Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 07/37/08. The contractual start date was in February 2009. The draft report began editorial review in June 2010 and was accepted for publication in October 2010. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2011. This work was produced by Pandor et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2011 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Description of health problem
Head injuries account for over 700,000 emergency department (ED) attendances every year in England and Wales1 (with about 20% of head-injured patients being admitted to hospital for further assessment and treatment),2 and are responsible for a significant proportion of the ED workload. In the UK, 70–88% of all people who sustain a head injury are male, 10–19% are aged ≥ 65 years and 40–50% are children. 1 The severity of head injury is directly related to the mechanism and cause. 2 Most minor head injuries (MHIs) in the UK result from falls (22–43%), assault (30–50%) or road traffic accidents (25%). 1 Alcohol may also be involved in up to 65% of adult head injuries. Motor vehicle accidents (MVAs) account for most fatal and severe head injuries. 3 There are, however, marked variations in aetiology across the UK, particularly by age, gender, area of residence and socioeconomic status. 3–5
Injury severity can be classified according to the patient’s consciousness level, as measured on the Glasgow Coma Scale (GCS) when they present to the emergency care services. Most patients (90%) present with a minor injury (GCS 13–15), whereas 10% present with either moderate (GCS 9–12) or severe (GCS 3–8) head injury. 6 Patients with a MHI are conscious and responsive, but may be confused or drowsy. Initial management of MHI may involve identification and treatment of other injuries, or first aid for scalp bruising or bleeding, but MHIs are typically isolated so initial treatment is limited to analgesia and reassurance.
The main challenge in the management of MHI is identification of the minority of patients with significant intracranial injury (ICI), especially those who require urgent neurosurgery. Head injury can result in a range of intracranial lesions, including extradural or subdural haematoma, subarachnoid haemorrhage, cerebral contusion or intracerebral haematoma. Although patients with intracranial lesions often present with moderate or severe head injury according to their GCS, some present with apparently MHI. Subsequent progression of the intracranial lesion can result in a decreasing consciousness level, brain damage, disability and even death.
Early identification of an intracranial lesion can reduce the risk of brain damage and death. First, some intracranial lesions (typically extradural haematoma) can rapidly expand if untreated, leading to raised intracranial pressure, brain damage and death. Emergency neurosurgery to evacuate the haematoma and relieve increased pressure can allow most patients to make a full recovery,7–11 whereas delayed neurosurgery is associated with poorer outcomes. 11,12 Second, a proportion of patients with an ICI that does not require urgent neurosurgery (i.e. a non-neurosurgical injury, such as an intracerebral haematoma) will subsequently deteriorate and require critical care support and/or neurosurgery. These patients may have better outcomes if they are admitted to hospital and managed in an appropriate setting. 13 We have defined the former group as having ‘neurosurgical’ injuries and the latter as having ‘non-neurosurgical’ injuries. However, it should be recognised that our definition is based upon the emergency treatment required rather than all subsequent treatment. Many patients with injuries that we define as having ‘non-neurosurgical’ injuries will benefit from general neurosurgical care and may require later neurosurgical interventions.
Outcome from head injury can be assessed using the Glasgow Outcome Score (GOS). The scale has the following categories:
-
dead
-
vegetative state – unresponsive and unable to interact with environment
-
severe disability – able to follow commands, but unable to live independently
-
moderate disability – able to live independently, but unable to return to work or school
-
good recovery – able to return to work or school.
The scale has subsequently been extended to eight categories by subdividing the severe disability, moderate disability and good recovery categories into upper and lower divisions [known as the extended GOS (GOS-E)].
Most patients with MHI have no intracranial lesion (or at least no lesion detectable by currently used imaging modalities) and will make a good recovery, although post-traumatic symptoms, such as headaches, depression and difficulty concentrating, are relatively common and often underestimated. There is some evidence that early educational intervention can improve these symptoms,14–17 but this does not rely upon initial diagnostic management. Most patients with a MHI and a neurosurgical or non-neurosurgical intracranial lesion will make a good recovery with appropriate timely treatment, although a significant proportion will suffer disability or die. 7–11,18 Failure to provide appropriate timely treatment appears to be associated with a higher probability of disability or death. 11,12
The incidence of death from head injury is estimated to be 6–10 per 100,000 population per annum. 2 This low incidence is owing to most patients having MHI with no significant intracranial lesion and the good outcomes associated with ICI in patients presenting with MHI when treated appropriately. However, when death or disability does occur following MHI, it often affects young people and, therefore, results in a substantial loss of health utility and years of life. As such outcomes are potentially avoidable, clinicians typically have a low threshold for investigation.
Current service provision
Patients with MHI present to the ED, where a doctor or nurse practitioner will assess them and, if appropriate, arrange investigation. Clinical assessment may consist of an unstructured assessment of the patient history and examination or may use a structured assessment to combine features of the clinical history and examination in a clinical decision rule. Investigations include skull radiography and computerised tomography (CT) of the head. After assessment and investigation, patients may be discharged home, admitted to hospital for observation or referred for emergency neurosurgery. The aim of diagnostic management is to identify as many patients with ICI as possible (particularly those with neurosurgical injury), while avoiding unnecessary investigation or hospital admission for those with no significant ICI.
Guidelines for managing head injury in the NHS were drawn up by the National Institute for Health and Clinical Excellence (NICE) in 200319 and revised in 2007. 1 These guidelines use clinical decision rules to determine which patients should receive CT scanning and which should be admitted to hospital. Similar guidelines from the Scottish Intercollegiate Guidelines Network (SIGN) are used in Scotland. 20
The NICE guidelines were based upon a literature review and expert consensus. Cost-effectiveness analysis was not used to develop the guidelines, but was used to explore the potential impact on health service costs. The guidelines were expected to reduce the use of skull radiography, increase the use of CT scanning and reduce hospital admissions, thus reducing overall costs. Data from a number of studies have since confirmed that more CT scans and less skull radiography are being performed. 21–23 However, Hospital Episode Statistics (HES) for England show that the annual number of admissions for head injury increased from 114,769 in 2001–2 to 155,996 in 2006–7. As average length of stay remained relatively constant, bed-days increased from 348,032 in 2001–2 to 443,593 in 2006–7. Figure 1 shows that the increase in admissions has been seen in adults rather than in children. 24
FIGURE 1.
Head injury admissions in England, 1998–2007.24
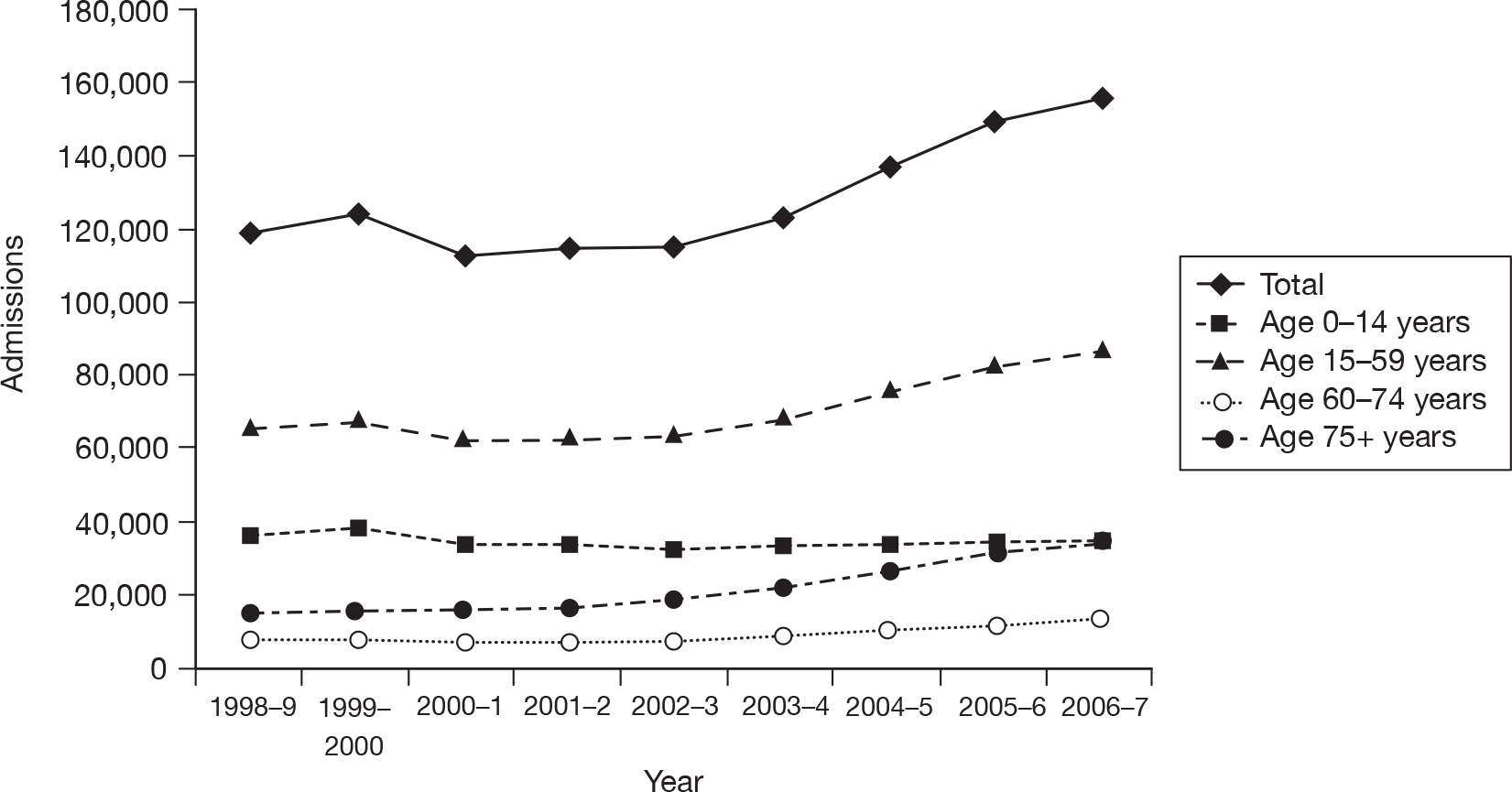
These data suggest that the annual costs of admission for head injury have increased from around £170M to £213M since the guidelines were introduced.
The increase in admissions could be indirectly due to the NICE guidance. If, for example, clinicians were ordering more CT scans, but lacked the ability to interpret them or access to a radiological opinion then this could result in more admissions. However, changes in NHS emergency care occurring around 2003 other than NICE guidance could have been responsible for the increase in admissions. For example, the introduction of a target limiting the time spent in the ED to 4 hours could have resulted in patients being admitted to hospital rather than undergoing prolonged assessment in the ED. Furthermore, a general trend away from surgical specialties and towards emergency physicians in the responsibility for MHI admissions may have changed the threshold for hospital admission.
Description of technology under assessment
Diagnostic strategies for MHI include clinical assessment, clinical decision rules, skull radiography, CT scanning and biochemical markers. Clinical assessment can be used to identify patients with an increased risk of ICI and select patients for imaging or admission. A recent meta-analysis of 35 studies reporting data from 83,636 adults with head injury25 found that severe headache (relative risk 2.44), nausea (2.16), vomiting (2.13), loss of consciousness (LOC) (2.29), amnesia (1.32), post-traumatic seizure (PTS) (3.24), old age (3.70), male gender (1.26), fall from a height (1.61), pedestrian crash victim (1.70), abnormal GCS (5.58), focal neurology (1.80) and evidence of alcohol intake (1.62) were all associated with intracranial bleeding. A similar analysis of 16 studies reporting data from 22,420 children with head injury25 found that focal neurology (9.43), LOC (2.23) and abnormal GCS (5.51) were associated with intracranial bleeding.
Clinical features have been combined in a number of studies to develop a structured clinical decision rule. Initially, clinical decision rules were developed to determine which patients should be admitted to hospital for observation. More recently, clinical decision rules have been developed to determine which patients should receive CT scanning. A systematic review undertaken for the NICE guidance19 identified four studies of four different clinical decision rules. The studies of the Canadian CT Head Rule (CCHR) criteria26 and the New Orleans Criteria (NOC) rule27 were both high quality, applicable to the NHS and reported 100% sensitivity for the need for neurosurgical intervention. Of the other two studies, one28 reported poor sensitivity and one29 was not applicable to the NHS. On this basis, the NICE guidance adapted the CCHR for use in the NHS and recommended this for adults and children, effectively as the NICE clinical decision rule. 19 In 2007, the guidance was updated1 to recommend using a rule developed specifically for children – the Children’s Head injury Algorithm for the prediction of Important Clinical Events (CHALICE) rule30 – although a modified version of the original rule continued to be recommended for adults.
Skull radiography can identify fractures that are associated with a substantially increased risk of intracranial bleeding, but cannot identify intracranial bleeding itself. Skull radiography is therefore used as a screening tool to select patients for investigation or admission, but not for definitive imaging. A meta-analysis31 found that skull fracture detected on a radiograph had a sensitivity of 38% and specificity of 95% for intracranial bleeding. More recent meta-analyses in adults25 and children32 reported relative risks of 4.08 and 6.13, respectively, for the association between skull fracture and intracranial bleeding. The NICE guidance only identifies a very limited role for skull radiography and use in the NHS has decreased accordingly. 21–23
Computerised tomography scanning definitively shows significant bleeding and a normal CT scan effectively excludes a significant bleed at the time of scanning. Magnetic resonance imaging (MRI) can detect some lesions that are not evident on CT,33 but arguably none that is of clinical importance and certainly none that influences early management. CT can therefore be considered as a reference standard investigation for detecting injuries of immediate clinical importance. Liberal use of CT scanning will minimise the risk of missed ICI. However, this has to be balanced against the cost of performing large numbers of CT scans on patients with no ICI and the potential for harm from radiation exposure, particularly in children.
Hospital admission and observation may be used to identify intracranial bleeding by monitoring the patient for neurological deterioration. Although commonly used in the past, the effectiveness of this approach has not been studied extensively and has the disadvantage that neurosurgical intervention is delayed until after patient deterioration has occurred. Hospital admission and observation are usually used selectively, based upon clinical assessment or skull radiography findings. As with CT scanning, the use of hospital admission involves a trade-off between the benefits of early identification of patients who deteriorate owing to ICI and the costs of hospital admission for patients with no significant ICI.
Studies have compared CT-based strategies to skull radiography and/or admission to conclude that CT-based strategies are more likely to detect intracranial bleeding and less likely to require hospital admission. 34,35 Both cost analyses based upon randomised controlled trial (RCT) data36 and economic modelling37 suggest that a CT-based strategy is cheaper. However, admission-based strategies may be an inappropriate comparator for cost-effectiveness analyses because they appear to be expensive and of limited effectiveness, particularly if applied unselectively.
More recently, the role of biochemical markers for the identification of brain injury has been investigated. The focus of these research efforts has been on a rule-out test, of high sensitivity and negative predictive value, such that patients with a negative test can be discharged without the radiation exposure associated with CT scanning. The most widely researched biomarker is the astroglial cell S100 calcium-binding protein beta subunit (S100B). Although it has been identified in non-head-injured patients,38 following isolated head injury a measurable concentration less than the currently used cut-off of 0.1 µg/l measured within 4 hours of injury39 has been linked to negative CT scans with a sensitivity of 96.8% and specificity of 42.5%. So far, inconsistency of sensitivity and specificity results has limited its widespread application. The question of clinical applicability and cost-effectiveness has also yet to be addressed adequately. Other biochemical markers, such as neuron-specific enolase (NSE), dopamine and adrenaline, have been studied but less extensively and without validation or consistent results, rendering it impossible to draw any evidence-based conclusions about their utilisation.
Chapter 2 Research questions
Rationale for the study
The diagnostic management of MHI, particularly the use of CT scanning and hospital admission, involves a trade-off between the benefits of early accurate detection of ICI and the costs and harms of unnecessary investigation and admission for patients with no significant ICI. Clinical assessment, particularly if structured in the form of a decision rule, can be used to select patients for CT scanning and/or admission. Selective use of investigations or admission can reduce resource use, but may increase the risk of missed pathology. Cost-effectiveness analysis is therefore necessary to determine what level of investigation represents the most efficient use of health-care resources.
Although primary research can provide accurate estimates of the cost-effectiveness of alternative strategies, it can only compare a limited number of alternatives and is often restricted by ethical and practical considerations. Economic modelling allows comparison of a wide range of different strategies, including those that might currently be considered impractical or unethical, but may be revealed to be appropriate alternatives. Economic modelling is also a much cheaper and quicker way of comparing alternative strategies than primary research, so it can be used to identify which alternatives are most promising and where uncertainty exists and, thus, where primary research is best focused.
Economic modelling needs to be based upon systematic synthesis of robust and relevant data. We therefore planned to systematically review the literature to identify studies that evaluated the diagnostic accuracy of clinical assessment, decision rules and diagnostic tests used in MHI and studies that compared the outcomes of different diagnostic management strategies. These data could then be used to populate an economic model that estimated the costs and outcomes of potential strategies for managing patients with MHI and identify the optimal strategy for the NHS.
We limited our study to the diagnosis of acute conditions arising from MHI (the accuracy of tests for identifying acute injuries and the costs and benefits of identifying and treating acute injuries). Chronic subdural haematoma can develop weeks after MHI with an initially normal CT scan. As diagnosis and management of this condition occurs after initial presentation, it is more appropriately analysed as part of a separate decision-making process that is beyond the scope of this review. Similarly, we did not explore issues related to diffuse brain injury or persistent symptoms related to mild traumatic brain injury (TBI).
Overall aims and objectives of assessment
The overall aim was to use secondary research methods to determine the most appropriate diagnostic management strategy for adults and children with minor (GCS 13–15) head injury in the NHS. More specifically, the objectives were:
-
To undertake systematic reviews to determine (1) the diagnostic performance of published clinical decision rules for identifying ICI (including the need for neurosurgery) in adults and children with MHI; (2) the diagnostic accuracy of individual clinical characteristics for predicting ICI (including the need for neurosurgery) in adults and children with MHI; and (3) the comparative effectiveness of different diagnostic management strategies for MHI in terms of process measures (hospital admissions, length of stay, time to neurosurgery) or patient outcomes.
-
To use a cross-sectional survey and routinely available data to describe current practice in the NHS, in terms of guidelines and management strategies used and hospital admission rates.
-
To develop an economic model to (1) estimate the cost-effectiveness of diagnostic strategies for MHI, in terms of the cost per quality-adjusted life-year (QALY) gained by each strategy; (2) identify the optimal strategy for managing MHI in the NHS, defined as the most cost-effective strategy at the NICE threshold for willingness to pay per QALY gained; and (3) identify the critical areas of uncertainty in the management of MHI, where future primary research would produce the most benefit.
Chapter 3 Assessment of diagnostic accuracy
A systematic review of the literature and meta-analysis (where appropriate) was undertaken to evaluate the diagnostic performance of clinical decision rules and to measure the diagnostic accuracy of key elements of clinical assessment for identifying intracranial injuries in adults and children with MHI.
The systematic review and meta-analysis was undertaken in accordance with the guidelines published by the Centre for Reviews and Dissemination (CRD) for undertaking systematic reviews40 and the Cochrane Diagnostic Test Accuracy Working Group on the meta-analysis of diagnostic tests. 41,42
Methods for reviewing diagnostic accuracy
Identification of studies
Electronic databases
Studies were identified by searching the following electronic databases:
-
MEDLINE (via OvidSP) 1950 to March 2010
-
MEDLINE In-Process & Other Non-Indexed Citations (via OvidSP) 1950 to March 2010
-
Cumulative Index of Nursing and Allied Health Literature (CINAHL) (via EBSCO) 1981 to April 2009
-
EMBASE (via OvidSP) 1980 to April 2009
-
Web of Science (WoS) [includes Science Citation Index (SCI) and Conference Proceedings Citation Index (CPCI)] [via Web of Knowledge (WoK) Registry] 1899 to April 2009
-
Cochrane Central Registry of Controlled Trials (CENTRAL) (via Cochrane Library Issue 2, 2009)
-
Cochrane Database of Systematic Reviews (CDSR) (via Cochrane Library Issue 2, 2009)
-
NHS Database of Abstracts of Reviews of Effects (DARE) (via Cochrane Library Issue 2, 2009)
-
Health Technology Assessment (HTA) database (via Cochrane Library Issue 2, 2009)
-
Research Findings Register (ReFeR)
-
National Institute for Health Research (NIHR) databases
-
International Network of Agencies for Health Technology Assessment (INAHTA)
-
Turning Research Into Practice (TRIP) database.
Sensitive keyword strategies using free text and, where available, thesaurus terms using Boolean operators and database-specific syntax were developed to search the electronic databases. Synonyms relating to the condition (e.g. head injury) were combined with a search filter aimed at restricting results to diagnostic accuracy studies (used in the searches of MEDLINE, CINAHL and EMBASE). Date limits or language restrictions were not used on any database. All resources were searched from inception to April 2009. Updated searches to March 2010 were conducted on the MEDLINE databases only. An example of the MEDLINE search strategy is provided in Appendix 1.
Other resources
To identify additional published, unpublished and ongoing studies, the reference lists of all relevant studies (including existing systematic reviews) were checked and a citation search of relevant articles [using WoK’s SCI and Social Science Citation Index (SSCI)] was undertaken to identify articles that cite the relevant articles. In addition, systematic keyword searches of the world wide web (WWW) were undertaken using the Copernic Agent™ Basic (version 6.12; Copernic, Quebec City, QC, Canada) meta-search engine and key experts in the field were contacted.
All identified citations from the electronic searches and other resources were imported into and managed using the Reference Manager bibliographic software version 12.0 (Thomson Reuters, Philadelphia, PA, USA).
Inclusion and exclusion criteria
The inclusion of potentially relevant articles was undertaken using a three-step process. First, two experienced systematic reviewers (APa and SH) independently screened all titles and excluded any citations that clearly did not meet the inclusion criteria (i.e. non-human, unrelated to MHI). Second, the list of included abstracts that were identified as possibly relevant by title (or when uncertainty existed) was divided equally between two pairs of authors (comprising an experienced reviewer and a clinical expert – APa and APi, respectively, or SH and SG, respectively) and assessed independently by each reviewer for inclusion. The full manuscript of all potentially eligible articles that were considered relevant by either pair of authors was obtained, where possible. Third, two review authors (APa and SH) independently assessed the full-text articles for inclusion. This was then checked by two clinical experts (SG and APi) separately. Blinding of journal, institution and author was not performed. Any disagreements in the selection process (within or between pairs) were resolved through discussion and included by consensus between the four reviewers. The relevance of each article for the diagnostic accuracy review was assessed according to the following criteria.
Study design
All diagnostic cohort studies (prospective or retrospective) with a minimum of 20 patients were included. Case–control studies (i.e. studies in which patients were selected on the basis of the results of their reference standard test) were excluded.
Reviews of primary studies were not included in the analysis, but were retained for discussion and identification of additional studies. The following publication types were excluded from the review: animal studies, narrative reviews, editorials, opinions, non-English-language papers and reports in which insufficient methodological details are reported to allow critical appraisal of the study quality.
Population
All studies of adults and children (of any age) with MHI (defined as patients with a blunt head injury and a GCS of 13–15 at presentation) were included. Studies of patients with moderate or severe head injury (defined as patients with a GCS of ≤ 12 at presentation) or no history of injury were excluded. Studies that recruited patients with a broad range of head injury severity were included only if > 50% of the patients had MHI.
Index test
Any test for ICI. This included clinical assessment (e.g. history, physical examination, clinical observation), laboratory testing (e.g. biochemical markers) or application of a clinical decision rule (defined as a decision-making tool that incorporates three or more variables obtained from the history, physical examination or simple diagnostic tests). 43
Target condition
The target conditions of this review were:
-
the need for neurosurgical intervention (defined as any ICI seen on CT or MRI scanning that required neurosurgery)
-
any ICI (defined as any intracranial abnormality detected on CT or MRI scan due to trauma).
Reference standard
The following reference standards were used to define the target conditions:
-
CT scan
-
combination of CT scan and follow-up for those with no CT scan
-
MRI scan.
Computerised tomography scanning is the diagnostic reference standard for detecting intracranial injuries that require immediate neurosurgical intervention, as well as those that require in-hospital observation and medical management. 1 Despite considerable variability in the use of CT scanning,44,45 performing a CT scan on all patients with MHI is costly and exposes most patients with normal CT scan to unnecessary radiation. 46 Therefore, CT scanning or follow-up for those not scanned was also deemed to be an acceptable reference standard.
Magnetic resonance imaging is considered to be more sensitive than CT scanning in detecting acute traumatic ICI in patients with MHI (i.e. can detect some lesions that are not evident on CT). 33 However, the lesions that are detected on MRI as opposed to CT are not likely to influence early neurosurgical management39 and its widespread use is constrained by costs, availability and accessibility issues. 39 Nevertheless, it can still be regarded as an appropriate reference standard.
Outcomes
Sufficient data to construct tables of test performance [numbers of true-positives (TPs), false-negatives (FNs), false-positives (FPs) and true-negatives (TNs) or sufficient data to allow their calculation]. Studies not reporting these outcomes were identified, but not incorporated in the analyses.
Data abstraction strategy
Data abstraction was performed by one reviewer (SH) into a standardised data extraction form and independently checked for accuracy by a second (APa). Discrepancies were resolved by discussion between the two reviewers and, if agreement could not be reached, a third or fourth reviewer was consulted (SG and APi). Where multiple publications of the same study were identified, data were extracted and reported as a single study. The authors of the studies were contacted to provide further details in cases where information was missing from the articles.
The following information was extracted for all studies when reported: study characteristics (author, year of publication, journal, country, study design and setting), participant details (age, gender, percentage with MHI, GCS, inclusion and exclusion criteria), test details, reference standard details, prevalence of each outcome [clinically significant ICI and need for neurosurgery (including definitions)] and data for a two-by-two table (TP, FN, FP, TN). Where a study presented several different versions of a clinical decision rule (i.e. developed during the derivation phase), all test performance data were extracted. However, the analyses considered data from only the rule endorsed by the authors or the rule derived for the most appropriate outcome.
Quality assessment strategy
The methodological quality of each included study was assessed by one reviewer (SH) and checked by another (APa) using a modified version of the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool47 (a generic, validated, quality assessment instrument for diagnostic accuracy studies). In case of doubt, a third and fourth reviewer (SG and APi) were consulted.
The quality assessment items in QUADAS include the following: spectrum composition, description of selection criteria and reference standard, disease progression bias (this item was not applicable to this review as the reference standard was defined as CT or MRI within 24 hours of admission), partial and differential verification bias, test and reference standard review bias, clinical review bias, incorporation bias (this item was not applicable to this review as the reference standard was always independent of the index test), description of index and reference test execution, study withdrawals and description of indeterminate test results. For studies reporting decision rules, three items relating to the reference standard (adequacy of reference standard, partial and differential verification bias) were included twice, once for each target condition. For studies reporting clinical characteristics, these items were included once and scored negatively if either reference standard was inadequate. Study quality was assessed with each item scored as ‘yes’, ‘no’ or ‘unclear’. A summary score estimating the overall quality of an article was not calculated as the interpretation of such summary scores is problematic and potentially misleading. 48,49 Further details on the modified version of the QUADAS tool are provided in Appendix 2.
Methods of data synthesis
Indices of test performance were extracted or derived from data presented in each primary study of each test. Two-by-two contingency tables of TP cases, FN cases, FP cases and TN cases were constructed. Data from cohorts of children were analysed separately. Data from cohorts of adults, mixed cohorts and cohorts with no clear description of the age range included were analysed together.
For the diagnostic performance of published clinical prediction rules (for diagnosing intracranial bleeding requiring neurosurgery or any clinically significant ICI), the data of the two-by-two tables were used to calculate sensitivity and specificity [and their 95% confidence intervals (CIs) for each study]. We planned to undertake meta-analysis if there were a sufficient number of validation studies of the same rule in cohorts that were not markedly heterogeneous. However, after searches were completed it was apparent that no rule had been studied sufficiently to allow a meaningful meta-analysis. Therefore, results were presented in a narrative synthesis and illustrated graphically (forest plots) using the Cochrane Collaboration Review Manager software (version 5.0; The Nordic Cochrane Centre, Copenhagen, Denmark). 50
For the diagnostic accuracy of clinical assessment, a different approach was used. We selected clinical characteristics that had been defined in a reasonably homogeneous and clinically meaningful way. Where applicable, three different approaches were used to meta-analyse the data. If data from only one study were available, no meta-analyses were undertaken, and the analysis produced estimates of sensitivity, specificity, negative likelihood ratio (NLR) and positive likelihood ratio (PLR), and corresponding 95% CIs. The last were calculated assuming that the statistics were normally distributed on the logit scale (sensitivity, specificity) and on the logarithm scale (NLR, PLR).
The PLR is the proportion with the outcome (neurosurgery or ICI) given that the risk factor is ‘positive’, divided by the proportion without the outcome given that the risk factor is ‘positive’, i.e. the PLR is the odds of having the outcome, given a positive risk factor. By a similar argument, the NLR is the odds of having the outcome given a negative risk factor. 51 Thus, the PLR and NLR are two potentially useful clinical diagnostic measures, depending on whether or not a patient is risk factor positive or risk factor negative.
If there were data from two studies, a fixed-effects meta-analysis was conducted using the DerSimonian and Laird method,52 weighted by the inverse of study variance estimate, and, as before, estimates of sensitivity, specificity, NLR, PLR and corresponding 95% CI. Note, that the correlation between outcomes cannot be taken into account in this case as there were insufficient data.
For data from three or more studies, a full Bayesian meta-analysis was conducted. The bivariate random-effects method of Reitsma et al. 53 was used. The Bayesian approach was chosen because the between-studies uncertainty can be modelled directly, which is important in any random effects meta-analysis where there are small numbers of studies and potential heterogeneity. Correlation between sensitivity and specificity was modelled at the logit level and the correlation was modelled separately. In addition to the estimated sensitivity, specificity, NLR, PLR and corresponding 95% highest-density regions (HDRs), results also included estimated heterogeneity (Q) statistics and corresponding p-values for sensitivity and specificity, calculated using a fixed-effects approach.
Results of the review of diagnostic accuracy
This section presents the results of the following systematic reviews separately:
-
the diagnostic performance of published clinical decision rules for identifying ICI or the need for neurosurgery in adults and children with MHI (see Clinical decision rules)
-
the diagnostic accuracy of individual clinical characteristics for predicting ICI or the need for neurosurgery in adults and children with MHI (see Individual characteristics)
-
the diagnostic accuracy of various biochemical markers for predicting ICI or the need for neurosurgery in adults and children with MHI (see Biomarkers).
Studies included in the review
Overall, the literature searches identified 8003 citations. Of the titles and abstracts screened, 222 relevant full papers were retrieved and assessed in detail. A flow chart describing the process of identifying relevant literature can be found in Appendix 3. A total of 93 papers evaluating the diagnostic performance and/or accuracy of clinical decision rules, individual clinical characteristics (symptoms, signs and plain imaging) and biochemical markers met the inclusion criteria. Table 1 shows the number of studies included for each systematic review of diagnostic accuracy. Studies excluded from the review are listed in Appendix 4.
| Diagnostic review | No. of included studies | |
|---|---|---|
| Adults | Children and/or infants | |
| Clinical decision rules | 19 | 14 |
| Individual clinical characteristics | 42 | 29 |
| Biomarkers | 11 | 1 |
Clinical decision rules
Description of included studies
Adults
The design and patient characteristics of the 19 studies (representing 22 articles)26,27,29,46,54–71 that evaluated the diagnostic performance of clinical decision rules for identifying ICI or need for neurosurgery in adults with MHI are summarised in Table 2. Eight studies were from the USA,27,29,55,58,59,61,62,64 two each from Italy,54,57,71 Canada26,46 and the Islamic Republic of Iran,66,67 and one each from the Netherlands,68–70 Australia,65 Japan,63 Spain60 and Denmark. 56 Six were multicentre studies. 26,46,62,66–70 Cohorts ranged in size from 16863 to 13,728. 62 Fourteen studies derived a new rule. 26,27,29,54–56,60,61–64,66,67,69 Four studies46,57,60,68–71 reported validation results for more than one rule in the same cohort. Data were collected prospectively in 15 studies,26,27,29,46,56–63,66–71 of which participants were recruited consecutively in 13,26,27,29,56–60,62,63,66–71 as a convenience sample in one,46 and one did not report the method of participant recruitment. 61 The remaining four studies were retrospective. 54,55,64,65 Of the 19 studies, three reported both a derivation and a validation cohort,27,61,63 making a total of 22 different cohorts.
| Author, year | Rule(s) derived | Rule(s) validated | Country | Design | No. of patients, n | Mean or median age, years (range) | Prevalence of neurosurgery | Prevalence of ICI | CT as inclusion? (yes/no) | Male, n | Patients with MHI, n | Prevalence of GCS 15, n | Other significant inclusion criteria | Other significant exclusion criteria |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Arienta et al. 199754 | Arienta et al. 199754 | Italy | R | 9917 | NR | 24/9917 (0.2%) | 85/9917 (0.86%) | No | NR for this subgroup | 9917/9917 (100%) | 9833/9917 (99%) | ≥ 6 years of age. Presenting to the ED directly | Children < 6 years of age | |
| Borczuk 199555 | Borczuk 199555 | USA | R | 1448 | NR | 119/1448 (8.2%) | Yes | 999/1448 (68%) | 1448/1448 (100%) | 1211/1448 (83.6%) | ≥ 17 years of age. GCS ≥ 13, blunt head trauma, had CT scan | ≤ 16 years. Patients with penetrating cranial trauma | ||
| Duus et al. 199456 | Duus et al. 199456 | Denmark | P, Cs | 2204 | Mean: 23.7 (0 to 108) | 4/2204 (0.18%) | No | 1378/2204 (62.5%) | 2204/2204 (100%) | NR | MHI, able to walk and talk | Comatose, unable to identify themselves or unresponsive to pain | ||
| Fabbri et al. 2005;57 aStein et al. 200971 | CCHR,26 NCWFS,72 NICE,19 NOC,27 NEXUS II,62 Scandinavian73 | Italy | P, Cs | 7955 | Median: 44 | 108/7955 (1.4%, reported as 1.3%) | 542/7955 (6.8%) | No | 4415/7955 (55.5%) | 7955/7955 (100%) | 7426/7955 (93.4%) | ≥ 10 years. Acute MHI within 24 hours of injury | Unclear history, unstable vital signs, GCS < 14, penetrating injuries, voluntary discharge, reattendances | |
| Falimirski et al. 200358 | Falimirski et al. 200358 | USA | P, Cs | 331 | Mean: 39.21 (16 to 95) | 40/331 (12.1%) | No | 214/337 (65%) | 331/331 (100%) | 302/331 (91.2%) | ≥ 16 years of age. Blunt injury, witnessed LOC or amnesia, GCS 14–15 | GCS 13, or transferred with a CT scan | ||
| Haydel et al. 200027 | NOC27 | USA | P, Cs | 520 | Mean: 36 (3 to 97) | 36/520 (6.9%) | No | 338/520 (65%) | 520/520 (100%) | 520/520 (100%) | > 3 years of age. GCS 15, LOC/amnesia, normal by brief neurological examination, injury within last 24 hours | Declined CT, concurrent injuries that preclude CT | ||
| NOC27 | P, Csb | 909b | Mean: 36 (3 to 94)b | 57/909 (6.3%)b | Nob | 591/909 (65%)b | 909/909 (100%)b | 909/909 (100%)b | As above | As above | ||||
| Holmes et al. 199759 | Miller et al. 199729 | USA | P, Cs | 264 | Mean: 39.5 | 4/264 (1.5%) | 35/264 (13.3%, reported as 13.2%) | Yes | 181//264 (68.5%) | 264/264 (100%) | 0 (all GCS 14) | Closed head injury, evidence of LOC or amnesia after head trauma and GCS 14. Had CT scan | Delay in presentation > 4 hours after injury | |
| Ibanez and Arikan 200460 | Ibanez and Arikan 200460 | Stein 1996,74 Tomei et al. 1996,75 Arienta et al. 1997,54 Lapierre 1998,76 Murshid 1998,77 NOC,27 Scandinavian,73 SIGN 2000,78 NCWFNS,72 CCHR,26 EFNS79 | Spain | P, Cs | 1101 | Mean: 46.7 (15 to 99) | 83/1101 (7.5%) | No | 573/1101 (52%) | 1101/1101 (100%) | 978 (88.8%) | > 14 years. MHI (GCS 14 or 15), with or without LOC | Referrals from other hospitals | |
| Madden et al. 199561 | Madden et al. 199561 | USA | P, NR | 537 | NR | 91/537 (17%) | Yes | NR | NR | All | All patients with acute head trauma presenting to the ED with head CT | Patients who received facial CT scans without cerebral studies | ||
| Madden et al. 199561 | P, NRb | 273b | 44/273 (16.1%)b | Yesb | NRb | NRb | Allb | As aboveb | As aboveb | |||||
| Miller et al. 199729 | Miller et al. 199729 | USA | P, Cs | 2143 | NR | 5/2143 (0.2%) | 138/2143 (6.4%) | Yes | NR | 2143/2143 (100%) | 2143/2143 (100%) | Normal mental status, LOC/amnesia, CT after blunt head trauma. Within 24 hours of injury, < 2 hours prior to presenting to the ED | No exclusion criteria applied | |
| Mower et al. 200562 | NEXUS II62 | USA | P, Cs | 13,728 | NR | 917/13,728 (6.7%) | Yes | 8988/13,728 (66%) | NR | All | All ages. Had CT scan, acute blunt head trauma | Delayed presentation, penetrating trauma | ||
| Ono et al. 200763 | Ono et al. 200763 | Japan | P, Cs | 1064 | Mean: 46 | 50/1064 (4.7%) | No | 621/1064 (58.4%) | 1064/1064 (100%) | 912 (85.7%) | ≥ 10 years. With head injury, within 6 hours of injury, GCS ≥ 14 | Extremely trivial injury (scalp or facial wounds), those who refused examination | ||
| Ono et al. 200763 | NRb | 168b | NRb | 13/168 (7.7%)b | Nob | NRb | 168/168 (100%)b | NRb | As above (assumed) | As above (assumed) | ||||
| Reinus et al. 199364 | Reinus et al. 199364 | USA | R | 355 | Mean: 39 (15 to 93) | 44/355 (12.4%) | Yes | 234/373 (62.7%) | NR | NR | > 15 years of age. Referred for CT scan from ED for closed or penetrating trauma to the head | Patients referred only for evaluation of facial bone fractures | ||
| Rosengren et al. 200465 | CCHR26 | Australia | R | 240 | Mean: 38 (14 to 95) | 1/240 (0.42%) | 10/240 (4.17%) | Yes | 168/240 (70%) | 240/240 (100%) | 240/240 (100%) | Adults, history of blunt trauma, GCS 15, history of LOC or amnesia | None reported | |
| Saadat et al. 200966 | Saadat et al. 200966 | Saadat et al. 200966 | Islamic Republic of Iran | P,Cs | 318 | NR | 20/318 (6.3%) | No | 242/318 (76%) | 318/318 (100%) | 285 (89.5%) | 15–70 years old with blunt head trauma within 12 hours of presentation and GCS ≥ 13 | Opium-addicted, concurrent major injuries that necessitated specialised care, unstable, suspected of malingering, or refused to participate in the study | |
| Saboori et al. 200767 | Saboori et al. 200767 | Islamic Republic of Iran | P, Cs | 682 | Mean: 29 (6 to 85) | 46/682 (6.7%) | No | 534/682 (78.3%) | 682/682 (100%) | 682 (100%) | ≥ 6 years of age. GCS 15 | > 24 hours post injury, no clear history of trauma, obvious penetrating skull injury or obvious depressed fracture | ||
| Smits et al. 2005,68 2007,69 200770 | CHIP69 | CCHR,26 NOC,27 Dutch, NCWFNS,72 EFNS,79 NICE,19 SIGN,78 Scandinavian73 | Nether-lands | P, Cs | 3181 | Mean: 41.4 (16 to 102) | 17/3181 (0.5%) | 243/3181 (7.6%) | No | 2244/3181 (70.5%) | 3181/3181 (100%) | 2462/3181 (77.4%) | ≥ 16 years. Presentation < 24 hours, GCS score 13–14 at presentation, or GCS 15 and one risk factor | Concurrent injuries precluded head CT within 24 hours of injury, contraindications to CT scanning, transfer from another hospital |
| CCHR26 | P, Csc | 1307c | 2/1307 (0.15%)c | 117/1307 (9%)c | Noc | NRc | 1307/1307 (100%)c | NRc | Subset (GCS score 13–15, LOC, no neurological deficit, no seizure, no anticoagulation, age > 16 years) selected from original cohort | |||||
| NOC27 | P, Csc | 2028c | 7/2028 (0.3%)c | 205/2028 (10.1%)c | Noc | NRc | 2028/2028 (100%)c | NRc | Subset (GCS 15, LOC, no neurological deficit, age > 3 years) selected from original cohort | |||||
| Stiell et al. 200126 | CCHR26 | Canada | P, Cs | 3121 | Mean: 38.7 ± (16 to 99) | 44/3121 (1.41%) | 254/3121 (8.14%) | No | 2135/3121 (68.4%) | 3121/3121 (100%) | 2489/3121 (80%) | ≥ 16 years. Witnessed LOC or amnesia or disorientation and GCS ≥ 13 and injury in last 24 hours | < 16 years. Minimal injury, no history of trauma as primary event, penetrating injury, obvious depressed skull fracture, focal neurological deficit, unstable vital signs, seizure, bleeding disorder/anticoagulants, reassessment of previous injury, pregnant | |
| Stiell et al. 200546 | CCHR,26 NOC27 | Canada | P, Cv | 2707 | Mean: 38.4 (16 to 99) | 41/2707 (1.5%) | 231/2707 (8.5%) | No | 1884/2707 (69.6%) | 2707/2707 (100%) | 2049/2707 (75.7%) | As per Stiell et al. 200126 | As per Stiell et al. 200126 | |
| CCHR,26 NOC27 | P, Cvc | 1822c | Mean: 37.7 (16 to 99)c | 8/1822 (0.4%)c | 97/1822 (5.3%)c | 1246/1822 (68.4%)c | 1822/1822 (100%)c | Subset (GCS 15) |
Median prevalence of neurosurgical injury was 0.95% [interquartile range (IQR) 0.3% to 1.5%]. Median prevalence of ICI was 7.2% (IQR 6.3% to 8.5%). Variations in prevalence may be owing to differences in inclusion criteria, reference standards and outcome definitions. Participant inclusion ages ranged from > 3 years27 to adults aged ≥ 17 years,55 with five studies including all ages or not reporting an age limit. 29,56,59,61,62 In seven studies,29,55,59,61,62,64,65 patients were enrolled only if they had a CT scan and in nine studies26,27,29,46,55,58,59,65,68–70 patients were selected on the basis of clinical characteristics, such as amnesia or LOC at presentation, which, in some studies, were used as criteria for having a CT scan. Five studies defined MHI as GCS 14–1554,57,58,60,63,71 and included only patients presenting within this range. Four studies collected data only on those with GCS 15,27,29,65,67 one study collected data on GCS 14 only,59 two studies61,62 included data from all GCS categories and two did not report GCS status. 56,64 The remaining five studies26,46,55,66,68–70 included patients with GCS 13–15. Ten studies26,27,29,46,57,59,63,66–71 stated that they enrolled people who presented within 48 hours of injury, although the more usual figure was within 24 hours of injury.
Definitions of outcomes and the reference standards used varied across studies (Table 3). If CT was not an inclusion criterion and was not performed on all then the reference standard used telephone follow-up and/or review of hospital records to identify clinically significant lesions. This method would not be expected to accurately identify all intracranial injuries and would potentially affect estimates of sensitivity and specificity. 80 Eight studies reported neurosurgery as an outcome. 26,29,46,54,57,59,65,68–71 The length of follow-up for neurosurgery varied from being not reported to up to 30 days after injury. The main difference in outcome definition for ICI involved the perception of clinical significance, with five cohorts defining this and 16 identifying any common acute lesion (listed in Table 3). Definitions of surgical lesions also varied, but most definitions included haematoma evacuation, elevation of depressed skull fracture and intracranial pressure monitoring.
| Author, year | Rule(s) tested | Definition of ICI | Reference standard used for ICI | Patients who had CT, n | Definition of need for neurosurgery | Reference standard used for need for neurosurgery |
|---|---|---|---|---|---|---|
| Arienta et al. 199754 | Arienta et al. 199754 | Intracranial lesion: not defined. Injuries listed include extradural haematoma, cortical contusion, subarachnoid haemorrhage, pneumocephalus, depressed fracture with contusion, intracerebral haematoma and subdural haematoma | CT scan or follow-up telephone call. Further details NR | 762/9917 (7.7%) | Neurosurgery or death | Retrospective chart review, telephone follow-up |
| Borczuk 199555 | Borczuk 199555 | ICI: abnormalities believed to be related to the trauma | CT scan | 1448/1448 (100%) | NA | NA |
| Duus et al. 199456 | Duus et al. 199456 | Intracranial complications: not defined |
If admitted: observation, CT scan if deteriorating level of consciousness and/or neurological signs If discharged: information sheet advising return if deterioration National Danish Patient Register checked for anyone diagnosed with appropriate ICD codes |
21/2204 (1%) | NA | NA |
| Fabbri et al. 2005;57 Stein et al. 200971 | CCHR,26 NCWFNS,72 NICE,19 NOC,27 Nexus II,62 Scandinavian73 |
Stein et al. 200971 – any lesion: surgical (intracranial haematoma large enough to require surgical evacuation) or non-surgical (other intracranial abnormality diagnosed on CT) Fabbri et al. 200557 – any post-traumatic lesion at CT within 7 days from trauma: depressed skull fracture, intracerebral haematoma/brain contusions, subarachnoid haemorrhage, subdural haematoma, epidural haematoma, intraventricular haemorrhage |
Patients were managed accord to NCWFS guidelines where low-risk patients sent home without CT, medium-risk patients given CT and observed for 3–6 hours if negative then discharged, high-risk patients given CT and observed 24–48 hours. All discharged with written advice of signs and symptoms with which they should return | 4177/7955 (52.5%) |
Stein et al. 200971 – surgical intracranial lesion: intracranial haematoma large enough to require surgical evacuation Fabbri et al. 2005:57 haematoma evacuation, skull fracture elevation within first 7 days of injury. Injuries after this period not considered in this analysis |
Assume hospital records |
| Falimirski et al. 200358 | Falimirski et al. 200358 | Significant ICI: not defined. Injuries recorded include subarachnoid haemorrhage, subdural haematoma, epidural haematoma, intracerebral haemorrhage, contusion, pneumocephaly, skull fracture | CT scan | 331/331 (100%) | NA | NA |
| Haydel et al. 200027 | NOC27 | ICI – presence of acute traumatic ICI: a subdural, epidural or parenchymal haematoma, subarachnoid haemorrhage, cerebral contusion or depressed skull fracture | CT scan |
520/520 (100%) 909/909 (100%)a |
NA | NA |
| Holmes et al. 199759 | Miller et al. 199729 | Abnormal CT scan: any CT scan showing an acute traumatic lesion (skull fractures or intracranial lesions: cerebral oedema, contusion, parenchymal haemorrhage, epidural haematoma, subdural haematoma, subarachnoid haemorrhage or intraventricular haemorrhage) | CT scan: patients with abnormal CT scan followed to discharge; those with normal CT not studied further | 264/264 (100%) | Neurosurgery |
Patients with abnormal CT scan followed to discharge Those with normal CT not studied further |
| Ibanez and Arikan 200460 |
Ibanez and Arikan 2004,60 Stein 1996,74 Tomei et al. 1996,75 Arienta et al. 1997,54 Lapierre 1998,76 Murshid 1998,77 NOC,27 Scandinavian,73 SIGN 2000,78 NCWFNS,72 CCHR,26 EFNS79 |
Relevant positive CT scan: acute intracranial lesion, not including isolated cases of linear skull fractures or chronic subdural effusions | CT scan | 1101/1101 (100%) | NA | NA |
| Madden et al. 199561 | Madden et al. 199561 | Clinically significant scan: pathology related to trauma affecting the bony calvaria or cerebrum (including non-depressed skull fractures, excluding scalp haematomas, those with no bony skull or intracerebral pathology) | CT scan: scans examined for bony and soft tissue injury, herniation, pneumocephalus, penetrating injury and the size and location of any cortical contusions, lacerations or external axial haematomas |
537/537 (100%) 273/273 (100%)a |
NA | NA |
| Miller et al. 199729 | Miller et al. 199729 | Abnormal CT scan: acute traumatic intracranial lesion (contusion, parenchymal haematoma, epidural haematoma, subdural haematoma, subarachnoid haemorrhage) or a skull fracture | CT scan: within 8 hours of injury | 2143/2143 (100%) | Surgical intervention: craniotomy to repair an acute traumatic injury or placement of a monitoring bolt | Hospital records of those with positive CT scan followed until discharge |
| Mower et al. 200562 | NEXUS II62 | Significant ICI: any injury that may require neurosurgical intervention, (craniotomy, intracranial pressure monitoring, mechanical ventilation), lead to rapid clinical deterioration or result in significant long-term neurological impairment | CT scan | 13,728/13,728 (100%) | NA | NA |
| Ono et al. 200763 | Ono et al. 200763 | Intracranial lesion: not defined. Injuries listed include subdural and epidural haematoma, subarachnoid haemorrhage, contusion, pneumocephalus | CT scan |
1064/1064 (100%), 152/168 (90.5%)a |
NA | NA |
| Reinus et al. 199364 | Reinus et al. 199364 | CT outcome: intracalvarial abnormalities, either axial or extra-axial, which could not be shown to be chronic | CT scan | 355/355 (100%) | NA | NA |
| Rosengren et al. 200465 | CCHR26 | Clinically significant ICI: CT abnormalities not significant if patient neurologically intact and had only one of the following: solitary contusion < 5 mm in diameter, localised subarachnoid blood < 1 mm thick, smear subdural haematoma < 4 mm thick, isolated pneumocephaly, closed depressed skull fracture not through the inner table (as per Stiell et al. 2001)26 | CT scan | 240/240 (100%) | Neurological intervention: not defined | NR |
| Saadat et al. 200966 | Saadat et al. 200966 | Positive CT scan: skull fracture (including depressed, linear, mastoid, comminuted, basilar, and sphenoid fracture), intracranial haemorrhage (including epidural, subdural, subarachnoid, intraparenchymal and petechial haemorrhage), brain contusion, pneumocephalus, midline shift and the presence of an air–fluid level | CT scan | 318/318 (100%) | NA | NA |
| Saboori et al. 200767 | Saboori et al. 200767 | Intracranial lesion: all acute abnormal finding on CT |
Normal CT: discharged with advice to return if symptoms occur, 1-week follow-up call Abnormal CT: admission, treatment. Evaluation at 2 weeks and 1 month after discharge |
682/682 (100%) | NA | NA |
| Smits et al. 200568–70 | CCHR,26 NOC,27 Dutch, NCWFNS,72 EFNS,79 NICE,19 SIGN, 78 Scandinavian,73 CHIP69 |
Any neurocranial traumatic finding on CT: any skull or skull base fracture and any intracranial traumatic lesion Smits et al. 2007 (CHIP derivation) definition differs: any intracranial traumatic findings on CT that included all neurocranial traumatic findings except for isolated linear skull fractures |
CT scan |
3181/3181 (100%) 1307/1307 (100%)b |
Neurosurgery: a neurosurgical intervention was any neurosurgical procedure (craniotomy, intracranial pressure monitoring, elevation of depressed skull fracture or ventricular drainage) performed within 30 days of the event | Assume patient records |
| Stiell et al. 200126 | CCHR26 | Clinically important brain injury on CT: all injuries unless patient neurologically intact and had one of following: solitary contusion < 5 mm, localised subarachnoid blood < 1 mm thick, smear subdural haematoma < 4 mm thick, closed depressed skull fracture not through inner table |
1. CT scan ordered on basis of judgement of physician in ED or result of follow-up telephone interview 2. Proxy telephone interview performed by registered nurse (24.4%). For those whose responses did not warrant recall for a CT scan this was the only reference standard |
2078/3121 (67%) | Within 7 days: death due to head injury, craniotomy, elevation of skull fracture, intracranial pressure monitoring, intubation for head injury demonstrated on CT | Performance of neurosurgery as reported in patient records and 14-day follow-up telephone interview (interview 100% sensitive for need for neurosurgery) |
| Stiell et al. 200546 | CCHR,26 NOC27 | As per Stiell et al. 200126 | As per Stiell et al. 200126 |
2171/2707 (80.2%) 1378/1822 (75.6%)b |
As per Stiell et al. 200126 | As per Stiell et al. 200126 |
Children and infants
The design and patient characteristics of the 14 studies (representing 16 papers)30,81–95 that evaluated the diagnostic performance of clinical decision rules for identifying ICI or need for neurosurgery in children and/or infants with MHI are summarised in Table 4. Six studies82,84–86,90,91,93,95 recruited only infants or reported a subset of infants-only data. Eight studies were from the USA,82,84–6,88,90,91,93–95 one from the USA and Canada,81 and one each from Italy,83 the UK,30 Turkey,87 Finland89 and Canada. 92 Nine studies30,81–87,89,90,92–94 derived a new rule or rules and five validated existing rules. 30,88–91,95 Three studies both derived and validated rules. 30,89,90 Six studies30,81,83,90–92,95 were multicentre studies. Eleven studies30,81,83–86,88,90–95 were prospective, one of which used a convenience sample,81 seven83–86,88,91,92,94,95 of which recruited consecutive patients, and three30,90,93 did not report how the sample was recruited. Three further studies82,87,89 used retrospective data. Two studies30,90 were very large with cohorts over 20,000. The smallest study was 97 patients. 82
| Author, year | Rule(s) derived | Rule(s) validated | Country | Design | No. of patients, n | Mean or median age, years (range) | Prevalence of neurosurgery | Prevalence of ICI | CT as inclusion? (yes/no) | Male, n | Patients with MHI, n | Prevalence of GCS 15, n | Other significant inclusion criteria | Other significant exclusion criteria |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Atabaki et al. 200881 | Atabaki et al. 200881 | USA, Canada | P, Cv | 1000 | Mean: 8.9 years (NR) | 6/1000 (0.6%) | 65/1000 (6.5%) | Yes | 641/1000 (64.1%) | 1000/1000 (100%) | 852/1000 (85.2%) | Birth to 21 years. Closed head trauma, undergoing CT | Prior CT at referring hospital, GCS < 13 | |
| Buchanich 200782 | Buch-anich 2007 | USA | R | 97 | Mean: 15.2 months (NR) | 22/97 (22.7%) | No | 97/97(100%) | NR | < 3 years old. GCS 14–15 | Penetrating injuries, depressed skull fractures, intentional injuries, CT scan > 24 hours after injury | |||
| Da Dalt et al. 200683 | Da Dalt et al. 200683 | Italy | P, Cs | 3806 | NR | 22/3806 (0.6%) | No | 2315/3806 (60.8%) | NR | 14 or normal value for age; 3749/3800 (98.7%) | < 16 years, history of blunt head trauma of any severity | Admitted > 24 hours after trauma, open injuries, previous history of neurological disorders or bleeding diathesis | ||
| Dietrich et al. 199384 | Dietrich et al. 199384 | USA | P, Cs | 166a | NR for this subgroupa | 16/166 (9.64%)a | Yesa | NR for this subgroupa | NR for this subgroupa | NR for this subgroupa | ≥ 2 years to 20 years, head trauma, with CT scana | Unable to answer questions because of age or altered mental statusa | ||
| 71a | NR for this subgroupa | 3/71 (4.2%)a | Yesa | NR for this subgroupa | NR for this subgroupa | NR for this subgroupa | < 2 years, as abovea | As abovea | ||||||
| Dunning et al. 200630 | CHALICE30 | RCS guidelines96 | UK | P, NR | 22,772 | Mean: 5.7 (NR) | 137/22,772 (0.6%) | 168/22,579 (0.744%) | No | 14,767/22,772 (64.8%) | 22,298/22,772 (97.9%) | 21,996/22,772 (96.6%) | < 16 years. History/signs of injury to the head. LOC or amnesia was not a requirement | Refusal to consent to entry into the study |
| Greenes and Schutzman 1999,85 b200186 | Greenes and Schutzman 199985 | USA | P, Cs | 608 | Mean: 11.2 months ± 6.8 months (NR) | 63/608 (10%) | No | 344/608 (57%) | NR | NR | < 2 years. Head trauma (symptomatic and asymptomatic) | NR | ||
| bGreenes and Schutzman 200186 | 172b | Mean: 11.6 months (3 days to 23 months)b | 13/172 (7.6%)b | Yesb | NRb | 100% (assumed from inclusion criteria)b | NRb | Asymptomatic subset of above cohort. With head CT scanb | Symptomaticb patients with any of history of LOC, lethargy, irritability, seizures, three or more episodes of emesis, irritability or depressed mental status, bulging fontanelle, abnormal vital signs indicating increased intracranial pressure or focal neurological findings | |||||
| Guzel et al. 200987 | Guzel et al. 200987 | Turkey | R | 337 | NR | 67/337 (19.9%) | Yes (applied at data extraction stage) | 223/337 (66.2%) | 337/337 (100%) | 304/337 (90.2%), | < 16 years. GCS 13–15. Had CT (applied at data extraction stage) | > 16 years, moderate or severe head injury, no clear history of trauma, obvious penetrating skull injury, unstable vital signs, seizure before assessment, bleeding disorder/anticoagulants, reattendances | ||
| Haydel and Schembekar 200388 | Noc27 | USA | P, Cs | 175 | Mean: 12.8 (range NR) | 6/175 (3.4%) | 14/175 (8%) | Yes | 114/175 (67%) | 100% (assumed from inclusion criteria) | 175/175 (100%) | 5–17 years. Within 24 hours of injury, blunt trauma with LOC, non-trivial mechanism of injury, CT scan | Trivial injuries, refused CT, concurrent injuries precluded CT, irritable or agitated (GCS < 15) | |
| Klemetti et al. 200989 | Klemetti et al. 200989 | CHALICE,30 NEXUS II,62 UCD93 | Finland | R | 485 | NR | 83/485 (17.1%) | No | 313/485 (65%) | NR | NR | ≤ 16 years. Admitted to paediatrics (usually hospitalised even after MHI), history of head trauma. Patients identified by reference to discharge diagnosis | NR | |
| cKupperman et al. 200990 | cPECARN (≥ 2 years to < 18 years)90 | USA | P, NR | 25,283c | NR for this subsetc | 215/25,283 (0.9%)c | Noc | NRc | 25,283/25,283 (100%)c | 24,563/25,283 (97.2%)c | ≥ 2 years to < 18 years. Children presenting within 24 hours GCS ≥ 14c | Trivial injuries, penetrating trauma, known brain tumours, pre-existing neurological disorders, or neuroimaging before transfer. Coagulopathy, shunts, GCS < 14c | ||
| cPECARN (< 2 years)90 | 8502c | 73/8502 (0.9%)c | Noc | NRc | 8502/8502 (100%)c | 8136/8502 (95.7%)c | As above, < 2 yearsc | As abovec | ||||||
| PECARN (2 years to < 18 years)90 | 6411c | 11/6411 (0.2%)c | 63/6411 (1%)c | Noc | NRc | 6411/6411 (100%)c | 6248/6411 (97.5%)c | As for derivation cohortc | As for derivation cohortc | |||||
| PECARN (< 2 years)90 | 2216c | 5/2216 (0.2%)c | 25/2216 (1.1%)c | Noc | NRc | 2216/2216 (100%)c | 2124/2216 (95.8%)c | As for derivation cohortc | As for derivation cohortc | |||||
| dOman 2006;91 dSun et al. 200795 | dNEXUS II,62 UCD93 | USA | P, Cs | 1666d | NRd | 138/1666 (8.3%)d | Yesd | 1072/1666 (64%)d | NRd | NRd | < 18 years. Had CT scan (physicians discretion), acute blunt head traumad | Delayed presentation, without blunt trauma (penetrating trauma)d | ||
| dNEXUS II91 | 309d | 25/309 (8.1%)d | Yesd | 170/309 (55%)d | NRd | NRd | Subset of above, < 3 years of aged | As aboved | ||||||
| dUCD95 | 208d | 7/208 (3.4%)d | Yesd | NR for this subgroupd | NRd | NRd | Subset of above, < 2 years of aged | As aboved | ||||||
| Osmond et al. 200692 | CATCH for ICI,92 CATCH for Neurosurgery92 | Canada | P, Cs | 3781 | Mean: 9.2 (NR) | 27/3781 (0.7%) | 170/3781 (4.5%) | No | 2458 (65%) | 3781/3781 (100%) | 3414/3781 (90.3%) | ≤ 16 years. GCS 13–15, documented LOC, amnesia, disorientation, persistent vomiting or irritability (if ≤ 2 years of age)e | NR | |
| Palchak et al. 200393 | UCD (neurosurgery),93 UCD (intervention or brain injury)93 | USA | P, NR | 2043 | Mean: 8.3 ± 5.3 (10 days to 17.9 years) | 29/2043 (1.4%) | No | 1323/2043 (65%) | NR | GCS 14 or 15: 1859/2043 (91%) | < 18 years. History of non-trivial blunt head trauma with findings consistent with head trauma: LOC, amnesia, seizures, vomiting, current headache, dizziness, nausea or vision change or physical examination findings of abnormal mental status, focal neurological deficits, clinical signs of skull facture or scalp trauma | Trivial injuries, neuroimaging before transfer | ||
| UCD (TBI)93 | 1098 | NR for this subset | 39/1098 (3.6%) | Yes | NR for this subset | 1098/1098 (100%) | GCS 14 or 15: 1098/1098 (100%) | Subset of above cohort; GCS 14–15 and had CT scan only | As above | |||||
| UCD (TBI)93 | 194 | NR for this subset | 15/194 (7.73%) | Yes | NR for this subset | 194/194 (100%) | NR for this subset | Subset of above cohort (had CT scan GCS 14 or 15), ≤ 2 years | As above | |||||
| Quayle et al. 199794 | Quayle et al. 199794 | USA | P, Cs | 321 | Mean: 4 years 10 months (2 weeks to 17.75 years) | 27/321 (8.4%) | Yes |
189/321 (59%) |
NR | NR | < 18 years. Non-trivial injury: symptoms such as headache, amnesia, vomiting, drowsiness, LOC, seizure, dizziness or significant physical findings including altered mental status, neurological deficit and altered surface anatomy. Scalp laceration or abrasion in infants < 12 months, scalp haematoma in infants < 24 months | Trivial head injuries, penetrating head injuries |
The median value for the prevalence of neurosurgery was 1.2% (IQR 0.2% to 1.4%). The median value for the prevalence of ICI was 6.5% (IQR 1.0% to 9.8%). Cohorts were not similar in terms of inclusion and exclusion criteria. For studies of children, the upper age limit ranged between 1630,83,87,89,92 and 21 years,81 and the lower limit between 081 and 5 years. 88 For infants, the upper age limit was usually 2 years, but in one case was 3 years82 of age. Eight studies30,83–85,89,91,93–95 included all severities of head injury; six81,82,87,88,90,92 recruited those with MHI. Two of these studies reported results for a MHI subset of the larger cohort. 86,93 Five studies excluded those with trivial head injury and/or recruited only those with clinical characteristics consistent with head trauma. 88,90,92,93,94 Six studies81,84,87,88,91,94 included only those who had a CT scan and two reported a subset, all of whom underwent CT. 86,93 Selection of patients on the basis of having had a CT scan and exclusion on the basis of trivial injury or not presenting with clinical characteristics is likely to recruit a patient spectrum with greater risk of ICI.
Definitions of outcomes and the reference standards used varied across studies (Table 5). The predominant differences in outcome definition for ICI involve the perception of clinical significance, with four cohorts30,89–91,95 having this defined and the remaining ten studies81–88,92–94 failing to define a positive outcome or just identifying any common acute lesion. The reference standards used where CT was not possible for all, and was not an inclusion criterion, usually comprised telephone follow-up, review of hospital records or both. The length of follow-up for neurosurgery varied from being not reported to following up until discharge, which may not capture all neurosurgical procedures leading to inaccurate estimations of diagnostic accuracy. Definitions of surgical lesions also varied or were not reported, but most definitions included haematoma evacuation and intracranial pressure monitoring; only one mentioned elevation of skull fracture explicitly.
| Author, year | Rule(s) tested | Definition of ICI | Reference standard used for ICI | Patients who had CT, n | Definition of need for neurosurgery | Reference standard used for need for neurosurgery |
|---|---|---|---|---|---|---|
| Atabaki et al. 200881 | Atabaki et al. 200881 | ICI: subdural, epidural, subarachnoid, intraparenchymal and intraventricular haemorrhages as well as contusion and cerebral oedema | CT scan | 1000/1000 (100%) | Neurosurgery, including craniotomy, craniectomy, evacuation or intracranial pressure monitoring | Medical record review (unclear when performed) |
| Buchanich 200782 | Buchanich 200782 | ICI: intracranial haematoma, intracranial haemorrhage, cerebral contusion and/or cerebral oedema |
CT scan Follow-up questionnaire/telephone interview |
97/97 (100%) | NA | NA |
| Da Dalt et al. 200683 | Da Dalt et al. 200683 | ICI: identified on CT either at initial ER presentation or during any hospital admission or readmission |
CT scan obtained at discretion of treating physician All children discharged immediately from ER or after short observation received a follow-up telephone interview approximately 10 days later. Hospital records were checked for readmissions for 1 month after conclusion of study |
79/3806 (2%) | NA | NA |
| Dietrich et al. 199384 | Dietrich et al. 199384 | Intracranial pathology: epidural or subdural haematoma, cerebral contusions or lacerations, intraventricular haemorrhage pneumocephaly or cerebral oedema, with or without skull fracture | CT scan |
166/166 (100%) 71/71 (100%)a |
NA | NA |
| Dunning et al. 200630 | CHALICE,30 RCS guidelines96 | Clinically significant ICI: death as a result of head injury, requirement for neurosurgical intervention or marked abnormalities on the CT scan |
All patients treated according to RCS guidelines. This recommends admission for those at high risk and CT scan for those at highest risk Follow-up: all patients who were documented as having had a skull radiograph, admission to hospital, CT scan or neurosurgery were followed up |
744/22,772 (3.3%) | NR | NR, assume as for ICI |
| Greenes and Schutzman 1999,85 200186 | Greenes and Schutzman 1999,85 200186 |
Greenes and Schutzman 1999 85 ICI: acute intracranial haematoma, cerebral contusion and/or diffuse brain swelling evident on head CT Greenes and Schutzman 2001 86 ICI: cerebral contusion, cerebral oedema or intracranial haematoma noted on CT |
Greenes and Schutzman 199985 CT scan, follow-up calls, review of medical records Greenes and Schutzman 200186 CT scan |
188/608 (31%). 73 symptomatic patients did not receive CT85 |
NA | NA |
| Guzel et al. 200987 | Guzel et al. 200987 | Positive CT scan: definition NR | CT scan | 337/337 (100%) | NA | NA |
| Haydel and Schembekar 200388 | NOC27 | ICI on head CT: any acute traumatic intracranial lesion, including subdural epidural or parenchymal haematoma, subarachnoid haemorrhage, cerebral contusion or depressed skull fracture | CT scan | 175/175 (100%) | Need for neurosurgical or medical intervention in patients with ICI on CT | All patients with abnormal CT scan admitted and followed until discharge |
| Klemetti et al. 200989 | Klemetti et al. 2009,89 CHALICE,30 NEXUS II,62 UCD93 | Complicated or severely complicated head trauma: brain contusion, skull base fracture, skull fracture. Patients who required neurosurgical intervention, patients who succumbed, epidural haematoma, subdural haematoma, subarachnoid haematoma, intracerebral haematoma | Hospital records | 242/485 (49.9%) | NA | NA |
| Kupperman et al. 200990 | Kupperman et al. 200990 | Clinically important brain injury: death from TBI, neurosurgery, intubation for > 24 hours for TBI, or hospital admission of two nights or more associated with TBI on CT. Brief intubation for imaging and overnight stay for minor CT findings not included |
CT scans, medical records, and telephone follow-up. Those admitted: medical records, CT scan results Those discharged: telephone survey 7 to 90 days after the ED visit, and medical records and county morgue records check for those uncontactable |
9420/25,283 (37.3%)c 2632/8502 (31.0%)c 2223/6411 (34.7%)c 694/2216 (31.3%)c |
NR | NR for neurosurgery. Assume as for ICI |
| Oman 2006;91 aSun et al. 200795 | NEXUS II,62 UCD93 | Clinically important/significant ICI: any injury that may require neurosurgical intervention, lead to rapid clinical deterioration, or result in significant long-term neurological impairment | CT scan |
1666/1666 (100%)d 309/309 (100%)d 208/208 (100%)d |
NA | NA |
| Osmond et al. 200692 | CATCH92 | Brain injury |
CT scan 14-day telephone interview |
NR | Neurosurgery: craniotomy, elevation of skull fracture, intubation, intracranial pressure monitor and/or anticonvulsants within 7 dayse | NR |
| Palchak et al. 200393 | UCD93 | TBI identified on CT scan or TBI requiring acute intervention or intervention by one or more of: neurosurgical procedure, ongoing antiepileptic pharmacotherapy beyond 7 days, the presence of a neurological deficit that persisted until discharge from the hospital, or two or more nights of hospitalisation because of treatment of the head injury | CT or performance of intervention |
1271/2043 (62.2%) 1098/1098 (100%) 194/194 (100%) |
Need for neurosurgical intervention | NR |
| Quayle et al. 199794 | Quayle et al. 199794 | ICI: definition NR | CT scan | 321/321 (100%) | NA | NA |
Quality of included studies
Adults
The methodological quality assessment of each included study is summarised in Figures 2 and 3. Overall, most of the included studies were well reported and generally satisfied the majority of the quality assessment items of the QUADAS tool, but with notable exceptions. 54–57,71 Despite poor reporting of the reference standards in most studies, the main source of variation was for patient spectrum, which will affect comparability across cohorts and application of conclusions to practice.
FIGURE 2.
Decision rules for adults with MHI – methodological quality graph. Review authors’ judgements about each methodological quality item presented as percentages across all included studies.
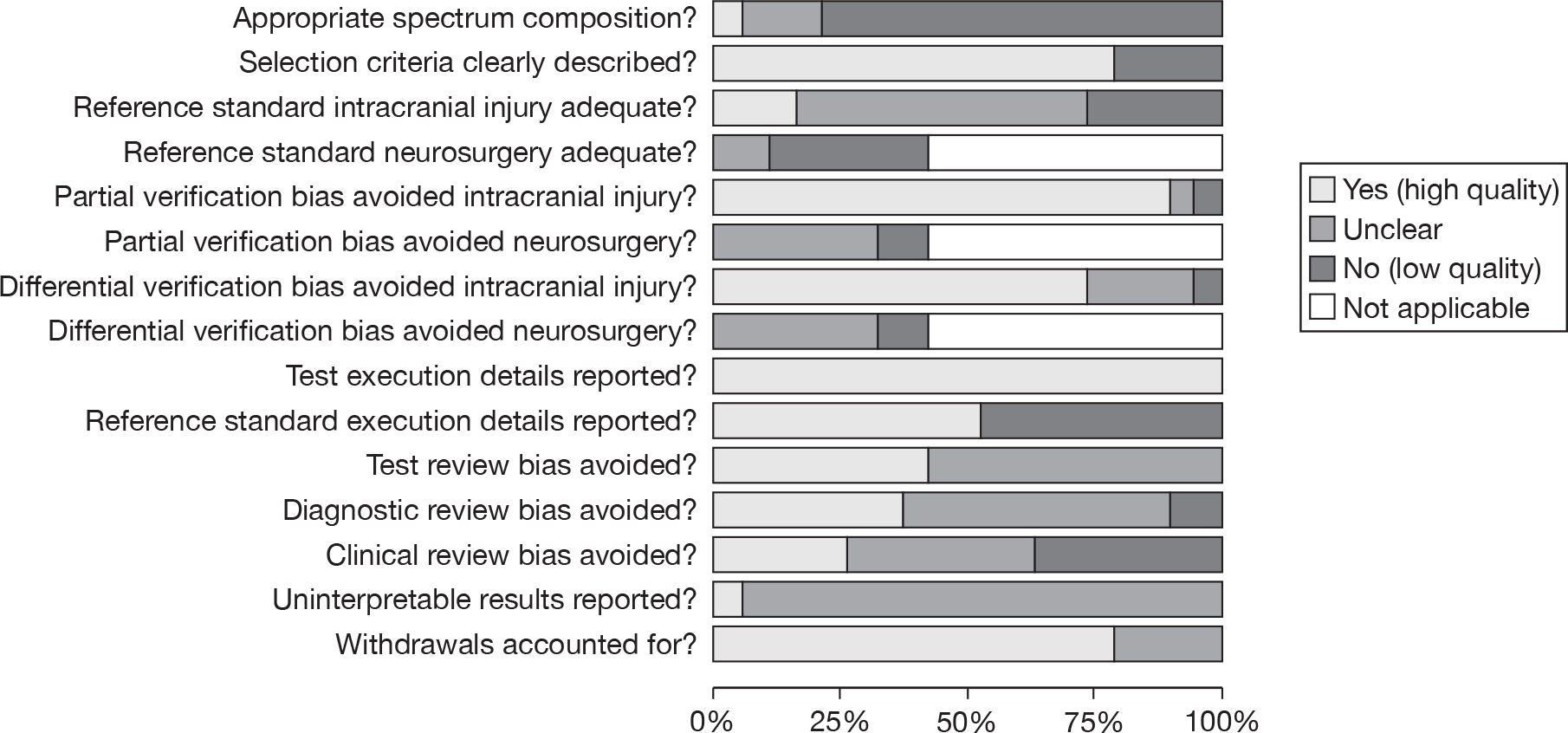
FIGURE 3.
Decision rules for adults with MHI – methodological quality summary. Review authors’ judgements about each methodological quality item for each included study. Minus sign, negative score; plus sign, positive score; question mark, unclear whether item scores negatively or positively; blank space, not applicable. a, Data from Fabbri et al. 57 and Stein et al. 71 b, Ono et al. 63 recruited two separate cohorts for validation and derivation. The derivation cohort was treated differently for the ICI outcome: the reference standard was not adequate, it was unclear whether partial verification bias was avoided and differential verification bias was not avoided. c, Smits et al. 68–70
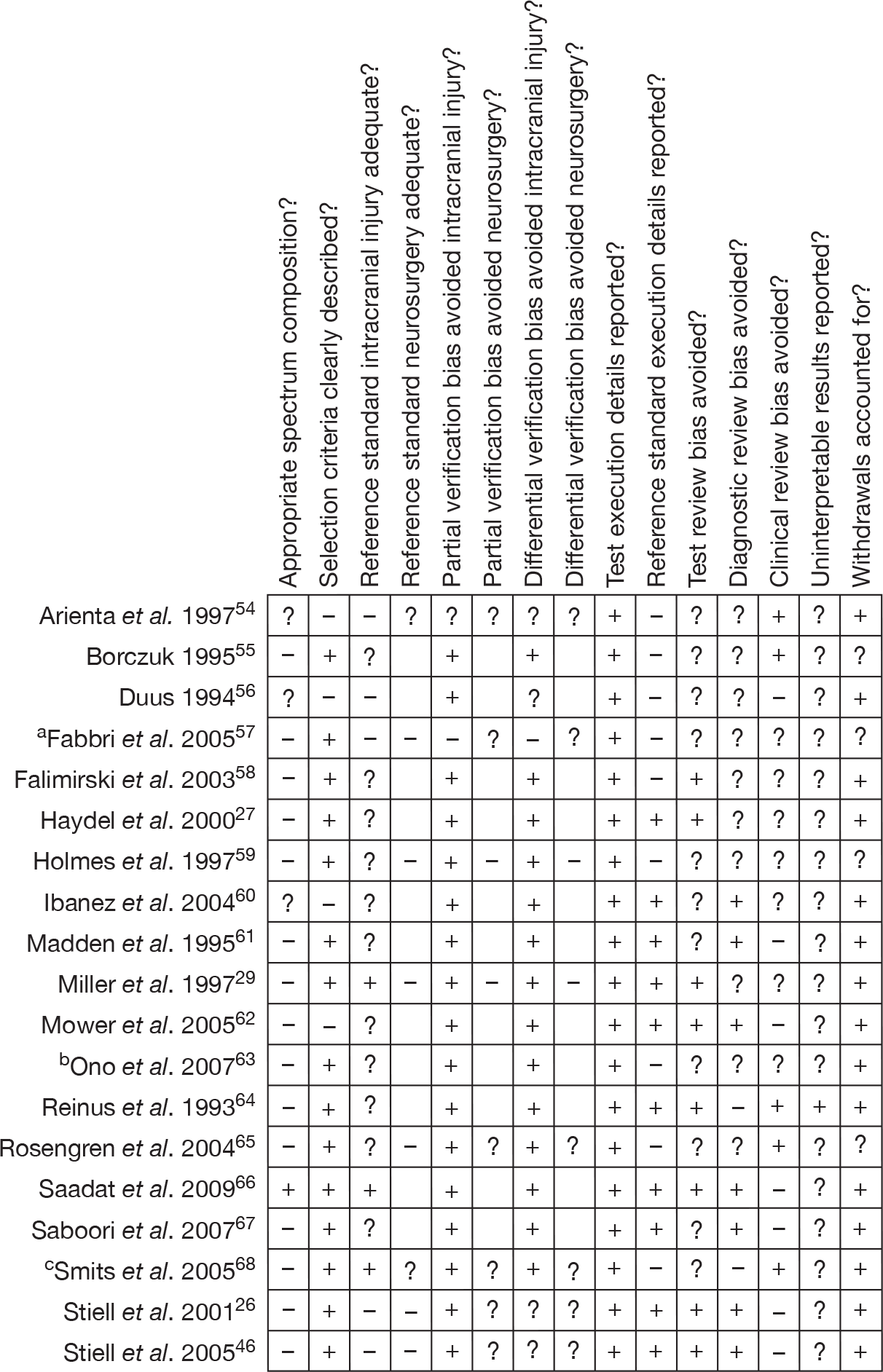
The spectrum of patients was appropriate in only one study,66 was unclear in three studies54,56,60 and did not completely match the desired patient spectrum in the remaining 15 studies, often because patients were selected on the basis of having a clinical characteristic at presentation (Table 2). Although 11 studies carried out CT in all participants,27,55,58–65,67 they did not state whether CT was performed within 24 hours and were therefore rated as unclear for the ICI reference standard quality assessment item. A further three cohorts performed CT on all participants within 24 hours and so scored well. 29,66,68–70 The remaining five studies did not perform CT in all participants and so scored negatively for this item. 26,46,54,56,57 The reference standard for neurosurgery was not reported for two studies54,68–70 and not considered adequate in the remaining six. 26,29,46,57,59,65,71 This was usually because not all patients were followed up.
Partial verification bias was largely avoided, with only two cohorts scoring unclear54 or negatively. 57,71 However, these two cohorts were large, and one reported results for a number of rules. 71 Partial verification bias may be more of an issue for the neurosurgery data as no cohort scored well. Differential verification bias for ICI may have affected results in the same large cohort reporting several rules. 57,71 Here participants received different reference standards according to clinical characteristics at presentation or the judgement of the treating physician. Criteria for CT were identical to the rule being tested in the case of the Neurotraumatology Committee of the World Federation of Neurosurgical Societies (NCWFNS)72 rule. In four cases26,46,54,56 it was unclear, although the majority avoided differential verification bias. For neurosurgery, it was unclear if differential verification bias was avoided in six cohorts26,46,54,57,65,68–71 and was scored negatively in two cohorts. 29,59
The execution of the index test was well described in all studies. The execution of the reference standards (either one or both) was not reported well in nine studies54–59,63,65,68 and scored negatively for this item. Diagnostic and test review biases may affect results as less than half of the studies scored well for blinding; the index test was interpreted blind in eight cases,26,27,29,46,58,62,64,66, but blinding status was unclear in 11. 54–57,59,60,61,63,65,67–70 The reference standard was interpreted blind in seven cases,26,46,60–62,66,67 and was not interpreted blind in two cases;64,68–70 blinding status was unclear in ten cases. 27,29,54–59,63,65 Studies were of mixed quality for clinical review bias, with almost equal numbers scoring in each quality category. Information about uninterpretable results was only given in one study,64 with all other studies scoring unclear for this item. Studies scored well for withdrawals, with only four studies55,57,59,65,71 scoring unclear because it was not apparent whether all patients were accounted for at the end of the study.
Children and infants
The methodological quality assessment of each included study is summarised in Figures 4 and 5. Overall, most of the included studies were poorly reported and did not satisfy the majority of the quality assessment items of the QUADAS tool. The study30 that scored the most negatives and fewest positives was also one of the two large cohorts (> 20,000), and consequently has the potential to influence the results. This study scored poorly mainly owing to the use of pragmatic reference standards.
FIGURE 4.
Decision rules for children and infants with MHI – methodological quality graph. Review authors’ judgements about each methodological quality item presented as percentages across all included studies.
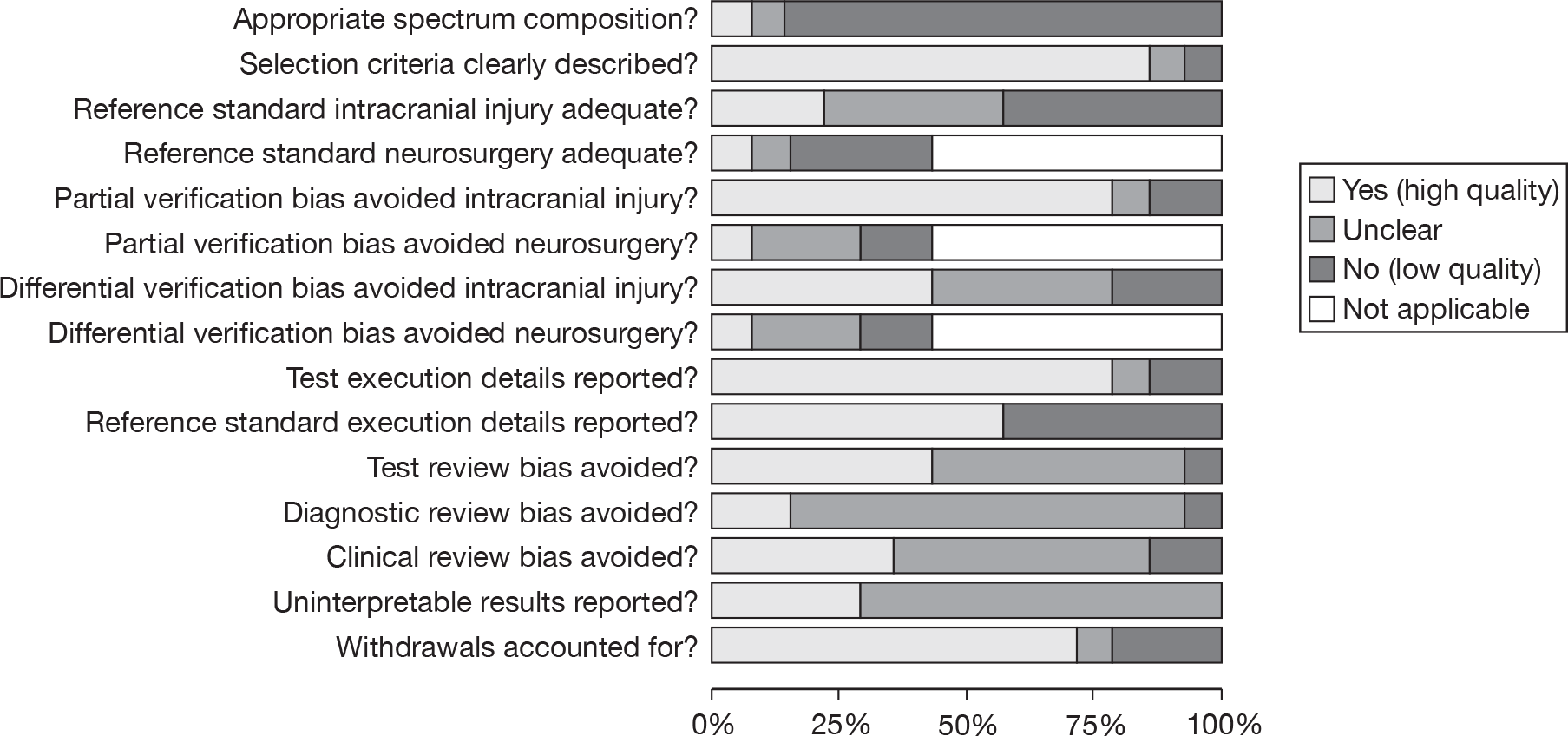
FIGURE 5.
Decision rules for children and infants with MHI: methodological quality summary. Review authors’ judgements about each methodological quality item for each included study. Minus sign, negative score; plus sign, positive score; question mark, unclear whether item scores negatively or positively; blank space, not applicable.
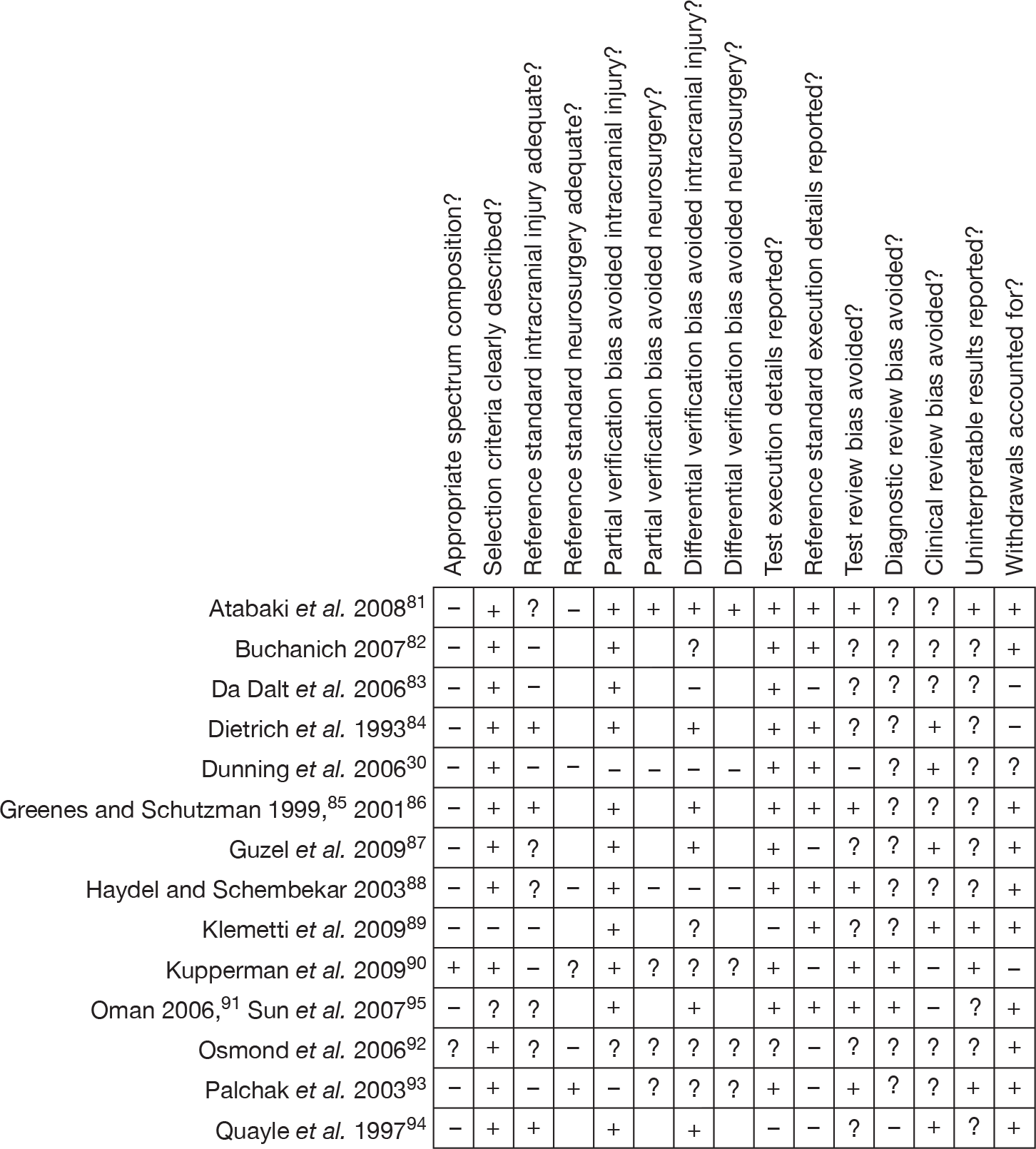
The patient spectrum item scored worst overall, with only one study (which was one of the large studies) scoring positively. 90 Studies failed this quality item for a range of reasons and sometimes for multiple reasons. Problems included selecting only patients who had had a CT scan or those who presented with clinical characteristics, including patients with all severities of head injury, recruiting patients regardless of time since injury and using a retrospective design.
The reference standard for ICI was of a mixed standard: only three scored positively. 84–86,94 Although, a further four81,87,88,91,95 did undertake CT in all participants, they failed to state whether this was within 24 hours and so scored unclear. The remaining seven studies scored negatively30,82,83,89,90,93 or unclear. 92 This represents a potential source of bias. Equally, the reference standards for neurosurgery scored negatively or unclear in all but one study. 93
Studies were well reported in terms of description of selection criteria and test execution details, with 1230,81–88,90,92–94 and 1130,81–88,90,91,93 studies, respectively, reporting these criteria adequately. Descriptions of the execution of the reference standard were mixed, with just over half scoring well. 30,81,82,84–86,88,89,91,95 Uninterpretable results were not reported in 10 studies81–83,85,86,88,92,93 and so scored unclear for this item.
Partial verification bias was generally avoided (11 studies scored well)81–91,94,95 for ICI where a reference standard was applied to all participants, but not for neurosurgical outcomes, for which only one study scored well. 81 The picture was less clear for differential verification bias of ICI, with three scoring negatively30,83,88 and almost equal numbers scoring well81,84–87,91,94,95 and unclear82,89,90,92,93 where, for example, it was not clear whether or not clinical characteristics (index test) may have contributed to the decision to give CT rather than follow-up as a reference standard. There is some potential for this bias to affect the results, especially as neither large cohort30,90 scored well. For neurosurgical outcomes only one study scored well. 81 Blinding was generally poorly reported, with seven studies scoring unclear82–84,87,89,92,94 for the test review bias and 11 studies30,81–89,92,93 scoring unclear for the diagnostic review bias. However, six studies scored well for test review bias. 81,85,86,88,90,91,93,95 Clinical review bias was avoided in retrospective studies by definition, but for most it was unclear81–83,85,86,88,92,93 or negative. 90,91,95 There is potential for these biases to affect the results. Few studies reported withdrawals and so most scored well for this item. 81,82,85–89,91–95
Summary of test accuracy results: clinical decision rules
Adults
From the 19 studies reporting diagnostic data for decision rules for adults with MHI, a total of 25 decision rules1,19,20,26,27,29,54–56,58,60–64,66,67,69,72–77,79 were identified and are outlined in Tables 6 and 7a and b. Eleven rules1,19,26,27,54,61–63,72,73,78,79 were evaluated in more than one data set and one further rule29 was evaluated in two cohorts: one of GCS 15 (derivation cohort)29 and one of GCS 14. 59 Nine of the decision rules1,19,26,70,72–75,78,79 existed in two forms: one to identify those most at risk (termed variously as high risk, mandatory, emergency, moderate and strict) and a second more inclusive version to identify those at medium risk (termed variously as medium risk, recommended, urgent, mild and lenient). These two risk categories were often intended to identify those at risk of needing neurosurgery (high risk) and those at risk of ICI (medium risk).
| Criteria | CCHR26 | NOC27 | aNICE 2003,19 20071 | NCWFNS72 | bArienta groups β and γ54 | ||||
|---|---|---|---|---|---|---|---|---|---|
| Decision rule | |||||||||
| Risk category | High risk | Medium risk | Lenient | Strict | High risk | Medium risk | |||
| Tested in study by | Stiell et al. 2001,26 2005;46 Stein et al. 2009;71 Rosengren et al. 200465 | Stiell et al. 2001,26 2005;46 Stein et al. 2009;71 Rosengren et al. 2004;65 Smits et al. 2005;68 cIbanez and Arikan 200460 | Haydel et al. 2000;27 Ibanez and Arikan 2004;60 Smits et al. 2005;68 Stiell et al. 2005;46 Rosengren et al. 200465 | Fabbri et al. 200557 (NICE 2003);Smits et al. 200770 (NICE 2003); Stein et al. 2009 (NICE 2007)71 | Smits et al. 200770 | Smits et al. 200769 | Fabbri et al. 2005;57 Smits et al. 2007;69 Stein et al. 2009;71 cIbanez and Arikan 200460 | Arienta et al. 1997;54 cIbanez and Arikan 200460 | |
| Eligibility criteriad | GCS 13–15, clinical characteristics. Some significant exclusions | GCS 15, clinical characteristicse–g | Sustained head injury | Mild, minor or trivial head injury (GCS 14–15h) | Head injury (GCS 9–15) | ||||
| Mental status | Impaired consciousness | ||||||||
| Focal/neurological deficits | Any | Neurological deficits | Neurological deficits | ||||||
| Skull fracture | Suspected open, depressed or basal | Suspected open, depressed or basali | Any | Otorrhagia/otorrhoea, rhinorrhoea, signs of basal skull fracture | |||||
| LOC | Any | Transitory | |||||||
| Vomiting | ≥ 2 | Any | Recurrenti | Any | Any | ||||
| Age | ≥ 65 years | > 60 years | ≥ 65 years if with LOC/amnesiaa,i | > 60 yearsj,k | |||||
| Amnesia | Amnesia before impact of ≥ 30 minutes | Amnesia before impact of ≥ 30 minutes | Any | Any | |||||
| Coagulopathy | If with LOC/amnesiai | Any | Anticoagulant therapy or coagulopathy | ||||||
| Seizures | Any | PTS | Pre-trauma epilepsy | Any or epileptic | |||||
| Visible injury | Trauma above clavicles | Penetrating or perforated wounds | |||||||
| Intoxication | Any | Any | Alcoholic patients | ||||||
| Behaviour | Uncooperative | ||||||||
| Headache | Any | Diffuse | |||||||
| Previous neurosurgery | Any | Intracranial operations | |||||||
| Failure to improve | GCS < 15 at 2 hours after injury | GCS < 15 at 2 hours after injuryi | |||||||
| Mechanism of injury | Dangerousl | Dangerous, if with LOC/amnesiai | |||||||
| Deterioration in mental status | |||||||||
| Other | Subgaleal swelling | ||||||||
| Criteria | mEFNS79 | Madden et al. 199561 | Ono et al. 200763 | Scandinavian73 | SIGN 200078 | NEXUS II62 | |||
| Decision rule | |||||||||
| Risk category | CT mandatory | CT recommended | CT mandatory | CT recommended | CT as emergency | CT urgently | |||
| Tested in study by | Smits et al. 200770 | cIbanez and Arikan 2004;60 Smits et al. 200770 | Madden et al. 199561 | Ono et al. 200763 | Smits et al. 200770 | Smits et al. 2007,70 2009;71 cIbanez and Arikan 200460 | Smits et al. 200770 | Smits et al. 2007;70 cIbanez and Arikan 200460 | Stein et al. 2009;71 Mower et al. 200562 |
| Eligibility criteriad | Mild TBI, GCS 13–15 | Acute head trauma | MHI | Minimal, mild and moderate head injury | Patients with head injury | Blunt head trauma | |||
| Mental status | GCS 13–15 | GCS 15p | GCS < 15 | JCS > 0 | GCS 9–13 | GCS 14–15n | GCS ≤ 12o | GCS < 15 with failure to improve within 4 hours (see below) | Altered level of alertness |
| Focal/neurological deficits | Present | p | Acute pupillary inequality | Present | Progressive signs | New signs that are not getting worse | Neurological deficit | ||
| Skull fracture | Clinical signs skull fracture (skull base or depressed) | p | Palpable depressed skull fracture, signs of basilar skull fracture | Radiographically demonstrated skull fracture or clinical signs of depressed or basal skull fracture | Radiological/clinical evidence of a fracture, whatever the level of consciousness | Evidence of significant skull fracture | |||
| LOC | < 30 minutesp | History of LOC or LOC > 5mins | Any | > 5 minutes | ≤ 5 minutes | o | |||
| Vomiting | Any | p | Vomiting or nausea | Nausea or vomiting | Persistent | ||||
| Age | < 2 yearsp or > 60 years | 60 years | ≥ 65 years | ||||||
| Amnesia | Continued PTA | PTA < 60 minutesp | Any | o | |||||
| Coagulopathy | Coagulation disorders | p | Therapeutic anticoagulation or haemophilia | Coagulopathy | |||||
| Seizures | Any | p | PTS | Any | |||||
| Visible injury | Trauma above clavicles | p | Facial injury, penetrating skull injury | o | Scalp haematoma | ||||
| Intoxication | Alcohol/drugs | p | |||||||
| Behaviour | Combativeness | Irritability/altered behaviour | Abnormal behaviour | ||||||
| Headache | Severe | p | Any | Severe or persistent | |||||
| Previous neurosurgery | Shunt-treated hydrocephalus | ||||||||
| Failure to improve | Failure to improve (from GCS < 15) within 4 hours of clinical observation | ||||||||
| Mechanism of injury | High-energy accidentq | p | o | ||||||
| Deterioration in mental status | Decreasing level of consciousness | Deteriorating level of consciousness | |||||||
| Other | Unclear or ambiguous accident history | p | Multiple injuries |
‘Other features’ are not fully enumerated |
|||||
Figures 6 and 7 show the sensitivities and specificities for any ICI and neurosurgical injury, respectively, for rules that have been evaluated in multiple cohorts. Figures 8 and 9 show the corresponding parameters for rules that have been evaluated in only one cohort.
FIGURE 6.
Decision rules for adults with MHI – sensitivity and specificity of decision rules for which more than one data set is available for the outcome ICI. NEXUS II, National Emergency X-Radiography Utilization Study II.
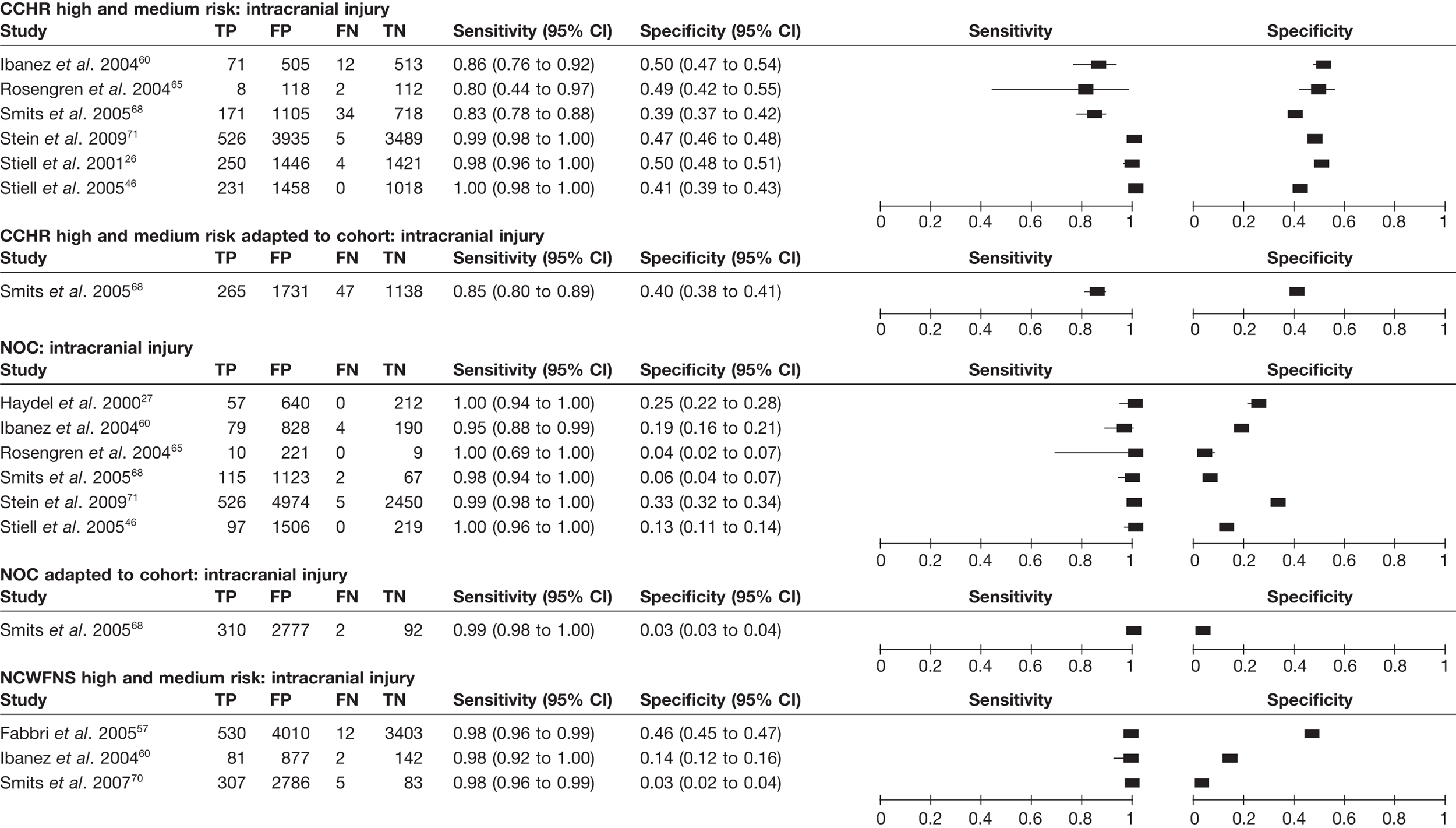
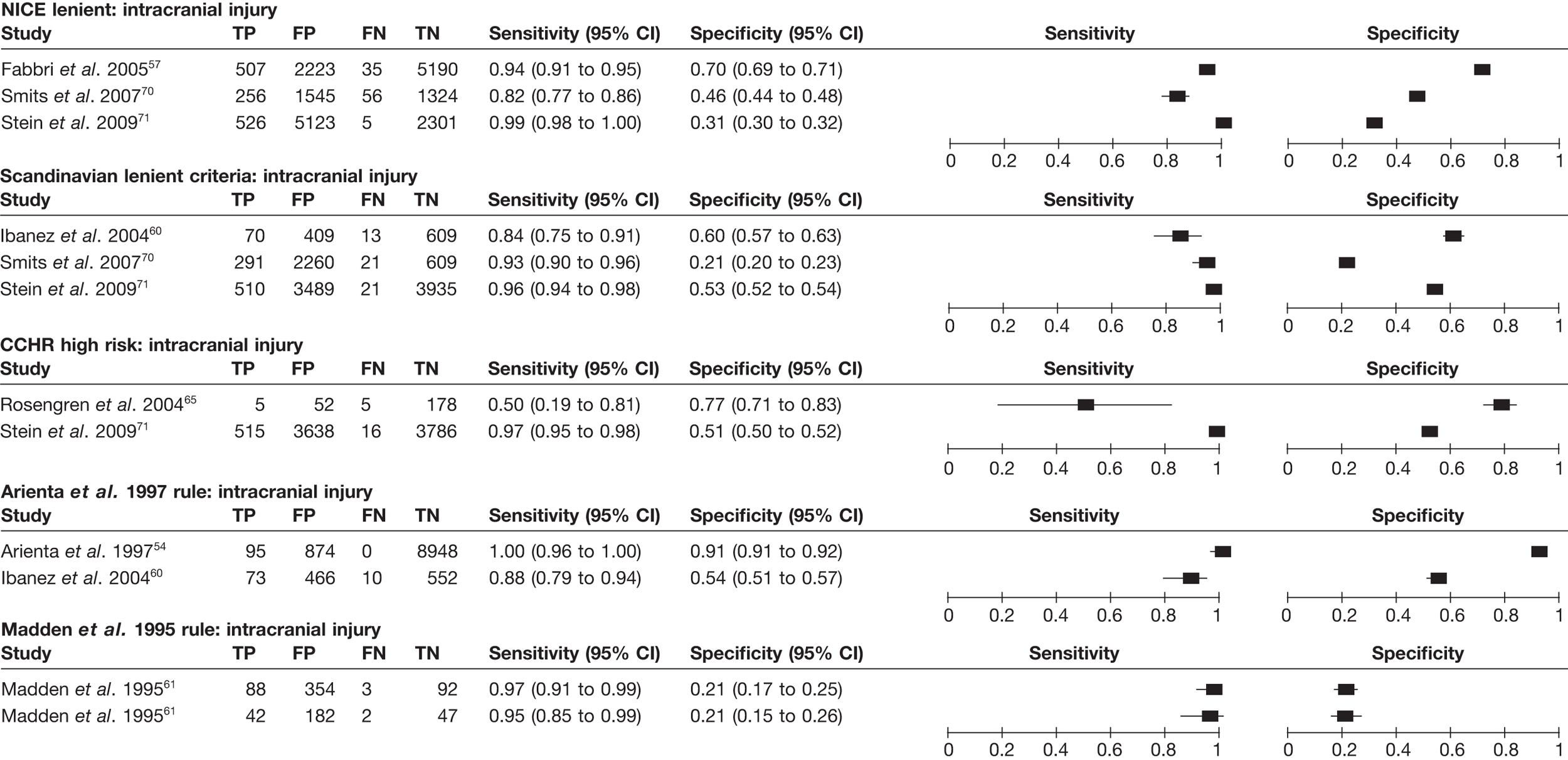
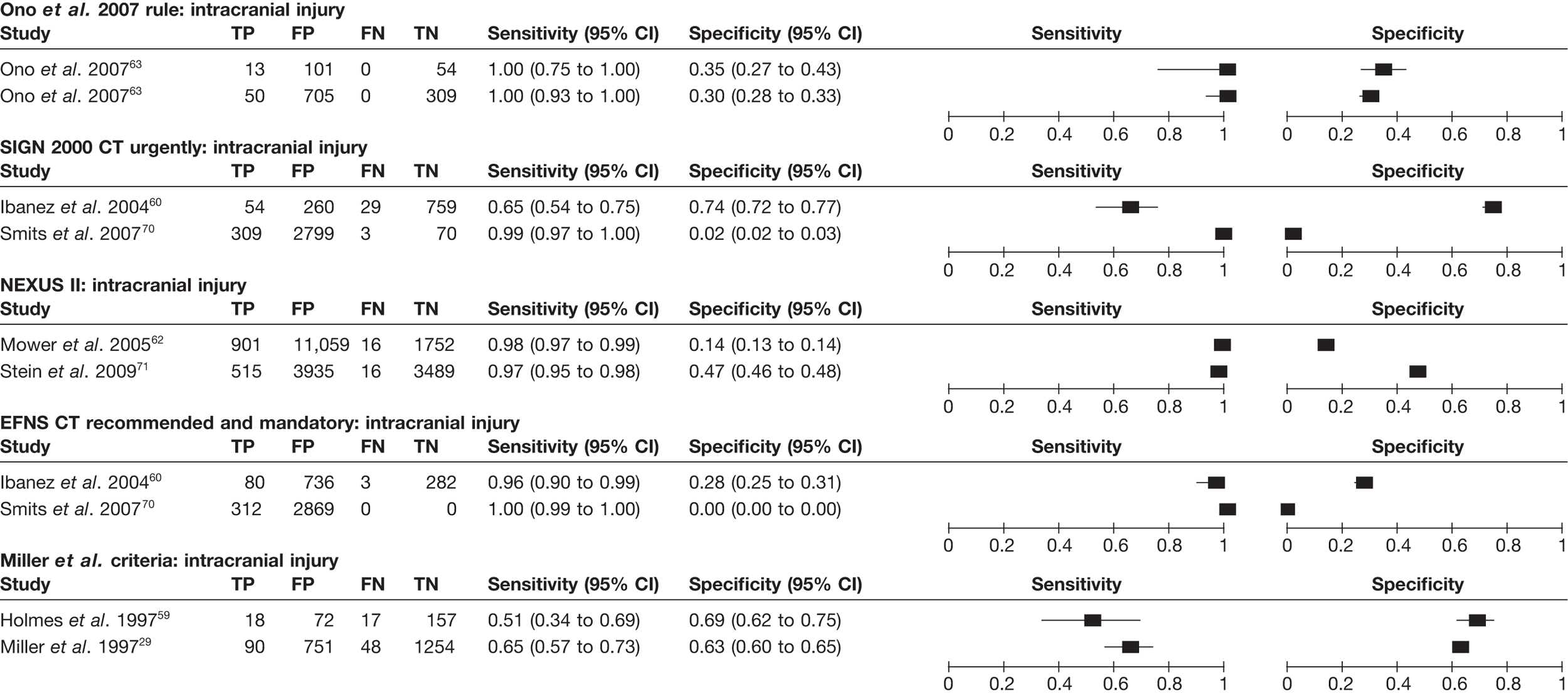
FIGURE 7.
Decision rules for adults with MHI – sensitivity and specificity of decision rules for which more than one data set is available for the outcome need for neurosurgery.
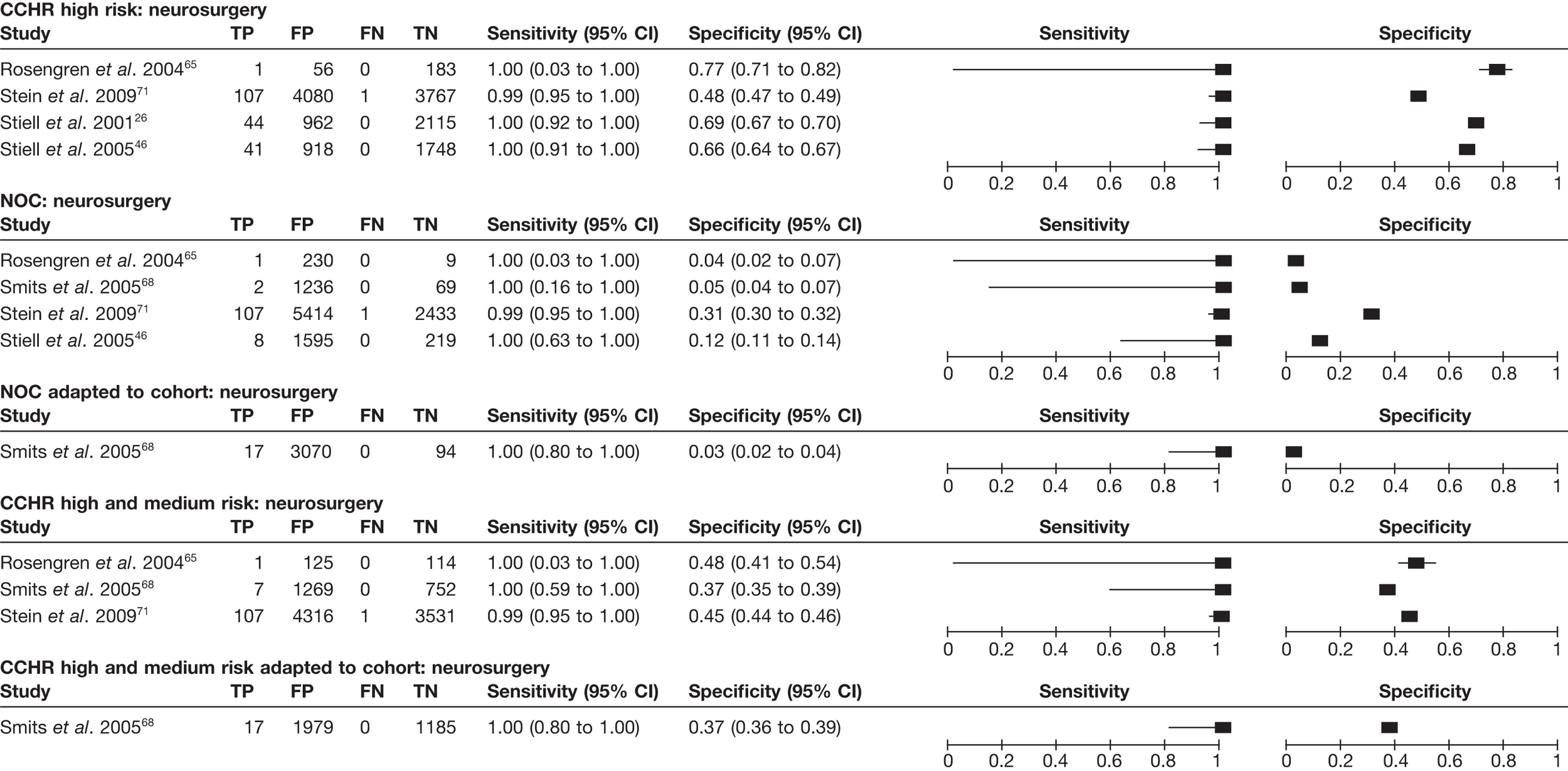
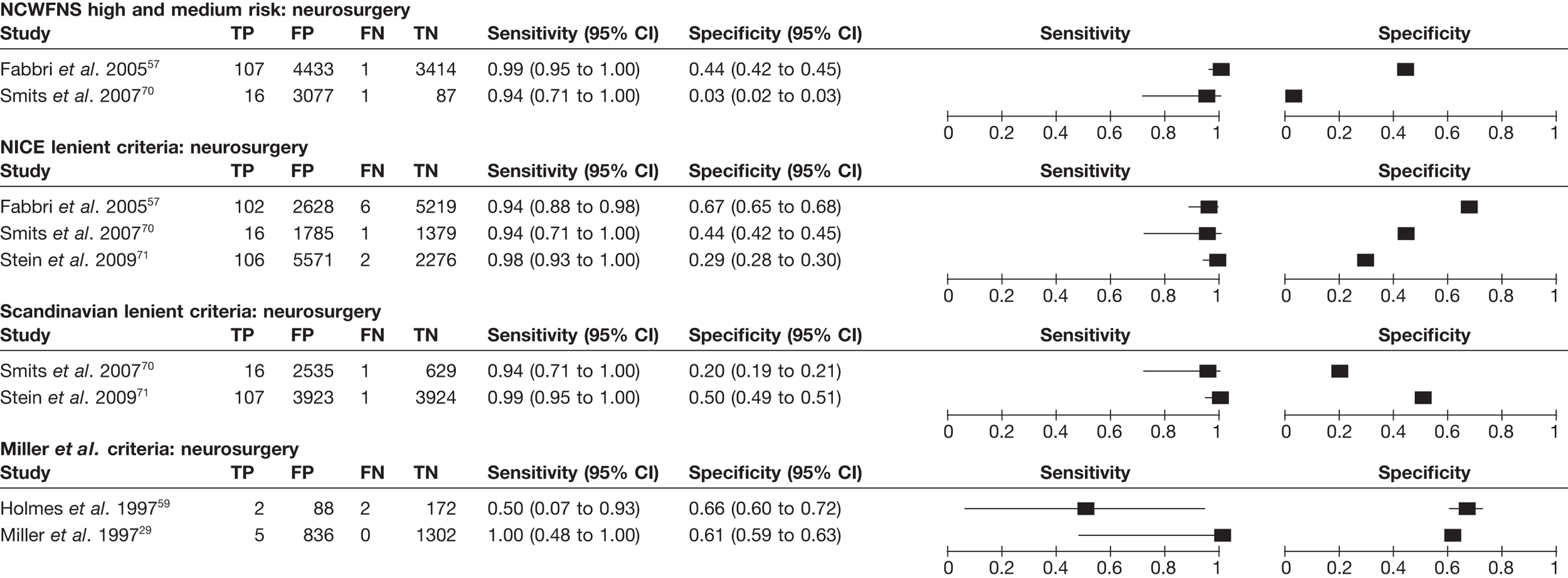
FIGURE 8.
Decision rules for adults with MHI – sensitivity and specificity of decision rules for which only one data set is available for the outcome ICI.
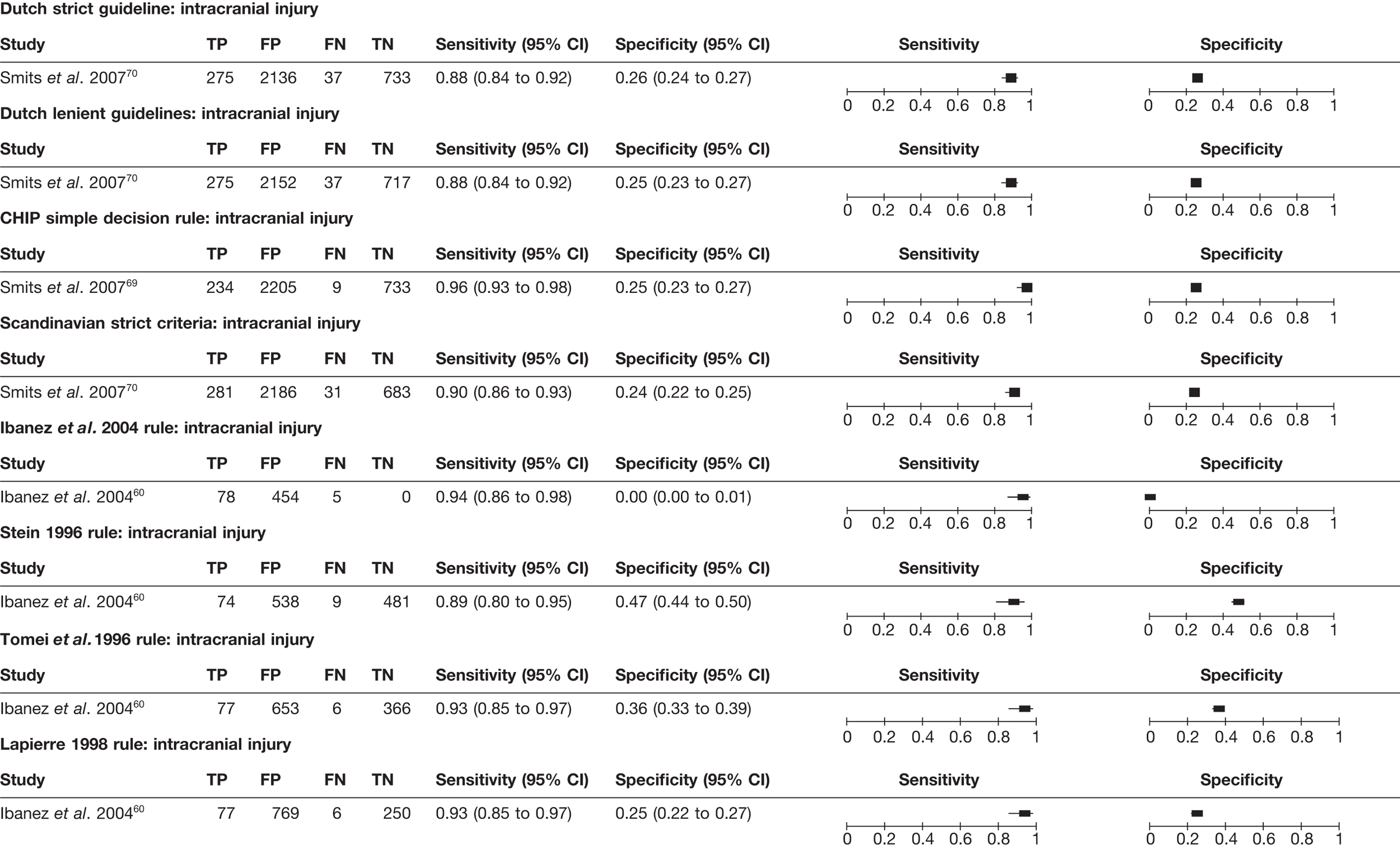
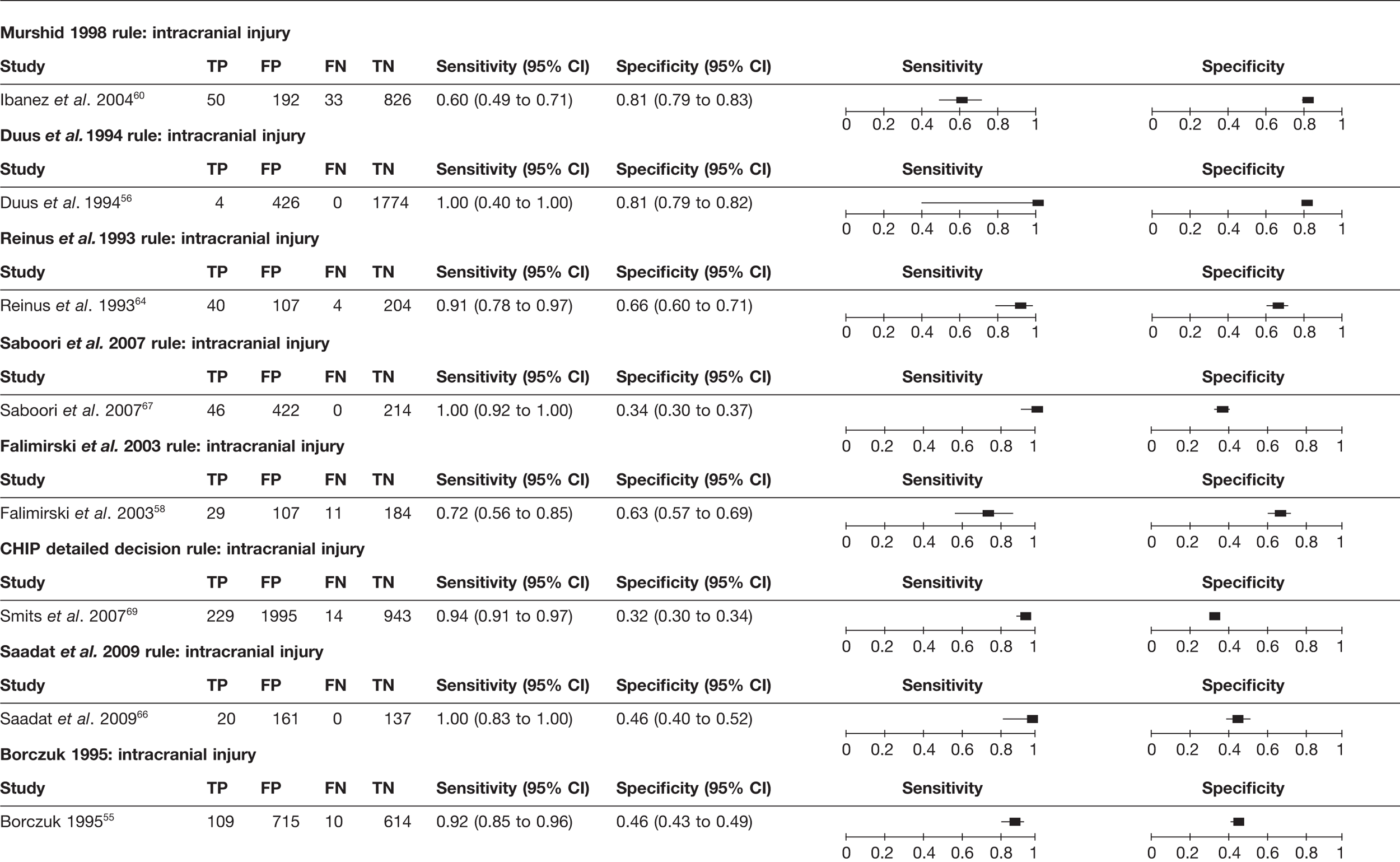
FIGURE 9.
Decision rules for adults with MHI – sensitivity and specificity of decision rules for which only one data set is available for the outcome need for neurosurgery. NEXUS II, National Emergency X-Radiography Utilization Study II.
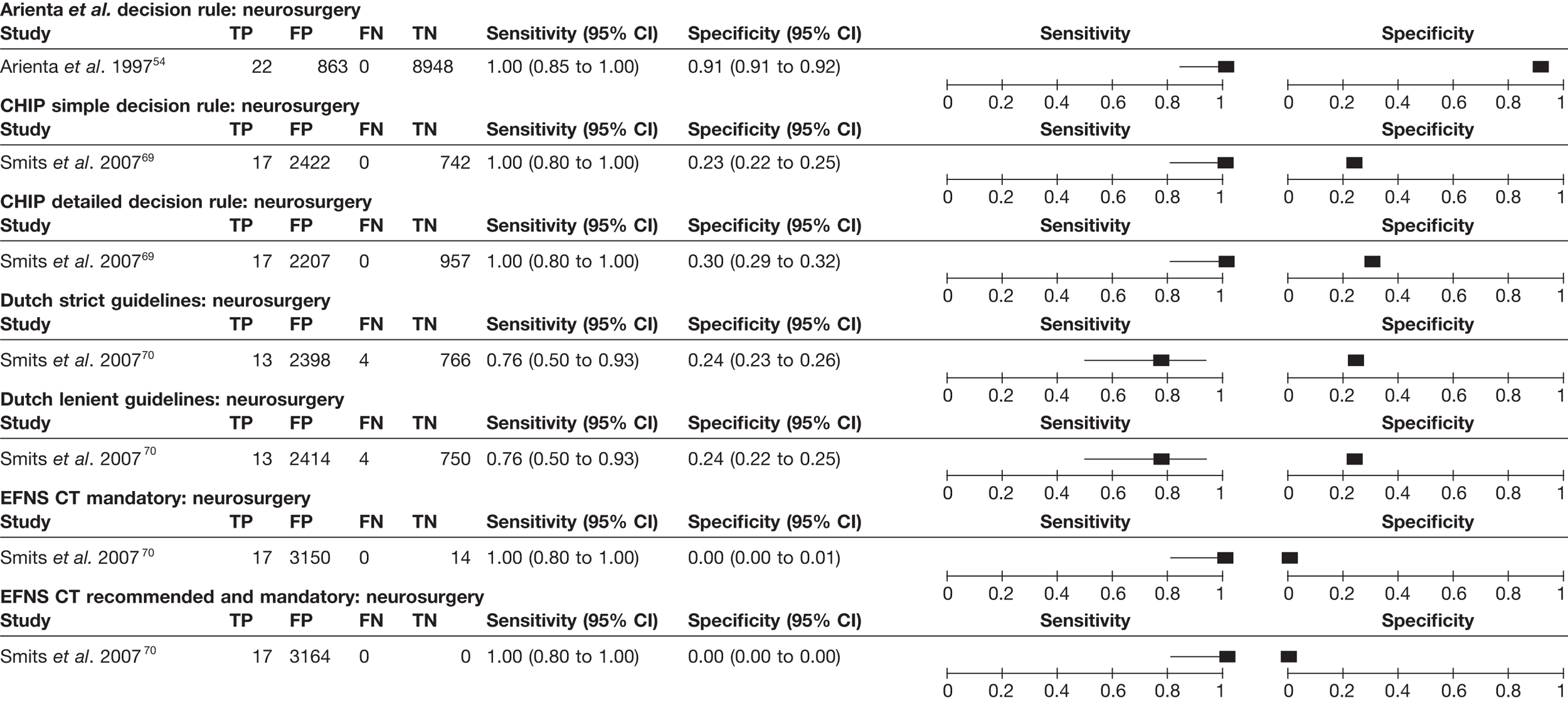
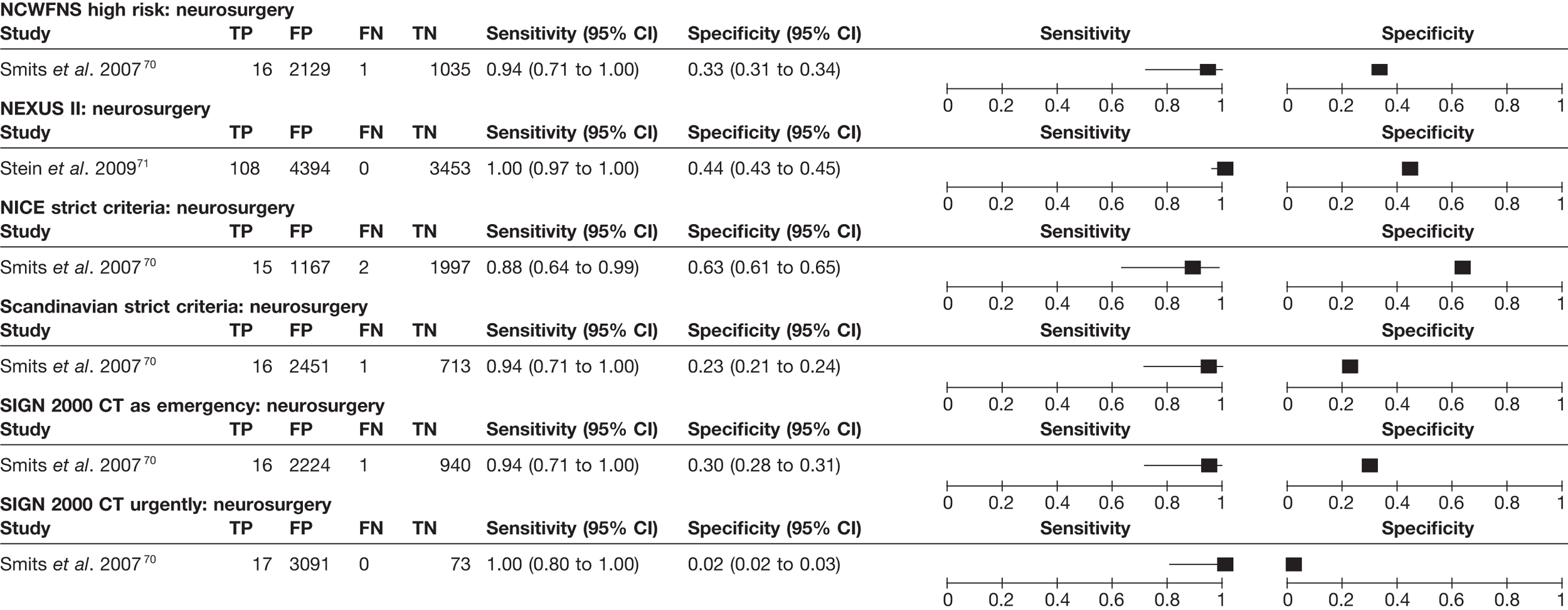
The CCHR26 has been validated in a number of studies26,46,60,65,68,71 and tested using either the high-risk criteria as a threshold or high- and medium-risk criteria. Using the high-risk criteria alone it has a sensitivity of 99–100% and a specificity of 48–77% for neurosurgical injury. 26,46,65,71 The high-risk criteria were derived to identify neurosurgical injury and were not tested to identify any intracranial injuries by the original researchers. Two other studies,65,71 however, used the high-risk rule to identify intracranial injuries. Results varied dramatically between the two studies, so no useful conclusions can be drawn.
Using the high- or medium-risk criteria, the CCHR has a sensitivity of 99–100%65,68,71 and 80–100%26,46,60,65,68,71 for neurosurgical and any ICI, respectively, and corresponding specificities of 37–48% and 39–50%, respectively. The variation in sensitivity for any ICI is probably due to variation in the reference standard: sensitivity was 98–100% in studies in which clinically low-risk patients received telephone follow-up rather than CT,26,46,71 but was 80–86% in studies in which all patients had CT. 60,65,68 This likely reflects differential identification of false-negative patients who were at low clinical risk and suffered no complication, but had ICI on CT.
Overall, it therefore appears that the CCHR has high sensitivity for detecting neurosurgical injuries, whether high-risk or high- and medium-risk criteria are used. This was consistent when some of the original patient exclusion criteria were included as risk factors (see Figure 6, CCHR high and medium risk adapted to cohort). 68 Sensitivity for any ICI is probably more modest, but the missed cases are unlikely to be clinically significant. Specificity is adequate to allow a meaningful proportion of patients to avoid CT scanning.
The NOC27 rule has been validated in several studies and shown to have excellent sensitivity for neurosurgical lesion (99–100%)46,65,68,71 and any intracranial lesion (95–100%). 27,46,60,65,68,71 However, specificity for neurosurgical lesions (3–31%) and any intracranial lesion (3–33%) was generally poor. In most cohorts, application of the NOC rule would have resulted in all patients having a CT scan.
The NICE guidelines1,19 were developed using the CCHR high- and medium-risk criteria. Sensitivity for neurosurgical injury and any injury varied from 88% to 98%57,70,71 and from 67% to 99%57,70,71 respectively, while corresponding specificities varied from 29% to 66% and from 31% to 70%, depending upon whether the 200319 or 20071 guidelines were tested and whether strict or lenient criteria were used. Amendment of the guidelines in 20071 entailed new recommendations for children and a change to management of patients over 65 years with LOC or amnesia. The revised NICE guidelines1 appeared to improve sensitivity at the cost of specificity, although the latter was still acceptable at 31%. The two versions of the rule were tested in the same cohort,57,71 which included adolescents over 10 years of age. It is possible that the improvement in performance of the rule is driven by the changes to the management of children rather than the relatively minor change in the management of adults.
Both the NCWFNS guidelines72 and the SIGN guidelines20 have sensitivities in a similar range to the CCHR when lenient criteria are used, but results for specificity are very variable and generally much lower. The Scandinavian lenient criteria73 have diagnostic parameters in the same range, but with more variation in sensitivity for neurosurgical injury (94–99%)69,74 and specificity for neurosurgical (20–50%) or any injury (21–60%). 60,69,74 The NEXUS II (National Emergency X-Radiography Utilization Study II) rule62 appears to have high sensitivity for both neurosurgical and any injury, but variable specificity and very limited validation. Other rules have not been validated in sufficient cohorts and settings to draw meaningful conclusions.
Children
From the 14 studies reporting diagnostic data for decision rules for children with MHI, a total of 15 decision rules30,81–94,96 were identified and are outlined in Table 8 a and b. Four studies presented more than one version of a rule: Greenes and Schutzman derived a decision rule85 for any severity of injury and a scoring system86 for asymptomatic patients from the same cohort; Kupperman et al. 90 reported a second rule for those aged < 2 years; the Canadian Assessment of Tomography for Childhood Injury (CATCH)92 rule had a high and a medium- and high-risk format; the University of California–Davis rule (UCD)93 had three versions, each designed to identify a different outcome (need for neurosurgery, brain injury and intervention or brain injury). Four of the rules or their versions were specifically for infants. 82,85,86,90
| Criteria | Decision rules | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Atabaki et al. 200881 | Buchanich 200782 | Da Dalt et al. 200683 | Dietrich et al. 199384 | CHALICE30 | CATCH92 | Greenes and Schutzman | Guzel et al. 200987 | Klemetti et al. 200989 | |||
| Medium risk | High risk | 199985 | 200186 | ||||||||
| Version of rule | Medium-risk factors | High-risk factors | Decision rule | Scoring system | |||||||
| Reported in | Atabaki et al. 200881 | Buchanich 200782 | Da Dalt et al. 200683 | Dietrich et al. 199384 | Dunning et al. 200630 | Osmond et al. 200692 | Osmond et al. 200692 | Greenes and Schutzman 199985 | Greenes and Schutzman 200186 | Guzel et al. 200987 | Klemetti et al. 200989 |
| Eligibility criteriaa | < 21 years, all severity | < 3 years, GCS 14–15 | < 16 years, all severity, some exclusions | ≥ 2 years to 20 years, all severity, some exclusions | < 16 years, all severity | ≤ 16 years, GCS 13–15, with clinical characteristics | ≤ 16 years, GCS 13–15, with clinical characteristics | < 2 years, all severity | Asymptomatic < 2 years | < 16 years, GCS 13–15 | ≤ 16, all severity |
| Mental status | GCS < 15 | Abnormal GCS | GCS < 15 | Abnormal, GCS < 14 or GCS < 15 if < 1-year-old | Depressed | Abnormal | |||||
| Focal/neurological deficits | Sensory deficit | Abnormal neurological examination | Focal neurological deficits | Abnormal vital signs indicating possible increased intracranial pressure or focal neurological findings | Neurological deficit | ||||||
| Skull fracture | Defect or signs of basilar skull fracture | Clinical signs in risk area, skull base fracture | Clinical signs of skull fracture | Signs of basal skull fractureb | Suspected open skull fracture | Clinical signs of skull fracture | |||||
| LOC | Prolonged | LOC | LOC | LOC | LOC | LOC | |||||
| Vomiting | Vomiting | Vomiting | Vomiting | Two or more | Vomiting | Vomiting | |||||
| Age | < 2 years | Risk factorc | |||||||||
| Amnesia | Persistent | For the event | Amnesia | PTA | |||||||
| Coagulopathy | |||||||||||
| Seizures | Seizures | Seizures | Seizures | Seizures | |||||||
| Visible injury | Scalp lacerations | Scalp trauma | Large boggy scalp haematoma | Scalp haematoma location and sizec | Scalp trauma | ||||||
| Behaviour | Inconsolable | Persistent drowsiness | b | Irritability on examination | Lethargy or irritability | ||||||
| Headache | Persistent | Headache | b | Worsening headache | Headache | ||||||
| Previous neurosurgery | |||||||||||
| Failure to improve | b | Failure to reach GCS 15 in 2 hours | |||||||||
| Mechanism of injury | Bicycle-related injury | High speed road traffic, or high speed or fall > 3 m | Dangerous | ||||||||
| Deterioration in mental status | Mental status change | ||||||||||
| Other | Dizziness | Vision changes, gender, area of residence | Suspicion of non-accidental injury | Bulging fontanelle | Blurred vision | Vertigo | |||||
| Criteria | Decision rules | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| NEXUS II91 | NOC88 | PECARN90 | Quayle et al. 199794 | aRCS guidelines96 | UCD93 | ||||
| (≥ 2 years to < 18 years) | (< 2 years) | Neurosurgery | Intervention or brain injury | TBI | |||||
| Version of rule | ≥ 2 years to < 18 years90 | < 2 years90 | Neurosurgery93 | Intervention or brain injury93 | TBI93 | ||||
| Reported in | Klemetti et al. 2009;89 Oman 200691 | Haydel and Schembekar 200388 | Kupperman et al. 200990 | Kupperman et al. 200990 | Quayle et al. 199794 | Dunning et al. 200630 | Palchak et al. 2003;93 Klemetti et al. 200989 | Palchak et al. 2003;93 Sun et al. 200795 | Palchak et al. 200393 |
| Eligibility criteriab | All ages, blunt head trauma | 5–17 years, GCS 15 with clinical characteristics, some exclusion | ≥ 2 years to < 18 years, GCS 14–15, some exclusions (e.g. trivial injury) | < 2 years, GCS 14–15, some exclusions (e.g. trivial injury) | < 18 years, non-trivial injury (with clinical characteristics) | All severities and ages,a with additional protocol for children | < 18 years, non-trivial head injury, with clinical characteristic, some exclusions | < 18 years, not trivial head injury, with clinical characteristic, some exclusions | < 18 years, GCS 14–15, non-trivial, with clinical characteristic, some exclusions |
| Mental status | Altered level of alertness | Altered | Altered | Altered | Abnormalc | Abnormalc | Abnormalc | ||
| Focal/neurological deficits | Neurological deficit | Focal neurological deficit | Focal neurological deficit | ||||||
| Skull fracture | Evidence of significant skull fracture | Clinically suspected skull fracture | Clinical signs of basilar skull fracture | Palpable or unclear | Signs of basilar skull fracture | Clinical signs of skull fracture | Clinical signs of skull fracture | ||
| LOC | LOC | LOC | LOCd | ||||||
| Vomiting | Persistent | Vomiting | Vomiting | Persistentd | Vomiting | Vomitinge | Vomiting | ||
| Age | N/A to children (≥ 65 years) | ||||||||
| Amnesia | Amnesiad | ||||||||
| Coagulopathy | Coagulopathy | ||||||||
| Seizures | PTS | ||||||||
| Visible injury | Scalp haematoma | Trauma above the claviclesf | Scalp haematoma |
Scalp laceration, bruise or swellingd Significant maxillofacial injuriesd |
Scalp haematoma in a child ≤ 2 years | Scalp haematoma in a child ≤ 2 years | |||
| Intoxication | Drug or alcohol | ||||||||
| Behaviour | Abnormal behaviour | Acting abnormally according to parent | |||||||
| Headache | Headache | Severe | Persistentd | Headachee | |||||
| Previous neurosurgery | |||||||||
| Failure to improve | |||||||||
| Mechanism of injury | Severeg | Severeh |
Violentd |
||||||
| Deterioration in mental status | |||||||||
| Other | Short-term memory deficitsj |
Tense fontanellei Suspected non-accidental injuryi |
|||||||
Of studies reporting prediction of ICI, only four rules30,90,91,93 were tested in more than one cohort (Figure 10). Of these four rules, the UCD rule93 for identifying patients with TBI or who needed acute intervention (which equates to ‘any ICI’) had the highest sensitivity (99% and 100%)89,93 with variable values for specificity (12% and 43%). A modified version of the UCD rule reported in Sun et al. ,95 in which ‘headache’ and ‘vomiting’ were redefined as ‘severe headache’ and ‘severe vomiting’, produced lower sensitivity (91%) but similar specificity (43%).
FIGURE 10.
Decision rules for children with MHI – sensitivity and specificity of decision rules for which more than one data set is available for the outcome ICI. a, Sun et al. 95 give a stricter definition of headache and vomiting than the original rule; b, derivation and validation cohorts reported in the same article.
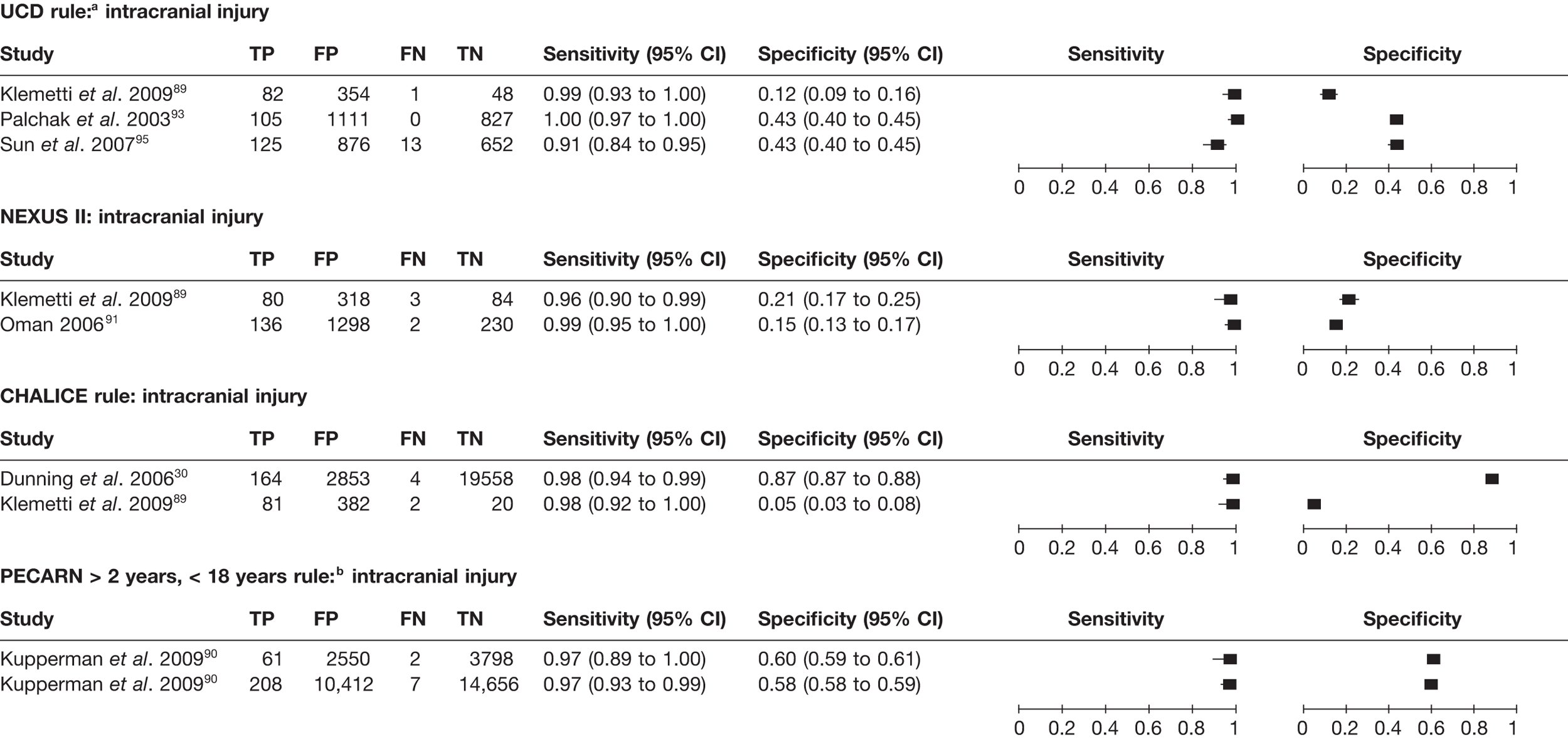
The CHALICE rule30 had the next best sensitivity (98% and 98%), but very variable specificity (87% and 5%). The derivation cohort30 used a poor reference standard (3% given CT) and the other cohort89 had different patient inclusion criteria (selecting only those admitted), both of which may contribute to the difference in specificity.
The Paediatric Emergency Care Applied Research Network (PECARN) rule for children ≥ 2 years to < 18 years was tested in two cohorts, a derivation and a validation cohort, reported in the same paper. 90 Sensitivity (97% and 97%) and specificity (58% and 60%) were very consistent. The rule appears to sacrifice a small degree of sensitivity for a higher specificity when compared with other rules.
The NEXUS II rule was tested in two studies. 89,91 These reported similar sensitivity (96% and 99%) and specificity (15% and 21%), despite differences in the adequacy of the reference standard in one study, and differences in cohort selection and outcome definitions. Although these results seem less promising than the rules discussed earlier, further validation work in a different setting is warranted before conclusions can be drawn.
Nine further rules81,83,84,87–89,92,94,96 were tested in only one cohort (Figure 11) against the outcome of ICI. Of these, one rule (that of Da Dalt et al. 83) had excellent sensitivity (100%) and specificity (87%). Further validation studies are needed before conclusions can be drawn regarding this rule. The Royal College of Surgeons (RCS) guidelines96 appeared to have excellent diagnostic accuracy. 30 However, the reference standard used was management according to the RCS guidelines with only some patients followed up. This is likely to significantly increase the estimates of sensitivity and specificity.
FIGURE 11.
Decision rules for children with MHI – sensitivity and specificity of decision rules for which only one data set is available for the outcome ICI.
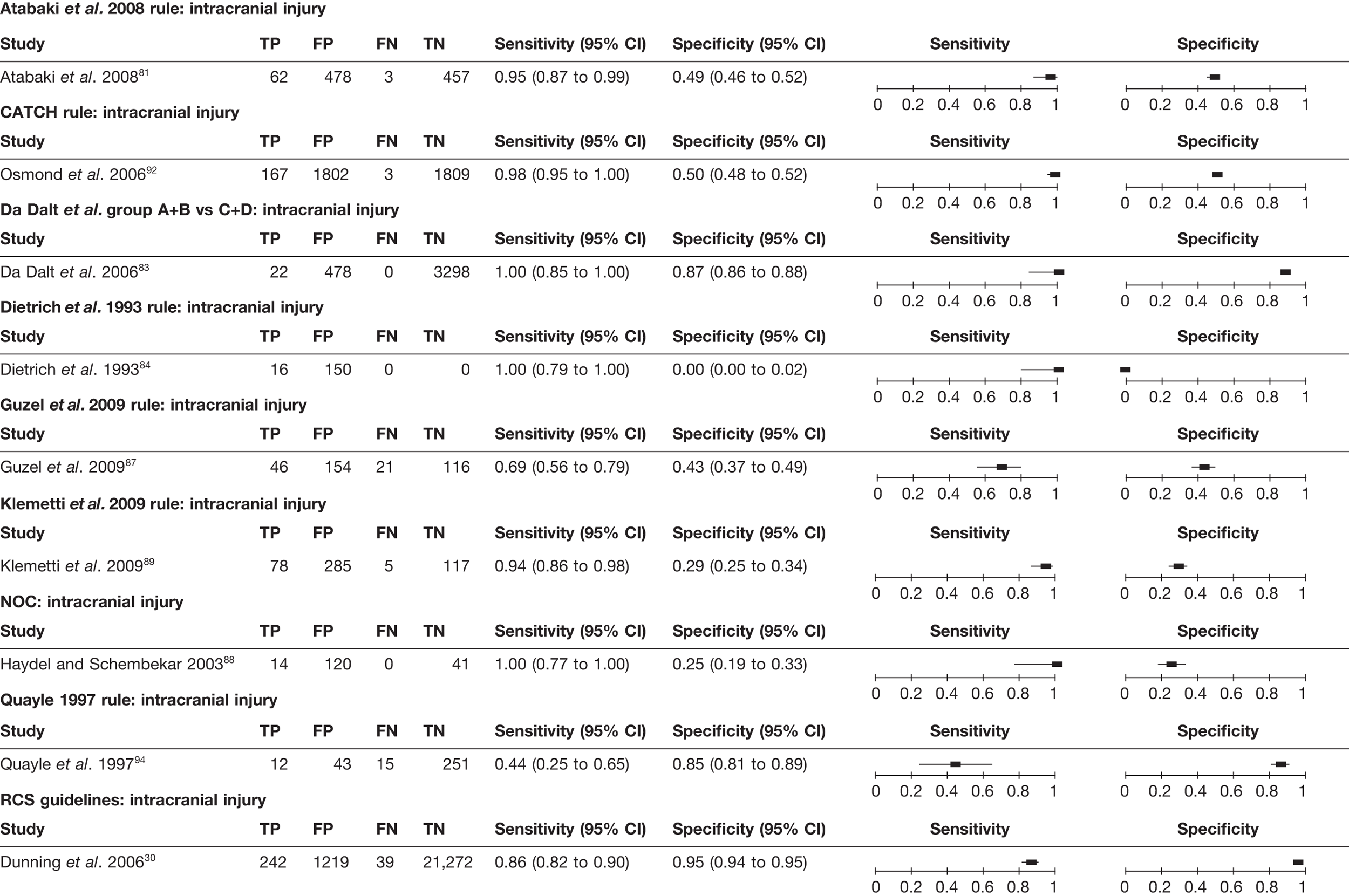
Six rules30,8188,90,92,93 were tested for prediction of the need for neurosurgery (Figure 12) and all in only one cohort. All had very good sensitivity (98–100%), but variable specificity (24–86%). The CHALICE rule30 had the highest specificity, but the lowest sensitivity. As observed with the PECARN criteria90 for children ≥ 2 years, the CHALICE rule30 appeared to sacrifice a degree of sensitivity for an improved specificity. All of these rules need further investigation and validation testing in other settings before firm conclusions can be drawn.
FIGURE 12.
Decision rules for children with MHI – sensitivity and specificity for the outcome neurosurgery.
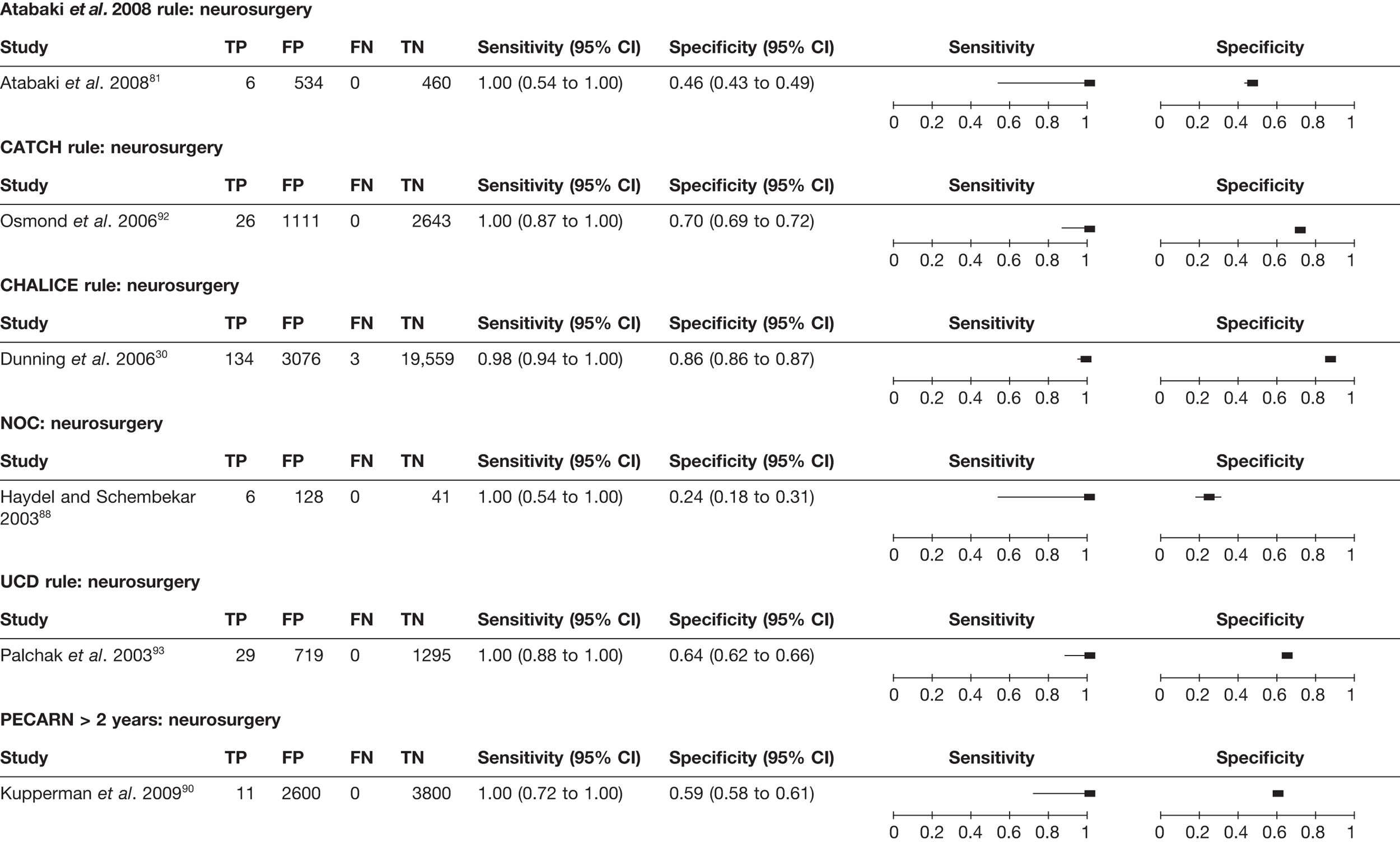
For infants (Figure 13), only the PECARN rule was tested in two cohorts against the outcome ICI. 90 This rule gave the most promising results out of the seven rules identified for ICI. 82,84–86,90,91,93,95 Only the PECARN90 rule (Figure 14) was tested against the outcome of need for neurosurgery in infants. All of these rules require further investigation and validation testing in other settings before firm conclusions can be drawn.
FIGURE 13.
Decision rules for infants with MHI – sensitivity and specificity for the outcome ICI. a, derivation and validation cohorts reported in the same article; b, Sun et al. 95 give a stricter definition of headache and vomiting than the original rule.
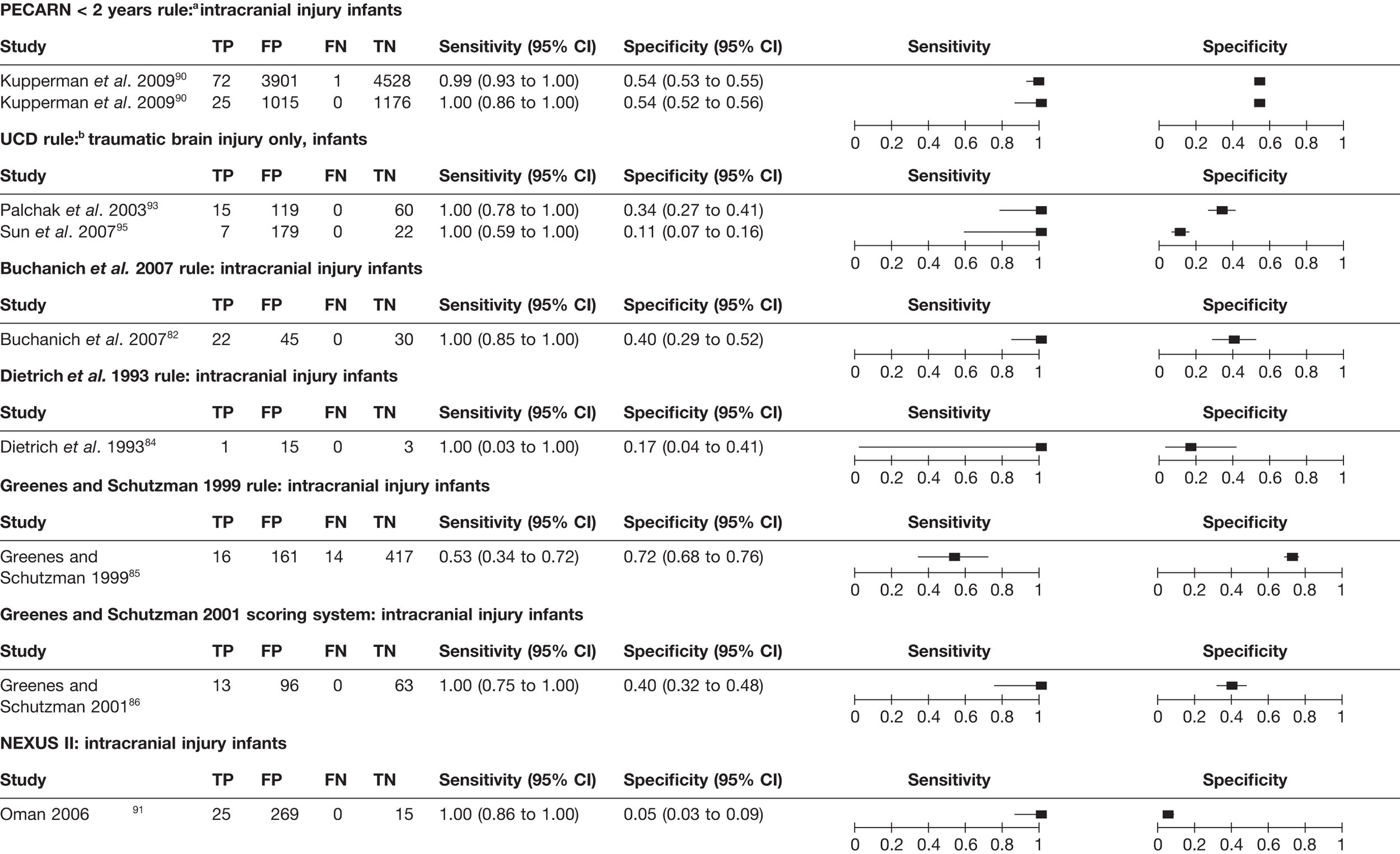
FIGURE 14.
Decision rules for infants with MHI – sensitivity and specificity for the outcome neurosurgery.
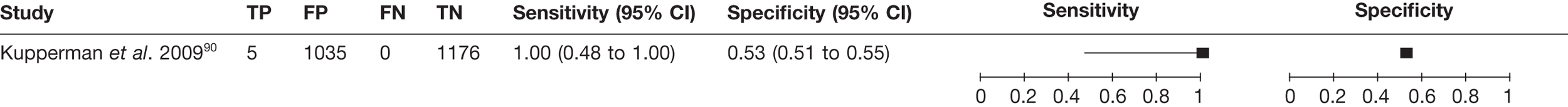
Individual characteristics
Description of included studies
Adults
The design and patient characteristics of the 42 studies (representing 44 papers)26,27,29,46,54,55,57–63,67,77,98–126 that evaluated the diagnostic accuracy of individual characteristics for identifying ICI or need for neurosurgery in adults with MHI are summarised in Table 9. Twenty-three studies were from the USA,27,29,55,58,59,61,62,100–102,104,107–112,116,118–123,126 two each from Italy,54,57 Germany,98,115 Spain,60,103 Japan,63,106 Canada,26,46 and India,120,124 and one from each of Saudi Arabia,77,114 Malaysia,99 Hong Kong,105 Islamic Republic of Iran,67 Denmark117 and Taiwan. 125 One further study was an international collaboration. 113 Ten studies were multicentre. 26,46,67,98,106,108,62,113,118,119 Of the 42 studies, 22 were prospective; 16 recruited consecutive patients,26,27,29,57–60,62,67,98,100,101,105,108,111,115,124 whereas two selected a convenience sample46,126 and four did not report the method of selection. 61,109,113,118 Sixteen studies were retrospective54,55,67,102–106,110,112,114,116,117,119,121–123,125 and four63,107,120,127 did not report the mode of data collection.
| Author, year | Country | Design | No. of patients, n | Mean or median age, years (range) | Prevalence of neurosurgery | Prevalence of ICI | CT as inclusion? (yes/no) | Male, n | Patients with MHI, n | Age group | Prevalence of GCS 15, n | Other significant inclusion criteria | Other significant exclusion criteria |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adults (any cohort selecting patients above a given age) | |||||||||||||
| Arienta et al. 199754 | Italy | R | 10,000 | Mean NR (6 to 95) | 154/10,000 (1.54%) | No | 54% | 9917/10,000 (99%) | Adults | 9833/10,000 (98.3%) | ≥ 6 years of age. Presenting to the ED directly | Children < 6 years of age | |
| 9917 (subset of above) | 24/9917 (0.2%) | 85/9917 (0.86%) | No | NR for this subset | 991/991 (100%) | Adults | 9833/9917 (99%) | Subset of above, GCS 13–15 (applied at data extraction stage) | Subset of above, patients in a coma excluded at data extraction stage | ||||
| Biberthaler et al. 200698 | Germany | P, Csa | 1309 | Median: 47 (IQR 32 to 65) | 93/1309 (7.1%) | No | 855/1309 (65%) | 1309/1309 (100%) | Adults | 1152/1309 (88%) | ≥ 18 years. Isolated head trauma, admitted within 3 hours, GCS 13–15 at admission, one or more of: brief LOC, PTA, nausea, vomiting, severe headache, dizziness, vertigo, intoxication, anticoagulation and age > 60 years | Pregnant women, prisoners and multiple-injured patients | |
| Borczuk 199555 | USA | R | 1448 | Mean NR (16 to 99) | 119/1448; (8.2%) | Yes | 999/1448 (69%) | 1448/1448 (100%) | Adults | 1211/1448 (83.6%) | ≥ 17 years of age. GCS 13 or more, blunt head trauma, had CT scan | ≤ 16 years, patients with penetrating cranial trauma | |
| Chan et al. 200599 | Malaysia | NR | 105 | Whole cohort mean: 30.4 (12 to 81) | 82/105 (78.1%) | Yes (applied at data extraction stage) | 78/105 (74.3%) | 105/105 (100%) | Adults | 37/105 (35.2%) | > 12 years. Malaysian ID cards, GCS 13–15, haemodynamically stable, with CT scan | NR | |
| 92 (subset of above) | As above | 71/92 (77.2%) | Yes (applied at data extraction stage) | NR | NR | Adults | NR | Subset of above who also underwent radiography | |||||
| Cook et al. 1994100 | USA | P, Cs | 107 | Mean NR (16 to NR) | 9/107 (8.4%) | No | NR | NR | Adults | NR | > 16 years. Evidence of alcohol intoxication (confirmed by blood test), presumed MHI, GCS ≥ 13 or < 13 with ethanol levels ≥ 200 mg/dl) | Penetrating head trauma | |
| Fabbri et al. 200557 | Italy | P, Csb | 7955 | Median: 44 (IQR 27 to 71) | 108/7955 (1.4%, reported as 1.3%) | 542/7955 (6.8%) | No | 4415/7955 (55.5%)b | 7955/7955 (100%) | Adults | 7426/7955 (93.4%) | ≥ 10 years. Acute MHI within 24 hours of injury | Unclear history, unstable vital signs, GCS < 14, penetrating injuries, voluntary discharge, re-attendances |
| Falimirski et al. 200358 | USA | P, Cs | 331 | Mean: 39.21 (16 to 95) | 40/331 (12.1%) | No | 214/331 (65%) | 331/331 (100%) | Adults | 302/331 (91.2%) | ≥ 16 years of age. Blunt injury, witnessed LOC or amnesia, GCS 14–15 | GCS 13, or transferred with a CT scan | |
| Feuerman et al. 1988102 | USA | R | 373 | Mean NR (18 to 80) | 8/373 (2%) | No | 303/373 (81%) | 373/373 (100%) | Adults | 236/373 (63%) | ≥ 16 years. Admitted for MHI, presenting to the ED within 24 hours of injury | NR | |
| 129 (subset of above) | NR for this subgroup | 8/129 (6.2%) | 53/129 (41.1%) | Yes (applied at data extraction stage) | NR for this subgroup | 129/129 (100%) | Adults | 59/129 (45.7%) | As above, with CT scan (applied at data extraction stage) | NR | |||
| Gomez et al. 1996103 | Spain | R | 2484 | Mean: 39.8 (NR) | 30/2484 (1.2%) | No | NR | 2484/2484 (100%) | Adults | 2351/2484 (94.6%) | > 15 years. Patients over 15 years classified as suffering a MHI with or without signs of brain dysfunction | Isolated facial trauma, deterioration to GCS < 13 within 4 hours of injury, those showing a lucid interval who were referred from local hospitals after they developed neurological deterioration | |
| Haydel et al. 200027 | USA | P, Cs | 520 | Mean: 36 (3 to 97) | 36/520 (6.9%) | No | 338/520 (65%) | 520/520 (100%) | Adults | 520/520 (100%) | > 3 years old. GCS 15, LOC/amnesia, normal by brief neurological examination, injury within last 24 hours | Declined CT, concurrent injuries that preclude CT | |
| Hsiang et al. 1997105 | Hong Kong | P, Cs | 1360 | Mean NR (11 to 92) | 42/1360 (3.1%) | 293/1360 (21.5%) | No | 983/1360 (72.3%) | 1360/1360 (100%) | Adults | 1177/1360 (86.5%) | ≥ 11 years, admitted to hospital with MHI (GCS 13–15 with or without LOC) | Patients treated in emergency room, but not admitted and patients < 11 years of age |
| 736 | NR for this subgroup | 162/736 (22%) | NR | NR for this subgroup | 736/736 (100%) | Adults | 635/736 (86.3%) | Subset of above; those with data on vomiting available | As above | ||||
| Ibanez and Arikan 200460 | Spain | P, Cs | 1101 | Mean: 46.7 (15 to 99) | 83/1101 (7.5%) | No | 573/1101 (52%) | 1101/1101 (100%) | Adults | 978 (88.8%) | > 14 years. MHI (GCS 14 or 15) with or without LOC | Referrals from other hospitals | |
| Jeret et al. 1993107 | USA | NR | 712 | Mean: 35.6 (18 to 90) | 67/712 (9.4%) | No | 520/712 (73%) | 712/712 (100%) | Adults | 712/712 (100%) | ≥ 18 years. GCS 15 as determined by consultant, blunt head trauma, those with LOC or amnesia | Patients transferred from other hospitals, < 18 years of age, no amnesia or LOC, penetrating cranial trauma or presenting more that 24 hours after the event. Those who refused CT | |
| Livingston et al. 1991109 | USA | P, NR | 60 | Mean: 29 (16 to 70) | 11/60 (18.3%) | No | 49/60 (81.7%) | 60/60 (100%) | Adults | 38/60 (63.3%) | > 16 years.a All patients with MHI (transient LOC or significant post-traumatic amnesia GCS 14 or 15, normal neurological examination) | GCS < 14, signs of basilar skull fracture, admitted for other injuries | |
| 111(separate cohort) | Mean NR (17 to 79) | 15/111 (13.5%) | No | 89/111 (80%) | 111/111 (100%) | Adults | 91/111 (82.0%) | As above | As above | ||||
| Livingston et al. 2000108 | USA | P, Cs | 2152 | Mean: 35.8 | 336/2152 (15.6%) | No | 1490/2152 (69.2%) | 2152/2152 (100%) | Adults | NR | ≥ 16 years. All patients with MHI (transient LOC or post-traumatic amnesia, ED recorded GCS 14 or 15) | Discharged < 20 hours, CT data missing, CT scan > 12 hours after injury, died < 20 hours after injury | |
| Muller et al. 2007113 | Multinational (Norway, UK, Switzerland and Sweden) | P, NR | 226 | Mean: 39 (18 to 92) | 21/226 (9%) | Yes | 168/226 (74.3%) | 226/226 (100%) | Adults | 180/226 (79.6%) | ≥ 18 years. Head injury, LOC or retrograde amnesia, GCS 13–15, blood sample and CT scan within 12 hours of trauma | Neurological or psychiatric disorder, focal neurological deficit, multiple injuries requiring immediate intervention, renal or liver disease | |
| Nelson et al. 1992116 | USA | Ra | 131 | Mean NR (16 to NR) | 20/131 (15.3%) | Yes | NR | NR | Adults | NR | ≥ 15 years. NR; however, major indicators for CT scanning include LOC, abnormal neurological examination, physical or historic evidence of head trauma | NR | |
| Ono et al. 200763 | Japan | NR | 1064 | Mean: 46 (10 to 104) | 50/1064 (4.7%) | No | 621/1064 (58.4%) | 1064/1064 (100%) | Adults | 912/1064 (85.7%) | ≥ 10 years. With head injury, within 6 hours of injury, GCS ≥ 14 | Extremely trivial injury (scalp or facial wounds), those who refused examination | |
| Saboori et al. 200767 | Islamic Republic of Iran | P, Cs | 682 | Mean: 29 (6 to 85) | 46/682 (6.7%) | No | 534/682 (78.3%) | 682/682 (100%) | Adults | 682/682 (100%) | ≥ 6 years of age, GCS 15 | > 24 hours post injury, no clear history of trauma, obvious penetrating skull injury or obvious depressed fracture | |
| Stiell et al. 200126 | Canada | P, Cs | 3121 | Mean: 38.7 (16 to 99) | 254/3121 (8.14%) | No | 2135/3121 (68.4%) | 3121/3121 (100%) | Adults | 2489/3121 (79.8%) | ≥ 16 years. Witnessed LOC or amnesia or disorientation and GCS ≥ 13 and injury in last 24 hours | < 16 years. Minimal injury, no history of trauma as primary event, penetrating injury, obvious depressed skull fracture, focal neurological deficit, unstable vital signs, seizure, bleeding disorder/anticoagulants, reassessment of previous injury, pregnant | |
| Stiell et al. 200546 | Canada | P, Cv | 2707 | Mean: 38.4 (16 to 99) | 41/2707 (1.5%) | 231/2707 (8.5%) | No | 1884/2707 (69.6%) | 2707/2707 (100%) | Adults | 2049/2707 (75.7%) | As per Stiell et al. 200126 | As per Stiell et al. 200126 |
| 1822 (subset of above) | Mean: 37.7 (16 to 99) | 8/1822 (0.4%) | 97/1822 (5.3%) | No | 1246/1822 (68.4%) | Adults | 1822/1822 (100%) | Subset (GCS 15) | |||||
| Vilke et al. 2000126 | USA | P, Cva | 58 | 37.4 (17 to 77) | 1/58 (1.7%) | 3/58 (5.2%) | Yes | 42/58 (72%) | 58/58 (100%) | Adults | 58/58 (100%) | > 14 years. Any patients 14 years or older who is getting a head CT for non-penetrating head trauma | No LOC or amnesia for the event, pregnancy, clinical intoxication, other significant trauma with competing pain or GCS score ≤ 14 |
| Dunham et al. 1996101 | USA | P, Cs | 2032 | Mean NR (14 to 60) | 128/2032 (6.3%) | No | NR | 2032/2032 (100%) | Adults, excluding older adults | 1481/2032 (72.9%) | 14–60 years. Mild cognitive impairment, transported to ED by Maryland emergency services. GCS 15 with amnesia, and/or witnessed LOC or GCS 14/13 with or without LOC or amnesia | Transferred from another hospital. Those > 60 years | |
| P, Cs | 220 | Mean: 72.5 | 35/220 (15.9%) | NR | NR | 220/220 (100%) | Adults, older | 150/220 (68.2%) | > 60 years, as above | As above | |||
| Mack et al. 2003110 | USA | R | 133 | Mean: 80.4 (65 to NR) | 19/133 (14.3%) | Yes | 45/133 (33.8%) | 133/133 (100%) | Adults, older | 113/133 (85%) | ≥ 65 years. Had CT scan, had minor head trauma (GCS 13–15) | Those who did not sustain head trauma | |
| All ages (any cohort reporting a cohort with no age limits) | |||||||||||||
| cMiller et al. 1996,111 c199729 | USA | P, Cs | c1382111 | 32.6 (NR) | 3/1382 (0.2%) | 84/1382 (6.1%) | Yes | NR | 1382/1382 (100%) | All ages | 1382/1382 (100%) | All ages. GCS 15 or age-appropriate behaviour in children, LOC/amnesia, CT after blunt head trauma. Within 24 hours of injury29 | NR |
| 214329 (some crossover with above cohort)c | NR | 5/2143 (0.2%)c | 138/2143 (6.4%)c | Yesc | NR | 2143/2143 (100%)c | All agesc | 2143/2143 (100%)c | As abovec | As abovec | |||
| Moran et al. 1994112 | USA | R | 200 | Mean: 33.4 (6 to 83) | 8/200; (4%) | No | 126/200 (63%) | 200/200 (100%) | All ages | NR | All ages. GCS 13–15 at both the scene and in the ED. Potential head injury. Transported to facility by air ambulance | NR | |
| dMower et al. 200562 | USA | P, Cs | 13,728 | NR | 917/13,728 (6.7%) | Yes | 8988/13,728 (66%) | NR | All ages | NR | All ages. Had CT scan, acute blunt head trauma | Delayed presentation, penetrating trauma | |
| eMurshid 1994,114 e199877 | Saudi Arabia | R | e566114 | Mean: 17 (1 month to 80 years) | 7/566 (1.2%) | NR | No | 396/566 (70%) | 566/566 (100%) | All ages | NR | All ages, admitted for MHI, within 24 hours of the injury. Had CT scan (applied at data extraction stage) | NR |
| 13177 (some crossover with above cohort)e | Mean: 17 (1 month to 80 years)e | 30/131 (22.9%)e | Yes (applied at data extraction stage)e | 91/131 (69.2%)e | 100%e | All agese | 112/131 (85.5%)e | As above. Had a CT scan and radiography (applied at data extraction stage)e | NRe | ||||
| Shackford et al. 1992119 | USA | R | 423 | NR | 97/423 (22.9%) | No | NR | 423/423 (100%) | All ages | NR | All ages. LOC, PTA and GCS > 12 | Significant non-CNS injuries – extensive definition given | |
| Schynoll et al. 1993118 | USA | P, NR | 264 | NR | 32/264 (12.12%) | Yes | 139/264 (53%) | 244/264 (92.4%) | All ages | 213/264 (80.7%) | All ages. Blunt head trauma, had head CT (at discretion of physician) | Penetrating head trauma | |
| Tender and Awasthi 2003123 | USA | R | 255 | 35 (1 to 97) | 153/255 (60%) | No | 219/255 (85.9%) | 255/255 (100%) | All ages | 194/255 (76.1%) | All ages. GCS 13–15, evaluated in the ED and admitted to the neurosurgery service | Penetrating missile injury, those treated but not admitted from the accident room | |
| Thiruppathy and Muthukumar 2004124 | India | P, Cs | 381 | Mean NR (3 months – 78 years) | 27/381 (7.09%) | 148/381 (38.9% reported, 38.8% calculated) | No | NR | 381/381 (100%) | All ages | 285/381 (74.8%) | All ages. GCS 13–15. Referred from ED. Most ED physicians refer to head injury unit irrespective of severity | Severe polytrauma, alcoholic intoxication, known history of seizure disorder or coagulation disorder, patients referred with CT scan |
| Age limit not reported | |||||||||||||
| Harad and Kerstein 1992104 | USA | Ra | 497 | NR | 172/497 (34.6%) | Yes | 362/497 (73%) | 302/497 (60.8%) | NR | 251/497 (50.5%) | Those who had CT (LOC, amnesia, focal deficits, depressed or open skull fracture, deteriorating mental status and pupillary inequality) and LOC status was known | LOC status not known | |
| 302 | NR | 55/302 (18.2%) | Yes | NR for this subset | 302/302 (100%) | NR | 251/302 (83.1%) | GCS 13–15 and had CT (LOC, amnesia, focal deficits, depressed or open skull fracture, deteriorating mental status and pupillary inequality) | |||||
| Holmes et al. 199759 | USA | P, Cs | 264 | NR | 4/264 (1.5%) | 35/264 (13.3%, reported as 13.2%) | Yes | 181/264 (68.6%) | 264/264 (100%) | NR | 0/264 (0%) | Closed head injury, evidence of LOC or amnesia after head trauma and GCS 14. Had CT scan | Delay in presentation > 4 hours after injury |
| Hung et al. 1996106 | Japan | Ra | 7000 | NR | 476/7000 (6.8%) | NR | NR for this subgroup | 7000/7000 (100%) | NR | NR | NR | NR | |
| Madden et al. 199561 | USA | P, NR | 537 | NR | 91/537 (17%) | Yes | NR | NR | NR | 354/537 (65.9%) | All patients with acute head trauma presenting to the ED with head CT | Patients who received facial CT scans without cerebral studies | |
| Mussack et al. 2002115 | Germany | P, Cs | 139 | Mean: 36 (28 to 60.1) | 19/139 (13.7%) | No | 106/139 (76.3%) | 139/139 (100%) | NR | 129/139 (92.8%) | History of trauma, GCS 13–15, one or more of: LOC (< 5 minutes), amnesia, nausea, vomiting or vertigo | Refused CT, blood-drawing, concurrent injuries that precluded CT | |
| Rosenorn et al. 1991117 | Denmark | R | 1876 | NR | 9/1876 (0.48%) | No | NR | NR | NR | NR | MHI patients admitted (neurosurgical, orthopaedic, paediatric) | Those discharged directly | |
| Sharma et al. 2001120 | India | NR, Cs | 39 | NR | 18/39 (46.2%) | NR | NR | 39/39 (100%) | NR | NR | Admitted for head injury. GCS 13–15 data extracted | Left against advice, no CT done, died | |
| Stein and Ross1990122 | USA | R | 658 | NR | 19/658 (2.9%) | 116/658 (17.6%) | Yes | NR | 658/658 (100%) | NR | 454/658 (69%) | MHI with LOC/amnesia for the event, GCS score ≥ 13. CT scan within 6 hours of injury | NR |
| Stein and Ross 1992121 | USA | R | 1538 | NR | 58/1538 (3.8%) | No | NR | 1538/1538 (100%) | NR | 1117/1538 (72.6%) | GCS 13–15, no focal neurological deficits. Probably only those with history of LOC/amnesia | NR | |
| Tsai 1994125 | Taiwan | R | 186 | NR | 40/186 (21.5%) | Yes | NR for this group | 186/186 (100%) | NR | 112/186 (60.2) | Had CT scan. GCS 13–15 | ||
The cohort sizes of the included studies ranged from 39120 to 13,728. 62 The mean age of the cohorts ranged from 17114 to 4760 years, with two cohorts108,110 reporting older patients separately, with mean ages in excess of 70 years. The variation in mean age range appeared to be influenced by the minimum age for inclusion in the study; some studies included all ages29,62,77,111,112,114,118,119,123,124 or did not report an age restriction,59,61,104,106,115,117,120–122,125 whereas others set a lower age limit. 26,27,46,54,55, 57,58,60,63,67,98–103,105,107–110,113,116,126 The median prevalence of need for neurosurgery was 1.7% (IQR 1.2% to 3.8%). The prevalence of ICI ranged from 0.48%117 to 78.1%99 with a median prevalence of 9.4% (IQR 6.8% to 18%). This wide variation is likely to be owing to differences in patient selection criteria, adequacy of reference standards and definitions of ICI, and neurosurgery. There was no study that clearly selected the whole population of interest. As detailed in Table 9, patients were excluded based on GCS score, absence or presence of clinical characteristics at presentation or because they had not had a CT scan; alternatively, selection criteria were rendered unclear by phrases such as ‘those admitted’. Twenty studies selected only patients with GCS 13–15,26,46,55,98,99,101–103,105,110,112,113,115,119–125 six only patients with GCS 14 or 15,57,58,60,63,108,109 another five only patients with GCS 15,27,29,67,107,111,126 one only those with GCS 14,59 three studies54,104,118 selected all severities of injury (with data available for a GCS 13–15 subgroup in two studies)54,104 and six did not report GCS scores. 61,62,77,106,114,116,117 One further study included GCS 13–15 or GCS < 13 if intoxicated. 100 In 26 studies26,27,46,54,57,58,60,63,67,98,100–103,105,107–109,112,114,115,117,119,121,123,124 patients were not selected on the basis of having had a CT scan, whereas in 14 studies29,55,59,61,62,99,104,110,111,113,116,118,122,125,126 patients were only enrolled if they had a CT scan. The remaining two studies106,120 did not state whether this was used as an inclusion criterion. Selection of patients based on clinical characteristics at presentation varied widely.
Definitions of outcomes and the reference standards used varied across the 42 studies (Table 10). For ICI, 21 studies54,55,58,63,67,77,99,101,102,107–110,112,113,116,118,120,122,125,126 gave only a very general description of the outcome, such as ICI or positive CT findings, with no definition. The remainder varied in the level of detail provided and the type of injuries included, with some including all common acute lesions including skull fractures (e.g. Biberthaler et al. ),98 and others defining injury in terms of severity and clinical significance (e.g. Mower et al. ;62 Stiell et al. 26,46). 62 For the outcome, ‘need for neurosurgery’ there was again a variety of definitions across the 16 studies, including narrow definitions which, for example, only included ‘urgent surgery’122 or specified a timescale,105,121 and definitions that included any neurosurgical procedure, including fitting an intracranial pressure monitor. 119
| Study | Definition of ICI | Reference standard for ICI | Patients receiving CT, n | Definition of need for neurosurgery | Reference standard for need for neurosurgery |
|---|---|---|---|---|---|
| Adults (any cohort selecting patients above a given age) | |||||
| Arienta et al. 199754 | Intracranial lesion: not defined | CT scan or follow-up telephone call. Details NR | 762/9917 (7.7%) | Neurosurgery or death: not defined further | Retrospective chart review, telephone follow-up |
| Biberthaler et al. 200698 | CT abnormality: epidural, subdural, subarachnoid, intracerebral, cerebellar or brainstem haemorrhage, cortex contusion (haemorrhagic or non-haemorrhagic), fracture (skull cap, skull base, mastoid) or intracranial pressure (focal or generalised brain oedema) | CT scan | 1309/1309 (100%) | NA | NA |
| Borczuk 199555 | ICI: abnormalities believed to be related to the trauma | CT scan | 1448/1448 (100%) | Neurosurgery: placement of an intracranial pressure monitoring device alone was not considered a neurosurgical intervention | Review of ED and hospital charts |
| Chan et al. 200599 | ICI: not defined | CT scan | 105/105 (100%), 92/92 (100%) | NA | NA |
| Cook et al. 1994100 | Positive CT scan: evidence of acute intracerebral injury, such as a haematoma or a contusion or a depressed skull fracture | CT scan: obtained after 1 hour’s observation or sooner if patient deteriorated | 107/107 (100%) | NA | NA |
| Fabbri et al. 200557 | Any post-traumatic lesion at CT within 7 days from trauma: depressed skull fracture, intracerebral haematoma/brain contusions, subarachnoid haemorrhage, subdural haematoma, epidural haematoma, intraventricular haemorrhage | Patients were managed according to NCWFS guidelines where low-risk patients were sent home without CT, medium-risk patients underwent CT and observed for 3–6 hours if negative, then discharged, high-risk patients underwent CT and were observed for 24–48 hours. All those discharged were given written advice about signs and symptoms with which they should return | 4177/7955 (52.5%)a | NA | NA |
| Falimirski et al. 200358 | Significant ICI: not defined | CT scan | 331/331 (100%) | NA | NA |
| Feuerman et al. 1988102 | Positive CT findings: not defined | CT scan | 129/373 (35%) 129/129 (100%) | Neurosurgery: operative haematoma or deterioration | Neurosurgery |
| Gomez et al. 1996103 | 2351/2484 (94.6%) | Neurosurgery: operation. Patients with focal mass intracranial lesions causing brain shift | Chart review: data entered into a database | ||
| Haydel et al. 200027 | ICI: presence of acute traumatic ICI (a subdural, epidural or parenchymal haematoma, subarachnoid haemorrhage, cerebral contusion or depressed skull fracture) | CT scan | 520/520 (100%) | NA | NA |
| Hsiang et al. 1997105 | Abnormal radiographic findings: skull fracture (including depressed skull fracture), intracranial haematoma or contusion, traumatic subarachnoid haemorrhage | CT scan and/skull radiography: at discretion of admitting neurosurgeon | 842/1360 (61.9%), NR for subgroup of 736 | Neurosurgery: neurosurgical intervention in first 48 hours | Patient records |
| Ibanez and Arikan 200460 | Relevant positive CT scan: acute intracranial lesion, not including isolated cases of linear skull fractures or chronic subdural effusions | CT scan | 1101/1101 (100%) | NA | NA |
| Jeret et al. 1993107 | Abnormal CT: not defined | CT scan | 712/712 (100%) | NA | NA |
| Livingston et al. 1991109 | Positive CT scan: not defined | CT scan | NR | NA | NA |
| Livingston et al. 2000108 | Positive CT scan: presence of ICI | CT scan | 2152/2152 (100%) | NA | NA |
| Muller et al. 2007113 | Intracranial abnormality: not defined | CT scan: within 12 hours of injury | 226/226 (100%) | NA | NA |
| Nelson et al. 1992116 | Abnormal CT scan: not defined | CT scan | 131/131 (100%) | NA | NA |
| Ono et al. 200763 | Intracranial lesion: not defined | CT scan | 1064/1064 (100%) | NA | NA |
| Saboori et al. 200767 | Intracranial lesion: all acute abnormal finding on CT |
CT scan Normal CT: discharged with advice to return if symptoms occur. One-week follow-up call Abnormal CT: admission, treatment. Evaluation at 2 weeks and 1 month after discharge |
682/682 (100%) | NA | NA |
| Stiell et al. 200126 | Clinically important brain injury on CT: all injuries unless patient neurologically intact and had one of the following: solitary contusion > 5 mm, localised subarachnoid blood > 1 mm thick, smear subdural haematoma > 4 mm thick, closed depressed skull fracture not through inner table |
|
2078/3121 (67%) | NA | NA |
| Stiell et al. 200546 | As Stiell et al. 200126 | As Stiell et al. 200126 | 2171/2707 (80.2%), 1378/1822 (75.6%)b | NA | NA |
| Vilke et al. 2000126 | ICI: not defined | CT scan: selected for CT at attending physician’s discretion | 58/58 (100%) | Neurosurgery: not defined | NR |
| Dunham et al. 1996101 | CT detected intracranial haemorrhage: not defined | CT scan for 91.4%, NR for remainder | 1857/2032 (91.4%), NR for 220, age > 60 years | NA | NA |
| Mack et al. 2003110 | ICI: not defined | CT scan | 133/133 (100%) | NA | NA |
| All ages (any cohort reporting a cohort with no age limits) | |||||
| Miller et al. 1996111 | Abnormal CT scan: acute traumatic intracranial lesion (contusion, parenchymal haematoma, epidural haematoma, subdural haematoma, subarachnoid haemorrhage) or a skull fracture | CT scan: within 8 hours of injury | 1382/1382 (100%) | Neurosurgery: surgical intervention (craniotomy to repair an acute traumatic injury or placement of a monitoring bolt) | Hospital records of those with positive CT scan followed until discharge |
| Miller et al. 199729 | Abnormal CT scan: acute traumatic intracranial lesion (contusion, parenchymal haematoma, epidural haematoma, subdural haematoma, subarachnoid haemorrhage) or a skull fracture | CT scan: within 8 hours of injury | 2143/2143 (100%) | Neurosurgery: surgical intervention (craniotomy to repair an acute traumatic injury or placement of a monitoring bolt) | Hospital records of those with positive CT scan followed until discharge |
| Moran et al. 1994112 | Positive CT scan: not defined | CT scan NR for those who did not have CT scan | 96/200 (48%) | NA | NA |
| Mower et al. 200562 | Significant ICI: any injury that may require neurosurgical intervention, lead to rapid clinical deterioration, or result in significant long-term neurological impairment | CT scan | 13,728/13,728 (100%) | NA | NA |
| Murshid 1994114 | NA | NA | N/A | Neurosurgery: not defined. Those reported positive had burr holes, craniotomy, ventilation, conservative treatment (assume not elevation of fracture) | NR |
| Murshid 199877 | ICI on CT scan; not defined | CT scan | 127/566 (22%) | NA | NA |
| Shackford et al. 1992119 | N/A | NA | N/A | Surgical intervention: craniotomy or ICP monitor | Hospital records |
| Schynoll et al. 1993118 | Abnormal CT scan: not defined | CT scan: at discretion of evaluating physician | 264/264 (100%) | NA | NA |
| Tender and Awasthi 2003123 | Abnormality on CT: intracranial haematoma, contusion, traumatic subarachnoid haemorrhage and skull fracture with an underlying lesion | CT scan | 255/255 (100%) | NA | NA |
| Thiruppathy and Muthukumar 2004124 | Positive CT scan: acute pathological state in the skull or brain attributable to head injury (vault or basilar fractures, epidural, subdural, intracerebral haematomas, contusions, intraventricular haemorrhage, pneumocephalus) | CT scan | 381/381 (100%) | Neurosurgery: not defined | Neurosurgery |
| Age limit not reported | |||||
| Harad and Kerstein 1992104 | Abnormal CT scan: contusion, depressed skull fracture, diffuse axonal injury, epidural/subdural haematoma, subarachnoid haemorrhage and oedema | CT scan | 497/497 (100%), 302/302 (100%) | Craniotomy | NR |
| Holmes et al. 199759 | Abnormal CT scan defined as any CT scan showing an acute traumatic lesion (skull fractures or intracranial lesions: cerebral oedema, contusion, parenchymal haemorrhage, epidural haematoma, subdural haematoma, subarachnoid haemorrhage or intraventricular haemorrhage) | CT scan | 264/264 (100%) | Neurosurgery | Neurosurgery: Patients with abnormal CT scan followed to discharge. Those with normal CT not studied further |
| Hung et al. 1996106 | NA | NA | NA | Surgically significant ICI | NR |
| Madden et al. 199561 | Clinically significant scan: pathology related to trauma affecting the bony calvaria or cerebrum (including non-depressed skull fractures, excluding scalp haematomas, those with no bony skull or intracerebral pathology) | CT scan | 537/537 (100%) | ||
| Mussack et al. 2002115 | Post-traumatic lesion: skull fracture, subarachnoid haemorrhage, epidural or subdural haematoma, intracerebral haemorrhage or diffuse brain oedema | CT scan | 139/139 (100%) | ||
| Rosenorn et al. 1991117 | Intracranial complication: intracerebral haematoma, subdural haematoma, cerebral contusion, traumatic subarachnoid haemorrhage | CT scan or admission and observation | NR | ||
| Sharma et al. 2001120 | Intracranial complications: not defined | CT scan | 39/39 (100%) | ||
| Stein and Ross 1990122 | Abnormal CT scan: not defined | CT scan | 658/658 (100%) | Urgent surgery: urgent surgery because of finding on CT scan – haematoma or previously unsuspected depressed fracture large enough to require surgery on an urgent basis (not those who deteriorated subsequently) | NR |
| Stein and Ross 1992121 | NA | NA | NA | Immediate neurosurgery or subsequent deterioration: not defined | Records searched |
| Tsai 1994125 | CT scan findings: not defined | CT scan | 186/186 (100%) | ||
In the 10 studies26,46,54,57,67,77,101,105,112,117 in which CT was not possible for all and was not an inclusion criterion, the reference standard varied, with four studies26,46,54,67 using telephone follow-up and five57,77,101,105,112 not reporting how ICI was identified in those not undergoing CT. One study admitted those not undergoing CT. 117 Telephone follow-up and no follow-up are both likely to miss some intracranial injuries, affecting estimates of diagnostic accuracy. The length of follow-up for neurosurgery varied from being not reported to following until discharge, which may not capture all neurosurgical procedures, again leading to inaccurate estimations of diagnostic accuracy.
Children and infants
The design and patient characteristics of the 29 studies (representing 30 papers)30,81–84,86–91,93–95,127–142 that evaluated the diagnostic accuracy of individual clinical characteristics for identifying ICI (including the need for neurosurgery) in children and/or infants with MHI are summarised in Table 11. Three studies84,90,135 provided separate data for children and infants, whereas two studies82,86 provided data for infants only, and one study84 provided data for infants as a subset of data from a cohort of children up to age 18 years. In one study only adolescents were selected. 127 Eighteen studies were from the USA,82,84,86,88,90,91,93,94,129–131,135,137–142 three from Turkey,87,128,132 two from the UK,30,136 one a USA–Canadian collaboration81 and one each from Italy,83 Finland,89 Poland,133 Australia134 and Hong Kong. 127 Eight studies30,81,83,90,91,95,129,135,140 were multicentre. Cohorts ranged in size from 39136 to 31,69490 patients with two cohorts30,90 providing a large data set of over 20,000 participants. Seventeen30,81,83,84,86,88,90,91,93–95,127,128,130,131,135,141,142 studies were prospective, seven of which were consecutive,83,84,86,88,91,94,95,127 one convenience81 and the remaining nine30,90,93,128,130,–131,135,141,142 did not report the method of patient recruitment. Twelve82,89,129,132–134,136–140 studies were retrospective.
| Author, year | Country | Design | No. of patients, n | Mean or median age, years (range) | Prevalence of neurosurgery | Prevalence of ICI | CT as inclusion? (yes/no) | Male, n | Patients with MHI, n | Prevalence of GCS 15, n | Other significant inclusion criteria | Other significant exclusion criteria |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Atabaki et al. 200881 | USA, Canada | P, Cv | 1000 | Mean: 8.9 (0 to 21) | 65/1000 (6.5%) | Yes | 641/1000 (64.1%) | 1000/1000 (100%) | 852/1000 (85.2%) | Birth to 21 years. Closed head trauma, undergoing CT | Prior CT at referring hospital, GCS < 13 | |
| Boran et al. 2006128 | Turkey | P, NR | 421 | Mean: 5.1 (0 to 16) | 37/421 (8.8%) | No | 239/421 (56.8%) | 421/421 (100%) | 421/421 (100%) | < 16 years. Head trauma, GCS 15, no focal neurological deficit | Penetrating skull injury, gunshot wounds and multiple trauma | |
| Da Dalt et al. 200683 | Italy | P, Cs | 3806 | Mean NR(0 to 16) | 22/3806 (0.58%) | No | 2315/3806 (60.8%) | NR | NR | < 16 years, history of blunt head trauma of any severity | Admitted > 24 hours after trauma, open injuries, previous history of neurological disorders or bleeding diathesis | |
| Davis et al. 1994129 | USA | R | 168 | Mean: 11.4 (2 to 17) | 12/168 (7.1%) | Yes | 118/168 (70.2%) | 168/168 (100%) | 168/168 (100%) | 2–17 years, CT scans, acute closed-head injury, LOC/amnesia, GCS 15 | Ventriculoperitoneal shunt in place, depressed skull fracture or basilar skull fractures | |
| Dietrich et al., 199384 | USA | P, Cs | 253 (some data missing in some cases – range 58 to 253) | Mean NR (2 to 20) | 36/253 (14.23%) | Yes | NR for this subgroup | NR for this subgroup | 176/253 (69.6%) | ≥ 2 years to 20 years, head trauma, with CT scan | Unable to answer questions because of age or altered mental status | |
| 71 (range 19 to 71) | Mean NR (10 days to < 2 years) | 3/71 (4.2%) | NR for this subgroup | NR for this subgroup | 57/71 (80.3%) | < 2 years, head trauma, with CT scan | Unable to answer questions because of age or altered mental status | |||||
| Dunning et al. 200630 | UK | P, NR | 22,772 | Mean: 5.7 (0 to 16) | 168/22,579 (0.744%) | No | 14,767/22,772 (64.8%) | 22,298/22,772 (97.9%) | 21,996/22,772 (96.6%) | < 16 years. History/signs of injury to the head. LOC or amnesia was not a requirement | Refusal to consent to entry into the study | |
| Fisher 1997141 | USA | P, NR | 42 | Mean: 5.8 months (1 to 153 months) | 9/42 (21%) | No | NR | NR | NR | < 12 years. Symptomatic blunt head trauma within 48 hours with any of LOC, amnesia, PTS, or any of vomiting headache and somnolence > 1 hour after injury | Cardiac arrest in pre-hospital course, pre-existing neurological deficit or suspicion of impairment due to toxins | |
| Fridriksson et al. 2000130 | USA | P, NR | 49 | Mean NR (2 months to 16 years) | 22/49 (44.9%) | Yes | 55% | 39/49 (79.6%) | NR | 0–18 years. Within 24 hours of injury, blunt trauma, requiring head CT | Penetrating trauma, bleeding disorders, longer than 24 hours since injury | |
| Guzel et al. 200987 | Turkey | R | 337 | NR | 67/337 (19.9%) | Yes (applied at data extraction stage) | 223/337 (66.2%) | 337/337 (100%) | 304/337 (90.2%), | < 16 years. GCS 13–15. Had CT (applied at data extraction stage) | > 16 years, moderate or severe head injury, no clear history of trauma, obvious penetrating skull injury, unstable vital signs, seizure before assessment, bleeding disorder/anticoagulants, re-attendances | |
| Hahn and McLone 1993131 | USA | P, NR | 791 | Mean: 5.5 (0 to 16) | 67/791 (8.5%) | No | 527/791 (66.6%) | 791/791 (100%) | 549/791 (69.4%) | 0–16 years. GCS 13–15 and LOC, neurological deficits, headache, vomiting or nausea, a major or minor skull fracture shown on a radiograph or abnormal finding on CT scans, suspected child abuse, caretaker unreliable or home observation unrealistic | NR | |
| Halley et al. 2004142 | USA | P, NR | 98 | Mean NR (2 to 16) | 13/98 (13.3%) | Yes | 73/98 (74%) | 98/98 (100%) | 76/98 (77.6%) | 2–16 years with minor closed head injury (GCS 13–15), LOC/amnesia | Age < 2 or > 16 years, painfully distracting injury, intoxication, history of previous neurological abnormality, suspicious history of non-accidental injury, or not undergoing CT | |
| Haydel and Schembekar 2003,88 | USA | P, Cs | 175 | Mean: 12.8 (5 to 17) | 6/175 (3.4%) | 14/175 (8%) | Yes | 114/175 (67%) | 100% (assumed from inclusion criteria) | 175/175 (100%) | 5–17 years. Within 24 hours of injury, blunt trauma with LOC, non-trivial mechanism of injury, CT scan | Trivial injuries, refused CT, concurrent injuries precluded CT, irritable or agitated (GCS < 15) |
| Keskil et al. 1995132 | Turkey | R | 257 | Mean NR (0 to 15) | 30/257 (11.7%) | No | 149/257 (58%) | 100% | 174/257 (67.7%) | ≤ 15 years. GCS 14–15. Those who performed normally after brief LOC (< 20 minutes) and/or history of PTA | Chronic subdural haematomas, unless history of acute injury or acute haematoma present also. Dead on arrival, brain-dead in ED, gunshot wounds | |
| Klemetti et al. 200989 | Finland | R | 485 | Mean: 7.7 (2 days to 16 years | 83/485 (17.1%) | No | 313/485 (65%) | NR | NR | ≤ 16 years. Admitted to paediatrics (usually hospitalised even after MHI), history of head trauma. Patients identified by reference to discharge diagnosis | NR | |
| Kupperman et al. 200990 | USA | P, NR | 31,694 (children’s cohort) | Mean NR (2 to < 18) | 278/31,694 (0.88%) | No | NR | 31,694/31,694 (100%) | 30,811/31,694 (97.2%) | ≥ 2 years to < 18 years. Children presenting within 24 hours GCS ≥ 14 | Trivial injuries, penetrating trauma, known brain tumours, pre-existing neurological disorders, or neuroimaging before transfer. Coagulopathy, shunts, GCS < 14 | |
| 10,718 (infant’s cohort) | Mean NR (0 to 2) | 98/10,718 (0.914%) | 10,718/10,718 (100%) | 10,260/10,718 (95.7%) | < 2 years. Children presenting within 24 hours GCS ≥ 14 | As above | ||||||
| Mandera 2000133 | Poland | R | 166 | Mean: 8 (0 to 17) | 68/166 (40.9%) | NR | 111/166 (66.6%) | 166/166 (100%) | 95/166 (57%) | < 17 years. GCS 13–15, records available | NR | |
| Ng et al. 2002134 | Australia | R | 119 | NR | 65/119 (54.6%) | Yes | NR for this subset, whole cohort: 184/311 (59%) | NR for this subset, whole cohort: 283/311 (91%) | NR | ≤ 14 years. Diagnosis of acute head injury. Within 24 hours of injury. Had CT scan | NR | |
| aOman 2006;91 aSun et al. 200795 | USA | P, Cs | 1666 | Mean NR (0 to 18) | 138/1666 (8.3%) | Yes | 1072/1666 (64%) | NR | 1296/1666 (77.8%) | < 18 years. Had CT scan (physician’s discretion), acute blunt head trauma | Delayed presentation, without blunt trauma (penetrating trauma) | |
| 309 (subset of above) | Mean NR (0 to 3) | 25/309 (8.1%) | Yes | NR | NR | 172/309 (55.7%) | Subset of above, 0–3 years | As above | ||||
| Palchak et al. 200393 | USA | P, NR | 1098 | NR for this subset | 39/1098 (3.6%) | Yes | NR for this subset | 1098/1098 (100%) | GCS 14 or 15: 1098/1098 (100%) | < 18 years. History of non-trivial blunt head trauma with findings consistent with head trauma: LOC, amnesia, seizures, vomiting, current headache, dizziness, nausea or vision change or physical examination findings of abnormal mental status, focal neurological deficits, clinical signs of skull fracture or scalp trauma | Trivial injuries, neuroimaging before transfer | |
| Quayle et al. 199794 | USA | P, Cs | 321 | Mean: 4 years 10 months (2 weeks to 17.75 years) | 27/321 (8.4%) | Yes | 189/321 (59%) | NR | NR | < 18 years. Non-trivial injury: symptoms such as headache, amnesia, vomiting, drowsiness, LOC, seizure, dizziness or significant physical findings including altered mental status, neurological deficit and altered surface anatomy. Scalp laceration or abrasion in infants < 12 months, scalp haematoma in < 24 months | Trivial head injuries, penetrating head injuries | |
| Ramundo et al. 1995135 | USA | P, NR | 261 (children’s cohort) | Mean NR (2 to 18) | 45/261 (17.2%) | Yes | NR for subgroup. Whole cohort 207/300 (69%) | NR | NR | 2 to ≤ 18 years. Closed head injury, those with CT | Where clinical data not recorded | |
| 37 (infant’s cohort) | Mean NR (NR to < 2) | 8/37 (22%) | Yes | NR | 28/37 (75.7%) | < 2 years. As above | As above | |||||
| Reed et al. 2005136 | UK | R | 39 | NR for this subset | 10/39 (25.6%) | Yes | NR for this subset | NR | NR | > 1 year, < 14 years. CT scan | NR | |
| Schunk 1996137 | USA | R | 313 | Median: 5.4 (2 weeks to 18 years) | 3/313 (1%) | 13/313 (4.2%) | Yes | 190/313 (61%) | 313/313 (100%) | 313/313 (100%) | < 18 years. Traumatic injury, CT scans for GCS 15/infant equivalent | Abnormal neurological examination (GCS < 15 or infant equivalent), known depressed skull fracture, bleeding diathesis, or developmental delay |
| Simon et al. 2001138 | USA | R | 569 | NR (NR to 16) | 84/569 (14.8%) | Yes | NR | 569/569 (100%) | 499/569 (87.7%) | < 16 years. GCS 14/15, high-risk mechanism of injury, CT scan | NR | |
| 429 (subset of above) | NR for this subset | 62/429 (14.5%) | Yes | NR | 429/429 (100%) | 377/429 (87.9%) | Subset of above, where LOC reliably known | NR | ||||
| Stein 1995 and Doolin139 | USA | R, Cs | 751 | NR | 24/751 (3.2%) | 94/751 (12.5%) | No | NR | 751/751 (100%) | 582/751 (77.5%) | ≤ 19 years. Admitted for mild closed head injury. GCS 13–15 (applied at data extraction stage) | Applied at data extraction phase: moderate head injury minimal head injury |
| Wang et al. 2000140 | USA | Retrospective (reported: prospective) | 157 | NR | 43/157 (27.4%) | Yes (applied at data extraction phase) | NR | 157/157 (100%) | NR | ≤ 15 years. Field GCS 13 or 14, blunt trauma. Had CT (applied at data extraction stage) | Stab or gunshot wounds | |
| Chan et al. 1990127 | Hong Kong | P, Cs | 418 | Mean NR (11 to 15) | 13/418 (3.1%) | NR | NR | NR | 397/418 (95.0%) | 11–15 years. Admitted. Admission criteria were GCS < 15, skull fracture detected radiologically and/or suspected clinically, including base of skull, associated injuries, post-traumatic epilepsy, neurological signs, history of LOC, headache and vomiting, scalp lacerations requiring treatment, drugs or alcohol | Those discharged home who did not re-attend. Those referred from other hospitals | |
| Buchanich 200782 | USA | R | 97 | Mean 15.2 months (NR to 2.9 years) | 22/97 (22.7%) | No | 52/97 (53.6%) | 100% | NR | < 3 years old. GCS 14–15 | Penetrating injuries, depressed skull fractures requiring surgery, injuries suspected to be intentional and initial CT scan > 24 hours after injury | |
| Greenes and Schutzman 200186 | USA | P, Cs | 422 | 11.6 months (3 days to 23 months) | 13/422 (3.1%) | No | NR | 422/422 (100%) (assumed) | NR, but all asymptomatic so assume GCS 15 | < 2 years. Asymptomatic, head trauma | Symptomaticb patients with any of: history of LOC, lethargy, irritability, seizures, three or more episodes of emesis, irritability or depressed mental status, bulging fontanelle, abnormal vital signs indicating increased intracranial pressure or focal neurological findings |
For studies of children, the upper age limit ranged between 12141 and 21 years,81 and the lower limit between 081 and 5 years. 88 For infants, the upper age limit was 284,86,90,135 or 3 years. 82,91 Mean age was not reported in the majority of cases; where it was reported it ranged from 4 years 10 months94 to 12 years 10 months. 88 Prevalence of neurosurgery ranged from 1.0%137 to 8.5%131 (median 3.3%, IQR 1.55% to 7.23%) and prevalence of ICI ranged from 0.58%83 to 54.6%134 (median 12.1%, IQR 4.1% to 21.0%). It was clear in only one study30 that only the whole population of interest had been selected. Variations in selection criteria include selection of patients on the basis of having had a CT scan,81,84,87,88,91,93–95,129,130,134–138,140,142 selecting only patients presenting with some clinical characteristics,83,88,90,93,94,127–129,131,132,138,139,141,142 selecting only those admitted89,127,139 and selecting a spectrum of patients with a wider or narrower range of GCS scores. Five studies selected only those with GCS 15,86,88,128,129,137 five only those with GCS 14 or 15,82,90,93,132,138 one only those with GCS 13 or 14140 and 1283,84,89,91,94,95,127,130,134–136,141 either did not report selection on the basis of GCS or selected all severities. The remaining six81,87,131,133,139,142 selected or reported a subset of patients with GCS 13–15.
Definitions of outcomes and the reference standards used varied across the 29 studies (Table 12). 30,81–84,86–91,93–95,127–142 The outcome definition for ICI differed across the 28 studies30,81–84,86–91,93–95,127–130,132–142 that reported this outcome. Four studies30,89–91,95 defined this as injuries of clinical significance, 13 studies81,82,84,86,88,93,128,130,132–135,138 had more general definitions including common acute lesions (listed in Table 12) and 11 studies83,87,94,127,129,136,137,139–142 did not give a definition. The reference standards used where CT was not possible for all and was not an inclusion criterion was unclear in five cases. 30,89,127,132,140 Other reference standards comprised telephone follow-up, review of hospital records or both. Neurosurgery was poorly defined in most cases; one study included other medical interventions88 and one study excluded skull fracture surgery,137 but it was unclear if these were included or excluded in other studies. The length of follow-up for neurosurgery varied from being not reported to following until discharge88 or at an outpatients clinic. 131
| Author, year | Definition of ICI | Reference standard for ICI | Patients receiving CT, n | Definition of need for neurosurgery | Reference standard for need for neurosurgery |
|---|---|---|---|---|---|
| Atabaki et al. 200881 | ICI: subdural, epidural, subarachnoid, intraparenchymal and intraventricular haemorrhages, as well as contusion and cerebral oedema | CT scan | 1000/1000 (100%) | NA | NA |
| Boran et al. 2006128 | Intracranial lesions: not including soft tissue swelling and linear skull fractures | CT scan | 421/421 (100%) | NA | NA |
| Da Dalt et al. 200683 | ICI: identified on CT either at initial ER presentation or during any hospital admission or readmission |
CT scan obtained at discretion of treating physician All children discharged immediately from ER or after short observation received a follow-up telephone interview approximately 10 days later. Hospital records were checked for readmissions for 1 month after conclusion of study |
79/3806 (2%) | NA | NA |
| Davis et al. 1994129 | Intracranial haemorrhage: not defined | CT scan | 168/168 (100%) | NA | NA |
| Dietrich et al. 199384 | Intracranial pathology: epidural or subdural haematoma, cerebral contusions or lacerations, intraventricular haemorrhage pneumocephaly or cerebral oedema, with or without skull fracture | CT scan | 166/166 (100%) | NA | NA |
| Dunning et al. 200630 | Clinically significant ICI: death as a result of head injury, requirement for neurosurgical intervention or marked abnormalities on the CT scan |
All patients treated according to RCS guidelines. This recommends admission for those at high risk and CT scan for those at highest risk Follow-up: all patients who were documented as having had a skull radiograph, admission to hospital, CT scan or neurosurgery were followed up |
744/22,772 (3.3%) | NA | NA |
| Fisher 1997141 | ICI: not defined | CT scan | 42/42 (100%) | NA | NA |
| Fridriksson et al. 2000130 | Intracranial lesion: cerebral oedema, parenchymal bleeding, cerebral contusion or subarachnoidal subdural or epidural bleeding | CT scan | 49/49 (100%) | NA | NA |
| Guzel et al. 200987 | Positive CT scan: definition NR | CT scan | 337/337 (100%) | NA | NA |
| Hahn and McLone 1993131 | 632/791 (79.9%) | Neurosurgical intervention: mass lesions (epidural or subdural haematoma requiring surgery) | CT scan, neurosurgery and follow-up at outpatient trauma clinic of those asymptomatic with clear CT | ||
| Halley et al. 2004142 | ICI: abnormality on CT scan | CT scan | 98/98 (100%) | NA | NA |
| Haydel and Schembekar 200388 | ICI on head CT: any acute traumatic intracranial lesion, including subdural epidural or parenchymal haematoma, subarachnoid haemorrhage, cerebral contusion or depressed skull fracture | CT scan | 175/175 (100%) | Need for neurosurgical or medical intervention in patients with ICI on CT | All patients with abnormal CT scan admitted and followed until discharge |
| Keskil et al. 1995132 | Epidural or subdural haematoma | Observed at operation or CT | NR | NA | NA |
| Klemetti et al. 200989 | Complicated or severely complicated head trauma: brain contusion, skull base fracture, skull fracture. Patients who required neurosurgical intervention, patients who succumbed, epidural haematoma, subdural haematoma, subarachnoid haematoma, intracerebral haematoma | Hospital records | 242/485 (49.9%) | NA | NA |
| Kupperman et al. 200990 | Clinically important brain injury: death from TBI, neurosurgery, intubation for > 24 hours for TBI or hospital admission of two nights or more associated with TBI on CT. Brief intubation for imaging and overnight stay for minor CT findings NOT included | CT scans, medical records, and telephone follow-up. Those admitted: medical records, CT scan results. Those discharged: telephone survey 7–90 days after the ED visit, and medical records and county morgue records check for those who were not contactable |
11,643/31,694 (36.7%) (children) 3326/10,718 (31.0%) (infants) |
NA | NA |
| Mandera 2000133 | ICI: mass lesion (epidural, subdural or intracerebral haematoma seen on CT) | CT scan | 166/166 (100%) | NA | NA |
| Ng et al. 2002134 | Abnormal CT scan: isolated fractures and intracranial pathology (epidural, subdural or parenchymal haematoma, cerebral contusion, intraventricular or subarachnoid haemorrhage, cerebral oedema) with or without a fracture | CT scan: at physician’s discretion | 119/119 (100%) | NA | NA |
| aOman 2006;91 aSun et al. 200795 | Clinically important/significant ICI: any injury that may require neurosurgical intervention, lead to rapid clinical deterioration or result in significant long-term neurological impairment | CT scan | 1666/1666 (100%) | NA | NA |
| Palchak et al. 200393 | TBI identified on CT scan or TBI requiring acute intervention OR intervention by one or more of: neurosurgical procedure, ongoing antiepileptic pharmacotherapy beyond 7 days, the presence of a neurological deficit that persisted until discharge from the hospital, or two or more nights of hospitalisation because of treatment of the head injury | CT or performance of intervention | 1098/1098 (100%) | NA | NA |
| Quayle et al. 199794 | ICI: definition NR | CT scan | 321/321 (100%) | NA | NA |
| Ramundo et al. 1995135 | Depressed or basilar skull fractures, brain contusion, epidural or subdural haematomas, subarachnoid haemorrhage, intraparenchymal or intraventricular haemorrhage, pneumocephaly, cerebral oedema | CT scan |
261/261 (100%) (children) 37/37 (100%) (infants) |
NA | NA |
| Reed et al. 2005136 | ICI: not defined | CT scan | 39/39 (100%) | ||
| Schunk et al. 1996137 | ICI: not defined | CT scan | 313/313 (100%) | ICI requiring neurosurgery, excluding skull fracture surgery | Records check |
| Simon et al. 2001138 | ICI: subarachnoid haemorrhage, subdural haematoma, epidural haematoma and contusion | CT scan |
569/569 (100%) 429/429 (100%) (subset) |
||
| Stein and Doolin 1995139 | Intracranial lesion on CT: not defined | CT scan | 751/751 (100%) | Neurosurgical procedure | NR |
| Wang et al. 2000140 | CT scan abnormality: any evidence of traumatic injury to the cranial bones or brain (haemorrhages classified as epidural, subdural, subarachnoid or intraparenchymal spaces) |
CT scan NR for those who did not have a CT scan |
134/157 (85.4%) | NA | NA |
| Chan et al. 1990127 | Intracranial haemorrhage: development of acute intracranial haemorrhage within 48 hours of injury | CT scan | NR | NA | NA |
| Buchanich 200782 | ICI: intracranial haematoma, intracranial haemorrhage, cerebral contusion and/or cerebral oedema |
CT scan Follow-up questionnaire/telephone interview: questions regarding child’s symptoms and behaviour following injury |
97/97 (100%) | NA | NA |
| Greenes and Schutzman 200186 | ICI: cerebral contusion, cerebral oedema or intracranial haematoma noted on CT | CT scan | 172/172 (100%) | NA | NA |
Quality of included studies
Adults
The methodological quality assessment of each included study is summarised in Figures 15 and 16. Overall, most of the included studies were poorly reported and did not satisfy the majority of the quality assessment items of the QUADAS tool.
FIGURE 15.
Individual clinical characteristics in adults with MHI – methodological quality graph. Review authors’ judgements about each methodological quality item presented as percentages across all included studies.
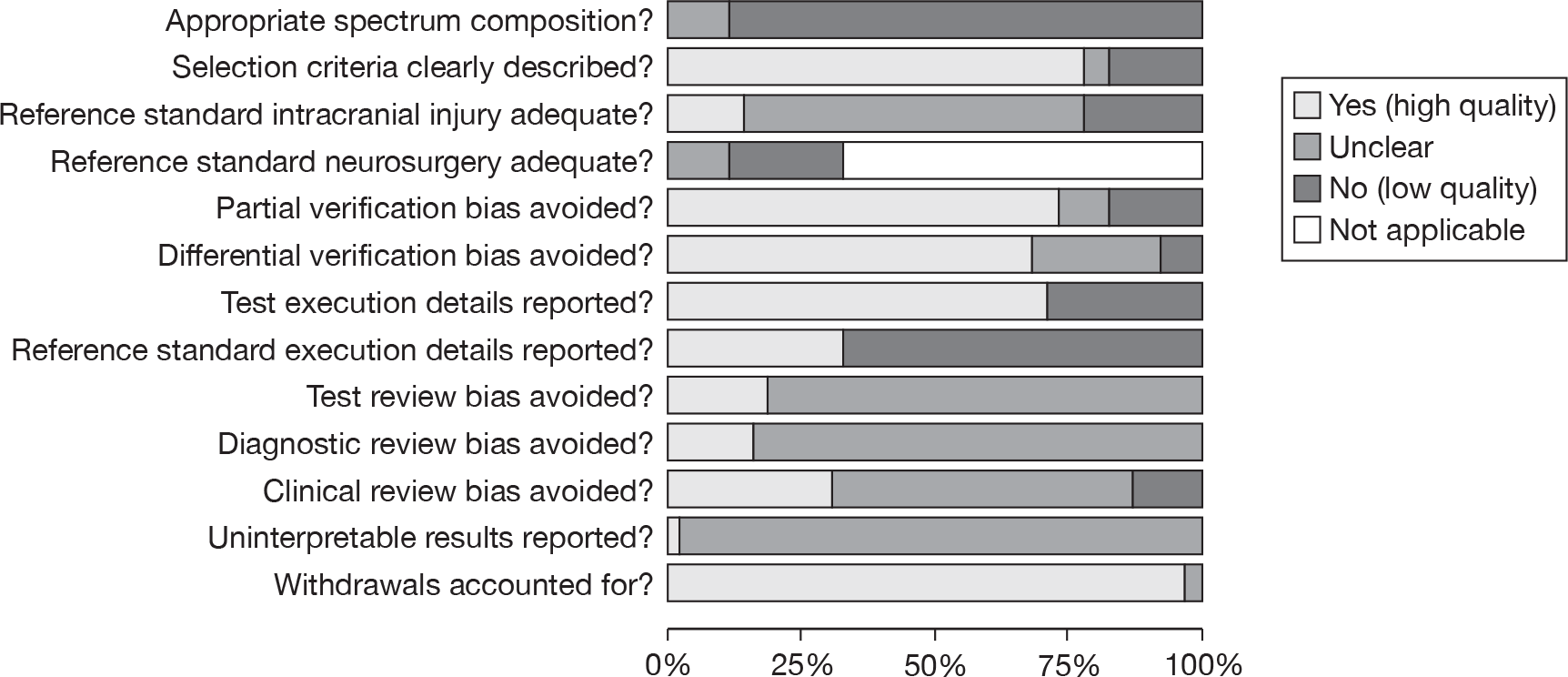
FIGURE 16.
Individual clinical characteristics in adults with MHI – methodological quality summary. Review authors’ judgements about each methodological quality item for each included study. Minus sign, negative score; plus sign, positive score; question mark, unclear whether item scores negatively or positively; blank space, not applicable.
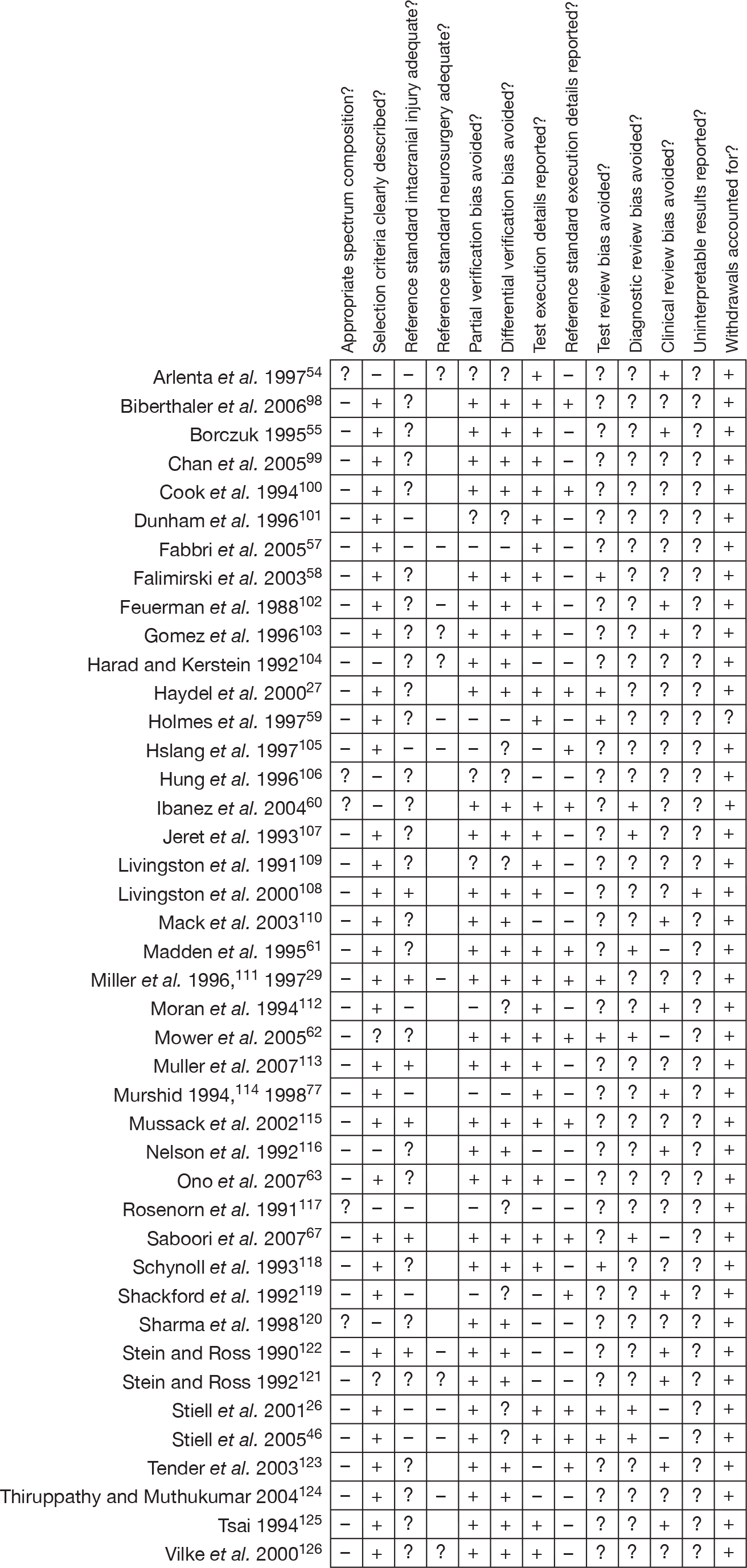
The main source of variation was patient spectrum, for which no study scored positively (further details are provided in Description of included studies). Fewer than one-quarter of the studies used an adequate reference standard for ICI,29,67,108,111,113,115,122 with the majority scoring unclear or negatively. Although 21 studies27,55,58–63,99,100,102,104,107,110,116,118,120,123–126 carried out CT in all participants, they failed to state whether this was done within 24 hours and were therefore scored unclear. Of the 14 studies26,29,46,54,57,59,102–105,111,121,122,124,126 that reported the outcome neurosurgery, all either reported an inadequate reference standard or were unclear on this point. Poor scores were usually given because length of follow-up was not adequate.
Partial verification bias was largely avoided. Similarly, studies scored well generally for differential verification bias, with reference standards being applied to the whole cohort in 29 cases. 26,27,29,46,55,58,60,62,63,67,69,98–100,102–104,107,108,110,111,113,115,116,118,120–126 However, it should be noted that three54,57,106 of the four largest cohorts scored negatively or unclear across the reference standard and verification items, and two54,57 of these report data for a large number of clinical characteristics. There is the potential for bias in these studies to influence results.
The execution of the index test was reported more often than the reference standard. This probably reflects the routine nature of CT scanning, whereas the index tests required more explanation. Test review and diagnostic review biases were largely unreported. This may have been considered an unnecessary detail to report as it is likely that clinical characteristics will have been assessed prior to CT scanning and, therefore, blinded by default. However, where it is not clear that this is the case, studies have been scored unclear. Blinding of the index test results when reading the reference standard may have been thought unethical, although no study examined this issue. It was difficult to assess to what extent a lack of blinding has influenced results. Clinical review bias scored a little better as retrospective studies by definition reflect real-life practice, but overall scored poorly or unclear. Uninterpretable results were rarely discussed. In the one case where they were,108 it was unclear how these results were treated for analysis. Withdrawals were generally not reported and, as there was no evidence to suggest that there were any withdrawals to report, all but one study59 scored well for this item.
Children
The methodological quality assessment of each included study is summarised in Figures 17 and 18. Overall, most of the included studies were poorly reported and did not satisfy the majority of the quality assessment items of the QUADAS tool.
FIGURE 17.
Individual clinical characteristics in children and infants with MHI – methodological quality graph. Review authors’ judgements about each methodological quality item presented as percentages across all included studies.
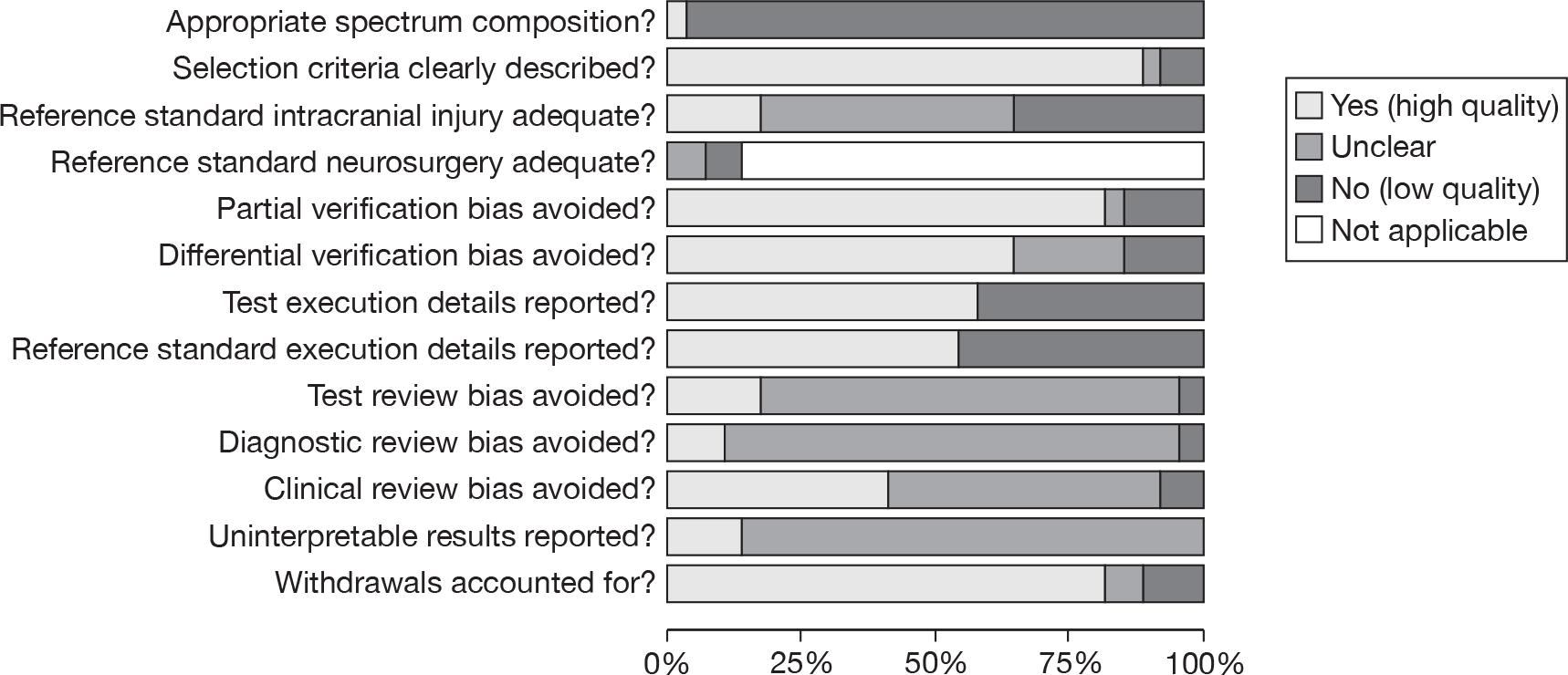
FIGURE 18.
Individual clinical characteristics in children and infants with MHI – methodological quality summary. Review authors’ judgements about each methodological quality item for each included study. Minus sign, negative score; plus sign, positive score; question mark, unclear whether item scores negatively or positively; blank space, not applicable.
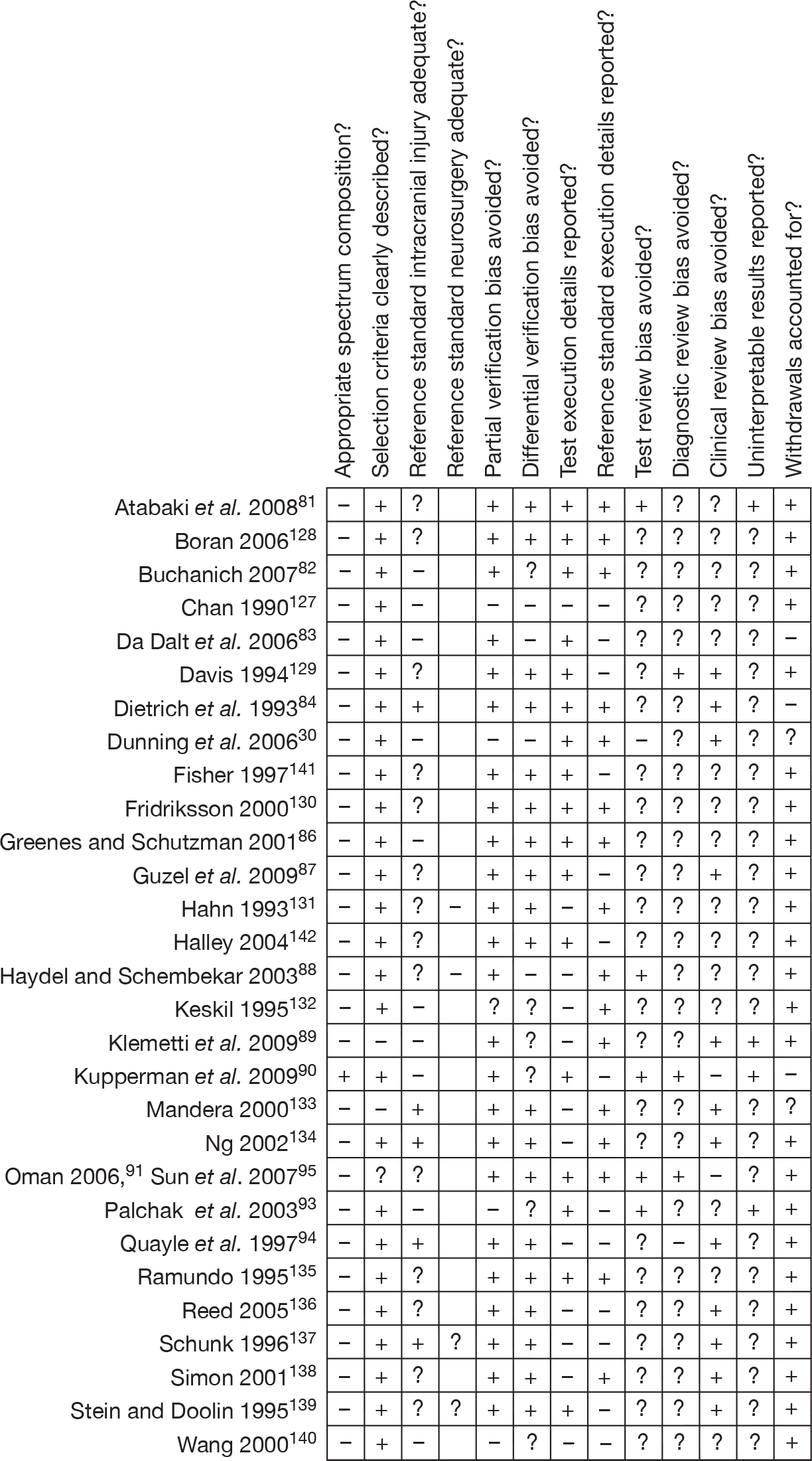
The main source of variation was patient spectrum, for which only one study scored positively90 (further details are in Description of included studies). Only five studies used an adequate reference standard for ICI,84,94,133,134,137 with the majority scoring unclear or negatively, including the two very large cohorts. 30,90 Although 13 studies81,87,88,91,95,128–130,135,136,138,139,141,142 did carry out CT in all participants, they failed to state whether this was within 24 hours and were therefore scored unclear. Of the four88,131,137,139 studies that reported the outcome data for neurosurgery, none reported an adequate reference standard: two reported an inadequate reference standard and two were unclear on this point.
Partial verification bias was largely avoided, with 24 studies81–84,86–91,94,128–131,133–139,141,142 scoring well for this item, although one of the large cohorts scored negatively. 30 Similarly, studies scored well generally for differential verification bias, with reference standards being applied to the whole cohort in 19 cases. 81,84,86,87,91,94,128–131,133–139,141,142 For the two very large cohorts, one study scored negatively for this item,30 whereas for the other study90 the reference standard was determined at the physician’s discretion so the item scored unclear.
The execution of the index test was reported more often than the reference standard. Test review and diagnostic review biases were largely unreported. Blinding of the index test results when reading the reference standard may have been thought unethical, though no study examined this issue. Clinical review bias scored a little better as retrospective studies by definition reflect real-life practice, but over half scored poorly or unclear. Uninterpretable results were discussed in only one study,81 with reference to a single uninterpretable CT scan that was treated as a positive. Withdrawals were generally not reported and, as there was no evidence to suggest that there were any withdrawals to report, most studies scored well for this item.
Summary of test accuracy results: individual characteristics
Adults
Tables 13 and 14 show the sensitivity, specificity, PLR and NLR for each individual clinical characteristic for predicting ICI or need for neurosurgery in adults. Further details are provided in Appendix 5. Only individual clinical characteristics that were defined consistently and in a clinically meaningful way were included in the meta-analysis. Two studies108,126 were excluded from the meta-analysis because they did not define the characteristics they reported (neurological examination) in a way similar enough to other studies to be meaningfully meta-analysed.
| Clinical characteristic | No. of studies | Heterogeneity test p-valuea | Pooled estimates | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Intoxication | 10 | < 0.001 | < 0.001 | 21.4 | 13.5 to 31.4 | 84.6 | 76.7 to 90.3 | 0.931 | 0.844 to 1.007 | 1.38 | 0.97 to 1.99 |
| Fall – any | 10 | < 0.001 | < 0.001 | 31.3 | 20.3 to 44.3 | 72.0 | 62.2 to 80.2 | 0.953 | 0.871 to 1.024 | 1.12 | 0.93 to 1.29 |
| Fall from a height | 1 | NA | NA | 28.0 | 17.3 to 41.9 | 87.8 | 85.6 to 89.6 | 0.820 | 0.689 to 0.977 | 2.29 | 1.43 to 3.68 |
| Dizziness | 3 | 0.482 | 0.267 | 18.7 | 11.9 to 27.3 | 73.8 | 70.2 to 78.1 | 1.101 | 0.970 to 1.217 | 0.72 | 0.44 to 1.09 |
| Coagulopathy | 8 | < 0.001 | < 0.001 | 4.9 | 0.6 to 16.0 | 98.2 | 93.3 to 99.8 | 0.968 | 0.897 to 0.999 | 3.27 | 1.21 to 7.52 |
| Chronic alcohol | 4 | < 0.001 | < 0.001 | 5.9 | 0.7 to 40.8 | 97.6 | 49.5 to 99.8 | 0.973 | 0.933 to 1.186 | 2.00 | 0.79 to 9.03 |
| Assault | 8 | < 0.001 | < 0.001 | 14.1 | 3.9 to 36.0 | 86.2 | 67.4 to 95.4 | 0.997 | 0.924 to 1.038 | 1.02 | 0.68 to 1.33 |
| Age > 60 years | 7 | < 0.001 | < 0.001 | 23.9 | 14.5 to 36.5 | 88.0 | 78.1 to 93.8 | 0.868 | 0.785 to 0.925 | 1.97 | 1.48 to 2.81 |
| Visual symptoms | 3 | 0.265 | < 0.001 | 2.4 | 0.0 to 21.4 | 94.2 | 70.7 to 99.3 | 1.033 | 0.940 to 1.199 | 0.39 | 0.00 to 2.49 |
| Prior neurosurgery | 3 | 0.231 | < 0.001 | 1.9 | 0.3 to 5.1 | 99.8 | 92.3 to 100.0 | 0.985 | 0.969 to 1.030 | 8.67 | 0.62 to 308.90 |
| Motor vehicle collision – pedestrian | 6 | 0.182 | < 0.001 | 15.9 | 10.9 to 21.3 | 95.4 | 91.9 to 97.8 | 0.882 | 0.836 to 0.923 | 3.43 | 2.27 to 6.45 |
| Motor vehicle collision – in car | 10 | < 0.001 | < 0.001 | 17.7 | 8.7 to 31.0 | 74.4 | 57.7 to 86.0 | 1.108 | 1.031 to 1.218 | 0.69 | 0.53 to 0.86 |
| Motor vehicle collision with bicycle | 2 | 0.011 | < 0.001 | 10.6 | 6.4 to 16.9 | 89.0 | 87.3 to 90.5 | 0.963 | 0.601 to 1.543 | 1.67 | 1.01 to 2.75 |
| Any seizure | 10 | 0.262 | < 0.001 | 2.8 | 1.1 to 5.1 | 99.0 | 96.2 to 99.7 | 0.984 | 0.970 to 0.996 | 2.59 | 1.20 to 6.40 |
| Any LOC | 17 | < 0.001 | < 0.001 | 59.9 | 43.0 to 75.8 | 58.0 | 39.5 to 74.1 | 0.698 | 0.532 to 0.871 | 1.41 | 1.14 to 1.84 |
| Any headache | 13 | < 0.001 | < 0.001 | 36.8 | 25.5 to 50.5 | 70.3 | 57.3 to 79.8 | 0.901 | 0.792 to 1.005 | 1.23 | 0.99 to 1.55 |
| Undefined vomiting | 10 | < 0.001 | < 0.001 | 20.2 | 13.7 to 28.3 | 92.2 | 85.8 to 95.9 | 0.868 | 0.794 to 0.935 | 2.58 | 1.52 to 4.49 |
| Undefined or mixed amnesia | 7 | < 0.001 | < 0.001 | 50.9 | 24.5 to 77.9 | 60.0 | 35.3 to 79.7 | 0.815 | 0.579 to 1.008 | 1.27 | 0.98 to 1.59 |
| PTS | 2 | 0.002 | 0.002 | 7.9 | 6.0 to 10.4 | 99.4 | 99.2 to 99.5 | 0.921 | 0.841 to 1.009 | 12.39 | 8.41 to 18.24 |
| Severe or persistent headache | 2 | < 0.001 | < 0.001 | 19.4 | 16.8 to 22.2 | 80.5 | 79.9 to 81.2 | 1.028 | 0.959 to 1.101 | 1.00 | 0.86 to 1.16 |
| Persistent vomiting | 4 | < 0.001 | < 0.001 | 16.1 | 3.0 to 50.7 | 97.2 | 69.3 to 99.9 | 0.871 | 0.659 to 0.983 | 5.53 | 1.33 to 30.12 |
| Retrograde amnesia | 4 | < 0.001 | < 0.001 | 44.3 | 36.9 to 55.2 | 81.6 | 56.7 to 91.6 | 0.687 | 0.635 to 0.848 | 2.41 | 1.21 to 4.55 |
| Anterograde or post-traumatic amnesia | 6 | < 0.001 | < 0.001 | 16.2 | 6.8 to 30.9 | 91.9 | 83.2 to 96.4 | 0.912 | 0.825 to 0.972 | 1.95 | 1.48 to 2.62 |
| GCS < 15 | 25 | < 0.001 | < 0.001 | 44.9 | 37.7 to 51.8 | 86.7 | 80.6 to 91.2 | 0.638 | 0.557 to 0.722 | 3.35 | 2.31 to 5.03 |
| GCS < 14 | 12 | < 0.001 | < 0.001 | 15.0 | 11.4 to 18.9 | 96.0 | 94.3 to 97.4 | 0.885 | 0.853 to 0.915 | 3.81 | 2.87 to 4.93 |
| GCS decrease | 3 | 0.024 | < 0.001 | 27.3 | 20.8 to 36.7 | 95.7 | 83.4 to 98.8 | 0.763 | 0.711 to 0.822 | 6.39 | 2.05 to 19.33 |
| Focal neurological deficit | 8 | < 0.001 | < 0.001 | 6.6 | 1.2 to 16.9 | 98.6 | 95.2 to 99.8 | 0.95 | 0.84 to 1.01 | 9.671 | 0.663 to 38.950 |
| Depressed skull fracture | 2 | 0.004 | 0.452 | 9.1 | 5.5 to 14.5 | 99.9 | 99.6 to 100.0 | 0.967 | 0.819 to 1.141 | 102.15 | 13.13 to 794.41 |
| Basal skull fracture | 8 | < 0.001 | < 0.001 | 21.1 | 8.4 to 33.9 | 98.4 | 90.5 to 100.0 | 0.80 | 0.72 to 0.92 | 54.070 | 3.594 to 353.700 |
| Radiological skull fracture | 8 | < 0.001 | < 0.001 | 29.8 | 9.8 to 55.9 | 97.4 | 94.2 to 99.2 | 0.720 | 0.455 to 0.923 | 14.26 | 3.68 to 38.43 |
| Clinical characteristic | No. of studies | Heterogeneity test p-valuea | Pooled estimates | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Fall – any | 2 | 0.952 | 0.002 | 17.9 | 5.2 to 46.1 | 74.4 | 72.3 to 76.5 | 1.027 | 0.334 to 3.159 | 0.91 | 0.29 to 2.83 |
| Assault | 1 | NA | NA | 63.6 | 33.9 to 85.7 | 83.2 | 78.4 to 87.0 | 0.437 | 0.200 to 0.957 | 3.78 | 2.26 to 6.32 |
| Motor vehicle collision – pedestrian | 1 | NA | NA | 4.5 | 0.3 to 44.8 | 85.9 | 81.4 to 89.5 | 1.111 | 0.969 to 1.274 | 0.32 | 0.02 to 4.91 |
| Motor vehicle collision – in car | 2 | 0.498 | 0.291 | 8.5 | 1.2 to 42.5 | 58.4 | 56.1 to 60.8 | 1.546 | 0.243 to 9.826 | 0.21 | 0.03 to 1.36 |
| GCS < 15 | 7 | 0.026 | < 0.001 | 53.1 | 34.8 to 73.1 | 86.8 | 62.3 to 96.2 | 0.546 | 0.310 to 0.881 | 4.00 | 1.24 to 14.61 |
| GCS < 14 | 5 | 0.271 | < 0.001 | 21.0 | 10.0 to 33.4 | 94.3 | 84.9 to 98.0 | 0.839 | 0.684 to 1.042 | 3.67 | 0.75 to 15.81 |
| Focal neurological deficit | 1 | NA | NA | 50.0 | 20.0 to 80.0 | 93.7 | 90.7 to 95.8 | 0.534 | 0.125 to 2.272 | 7.93 | 1.86 to 33.79 |
| Depressed skull fracture | 1 | NA | NA | 60.0 | 20.0 to 90.0 | 99.98 | 99.6 to 100.0 | 0.400 | 0.137 to 1.171 | 2.56 | 146.6 to 44,909 |
| Any LOC | 1 | NA | NA | 16.7 | 1.0 to 80.6 | 38.7 | 36.1 to 41.3 | 2.156 | 0.103 to 44.998 | 0.27 | 0.01 to 5.67 |
| Any headache | 1 | NA | NA | 25.0 | 3.4 to 76.2 | 78.5 | 73.0 to 83.0 | 0.956 | 0.098 to 9.368 | 1.16 | 0.12 to 11.38 |
| Undefined vomiting | 2 | 0.858 | 0.015 | 22.3 | 5.6 to 58.1 | 94.6 | 93.6 to 95.4 | 0.811 | 0.386 to 1.706 | 6.41 | 1.50 to 27.33 |
| Undefined or mixed amnesia | 1 | NA | NA | 16.7 | 1.0 to 80.6 | 61.1 | 58.5 to 63.7 | 1.363 | 0.065 to 28.451 | 0.43 | 0.02 to 8.95 |
| Severe or persistent headache | 1 | NA | NA | 20.0 | 2.7 to 69.1 | 67.7 | 65.7 to 69.6 | 1.182 | 0.132 to 10.596 | 0.62 | 0.07 to 5.55 |
| Radiological skull fracture | 3 | 0.004 | < 0.001 | 43.1 | 31.0 to 58.6 | 91.3 | 87.3 to 94.1 | 0.623 | 0.444 to 0.788 | 4.99 | 2.48 to 9.48 |
| PTS | 1 | NA | NA | 8.3 | 0.5 to 62.2 | 96.3 | 92.0 to 98.3 | 0.952 | 0.924 to 0.982 | 0.09 | 0.01 to 1.38 |
The PLR indicates how useful each characteristic is for ruling injury in, whereas the NLR indicates how useful it is for ruling injury out. In general, clinical assessment contributes to diagnosis by identifying features that increase the risk of ICI. There are no clinical or radiological characteristics that can be used individually to rule out ICI. The only test that does have a rule-out role is S100B with a NLR of 0.076 (further details are provided – see Biomarkers).
Depressed, basal or radiological skull fracture and PTS each substantially increased the likelihood of ICI (PLR > 10). These findings are of mainly historical interest, as CT scanning has generally replaced skull radiology. Skull fractures are now usually identified on CT scanning, which will also show the ICI.
Clinical characteristics appear to be more useful if they are precisely defined. Focal neurological deficit, persistent vomiting, decrease in GCS and previous neurosurgery all markedly increased the likelihood of ICI (PLR 5–10). However, the last was only assessed in three studies, was subject to significant heterogeneity and had a CI for the PLR crossing 1. Fall from a height, coagulopathy, chronic alcohol use, age over 60 years, pedestrian MVA, any seizure, undefined vomiting, retrograde or anterograde amnesia GCS < 14 and GCS < 15 moderately increased the risk of ICI (PLR 2–5). Meanwhile, LOC and headache (even if severe) appear to be of little value in diagnosing ICI.
Only a few studies have assessed the value of individual characteristics to diagnose specifically neurosurgical injury, so only limited conclusions can be drawn. GCS < 15 has some limited value for both ruling in and ruling out neurosurgical injury (i.e. a normal GCS reduces the likelihood of neurosurgical injury). Focal neurological injury, vomiting and radiological skull fracture all increased the likelihood of neurosurgical injury. The failure to demonstrate diagnostic value of many characteristics for diagnosing neurosurgical injury probably reflects the limited data available for this outcome and should not be interpreted as showing that individual characteristics are of limited value. There are good theoretical reasons to anticipate that characteristics that are useful for diagnosing any ICI will also be valuable for diagnosing specifically neurosurgical injury.
Children
Tables 15 and 16 show the sensitivity, specificity, PLR and NLR for each individual clinical characteristic for predicting ICI or need for neurosurgery in children. Further details are provided in Appendix 6. Corresponding data are provided in Table 17 for infants; however, no studies evaluated the diagnostic accuracy of individual clinical characteristics for predicting the need for neurosurgery in infants. Further details are also provided in Appendix 6.
| Clinical characteristic | No. of studies | Heterogeneity test p-valuea | Pooled estimates | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Intoxication | 4 | 0.689 | < 0.001 | 3.8 | 1.8 to 6.4 | 98.6 | 90.2 to 99.8 | 0.976 | 0.946 to 1.072 | 2.72 | 0.29 to 26.06 |
| Fall – any | 5 | < 0.001 | < 0.001 | 34.7 | 17.0 to 56.5 | 54.7 | 49.1 to 60.6 | 1.206 | 0.726 to 1.683 | 0.78 | 0.34 to 1.41 |
| Fall from a height | 2 | 0.423 | 0.421 | 20.0 | 15.8 to 25.0 | 80.2 | 79.7 to 80.7 | 0.991 | 0.787 to 1.247 | 1.01 | 0.80 to 1.28 |
| Dizziness | 3 | 0.881 | 0.012 | 5.2 | 0.6 to 13.3 | 93.5 | 85.7 to 98.5 | 1.014 | 0.910 to 1.109 | 0.79 | 0.11 to 4.30 |
| Coagulopathy | 2 | 0.010 | < 0.001 | 5.8 | 3.2 to 10.5 | 99.7 | 99.6 to 99.8 | 0.942 | 0.520 to 1.706 | 6.56 | 3.08 to 14.00 |
| Assault | 2 | 0.648 | 0.017 | 3.4 | 1.9 to 6.0 | 95.9 | 95.6 to 96.1 | 1.010 | 0.565 to 1.805 | 0.79 | 0.44 to 1.42 |
| Visual symptoms | 2 | < 0.001 | 0.933 | 9.1 | 5.6 to 14.5 | 98.9 | 98.8 to 99.1 | 0.864 | 0.549 to 1.360 | 3.51 | 1.63 to 7.57 |
| Prior neurosurgery | 1 | NA | NA | 0.7 | 0.2 to 2.8 | 99.9 | 99.8 to 99.9 | 0.994 | 0.984 to 1.004 | 5.93 | 1.42 to 24.81 |
| Motor vehicle collision – pedestrian | 6 | < 0.001 | < 0.001 | 19.4 | 9.0 to 30.2 | 91.9 | 81.7 to 96.6 | 0.883 | 0.754 to 1.043 | 2.32 | 0.75 to 6.56 |
| Motor vehicle collision – in car | 5 | < 0.001 | < 0.001 | 15.2 | 5.6 to 31.7 | 90.0 | 67.9 to 98.4 | 0.947 | 0.870 to 1.065 | 1.99 | 0.82 to 4.30 |
| Motor vehicle collision with bicycle | 1 | NA | NA | 15.3 | 11.5 to 20.0 | 96.7 | 96.5 to 96.9 | 0.876 | 0.833 to 0.921 | 4.63 | 3.49 to 6.15 |
| Any seizure | 9 | 0.602 | < 0.001 | 10.0 | 7.3 to 13.3 | 96.3 | 91.9 to 98.3 | 0.935 | 0.899 to 0.987 | 2.69 | 1.17 to 6.24 |
| Any LOC | 17 | < 0.001 | < 0.001 | 45.9 | 36.4 to 55.6 | 80.1 | 67.4 to 87.3 | 0.679 | 0.566 to 0.814 | 2.30 | 1.46 to 3.47 |
| Any headache | 14 | < 0.001 | < 0.001 | 33.9 | 22.9 to 47.6 | 73.3 | 62.1 to 81.3 | 0.905 | 0.784 to 1.010 | 1.26 | 0.97 to 1.61 |
| Undefined vomiting | 14 | < 0.001 | < 0.001 | 30.9 | 21.6 to 40.1 | 76.0 | 68.1 to 83.8 | 0.910 | 0.774 to 1.059 | 1.29 | 0.85 to 1.99 |
| Undefined or mixed amnesia | 8 | < 0.001 | < 0.001 | 33.4 | 17.8 to 52.4 | 81.4 | 63.1 to 93.3 | 0.821 | 0.642 to 0.998 | 1.82 | 1.00 to 3.74 |
| Undefined or mixed amnesia | 8 | < 0.001 | < 0.001 | 33.4 | 17.8 to 52.4 | 81.4 | 63.1 to 93.3 | 0.821 | 0.642 to 0.998 | 1.82 | 1.00 to 3.74 |
| Severe or persistent headache | 5 | < 0.001 | < 0.001 | 13.5 | 7.8 to 21.5 | 94.9 | 81.8 to 99.3 | 0.916 | 0.872 to 0.986 | 4.35 | 1.07 to 12.35 |
| Persistent vomiting | 4 | 0.028 | < 0.001 | 22.1 | 10.7 to 40.6 | 92.9 | 87.4 to 96.8 | 0.840 | 0.635 to 0.969 | 3.14 | 1.30 to 8.05 |
| Anterograde or post-trauma amnesia | 1 | NA | NA | 20.9 | 12.8 to 32.3 | 93.0 | 89.2 to 95.5 | 0.851 | 0.401 to 1.804 | 2.97 | 1.40 to 6.29 |
| PTS | 5 | 0.493 | 0.810 | 8.7 | 4.2 to 15.7 | 98.0 | 94.5 to 99.6 | 0.932 | 0.849 to 1.004 | 8.49 | 0.93 to 31.66 |
| Scalp laceration | 3 | 0.002 | 0.051 | 7.4 | 0.1 to 33.7 | 89.1 | 83.0 to 94.7 | 1.040 | 0.782 to 1.107 | 0.67 | 0.02 to 2.27 |
| Scalp haematoma | 5 | < 0.001 | < 0.001 | 45.4 | 27.0 to 57.6 | 73.1 | 64.9 to 82.5 | 0.745 | 0.615 to 0.918 | 1.70 | 1.30 to 2.23 |
| GCS < 15 | 12 | < 0.001 | < 0.001 | 46.3 | 29.6 to 64.2 | 89.6 | 81.1 to 94.7 | 0.602 | 0.418 to 0.765 | 4.42 | 2.63 to 7.66 |
| GCS < 14 | 5 | < 0.001 | < 0.001 | 40.4 | 12.8 to 77.5 | 89.1 | 18.9 to 99.6 | 0.718 | 0.429 to 1.674 | 3.58 | 0.80 to 46.84 |
| Focal neurological deficit | 10 | < 0.001 | < 0.001 | 21.1 | 8.8 to 41.1 | 99.0 | 95.4 to 99.8 | 0.798 | 0.615 to 0.915 | 20.46 | 7.40 to 54.24 |
| Depressed skull fracture | 2 | 0.032 | < 0.001 | 16.0 | 12.4 to 20.5 | 99.8 | 99.7 to 99.9 | 0.855 | 0.756 to 0.966 | 73.82 | 46.45 to 117.32 |
| Basal skull fracture | 5 | < 0.001 | < 0.001 | 17.8 | 7.8 to 31.7 | 98.7 | 96.5 to 99.6 | 0.833 | 0.703 to 0.929 | 16.90 | 6.13 to 32.44 |
| Radiological skull fracture | 7 | < 0.001 | < 0.001 | 48.4 | 40.8 to 57.3 | 89.3 | 67.7 to 97.3 | 0.585 | 0.516 to 0.708 | 4.55 | 1.64 to 15.73 |
| Clinical characteristic | No. of studies | Heterogeneity test p-valuea | Pooled estimates | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| GCS < 14 | 2 | 0.912 | < 0.001 | 24.2 | 16.5 to 34.0 | 88.9 | 87.2 to 90.5 | 0.863 | 0.677 to 1.102 | 2.10 | 1.34 to 3.28 |
| Any seizure | 1 | NA | NA | 33.3 | 4.3 to 84.6 | 92.3 | 88.7 to 94.8 | 0.723 | 0.324 to 1.610 | 4.31 | 0.83 to 22.33 |
| PTS | 1 | NA | NA | 8.3 | 0.5 to 62.2 | 96.3 | 92.0 to 98.3 | 0.952 | 0.924 to 0.982 | 0.09 | 0.01 to 1.38 |
| Any LOC | 1 | NA | NA | 16.7 | 1.0 to 80.6 | 73.9 | 68.7 to 78.5 | 1.128 | 0.054 to 23.748 | 0.64 | 0.03 to 13.43 |
| Any headache | 2 | 0.161 | 0.479 | 64.2 | 26.6 to 89.9 | 68.9 | 64.6 to 72.9 | 0.267 | 0.186 to 0.384 | 2.39 | 1.60 to 3.58 |
| Undefined vomiting | 2 | 0.638 | < 0.001 | 55.3 | 24.6 to 82.4 | 70.4 | 66.1 to 74.4 | 0.558 | 0.316 to 0.986 | 2.36 | 0.96 to 5.83 |
| Undefined or mixed amnesia | 1 | NA | NA | 16.7 | 1.0 to 80.6 | 80.0 | 75.2 to 84.1 | 1.042 | 0.049 to 21.976 | 0.83 | 0.04 to 17.58 |
| Radiological skull fracture | 1 | NA | NA | 73.1 | 61.3 to 82.4 | 53.3 | 49.7 to 56.9 | 0.504 | 0.337 to 0.752 | 1.57 | 1.33 to 1.85 |
| GCS < 15 | 2 | 0.298 | < 0.001 | 45.1 | 35.1 to 55.4 | 74.3 | 72.0 to 76.5 | 0.763 | 0.573 to 1.015 | 1.71 | 1.24 to 2.36 |
| Clinical characteristic | No. of studies | Heterogeneity test p-valuea | Pooled estimates | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Fall – any | 2 | 0.771 | 0.620 | 66.6 | 48.3 to 81.0 | 24.1 | 16.8 to 33.3 | 1.365 | 0.893 to 2.085 | 0.88 | 0.67 to 1.16 |
| Motor vehicle collision – in car | 1 | NA | NA | 25.0 | 6.3 to 62.3 | 93.1 | 76.2 to 98.3 | 0.806 | 0.533 to 1.216 | 3.63 | 0.60 to 21.86 |
| Coagulopathy | 1 | NA | NA | 4.0 | 0.6 to 23.5 | 97.0 | 94.2 to 98.5 | 0.990 | 0.911 to 1.075 | 1.33 | 0.17 to 10.16 |
| Any seizure | 2 | 0.858 | 0.017 | 13.7 | 2.8 to 47.2 | 84.3 | 69.5 to 92.7 | 1.066 | 0.240 to 4.730 | 1.32 | 0.23 to 7.55 |
| Any LOC | 4 | < 0.001 | < 0.001 | 39.4 | 20.6 to 65.2 | 84.1 | 56.2 to 95.5 | 0.730 | 0.519 to 0.901 | 2.51 | 1.23 to 5.28 |
| Undefined vomiting | 2 | 0.858 | 0.991 | 13.7 | 2.8 to 47.2 | 79.4 | 70.2 to 86.3 | 1.155 | 0.583 to 2.289 | 0.67 | 0.12 to 3.65 |
| PTS | 1 | NA | NA | 8.0 | 2.0 to 26.9 | 91.0 | 87.1 to 93.8 | 1.011 | 0.896 to 1.141 | 0.89 | 0.22 to 3.53 |
| Persistent vomiting | 1 | NA | NA | 13.0 | 4.5 to 32.4 | 87.0 | 82.6 to 90.4 | 1.000 | 0.296 to 3.373 | 1.00 | 0.30 to 3.37 |
| GCS < 15 | 3 | 0.004 | < 0.001 | 51.9 | 34.4 to 75.8 | 84.5 | 45.8 to 95.2 | 0.586 | 0.377 to 0.791 | 3.38 | 1.24 to 8.02 |
| Scalp haematoma | 2 | 0.927 | 0.312 | 65.8 | 56.9 to 73.6 | 56.1 | 55.1 to 57.0 | 0.605 | 0.531 to 0.689 | 1.51 | 1.33 to 1.73 |
| Focal neurological deficit | 1 | NA | NA | 33.3 | 4.3 to 84.6 | 97.1 | 89.0 to 99.3 | 0.687 | 0.043 to 11.098 | 11.33 | 0.70 to 183.11 |
| Radiological skull fracture | 2 | 0.058 | < 0.001 | 64.7 | 44.8 to 80.5 | 81.4 | 76.8 to 85.3 | 0.051 | 0.046 to 0.057 | 4.51 | 3.45 to 5.88 |
| Depressed skull fracture | 1 | NA | NA | 25.0 | 6.3 to 62.3 | 98.3 | 78.0 to 99.9 | 0.763 | 0.510 to 1.142 | 14.50 | 0.72 to 290.82 |
Only individual clinical characteristics that were defined consistently and in a clinically meaningful way were included in the meta-analyses. Three studies93,141,142 were excluded from the meta-analysis because they did not define the characteristics they reported (neurological examination,141 clinical signs of skull fracture93 and physical examination)142 in a way similar enough to other studies to be meaningfully meta-analysed.
As with adults, clinical assessment is generally used to identify features that increase the likelihood of ICI, although both the absence of any LOC and a normal GCS moderately reduced the likelihood of ICI. The most useful characteristics were depressed or basal skull fracture and focal neurological deficit (PLR > 10), although, as mentioned above, skull fractures are usually identified on CT scanning, so the clinical utility of the impressive PLR is limited. Coagulopathy, PTS and previous neurosurgery (albeit in only one study) all markedly increased the likelihood of ICI (PLR 5–10). Visual symptoms, bicycle and pedestrian MVA, any seizure, LOC, vomiting, severe or persistent headache, anterograde or retrograde amnesia, GCS < 14, GCS < 15 and radiological skull fracture all moderately increased the likelihood of ICI (PLR 2–5). Meanwhile, headache (other than severe or persistent), scalp haematoma and scalp laceration were not diagnostically useful.
There were only four studies88,131,137,139 that reported neurosurgical injury as an outcome, so only very limited conclusions can be drawn and, as suggested with adults, it may be more appropriate to simply extrapolate from estimates for any ICI. The absence of radiological fracture had some value for ruling out neurosurgical injury. GCS < 14, seizure, headache and vomiting each moderately increased the likelihood of neurosurgical injury.
The results for infants were based on a small number of heterogeneous studies, so the results should be interpreted with caution. The failure to show diagnostic value for some characteristics may reflect the limitations of the data rather than a genuine lack of value. Both depressed skull fracture and focal neurological deficit substantially increased the likelihood of ICI. Radiological skull fracture, GCS < 15 and any LOC moderately increased the likelihood of ICI.
Biomarkers
Description of included studies (design and patient characteristics)
The design and patient characteristics of the 12 studies98,113,115,130,143–150 that evaluated the diagnostic accuracy of various biochemical markers for diagnosing ICI (including the need for neurosurgery) in adults and children with MHI are summarised in Table 18. Nine studies provided diagnostic data on protein S100B only,98,113,115,143–149 one on NSE only115,130 and one on other markers [creatine kinase isozyme (CK-BB), noradrenaline, adrenaline, dopamine, amylase and total catecholamines]. 150 One study115 provided diagnostic data on both protein S100B and NSE levels.
| Author, year | Derivation or validation cohort | Country | Setting | Design | Patients included, n | Mean age, years (range) | Prevalence of ICI, n | CT as inclusion? (yes/no) | Male, n | Patients with MHI, n | GCS, n | Other significant inclusion criteria | Other significant exclusion criteria |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Biochemical marker – S100B only | |||||||||||||
| Biberthaler et al. 2001149 | Derivation | Germany | ED | P, Cs | 52 | NR | 15/52 (28.8%) | No | 38/52 (73%) | 52/52 (100%) | NR | Isolated MHI (GCS 13–15 on admission) and one or more of amnesia, LOC, nausea, vomiting, vertigo or severe headache | Focal neurological deficits |
| Biberthaler et al. 2002143 | Derivation | Germany | ED | P, NR | 104 | NR | 24/104 (23.1%) | No | NR | 104/104 (100%) | NR | GCS 13–15, history of isolated minor head trauma, and at least one symptom: transient LOC (< 5 minutes), amnesia for the traumatic event, nausea, vomiting, vertigo and severe headache | |
| Biberthaler et al. 200698 | Derivation | Germany | Three trauma centres | P, Cs | 1309 | 47 (IQR 32–65) | 93/1309 (7.1%) | No | 855/1309 (65%) | 1309/1309 (100%) |
GCS 15: 1152/1309 (88%) GCS 14: 122/1309 (9.3%) GCS 13: 35/1309 (2.7%) |
Aged ≥ 18 years. Isolated head trauma, admitted within 3 hours, GCS 13–15 at admission, one or more of: brief LOC, PTA, nausea, vomiting, severe headache, dizziness, vertigo, intoxication, anticoagulation and age > 60 years | Pregnant women, prisoners and multiple-injured patients |
| Ingebrigtsen et al. 2000145 | Validation | Scandinavia | Neurology | P, NR | 182 | 33 (15–78) | 10/182 (5.5%) | No | 111 (61%) | 182/182 (100%) |
GCS 15: 138/182 (75.8%) GCS 14: 34/182 (18.7%) GCS 13:10/182 (5.5%) |
Aged 15–80 years. Head injury with brief (≤ 10 minutes) LOC/amnesia, GCS 13–15 at admission, no focal neurological deficits, patient admitted within 12 hours post injury, CT scan within 24 hours post injury | History of neurological disease |
| Muller et al. 2007113 | Derivation | Multi-national (Norway, UK, Switzerland, and Sweden) | Neurosurgery × 2, ED × 1, orthopaedics × 1 | P, NR | 226 | 39 (18–92) | 21/226 (9%) | No | 168/226 (74.3%) | 226/226 (100%) |
GCS 15: 180/226 (78%) GCS 14: 30/226 (13%) GCS 13: 16/226 (7%) |
Aged ≥18 years. Head injury, LOC or retrograde amnesia, GCS 13–15,blood sample and CT scan within 12 hours of trauma | Neurological or psychiatric disorder, focal neurological deficit, multiple injuries requiring immediate intervention, renal or liver disease |
| Poli-de-Figueiredo et al. 2006147 | Validation | Brazil | ED | P, Cs | 50 | NR | 6/50 (12%) | No | 28/50 (56%) | 50/50 (100%) |
GCS 15: 37/50 (74%) GCS 14: 11/50 (22%) GCS 13: 2/50 (4%) |
GCS 13–15 and at least one of amnesia, LOC, nausea, vomiting, vertigo or severe headache on admission | Patients with focal neurological deficits |
| Romner et al. 2000148 | Validation | Scandinavia | Neurology | P, NR | 278 | 32 (1–84) | 25/278 (9%) | No | 175/278 (63%) | 254/278 (91.4%) | NR | All ages. Mild, moderate and severe patients, with:
|
History of neurological disease |
| Morochovic et al. 2009146 | Validation | Slovakia | ED | P, Cs | 102 | 42 (12–84) | 18/102 (17.6%) | No | 71 (70%) |
102/102 (100%) |
GCS 15: 76/102 (74.6%) GCS 14: 23/102 (22.5%) GCS 13: 3/102 (2.9%) |
Mild TBI category 1–3 of EFNS classification (category 1: GCS 15, LOC < 30 minutes, PTA < 1 hour, no risk factors;a category 2: GCS 15 and risk factors;a category 3: GCS 13–14, LOC < 30 minutes, PTA < 1 hour ± risk factors)a |
Unknown time of injury/acute non-traumatic intracerebral lesions Category 0 of EFNS classification |
| Castellani et al. 2009144 | Validation | Austria | Paediatric | P, Sel | 109 | 9.5 (0.4–17.5) | 14/109 (12.8%) | Yes | 73 (67%) | 109/109 (100%) |
GCS 15: 86/109 (78.9%) GCS 14: 13/109 (11.9%) GCS 13: 10/109 (9.2%) |
Age < 18 years, blunt trauma, mild TBI (GCS 13–15 and vomiting, LOC, if > 4 years – persisting headache, retrograde amnesia, vertigo) | NR |
| Biochemical marker – NSE only | |||||||||||||
| Fridriksson et al. 2000130 | Derivation | USA | Paediatric ED | P, NR | 49 | NR (0.2–16) | 22/49 (45%) | Yes | 27/49 (55%) | 39/49 (79.6%) | NR | Blunt trauma (within 24 hours of injury) requiring head CT | Penetrating trauma, bleeding disorders, longer than 24 hours since injury |
| Biochemical marker – S100B and NSE only | |||||||||||||
| Mussack et al. 2002115 | Derivation | Germany | ED | P, Cs | 139 | 36 (28–60.1) | 19/139 (13.7%) | No | 106/139 (76.3%) | 139/139 (100%) |
GCS 15: 129/139 (92.8%), GCS 13/14: 10/129 (7.2%) |
History of trauma, GCS 13–15, at least one of following: transient LOC ( < 5 minutes), anterograde or retrograde amnesia, nausea, vomiting or vertigo | Those who refused CT, blood-drawing or suffered concurrent injuries that precluded CT |
| Biochemical marker – other multiple markers (CK-BB, noradrenaline, adrenaline, dopamine, amylase and total catecholamines) | |||||||||||||
| Levitt et al. 1995150 | Derivation | USA | ED | P, NR | 107 | NR | 9/107 (8.4%) | No | NR | NR | NR | Evidence of ethanol intoxication (odour on breath and confirmed with Alco-sensor intoximeter reading, serum levels gave exact levels) and apparently minor head trauma (external evidence such as laceration, contusion, haematoma, abrasion or history of injury by witnesses or out of hospital care personnel) | NR |
Of the 10 S100B studies, four were from Germany,98,115,143,149 three from Scandinavia (including one multinational project),113,145,148 and one each from Austria,144 Brazil147 and Slovakia. 146 Half of the studies were derivation studies, using receiver-operating characteristic (ROC) curve analysis of the study data to derive a best-fit value for optimising sensitivity and specificity. 98,113,115,143,149 The other five could be classed as validation studies, where a predefined cut-off value, based on derivation studies, was used to dichotomise patients into positive and negative for S100B. 98,113,115,143–149 Only one study looked exclusively at paediatric patients (0–18 years),144 with some specifically excluding them and other authors not reporting this parameter. Patients were recruited prospectively, mostly consecutively, although in some cases it was not reported if they had sustained an isolated head injury and presented to the hospital with GCS 13–15 and one or more additional symptoms including amnesia, LOC, nausea, vomiting, dizziness/vertigo and severe headache. These criteria were universal to all studies. Patients with focal neurological deficits, multiple injuries or a history of neurological disease were mostly excluded.
As technology has advanced, the methods for analysing blood samples for biomarkers have improved. Initial studies145,148 used the Sangtec 100 immunoradiometric assay kit (Sangtec Medical, Bromma, Sweden) with a detection limit of 0.2 µg/l. Subsequent researchers have advanced to more precise technology, such as the LIA-mat luminescence immunoassay115,149 (Byk-Sangtec Diagnostica, Dietzenbach FRG) or attempted to achieve more rapid results with the DiaSorin automated immunoluminometric Liaison assay113,115,143 (DiaSorin, Saluggia, Italy) or the Roche Elecsys S100 electrochemiluminometric assay (Roche, Basel, Switzerland). 143,144,146,147 Initial studies describe a delay of up to 24 hours between injury and blood sampling,148 but more recently it has been recognised that the short half-life of protein S100B necessitates more rapid sampling and analysis. Studies report this differently, but the majority of patients had blood samples taken within 3 hours, with only the two most recent studies extending this to up to 6 hours following injury.
One study115 investigating protein S100B also used separate samples to analyse NSE. This was in intoxicated adult patients presenting consecutively to the ED following symptomatic MHI, during Oktoberfest in Germany. Subjects who refused consent or had sustained extracranial injuries were excluded. Samples were taken in < 2 hours and all patients received a subsequent cranial CT. Samples were processed to citrated plasma and analysed using the fully automated electrochemiluminescence Elecsys NSE assay (Roche, Basel, Switzerland). Sample concentrations for CT-positive and CT-negative groups were compared for any statistically significant difference. A subsequent ROC curve was generated. The second study into NSE prospectively recruited 49 children, age 0–18 years, presenting within 24 hours of any severity head injury (39 mild and 10 moderate/severe) and selected patients on the basis of requiring CT. The mean time from injury to sample was around 4 hours (± 3 hours) and samples were processed using a radioimmunoassay technique. CT-positive and CT-negative group results were compared using the Student’s t-test and a subsequent ROC curve was generated.
In the only study identified investigating other biochemical markers,150 patients were recruited consecutively if they presented following a MHI (evidence of external head trauma or witnessed injury) and demonstrated evidence of alcohol intoxication (clinically or upon investigation). Serum samples were taken upon recruitment and prior to CT scan with a mean time from injury to evaluation of 1.5 ± 0.2 hours. All subjects received a CT scan, which was assessed for any acute ICI. Multiple biomarkers were tested for in each sample and results were analysed independently of CT findings. ROC curves were generated for each biomarker, with a statistically significant difference in CT-positive and CT-negative groups (unpaired t-test) and, from these, different values were calculated to optimise both sensitivity and specificity and then to achieve a sensitivity of 100%.
Quality of included studies
The quality assessment of each included study is summarised in Figures 19 and 20. Although the patient selection criteria were consistent and clearly described across all studies, no study met all of the QUADAS criteria, as nearly all patients were chosen selectively by being symptomatic at presentation. Although an argument could be made for the fact that these biochemical markers should be used in conjunction with clinical assessment, from a quality-control perspective testing should take place in an undifferentiated sample of subjects for whom the condition has been universally applied, in this case any patient having suffered a MHI.
FIGURE 19.
Biochemical markers for MHI – methodological quality graph. Review authors’ judgements about each methodological quality item presented as percentages across all included studies.
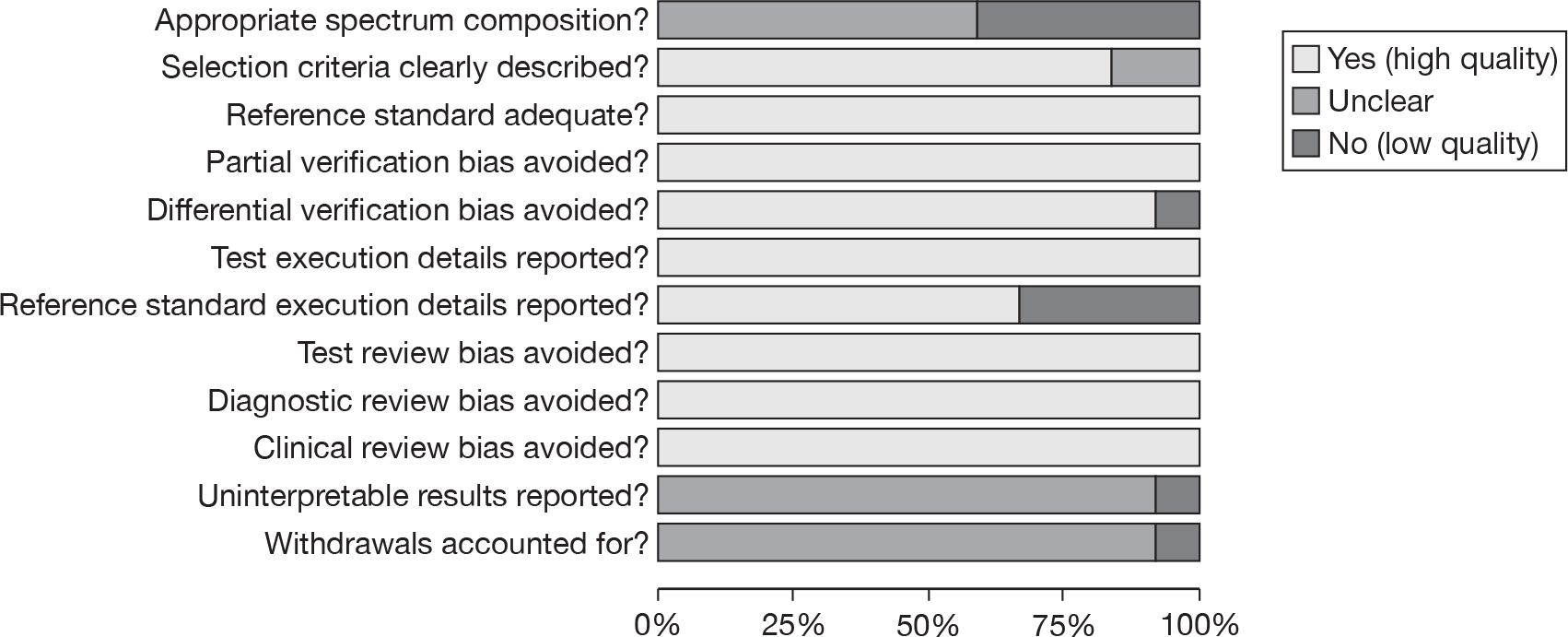
FIGURE 20.
Biochemical markers for MHI – methodological quality summary. Review authors’ judgements about each methodological quality item for each included study. Minus sign, negative score; plus sign, positive score; question mark, unclear whether item scores negatively or positively; blank space, not applicable.
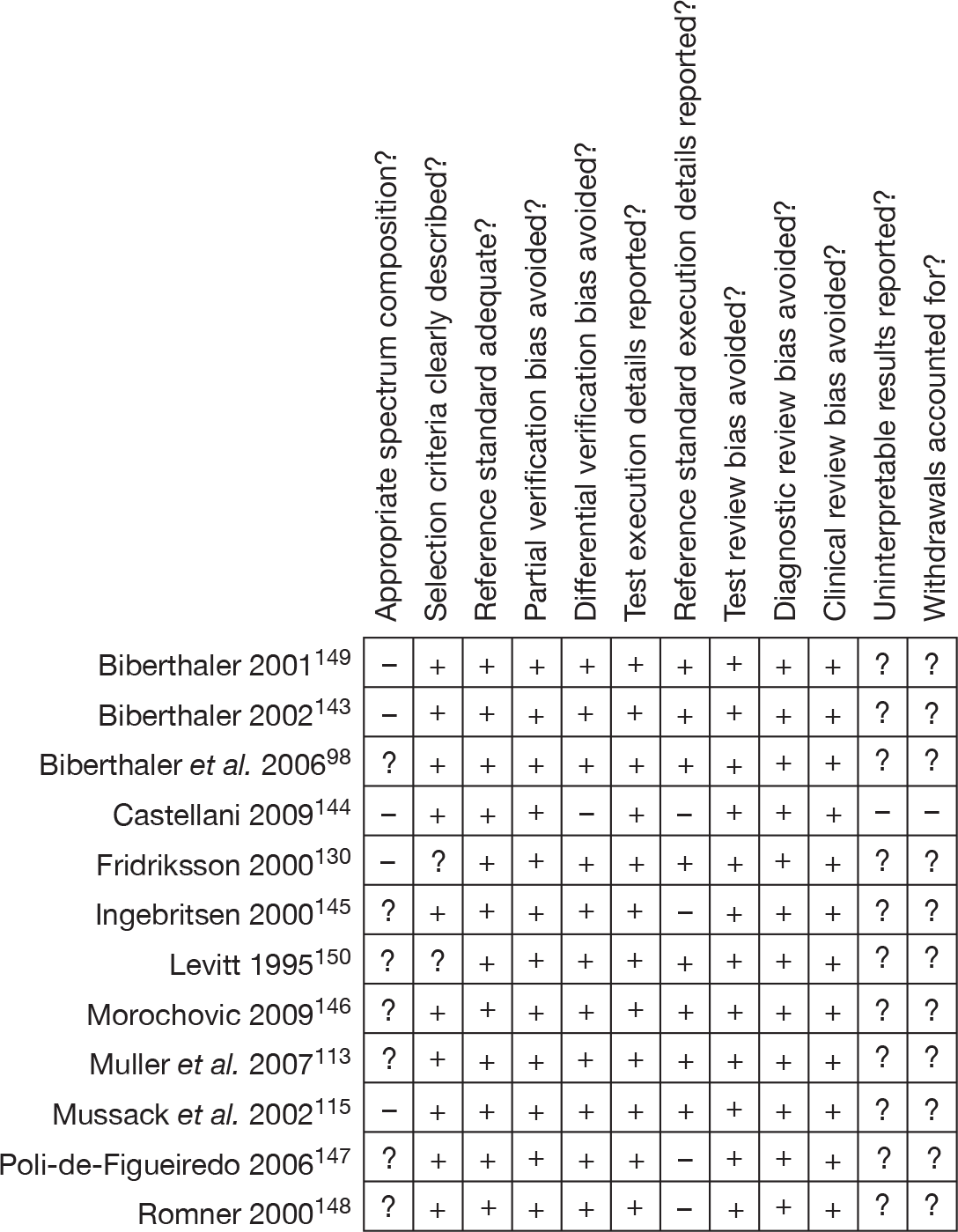
All patients received both the index test and reference standard, with the results being interpreted independently. Castellani et al. 144 selectively included those patients undergoing CT from a larger cohort of potential subjects, contributing to patient spectrum bias. Differential verification bias was generally avoided for ICI, with no studies focusing on neurosurgical injury. Test execution was inconsistently described across all studies, particularly the details of CT scan method, although sampling and biomarker analysis were well described and repeatable from such descriptions. Positive CT scans were considered as any visible acute ICI and no definition of clinical significance or neurosurgical injury was attempted. Clinical data were available as for normal practice, but in all studies it was unclear whether there were any uninterpretable results or subject withdrawal.
Summary of test accuracy results: biochemical markers
Protein S100B
Tables 19 and 20 show a summary of the test characteristics and raw data with calculated sensitivities, specificities and (negative and positive) likelihood ratios for each study of adults with ICI. Pooling all the raw data for meta-analysis, using dichotomised S100B results (not accounting for delay until sampling, method of biochemical analysis or cut-off value) gives an estimated sensitivity of 96.8% (95% HDR 93.8% to 98.6%) and specificity of 42.5% (95% HDR 31.0% to 54.2%). Bayesian analysis of these data gives a NLR of 0.076 (95% HDR 0.031 to 0.156) and PLR of 1.68 (95% HDR 1.40 to 2.11).
| Author, year | Sample | How obtained | Cut-off value | Time to sample | Analyser | Positive CT (%) | TP | FP | FN | TN | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adults | ||||||||||||
| Poli-de-Figueiredo et al. 2006147 | S100B serum | Venous blood sample drawn on admission (average 82 minutes post trauma) and processed to serum, deep frozen and analysed in Germany using heterogeneous immunoassay [Elecsys 2010(R)] | > 0.10 µg/l | 82 minutes | Elecsys | 6/50 (12%) | 6 | 35 | 0 | 9 | 100 | 20.5 |
| Biberthaler et al. 200698 | S100B serum | Venous blood samples processed to serum and deep frozen, assay with electrochemiluminescence immunoassay kit (Elecsys S100) | > 0.10 µg/l | 60 minutes | Elecsys | 93/1309 (7.1%) | 92 | 855 | 1 | 361 | 98.9 | 29.7 |
| Morochovic et al. 2009146 | S100B serum | Peripheral venous samples taken < 6 hours and sent to lab. Processed on electrochemiluminometric immunoassay by Roche Elecsys S100 | > 0.10 µg/l | < 6 hours | Elecsys | 18/102 (17.6%) | 15 | 59 | 3 | 25 | 83.3 | 29.8 |
| Muller et al. 2007113 | S100B serum | Blood sample taken within 12 hours of injury. Analysed using fully automated Liaison system. Analytical sensitivity is 0.013 µg/l. Results in final analysis not adjusted for half-life of S100B | ≥ 0.10 µg/l | < 3 hours | Liaison | 21/226 (9%) | 20 | 141 | 1 | 64 | 95.2 | 31.2 |
| Biberthaler et al. 2002143 | S100B serum | Blood drawn, processed to serum and citrated plasma and stored at –8 °C for later analysis. LIA-mat or Liaison assay procedures | > 0.12 ng/ml | < 2 hours | Liaison | 24/104 (23.1%) | 24 | 43 | 0 | 37 | 100 | 46.3 |
| S100B plasma | Blood drawn, processed to serum and citrated plasma respectively and stored at –8°C for later analysis. LIA-mat or Liaison assay procedures. | > 0.18 ng/ml | < 2 hours | Liaison | 24/104 (23.1%) | 24 | 43 | 0 | 37 | 100 | 46.3 | |
| Mussack et al. 2002115 | S100B plasma | Blood drawn immediately after admission plus consent. Processed to serum. Citrated. Fully automated immunoluminometric assay (Liaison Sangtec100), lower detection limit 0.02 ng/ml | > 0.21 ng/ml | < 40 minutes | Liaison | 19/139 (13.7%) | 19 | 60 | 0 | 60 | 100 | 50.0 |
| Biberthaler et al. 2001149 | S100B serum | Blood taken on admission and processed to serum. Immunoluminometric assay (LIA-mat Sangtec) | > 0.12 ng/ml | 75 minutes | Liamat | 15/52 (28.8%) | 15 | 22 | 0 | 15 | 100 | 40.5 |
| Romner et al. 2000148 | S-100B serum | Serum sample drawn immediately after admission to ED, analysed with immunoradiometric assay kit | > 0.2 µg/l | < 24 hours | Sangtec | 25/278 (9%) | 23 | 85 | 2 | 168 | 92 | 66.4 |
| Ingebrigtsen et al. 2000145 | S-100B serum | Serum sample drawn immediately after admission to ED, immunoradiometric assay kit [Sangtec 100(R)]. | > 0.2 µg/l | < 12 hours | Sangtec | 10/182 (5.5%) | 9 | 60 | 1 | 112 | 90 | 65.1 |
| Children | ||||||||||||
| Castellani et al. 2009144 | S100B serum | Serum sample within 6 hours of trauma Roche Modular analytics | > 0.16 µg/l | < 6 hours | Elecsys | 36/109 (30.3%) | 36 | 42 | 0 | 31 | 100 | 42.5 |
| Study | No. of patients | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Ingebrigtsen et al. 2000145 | 182 | 90.0 | 65.1 | 97.0 | 89.8 to 99.0 | 63.7 | 56.4 to 70.7 | 0.048 | 0.015 to 0.158 | 2.65 | 2.20 to 3.29 |
| Romner et al. 2000148 | 278 | 92.0 | 66.4 | 97.0 | 89.4 to 99.1 | 65.3 | 59.4 to 71.1 | 0.047 | 0.014 to 0.162 | 2.78 | 2.35 to 3.33 |
| Biberthaler et al. 2001149 | 52 | 100.0 | 40.5 | 96.8 | 93.8 to 98.7 | 40.9 | 27.6 to 55.3 | 0.078 | 0.031 to 0.170 | 1.64 | 1.33 to 2.17 |
| Biberthaler et al. 2002143 | 104 | 100.0 | 46.3 | 96.9 | 93.8 to 98.7 | 45.8 | 35.6 to 56.1 | 0.070 | 0.028 to 0.141 | 1.78 | 1.50 to 2.21 |
| Mussack et al. 2002115 | 139 | 100.0 | 50.0 | 96.9 | 93.4 to 98.7 | 49.3 | 40.7 to 58.0 | 0.065 | 0.026 to 0.135 | 1.90 | 1.63 to 2.31 |
| Biberthaler et al. 200698 | 1309 | 98.9 | 29.7 | 96.7 | 93.4 to 98.8 | 29.8 | 27.3 to 32.4 | 0.110 | 0.040 to 0.222 | 1.38 | 1.31 to 1.44 |
| Poli-de-Figueiredo et al. 2006147 | 50 | 100.0 | 20.5 | 96.7 | 92.2 to 99.1 | 25.0 | 14.3 to 37.7 | 0.129 | 0.039 to 0.405 | 1.29 | 1.11 to 1.56 |
| Muller et al. 2007113 | 226 | 95.2 | 31.2 | 96.7 | 93.5 to 98.7 | 31.8 | 25.8 to 38.3 | 0.102 | 0.040 to 0.215 | 1.42 | 1.29 to 1.57 |
| Morochovic et al. 2009146 | 102 | 83.3 | 29.8 | 96.7 | 93.5 to 98.6 | 33.9 | 24.8 to 44.0 | 0.098 | 0.040 to 0.219 | 1.46 | 1.27 to 1.73 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 9 | 0.334 | < 0.001 | 96.8 | 93.8 to 98.6 | 42.5 | 31.0 to 54.2 | 0.076 | 0.031 to 0.156 | 1.68 | 1.40 to 2.11 | |
The single study identified investigating this biomarker in the paediatric population found 14 out of 109 patients with ICI and a further 22 patients with isolated skull fracture on CT. All 36 patients had elevated S100B concentrations, resulting in a sensitivity of 100% (95% CI 92% to 100%) and a negative predictive value of 100% (95% CI 90% to 100%). Only 31 subjects had a negative sample giving the 42 remaining a false-positive result. This gives a specificity of 42% (95% CI 38% to 43%). These data have not been included in the likelihood ratio calculations.
Neuron-specific enolase
Two studies115,130 (not meta-analysable) investigated the role of NSE in triage for CT in different age groups. Mussack et al. 115 analysed samples in 139 adults alongside their study on S100B, identified a cut-off value (using ROC curve data) of 12.28 ng/ml, giving a sensitivity of 100%, but a specificity of only 6.9%. The area under the curve (AUC) was 0.589, demonstrating an almost complete lack of differentiation. Fridriksson et al. 130 studied 49 children aged 0–18 years, selecting patients by the need for CT scan following blunt head trauma (severity not defined). Using a different radioimmunoassay technique, they identified a cut-off value of 15.3 ng/ml from their ROC curve analysis. This resulted in a sensitivity of 77% with a specificity of 52%. These two studies have not been validated elsewhere, but suggest that NSE is a poor marker for predicting ICI, or the lack of, on cranial CT.
Other markers
In 1995 Levitt et al. 150 studied 107 intoxicated patients following MHI, all of whom received a CT scan and had a sample of blood taken within 3 hours. Of the potential biochemical markers under investigation (CK-BB, noradrenaline, adrenaline, dopamine, amylase and total catecholamines) only adrenaline and dopamine were associated with positive CT findings. From these data, the authors generated ROC curves calculating a cut-off value of 116 pg/ml for adrenaline and 104 pg/ml for dopamine that gave a sensitivity for ICI of 100% (95% CI 66% to 100%) with an acceptable specificity of 57% (95% CI 47% to 67%) and 58% (95% CI 48% to 68%), respectively. These findings do not appear to have been validated elsewhere in the literature.
Chapter 4 Review of studies evaluating diagnostic management strategies
A systematic review of the literature was undertaken to identify studies that evaluated alternative diagnostic management strategies for MHI. We sought studies that compared the effect upon processes or outcomes for patients with MHI of two or more alternative strategies. The systematic review was undertaken in accordance with the standard guidelines published by the Cochrane Effective Practice and Organisation of Care (EPOC) Review Group (www.epoc.uottawa.ca).
Methods for reviewing management practices
Identification of studies
Electronic databases
Studies were identified by searching the following electronic databases:
-
MEDLINE (via OvidSP) 1950 to March 2010
-
MEDLINE In-Process & Other Non-Indexed Citations (via OvidSP) 1950 to March 2010
-
CINAHL (via EBSCO) 1981 to April 2009
-
EMBASE (via OvidSP) 1980 to April 2009
-
WoS (includes SCI and CPCI) (via WOK) 1899 to April 2009
-
CENTRAL (via Cochrane Library Issue 2, 2009)
-
CDSR (via Cochrane Library Issue 2, 2009)
-
NHS DARE (via Cochrane Library Issue 2, 2009)
-
HTA Database (via Cochrane Library Issue 2, 2009)
-
ReFeR
-
NIHR databases
-
INAHTA
-
TRIP database.
Sensitive keyword strategies using free text and, where available, thesaurus terms using Boolean operators and database-specific syntax were developed to search the electronic databases. Synonyms relating to the condition (e.g. head injury) were combined with a search filter aimed at restricting results to prognostic studies (used in the searches of MEDLINE, CINAHL and EMBASE). Date limits or language restrictions were not used on any database. All resources were searched from inception to April 2009. Updated searches to March 2010 were conducted on the MEDLINE databases only. An example of the MEDLINE search strategy is provided in Appendix 1.
Other resources
To identify additional published, unpublished and ongoing studies, the reference lists of all relevant studies (including existing systematic reviews) were checked and a citation search of relevant articles (using the WOK’s SCI and SSCI) was undertaken to identify articles that cite the relevant articles. In addition, systematic keyword searches of the WWW were undertaken using the Copernic Agent Basic (version 6.12) meta-search engine and key experts in the field were contacted.
All identified citations from the electronic searches and other resources were imported into, and managed using, the Reference Manager (version 12.0) bibliographic software.
Inclusion and exclusion criteria
The inclusion of potentially relevant articles was undertaken using the method described in Chapter 3 (see Inclusion and exclusion criteria). However, the relevance of each article was assessed according to the following criteria.
Study design
Randomised controlled trials, controlled clinical trials (CCTs) and controlled before/after (CBA) studies (with a minimum of 20 patients) were included. We did not include uncontrolled before/after studies or cohort studies, but recorded when such studies were identified. Studies that compared alternative strategies in the same group of patients (i.e. by applying a new rule to existing data) and studies that compared strategies in theoretical cohorts were excluded.
Reviews of primary studies were not included in the analysis, but were retained for discussion and identification of additional studies. The following publication types were excluded from the review: animal studies, narrative reviews, editorials, opinions and non-English-language papers.
Population
All studies of adults and children (of any age) with MHI (defined as blunt head injury with a GCS of 13–15 at presentation) were included. Studies of patients with moderate or severe head injury (defined by a GCS ≤ 12 at presentation) or no history of injury were excluded. Studies that recruited patients with a broad range of head injury severity were included only if > 50% of the patients had MHI.
Intervention
Any diagnostic management or organisational change strategy for MHI was included.
Comparator
Any alternative comparators were included.
Outcomes
The main outcomes of interest were:
-
hospital admissions
-
length of stay
-
time to neurosurgery
-
patient outcomes [e.g. quality of life (QoL), headaches].
Data abstraction strategy
Data abstraction was performed by one reviewer (APa) into a standardised data extraction form and independently checked for accuracy by a second (SG). Discrepancies were resolved by discussion. Where multiple publications of the same study were identified, data were extracted and reported as a single study. The authors of the relevant studies were contacted to provide further details in cases where information was missing from the articles.
The following information was extracted for all studies when reported:
-
study design (RCT, CCT, CBA)
-
description of intervention
-
description of control
-
types of study participants (age, gender, patients included, hospitals included)
-
study setting (country)
-
methods (unit of allocation, unit of analysis, study power)
-
main outcome measures (process measures, patient outcomes and length of time during which outcomes were measured after initiation of intervention)
-
results for the main outcome measures.
Quality assessment strategy
The methodological quality of each included study was assessed by one reviewer (APa) and checked by another (SG) using the quality criteria recommended by EPOC. 151 Disagreements between assessors were discussed and resolved by consensus. In the case of no consensus agreement, a third reviewer (APi) was consulted.
The quality assessment criteria (as described in the EPOC data collection checklist) to assess RCTs or CCTs were: concealment of allocation, follow-up of professionals, follow-up of patients or episodes of care, blinded assessment of primary outcome(s), baseline measurement, reliable primary outcomes measure(s) and protection against contamination. The criteria to assess CBA studies were: baseline measurement, characteristics of studies using second site as control, blinded assessment of primary outcome(s), protection against contamination, reliable primary outcomes measure(s), follow-up of professionals and follow-up of patients.
Study quality was assessed, with each item scored as ‘done’, ‘not done’ or ‘not clear’. A study was judged as having a low risk of bias if all criteria were rated as done or not applicable; a moderate risk of bias was assigned if one or two criteria were not done, partially done or not clear; and a high risk of bias was assigned if three or more criteria were not done, partially done or not clear.
Methods of data synthesis
The extracted data and quality assessment variables were presented for each study, both in structured tables and as narrative description. No meta-analysis was planned owing to the anticipated limited number of studies of sufficient quality and homogeneity.
Results of the review of management practices
Studies included in the review
The literature searches identified 8003 citations. Of the titles and abstracts screened, 12 relevant full papers were retrieved and assessed in detail. 21,22,37,136,152–159 One RCT37 comparing immediate CT during triage with observation in hospital for patients with MHI fulfilled the inclusion criteria. A flow chart describing the process of identifying relevant literature can be found in Appendix 7. Studies excluded from the review are listed in Appendix 8.
Description of included studies
The included study37 was a large, randomised, multicentre, pragmatic, non-inferiority, controlled trial. A summary of the design and patient characteristics is presented in Table 21.
| Author, year | Study details | Description of intervention | Description of control | Type of study participants | Methods | Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|
| Inclusion criteria | Patients included (n) | Mean age (years ± SD) and gender (n) | Unit of allocation and analysis | Study power | Process measures (including time)a and patient outcomes | ||||
| Af Geijerstam et al. 200637 |
Design: multicentre, RCT Setting: 39 acute hospitals in Sweden |
Immediate CT strategy: CT given to patients after randomisation. Scans were reported and interpreted according to local practice. If the scan was interpreted as normal, the patient was discharged home. Attending physicians could admit patients despite normal findings, for other medical or social reasons |
Observation in hospital strategy: Patients admitted for observation as inpatients according to local guidelines. The attending physician could decide to perform CT if this seemed to be clinically necessary |
Patients (aged ≥ 6 years) with MHI (defined as head trauma within 24 hours; confirmed or suspected LOC or amnesia, or both; normal results on neurological examination, GCS 15 and no associated injuries that required admission) who attended for acute care |
All patients: 2602 Numbers randomised: CT group: 1316 Observation group: 1286 |
Mean age (± SD), years: CT group: 30.9 (± 22.1) Observation group: 32.0 (±22.4) Male/female: CT group: 787 (59.8%)/529 (40.2%) Observation group: 752 (58.5%)/534 (41.5%) |
Allocation: patient Analysis: patient |
Non-inferiority. Limit for acceptability was a 5% difference against CT. A sample size of 2000 patients would have 80% power to get a one-sided 95% CI that excluded the non-inferiority limit |
Primary outcome (non-inferiority): dichotomised extended GOS [1–7 (not fully recovered) vs 8 (fully recovered)] Other: same scores dichotomised in six different ways Patient satisfaction |
The RCT recruited 2602 patients between May 2001 and January 2004 at 36 acute hospitals in Sweden. The trial included patients aged ≥ 6 years with MHI (within 24 hours) who attended EDs. Patients were randomly assigned to immediate CT or observation in hospital. The study was designed to demonstrate that a management strategy based on CT and early discharge leads to similar clinical outcomes compared with observation in hospital. The primary end point was an outcome according to a dichotomised GOS-E, 3 months after the injury [8 (fully recovered) vs 1–7 (not fully recovered)]. Secondary end points were the same scores dichotomised in six other possible ways. 37
Quality of included studies
The included RCT37 was considered to be at moderate risk of bias (Table 22). Patients and carers were inevitably not blinded so subjective outcomes may have been influenced by awareness of treatment group. Individual patient randomisation in a trial of different methods of service delivery raises the possibility of bias owing to contamination of the intervention or control group. However, crossover rates were low, with only 8.9% (117/1316) of the CT group being admitted for observation and 8.6% (111/1286) of the observation group receiving CT.
| Author, year | Concealment of allocation (protection against selection bias) | Follow-up | Baseline measurement | Reliable primary outcome measure(s) | Protection against contamination | Risk of bias | ||
|---|---|---|---|---|---|---|---|---|
| Protection against exclusion bias | Protection against detection bias | |||||||
| Professionals | Patients or episodes of care | Blinded assessment of primary outcome | ||||||
| Af Geijerstam et al. 200637 | Done | NA | Done | Patients and carers were aware of allocated group. Deaths and complications were assessed by blinded reviewers | Done | Not clear | Not done | Moderate |
Summary of management practice results
The main findings from this trial37 were that at 3 months 21.4% (275/1283) of patients in the CT group had not recovered completely compared with 24.2% (300/1240) admitted for observation. The difference was found to be not significant in favour of CT (95% CI –6.1% to 0.6%). The worst outcomes (mortality and severe loss of function) were similar between the groups. None of the patients with normal findings on immediate CT had complications later. The authors37 concluded that the use of CT in the management of patients with MHI is feasible and leads to similar outcomes compared with observation in hospital. An associated cost analysis36 reports a mean cost per patient of €461 (£314, US$582) in the CT group and €677 (£462, $854) in the observation group (difference €216, 95% CI –€272 to –€164; p < 0.001), leading the authors to conclude that CT is more cost-effective than hospital admission for MHI.
The single trial identified in this review provides good evidence that early CT and discharge of patients with MHI is at least as effective as hospital admission and costs less. The main limitation is that a trial can only feasibly compare a limited number of alternatives – in this case two. It is possible that other strategies, such as those using clinical decision rules to select patients for CT or hospital admission, could achieve comparable outcomes at similar cost.
Additional evidence
Eleven studies were identified (two contemporaneous cohort studies152,153 and nine uncontrolled before/after studies)21,22,136,154–159 that did not fulfil the inclusion criteria of the systematic review, but are reported here as additional evidence (i.e. data presented as structured tables with a narrative description, but without a formal quality assessment). The two contemporaneous cohort studies152,153 compared alternative hospital admission policies, whereas nine uncontrolled before/after studies21,22,136,154–159 evaluated the effect of introducing guidelines for head injury management. A summary of the study and patient characteristics is presented in Table 23.
| Author, year | Study details | Description of interventions | Data collection period | Type of study participants | Methods | Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|
| Inclusion criteria | Patients included (n) | Mean age (years ± SD) and gender (n) | Unit of allocation and analysis | Study power | Process measures (including time)a and/or patient outcomes | ||||
| Cohort studies (prospective or retrospective) | |||||||||
| Brown et al. 1994152 |
Design: prospective cohort study Setting: ED of two teaching hospitals in Scotland, UK |
Control group (Edinburgh): no access to short-stay ward Study group (Glasgow): access to short-stay observation ward |
Control group: 16 November 1992 to 13 December 1992 Study group: 16 November 1992 to 13 December 1992 |
Patients (aged > 13 years at time of presentation) with MHI |
All patients: 483 Control group: 206 Study group: 277 |
Mean age: NR Male/female: Before group: NR After group: NR |
Allocation: group, allocated according to hospital attended Analysis: patient |
NR | Admission for observation |
| Fabbri et al. 2004153 |
Design: prospective cohort study Setting: ED of district hospital, Ravenna, Italy |
Control group: 24–28 hours in-hospital observation followed by home monitoring Study group: up to 12 hours in-hospital observation and early home monitoring |
Control group: 1999 to 2001 Study group: 1999 to 2001 |
Patients (aged ≥ 10 years) with MHI within the past 24 hours and early negative CT scan |
All patients: 1480 Control group: 646 Study group: 834 |
Mean age: NR Male/female: Control group: 387 (60%)/ 259 (40%) Study group: 415 (50%)/419 (50%) |
Allocation: patient, allocated according to clinician judgement Analysis: patient |
NR | Post-traumatic ICI at CT, the need for neurosurgical intervention and an unfavourable outcome (death or disability) |
| Before/after studies without concurrent control group | |||||||||
| Browning et al. 2005154 |
Design: uncontrolled before/after study Setting: ED of a paediatric teaching hospital, Edinburgh, UK |
Before group: guidelines advise skull radiography for all After group: guidelines advise skull radiography only if visible evidence of head injury or suspicious history for non-accidental injury |
Before group: 1 August 1998 to 31 July 1999 After group: 1 August 2002 to 31 July 2003 |
Patients (aged < 1 year at time of presentation or diagnosis) with head injury |
All patients: 371 Before group: 181 After group: 190 |
Mean age: NR Male/female: Before group: 94 (52%)/87 (48%) After group: 98 (52%)/92 (48%) |
Allocation: group, allocated according to date Analysis: patient |
NR |
Admissions, skull radiographs, total radiation dose NR |
| Fong et al. 2008155 |
Design: uncontrolled before/after study Setting: ED of tertiary referral hospital, Melbourne, Australia |
Before group: pre-guideline After group: post guideline (Southernhealth Head Injury Guideline, based on CCHR) |
Before group: September 2002 to January 2003 After group: February 2003 to August 2003 |
Patients aged over 16 years who presented to the ED following a non-trivial blunt or penetrating trauma to the head |
N = 637 Before group: n = 311 After group: n = 326 |
Mean age: Before group: 46.3 (± 24.5) After group: 51 (± 26.1) Male/female: Before group: 975 (64%)/560 (36%) After group: 1248 (67%)/619 (33%) |
Allocation: group, allocated according to date Analysis: patient |
Assuming 20% reduction from a 50% baseline head CT ordering rate, a sample size of 300 will provide 94.6% power (α = 0.05) | Admissions, CT rates, neuro-observations an asymptomatic treatment, neurosurgery and death |
| Hassan et al. 200522 |
Design: uncontrolled before/after study Setting: ED of a teaching (North Tyneside) and district hospital (Salford) in England, UK |
Before group: pre-NICE 2003 guidelines After group: post NICE 2003 guidelines |
Before group 1 (North Tyneside): 1 November 2002 to 30 November 2002 After group 1: 1 May 2003 to 31 May 2003 Before group 2 (Salford): 1 May 2003 to 31 May 2003 After group 2: 1 January 2004 to 31 January 2004 |
Any patient with head injury (defined as any injury around the head and upper part of face) presenting to the ED |
N = 1130: Before group 1: n = 276 After group 1: n = 351 Before group 2: n = 221 After group 1: n = 282 |
Mean age: NR Male/female: Before group 1: 181 (66%)/95 (34%) After group 1: 223 (64%)/128 (36%) Before group 2: 150 (68%)/71(32%) After group 2: 181(64%)/101 (36%) |
Allocation: group, allocated according to date Analysis: patient |
NR | Rates of admission, CT and skull radiography, costs |
| Kerr et al. 2005156 |
Design: uncontrolled before/after study Setting: ED of teaching hospital in Edinburgh, UK |
Before group: pre-SIGN 2000 guidelines After group: post SIGN 2000 guidelines |
Before group: 1 November 1999 to 30 November 1999 After group: 1 May 2001 to 31 May 2001 |
All patients with blunt force trauma above the neck (including patients with facial lacerations) |
N = 1607 Before group: n = 788 After group: n = 819 |
Mean age: NR Male/female: Before group: 575 (73%)/213 (27%) After group: 566 (69%)/253 (31%) |
Allocation: group, allocated according to date Analysis: patient |
NR | Admissions for observations, discharge |
| Loroni et al. 1996157 |
Design: uncontrolled before/after study Setting: ED of district hospital, Ravenna, Italy |
Before group: no clinical diagnostic protocol After group: clinical diagnostic protocol with indications for hospital admission and diagnostic procedures |
Before group: 1 April 1984 to 31 March 1985 After group: 1 June 1988 to 31 December 1990 |
Patients (aged ≤ 14 years at time of presentation or diagnosis) with head injury |
N = 942: Before group: n = 233 After group: n = 709 |
Mean age: Before group: 5.4 (± NR) After group: 4.3 (± NR) Male/female: Control group: 140 (67%)/ 93 (33%) Study group: 456(64%)/253(36%) |
Allocation: group, allocated according to date Analysis: patient |
NR | Admissions for observations, CT rates, skull radiography, neurosurgical admission |
| Reed et al. 2005136 |
Design: uncontrolled before/after study Setting: ED of a paediatric teaching hospital, Edinburgh, UK |
Before group: guidelines advise skull radiography for all After group: guidelines advise no skull radiography |
Before group: 1 August 1998 to 31 July 1999 After group: 1 August 2002 to 31 July 2003 |
Patients (aged between 1 and 14 years at time of presentation or diagnosis) with head injury |
N = 3402: Before group: n = 1535 After group: n = 1867 |
Mean age: NR Male/female: Before group: 975 (64%)/560 (36%) After group: 1248 (67%)/619 (33%) |
Allocation: group, allocated according to date Analysis: patient |
NR |
Admissions, skull radiographs, CT rates, total radiation dose NR |
| Shravat et al. 2006158 |
Design: uncontrolled before/after study Setting: ED of district hospital, London, UK |
Before group: pre-NICE 2003 guidelines After group: post NICE 2003 guidelines |
Before group: NR/NR/2003 After group: 01 June 2004 to 31 August 2004 |
All patients with head injury presenting to the ED |
N = 992: Before group: n = 520 After group: n = 472 |
Mean age: NR Male/female: Before group: NR After group: 271 (57.4%)/201 (42.6%) |
Allocation: group, allocated according to date Analysis: patient |
NR | Admissions for observations, CT rates, skull radiography, cost |
| Sultan et al. 200421 |
Design: uncontrolled before/after study Setting: ED of teaching hospital, Cambridge, UK |
Before group: RCS ‘Galasko’ guideline (1999) After group: Cambridge protocol (based on CCHR) |
Before group: 1 April 2001 to 31 October 2001 After group: 1 January 2002 to 30 September 2002 |
Adult patients (aged > 15 years) with MHIs presenting to the ED |
N = 597 Before group: n = 330 After group: n = 267 |
Mean age: NR Male/female: Before group: NR After group: NR |
Allocation: group, allocated according to date Analysis: patient |
NR | Admissions for observations, CT rates, discharge, skull radiography |
| Thomson et al. 1994159 |
Design: uncontrolled before/after study Setting: ED of two hospitals in Northern region of England, UK |
Before group: pre-Group of Neurosurgeon guidelines, 1984 After group: post Group of Neurosurgeon guidelines, 1984 |
Before group: 1 February 1987 to 31 May 1987 After group: 1 February 1990 to 31 May 1990 |
Adult patients (aged > 16 years) with head injuries or altered consciousness after a relevant injury or with a scalp or forehead laceration presenting to the ED |
N = 1880 Before group 1: n = 533 After group 1: n = 613 Before group 2: n = 370 After group 2: n = 364 |
Mean age: Before group 1: 37.1 (± NR) After group 1: 38.4 (± NR) Before group 2: 39.7 (± NR) After group 2: 38.4 (± NR) Male/female: Before group 1: 316 (59%)/217 (41%) After group 1: 402 (66%)/211 (34%) Before group 2: 225 (61%)/145 (39%) After group 2: 275 (76%)/89 (24%) |
Allocation: group, allocated according to date Analysis: patient |
NR | Admissions for observations, skull radiography |
Cohort studies
Two prospective cohort studies152,153 determined the effect of a change in admission policy in the management of MHIs. Fabbri et al. 153 evaluated early home monitoring (up to 12 hours in hospital observation and early home monitoring) with in-hospital observation (24–48 hours in hospital observation followed by home monitoring). The results showed that in the in-hospital arm 1.4% (of these 0.5% after discharge) developed intracranial injuries compared with 0.7% in the early home monitoring group. No patients with previously undiagnosed intracranial injuries had a neurosurgical intervention. After 6 months, five patients (0.8%) died in the home monitoring group compared with eight patients (1.0%) in the hospital arm. No permanent disability or vegetative state was observed. The authors concluded that early home monitoring may be safely proposed to select high-risk individuals with an early negative CT, normal clinical examination and feasible home monitoring. The study was limited by allocation to intervention group being based on clinical judgement of severity and lack of power to detect rare, but serious events.
Brown et al. 152 determined whether access to a short-stay ward significantly affected the threshold for admission of patients with MHIs and the implementation of head injury admission guidelines. The results showed that 49/83 (59%) patients who met accepted guidelines for hospital admission were admitted to a hospital with an observation ward, compared with 10/49 (34%) admitted to a hospital with no observation ward (p < 0.001). The authors concluded that access to a short-stay ward has a considerable bearing on whether or not a minor head-injured patient is admitted to hospital. The study involved only two hospitals, so it is uncertain whether the findings can be generalised to other hospitals.
Before/after studies without concurrent control group
These studies have evaluated the effect of implementing guidelines and changes in policy upon hospital admission policy, use of skull radiography and/or use of CT scanning. The absence of a control group to record concurrent changes over time means that we cannot be sure that the changes observed in these studies were due to the intervention rather than to temporal trends, concurrent changes or a Hawthorne effect. They, therefore, represent very weak evidence of effectiveness.
Sultan et al. 21 evaluated the effects of a protocol based on the CCHR (the Cambridge protocol) for managing MHIs compared with guidelines published by the Society of British Neurological Surgeons, 1998, and Royal College of Surgeons for England, 1999. The results showed that CT rates increased significantly from 14% to 20% (p < 0.05), and admissions for observation increased from 34% to 45% (p < 0.05). Skull radiography rates decreased considerably from 33% of all patients with head injuries in 2001 to 1.6% in 2002 (p-value not reported), without any adverse effect. The authors21 concluded that it was possible to replace the practice of risk stratification of adults with MHI based on skull radiography with a slightly modified version of the CCHR. Fong et al. 155 reported a similar effect in their evaluation of a guideline based on the CCHR and the NOC for MHI (the Southernhealth Head Injury Guideline). The results showed that after implementation of the new guidelines, the CT ordering rate increased from 31.6% to 59% (p-value not reported), and admissions for observation increased from 21.9% to 27% (p = 0.08). Abnormal head CT was reported in 6.8% in the pre-guideline group compared with 5% in the post guideline group. The authors155 concluded that, although CT head scanning rates were increased, the Southernhealth Head Injury Guidelines were safe and easy to apply to major and MHIs.
Hassan et al. 22 and Shravat et al. 158 evaluated the effect of implementation of the NICE head injury guidance, which was also based upon the CCHR. Hassan et al. 22 studied two hospitals and reported that after implementation of the NICE guidance at the teaching hospital the CT scan rate increased from 3% to 7%, the skull radiography declined from 37% to 4% and the admission rate decreased from 9% to 4%, whereas at the non-teaching hospital the CT scan rate increased from 1.4% to 9%, the skull radiography rate decreased from 19% to < 1% and the admission rate declined from 7% to 5%. Shavrat et al. 158 studied one hospital and reported that the CT scan rate increased significantly, the skull radiography rate fell and the admission rate was unchanged.
Kerr et al. 156 evaluated the effect of implementing the SIGN guidelines at a Scottish hospital. After guideline implementation the proportion of patients admitted to hospital increased from 20% to 26%, but there were no significant changes in the proportion of patients undergoing skull radiography or CT.
Two papers from the same UK paediatric teaching hospital evaluated the effect of a policy change to restrict the use of skull radiography in infants154 and children136 with a head injury presenting to the ED between 1998–9 and 2002–3. Abandoning the use of skull radiography in children aged between 1 and 14 years did not lead to a significant increase in admission rates (10.1% vs 10.9%; p = 0.43), missed ICI (0.20% vs 0.37%; p = 0.53) or neurosurgical intervention (0% vs 0.1%; p = 0.30), but doubled the proportion of children who received a CT scan from 1.0% to 2.1% (p = 0.02). 136 Limitation of skull radiography in infants led to a substantial decrease in skull radiography rates (77.3% to 29.5%; p-value not reported) with no detriment to the infant in terms of missed injury or admissions (13.8% vs 10%; p-value not reported). 154
Loroni et al. 157 compared the management of children (≤ 14 years) with head injury (all severities) in an Italian general hospital in two different periods (1984–5 and 1988–90), one before and one after the introduction of a protocol for the management of children with head injury (with indications for hospital admission and diagnostic procedures). The results showed that, among the clinical cases with milder symptoms of head injury, hospital admissions for observation decreased significantly from 40.3% to 27.8% (p < 0.05) and skull radiography from 86.7% to 36.1% (p < 0.05), without an increase in the number of diagnostic errors. Data on CT rates and neurosurgical admission were limited. The authors157 concluded that it was possible to reduce the number of radiographical examinations and admissions without increasing the number of diagnostic errors with a management protocol with indications for hospital admission and diagnostic procedures for children with head injury.
Thomson et al. 159 compared the management of adults with head injury before and after the introduction in two hospitals of guidelines drawn up in 1984 by a group of neurosurgeons. After implementation of the guidelines the proportion receiving skull radiography increased from 49% to 60% in one hospital, but decreased from 34% to 25% in the other. The proportion admitted remained constant in one department (34% vs 36%), but decreased from 33% to 15% in the other.
Overall, these studies show that implementation of guidelines may change the management of patients with MHI, although the effects are varied and not always as anticipated. The findings may be specific to the hospitals concerned or may be owing to the potential biases outlined above.
Chapter 5 Assessment of cost-effectiveness evidence
This section of the assessment focuses on the health economics of diagnostic strategies for the management of MHI. It includes a brief review of existing economic evaluations and a detailed explanation of the methodologies and results of a de novo economic model. The section Systematic review of existing cost-effectiveness evidence, presents the results of the systematic review of economic literature. The modelling approach adopted for this study is described (see Independent economic assessment), along with the results of the analysis (see Results).
Systematic review of existing cost-effectiveness evidence
The primary objective of this review was to identify and evaluate studies exploring the cost-effectiveness of different diagnostic strategies for the management of MHI. The secondary objective was to evaluate methodologies used to inform our own economic evaluation.
Identification of studies
Electronic databases
Studies were identified by searching the following electronic databases:
-
MEDLINE (via OvidSP) 1950 to March 2010
-
MEDLINE In-Process & Other Non-Indexed Citations (via OvidSP) 1950 to March 2010
-
CINAHL (via EBSCO) 1981 to April 2009
-
EMBASE (via OvidSP) 1980 to April 2009
-
WOS (includes SCI and CPCI) (via WOK) 1899 to April 2009
-
NHS DARE (via CRD databases) Approximately 1994 to April 2009
-
NHS Economic Evaluation Database (NHS EED) (via CRD databases) approximately 1994 to April 2009
-
HTA database (via CRD databases) approximately 1994 to April 2009
-
Health Economic Evaluation Database (via Wiley InterScience) 1967 to April 2009.
Sensitive keyword strategies using free text and, where available, thesaurus terms using Boolean operators and database-specific syntax were developed to search the electronic databases. Synonyms relating to the condition (e.g. head injury) were combined with a search filter aimed at restricting results to economic and cost-related studies (used in the searches of MEDLINE, CINAHL and EMBASE). Date limits or language restrictions were not used on any database. All resources were searched from inception to April 2009. Updated searches to March 2010 were conducted on the MEDLINE databases only. An example of the MEDLINE search strategy is provided in Appendix 9.
Other resources
To identify additional published, unpublished and ongoing studies, the reference lists of all relevant studies were checked and a citation search of relevant articles (using the WOK’s SCI and SSCI) was undertaken to identify articles that cite the relevant articles. In addition, systematic keyword searches of the WWW were undertaken using the Copernic Agent Basic (version 6.12) meta-search engine.
All identified citations from the electronic searches and other resources were imported into and managed using the Reference Manager bibliographic software (version 12.0).
Inclusion and exclusion criteria
Studies were selected for inclusion according to pre-determined inclusion and exclusion criteria. Studies were included if they reported the cost-effectiveness of diagnostic management strategies for MHI, included CT scanning in a patient management strategy and estimated the benefits in terms of life-years gained or QALYs. Studies that were considered to be methodologically unsound (including abstracts), that were not reported in sufficient detail to extract costs and outcome estimates or that did not report an estimate of cost-effectiveness (e.g. costing studies) were excluded. Papers not published in the English language were also excluded.
One reviewer (MH) independently screened all titles and abstracts. Any discrepancies were resolved by discussion, with involvement of a second reviewer (SG) when necessary. Full papers were obtained for any titles/abstracts that were considered relevant or where the title/abstract information was not sufficient to make a decision.
Quality assessment strategy
The quality of studies was assessed using a combination of key components of the Drummond and Jefferson checklist for economic evaluations,160 together with the Eddy checklist on mathematical models used in technology assessments. 161 The use of the checklist ensures a consistent approach to assessing the quality of each economic evaluation.
Results of cost-effectiveness review
The systematic searches identified 1263 potentially relevant citations. Of the titles and abstracts screened, six relevant full-text papers were retrieved and assessed in detail. A flow chart describing the process of identifying relevant literature can be found in Appendix 10. A total of three studies162–164 were identified as meeting the inclusion criteria. Although, no UK cost-effectiveness studies were found, one study162 did repeat the analysis using UK modelling recommendations. Studies excluded from the review are listed in Appendix 11.
Cost-effectiveness review
Stein et al.163
Overview
Stein et al. 163 developed a decision-analytic model to compare the cost-effectiveness of six strategies for the management of mild traumatic head injury: selective CT scanning based largely on the CCHR; CT for all patients; skull radiography for all patients; prolonged ED observation; 24-hour hospital admission; and no treatment.
A decision tree approach was used to compare the strategies. Patients having no intracranial lesion were either correctly diagnosed and discharged or incorrectly diagnosed and received unnecessary treatment. Patients with an intracranial lesion were either correctly diagnosed and received prompt treatment or incorrectly diagnosed and received delayed treatment that was associated with worse outcomes. Outcomes were described by the GOS. The base case represented a 20-year-old patient with a GCS of 14 or 15. Epidemiological data were derived from a MEDLINE search. The setting of the model was the US health service with a societal perspective. The economic outcome was incremental cost per QALY discounted at 3% annually. Health-related utility values were taken from a study that used standard gamble techniques to elicit utility values for GOS outcomes 2–4 from 52 health professionals and 83 medical students. 165 Utility scores of 0 and 1 were assigned to GOS 1 and GOS 5, respectively. Univariate sensitivity analysis and probabilistic sensitivity analysis (PSA) were undertaken and the analysis was repeated for patients aged 40, 60 and 80 years. In the deterministic analysis the selective CT scanning strategy dominated all other strategies, and in the PSA, for willingness-to-pay thresholds of between $50,000 and $150,000 per QALY, there was a 68–90% probability that selective CT scanning would be cost-effective. The PSA incremental cost per QALY is not reported. In the univariate analysis, the results were most sensitive to the outcome of prompt surgery; however, no parameter changes altered the conclusion. In the higher age group analysis, selective CT scanning remained dominant, although the magnitude of the incremental costs and QALYs reduced with older age.
Comments
This appears to be a well-constructed model, parameterised by relevant data at the time. The authors acknowledged that a limitation of their model was that the risk of cancer due to CT scanning was not modelled. However, they appeared to have conducted a sensitivity analysis in which they adjusted for the published risk of cancer for a 20-year-old patient and this did not alter the conclusion.
Stein et al.164
Overview
Stein and colleagues164 examined the cost-effectiveness of routinely re-scanning patients, compared with repeating the scan only after clinical deterioration, in a patient group with MHI in whom the admission CT scan revealed a non-neurosurgical lesion. A decision tree approach was used to compare the two strategies. Patients in the ‘routine repeat CT’ pathway either developed a haematoma or did not; those developing a haematoma were assumed to receive prompt surgery. In the ‘CT only if deteriorates’ pathway, patients deteriorated and received prompt surgery, deteriorated and received delayed surgery or did not deteriorate. In both pathways, patients who do not deteriorate have an uneventful recovery. The base case was a 20-year-old with mild TBI with a GCS of 14 or 15. Patient outcomes were measured by the GOS, with prompt surgery having a better outcome than delayed surgery. Epidemiology data were derived from a MEDLINE search. The setting of the model was the US health service with a societal perspective. The economic outcome was the cost/QALY discounted at 3% annually. Health-related utility values were taken from the same study used by the earlier Stein et al. study163 described above. Utility scores of 0 and 1 were assigned to GOS 1 and GOS 5, respectively. Both univariate and PSA were carried out. The incremental cost-effectiveness ratio (ICER) of routine CT scanning compared with CT scanning after deterioration was $12,670 (95% CI –$76,038 to $80,693). The study found that the ICER increased exponentially as patients’ age increased and the mean ICER at age 80 years was around $80,000. The authors concluded that there is a case for routine follow-up CT scanning; however, the uncertainty around the results was substantial.
Comments
This evaluation satisfied the majority of items used to assess the overall quality and appeared to be well conducted using the evidence available at the time. However, as the authors remark, the mean cost per QALY had considerable uncertainty ranging from routine CT scanning dominating to being dominated. Unfortunately, the published table of results had mistakes, so the costs and QALYs that contribute to this uncertainty were not transparent and the authors did not elaborate on the possible reasons for this uncertainty. The authors acknowledged that omitting the risk of cancer from CT scanning was a limitation of their study, especially in children. The authors concluded that routine CT scanning should be considered as an option by decision-makers. We would conclude that more clarification around the considerable uncertainty is needed before this decision can be made.
Smits et al.162
Overview
This study compared the cost-effectiveness of various CT scanning strategies with CT scanning all patients with MHI. Strategies included are the NOC,27 CCHR,26 CT in Head Injury Patients (CHIP)69 and CT for no patients. A Markov model was developed to assess long-term costs and QALYs. The model was based on data from the CHIP study69 (n = 3181) and from literature reviews. The correct identification of patients with a neurosurgical lesion, a non-neurosurgical lesion or no lesion was based on the sensitivity and specificity of the decision rules. Patients with delayed surgery were estimated to have worse outcomes than patients treated without delay. Patient outcomes are measured by the GOS. QoL estimates were derived from European Quality of Life-5 Dimensions (EQ-5D) questionnaires (n = 87) administered as part of the CHIP study and converted to utilities. The perspective of the model is the Dutch health-care system; both direct health-care and direct non-health-care costs are included. The base-case analysis was a cohort of 41-year-old men, representative of the typical patient in the CHIP study. The time horizon was 1 and 25 years. Costs and benefits were discounted at 3%. Univariate and multivariate sensitivity analysis and PSA were carried out. The risk of cancer from a CT scan was included; however, the authors give no information on the parameters used. Expected value of perfect information (EVPI) for further research was undertaken. The EVPI for further research was $1759 per patient, which, for the US population, over a period of 5 years, was estimated to amount to $7B. The analysis was repeated using cost-effectiveness modelling recommendations from the UK (health-care perspective, discounting rate of 3.5% for both costs and outcomes) and the Dutch (societal perspective, costs and outcomes discounted at 4% and 1.5%, respectively). In the base-case analysis, the NOC, ‘CT all patients’ and ‘CT not performed’ strategies were dominated by the other strategies. The ICER for the CHIP rule versus CCHR was $3M. In the PSA, the probability that performing selective CT was cost-effective compared with performing CT in all patients was 0.51–0.64, depending on the willingness-to-pay threshold (maximum of $75,000). The incremental cost per QALY results from the PSA were not reported. The authors state that similar results were found when using UK and Dutch modelling recommendations. The value of information (VOI) analysis indicated that further research was justified to reduce uncertainty about long-term functional outcomes after MHI.
Comments
This was a well-constructed model that scored highly on the assessment criteria. A particular strength of this model was that it was based on good-quality trial data with minimum input from the literature. The authors recognised that there was uncertainty around some of the rare events in the model.
Cost-effectiveness review summary
Comparison of the results from the three studies is not straightforward owing to the different objectives, comparators, populations and costings used. However, both the Smits et al. 162 and Stein et al. 163 studies agreed that the CCHR prediction tool was cost-effective compared with other strategies, although the comparator strategies used were different in these studies.
Independent economic assessment
This section details the methods and results of our health economic model, constructed to compare CT scanning management strategies for patients with a MHI. The strategies evaluated in adults were ‘CT all’ (theoretical), abnormal arrival GCS (theoretical), CCHR (high risk),26 CCHR (high or medium risk),26 NCWFNS,72 NOC,27 NEXUS II,62 NICE1 and the Scandinavian rule. 73 The decision rules evaluated in children were ‘CT all’ (theoretical), CHALICE,30 PECARN,90 UCD93 and the rule of Atabaki et al. 2008. 81 The analysis was undertaken to address the lack of any published cost-effectiveness evidence from the perspective of the NHS in England and Wales. The key aim was to determine the optimal CT scanning management strategy in terms of cost-effectiveness.
Methods of independent economic analysis
Objectives
The objectives of the cost-effectiveness analysis were to:
-
estimate the cost-effectiveness of diagnostic strategies for MHI, in terms of the cost per QALY gained by each strategy
-
identify the optimal strategy for managing MHI in the NHS, defined as the most cost-effective strategy at a willingness to pay per QALY gained threshold of £30,000
-
identify the critical areas of uncertainty in the management of MHI, where future primary research would produce the most benefit.
The costs and benefits of diagnostic management of minor head injuries
The main benefits of diagnostic management relate to rapid identification and treatment of patients with intracranial lesions that require urgent neurosurgery (neurosurgical lesions) and the identification of patients with non-neurosurgical lesions, so that they can be monitored and receive timely treatment if they subsequently deteriorate. The main disbenefit is the risk of cancer associated with CT radiation, particularly in children. The direct costs of diagnostic management include the costs of investigation, particularly CT scanning, and hospital admission for observation, and the subsequent costs of providing neurosurgical treatment, intensive care, rehabilitation and, for those with persistent disability, long-term social care. We built a model to allow us to analyse the effect of different diagnostic management strategies on these costs and benefits.
The decision-analysis model structure
We developed a decision-analysis model to estimate the costs and QALYs accrued by each potential management strategy for MHI, including a theoretical ‘zero option’ strategy of discharging all patients home without investigation. Each strategy was applied to a hypothetical cohort of patients attending the ED with MHI. We assumed that a proportion of the cohort would have an intracranial lesion requiring neurosurgery (typically an extradural haemorrhage) and another proportion would have an intracranial lesion that did not require neurosurgery. The remainder would have no intracranial haemorrhage. These proportions were estimated from the study of patients with MHI by Smits et al. 166 (Table 24). This was a large study of patients with GCS 13–15 head injury in which all patients underwent CT scanning, and was thus judged to provide a reliable and relevant estimate of the prevalence of ICI. We also undertook a sensitivity analysis in which we used estimates from another study, that of Stein et al. 71 This was also a large well-conducted study, but was limited to patients with GCS 14–15 and not all had CT scanning.
| Author | Neurosurgical injury | Non-neurosurgical injury | ||||
|---|---|---|---|---|---|---|
| n | % | 95% CI (%) | n | % | 95% CI (%) | |
| Smits et al.166 | 17/3181 | 0.53 | 0.33 to 0.85 | 226/3181 | 7.10 | 6.26 to 8.05 |
| Stein et al.71 | 108/7955 | 1.36 | 1.13 to 1.64 | 423/7955 | 5.32 | 4.85 to 5.83 |
We assumed that the strategy would determine which patients underwent CT scanning and that the probability of detecting a neurosurgical lesion was determined by the sensitivity of the strategy for neurosurgical lesions. We assumed that patients with a neurosurgical lesion detected on CT would be managed promptly (before any deterioration occurred), while those who did not undergo CT according to the strategy would receive delayed treatment (after deterioration had occurred).
We assumed that a proportion of patients with a non-neurosurgical lesion would deteriorate over the following 48 hours and require intervention (critical care support and/or neurosurgery), whereas the remainder would remain well. If the strategy led to CT being performed and the lesion detected then we assumed that the patient would be admitted to hospital and would receive prompt appropriate treatment. If the strategy did not lead to CT being performed we assumed that the patient would be discharged home and would receive delayed treatment. The proportion of patients undergoing CT was determined by the sensitivity of the strategy for detecting a non-neurosurgical lesion.
We assumed that patients without an intracranial lesion remained well and did not deteriorate. These patients would not therefore benefit from investigation and treatment.
The model assigned each patient to a GOS category depending upon whether or not he or she had an intracranial lesion (neurosurgical or non-neurosurgical) and how quickly it was treated. Each patient then accrued lifetime QALYs and health-care costs according to his or her GOS category. Costs were also accrued according to whether or not the strategy resulted in the patient receiving investigation with a CT scan, hospital admission for observation, or neurosurgery. Finally, we applied a QALY decrement and additional cost to every patient who received a CT scan to reflect the potential effect of radiation exposure upon long-term health. Details of each of these processes are outlined below.
Selection of strategies
The literature review identified a number of clinical decision rules for MHI. The national survey revealed that most hospitals used either the NICE1 or SIGN20 guidelines. Clinical decision rules for adults had been more extensively validated than those developed for children. We therefore selected clinical decision rules for adults only if they had been validated in a different cohort from the derivation cohort, whereas clinical decision rules for children were included if they had any accuracy parameters at the time we developed the model, even if they were from the derivation cohort.
The clinical decision rules were typically developed to determine whether or not patients should receive CT scanning. We therefore made the following assumptions about how they would be put into practice, based on clinical expertise:
-
patients with a neurosurgical lesion diagnosed on CT are admitted and operated on
-
patients with a non-neurosurgical lesion diagnosed on CT are admitted for observation
-
patients with a normal CT and those who do not receive a CT are discharged to the care of a responsible adult.
We also included several theoretical strategies:
-
a ‘zero option’ of discharging all patients without CT, to determine whether or not investigation and management of MHIs is cost-effective in general
-
CT scan for all patients, to determine whether this is more cost-effective than any attempt to select patients for CT
-
a ‘high specificity’ strategy of CT scanning only patients with an abnormal GCS at presentation.
The ‘discharge all’ and ‘CT all’ strategies are included as theoretical strategies to explore the overall cost-effectiveness of diagnostic testing. The former would not be considered acceptable and the latter not currently feasible. However, their inclusion allows the model to explore theoretical issues, such as whether CT scanning in itself, or attempts to select patients for scanning, are cost-effective. The last strategy was included because clinical decision rules have been developed to optimise sensitivity at the expense of specificity. Health economic modelling gave us the opportunity to test the assumption that sensitivity should always be optimised. We assumed that a strategy based on GCS alone could have reasonably high specificity, albeit with sacrifice of sensitivity.
We did not use the modelling to compare strategies that admitted patients for observation (without CT) to those that used CT. Hospital admission costs slightly more than CT and there is no theoretical reason to expect better outcomes with hospital admission on the basis of our assumptions. Indeed, as CT allows neurosurgical intervention before deterioration, whereas admission uses patient deterioration to detect neurosurgical lesions, there are strong reasons to expect CT-based strategies to be more effective and cheaper. This is supported by several primary studies that have compared CT-based strategies with skull radiography and/or admission to conclude that CT-based strategies are more likely to detect intracranial bleeding and less likely to require hospital admission. 35,34 Cost analyses based upon trial data36 and modelling37 both suggest that a CT-based strategy is cheaper.
However, there are a number of circumstances in which hospital admission can be used in CT-based strategies and several questions arise:
-
Is it cost-effective to admit clinically normal patients with a normal CT scan? Patients with a MHI and a normal CT scan have a very low (0.006%) risk of deterioration,167 so it is usually considered appropriate to discharge these patients home. We used our model to test the assumption that admission is not cost-effective for these patients.
-
Is it cost-effective to admit patients with a non-neurosurgical lesion on CT scan? These patients have a significant (13.5%)18 risk of deterioration requiring critical care or neurosurgical intervention, so hospital admission is typically considered appropriate. We used our model to determine whether or not admission is cost-effective for these patients.
-
Is it cost-effective to admit patients with a normal CT scan if no responsible adult is available to care for them? We assumed in the main analysis that patients with a normal CT scan would be discharged to the care of a responsible adult and would be brought back if they deteriorated. However, some patients do not have a responsible adult available and in the worst-case scenario a patient who deteriorated after discharge might die before being brought to medical attention. We used our model to test whether hospital admission for patients with a normal CT would be cost-effective if no responsible adult was available.
Finally, leading on from the last issue, we planned a secondary analysis to determine whether the optimal strategy remained so in the absence of a responsible adult. In these circumstances the potential benefit of CT scanning is enhanced because the consequences of missed intracranial lesion are more severe. The worst-case scenario would be that any patient discharged with an intracranial lesion would die before being brought to medical attention. We used the model to determine which strategy would be most cost-effective in this situation. This analysis and the third analysis above were only undertaken for adults because it was assumed that, in the case of children, a responsible adult would always be available.
Diagnostic parameters of each strategy
For each strategy, we estimated the sensitivity for neurosurgical intracranial lesion, the sensitivity for non-neurosurgical intracranial lesion and the specificity for no lesion. In the main analysis we assumed that CT scanning was 100% accurate for identifying significant intracranial lesions and that the only relevant lesions were those related to the head injury (i.e. we did not consider incidental findings unrelated to the injury). The ‘CT all’ strategy, therefore, had 100% sensitivity for both neurosurgical and non-neurosurgical lesions and 100% specificity. The ‘zero option’ strategy had zero sensitivity and 100% specificity.
The literature review identified that most clinical decision rules for adults had estimates of diagnostic parameters from validation cohorts, although often in different settings from the derivation cohort. Decision rules would be expected to perform better in a derivation cohort and in a validation cohort from the same setting as the derivation cohort, so a validation study undertaken in a different setting could provide the most appropriate estimate of diagnostic performance. However, using different cohorts to estimate parameters for different decision rules could introduce selection bias. We therefore decided to use data from a validation study by Stein et al. 71 to estimate parameters for all adult decision rules. This study reported a large, unselected cohort in which all of the main clinical decision rules were validated. All but one of them (the NWFCS rule)72 had been developed in a different population. Further details of the parameters used are provided below (see Transition possibilities).
The literature review identified that there has been very little validation of decision rules for children. We therefore used the derivation cohorts to provide estimates of diagnostic parameters for each of the decision rules for children, with the exception of Kupperman et al.,90 where we combined data from the derivation and validation cohorts. Further details are provided below (see Transition possibilities). We included decision rules only where data were available to calculate the sensitivity of the rule for neurosurgical and non-neurosurgical lesions separately, and where there were sufficient numbers of neurosurgical lesions to provide a meaningful estimate of sensitivity. The differences between the parameters reported for children’s decision rules may be due to differences in the cohorts and the reference standard used (particularly for non-neurosurgical injury) rather than performance of the rules. During the project we identified a study that had compared multiple decision rules for children in a validation cohort. 89 We used the estimates of diagnostic accuracy for the UCD,93 NEXUS II62 and CHALICE30 rules from this study to undertake a sensitivity analysis using validation data. Further details of the estimated diagnostic parameters used are provided below (see Transition possibilities).
To estimate the cost-effectiveness of hospital admission compared with discharge home for clinically well patients with a normal CT scan we used data from a published review of studies that followed up patients with a MHI and a normal CT scan. 167 This study reported that 4/66,121 (0.006%) patients subsequently deteriorated and required neurosurgery. We assumed that the effect of early intervention associated with admitting these patients was similar to the effect modelled in patients with a non-neurosurgical lesion on CT (see below). We therefore modelled a comparison between admission and discharge of a cohort of patients who received CT scan and then had a 0.006% probability of subsequent deterioration.
To estimate the cost-effectiveness of hospital admission compared with discharge home for patients with a non-neurosurgical lesion on CT we modelled a comparison between admission and discharge for a cohort of patients with a non-neurosurgical lesion on CT. We used data from Fabbri et al. 18 to estimate the risk of subsequent deterioration and an estimate of the relative risk of adverse outcome after discharge home (details outlined below).
To estimate the cost-effectiveness of hospital admission for patients with a normal CT scan and no responsible adult we repeated the analysis used to determine the cost-effectiveness of admission in those with a normal CT, but assumed that patients who deteriorated after discharge died and accrued no QALYs.
To determine the optimal strategy for adults when no responsible adult is available we repeated the main analysis, but assumed that all patients who had a missed ICI (neurosurgical or non-neurosurgical) died and accrued no QALYs.
Glasgow Outcome Score categorisation
The model allocated each patient to a GOS category according to whether they had an intracranial lesion and how quickly it was treated. This involved estimating the probabilities that patients with neurosurgical and non-neurosurgical lesions would end up in each GOS category depending on the extent of treatment delay.
Outcomes of neurosurgical lesions
As outlined in the previous section (see Glasgow Outcome Score categorisation), we needed to estimate the effect of delayed intervention upon the probability of ending up in each GOS category after suffering a neurosurgical intracranial lesion. Treatment without significant delay should correspond to current best practice. We therefore estimated outcomes from published studies reporting GOS after operation for extradural haemorrhage in cohorts of patients exclusively or predominantly presenting with GCS 13–15. These are summarised in Table 25.
| Author, year | Patients | GCS score | n | GOS score | ||||
|---|---|---|---|---|---|---|---|---|
| 5 | 4 | 3 | 2 | 1 | ||||
| Lee et al. 19987 | All | 13–15 | 77 | 63 | 4 | 3 | 4 | 3 |
| Cheung et al. 20078 | All | 13–15 | 21 | 14 | 5 | 1 | 0 | 1 |
| Cook et al. 19889 | All | 14–15 | 34 | 33 | 0 | 0 | 0 | 1 |
| Gerlach et al. 200910 | Children | 13–15 | 23 | 23 | 0 | 0 | 0 | 0 |
| Haselberger et al. 198811 | All | 8–15 | 22 | 13 | 7 | 1 | 0 | 1 |
A fixed-effects meta-analysis was conducted to estimate the proportions of patients categorised into each of the five GOS categories. The outcome data from each study were assumed to come from a multinomial distribution and the same degree of heterogeneity was assumed for each of the five states. The analysis was conducted in the Bayesian software Winbugs Version 1.4 (MRC Biostatistics Unit, Cambridge, UK) using vague prior distributions. In order for the pooled proportions to add up to approximately 1, constraints similar to those used previously for relative risks and risk differences were applied. 168 The results are shown in Table 26.
| GOS state | n | % | 95% CrI (%) |
|---|---|---|---|
| 5 | 146/177 | 81.00 | 74.7 to 86.1 |
| 4 | 16/177 | 9.30 | 5.6 to 13.9 |
| 3 | 5/177 | 3.20 | 1.2 to 6.3 |
| 2 | 4/177 | 2.70 | 0.9 to 5.5 |
| 1 | 6/177 | 3.80 | 1.6 to 7.9 |
Estimating the effect of delay upon outcome is difficult. Studies have analysed the association between time delay before surgery and outcome, generally reporting either no association or a negative association (i.e. longer time delays are associated with lower mortality). One would expect delays before neurosurgery to be associated with higher mortality, so this association is likely to be confounded by disease severity, with more severe cases receiving more urgent treatment.
We identified one study12 reporting the association between time delay and outcome where the time delay was due to long-distance interhospital transfer and thus presumably not related to disease severity. The outcomes for the patients who went directly to the neurosurgical centre (non-delayed) and those transferred before operation (delayed) are outlined in Table 27.
| Median timea | GOS 5, n (%) | GOS 4, n (%) | GOS 3, n (%) | GOS 2, n | GOS 1, n (%) | |
|---|---|---|---|---|---|---|
| Direct | 4 hours 19 minutes | 16 (69.6) | 5 (21.7) | 2 (8.7) | 0 | 0 |
| Transfer | 8 hours 5 minutes | 30 (68.1) | 5 (11.4) | 4 (9.1) | 0 | 5 (11.4) |
Using the probabilities for transferred patients directly would be problematic because of the small numbers. In particular, no transferred patients ended up in a vegetative state (GOS 2), whereas intuitively we would expect this outcome to be more common after delayed treatment. We therefore dichotomised GOS into good outcome (GOS 4 or 5) versus poor outcome (GOS 1–3) and used this to estimate the relative risk of a poor outcome following delayed treatment, which was 2.4.
Another study11 showed the association between outcome and time delay from LOC to operation. In this circumstance we would not expect confounding by disease severity to have a major influence because all patients who required neurosurgery after LOC would be treated as urgent and any delays would more likely be due to logistic factors. The results of this study are shown in Table 28.
| Delay | GOS 5, n (%) | GOS 4, n (%) | GOS 3, n (%) | GOS 2, n | GOS 1, n (%) |
|---|---|---|---|---|---|
| < 2 hours | 6 (33.3) | 6 (33.3) | 3 (16.7) | 0 | 3 (16.7) |
| > 2 hours | 1 (6.7) | 1 (6.7) | 4 (26.7) | 0 | 9 (60.0) |
Dichotomising the data between good outcome (GOS 4 or 5) and poor outcome (GOS 1–3) produced a relative risk for additional time delay causing an adverse outcome of 2.6, suggesting a similar effect to that calculated from the Deverill and Aitken12 data, albeit in a different scenario.
The relative risk for delay was calculated by assuming the proportion of patients with a poor outcome (GOS 1–3) was distributed binomially (and independently) for the two groups and treated as a stochastic variable in the calculations that follow. The proportions of patients in GOS categories 3, 2 and 1 above (i.e. with prompt treatment) were multiplied by the relative risk and the proportions in categories 4 and 5 were divided by the relative risk. Then the five probabilities were adjusted by dividing them by the sum of the probabilities for all categories to ensure that the proportions in each category for the delayed group added up to 1. These calculations were done in Winbugs to ensure that all variables were treated as stochastic (i.e. with uncertainty) for all calculations. The probabilities for each GOS category after delayed treatment are shown in Table 29.
| GOS state | Percentage | 95% CrI (%) |
|---|---|---|
| 5 | 57.0 | 7.3 to 87.5 |
| 4 | 6.8 | 0.8 to 12.4 |
| 3 | 12.0 | 0.9 to 38.2 |
| 2 | 9.9 | 0.7 to 33.2 |
| 1 | 14.3 | 1.1 to 43.1 |
The economic model of Smits et al. 162 was published while we were developing our model. This used data from a study of the CHIP rule to estimate GOS outcomes after prompt treatment and historical data from Cordobés et al. 169 (before the routine use of CT scanning) to estimate outcomes after delayed treatment. Having established our own approach we decided not to copy the approach used by Smits et al. 162 or use the CHIP data, but to retain our own approach and see if the two different models would use similar parameter estimates and generate similar outcomes. Table 30 shows the estimates used in our model alongside those used in a similar model by Smits et al. 162 This shows that although we estimated that more patients in both scenarios would make a full recovery, the absolute effect of delayed care (in terms of the proportion who would make a full recovery) was less.
| GOS state | Our study % (95% CI) | Smits et al. % (95% CI) | ||
|---|---|---|---|---|
| Immediate | Delayed | Immediate | Delayed | |
| 5 | 80.9 (74.7 to 86.1) | 56.3 (7.3 to 87.5) | 63 (19 to 95) | 39 (5 to 82) |
| 4 | 9.2 (5.6 to 13.9) | 6.1 (0.8 to 12.4) | 31.0 (2 to 26) | 22.0 (0 to 73) |
| 3 | 3.1 (1.2 to 6.3) | 11.3 (0.9 to 38.2) | 0 | 10 (0 to 68) |
| 2 | 2.6 (0.9 to 5.5) | 9.2 (0.7 to 33.2) | 0 | 0 |
| 1 | 3.7 (1.6 to 7.9) | 13.5 (1.1 to 43.1) | 6 (0 to 20) | 29 (1 to 76) |
Outcome of non-neurosurgical lesions
We needed to estimate what proportion of patients with a non-neurosurgical lesion on CT subsequently deteriorated and needed intervention. We also needed to estimate the probability of ending up in each GOS category if (1) the lesion is detected on CT and the patient admitted and treated appropriately and (2) CT is not performed and the patient discharged home without appropriate treatment.
The first scenario corresponds to best current practice and was therefore estimated from studies of outcome for patients admitted with GCS 13–15 and a non-neurosurgical lesion on CT. We found one relevant study (Fabbri et al. 18) that reported on 865 patients admitted with GCS 9–15 (700/865 with GCS 14–15) and ICI who did not require immediate neurosurgery. Of these 177/865 (13.5%) deteriorated and required neurosurgical intervention. The outcomes for these patients are reported in Table 31. GOS categories 4 and 5 were reported together for these 117 patients so we assumed that the relative proportions of GOS 4 and 5 among those receiving intervention were similar to those of the overall cohort, i.e. 12% had GOS 4.
| GOS state | n | Percentage | 95% CI (%) |
|---|---|---|---|
| 5 | 95/117 | 81.2 | 73.2 to 87.2 |
| 4 | 13/117 | 11.1 | 6.6 to 18.1 |
| 3 | 8/117 | 6.8 | 3.5 to 12.9 |
| 2 | 0/117 | 0. | 0. to 3.2 |
| 1 | 1/117 | 0.9 | 0.2 to 4.7 |
We could not find any studies that reported the effect of time delay upon outcome in these patients. We therefore assumed that time delay had a similar effect to time delay in the treatment of lesions requiring immediate surgery, i.e. a relative risk of 2.4 for adverse outcome. The probability estimates for GOS after missed lesion and delayed treatment are shown in Table 32.
| GOS state | Point estimate (%) | 95% CI (%) |
|---|---|---|
| 5 | 55.96 | 7.2 to 85.8 |
| 4 | 8.26 | 1.0 to 15.7 |
| 3 | 27.66 | 2.1 to 74.1 |
| 2 | 2.66 | 0. to 15.8 |
| 1 | 5.46 | 0.2 to 24.7 |
Most patients with non-neurosurgical lesions do not deteriorate, but these patients could potentially benefit from hospital admission if this allowed structured provision of information and planning of follow-up. We searched the literature to identify studies that estimated the benefit of such an intervention. A systematic review to examine the evidence for non-surgical intervention following mild TBI revealed only 16 acceptable studies. 14 The authors concluded that the evidence supported a minimal educational strategy and encouragement of early return to normal activity. Routine use of intensive assessment and intervention did not improve outcomes when compared with simple interventions. In particular, there was no evidence that hospital admission was any better or worse in the prediction of adverse outcomes in this group. The most efficient and effective intervention was explanation and education for the patient about expected symptoms, but no figures for degree of effect are quoted. We therefore assumed that patients with non-neurosurgical lesions who did not deteriorate did not benefit from detection of their lesion or hospital admission.
Modelling methodology
A decision tree model was developed using Simul8 Professional software (Simul8 Corporation, Boston, MA, USA) to explore the costs and health outcomes associated with a MHI. The analysis was conducted for patients aged 1, 10, 40 and 75 years when presenting to the ED. The model takes a lifetime horizon, with mean life expectancy based on UK interim life tables. 170 The analysis did not consider males and females separately. The economic perspective of the model is the NHS in England and Wales. Figure 21 shows the treatment pathways in the model.
FIGURE 21.
Treatment pathway in the economic model.
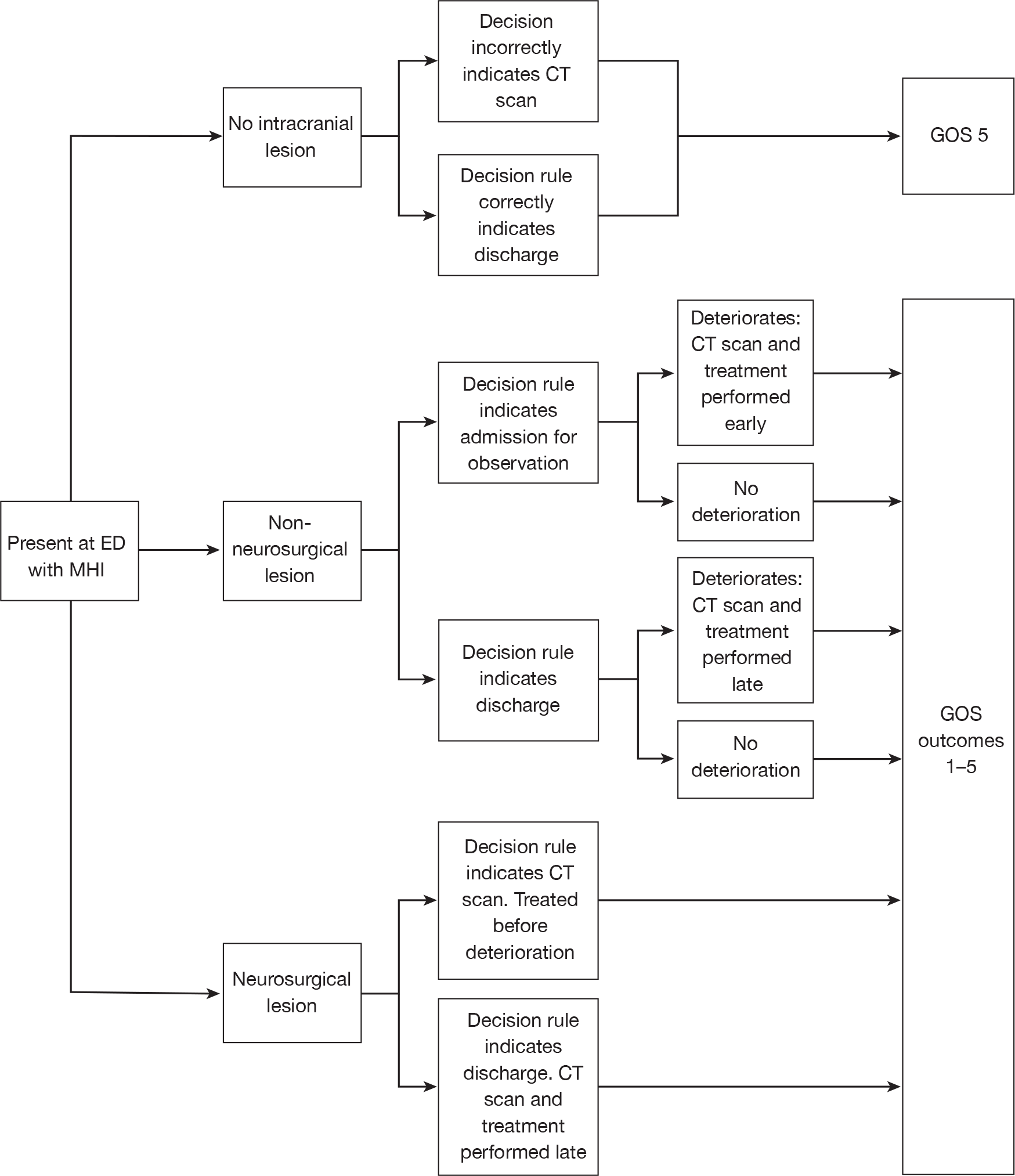
Baseline and comparator decision rules
The decision rules evaluated in adults were ‘CT all’ (theoretical), ‘abnormal arrival’ GCS (theoretical), CCHR (high risk),26 CCHR (high or medium risk),26 NCWFNS,72 NOC,27 NEXUS II,62 NICE1 and Scandinavian. 73 The decision rules evaluated in children were ‘CT all’ (theoretical), CHALICE,30 PECARN,90 UCD93 and the rule of Atabaki et al. 2008. 81
Movement between Glasgow Outcome Score states over time
A literature review was conducted to identify studies that investigated progression and regression between GOS states over time. One study was found: Whitnall et al. 171 determined the outcomes at 5–7 years compared with outcomes at 1 year of a cohort of patients (n = 219) admitted to hospital after a head injury. The cohort was recruited from five hospitals in Glasgow in 1995–6. The index used to assess outcomes was the GOS-E. The comparison of outcomes (converted to GOS) between 1 and 5–7 years after injury is shown in Table 33. As the transition time is between 5 and 7 years, each patient is randomly assigned a time between 5 and 7 years at which point they will change states according to the Whitnall et al. 171 findings; thereafter, they are assumed to stay in that state for life.
| GOS state at 1 year | GOS at follow-up years 5–7 (%) | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| 1 | NA | NA | NA | NA | NA |
| 2 | 100 | 0 | 0 | 0 | 0 |
| 3 | 46 | 0 | 31 | 16 | 7 |
| 4 | 30 | 0 | 6 | 41 | 23 |
| 5 | 28 | 0 | 4 | 14 | 54 |
Vegetative state
The Multi-Society Task Force on Persistent Vegetative State reported the mean length of survival for adults and children in a vegetative state as 3.6 and 7.4 years, respectively. Patients in GOS 2 accrued the costs associated with a vegetative state for this length of time and were then assumed to have died. The QoL associated with a vegetative state in our model is zero.
Costs
Costs included in the model are the direct costs of diagnostic management including the costs of investigation, including CT scanning, and the subsequent costs of providing neurosurgical treatment and intensive care. A literature review was conducted to find costs for patients whose outcomes are represented by GOS states 2–5. Only one study was found. This study by the Personal Social Services Research Unit172 (PSSRU) aimed to identify the health and social care services used by young adults aged 18–25 years with acquired brain injury. The study used literature reviews, surveys and expert opinion to identify the annual incidence of acquired brain injury and then estimated likely pathways of care over a notional 12-month period. The study estimated average costs per person in four groups of patients, which correspond closely to the descriptions of GOS scores 3–5. As acknowledged in the above study, there is a ‘dearth of literature’ in this area and we have been unable to find any cost data for children or older people and have therefore assumed that the costs are the same as for age 18–25 years. The effect of differential cost by age will be tested in the sensitivity analysis. No cost data were found for patients in a vegetative state. We have, therefore, based our estimates on expert opinion. 173 This estimate is based on 2 weeks in intensive care, followed by 4 months of rehabilitation and then transfer to a nursing home for the rest of the patient’s life. No nursing home care cost for children is available in the PSSRU Unit Costs of Health and Social Care 2009 and we have, therefore, assumed it is the same as for adults. Gamma distributions were used for all costs in the PSA.
Costs were discounted at an annual rate of 3.5% and were varied between 0% and 6% in the sensitivity analysis, as recommended by the NICE guide to the methods of technology appraisal). 182 Costs used in the model are shown in Table 34.
| Description | Cost (£) | 95% CI (£) | Horizon | Source |
|---|---|---|---|---|
| ED visit | 126 | 67 to 170 | One off | National Schedule of Reference Costs 2007–08 174 |
| CT scan | 100 | 80 to 117 | One off | National Schedule of Reference Costs 2007–08 174 |
| Admission with no deterioration or neurosurgery: head Injury without ICI without complications | 847 | 490 to 997 | One off | National Schedule of Reference Costs 2007–08 174 |
| Neurosurgical intervention after deterioration: intracranial procedures for trauma with intermediate diagnosis | 5805 | 3605 to 6616 | One off | National Schedule of Reference Costs 2007–08 174 |
| Neurosurgical intervention before deterioration: intracranial procedures for trauma with minor diagnosis | 5273 | 3758 to 6374 | One off | National Schedule of Reference Costs 2007–08 174 |
| Long-term costs – GOS 4 | 17,160 | –10% to 20% | 1 year | Beecham et al.172 |
| Long-term costs – GOS 3 | 33,900 | –10% to 20% | 1 year | Beecham et al.172 |
| GOS 2 – intensive care | 15,469 | 12,781 to 17,561 | 14 days of care | National Schedule of Reference Costs 2007–08 174 |
| GOS 2 – rehabilitation | 27,960 | –10% to 20% | 4 months | PSSRU 2009. NLIU for intermediate care175 |
| GOS 2 – nursing home | 893/week | –10% to 20% | Rest of life | PSSRU 2009. Local authority residential care for older people175 |
Quality-of-life utility values
A literature review was conducted to identify studies that estimated utility values for GOS scores. Two studies were found: Smits et al. 162 obtained long-term GOS outcomes and QoL scores using the EQ-5D questionnaire from a subset of patients from the study of CT in head injury patients. 166 These were converted to utility scores and reported in the publication. QoL data were available for 87 patients. Aoki and Kitahara165 used standard gamble methods to elicit QoL utilities for GOS states 2–5 from 140 members of staff and students at a hospital in Japan.
These studies were assessed for methodological compliance with the NICE reference case, which stipulates that utilities should be measured in patients using a generic and validated classification system for which reliable UK population reference values, elicited using a choice-based method such as the time trade-off or standard gamble, are available. The Smits et al. study162 was considered to comply most closely with the NICE reference case. Table 35 shows the results from this study.
| GOS state | QoL point estimate | 95% CI |
|---|---|---|
| 3 | 0.15 | 0.06 to 0.28 |
| 4 | 0.51 | 0.39 to 0.63 |
| 5 | 0.88 | 0.74 to 0.97 |
The GOS state 2 represents patients in a vegetative state and, therefore, no QoL data can be collected from these patients. We have assumed that the QoL of these patients is the same as death (GOS 1) and is zero. The Smits et al. study162 did not report the age distribution of those patients used to estimate QoL utilities. We have, therefore, assumed that QoL for GOS 3 and GOS 4 is not age related. We have also assumed that QoL for GOS 5 is not age related; this is a potential weakness of the model. However, it is likely that the QoL lost through the ageing process will be proportionately comparable across all management strategies and the conclusions will be unaltered.
Cancer risk due to radiation from computerised tomography scans
Computerised tomography scans expose the patient to radiation, which causes cancer in a proportion of patients. This will have cost and QoL implications that have been accounted for in the model. The additional lifetime risk of cancer in adult patients is estimated at 1 in 10,000. 176 However, the risk decreases with age. 177 A study by Stein et al. 178 used modelling techniques and data from a literature review to estimate the risks of radiation exposure from a single CT scan to children of different ages. 178 The study also estimated mean QALYs lost attributable to radiation (discounted at 3% per annum) and the types and relative prevalence of radiation-induced cancers. The Stein et al. 178 data estimate tumour risk and QALY loss up to the age of 20 years and, in order to include the tumour risk and QALY loss for adults in our model, we used the Stein et al. 178 data from ages 5–20 years and predicted these forward using regression techniques (model R2 = 0.98). Table 36 shows the Stein et al. 178 data and our predictions. The tumour-risk prediction from age 35 years is the same as the best available evidence for the lifetime risk of cancer in adult patients. 176 A potential limitation of the model is using data from ages 5–20 years to predict QALY loss in adults. It is possible that our predictions do not sufficiently take into account the effects of discounting on QALY loss, which could mean that our predictions overestimate QALY loss in adults, especially the 75-year-old patient. This limitation, however, is expected to have little effect, as any inaccuracies around the QALY loss are likely to be small, but would favour those policies that perform fewer CT scans.
| Age at exposure (years) | Tumour risk | Discounted QALY loss | |
|---|---|---|---|
| Mean | SD | ||
| Stein et al. data178 | |||
| 1 | 0.0022 | 0.0221 | 0.0018 |
| 2 | 0.0015 | 0.0156 | 0.0018 |
| 5 | 0.0012 | 0.0130 | 0.0014 |
| 10 | 0.0008 | 0.0093 | 0.0014 |
| 15 | 0.0005 | 0.0062 | 0.0012 |
| 20 | 0.0004 | 0.0052 | 0.0010 |
| Predicted values | |||
| 25 | 0.0003 | 0.005 | 0.0010 |
| 30 | 0.0002 | 0.004 | 0.0009 |
| 35 | 0.0001 | 0.004 | 0.0009 |
| 40 | 0.0001 | 0.003 | 0.0008 |
| 45 | 0.0001 | 0.003 | 0.0008 |
| 50 | 0.0001 | 0.003 | 0.0008 |
| 55 | 0.0001 | 0.003 | 0.0008 |
| 60 | 0.0001 | 0.003 | 0.0007 |
| 65 | 0.0001 | 0.002 | 0.0007 |
| 70 | 0.0001 | 0.002 | 0.0007 |
| 75 | 0.0001 | 0.002 | 0.0007 |
Table 37 shows the types and relative prevalence of radiation-induced cancers in children as estimated in the Stein et al. 178 study. We were unable to find similar evidence relating to adults and our model, therefore, assumes that the types and relative prevalence of cancer are the same in adults as in children. We conducted a literature review to identify the mean expected cost of thyroid carcinoma, meningioma and glioma. The mean cost of glioma is taken from a Health Technology Assessment journal publication; this was the only reliable UK data source identified. 179 No reliable UK data source was identified for the cost of thyroid carcinoma or meningioma; in the absence of information, the cost of glioma has been used. We have also included a cost for palliative care for terminally ill patients in the UK. 179
| Cancer type | Relative incidence | Cost (£) | Assumed lower and upper bounds |
|---|---|---|---|
| Thyroid carcinoma | 0.47 | 23,651 | ± 10% |
| Meningioma | 0.35 | 23,651 | ± 10% |
| Glioma | 0.19 | 23,651 | ± 10% |
| Cost of palliative care | 3087 | ± 10% | |
| Overall cost of cancer | 26,738 | ± 10% |
The cost of cancer for each person in the model is estimated by tumour risk × mean cost of cancer × number of scans received. The Stein et al. 178 study reports that the latency between radiation exposure and tumour diagnosis is > 5 years in the majority of cases; based on this, we have assumed a mean latency period of 10 years and the cost of cancer is therefore discounted for this time period.
Transition probabilities
Transition probabilities in the model are determined by the sensitivity and specificity of each decision rule. Further details are provided in Table 38 for adults and Tables 39 and 40 for children. Column ‘R’ denotes the row number for simplicity. ‘R1’ is the probability that a neurosurgical lesion is correctly identified; these patients receive prompt surgery. ‘R2’ is 1 – R1, these patients have an intracranial lesion and are discharged with a responsible adult. ‘R3’ is the probability that a non-neurosurgical lesion is correctly identified; these patients are admitted and those that deteriorate are given prompt treatment. ‘R4’ is 1 – R3; these patients are discharged and receive delayed treatment if they deteriorate. ‘R5’ is the probability that patients with no intracranial lesion are correctly identified and discharged. ‘R6’ is 1 – R5; these patients have an unnecessary CT scan. The transition probabilities for GOS outcomes are described above (see Glasgow Outcome Score categorisation).
| R | Type of sensitivity or specificity | Probability of sensitivity or specificity of each strategy (95% CI) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Discharge all | CT all, admit positive, discharge negative | Abnormal arrival GCS | CCHR (high risk)26 | CCHR (high or medium risk)26 | NCWFNS72 | NOC27 | NEXUS II62 | NICE1 | Scandinavian73 | ||
| 1 | Strategy sensitivity for NS injury | 0 | 1 |
0.91 (0.84 to 0.95) |
0.99 (0.94 to 1.00) |
0.99 (0.94 to 1.00) |
0.99 (0.94 to 1.00) |
0.99 (0.94 to 1.00) |
1.00 (0.97 to 1.00) |
0.98 (0.93 to 1.00) |
0.99 (0.94 to 1.00) |
| 2 | 1 – sensitivity for NS injury | 1 | 0 | 0.09 | 0.01 | 0.01 | 0.01 | 0.01 | 0.00 | 0.02 | 0.01 |
| 3 | Strategy sensitivity for NNS injury | 0 | 1 |
0.72 (0.68 to 0.76) |
0.97 (0.94 to 0.98) |
0.99 (0.97 to 1.00) |
0.95 (0.93 to 0.97) |
0.99 (0.97 to 1.00) |
0.97 (0.94 to 0.98) |
1.00 (0.99 to 1.00) |
0.95 (0.92 to 0.97) |
| 4 | 1 – sensitivity for NNS injury | 1 | 0 | 0.28 | 0.03 | 0.01 | 0.05 | 0.01 | 0.03 | 0.00 | 0.05 |
| 5 | Strategy specificity | 1 | 0 |
0.97 (0.96 to 0.98) |
0.51 (0.49 to 0.52) |
0.47 (0.46 to 0.48) |
0.47 (0.46 to 0.48) |
0.33 (0.32 to 0.34) |
0.47 (0.46 to 0.48) |
0.31 (0.30 to 0.32) |
0.53 (0.52 to 0.54) |
| 6 | 1 – specificity | 0 | 1 | 0.03 | 0.49 | 0.53 | 0.53 | 0.67 | 0.53 | 0.69 | 0.47 |
| R | Type of sensitivity or specificity | Probability of sensitivity or specificity of each strategy (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| Discharge all | CT all, admit positive, discharge negative | CHALICE30 | PECARN90 | Atabaki et al. 200881 | UCD93 | ||
| 1 | Strategy sensitivity for NS injury | 0 | 1 |
134/137 0.98 (0.94 to 0.99) |
41/41 1.00 (0.91 to 1.00) |
6/6 1.00 (0.61 to 1.00) |
29/29 1.00 (0.88 to 1.00) |
| 2 | 1 – sensitivity for NS injury | 1 | 0 |
3/137 0.02 |
0/41 0.00 |
0/6 0.00 |
0/29 0.00 |
| 3 | Strategy sensitivity for NNS injury | 0 | 1 |
142/143 0.99 (0.96 to 1.00) |
228/237 0.96 (0.93 to 0.98) |
56/59 0.95 (0.86 to 0.98) |
97/98 0.99 (0.94 to 0.99) |
| 4 | 1 – sensitivity for NNS injury | 1 | 0 |
1/143 0.01 |
9/237 0.04 |
3/59 0.05 |
1/98 0.01 |
| 5 | Strategy specificity | 1 | 0 |
19,558/22,491 0.87 (0.86 to 0.88) |
18,454/31,416 0.59 (0.58 to 0.60) |
457/935 0.49 (0.46 to 0.52) |
827/1938 0.43 (0.40 to 0.45) |
| 6 | 1 – specificity | 0 | 1 |
2933/22,491 0.13 |
12,871/31,416 0.41 |
478/935 0.51 |
1111/1938 0.57 |
| R | Type of sensitivity or specificity | Probability of sensitivity or specificity of each strategy (95% CI) | ||||
|---|---|---|---|---|---|---|
| Discharge all | CT all, admit positive, discharge negative | CHALICE30 | NEXUS II62 | UCD93 | ||
| 1 | Strategy sensitivity for NS injury | 0 | 1 |
1.00 (0.88–1.00) |
1.00 (0.88–1.00) |
1.00 (0.88–1.00) |
| 2 | 1 – sensitivity for NS injury | 1 | 0 | 0.00 | 0.00 | 0.00 |
| 3 | Strategy sensitivity for NNS injury | 0 | 1 |
0.98 (0.92–1.00) |
0.96 (0.93–1.00) |
0.99 (0.93–1.00) |
| 4 | 1 – sensitivity for NNS injury | 1 | 0 | 0.02 | 0.04 | 0.01 |
| 5 | Strategy specificity | 1 | 1 |
0.05 (0.03–0.07) |
0.21 (0.17–0.26) |
0.12 (0.09–0.16) |
| 6 | 1 – specificity | 0 | 0 | 0.95 | 0.79 | 0.88 |
Model stability
The number of patients in each model run determines the stability of the results for estimating the optimal management strategy. This instability is a result of some events having a rare occurrence and stability can only be achieved by having sufficient numbers of patients to account for these rare events. With < 100,000 patients the model results were unstable in as far as the optimal management strategy would sometimes differ. With ≥ 100,000 patients in the model run, the optimal strategy was unchanged for all age groups despite the same input data.
Results
Deterministic results
Adult aged 40 years
Table 41 shows the mean costs and QALYs per patient according to whether or not the patient had an intracranial lesion, and then all cases combined. Costs and QALYs for patients with an intracranial lesion were determined by the sensitivity of the strategy for detecting lesions. Higher sensitivity was associated with higher QALYs and lower costs, the latter being due to the costs of care for those with GOS 2–4. Costs and QALYs for patients without an intracranial lesion were determined by the specificity of the strategy. Higher specificity was associated with lower costs and higher QALYs, the latter due to the effect of radiation exposure (the fewer CT scans performed, the less the radiation exposure and associated QALY loss).
| Strategy | Intracranial lesion | No intracranial lesion | All patients | |||
|---|---|---|---|---|---|---|
| Mean costs (£) | Mean QALYs | Mean costs (£) | Mean QALYs | Mean costs (£) | Mean QALYs | |
| Discharge all | 41,795 | 12.699 | 126 | 19.1560 | 3305 | 18.6633 |
| NICE1 | 35,930 | 13.052 | 196 | 19.1537 | 2923 | 18.6881 |
| CT all | 35,972 | 13.047 | 228 | 19.1526 | 2955 | 18.6868 |
| Abnormal arrival GCS | 37,635 | 12.970 | 129 | 19.1559 | 2991 | 18.6839 |
| CCHR (high risk)26 | 36,113 | 13.045 | 176 | 19.1543 | 2918 | 18.6882 |
| CCHR (high or medium risk)26 | 35,946 | 13.055 | 180 | 19.1542 | 2909 | 18.6888 |
| NCWFNS72 | 35,974 | 13.041 | 180 | 19.1542 | 2911 | 18.6878 |
| NOC27 | 35,946 | 13.055 | 194 | 19.1537 | 2922 | 18.6884 |
| NEXUS II62 | 35,937 | 13.045 | 180 | 19.1542 | 2908 | 18.6880 |
| Scandinavian73 | 35,974 | 13.041 | 174 | 19.1544 | 2905 | 18.6880 |
Variation in specificity between the strategies leads to only small differences in the mean cost per patient for those with no intracranial lesion (about £100 per patient difference between the cheapest and most expensive) compared with the cost differences between those with intracranial lesion associated with variation in sensitivity (> £6000 per patient difference). This reflects the modest cost of CT scanning compared with the substantial costs of long-term care. Similarly, the QALY differences associated with variation in specificity are small (range of 0.0034 QALYs) compared with the QALY differences associated with variation in sensitivity (range of 0.3540 QALYs). These observations mean that when all patients are examined together, sensitivity is a greater determinant of both costs and QALYs, despite the relatively low prevalence of ICI. However, the increased costs and reduced QALYs observed in patients with no intracranial lesion with the ‘CT all’ strategy are still significant enough to reduce the cost-effectiveness of this strategy compared with more selective strategies.
Table 42 shows the strategies ordered by ascending effectiveness (QALYs gained) and reports whether or not they are dominated by a cheaper and more effective strategy or subject to extended dominance. Where a strategy is neither dominated nor extendedly dominated an ICER is reported. The theoretical strategies (‘discharge all’, ‘CT all’ and ‘CT only if abnormal GCS’) are all clearly dominated, confirming that selective CT use based upon sensitive decision rules is likely to represent a cost-effective use of health-care resources. The NCWFNS,72 NICE,1 CCHR26 (high risk) and NOC27 strategies were all dominated. The NEXUS II62 strategy was extendedly dominated by the Scandinavian73 and CCHR26 (high or medium risk) strategies. The CCHR26 (with CT for high- and medium-risk cases) is the most cost-effective on deterministic analysis, although the differences in mean costs and QALYs between the various rules were small and determined by differences in point estimates for sensitivity that were not statistically significant in the primary data.
| Strategy | Mean costs (£) | Mean QALYs | Incremental cost (£) | Incremental QALYs | ICER compared with next last effective treatment on the CE frontier |
|---|---|---|---|---|---|
| Discharge all | 3305 | 18.6633 | Dom | ||
| Abnormal arrival GCS | 2991 | 18.6839 | Dom | ||
| CT all | 2955 | 18.6868 | Dom | ||
| NCWFNS72 | 2911 | 18.6878 | Dom | ||
| Scandinavian73 | 2905 | 18.6880 | NA | ||
| NEXUS II62 | 2908 | 18.6880 | ExtDoma | ||
| NICE | 2923 | 18.6881 | Dom | ||
| CCHR26 (high risk) | 2918 | 18.6882 | Dom | ||
| NOC27 | 2922 | 18.6884 | Dom | ||
| CCHR26 (high or medium risk) | 2909 | 18.6888 | 3 | 0.00089 | £3879 |
Adult aged 75 years
Table 43 reports the main deterministic analysis for an adult aged 75 years. Mean QALYs and mean costs are both lower than in the analysis for a 40-year-old adult, reflecting reduced life expectancy, and thus reduced long-term costs and QALYs. However, long-term costs of care for patients with GOS 2–4 remain the main cost driver and the QALY gain from accurate identification of intracranial lesion still outweighs the proportionately reduced QALY loss from irradiation. The CCHR, therefore, remains the most cost-effective, with the theoretical strategies clearly dominated.
| Strategy | Mean costs (£) | Mean QALYs | Incremental cost (£) | Incremental QALYs | ICER compared with next last effective treatment on the CE frontier |
|---|---|---|---|---|---|
| Discharge all | 1716 | 7.8277 | Dom | ||
| Abnormal arrival GCS | 1543 | 7.8363 | Dom | ||
| CT all | 1567 | 7.8368 | Dom | ||
| NCWFNS72 | 1523 | 7.8376 | Dom | ||
| NICE1 | 1535 | 7.8376 | Dom | ||
| NEXUS II62 | 1520 | 7.8377 | Dom | ||
| Scandinavian73 | 1517 | 7.8377 | NA | ||
| NOC27 | 1534 | 7.8378 | Dom | ||
| CCHR (high risk)26 | 1521 | 7.8378 | Dom | ||
| CCHR (high or medium risk)26 | 1521 | 7.8381 | 3 | 0.00033 | £10,397 |
Child aged 10 years
Table 44 reports the mean costs and QALYs for a child aged 10 years ‘with an intracranial lesion’, ‘without’ and ‘all patients’. Mean costs and QALYs are generally higher, reflecting longer life expectancy. However, the variation in the differences in mean costs and QALYs are only moderately greater than the variation observed in the adult case, owing to the effect of discounting. The variation in costs and QALYs for those with an intracranial lesion is again much greater than the variation in those without an intracranial lesion. So, although the potential effect of irradiation in children is greater than in adults, the costs and QALYs lost by misdiagnosis of intracranial lesion are correspondingly increased. The CHALICE30 rule dominates the other strategies by virtue of gaining more QALYs with lower costs.
| Strategy | Intracranial lesion | No intracranial lesion | All patients | |||
|---|---|---|---|---|---|---|
| Mean costs (£) | Mean QALYs | Mean costs (£) | Mean QALYs | Mean costs (£) | Mean QALYs | |
| CHALICE30 | 45,038 | 15.6795 | 141 | 22.9720 | 3567 | 22.4156 |
| PECARN90 | 45,221 | 15.6639 | 174 | 22.9693 | 3611 | 22.4119 |
| UCD93 | 44,961 | 15.6717 | 192 | 22.9679 | 3608 | 22.4112 |
| Atabaki et al.81 | 45,225 | 15.6604 | 185 | 22.9684 | 3621 | 22.4108 |
| CT all | 45,122 | 15.6680 | 241 | 22.9639 | 3666 | 22.4072 |
| Discharge all | 52,405 | 15.2597 | 126 | 22.9732 | 4115 | 22.3847 |
Child aged 1 year
Table 45 reports mean costs and QALYs for a child aged 1 year ‘with an intracranial lesion’, ‘without’ and ‘all patients’. The results do not differ markedly from those for a child aged 10 years and, again, CHALICE30 is the dominant strategy.
| Strategy | Intracranial lesion | No intracranial lesion | All patients | |||
|---|---|---|---|---|---|---|
| Mean costs (£) | Mean QALYs | Mean costs (£) | Mean QALYs | Mean costs (£) | Mean QALYs | |
| CHALICE30 | 46,066 | 16.0746 | 144 | 23.5566 | 3648 | 22.9857 |
| PECARN90 | 46,252 | 16.0583 | 185 | 23.5503 | 3699 | 22.9787 |
| UCD93 | 45,985 | 16.0665 | 207 | 23.5568 | 3700 | 22.9760 |
| Atabaki et al.81 | 46,257 | 16.0545 | 198 | 23.5482 | 3713 | 22.9764 |
| CT all | 46,179 | 16.0526 | 268 | 23.5374 | 3771 | 22.9663 |
| Discharge all | 53,605 | 15.6364 | 126 | 23.5595 | 4206 | 22.9549 |
Sensitivity analysis
Sensitivity analysis using Stein et al.’s prevalence estimates
We repeated the deterministic analysis using the estimates of prevalence of neurosurgical lesion and non-neurosurgical lesion from Stein et al. 71 (Tables 46–49). The CHALICE30 rule remained dominant for children, but the NEXUS II62 rule was dominant for adults. This reflects our estimates of sensitivity for neurosurgical and non-neurosurgical injury. The CCHR (high- and medium-risk criteria) had higher sensitivity than NEXUS II for non-neurosurgical injury, and was more cost-effective in the baseline analysis, which used a higher estimated prevalence of non-neurosurgical injury. However, the NEXUS II62 rule had higher sensitivity for neurosurgical injury and was thus dominant when the Stein et al. data71 (with higher prevalence for neurosurgical injury) were used. The absolute cost and QALY differences between the CCHR and NEXUS II62 rules were very small in both analyses and attributable to small differences in point estimates of sensitivity.
| Strategy | Mean costs (£) | Mean QALYs | ICER compared with the next last effective treatment on the CE frontier |
|---|---|---|---|
| Discharge all | 4979 | 22.9426 | Dom |
| CT all | 4512 | 22.9552 | Dom |
| UCD93 | 4440 | 22.9653 | Dom |
| Atabaki et al.81 | 4415 | 22.9670 | Dom |
| PECARN90 | 4429 | 22.9690 | Dom |
| CHALICE30 | 4400 | 22.9735 | Dominant strategy |
| Strategy | Mean costs (£) | Mean QALYs | ICER compared with the next last effective treatment on the CE frontier |
|---|---|---|---|
| Discharge all | 4874 | 22.3725 | Dom |
| CT all | 4393 | 22.3965 | Dom |
| UCD93 | 4333 | 22.4009 | Dom |
| Atabaki et al.81 | 4310 | 22.4019 | Dom |
| PECARN90 | 4326 | 22.4027 | Dom |
| CHALICE30 | 4304 | 22.4038 | Dominant strategy |
| Strategy | Mean costs (£) | Mean QALYs | ICER compared with the next last effective treatment on the CE frontier |
|---|---|---|---|
| Discharge all | 3757 | 18.6512 | Dom |
| Abnormal arrival GCS | 3394 | 18.6730 | Dom |
| CT all | 3391 | 18.6761 | Dom |
| NOC27 | 3339 | 18.6774 | Dom |
| CCHR (high risk)26 | 3346 | 18.6775 | Dom |
| NICE1 | 3364 | 18.6775 | Dom |
| CCHR (high or medium risk)26 | 3326 | 18.6778 | Dom |
| NCWFNS72 | 3350 | 18.6778 | Dom |
| Scandinavian73 | 3344 | 18.6780 | Dom |
| NEXUS II62 | 3312 | 18.6783 | Dominant strategy |
| Strategy | Mean costs (£) | Mean QALYs | ICER compared with the next last effective treatment on the CE frontier |
|---|---|---|---|
| Discharge all | 1954 | 7.8226 | Dom |
| Abnormal arrival GCS | 1748 | 7.8318 | Dom |
| CT all | 1788 | 7.8323 | Dom |
| NOC27 | 1746 | 7.8332 | Dom |
| NICE1 | 1757 | 7.8332 | Dom |
| CCHR (high risk)26 | 1739 | 7.8333 | Dom |
| CCHR (high or medium risk)26 | 1732 | 7.8334 | Dom |
| NCWFNS72 | 1743 | 7.8334 | Dom |
| Scandinavian73 | 1738 | 7.8336 | Dom |
| NEXUS II62 | 1727 | 7.8336 | Dominant strategy |
Univariate
A univariate sensitivity analysis was conducted to identify those parameters that were most likely to alter the choice of which management strategy was optimal. Each parameter was assigned the lowest and highest value according to the 95% CI. For all ages, no parameter change altered the optimal strategy decision. Discount rates were varied between 0% and 6% in accordance with the NICE methods guide;182 these rates had no effect on the optimal strategy decision for all ages.
Sensitivity analysis using validation data for children
We repeated the deterministic analysis for children using data from the study that validated the NEXUS II,62 UCD93 and CHALICE30 rules. 89 The results are shown for children aged 1 year (Table 50) and children aged 10 years (Table 51). All three rules dominate the ‘CT all’ and ‘discharge all’ strategies at both ages. The CHALICE30 rule is dominated by the NEXUS II62 and UCD93 rules. The NEXUS II62 rule is more effective and more expensive than the UCD rule93 with an ICER of £3363 per QALY in the age 1 year analysis and £7471 in the age 10 years analysis. Assuming a threshold for willingness to pay of £20,000 or 30,000 per QALY, the NEXUS II62 rule is optimal.
| Strategy | Mean costs (£) | Mean QALYs | Incremental cost (£) | Incremental QALYs | ICER compared with the next last effective treatment on the CE frontier |
|---|---|---|---|---|---|
| Discharge all | 4206 | 22.955 | Dom | ||
| CT all | 3771 | 22.966 | Dom | ||
| CHALICE30 | 3759 | 22.968 | Dom | ||
| UCD93 | 3740 | 22.970 | |||
| NEXUS II62 | 3749 | 22.972 | 8 | 0.002 | £3556 |
| Strategy | Mean costs (£) | Mean QALYs | Incremental cost (£) | Incremental QALYs | ICER compared with the next last effective treatment on the CE frontier |
|---|---|---|---|---|---|
| Discharge all | 4115 | 22.3847 | Dom | ||
| CT all | 3666 | 22.4072 | Dom | ||
| CHALICE30 | 3658 | 22.4073 | Dom | ||
| UCD93 | 3641 | 22.4085 | |||
| NEXUS II62 | 3651 | 22.4098 | 10 | 0.001 | £7755 |
| Parameter | Mean probability or per cent | 95% CI probability or per cent | Distribution |
|---|---|---|---|
| Clinical outcomes | |||
| NS injury | 0.0053 | 0.0033 to 0.0085 | Beta |
| NNS injury | 0.0710 | 0.0626 to 0.0805 | Beta |
| NS lesion: GOS outcomes after immediate intervention | |||
| GOS 5 | 81.00% | 74.7% to 86.1% | Dirichlet |
| GOS 4 | 9.30% | 5.6% to 13.9% | Dirichlet |
| GOS 3 | 3.20% | 1.2% to 6.3% | Dirichlet |
| GOS 2 | 2.70% | 0.9% to 5.5% | Dirichlet |
| GOS 1 | 3.80% | 1.6% to 7.9% | Dirichlet |
| NS lesion: GOS outcomes after late intervention | |||
| GOS 5 | 57.0% | 7.3% to 87.5% | Dirichlet |
| GOS 4 | 6.8% | 0.8% to 12.4% | Dirichlet |
| GOS 3 | 12.0% | 0.9% to 38.2% | Dirichlet |
| GOS 2 | 9.9% | 0.7% to 33.2% | Dirichlet |
| GOS 1 | 14.3% | 1.1% to 43.1% | Dirichlet |
| NNS lesion: GOS outcomes after immediate intervention | |||
| GOS 5 | 81.2% | 73.2% to 87.2% | Dirichlet |
| GOS 4 | 11.1% | 6.6% to 18.1% | Dirichlet |
| GOS 3 | 6.8% | 3.5% to 12.9% | Dirichlet |
| GOS 2 | 0% | 0.0% to 3.2% | Dirichlet |
| GOS 1 | 0.9% | 0.2% to 4.7% | Dirichlet |
| NNS lesion: GOS outcomes after late intervention | |||
| GOS 5 | 55.96% | 7.2% to 85.8% | Dirichlet |
| GOS 4 | 8.26% | 1.0% to 15.7% | Dirichlet |
| GOS 3 | 27.66% | 2.1% to 74.1% | Dirichlet |
| GOS 2 | 2.66% | 0.0% to 15.8% | Dirichlet |
| GOS 1 | 5.46% | 0.2% to 24.7% | Dirichlet |
| QoL utilities | |||
| GOS 3 | 0.15 | 0.06 to 0.28 | Beta |
| GOS 4 | 0.51 | 0.39 to 0.63 | Beta |
| GOS 5 | 0.88 | 0.74 to 0.97 | Beta |
| Age-related effect of a single paediatric head CT scan on tumour occurrence | |||
| Age 1 year | 0.0022 | ± 10% | Normal |
| Age 10 years | 0.0008 | ± 10% | Normal |
| Age 40 years | 0.0001 | ± 10% | Normal |
| Age 75 years | 0.0001 | ± 10% | Normal |
| Age-related effect of a single paediatric head CT scan on QoL decrement | |||
| Age 1 year | 0.0221 | 0.0185 to 0.0257 | Beta |
| Age 10 years | 0.0093 | 0.0066 to 0.012 | Beta |
| Age 40 years | 0.0030 | 0.0018 to 0.005 | Beta |
| Age 75 years | 0.0020 | 0.001 to 0.0035 | Beta |
| Cancer latency (years) | 10 | ± 5 | Normal |
| PVS mean survival | |||
| Age 1 and 10 years | 7.4 | ± 10% | Normal |
| Age 40 and 75 years | 3.59 | ± 10% | Normal |
| Costs (£) | 95% CI or assumed limit | ||
| Costs | |||
| ED visit | 126 | £67 to 170 | Gamma |
| CT scan | 100 | £80 to 117 | Gamma |
| Admission with no deterioration or neurosurgery: head Injury without ICI without complications | 847 | £490 to 997 | Gamma |
| NS intervention after deterioration: intracranial procedures for trauma with intermediate diagnosis | 5805 | £3605 to 6616 | Gamma |
| NS intervention before deterioration: intracranial procedures for trauma with minor diagnosis | 5273 | £3758 to 6374 | Gamma |
| Long-term costs – GOS 4 | 17,160 | –10% to 20% | Gamma |
| Long-term costs – GOS 3 | 33,900 | –10% to 20% | Gamma |
| GOS 2 – intensive care | 15,469 | £12,781 to 17,561 | Gamma |
| GOS 2 – rehabilitation | 27,960 | –10% to 20% | Gamma |
| GOS 2 – nursing home | 893/week | –10% to 20% | Gamma |
| Cost of cancer | 26,738 | ± 10% | Gamma |
Probabilistic sensitivity analysis
Table 52 shows the parameters and distributions used in the PSA.
Probabilistic sensitivity analysis results
Tables 53–56 show the mean PSA values for ages 1, 10, 40 and 75 years, respectively. In the PSA, the CHALICE30 rule is the dominant strategy for children, as was the case in the deterministic analysis. For adults, the CCHR26 (high or medium risk) rule was the most cost-effective in the deterministic analysis, with ICERs of approximately £4000 and £10,000 for ages 40 and 75 years, respectively. However, in the PSA this decision rule dominates the other rules for both ages.
| Strategy | Mean costs (£) | Mean QALYs | ICER compared with next last effective treatment on the CE frontier |
|---|---|---|---|
| Discharge all | 14,743 | 22.9599 | Dom |
| CT all | 13,046 | 22.9706 | Dom |
| Atabaki et al.81 | 13,056 | 22.9804 | Dom |
| UCD93 | 13,003 | 22.9804 | Dom |
| PECARN90 | 13,014 | 22.9832 | Dom |
| CHALICE30 | 12,936 | 22.9896 | Dominant strategy |
| Strategy | Mean costs (£) | Mean QALYs | ICER compared with the next last effective treatment on the CE frontier |
|---|---|---|---|
| Discharge all | 14,403 | 22.3895 | Dom |
| CT all | 12,723 | 22.4114 | Dom |
| Atabaki et al.81 | 12,746 | 22.4147 | Dom |
| UCD93 | 12,693 | 22.4154 | Dom |
| PECARN90 | 12,707 | 22.4164 | Dom |
| CHALICE30 | 12,636 | 22.4194 | Dominant strategy |
| Strategy | Mean costs (£) | Mean QALYs | ICER compared with the next last effective treatment on the CE frontier |
|---|---|---|---|
| Discharge all | 11,540 | 18.6674 | Dom |
| Abnormal arrival GCS | 10,538 | 18.6863 | Dom |
| CT all | 10,232 | 18.6902 | Dom |
| NCWFNS72 | 10,232 | 18.6911 | Dom |
| NICE1 | 10,212 | 18.6912 | Dom |
| Scandinavian73 | 10,226 | 18.6913 | Dom |
| NOC27 | 10,205 | 18.6913 | Dom |
| NEXUS II62 | 10,214 | 18.6914 | Dom |
| CCHR (high risk)26 | 10,210 | 18.6915 | Dom |
| CCHR (high or medium risk)26 | 10,192 | 18.6917 | Dominant strategy |
| Strategy | Mean costs (£) | Mean QALYs | ICER compared with the next last effective treatment on the CE frontier |
|---|---|---|---|
| Discharge all | 5466 | 7.82941 | Dom |
| Abnormal arrival GCS | 5008 | 7.83736 | Dom |
| CT all | 4919 | 7.83823 | Dom |
| NICE1 | 4891 | 7.83895 | Dom |
| NOC27 | 4887 | 7.83899 | Dom |
| NCWFNS72 | 4892 | 7.83903 | Dom |
| Scandinavian73 | 4886 | 7.83913 | Dom |
| NEXUS II62 | 4884 | 7.83914 | Dom |
| CCHR (high risk)26 | 4880 | 7.83921 | Dom |
| CCHR CT (high or medium risk)26 | 4874 | 7.83928 | Dominant strategy |
Figures 22–25 show the graphical results of the PSA for each age group. These are presented as cost-effectiveness acceptability curves,181 with the probability of each strategy being the most cost-effective plotted against values of willingness to pay for health gain ranging from £0 (where the cheapest strategy is the most cost-effective) to £50,000 per QALY. The usual threshold for decision-making is £20,000–30,000 per QALY. 182
FIGURE 22.
Cost-effectiveness acceptability curve for a child aged 1 year.
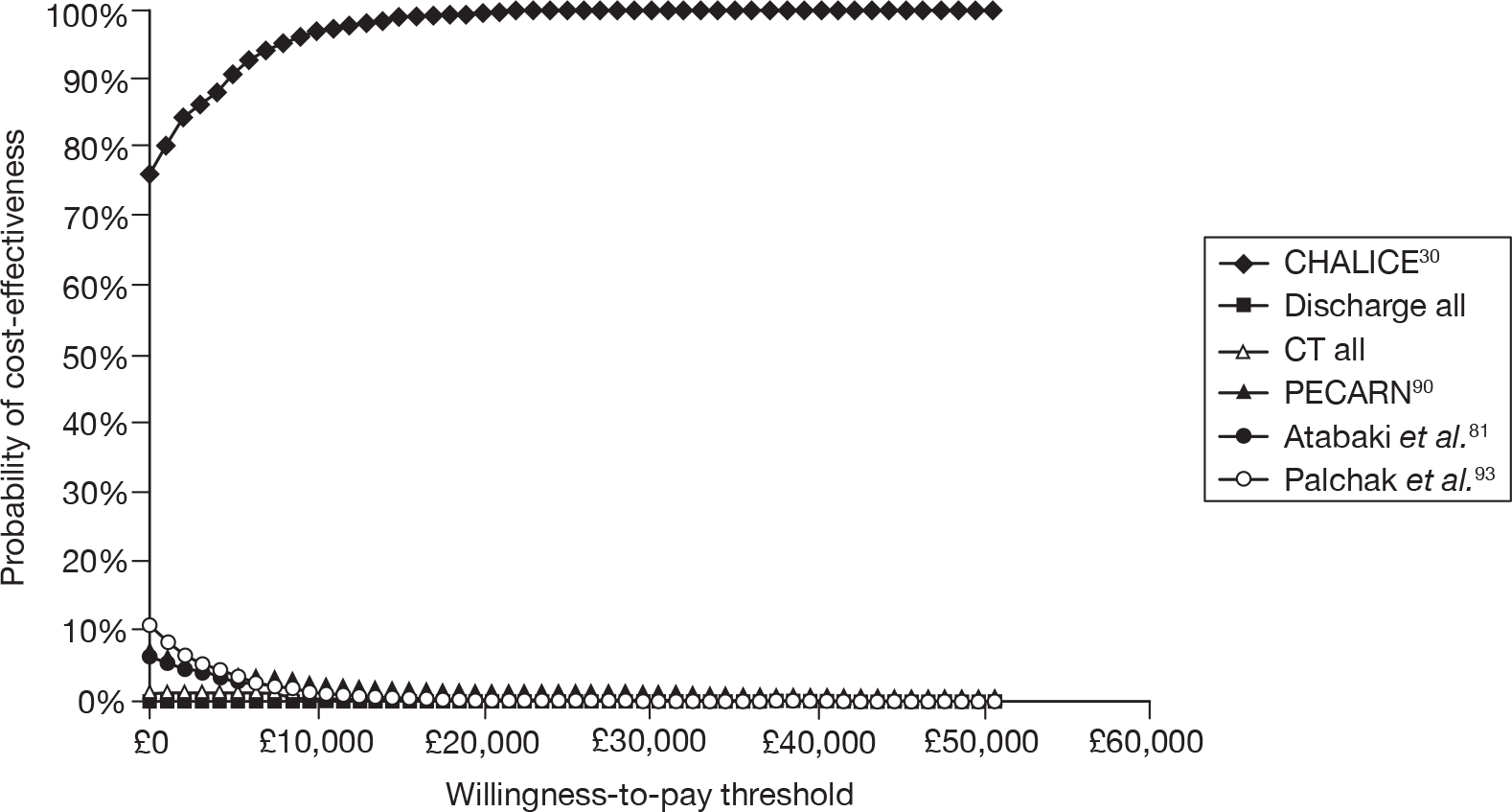
FIGURE 23.
Cost-effectiveness acceptability curve for a child aged 10 years.
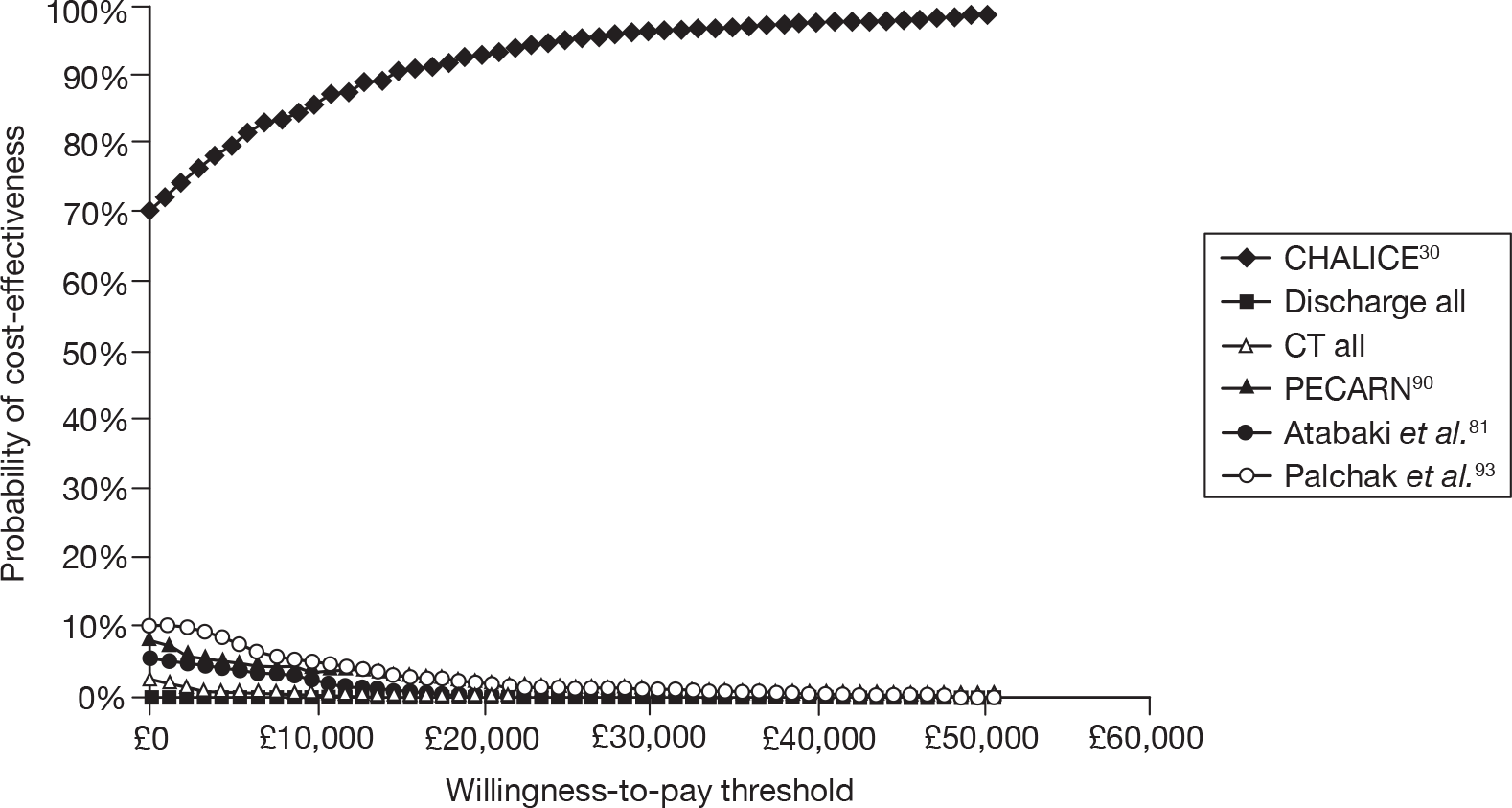
FIGURE 24.
Cost-effectiveness acceptability curve for an adult aged 40 years. H/M, high/medium.
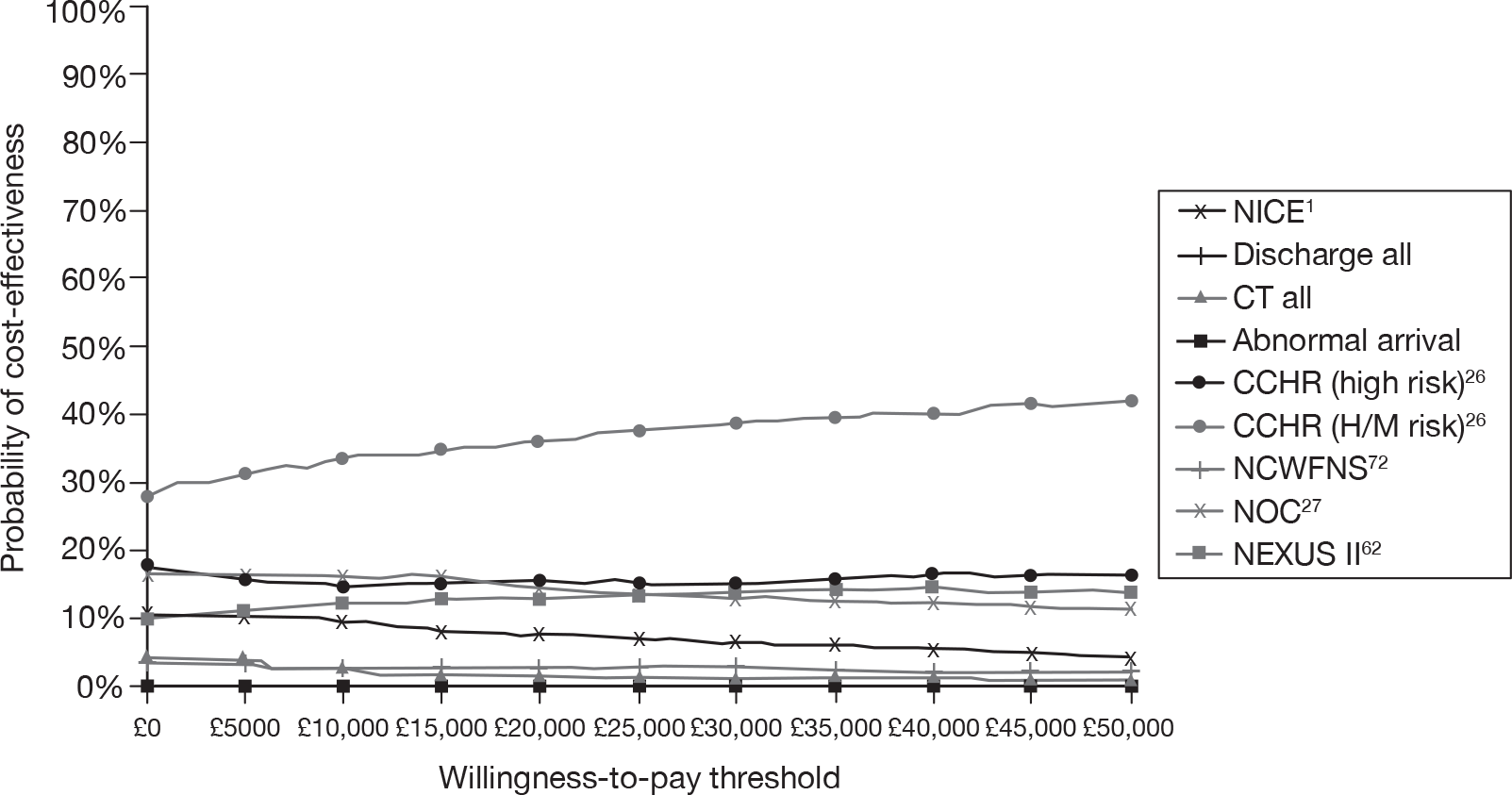
FIGURE 25.
Cost-effectiveness acceptability curve for an adult aged 75 years. H/M, high/medium.
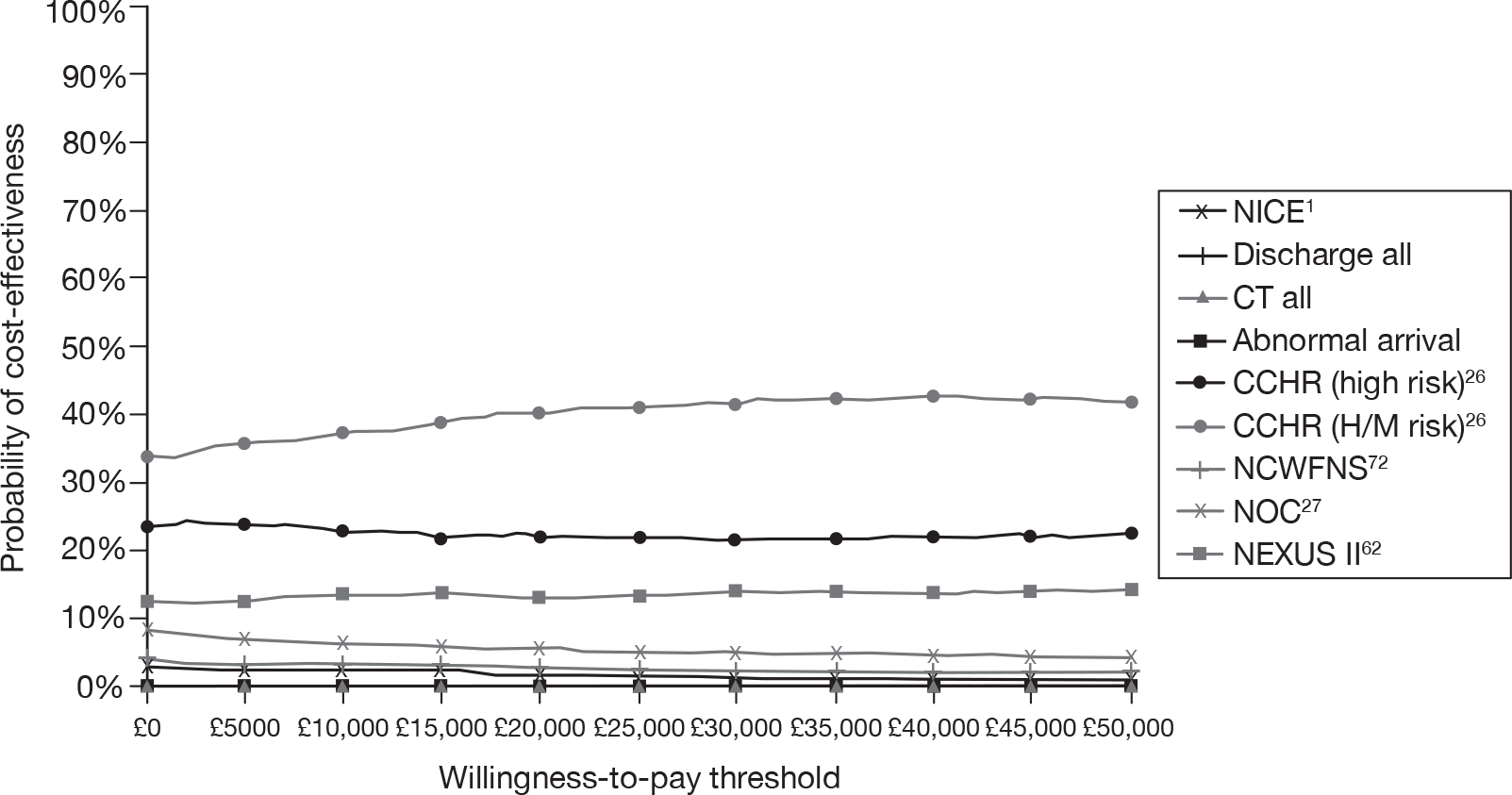
For children, the optimal management strategy is the CHALICE30 rule. For willingness-to-pay thresholds between £0 and £50,000, the probability that this management strategy is cost-effective is 75–100% for children aged 1 year and 70–100% for children aged 10 years.
For adults, the optimal management strategy is the CCHR (medium to high risk). For willingness-to-pay thresholds between £0 and £50,000, the probability that this management strategy is cost-effective is 28–42% for adults aged 40 years and 34–42% for adults aged 75 years.
Analysis of optimal sensitivity and specificity
The CCHR (high and medium risk), with sensitivity of 99% and specificity of 47%, was the optimal strategy for adults. To explore whether this represents an appropriate trade-off between sensitivity and specificity, we undertook a secondary deterministic analysis to identify the extent to which specificity could be sacrificed to produce a more cost-effective rule with 100% sensitivity and the extent to which sensitivity could be sacrificed to produce a more cost-effective rule with markedly increased (70%) specificity. We compared a theoretical rule with 100% sensitivity and varying specificity to the CCHR, and then compared a theoretical rule with 70% specificity and varying sensitivity to the CCHR. The results are shown in Table 57.
| Specificity of 100% sensitive rule | Dominates or ICER | Sensitivity of 70% specific rule | Dominates or ICER |
|---|---|---|---|
| 0.47 | Dominates | 0.99 | Dominates |
| 0.40 | Dominates | 0.98 | Dominates |
| 0.39 | £11,288 | 0.97 | Dominates |
| 0.38 | £29,061 | 0.96 | Dominates |
| 0.37 | £51,828 | 0.95 | £64,714 |
| 0.36 | £82,036 | 0.94 | £152,631 |
| 0.29 | Dominated | 0.93 | Dominated |
The results show that the rule with 100% sensitivity would dominate the CCHR if specificity were ≥ 40%. It would be cost-effective with 38–39% specificity if we were willing to pay £30,000 per QALY gained, but would not be cost-effective using this threshold if specificity were ≤ 37%. The rule with 70% specificity would dominate the CCHR if sensitivity were ≥ 96%. It would be cost-effective with 94–95% specificity unless we were willing to pay more than the £30,000 per QALY threshold, but if sensitivity were ≤ 93% it would be dominated. This analysis suggests that the CCHR26 has an appropriate ratio of sensitivity to specificity and one should not be sacrificed to any great extent to optimise the other.
Admission strategies
Table 58 shows the costs, QALYs, discounted life-years gained (DLYG) and ICER for the strategy of admitting patients with a normal CT to hospital compared with discharge home with a responsible adult. Hospital admission gains a very small number of QALYs compared with discharge home, reflecting the low risk of subsequent deterioration and thus the low potential benefit from admission. Hospital admission is markedly more expensive than discharge home, so the ICER of admission is almost £39M per QALY. Hospital admission for patients with a normal CT scan would not therefore be considered a cost-effective use of health-care resources on the basis of detecting subsequent deterioration.
| Management policy | Cost (£) | QALY | DLYG | Incremental cost (£) | Incremental QALY | ICER |
|---|---|---|---|---|---|---|
| Admit | 467,668,501 | 8,706,969 | 10,883,914 | 441,432,181 | 11 | 38,997,739 |
| Discharge | 26,236,319 | 8,706,958 | 10,883,870 |
Table 59 shows the costs, QALYs, DLYG and ICER for the same strategy, but compared with discharge home without a responsible adult. The admission strategy gains more QALYs because it is assumed that discharged patients who deteriorate are not brought to medical attention and die. As a result, the ICER drops to £2.5M per QALY, but is still much higher than current thresholds for willingness to pay.
| Management policy | Cost (£) | QALY | DLYG | Incremental cost (£) | Incremental QALY | ICER |
|---|---|---|---|---|---|---|
| Admit | 467,668,501 | 8,706,969 | 10,883,914 | 467,668,501 | 186 | 2,507,834 |
| Discharge | 0 | 8,706,783 | 10,883,478 |
Table 60 shows the costs, QALYs, DLYG and ICER for the strategy of admitting patients with a non-neurosurgical lesion on CT scan. The admission strategy gains QALYs by providing earlier treatment of patients who deteriorate. It also costs less because earlier treatment results in fewer cases requiring long-term care, which compensates for the costs of hospital admission. The admission strategy is, therefore, cheaper and more effective than discharge home.
| Cost (£) | QALY | DLYG | Incremental cost (£) | Incremental QALY | ICER | |
|---|---|---|---|---|---|---|
| Admit | 60,659,174,150 | 7,974,524 | 10,365,266 | –3,387,557,645 | 37,543 | Dominates |
| Discharge | 64,046,731,795 | 7,936,981 | 10,317,224 |
Table 61 shows the base-case analysis for a 40-year-old adult repeated with the assumption that patients who are discharged home have no responsible adult and are, therefore, not brought to medical attention when they deteriorate. It is assumed that patients with a missed neurosurgical lesion or a missed non-neurosurgical lesion and who deteriorate will not receive treatment and die. The ‘discharge all’ strategy is therefore cheaper and less effective than in the main model and is not dominated by other strategies. The NCWFNS,72 Scandinavian,73 ‘CT all’, NEXUS II62 and NOC27 strategies are all dominated and the Abnormal arrival GCS and CCHR (high risk)26 are both extendedly dominated by the CCHR (high or medium risk)26 and the NICE1 strategies. The NICE1 strategy is therefore compared with the CCHR (high or medium risk)26 strategy and is cost-effective with an ICER of £8508.
| Strategy | Mean cost (£) | Mean QALY | Incremental cost (£) | Incremental QALY | ICER compared with the next least effective treatment on the CE frontier |
|---|---|---|---|---|---|
| Discharge all | 2055 | 18.5508 | |||
| Abnormal arrival GCS | 2830 | 18.6599 | ExtDoma | ||
| NCWFNS72 | 2910 | 18.6847 | Dom | ||
| Scandinavian73 | 2904 | 18.6849 | Dom | ||
| CT all | 2955 | 18.6868 | Dom | ||
| CCHR (high risk) | 2896 | 18.6868 | ExtDoma | ||
| NEXUS II62 | 2913 | 18.6869 | Dom | ||
| NOC27 | 2914 | 18.6872 | Dom | ||
| CCHR (high or medium risk)26 | 2901 | 18.6876 | 846 | 0.13683 | £6,182 |
| NICE1 | 2904 | 18.6880 | 3 | 0.00040 | £8,508 |
Expected value of perfect information analysis
The EVPI is the expected outcome with perfect information minus the expected outcome without perfect information. 183 Per-person EVPI for each age is shown in Table 62. An estimated 700,000 patients per year attend the ED with a MHI. Assuming a 10-year horizon for the value of further research, the maximum amount of research funding to achieve perfect information is calculated as the EVPI per person × 700,000 × 10.
| Age (years) | EVPI per person (£) | Maximum funding (£) |
|---|---|---|
| 1 | 0 | 0 |
| 10 | 0.6 | 4,200,000 |
| 40 | 24 | 168,000,000 |
| 75 | 14.1 | 98,700,000 |
The EVPI analysis appears to show that research funding will provide little value for money for children. However, this reflects failure of the model to appropriately quantify uncertainty around estimates of diagnostic accuracy for clinical decision rules in children. These estimates were obtained from large derivation studies that generated estimates of sensitivity and specificity that were precise, but arguably not accurate. Derivation studies may overestimate sensitivity and specificity. If this is the case then the CI from a large derivation study will not encompass the true value and will not reflect the uncertainty around diagnostic parameters.
For adults there appears to be a considerable sum of money available to be spent in order to remove all uncertainty from the model. However, such trials may need to be exceedingly large to remove a considerable proportion of uncertainty and may be of questionable ethical status. Formal expected value of sample information techniques185 would be an area for future research.
Expected value of partial perfect information analysis
An expected value of partial perfect information (EVPPI)184 analysis was not undertaken as this relies on two nested Monte Carlo simulations. The model takes approximately 1–2 hours to run a PSA of 1000 runs, depending on the processor speed. There are over 60 parameters in the model, each with 1000 PSA values. A full EVPPI analysis would therefore take approximately 90,000 (1.5 × 60 × 1000) hours, which was deemed impractical.
Chapter 6 Survey of current NHS practice
We aimed to evaluate current NHS practice in the management of isolated MHI, review national statistics relating to head injury and then correlate these two data sources to determine whether or not methods of service delivery are associated with differences in admission rates for head injury.
Methods of the survey
Data sources
Data were sought from two sources: (1) postal survey of the lead clinician of all major acute hospital EDs in the UK and (2) HES for England and Wales.
Questionnaire specification
A simple postal questionnaire survey was developed to identify key elements of service provision for isolated MHI. The survey was designed to be completed within 5 minutes by the lead clinician, based entirely upon his/her working knowledge of the department. The clinician was not asked to seek out data or estimate any parameters, such as proportions of patients receiving a particular form of care. The aim of this approach was to maximise response rates, data completion and reliability of responses. Two copies of the questionnaire were sent to each consultant, one for adults and one for children, except for departments known to only routinely receive adults or children. The two copies differed only in the patient group of interest. An example of the adult questionnaire is outlined in Appendix 12. Two further reminders, sent at 3-week intervals, were sent to non-responders.
Hospital Episode Statistics data requests
The HES is a data warehouse containing details of all admissions to NHS hospitals in England and is openly accessible online (www.hesonline.org.uk). Data on all acute hospital episodes from 1998 have been collected, assembled and made available online. Data on ED attendances have recently started to be collected and are available on request. HES data were formally requested from the Health and Social Care Information Centre for all records between 2007 and 2008 containing the ED diagnosis ‘head injury’ and attendance disposal (e.g. admission or discharge) by each provider (e.g. hospital or trust) in the UK.
Data analysis
The questionnaire survey responses were entered onto a Microsoft Excel 2007 (Microsoft Corporation, Redmond, WA, USA) spreadsheet and simple descriptive analysis of proportions in each response category were undertaken. The HES data were received on a Microsoft excel spreadsheet and were also analysed descriptively. Cases were divided into children (age 0–14 years) and adults (age > 14 years) and analysed separately. The proportions of adults and children at each trust who were admitted, discharged or had an unknown disposal from the ED were calculated, and then the proportion of cases in each category was determined. The following were excluded: trusts through which all patients were admitted, all were discharged or > 50% were unknown. This was because it was suspected that such trusts were seeing a selected patient group (such as referrals), were unable to admit patients or were providing unreliable data. The median proportion of patients admitted and discharged was then estimated.
Finally, each trust with analysable HES data was matched to an acute hospital associated with those trusts that had been sent and returned a questionnaire. Data were analysed using spss for Windows version 15.0 (SPSS Inc., Chicago, IL, USA). The median and IQR of the proportion of patients admitted between different types of service delivery were compared, and the Mann–Whitney U-test was used to assess the association between the proportions admitted and the type of service delivery. Data were presented separately for adults and children.
Results of the survey
Adults
Completed questionnaires were returned from 174/250 hospitals (69.6%). Table 63 summarises the questionnaire responses. Nearly all hospitals had unrestricted CT access. NICE guidelines were followed by 147/174 hospitals (84.5%), although amendments had been made to 33/147 (22.4%). Of the 33 hospitals that had made modifications to formal guidelines for local use, 17 provided further details on the changes undertaken. These typically took the form of additional criteria (not specified in the NICE guidelines) for CT scanning, including immediate CT for any reduction in GCS at presentation, delayed CT for patients that make assessment difficult while under the influence of alcohol and drugs, considering CT for severe (persistent/prolonged) headache and CT indicated in patients who return to the ED within 48 hours. The admission location varied between hospitals, but most hospitals admitted adults under the ED staff, and most required approval for admission by a senior or specialist doctor.
| Question | Response | n (%) |
|---|---|---|
| Guidelines | NICE (not specified) | 12 (6.9) |
| NICE (2003) | 7 (4.0) | |
| NICE (2007) | 128 (73.6) | |
| Other, including SIGN | 24 (13.8) | |
| None | 3 (1.7) | |
| CT access | Yes | 167 (96.0) |
| No | 6 (3.4) | |
| Not completed | 1 (0.6) | |
| Admission location | ED observation | 69 (39.7) |
| Clinical decision unit | 36 (20.7) | |
| Formal admission | 69 (39.7) | |
| Admission team | ED staff | 122 (70.1) |
| Inpatient team | 50 (28.7) | |
| Not completed | 2 (1.2) | |
| Admission approval | Any doctor | 53 (30.5) |
| Senior doctor | 94 (54.0) | |
| Senior or specialist | 11 (6.3) | |
| Specialist | 14 (8.0) | |
| Not completed | 2 (1.1) |
Hospital Episode Statistics data relating to adults were available from 121 trusts. We excluded 21 from further analysis because they either recorded that all patients were discharged, all were admitted, or had no admission or discharge data for over one-half of the patients. The number of adult cases attending the remaining 100 trusts ranged from 15 to 5630 (median 1050). The proportion discharged ranged from 54% to 95% (median 80%) and the proportion admitted from 1% to 45% (median 18%).
A total of 91 trusts that supplied usable adult HES data were matched with hospitals that had been sent a questionnaire, 72 of which had returned a completed questionnaire. Table 64 summarises the tests for association between questionnaire data and proportion admitted. There was a slight trend towards a lower proportion being admitted at hospitals requiring formal admission, where admission was under an inpatient team and where admission required senior or specialist approval. However, the differences were small (1–2%) and none of the associations approached statistical significance.
| Subgroup | n | Median % admitted | IQR (%) | p-value |
|---|---|---|---|---|
| Formal admission | 27 | 18.0 | 14.00 to 24.00 | 0.194 |
| Observation ward or CDU | 43 | 20.0 | 14.00 to 28.00 | |
| Admitted by ED staff | 51 | 20.0 | 15.00 to 27.00 | 0.349 |
| Admitted by inpatient team | 18 | 18.5 | 13.25 to 24.00 | |
| Senior or specialist | 49 | 19.0 | 14.00 to 25.00 | 0.964 |
| Any doctor can admit | 21 | 20.0 | 14.50 to 24.50 |
Children
Completed questionnaires were returned from 181/250 hospitals (72.4%). Table 65 summarises the questionnaire responses. Nearly all hospitals had unrestricted CT access. NICE guidelines were followed by 153/181 hospitals (84.5%), although amendments had been made to 35/153 (22.9%). Of the 35 hospitals that had made modifications to formal guidelines for local use, 20 provided further details on the changes undertaken. Of those hospitals that had modified the NICE guidelines for CT scanning (n = 16) in children, amendments were generally around the timing of performing CT, i.e. immediate CT versus delayed CT. The most common features that were amended for local use included delaying CT in patients with amnesia (anterograde or retrograde) lasting > 5 minutes, and dangerous mechanism of injury or presence of bruise, swelling or laceration > 5 cm on head in children < 1 year of age, as opposed to immediate CT as indicated in the NICE guidelines. Additional criteria for considering CT scanning included LOC or amnesia and coagulopathy or severe (persistent) headache. Unlike adults, most hospitals formally admitted children under an inpatient team. Most hospitals required approval for admission by a senior or specialist doctor.
| Question | Response | n (%) |
|---|---|---|
| Guidelines | NICE (not specified) | 6 (3.3) |
| NICE (2003) | 7 (3.9) | |
| NICE (2007) | 140 (77.3) | |
| Other, including SIGN | 25 (13.8) | |
| None | 3 (1.7) | |
| CT access | Yes | 171 (94.5) |
| No | 9 (5.0) | |
| Not completed | 1 (0.5) | |
| Admission location | ED observation | 10 (5.5) |
| Clinical decision unit | 11 (6.1) | |
| Formal admission | 157 (86.7) | |
| Not completed | 3 (1.7) | |
| Admission team | ED staff | 37 (20.4) |
| Inpatient team | 142 (78.5) | |
| Not completed | 2 (1.1) | |
| Admission approval | Any doctor | 63 (34.8) |
| Senior doctor | 64 (35.4) | |
| Senior or specialist | 7 (3.9) | |
| Specialist | 45 (24.9) | |
| Not completed | 2 (1.1) |
The HES data relating to children were available from 118 trusts. Data from 32 were excluded from further analysis because they recorded either that all patients were discharged or that all patients were admitted or because they had no admission or discharge data for over half the patients. The number of child cases ranged from 14 to 3202 (median 753). The proportion discharged ranged from 53% to 97% (median 90%) and the proportion admitted from 3% to 43% (median 9%).
A total of 78 trusts that supplied useable child HES data were matched with hospitals that had been sent a questionnaire, 64 of which had returned a completed questionnaire. Table 66 summarises the tests for association between questionnaire data and proportion admitted. The trend in children was the opposite of that in adults, with slightly more being admitted at hospitals requiring formal admission and/or admission under an inpatient team. However, the differences were again small and none of the associations approached statistical significance.
| Subgroup | n | Median % admitted | IQR (%) | p-value |
|---|---|---|---|---|
| Formal admission | 54 | 9.5 | 6.00 to 12.00 | 0.367 |
| Observation ward or CDU | 7 | 7.0 | 4.00 to 11.00 | |
| Admitted by ED staff | 14 | 8.5 | 4.00 to 11.00 | 0.282 |
| Admitted by inpatient team | 48 | 10.0 | 6.00 to 12.00 | |
| Senior or specialist | 40 | 8.5 | 6.00 to 11.00 | 0.559 |
| Any doctor can admit | 22 | 10.5 | 6.50 to 12.25 |
Chapter 7 Discussion
Statement of principal findings
Diagnostic accuracy studies
Clinical decision rules
Clinical decision rules for adults have generally been more widely validated than those for children. The CCHR criterion26 is the most widely validated rule for adults and appears to have consistently high sensitivity for neurosurgical injury whether or not the high- and medium-risk criteria or the high-risk criteria alone are used. Specificity has been sacrificed to optimise sensitivity, but is still adequate for a substantial proportion of patients to test negative in a typical population. Sensitivity of the rule for any ICI is more variable and estimates may reflect definition and application of the reference standard. Sensitivity of the criterion26 for any ICI may be lower if the definition of any ICI includes all potentially significant CT abnormalities. Other clinical decision rules have not been as widely tested as the CCHR and/or do not perform as well.
Clinical decision rules for children following MHI have increased in number from the eight identified in the recent review by Maguire et al. 186 The conclusion of Maguire et al. 186 that more research is needed has been accepted, although with new rules being derived but little validation there remains substantial uncertainty. Our review has identified a number of rules with derivation and validation data for both infants and children following MHI. Four rules have now been validated,30,90,91,93 three in an independent cohort. 30,91,93 All four rules have high sensitivity, but specificity is variable. The CHALICE30 rule in particular had 87% specificity in a derivation cohort30 with a limited reference standard but poor specificity in the validation study. 89 Currently, the PECARN rule90 appears to have the best specificity, but this may be because it has only been validated in a cohort from the same setting as the derivation cohort and not in a new setting.
Individual characteristics
Overall, it is apparent that nearly all the individual clinical features that have diagnostic value are useful for diagnosing ICI, rather than ruling out (i.e. they have high specificity and PLR, but poor sensitivity and NLR). Thus an unstructured approach to clinical evaluation would involve identifying positive clinical findings that raise the probability of ICI.
In adults, a depressed skull fracture, basal skull fracture, radiological skull fracture, PTS, focal neurological deficit, decrease in GCS or persistent vomiting all indicate a markedly increased risk of ICI (PLR > 5), whereas fall from a height, coagulopathy, chronic alcohol abuse, age over 60 years, pedestrian MVA, GCS < 14, GCS < 15, any seizure, any vomiting, anterograde amnesia or retrograde amnesia indicate a moderately increased risk of ICI (PLR 2–5). Other features, such as LOC and headache, appear to add little diagnostic value. However, LOC is sometimes used as an inclusion criterion for studies, so its diagnostic value may be underestimated. Only a few studies report data specifically for neurosurgical injuries, so it is difficult to draw reliable conclusions; however, the diagnostic value of characteristics for neurosurgical injuries does not appear to differ markedly from that of characteristics for any injury.
In children, a depressed skull fracture, basal skull fracture, focal neurological deficit, coagulopathy or PTS all indicate a substantially increased risk of ICI (PLR > 5), whereas visual symptoms, bicycle and pedestrian MVA, any seizure, any LOC, persistent vomiting, severe or persistent headache, anterograde/retrograde amnesia, GCS < 14, GCS < 15, intoxication and radiological skull fracture indicate a moderately increased risk of ICI (PLR 2–5). Other features, such as any headache or scalp laceration or haematoma, appear to add little diagnostic value. Only two studies report data for neurosurgical injuries and examined a limited range of characteristics. As with adults, there was no clear evidence that any characteristic had different diagnostic performance for neurosurgical injury as opposed to any ICI.
In infants, a depressed skull fracture or focal neurological deficit indicates a substantially increased risk of ICI, whereas radiological skull fracture, GCS < 15 and any LOC indicate a moderately increased risk.
Clinical decision rules for MHI are based on individual clinical characteristics, with the presence of a criterion indicating the need for CT scanning (or hospital admission prior to the widespread use of CT). There is substantial variation in the criteria used by each rule and it is interesting to examine the diagnostic value of each item, as estimated in our meta-analysis.
Most adult rules use GCS < 15, focal neurological deficit, LOC, vomiting and amnesia. Our meta-analysis of these individual characteristics suggested that LOC has little diagnostic value, although this may reflect its use as a selection criterion in many studies. The other four criteria were supported by our meta-analysis, although vomiting was only useful if it was persistent. Most rules did not specify that vomiting had to be persistent. Only around half of the rules specified suspected basal or depressed skull fracture, age, seizure, decreasing GCS, mechanism of injury or coagulopathy as criteria. Our meta-analysis suggested that these were useful criteria (or at least fall from a height and bicycle or pedestrian MVA were useful with regards to mechanism of injury). Conversely, several rules used headache as a criterion, whereas our meta-analysis suggested that this was of limited diagnostic value. Interestingly, this criterion also seems to have been added to NICE guidelines1,19 by some NHS trusts. Overall it appeared that NICE guidelines1,19 matched the findings of our meta-analysis very well (perhaps better than any other decision rule) in terms of including criteria that are diagnostically useful and excluding those that are not. We found little evidence to support the application of additional criteria to the NICE guidelines. 1,19
Most rules for children use LOC, GCS < 15, skull fracture, vomiting, headache and visible injury as criteria. Our meta-analysis of the individual characteristics supported the use of LOC, GCS < 15, skull fracture, vomiting and headache (if severe or persistent), but suggested that scalp laceration/haematoma or an undefined headache were of little diagnostic value. Less than half of the rules used focal neurological deficit, amnesia or seizures as criteria, few used mechanism of injury and only one used coagulopathy as criteria. Yet our meta-analysis suggested that all these criteria were potentially diagnostically useful. Overall the CHALICE30 and NEXUS II62 rules appeared to be most consistent with the findings of our meta-analysis, in terms of including criteria that are diagnostically useful and excluding those that are not.
Biomarkers
The only biomarker to be widely evaluated to date is S100B. Our meta-analysis shows that sensitivity has the potential to be clinically acceptable, whereas specificity could be adequate to significantly reduce the number of negative scans being performed. These findings are consistent with other non-systematic reviews on protein S100B. We identified more relevant studies than have previously been described and have formally assessed their quality. In general, these studies have been of high quality. However, there are some inconsistencies between the studies (see Strengths and limitation of the assessment, Clinical evaluation) in terms of timing of the sample and analyser used that may limit our ability to draw general conclusions.
It is likely that S100B will need to develop a role alongside or as part of a clinical decision rule. Two studies were identified that specifically used S100B in conjunction with current clinical decision rules, with the selection of symptomatic patients based on two previously reported guidelines26,27 for cranial CT in one study98 and using the European Federation of Neurological Societies guidelines for CT in another. 146 The sensitivity and specificity of a number of international decision rules published are better than those quoted for S100B alone, but these two studies provide support for an additional level of screening for intracranial abnormality.
Analysis of urine samples for elevated protein S100B has been performed in both adults and children as an alternative to blood sampling following head injury, although these data are not presented here. None of these studies has demonstrated a potential role for early urine sampling as a screening tool for cranial CT. 187–189
As an objective tool in the management of MHI, protein S100B has a potential role in reducing unnecessary radiation exposure. Meta-analysis data reveal clinically significant results that would permit an acceptable reduction in the rate of CT scan use while still identifying those with intracranial trauma. Clarification is required on the optimum time following injury for testing (evidence currently suggests < 3 hours) and acceptance that a local discriminative value is necessary to ensure patient safety, dependent on which analyser and sample type is used.
Diagnostic management studies
We found only one appropriately controlled study of alternative diagnostic management strategies for MHI. 37 It showed that early CT and discharge of patients with MHI is at least as effective as hospital admission and costs less. This provides empirical evidence for one of the assumptions behind our modelling strategy – that CT scanning is cheaper and more effective than hospital admission and will, therefore, dominate a direct comparison of these two strategies. This is why we did not use modelling to directly compare CT scanning with hospital admission, but instead used the modelling to explore alternative strategies that involved selecting patients for CT scanning using a clinical decision rule or alternative admission strategies based on CT findings. The main limitation of the diagnostic management study was that it could only reasonably compare two alternative strategies, whereas modelling allows comparison of multiple alternatives.
Eleven other studies (two contemporaneous cohort studies152,153 and nine uncontrolled before/after studies)21,22,136,154–159 were identified, but not formally included in the review as they lacked adequate control groups. Overall, these studies showed that implementation of guidelines may change the management of patients with MHI, although the effects are varied and not always as anticipated. The changes identified may be due to inherent biases in studies with limited control groups and may not be generalisable to other settings.
It is perhaps surprising that there have not been more appropriately controlled studies of diagnostic management strategies in MHI, particularly of clinical decision rules. Accuracy studies may be subject to selection biases and do not show whether and how decision rules are put into practice by clinicians. Furthermore, it should not be assumed that an accurate clinical decision rule is better than an unstructured clinical assessment undertaken by a qualified and experienced clinician. Properly controlled management studies could determine whether or not the potential benefits of using clinical decision rules are realised in practice.
Economic evaluation
Economic evaluations from the perspectives of the Dutch162–164 and US162–164 health-care systems have concluded that selective CT use is more cost-effective than CT for all patients or no investigation. Our economic analysis confirmed this finding from the NHS perceptive and showed that the use of CT scanning as determined by a clinical decision rule is a cost-effective use of NHS resources. Indeed, the substantial costs of long-term care for patients with delayed treatment means that using CT selectively or in all patients is not only more effective than not investigating, but also is cheaper. Effective care for MHIs is a cost saving.
Selective CT use according to a clinical decision rule was also cost-effective compared with CT for all patients. This is because the clinical decision rules we evaluated are all highly sensitive, so using CT for all patients resulted in a substantial increase in the number of normal CT scans being performed for a small benefit in terms of additional cases detected. The disbenefit associated with increased radiation exposure offset the benefit of detecting a few extra cases and the additional costs rendered the ‘CT all’ strategy more expensive than the selective strategies. Our conclusion that selective CT use is cost-effective compared with CT for all may not hold if the strategy used to select patients is not sufficiently sensitive. The base-case analysis showed that CT for all dominated a theoretical strategy with 91% sensitivity for neurosurgical lesion, 72% sensitivity for non-neurosurgical lesion and 97% specificity.
Development of a clinical decision rule with less than perfect diagnostic accuracy will inevitably involve a trade-off between sensitivity and specificity. Established clinical decision rules typically sacrifice specificity to achieve high sensitivity (98–99%). Our analysis suggests that accepting 40–50% specificity to ensure high sensitivity provides an appropriate trade-off in terms of cost-effectiveness. It did not appear to be cost-effective to allow specificity to drop below 38% to achieve 100% sensitivity. Conversely, it did not appear to be cost-effective to allow sensitivity to drop below 94% to achieve 70% specificity. This has implications for the development of new or refined decision rules. We should continue to search for more accurate strategies, but studies need to be powered to show equivalent sensitivity to existing rules. This means they will need to recruit thousands or even tens of thousands of patients.
The most cost-effective rule for adults was the CCHR criterion26 using high- and medium-risk factors to guide CT use. The costs and outcomes associated with each rule were broadly similar, so the superiority of the CCHR26 may simply reflect a small difference in the estimate of diagnostic accuracy that was not statistically significant in the primary data. 71 Indeed, sensitivity analysis using different prevalence estimates for neurosurgical and non-neurosurgical injuries suggested that the NEXUS II rule62 was more cost-effective. However, our systematic review suggested that the CCHR criterion26 is the most well-validated rule and has estimates of diagnostic accuracy that are reasonably consistent across a number of cohorts. It therefore seems appropriate to conclude that the CCHR criterion26 has the best evidence to support its use.
The picture is less clear for children because the rules are less well validated. Our main analysis used estimates of diagnostic accuracy from derivation cohorts. These may overestimate diagnostic accuracy and the estimate of specificity from the derivation cohort of the CHALICE30 rule is much higher than that from a validation cohort. 89 The CHALICE30 rule appeared to be the most cost-effective rule for children in the main analysis, but this probably reflects superior estimates of diagnostic accuracy from a derivation cohort. A sensitivity analysis using data from the validation cohort89 showed that the CHALICE rule30 was dominated by the NEXUS II62 and UCD93 rules. However, in the PSA, the CHALICE rule30 was the dominant strategy.
Our analysis showed that admission of patients with a normal CT scan would not be cost-effective, with an ICER of £39M per QALY compared with discharge home with a responsible adult. If the alternative to admission is discharge home with no responsible adult then the ICER is lower, at £2.5M per QALY, but would still not be considered cost-effective. This analysis is based upon data suggesting a very low (0.006%) risk of deterioration167 and it is assumed that patients are clinically well and would not benefit from general hospital care. The conclusion that patients with a normal CT scan should not be admitted to hospital does not apply to those with, for example, repeated vomiting or significant amnesia who may benefit from symptomatic treatment, nursing care or a safe environment. However, if the patient is orientated, comfortable and able to self care then our analysis suggests that hospital admission for observation is not a cost-effective use of NHS resources, even if the alternative is discharge home without a responsible adult to observe them at home.
Hospital admission for those with a non-neurosurgical lesion on CT was cost-effective. Indeed it was cost saving, as the costs of long-term care for those who deteriorated and received late treatment outweighed the costs of hospital admission. This analysis was limited by the lack of a standard definition as to what constitutes a significant non-neurosurgical lesion on CT and the limited data relating to outcomes from non-neurosurgical lesions. The prognosis of different non-neurosurgical lesions varies markedly, so cost-effectiveness could potentially be improved by selecting those at highest risk of deterioration for admission while discharging those at lower risk. Currently, however, we do not have sufficient data to evaluate this approach.
A willingness-to-pay threshold of £30,000 was used to compare the cost-effectiveness of the strategies. However, with a lower threshold of £20,000 the results and conclusions would be the same.
Survey of current practice
The survey of NHS EDs showed that nearly all had unrestricted access to CT scanning (adults 96%, children 94.5%). Most hospitals followed the NICE guidelines, although 22% had made their own local amendments. In adults these included immediate CT for any reduction in GCS at presentation and considering CT for severe (persistent/prolonged) headache. Our meta-analysis suggests that immediate CT for any reduction in GCS at presentation would be a reasonable amendment, with a PLR of 3.2 for ICI in adults, but that headache, even if severe or persistent, was a poor predictor of ICI.
The most common features that were amended for local use in children involved delayed instead of immediate CT for patients with amnesia lasting > 5 minutes and dangerous mechanism of injury or presence of bruising, swelling or laceration > 5 cm on heads of children < 1 year of age. Additional criteria for considering CT scanning included LOC or amnesia and coagulopathy or severe (persistent) headache. Our meta-analysis suggested that anterograde or post-traumatic amnesia (PTA) (PLR 3.0), dangerous mechanism of injury (2.0–4.6), LOC (2.2), coagulopathy (6.6) and severe or persistent headache (4.3) predicted ICI to varying degrees in children, but that the presence of scalp bruising or laceration was not very useful.
Adults were usually admitted to an observation ward or clinical decision unit (61.4%), whereas children were usually admitted to an inpatient ward (86.7%). The median proportion of attendances admitted was higher for adults (18%) than for children (9%). This difference may reflect differences in the prevalence of ICI in adults and children, or lack of a responsible adult to look after injured adults. It is conceivable that admissions practice could influence admission rates, with more accessible locations (such as observation wards or clinical decision units) being associated with higher admission rates. However, we found no evidence of an association between the proportion admitted and the admission team, location or requirement for senior or specialist approval (all p > 0.1). This may reflect inadequacies in current HES data. As these data improve there may be further opportunities to explore for associations between admission practices and the proportion admitted.
Strengths and limitations of the assessment
Clinical evaluation
Decision rules
The data evaluating decision rules are strongest for adults, particularly the CCHR, which has been validated in a number of new cohorts and in different settings. Studies by Stein et al. ,71 Ibanez et al. 60 and Smits et al. 68 have compared multiple decision rules in large cohorts to provide powerful evidence of comparative diagnostic performance. Validation of decision rules for children, by contrast, is much more limited. Where validation has been undertaken it has shown that specificity may be much lower than estimated in the derivation cohort. This could have important implications if implementation of decision rules leads to increases in unnecessary CT scanning.
Studies of clinical decision rules have inevitable limitations. Most patients with MHI do not routinely receive CT scanning. Indeed the aim of developing a decision rule is to formalise the selection process for scanning. So, although a CT scan might be considered the ideal reference standard, it is unlikely to be performed on all patients if an appropriate patient spectrum is recruited. Studies may increase the proportion receiving CT scanning by limiting patient selection, but this may lead to spectrum bias. An associated limitation is that there seems to be inconsistency in what is considered a clinically significant intracranial abnormality on CT. If liberal criteria for clinical significance are used then sensitivity will be apparently reduced, but the addition FNs may not be clinically significant. The best way of determining clinical significance is to undertake follow-up studies and identify whether or not particular lesions are associated with an adverse outcome.
These limitations are less important with regard to neurosurgical injury, where adequate clinical follow-up should identify cases regardless of CT findings. The main limitation with regard to neurosurgical injury is the small number of cases in even very large cohorts, limiting the precision with which sensitivity can be estimated. The few large cohorts of minor head-injured patients assembled have been invaluable in providing precise estimates of sensitivity for this very important outcome.
Most studies of clinical decision rules have evaluated children and adults separately. However, within the age ranges used to define children there is substantial variation from infants at one extreme to adolescents at the other. This variation will be reflected in variation in ability to express symptoms and co-operate with examination. The limitations of attempting to develop a clinical decision rule for all children need to be considered when applying findings to an individual child.
Individual clinical characteristics
There are substantial data evaluating individual clinical characteristics in both adults and children. Frequently used clinical characteristics, such as LOC, headache and vomiting, have been widely studied, although not always clearly defined. This may be important because clinical characteristics appeared to be more diagnostically useful when they were clearly defined. Other clinical characteristics, such as decreasing GCS, visual symptoms and specific mechanisms of injury, have been less widely studied. We should be cautious about drawing conclusions from only two or three studies, particularly when the findings are inconsistent.
There was usually statistically significant heterogeneity between studies, wherever sufficient numbers of studies existed to allow analysis. It could be argued that it is inappropriate to calculate a pooled likelihood ratio in the presence of significant heterogeneity. However, not reporting a pooled estimate can make interpretation difficult and reduce the clinical value of a systematic review. The pooled estimate should, therefore, be regarded as a very general estimate of the diagnostic value of a characteristic that may actually vary substantially between settings and populations.
Biomarkers
The results of our meta-analysis appear positive and would superficially support use of this test in the MHI population described. However, care must always be taken in interpreting such meta-analysis results. These studies may appear similar, but it has been demonstrated by two groups that the results produced by the Liaison and Elecsys analysers are only moderately correlated when analysing the same samples. 165,190,191 Results are not interchangeable and as concentrations increase the difference between the two analysers also increases, often with the Liaison giving higher concentration results. This would imply that the universal application of a single discriminative value, as suggested by the American College of Emergency Physicians (ACEP),39 is inappropriate.
Time delay significantly influences these results. The specificity of a higher cut-off value in early studies, measuring concentrations later after injury, positively skews the specificity when analysed in this pooled format. This improvement in specificity was at the cost of sensitivity, which would be the more appropriate value to consider for this test in its potential role as an exclusion tool, although the specificity being too low would render this biomarker clinically useless in this field. A serum measurement within 4 hours was suggested by the ACEP report. Six of the studies took their samples within 3 hours and achieved a sensitivity ranging from 95% to 100% and a specificity of 20% to 50%, two analysing plasma concentrations on the Liaison, two analysing sera on the Liaison and two analysing sera on the Elecsys.
Diagnostic management studies
The single RCT identified by our review provides powerful evidence that CT scanning is more clinically effective and cost-effective than hospital admission for MHI. However, it can only compare two alternatives and does not estimate the clinical effectiveness or cost-effectiveness of selective strategies based on a decision rule. The other studies mentioned, but not formally included in the review, have clear methodological limitations described in the relevant section and should not be used to draw general conclusions.
Economic evaluation
The economic analysis used current best practice to develop the model and followed recommendations produced by NICE. 182 We included aspects of intervention, such as the benefits of treating non-neurosurgical intracranial lesions and the disbenefit associated with radiation exposure, that have not always been included in previous models. However, economic models are inevitably limited by the need to make assumptions in developing the model and by the limitations of the primary data.
Estimating the benefit of treating neurosurgical and non-neurosurgical lesions was inevitably difficult and relied upon observational data with small numbers. Experienced neurosurgeons and emergency physicians checked our estimates and felt that they were appropriate, but it is almost impossible to determine whether they are accurate. In particular, the probabilities of GOS 2 or 3 are subject to substantial uncertainty and have a potentially powerful effect upon cost-effectiveness. The expectation that delayed treatment will increase the probability of GOS 2 or 3 seems intuitively reasonable, but is very difficult to prove empirically.
As discussed previously, the potential benefit of treating non-neurosurgical intracranial lesions is uncertain and probably dependent on the definition used. We assumed that benefit was related to the risk of subsequent deterioration. However, this risk will depend upon the type and extent of injury. Conversely, we assumed that hospital admission and treatment provided no benefit for patients with a non-neurosurgical lesion that did not deteriorate or those with a normal CT scan. This was based upon our literature search finding no clear evidence of benefit. However, absence of evidence of benefit does not equate to evidence of absence of benefit. Further research would be helpful to determine whether early intervention helps to reduce persistent symptoms in patients with non-neurosurgical lesions or even those with normal CT scans.
Limitations of the primary data were particularly important in children, in whom there has been very little validation of clinical decision rules. The cost-effectiveness of each decision rule was determined by its diagnostic parameters, yet these (especially specificity) varied between the derivation data and (admittedly very limited) validation data. The conclusions regarding the optimal decision rule for children are, therefore, much less clear than for adults.
There were insufficient data for us to model strategies for specific patient groups, such as those receiving anticoagulant medication. These patients represent an increasing group with MHI. They have a higher risk of ICI and have a higher risk of adverse outcome, but the potential benefits of neurosurgery are less certain. Development of a specific model for these patients may be helpful when better data are available.
The model assumed that patients in GOS states maintained the associated utility throughout the modelling horizon. This could mean that those in GOS 5 have a higher utility than the average person of that age. This limitation, however, is expected to have little bias as the effects of discounting will mean any inaccuracies are small, but would favour those policies that provided treatment more promptly.
Finally, a potential limitation is the method used to estimate QALY loss in adults owing to the risk of cancer from performing a CT scan. This limitation, however, is expected to have little effect as any inaccuracies around the QALY loss are likely to be small, but would favour those policies that perform fewer CT scans.
Survey of current practice
Most of the hospitals surveyed (70%) responded, ensuring that the survey was reasonably representative of NHS practice. However, it is possible that hospitals that did not follow the guidelines or lacked a lead clinician with interest in management of MHI were under-represented. Furthermore, the survey could only determine what the respondent thought was supposed to happened, not what actually happened in practice. In particular, the estimate of CT availability may be an overestimate and the survey may be a poor reflection of what actually happens out of normal working hours.
The HES data were limited and often poor quality, so the absence of any association between reported practice and proportion of patients admitted may reflect data quality rather than absence of any such association. This was the first year that such data were available from HES, so, hopefully, data quality will improve as more hospitals record and report their ED data. We would have liked to use the survey and HES data to explore whether or not differences in admissions practice could be explained by characteristics of the hospitals, but unfortunately the data were inadequate for this purpose.
Uncertainties
The main uncertainties identified in this report are:
-
How do clinical decision rules for children perform outside their derivation setting?
-
What is the prognosis of different non-neurosurgical injuries?
-
Does S100B provide useful diagnostic information when used alongside clinical decision rules?
-
How do diagnosis and outcomes of MHI in anticoagulated patients differ from the general population?
-
What is the clinical effect (and cost-effectiveness) of implementing guidelines, decision rules and diagnostic management strategies?
Clinical decision rules for children have only received very limited validation. Where this has occurred it has raised concerns about the specificity of the rules. Our analysis suggests that optimising sensitivity is more important than optimising specificity. However, if specificity is too low then the radiation exposure and costs associated with normal CT scanning will reduce cost-effectiveness. Evaluation of clinical decision rules for children (CHALICE,30 PECARN,90 UCD93 and NEXUS II62) in a large representative cohort presenting to the ED with MHI would provide valuable validation and more reliable estimates of diagnostic accuracy for ICI. Planning such a study will require careful consideration of inclusion criteria, reference standard and outcome definition. It will need to be very large to provide precise estimates of sensitivity.
Our economic model was limited by uncertainties surrounding the benefit of treatment for patients with non-neurosurgical injury. Benefits are clearly likely for patients who deteriorate if their deterioration can be predicted, prevented or treated. Research is required to better estimate the risk of deterioration with different non-neurosurgical injuries and the benefit of different treatments for these injuries. This research would be helpful for determining the definition of a clinically significant injury on CT and, thus, defining the important outcomes for future studies of decision rules. Research is also required to determine what benefits, if any, patients with non-neurosurgical injury can gain from treatment even if they do not deteriorate. These patients often have significant and persistent symptoms, yet we were unable to find any strong evidence of treatment benefit.
Our meta-analysis suggested that S100B might have a role in ruling out ICI and reducing CT use. It is unlikely to be cost-effective when used as a single test because clinical decision rules can already reduce CT use without compromising sensitivity excessively and without incurring significant additional costs. However, S100B may have a role in further reducing CT use after application of (or as part of) a clinical decision rule. Defining this role would require evaluation of S100B alongside a widely used and well-validated clinical decision rule in a representative cohort of patients with MHI. This cohort would need to be large enough to estimate sensitivity with a high degree of precision.
An increasing number of patients with MHI have been prescribed anticoagulants to reduce their thromboembolic risk. We found that coagulopathy was associated with an increased likelihood of ICI. Beyond this finding there was very little research into the value of clinical assessment, use of diagnostic tests and outcome of MHI in this patient group. Research is required to determine the diagnostic accuracy of clinical characteristics, decision rules and biomarkers in patients receiving anticoagulants, the prognosis associated with different CT appearances (including normal) and the risks and benefits of different approaches to treatment, including reversal of anticoagulation and neurosurgery.
We found only one acceptable quality study evaluating the implementation of alternative strategies for managing MHI. 37 We identified a number of studies that did not meet our inclusion criteria and were only able to draw limited conclusions. Implementation studies are challenging to undertake, but can provide valuable insights and powerful evidence of the real-practice effects of management strategies. The implementation of NICE head injury guidance may not have had the anticipated effect of reducing hospital admissions. 24 This may be owing to cautious framing or interpretation of guidance. Studies of guideline implementation would provide valuable insights into their intended and unintended consequences. Furthermore, there have been no studies comparing structured clinical care following guidelines, decision rules or diagnostic strategies to unstructured care based on clinician assessment of the individual patient.
Assessment of factors relevant to the NHS and other parties
Management of MHI in the NHS is subject to guidance issued by NICE in 200319 and was updated in 2007. 1 Our national survey found that most NHS EDs follow NICE guidance, albeit with some local modifications. A previous analysis of HES admissions data suggested that head injury admissions had increased following the introduction of NICE guidance and questioned whether or not this represented cost-effective care. 24 Our analyses, and in particular the economic analysis, generally support the guidance provided by NICE,1 although the implementation of NICE guidance in practice has not yet been subject to a detailed evaluation.
Selection of patients for CT scanning in the NICE guidance for adults is based on the CCHR criterion. 26 We found that the criteria for CT scanning are supported by meta-analysis showing that these criteria are all useful predictors of ICI. The CCHR criterion26 is the most widely validated decision rule, with high sensitivity and acceptable specificity for ICI, and appears to be the most cost-effective strategy.
The NICE criteria for CT scanning for children generally correspond to the features that were found to be most useful in our meta-analysis, although there were a few exceptions. Our meta-analysis suggested that severe or persistent headache and coagulopathy may be useful additional criteria. The NICE criteria1 were based on the CHALICE rule30 and an economic analysis using derivation cohort data, which suggested that this was the optimal strategy. However, analysis based on validation data89 suggested that the CHALICE rule30 was dominated by the NEXUS II62 and UCD93 rules. Further research is required to determine the diagnostic parameters of these rules in large validation studies, which could then be used to refine our model.
The NICE guidelines1 suggest that patients with new clinically significant abnormalities on imaging should be admitted. Our economic analysis suggests that admission for patients with non-neurosurgical injury is not only cost-effective, but also cost saving. However, further research is required to determine which non-neurosurgical injuries are clinically significant, thus refining admissions policies.
The NICE guidance1 states that with ‘Normal imaging of the head: clinician may conclude risk is low enough to allow discharge if patient has returned to GCS 15, no other factors warrant admission and there are appropriate support structures for safe transfer and subsequent care’. Our economic analysis suggested that admission for patients with a normal CT scan represents very poor value for money for the health service, assuming that admission is to observe for deterioration rather than provide symptom control or general care. The results of this analysis would support a clear statement in clinical guidance that hospital admission is not recommended for those with a normal CT scan unless they are unable to self-care or require treatment of symptoms.
Chapter 8 Conclusions
Implications for service provision
The CCHR is the most well-validated rule in adults and, when high- and medium-risk criteria are used, has high sensitivity and acceptable specificity. The CCHR and related NICE guideline are based upon the clinical characteristics that our meta-analysis suggests are the most powerful predictors of ICI. The use of headache as an additional criterion for CT scanning (as used in some hospitals) was not supported by our meta-analysis. Decision rules for children have not been widely validated, so conclusions are less clear. Three rules have been validated in a different setting from the derivation cohort and one in the same setting. Specificity appears to be worse in validation cohorts. The CHALICE and NEXUS II rules appeared to be based on characteristics that our meta-analysis suggested were the most powerful predictors of ICI.
Our economic analysis confirms that the recent extension of access to CT scanning for MHI is appropriate. Liberal use of CT scanning based on a high-sensitivity decision rule is not only effective, but also a cost saving. The cost of CT scanning is very small compared with the estimated cost of caring for patients with brain injury worsened by delayed treatment. The analysis supports the view that all hospitals receiving patients with MHI should have unrestricted access to CT scanning. Our survey suggests that this is achieved by around 95% of NHS EDs.
High-sensitivity clinical decision rules that selected patients for CT were more cost-effective than CT for all. We found that the CCHR (high or medium criteria) was the optimal rule for adults. The optimal rule for children was less certain, with either the CHALICE or NEXUS II rules appearing optimal, but based on very limited validation data. Attempts to improve the specificity of decision rules for MHI would be worthwhile, but must not compromise sensitivity. Although promising, there is currently insufficient evidence to recommend the use of S100B and other biomarkers for patients with MHI outside appropriately designed and powered research studies.
Hospital admission appears to be cost-effective for patients with an intracranial lesion on CT scanning, but not for those with a normal CT. It might be hoped that more liberal CT use would lead to less need for hospital admission, but this does not seem to be the case. The reasons for this are not clear and routine data sources are not yet sufficient to allow detailed investigation of admission rates and associations with different methods of service delivery. However, there is clearly potential for more cost-effective practice in relation to hospital admission for MHI and further research in this area could represent a worthwhile investment for the NHS. Moreover, not all intracranial lesions are likely to benefit from hospital admission and research is needed to identify those that do.
Suggested research priorities
The main research priorities suggested by this report are:
-
Evaluation of the diagnostic accuracy for clinically significant ICI of the CHALICE,30 PECARN,90 NEXUS II62 and UCD93 decision rules for children in a large representative cohort presenting to the ED with MHI.
-
Evaluation of the effects (and cost-effectiveness) of implementing guidelines, decision rules and diagnostic management strategies, including comparison to unstructured clinical care.
-
Evaluation of the outcomes of intracranial injuries identified on CT that do not require immediate neurosurgery, in terms of risk of subsequent deterioration leading to neurosurgical or critical care intervention, persistent symptoms, return to normal activities and QoL. This could involve development of definitions of what constitutes clinically significant injury and adverse outcome.
-
Evaluation of the diagnostic accuracy of S100B alongside validated clinical decision rules to determine whether it can improve decision rule specificity without compromising specificity.
-
Evaluation of the diagnostic performance of clinical characteristics, decision rules and biomarkers, along with the prognostic value of a normal CT scan and outcomes of MHI in anticoagulated patients.
These research priorities mostly require a large patient cohort and thus substantial funding. Where possible attempts should be made to address multiple objectives in the same cohort, i.e. data and blood samples should be collected to allow comparison of all potentially worthwhile decision rules and biomarkers. Decision rules for adults are reasonably accurate, well validated and cost-effective, so any research to further develop or refine diagnostic strategies for adults may benefit from expected value of sample information analysis using our model to determine whether the benefits of further research justify the costs.
Acknowledgements
We would like to thank the following people for their help with this project:
Professor Timothy J Coats, Academic Unit of Emergency Medicine, Leicester University, Leicester, UK.
Dr David Hughes, Department of Neuroradiology, Hope Hospital, Salford, UK.
Dr Fiona Lecky, Trauma Audit and Research Network, University of Manchester, Manchester, UK.
Tim Pigott, Walton Centre for Neurology and Neurosurgery, Fazakerley, Liverpool, UK.
Jake Timothy, Department of Neurosurgery, Leeds General Infirmary, Leeds, UK, for providing clinical expertise.
Professor Alex Sutton, Department of Health Sciences, University of Leicester, Leicester, UK, for providing statistical advice.
Thanks also to Joanne Turner for clerical assistance.
Contributions of authors
Abdullah Pandor (Research Fellow) co-ordinated the review and was responsible for the acquisition of data, analysis and interpretation of data (for the systematic reviews and postal survey of UK hospitals) and drafting/revising of the final report.
Steve Goodacre (Professor of Emergency Medicine) was responsible for conception and design, acquisition of data, analysis and interpretation of data (for the systematic reviews, postal survey of UK hospitals and health economic evaluations) and drafting/revising the final report.
Sue Harnan (Research Associate) was responsible for the acquisition of data, analysis and interpretation of data (for the systematic reviews) and drafting/revising the final report.
Mike Holmes (Operational Research Analyst) was responsible for the acquisition of data, analysis and interpretation of data (for the health economic evaluations) and drafting/revising the final report.
Alastair Pickering (Clinical Lecturer in Emergency Medicine) was responsible for the acquisition of data, analysis and interpretation of data (for the systematic reviews) and drafting/revising the final report.
Patrick Fitzgerald (Research Fellow in Health Economics) provided statistical support and undertook the meta-analyses.
Angie Rees (Information Specialist) was responsible for the development and undertaking of the electronic literature searches.
Matt Stevenson (Mathematical Modeller) oversaw the modelling and reviewed the final report.
Publications
-
Goodacre SW, Pandor A, Pickering A. Management of isolated minor head injury in the UK. Emerg Med J 2010;27:856–9.
-
Pickering A, Harnan S, Fitzgerald P, Pandor A, Goodacre S. Clinical decision rules for children with minor head injury: a systematic review. Arch Dis Child 2011;96:414–21.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- National Institute for Health and Clinical Excellence (NICE) . Head Injury – Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adults 2007.
- Kay A, Teasdale G. Head injury in the United Kingdom. World J Surg 2001;25:1210-20.
- Jennett B. Epidemiology of head injury. J Neurol Neurosurg Psychiatry 1996;60:362-9.
- Tennant A. Admission to hospital following head injury in England: incidence and socio-economic associations. BMC Public Health 2005;5.
- Yates PJ, Williams WH, Harris A, Round A, Jenkins R. An epidemiological study of head injuries in a UK population attending an emergency department. J Neurol Neurosurg Psychiatry 2006;77:699-701.
- Swann IJ, Teasdale GM. Current concepts in the management of patients with so-called ‘minor’ or ‘mild’ head injury. Trauma 1999;1:143-55.
- Lee EJ, Hung YC, Wang LC, Chung KC, Chen HH. Factors influencing the functional outcome of patients with acute epidural hematomas: analysis of 200 patients undergoing surgery. J Trauma 1998;45:946-52.
- Cheung PSY, Lam MY, Yeung JHH, Graham CA, Rainer TH. Outcome of traumatic extradural haematoma in Hong Kong. Injury 2007;38:76-80.
- Cook RJD, Dorsch NWC, Fearnside MR, Chaseling R. Outcome prediction in extradural haematomas. Acta Neurochir 1988;95:90-4.
- Gerlach R, Dittrich S, Schneider W, Ackermann H, Seifert V, Kieslich M. Traumatic epidural hematomas in children and adolescents outcome analysis in 39 consecutive unselected cases. Pediatr Emerg Care 2009;25:164-9.
- Haselsberger K, Pucher R, Auer LM. Prognosis after acute subdural or epidural haemorrhage. Acta Neurochir 1988;90:111-16.
- Deverill J, Aitken LM. Treatment of extradural haemorrhage in Queensland: interhospital transfer, preoperative delay and clinical outcome. Emerg Med Australasia 2007;19:325-32.
- Hannan ELF, Farell LS, Cooper A, Henry M, Simon B, Simon R. Physiologic trauma triage criteria in adult trauma patients: are they effective in saving lives by transporting patients to trauma centers?. J Am Coll Surg 2005;200:584-92.
- Borg J, Holm L, Peloso PM, Cassidy JD, Carroll LJ, von Holst H, et al. Non-surgical intervention and cost for mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehab Med 2004;36:76-83.
- Ponsford J, Willmott C, Rothwell A, Cameron P, Kelly AM, Nelms R, et al. Impact of early intervention on outcome following mild head injury in adults. J Neurol Neurosurg Psychiatry 2002;73:330-2.
- Ponsford J, Willmott C, Rothwell A, Cameron P, Ayton G, Nelms R, et al. Impact of early intervention on outcome after mild traumatic brain injury in children. Pediatrics 2001;108:1297-303.
- Andersson E, Emanuelson I, Bjorklund R, Stalhammar DA. Mild traumatic brain injuries: the impact of early intervention on late sequelae. A randomized controlled trial. Acta Neurochir 2007;149:151-9.
- Fabbri A, Servadei F, Marchesini G, Stein SC, Vandelli A. Observational approach to subjects with mild-to-moderate head injury and initial non-neurosurgical lesions. J Neurol Neurosurg Psychiatry 2008;79:1180-5.
- National Institute for Health and Clinical Excellence (NICE) . Head Injury – Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adults 2003.
- Scottish Intercollegiate Guidelines Network (SIGN) . Early Management of Patients With a Head Injury 2009.
- Sultan HY, Boyle A, Pereira M, Antoun N, Maimaris C. Application of the Canadian CT head rules in managing minor head injuries in a UK emergency department: implications for the implementation of the NICE guidelines. Emerg Med J 2004;21:420-5.
- Hassan Z, Smith M, Littlewood S, Bouamra O, Hughes D, Biggin C, et al. Head injuries: a study evaluating the impact of the NICE head injury guidelines. Emerg Med J 2005;22:845-9.
- Shravat BP, Hynes KA. The impact of NICE guidelines for the management of head injury on the workload of the radiology department. Emerg Med J 2004;21:521-2.
- Goodacre S. Hospital admissions with head injury following publication of NICE guidance. Emerg Med J 2008;25:556-7.
- Dunning J, Stratford-Smith P, Lecky F, Batchelor J, Hogg K, Browne J, et al. A meta-analysis of clinical correlates that predict significant intracranial injury in adults with minor head trauma. J Neurotrauma 2004;21:877-85.
- Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet 2001;357:1391-6.
- Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux MC. Indications for computed tomography in patients with minor head injury. N Engl J Med 2000;343:100-5.
- Richless LK, English K, Heller MB, Rachlin J, McClean P, Auble TE. A prospective evaluation of radiologic criteria for head injury patients in a community emergency department. Am J Emerg Med 1993;11:327-30.
- Miller EC, Holmes JF, Derlet RW. Utilizing clinical factors to reduce head CT scan ordering for minor head trauma patients. J Emerg Med 1997;15:453-7.
- Dunning J, Daly JP, Lomas JP, Lecky F, Batchelor J, Mackway-Jones. Derivation of the children’s head injury algorithm for the prediction of important clinical events decision rule for head injury in children. Arch Dis Child 2006;91:885-91.
- Hofman PA, Nelemans P, Kemerink, GJ, Wilmink JT. Value of radiological diagnosis of skull fracture in the management of mild head injury: meta-analysis. J Neurol Neurosurg Psychiatry 2000;68:416-22.
- Dunning J, Batchelor J, Stratford-Smith P, Teece S, Browne J, Sharpin C, et al. A meta-analysis of variables that predict significant intracranial injury in minor head trauma. Arch Dis Child 2004;89:653-9.
- Kelly AB, Zimmerman RD, Snow RB, Gandy SE, Heier LA, Deck MD. Head trauma: comparison of MR and CT – experience in 100 patients. AJNR Am J Neuroradiol 1988;9:699-708.
- Ingebrigtsen T, Romner B. Routine early CT-scan is cost saving after minor head injury. Acta Neurol Scand 1996;93:207-10.
- Af Geijerstam JL, Oredsson S, Britton M. Octopus Study Investigators . Medical outcome after immediate computed tomography or admission for observation in patients with mild head injury: randomised controlled trial. BMJ 2006;333.
- Norlund A, Marke LA, af Geijerstam JL, Oredsson S, Britton M. Immediate computed tomography or admission for observation after mild head injury: cost comparison in randomised controlled trial. BMJ 2006;333.
- Af Geijerstam J-L, Britton M, Marke L-A. Mild head injury: observation or computed tomography? Economic aspects by literature review and decision analysis. Emerg Med J 2004;21:54-8.
- Savola O, Pyhtinen J, Leino TK, Siitonen S, Niemela O, Hillbom M, et al. Effects of head and extracranial injuries on serum protein S100B levels in trauma patients. J Trauma 2004;56:1229-34.
- Jagoda AS, Bazarian JJ, Bruns JJ, Cantrill SV, Gean AD, Howard PK, et al. Clinical policy: neuroimaging and decision-making in adult mild traumatic brain injury in the acute setting. J Emerg Nurs 2009;35:e5-40.
- Centre for Reviews and Dissemination (CRD) . Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care 2008.
- Leeflang MM, Deeks JJ, Gatsonis C, Bossuyt PM. Cochrane Diagnostic Test Accuracy Working Group . Systematic reviews of diagnostic test accuracy. Ann Intern Med 2008;149:889-97.
- Deeks JJ, Bossuyt PM, Gatsonis C. Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy, Version 1.0 2009. http://srdta.cochrane.org.
- Stiell IG, Wells GA. Methodologic standards for the development of clinical decision rules in emergency medicine. Ann Emerg Med 1999;33:437-47.
- Ryu WH, Feinstein A, Colantonio A, Streiner DL, Dawson D. Regional variability in the use of CT for patients with suspected mild traumatic brain injury. Can J Neurol Sci 2009;36:42-6.
- Stiell IG, Wells GA, Vandemheen K, Laupacis A, Brison R, Eisenhauer MA, et al. Variation in ED use of computed tomography for patients with minor head injury. Ann Emerg Med 1997;30:14-22.
- Stiell IG, Clement CM, Rowe BH, Schull MJ, Brison R, Cass D. Comparison of the Canadian CT head rule and the New Orleans criteria in patients with minor head injury. JAMA 2005;294:1511-18.
- Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3.
- Juni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA 1999;282:1054-60.
- Whiting P, Harbord R, Kleijnen J. No role for quality scores in systematic reviews of diagnostic accuracy studies. BMC Med Res Methodol 2005;5.
- Review Manager (REVMAN). Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2008.
- Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ 2004;329:168-9.
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Clin Trials 1986;7:177-88.
- Reitsma JB, Glas AS, Rutjes AW, Scholten RJ, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 2005;58:982-90.
- Arienta C, Caroli M, Balby S. Management of head-injured patients in the emergency department: a practical protocol. Surg Neurol 1997;48:213-19.
- Borczuk P. Predictors of intracranial injury in patients with mild head trauma. Ann Emerg Med 1995;25:731-6.
- Duus BR, Lind B, Christensen H, Nielsen OA. The role of neuroimaging in the initial management of patients with minor head injury. Ann Emerg Med 1994;23:1279-83.
- Fabbri A, Servadei F, Marchesini G, Dente M, Lervese T, Spada M, et al. Clinical performance of NICE recommendations versus NCWFNS proposal in patients with mild head injury. J Neurotrauma 2005;22:1419-27.
- Falimirski ME, Gonzalez R, Rodriguez A, Wilberger J. The need for head computed tomography in patients sustaining loss of consciousness after mild head injury. J Trauma 2003;55:1-6.
- Holmes JF, Baier ME, Derlet RW. Failure of the Miller criteria to predict significant intracranial injury in patients with a Glasgow Coma Score of 14 after minor head trauma. Acad Emerg Med 1997;4:788-92.
- Ibanez J, Arikan F. Reliability of clinical guidelines in the detection of patients at risk following mild head injury: results of a prospective study. J Neurosurg 2004;100:825-34.
- Madden C, Witzkc DB, Arthur, Sanders B, Valente J, Fritz M, . High-yield selection criteria for cranial computed tomography after acute trauma. Acad Emerg Med 1995;2:248-53.
- Mower WRH, Hoffman HJ, Herbert M, Wolfson AB, Pollack CV, Zucker MI, et al. Developing a decision instrument to guide computed tomographic imaging of blunt head injury patients. J Trauma 2005;59:954-9.
- Ono K, Wada K, Takahara T, Shirotani T. Indications for computed tomography in patients with mild head injury. Neurol Med Chir 2007;47:291-7.
- Reinus WR, Wippold FJ, Erickson KK. Practical selection criteria for noncontrast cranial computed tomography in patients with head trauma. Ann Emerg Med 1993;22:1148-55.
- Rosengren D, Rothwell S, Brown AF, Chu K, Rosengren D, Rothwell S. The application of North American CT scan criteria to an Australian population with minor head injury. Emerg Med Australas 2004;16:195-200.
- Saadat S, Ghodsi SM, Naieni KH, Firouznia K, Hosseini M, Kadkhodaie HR, et al. Prediction of intracranial computed tomography findings in patients with minor head injury by using logistic regression. J Neurosurg 2009;111:688-94.
- Saboori M, Ahmadi J, Farajzadegan Z. Indications for brain CT scan in patients with minor head injury. Clin Neurol Neurosurg 2007;109:399-405.
- Smits M, Dippel DW, de Haan GG, Dekker HM, Vos PE, Nederkoorn PJ, et al. External validation of the Canadian Head Rule and the New Orleans Criteria for CT scanning in patients with minor head injury. JAMA 2005;294:1519-25.
- Smits M, Dippel DW, Steyerberg EW, de Haan GG, Dekker HM, Vos PE, et al. Predicting intracranial traumatic findings on computed tomography in patients with minor head injury: the CHIP prediction rule. Ann Intern Med 2007;146:397-405.
- Smits M, Dippel DW, Steyerberg EW, de Haan GG, Dekker HM, Vos PE, et al. Minor head injury: Guidelines for the use of CT: a multicenter validation study. Radiology 2007;245:831-8.
- Stein SC, Fabbri A, Servadei F, Glick HA. A critical comparison of clinical decision instruments for computed tomographic scanning in mild closed traumatic brain injury in adolescents and adults. Ann Emerg Med 2009;53:180-8.
- Servadei F, Teasdale G, Merry G. Neurotraumatology Committee of the World Federation of Neurosurgical Societies . Defining acute mild head injury in adults: a proposal based on prognostic factors, diagnosis, and management. J Neurotrauma 2001;18:657-64.
- Ingebrigtsen T, Romner B, Kock-Jensen C. Scandinavian guidelines for initial management of minimal, mild, and moderate head injuries. The Scandinavian Neurotrauma Committee. J Trauma 2000;48:760-6.
- Stein SC. Management of minor closed head injury. Neurosurg Quart 1996;6:108-15.
- Tomei G, Brambilla GL, Delfini R, Servadei F, Ambrosio A, Acampora S, et al. Guidelines for minor head injured patient’s management in adult age. J Neurosurg Sci 1996;40:11-5.
- Lapierre F. Guide-lines for head injured patients management in adult age. Neurosurgical Society of France. Neurochirurgie 1998;44:55-6.
- Murshid WR. Management of minor head injuries: admission criteria, radiological evaluation and treatment of complications. Acta Neurochir 1998;140:56-64.
- Teasdale G, Gentleman D, Andrews P. Early management of patients with head injury. Edinburgh: SIGN; 2000.
- Vos PE, Battistin L, Birbamer G, Gerstenbrand F, Potapov A, Prevec T, et al. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol 2002;9:207-19.
- Whiting P, Rutjes AW, Reitsma JB, Glas AS, Bossuyt PM, Kleijnen J. Sources of variation and bias in studies of diagnostic accuracy: a systematic review. Ann Intern Med 2004;140:189-202.
- Atabaki SM, Stiell IG, Bazarian JJ, Daow KE, Vu TT, Camarca MA, et al. A clinical decision rule for cranial computed tomography in minor pediatric head trauma. Arch Pediatr Adolesc Med 2008;162:439-45.
- Buchanich JM. A Clinical Decision-Making Rule for Mild Head Injury in Children Less Than Three Years Old 2007.
- Da Dalt L, Marchi AG, Laudizi L, Crichiutti G, Messi G, Pavanello L, et al. Predictors of intracranial injuries in children after blunt head trauma. Eur J Pediatr 2006;165:142-8.
- Dietrich AM, Bowman MJ, Ginn-Pease ME, Kosnik E, King D.R. Pediatric head injuries: can clinical factors reliably predict an abnormality on computed tomography?. Ann Emerg Med 1993;22:1535-40.
- Greenes DS, Schutzman SA. Clinical indicators of intracranial injury in head-injured infants. Pediatrics 1999;104:861-7.
- Greenes DS, Schutzman SA. Clinical significance of scalp abnormalities in asymptomatic head-injured infants. Pediatr Emerg Care 2001;17:88-92.
- Guzel A, Hicdonmez T, Temizoz O, Aksu B, Aylanc H, Karasalihoglu S. Indications for brain computed tomography and hospital admission in pediatric patients with minor head injury: how much can we rely upon clinical findings?. Pediatr Neurosurg 2009;45:262-70.
- Haydel MJ, Shembekar AD. Prediction of intracranial injury in children aged five years and older with loss of consciousness after minor head injury due to nontrivial mechanisms. Ann Emerg Med 2003;42:507-14.
- Klemetti S, Uhari M, Pokka T, Rantala H. Evaluation of decision rules for identifying serious consequences of traumatic head injuries in pediatric patients. Pediatr Emerg Care 2009;25:811-15.
- Kuppermann N, Holmes JF, Dayan PS, Hoyle JD, Atabaki SM, Holubkov R, et al. Identification of children at very low risk of clinically important brain injuries after head trauma: a prospective cohort study. Lancet 2009;374:1160-70.
- Oman JAC. Performance of a decision rule to predict need for computed tomography among children with blunt head trauma. Pediatrics 2006;117:e238-46.
- Osmond MH, Klassen TP, Stiell IG, Correll R. The CATCH Rule: a clinical decision rule for the computed tomography of the head in children with minor head injury. Acad Emerg Med 2006;13.
- Palchak MJ, Holmes JF, Vance CW, Gelber RE, Schauer BA, Harrison MJ, et al. A decision rule for identifying children at low risk for brain injuries after blunt head trauma. Ann Emerg Med 2003;42:492-506.
- Quayle KS, Jaffe DM, Kuppermann N, Kaufman BA, Lee BC, Park TS, et al. Diagnostic testing for acute head injury in children: when are head computed tomography and skull radiographs indicated?. Pediatrics 1997;9:E1-8.
- Sun BCH, Hoffman JR, Mower WR. Evaluation of a modified prediction instrument to identify significant pediatric intracranial injury after blunt head trauma. Ann Emerg Med 2007;49:325-32.
- Royal College of Surgeons of England (RCSENG) . Report of the Working Party on the Management of Patients With Head Injury 1999.
- Mehta S. Neuroimaging for paediatric minor closed head injuries. Paediatr Child Health 2007;12:482-4.
- Biberthaler P, Linsenmeier U, Pfeifer K, Kroetz M, Mussack T, Kanz K, et al. Serum S-100B concentration provides additional information for the indication of computed tomography in patients after minor head injury a prospective multicenter study. Shock 2006;25:446-53.
- Chan HC, Adnan WA, Jaalam K, Abdullah MR, Abdullah J. Which mild head injured patients should have follow-up after discharge from an accident and emergency ward? A study in a university hospital setting in Kelantan, Malaysia. Southeast Asian J Trop Med Public Health 2005;36:982-93.
- Cook LS, Levitt MA, Simon B, Williams VL. Identification of ethanol-intoxicated patients with minor head trauma requiring computed tomography scans. Acad Emerg Med 1994;1:227-34.
- Dunham CM, Coates S, Cooper C. Compelling evidence for discretionary brain computed tomographic imaging in those patients with mild cognitive impairment after blunt trauma. J Trauma 1996;41:679-86.
- Feuerman T, Wackym PA, Gade GF, Becker DP. Value of skull radiography, head computed tomographic scanning, and admission for observation in cases of minor head injury. Neurosurgery 1988;22:449-53.
- Gomez PA, Lobato RD, Ortega JM. Mild head injury: differences in prognosis among patients with a Glasgow Coma Scale score of 13 to 15 and analysis of factors associated with abnormal CT findings. Br J Neurosurg 1996;10:453-60.
- Harad FT, Kerstein MD. Inadequacy of bedside indicators in identifying intracranial injury in trauma patients. J Trauma 1992;32:359-61.
- Hsiang JN, Yeung T, Yu AL, Poon WS. High-risk mild head injury. J Neurosurg 1997;87:234-8.
- Hung CC, Chiu WT, Lee LS, Lin LS, Shih CJ. Risk factors predicting surgically significant intracranial hematomas in patients with head injuries. J Formos Med Assoc 1996;95:294-7.
- Jeret JS, Mandell M, Anzistka B. Clinical predictors of abnormality disclosed by computed tomography after mild head trauma. Neurosurgery 1993;32:9-15.
- Livingston DH, Lavery RF, Passanannte MR. Emergency department discharge of patients with a negative cranial computed tomography scan after minimal head injury. Ann Surg 2000;232:126-32.
- Livingston DH, Loder PA, Koziol J, Hunt CD. The use of CT scanning to triage patients requiring admission following minimal head injury. J Trauma 1991;31:483-9.
- Mack LR, Chan SB, Silva JC, Hogan TM. The use of head computed tomography in elderly patients sustaining minor head trauma. J Emerg Med 2003;24:157-62.
- Miller EC, Derlet RW, Kinser D. Minor head trauma: is computed tomography always necessary?. Ann Emerg Med 1996;27:290-4.
- Moran SG, McCarthy MC, Uddin DE, Poelstra RJ. Predictors of positive CT scans in the trauma patient with minor head injury. Am Surg 1994;60:533-5.
- Muller K, Townend W, Biasca N, Unden J, Waterloo K, Romner B, et al. S100B serum level predicts computed tomography findings after minor head injury. J Trauma 2007;62:1452-6.
- Murshid WR. Role of skull radiography in the initial evaluation of minor head injury: a retrospective study. Acta Neurochir 1994;129:11-4.
- Mussack T, Biberthaler P, Kanz KG, Heckl U, Gruber R, Linsenmaier U, et al. Immediate S-100B and neuron-specific enolase plasma measurements for rapid evaluation of primary brain damage in alcohol-intoxicated, minor head-injured patients. Shock 2002;18:395-400.
- Nelson JB, Bresticker MA, Nahrwold DL. Computed tomography in the initial evaluation of patients with blunt trauma. J Trauma 1992;33:722-7.
- Rosenorn J, Duus B, Nielsen K, Kruse K, Boesen T. Is a skull X-ray necessary after milder head trauma?. Br J Neurosurg 1991;5:135-9.
- Schynoll W, Overton D, Krome R, Wesolowski D, Wang AM, Wilson A, et al. A prospective study to identify high-yield criteria associated with acute intracranial computed tomography findings in head-injured patients. Am J Emerg Med 1993;11:321-6.
- Shackford SR, Wald SL, Rose SE. The clinical utility of computed tomographic scanning and neurologic examinations in the management of patients with minor head injuries. J Trauma 1992;33:385-94.
- Sharma P, Dahiya RS, Dass B, Dewan Y, Arora AL, Sharma P, et al. How important is history of unconsciousness in head injury patients?. J Indian Med Assoc 2001;99:81-3.
- Stein SC, Ross SE. Mild head injury: a plea for routine early CT scanning. J Trauma 1992;33:11-3.
- Stein SC, Ross SE. The value of computed tomographic scans in patients with low-risk head injuries. Neurosurgery 1990;26:638-40.
- Tender GC, Awasthi D. Risk stratification in mild head injury patients: the head injury predictive index. J La State Med Soc 2003;155:338-42.
- Thiruppathy SP, Muthukumar N. Mild head injury: revisited. Acta Neurochir 2004;146:1075-83.
- Tsai EA. Value of emergency room computed tomography brain scan in mild head injury patients. J Surg Assoc Repub China 1994;27:2278-82.
- Vilke GM, Chan TC, Guss DA, Vilke GM. Use of a complete neurological examination to screen for significant intracranial abnormalities in minor head injury. Am J Emerg Med 2000;18:159-63.
- Chan KH, Mann KS, Yue CP, Fan YW, Cheung M. The significance of skull fracture in acute traumatic intracranial hematomas in adolescents: a prospective study. J Neurosurg 1990;72:189-94.
- Boran BO, Boran P, Barut N, Akgun C, Celikoglu E, Bozbuga M. Evaluation of mild head injury in a pediatric population. Pediatr Neurosurg 2006;42:203-7.
- Davis RL, Mullen N, Makela M, Taylor JA, Cohen W, Rivara FP. Cranial computed tomography scans in children after minimal head injury with loss of consciousness. Ann Emerg Med 1994;24:640-5.
- Fridriksson T, Kini N, Walsh-Kelly C, Hennes H. Serum neuron-specific enolase as a predictor of intracranial lesions in children with head trauma: A pilot study. Acad Emerg Med 2000;7:816-20.
- Hahn YS, McLone DG. Risk factors in the outcome of children with minor head injury. Pediatr Neurosurg 1993;19:135-42.
- Keskil IS, Baykaner MK, Ceviker N, Kaymaz M. Assessment of mortality associated with mild head-injury in the pediatric age group. Childs Nerv Syst 1995;11:467-73.
- Mandera M, Wencel T, Bazowski P, Krauze J. How should we manage children after mild head injury?. Childs Nerv Syst 2000;16:156-60.
- Ng SM, Toh EM, Sherrington CA. Clinical predictors of abnormal computed tomography scans in paediatric head injury. J Paediatr Child Health 2002;38:388-92.
- Ramundo ML, McKnight T, Kempf J, Satkowiak L. Clinical predictors of computed tomographic abnormalities following pediatric traumatic brain injury. Pediatr Emerg Care 1995;11:1-4.
- Reed MJ, Browning JG, Wilkinson AG, Beattie T. Can we abolish skull x-rays for head injury?. Arch Dis Child 2005;90:859-64.
- Schunk JE, Rodgerson JD, Woodward GA. The utility of head computed tomographic scanning in pediatric patients with normal neurologic examination in the emergency department. Pediatr Emerg Care 1996;12:160-5.
- Simon B, Letourneau P, Vitorino E, McCall J. Pediatric minor head trauma: Indications for computed tomographic scanning revisited. J Trauma 2001;51:231-8.
- Stein SC, Doolin EJ. Management of minor closed head injury in children and adolescents. Pediatr Surg Int 1995;10:465-71.
- Wang MY, Griffith P, Sterling J, McComb J, Levy M. A prospective population-based study of pediatric trauma patients with mild alterations in consciousness (Glasgow Coma Scale score of 13–14). Neurosurgery 2000;46:1093-9.
- Fisher JD. Symptomatic blunt head injury in children: a prospective, single-investigator study. Clin Pediatr 1997;36:461-5.
- Halley MK, Silva PD, Foley J, Rodarte A. Loss of consciousness: when to perform computed tomography?. Pediatr Crit Care Med 2004;5:230-3.
- Biberthaler P, Mussack T, Wiedemann E, Kanz KG, Mutschler W, Linsenmaier U, et al. Rapid identification of high-risk patients after minor head trauma (MHT) by assessment of S-100B: ascertainment of a cut-off level. Eur J Med Res 2002;7:164-70.
- Castellani C, Bimbashi P, Ruttenstock E, Sacherer P, Stojakovic T, Weinberg AM. Neuroprotein S-100B: a useful parameter in paediatric patients with mild traumatic brain injury?. Acta Pediatr 2009;98:1607-12.
- Ingebrigtsen T, Romner B, Marup-Jensen S, Dons M, Lundqvist C, Bellner J, et al. The clinical value of serum S-100 protein measurements in minor head injury: a Scandinavian multicentre study. Brain Injury 2000;14:1047-55.
- Morochovic R, Racz O, Kitka M, Pingorova S, Cibur P, Tomkova D, et al. Serum S100B protein in early management of patients after mild traumatic brain injury. Eur J Neurol 2009;16:1112-17.
- Poli-de-Figueiredo LF, Biberthaler P, Simao, Filho C, Hauser C, Mutschler W, et al. Measurement of S-100B for risk classification of victims sustaining minor head injury: first pilot study in Brazil. Clinics 2006;61:41-6.
- Romner B, Ingebrigtsen T, Kongstad P, Borgesen SE. Traumatic brain damage: Serum S-100 protein measurements related to neuroradiological findings. J Neurotrauma 2000;17:641-7.
- Biberthaler P, Mussack T, Wiedemann E, Kanz K, Koelsch M, Gippner-Steppert C, et al. Evaluation of S-100b as a specific marker for neuronal damage due to minor head trauma. World J Surg 2001;25:93-7.
- Levitt MA, Cook LA, Simon BC, Williams V, Levitt MA, Cook LA, et al. Biochemical markers of cerebral injury in patients with minor head trauma and ethanol intoxication. Acad Emerg Med 1995;2:675-80.
- Cochrane Effective Practice and Organisation of Care Group . Data Collection Checklist 2010. www.epoc.cochrane.org/Files/Website%20files/Documents/Reviewer%20Resources/datacollectionchecklist.pdf.
- Brown SR, Raine C, Robertson CE, Swann IJ. Management of minor head injuries in the accident and emergency department: the effect of an observation ward. J Accident Emerg Med 1994;11:144-8.
- Fabbri A, Servadei F, Marchesini G, Dente M, Iervese T, Spada M, et al. Which type of observation for patients with high-risk mild head injury and negative computed tomography?. Eur J Emerg Med 2004;11:65-9.
- Browning JG, Reed MJ, Wilkinson AG, Beattie T. Imaging infants with head injury: effect of a change in policy. Emerg Med J 2005;22:33-6.
- Fong C, Chong W, Villaneuva E, Segal AY. Implementation of a guideline for computed tomography head imaging in head injury: a prospective study. Emerg Med Australas 2008;20:410-19.
- Kerr J, Smith R, Gray S, Beard D, Robertson CE. An audit of clinical practice in the management of head injured patients following the introduction of the Scottish Intercollegiate Guidelines Network (SIGN) recommendations. Emerg Med J 2005;22:850-4.
- Loroni L, Ciucci G, Piccinini G, Cuscini M, Scorza P, Piola C, et al. Approach to head trauma in childhood in a district general hospital. Eur J Emerg Med 1996;3:141-8.
- Shravat BP, Huseyin TS, Hynes KA. NICE guideline for the management of head injury: an audit demonstrating its impact on a district general hospital, with a cost analysis for England and Wales. Emerg Med J 2006;23:109-13.
- Thomson R, Gray J, Madhok R, Mordue A, Mendelow AD. Effect of guidelines on management of head injury on record keeping and decision making in accident and emergency departments. Qual Health Care 1994;3:86-91.
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 1996;313:275-83.
- Eddy DM. Assessing Medical Technology. Washington, DC: National Academy Press; 1985.
- Smits M, Dippel DW, Nederkoorn PJ, Dekker HM, Vos PE, Kool DR, et al. Minor head injury: CT-based strategies for management: a cost-effectiveness analysis. Radiology 2010;254:532-40.
- Stein SC, Burnett MG, Glick HA. Indications for CT scanning in mild traumatic brain injury: a cost-effectiveness study. J Trauma 2006;61:558-66.
- Stein SC, Fabbri A, Servadei F. Routine serial computed tomographic scans in mild traumatic brain injury: when are they cost-effective?. J Trauma 2008;65:66-72.
- Aoki N, Kitahara T. Management of unruptured intracranial aneurysm in Japan: a Markovian decision analysis with utility measurements based on the Glasgow Outcome Scale. Med Decis Making 1998;18:357-64.
- Smits M, Dippel DW, Nederkoorn PJ, Dekker HM. Predicting intracranial traumatic findings on computed tomography in patients with minor head injury: the CHIP prediction rule. Ann Intern Med 2007;146:397-405.
- Af Geijerstam JL, Britton M. Mild head injury: reliability of early computed tomographic findings in triage for admission. Emerg Med J 2005;22:103-7.
- Warn DE, Thompson SG, Spiegelhalter DJ. Bayesian random effects meta-analysis of trials with binary outcomes: methods for the absolute risk difference and relative risk scales. Stat Med 2002;21:1601-23.
- Cordobés F, Lobato RD, Rivas JJ, Muñoz MJ, Chillón D, Portillo J, et al. Observations on 82 patients with extradural haematoma: comparison of results before and after the advent of computerized tomography. J Neurosurg 1981;54:179-86.
- Office for National Statistics (ONS) . United Kingdom, Interim Life Tables 1980–82 to 2006–2008 2008.
- Whitnall L, McMillan TM, Murray GD, Teasdale GM. Disability in young people and adults after head injury: 5–7 year follow up of a prospective cohort study. J Neurol Neurosurg Psychiatry 2006;77:640-5.
- Beecham J, Perkins M, Snell T, Knapp M. Treatment paths and costs for young adults with acquired brain injury in the United Kingdom. Brain Injury 2009;23:30-8.
- Duport S. Royal Hospital for Neuro Disability 2010.
- Department of Health . National Schedule of Reference Costs 2007–08 for NHS Trusts 2010.
- Curtis L. Unit Costs of Health and Social Care 2009. Personal Social Services Research Unit (PSSRU): University of Kent; 2009.
- National Radiological Protection Board (NRPB) . X-Rays, How Safe Are They? 2001.
- Berrington de González A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet 2004;363:345-51.
- Stein SC, Hurst RW, Sonnad SS. Meta-analysis of cranial CT scans in children. A mathematical model to predict radiation-induced tumors. Pediatr Neurosurg 2008;44:448-57.
- Garside R, Pitt M, Anderson R, Rogers G, Dyer M, Mealing S, et al. The effectiveness and cost-effectiveness of carmustine implants and temozolomide for the treatment of newly diagnosed high-grade glioma: a systematic review and economic evaluation. Health Technol Assess 2007;11.
- Stein SC, Fabbri A, Servadei F. A critical comparison of clinical decision instruments for computed tomographic scanning in mild closed traumatic brain injury in adolescents and adults. Ann Emerg Med 2009;53:180-8.
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87.
- National Institute for Health and Clinical Excellence . Guide to the Methods of Technology Appraisal 2008. www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdatedJune2008.pdf.
- Claxton K, Posnett J. An economic approach to clinical trial design and research priority-setting. Health Econ 1996;5:513-24.
- Felli JC, Hazen GB. Sensitivity analysis and the expected value of perfect information. Med Decis Making 1998;18:95-109.
- Ades AE, Lu G, Claxton K. Expected value of sample information calculations in medical decision modeling. Med Decis Making 2004;24:207-27.
- Maguire JL, Boutis K, Uleryk EM, Laupacis A, Parkin PC. Should a head-injured child receive a head CT scan? A systematic review of clinical prediction rules. Pediatrics 2009;124:e145-54.
- Berger RP, Kochanek PM. Urinary S100B concentrations are increased after brain injury in children: a preliminary study. Pediatr Crit Care Med 2006;7:557-61.
- Pickering A, Carter J, Hanning I, Townend W. Emergency department measurement of urinary s100B in children following head injury: can extracranial injury confound findings?. Emerg Med J 2008;25:88-9.
- Schultke E, Sadanand V, Kelly ME, Griebel RW, Juurlink BH. Can admission S-100beta predict the extent of brain damage in head trauma patients?. Can J Neurol Sci 2009;36:612-16.
- Muller K, Elverland A, Romner B, Waterloo K, Langbakk B, Unden J, et al. Analysis of protein S-100B in serum: a methodological study. Clin Chem Lab Med 2006;44:1111-14.
- Hallen M, Carlhed R, Karlsson M, Hallgren T, Bergenheim M. A comparison of two different assays for determining S-100B in serum and urine. Clin Chem Lab Med 2008;46:1025-9.
- Adams J, Frumiento C, Shatney-Leach L, Vane DW. Mandatory admission after isolated mild closed head injury in children: is it necessary?. J Pediatr Surg 2001;36:119-21.
- Andronikou S, Kilborn T, Patel M, Fieggen AG. Skull fracture as a herald of intracranial abnormality in children with mild head injury: is there a role for skull radiographs?. Australas Radiol 2003;47:381-5.
- Anglin D, Hutson HR, Luftman J, Qualls S, Moradzadeh D. Intracranial hemorrhage associated with tangential gunshot wounds to the head. Acad Emerg Med 1998;5:672-8.
- Anonymous . Which of the following selection criteria predict positive results on computed tomography scans for patients with traumatic head injury? Focal neurologic deficit. Alcohol intoxication. Depressed sensorium. Can Fam Physician 1994;40:1540-3.
- Anonymous . Clinical criteria predict serious head injury risk in kids. J Fam Pract 2007;56.
- Ariel VH, Guillermo PC, Guillermo PC. Optimización de la tomografía computarizada de crbneo en el trauma craneoencefalico leve. Rev Mex Neuroci 2006;7:194-9.
- Atif, MKS, Qureshi NA. Post-traumatic vomiting: a predictor of severity of head injury. J Coll Physicians Surg Pak 2001;11:349-51.
- Baglaj M, Czernik J, Ladogorska J. Minor head injuries in children: are radiological examinations and hospitalization necessary in every case?. Pol J Surg 2005;77:672-89.
- Balla JI, Elstein AS. Skull X-ray assessment of head injuries: a decision-analytic approach. Methods Inf Med 1984;23:135-8.
- Bamvita JM, Lavoie A, Clas D, Demers J, Trottier E, Bergeron E. Centre de Recherche de l’Hopital Charles-LeMoyne . The use of head CT scan in adult trauma victims: an algorithm. Ann Chir 2006;131:250-5.
- Bazarian JJ, Beck C, Blyth B, von Ahsen N, Hasselblatt M. Impact of creatine kinase correction on the predictive value of S-100B after mild traumatic brain injury. Restor Neurol Neurosci 2006;24:163-72.
- Beaudin M, Saint-Vil D, Ouimet A, Mercier C, Crevier L. Clinical algorithm and resource use in the management of children with minor head trauma. J Pediatr Surg 2007;42:849-52.
- Benito Fernández J, Mintegui Raso S, Sánchez Echániz J, Martinez González MJ, Fernández Cuesta MA. Head injuries in children: can clinical features identify patients with high or low risk for intracranial injury?. An Esp Pediatr 1998;48:122-6.
- Berger RP, Pierce MC, Wisniewski S, Adelson P, Kochanek P. Serum S100B concentrations are increased after closed head injury in children: A preliminary study. J Neurotrauma 2002;19:1405-9.
- Bernard C, Noiret A, Oswald P, Hoeffel JC, Bernard C, Noiret A, et al. What is the value of emergency cranial radiography in craniofacial injuries?. Sem Hop 1983;59:2567-9.
- Biberthaler P, Mussack T, Wiedemann E, Gilg T, Soyka M, Koller G, et al. Elevated serum levels of S-100B reflect the extent of brain injury in alcohol intoxicated patients after mild head trauma. Shock 2001;16:97-101.
- Biberthaler P, Mussack T, Kanz KG, Linsenmaier U, Pfeifer KJ, Mutschler W, et al. Identification of high-risk patients after minor craniocerebral trauma. Measurement of nerve tissue protein S 100. Unfallchirurg 2004;107:197-202.
- Block R. A decision rule with 7 clinical criteria identified patients with minor head injury who did not need computed tomography. Evid-Based Med 2001;6.
- Boran BO, Barut N, Akgun C, Celikoglu E, Bozbuga M. Indications for computed tomography in patients with mild head injuries. Ulusal Travma Ve Acil Cerrahi Dergisi 2005;11:218-24.
- Bouvier D, Oddoze C, Ben Haim D, Moustafa F, Legrand A, Alazia M, et al. Interest of S100B protein blood level determination for the management of patients with minor head trauma. Ann Biol Clin (Paris) 2009;67:425-31.
- Chan KH, Yue CP, Mann KS. The risk of intracranial complications in pediatric head injury. Results of multivariate analysis. Childs Nerv Syst 1990;6:27-9.
- Chan HC, Aasim WA, Abdullah NM, Naing NN, Abdullah JM, Saffari MH, et al. Characteristics and clinical predictors of minor head injury in children presenting to two Malaysian accident and emergency departments. Singapore Med J 2005;46:219-23.
- Clement CM, Stiell IG, Schull MJ, Rowe BH, Brison R, Lee JS, et al. Clinical features of head injury patients presenting with a Glasgow Coma Scale Score of 15 and who require neurosurgical intervention. Ann Emerg Med 2006;48:245-51.
- Cummins BH. The management of minor head injuries. Curr Orthop 1992;6:240-4.
- Dahl-Grove DL, Chande VT, Barnoski A. Closed head injuries in children: Is hospital admission always necessary?. Pediatr Emerg Care 1995;11:86-8.
- de Andrade AF, de Almeida AN, Bor-Seng-Shu E, Lourenco L, Mandel M, Marino R. The value of cranial computed tomography in high-risk, mildly head-injured patients. Surg Neurol 2006;65.
- de Boussard CN, Lundin A, Karlstedt D, Edman G, Bartfai A, Borg J. S100 and cognitive impairment after mild traumatic brain injury. J Rehab Med 2005;37:53-7.
- de Boussard CN, Bellocco R, af Geijerstam JLA, Borg J, Adami J. Delayed intracranial complications after concussion. J Trauma 2006;61:577-81.
- Dunning J, Daly JP, Malhotra R, Stratford-Smith P, Lomas JP, Lecky F, et al. The implications of NICE guidelines on the management of children presenting with head injury. Arch Dis Child 2004;89:763-7.
- Duus BR, Boesen T, Kruse KV, Nielsen KB. Prognostic signs in the evaluation of patients with minor head injury. Br J Surg 1993;80:988-91.
- Edna TH. Acute traumatic intracranial haematoma and skull fracture. Acta Chir Scand 1983;149:449-51.
- Edna TH. Risk factors in traumatic head injury. Acta Neurochir 1983;69:15-21.
- Edna TH, Cappelen J. Hospital admitted head injury. A prospective study in Trondelag, Norway, 1979–80. Scand J Soc Med 1984;12:7-14.
- Espersen JO, Petersen OF, Espersen JO, Petersen OF. Computerized tomography (CT) in patients with head injuries. Assessment of outcome based upon initial clinical findings and initial CT scans. Acta Neurochir 1982;65:81-9.
- Fabbri A, Servadei F, Marchesini G. Prospective validation of a proposal for diagnosis and management of patients attending the emergency department for mild head injury. J Neurol Neurosurg 2004;75:410-16.
- Geyer C, Ulrich A, Grafe G, Stach B, Till H. Diagnostic value of S100B and neuron-specific enolase in mild pediatric traumatic brain injury. J Neurosurg 2009;4:339-44.
- Gonzalez IC, Hernandez JAF. Analysis of minor head injuries treated in an Accident & Emergency Department. Emergencias 2007;19:21-4.
- Gorelick MH, Atabaki SM, Hoyle J, Dayan DS, Holmes JF, Holubkov R, et al. Interobserver agreement in assessment of clinical variables in children with blunt head trauma. Acad Emerg Med 2008;15:812-18.
- Greenes DS, Schutzman SA. Occult intracranial injury in infants. Ann Emerg Med 1998;32:680-6.
- Gruskin KD, Schutzman SA, Gruskin KD, Schutzman SA. Head trauma in children younger than 2 years: are there predictors for complications?. Arch Pediatr Adolesc Med 1999;153:15-20.
- Gupta R, Taha MD, McCarroll K, Blair H, Wu J. Head CT evaluation in clinically stable motor vehicle collision patients. Emerg Radiol 2005;11:328-35.
- Gutman MB, Moulton RJ, Sullivan I, Hotz G, Tucker WS, Muller PJ. Risk-factors predicting operable intracranial hematomas in head-injury. J Neurosurg 1992;77:9-14.
- Harris OA, Bruce CA, Reid M, Cheeks R, Easley K, Surles MC, et al. Examination of the management of traumatic brain injury in the developing and developed world: focus on resource utilization, protocols, and practices that alter outcome. J Neurosurg 2008;109:433-8.
- Hoffmann ME, Ma J, Gaddis G. Utility of an initial d-dimer assay in screening for traumatic or spontaneous intracranial hemorrhage. Acad Emerg Med 2001;8:859-65.
- Hollingworth W, Vavilala M, Jarvik S. The use of repeated head computed tomography in pediatric blunt head trauma: Factors predicting new and worsening brain injury. Pediatr Crit Care Med 2007;8:348-56.
- Holsti M, Kadish HA, Sill BL, Firth SD, Nelson DS. Pediatric closed head injuries treated in an observation unit. Pediatr Emerg Care 2005;21:639-44.
- Benito Fernández J, Mintegui Raso S, Sanchez Echaniz J, Martinez Gonzales MJ, Fernandez Cuesta MA. Pediatric head trauma: Can clinical features predict the presence of an intracranial injury?. An Esp Pediatr 1998;48:122-6.
- Jones PA, Chambers IR, Minns RA, Lo TY, Myles LM, Steers AJ. Are head injury guidelines changing the outcome of head injured children? A regional investigation. Acta Neurochir 2008;102:S81-4.
- Kahraman S, Kayali H, Atabey C, Acar F, Gocmen S. The accuracy of near-infrared spectroscopy in detection of subdural and epidural hematomas. J Trauma 2006;61:1480-3.
- Kakarieka A, Braakman R, Schakel EH. Clinical significance of the finding of subarachnoid blood on CT scan after head injury. Acta Neurochir 1994;129:1-5.
- Kavalci C, Pekdemir M, Durukan P, Ilhan N, Yildiz M, Serhatlioglu S, et al. The value of serum tau protein for the diagnosis of intracranial injury in minor head trauma. Am J Emerg Med 2007;25:391-5.
- King J, Haddock G. Neonatal head injuries revisited. Scottish Med J 2009;54:34-6.
- Knuckey NW, Gelbard S, Epstein MH. The management of ‘asymptomatic’ epidural hematomas. J Neurosurg 1989;70:392-6.
- Kuhne CA, Homann M, Ose C, Waydhas C, Nast-Kolb D, Ruchholtz S. Emergency room patients. Unfallchirurg 2003;106:380-6.
- Kuppermann N, Holmes JF, Dayan PS, Hoyle JD, Atabaki S, Dean DM, et al. and PECARN . Blunt head trauma in the Pediatric Emergency Care Applied Research Network (PECARN). Acad Emerg Med 2007;14:S94-5.
- Lehmann U, Regel G, Ellendorf B, Rickels E, Lorenz M, Becker H, et al. Initial cranial CT for evaluating the prognosis of craniocerebral trauma. Unfallchirurg 1997;100:705-10.
- Levi L, Guilburd JN, Linn S, Feinsod M. The association between skull fracture, intracranial pathology and outcome in pediatric head injury. Br J Neurosurg 1991;5:617-25.
- Livingston DH, Loder PA, Hunt CD. Minimal head injury: is admission necessary?. Am Surg 1991;57:14-7.
- Lloyd DA, Carty H, Patterson M, Butcher CK, Roe D. Predictive value of skull radiography for intracranial injury in children with blunt head injury. Lancet 1997;349:821-4.
- Lucchi S, Giua G, Bettinelli A, Farabola M, Sina C, Mangiagalli E. The role of computerized tomography in the management of mild head injury patients. Riv Neuroradiol 1995;8:415-28.
- Mahmood KSA. Post-traumatic vomiting: a predictor of severity of head injury. Med Forum 2000;11:1-5.
- Mandera M, Zralek C, Zycinski A, Wencel T, Bazowski P. Surgery or conservative treatment in children with traumatic intracerebral haematoma. Childs Nerv Syst 1999;15:267-9.
- Markle J, Cayten CG, Byrne DW, Murphy JG. Comparison between TRISS and ASCOT methods in controlling for injury severity. J Trauma 1992;33:326-32.
- Marshall LF, Maas AI, Marshall SB, Bricolo A, Fearnside M, Iannotti F, et al. A multicenter trial on the efficacy of using tirilazad mesylate in cases of head injury. J Neurosurg 1998;89:519-25.
- Marti-Fabregas J, Belvis R, Guardia E, Cocho D, Munoz J, Marruecos L, et al. Prognostic value of Pulsatility Index in acute intracerebral hemorrhage. Neurology 2003;61:1051-6.
- Martinot A, Chartier A, Hue V, Dubos F. Performance of decision rules to predict need for computed tomography among children with blunt head trauma. Arch Pediatr 2008;15:721-3.
- Massaro F, Lanotte M, Faccani G, Triolo C. One hundred and twenty-seven cases of acute subdural haematoma operated on: correlation between CT scan findings and outcome. Acta Neurochir 1996;138:185-91.
- Masters SJ. Evaluation of head trauma: efficacy of skull films. AJR Am J Roentgenol 1980;135:539-47.
- Matsumoto M, Sanpei K, Nishikawa H, Seki T, Shibata I, Terao H. Characteristics of traumatic intracerebral hematomas in children. Neurol Med Chir 1988;28:1081-8.
- Mattox KL, Bickell W, Pepe PE, Burch J, Feliciano D. Prospective MAST study in 911 patients. J Trauma 1989;29:1104-11.
- Meier EM. Evaluating head trauma in infants and children. MCN Am J Matern Child Nurs 1983;8:54-7.
- Memon ZI, Altura BT, Benjamin JL, Cracco RQ, Altura BM. Predictive value of serum ionized but not total magnesium levels in head injuries. Scand J Clin Lab Invest 1995;55:617-77.
- Mendelow AD, Teasdale GM, Barer D, Fernandes HM, Murray GD, Gregson BA. Outcome assignment in the International Surgical Trial of Intracerebral Haemorrhage. Acta Neurochir 2003;145:679-81.
- Mendelow AD, Timothy J, Steers JW, Lecky F, Yates D, Bouamra O, et al. Management of patients with head injury. Lancet 2008;372:685-7.
- Menon D, Harrison D. Prognostic modelling in traumatic brain injury. BMJ 2008;336:397-8.
- Meyer P, Ducrocq S, Baugnon T, Thelot B, Orliaguet G, Carli P, et al. Head injury in children less than 2 years of age. Arch Pediatr 2006;13:737-40.
- Mikhail MG, Levitt MA, Christopher TA, Sutton MC. Intracranial injury following minor head trauma. Am J Emerg Med 1992;10:24-6.
- Miller JD, Murray LS, Teasdale GM, Miller JD, Murray LS, Teasdale GM. Development of a traumatic intracranial hematoma after a ‘minor’ head injury. Neurosurgery 1990;27:669-73.
- Mohanty SK, Thompson W, Rakower S. Are CT scans for head injury patients always necessary?. J Trauma 1991;31:801-4.
- Murgio A, Herrera EJ, Mutluer S, Fong D. Mild closed head injury in children and adolescents. SAGGI Child Dev Disabil 2003;29.
- Mussack T, Biberthaler P, Wiedemann E, Kanz KG, Englert A, Gippner-Steppert C, et al. S-100b as a screening marker of the severity of minor head trauma (MHT): a pilot study. Acta Neurochir 2000;76:S393-6.
- Muszynski CA, Hayman LA, Weingarten K, Prow HW, Cole JW, Contant CF. Conservative management of extra-axial hematomas diagnosed by CT. Neuroradiology 1999;41:875-81.
- Muthukumar N, Srinivasan US, Sampathkumar M, Gajendran R, Nakamura N, Hashimoto T, et al. Recent advances in neurotraumatology. Tokyo: Springer–Verlag; 1993.
- Naeimi ZS, Weinhofer A, Sarahrudi K, Heinz T, Vecsei V. Predictive value of S-100B protein and neuron specific-enolase as markers of traumatic brain damage in clinical use. Brain Inj 2006;20:463-8.
- Nagy KK, Joseph KT, Krosner SM. The utility of computed tomography after minimal head injury. J Trauma 1999;46:268-70.
- Oertel M, Kelly DF, McArthur D, Boscardin WJ, Glenn TC, Lee JH, et al. Progressive hemorrhage after head trauma: predictors and consequences of the evolving injury. J Neurosurg 2002;96:109-16.
- Oh EJ, Kim YM, Jegal DW, Kahng J, Park YJ, Han K. Diagnostic value of Elecsys S100 as a marker of acute brain injury in the emergency department. J Clin Lab Anal 2007;21:387-92.
- Orrison WW, Gentry LR, Stimac GK, Tarrel RM, Espinosa MC, Cobb LC. Blinded comparison of cranial CT and MR in closed head injury evaluation. Am J Neuroradiol 1994;15:351-6.
- Ortiz HJL, Guerra P, Sanchez G. Las fracturas lineales de crbneo como factor de riesgo en pacientes con traumatismo craneoencefblico menor. Rev Chil Neurocirug 2006;26:38-43.
- Ortiz HJL, Paneque GS. Valor pronstico del sexo y la edad en el traumatismo craneoencefblico no grave del adulto [Prognostic value of the age and gender in the mild head trauma of the adult]. Rev Chil Neuropsiquiatr 2005;25:48-52.
- Owings JT, Wisner DH, Battistella FD. Isolated transient loss of consciousness is an indicator of significant injury. Arch Surg 1998;133:941-6.
- Palchak MJ, Holmes JF, Kuppermann N. Clinician judgment versus a decision rule for identifying children at risk of traumatic brain injury on computed tomography after blunt head trauma. Pediatr Emerg Care 2009;25:61-5.
- Pasman P, Twijnstra A, Wilmink J, Leffers P. The value of skull radiography in patients with head trauma. J Belge Radiol 1995;78:169-71.
- Pretto Flores L, De Almeida CS, Casulari LA. Positive predictive values of selected clinical signs associated with skull base fractures. J Neurosurg Sci 2000;44:77-82.
- Rathlev NK, Medzon R, Lowery D, Pollack C, Bracken M, Barest G, et al. Intracranial pathology in elders with blunt head trauma. Acad Emerg Med 2006;13.
- Reinus WR, Zwemer FLJ. Clinical prediction of emergency cranial computed tomography results. Ann Emerg Med 1994;23:1271-8.
- Rivas JJ, Lobato RD, Sarabia R. Extradural hematoma: analysis of factors influencing the courses of 161 patients. Neurosurgery 1988;23:44-51.
- Sainsbury CPQ, Sibert JR. How long do we need to observe head injuries in hospital?. Arch Dis Child 1984;59:856-9.
- Sanus GZ, Tanriverdi T, Alver I, Aydin S, Uzan MT. Evolving traumatic brain lesions: Predictors and results of ninety-eight head-injured patients. Neurosurg Quart 2004;14:97-104.
- Savastio G, Golfieri R, Pastore, Trossello M, Venturoli L. Cranial trauma: the predictability of the presentation symptoms as a screening for radiologic study. Radiol Med 1991;82:769-75.
- Servadei F, Faccani G, Roccella P, Seracchioli A, Godano U, Ghadirpor R, et al. Asymptomatic extradural haematomas. Results of a multicenter study of 158 cases in minor head injury. Acta Neurochir 1989;96:39-45.
- Shane SA, Fuchs SM. Skull fractures in infants and predictors of associated intracranial injury. Pediatr Emerg Care 1997;13:198-203.
- Sifri ZC, Homnick AT, Vaynman A, Lavery R, Liao W, Mohr A, et al. A prospective evaluation of the value of repeat cranial computed tomography in patients with minimal head injury and an intracranial bleed. J Trauma 2006;61:862-7.
- Smits M, Hunink MG, Nederkoorn PJ, Dekker HM, Vos PE, Kool DR, et al. A history of loss of consciousness or post-traumatic amnesia in minor head injury: ‘Conditio sine qua non’ or one of the risk factors?. J Neurol Neurosurg Psychiatry 2007;78:1359-64.
- Stein SC, Spettell C, Young G, Ross SE. Limitations of neurological assessment in mild head injury. Brain Inj 1993;7:425-30.
- Taheri PA, Karamanoukian H, Gibbons K. Can patients with minor head injuries be safely discharged home?. Arch Surg 1993;128:289-92.
- Teasdale GM, Murray G, Anderson E, Mendelow AD, MacMillan R, Jennett B, et al. Risks of acute traumatic intracranial haematoma in children and adults: implications for managing head injuries. BMJ 1990;300:363-7.
- Turedi S, Hasanbasoglu A, Gunduz A, Yandi M. Clinical decision instruments for CT scan in minor head trauma. J Emerg Med 2008;34:253-9.
- Velmahos GC, Gervasini A, Petrovick L, Dorer DJ, Doran ME, . Routine repeat head CT for minimal head injury is unnecessary. J Trauma 2006;60:494-9.
- Vogelbaum MA, Kaufman BA, Park TS, Winthrop AL. Management of uncomplicated skull fractures in children: Is hospital admission necessary?. Pediatr Neurosurg 1998;29:96-101.
- Voss M, Knottenbelt JD, Peden MM. Patients who reattend after head injury: a high risk group. BMJ 1995;311:1395-8.
- Willis AP, Latif SAA, Chandratre S, Stanhope B, Johnson K. Not a NICE CT protocol for the acutely head injured child. Clin Radiol 2008;63:165-9.
- Yamamoto T, Ogata M. Intraventricular hemorrhage in blunt head injury (author’s translation). Nippon Geka Hokan 1981;50:526-33.
- Yanagawa Y, Tsushima Y, Tokumaru A, Un-no Y, Sakamoto T, Okada Y, et al. A quantitative analysis of head injury using T2*-weighted gradient-echo imaging. J Trauma 2000;49:272-7.
- Zimmerman RA, Bilaniuk LT, Hackney DB, Goldberg HI, Grossman RI. Head injury: Early results of comparing CT and high-field MR. Am J Roentgenol 1986;147:1212-22.
- Burnett MG, Stein SC, Mickel HS. Safety and cost-effectiveness of common management strategies for treating mild closed head injuries: should all patients be evaluated with the use of computed tomography?. Neurosurgery 2002;51:542-95.
Appendix 1 Diagnostic accuracy and management strategies for minor head injury review: literature search strategies – a MEDLINE example
Database searched: Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R)
Platform or provider used: OvidSP
Date of coverage: 1950 to March 2010
Search undertaken: initial search 20 April 2009
Updated search: 11 March 2010
-
*Craniocerebral Trauma/
-
head injur$.tw.
-
1 or 2
-
prognosis.sh.
-
diagnosed.tw.
-
cohort:.mp.
-
predictor:.tw.
-
death.tw.
-
exp models, statistical/
-
(clinical assess* or decision rule* or prediction rule*).tw.
-
4 or 5 or 6 or 7 or 8 or 9 or 10
-
exp “Sensitivity and Specificity”/
-
sensitivity.tw.
-
specificity.tw.
-
((pre-test or pretest) adj probability).tw.
-
post-test probability.tw.
-
predictive value$.tw.
-
likelihood ratio$.tw.
-
12 or 13 or 14 or 15 or 16 or 17 or 18
-
3 and (11 or 19)
Appendix 2 The modified QUADAS tool for the methodological assessment of diagnostic studies
| QUADASa criterion | Criteria met | Criteria defined | |
|---|---|---|---|
| 1 | Was the spectrum of patients representative of the patients who will receive the test in practice? | Yes | Unselected, prospective patients (children or adults) with early head injury (GCS 13–15, within 48 hours of presentation) |
| No | All other patient spectra including retrospectively selected patient spectra, and spectra including only those who had CT | ||
| Unclear | If insufficient details were provided to make a judgement as to whether the patient spectrum would be scored as ‘yes’ | ||
| 2 | Were selection criteria clearly described? | Yes | Enough details are provided of how patients were selected so that the selection process could be replicated |
| No | Insufficient details are presented | ||
| Unclear | NA | ||
| 3a |
Criteria modified Is the reference standard likely to correctly classify ICI? (Where ICI is not an outcome, this item may be classed as not applicable) |
Yes | ICI: All of cohort have CT or MRI within 24 hours of admission |
| No | All other reference standards | ||
| Unclear | If details of the reference standard are not reported | ||
| 3b |
Criteria modified Is the reference standard likely to correctly classify need for neurosurgery? (Where need for neurosurgery is not an outcome, this item may be classed as not applicable) |
Yes | Neurosurgery: all of the cohort have follow-up 30 days or more after the injury |
| No | All other reference standards | ||
| Unclear | If details of the reference standard are not reported | ||
| 4 |
Not used: not relevant to this reviewb Is the time period between reference standard and index test short enough to be reasonably sure that the target condition did not change between the two tests? |
Yes | |
| No | |||
| Unclear | |||
| 5a |
Criteria modified Partial verification bias. Did the whole sample or a random selection of the sample, receive verification using a reference standard of diagnosis for ICI? |
Yes | If the whole sample or random selection of the sample received a reference standard |
| No | If only a selected sample received a reference standard | ||
| Unclear | If it was not clear whether or not all the patients received a reference standard | ||
| 5b |
Criteria modified Partial verification bias. Did the whole sample or a random selection of the sample, receive verification using a reference standard of diagnosis for neurosurgery? |
Yes | If the whole sample or random selection of the sample received a reference standard |
| No | If only a selected sample received a reference standard | ||
| Unclear | If it was not clear whether or not all the patients received a reference standard | ||
| 6a |
Criteria modified Differential verification bias. Did all patients receive the same reference standard for ICI regardless of the index test result? |
Yes | If patients received a reference standard regardless of the index test result |
| No | If patients received a reference standard based on part or all of the index test result | ||
| Unclear | If it was not clear whether or not the index test result influenced which reference standard was used, including where physician discretion may incorporate part or all of the index test | ||
| 6b |
Criteria modified Differential verification bias. Did all patients receive the same reference standard for neurosurgery regardless of the index test result? |
Yes | If patients received a reference standard regardless of the index test result |
| No | If patients received a reference standard based on part or all of the index test result | ||
| Unclear | If it was not clear whether the index test result influenced which reference standard was used, including where physician discretion may incorporate part or all of the index test | ||
| 7 |
Not used: not relevant to this reviewc Was the reference standard independent of the index test (i.e. the index test did not form part of the reference standard)? |
Yes | |
| No | |||
| Unclear | |||
| 8 | Was the execution of the index test described in sufficient detail to permit replication of the test? | Yes | If sufficient details of test standard execution were reported so that the test/reference standard could reasonably be replicated |
| No | If sufficient details are not reported | ||
| Unclear | NA | ||
| 9 | Was the execution of the reference standard described in sufficient detail to permit its replication? | Yes | If sufficient details of reference standard execution were reported so that the test/reference standard could reasonably be replicated |
| No | If sufficient details are not reported | ||
| Unclear | NA | ||
| 10 | Test review bias. Were the index test results interpreted without knowledge of the results of the reference standard? | Yes |
If the index test was interpreted without knowledge (blinding) of the results of the reference standard and vice versa If one test was clearly interpreted before the results of the other test were available then this should be scored as ‘yes’ |
| No | If the person interpreting the index test was aware of the results of the reference standard or vice versa | ||
| Unclear | If no information is provided regarding whether tests were interpreted blindly | ||
| 11 | Diagnostic review bias. Were the reference standard results interpreted without knowledge of the results of the index test? | Yes |
If the index test was interpreted without knowledge (blinding) of the results of the reference standard and vice versa If one test was clearly interpreted before the results of the other test were available then this should be scored as ‘yes’ |
| No | If the person interpreting the index test was aware of the results of the reference standard or vice versa | ||
| Unclear | If no information is provided regarding whether tests were interpreted blindly | ||
| 12 | Clinical review bias. Were the same clinical data available when test results were interpreted as would be available when the test is used in practice? | Yes | If the article states the following information was available: description of symptoms, site of injury, patient characteristics, e.g. clinician may be blinded to data that are normally available to them |
| No | If not as above | ||
| Unclear | If details on the availability of clinical data were not reported | ||
| 13 | Were uninterpretable/intermediate test results reported? | Yes | If details are provided on uninterpretable/intermediate test results |
| No | If there appear to be some on uninterpretable/intermediate but the results of those are not reported | ||
| Unclear | If it is not clear whether there were any uninterpretable/intermediate test results | ||
| 14 | Were withdrawals from the study explained? | Yes | If all patients who entered into the study were accounted for |
| No | If it appears that some of the participants who entered the study did not complete the study, i.e. did not receive both the index test and reference standard, and these patients were not accounted for | ||
| Unclear | If it is not clear whether all patients who entered the study were accounted for |
Appendix 3 Diagnostic accuracy review – PRISMA (adapted) flow chart
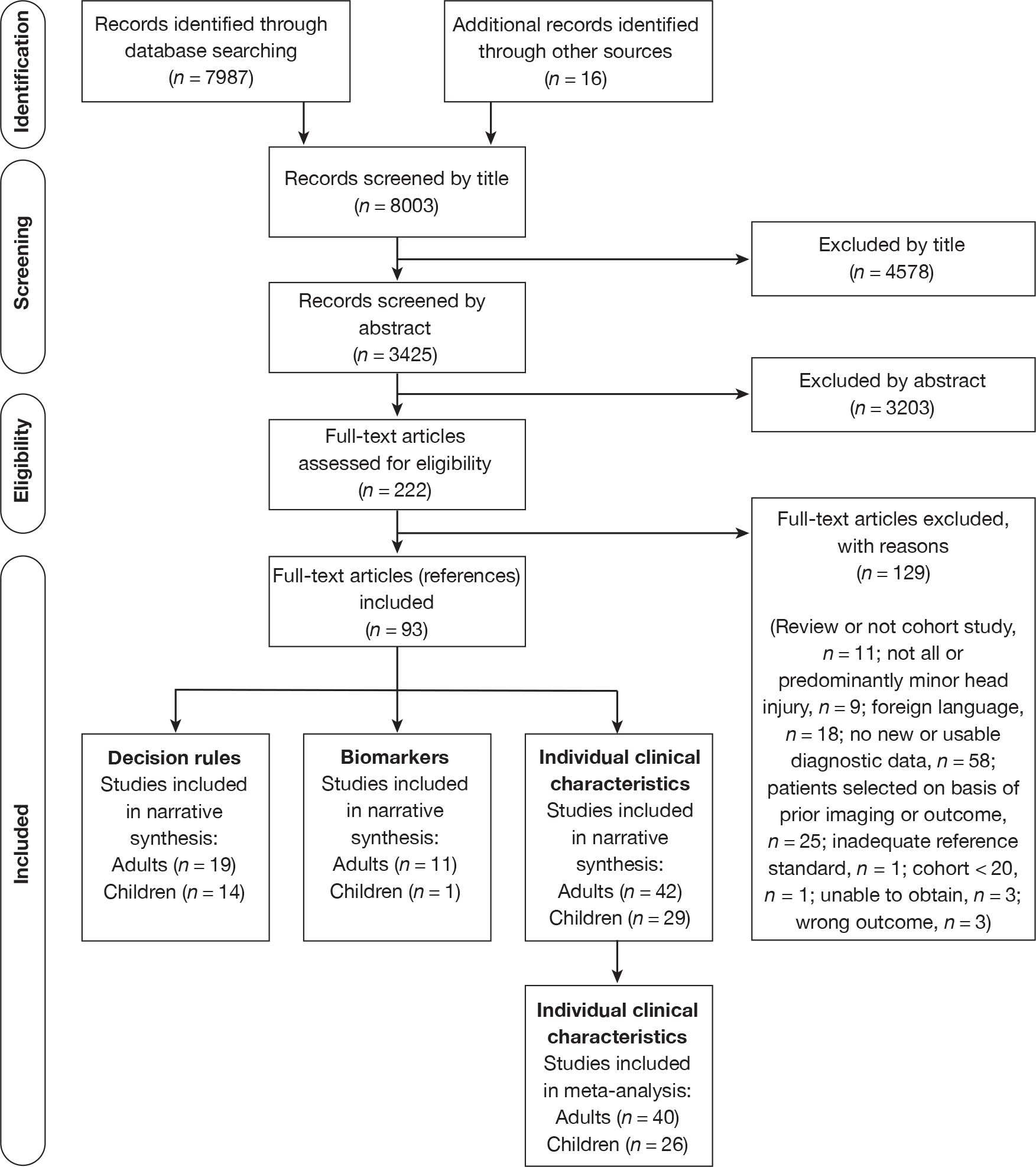
Appendix 4 Diagnostic accuracy review – table of excluded studies with rationale
| Author, year | Reason for exclusion |
|---|---|
| Adams et al. 2001192 | No useable diagnostic data |
| Andronikou et al. 2003193 | No useable diagnostic data |
| Anglin et al. 1998194 | Not all or predominantly MHI: gunshot wounds |
| Anonymous 1994195 | No useable diagnostic data |
| Anonymous 2007196 | Review |
| Ariel et al. 2006197 | Foreign language |
| Atif and Qureshi 2001198 | Wrong outcome – predicting skull fracture |
| Baglaj et al. 2005199 | Unable to obtain |
| Balla and Elstein 1984200 | Review |
| Bamvita et al. 2006201 | Foreign language |
| Bazarian et al. 2006202 | No useable diagnostic data |
| Beaudin et al. 2007203 | No useable diagnostic data |
| Benito Fernández et al. 1998204 | No useable diagnostic data |
| Berger et al. 2002205 | Not cohort study (case control); no useable diagnostic data |
| Bernard et al. 1983206 | Foreign language |
| Biberthaler et al. 2001207 | No useable diagnostic data |
| Biberthaler et al. 2004208 | Foreign language |
| Block 2001209 | Review |
| Boran et al. 2005210 | Foreign language |
| Bouvier et al. 2009211 | Foreign language |
| Brown et al. 1994152 | No useable diagnostic data |
| Browning et al. 2005154 | No useable diagnostic data |
| Chan et al. 1990212 | Patients selected on the basis of outcome |
| Chan et al. 2005213 | No useable diagnostic data |
| Clement 2006214 | No new data |
| Cummins 1992215 | Review |
| Dahl-Grove et al. 1995216 | Patients selected on the basis of outcome: negative CT scan |
| de Andrade et al. 2006217 | No useable diagnostic data |
| de Boussard et al. 2005218 | Wrong outcome – symptoms and signs of cognitive impairment |
| de Boussard et al. 2006219 | Not cohort study |
| Dunning et al. 2004220 | No useable diagnostic data |
| Duus et al. 1993221 | No useable diagnostic data |
| Edna 1983222 | Patients selected on the basis of outcome |
| Edna 1983223 | Patients selected on the basis of outcome |
| Edna and Cappelen 1984224 | Patients selected on the basis of outcome |
| Espersen and Petersen 1982225 | No useable diagnostic data |
| Fabbri et al. 2004226 | No new data |
| Fabbri et al. 2004153 | No useable diagnostic data |
| Fong et al. 2008155 | No useable diagnostic data |
| Af Geijerstam et al. 200637 | Wrong outcome – GOS |
| Geyer et al. 2009227 | No useable diagnostic data |
| Gonzalez et al. 2007228 | Foreign language |
| Gorelick et al. 2008229 | No useable diagnostic data |
| Greenes and Schutzman 1998230 | Patients selected on the basis of outcome |
| Gruskin et al. 1999231 | Patients selected on the basis of outcome |
| Gupta et al. 2005232 | No useable diagnostic data |
| Gutman et al. 1992233 | No useable diagnostic data |
| Harris et al. 2008234 | No useable diagnostic data |
| Hassan et al. 200522 | No useable diagnostic data |
| Hoffmann et al. 2001235 | Not all or predominantly MHI: includes spontaneous injury |
| Hollingworth et al. 2007236 | Not all or predominantly MHI: progressive injury |
| Holsti et al. 2005237 | Patients selected on the basis of outcome |
| Benito Fernández 1998238 | Foreign language |
| Jones et al. 2008239 | No useable diagnostic data |
| Kahraman et al. 2006240 | Patients selected on the basis of outcome |
| Kakarieka et al. 1994241 | Patients selected on the basis of outcome |
| Kavalci et al. 2007242 | No useable diagnostic data |
| Kelly et al. 198833 | Patients selected on the basis of outcome |
| Kerr et al. 2005156 | No useable diagnostic data |
| King and Haddock 2009243 | No useable diagnostic data |
| Knuckey et al. 1989244 | Patients selected on the basis of outcome |
| Kuhne et al. 2003245 | Foreign language |
| Kuppermann et al. 2007246 | No useable diagnostic data. Protocol only, full study being prepared for publication |
| Lehmann et al. 1997247 | Foreign language |
| Levi et al. 1991248 | No useable diagnostic data |
| Livingston et al. 1991249 | No useable diagnostic data |
| Lloyd et al. 1997250 | Not all or predominantly MHI (assumed) |
| Loroni et al. 1996157 | No useable diagnostic data |
| Lucchi et al. 1995251 | Foreign language |
| Mahmood 2000252 | Unable to obtain |
| Mandera et al. 1999253 | Patients selected on the basis of outcome |
| Markle et al. 1992254 | No useable diagnostic data |
| Marshall et al. 1998255 | No useable diagnostic data |
| Marti-Fabregas et al. 2003256 | Patients selected on the basis of outcome |
| Martinot et al. 2008257 | Foreign language |
| Massaro et al. 1996258 | Patients selected on the basis of outcome |
| Masters 1980259 | Inadequate reference standard |
| Matsumoto et al. 1988260 | Foreign language |
| Mattox et al. 1989261 | No useable diagnostic data |
| Meier 1983262 | Review |
| Memon et al. 1995263 | No useable diagnostic data |
| Mendelow et al. 2003264 | Review |
| Mendelow et al. 2008265 | Review |
| Menon and Harrison 2008266 | Review |
| Meyer et al. 2006267 | Foreign language |
| Mikhail et al. 1992268 | No useable diagnostic data |
| Miller et al. 1990269 | Patients selected on the basis of outcome |
| Mohanty et al. 1991270 | No useable diagnostic data |
| Murgio et al. 2003271 | Unable to obtain |
| Mussack et al. 2000272 | No useable diagnostic data |
| Muszynski et al. 1999273 | Patients selected on the basis of outcome |
| Muthukumar et al. 1993274 | Not all or predominantly MHI |
| Naeimi et al. 2006275 | Not all or predominantly MHI |
| Nagy et al. 1999276 | No useable diagnostic data |
| Oertel et al. 2002277 | Not all or predominantly MHI: progressive injury |
| Oh et al. 2007278 | Not all or predominantly MHI: includes chronic injury |
| Orrison et al. 1994279 | No useable diagnostic data |
| Ortiz et al. 2006280 | Foreign language |
| Ortiz and Paneque 2006281 | Foreign language |
| Owings et al. 1998282 | No useable diagnostic data |
| Palchak et al. 2009283 | No new data |
| Pasman et al. 1995284 | No useable diagnostic data |
| Pretto et al. 2000285 | No useable diagnostic data |
| Rathlev et al. 2006286 | No new data |
| Reinus et al. 1994287 | Not all or predominantly MHI: includes chronic or spontaneous head injury |
| Richless et al. 199328 | No useable diagnostic data |
| Rivas et al. 1988288 | Patients selected on the basis of outcome |
| Sainsbury and Sibert 1984289 | Patients selected on the basis of outcome |
| Sanus et al. 2004290 | Patients selected on the basis of outcome |
| Savastio et al. 1991291 | Foreign language |
| Schultke et al. 2009189 | No useable diagnostic data |
| Servadei et al. 1989292 | Patients selected on the basis of outcome |
| Shane and Fuchs 1997293 | Patients selected on the basis of prior imaging or outcome |
| Shravat et al. 2006158 | No useable diagnostic data |
| Sifri et al. 2006294 | Patients selected on the basis of prior imaging or outcome |
| Smits et al. 2007295 | No new data |
| Stein et al. 1993296 | No useable diagnostic data |
| Sultan et al. 200421 | No useable diagnostic data |
| Taheri et al. 1993297 | No useable diagnostic data |
| Teasdale et al. 1990298 | No useable diagnostic data |
| Thompson et al. 2005159 | No useable diagnostic data |
| Turedi et al. 2008299 | Not cohort study (patients selected on basis of age) |
| Velmahos et al. 2006300 | Patients selected on the basis of outcome |
| Vogelbaum et al. 1998301 | No useable diagnostic data |
| Voss et al. 1995302 | No useable diagnostic data |
| Willis et al. 2008303 | No useable diagnostic data |
| Yamamoto and Ogata 1981304 | Foreign language |
| Yanagawa et al. 2000305 | Patients selected on the basis of outcome (survived for 1 week) |
| Zimmerman et al. 1986306 | Cohort of < 20 |
Appendix 5 Individual clinical characteristics in adults – data for meta-analysis
Intracranial injury in adults
Intoxication (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schynoll 1993118 | 264 | 18.8 | 87.9 | 18.5 | 9.8 to 30.2 | 87.8 | 83.4 to 91.4 | 0.930 | 0.797 to 1.033 | 1.51 | 0.79 to 2.64 |
| Borczuk 199555 | 1448 | 25.2 | 68.5 | 26.4 | 19.5 to 34.3 | 68.8 | 66.3 to 71.2 | 1.070 | 0.950 to 1.180 | 0.85 | 0.62 to 1.11 |
| Haydel 200027 | 520 | 61.1 | 67.4 | 51.6 | 36.2 to 67.2 | 67.3 | 63.1 to 71.4 | 0.720 | 0.486 to 0.953 | 1.58 | 1.09 to 2.12 |
| Stiell 200126 | 3121 | 18.1 | 88.2 | 18.0 | 13.9 to 22.8 | 88.2 | 87.0 to 89.4 | 0.929 | 0.875 to 0.977 | 1.53 | 1.17 to 1.97 |
| Mack 2003110 | 133 | 15.8 | 94.7 | 13.6 | 5.5 to 26.9 | 93.2 | 88.3 to 96.7 | 0.929 | 0.790 to 1.015 | 1.98 | 0.83 to 4.71 |
| Ibanez and Arikan 200460 | 1101 | 6.0 | 94.0 | 8.2 | 3.9 to 14.4 | 94.0 | 92.4 to 95.3 | 0.977 | 0.911 to 1.026 | 1.36 | 0.63 to 2.46 |
| Fabbri 200557 | 7955 | 26.9 | 91.6 | 26.2 | 22.6 to 30.0 | 91.6 | 90.9 to 92.2 | 0.806 | 0.764 to 0.846 | 3.10 | 2.63 to 3.63 |
| Mower 200562 | 13,728 | 19.0 | 75.6 | 19.3 | 16.8 to 21.9 | 75.7 | 74.9 to 76.4 | 1.067 | 1.031 to 1.101 | 0.79 | 0.69 to 0.90 |
| Stiell 200546 | 1822 | 13.4 | 84.4 | 15.4 | 9.6 to 22.4 | 84.5 | 82.8 to 86.2 | 1.002 | 0.918 to 1.074 | 0.99 | 0.61 to 1.46 |
| Ono 200763 | 1064 | 36.0 | 72.7 | 34.1 | 23.5 to 46.5 | 72.8 | 70.0 to 75.5 | 0.905 | 0.736 to 1.055 | 1.25 | 0.86 to 1.7 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 10 | < 0.001 | < 0.001 | 21.4 | 13.5 to 31.4 | 84.6 | 76.7 to 90.3 | 0.931 | 0.844 to 1.007 | 1.38 | 0.97 to 1.99 | |
Fall – any (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Harad 1992104 | 302 | 16.4 | 81.4 | 19.3 | 12.7 to 26.3 | 81.6 | 77.1 to 85.6 | 0.990 | 0.921 to 1.060 | 1.05 | 0.74 to 1.4 |
| Jeret 1993107 | 712 | 6.0 | 90.9 | 8.6 | 4.3 to 14.7 | 90.7 | 88.3 to 92.7 | 1.008 | 0.943 to 1.058 | 0.92 | 0.47 to 1.59 |
| Schynoll 1993118 | 264 | 56.3 | 44.8 | 61.3 | 49.7 to 72.6 | 47.0 | 40.8 to 53.1 | 0.822 | 0.597 to 1.077 | 1.16 | 0.94 to 1.4 |
| Cook 1994100 | 107 | 22.2 | 71.6 | 30.7 | 19.8 to 42.5 | 72.4 | 64.1 to 79.8 | 0.956 | 0.867 to 1.051 | 1.12 | 0.86 to 1.32 |
| Tsai 1994125 | 186 | 22.5 | 75.3 | 26.0 | 17.9 to 34.4 | 76.1 | 70.1 to 81.6 | 0.971 | 0.902 to 1.053 | 1.09 | 0.83 to 1.3 |
| Borczuk 199555 | 1448 | 36.1 | 70.0 | 34.5 | 29.3 to 40.0 | 69.8 | 67.5 to 72.2 | 0.938 | 0.866 to 1.008 | 1.14 | 0.98 to 1.31 |
| Miller 1996111 | 1382 | 25.0 | 73.0 | 29.3 | 23.0 to 34.6 | 73.4 | 71.0 to 75.6 | 0.964 | 0.899 to 1.048 | 1.10 | 0.87 to 1.3 |
| Stiell 200126 | 3121 | 42.1 | 70.1 | 36.5 | 31.9 to 42.3 | 69.6 | 67.9 to 71.2 | 0.914 | 0.827 to 0.978 | 1.20 | 1.05 to 1.40 |
| Mack 2003110 | 133 | 42.1 | 58.8 | 45.1 | 34.4 to 57.3 | 60.8 | 52.6 to 68.3 | 0.902 | 0.759 to 1.039 | 1.16 | 0.94 to 1.36 |
| Ono 200763 | 1064 | 32.0 | 63.2 | 40.8 | 32.8 to 48.0 | 63.9 | 61.0 to 66.7 | 0.927 | 0.824 to 1.052 | 1.13 | 0.91 to 1.31 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 10 | < 0.001 | < 0.001 | 31.3 | 20.3 to 44.3 | 72.0 | 62.2 to 80.2 | 0.953 | 0.871 to 1.024 | 1.12 | 0.93 to 1.29 | |
Fall from a height (intracranial injury – adults)
| Study | Observed estimates | Fixed effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Ono 200763 | 28.0 | 87.8 | 28.0 | 17.3 to 41.9 | 87.8 | 85.6 to 89.6 | 0.820 | 0.689 to 0.977 | 2.29 | 1.43 to 3.68 |
Dizziness (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Cook1994100 | 107 | 12.5 | 73.2 | 18.7 | 11.7 to 27.3 | 73.7 | 69.4 to 78.1 | 1.103 | 0.969 to 1.227 | 0.71 | 0.43 to 1.10 |
| Mack 2003110 | 133 | 10.5 | 79.8 | 18.9 | 11.8 to 27.6 | 74.3 | 70.5 to 80.2 | 1.091 | 0.946 to 1.208 | 0.74 | 0.45 to 1.19 |
| Ibanez and Arikan 200460 | 1101 | 21.7 | 72.7 | 18.6 | 12.1 to 26.8 | 73.3 | 70.7 to 75.8 | 1.109 | 0.995 to 1.210 | 0.70 | 0.45 to 1.02 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 3 | 0.482 | 0.267 | 18.7 | 11.9 to 27.3 | 73.8 | 70.2 to 78.1 | 1.101 | 0.970 to 1.217 | 0.72 | 0.44 to 1.09 | |
Coagulopathy (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Borczuk 199555 | 1448 | 6.7 | 96.8 | 7.2 | 4.0 to 11.7 | 96.9 | 95.9 to 96.9 | 0.958 | 0.913 to 0.992 | 2.29 | 1.22 to 3.88 |
| Arienta 199754 | 10,000 | 0.6 | 100.0 | 0.2 | 0.0 to 1.3 | 100.0 | 99.9 to 100.0 | 0.998 | 0.988 to 1.000 | 5.41 | 0.42 to 40.81 |
| Haydel 200027 | 520 | 0.0 | 99.8 | 0.7 | 0.0 to 3.5 | 99.8 | 99.2 to 99.8 | 0.995 | 0.970 to 1.001 | 3.53 | 0.50 to 21.92 |
| Mack 2003110 | 133 | 15.8 | 86.8 | 20.1 | 8.9 to 36.0 | 88.4 | 81.9 to 88.4 | 0.904 | 0.734 to 1.044 | 1.75 | 0.73 to 3.36 |
| Ibanez and Arikan 200460 | 1101 | 32.5 | 90.3 | 29.2 | 20.6 to 39.3 | 90.2 | 88.2 to 90.2 | 0.786 | 0.673 to 0.882 | 2.96 | 2.02 to 4.22 |
| Fabbri 200557 | 7955 | 12.4 | 97.3 | 11.7 | 9.2 to 14.6 | 97.3 | 96.9 to 97.3 | 0.908 | 0.878 to 0.934 | 4.33 | 3.28 to 5.62 |
| Mower 200562 | 13,728 | 5.0 | 96.1 | 5.4 | 4.1 to 7.1 | 96.1 | 95.8 to 96.1 | 0.984 | 0.967 to 0.999 | 1.39 | 1.03 to 1.85 |
| Saboori 200767 | 682 | 0.0 | 99.8 | 0.6 | 0.0 to 2.9 | 99.9 | 99.4 to 99.9 | 0.996 | 0.974 to 1.001 | 3.64 | 0.46 to 23.50 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 8 | < 0.001 | < 0.001 | 4.9 | 0.6 to 16.0 | 98.2 | 93.3 to 99.8 | 0.968 | 0.897 to 0.999 | 3.27 | 1.21 to 7.52 | |
Chronic alcohol (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Arienta 199754 | 10,000 | 0.6 | 100.0 | 0.4 | 0.0 to 2.1 | 100.0 | 99.9 to 100.0 | 0.996 | 0.979 to 1.000 | 9.52 | 0.95 to 62.07 |
| Stiell 200126 | 3121 | 17.3 | 89.7 | 14.0 | 11.2 to 17.4 | 89.5 | 88.4 to 90.6 | 0.961 | 0.923 to 0.993 | 1.34 | 1.06 to 1.68 |
| Ibanez and Arikan 200460 | 1101 | 2.4 | 95.8 | 7.4 | 4.2 to 10.8 | 96.1 | 94.8 to 97.1 | 0.964 | 0.931 to 0.996 | 1.86 | 1.11 to 2.82 |
| Stiell 200546 | 2707 | 15.2 | 85.1 | 16.9 | 13.3 to 21.0 | 85.2 | 83.8 to 86.6 | 0.975 | 0.926 to 1.019 | 1.15 | 0.89 to 1.4 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 4 | < 0.001 | < 0.001 | 5.9 | 0.7 to 40.8 | 97.6 | 49.5 to 99.8 | 0.973 | 0.933 to 1.186 | 2.00 | 0.79 to 9.03 | |
Assault (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Harad 1992104 | 302 | 27.3 | 83.4 | 19.4 | 14.1 to 26.1 | 81.6 | 77.1 to 85.8 | 0.987 | 0.928 to 1.036 | 1.06 | 0.85 to 1.32 |
| Jeret 1993107 | 712 | 37.3 | 70.1 | 10.5 | 7.6 to 13.9 | 89.3 | 88.1 to 90.4 | 1.002 | 0.964 to 1.036 | 0.98 | 0.71 to 1.31 |
| Schynoll 1993118 | 264 | 3.1 | 88.8 | 9.9 | 5.4 to 15.4 | 89.8 | 85.9 to 93.1 | 1.003 | 0.962 to 1.039 | 0.97 | 0.64 to 1.35 |
| Cook 1994100 | 107 | 66.7 | 37.8 | 66.8 | 48.6 to 82.9 | 39.1 | 30.1 to 48.4 | 0.847 | 0.469 to 1.315 | 1.10 | 0.81 to 1.36 |
| Tsai 1994125 | 186 | 5.0 | 96.6 | 3.7 | 1.3 to 7.9 | 95.9 | 92.4 to 98.1 | 1.005 | 0.974 to 1.028 | 0.89 | 0.43 to 1.72 |
| Borczuk 199555 | 1448 | 22.7 | 74.9 | 26.0 | 20.9 to 31.8 | 75.4 | 73.1 to 77.6 | 0.982 | 0.907 to 1.051 | 1.06 | 0.85 to 1.29 |
| Stiell 200126 | 3121 | 10.2 | 89.3 | 1.2 | 0.1 to 4.7 | 98.5 | 95.5 to 99.8 | 1.002 | 0.983 to 1.017 | 0.79 | 0.22 to 2.26 |
| Mack 2003110 | 133 | 0.0 | 99.1 | 33.1 | 25.9 to 41.7 | 69.7 | 66.3 to 73.0 | 0.960 | 0.843 to 1.062 | 1.09 | 0.86 to 1.37 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 8 | < 0.001 | < 0.001 | 14.1 | 3.9 to 36.0 | 86.2 | 67.4 to 95.4 | 0.997 | 0.924 to 1.038 | 1.02 | 0.68 to 1.33 | |
Age > 60 years (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Jeret 1993107 | 712 | 19.4 | 94.7 | 15.7 | 10.4 to 23.1 | 94.3 | 92.4 to 95.9 | 0.895 | 0.815 to 0.948 | 2.73 | 1.80 to 4.42 |
| Haydel 200027 | 520 | 16.7 | 92.6 | 17.4 | 11.2 to 25.5 | 92.5 | 90.0 to 92.5 | 0.894 | 0.810 to 0.957 | 2.29 | 1.51 to 3.50 |
| Ibanez and Arikan 200460 | 1101 | 45.8 | 71.9 | 42.5 | 33.4 to 52.6 | 71.9 | 69.1 to 71.9 | 0.799 | 0.661 to 0.928 | 1.52 | 1.18 to 1.90 |
| Mower 200562 | 13,728 | 19.0 | 86.4 | 20.2 | 17.5 to 23.2 | 86.4 | 85.8 to 86.4 | 0.924 | 0.888 to 0.956 | 1.49 | 1.28 to 1.73 |
| Stiell 200546 | 2707 | 27.3 | 90.7 | 24.2 | 18.7 to 30.3 | 90.5 | 89.3 to 90.5 | 0.838 | 0.770 to 0.901 | 2.55 | 1.90 to 3.30 |
| Ono 200763 | 1064 | 48.0 | 67.6 | 45.2 | 34.6 to 57.1 | 67.7 | 64.8 to 67.7 | 0.810 | 0.635 to 0.969 | 1.40 | 1.06 to 1.78 |
| Saboori 200767 | 682 | 10.9 | 94.5 | 13.6 | 8.1 to 20.5 | 94.5 | 92.6 to 94.5 | 0.915 | 0.844 to 0.971 | 2.45 | 1.48 to 3.85 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 7 | < 0.001 | < 0.001 | 23.9 | 14.5 to 36.5 | 88.0 | 78.1 to 93.8 | 0.868 | 0.785 to 0.925 | 1.97 | 1.48 to 2.81 | |
Vision (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schynoll 1993118 | 226 | 13.0 | 82.8 | 8.0 | 1.2 to 24.4 | 83.1 | 77.8 to 88.0 | 1.104 | 0.905 to 1.223 | 0.48 | 0.07 to 1.51 |
| Cook1994100 | 107 | 0.0 | 92.9 | 2.5 | 0.0 to 9.9 | 93.2 | 87.8 to 97.0 | 1.042 | 0.970 to 1.106 | 0.37 | 0.00 to 1.55 |
| Falimirski 200358 | 331 | 0.0 | 98.6 | 0.6 | 0.0 to 7.2 | 98.4 | 96.4 to 99.5 | 1.008 | 0.946 to 1.030 | 0.39 | 0.00 to 5.20 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 3 | 0.265 | < 0.001 | 2.4 | 0.0 to 21.4 | 94.2 | 70.7 to 99.3 | 1.033 | 0.940 to 1.199 | 0.39 | 0.00 to 2.49 | |
Prior neurosurgery (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Arienta 199754 | 10,000 | 0.6 | 100.0 | 0.9 | 0.1 to 3.1 | 99.99 | 100.0 to 100.0 | 0.991 | 0.969 to 0.999 | 69.80 | 7.66 to 918.60 |
| Ibanez and Arikan 200460 | 1101 | 2.4 | 99.7 | 2.0 | 0.8 to 3.5 | 99.7 | 99.3 to 99.9 | 0.983 | 0.968 to 0.994 | 7.13 | 2.64 to 27.08 |
| Fabbri 200557 | 7955 | 3.5 | 98.0 | 3.4 | 2.1 to 5.1 | 98.0 | 97.6 to 98.3 | 0.986 | 0.968 to 1.000 | 1.67 | 1.01 to 2.60 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 3 | 0.231 | < 0.001 | 1.9 | 0.3 to 5.1 | 99.8 | 92.3 to 100.0 | 0.985 | 0.969 to 1.030 | 8.67 | 0.62 to 308.90 | |
Motor vehicle collision – pedestrian (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Jeret 1993107 | 712 | 26.9 | 87.3 | 22.9 | 13.4 to 33.5 | 87.8 | 85.1 to 90.2 | 0.878 | 0.759 to 0.987 | 1.88 | 1.09 to 2.84 |
| Schynoll 1993118 | 264 | 15.6 | 96.6 | 14.9 | 9.6 to 19.8 | 96.3 | 93.8 to 98.1 | 0.886 | 0.837 to 0.930 | 3.88 | 2.58 to 7.26 |
| Cook 1994100 | 107 | 0.0 | 98.6 | 12.6 | 4.5 to 19.8 | 97.7 | 94.6 to 99.5 | 0.898 | 0.826 to 0.965 | 5.05 | 2.78 to 17.29 |
| Borczuk 199555 | 1448 | 14.3 | 93.8 | 17.3 | 13.7 to 21.4 | 94.0 | 92.7 to 95.2 | 0.880 | 0.838 to 0.919 | 2.90 | 2.17 to 3.74 |
| Stiell 200126 | 3121 | 16.9 | 96.0 | 15.3 | 12.0 to 19.1 | 95.9 | 95.2 to 96.6 | 0.883 | 0.843 to 0.918 | 3.77 | 2.84 to 5.03 |
| Ono 200763 | 1064 | 10.0 | 96.6 | 14.2 | 9.5 to 19.0 | 96.6 | 95.5 to 97.6 | 0.889 | 0.839 to 0.933 | 4.15 | 2.89 to 6.3 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 6 | 0.182 | < 0.001 | 15.9 | 10.9 to 21.3 | 95.4 | 91.9 to 97.8 | 0.882 | 0.836 to 0.923 | 3.43 | 2.27 to 6.45 | |
Motor vehicle collision – in car (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Harad 1992104 | 302 | 27.3 | 53.8 | 32.2 | 26.0 to 39.5 | 55.3 | 49.4 to 61.0 | 1.223 | 1.112 to 1.360 | 0.72 | 0.60 to 0.86 |
| Jeret 1993107 | 712 | 22.4 | 60.5 | 27.4 | 22.4 to 33.0 | 61.1 | 57.4 to 64.7 | 1.187 | 1.106 to 1.277 | 0.71 | 0.59 to 0.83 |
| Schynoll 1993118 | 264 | 25.0 | 78.9 | 15.5 | 10.7 to 21.1 | 77.6 | 72.2 to 82.5 | 1.089 | 1.022 to 1.149 | 0.69 | 0.52 to 0.91 |
| Cook 1994100 | 107 | 33.3 | 85.3 | 11.4 | 6.0 to 18.2 | 83.5 | 75.7 to 89.6 | 1.063 | 0.998 to 1.124 | 0.68 | 0.46 to 1.01 |
| Tsai 1994125 | 186 | 60.0 | 37.7 | 50.7 | 39.4 to 63.0 | 36.4 | 29.5 to 43.7 | 1.353 | 1.031 to 1.727 | 0.80 | 0.63 to 1.0 |
| Borczuk 199555 | 1448 | 19.3 | 65.3 | 23.7 | 19.4 to 28.0 | 65.7 | 63.2 to 68.2 | 1.161 | 1.098 to 1.229 | 0.69 | 0.57 to 0.81 |
| Miller 1996111 | 1382 | 39.3 | 59.0 | 30.4 | 25.4 to 37.3 | 58.5 | 55.9 to 61.2 | 1.188 | 1.076 to 1.275 | 0.73 | 0.62 to 0.89 |
| Stiell 200126 | 3121 | 16.1 | 73.4 | 18.0 | 14.6 to 21.6 | 73.5 | 71.9 to 75.1 | 1.117 | 1.065 to 1.165 | 0.68 | 0.55 to 0.82 |
| Mack 2003110 | 133 | 5.3 | 95.6 | 4.0 | 1.3 to 8.9 | 94.3 | 89.3 to 97.5 | 1.018 | 0.978 to 1.057 | 0.68 | 0.30 to 1.47 |
| Ono 200763 | 1064 | 4.0 | 94.7 | 3.7 | 1.6 to 7.6 | 94.5 | 93.1 to 95.8 | 1.018 | 0.978 to 1.044 | 0.68 | 0.30 to 1.39 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 10 | < 0.001 | < 0.001 | 17.7 | 8.7 to 31.0 | 74.4 | 57.7 to 86.0 | 1.108 | 1.031 to 1.218 | 0.69 | 0.53 to 0.86 | |
Motor vehicle collision with bicycle (intracranial injury – adults)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Borczuk 199555 | 1448 | 5.0 | 98.4 | 5.0 | 2.3 to 10.8 | 98.4 | 97.6 to 99.0 | 0.965 | 0.442 to 2.104 | 3.19 | 1.31 to 7.75 |
| Ono 200763 | 1064 | 18.0 | 85.3 | 18.0 | 9.6 to 31.1 | 85.3 | 83.0 to 87.4 | 0.961 | 0.532 to 1.738 | 1.22 | 0.67 to 2.25 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.011 | < 0.001 | 10.6 | 6.4 to 16.9 | 89.0 | 87.3 to 90.5 | 0.963 | 0.601 to 1.543 | 1.67 | 1.01 to 2.75 | |
Persistent vomiting (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Arienta 199754 | 10,000 | 3.9 | 99.9 | 3.3 | 1.2 to 7.0 | 99.9 | 99.8 to 100.0 | 0.968 | 0.931 to 0.989 | 35.77 | 11.13 to 104.50 |
| Stiell 200126 | 3121 | 30.3 | 92.2 | 29.9 | 24.7 to 35.7 | 92.2 | 91.2 to 93.1 | 0.760 | 0.698 to 0.817 | 3.83 | 3.06 to 4.76 |
| Stiell 200546 | 2707 | 45.9 | 86.7 | 44.9 | 38.5 to 51.3 | 86.7 | 85.3 to 88.0 | 0.636 | 0.561 to 0.710 | 3.37 | 2.82 to 3.99 |
| Mower 200562 | 13,728 | 10.0 | 94.3 | 10.4 | 8.5 to 12.6 | 94.3 | 93.9 to 94.7 | 0.950 | 0.927 to 0.970 | 1.83 | 1.48 to 2.24 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 4 | < 0.001 | < 0.001 | 16.1 | 3.0 to 50.7 | 97.2 | 69.3 to 99.9 | 0.871 | 0.659 to 0.983 | 5.53 | 1.33 to 30.12 | |
Glasgow Coma Scale < 15 (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Feuerman 1988102 | 129 | 62.3 | 51.3 | 26.3 | 21.6 to 31.4 | 89.9 | 88.0 to 91.6 | 0.820 | 0.761 to 0.876 | 2.60 | 2.01 to 3.4 |
| Stein 1990122 | 658 | 49.1 | 72.9 | 25.8 | 16.3 to 37.3 | 84.5 | 79.7 to 88.6 | 0.878 | 0.738 to 1.004 | 1.66 | 0.98 to 2.7 |
| Livingston 1991109 | 111 | 40.0 | 85.4 | 37.6 | 25.9 to 50.2 | 86.8 | 84.7 to 88.8 | 0.719 | 0.573 to 0.855 | 2.85 | 1.91 to 4.0 |
| Livingston 1991109 | 60 | 72.7 | 71.4 | 52.9 | 46.8 to 58.8 | 82.7 | 81.3 to 84.1 | 0.570 | 0.498 to 0.645 | 3.05 | 2.64 to 3.5 |
| Harad 1992104 | 302 | 21.8 | 84.2 | 22.8 | 15.1 to 32.0 | 96.6 | 95.4 to 97.6 | 0.799 | 0.704 to 0.879 | 6.72 | 4.06 to 10.9 |
| Stein 1992121 | 1538 | 44.5 | 76.2 | 61.0 | 39.5 to 80.3 | 72.6 | 59.5 to 83.4 | 0.541 | 0.272 to 0.865 | 2.21 | 1.27 to 3.9 |
| Schynoll 1993118 | 264 | 53.1 | 85.3 | 34.7 | 27.5 to 42.3 | 80.6 | 75.2 to 85.2 | 0.811 | 0.708 to 0.917 | 1.78 | 1.28 to 2.5 |
| Tsai 1994125 | 186 | 50.0 | 63.0 | 50.1 | 36.4 to 63.9 | 63.8 | 55.8 to 71.2 | 0.784 | 0.560 to 1.032 | 1.38 | 0.95 to 1.9 |
| Borczuk 199555 | 1448 | 39.5 | 85.7 | 40.0 | 31.9 to 48.5 | 85.7 | 83.8 to 87.6 | 0.701 | 0.600 to 0.797 | 2.80 | 2.16 to 3.56 |
| Madden 199561 | 537 | 78.0 | 74.9 | 26.7 | 13.1 to 44.2 | 85.7 | 78.7 to 91.2 | 0.856 | 0.651 to 1.033 | 1.87 | 0.84 to 3.7 |
| Dunham 1996101 | 2032 | 64.8 | 75.4 | 65.9 | 61.8 to 69.7 | 97.7 | 97.3 to 98.0 | 0.350 | 0.310 to 0.391 | 28.59 | 24.41 to 33.68 |
| Arienta 199754 | 9917 | 42.1 | 99.6 | 40.9 | 31.7 to 50.6 | 99.5 | 99.4 to 99.7 | 0.594 | 0.496 to 0.687 | 86.43 | 59.80 to 125.10 |
| Hsiang 1997105 | 1360 | 25.6 | 89.9 | 42.1 | 24.2 to 61.5 | 85.8 | 78.1 to 91.6 | 0.678 | 0.449 to 0.897 | 2.94 | 1.49 to 5.6 |
| Murshid 199877 | 131 | 43.3 | 94.1 | 51.2 | 36.2 to 66.0 | 85.4 | 80.5 to 89.5 | 0.572 | 0.397 to 0.750 | 3.50 | 2.26 to 5.3 |
| Stiell 200126 | 3121 | 53.1 | 82.7 | 74.7 | 65.7 to 82.6 | 74.9 | 70.8 to 78.8 | 0.337 | 0.231 to 0.462 | 2.98 | 2.44 to 3.6 |
| Mussack 2002115 | 139 | 47.4 | 99.2 | 49.1 | 40.5 to 57.7 | 73.0 | 69.2 to 76.7 | 0.698 | 0.577 to 0.823 | 1.82 | 1.44 to 2.3 |
| Mack 2003110 | 133 | 15.8 | 85.1 | 63.5 | 55.3 to 71.3 | 75.4 | 73.5 to 77.3 | 0.484 | 0.381 to 0.594 | 2.59 | 2.21 to 3.0 |
| Tender 2003123 | 255 | 27.5 | 81.4 | 43.4 | 26.3 to 62.2 | 98.1 | 94.9 to 99.5 | 0.578 | 0.387 to 0.753 | 21.98 | 7.67 to 86.3 |
| Ibanez 200460 | 1101 | 20.5 | 96.7 | 47.1 | 30.4 to 64.5 | 82.7 | 77.1 to 87.4 | 0.641 | 0.428 to 0.850 | 2.71 | 1.63 to 4.2 |
| Thiruppathy 2004124 | 381 | 33.8 | 80.3 | 44.6 | 38.8 to 50.5 | 76.3 | 73.9 to 78.6 | 0.726 | 0.646 to 0.807 | 1.88 | 1.59 to 2.2 |
| Chan 200599 | 105 | 69.5 | 52.2 | 67.4 | 57.4 to 76.5 | 56.2 | 36.9 to 74.3 | 0.582 | 0.379 to 0.945 | 1.54 | 1.04 to 2.64 |
| Fabbri 200557 | 7955 | 66.4 | 97.7 | 60.6 | 48.2 to 72.2 | 52.8 | 41.8 to 63.7 | 0.746 | 0.506 to 1.066 | 1.28 | 0.94 to 1.75 |
| Biberthaler 200698 | 1309 | 32.3 | 89.6 | 33.4 | 24.7 to 42.8 | 89.6 | 87.8 to 91.2 | 0.744 | 0.638 to 0.841 | 3.20 | 2.29 to 4.34 |
| Muller 2007113 | 226 | 47.6 | 82.4 | 42.8 | 28.2 to 58.3 | 93.7 | 88.2 to 97.2 | 0.613 | 0.446 to 0.772 | 6.73 | 3.26 to 15.9 |
| Ono 200763 | 1064 | 36.0 | 86.8 | 28.7 | 22.2 to 36.0 | 82.2 | 74.2 to 88.6 | 0.868 | 0.761 to 0.994 | 1.61 | 1.02 to 2.6 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 25 | < 0.001 | < 0.001 | 44.9 | 37.7 to 51.8 | 86.7 | 80.6 to 91.2 | 0.638 | 0.557 to 0.722 | 3.35 | 2.31 to 5.03 | |
Glasgow Coma Scale < 14 (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Feuerman 1988102 | 129 | 24.5 | 89.5 | 22.0 | 15.7 to 31.2 | 92.0 | 86.2 to 95.5 | 0.849 | 0.766 to 0.911 | 2.81 | 1.70 to 4.21 |
| Stein 1990122 | 658 | 21.6 | 93.2 | 20.0 | 15.7 to 25.8 | 93.4 | 91.3 to 95.1 | 0.856 | 0.799 to 0.900 | 3.06 | 2.24 to 4.10 |
| Harad 1992104 | 302 | 5.5 | 96.8 | 12.0 | 6.9 to 16.7 | 97.2 | 95.3 to 98.5 | 0.905 | 0.868 to 0.953 | 4.33 | 2.53 to 6.5 |
| Stein 1992121 | 1538 | 17.0 | 94.1 | 18.0 | 14.6 to 21.7 | 94.4 | 93.1 to 95.5 | 0.869 | 0.831 to 0.905 | 3.22 | 2.45 to 4.08 |
| Tsai 1994125 | 186 | 20.0 | 88.4 | 22.9 | 16.2 to 31.9 | 91.1 | 86.1 to 94.5 | 0.847 | 0.761 to 0.922 | 2.60 | 1.61 to 3.82 |
| Dunham 1996101 | 2032 | 22.7 | 95.4 | 17.3 | 14.2 to 22.8 | 95.3 | 94.3 to 96.1 | 0.869 | 0.811 to 0.899 | 3.65 | 2.95 to 5.0 |
| Hsiang 1997105 | 1360 | 8.9 | 98.2 | 9.8 | 7.1 to 12.8 | 98.1 | 97.3 to 98.8 | 0.919 | 0.890 to 0.946 | 5.23 | 3.47 to 8.0 |
| Stiell 200126 | 3121 | 17.7 | 97.7 | 12.7 | 10.2 to 17.4 | 97.4 | 96.8 to 98.0 | 0.896 | 0.847 to 0.921 | 4.91 | 3.80 to 7.40 |
| Mack 2003110 | 133 | 5.3 | 97.4 | 12.3 | 6.2 to 18.4 | 97.2 | 94.5 to 98.9 | 0.902 | 0.857 to 0.954 | 4.36 | 2.66 to 7.3 |
| Tender 2003123 | 255 | 7.8 | 94.1 | 12.1 | 7.7 to 16.5 | 97.1 | 94.4 to 98.5 | 0.905 | 0.872 to 0.952 | 4.19 | 2.08 to 6.52 |
| Biberthaler 200698 | 1309 | 6.5 | 97.6 | 10.9 | 6.8 to 14.3 | 97.7 | 96.8 to 98.4 | 0.912 | 0.881 to 0.954 | 4.71 | 2.88 to 6.5 |
| Muller 2007113 | 226 | 23.8 | 94.6 | 17.6 | 12.4 to 25.5 | 94.8 | 91.7 to 97.0 | 0.870 | 0.799 to 0.912 | 3.44 | 2.37 to 4.9 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 12 | < 0.001 | < 0.001 | 15.0 | 11.4 to 18.9 | 96.0 | 94.3 to 97.4 | 0.885 | 0.853 to 0.915 | 3.81 | 2.87 to 4.93 | |
Glasgow Coma Scale decrease (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Madden 199561 | 537 | 33.0 | 93.9 | 29.1 | 24.7 to 34.4 | 94.0 | 91.5 to 95.9 | 0.754 | 0.703 to 0.801 | 4.84 | 3.47 to 6.86 |
| Stiell 200126 | 3121 | 21.3 | 98.7 | 22.0 | 17.2 to 27.4 | 98.6 | 98.2 to 99.0 | 0.791 | 0.737 to 0.839 | 16.11 | 11.04 to 23.82 |
| Stiell 200546 | 2707 | 30.7 | 91.0 | 31.2 | 25.9 to 36.8 | 91.1 | 89.9 to 92.2 | 0.755 | 0.693 to 0.814 | 3.50 | 2.81 to 4.31 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 3 | 0.024 | < 0.001 | 27.3 | 20.8 to 36.7 | 95.7 | 83.4 to 98.8 | 0.763 | 0.711 to 0.822 | 6.39 | 2.05 to 19.33 | |
Focal neurological deficit (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Cook 1994100 | 107 | 0.0 | 98.5 | 2.8 | 0.1 to 17.5 | 99.2 | 96.4 to 99.9 | 0.981 | 0.833 to 1.021 | 3.44 | 0.08 to 64.34 |
| Borczuk 199555 | 1448 | 3.4 | 85.9 | 3.5 | 1.2 to 7.7 | 86.0 | 84.0 to 87.7 | 1.122 | 1.070 to 1.161 | 0.25 | 0.08 to 0.56 |
| Arienta 199754 | 10,000 | 7.1 | 99.9 | 6.8 | 3.6 to 11.5 | 99.9 | 99.8 to 100.0 | 0.933 | 0.886 to 0.965 | 71.02 | 30.16 to 170.3 |
| Falimirski 200358 | 331 | 0.0 | 97.6 | 1.5 | 0.1 to 7.2 | 97.8 | 95.7 to 99.1 | 1.007 | 0.948 to 1.035 | 0.69 | 0.03 to 4.09 |
| Ibanez and Arikan 200460 | 1101 | 4.8 | 99.3 | 4.7 | 1.6 to 10.3 | 99.3 | 98.7 to 99.7 | 0.960 | 0.903 to 0.992 | 6.96 | 2.00 to 22.04 |
| Chan 200599 | 105 | 12.2 | 87.0 | 11.5 | 5.9 to 19.4 | 91.0 | 75.4 to 98.0 | 0.973 | 0.862 to 1.180 | 1.28 | 0.38 to 6.26 |
| Fabbri 200557 | 7955 | 54.4 | 98.8 | 54.1 | 49.9 to 58.3 | 98.8 | 98.5 to 99.0 | 0.465 | 0.422 to 0.507 | 44.70 | 36.11 to 56.08 |
| Saboori 200767 | 682 | 2.2 | 100.0 | 2.5 | 0.3 to 8.9 | 99.9 | 99.5 to 100.0 | 0.976 | 0.912 to 0.998 | 30.36 | 2.15 to 1392.00 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 8 | < 0.001 | < 0.001 | 6.6 | 1.2 to 16.9 | 98.6 | 95.2 to 99.8 | 0.95 | 0.84 to 1.01 | 9.671 | 0.663 to 38.950 | |
Depressed skull fracture (intracranial injury – adults)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Madden 199561 | 537 | 13.2 | 100.0 | 13.2 | 7.6 to 21.8 | 99.9 | 98.2 to 100.0 | 0.868 | 0.512 to 1.471 | 117.63 | 7.01 to 1973.44 |
| Miller 199729 | 2143 | 2.2 | 100.0 | 2.2 | 0.7 to 6.5 | 99.98 | 99.6 to 100.0 | 0.978 | 0.822 to 1.165 | 87.17 | 4.39 to 1731.74 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.004 | 0.452 | 9.1 | 5.5 to 14.5 | 99.9 | 99.6 to 100.0 | 0.967 | 0.819 to 1.141 | 102.15 | 13.13 to 794.41 | |
Basal skull fracture (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schynoll 1993118 | 264 | 21.9 | 94.0 | 30.8 | 25.6 to 36.0 | 94.4 | 91.2 to 96.9 | 0.733 | 0.687 to 0.780 | 5.85 | 3.67 to 9.19 |
| Madden 199561 | 537 | 28.6 | 93.9 | 31.2 | 26.8 to 35.8 | 94.2 | 91.9 to 96.1 | 0.730 | 0.686 to 0.774 | 5.50 | 3.89 to 7.63 |
| Dunham 1996101 | 2032 | 27.3 | 96.6 | 28.1 | 24.5 to 31.7 | 96.7 | 95.8 to 97.4 | 0.744 | 0.708 to 0.779 | 8.53 | 6.69 to 10.76 |
| Arienta 199754 | 10,000 | 0.6 | 100.0 | 4.5 | 1.7 to 8.2 | 100.0 | 100.0 to 100.0 | 0.955 | 0.918 to 0.983 | 13,090 | 429.40 to 77,610 |
| Stiell 200126 | 3121 | 30.3 | 95.4 | 30.1 | 26.6 to 33.8 | 95.4 | 94.6 to 96.1 | 0.733 | 0.696 to 0.769 | 6.53 | 5.40 to 7.82 |
| Ibanez 200460 | 1101 | 19.3 | 97.9 | 24.9 | 20.7 to 28.6 | 98.1 | 97.2 to 98.8 | 0.766 | 0.731 to 0.806 | 13.42 | 9.03 to 19.51 |
| Fabbri 200557 | 7955 | 16.6 | 99.9 | 14.1 | 11.7 to 16.7 | 99.9 | 99.8 to 99.9 | 0.860 | 0.834 to 0.884 | 129.10 | 64.37 to 256.80 |
| Stiell 200546 | 2707 | 29.9 | 96.4 | 28.7 | 25.4 to 32.3 | 96.4 | 95.6 to 97.1 | 0.740 | 0.704 to 0.773 | 8.01 | 6.49 to 9.85 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 8 | < 0.001 | < 0.001 | 21.1 | 8.4 to 33.9 | 98.4 | 90.5 to 100.0 | 0.80 | 0.72 to 0.92 | 54.070 | 3.594 to 353.700 | |
Any seizure (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schynoll 1993118 | 264 | 3.1 | 96.1 | 4.7 | 3.0 to 7.0 | 96.5 | 93.8 to 98.3 | 0.987 | 0.972 to 1.008 | 1.37 | 0.85 to 2.22 |
| Cook 1994100 | 107 | 0.0 | 97.2 | 3.9 | 1.7 to 6.8 | 97.7 | 93.7 to 99.4 | 0.985 | 0.970 to 1.007 | 1.67 | 0.89 to 4.18 |
| Arienta 199754 | 10,000 | 0.6 | 100.0 | 0.4 | 0.0 to 1.8 | 100.0 | 100.0 to 100.0 | 0.996 | 0.982 to 1.000 | 29.56 | 2.39 to 501.40 |
| Haydel 200027 | 520 | 11.1 | 95.9 | 5.1 | 3.6 to 7.4 | 95.8 | 93.8 to 97.3 | 0.989 | 0.971 to 1.009 | 1.25 | 0.84 to 1.79 |
| Falimirski 200358 | 331 | 2.5 | 99.3 | 2.3 | 0.8 to 4.1 | 99.3 | 98.1 to 99.9 | 0.984 | 0.970 to 0.996 | 3.26 | 1.47 to 11.16 |
| Ibanez and Arikan 200460 | 1101 | 1.2 | 99.4 | 2.1 | 0.8 to 3.7 | 99.5 | 98.9 to 99.8 | 0.985 | 0.970 to 0.997 | 3.69 | 1.61 to 8.85 |
| Chan 200599 | 105 | 3.7 | 95.7 | 3.9 | 1.6 to 7.2 | 97.8 | 91.1 to 99.7 | 0.986 | 0.971 to 1.028 | 1.70 | 0.69 to 6.54 |
| Mower 200562 | 13,728 | 5.0 | 96.1 | 5.0 | 3.8 to 6.4 | 96.1 | 95.7 to 96.4 | 0.989 | 0.974 to 1.002 | 1.27 | 0.96 to 1.66 |
| Stiell 200546 | 1822 | 4.3 | 98.1 | 3.6 | 2.4 to 4.9 | 98.1 | 97.4 to 98.7 | 0.983 | 0.970 to 0.994 | 1.89 | 1.29 to 2.79 |
| Saboori 200767 | 682 | 0.0 | 99.7 | 1.6 | 0.4 to 3.3 | 99.7 | 99.1 to 99.9 | 0.987 | 0.971 to 0.998 | 5.19 | 1.72 to 21.4 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 10 | 0.262 | < 0.001 | 2.8 | 1.1 to 5.1 | 99.0 | 96.2 to 99.7 | 0.984 | 0.970 to 0.996 | 2.59 | 1.20 to 6.40 | |
Any loss of consciousness (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Nelson 1992116 | 131 | 90.0 | 21.6 | 88.0 | 74.6 to 95.7 | 21.8 | 15.0 to 29.8 | 0.553 | 0.201 to 1.203 | 1.12 | 0.95 to 1.3 |
| Schynoll 1993118 | 264 | 50.0 | 66.8 | 50.4 | 35.3 to 65.4 | 66.8 | 60.7 to 72.6 | 0.742 | 0.519 to 0.979 | 1.52 | 1.04 to 2.1 |
| Cook 1994100 | 107 | 44.4 | 48.5 | 56.0 | 31.0 to 77.0 | 50.1 | 40.4 to 59.7 | 0.877 | 0.467 to 1.413 | 1.12 | 0.62 to 1.6 |
| Moran 1994112 | 200 | 100.0 | 55.7 | 78.0 | 56.3 to 93.8 | 55.0 | 48.0 to 61.8 | 0.402 | 0.114 to 0.795 | 1.72 | 1.24 to 2.2 |
| Borczuk 199555 | 1448 | 77.3 | 36.8 | 77.2 | 69.6 to 83.8 | 36.8 | 34.3 to 39.4 | 0.618 | 0.439 to 0.835 | 1.22 | 1.09 to 1.3 |
| Madden 199561 | 537 | 94.5 | 30.9 | 91.8 | 85.5 to 96.2 | 30.6 | 26.5 to 34.9 | 0.267 | 0.121 to 0.479 | 1.32 | 1.21 to 1.4 |
| Miller 1996111 | 1382 | 65.5 | 39.1 | 66.7 | 56.6 to 75.7 | 39.2 | 36.5 to 41.8 | 0.851 | 0.617 to 1.117 | 1.10 | 0.93 to 1.25 |
| Arienta 199754 | 10,000 | 3.9 | 98.7 | 3.9 | 1.8 to 7.6 | 98.7 | 98.5 to 98.9 | 0.973 | 0.936 to 0.995 | 3.10 | 1.36 to 6.1 |
| Sharma 2001120 | 39 | 44.4 | 19.0 | 58.1 | 36.4 to 76.6 | 31.3 | 15.4 to 50.7 | 1.324 | 0.696 to 2.958 | 0.85 | 0.52 to 1.2 |
| Stiell 200126 | 3121 | 52.0 | 54.6 | 52.4 | 46.4 to 58.4 | 54.6 | 52.8 to 56.4 | 0.872 | 0.760 to 0.987 | 1.15 | 1.02 to 1.30 |
| Mack 2003110 | 133 | 42.1 | 72.8 | 70.7 | 60.8 to 79.6 | 70.0 | 67.2 to 72.8 | 0.419 | 0.291 to 0.562 | 2.36 | 1.98 to 2.75 |
| Ibanez 200460 | 1101 | 73.5 | 70.2 | 88.5 | 81.0 to 93.9 | 14.3 | 5.4 to 28.7 | 0.800 | 0.356 to 2.220 | 1.03 | 0.92 to 1.2 |
| Chan 200599 | 105 | 87.8 | 8.7 | 53.3 | 49.1 to 57.5 | 82.4 | 81.6 to 83.3 | 0.566 | 0.516 to 0.618 | 3.04 | 2.76 to 3.3 |
| Fabbri 200557 | 7955 | 53.7 | 82.5 | 63.1 | 59.9 to 66.1 | 53.1 | 52.2 to 53.9 | 0.696 | 0.638 to 0.756 | 1.34 | 1.27 to 1.4 |
| Mower 200562 | 13,728 | 63.0 | 53.1 | 53.7 | 47.4 to 60.0 | 53.0 | 51.0 to 54.9 | 0.874 | 0.754 to 0.999 | 1.14 | 1.00 to 1.3 |
| Stiell 200546 | 2707 | 53.2 | 52.9 | 43.1 | 25.7 to 61.9 | 72.8 | 64.4 to 80.2 | 0.782 | 0.526 to 1.032 | 1.58 | 0.93 to 2.5 |
| Saboori 200767 | 682 | 8.7 | 88.4 | 12.8 | 5.6 to 23.0 | 88.5 | 85.9 to 90.8 | 0.985 | 0.869 to 1.071 | 1.11 | 0.48 to 2.1 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 17 | < 0.001 | < 0.001 | 59.9 | 43.0 to 75.8 | 58.0 | 39.5 to 74.1 | 0.698 | 0.532 to 0.871 | 1.41 | 1.14 to 1.84 | |
Any headache (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schynoll 1993118 | 228 | 40.9 | 26.7 | 61.2 | 37.5 to 79.2 | 29.6 | 23.5 to 36.4 | 1.311 | 0.686 to 2.288 | 0.87 | 0.52 to 1.15 |
| Cook 1994100 | 107 | 75.0 | 41.7 | 64.8 | 46.3 to 81.9 | 42.4 | 33.3 to 51.9 | 0.830 | 0.436 to 1.277 | 1.13 | 0.81 to 1.46 |
| Borczuk 199555 | 1448 | 50.4 | 61.2 | 48.7 | 41.2 to 57.3 | 61.1 | 58.5 to 63.7 | 0.841 | 0.697 to 0.965 | 1.25 | 1.05 to 1.49 |
| Holmes 199759 | 261 | 45.7 | 75.2 | 38.1 | 27.3 to 53.6 | 74.2 | 68.5 to 79.5 | 0.837 | 0.623 to 0.972 | 1.47 | 1.07 to 2.22 |
| Haydel 200027 | 520 | 33.3 | 77.1 | 31.1 | 21.7 to 44.1 | 76.9 | 73.1 to 80.4 | 0.899 | 0.727 to 1.018 | 1.34 | 0.94 to 2.0 |
| Falimirski 200358 | 331 | 22.5 | 85.2 | 21.7 | 13.7 to 33.0 | 84.8 | 80.6 to 88.5 | 0.927 | 0.790 to 1.018 | 1.41 | 0.91 to 2.30 |
| Mack 2003110 | 133 | 31.6 | 79.8 | 28.8 | 17.6 to 44.5 | 79.1 | 71.7 to 85.4 | 0.907 | 0.709 to 1.042 | 1.35 | 0.86 to 2.26 |
| Ibanez 200460 | 1101 | 69.9 | 45.6 | 65.9 | 56.4 to 75.5 | 45.4 | 42.4 to 48.5 | 0.752 | 0.535 to 0.965 | 1.21 | 1.03 to 1.40 |
| Chan 200599 | 105 | 43.9 | 69.6 | 42.6 | 33.1 to 52.6 | 66.8 | 52.9 to 80.0 | 0.866 | 0.680 to 1.074 | 1.27 | 0.90 to 2.12 |
| Fabbri 200557 | 7955 | 17.2 | 83.4 | 18.0 | 14.8 to 21.7 | 83.5 | 82.6 to 84.3 | 0.982 | 0.937 to 1.023 | 1.09 | 0.89 to 1.32 |
| Stiell 200546 | 1822 | 37.1 | 64.8 | 39.0 | 30.2 to 46.9 | 64.9 | 62.7 to 67.2 | 0.938 | 0.818 to 1.080 | 1.11 | 0.86 to 1.34 |
| Ono 200763 | 1064 | 38.0 | 85.8 | 29.1 | 17.3 to 43.9 | 85.3 | 83.0 to 87.4 | 0.831 | 0.657 to 0.972 | 1.99 | 1.16 to 3.10 |
| Saboori to 200767 | 682 | 4.3 | 85.5 | 14.0 | 5.6 to 22.0 | 85.9 | 83.1 to 88.5 | 0.999 | 0.911 to 1.105 | 1.01 | 0.39 to 1.57 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 13 | < 0.001 | < 0.001 | 36.8 | 25.5 to 50.5 | 70.3 | 57.3 to 79.8 | 0.901 | 0.792 to 1.005 | 1.23 | 0.99 to 1.55 | |
Anterograde or post-trauma amnesia (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schynoll 1993118 | 239 | 27.3 | 91.2 | 18.6 | 12.0 to 26.2 | 90.6 | 86.7 to 93.7 | 0.900 | 0.840 to 0.950 | 1.95 | 1.53 to 2.53 |
| Arienta 199754 | 10,000 | 2.6 | 98.6 | 3.1 | 1.4 to 5.8 | 98.6 | 98.3 to 98.8 | 0.984 | 0.956 to 1.000 | 2.11 | 0.97 to 4.08 |
| Stiell 200126 | 3121 | 40.2 | 76.8 | 39.7 | 34.3 to 45.3 | 76.8 | 75.3 to 78.4 | 0.785 | 0.712 to 0.856 | 1.71 | 1.47 to 1.98 |
| Ibanez and Arikan 200460 | 1101 | 21.7 | 91.1 | 18.2 | 13.7 to 23.0 | 90.8 | 89.0 to 92.4 | 0.902 | 0.853 to 0.945 | 1.97 | 1.54 to 2.5 |
| Stiell 200546 | 1822 | 23.7 | 85.0 | 27.1 | 22.3 to 32.2 | 85.2 | 83.6 to 86.8 | 0.855 | 0.800 to 0.908 | 1.84 | 1.53 to 2.16 |
| Saboori 200767 | 682 | 8.7 | 93.7 | 12.2 | 7.7 to 17.4 | 94.0 | 92.1 to 95.5 | 0.935 | 0.888 to 0.975 | 2.01 | 1.39 to 2.76 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 6 | < 0.001 | < 0.001 | 16.2 | 6.8 to 30.9 | 91.9 | 83.2 to 96.4 | 0.912 | 0.825 to 0.972 | 1.95 | 1.48 to 2.62 | |
Undefined vomiting (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schynoll 1993118 | 261 | 25.0 | 69.9 | 27.1 | 15.5 to 41.1 | 70.9 | 64.7 to 76.5 | 1.028 | 0.824 to 1.223 | 0.93 | 0.52 to 1.48 |
| Holmes 199759 | 261 | 14.3 | 97.8 | 14.2 | 7.1 to 24.9 | 97.4 | 95.0 to 98.9 | 0.882 | 0.773 to 0.955 | 5.36 | 2.26 to 13.71 |
| Miller 199729 | 2143 | 15.2 | 95.0 | 15.6 | 10.7 to 21.7 | 95.0 | 93.9 to 95.9 | 0.889 | 0.825 to 0.941 | 3.10 | 2.04 to 4.52 |
| Haydel 200027 | 520 | 11.1 | 91.1 | 15.4 | 7.7 to 25.7 | 91.3 | 88.6 to 93.6 | 0.926 | 0.814 to 1.016 | 1.78 | 0.85 to 3.16 |
| Mussack 2002115 | 139 | 21.1 | 91.7 | 20.6 | 10.5 to 35.0 | 91.9 | 86.5 to 95.7 | 0.866 | 0.710 to 0.982 | 2.54 | 1.16 to 5.40 |
| Ibanez and Arikan 200460 | 1101 | 22.9 | 93.2 | 21.9 | 14.8 to 30.5 | 93.2 | 91.6 to 94.6 | 0.839 | 0.746 to 0.915 | 3.21 | 2.08 to 4.8 |
| Chan 200599 | 105 | 45.1 | 69.6 | 41.9 | 32.0 to 52.5 | 73.7 | 54.9 to 87.6 | 0.790 | 0.613 to 1.079 | 1.59 | 0.89 to 3.41 |
| Fabbri 200557 | 7955 | 16.1 | 97.4 | 15.9 | 13.0 to 19.1 | 97.4 | 97.0 to 97.8 | 0.863 | 0.830 to 0.893 | 6.14 | 4.84 to 7.75 |
| Stiell 200546 | 1822 | 20.6 | 90.1 | 20.7 | 14.2 to 28.5 | 90.1 | 88.7 to 91.5 | 0.880 | 0.794 to 0.954 | 2.10 | 1.41 to 2.97 |
| Saboori 200767 | 682 | 17.4 | 95.1 | 17.4 | 9.9 to 27.3 | 95.1 | 93.3 to 96.6 | 0.870 | 0.766 to 0.949 | 3.52 | 1.90 to 6.20 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 10 | < 0.001 | < 0.001 | 20.2 | 13.7 to 28.3 | 92.2 | 85.8 to 95.9 | 0.868 | 0.794 to 0.935 | 2.58 | 1.52 to 4.49 | |
Undefined or mixed amnesia (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Borczuk 199555 | 1448 | 31.1 | 81.7 | 28.9 | 22.0 to 36.7 | 81.5 | 79.3 to 83.5 | 0.874 | 0.776 to 0.960 | 1.55 | 1.17 to 2.02 |
| Miller 1996111 | 1382 | 34.5 | 60.9 | 40.1 | 29.4 to 53.0 | 61.4 | 58.7 to 64.0 | 0.977 | 0.759 to 1.159 | 1.04 | 0.75 to 1.40 |
| Stiell 200126 | 3121 | 92.9 | 13.3 | 93.2 | 89.8 to 95.7 | 13.4 | 12.2 to 14.6 | 0.513 | 0.318 to 0.775 | 1.08 | 1.03 to 1.11 |
| Mussack 2002115 | 139 | 63.2 | 40.8 | 68.7 | 51.9 to 80.6 | 42.1 | 33.9 to 50.5 | 0.739 | 0.486 to 1.149 | 1.19 | 0.90 to 1.4 |
| Mack 2003110 | 133 | 15.8 | 79.8 | 22.6 | 10.5 to 36.8 | 80.7 | 73.4 to 86.8 | 0.957 | 0.804 to 1.119 | 1.19 | 0.56 to 1.88 |
| Chan 200599 | 105 | 9.8 | 87.0 | 11.2 | 5.8 to 18.7 | 89.6 | 79.1 to 95.5 | 0.990 | 0.916 to 1.115 | 1.09 | 0.49 to 2.20 |
| Fabbri 200557 | 7955 | 67.2 | 57.3 | 66.0 | 61.6 to 70.1 | 57.3 | 56.1 to 58.4 | 0.593 | 0.522 to 0.672 | 1.55 | 1.43 to 1.65 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 7 | < 0.001 | < 0.001 | 50.9 | 24.5 to 77.9 | 60.0 | 35.3 to 79.7 | 0.815 | 0.579 to 1.008 | 1.27 | 0.98 to 1.59 | |
Severe or persistent headache (intracranial injury – adults)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Miller 199729 | 2143 | 54.3 | 69.2 | 54.3 | 46.0 to 62.5 | 69.2 | 67.2 to 71.2 | 0.659 | 0.512 to 0.849 | 1.77 | 1.39 to 2.24 |
| Mower 200562 | 13,728 | 12.0 | 82.6 | 12.0 | 10.1 to 14.3 | 82.6 | 82.0 to 83.3 | 1.065 | 0.991 to 1.144 | 0.69 | 0.57 to 0.84 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | < 0.001 | < 0.001 | 19.4 | 16.8 to 22.2 | 80.5 | 79.9 to 81.2 | 1.028 | 0.959 to 1.101 | 1.00 | 0.86 to 1.16 | |
Retrograde amnesia (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schynoll 1993118 | 240 | 50.0 | 68.3 | 49.6 | 43.6 to 56.6 | 68.9 | 62.5 to 74.6 | 0.732 | 0.637 to 0.832 | 1.60 | 1.31 to 1.95 |
| Stiell 200126 | 3121 | 38.2 | 80.7 | 44.0 | 39.1 to 48.1 | 80.9 | 79.4 to 82.3 | 0.692 | 0.641 to 0.754 | 2.30 | 2.01 to 2.6 |
| Fabbri 200557 | 7955 | 33.9 | 95.4 | 33.4 | 29.5 to 37.4 | 95.4 | 94.9 to 95.8 | 0.698 | 0.656 to 0.739 | 7.21 | 6.14 to 8.41 |
| Stiell 200546 | 2707 | 54.5 | 71.1 | 49.4 | 44.2 to 55.3 | 71.0 | 69.2 to 72.7 | 0.713 | 0.629 to 0.787 | 1.70 | 1.51 to 1.93 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 4 | < 0.001 | < 0.001 | 44.3 | 36.9 to 55.2 | 81.6 | 56.7 to 91.6 | 0.687 | 0.635 to 0.848 | 2.41 | 1.21 to 4.55 | |
Radiological skull fracture (intracranial injury – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Rosenorn 1991117 | 1876 | 11.1 | 98.7 | 16.5 | 2.5 to 39.9 | 98.7 | 98.1 to 99.2 | 0.846 | 0.609 to 0.988 | 13.13 | 1.88 to 33.53 |
| Shackford 1992119 | 423 | 60.8 | 72.1 | 60.6 | 50.7 to 70.0 | 72.8 | 67.8 to 77.5 | 0.542 | 0.409 to 0.686 | 2.24 | 1.74 to 2.83 |
| Moran 1994112 | 200 | 62.5 | 97.9 | 52.4 | 23.9 to 81.5 | 97.7 | 95.3 to 99.2 | 0.487 | 0.190 to 0.779 | 27.94 | 8.50 to 72.56 |
| Dunham 1996101 | 2032 | 27.3 | 97.5 | 33.9 | 26.5 to 41.9 | 97.5 | 96.7 to 98.1 | 0.678 | 0.597 to 0.754 | 13.72 | 9.45 to 19.37 |
| Mack 2003110 | 133 | 0.0 | 97.4 | 7.3 | 0.3 to 21.5 | 97.7 | 94.6 to 99.5 | 0.949 | 0.803 to 1.030 | 4.41 | 0.14 to 17.68 |
| Chan 200599 | 92 | 54.9 | 100.0 | 53.6 | 42.2 to 65.0 | 97.4 | 90.9 to 99.9 | 0.476 | 0.358 to 0.597 | 105.10 | 5.84 to 385.30 |
| Ono 200763 | 1064 | 48.0 | 99.4 | 45.8 | 32.2 to 59.6 | 99.3 | 98.7 to 99.7 | 0.546 | 0.407 to 0.683 | 72.05 | 30.90 to 155.10 |
| Saboori 200767 | 682 | 4.3 | 98.4 | 7.2 | 1.6 to 16.5 | 98.4 | 97.4 to 99.2 | 0.942 | 0.848 to 1.001 | 5.13 | 0.95 to 13.76 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 8 | < 0.001 | < 0.001 | 29.8 | 9.8 to 55.9 | 97.4 | 94.2 to 99.2 | 0.720 | 0.455 to 0.923 | 14.26 | 3.68 to 38.43 | |
Post-trauma seizure (intracranial injury – adults)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Stiell 200126 | 3121 | 0.4 | 99.9 | 0.4 | 0.1 to 2.7 | 99.9 | 99.7 to 100.0 | 0.997 | 0.141 to 7.052 | 3.76 | 0.39 to 36.04 |
| Fabbri 200557 | 7955 | 8.5 | 99.3 | 8.5 | 6.4 to 11.1 | 99.3 | 99.1 to 99.5 | 0.921 | 0.841 to 1.009 | 12.84 | 8.67 to 19.02 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.002 | 0.002 | 7.9 | 6.0 to 10.4 | 99.4 | 99.2 to 99.5 | 0.921 | 0.841 to 1.009 | 12.39 | 8.41 to 18.24 | |
Need for neurosurgery in adults
Fall – any (neurosurgery – adults)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Harad 1992104 | 302 | 18.2 | 81.8 | 18.2 | 4.6 to 50.7 | 81.8 | 76.9 to 85.8 | 1.000 | 0.285 to 3.508 | 1.00 | 0.28 to 3.58 |
| Miller 1996111 | 1382 | 0.0 | 73.1 | 16.7 | 1.0 to 80.6 | 73.1 | 70.7 to 75.4 | 1.140 | 0.091 to 14.319 | 0.62 | 0.05 to 7.79 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.952 | 0.002 | 17.9 | 5.2 to 46.1 | 74.4 | 72.3 to 76.5 | 1.027 | 0.334 to 3.159 | 0.91 | 0.29 to 2.83 | |
Assault (neurosurgery – adults)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Harad 1992104 | 63.6 | 83.2 | 63.6 | 33.9 to 85.7 | 83.2 | 78.4 to 87.0 | 0.437 | 0.200 to 0.957 | 3.78 | 2.26 to 6.32 |
Motor vehicle collision – pedestrian (neurosurgery – adults)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Harad 1992104 | 0.0 | 85.9 | 4.5 | 0.3 to 44.8 | 85.9 | 81.4 to 89.5 | 1.111 | 0.969 to 1.274 | 0.32 | 0.02 to 4.91 |
Motor vehicle collision – in car (neurosurgery – adults)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Harad 1992104 | 302 | 0.0 | 55.7 | 16.7 | 0.3 to 44.8 | 55.7 | 49.9 to 61.3 | 1.715 | 0.114 to 25.772 | 0.10 | 0.01 to 1.54 |
| Miller 1996111 | 1382 | 0.0 | 59.0 | 4.5 | 1.0 to 80.6 | 59.0 | 56.4 to 61.6 | 1.412 | 0.112 to 17.735 | 0.41 | 0.03 to 5.11 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.498 | 0.291 | 8.5 | 1.2 to 42.5 | 58.4 | 56.1 to 60.8 | 1.546 | 0.243 to 9.826 | 0.21 | 0.03 to 1.36 | |
Glasgow Coma Scale < 15 (neurosurgery – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Feuerman 1988102 | 129 | 75.0 | 47.1 | 62.1 | 34.7 to 87.2 | 47.9 | 39.2 to 56.7 | 0.790 | 0.266 to 1.419 | 1.19 | 0.65 to 1.76 |
| Stein 1990122 | 658 | 36.8 | 69.2 | 41.1 | 22.7 to 60.7 | 69.3 | 65.6 to 72.8 | 0.851 | 0.568 to 1.122 | 1.34 | 0.73 to 2.01 |
| Borczuk 199555 | 1448 | 90.9 | 84.2 | 73.8 | 49.9 to 93.2 | 84.2 | 82.3 to 86.1 | 0.311 | 0.082 to 0.596 | 4.67 | 3.11 to 6.10 |
| Gomez 1996103 | 2484 | 53.3 | 95.2 | 53.8 | 37.7 to 69.5 | 95.2 | 94.3 to 96.0 | 0.486 | 0.320 to 0.655 | 11.24 | 7.60 to 15.41 |
| Arienta 199754 | 9917 | 62.5 | 99.3 | 61.5 | 42.1 to 78.3 | 99.3 | 99.1 to 99.4 | 0.388 | 0.219 to 0.583 | 86.30 | 56.30 to 123.10 |
| Hsiang 1997105 | 1360 | 38.1 | 87.3 | 40.7 | 27.4 to 54.6 | 87.3 | 85.5 to 89.1 | 0.679 | 0.520 to 0.833 | 3.21 | 2.12 to 4.46 |
| Thiruppathy 2004124 | 381 | 33.3 | 75.4 | 37.8 | 22.2 to 54.7 | 75.6 | 70.9 to 79.8 | 0.823 | 0.596 to 1.041 | 1.55 | 0.88 to 2.4 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 7 | 0.026 | < 0.001 | 53.1 | 34.8 to 73.1 | 86.8 | 62.3 to 96.2 | 0.546 | 0.310 to 0.881 | 4.00 | 1.24 to 14.61 | |
Glasgow Coma Scale < 14 (neurosurgery – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Feuerman 1988102 | 129 | 25.0 | 84.3 | 14.0 | 6.8 to 24.9 | 85.8 | 79.0 to 91.2 | 1.001 | 0.856 to 1.143 | 0.99 | 0.39 to 2.24 |
| Stein 1990122 | 658 | 15.8 | 90.8 | 17.1 | 9.9 to 26.5 | 90.9 | 88.5 to 92.9 | 0.912 | 0.806 to 1.000 | 1.88 | 1.00 to 3.20 |
| Gomez 1996103 | 2484 | 40.0 | 98.7 | 34.8 | 22.8 to 48.5 | 98.6 | 98.1 to 99.0 | 0.662 | 0.522 to 0.784 | 25.06 | 14.50 to 42.66 |
| Hsiang 1997105 | 1360 | 21.4 | 97.3 | 27.0 | 18.9 to 36.3 | 97.1 | 96.2 to 97.9 | 0.752 | 0.654 to 0.837 | 9.42 | 5.72 to 15.24 |
| Thiruppathy 2004124 | 381 | 18.5 | 89.8 | 16.6 | 9.4 to 26.1 | 90.2 | 86.9 to 92.9 | 0.925 | 0.813 to 1.020 | 1.70 | 0.85 to 3.09 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 5 | 0.271 | < 0.001 | 21.0 | 10.0 to 33.4 | 94.3 | 84.9 to 98.0 | 0.839 | 0.684 to 1.042 | 3.67 | 0.75 to 15.81 | |
Focal neurological deficit (neurosurgery – adults)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Feuerman 1988102 | 50.0 | 93.7 | 50.0 | 20.0 to 80.0 | 93.7 | 90.7 to 95.8 | 0.534 | 0.125 to 2.272 | 7.93 | 1.86 to 33.79 |
Depressed skull fracture (neurosurgery – adults)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Miller 199729 | 60.0 | 100.0 | 60.0 | 20.0 to 90.0 | 99.98 | 99.6 to 100.0 | 0.400 | 0.137 to 1.171 | 2565.6 | 146.6 to 44,909 |
Any loss of consciousness (neurosurgery – adults)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Miller 1996111 | 0.0 | 38.7 | 16.7 | 1.0 to 80.6 | 38.7 | 36.1 to 41.3 | 2.156 | 0.103 to 44.998 | 0.27 | 0.01 to 5.67 |
Any headache (neurosurgery – adults)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Holmes 199759 | 25.0 | 78.5 | 25.0 | 3.4 to 76.2 | 78.5 | 73.0 to 83.0 | 0.956 | 0.098 to 9.368 | 1.16 | 0.12 to 11.38 |
Undefined vomiting (neurosurgery – adults)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Holmes 199759 | 264 | 25.0 | 98.1 | 25.0 | 3.4 to 76.2 | 98.1 | 95.5 to 99.2 | 0.765 | 0.245 to 2.387 | 13.00 | 1.52 to 111.28 |
| Miller 199729 | 2143 | 20.0 | 94.3 | 20.0 | 2.7 to 69.1 | 94.3 | 93.3 to 95.2 | 0.848 | 0.318 to 2.262 | 3.53 | 0.49 to 25.29 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.858 | 0.015 | 22.3 | 5.6 to 58.1 | 94.6 | 93.6 to 95.4 | 0.811 | 0.386 to 1.706 | 6.41 | 1.50 to 27.33 | |
Undefined or mixed amnesia (neurosurgery – adults)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Miller 1996111 | 0.0 | 61.1 | 16.7 | 1.0 to 80.6 | 61.1 | 58.5 to 63.7 | 1.363 | 0.065 to 28.451 | 0.43 | 0.02 to 8.95 |
Severe or persistent headache (neurosurgery – all ages)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Miller 199729 | 20.0 | 67.7 | 20.0 | 2.7 to 69.1 | 67.7 | 65.7 to 69.6 | 1.182 | 0.132 to 10.596 | 0.62 | 0.07 to 5.55 |
Radiological skull fracture (neurosurgery – adults)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Murshid 1994114 | 566 | 57.1 | 89.3 | 39.5 | 30.1 to 49.8 | 90.2 | 87.6 to 92.1 | 0.671 | 0.549 to 0.791 | 4.00 | 2.54 to 6.12 |
| Hung 1996106 | 7000 | 37.8 | 90.2 | 39.1 | 34.7 to 43.5 | 90.1 | 89.4 to 90.8 | 0.676 | 0.627 to 0.725 | 3.96 | 3.45 to 4.52 |
| Stein 1992121 | 1538 | 60.3 | 93.5 | 51.4 | 41.5 to 65.5 | 93.3 | 91.9 to 94.6 | 0.520 | 0.369 to 0.631 | 7.79 | 5.50 to 10.82 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 3 | 0.004 | < 0.001 | 43.1 | 31.0 to 58.6 | 91.3 | 87.3 to 94.1 | 0.623 | 0.444 to 0.788 | 4.99 | 2.48 to 9.48 | |
Appendix 6 Individual clinical characteristics in children and infants – data for meta-analysis
Intracranial injury in children
Intoxication (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Haydel 200388 | 175 | 7.1 | 93.8 | 3.4 | 1.3 to 7.0 | 94.4 | 90.2 to 97.2 | 1.022 | 0.977 to 1.078 | 0.61 | 0.19 to 1.63 |
| Dunning 200630 | 22,772 | 4.6 | 99.8 | 4.5 | 2.5 to 7.3 | 99.8 | 99.8 to 99.9 | 0.957 | 0.929 to 0.976 | 28.10 | 14.69 to 50.93 |
| Oman 200691 | 1666 | 4.0 | 95.0 | 3.4 | 1.4 to 6.9 | 95.1 | 93.9 to 96.1 | 1.015 | 0.978 to 1.040 | 0.70 | 0.28 to 1.5 |
| Atabaki 200881 | 1000 | 1.5 | 99.1 | 3.9 | 2.3 to 6.0 | 99.1 | 98.4 to 99.6 | 0.970 | 0.948 to 0.988 | 4.57 | 1.92 to 11.25 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 4 | 0.689 | < 0.001 | 3.8 | 1.8 to 6.4 | 98.6 | 90.2 to 99.8 | 0.976 | 0.946 to 1.072 | 2.72 | 0.29 to 26.06 | |
Fall – any (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Ramundo 1995135 | 249 | 26.7 | 53.4 | 28.2 | 18.1 to 39.9 | 53.0 | 49.0 to 57.0 | 1.360 | 1.076 to 1.647 | 0.60 | 0.36 to 0.90 |
| Boran 2006128 | 421 | 40.5 | 60.2 | 44.5 | 32.1 to 57.7 | 57.7 | 54.0 to 61.6 | 0.965 | 0.707 to 1.228 | 1.06 | 0.72 to 1.44 |
| Dunning 200630 | 22,772 | 11.7 | 46.5 | 12.4 | 8.7 to 16.5 | 46.6 | 45.9 to 47.2 | 1.883 | 1.791 to 1.966 | 0.23 | 0.16 to 0.31 |
| Atabaki 200881 | 1000 | 61.5 | 56.8 | 52.7 | 40.9 to 64.8 | 58.6 | 55.7 to 61.3 | 0.809 | 0.597 to 1.023 | 1.27 | 0.97 to 1.59 |
| Guzel 200987 | 337 | 40.3 | 61.5 | 43.1 | 32.9 to 53.7 | 57.4 | 53.8 to 61.7 | 0.993 | 0.777 to 1.223 | 1.02 | 0.73 to 1.34 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 5 | < 0.001 | < 0.001 | 34.7 | 17.0 to 56.5 | 54.7 | 49.1 to 60.6 | 1.206 | 0.726 to 1.683 | 0.78 | 0.34 to 1.41 | |
Fall from a height (intracranial injury – children)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Reed 2005136 | 39 | 30.0 | 86.2 | 30.0 | 10.0 to 62.4 | 86.2 | 68.5 to 94.7 | 0.812 | 0.312 to 2.116 | 2.18 | 0.59 to 8.09 |
| Dunning 200630 | 22,772 | 19.6 | 80.2 | 19.6 | 15.3 to 24.6 | 80.2 | 79.7 to 80.7 | 1.003 | 0.791 to 1.271 | 0.99 | 0.78 to 1.26 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.423 | 0.421 | 20.0 | 15.8 to 25.0 | 80.2 | 79.7 to 80.7 | 0.991 | 0.787 to 1.247 | 1.01 | 0.80 to 1.28 | |
Dizziness (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Davis 1994129 | 168 | 0.0 | 98.1 | 5.6 | 0.1 to 16.2 | 96.4 | 90.9 to 99.0 | 0.986 | 0.862 to 1.054 | 1.35 | 0.05 to 8.42 |
| Reed 2005136 | 39 | 0.0 | 93.1 | 5.1 | 0.6 to 12.4 | 93.0 | 85.7 to 98.1 | 1.018 | 0.920 to 1.117 | 0.74 | 0.11 to 3.57 |
| Atabaki 200881 | 1000 | 7.7 | 89.9 | 5.3 | 1.8 to 11.6 | 90.3 | 88.3 to 92.2 | 1.048 | 0.977 to 1.095 | 0.55 | 0.18 to 1.23 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 3 | 0.881 | 0.012 | 5.2 | 0.6 to 13.3 | 93.5 | 85.7 to 98.5 | 1.014 | 0.910 to 1.109 | 0.79 | 0.11 to 4.30 | |
Coagulopathy (intracranial injury – children)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Dunning 200630 | 22,772 | 0.0 | 99.9 | 0.2 | 0.001 to 2.8 | 99.9 | 99.9 to 100.0 | 0.999 | 0.063 to 15.930 | 2.86 | 0.17 to 47.88 |
| Oman 200691 | 1666 | 7.0 | 99.0 | 7.0 | 3.8 to 12.6 | 99.0 | 98.4 to 99.4 | 0.939 | 0.511 to 1.726 | 7.00 | 3.19 to 15.37 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.010 | < 0.001 | 5.8 | 3.2 to 10.5 | 99.7 | 99.6 to 99.8 | 0.942 | 0.520 to 1.706 | 6.56 | 3.08 to 14.00 | |
Assault (intracranial injury – children)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Dunning 200630 | 22,772 | 3.6 | 95.9 | 3.6 | 1.9 to 6.5 | 95.9 | 95.6 to 96.1 | 1.006 | 0.547 to 1.848 | 0.87 | 0.47 to 1.60 |
| Ramundo 1995135 | 261 | 2.2 | 92.6 | 2.2 | 0.3 to 14.2 | 92.6 | 88.3 to 95.4 | 1.056 | 0.152 to 7.337 | 0.30 | 0.04 to 2.20 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.648 | 0.017 | 3.4 | 1.9 to 6.0 | 95.9 | 95.6 to 96.1 | 1.010 | 0.565 to 1.805 | 0.79 | 0.44 to 1.42 | |
Vision (intracranial injury – children)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Dunning 200630 | 22,772 | 1.4 | 98.9 | 1.4 | 0.5 to 3.7 | 98.9 | 98.8 to 99.1 | 0.996 | 0.377 to 2.636 | 1.35 | 0.50 to 3.59 |
| Guzel 200987 | 337 | 17.9 | 98.9 | 17.9 | 10.5 to 28.9 | 98.9 | 96.6 to 99.6 | 0.830 | 0.497 to 1.386 | 16.12 | 4.68 to 55.51 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | < 0.001 | 0.933 | 9.1 | 5.6 to 14.5 | 98.9 | 98.8 to 99.1 | 0.864 | 0.549 to 1.360 | 3.51 | 1.63 to 7.57 | |
Prior neurosurgery (intracranial injury – children)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Dunning 200630 | 0.7 | 99.9 | 0.7 | 0.2 to 2.8 | 99.9 | 99.8 to 99.9 | 0.994 | 0.984 to 1.004 | 5.93 | 1.42 to 24.81 |
Motor vehicle collision – pedestrian (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Harad 1992104 | 302 | 18.2 | 87.4 | 18.4 | 10.9 to 27.0 | 87.8 | 83.4 to 91.4 | 0.930 | 0.826 to 1.029 | 1.50 | 0.83 to 2.55 |
| Tsai 1994125 | 186 | 5.0 | 91.8 | 13.7 | 3.0 to 23.8 | 91.6 | 86.6 to 95.4 | 0.945 | 0.819 to 1.072 | 1.58 | 0.35 to 3.90 |
| Boran 2006128 | 421 | 43.2 | 80.2 | 28.9 | 13.2 to 51.8 | 80.8 | 76.7 to 84.6 | 0.883 | 0.597 to 1.088 | 1.48 | 0.67 to 2.80 |
| Dunning 200630 | 22,772 | 28.1 | 98.7 | 27.3 | 22.2 to 32.8 | 98.7 | 98.5 to 98.8 | 0.737 | 0.681 to 0.788 | 20.79 | 16.46 to 25.85 |
| Atabaki 200881 | 1000 | 4.6 | 91.2 | 11.5 | 3.0 to 23.4 | 91.2 | 89.3 to 92.9 | 0.969 | 0.837 to 1.067 | 1.34 | 0.34 to 2.87 |
| Guzel 200987 | 337 | 23.9 | 88.1 | 20.7 | 14.5 to 31.7 | 88.5 | 84.4 to 91.9 | 0.894 | 0.768 to 0.983 | 1.84 | 1.11 to 3.1 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 6 | < 0.001 | < 0.001 | 19.4 | 9.0 to 30.2 | 91.9 | 81.7 to 96.6 | 0.883 | 0.754 to 1.043 | 2.32 | 0.75 to 6.56 | |
Motor vehicle collision – in car (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Ramundo 1995135 | 261 | 51.1 | 76.4 | 31.7 | 19.5 to 53.4 | 74.6 | 68.5 to 80.3 | 0.918 | 0.611 to 1.094 | 1.27 | 0.76 to 2.36 |
| Boran 2006128 | 421 | 13.5 | 83.9 | 19.2 | 10.0 to 26.9 | 84.3 | 80.5 to 87.7 | 0.959 | 0.871 to 1.075 | 1.23 | 0.62 to 1.76 |
| Dunning 200630 | 22,772 | 5.0 | 99.2 | 4.6 | 2.6 to 7.2 | 99.2 | 99.1 to 99.3 | 0.962 | 0.935 to 0.982 | 5.87 | 3.20 to 9.43 |
| Atabaki 200881 | 1000 | 10.8 | 78.9 | 20.8 | 9.2 to 29.8 | 79.4 | 76.7 to 81.9 | 0.999 | 0.882 to 1.152 | 1.01 | 0.44 to 1.47 |
| Guzel 200987 | 337 | 7.5 | 96.3 | 9.2 | 4.8 to 13.8 | 96.4 | 94.0 to 98.1 | 0.942 | 0.901 to 0.989 | 2.68 | 1.26 to 4.56 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 5 | < 0.001 | < 0.001 | 15.2 | 5.6 to 31.7 | 90.0 | 67.9 to 98.4 | 0.947 | 0.870 to 1.065 | 1.99 | 0.82 to 4.30 | |
Motor vehicle collision with bicycle (intracranial injury – children)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Dunning 200630 | 15.3 | 96.7 | 15.3 | 11.5 to 20.0 | 96.7 | 96.5 to 96.9 | 0.876 | 0.833 to 0.921 | 4.63 | 3.49 to 6.15 |
Persistent vomiting (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Da Dalt 200683 | 3803 | 14.3 | 94.4 | 17.8 | 7.2 to 32.7 | 94.4 | 93.6 to 95.0 | 0.871 | 0.713 to 0.984 | 3.15 | 1.26 to 5.89 |
| Dunning 200630 | 22,772 | 29.2 | 94.1 | 28.7 | 23.7 to 34.1 | 94.1 | 93.7 to 94.4 | 0.758 | 0.701 to 0.812 | 4.83 | 3.96 to 5.78 |
| Oman 200691 | 1666 | 24.0 | 89.0 | 23.6 | 17.3 to 30.9 | 89.1 | 87.5 to 90.6 | 0.857 | 0.774 to 0.930 | 2.18 | 1.55 to 3.0 |
| Kupperman 200990 | 31,292 | 18.8 | 92.4 | 19.0 | 14.7 to 23.8 | 92.4 | 92.1 to 92.7 | 0.877 | 0.824 to 0.923 | 2.51 | 1.93 to 3.16 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 4 | 0.028 | < 0.001 | 22.1 | 10.7 to 40.6 | 92.9 | 87.4 to 96.8 | 0.840 | 0.635 to 0.969 | 3.14 | 1.30 to 8.05 | |
Glasgow Coma Scale < 15 (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Chan 1990212 | 418 | 23.1 | 95.6 | 26.2 | 10.2 to 48.5 | 95.5 | 93.2 to 97.2 | 0.774 | 0.540 to 0.941 | 5.78 | 2.17 to 12.36 |
| Dietrich 199384 | 253 | 75.0 | 77.0 | 73.0 | 58.3 to 84.9 | 77.2 | 71.4 to 82.4 | 0.351 | 0.197 to 0.543 | 3.18 | 2.35 to 4.30 |
| Ramundo 1995135 | 259 | 76.7 | 70.8 | 75.3 | 62.0 to 86.1 | 71.2 | 65.0 to 76.9 | 0.348 | 0.196 to 0.539 | 2.60 | 1.99 to 3.37 |
| Stein 1995139 | 751 | 40.4 | 80.1 | 41.3 | 31.9 to 51.2 | 80.3 | 77.1 to 83.2 | 0.731 | 0.606 to 0.852 | 2.09 | 1.56 to 2.73 |
| Mandera 2000133 | 166 | 61.8 | 70.4 | 62.1 | 50.5 to 72.6 | 71.6 | 62.3 to 79.8 | 0.531 | 0.377 to 0.713 | 2.18 | 1.55 to 3.16 |
| Simon 2001138 | 569 | 17.9 | 88.7 | 19.8 | 12.4 to 29.0 | 88.9 | 85.9 to 91.5 | 0.902 | 0.796 to 0.991 | 1.79 | 1.06 to 2.84 |
| Reed 2005136 | 39 | 90.0 | 82.8 | 77.4 | 52.8 to 93.7 | 82.3 | 67.1 to 92.3 | 0.277 | 0.079 to 0.577 | 4.27 | 2.22 to 9.9 |
| Dunning 200630 | 22,772 | 55.5 | 98.5 | 54.8 | 49.0 to 60.5 | 98.5 | 98.3 to 98.6 | 0.459 | 0.401 to 0.518 | 36.04 | 30.97 to 41.7 |
| Oman 200691 | 1666 | 68.8 | 82.0 | 68.4 | 60.5 to 75.7 | 82.0 | 80.0 to 83.9 | 0.386 | 0.296 to 0.483 | 3.80 | 3.24 to 4.4 |
| Atabaki 200881 | 1000 | 29.2 | 86.2 | 30.9 | 20.7 to 42.2 | 86.3 | 84.0 to 88.4 | 0.801 | 0.668 to 0.922 | 2.26 | 1.47 to 3.2 |
| Guzel 200987 | 337 | 10.4 | 97.0 | 12.3 | 6.2 to 21.2 | 97.0 | 94.6 to 98.5 | 0.905 | 0.813 to 0.972 | 4.09 | 1.67 to 9.7 |
| Kupperman 200990 | 31,694 | 26.6 | 97.4 | 26.6 | 21.6 to 31.9 | 97.4 | 97.2 to 97.6 | 0.754 | 0.699 to 0.804 | 10.30 | 8.32 to 12.5 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 12 | < 0.001 | < 0.001 | 46.3 | 29.6 to 64.2 | 89.6 | 81.1 to 94.7 | 0.602 | 0.418 to 0.765 | 4.42 | 2.63 to 7.66 | |
Glasgow Coma Scale < 14 (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Stein 1995139 | 751 | 18.1 | 94.1 | 19.4 | 12.4 to 27.9 | 94.2 | 92.2 to 95.8 | 0.856 | 0.765 to 0.933 | 3.33 | 1.95 to 5.41 |
| Mandera 2000133 | 166 | 22.1 | 85.7 | 24.0 | 15.0 to 34.8 | 86.6 | 79.0 to 92.3 | 0.879 | 0.746 to 1.014 | 1.78 | 0.94 to 3.43 |
| Dunning 200630 | 22,772 | 45.9 | 99.4 | 45.1 | 39.3 to 51.0 | 99.4 | 99.3 to 99.5 | 0.552 | 0.493 to 0.611 | 73.48 | 59.56 to 91.00 |
| Atabaki 200881 | 1000 | 90.8 | 2.7 | 89.7 | 80.7 to 95.6 | 2.7 | 1.8 to 3.8 | 3.858 | 1.534 to 8.154 | 0.92 | 0.83 to 0.98 |
| Guzel 200987 | 337 | 20.9 | 98.5 | 21.1 | 12.9 to 31.3 | 98.6 | 96.8 to 99.6 | 0.802 | 0.697 to 0.885 | 14.90 | 5.78 to 48.58 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 5 | < 0.001 | < 0.001 | 40.4 | 12.8 to 77.5 | 89.1 | 18.9 to 99.6 | 0.718 | 0.429 to 1.674 | 3.58 | 0.80 to 46.84 | |
Focal neurological deficit (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Chan 1990212 | 418 | 7.7 | 96.0 | 33.8 | 9.9 to 45.7 | 96.6 | 94.6 to 98.1 | 0.683 | 0.568 to 0.935 | 10.07 | 2.63 to 16.23 |
| Dietrich 199384 | 252 | 28.6 | 94.5 | 37.8 | 21.2 to 49.3 | 95.6 | 92.4 to 97.6 | 0.648 | 0.538 to 0.831 | 8.75 | 3.69 to 14.70 |
| Ramundo 1995135 | 261 | 11.1 | 99.5 | 12.1 | 5.4 to 21.5 | 99.7 | 98.8 to 99.9 | 0.883 | 0.791 to 0.948 | 36.64 | 9.68 to 112.20 |
| Quayle 199794 | 321 | 40.7 | 85.0 | 56.6 | 32.3 to 67.4 | 86.1 | 81.8 to 89.7 | 0.500 | 0.384 to 0.793 | 4.03 | 2.14 to 5.55 |
|
Ng 2002134 |
119 | 12.3 | 100.0 | 12.1 | 5.9 to 20.6 | 99.7 | 98.4 to 100.0 | 0.883 | 0.800 to 0.943 | 39.00 | 8.33 to 148.00 |
| Da Dalt 200683 | 3796 | 25.0 | 99.8 | 12.2 | 6.7 to 25.9 | 99.8 | 99.6 to 99.9 | 0.880 | 0.743 to 0.935 | 48.31 | 26.62 to 125.20 |
| Dunning 200630 | 22,772 | 19.2 | 99.6 | 16.9 | 12.9 to 22.0 | 99.6 | 99.5 to 99.6 | 0.835 | 0.783 to 0.874 | 38.00 | 27.43 to 54.56 |
| Oman 200691 | 1666 | 81.0 | 68.0 | 76.9 | 69.2 to 84.4 | 67.8 | 65.5 to 70.2 | 0.340 | 0.230 to 0.456 | 2.39 | 2.11 to 2.70 |
| Atabaki 200881 | 1000 | 3.1 | 99.6 | 8.1 | 2.8 to 15.0 | 99.8 | 99.3 to 99.9 | 0.921 | 0.854 to 0.975 | 41.38 | 6.97 to 102.6 |
| Guzel 200987 | 337 | 3.0 | 100.0 | 3.8 | 1.0 to 9.5 | 100.0 | 99.7 to 100.0 | 0.962 | 0.907 to 0.990 | 87.38 | 12.21 to 503.50 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 10 | < 0.001 | < 0.001 | 21.1 | 8.8 to 41.1 | 99.0 | 95.4 to 99.8 | 0.798 | 0.615 to 0.915 | 20.46 | 7.40 to 54.24 | |
Depressed skull fracture (intracranial injury – children)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Ramundo 1995135 | 261 | 26.7 | 96.8 | 26.7 | 15.8 to 41.3 | 96.8 | 93.4 to 98.4 | 0.758 | 0.467 to 1.231 | 8.23 | 3.43 to 19.74 |
| Dunning 200630 | 22,772 | 13.9 | 99.9 | 13.9 | 10.3 to 18.4 | 99.9 | 99.9 to 99.9 | 0.862 | 0.759 to 0.978 | 173.42 | 100.4 to 299.3 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.032 | < 0.001 | 16.0 | 12.4 to 20.5 | 99.8 | 99.7 to 99.9 | 0.855 | 0.756 to 0.966 | 73.82 | 46.45 to 117.32 | |
Basal skull fracture (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Reed 2005136 | 39 | 30.0 | 93.1 | 28.1 | 11.6 to 49.9 | 96.6 | 90.0 to 99.3 | 0.744 | 0.535 to 0.913 | 11.12 | 2.53 to 24.08 |
| Da Dalt 200683 | 3806 | 9.1 | 99.8 | 8.7 | 3.1 to 18.3 | 99.7 | 99.6 to 99.9 | 0.916 | 0.820 to 0.972 | 35.58 | 12.71 to 88.00 |
| Dunning 200630 | 22,772 | 30.2 | 98.0 | 27.5 | 21.9 to 33.6 | 98.0 | 97.8 to 98.2 | 0.740 | 0.678 to 0.797 | 13.64 | 10.65 to 17.01 |
| Atabaki 200881 | 1000 | 4.6 | 97.6 | 17.2 | 4.7 to 26.4 | 98.3 | 97.1 to 99.1 | 0.843 | 0.751 to 0.975 | 11.07 | 2.10 to 18.86 |
| Kupperman 200990 | 31,396 | 13.5 | 99.4 | 13.4 | 9.7 to 17.5 | 99.4 | 99.3 to 99.5 | 0.872 | 0.831 to 0.909 | 21.53 | 15.26 to 29.07 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 5 | < 0.001 | < 0.001 | 17.8 | 7.8 to 31.7 | 98.7 | 96.5 to 99.6 | 0.833 | 0.703 to 0.929 | 16.90 | 6.13 to 32.44 | |
Any seizure (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Dietrich 199384 | 253 | 11.1 | 94.5 | 10.0 | 7.0 to 13.7 | 94.8 | 91.4 to 97.1 | 0.949 | 0.907 to 0.999 | 1.92 | 1.02 to 3.70 |
| Ramundo 1995135 | 256 | 11.9 | 95.8 | 10.0 | 7.3 to 13.3 | 96.0 | 93.0 to 98.0 | 0.937 | 0.900 to 0.981 | 2.51 | 1.29 to 5.21 |
| Schunk 1996137 | 313 | 7.7 | 92.0 | 10.0 | 6.7 to 14.3 | 92.3 | 89.0 to 95.0 | 0.975 | 0.924 to 1.028 | 1.31 | 0.74 to 2.22 |
| Fridriksson 2000130 | 49 | 22.7 | 88.9 | 10.0 | 6.8 to 14.7 | 92.4 | 80.2 to 97.8 | 0.973 | 0.909 to 1.120 | 1.33 | 0.47 to 4.69 |
| Ng 2002134 | 119 | 6.2 | 88.9 | 9.9 | 6.5 to 14.3 | 91.1 | 82.2 to 96.4 | 0.987 | 0.918 to 1.107 | 1.13 | 0.47 to 2.97 |
| Reed 2005136 | 39 | 20.0 | 96.6 | 10.1 | 7.3 to 13.6 | 96.7 | 89.0 to 99.4 | 0.931 | 0.889 to 1.014 | 3.07 | 0.88 to 16.95 |
| Dunning 200630 | 22,772 | 10.0 | 99.6 | 10.1 | 7.2 to 13.8 | 99.6 | 99.5 to 99.7 | 0.902 | 0.866 to 0.932 | 27.40 | 18.36 to 40.06 |
| Atabaki 200881 | 1000 | 10.8 | 94.7 | 10.0 | 7.0 to 13.6 | 94.7 | 93.2 to 96.0 | 0.950 | 0.911 to 0.985 | 1.90 | 1.22 to 2.85 |
| Guzel 200987 | 337 | 7.5 | 98.1 | 10.0 | 7.6 to 12.8 | 98.0 | 96.0 to 99.2 | 0.919 | 0.888 to 0.950 | 5.05 | 2.36 to 12.58 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 9 | 0.602 | < 0.001 | 10.0 | 7.3 to 13.3 | 96.3 | 91.9 to 98.3 | 0.935 | 0.899 to 0.987 | 2.69 | 1.17 to 6.24 | |
Any loss of consciousness (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Chan 1990212 | 418 | 61.5 | 67.4 | 56.2 | 36.4 to 75.3 | 67.5 | 62.9 to 72.0 | 0.650 | 0.366 to 0.950 | 1.73 | 1.10 to 2.4 |
| Dietrich 199384 | 179 | 67.9 | 60.3 | 63.2 | 47.3 to 77.7 | 60.6 | 52.6 to 68.1 | 0.608 | 0.366 to 0.893 | 1.60 | 1.14 to 2.2 |
| Davis 1994129 | 138 | 60.0 | 68.8 | 54.6 | 33.3 to 75.3 | 69.1 | 60.8 to 76.5 | 0.659 | 0.356 to 0.982 | 1.76 | 1.04 to 2.7 |
| Ramundo 1995135 | 212 | 70.6 | 59.0 | 65.9 | 51.3 to 79.1 | 59.2 | 51.9 to 66.2 | 0.577 | 0.351 to 0.839 | 1.61 | 1.21 to 2.10 |
| Schunk 1996137 | 313 | 15.5 | 73.7 | 30.9 | 13.5 to 50.8 | 74.0 | 68.9 to 78.7 | 0.935 | 0.663 to 1.181 | 1.19 | 0.51 to 2.0 |
| Fridriksson 2000130 | 49 | 45.5 | 66.7 | 46.9 | 30.1 to 64.0 | 69.0 | 51.3 to 83.3 | 0.774 | 0.508 to 1.130 | 1.50 | 0.83 to 3.0 |
| Simon 2001138 | 429 | 38.7 | 52.9 | 41.1 | 30.0 to 52.8 | 53.3 | 48.1 to 58.3 | 1.106 | 0.873 to 1.351 | 0.88 | 0.63 to 1.2 |
| Ng 2002134 | 119 | 47.7 | 61.1 | 48.3 | 37.2 to 59.5 | 62.7 | 49.8 to 74.4 | 0.826 | 0.618 to 1.108 | 1.29 | 0.88 to 2.0 |
| Reed 2005136 | 39 | 50.0 | 86.2 | 46.3 | 25.8 to 68.5 | 85.5 | 71.5 to 94.4 | 0.632 | 0.372 to 0.890 | 3.17 | 1.40 to 8.46 |
| Boran 2006128 | 421 | 37.8 | 97.7 | 36.3 | 23.5 to 51.0 | 97.3 | 95.4 to 98.6 | 0.655 | 0.505 to 0.787 | 13.35 | 6.81 to 27.5 |
| Da Dalt 200683 | 3793 | 38.1 | 97.4 | 35.9 | 20.6 to 54.1 | 97.3 | 96.8 to 97.8 | 0.659 | 0.472 to 0.816 | 13.44 | 7.56 to 21.3 |
| Dunning 200630 | 22,772 | 51.2 | 95.4 | 50.6 | 44.8 to 56.3 | 95.4 | 95.1 to 95.6 | 0.519 | 0.458 to 0.579 | 10.91 | 9.56 to 12.4 |
| Oman 200691 | 1666 | 75.0 | 45.0 | 73.3 | 65.8 to 80.0 | 45.1 | 42.6 to 47.6 | 0.592 | 0.441 to 0.764 | 1.33 | 1.19 to 1.5 |
| Atabaki 200881 | 1000 | 23.1 | 66.7 | 27.4 | 17.8 to 38.4 | 66.9 | 63.8 to 69.9 | 1.086 | 0.916 to 1.240 | 0.83 | 0.53 to 1.2 |
| Guzel 200987 | 337 | 13.4 | 93.7 | 17.6 | 9.9 to 27.3 | 93.8 | 90.5 to 96.2 | 0.879 | 0.775 to 0.967 | 2.81 | 1.40 to 5.4 |
| Klemetti 200989 | 485 | 53.0 | 68.7 | 51.4 | 41.2 to 61.6 | 91.1 | 87.7 to 94.0 | 0.534 | 0.421 to 0.647 | 5.79 | 3.93 to 8.8 |
| Kupperman 200990 | 28,195 | 36.6 | 87.6 | 37.0 | 30.1 to 44.4 | 87.6 | 87.2 to 88.0 | 0.719 | 0.635 to 0.798 | 2.98 | 2.42 to 3.58 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 17 | < 0.001 | < 0.001 | 45.9 | 36.4 to 55.6 | 80.1 | 67.4 to 87.3 | 0.679 | 0.566 to 0.814 | 2.30 | 1.46 to 3.47 | |
Any headache (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Chan 1990212 | 418 | 15.4 | 75.6 | 25.8 | 12.5 to 41.8 | 75.9 | 71.6 to 79.9 | 0.978 | 0.772 to 1.159 | 1.07 | 0.52 to 1.73 |
| Dietrich 199384 | 194 | 50.0 | 51.7 | 52.7 | 34.7 to 69.6 | 52.7 | 45.6 to 59.7 | 0.898 | 0.584 to 1.259 | 1.11 | 0.73 to 1.49 |
| Davis 1994129 | 168 | 33.3 | 77.6 | 30.4 | 16.4 to 48.9 | 77.3 | 70.6 to 83.2 | 0.901 | 0.671 to 1.080 | 1.34 | 0.74 to 2.21 |
| Ramundo 1995135 | 185 | 66.7 | 32.9 | 69.6 | 49.6 to 84.6 | 34.4 | 27.7 to 41.6 | 0.881 | 0.455 to 1.507 | 1.06 | 0.76 to 1.31 |
| Schunk 1996137 | 313 | 38.4 | 70.3 | 37.3 | 22.0 to 55.1 | 70.4 | 65.2 to 75.3 | 0.890 | 0.641 to 1.109 | 1.26 | 0.75 to 1.88 |
| Fridriksson 2000130 | 49 | 40.9 | 66.7 | 40.1 | 24.8 to 57.0 | 67.8 | 52.7 to 80.5 | 0.886 | 0.655 to 1.153 | 1.24 | 0.77 to 2.0 |
| Ng 2002134 | 119 | 12.3 | 85.2 | 14.6 | 8.1 to 23.2 | 86.2 | 77.5 to 92.5 | 0.990 | 0.891 to 1.107 | 1.06 | 0.55 to 1.98 |
| Haydel 200388 | 175 | 50.0 | 66.5 | 44.5 | 27.9 to 62.8 | 66.3 | 59.1 to 73.0 | 0.838 | 0.568 to 1.089 | 1.32 | 0.84 to 1.91 |
| Reed 2005136 | 39 | 10.0 | 100.0 | 9.7 | 2.1 to 26.0 | 93.5 | 84.1 to 98.4 | 0.970 | 0.822 to 1.046 | 1.45 | 0.51 to 4.77 |
| Da Dalt 200683 | 3800 | 25.0 | 91.1 | 16.4 | 7.6 to 32.0 | 91.0 | 90.1 to 91.9 | 0.918 | 0.748 to 1.015 | 1.83 | 0.85 to 3.60 |
| Dunning 200630 | 22,772 | 20.3 | 79.0 | 21.0 | 16.6 to 25.9 | 79.0 | 78.5 to 79.5 | 1.000 | 0.938 to 1.056 | 1.00 | 0.79 to 1.23 |
| Atabaki 200881 | 1000 | 26.2 | 61.7 | 31.4 | 21.2 to 42.8 | 62.2 | 59.0 to 65.2 | 1.103 | 0.916 to 1.282 | 0.83 | 0.55 to 1.14 |
| Guzel 200987 | 337 | 32.8 | 83.7 | 29.7 | 20.7 to 40.5 | 82.8 | 78.2 to 86.9 | 0.850 | 0.717 to 0.966 | 1.72 | 1.15 to 2.57 |
| Kupperman 200990 | 27,495 | 73.4 | 54.1 | 71.3 | 64.9 to 77.1 | 54.1 | 53.5 to 54.7 | 0.531 | 0.424 to 0.648 | 1.55 | 1.41 to 1.68 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 14 | < 0.001 | < 0.001 | 33.9 | 22.9 to 47.6 | 73.3 | 62.1 to 81.3 | 0.905 | 0.784 to 1.010 | 1.26 | 0.97 to 1.61 | |
Anterograde or post-trauma amnesia (intracranial injury – children)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Guzel 200987 | 20.9 | 93.0 | 20.9 | 12.8 to 32.3 | 93.0 | 89.2 to 95.5 | 0.851 | 0.401 to 1.804 | 2.97 | 1.40 to 6.29 |
Undefined vomiting (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Chan 1990212 | 418 | 38.5 | 73.8 | 34.7 | 18.2 to 55.4 | 73.9 | 69.5 to 78.0 | 0.883 | 0.603 to 1.117 | 1.33 | 0.69 to 2.19 |
| Dietrich 199384 | 253 | 27.8 | 59.4 | 28.9 | 17.3 to 43.0 | 60.2 | 53.7 to 66.3 | 1.181 | 0.932 to 1.431 | 0.73 | 0.42 to 1.11 |
| Davis 1994129 | 168 | 8.3 | 93.6 | 18.8 | 5.7 to 38.2 | 92.4 | 87.7 to 95.8 | 0.880 | 0.669 to 1.027 | 2.46 | 0.72 to 6.14 |
| Ramundo 1995135 | 218 | 13.9 | 79.7 | 18.7 | 9.0 to 31.2 | 79.7 | 73.6 to 85.0 | 1.021 | 0.856 to 1.172 | 0.92 | 0.43 to 1.65 |
| Schunk 1996137 | 313 | 46.1 | 65.7 | 39.3 | 21.6 to 60.9 | 66.0 | 60.6 to 71.1 | 0.920 | 0.590 to 1.206 | 1.16 | 0.62 to 1.84 |
| Fridriksson 2000130 | 49 | 63.6 | 66.7 | 52.6 | 35.2 to 71.2 | 68.4 | 51.0 to 82.4 | 0.696 | 0.411 to 1.050 | 1.66 | 0.93 to 3.2 |
| Ng 2002134 | 119 | 41.5 | 50.0 | 40.2 | 29.4 to 51.7 | 53.2 | 40.4 to 65.6 | 1.122 | 0.834 to 1.542 | 0.86 | 0.58 to 1.28 |
| Haydel 200388 | 175 | 42.9 | 82.6 | 36.5 | 19.9 to 57.4 | 82.3 | 76.1 to 87.5 | 0.773 | 0.516 to 0.987 | 2.05 | 1.05 to 3.64 |
| Reed 2005136 | 39 | 0.0 | 72.4 | 18.2 | 5.1 to 36.9 | 74.3 | 58.2 to 86.6 | 1.099 | 0.825 to 1.457 | 0.71 | 0.19 to 1.79 |
| Da Dalt 200683 | 3803 | 23.8 | 87.1 | 25.8 | 12.8 to 42.4 | 87.1 | 86.0 to 88.2 | 0.852 | 0.661 to 1.002 | 2.00 | 0.99 to 3.32 |
| Dunning 200630 | 22,772 | 40.9 | 89.4 | 40.3 | 34.7 to 46.1 | 89.4 | 89.0 to 89.8 | 0.668 | 0.603 to 0.731 | 3.80 | 3.26 to 4.38 |
| Atabaki 200881 | 1000 | 26.2 | 66.3 | 27.1 | 17.9 to 37.8 | 66.4 | 63.4 to 69.4 | 1.098 | 0.932 to 1.248 | 0.81 | 0.53 to 1.14 |
| Guzel 200987 | 337 | 25.4 | 54.8 | 26.7 | 17.6 to 37.1 | 55.5 | 49.6 to 61.3 | 1.321 | 1.101 to 1.557 | 0.60 | 0.39 to 0.86 |
| Kupperman 200990 | 31,476 | 35.5 | 87.5 | 35.2 | 29.8 to 40.9 | 87.5 | 87.1 to 87.9 | 0.740 | 0.676 to 0.803 | 2.82 | 2.38 to 3.28 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 14 | < 0.001 | < 0.001 | 30.9 | 21.6 to 40.1 | 76.0 | 68.1 to 83.8 | 0.910 | 0.774 to 1.059 | 1.29 | 0.85 to 1.99 | |
Undefined or mixed amnesia (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Dietrich 199384 | 159 | 87.1 | 45.3 | 77.7 | 54.5 to 90.9 | 44.9 | 36.4 to 53.5 | 0.497 | 0.201 to 1.059 | 1.41 | 0.96 to 1.78 |
| Ramundo 1995135 | 178 | 56.3 | 49.4 | 54.3 | 34.9 to 74.3 | 49.9 | 42.3 to 57.5 | 0.915 | 0.512 to 1.346 | 1.08 | 0.69 to 1.53 |
| Schunk 1996137 | 313 | 22.9 | 80.3 | 28.8 | 12.2 to 48.3 | 80.6 | 75.9 to 84.8 | 0.884 | 0.643 to 1.097 | 1.48 | 0.62 to 2.58 |
| Fridriksson 2000130 | 49 | 31.8 | 74.1 | 33.8 | 18.7 to 51.0 | 76.3 | 59.8 to 88.5 | 0.869 | 0.638 to 1.165 | 1.42 | 0.68 to 3.01 |
| Ng 2002134 | 119 | 15.4 | 87.0 | 17.9 | 10.0 to 28.6 | 88.5 | 78.9 to 94.8 | 0.929 | 0.794 to 1.072 | 1.56 | 0.68 to 3.82 |
| Reed 2005136 | 39 | 20.0 | 100.0 | 17.2 | 4.6 to 38.9 | 96.7 | 88.2 to 99.6 | 0.863 | 0.643 to 0.987 | 5.05 | 1.22 to 39.56 |
| Dunning 200630 | 22,772 | 24.6 | 97.1 | 23.8 | 19.0 to 29.0 | 97.1 | 96.9 to 97.3 | 0.785 | 0.731 to 0.835 | 8.20 | 6.46 to 10.16 |
| Atabaki 200881 | 1000 | 23.1 | 67.8 | 26.5 | 16.6 to 39.5 | 68.0 | 65.0 to 71.0 | 1.081 | 0.886 to 1.236 | 0.83 | 0.52 to 1.25 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 8 | < 0.001 | < 0.001 | 33.4 | 17.8 to 52.4 | 81.4 | 63.1 to 93.3 | 0.821 | 0.642 to 0.998 | 1.82 | 1.00 to 3.74 | |
Severe or persistent headache (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Reed 2005136 | 39 | 0.0 | 75.9 | 20.4 | 13.8 to 29.2 | 80.6 | 64.8 to 92.2 | 0.994 | 0.876 to 1.206 | 1.17 | 0.58 to 2.19 |
| Da Dalt 200683 | 3800 | 25.0 | 98.1 | 11.1 | 8.5 to 14.0 | 98.1 | 97.6 to 98.5 | 0.907 | 0.878 to 0.933 | 5.80 | 4.27 to 7.73 |
| Dunning 200630 | 22,772 | 6.0 | 99.7 | 7.0 | 4.5 to 10.0 | 99.7 | 99.6 to 99.7 | 0.933 | 0.904 to 0.958 | 20.26 | 12.56 to 30.44 |
| Oman 200691 | 1666 | 20.0 | 85.0 | 19.3 | 13.9 to 25.4 | 85.0 | 83.2 to 86.8 | 0.949 | 0.876 to 1.016 | 1.29 | 0.92 to 1.74 |
| Kupperman 200990 | 26,494 | 12.7 | 97.0 | 12.4 | 9.8 to 15.3 | 97.0 | 96.8 to 97.2 | 0.903 | 0.873 to 0.929 | 4.19 | 3.29 to 5.20 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 5 | < 0.001 | < 0.001 | 13.5 | 7.8 to 21.5 | 94.9 | 81.8 to 99.3 | 0.916 | 0.872 to 0.986 | 4.35 | 1.07 to 12.35 | |
Radiological skull fracture (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Chan 1990212 | 418 | 100.0 | 96.8 | 43.9 | 38.5 to 51.5 | 96.5 | 94.4 to 98.0 | 0.583 | 0.506 to 0.635 | 12.43 | 8.03 to 21.53 |
| Quayle 199794 | 321 | 51.9 | 87.8 | 49.0 | 43.2 to 55.5 | 87.8 | 83.8 to 91.3 | 0.581 | 0.509 to 0.649 | 4.04 | 3.01 to 5.57 |
| Mandera 2000133 | 166 | 51.7 | 32.1 | 59.5 | 49.9 to 68.8 | 33.7 | 25.2 to 43.0 | 1.199 | 0.849 to 1.725 | 0.90 | 0.73 to 1.10 |
| Wang 2000140 | 157 | 46.7 | 88.2 | 48.7 | 42.7 to 55.1 | 88.5 | 82.3 to 93.2 | 0.581 | 0.512 to 0.652 | 4.24 | 2.79 to 6.90 |
| Boran 2006128 | 421 | 43.2 | 93.0 | 46.4 | 41.0 to 52.2 | 93.1 | 90.2 to 95.3 | 0.577 | 0.517 to 0.634 | 6.67 | 4.77 to 9.7 |
| Dunning 200630 | 22,772 | 34.9 | 99.3 | 37.0 | 31.7 to 42.4 | 99.3 | 99.2 to 99.4 | 0.635 | 0.581 to 0.688 | 51.58 | 41.74 to 63.64 |
| Keskil 1995132 | 257 | 70.0 | 61.2 | 55.4 | 47.5 to 64.2 | 61.2 | 54.8 to 67.4 | 0.728 | 0.580 to 0.879 | 1.43 | 1.16 to 1.77 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 7 | < 0.001 | < 0.001 | 48.4 | 40.8 to 57.3 | 89.3 | 67.7 to 97.3 | 0.585 | 0.516 to 0.708 | 4.55 | 1.64 to 15.73 | |
Post-trauma seizure (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Davis 1994129 | 168 | 8.3 | 96.2 | 6.9 | 3.4 to 11.5 | 96.6 | 93.4 to 98.6 | 0.965 | 0.904 to 1.023 | 2.49 | 0.64 to 7.08 |
| Haydel 200388 | 175 | 0.0 | 96.3 | 6.7 | 3.3 to 11.2 | 96.4 | 93.2 to 98.6 | 0.968 | 0.908 to 1.026 | 2.32 | 0.60 to 6.51 |
| Boran 2006128 | 421 | 13.5 | 99.7 | 13.5 | 6.4 to 23.3 | 99.4 | 98.6 to 99.9 | 0.870 | 0.770 to 0.943 | 39.81 | 6.41 to 164.30 |
| Da Dalt 200683 | 3803 | 13.6 | 99.4 | 12.9 | 6.3 to 22.3 | 99.4 | 99.2 to 99.6 | 0.876 | 0.781 to 0.943 | 23.20 | 9.59 to 47.78 |
| Oman 200691 | 1666 | 6.0 | 94.0 | 5.4 | 2.7 to 9.1 | 94.1 | 92.9 to 95.2 | 1.006 | 0.965 to 1.038 | 0.92 | 0.45 to 1.61 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 5 | 0.493 | 0.810 | 8.7 | 4.2 to 15.7 | 98.0 | 94.5 to 99.6 | 0.932 | 0.849 to 1.004 | 8.49 | 0.93 to 31.66 | |
Scalp laceration (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Davis 1994129 | 168 | 41.7 | 84.0 | 12.3 | 3.8 to 56.2 | 86.4 | 79.4 to 90.7 | 1.001 | 0.521 to 1.114 | 0.99 | 0.31 to 3.85 |
| Reed 2005136 | 39 | 0.0 | 96.6 | 5.7 | 0.0 to 14.9 | 90.6 | 86.0 to 97.5 | 1.045 | 0.946 to 1.108 | 0.54 | 0.00 to 1.58 |
| Atabaki 200881 | 1000 | 3.1 | 89.7 | 6.0 | 1.1 to 13.5 | 89.5 | 87.5 to 91.4 | 1.050 | 0.966 to 1.107 | 0.57 | 0.11 to 1.31 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 3 | 0.002 | 0.051 | 7.4 | 0.1 to 33.7 | 89.1 | 83.0 to 94.7 | 1.040 | 0.782 to 1.107 | 0.67 | 0.02 to 2.27 | |
Scalp haematoma (intracranial injury – children)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Davis 1994129 | 168 | 25.0 | 84.0 | 33.6 | 15.6 to 52.3 | 81.7 | 75.4 to 87.4 | 0.813 | 0.591 to 1.017 | 1.86 | 0.92 to 3.07 |
| Reed 2005136 | 39 | 20.0 | 72.4 | 41.3 | 21.1 to 56.4 | 75.6 | 64.7 to 85.3 | 0.775 | 0.618 to 0.968 | 1.71 | 1.12 to 2.46 |
| Oman 200691 | 1666 | 59.0 | 63.0 | 57.6 | 49.7 to 65.3 | 63.3 | 60.8 to 65.7 | 0.670 | 0.548 to 0.796 | 1.57 | 1.34 to 1.80 |
| Atabaki 200881 | 1000 | 43.1 | 73.5 | 45.2 | 35.5 to 54.2 | 73.5 | 70.7 to 76.2 | 0.747 | 0.625 to 0.875 | 1.71 | 1.34 to 2.08 |
| Guzel 200987 | 337 | 56.7 | 68.9 | 52.2 | 44.4 to 60.2 | 68.4 | 63.5 to 73.2 | 0.699 | 0.596 to 0.799 | 1.66 | 1.41 to 1.94 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 5 | < 0.001 | < 0.001 | 45.4 | 27.0 to 57.6 | 73.1 | 64.9 to 82.5 | 0.745 | 0.615 to 0.918 | 1.70 | 1.30 to 2.23 | |
Need for neurosurgery in children
Glasgow Coma Scale < 15 (neurosurgery – children)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Hahn 1993131 | 791 | 41.8 | 70.4 | 41.8 | 30.6 to 53.8 | 70.4 | 67.0 to 73.7 | 0.826 | 0.597 to 1.144 | 1.41 | 0.95 to 2.10 |
| Stein 1995139 | 751 | 54.2 | 78.5 | 54.2 | 34.6 to 72.5 | 78.5 | 75.4 to 81.4 | 0.584 | 0.321 to 1.060 | 2.52 | 1.43 to 4.44 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.298 | < 0.001 | 45.1 | 35.1 to 55.4 | 74.3 | 72.0 to 76.5 | 0.763 | 0.573 to 1.015 | 1.71 | 1.24 to 2.36 | |
Glasgow Coma Scale < 14 (neurosurgery – children)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Hahn 1993131 | 791 | 23.9 | 85.9 | 23.9 | 15.2 to 35.5 | 85.9 | 83.2 to 88.3 | 0.886 | 0.666 to 1.179 | 1.70 | 1.00 to 2.87 |
| Stein 1995139 | 751 | 25.0 | 93.1 | 25.0 | 11.7 to 45.6 | 93.1 | 91.0 to 94.7 | 0.805 | 0.504 to 1.286 | 3.64 | 1.56 to 8.48 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.912 | < 0.001 | 24.2 | 16.5 to 34.0 | 88.9 | 87.2 to 90.5 | 0.863 | 0.677 to 1.102 | 2.10 | 1.34 to 3.28 | |
Any seizure (neurosurgery – children)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Schunk 1996137 | 33.3 | 92.3 | 33.3 | 4.3 to 84.6 | 92.3 | 88.7 to 94.8 | 0.723 | 0.324 to 1.610 | 4.31 | 0.83 to 22.33 |
Post-trauma seizure (neurosurgery – children)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Haydel 200388 | 0.0 | 96.3 | 8.3 | 0.5 to 62.2 | 96.3 | 92.0 to 98.3 | 0.952 | 0.924 to 0.982 | 0.09 | 0.01 to 1.38 |
Any loss of consciousness (neurosurgery – children)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Schunk 1996137 | 0.0 | 73.9 | 16.7 | 1.0 to 80.6 | 73.9 | 68.7 to 78.5 | 1.128 | 0.054 to 23.748 | 0.64 | 0.03 to 13.43 |
Any headache (neurosurgery – children)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schunk 1996137 | 313 | 33.3 | 70.0 | 33.3 | 4.3 to 84.6 | 70.0 | 64.7 to 74.8 | 0.952 | 0.192 to 4.727 | 1.11 | 0.22 to 5.56 |
| Haydel 200388 | 175 | 83.3 | 66.9 | 83.3 | 36.9 to 97.7 | 66.9 | 59.4 to 73.5 | 0.249 | 0.172 to 0.362 | 2.51 | 1.66 to 3.82 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.161 | 0.479 | 64.2 | 26.6 to 89.9 | 68.9 | 64.6 to 72.9 | 0.267 | 0.186 to 0.384 | 2.39 | 1.60 to 3.58 | |
Undefined vomiting (neurosurgery – children)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Schunk 1996137 | 313 | 66.7 | 65.5 | 66.7 | 15.4 to 95.7 | 65.5 | 60.0 to 70.6 | 0.509 | 0.228 to 1.138 | 1.93 | 0.48 to 7.82 |
| Haydel 200388 | 175 | 50.0 | 81.7 | 50.0 | 16.8 to 83.2 | 81.7 | 75.1 to 86.8 | 0.612 | 0.274 to 1.367 | 2.73 | 0.83 to 8.92 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.638 | < 0.001 | 55.3 | 24.6 to 82.4 | 70.4 | 66.1 to 74.4 | 0.558 | 0.316 to 0.986 | 2.36 | 0.96 to 5.83 | |
Undefined or mixed amnesia (neurosurgery – children)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Schunk 1996137 | 0.0 | 80.0 | 16.7 | 1.0 to 80.6 | 80.0 | 75.2 to 84.1 | 1.042 | 0.049 to 21.976 | 0.83 | 0.04 to 17.58 |
Radiological skull fracture (neurosurgery – children)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Hahn 1993131 | 73.1 | 53.3 | 73.1 | 61.3 to 82.4 | 53.3 | 49.7 to 56.9 | 0.504 | 0.337 to 0.752 | 1.57 | 1.33 to 1.85 |
Intracranial injury in infants
Fall – any (intracranial injury – infants)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Ramundo 1995135 | 37 | 62.5 | 20.7 | 62.5 | 28.5 to 87.5 | 20.7 | 9.6 to 39.0 | 1.813 | 0.743 to 4.423 | 0.79 | 0.45 to 1.39 |
| Buchanich 200782 | 97 | 68.2 | 25.3 | 68.2 | 46.6 to 84.0 | 25.3 | 16.8 to 36.3 | 1.256 | 0.776 to 2.034 | 0.91 | 0.67 to 1.25 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.771 | 0.620 | 66.6 | 48.3 to 81.0 | 24.1 | 16.8 to 33.3 | 1.365 | 0.893 to 2.085 | 0.88 | 0.67 to 1.16 | |
Coagulopathy (intracranial injury – infants)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Oman 200691 | 4.0 | 97.0 | 4.0 | 0.6 to 23.5 | 97.0 | 94.2 to 98.5 | 0.990 | 0.911 to 1.075 | 1.33 | 0.17 to 10.16 |
Motor vehicle collision – in car (intracranial injury – infants)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Ramundo 1995135 | 25.0 | 93.1 | 25.0 | 6.3 to 62.3 | 93.1 | 76.2 to 98.3 | 0.806 | 0.533 to 1.216 | 3.63 | 0.60 to 21.86 |
Persistent vomiting (intracranial injury – infants)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Oman 200691 | 13.0 | 87.0 | 13.0 | 4.5 to 32.4 | 87.0 | 82.6 to 90.4 | 1.000 | 0.296 to 3.373 | 1.00 | 0.30 to 3.37 |
Glasgow Coma Scale < 15 (intracranial injury – infants)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Ramundo 1995135 | 37 | 50.0 | 82.8 | 52.0 | 38.0 to 68.7 | 84.0 | 69.2 to 93.2 | 0.574 | 0.404 to 0.719 | 3.30 | 1.82 to 6.33 |
| Oman 200691 | 309 | 72.0 | 58.1 | 67.9 | 49.0 to 84.3 | 58.4 | 52.6 to 64.0 | 0.551 | 0.268 to 0.885 | 1.63 | 1.15 to 2.13 |
| Kupperman 200990 | 10,718 | 33.7 | 96.0 | 34.6 | 25.5 to 44.3 | 96.0 | 95.6 to 96.4 | 0.682 | 0.580 to 0.776 | 8.62 | 6.29 to 11.24 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 3 | 0.004 | < 0.001 | 51.9 | 34.4 to 75.8 | 84.5 | 45.8 to 95.2 | 0.586 | 0.377 to 0.791 | 3.38 | 1.24 to 8.02 | |
Focal neurological deficit (intracranial injury – infants)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Dietrich 199384 | 33.3 | 97.1 | 33.3 | 4.3 to 84.6 | 97.1 | 89.0 to 99.3 | 0.687 | 0.043 to 11.098 | 11.33 | 0.70 to 183.11 |
Radiological skull fracture (intracranial injury – infants)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Greenes 200186 | 422 | 100.0 | 92.2 | 96.2 | 59.7 to 99.8 | 92.2 | 89.1 to 94.4 | 0.042 | 0.037 to 0.047 | 12.29 | 8.66 to 17.44 |
| Buchanich 200782 | 97 | 59.1 | 48.0 | 59.1 | 38.2 to 77.2 | 48.0 | 37.0 to 59.2 | 0.852 | 0.560 to 1.297 | 1.14 | 0.75 to 1.71 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.058 | < 0.001 | 64.7 | 44.8 to 80.5 | 81.4 | 76.8 to 85.3 | 0.051 | 0.046 to 0.057 | 4.51 | 3.45 to 5.88 | |
Depressed skull fracture (intracranial injury – infants)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Ramundo 1995135 | 25.0 | 100.0 | 25.0 | 6.3 to 62.3 | 98.3 | 78.0 to 99.9 | 0.763 | 0.510 to 1.142 | 14.50 | 0.72 to 290.82 |
Any seizure (intracranial injury – infants)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Dietrich 199384 | 71 | 0.0 | 100.0 | 16.7 | 1.0 to 80.6 | 100.0 | 89.3 to 100.0 | 1.000 | 0.080 to 12.564 | 22.67 | 0.54 to 959.56 |
| Ramundo 1995135 | 37 | 12.5 | 79.3 | 12.5 | 1.7 to 53.7 | 79.3 | 61.0 to 90.4 | 1.103 | 0.175 to 6.966 | 0.60 | 0.08 to 4.32 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.858 | 0.017 | 13.7 | 2.8 to 47.2 | 84.3 | 69.5 to 92.7 | 1.066 | 0.240 to 4.730 | 1.32 | 0.23 to 7.55 | |
Any loss of consciousness (intracranial injury – infants)
| Study | n | Observed estimates | Posterior median estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Dietrich 199384 | 58 | 50.0 | 83.9 | 37.8 | 25.4 to 54.1 | 84.1 | 73.3 to 92.0 | 0.741 | 0.576 to 0.873 | 2.41 | 1.47 to 4.07 |
| Ramundo 1995135 | 31 | 16.7 | 64.0 | 47.1 | 31.9 to 65.3 | 69.7 | 49.7 to 85.0 | 0.759 | 0.519 to 1.075 | 1.57 | 0.90 to 2.85 |
| Oman 200691 | 309 | 64.0 | 68.0 | 49.1 | 34.0 to 67.5 | 67.6 | 62.0 to 72.9 | 0.754 | 0.480 to 0.986 | 1.52 | 1.03 to 2.17 |
| Kupperman 200990 | 10,215 | 19.5 | 96.4 | 21.9 | 13.6 to 31.4 | 96.4 | 96.1 to 96.8 | 0.810 | 0.711 to 0.896 | 6.15 | 3.77 to 8.92 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 4 | < 0.001 | < 0.001 | 39.4 | 20.6 to 65.2 | 84.1 | 56.2 to 95.5 | 0.730 | 0.519 to 0.901 | 2.51 | 1.23 to 5.28 | |
Undefined vomiting (intracranial injury – infants)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Dietrich 199384 | 71 | 0.0 | 79.4 | 16.7 | 1.0 to 80.6 | 79.4 | 68.2 to 87.4 | 1.259 | 0.394 to 4.027 | 0.81 | 0.05 to 13.59 |
| Ramundo 1995135 | 37 | 12.5 | 79.3 | 12.5 | 1.7 to 53.7 | 79.3 | 61.0 to 90.4 | 1.103 | 0.473 to 2.571 | 0.60 | 0.07 to 5.02 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.858 | 0.991 | 13.7 | 2.8 to 47.2 | 79.4 | 70.2 to 86.3 | 1.155 | 0.583 to 2.289 | 0.67 | 0.12 to 3.65 | |
Post-trauma seizure (intracranial injury – infants)
| Study | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | |
| Oman 200691 | 8.0 | 91.0 | 8.0 | 2.0 to 26.9 | 91.0 | 87.1 to 93.8 | 1.011 | 0.896 to 1.141 | 0.89 | 0.22 to 3.53 |
Scalp haematoma (intracranial injury – infants)
| Study | n | Observed estimates | Fixed-effects estimatesa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivityb | Specificityb | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| Oman 200691 | 309 | 65.0 | 59.0 | 65.0 | 44.9 to 80.9 | 59.0 | 53.2 to 64.6 | 0.593 | 0.438 to 0.804 | 1.59 | 1.15 to 2.18 |
| Kupperman 200990 | 10,659 | 66.0 | 56.0 | 66.0 | 56.0 to 74.7 | 56.0 | 55.0 to 56.9 | 0.608 | 0.526 to 0.702 | 1.50 | 1.30 to 1.73 |
| No. of studies | Heterogeneity test p-valuec | Pooled estimates | |||||||||
| Sensitivity | Specificity | Sensitivity | 95% HDR | Specificity | 95% HDR | NLR | 95% HDR | PLR | 95% HDR | ||
| 2 | 0.927 | 0.312 | 65.8 | 56.9 to 73.6 | 56.1 | 55.1 to 57.0 | 0.605 | 0.531 to 0.689 | 1.51 | 1.33 to 1.73 | |
Appendix 7 Management practices review – PRISMA (adapted) flow chart
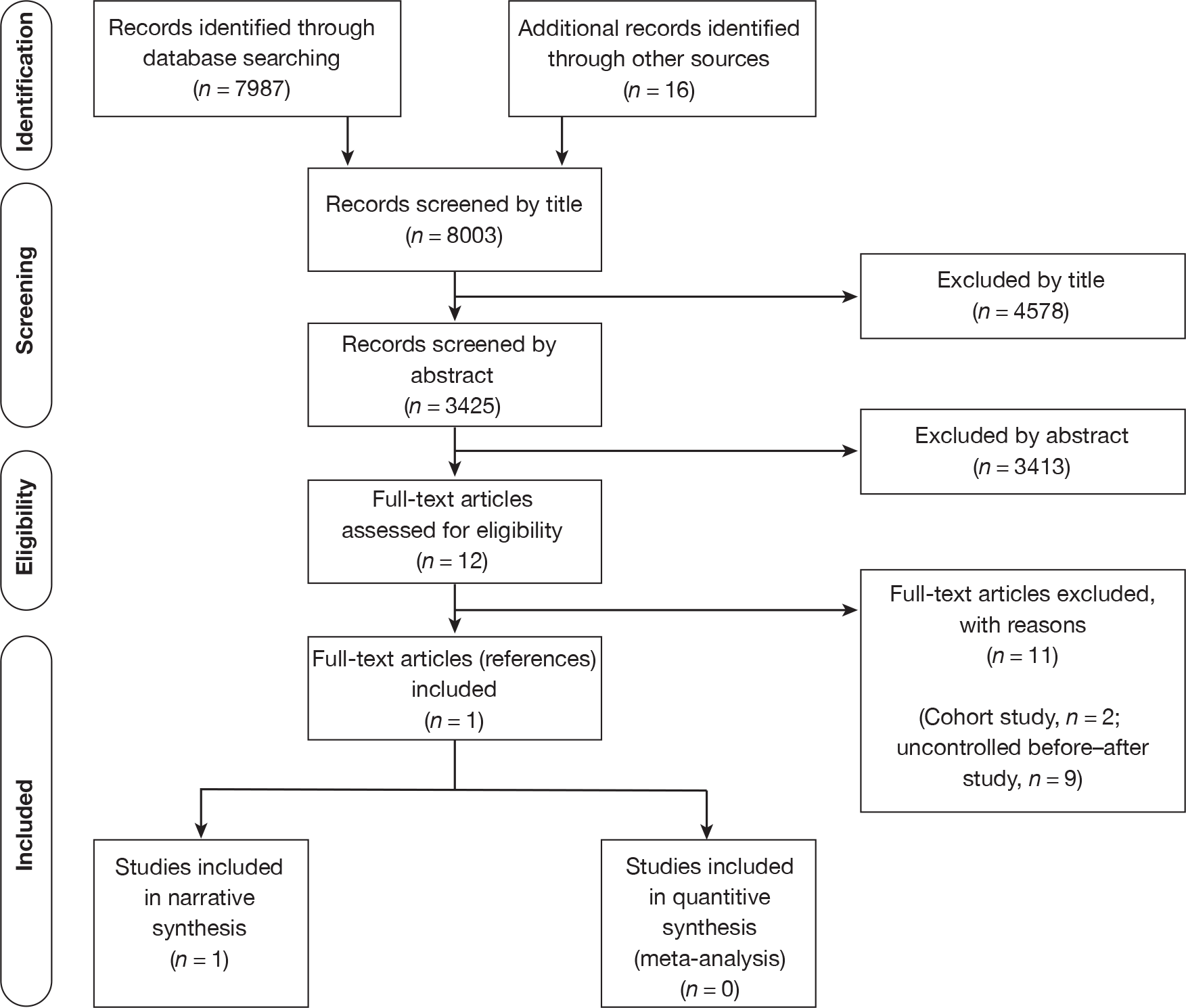
Appendix 8 Management practices review – table of excluded studies with rationale
| Author, year | Reason for exclusion |
|---|---|
| Brown et al. 1994152 | Cohort study |
| Fabbri et al. 2004153 | Cohort study |
| Browning et al. 2005154 | Before–after study without concurrent control group |
| Fong et al. 2008155 | Before–after study without concurrent control group |
| Hassan et al. 200522 | Before–after study without concurrent control group |
| Kerr et al. 2005156 | Before–after study without concurrent control group |
| Loroni et al. 1996157 | Before–after study without concurrent control group |
| Reed et al. 2005136 | Before–after study without concurrent control group |
| Shravat et al. 2006158 | Before–after study without concurrent control group |
| Sultan et al. 200421 | Before–after study without concurrent control group |
| Thomson et al. 1994159 | Before–after study without concurrent control group |
Appendix 9 Cost-effectiveness review: literature search strategies – a MEDLINE example
Database searched: Ovid MEDLINE(R) In-Process and Other Non-Indexed Citations and Ovid MEDLINE(R)
Platform or provider used: OvidSP
Date of coverage: 1950 to March 2010
Search undertaken: initial search 20 April 2009
Updated search: 11 March 2010
-
*Craniocerebral Trauma/
-
head injur$.tw.
-
1 or 2
-
Economics/
-
“costs and cost analysis”/
-
Cost allocation/
-
Cost–benefit analysis/
-
Cost control/
-
Cost savings/
-
Cost of illness/
-
1Cost sharing/
-
“deductibles and coinsurance”/
-
Medical savings accounts/
-
Health care costs/
-
Direct service costs/
-
Drug costs/
-
Employer health costs/
-
Hospital costs/
-
Health expenditures/
-
Capital expenditures/
-
Value of life/
-
exp economics, hospital/
-
exp economics, medical/
-
Economics, nursing/
-
Economics, pharmaceutical/
-
exp “fees and charges”/
-
exp budgets/
-
(low adj cost).mp.
-
(high adj cost).mp.
-
(health?care adj cost$).mp.
-
(fiscal or funding or financial or finance).tw.
-
(cost adj estimate$).mp.
-
(cost adj variable).mp.
-
(unit adj cost$).mp.
-
(economic$or pharmacoeconomic$or price$or pricing).tw.
-
4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35
-
3 and 36
Appendix 10 Cost-effectiveness review – PRISMA (adapted) flow chart
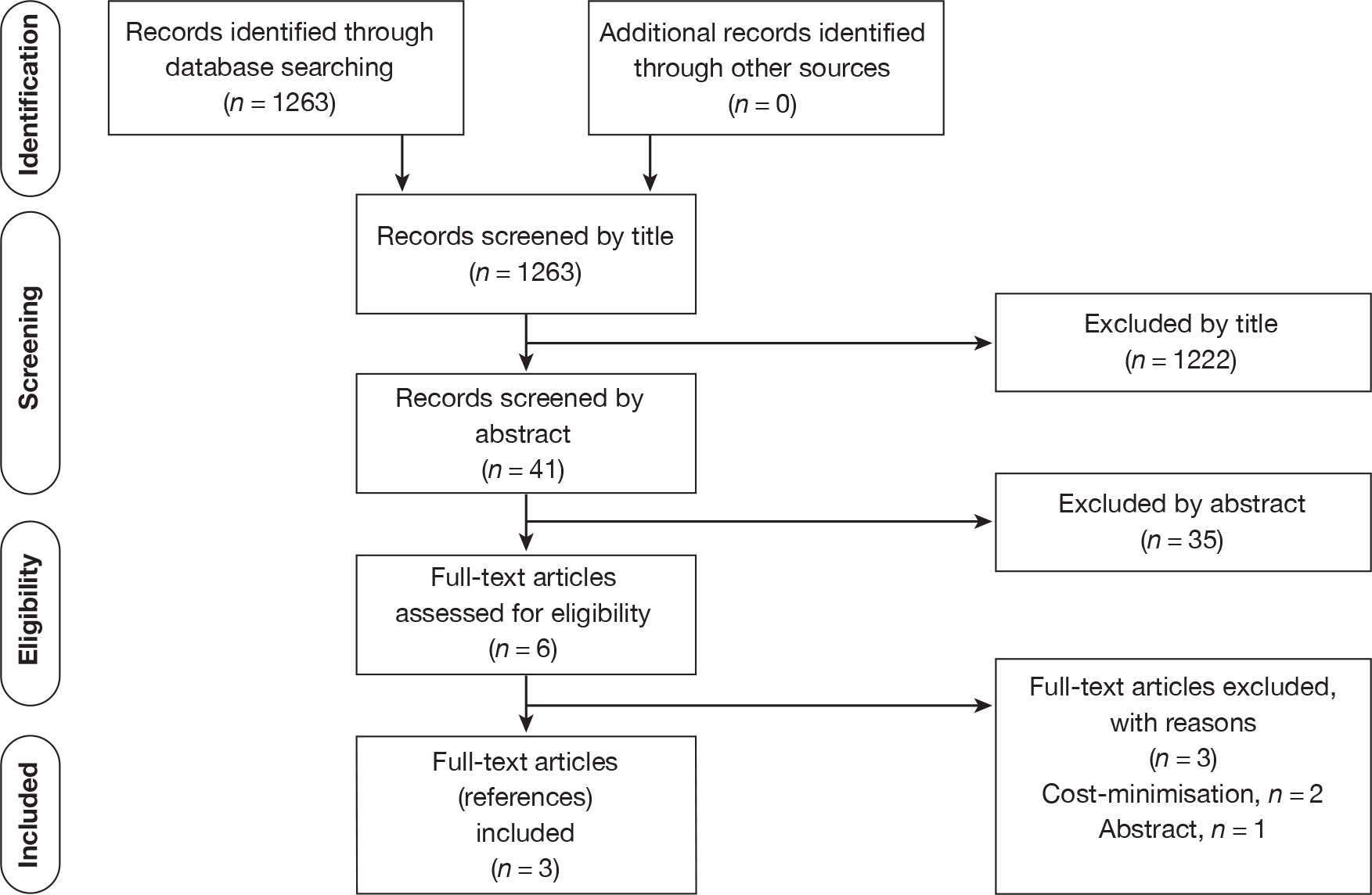
Appendix 11 Cost-effectiveness review – table of excluded studies with rationale
Appendix 12 Questionnaire survey (adults) sent to lead clinician
| 1. What guidelines, if any, do you use to assess, investigate and manage MHI in adults? | |||
| NICE clinical guidelines | [ ] | If NICE clinical guidelines, please clarify | |
| NICE 2007 | [ ] | ||
| NICE 2003 | [ ] | ||
| No guidelines | [ ] | ||
| Other | [ ] | If ‘Other’, please could you enclose a copy | |
| 2. If these are formal guidelines, have you made amendments for local use? Please only tick yes if you have amended the actual guidelines, not simply formatting or presentation. | |||
| Yes [ ] | No [ ] | If yes, please could you enclose a copy | |
| 3. Do you have access to a CT head scan for head injured patients ( adults ) within 4 hours at any time (24 hours per day, 7 days per week) of presentation? | |||
| Yes [ ] | No [ ] | If no, please state what restrictions apply | |
| 4a. Where are MHI patients ( adults ) admitted in hospital? | |||
| CDU | [ ] | ||
| accident and emergency observation | [ ] | ||
| formal admission | [ ] | ||
| 4b. Who are they admitted under? | |||
| accident and emergency staff | [ ] | ||
| inpatient team | [ ] | ||
| 4c. Who has to approve admission? | |||
| any doctor | [ ] | ||
| senior doctor | [ ] | ||
| specialist | [ ] | ||
Appendix 13 Protocol
Project title
The cost-effectiveness of investigation and hospital admission for minor (Glasgow Coma Scale 13–15) head injury.
Planned investigation
Research objectives
We aim to identify the optimal strategy for managing adults and children with minor [Glasgow Coma Scale (GCS) 13–15] head injury. Our specific objectives are to:
-
estimate the diagnostic accuracy of clinical assessment, clinical decision rules, skull radiography, cranial computerised tomography (CT) and inpatient observation for identifying intracranial bleeding requiring neurosurgery in adults and children with minor (GCS 13–15) head injury
-
estimate the cost-effectiveness of diagnostic strategies for minor head injury (MHI), in terms of the cost per quality-adjusted life-year (QALY) gained by each strategy
-
identify the optimal strategy for managing MHI in the NHS, defined as the most cost-effective strategy at the National Institute for Health and Clinical Excellence (NICE) threshold for willingness to pay per QALY gained
-
identify the critical areas of uncertainty in the management of MHI, where future primary research would produce the most benefit.
Existing research
Head injury is responsible for around 700,000 emergency department (ED) attendances per year in England and Wales, most of which (90%) will be minor (GCS 13–15) and will not need immediate neurosurgical intervention or inpatient care. 1 These patients have a small (< 1%), but important risk of subsequent deterioration due to intracranial bleeding. If these cases are recognised and treated early then a full recovery can be expected; if not then severe disability or death may ensue.
Potential diagnostic management strategies for MHI typically use a combination of clinical assessment, skull radiography, CT scanning and hospital admission for observation to detect intracranial bleeding. The choice of strategy will have substantial cost implications for the NHS because it will be applied to hundreds of thousands of patients each year. Only a small proportion of patients will have intracranial bleeding, but those who do have a huge potential to benefit from early diagnosis and treatment.
Guidelines for managing head injury were drawn up by NICE in 20031 and revised in 2007. 2 These guidelines were based upon literature review and expert consensus. Cost-effectiveness analysis was not used to develop the guidelines, but was used to explore the potential impact upon health service costs. The guidelines were expected to potentially reduce costs, but recent data (outlined below) suggest that costs may have substantially increased. Additional expenditure on MHI may represent a worthwhile use of NHS resources but there are currently no relevant analyses to support this. An extensive evidence synthesis and economic evaluation is thus needed to inform future NICE guidance.
Clinical assessment can be used to identify patients with an increased risk of intracranial bleeding and select patients for imaging or admission. A recent meta-analysis of 35 studies reporting data from 83,636 adults with head injury3 found that severe headache (relative risk 2.44), nausea (2.16), vomiting (2.13), loss of consciousness (LOC) (2.29), amnesia (1.32), post-traumatic seizure (PTS) (3.24), old age (3.70), male gender (1.26), fall from a height (1.61), pedestrian crash victim (1.70), abnormal GCS score (5.58), focal neurology (1.80) and evidence of alcohol intake (1.62) were all associated with intracranial bleeding. A similar analysis of 16 studies reporting data from 22,420 children with head injury4 found that focal neurology (9.43), LOC (2.23) and abnormal GCS score (5.51) were associated with intracranial bleeding.
Clinical features have been combined in a number of studies to develop a structured clinical decision rule. A systematic review undertaken for the NICE guidance1 identified four studies of four different clinical decision rules. The studies of the Canadian CT rule5 and the New Orleans rule6 were both high quality, applicable to the NHS and reported 100% sensitivity for the need for neurosurgical intervention. The other two studies,7,8 respectively, reported poor sensitivity and were not applicable to the NHS.
Several further studies have been published and new rules developed since the NICE review. A comparison of the Canadian CT and New Orleans rules undertaken by the researchers who developed the Canadian rule9 showed that both rules had 100% sensitivity for predicting neurosurgical intervention and clinically important brain injury, but the Canadian rule had higher specificity (76.3% vs 12.1% and 50.6% vs 12.7%). A comparison by an independent team10 found that both rules had 100% sensitivity for neurosurgical intervention, but the New Orleans rule had higher sensitivity for clinically significant brain injury (99.4% vs 87.2%), while the Canadian rule had higher specificity (39.7% vs 5.6%). This team also developed a new rule, the CT in Head Injury Patients (CHIP) rule, with 100% sensitivity and 30% specificity for neurosurgical intervention. 11
New rules have also been developed for children with head injury. The National Emergency X-Radiography Utilization Study II (NEXUS II) rule, was developed and shown to have 98.6% sensitivity and 15.1% specificity for significant ICI,12 whereas the Children’s Head injury Algorithm for the prediction of Important Clinical Events (CHALICE) rule had 98.6% sensitivity and 86.9% specificity. 13 The striking difference in specificity may be due to the use of broader selection criteria in the CHALICE study (and thus lower prevalence). Both studies had similar positive predictive value (9.5% vs 8.6%) and negative predictive value (99.1% vs 99.9%).
Skull radiography can identify fractures that are associated with a substantially increased risk of intracranial bleeding, but cannot identify intracranial bleeding itself. Skull radiography is therefore used as a screening tool to select patient for investigation or admission, but not for definitive imaging. A meta-analysis14 found that skull fracture detected on radiograph had a sensitivity of 38% and specificity of 95% for intracranial bleeding. More recent meta-analyses in adults3 and children4 reported relative risks of 4.08 and 6.13, respectively, for the association between skull fracture and intracranial bleeding.
Computerised tomography definitively shows significant bleeding and a normal CT scan effectively excludes a significant bleed at the time of scanning. MRI scanning can detect some lesions that are not evident on CT,15 but arguably none that is of clinical importance and certainly none that influences early management. CT can therefore be considered a reference standard investigation for detecting injuries of immediate clinical importance.
Hospital admission and observation may be used to identify intracranial bleeding by monitoring the patient for neurological deterioration. Although commonly used in the past, the effectiveness of this approach has not been studied extensively and has the disadvantage that neurosurgical intervention is delayed until after patient deterioration has occurred. Hospital admission and observation are usually used selectively, based upon clinical assessment or skull radiography findings.
Theoretically, patients without intracranial bleeding on their CT scan do not require hospital admission. In practice, however, patients may be admitted for a number of reasons (1) CT scanning may identify abnormalities, such as minor cerebral contusions, which do not require neurosurgery and are of uncertain significance, but prompt hospital admission; (2) patients may be admitted pending CT scanning because they are deemed to need imaging but are unable to have imaging, either due to lack of availability or lack of ability to cooperate; and (3) patients may be admitted despite a normal CT because of concern about continuing symptoms, such as severe headache or vomiting, or with drug or alcohol intoxication.
Studies have compared CT-based strategies to skull radiography and/or admission to conclude that CT-based strategies are more likely to detect intracranial bleeding and less likely to require hospital admission. 16,17 Cost analyses based upon trial data18 and modelling19 both suggest that a CT-based strategy is cheaper. However, admission-based strategies may be an inappropriate comparator for cost-effectiveness analysis because they appear to be expensive and ineffective, particularly if applied unselectively.
Computerised tomography may be used unselectively (in all patients) or selectively, based upon clinical assessment or a decision rule. A strategy of CT scanning all patients would clearly be very effective, but would have a low yield of positive results and would be expensive. The more selective the use of investigations or admission the cheaper the strategy, but the higher the risk of missed pathology. Cost-effectiveness analysis is therefore necessary to determine what level of investigation represents the most efficient use of health-care resources.
A study from the USA20 used decision analysis modelling to examine the cost-effectiveness of strategies for managing MHI and concluded that strategies involving selective CT use or CT for all, followed by discharge if negative, were cost-effective, whereas admission-based strategies were not. There was only limited exploration of uncertainty, particularly around the estimate of the effect of early versus delayed neurosurgery, and it is not clear whether the results are applicable to the NHS.
Despite the economic importance of MHI there has been little evaluation of cost-effectiveness in the NHS. Recent NICE head injury guidance was based upon the Canadian CT head rule9 and was anticipated to lead to more CT scans being performed, but fewer skull radiographs and admissions. A cost analysis1 suggested that the guidelines would be cost saving, by virtue of decreasing skull radiography and admissions while increasing CT scanning. Patient outcomes were not examined and the discussion cautioned that the assumption that increased CT scanning would reduce admissions might not hold in practice.
Data from a number of studies have since confirmed that more CT scans are being performed and less skull radiography is being undertaken. 21–23 However, Hospital Episode Statistics (HES) for England show that the annual number of admissions for head injury has increased from 114,769 in 2001–2 to 155,996 in 2006–7. As average length of stay has remained relatively constant, bed-days have increased from 348,032 in 2001–2 to 443,593 in 2006–7. As Figure 1 shows, the increase in admissions has been seen in adults rather than children. 24
FIGURE 1.
Head injury admissions in England, 1998–2007.
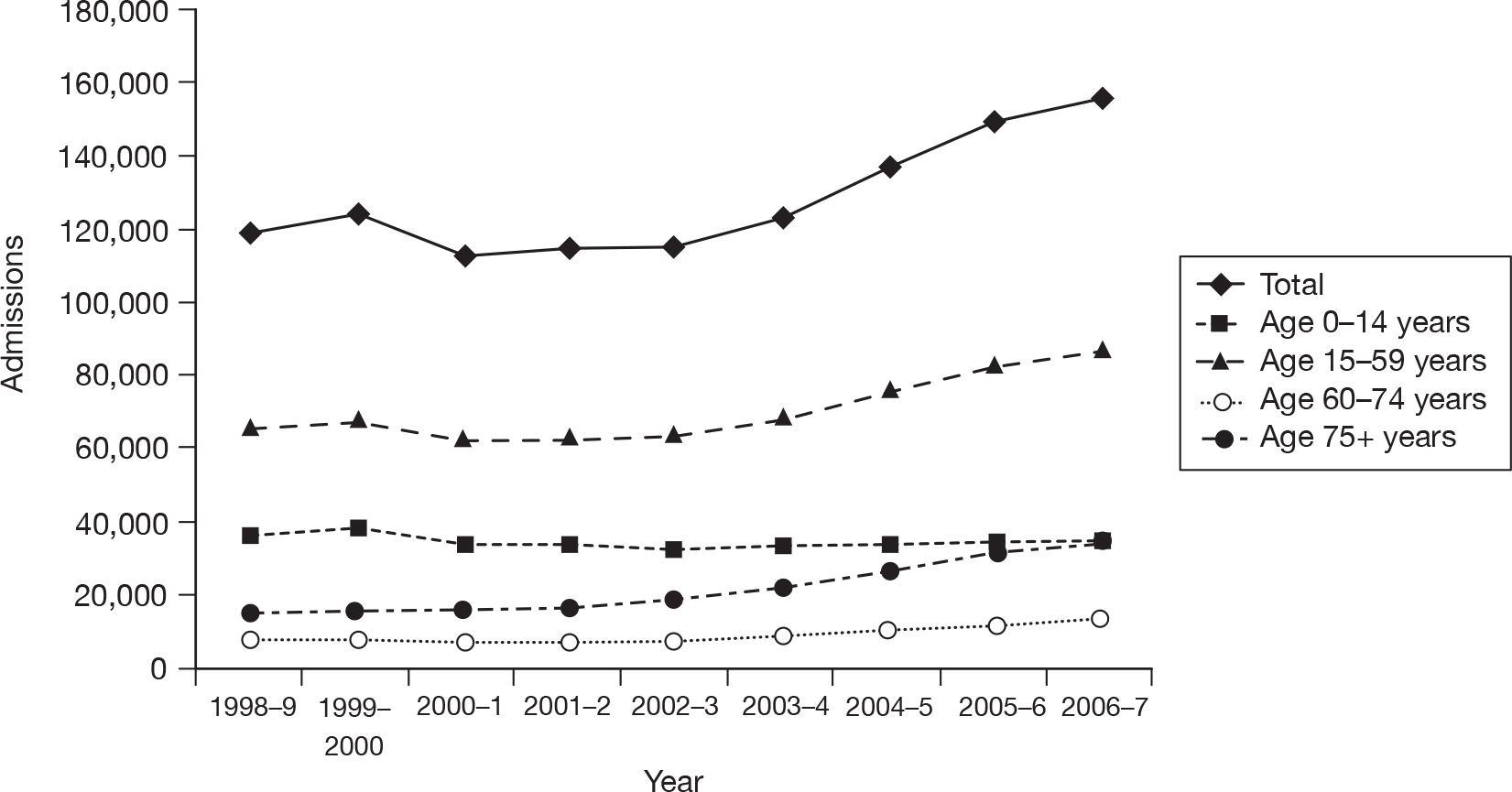
These data suggest that the annual costs of admission for head injury have increased from around £170M to £213M since the guidelines were introduced. Additional expenditure may be justified if associated with improved outcomes, but the anticipated effect of the guidelines was originally estimated only in resource terms and published studies have not examined effects upon patient health. It is therefore not clear whether this additional expenditure has produced any health benefits.
Management guidelines of the NHS should be based upon rigorous cost-effectiveness analysis. This is particularly important for MHI, where guideline development involves a trade-off between the costs of investigation and the benefits of detecting pathology, and where guideline implementation has substantial resource implications for the NHS.
Research methods
Design
We plan to undertake a cost-effectiveness analysis based on secondary research (systematic review, meta-analysis and decision-analysis modelling), along with a national survey and analysis of routine data sources to determine the most appropriate diagnostic management strategy for adults and children with minor head injuries in the NHS.
Systematic review and meta-analysis
Using standard methodology, we will undertake systematic literature reviews to identify:
-
cohort studies of patients with head injury that measure the diagnostic accuracy of any element of clinical assessment, any clinical decision rule, skull radiography, cranial CT or observation strategy for identifying intracranial injuries that require neurosurgery
-
observational or experimental studies that evaluate diagnostic management strategies for MHI in terms of process measures (hospital admissions, length of stay, time to neurosurgery) or patient outcomes
-
studies that report data to estimate key parameters in the decision-analysis model: prevalence of intracranial bleeding in MHI, survival and QoL after early or delayed neurosurgery for intracranial bleeding and long-term costs of care after neurosurgery for intracranial bleeding.
Search strategy
Relevant studies will be identified through electronic searches of key databases including MEDLINE, EMBASE, Science Citation Index (SCI) and Biological Abstracts. Recent published empirical work will be used to identify optimal strategies for prognosis and diagnosis on MEDLINE and EMBASE. 25–28
Search terms will include:
-
head injur$, craniocerebral trauma (including brain injuries, coma, post-head injur, cranial nerve injuries, head injuries (closed), brain concussion, head injuries (penetrating), intracranial haemorrhage (traumatic) and skull fracture)
-
clinical assessment, clinical decision rule$, guideline$, Canadian CT, CHIP, NEXUS, New Orleans, skull radiograph$, skull X-ray$, CT scanning, and hospital admission; plus such terms as
-
cohort studies, longitudinal studies, follow-up studies, time factors, long term, sequela$, prognosis
-
diagnostic terms such as specificity and sensitivity, false positive$, false negative$, true positive$, true negative$.
References will also be located through review of reference lists for relevant articles and through use of citation search facilities through WoK’s SCI and Social Science Citation Index. Where existing systematic reviews already exist, these will be used both to identify relevant studies and to inform subsequent analysis. In addition, systematic searches of the internet the Copernic meta-search engine will be used to identify unpublished materials and work in progress. Key authors and professional and academic research groups will also be contacted and asked for unpublished material.
Review strategy
The stages of the review for diagnostic cohort studies will include:
-
Accumulation of references, entry and tagging on a Reference Manager database, enabling studies to be retrieved in each of the above categories by either keyword or textword searches.
-
Two reviewers will independently undertake preliminary review to identify any potentially relevant article based on titles, abstracts and subject indexing. All studies identified for inclusion, together with those for which a decision on inclusion is not possible from these brief details, will be obtained for more detailed appraisal.
-
Two reviewers will make decisions on the final composition of included studies, assessed from a hard copy of the item. The decisions will be coded and recorded on the Reference Manager database by the project manager.
-
Authors will be contacted, if appropriate, to clarify details and obtain missing data.
-
The quality of each study will be assessed against recognised criteria. 29,30
-
Data extraction will be undertaken independently with discrepancies being discussed by the data extractors. Those that cannot be resolved at this stage will be referred to the rest of the project team.
These methods will also be used to identify studies of the management of head injuries and studies reporting data to inform the decision analysis model, but search terms, filters, selection criteria and quality assessments will be adapted to suit the purpose of each literature search.
Data extraction
The following data will be extracted from each study: population characteristics (age, gender, mechanism of injury, median GCS), setting (ED, general ward, neurosurgical centre), characteristics of the assessment or intervention (e.g. method of recording clinical features or decision score, staff training), definition of each outcome used, methods used to measure outcomes, study quality criteria (independence of the reference standard, blinding of the intervention and reference standard), prevalence of each outcome (clinically significant brain injury and need for neurosurgery), and true-positives, false-positives, false-negatives and true-positives for each outcome.
Data synthesis
Where appropriate, we will combine diagnostic data to provide pooled estimates of the diagnostic accuracy of clinical characteristics or clinical decision rules for diagnosing intracranial bleeding. For each modality, we will estimate the diagnostic performance (together with associated uncertainty) for diagnosing (1) intracranial bleeding requiring neurosurgery and (2) any clinically significant brain injury.
We will analyse data from adults and children separately wherever possible. Although we are specifically interested in diagnostic performance in patients with MHI we anticipate that most studies will report cohorts that include a range of severity. We will explore the applicability of findings to patients with MHI as part of our analysis of heterogeneity (see below).
The model used to analyse the data will depend on characteristics of the data obtained. For example, if diagnostic thresholds can be assumed constant across studies then simple methods of pooling sensitivity and specificity will be conducted. 31 If there is implicit or explicit evidence that diagnostic thresholds differ between primary studies then sensitivity and specificity cannot be considered independent and simultaneous modelling will be required. 32 A detailed assessment of heterogeneity will be conducted in all instances. If possible, meta-regression will be used to explore whether heterogeneity can be explained by study population characteristics, the method of implementation of the intervention, the definition of the outcome or the study quality, although the feasibility of this will depend on the number of individual studies identified and the quality of reporting. Where exploration of covariates is not possible or (unexplained) heterogeneity remains after the incorporation of covariates into the model(s), random effects will be incorporated to allow for such variability in results between studies.
Covariate effects, unexplainable variability and uncertainty in parameter estimates will all be reflected in the results using cutting-edge meta-analysis approaches. As the outputs from these analyses will be used in the decision modelling, all such sources of variation and uncertainty will be accurately reflected in the decision modelling. 33
Standard meta-analysis methods will be used to combine multiple estimates, where they exist, for other parameters in the decision model.
A combination of Stata and the Meta-Disc statistical software34 (version Beta 1.0.10) will be used for this analysis.
Identification of potential management strategies
We will identify potential management strategies for MHI using the following methods:
-
Literature review As outlined above, we will identify any diagnostic management strategies evaluated in previous studies, particularly those based upon clinical decision rules.
-
Expert panel review We will constitute an expert panel of emergency physicians, neurosurgeons and neuroradiologists, who will review emerging data from the systematic reviews and then use consensus methods to develop potential diagnostic management strategies that would be appropriate for the NHS. These may be based upon established strategies or clinical decision rules, or theoretical combinations of clinical features and diagnostic tests identified as being diagnostically useful in the systematic reviews.
-
National survey We will undertake a national survey, as outlined below, to identify diagnostic management strategies that are currently being used in the NHS. These will then be reviewed by the expert panel and consensus methods used to select those with the potential for widespread use throughout the NHS.
National survey and routine data sources
We will undertake a national survey of EDs to identify formal guidelines used for MHI, clinical assessment strategies, policies for access to skull radiography and cranial CT, hospital admission policies (e.g. clinical decision unit, A&E observation or formal admission), bed availability, specialty responsible for inpatient care, staffing and senior supervision. This will be correlated with data from routine sources (e.g. HES).
We used a national survey in this way in our previous National Coordinating Centre for Health Technology Assessment (NCCHTA)-funded secondary research on diagnostic tests for deep vein thrombosis35 and found it to be a valuable source of data, and well worth the relatively trivial outlay of resources required to undertake it. Data from the national survey will provide the following:
-
identification of potential management strategies that are feasible in the NHS and can be evaluated by the decision-analysis model
-
data to inform the structure and populate key parameters of the decision-analysis model
-
context for our analysis, thus ensuring that the output of our research is relevant to the NHS.
Decision-analysis modelling
We will develop a decision-analysis model to estimate the costs and QALYs accrued by each potential management strategy for MHI, including a theoretical ‘zero option’ strategy of discharging all patients home without investigation. Each strategy will be applied to a theoretical cohort of patients attending the ED, with MHI allowing a direct comparison of results. For each strategy, sensitivity and specificity estimates from the literature review will determine the proportion of patients with intracranial bleeding who receive early or delayed neurosurgery and the proportion with no neurosurgical lesion who undergo diagnostic testing and/or admission to hospital.
The following costs will be estimated using data from the literature review, national survey, routine data sources and, if necessary, an expert panel: initial assessment, diagnostic tests (CT and skull radiography), hospital admission, neurosurgical intervention, long-term health and social care, and productivity losses.
Outcomes will be estimated as QALYs accrued following the decision to employ each management strategy. The expected utility associated with early or delayed neurosurgery will be taken from previous studies or, if necessary, expert panel opinion. We will search the literature to identify studies reporting survival and quality of life (QoL) after uncomplicated MHI (no bleeding), intracranial bleeding with early surgery, intracranial bleeding with delayed surgery and the disutility of the surgical procedure.
We will also use data from the Health And Long term Outcomes (HALO) study of patients with trauma. Researchers at the Medical Care Research Unit have been collecting diagnosis and baseline GCS, along with costs and QoL data up to 15 years after significant injury (including head injury). Where data from the existing literature are limited or inadequate we will ask the expert panel to review potential alternative data sources, for example extrapolating QoL data from other disabling neurological conditions. We will also use expert panel input to ensure that parameters are used in the model with appropriate estimates of uncertainty.
The time frame for the model will be the lifetime of the patient. We will assume that only patients with intracranial bleeding will incur long-term costs that are likely to be influenced by their initial diagnostic management, so long-term costs will be estimated only for patients in the model who survive intracranial bleeding. We will estimate discounted long-term costs by extrapolating follow-up costs from patients with significant head injury to the HALO study over the anticipated lifetime of the patient. Sensitivity analysis will be used to explore uncertainty in estimates of long-term costs. The baseline analysis will not include productivity losses but secondary analysis will be undertaken, including productivity losses to explore the effect of changing assumptions regarding the role of productivity losses. We will value productivity losses in the model by applying an average salary cost to estimated time off work as a result of intracranial bleeding.
We will undertake a literature review to estimate the effects of radiation exposure associated with radiological investigations (CT brain and skull radiography). We will then model these data to estimate a QALY loss and/or cost associated with each radiological investigation. This QALY loss and/or cost will then be applied to every patient in the model who receives a radiological investigation.
Analysis will be conducted in accordance with the NICE reference case. 36 Net benefit analysis will be used to identify the most cost-effective option at varying thresholds of willingness to pay. 37 The optimal strategy at the threshold currently used by NICE for decision-making will be presented as the optimal strategy for the NHS. The methodology used in the decision-analytic model will be dependent on the data that are available and the number of health states following the minor head injuries that are necessary to incorporate, with the most appropriate technique selected.
The exact modelling methodology to be used will be chosen once key data have been identified as attempting to manipulate data to fit a prespecified modelling structure will not be as accurate as choosing the method that can best represent the decision problem. The lead modeller has published papers using a wide range of decision methodologies, including discrete event simulation,38 meta-modelling,39 transition-state modelling,40 decision-tree modelling,35 and infectious disease modelling incorporating herd immunity,41 and we are confident that whatever modelling methodology is most appropriate will be able to be constructed. If possible, we shall attempt to calibrate the mathematical model with published data during the construction phase.
Probabilistic sensitivity analyses (PSAs) will be conducted in order that any interactions and non-linearities within the modelling are properly considered. Jack-knife techniques42 will be conducted to ensure that a sufficient number of PSA runs have been conducted to ensure that the average calculated from all runs for a management strategy is robust. Additionally the uncertainty associated in the actual mean net benefit will be provided using the percentile method in order that the full uncertainty in the results is reported. These analyses will facilitate the calculation of both full and partial expected value of perfect information, and if it is deemed appropriate an evaluation of the expected value of sample information will also be conducted.
The value of information analysis will help us to determine where funders of primary research in this important area (such as health technology assessment) should direct future studies to ensure that recommendations for policy and practice are more robust.
- National Institute for Health and Clinical Excellence (NICE) . Head Injury: Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adults 2003.
- National Institute for Health and Clinical Excellence (NICE) . Head Injury: Triage, Assessment, Investigation and Early Management of Head Injury in Infants, Children and Adults 2007.
- Dunning J, Stratford-Smith P, Lecky F, Batchelor J, Hogg K, Browne J, et al. Emergency Medicine Research Group . A meta-analysis of clinical correlates that predict significant intracranial injury in adults with minor head trauma. J Neurotrauma 2004;21:877-85.
- Dunning J, Batchelor J, Stratford-Smith P, Teece S, Browne J, Sharpin C, et al. A meta-analysis of variables that predict significant intracranial injury in minor head trauma. Arch Dis Child 2004;89:653-9.
- Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, et al. The Canadian CT Head rule for patients with minor head injury. Lancet 2001;357:1391-6.
- Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM. Indications for computed tomography in patients with minor head injury. N Engl J Med 2000;343:100-5.
- Richless LK, English K, Heller MB, Rachlin J, McClean P, Auble TE. A prospective evaluation of radiologic criteria for head injury patients in a community emergency department. Am J Emerg Med 1993;11:327-30.
- Miller EC, Holmes JF, Derlet RW. Utilizing clinical factors to reduce head CT scan ordering for minor head trauma patients. J Emerg Med 1997;15:453-7.
- Stiell IG, Clement CM, Rowe BH, Schull MJ, Brison R, Cass D, et al. Comparison of the Canadian CT Head rule and the New Orleans criteria in patients with minor head injury. JAMA 2005;294:1511-18.
- Smits M, Dippel DW, de Haan GG, Dekker HM, Vos PE, Kool DR, et al. External validation of the Canadian CT Head rule and New Orleans criteria for CT scanning in patients with minor head trauma. JAMA 2005;294:1519-25.
- Smits M, Dippel DW, Steyerberg EW, de Haan GG, Dekker HM, Vos PE, et al. Predicting intracranial traumatic findings on computed tomography in patients with minor head injury: the CHIP prediction rule. Ann Intern Med 2007;146:397-405.
- Oman JA, Cooper RJ, Holmes JF, Viccellio P, Nyce A, Ross SE, et al. Performance of a decision rule to predict need for CT among children with blunt head trauma. Pediatrics 2006;117:e238-46.
- Dunning J, Daly JP, Lomas J-P, Lecky F, Batchelor K, Mackway-Jones K. Derivation of the children's head injury algorithm for the prediction of important clinical events decision rule for head injury in children. Arch Dis Child 2006;91:885-91.
- Hofman PA, Nelemans P, Kemerink GJ, Wilmink JT. Value of radiological diagnosis of skull fracture in the management of mild head injury: meta-analysis. J Neurol Neurosurg Psychiatry 2000;68:416-22.
- Kelly AB, Zimmerman RD, Snow RB, Gandy SE, Heier LBA, Deck MDF. Head trauma – comparison of MR and CT – experience of 100 patients. Am J 1988;9:699-708.
- Ingebrigtsen T. Routine early CT-scan is cost saving after minor head injury. Acta Neurol Scand 1996;93:207-10.
- Af Geijerstam J-L, Britton M, Marke LA. Minor head injury: observation or computer tomography? Economic aspects by literature review and economic analysis. Emerg Med J 2004;21:54-8.
- Norlund A, Marke LA, af Geijerstam J-L, Oredsson S. Britton M and the OCTOPUS study investigators. Immediate computed tomography or admission for observation after mild head injury: cost comparison in randomised controlled trial. BMJ 2006;333.
- Af Geijerstam J-L, Oredsson S. Britton M and the OCTOPUS study investigators. Medical outcome after immediate computed tomography or admission for observation in patients with mild head injury: randomised controlled trial. BMJ 2006;333:465-8.
- Stein SC. Indications for CT scanning in mild traumatic brain injury: a cost-effectiveness study. J Trauma 2006;61:558-66.
- Sultan HY, Boyle A, Pereira M, . Application of the Canadian CT head rules in managing minor head injuries in a UK emergency department: implications for the implementation of the NICE guidelines. Emerg Med J 2004;21:420-5.
- Hassan Z, Smith M, Littlewood S, Bouamra O, Hughes D, Biggin C, et al. Head injuries: a study evaluating the impact of the NICE head injury guidelines. Emerg Med J 2005;22:845-9.
- Shravat BP, Hynes KA. The impact of NICE guidelines for the management of head injury on the workload of the radiology department. Emerg Med J 2004;21:521-2.
- Goodacre S. Hospital admissions with head injury following publication of NICE guidance. Emerg Med J 2008;25:556-7.
- Westwood ME, Whiting PF, Kleijen J. How does study quality affect the results of a diagnostic meta-analysis?. BMC Med Res Methodol 2005;5.
- Whiting P, Harbord R, Kleijnen J. No role for quality scores in systematic reviews of diagnostic accuracy studies. BMC Med Res Methodol 2005;5.
- Whiting P, Rutjes AW, Dinnes J, Reitsma JB, Bossuyt PM, Kleijnen J. A systematic review finds that diagnostic reviews fail to incorporate quality despite available tools. J Clin Epidemiol 2005;58:1-12.
- Whiting P, Rutjes AW, Dinnes J, Reitsma J, Bossuyt PM, Kleijnen J. Development and validation of methods for assessing the quality of diagnostic accuracy studies. Health Technol Assess 2004;8.
- Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: The STARD initiative. Department of Clinical Epidemiology and Biostatistics Academic Medical Centre, University of Amsterdam, the Netherlands; 2003.
- Lijmer JG, Mol JJ, Heisterkamp S, Bonsel GJ, van der Meulen JHP, Bossuyt PMM. Empirical evidence of design-related bias in studies of diagnostic tests. JAMA 1999;282:1061-6.
- Deeks JJ, Egger M, Davey Smith G, Altman DG. Systematic reviews in health care: meta-analysis in context. London: BMJ Publishing Group; 2001.
- Harbord RM, Deeks JJ, Egger M, Whiting P, Sterne JA. A unification of models for meta-analysis of diagnostic accuracy studies. Biostatistics 2007;8:239-51.
- Sutton AJ, Cooper NJ, Goodacre S, Stevenson M. Integration of meta-analysis and economic decision modelling for evaluating diagnostic tests. Med Decis Making 2008;28:650-67.
- Zamora J, Abraira V, Muriel A, Khan KS, Coomavasamy A. Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 2006;6.
- Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton AJ, Thomas S, et al. Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis. Health Technol Assess 2006;10.
- National Institute of Clinical Excellence (NICE) . Guide to the Methods of Technology Appraisal 2004.
- Fenwick E, Claxton K, Sculpher M. (2001). Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ n.d.;10:779-87.
- Stevenson MD, Oakley JE, Chick SE, Chalkidou K. The cost-effectiveness of surgical instrument management policies to reduce the risk of vCJD transmission to humans. JORS 2009;60:506-18.
- Stevenson MD, Brazier JE, Calvert NW, Lloyd-Jones M, Oakley J, Kanis JA. Description of an individual patient methodology for calculating the cost-effectiveness of treatments for osteoporosis in women. JORS 2005;56:214-21.
- Wardlaw JM, Chappell FM, Stevenson M, De Nigris E, Thomas S, Gillard J, et al. Accurate, practical and cost-effective assessment of carotid stenosis in the UK. Health Technol Assess 2006;10.
- Stevenson MD, Beard SM, Finn A, Brennan A. Estimating the potential health gain and cost consequences of introducing a pre-school pertussis booster into the UK child vaccination schedule. Vaccine 2002;20:1778-86.
- Inglehart DL. Simulating stable stochastic systems, V: comparison of ratio estimators. Naval Res Logist Quart 1975;22:553-65.
Glossary
Technical terms and abbreviations are used throughout this report. The meaning is usually clear from the context, but a glossary is provided for the non-specialist reader. In some cases, usage differs in the literature, but the term has a constant meaning throughout this review.
- Basal skull fracture
- A fracture involving the base of the cranium.
- Battle’s sign
- Bruising that sometimes occurs behind the ear in cases of fracture of the base of the skull (basal skull fracture).
- Clinical decision rule
- A rule that uses standardised information from the patient history, examination and investigations to direct a clinical management decision.
- Coagulopathy
- A condition affecting the blood’s ability to form a clot.
- Consciousness
- An alert cognitive state in which you are aware of yourself and your situation.
- Cost-effectiveness acceptability curve
- A way of illustrating cost-effectiveness results by plotting the probability that the intervention is cost-effective (y-axis) against the maximum that society is willing to pay for an improvement in health (x-axis).
- Cost-effectiveness plane
- A way of illustrating cost-effectiveness results by plotting the mean incremental cost and effectiveness on a four-quadrant graph. Interventions that are more costly and more effective fall in the north-east quadrant.
- Diagnostic case–control study
- Diagnostic accuracy study in which the test results of a series of patients with an established diagnosis are compared with those of a non-diseased control group.
- Diagnostic cohort study
- Diagnostic accuracy study in which a group of individuals with a suspected disease undergo both the index test and the reference standard, and the results of the two tests are compared.
- Drowsiness
- A state of impaired awareness associated with a desire or inclination to sleep.
- False-negative
- A patient with a condition who is wrongly diagnosed as not having it.
- False-positive
- A patient without a condition who is wrongly diagnosed as having it.
- Focal neurological deficit
- A neurological abnormality that is restricted to a particular part of the body or a particular activity.
- Glasgow Coma Scale (GCS)
- A standardised system that is used to assess the degree of brain impairment and to identify the seriousness of injury in relation to outcome. The system involves three determinants – eye opening, verbal responses and motor response – all of which are evaluated independently according to a numerical value that indicates the level of consciousness and degree of dysfunction.
- Highest-density region (HDR)
- The Bayesian equivalent of a confidence interval.
- Incremental cost-effectiveness ratio (ICER)
- The difference in costs between one intervention and an alternative, divided by the difference in outcomes.
- Intracranial haematoma
- A collection of blood inside the cranium, caused by damage to brain tissue or the rupture of a blood vessel. The resulting swelling can compress the brain.
- Likelihood ratio
- Describes how many times more likely a person with a disease is to receive a particular test result than a person without disease. A likelihood ratio of a positive test result is usually a number > 1; a likelihood ratio of a negative test result usually lies between 0 and 1.
- Neurosurgery
- A surgical specialty for the treatment of diseases and disorders of the brain, spinal cord and nerves.
- Quality-adjusted life-year (QALY)
- A measure of benefit of health care combining the impact of both expected length of life and quality of life.
- Receiver-operating characteristic (ROC)
- A receiver-operating characteristic curve represents the relationship between ‘true-positive fraction’ (sensitivity) and ‘false-positive fraction’ (1–specificity). It displays the trade-offs between sensitivity and specificity as a result of varying the cut-off value for positivity in case of a continuous test result.
- Reference standard
- Established test(s) against which the accuracy of a new test for detecting a particular condition can be evaluated.
- Sensitivity (true-positive rate)
- The proportion of individuals with the target condition in a population who are correctly identified by a diagnostic test.
- Specificity (true-negative rate)
- The proportion of individuals free of the target condition in a population who are correctly identified by a diagnostic test.
- Test accuracy
- The proportion of test results that is correctly identified by the test.
- True-negative (TN)
- A patient without a condition who is correctly diagnosed as not having it.
- True-positive (TP)
- A patient with a condition who is correctly diagnosed as having it.
List of abbreviations
- ACEP
- American College of Emergency Physicians
- AUC
- area under curve
- CATCH
- Canadian Assessment of Tomography for Childhood Injury
- CBA
- controlled before/after
- CCHR
- Canadian CT Head Rule
- CCT
- controlled clinical trial
- CDSR
- Cochrane Database of Systematic Reviews
- CENTRAL
- Cochrane Central Registry of Controlled Trials
- CHALICE
- Children’s Head injury Algorithm for the prediction of Important Clinical Events
- CHIP
- CT in Head Injury Patients
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CI
- confidence interval
- CK-BB
- creatine kinase isozyme
- CPCI
- Conference Proceedings Citation Index
- CRD
- Centre for Reviews and Dissemination
- CT
- computerised tomography
- DARE
- Database of Abstracts of Reviews of Effects
- DLYG
- discounted life-year gained
- ED
- emergency department
- EFNS
- European Federation of Neurological Societies
- EPOC
- Effective Practice and Organisation of Care
- EQ-5D
- European Quality of Life-5 Dimensions
- EVPI
- expected value of perfect information
- EVPPI
- expected value of partial perfect information
- FN
- false-negative
- FP
- false-positive
- GCS
- Glasgow Coma Scale
- GOS
- Glasgow Outcome Score
- GOS-E
- Extended Glasgow Outcome Score
- HDR
- highest-density region
- HES
- Hospital Episode Statistics
- HTA
- health technology assessment
- ICER
- incremental cost-effectiveness ratio
- ICI
- intracranial injury
- INAHTA
- International Network of Agencies for Health Technology Assessment
- IQR
- interquartile range
- LOC
- loss of consciousness
- MHI
- minor head injury
- MRI
- magnetic resonance imaging
- MVA
- motor vehicle accident
- NCWFNS
- Neurotraumatology Committee of the World Federation of Neurosurgical Societies
- NEXUS II
- National Emergency X-Radiography Utilization Study II
- NICE
- National Institute for Health and Clinical Excellence
- NIHR
- National Institute for Health Research
- NLR
- negative likelihood ratio
- NOC
- New Orleans Criteria
- NSE
- neuron-specific enolase
- PECARN
- Paediatric Emergency Care Applied Research Network
- PLR
- positive likelihood ratio
- PSA
- probabilistic sensitivity analysis
- PSSRU
- Personal Social Services Research Unit
- PTA
- post-traumatic amnesia
- PTS
- post-traumatic seizure
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- QUADAS
- Quality Assessment of Diagnostic Accuracy Studies
- RCS
- Royal College of Surgeons
- RCT
- randomised controlled trial
- ReFeR
- Research Findings Register
- ROC
- receiver-operating characteristic
- S100B
- S100 calcium-binding protein B
- SCI
- Science Citation Index
- SIGN
- Scottish Intercollegiate Guidelines Network
- SSCI
- Social Science Citation Index
- TBI
- traumatic brain injury
- TN
- true-negative
- TP
- true-positive
- TRIP
- Turning Research into Practice
- UCD
- University of California–Davis rule
- VOI
- value of information
- WoK
- Web of Knowledge
- WoS
- Web of Science
- WWW
- world wide web
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
Prioritisation Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Imti Choonara, Professor in Child Health, Academic Division of Child Health, University of Nottingham
Chair – Pharmaceuticals Panel
-
Dr Bob Coates, Consultant Advisor – Disease Prevention Panel
-
Dr Andrew Cook, Consultant Advisor – Intervention Procedures Panel
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Dr Nick Hicks, Consultant Adviser – Diagnostic Technologies and Screening Panel, Consultant Advisor–Psychological and Community Therapies Panel
-
Ms Susan Hird, Consultant Advisor, External Devices and Physical Therapies Panel
-
Professor Sallie Lamb, Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick
Chair – HTA Clinical Evaluation and Trials Board
-
Professor Jonathan Michaels, Professor of Vascular Surgery, Sheffield Vascular Institute, University of Sheffield
Chair – Interventional Procedures Panel
-
Professor Ruairidh Milne, Director – External Relations
-
Dr John Pounsford, Consultant Physician, Directorate of Medical Services, North Bristol NHS Trust
Chair – External Devices and Physical Therapies Panel
-
Dr Vaughan Thomas, Consultant Advisor – Pharmaceuticals Panel, Clinical
Lead – Clinical Evaluation Trials Prioritisation Group
-
Professor Margaret Thorogood, Professor of Epidemiology, Health Sciences Research Institute, University of Warwick
Chair – Disease Prevention Panel
-
Professor Lindsay Turnbull, Professor of Radiology, Centre for the MR Investigations, University of Hull
Chair – Diagnostic Technologies and Screening Panel
-
Professor Scott Weich, Professor of Psychiatry, Health Sciences Research Institute, University of Warwick
Chair – Psychological and Community Therapies Panel
-
Professor Hywel Williams, Director of Nottingham Clinical Trials Unit, Centre of Evidence-Based Dermatology, University of Nottingham
Chair – HTA Commissioning Board
Deputy HTA Programme Director
HTA Commissioning Board
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
-
Department of Public Health and Epidemiology, University of Birmingham
-
Professor of Clinical Pharmacology, Director, NIHR HTA programme, University of Liverpool
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Peter Brocklehurst, Professor of Women’s Health, Institute for Women’s Health, University College London
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Jonathan Green, Professor and Acting Head of Department, Child and Adolescent Psychiatry, University of Manchester Medical School
-
Professor John W Gregory, Professor in Paediatric Endocrinology, Department of Child Health, Wales School of Medicine, Cardiff University
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, Head of Nuffield Department of Surgery, University of Oxford
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor Irwin Nazareth, Professor of Primary Care and Head of Department, Department of Primary Care and Population Sciences, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norrie, Chair in Clinical Trials and Biostatistics, Robertson Centre for Biostatistics, University of Glasgow
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Martin Underwood, Professor of Primary Care Research, Warwick Medical School, University of Warwick
-
Professor Marion Walker, Professor in Stroke Rehabilitation, Associate Director UK Stroke Research Network, University of Nottingham
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Dr Tom Foulks, Medical Research Council
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
HTA Clinical Evaluation and Trials Board
-
Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick and Professor of Rehabilitation, Nuffield Department of Orthopaedic, Rheumatology and Musculoskeletal Sciences, University of Oxford
-
Professor of the Psychology of Health Care, Leeds Institute of Health Sciences, University of Leeds
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Keith Abrams, Professor of Medical Statistics, Department of Health Sciences, University of Leicester
-
Professor Martin Bland, Professor of Health Statistics, Department of Health Sciences, University of York
-
Professor Jane Blazeby, Professor of Surgery and Consultant Upper GI Surgeon, Department of Social Medicine, University of Bristol
-
Professor Julia M Brown, Director, Clinical Trials Research Unit, University of Leeds
-
Professor Alistair Burns, Professor of Old Age Psychiatry, Psychiatry Research Group, School of Community-Based Medicine, The University of Manchester & National Clinical Director for Dementia, Department of Health
-
Dr Jennifer Burr, Director, Centre for Healthcare Randomised trials (CHART), University of Aberdeen
-
Professor Linda Davies, Professor of Health Economics, Health Sciences Research Group, University of Manchester
-
Professor Simon Gilbody, Prof of Psych Medicine and Health Services Research, Department of Health Sciences, University of York
-
Professor Steven Goodacre, Professor and Consultant in Emergency Medicine, School of Health and Related Research, University of Sheffield
-
Professor Dyfrig Hughes, Professor of Pharmacoeconomics, Centre for Economics and Policy in Health, Institute of Medical and Social Care Research, Bangor University
-
Professor Paul Jones, Professor of Respiratory Medicine, Department of Cardiac and Vascular Science, St George‘s Hospital Medical School, University of London
-
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, Queen Mary, University of London
-
Professor Richard J McManus, Professor of Primary Care Cardiovascular Research, Primary Care Clinical Sciences Building, University of Birmingham
-
Professor Helen Rodgers, Professor of Stroke Care, Institute for Ageing and Health, Newcastle University
-
Professor Ken Stein, Professor of Public Health, Peninsula Technology Assessment Group, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Jonathan Sterne, Professor of Medical Statistics and Epidemiology, Department of Social Medicine, University of Bristol
-
Mr Andy Vail, Senior Lecturer, Health Sciences Research Group, University of Manchester
-
Professor Clare Wilkinson, Professor of General Practice and Director of Research North Wales Clinical School, Department of Primary Care and Public Health, Cardiff University
-
Dr Ian B Wilkinson, Senior Lecturer and Honorary Consultant, Clinical Pharmacology Unit, Department of Medicine, University of Cambridge
-
Ms Kate Law, Director of Clinical Trials, Cancer Research UK
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, University of Manchester
-
Mr Angus S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital, Birmingham
-
Dr Diana Baralle, Consultant and Senior Lecturer in Clinical Genetics, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Diane Eccles, Professor of Cancer Genetics, Wessex Clinical Genetics Service, Princess Anne Hospital
-
Dr Trevor Friedman, Consultant Liason Psychiatrist, Brandon Unit, Leicester General Hospital
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Public contributor
-
Professor Anthony Robert Kendrick, Associate Dean for Clinical Research and Professor of Primary Medical Care, University of Southampton
-
Dr Nicola Lennard, Senior Medical Officer, MHRA
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee, London
-
Mr David Mathew, Public contributor
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mrs Una Rennard, Public contributor
-
Dr Stuart Smellie, Consultant in Clinical Pathology, Bishop Auckland General Hospital
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr Allison Streetly, Programme Director, NHS Sickle Cell and Thalassaemia Screening Programme, King’s College School of Medicine
-
Dr Matthew Thompson, Senior Clinical Scientist and GP, Department of Primary Health Care, University of Oxford
-
Dr Alan J Williams, Consultant Physician, General and Respiratory Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Joanna Jenkinson, Board Secretary, Neurosciences and Mental Health Board (NMHB), Medical Research Council
-
Professor Julietta Patrick, Director, NHS Cancer Screening Programme, Sheffield
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Disease Prevention Panel
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook, Clinical Programmes Director, Bazian Ltd, London
-
Dr Colin Greaves, Senior Research Fellow, Peninsula Medical School (Primary Care)
-
Mr Michael Head, Public contributor
-
Professor Cathy Jackson, Professor of Primary Care Medicine, Bute Medical School, University of St Andrews
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Julie Mytton, Consultant in Child Public Health, NHS Bristol
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Dr Richard Richards, Assistant Director of Public Health, Derbyshire County Primary Care Trust
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Dr Kenneth Robertson, Consultant Paediatrician, Royal Hospital for Sick Children, Glasgow
-
Dr Catherine Swann, Associate Director, Centre for Public Health Excellence, NICE
-
Mrs Jean Thurston, Public contributor
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust
-
Reader in Wound Healing and Director of Research, University of Leeds
-
Professor Bipin Bhakta, Charterhouse Professor in Rehabilitation Medicine, University of Leeds
-
Mrs Penny Calder, Public contributor
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol
-
Mrs Anthea De Barton-Watson, Public contributor
-
Professor Nadine Foster, Professor of Musculoskeletal Health in Primary Care Arthritis Research, Keele University
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester
-
Professor Christine Norton, Professor of Clinical Nursing Innovation, Bucks New University and Imperial College Healthcare NHS Trust
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham
-
Dr Kate Radford, Senior Lecturer (Research), University of Central Lancashire
-
Mr Jim Reece, Public contributor
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton
-
Dr Pippa Tyrrell, Senior Lecturer/Consultant, Salford Royal Foundation Hospitals’ Trust and University of Manchester
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Interventional Procedures Panel
-
Professor of Vascular Surgery, University of Sheffield
-
Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Mrs Isabel Boyer, Public contributor
-
Mr Sankaran Chandra Sekharan, Consultant Surgeon, Breast Surgery, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Ms Leonie Cooke, Public contributor
-
Mr Seumas Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor Sam Eljamel, Consultant Neurosurgeon, Ninewells Hospital and Medical School, Dundee
-
Dr Adele Fielding, Senior Lecturer and Honorary Consultant in Haematology, University College London Medical School
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Fiona Lecky, Senior Lecturer/Honorary Consultant in Emergency Medicine, University of Manchester/Salford Royal Hospitals NHS Foundation Trust
-
Dr Nadim Malik, Consultant Cardiologist/Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Professor Jon Moss, Consultant Interventional Radiologist, North Glasgow Hospitals University NHS Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Dr Matthew Wilson, Consultant Anaesthetist, Sheffield Teaching Hospitals NHS Foundation Trust
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Dr Martin Ashton-Key, Medical Advisor, National Commissioning Group, NHS London
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr James Gray, Consultant Microbiologist, Department of Microbiology, Birmingham Children’s Hospital NHS Foundation Trust
-
Dr Jurjees Hasan, Consultant in Medical Oncology, The Christie, Manchester
-
Dr Carl Heneghan, Deputy Director Centre for Evidence-Based Medicine and Clinical Lecturer, Department of Primary Health Care, University of Oxford
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Maria Kouimtzi, Pharmacy and Informatics Director, Global Clinical Solutions, Wiley-Blackwell
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Ms Amanda Roberts, Public contributor
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Professor Donald Singer, Professor of Clinical Pharmacology and Therapeutics, Clinical Sciences Research Institute, CSB, University of Warwick Medical School
-
Mr David Symes, Public contributor
-
Dr Arnold Zermansky, General Practitioner, Senior Research Fellow, Pharmacy Practice and Medicines Management Group, Leeds University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick, Coventry
-
Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Public contributor
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Peter Langdon, Senior Clinical Lecturer, School of Medicine, Health Policy and Practice, University of East Anglia
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician and Cardiologist, County Durham and Darlington Foundation Trust
-
Dr Richard Neal, Clinical Senior Lecturer in General Practice, Cardiff University
-
Mr John Needham, Public contributor
-
Ms Mary Nettle, Mental Health User Consultant
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry and Warwickshire Partnership Trust
-
Dr Lesley Stockton, Lecturer, School of Health Sciences, University of Liverpool
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation of Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Professor Bruce Campbell, Consultant Vascular & General Surgeon, Royal Devon & Exeter Hospital, Wonford
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Neill McIntosh, Edward Clark Professor of Child Life and Health, University of Edinburgh
-
Professor Rajan Madhok, Consultant in Public Health, South Manchester Primary Care Trust
-
Professor Sir Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, Director, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Philip Shackley, Senior Lecturer in Health Economics, Sheffield Vascular Institute, University of Sheffield
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Dr Nick Summerton, GP Appraiser and Codirector, Research Network, Yorkshire Clinical Consultant, Primary Care and Public Health, University of Oxford
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Dr Ross Taylor, Senior Lecturer, University of Aberdeen
-
Dr Richard Tiner, Medical Director, Medical Department, Association of the British Pharmaceutical Industry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington