creatinine ratio verified |
| Secker-Walker et al. (1998)72 | USA, method of randomisation not stated | 125 women who had quit smoking during pregnancy |
Structured intervention from physician and individual counselling by nurse at the first, second, third, fifth and the 36-week prenatal visits Usual care |
Point prevalence abstinence at the end of pregnancy | Carbon monoxide verified abstinence |
| Severson et al. (1997)73 | USA, cluster randomisation by practice | 1026 abstinent new mothers |
Extended condition: written materials provided at the first paediatrician’s visit and a letter to the mother signed by the paediatrician, counselling at the first four well-baby visits and a specially developed video shown at one of the visits Minimal condition: written materials at first visit only |
Continuous abstinence at long term | Self-reported abstinence only |
| Van’t Hof et al. (2000)74 | USA, randomisation method not stated | 277 women who had quit during pregnancy |
A 5- to 30-minute relapse prevention intervention from a Visiting Nurse Association nurse at baseline and reinforcements at 2-week, 2-month and 4-month well-baby visits Standard care from paediatric provider |
Point prevalence abstinence at medium term | Self-reported abstinence only |
Characteristics of interventions
Two trials used three interventions of varying intensities,65,66 one investigated two interventions of different intensities73 and the remaining 11 trials compared one intervention with usual care control groups. In two studies, interventions were delivered in women’s homes,64,70 two mailed interventions to women,65,75 two used telephone interventions64,69 and two involved interventions delivered in paediatricians offices and well-baby clinics. 73,74 Six studies delivered interventions during pregnancy only,40,63,68,70,72,75 examining the effect of individual behavioural counselling on abstinence at various follow-up points. Four trials delivered smoking RPIs postpartum;64,69,73,74 two investigated the effectiveness of individual behavioural counselling73,74 and the remainder assessed the combined effect of individual behavioural counselling and telephone booster sessions. 64,69 Four trials65–67,71 initiated smoking relapse prevention interventions during pregnancy and continued postpartum; one of these delivered a combination of self-help interventions and telephone counselling,65 another investigated individual behavioural counselling71 and two trials compared individual and telephone counselling with control groups. 66,67
Outcome assessment
Self-reported smoking status was validated in 10 studies. 40,63,65,67–72,75 Five studies reported smoking status at delivery,40,63,67,72,75 nine studies presented abstinence at 6 months’ follow-up63–70,74 and four studies reported abstinence at both 6 and 12 months’ follow-up. 63,65,69,70 Nine studies presented point prevalence abstinence,40,65,67,68,70–72,74,75 while five presented continuous or sustained abstinence. 63,64,66,69,73
Effectiveness of interventions
One study reported that the intervention administered appeared effective at 6 months, an effect which diminished over time and disappeared at 12 months’ follow-up. 73 The other 13 studies reported that interventions designed to reduce relapse in pregnant and/postpartum women did not appear effective. 40,63–72,74,75
Analyses
Interventions delivered during pregnancy
Pooled analyses of behavioural interventions delivered during pregnancy at delivery/the longest follow-up prior to delivery failed to detect a significant effect (pooled OR 1.18, 95% CI 0.85 to 1.62, I2 = 0%, five studies; Figure 2). Three of these studies40,63,75 do not provide details of the exact follow-up point, and abstinence was measured at delivery. One study reported abstinence during the 34th week of pregnancy,75 while the last study in this category measured abstinence at 36 weeks. 72 Only one study in this category assessed abstinence at short-term follow-up68 and the intervention did not appear to have an effect on abstinence (OR 0.83, 95% CI 0.43 to 1.58). Pooled analysis of three studies at the medium-term follow-up was not performed due to significant levels of heterogeneity between the studies (I2 = 81%). In all three studies individual behavioural counselling did not significantly appear effective at reducing relapse (OR 0.88, 95% CI 0.49 to 1.58),63 (OR 0.35, 95% CI 0.18 to 0.70)68 and (OR 3.45, 95% CI 0.95 to 12.62)70 respectively. Only one study reported data at long-term follow-up72 that found no significant effect with individual counselling (OR 0.76, 95% CI 0.36 to 1.57).
FIGURE 2.
Behavioural relapse prevention interventions in pregnant and postpartum women. (a) Individual counselling delivered during pregnancy at longest follow-up prior to delivery; (b) individual and telephone counselling delivered postpartum at long-term follow-up; (c) individual and telephone counselling delivered during pregnancy and postpartum at longest follow-up prior to delivery; and (d) individual and telephone counselling delivered during pregnancy and postpartum at medium-term follow-up.
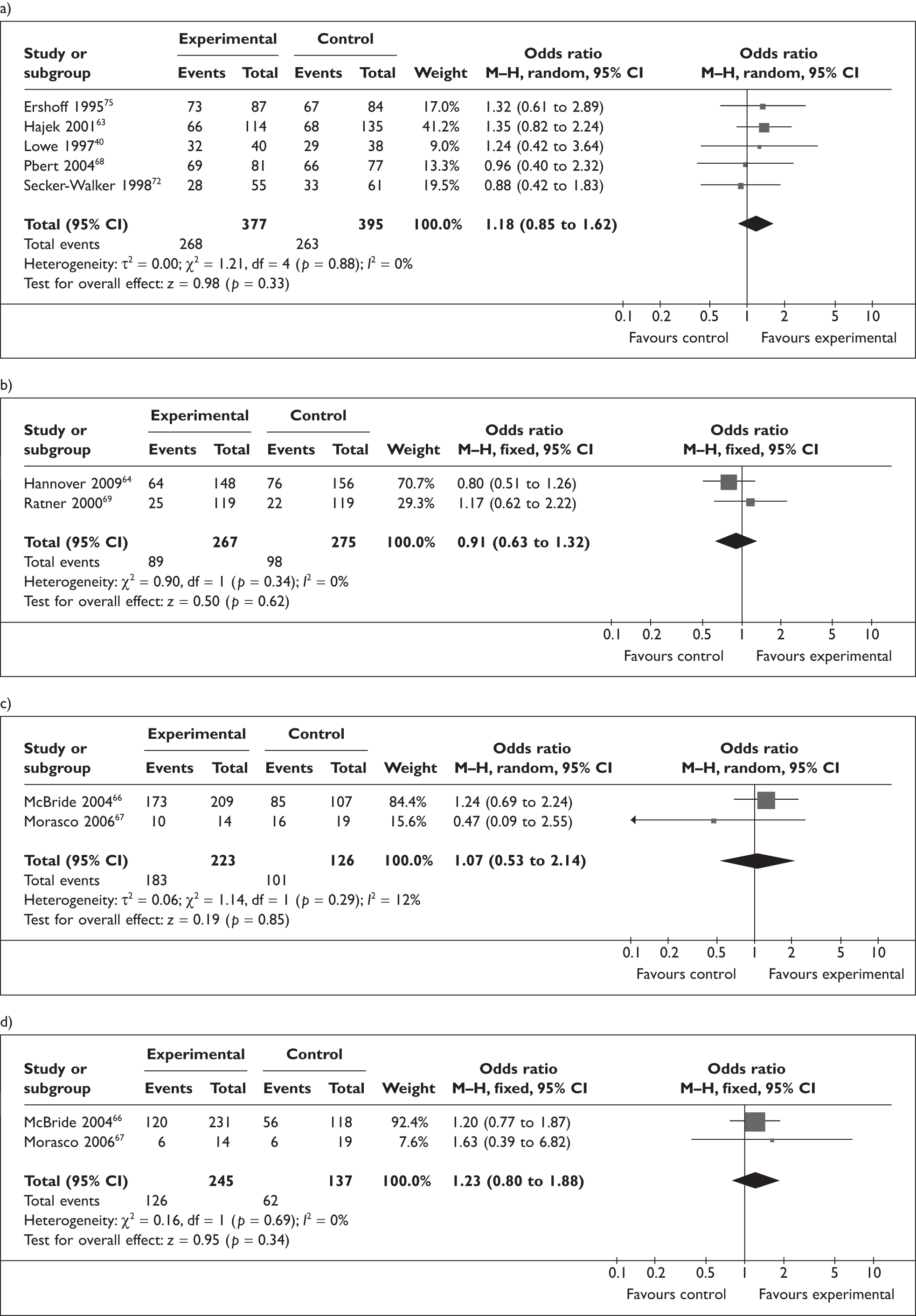
Interventions delivered postpartum
Individual behavioural counselling did not appear effective at the medium-term follow-up in one study (OR 0.83, 95% CI 0.51 to 1.34)74 but appeared effective in the long term in one large trial (OR 1.38, 95% CI 1.05 to 1.82). 73 No data were available for short-term follow-up in either study.
Two trials64,69 randomised participants to receive individual counselling plus telephone booster sessions. Pooled analysis of both trials failed to detect a significant effect at medium-term follow-up (pooled OR 1.33, 95% CI 0.94 to 1.90, I2 = 4%), and at long-term follow-up (pooled OR 0.91, 95% CI 0.63 to 1.32, I2 = 0%, Figure 2). No data were available for short-term follow-up.
Interventions delivered during pregnancy and continued postpartum
A combination of self-help booklets (written materials intended to prevent relapse) and pre- and postpartum telephone counselling exerted a moderately significant effect on abstinence rates at short-term follow-up in one study (OR 1.60, 95% CI 1.15 to 2.23) and in the medium term (OR 1.60, 95% CI 1.16 to 2.21). 65 This effect was not present at long-term follow-up (OR 1.04, 95% CI 0.76 to 1.44).
One study71 delivered individual behavioural counselling to participants during pregnancy and postpartum, but failed to detect evidence for an effect at the longest follow-up prior to delivery (OR 0.91, 95% CI 0.46 to 1.79) and at long-term follow-up (OR 1.02, 95% CI 0.53 to 1.96). No data were available for short- and medium-term follow-ups.
Two trials66,67 examined the effectiveness of individual counselling followed by pre- and postpartum telephone counselling calls. The interventions did not appear effective at delivery (pooled OR 1.07, 95% CI 0.53 to 2.14, I2 = 12%) or at medium-term follow-up (pooled OR 1.23, 95% CI 0.80 to 1.88, I2 = 0%; Figure 2). Only one study reported data at short- and long-term follow-ups66 that found no significant effect at either follow-up.
Behavioural interventions in other population groups
There were 14 studies in this category41,76–88 and Table 5 summarises these.
| Study | Setting/randomisation | Participants | Interventions | Outcome measure/follow-up points | Verification |
|---|---|---|---|---|---|
| Borland et al. (2004)76 | Australia, randomisation by computer-generated numbers | 286 smokers who were quit at baseline |
Tailored advice letters based on standardised telephone assessment, control group received No extra treatment, sent printed self-help materials for 12 months |
Continuous abstinence at medium and long term | None, self-report only |
| Brandon et al. (2000)77 | USA, randomisation method not stated | 446 ex-smokers, abstinent at least 7 days at baseline |
Four groups: Single booklet at the time of enrolment Single booklet and hotline number Eight booklets mailed at enrolment, 1, 2, 3, 5, 7, 9 and 12 months Eight booklets and hotline number |
Point prevalence abstinence at long term | None, self-report only |
| Brandon et al. (2004)78 | USA, randomisation method not stated | Community volunteers, 431 abstinent at time of baseline assessment |
Four groups: Single booklet at time of enrolment Repeated mailings at enrolment, 1, 2, 3, 5, 7, 9 and 12 months Massed mailing of all eight booklets at once Repeated letters at same intervals as repeated mailings and single booklet at enrolment |
Continuous abstinence at long term only | Carbon monoxide verified self-reported abstinence |
| Conway et al. (2004)41 | USA, naval training, cluster randomisation by division | 1682 female navy recruits, abstinent for 2 months during training |
Three groups: Standard treatment (control): the recruit training ban and small amount of health education Mail Intervention group: regular mailings with incentive items and standard treatment Telephone helpline group: access to helpline and standard treatment Smoking was banned for 8 weeks |
Point prevalence abstinence at short, medium and long term | Self-report only |
| Copeland et al. (2006)79 | USA, random assignment sequence generated by statisticians | 76 abstinent participants at the end of initial smoking cessation treatment |
A 2-week smoking cessation treatment. At the end of 2 weeks, participants were randomised to: Individually tailored cessation maintenance and dietary and weight-control intervention Group cessation therapy and dietary and weight-control intervention Interventions were delivered in six sessions spread over 38 weeks |
Continuous abstinence at short and medium terms | Carbon monoxide verified self-reported abstinence |
| Hajek et al. (2002)80 | UK, randomisation via serially numbered opaque, sealed envelopes | 540 smokers or recent quitters who had not smoked since hospital admission |
Single session intervention lasting 20–30 minutes including carbon monoxide reading, booklet on smoking and cardiac recovery, commitment, reminders Verbal advice, smoking cessation booklet |
Continuous abstinence at short and long term | Carbon monoxide verified abstinence |
| Hasuo et al. (2004)81 | Japan, computer-generated randomisation | 106 hospital in-patient volunteers who had quit smoking 31 days prior to recruitment |
Telephone counselling at 7, 21 and 42 days postdischarge Control: no additional contact. All received nurse-mediated behaviourally oriented in-patient counselling focused on relapse prevention |
Point prevalence abstinence at short, medium and long term | Urine cotinine verified |
| Klesges et al. (1999)82 | USA, cluster randomisation | 18,010 air force recruits, underwent enforced abstinence during training |
Single, adjunctive 50-minute intervention geared to convince recruits to stay quit after smoking ban Smoking ban |
Point prevalence abstinence at long term | Self-reported only |
| Mayer et al. (2006)83 | Belgium, randomisation by company | 275 workers at 42 companies who had undergone cessation treatment with 3-month smoking cessation programme |
Workplace group counselling: 10 sessions bimonthly during the first month, and monthly in the remaining 8 months; each session lasted 1 hour 30 minutes Proactive telephone counselling: 10 sessions, bimonthly during the first month, and monthly afterwards; each telephone call lasted a minimum of 10 minutes |
Point prevalence abstinence at medium term | Carbon monoxide verified abstinence |
| Mermelstein et al. (2003)84 | USA, cluster randomisation by group | 341 abstinent participants at the end of 7-week group cessation programme |
Weekly proactive, intensive telephone calls for 3 weeks, followed by three telephone calls on alternate weeks, 15 minutes per call Non-specific guidance, words of encouragement at same times as above |
Point prevalence abstinence at long term | Carbon monoxide verified |
| Powell and McCann (1981)85 | USA, randomisation method not stated | 51 abstinent community volunteers |
Three groups: 4-week support group Telephone contact system which allowed subjects to telephone one another No contact control group |
Point prevalence abstinence at short, medium and long terms | Self-reported abstinence only |
| Razavi et al. (1999)86 | Belgium, randomisation by company, using random numbers | 344 participants abstinent at the end of 3-month cessation programme |
10 monthly sessions led by trained counsellor 10 monthly group sessions led by former group smokers No relapse prevention treatment |
Continuous abstinence at medium term | Carbon monoxide verified abstinence |
| Smith et al. (2001)87 | USA, randomisation method not stated | 677 community volunteers, abstinent at the end of 1-week group orientation meetings and two individual counselling sessions |
Three groups: CBT – six 90-minute sessions in 4 weeks MI – six 90-minute sessions in 4 weeks No additional treatment |
Point prevalence abstinence at medium and long term | Carbon monoxide verified abstinence |
| Stevens and Hollis (1989)88 | USA, randomisation by predetermined number list | 587 abstinent smokers after 4-day cessation programme |
Skills training programme, three sessions, subjects developed coping strategies for likely relapse situations Discussion control condition, three sessions, subjects discussed maintenance, and not relapse prevention No treatment control |
Continuous abstinence at short, medium and long term | Carbon monoxide verified abstinence |
Details of included studies
Two studies involved military recruits41,82 and eight studies community volunteers,76–79,84,85,87,88 two trials were conducted in hospital in-patients80,81 and two were conducted in the workplace;83,86 two studies were conducted in women only. 41,79 We have divided studies in this section according to three types of participant: unaided abstinent smokers (five studies);76–78,80,81 aided abstinent smokers (seven studies in which participants had achieved abstinence with support from a formal smoking cessation programme);79,83–88 and individuals undergoing enforced abstinence (two studies). 41,82 The length of abstinence prior to randomisation in trials of unaided abstinent smokers ranged from 1 week to 1 month.
Unaided abstinent smokers
These five studies examined the effectiveness of self-help booklets and letters, telephone counselling and individual counselling. 76–78,80,81
Three trials assessed the effectiveness of repeated mailings of relapse prevention-orientated booklets and letters:76–78 one investigated the impact of booklets’ content and mailing frequency in a 2 × 2 factorial design;78 a second compared mailing of booklets with a ‘non-mailing’ control group;77 and a third compared computer-generated (tailored) letters and standard self-help materials. 76 In the former two studies above, participants had achieved at least 1 weeks’ abstinence prior to enrolment and in the latter study participants required at least 24 hours’ abstinence to participate.
One study examined the effectiveness of postdischarge telephone counselling in hospital in-patients who had stopped smoking within 31 days of admission into hospital. 81
One study examined the effect of a combination of individual behavioural interventions in individuals admitted to hospital after myocardial infarction (MI) or for cardiac bypass surgery, and who had not smoked since admission. Interventions included verbal advice, a self-help booklet, a written quiz on the contents of the booklet, carbon monoxide readings, signed declaration of commitment, contact with other people giving up and a sticker in hospital notes. 80
Two studies present point prevalence abstinence only;77,81 three validated smoking status biochemically;77,80,81 and two reported abstinence at one follow-up point only. 77,78
Two trials detected no effect79,80 and three studies reported that the interventions appeared effective at preventing relapse to smoking. 76–78
Pooled analysis of data from the three studies of self-help booklets and letters at long-term follow-up indicated a significant effect on abstinence rates76–78 (pooled OR 1.52, 95% CI 1.15 to 2.01, I2 = 0%, NNT = 14; Figure 3); and one study found significant increases in abstinence rates at medium-term follow-up (OR 1.72; 95% CI 1.01 to 2.92). 76 No data were available for short-term follow-up.
FIGURE 3.
Behavioural relapse prevention interventions in unaided abstinent smokers. Self-help booklets and letters at long-term follow-up.
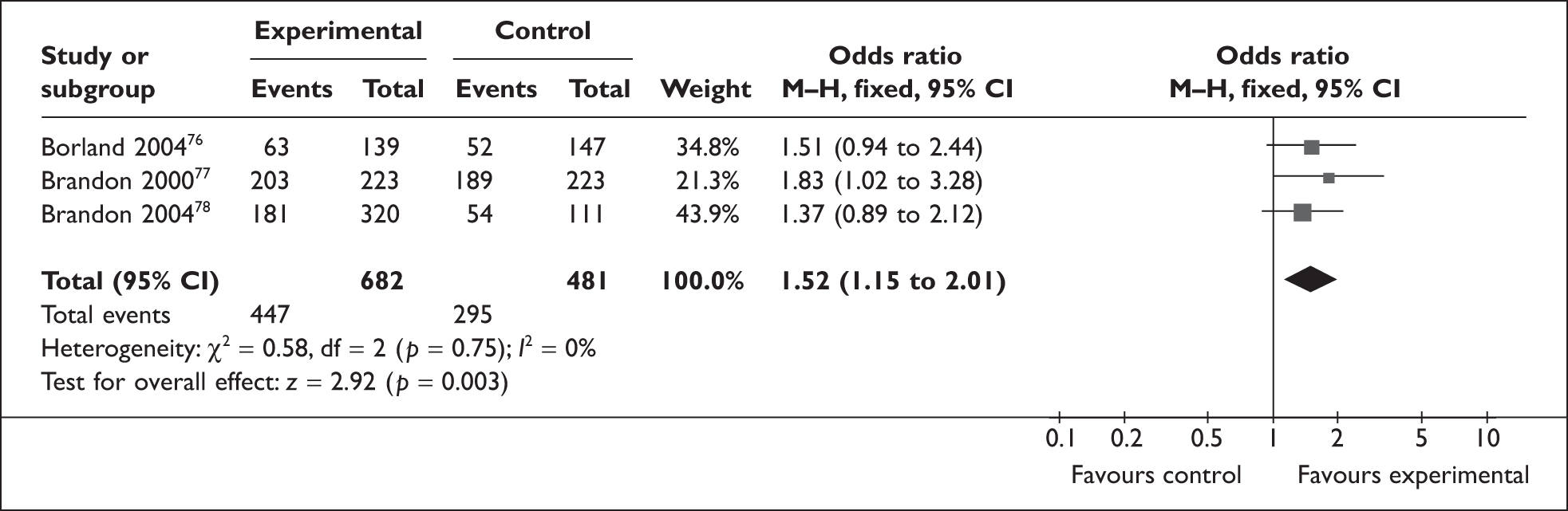
Telephone counselling did not have an effect on abstinence rates at any of the three follow-ups respectively (short term, OR 1.52, 95% CI 0.59 to 3.92; medium term, OR 1.06, 95% CI 0.47 to 2.38; long term, OR 1.23, 95% CI 0.57 to 2.64).
Individual counselling did not appear to have an effect on abstinence rates in the short and long terms respectively (OR 1.04, 95% CI 0.73 to 1.47; OR 0.86, 95% CI 0.60 to 1.23). No data were available for medium-term follow-up.
Aided abstinent smokers
Of these seven studies,79,83–88 four investigated behavioural counselling delivered to groups,85–88 one84 studied the effect of telephone call content, one83 compared proactive telephone counselling to workplace group counselling and another79 examined the effect of individual behavioural counselling.
These four trials compared group behavioural counselling to usual care or no intervention. 85–88 One study randomised participants who had achieved 1 weeks’ abstinence with counselling and NRT,87 two after 1 week88 and 5 days85 of group counselling and, in one trial, 3 months’ abstinence, achieved with group behavioural support and NRT,86 were required before randomisation.
One study assessed the effect of the content of telephone calls, randomising participants into a ‘basic’ content group or ‘enhanced’ content group;84 they received group counselling and pharmacotherapy in a 7-week abstinence period prior to randomisation.
One study83 compared workplace group counselling to proactive telephone counselling; participants were abstinent for 3 months, using a smoking cessation programme prior to randomisation.
One study50 randomised abstinent smokers who had achieved abstinence with 2 weeks of group counselling to receive either group-based or individually-tailored relapse prevention treatment; the authors hypothesised that smoking abstinence rates would be higher in individuals assigned to the individually-tailored intervention.
One study reported point prevalence and continuous abstinence rates,79 four trials reported point prevalence only83–85,87 and two studies presented continuous abstinence only;86,88 all trials biochemically validated outcomes.
Interventions in four trials were reportedly effective at reducing relapse rates,79,84,85,88 but the remaining trials had negative outcomes. 83,86,87
Pooled analysis of data from two studies of group behavioural counselling at short-term follow-up appeared to have a significant effect (pooled OR 2.55, 95% CI 1.58 to 4.11, I2 = 0%),85,88 but a pooled analysis of data from four studies at the medium-term follow-up did not detect a significant effect (pooled OR 1.20; 95% CI 0.72 to 2.00, I2 = 68%),85–88 and a pooled analysis of data from three of the studies at the long-term follow-up point also did not detect a significant effect (pooled OR 0.98, 95% CI 0.55 to 1.76, I2 = 63%; Figure 4). 85,87,88
FIGURE 4.
Behavioural relapse prevention interventions in aided abstinent smokers. (a) Group counselling at short-term follow-up; (b) group counselling at medium-term follow-up; and (c) group counselling at long-term follow-up.
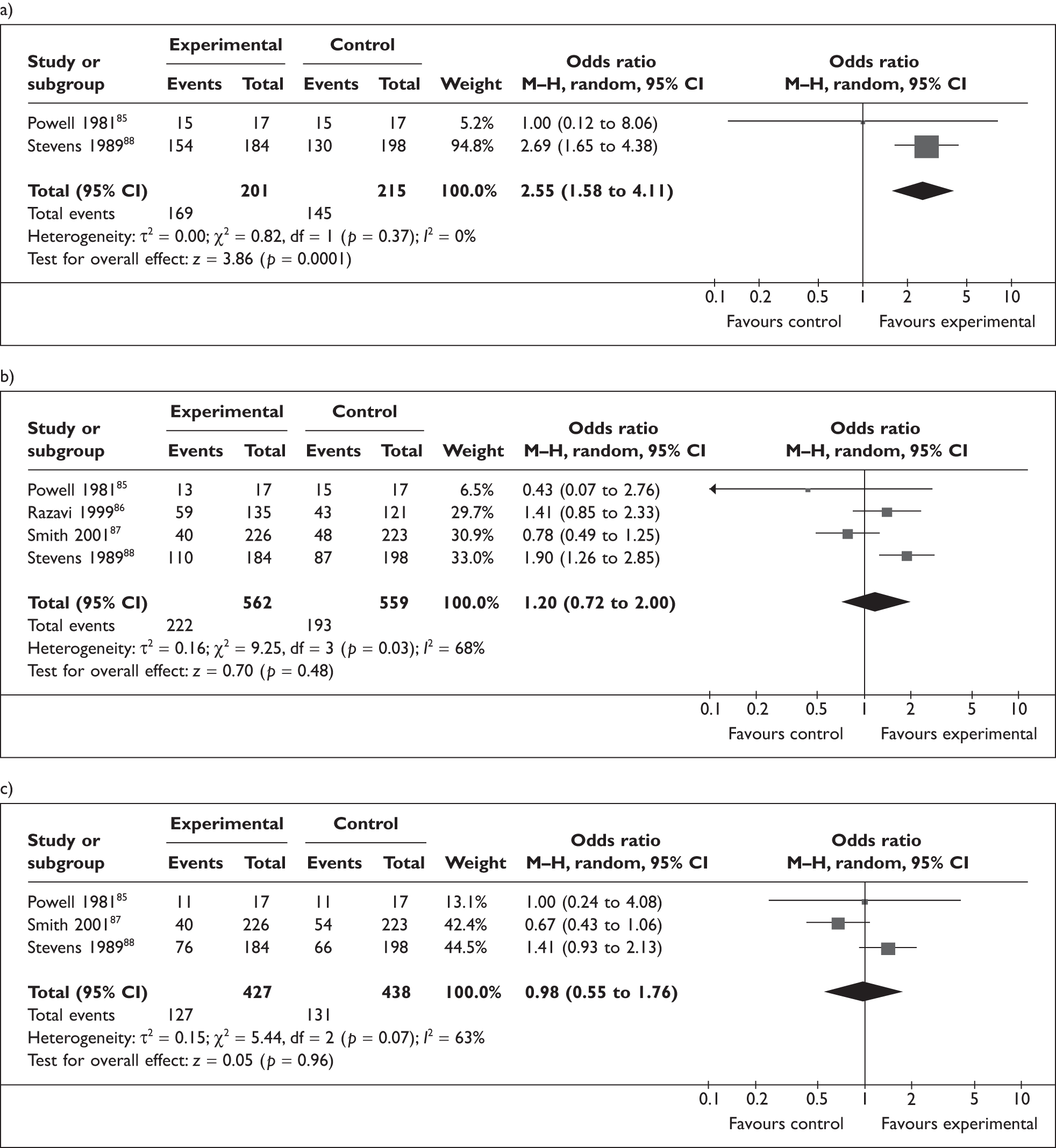
Enforced abstinent smokers
Two studies41,82 assessed the effect of behavioural interventions in individuals that were undergoing enforced abstinence.
One study82 randomised military personnel after 6 weeks of a smoking ban and presented abstinence at long-term follow-up only.
One study41 randomised military personnel into either a telephone counselling group, a self-help group and a control group after 8 weeks of a smoking ban respectively.
Both trials presented point prevalence abstinence, and neither validated outcomes.
The group counselling intervention did not appear effective at long-term follow-up (OR 0.93, 95% CI 0.85 to 1.02). Telephone counselling was effective in the short term (OR 1.26, 95% CI 1.06 to 1.49); however, the effect was lost in the medium term (OR 0.89, 95% CI 0.76 to 1.05) and in the long term (OR 0.96, 95% CI 0.82 to 1.13).
Pharmacotherapy interventions
Table 6 gives details of all trials involving pharmacotherapy interventions.
| Study | Setting/randomisation | Participants | Interventions | Outcome measure/follow-up points | Verification |
|---|---|---|---|---|---|
| Covey et al. (2007)33 | USA, computer-generated randomisation | 294 abstinent smokers at the end of 8-week open-label bupropion and nicotine patch |
All abstinent at the end of 8 weeks randomised to 16 weeks of: Bupropion and nicotine gum Bupropion and placebo gum Nicotine gum and placebo pill Placebo pill and placebo gum |
Point prevalence abstinence at medium and long term | Carbon monoxide verified self-reported abstinence |
| Croghan et al. (2007)34 | USA, Pocock–Simon randomisation, stratified | 405 smokers who were quit after 3 months of open-label treatment with either bupropion (300-mg SR); or nicotine inhaler (16 cartridges/day) or both |
Nicotine inhaler or placebo Bupropion or placebo Nicotine inhaler combined with placebo bupropion Placebo inhaler combined with bupropion Nicotine inhaler combined with bupropion Placebo inhaler combined with placebo bupropion. Additional counselling was provided, all participants received smoking cessation booklet. All treatments were administered for 36 weeks |
Point prevalence abstinence at medium and long term | Carbon monoxide verified self-reported abstinence |
| Fortmann and Killen (1995)35 | USA, randomisation method not stated | 1044 smokers quit for 24 hours |
Participants randomised into: Nicotine gum only Self-help materials Nicotine gum and self-help materials Monetary incentive only Interventions administered for 6 months |
Point prevalence abstinence at short, medium and long term | Carbon monoxide verified self-reported abstinence |
| Hays et al. (2001)36 | USA, computer-generated randomisation | 429 smokers who were quit after 7 weeks open-label bupropion |
Bupropion, 300 mg/day for 45 weeks Placebo All received physician advice, self-help booklets and brief individual counselling at follow-ups |
Continuous abstinence at short, medium and long term | Carbon monoxide verified abstinence |
| Hurt et al. (2003)37 | USA, randomisation by dynamic allocation, stratified | 176 smokers who were abstinent after 8 weeks of nicotine patch therapy |
Bupropion 300 mg/day for 6 months Placebo |
Point prevalence abstinence at short, medium and long term | Carbon monoxide verified abstinence |
| Killen et al. (1990)38 | USA, method of randomisation not stated | 1218 smokers who had quit for 48 hours |
Nicotine gum ad lib (whenever there’s urge to smoke) Nicotine gum fixed (one piece for at least 12 hour/day) Placebo gum No gum Interventions administered for 6 months |
Point prevalence abstinence at short, medium and long term | Carbon monoxide verified abstinence |
| Niaura (2005)39 | Multiple country study | 1661 successful quitters after 10 weeks of 5-mg or 20-mg rimonabant |
Rimonabant 20 mg/day Rimonabant 5 mg/day Placebo Treatment was for 1 year |
Point prevalence abstinence at short and medium term | Carbon monoxide verified |
| Tonstad et al. (2006)89 | Multiple country, computer-generated randomisation sequence, stratified by centre | 1210 abstinent participants at the end of 12 weeks of open-label treatment with varenicline |
All participants received 10-minute counselling sessions at each clinic visit Varenicline, 1 mg twice daily for additional 12 weeks Placebo, 1 mg twice daily for additional 12 weeks |
Continuous abstinence at short and medium term | Carbon monoxide verified abstinence |
Pharmacotherapy interventions – bupropion
Details of included studies
Of the eight pharmacotherapy trials,33–39,89 four assessed the effectiveness of bupropion for relapse prevention;33,34,36,37 two of these also examined the effects of bupropion and NRT combined, and NRT alone. 33,34 Participants in all trials were community volunteers and participants were treated in the following ways prior to randomisation: bupropion and NRT for 8 weeks,33 NRT patch for 8 weeks37 or bupropion treatment for 7 weeks36 or 3 months. 34 In two studies, participants still smoking at the end of open-label treatment were treated for an additional 3 months,34 and 8 weeks37 respectively until they became abstinent.
Characteristics of interventions
Abstinent participants at the end of open-label treatment received bupropion for 16 weeks,33 6 months,37 9 months34 and 45 weeks. 36 Identical placebos and additional behavioural counselling were used in all four studies.
Outcome assessment
All trials validated self-reported smoking status biochemically. One reported both point prevalence and continuous abstinence as primary outcomes,36 two presented point prevalence abstinence34,37 and one reported time to relapse as a primary outcome. 33 Two studies reported abstinence data at seven follow-up points after randomisation,36,37 one at 12 follow-up points after randomisation34 and another at 14 follow-up points after randomisation. 37
Effectiveness of interventions
In three studies33,34,36 maintenance treatment with bupropion appeared to exert a modest benefit for preventing relapse. In two studies,33,36 bupropion’s advantage diminished when the treatment period ended. In the two trials that also combined NRT and bupropion, one found that the combination did not reduce relapse rates,33 while the other study reported that NRT and bupropion combination reduced relapse rates. 34
Analyses
Pooled analysis of two heterogeneous trials of bupropion did not detect any effect in the short term (pooled OR 1.38, 95% CI 0.64 to 2.96; I2 = 76%; Figure 5),36,37 or with the inclusion of other studies, in the medium term (pooled OR 1.56, 95% CI 0.95 to 2.56, I2 = 56%). However, the estimated effect for relapse prevention treatment with bupropion reached statistical significance when assessed at long-term follow-up (pooled OR 1.49, 95% CI 1.10 to 2.01, I2 = 0%; NNT = 11, four studies). Pooled analysis of two trials that combined bupropion and NRT did not show any effect in either the medium term (pooled OR 1.94, 95% C1 0.50 to 7.51, I2 = 64%; Figure 6) or long term (pooled OR 1.31, 95% CI 0.46 to 3.79, I2 = 30%; Figure 6). No data were available for short-term follow-up analysis.
FIGURE 5.
Bupropion for relapse prevention. Participants were randomised after variable treatment periods with either open-label bupropion and/or nicotine replacement patch. (a) Short-term follow-up; (b) medium-term follow-up; and (c) long-term follow-up.
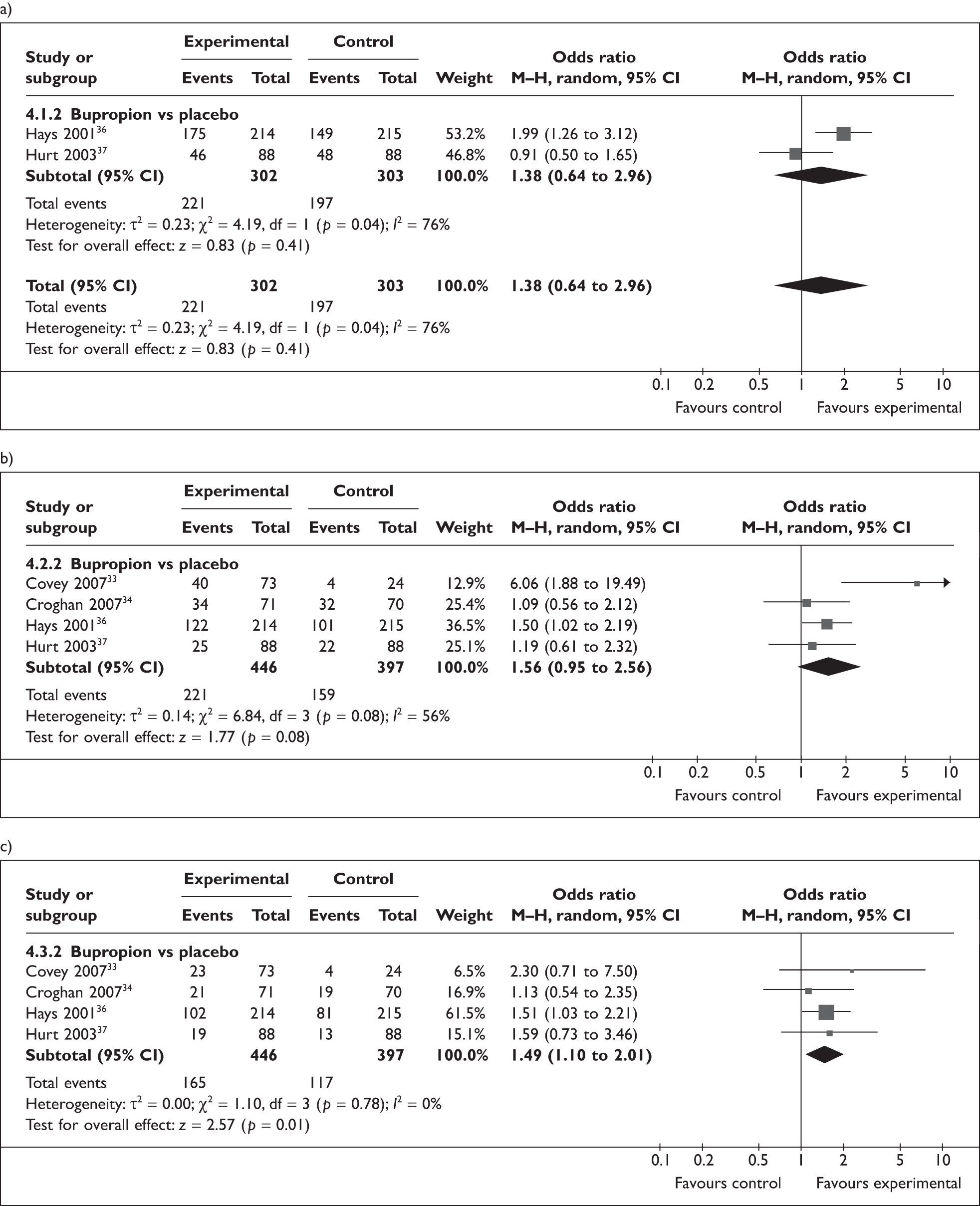
FIGURE 6.
Bupropion and NRT for relapse prevention. Participants were randomised after variable treatment periods with bupropion and NRT. (a) Medium-term follow-up; and (b) long-term follow-up.
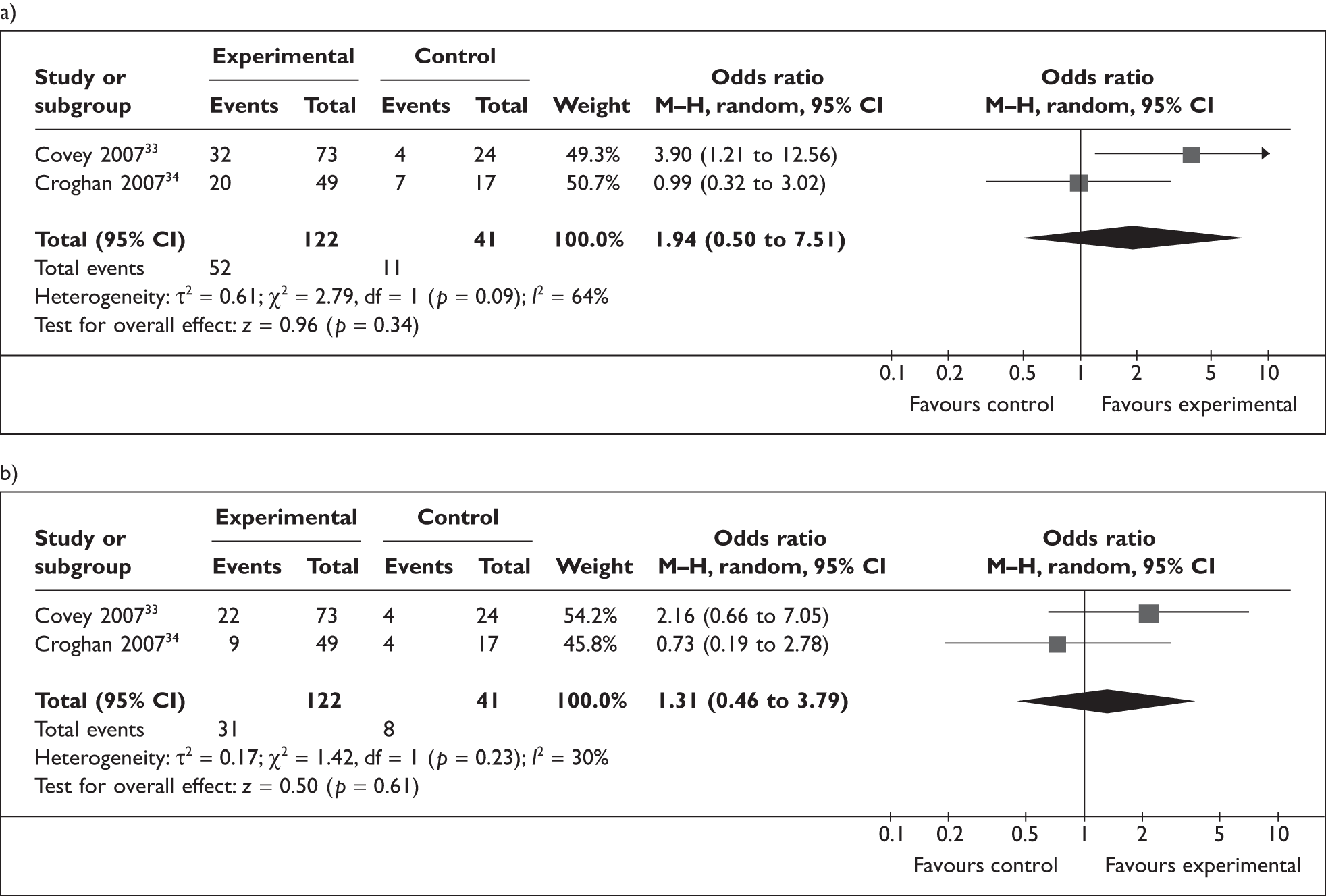
Pharmacotherapy interventions – nicotine replacement therapy
Details of included studies
Four trials assessed the impact of NRT on relapse rates;33–35,38 two used factorial designs,33,34 one was a 2 × 2 factorial design35 and the other a 4 × 3 crossed factorial design. 38 All randomised community volunteers; two included participants who had achieved unaided abstinence for 24 hours35 and 48 hours38 respectively. In the remaining two trials, participants received open-label treatment with bupropion and NRT patch for 8 weeks33 or NRT inhaler for 3 months34 to achieve abstinence. NRT gum was the relapse prevention treatment in two trials,35,38 one used NRT inhaler34 and the final trial used NRT patch;33 and one trial provided a monetary incentive for participants. 35
Characteristics of interventions
One trial was not a placebo RCT and compared different doses of NRT gum and different intensities of behavioural self-help interventions with each other;35 the behavioural interventions compared comprised self-help relapse prevention materials and no intervention. One study randomised participants into four different NRT gum-dosing regimens and three levels of self-guided behavioural intervention;38 participants received NRT gum for 16 weeks after randomisation,33 and NRT inhaler for 9 months after randomisation34 in two studies respectively.
Outcome assessment
Three studies reported point prevalence abstinence34,35,38 and all validated self-reported outcomes biochemically. One study reported abstinence data at 12 follow-up points after randomisation,34 another at 14 follow-up points33 and remaining trials reported abstinence at three follow-up points. 35,38
Effectiveness of interventions
In one trial,33 gum use was reported as low, but this appeared effective at reducing relapse rates and in another, NRT had no statistically significant effect34 and in two studies NRT appeared effective in reducing relapse to smoking in the long term. 35,38
Analyses
Pooled analysis of the two trials of NRT which assessed effectiveness at short-term follow-up was not performed due to high levels of heterogeneity (I2 = 85%), but results from these individual studies both showed statistically significant increases in the odds of abstinence (Figure 7). 35,38 More conclusive evidence of an effect for NRT was seen in a pooled analysis of these studies and two more smaller trials with low levels of heterogeneity, at the medium- (pooled OR 1.56, 95% CI 1.16 to 2.11, I2 = 37%, NNT = 14, four trials) and long-term follow-ups (pooled OR 1.33, 95% CI 1.08 to 1.63, I2 = 0%, NNT = 20, four trials).
FIGURE 7.
Nicotine replacement therapy for relapse prevention. Participants randomised after unassisted abstinence or variable treatment periods with nicotine inhaler or bupropion plus nicotine replacement patch. (a) Short-term follow-up; (b) medium-term follow-up; and (c) long-term follow-up.
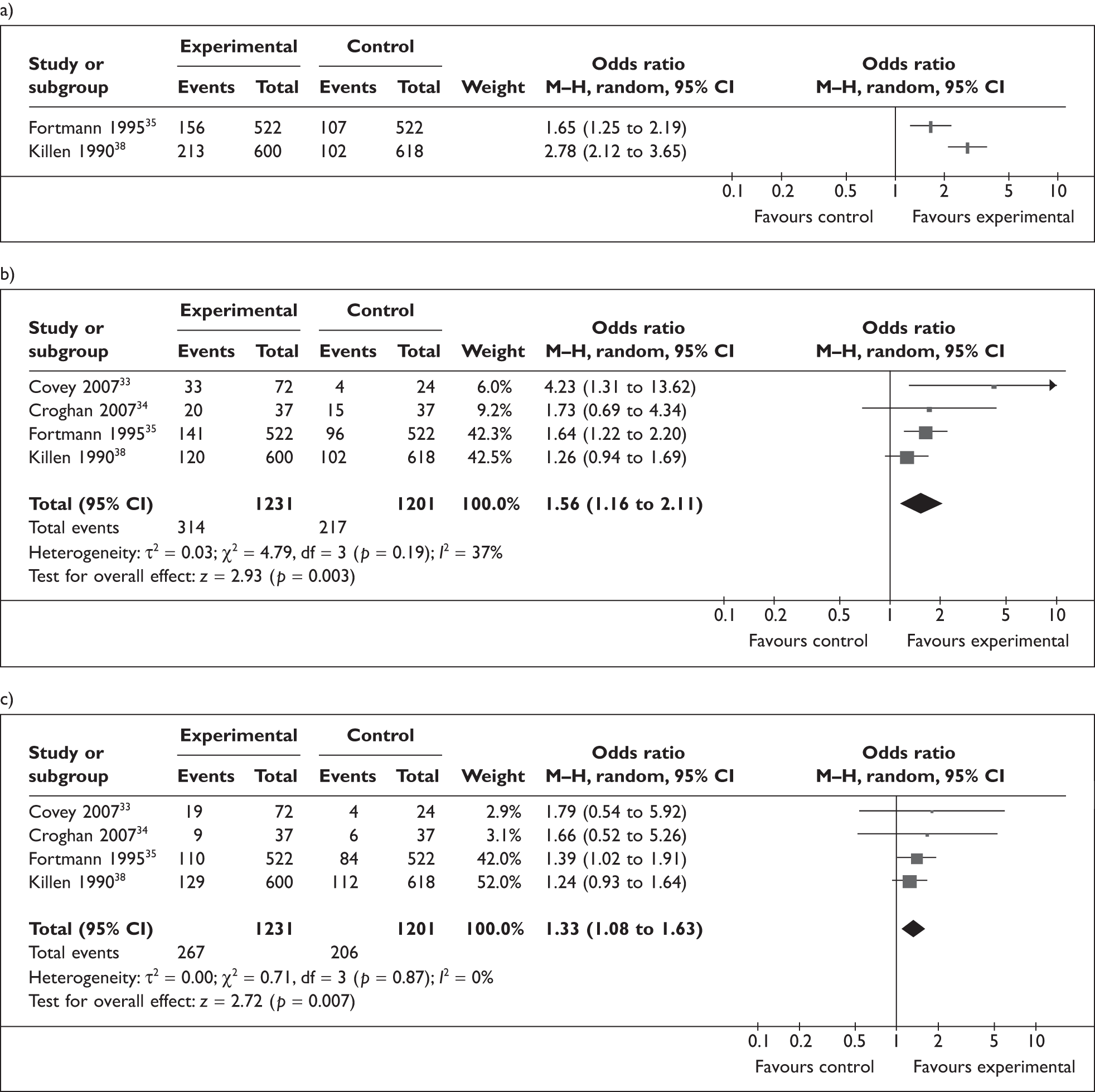
Pharmacotherapy interventions – varenicline
Details of included study
One trial of varenicline89 was included; community volunteers treated at multiple medical clinics in seven countries were enrolled.
Characteristics of intervention
Participants received smoking cessation counselling at each clinic visit and either varenicline 1 mg or identical placebo twice daily for 12 weeks after an initial 12 weeks of open-label treatment (0.5 mg varenicline for the first 3 days, 0.5 mg twice daily for the next 4 days, and 1 mg twice daily for 11 weeks).
Outcome assessment
Point prevalence and continuous abstinence were reported at 10 follow-up points and biochemically validated.
Effectiveness of intervention
A significant effect for varenicline was detected in the short-term (OR 2.54, 95% CI 1.93 to 3.36, NNT = 6) and medium-term (OR 1.40, 95% CI 1.12 to 1.76, NNT = 12) follow-ups. No data were available for longer-term follow-up.
Pharmacotherapy interventions – rimonabant
Details of included study
One study of rimonabant, conducted in three countries, was included. 39
Characteristics of intervention
Smokers were initially randomised to receive either 5-mg rimonabant or 20-mg rimonabant for 10 weeks and those who achieved abstinence were rerandomised to either 5-mg or 20-mg rimonabant daily or identical placebos for 42 weeks, followed by a 50-week non-treatment follow-up period.
Outcome assessment
Self-reported abstinence from smoking was verified biochemically, with abstinence data reported at 18 follow-up points.
Effectiveness of intervention
Treatment with rimonabant appeared to reduce rates of relapse to smoking, with OR 1.67 (95% CI 1.14 to 2.46) in the short term and OR 1.48 (95% CI 1.14 to 1.93) in the medium term.
Studies randomising smokers
Behavioural interventions matched for programme length
Details of included studies
Nine of the 18 trials that randomised smokers tested relapse prevention-orientated interventions in behavioural programmes, investigating the impact of RPI programme content by matching programme length but varying contents in intervention and control groups;42–46,48–51 details are given in Table 7. One study included only women with either confirmed coronary artery disease or risk factors for this,50 another enrolled workplace volunteers in four local businesses. 51 The seven remaining studies recruited community volunteers. 42–46,48,49 All studies in this category reported demographic characteristics of participants except one. 43 One trial used a 2 × 2 factorial design. 48
| Study | Setting/randomisation | Participants | Interventions | Outcome measure/follow-up points | Verification |
|---|---|---|---|---|---|
| Becona and Vazquez (1997)42 | Spain, randomisation method not stated | 76 community volunteers, all smokers at baseline |
Standard behavioural intervention (control group) Relapse prevention group Interventions administered for 8 weeks |
Point prevalence abstinence at short, medium and long term | Carbon monoxide verified self-report |
| Buchkremer et al. (1991)43 | Germany, randomisation method not stated | 74 community volunteers |
Self management with training in relapse coping strategies Self management without training in relapse coping strategies Interventions administered for 9 weeks |
Point prevalence abstinence at short, medium and long term | Self-report only |
| Curry et al. (1988)44 | USA, randomisation method described | 139 community volunteers, 48 randomised to two types of group treatment |
Relapse prevention group Absolute abstinence group |
Point prevalence abstinence at medium and long term | Saliva thiocyanate verified abstinence |
| Davis and Glaros (1986)45 | Canada, randomisation method described | 45 community volunteers |
Experimental Enhanced control Control Interventions administered for 8 weeks in all three groups |
Point prevalence abstinence at short, medium and long term | Carbon monoxide verified self-report |
| Emmons et al. (1988)46 | USA, randomisation method described | 49 community volunteers |
Broad spectrum group Relapse prevention group Interventions administered for 8 weeks in both groups |
Point prevalence abstinence at medium and long term | Saliva thiocyanate verified self-reported abstinence |
| Hall et al. (1984)48 | USA, randomisation method not stated | 135 community volunteers |
Skills training Discussion control Interventions administered for 6 weeks in both groups |
Point prevalence abstinence at medium and long term | Carbon monoxide verified self-reported smoking status |
| Niaura et al. (1999)49 | USA, randomisation method not stated | 129 community volunteers |
Brief cognitive behavioural group Cognitive behavioural with nicorette gum Cognitive behavioural and cue exposure Cognitive behavioural, cue exposure and nicorette gum Interventions administered in six sessions over 3 weeks in all four groups |
Point prevalence abstinence at short, medium and long term | Carbon monoxide verified self-reported smoking status |
| Schmitz et al. (1999)50 | USA, randomisation method not stated | 160 women with either coronary artery disease or risk factors for coronary artery disease |
Coping skills relapse prevention Health belief model Interventions administered over 6 weeks |
Point prevalence abstinence at short and medium terms | Carbon monoxide verified self-report |
| Schroter et al. (2006)51 | Germany, randomisation method described | 79 workplace volunteers at four businesses |
Relapse prevention Standard behavioural treatment Interventions administered over 8 weeks. Participants also received NRT |
Continuous abstinence at short and long term | Self-report only |
Characteristics of interventions
Seven studies randomised participants into either a treatment or control group;42–44,46,48,50,51 one trial had four treatment groups,49 and one, three. 45 Participants in three trials received NRT in addition to behavioural treatment. 43,49,51 In one trial,48 eight of the 14 treatment sessions also involved 6 and 30 second aversive smoking. Subjects were instructed to inhale on three consecutive cigarettes of their usual brand either every 6 or 30 seconds. The subjects were encouraged while smoking, to focus on the negative aspects of smoking, and subjects were videotaped, and replayed to the subject after the session. The remaining six sessions comprised either a skills training treatment or a discussion control.
One trial compared a behavioural programme that placed emphasis on absolute abstinence to a RPI and evaluated each programme in group and self-help formats. 44 One study randomised participants into a control group that received standard treatment, an enhanced control group that received standard treatment in addition to discussions of 11 problem situations and an experimental group that received cognitive behavioural skills training aimed specifically at preventing relapse. 45 Another study in this category randomised smokers to receive, for 8 weeks, either in the relapse prevention group, 12 hours of treatment and self-help booklets containing homework exercises, and a ‘broad spectrum’ group in which participants were provided with group support during times when the most difficulty with cessation was anticipated. 46 In one study, participants in the workplace received either a standard behavioural treatment over 8 weeks which focused on monitoring smoking behaviour and setting a quit date, or a RPI which focused on analysis of, and development of, coping strategies for prototypical high-risk situations. 51
Outcome assessment
Five trials validated abstinence with exhaled carbon monoxide,42,45,48–50 two used saliva thiocyanate,44,46 and two used no validation. 43,51 One study reported both point prevalence and continuous abstinence51 and remaining studies reported point prevalence abstinence only.
Effectiveness of interventions
One trial reported that the interventions were effective in reducing relapse to smoking48 and the remaining trials had negative results.
Analyses
Pooled analysis of nine trials42–46,48–51 in the short term did not detect evidence for the effectiveness of behavioural interventions among smokers; OR 0.67 (CI 0.44 to 1.01, I2 = 14%). No evidence for the effectiveness of these interventions was detected in the medium- and long-term analyses; OR 0.99 (CI 0.71 to 1.39, I2 = 0%, seven trials) and OR 1.09 (CI 0.72 to 1.67, I2 = 14%, seven trials) respectively (Figure 8).
FIGURE 8.
Studies randomising smokers with interventions matched for programme length. Interventions were administered for equal durations in both control and intervention groups. (a) Short-term follow-up; (b) medium-term follow-up; and (c) long-term follow-up.
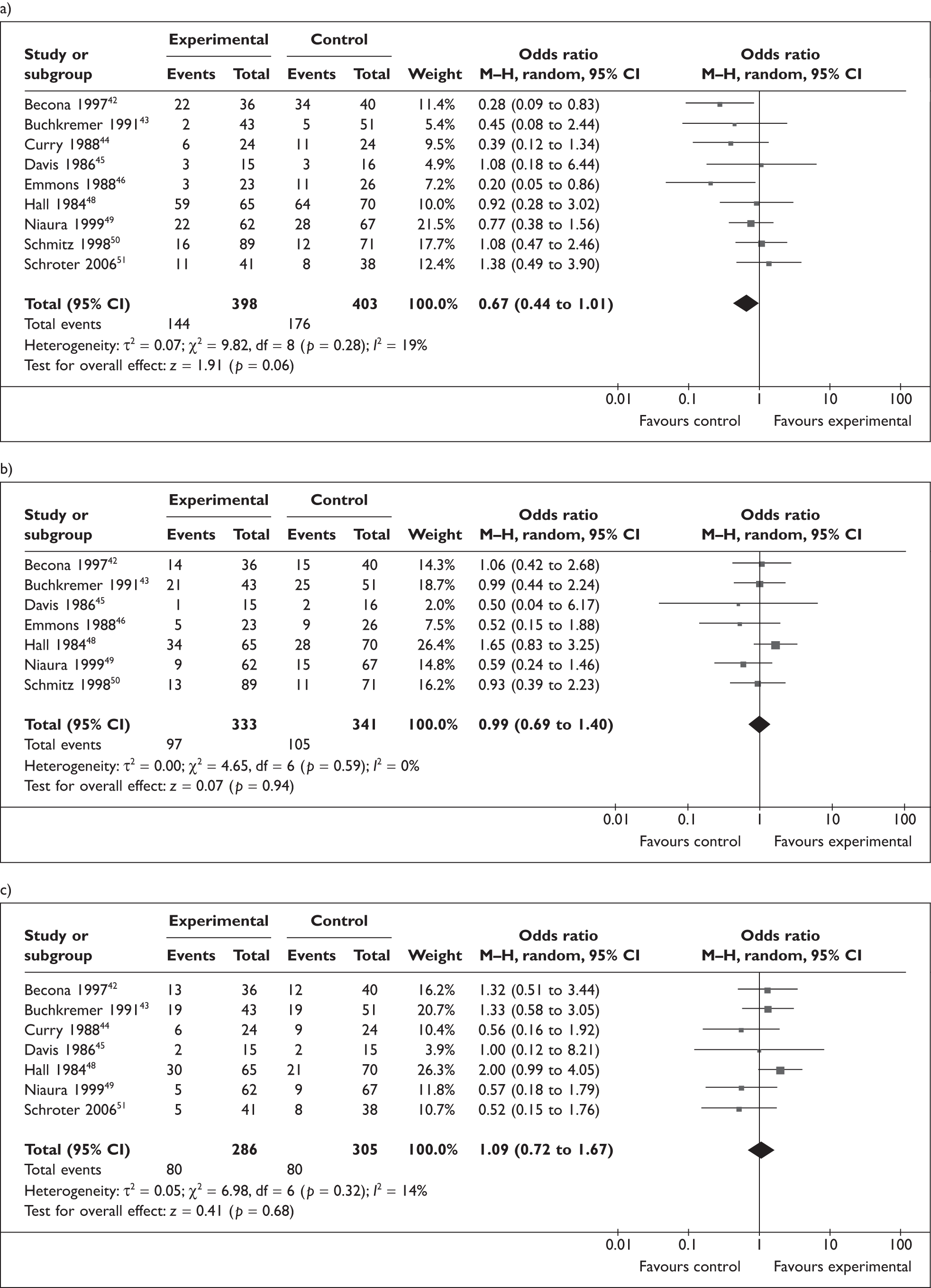
Studies investigating behavioural interventions of differing intensities
Six studies (Table 8) randomised participants into intervention and control groups of varying intensities. 52–71 These studies investigated the impact of behavioural RPIs delivered to smokers as additional components of cessation programmes which resulted in longer treatment programmes; trials in this category do not have intervention and control groups matched for length, rather intervention group programmes are administered for longer periods because of additional relapse prevention content, or deliver content with additional components not included in control group treatments.
| Study | Setting/Randomisation | Participants | Interventions | Outcome measure/follow-up points | Verification |
|---|---|---|---|---|---|
| Brandon et al. (1987)52 | USA, randomisation method not stated | 57 community volunteers, heavy smokers only |
Maintenance treatment plus rapid puffing Maintenance treatment alone Counselling only Interventions administered over 2 weeks. Subjects in maintenance groups had four meetings each lasting an hour. Subjects in control group had one meeting only |
Point prevalence abstinence at short, medium and long term | Carbon monoxide verified self-report |
| Hall and Killen (1985)53 | USA, randomisation method not stated | 84 community volunteers in relevant arms |
Intensive behavioural treatment Same as 1. With NRT gum Low contact with nicotine gum (control) Interventions were administered over 8 weeks |
Point prevalence abstinence at short, medium and long term | Plasma thiocyanate verified self-report |
| Hall et al. (1987)54 | USA, randomisation method not stated | 139 community volunteers |
2 × 2 factorial design Low contact group: five sessions Intensive behavioural group: 14 sessions |
Point prevalence abstinence at short, medium and long term | Serum thiocyanate and carbon monoxide verified abstinence |
| Killen et al. (1984)55 | USA, randomisation method not stated | 44 community volunteers in relevant arms |
Nicotine gum in addition to 20 minute weekly clinic attendance for 7 weeks Skills training only plus once a week therapist led meetings for 7 weeks Combined (1 and 2) |
Continuous abstinence at short and medium term | Saliva thiocyanate and carbon monoxide verified abstinence |
| Lifrak et al. (1996)56 | USA, randomisation method not stated | 69 community volunteers |
High-intensity group, interventions administered weekly for 16 weeks Moderate-intensity group, interventions administered weekly for 4 weeks |
Point prevalence abstinence at short, medium and long term | Urine cotinine verified abstinence |
| Shoptaw et al. (2002)57 | USA, randomisation method stated | 175 clinic volunteers at three narcotic treatment centres |
Group counselling weekly for 12 weeks NRT only |
Point prevalence abstinence at medium and long term | Carbon monoxide verified abstinence |
Details of included studies
One study only enrolled heavy smokers, five trials recruited community volunteers and one recruited clinic volunteers. 57 Two trials used a 2 × 2 factorial design. 54,57
Characteristics of interventions
In four studies, participants received nicotine patch therapy or nicotine gum in addition to behavioural treatment. 52–55 The intervention condition in one trial54 included 6 second aversive smoking of three cigarettes, relapse prevention training and written exercises. Treatment was provided in 14 75-minute sessions. Participants in the control condition completed exercises, read educational materials and participated in group discussions. Treatment was provided in five sessions and meetings lasted 60 minutes. In another study,53 participants in the intervention group completed eight 30-second aversive smoking sessions, and received videotaped feedback of the sessions in addition to behavioural relapse prevention treatment. Participants in the control group received nicotine gum and four treatment sessions which involved discussion of reading materials only. One trial52 randomised participants into one of two treatment conditions or a control condition. All participants received six treatment sessions which included 30 minutes rapid smoking at each session. Thereafter, subjects in one treatment condition received counselling and three rapid-puffing trials with three cigarettes and met at 2, 4, 8 and 12 weeks’ post-treatment follow-up. Subjects assigned to the second treatment condition met at the same intervals post-treatment and received behavioural counselling only. Subjects in the control group met once, at the 12-week post-treatment follow-up.
All subjects in another trial55 received behavioural counselling for 1 week and an aversive smoke-holding procedure designed to create aversion to smoking. One treatment condition in this trial consisted of nicotine gum and attendance at a drop-in clinic weekly for 6 weeks. Individuals in the second treatment condition attended two therapist-led weekly meetings for 6 weeks and did not receive nicotine gum. Participants in the third treatment condition received a combination of both treatments.
A further study56 randomised participants to receive either moderate intensity behavioural intervention in addition to nicotine patch treatment. The behavioural intervention was administered in four sessions. Individuals in the intervention group received 16 sessions of high intensity cognitive behavioural relapse prevention treatment.
Participants in one trial57 were assigned to one of four treatment conditions – patch only, relapse prevention and patch, patch plus contingency management, and patch plus the combination of relapse prevention and contingency management. Relapse prevention treatment used psychosocial techniques to enhance coping skills, while contingency management allowed participants to earn money for every breath sample provided at or below 8 parts per million (p.p.m.).
Outcome assessment
Two studies validated abstinence with exhaled carbon monoxide and serum thiocyanate,54,55 plasma thiocyanate was used in one53 exhaled carbon monoxide was used alone in two,52,57 and urinary cotinine in one trial. 56
Effectiveness of interventions
In the two trials which simultaneously used NRT as a cessation treatment, behavioural RPIs appeared to be effective at preventing relapse. 53,54 Two studies reported that participants in intervention groups had lower relapse rates than their control counterparts,55,57 but evidence for efficacy was not maintained in the long term in one study. 57 Two studies reported that interventions were not effective in reducing relapse to smoking. 52,56
Analyses
Pooled analysis revealed that the interventions were not effective in the short, medium and long term respectively with pooled OR 1.11 (95% CI 0.49 to 2.49, I2 = 69%, six studies, short term), 1.01 (95% CI 0.57 to 1.80, I2 = 47%, six studies, medium term) and 0.86 (95% CI 0.56 to 1.31, I2 = 0%, five studies, long term; Figure 9).
FIGURE 9.
Studies randomising smokers with different intensity programmes. Interventions varied in intensity and timing. (a) Short-term follow-up; (b) medium-term follow-up; and (c) long-term follow-up.
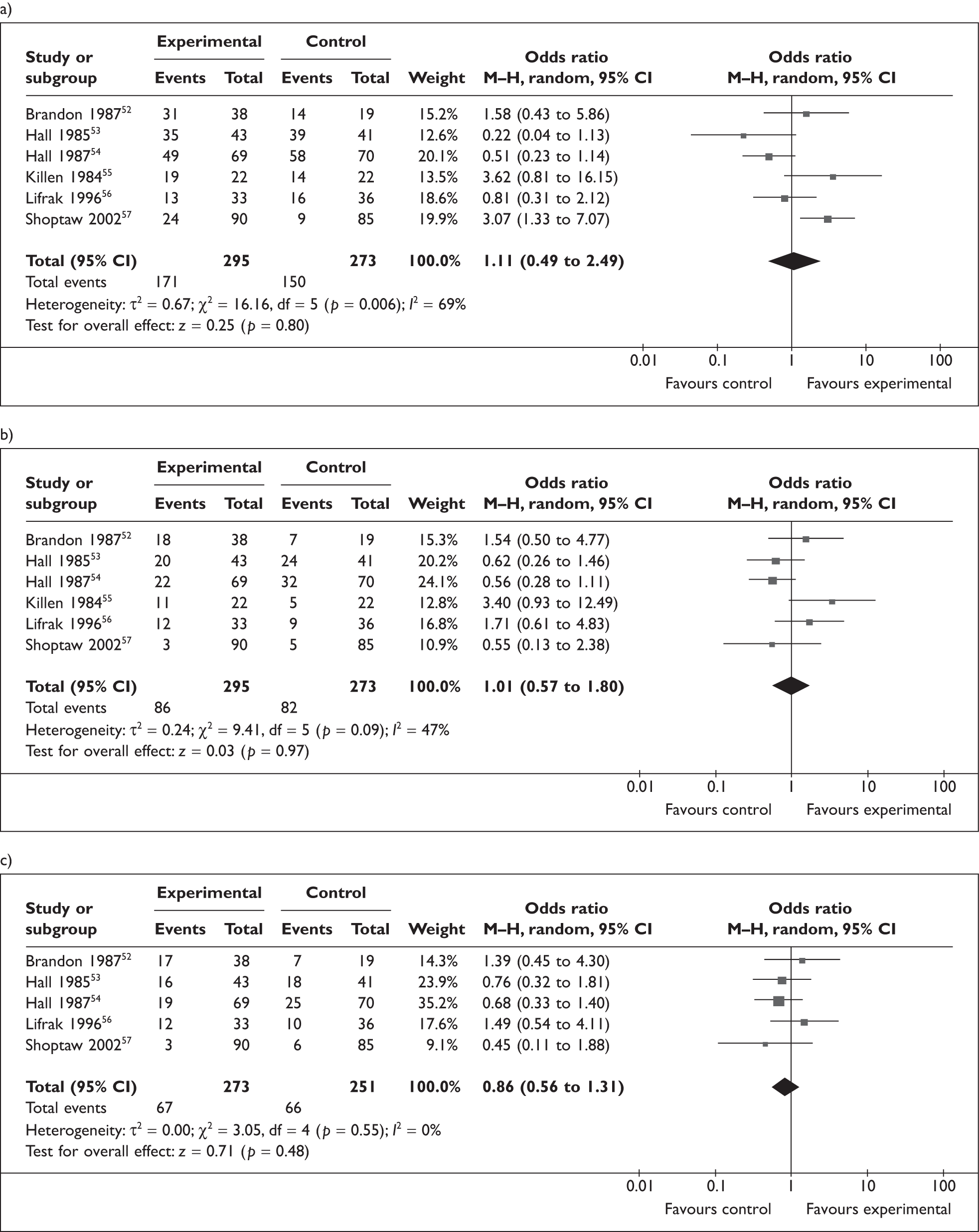
Relapse prevention adjuncts to cessation programmes
Two studies (Table 9) provided adjunctive interventions, aimed at preventing relapse to smoking, in addition to smoking cessation treatments. One provided telephone support at specific intervals after a multisession smoking cessation clinic and the other provided access to a specially designed computer program in addition to the control condition components.
| Study | Setting/randomisation | Participants | Interventions | Outcome measure/follow-up points | Verification |
|---|---|---|---|---|---|
| Japuntich et al. (2006)58 | USA, randomisation method not stated | 284 community volunteers |
Bupropion, behavioural counselling and internet intervention Bupropion and counselling only |
Point prevalence abstinence at short and medium term | Carbon monoxide verified abstinence |
| Lando et al. (1996)59 | USA, community volunteers, randomisation method not stated | 1083 heavy smokers, community volunteers |
Telephone support with calls at 3, 9 and 21 months after target quit date Comparison group All subjects attended cessation clinic for 8 weeks. Interventions began in third week |
Point prevalence abstinence at medium and long term | Saliva cotinine verified self-reported smoking abstinence |
Additional proactive telephone contact
Details of included study and characteristics of intervention
One study59 is included in this category. It randomised community volunteers into either a telephone support group or a no-contact comparison that they received after an initial 8-week smoking cessation programme. Participants attended 15 smoking cessation sessions with a 3-week preparation phase and a 5-week maintenance phase. Subjects in intervention group received telephone calls at 3, 9 and 21 months after targeted quit date.
Outcome assessment
Abstinence was recorded at 6, 12, 24 and 34 months after target quit date and was verified by saliva cotinine.
Effectiveness of intervention
Telephone intervention appeared effective at 6 and 24 months but this effect was lost at 34 months’ follow-up.
Additional internet intervention
Details of included study and characteristics of intervention
One study58 examined the effectiveness of an internet-based smoking cessation intervention in addition to bupropion and behavioural counselling compared to a bupropion and behavioural counselling only control group. The study tested the efficacy of an internet intervention, the Comprehensive Health Enhancement Support System for Smoking Cessation and Relapse Prevention, as an adjuvant to standard care. Participants in the intervention condition received 9 weeks of twice-daily bupropion, three brief behavioural counselling sessions, five follow-up visits and access to the internet intervention for 90 days, and were instructed to log into the program daily.
Outcome assessment
Point prevalence abstinence was reported at 3 and 6 months from the start of the study. Abstinence was verified using carbon monoxide measurements.
Effectiveness of intervention
The intervention did not appear effective at either 3 or 6-month follow-up points.
Pharmacotherapy interventions – bupropion
Table 10 gives details of the single study that randomised smokers and then tested a pharamacotherapy (bupropion) intervention plus 30 minutes of behavioural counselling at clinic visits after open-label bupropion treatment. 60
| Study | Setting/randomisation | Participants | Interventions | Outcome measure/follow-up points | Verification |
|---|---|---|---|---|---|
| Killen et al. (2006)60 | USA, community volunteers, permuted block randomisation | 362 adult smokers, community volunteers |
Bupropion 150 mg/day for 14 weeks Matching placebo |
Point prevalence abstinence at medium and long term | Carbon monoxide verified abstinence |
Outcome assessment
Point prevalence and continuous abstinence rates were reported. Abstinence was verified using carbon monoxide measurements.
Effectiveness of interventions
The intervention appeared effective at reducing relapse to smoking.
Discussion
In this review, data from multiple trials suggest that bupropion prevent relapse to smoking when used by smokers who have already achieved abstinence using drug cessation treatments; four trials suggest NRT prevents relapse to smoking, although two of these trials involved smokers who were unsupported quitters after only a very short period of abstinence; based on data from one trial, varenicline also appears effective. Observed effects are long term; for every 11 abstinent smokers who use bupropion to prevent relapse, one extra non-smoker can be expected at 12 months and the corresponding NNT for NRT is 20 abstinent smokers. When used by smokers who have managed to stop smoking without accessing any support, self-help, behavioural interventions also appear effective in preventing relapse at 12 months.
By categorising trials according to their participants’ characteristics and the nature of interventions delivered and combining outcome data collected only at similar time points, we have produced findings that would not have been obvious had we merely replicated previous Cochrane review methods. These combined smoking outcome data obtained between 6 and 24 months that, we believe, may have contributed to a less statistically powerful meta-analysis than ours. Statistical power refers to the likelihood of detecting within a sample an effect or relationship that exists within a population. Meta-analysis of individual studies can increase statistical power by reducing the standard error of the weighted average effect size. Combining different outcome time points compromises the validity and precision of the weighted average effect size and ultimately produces a less powerful meta-analysis, as is the case with the Cochrane review.
In contrast we have minimised methodological heterogeneity that might otherwise have obscured the real effects of interventions and this has probably given rise to our different findings. Additionally, the Cochrane reviews analysed trials that investigated NRT and bupropion, delivered as a combined intervention, together with those of bupropion alone. We could think of no theoretical reason for combining data in this way and conducted separate analyses for these different interventions; this may also account for differences between our findings and those of Cochrane reviews. In addition, the Cochrane reviews combined trials testing a variety of different behavioural interventions; however, we examined behavioural interventions according to their delivery modality and by population group separately. This separating out of interventions resulted in a key difference between our analyses and the Cochrane review, namely that self-help booklets and letters were effective for preventing relapse when used by abstainers who have managed to stop smoking without using any smoking cessation support.
Trials included in this review evaluated the effectiveness of the interventions both while treatment was ongoing and after this had ended and our short- and medium-term follow-up abstinence rates may, therefore, reflect the fact that some participants were still receiving treatment at these times. For bupropion, a significant effect was not detected in the short and medium term, but only in the long term after treatment had ended whereas NRT appeared to exert an effect both during treatment and in the long term when treatment had concluded. These findings highlight a need for drug relapse prevention trials that measure specifically, abstinence at follow-up points during the non-treatment follow-up phase.
Evidence for the use of pharmacotherapies, and particularly of bupropion, to prevent relapse seems most relevant to the UK NHS. In relapse prevention trials, bupropion was introduced only after smokers had used pharmacological cessation therapies to achieve relatively sustained abstinence periods; similarly any relapse prevention treatment introduced in the UK, would be likely to follow cessation support delivered by NHS SSS which usually includes drug treatments. Although effective for relapse prevention, the way NRT was used in relapse prevention trials would not, perhaps, translate so readily to the UK context; in two NRT trials, NRT was used by smokers after only very short abstinence periods (maximum length 48 hours), without the use of evidence based support or treatments. These two trials, therefore, enrolled ‘unsupported quitters’ and although these trials contributed substantially to the observed efficacy of NRT, smokers who are motivated enough to access evidence-based cessation support, like routinely-delivered NHS SSS support, might respond differently to NRT used for relapse prevention. However, NRT is the most frequently used pharmacotherapy among smokers who access NHS SSS support and this popularity indicates that further evaluation of its potential role for relapse prevention is warranted. Varenicline shows promise as a relapse prevention treatment; one trial demonstrated medium-term efficacy when this was used as NHS SSS might do so, but further studies are required to confirm or refute this. Finally, it is noteworthy that self-help RPIs are effective for smokers who have achieved abstinence without the use of any cessation support (called ‘unsupported quitters’). Such interventions might also have an adjunctive effect when used by smokers who have achieved abstinence after using evidence based cessation interventions, like those delivered by NHS SSS, and research is needed to investigate this issue and also further investigate the potential of self-help to reduce relapse among ‘unsupported quitters’.
Data are presented as ORs abstinence of smoking at end of pregnancy/longest follow-up before delivery, short- (1–3 months), medium- (6–9 months), and long- (12–18 months) term follow-up for behavioural relapse prevention intervention as compared to control. Data are presented for continuous abstinence where available. Squares represent ORs and horizontal lines denote 95% CIs. The size of the square corresponds to the weight of the study in the meta-analysis.
Chapter 4 Cost-effectiveness of interventions to reduce relapse following smoking cessation
Introduction
Meta-analyses presented in Chapter 3 suggest that extending treatment with bupropion, NRT and varenicline may be effective at preventing smokers who have recently achieved abstinence from relapsing back to smoking. Smoking cessation interventions are among the most cost-effective that any health care system can employ and, as RPIs enhance cessation rates, these are also potentially very cost-effective. However, as drug treatments for relapse prevention are issued for much longer than standard periods, the costs of delivering RPIs will be far higher than those attributed to smoking cessation interventions, reducing cost-effectiveness ratios. Consequently, in this chapter, we present a formal cost-effectiveness analysis of those RPIs identified as potentially effective by our systematic review and which could also be incorporated into current NHS clinical care.
Aims and objectives
The aim of this chapter was to determine the cost-effectiveness of interventions for preventing smokers, who have recently become abstinent, from relapsing back to smoking. Specifically, the model will assess the costs and outcomes associated with the following interventions, compared to no intervention:
-
bupropion
-
NRT
-
varenicline.
These interventions were selected because our systematic review (see Chapter 3) demonstrated evidence that each could be effective when used by smokers who had stopped smoking after using evidence-based cessation support (i.e. smokers who are similar to those who access and use NHS SSS cessation support in quit attempts). The analysis aims to estimate the lifetime costs (including the intervention costs and those associated with smoking-related comorbidities) and the lifetime health outcomes [measured using quality-adjusted life-years (QALYs)] of a cohort of patients who have recently quit smoking; incremental cost-effectiveness ratios (ICERs) are provided to help inform decisions about the best ‘value-for-money’ options for using RPIs within the UK NHS.
Methods
Overview of methods
A cohort simulation model was designed to estimate the costs and QALYs associated with interventions to reduce relapse following initial smoking cessation and to determine and compare different interventions’ relative cost-effectiveness. A hypothetical cohort of 1000 smokers who had recently initiated quit attempts (‘recent quitters’) was assembled; this was intended for use in a simulated ‘population cohort’ approach with modelling in 6-monthly cycles over cohort smokers’ lifetimes. In each cycle, ‘recent quitters’ could:
-
relapse (i.e. become a ‘smoker’)
-
remain a non-smoker (i.e. a ‘former smoker’)
-
die.
Figure 10 demonstrates the relationships between smoking status and smokers’ comorbidities permitted by the model which are explained further below.
FIGURE 10.
Movement between health states (note that a smoker can have more than one comorbidity).
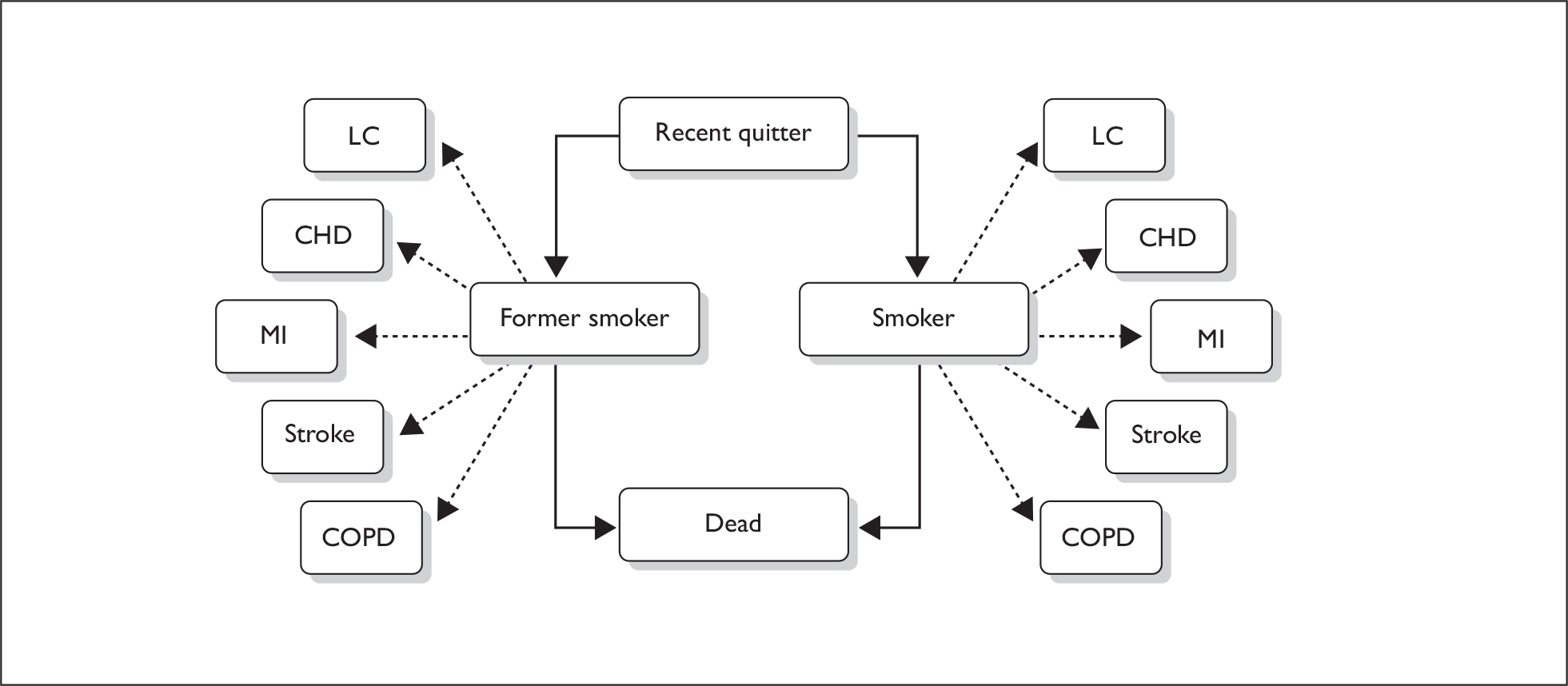
In each cycle, smokers and former smokers have a chance of experiencing one or more of five potential comorbidities:
-
lung cancer (LC)
-
coronary heart disease (CHD)
-
chronic obstructive pulmonary disease (COPD)
-
MI
-
stroke.
First, estimates for the prevalences of each comorbidity within regular and former smokers of different ages and genders were calculated; below, further details of methods used are given. To calculate the number of people with comorbidities, in each cycle, the numbers of smokers and former smokers were multiplied by the estimated prevalences (e.g. to calculate the number of smokers with LC, the number of smokers in each cycle was multiplied by the prevalence of LC among smokers). One qualification is that, as there were insufficient available data on the relative risks (RRs) of former smokers experiencing comorbidities, the model could not take into account the impact of the length of abstinence from smoking amongst former smokers; therefore, the same smoking-related costs are attributed to recent or long-term ex-smokers.
The likelihood of a cohort individual being a smoker or former smoker and also of developing one or more comorbidities in each cycle varies with their age. Each comorbidity has an associated cost and utility [quality of life (QoL)]; to enable the total costs and utilities of the interventions to be compared with ‘no intervention’, the number of people with each comorbidity was, within each cycle, multiplied by the associated cost/utility of that comorbidity, giving an estimated cost/utility for each comorbidity, and these were summed together to calculate an overall estimate for total cost/utility. The cost-effectiveness of individual relapse prevention treatments were determined by inputting the costs of these treatments into the simulation cohort and modelling their impact on cohort utilities, using estimates for effectiveness derived from Chapter 3.
Study population
The cohort is flexible and the cost and QALY outcomes for each combination of age and gender were estimated (e.g. for a 16-year-old man, 16-year-old woman, 17-year-old man, 17-year-old woman, etc.). Population weights derived from population estimates provided by the Office for National Statistics101 (see Appendix 4) were then applied to each cohort group, to ensure that the cohort was representative of the England and Wales population. The costs and QALY outcomes for each age–gender group were also multiplied by these weights to ensure overall QALY outcomes were similarly representative. We did not weight cohort simulations to reflect the sociodemographic characteristics; theoretically this would only have been possible using data on variations in model parameters (e.g. rates of complications, comorbidities, smoking status, etc.) with these characteristics, but such data were unavailable.
Data
This section describes the data sources from which estimates for parameters used in the cohort simulation were derived.
Literature search
Electronic databases (MEDLINE and PubMed), the Worldwide Web and references listed in identified articles were searched for relevant studies (see Appendix 5). Where there were any gaps, the Centre for Reviews and Dissemination (CRD, University of York, York, UK) carried out further searches. Data were required for the following areas:
-
mortality, by age, gender and smoking status
-
prevalence of each comorbidity, by age, gender and smoking status
-
utilities for each comorbidity
-
costs for each comorbidity.
Mortality
We estimated mortality by age, gender and smoking status, reflecting general population mortality rates for the cohort (see Appendix 6),102 using a number of data sources. Firstly, mortality rates per 1000 men and smoking exposure data from Doll et al. ,103 a study of doctors’ mortality, were used to derive ORs for mortality among former (A) and non-smokers (B), compared with current smokers (Table 11). The Actuary Life Tables102 provide the ‘real’ mortality for each age (C) and the prevalence of smoking for each age and gender (D) was taken from the Health Survey for England105 (Table 12). These data were used to calculate the actual mortality rates for smokers (E), former smokers (F) and non-smokers (G), by ensuring that the following equation was satisfied:
| Age at death (years) | Doll et al. (1994)103 | Doll et al. (2004)104 | ||||||
|---|---|---|---|---|---|---|---|---|
| Current smoker | Former | Non-smoker | Current smoker | Former smoker, by age stopped (years) | Non-smoker | |||
| 35–44 | 45–54 | 55–64 | ||||||
| 35–44 | 2.8 | 2 | 1.60 | 2.7 | 1.6 | |||
| 45–54 | 8.1 | 4.9 | 4.00 | 8.5 | 5.4 | 3.8 | ||
| 55–64 | 20.3 | 13.4 | 9.50 | 21.4 | 9.0 | 16.4 | 8.4 | |
| 65–74 | 47 | 31.6 | 23.70 | 50.7 | 22.7 | 31.7 | 36.4 | 18.6 |
| 75–84 | 106 | 77.3 | 67.40 | 112.2 | 53.1 | 39.1 | 78.9 | 51.7 |
| 85 + | 218.7 | 179.7 | 168.60 | |||||
| Age (years) | Current cigarette smoker (D1)a |
Ex-regular cigarette smoker (D2)a |
Never regularly smoked cigarettes (D3)a |
|---|---|---|---|
| 16–24 | 0.25 (0.29) | 0.05 (0.07) | 0.69 (0.64) |
| 25–34 | 0.37 (0.28) | 0.14 (0.16) | 0.49 (0.56) |
| 35–44 | 0.26 (0.27) | 0.21 (0.18) | 0.53 (0.55) |
| 45–54 | 0.25 (0.25) | 0.30 (0.24) | 0.44 (0.51) |
| 55–64 | 0.19 (0.20) | 0.44 (0.30) | 0.36 (0.50) |
| 65–74 | 0.10 (0.13) | 0.56 (0.29) | 0.34 (0.57) |
| 75 + | 0.07 (0.09) | 0.61(0.34) | 0.32 (0.57) |
| All ages | 0.24 (0.23) | 0.29 (0.22) | 0.47 (0.56) |
Where E : F = the OR, A; E : G = B
This calculation is best illustrated by example; taking a 44 year old and substituting the prevalence of smoking and the actual mortality rate into the equation gives:
Further substituting the ORs reduces the equation to:
This allows the equation to be solved as follows, to give an accurate estimate of the mortality for a 44-year-old smoker, former smoker and non-smoker:
This process was repeated for all ages.
Calculation of the prevalence by smoking status of each comorbidity
We searched for information concerning: (1) the prevalence, by age, of each comorbidity in the general population, regardless of smoking status (A), (2) the RR of each comorbidity by smoking status [i.e. smokers vs former (B) and non-smokers (C)] and (3) the prevalence of smoking in England and Wales (D) (Appendix 5). These data were used to calculate the prevalence of each comorbidity within current (E), former (F) and non-smokers (G), by ensuring that the following equation was satisfied:
Where E : F = the OR, B; G : F = the OR, C.
This can be illustrated using the example of a 60-year-old person with LC. The prevalence of LC comes from Table 13,106 the RR of LC from Table 14107 and the prevalence of smoking, as above from Table 12. 105
| Age (years) | Prevalence |
|---|---|
| 0–44 | 0.00% |
| 45–64 | 0.15% |
| 65 + | 0.80% |
| All ages | 0.14% |
| Current smoker | Former | Non-smoker | |
|---|---|---|---|
| RR | 1 | 0.44 | 0.03 |
-
Substituting the prevalence of smoking and the actual prevalence rate:(E×0.19)+(F×0.44)+(G×0.36)=0.15
-
Substituting the ORs:
This process was repeated for all age and gender categories within each comorbidity. The prevalence of each comorbidity, the RR by smoking status and resulting prevalence by age, gender and smoking status are shown in Appendices 7–11.
Deriving utility weights
Comorbidities within our cohort were each allocated an associated utility and, for every cohort cycle, the number of people with each comorbidity was multiplied by the associated utility and adjusted for the time period spent in the morbid health state. Where someone had more than one comorbidity, we used the lowest utility value, so ‘double counting’ of morbidities resulting in false multiplicative or additive assumptions would not have occurred. Attaching utilities to morbidities in this way permitted our model to determine estimates for the utilities of morbidities when no intervention was used, enabling comparison of the total QALYs attributable to interventions and ‘no intervention’.
The following procedure was used to derive utilities for our cohort. Tengs and Wallace reviewed studies that included original QoL weights with the aim of compiling a list of QoL weights for 1000 disease areas. 108 A search of Tengs and Wallace’s database, the NHS Economic Evaluation Database, MEDLINE and of bibliographies in retrieved papers identified 1100 potential studies, of which, 243 contained potentially relevant information on utilities and 154 reported original data. Tengs and Wallace calculated the average values for utility scores and these were used in our model for LC, CHD, MI and stroke. We did not attempt to combine these with scores from other sources due to a lack of sufficient evidence on the quality of the respective data.
Lung cancer utilities
Six utility values were provided for LC covering the following areas, an average of which was calculated:
-
small cell LC with one cycle course of radiation
-
small cell LC with one cycle course of cyclophosphamide, doxorubicin and vincristine (CAV) chemotherapy
-
small cell LC with one cycle course of etoposide (VP-16)/cisplatin
-
small cell LC after disease progression
-
small cell LC that is in complete remission
-
small cell LC in partial remission of treatment.
Stroke utilities
Tengs and Wallace108 identified 28 papers with QoL stroke weights, including patients in the following health states:
-
Minor stroke:
-
– with or without cognitive deficit
-
– first year after stroke
-
– left with residual cerebral arteriovenous malformations after treatment.
-
-
Moderate stroke:
-
– with or without cognitive deficit
-
– residual deficit in patients with prior MI
-
– language deficit
-
– motor deficit.
-
-
Acute requiring hospitalisation.
-
Major stroke:
-
– with or without the ability to speak
-
– first year after stroke
-
– left with residual cerebral arteriovenous malformations after treatment
-
– severe residual deficit in patients with prior MI
-
– with or without cognitive deficit
-
– language deficit
-
– motor deficit.
-
Coronary heart disease and myocardial infarction utilities
Tengs and Wallace108 identified only one paper for CHD (utility = 0.8) and 83 for health status after MI; the MI papers covered the following health states:
-
All MIs (no further details provided).
-
MI treated with streptokinase or recombinant tissue plasminogen activator, no dyspnoea at rest/on mild exertion or on strenuous exertion.
-
MI patients unable to care for themselves.
-
MI patients who did not experience a stroke or refraction.
-
MI patients where rehabilitation had been provided.
Chronic obstructive pulmonary disease utilities
Rutten-van Molken et al. 109 investigated the differences in COPD utility measured in 13 countries using data from a subset of 1235 trial patients (from 6000 participants) who completed a baseline European Quality of Life-5 Dimensions (EQ-5D) questionnaire110 as part of a double-blind, placebo-RCT investigating whether dopropium reduces the rate of decline in forced expiratory volume. EQ-5D utility score was 0.76 at baseline; scores were split into six groups based on the severity of COPD (moderate, severe and very severe) and location (UK/USA); our model used an average of UK scores for all severities of COPD.
Utility of current and former smoking: no comorbidity
Tillmann and Silcock111 assessed differences in health status between Scottish current and former smokers (abstinent for > 5 years), registered with nine general medical practices using the EQ-5D, and EQ-5D scores were 0.78 for former and 0.75 for current smokers.
Summary of utility scores used
The utility scores used in the model are shown in Table 15. There were insufficient data on how comorbidity severity might be distributed among smokers, former smokers and non-smokers so, as per Tengs and Wallace,108 we used average utility scores rather than scores intended to reflect varied severity of comorbidity.
| Comorbidity | Utility | Source (reference number) |
|---|---|---|
| LC | 0.58 | 107 |
| Stroke | 0.48 | 107 |
| CHD | 0.80 | 107 |
| MI | 0.80 | 107 |
| COPD | 0.73 | 108 |
| No comorbidities | 0.75 current smoker | 110 |
| 0.78 former smoker |
Deriving comorbidity costs
Summary of comorbidity costs used in model
For cohort simulations we required a cost attributable to each comorbidity and, to permit comparisons with ‘no intervention’, we needed to calculate the annual total costs for each comorbidity. Total annual costs were derived by multiplying, for each cohort cycle, the number of people with each comorbidity and attributable costs; annual comorbidity costs, inflated to 2008 prices, are shown in Table 16 and explanations of the rationale for deriving these follow.
| Disease | Average annual cost (2008 £) | Source (reference number) |
|---|---|---|
| LC | 5501 | 111 |
| Stroke | 2061 | 104, 112, 113 |
| CHD | 1063 | 104, 113, 114 |
| MI | 2175 | 115, 116, 117 |
| COPD | 926 | 118 |
Rationale for deriving costs attributable to each comorbidity
The Health Care Needs Assessment provides evidence for cost, cost-effectiveness and optimum service configuration for treatment of diseases including LC. 112 The authors acknowledge that there is uncertainty surrounding the cost of palliative and terminal LC care, but estimate it to be between £2000 and £7100 per person (1998 UK sterling); we used average figures in the model, £4550 (£5501 at current prices). It is unclear whether reported costs figure take account of gender differences in the number of people with LC.
The National Audit Office (NAO)113 estimated that the direct cost of stroke was £2.8B each year (in 2005). The total cost per person was calculated by dividing the NAO estimated cost by the number of people with stroke in the UK, giving an estimated annual 2006 cost of £2061;105,114 it was assumed that the same definition of stroke was used for both data sources. A similar approach was used for the cost of CHD with the annual cost provided by the British Heart Foundation;115 stroke and CHD costs are shown in Table 17.
| Stroke | CHD | |
|---|---|---|
| Total cost per year (£) | 2,867,200,000 | 3,809,320,747 |
| Total population (male) | 29,668,033 | 29,668,033 |
| Total population (female) | 30,864,468 | 30,864,468 |
| % with stroke/CHD (male) | 2.40 | 7.00 |
| % with stoke/CHD (female) | 2.20 | 5.00 |
| Average cost per person (£) | 2061 | 1063 |
The cost of MI has two components; those of the acute event and ongoing annual health-care costs. Event costs were taken from national published databases and the calculation of long-term costs assumed monthly general practitioner (GP) and 3-monthly cardiology follow-up visits, with use of cholesterol lowering drugs. 116–118
The annual cost of COPD care was taken from Appendix D of the Chronic Obstructive Pulmonary Disease: National Clinical Guideline on Management of Chronic Obstructive Pulmonary Disease in Adults in Primary and Secondary Care. 119 This includes GP visits, medication, oxygen, inpatient stay and emergency admission; it is unclear whether this takes account of the gender distribution amongst people with COPD.
Cohort simulations and model assumptions
The virtual cohort assembled 1000 smokers who had recently started a quit attempt and simulations aimed to determine the cost-effectiveness of RPIs used within this population.
The following assumptions were made in the base-case model:
-
A background (i.e. spontaneous) rate of quitting smoking of 2% among all smokers.
-
RPIs used by this population of smokers would have the same efficacy as in clinical trials.
-
Costs of RPIs were as recorded in the British National Formulary (BNF).
-
Age, gender and smoking-specific cohort mortality and morbidity rates are accurately calculated using procedures outlined above.
-
Costs incurred by exposure to morbidities are adequately calculated as described above.
Analysis of intervention effectiveness
For all interventions, the most influential parameter within the model was the proportion abstinent from smoking during each 6-monthly cohort cycle. In all cases, the proportion abstinent at time zero was 100%, because RPIs are provided to smokers who have recently stopped smoking; parameters representing the likely proportions remaining abstinent at 6 and 12 months (Table 18, Figure 11) are from control and intervention groups within trials included in the Chapter 3 systematic review, conducted to estimate the effectiveness of RPIs for relapse prevention. Model parameters (estimates) representing the effectiveness of bupropion, varenicline and NRT for preventing relapse to smoking amongst abstinent smokers are also from this review.
FIGURE 11.
Proportion abstinent at baseline, 6 months and 12 months with relapse prevention intervention and in comparable ‘no intervention’ groups.
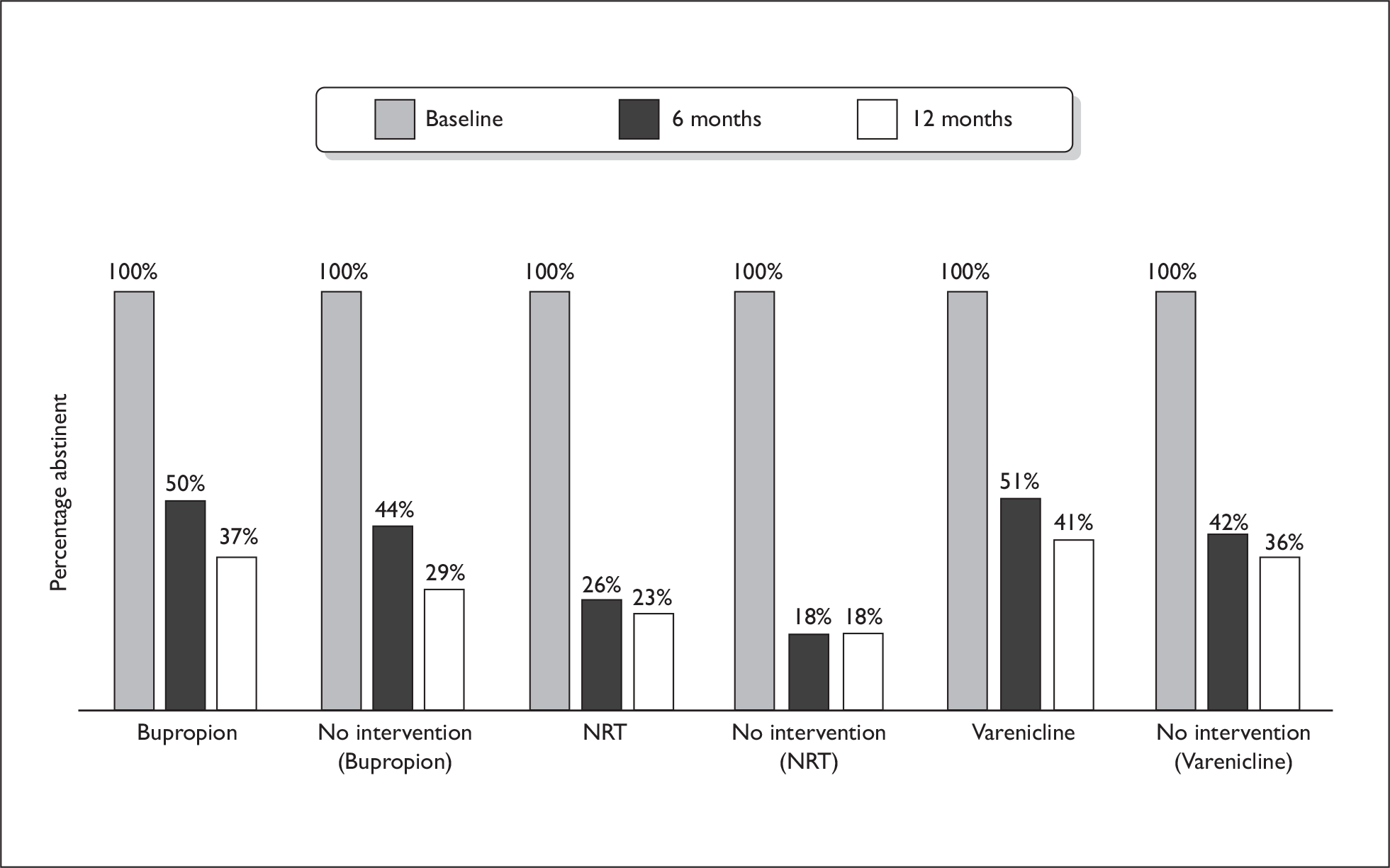
| Bupropion | NRT | Varenicline | ||||
|---|---|---|---|---|---|---|
| Bupropion | No intervention | NRT | No intervention | Varenicline | No intervention | |
| Cost of intervention (£) | 69 | 0 | 100 | 0 | 177 | 0 |
| % abstinent at 0 months | 100 | 100 | 100 | 100 | 100 | 100 |
| % abstinent at 6 months | 50 | 44 | 26 | 18 | 51 | 42 |
| % abstinent at 12 months | 37 | 29 | 23 | 18 | 41 | 36 |
Trials investigating RPIs have followed up participants for a maximum of 12 months, so we only have data on the effectiveness of interventions over this length of time. However, some relapse to smoking will occur after 1 year and, hence, in the longer term, the impact of RPIs may diminish as time passes if relapse rates are higher in those who have used RPIs. To estimate the potential long-term impact of RPIs, we made three different assumptions about the likely persistence of short-term benefits from use of RPIs and incorporated these into our model. These assumptions were that differences between the RPI-treated and non-treated groups observed after 1 year would:
-
Diminish with the same annual ‘background’ relapse rate (2% of non-smokers relapsing to smoking each year in ‘treated’ and ‘non-treated’ groups).
-
Persist for 10 years but then disappear.
-
Disappear completely after 1 year.
Assumption 1, above, was used in the base-case scenario and assumptions 2 and 3 were used in sensitivity analyses.
Table 18 gives (1) the estimated costs of delivering interventions (full details explaining calculations follow) and (2) the proportions of smokers abstinent at different time points after quitting, as derived from our review in Chapter 3 that the costs of ‘no intervention’ accrue with time, as the amount of relapse to smoking increases.
The cost of bupropion was calculated using a price per 150-mg tablet of £0.66120 with patients receiving one daily tablet for 6 days followed by 150 mg twice daily for a period of 7 weeks. NRT costs were calculated by combining dosing provided in a previous analysis121 with costs from the BNF120 and a study by Parrott calculated that smokers received 60.48 units of NRT during a course of treatment. 121 Varenicline was calculated using a cost per initial pack of £27.30, followed by two tablets per day (at a cost of £0.97 per tablet) for a period of 77 days. 120
For NRT trials, a further sensitivity analysis was undertaken, excluding two trials in which participants had been abstinent from smoking for only very short periods (24 and 48 hours, respectively) prior to NRT being introduced as relapse prevention therapy. As most relapse was expected to occur in the first few days after abstinence, relapse prevention treatments might be expected, therefore, to have lower efficacy amongst participants of these trials. The cost and effectiveness inputs for remaining NRT trials that required longer abstinence periods prior to the onset of relapse prevention treatment are shown in Table 19.
| NRT | ||
|---|---|---|
| NRT | No intervention | |
| Cost of intervention (£) | 100 | 0 |
| % abstinent at 0 months | 100 | 100 |
| % abstinent at 6 months | 48.62 | 31.15 |
| % abstinent at 12 months | 25.69 | 16.39 |
Economic evaluation
Cost-effectiveness models are used to assess the relative benefits of a given treatment using patient outcomes and the costs incurred in achieving those outcomes. The calculation of the additional cost per additional unit gain of benefit (i.e. QALYs) is known as the incremental analysis and results are presented as ICERs. After incremental costs and QALYs were estimated, the ICERs were calculated using the following formula:
The incremental cost per QALY is calculated for all the interventions modelled, allowing the user to compare any two interventions.
Discounting
Costs and outcomes were discounted at 3.5% per year. 122
Sensitivity analyses
Sensitivity analyses were carried out for each intervention to examine the impact of changing model values for:
-
background quit rate
-
cost and effectiveness
-
persistence of intervention benefits.
Model background quit rates of 2% (base case), 1.2% and 2.8% were investigated, as was varying intervention costs between – 50% and + 50% of the base-case value. For effectiveness data, the proportion of additional abstainers at 6 and 12 months was assessed using a range between 10% and 150% of the original value for additional abstainers. For example if, in the control group, the number of abstainers in the control group is 40% and the number of abstainers in the treatment group is 50%, then this equates to an additional 10% of abstainers. Therefore, the sensitivity analysis would assess the impact of changing this value between 1% (i.e. 41% abstaining) and 15% (i.e. 55% abstaining). The persistence of short-term benefits from interventions was investigated as described for the three scenarios outlined above (see Analysis of intervention effectiveness).
Results
Base-case results
Table 20 provides the base-case costs and QALYs, per person, associated with each intervention, using a 2% background cessation rate.
| Intervention | Background cessation = 2% | |
|---|---|---|
| Cost (£) | QALY | |
| Bupropion | 6755 | 12.76 |
| No intervention (bupropion trial) | 6822 | 12.69 |
| NRT | 7050 | 12.63 |
| No intervention (NRT trial) | 7039 | 12.58 |
| Varenicline | 6794 | 12.79 |
| No intervention (varenicline trial) | 6704 | 12.75 |
| No intervention (pooled data) | 6981 | 12.61 |
All interventions result in increased QALYs compared with ‘no intervention’ and net costs, including all medical costs incorporated in the model and intervention costs, generally increased, with the exception of bupropion.
Figure 12 illustrates the total cost and total QALYs for all the interventions and ‘no intervention’.
FIGURE 12.
Total cost and total QALY results.
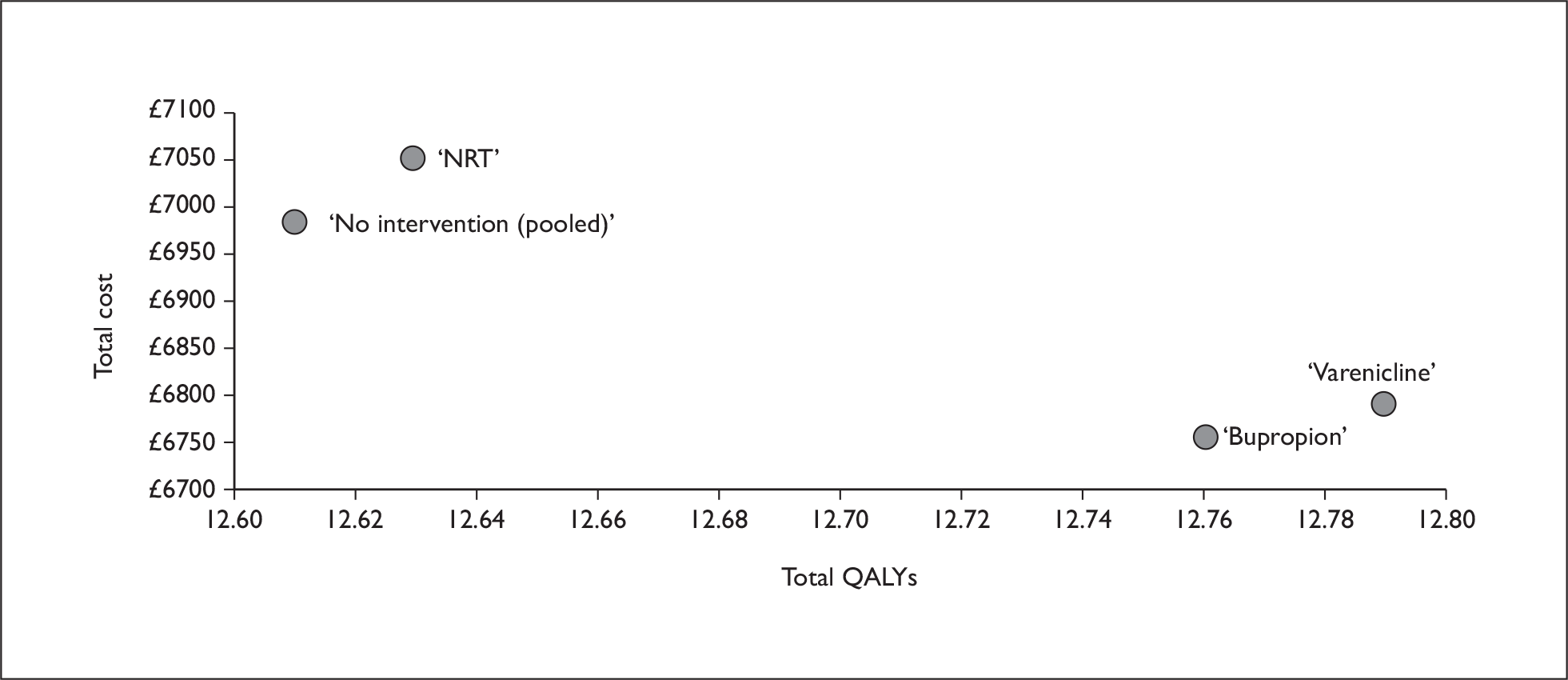
Incremental analysis – comparison against ‘no intervention’ using trial data
Incremental analysis was carried out to compare each intervention to ‘no intervention’ in terms of the total costs and QALYs. All treatments show a very low cost per QALY (maximum = £2106), therefore, they can be considered cost-effective against a willingness-to-pay threshold of £20,000. However, bupropion is the cheapest and the most effective intervention and, therefore, assuming that the interventions are mutually exclusive it dominates all the other interventions (i.e. is more effective and less costly).
Should any decision maker/health service commissioner wish to choose between the different interventions included in the analysis, the incremental costs and benefits should be assessed. For example, if varenicline was compared against, say, bupropion, we can see that it produces an additional 0.03 QALYs at an additional cost of around £45 (Figure 13). The ICER for varenicline versus bupropion is, therefore, £1500 per QALY and varenicline would be considered cost-effective compared to bupropion. However, as mentioned below, caution should be taken when comparing results from different trials; robust data comparing interventions is best obtained from head-to-head comparisons are made within studies and none were available for bupropion and varenicline.
FIGURE 13.
Hypothetical example of long-term benefits (as assumed in ‘base-case’ model). Assuming abstinence rates observed at 1 year continue for a further 10 years.
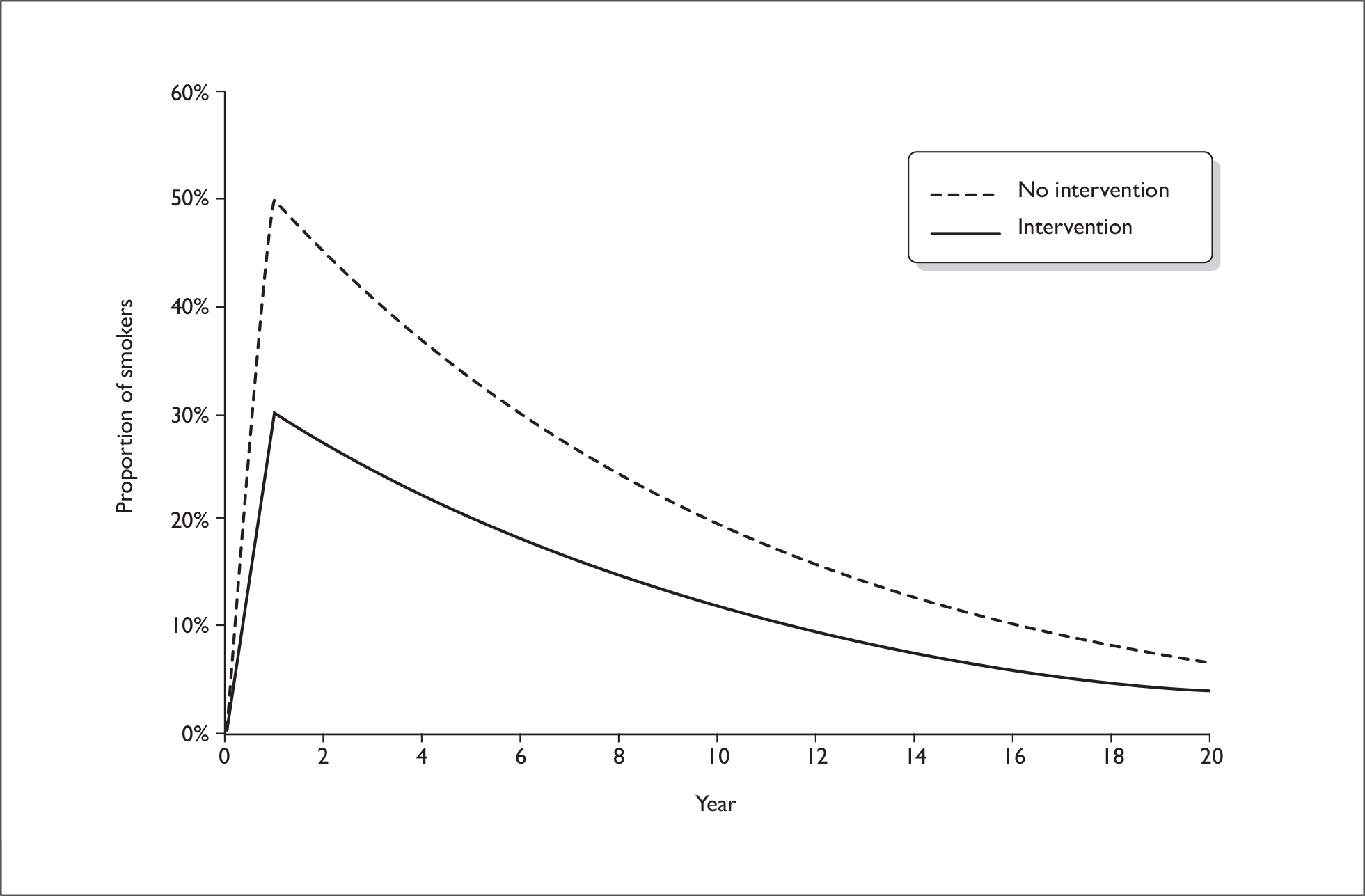
Table 21 shows the results of comparing each intervention to ‘no intervention’. Note that the effectiveness of ‘no intervention’ varies, as each treatment was modelled against the relevant ‘no intervention’ abstinence rate derived from control groups in trials of that treatment. However, as baseline differences may exist between different trial participants, comparisons between drugs are, indirect and need to be treated with caution. Incremental costs and QALYs are shown, as well as the ICER.
| Compared with ‘no intervention’ | Background cessation = 2% | ||
|---|---|---|---|
| Incremental cost (£) | Incremental QALY | ICER (£) | |
| ‘Bupropion’ vs ‘no intervention’a | –68 | 0.07 | Dominantb |
| ‘NRT’ vs ‘no intervention’ | 12 | 0.04 | 265 |
| ‘Varenicline’ vs ‘no intervention’ | 90 | 0.04 | 2106 |
When we excluded those NRT trials, which recruited participants who had been abstinent for very short periods and compared remaining trials with ‘no intervention’, there was very little change in findings for NRT; the incremental QALYs gained were 0.08 (12.66 compared to 12.58) and NRT was also associated with an overall reduction in total costs of £47 (of which, the £100 cost of NRT was offset by £147 savings on other costs). As such, NRT (when used for relapse prevention with smokers who have been abstinent for longer periods) dominated ‘no intervention’ in terms of cost-effectiveness.
Sensitivity analyses
Background quit rate variation
Background quit rate is 1.2% or 2.8%
Table 22 shows the results of comparing each intervention to ‘no intervention’ with a lower background cessation of 1.2%, but keeping everything else the same; findings are very similar to the base case (2% in the base case). All interventions follow the pattern of the base-case results and can be considered cost-effective against a willingness-to-pay threshold of £20,000 per QALY. Bupropion remains the cheapest and the most effective intervention and dominates all the other interventions (more effective and less costly).
| Compared with ‘no intervention’ | Background cessation = 1.2% | ||
|---|---|---|---|
| Incremental cost (£) | Incremental QALY | ICER (£) | |
| ‘Bupropion’ vs ‘no intervention (bupropion trial)’ | – 85 | 0.07 | Dominant |
| ‘NRT’ vs ‘no intervention (NRT trial)’ | 1 | 0.05 | 11 |
| ‘Varenicline’ vs ‘no intervention (varenicline trial)’ | 79 | 0.04 | 1676 |
Table 23 demonstrates that all treatments are still cost-effective when compared against ‘no intervention’ at a background quit rate of 2.8%.
| Compared with ‘no intervention’ | Background cessation = 2.8% | ||
|---|---|---|---|
| Incremental cost (£) | Incremental QALY | ICER (£) | |
| ‘Bupropion’ vs ‘no intervention (bupropion trial)’ | – 54 | 0.06 | Dominant |
| ‘NRT’ vs ‘no intervention (NRT trial)’ | 21 | 0.04 | 520 |
| ‘Varenicline’ vs ‘no intervention (varenicline trial)’ | 99 | 0.04 | 2538 |
Intervention costs
For each of the three interventions, cost and effectiveness parameters were varied to assess their impact upon the cost-effectiveness results in the model. Tables 24–26 detail the impact of changing the attributable costs of the three interventions. Bupropion remains dominant, and hence cost-effective at all projected costs (i.e. ± 50% of those included in the base case) while NRT is more sensitive to cost changes, becoming dominant at an intervention cost of £70, which is below that in the base case. At the highest projected intervention cost, varenicline appears less cost-effective; however, all interventions remain cost-effective as judged by the National Institute for Health and Clinical Excellence (NICE) cost-effectiveness benchmark of £20,000 per QALY.
| Intervention cost (£) | Incremental cost (£) | Incremental QALYs | ICER |
|---|---|---|---|
| 35 | –83 | 0.07 | Dominant |
| 41 | –76 | 0.07 | Dominant |
| 48 | –69 | 0.07 | Dominant |
| 55 | –62 | 0.07 | Dominant |
| 62 | –55 | 0.07 | Dominant |
| 69 | –48 | 0.07 | Dominant |
| 76 | –41 | 0.07 | Dominant |
| 83 | –35 | 0.07 | Dominant |
| 90 | –28 | 0.07 | Dominant |
| 97 | –21 | 0.07 | Dominant |
| 104 | –14 | 0.07 | Dominant |
| Intervention cost (£) | Incremental cost (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|
| 50 | –26 | 0.04 | Dominant |
| 60 | –16 | 0.04 | Dominant |
| 70 | –6 | 0.04 | Dominant |
| 80 | 4 | 0.04 | 92 |
| 90 | 14 | 0.04 | 323 |
| 100 | 24 | 0.04 | 554 |
| 110 | 34 | 0.04 | 785 |
| 120 | 44 | 0.04 | 1016 |
| 130 | 54 | 0.04 | 1247 |
| 140 | 64 | 0.04 | 1478 |
| 150 | 74 | 0.04 | 1710 |
| Intervention cost (£) | Incremental cost (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|
| 89 | 14 | 0.04 | 319 |
| 106 | 31 | 0.04 | 734 |
| 124 | 49 | 0.04 | 1149 |
| 142 | 67 | 0.04 | 1565 |
| 159 | 85 | 0.04 | 1980 |
| 177 | 102 | 0.04 | 2395 |
| 195 | 120 | 0.04 | 2810 |
| 212 | 138 | 0.04 | 3226 |
| 230 | 156 | 0.04 | 3641 |
| 248 | 173 | 0.04 | 4056 |
| 266 | 191 | 0.04 | 4472 |
Effectiveness of interventions
Tables 27–29 demonstrate the impact of changing the level of effectiveness of each intervention. As described above, the proportion of additional abstainers at 6 and 12 months was assessed using a range between 10% and 150% of the original value for additional abstainers. For example if, in the control group, the number of abstainers in the control group was 40% and the number of abstainers in the treatment group was 50%, then this equates to an additional 10% of abstainers. Therefore, the sensitivity analysis would assess the impact of changing this value between 1% (i.e. 41% abstaining) and 15% (i.e. 55% abstaining). Changes in the postulated effectiveness of interventions affects RPIs’ cost-effectiveness more than alterations in cost. Bupropion dominates unless hypothesised effectiveness falls below 50% of used in the base case, and cost-effectiveness falls with decreasing effectiveness as shown by an incremental cost-effectiveness ratio of £8831 per QALY at 10% of base-case effectiveness. NRT only dominates when effectiveness is set at a higher level than estimated from clinical trials and used in the base case, but the ICER for NRT would exceed the NICE threshold if this were to fall below 10% of the base-case level. Varenicline is never dominant and although the NICE benchmark is only exceeded when effectiveness falls below 20% of observed, it appears less cost-effective than either NRT or bupropion with consistently higher ICER values throughout the range of effectiveness explored.
| Increase in abstainers (%) | Incremental cost (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|
| 10 | 57 | 0.01 | 8331 |
| 20 | 46 | 0.01 | 3376 |
| 30 | 34 | 0.02 | 1682 |
| 40 | 22 | 0.03 | 826 |
| 50 | 10 | 0.03 | 311 |
| 60 | –1 | 0.04 | Dominant |
| 70 | –13 | 0.05 | Dominant |
| 80 | –25 | 0.05 | Dominant |
| 90 | –37 | 0.06 | Dominant |
| 100 | –48 | 0.07 | Dominant |
| 110 | –60 | 0.07 | Dominant |
| 120 | –72 | 0.08 | Dominant |
| 130 | –84 | 0.09 | Dominant |
| 140 | –95 | 0.09 | Dominant |
| 150 | –107 | 0.10 | Dominant |
| Increase in abstainers (%) | Incremental cost (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|
| 10 | 93 | 0.00 | 20,097 |
| 20 | 85 | 0.01 | 9533 |
| 30 | 78 | 0.01 | 5851 |
| 40 | 70 | 0.02 | 3979 |
| 50 | 62 | 0.02 | 2845 |
| 60 | 55 | 0.03 | 2085 |
| 70 | 47 | 0.03 | 1540 |
| 80 | 39 | 0.03 | 1130 |
| 90 | 32 | 0.04 | 810 |
| 100 | 24 | 0.04 | 554 |
| 110 | 16 | 0.05 | 344 |
| 120 | 9 | 0.05 | 169 |
| 130 | 1 | 0.06 | 21 |
| 140 | –6 | 0.06 | Dominant |
| 150 | –14 | 0.07 | Dominant |
| Increase in abstainers (%) | Incremental cost (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|
| 10 | 170 | 0.00 | 37,909 |
| 20 | 162 | 0.01 | 18,600 |
| 30 | 155 | 0.01 | 11,933 |
| 40 | 147 | 0.02 | 8554 |
| 50 | 140 | 0.02 | 6512 |
| 60 | 132 | 0.03 | 5145 |
| 70 | 125 | 0.03 | 4165 |
| 80 | 117 | 0.03 | 3429 |
| 90 | 110 | 0.04 | 2855 |
| 100 | 102 | 0.04 | 2395 |
| 110 | 95 | 0.05 | 2019 |
| 120 | 87 | 0.05 | 1705 |
| 130 | 80 | 0.06 | 1439 |
| 140 | 72 | 0.06 | 1211 |
| 150 | 65 | 0.06 | 1013 |
Additional analysis: varying persistence of intervention benefits
It is recognised that the benefits of smokers achieving permanent abstinence are greater than those arising from temporary abstinence periods, but there were no available data with which to predict the long-term smoking status of those smokers who achieved temporary abstinence but subsequently relapsed to smoking. Consequently, we assessed three different potential scenarios for the persistence of benefits arising from intervention delivery (described above) and findings are related below for the base case (i.e. a constant ‘background’ relapse rate occurring after all interventions), assuming abstinence rates observed at 1 year continue for a further 10 years and assuming that differences in abstinence rates attributable to interventions persist for only 1 year.
For this analysis, it was assumed that abstinence rates observed at 1 year would continue for a further period of 10 years, after which the ‘background’ rate would be observed for each treatment arm (Figure 14). As expected, increasing the level of effectiveness of the treatments to 10 years increases the cost-effectiveness of each intervention (Table 30). However, it should be recognised that abstinence rates usually decline with time,123 so this scenario is likely to overestimate the cost-effectiveness of treatments.
FIGURE 14.
Hypothetical example of benefits remaining for 10 years.
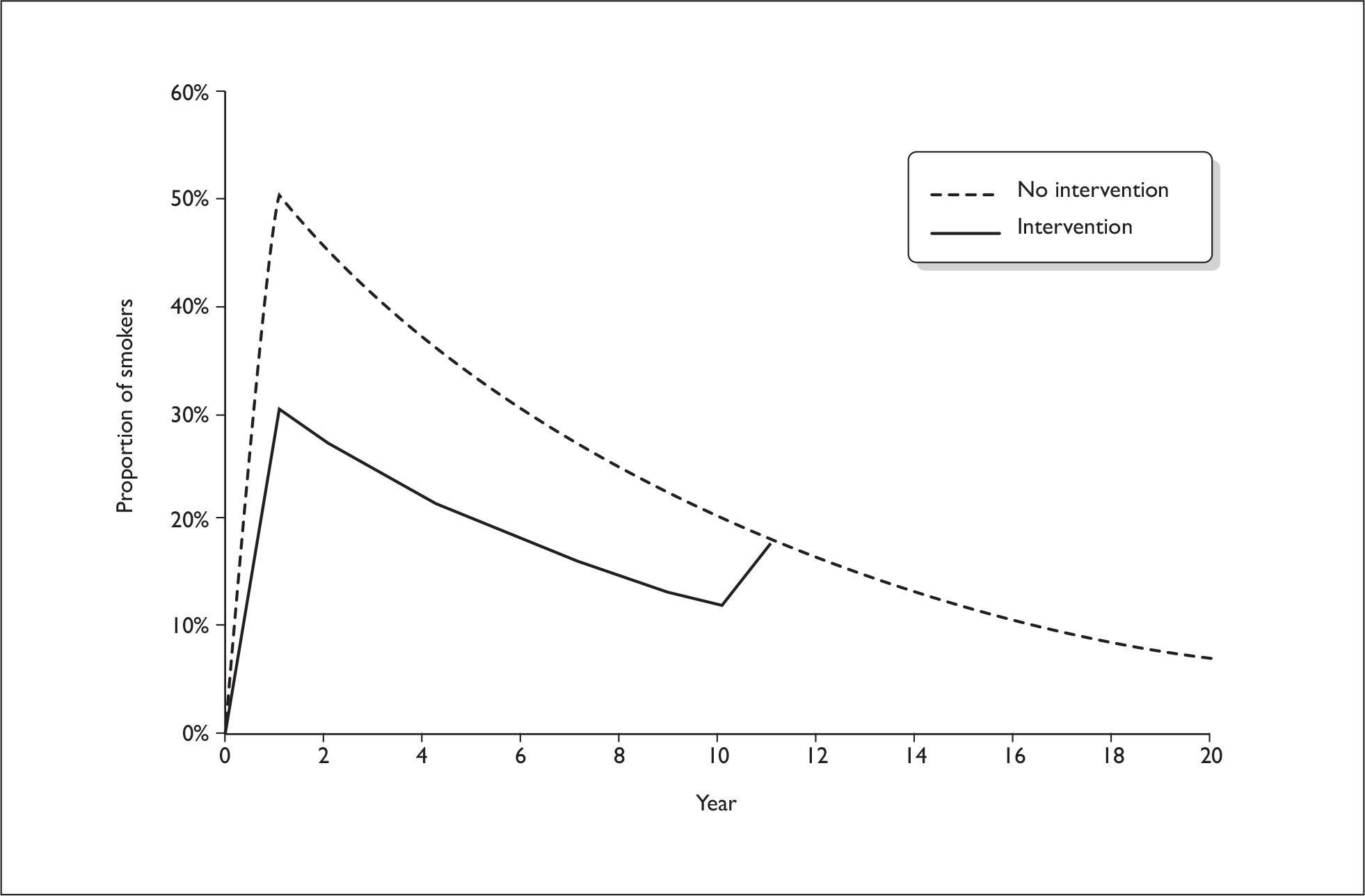
| Compared with ‘no intervention’ | Background cessation = 2% | ||
|---|---|---|---|
| Incremental cost (£) | Incremental QALY | ICER (£) | |
| ‘Bupropion’ vs ‘no intervention (bupropion trial)’ | –102 | 0.091 | Dominant |
| ‘NRT’ vs ‘no intervention (NRT trial)’ | –38 | 0.074 | Dominant |
| ‘Varenicline’ vs ‘no intervention (varenicline trial)’ | 26 | 0.081 | 322 |
Assuming abstinence rates at 1 year do not persist beyond this and differences between groups disappear
In this scenario, we assumed that the benefits of an intervention would last only 1 year, after which there would be no differences between intervention and ‘no intervention’ groups (Figure 15). Table 31 shows that, in this instance, interventions do not appear to be cost-effective as judged by the usual NICE benchmark. This makes intuitive sense, since the benefits are only accrued for 1 year, while the cost of the intervention has remained at its full amount. However, it is very unlikely that the benefits of averting relapse would not be apparent after the first year and, as such, these results represent a highly unlikely worst-case scenario. Differences in abstinence rates between arms of smoking cessation trials have been observed up to 8 years after randomisation. 123
FIGURE 15.
Hypothetical example of benefits remaining for 1 year.
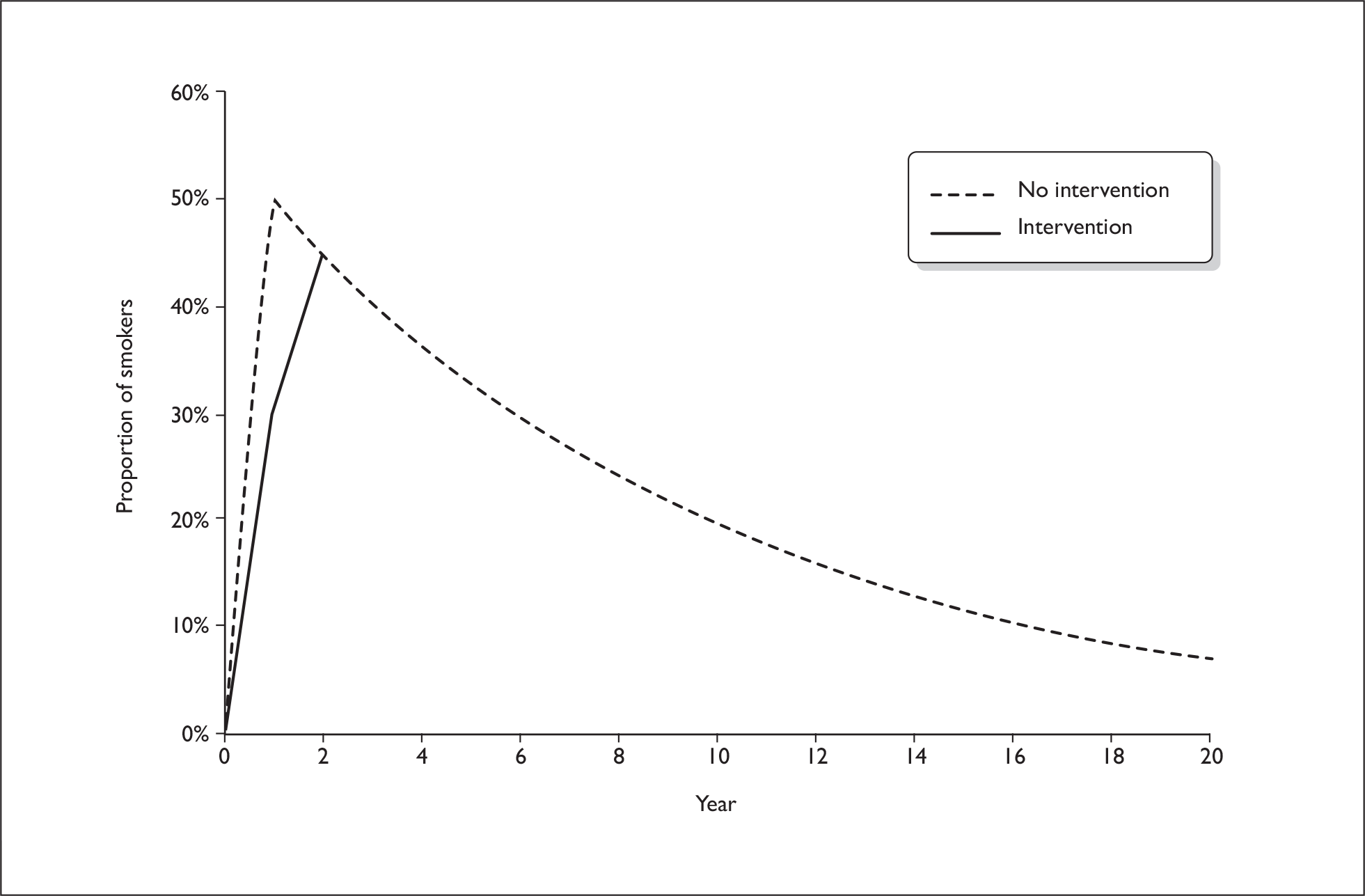
| Compared with ‘no intervention’ | Background cessation = 2% | ||
|---|---|---|---|
| Incremental cost (£) | Incremental QALY | ICER (£) | |
| ‘Bupropion’ vs ‘no intervention (bupropion trial)’ | 59 | 0.002 | 25,098 |
| ‘NRT’ vs ‘no intervention (NRT trial)’ | 93 | 0.002 | 49,731 |
| ‘Varenicline’ vs ‘no intervention (varenicline trial)’ | 170 | 0.002 | 91,189 |
Discussion and conclusions
Findings indicate that, in common with other interventions which reduce smoking, RPIs are also likely to be highly cost-effective; the economic and health costs of smoking are so great that reducing this, even moderately, produces substantial benefits. Compared with ‘no intervention’, using bupropion for relapse prevention resulted in an incremental QALY increase of 0.07 with a concurrent NHS cost saving of £68; for NRT, spending £12 resulted in a 0.04 incremental QALY increase (see Table 21). Varenicline, produced the same incremental QALY increase as NRT, but at over seven times the cost, however, as these figures are derived from a single trial, they, require cautious interpretation and cost-effectiveness estimates for interventions should not be directly compared as they were obtained from different, heterogenic trials conducted in varied populations. Extensive sensitivity analyses demonstrated that cost-effectiveness ratios were more sensitive to variations in RPI effectiveness than cost and that; for bupropion and NRT, cost-effectiveness generally remained, even when input parameters are varied greatly. For varenicline, cost-effectiveness, as judged by the £20,000 per QALY benchmark remained at all but the minimum of the effectiveness range, but ICERs remained substantially higher than for bupropion and NRT throughout the range of costs and effects inputted. Cost-effectiveness was robust to the projected persistence of longer-term benefits from RPIs and base-case cost-effectiveness ratios only exceeded £20,000 per QALY when intervention effects were projected to last for only 1 year (Table 31). However, this scenario is highly unlikely as cessation intervention benefits can last for up to 8 years123 and we can think of no reason why similar patterns of relapse to smoking would not be experienced after RPIs, and the effectiveness of NRT and varenicline is not likely to vary as markedly as was tested in analyses. The results of this study are comparable to those from economic evaluations of smoking cessation interventions; smoking cessation interventions have, in general, also been shown to result in greater benefits at lower or marginally higher costs than ‘no intervention’. 121,124,125
Limitations
There are a number of limitations inherent within the model. A lack of data on how comorbidities varied with smoking status made it impossible to categorise former smokers as achieving either ‘recent’ or ‘long-term’ abstinence and the impact of this on our findings is unclear. If at some point after permanently stopping smoking, the probability of developing some or all of the model comorbidities returns to that of non-smokers, the model will have overestimated the numbers of people with comorbidities and, hence, comorbidity costs, resulting in an underestimation of interventions’ cost-effectiveness.
The model assumes that smokers use only one type of cessation intervention in any one quit attempt but, in ‘real life’, some smokers try stopping smoking repeatedly and some use many different cessation methods. However, the incorporation of a background quit rate into the model addresses this limitation, and sensitivity analysis demonstrated that RPIs appeared effective across a wide range of different background rates.
Model estimates for the effectiveness of interventions were taken from RCTs but interventions often show greater efficacy in trials than in routine clinical care and this could have contributed to an overestimation of cost-effectiveness. Also most pharmacotherapy relapse prevention trials required between 2 and 3 months abstinence from smoking before relapse prevention treatments were started and abstinence was generally achieved with the help of evidence-based support, so the model relates primarily to interventions used in this context. NRT trials provide some insight into the potential influences of abstinence period length and the use of support to achieve abstinence on cost-effectiveness. When trials with very short abstinence periods (< 48 hours), achieved without cessation support, were excluded from NRT analyses, NRT appeared to be even more cost-effective. Consequently, the effectiveness and cost-effectiveness of NRT, and perhaps of other RPIs, is likely to be dependent upon abstinent smokers’ characteristics, such as how they achieved abstinence and also upon the timing of relapse prevention intervention delivery in relation to the start of any quit attempt. Unfortunately, the model cannot investigate these issues in the absence of sufficient empirical trial data.
Again, due to a lack of available data, the model assumed that, when a person had multiple comorbidities, their QoL was equivalent to that experienced with the most severe of these. From the perspective of assessing the impact of the interventions, this is a conservative assumption as each intervention, by encouraging abstinence from smoking, is likely to reduce the prevalence of combinations of comorbidities (e.g. LC and CHD would both become less likely in the event of smoking cessation). Improvements in the QoL experienced by some of those people with more than one comorbidity who remain abstinent would, therefore, be greater than the model predicts; QALY gains from eliminating such comorbidity combinations would be greater than predicted within the model and interventions would appear even more cost-effective.
One interesting aspect of this model is that, as recommended by the UK Treasury, all future costs and health outcomes have been discounted at 3.5% per year. However, it should be noted that the costs of RPIs are borne in the immediate future (i.e. undiscounted), while the benefits are likely to be accrued in the long-term future and hence, discounted. With discounting at 3.5% rate, one QALY today is equivalent to around 0.25 QALYs in 40 years’ time and health gains experienced at this future time are, therefore, reduced fourfold. Recommended discount rates vary between different countries and even within countries over time; NICE’s recommended rate for health outcomes was 1.5% until 2003. Because the costs of the interventions are accrued in the short-term and the benefits (i.e. reduced comorbidities) occur in the future, the results of this analysis will underestimate the undiscounted outcomes.
Summary
Our model shows that bupropion, NRT and varenicline (based on one trial) used by recently abstinent quitters to prevent relapse to smoking are cost-effective when, compared with ‘no intervention’ and judged against a ‘willingness-to-pay’ threshold of £20,000 per QALY. A direct comparison of the incremental cost-effectiveness of these treatments was not possible because data underpinning analyses were generally derived from mutually-exclusive trials, with insufficient data comparing interventions within trials to permit direct comparisons and any comparisons, therefore, must be indirect. All three of these pharmacological interventions for relapse prevention appear to have a similar magnitude of cost-effectiveness as smoking cessation-orientated interventions.
Chapter 5 Systematic review to derive abstinence curves for smokers attempting to stop smoking with the use of evidence-based treatments
Introduction
Understanding relapse patterns for smokers attending the NHS SSS is necessary to help estimate the likely impact that effective RPIs might have, if introduced into routine NHS SSS care. Unfortunately, routinely-available NHS SSS data cannot be used to accurately describe such relapse patterns because, in the NHS, smoking status is recorded at very few times after smokers’ start quit attempts. 126,127 However, smokers attempting to quit using evidence-based cessation treatments are likely to have similar relapse behaviours and their patterns can be used as a proxy for those of smokers who use NHS support to assist cessation attempts.
Relapse patterns among smokers who attempt smoking cessation without support, the ‘natural history’ of relapse, have been described; most such untreated smokers return to smoking within 8 days of starting a quit attempt and only 3–5% are still abstinent at 6–12 months. 128 However, the patterns of relapse among smokers who use optimal, evidence-based treatments, such as those delivered through the NHS SSS, to help them try stopping have not been clearly defined. Individual trials have presented abstinence and/or relapse rates, but no systematic attempt has been made to locate and synthesise data from these diverse studies. Supported quit attempts are more successful than unsupported ones;129 trials of pharmacotherapies and behavioural support for smoking cessation and their delivery in routine health-care result in higher 1 year abstinence rates of around 25%130–133 and 18%127 respectively. Relapse is, therefore, less frequent in supported quit attempts, but we currently do not know how smoking cessation treatments might exert effects on relapse. For example, cessation treatments may make relapse less frequent without affecting the actual process of relapse itself; in this situation, variations over time in relapse rates of untreated and treated smokers would be identical and, hence, the shapes of relapse curves for both would be the same. However, the proportion of smokers remaining abstinent from smoking at any given time after quitting would be higher after cessation had been achieved with treatment. Alternatively, if cessation treatments affected the processes involved in relapse to smoking, then relapse curves for treated smokers would have different shapes to those derived for untreated ones.
Only two studies have investigated relapse patterns after cessation had been achieved, using evidence-based treatments. A systematic review investigated relapse to smoking after use of NRT, but did not adequately describe relapse patterns immediately after smokers’ quit dates when relapse rates are highest. 134 Also, a non-systematic review has, using data from a small number of trials, qualitatively compared relapse curves after cessation with NRT and behavioural support; the authors hypothesised that most variation in relapse patterns or rates of relapse happened in the very early stages of quit attempts and that such differences were attributable to different cessation treatments used. 135 Clearly more rigorous synthesis of available data would determine whether such hypotheses are valid. To investigate patterns of relapse among smokers who have used cessation support, we conducted a systematic review to determine the timing and rate of relapse among smokers who attempt to stop smoking while accessing evidence-based support, and derived relapse curves reflecting their experiences. We define ‘relapse’ in this chapter to mean any return to smoking after quit date.
Aim
To derive ‘relapse to smoking’ (abstinence) curves for smoking cessation attempts made with NHS SSS using (1) prolonged and (2) point abstinence from smoking as outcome measures.
Objectives
-
To systematically search for and identify RCTs in which intervention group smokers receive evidence-based interventions similar to those provided by NHS SSS, including trials of NRT, bupropion varenicline and nortriptyline delivered with behavioural support.
-
To select from identified trials, those including sufficient data for accurate relapse curves, reflecting relapse patterns in the first year after smokers’ quit dates, to be drawn; those involving adult smokers with a clearly reported quit date and at least 12 months’ subsequent follow-up, with smoking status being recorded at least three times in the first month after quitting.
-
To extract and synthesise smoking status data from intervention groups of selected trials, above enabling relapse curves to be drawn.
Methods
Rationale for studies’ inclusion
We anticipated that the most robust data on the frequency of relapse by smokers in quit attempts would be collected during clinical trials and used the following considerations to decide which clinical trials were appropriate for consideration.
Interventions
We wanted to derive a relapse curve for smokers receiving optimal, evidence-based smoking cessation support and used Cochrane Collaboration systematic review evidence to define this. Cochrane reviews show that behavioural support provided outside of routine clinical care is effective for smoking cessation136,137 as are NRT,138 bupropion,139 varenicline140 and nortriptyline. 139 Consequently, we defined optimal, evidence-based smoking cessation support as the following two interventions combined, being provided in addition to routine clinical health care: (1) if behavioural support, defined as either the duration of time spent with a smoker (including assessment for trial entry), exceeded 30 minutes at the initial consultation and the number of further assessment and re-enforcement visits exceeded two or at least four appointments in total occurred in which brief support (5–10 minutes’ duration) was given plus (2) any single pharmacotherapy treatment for which there was Cochrane review evidence for efficacy and a side effect profile which has enabled it to have widespread use in at least one country; eligible pharmacotherapies were NRT, bupropion, varenicline and nortriptyline. We excluded trials that assessed relapse prevention.
Relapse curves
Although we wanted to derive a ‘survival’-type relapse curve, we anticipated some difficulty in obtaining data for this. A ‘survival’-type relapse curve uses the exact date that a smoker returns to smoking to plot the proportion remaining abstinent from smoking over time,128,141 but such plots or the data to draw them are not often reported. 128 Many trials either provide line graphs connecting the percentage or number of participants still abstinent at different time points or data with which these can be drawn142 and due to a lack of ‘survival’-type relapse curves and data in trial reports, these were used in a recent attempt to derive a relapse curve for ‘untreated’ smokers. 128 Consequently, for estimating our relapse curve, we decided to use trial reports which included both types of curve or data from which either could be derived.
Smoking outcomes and frequency of ascertainment
In smoking cessation trials, participants usually set a target quit date and have abstinence from smoking recorded as point prevalence or prolonged measures143 at set time points afterwards; trials do not usually identify those participants who fail to stop smoking on the intended quit date (i.e. who quit for < 24 hours). Ideally, for constructing relapse curves, one would use a continuous or prolonged measure of smoking abstinence, but we anticipated that, in many trials, such measures would not be available and repeated point prevalence was more likely to be recorded at multiple follow-up points. We therefore decided to use trials which reported either prolonged or point prevalence abstinence from smoking, but present curves for these separately. Also, we anticipated, as has been found in ‘untreated’ smokers, that a large proportion of relapse would occur soon into any quit attempt,128 so we sought trials which ascertained smoking status at least three times in the month following smokers’ quit dates (preferably recorded at 2, 3 and 4 weeks after the start of treatment) and which had a final follow-up point at least 12 months after randomisation by which time most relapse to smoking would have occurred.
Process for identifying studies
The Cochrane Database of Systematic Reviews was searched in December 2009 to identify all reviews that potentially assessed the impact of smoking cessation treatments using the term ‘smoking cessation’. Forty-one systematic reviews were identified, of which 12 focused on pharmacotherapies for smoking cessation. 138–140,144–152 The 12 systematic reviews were screened to identify studies that assessed specific pharmacotherapies with evidence of effectiveness. The full texts of the papers identified from the included Cochrane reviews were then screened independently by two authors (JL-B and SA or AMcN and TC) using a specially designed data extraction form to assess whether they fulfilled the pre-specified inclusion criteria (see Box 7, Figure 16).
RCTs
Types of participantsAdult daily smokers with a clearly defined quit date
Types of interventionsIntensive behavioural support [defined as either the duration of time spent with a smoker (including assessment for the trial) exceeded 30 minutes at the initial consultation and the number of further assessment and re-enforcement visits exceeds two; or a large number of visits to clinic/trial centre (at least four) where often brief (5–10 minutes) support is given over an extended period during treatment and follow-up], in addition to NRT, bupropion, varenicline, or nortriptyline
Frequency of smoking outcome ascertainmentA minimum follow-up period of 12 months and at least three follow-up points in the first month after quit date
Nature of smoking outcomesSelf-reported, prolonged or point prevalence abstinence from smoking between a quit date and follow-up points, where possible verified by biochemical assessment
FIGURE 16.
Flow chart for included studies.
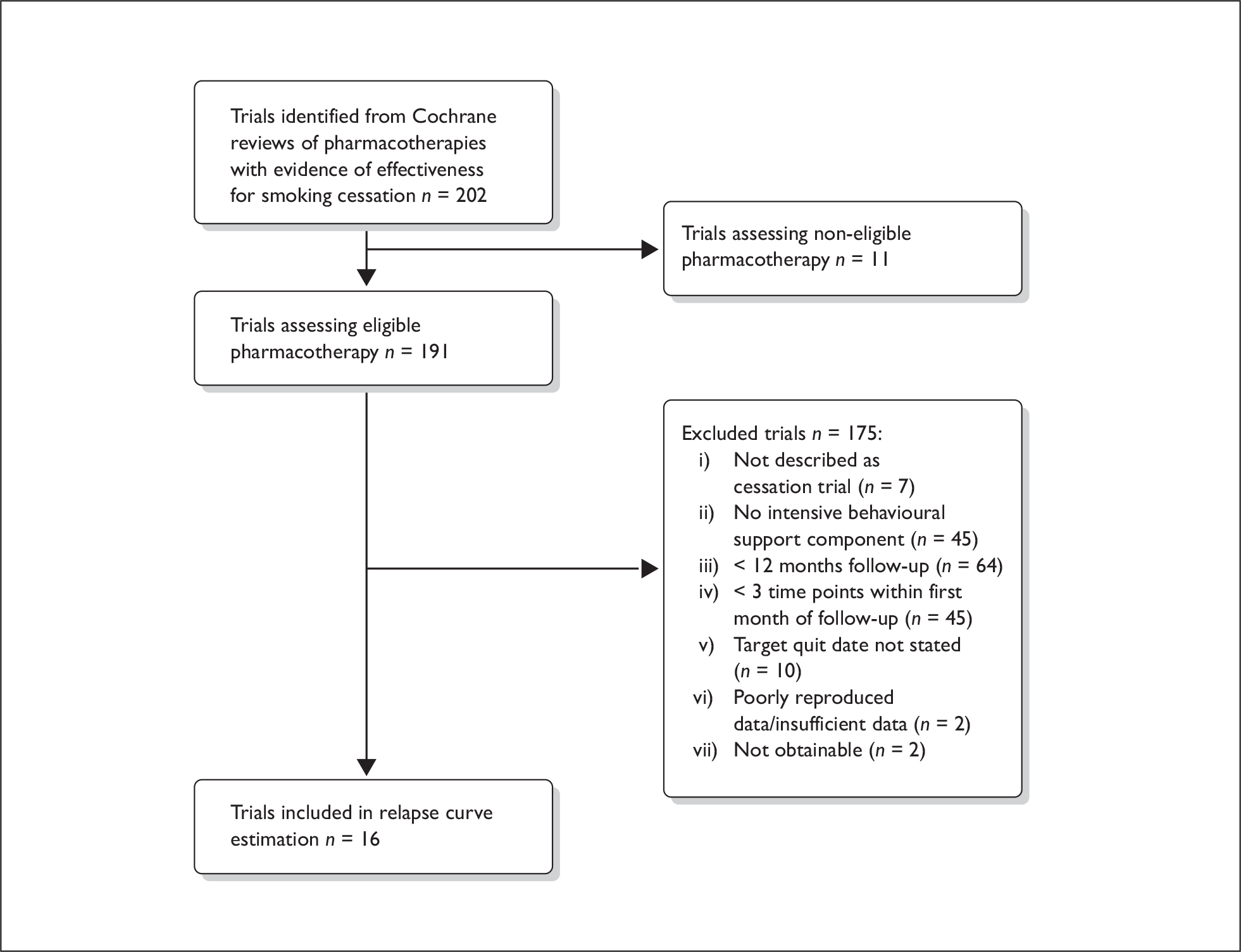
Assessment of methodological quality
Two authors (JL-B and SA) independently assessed the methodological quality of the eligible primary trials. The quality assessment for each trial included an evaluation of the method of generation of the randomisation sequence, the method of allocation concealment, whether blinding was used, percentage of participants lost to follow-up in the treatment group, and whether the participants were analysed using the intention to treat principle.
Data extraction
Two authors (JL-B and SA) performed data extraction independently and any differences were resolved through discussion. To derive curves for relapse to smoking by smokers using optimal, evidence-based smoking cessation treatments (as defined above), the following data were extracted from the arms of all included trials in which participants used such support:
-
(a) Where survival curves were reported, these were converted to abstinence rates at the pre-specified time points using visual assessment.
-
(b) Proportion of trial participants reporting continuous abstinence from smoking at all pre-specified time points between quit date and final follow-up.
-
(c) Proportion of trial participants reporting point abstinence from smoking at pre-specified time points between quit date and final follow-up.
-
(d) Number enrolled into the pharmacotherapy treatment group at randomisation.
The standard error for the prevalence of abstinence from smoking was estimated using the following formula:
If possible, missing data were obtained by contacting the authors of the primary papers. One author (JL-B) entered the data, and double-checking was performed by another author (SA).
Statistical analysis
Meta-analyses were performed to calculate a weighted prevalence of abstinence in the cessation treatment groups across trials using a random effect model (DerSimonian and Laird model) at each pre-specified time point to allow for heterogeneity being anticipated between the studies. The results are presented as prevalence of abstinence estimates with 95% CIs. Statistical heterogeneity between the trials was quantified using I2. 153 Separate pooled analyses were conducted based on the method used to report abstinence from smoking (point prevalence or continuous abstinence) were performed. Sensitivity analyses were conducted to assess the effect of excluding trials which yielded heterogeneous findings. The pooled estimates were then plotted to derive relapse curves for prolonged/continuous abstinence, and abstinence curves for point prevalence abstinence. Meta-analyses were conducted using review manager 5.
Results
Three Cochrane systematic reviews that assessed pharmacotherapy trials for evidence of effectiveness were identified;138–140 these included 202 articles and provided strong evidence that NRT, bupropion, varenicline and nortryptiline are all effective for smoking cessation (Box 7, Figure 16). Eleven trials were excluded due to having assessed a pharmacotherapy for which there was no evidence of effectiveness or one with a side effect profile that precluded its widespread use in at least one country (fluoxetine, n = 2; paroxetine, n = 1; sertraline, n = 1; moclobemide, n = 1; selegilline, n = 2; venlafaxine, n = 1; cytisine, n = 1;) or having assessed combinations of cessation treatments for which there was no evidence of effectiveness (n = 2). From the remaining 191 studies, 175 were excluded, in the following order, for not being described as a cessation trial (n = 7), not incorporating an intensive behavioural support component (n = 45), not having at least 12 months follow-up (n = 64), not having at least three time points measured in the first month since quit date (n = 45), not having stated using a target quit date (n = 10), insufficient/poorly reproduced data presented to allow data extraction (n = 2), or not being obtainable through interlibrary loan (n = 2). Thus 16 RCTs were included130–133,154–165 (Table 32, Figure 17) and 8679 participants were included in analyses. Ten trials were conducted in the USA, one in the UK, three in Iceland, one in Japan, and the remaining study was conducted in both the UK and the USA.
| Trial | Pharmacotherapy and dose | Duration of pharmacotherapy treatment | Setting, number and characteristics of participants | Time points used within first month of follow-up | Verification method for abstinence | Ascertainment of abstinence | ||
|---|---|---|---|---|---|---|---|---|
| Blondal et al. (1997)160 | NRT: 1-mg nicotine vapour maximum 5 doses/day | Recommended 3-month use | Iceland, n = 79 (40 male), mean (range) age = 42 years (22–67), mean (range) CPD = 26 (4–50), mean (range) FTQ score = 7.1 (3–10), mean (range) exhaled CO (p.p.m.) = 29 (3–80) | 6 days | 15 days | 22 days | CO < 10 p.p.m. | Continuous |
| Blondal et al. (1999a)132 | NRT: 0.5-mg nicotine spray/dose and 15 mg patch |
Spray: 1 year Patch: 5 months |
Iceland, n = 120 (43 male), mean (range) age = 41 years (23–62), mean (SD) grammes tobacco per day = 25.6 (15.7), mean FTQ score = 5.7, mean (SD) exhaled CO (p.p.m.) = 24.6 (12.3) | 1 day | 15 days | 43 days | CO < 10 p.p.m. | Continuous |
| Blondal et al. (1999b)133 | NRT: 15-µg nicotine vapour 6–12 times/day | Recommended maximum of 6 months | Iceland, n = 52 (21 male), mean (range) age = 42 years (25 –63), CPD mean (SE) = 29 (1) mean (SE) FTND = 6.5 (0.22) | 15 days | 22 days | 43 days | CO < 10 p.p.m. | Continuous |
| Gonzales et al. (2001)155 | Bupropion SR: 150 mg twice/day | 12 weeks | USA, n = 226 (48% female), mean (SD) age 44.5 years (11.8), mean (SD) FTQ = 7.0 (1.7) | 2 weeks | 3 weeks | 4 weeks | CO ≤ 10 p.p.m. | 7-day PP (only reports continuous at 12 months) |
| Gonzales et al. (2006)154 |
Varenicline: 1 mg twice/day Bupropion SR: 150 mg twice/day |
12 weeks |
US study Varenicline arm: n = 352 (176 male – 50%), mean (SD) age = 42.5 years (11.1), mean (SD) CPD = 21.1 (9.47), mean (SD) FTND = 5.18 (2.16) Bupropion arm: n = 329 (192 male – 58.4%), mean (SD) age = 42.0 years (11.7), mean (SD) CPD = 21.0 (8.52), mean (SD) FTND = 5.19 (2.08) |
2 weeks | 3 weeks | 4 weeks | CO < 10 p.p.m. | 7-day PP |
| Hurt et al. (1994)161 | NRT: 22-mg patch | 8 weeks | USA, n = 120 (51.7% female), mean (SD) age = 42.8 years (11.1), mean (SD) CPD = 28.8 (9.4), mean (SD) FTQ = 7 (1.8), FTND = 6.3 (2), mean (SD) exhaled CO (p.p.m.) = 28.1 (11.7) | 2 weeks | 3 weeks | 4 weeks | CO ≤ 8 p.p.m. | 7-day PP |
| Hurt et al. (1997)162 |
Bupropion SR: 50 mg twice/day 150 mg once/day 150 mg twice/day |
7 weeks |
US study 50 mg twice/day arm: n = 153 (58.2% female), mean (SD) age = 44.1 years (10.5), mean (SD) CPD = 26.2 (8.5), mean (SD) FTQ = 7.3 (1.6) 150 mg once/day arm: n = 153 (50.3% female), mean (SD) age = 42.3 years (11.3), mean (SD) CPD = 27.5 (9.6), mean (SD) FTQ = 7.3 (1.6) 150 mg twice/day arm: n = 156 (50.6% female), mean (SD) age = 45.0 years (11.8), mean (SD) CPD = 27.2 (10.8), mean (SD) FTQ = 7.1 (1.7) |
2 weeks | 3 weeks | 4 weeks | CO ≤ 10 p.p.m. | Continuous (first month), then 7 day PP |
| Jarvis et al. (1982)163 | NRT: 2-mg gum | Recommended minimum of 3 months | UK, n = 58 (29/50% male), mean age = 41.0 years, mean CPD = 30.9. No nicotine addiction measure reported | 1 week | 2 weeks | 4 weeks | Not used | PP (days not specified) |
| Jorenby et al. (1999)164 |
NRT: 21-mg patch Bupropion SR: 150 mg twice/day |
Patch: 8 weeks Tablets: 9 weeks |
US study NRT arm: n = 244 (51.6% female), mean (SD) age 44.0 years (10.9), mean (SD) CPD = 26.5 (9.4), mean (SD) FTQ = 7.4 (1.7), mean (SD) exhaled CO (p.p.m.) = 28.3 (9.9) Bupropion arm: n = 244 (51.6% female), mean (SD) age = 42.3 years (10.2), mean (SD) CPD = 25.5 (8.8), mean (SD) FTQ = 7.4 (1.6), mean (SD) exhaled CO (p.p.m.) = 28.4 (11.1) |
2 weeks | 3 weeks | 4 weeks | CO < 10 p.p.m. | PP (days not specified) |
| Jorenby et al. (2006)130 |
Bupropion SR: 150 mg twice/day Varenicline: 1 mg twice/day |
12 weeks |
US study Bupropion arm: n = 342 (60.2% male), mean (SD) age = 42.9 years (11.9), mean (SD) CPD = 21.8 (8.7), mean (SD) FTND = 5.39 (2.19) Varenicline arm: n = 344 (55.2% male), mean (SD) age = 44.6 years (11.4), mean (SD) CPD = 27.1 (11.5), mean (SD) FTND = 5.39 (2.21) |
2 weeks | 3 weeks | 4 weeks | CO ≤ 10 p.p.m. | 7-day PP |
| Nakamura et al. (2007)159 |
Varenicline: 0.25 mg twice/day 0.5 mg twice/day 1 mg twice/day |
12 weeks |
Japan study 0.25 mg twice/day arm: n = 153 (93 male – 72.7%), mean (SD) age = 40.2 years (12.3), mean (SD) CPD = 24.9 (10.3), mean (SD) FTND = 5.6 (2.1) 0.5 mg twice/day arm: n = 128 (91 male – 71.1%), mean (SD) age = 39.0 years (12.0), mean (SD) CPD = 23.8 (10.5), mean (SD) FTND = 5.5 (2.1) 1.0 mg twice/day arm: n = 130 (103 male – 79.2%), mean (SD) age = 40.1 years (11.6), mean (SD) CPD = 24.0 (9.8), mean (SD) FTND = 5.4 (2.1) |
2 weeks | 3 weeks | 4 weeks | CO ≤ 10 p.p.m. | 7-day PP |
| Oncken et al. (2006)156 |
Varenicline: 0.5 mg twice/day (non-titrated) 0.5 mg twice/day (titrated) 1.0 mg twice/day (non-titrated) 1.0 mg twice/day (titrated) |
12 weeks |
US study 0.5 mg twice/day (non-titrated) arm: n = 129 (45.0% male), mean (SD) age = 42.9 years (10.1), mean (SD) CPD = 20.9 (8.1), mean (SD) FTND = 5.5 (2.0) 0.5 mg twice/day (titrated) arm: n = 130 (53.1% male), mean (SD) age = 43.5 years (10.5), mean (SD) CPD = 21.3 (8.1), mean (SD) FTND = 5.4 (1.9) 1.0 mg twice/day (non-titrated) arm: n = 129 (48.8% male), mean (SD) age = 43.7 years (10.0), mean (SD) CPD = 20.8 (10.1), mean (SD) FTND = 5.5 (2.0) 1.0 mg twice/day (titrated) arm: n = 130 (48.5% male), mean (SD) age = 42.2 years (10.7), mean (SD) CPD = 20.9 (7.0), mean (SD) FTND = 5.3 (2.1) |
2 weeks | 3 weeks | 4 weeks | CO ≤ 10 p.p.m. | 7-day PP |
| Piper et al. (2007)131 | Bupropion: 150 mg twice/day plus placebo gum | 8 weeks | USA, n = 224 (135 female – 60.3%), mean (SD) age = 42.3 years (11.4), mean (SD) CPD = 23.4 (10.8), mean (SD) FTND = 5.7 (2.04), mean (SD) exhaled CO (p.p.m.) = 27.3 (11.2) | 2 weeks | 3 weeks | 4 weeks | CO at 6 and 12 months only | 3 consecutive day PP |
| Schneider et al. (1983)165 | NRT: 2-mg gum | Ad lib, up to 1 year | USA, n = 30 (17 female – 57%), mean age = 40 years, mean CPD = 35. No nicotine addiction measure reported | 2 weeks | 3 weeks | 4 weeks | CO at 4, 6 and 12 months only | PP (days not specified) |
| Shiffman et al. (2002)157 |
NRT: 4-mg gum NRT: 2-mg gum |
12 weeks, but could extend to 24 weeks if required |
UK and US study 4-mg gum arm: n = 450 (43.3% male), mean (SD) age = 44.28 years (11.78), mean (SD) CPD = 26.3 (11.2), mean (SD) FTND = 6.1 (1.8), mean (SD) exhaled CO (p.p.m.) = 27.16 (13.83) 2-mg gum arm: n = 459 (42.9% male), mean (SD) age 41.11 years (12.06), mean (SD) CPD = 17.7 (8.2), mean (SD) FTND = 2.6 (1.8), mean (SD) exhaled CO (p.p.m.) = 19.36 (12.02) |
2 weeks | 3 weeks | 4 weeks | CO ≤ 10 p.p.m. | Continuous, had to be abstinent during first 2 weeks of follow-up to be eligible as abstinent at further follow-up |
| Williams et al. (2007)158 | Varenicline: 1 mg twice/day | 52 weeks | USA, n = 251 (127 male – 50.6%), mean (SD) age 48.2 years (12.3), mean (range) CPD = 23.2 (10–90), mean (SD) FTND = 5.50 (2.07) | 2 weeks | 3 weeks | 4 weeks | CO ≤ 10 p.p.m. | 7-day PP |
FIGURE 17.
Prevalence of continuous/prolonged abstinence after using NRT for smoking cessation in addition to behavioural support using a meta-analysis of RCTs. Data are presented as prevalence of abstinence and are pooled using random effect models. Squares represent the point estimate and the horizontal lines denote 95% CIs. Size of the data markers correspond to the weight of the study in the meta-analysis.
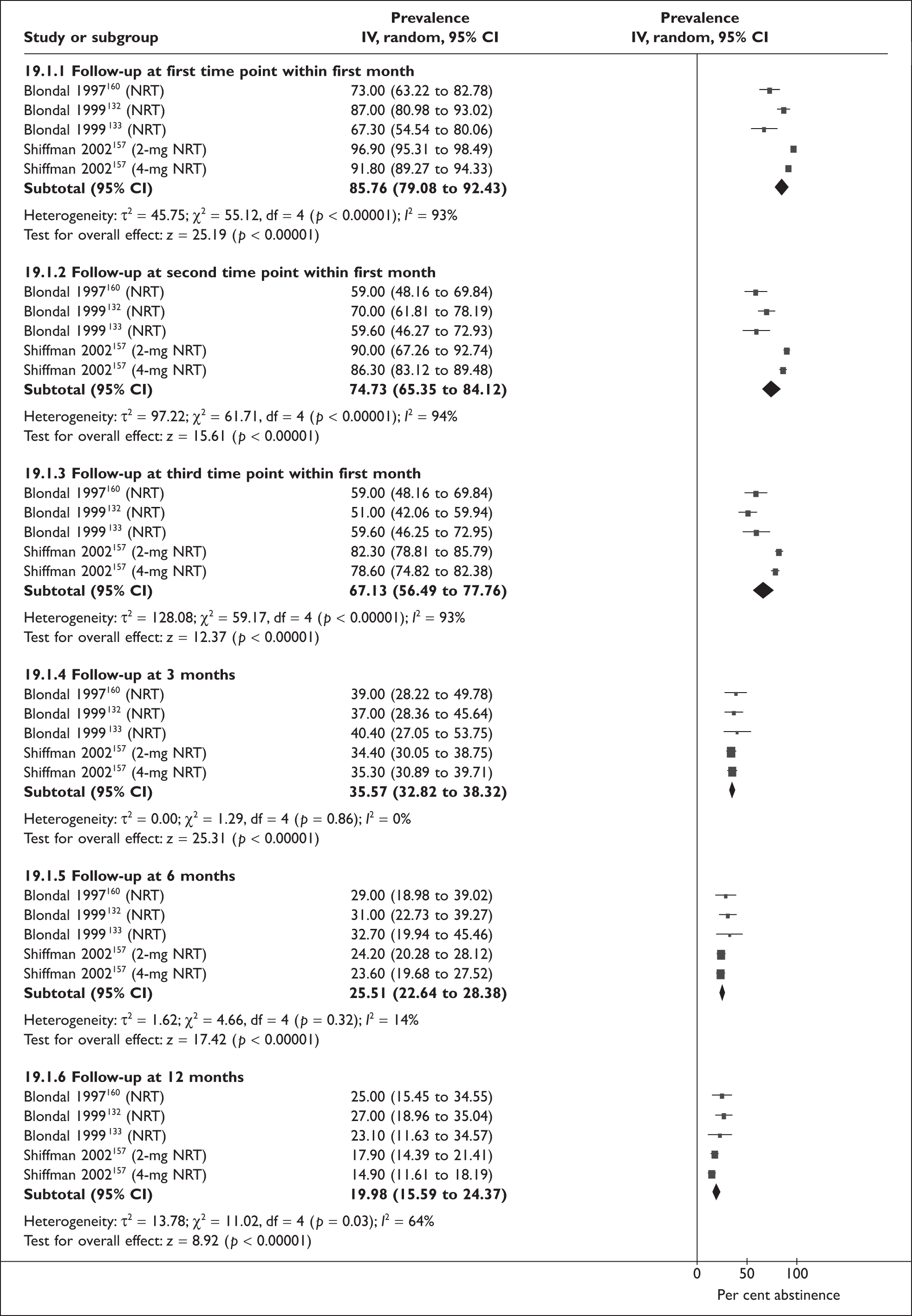
All included studies were published and assessed the individual effects of NRT,132,133,157,160,161,163–165 bupropion,130,131,154,155,162,164 or varenicline;130,154,156,158,159 no eligible nortriptyline studies were identified. Eight trials used a two-arm, parallel group design and eight had multiple arms; four of which assessed the effect of two cessation treatments130,131,154,164 and four trials were dose-ranging studies. 156,157,159,162
Definition of abstinence
The majority of the included trials used point prevalence estimates to ascertain abstinence from smoking; 3-day point prevalence was used by one trial,131 7-day point prevalence by six,130,154,156,158,159,161 and three did not report a minimum abstinence period required for point prevalence to be considered achieved. 163–165 Four trials used continuous abstinence from quit date,132,133,157,160 one trial used continuous abstinence for the first month of follow-up followed by 7-day point prevalence,162 and the remaining trial used 7-day point prevalence for all time points, except at 12 months when prolonged abstinence was reported. 155 None of the four trials reporting continuous abstinence reported point prevalence abstinence. 132,133,157,160 All of the included studies used biochemical verification to confirm non-smoking status.
Behavioural support
In addition to drug treatments, all included trials provided behavioural support (see definition above) outside of routine clinical care; four used group-based sessions and remaining studies used individual consultations to deliver this support. Further details are given in Table 33.
| Trial | Details of behavioural support |
|---|---|
| Blondal et al. (1997)160 | Group sessions. Each session 60 minutes. Six sessions over 43 days. Supportive treatment emphasised change in attitude towards smoking, discussion of various methods to remain smoker free and how to cope with difficult situations. Instructional booklet on how to stop smoking |
| Blondal et al. (1999)132 | Group sessions. Supportive meetings attended on days 1, 8, 15 and 22 days post-quit |
| Blondal et al. (1999)133 | Group sessions. Each session 60 minutes. Five sessions up to day 22 post-quit. Support delivered by two therapists experienced in smoking cessation. Change in self-image from a smoker to a non-smoker was emphasised and coping strategies |
| Gonzales et al. (2001)155 | Individual sessions. Brief counselling from trained research counsellors based on a standard intervention to encourage smoking cessation and to prevent relapse for nine visits to week 12 |
| Gonzales et al. (2006)154 | Individual sessions. Up to 10 minutes of brief standardised counselling to assist in problem solving and skills training for relapse prevention for 12 weeks |
| Hurt et al. (1994)161 | Individual sessions. Brief counselling by study nurse then weekly telephone calls for counselling to week 12, further follow-up visits with counselling made at 6, 9 and 12 months |
| Hurt et al. (1997)162 | Individual sessions. Each session 10–15 minutes lead by study assistant |
| Jarvis et al. (1982)163 | Group sessions. Each session 60 minutes. Weekly meeting for 6 weeks |
| Jorenby et al. (1999)164 | Individual sessions. Each session up to 15 minutes. Weekly sessions. Motivation, identification of smoking triggers, coping responses, weight management, use of medications, using standardised treatment. Supportive telephone call from counsellor approximately 3 days post-quit date |
| Jorenby et al. (2006)130 | Individual sessions. Up to 10 minutes of brief smoking-cessation counselling at each clinic visit for 12 weeks. Up to 5 minute telephone call 3 days post-target quit date |
| Nakamura et al. (2007)159 | Individual sessions. Up to 10 minutes of brief smoking-cessation counselling at each clinic visit for 12 weeks. Up to 5 minute telephone call 3 days post-target quit date |
| Oncken et al. (2006)156 | Individual sessions. Up to 10 minutes of brief smoking-cessation counselling at each clinic visit for 12 weeks. Up to 5 minute telephone call 3 days post-target quit date |
| Piper et al. (2007)131 | Individual sessions. Participants attended one session per week for 4 weeks then two more sessions every other week. Brief counselling at quit date and first post-quit session for a total of three 10-minute counselling sessions over 3 weeks |
| Schneider (1983)165 | Individual sessions. Each session approximately 45 minutes. Clinic support system. Discussed daily progress and problems |
| Shiffman et al. (2002)157 | Individual sessions. Each session 5–10 minutes for first four weekly visits. Study co-ordinator reviewed behavioural tips and directing participant’s attention to user guide |
| Williams et al. (2007)158 | Individual sessions. Each session up to 10 minutes of brief counselling at randomisation and at each visit |
Risk of bias in included studies
Of the 16 included trials, eight reported methods used to generate their randomisation sequence, with five using computer-generated lists,130,132,133,159,160 one stratified randomisation162 and two block randomisation. 131,154 Only seven studies reported using an adequate method for allocation concealment, using centrally performed systems. 130,132,133,154,155,159,160 Thirteen studies used double-blinding,130–133,154–157,159,160,162,163,165 all studies reported the proportion of loss to follow-up, and 11 stated using an intention-to-treat analysis. 130,131,154–159,161,162,164
Pooled estimates for prevalences of abstinence by treatment
Nine estimates of prevalence from eight studies contributed to a pooled analysis which assessed the prevalence of abstinence from smoking after using NRT as a smoking cessation treatment; five assessed continuous/prolonged abstinence and the remaining four assessed point prevalence abstinence. In studies that reported continuous/prolonged estimates, abstinence decreased over time from 86% (95% CI 79% to 92%) at the first time point in the first month to 20% (95% CI 16% to 24%) at 12 months’ follow-up (Table 34, Figure 18). Very high levels of heterogeneity were seen in the analyses conducted at the first three time points within the first month (I2 = 93%, 94% and 93%, respectively). In studies that reported point prevalence estimates, smaller reductions in abstinence were seen over time, which decreased from 51% (95% CI 42% to 61%) at the first time point in the first month to 30% (95% CI 17% to 42%; Figure 19). Substantially lower levels of heterogeneity were seen between the studies. Studies that reported continuous abstinence for all timings showed higher abstinence rates than studies which reported point prevalence abstinence rates. This is slightly unusual because point prevalence estimates for smoking cessation are usually higher than prolonged/continuous ones, however, these abstinence estimates were obtained from different trials, so comparisons are indirect and must be made cautiously because outcome differences may reflect the different characteristics of smokers within and settings of trials.
| Pooled point prevalence of abstinence (95% CI, I2) | ||||
|---|---|---|---|---|
| NRT | Bupropion sustained release | Varenicline | Combined | |
| Number of trials included | 5 | 6 | 5 | 16 |
| First time point within first month | 51.1 (41.7 to 60.5, I2 = 67%) | 34.7 (20.7 to 48.8, I2 = 98%) | 35.9 (32.2 to 39.6, I2 = 64%) | 47.0 (33.7 to 60.3, I2 = 99%) |
| Second time point within first month | 54.0 (46.0 to 62.0, I2 = 59%) | 37.0 (27.6 to 46.3, I2 = 95%) | 46.0 (43.1 to 48.8, I2 = 32%) | 49.8 (40.7 to 58.8, I2 = 98%) |
| Third time point within first month | 50.3 (45.2 to 55.5, I2 = 13%) | 37.3 (27.3 to 47.3, I2 = 95%) | 48.5 (45.0 to 52.0, I2 = 55%) | 49.0 (41.7 to 56.3, I2 = 97%) |
| 3 months | 40.8 (34.4 to 47.3, I2 = 40%) | 34.8 (29.1 to 40.4, I2 = 85%) | 55.3 (49.9 to 60.6, I2 = 82%) | 43.9 (39.6 to 48.2, I2 = 90%) |
| 6 months | 32.2 (21.8 to 42.6, I2 = 79%) | 27.2 (24.0 to 34.3, I2 = 57%) | 35.1 (30.6 to 37.0, I2 = 77%) | 30.6 (27.9 to 33.3, I2 = 77%) |
| 12 months | 29.3 (16.6 to 42.0, I2 = 87%) | 21.9 (16.6 to 27.2, I2 = 88%) | 31.4 (27.5 to 35.2, I2 = 69%) | 26.2 (22.9 to 29.4, I2 = 87%) |
FIGURE 18.
Prevalence of point abstinence after using NRT for smoking cessation in addition to behavioural support using a meta-analysis of RCTs. Data are presented as prevalence of abstinence and are pooled using random effect models. Squares represent the point estimate and the horizontal lines denote 95% CIs. Size of the data markers correspond to the weight of the study in the meta-analysis.
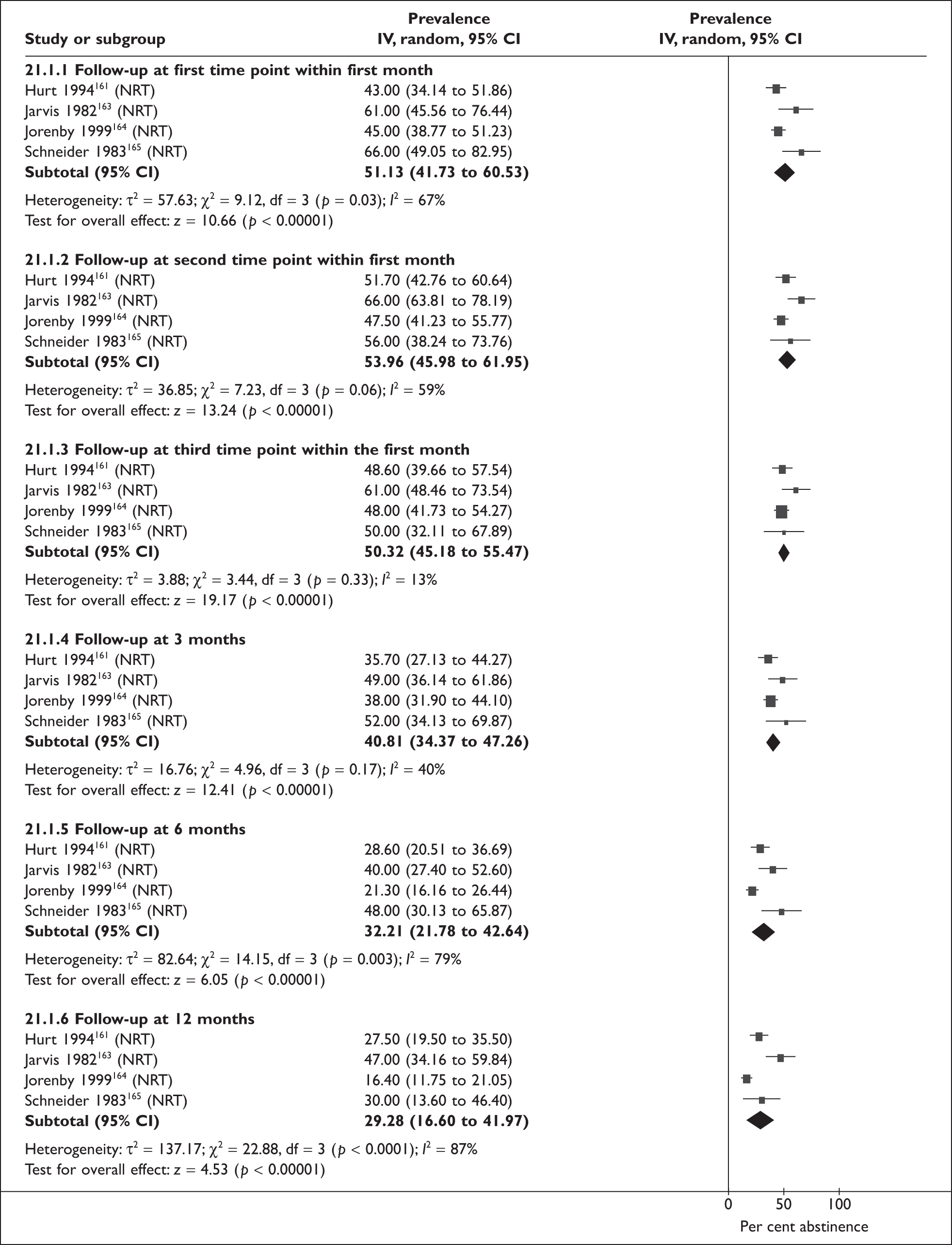
FIGURE 19.
Prevalence of point abstinence after using bupropion SR for smoking cessation in addition to behavioural support using a meta-analysis of RCTs. Data are presented as prevalence of abstinence and are pooled using random effect models. Squares represent the point estimate and the horizontal lines denote 95% CIs. Size of the data markers correspond to the weight of the study in the meta-analysis.
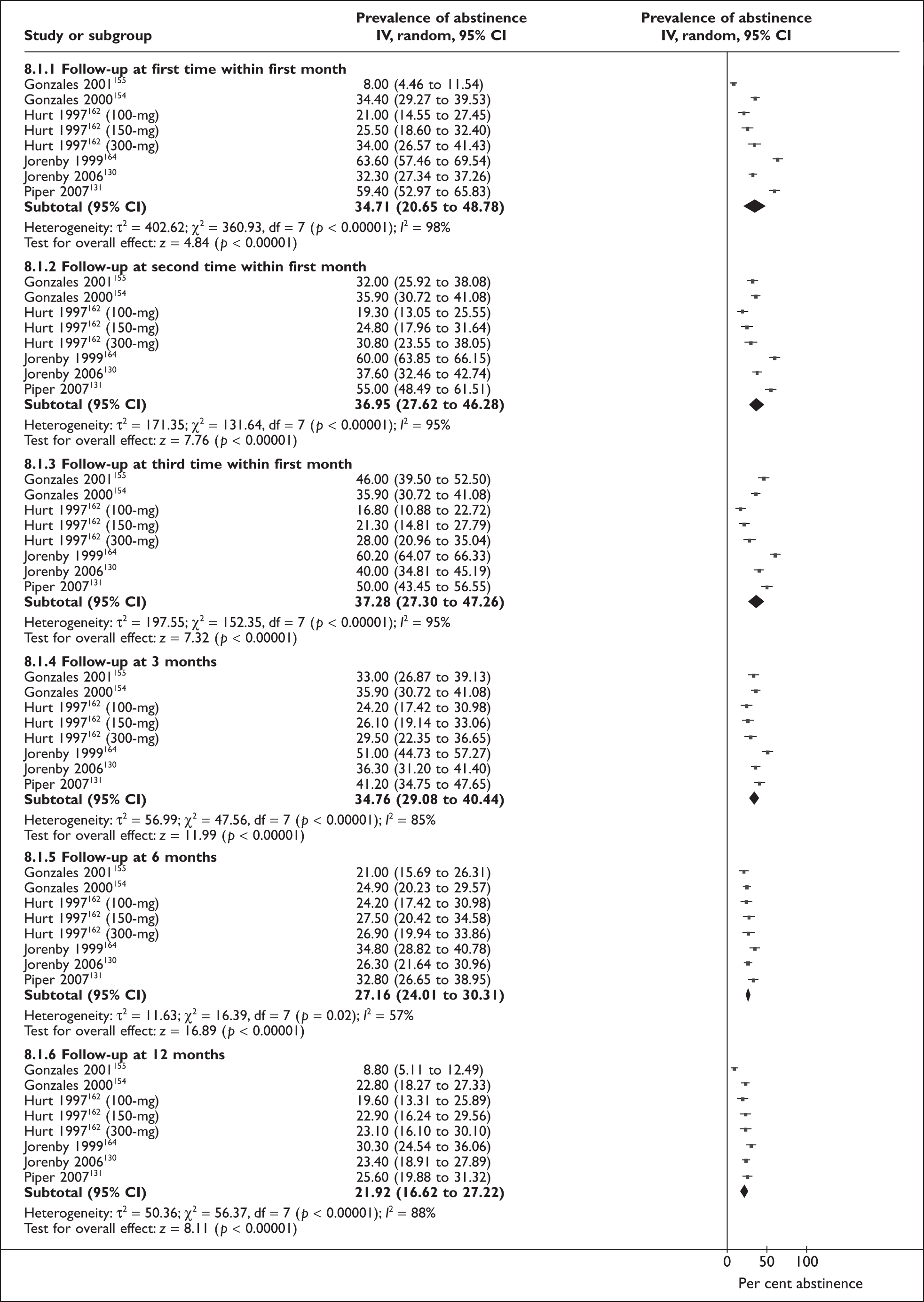
Six trials provided eight point prevalence of abstinence estimates that contributed to the pooled analysis assessing relapse after using bupropion; abstinence decreased over time from 35% (95% CI 21% to 49%) at the first time point within the first month to 22% (95% CI 17% to 27%) at 12 months’ follow-up (Figure 20). Very high levels of heterogeneity were seen in the analyses conducted for the three follow-up points within the first month, at 3 months’ and 12 months’ follow-up (I2 = 98%, 95%, 95%, 85%, 88%, respectively). A subgroup analysis based on studies that reported continuous abstinence for all timings could not be performed as all of the included studies reported point prevalence of abstinence only. However, when a sensitivity analysis based on excluding outlier results131,155,164 was performed, the estimates for pooled prevalence were generally less heterogeneous and abstinence rates were lower (first month: first time point = 30%, second time point = 30%, third time point = 29%; 3 months = 31%; 6 months = 26%; 12 months = 23%).
FIGURE 20.
Prevalence of point abstinence after using varenicline for smoking cessation in addition to behavioural support using a meta-analysis of RCTs. Data are presented as prevalence of abstinence and are pooled using random effect models. Squares represent the point estimate and the horizontal lines denote 95% CIs. Size of the data markers correspond to the weight of the study in the meta-analysis. BID, twice per day; NT, non-titrated; T, titrated.
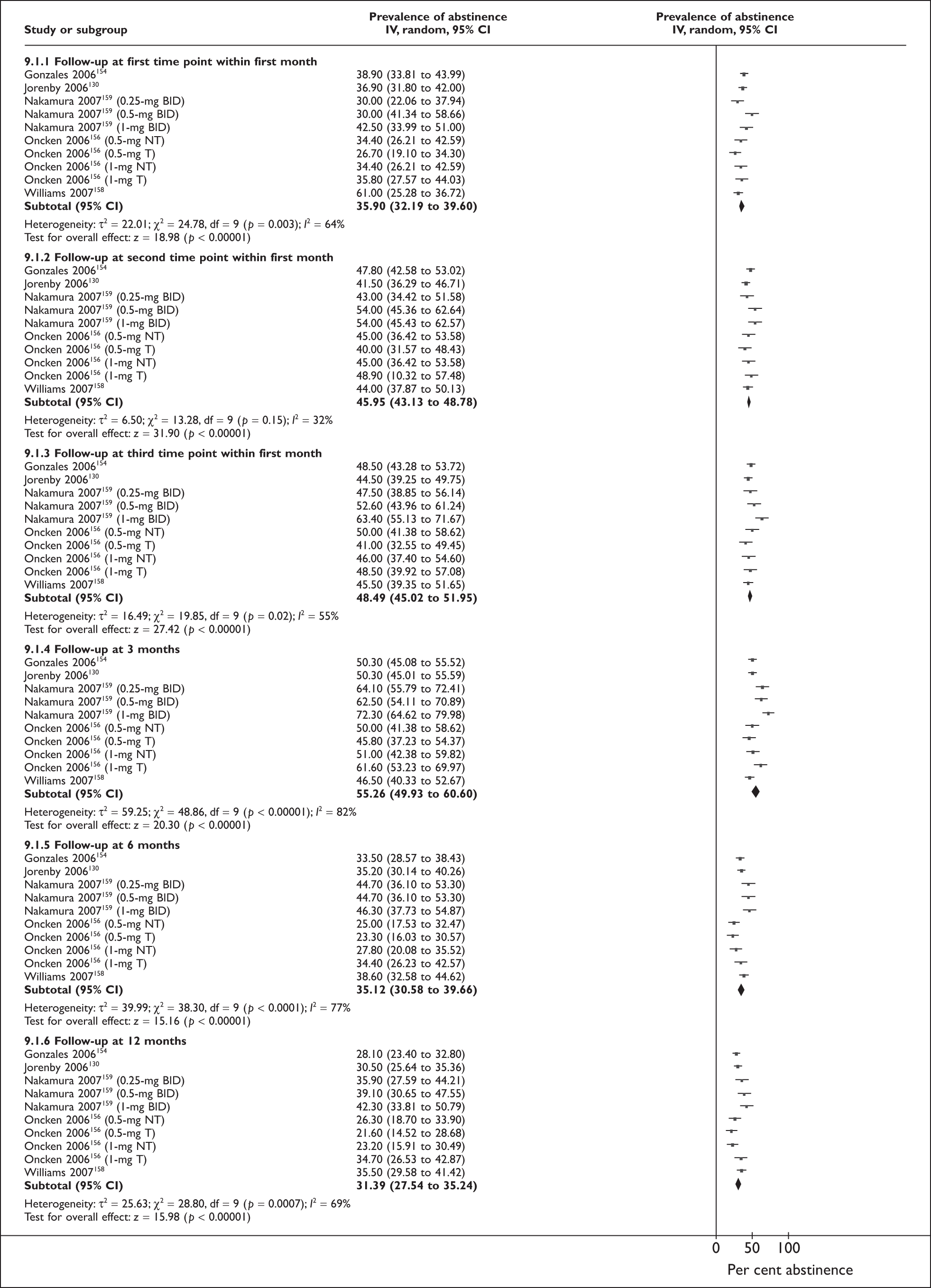
Five trials provided 10-point prevalence of abstinence estimates that contributed to the analysis-assessing relapse after varenicline use. Abstinence did not decrease appreciably over time; it was 36% (95% CI 32% to 40%) at the first time point within the first month and 31% (95% CI 28% to 35%) at 12-month follow-up (Figure 21) with moderate levels of heterogeneity in analyses. A sensitivity analysis based on methods of ascertainment of smoking cessation outcome was not possible because all studies reported only point prevalence abstinence, and a sensitivity analysis excluding ‘outliers’ was not performed as no studies were deemed to have outlier results.
FIGURE 21.
Abstinence curves (shown as line graph) in participants from the included trials of evidence-based smoking cessation treatments using pooled estimates of point prevalence of abstinence from meta-analyses of RCTs. Crosses represent the point estimates for NRT, squares represent the point estimates for bupropion, triangles represent the point estimates for varenicline, and stars represent the point estimate for the combined medications derived from the meta-analyses. Horizontal lines denote the 95% CIs for the combined medications estimate at each of the pre-specified points of follow-up.
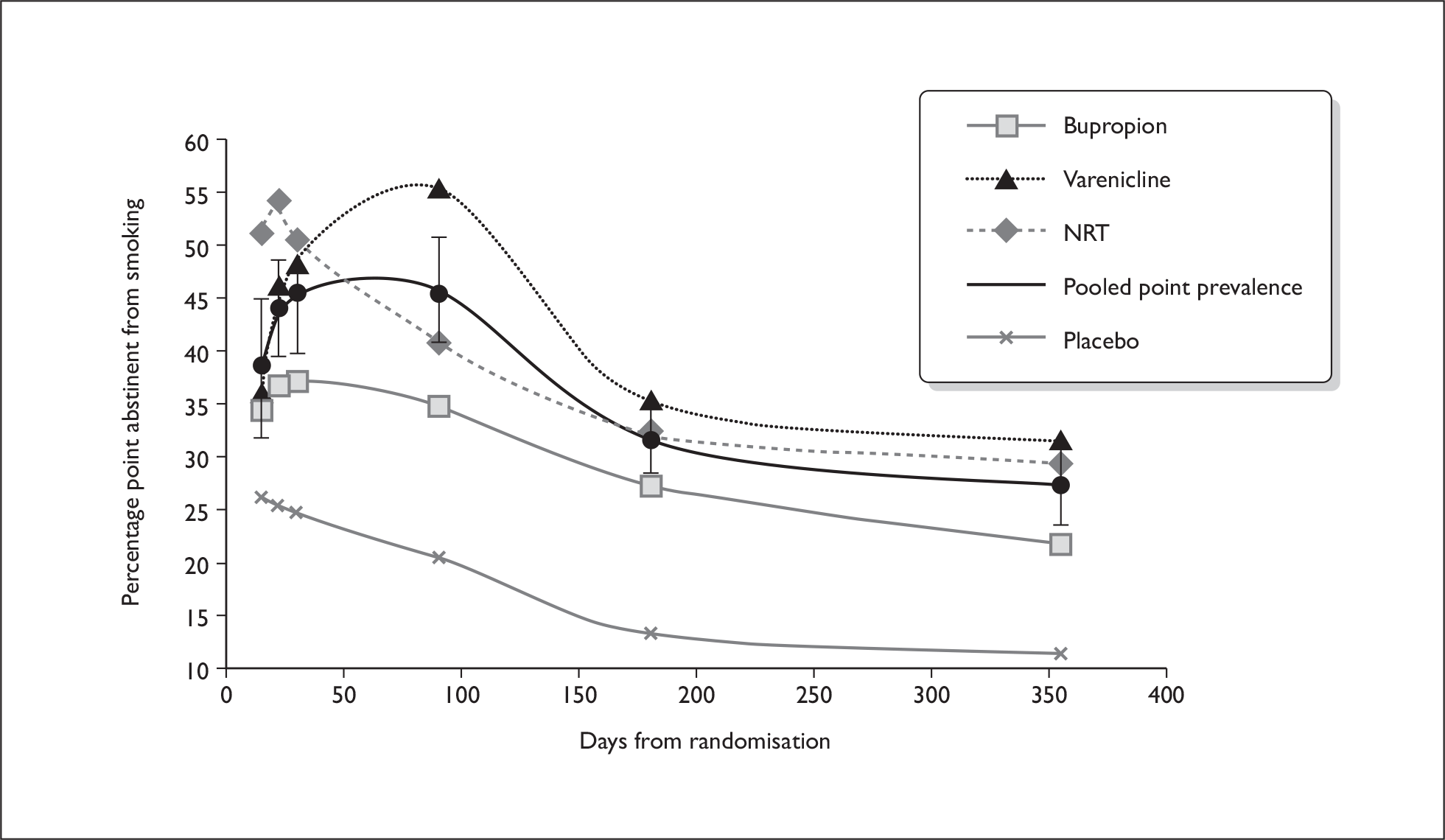
Comparison of relapse patterns, measured by point prevalence, for different cessation treatments
The smoking abstinence patterns for NRT, bupropion and varenicline, as measured by point prevalence estimation, differed markedly over the first 3 months after quitting, became similar after this and showed a similar pattern of steady decline from 6 months onwards (Figure 21). One caveat was that, when drawing smoking abstinence curves from point prevalence estimates, imputation of data between the discrete time points at which prevalence’s were obtained is necessary. However, Figure 21 summarises the best currently available data for considering smoking abstinence patterns after supported cessation attempts.
Treatment with NRT resulted in most abstinence at the first follow-up point after quitting; approximately 51% of those receiving NRT were abstinent at around 2 weeks into quit attempts, compared with approximately 35% of those receiving bupropion and varenicline. The abstinence rate with NRT then remained fairly constant, and much higher than with other treatments, for the rest of the first month after quitting, followed by a smooth decline for the remainder of the year. In contrast, the proportion abstinent with bupropion changed little over the initial 3 months and subsequently followed a near-identical pattern of decline to that with NRT. Abstinence patterns with varenicline were different again; varenicline treatment resulted in a sharp increase in the proportion abstinent within the first month of treatment followed by a slower rate of increase in abstinence until around 3 months, when over half were abstinent (55%). After 3 months, point prevalence abstinence rates after varenicline began declining and did so at a similar rate to those after treatment with on bupropion and NRT, but with higher overall abstinence rates recorded. This is demonstrated by the varenicline curve having a very similar shape to others after the 3-month point, but being higher in relation to the y-axis.
Discussion
We have described, for the first time, abstinence patterns over 12 months after quitting with NRT, bupropion or varenicline; the three cessation treatments used most frequently used by NHS SSS; combined with behavioural support. Abstinence rates differed markedly initially but became comparable after 3 months. For NRT, the complete abstinence curve followed a similar trajectory to untreated smokers’ relapse curves128 with highest abstinence rates at the very start of smokers’ quit attempts; for bupropion minimal smoking occurred before 3 months and, for varenicline, little return to smoking occurred in the whole 12-month period. Compared to untreated smokers’ curves,128 those derived in this study suggest that evidence-based cessation treatments postpone returning to smoking; returning to smoking continued throughout the first year of treated quit attempts but in untreated ones almost all returning to smoking occurs within 3 months.
Limitations
Comparisons across treatments require caution because most studies used only point prevalence measures to ascertain smoking status and few trials reported prolonged abstinence measures, such as continuous cessation between quit dates and follow-up points. Point prevalence measures can be more volatile than continuous or prolonged measures of abstinence and the latter are more appropriate for deriving relapse curves, however, in the absence of continuous outcome data being reported at all time points we have been restricted to using point prevalence to derive our abstinent curve. We have only been able to contrast curves derived from prolonged and point prevalence abstinence measures for NRT trials and curves presented are derived from different trials as, within individual studies, continuous and point prevalence outcome measures were often not reported for simultaneous follow-up points. However, apart from within the first month where an increase in abstinence was seen in the abstinence curves, the curves derived using these two different outcome measures had broadly similar shapes. When comparing the shapes of the abstinent curves derived using prevalence data, very different relapse patterns are seen within the first 3 months of quit attempts assisted by bupropion or varenicline as compared to NRT. This difference may be real and due to differences in the responses of patients to these treatments or perhaps in the characteristics of smokers using them. Another caveat is that 14 of the 16 included studies assumed participants with missing outcome data or who were lost to follow-up had returned to smoking; this could have had an impact on our findings by artificially lowering the abstinence rates at the later follow-up time points since the percentage of participants not completing the studies ranged from 0% to 50%, although a third of studies had less than 10% non-completers.
A further caveat is that no trials reported the proportion of participants who did not attempt to stop smoking on their quit date and none explicitly reported that patients must attempt cessation on their intended quit dates (though this is implied in many cessation studies). Consequently, by including in our analyses those who fail to stop smoking at all, our relapse curves may overestimate initial relapse rates at the outset of cessation attempts; future trials should consider reporting such data. Findings should be seen as preliminary due to observed heterogeneity between some prevalence estimates. By only including trials that satisfied Cochrane review standards, heterogeneity attributable to interventions employed is likely to have been minimised, but different doses of drug treatments and/or intensities of behavioural support may still have contributed towards this, as there were no striking differences in participants’ demographic characteristics or nicotine addiction levels to help explain it. We believe that most heterogeneity has arisen from trials’ use of slightly different follow-up time points within the first month after quitting which explains the more acceptable heterogeneity levels observed at the later, more uniform follow-up time points. We attempted to account for heterogeneity by using random effect models in analyses, though these methods may still result in confidence intervals which are too narrow and hence insufficiently conservative. 166 However, it is unlikely that bias was introduced into the meta-analysis since we identified eligible studies from published Cochrane reviews and included only relevant RCTs which collect data prospectively and are the most robust form of research evidence. Finally, the generalisibility of our findings to NHS SSS might be questioned; while all three pharmacotherapies studied are used frequently by NHS SSS, treatment protocols for the delivery of behavioural support are likely to differ and interventions used in clinical trials often demonstrate less effectiveness when translated into routine care.
A key finding of this review is that, irrespective of what happens in the very early stages of quit attempts, for all three treatments considered, substantial relapse occurs after 3 months and most cessation treatments will have been discontinued either prior to or at this time point. Eliminating relapse after 3 months could potentially increase 12-month quit rates by 13%, 14% and 19% for NRT, bupropion and varenicline respectively (estimates taken from Figures 2, 4 and 5 but are preliminary due to heterogeneity levels). This illustrates the potential impact of extending cessation treatment and complements the findings from Chapter 3 in which we demonstrated the efficacy, for smoking cessation, of extending the provision of smoking cessation medications beyond the usual acute cessation treatment period. Clearly, for the three treatments considered here and in Chapter 3, an extension of therapy periods, as previously suggested for NRT134 might reduce relapse to smoking, facilitating higher rates of permanent smoking cessation. Additionally, as the rate of relapse early in quit attempts involving NRT is so rapid, any relapse prevention treatments that have an adjunctive impact at this time could have the substantial effects.
Chapter 6 Discussion
The strengths and weaknesses of the methodologies used in this review have been discussed within the chapters in which research methods were described; here we summarise the findings from the individual studies and discuss their implications, with particular reference to the potential integration of RPIs with smoking cessation support currently delivered by the NHS SSS.
Qualitative work and survey
Qualitative research with 16 health professionals working in NHS SSS indicated that there was no shared understanding of what relapse prevention meant or the kinds of interventions that should be used for this. Despite this, managers were positively orientated towards their use and indicated a willingness to provide them within the routine care delivered by their services. In the online survey, 96 NHS SSS managers from across the UK returned completed survey questionnaires (52% response rate). Of these, 58.3% (n = 56) reported running services that already provided RPIs for clients (RPI definition provided within survey), despite the absence of evidence for RPI effectiveness at the time of survey completion. The most commonly provided RPIs were behavioural support delivered by telephone (77%), in group settings (73%), or to individuals (54%). Pharmacotherapy was less frequently used for relapse prevention; just under half of managers reported that their services offered NRT (48%, n = 27) and 21.4% (n = 12) bupropion. Performance management targets for NHS SSS that focus on achieving relatively short (4-week) periods of cessation and inadequate funding for provision of RPIs were reported barriers to introducing such interventions into routine care.
Effectiveness of relapse prevention interventions
The systematic review that investigated the effectiveness of RPIs included 36 studies that randomised and delivered interventions to smokers who had recently achieved abstinence (‘abstainers’). ‘Self-help’ behavioural interventions delivered to abstainers who had become abstinent without using any form of cessation support were effective for preventing relapse to smoking at long-term follow-up (OR 1.52, 95% CI 1.15 to 2.01). The following pharmacotherapies were also effective as RPIs after their successful use as cessation treatments: bupropion at long-term follow-up (pooled OR 1.49, 95% CI 1.10 to 2.01); NRT at medium- (pooled OR 1.56, 95% CI 1.16 to 2.11) and long-term follow-ups (pooled OR 1.33, 95% CI 1.08 to 1.63) and one trial of varenicline also indicated effectiveness. Eighteen studies randomised smokers and delivered behavioural RPIs to them as additional components to cessation treatment. Although a few individual trials reported some statistically significant findings, where pooled analyses were possible there was no evidence for the effectiveness of any interventions delivered at this time.
Cost-effectiveness of relapse prevention interventions
We conducted a health economic analysis for those interventions which, in our effectiveness review, appeared effective at preventing relapse when used by smokers who had achieved abstinence in ‘supported’ quit attempts, as would occur in routine NHS SSS care. We found that, in common with other interventions that reduce smoking, RPIs are highly cost-effective. Compared with ‘no intervention’; using bupropion resulted in an incremental QALY increase of 0.07, with a concurrent NHS cost saving of £68; for NRT, spending £12 resulted in a 0.04 incremental QALY increase; varenicline resulted in a similar QALY increase as NRT but at almost seven times the cost; however, findings were derived from a single trial and require cautious interpretation. Extensive sensitivity analyses demonstrated that cost-effectiveness ratios were more sensitive to variations in effectiveness than cost and that, for bupropion and NRT, cost-effectiveness generally remained, even when input parameters are varied greatly, suggesting that this will be apparent in routine clinical practice. Varenicline also generally demonstrated cost-effectiveness at a ‘willingness-to-pay’ threshold of £20,000 per QALY, but exceeded this when inputted values for potential effectiveness were at the lower end of the range explored. With available data, only indirect comparisons between RPIs are possible and, therefore, assessments of their relative cost-effectiveness should only be made with caution.
Relapse curves for smokers in supported quit attempts
There were no data available from smokers attending NHS SSS which could be used to draw relapse curves to reflect their experiences of relapse to smoking; curves derived were therefore based entirely on data from cessation trials in which smokers received interventions similar to those delivered by NHS SSS. Systematic searching and consideration of retrieved articles identified 16 RCTs meeting all review inclusion criteria and these investigated NRT, bupropion or varenicline combined with intensive behavioural support. For all drugs, there was substantial relapse to smoking after treatment courses had finished (i.e. between 3 and 12 months into quit attempts). Eliminating such relapse would improve cessation rates at 12 months by 13%, 14% and 19% for NRT, bupropion and varenicline respectively (though these figures are derived using some pooled abstinence estimates which have substantial heterogeneity). Quit attempts involving NRT appeared to have the highest early relapse rates, when trial participants would be expected to still be on treatment, but for those involving bupropion and varenicline little relapse was apparent during this time. However, this observation could have arisen because bupropion and varenicline trials assessed smoking cessation by repeatedly assessing short periods of abstinence from smoking, rather than asking about continuous cessation between participants’ quit dates and all follow-up points.
Interpretation
Research with health professionals and managers working in the NHS SSS across the UK, indicated that a small majority were already providing RPIs, and there was a keenness to continue to do so or, in services which did not currently offer RPIs, to start to provide such interventions in the future. However, a lack of a shared understanding of what relapse prevention meant and a lack of evidence for the effectiveness of RPIs at the time of the survey meant that RPIs provided at that time were being delivered in the absence of any convincing evidence for their effectiveness. Additionally, in our efficacy review, we found no evidence that the most frequently-provided RPIs (counselling by telephone or in person) by the NHS SSS have any positive impacts. Should the NHS decide to fund RPI delivery by the NHS SSS, clear guidance on the kinds of interventions which should be delivered and which is informed by this report is required. Additionally, performance-management of NHS SSS would need altering, such that importance of sustaining quit attempts beyond 4 weeks is incentivised.
Our refined approach to reviewing the effectiveness of RPIs, found evidence for long-term effectiveness of bupropion, NRT and varenicline which had not previously been apparent. These medications are commonly used in NHS SSS and introducing them as relapse prevention treatments after a period of sustained abstinence reflects how relapse prevention would be likely to work within NHS SSS. Findings for bupropion are probably the most robust and the most generalisable to potential RPI use in the NHS as all the bupropion trials employed this model of ‘extended treatment’ after prolonged abstinence achieved with support. Greater caution is needed with respect to NRT because two of the four NRT trials, began relapse treatment with NRT after very short periods of unsupported abstinence (maximum 48 hours); it is not clear how generalisable findings from these trials are to the NHS SSS. Also as varenicline findings are based on only one trial, these should also be seen as preliminary, although since our review searches were conducted, further varenicline relapse prevention trials have also reported positively. It’s worth noting that, none of the pharmacotherapy studies were conducted in countries which, like the UK, have had organised smoking cessation services for some years; it is possible that RPIs might be less effective in the UK where more ‘resistant’ smokers avail themselves for support. Self-help RPIs were also found to be effective for unsupported quitters and it is possible that these interventions could also be effective for smokers, like those accessing NHS SSS, who are supported in cessation attempts. However, this needs formal testing as it is entirely possible for self-help materials to have a much smaller treatment effect for preventing relapse when used by smokers who, early in quit attempts, are also receiving either pharmaceutical of behavioural treatments to try to stop smoking.
As might be expected for interventions which reduce smoking; NRT, bupropion and varenicline all appear very cost-effective as judged by the £20,000 per QALY, NICE benchmark and, for bupropion and NRT, with highly favourable cost-effectiveness ratios generally being maintained in the face of substantial sensitivity analyses, such that this is very likely to be maintained in routine clinical practice. Our economic analyses were limited by the empirical data from trials included in the RPI effectiveness review and, as such, there were too few direct comparisons between the different RPIs to enable comparisons about their relative cost efficacy to be made; available comparisons are indirect and must be viewed with caution. Similarly, most interventions were introduced after 2–3 months of supported abstinence, so it is not possible to be confident about the optimal time after quit attempts begin for relapse prevention treatments to be introduced. However, the relapse curves that were drawn as proxies for the relapse experiences of NHS SSS users suggest that merely extending treatment periods could have a significant impact. Additionally, the sensitivity analysis for NRT trials in the cost-effectiveness analysis suggests that RPIs delivered to supported quitters after longer abstinence periods might be more cost-effective than those delivered to unsupported smokers who have maintained only very short abstinences; this supports a model of extending treatment periods beyond currently delivered smoking cessation treatments in the NHS SSS.
To our knowledge, this is the first systematic attempt to describe relapse patterns for supported quit attempts; although relapse curves were not produced from routine NHS SSS data, they are the most appropriate to NHS SSS users’ experiences yet produced. Curves show that initial patterns of relapse while smokers are likely to be on either NRT, bupropion or varenicline, differ markedly, but rates of relapse became comparable, and then converge after 3 months when most users are no longer being treated. Extended treatment periods with these medications past the 3-month point could potentially increase 12-month quit rates by between 10% and 20%. Given the uncertainties in some of our prevalence estimates, further research is needed to explore whether the varied trajectories observed early in quit attempts on different treatments are real or, alternatively, an artefact of how cessation was measured. However, as the high rates of relapse that were observed early in quit attempts using NRT appear independent of how trials assessed smoking cessation, the use of non-drug, behavioural RPIs, alongside NRT and behavioural support in such attempts, merits research.
Conclusions
In summary, our findings have identified that RPIs are likely to be very good value for money if incorporated into routine treatment within the NHS SSS. While staff within the NHS SSS were largely favourably inclined towards providing RPIs, guidance would be needed to encourage the adoption of the most effective RPIs as would incentives that focused on the importance of sustaining quit attempts beyond the currently monitored 4-week targets.
Recommendations
Research
-
Further research investigating the use of NRT, bupropion and varenicline (the three pharmacotherapies used in the NHS SSS) for relapse prevention is required, including the following:
-
Placebo RCTs to investigate the (cost) effectiveness of these RPIs as an extension to current NHS SSS cessation support – most review trials were conducted in countries without organised cessation services and, hence relapse prevention interventions may have different outcomes in the UK.
-
Studies of the acceptability of extended use of pharmacotherapies for relapse prevention in NHS SSS users, and particularly of bupropion, which is the least frequently used cessation therapy in England; the acceptability of these pharmacotherapies for relapse prevention will influence their uptake.
-
Whether or not the addition of behavioural relapse prevention interventions, delivered in the early stages of quit attempts using NRT can have an adjunctive, positive impact on cessation rates.
-
Confirmation of whether the different trajectories of relapse that we observed for NRT, bupropion and varenicline are valid (i.e. a more rapid relapse rate for users of NRT in the first month compared with the other two drug treatments) and occur when these treatments are used in routine NHS SSS clinical practice.
-
-
The following research into behavioural relapse prevention interventions is required:
-
RCTs to confirm or refute the finding that self-help interventions, delivered to smokers who have achieved abstinence unsupported, have long-term effectiveness for preventing relapse to smoking.
-
RCTs to investigate whether or not self-help interventions delivered to smokers who have achieved abstinence with NHS SSS support are effective.
-
Further research to refine interventions that showed potential in our effectiveness review, such as individual counselling for pregnant women and the use of telephone support after cessation treatment and test whether or not these might have long-term effectiveness.
-
-
Methodological standardisation: among relapse prevention trials identified for this report, there was huge variation in the definition of RPIs, the characteristics of smokers these were delivered to, follow-up periodicity, and outcome measurement after randomisation. Also among cessation trials used to derive relapse curves, reporting of outcomes seriously restricted the data available. In order to permit coherent synthesis of future research findings in this important field, we recommend that practitioners and researchers investigating this field agree common standards for:
-
The definition of RPI: in particular, consensus is needed as to whether behavioural RPIs, delivered alongside smoking cessation interventions to smokers either prior to or soon after quit attempts have started can or should be categorised as different to smoking cessation interventions. If there is consensus about such interventions being different, clear definitions for both are required.
-
Methodological standards for the conduct and reporting of behavioural and pharmacological relapse prevention trials.
-
Cessation trials should report the percentage of participants who make no attempt to stop smoking on target quit dates and should report continuous and point prevalence smoking cessation measures simultaneously at all follow-ups.
-
Implications for health care
Some NHS SSS are providing RPIs, but where this occurs, those with the weakest evidence base are generally used, illustrating a requirement for the emerging evidence base, and guidance, to be made available as soon as possible. Should the NHS decide to encourage and fund the use of RPIs for smokers who have become abstinent with NHS SSS support, new incentives are likely to be required before NHS SSS will substantially adopt their use. Currently, NHS SSS are performance-managed on their ability to achieve targets set for short-term (i.e. 4-week) periods of cessation; managers perceived these targets were a clear disincentive to spending on interventions such as RPIs, which might enhance longer term abstinence but not their clients’ initial, monitored cessation rates. Any integration of RPIs into NHS SSS care should include sufficient monitoring such that an assessment of their cost-effectiveness in routine use can be made.
Acknowledgements
The authors would like to thank the professionals who agreed to be interviewed in the qualitative research study and the managers of the NHS SSS in the UK who responded to our request to complete the survey. The authors would also like to thank Lindsay Stead, from the Tobacco Addiction Cochrane Review Group for support in identifying and accessing journal articles from Cochrane reviews on relapse prevention interventions. We are also grateful to Professor Linda Bauld for sharing NHS SSS monitoring datasets for projects that she was involved in; these datasets were not used in the study as there were not enough data points from which to be able to draw relapse curves. The authors would also like to thank Professor John Britton and Professor Christine Godfrey for their helpful comments during the writing of the grant proposal. The authors would like to thank Clare Randall for help with formatting the final report.
TC and AMcN are members of the UK Centre for Tobacco Control Studies, a UKCRC Public Health Research Centre of Excellence, with core funding from the British Heart Foundation, Cancer Research UK Economic and Social Research Council, Medical Research Council and the Department of Health under the auspices of the UK Clinical Research Collaboration.
Contribution of authors
Tim Coleman was the lead applicant at funding stage and participated in design, conduct, analysis and write up of all studies within report. Shade Agboola led the design, conduct analysis and write up of the qualitative and survey research and effectiveness review and participated in the conduct, analysis and write up of the systematic review. Jo Leonardi-Bee was a co-applicant at funding stage, participated in design, conduct, analysis and write up of systematic reviews and survey work, and led the ‘relapse curves’ review. Matthew Taylor designed, led, conducted and wrote up the health economic aspects of the report. Andy McEwan participated in design, conduct, analysis and write up of survey work. Ann McNeill was a co-applicant at funding stage, was the project manager following the grant award, and participated in design, conduct, analysis and write up of all studies within the report.
Publications
Agboola SA, Coleman TJ, McNeill AD. Relapse Prevention in UK Stop Smoking Services: a qualitative study of health professionals’ views and beliefs. BMC Health Serv Res 2009;9:67.
Agboola S, McNeill A, Coleman T, Leonardi-Bee J. A systematic review of the effectiveness of smoking relapse prevention interventions for abstinent smokers. Addiction 2010;105:1362–80.
Agboola S, Coleman T, Leonardi-Bee J, McEwan A, McNeill A. Provision of relapse prevention interventions in UK NHS Stop Smoking Services: A survey. BMC Health Serv Res 2010;10:214.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Royal College of Physicians Tobacco Advisory Group . Nicotine Addiction in Britain 2000.
- Department of Health . Smoking Kills 1998.
- McNeill A, Raw M, Whybrow J, Bailey P. A national strategy for smoking cessation treatment in England. Addiction 2005;100:1-11.
- Godfrey C, Parrott S, Coleman T, Pound E. The cost-effectiveness of the English smoking treatment services: evidence from practice. Addiction 2005;100:70-83.
- Department of Health . A Smokefree Future: A Comprehensive Tobacco Control Strategy for England 2010.
- Ferguson J, Bauld L, Chesterman J, Judge K. The English smoking treatment services: one-year outcomes. Addiction 2005;100:59-6.
- Cami J, Farre M. Drug addiction. N Engl J Med 2003;349:975-86.
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction 2004;99:29-38.
- Hughes JR, Gust SW, Skoog K, Keenan RM, Fenwick JW. Symptoms of tobacco withdrawal. A replication and extension. Arch Gen Psychiatry 1991;48:52-9.
- Kenford SL, Flore MC, Jorenby DE, Smith SS, Wetter D, Baker TB. Predicting smoking cessation. Who will quit with and without the nicotine patch. JAMA 1994;271:589-94.
- Herd N, Borland R. The Natural History of Quitting Smoking: findings from the International Tobacco Control (ITC) Four Country Project. Addiction 2009;104:2088-99.
- Marlatt A, Gordon J. Relapse prevention: maintenance strategies in the treatment of addictive behaviours. New York, NY: Guilford Press; 1985.
- Shiffman S. How when matters for quitting and relapse. Addiction 2008;103:822-3.
- Gwaltney CJ, Metrik J, Kahler CW, Shiffman S. Self-efficacy and smoking cessation: a meta-analysis. Psychol Addict Behav 2009;23:56-6.
- Shiffman S, Scharf DM, Shadel WG, Gwaltney CJ, Dang Q, Paton SM, et al. Analysing milestones in smoking cessation: illustration in a nicotine patch trial in adult smokers. J Consult Clin Psychol 2006;74:275-85.
- Piasecki TM. Relapse to smoking. Clin Psychol Rev 2006;26:196-215.
- Hajek P, Stead LF, West R, Jarvis M, Lancaster T. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev 2009;1.
- West R, McNeill A, Raw M. Smoking cessation guidelines for Scotland: 2004 Update. Edinburgh: NHS Health Scotland and ASH Scotland; 2004.
- Department of Health . NHS Stop Smoking Services. Service and Monitoring Guidance 2010–2011 2009.
- West R, McNeill A, Raw M. Smoking cessation guidelines for health professionals: an update. Thorax 2000;55:987-99.
- Department of Health . Improvement, Expansion and Reform – the Next 3 Years: Priorities and Planning Framework 2003–6 2002.
- O’Brien CP, McLellan AT. Myths about the treatment of addiction. Lancet 1996;347:237-40.
- Hajek P, Stead LF, West R, Jarvis M, Lancaster T. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev 2005;1.
- Lancaster T, Hajek P, Stead LF, West R, Jarvis MJ. Prevention of relapse after quitting smoking: a systematic review of trials. Arch Int Med 2006;166:828-35.
- Medioni J, Berlin I, Mallet A. Increased risk of relapse after stopping nicotine replacement therapies: a mathematical modelling approach. Addiction 2005;100:247-54.
- Ritchie J, Spencer L, O’Connor W, Ritchie J, Lewis J. Qualitative research practice: a guide for social science students and researchers. London: Sage Publications; 2006.
- Fitzpatrick R, Boulton M. Qualitative research in health care. The scope and validity of methods. J Eval Clin Pract 1996;2:123-30.
- Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Sage Publications; 1998.
- Shiffman S, Hickcox M, Paty JA, Gnys M, Kassel JD, Richards TJ. Progression from smoking lapse to relapse:prediction from abstinence violation effects, nicotine dependence and lapse characteristics. J Consult Clin Psychol 1996;64:993-1002.
- National Institute for Health and Clinical Excellence (NICE) . Public Health Guidance 10:Smoking Cessation Services in Primary Care, Pharmacies, Local Authorities and Workplaces, Particularly for Manual Working Groups, Pregnant Women and Hard to Reach Communities 2008:2-87.
- West W, McNeill A, Raw M. Meeting Department of Health smoking cessation targets. Recommendations for service providers. London: Health Development Agency; 2003.
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistencies in meta-analysis. BMJ 2003;327:557-60.
- Covey LS, Glassman AH, Jiang H, Fried J, Masmela J, LoDuca C, et al. A randomised trial of bupropion and/or nicotine gum as maintenance treatment for preventing smoking relapse. Addiction 2007;102:1292-302.
- Croghan IT, Hurt RD, Dakhil SR, Croghan GA, Sloan JA, Novotny PJ, et al. Randomised comparison of a nicotine inhaler and bupropion for smoking cessation and relapse prevention. Mayo Clin Proc 2007;82:186-95.
- Fortmann SP, Killen JD. Nicotine gum and self-help behavioural treatment for smoking relapse prevention: results from a trial using population-based recruitment. J Consult Clin Psychol 1995;63:460-8.
- Hays JT, Hurt RD, Rigotti NA, Niaura R, Gonzales D, Durcan MJ, et al. Sustained-release bupropion for pharmacologic relapse prevention after smoking cessation. Ann Intern Med 2001;135:423-33.
- Hurt RD, Krook JE, Croghan IT, Loprinzi CL, Sloan JA, Novotny PJ, et al. Nicotine patch therapy based on smoking rate followed by bupropion for prevention of relapse tosmoking. J Clin Oncol 2003;21:914-20.
- Killen JD, Fortmann SP, Newman B, Varady A. Evaluation of a treatment approach combining nicotine gum with self-guided behavioural treatments for smoking relapse prevention. J Consult Clin Psychol 1990;58:85-92.
- Niaura R. Long-Term Treatment With Rimonabant for Smoking Cessation and the Maintenance of Abstinence: Results from STRATUS-WORLDWIDE Trial n.d.
- Lowe JB, Windsor R, Balanda KP, Woodby L. Smoking relapse prevention methods for pregnant women: a formative evaluation. Am J Health Promot 1997;11:244-6.
- Conway TL, Woodruff S, Edwards CC, Elder JP, Hurtado SL, Hervig LK. Operation stay quit: evaluation of two smoking relapse prevention strategies for women after involuntary cessation during US Navy recruit training. Mil Med 2004;169:236-42.
- Becona EVF. Does using relapse prevention increase the efficacy of a program for smoking cessation? An empirical study. Psychol Rep 1997;81:291-6.
- Buchkremer G, Minneker E, Block M. Smoking cessation treatment combining transdermal nicotine substitution with behavioural therapy. Pharmacopsychiatry 1991;24:96-102.
- Curry SJ, Marlatt G, Gordon J, Baer JS. A comparison of alternative theoretical approaches to smoking cessation and relapse. Health Psychol 1988;7:545-56.
- Davis JR, Glaros A. Relapse prevention and smoking cessation. Addict Behav 1986;11:104-14.
- Emmons KM, Emont S, Weidner G. Relapse prevention versus broad spectrum treatment for smoking cessation: a comparison of efficacy. J Subst Abuse 1988;1:79-8.
- George TP, Douglas Z, Feingold A, Pepper WT, Satterburg CA, Winkel J, et al. Nicotine transdermal patch and atypical antipsychotic medications for smoking cessation in schizophrenia. Am J Psychiatry 2000;157:1835-42.
- Hall SM, Rugg D, Tunstall C, Jones RT. Preventing relapse to cigarette smoking by behavioural skill training. J Consult Clin Psychol 1984;52:372-82.
- Niaura R, Abrams D, Shadel WG, Rohsenow DJ, Monti PM, Sirota AD. Cue exposure treatment for smoking relapse prevention: a controlled clinical trial. Addiction 1999;94:685-95.
- Schmitz JM, Spiga R, Rhoades HM, Fuentes F, Grawbowski J. Smoking cessation in women with cardiac risk: a comparative study of two theoretically based therapies. Nicotine Tob Res 1999;1:87-94.
- Schroter M, Collins S, Frittrang T, Buchkremer G, Batra A. Randomised controlled trial of relapse prevention and a standard behavioural intervention with adult smokers. Addict Behav 2006;31:1259-64.
- Brandon TH, Zelman D, Baker TB. Effects of maintenance sessions on smoking relapse: delaying the inevitable?. J Consult Clin Psychol 1987;55:780-2.
- Hall SM, Killen J. Psychological and pharmacological approaches to smoking relapse prevention. NIDA Res Monogr 1985;53:131-41.
- Hall SM, Tunstall C, Ginsberg D, Benowitz NL, Jones RT. Nicotine gum and behavioural treatment: a placebo controlled trial. J Consult Clin 1987;55:603-5.
- Killen JD, Maccoby N, Taylor CB. Nicotine gum and self-regulation training in smoking relapse prevention. Behav Ther 1984;15:234-48.
- Lifrak P, Gariti P, Alterman AI, McKay J, Volpicelli J, Sparkman T, et al. Results of two levels of adjunctive treatment used with nicotine patch. Am J Addict 1996;6:93-8.
- Shoptaw S, Rotheram-Fuller E, Yang X, Frosch D, Nahom D, Jarvik ME, et al. Smoking cessation in methadone maintenance. Addiction 2002;97:1317-28.
- Japuntich SJ, Zehner M, Smith SS, Jorenby DE, Valdez JA, Fiore MC, et al. Smoking cessation via the internet: a randomised clinical trial of an internet intervention as adjuvant treatment in smoking cessation intervention. Nicotine Tob Res 2006;8:S59-S67.
- Lando HA, Pirie P, Roski J, McGovern PG, Schmid LA. Promoting abstinence among relapsed chronic smokers: the effect of telephone support. Am J Public Health 1996;86:1786-90.
- Killen JD, Fortmann S, Murphy GM, Hayward C, Arredondo C, Cromp D, et al. Extended treatment with bupropion SR for cigarette smoking cessation. J Consult Clin 2006;74:286-94.
- Juliano LM, Houtsmuller E, Stitzer ML. A preliminary investigation of rapid smoking as a lapse-responsive treatment for tobacco dependence. Exp Clin Psychopharmacol 2006;14:429-38.
- Klesges RC, Vander Weg MW, Lando HA, Peterson AL, DeBon M, Haddock CK, et al. Efficacy of a tailored tobacco control program on long-term use in a population of U.S military troops. J Consult Clin 2006;74:295-306.
- Hajek P, West R, Lee A, Foulds J, Owen L, Eiser JR. Randomised controlled trial of a midwife-delivered brief smoking cessation intervention in pregnancy. Addiction 2001;96:485-94.
- Hannover W, Thyrian J, Roske K, Grempler J, Rumpf H, John U, et al. Smoking cessation and relapse prevention for postpartum women: results from a randomised controlled trial at 6, 12, 18 and 24 months. Addict Behav 2009;34:1-8.
- McBride CM, Lando HA, Pirie PL, Grothaus LC, Nelson JC. Prevention of relapse in women who quit smoking during pregnancy. Am J Public Health 1999;89:706-11.
- McBride CM, Baucom D, Peterson BL, Pollak KI, Palmer C, Westman E, et al. Prenatal and postpartum smoking abstinence a partner-assisted approach. Am J Prev Med 2004;27:232-38.
- Morasco BJ, Dornelas E, Fischer EH, Oncken C, Lando HA. Spontaneous smoking cessation during pregnancy among ethnic minority women: a preliminary investigation. Addict Behav 2006;31:203-10.
- Pbert L, Ockene J, Zapka J, Ma Y, Goins KV, Oncken C, et al. A community health center smoking-cessation intervention for pregnant and postpartum women. Am J Prev Med 2004;26:377-85.
- Ratner PA, Johnson J, Bottorff JL, Dahinten S, Hall W. Twelve-month follow-up of a smoking relapse prevention intervention for postpartum women. Addict Behav 2000;25:81-92.
- Ruger JP, Weinstein M, Hammond SK, Kearney MH, Emmons KM. Cost-effectiveness of motivational interviewing for smoking cessation and relapse prevention among low-income pregnant women: a randomised controlled trial. Value Health 2008;11:191-8.
- Secker-Walker RH, Solomon L, Flynn BS, Skelly JM. Smoking relapse prevention counseling during prenatal and early postnatal care. Am J Prev Med 1995;11:86-93.
- Secker-Walker RH, Solomon L, Flynn BS, Skelly JM, Mead PB. Smoking relapse prevention during pregnancy. Am J Prev Med 1998;15:25-31.
- Severson HH, Andrews J, Lichtenstein E, Wall M, Akers L. Reducing maternal smoking and relapse: long-term evaluation of a paediatric intervention. Prev Med 1997;26:120-30.
- Van’t Hof M, Wall M, Dowler D, Stark MJ. Randomised controlled trial of a postpartum relapse prevention intervention. Tob Control 2000:64-6.
- Ershoff DH, Quinn V, Patricia DM. Relapse prevention among women who stop smoking early in pregnancy: a randomised clinical trial of a self-help intervention. Am J Prev Med 1995;11:178-84.
- Borland R, Balmford J, Hunt D. The effectiveness of personally tailored computer-generated advice letters for smoking cessation. Addiction 2004;99:369-77.
- Brandon TH, Collins B, Juliano LM, Lazev AB. Preventing relapse among former smokers: a comparison of minimal interventions through telephone and mail. J Consult Clin Psychol 2000;68:103-13.
- Brandon TH, Meade C, Herzog TA, Chirikos TN, Webb MS, Cantor AB. Efficacy and cost-effectiveness of a minimal intervention to prevent smoking relapse: dismantling the effects of amount of content versus contact. J Consult Clin Psychol 2004;72:797-808.
- Copeland AL, Martin P, Geiselman PJ, Rash CJ, Kendzor DE. Smoking cessation for weight-concerned women: group vs. individually tailored, dietary, and weight-control follow-up sessions. Addict Behav 2006;31:115-27.
- Hajek P, Taylor T, Mills P. Brief Intervention during hospital admission to help patients to give up smoking after myocardial infarction and bypass surgery: randomised controlled trial. BMJ 2002;324:87-9.
- Hasuo S, Tanaka H, Oshima A. Efficacy of a smoking relapse prevention program by postdischarge telephone contacts: a randomised trial. Kosei Kagaku Jpn J Public Health 2004;51:403-12.
- Klesges RC, Lando H, Haddock CK, Talcott GW. Efficacy of forced smoking cessation and an adjunctive behavioural treatment on long-term smoking rates. J Consult Clin Psychol 1999;67:952-8.
- Mayer C, Slachmuylder J, Vandecasteele H, Bodo M, Razavi D. Smoking relapse prevention programs and factors which predict abstinence: a controlled study comparing the efficacy of workplace group counselling arid proactive phone counselling. Psychooncology n.d.;2006:S319-S320.
- Mermelstein R, Hedeker D, Wong SC. Extended telephone counselling for smoking cessation: does content matter?. J Consult Clin Psychol 2003;71:565-74.
- Powell DR, McCann B. The effects of a multiple treatment program and maintenance procedures on smoking cessation. Prev Med 1981;10:94-104.
- Razavi D, Vandecasteele H, Primo C, Bodo M, Debrier F, Verbist H, et al. Maintaining abstinence from cigarette smoking: effectiveness of group counselling and factors predicting outcome. Eur J Cancer 1999;35:1238-47.
- Smith SS, Jorenby D, Fiore MC, Anderson JE, Mielke MM, Beach KE, et al. Strike while the iron is hot: can stepped care treatments resurrect relapsing smokers?. J Consult Clin Psychol 2001;69:429-39.
- Stevens VJ, Hollis J. Preventing smoking relapse using an individually tailored skills-training technique. J Consult Clin Psychol 1989;57.
- Tonstad S, Tønnesen P, Hajek P, Williams KE, Billing CB, Reeves KR, et al. Effect of maintenance therapy with varenicline on smoking cessation: a randomised controlled trial. JAMA 2006;296:64-71.
- Boyle RG, Solberg L, Asche SE, Maciosek MV, Boucher JL, Pronk NP. Proactive recruitment of health plan smokers into telephone counselling. Nicotine Tob Res 2007;9:581-9.
- Chirikos TN, Herzog T, Meade CD, Webb MS, Brandon TH. Cost-effectiveness analysis of a complementary health intervention: the case of smoking relapse prevention. Int J Technol Assess 2004;20:475-80.
- Cox LS, Patten C, Niaura R, Decker PA, Rigotti NA, Sachs DP, et al. Efficacy of bupropion for relapse prevention in smokers with and without a past history of major depression. J Genl Intern Med 2004;19:828-34.
- Fang WL, Goldstein A, Butzen AY, Hartsock SA, Hartmann KE, Helton M, et al. Smoking cessation in pregnancy: a review of postpartum relapse prevention strategies. J Am Board Fam Pract 2004;17:264-75.
- George TP, Ziedonis D, Feingold A, Pepper WT, Satterburg CA, Winkel J, et al. Nicotine transdermal patch and atypical antipsychotic medications for smoking cessation in schizophrenia. Am J Psychiatry 2000;157:1835-42.
- Hoving EF, Mudde A, deVries H. Predictors of smoking relapse in a sample of Dutch adult smokers; the roles of gender and action plans. Addictive Behaviors 2006;31:1177-89.
- Ma Y, Goins K, Pbert L, Ockene J. Predictors of smoking cessation in pregnancy and maintenance postpartum in low-income women. Matern Child Health J 2005;9:393-402.
- Partin MR, An L, Nelson DB, Nugent S, Snyder A, Fu SS, et al. Randomised trial of an intervention to facilitate recycling for relapsed smokers. Am J Prev Med 2006;31:293-9.
- Rigotti NA, Park E, Regan S, Chang Y, Perry C, Loudin B, et al. Efficacy of telephone counselling for pregnant smokers. J Obstet Gynaecol 2006;108:83-92.
- Suplee PD. The importance of providing smoking relapse counseling during the postpartum hospitalization. JOGNN 2005;34:703-12.
- Sutton S, Gilbert H. Effectiveness of individually tailored smoking cessation advice letters as an adjunct to telephone counseling and generic self-help materials: randomised control trial. Addiction 2007;102:994-1000.
- Office for National Statistics . Interim Revised Population Estimates: England and Wales 2000 2006.
- Government Actuary's Department . Life Tables 2006. www.gad.gov.uk/Demography%20Data/Life%20Tables/Historic_interim_life_tables.html (accessed 16 May 2008).
- Doll R, Peto R, Wheatley K, Gray R, Sutherland I. Mortality in relation to smoking – 40 years observations on male British doctors. BMJ 1994;309:901-11.
- Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years' observations on male British doctors. BMJ 2004;328.
- Department of Health . Health Survey for England 2004 2006.
- Forman D, Stockton D, Møller H, Quinn M, Babb P, De Angelis R, et al. Cancer prevalence in the UK: results from the EUROPREVAL study. Ann Oncol 2003;14:648-54.
- Peto R, Darby S, Deo H, Silcocks P, Whitley E, Doll R. Smoking, smoking cessation, and lung cancer in the UK since 1950: combination of national statistics with two case-control studies. BMJ 2000;321:323-9.
- Tengs T, Wallace A. One thousand health-related quality of life estimates. Med Care 2000;38:583-637.
- Rutten-van Molken M, Oostenbrink JB, Tashkin DP, Burkhart D, Monz BU. Does quality of life of COPD patients as measured by the generic EuroQol five-dimension questionnaire differentiate between COPD severity stages?. Chest 2006;130:1117-28.
- Szende A, Oppe M, Devlin N. EQ-5D value sets: inventory, comparative review and user guide. Dordrecht: Springer; 2007.
- Tillmann M, Silcock J. A comparison of smokers' and ex-smokers' health-related quality of life. J Public Health 1997;19.
- Sanderson H, Spiro S, In Stevens A, Raftery J, Mant J, Simpson S. Health Care Needs Assessment. Oxford: Radcliffe Publishing; 1998.
- Bourn J. Reducing Brain Damage: Faster Access to Better Stroke Care 2005. www.nao.org.uk/publications/0506/reducing_brain_damage.aspx (accessed 17 November 2006).
- Government Actuary's Department . Population Projections by the Government Actuary 2006. www.gad.gov.uk/Demography%20Data/Population/index.aspx?y=2006%26v=Principal (accessed 17 November 2006).
- Petersen S, Peto V, Rayner M, Leal J, Luengo-Fernandez R, Gray A. Health Care Costs of CVD and CHD 2005. www.heartstats.org/datapage.asp?id=1570 (accessed 17 November 2006).
- Department of Health . NHS Reference Costs 2005 2006.
- Curtis L, Netten A. Unit Cost of Health and Social Care 2005. www.pssru.ac.uk/uc/uc2005contents.htm (accessed 21 November 2006).
- Health & Social Care Information Centre . Prescription Cost Analysis England 2005 2006. www.ic.nhs.uk/pubs/prescostanalysis2005 (accessed 17 November 2006).
- National Collaborating Centre for Chronic Conditions . Chronic obstructive pulmonary disease: National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax 2004;59:1-232.
- British Medical Association and Royal Pharmaceutical Society of Great Britain . British National Formulary 2008.
- Parrott S, Godfrey C, Raw M, West R, McNeill A. Guidance for commissioners on the cost-effectiveness of smoking cessation interventions. Thorax 1998;53:1-38.
- HM Treasury . Trend Growth: Recent Developments and Prospects 2002.
- Yudkin P, Hey K, Roberts S, Welch S, Murphy M, Walton R. Abstinence from smoking eight years after participation in randomised controlled trial of nicotine patch. BMJ 2003;327:28-9.
- McGhan W, Dix Smith M. Pharmacoeconomic analysis of smoking-cessation interventions. Am J Health Syst Pharm 1996;53:45-52.
- Song F, Raftery J, Aveyard P, Hyde C, Barton P, Woolacott N. Cost-effectiveness of pharmacological interventions for smoking cessation: a literature review and a decision analytic analysis. Med Decis Making 2002;22:26-37.
- Bauld L, Chesterman J, Ferguson J, Judge K. A comparison of the effectiveness of group-based and pharmacy-led smoking cessation treatment in Glasgow. Addiction 2009;104:308-16.
- Ferguson J, Bauld J, Chesterman J, Judge K. The English smoking treatment services: one-year outcomes. Addiction 2005;100:59-6.
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among treated smokers. Addiction 2004;99:29-38.
- Zhu S, Melcer T, Sun J, Rosbrook B, Pierce J. Smoking cessation with and without assistance: a population-based analysis. AJPM 2000;18:305-11.
- Jorenby DE, Hays T, Rigotti N, Azoulay S, Watsky E, Williams K, et al. Efficacy of varenicline, an α4β2 nicotinic acetylocholine receptor partial agonist, versus placebo or sustained-release bupropion for smoking cessation. A randomised controlled trial. JAMA 2006;296.
- Piper ME, Federman FB, McCarthy DE, Bolt DM, Smith SS, Flore MC, et al. Efficacy of bupropion alone and in combination with nicotine gum. Nicotine Tob Res 2007;9:947-54.
- Blondal T, Gudmundsson LJ, Olafsdottir I, Gustavsson G, Westin A. Nicotine nasal spray with nicotine patch for smoking cessation: randomised trial with six year follow up. BMJ 1999;318:285-9.
- Blondal T, Gudmundsson LJ, Tomasson K, Jonsdottir D, Hilmarsdottir H, Kristjansson F, et al. The effects of fluoxetine combined with nicotine inhalers in smoking cessation – a randomised trial. Addiction 1999;94:1007-15.
- Medioni J, Berlin I, Mallet A. Increased risk of relapse after stopping nicotine replacement therapies: a mathematical modelling approach. Addiction 2005;100:247-54.
- Piasecki TM, Flore MC, McCarthy DE, Baler TB. Have we lost our way? The need for dynamic formulations of smoking relapse proneness. Addiction 2002;97:1093-108.
- Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev 2005;2.
- Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev 2005;2.
- Stead LF, Perera R, Bullen C, Mant D, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 10.1002/14651858.CD000146.pub3.
- Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev 2007;1. 10.1002/14651858.CD000031.pub3.
- Cahill K, Ussher MH. Cannabinoid type 1 receptor antagonists (rimonabant) for smoking cessation. Cochrane Database Syst Rev 2007;4. 10.1002/14651858.CD005353.pub3.
- Koehler KJ, McGovern PG. An application of the LFP survival model to smoking cessation data. Stat Med 1990;9:409-21.
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine Tob Res 2003;5:13-25.
- SRNT Subcommittee on Biochemical Verification . Biochemical verification of tobacco use and cessation. Nicotine Tob Res 2002;4:149-59.
- David S, Lancaster T, Stead LF, Evins AE, Cahill K. Opioid antagonists for smoking cessation. Cochrane Database Syst Rev 2006;4. 10.1002/14651858.CD003086.pub2.
- Gourlay SG, Stead LF, Benowitz N. Clonidine for smoking cessation. Cochrane Database Syst Rev 2004;3. 10.1002/14651858.CD000058.pub2.
- Grimshaw GM, Stanton A. Tobacco cessation interventions for young people. Cochrane Database Syst Rev 2006;4. 10.1002/14651858.CD003289.pub4.
- Hughes JR, Stead LF, Lancaster T. Anxiolytics for smoking cessation. Cochrane Database Syst Rev 2000;4. 10.1002/14651858.CD002849.
- Lancaster T, Sachs DPL. Silver acetate for smoking cessation. Cochrane Database Syst Rev 1997;3. 10.1002/14651858.CD000191.
- Lancaster T, Stead LF. Mecamylamin (a nicotine antagonist) for smoking cessation. Cochrane Database Syst Rev 1998;2. 10.1002/14651858.CD001009.
- Stead LF, Hughes JR. Lobeline for smoking cessation. Cochrane Database Syst Rev 1997;3. 10.1002/14651858.CD000124.
- Stead LF, Lancaster T. Nicobrevin for smoking cessation. Cochrane Database Syst Rev 2006;2. 10.1002/14651858.CD005990.
- Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev 2007;1. 006110.001002/14651858.CD14006103.pub14651852.
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58.
- Gonzales D, Rennard SI, Nides M, Oncken C, Azoulay S, Billing CB, et al. Varenicline, an alpha4beta2 nicotinic acetylcholine receptor agonist, vs sustained-release bupropion and placebo for smoking cessation. JAMA 2006;296.
- Gonzales DH, Nides MA, Ferry LH, Kustra RP, Jamerson BD, Segall N, et al. Bupropion SR as an aid to smoking cessation in smokers treated previously with bupropion: a randomised placebo-controlled study. Clin Pharmacol Ther 2001;69:438-44.
- Oncken C, Gonzales D, Nides M, Renard S, Watsky E, Billing CB, et al. Efficacy and safety of the novel selective nicotinic acetylcholine receptor partial agonist, varenicline, for smoking cessation. Arch Intern Med 2006;166:1571-7.
- Shiffman S, Dresler CM, Hajek P, Gilburt SJ, Targett DA, Strahs. Efficacy of a nicotine lozenge for smoking cessation. Arch Intern Med 2002;162:1267-76.
- Williams KE, Reeves K, Billing C, Pennington A, Gong J. A double-blind study evaluating the long-term safety of varenicline for smoking cessation. Curr Med Res Opin 2007;23:793-801.
- Nakamura M, Oshima A, Fujimoto Y, Maruyama N, Ishibashi T, Reeves KR. Efficacy and tolerability of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, in a 12-week randomised, placebo-controlled, dose–response study with 40-week follow-up for smoking cessation in Japanese smokers. Clin Ther 2007;29:1040-56.
- Blondal T, Franzon M, Westin A. A double-blind randomised trial of nicotine nasal spray as an aid in smoking cessation. Eur Respir J 1997;10:1585-90.
- Hurt RD, Dale LC, Fredrickson PA, Caldwell CC, Lee GA, Offord KP, et al. Nicotine patch therapy for smoking cessation combined with physician advice and nurse follow-up. One year outcome and percentage of nicotine replacement. JAMA 1994;271:595-600.
- Hurt RD, Sachs DP, Glover ED, Offord KP, Johnston JA, Dale LC, et al. A comparison of sustained-release bupropion and placebo for smoking cessation. New Engl J Med 1997;337:1195-202.
- Jarvis MJ, Raw M, Russell MA, Feyerabend C. Randomised controlled trial of nicotine chewing-gum. Br Med J 1982;285:537-40.
- Jorenby DE, Leischow SJ, Nides MA, Rennard SI, Johnston JA, Hughes AR, et al. A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. New Engl J Med 1999;340:685-91.
- Schneider NG, Jarvik ME, Forsythe AB, Read LL, Elliott ML, Schweiger A. Nicotine gum in smoking cessation: a placebo-controlled, double-blind trial. Addict Behav 1983;8:253-61.
- Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F. Systematic reviews of trials and other studies. Health Technol Assess 1998;2.
Appendix 1 Interview questions (Chapter 2)
-
What interventions are currently being used by your service to help smokers who wish to stop smoking?
-
In your experience, at what point do smokers who have quit smoking most often relapse to smoking?
-
What do you understand by smoking relapse prevention interventions?
Experiences of delivering relapse prevention interventions within Stop Smoking Services
-
Do you routinely provide relapse prevention interventions to smokers in your service?
-
What types? (Content)
-
To whom, is it to those who have already relapsed or to all smokers after the four week quit date, regardless of smoking status at the time?
-
For how long is the relapse prevention intervention provided for? (Duration)
-
What percentage of smokers who relapse to smoking take advantage of relapse prevention treatments? (Uptake)
-
Are your staff trained to provide relapse prevention support?
-
Do you collect any data so as to monitor the effectiveness of relapse prevention support you provide?
Feasibility
-
What do you think about the effectiveness of…? Varenicline (champix); bupropion (zyban); extended treatment with NRT; behavioural sessions after the 4 week quit date; extended telephone contact after the 4 week quit date (This question depends on the answer to question 4)
Challenges experienced
-
Is it difficult to get smokers to attend any clinics or sessions after the 4-week quit date?
-
Are there any groups of smokers who pose a challenge in particular?
-
What other challenges do you face with respect to preventing relapse in smokers?
Service provision
-
What is the nature and number of sessions offered?
-
What is the length and timing of these sessions?
-
What is the actual uptake of these treatment sessions by smokers?
-
What kind of staff are involved in providing these services for smokers who wish to quit?
Appendix 2 Relapse prevention intervention questionnaire
Appendix 3 Search strategies and results
MEDLINE (Ovid Web); 2004–7/August week 1; 8 August 2007
579 records were retrieved.
-
Smoking Cessation/
-
“Tobacco Use Disorder”/
-
Tobacco/
-
Nicotine/
-
Tobacco, Smokeless/
-
Smoking/pc, th
-
((quit$or stop$or ceas$or giv$) adj smok$).ti,ab.
-
Tobacco Smoke Pollution/
-
or/1-8
-
Randomised controlled trial.pt.
-
controlled clinical trial.pt.
-
Randomised Controlled Trials/
-
Random Allocation/
-
Double-Blind Method/
-
Single-Blind Method/
-
clinical trial.pt.
-
exp Clinical Trials/
-
(clin$adj trial$).ti,ab.
-
Placebos/
-
placebo$.ti,ab.
-
random$.ti,ab.
-
Research Design/
-
((singl$or doubl$or trebl$or tripl$) adj (blind$or mask$)).ti,ab.
-
(volunteer$or prospectiv$).ti,ab.
-
exp Evaluation Studies/
-
exp Cross-Sectional Studies/
-
Prospective Studies/
-
Retrospective Studies/
-
Follow-Up Studies/
-
exp Health Education/
-
exp Health Behaviour/
-
exp Community Health Services/
-
Health Promotion/
-
exp Behaviour Therapy/
-
or/10-34
-
Recurrence/
-
(relaps$or recurr$).ti,ab.
-
(resum$or restart$or re start$or lapse$).ti,ab.
-
maintenance.ti,ab.
-
(maintain$or sustain$).ti,ab.
-
or/36-40
-
9 and 35 and 41
-
Animals/
-
Humans/
-
43 not (43 and 44)
-
42 not 45
-
(2004$or 2005$or 2006$or 2007$).ed.
-
46 and 47
EMBASE (Ovid Web); 2004–7/week 31; 8 August 2007
406 records were retrieved.
-
(random$or factorial$or crossover$or cross over$or cross-over$or placebo$or (doubl$adj blind$) or (singl$adj blind$) or assign$or allocat$or volunteer$).ti,ab.
-
crossover procedure/or double-blind procedure/or Randomised controlled trial/or single-blind procedure/
-
1 or 2
-
smoking cessation.mp.
-
exp Smoking Cessation/
-
exp SMOKING/
-
((quit$or stop$or ceas$or giv$or prevent$) adj smok$).mp.
-
exp Passive Smoking/or exp Smoking Habit/or exp Cigarette Smoking/
-
or/4-8
-
Relapse/
-
(relaps$or recurr$).ti,ab.
-
(resum$or restart$or re start$or lapse$).ti,ab.
-
maintenance therapy/
-
maintenance.ti,ab.
-
(maintain$or sustain$).ti,ab.
-
or/10-15
-
3 and 9 and 16
-
exp animal/
-
Nonhuman/
-
(rat or rats or mouse or mice or hamster or hamsters or animal or animals or dogs or dog or cats or bovine or sheep or ovine or pig or pigs or porcine).ti,ab, sh.
-
or/18-20
-
exp human/or exp human experiment/
-
21 not (21 and 22)
-
17 not 23
-
(2004$or 2005$or 2006$or 2007$).em.
-
24 and 25
CENTRAL (Cochrane Library/Wiley); 2007:3; 8 August 2007
228 records were retrieved.
-
#1 MeSH descriptor Tobacco Use Disorder explode all trees
-
#2 MeSH descriptor Tobacco, Smokeless explode all trees
-
#3 MeSH descriptor Tobacco Smoke Pollution explode all trees
-
#4 MeSH descriptor Tobacco Use Cessation explode all trees
-
#5 MeSH descriptor Nicotine explode all trees
-
#6 (smoking AND cessation)
-
#7 (antismok*)
-
#8 (quit*):ti
-
#9 (smok*):ti
-
#10 (cigar*):ti
-
#11 (tobacco):ti
-
#12 (nicotine):ti
-
#13 MeSH descriptor Smoking explode all trees
-
#14 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13)
-
#15 MeSH descriptor Recurrence explode all trees
-
#16 (relaps* or recurr*)
-
#17 (resum* or restart* or (re start*) or lapse*)
-
#18 (maintenance)
-
#19 (maintain* or sustain*)
-
#20 (#15 OR #16 OR #17 or #18 or #19)
-
#21 (#14 AND #20), from 2004 to 2007
PsycINFO (Ovid Web); 2004–7/July week 5; 8 August 2007
555 records were retrieved.
-
smoking cessation.mp. or exp Smoking Cessation/
-
(antismoking or anti-smoking).mp.
-
(quit$or cessat$).mp.
-
(abstin$or abstain$).mp.
-
(control$adj smok$).mp. [mp = title, abstract, heading word, table of contents, key concepts]
-
exp Behaviour Modification/
-
2 or 3 or 4 or 5 or 6
-
exp Tobacco Smoking/
-
(smok$or cigar$or tobacco$).mp.
-
exp Prevention/
-
8 or 9
-
7 and 11
-
10 and 11
-
1 or 12 or 13
-
relapse prevention/
-
exp Maintenance Therapy/
-
(relaps$or recurr$).ti,ab.
-
(resum$or restart$or re start$or lapse$).ti,ab.
-
maintenance.ti,ab.
-
(maintain$or sustain$).ti,ab.
-
or/15-20
-
14 and 21
-
(2004$or 2005$or 2006$or 2007$).up.
-
22 and 23
Science Citation and Social Science Citation Index (ISI Web of Science); 2004–7/August 8; 8 August 2007
646 records were retrieved.
(((smoking cessation) OR (smok* SAME (quit or stop or prevent*))) AND (random* or trial or control* or (study same smok*)) AND (relaps* or recur* or resum* or restart* or (re start*) or lapse* or maintenance or maintain or sustain)) NOT (rat or rats or mouse or mice or hamster or hamsters or animal or animals or dogs or dog or cats or bovine or sheep or ovine or pig or pigs or porcine)
Time span = 2004–7
Appendix 4 Population weights
| Age (years) | Total (%) | Male (%) | Female (%) |
|---|---|---|---|
| 16 | 0.87 | 0.43 | 0.44 |
| 17 | 0.87 | 0.43 | 0.44 |
| 18 | 0.87 | 0.43 | 0.44 |
| 19 | 0.87 | 0.43 | 0.44 |
| 20 | 0.87 | 0.43 | 0.44 |
| 21 | 0.87 | 0.43 | 0.44 |
| 22 | 0.87 | 0.43 | 0.44 |
| 23 | 0.87 | 0.43 | 0.44 |
| 24 | 0.87 | 0.43 | 0.44 |
| 25 | 1.85 | 0.93 | 0.93 |
| 26 | 1.85 | 0.93 | 0.93 |
| 27 | 1.85 | 0.93 | 0.93 |
| 28 | 1.85 | 0.93 | 0.93 |
| 29 | 1.85 | 0.93 | 0.93 |
| 30 | 2.10 | 1.05 | 1.05 |
| 31 | 2.10 | 1.05 | 1.05 |
| 32 | 2.10 | 1.05 | 1.05 |
| 33 | 2.10 | 1.05 | 1.05 |
| 34 | 2.10 | 1.05 | 1.05 |
| 35 | 2.09 | 1.03 | 1.05 |
| 36 | 2.09 | 1.03 | 1.05 |
| 37 | 2.09 | 1.03 | 1.05 |
| 38 | 2.09 | 1.03 | 1.05 |
| 39 | 2.09 | 1.03 | 1.05 |
| 40 | 1.84 | 0.92 | 0.92 |
| 41 | 1.84 | 0.92 | 0.92 |
| 42 | 1.84 | 0.92 | 0.92 |
| 43 | 1.84 | 0.92 | 0.92 |
| 44 | 1.84 | 0.92 | 0.92 |
| 45 | 1.69 | 0.84 | 0.85 |
| 46 | 1.69 | 0.84 | 0.85 |
| 47 | 1.69 | 0.84 | 0.85 |
| 48 | 1.69 | 0.84 | 0.85 |
| 49 | 1.69 | 0.84 | 0.85 |
| 50 | 1.83 | 0.91 | 0.92 |
| 51 | 1.83 | 0.91 | 0.92 |
| 52 | 1.83 | 0.91 | 0.92 |
| 53 | 1.83 | 0.91 | 0.92 |
| 54 | 1.83 | 0.91 | 0.92 |
| 55 | 1.48 | 0.73 | 0.75 |
| 56 | 1.48 | 0.73 | 0.75 |
| 57 | 1.48 | 0.73 | 0.75 |
| 58 | 1.48 | 0.73 | 0.75 |
| 59 | 1.48 | 0.73 | 0.75 |
| 60 | 1.31 | 0.64 | 0.67 |
| 61 | 1.31 | 0.64 | 0.67 |
| 62 | 1.31 | 0.64 | 0.67 |
| 63 | 1.31 | 0.64 | 0.67 |
| 64 | 1.31 | 0.64 | 0.67 |
| 65 | 1.18 | 0.56 | 0.61 |
| 66 | 1.18 | 0.56 | 0.61 |
| 67 | 1.18 | 0.56 | 0.61 |
| 68 | 1.18 | 0.56 | 0.61 |
| 69 | 1.18 | 0.56 | 0.61 |
| 70 | 1.06 | 0.48 | 0.58 |
| 71 | 1.06 | 0.48 | 0.58 |
| 72 | 1.06 | 0.48 | 0.58 |
| 73 | 1.06 | 0.48 | 0.58 |
| 74 | 1.06 | 0.48 | 0.58 |
| 75 | 0.92 | 0.38 | 0.54 |
| 76 | 0.92 | 0.38 | 0.54 |
| 77 | 0.92 | 0.38 | 0.54 |
| 78 | 0.92 | 0.38 | 0.54 |
| 79 | 0.92 | 0.38 | 0.54 |
| 80 | 0.57 | 0.21 | 0.36 |
| 81 | 0.57 | 0.21 | 0.36 |
| 82 | 0.57 | 0.21 | 0.36 |
| 83 | 0.57 | 0.21 | 0.36 |
| 84 | 0.57 | 0.21 | 0.36 |
| 85 | 0.35 | 0.10 | 0.24 |
| 86 | 0.35 | 0.10 | 0.24 |
| 87 | 0.35 | 0.10 | 0.24 |
| 88 | 0.35 | 0.10 | 0.24 |
| 89 | 0.35 | 0.10 | 0.24 |
| 90 | 0.08 | 0.02 | 0.06 |
| 91 | 0.08 | 0.02 | 0.06 |
| 92 | 0.08 | 0.02 | 0.06 |
| 93 | 0.08 | 0.02 | 0.06 |
| 94 | 0.08 | 0.02 | 0.06 |
| 95 | 0.08 | 0.02 | 0.06 |
| 96 | 0.08 | 0.02 | 0.06 |
| 97 | 0.08 | 0.02 | 0.06 |
| 98 | 0.08 | 0.02 | 0.06 |
| 99 | 0.08 | 0.02 | 0.06 |
| 100 | 0.08 | 0.02 | 0.06 |
| Total | 100.00 | 48.00 | 52.00 |
Appendix 5 Search strategies
Productivity losses and absenteeism
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations; 2000–6/Sep week 3; searched 2 October 2006
-
Smoking/
-
(smoke or smoker or smokers or smoking).ti,ab.
-
(tobacco or cigar$).ti,ab.
-
or/1-3
-
((loss$or lost or reduc$) adj3 productivity).ti,ab.
-
((loss$or lost or reduc$) adj3 output$).ti,ab.
-
5 or 6
-
4 and 7
-
Absenteeism/
-
Sick Leave/
-
(sick$adj3 (certificat$or absence or leave or work)).ti,ab.
-
absenteeism.ti,ab.
-
or/9-12
-
4 and 13
-
18 or 14
EMBASE; 2000–6/week 39; searched 2 October 2006
-
SMOKING/
-
(smoke or smoker or smokers or smoking).ti,ab.
-
(tobacco or cigar$).ti,ab.
-
or/1-3
-
PRODUCTIVITY/
-
((loss$or lost or reduc$) adj3 productivity).ti,ab.
-
((loss$or lost or reduc$) adj3 output$).ti,ab.
-
or/5-7
-
4 and 8
-
ABSENTEEISM/
-
Medical Leave/
-
(sick$adj3 (certificat$or absence or leave or work)).ti,ab.
-
absenteeism.ti,ab.
-
or/10-13
-
4 and 14
-
9 or 15
CINAHL; 2000–6/Sep week 4; searched 2 October 2006
-
SMOKING/
-
(smoke or smoker or smokers or smoking).ti,ab.
-
(tobacco or cigar$).ti,ab.
-
or/1-3
-
((loss$or lost or reduc$) adj3 productivity).ti,ab.
-
((loss$or lost or reduc$) adj3 output$).ti,ab.
-
PRODUCTIVITY/
-
or/5-7
-
4 and 8
-
ABSENTEEISM/
-
Sick Leave/
-
(sick$adj3 (certificat$or absence or leave or work)).ti,ab.
-
absenteeism.ti,ab.
-
or/10-13
-
4 and 14
-
9 or 15
Health Management Information Consortium (HMIC); 2000–6/September; searched 2 October 2006
-
exp SMOKING/
-
(smoke or smoker or smokers or smoking).ti,ab.
-
(tobacco or cigar$).ti,ab.
-
or/1-3
-
exp PRODUCTIVITY/
-
((loss$or lost or reduc$) adj3 productivity).ti,ab.
-
((loss$or lost or reduc$) adj3 output$).ti,ab.
-
or/5-7
-
4 and 8
-
exp ABSENTEEISM/
-
exp SICK LEAVE/
-
(sick$adj3 (certificat$or absence or leave or work)).ti,ab.
-
absenteeism.ti,ab.
-
or/10-13
-
4 and 14
-
9 or 15
NHS Economic Evaluation Database (NHS EED); CRD internal database; 2000–6/September; searched 2 October 2006
s smoke or smoker or smokers or smoking
s tobacco or cigar$
s s1 or s2
s (loss$or lost or reduc$)(w3)productivity
s (loss$or lost or reduc$)(w3)output$
s s4 or s5
s s3 and s6
s sick$(w3)(certificat$or absence or leave or work)
s absenteeism
s s8 or s9
s s3 and s10
Annual costs of lung cancer and stroke in the UK
Lung cancer
Sanderson H, Spiro S. Cancer of the lung. In. Stevens A, Raftery J, Mant J, Simpson S. Health care needs assessment: the epidemiologically based needs assessment reviews: Volume 1. Second Edition. Abingdon: Radcliffe Publishing, 2004. pp. 503–48.
Stroke
Mant J, Wade D, Winner S. Stroke. In. Stevens A, Raftery J, Mant J, Simpson S. Health care needs assessment: the epidemiologically based needs assessment reviews: Volume 1. Second Edition. Abingdon: Radcliffe Publishing, 2004. pp. 141–244.
National Audit Office. Reducing brain damage: faster access to better stroke care. London: Stationery Office, 2005.
Utilities: myocardial infarction; chronic obstructive pulmonary disease; lung cancer; coronary heart disease; and stroke
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations; 1996–2006/November week 1; searched 15 November 2006
-
exp Quality-Adjusted Life Years/
-
quality adjusted life year$.ti,ab.
-
qaly$.ti,ab.
-
(utility or utilities).ti,ab.
-
(preference or preferences).ti,ab.
-
(time adj2 trade).ti,ab.
-
standard gamble.ti,ab.
-
rating scale.ti,ab.
-
or/1-8
-
*Myocardial Infarction/
-
9 and 10
-
*Pulmonary Disease, Chronic Obstructive/
-
9 and 12
-
*Lung Neoplasms/
-
9 and 14
-
*Coronary Disease/
-
9 and 16
-
*Cerebrovascular Accident/
-
9 and 18
EMBASE; 1996–2006/week 45; searched 15 November 2006
-
exp quality adjusted life year/
-
quality adjusted life year$.ti,ab.
-
qaly$.ti,ab.
-
(utility or utilities).ti,ab.
-
(preference or preferences).ti,ab.
-
standard gamble.ti,ab.
-
rating scale.ti,ab.
-
or/1-7
-
*Heart Infarction/
-
8 and 9
-
*Chronic Obstructive Lung Disease/
-
8 and 11
-
*Lung Cancer/
-
8 and 13
-
*Ischemic Heart Disease/
-
8 and 15
-
*STROKE/
-
8 and 17
NHS Economic Evaluation Database (NHS EED); CRD internal database. 2006/October; searched 15 November 2006
s quality(w)adjusted(w)life(w)year$
s qaly$
s utility or utilities
s preference or preferences
s time(w2)trade
s standard(w)gamble
s rating(w)scale
s s1 or s2 or s3 or s4 or s5 or s6 or s7
s myocardial(w)infarct$
s s8 and s9
s chronic(w)obstructive(w)pulmonary(w)disease$or COPD
s s8 and s11
s lung(w)(cancer$or neoplasm$)
s s8 and s13
s coronary(w2)disease or CHD
s s8 and s15
s stroke
s s8 and s17
Health Economic Evaluation Database (HEED); CD-ROM; September 2006; searched 15 November 2006
AX = (quality adjusted life year) or (quality adjusted life years)
AX = qaly or qalys
AX = utility or utilities
AX = preference or preferences
AX = (time trade off)
AX = (standard gamble)
AX = (rating scale)
CS = 1 or 2 or 3 or 4 or 5 or 6 or 7
AX = (myocardial infarction)
CS = 8 and 9
AX = (chronic obstructive pulmonary disease) or COPD
CS = 8 and 11
AX = (lung cancer) or (lung cancers) or (lung neoplasm) or (lung neoplasms)
CS = 8 and 13
AX = “coronary disease” within 2 OR CHD
CS = 8 and 15
AX = stroke
CS = 8 and 17
The Cost-Effectiveness (CEA) Registry. Internet. Comprehensive Table of Cost-Utility Ratios 2002–2003 and Comprehensive Table of Cost-Utility Ratios 1976–2001. Searched 15 November 2006
Association between smoking and COPD/stroke: separated into current, former and never smokers
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations; 1996–2006/November week 2; searched 20 November 2006
-
Smoking/
-
(former$and never and current$).ti,ab.
-
(smoking status).ti,ab.
-
1 and (2 or 3)
-
Pulmonary Disease, Chronic Obstructive/
-
((chronic adj2 pulmon$) or copd).ti,ab.
-
5 or 6
-
4 and 7
-
Cerebrovascular Accident/
-
stroke.ti,ab.
-
9 or 10
-
4 and 11
EMBASE; 1996–2006/week 46; searched 20 November 2006
-
SMOKING/
-
(former$and never and current$).ti,ab.
-
smoking status.ti,ab.
-
1 and (2 or 3)
-
Chronic Obstructive Lung Disease/
-
((chronic adj2 pulmon$) or copd).ti,ab.
-
5 or 6
-
4 and 7
-
STROKE/
-
stroke.ti,ab.
-
9 or 10
-
4 and 11
NHS Economic Evaluation Database (NHS EED); CRD internal database; 2006/October; searched 20 November 2006
s smoking
s former$and never and current$
s smoking(w)status
s s1 and (s2 or s3)
s chronic(w2)pulmon$or copd
s s4 and s5
s stroke
s s4 and s7
Health Economic Evaluation Database (HEED); CD-ROM; October 2006; searched 20 November 2006
AX = smoking
AX = (former and never and current)
AX = (smoking status)
CS = 1 and (2 or 3)
AX = “chronic pulmonary” within 2 OR COPD
CS = 4 and 5
AX = stroke
CS = 4 and 7
Appendix 6 Male mortality in the general population
| Age (years) | Mortality |
|---|---|
| 0 | 0.005709 |
| 1 | 0.000414 |
| 2 | 0.000243 |
| 3 | 0.000182 |
| 4 | 0.000145 |
| 5 | 0.000114 |
| 6 | 0.000122 |
| 7 | 0.000101 |
| 8 | 0.000106 |
| 9 | 0.000117 |
| 10 | 0.000106 |
| 11 | 0.000122 |
| 12 | 0.000142 |
| 13 | 0.000173 |
| 14 | 0.000192 |
| 15 | 0.000254 |
| 16 | 0.000321 |
| 17 | 0.000486 |
| 18 | 0.000644 |
| 19 | 0.000612 |
| 20 | 0.000738 |
| 21 | 0.000665 |
| 22 | 0.000778 |
| 23 | 0.000759 |
| 24 | 0.000716 |
| 25 | 0.000820 |
| 26 | 0.000786 |
| 27 | 0.000765 |
| 28 | 0.000815 |
| 29 | 0.000851 |
| 30 | 0.000923 |
| 31 | 0.000937 |
| 32 | 0.001037 |
| 33 | 0.001027 |
| 34 | 0.001052 |
| 35 | 0.001124 |
| 36 | 0.001217 |
| 37 | 0.001302 |
| 38 | 0.001279 |
| 39 | 0.001457 |
| 40 | 0.001595 |
| 41 | 0.001648 |
| 42 | 0.001822 |
| 43 | 0.002132 |
| 44 | 0.002144 |
| 45 | 0.002345 |
| 46 | 0.002623 |
| 47 | 0.002956 |
| 48 | 0.003201 |
| 49 | 0.003554 |
| 50 | 0.003901 |
| 51 | 0.004234 |
| 52 | 0.004641 |
| 53 | 0.004968 |
| 54 | 0.005386 |
| 55 | 0.005915 |
| 56 | 0.006354 |
| 57 | 0.007306 |
| 58 | 0.007891 |
| 59 | 0.008734 |
| 60 | 0.010033 |
| 61 | 0.010965 |
| 62 | 0.012447 |
| 63 | 0.013166 |
| 64 | 0.014799 |
| 65 | 0.016079 |
| 66 | 0.017600 |
| 67 | 0.019556 |
| 68 | 0.021774 |
| 69 | 0.024228 |
| 70 | 0.026342 |
| 71 | 0.029574 |
| 72 | 0.032947 |
| 73 | 0.036459 |
| 74 | 0.040973 |
| 75 | 0.045751 |
| 76 | 0.050710 |
| 77 | 0.056151 |
| 78 | 0.061724 |
| 79 | 0.069489 |
| 80 | 0.075742 |
| 81 | 0.083605 |
| 82 | 0.091501 |
| 83 | 0.097921 |
| 84 | 0.106861 |
| 85 | 0.118207 |
| 86 | 0.135494 |
| 87 | 0.148454 |
| 88 | 0.161954 |
| 89 | 0.175991 |
| 90 | 0.185602 |
| 91 | 0.200472 |
| 92 | 0.220085 |
| 93 | 0.239483 |
| 94 | 0.251598 |
| 95 | 0.280321 |
| 96 | 0.292331 |
| 97 | 0.310996 |
| 98 | 0.331163 |
| 99 | 0.345437 |
| 100 | 0.362748 |
Appendix 7 Lung cancer
| Age (years) | Prevalence (%) |
|---|---|
| 0–44 | 0.00 |
| 45–64 | 0.15 |
| 65 + | 0.80 |
| All ages | 0.14 |
| Gender | Current smoker | Former | Non-smoker |
|---|---|---|---|
| Men | 1 | 0.44 | 0.03 |
| Women | 1 | 0.21 | 0.05 |
| Age (years) | Men | Women | ||||
|---|---|---|---|---|---|---|
| Current smoker | Former | Non-smoker | Current smoker | Former | Non-smoker | |
| 16 | 0.00007 | 0.00003 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 17 | 0.00007 | 0.00003 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 18 | 0.00007 | 0.00003 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 19 | 0.00007 | 0.00003 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 20 | 0.00007 | 0.00003 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 21 | 0.00007 | 0.00003 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 22 | 0.00007 | 0.00003 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 23 | 0.00007 | 0.00003 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 24 | 0.00007 | 0.00003 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 25 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 26 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 27 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 28 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 29 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 30 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 31 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 32 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 33 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 34 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 35 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 36 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 37 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 38 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 39 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 40 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 41 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 42 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 43 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 44 | 0.00005 | 0.00002 | 0.00000 | 0.00006 | 0.00001 | 0.00000 |
| 45 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 46 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 47 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 48 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 49 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 50 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 51 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 52 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 53 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 54 | 0.00383 | 0.00169 | 0.00012 | 0.00214 | 0.00045 | 0.00011 |
| 55 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 56 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 57 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 58 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 59 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 60 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 61 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 62 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 63 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 64 | 0.00384 | 0.00169 | 0.00012 | 0.00241 | 0.00051 | 0.00012 |
| 65 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 66 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 67 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 68 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 69 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 70 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 71 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 72 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 73 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 74 | 0.02236 | 0.00984 | 0.00067 | 0.01007 | 0.00211 | 0.00050 |
| 75 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 76 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 77 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 78 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 79 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 80 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 81 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 82 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 83 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 84 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 85 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 86 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 87 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 88 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 89 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 90 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 91 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 92 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 93 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 94 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 95 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 96 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 97 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 98 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 99 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
| 100 | 0.02304 | 0.01014 | 0.00069 | 0.01167 | 0.00245 | 0.00058 |
Appendix 8 Coronary heart disease
| Age (years) | Prevalence (%) |
|---|---|
| 16–24 | 0.00 |
| 25–34 | 0.00 |
| 35–44 | 0.90 |
| 45–54 | 3.50 |
| 55–64 | 11.10 |
| 65–74 | 21.50 |
| 75 + | 26.40 |
| Current smoker | Former | Non-smoker | |
|---|---|---|---|
| RR | 3.12 | 1.55 | 1 |
| Age (years) | Men | Women | ||||
|---|---|---|---|---|---|---|
| Current smoker | Former | Non-smoker | Current smoker | Former | Non-smoker | |
| 16 | 0.00000 | 0.00000 | 0.00000 | 0.00378 | 0.00188 | 0.00121 |
| 17 | 0.00000 | 0.00000 | 0.00000 | 0.00378 | 0.00188 | 0.00121 |
| 18 | 0.00000 | 0.00000 | 0.00000 | 0.00378 | 0.00188 | 0.00121 |
| 19 | 0.00000 | 0.00000 | 0.00000 | 0.00378 | 0.00188 | 0.00121 |
| 20 | 0.00000 | 0.00000 | 0.00000 | 0.00378 | 0.00188 | 0.00121 |
| 21 | 0.00000 | 0.00000 | 0.00000 | 0.00378 | 0.00188 | 0.00121 |
| 22 | 0.00000 | 0.00000 | 0.00000 | 0.00378 | 0.00188 | 0.00121 |
| 23 | 0.00000 | 0.00000 | 0.00000 | 0.00378 | 0.00188 | 0.00121 |
| 24 | 0.00000 | 0.00000 | 0.00000 | 0.00378 | 0.00188 | 0.00121 |
| 25 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 26 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 27 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 28 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 29 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 30 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 31 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 32 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 33 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 34 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 35 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 36 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 37 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 38 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 39 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 40 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 41 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 42 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 43 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 44 | 0.01677 | 0.00833 | 0.00538 | 0.00747 | 0.00371 | 0.00239 |
| 45 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 46 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 47 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 48 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 49 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 50 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 51 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 52 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 53 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 54 | 0.06416 | 0.03188 | 0.02057 | 0.03767 | 0.01871 | 0.01207 |
| 55 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 56 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 57 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 58 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 59 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 60 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 61 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 62 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 63 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 64 | 0.20977 | 0.10421 | 0.06724 | 0.11597 | 0.05761 | 0.03717 |
| 65 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 66 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 67 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 68 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 69 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 70 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 71 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 72 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 73 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 74 | 0.44038 | 0.21878 | 0.14115 | 0.20962 | 0.10414 | 0.06718 |
| 75 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 76 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 77 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 78 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 79 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 80 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 81 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 82 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 83 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 84 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 85 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 86 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 87 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 88 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 89 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 90 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 91 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 92 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 93 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 94 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 95 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 96 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 97 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 98 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 99 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
| 100 | 0.55568 | 0.27606 | 0.17810 | 0.41478 | 0.20606 | 0.13294 |
Appendix 9 Chronic obstructive pulmonary disease
| Age (years) | Prevalence (%) |
|---|---|
| 0–64 | 1.00 |
| 65–74 | 5.00 |
| 75 + | 10.00 |
| Current smoker | Former | Non-smoker | |
|---|---|---|---|
| Men | 1 | 0.84 | 0.68 |
| Women | 1 | 0.96 | 0.92 |
| Age (years) | Men | Women | ||||
|---|---|---|---|---|---|---|
| Current smoker | Former | Non-smoker | Current smoker | Former | Non-smoker | |
| 16 | 0.01299 | 0.01091 | 0.00883 | 0.01057 | 0.01015 | 0.00973 |
| 17 | 0.01299 | 0.01091 | 0.00883 | 0.01057 | 0.01015 | 0.00973 |
| 18 | 0.01299 | 0.01091 | 0.00883 | 0.01057 | 0.01015 | 0.00973 |
| 19 | 0.01299 | 0.01091 | 0.00883 | 0.01057 | 0.01015 | 0.00973 |
| 20 | 0.01299 | 0.01091 | 0.00883 | 0.01057 | 0.01015 | 0.00973 |
| 21 | 0.01299 | 0.01091 | 0.00883 | 0.01057 | 0.01015 | 0.00973 |
| 22 | 0.01299 | 0.01091 | 0.00883 | 0.01057 | 0.01015 | 0.00973 |
| 23 | 0.01299 | 0.01091 | 0.00883 | 0.01057 | 0.01015 | 0.00973 |
| 24 | 0.01299 | 0.01091 | 0.00883 | 0.01057 | 0.01015 | 0.00973 |
| 25 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 26 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 27 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 28 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 29 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 30 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 31 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 32 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 33 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 34 | 0.01216 | 0.01022 | 0.00827 | 0.01054 | 0.01012 | 0.00970 |
| 35 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 36 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 37 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 38 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 39 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 40 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 41 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 42 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 43 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 44 | 0.01254 | 0.01053 | 0.00853 | 0.01054 | 0.01012 | 0.00970 |
| 45 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 46 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 47 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 48 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 49 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 50 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 51 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 52 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 53 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 54 | 0.01236 | 0.01038 | 0.00840 | 0.01053 | 0.01011 | 0.00969 |
| 55 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 56 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 57 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 58 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 59 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 60 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 61 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 62 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 63 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 64 | 0.01231 | 0.01034 | 0.00837 | 0.01055 | 0.01013 | 0.00971 |
| 65 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 66 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 67 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 68 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 69 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 70 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 71 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 72 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 73 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 74 | 0.06235 | 0.05237 | 0.04240 | 0.05306 | 0.05093 | 0.04881 |
| 75 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 76 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 77 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 78 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 79 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 80 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 81 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 82 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 83 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 84 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 85 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 86 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 87 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 88 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 89 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 90 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 91 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 92 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 93 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 94 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 95 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 96 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 97 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 98 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 99 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
| 100 | 0.12504 | 0.10504 | 0.08503 | 0.10627 | 0.10202 | 0.09777 |
Appendix 10 Myocardial infarction
| Age (years) | Prevalence (%) |
|---|---|
| 0–54 | 0.00 |
| 55–64 | 6.70 |
| 65–74 | 12.10 |
| Current smoker | Former | Non-smoker | |
|---|---|---|---|
| Men | 1.6 | 1.11 | 1.00 |
| Women | 2.76 | 1.05 | 1 |
| Age (years) | Men | Women | ||||
|---|---|---|---|---|---|---|
| Current smoker | Former | Non-smoker | Current smoker | Former | Non-smoker | |
| 16 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 17 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 18 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 19 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 20 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 21 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 22 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 23 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 24 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 25 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 26 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 27 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 28 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 29 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 30 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 31 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 32 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 33 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 34 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 35 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 36 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 37 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 38 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 39 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 40 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 41 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 42 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 43 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 44 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 45 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 46 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 47 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 48 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 49 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 50 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 51 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 52 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 53 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 54 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 | 0.00000 |
| 55 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 56 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 57 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 58 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 59 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 60 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 61 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 62 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 63 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 64 | 0.09210 | 0.06390 | 0.05756 | 0.04250 | 0.01617 | 0.01540 |
| 65 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 66 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 67 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 68 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 69 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 70 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 71 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 72 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 73 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 74 | 0.17246 | 0.11965 | 0.10779 | 0.09283 | 0.03532 | 0.03363 |
| 75 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 76 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 77 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 78 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 79 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 80 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 81 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 82 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 83 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 84 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 85 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 86 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 87 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 88 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 89 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 90 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 91 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 92 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 93 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 94 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 95 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 96 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 97 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 98 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 99 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
| 100 | 0.17463 | 0.12115 | 0.10914 | 0.09811 | 0.03732 | 0.03555 |
Appendix 11 Stroke
| Age (years) | Prevalence (%) |
|---|---|
| 16–24 | 0.00 |
| 25–34 | 0.00 |
| 35–44 | 0.30 |
| 45–54 | 1.20 |
| 55–64 | 2.20 |
| 65–74 | 7.60 |
| 75 + | 13.30 |
| Current smoker | Former | Non-smoker | |
|---|---|---|---|
| RR | 1.37 | 1.11 | 1.00 |
| Age (years) | Men | Women | ||||
|---|---|---|---|---|---|---|
| Current smoker | Former | Non-smoker | Current smoker | Former | Non-smoker | |
| 16 | 0.00125 | 0.00101 | 0.00091 | 0.00246 | 0.00199 | 0.00179 |
| 17 | 0.00125 | 0.00101 | 0.00091 | 0.00246 | 0.00199 | 0.00179 |
| 18 | 0.00125 | 0.00101 | 0.00091 | 0.00246 | 0.00199 | 0.00179 |
| 19 | 0.00125 | 0.00101 | 0.00091 | 0.00246 | 0.00199 | 0.00179 |
| 20 | 0.00125 | 0.00101 | 0.00091 | 0.00246 | 0.00199 | 0.00179 |
| 21 | 0.00125 | 0.00101 | 0.00091 | 0.00246 | 0.00199 | 0.00179 |
| 22 | 0.00125 | 0.00101 | 0.00091 | 0.00246 | 0.00199 | 0.00179 |
| 23 | 0.00125 | 0.00101 | 0.00091 | 0.00246 | 0.00199 | 0.00179 |
| 24 | 0.00125 | 0.00101 | 0.00091 | 0.00246 | 0.00199 | 0.00179 |
| 25 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 26 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 27 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 28 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 29 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 30 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 31 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 32 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 33 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 34 | 0.00475 | 0.00385 | 0.00347 | 0.00367 | 0.00297 | 0.00268 |
| 35 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 36 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 37 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 38 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 39 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 40 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 41 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 42 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 43 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 44 | 0.00367 | 0.00297 | 0.00268 | 0.00734 | 0.00595 | 0.00536 |
| 45 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 46 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 47 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 48 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 49 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 50 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 51 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 52 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 53 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 54 | 0.01459 | 0.01182 | 0.01065 | 0.01103 | 0.00894 | 0.00805 |
| 55 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 56 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 57 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 58 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 59 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 60 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 61 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 62 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 63 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 64 | 0.02691 | 0.02181 | 0.01965 | 0.03095 | 0.02507 | 0.02259 |
| 65 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 66 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 67 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 68 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 69 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 70 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 71 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 72 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 73 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 74 | 0.09473 | 0.07675 | 0.06914 | 0.06840 | 0.05542 | 0.04993 |
| 75 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 76 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 77 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 78 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 79 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 80 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 81 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 82 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 83 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 84 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 85 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 86 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 87 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 88 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 89 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 90 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 91 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 92 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 93 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 94 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 95 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 96 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 97 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 98 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 99 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
| 100 | 0.16675 | 0.13510 | 0.12172 | 0.11377 | 0.09218 | 0.08304 |
Appendix 12 Protocol submitted for study funding
1 TITLE: Relapse prevention in UK Stop Smoking Services: current practice, potential effectiveness and cost-effectiveness
2 Planned investigation
2.1 Existing research
2.1.1 Introduction
Smoking remains a major, international cause of morbidity and mortality and reducing smoking should be a priority for health systems like the UK National Health Service (NHS). 1 Although behavioural support, bupropion and nicotine replacement therapy (NRT) are effective treatments provided by the NHS,2 many smokers who stop after using these subsequently relapse to smoking (‘relapsers’). The proportion of relapsers increases with time elapsed after any initial cessation attempt, diminishing the impact of effective therapies on eventual cessation. Interventions that aim to decrease the proportion of relapsers are termed ‘relapse prevention’ interventions (RPIs). This project proposes an investigation into the potential effectiveness and cost-effectiveness of such interventions within the context of UK clinical practice and an assessment of which RPIs are most feasible for trialling within NHS Stop Smoking Services.
2.1.2 Effectiveness of relapse prevention interventions
A Cochrane review, updated in October 2004,3 (and summary journal article with searching until August 20054) found no evidence for the effectiveness of any specific type of relapse prevention intervention (RPI), but also noted that there was only a small evidence base from which this conclusion was drawn. Most included trials tested interventions which taught smokers the skills to identify situations that may increase their risk of relapsing and provided them with cognitive and behavioural strategies for coping with these. More intensive RPIs were usually delivered face to face and less intensive ones, involved briefer, minimal contact or self-help versions of these ‘skills-equipping’ interventions. As included trials involved a variety of RPIs delivered to smokers with varied characteristics both before and after quit attempts, a pooled estimate for the general effectiveness of RPIs is not available and instead review authors pooled analyses for trials in subgroups where comparisons were valid. Trials which recruited smokers who had completed smoking cessation programmes, perhaps provide data which are most relevant to the UK context (see below). 3,4 Among these, five studies found no evidence that RPIs could reduce relapse rates (n = 1121; OR, 1.00; 95% CI, 0.80–1.25), whereas two trials found some evidence for the effectiveness of NRT (n = 2261; OR, 1.30; 95% CI, 1.06–1.61) and two found no evidence for use of bupropion in relapse prevention (n = 605; OR, 1.25; 95% CI, 0.86–1.81). It is possible that further trials have either concluded or been published since the above review searches were conducted. 3,4 This is particularly likely for investigations of newer drug treatments being used for RP, as trials of a new therapeutic agent, varenicline, have reported in this period and in at least one of these studies, this drug was used effectively for relapse prevention. 5
2.1.3 Clinical practice of smoking cessation in NHS Stop Smoking Services
In 2000, the NHS introduced Stop Smoking Services (SSS) in England after piloting these in a small number of areas2 and similar services were set up in other UK countries. Between April 2003 and March 2006, 1.5 million smokers set quit dates with English SSS and 832,900 successfully stopped for at least 4 weeks. 6 Around 15% of smokers attending English SSS stop smoking for at least one year7 at an average cost per life year saved of £438, after allowance for future health care savings. 8 Unfortunately, relapse rates within SSS are high and 75% of smokers who are abstinent 4 weeks after their quit date relapse to smoking by 12 months. 7 Clearly, compared to other health-care interventions SSS are already very cost-effective but this could be further increased by the addition of any effective relapse prevention intervention (RPI) to current, routine SSS smoking cessation treatment.
2.1.4 Provision or trialling of relapse prevention interventions within SSS
There is no current evidence to support the routine provision of RPIs by SSS but because large numbers of motivated smokers access these services, they could provide an ideal environment for conducting RCTs to investigate RPIs’ effectiveness. Additionally, if any RPIs were proven to be effective then delivering these via NHS SSS would ensure that the maximum number of abstinent smokers received these. Consequently, it is important to consider how the ways in which current standard drug and behavioural treatments offered by SSS are provided might affect the feasibility of conducting trials for additional RPIs or introducing these into routine clinical practice.
All SSS are required to monitor the numbers of smokers who (i) access services and set a quit date and (ii) are abstinent from smoking for at least 4 weeks,9 but there are no other criteria governing how services should be structured and there is a paucity of contemporary data about this. Shortly after SSS were introduced, most offered 6 (for individuals) or 7 (for groups) session programmes of behavioural support to smokers. 10 However, there are no up to date information available about what constitutes ‘treatment’ for smoking cessation in UK NHS Stop Smoking services such as the numbers and nature of sessions offered, their length and timing and who delivers these. Additionally, we have no idea about smokers’ actual uptake of treatment sessions that they are offered by SSS. However, the length and timing of treatment programmes offered by SSS and the completeness of smokers’ attendance at these are determinants of how RPIs could be delivered in addition to SSS current treatment programmes and the likely costs of this to the NHS. For example, if most abstinent smokers actually attend most SSS treatment sessions offered soon after their quit dates, then trialling or providing additional RPIs early in quit attempts would not necessarily involve extra contacts with SSS staff and increased NHS costs. Alternatively, if few abstinent smokers attend treatment sessions after their smoking status is ascertained at 4 weeks, introducing additional RPIs after this time would involve increased costs to the NHS (extra patient contact). Also persuading abstinent smokers to attend SSS for any RPIs being trialled at this time point might be difficult. Finally, if drug treatments were to be trialled or provided for RP in addition to standard smoking cessation, knowing exactly how SSS currently use or recommend nicotine addiction therapies is necessary. Other service provision issues also have the potential to impact on the feasibility to trial the effectiveness of RPIs within NHS Stop Smoking Services and current information on both the nature of treatments provided by SSS and the structure of service provision will help decide priorities for relapse prevention research.
2.1.5 Natural history of relapse to smoking in NHS stop smoking service users
Any trials of RPI conducted within SSS would need to demonstrate improvement in relapse to smoking rates compared to those already experienced by smokers trying to quit with SSS support. Additionally, the timing of relapse after quit attempts begin is important because, for RPIs to have maximum effect, these need to be delivered when most quitters are still abstinent. Consequently, ‘relapse curves’ which plot abstinence from smoking against time (t) [where t = 0 at the initiation of a quit attempt] would assist decisions about the optimal time for delivery of RPIs in any trial. Relapse curves would also provide information for health economic modelling aimed at determining the treatment effects that any RPIs delivered by SSS might need in order to be cost-effective.
Unfortunately, SSS do not routinely record data on smoking behaviour at sufficient time points to provide data from which relapse curves could be constructed. 9 However, more detailed, individual-level data collected from SSS users during an earlier evaluation of English SSS and which includes biochemically-validated smoking status data at 4 and 52 weeks after quitting and self report data of when relapse occurred, is available to the research team. 7 These data are the most relevant available on SSS users, but to derive relapse curves, smoking status information from more time points is required, so we propose using these data in conjunction with data from clinical trials to derive ‘best estimate’ relapse curves for SSS users. Smokers who use SSS are motivated to quit and all receive an intensive behavioural intervention with most also receiving NRT or bupropion. 7 Trial participants who are also treated with intensive behavioural support and NRT or bupropion with might, therefore, be expected to have similar relapse trajectories as SSS users, but the relapse rates from clinical trials may differ from those obtained by SSS. Consequently, this proposal includes a methodology for combining data from participants in these trials with SSS-user data to estimate accurate relapse curves for SSS users.
Overall, this project will reassess the evidence for the effectiveness of relapse prevention interventions from a UK perspective and produce baseline information on the pattern and scale of relapse prevention practice that currently occurs within UK SSS. The feasibility of trialling RPIs within SSS and estimates for the potential cost-effectiveness of RPIs will be provided. Together, this information will be essential for funding bodies to determine relapse prevention research priorities and for researchers planning UK trials for relapse prevention interventions.
2.2 Research objectives
-
To update estimates of effectiveness in the Cochrane review on interventions for preventing relapse to smoking
-
To assess which studies included in 1 above, provide findings that are generalisable to NHS Stop Smoking Services and which test interventions that might be acceptable to introduce within the UK.
-
To derive ‘relapse to smoking’ curves for smoking cessation attempts made with NHS Stop Smoking Services using (i) prolonged and (ii) point abstinence from smoking as outcome measures.
-
To survey NHS stop smoking services in order to:
-
describe and categorise relapse prevention interventions which are currently used in UK NHS Stop Smoking Services
-
describe the current treatment provided by UK NHS stop smoking services for smokers who are trying to stop
-
describe how treatment in (ii) above is provided (e.g. number and nature of staff involved)
-
to ascertain barriers to the trialling or introduction of relapse prevention interventions within current clinical practice.
-
-
To determine the potential cost-effectiveness of relapse prevention interventions, delivered to smokers using NHS Stop Smoking Services.
-
To identify deficiencies in the evidence base concerning the use of relapse prevention interventions for smoking cessation and to identify priorities for future research.
3 Research methods
The proposed project is divided into four distinct phases and initials here refer to research team members named in a later section:
-
Systematic review to update previous Cochrane review.
-
Systematic review to derive relapse curves for NHS Stop Smoking Service users.
-
Survey of UK NHS Stop Smoking Services.
-
Economic analysis.
3.1 Systematic review to update and augment Cochrane review of RPI effectiveness
Specific objectives are to:
-
(a) Update estimates of effectiveness from the Cochrane review on effectiveness of interventions for preventing relapse to smoking.
-
(b) For studies included in (a), assess which provide findings that are generalisable to NHS Stop Smoking Services interventions and which interventions might be acceptable to introduce within the UK.
3.1.1 Search strategy
We will obtain copies of all papers included in the Cochrane review of RPI11 and use the search strategy from this to identify papers published since the final Cochrane review searches were undertaken (Oct 2004). We aim to find all new, relevant trials including those of new drug therapies (e.g. varenicline). 5 To ensure that we do not miss any relevant studies since October 2004 that are either concluded or ongoing, we will add to the Cochrane review search strategy11 by (i) conducting a ‘review of reviews’, looking for similar studies in all of the relevant reviews that have been produced recently (e.g. rapid reviews for NICE guidance), (ii) searching the NRR and trial registers (e.g. Controlled Clinical Trials) and where necessary contacting triallists to ascertain whether results can be provided, (iii) contacting, for information, members of the Society for Research on Nicotine and Tobacco e-mail discussion list, (iv) hand searching abstracts of relevant conferences that are not included in specialist registers of the Cochrane Tobacco Addiction Review Group, (v) searching the reference lists of relevant papers (vi) contacting pharmaceutical companies that produce pharmacotherapies and enquiring about relevant studies. JLB will supervise a research assistant (RA) to conduct searches and will liaise with LS, an author of the original Cochrane review, to ensure that this and other aspects of updating the Cochrane review are properly-conducted.
3.1.2 Updating Cochrane estimates
We will follow the same plan for extracting data, categorising interventions, and data synthesis as in the original review,11 which defined relapse very broadly and permitted RPIs to be delivered to smokers who had been abstinent for as little as 24 hours. This also allowed inclusion of studies with self-reported smoking cessation as an outcome and required that follow up occurred for 6 months after the RPI intervention was delivered. Updated analyses of the effectiveness of RP interventions will be performed, as necessary but, given that 38 out of 40 trials in the 2004 review yielded negative findings, it is unlikely that different conclusions will be reached unless significant new data are available. At the conclusion of this process, we will provide data and analyses to LS and other Cochrane review authors for them to include in their biannual review update.
3.1.3 Additional analyses
In addition to updating Cochrane estimates, we will also undertake the following analyses. The Cochrane review used a fixed effects method to pool estimates for the effectiveness of RPIs in sub groups. However, if after considering interventions employed in the sub groups of trials that the Cochrane analysis employed, we consider that heterogeneity between studies is likely (e.g. where treatments of differing intensities are delivered at different times during abstinence after smoking cessation has begun), we will conduct an analysis using a random effects model. We will use I2 to estimate variability between trials12 and if I2 is >85%, this will be taken to be excessive heterogeneity and we will not perform a meta-analysis of sub groups but will restrict our report to individual trial estimates rather than pooled sub group estimates. Where pooling is permissible, we will attempt (data permitting) to conduct analyses to determine effects of RPIs on relapse rates at the following times after provision of relapse prevention interventions: around 1 month (short term), around 6 months (medium term) and 1 year and over (longer term), reporting pooled effectiveness of interventions as odds ratios with 95% confidence intervals. Additionally, we will attempt to report the impact of RPIs on time taken to relapse, using hazard ratios with 95% CIs assessed at 1 year and over.
If updated estimates suggest that RPI are effective in any one context (e.g. for pregnant women or with smokers who have completed treatment programmes), we will investigate data further to determine whether differential effectiveness is observed in sub-groups of trial subjects (e.g. ethnic group or different socioeconomic groups)(Note: the research brief suggests that such analyses should be undertaken, if appropriate). However, we will not pursue these analyses if the overall estimates for effectiveness of RPI remain negative because, in this instance, these would not be scientifically justified.
3.1.4 Generalisability and acceptability of review RPIs to NHS SSS
For all studies included in our updated review, we will extract data describing interventions as per the initial review, taking particular care to ensure that we note:
-
Length of quit attempt prior to delivery of RPI.
-
Whether or not RPI interventions are delivered to abstainers who have attended smoking cessation programmes.
These data will be used in conjunction with survey findings (section, 3.3) to assess relevance of study interventions to the UK and judge the feasibility of trialling or introducing these into SSS.
Generalisability of trial findings:
The Cochrane review used a broad definition of relapse which included, for example, failed quit attempts of 24 hours13 or more and patients who had stopped smoking during hospital admissions. 14 This and other factors could mean that some trials in the review may have findings that are not generalisable to all smokers who engage in quit attempts whilst using NHS SSS. In tandem with the process above, the study team will inspect trial details to determine how generalisable findings are to the NHS SSS and will provide an assessment of this in the final study report. For example, the timing of RPI delivery in relation to period of abstinence from smoking important may be an important determinant of the potential external validity of trial findings.
Acceptability of intervention:
This will be assessed in the context of current NHS SSS ‘standard treatment and practice’ for smoking cessation as revealed in the survey (3.3) and using a research-based model for assessing the feasibility of introducing complex interventions into routine clinical care. 15 Acceptability (or the likelihood that any intervention can become ‘normalised’15 within routine care will be judged against the four constructs of this model: interactional workability; relational integration; skill set workability and contextual integration. 15 The exact criteria for judging feasibility will depend upon survey findings and be derived after discussion of survey findings by the research team but before the assessment process begins. Explicit written criteria for judgements will be produced and these criteria will facilitate judgements in the context of the May criteria. 15 For example, the level of difficulty that introducing RPIs would entail in terms of providing extra resources for SSS delivery (e.g. human or financial resources) or necessitating changes in current clinical practice will be important considerations. Judgements about feasibility will be made by independently by the RA, TC and AMcN and disagreements will be resolved by a group meeting to achieve consensus. Where possible, studies will be grouped into different categories, based on the feasibility of implementing interventions described and the final study report will contain an assessment of the pros and cons of introducing different RPIs into SSS.
3.2 Deriving relapse curves for NHS Stop Smoking Service users
Objective: To derive relapse to smoking curves for smoking cessation attempts made with NHS Stop Smoking Services using (i) prolonged and (ii) point abstinence from smoking as outcome measures.
Technical note: A relapse curve (survival curve) uses data on smoking status, collected from the time that smokers start quit attempts and subtracts the number of ‘relapsers’ from the total number of smokers enrolled into a study to derive the number still abstinent as time elapses. 16
3.2.1 Systematic search for trial data
This literature search will aim to find trials which include at least one treatment group that includes smokers who receive intensive behavioural support, plus a drug treatment for nicotine addiction (e.g. varenicline, NRT or bupropion). Additionally, we will look for any observational studies in which smokers’ abstinence over time is monitored, but we will exclude studies reporting analyses of the data contained in the databases that are proposed for use in conjunction with trial data to produce relapse curves7). JLB will determine the exact search criteria in conjunction with LS and the RA will conduct searches. LS is Cochrane Tobacco Addiction Group Review Group co-ordinator and has substantial experience of conducting systematic reviews for smoking cessation interventions.
3.2.2 Selecting trials for inclusion in analysis:
Two members of the research team will independently inspect the titles and abstracts of all selected studies to determine whether or not these should be included in the review at this stage and any disagreements will be resolved by a third researcher. The full text of all included and potentially relevant studies will be obtained and two researchers will independently assess, using criteria below, whether or not these should be included in the review with the third researcher participating as necessary to ensure that disagreements are resolved by consensus.
We will assess the quality of included studies using accepted criteria17 including:
-
(a) method for generating randomisation sequence
-
(b) method of allocation concealment – considered ‘adequate’ if the assignment could not be foreseen
-
(c) who was blinded/not blinded (participants, clinicians, outcome assessors) if this is appropriate
-
(d) how many participants were lost to follow up in each arm, and whether reasons for losses were adequately reported
-
(e) whether all participants were analysed in the groups to which they were originally randomised.
We will assume that any trial participants who withdraw from trials have relapsed to smoking.
The following inclusion criteria have been informed by a previous review which attempted to construct relapse curves for smokers who were attempting to stop smoking without any form of treatment or support. 18 Study subjects will need to (i) be followed prospectively, (ii) be adult daily smokers [> 18], (iii) have received behavioural support plus one or more drug treatment for smoking cessation (iv) have reported a clearly defined quit date and subsequent follow-ups associated with this (v) have follow up data recorded for at least 12 months and on at least three occasions in the first month after their quit date. This final criterion is important because previous work suggests that most relapse occurs early in quit attempts. 16
3.2.3 Data extraction
For all included studies, the RA will extract the following data to derive survival curves for relapse to smoking amongst trial participants:
-
where survival curves are reported, these will be converted into daily abstinence rates from these using ‘digimatic™’ software (scans graphical plots and converts into numerical data)
-
proportion of trial participants reporting prolonged abstinence19 from smoking at all time points when this data collected between quit date and final follow up
-
proportion of trial participants reporting point abstinence19 from smoking at all time points when this data collected between quit date and final follow up
-
number enrolled into trial at randomisation
-
number of smokers followed up at each point (for studies where survival curve not reported)
-
demographic characteristics of trial sample (i.e. age, sex, ethnicity and socioeconomic characteristics)
-
trial setting
-
proportions of trial participants in different demographic groups (i.e. age, sex, ethnicity and socioeconomic characteristics) reporting prolonged abstinence19 or point abstinence19 from smoking at all time points when this data collected between quit date. (Note: we anticipate that very few trials will publish detailed data on smoking cessation in different demographic groups.)
Extracted data will be double checked by AMcN and consensus will be achieved about disagreements by referring to TC, as appropriate.
3.2.4 Derivation of relapse curves using trial data
A previous study which tried to derive relapse curves for smokers who stop without any sort of support found that few trials in this group of smokers published sufficient data from which relapse curves could be constructed. 18 Consequently, although reported prolonged abstinence from smoking is the most relevant outcome for our purposes, we also propose deriving relapse curves using reported point prevalence (i.e. short periods of smoking cessation) at time points after quit date.
For both outcomes, the proportion of trial subjects reported to be abstinent (point or prolonged) at different time points will be combined, taking into account the size of individual trials and a pooled value for abstinence at different time points after quit date will be determined. We will use the same approach towards testing for heterogeneity as outlined in 3.1.3. and if there is too much heterogeneity or insufficient data to allow pooled relapse curves to be drawn, relapse curves from individual trials will be presented together.
If individual curves are presented, we will explore whether variability in relapse curves shapes is affected by the final effectiveness of smoking cessation interventions in individual trials by replotting curves so that the final point on each is zero. Additionally, we will group together trials of different interventions (e.g. NRT vs bupropion) to determine whether or not these have similar relapse curve shapes.
It is possible that there will be insufficient data to determine the characteristics of relapse curves in the first month after quitting, which is the time period during which the majority of relapse is thought to occur. In this is eventuality, we will access and investigate the use of data from the publicly-available GlaxoSmithKline (GSK) Clinical Trial Register which is available at: http://ctr.glaxowellcome.co.uk/Summary/bupropion/studylist.asp. This contains summaries of all GSK trials investigating the drug bupropion (a.k.a. Wellbutrin) and includes over 20 trials with smoking cessation as an outcome. Some of these trials have not been published in conventional medical journals and contain potentially-useful data. However, if such data were to be used then these trials would need an identical (i.e. to published data) assessment of methodological quality and the origin and quality of the data used for deriving different sections of relapse curves would be made explicit. Additionally, if these data are used, the study team will need to ensure that these data compliment that which is available in published reports and there is no ‘double-counting’ of trial register report data which is also contained in papers identified by literature searching.
If, after the above procedure has been followed, it is still not possible to derive complete relapse curves, we will attempt to obtain further data from pharmaceutical companies that produce NRT and/or varenicline. Obtaining NRT trial data might be problematic because most NRT trials were conducted some time ago and there have been many pharmaceutical company mergers since then. It is more likely that Pfizer would be able to provide data from unpublished varenicline trials, but the trial team do not believe that it is appropriate to approach Pfizer with such a request at this point for the following reasons:
(i) There may be enough published literature in peer review journals from which relapse curves can be drawn.
(ii) Any request for data would be best made when the research team’s exact data needs are clearly defined [i.e. which part(s) of the relapse curve require further data]. This would enable focused question(s) to be asked of Pfizer rather than a broad request for data from trials of a new product which could be considered ‘sensitive’.
3.2.5 Derivation of relapse curves for special populations of smokers
If possible, we will repeat the analyses conducted in 3.2.4 for sub-groups smokers defined by demographic characteristics. However, it is very likely that trial reports will not contain enough data to permit this and the next section indicates how we can produce estimates for the shape of relapse curves within these groups.
3.2.6 Combining trial and routine data on patients attending NHS Stop Smoking Services
Although the participants in trials used to derive relapse curves above are similar to SSS users, we cannot assume that relapse curves for both groups will be identical because participants in trials often differ from the wider patient community. Consequently, we propose comparing individual-level data on relapse that has been obtained from SSS users attending two English7 and a number of Scottish SSSs20 with trial data to obtain ‘best-estimate’ relapse curves for SSS attenders. We propose that the analysis above (3.2.4/5) should determine the shape of relapse curves in this group and that data collected from SSS users will indicate the likely abstinence rates for patients form different demographic groups at one and 12 months.
The English SSS database contains data from 6959 SSS attenders, who set quit dates between May and November 20027 and the Scottish database, similar data collected between October 2004 and February 2005. 20 The English database includes data from three time points (enrolment, four weeks and one year) and the Scottish from two (enrolment and four weeks), so relapse curves could not be constructed from these data alone. Nevertheless, these databases contain individual-level data on a wide range of variables for SSS attenders (e.g. age, gender, ethnic group, socioeconomic status, motivation to stop smoking) and to the authors’ knowledge, these are the main sources of data from which relapse rates of different SSS client groups could be determined. It should be noted that this research team has unrestricted access to databases needed for these analyses. In addition, the research team are aware that a small number of SSS have recently begun to collect data on smoking status at more time points after their quit attempts than they are required to do for monitoring purposes (personal communication, A McEwen). A research collaborator, Dr Andy McEwen, who manages the Smoking Cessation Service Research Network (SCSRN) will investigate the feasibility of using these data too.
LB will provide the two databases which will be combined and from these data we will calculate the proportions of SSS users who set quit dates and were subsequently recorded as not smoking (with biochemical verification) at 4 and 52 weeks after this. Next, we will recalculate these rates by age, gender, ethnic group, level of nicotine addiction, level of initial motivation to stop and socioeconomic status. Using these data and imputing data for other time points based on the overall shape of relapse curves derived in 3.2.4/5 above, we will draw estimated relapse curves for SSS users from with these different characteristics.
3.3 Survey of UK NHS Stop Smoking Services
Specific objectives are to:
(i) describe and categorise relapse prevention interventions which are currently used by UK NHS Stop Smoking Services
(ii) describe the current treatment provided by UK NHS stop smoking services to smokers who are trying to stop
(iii) describe how treatment in (ii) above is provided (e.g. number and nature of staff involved)
(iv) to ascertain barriers to the trialling or introduction of relapse prevention interventions within current clinical practice.
The feasibility of trialling or introducing RPIs into clinical practice and also their potential cost-effectiveness will vary with current UK SSS clinical practice. Consequently, we will conduct a postal survey of English and Scottish NHS stop smoking services to determine current practice and provision of relapse prevention interventions in these services and make an estimate of the costs associated with delivering these. To ensure that the survey asks valid questions, we will first undertake qualitative interviews with a selection of NHS stop smoking service staff.
3.3.1 Qualitative pilot work
NHS SSS staff will be recruited at the Third UK National Smoking Cessation Conference (UKNSCC) which is to be held in June 2007 in London and is organised by AMcE, a study collaborator. This large conference is held for health professionals working in NHS SSS and is well attended by representatives from many such services throughout the UK. The lead applicant successfully recruited smoking cessation advisors for research in a similar way during the 2006 conference. If, for any reason recruitment is not possible at this conference, we will seek health professionals for interview from contributors to the Smoking Cessation Service Research Network (network of NHS SSS that are interested in research and run by AMcE). Both proposed methods of recruiting health professionals for interview avoid the need to obtain research governance approval from R&D departments.
The research team will offer to run or contribute to a workshop on relapse prevention at this conference and during this will inform workshop attenders about the proposed survey and invite them to be interviewed to assist with the development of the survey questionnaire. We will recruit, for individual interviews (face to face or telephone), twenty health professionals who work for SSS as smoking cessation advisors or managers. Where possible, interviews will be held during or soon after the conference with the aim of all being completed within one month. Interviews will be semi-structured,21 conducted by a research assistant, audio taped and transcribed. Interviewees’ perceptions of what relapse prevention entails will be explored. As there is no universally accepted definition of relapse prevention, interviewees’ perceptions will be used to ensure that the subsequent survey uses a definition of RP that is clearly understandable to SSS staff. Interviews will explore experiences of delivering RPIs within stop smoking service (if indeed this is happening) including interventions’ content and timing in relation to other aspects of SSS treatment for smokers. Health professionals who have first hand experience of delivering relapse prevention support will be asked about the challenges experienced (e.g. lack of patient motivation). With all interviewees we will ascertain their opinion on the factors which could hinder or help the introduction of relapse prevention support within their service. Additionally if, in our review (3.1), we identify interventions we believe are feasible for introduction within the UK, we will ascertain interviewees’ opinions about these. Interviews will be analysed by at least two researchers who will read and reread transcripts in an iterative process to identify key themes arising from data and also categories within themes. Interpretation of findings from interviews will be cross checked between researchers conducting the analysis and a systematic approach will be taken to reintegrating coded data. 22,23 At the end of this process, key themes arising from interview data and categories within these will be summarised.
3.3.2 Postal survey
The survey will be administered by the Nottingham-based research assistant and the questionnaire used will be designed after input from Ann McNeill, Tim Coleman, John Britton, Paul Trueman, Linda Bauld (all co-applicants) and Andrew McEwen (collaborator). Bauld, Coleman and Mc Neill have previously conducted surveys of smoking cessation services and will use this experience to ensure that the proposed survey has the highest possible response rate.
Our aim is for all managers of PCT-run (CHP-run in Scotland) smoking cessation services to receive and potentially complete one questionnaire. Generally, in England and Scotland, each PCT/CHP runs one NHS Stop Smoking Service (SSS), though in some areas these may share one manager and associated administrative services. Primary care health service administration is currently being reorganised and consequently NHS SSS in some areas are being either combined or disaggregated depending upon the re-configuration of the PCTs in which they are located. For example, in Nottingham City before reconfiguration one smoking cessation service served four PCTs, but this is set to increase to two services working within the same area. Care will, therefore, be required in deriving a sampling frame for the survey and our procedure for doing this is described below. One cannot be certain of the exact sample size for the survey, though this should not exceed the combined number of PCTs and CHPs in England and Scotland and the unit of analysis for the questionnaire will be the smoking cessation service. The survey will commence approximately 9 months after the start of the project (around Dec 07 if the project commences in April 07).
Interview data and relevant systematic review findings will be combined to design a postal questionnaire, which will be piloted on interviewees before distribution to all SSS managers in England and Scotland. For this survey to be successful, it is vital that addressees are appropriate and their contact details correct. There is currently no up to date list of SSS managers in the UK, so initially the RA will contact the English DH/Scottish Office to determine which Primary Care Trusts (Community Health Partnerships in Scotland) return statistics for NHS Stop Smoking Services. Then the RA will telephone and/or e-mail these PCTs/CAPs to obtain postal and e-mail contact details for SSS managers and hence a sampling frame for the survey, so that both contact modalities can be used for an initial mailing. Research team members have previously conducted similar surveys of SSS and have found this approach results in questionnaires reaching the relevant professionals. 10,24 One postal/e-mail and one telephone reminder will be used to secure healthy response rates.
Items for the survey questionnaire will, to an extent, be determined by the outcome of qualitative pilot work (Section 3.3.1). However, we will aim to ask about the delivery of relapse prevention interventions by SSS in terms that respondents are familiar with and understand, but which also facilitate comparison with other research on relapse prevention interventions. The survey will investigate the feasibility of introducing effective but unused relapse prevention interventions (identified in the earlier review) into routine care by SSS. It will also be important for the survey to produce information for estimation of costs involved in the delivery of interventions. Consequently, respondents will be asked to indicate the nature of interventions that SSS deliver to smokers, the time involved and any other potential costs. Questions on cost will be designed in conjunction with Paul Trueman and based upon those used in a previous survey of Stop Smoking Services and which contributed to an analysis of their cost-effectiveness.
The brief survey instrument will ask about size and location of SSS, current provision of both smoking cessation and relapse prevention interventions, who delivers these and an estimate of the time involved and other potential costs (e.g. prescription or advisor travel costs). Questions concerning costs of interventions will be informed by relevant items from a similar survey that contributed to an assessment of the cost-effectiveness of SSS which was conducted by study team members. 10 Additionally, respondents will be asked their perceptions of organisational factors (relevant to their particular SSS) which could influence the introduction of any new relapse prevention interventions into their services.
3.3.3 Survey analysis:
As the survey is predominantly descriptive, data analysis will reflect this and quantitative data will be presented as summary statistics with measures of spread. No hypotheses generating analyses are planned. We expect that the survey will provide (i) clear descriptions, with quantification, of RPIs (if any) that SSS currently employ, (ii) a clear summary of how current treatments for smoking cessation by SSS are provided (i.e. length of treatment courses, group or individual sessions etc.), (iii) likely costs of providing RPIs, (iv) the structure and organisation of SSS (i.e. how many staff, staff salaries etc.) and (v) organisational factors within SSS that may hinder trialling of RPIs or their introduction into routine clinical practice. Consequently, survey findings will provide a clear snapshot of current practice in relapse prevention, with data to help assess the feasibility of how RPIs might be trialled or even introduced into clinical practice.
3.4 Health economic analysis
Objective: To determine the potential cost-effectiveness of relapse prevention interventions, delivered to smokers using NHS Stop Smoking Services.
Input to this exercise will be dependent upon project outcomes prior to this point. If RPIs have been found to be effective with some patient sub-groups or relapse rates have been found to differ between sub groups of SSS attenders, then modelling will also investigate the potential for different RPIs to be more or less cost-effective with different SSS client groups. It is envisaged that the following inputs would be used in a modelling exercise:
-
Description of RPIs derived from review (3.1) and survey (3.3).
-
Estimated costs of delivering RPIs within UK NHS SSS.
-
Potential treatment effects for RPIs described in 1 & 2.
-
Relapse curves derived in 3.2 – Potential cost-effectiveness of RPIs will vary with timing of their delivery after quit attempts have started, as the numbers of smokers who are abstinent from smoking (and in whom relapse can be prevented) will decrease with time elapsed after quit attempts began.
3.4.1: Data analysis
The description of RPIs will come from categorisation of interventions in the review (3.1). In addition to describing RPIs, we will indicate the feasibility of introducing each into clinical practice based on our assessment made in section 3.1 in conjunction with survey data from 3.3. The estimated costs of delivering RPIs will be dependant on configurations of SSS revealed in our survey and we will use a similar approach to costing delivery of RPIs as was used in our analysis of the cost-effectiveness of English smoking cessation services. 8 Costs are dependant on, for example, whether or not (i) interventions are delivered to groups or individuals, (ii) the salaries of those delivering them and (iii) whether or not drug treatments are provided.
Current systematic review evidence suggests that no interventions reduce relapse to smoking at 6 months of follow up, so economic modelling will involve sensitivity analyses using imputation of potential treatment effects, based on the most likely values as per systematic review findings. If, however, our updated review indicates that any type of RPI is/are effective, then modelling for these will be based around newly derived treatment effects. We will also investigate the potential impact on cost-effectiveness of delivering RPIs at different times after smokers become abstinent and hence to different proportions of smokers who have not yet relapsed to smoking.
The economics of the RPIs will be analysed using economic modelling techniques to extrapolate data on the short-term impact of the interventions to longer-term outcomes. The model is expected to build on previously completed models for smoking cessation, which may be adapted to review relapse prevention. The research team at the University of York are currently in the process of developing an economic model of smoking cessation interventions to inform the development of the NICE guideline on smoking cessation. It is hoped that it will be possible to adapt this model to help determine the cost-effectiveness of smoking relapse interventions.
The data on the effectiveness of the RPIs will be derived from the systematic review conducted at the earlier stage of this research. The resources involved in the provision of the RPIs under review are expected to be drawn from the survey of current practice. Unit costs will be applied to these resources in order to estimate the costs of providing the interventions. Unit costs will be drawn from widely used sources (e.g. Unit Costs of Health & Social Care, PSSRU).
In order to determine the cost-effectiveness of the interventions under consideration, it will be necessary to extrapolate the short-term outcomes of RPIs over a longer-term, possibly the lifetime of an individual. The extrapolation of findings will be based on biologically plausible models which, wherever possible, will be drawn from published research identified as part of the systematic review. However, where such models are unavailable in the published evidence, it may be necessary to draw on clinical expertise both within and outside of the research team, for assumptions on the longer-term impact of RPIs. Any assumptions used to inform the modelling exercise will be clearly reported and subject to sensitivity analysis. Sensitivity analysis will also be conducted on other key parameters identified from the systematic review, if there is cause to believe that there is uncertainty around the reported estimates. Univariate and multi-variate sensitivity analysis will be conducted as part of the research. It may also be appropriate to consider undertaking probabilistic sensitivity analysis, in order to report the cost-effectiveness acceptability curves.
Outcomes of the model will be presented as cost per life year saved and cost per quality adjusted life year saved. Disaggregated findings, such as number of attendees remaining abstinent at a particular time, may also be reported.
The approach to modelling will adhere to best practice principles, such as those set out by Drummond25 and the NICE reference case.
4 Ethical issues
Any delays encountered in obtaining necessary ethical permissions are unlikely to delay the project as systematic reviews will be conducted before the SSS survey. Ethical approval will be required to conduct qualitative interviews with SSS professionals but, as these are not recruited via NHS organisations, formal R&D approval will not be required. Patient information from the English and Scottish databases will be provided to the research team in an anonymous format and all patients enrolled into these databases have previously consented for these data to be used for research. Consequently, obtaining ethical approval to use these data for the proposed analyses is not likely to be problematic. If data from other NHS SSS has been obtained using similar consent procedures and these data can be provided anonymously to the research team, then ethical permission to use such data should not be problematic and accessing the data will be within the resources of the proposed project. If, however, this is not the case, then we will not use these data for our analyses. As part of our ethical approval application, we will highlight, drawing attention to COREC definitions of audit and research, our belief that the proposed survey of NHS stop smoking services is an audit of service provision, rather than original research. This will ensure that research governance approval is not needed. If this argument is not accepted by the REC, however, and the research team need to obtain R&D approval from the many PCTs in which SSS are located, then completion of this project within the timescale below will be less feasible.
5 Project timetable and milestones
| Tasks | Months | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-funding | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
| Protocol development | |||||||||||||||||||
| MREC approval | |||||||||||||||||||
| Appointment of RA (Nottingham) | |||||||||||||||||||
| RPI and relapse curve derivation reviews | |||||||||||||||||||
| Qualitative interviews/analysis | |||||||||||||||||||
| Design and piloting of questionnaire | |||||||||||||||||||
| Construction of survey sampling frame | |||||||||||||||||||
| SSS survey | |||||||||||||||||||
| Health economic analysis | |||||||||||||||||||
| Write up (general) | |||||||||||||||||||
| Write up (incorporation of HE analysis) | |||||||||||||||||||
6 Expertise of research team
Co-applicants
Linda Bauld Linda Bauld has substantial experience of research involving NHS stop smoking services. She was a member of a DH team which evaluated English SSS, has completed a similar project for Scotland and is an author of the recent NICE rapid review of the effectiveness of NHS Stop Smoking Services. Dr Bauld has access to data for use in 3.2. John Britton is an epidemiologist and triallist with an interest in smoking cessation and currently works with a local NHS SSS to execute a clinical trial investigating the effectiveness of Varenicline for smoking cessation. He Chairs the Royal College of Physician’s Tobacco Advisory Group, has a broad interested in smoking cessation trials and will provide strategic level input. Tim Coleman also worked on the English SSS evaluation and currently is chief investigator for a trial of NRT in pregnancy that involves close liaison with a number of NHS stop smoking services. Jo Leonardi-Bee is a medical statistician with experience of systematic review methodology and provides valuable relevant expertise in both areas. Ann McNeill is a recent (September 2006) appointment to The University of Nottingham. She is an internationally-renowned expert on smoking cessation and tobacco control and has completed numerous projects in this area, including being a key member of the English evaluation of smoking cessation services mentioned above. More recently, Prof McNeill produced an exhaustive NICE rapid review into the effectiveness of brief interventions. Although she is a new appointment to Nottingham, Professor McNeill has a strong history of collaboration with other members of the research team. Paul Trueman is the Director of the York Health Economics Consortium at the University of York. Paul is an experienced health economist who specialises in the conduct of economic evaluations using modelling techniques as well as analysis alongside clinical trials. Paul is currently leading a research team at the University of York in undertaking a rapid review and economic model of smoking cessation services for input to the NICE guideline on this topic. Paul will be supported by Matthew Taylor (not a named applicant) who has expertise in economic modelling techniques and has worked on models in a wide range of diseases including, coronary heart disease, rheumatology and nephrology. Matthew has a particular interest in the application of probabilistic sensitivity analysis.
Collaborators
Christine Godfrey is a Health Economist with a particular interest in smoking cessation. She has lead on the health economic components of the DH-funded English evaluation of the English smoking cessation services, the Thorax smoking cessation guidelines and, more recently, a NICE rapid review of the cost-effectiveness of brief interventions for smoking cessation. Lindsay Stead is an information scientist who is expert in systematic review and has worked within the Cochrane Collaboration Review Group for many years, producing a wide range of reviews on smoking-related topics, including the initial relapse prevention review. 3 Andy McEwen is a Senior Research Nurse at the CRUK Health Behaviour Unit with strong research and clinical links with NHS SSS; he is also Programme Director of the UKNSCC and is developing the Smoking Cessation Service Research Network (SCSRN) in which a small group of SSS collect comprehensive data on service attenders.
7 Justification of support required
One research assistant (RA) is required for 18 months to ensure that primary data collection is conducted thoroughly and the diverse data retrieved from literature searches is synthesised appropriately into a coherent research report. The RA will conduct literature research and lead on data extraction. (S)he will conduct pilot qualitative interviews with smoking cessation health professionals and conduct the postal survey of NHS stop smoking services. (S)he will lead on and co-ordinate collaboration with the health economic team at York and will co-ordinate writing of the final project report. Contributions for the academic time of all team members are written proposal.
Office costs: The research assistant will require a computer, monitor, printer, ‘Digimatic™’ and qualitative analysis data software, office consumables and access to a telephone and shared IT systems. Recording and transcription equipment will also be required. Travel: Rail travel for meetings (6 individual journeys), travel within Nottingham (as the research team work on different sites) and for the RA to conduct up to half the 20 interviews is required. Teleconference: 4 teleconferences are required to ensure that the expertise of all researchers is effectively utilised, and in particular for the model building and testing stage of the HE analysis. Dissemination: Travel and conference registration for one international conference is included. Postage: is primarily required for the survey of SSS and costs for undertaking 2 literature reviews are included.
The York team conducting the health economic analysis are a self-funding unit and are not subject to FEC. Consequently, their costs have been entered onto the application form as a consumable which will be supplied on a sub-contract basis to the UoN. The Paul Trueman’s and Matthew Taylor’s time is costed in at £850 and £750 per day respectively and the time of a third data analyst is also required at a daily rate of £650. The table below indicates days spent on the various activities involved in the HE analysis. Total = £26,200
| Activity | Days contributed by staff HE team member | ||
|---|---|---|---|
| PT | MT | Data analyst | |
| Development of model | 1 | 2 | |
| Build model in excel | 1 | 3 | 3 |
| Populate model | 2 | 5 | |
| Run model | 0.5 | 2 | |
| Sensitivity analysis | 0.5 | 5 | |
| Report writing | 3 | 5 | |
| Quality assurance | 1 | 1 | |
| Total | 7 | 20 | 15 |
8 Projected outputs
The following outputs are anticipated: (i) HTA monograph, (ii) data for updating Cochrane RPI review provided to authors, (iii) paper describing relapse curves for attenders at smoking cessation services, (iv) paper describing current treatment for smoking cessation provided by NHS SSS, (v) paper describing the potential cost-effectiveness of RPI interventions delivered via NHS Stop Smoking services.
- Tobacco Advisory Group of the Royal College of Physicians . Nicotine Addiction in Britain 2000.
- McNeill A, Raw M, Whybrow J, Bailey P. A national strategy for smoking cessation treatment in England. Addiction 2005;100:1-11.
- Hajek P, Stead LF, West R, Jarvis M, Hajek P, Stead LF, et al. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev 2005.
- Lancaster T, Hajek P, Stead LF, West R, Jarvis MJ, Lancaster T, et al. Prevention of relapse after quitting smoking: a systematic review of trials. Arch Intern Med 2006;166:828-35.
- Tonstad S, Tonnesen P, Hajek P, Williams KE, Billing CB, Reeves KR, et al. Effect of maintenance therapy with varenicline on smoking cessation: a Randomised controlled trial. JAMA 2006;296:64-71.
- Anonymous . Statistics on NHS Stop Smoking Services in England, April 2005 to March 2006. Q4 – Quarterly Report 2006.
- Ferguson J, Bauld L, Chesterman J, Judge K. The English smoking treatment services: one-year outcomes. Addiction 2005;100:59-6.
- Godfrey C, Parrott S, Coleman T, Pound E. The cost-effectiveness of the English smoking treatment services: evidence from practice. Addiction 2005;100:70-83.
- Department of Health . NHS Smoking Cessation Services: Service and Monitoring Guidance 2001 02 2001.
- Pound E, Coleman T, Cheater F, McNeil. National survey of the new smoking cessation services in England. Health Edu J 2003;62:246-55.
- Hajek P, Stead LF, West R, Jarvis M, Hajek P, Stead LF, et al. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev 2005.
- Higgins J, Thompson S. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58.
- Fortmann SP, Killen JD, Fortmann SP, Killen JD. Nicotine gum and self-help behavioral treatment for smoking relapse prevention: results from a trial using population-based recruitment. J Consult Clin Psychol 1995;63:460-8.
- Hajek P, Taylor TZ, Mills P. Brief intervention during hospital admission to help patients to give up smoking after myocardial infarction and bypass surgery: randomised controlled trial. BMJ 2002;324:87-9.
- May C. A rational model for assessing and evaluating complex interventions in health care. BMC Health Serv Res 2006;6.
- Koehler KJ, McGovern PG. An application of the LFP survival model to smoking cessation data. Stat Med 1990;9:409-21.
- Juni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ 2001;323:42-6.
- Hughes JR, Keely J, Naud S, Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction 2004;99:29-38.
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine Tob Res 2003;5:13-25.
- Bauld L, Ferguson J, Lawson L, Judge K. Tackling Smoking in Glasgow: Final Report 2006.
- Britten N. Qualitative interviews in medical research. BMJ 1995;311:251-3.
- Fitzpatrick R, Boulton M. Qualitative research in health care: I. The scope and validity of methods. J Eval Clin Pract 1996;2:123-30.
- Strauss A, Corbin J. Basics of qualitative research: grounded theory proceedures and tecniques. Newbury Park, CA: SAGE Publications Inc; 1998.
- Pound E, Coleman T, Adams C, Bauld L, Ferguson J. Targeting smokers in priority groups: the influence of government targets and policy statements. Addiction 2005;100:28-35.
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 1996;313:275-83.
List of abbreviations
- BNF
- British National Formulary
- CHD
- coronary heart disease
- CI
- confidence interval
- COPD
- chronic obstructive pulmonary disease
- CRD
- Centre for Reviews and Dissemenation
- DoH
- Department of Health
- EQ-5D
- European Quality of Life-5 Dimensions
- ICER
- incremental cost-effectiveness ratio
- LC
- lung cancer
- MI
- myocardial infarction
- NHS SSS
- NHS Stop Smoking Service
- NICE
- National Institute for Health and Clinical Excellence
- NNT
- number needed to treat
- NRT
- nicotine replacement therapy
- OR
- odds ratio
- PCT
- primary care trust
- p.p.m.
- parts per million
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCT
- randomised controlled trial
- RPI
- relapse prevention intervention/treatment
- RR
- relative risk
- SCSC
- Smoking Cessation Service Co-ordinator
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment reports published to date
-
Home parenteral nutrition: a systematic review.
By Richards DM, Deeks JJ, Sheldon TA, Shaffer JL.
-
Diagnosis, management and screening of early localised prostate cancer.
A review by Selley S, Donovan J, Faulkner A, Coast J, Gillatt D.
-
The diagnosis, management, treatment and costs of prostate cancer in England and Wales.
A review by Chamberlain J, Melia J, Moss S, Brown J.
-
Screening for fragile X syndrome.
A review by Murray J, Cuckle H, Taylor G, Hewison J.
-
A review of near patient testing in primary care.
By Hobbs FDR, Delaney BC, Fitzmaurice DA, Wilson S, Hyde CJ, Thorpe GH, et al.
-
Systematic review of outpatient services for chronic pain control.
By McQuay HJ, Moore RA, Eccleston C, Morley S, de C Williams AC.
-
Neonatal screening for inborn errors of metabolism: cost, yield and outcome.
A review by Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leonard JV, et al.
-
Preschool vision screening.
A review by Snowdon SK, Stewart-Brown SL.
-
Implications of socio-cultural contexts for the ethics of clinical trials.
A review by Ashcroft RE, Chadwick DW, Clark SRL, Edwards RHT, Frith L, Hutton JL.
-
A critical review of the role of neonatal hearing screening in the detection of congenital hearing impairment.
By Davis A, Bamford J, Wilson I, Ramkalawan T, Forshaw M, Wright S.
-
Newborn screening for inborn errors of metabolism: a systematic review.
By Seymour CA, Thomason MJ, Chalmers RA, Addison GM, Bain MD, Cockburn F, et al.
-
Routine preoperative testing: a systematic review of the evidence.
By Munro J, Booth A, Nicholl J.
-
Systematic review of the effectiveness of laxatives in the elderly.
By Petticrew M, Watt I, Sheldon T.
-
When and how to assess fast-changing technologies: a comparative study of medical applications of four generic technologies.
A review by Mowatt G, Bower DJ, Brebner JA, Cairns JA, Grant AM, McKee L.
-
Antenatal screening for Down’s syndrome.
A review by Wald NJ, Kennard A, Hackshaw A, McGuire A.
-
Screening for ovarian cancer: a systematic review.
By Bell R, Petticrew M, Luengo S, Sheldon TA.
-
Consensus development methods, and their use in clinical guideline development.
A review by Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Askham J, et al.
-
A cost–utility analysis of interferon beta for multiple sclerosis.
By Parkin D, McNamee P, Jacoby A, Miller P, Thomas S, Bates D.
-
Effectiveness and efficiency of methods of dialysis therapy for end-stage renal disease: systematic reviews.
By MacLeod A, Grant A, Donaldson C, Khan I, Campbell M, Daly C, et al.
-
Effectiveness of hip prostheses in primary total hip replacement: a critical review of evidence and an economic model.
By Faulkner A, Kennedy LG, Baxter K, Donovan J, Wilkinson M, Bevan G.
-
Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials.
By Song F, Glenny AM.
-
Bone marrow and peripheral blood stem cell transplantation for malignancy.
A review by Johnson PWM, Simnett SJ, Sweetenham JW, Morgan GJ, Stewart LA.
-
Screening for speech and language delay: a systematic review of the literature.
By Law J, Boyle J, Harris F, Harkness A, Nye C.
-
Resource allocation for chronic stable angina: a systematic review of effectiveness, costs and cost-effectiveness of alternative interventions.
By Sculpher MJ, Petticrew M, Kelland JL, Elliott RA, Holdright DR, Buxton MJ.
-
Detection, adherence and control of hypertension for the prevention of stroke: a systematic review.
By Ebrahim S.
-
Postoperative analgesia and vomiting, with special reference to day-case surgery: a systematic review.
By McQuay HJ, Moore RA.
-
Choosing between randomised and nonrandomised studies: a systematic review.
By Britton A, McKee M, Black N, McPherson K, Sanderson C, Bain C.
-
Evaluating patient-based outcome measures for use in clinical trials.
A review by Fitzpatrick R, Davey C, Buxton MJ, Jones DR.
-
Ethical issues in the design and conduct of randomised controlled trials.
A review by Edwards SJL, Lilford RJ, Braunholtz DA, Jackson JC, Hewison J, Thornton J.
-
Qualitative research methods in health technology assessment: a review of the literature.
By Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P.
-
The costs and benefits of paramedic skills in pre-hospital trauma care.
By Nicholl J, Hughes S, Dixon S, Turner J, Yates D.
-
Systematic review of endoscopic ultrasound in gastro-oesophageal cancer.
By Harris KM, Kelly S, Berry E, Hutton J, Roderick P, Cullingworth J, et al.
-
Systematic reviews of trials and other studies.
By Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F.
-
Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prostheses.
A review by Fitzpatrick R, Shortall E, Sculpher M, Murray D, Morris R, Lodge M, et al.
-
Informed decision making: an annotated bibliography and systematic review.
By Bekker H, Thornton JG, Airey CM, Connelly JB, Hewison J, Robinson MB, et al.
-
Handling uncertainty when performing economic evaluation of healthcare interventions.
A review by Briggs AH, Gray AM.
-
The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H.
-
A randomised controlled trial of different approaches to universal antenatal HIV testing: uptake and acceptability. Annex: Antenatal HIV testing – assessment of a routine voluntary approach.
By Simpson WM, Johnstone FD, Boyd FM, Goldberg DJ, Hart GJ, Gormley SM, et al.
-
Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review.
By Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ.
-
Assessing the costs of healthcare technologies in clinical trials.
A review by Johnston K, Buxton MJ, Jones DR, Fitzpatrick R.
-
Cooperatives and their primary care emergency centres: organisation and impact.
By Hallam L, Henthorne K.
-
Screening for cystic fibrosis.
A review by Murray J, Cuckle H, Taylor G, Littlewood J, Hewison J.
-
A review of the use of health status measures in economic evaluation.
By Brazier J, Deverill M, Green C, Harper R, Booth A.
-
Methods for the analysis of quality-of-life and survival data in health technology assessment.
A review by Billingham LJ, Abrams KR, Jones DR.
-
Antenatal and neonatal haemoglobinopathy screening in the UK: review and economic analysis.
By Zeuner D, Ades AE, Karnon J, Brown J, Dezateux C, Anionwu EN.
-
Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses.
A review by Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al.
-
‘Early warning systems’ for identifying new healthcare technologies.
By Robert G, Stevens A, Gabbay J.
-
A systematic review of the role of human papillomavirus testing within a cervical screening programme.
By Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, et al.
-
Near patient testing in diabetes clinics: appraising the costs and outcomes.
By Grieve R, Beech R, Vincent J, Mazurkiewicz J.
-
Positron emission tomography: establishing priorities for health technology assessment.
A review by Robert G, Milne R.
-
The debridement of chronic wounds: a systematic review.
By Bradley M, Cullum N, Sheldon T.
-
Systematic reviews of wound care management: (2) Dressings and topical agents used in the healing of chronic wounds.
By Bradley M, Cullum N, Nelson EA, Petticrew M, Sheldon T, Torgerson D.
-
A systematic literature review of spiral and electron beam computed tomography: with particular reference to clinical applications in hepatic lesions, pulmonary embolus and coronary artery disease.
By Berry E, Kelly S, Hutton J, Harris KM, Roderick P, Boyce JC, et al.
-
What role for statins? A review and economic model.
By Ebrahim S, Davey Smith G, McCabe C, Payne N, Pickin M, Sheldon TA, et al.
-
Factors that limit the quality, number and progress of randomised controlled trials.
A review by Prescott RJ, Counsell CE, Gillespie WJ, Grant AM, Russell IT, Kiauka S, et al.
-
Antimicrobial prophylaxis in total hip replacement: a systematic review.
By Glenny AM, Song F.
-
Health promoting schools and health promotion in schools: two systematic reviews.
By Lister-Sharp D, Chapman S, Stewart-Brown S, Sowden A.
-
Economic evaluation of a primary care-based education programme for patients with osteoarthritis of the knee.
A review by Lord J, Victor C, Littlejohns P, Ross FM, Axford JS.
-
The estimation of marginal time preference in a UK-wide sample (TEMPUS) project.
A review by Cairns JA, van der Pol MM.
-
Geriatric rehabilitation following fractures in older people: a systematic review.
By Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Gillespie W, et al.
-
Screening for sickle cell disease and thalassaemia: a systematic review with supplementary research.
By Davies SC, Cronin E, Gill M, Greengross P, Hickman M, Normand C.
-
Community provision of hearing aids and related audiology services.
A review by Reeves DJ, Alborz A, Hickson FS, Bamford JM.
-
False-negative results in screening programmes: systematic review of impact and implications.
By Petticrew MP, Sowden AJ, Lister-Sharp D, Wright K.
-
Costs and benefits of community postnatal support workers: a randomised controlled trial.
By Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A.
-
Implantable contraceptives (subdermal implants and hormonally impregnated intrauterine systems) versus other forms of reversible contraceptives: two systematic reviews to assess relative effectiveness, acceptability, tolerability and cost-effectiveness.
By French RS, Cowan FM, Mansour DJA, Morris S, Procter T, Hughes D, et al.
-
An introduction to statistical methods for health technology assessment.
A review by White SJ, Ashby D, Brown PJ.
-
Disease-modifying drugs for multiple sclerosis: a rapid and systematic review.
By Clegg A, Bryant J, Milne R.
-
Publication and related biases.
A review by Song F, Eastwood AJ, Gilbody S, Duley L, Sutton AJ.
-
Cost and outcome implications of the organisation of vascular services.
By Michaels J, Brazier J, Palfreyman S, Shackley P, Slack R.
-
Monitoring blood glucose control in diabetes mellitus: a systematic review.
By Coster S, Gulliford MC, Seed PT, Powrie JK, Swaminathan R.
-
The effectiveness of domiciliary health visiting: a systematic review of international studies and a selective review of the British literature.
By Elkan R, Kendrick D, Hewitt M, Robinson JJA, Tolley K, Blair M, et al.
-
The determinants of screening uptake and interventions for increasing uptake: a systematic review.
By Jepson R, Clegg A, Forbes C, Lewis R, Sowden A, Kleijnen J.
-
The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth.
A rapid review by Song F, O’Meara S, Wilson P, Golder S, Kleijnen J.
-
Ultrasound screening in pregnancy: a systematic review of the clinical effectiveness, cost-effectiveness and women’s views.
By Bricker L, Garcia J, Henderson J, Mugford M, Neilson J, Roberts T, et al.
-
A rapid and systematic review of the effectiveness and cost-effectiveness of the taxanes used in the treatment of advanced breast and ovarian cancer.
By Lister-Sharp D, McDonagh MS, Khan KS, Kleijnen J.
-
Liquid-based cytology in cervical screening: a rapid and systematic review.
By Payne N, Chilcott J, McGoogan E.
-
Randomised controlled trial of non-directive counselling, cognitive–behaviour therapy and usual general practitioner care in the management of depression as well as mixed anxiety and depression in primary care.
By King M, Sibbald B, Ward E, Bower P, Lloyd M, Gabbay M, et al.
-
Routine referral for radiography of patients presenting with low back pain: is patients’ outcome influenced by GPs’ referral for plain radiography?
By Kerry S, Hilton S, Patel S, Dundas D, Rink E, Lord J.
-
Systematic reviews of wound care management: (3) antimicrobial agents for chronic wounds; (4) diabetic foot ulceration.
By O’Meara S, Cullum N, Majid M, Sheldon T.
-
Using routine data to complement and enhance the results of randomised controlled trials.
By Lewsey JD, Leyland AH, Murray GD, Boddy FA.
-
Coronary artery stents in the treatment of ischaemic heart disease: a rapid and systematic review.
By Meads C, Cummins C, Jolly K, Stevens A, Burls A, Hyde C.
-
Outcome measures for adult critical care: a systematic review.
By Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al.
-
A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.
By Fairbank L, O’Meara S, Renfrew MJ, Woolridge M, Sowden AJ, Lister-Sharp D.
-
Implantable cardioverter defibrillators: arrhythmias. A rapid and systematic review.
By Parkes J, Bryant J, Milne R.
-
Treatments for fatigue in multiple sclerosis: a rapid and systematic review.
By Brañas P, Jordan R, Fry-Smith A, Burls A, Hyde C.
-
Early asthma prophylaxis, natural history, skeletal development and economy (EASE): a pilot randomised controlled trial.
By Baxter-Jones ADG, Helms PJ, Russell G, Grant A, Ross S, Cairns JA, et al.
-
Screening for hypercholesterolaemia versus case finding for familial hypercholesterolaemia: a systematic review and cost-effectiveness analysis.
By Marks D, Wonderling D, Thorogood M, Lambert H, Humphries SE, Neil HAW.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists in the medical management of unstable angina.
By McDonagh MS, Bachmann LM, Golder S, Kleijnen J, ter Riet G.
-
A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma.
By Turner J, Nicholl J, Webber L, Cox H, Dixon S, Yates D.
-
Intrathecal pumps for giving opioids in chronic pain: a systematic review.
By Williams JE, Louw G, Towlerton G.
-
Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review.
By Shepherd J, Waugh N, Hewitson P.
-
A systematic review of comparisons of effect sizes derived from randomised and non-randomised studies.
By MacLehose RR, Reeves BC, Harvey IM, Sheldon TA, Russell IT, Black AMS.
-
Intravascular ultrasound-guided interventions in coronary artery disease: a systematic literature review, with decision-analytic modelling, of outcomes and cost-effectiveness.
By Berry E, Kelly S, Hutton J, Lindsay HSJ, Blaxill JM, Evans JA, et al.
-
A randomised controlled trial to evaluate the effectiveness and cost-effectiveness of counselling patients with chronic depression.
By Simpson S, Corney R, Fitzgerald P, Beecham J.
-
Systematic review of treatments for atopic eczema.
By Hoare C, Li Wan Po A, Williams H.
-
Bayesian methods in health technology assessment: a review.
By Spiegelhalter DJ, Myles JP, Jones DR, Abrams KR.
-
The management of dyspepsia: a systematic review.
By Delaney B, Moayyedi P, Deeks J, Innes M, Soo S, Barton P, et al.
-
A systematic review of treatments for severe psoriasis.
By Griffiths CEM, Clark CM, Chalmers RJG, Li Wan Po A, Williams HC.
-
Clinical and cost-effectiveness of donepezil, rivastigmine and galantamine for Alzheimer’s disease: a rapid and systematic review.
By Clegg A, Bryant J, Nicholson T, McIntyre L, De Broe S, Gerard K, et al.
-
The clinical effectiveness and cost-effectiveness of riluzole for motor neurone disease: a rapid and systematic review.
By Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al.
-
Equity and the economic evaluation of healthcare.
By Sassi F, Archard L, Le Grand J.
-
Quality-of-life measures in chronic diseases of childhood.
By Eiser C, Morse R.
-
Eliciting public preferences for healthcare: a systematic review of techniques.
By Ryan M, Scott DA, Reeves C, Bate A, van Teijlingen ER, Russell EM, et al.
-
General health status measures for people with cognitive impairment: learning disability and acquired brain injury.
By Riemsma RP, Forbes CA, Glanville JM, Eastwood AJ, Kleijnen J.
-
An assessment of screening strategies for fragile X syndrome in the UK.
By Pembrey ME, Barnicoat AJ, Carmichael B, Bobrow M, Turner G.
-
Issues in methodological research: perspectives from researchers and commissioners.
By Lilford RJ, Richardson A, Stevens A, Fitzpatrick R, Edwards S, Rock F, et al.
-
Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy.
By Cullum N, Nelson EA, Flemming K, Sheldon T.
-
Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review.
By Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, et al.
-
Effectiveness of autologous chondrocyte transplantation for hyaline cartilage defects in knees: a rapid and systematic review.
By Jobanputra P, Parry D, Fry-Smith A, Burls A.
-
Statistical assessment of the learning curves of health technologies.
By Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT.
-
The effectiveness and cost-effectiveness of temozolomide for the treatment of recurrent malignant glioma: a rapid and systematic review.
By Dinnes J, Cave C, Huang S, Major K, Milne R.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of debriding agents in treating surgical wounds healing by secondary intention.
By Lewis R, Whiting P, ter Riet G, O’Meara S, Glanville J.
-
Home treatment for mental health problems: a systematic review.
By Burns T, Knapp M, Catty J, Healey A, Henderson J, Watt H, et al.
-
How to develop cost-conscious guidelines.
By Eccles M, Mason J.
-
The role of specialist nurses in multiple sclerosis: a rapid and systematic review.
By De Broe S, Christopher F, Waugh N.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of orlistat in the management of obesity.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The clinical effectiveness and cost-effectiveness of pioglitazone for type 2 diabetes mellitus: a rapid and systematic review.
By Chilcott J, Wight J, Lloyd Jones M, Tappenden P.
-
Extended scope of nursing practice: a multicentre randomised controlled trial of appropriately trained nurses and preregistration house officers in preoperative assessment in elective general surgery.
By Kinley H, Czoski-Murray C, George S, McCabe C, Primrose J, Reilly C, et al.
-
Systematic reviews of the effectiveness of day care for people with severe mental disorders: (1) Acute day hospital versus admission; (2) Vocational rehabilitation; (3) Day hospital versus outpatient care.
By Marshall M, Crowther R, Almaraz- Serrano A, Creed F, Sledge W, Kluiter H, et al.
-
The measurement and monitoring of surgical adverse events.
By Bruce J, Russell EM, Mollison J, Krukowski ZH.
-
Action research: a systematic review and guidance for assessment.
By Waterman H, Tillen D, Dickson R, de Koning K.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of gemcitabine for the treatment of pancreatic cancer.
By Ward S, Morris E, Bansback N, Calvert N, Crellin A, Forman D, et al.
-
A rapid and systematic review of the evidence for the clinical effectiveness and cost-effectiveness of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer.
By Lloyd Jones M, Hummel S, Bansback N, Orr B, Seymour M.
-
Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature.
By Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al.
-
The cost-effectiveness of magnetic resonance imaging for investigation of the knee joint.
By Bryan S, Weatherburn G, Bungay H, Hatrick C, Salas C, Parry D, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of topotecan for ovarian cancer.
By Forbes C, Shirran L, Bagnall A-M, Duffy S, ter Riet G.
-
Superseded by a report published in a later volume.
-
The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial.
By Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M.
-
Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients.
By McColl E, Jacoby A, Thomas L, Soutter J, Bamford C, Steen N, et al.
-
A rapid and systematic review of the clinical effectiveness and cost-effectiveness of paclitaxel, docetaxel, gemcitabine and vinorelbine in non-small-cell lung cancer.
By Clegg A, Scott DA, Sidhu M, Hewitson P, Waugh N.
-
Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives.
By Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G.
-
Depot antipsychotic medication in the treatment of patients with schizophrenia: (1) Meta-review; (2) Patient and nurse attitudes.
By David AS, Adams C.
-
A systematic review of controlled trials of the effectiveness and cost-effectiveness of brief psychological treatments for depression.
By Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al.
-
Cost analysis of child health surveillance.
By Sanderson D, Wright D, Acton C, Duree D.
-
A study of the methods used to select review criteria for clinical audit.
By Hearnshaw H, Harker R, Cheater F, Baker R, Grimshaw G.
-
Fludarabine as second-line therapy for B cell chronic lymphocytic leukaemia: a technology assessment.
By Hyde C, Wake B, Bryan S, Barton P, Fry-Smith A, Davenport C, et al.
-
Rituximab as third-line treatment for refractory or recurrent Stage III or IV follicular non-Hodgkin’s lymphoma: a systematic review and economic evaluation.
By Wake B, Hyde C, Bryan S, Barton P, Song F, Fry-Smith A, et al.
-
A systematic review of discharge arrangements for older people.
By Parker SG, Peet SM, McPherson A, Cannaby AM, Baker R, Wilson A, et al.
-
The clinical effectiveness and cost-effectiveness of inhaler devices used in the routine management of chronic asthma in older children: a systematic review and economic evaluation.
By Peters J, Stevenson M, Beverley C, Lim J, Smith S.
-
The clinical effectiveness and cost-effectiveness of sibutramine in the management of obesity: a technology assessment.
By O’Meara S, Riemsma R, Shirran L, Mather L, ter Riet G.
-
The cost-effectiveness of magnetic resonance angiography for carotid artery stenosis and peripheral vascular disease: a systematic review.
By Berry E, Kelly S, Westwood ME, Davies LM, Gough MJ, Bamford JM, et al.
-
Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’.
By Carroll B, Ali N, Azam N.
-
Zanamivir for the treatment of influenza in adults: a systematic review and economic evaluation.
By Burls A, Clark W, Stewart T, Preston C, Bryan S, Jefferson T, et al.
-
A review of the natural history and epidemiology of multiple sclerosis: implications for resource allocation and health economic models.
By Richards RG, Sampson FC, Beard SM, Tappenden P.
-
Screening for gestational diabetes: a systematic review and economic evaluation.
By Scott DA, Loveman E, McIntyre L, Waugh N.
-
The clinical effectiveness and cost-effectiveness of surgery for people with morbid obesity: a systematic review and economic evaluation.
By Clegg AJ, Colquitt J, Sidhu MK, Royle P, Loveman E, Walker A.
-
The clinical effectiveness of trastuzumab for breast cancer: a systematic review.
By Lewis R, Bagnall A-M, Forbes C, Shirran E, Duffy S, Kleijnen J, et al.
-
The clinical effectiveness and cost-effectiveness of vinorelbine for breast cancer: a systematic review and economic evaluation.
By Lewis R, Bagnall A-M, King S, Woolacott N, Forbes C, Shirran L, et al.
-
A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease.
By Vale L, Wyness L, McCormack K, McKenzie L, Brazzelli M, Stearns SC.
-
The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation.
By Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al.
-
A systematic review of effectiveness and economic evaluation of new drug treatments for juvenile idiopathic arthritis: etanercept.
By Cummins C, Connock M, Fry-Smith A, Burls A.
-
Clinical effectiveness and cost-effectiveness of growth hormone in children: a systematic review and economic evaluation.
By Bryant J, Cave C, Mihaylova B, Chase D, McIntyre L, Gerard K, et al.
-
Clinical effectiveness and cost-effectiveness of growth hormone in adults in relation to impact on quality of life: a systematic review and economic evaluation.
By Bryant J, Loveman E, Chase D, Mihaylova B, Cave C, Gerard K, et al.
-
Clinical medication review by a pharmacist of patients on repeat prescriptions in general practice: a randomised controlled trial.
By Zermansky AG, Petty DR, Raynor DK, Lowe CJ, Freementle N, Vail A.
-
The effectiveness of infliximab and etanercept for the treatment of rheumatoid arthritis: a systematic review and economic evaluation.
By Jobanputra P, Barton P, Bryan S, Burls A.
-
A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety.
By Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J.
-
A systematic review and economic evaluation of pegylated liposomal doxorubicin hydrochloride for ovarian cancer.
By Forbes C, Wilby J, Richardson G, Sculpher M, Mather L, Riemsma R.
-
A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change.
By Riemsma RP, Pattenden J, Bridle C, Sowden AJ, Mather L, Watt IS, et al.
-
A systematic review update of the clinical effectiveness and cost-effectiveness of glycoprotein IIb/IIIa antagonists.
By Robinson M, Ginnelly L, Sculpher M, Jones L, Riemsma R, Palmer S, et al.
-
A systematic review of the effectiveness, cost-effectiveness and barriers to implementation of thrombolytic and neuroprotective therapy for acute ischaemic stroke in the NHS.
By Sandercock P, Berge E, Dennis M, Forbes J, Hand P, Kwan J, et al.
-
A randomised controlled crossover trial of nurse practitioner versus doctor-led outpatient care in a bronchiectasis clinic.
By Caine N, Sharples LD, Hollingworth W, French J, Keogan M, Exley A, et al.
-
Clinical effectiveness and cost – consequences of selective serotonin reuptake inhibitors in the treatment of sex offenders.
By Adi Y, Ashcroft D, Browne K, Beech A, Fry-Smith A, Hyde C.
-
Treatment of established osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd Jones M.
-
Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial.
By Elliott RA, Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al.
-
Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice.
By Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al.
-
The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature.
By Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al.
-
The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review.
By Garside R, Round A, Dalziel K, Stein K, Royle R.
-
A comparative study of hypertonic saline, daily and alternate-day rhDNase in children with cystic fibrosis.
By Suri R, Wallis C, Bush A, Thompson S, Normand C, Flather M, et al.
-
A systematic review of the costs and effectiveness of different models of paediatric home care.
By Parker G, Bhakta P, Lovett CA, Paisley S, Olsen R, Turner D, et al.
-
How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study.
By Egger M, Jüni P, Bartlett C, Holenstein F, Sterne J.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of home versus hospital or satellite unit haemodialysis for people with end-stage renal failure.
By Mowatt G, Vale L, Perez J, Wyness L, Fraser C, MacLeod A, et al.
-
Systematic review and economic evaluation of the effectiveness of infliximab for the treatment of Crohn’s disease.
By Clark W, Raftery J, Barton P, Song F, Fry-Smith A, Burls A.
-
A review of the clinical effectiveness and cost-effectiveness of routine anti-D prophylaxis for pregnant women who are rhesus negative.
By Chilcott J, Lloyd Jones M, Wight J, Forman K, Wray J, Beverley C, et al.
-
Systematic review and evaluation of the use of tumour markers in paediatric oncology: Ewing’s sarcoma and neuroblastoma.
By Riley RD, Burchill SA, Abrams KR, Heney D, Lambert PC, Jones DR, et al.
-
The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discrete-event simulation model.
By Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Bhandari P, et al.
-
The clinical effectiveness and cost-effectiveness of routine dental checks: a systematic review and economic evaluation.
By Davenport C, Elley K, Salas C, Taylor-Weetman CL, Fry-Smith A, Bryan S, et al.
-
A multicentre randomised controlled trial assessing the costs and benefits of using structured information and analysis of women’s preferences in the management of menorrhagia.
By Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Horsley S, et al.
-
Clinical effectiveness and cost–utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation.
By Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C.
-
Evaluation of molecular tests for prenatal diagnosis of chromosome abnormalities.
By Grimshaw GM, Szczepura A, Hultén M, MacDonald F, Nevin NC, Sutton F, et al.
-
First and second trimester antenatal screening for Down’s syndrome: the results of the Serum, Urine and Ultrasound Screening Study (SURUSS).
By Wald NJ, Rodeck C, Hackshaw AK, Walters J, Chitty L, Mackinson AM.
-
The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation.
By Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A.
-
A systematic review of atypical antipsychotics in schizophrenia.
By Bagnall A-M, Jones L, Lewis R, Ginnelly L, Glanville J, Torgerson D, et al.
-
Prostate Testing for Cancer and Treatment (ProtecT) feasibility study.
By Donovan J, Hamdy F, Neal D, Peters T, Oliver S, Brindle L, et al.
-
Early thrombolysis for the treatment of acute myocardial infarction: a systematic review and economic evaluation.
By Boland A, Dundar Y, Bagust A, Haycox A, Hill R, Mujica Mota R, et al.
-
Screening for fragile X syndrome: a literature review and modelling.
By Song FJ, Barton P, Sleightholme V, Yao GL, Fry-Smith A.
-
Systematic review of endoscopic sinus surgery for nasal polyps.
By Dalziel K, Stein K, Round A, Garside R, Royle P.
-
Towards efficient guidelines: how to monitor guideline use in primary care.
By Hutchinson A, McIntosh A, Cox S, Gilbert C.
-
Effectiveness and cost-effectiveness of acute hospital-based spinal cord injuries services: systematic review.
By Bagnall A-M, Jones L, Richardson G, Duffy S, Riemsma R.
-
Prioritisation of health technology assessment. The PATHS model: methods and case studies.
By Townsend J, Buxton M, Harper G.
-
Systematic review of the clinical effectiveness and cost-effectiveness of tension-free vaginal tape for treatment of urinary stress incontinence.
By Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al.
-
The clinical and cost-effectiveness of patient education models for diabetes: a systematic review and economic evaluation.
By Loveman E, Cave C, Green C, Royle P, Dunn N, Waugh N.
-
The role of modelling in prioritising and planning clinical trials.
By Chilcott J, Brennan A, Booth A, Karnon J, Tappenden P.
-
Cost–benefit evaluation of routine influenza immunisation in people 65–74 years of age.
By Allsup S, Gosney M, Haycox A, Regan M.
-
The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors.
By Wight J, Chilcott J, Holmes M, Brewer N.
-
Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment.
By Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT.
-
Evaluating non-randomised intervention studies.
By Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al.
-
A randomised controlled trial to assess the impact of a package comprising a patient-orientated, evidence-based self- help guidebook and patient-centred consultations on disease management and satisfaction in inflammatory bowel disease.
By Kennedy A, Nelson E, Reeves D, Richardson G, Roberts C, Robinson A, et al.
-
The effectiveness of diagnostic tests for the assessment of shoulder pain due to soft tissue disorders: a systematic review.
By Dinnes J, Loveman E, McIntyre L, Waugh N.
-
The value of digital imaging in diabetic retinopathy.
By Sharp PF, Olson J, Strachan F, Hipwell J, Ludbrook A, O’Donnell M, et al.
-
Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy.
By Law M, Wald N, Morris J.
-
Clinical and cost-effectiveness of capecitabine and tegafur with uracil for the treatment of metastatic colorectal cancer: systematic review and economic evaluation.
By Ward S, Kaltenthaler E, Cowan J, Brewer N.
-
Clinical and cost-effectiveness of new and emerging technologies for early localised prostate cancer: a systematic review.
By Hummel S, Paisley S, Morgan A, Currie E, Brewer N.
-
Literature searching for clinical and cost-effectiveness studies used in health technology assessment reports carried out for the National Institute for Clinical Excellence appraisal system.
By Royle P, Waugh N.
-
Systematic review and economic decision modelling for the prevention and treatment of influenza A and B.
By Turner D, Wailoo A, Nicholson K, Cooper N, Sutton A, Abrams K.
-
A randomised controlled trial to evaluate the clinical and cost-effectiveness of Hickman line insertions in adult cancer patients by nurses.
By Boland A, Haycox A, Bagust A, Fitzsimmons L.
-
Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs.
By MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al.
-
Estimating implied rates of discount in healthcare decision-making.
By West RR, McNabb R, Thompson AGH, Sheldon TA, Grimley Evans J.
-
Systematic review of isolation policies in the hospital management of methicillin-resistant Staphylococcus aureus: a review of the literature with epidemiological and economic modelling.
By Cooper BS, Stone SP, Kibbler CC, Cookson BD, Roberts JA, Medley GF, et al.
-
Treatments for spasticity and pain in multiple sclerosis: a systematic review.
By Beard S, Hunn A, Wight J.
-
The inclusion of reports of randomised trials published in languages other than English in systematic reviews.
By Moher D, Pham B, Lawson ML, Klassen TP.
-
The impact of screening on future health-promoting behaviours and health beliefs: a systematic review.
By Bankhead CR, Brett J, Bukach C, Webster P, Stewart-Brown S, Munafo M, et al.
-
What is the best imaging strategy for acute stroke?
By Wardlaw JM, Keir SL, Seymour J, Lewis S, Sandercock PAG, Dennis MS, et al.
-
Systematic review and modelling of the investigation of acute and chronic chest pain presenting in primary care.
By Mant J, McManus RJ, Oakes RAL, Delaney BC, Barton PM, Deeks JJ, et al.
-
The effectiveness and cost-effectiveness of microwave and thermal balloon endometrial ablation for heavy menstrual bleeding: a systematic review and economic modelling.
By Garside R, Stein K, Wyatt K, Round A, Price A.
-
A systematic review of the role of bisphosphonates in metastatic disease.
By Ross JR, Saunders Y, Edmonds PM, Patel S, Wonderling D, Normand C, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda®) for locally advanced and/or metastatic breast cancer.
By Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R.
-
Effectiveness and efficiency of guideline dissemination and implementation strategies.
By Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al.
-
Clinical effectiveness and costs of the Sugarbaker procedure for the treatment of pseudomyxoma peritonei.
By Bryant J, Clegg AJ, Sidhu MK, Brodin H, Royle P, Davidson P.
-
Psychological treatment for insomnia in the regulation of long-term hypnotic drug use.
By Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: development of a patient-based measure of outcome.
By Hobart JC, Riazi A, Lamping DL, Fitzpatrick R, Thompson AJ.
-
A systematic review and economic evaluation of magnetic resonance cholangiopancreatography compared with diagnostic endoscopic retrograde cholangiopancreatography.
By Kaltenthaler E, Bravo Vergel Y, Chilcott J, Thomas S, Blakeborough T, Walters SJ, et al.
-
The use of modelling to evaluate new drugs for patients with a chronic condition: the case of antibodies against tumour necrosis factor in rheumatoid arthritis.
By Barton P, Jobanputra P, Wilson J, Bryan S, Burls A.
-
Clinical effectiveness and cost-effectiveness of neonatal screening for inborn errors of metabolism using tandem mass spectrometry: a systematic review.
By Pandor A, Eastham J, Beverley C, Chilcott J, Paisley S.
-
Clinical effectiveness and cost-effectiveness of pioglitazone and rosiglitazone in the treatment of type 2 diabetes: a systematic review and economic evaluation.
By Czoski-Murray C, Warren E, Chilcott J, Beverley C, Psyllaki MA, Cowan J.
-
Routine examination of the newborn: the EMREN study. Evaluation of an extension of the midwife role including a randomised controlled trial of appropriately trained midwives and paediatric senior house officers.
By Townsend J, Wolke D, Hayes J, Davé S, Rogers C, Bloomfield L, et al.
-
Involving consumers in research and development agenda setting for the NHS: developing an evidence-based approach.
By Oliver S, Clarke-Jones L, Rees R, Milne R, Buchanan P, Gabbay J, et al.
-
A multi-centre randomised controlled trial of minimally invasive direct coronary bypass grafting versus percutaneous transluminal coronary angioplasty with stenting for proximal stenosis of the left anterior descending coronary artery.
By Reeves BC, Angelini GD, Bryan AJ, Taylor FC, Cripps T, Spyt TJ, et al.
-
Does early magnetic resonance imaging influence management or improve outcome in patients referred to secondary care with low back pain? A pragmatic randomised controlled trial.
By Gilbert FJ, Grant AM, Gillan MGC, Vale L, Scott NW, Campbell MK, et al.
-
The clinical and cost-effectiveness of anakinra for the treatment of rheumatoid arthritis in adults: a systematic review and economic analysis.
By Clark W, Jobanputra P, Barton P, Burls A.
-
A rapid and systematic review and economic evaluation of the clinical and cost-effectiveness of newer drugs for treatment of mania associated with bipolar affective disorder.
By Bridle C, Palmer S, Bagnall A-M, Darba J, Duffy S, Sculpher M, et al.
-
Liquid-based cytology in cervical screening: an updated rapid and systematic review and economic analysis.
By Karnon J, Peters J, Platt J, Chilcott J, McGoogan E, Brewer N.
-
Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement.
By Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al.
-
Autoantibody testing in children with newly diagnosed type 1 diabetes mellitus.
By Dretzke J, Cummins C, Sandercock J, Fry-Smith A, Barrett T, Burls A.
-
Clinical effectiveness and cost-effectiveness of prehospital intravenous fluids in trauma patients.
By Dretzke J, Sandercock J, Bayliss S, Burls A.
-
Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation.
By Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, et al.
-
Development and validation of methods for assessing the quality of diagnostic accuracy studies.
By Whiting P, Rutjes AWS, Dinnes J, Reitsma JB, Bossuyt PMM, Kleijnen J.
-
EVALUATE hysterectomy trial: a multicentre randomised trial comparing abdominal, vaginal and laparoscopic methods of hysterectomy.
By Garry R, Fountain J, Brown J, Manca A, Mason S, Sculpher M, et al.
-
Methods for expected value of information analysis in complex health economic models: developments on the health economics of interferon-β and glatiramer acetate for multiple sclerosis.
By Tappenden P, Chilcott JB, Eggington S, Oakley J, McCabe C.
-
Effectiveness and cost-effectiveness of imatinib for first-line treatment of chronic myeloid leukaemia in chronic phase: a systematic review and economic analysis.
By Dalziel K, Round A, Stein K, Garside R, Price A.
-
VenUS I: a randomised controlled trial of two types of bandage for treating venous leg ulcers.
By Iglesias C, Nelson EA, Cullum NA, Torgerson DJ, on behalf of the VenUS Team.
-
Systematic review of the effectiveness and cost-effectiveness, and economic evaluation, of myocardial perfusion scintigraphy for the diagnosis and management of angina and myocardial infarction.
By Mowatt G, Vale L, Brazzelli M, Hernandez R, Murray A, Scott N, et al.
-
A pilot study on the use of decision theory and value of information analysis as part of the NHS Health Technology Assessment programme.
By Claxton K, Ginnelly L, Sculpher M, Philips Z, Palmer S.
-
The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas.
By Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al.
-
Psychosocial aspects of genetic screening of pregnant women and newborns: a systematic review.
By Green JM, Hewison J, Bekker HL, Bryant LD, Cuckle HS.
-
Evaluation of abnormal uterine bleeding: comparison of three outpatient procedures within cohorts defined by age and menopausal status.
By Critchley HOD, Warner P, Lee AJ, Brechin S, Guise J, Graham B.
-
Coronary artery stents: a rapid systematic review and economic evaluation.
By Hill R, Bagust A, Bakhai A, Dickson R, Dündar Y, Haycox A, et al.
-
Review of guidelines for good practice in decision-analytic modelling in health technology assessment.
By Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al.
-
Rituximab (MabThera®) for aggressive non-Hodgkin’s lymphoma: systematic review and economic evaluation.
By Knight C, Hind D, Brewer N, Abbott V.
-
Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation.
By Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al.
-
Pegylated interferon α-2a and -2b in combination with ribavirin in the treatment of chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Brodin H, Cave C, Waugh N, Price A, Gabbay J.
-
Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment- elevation acute coronary syndromes: a systematic review and economic evaluation.
By Main C, Palmer S, Griffin S, Jones L, Orton V, Sculpher M, et al.
-
Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups.
By Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al.
-
Involving South Asian patients in clinical trials.
By Hussain-Gambles M, Leese B, Atkin K, Brown J, Mason S, Tovey P.
-
Clinical and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes.
By Colquitt JL, Green C, Sidhu MK, Hartwell D, Waugh N.
-
Identification and assessment of ongoing trials in health technology assessment reviews.
By Song FJ, Fry-Smith A, Davenport C, Bayliss S, Adi Y, Wilson JS, et al.
-
Systematic review and economic evaluation of a long-acting insulin analogue, insulin glargine
By Warren E, Weatherley-Jones E, Chilcott J, Beverley C.
-
Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis.
By McCarthy CJ, Mills PM, Pullen R, Richardson G, Hawkins N, Roberts CR, et al.
-
Clinical and cost-effectiveness of once-daily versus more frequent use of same potency topical corticosteroids for atopic eczema: a systematic review and economic evaluation.
By Green C, Colquitt JL, Kirby J, Davidson P, Payne E.
-
Acupuncture of chronic headache disorders in primary care: randomised controlled trial and economic analysis.
By Vickers AJ, Rees RW, Zollman CE, McCarney R, Smith CM, Ellis N, et al.
-
Generalisability in economic evaluation studies in healthcare: a review and case studies.
By Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al.
-
Virtual outreach: a randomised controlled trial and economic evaluation of joint teleconferenced medical consultations.
By Wallace P, Barber J, Clayton W, Currell R, Fleming K, Garner P, et al.
-
Randomised controlled multiple treatment comparison to provide a cost-effectiveness rationale for the selection of antimicrobial therapy in acne.
By Ozolins M, Eady EA, Avery A, Cunliffe WJ, O’Neill C, Simpson NB, et al.
-
Do the findings of case series studies vary significantly according to methodological characteristics?
By Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L.
-
Improving the referral process for familial breast cancer genetic counselling: findings of three randomised controlled trials of two interventions.
By Wilson BJ, Torrance N, Mollison J, Wordsworth S, Gray JR, Haites NE, et al.
-
Randomised evaluation of alternative electrosurgical modalities to treat bladder outflow obstruction in men with benign prostatic hyperplasia.
By Fowler C, McAllister W, Plail R, Karim O, Yang Q.
-
A pragmatic randomised controlled trial of the cost-effectiveness of palliative therapies for patients with inoperable oesophageal cancer.
By Shenfine J, McNamee P, Steen N, Bond J, Griffin SM.
-
Impact of computer-aided detection prompts on the sensitivity and specificity of screening mammography.
By Taylor P, Champness J, Given- Wilson R, Johnston K, Potts H.
-
Issues in data monitoring and interim analysis of trials.
By Grant AM, Altman DG, Babiker AB, Campbell MK, Clemens FJ, Darbyshire JH, et al.
-
Lay public’s understanding of equipoise and randomisation in randomised controlled trials.
By Robinson EJ, Kerr CEP, Stevens AJ, Lilford RJ, Braunholtz DA, Edwards SJ, et al.
-
Clinical and cost-effectiveness of electroconvulsive therapy for depressive illness, schizophrenia, catatonia and mania: systematic reviews and economic modelling studies.
By Greenhalgh J, Knight C, Hind D, Beverley C, Walters S.
-
Measurement of health-related quality of life for people with dementia: development of a new instrument (DEMQOL) and an evaluation of current methodology.
By Smith SC, Lamping DL, Banerjee S, Harwood R, Foley B, Smith P, et al.
-
Clinical effectiveness and cost-effectiveness of drotrecogin alfa (activated) (Xigris®) for the treatment of severe sepsis in adults: a systematic review and economic evaluation.
By Green C, Dinnes J, Takeda A, Shepherd J, Hartwell D, Cave C, et al.
-
A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy.
By Dinnes J, Deeks J, Kirby J, Roderick P.
-
Cervical screening programmes: can automation help? Evidence from systematic reviews, an economic analysis and a simulation modelling exercise applied to the UK.
By Willis BH, Barton P, Pearmain P, Bryan S, Hyde C.
-
Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation.
By McCormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al.
-
Clinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: a systematic review and economic evaluation.
By Wilby J, Kainth A, Hawkins N, Epstein D, McIntosh H, McDaid C, et al.
-
A randomised controlled trial to compare the cost-effectiveness of tricyclic antidepressants, selective serotonin reuptake inhibitors and lofepramine.
By Peveler R, Kendrick T, Buxton M, Longworth L, Baldwin D, Moore M, et al.
-
Clinical effectiveness and cost-effectiveness of immediate angioplasty for acute myocardial infarction: systematic review and economic evaluation.
By Hartwell D, Colquitt J, Loveman E, Clegg AJ, Brodin H, Waugh N, et al.
-
A randomised controlled comparison of alternative strategies in stroke care.
By Kalra L, Evans A, Perez I, Knapp M, Swift C, Donaldson N.
-
The investigation and analysis of critical incidents and adverse events in healthcare.
By Woloshynowych M, Rogers S, Taylor-Adams S, Vincent C.
-
Potential use of routine databases in health technology assessment.
By Raftery J, Roderick P, Stevens A.
-
Clinical and cost-effectiveness of newer immunosuppressive regimens in renal transplantation: a systematic review and modelling study.
By Woodroffe R, Yao GL, Meads C, Bayliss S, Ready A, Raftery J, et al.
-
A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis.
By Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J.
-
A systematic review to examine the impact of psycho-educational interventions on health outcomes and costs in adults and children with difficult asthma.
By Smith JR, Mugford M, Holland R, Candy B, Noble MJ, Harrison BDW, et al.
-
An evaluation of the costs, effectiveness and quality of renal replacement therapy provision in renal satellite units in England and Wales.
By Roderick P, Nicholson T, Armitage A, Mehta R, Mullee M, Gerard K, et al.
-
Imatinib for the treatment of patients with unresectable and/or metastatic gastrointestinal stromal tumours: systematic review and economic evaluation.
By Wilson J, Connock M, Song F, Yao G, Fry-Smith A, Raftery J, et al.
-
Indirect comparisons of competing interventions.
By Glenny AM, Altman DG, Song F, Sakarovitch C, Deeks JJ, D’Amico R, et al.
-
Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling.
By Robinson M, Palmer S, Sculpher M, Philips Z, Ginnelly L, Bowens A, et al.
-
Outcomes of electrically stimulated gracilis neosphincter surgery.
By Tillin T, Chambers M, Feldman R.
-
The effectiveness and cost-effectiveness of pimecrolimus and tacrolimus for atopic eczema: a systematic review and economic evaluation.
By Garside R, Stein K, Castelnuovo E, Pitt M, Ashcroft D, Dimmock P, et al.
-
Systematic review on urine albumin testing for early detection of diabetic complications.
By Newman DJ, Mattock MB, Dawnay ABS, Kerry S, McGuire A, Yaqoob M, et al.
-
Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis.
By Cochrane T, Davey RC, Matthes Edwards SM.
-
Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain.
By Thomas KJ, MacPherson H, Ratcliffe J, Thorpe L, Brazier J, Campbell M, et al.
-
Cost-effectiveness and safety of epidural steroids in the management of sciatica.
By Price C, Arden N, Coglan L, Rogers P.
-
The British Rheumatoid Outcome Study Group (BROSG) randomised controlled trial to compare the effectiveness and cost-effectiveness of aggressive versus symptomatic therapy in established rheumatoid arthritis.
By Symmons D, Tricker K, Roberts C, Davies L, Dawes P, Scott DL.
-
Conceptual framework and systematic review of the effects of participants’ and professionals’ preferences in randomised controlled trials.
By King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al.
-
The clinical and cost-effectiveness of implantable cardioverter defibrillators: a systematic review.
By Bryant J, Brodin H, Loveman E, Payne E, Clegg A.
-
A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study.
By Kendrick T, Simons L, Mynors-Wallis L, Gray A, Lathlean J, Pickering R, et al.
-
The causes and effects of socio-demographic exclusions from clinical trials.
By Bartlett C, Doyal L, Ebrahim S, Davey P, Bachmann M, Egger M, et al.
-
Is hydrotherapy cost-effective? A randomised controlled trial of combined hydrotherapy programmes compared with physiotherapy land techniques in children with juvenile idiopathic arthritis.
By Epps H, Ginnelly L, Utley M, Southwood T, Gallivan S, Sculpher M, et al.
-
A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study.
By Hobbs FDR, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al.
-
Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty.
By Keating JF, Grant A, Masson M, Scott NW, Forbes JF.
-
Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland.
By Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al.
-
The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation.
By Castelnuovo E, Stein K, Pitt M, Garside R, Payne E.
-
Newborn screening for congenital heart defects: a systematic review and cost-effectiveness analysis.
By Knowles R, Griebsch I, Dezateux C, Brown J, Bull C, Wren C.
-
The clinical and cost-effectiveness of left ventricular assist devices for end-stage heart failure: a systematic review and economic evaluation.
By Clegg AJ, Scott DA, Loveman E, Colquitt J, Hutchinson J, Royle P, et al.
-
The effectiveness of the Heidelberg Retina Tomograph and laser diagnostic glaucoma scanning system (GDx) in detecting and monitoring glaucoma.
By Kwartz AJ, Henson DB, Harper RA, Spencer AF, McLeod D.
-
Clinical and cost-effectiveness of autologous chondrocyte implantation for cartilage defects in knee joints: systematic review and economic evaluation.
By Clar C, Cummins E, McIntyre L, Thomas S, Lamb J, Bain L, et al.
-
Systematic review of effectiveness of different treatments for childhood retinoblastoma.
By McDaid C, Hartley S, Bagnall A-M, Ritchie G, Light K, Riemsma R.
-
Towards evidence-based guidelines for the prevention of venous thromboembolism: systematic reviews of mechanical methods, oral anticoagulation, dextran and regional anaesthesia as thromboprophylaxis.
By Roderick P, Ferris G, Wilson K, Halls H, Jackson D, Collins R, et al.
-
The effectiveness and cost-effectiveness of parent training/education programmes for the treatment of conduct disorder, including oppositional defiant disorder, in children.
By Dretzke J, Frew E, Davenport C, Barlow J, Stewart-Brown S, Sandercock J, et al.
-
The clinical and cost-effectiveness of donepezil, rivastigmine, galantamine and memantine for Alzheimer’s disease.
By Loveman E, Green C, Kirby J, Takeda A, Picot J, Payne E, et al.
-
FOOD: a multicentre randomised trial evaluating feeding policies in patients admitted to hospital with a recent stroke.
By Dennis M, Lewis S, Cranswick G, Forbes J.
-
The clinical effectiveness and cost-effectiveness of computed tomography screening for lung cancer: systematic reviews.
By Black C, Bagust A, Boland A, Walker S, McLeod C, De Verteuil R, et al.
-
A systematic review of the effectiveness and cost-effectiveness of neuroimaging assessments used to visualise the seizure focus in people with refractory epilepsy being considered for surgery.
By Whiting P, Gupta R, Burch J, Mujica Mota RE, Wright K, Marson A, et al.
-
Comparison of conference abstracts and presentations with full-text articles in the health technology assessments of rapidly evolving technologies.
By Dundar Y, Dodd S, Dickson R, Walley T, Haycox A, Williamson PR.
-
Systematic review and evaluation of methods of assessing urinary incontinence.
By Martin JL, Williams KS, Abrams KR, Turner DA, Sutton AJ, Chapple C, et al.
-
The clinical effectiveness and cost-effectiveness of newer drugs for children with epilepsy. A systematic review.
By Connock M, Frew E, Evans B-W, Bryan S, Cummins C, Fry-Smith A, et al.
-
Surveillance of Barrett’s oesophagus: exploring the uncertainty through systematic review, expert workshop and economic modelling.
By Garside R, Pitt M, Somerville M, Stein K, Price A, Gilbert N.
-
Topotecan, pegylated liposomal doxorubicin hydrochloride and paclitaxel for second-line or subsequent treatment of advanced ovarian cancer: a systematic review and economic evaluation.
By Main C, Bojke L, Griffin S, Norman G, Barbieri M, Mather L, et al.
-
Evaluation of molecular techniques in prediction and diagnosis of cytomegalovirus disease in immunocompromised patients.
By Szczepura A, Westmoreland D, Vinogradova Y, Fox J, Clark M.
-
Screening for thrombophilia in high-risk situations: systematic review and cost-effectiveness analysis. The Thrombosis: Risk and Economic Assessment of Thrombophilia Screening (TREATS) study.
By Wu O, Robertson L, Twaddle S, Lowe GDO, Clark P, Greaves M, et al.
-
A series of systematic reviews to inform a decision analysis for sampling and treating infected diabetic foot ulcers.
By Nelson EA, O’Meara S, Craig D, Iglesias C, Golder S, Dalton J, et al.
-
Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial).
By Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, Ratcliffe J, et al.
-
The cost-effectiveness of screening for oral cancer in primary care.
By Speight PM, Palmer S, Moles DR, Downer MC, Smith DH, Henriksson M, et al.
-
Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis.
By Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al.
-
Systematic review of the effectiveness and cost-effectiveness of HealOzone® for the treatment of occlusal pit/fissure caries and root caries.
By Brazzelli M, McKenzie L, Fielding S, Fraser C, Clarkson J, Kilonzo M, et al.
-
Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment.
By Lewis SW, Davies L, Jones PB, Barnes TRE, Murray RM, Kerwin R, et al.
-
Diagnostic tests and algorithms used in the investigation of haematuria: systematic reviews and economic evaluation.
By Rodgers M, Nixon J, Hempel S, Aho T, Kelly J, Neal D, et al.
-
Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial.
By Kennedy TM, Chalder T, McCrone P, Darnley S, Knapp M, Jones RH, et al.
-
A systematic review of the clinical effectiveness and cost-effectiveness of enzyme replacement therapies for Fabry’s disease and mucopolysaccharidosis type 1.
By Connock M, Juarez-Garcia A, Frew E, Mans A, Dretzke J, Fry-Smith A, et al.
-
Health benefits of antiviral therapy for mild chronic hepatitis C: randomised controlled trial and economic evaluation.
By Wright M, Grieve R, Roberts J, Main J, Thomas HC, on behalf of the UK Mild Hepatitis C Trial Investigators.
-
Pressure relieving support surfaces: a randomised evaluation.
By Nixon J, Nelson EA, Cranny G, Iglesias CP, Hawkins K, Cullum NA, et al.
-
A systematic review and economic model of the effectiveness and cost-effectiveness of methylphenidate, dexamfetamine and atomoxetine for the treatment of attention deficit hyperactivity disorder in children and adolescents.
By King S, Griffin S, Hodges Z, Weatherly H, Asseburg C, Richardson G, et al.
-
The clinical effectiveness and cost-effectiveness of enzyme replacement therapy for Gaucher’s disease: a systematic review.
By Connock M, Burls A, Frew E, Fry-Smith A, Juarez-Garcia A, McCabe C, et al.
-
Effectiveness and cost-effectiveness of salicylic acid and cryotherapy for cutaneous warts. An economic decision model.
By Thomas KS, Keogh-Brown MR, Chalmers JR, Fordham RJ, Holland RC, Armstrong SJ, et al.
-
A systematic literature review of the effectiveness of non-pharmacological interventions to prevent wandering in dementia and evaluation of the ethical implications and acceptability of their use.
By Robinson L, Hutchings D, Corner L, Beyer F, Dickinson H, Vanoli A, et al.
-
A review of the evidence on the effects and costs of implantable cardioverter defibrillator therapy in different patient groups, and modelling of cost-effectiveness and cost–utility for these groups in a UK context.
By Buxton M, Caine N, Chase D, Connelly D, Grace A, Jackson C, et al.
-
Adefovir dipivoxil and pegylated interferon alfa-2a for the treatment of chronic hepatitis B: a systematic review and economic evaluation.
By Shepherd J, Jones J, Takeda A, Davidson P, Price A.
-
An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial.
By Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al.
-
Accurate, practical and cost-effective assessment of carotid stenosis in the UK.
By Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al.
-
Etanercept and infliximab for the treatment of psoriatic arthritis: a systematic review and economic evaluation.
By Woolacott N, Bravo Vergel Y, Hawkins N, Kainth A, Khadjesari Z, Misso K, et al.
-
The cost-effectiveness of testing for hepatitis C in former injecting drug users.
By Castelnuovo E, Thompson-Coon J, Pitt M, Cramp M, Siebert U, Price A, et al.
-
Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation.
By Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C, et al.
-
Cost-effectiveness of using prognostic information to select women with breast cancer for adjuvant systemic therapy.
By Williams C, Brunskill S, Altman D, Briggs A, Campbell H, Clarke M, et al.
-
Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation.
By Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al.
-
Clinical effectiveness and cost-effectiveness of tests for the diagnosis and investigation of urinary tract infection in children: a systematic review and economic model.
By Whiting P, Westwood M, Bojke L, Palmer S, Richardson G, Cooper J, et al.
-
Cognitive behavioural therapy in chronic fatigue syndrome: a randomised controlled trial of an outpatient group programme.
By O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A.
-
A comparison of the cost-effectiveness of five strategies for the prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal toxicity: a systematic review with economic modelling.
By Brown TJ, Hooper L, Elliott RA, Payne K, Webb R, Roberts C, et al.
-
The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: systematic review.
By Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G.
-
What are the clinical outcome and cost-effectiveness of endoscopy undertaken by nurses when compared with doctors? A Multi-Institution Nurse Endoscopy Trial (MINuET).
By Williams J, Russell I, Durai D, Cheung W-Y, Farrin A, Bloor K, et al.
-
The clinical and cost-effectiveness of oxaliplatin and capecitabine for the adjuvant treatment of colon cancer: systematic review and economic evaluation.
By Pandor A, Eggington S, Paisley S, Tappenden P, Sutcliffe P.
-
A systematic review of the effectiveness of adalimumab, etanercept and infliximab for the treatment of rheumatoid arthritis in adults and an economic evaluation of their cost-effectiveness.
By Chen Y-F, Jobanputra P, Barton P, Jowett S, Bryan S, Clark W, et al.
-
Telemedicine in dermatology: a randomised controlled trial.
By Bowns IR, Collins K, Walters SJ, McDonagh AJG.
-
Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model.
By Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C.
-
Clinical effectiveness and cost-effectiveness of laparoscopic surgery for colorectal cancer: systematic reviews and economic evaluation.
By Murray A, Lourenco T, de Verteuil R, Hernandez R, Fraser C, McKinley A, et al.
-
Etanercept and efalizumab for the treatment of psoriasis: a systematic review.
By Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Bravo Vergel Y, et al.
-
Systematic reviews of clinical decision tools for acute abdominal pain.
By Liu JLY, Wyatt JC, Deeks JJ, Clamp S, Keen J, Verde P, et al.
-
Evaluation of the ventricular assist device programme in the UK.
By Sharples L, Buxton M, Caine N, Cafferty F, Demiris N, Dyer M, et al.
-
A systematic review and economic model of the clinical and cost-effectiveness of immunosuppressive therapy for renal transplantation in children.
By Yao G, Albon E, Adi Y, Milford D, Bayliss S, Ready A, et al.
-
Amniocentesis results: investigation of anxiety. The ARIA trial.
By Hewison J, Nixon J, Fountain J, Cocks K, Jones C, Mason G, et al.
-
Pemetrexed disodium for the treatment of malignant pleural mesothelioma: a systematic review and economic evaluation.
By Dundar Y, Bagust A, Dickson R, Dodd S, Green J, Haycox A, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer.
By Collins R, Fenwick E, Trowman R, Perard R, Norman G, Light K, et al.
-
A systematic review of rapid diagnostic tests for the detection of tuberculosis infection.
By Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, et al.
-
The clinical effectiveness and cost-effectiveness of strontium ranelate for the prevention of osteoporotic fragility fractures in postmenopausal women.
By Stevenson M, Davis S, Lloyd-Jones M, Beverley C.
-
A systematic review of quantitative and qualitative research on the role and effectiveness of written information available to patients about individual medicines.
By Raynor DK, Blenkinsopp A, Knapp P, Grime J, Nicolson DJ, Pollock K, et al.
-
Oral naltrexone as a treatment for relapse prevention in formerly opioid-dependent drug users: a systematic review and economic evaluation.
By Adi Y, Juarez-Garcia A, Wang D, Jowett S, Frew E, Day E, et al.
-
Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis.
By Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M.
-
Epidemiological, social, diagnostic and economic evaluation of population screening for genital chlamydial infection.
By Low N, McCarthy A, Macleod J, Salisbury C, Campbell R, Roberts TE, et al.
-
Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation.
By Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al.
-
Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only.
By Isaacs AJ, Critchley JA, See Tai S, Buckingham K, Westley D, Harridge SDR, et al.
-
Interferon alfa (pegylated and non-pegylated) and ribavirin for the treatment of mild chronic hepatitis C: a systematic review and economic evaluation.
By Shepherd J, Jones J, Hartwell D, Davidson P, Price A, Waugh N.
-
Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer.
By Tappenden P, Jones R, Paisley S, Carroll C.
-
A systematic review and economic evaluation of epoetin alfa, epoetin beta and darbepoetin alfa in anaemia associated with cancer, especially that attributable to cancer treatment.
By Wilson J, Yao GL, Raftery J, Bohlius J, Brunskill S, Sandercock J, et al.
-
A systematic review and economic evaluation of statins for the prevention of coronary events.
By Ward S, Lloyd Jones M, Pandor A, Holmes M, Ara R, Ryan A, et al.
-
A systematic review of the effectiveness and cost-effectiveness of different models of community-based respite care for frail older people and their carers.
By Mason A, Weatherly H, Spilsbury K, Arksey H, Golder S, Adamson J, et al.
-
Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial.
By Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ.
-
Screening for type 2 diabetes: literature review and economic modelling.
By Waugh N, Scotland G, McNamee P, Gillett M, Brennan A, Goyder E, et al.
-
The effectiveness and cost-effectiveness of cinacalcet for secondary hyperparathyroidism in end-stage renal disease patients on dialysis: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Mealing S, Roome C, Snaith A, et al.
-
The clinical effectiveness and cost-effectiveness of gemcitabine for metastatic breast cancer: a systematic review and economic evaluation.
By Takeda AL, Jones J, Loveman E, Tan SC, Clegg AJ.
-
A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease.
By Collins R, Cranny G, Burch J, Aguiar-Ibáñez R, Craig D, Wright K, et al.
-
The clinical effectiveness and cost-effectiveness of treatments for children with idiopathic steroid-resistant nephrotic syndrome: a systematic review.
By Colquitt JL, Kirby J, Green C, Cooper K, Trompeter RS.
-
A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions.
By Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, et al.
-
Systematic review of the effectiveness of preventing and treating Staphylococcus aureus carriage in reducing peritoneal catheter-related infections.
By McCormack K, Rabindranath K, Kilonzo M, Vale L, Fraser C, McIntyre L, et al.
-
The clinical effectiveness and cost of repetitive transcranial magnetic stimulation versus electroconvulsive therapy in severe depression: a multicentre pragmatic randomised controlled trial and economic analysis.
By McLoughlin DM, Mogg A, Eranti S, Pluck G, Purvis R, Edwards D, et al.
-
A randomised controlled trial and economic evaluation of direct versus indirect and individual versus group modes of speech and language therapy for children with primary language impairment.
By Boyle J, McCartney E, Forbes J, O’Hare A.
-
Hormonal therapies for early breast cancer: systematic review and economic evaluation.
By Hind D, Ward S, De Nigris E, Simpson E, Carroll C, Wyld L.
-
Cardioprotection against the toxic effects of anthracyclines given to children with cancer: a systematic review.
By Bryant J, Picot J, Levitt G, Sullivan I, Baxter L, Clegg A.
-
Adalimumab, etanercept and infliximab for the treatment of ankylosing spondylitis: a systematic review and economic evaluation.
By McLeod C, Bagust A, Boland A, Dagenais P, Dickson R, Dundar Y, et al.
-
Prenatal screening and treatment strategies to prevent group B streptococcal and other bacterial infections in early infancy: cost-effectiveness and expected value of information analyses.
By Colbourn T, Asseburg C, Bojke L, Philips Z, Claxton K, Ades AE, et al.
-
Clinical effectiveness and cost-effectiveness of bone morphogenetic proteins in the non-healing of fractures and spinal fusion: a systematic review.
By Garrison KR, Donell S, Ryder J, Shemilt I, Mugford M, Harvey I, et al.
-
A randomised controlled trial of postoperative radiotherapy following breast-conserving surgery in a minimum-risk older population. The PRIME trial.
By Prescott RJ, Kunkler IH, Williams LJ, King CC, Jack W, van der Pol M, et al.
-
Current practice, accuracy, effectiveness and cost-effectiveness of the school entry hearing screen.
By Bamford J, Fortnum H, Bristow K, Smith J, Vamvakas G, Davies L, et al.
-
The clinical effectiveness and cost-effectiveness of inhaled insulin in diabetes mellitus: a systematic review and economic evaluation.
By Black C, Cummins E, Royle P, Philip S, Waugh N.
-
Surveillance of cirrhosis for hepatocellular carcinoma: systematic review and economic analysis.
By Thompson Coon J, Rogers G, Hewson P, Wright D, Anderson R, Cramp M, et al.
-
The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Homebased compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence.
By Jolly K, Taylor R, Lip GYH, Greenfield S, Raftery J, Mant J, et al.
-
A systematic review of the clinical, public health and cost-effectiveness of rapid diagnostic tests for the detection and identification of bacterial intestinal pathogens in faeces and food.
By Abubakar I, Irvine L, Aldus CF, Wyatt GM, Fordham R, Schelenz S, et al.
-
A randomised controlled trial examining the longer-term outcomes of standard versus new antiepileptic drugs. The SANAD trial.
By Marson AG, Appleton R, Baker GA, Chadwick DW, Doughty J, Eaton B, et al.
-
Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anti-coagulation therapy: a systematic review and economic modelling.
By Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al.
-
A systematic review and economic model of the clinical effectiveness and cost-effectiveness of interventions for preventing relapse in people with bipolar disorder.
By Soares-Weiser K, Bravo Vergel Y, Beynon S, Dunn G, Barbieri M, Duffy S, et al.
-
Taxanes for the adjuvant treatment of early breast cancer: systematic review and economic evaluation.
By Ward S, Simpson E, Davis S, Hind D, Rees A, Wilkinson A.
-
The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation.
By Burr JM, Mowatt G, Hernández R, Siddiqui MAR, Cook J, Lourenco T, et al.
-
Acceptability, benefit and costs of early screening for hearing disability: a study of potential screening tests and models.
By Davis A, Smith P, Ferguson M, Stephens D, Gianopoulos I.
-
Contamination in trials of educational interventions.
By Keogh-Brown MR, Bachmann MO, Shepstone L, Hewitt C, Howe A, Ramsay CR, et al.
-
Overview of the clinical effectiveness of positron emission tomography imaging in selected cancers.
By Facey K, Bradbury I, Laking G, Payne E.
-
The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation.
By Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al.
-
Drug-eluting stents: a systematic review and economic evaluation.
By Hill RA, Boland A, Dickson R, Dündar Y, Haycox A, McLeod C, et al.
-
The clinical effectiveness and cost-effectiveness of cardiac resynchronisation (biventricular pacing) for heart failure: systematic review and economic model.
By Fox M, Mealing S, Anderson R, Dean J, Stein K, Price A, et al.
-
Recruitment to randomised trials: strategies for trial enrolment and participation study. The STEPS study.
By Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al.
-
Cost-effectiveness of functional cardiac testing in the diagnosis and management of coronary artery disease: a randomised controlled trial. The CECaT trial.
By Sharples L, Hughes V, Crean A, Dyer M, Buxton M, Goldsmith K, et al.
-
Evaluation of diagnostic tests when there is no gold standard. A review of methods.
By Rutjes AWS, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PMM.
-
Systematic reviews of the clinical effectiveness and cost-effectiveness of proton pump inhibitors in acute upper gastrointestinal bleeding.
By Leontiadis GI, Sreedharan A, Dorward S, Barton P, Delaney B, Howden CW, et al.
-
A review and critique of modelling in prioritising and designing screening programmes.
By Karnon J, Goyder E, Tappenden P, McPhie S, Towers I, Brazier J, et al.
-
An assessment of the impact of the NHS Health Technology Assessment Programme.
By Hanney S, Buxton M, Green C, Coulson D, Raftery J.
-
A systematic review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for surgery.
By Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins N, Myers L, et al.
-
‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis.
By Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D.
-
A systematic review of the effectiveness of strategies for reducing fracture risk in children with juvenile idiopathic arthritis with additional data on long-term risk of fracture and cost of disease management.
By Thornton J, Ashcroft D, O’Neill T, Elliott R, Adams J, Roberts C, et al.
-
Does befriending by trained lay workers improve psychological well-being and quality of life for carers of people with dementia, and at what cost? A randomised controlled trial.
By Charlesworth G, Shepstone L, Wilson E, Thalanany M, Mugford M, Poland F.
-
A multi-centre retrospective cohort study comparing the efficacy, safety and cost-effectiveness of hysterectomy and uterine artery embolisation for the treatment of symptomatic uterine fibroids. The HOPEFUL study.
By Hirst A, Dutton S, Wu O, Briggs A, Edwards C, Waldenmaier L, et al.
-
Methods of prediction and prevention of pre-eclampsia: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Meads CA, Cnossen JS, Meher S, Juarez-Garcia A, ter Riet G, Duley L, et al.
-
The use of economic evaluations in NHS decision-making: a review and empirical investigation.
By Williams I, McIver S, Moore D, Bryan S.
-
Stapled haemorrhoidectomy (haemorrhoidopexy) for the treatment of haemorrhoids: a systematic review and economic evaluation.
By Burch J, Epstein D, Baba-Akbari A, Weatherly H, Fox D, Golder S, et al.
-
The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.
By Loveman E, Frampton GK, Clegg AJ.
-
Payment to healthcare professionals for patient recruitment to trials: systematic review and qualitative study.
By Raftery J, Bryant J, Powell J, Kerr C, Hawker S.
-
Cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs (etodolac, meloxicam, celecoxib, rofecoxib, etoricoxib, valdecoxib and lumiracoxib) for osteoarthritis and rheumatoid arthritis: a systematic review and economic evaluation.
By Chen Y-F, Jobanputra P, Barton P, Bryan S, Fry-Smith A, Harris G, et al.
-
The clinical effectiveness and cost-effectiveness of central venous catheters treated with anti-infective agents in preventing bloodstream infections: a systematic review and economic evaluation.
By Hockenhull JC, Dwan K, Boland A, Smith G, Bagust A, Dundar Y, et al.
-
Stepped treatment of older adults on laxatives. The STOOL trial.
By Mihaylov S, Stark C, McColl E, Steen N, Vanoli A, Rubin G, et al.
-
A randomised controlled trial of cognitive behaviour therapy in adolescents with major depression treated by selective serotonin reuptake inhibitors. The ADAPT trial.
By Goodyer IM, Dubicka B, Wilkinson P, Kelvin R, Roberts C, Byford S, et al.
-
The use of irinotecan, oxaliplatin and raltitrexed for the treatment of advanced colorectal cancer: systematic review and economic evaluation.
By Hind D, Tappenden P, Tumur I, Eggington E, Sutcliffe P, Ryan A.
-
Ranibizumab and pegaptanib for the treatment of age-related macular degeneration: a systematic review and economic evaluation.
By Colquitt JL, Jones J, Tan SC, Takeda A, Clegg AJ, Price A.
-
Systematic review of the clinical effectiveness and cost-effectiveness of 64-slice or higher computed tomography angiography as an alternative to invasive coronary angiography in the investigation of coronary artery disease.
By Mowatt G, Cummins E, Waugh N, Walker S, Cook J, Jia X, et al.
-
Structural neuroimaging in psychosis: a systematic review and economic evaluation.
By Albon E, Tsourapas A, Frew E, Davenport C, Oyebode F, Bayliss S, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in adults and children aged 12 years and over.
By Shepherd J, Rogers G, Anderson R, Main C, Thompson-Coon J, Hartwell D, et al.
-
Systematic review and economic analysis of the comparative effectiveness of different inhaled corticosteroids and their usage with long-acting beta2 agonists for the treatment of chronic asthma in children under the age of 12 years.
By Main C, Shepherd J, Anderson R, Rogers G, Thompson-Coon J, Liu Z, et al.
-
Ezetimibe for the treatment of hypercholesterolaemia: a systematic review and economic evaluation.
By Ara R, Tumur I, Pandor A, Duenas A, Williams R, Wilkinson A, et al.
-
Topical or oral ibuprofen for chronic knee pain in older people. The TOIB study.
By Underwood M, Ashby D, Carnes D, Castelnuovo E, Cross P, Harding G, et al.
-
A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial.
By George S, Pockney P, Primrose J, Smith H, Little P, Kinley H, et al.
-
A review and critical appraisal of measures of therapist–patient interactions in mental health settings.
By Cahill J, Barkham M, Hardy G, Gilbody S, Richards D, Bower P, et al.
-
The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation.
By Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J.
-
A systematic review of the clinical effectiveness and cost-effectiveness and economic modelling of minimal incision total hip replacement approaches in the management of arthritic disease of the hip.
By de Verteuil R, Imamura M, Zhu S, Glazener C, Fraser C, Munro N, et al.
-
A preliminary model-based assessment of the cost–utility of a screening programme for early age-related macular degeneration.
By Karnon J, Czoski-Murray C, Smith K, Brand C, Chakravarthy U, Davis S, et al.
-
Intravenous magnesium sulphate and sotalol for prevention of atrial fibrillation after coronary artery bypass surgery: a systematic review and economic evaluation.
By Shepherd J, Jones J, Frampton GK, Tanajewski L, Turner D, Price A.
-
Absorbent products for urinary/faecal incontinence: a comparative evaluation of key product categories.
By Fader M, Cottenden A, Getliffe K, Gage H, Clarke-O’Neill S, Jamieson K, et al.
-
A systematic review of repetitive functional task practice with modelling of resource use, costs and effectiveness.
By French B, Leathley M, Sutton C, McAdam J, Thomas L, Forster A, et al.
-
The effectiveness and cost-effectivness of minimal access surgery amongst people with gastro-oesophageal reflux disease – a UK collaborative study. The reflux trial.
By Grant A, Wileman S, Ramsay C, Bojke L, Epstein D, Sculpher M, et al.
-
Time to full publication of studies of anti-cancer medicines for breast cancer and the potential for publication bias: a short systematic review.
By Takeda A, Loveman E, Harris P, Hartwell D, Welch K.
-
Performance of screening tests for child physical abuse in accident and emergency departments.
By Woodman J, Pitt M, Wentz R, Taylor B, Hodes D, Gilbert RE.
-
Curative catheter ablation in atrial fibrillation and typical atrial flutter: systematic review and economic evaluation.
By Rodgers M, McKenna C, Palmer S, Chambers D, Van Hout S, Golder S, et al.
-
Systematic review and economic modelling of effectiveness and cost utility of surgical treatments for men with benign prostatic enlargement.
By Lourenco T, Armstrong N, N’Dow J, Nabi G, Deverill M, Pickard R, et al.
-
Immunoprophylaxis against respiratory syncytial virus (RSV) with palivizumab in children: a systematic review and economic evaluation.
By Wang D, Cummins C, Bayliss S, Sandercock J, Burls A.
-
Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation.
By McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al.
-
Thrombophilia testing in people with venous thromboembolism: systematic review and cost-effectiveness analysis.
By Simpson EL, Stevenson MD, Rawdin A, Papaioannou D.
-
Surgical procedures and non-surgical devices for the management of non-apnoeic snoring: a systematic review of clinical effects and associated treatment costs.
By Main C, Liu Z, Welch K, Weiner G, Quentin Jones S, Stein K.
-
Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea–hypopnoea syndrome: a systematic review and economic analysis.
By McDaid C, Griffin S, Weatherly H, Durée K, van der Burgt M, van Hout S, Akers J, et al.
-
Use of classical and novel biomarkers as prognostic risk factors for localised prostate cancer: a systematic review.
By Sutcliffe P, Hummel S, Simpson E, Young T, Rees A, Wilkinson A, et al.
-
The harmful health effects of recreational ecstasy: a systematic review of observational evidence.
By Rogers G, Elston J, Garside R, Roome C, Taylor R, Younger P, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of oesophageal Doppler monitoring in critically ill and high-risk surgical patients.
By Mowatt G, Houston G, Hernández R, de Verteuil R, Fraser C, Cuthbertson B, et al.
-
The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports.
By Taylor RS, Elston J.
-
Controlling Hypertension and Hypotension Immediately Post Stroke (CHHIPS) – a randomised controlled trial.
By Potter J, Mistri A, Brodie F, Chernova J, Wilson E, Jagger C, et al.
-
Routine antenatal anti-D prophylaxis for RhD-negative women: a systematic review and economic evaluation.
By Pilgrim H, Lloyd-Jones M, Rees A.
-
Amantadine, oseltamivir and zanamivir for the prophylaxis of influenza (including a review of existing guidance no. 67): a systematic review and economic evaluation.
By Tappenden P, Jackson R, Cooper K, Rees A, Simpson E, Read R, et al.
-
Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods.
By Hobart J, Cano S.
-
Treatment of severe ankle sprain: a pragmatic randomised controlled trial comparing the clinical effectiveness and cost-effectiveness of three types of mechanical ankle support with tubular bandage. The CAST trial.
By Cooke MW, Marsh JL, Clark M, Nakash R, Jarvis RM, Hutton JL, et al. , on behalf of the CAST trial group.
-
Non-occupational postexposure prophylaxis for HIV: a systematic review.
By Bryant J, Baxter L, Hird S.
-
Blood glucose self-monitoring in type 2 diabetes: a randomised controlled trial.
By Farmer AJ, Wade AN, French DP, Simon J, Yudkin P, Gray A, et al.
-
How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria.
By Feder G, Ramsay J, Dunne D, Rose M, Arsene C, Norman R, et al.
-
Spinal cord stimulation for chronic pain of neuropathic or ischaemic origin: systematic review and economic evaluation.
By Simpson EL, Duenas A, Holmes MW, Papaioannou D, Chilcott J.
-
The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost-effectiveness and natural history.
By Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al.
-
Dipsticks and diagnostic algorithms in urinary tract infection: development and validation, randomised trial, economic analysis, observational cohort and qualitative study.
By Little P, Turner S, Rumsby K, Warner G, Moore M, Lowes JA, et al.
-
Systematic review of respite care in the frail elderly.
By Shaw C, McNamara R, Abrams K, Cannings-John R, Hood K, Longo M, et al.
-
Neuroleptics in the treatment of aggressive challenging behaviour for people with intellectual disabilities: a randomised controlled trial (NACHBID).
By Tyrer P, Oliver-Africano P, Romeo R, Knapp M, Dickens S, Bouras N, et al.
-
Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study.
By Kendrick T, Chatwin J, Dowrick C, Tylee A, Morriss R, Peveler R, et al.
-
Diagnostic strategies using DNA testing for hereditary haemochromatosis in at-risk populations: a systematic review and economic evaluation.
By Bryant J, Cooper K, Picot J, Clegg A, Roderick P, Rosenberg W, et al.
-
Enhanced external counterpulsation for the treatment of stable angina and heart failure: a systematic review and economic analysis.
By McKenna C, McDaid C, Suekarran S, Hawkins N, Claxton K, Light K, et al.
-
Development of a decision support tool for primary care management of patients with abnormal liver function tests without clinically apparent liver disease: a record-linkage population cohort study and decision analysis (ALFIE).
By Donnan PT, McLernon D, Dillon JF, Ryder S, Roderick P, Sullivan F, et al.
-
A systematic review of presumed consent systems for deceased organ donation.
By Rithalia A, McDaid C, Suekarran S, Norman G, Myers L, Sowden A.
-
Paracetamol and ibuprofen for the treatment of fever in children: the PITCH randomised controlled trial.
By Hay AD, Redmond NM, Costelloe C, Montgomery AA, Fletcher M, Hollinghurst S, et al.
-
A randomised controlled trial to compare minimally invasive glucose monitoring devices with conventional monitoring in the management of insulin-treated diabetes mellitus (MITRE).
By Newman SP, Cooke D, Casbard A, Walker S, Meredith S, Nunn A, et al.
-
Sensitivity analysis in economic evaluation: an audit of NICE current practice and a review of its use and value in decision-making.
By Andronis L, Barton P, Bryan S.
-
Trastuzumab for the treatment of primary breast cancer in HER2-positive women: a single technology appraisal.
By Ward S, Pilgrim H, Hind D.
-
Docetaxel for the adjuvant treatment of early node-positive breast cancer: a single technology appraisal.
By Chilcott J, Lloyd Jones M, Wilkinson A.
-
The use of paclitaxel in the management of early stage breast cancer.
By Griffin S, Dunn G, Palmer S, Macfarlane K, Brent S, Dyker A, et al.
-
Rituximab for the first-line treatment of stage III/IV follicular non-Hodgkin’s lymphoma.
By Dundar Y, Bagust A, Hounsome J, McLeod C, Boland A, Davis H, et al.
-
Bortezomib for the treatment of multiple myeloma patients.
By Green C, Bryant J, Takeda A, Cooper K, Clegg A, Smith A, et al.
-
Fludarabine phosphate for the firstline treatment of chronic lymphocytic leukaemia.
By Walker S, Palmer S, Erhorn S, Brent S, Dyker A, Ferrie L, et al.
-
Erlotinib for the treatment of relapsed non-small cell lung cancer.
By McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al.
-
Cetuximab plus radiotherapy for the treatment of locally advanced squamous cell carcinoma of the head and neck.
By Griffin S, Walker S, Sculpher M, White S, Erhorn S, Brent S, et al.
-
Infliximab for the treatment of adults with psoriasis.
By Loveman E, Turner D, Hartwell D, Cooper K, Clegg A
-
Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial.
By Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al.
-
The effect of different treatment durations of clopidogrel in patients with non-ST-segment elevation acute coronary syndromes: a systematic review and value of information analysis.
By Rogowski R, Burch J, Palmer S, Craigs C, Golder S, Woolacott N.
-
Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care.
By Mant J, Doust J, Roalfe A, Barton P, Cowie MR, Glasziou P, et al.
-
A multicentre randomised controlled trial of the use of continuous positive airway pressure and non-invasive positive pressure ventilation in the early treatment of patients presenting to the emergency department with severe acute cardiogenic pulmonary oedema: the 3CPO trial.
By Gray AJ, Goodacre S, Newby DE, Masson MA, Sampson F, Dixon S, et al. , on behalf of the 3CPO study investigators.
-
Early high-dose lipid-lowering therapy to avoid cardiac events: a systematic review and economic evaluation.
By Ara R, Pandor A, Stevens J, Rees A, Rafia R.
-
Adefovir dipivoxil and pegylated interferon alpha for the treatment of chronic hepatitis B: an updated systematic review and economic evaluation.
By Jones J, Shepherd J, Baxter L, Gospodarevskaya E, Hartwell D, Harris P, et al.
-
Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis.
By Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al.
-
A double-blind randomised placebo-controlled trial of topical intranasal corticosteroids in 4- to 11-year-old children with persistent bilateral otitis media with effusion in primary care.
By Williamson I, Benge S, Barton S, Petrou S, Letley L, Fasey N, et al.
-
The effectiveness and cost-effectiveness of methods of storing donated kidneys from deceased donors: a systematic review and economic model.
By Bond M, Pitt M, Akoh J, Moxham T, Hoyle M, Anderson R.
-
Rehabilitation of older patients: day hospital compared with rehabilitation at home. A randomised controlled trial.
By Parker SG, Oliver P, Pennington M, Bond J, Jagger C, Enderby PM, et al.
-
Breastfeeding promotion for infants in neonatal units: a systematic review and economic analysis.
By Renfrew MJ, Craig D, Dyson L, McCormick F, Rice S, King SE, et al.
-
The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation.
By Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, Baxter L, et al.
-
Rapid testing for group B streptococcus during labour: a test accuracy study with evaluation of acceptability and cost-effectiveness.
By Daniels J, Gray J, Pattison H, Roberts T, Edwards E, Milner P, et al.
-
Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling.
By Honest H, Forbes CA, Durée KH, Norman G, Duffy SB, Tsourapas A, et al.
-
The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model.
By Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, et al.
-
Gemcitabine for the treatment of metastatic breast cancer.
By Jones J, Takeda A, Tan SC, Cooper K, Loveman E, Clegg A.
-
Varenicline in the management of smoking cessation: a single technology appraisal.
By Hind D, Tappenden P, Peters J, Kenjegalieva K.
-
Alteplase for the treatment of acute ischaemic stroke: a single technology appraisal.
By Lloyd Jones M, Holmes M.
-
Rituximab for the treatment of rheumatoid arthritis.
By Bagust A, Boland A, Hockenhull J, Fleeman N, Greenhalgh J, Dundar Y, et al.
-
Omalizumab for the treatment of severe persistent allergic asthma.
By Jones J, Shepherd J, Hartwell D, Harris P, Cooper K, Takeda A, et al.
-
Rituximab for the treatment of relapsed or refractory stage III or IV follicular non-Hodgkin’s lymphoma.
By Boland A, Bagust A, Hockenhull J, Davis H, Chu P, Dickson R.
-
Adalimumab for the treatment of psoriasis.
By Turner D, Picot J, Cooper K, Loveman E.
-
Dabigatran etexilate for the prevention of venous thromboembolism in patients undergoing elective hip and knee surgery: a single technology appraisal.
By Holmes M, C Carroll C, Papaioannou D.
-
Romiplostim for the treatment of chronic immune or idiopathic thrombocytopenic purpura: a single technology appraisal.
By Mowatt G, Boachie C, Crowther M, Fraser C, Hernández R, Jia X, et al.
-
Sunitinib for the treatment of gastrointestinal stromal tumours: a critique of the submission from Pfizer.
By Bond M, Hoyle M, Moxham T, Napier M, Anderson R.
-
Vitamin K to prevent fractures in older women: systematic review and economic evaluation.
By Stevenson M, Lloyd-Jones M, Papaioannou D.
-
The effects of biofeedback for the treatment of essential hypertension: a systematic review.
By Greenhalgh J, Dickson R, Dundar Y.
-
A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: the BELLS study.
By Sullivan FM, Swan IRC, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al.
-
Lapatinib for the treatment of HER2-overexpressing breast cancer.
By Jones J, Takeda A, Picot J, von Keyserlingk C, Clegg A.
-
Infliximab for the treatment of ulcerative colitis.
By Hyde C, Bryan S, Juarez-Garcia A, Andronis L, Fry-Smith A.
-
Rimonabant for the treatment of overweight and obese people.
By Burch J, McKenna C, Palmer S, Norman G, Glanville J, Sculpher M, et al.
-
Telbivudine for the treatment of chronic hepatitis B infection.
By Hartwell D, Jones J, Harris P, Cooper K.
-
Entecavir for the treatment of chronic hepatitis B infection.
By Shepherd J, Gospodarevskaya E, Frampton G, Cooper K.
-
Febuxostat for the treatment of hyperuricaemia in people with gout: a single technology appraisal.
By Stevenson M, Pandor A.
-
Rivaroxaban for the prevention of venous thromboembolism: a single technology appraisal.
By Stevenson M, Scope A, Holmes M, Rees A, Kaltenthaler E.
-
Cetuximab for the treatment of recurrent and/or metastatic squamous cell carcinoma of the head and neck.
By Greenhalgh J, Bagust A, Boland A, Fleeman N, McLeod C, Dundar Y, et al.
-
Mifamurtide for the treatment of osteosarcoma: a single technology appraisal.
By Pandor A, Fitzgerald P, Stevenson M, Papaioannou D.
-
Ustekinumab for the treatment of moderate to severe psoriasis.
By Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A.
-
Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model.
By Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al.
-
Clinical and cost-effectiveness of epoprostenol, iloprost, bosentan, sitaxentan and sildenafil for pulmonary arterial hypertension within their licensed indications: a systematic review and economic evaluation.
By Chen Y-F, Jowett S, Barton P, Malottki K, Hyde C, Gibbs JSR, et al.
-
Cessation of attention deficit hyperactivity disorder drugs in the young (CADDY) – a pharmacoepidemiological and qualitative study.
By Wong ICK, Asherson P, Bilbow A, Clifford S, Coghill D, R DeSoysa R, et al.
-
ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening.
By Kitchener HC, Almonte M, Gilham C, Dowie R, Stoykova B, Sargent A, et al.
-
The clinical effectiveness of glucosamine and chondroitin supplements in slowing or arresting progression of osteoarthritis of the knee: a systematic review and economic evaluation.
By Black C, Clar C, Henderson R, MacEachern C, McNamee P, Quayyum Z, et al.
-
Randomised preference trial of medical versus surgical termination of pregnancy less than 14 weeks’ gestation (TOPS).
By Robson SC, Kelly T, Howel D, Deverill M, Hewison J, Lie MLS, et al.
-
Randomised controlled trial of the use of three dressing preparations in the management of chronic ulceration of the foot in diabetes.
By Jeffcoate WJ, Price PE, Phillips CJ, Game FL, Mudge E, Davies S, et al.
-
VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers.
By Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al.
-
A prospective randomised controlled trial and economic modelling of antimicrobial silver dressings versus non-adherent control dressings for venous leg ulcers: the VULCAN trial.
By Michaels JA, Campbell WB, King BM, MacIntyre J, Palfreyman SJ, Shackley P, et al.
-
Communication of carrier status information following universal newborn screening for sickle cell disorders and cystic fibrosis: qualitative study of experience and practice.
By Kai J, Ulph F, Cullinan T, Qureshi N.
-
Antiviral drugs for the treatment of influenza: a systematic review and economic evaluation.
By Burch J, Paulden M, Conti S, Stock C, Corbett M, Welton NJ, et al.
-
Development of a toolkit and glossary to aid in the adaptation of health technology assessment (HTA) reports for use in different contexts.
By Chase D, Rosten C, Turner S, Hicks N, Milne R.
-
Colour vision testing for diabetic retinopathy: a systematic review of diagnostic accuracy and economic evaluation.
By Rodgers M, Hodges R, Hawkins J, Hollingworth W, Duffy S, McKibbin M, et al.
-
Systematic review of the effectiveness and cost-effectiveness of weight management schemes for the under fives: a short report.
By Bond M, Wyatt K, Lloyd J, Welch K, Taylor R.
-
Are adverse effects incorporated in economic models? An initial review of current practice.
By Craig D, McDaid C, Fonseca T, Stock C, Duffy S, Woolacott N.
-
Multicentre randomised controlled trial examining the cost-effectiveness of contrast-enhanced high field magnetic resonance imaging in women with primary breast cancer scheduled for wide local excision (COMICE).
By Turnbull LW, Brown SR, Olivier C, Harvey I, Brown J, Drew P, et al.
-
Bevacizumab, sorafenib tosylate, sunitinib and temsirolimus for renal cell carcinoma: a systematic review and economic evaluation.
By Thompson Coon J, Hoyle M, Green C, Liu Z, Welch K, Moxham T, et al.
-
The clinical effectiveness and cost-effectiveness of testing for cytochrome P450 polymorphisms in patients with schizophrenia treated with antipsychotics: a systematic review and economic evaluation.
By Fleeman N, McLeod C, Bagust A, Beale S, Boland A, Dundar Y, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of photodynamic diagnosis and urine biomarkers (FISH, ImmunoCyt, NMP22) and cytology for the detection and follow-up of bladder cancer.
By Mowatt G, Zhu S, Kilonzo M, Boachie C, Fraser C, Griffiths TRL, et al.
-
Effectiveness and cost-effectiveness of arthroscopic lavage in the treatment of osteoarthritis of the knee: a mixed methods study of the feasibility of conducting a surgical placebo-controlled trial (the KORAL study).
By Campbell MK, Skea ZC, Sutherland AG, Cuthbertson BH, Entwistle VA, McDonald AM, et al.
-
A randomised 2 × 2 trial of community versus hospital pulmonary rehabilitation for chronic obstructive pulmonary disease followed by telephone or conventional follow-up.
By Waterhouse JC, Walters SJ, Oluboyede Y, Lawson RA.
-
The effectiveness and cost-effectiveness of behavioural interventions for the prevention of sexually transmitted infections in young people aged 13–19: a systematic review and economic evaluation.
By Shepherd J, Kavanagh J, Picot J, Cooper K, Harden A, Barnett-Page E, et al.
-
Dissemination and publication of research findings: an updated review of related biases.
By Song F, Parekh S, Hooper L, Loke YK, Ryder J, Sutton AJ, et al.
-
The effectiveness and cost-effectiveness of biomarkers for the prioritisation of patients awaiting coronary revascularisation: a systematic review and decision model.
By Hemingway H, Henriksson M, Chen R, Damant J, Fitzpatrick N, Abrams K, et al.
-
Comparison of case note review methods for evaluating quality and safety in health care.
By Hutchinson A, Coster JE, Cooper KL, McIntosh A, Walters SJ, Bath PA, et al.
-
Clinical effectiveness and cost-effectiveness of continuous subcutaneous insulin infusion for diabetes: systematic review and economic evaluation.
By Cummins E, Royle P, Snaith A, Greene A, Robertson L, McIntyre L, et al.
-
Self-monitoring of blood glucose in type 2 diabetes: systematic review.
By Clar C, Barnard K, Cummins E, Royle P, Waugh N.
-
North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): a pragmatic randomised controlled trial with a parallel non-randomised preference study.
By Lock C, Wilson J, Steen N, Eccles M, Mason H, Carrie S, et al.
-
Multicentre randomised controlled trial of the clinical and cost-effectiveness of a bypass-surgery-first versus a balloon-angioplasty-first revascularisation strategy for severe limb ischaemia due to infrainguinal disease. The Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial.
By Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FGR, Gillespie I, et al.
-
A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability – the TOuCAN trial.
By Gowers SG, Clark AF, Roberts C, Byford S, Barrett B, Griffiths A, et al.
-
Randomised controlled trials for policy interventions: a review of reviews and meta-regression.
By Oliver S, Bagnall AM, Thomas J, Shepherd J, Sowden A, White I, et al.
-
Paracetamol and selective and non-selective non-steroidal anti-inflammatory drugs (NSAIDs) for the reduction of morphine-related side effects after major surgery: a systematic review.
By McDaid C, Maund E, Rice S, Wright K, Jenkins B, Woolacott N.
-
A systematic review of outcome measures used in forensic mental health research with consensus panel opinion.
By Fitzpatrick R, Chambers J, Burns T, Doll H, Fazel S, Jenkinson C, et al.
-
The clinical effectiveness and cost-effectiveness of topotecan for small cell lung cancer: a systematic review and economic evaluation.
By Loveman E, Jones J, Hartwell D, Bird A, Harris P, Welch K, et al.
-
Antenatal screening for haemoglobinopathies in primary care: a cohort study and cluster randomised trial to inform a simulation model. The Screening for Haemoglobinopathies in First Trimester (SHIFT) trial.
By Dormandy E, Bryan S, Gulliford MC, Roberts T, Ades T, Calnan M, et al.
-
Early referral strategies for management of people with markers of renal disease: a systematic review of the evidence of clinical effectiveness, cost-effectiveness and economic analysis.
By Black C, Sharma P, Scotland G, McCullough K, McGurn D, Robertson L, et al.
-
A randomised controlled trial of cognitive behaviour therapy and motivational interviewing for people with Type 1 diabetes mellitus with persistent sub-optimal glycaemic control: A Diabetes and Psychological Therapies (ADaPT) study.
By Ismail K, Maissi E, Thomas S, Chalder T, Schmidt U, Bartlett J, et al.
-
A randomised controlled equivalence trial to determine the effectiveness and cost–utility of manual chest physiotherapy techniques in the management of exacerbations of chronic obstructive pulmonary disease (MATREX).
By Cross J, Elender F, Barton G, Clark A, Shepstone L, Blyth A, et al.
-
A systematic review and economic evaluation of the clinical effectiveness and cost-effectiveness of aldosterone antagonists for postmyocardial infarction heart failure.
By McKenna C, Burch J, Suekarran S, Walker S, Bakhai A, Witte K, et al.
-
Avoiding and identifying errors in health technology assessment models: qualitative study and methodological review.
By Chilcott JB, Tappenden P, Rawdin A, Johnson M, Kaltenthaler E, Paisley S, et al.
-
BoTULS: a multicentre randomised controlled trial to evaluate the clinical effectiveness and cost-effectiveness of treating upper limb spasticity due to stroke with botulinum toxin type A.
By Shaw L, Rodgers H, Price C, van Wijck F, Shackley P, Steen N, et al. , on behalf of the BoTULS investigators.
-
Weighting and valuing quality-adjusted life-years using stated preference methods: preliminary results from the Social Value of a QALY Project.
By Baker R, Bateman I, Donaldson C, Jones-Lee M, Lancsar E, Loomes G, et al.
-
Cetuximab for the first-line treatment of metastatic colorectal cancer.
By Meads C, Round J, Tubeuf S, Moore D, Pennant M, Bayliss S.
-
Infliximab for the treatment of acute exacerbations of ulcerative colitis.
By Bryan S, Andronis L, Hyde C, Connock M, Fry-Smith A, Wang D.
-
Sorafenib for the treatment of advanced hepatocellular carcinoma.
By Connock M, Round J, Bayliss S, Tubeuf S, Greenheld W, Moore D.
-
Tenofovir disoproxil fumarate for the treatment of chronic hepatitis B infection.
By Jones J, Colquitt J, Shepherd J, Harris P, Cooper K.
-
Prasugrel for the treatment of acute coronary artery syndromes with percutaneous coronary intervention.
By Greenhalgh J, Bagust A, Boland A, Saborido CM, Fleeman N, McLeod C, et al.
-
Alitretinoin for the treatment of severe chronic hand eczema.
By Paulden M, Rodgers M, Griffin S, Slack R, Duffy S, Ingram JR, et al.
-
Pemetrexed for the first-line treatment of locally advanced or metastatic non-small cell lung cancer.
By Fleeman N, Bagust A, McLeod C, Greenhalgh J, Boland A, Dundar Y, et al.
-
Topotecan for the treatment of recurrent and stage IVB carcinoma of the cervix.
By Paton F, Paulden M, Saramago P, Manca A, Misso K, Palmer S, et al.
-
Trabectedin for the treatment of advanced metastatic soft tissue sarcoma.
By Simpson EL, Rafia R, Stevenson MD, Papaioannou D.
-
Azacitidine for the treatment of myelodysplastic syndrome, chronic myelomonocytic leukaemia and acute myeloid leukaemia.
By Edlin R, Connock M, Tubeuf S, Round J, Fry-Smith A, Hyde C, et al.
-
The safety and effectiveness of different methods of earwax removal: a systematic review and economic evaluation.
By Clegg AJ, Loveman E, Gospodarevskaya E, Harris P, Bird A, Bryant J, et al.
-
Systematic review of the clinical effectiveness and cost-effectiveness of rapid point-of-care tests for the detection of genital chlamydia infection in women and men.
By Hislop J, Quayyum Z, Flett G, Boachie C, Fraser C, Mowatt G.
-
School-linked sexual health services for young people (SSHYP): a survey and systematic review concerning current models, effectiveness, cost-effectiveness and research opportunities.
By Owen J, Carroll C, Cooke J, Formby E, Hayter M, Hirst J, et al.
-
Systematic review and cost-effectiveness evaluation of ‘pill-in-the-pocket’ strategy for paroxysmal atrial fibrillation compared to episodic in-hospital treatment or continuous antiarrhythmic drug therapy.
By Martin Saborido C, Hockenhull J, Bagust A, Boland A, Dickson R, Todd D.
-
Chemoprevention of colorectal cancer: systematic review and economic evaluation.
By Cooper K, Squires H, Carroll C, Papaioannou D, Booth A, Logan RF, et al.
-
Cross-trimester repeated measures testing for Down’s syndrome screening: an assessment.
By Wright D, Bradbury I, Malone F, D’Alton M, Summers A, Huang T, et al.
-
Exploring the needs, concerns and behaviours of people with existing respiratory conditions in relation to the H1N1 ‘swine influenza’ pandemic: a multicentre survey and qualitative study.
By Caress A-L, Duxbury P, Woodcock A, Luker KA, Ward D, Campbell M, et al.
-
Influenza A/H1N1v in pregnancy: an investigation of the characteristics and management of affected women and the relationship to pregnancy outcomes for mother and infant.
By Yates L, Pierce M, Stephens S, Mill AC, Spark P, Kurinczuk JJ, et al.
-
The impact of communications about swine flu (influenza A H1N1v) on public responses to the outbreak: results from 36 national telephone surveys in the UK.
By Rubin GJ, Potts HWW, Michie S.
-
The impact of illness and the impact of school closure on social contact patterns.
By Eames KTD, Tilston NL, White PJ, Adams E, Edmunds WJ.
-
Vaccine effectiveness in pandemic influenza – primary care reporting (VIPER): an observational study to assess the effectiveness of the pandemic influenza A (H1N1)v vaccine.
By Simpson CR, Ritchie LD, Robertson C, Sheikh A, McMenamin J.
-
Physical interventions to interrupt or reduce the spread of respiratory viruses: a Cochrane review.
By Jefferson T, Del Mar C, Dooley L, Ferroni E, Al-Ansary LA, Bawazeer GA, et al.
-
Randomised controlled trial and parallel economic evaluation of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR).
By Peek GJ, Elbourne D, Mugford M, Tiruvoipati R, Wilson A, Allen E, et al.
-
Newer agents for blood glucose control in type 2 diabetes: systematic review and economic evaluation.
By Waugh N, Cummins E, Royle P, Clar C, Marien M, Richter B, et al.
-
Barrett’s oesophagus and cancers of the biliary tract, brain, head and neck, lung, oesophagus and skin.
By Fayter D, Corbett M, Heirs M, Fox D, Eastwood A.
-
Towards single embryo transfer? Modelling clinical outcomes of potential treatment choices using multiple data sources: predictive models and patient perspectives.
By Roberts SA, McGowan L, Hirst WM, Brison DR, Vail A, Lieberman BA.
-
Sugammadex for the reversal of muscle relaxation in general anaesthesia: a systematic review and economic assessment.
By Chambers D, Paulden M, Paton F, Heirs M, Duffy S, Craig D, et al.
-
Systematic review and economic modelling of the effectiveness and cost-effectiveness of non-surgical treatments for women with stress urinary incontinence.
By Imamura M, Abrams P, Bain C, Buckley B, Cardozo L, Cody J, et al.
-
A multicentred randomised controlled trial of a primary care-based cognitive behavioural programme for low back pain. The Back Skills Training (BeST) trial.
By Lamb SE, Lall R, Hansen Z, Castelnuovo E, Withers EJ, Nichols V, et al.
-
Recombinant human growth hormone for the treatment of growth disorders in children: a systematic review and economic evaluation.
By Takeda A, Cooper K, Bird A, Baxter L, Frampton GK, Gospodarevskaya E, et al.
-
A pragmatic randomised controlled trial to compare antidepressants with a community-based psychosocial intervention for the treatment of women with postnatal depression: the RESPOND trial.
By Sharp DJ, Chew-Graham C, Tylee A, Lewis G, Howard L, Anderson I, et al.
-
Group cognitive behavioural therapy for postnatal depression: a systematic review of clinical effectiveness, cost-effectiveness and value of information analyses.
By Stevenson MD, Scope A, Sutcliffe PA, Booth A, Slade P, Parry G, et al.
-
Screening for hyperglycaemia in pregnancy: a rapid update for the National Screening Committee.
By Waugh N, Royle P, Clar C, Henderson R, Cummins E, Hadden D, et al.
-
Open-label, randomised, parallel-group, multicentre study to evaluate the safety, tolerability and immunogenicity of an AS03B/oil-in-water emulsion-adjuvanted (AS03B) split-virion versus non-adjuvanted wholevirion H1N1 influenza vaccine in UK children 6 months to 12 years of age.
By Waddington CS, Andrews N, Hoschler K, Walker WT, Oeser C, Reiner A, et al.
-
Evaluation of droplet dispersion during non-invasive ventilation, oxygen therapy, nebuliser treatment and chest physiotherapy in clinical practice: implications for management of pandemic influenza and other airborne infections.
By Simonds AK, Hanak A, Chatwin M, Morrell MJ, Hall A, Parker KH, et al.
-
Evaluation of triage methods used to select patients with suspected pandemic influenza for hospital admission: cohort study.
By Goodacre S, Challen, K, Wilson R, Campbell M.
-
Virus shedding and environmental deposition of novel A (H1N1) pandemic influenza virus: interim findings.
By Killingley B, Greatorex J, Cauchemez S, Enstone JE, Curran M, Read R, et al.
-
Neuraminidase inhibitors for preventing and treating influenza in healthy adults: a Cochrane review.
By Jefferson T, Jones M, Doshi P, Del Mar C, Dooley L, Foxlee R.
-
Intensity-modulated radiotherapy for the treatment of prostate cancer: a systematic review and economic evaluation.
By Hummel S, Simpson EL, Hemingway P, Stevenson MD, Rees A.
-
Computerised decision support systems in order communication for diagnostic, screening or monitoring test ordering: systematic reviews of the effects and cost-effectiveness of systems.
By Main C, Moxham T, Wyatt JC, Kay J, Anderson R, Stein K.
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
Prioritisation Strategy Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Medical Care Research Unit, University of Sheffield
-
Dr Bob Coates, Consultant Advisor, NETSCC, HTA
-
Dr Andrew Cook, Consultant Advisor, NETSCC, HTA
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Professor Robin E Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Professor Paul Glasziou, Professor of Evidence-Based Medicine, University of Oxford
-
Dr Nick Hicks, Consultant Adviser, NETSCC, HTA
-
Dr Edmund Jessop, Medical Adviser, National Specialist, National Commissioning Group (NCG), Department of Health, London
-
Ms Lynn Kerridge, Chief Executive Officer, NETSCC and NETSCC, HTA
-
Professor Ruairidh Milne, Director of NETSCC External Relations
-
Ms Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Ms Pamela Young, Specialist Programme Manager, NETSCC, HTA
HTA Commissioning Board
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Director, Warwick Clinical Trials Unit
-
Director, Nottingham Clinical Trials Unit
-
Senior Lecturer in General Practice, Department of Primary Health Care, University of Oxford
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Deborah Ashby, Professor of Medical Statistics, Queen Mary, University of London
-
Professor John Cairns, Professor of Health Economics, London School of Hygiene and Tropical Medicine
-
Professor Peter Croft, Director of Primary Care Sciences Research Centre, Keele University
-
Professor Nicky Cullum, Director of Centre for Evidence-Based Nursing, University of York
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, University of Sheffield
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford?
-
Professor Stuart Logan, Director of Health & Social Care Research, The Peninsula Medical School, Universities of Exeter and Plymouth
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor Ian Roberts, Professor of Epidemiology & Public Health, London School of Hygiene and Tropical Medicine
-
Professor Mark Sculpher, Professor of Health Economics, University of York
-
Professor Helen Smith, Professor of Primary Care, University of Brighton
-
Professor Kate Thomas, Professor of Complementary & Alternative Medicine Research, University of Leeds
-
Professor David John Torgerson, Director of York Trials Unit, University of York
-
Ms Kay Pattison, NHS R&D Programme/DH, Leeds
-
Dr Morven Roberts, Clinical Trials Manager, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Professor of Evidence-Based Medicine, University of Oxford
-
Consultant Paediatrician and Honorary Senior Lecturer, Great Ormond Street Hospital, London
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, Imaging Science and Biomedical Engineering, Cancer & Imaging Sciences, University of Manchester
-
Mr A S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital
-
Dr Dianne Baralle, Consultant & Senior Lecturer in Clinical Genetics, Human Genetics Division & Wessex Clinical Genetics Service, Southampton, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Service User Representative
-
Professor Anthony Robert Kendrick, Professor of Primary Medical Care, University of Southampton
-
Dr Susanne M Ludgate, Director, Medical Devices Agency, London
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee
-
Dr David Mathew Service User Representative
-
Dr Michael Millar, Lead Consultant in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mr Stephen Pilling, Director, Centre for Outcomes, Research & Effectiveness, University College London
-
Mrs Una Rennard, Service User Representative
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Ultrasound Department, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr W Stuart A Smellie, Consultant, Bishop Auckland General Hospital
-
Professor Lindsay Wilson Turnbull, Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Dr Alan J Williams, Consultant in General Medicine, Department of Thoracic Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Catherine Moody, Programme Manager, Neuroscience and Mental Health Board
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Disease Prevention Panel
-
Medical Adviser, National Specialist Commissioning Advisory Group (NSCAG), Department of Health
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook Clinical Programmes Director, Bazian Ltd, London
-
Dr Elizabeth Fellow-Smith, Medical Director, West London Mental Health Trust, Middlesex
-
Dr Colin Greaves Senior Research Fellow, Peninsular Medical School (Primary Care)
-
Dr John Jackson, General Practitioner, Parkway Medical Centre, Newcastle upon Tyne
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Chris McCall, General Practitioner, The Hadleigh Practice, Corfe Mullen, Dorset
-
Miss Nicky Mullany, Service User Representative
-
Dr Julie Mytton, Locum Consultant in Public Health Medicine, Bristol Primary Care Trust
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Professor Carol Tannahill, Glasgow Centre for Population Health
-
Mrs Jean Thurston, Service User Representative
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Caroline Stone, Programme Manager, Medical Research Council
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust, Bristol
-
Reader in Wound Healing and Director of Research, University of Leeds, Leeds
-
Professor Bipin Bhakta Charterhouse Professor in Rehabilitation Medicine, University of Leeds, Leeds
-
Mrs Penny Calder Service User Representative
-
Professor Paul Carding, Professor of Voice Pathology, Newcastle Hospital NHS Trust, Newcastle
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry, London
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol, Bristol
-
Mrs Anthea De Barton-Watson, Service User Representative
-
Professor Christopher Griffiths, Professor of Primary Care, Barts and the London School of Medicine and Dentistry, London
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester, Manchester
-
Dr Peter Martin, Consultant Neurologist, Addenbrooke’s Hospital, Cambridge
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham, Nottingham
-
Dr Kate Radford, Division of Rehabilitation and Ageing, School of Community Health Sciences. University of Nottingham, Nottingham
-
Mr Jim Reece, Service User Representative
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton, Southampton
-
Dr Pippa Tyrrell, Stroke Medicine, Senior Lecturer/Consultant Stroke Physician, Salford Royal Foundation Hospitals’ Trust, Salford
-
Dr Sarah Tyson, Senior Research Fellow & Associate Head of School, University of Salford, Salford
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University, Cardiff
-
Dr Phillip Leech, Principal Medical Officer for Primary Care, Department of Health , London
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, MRC, London
-
Dr Ursula Wells PRP, DH, London
Interventional Procedures Panel
-
Consultant Surgeon & Honorary Clinical Lecturer, University of Sheffield
-
Mr David P Britt, Service User Representative, Cheshire
-
Mr Sankaran ChandraSekharan, Consultant Surgeon, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Mr Seamus Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor David Taggart, Consultant Cardiothoracic Surgeon, John Radcliffe Hospital
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Nadim Malik, Consultant Cardiologist/ Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Mr Michael Thomas, Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Mrs Isabel Boyer, Service User Representative, London
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Unit Manager, Pharmacoepidemiology Research Unit, VRMM, Medicines & Healthcare Products Regulatory Agency
-
Mrs Nicola Carey, Senior Research Fellow, School of Health and Social Care, The University of Reading
-
Mr John Chapman, Service User Representative
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Professor Robin Ferner, Consultant Physician and Director, West Midlands Centre for Adverse Drug Reactions, City Hospital NHS Trust, Birmingham
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr Bill Gutteridge, Medical Adviser, London Strategic Health Authority
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Yoon K Loke, Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Dr Martin Shelly, General Practitioner, Leeds, and Associate Director, NHS Clinical Governance Support Team, Leicester
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Mr David Symes, Service User Representative
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Dr Ursula Wells, Principal Research Officer, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Service User Representative, Gloucestershire
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician & Cardiologist, County Durham & Darlington Foundation Trust
-
Mr John Needham, Service User, Buckingmashire
-
Ms Mary Nettle, Mental Health User Consultant, Gloucestershire
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Howard Ring, Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry & Warwickshire Partnership Trust
-
Dr Alastair Sutcliffe, Senior Lecturer, University College London
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Ms Kay Pattison Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, MRC, London
-
Professor Tom Walley, HTA Programme Director, Liverpool
-
Dr Ursula Wells, Policy Research Programme, DH, London
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation for Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Dr Katherine Darton, Information Unit, MIND – The Mental Health Charity, London
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Mr George Levvy, Chief Executive, Motor Neurone Disease Association, Northampton
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Rajan Madhok, Medical Director and Director of Public Health, Directorate of Clinical Strategy & Public Health, North & East Yorkshire & Northern Lincolnshire Health Authority, York
-
Professor Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, National Co-ordinator, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Susan Schonfield, Consultant in Public Health, Hillingdon Primary Care Trust, Middlesex
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington