Notes
Article history
The research reported in this issue of the journal was commissioned by the National Coordinating Centre for Research Methodology (NCCRM), and was formally transferred to the HTA programme in April 2007 under the newly established NIHR Methodology Panel. The HTA programme project number is 06/90/12. The contractual start date was in May 2002. The draft report began editorial review in November 2010 and was accepted for publication in July 2011. The commissioning brief was devised by the NCCRM who specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Nicky Britten and Catherine Pope have both run workshops using some material from this research. Some have charged attendance fees and generated a small surplus which was paid to their universities. They have not received any personal payment for these workshops. Catherine Pope also co-authored a textbook entitled Synthesising qualitative and quantitative health evidence: a guide to methods, which contains material about metaethnography and cites the research on which this report is based. Pandora Pound was training to be an acupuncturist while also conducting this research and currently practises as an acupuncturist.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2011. This work was produced by Campbell et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2011 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Although it is widely acknowledged that science is cumulative, people have only very recently begun to acknowledge that scientists have a responsibility to cumulate scientifically.
Chalmers et al. 1
Evidence-based medicine and a science of synthesis
Recognition of the need for research syntheses has existed for over two centuries,1 but a ‘science of synthesis’ has been slow to advance. In the field of health care, much of the momentum for the development of methods of synthesis has come from the move towards evidence-based medicine: a shift that has had a variety of antecedents. One was apprehension about the rapidity of technological change and the impossibility of individual clinicians reading and appraising all the journal articles relevant to their specialty. 2 Another factor was unease about the quality of primary research testing the effectiveness of clinical and health-care interventions. 3 Foremost, however, was recognition that all the best available scientific evidence should primarily inform clinical decision-making and that changes in medical practice should not simply rely on expert opinion.
Narrative literature reviews have been the traditional method for bringing together existing knowledge in a particular area. From the mid-1980s onwards, however, a number of questions about the adequacy of this method for compiling research evidence on health-care interventions were raised. The narrative review was criticised for being unscientific and, as a consequence, it was suggested ‘the results and conclusions would often be susceptible to and reflect the biases of the reviewer’. 4 In addition, seminal studies such as that by Antman et al. 5 provided powerful demonstrations of the value of a systematic approach to all the components of a review including the selection of studies for inclusion, the appraisal of the quality of the research and the application of relevant statistical methods for pooling data from a number of studies. Using meta-analysis to synthesise randomised controlled trial (RCT) evidence about the effectiveness of treatments in preventing death following heart attack, and contrasting this with expert recommendations in textbooks and review articles, these authors showed that some treatments were still being promoted when there was clear evidence that they were harmful, and that thrombolytic drugs were still not being recommended for use by more than half of clinical experts 13 years after cumulative meta-analyses showed them to be highly effective in reducing mortality. 5
In the late 1980s, international collaborations of researchers, responding both to Archie Cochrane’s6 championing of the value of the RCT in health-care evaluation and to his stinging criticism of health-care professionals’ failure to use scientific evidence as the primary basis for making choices about which preventive measures, diagnostic tests and treatments to use, began to publish the first systematic reviews of health care. Foremost among these was a two-volume publication containing hundreds of reviews about different aspects of the care of women and infants during pregnancy and childbirth. 7 There were two notable features of this review. Firstly, it was acknowledged that there would be different audiences for such reviews, and so a much shorter, more accessible, summary was also published. 8 Secondly, it was recognised that such a review would need to be regularly updated and that electronic publishing could facilitate this requirement. Rapid adoption of systematic reviews followed this pioneering work and global systematic reviewing networks have gradually developed, with the Cochrane Collaboration being the best known.
Health technology assessment
By the late 1990s, with the systematic review firmly established as a scientific method for bringing together findings from quantitative studies of effectiveness, interest was beginning to shift towards how qualitative data could be brought into the evidence base and a ‘science of synthesis’ developed for qualitative research. Whereas bringing together research information on effectiveness, costs and acceptability has always been fundamental to the health technology assessment (HTA) enterprise, the use of qualitative research methods within HTA has been a more recent development. In the mid-1990s, the HTA Methodology programme commissioned a review of the literature on the use of qualitative research methods in HTA, which noted that application of conventional systematic review methodology to qualitative research presented both philosophical and practical challenges. 9 Following publication of this report, the HTA recognised that further work was required to enable ‘users of qualitative research to be able to both appraise and to synthesise qualitative studies in a rigorous, replicable and formalised way’. 10
Synthesis of qualitative research
The possibility of synthesising qualitative research immediately raises a range of important epistemological, methodological and practical questions. The most fundamental of these is what ‘synthesis’ means in this context. Strike and Posner11 have suggested that ‘synthesis is usually held to be activity or the product of activity where some set of parts is combined or integrated into a whole… [Synthesis] involves some degree of conceptual innovation, or the invention or employment of concepts not found in the characterization of the parts as means of creating the whole’. Thus, synthesis of qualitative research could be envisaged as the bringing together of findings on a chosen theme, the results of which should, in conceptual terms, be greater than the sum of parts. This implies that qualitative synthesis would go beyond the description and summarising usually associated with a narrative literature review, as it would involve conceptual development and would be distinct from a quantitative meta-analysis in that it would not simply entail the aggregation of findings from individual, high-quality research studies. Qualitative synthesis should involve reinterpretation but, unlike secondary analysis, it would be based on published findings rather than primary data.
The impetus for developing methods of qualitative synthesis has arisen from recognition of the importance of qualitative evidence in complementing quantitative research and in particular its ability to provide a more complete understanding of phenomena, especially in terms of processes involved in the organisation and provision of services and influences on behaviours. 12 Another driver has been acknowledgement that the considerable expansion of the qualitative research literature over recent years has produced little accumulated understanding, highlighting a need to bring together isolated studies. 13 Thus, if qualitative research is to be made accessible to health policy-makers and planners, in a manageable form, then developing and evaluating methods of qualitative synthesis, as in this project, would seem to be an important and timely endeavour.
Despite recognition of the potential value of qualitative synthesis, it is a contentious enterprise. From a social science perspective, the notion of qualitative research synthesis best agrees with what is termed a ‘subtle realist’ position. This stance maintains that phenomena exist independently of the investigators’ claims about them, but also acknowledges the possibility of multiple, non-competing valid descriptions and explanations of the same phenomena. Subtle realism, therefore, enables the different constructions people make of reality to be studied, without accepting that particular beliefs are true; thus, qualitative synthesis can be regarded as potentially promoting such understanding. By contrast, an extreme relativist or radical constructionist perspective is based on a belief that reality is only what we make it and it is therefore not possible to have any knowledge of phenomena apart from our own experience of them. The aim of qualitative research arising from within this influential tradition is to describe unique particularities and present an ideographic account. The process of synthesis could thus be regarded as destroying the integrity of individual studies in the pursuit of some unattainable more ‘complete’ or ‘true’ account. As Sandelowski et al. 13 explained, from this perspective the summary of qualitative findings is regarded as thinning out the desired thickness of particulars, which may therefore ‘lose the vitality, viscerality, and vicariism (sic) of the human experiences represented in the original studies’. From a radical constructionist perspective, the aim of qualitative research is to produce fit descriptions of unique cases and leave it to the reader to engage in ‘naturalistic generalisation’ using these individual descriptions. However, as Hammersley14 observed, in practice it is rare for researchers not to hint at general conclusions from the unique cases that they study.
There are no standard or agreed methods for conducting syntheses of qualitative research. The review presented in Chapter 2 of this report illustrates a number of possible methods that have been identified and applied. Meta-ethnography, developed and used first in educational research, is one approach. 15 It involves taking relevant empirical studies to be synthesised, reading them repeatedly and noting down key concepts (interpretive metaphors). These key concepts are the raw data for the synthesis. Noblit and Hare15 suggested that the process by which a synthesis is achieved is one of translation. This entails examining the key concepts in relation to others in the original study and across studies. The way of translating key concepts or interpretive metaphors from one study to another involves an idiomatic rather than a word-for-word translation. The purpose of the translation is to try to derive concepts that can encompass more than one of the studies being synthesised. The synthesised concepts may not have been explicitly identified in any of the original empirical studies. As perhaps the best developed method for synthesising qualitative data, and one which clearly had its origins in the interpretive paradigm from which most methods of primary qualitative research evolved, this was the method selected for evaluation in this HTA project.
Prior to the research reported on here, this research group had undertaken a pilot synthesis of four papers concerned with the lay meanings of medicines, which demonstrated that it was possible to use meta-ethnography to synthesise qualitative research. 16 A feasibility study followed that included the formative evaluation of a set of criteria for assessing qualitative research studies followed by a synthesis of selected studies on patient experiences of diabetes mellitus. 17 This second pilot synthesis proved to be successful and illuminating; as none of the research papers included it in contained any references to each other, it demonstrated the need for primary researchers to search and read the existing literature more carefully and indicated that it would be helpful to bring the findings of qualitative research together. This second synthesis also confirmed the effectiveness of meta-ethnography as a method of synthesis. In addition, a practical method of qualitative research assessment and data extraction evolved from it. However, this process required further testing and evaluation before it could be recommended for widespread adoption by those undertaking HTA, as a number of important questions remained to be answered, for example, in terms of the selection of studies, how many studies can be included and how reproducible syntheses are. It is this more detailed evaluation that is the subject of this report.
Aims and objectives
Aim
To appraise and synthesise qualitative health research for HTA using a meta-ethnographic approach.
Objectives
Primary
-
To conduct, using the meta-ethnographic method, syntheses of qualitative research studies in two applied health-care contexts:
-
living with rheumatoid arthritis (RA) (patient experiences of a chronic illness)
-
lay beliefs about medicine-taking in chronic disease.
-
-
To test a modified version of the Critical Appraisal Skills Programme (CASP)18 criteria for appraising qualitative research for appropriateness, ease of use and inter-reviewer agreement.
-
To evaluate the reproducibility of the meta-ethnographic method of synthesis.
Secondary
-
To complete a review of the methods available for appraising and synthesising qualitative research.
-
To document the effectiveness of different elements in the search strategies in identifying relevant qualitative research studies.
Content of this report
This report continues in Chapter 2 with a review of the methods of qualitative synthesis. We did not complete a review of methods of appraisal as two other projects commissioned by other bodies at a similar time had such a review within their remit. 19,20 To avoid unnecessary duplication, we focused our efforts on reviewing methods for the synthesis of qualitative research. Chapter 3 describes the literature searching strategies employed in the two meta-ethnographic syntheses undertaken. An evaluation of the methods of appraisal used in the syntheses is reported in Chapter 4. The precise methods used to conduct the syntheses are described in Chapter 5 together with an assessment of the reproducibility of the meta-ethnographic method. The two syntheses are presented in Chapters 6 and 7. Chapter 8 contains a discussion of all the issues raised by this evaluation of meta-ethnography, and a number of conclusions are drawn about its value as a method of qualitative synthesis and its potential role in HTA.
Chapter 2 Methods of qualitative synthesis
The relative inattention towards integrating qualitative findings stands in sharp contrast to the considerable attention given to the development of techniques for conducting syntheses of quantitative research.
Sandelowski et al. 13
Introduction
Methods for the synthesis of qualitative research have been slow to develop, as the above quote suggests, but a number have emerged in recent years. These methods are still evolving, but are doing so in the shadow of widely used and well-developed methods for quantitative research synthesis. The result is that there is sometimes an expectation or assumption that qualitative syntheses will proceed in a manner similar to their quantitative counterparts, despite the very obvious differences between the quantitative and qualitative research traditions. This chapter begins by considering the distinctions between different types of research syntheses before going on to review methods of qualitative synthesis.
One of the confusing features of the research synthesis literature is that the terms ‘review’ and ‘synthesis’ are often used interchangeably,21 yet a distinction can be made between these two activities. A process of review can be said to be one of seeking out, sifting through, reading, appraising and describing relevant research evidence. The synthesis of evidence, on the other hand, involves a process of extracting data from individual research studies and interpreting and representing them in a collective form. According to this distinction, conventional literature reviews are generally reviews, whereas systematic reviews usually combine elements of review and synthesis.
Within systematic reviews, Hammersley14 identified three types of synthesis: aggregative (involving the accumulation and generalisation of evidence); comparative or replicative (determining the extent to which different sources of evidence reinforce each other by comparison between sources); and developmental (overarching theory development). Although these have evolved within a quantitative research tradition, Hammersley14 suggested that none of these types of synthesis is incompatible with qualitative synthesis. Hammersley14 also suggested convenience mapping synthesis as a fourth category. This category drew on Howard Becker’s notion of a mosaic of different studies being put together in order to see the bigger picture, with each study providing a context for the next.
Noblit and Hare (p. 15)15 also made a distinction between integrative reviews, in which data from different studies are pooled or aggregated, and interpretive reviews, which bring together the findings from different studies using induction and interpretation to gain deeper understandings of a particular phenomenon. They noted how integrative reviews require an etic approach (working with a pre-existing frame of reference), thereby enabling the aggregation of findings by ensuring that there is ‘a basic comparability between phenomena’. 15 Drawing on work by Spicer,22 interpretative reviews were contrastingly characterised as using an emic approach with concepts and explanatory frameworks emerging through a process of induction.
This chapter examines the assumptions and procedures of different methods of synthesising qualitative research drawing on the framework proposed by Hammersley14 as a means of distinguishing different methods of qualitative synthesis. Particular attention is given to Noblit and Hare’s15 meta-ethnography, as this forms the main approach to qualitative synthesis employed in the health field and is the focus of this report. Methods for the formal integration and synthesis of quantitative and qualitative studies are beyond the scope of this report and have been considered in detail elsewhere. 21,23,24
Types of qualitative synthesis
Methods of qualitative synthesis are at an early stage of development and considerable methodological work is ongoing, particularly within health and educational research. The rapid expansion of the field has resulted in a lack of standard terminology, with the terms ‘meta-ethnography’, ‘meta-interpretation’, ‘meta-analysis’, ‘narrative synthesis’, ‘meta-synthesis’ and other descriptors being widely used to describe similar approaches. Conversely, the same terms are frequently employed to describe different approaches. This suggests a need to look beyond labels when searching and reviewing this area of work and for developing an agreed terminology.
The term ‘synthesis’ also has varying meanings and fuzzy boundaries in relation to qualitative research and involves a range of activities. At present, there is no single agreed classification of different types of qualitative synthesis and different authors adopt varying frameworks. Based on their main aims and approaches to synthesis, this chapter identifies the different types of synthesis that may be undertaken in relation to qualitative studies (i.e. secondary data) as numeric, narrative and interpretive (Box 1). In practice, however, these different methods may overlap and can be viewed as forming part of a continuum that ranges from numeric syntheses at one end to interpretive approaches based on a qualitative paradigm at the other. Some forms of secondary analysis of primary data across studies can also be regarded as a form of qualitative synthesis.
Case survey method
Bayesian methods
Narrative synthesisNarrative review
Thematic analysis
Cross-case analysis
Interpretive synthesisMeta-ethnography
Meta-study
Grounded theory
Realist synthesis
Primary data Secondary data analysisAggregative synthesis
It seems paradoxical to begin this review of methods for synthesising qualitative research with numeric approaches. Nevertheless, a variety of methods have been proposed for converting data from qualitative research studies into a quantitative form for the purposes of analysis and synthesis. An early example is Yin’s25 case survey method, which was developed for the synthesis of case studies based on a qualitative or mixed-method approach. This method involves the initial application of a closed-ended coding instrument to each qualitative case study to abstract and record relevant data. The collective data from these codes are then tallied and analysed in much the same way as traditional survey data. Examples are analyses by Yin25 and colleagues of citizen participation in urban services26 and of innovations in urban services. 27,28 This approach to the synthesis of qualitative data mimics quantitative meta-analysis in which findings (usually from individual RCTs) are aggregated in order to have sufficient statistical power to detect a cause and effect relationship between a particular treatment and specific health outcomes. 28
Current interest in combining qualitative and quantitative syntheses has led to other types of numeric methods, with a key example being the Bayesian synthesis of qualitative and quantitative evidence. This involves pooling of the data and is illustrated by Roberts et al. ’s29 investigation of childhood immunisation and the probable effects of a variety of factors on uptake. Their approach involved the initial extraction of factors influencing the uptake of childhood immunisation identified from qualitative studies. These factors were then classified in terms of broader descriptive categories (e.g. ‘lay beliefs’ was used to capture such concepts as ‘parents’ beliefs’ and ‘opinions of parents and other family members about the value of immunisation’). Rankings of the relative importance of each factor by each reviewer yielded a probability of that factor being important in determining uptake. These factors were then combined with evidence from the quantitative data to form a posterior probability that each factor identified (e.g. lay beliefs) was important in determining uptake of immunisation. This synthesis, therefore, provided a more complete enumeration of factors associated with the uptake of immunisation through combining quantitative and qualitative studies. Bayes factor methods were then employed to compare two possible meta-regression models in explaining the log-odds of immunisation uptake for each possible factor. This approach forms an important attempt to combine qualitative and quantitative evidence using numeric methods and pooling data, but like other numeric methods is mainly concerned with what Hammersley14 identified as aggregative purposes in terms of the accumulation and generalisation of evidence.
Other approaches to the systematic analysis/synthesis of studies derive from Miles and Huberman’s30 cross-case techniques, which involve developing summary tables based on content analysis and noting commonalities and differences between studies.
Narrative synthesis
The aims of narrative synthesis are generally to achieve an aggregation of findings or check the comparability and replication of findings, based on narrative rather than numeric methods. A narrative synthesis may also lead to new insights and form the basis for further interpretive analysis and conceptual development, although this is not the primary focus.
There are two broad approaches to qualitative narrative synthesis. One is based on the traditional literature review and involves the use of informal but critical and reflective methods. This approach, lately described as ‘narrative review’,20 unusually aims to provide a commentary and summary of the main features and findings of a body of literature using methods that are not explicitly pre-defined and transparent. This method has been distinguished from ‘narrative synthesis’, which employs more transparent and systematic methods to identify studies, assess study quality and synthesise the findings. It usually involves a form of thematic analysis to identify the main, recurrent or most important themes in the literature, thus allowing the findings of studies to be summarised and grouped. Examples of narrative syntheses include McNaughton’s31 review of research reports describing the home-visiting practice of public-health nurses to identify common elements and differences between studies, and Finfgeld’s32 review of studies to better clarify how individuals overcome drug and alcohol problems without participating in 12-step-type self-help groups or formal treatment.
Narrative synthesis is an approach that has evolved largely from within the quantitative systematic reviewing tradition. Indeed, the Centre for Reviews and Dissemination at York University33 now encourages reviewers to first undertake a ‘descriptive or non-quantitative synthesis’ of studies to be included in a review, in other words a narrative synthesis, to help them think about what the ultimate method of synthesis should be. In order to further assist this development, a report has recently been compiled to provide detailed guidance on how to undertake narrative synthesis in systematic reviews. 34
Interpretive synthesis
This is generally regarded as ‘the’ approach to the synthesis of qualitative research, and has as its specific aim the achievement of the developmental goal of qualitative synthesis in terms of producing interpretations that go beyond individual studies and thus contribute to conceptual and theoretical development in the field14 and accords with Strike and Posner’s11 notion of qualitative synthesis as achieving ‘conceptual innovation’ or the ‘invention or employment of concepts not found in the characterization of the parts as a means of creating the whole’ (p. 346). The output is, therefore, a new interpretation or theory that goes beyond the findings of any individual study.
A number of approaches to the conduct of interpretive synthesis have been developed. These include meta-ethnography, meta-study, critical interpretive synthesis, realist synthesis and grounded formal theory. Each of these approaches is examined in detail in Approaches to interpretive synthesis, but a general feature is that the synthesis builds interpretation from original studies by firstly identifying interpretations offered by the original researchers (second-order constructs) and, secondly, enabling the development of new interpretations (third-order constructs) that go beyond those offered in individual primary studies.
Secondary data analysis
This approach is concerned with the analysis and interpretation of primary (i.e. ‘raw’) data rather than the findings of published studies. Secondary data analysis may be regarded as a form of interpretive synthesis if it fulfils two requirements: it involves multiple qualitative data sets rather than a single data set; and the aim is to provide a new perspective or conceptual focus rather than to undertake an additional in-depth or subset analysis of existing data.
There are currently only a few examples of secondary analysis of multiple qualitative data sets. These have mainly involved the re-analysis by researchers of their own data. An example is Bloor and MacIntosh’s35 study of techniques of client resistance to surveillance based on two earlier studies they conducted. Interest in the secondary analysis of qualitative data is growing, and the capacity to undertake such work is considerably enhanced by the establishment by the Economic and Social Research Council’s (ESRC’s) UK Data Archive of an archive of data from qualitative studies.
Secondary analysis of qualitative data raises a number of ethical and methodological issues, including issues of consent in relation to the reuse of another researcher’s data for a different purpose,36,37 and methodological questions such as the effects of distance from the data collection and of possible variations in study design on interpretation. 38 It is likely that the greater availability of qualitative data sets and increasing interest in secondary analysis will lead to new protocols and strategies to address these issues, thus, enhancing this approach to the synthesis of qualitative research.
Approaches to interpretive synthesis
This section provides a more detailed consideration of four approaches to interpretive synthesis: meta-ethnography, meta-study, grounded formal theory and realist synthesis.
Meta-ethnography
Noblit and Hare’s15 method of meta-ethnography was published in 1988 and is described as ‘an attempt to develop an inductive and interpretive form of knowledge synthesis’. Noblit and Hare15 developed meta-ethnography in response to the perceived failure of a synthesis of five ethnographic studies of educational desegregation that were undertaken to convey information to policy-makers. This educational synthesis took an aggregative, thematic approach that involved abstracting data and isolating factors in each study that appeared to be responsible for the failure of schools to desegregate. This process of abstraction de-emphasised the uniqueness of each site. The context therefore merely became a confounding variable in the search for common findings rather than contributing to an explanation of these findings. As a result, the synthesis did not provide researchers or policy-makers with an understanding of what went wrong and what could be done about it. Noblit and Hare15 aimed to overcome these limitations through developing a distinct method for the synthesis of qualitative studies that was informed by Turner’s39 theory of social explanation and is interpretive rather than aggregative. As they stated:
The nature of interpretive explanation is such that we need to construct an alternative to the aggregative theory of synthesis entailed in integrative research reviews and meta-analysis and be explicit about it.
Noblit and Hare15 (p. 18)
This aim of constructing adequate interpretive explanations required developing a way of ‘reducing’ and deriving understanding from multiple cases, accounts, narratives or studies while retaining the sense of the account. Noblit and Hare15 were themselves ethnographers who were concerned with long-term intensive studies that employed observation, interviews and documents, and termed the approach that they developed ‘meta-ethnography’. However, they described meta-ethnography as being applicable to qualitative research generally and as forming ‘a rigorous procedure for deriving substantive interpretations about any set of ethnographic or interpretive studies’ (p. 9). Noblit and Hare15 also noted that their particular approach was ‘a’ meta-ethnography and that it formed ‘but one of many possible approaches’ (p. 25).
Noblit and Hare15 identified seven phases in undertaking meta-ethnography (Box 2), but observed that in practice these phases may occur in parallel and overlap. The phases broadly correspond with other methods of synthesis, but differ in the assumptions and procedures involved. One difference is that the sample for research is purposively selected in relation to the topic of interest (and may involve maximum variation sampling), rather than being exhaustive. This reflects the general approach of qualitative methods and the aim of achieving interpretive explanation. A second difference is that the interpretations and explanations contained in the original studies are treated as data through the selection and analysis of key ‘metaphors’ (i.e. the themes, perspectives or concepts revealed by qualitative studies), with the aim of reducing accounts while preserving the sense of the account. Preparation for comparison between studies requires listing and juxtaposing the key metaphors, phases, ideas and/or concepts used in each account but retaining, as far as possible, the terminology used by the authors to remain faithful to the original meanings (phase 4). A third difference is that comparison between studies involves processes of ‘translation’, with the metaphors/concepts and their interrelationships in one account being compared with those in another account. This process of translation is idiomatic and focuses on translating the meaning of the text rather than a literal translation, with the aim of preserving original meanings and contextualisation. Noblit and Hare15 identified three possible types of relationship that guide translation and subsequent synthesis:
-
Reciprocal: when studies are about similar things, they can be synthesised as direct translations (i.e. in an iterative fashion each study is translated into the metaphors of the others – see Chapter 5 for a detailed description and illustration of this process). ‘These reciprocal translations may reveal that the metaphors of one study are better than those of others in representing both studies, or that some other set of metaphors not drawn from these studies seems reasonable.’ Noblit and Hare15 pointed out that the ‘uniqueness of studies may not make it possible for a single set of metaphors to adequately express the studies’, in which case more is often learned from the process of translation than from the metaphors alone.
-
Refutational: this is undertaken when studies refute each other. It requires a more elaborate set of translations ‘involving’ translations of both the ethnographic account and the refutations to examine the implied relationship between competing explanations.
-
Lines-of-argument: many studies suggest a lines-of-argument or inference about some larger issue or phenomenon. This involves first translating studies into each other and then constructing an interpretation (‘lines-of-argument’) that may serve to reveal what was hidden in individual studies (discovering a ‘whole’ among a set of parts). This is achieved through the use of the comparison and theory generation aspects of grounded theory as described by Glaser and Straus,40 and involves the detailed study of differences and similarities among studies to be synthesised with the aim of producing an integrated scheme and new interpretive context.
Phase 1: Getting started – ‘identifying an intellectual interest that qualitative research might inform’. This may be changed/modified as interpretive accounts are read.
Phase 2: Describing what is relevant to initial interest – an exhaustive search for relevant accounts can be undertaken followed by selection of research relevant to the topic of interest (they observe that employing all studies of a particular setting often yields trite conclusions).
Phase 3: Reading the studies – the repeated reading and noting of metaphors is required and continues as the synthesis develops.
Phase 4: Determining how the studies are related – the task of putting together the studies requires creating a list of key metaphors, phrases, ideas or concepts (and their relations) used in each account, and juxtaposing them. This leads to initial assumptions about relations between studies.
Phase 5: Translating the studies into one another – the metaphors and/or concepts in each account and their interactions are compared with the metaphors and/or concepts and their interactions in other accounts. These translations are one level of meta-ethnographic synthesis.
Phase 6: Synthesizing translations – ‘the various translations can be compared with one another to determine if there are types of translation or if some metaphors/concepts are able to encompass those of other accounts. In these cases, a second level of synthesis is possible, analysing types of competing interpretation and translating them into each other’ to produce a new interpretation/conceptual development.
Phase 7: Expressing the synthesis – for the proposed synthesis to be communicated effectively it needs to be expressed in a medium that takes account of the intended audience’s own culture and so uses concepts and language they can understand.
How translations are synthesised (phase 6), and the product of this process, depends on how studies relate to each other. Both translation and synthesis involve a continuous comparative analysis of texts until a comprehensive understanding of the phenomena is realised and the synthesis is then complete. Noblit and Hare15 did not specify this process in detail, but regarded it as akin to the general processes of qualitative research. The main difference is that the ‘data’ of meta-ethnography are the substance of several qualitative studies.
The final stage of meta-ethnography is ‘expressing the synthesis’ or communicating with an audience. This was given considerable emphasis by Noblit and Hare,15 who stated that ‘the worth of any synthesis is in its comprehensibility to some audience’ (p. 82). They described the needs of the audience (e.g. researchers, policy-makers) as influencing both the form and substance of the synthesis. Some understanding of the audience’s culture is therefore required to ensure that the translation of studies for the synthesis uses intelligible concepts to inform the final presentation of synthesis. They observed that if the data are inadequate or if the audience cannot see the connection between data and the argument then the study becomes unbelievable. Comprehensibility and believability are thus central to determining worth.
Noblit and Hare’s15 approach to meta-ethnography was based on a literary tradition of interpretivism and was, therefore, driven by a desire to achieve adequate interpretive explanations rather than by technical interests. This means that the authors were critical of the emphasis given by some qualitative researchers to the explicitness of processes employed to analyse data and refer to what Marshall41 described as the ‘bureaucratization of data analysis’. 15 Instead they emphasised the fluidity and interpretive aspects, and described the conduct of meta-ethnography as an ongoing process in which substantive interests may change as the synthesis proceeds. Similarly, translations were regarded as emergent and interactive, with the stages of translation and synthesis often interweaving rather than forming distinct phases.
Noblit and Hare15 illustrated the methods of meta-ethnography using brief excerpts of material from educational studies. Following publication of their monograph, there has been considerable interest in the application of meta-ethnography to a variety of fields including education, public policy and health. The greatest number of recent meta-ethnographic syntheses have come from nursing, reflecting the large number of qualitative studies in nursing and the particular interests and contributions of schools of nursing in the USA and Canada.
The present review involved a search for examples of meta-ethnography and other methods of interpretive synthesis in the health field. This initially involved a computer search undertaken in spring 2003 and updated in the summer of 2006 using MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), EMBASE, Web of Science (Social Science Citation Index and Science Citation Index), PsychINFO and Zetoc (British Library’s Electronic Table of Contents) electronic databases. A simple search strategy was used that combined the term ‘qualitative research’ with the terms ‘meta analysis’, ‘meta synthesis’, ‘meta ethnography’, ‘systematic review’, ‘data synthesis’ and ‘meta study’. Hyphenated terms (e.g. meta-ethnography) were also used. Further syntheses were identified via a published textbook of methods of qualitative meta-synthesis42 and later compared with Finfgeld’s43 review. However, the aim was not so much to achieve an exhaustive list as to identify representative syntheses using meta-ethnography and to examine their practical applications.
A total of 41 reports were identified that appeared to be qualitative syntheses. 16,17,44–82 The authors used various terms to describe the methods employed and occasionally used more than one term. We therefore broadly grouped syntheses according to what appeared to be their main approach. Syntheses employing meta-ethnography prior to the beginning of the present project demonstrated the potential value of this approach in producing conceptual developments. This is illustrated by the development of a wellness–illness model,61 a model of caring,74 models of diabetes management17,70 and explanations of states and behaviours such as moral distress among nurses, non-adherence among patients, the experience of post partum depression and help-seeking behaviours (Table 1). The studies included in these syntheses mainly collected data through interviews with only a few including focus groups or observational methods. They also exhibited a limited variety of theoretical perspectives, reflecting the dominant approaches to qualitative research in the field of health and illness.
| Authors and title | Number of reports included | Authors’ description | Appraisal criteria | Main concepts/explanations | Comments |
|---|---|---|---|---|---|
| Meta-ethnography | |||||
|
Britten et al. , 200216 Using meta-ethnography to synthesise qualitative research: a worked example |
Four papers, arbitrarily chosen (included three by authors) | Use of Noblit and Hare’s15 meta-ethnography | No | Developed a line of argument that accounts for patients’ medicine-taking behaviour and communication with health professionals in different settings based on notions of self-regulation and selective disclosure | Aimed to assess benefits of meta-ethnography through a worked example |
|
Campbell et al. , 200317 Evaluating meta-ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care |
10 reports, purposively selected | Use of Noblit and Hare’s15 meta-ethnography |
Questions from CASP18 Two papers excluded because of methods and one because of an overlap with another paper |
Identified a model of diabetes management involving strategic non-compliance which was associated with being in control of diabetes, ‘coping’, achieving a balance between quality of life and illness, improved glucose levels and a feeling of well-being | Aimed to provide a formative assessment of meta-ethnography and of a qualitative assessment tool |
|
Feder et al. , 200644 Women exposed to intimate partner violence: expectations and experiences when they encounter health-care professionals: a meta-analysis of qualitative studies |
29 articles, computer search | Meta-analysis of qualitative studies. Use of Schulz et al.’s3 framework of constructs for meta-analysis. Meta-ethnography method used by Campbell et al.,17 and first used by Noblit and Hare15 | No | Use of first-, second- and third-order constructs to identify desirable characteristics of health-care professionals in consultations in which partner violence is raised | Table of third-order constructs in terms of recommendations to health-care providers by stage of interaction with abused women |
|
Smith et al. , 200545 Delay in presentation of cancer: a synthesis of qualitative research on cancer patients’ help-seeking experiences |
32 papers, computer search | Use of Noblit and Hare’s15 meta-ethnography | No | Use of second- and third-order constructs. Similarities in help-seeking in patients with different cancer types. Key concepts were recognition and interpretation of symptoms, and fear of consultation. Fear of embarrassment and fear of cancer. Patient’s gender and the sanctioning of help-seeking were important factors in prompt consultation | Provides international overview through the systematic synthesis of a diverse group of small-scale qualitative studies |
|
Walter et al. , 200446 Lay understanding of familial risk of common chronic diseases: a systematic review and synthesis of qualitative research |
11 qualitative articles, computer search and reference lists |
Meta-analysis using meta-ethnographic methods and drawing on Schulz et al. 3 Three stages: first-order constructs (key concepts from each article); second-order constructs (translating first-order constructs); third-order constructs (synthesising second-order constructs to produce overarching concepts) |
Articles assessed using appraisal scoring system (CASP). None excluded | Second-order constructs included diseases running in my family; experiencing a relative’s illness; personal mental models; personalising vulnerability; and control of familial risk. Led to three main third-order constructs: salience; personalising process; and personal sense of vulnerability | Identifies third-order constructs for health professionals to explore with patients that may improve the effectiveness of communication about disease risk and management |
| Meta-synthesis | |||||
|
Attree, 200547 Parenting support in the context of poverty: a meta-synthesis of the qualitative evidence |
12 studies, search methods not given | Use of Noblit and Hare’s15 meta-ethnographic methods to produce meta-synthesis of findings | Quality appraised using checklist that drew on earlier models of assessing qualitative research: Popay et al.,83 Seale,84 Mays and Pope,85 CASP,18 Spencer et al.19 Studies graded A–D. A–C grades were included | Systematic review of qualitative studies of low-income parents to explore informal and formal support networks. Two main themes were found: informal and formal support | Difficult to identify any of the key components of a meta-ethnography, e.g. reciprocal translation, refutation or lines-of-argument |
|
Barroso and Sandelowski, 200448 Substance abuse in HIV-positive women |
74 reports, search methods not given | Qualitative meta-synthesis of studies | No | Qualitative meta-synthesis of studies containing information on abuse among HIV-positive women. Three main themes found: diagnosis as a turning point; complications of motherhood for dually diagnosed women; and benefits of recovery – beyond stopping substance abuse | Constructs trajectory that describes events of women’s lives with regard to substance abuse and its intersection with HIV infection |
|
Barroso and Powell-Cope, 200049 Meta-synthesis of qualitative research on living with HIV infection |
21 studies, computer search | Meta-synthesis | Burns86 standards: led to ‘some exclusions’ | Identified importance of finding meaning in HIV infection/AIDS which led to being able to establish human connectedness, focusing on the self, negotiating health care and dealing with stigma. Those for whom HIV infection had shattered meaning were unable to establish a framework for coping |
Conducted a post-review validity check on a random sample of a further 33 studies published 1996–8 to determine that their metaphors were still valid in these studies Many extracts of interviews with HIV-positive people |
|
Beck, 200250 Mothering multiples: a meta-synthesis of qualitative research |
Six qualitative studies, computer search | Use of Noblit and Hare’s15 meta-ethnography | No | Synthesis produced five themes: bearing the burden; riding the emotional roller coaster; lifesaving support; striving for maternal justice; and acknowledging individuality | Synthesis conducted to illustrate the method |
|
Beck, 200251 Post partum depression: a meta-synthesis |
18 studies, computer search | Use of Noblit and Hare’s15 meta-ethnography | No | Identified four overarching themes with their subsumed metaphors in relation to the experience of post partum depression: incongruity between expectations and reality of motherhood; spiralling downward; pervasive loss; and making gains. Coping involved seeking professional help, adjusting unrealistic expectations and regaining control in their lives | Described the end product as a comprehensive and thickly descriptive account that is the foundation for theory development |
|
Carrol, 200452 Nonvocal ventilated patients’ perceptions of being understood |
12 studies, computer search | Meta-synthesis following Noblit and Hare’s15 meta-ethnography | No | Found five overarching themes and divided them into two groups: characteristics of non-vocal ventilated patients’ communication experience; type of nursing care desired by non-vocal patients in order to be understood | Data translated into second-order interpretations, but not constructed into third-order interpretations |
|
Clemmens, 200353 Adolescent motherhood: a meta-synthesis of qualitative studies |
18 studies, computer search | Meta-synthesis following Noblit and Hare’s15 meta-ethnography | No | Five metaphors were found: reality of motherhood brings hardship; living in the two worlds of adolescence and motherhood; motherhood as positively transforming; baby as stabilising influence; and supportive context as turning point for future. Clinical implications of study | |
|
Coffey, 200654 Parenting a child with chronic illness: a meta-synthesis |
11 studies, computer search | Meta-synthesis following Noblit and Hare’s15 meta-ethnography | No | Two of the 11 studies were triangulated. Seven themes were found: living worried; staying in the struggle; carrying the burden; survival as a family; bridge to the outside world; critical times; and taking charge | |
|
Coffman M, 200455 Cultural caring in nursing practice: a meta-synthesis of qualitative research |
13 studies, computer search | Meta synthesis following Noblit and Hare’s15 meta-ethnography | No | Findings reduced to six overall themes: connecting with the client; cultural discovery; the patient in context; in their world, not mine; roadblocks; and the cultural lens | |
|
Evans and FitzGerald, 200256 The experience of physical restraint: a systematic review of qualitative research |
Four qualitative studies, computer search | Using meta-ethnography Noblit and Hare;15 meta-synthesis Jenson and Allen;61 content analysis (Suikkala and Leino-Kilpi87). Identify the key themes and compare these across studies | Locally developed tool to appraise: methodology; clear descriptions; adequate result information; information supported by exemplars from study participants | Summarises current evidence on the experience of being physically restrained, and the experience of having a relative subject to restraint in an acute or residential care facility | References a number of approaches to qualitative synthesis, but does not seem to apply them |
|
Finfgeld-Connett, 200557 Clarification of social support |
47 studies, computer search (3 linguistic analyses and 44 qualitative studies) | Meta-synthesis. Use of the Template Verification and Expansion Model (Finfgeld88) of concept development, based on meta-synthesis of findings from qualitative studies and linguistic analyses to inductively clarify and expand existing conceptual models and triangulate findings | No | Aimed to clarify the concept of social support. Findings placed in a matrix organised by Walker and Avant’s89 broad concept analysis categories: antecedents, critical attributes and consequences. Three themes found: types of social support; attributes of social support; and antecedents of social support | |
|
Finfgeld-Connett, 200658 Meta-synthesis of presence in nursing |
18 studies, computer search (14 qualitative studies and 4 linguistic-concept analyses) | Finfgeld’s43 meta-synthesis methods. Grounded theory (Strauss and Corbin90) | No | Presence is an interpersonal process that is characterised by sensitivity, holism, intimacy, vulnerability and adaptation to unique circumstances. Created chart: ‘process of presence’ | |
|
Goodman, 200559 Becoming an involved father of an infant |
10 articles, computer search | Meta-synthesis using Noblit and Hare’s15 meta-ethnography | No | Fathers of infants experienced four phases: entering with expectations and intentions; confronting reality; creating one’s role of involved father; and reaping rewards. Implications for theory development, research and clinical practice are discussed | |
|
Howell and Brazil, 200560 Reaching common ground: a patient-family-based conceptual framework of quality EOL care |
Seven studies, computer search | Descriptive meta-synthesis in systematic review. Linking metaphors in a Venn diagram, Miles and Huberman30 | Excluded if inductive reasoning not used/lack of evidentiary support. Sandelowski and Barroso’s91 typology used for classifying studies on the basis of their interpretive analysis to determine their methodological comparability | Found eight themes: pain and symptom control; dying process not prolonged; prepared for death; support of family or friends; supported decision-making; spiritual support and meaning; holistic and individualised care; death in a supportive environment in location of choice | Grounded theory methods were used for developing metaphors and themes in four studies; unspecified content analysis was described in the remaining studies |
|
Jensen and Allen, 199461 A synthesis of qualitative research on wellness–illness |
112 studies, search methods not given (included 63 dissertations and theses) | Use of Noblit and Hare’s15 meta-ethnography and grounded theory | No | Derived overall model of wellness–illness based on lived experience involving abiding vitality (when one is healthy); transitional harmony (experience of unity disrupted by disease); rhythmical connectedness (disease results in detachment or disconnection from oneself, others and environment); unfolding fulfilment; active optimism; and reflective transformation | |
|
Kärkkäinen et al. , 200562 Documentation of individualized patient care: a qualitative metasynthesis |
14 research reports, computer search | Qualitative meta-synthesis | Data management followed Gadamer’s hermeneutic empirical theory:a a new understanding of investigated matter occurs when a concept conveyed by the studied text by means of hermeneutic dialogue is added to the researchers view. Results of analysed articles can be interpreted in a different way | Three themes emerged that affected the content of nursing-care documentation: reflecting the demands on an organisation; reflecting nurses attitudes and duties; and reflecting patients’ involvement in their care | |
|
Kennedy et al. , 200363 An exploration meta-synthesis of midwifery practice in the United States |
Six studies, search methods not given | Meta-synthesis | No | Four themes identified, conceptually arrayed into a helix model to portray their dynamic and overlapping nature: the term midwife as an instrument of care; the woman as a partner in care; alliance in midwifery care; and the environment in the process of midwifery care | Uses some of the stages in meta-ethnography as described by Noblit and Hare15 |
|
Kylma, 200564 Despair and hopelessness in the context of HIV infection – a meta-synthesis on qualitative research findings |
Five qualitative studies by the same author, computer search | Meta-synthesis method: extraction, comparing extracted factors, coding, gathering categories together | No | Despair consists of two subprocesses – downwards and upwards. Downwards: being stuck in a situation, losing perspective. Upwards: fighting against sinking, rising up | Five studies were all by the same author |
|
Kylma, 200565 Dynamics of hope in adults living with HIV infection/AIDS: a substantive theory |
Five articles by the same author, computer search | Meta-synthesis: read articles, extraction, comparing extracted factors, coding, gathering categories together | No | Dynamically altering balance between interconnected hope, despair and hopelessness based on folding and unfolding possibilities with regard to the dynamics of hope in dealing with the changing self and life with HIV infection/AIDS | Five grounded theory studies – all by the same author |
|
Lefler and Bondy, 200466 Women’s delay in seeking treatment with myocardial infarction: a meta-synthesis |
48 reports, computer search (39 descriptive studies, 4 experimental in design, 5 used qualitative methodology) | Meta-synthesis of the literature using Cooper’s92 five stages: problem formation; data collection; data evaluation; analysis and interpretation; and presentation of results | Articles representing opinions/discussions were excluded | Three factors explain why women delay in seeking treatment: clinical; sociodemographic; and psychosocial | |
|
Meadows-Oliver, 200367 Mothering in public: a meta-synthesis of homeless women with children living in shelters |
18 studies, search methods not given | Meta-synthesis | No | Six reciprocal translations of homeless mothers caring for children in shelters: becoming homeless; protective mothering; loss; stressed and depressed; survival strategies; and strategies for resolution | Uses some of the stages in meta-ethnography as described by Noblit and Hare15 |
|
Nelson, 200368 Transition to motherhood |
Nine studies, computer search | Meta-synthesis | No | Two processes inherent in maternal transition were identified: engagement, and growth and transformation. In addition, five thematic categories identified signifying areas of disruption present in the maternal transition: commitment; daily life; relationships; work; and self | |
|
Nelson, 200269 A meta-synthesis mothering other-than-normal children |
12 studies, search methods not given | Use of Noblit and Hare’s15 meta-ethnography | No (three exclusions as not qualitative and two not relevant) | 13 themes/metaphors reduced to four steps common to the mothering experience: becoming a mother of a disabled child, negotiating a new kind of mothering, dealing with daily life; and the process of acceptance/denial | |
|
Paterson et al. , 199870 Adapting to and managing diabetes |
43 papers (38 studies), computer search | Use of Noblit and Hare’s15 meta-ethnography | No | Identifies ‘balance’ as the main metaphor in the experience of diabetes, and examines process and requirements for learning to balance | Use of prior organising framework: Curtin and Lubkin93 conceptualisation of the experience of chronic illness. Several methods used to achieve trustworthiness including other members of team reviewing/agreeing analysis; identifying negative/disconfirming cases; testing rival hypotheses |
|
Roux et al. , 200271 Inner strength in women: meta-synthesis of qualitative findings in theory development |
Five studies, search methods not given | Meta-synthesis using Walker and Avant.89 Meta-synthesis used is similar to qualitative analysis or constant comparison, the selected literature was read, reread and examined for patterns of similarities among study findings that could be categorised or grouped together | No | ‘Conceptual model of inner strength in women revealed in the following constructs: knowing and searching; nurturing through connection; dwelling in a different place by recreating the spirit within; healing through movement in the present; and connecting with the future by living a new normal’71 | |
|
Sandelowski et al. , 200472 Stigma in HIV-positive women |
93 studies, search methods not given | Meta-synthesis. Worked inductively to create a taxonomy to depict the conceptual range of findings | No | Key findings included pervasiveness of both felt and enacted stigma; gender-linked intensification of HIV infection-related stigma; and unending work and care of stigma management | |
|
Sandelowski and Barroso, 200573 The travesty of choosing after positive prenatal diagnosis |
17 studies, computer search | Meta-summary techniques included the calculation of frequency effect sizes, used to aggregate findings. Meta-synthesis techniques included the reciprocal translation of concepts (Noblit and Hare15 used to interpret the findings) | No | Emphasis in findings is on the termination of pregnancy following positive diagnosis. The thematic emphasis is on the dilemmas of choice and decision-making. For couples, positive prenatal diagnosis was an experience of chosen losses and lost choices | |
|
Sherwood, 199774 Meta-synthesis of qualitative analyses of caring: defining a therapeutic model of nursing |
16 studies, search methods not given | Use of Noblit and Hare’s15 meta-ethnography | Burns86 and Roberts and Burke94 applied to each study. None excluded | Developed a therapeutic model of caring that identifies relationships between caregivers and receivers of care in producing therapeutic outcomes (involves the interaction context, nurses’ knowledge and nurses’ response patterns) | Consultation with two independent caring experts to validate the findings |
|
Steeman et al. , 200675 Living with early-stage dementia: a review of qualitative studies |
33 articles (28 studies), computer search, manually searched reference lists | Meta-synthesis aimed at an integrative interpretation of findings from single qualitative studies to synthesise a more substantive description of the phenomenon43,95,96 | Studies meeting inclusion criteria were appraised using Sandelowski and Barrosso97 guide for qualitative research | Living with dementia is described from the stage at which a person discovers the memory impairment, through the stage of being diagnosed with dementia, to that of the person’s attempts to integrate the impairment into everyday life | |
|
Swartz, 200576 Parenting preterm infants: a meta-synthesis |
10 studies, computer search | Meta-synthesis. Use of Noblit and Hare’s15 meta-ethnography | No | Five themes of parenting preterm infants emerged: adapting to risk; protecting fragility; preserving the family; compensating for the past; and cautiously affirming the future. Clinical implications | |
|
Varcoe et al. , 200377 Health-care relationships in context: an analysis of three ethnographies |
Three reports (based on own studies) | Qualitative meta-data analysis influenced by Noblit and Hare’s15 meta-ethnography | No | Importance of ‘moral distress’ for nurses due to experience of structural and personal constraints (e.g. excessive workloads, absence of interdisciplinary team rounds, conflict between team members and conflict with patients and families) and may lead to coercive practices | All studies conducted within 5-year period in four acute hospitals in same geographical location in western Canada. Studies based on different theoretical perspectives |
|
Werner, 200278 Human response outcomes influenced by nursing care |
42 studies, computer search | Meta-synthesis | No | Use of Loomis and Wood’s98 model of the seven human response systems which has three dimensions: health and illness; human-response systems; and nursing clinical decision-making. Findings organised into categories: physical human responses influenced by nurse caring; emotional human responses influenced by nurse caring; cognitive human responses influenced by nurse caring; family human responses influenced by nurse caring; social human responses influenced by nurse caring; spiritual human responses influenced by nurse caring | |
| Meta-studies | |||||
|
Paterson et al. , 200379 Embedded assumptions in qualitative studies of fatigue |
35 primary research reports, computer search | Meta-study (analysis in three stages): meta-data analysis, meta-method and meta-theory. Synthesis is a creative interpretation of the primary research to produce new and expanded understandings of the phenomenon under study | No | Four key assumptions found in the data: fatigue as exclusively attributed to disease; fatigue as a unitary phenomenon across human experiences; fatigue as inherently and necessarily problematic; and fatigue as isolated from the context in which it occurs | |
|
Paterson, 200180 The shifting perspectives model of chronic illness |
292 studies that met inclusion criteria from 1000 computer and manual search and professional networks | Meta-study including meta-ethnography |
Yes Burns standards86 |
Depicts people with chronic illness as shifting between illness and wellness in the foreground. Also identifies major factors leading to shift to illness in the foreground and process of ‘bouncing back’ to wellness in the foreground | Data synthesised to create model |
|
Thorne and Paterson, 199881 Shifting images of chronic illness |
158 reports that met inclusion criteria from 400 identified, computer and manual search (included dissertations) | Meta-study |
Yes Burns standards86 |
Describes shifting conceptualisations of individuals with chronic illness and parallel shifts in conceptualisations of health-care relationships appropriate to chronic illness from client-as-patient to client-as-partner | |
| Critical interpretative synthesis | |||||
|
Dixon Woods et al. , 200682 Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups |
119 papers, computer search, websites, reference chaining, contacting experts | Development and use of the method of CIS. Identified their method as reciprocal translational analysis; refutational syntheses and lines of argument synthesis | NHS National Electronic Library for Health for the evaluation of qualitative research, to inform judgements on the quality of papers. 20 excluded on grounds of being ‘fatally flawed’ | Created synthesis including critique of utilisation as a measure of access; candidacy; identification of candidacy; navigation; permeability of services; appearances at health services; adjudications; offers and resistance; operating conditions; and the local production of candidacy | |
Altogether we identified six syntheses that were clearly labelled as employing the methods of meta-ethnography. These included two papers on preliminary work published by the present team;16,17 a synthesis of 43 papers concerned with the experience of diabetes;70 a meta-ethnographic synthesis by Smith et al. 45 examining cancer patients’ help-seeking experiences; a synthesis by Feder et al. 44 of health-care professionals’ interactions with women in violent relationships; and another by Walter et al. 46 which was concerned with lay understandings of familial risk in common cancers.
The largest group of qualitative syntheses that we identified were labelled as meta-synthesis. Qualitative meta-synthesis was defined by Sandelowski et al. 13 as ‘the theories, grand narratives, generalizations, or interpretative translations produced from the integration or comparisons of qualitative synthesis’. Meta-synthesis, thus, seems to be, in effect, another term for qualitative synthesis and one that is not identified with any particular method. Many of the syntheses included within this category cited Noblit and Hare15 and claimed to be using meta-ethnographic methods, but what seemed to distinguish this group of studies from those labelling themselves explicitly as meta-ethnographies was that the latter group adhered more closely to the approach described by Noblit and Hare,15 included a smaller number of studies (maximum of 32) and, in general, achieved a higher degree of conceptual development. Meta-study and critical interpretative synthesis, which have their origins in meta-ethnography, are more recent developments and to date have been used only by their creators. The general tendency among all these syntheses was not to formally assess the quality of the research prior to synthesis. Where this did occur it was liable to result in just a couple of exclusions or in none at all. The reports of most syntheses aimed to draw out the implications for policy-makers and practitioners, but there was little evidence of wider policy/practitioner responses to these findings and assessment of worth in these terms.
The next section considers a development of Noblit and Hare’s15 meta-ethnography through its use as one aspect of a wider meta-study.
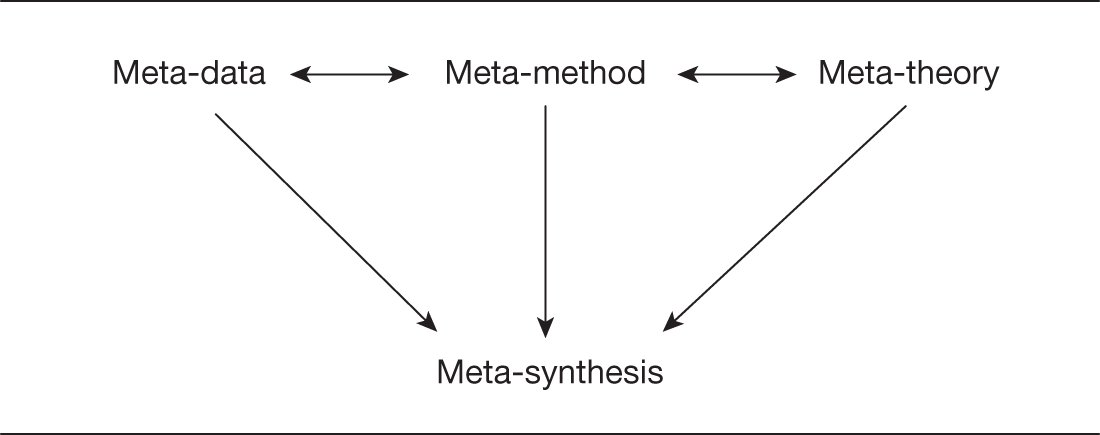
Meta-study
Paterson et al. 42 described an approach to synthesis that incorporates Noblit and Hare’s15 meta-ethnography as part of a meta-study. 70 Meta-study aims to go beyond meta-ethnography (or other methods of what they term meta-data analysis), as Paterson and colleagues do not regard meta-ethnography as giving sufficient attention to the way that theories and methods shape knowledge and confer meaning on findings. The enlarged framework of meta-study that Paterson and colleagues present derives from earlier sociological work that was concerned about understanding the ways in which theoretical, methodological or societal contexts shape reported results and bodies of knowledge. They draw particularly on the writings of Ritzer99 and of Zhao,100 who introduced the term meta-study and described its components: meta-data analysis (study of the processed data based on meta-ethnography or other methods of data analysis), meta-method (study of the appropriateness and rigour of particular methods used in the research studies and the implications of a range of epistemologically sound approaches for emerging data and interpretations) and meta-theory (analysis of the philosophical, cognitive and theoretical perspectives underlying the research that influences emerging data and interpretations). Paterson et al. 42 described each of these components as providing a unique angle of vision from which to deconstruct and interpret a body of qualitatively derived knowledge about a particular phenomenon, and suggests that meta-synthesis ‘… brings back together those ideas that have been taken apart or deconstructed in these three analytic meta-study processes’ (p. 13). Meta-synthesis, therefore, represents ‘the creation of a new interpretation of a phenomenon that accounts for the data, method and theory by which the phenomenon has been studied by others’ (p. 13) (Figure 1).
Paterson et al. 42 outlined the assumptions and methods for conducting a meta-study in their book, Meta-study of qualitative health research,42 and illustrated this in terms of the conduct of their own synthesis of the subjective experience of chronic illness. 70,101 Their initial phase of meta-data analysis was based on the methods of meta-ethnography, but whereas Noblit and Hare15 focused on the in-depth study of a small number of cases, Paterson et al. ’s42 synthesis began with the identification of close to 1000 reports, books, dissertations and research articles published during a 16-year period. These initial publications were reduced to 292 through assessment of their relevance to the review and appraisal of the sampling, data analysis and interpretation that was undertaken using Burns’86 standards for qualitative research. This appraisal involved at least three members of the team reviewing each report and reaching a consensus. Paterson et al. 42 stated that the number of studies was not reduced further as they regarded this number as necessary to achieve all components of the meta-study. The decision to include such a large number of studies required a systematised approach to meta-ethnography (i.e. meta-data analysis component) and was undertaken by the use of coded categories of themes, patterns, processes, etc. This was followed by a computer-based analysis in much the same way as the analysis of the original primary data. The use of computer software also facilitated comparisons between different groups (e.g. whether or not the disease was considered terminal, the method of sampling, gender, etc.). Paterson et al. 42 acknowledged that the handling of large numbers of reports in this way meant that there was an element of context stripping at this level, although their overall aim was to achieve greater contextualisation through finally integrating the different elements of a meta-synthesis (see Figure 1).
Although Paterson et al. 42 provided a clear and fairly detailed description of their approach to meta-data analysis, the stages of meta-method and meta-theory are less fully developed (particularly meta-theory). They also gave little guidance as to how the three components were to be integrated in the final stage of the meta-synthesis. Indeed, in terms of achieving the synthesis, they stated that they ‘… resist definitive procedural steps and encourage instead a dynamic and iterative process of thinking, interpreting, creating, theorising, and reflecting’. 42
Paterson et al. ’s42 own experience of conducting a meta-study has been their work on the subjective experience of chronic illness. 101 They acknowledged that the vast size of this undertaking presented considerable demands of organisation and data management, as well as requiring much time and a large team of researchers. What they termed the meta-data analysis component led to the depiction of the shifting perspective experienced by people with chronic illness from ‘wellness’ in the foreground to ‘illness’ in the foreground and the factors responsible for this shift and ‘bouncing back’. 80 Their attempt to achieve a meta-synthesis based on the three components of meta-study has not, however, led to a major new understanding of chronic illness, although they described the changes that have occurred in the conceptualisation of chronic illness over time. The approach they adopted to meta-synthesis also raises issues of practicability, with considerable time and resources required by the processes involved in first deconstructing and then reconstructing and synthesising the distinct components of meta-study; their own study involved seven researchers who contributed time over several years. Nevertheless, their work is important in its emphasis on the need for syntheses to take account of wider contextual factors, including the influence of theories and methods on the questions addressed and the interpretations developed. This is of particular importance in relation to the syntheses of studies conducted over a long time period and involving a broad area of research, as with Paterson et al. ’s42 own study of chronic illness. Their work also draws attention to the importance of meta-theory in terms of the study of the influence of cognitive, philosophical and theoretical perspectives on the questions addressed and interpretations as an aspect of study in its own right to complement more empirical data-based approaches.
Critical interpretive synthesis
More recently, Dixon-Woods et al. 102 used meta-ethnography to synthesise the diverse quantitative and qualitative literature on access to health care by vulnerable groups. In doing so, they suggest that it was necessary to introduce a number of innovations that were judged to be of sufficient substance to produce what they regard as a new methodological approach that they titled critical interpretive synthesis.
This synthesis was truly innovative in that it used meta-ethnography to synthesise a wide range of different paper types including primary quantitative, primary qualitative, mixed methods, editorial, review and theoretical papers. Books and reports were also included. Dixon-Woods et al. , citing Glaser and Strauss,40 present a compelling argument for there being no reason in principle why interpretive syntheses should not include different forms of evidence. The end result was that six syntheses were produced. The first was a synthesis that set out ‘a general taxonomic framework within which the literature on access to health care can usefully be organised’. 102 The remaining five syntheses comprised interpretive syntheses of access to health care for specific vulnerable groups (socioeconomically disadvantaged people, people of minority ethnicity, children and young people, and older people) and a synthesis examining the effects of gender. These syntheses led to a substantial number of findings and specific recommendations for policy and practice. In addition, concepts of candidacy and the porosity or permeability of services were proposed as useful aids to understanding access to health care. Candidacy was characterised as the processes of negotiation between people and health-care providers by which people’s eligibility for health care is established. Service porosity signalled ease of use and the number of qualifications for candidacy: the more porous a service the more comfortable it is for people to use and the fewer the qualifications required for candidacy. 102
Much of the claimed novelty of critical interpretive synthesis (CIS) rests on the way in which the three different types of syntheses identified by Noblit and Hare15 (reciprocal translation, refutational and lines-of-argument) were interpreted and understood within this particular synthesis. In terms of reciprocal translation, Dixon-Woods et al. 102 reported two problems. Firstly, they found it difficult to operationalise this process with such a large collection of papers. Although not specifically mentioned, given the wide variation in the types of papers included it seems possible that incommensurability was a problem. In other words, it is likely that the very different kinds of papers included had incompatible aims and therefore could not be integrated within the same frameworks. As we indicated after our first worked example of meta-ethnography, a key assumption of the process is that the studies are commensurable. 16 A second issue raised by Dixon-Woods102 et al. was that their experience suggested that reciprocal translation ‘provides primarily a demonstration of the extent to which concepts reported in papers are “translatable” into each other, but offers little in the way of insight … it provides only a summary in terms that have already been used in the literature, and the extent to which demonstrating “reciprocity” between the various terms and concepts is a useful exercise is questionable’. However, the authors also noted that in producing a lines-of-argument synthesis it may be necessary to employ ‘found’ or second-order constructs that are already reported in the literature ‘… to code evidence that was not previously categorised using such a construct’. 102 This use of second-order constructs from one study to code findings reported in another study102 which may not have been explicitly labelled in this way is, however, part of what we would recognise as reciprocal translation. In a more recent paper providing a reflexive account of the process of producing this synthesis, Dixon-Woods et al. 82 reflected further on the difficulties that they experienced with reciprocal translation and suggested that it may not have worked for them because of the ‘large and diverse body of literature’ that they were attempting to synthesise.
A further part of the uniqueness claimed for CIS is that it produces a ‘synthesising argument’ that ‘integrates evidence from across the studies in the review into a coherent theoretical framework comprising a network of constructs and the relationships between them’. 103 It is difficult, however, to see how this differs substantially from Noblit and Hare’s15 eloquent description of a lines-of-argument synthesis as having as its goal ‘to discover a “whole” in a set of parts’ and being akin to ethnographic accounts in that ‘it is emic … in its allegiance to the studies being synthesized; it is historical in that it uses time to give order and history-in-use to give context; it is comparative in that it constructs an analogy of relationships among studies and it is holistic in that it constructs an interpretation of all the studies; their interrelations, and contexts’. 15
The final original aspect of CIS, and the main rationale for use of the term critical, relates to refutation synthesis. In this new approach it is suggested that the synthesiser should ‘consider contradictions in the evidence in the course of producing the synthesising argument, in the same way as deviant or negative cases would be considered as part of the analysis that produces the theoretical output in primary research’. 103 Again this does not seem very different from Noblit and Hare’s15 suggestion that ‘the synthesis must “take into account” the implied relationship between the competing explanations. The implied refutation, then, is analyzed substantively and subsequently incorporated into the synthesis. Our approach treats the refutation itself as part of the interpretation to be synthesised’. 15
In their monograph, Noblit and Hare15 did appear to suggest, through the examples that they provided, that any individual synthesis would take just one of the three forms (i.e. reciprocal translation, refutational or lines-of-argument). In practice what we, and Dixon-Woods et al. ,103 have found is that one meta-ethnography may include elements of these different types of synthesis. The point at which variations on an existing method become sufficient to justify it being labelled as a new method is a matter or judgement.
The next sections describe two other approaches to meta-synthesis: grounded formal theory, that is closely linked with meta-ethnography; and realist synthesis, that describes an integrative theory-building approach developed in the health-policy field.
Grounded formal theory
Grounded formal theory is an approach to meta-synthesis that shares a common framework with Noblit and Hare’s15 meta-ethnography, but is specifically concerned with theory development and gives greater emphasis to the analysis and reporting of verbatim data. Examples of the synthesis of qualitative research using grounded formal theory are Kearney’s104 research aiming to develop a grounded theory of women’s addiction and recovery, and Finfgeld’s105 synthesis of courage among people with long-term threats to well-being that describes a grounded theory approach as forming the ‘epistemological and methodological basis’ for the study.
Kearney104 and Finfgeld105 both included dissertations in the reports that they synthesised because these include more first-hand data. Kearney104 described how she analysed the research reports as if each one was an interview transcript and coded descriptively (verbatim data) and theoretically. She developed a formal theory using a constant comparative approach that involved consulting the verbatim descriptions and the sociocultural and historical context. Following the requirements of grounded theory, once the formal theory was developed other kinds of qualitative reports on addiction and recovery were examined for relevance and to support or challenge the theory (e.g. personal accounts, autobiographies and ethnographies). This led to the development of a theory of truthful self-nurturing that regards the basic problem of addiction as self-destructive self-nurturing, and the basic process of recovery as truthful self-nurturing in which addiction gains meaning as a problem. Recovery work therefore involved three areas of psychological change: abstinence work, self-work and connection work. The analysis is illustrated by substantial reference to original data and the inclusion of verbatim material from the studies in terms of the respondent’s own words. Finfgeld’s105 approach gives a similar emphasis to coding verbatim data from the included reports. This material was then grouped into metaphorical codes and a process model was developed that consisted of the causal and contextual conditions of the phenomenon of becoming and being courageous.
Realist synthesis
This term was introduced by Pawson106 to describe a new methodology developed in the field of evidence-based policy to understand the changes introduced by programmes in terms of their generative mechanisms. Realist synthesis aims to achieve this through a process of theory building rather than assembling empirical generalisations, and draws on material regarding the workings of the same underlying mechanism (such as the public disclosure of information on performance) in different contexts. It therefore differs from other forms of synthesis in bringing together material from diverse sources that may include health, education, social policy or other sectors. In addition, the explicit aim of realist synthesis is theory development. Realist synthesis has so far not been widely employed, but forms one of the increasing armoury of approaches to developing new conceptualisations by drawing together the findings of individual studies and shares with other interpretive approaches the aim of going beyond individual studies to develop new theories and conceptualisations.
Summary
In this chapter we sought to identify the various approaches and methods that can and have been used to synthesise the findings from individual qualitative research studies. Both Hammersley14 and Noblit and Hare15 differentiated integrative syntheses, which involve the aggregation, pooling or comparison of findings from qualitative studies, from interpretative syntheses, whose methods involve induction and interpretation and whose aim is to achieve conceptual and theoretical development and, hence, greater insight into particular phenomena or issues.
The method that has received the greatest attention to date is meta-ethnography. This method has been applied by some in a way that appears to be fairly consistent with the approach to qualitative synthesis described by its architects, Noblit and Hare. 15 Others, notably Paterson et al. ,42 have sought to use meta-ethnography as a procedure within a more all-encompassing form of synthesis which they call meta-study. In addition, Dixon-Woods et al. 102 have tested whether or not meta-ethnography can be used to bring together a large and methodologically diverse group of studies and in the process have evolved what they consider to be a new method, CIS.
The subsequent chapters consist of a detailed evaluation of meta-ethnography as a method of qualitative synthesis. To accomplish this evaluation, two substantial syntheses were undertaken: the first was a synthesis of studies of medicine-taking and the second a synthesis of patients’ experiences of RA. In both cases the intention was to apply the method as depicted by Noblit and Hare. 15 The next chapter describes how relevant qualitative studies on these topics were identified.
Chapter 3 Literature searching
Introduction
Although the potential relevance and importance of qualitative research is being increasingly acknowledged by policy-makers and those concerned with establishing evidence-based medicine and social care, there is consensus that searching for and identifying appropriate qualitative research remains frustrating and difficult. 17,91,107–109 The problem becomes particularly acute when attempting a synthesis of the studies on a given topic – the task that we have set ourselves here. Naturally, one would wish to locate the maximum amount of primary research in the most efficient way before undertaking further assessment of the material. However, it is becoming ever clearer that it is no easy task to develop a search strategy that maximises recall and precision, while ensuring that expenditure of resources is kept within manageable limits.
Considerable effort has already been expended to produce guidelines and procedures for retrieval33 and, to a lesser extent, to evaluate their usefulness and relative efficiency. Nevertheless, it is apparent that even when the focus is on studies using quantitative methods reported in the medical literature (and hence perhaps more systematically indexed), retrieval rates can be surprisingly low. Limitations with searching bibliographic databases led the Cochrane Collaboration to search European general health-care journals by hand for reports of controlled trials: only 17% of those identified were indexed in MEDLINE as controlled trials and 30% were not indexed in MEDLINE at all. 110 Accordingly, a multipronged approach is currently advocated: searching a range of databases; hand-searching of relevant journals; contacting experts in the field of enquiry for curricula vitae and information; and examination of the ‘grey literature’, conference proceedings and the like. Decisions have to be made at each stage depending on the resources available.
Whatever problems are encountered in searching for studies employing quantitative methods, they are multiplied when searching for relevant qualitative research. For example, Evans108 highlighted the particular difficulties of searching electronic databases for reports of qualitative studies arising because of the nature of the titles, the content of the abstracts and the indexing practices111 of those preparing the databases. Evans108 pointed out that the titles given to qualitative work, although often very descriptive of the study’s focus, may not easily lend themselves to the selection of specific key terms. Moreover, the content of the abstracts can also vary greatly and the research method may not be stated in the title or the abstract. Such studies run the risk of failing to be identified.
For this reason, it is important to include a range of databases as they vary in the extent to which they use methodological indexing terms that accurately describe qualitative study design. 112 In addition, the more diffuse or broad the topic for review or synthesis is – and this may often be the case where qualitative research is involved – the more necessary it is to throw the net wider and include more databases. 113 However, the more varied the databases, the more problematic the notion becomes of a ‘standard’ search filter suitable for application to all. Search strings to identify qualitative studies probably need to be adapted to the idiosyncrasies of each synthesis to achieve the best results. Moreover, qualitative research lacks the more standardised keywords associated with quantitative research in medicine. An evaluation of three different electronic search strategies for finding qualitative research (using thesaurus, free-text or broad-based terms) by Shaw et al. 114 found that relying on one strategy alone would have resulted in failure to identify some relevant records. This evaluation also highlighted the low level of precision of all three strategies, with only 4% of papers initially identified as potentially relevant actually proving to be so.
In addition to the need to include a range of databases and search strategies in order to maximise the yield of relevant qualitative research papers comes the further complication that social science literature is much more diverse in terms of its publication media than medical literature. 115 This suggests a requirement for the effective qualitative literature search not simply to be confined to electronic searches for journal articles.
In the following sections we describe the choices made and the strategies adopted for the retrieval of material for the two synthesis studies undertaken, one being a relatively diffuse topic, whereas the other had a specific disease focus. In both cases, the decision was made at the beginning not to explore the ‘grey literature’ or to consider unpublished theses. The decision to restrict ourselves to published work was made in order to keep the number of papers manageable, as we anticipated that these would be high, particularly in the case of the medicines synthesis. It was also part of the purpose to investigate the usefulness of the methodology for HTA and health-services research in which published research would be easier and quicker to access. The literature searches for both syntheses were conducted in July and August 2002.
Methods
The research group formed into two subgroups, one for each of the syntheses. PP led the medicines synthesis and GDW led the RA synthesis. Each subgroup managed the process of searching, appraising and synthesising separately, although the whole group got together regularly to discuss progress and general issues arising from the projects.
Medicines synthesis
Defining the topic
We used the following definition when searching: ‘Papers whose primary focus is patients’ views of medicines prescribed and taken for the treatment of a long- or short-term condition (excluding medicines only taken for preventive purposes)’. The study had to use qualitative methods of data collection and analysis and be published in the English language.
Sampling strategy
We chose the 10-year period from 1 January 1992 to 31 December 2001 (the study began in spring 2002), believing that most of the relevant studies would be found within this period. We were aware that a small number of important early studies would be missed, e.g. Arluke,116 Trostle et al. 117 and Conrad,118 but needed to set limits on what was a potentially large number of available studies.
Electronic search strategies
We used the following electronic databases: MEDLINE, EMBASE, CINAHL, Web of Science, PsycINFO and Zetoc. The initial MEDLINE search was very detailed (Table 2) and produced a large pool of papers. Hoping for a more sensitive and focused search, we tried simply using the terms ‘patient compliance’, ‘adherence’, ‘medicine’, ‘medication’ and ‘qualitative’ (Table 3). The second, simpler, MEDLINE search produced a much smaller pool of potential papers, but all the relevant papers that had been identified in the first search (this simpler search produced no additional relevant papers). We repeated these two searches in EMBASE. Again, the second, simpler, search produced all the relevant papers that had been identified in the first, more detailed EMBASE search. The same strategy in CINAHL resulted in the second, simpler, search producing an additional three relevant papers to the first. Thus, the simple search was just as sensitive as the more comprehensive search in MEDLINE and EMBASE, and more sensitive in CINAHL.
| # | Search history | Results |
|---|---|---|
| 1 | exp *Prescriptions, Drug/ | 1852 |
| 2 | Pharmaceutical Preparations/ad, ae, ct, du [Administration & Dosage, Adverse Effects, Contraindications, Diagnostic Use] | 1144 |
| 3 | Drugs, Non-Prescription/ad, ae, ct, tu [Administration & Dosage, Adverse Effects, Contraindications, Therapeutic Use] | 376 |
| 4 | Drug Therapy/ae, nu, px, ut [Adverse Effects, Nursing, Psychology, Utilization] | 865 |
| 5 | Drug Utilization/ | 2620 |
| 6 | prescrib$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 11,166 |
| 7 | prescription$1.mp [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 7383 |
| 8 | non-prescription$1.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 190 |
| 9 | over the counter.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 870 |
| 10 | OTC$1.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 503 |
| 11 | dispens$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 2795 |
| 12 | pharmaceutical$1.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 10,561 |
| 13 | drugs$1.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 14,959 |
| 14 | medicin$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 37,736 |
| 15 | medication$1.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 23,725 |
| 16 | drug therapy.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 6123 |
| 17 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 | 215,999 |
| 18 | Patient Compliance/ | 6509 |
| 19 | Treatment Refusal/ | 2126 |
| 20 | Self Medication/ae, px, ct, nu [Adverse Effects, Psychology, Contraindications, Nursing] | 132 |
| 21 | Self Administration/ae, px, nu [Adverse Effects, Psychology, Nursing] | 162 |
| 22 | complian$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 13,108 |
| 23 | complying.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 225 |
| 24 | adher$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 14,055 |
| 25 | treatment refusal.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 2144 |
| 26 | self-administ$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 4750 |
| 27 | concord$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 5522 |
| 28 | Attitude to Health/ | 10,643 |
| 29 | Knowledge, Attitudes, Practice/ | 9853 |
| 30 | Patient Acceptance of Health Care/eh, px [Ethnology, Psychology] | 951 |
| 31 | Physician-Patient Relations/ | 8459 |
| 32 | Adaptation, Psychological/de [Drug Effects] | 43 |
| 33 | Nonverbal communication/or communication/or persuasive communication/or communication barriers/ | 8415 |
| 34 | Health Behavior/or Life Style/or Stress, Psychological/ | 17,403 |
| 35 | Self Care/ae, px, ut [Adverse Effects, Psychology, Utilization] | 496 |
| 36 | Risk Taking/ | 2677 |
| 37 | Decision Making/de [Drug Effects] | 11 |
| 38 | Decision Support Techniques/ | 1906 |
| 39 | Sick Role/ | 1831 |
| 40 | Self Concept/ | 4901 |
| 41 | medicine taking.mp. | 22 |
| 42 | 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 | 96,869 |
| 43 | focus group$1.mp | 2414 |
| 44 | Interviews/or interview$.mp. or Research/ | 43,854 |
| 45 | Nursing Methodology Research/mt [Methods] | 258 |
| 46 | patient experience.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 134 |
| 47 | patients’ experiences.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 188 |
| 48 | patient perception.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 112 |
| 49 | patients’ perceptions.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 402 |
| 50 | patient perspective.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 79 |
| 51 | patients’ perspectives.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 77 |
| 52 | ethnograph$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 667 |
| 53 | content analysis.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 943 |
| 54 | grounded theory.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 555 |
| 55 | qualitative.mp. or Health Services Research/or Research Design/ | 26,939 |
| 56 | 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 | 70,155 |
| 57 | qualitative.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 12,358 |
| 58 | 17 and 42 and 56 | 2105 |
| 59 | 57 and 58 | 305 |
| 60 | limit 59 to yr=1997 to 2001 | 268 |
| # | Search history | Results |
|---|---|---|
| 1 | Patient Compliance/or patient compliance.mp. | 7154 |
| 2 | adherence.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 6563 |
| 3 | medicin$.mp. | 37,736 |
| 4 | medication$1.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 23,725 |
| 5 | qualitative$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] | 16,190 |
| 6 | 1 or 2 | 12,812 |
| 7 | 3 or 4 | 60,560 |
| 8 | 5 and 6 and 7 | 37 |
| 9 | Limit 8 to yr=1997-2001 | 32 |
For Zetoc, the search terms used were ‘prescri*’ and ‘qualitative’. For Web of Science, the following search was conducted: (medicine* or medication* or prescription*) and (compliance or adherence or concordance) and (qualitative or grounded same theory or patient* same interview* or patient* same perception* or patient* same experience* or content same analysis or ethnography). The databases searched were SCI-EXPANDED, Social Sciences Citation Index, Arts and Humanities Citation Index. The following search was conducted for PsycINFO: (medicine* or medication* or prescription*) and (compliance or adherence or concordance) and (qualitative or (grounded adj theory) or (patient* adj interview*) or (patient* adj perception*) or (patient* adj experience*) or (content adj analysis) or ethnography) and (PO= HUMAN).
Hand-searching strategies
For the hand-searches we asked colleagues and team members to suggest any papers they might think relevant, we searched the departmental Reference Manager (version 8; Thomson Research Soft, Carlsbad, CA, USA) database (which includes a record of all references held by academic and research staff in the School of Social and Community Medicine at University of Bristol), we checked reference lists of obtained papers and we searched the Medicines Partnership website. We also hand-searched the Arts and Humanities Library and the Medical Library of University of Bristol. All books in the RA–RC (medical) section and in the HM–HV (general sociology) section were searched, as were short-loan collections for the same class marks.
The key journals were hand-searched in case the electronic searches were not sufficiently sensitive or in case the individual articles had not been given adequate keywords. Hand-searching of journals was conducted for either the online or paper versions of journals and was shared between members of the team. The journals we hand-searched were Qualitative Health Research; Sociological Review; Psychology and Health; Journal of Health Psychology; Journal of Advanced Nursing; Medical Anthropology Quarterly; Culture, Medicine and Psychiatry; Medical Anthropology; Patient Education and Counselling; Family Practice; Sociology of Health and Illness; Social Science and Medicine; and Health.
The process of selecting/rejecting
For the electronic searching, PP was responsible for deciding whether or not to include studies. She examined titles and abstracts and obtained full copies of papers that looked promising. For hand-searching, the decision-making process was shared among team members and occurred as we went along. The process of selecting/rejecting was lengthy but was conducted thoroughly at this stage (rather than being initially overinclusive as with the RA synthesis), because of the much larger number of studies involved.
Results of searches
The electronic searches produced 21 studies for appraisal and the hand-searches 21, giving a total of 42 studies to be appraised for inclusion in the synthesis. (Further exclusions could be made following the appraisal.) Figure 2 gives a breakdown of the yield from each of the different databases.
FIGURE 2.
Search yields (medicines synthesis) for the 43 papers. aPapers could appear on more than one electronic database. Hnd, hand-searching; Med, MEDLINE; Emb, EMBASE; Cin, CINAHL; WoS, Web of Science; Psy, PsycINFO; Zet, Zetoc.
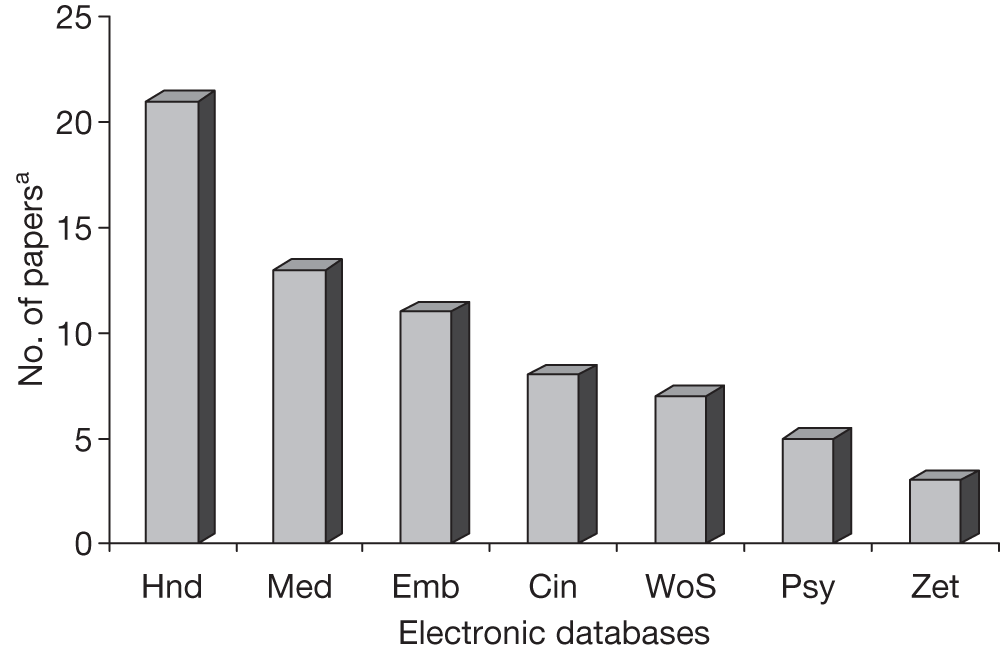
Reproducibility of electronic search strategy
A second researcher, GDW, conducted the electronic searches independently in order to assess the reproducibility of the selection/rejection process. GDW used the same search strategy with the same databases and examined titles and abstracts before drawing up a list of papers for possible inclusion (Box 3). Of the 21 papers that PP found electronically, GDW found 18. He also identified one additional useful paper that PP had missed, bringing the final number of studies to be appraised to 43 (22 produced electronically and 21 from hand-searching) (Box 3). (GDW also identified 22 other papers which PP had rejected. This may be accounted for by the fact that PP had time to obtain papers that she was not sure about and look at them in more detail, but for the purposes of this exercise, GDW was working with titles and abstracts only.)
| Electronic searches (PP) | 21 |
| Additional paper identified by GDW as a result of reproducibility exercise (electronic) | 1 |
| Hand-searches (whole team) | 21 |
| Total papers for appraisal | 43 |
Success of search strategy
As indicated above, the double screening of titles and abstracts ensured that one relevant study that might otherwise have been missed was included. Time limitations meant that only one person hand-searched any one journal. Late in the course of conducting the synthesis, we came across a study that could have been included and which should have been identified during the hand-searching. 119 Given that this discovery was made at a point at which the synthesis was well advanced, we did not feel it appropriate to try and incorporate it post hoc.
Rheumatoid arthritis synthesis
Defining the topic
Papers were sought that reported the results of qualitative studies concerned with lay experiences of RA, or lay perceptions of aetiology, treatment or management. The study had to use both qualitative methods of data collection and analysis. Papers were not restricted to English language only, because initial scoping exercises suggested that the number of papers produced for the RA synthesis would be manageable.
Sampling strategy
We searched intensively for papers published between January 1992 and December 2001, using the strategies below. However, because we knew that important work had been published before 1992, and because initial searches suggested that the number of potential papers would be manageable, we decided to further include so-called ‘classic’ studies in the field that were published prior to 1992. To decide which ‘classic’ papers to include, we consulted relevant experts in medical sociology, nursing, occupational therapy and rheumatology, including authors of some of the papers identified as a result of our searches below.
Electronic search strategies
We used the following electronic databases: MEDLINE, EMBASE, CINAHL, Web of Science, PsycINFO and Zetoc. The MEDLINE searches are detailed in Tables 4 (the detailed search) and 5 (the simpler one). The two different searches were conducted in order to maximise yield. Although they produced some of the same papers, they also each produced a distinct list of papers that met the inclusion criteria. The same searches were run in EMBASE and CINAHL. For PsycINFO and the Web of Science (Science Citation Index and Social Science Citation Index), the search terms were ‘arthritis and (qualitative or focus group or grounded theory or lay or perception or experience)’ for the period 1992–2001. For Zetoc, six separate simple searches were conducted:
-
arthritis qualitative
-
arthritis grounded theory
-
arthritis focus group
-
arthritis lay
-
arthritis interview
-
arthritis perception.
| # | Search history |
|---|---|
| 1 | attitude to health/or knowledge, attitudes, practice/ |
| 2 | Patient Satisfaction/ |
| 3 | lay.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 4 | patient$experience$.mp [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 5 | arthritis/or exp arthritis, rheumatoid |
| 6 | exp Arthritis, Rheumatoid |
| 7 | arthritis.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 8 | qualitative research.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 9 | qualitative.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 10 | interviews/or focus groups/ |
| 11 | interview$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 12 | focus group$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 13 | patient perception.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 14 | social sciences/or anthropology/or anthropology, cultural/ |
| 15 | ethnograph$.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 16 | content analysis.mp. |
| 17 | grounded theory.mp. [mp=title, abstract, cas registry/ec number word, mesh subject heading] |
| 18 | Nursing Methodology Research/ |
| 19 | Adaptation, Psychological/ |
| 20 | Activities of Daily Living/ |
| 21 | Rheumatic Diseases/ |
| 22 | 1 or 2 or 3 or 4 or 13 or 19 or 20 |
| 23 | 5 or 6 or 7 or 21 |
| 24 | 8 or 9 or 10 or 11 or 12 or 14 or 15 or 16 or 17 or 18 |
| 25 | 22 and 23 and 24 |
| # | Search history |
|---|---|
| 1 | exp ARTHRITIS, RHEUMATOID/or arthritis.mp. or *ARTHRITIS/ |
| 2 | qualitative.mp. or exp Knowledge, Attitudes, Practice/or exp Health Services Research |
| 3 | 1 and 2 limit 3 to human |
Hand-searching strategies
For the RA synthesis, the hand-searches were conducted in the same way as for the medicines synthesis, the only differences being that the journal Family Practice was not hand-searched for the RA synthesis, nor was the Medicines Partnership website.
The process of selecting/rejecting
For the electronic searching, GDW was responsible for deciding whether or not to include studies. He examined titles and abstracts and obtained full copies of papers that looked promising. For the hand-searching, decisions were shared among team members and were made as we went along. Because of the manageable number of papers, we erred on the side of inclusivity at this stage.
Results of searches
The electronic searches produced 38 papers for appraisal and the hand-searches four. A further nine ‘classics’ were obtained, giving a total of 51 studies to be appraised. (Further exclusions could be made following the appraisal.) Figure 3 provides a breakdown of the yield from each of the different databases.
FIGURE 3.
Search yields (RA synthesis) for 51 papers. aPapers could appear on more than one electronic database. Zet, Zetoc; Cin, CINAHL; Med, MEDLINE; Emb, EMBASE; WoS, Web of Science; Hnd, hand-searching; Psy, PsycINFO.
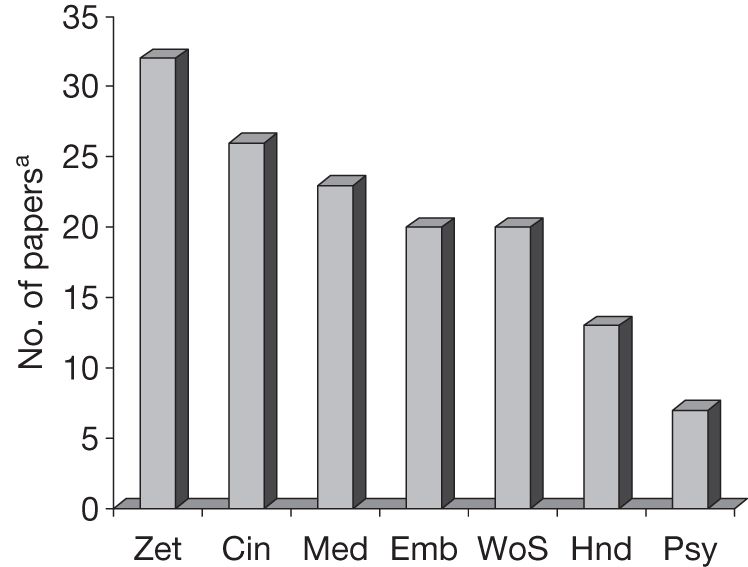
Reproducibility of electronic search strategy
The electronic searches were conducted independently by a second researcher, RC, in order to assess the reproducibility of the selection/rejection process. RC used the same search strategy with the same databases and examined titles and abstracts before drawing up a list of papers for possible inclusion (Box 4). RC’s searches did not produce any additional relevant papers.
| Electronic searches (GDW) | 38 |
| Hand-searches (whole team) | 13 (of which 9 ‘classics’) |
| Reproducibility exercise | 0 |
| Total papers for appraisal | 51 |
Conclusion
When searching for qualitative reports, the policy of a ‘belt and braces’ strategy was certainly vindicated for both syntheses. Perhaps the most striking feature of the results of our searches was the demonstration of the importance of hand-searching and consultation with experts, and the difference between the two topic areas. For the medicines synthesis, a more diffuse topic, these sources contributed as many papers as did the electronic searching. For the disease-based synthesis on RA, electronic searching identified three-quarters of the papers considered for appraisal. The yield from the various electronic databases also differed between the two topic areas, with MEDLINE being most successful for the medicines synthesis and Zetoc the most successful for RA.
Our strategy included a limited search of library books, but excluded theses. One book was included in the RA synthesis and one book chapter, and two book chapters were included in the medicines synthesis. Searching for books and theses is challenging as they are not indexed in the same way as journal papers, and may be accessible only from experts who know the field. Qualitative researchers have often chosen to publish their work in book form as this is far less constraining than publishing in journal articles. Searches confined to journal articles may produce a ‘truncation’ bias as the full details of a descriptive qualitative study are unlikely to be published in a short article. The deciding factor is likely to be the resources available in any individual project. If resources are available to include theses, one strategy would be to identify recent theses on the grounds that they are less likely to have been published in journal form.
This experience has reinforced our commitment to an eclectic approach to the issue of searching and the need to remain alert to the distinct possibility that what worked last time will not necessarily work for the next retrieval exercise. What is clear is that this is never going to be a process capable of being regulated and therefore totally delegated. This vital initial part of any synthesis requires experienced skills of judgement and persistence, just as much as at the later stages.
Although it is too early to make authoritative recommendations, we can make some observations that may be helpful to others attempting a similar task. A multiple search strategy is more likely to identify relevant qualitative research than one relying solely on electronic searching. However, the purpose of the synthesis will determine the most appropriate search strategy. In the synthesis of quantitative research, the purpose is usually to be comprehensive, and to identify all the published and grey literature on a particular question in order to calculate a precise and unbiased estimate. In qualitative synthesis, the aims may be different. One aim might be the mapping out of key conceptual developments in a particular field. For this purpose, a grounded theory and/or purposeful sampling approach may be appropriate. 120 If the aim is not to produce an aggregative synthesis, the omission of some papers is unlikely to have a dramatic effect on the results. Our experience suggests that a maximum of about 40 papers is realistic because it is difficult to maintain sufficient familiarity with > 40 papers when trying to synthesise them all and that it is, therefore, best not to be overambitious in terms of numbers.
Chapter 4 Appraisal of papers
Introduction
Conventional models for conducting quantitative systematic reviews first require the application of criteria for assessing the quality of the research in the literature. Study quality in this context largely equates to methodological quality. The highest quality quantitative research is usually deemed to be that in which the study design minimises bias (systematic error) and, hence, maximises internal validity. The more internally valid a study is, the argument runs, the more likely its results are ‘to approximate to the truth’. 121 Within quantitative systematic reviews, a minimum quality threshold is normally set to ensure the exclusion of studies so methodologically weak that their results are likely to be very biased. The quality grade of studies included can also be used to weight the findings of studies contributing to cumulative meta-analyses and be used to explore heterogeneity in study results.
Over the past 30 years, there has been considerable debate about quality assessment in qualitative research. This debate centres on two related questions: firstly, whether or not there is a plausible philosophical rationale for undertaking such assessments; and, secondly, if such a rationale exists, what criteria should be used to inform judgements about quality. Fundamental issues of ontology, epistemology and methodology underpin this, and debates about the nature and practice of qualitative research have been described, explained and analysed in considerable detail by Murphy et al. 9 Quality assessment of qualitative research was part of the brief for this methodological research, making it necessary to include a brief summary of the main positions taken in this debate.
Taking the view that there is no single, unequivocal social reality or truth independent of the researcher or the research process, extreme relativists argue that it is impossible to judge research against external criteria. They contend that the multiple realities produced by different styles of research, and from different studies, provide unique but equally valid perspectives. Lincoln and Guba,122 although rejecting the conventional quantitative criteria of reliability, validity and generalisability, took a less extreme stance when they maintained that it was possible to develop alternative criteria better suited to the assessment of qualitative work. They suggested a focus on credibility (as confirmed by the participants or subjects through member validation); transferability (how far the ideas are transferable to another context); consistency or dependability (how well the researchers have taken into account ways in which the phenomenon studied have changed over time); and confirmability (the ability to follow how the conclusions were reached). Later they argued for qualitative work to be judged on its authenticity, which rests on the researchers themselves demonstrating the fairness and strength of the interpretation and the impact on the participants. 123
Against these relativist perspectives, others124,125 have argued that the same criteria can be used to assess quantitative and qualitative research. Hammersley126 proposed subtle realism as a variant of this position, accepting that similar criteria apply, but suggesting that some of the methods used to assess quality in quantitative research styles may need to be adapted for qualitative work. He argued that the central issues for all research are validity and relevance. Validity can be judged from the clarity of the account of data collection and analysis; the researchers’ sensitivity to, and reflection on, the ways in which the researcher/research has shaped the data; fairness or balance in the account; and attention to negative or deviant cases that disprove or develop the interpretation. Relevance is concerned with whether or not the research adds to the sum of knowledge and the extent to which findings can be generalised beyond the setting in which they were generated. 126
Taking account of this debate, but also as a pragmatic response to requests from publishers, funding bodies and those in the health service who wanted guidance on how to assess qualitative research, a substantial number of authors have produced sets of criteria and checklists. 83,127–132 Indeed, research to examine how systematic reviews can incorporate qualitative research identified > 100 such sets of criteria. 20 To our knowledge none of these lists of criteria has, however, been designed specifically as a precursor to conducting any secondary analysis or synthesis of qualitative research. The Joanna Briggs Institute at the University of Adelaide, Australia, has, however, developed systematic review software that includes a module ‘designed to manage, appraise, extract and synthesise qualitative data as part of a systematic review of evidence’ [www.joannabriggs.edu.au/Appraise%20Evidence/JBI%20SUMARI%20(systematic%20review%20software)%20FREE].
As the review in Chapter 2 of qualitative research syntheses employing meta-ethnography or related methods illustrates, only a small minority of researchers have undertaken an appraisal of the quality of individual research papers as a precursor to the synthesis. Sandelowski et al. 13 argued against assessing papers for methodological quality because of concern that relatively minor methodological flaws may result in insightful studies being excluded from syntheses. They suggested that the qualitative synthesiser needs to apply careful judgement in order to distinguish between superficial mistakes and flaws of such magnitude that the findings are rendered invalid. In their recent review of vulnerable groups and access to health care, Dixon-Woods et al. 82 followed this prescription and used a very brief appraisal tool to identify papers that were ‘fatally flawed’ and therefore unsuitable for inclusion.
The recent drive within the UK government towards evidence-based policy-making has also focused attention on the quality of the qualitative research because government policy-makers are substantial consumers of qualitative social research. As a result, the Strategy Unit in the Cabinet Office commissioned the National Centre for Social Research (NatCen) to produce guidance on quality assessment in qualitative research. 19 After conducting a number of review exercises, the NatCen team proposed a new generic assessment framework for qualitative research. Drawing on 29 sets of previously suggested assessment criteria, it comprises a series of 18 appraisal questions underpinned by four ‘guiding principles’. For each question, a set of points for consideration is suggested. This new framework was still under development when we began our evaluation of meta-ethnography and so we continued to use the modified version of the CASP criteria for quality appraisal18 that we had used in our pilot synthesis on lay experiences of diabetes. 17 We originally chose the CASP criteria18 because they had been developed and tested over a period of time and because they were widely recommended for use within the NHS. 18
Appraisal process
For our present syntheses, we further modified the CASP criteria18 for quality appraisal (see Appendix 1). These criteria were entered onto a Microsoft Access 2000 database (Microsoft Corporation, Redmond, WA, USA), which meant that papers could be appraised online. The papers for the medicine-taking synthesis were first appraised by PP and the papers for the RA synthesis were first appraised by GDW.
Prior to the quality appraisal, two screening questions were asked:
-
Does the paper report on findings from qualitative research and did that work involve both qualitative methods of data collection and analysis?
-
Is the research relevant to the synthesis topic?
If one of the answers to these questions was ‘no’, the paper was excluded. The first question effectively excluded those papers that could be regarded as ‘fatally flawed’. If both answers were ‘yes’, the appraisal could proceed. This involved answering questions (both yes/no answers and an elaboration on these) about each paper for each of the following categories: aims, methodology, theoretical perspective, sampling, data collection, data analysis, research relations, data interpretation, transferability, relevance and usefulness. The data recorded were both quantitative (the yes/no answers) and qualitative (the elaboration on those answers). A key part of the appraisal was to outline, in detail, the main findings and concepts. These were recorded in large free-text boxes on the database.
Assessing reproducibility of appraisals
A second reviewer from the research team also appraised each of the papers, blind to the first appraisal, in order to assess the reproducibility of the process. (The results of this process are described in detail below.) The independent reviewers were allocated to each paper in a random manner using an allocation schedule drawn up in advance. This used random number tables and randomisation blocks of nine. If independent reviewers were allocated a paper that they had themselves authored, a different reviewer was chosen randomly from those remaining. The independent reviewers were MM, NB and LY for the medicine-taking synthesis and RC, RP and JD for the RA synthesis.
Inclusions/exclusions
Four of the papers in the medicine-taking synthesis were the subjects of disagreement (between the first and second reviewers) about whether or not to include them. This was because they were considered borderline, either in terms of methodology (were they sufficiently qualitative?) or because the findings were somewhat slight. Disagreements were resolved through a process of negotiation (by e-mail), with the result that one paper was excluded and three were included with the proviso that if they contributed nothing to the synthesis they would ‘fall out’ later on. In the RA synthesis, a team meeting was held to decide the fate of papers over which there was disagreement. If disagreement persisted or if studies were considered borderline according to the inclusion criteria, they were included.
For the medicine-taking synthesis, five papers were excluded following appraisal; for the RA synthesis, 22 papers were excluded following appraisal. The larger number of exclusions in the RA synthesis is largely because, at the literature searching stage, GDW decided to retain any papers that might prove relevant and enter them into the appraisal process. Papers in the medicine-taking synthesis were more heavily screened for relevance by PP at the literature searching stage. Thirty-eight papers were finally included in the medicine-taking synthesis and 29 papers in the RA synthesis, although further exclusions were made during the synthesis (Box 5).
| Number of papers for appraisal | 43 |
| Number of papers excluded following appraisal | 5 |
| Number of papers included in synthesis | 38 |
| Number of papers for appraisal | 51 |
| Number of papers excluded following appraisal | 22 |
| Number of papers included in synthesis | 29 |
Quality
We did not exclude papers on grounds of quality. The only reasons for excluding papers were either that they were not sufficiently focused on the topic or that they did not actually report qualitative research. Sometimes this was not immediately obvious. For example, some papers described work where qualitative data had been collected, but on closer examination it became clear that the data were not analysed qualitatively. In several papers that, strictly speaking, were relevant and the methodology was qualitative, the analysis was considered to be very superficial or few findings were reported. In these cases we did not exclude papers, but attempted to synthesise them.
Sometimes, it was an absence of adequate reporting that could confuse matters. For example, in the RA synthesis, some of the better theoretical papers (the ‘classics’) scarcely reported their research methods. These papers were conceptually very useful to the synthesis, but if strict quality screening had been employed these papers would have been excluded. Indeed, many of the RA studies would have been so excluded. Only four papers in the RA synthesis were characterised both by good reporting of the use of qualitative methods of data collection and by analysis. (This is discussed further in relation to specific studies in Chapter 7 in which the RA synthesis is reported.) On the other hand, for both topic areas there were papers that reported on methodology in great detail, but produced very superficial findings. We remained inclusive in our approach because, although some of the papers were slight, they were synthesisable in that at least they were descriptively confirmatory of previous findings.
In the medicine-taking synthesis we did not attach greater or lesser importance to any of the papers, we simply tried to put all the findings together. Some papers contributed more in terms of findings than others, but this is not necessarily a comment on their significance. Some papers were more interesting to read than others – usually implying that they interpreted their data rather than simply offering description and content analysis – but all papers were treated in the same way. Whatever they offered, whether description or interpretation, was synthesised. Some papers contributed more to particular areas than others. For example, the asthma papers contributed the least overall, but they made a strong contribution in one area, that of identity and the psychological aspects of medicine-taking.
Several of the individual questions posed in the appraisal were difficult to interpret (e.g. some of those on sampling) and others were felt to be redundant (e.g. one on the setting in which data collection occurred). The question on theoretical perspective was felt to be of limited value, particularly as many of the later studies that we found were primarily descriptive.
Appraising the papers in Access
After conducting the appraisals, both PP and GDW found it easier to import the findings and concepts from the Access database into Microsoft Word and work with the data in this format. Only one of the researchers (LY) found it necessary to access the database thereafter, in order to analyse the reproducibility of the appraisals. For quantitative analyses, therefore, the database was useful. However, the majority of the data were qualitative. Given the time that we invested in setting up the database and the small returns we obtained from doing so, we do not consider that it was a worthwhile endeavour to have conducted the appraisals in Access 2000. After conducting the appraisals, both PP and GDW found it much easier to revisit the papers themselves, rather than access the database, for any information that was subsequently needed. Those independent second reviewers who did not have access to the database conducted their appraisals in Word and reported that this was acceptable.
Reproducibility of appraisals
To evaluate the reproducibility of our quality assessment procedure, data from the Access 2000 database were exported to an Spss (version 12; SPSS Inc., Chicago, IL, USA) save file for analysis.
Inter-rater agreement
The data were firstly examined to determine inter-rater agreement (Cohen’s kappa) for each item. This calculation was based on six pairings of assessors, as there were two first assessors, each of whom was paired with three different second assessors. The number of papers rated by each of the six pairs for which complete data were available was too low (ranging from 6 to 14) to permit meaningful statistical comparison of the differences between kappa values for each pair of assessors, and so averaged kappa values for all pairs are presented in Tables 6–10.
| CASP question | Kappa | % ‘Yes’ | r |
|---|---|---|---|
| Is there a clear statement of the aims of the research? | 0.17 | 91.2 | 0.02 |
| Is a qualitative methodology appropriate for authors’ stated aims? | N/Aa | 96.6 | 0.06 |
| Is a theoretical perspective identified? | 0.70 | 43.9 | –0.01 |
| Is it clear which setting(s) the sample was selected from (e.g. hospital)? | 0.63 | 91.2 | 0.29 |
| Is it clear why this setting was chosen? | 0.09 | 70.1 | 0.21 |
| Is clear and adequate information given on who was selected? | 0.23 | 76.4 | 0.13 |
| Is it clear why these samples were selected? | 0.17 | 69.9 | 0.17 |
| Is it clear how the sample was recruited? | 0.52 | 55.1 | 0.06 |
| Is the sample size justified by the authors? | 0.43 | 17.6 | 0.10 |
| Is it clear how many people accepted or refused to take part? | 0.80 | 24.5 | 0.07 |
| Is it clear why some participants chose not to take part? | 0.65 | 5.8 | –0.04 |
| Overall, is the sampling strategy appropriate to address the aims? | 0.18 | 74.7 | 0.32 |
| CASP question | Kappa | % ‘Yes’ | r |
|---|---|---|---|
| Is it clear where the setting of the data collection was? | 0.74 | 59.2 | 0.21 |
| Is it clear why that setting was chosen? | 0.17 | 27.5 | 0.18 |
| Is it clear how the purpose of the research was explained to the participants? | 0.23 | 14.3 | –0.03 |
| Is it clear how the data were collected and why (e.g. interviews, focus groups)? | –0.04 | 96.6 | –0.06 |
| Is it clear how the data were recorded (e.g. audio/video/notes, etc.)? | 0.36 | 88.4 | 0.00 |
| Is there evidence of flexibility/an iterative process in how research was conducted? | 0.24 | 25.7 | 0.14 |
| Is it clear who collected the data? | 0.24 | 66.0 | 0.14 |
| Overall, do you consider that data collection addresses the research aims? | –0.07 | 91.8 | 0.37 |
| CASP question | Kappa | % ‘Yes’ | r |
|---|---|---|---|
| Is it clear how the analysis was done? | 0.55 | 71.7 | 0.00 |
| It is clear how the categories/themes were derived from the data? | 0.48 | 67.1 | 0.00 |
| Is there adequate description of the analysis? | 0.53 | 62.8 | –0.03 |
| Have attempts been made to feed results back to respondents? | 0.58 | 14.5 | 0.01 |
| Have different sources of data been compared where appropriate? | 0.36 | 24.7 | 0.00 |
| Was the analysis repeated by more than one researcher to ensure reliability? | 0.70 | 43.1 | –0.08 |
| Overall, is the data analysis sufficiently rigorous to address the aims? | 0.31 | 69.9 | 0.36 |
| CASP question | Kappa | % ‘Yes’ | r |
|---|---|---|---|
| Is it clear whether researchers critically examined own role, bias, influence? | 0.32 | 19.3 | 0.14 |
| Is the relationship between researchers and participants adequately considered? | 0.25 | 14.6 | 0.18 |
| Were the findings explicit and easy to understand? | 0.20 | 93.5 | 0.22 |
| Are sufficient data presented to support the descriptive findings? | 0.23 | 73.6 | 0.39 |
| Are quotes numbered/identified? | 0.71 | 48.3 | 0.24 |
| Do the researchers explain how the data presented were selected? | 0.52 | 17.2 | 0.10 |
| Do researchers say how they developed their conceptual interpretations? | 0.23 | 27.4 | 0.44 |
| Are negative, unusual or contradictory cases presented? | 0.19 | 36.1 | 0.28 |
| Is there adequate discussion of evidence for/against interpretations? | 0.10 | 28.3 | 0.35 |
| Overall, are you confident that all the data were taken into account? | 0.25 | 60.0 | 0.37 |
| CASP question | Kappa | % ‘Yes’ | r |
|---|---|---|---|
| Is there descriptive, conceptual or theoretical congruence with other work? | 0.00 | 86.9 | 0.27 |
| Are the findings of this study transferable to a wider population? | –0.02 | 71.1 | 0.38 |
| Does the study add to knowledge or theory in the field? | 0.38 | 69.7 | 0.63 |
| How important are these findings to practice? | 0.42 | N/A | 0.74 |
| What is your overall view of this study? | 0.42 | N/A | N/A |
It is evident that inter-rater agreement was typically rather low, albeit better for some classes of questions than others. There was moderate-to-good agreement on the majority of questions relating to design, sampling and recruitment (see Table 6), and modest agreement for all those relating to data analysis (see Table 8) and the value of the study (see Table 10). However, agreement was poor for questions concerning data collection (see Table 7), the interpretation and presentation of data (see Table 9) and the transferability of results (see Table 10).
Pooled ratings of papers
For all subsequent analyses, the data were pooled, such that ratings of the papers by all assessors were combined. The pooled data thus aggregated two sets of ratings for each paper: one set was derived from the two first assessors, and the second from the six second assessors. Consequently, it should be noted that the ratings of the two first assessors had a greater influence on the aggregated results than the ratings of the six second assessors, as each of the first assessors rated approximately three times as many papers as each of the second assessors.
Tables 6–10 show the percentage of pooled ratings that indicated that the assessors replied affirmatively to each of the CASP18 questions. The assessors answered positively to most questions about design and sampling (see Table 6); reporting of the setting of data collection and how data were recorded (see Table 7); clarity about how the analysis was conducted (see Table 8); satisfactory presentation of data and findings (see Table 9); and the value of the studies (see Table 10). However, few studies provided details such as justification of sample size, explanation of refusals to take part, how the research was explained to the participants or how the data presented were selected. Nonetheless, most papers were given positive ratings regarding the global evaluations (see emboldened question on the bottom row of each table) of their sampling strategy, data collection and data analysis. There was, however, little inter-rater agreement concerning which papers could not be rated positively on these questions. This pattern of findings may largely reflect the publication process, whereby papers would not normally be accepted unless the basic design, collection and presentation of data and value of the study were generally considered satisfactory, but space limitations may have prevented authors from providing more detail of the research process. It is perhaps of more concern that few studies appeared to have engaged in flexible or iterative data collection, reflexive consideration of the role of the researchers and their relationship to the participants, feeding back results to participants, or consideration of contradictory evidence or alternative interpretations. However, it must be noted that not all of these procedures for increasing the credibility and rigor of the research process would be appropriate for every study or would have been expected over the period of publication.
Correlations with ratings of the overall value of the papers
Ratings of the overall value of the papers had an approximately normal distribution, and so correlations were calculated between this item (see bottom line of Table 10) and all the other CASP18 items, in order to determine which aspects of the studies assessed by the CASP18 questions were associated with positive global evaluations (see final column of Tables 6–10). All those items that were significantly correlated with the global evaluation were then entered into a stepwise multiple regression (Table 11) in order to determine which items independently predicted the global evaluation of overall value.
| Step | Predictor variables | Adjusted R2 | Change in R2 | F R2 Change |
Beta |
|---|---|---|---|---|---|
| 1 | How important are these findings to practice? | 0.49 | 0.490 | 99.9a | 0.44a |
| 2 | Do researchers say how they developed their conceptual interpretations? | 0.59 | 0.104 | 26.4a | 0.23a |
| 3 | Does the study add to knowledge or theory in the field? | 0.63 | 0.049 | 14.1a | 0.20a |
| 4 | Is there adequate discussion of evidence for/against interpretations? | 0.66 | 0.028 | 8.6b | 0.13c |
| 5 | Are quotes numbered/identified? | 0.67 | 0.014 | 4.6c | 0.16b |
| 6 | Overall, do you consider that data collection addresses the research aims? | 0.68 | 0.015 | 4.9c | 0.12c |
| 7 | Were the findings explicit and easy to understand? | 0.69 | 0.013 | 4.3c | 0.12c |
These results show that the assessors’ global ratings of the value of the study were, unsurprisingly, associated with their judgements of its importance and contribution to knowledge. More significantly, global evaluations were related to positive ratings of a clear description of how conceptual interpretations were developed, adequate discussion of evidence for and against the interpretations presented, and a method of data collection appropriate to the aims of the research. Papers that had clearly identified quotations and whose findings were presented in an explicit and easy to follow manner were also more likely to be positively rated.
A later date of publication was correlated with more positive global evaluations (r = 0.24, p < 0.001). Additional features of the paper weakly associated (p < 0.05) with more negative global evaluations were type of publication other than peer-reviewed article and a later date of appraisal (possibly indicating papers identified by means other than electronic database searching).
Discussion
The analysis of the quantifiable data from the appraisal process indicates that inter-rater agreement was rather low. Some of this unreliability was probably due to the poor reporting of research methods in papers, which meant that reviewers were often giving a qualified ‘yes’ or ‘no’ which is not reflected in this quantitative analysis. Our findings concur with those of Dixon-Woods,24 who found ‘slight’ levels of agreement when comparing three approaches with appraisal: CASP,18 the quality framework devised by the NatCen and unprompted judgement by two experienced qualitative researchers. 24 This research also found that using a structured approach did not result in a higher level of agreement.
As we progressed with our study, it became clear to us that, that despite having conducted very detailed appraisals, we were not excluding papers on the basis of quality. If we were to conduct another synthesis in the future, therefore, we would be unlikely to conduct such a detailed appraisal beforehand. We would not, however, recommend abandoning appraisal altogether because it has advantages in terms of encouraging the reviewers to read the papers carefully and systematically, and serves as a reminder to treat the papers as data for the synthesis.
We did not ultimately find our modified version of the CASP18 tool to be especially helpful as an appraisal framework prior to a synthesis. Although it did facilitate a structured reading of papers, the questions it poses place a good deal of emphasis on methodological quality. From the point of view of a synthesis, it is conceptual quality that is most important, as was highlighted in our quantitative analysis of what items contributed most to assessors’ global ratings of the value of the study, As we observed, particularly in the case of the RA synthesis, there appears almost to be an inverse correlation between methodological quality and the quality of insight and theory-building displayed in many papers. This is, in part, related to the often inadequate reporting of qualitative research methods in the past. The current requirements of funding bodies, ethics committees and publishers for greater transparency in these matters should ensure that this is less of a problem with more recent work, but it leaves the qualitative synthesiser with a dilemma about whether or not to include older ‘classic’ papers for which there may be almost no detail given about how the research was conducted. In these cases, we would suggest that the methodological integrity of the work might have to be assumed. If the work concerned turns out to be very difficult or impossible to synthesise, then that may be a strong indication that it was not well grounded empirically.
We would endorse the stance taken by Sandelowski et al. 13 and Dixon-Woods et al. 82 that where possible it is important to expose and exclude papers that are, methodologically speaking, ‘fatally flawed’. Beyond that, what is required is an appraisal tool that aids the identification of findings, interpretations and concepts. The consensus within our research team was that any future appraisal process could be much shorter, with just a few key questions. We would retain the two initial screening questions about the relevance of the paper to the topic of the synthesis, and the question about whether or not qualitative methods of data collection and analysis were employed. Beyond that, we would include questions about the clear identification of the aim and objectives of the research; whether or not the data were collected in a way that addressed the research aim; whether or not the data analysis was sufficiently rigorous to address the aims; confidence that all the data were taken into account; whether or not there were enough data presented to support the interpretations made; and whether the paper demonstrated theoretical insight, novel findings or perspectives. In addition, we would include questions that enabled the data for the synthesis to be extracted and recorded.
The exercise of judgement is crucial to a number of stages of the synthesis. This includes making decisions about what constitutes a ‘fatal flaw’ as well as decisions about which papers should and should not be entered into the synthesis on the grounds of relevance. We would suggest that teamwork facilitates the exercise of sound judgement, as does a high level of qualitative research expertise.
Ultimately, the purpose of qualitative synthesis is to achieve a greater level of understanding and insight into particular phenomena and to generate and test theory. This is very different from quantitative syntheses in health care, where the objectives are to establish whether or not an intervention does more good than harm and to calculate an effect size. In the latter case, including biased findings or giving equal weight to all study findings irrespective of their methodological quality may result in an incorrect assessment of an intervention’s effectiveness, with potentially deleterious consequences for human health. The inclusion of poorer quality qualitative research in a synthesis is unlikely to be as damaging. As can be seen in the two syntheses reported in Chapters 6 and 7, those studies whose findings were slight contributed minimally to the synthesis. When describing their meta-ethnographic method, Noblit and Hare15 did not advocate any form of quality appraisal prior to a synthesis. Instead they cited Hunter et al. ,133 who argued against excluding ‘methodologically deficient’ studies, and they suggested that ‘the worth of studies … is determined in the process of achieving a synthesis’. 15 The lack of consistency in judgements about the quality of qualitative research that we and others have identified, and the evidence garnered thus far that the inclusion of poorer quality studies is unlikely to have a very distorting impact on a qualitative synthesis, suggest that this is wise counsel.
Chapter 5 Synthesis methodologies
Introduction
In this chapter, we describe the methods used to conduct our two syntheses. Before embarking on the syntheses, each subgroup – one for the medicine-taking synthesis and the other for the RA synthesis – conducted a preliminary study to assess the reproducibility of the synthesis process. We present these preliminary syntheses first, before going on to describe, in some detail, the methods employed to conduct the two full syntheses.
Preliminary syntheses
Concerns are frequently expressed about whether or not qualitative research can be subjected to an assessment of its reproducibility. This area is heavily contested, with extremes of opinion taking the view either that reproducibility cannot be expected as different qualitative researchers will interpret the same papers differently, depending on their perspectives and background, or that reproducibility must be shown for such work to be taken seriously alongside quantitative research. There are many positions in between. We investigated the degree to which these syntheses might be comparable or reproducible.
Each of the subgroups managed the process of searching and selecting relevant articles. Four items (papers or book chapters) were identified for each preliminary synthesis, either by chronology (RA synthesis) or by disease area (medicines synthesis). Each of the two lead researchers (PP and GDW) then synthesised the four RA papers and the four medicines papers. They did this blind, i.e. without any contact between them to discuss the methods to be employed, emergent findings or methods of presentation. PP had completed a synthesis previously, but GDW had not. Each researcher submitted his or her synthesis of both sets of papers to the overall lead researcher (RC).
Medicine-taking (PP lead)
PP’s synthesis
The four papers134–137 focused on antihypertensive medications, with the aim of describing the experiences of patients taking these medications and providing reasons for not taking medicines as prescribed. For PP, the first published, by Morgan,134 was the ‘index’ paper against which the others were compared. Morgan’s134 publication was a book chapter, and the others were articles published in journals: nursing (two135,136) and clinical (one137). PP then summarised and combined the findings from each of the papers around 13 issues that she felt emerged from the papers, some of which were inter-related. PP described the combined findings on issues such as the extent of taking and not taking medications as prescribed, lay testing of medication, and characteristics of patients taking and not taking medications as prescribed. In each case, she summarised the common findings from the four papers and indicated contrary or additional findings from particular papers. She began the process of exploring ‘higher order’ concepts, for example noting that several papers indicated that patients appeared to purposefully not take medications, although this was not overtly stated.
PP produced a ‘map’ (Figure 4) that explored links between the issues identified, using labels to indicate which papers contained the categorisations, and attempted to coalesce findings into common labels. For example, in one instance, a finding that patients did not take hypertensive medication as prescribed because they wished to avoid certain side effects when engaged in a particular activity was described by the authors as ‘incidental non-adherence’. 136 This was reclassified by PP as ‘purposeful non-adherence’,136 as specified in another paper.
FIGURE 4.
Map of antihypertensive medication papers (pilot synthesis – PP). AC, African Caribbean.
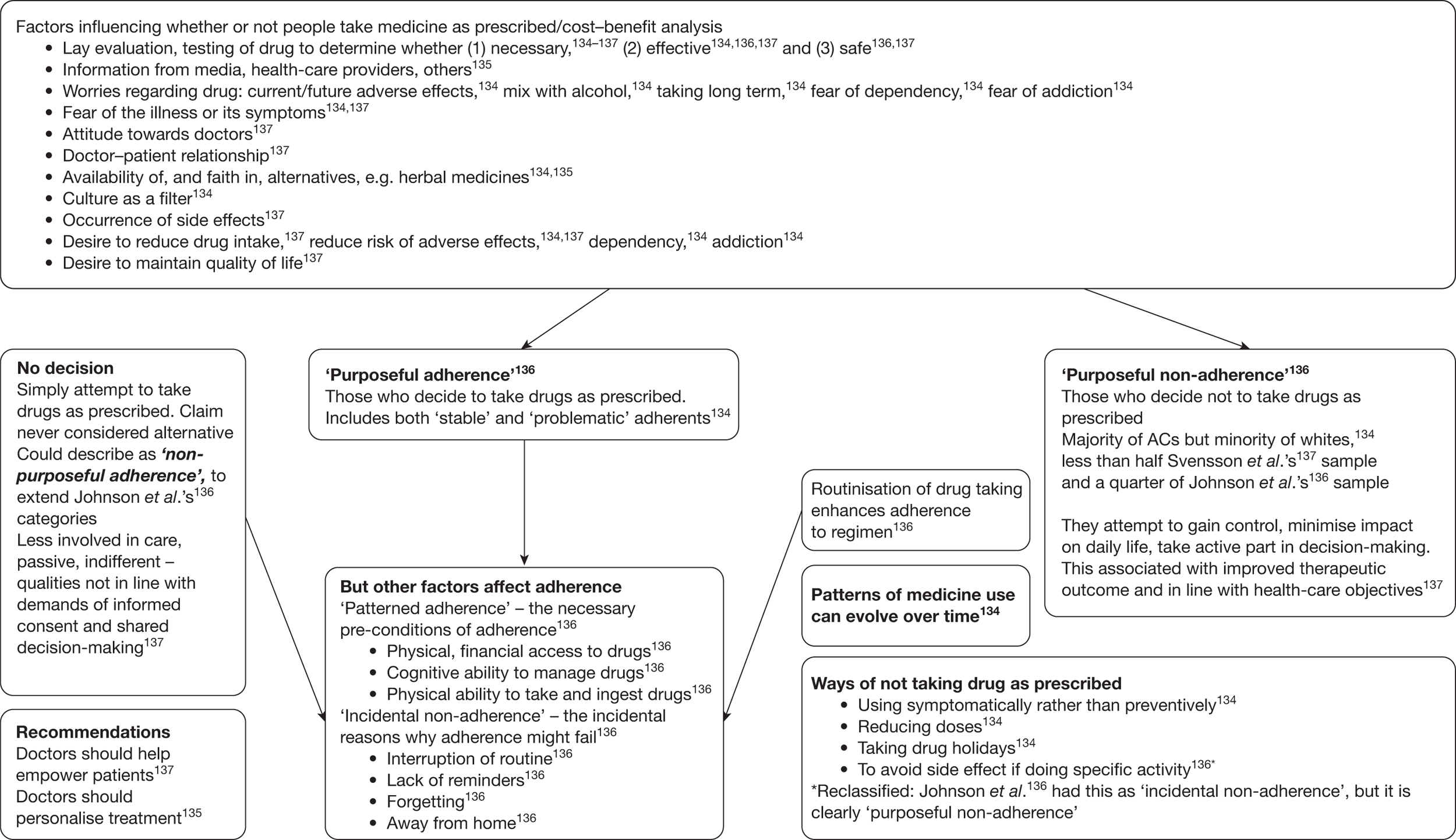
GDW’s synthesis
GDW indicated that the Morgan134 chapter would be the ‘index’ paper. GDW described each paper in turn in some detail, including the sample, methods of the study and the findings. He noted the main concepts emerging and issues that seemed particularly salient (e.g. ‘leaving off’ medication in Morgan’s chapter). At the end of each description of the paper, GDW listed key findings and associated interpretations. As the chapter by Morgan was the ‘index’ paper, GDW considered the findings of the other studies in the context of this first paper. These findings were compared with those from the index paper and presented in terms of those that were similar to, and those different from, the key findings that he elucidated from Morgan’s chapter. He termed this a ‘translation’ of the findings from each of the papers into those preceding. This also allowed the exploration of ideas emerging from later papers to be considered in the index paper – for example the related importance of blood pressure monitoring.
At the end of the description of the papers and their findings, GDW provided a ‘lines-of-argument’ synthesis, indicating that the four studies134–137 were essentially concerned with the same major issues about why people did or did not take the medications. He indicated that the studies did not refute each other, and that small differences between the studies related to the aims and samples in them. He presented interpretations emerging from the studies of relevance to clinical practice, as intended in most of the studies (Box 6). GDW also went on to observe what he regarded as a tension in the expression of the synthesis whereby it appeared that, on the one hand, those who adhered to their antihypertensive therapy took a passive approach, but that, on the other hand, those who experienced difficulties adhering used strategies to encourage their adherence, suggesting a proactive approach. GDW noted that, were he to have continued with the synthesis, he would have employed a grounded theory approach and searched for studies that could shed further light on this issue.
-
Patients took antihypertensive drugs to control symptoms of high blood pressure.
-
Adherence was associated with the recognition, interpretation and understanding of symptoms, whether felt subjectively or measured objectively by clinicians. This introduced ‘evolving’ variability in adherence over time.
-
Non-adherence was associated with fears about the strength, side effects and potential future dangers of prescription medicines, including dependence or addiction. These possible effects were seen to vary according to the amount of drugs prescribed.
-
Adherents took a passive approach (but see point 8, below) that involved faith in the role of the doctor and commitment to Western biomedical science to help them maintain control. There were trade-offs between costs and benefits of medicines. Adherence was associated with fears about the consequences of high blood pressure.
-
Non-adherents took an ‘active’ approach to the management of hypertension, where strategies such as ‘leaving off drugs’ were used to maintain autonomous control of the body and everyday life against the strength and power of biomedicine.
-
Patients adhered if they found personal evidence that their drugs were effective. This was mainly an issue of blood pressure monitoring, although irregular takers also checked their blood pressure regularly.
-
Adherence was problematic where people filtered the meanings of prescription drugs through alternative illness–treatment models (such as herbal medicine). Others outright disapproved of Western biomedical treatments.
-
Patients with psychosocial or lifestyle barriers to adherence used strategies to promote personal adherence (routinisation, acquiring knowledge about prescription regimens, modifying lifestyle). This implies that these people took an active approach to their adherence, which contradicts the idea that all adherents were ‘passive’ (cf. point 4, above).
-
Patients’ reasons for either adhering or not adhering centre on the subjective (and different) ways in which they seek to control their symptoms.
Similarities/differences between the two medication syntheses
The researchers undertook the syntheses in slightly different ways. Both identified Morgan’s134 chapter as the index paper, but then PP presented the work in terms of similarities and differences between the papers in relation to issues emerging from them, whereas GDW attempted to combine the findings of later papers with those preceding. Their written material therefore looks quite different, but the content, in terms of the major findings from the syntheses, is broadly similar. Both indicate that the papers are concerned with the factors affecting whether and why people do or do not take antihypertensive medications. They mention ‘active’ (GDW) or ‘purposeful’ (PP) non-compliance, which are different terms for the same concept. Both indicate that there were no great differences between the papers in terms of the key findings, although differences in samples, aims and publication format did lead to some different aspects, particularly of reasons for taking or not taking medications.
The process of synthesising was undertaken differently by the researchers and so the work is presented differently. GDW described his method in more detail and more explicitly, including taking into account the methods and samples of the papers. This difference is likely to be related, in part at least, to the fact that GDW was less familiar with undertaking a qualitative synthesis, and with this particular topic, than PP. This was GDW’s first attempt at a synthesis, and he was aware that he was not going to go on to complete this particular topic. He felt it important to describe the papers in detail and the process he undertook, both to gain greater familiarity with this topic but also to check that he was doing this in the way that the group wanted. PP, on the other hand, had completed previous syntheses and had more confidence in her process. It is probably also the case that PP’s ‘map’ was developed in detail to summarise the findings of the papers because she knew she would need this as the basis of her longer synthesis.
As indicated above, there was similarity between the two researchers in terms of interpretation. There were, however, some differences of detail. Most commonly, these were expressed in terms of differences in categorisations when attempting to combine concepts between papers. For example, in probably the starkest difference of interpretation, PP and GDW differed over whether to combine Morgan’s134 ‘problematic adherents’ with Johnson et al. ’s136 ‘adherents’ or ‘non-adherents’. Interestingly, both felt that Morgan’s134 ‘stable adherents’ could be combined with Johnson et al. ’s136 ‘purposeful adherents’. This difference most likely occurred because the concept ‘problematic’ contains the intention to both comply and not comply, and thus overlaps with both of Johnson et al. ’s136 categories. Such differences are small and related to the descriptive detail provided by the original authors of their concepts, which have to be reinterpreted by the synthesiser and compared with each other.
In summary, these pilot syntheses indicated some difference in approach by the two researchers. This may well be related to their experience and involvement in this work – PP had completed such work previously and was going on to complete this synthesis, whereas GDW had not done this before and was not going to continue with this topic. In terms of the accessibility of the approach, GDW’s is more explicit (which was helpful to the group), but PP’s diagram is easier to follow and a good basis from which to complete the remainder of the synthesis.
Rheumatoid arthritis (GDW lead)
PP’s synthesis
PP began with a short summary of the publications to be synthesised. 138–141 She felt that they fell into two groups: two were theoretical explorations of chronic illness,140,141 using RA as an example, whereas the other two focused on the day-to-day experiences of living with RA. 138,139 PP elucidated a number of key categories from the papers and then described each one, indicating how it was presented in each of the papers. PP indicated whether or not the concept was explicitly mentioned in each paper and then described how it was presented. For example, the concept ‘normalising’ was identified by two of the original authors explicitly138,140 and in terms of various activities in another. PP then drew several diagrams that placed the experience of RA on scales, with benefits and costs of normalising and renormalising presented as being in balance (Figure 5 and 6). There are then two tables (Tables 12 and 13), one presenting aspects of the key concept of uncertainty and the other focusing on issues related to medication use, its limitations and other resources which patients could draw on. PP focused the synthesis around the concepts of Wiener138 (the first and index paper) of normalising and renormalising, and synthesised the other papers around this. This produced the key concept of ‘achieving a balance’. She attempted to combine the papers around this concept, using a grounded theory approach, which appeared to work well.
FIGURE 5.
Normalising and costs of normalising (pilot RA synthesis – PP).
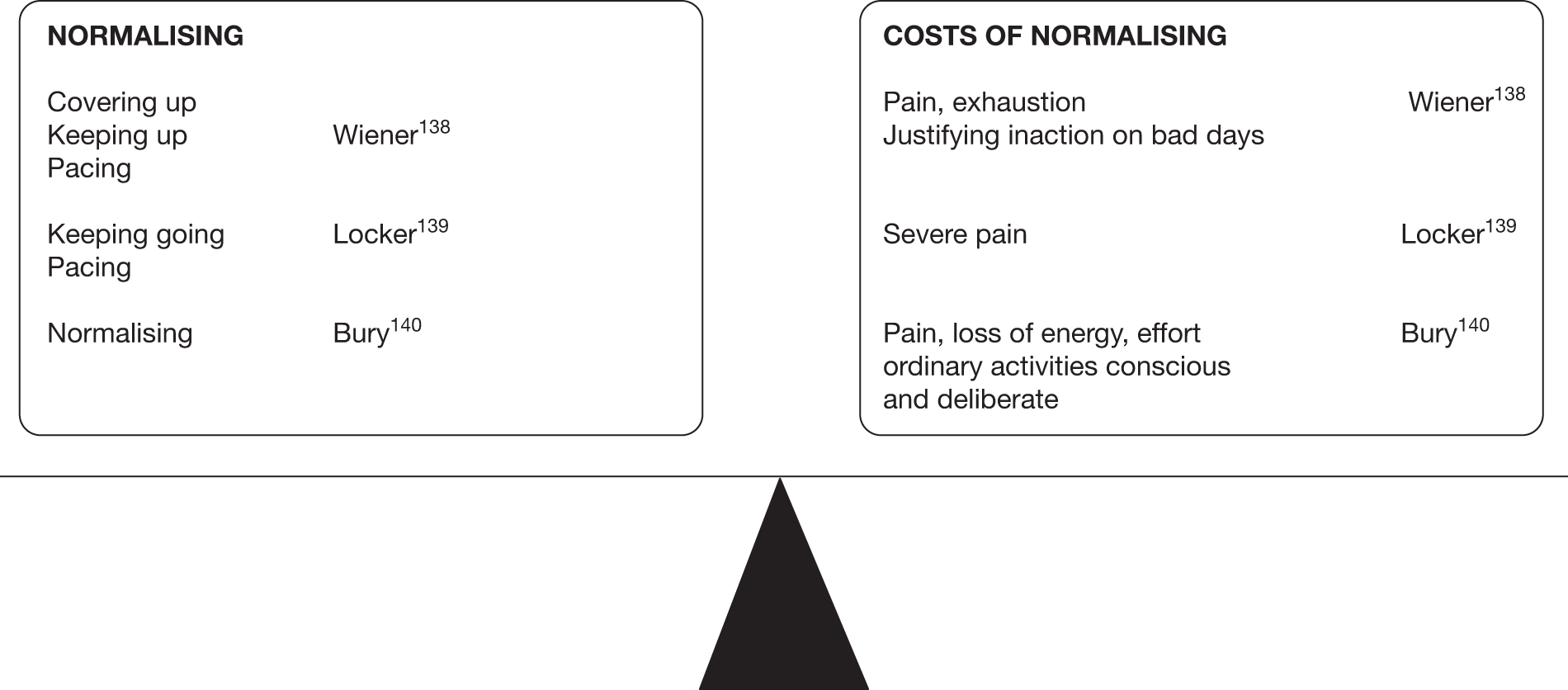
FIGURE 6.
Renormalising and costs of renormalising (pilot RA synthesis – PP). aRelated to resources.
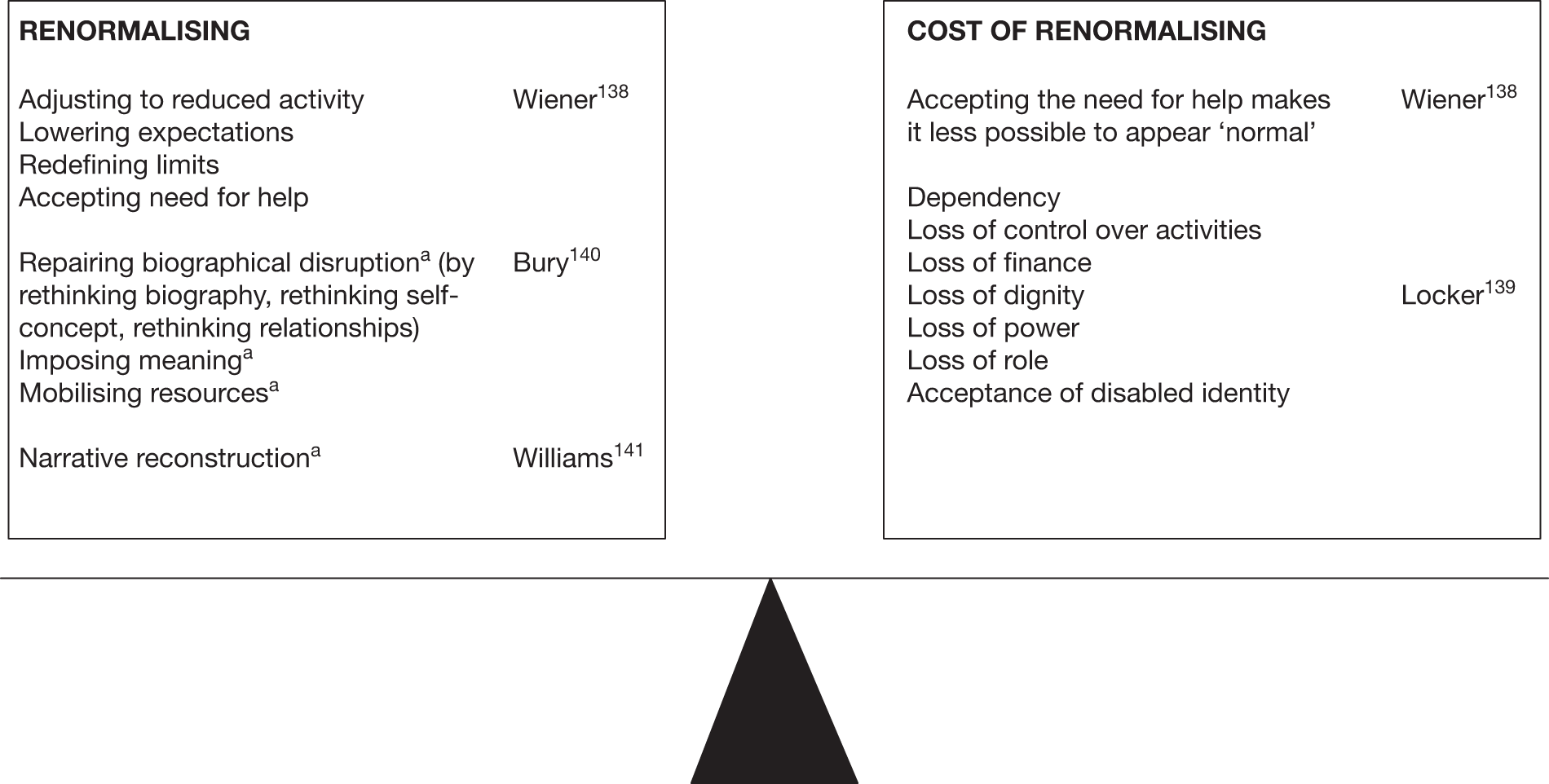
| Acute flare-up | Author | Uncertainty | Author | Remission/relief | Author |
|---|---|---|---|---|---|
|
When will it strike? How long will it last? How will it manifest? |
Wiener138 | Uncertainty about flare-ups and remission makes illness difficult to manage | Locker139 |
How long will it last? Timing? |
Wiener138 |
| What (if anything) will control symptoms? | Constant self-monitoring necessary | Remission mitigates against acceptance of disabled status | |||
| How much pain will there be? | Locker139 | Continuous testing of tolerance to activity is necessary | Hope for remission balanced against dread of disease progression | ||
|
How long will pain last? Which joints will be affected? When will it happen? |
|||||
| Which treatments (if any) will work? | Bury140 |
| Medicine | Author | Limitations of medicine | Author | Inner resources | Author |
|---|---|---|---|---|---|
|
Is a key cultural resource Referral to RA clinic and diagnosis gives relief and imposes order on symptoms |
Bury140 | People realise limits of medical knowledge regarding the cause and nature of RA | Locker139 and Bury140 | Patients left to draw own conclusions about whether or not RA is inherited | Bury140 |
| Diagnosis justifies people’s symptoms and behaviour | Locker139 and Bury140 | Medicine cannot answer questions regarding aetiology | Patients have to construct own theories. Might search past for reasons or search family/personal biographies, or reinterpret doctor’s explanation | Locker139 and Bury140 | |
| Narrative reconstruction | Williams141 | ||||
| People hope that medicine will provide information on how to manage RA, aetiology, fluctuating pain levels, prognosis | Locker139 |
Often medicine cannot provide satisfactory answers Medicine cannot allay fears about future with disability |
Locker139 and Bury140 | People have to impose own meaning and certainty in whatever ways possible | Locker139 and Bury140 |
| Medicine provides treatment | People realise that regimens are difficult to follow, not very effective | Bury140 | |||
| People hope it will help manage pain (because pain depletes energy, disrupts personal and social life, is difficult for others to understand, and is unpredictable and intangible, so it is difficult for sufferers to secure legitimacy) | Realisation that treatments are often unpleasant, painful, risky and of dubious efficacy | Locker139 | |||
| Realisation that pain can defy medical management | Development of own strategies to deal with pain (social withdrawal, hiding extent of pain to deal with problems of legitimation) | Locker139 | |||
| Worry regarding dependency on and side effects of painkillers | Adaptation of regimen to allow maximum relief with minimum side effects/dependency |
GDW’s synthesis
The synthesis was reported in several explicit stages: a description of the methods and samples in each paper, along with the major findings; tables to present the combination of findings in particular categories; a textual report of the synthesis, pointing to similarities and differences between the papers; and finally a table (Table 14) presenting the original concepts and higher order concepts derived from the synthesis. The descriptions of the papers help to set the scene for the synthesis, describing the main aims of the research, its methods and the citation of some papers by the other authors. Two of the papers are indicated to be theoretical in nature,140,141 drawing on experiences of RA as an example, whereas the others are more concerned with the lived experience of the disease. 138,139 GDW noted that a major concept in one paper,139 pain, was not mentioned in another, probably because of this different approach. GDW observed that one paper was described as very difficult to synthesise as it was so theoretical140 and commented that the methods of data collection and analysis were poorly described in the theoretical papers. 140,141
| Concepts | Second-order interpretations | Third-order interpretations | Fourth-order interpretations |
|---|---|---|---|
| DISEASE CONDITIONS: elusive aetiology; pain; crippling; absence of predictability; variability in progression and areas of involvement; lack of visible signs accompanying painful symptoms | Variability in the disease conditions of RA makes it difficult for people to maintain normal activities and be believed by others (e.g. family members, workmates) |
|
|
| IMPERATIVES: to identify the causes of arthritis/pain and disability; learning to live with it; avoiding embarrassment; maintaining a normal life and social roles | There is an evident tension between these IMPERATIVES and DISEASE CONDITIONS | Socially constructed norms, imperatives or expectations are a major source of the problems faced by people with RA | Coping with RA is as much about managing symptoms as it is about managing changing social expectations, norms and relationships |
| BURDENS: tolerating variable uncertainty; dread of dependency or invalidity; previously taken for granted actions require conscious and deliberate physical and psychological effort; biographical disruption; problems of legitimating changed behaviour; stigma; frustration; insecurity about dangers of everyday life; costs of treatment may outweigh the benefits |
|
In addition to the symptomatological burdens of RA, individuals face other burdens centred on changes in their relationships with their own physical bodies, other people and the medical system | |
| STRUCTURAL INFLUENCES: material resources; the limits of medical knowledge; emotional and social support networks; the organisation of paid employment; knowledge |
|
The everyday impact of RA is exacerbated by the organisation of society | |
| PSYCHOLOGICAL COPING STRATEGIES: hope of remission; dread of progression; accepting it; living with it; fighting it; keeping going/carrying on; mastering pain; withdrawal from others; reconstructing a sense of order; super-normalising (see below) | Psychological coping strategies involve ‘juggling’ opposites (hope/dread, accepting/fighting, carrying on/withdrawal) | Psychological coping strategies are limited by the unpredictable nature of the disease | |
| SOCIAL COPING STRATEGIES: normalising (pacing/thinking it out, covering up, keeping up); renormalising [adjusting to reduced activity: lowering expectations, developing a new set of norms for action (have to be constantly learned and relearned), eliciting help]; balancing the options; avoiding inappropriate behaviour; planning and routing | The ways that people with RA attempt to adjust to their illness are constrained by social norms and expectations about behaviour and social action | ||
| CONSEQUENCES: a sense of loss in relation to social roles and activities; a change from a participant in social life to an observer of it; eliciting help may give rise to feelings of dependency and decreases the possibilities of covering up and keeping up; medical knowledge is both resource and constraint; in acute phases, strategies of accepting it and keeping going break down; different aspects of biography are linked to realign the past with the present | The strategies used to cope with RA are undermined by the conditions of the disease itself |
In the synthesis, it was made clear that two papers138,139 were closest to the heart of the aim of the synthesis, whereas the others used the example of RA in their theoretical expositions. 140,141 On the whole, it was found that concepts were similar across the studies, although one paper141 was peripheral as it was concerned with the search for a cause of the condition rather than the experience of living with it. GDW reported the various burdens and coping strategies outlined by the authors, which are basically similar in concept. In the table of concepts (see Table 14), GDW focused on ‘disease conditions’ (symptoms, unpredictability), ‘imperatives’ (need to find cause of symptoms, learning to live with them), ‘burdens’ (tolerating uncertainty), ‘structural influences’ (resources such as medical and emotional), ‘coping strategies’ (psychological, social) and ‘consequences’ (loss and change). He produced this as a framework for the continuation of the synthesis.
Similarities/differences between the two arthritis syntheses
At the heart of both syntheses is the disruption to normal life by RA and the various strategies people employ to cope with it. Both researchers grouped the papers into two sets in the same way and noted the purpose of the papers identically. Both noted that all the papers referenced each other, with the exception of Williams,141 who refers only to Bury. 140 The two researchers used different terms for the core concepts. PP used Wiener’s138 thesis of normalising and renormalising, and identified that the concepts of uncertainty and balance were crucial. GDW focused more on the burdens and imperatives caused by the disease, the strategies employed and resulting consequences. PP, perhaps because of her in-depth involvement in the medicines synthesis, also focused on how those with RA became aware of the limitations of medicine and the treatments that it provides and had to draw on their own inner resources when coming to terms with the disease and its effects on them.
In summary, there are some similarities between the syntheses, but also notable differences. GDW was trying to establish a basis from which to continue the synthesis, and so displayed the information in more detail and in several ways. GDW presented a very detailed description of his attempt to synthesise these papers, probably because of his need to make this a firm foundation for the complete synthesis. He synthesised Wiener’s138 and Locker’s139 work first, as these were similar in presentation and focus, then integrated Bury’s140 findings, and attempted to include something of Williams’141 work, although this proved difficult. PP decided to focus on the key concepts from the index paper by Wiener,138 integrating the other findings into these, and this allowed the development of the higher order concept of ‘balance’. It is clear from the tables presented by both researchers that they found some aspects in common across the papers, although the terminology used was dissimilar and the syntheses were somewhat different.
The full syntheses
After the pilot syntheses had been completed, PP and GDW proceeded to conduct a full synthesis in the topic areas of medicine-taking and RA, respectively. Both synthesis subgroups reviewed and discussed the two pilot syntheses. Their experience of the pilot syntheses did not affect the way in which they conducted the full syntheses, although they used their initial syntheses as a starting point for the full synthesis. The methodologies used to conduct the full syntheses are now described in some detail.
Noblit and Hare15 suggested that there are seven stages to conducting a synthesis:
-
topic selection
-
selecting and finding the studies
-
reading the studies
-
determining how the studies are related
-
translating studies into one another
-
synthesising the translations
-
expressing the synthesis.
We described in Chapters 3 and 4 how Noblit and Hare’s15 first three stages of topic selection, literature searching and reading of the studies were conducted. As noted, we appraised our studies while reading them and part of that appraisal process required us to extract and outline in some detail the main findings and concepts for each of the papers. Thus, for us, Noblit and Hare’s15 third stage (reading the studies) expanded into reading, appraisal and initial data extraction. The subsequent stages varied for each of the syntheses and are described separately below. As will be seen, they did not necessarily conform to the stages outlined by Noblit and Hare. 15
Medicines synthesis
Initial extraction of data from papers
The findings and concepts that we outlined for each of the studies constituted the raw data for the initial stages of the syntheses. (The modified CASP18 appraisal tool that we used had separate questions about findings and concepts.) For the medicines synthesis, the extracted findings and concepts were compared between the two independent reviewers for each of the papers. In the rare cases in which the second reviewer had identified a finding or concept that was missed by the first, this was included to ensure that the final record of findings and concepts was comprehensive. The process of extracting the findings and concepts inevitably involves a degree of organising and summarising; thus, to some extent, an initial process of interpretation was already under way at this stage, especially when organising descriptive findings that had not been interpreted. At this stage, it also became apparent that the distinction between findings and concepts was neither simple to make nor useful, and because it was felt to be unnecessarily complicated it was abandoned.
Organising studies into medicine groups
As noted above, Noblit and Hare15 suggested that the fourth stage of the synthesis might be determining how the studies are related, followed by (5) translating studies into one another, (6) synthesising the translations and (7) expressing the synthesis. However, Noblit and Hare15 used much smaller samples in their syntheses (two or three studies at the most, although the reports were probably quite lengthy) and, with 38 studies to synthesise, the need to organise the studies in some preliminary way became imperative. For this reason, we began by organising the studies in what seemed to us to be the most immediately obvious way, into groups according to the medicine studied, and then within medicine groups, by the date of publication (Table 15). This gave us seven groups: antihypertensive medicine, which was also used for the preliminary synthesis (four studies); human immunodeficiency virus (HIV) infection medicine (11 studies); psychotropic medicine (six studies); asthma medicine (five studies); studies on medicine in general (five studies); a group of medicines for miscellaneous illnesses (five studies); and proton pump inhibitors (PPIs) (two studies). We then proceeded to translate studies into each other within each of the medicine groups.
| Medicine group | Papers |
|---|---|
| Antiretroviral therapy | Siegel and Gorey, 1997142 |
| Stone and Clarke, 1998143 | |
| Erlen and Mellors, 1999144 | |
| Halkitis and Kirton, 1999145 | |
| Proctor et al., 1999146 | |
| Siegel et al., 1999147 | |
| Siegel et al., 2000148 | |
| McDonald et al., 2000149 | |
| Murphy et al., 2000150 | |
| Johnston Roberts and Mann, 2000151 | |
| Barton Laws and Wilson, 2000152 | |
| Antihypertensives | Morgan, 1996134 |
| Van Wissen et al., 1998135 | |
| Johnson et al., 1999136 | |
| Svensson et al., 2000137 | |
| Psychotropic medicine | Kaljee and Beardsley, 1992153 |
| North et al., 1995154 | |
| Barter and Cormack, 1996155 | |
| Rogers et al., 1998156 | |
| Angermeyer et al., 2001157 | |
| Usher, 2001158 | |
| PPIs | Boath and Blenkinsopp, 1997159 |
| Pollock and Grime, 2000160 | |
| Asthma medicine | Adams et al., 1997161 |
| Prout et al., 1999162 | |
| Buston and Wood, 2000163 | |
| Walsh et al., 2000164 | |
| Pradel et al., 2001165 | |
| Miscellaneous medicines | Donovan and Blake, 1992166 |
| Dowell et al., 1996167 | |
| Ersek et al., 1999168 | |
| Atkin and Ahmad, 2000169 | |
| Smith et al., 2000170 | |
| Medicines in general | Roberson, 1992171 |
| Britten, 1996172 | |
| Dowell and Hudson, 1997173 | |
| Watson and Mitchell, 1998174 | |
| Lumme-Sandt et al., 2000175 |
Translating studies into each other within medicine groups
Noblit and Hare15 suggested that the process of translating findings into each other goes something like, ‘one case is like another, except that …’ (p. 38). We followed this process in a systematic way. For example, paper 1 in the psychotropic medicine group might have findings X, Y and Z. Paper 2 in the same group might have finding w (something new that was not in paper 1), findings x and y (findings similar to findings X and Y in paper 1) and nothing like finding Z from paper 1. So this would produce a synthesis of papers 1 and 2:
-
finding w (from paper 2)
-
findings X and x (from papers 1 and 2)
-
findings Y and y (from papers 1 and 2)
-
finding Z (from paper 1).
This synthesis of papers 1 and 2 would then be compared with paper 3 in the same way. Then the synthesis of papers 1, 2 and 3 would be compared with paper 4, and so on until all the studies within, for example, the psychotropic medicine group had been translated into each other. Then the process would begin again for the next medicine group, and so on. This process of translating the findings into each other is one of ‘reciprocal translation’, as described by Noblit and Hare. 15 The process of ‘reciprocal translation’ was employed because the majority of the studies are essentially about similar issues. Another possible method of translation is ‘refutational’,15 but in this case none of the findings from the studies refuted each other.
Determining how findings relate to each other within medicine groups
The translation of findings from the studies into each other for each of the medicine groups resulted in a raw textual synthesis for each of the groups. We then needed to know how the findings related to each other within each of the groups. Noblit and Hare (p. 28)15 wrote: ‘We think it makes sense to create a list of the key metaphors, phrases, ideas and/or concepts (and their relations) used in each account and to juxtapose them’. We did this by summarising the key findings for each of the illness groups so that they fitted on one page and then drew the relationships between them. This resulted in a ‘map’ for each of the groups (Figures 7–12). These ‘medicine maps’ summarised the key findings, the way in which they translated into each other and the relations between them, for each of the groups.
FIGURE 7.
Proton pump inhibitors synthesis. OTC, over the counter.
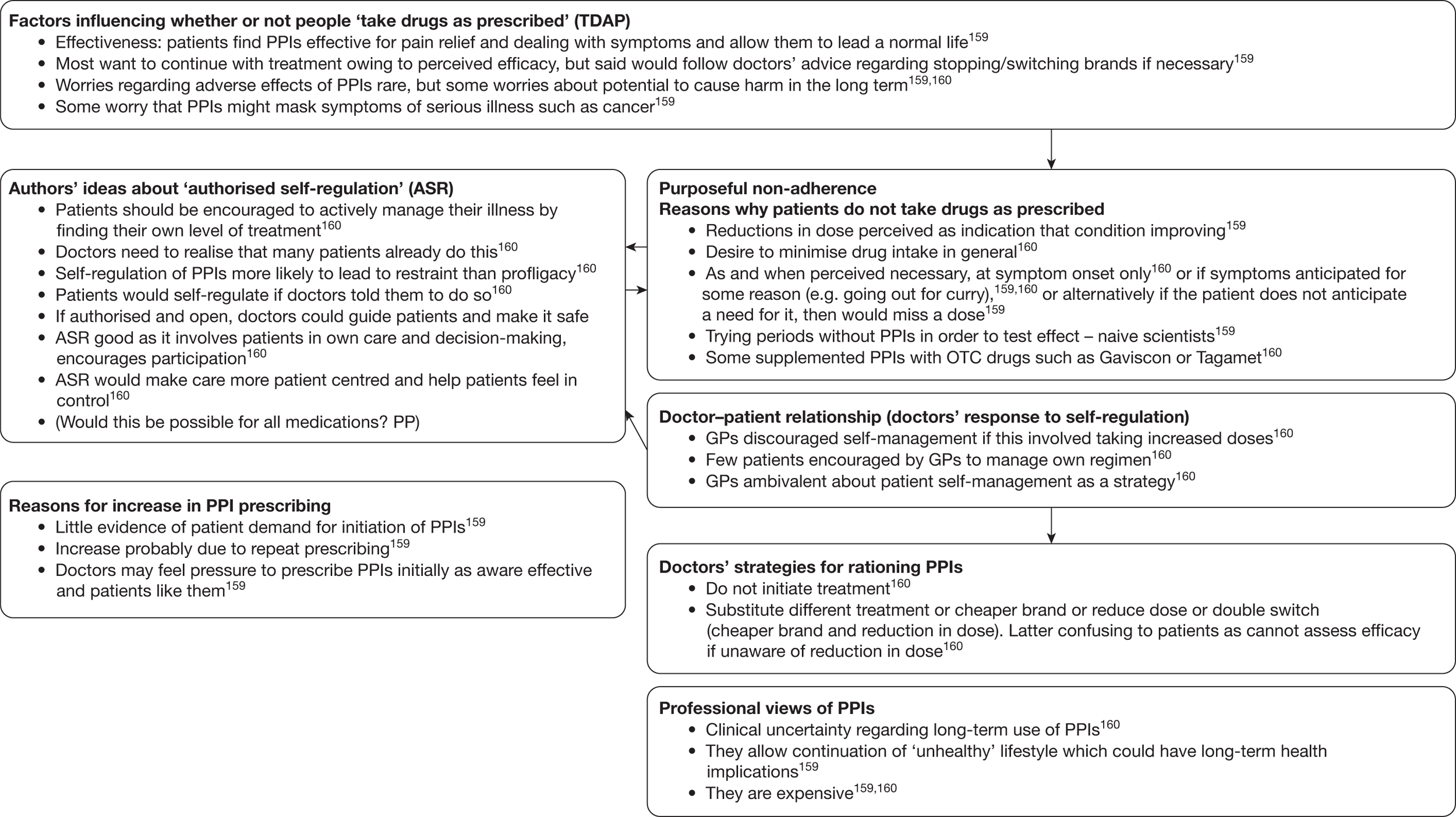
FIGURE 8.
Highly active antiretroviral therapy (HAART) synthesis. QoL, quality of life.
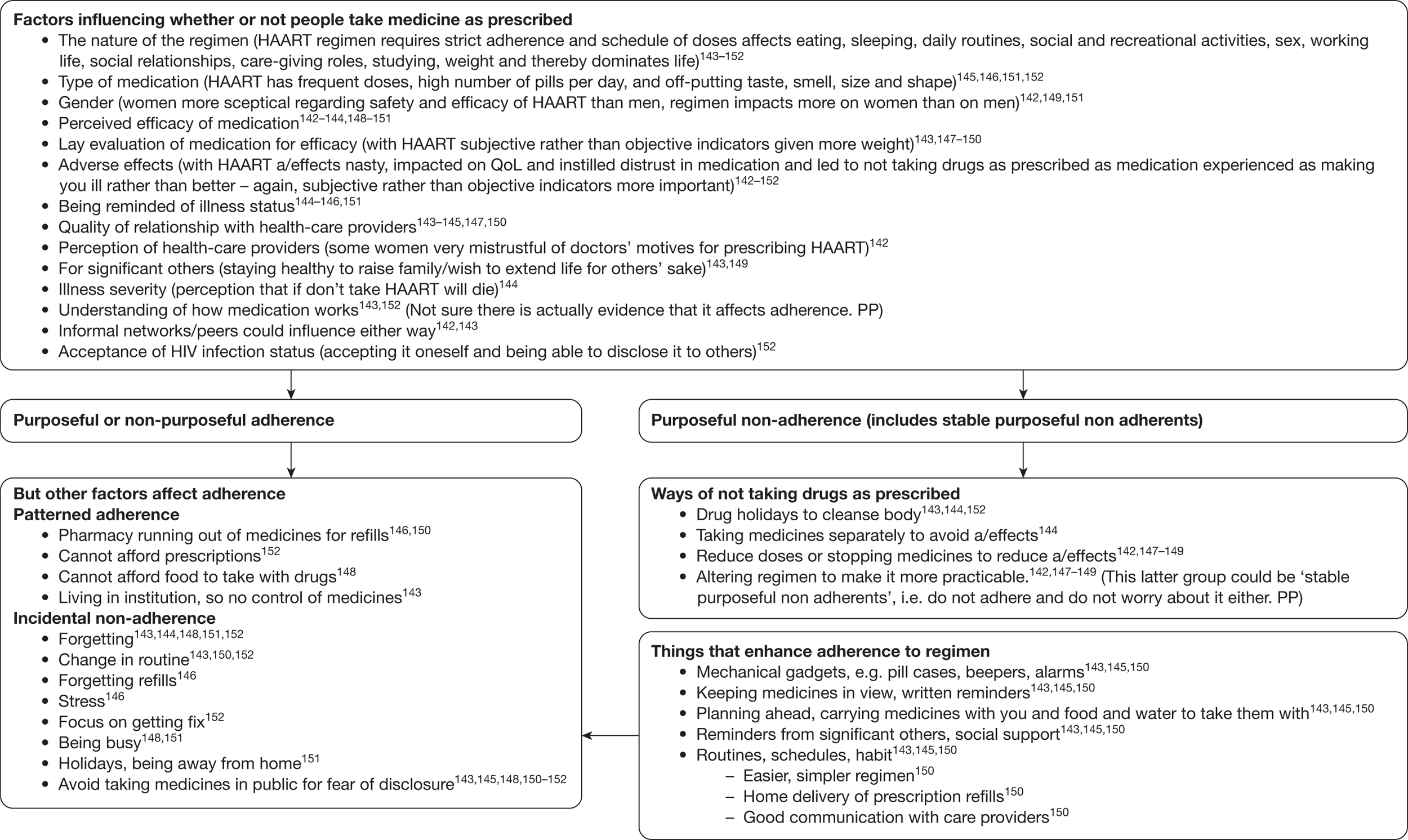
FIGURE 9.
Miscellaneous medication (including for arthritis, cancer pain, mental-health problems, thalassaemia major and respiratory disease) synthesis. ntdap, not taking drugs as prescribed.
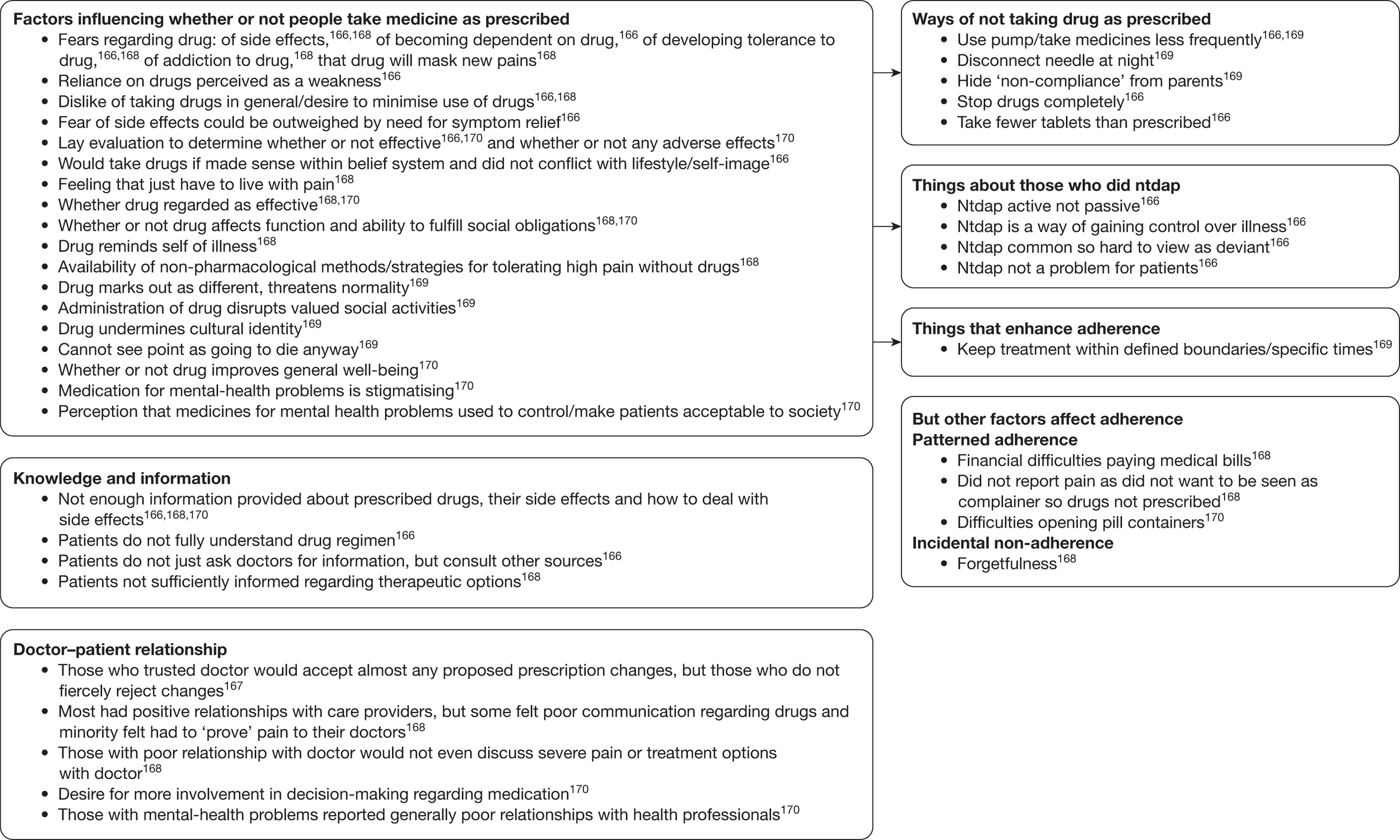
FIGURE 10.
General medication synthesis.
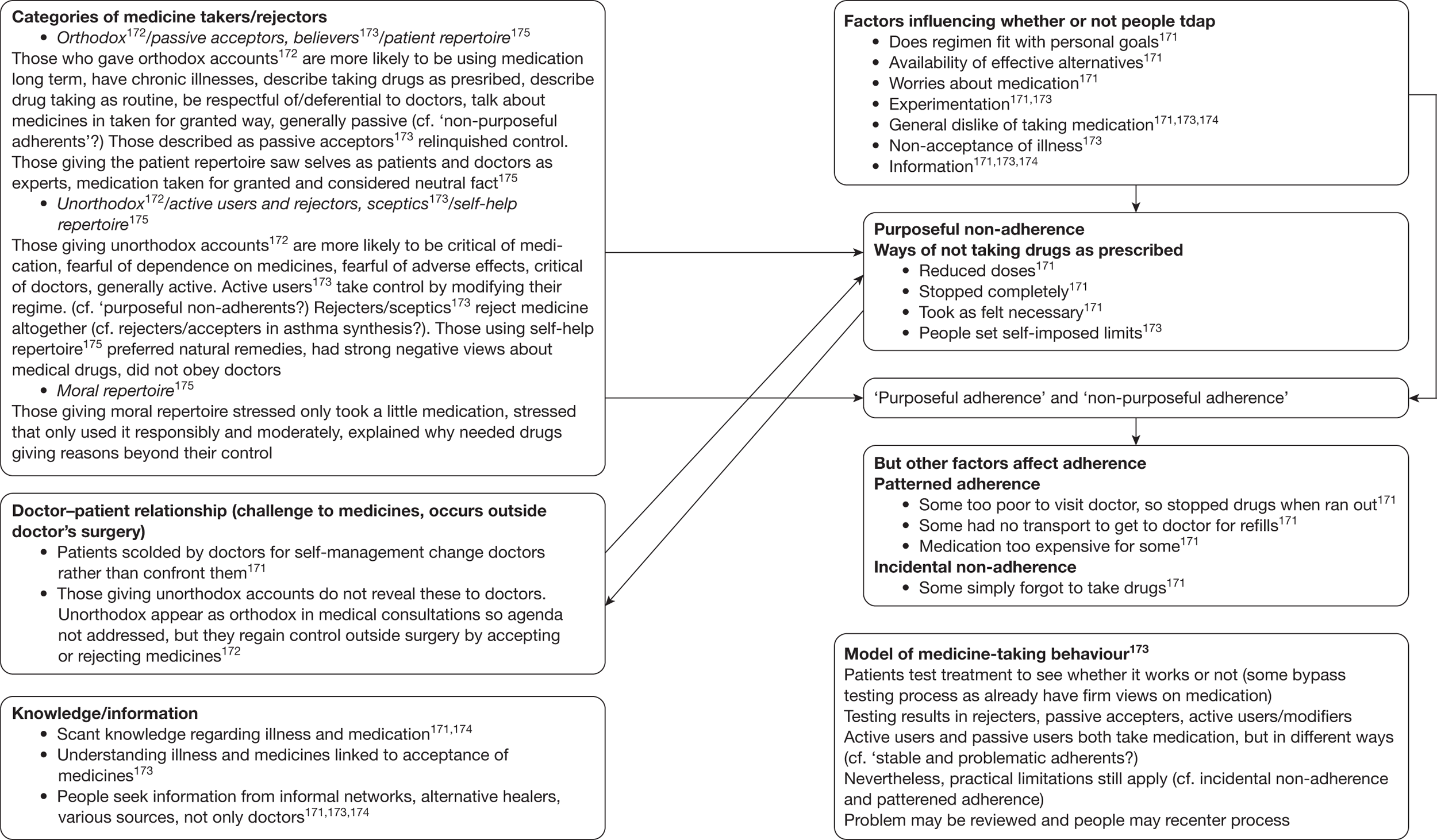
FIGURE 11.
Asthma medication synthesis.
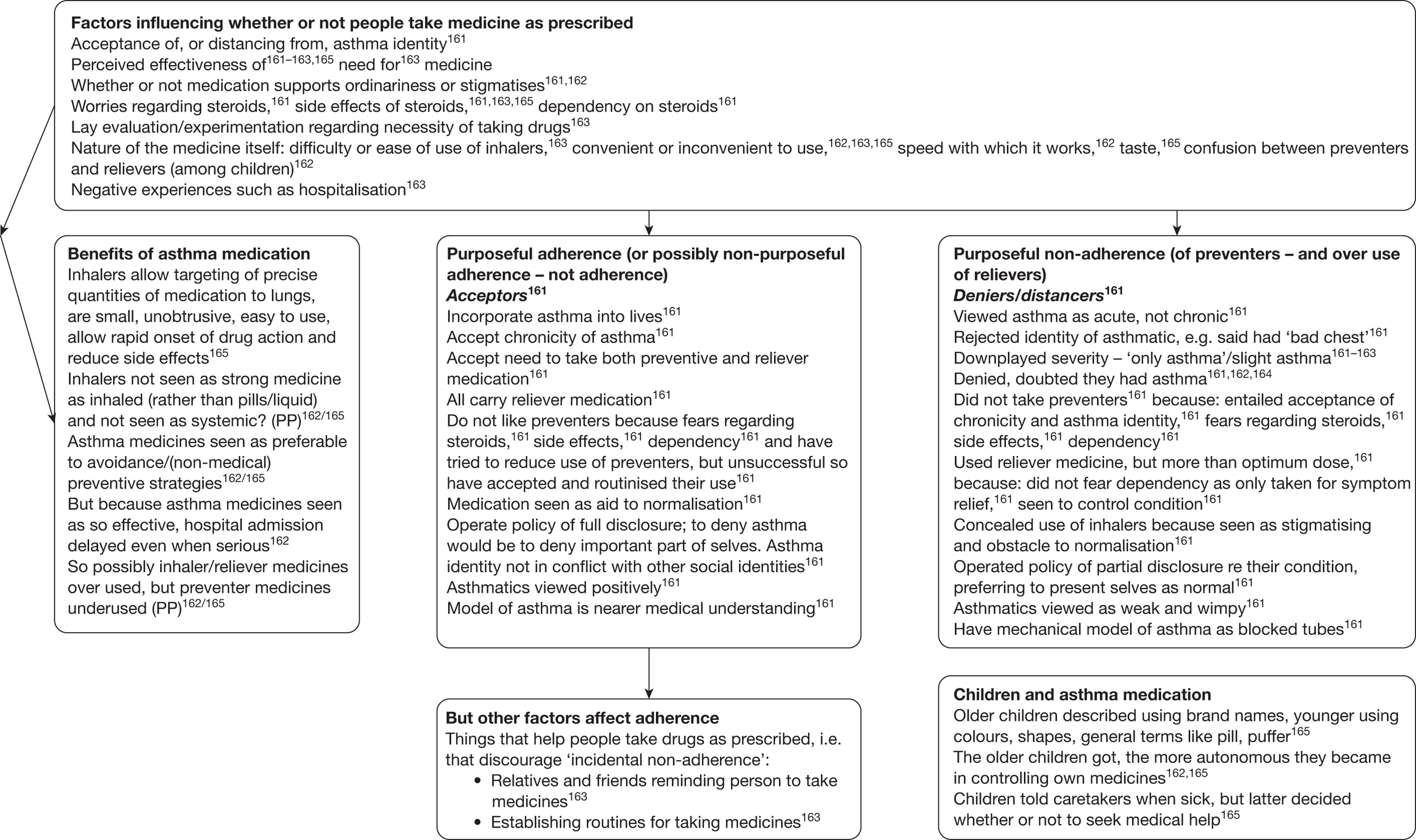
FIGURE 12.
Psychotropic medication synthesis. CPN, community psychiatric nurse; ntdap, not taking drugs as prescribed; PRN, prescribed as needed; QoL, quality of life.
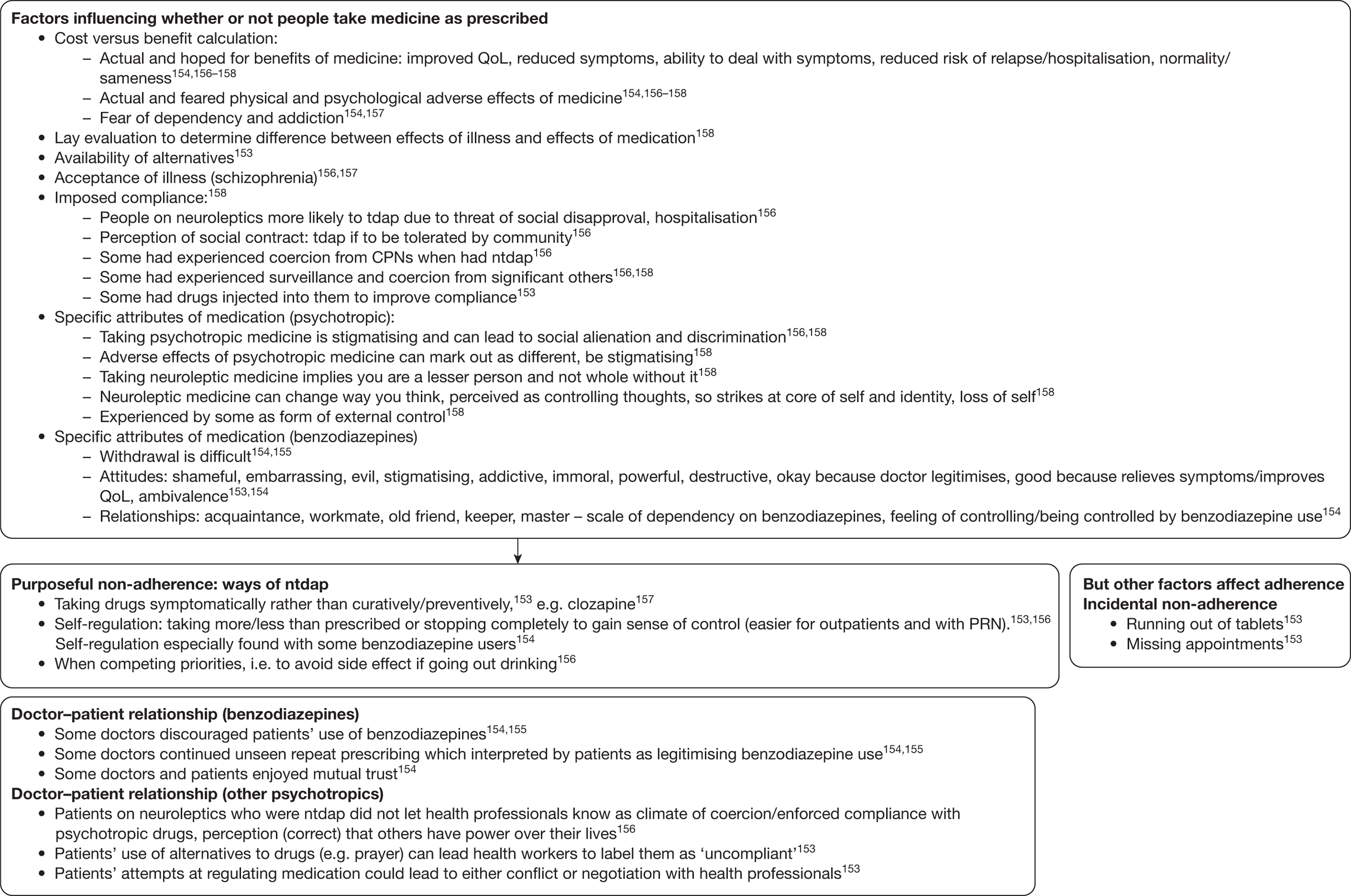
Determining how studies are related across the medicine groups
We now needed to know how the findings related to each other across the medicine groups. We determined this by comparing the medicine maps with each other, and developed a model that was able to encompass the findings from all of the studies in the synthesis. Some of North et al. ’s154 findings did ‘fit’ with this, but their typology of relationships to benzodiazepines did not. Our model changed slightly as we progressed with the synthesis, but the final version is shown in Figure 13. Dowell and Hudson,173 authors of one of the studies in the synthesis, had developed a model of medicine that was similar in many ways, but which was unable to ‘hold’, or account for all the findings from all the studies in our synthesis. Our model provides a useful overall map for the synthesis process. It was an invaluable organisational aid during the synthesis process, but it may also prove to be a useful model for understanding the route by which people decide whether or not and how to take their medicines. It also illustrates that seemingly disparate studies may be put together to create something new. The model, however, provides only an overview. As an abstract representation of the findings and the relationships between them, it lacks necessary detail.
FIGURE 13.
Model of medicine-taking.
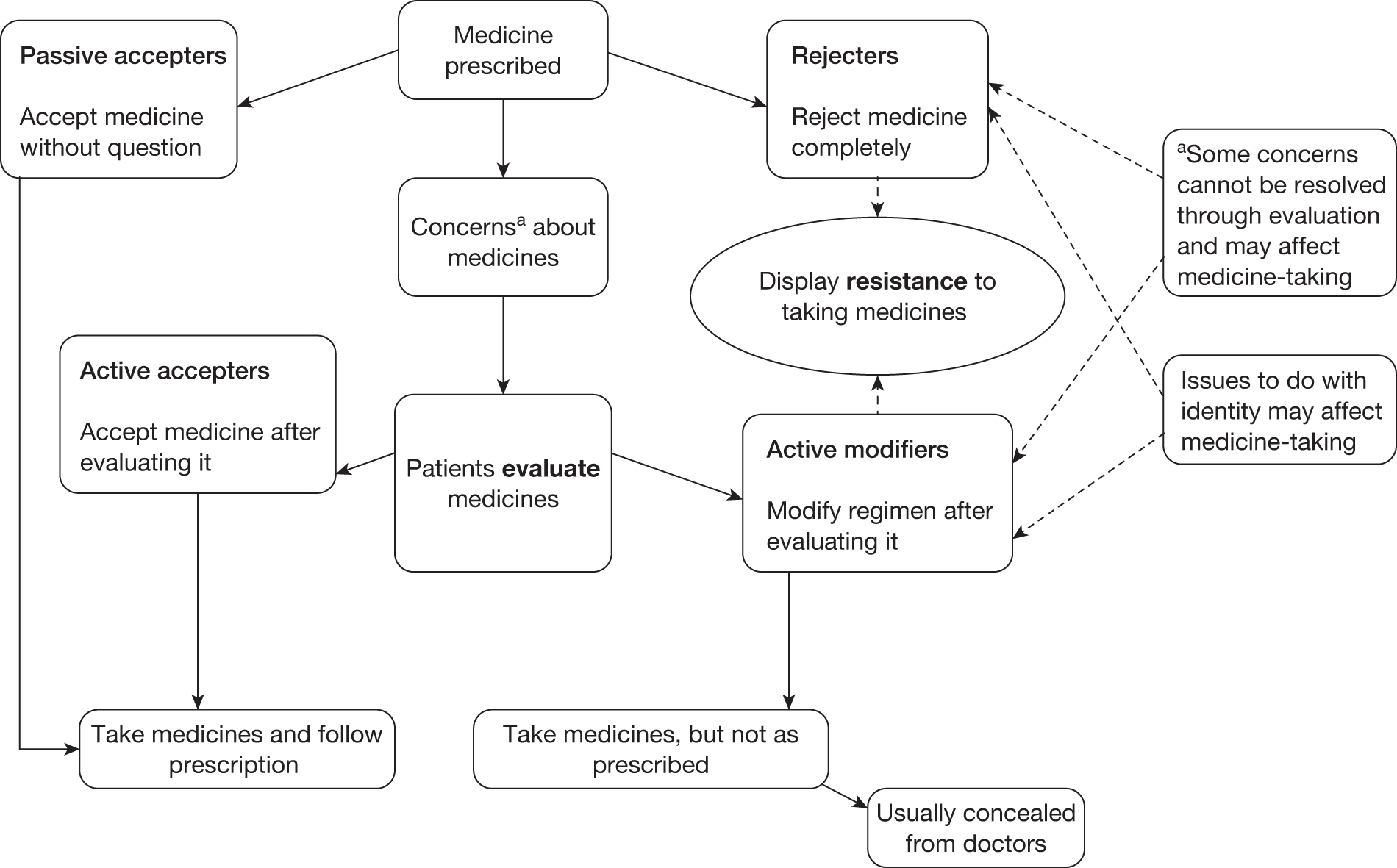
Synthesising translations across the illness groups
The next stage was to return to the detail, to the textual translations that were conducted for each of the medicine groups, and synthesise these across the medicine groups. So whereas the medicine maps were ‘brought together’ to provide our overall model of medicine-taking, now the textual syntheses for each of the medicine groups were ‘brought together’, or synthesised, to provide an overall synthesis of medicine-taking. This initially involved reading and rereading the textual syntheses for each of the medicine groups (referring back to the original papers where clarification was necessary), then bringing together the data thematically. So, for example, if ‘worries about medicine-taking’ were identified in the asthma, HIV infection and hypertension textual syntheses, these data were brought together beneath this heading in the overall synthesis. Thus, the data for the overall synthesis were analysed thematically rather than according to medicine group. This overall synthesis is a ‘lines-of-argument’ synthesis,15 in that it says something about the whole based on studies of the parts.
Noblit and Hare (p. 64)15 explained the relationship between the translating of cases into each other and the subsequent expression of the synthesis as ‘lines-of-argument’: ‘In short, the translation of cases into one another sets the stage for a second-level inference about the relationship between the studies. It is the second-level inference that assigns interpretive significance to each study to be synthesized’. The ‘lines-of-argument’ synthesis, therefore, essentially involves a process of interpretation and conceptual advancement and is at the same level as Britten et al. ’s16 ‘third-order interpretations’. The entire process of the medicine-taking synthesis is summarised in Box 7.
-
Topic selection.
-
Searching for the studies.
-
Reading and appraising the studies, including initial extraction of main findings/concepts.
-
Organising studies into medicine groups.
-
Translating studies into each other within medicine groups; produces a raw textual synthesis for each medicine group (‘reciprocal translations’).
-
Determining how findings relate to each other within medicine groups; produces ‘medicine maps’.
-
Determining how studies are related across the medicine groups; produces an overall model of medicine-taking.
-
Synthesising translations across the medicine groups; produces an overall textual synthesis of medicine-taking (‘lines-of-argument’ synthesis/‘third order’ interpretation).
Exclusions during synthesis
At the end of the synthesis, it became apparent that one of the papers in the medicines synthesis165 had contributed nothing at all to the final synthesis even though it had been included in the asthma medications map. The paper had been borderline because much of it was about children’s response to asthma as well as asthma medicine. On further reading, it became clear that its emphasis precluded it from contributing to the synthesis. The final number of papers that contributed to the medicines synthesis was therefore 37 (Box 8).
| Number of papers initially included in synthesis | 38 |
| Number of papers excluded during synthesis | 1 |
| Number of papers in final synthesis | 37 |
Rheumatoid arthritis synthesis
The papers were read and synthesised chronologically, according to publication date. The earliest paper in the series138 was used as an index paper, i.e. subsequent papers were compared with this one. The synthesis proceeded as ‘reciprocal translations of each case (i.e. paper) into each of the other cases’. 15 There was a conceptual coherence among the majority of the studies that eased the synthesis process. The synthesis was conducted in a cyclical fashion. The papers were read carefully three times by the first author: once for appraisal and data extraction; once during the reciprocal translation phase; and once to fill in any holes in the emerging theory. As noted above, the papers were also read once independently by second assessors. Thus, each paper was read in detail on four different occasions by two different people.
Reciprocal translation involves comparing the findings and concepts from each included paper with those of the others. The coherence of the papers in the RA synthesis meant that it was possible to do this simply by means of a table, with columns representing all of the included studies, and rows representing differently themed groups of findings or concepts. The whole table is too large to be included here, although an extract of some of the studies and theme groups has been given (Table 16) by way of example. Some theme groups were renamed, added to, merged or deleted during the reciprocal translation process. In order to preserve the authors’ own findings and concepts, verbatim quotations from the papers were retained at this stage of the synthesis, and the page numbers in the cells in the table refer to the pages from which the quotations were taken. The concepts and findings in the table derived primarily from those listed by the first and second assessors when the papers were read and appraised. The initial framework extracted information from the studies into the following headings: sample, data collection setting, data collection method, data analysis method, disease conditions, imperatives, burdens, structural factors, psychological (‘coping’) strategies and social (‘coping’) strategies. However, it was necessary in some cases to return to the original papers at this stage, both for clarification, and for further elucidation of findings or concepts which achieved added importance only during the reciprocal translation stage itself. The initial framework was adapted to fit the reciprocal translations as the synthesis progressed.
| Bury, 1982140 | Stenström et al., 1993176 | Shaul, 1995177 | |
|---|---|---|---|
| Disease conditions |
Signs and symptoms (p. 170) Implies premature ageing (p. 171, after Singer, 1974)a ‘An outside force … [invading] … all aspects of life’ (p. 173) ‘A crippling disease’ (p. 173) ‘Nature of the disease remains elusive’ (p. 173) |
‘The respondents were uncertain about themselves and their own interpretations of their symptoms, and whether they would be able to get adequate help to master the disease and manage their everyday lives’ (p. 237) |
‘Most common symptoms involved the hands, wrists, shoulders, and feet. In some cases, pain and swelling occurred simultaneously, in others, pain occurred alone, followed by swelling. In either case, there was usually weakness in the affected limb and general fatigue’ (p. 292) ‘Fatigue and pain were cited as the most distressing of the symptoms and contributory to an increase in depressive symptoms’ (p. 293) Weakness (p. 293) ‘Of all the physical symptoms that the women described, none were as pervasive as fatigue. Fatigue was often the first sign of an impending flare, and continued long after the flare had subsided. Some women commented on being “always tired” ’ (p. 294) |
| Burdens or needs (added while synthesising Stenström et al.176) |
‘Many saw a future of growing dependency and invalidity’ (p. 173) ‘Functional limitations’ (p. 175) ‘The erstwhile taken-for-granted world of everyday life becomes a burden of conscious and deliberate action’ (p. 176) Chronic illness as a disruptive experience (biography, relationships) Problems of legitimating changed behaviour; stigma |
Needs accentuated after disease onset: ‘Maintenance of one’s identity, personal integrity, mental balance, practical help, support from significant others, social support, communication about the disease, social contacts’ (p. 237) | |
| Psychological strategies | ‘The search for a more comprehensive level of explanation, a more certain basis of coping with the illness is often a long and profound one’ (p. 174) |
Strategies/attitudes used to reduce uncertainty, regain control and achieve security in everyday life: ignore; mental and physical struggle; solve problems; distract; enjoy; hope; adjust/accept; reappraise; escape/deny/suppress; be resigned (p. 239) ‘Sometimes it is possible to confront the disease, whereas at other times the only thing to do is hope for better times’ (p. 240) |
Denial (p. 292) ‘Learning to live with it’ (p. 293) ‘They incorporated the illness into their self-image, and although they could not predict the course of the illness or when another flare would occur, they were better prepared to cope with it when it came’ (p. 293) ‘The thought of death seemed to bring some form of relief, even as a fantasy’ (p. 294) |
| Social strategies |
‘The attempt to normalise in the face of disruption’ (p. 177) ‘Departing from behaviour which is deemed appropriate carries it’s own specific disadvantages and thus is avoided as far as possible’ (p. 177) |
||
| Coping strategies (added while synthesising Williams and Wood178) | ‘Strategies labelled “confrontation,” “expectation,” and “redefinition” all seem helpful in reducing uncertainty by taking into account RA patients’ needs and somehow trying to satisfy them’ (p. 240) | ‘The women in this study became experts at recognizing the cues that signal the onset of a flare, of overwork, or the need to change a pattern of activity through the acquisition of knowledge about the disease, its treatment, and experience of living with it’ (p. 295) | |
| Consequences |
‘Much depends on the degree of flexibility which both formal institutions and informal relationships are prepared to allow’ (p. 177) Medical knowledge is both resource and constraint |
‘There is an indication in the data that the frequent use of defence (i.e. denial that you have the disease/any problem) or resignation reflects a neglect of one’s needs while trying to reduce uncertainty. Thus, defence might be a ‘dead end’ resulting only in an illusory reduction in uncertainty’ (p. 240) The results are said to be ‘largely consistent with coping theory’ (p. 241) Needs in RA are mediated by the uncertain course of the disease (I don’t think this finding is new?) |
‘feeling alienated from friends, family and coworkers’ (p. 293) |
The synthesis was concerned with perceptions of aetiology, experience and treatment. However, the substance of the studies, and their main theoretical significance, concerned the ‘experience’ of daily life with RA following the changes brought by the condition. Although issues around aetiology and treatment did feature, the papers that focused on these issues felt marginal to the wider collective voice of the papers. In expressing the synthesis here, the three areas of aetiology, experience and treatment are separated out, although far more attention is devoted to ‘experience’ as it was the focus of most of the studies. This process resulted in two sociological models, one concerned with gender relations and one concerned with adaptation to RA, which were constructed after the reciprocal translations, perhaps in a manner akin to moving to a ‘higher’ level of conceptual development (although not in the ‘by theme’ manner exemplified by Britten et al. 16).
Exclusions during synthesis
Four papers were excluded at the synthesis stage,179–182 leaving a total of 25 papers in the RA synthesis, describing 22 studies (Box 9). One was excluded because the focus was doctor–patient communication, rather than the lived experience of RA. 179 Another was excluded because it focused on conditions other than RA,180 whereas the remaining two181,182 were marginal in terms of whether or not the research methods employed meant that the study fell within our definition of qualitative research.
| Number of papers initially included in synthesis | 29 |
| Number of papers excluded during synthesis | 4 |
| Number of papers in final synthesis | 25 (describing 22 studies) |
Discussion
Preliminary studies of reproducibility
Reproducibility of qualitative research is difficult to assess as it is not possible to collapse the detail and richness of the data into simple quantified components. Assessing the reproducibility of qualitative research is, then, a matter of judgement. There is considerable debate in the methodological literature about whether or not ‘reproducibility’ is a reasonable concept with which to assess qualitative research. It is always likely that different researchers with different backgrounds and different levels of experience will interpret qualitative data in different ways. It is likely, therefore, that the reproducibility of syntheses of qualitative research is also likely to be variable and related to the particular researchers involved. This can be seen in the comparison above, particularly in relation to researchers’ different levels of experience of synthesising: PP had undertaken this before and so did not feel the need to describe the process in as much detail as GDW who was doing this for the first time. Similarly, as the two researchers were going on to complete only one of the syntheses each, there were differences in their preparation of the material for continuing to synthesise beyond the first four papers.
Many of the concepts and findings in these two syntheses were nevertheless combined similarly by the researchers. There were differences of detail, but often these were related to the way in which the original authors presented the concepts, which presented the opportunity for terminology to be interpreted differently. The approaches to the syntheses were somewhat different. GDW, for example, preferred to place the findings in tables to facilitate comparison, whereas PP preferred to describe the process of combining findings more textually. Such differences are reflective of individuals’ particular modes of working, and it is unlikely that a single approach could be deduced and applied universally. Indeed, this is also true of primary qualitative research. The key to synthesising qualitative research lies in becoming immersed in the findings and concepts presented by the original authors, and then attempting to combine these to reach summaries of findings and higher level concepts.
Overall, this preliminary and exploratory attempt to investigate the reproducibility of the first stage of a qualitative synthesis has shown that the combination of concepts and findings is fairly similar, even when the approach to synthesising is quite different. It is possible to deduce reasons for differences related to approach and background of the researchers and a lack of explicitness on the part of the original authors. This investigation involved experienced qualitative researchers. The complexity of the task suggests to us that it should always be undertaken by experienced researchers. It is our view that less experienced researchers would find the tasks of translating concepts more difficult, with the likely result of less coherent syntheses – although, this remains to be tested. This investigation examined reproducibility only at an early stage with only four papers, and it is not clear whether the syntheses would have become more or less similar with the inclusion of further papers. Only two researchers independently synthesising the same full set of papers would show this. We would suggest that the evidence from this investigation of reproducibility should assure researchers and policy-makers that the process of qualitative synthesis is reasonably robust when undertaken by experienced researchers.
Full syntheses
As with the preliminary syntheses, the two full syntheses were conducted differently from each other, primarily reflecting the differing amounts of literature to be synthesised. Because there was more literature for the medicines topic, additional work had to be done to organise the literature and make the synthesis process manageable. Another research group might simply have synthesised the medicine papers chronologically, but it is likely that an analysis by medicine or disease would still have been conducted at some later stage. More detailed reflections on the full syntheses will be offered at the conclusion of the synthesis findings (see Chapter 6).
Chapter 6 Resisting medicines: a synthesis of qualitative studies of medicine-taking
Introduction
The year 2003 saw the publication of three high-profile reports on medicine-taking: one from the World Health Organization (WHO),183 one from the government-funded Medicines Partnership184 and the last from the King’s Fund. 185 Meanwhile, an initiative called ‘Ask about Medicines Week’ (www.askaboutmedicines.org) was launched to ‘help promote partnership in medicine-taking between medicine users, carers and health professionals’. During ‘Ask About Medicines Week’, the British Medical Journal dedicated an issue to the theme of ‘concordance’,186 as did the official journal of the Royal Pharmaceutical Society, The Pharmaceutical Journal. 187 Additionally, the NHS Service Delivery and Organisation Research and Development programme commissioned a scoping exercise to review ‘Concordance, adherence and concordance in medicine taking’ which reported in 2005. 188 What prompted this attention?
The WHO183 report aimed to improve worldwide rates of ‘adherence’ to long-term treatments for chronic conditions, which the authors of the report currently estimated to be 50%. They argued that the consequences of low adherence to long-term treatments were firstly poor health and secondly increased costs of health care, claiming: ‘Poor adherence is the primary reason for sub-optimal clinical benefit. It causes medical and psychosocial complications of disease, reduces patients’ quality of life and wastes health care resources’ (p. 25). Likewise, the Medicines Partnership cited ‘a rising drugs bill and the key role of medicines in promoting health’184 as the key reasons for improving compliance. The editor of The Pharmaceutical Journal explained that the themed issue aimed to clarify the concept of concordance because, if concordance can be achieved,187 ‘… people are more likely to take the medicines prescribed for them and stick to the regimen’ (p. 480). Although noting that the result may also be a refusal of the medicine, the editor went on to remind readers that many medicines are taken by less than half the patients to whom they are prescribed and that ‘… the waste alone should make them think again’ (p. 480).
The reports by the WHO183 and by the Medicines Partnership were wide-ranging and reviewed the literature to establish what was known about medicine-taking, the factors affecting it and interventions that could enhance it. The Medicines Partnership report noted that several factors can affect medicine-taking, including demographic factors, issues surrounding the medicine itself (including adverse effects and the complexity of the regimen), ‘beliefs’ about medicines, concerns about the value or appropriateness of medicines, psychosocial issues, confusion and physical difficulties. The WHO183 report suggested that the main influences on medicine-taking were a wide range of social and economic factors (including poverty, lack of education and ‘culture’), health-care team and system-related factors (such as the patient–provider relationship and the quality of the health services offered), condition-related factors (for example, the severity of the illness and its symptoms), therapy-related factors (i.e. the efficacy of the treatment itself and whether or not it has adverse effects) and, finally, patient-related factors (such as anxieties about the treatment, stress, perceptions that the medicine is not needed or not effective, and non-acceptance of illness).
The independent King’s Fund report was quite different. 185 It was written in response to a ‘growing recognition’ that the interests of those who provide health care do not necessarily coincide with the needs of those who use it. Harrison185 suggested that at present an implicit public–private partnership exists between the NHS and the pharmaceutical industry, but that the pharmaceutical industry is largely free to provide products it considers will be profitable, whereas the NHS is a passive purchaser. Harrison185 argued that this has led to an emphasis on pharmaceutical products at the expense of non-pharmaceutical approaches to health care such as behavioural therapies, illness prevention, public-health interventions and ‘alternative therapies’. Furthermore, because research priorities are not determined by consumers, the needs of major groups, including women, children and older people, have been ignored, and important therapeutic areas have been neglected. ‘These circumstances have produced health care systems that are highly drug dependent and that in general cannot see themselves being any different.’185
The reports by the WHO183 and the Medicines Partnership are, arguably, products of this type of health-care system and culture, where health is seen to depend upon pharmaceutical medicine. Both reports assumed that adherence to medicine will lead to better health. Yet, a systematic review of interventions to increase adherence to medicines found that successful interventions (of which there were 19 out of 39) did not lead to large improvements in adherence or treatment outcomes. 189
The bulk of the research upon which both reports relied is quantitative and much of it has been conducted from the professional or systems perspective, taking little account of lay perspectives. Vermeire et al. 190 observed that during three decades of quantitative research into non-compliance, > 200 variables have been studied, but none consistently predicts compliance. The authors suggested that despite continuing research, there have been few insights since the 1980s. Most of the research has been on the extent and determinants of non-compliance, but Vermeire et al. 190 argued that this research has been fragmented, of variable methodological quality and lacking an integrating model or theory. The authors attributed the lack of success in this field to neglect of patients’ perspectives and beliefs, as well as to an absence of qualitative research.
In 1996, Blaxter and Britten191 reviewed lay beliefs in the context of medicine-taking and concluded, usefully, that lay people do not view medicine as something to be taken ‘as prescribed’, but rather as a resource for use as they themselves see fit. The theory that medicines are used as a lay resource provides an alternative perspective on the behaviour that professionals find bewildering. If lay people use medicines as a resource then it is understandable that they might modify their regimens to suit their daily routines, take medicine only when they experience symptoms, cease taking it if they experience adverse effects or draw upon other resources, such as ‘natural remedies’ alongside it. Blaxter and Britten191 suggested that more research, especially qualitative research, is needed to understand lay theories of bodily systems, the actions of medicines, the origins of lay beliefs about medicines and the influence of the media on public perceptions of medicines.
Our synthesis brings together 10 years of qualitative research into lay experiences of medicine-taking and we hope that the emphasis on lay perspectives will shed new light on this field. Before outlining the various perspectives of the studies, however, a brief discussion of the terminology of medicine-taking is necessary because, as can be seen, this varies. Medicine-taking has been characterised in three different ways during the last few decades: compliance, adherence and now concordance. Compliance is traditionally assumed to refer to doctors’ desire for patients to comply with their instructions about taking medicine. Adherence was subsequently offered as a more neutral expression, in the hope of avoiding the paternalism for which compliance came to be criticised. The tone remained prescriptive, however, and a new model, that of concordance, was proposed. 192 Concordance refers to the anticipated outcome of the consultation between doctors and patients about medicine-taking, if both parties can be encouraged to work together as partners. In practice, the three terms are often used interchangeably, despite the subtle differences in meaning and perspective.
The studies
Key features of the studies in this synthesis are summarised in Table 17 and the citation tracking of papers is recoded in Table 18. As can be seen, most studies are concerned with medicines taken on a long-term basis for chronic illnesses.
| Source paper (n = 38) | Country setting | Participants (female) | Sample origins | Medicines/condition | Data collection |
|---|---|---|---|---|---|
| Donovan and Blake, 1992166 | UK | 54 (39) people | Hospitals | Miscellaneous (inflammatory arthropathy/osteoarthritis/minor rheumatology complaints | Semi-structured interviews, before and after recorded consultation with doctor |
| Kaljee and Beardsley, 1992153 | USA | 70 people | Rural mental-health clinic | Psychotropic medicine | Observation of meetings, group sessions, in-depth interviews |
| Roberson, 1992171 | USA | 23 (14) black adults aged 19–77 years, varied education; 18 hypertension, 8 arthritis, 5 diabetes, 1 asthma, 1 hepatitis, 1 erythema multiforme | Southern rural African American community population | Medicines in general | Unstructured interviews |
| North et al., 1995154 | New Zealand | 22 Europeans (11) aged from 34 to 82 years | One group from the community and one from self-help group | Psychotropic medicine | In-depth interviews |
| Barter and Cormack, 1996155 | UK | 11 (10) aged 60–90 years. Also sample of 20 (12) elderly people ‘randomly’ sampled on street, not on benzodiazepines | Community (those in receipt of benzodiazepines for at least 1 year) | Psychotropic medicine | Semi-structured interviews |
| Britten et al., 199616 | UK | 30 (11) aged 20–70 years, 27 white, 2 black and 1 Middle Eastern | Two London GP practices: poor area (9 patients), affluent (21) | Medicines in general | Semi-structured interviews |
| Dowell et al., 1996167 | UK | 17 people | Urban Scottish general practice | Miscellaneous (rapid prescribing changes) | In-depth interviews, twice over 6 months |
| Morgan, 1996130 | UK | 60 (30): 30 white, 30 African Caribbean (30) all aged at least 35 years | 15 general practices in London Borough of Lambeth | Antihypertensive medicine | Semi-structured interviews |
| Adams et al., 1997161 | UK | 30: 14 women (10 working class, 4 middle class) and 16 men (8 working class and 8 middle class). Aged 19–57 years | Single general practice in south Wales (former mining) town | Asthma medicine | In-depth interviews |
| Boath and Blenkinsopp, 1997159 | UK | 20 (11) aged 28–68 years, 15 married, 10 working, 1 unemployed, 1 housewife, 4 unable to work and 4 retired | One fund-holding group medical practice | PPIs | Semi-structured interviews |
| Dowell and Hudson, 1997173 | UK | 44 (24), 23 aged > 65 years, 12 living alone | Two samples, both from GP registers | Medicines in general | In-depth interviews |
| Siegel and Gorey, 1997142 | USA | 71 women, 42% black, 17% white, 40% Puerto Rican. Mean age 34.9 years. 37% working. 82% were parents. Median household income low (US$12,500 per annum) | HIV organisations, including hospitals and community organisations | Antiretroviral medicine | Unstructured interviews |
| Rogers et al., 1998156 | UK | 34 (12) aged 18–56 years, varied social class | Voluntary groups, MIND centres/outpatient centres, inpatients | Psychotropic medicine | In-depth interviews |
| Stone and Clarke, 1998143 | USA | 56 (28), 50% white, 29% black, 21% Latino, mean age 37 years, varied education | Five hospital and community centres in Boston, MA, USA and Providence, RI, USA | Antiretroviral medicine | Focus groups |
| Van Wissen et al., 1998135 | New Zealand | 19 (15), 2 Maori, 17 European. Age range 41–67 years, mean age 54 years | Register of people previously involved in hypertension research | Antihypertensive medicine | In-depth interviews |
| Watson and Mitchell, 1998174 | Australia | 37 women aged 59–83 years living independently in the community | Two community pharmacies | Medicines in general | Semi-structured interviews |
| Erlen and Mellors, 1999144 | USA | Six (two), five ‘on disability’, one employed, three white, three black, all high school educated | University trial unit/community AIDS ministry/private practice | Antiretroviral medicine | Semi-structured interviews |
| Ersek et al., 1999168 | USA | 21 (18), mean age 60 (range 42–79) years, mostly white, educated, married | Larger longitudinal study (not known where patients from) | Miscellaneous (cancer) | Semi-structured interviews |
| Halkitis and Kirton,1999145 | USA | 37, 22% female, mean age 42 years. Men: 24% heterosexual, 76% bisexual or gay. Women: majority heterosexual, 38% black, 24% Latino, 35% white | Attendants of large city AIDS service organisation | Antiretroviral medicine | Focus groups |
| Johnson et al., 1999136 | USA | 21 (17), aged 65–92 years, Caucasian, retired | Local emergency centres and physicians’ offices | Antihypertensive medicine | Semi-structured interviews |
| Proctor et al., 1999146 | USA | 39: 27 men age 30–69 years, 12 women age 29–60 years. 9 white, 16 black, 4 Hispanic. 10 gay men, 9 heterosexual men, 9 heterosexual women, 11 injecting drug users | Five New York institutions providing AIDS services: three state, one federal and one private | Antiretroviral medicine | Focus groups |
| Prout et al., 1999162 | UK | Nine families: five middle class, four working class, including four girls, five boys aged 10–12 years | Larger European Union Biomed project. Asthma clinics in two general practices in towns in Midlands | Asthma medicine | Repeated interviews, some open-ended some using check list |
| Siegel et al., 1999147 | USA | 78 (20), age 50–68 years, 41% black, 19% Puerto Ricans, 40% non-Hispanic white. Majority single, most living alone. 51% heterosexual, 42% gay. Varied education, low income (only 18% on > US$20,000 per annum) | Community-based health and social organisations, support groups, advocacy groups and drug treatment centres in New York, NY | Antiretroviral medicine | Questionnaires and semi-structured interviews |
| Atkin and Ahmad, 2000169 | UK | 25 children: 12 boys, 13 girls, average age 13.9 years. 22 Pakistani Muslim, 1 Bangladeshi Muslim, 1 Iranian Muslim, 1 Indian Hindu. 15 school, 7 college, 2 unemployed, 1 university | Health professionals’ records, e.g. paediatricians/specialist haemoglobinopathy workers in six localities in Midlands/northern England | Miscellaneous (thalassaemia major) | In-depth interviews, twice over 6 months |
| Barton Laws and Wilson, 2000152 | USA | 25 (8) aged 27–57 years, 9 white, 3 black, 12 Latino, 1 Portuguese | AIDS groups in Boston and other parts of Massachussets, word of mouth | Antiretroviral medicine | Semi-structured interviews |
| Buston and Wood, 2000163 | UK | 49 (29), mean age 15.6 years. Mean age of diagnosis 4.9 years. 35 at school, 7 in further education, 5 unemployed and 2 employed | Hospital asthma clinics in Greater Glasgow | Asthma medicine | Semi-structured interviews |
| Lumme-Sandt et al., 2000175 | Finland | No information, except originally 448 people aged > 90 years. 250 interviewed. Data from 151 interviews referring to medication | All people > 90 years living in the city of Tampere in southern Finland | Medicines in general | Narrative/biographical interviews |
| McDonald et al., 2000149 | Australia | 76 (13) aged 25–62 years. 52 gay men, 2 women and 6 men bisexual, 11 women and 5 men heterosexual. 84% of interviewees currently using antiretroviral medicine | Larger HIV Futures Study of people with AIDS/HIV in Australia. AIDS organisations/mailing lists, hospitals, doctors’ surgeries, adverts | Antiretroviral medicine | Semi-structured interviews |
| Murphy et al., 2000150 | USA | 39, aged 33–54 years, 69% male. 44% black, 39% white, 6% other/mixed race, 6% Latino (16% graduate college degrees, 24% undergraduate college degrees, 32% some college, 19% high school, 8% less than a high school education) | HIV infection clinic and advertisement in an AIDS publication | Antiretroviral medicine | Focus groups |
| Johnston Roberts and Mann, 2000151 | USA | 20 women aged 25–54 years. 50% Hispanic, 35% black, 15% white. Varied education. Two-thirds with more than one child | Los Angeles, CA, USA, HIV infection/AIDS clinic | Antiretroviral medicine | Participants kept a journal |
| Siegal et al., 2000148 | USA | 49 (9) HIV-positive adults aged 50–67 years, in New York, NY metropolitan area. 45% black, 51% white, 4% Latino. 51% heterosexual, 18% bisexual, 31% gay/lesbian. Education varied, 86% unemployed. 63% live alone | Community-based health and social organisations, HIV infection support groups and HIV infection advocacy organisations in New York, NY | Antiretroviral medicine | Semi-structured interviews |
| Smith et al., 2000170 | UK | No information on participants | Relevant national and local voluntary organisations | Miscellaneous (arthritis/respiratory disease/mental health) | Focus groups |
| Svensson et al., 2000137 | Sweden | 33 (15), mean age 58 (range 35–83) years, mean duration of hypertension 10 (range 1–30) years | Rural GP centre and specialist hypertension unit in major hospital, both in southern Sweden | Antihypertensive medicine | Semi-structured interviews |
| Walsh et al., 2000164 | UK | 35 people, no other information given | One general practice | Asthma medicine | In-depth interviews |
| Pollock and Grime, 2000160 | UK | 82 (43), aged 28–83 years, 88% aged > 45 years. 77% economically inactive, mainly working class | General practices in North Staffordshire Health Authority | PPIs | Semi-structured interviews |
| Angermeyer et al., 2001157 | Germany | 80, 60% male. One-third aged < 30 years; one-third 30–40 years; one-third > 40 years. 74% single; 37.5% live alone, 20% with parents, 17.5% with partners | Four hospitals | Psychotropic medicine | Semi-structured interviews |
| Usher, 2001158 | Australia | 10, mostly male, being treated for schizophrenia and taking neuroleptic medication. No other information | Consumer groups/advertising in relevant newsletters | Psychotropic medicine | Two in-depth interviews each |
| Medicine | Author citing | Date | Author cited |
|---|---|---|---|
| HIV infection | Siegel and Gorey142 | 1997 | None |
| Stone and Clarke143 | 1998 | None | |
| Erlen and Mellors144 | 1999 | None | |
| Halkitis and Kirton145 | 1999 | None | |
| Proctor et al.146 | 1999 | None | |
| Siegel et al.147 | 1999 | Siegel and Gorey, 1997142 | |
| Siegal et al.148 | 2000 | Siegel and Gorey, 1997;142 Siegel et al., 1999147 | |
| McDonald et al.149 | 2000 | None | |
| Murphy et al.150 | 2000 | None | |
| Johnston Roberts and Mann151 | 2000 | None | |
| Barton Laws and Wilson152 | 2000 | Stone and Clarke, 1998143 | |
| Antihypertensives | Morgan134 | 1996 | Donovan and Blake, 1992166 |
| Van Wissen et al.135 | 1998 | Roberson, 1992171 | |
| Johnson et al.136 | 1999 | Dowell and Hudson, 1997;173 Van Wissen et al., 1998135 | |
| Svensson et al.137 | 2000 | None | |
| Psychotropic medicines | Kaljee and Beardsley153 | 1992 | None |
| North et al.154 | 1995 | None | |
| Barter and Cormack155 | 1996 | None | |
| Rogers et al.156 | 1998 | None | |
| Angermeyer et al.157 | 2001 | None | |
| Usher158 | 2001 | None | |
| PPIs | Boath and Blenkinsopp159 | 1997 | Dowell et al., 1996167 |
| Pollock and Grime160 | 2000 | Boath and Blenkinsopp, 1997;159 Donovan and Blake, 1992166 | |
| Asthma medicine | Adams et al.161 | 1997 | Donovan and Blake, 1992;166 Morgan, 1996134 |
| Prout et al.162 | 1999 | Adams et al., 1997161 | |
| Buston and Wood163 | 2000 | None | |
| Walsh et al.164 | 2000 | Adams et al., 1997;161 Donovan and Blake, 1992166 | |
| Miscellaneous medicines | Donovan and Blake166 | 1992 | None |
| Dowell et al.167 | 1996 | None | |
| Ersek et al.168 | 1999 | None | |
| Atkin and Ahmad169 | 2000 | Prout et al., 1999162 | |
| Smith et al.170 | 2000 | None | |
| Medicines in general | Roberson171 | 1992 | None |
| Britten172 | 1996 | Donovan and Blake, 1992166 | |
| Dowell and Hudson173 | 1997 | None | |
| Watson and Mitchell174 | 1998 | None | |
| Lumme-Sandt et al.175 | 2000 | Donovan and Blake, 1992;166 Britten 1996;172 Adams et al., 1997161 |
Sociological and anthropological studies challenging compliance
The earlier sociological and anthropological studies in this synthesis challenged decades of quantitative research that had worked within the paradigm of compliance. The first three studies153,166,171 noted that previous research rested on an ideology of compliance which implied medical dominance. Donovan and Blake,166 in the context of a study into lay experiences of treatment for RA, argued that the concept of ‘compliance’ lays the responsibility squarely on the patient, and questioned the assumption that patients should comply with their medical treatment, observing that ‘non-compliance’ is a problem for doctors, not patients. Roberson,171 whose study is about general experiences of taking medicine, also highlighted the assumptions upon which earlier research was based: that people’s health will improve if they follow their doctors’ orders, that biomedicine is the only option and that those who do not follow medical advice are irrational, deviant or uncooperative. Kaljee and Beardsley,153 writing about psychotropic medicines, noted that the term ‘compliance’ assumes the authority of doctors over patients, the latter being represented as ignorant and unable to understand the doctors’ orders. Like Roberson,171 Kaljee and Beardsley153 noted that the biomedical approach is only one among many other ways of achieving health (a point that is seldom made after these two early papers). Both Roberson171 and Kaljee and Beardsley153 concluded that if health professionals want to understand compliance it is important to understand the patients’ perspective, and Donovan and Blake166 recommended the ‘development of active, co-operative relationships between patients and doctors’ (p. 512).
Later studies by sociologists Adams et al. 161 of treatment for asthma, Rogers et al. 156 of neuroleptic medicine, Lumme-Sandt et al. 175 of older people’s experiences of medicine-taking and Atkin and Ahmad169 of the ways in which young people respond to chelation therapy for thalassaemia major also gave primacy to lay perspectives and tried to illustrate that patients’ behaviour could be understood as rational and strategic, rather than passive and powerless. Like the earlier studies, they suggested that qualitative investigations of lay explanations and experiences would provide clues as to how people can be better supported in taking their medicine. Thus, although they challenged the ideology of compliance for its paternalism, these studies nevertheless displayed varying levels of attachment to the biomedical paradigm.
Sociological studies not focusing on compliance
A small number of sociological studies investigated medicine-taking, but without a focus on compliance. North et al. 154 developed a typology of relationships to benzodiazepines in order to understand how people use them, whereas Britten172 took Cornwell’s193 work on ‘private’ and ‘public’ accounts as a starting point for her analysis of ‘orthodox’ and ‘unorthodox’ lay accounts of medicine-taking. Morgan134 was primarily concerned with how ethnicity influences the way people manage their antihypertensive medicines. She noted that reducing blood pressure through antihypertensive medicines was regarded as a major preventive strategy for decreasing stroke and heart disease, but she did not ally herself with attempting to resolve what the medical profession regarded as a problem of ‘non-compliance’. Rather, she suggested that reliance on medicine as a response to ill health can be regarded as culturally rooted. Prout et al. 162 investigated the role of medicine in the lives of families with asthma and concluded that people much prefer it to the ‘non-medical’ preventive strategies that are advocated alongside the use of inhalers.
Nursing study not focusing on compliance
Usher,158 writing in a nursing journal, explored the experience of taking neuroleptic medicine. She considered the issue of compliance, but her focus was on understanding what it is like to take the medicine.
Economically motivated studies
Four studies set out to answer specific and largely economically motivated questions about medicines. 155,159,160,167 All but the first of these were published in the journal Social Science and Medicine. Aiming to reduce benzodiazepine use, Barter and Cormack155 investigated why people continue to take this medicine despite a reduction in prescribing. Dowell et al. 167 explored patients’ experiences of having their prescriptions changed in order to determine whether or not expensive prescriptions can be switched for cheaper ones without upsetting too many people. Boath and Blenkinsopp159 and Pollock and Grime160 set out to discover, respectively, an explanation for the dramatic increase in prescribing for PPIs and ways of decreasing the costs of PPI prescribing.
Professional agendas
Watson and Mitchell,174 writing in a nursing journal, investigated how older women use medicines, claiming a dearth of information on women’s health. Their discussion, however, was more suggestive of an interest in expanding the role of community nurses in the care of older women. Similarly, Smith et al. ,170 writing in a pharmacy journal, investigated long-term users’ experiences of medicine use, but they seemed most interested in whether or not there was an opportunity for pharmacists to extend their information-giving role.
Increasing adherence
Just over half of the studies in the synthesis were primarily concerned with finding out how to increase people’s use of medicines. These papers were published mainly in medical or nursing journals and varied in the extent to which they questioned the concept of compliance.
Dowell and Hudson173 writing in Family Practice about medicine-taking in primary care, noted that compliance is based upon problematic assumptions and acknowledged that many people have good reasons for not taking their medicine as prescribed. Nevertheless, they aimed to increase compliance as long as this is effective, safe and acceptable to patients and they suggested that doctors could help by supervising the changes patients make to their regimens. Ersek and Miller,168 writing in Cancer Practice, aimed to find ways of overcoming cancer patients’ non-adherence to analgesic therapy. They concluded, somewhat unusually, that although patient education may help some, assisting people to use non-pharmacologic pain strategies may be more successful. Angermeyer et al. ’s157 study published in a psychology journal investigated people’s perceptions of neuroleptic medicine in order to find ‘hints’ for increasing compliance with treatment.
In addition to Morgan’s134 study, three other studies investigated the experience of taking antihypertensive medicine. 135–137 The first two were published in nursing journals and the third in a cardiology journal. All encouraged adherence and none questioned the assumption that medicines are the only way of managing high blood pressure and preventing strokes and heart disease. Van Wissen et al. 135 took the view that ‘Compliance with treatment is a fundamental prerequisite for therapeutic benefit’ (p. 568) whereas Johnson et al. 136 suggested, ‘Poor adherence to prescribed hypertensive pharmacotherapy is responsible for unnecessary complications, leading to increased health care spending, premature progression of complications, and early death’ (p. 319). Interestingly, Johnson et al. 136 seemed to be attributing the morbidity and mortality to non-adherence rather than to the hypertension itself, illustrating the extent to which health is seen to be allied to taking medicine. Svensson et al. ,137 on the other hand, although promoting adherence, suggested that modifying the regimen was ‘sound behaviour’ and should be encouraged if it represented an attempt to gain control of the condition.
In addition to the studies by Adams et al. 161 and Prout et al. 162 (above), two further studies dealt with taking medicine for asthma. Buston and Wood,163 writing in Family Practice, were concerned with surmounting the barriers to compliance in the case of adolescents with asthma, and Walsh et al. 164 were interested in how the doctor–patient relationship influenced compliance. Although the psychotherapeutic framework they adopted was unique in the synthesis, Walsh et al. 164 shared with Buston and Wood163 the assumption that compliance is desirable. However, Walsh et al. ’s164 emphasis that patients’ behaviour is rational and ‘sense making’ recalled the earlier sociological studies that stressed the importance of lay meanings.
Eleven studies142–152 (10 of which were American142–148,150–152) focused on adherence to antiretroviral therapy for HIV infection. Most of the authors of these studies took a fairly strong position, repeatedly citing the benefits of taking the medicine (increased survival, delayed disease progression, improved immune functioning, reduced incidence of opportunistic infections) and the problems associated with not taking it (vertical transmission to babies, viral resistance, limited future treatment options). Siegel and Gorey142 investigated women’s experiences of, and views about, taking azidothymidine (AZT; zidovudine) in the hope of increasing their uptake of the drug. Stone and Clarke143 recommended simplifying the antiretroviral regimen to improve adherence but suggested that only patients who committed themselves to the regimen should be treated. Erlen and Mellors144 suggested that health professionals need to know what patients’ experiences are so that they can individualise regimens to suit the patient. Both Halkitis and Kirton145 and Proctor et al. 146 focused on the obstacles that prevent adherence to antiretroviral therapies and the strategies people use to enhance adherence.
Siegel et al. 147 took the position that patients were misinterpreting the symptoms of HIV infection as the adverse effects of antiretroviral therapy, either through ignorance or because they could not accept that the HIV infection was progressing. They recommended that health professionals help people distinguish between symptoms and adverse effects, provide strategies for alleviating symptoms and educate patients about the harmful consequences of non-adherence. Siegel et al. 147 categorised those who did not adhere to antiretroviral therapy as offering ‘excuses’ or ‘justifications’ for their behaviour and recommended that misconceptions be debunked and the importance of adherence promoted. They noted that ‘… a set of beliefs may be growing among patients that may support non-adherence’ (p. 39). Similarly, Barton Laws and Wilson152 explored people’s experience of taking antiretroviral therapy and concluded that people come to believe that whatever standard of adherence they can achieve is good enough. Murphy et al. 150 investigated factors that facilitate and prevent adherence, and McDonald et al. 149 investigated the differences between men’s and women’s experiences of treatment. Noting that women with HIV are less likely than their male counterparts to use antiretroviral therapy, the authors concluded that this is because women are less likely to believe in the treatment’s efficacy. Johnston Roberts and Mann150 set out to explore the unique barriers to adherence to antiretroviral therapy faced by women. They wrote from the standpoint that adherence should be encouraged, but were sensitive to the social factors that impinge uniquely on women, such as motherhood.
In summary, the earlier studies in the synthesis can be understood as reacting to the concept of compliance that had held sway in the preceding decades. They advocated a qualitative methodology for the purpose of providing an alternative, lay perspective and emphasised the rationality of lay behaviour. A small number of sociological studies investigated medicine-taking in its own right, but the absence of compliance as a starting point was rare in the studies. A few studies answered specific economic questions and a couple seemed to be influenced by specific professional agendas. Among the later studies, few were sociological and more were conducted from the perspective of increasing adherence. Taken as a whole, the studies in this synthesis illustrated that the employment of a qualitative methodology, or a sociological perspective, does not necessarily imply abandonment of the medical agenda. The majority of the studies focused on the reasons why people do not take their medicine as prescribed. Few considered the experience of those who reject medicine outright or those who accept it uncritically. Additionally, the vast majority of studies were concerned with chronic illness. Because the protracted nature of chronic illness presents more challenges to Western medicine than acute illness, this is probably a reflection of medical concerns. The ideology that people should take their medicines as prescribed remained dominant in the studies.
Findings
Our findings fall into four parts. We begin with the ways in which people evaluate their medicines: trying out the medicine and weighing up its costs and benefits, stopping the medicine and observing the effect, observing others and obtaining information. We also detail the lay use of subjective and objective indicators, the way in which gender influences evaluations and the several difficulties lay people face in the process of evaluating their medicines. Secondly, we describe the concerns that cannot be resolved through lay evaluation, including concerns about dependence, tolerance and addiction, the potential harm from using medicine on a long-term basis and the possibility of medicine masking other symptoms. The ways in which medicine and identity are linked is the third aspect. Here we considered non-acceptance of illness and consequently of the medicine, medicine as a reminder of being ill, medicine presenting problems of disclosure and also the stigmatising potential of some medicines. The last section presents the ways in which some authors have categorised medicine-taking before going on to detail the various methods that people use to modify their regimens. Attempts to minimise medicine intake were common, and this was reflected in many of the reasons why people modified their regimens: to decrease unwanted effects, to make the regimen more acceptable and for financial reasons. People were also found to take their medicines symptomatically and, in some cases, strategically. Others replaced or supplemented their regimens with non-pharmacological treatments. Additionally, there were incidental reasons for regimen breaks. Finally, we consider the communication between doctors and patients about regimen modifications.
Lay evaluation of medicines and its difficulties and limits
Trying out the medicine and weighing up the costs and benefits
People weighed up the benefits of taking the medicine against the costs of doing so. The costs included adverse effects and the difficulties faced when trying to incorporate the regimen into daily life. In general, the studies focused less on the benefits of medicines than their costs. Nevertheless, it was clear that people did place hope in their medicines and that these hopes varied according to the medicine in question. The most common reason for taking medicine was to relieve symptoms, whether physical, as in the case of digestive disorders159,160 and RA,166 or mental. 154–156,158,170 However, in the case of neuroleptic medicine, people with schizophrenia hoped to avoid relapse and hospitalisation in addition to obtaining symptom relief. 156 With treatment for HIV infection, people hoped to slow down or halt the progression of the disease;142–144 asthma medicine was taken both to relieve physical symptoms163,164 and in the hope of sustaining normality. 161,162 Those with hypertension hoped that antihypertensive medicine would prevent or reduce the risk of a future illness such as heart attack or stroke134 and control blood pressure and symptoms. 137
The costs, or undesired outcomes, of taking medicines were reported more frequently. Adverse effects were a significant issue for people taking medicine and a key criterion in the evaluation of treatment. Worries about adverse effects were found in the context of RA,166 cancer,168 asthma,161 digestive disorders,159,160 high blood pressure136,137 and schizophrenia. 156,158 In the last case, the considerable physical and psychological effects of neuroleptic medicine were highlighted by participants in both studies: effects that could alter thoughts, inhibit social interaction and identify the person as having schizophrenia. However, it was the studies on HIV infection that stood out because of their participants’ emphasis on the undesirable effects of antiretroviral therapy.
All of the 11142–152 studies on antiretroviral therapy reported people’s experiences of adverse events while having treatment, which included nausea, vomiting, gastrointestinal distress, kidney stones, insomnia, headaches, rashes, dry skin, diarrhoea, dizziness, numbness, feeling generally lousy, a bad taste in mouth, neuropathy, anaemia, breathing difficulties, fatigue, stiffness, mood swings, visual problems, leg pain, hair loss, liver damage, cancers, blackening of fingertips and nails, loss of appetite, general ill health and sweating. These reactions were experienced as unpleasant and challenging in their own right, but because they could be so frequent, severe and unpredictable they were also described as instilling fear and distrust of the medicine. Furthermore, they could have the effect of restricting social activities, affecting friendships, relationships and work, making it difficult to look after families and sometimes necessitating disclosure of the illness. 141,143–145,148–150 One man described the effect of his regimen:146
The first regimen that I was on was Norvir [ritonavir]. I found out that it was almost next to impossible to stay on it. I literally told my doctor, ‘I’m not taking this stuff any more. I don’t care if I die’. It made me feel 10 times sicker when I took it than when I didn’t take it.
With such overwhelming undesirable effects, it is not surprising that many people viewed their medicine negatively. The following are excerpts from diaries kept by HIV-positive women in Johnston Roberts and Mann’s study:151
… I choke down the Viracept [nelfinavir] and it’s stuck in my throat again, chalky and grainy, so it drops into my stomach … like a ton of bricks … The poison that’s supposed to save my life makes me miserable.
(p. 380)
I actually feel as though I am damaging my body with each pill that I take. I believe these medicines are too toxic and powerful and I do not feel comfortable taking them.
(p. 381)
Many of the women in Siegel and Gorey’s142 study, especially the African American women, also had very negative attitudes to their treatment (AZT), claiming that at best the drug did more harm than good and at worst it did serious harm. They feared that the drug’s high toxicity was damaging to the internal organs and that the drug could not discriminate between HIV cells and healthy cells.
Acceptability of regimen
In addition to the occurrence of adverse effects, people evaluated their regimen in terms of whether it was feasible or acceptable given their daily schedules. All of the studies on HIV infection, except two,142,147 described the impact of the regimen in strikingly similar ways. Stone and Clarke’s143 participants found the regimen highly demanding because of the need to take the protease inhibitors exactly as prescribed. The regimen required people to radically alter their daily routines of sleeping and eating and was experienced as interrupting life’s normal flow. Participants described it as becoming ‘the central organising principle’ and it was experienced as being so overwhelming that they were no longer in control of their lives:143
Everything is amplified. I’m more aware of, ‘Oh I ate that cheeseburger. Now I’ve got to wait another two hours before it digests to take my pills’. I feel very out of control with the regime that I have to follow. My life is focusing around that, rather than the other way round.
McDonald et al. ’s149 sample found that the drug regimen had a long-term impact on social relationships, employment and studying, not just the daily routines of sleeping and eating. The authors found that the regimen had a different impact according to gender: for men the social world was made to fit round their medical regimen, whereas for women the social world took priority and impinged on the regimen. The authors also suggested that men were more concerned with the impact of the regimen on themselves, whereas women were more concerned about its impact on relationships. The women in their study were found to be more resistant to the demands of the regimen than men and less worried about not taking the drugs as prescribed. Johnston Roberts and Mann151 also reported that their women-only sample found the regimen exceptionally difficult to follow. In addition to reporting that it took away their freedom regarding daily routines and activities, the women found that it competed with other goals such as losing or gaining weight, forming relationships and fulfilling their care-giving roles. As one woman wrote in her study journal:151
I am a single parent of three children. So being a mother and father put into one and living with this illness, well, I’m sure people must have easier lives. I take eight different medicines three times a day. Some on an empty stomach and some with food. Some 8 hours apart. It’s extremely hard to stay focused on my medicine being a full-time mother and, on the other hand, it’s hard to stay a full-time mother while fighting for my life.
The frequency of doses and the sheer number of pills (sometimes between 25 and 35 per day) were also found to be problematic in the case of antiretroviral therapy,145,151,152 as was the nature of the pills themselves – their taste, smell, size and shape. 151,152
None of the other regimens seemed to have as great an impact as antiretroviral therapy, although the one study on young people with thalassaemia major suggested that chelation therapy was found to be profoundly disruptive. 169 As Atkin and Ahmad169 described, an infusion pump delivers a drug that helps excrete the excess iron that accumulates as a result of the frequent blood transfusions that people with thalassaemia major need. The pump has to be used five to seven nights a week, for 8–12 hours each time. Nearly all of the young people in the sample cited the use of the pump as the most difficult and hated aspect of their illness. Older children especially hated it because it disrupted their social life and marked them out as different from their peers. For this reason, some decided not to pursue the treatment. One boy said, ‘To be honest I couldn’t be arsed [sic] to use it. I just got fed up. I wanted to be like everyone else’. 169 In such cases, the regimen is assessed as being more problematic than the condition it is meant to treat. Roberson171 found that some of her participants similarly concluded that their regimens (for a variety of illnesses) were too disruptive.
The process of weighing and balancing
As noted above, when assessing whether or not to persevere with a regimen, people had to weigh up the costs and benefits. Most of the studies that referred to this weighing-up process were those that had outlined severe costs as a result of taking the medicine, i.e. those relating to treatment for HIV infection and mental illnesses. In the case of antiretroviral therapy, the undesirable effects of the treatment could be so bad that some people had to seriously question whether or not it was worth continuing with the medicine. Five of the HIV studies noted this and outlined the stark choices involved. 142,146,147,149,152 McDonald et al. 149 noted that the overwhelming impact of adverse effects affected people’s evaluations of antiretroviral therapy because it was difficult to appreciate the potential benefits when experiencing such unpleasant symptoms. Some of the women in Siegel and Gorey’s142 study felt that, despite the possible benefits of AZT, the effects were too debilitating to make it worthwhile; others felt that ‘alternative’ treatments were better for quality of life. In Siegel et al. ’s147 study, some of the participants described the medicine as more threatening to their well-being than the disease for which they took it. Similarly, Proctor et al. 146 found that some of their participants chose quality of life with HIV infection in preference to taking antiretroviral therapy.
People had to balance the costs and benefits in the case of psychotropic medicine too. North et al. 154 reported that some of their participants weighed up the costs of taking benzodiazepines (adverse effects, dependence and social alienation) against the benefits (improved quality of life). Both studies of neuroleptic medicine for schizophrenia156,158 found high gains associated with taking the medicine in terms of reduced symptoms, improved ability to deal with symptoms and reduced risk of relapse, but also high costs in terms of physical and psychological adverse effects, the stigma of taking neuroleptic medicine and the consequent discrimination. Similarly, Angermeyer et al. ’s157 participants had to weigh up the benefits of clozapine (improved sleep, feeling calmer, less depressed, less anxious, reduced risk of relapse, perceived protection against mental illness) against its undesirable effects which included feelings of sedation, fatigue and lack of motivation, difficulty getting up in the morning, lethargy, passivity, hypersalivation, constipation, weight gain, sexual ‘dysfunction’, increased perspiration and restlessness.
Although the losses and gains experienced by those taking other medicines may appear less extreme than in the cases of HIV infection and mental illness, the process of weighing up the costs and benefits still occurred. Donovan and Blake166 found, in the context of RA, that the costs included the unpleasantness or stigma of having to take drugs or wear supports, the need to attend clinics for tests and the risks of adverse effects and dependence upon drugs:166
I had Naprosyn [naproxen] and they made [the arthritis] a bit easier, but not much, so I stopped them. To me, the odds, the results from the tablets didn’t balance the risks of taking them. The risk was higher than the result.
The benefits of taking drugs in the case of RA were the immediate relief of symptoms or the anticipation of relief in the long term. Donovan and Blake166 noted that some people decided whether or not to accept the medicine without even trying it, whereas others made a decision based on the results of tests.
Stopping the medicine and observing the effect
Siegel et al. ,147 referring to patients as ‘naive scientists’, suggested that people formulate hypotheses about medicines causing effects and then test these hypotheses by altering the dose or stopping the medicine in order to observe the effects. This seems to be a popular method with several different types of medicine: antiretroviral therapy,148 PPIs,159 antihypertensive medicine,136 inhalers163 and non-steroidal anti-inflammatory drugs. 166 Although several of these studies implicitly referred to this type of test, none outlined it in much detail. Dowell and Hudson173 suggested that the lay testing of medicines may be either an explicit or a subconscious act and that people are more likely to conduct tests if the medicine is to be taken in the long term. They gave an example of a woman with systemic lupus erythematosus who was trying to manage without her steroid therapy:174
Prednisolone, I felt that I could be off them, I thought you know, I was feeling well at the time, I didn’t need to be taking this lot (…) and, err, I mean I did it, they knew I was doing it but it didnae work and I mean I had to go back on them.
This woman suffered rapid weight loss following the cessation of her medicine, which convinced her that she needed to commit herself to the regimen. Another woman, quoted by Buston and Wood,163 reached the same conclusion after experimenting with her asthma medicine:163
I stopped taking my inhalers for a while [laughs] cos I thought I didnae need them so I just stopped taking them. I never told anyone but I just stopped taking them. I’d been all right for a wee while but then I was in hospital. I was in hospital at the end of the year and I think it’s because I stopped taking them for a wee while and then it just built up.
Donovan and Blake166 found that many of the people with RA in their sample conducted a process of testing or evaluating their medicines before deciding whether or not to take the medicine as prescribed. The authors found that 4 of 41 people taking non-steroidal anti-inflammatory drugs eventually reduced their doses and six gave up altogether. One woman said:166
Feldene [piroxicam] worked OK but they make me feel sick and dizzy. I just stopped taking them because I couldn’t do anything when I was feeling giddy … I’d rather just cope with the pain than the pain and the side effects as well.
The authors gave another example of a person who gave up the drug having experimented with it:166
[The doctor] gave me anti-inflammatory tablets. I tried them for a week and they didn’t seem to help at all and I don’t particularly like taking tablets anyway, so I stopped taking them a week after I started.
Donovan and Blake166 noted that some people did not give the drugs sufficient time to work, but were unaware of this.
Observing others
One study,142 of women’s experiences of, and attitudes towards, taking AZT found that some women relied on observations of how others fared on AZT in order to come to a decision about whether or not to take it. Siegel and Gorey’s142 participants felt that AZT was experimental and consequently they placed more faith in their observations than in their doctors’ advice, as the following two quotes illustrate:142
The doctors try to tell me, ‘Oh it depends on the person’, or ‘They took it too late’. Well, I’ve made my own research, and my research has told me that those who don’t take it live longer than those who take it. I would not take it … They are experimenting. They are not sure themselves, but they don’t want to say it.
I don’t want to take it [AZT] because from what I, from what I’ve seen, friends of mine that have taken it, they just die quicker, or all of a sudden start getting sick.
Observation of others as a form of evaluation was found only in this one case.
Obtaining information about medicines
Both Dowell and Hudson173 and Donovan and Blake166 noted that before accepting their medicines people consult a variety of sources and do not rely solely on their doctors’ advice. Some of Roberson’s171 sample used ‘root’ doctors as well as informal networks, while Watson and Mitchell’s173 participants sought information about medicine from pharmacists, friends, peers, relatives and the media, as well as from their GPs. Erlen and Mellors144 found that information was obtained from support groups, peers, books and the internet when participants were deciding whether or not to take the medicine.
Objective and subjective indicators used in lay evaluation
Johnson et al. 136 found that people used blood pressure monitoring to help them evaluate their antihypertensive medicine. They noted that in order to establish the efficacy of the medicine, ‘Participants needed to sense a reduction in blood pressure and, preferably, controlled blood pressure readings’ (p. 327). Roberson’s171 study was of medicine in general, but most of her participants were on antihypertensive medication for high blood pressure. She noted that people would use their own or their doctor’s blood pressure readings to help them decide whether or not the medicine was working. This finding was confirmed by Morgan134 and Van Wissen et al. 135 Blood pressure readings were, therefore, a key tool for monitoring the effectiveness of the antihypertensive medicine.
However, in the case of antiretroviral therapy for HIV infection, there was evident tension between objective and subjective indicators of health, the objective indicators in this case being laboratory results such as T-cell counts. A 46-year-old woman in McDonald et al. ’s149 study illustrates the problem:
… the incentive, I suppose, for somebody to go on to tablets is if they are going to make you feel better, and my experience is that whilst they are physically making me better, and my viral load has dropped and my T-cell count has gone up, so they are obviously doing my immune system good, I don’t feel better on them, and that’s the difficult thing to weigh up.
Siegel et al. 147 and Stone and Clarke143 found likewise, with a participant in Stone and Clarke’s study making a similar point:143
You know, it might serve the purpose, okay, make your T-cells go up or whatever, or make your viral load get to where it’s supposed to, but what about the way you’re feelin’ overall?
People that were affected with HIV were more influenced by subjective indicators, such as symptom alleviation and a sense of health and well-being, than by laboratory results. Siegel et al. 147 noted ‘… participants seemed to rely heavily on their subjective sense of how they were feeling and their perception of how symptomatic they were in order to assess the efficacy, benefits, and risks of the antiviral medicines they had been prescribed’ (p. 251).
Gender differences in evaluating medicines
A few studies141,142,149,151 found that women were more sceptical than men about antiretroviral therapy. Only a few (mainly white) women believed that the drug could be beneficial under some circumstances. Additionally, women were more sceptical about the scientific basis of drugs for treating HIV infection, arguing that trials had not been conducted with women, so its effectiveness in women was unknown. 142,149,151 Both Siegel and Gorey142 and Johnston Roberts and Mann151 found that distrust of drugs was associated with not taking the drugs as prescribed. Some of the women in Siegel and Gorey’s142 study suggested that doctors were ill informed about the drug, yet failed to acknowledge the limits of their knowledge. Stone and Clarke143 pointed out that, unlike gay men or injecting drug users, women do not belong to the social networks that people infected with HIV form. They argued that informal social networks are important in promoting confidence in drugs and for circulating up-to-date information about treatments, but women’s lack of access to these networks may account for women’s greater negativity towards the medicine.
Difficulties with evaluating medicines
A small number of studies noted that, in the course of evaluating their medicine, a few people had difficulty distinguishing the effects of their medicine from the effects of their illness. Morgan134 found this in the case of antihypertensive medicine, but Usher158 found, in the case of neuroleptic medicine, that some people with schizophrenia learned to monitor their bodies in order to discern the difference between the symptoms of their illness and the effects of the medicine. One person explained: ‘… lots of times you get confused; what’s the side effects and what’s the illness? You have to focus on your body and try to work it out, but it’s not easy … the side effects would also get confused with my thinking and get linked to my illness’. 158 In the case of antiretroviral therapy, Siegel et al. 147 suggested that patients wrongly interpreted the symptoms of the disease as the undesirable effects of their treatment and, as a result, rejected the treatment mistakenly. Whether or not this is the case is hard to say, but it does highlight the difficulty patients faced when attempting to evaluate their medicine. Particularly with HIV infection, people found it confusing if objective indicators indicated improvement after taking the medicine, but they felt no better or felt worse. In such cases, there might also be disparity between professional and lay assessments of the efficacy of treatment, in which cases patients might feel compelled to ignore their doctors’ advice to continue with treatment.
Dowell and Hudson173 noted that the method of testing depends on the person’s understanding of the medicine’s function; thus, analgesics with a short-term, symptomatic effect may be easily assessed, but other medicines which cannot be assessed using the presence or absence of symptoms may still be evaluated by conferring with doctors or obtaining information from friends or the media. With preventive medicine, the evaluative process is difficult for patients because immediate symptoms cannot be used as indicators of efficacy. Although health professionals can evaluate medicine in terms of its long-term and preventive effect, lay people can evaluate it only in terms of its immediate impact on their lives. For example, Angermeyer et al. 157 found that health professionals prescribed clozapine to reduce psychotic symptoms, but also to prevent relapse, whereas patients primarily evaluated it in terms of its effect on symptoms: the fact that it was calming, relaxing and helped them sleep. Again, it is difficult for lay people to evaluate the effectiveness of antihypertensive medicine given that the anticipated benefits are long term. Because they cannot assess its impact, some people may also be uncertain about whether or not the medicine is necessary, in other words whether or not they actually have hypertension; this uncertainty was an issue in all four studies of hypertension. 134–137
Occasionally, people might have difficulty evaluating their medicine because they lack information. In one case, where doctors were replacing patients’ usual brand of PPIs for a cheaper brand,160 they ‘double-switched’ by reducing the dose at the same time as changing the brand. The authors noted that this confused patients because, being unaware of the dose reduction, they could not accurately assess the efficacy of the new drug, so many rejected it as being less effective than their original brand. There was also a lack of desired information on adverse effects. Smith et al. 170 found that people with respiratory diseases had to educate themselves about the adverse effects of asthma medicine and lacked knowledge about the appropriate doses of inhalers. They also found that people with arthritis were given inadequate and superficial information on the adverse effects of arthritis drugs and what to do about them. Donovan and Blake166 found the same in the context of arthritis, and Ersek et al. 168 noted that few people with cancer knew how to deal with adverse effects, that some confused tolerance, dependence and addiction and others were unaware that analgesics did not always provide immediate pain relief. The absence of such basic information on medicines and their adverse effects cannot have helped people with their evaluations.
Worries about medicine that lay testing and evaluation cannot resolve
Although many of the concerns that people have can be resolved through lay evaluation of medicines, some are less easily resolved and may linger, affecting decisions about medicine-taking.
Dependence, tolerance and addiction
Dislike of dependence upon medicines was noted in the context of medicines in general,171 asthma,161 cancer,168 hypertension,134 mental health154,155,157 and arthritis. 166 Both Donovan and Blake166 and Ersek et al. 168 noted that fear of dependence was a reason why some people did not take their medicines. These two studies166,168 also reported that participants were worried that they would become accustomed to the medicine and that it would thereby lose its effectiveness; again this resulted in people using less than the prescribed doses. As one woman with RA said:166
I have two tablets at night and I put two by the bed if I need them. But I don’t take them unless it is absolutely necessary. It’s no good taking tablets when you’re not in pain because when you are, your body will be used to them.
Some of Morgan’s134 participants feared that if they took their antihypertensive medicine as prescribed, they might become unable to manage without the drugs or become addicted to them. As one African Caribbean respondent said:134
Sometimes I remember and sometimes I do not because I don’t want to build my hopes on tablets. I don’t want to become an addict.
Similarly, Angermeyer et al. 157 found that a few people expressed fear about becoming addicted to clozapine. Benzodiazepines are well known for their addictive potential, and North et al. 154 referred to a spectrum of dependence in their sample, with people who felt that they could control their benzodiazepine use at one end and those who were completely reliant on the medicine at the other end. There also appeared to be a spectrum of attitudes to dependence, with participants at one end believing that constant low doses represented only ‘partial dependence’ as compared with dependence on escalating doses. Barter and Cormack155 found that only a small number of participants in their sample worried about dependence on benzodiazepines.
Potential harm from long-term use
Three studies134,159,160 reported people’s fears about taking medicines on a long-term basis. Morgan134 found this to be a major concern, expressed by both men and women, both white and African Caribbean, as the following quotes illustrate:134
I have thought about adverse effects. If you keep on with these tablets, what is it going to do eventually? That’s what bothers me.
I used to say to my friend at work that these tablets are going to affect my insides. She said don’t be silly … taking so much of them each day and for so long, they might do something to me.
Both of the studies on PPIs159,160 found that people’s generally positive opinions of the medicine were tempered by their concern about the potential for long-term harm. Pollock and Grime160 noted that the people in their study who were worried about the long-term effects of taking PPIs were more likely to experiment with their regimen to achieve the lowest possible dose. The authors noted that this is desirable ‘in view of the clinical uncertainty about possible hazards of long term acid suppression’ (p. 1837). 160
The possibility of medicine masking other symptoms
Two of Boath and Blenkinsopp’s159 participants were concerned about the potential of PPIs to mask symptoms that they should know about, symptoms that might indicate a more serious condition such as cancer. A woman with cancer in Ersek et al. ’s168 study was also worried about this. She was reluctant to take analgesics in case it masked new pains that might indicate an infection that she should be aware of.
Medicine and identity
Not accepting the illness
Dowell and Hudson173 found that acceptance of medicines was linked to acceptance of the illness in question. They suggested that taking medicine was equated with having an illness, so if people did not accept that they had the illness then they were unlikely to continue with or start the treatment. Acceptance was a strong theme in the asthma studies. Adams et al. 161 reported that some people with asthma denied that they had asthma, or distanced themselves from their asthma. Although these people – termed ‘deniers and distancers’ by the authors – had asthma that was just as severe as it was among those who accepted their asthma, the deniers/distancers tended to downplay its significance, claiming that they did not have asthma at all or that they had only slight or ‘not real’ asthma. They viewed their asthma as acute rather than chronic and did not take the preventive asthma medicine as this entailed acceptance of the asthma identity and the chronicity of the condition. However, they did take the reliever medicine ‘just in case they demonstrated symptoms in social/public situations’. 161 As such, they were found to use relievers and avoid preventers for the same purpose: maintenance of normality.
Prout et al. 162 also found a tendency among the people in their study to downplay the severity of asthma, as did Buston and Wood. 163 In Prout et al. ’s162 study, families did not define childhood asthma as a serious illness, preferring to stress the ordinariness of children instead. As with some of Adams et al. ’s161 sample, Prout et al. 162 found that some of their families doubted that their children actually had asthma. The authors argued that inhalers were enrolled into the task of maintaining this sense of ordinariness. Walsh et al. 164 identified three categories of people who did not take their asthma medicine as prescribed: those in denial, those in avoidance and those in depression. Those in denial did not want to see themselves as having a chronic illness and felt that they could manage the asthma on their own; they were therefore motivated to reduce their medicine. Those in avoidance felt that nothing helped resolve their breathing difficulties, so they did not attend clinic appointments and neglected their regimens. These two categories resemble the people in Adams et al. ’s161 study who denied or distanced themselves from the asthma, but those in Walsh et al. ’s162 third category, depression, are unlike any described in the other asthma studies. These people accepted that they had asthma and, in as far as this goes, they are similar to those in Adams et al. ’s163 study who accepted their asthma, but here the similarity ends because Walsh’s et al. ’s164 ‘depressed’ group keenly felt the loss of their previous abilities and also a vulnerability that led them to restrict their lives in order to avoid asthma attacks. They became more and more withdrawn and depressed until they neglected their regimen and became ill. By contrast, Adams et al. ’s161 ‘accepters’ appeared to be well balanced and had come to terms with the asthma and the need for medicine.
Only one152 of the HIV studies and one158 of the studies on psychotropic medicine dealt with the issue of illness acceptance. Barton Laws and Wilson152 suggested that the ability to confront the fact of being HIV positive is a key factor determining whether or not people take their drugs as prescribed, whereas Usher158 noted that the acceptance of schizophrenia is a necessary precursor to the acceptance of neuroleptic medicine. Usher158 observed that this acceptance occurs over time and is not easy as it entails taking on a stigmatised label, the unlikelihood of recovery and the need to take medicine long term.
Being reminded of the illness
Medicine can also be a constant and unwelcome reminder of illness, whether or not that illness is accepted. Four of the HIV studies found this. 144–146,151 One of the men in Halkitis and Kirton’s145 study said:
… it’s hard every time you take that pill, to recognize what you’re taking it for, and to know that this is going to be probably the course of my life …
One woman wrote in her journal for Johnston Roberts and Mann’s151 study:
Each time I take a pill it is a reminder that I am sick. I do not want to focus on my sickness or let it control my life. I want so badly to be ‘normal’ and healthy again.
Only one other study reported that taking medicine reminded people of their illness, in this case cancer. 168
Disclosing the illness to others
A separate but related issue in the case of HIV infection (and a significant reason why some people did not always take their medicine as prescribed) was fear of disclosing their illness to others. 143,145,148,150,151 Consequently, rather than take the medicine in front of people and risk disclosing their HIV status, people might postpone or forgo their medicine. 151 A participant in Stone and Clarke’s143 study said:
If you don’t want everybody to know, you know, you don’t take ‘em in front of people. It raises questions.
This could include public social situations such as parties and the work place, but also private, family life. One woman in Johnston Roberts and Mann’s151 study who had not disclosed her HIV status to her children found it hard to take all her pills because she had to do so out of sight of her children.
The stigmatising effects of medicine
Some of the people in Rogers et al. ’s156 study reported that neuroleptic medicine was stigmatising because it could mark out a person as having schizophrenia. Similarly, Smith et al. 170 found that those with mental-health problems reported feeling stigmatised and labelled by their medicine, as did Usher,158 again in the case of neuroleptic medicine. Her respondents reported that the adverse effects of the medicine drew attention to their illness, as one person illustrated:158
When you go out it’s like advertising you have a mental illness, so the side effects draw attention to the fact that you have a mental illness. And even though you might be quite well mentally, the side effects stigmatize you … you cannot even go over to your sister’s place and go out into the yard without the neighbours thinking she’s got someone there who is mentally ill … you know your legs are going up and down all the time and they think you’re a lunatic. It’s like wearing a sign on your forehead.
Other studies in the psychotropic medicine group did not cover this issue, although North et al. 154 noted that some people reported feeling ashamed of using benzodiazepines. In the context of HIV infection, Barton Laws and Wilson152 found that some people did not initiate treatment because they worried that the regimen would identify them as having HIV. Finally, Atkin and Ahmad169 found that for children with thalassaemia major, one of the most hated aspects of their chelation therapy was the fact that it marked them out as different from their peers.
Ways of taking medicine
A small number of studies categorised or characterised the various ways in which people take their medicines. This section begins with these studies, before going on to examine the range of modifications people make to their regimens, the reasons behind them and how far these are communicated to doctors.
Those who take their medicine as prescribed (Figure 14)
Passive accepters
Dowell and Hudson173 described people who accepted the regimen that they had been prescribed, who assumed a more passive role and who relinquished control to their doctors as ‘passive accepters’. Similarly, in the context of hypertension, Svensson et al. 137 reported that those who accepted the prescribed regimen were passive, indifferent and less involved in their care. The authors noted that many had ‘rather obscure motives for continuing with treatment, and often claimed not to have considered the possibility of changing or omitting medication’ (p. 162). 137
FIGURE 14.
Categories of those who do take their medicine as prescribed.
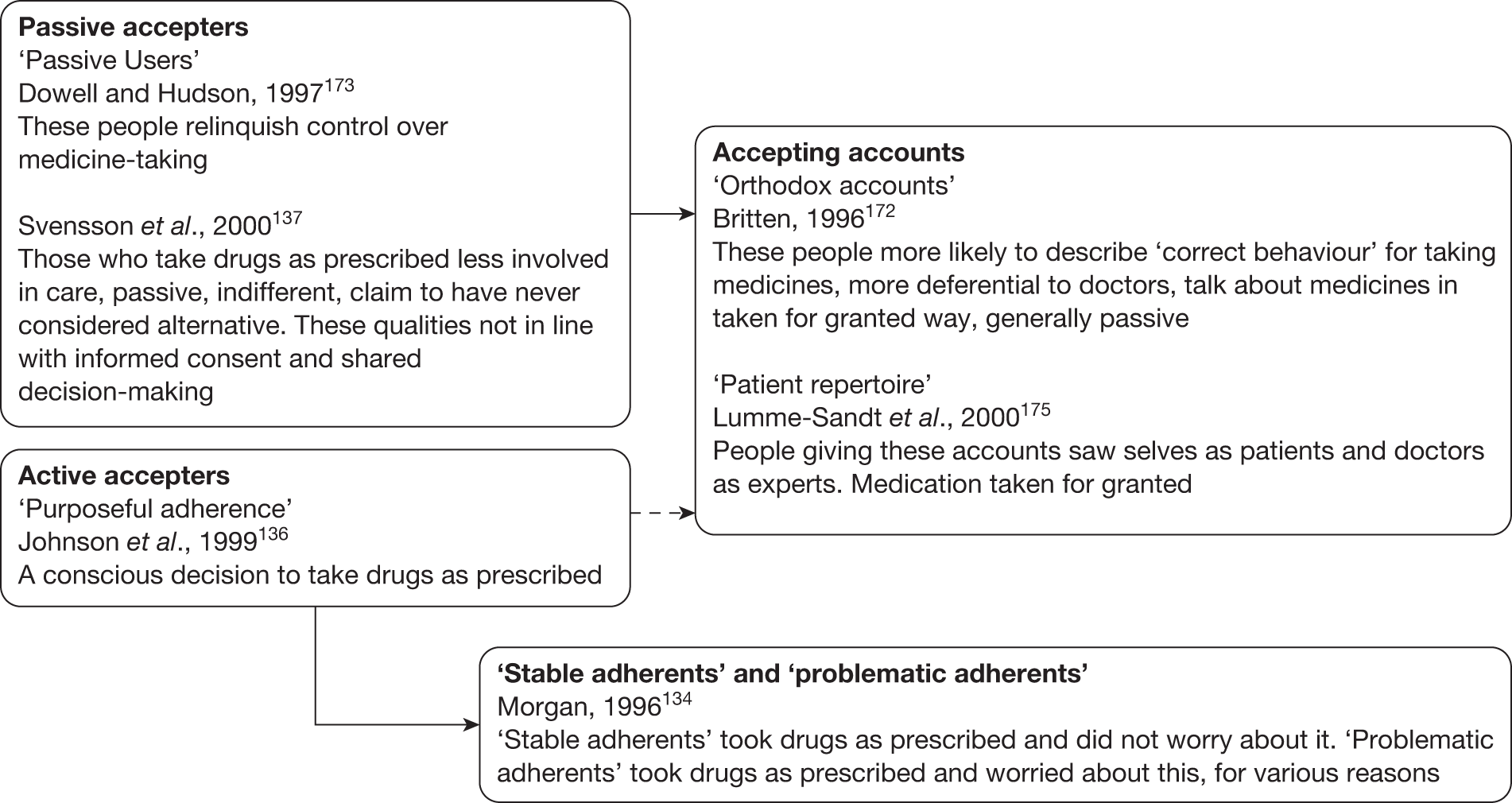
Active accepters
In the context of hypertension, Johnson et al. 136 developed a category of medicine-taking which they termed ‘purposeful adherence’. ‘Purposeful adherence’ followed a conscious decision to pursue the prescribed regimen and was dependent upon having first tested the medicine to ensure its effectiveness. Those Morgan134 described as ‘stable adherents’ and ‘problematic adherents’ – also in the context of hypertension – could be seen as practising ‘purposeful adherence’. These people took their medicine as prescribed but the ‘problematic adherents’ expressed concern about doing so and had worries about adverse effects and dependence, whereas the ‘stable adherents’ seemed unconcerned, even by the prospect of remaining on the tablets for all of their lives. Although ‘stable adherents’ seem similar to Dowell and Hudson’s173 ‘passive accepters’, they were not necessarily passive and may have reached their position after a period of testing their medicines.
Accepting accounts
Both active and passive accepters, but especially the latter, might give a more ‘orthodox’ account of their medicine-taking. In Britten’s172 study of lay accounts of medicine-taking, she developed an analysis based on ‘orthodox’ and ‘unorthodox’ accounts. Those giving ‘orthodox accounts’ were more likely to describe the ‘correct behaviour’ for taking medicines, such as cashing prescriptions, taking the medicine as prescribed, following the doctor’s advice even if they had doubts about it and not wasting the doctor’s time. These people appeared to be more deferential to doctors, talked about medicine in an unquestioning manner and were generally passive. Similarly, those offering what Lumme-Sandt et al. 175 described as the ‘patient repertoire’ offered ‘very traditional representations of themselves as patients’ (p. 1847) and regarded doctors as experts who should be obeyed. Medicine was simply taken for granted.
Those who do not take their medicine as prescribed (Figure 15)
Rejecters/sceptics
Dowell and Hudson173 reported that some people rejected their prescribed medicine outright, without testing it first. These people, whom the authors describe as ‘rejecters’ or ‘sceptics’, preferred to maintain control by using ‘alternative’ therapies or by tolerating their symptoms. They completely rejected Western medicine and its emphasis on drug taking. In the context of hypertension, Johnson et al. 136 noted that some people, whom they termed ‘purposeful non-adherers’, made a conscious decision not to take the medicine, but in this case possibly following a period of testing.
FIGURE 15.
Categories of those who do take their medicine as prescribed.
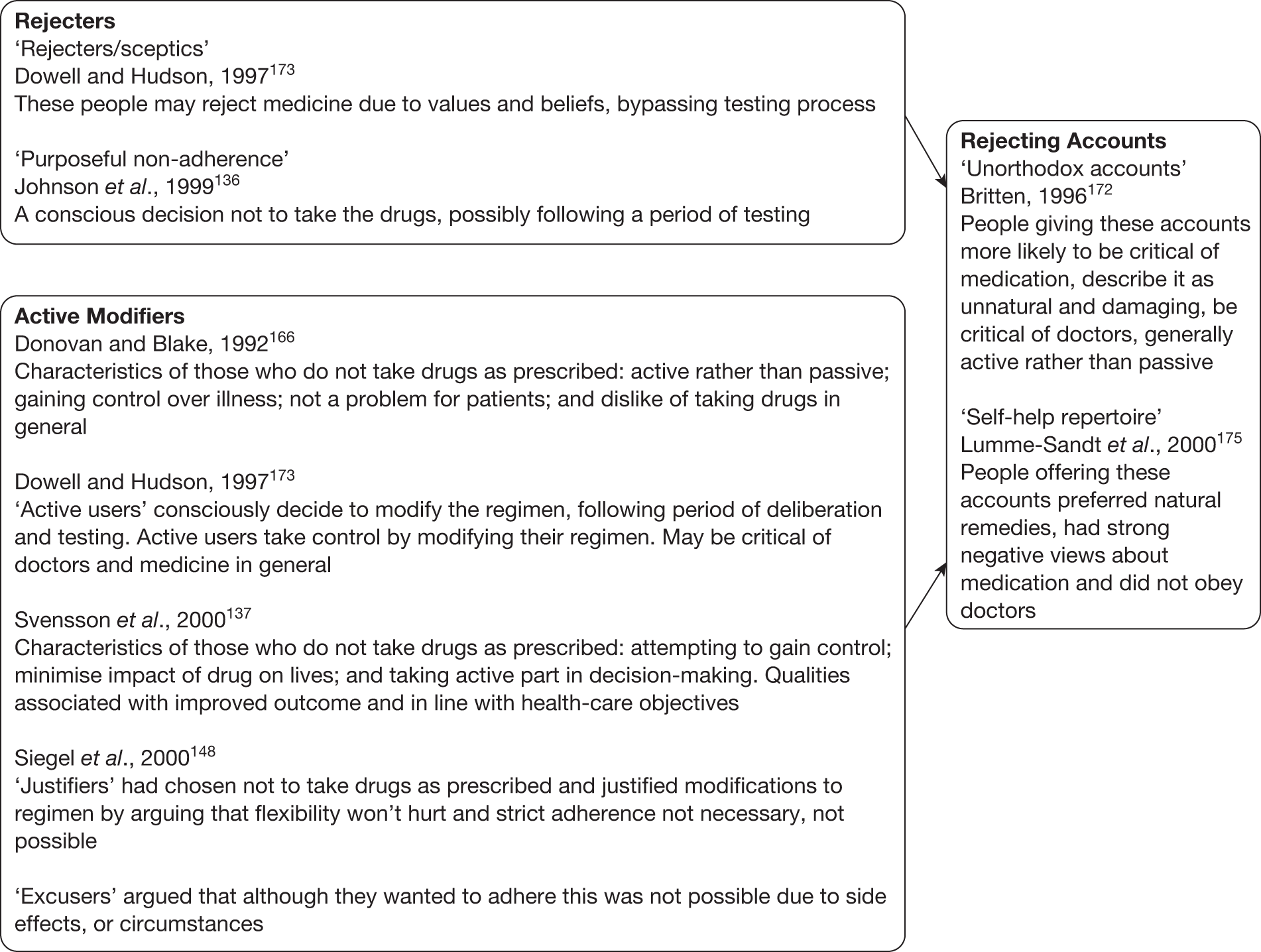
Rejecting accounts
Both the ‘active modifiers’ (see below) and the ‘rejecters’ (but more likely the ‘rejecters’) might give ‘unorthodox accounts’172 or draw on the ‘self-help repertoire’,175 both of which imply a rejection of modern medicine. Britten172 found that those giving ‘unorthodox accounts’ were ‘almost entirely negative’ (p. 60) about medicines in general. These people preferred not to take medicine, describing it as unnatural, damaging, dealing with symptoms rather than causes and not being tailored to individuals. They were critical of doctors, mainly because of overprescribing, and their criticisms of doctors and medicines went hand in hand. These people were generally active in their approach. Similarly, those drawing on the ‘self-help repertoire’ described by Lumme-Sandt et al. 175 had strong negative views about medicine, and some explicitly reported that they did not follow their doctors’ advice. They reported using both medical and home remedies side by side, but had greater confidence in the latter.
Those who modify their regimen – the ‘active modifiers’
Donovan and Blake’s166 study of RA is the earliest in the synthesis to describe the characteristics of those who do not take their medicine as prescribed. Most of Donovan and Blake’s166 sample stated that they disliked taking drugs, most chose to ignore advice or alter doses and few saw this as an issue. The authors suggested that modification of the regimen represented a means of gaining some control over the illness. Similarly, Dowell and Hudson173 found that a number of people in their sample took control by making a conscious decision to modify the regimen following a period of deliberation and testing. These people, whom the authors describe as ‘active users’, aimed to balance the benefits of the medicine against its perceived drawbacks, and to this end they adjusted the doses in order to take as little as possible. In the same way, Svensson et al. 137 suggested that those who modified their antihypertensive regimen did so following active reasoning and in an attempt to gain control and minimise the impact of the drug on their lives. In the context of HIV infection, Siegel et al. 148 categorised those who did not take their medicine as prescribed as ‘justifiers’ and ‘excusers’. ‘Justifiers’ were those who had chosen to modify their regimen on the basis that some flexibility would not hurt and that strict adherence was neither necessary nor possible, and ‘excusers’ claimed that they wanted to adhere to the regimen, but that various circumstances and adverse effects prevented them from doing so.
Before going on to look in detail at the various ways in which people modify their regimens, it should be noted that there is another category of medicine-taking that none of the above studies considered, but which came out strongly in the studies on mental illnesses: those who are forced or strongly coerced into taking their medicines.
‘Imposed compliance’
Usher158 used the term ‘imposed compliance’ to describe the result of the pressure exerted by relatives or health professionals to take medicine. Writing in the context of neuroleptic medicine for schizophrenia, she suggested that some people take their medicines only because they feel powerless to do otherwise. Some of her participants reported that friends and relatives surveyed them for signs of illness and, if they felt it necessary, exerted pressure on them to take their medicine. Rogers et al. 156 also found this to be true in the case of neuroleptic medicines. Some of their participants had experienced relatives or friends strongly encouraging or forcing them to take the medicine, as one of their participants illustrated:156
My husband is supposed to sort of see that I take it, I don’t see that it’s up to your husband to see that you take your medication, it’s up to you … but my husband gets blamed if I don’t take my medication.
A different type of pressure was found in the context of HIV infection. McDonald et al. 149 noted that some relatives or partners might encourage the HIV-positive person to take the medicine because they wanted their loved one’s lifespan to be extended. As one of their participants said:149
… I mean, when you’re in a relationship you have to take into consideration your partner’s thoughts and feelings on things and what she sees in tablets is ten or more years of being together … And that’s what she wants of course and to some extent of course I want it too but I don’t want it if I’m going to be sick all the time taking them.
At the other end of the scale, Kaljee and Beardsley153 noted that some patients with mental illness have no control at all over their medicine because it is administered by injection. This is the most extreme form of ‘imposed compliance’. Somewhere in between the two ends of the scale is the pressure to take medicine that is imposed by communities. Rogers et al. 156 suggested that people on neuroleptic medicine are more likely to take their drugs as prescribed because of the threat of social sanctions (for example social disapproval, withdrawal of acceptance, hospitalisation) if they do not. Their participants perceived the existence of an unwritten social contract: take the medicine in order to be tolerated by the community. Furthermore, some had experienced coercion from health professionals when in the past they had not taken their medicine, as a woman in Rogers et al. ’s156 study illustrated:
You’re supposed to do as they [doctors] tell you, you know, otherwise you get sectioned and I have been sectioned so er it’s not very nice, police bringing you down to [local psychiatric hospital], so, you take them to stop yourself from being sectioned.
Similarly, one of Usher’s158 participants said:
The community nurse comes to see if I’m taking my medicines … I call them the thought police … I felt like I didn’t have any choice.
Some of the people with mental illness in Smith et al. ’s170 study also felt that medicine was used to control them and make them acceptable to society. As the authors wrote, ‘Medicines for mental health problems were seen as a tool used by professionals to control individuals within a social context. The aim of treatment was viewed as a means to achieve behaviour acceptable to society’ (p. 93). 170 As can be seen then, imposed compliance was almost exclusively an issue for people with mental illnesses.
A general desire to minimise medicine intake
Dowell and Hudson173 suggested that people take medicine within limits, either those established by the doctor or self-imposed. They noted that people ‘… have a powerful drive to minimize treatment use. Indeed, the more powerful the drug, the more its importance is emphasized and the stronger may be the desire to reduce it’ (p. 375). 173 Few of the rural African Americans in Roberson’s171 study took their drugs as prescribed, and most talked openly about this. They regularly reduced the number of doses that they were supposed to have, for example by taking them once rather than twice daily. A general impulse to minimise the intake of tablets was also found in the context of treatment for arthritis. Donovan and Blake166 found that more than four-fifths of all the people in their sample spontaneously expressed their dislike at having to take drugs. Watson and Mitchell174 found that the older women in their sample avoided taking medicine unless they felt it to be essential. People taking PPIs also preferred to minimise their intake,159,160 despite PPI’s being regarded by doctors as a medicine that is overconsumed by patients. Similarly, North et al. 154 found that many people taking benzodiazepines, which are also regarded by doctors as being overused, set self-imposed limits on their consumption of this medicine.
Altough the above authors referred to a general desire to minimise the intake of medicine, many of the following strategies reflect a similar desire.
Adjusting doses to decrease adverse effects and addiction
As noted earlier, many of the HIV studies reported people’s concerns with the adverse effects of the antiretroviral regimen. The following studies illustrate the ways in which people adjusted their regimens to try and realise some therapeutic gain at the same time as reducing adverse effects. Siegel and Gorey142 found that many of the women who took or had taken AZT reduced the dosage, for example by taking it three or four times daily rather than five times, or by skipping a day here and there. Some of Siegel et al. ’s147 older respondents reported that if altering the dose reduced the adverse effects and improved their well-being, then they felt that such alterations were acceptable. Some would stop taking the medicine completely to reduce the debilitating adverse effects, whereas others would interrupt their regimen if the adverse effects were too severe, then continue once the effects had abated. One man, when asked if he took his medicine as prescribed, answered:148
No, it’s too strong … You’re not supposed to stop taking the medicine. It is supposed to be taken consecutively so that it can have effect. But since I start taking it and I see that it is attacking parts of my body, that is more dangerous. I will stop taking the medicine … if my liver begins to hurt, or my prostate, or this or that, I stop taking it for up to two days.
Some of Erlen and Mellors’144 participants who were infected with HIV reported taking their tablets separately instead of all together, to avoid adverse effects. Several of Siegel et al. ’s148 sample reported reducing their doses, or taking their medicine at different times, to reduce adverse effects. One man explained:148
Yes, I decided that I would double up [doses] at the end of the day because it [medication] was giving me diarrhoea so bad. And I figured like I didn’t want to be out in public and have to go, and not be able to have any place to go. So what I would do, I would take one at mid-day when it wouldn’t bother me too bad. But the morning dose, I would not take, because if I did and had to go out, then I would be in trouble.
Some people specifically referred to ‘drug holidays’ as a means of stopping the build-up of toxicity and of cleansing their bodies. 144,152 Several of Stone and Clarke’s143 participants reported going without medicine for periods ranging from 1 week to 1 month or more. One person said:143
Every once in a while I’d have drug holidays, and you do feel like a toxicity’s building up, and so on and so forth. That something just tells you to stop. And you stop for, like, a week.
One of Barton Laws and Wilson’s152 respondents reported taking a 6-week break during which his viral load had ‘shot up’, but he did not believe that the practice was harmful and was convinced that almost every person infected with HIV took drug holidays. Morgan134 found that people also took drug holidays in the context of antihypertensive medicine, in the hope of reducing the total drug intake and reducing the risk of adverse effects, dependence and addiction. She suggested that ‘leaving off’ the drugs took two forms: one method was to stop taking the medicine for a few days each week regularly and the other was to take a break of several weeks or months if the person was feeling well. Donovan and Blake166 suggested that people modified their regimen to reduce their fears about adverse effects. ‘They reasoned that there would be fewer side effects with fewer tablets, and so kept their doses to the minimum they could. In some cases, this meant them putting up with considerable amounts of pain and discomfort … ’ (p. 509). 166 North et al. 154 reported that many people tried to restrict their use of benzodiazepines in order to avoid addiction. The authors noted that doctors gave people a high degree of autonomy in the management of their benzodiazepines. Most people were found to set self-determined controls on their doses and many were trying alternative ways of managing their symptoms owing to their ambivalence about using benzodiazepines.
Adjusting the regimen to make it more acceptable
Some of Siegel et al. ’s147 participants amended their antiretroviral regimen to fit in with their daily schedule, arguing that complete adherence was not necessary for therapeutic gain. Similarly, some of those in Siegel et al. ’s148 study were not worried about straying from their regimen, feeling that some flexibility in the regimen was acceptable and harmless, as the optimum regimen was not known anyway. They argued that flexibility with the regimen allowed life to continue without too much disruption and that strict adherence to the regimen was neither an attainable nor realistic goal. In the same way, Barton Laws and Wilson152 found several people adjusted their doses or the timing of their doses to fit in with their daily routine rather than modifying their daily routine to accommodate the regimen. One person, who took his medicine whenever he ate rather than every 8 hours, said:152
They’re not spaced like they’re supposed to, but I know enough about the medication where I know that they still overlap … These medications don’t flush out of your system in 8 hours like they make … people believe.
Another intrusive regimen was the nightly infusion pump for administering chelation therapy to children with thalassaemia major. Atkin and Ahmad169 reported that some children would use the infusion pump less frequently than prescribed or would disconnect the needle at night. The authors suggested that children did this because the therapy dominated their lives and marked them out as different from their peers, thus making them feel physically and symbolically tied to the pump and the regimen.
Reducing doses for financial reasons
Johnson et al. 136 noted that in order to take medicines, people need insurance or sufficient personal income to purchase or access their treatment. Some of Roberson’s171 sample reduced doses because they could not afford the prescribed amounts. One of her respondents with hypertension, diabetes and arthritis was on a low income and had no health insurance. Her medicines cost between US$100 and US$125 per month. She said, ‘If I see I’m about to run out and I don’t have no money to get no more, I just cut down my pressure pills to once a day’ (p. 16). 171 Financial difficulties that impacted on medicine-taking were also reported by Ersek et al. ,168 Barton Laws and Wilson152 and Siegel et al. 148
Using medicine symptomatically
Morgan134 is the only person to have considered the influence of ethnicity on medicine-taking. She found that some of her African Caribbean respondents used their antihypertensive drugs in the same way as they used their herbal remedies, in other words, symptomatically. She noted that although high blood pressure is regarded as an asymptomatic condition, some of the people in her study described feelings of weakness or tiredness, eye problems, dizziness or hotness and perceived these as indications that their blood pressure was elevated. If this was the case, they might be prompted to take the medicine. One respondent said:134
Please don’t tell him [Dr] this, but I’m a person that if I find it’s stable and I’m not getting any funny feelings then I don’t take them. If I feel peaky again, then I go back on them.
Similarly, one of Johnson et al. ’s136 respondents reported taking his or her antihypertensive medicine sporadically, when his or her blood pressure readings was elevated. Roberson171 found likewise, that some people would check their blood pressure and decide on dosage accordingly. Some of the people with RA in Donovan and Blake’s166 study altered their doses according to the symptoms they experienced. As one woman put it:166
When [the arthritis] is bad, I take two [Feldene, i.e. piroxicam] because that’s how it’s directed, but otherwise, if I get a twinge, I only take the one. There is days I don’t take any. I’d rather not take them if I can.
Kaljee and Beardsley153 suggested that some people on psychotropic medicine manipulate their drug doses to control symptoms. One person diagnosed as having manic depression felt that his drugs provided immediate relief from his symptoms: ‘… a couple of sinking feelings, take a pill, (the feelings) would go away’. 153 A few of Rogers et al. ’s156 participants adjusted their doses of neuroleptic medicine to cope with distress when it arose, and Angermeyer et al. 157 also found that some people with schizophrenia used clozapine symptomatically.
Using medicine strategically
Some of Morgan’s134 respondents reported that they would not take their antihypertensive medicine if they intended to drink alcohol, for fear that the interaction would have severe consequences:134
I am a man that goes out to parties sometimes and has a nice drink. When you are taking drugs you have to limit your drinks. If I know that I’m going out on a Saturday night or Friday or Sunday I won’t take the tablets as you do not want to mix the drugs with the alcohol.
Why is that?
It is not something you should do, you can die if you mix them.
Similarly, Rogers et al. 156 found that several people adjusted their doses of neuroleptic medicine when they wanted to go out for a drink, because they knew that alcohol interacted poorly with their medicine. Most stopped taking their medicine on the day they drank alcohol; thus the need for social activity was weighed against the need for medicine. The authors of the studies on PPIs reported that some people took their medicine strategically rather than continuously. 159,160 Boath and Blenkinsopp159 found that some took PPIs as and when they thought it necessary, relating the dosage to their proposed diet. Thus, some might take a pill in advance of a planned indulgence, whereas others might miss a dose if they did not anticipate a need for it. Pollock and Grime160 also found that several of their participants took PPIs only at symptom onset, or if symptoms were anticipated.
Replacing or supplementing medicines with non-pharmacological treatments
Most of Roberson’s171 sample undertook ‘self-care activities’ in addition to their prescribed regimen. Vinegar, Epsom salts, lemon and garlic were taken for hypertension, BENGAY® (Johnson & Johnson, New Brunswick, NJ, USA) and copper wire bracelets were used for arthritis, horehound tea or buttermilk for diabetes and rabbit tobacco tea and pine top for asthma. A few people sought advice from ‘root doctors’, who are described as having an extensive knowledge of herbs and roots. However, although Roberson171 noted that people took traditional remedies in addition to their prescribed medicine, it is not clear whether or how this affected people’s drug regimens. Lumme-Sandt et al. 175 noted that their respondents who spontaneously talked about traditional remedies seemed to use them as their primary medicine. As one man said, ‘Yes, I have slight blood pressure and I eat garlic for that. I didn’t take any medicine when the doctor told me to. I cure it with garlic’ (p. 1847). 175 Others used both medical drugs and traditional remedies alongside each other.
Several of Ersek et al. ’s168 participants used non-pharmacological methods to reduce pain and also to lower their use of analgesics, and about half of the people in Donovan and Blake’s166 study used some sort of ‘alternative’ remedy either instead of or as well as their medicine. Kelp, cod liver oil, feverfew, dietary changes and homeopathy were mentioned. Morgan134 found that over half of the African Caribbean people in her study took herbal remedies. Respondents reported taking cerasee, which was described as good for reducing high blood pressure, and Constitution Bitters, a drink containing a blend of seven herbs. The African Caribbean women boiled grapefruit skins with garlic and drank the water to reduce blood pressure. Morgan134 noted that these herbal remedies formed an additional resource for many people and that they were taken either in addition to or instead of their prescribed medicines. Furthermore, she observed that people were familiar with these remedies and regarded them as potentially less harmful and powerful than prescribed drugs because they were seen as ‘natural’ substances. If people were worried about the potentially harmful effects of prescribed drugs they might take a break from them for a period and use natural remedies instead.
Temporary breaks in regimen for incidental reasons
Several studies reported forgetfulness to be a reason why some people occasionally did not take their medicine as prescribed,136,143,144,148,151,152,168,171 and three studies136,146,153 reported that occasionally people unintentionally ran out of tablets. Interruption in routine or an irregular daily schedule could lead to a break in the regimen. 136,143,148,150–152 Strategies for minimising what Johnson et al. 136 referred to as ‘incidental non-adherence’ were developed mainly by those infected with HIV. Stone and Clarke,143 Halkitis and Kirton145 and Murphy et al. 150 reported that people used mechanical reminders to take their pills (including beeper pill cases, weekly or monthly pill boxes, stopwatches or alarm clocks) or visible cues. Reminders from significant others were found to help in the context of asthma163 and HIV infection. 143,145,150 The routinisation of medicine-taking was a key strategy for those infected with HIV,143,145,150 hypertension136 or asthma. 163
Doctor–patient communication about regimen modifications
A small number of studies suggested that a better relationship with one’s doctor meant that patients were more likely to take their medicines as prescribed137,143,144,173 or accept prescription changes,167 whereas a poor relationship with the doctor could lead to not taking medicines as prescribed. 150 More specifically, with regard to regimen changes, some of Roberson’s171 respondents reported that they were scolded by their doctors for making their own decisions about their health care. However, instead of confronting them, patients would change doctors whom they were dissatisfied with. Britten172 also suggested that people who gave ‘unorthodox accounts’ tended not to mention their beliefs or criticisms to their doctors because they did not perceive their criticisms to have medical legitimacy. Thus, people giving ‘unorthodox’ accounts appeared ‘orthodox’ while in the surgery. Once outside the surgery, however, they regained control by modifying or rejecting their prescription, offering an unseen challenge to the medical system.
Most of Ersek et al. ’s168 sample reported positive relationships with care providers, but a minority felt that doctors did not communicate well about medicine. Smith et al. ,170 whose study included people with arthritis, respiratory disease and mental illness, found that people with arthritis varied in their attitude to involvement in decision-making about medicine, and those with respiratory disease wanted more involvement. People with mental-health problems reported having generally poor relationships with health professionals and participation in decision-making was rare for this group, particularly during the acute phases of their illnesses. Also in the context of mental illness, Rogers et al. 156 observed that people with schizophrenia who did not take their neuroleptic drugs as prescribed were unlikely to reveal this to health professionals because of their awareness or experience of coercion and their knowledge of the power that health professionals held over their lives. One person put it like this:156
He’s [psychiatrist] bawling and shouting at me in my own house, and quite a few other people have had this experience, he’s got a very poor personal style. I feel intimidated by him and he’s over-bearing and he’s got the power to section me, he’s got the power to do just whatever he wants to me so I’m very careful what I say to him.
Another of Rogers et al. ’s156 participants felt unable to discuss her use of ‘alternative’ remedies with the psychiatrist because she felt that he would consider this as further evidence of mental illness. Similarly, Kaljee and Beardsley153 noted that patients’ use of alternatives (e.g. prayer) to drugs for mental illness could lead care providers to label them as ‘uncompliant’.
Evidently then, although people are indirectly challenging medicine outside the surgery, in the day-to-day practice of using alternative remedies, discarding their prescriptions and modifying regimens to suit themselves, no resolution occurs between doctors and patients on this issue. Some suggestions about resolving the issue have been made. In the context of PPIs, Pollock and Grime160 argued that the best solution is to let people find their own dose and manage it themselves, given that their tendency is to under- rather than overmedicate. They recommended that patients be encouraged to actively manage their illness by finding their own level of treatment and suggested that doctors need to recognise that many patients do this already. They argued that more patients would self-regulate if doctors told them to do so and that if the practice were authorised and open, with doctors guiding patients, it would be safer than it is at present. They suggested that self-regulation would involve people in their own care and help them feel in control. Similarly, Dowell and Hudson173 suggested that as there is a powerful drive to minimise the use of medicines and as patients will continue to test and modify their medicines, doctors may as well assist them in doing so.
Svensson et al. 137 reached similar conclusions with regard to antihypertensive medicine. They suggested that ‘non-adherence’ should be encouraged because it is a way for patients to gain control and take an active part in decision-making. They suggested that it ‘must be considered sound behaviour, the danger of which is only apparent when it occurs frequently and is not communicated to health professionals’ (p. 162). 137 The authors further claimed that taking an active part in care and gaining control over illness are practices associated with improved therapeutic outcomes and are also in line with health-care objectives. Conversely, they noted that indifference and passivity may co-exist with adherence but are not qualities associated with informed consent or shared decision-making, which are assumed to be characteristics of good clinical practice.
Summary of main findings
A small number of sociological studies investigated medicine-taking in its own right,134,154,162,172,193 but the absence of compliance as a starting point was rare in the studies and the ideology that people should take their medicines as prescribed held sway. The majority of the studies focused on the reasons why people do not take their medicine as prescribed, with few considering the experience of those who reject medicine outright or those who accept it uncritically. Additionally, the vast majority of studies were concerned with chronic illness.
The synthesis revealed widespread caution about taking medicines and highlighted the lay practice of testing and evaluating medicines prior to accepting or rejecting them, principally owing to worries about adverse effects and other unwanted consequences of taking medicine. Although some concerns about medicines may be resolved through lay evaluation, many cannot be dealt with in this way. These include worries about dependence, tolerance and addiction, the potential harm from taking medicines in the long term and the possibility of medicines masking important symptoms. Additionally, it is clear that in some cases medicine has a significant impact on identity, presenting problems of disclosure and stigma, among others.
People were found to accept their medicine either passively or actively, or to reject it. Additionally, some were strongly coerced into taking medicines. Most of the studies focused on those who did not take their medicines as prescribed. Regimens might be modified symptomatically or strategically, adjusted in order to decrease adverse effects and other unwanted consequences, or adapted to fit more acceptably into daily life. Many of the modifications reflected a general desire to minimise the intake of medicines and this desire was echoed in some people’s use of non-pharmacological treatments to either supplant or supplement their prescribed regimen. Few discussed regimen modifications with their doctors.
The lines of argument presented in this synthesis, and summarised textually in this section, are displayed in the form of a model of medicine-taking in Figure 16.
FIGURE 16.
Model of medicine-taking.
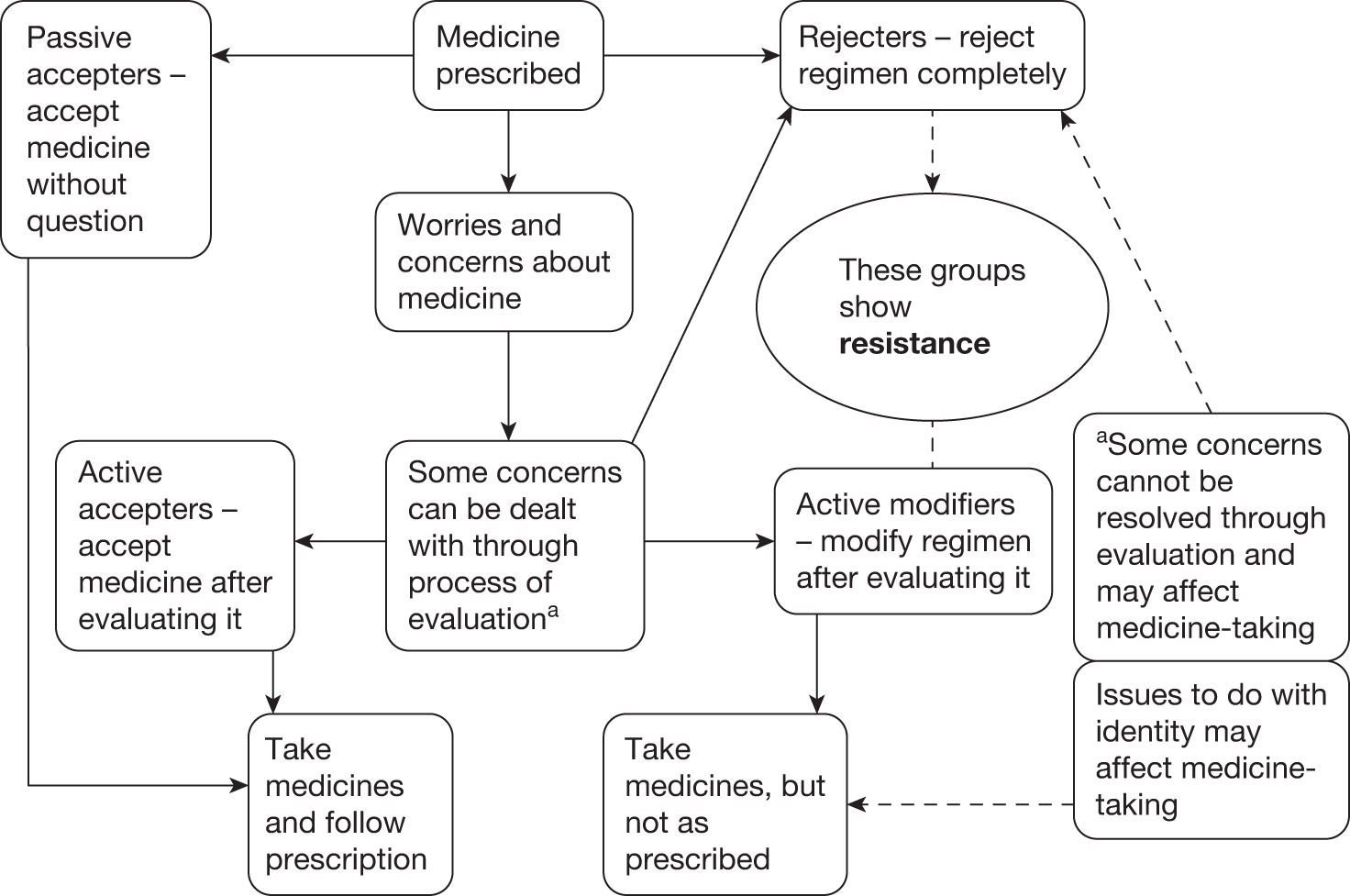
Discussion
It is important to remember that our sample of studies represented only a small range of medicines, taken mainly for chronic illnesses. Furthermore, the illness most frequently represented in the studies was HIV infection, which provided relatively extreme experiences of medicine-taking. A person’s experience of medicines is likely to differ according to the medicine in question and the nature of the illness for which it is taken. For example, it is possible that those classified in some of the studies as ‘rejecters’ could become ‘accepters’ if they were given a different medicine or vice versa. Equally, it is important to remember that in some cases the consequences of not taking medicines as prescribed can be serious or fatal.
Lay evaluation
At least two studies preceding our synthesis considered the topic of lay testing,118,194 but we found only one study that specifically set out to investigate this issue. In common with our findings, the participants in the study by Arluke,116 which also predated our synthesis, tested their medicines in a number of ways including observing the effect of stopping the drugs or reducing the dose, and observing the reactions of others on the same medicine. However, although some lay people conduct their own tests of medicines this does not imply that they are ‘experts’ in the field. Prior195 criticised the sociological inclination to treat lay knowledge as ‘every bit as valuable’ as professional knowledge, arguing instead that lay knowledge is often partial and restricted. An example from the synthesis that may support this is the gender difference evident in lay evaluations of treatment for HIV infection. McDonald et al. 149 argued that gay men collectively engaged with the AIDS (acquired immunodeficiency syndrome) epidemic and achieved an unusual level of biomedical expertise on the subjects of HIV infection and trial methodologies, as well as credibility within medical circles (see also Epstein196). On the other hand, women’s decisions tended to be based on ‘personal and idiosyncratic health histories or current or very recent health status. Women were simply unused to making judgements about the efficacy of HIV treatments and their frame of reference was not historically and communally situated, as it was for the men’. 149
However, we believe that the significance of the lay evaluation of medicines lies not simply in the fact that it occurs, but in the reasons why it does. The urge to evaluate suggests widespread caution with regard to taking medicine as well as the possibility that people do not completely trust what they have been told about their medicines. It may also reflect an (instinctive) understanding of the principle of individual treatment response and a desire to ensure that the medicine is suitable in their particular case. As Johannessen et al. 197 explained: ‘The controlled single subject trial is concerned with determining the efficacy of a drug compared with placebo or another drug in one particular patient. Such trials can also be employed to assess the optimal dose of a drug, to identify adverse effects, or to stop established, unnecessary treatment by convincing the patient that there is no benefit beyond the placebo effect. In N of 1 trials each subject serves as his or her own control’. 197
The principle of the ‘N of 1’ trial methodology is often compared with the strategy of ‘trial and error’ in clinical practice, where perhaps the effect of a therapy or the optimal dose is uncertain. Lay people, in the way in which they test their medicines, are attempting to determine whether or not there are any adverse effects and whether or not the medicine works for them and, if so, to establish the most suitable dose for themselves. This suggests that lay people may have an intuitive understanding that population set doses may not be appropriate for individuals. Recently, the worldwide vice president of GlaxoSmithKline acknowledged that most prescription medicines do not work on most people who take them. Steve Connor, the Science Editor for the Independent, wrote ‘It is an open secret within the drugs industry that most of its products are ineffective in most patients …’198 (see also Smith199). Although this may be an open secret within the drugs industry, it is well concealed from those who take the medicines. Fortunately, as this synthesis suggests, many lay people work this out for themselves and modify their regimens accordingly. In support of a flexible approach to medicine-taking, a study on the use of non-steroidal anti-inflammatory drugs found that an adaptable approach that involved varying the dose according to the presence of symptoms was less likely to result in hospital admission for upper gastrointestinal bleeding than was rigid compliance to prescribed doses. 200,201
Adverse drug reactions
The literature on adverse drug reactions (ADRs) suggests that people are right to be cautious about taking medicines. A meta-analysis of studies in the USA found the incidence of fatal ADRs (excluding those because of prescribing errors) to be between the fourth and sixth leading cause of death,202 whereas in England and Wales the Audit Commission estimated that just under 11% of hospitalised patients suffer an ADR, with mortality following ADR showing a marked upward trend. 203 Yet the very real risks involved in taking medicine are either ignored or treated dismissively in the literature. For example, the WHO183 report stated, ‘Concerns about medication typically arise from beliefs about side effects and disruption of lifestyle and from more abstract worries about the long term effects and dependence. They are related to negative views about medications as a whole and suspicions that doctors over-prescribe medicines …’ (p. 44, italics added).
It is worrying that the WHO183 is so dismissive of people’s concerns about medicines. The qualitative studies suggest that these concerns are real and sensible; they are not ‘beliefs’, ‘abstract worries’ or ‘suspicions’ and the statistics on ADRs bear testimony to this. Nevertheless, lay reports of the adverse effects of medicines are consistently dismissed, despite the fact that the current Yellow Card Scheme, which relies on doctors voluntarily reporting ADRs, has been estimated to capture only 1% of actual ADRs. 204,205 Heath206 pointed out that more people are admitted to hospital for ADRs than for problems relating to ‘non-compliance’. ‘Medication errors’ caused by poor prescribing, poor dispensing and poor labelling are also a significant problem for patients and the NHS, with the potential to cause death, morbidity, increased or extended hospital admissions, litigation and financial burden to the NHS. 199
Concordance
Pollock and Grime,160 Dowell and Hudson173 and Svensson et al. 137 suggested that doctors need to accept that patients modify their regimens and that the way forward is to encourage ‘authorised’ self-regulation. This is similar to Donovan and Blake’s166 earlier call for ‘active and co-operative relationships between patients and doctors’ and to the newer concept of concordance, which ‘… describes the process whereby the patient and doctor reach an agreement on how a drug will be used, if at all’. 207 The aim of ‘concordance’ is to involve patients in making decisions about their medicines, to ensure that they have enough information for doing this and to support them with any problems that they might have. Thus, doctors might help patients with their testing and their modifications, providing feedback and guidance. ‘Crucially, concordance advocates a sharing of power in the professional–patient interaction.’208
Concordance and related approaches would appear to make sense in cases where doctors can help patients determine appropriate individualised doses, and provide information on adverse effects and how to deal with them as well as the information necessary to conduct their evaluations safely and effectively. However, concordance depends on doctors sharing information honestly with patients. Unfortunately, Cox et al. 209 have found that doctors emphasise the benefits of treatment rather than discussing its possible harms or risks, despite patients regarding these topics as essential. Equally, the concordance model depends on patients sharing information with doctors, but a few of the studies in the synthesis found that people were unlikely to raise issues with their doctors that they felt would be frowned upon. 156,171,172 Furthermore, Rogers et al. 156 noted that people with mental illness were very cautious about what they revealed to doctors because they were aware of the power that health professionals held over their lives. This was confirmed more recently by Britten et al. 16 Socially excluded patient groups, such as those with poor mental health or HIV infection, may be less likely to achieve ‘concordance’ with their doctors. This could be because they are less normative in their attitudes or because they feel disempowered owing to their membership of marginalised groups. On the other hand, they might feel unable to reveal how they actually take their medicine; for example, people infected with HIV might feel unable to ‘admit’ modifying their regimen because of public health fears about viral mutation. This is not to suggest that health professionals should give up trying to acknowledge and deal with the concerns of marginalised groups, but to make the point that the power imbalance inherent in the doctor–patient relationship will not easily be resolved by the model of concordance.
It is has also been suggested that concordance is simply another way of encouraging people to take their medicine, except that, unlike the ‘compliance’ model, this time the coercion is concealed. 206 This is an important consideration. Nevertheless, although doctors hold the balance of power during the consultation, the medical profession is oddly powerless once the patient has left the surgery. Whether or not there is coercion and whether this is concealed or explicit, lay people have always exercised their power to reject prescriptions or modify their regimens. Undoubtedly they will continue to exercise this power, as this is ‘normal’ behaviour for them. Unless health professionals learn to acknowledge their lack of power over how people take their medicines, ‘concordance’ is unlikely to be achieved.
Relationship between health and medicine-taking
Arguably, the ideologies of compliance, adherence and concordance, because they revolve around the axis of pharmaceutical medicine, distract attention away from non-pharmaceutical approaches to health. Heath206 made the point that the rhetoric of both concordance and compliance uncritically endorses medicine-taking. This relates to the most profound and hidden assumptions in the medicine-taking debate: firstly, that taking medicine is good for you and, secondly, that taking medicine is the only way of achieving desired health outcomes. In fairness, the original conceptualisation of concordance, as set out in the Royal Pharmaceutical Society of Great Britain report,210 acknowledged that taking medicine was not always the best thing to do and that ‘Almost all medicines have the capacity to harm as well as to do good’. 210 However, the WHO182 report made unsubstantiated claims about the health effects of not taking medicines as prescribed: ‘Poor adherence to long term therapies severely compromises the effectiveness of treatment making this a critical issue in population health …’. 183
Both the WHO183 report and the Medicines Partnership report184 assumed that taking medicines as prescribed would lead to good health outcomes. The introduction to the latter report, for example, stated, ‘In the context of a rising drugs bill and the key role of medicines in promoting health, the review underlines the vital importance of maintaining a clear focus on improving compliance and making better use of medicines’ (p. 2). 184 Yet in the body of the report, the authors noted that the Cochrane Review of interventions to improve compliance (also published as a journal article)189 found little evidence that such interventions would lead to large improvements in treatment outcomes. 189 Similarly, the review of the literature contained in the report indicated that the evidence relating ‘adherence’ to improved biomedical outcomes varies according to the illness. 184 At the very least this suggests caution against generalising about the benefits of taking medicines, as clearly the evidence for the benefits of pharmacological treatments is stronger in some areas than in others.
Although the bulk of the medicine-taking literature uncritically assumes that pharmaceutical drugs and Western medicine are the only response to ill health, those people who reject their prescriptions outright clearly think otherwise. Presumably so too did the one in three Americans in 1990 who reported using at least one ‘unconventional therapy’ in the previous year, and who spent almost US$13.7B on alternative health treatments in the same year. 211 It is estimated that approximately half the general population in developed countries uses complementary and alternative medicine. 168 Harrison185 argued that user support for complementary and alternative medicines ‘… indicates in the clearest possible way that a significant number of people do not like conventional medicine or that it has failed them in particular ways’ (p. 36).
Sociology, qualitative methodologies and the adoption of the medical agenda
The sociological studies in this synthesis barely touched the assumptions underlying the compliance debate: firstly, that taking medicine leads to good health outcomes and, secondly, that it is the only possible response to ill health. As such, sociologists have to a large extent adopted the medical agenda. Only a few studies considered those who rejected medicine,172,173,175 despite the fact that it is this group that probably has the most to tell us about the reasons for the widespread reluctance to take medicine. Nevertheless, the early sociological and anthropological studies in this synthesis134,153,156,161,166,171 demonstrated that people have understandable and logical reasons for not taking their medicine as prescribed and challenged the assumptions inherent in the ideology of compliance. As such they undoubtedly influenced medical culture to the extent that, 10 years later, the term ‘compliance’ is no longer considered appropriate and there is a greater readiness to accept that some people will disregard their doctor’s advice and that they may be perfectly sensible for doing so.
There was a discernible tendency in some of the studies to regard qualitative methods as a means of obtaining information on the patient’s perspective that might ultimately be used to encourage people to take their medicine as prescribed. Broadly speaking, the sociological studies advocated the use of qualitative methods as a means of understanding why patients do not take their medicine as prescribed, whereas the medical and nursing studies advocated the methodology as a means of finding out why people did not comply. Angermeyer et al. 157 put it bluntly, ‘Our findings point to the necessity for psychiatrists to explore patients’ subjective views and motivations with regard to their medicine in order to improve treatment adherence’. 157 Given that qualitative methods are the preferred means of exploring ‘patients’ subjective views and motivations’ it is possible to argue that in some cases qualitative methods may have been used to advance the medical agenda.
Bringing medicine into the medicine-taking debate
In our view, one of the key conclusions produced by this synthesis is that the main reason why people do not take their medicines as prescribed is because of concerns about the medicines themselves. On the whole, the findings suggest that there is considerable reluctance to take medicine and a preference to take as little medicine as possible. This is in contrast to earlier theories that attributed ‘non-compliance’ to failings in patients, or current theories that attribute it to failures of the ‘system’ or the doctor–patient consultation. Although medicines are obviously at the centre of the medicine-taking debate and lay people have repeatedly demonstrated their wariness of medicines, their worries have tended to be marginalised or, as noted earlier, treated as ‘beliefs about medicines’, despite the well-documented existence of ADR and instances where concerns about the safety of medicines, for example over addiction to benzodiazepines, have been highlighted by patient groups based on their lay expertise, well before they were acknowledged by professionals (p. 145). 212
It is difficult to imagine how or why this most obvious factor has been overlooked, but it may be because of the dominance of the cultural belief in the benefit of pharmaceutical medicines. Or perhaps it was dismissed because of the view that patients, doctors and systems are easier to modify than medicines themselves. It may be because most of the research has ignored the lay perspective and has failed to involve consumers, resulting in a mismatch between the priorities of researchers and those of patients. 213,214 However, sociologists are also responsible here because we have tended to focus on ‘perceptions’ of medicines or the ‘meanings’ people attach to medicines. This tendency has significant consequences. It makes the person, rather than the medicine, the focus of attention, in much the same way as the WHO183 report (as noted in the introduction to this synthesis) considered anxieties about medicines to be ‘patient-related’ rather than ‘therapy-related’ factors. The result of this is that attempts are made to modify patient behaviour or the doctor–patient consultation rather than question the appropriateness of the medicine. Thus, because people’s accounts are not taken at face value, the more mundane issues about the physical reality of medicines and the effects that they have on people’s bodies and minds have become obscured, with the result that patients’ priorities and concerns are neglected.
Resisting medicines
We feel that many lay people’s response to medicine is best captured by the concept of resistance. In part this is because the term encapsulates the ways in which people take medicines at the same time as attempting to minimise their intake. However, the majority of people represented in this synthesis were not just unwilling or reluctant to take their medicines, nor simply cautious. The strategies they adopted to manage their medicine-taking indicate varying degrees of resistance to the prescription which they were given and, if the term resistance sounds strong, it should be remembered that the huge literature on ‘non-compliance’ exists only because so many people have continued to resist taking medicines in the face of sustained advice, interventions and admonitions. The term resistance also captures lay people’s active engagement with their medicines, as well as the ingenuity and energy that they bring to dealing with their medicines. Additionally, it carries the suggestion of a clandestine operation, which it is, as most people do not tell their doctors about the modifications they make to their regimens.
The term resistance is usually employed in relation to the exercise of power or coercion. As such, it entails acknowledging that the traditional approach to medicine-taking has been, and in varying degrees continues to be, coercive. In this context it should be noted that the noun ‘medicine’ refers both to the pharmacological substance as well as to the profession that prescribes it. Therefore, we could also consider the possibility that any resistance is not only to the pharmacological substance, but also to Western biomedicine. From this perspective, the evaluation and modification of drug regimens that people engage in could also be understood as ways of reasserting control over their bodies and the decisions about it.
Policy and practice implications
There is a need to accept that people are unlikely to stop resisting their medicines. Doctors could assist people in their lay evaluations of medicines by providing the necessary information, feedback and support and by prescribing safely. However, doctors will need training and support to do this effectively. The policy emphasis needs to be less on attempting to modify people’s behaviour and more on developing safer medicines. This huge undertaking involves questioning the present methods used to develop and test medicines215 and ensuring that more attention is paid to safety at the licensing stage, possibly by having a probationary period. Additionally, safer ways need to be found of administering medicines, and of monitoring their effectiveness and acceptability to individual patients. Effective ways of identifying ADR in all patients need to be developed and implemented. Furthermore, in recognition of the fact that many people prefer not to take medicines, funds should be allocated, firstly, to determine what sort of treatments patients prefer and, secondly, to evaluate the safety, efficacy and cost-effectiveness of those preferred treatments.
Chapter 7 A synthesis of qualitative studies about lay experiences and perceptions of rheumatoid arthritis
Introduction
This chapter presents a synthesis of published reports of qualitative studies concerning lay perceptions and experiences related to the aetiology, treatment, management and lived experience of RA. RA was chosen as a topic because it was known to be a field where published qualitative studies had impacted widely on medical sociology. 140,141 Furthermore, RA was selected as a narrow, disease-specific field in order to investigate what value qualitative synthesis might have for clinical practice for a particular condition.
RA, unlike the other main cause of arthritis, osteoarthritis, is not primarily a disease of ageing; the most common age of onset is between 30 and 50 years (www.arc.org.uk). RA is an inflammatory disease of the joints, which is experienced as a spectrum from minor twinges to destruction of joints, often with an uncertain pattern of flares and remissions. It is the potentially chronic and disabling nature of the condition and its uncertain course that has brought it to the attention of medical sociologists and others. RA affects women disproportionately (ratio 3 : 2 to men).
The central preoccupation of the studies, and their main theoretical significance, concerned the ‘experience’ of daily life with RA following the changes brought by the condition. Although issues of aetiology and treatment did feature, the papers that focused on these issues were marginal to the wider collective voice of the papers. Salient features of the included studies are detailed in Table 19. In expressing the synthesis here, the three areas of aetiology, experience and treatment are separated out, although far more attention is devoted to ‘experience’ as it was the focus of most of the studies.
| Source paper(s) (n = 25) | Country setting | Participants, male (female) | Sample origins | Type of study |
|---|---|---|---|---|
| Wiener, 1975138 | USA | 21 (16) | Hospital patients | Interviews |
| Bury, 1982;140 Bury, 1988216 | UK | 30 (25) | Hospital patients | Interviews |
| Locker, 1983139 | UK | 24 (16) | ‘Severely disabled by RA’ | Interviews |
| Williams, 1984;141 Williams and Wood, 1988178 | UK | 30 (19) | Hospital patients | Interviews |
| Donovan et al., 1989;217 Donovan, 1991218 | UK |
1989: 32 (ns) 1991: 54 (ns) |
Hospital patients | Interviews (twice each), observation of consultation |
| Bjørner and Hansen, 1993 (Danish)219 | Denmark | 8 + 3 sexual partners (ns) | Hospital patients | Interviews |
| Stenström et al., 1993176 | Sweden | 9 women | Hospital patients | Interviews |
| Rice and Young, 1994220 | USA | 50 (38) | Senior activity centre | Semi-structured questionnaire |
| Pinder, 1995221 | UK | 25 (18) | Snowballed, mainly voluntary group and hospital patients | Case studies developed from interviews |
| Brown and Williams, 1995222 | UK | 7 women | Hospital patients | Interviews |
| Shaul, 1995177 | USA | 30 women | Hospital patients | Interviews |
| Dildy, 1996223 | USA | 14 (9) | Hospital patients | Interviews (twice for seven patients) |
| Ryan, 1996224 | UK | 7 (ns) | Hospital patients | Interviews |
| Moss, 1997225 | Canada | 25 women | Hospital patients | Case studies developed from interviews |
| Rao et al., 1998226 | USA | 33 (ns) | Hospital patients | Focus groups |
| Williams and Barlow, 1998227 | UK | 14 (9) | From arthritis charities/research centre | Interviews |
| Archenholtz et al.,1999228 | USA | 50 women with SLE and 50 women with RA | Hospital patients | Structured telephone interviews |
| Stephens and Yoshida, 1999229 | Canada | 46 (32) | Arthritis charity | Interviews |
| Lambert and Butin, 2000230 | USA | 12 (?) | Hospital patients | Focus groups |
| Gilworth et al., 2001231 | UK | 47 (29) | Hospital patients | Interviews |
| Grant, 2001232 | UK | 4 mothers | Hospital patients | Case studies based on observation of OT sessions, interviews, OT case note analysis |
| McPherson et al., 2001233 | New Zealand | 10 women | Hospital patients | Interviews |
Methodological features of included papers
As noted in the methods chapter, of the studies initially included, only four were characterised by both good reporting of the use of qualitative methods of data collection and good analysis. 138,177,229,233 One further paper contained good reporting of qualitative methods of data collection and analysis,223 but in this case the reviewers were concerned that the methods described were not actually reflected in the way in which data were analysed or presented in the paper. Studies by Bury,140,216 Williams,141 Williams and Wood178 and Pinder221 were conceptually very useful to the synthesis, but were characterised by poor reporting of methods of data collection and/or analysis. These papers described various forms of case study approaches that sought to build lines of sociological argument. It might not even be obvious to the casual reader that these studies employed interpretive or qualitative research methods, as this was not always stated explicitly.
The synthesis was principally constructed on the seven following studies. The studies by Bury,140,216 Williams141 and Williams and Wood178 stood out for their theoretical contribution alone, whereas that by Stephens and Yoshida229 stood out for good reporting of methods. The studies by Wiener,138 Shaul177 and McPherson et al. 233 managed to combine conceptual coherence with good reporting and/or use of methods. The last two papers were both also grounded in the results of earlier ‘classic’ studies. The main value of Locker’s139 approach was that the book format allowed for a higher degree of ‘thick description’ and contextualisation of findings than that is found in the shorter journal articles.
The main contribution of three later studies to the synthesis was primarily as descriptive confirmation or elucidation of previous findings. 222,227,231 The value of the studies reported by Williams and Barlow227 and Brown and Williams222 became apparent only during the reciprocal translation stage. This is as an important point because, following initial ‘assessment by checklist’, the papers might have been rejected on grounds of quality or relevance. The studies by Rao et al. 226 and Archenholtz et al. 228 did not look as if they had employed an interpretive approach, although their findings did not conflict with other papers in the synthesis and they were not excluded, although they could have been on these grounds. In addition, neither paper was focused on RA, the latter also including patients with systemic lupus erythematosus, although both clearly incorporated the views of patients with inflammatory arthropathy. Three papers were characterised by poor reporting and/or poor methods, and also added little conceptually to the synthesis, although again they were not excluded on these grounds. 176,224,232 However, and in a similar manner to the Williams and Barlow227 paper mentioned above, the worth of the paper by Stenström et al. 176 became apparent only during the reciprocal translation stage. The importance of the paper by Bjørner and Hansen219 was that its topic – sexuality – was ignored in most of the other papers.
Findings
Lay perceptions of the causes of arthritis
Three of the five factors mentioned by Rice and Young’s220 respondents (damp and/or cold weather, ageing and injury) were also found in the two patient focus groups conducted by Lambert and Butin. 230 Rice and Young’s220 participants also mentioned heredity and diet. In the Lambert and Butin230 focus groups, diet was not mentioned as a cause of arthritis, but rather specific foods (red meat, coffee, sugar and junk food) were identified as exacerbating arthritis pain. Other causes mentioned only in the focus groups were viruses, bacteria, bursitis, close-fitting shoes and air pollution. However, in comparing the two studies, the main problem was that Rice and Young’s220 participants included people who did not have arthritis and these responses were not separated out from those of the other respondents.
Rice and Young220 noted that lay accounts of the aetiology of arthritis fell broadly into two types of explanation: firstly, just those that suggested internal, ‘mechanical breakdown’ as responsible, where ageing and injury were identified as factors; and secondly, those that saw arthritis as resulting from an outside agent that infected the body. It was reported both by Shaul,177 and Brown and Williams222 that people had attributed initial symptoms to ‘commonsense’ explanations like minor trauma or overexertion, which also pointed towards ‘mechanical’ explanations.
For people with RA, the search for an understanding of disease aetiology became a more personal matter, as part of the broader ‘attempt to establish points of reference between body, self and society, and to reconstruct a sense of order from the fragmentation produced by chronic illness’. 141 In the perceived absence of biomedical explanations for the disease,226,234 ‘the actual nature of the disease remains elusive’. 140 Without adequate scientific–medical explanations for such devastating ‘physical and social breakdown’,141 people turned to lay explanations reflecting that ‘the body is defined by its relationship to the world of social action not in isolation from it’ (p. 182). 141 In the account to follow, it will be shown that particular features external to the body become significant precisely because of characteristics within the individual, his or her place in society or his or her social milieu.
Living with the symptoms of rheumatoid arthritis
Pain dominated patients’ accounts of the illness experience in RA to such an extent that one could wonder whether pain was the issue at the heart of the matter, rather than RA itself. Many studies contained detailed accounts of the nature of pain in arthritis, although this concept was noticeably absent in Bury’s140 study. However, the abundance of work had fundamentally little to add to Wiener’s138 study of the sociological aspects of pain management in chronic illness. Wiener’s138 was also the earliest published study considered in the synthesis. Whether or not later studies referenced Wiener’s138 work, all those that contained findings about ‘pain’ demonstrated conceptual coherence with her framework and concepts.
Wiener138 noted four features of pain in RA. Firstly, there is an ‘absence of predictability’ to RA’s symptoms, including pain, which is characterised by ‘flare-ups’219 that come without signs or warning. Secondly, there is a ‘variability of progression, severity and areas of involvement’. 138 In other words, people with RA do not know from one day to the next whether they will be feeling better, worse or the same as they do today, or whether or not the disease will affect the same body part(s) as last time. However, the one ‘certainty’ is that sooner or later there will be pain. 139 Thirdly, Wiener138 also found that pain in RA had a ‘circuitous’ relationship with fatigue, such that ‘pain drains energy and fatigue produces more pain’ (p. 98). In later studies, ‘fatigue’ was sometimes mentioned as a separate symptom in its own right, rather than a concept in relationship with pain. Fourthly, Wiener138 noted that these features of pain in RA led to a ‘reduction in personal resources’ for the individual.
Wiener’s138 findings led her to two key interpretations. Firstly, the key concept in living with arthritis relates to ‘tolerating variable uncertainty’. Secondly, the disease conditions engender a ‘dread of [future] dependency [on others]’. Wiener’s138 twin theories were confirmed and rediscovered by most of the later published studies, but no single study has captured these concepts with such clarity and groundedness. Wiener’s138 findings were consistently validated by the findings of the other studies included in the synthesis. Furthermore, her reporting of research methods and methods of data analysis compared favourably with that found in other included studies.
Other work added further findings to Wiener’s138 basic schema. Locker139 completed detailed case histories and interviewed people twice, 1 year apart. He noted a further feature of pain in RA: that it ‘is often not accompanied by any signs which would help to verify the sufferer’s complaints’ (p. 132). 139 This is similar to Williams and Wood’s178 assertion that the symptoms of RA are ‘often vague’ although, for Brown and Williams,222 ‘vague’ was rather used to describe earlier symptoms, which were also characterised as ‘mild’ and ‘non-disabling’. Similarly, Pinder221 noted that both pain and fatigue provide considerable ambiguity, as they are not visible forms of disability.
Interestingly, apart from pain and fatigue, the only other typification of the condition of RA in the earlier literature reviewed was as a ‘crippling disease’ by Bury (p. 173),140 who also identified RA as ‘an outside force’ (see Lay perceptions of the causes of arthritis, above). The focus of earlier work was much more on coping strategies and the effects on social relations, which will be considered later. However, by 1989, Donovan et al. ,217 although still describing pain as the major symptom, also included ‘stiffness’ and ‘burning’ (p. 59). Bjørner and Hansen219 noted that flare-ups of arthritis were associated with reduced libido for some patients. Rice and Young’s220 folk model of arthritis identified ‘painful movement’ as a core concept, and also included ‘inflamed’ and ‘deformed’ joints as conditions, although their model was not necessarily applicable to specific types of arthritis.
From the mid-1990s, the practitioners of qualitative research into RA changed, and there was a discernible move towards descriptive studies highlighting the symptoms and conditions of the disease and their impact on physical and social functioning. This probably reflected the fact that these studies were being undertaken by people also involved in clinical practice, whereas earlier work had focused more on RA as an example of a painful, disrupting, disabling, chronic illness. Wiener138 was interested in the sociological aspects of pain management; Bury140 in the disruption to biography and relationships by chronic illness; Locker139 in RA as a form of social disadvantage; Williams141 in the application of the idea that people reconstruct their personal biographies in light of subsequent events; and Donovan217 in RA as a clinical encounter.
In later qualitative studies undertaken by nurses and others (although we should note that Wiener138 also came from a nursing background), there was a definite move towards a ‘disease-specific’ approach. At their best, these studies confirmed the findings of previous work while presenting results to clinical audiences. However, the reviewers characterised many of these studies as being of ‘poor’ methodological quality. One exception was the article by Shaul,176 which stood out as a far better study. Hers was the first paper to discuss areas of the body involved in RA symptomatology in any depth. For the women in Shaul’s study, ‘Most common symptoms involved the hands, wrists, shoulders and feet. In some cases pain and swelling occurred simultaneously, in others, pain occurred alone, followed by swelling. In either case, there was usually weakness in the affected limb and general fatigue’ (p. 292). 177 Shaul177 identified fatigue as the most ‘pervasive’ symptom, although both fatigue and pain were described as the most ‘distressing’ symptoms. These findings were further developed in a later study, where the root dissatisfaction with RA for female informants concerned the ‘visible swollen and disfigured appearance of these painful body parts’. 227 As one respondent to this study put it, ‘The swellings are like a physical effect of pain. You don’t want people to see the pain you are suffering’ (p. 131). 227 Although these findings seem partly to conflict with those of other studies which noted that the primary symptoms of RA are not obvious, they most probably reflect that in each case findings derived from people in different stages of the disease course (but see Discussion). The primary symptoms of arthritis lead to secondary symptoms, largely related to pain, and identified by: exhaustion, anger, depression, despair, self-pity and [perception of] loss of control. 223 Bjørner and Hansen219 similarly identified ‘low self confidence’, reduced libido and difficulties reaching orgasm.
Consequences for identity and problems maintaining taken-for-granted activities
This section is largely about the problems of maintaining ‘taken-for-granted’ actions and behaviours and the concomitant challenges to norms of behaviour (as perceived by self or others). The best term to capture these issues in the context of RA is probably Bury’s140 ‘biographical disruption’. In a later reflection on these data, he noted: ‘The onset and development of arthritis is simultaneously an assault on the body and a disruption of social life’. 216 This ‘biographical disruption’ centred on the loss of previous life and work identities, or in the metaphor employed by McPherson et al. ,233 loss of the individual’s ‘life definition’. Another metaphor related to these issues is Brown and Williams’222 ‘role incompetence’ (p. 699).
The experience of people with RA was mediated by certain sociological and physiological needs. The metaphors relating to these needs are detailed in Table 20 and are grouped according to the focus on symptoms, personal biography, presentation of self and social roles, and further categorised into intrinsic and interpersonal needs. The studies showed how RA brought previously taken-for-granted actions and behaviours into sharp focus. As Pinder221 put it, ‘The conditions under which people take themselves for granted may be compromised’ (p. 610). As important in this context were the conditions under which other people take the person with arthritis for granted. Some of these conditions were ‘expectations governing behaviour in the wider culture’. 216 As Williams and Wood178 noted, such social or cultural ‘norms’ may be unspoken, which seems to be a large part of the problem for the person with RA: ‘Informal structures like families contain unstated norms of reciprocity or give-and-take, and for many people the experience of disablement is one of having these norms upset’ (p. 130). It is evident that there are as many expectations governing physical functioning or the ability to do things as there are in relation to fulfilling social obligations. Table 21 shows that many of the factors causing disruption in the social lives of people are related to expectations governing social and cultural actions whether at home or in the workplace.
| Types of need | Study |
|---|---|
| Intrinsic | |
| Symptom focused (Wiener, 1975;138 Locker, 1983139) | |
| ‘Relief from pain’ | Rao et al., 1998, p. 256226 |
| ‘The feeling of being in control of the symptoms is vital’ | Gilworth et al., 2001, p. 345231 |
| Biographically focused (Bury, 1982) 140 | |
| ‘To identify the causes of her arthritis’ | Williams, 1984, p. 192141 |
| ‘To reaffirm telos and to reconstruct order in the presence of profound disruption in the biographical processes of daily life’ | Williams, 1984, p. 192141 |
| ‘To prevent the onset of disability and deformity’ | Donovan et al., 1989, p. 60217 |
| ‘Maintenance of one’s identity’ | Stenström et al., 1993, p. 237176 |
| Attitude focused | |
| ‘Learning to live with it’ | Bury, 1982, p. 173140 |
| ‘Learned to live with pain’ | Locker, 1983, p. 16139 |
| Does not ‘give in’ | Williams and Wood, 1988, p. 130178 |
| ‘Mental balance’ | Stenström et al.,1993, p. 237176 |
| Interpersonal | |
| ‘Presentation of self’ focused | |
| Avoid embarrassment | Bury, 1982, p. 175;140 Locker, 1983, p. 38139 |
| ‘Avoiding unpleasant reaction’ | Bury, 1988, p. 101216 |
| ‘You don’t want people to see the pain you are suffering’ | Williams and Barlow, 1998, p. 131227 |
| ‘To present themselves as morally competent actors in the workplace’ | Pinder, 1995, p. 624221 |
| Self-sufficiency | Stephens and Yoshida, 1999, p. 23229 |
| Social role focus (Bury, 1988;216 Williams and Wood, 1988178) | |
| ‘Reciprocate for favours or help’ | Bury, 1982, p. 175140 |
| ‘Personal integrity’ | Stenström et al., 1993, p. 237176 |
| ‘Overcoming isolation and maintaining contact with family, friends and neighbours’ | Moss, 1997, p. 27225 |
| ‘Trying to retain as much autonomy as possible’ | Stephens and Yoshida, 1999, p. 23229 |
| Type of Disruption | Studies |
|---|---|
| Changed appearance | ‘Visible changes … made them less attractive to their partners and potential partners’ (Williams and Barlow, 1998, p. 134);227 ‘People in their social worlds would see only the disease rather than the person within’ (Williams and Barlow, 1998, p. 131);227 Difficulties finding a sexual partner (Bjørner and Hansen, 1993)219 |
| Changed abilities | ‘Reduction of personal resources’ (Wiener, 1975, p. 98);138 warrantability of a person’s changed behaviour (Bury, 1982, p. 180);140 ‘Chronic illness undermines … autonomy and routine’ (Williams and Wood, 1988, pp. 130–1);178 ‘Their bodies appeared to have become detached, creating a hiatus between their wishes and their actions’ (Williams and Wood, 1988, p. 129);178 ‘Influences physical capacity’ (Stenström et al., 1993, p. 240);176 changes in the way work is tackled (Bjørner and Hansen, 1993);219 inhibits sexual activity, makes sex painful (Lambert and Butin, 2000;230 Bjørner and Hansen, 1993219); arthritis makes everyday life difficult (Lambert and Butin, 2000);230 ‘Implications for current life definition and self-perception relative to life without disability’ (McPherson et al., 2001, p. 710)233 |
| Interpersonal relationships | Dread of dependency (burden on others) (Wiener, 1975,138 key concept; Donovan et al., 1989;217 Brown and Williams, 1995, p. 699);222 loss of friends through difficulties keeping plans and having to cancel at the last minute (Williams and Wood, 1988;178 Brown and Williams, 1995, p. 699222); changes in roles/work sharing (Bjørner and Hansen, 1993);219 the partner needs to be trained in how to do new things (Bjørner and Hansen, 1993);219 ‘Makes social relationships more complicated’ (Stenström et al., 1993, p. 240)176 |
| Cultural impediments | ‘The illness is in many ways incompatible with the organisation of work’ (Locker, 1983, pp. 98–9);139 difficulties in maintaining the reciprocal nature of family relationships (Williams and Wood, 1988);178 ‘The burden they felt their physical care caused for others’ (Brown and Williams, 1995, p. 699);222 the way one is viewed by strangers (Moss, 1997, p. 30);225 bodily changes as a taboo area (Williams and Barlow, 1998, p. 131);227 responsibility for domestic chores still resides with the woman (Bjørner and Hansen, 1993);219 ‘The wider social and cultural significance of illness in the workplace’ (Pinder, 1995, p. 605);221 ‘Society at large is not organised to help disabled people’ (Archenholtz et al., 1999)228 |
| Changing social status | ‘Women frequently complained of their diminished roles as homemaker’ (Wiener, 1975, p. 102);138 ‘A deep sense of loss’ because ‘chronic illness caused them to fail in a valued role’ (Locker, 1983, p. 84);139 ‘Coming to terms with their own embarrassment about being “different,” as well as the discomfort it aroused in others’ (Williams and Wood, 1988, p. 131);178 ‘feeling alienated from friends, family and co-workers’ (Shaul, 1995, p. 293);177 partners of women ‘taking on aspects of what had hitherto been women’s domains’ (Brown and Williams, 1995, p. 699);222 ‘Illness carries … disturbing connotations relating to contagion, pollution and taboo’ (Pinder, 1995, p. 624);221 ‘Bodies which are flawed or conspicuously ill convey powerful symbolic messages concerning social order and disorder’ (Pinder, 1995, p. 624);221 ‘The presence of ‘visible disease’ was invasive, threatening their private and public selves’ (Williams and Barlow, 1998, p. 131)227 |
So far as ‘the material world’ and physical activities were concerned, the most detailed exposition of the effects of RA ‘as a disablement’ was that provided by Locker. 139 Usefully, he followed Wiener,138 and noted that the uncertain course of symptoms in RA called for ‘continuous monitoring and self-management since little can be taken for granted’. 139 ‘Activity, however minimal, requires physical and psychological effort’ (p. 19). 139 The ‘erstwhile, taken-for-granted world of everyday life’140 becomes ‘fraught with danger’ and ‘everyday objects and events take on an alarming character and may give rise to feelings of insecurity’. 139 One possible response to such dangers was to never leave the house, although such a response may leave people feeling that they were ‘locked-in’. 223
Responses and coping strategies
The studies showed that the main factors that affect people’s experiences of RA are the symptoms of the disease, the nature of the cultural backdrop, and expectations governing norms of social roles and behaviour. Certain consequences derive from these factors, which affect the ways in which people can or cannot cope with the disease. The psychologically oriented data also pointed towards a ‘career’ model of adaptation to RA, although an attempt to synthesise the studies along these lines was unsuccessful. However, the attempt yielded insights into both the nature of the studies themselves and the experience of adapting to life with RA. As with psychological coping strategies, it seemed as though the idea of an illness ‘career’ probably reflected more the professional and academic standpoint of the authors of the studies than it did the data gathered during the interviews. That is, concepts such as ‘mastery’177 or ‘taking charge’230 were more fundamentally associated with clinical imperatives surrounding treatment, cure and rehabilitation than they were patient perceptions. (Both reviewers felt that Shaul’s177 concept of ‘mastery’ of disease was not clearly evidenced by the findings presented in her paper.)
A further problem derived from the fact that many studies were cross-sectional in nature and were focused on people with more problematic or advanced disease, problems or disability. However, the failed attempt to synthesise the studies around the theme of illness career may say something about the nature of RA itself. Thus, it may be that the pervasive uncertainty and unpredictability of RA means that some people never manage to ‘master’ or ‘take charge’ in RA and, in effect, the disease ‘wins’. Alternatively, people may think that they will one day ‘master’ the disease, but repeated failed attempts lead to a sort of progressive disillusionment. So long as studies remain focused on captive clinical populations, we may never find answers to these questions, as the views of people who can cope, whose flare-ups are not so bad, or for whom the disease is ‘in remission’ were not included in the available research, which was more fundamentally concerned with describing the lives of chronically disabled people trying to cope with severe and debilitating disease.
Tables 22a and b outline the main coping strategies described in the studies. Those described in Table 22a seem to constitute ‘grand’ strategies related to activity in general. Those strategies presented in Table 22b are specific to different arenas: intrinsic strategies, interpersonal strategies, public strategies, and strategies relating to the environment.
|
‘Pacing/keeping up with normal activity’ (Wiener, 1975, p. 100)138 ‘Lowering expectations’ (Wiener, 1975, p. 101)138 ‘Developing a new set of norms for action’ (Wiener, 1975, p. 101)138 ‘Eliciting help’ (Wiener, 1975, p. 101;138 Donovan et al. , 1989, p. 60:217 ‘the last resort’) (decreases the potential of using other strategies) ‘Thinking it out’ (plan or avoid activities) (Locker, 1983, p. 71)139 ‘Individuals, families and others frequently test the limits of their relationships, particularly the amount of support and care they are able or willing to afford each other’ (Bury, 1988, p. 113)216 ‘Changing the way they did things, consciously or unconsciously’ (Donovan et al. , 1989, p. 60;217 also ‘modify tasks’ in Stephens and Yoshida, 1999, p. 239;229 ‘Changing or adapting their jobs’ in Gilworth et al. , 2001, p. 344)231 Some women react to renewed illness by isolating themselves (Bjørner and Hansen, 1993;219 also ‘self-imposed isolation’ in Dildy, 1996, p. 180)223 ‘[They] became experts at recognizing the cues that signal the onset of a flare, of overwork or the need to change a pattern of activity through the acquisition of knowledge about the disease, its treatment, and experience of living with it’ (Shaul, 1995, p. 295)177 ‘Not use an assistive device; or be selective in terms of where help or an aid is used’ (Stephens and Yoshida, 1999, p. 239)229 |
| Intrinsic | Interpersonal | Public/societal | Environmental |
|---|---|---|---|
|
Use alternative remedies (Donovan et al. , 1989)217 Take multiple medications (Rao et al. , 1998, p. 255)226 |
‘Concealing disability and/or pain’ (Wiener, 1975, p. 99)138 Concealment, grooming behaviours (Williams and Barlow, 1998)227 |
‘Modifying the dwelling structurally, using assistive devices, arranging physical space according to ability and adjusting the body to the environment’ (Moss, 1997, p. 27)225 | |
| ‘For Marilyn, the mystification underlying the disease can be gotten around through shifts and changes in the physical and social aspects of her home environment’ (Moss, 1997, p. 28)225 | |||
| ‘Pay for help rather than receive it informally’ (Stephens and Yoshida, 1999, p. 239)229 | |||
| ‘[Florence] continues to neglect her health in the face of maintaining social interaction’ (Moss, 1997, p. 29)225 | ‘Planning and routing not only reduce the physical difficulty of moving around the community, they do so in a manner which helps to preserve the person’s public identity’ (Locker, 1983, p. 87)139 | ||
| Men felt through regular exercise ‘they were able to play an active role in controlling their disease’ (Williams and Barlow, 1998, p. 136)227 | Flexibility in the couple’s roles, so that the partner can step in and take responsibility for tasks when necessary (Bjørner and Hansen, 1993)219 | ||
| ‘Self-determination and agency’; ‘Struggle to do difficult tasks by themselves’ (Stephens and Yoshida, 1999, p. 239)229 | ‘Refuse offers of assistance’; ‘Avoid people who give unwanted help’ (Stephens and Yoshida, 1999, p. 239)229 | ||
Perceptions and experiences of treatment
Surprisingly (given that the interview samples were derived largely from people in clinical settings), perceptions and experiences of care were not a major feature of these studies. An exception was Bury,140 who noted that as medical intervention appeared ‘both important and limited’ (p. 173), medical knowledge in the context of RA was both a resource and a constraint. In a similar manner, Locker139 found that because all treatments involved risks in terms of side effects, ‘the disadvantages may outweigh the advantages to be gained’ (p. 62). Within a focus on individuals’ needs to ‘identify the causes of arthritis’ (p. 191), Williams141 noted, ‘the limitations of medical science in delivering a satisfactory explanation’ (p. 175) and also asserted within this context that ‘medicine can support political bureaucracy in preventing the establishment of social justice’ (p. 185).
Similarly, Brown and Williams222 reported that some of the seven women nursed by the interviewer expressed frustration at the perceived ‘medical impotence’ (p. 698). However, they were also relieved at being referred to a specialist and receiving ‘an acceptable name or diagnosis for their symptoms’ (p. 698). Similar themes were evident in Shaul (p. 292):177 ‘In many cases, the first experiences of medical management were not helpful, as many were misdiagnosed or found that their complaints were not taken seriously’. Ryan224 reported complaints about ‘too much emphasis placed on the physical manifestations of the condition’ (p. 48), and not always being reviewed by the doctor, but these issues did not seem specific to patients with RA. Similarly, Archenholtz et al. 228 mentioned ‘lack of continuity of care, not always the same doctor, [and] difficulties making appointments’.
The most detailed consideration of the issues was that provided by Rao et al. ’s226 focus group study, which usefully compared RA patients with people with osteoarthritis. As in Lambert and Butin’s230 patient focus groups, ‘[some] believed that doctors could do very little to relieve pain or cure the underlying disease’ because ‘arthritis has no known cause or cure’. 226 Interestingly, when compared with the osteoarthritis patients, RA patients more frequently mentioned ‘their trust in the physician’s ability to treat their arthritis’ (p. 259). 226 Other findings were that medications were only effective for short periods of time (p. 255) and that ‘Several patients wished that a single medicine instead of multiple medications could be used to treat their arthritis’ (pp. 255–6). 226
Gender
Given that RA disproportionately affects women, it was perhaps unsurprising that gender roles were particularly emphasised in these studies. However, although some of the papers seemed to have chosen RA as a focus for study precisely because of the likely gender issues, the conceptual development in this field is weak and generally not related either to the existing studies in RA or to wider feminist or gender theory.
A generic weakness across the studies seemed to be the attempt to explain the experiences of women by analysing their accounts in isolation from those of men. A notable exception here was the study by Bjørner and Hansen. 219 It was particularly disappointing that the conceptually rich account provided by Pinder221 seemingly excluded men at the analysis stage. We suspect that the reason for excluding male accounts was ostensibly to ‘strengthen’ the focus of the accounts on the experiences of women, but it could be argued that this approach actually had the opposite effect.
Once again, the main issues were covered in Wiener’s138 ground-breaking study and related to the fact that, within the traditional domestic division of labour, men and children have a stake in women remaining active. Where men take on what were once women’s roles, ‘role reversal may result in a permanent change in the household’s division of labour’ (p. 102). 138 Ultimately, the relevant issues did not seem to point towards gender per se, but rather towards the more general loss of the ability to engage in activities once seen as mundane. Whether for worker221 or homemaker,222 it was precisely these taken-for-granted activities which constituted a large measure of self-identity. 222 Some of the women interviewed in the studies complained that the support they were receiving from partners was ‘too much’, as such support was felt to be eroding their social roles. 232 Reading across the studies, however, it was evident that similar issues also applied to men:223
I’m no longer the man I used to be. I am no longer the husband, the lover, you know, all of the aspects of my life, they’re no longer there.
The one attempt to seemingly systematically compare accounts from women with those from men was found in the study by Locker139 who, in contrast to the other studies already cited, Locker noted that ‘The women experienced job loss as acutely as the men and few were content to settle into the role of housewife’. Thus, we are left wondering whether or not the sorts of gender issues highlighted in the studies were particular to women, or whether or not they were made particular in the way that data were collected and analysed.
Interpersonal gender dynamics received more attention in the two Scandinavian studies,176,219 and the main findings seemed to further underline Bury’s140 assertion that much of the success in coping with RA seems to hinge upon the degree of flexibility possible in both formal institutions and informal relationships:219
In the beginning Soren was going to help me with the cooking, but that was no good. I wanted everything done my way. Now we each do our own things, but duties are not fixed. Soren just does the things he knows I can’t do, and when I am feeling rough he just takes over. It isn’t something we talk about much.
Discussion
The main findings of the studies concerning coping strategies in RA, and the experience of living with the illness were probably best represented in the earlier ‘classic’ studies. Although the synthesis has not added much conceptually in relation to these issues, one of the main reasons for this was that many later studies were confirmatory rather than offering conceptual development or innovation. They did not refine or develop the concepts of earlier studies, in relation to either gender or the different ‘stages’ of the disease. Most of the studies were cross-sectional in nature. Although some authors (e.g. Shaul,177 Bury140 and especially Locker139) did follow people over time, these respondents were seemingly already at the ‘chronic’ end of the spectrum to start with.
As we noted at the outset of this chapter, some of the earlier classic studies included in this synthesis were characterised by poor reporting of methods of data collection and/or analysis. Assuming the integrity of past classics, as we did, where transparency about the methods used is absent or poor is questionable. However, we feel that our decision was vindicated in this case because the later papers, for which the reporting of methods was much better, and in which there seemed to be no awareness of the earlier classic papers, nevertheless, produced very similar findings.
Our synthesis also raises all sorts of questions about the nature and value of qualitative research. Given the repetitive nature of the findings of the studies, and their large number, we would call into question the necessity of further work in this field, particularly work which fails to build on or develop what is already known. Although there was a conceptual coherence among these studies that rendered their synthesis easier, we found evidence that later studies had stopped referencing earlier work (Table 23). For example, Wiener138 was last referenced in Shaul’s177 paper and now seems to have been consigned to history, even though the synthesis has found that the findings of her study are still being rediscovered by more recent researchers. This could reflect a tendency in science and medicine to search only for more recent work, an implicit assumption of this approach being that previous authors will have already read and incorporated the salient aspects of relevant work. The implication for qualitative researchers is that they need to search back further for relevant studies before repeating work that has already been done. The implication for synthesists of qualitative studies is that they will need to have an open-ended attitude (date wise) when searching for relevant studies.
| Source papers | Source papers referenced |
|---|---|
| Wiener, 1975138 | |
| aBury, 1982;140 Bury, 1988216 | aWiener, 1975;138 Bury,1982;140 Locker, 1983;139 Williams, 1984141 |
| Locker, 1983139 | Wiener, 1975;138 Bury, 1982140 |
| aWilliams, 1984;141 Williams and Wood, 1988178 | aBury, 1982;140 Bury, 1988;216 Locker, 1983139 |
| aDonovan et al., 1989;217 Donovan, 1991218 | Locker, 1983;139 aWilliams, 1984141 |
| Bjørner and Hansen, 1993219 | Wiener, 1975138 |
| Stenström et al., 1993176 | Wiener, 1975;138 Williams and Wood, 1988178 |
| Rice and Young, 1994220 | |
| Pinder, 1995221 | Bury, 1988216 |
| Shaul, 1995177 | Wiener, 1975138 |
| Dildy, 1996223 | |
| Brown and Williams, 1995222 | Bury, 1988;216 Locker, 1983;139 Williams, 1984141 |
| Ryan, 1996224 | |
| Moss, 1997225 | Locker, 1983;139 Williams and Wood, 1988178 |
| Rao et al., 1998226 | |
| Williams and Barlow, 1998227 | Stenström et al., 1993176 |
| Archenholtz et al., 1999228 | |
| Stephens and Yoshida, 1999229 | Locker, 1983;139 Wiener, 1975;138 Williams and Wood, 1988178 |
| Lambert and Butin, 2000230 | |
| Gilworth et al., 2001231 | |
| Grant, 2001232 | |
| McPherson et al., 2001233 | Bury, 1982;140 Ryan, 1996224 |
We are likely to learn more about chronic illness through different forms of cross-cultural analysis, a point made by Wiener138 in 1975. She suggested that her theoretical framework could have been expanded by ‘sampling under different conditions, for example in another culture’ (p. 102). 138 Unfortunately, later qualitative researchers chose to ignore her advice and instead reinvented the theoretical wheel of experience and adaptation in RA in clinically captive Western populations. This synthesis underlined the value of Wiener’s138 paper, which to this day seems the best at capturing the essence of lay experiences of RA. However, this point emerged only when her work was systematically compared and synthesised with subsequent studies.
This synthesis raises questions about the usefulness of attempting to synthesise a body of qualitative research within a very narrowly defined clinical area. With hindsight, it may have been more fruitful to synthesise studies within a broader field, say ‘chronic illness’, which seemed to be the topic that interested some of the study authors in the first place. Nevertheless, it may be that our findings could be presented to clinicians and patients in a way that would be helpful in order to highlight the patient’s perspective or provide information relevant for self-help or professional care.
Following our experiences in this and other synthesis projects, and discussions with others, we feel that there will be much to gain from future synthesists searching for the ‘absences’ and the ‘audible silences’15 in reports of qualitative studies. This synthesis is based on the substance of what was present in the findings of the included papers, but we could have learned more by focusing on what was missing. For example, it is noteworthy that patient experiences of health care did not feature much, even though most interviewees were derived from patient settings. Further, despite statements in some of the papers to the effect that the insights of qualitative studies can inform and improve patient care, specific implications or recommendations for care or treatment were also largely notable by their absence. Although some of the practitioners’ papers were indicative of studies undertaken by researchers at the beginning of their research careers, or primarily for professional development purposes, others138,179,233 constituted substantive studies. However, even these studies failed to draw out implications for treatment and care.
With more absences in mind, and notwithstanding our earlier comments about the usefulness of further research, our synthesis points to those areas in which further work might be done. We have already pointed out a need for cross-cultural studies and more detailed work around gender. Perhaps, more fundamentally, there is a need to capture the views of people with RA who inhabit the world outside the treatment system, or those who can cope, perhaps with milder disease. At present, our understanding of lay ‘coping strategies’ is largely skewed towards samples of people who, by definition, cannot cope. Essential concepts derived from the synthesis point towards a narrative or biographical approach, but this needs to somehow extend into the time horizon preceding disruption or reconstruction.
Chapter 8 Discussion
The value of syntheses
At the outset of this evaluation, we noted a number of objectives that might be attained through qualitative syntheses. In particular, it was suggested that they could bring together isolated qualitative studies and provide an accumulated understanding on a particular theme; that they could go beyond the detailed summarising of the traditional narrative review by achieving fresh insights, conceptual development and theory building; and that they could complement quantitative research by providing a more comprehensive understanding of a variety of phenomena. A primary purpose of this evaluation was to complete two full-scale qualitative research syntheses using meta-ethnography. We succeeded in this by producing a detailed synthesis of qualitative studies of medicine-taking, and a synthesis of qualitative studies of people’s experiences of living with RA. In doing so, we have demonstrated that these objectives are achievable.
The synthesis into medicine-taking has produced major new insights. It has shown that the reason why patients do not take medicines as prescribed is not because of failures in the doctor–patient consultation, as volumes of previous work have suggested, but because people have real concerns about the medicines themselves. These concerns had been voiced in qualitative studies, but it was only when brought together through the painstaking process of reciprocal translation that the significance of this evidence became apparent. This synthesis, however, went beyond simply drawing attention to these findings. It also produced an explanation for why people’s concerns about medicines were overlooked for so long and went on to propose resistance to medicine as a concept which best encapsulates lay responses to medicine. Another product of this synthesis was the model of medicine-taking which describes the various pathways which people might follow after a medicine has been prescribed for them.
On the other hand, it is possible that syntheses will not always reveal new insights. Although the RA synthesis shed new light on the range of ways in which the social relationships of those with RA were disrupted (see Table 21) and the general and specific coping strategies that those with RA employed (see Table 22), there was little to add to the conceptually rich earlier ‘classic’ studies. Thus, this synthesis did not produce significant new insights, but it did serve an important function in demonstrating what cumulative knowledge there is in this area.
Both of the meta-ethnographies conducted demonstrate the value of qualitative synthesis in establishing what is known and what remains unknown or hidden about a topic at a given point in time. They also illustrate how it is possible to trace conceptual development, or the lack of it, within a field. Within the field of medicine-taking, many of the earlier sociological studies focused on challenging the concept of compliance, rather than developing new theory, whereas the later, practice-based literature has been mainly descriptive. Similarly, in the earlier studies in the RA synthesis, there was evidence of considerable conceptual development around both patients’ experiences of RA specifically and of chronic illness more generally, but little by way of theoretical advance detectable in the later papers.
Additionally, our work illustrates that qualitative syntheses can highlight the various positions adopted by authors and, in the case of the medicine-taking synthesis, the involvement of sociologists with the medical agenda became clear only as the papers were synthesised. Perhaps most importantly, syntheses can provide a weight of evidence. In the medicine-taking synthesis, for example, only one of the studies173 dealt explicitly with the lay evaluation of medicines in any detail, yet when synthesised, the studies revealed many data on this topic, substantially more than any individual study produced alone. The synthesis could not complete the detail for some aspects of the lay evaluation of medicines but has revealed the practice to be widespread. This synthesis also produced a weight of evidence about people’s concerns with the safety of their medicine that has not been found elsewhere. Single studies reporting worries about medicines are not taken to be sufficient evidence, yet when studies are brought together the weight of evidence is hard to ignore.
One of the great values of a qualitative synthesis, it seems to us, lies in the systematic and comprehensive approach that it brings to reviewing the literature. Both our syntheses revealed that only a minority of the studies referenced each other. This was the case in the medicine-taking synthesis even when papers were about the same medicines. We found a similar picture in our earlier pilot synthesis on patient experiences of diabetes. 17 This suggests that qualitative health research is not an evolving process whereby new studies build on earlier ones and research is conducted only after the relevant literature has been reviewed and important questions identified. Rather, among the later studies in each of the syntheses, there appeared to be little regard for earlier relevant studies and, certainly within the medicines for treating HIV infection and experience of RA literature, a tendency for studies to replicate each other. Another important aspect of a qualitative synthesis may therefore be to indicate when it is time to draw a line and strongly discourage further research on a particular topic. In making this judgement, it may be helpful to apply the notion of saturation, rather as one would in primary qualitative research. In the RA synthesis, it was clear that in more recent studies there was no new conceptual or theoretical development taking place, suggesting that ‘saturation point’ had been reached, at least as far as studies of the experiences of clinical groups of people with RA were concerned. While wishing to prevent ‘me too’ qualitative studies in this way, it is important to recognise the possibility that further research could lead to new directions and insights, if it was, for example, informed by a new theoretical approach.
The fact that we have found, in meta-ethnographies that we have conducted on three different topics, that only a minority of studies reference earlier work is not just an argument for the value of qualitative synthesis, but also a source of concern about the research practice of primary qualitative researchers. This finding indicates that those of us providing training in qualitative research methods evidently need to do more to emphasise the importance of a thorough literature review as a prelude to any qualitative research.
In the same way that qualitative syntheses could be useful in revealing where there has been sufficient research, they may also help to indicate where further research effort needs to be focused. Our experience of conducting the RA synthesis in particular taught us that it was important to pay attention to absences or, as Noblit and Hare15 termed them, ‘audible silences’. In the case of RA, it became clear that most of the qualitative studies had based their research on clinical groups of patients. Consequently, the strong focus in the research on the immense disruption that RA wrought on people’s lives may have been a reflection of this. The voices of those with RA who were not receiving clinical care for their RA, and for whom RA may have represented less of a disruptive and disabling experience, were not present. Syntheses are also able to reveal aspects of a body of literature that are disguised; the medicine-taking synthesis unveiled people’s real concerns about the safety of medicines which had in effect been rendered absent by their labelling as lay beliefs.
Meta-ethnography as a method of qualitative synthesis
Stages in a meta-ethnography
The studies in both syntheses were concerned with two specific topics but were conducted in several different countries, with disparate samples and methods and for varying readerships. In the case of the medicine-taking synthesis, they also involved a diverse group of medicines. Nevertheless, it was possible, using meta-ethnography, to systematically draw these studies together to present something new. Having completed three syntheses, it is our considered view that reciprocal translation is at the heart of why meta-ethnography is an effective method of qualitative synthesis. The requirement of systematically relating findings from different studies to each other makes it possible to establish new relationships between concepts, such that it is possible to conceptualise an issue in a coherent but fresh way. Following the reciprocal translation stage, the necessary reordering, relinking and reanalysis of material that a synthesis entails represents in itself new material or new findings and may in this case correspond to what Noblit and Hare15 called a ‘lines-of-argument’ synthesis. In the medicine-taking synthesis, the line of argument was both written and summarised and depicted diagrammatically in the model of medicine-taking (see Figure 16). However, further concepts may advance from this level, what Britten et al. 16 called ‘third-order’ concepts. In the medicine-taking synthesis, there were two such concepts: the notion that the medicines themselves needed to be brought back into the debate about medicine-taking and that the way in which many lay people respond to medicines is best characterised by the concept of resistance. In the RA synthesis, the lines-of-argument synthesis was presented in both a written and a tabular form.
Noblit and Hare15 suggested that there were three possible types of synthesis: reciprocal translation, refutational and lines-of-argument. As the preceding paragraph suggests, our experience is that there are three stages of qualitative synthesis in a meta-ethnography with reciprocal translation the first crucial stage. It requires the synthesiser to consider all the concepts and findings in each study in relation to all other studies. One of the concerns about qualitative synthesis is its potential to destroy the integrity of the initial studies. We consider that reciprocal translation protects against this because the method requires taking account of all the findings and concepts in each study and assiduously considering what each means. The next stage involves a process of reordering, relinking and reanalysis, finally leading to a representation of the synthesised material as line of argument. Beyond this there may be a further level of abstraction and conceptual development.
Identification of studies to be included
A key requirement of quantitative syntheses is to achieve an exhaustive search of the literature. Other research groups, using modified versions of meta-ethnography, have conducted extensive literature searches on broad topics. For example, Paterson80 followed the procedures of quantitative synthesis and retained all studies that satisfied the appraisal criteria, resulting in the meta-synthesis of 292 studies of chronic illness. Noblit and Hare15 regarded wide-ranging literature search as useful but not a requirement, depending on purpose of the meta-ethnography. They emphasised that the selection of studies should be made on the grounds of relevance to the topic and should include a range of studies likely to enable new insights. They warned that ‘… generalizing from all studies of a particular setting yields trite conclusions’ (p. 28). 15 We searched only for papers within a 10-year time frame for both the RA and medicine-taking syntheses, although in the case of the former we subsequently included a purposive sample of earlier ‘classic’ papers. In addition, the medicine-taking synthesis included only English-language papers, whereas in the RA synthesis non-English-language papers were considered, and one such included paper required translation, thus increasing the resources and time required.
The reciprocal translation stage is very time-consuming. It and the subsequent stages of synthesis also require the synthesiser to be immersed in all the studies. This places practical limits on the number of papers that can be synthesised. In the medicine-taking synthesis, it was necessary to begin by grouping the papers according to the type of medication as a way of making the task more manageable. Even so, it was difficult to conceive of synthesising many more than the 38 papers included in that synthesis without there being a trade-off between the breadth of papers included and the depth of the scrutiny and thought invested in the various stages of synthesis.
The practicalities of handling large numbers of studies may result in using processes of data selection, management and computing that lead to context stripping, and a less detailed immersion of researchers in the studies to be synthesised. Specialist computer packages are being developed to assist the synthesis of qualitative research, and these are likely to encourage the synthesis of greater numbers of studies, but this approach will potentially change the nature of the meta-ethnographic synthesis towards a more procedural and less interpretive approach.
Noblit and Hare15 were mainly concerned with identifying the relevance of studies and their potential contribution to the question of interest. As we noted in Chapter 4, most syntheses employing meta-ethnography, or methods of synthesis derived from meta-ethnography, have followed Noblit and Hare’s15 approach and not undertaken a formal appraisal of quality. From our experience, an important benefit of the use of formal appraisal criteria was to encourage the close reading of studies as an aid to interpretation. We also found it helpful to be able to discuss papers within the research team. We did exclude papers on the grounds of relevance, or because they did not conform to our definition of qualitative research as involving both qualitative methods of data collection and data analysis. This latter criterion ensured that we excluded qualitative work that was fatally flawed. Yet, in spite of our very detailed appraisal of studies, we did not exclude any studies on quality grounds. Some studies made an important contribution to the synthesis because of their conceptual strength, although their methods, as formally assessed, were weaker (or inadequately described), whereas other studies largely fulfilled the quality checklist in terms of methods but made little conceptual contribution to the synthesis.
We regard the quality of qualitative research as a very important issue. However, we look on the appraisal of qualitative research as more of a concern for the funders and publishers of qualitative research than for the qualitative synthesiser. This is because we have found that weak studies either will not synthesise or will contribute only minimally to a synthesis, adding weight to the better studies. Although there is an argument that including weak studies gives them an unwarranted credibility, such studies do not unduly distort a qualitative synthesis in the way that a poor-quality, highly biased quantitative study could influence a meta-analysis. In a qualitative synthesis, it is the power of ideas that matters.
Reproducibility and validity
The commissioning brief for this project was for methodological work ‘to enable users of qualitative work to both appraise and synthesise qualitative studies in a rigorous, replicable and formalised way’. 10 Meta-ethnography, as described by Noblit and Hare,15 is a rigorous approach to synthesis but it is also an interpretive approach. Consequently, a high level of reproducibility would not be expected. Indeed, the authors acknowledged this and did not view it as problematic, rather the contrary. They advised that ‘Like all interpretations, a meta-ethnography is but a “reading” of what is studied. Other readings are possible and are to be encouraged. However, all interpretations must be grounded in the texts to be synthesized’. 15 Evidence from the reproducibility exercise included within this evaluation is equivocal. Without repeating an entire synthesis, it is difficult to know whether the similarities and differences between the two sets of initial syntheses produced would have become more or less pronounced. (Since the work for this report was completed, we have undertaken an exercise to explore this issue. PP, the key author of the medicines synthesis, undertook a synthesis of all the papers in the RA synthesis. As expected her ‘reading’ of these papers was a little different, but the overall result was the same as the RA synthesis included in this report: it did not produce any substantial new insights.) Pilot syntheses and comparability/reproducibility exercises may have another valuable function, particularly for the first-time synthesiser, as a rehearsal for the full synthesis.
Noblit and Hare15 took a subtle relativist stance and accepted that an interpretation is but one possible interpretation, but also noted that the ethnographer reveals a limited relativism because the range of perceptions is influenced by context and socialisation. Noblit and Hare15 therefore adopted a position held by many qualitative researchers that worth is judged by the understandings and explanations derived rather than by assessments of the validity of processes. Noblit and Hare15 acknowledged that their approach may be regarded as overly relativist as they were essentially dealing with ‘interpretations of interpretation’. Nevertheless, they identified five criteria drawn from writings of qualitative researchers for what constitutes a good synthesis. These criteria related to the adequacy of metaphors (we have always understood metaphors to mean concepts in this context) in synthesising diverse studies which they suggested needed to be assessed according to the following criteria: economy – a metaphor is adequate when it is the simplest concept that accounts for the phenomena and has a superior ‘ease of representation’;234 cogency – a metaphor is adequate when it achieves the explanation without redundancy, ambiguity and contradiction;234 range – refers to the power of the metaphor in incorporating other symbolic domains;234 apparency – ability of language to (seemingly) ‘show’ us experience rather than merely refer to it;235 and credibility – adequate metaphors must be credible and understood by the audience. 236 Noblit and Hare,15 therefore, regarded the worth of a synthesis to be judged by the quality of its metaphors and whether or not the synthesis was regarded as useful and insightful by the intended audience.
Audiences
The issue of the audience for qualitative syntheses is an important one. There are a number of potential audiences for the two syntheses contained in this report. For the medicine-taking synthesis the relevant audiences are health policy-makers, clinicians, research funders, academic health researchers and those involved in the manufacture and control of medicines. In the case of the RA synthesis, the most relevant audiences are health practitioners and others caring for and working with people with RA (for example those providing social, educational, environmental, employment or housing services), people with RA and academic health researchers. These audiences are varied and the format for presenting the syntheses needs to vary accordingly. There is still work to be done on how to present and effectively disseminate the findings from qualitative syntheses. There are examples from within the quantitative review tradition that provide possible models, for example the ‘Guides for the public’ produced by the National Institute for Health and Clinical Excellence, which complement the formal guidance issued to health-care providers and any systematic reviews on which that guidance is based (www.nice.org.uk).
Place of meta-ethnography
Qualitative syntheses published prior to the present HTA project (and subsequently) have identified the value of this approach in informing policy and practice by contributing to conceptual and theoretical developments in the field. Qualitative syntheses may also advance the evidence base by achieving an accumulation of findings and enhancing individual studies by checking their comparability and replication. Moreover, qualitative synthesis has a potential empowering function, as it involves methods for combining multiple voices to seek new interpretations, rather than dismissing single case studies as locally bound. 237
Meta-ethnographies of qualitative health research could be stand-alone or could be a component part of a systematic review incorporating a variety of different types of evidence. This latter role may be particularly useful in HTA in which meta-ethnographies of qualitative research could complement quantitative systematic reviews of clinical effectiveness and cost-effectiveness, thus ensuring that patients’ views and experiences are fully represented in the evidence base. The benefits of this can clearly be seen in the case of a review of the neuroprotective drug riluzole in the treatment of motor neuron disease. 238 The review found that the cost of the drug to the NHS was greater than usually considered acceptable by the National Institute for Health and Clinical Excellence. Qualitative research found mixed views about the acceptability of the treatment for patients: some people with motor neuron disease were resistant to a drug that might marginally extend life without improving its quality; others felt that any extension of life was extremely important. On the basis of these findings, recommendations were made about the kind of information that should be given to patients about the possible benefits of the drug, so that they could make informed choices relating to their own requirements. It also highlighted to the policy-makers that there would be a limit to the number of people who would want the drug if it were made available. 238
Different approaches to meta-ethnography
The synthesis of qualitative research has opened up a very large agenda, reflecting the range of approaches and theoretical traditions that characterise qualitative research. This breadth and inclusiveness has led to the development of differing approaches to synthesis that reflect the varying assumptions and approaches to qualitative research. In addition, the fundamental distinctions between different schools of qualitative research have led to debates regarding appropriate methods for the conduct of each of the phases of study selection, appraisal and synthesis.
There is often a concern to identify a single ‘best’ approach to synthesis. As Barbour and Barbour239 observed, this may result in formalised, proceduralist approaches becoming dominant, and a corresponding neglect of the systematic and meticulous methods of qualitative research and its particular challenges for synthesis, thus leading to a kind of ‘mission drift’. We argue that it is important to acknowledge explicitly these differences and to distinguish between interpretive syntheses based on qualitative methods as developed by Noblit and Hare,15 and more structured proceduralist approaches that transpose checklists, standards and other terminology and procedures from quantitative research, with implications for appraisal, sample size, assessment of validity, etc. Whereas proceduralist approaches may be particularly suitable for conducting broadly focused syntheses involving large numbers of reports, or the synthesis of qualitative research for purposes of combining this with a quantitative synthesis, the strength of an interpretive approach based on the qualitative paradigm is in contributing to conceptual and theoretical development. As Hammersley14 stated, ‘I don’t think there is a single, all-purpose kind of research synthesis, whether we call it a systematic review or meta-ethnography. I think there are different kinds with different functions that make different demands on us’. We endorse this view, and believe that what is therefore of paramount importance is to be clear about the aims and purpose of the synthesis and to select methods that correspond to these goals.
The value and general feasibility of qualitative synthesis has been demonstrated, although the development of methods for the synthesis of qualitative research is at present at an early stage and there is a need for further methodological work. Specific issues requiring clarification and/or further research include:
-
A need for an agreed terminology, as the rapid development of new approaches in the field has meant that key terms such as meta-synthesis and meta-ethnography are employed to refer to differing approaches and there is no single classification of methods of qualitative synthesis.
-
Qualitative syntheses have tended to focus on research adopting thematic and phenomenological approaches, and there is a need for further work that synthesises research based on other theoretical traditions and methods.
-
Further experience of undertaking meta-ethnography is required to provide guidance regarding specific aspects of this process. In terms of a qualitative interpretive approach, this includes questions about the advantages of defining phenomena of interest a priori compared with a broader approach to the field; ways of assessing the worth of qualitative synthesis; and the value of approaching and feeding back interpretations to the original researchers. Other questions that are particularly applicable to a more proceduralist approach relate to forms of purposive sampling, the number of studies that are manageable, and ways of reducing context stripping and the decontextualisation of studies.
-
A wider question that requires a comparative methodology is the investigation of how different methods of synthesis influence the outcome of the synthesis in terms of its focus and emphasis, which in turn will help to clarify the applications and contributions of different methods of qualitative synthesis.
-
Further developmental work is required on how to take account of relevant quantitative syntheses while retaining an interpretative approach to the synthesis of qualitative research.
Conclusion
We conclude that meta-ethnography is an effective method of interpretive qualitative synthesis. It allows a body of qualitative research to be drawn together in a systematic way, and can produce novel and important insights, even in fields which appear to have been thoroughly investigated. However, failure to produce new insights does not necessarily mean that the synthesis, or the synthesiser, has failed. It may mean that the field of enquiry has already yielded very rich material in the primary studies. In terms of HTA, meta-ethnography offers a method for including the views of patients in technology assessments in a way that complements the involvement of users/consumers on panels. In particular, it offers a method for including the views of larger numbers of patients in different contexts, and of identifying underlying concepts and explanations. However, meta-ethnography requires considerable qualitative expertise and should be considered an advanced qualitative research method. Meta-ethnography has considerable potential as a method of qualitative synthesis, but it is still evolving and cannot be regarded as a standardised approach to be applied in a routinised way.
Acknowledgements
We would like to thank Jen Jamieson and Katrina Crook for secretarial support, Pete Shiarly for help setting up the database, Suzanne Audrey for her help with checking references cited and the formatting of this final report, and Sofie Akhurst for her assistance in compiling Table 2 and with checking references.
For the RA synthesis we are grateful to Guro Huby for conducting an initial assessment of the non-English-language papers, and to Lone Gale who translated the paper by Bjørner and Hansen218 from Danish to English. Experts consulted about ‘classic’ studies in the field of RA were Mike Bury, Gareth Williams, Muriel Shaul, Julie Barlow, John Weinman, Paul Dieppe, Caroline Sanders, Gillian Woolhead and Lucy Blenkiron. We are also grateful to Margaret Byron for helpful comments on the RA synthesis. For the medicines synthesis, we thank Andrew Herxheimer and Richard Martin for very helpful comments on earlier drafts.
The project as a whole benefited from the comments of George Noblit, and others, who attended a workshop on meta-ethnography held at the University of Bristol in July 2003, where the results of earlier versions of the syntheses were presented in an early, abridged form.
Contribution of authors
A team of people undertook this research project. In the report, where necessary, we have identified who did what. When it came to writing this report, specific people took responsibility for drafting particular chapters and their names are listed below. All authors then had the opportunity to contribute to the final drafts of all chapters.
-
Chapter 1 Rona Campbell and Myfanwy Morgan.
-
Chapter 2 Myfanwy Morgan, Gavin Daker-White and Rona Campbell.
-
Chapter 3 Nicky Britten, Roisin Pill, Pandora Pound and Rona Campbell.
-
Chapter 4 Rona Campbell, Lucy Yardley, Catherine Pope and Pandora Pound.
-
Chapter 5 Pandora Pound, Gavin Daker-White and Jenny Donovan.
-
Chapter 6 Pandora Pound, Nicky Britten, Myfanwy Morgan, Catherine Pope and Rona Campbell.
-
Chapter 7 Gavin Daker-White, Jenny Donovan, Roisin Pill and Rona Campbell.
-
Chapter 8 Rona Campbell, Myfanwy Morgan and Pandora Pound.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Chalmers I, Hedges LV, Cooper H. A brief history of research synthesis. Eval Health Prof 2002;25:12-37.
- Davidoff F, Haynes B, Sackett D, Smith R. Evidence based medicine (editorial). BMJ 1995;310:1085-6.
- Schulz KF, Chalmers I, Grimes DA, Altman D. Assessing the quality of randomization from reports of controlled trials published on obstetrics and gynecology journals. JAMA 1994;272:125-8.
- Sheldon TA. Making evidence synthesis more useful for management and policy-making. J Health Serv Res Pol 2005;10:1-5.
- Antman EM, Lau J, Kupelnick B, Mosteller F, Chalmers TC. A comparison of results of meta-analyses of randomized control trials and recommendations of clinical experts. JAMA 1992;268:240-8.
- Cochrane A. Effectiveness and efficiency. Random reflections on health services. London: Nuffield Provincial Hospital Trust; 1972.
- Chalmers I, Enkin M, Keirse MJNC, Chalmers I. Effective care in pregnancy and childbirth. 2. childbirth. Oxford: Oxford University Press; 1989.
- Enkin M, Keirse M, Chalmers I. A guide to effective care in pregnancy and childbirth. Oxford: Oxford University Press; 1989.
- Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P. Qualitative research methods in health technology assessment: a review of the literature. Health Technol Assess 1998;2.
- NHS R&D Methodology Programme . Developing Methods for Appraising and Reviewing Qualitative Research 1999.
- Strike K, Posner G, Ward S, Reed L. Knowledge structure and use. Philadelphia, PA: Temple University Press; 1983.
- Greenhalgh T. Meta-analysis and beyond: applying secondary research methods to primary care. Br J Gen Pract 1998;48:1540-1.
- Sandelowski M, Docherty S, Emden C. Qualitative metasynthesis: issues and techniques. Res Nurs Health 1997;20:365-71.
- Hammersley M. Talk Delivered at Meta-Ethnography Workshop Funded by HTA MRC, University of Bristol (chaired by R Campbell) 2003.
- Noblit G, Hare R. Meta-ethnography: synthesising qualitative studies. London: Sage Publications; 1988.
- Britten N, Campbell R, Pope C, Donovan J, Morgan M, Pill R. Using meta ethnography to synthesise qualitative research: a worked example. J Health Serv Res Policy 2002;7:209-15.
- Campbell R, Pound P, Pope C, Britten N, Pill R, Morgan M, et al. Evaluating meta-ethnography: a synthesis of qualitative research on lay experiences of diabetes and diabetes care. Soc Sci Med 2003;56:671-84.
- Critical Appraisal Skills Program . (CASP) Collaboration for Qualitative Methodologies 1998. www.casp-uk.net.
- Spencer L, Ritchie J, Lewis J, Dillon L. Quality in qualitative evaluation: a framework for assessing research evidence. London: Government Chief Social Researcher’s Office; 2003.
- Dixon-Woods M, Agarwal S, Young B, Jones D, Sutton S. Integrative approaches to qualitative and quantitative evidence. London: NHS Health Development Agency; 2004.
- Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy 2005;10:6-20.
- Spicer E. Beyond analysis and explanation. Hum Organ 1976;35:335-43.
- Thomas J, Harden A, Oakley A, Oliver S, Sutcliffe K, Rees R, et al. Integrating qualitative research with trials in systematic reviews. BMJ 2004;328:1010-12.
- Dixon-Woods M. How can systematic review incorporate qualitative research?. Swindon: Economic and Social Research Council; 2005.
- Yin RK. Case studies research: design and methods. Thousand Oaks, CA: Sage; 1989.
- Yin RK, Yates D. Street-level governments: assessing decentralization and urban services. Lexington, MA: Lexington books; 1975.
- Yin RK, Heald KA, Vogel M. Tinkering with the system: technological innovations in state and local services. Lexington, MA: Lexington books; 1997.
- Egger M, Davey Smith G, Sterne JAC. Meta-analysis: is moving the goal post the answer? (Letter). Lancet 1998;351.
- Roberts KA, Dixon-Woods M, Fitzpatrick R, Abrams KR, Jones DR. Factors affecting uptake of childhood immunisation: a Bayesian synthesis of qualitative and quantitative evidence. Lancet 2002;360:1596-9.
- Miles MB, Huberman AM. Qualitative data analysis: An expanded source book. Sage; 1994.
- McNaughton DB. A synthesis of qualitative home visiting research. Public Health Nurs 2000;17:405-16.
- Finfgeld DL. Self-resolution of drug and alcohol problems: a synthesis of qualitative findings. J Addict Nurs 2000;12:65-72.
- NHS Centre for Reviews and Dissemination (CRD) . Undertaking Systematic Reviews of Research on Effectiveness: CRD’s Guidance for Those Carrying Out or Commissioning Reviews 2001.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. Swindon: Economic and Social Research Council; 2006.
- Bloor M, MacIntosh J, Cunningham-Burleys S, McKeganey N. Medical sociology. London: Routledge; 1990.
- Heaton J. Secondary analysis of qualitative data. Soc Res Update 1998;22:1-7.
- Hinds PS, Vogel RJ, Clarke-Steffen L. The possibilities and pitfalls of doing a secondary analysis of a qualitative data set. Qual Health Res 1997;7:408-24.
- Thorne S, Morse JM. Qualitative research methods. London: Sage; 1994.
- Turner S. Sociological explanation as translation. New York, NY: Cambridge University Press; 1980.
- Glaser B, Strauss A. The discovery of grounded theory. Chicago, IL: Aldine; 1967.
- Marshall C. Appropriate criteria of trustworthiness and goodness for qualitative research on education organizations. Qual Quant 1985;19:353-73.
- Paterson BL, Thorne SE, Canam C, Jillings C. Meta-study of qualitative health research: a practical guide to meta-analysis and synthesis. Thousand Oaks, CA: Sage Publications Ltd; 2001.
- Finfgeld DL. Metasynthesis: the state of the art – so far. Qual Health Res 2003;13:893-904.
- Feder GS, Hutson M, Ramsay J, Taket AR. Women exposed to intimate partner violence: expectations and experiences when they encounter health care professionals: a meta-analysis of qualitative studies. Arch Intern Med 2006;166:22-37.
- Smith LK, Pope C, Botha JL. Delay in presentation of cancer: a synthesis of qualitative research on cancer patients’ help-seeking experiences. Lancet 2005;366:825-31.
- Walter FM, Emery J, Braithwaite D, Marteau TM. Lay understanding of familial risk of common chronic diseases: a systematic review and synthesis of qualitative research. Ann Fam Med 2004;2:583-94.
- Attree P. Parenting support in the context of poverty: a meta-synthesis of the qualitative evidence. Health Soc Care Community 2005;13:330-7.
- Barroso J, Sandelowski M. Substance abuse in HIV-positive women. J Assoc Nurses AIDS 2004;15:48-59.
- Barroso J, Powell-Cope GM. Metasynthesis of qualitative research on living with HIV infection. Qual Health Res 2000;10:340-53.
- Beck CT. Mothering multiples: a meta-synthesis of qualitative research. MCN Am J Matern Child Nurs 2002;27:214-21.
- Beck CT. Postpartum depression: a metasynthesis. Qual Health Res 2002;12:453-72.
- Carroll SM. Nonvocal ventilated patients perceptions of being understood. West J Nurs Res 2004;26:85-103.
- Clemmens D. Adolescent motherhood: a meta-synthesis of qualitative studies. MCN Am J Matern Child Nurs 2003;28:93-9.
- Coffey JS. Parenting a child with chronic illness: a metasynthesis. Pediatr Nurs 2006;32:51-9.
- Coffman MJ. Cultural caring in nursing practice: a meta-synthesis of qualitative research. J Cult Divers 2004;11:100-9.
- Evans D, FitzGerald M. The experience of physical restraint: a systematic review of qualitative research. Contemp Nurse 2002;13:126-35.
- Finfgeld-Connett D. Clarification of social support. Image J Nurs Sch 2005;37:4-9.
- Finfgeld-Connett D. Meta-synthesis of presence in nursing. J Adv Nurs 2006;55:708-14.
- Goodman JH. Becoming an involved father of an infant. J Obstet Gynecol Neonatal Nurs 2005;34:190-20.
- Howell D, Brazil K. Reaching common ground: a patient-family-based conceptual framework of quality EOL care. J Palliat Care 2005;21:19-26.
- Jensen LA, Allen MN. A synthesis of qualitative research on wellness-illness. Qual Health Res 1994;14:349-69.
- Kärkkäinen O, Bondas T, Eriksson K. Documentation of individualized patient care: a qualitative metasynthesis. Nurs Ethics 2005;12:123-32.
- Kennedy HP, Rousseau AL, Low LK. An exploratory metasynthesis of midwifery practice in the United States. Midwifery 2003;19:203-14.
- Kylma J. Despair and hopelessness in the context of HIV – a meta-synthesis on qualitative research findings. J Clin Nurs 2005;14:813-21.
- Kylma J. Dynamics of hope in adults living with HIV/AIDS: a substantive theory. J Adv Nurs 2005;52:620-30.
- Lefler LL, Bondy KN. Women’s delay in seeking treatment with myocardial infarction: a meta-synthesis. J Cardiovasc Nurs 2004;19:251-68.
- Meadows-Oliver M. Mothering in public: a meta synthesis of homeless women with children living in shelters. J Spec Pediatr Nurs 2003;8:130-6.
- Nelson AM. Transition to motherhood. J Obstet Gynecol Neonatal Nurs 2003;32:465-77.
- Nelson AM. A metasynthesis: mothering other-than-normal children. Qual Health Res 2002;12:515-30.
- Paterson BL, Thorne S, Dewis M. Adapting to and managing diabetes. Image J Nurs Sch 1998;30:57-62.
- Roux G, Dingsor E, Bush HA. Inner strength in women: metasynthesis of qualitative findings in theory development. J Theor Construct Test 2002;6:86-93.
- Sandelowski M, Lambe C, Barroso J. Stigma in HIV-positive women. J Nurs Scholarsh 2004;36:122-8.
- Sandelowski M, Barroso J. The travesty of choosing after positive prenatal diagnosis. J Obstet Gynecol Neonatal Nurs 2005;34:307-18.
- Sherwood GD. Meta-synthesis of qualitative analysis of caring: defining a therapeutic model of nursing. Adv Pract Nurse 1997;3:32-4.
- Steeman E, de Casterlé BD, Godderis J, Grypdonck M. Living with early-stage dementia: a review of qualitative studies. J Adv Nurs 2006;54:722-38.
- Swartz MK. Parenting preterm infants: a meta-synthesis. MCN Am J Matern Child Nurs 2005;31:115-20.
- Varcoe C, Rodney P, McCormick J. Health care relationships in context: an analysis of three ethnographies. Qual Health Res 2003;13:957-73.
- Werner JS, Wendler, MC, McCormick J, Paulus-Smith S, Jackson C, Nie J, et al. Human response outcomes influenced by nursing care. Int J Hum Caring 2002;6:15-23.
- Paterson B, Canam C, Joachim G, Thorne S. Embedded assumptions in qualitative studies of fatigue. West J Nurs Res 2003;25:119-33.
- Paterson BL. The shifting perspectives model of chronic illness. J Nurs Scholarsh 2001;33:21-6.
- Thorne S, Paterson B. Shifting images of chronic illness. Image J Nurs Sch 1998;30:173-8.
- Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6.
- Popay J, Rogers A, Williams G. Rationale and standards for the systematic review of qualitative literature in health services research. Qual Health Res 1998;8:341-51.
- Seale C. The quality of qualitative research. Thousand Oaks, CA: Sage; 1999.
- Mays N, Pope C. Assessing quality in qualitative research. BMJ 2000;330:50-2.
- Burns N. Standards for qualitative research. Nurs Sci Q 1989;2:44-52.
- Suikkala A, Leino-Kilpi H. Nursing student–patient relationships: a review of the literature from 1984 to 1998. J Adv Nurs 2001;33:42-50.
- Finfgeld DL. Empowerment of individuals with enduring mental health problems: perspectives from concept analysis and qualitative findings. Adv Nurs Sci 2004;27:44-52.
- Walker LO, Avant KC. Strategies for theory construction in nursing. Norwalk, CT: Appleton & Lange; 1995.
- Strauss A, Corbin J. Basics of qualitative research. Techniques and procedures for developing grounded theory. Thousand Oaks, CA; 1998.
- Sandelowski M, Barroso J. Classifying the findings in qualitative studies. Qual Health Res 2003;13:905-23.
- Cooper H. Synthesizing research. London: Sage; 1998.
- Curtis M, Lubkin I. What is chronicity? Chronic illness: impact and interventions. Boston, MA: Jones and Bartlett; 1990.
- Roberts CA, Burke SO. Nursing research: a quantitative and qualitative approach. Boston, MA: Jones & Bartlett; 1989.
- Sherwood G. Meta-synthesis: merging qualitative studies to develop nursing knowledge. Int J Hum Caring 1999;3:37-42.
- Evans D. Systematic review of interpretative research: interpretative data synthesis of processed data. Aust J Adv Nurs 2003;20:22-6.
- Sandelowski M, Barosso J. Reading qualitative studies (Article 5). Int J Qual Meth 2002;1:1-47.
- Loomis ME, Wood DJ. Cure: the potential outcome of nursing care. Image J Nurs Sch 1983;15:4-7.
- Ritzer G. Meta-theorizing in sociology. Lexington, MA: Lexington Books; 1991.
- Zhao S. Meta-theory, meta-method, meta-data-analysis: what, why, and how?. Sociol Perspect 1991;34:377-90.
- Thorne S, Paterson B, Acorn S, Canam C, Joachim G, Jillings C. Chronic illness experience: insights from a metastudy. Qual Health Res 2002;12:437-52.
- Dixon-Woods M, Kirk D, Agarwal S, Annandale E, Arthur T, Harvey J, et al. Report for the National Co-ordinating Centre for NHS Service Delivery and organisation R&D (NCCSDO). Vulnerable Groups and Access to Health Care: A Critical Interpretive Review 2005.
- Dixon-Woods M, Agarwal S, Jones D, Young B, Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy 2005;10:45-53.
- Kearney MH. Truthful Self-Nurturing: A grounded formal theory of women’s addiction recovery. Qual Health Res 1998;8:495-512.
- Finfgeld DL. Courage as a process of pushing beyond the struggle. Qual Health Res 1999;9:803-14.
- Pawson R. Evidence-based policy: the promise of ‘realist synthesis’. Evaluation 2002;8:340-58.
- Dixon-Woods M, Fitzpatrick R. Qualitative research in systematic reviews has establised a place for itself. BMJ 2001;323:765-6.
- Evans D. Database searches for qualitative research. J Med Libr Assoc 2002;90:290-3.
- Popay J, Roen K. Synthesis of Evidence from Research Using Diverse Study Designs: A Preliminary Review of Methodological Work 2003.
- McDonald S, Lefebvre C, Antes G, Galandi D, Gøtzsche P, Hammarquist C, et al. The contribution of handsearching European general health care journals to the Cochrane Controlled Trials Register. Eval Health Prof 2002;25:65-7.
- Murphy L, Reinsch S, Najm W, Dickerson V, Seffinger M, Adams A, et al. Searching biomedical databases on complementary medicine: the use of controlled vocabulary among authors, indexers and investigators. BMC Complement Altern Med 2003;3.
- Petticrew M, Roberts H. How to find the studies: the literature search. Systematic reviews in the social sciences: A practical guide. Malden, MA: Blackwell Publishing; 2006.
- Matthews EJ, Edwards AGK, Barker J, Bloor M, Covey J, Hood K, et al. Efficient literature searching in diffuse topics: lessons from a systematic review of research on communicating risk to patients in primary care. Health Libr Rev 1999;16:112-20.
- Shaw R, Booth A, Sutton A, Miller T, Smith J, Young B, et al. Finding qualitative research: an evaluation of search strategies. BMC Med Res Methodol 2004;4.
- Grayson L, Gomersall A. A difficult business: finding the evidence for social science reviews. ESRC UK Centre for Evidence Based Policy and Practice; 2003.
- Arluke A. judging drugs: patient’s conceptions of therapeutic efficacy in the treatment of arthritis. Hum Organ 1980;39:84-8.
- Trostle JA, Hauser WA, Susser IS. The logic of noncompliance: Management of epilepsy from the patient’s point of view. Cult Med Psychiatry 1983;7:35-56.
- Conrad P. The meaning of medications: another look at compliance. Soc Sci Med 1985;20:29-37.
- Erwin J, Peters B. Treatment issues for HIV+ Africans in London. Soc Sci Med 1999;49:1519-28.
- Booth A. Cochrane or Cock-Eyed? How Should We Conduct Systematic Reviews of Qualitative Research? n.d.
- Khan K, ter Riet G, Popay J, Nixon J, Kleijen J. Study Quality Assessment. CRD Report Number 4. Undertaking Systematic Reviews of Research on Effectiveness 2001.
- Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hill, CA: Sage Publications; 1985.
- Guba EG, Lincoln YS. Fourth generation evaluation. Newbury Park, CA: Sage; 1989.
- Cook TD, Campbell DT. Quasi-experimentation: Design and analysis issues for field testing. Boston, MA: Houghton Mifflin (Academic); 1979.
- Kirk J, Miller ML. Reliability and validity in qualitative research. London: Sage Publications; 1986.
- Hammersley M. What’s wrong with ethnography?. London: Routledge; 1992.
- Mays N, Pope C. Quality in qualitative health research. Qualitative research in health care. London: BMJ Books; 1999.
- Blaxter M. Criteria for the evaluation of qualitative research papers. Medical Sociology News 1996;22:68-71.
- Reid M, Armstrong D. Guidelines on evaluating qualitative research proposals in health services research. Produced for the Cancer Research Campaign Education and Psychosocial Research Commitee; 1998.
- Elliott R, Fischer CT, Rennie DL. Evolving guidelines for publication of qualitative research studies in psychology and related fields. Br J Clin Psychol 1999;38:215-29.
- Boulton M, Fitzpatrick R, Swinburn C. Qualitative research in health care: II. A structured review and evaluation of studies. J Eval Clin Pract 1996;2:171-9.
- Yardley L. Dilemmas in qualitative health research. Psychol Health 2000;15:215-28.
- Hunter JF, Schmidt F, Jackson G. Meta analysis. Newbury Park, CA: Sage; 1982.
- Morgan M, Williams SJ, Calnan M. Modern medicine. Lay perspectives and experiences. London: UCL Press; 1996.
- Van Wissen K, Litchfield M, Maling T. Living with high blood pressure. J Adv Nurs 1998;27:567-74.
- Johnson MJ, Williams M, Marshall ES. Adherent and non-adherent medication-taking in elderly hypertensive patients. Clin Nurs Res 1999;8:318-35.
- Svensson S, Kjellgren KI, Ahlner J, Saljo R. Reasons for adherence with antihypertensive medication. Int J Cardiol 2000;76:157-63.
- Wiener CL. The burden of rheumatoid arthritis: tolerating the uncertainty. Soc Sci Med 1975;9:97-104.
- Locker D. Disability and disadvantage: the consequences of chronic illness. London: Tavistock Publications; 1983.
- Bury M. Chronic illness as biographical disruption. Sociol Health Illness 1982;4:167-82.
- Williams G. The genesis of chronic illness: narrative re-construction. Sociol Health Illness 1984;6:175-200.
- Siegel K, Gorey E. HIV-infected women: barriers to AZT use. Soc Sci Med 1997;45:15-22.
- Stone VE, Clarke J. HIV/AIDS patients’ perspectives on adhering to regimens containing protease inhibitors. J Gen Intern Med 1998;13:586-93.
- Erlen JA, Mellors MP. Adherence to combination therapy in persons living with HIV: balancing the hardships and the blessings. J Assoc Nurses AIDS Care 1999;10:75-84.
- Halkitis PN, Kirton C. Self-strategies as means of enhancing adherence to HIV antiretroviral therapies: a Rogerian approach. J New York State Nurses Assoc 1999;30:22-7.
- Proctor VE, Tesfa A, Tompkins DC. Barriers to adherence to highly active antiretroviral therapy as expressed by people living with HIV/AIDS. AIDS Patient Care STDs 1999;13:535-44.
- Siegel K, Schrimshaw EW, Dean L. Symptom interpretation and medication adherence among late middle age and older HIV infected adults. J Health Psychol 1999;4:247-57.
- Siegel K, Schrimshaw EW, Raveis VH. Accounts for non-adherence to antiviral combination therapies among older HIV-infected adults. Psychol Health Med 2000;5:29-42.
- McDonald K, Bartos M, Rosenthal D. Australian women living with HIV/AIDS are more sceptical than men about antiretroviral treatment. AIDS Care 2001;13:15-26.
- Murphy DA, Johnston Roberts KJ, Martin DJ, Marelich W, Hoffman D. Barriers to antiretroviral adherence among HIV-infected adults. AIDS Patient Care STDs 2000;14:47-58.
- Johnston Roberts KJ, Mann T. Barriers to antiretroviral medication adherence in HIV-infected women. AIDS Care 2000;12:377-86.
- Barton Laws M, Wilson IB. Taking antiretroviral therapy for HIV infection: learning from patients’ stories. J Gen Intern Med 2000;15:848-58.
- Kaljee LM, Beardsley R. Psychotropic drugs and concepts of compliance in a rural mental health clinic. Med Anthropol Q 1992;6:271-87.
- North D, Davis P, Powell A. Patient responses to benzodiazepine medication: a typology of adaptive repertoires developed by long term users. Sociol Health Illness 1995;17:632-50.
- Barter G, Cormack M. The long-term use of benzodiazepines: patients’ views, accounts and experiences. Fam Pract 1996;13:491-7.
- Rogers A, Day JC, Williams B, Randall F, Wood P, Healy D, et al. The meaning and management of neuroleptic medicaiton: a study of patients with a diagnosis of schizophrenia. Soc Sci Med 1998;47:1313-23.
- Angermeyer MC, Loffler W, Muller P, Schulze B, Priebe S. Patients’ and relatives’ assessment of clozapine treatment. Psychol Med 2001;31:509-17.
- Usher K. Taking neuroleptic medications as the treatment for schizophrenia: a phenomenological study. Aust N Z J Ment Health Nurs 2001;10:145-55.
- Boath EH, Blenkinsopp A. The rise and rise of proton pump inhibitor drugs: patients’ perspectives. Soc Sci Med 1997;45:1571-9.
- Pollock K, Grime J. Strategies for reducing the prescribing of proton pump inhibitors (PPIs): patient self-regulation of treatment may be an under-exploited resource. Soc Sci Med 2000;51:1827-39.
- Adams S, Pill R, Jones A. Medication, chronic illness and identity: the perspective of people with asthma. Soc Sci Med 1997;45:189-201.
- Prout A, Hayes L, Gelder L. Medicines and the maintenance of ordinariness in the household management of childhood asthma. Sociol Health Illness 1999;21:137-62.
- Buston KM, Wood SF. Non-compliance amongst adolescents with asthma: listening to what they tell us about self-management. Fam Pract 2000;17:134-8.
- Walsh S, Hagan T, Gamsu D. Rescuer and rescued: applying a cognitive analytic perspective to explore the ‘mismanagement’ of asthma. Br J Med Psychol 2000;73:151-68.
- Pradel FG. Asthma self-management: the perspective of children. Patient Educ Counsel 2001;45:199-20.
- Donovan JL, Blake DR. Patient non-compliance: deviance or reasoned decision-making?. Soc Sci Med 1992;34:507-13.
- Dowell JS, Snadden D, Dunbar J. Rapid prescribing change, how do patients respond?. Soc Sci Med 1996;43:1543-9.
- Ersek M, Miller B, Du Pen A. Factors hindering patients’ use of medications for cancer pain. Cancer Pract 1999;7:226-32.
- Atkin K, Ahmad WIU. Pumping iron: compliance with chelation therapy among young people who have thalassaemia major. Sociol Health Illness 2000;22:500-24.
- Smith F, Francis S, Rowley E. Group interviews with people taking long-term medication: comparing the perspectives of people with arthritis, respiratory diseases and mental health problems. Int J Pharm Pract 2000;8:88-96.
- Roberson MHB. The meaning of complicance: patient perspectives. Qual Health Res 1992;2:7-26.
- Britten N, Williams S, Calnan M. Modern medicine. Lay perspectives and experiences. London: UCL Press; 1996.
- Dowell J, Hudson H. A qualitative study of medication-taking behaviour in primary care. Fam Pract 1997;14:369-75.
- Watson J, Mitchell T. Older women, medication use and nursing care. Int J Nurs Pract 1998;4:189-96.
- Lumme-Sandt K, Hervonen A, Jylha M. Interpretative repertoires of medication among the oldest-old. Soc Sci Med 2000;50:1843-50.
- Stenström CH, Bergman B, Dahlgren LO. Everyday life with rheumatoid arthritis: a phenomenographic study. Physiother Theor Pract 1993;9:235-43.
- Shaul MP. From early twinges to mastery: the process of adjustment in living with rheumatoid arthritis. Arthritis Care Res 1995;8:290-7.
- Williams GH, Wood PHN. Coming to terms with chronic illness: the negotiation of autonomy in rheumatoid arthritis. Int Disabil Stud 1988;10:128-33.
- Donovan JL, Blake DR. Qualitative study of interpretation of reassurance among patients attending rheumatology clinics: ‘just a touch of arthritis, doctor?’. BMJ 2000;320:541-4.
- Edwards J, Mulherin D, Ryan S, Jester R. The experience of patients with rheumatoid arthritis admitted to hospital. Arthritis Rheum 2001;45:1-7.
- De Vellis RF, Patterson CC. Do people with rheumatoid arthritis develop illness-related schemas?. Arthritis Care Res 1997;10:78-8.
- Barlow JH, Cullen LA. Does arthritis influence perceived ability to fulfil a parenting role? Perceptions of mothers, fathers and grandparents. Patient Educ Counsel 1999;37:141-51.
- World Health Organization . Adherence to Long-Term Therapies 2003.
- Carter S, Taylor D, Levenson R. A Question of Choice – Compliance in Medicine-Taking. A Preliminary Report 2003.
- Harrison A. Getting the right medicines? Putting public interests at the heart of health related research. London: Kings’s Fund; 2003.
- BMJ 2003;327.
- Pharmaceut J 2003;271.
- Horne R. Concordance, adherence and compliance in medicine taking. Report for the National Co-ordinating Centre for NHS Service Delivery and Organisation R & D (NCCSDO); 2005.
- McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions. JAMA 2002;288:2868-79.
- Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: three decades of research. A comprehensive review. J Clin Pharm Ther 2001;26:331-42.
- Blaxter M, Britten N. Lay beliefs about drugs and medicines and the implications for community pharmacy. Produced fot the Pharmacy Practice Research Resource Centre at the University of Manchester; 1996.
- Marinker M. From compliance to concordance: achieveing shared goals in medicine taking. London: Royal Pharmaceutical Society of Great Britain; 1997.
- Cornwell J. Hard-earned lives: accounts of health and illness from East London. London: Tavistock; 1984.
- Trostle JA. Medical compliance as an ideology. Soc Sci Med 1988;27:1299-308.
- Prior L. Belief, knowledge and expertise: the emergence of the lay expert in medical sociology. Sociol Health Illn 2003;25:41-57.
- Epstein S. The construction of lay expertise: AIDS activism and the forging of credibility in the reform of clinical trials. Sci Technol Human Values 1995;20:408-37.
- Johannessen T, Petersen H, Kristensen P, Fosstvedt D. The controlled single subject trial. Scand J Prim Health Care 1991;9:17-21.
- Connor S. Glaxo Chief: our drugs do not work on most patients. Independent 2003.
- Smith R. The drugs don’t work. BMJ 2003;327. www.bmj.com/content/327/7428/0.9short.
- Wynne HA, Long A. Patient awareness of the adverse effects of non-steroidal anti-inflammatory drugs (NSAIDs). Br J Clin Pharmacol 1996;42:253-6.
- Herxheimer A. Many NSAID users who bleed don’t know when to stop. BMJ 1998;316.
- Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients. JAMA 1998;279:1200-5.
- Eaton L. Adverse reactions to drugs increase. BMJ 2002;324.
- Medawar C, Herxheimer A. A comparison of adverse drug reaction report from professionals and users, relating to risk of dependence and suicidal behaviour with paroxetine. Int J Risk Saf Med 2004;16:5-9.
- Medawar C, Herxheimer A, Bell A, Jofre S. Paroxetine, Panorama and user reporting of ADRs: consumer intelligence matters in clinical practice and post-marketing drug surveillance. Int J Risk Saf Med 2002;15:161-9.
- Heath I. A wolf in sheep’s clothing: a critical look at the ethics of drug taking. BMJ 2003;327:856-8.
- Elwyn G, Edwards A, Britten N. ‘Doing prescribing’: how doctors can be more effective. BMJ 2003;327:864-7.
- Weiss M, Britten N. What is concordance?. Pharmaceut J 2003;271.
- Cox K, Stevenson F, Britten N, Dundar Y. A systematic review of communication between patients and health care professionals about medicine taking and prescribing. London: GKT Concordance Unit, King’s College; 2004.
- Blenkinsopp A, Bond C, Britten N, Feely M, George C, Green P, et al. From compliance to concordance: achieving shared goals in medicine taking. London: Royal Pharmaceutical Society of Great Britain; 1997.
- Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. N Engl J Med 1993;328:246-52.
- Rogers A, Pilgrim D. A sociology of mental health and illness. Maidenhead: Open University Press; 2005.
- Chalmers I. What do I want from health research and researchers when I am a patient?. BMJ 1995;310:1315-18.
- Tallon D, Chard JA, Dieppe PA. Relation between agendas of the research community and the research consumer. Lancet 2000;355:2037-40.
- Horrobin DF. Modern biomedical research: an internally self-consistent universe with little contact with medical reality?. Nat Rev Drug Discov 2003;2:151-4.
- Bury M, Anderson R, Bury M. Living with chronic illness: the experiences of patients and their families. London: Unwin Hyman Ltd; 1988.
- Donovan JL, Blake DR, Fleming WG. The patient is not a blank sheet: lay beliefs and their relevance to patient education. Br J Rheumatol 1989;28:58-61.
- Donovan J. Patient education and the consultation: the importance of lay beliefs. Ann Rheum Dis 1991;50:418-21.
- Bjørner JB, Hansen IR. Reumatoid artrit og samliv. En kvalitativ undersogelse [Rheumatoid arthritis and partner relationships: a qualitative study]. Nordisk Sexologi 1993;11:101-11.
- Rice GE, Young LH. A folk model of arthritis. Health Val 1994;18:15-27.
- Pinder R. Bringing back the body without the blame?: the experience of ill and disabled people at work. Sociol Health Illness 1995;17:605-31.
- Brown S, Williams A. Women’s experiences of rheumatoid arthritis. J Adv Nurs 1995;21:695-701.
- Dildy SP. Suffering in people with rheumatoid arthritis. Appl Nurs Res 1996;9:177-83.
- Ryan S. Living with rheumatoid arthritis: a phenomenological exploration. Nurs Stand 1996;10:45-8.
- Moss P. Negotiating spaces in home environments: older women living with arthritis. Soc Sci Med 1997;45:23-3.
- Rao JK, Arick R, Mihaliak K, Weinberger M. Using focus groups to understand arthritis patients’ perceptions about unconventional therapy. Arthritis Care Res 1998;11:253-60.
- Williams B, Barlow JH, Nettleton S, Watson J. The body in everyday life. London: Routledge; 1998.
- Archenholtz B, Burckhardt CS, Segesten K. Quality of life of women with systemic lupus erythematosus or rheumatoid arthritis: domains of importance and dissatisfaction. Qual Life Res 1999;8:411-16.
- Stephens M, Yoshida KK. Independence and autonomy among people with rheumatoid arthritis. Can J Rehabil 1999;12:229-43.
- Lambert BL, Butin DN. Arthritis care: comparison of physicians’ and patients’ views. Semin Arthritis Rheum 2000;30:100-10.
- Gilworth G, Woodhouse A, Tennant A, Chamberlain MA. The impact of rheumatoid arthritis in the workplace. Int J Ther Rehabil 2001;8:342-7.
- Grant M. Mothers with arthritis, child care and occupational therapy: insight through case studies. Br J Occup Ther 2001;64:322-9.
- McPherson KM, Brander P, Taylor WJ, McNaughton HK. Living with arthritis – what is important?. Disabil Rehabil 2001;23:706-21.
- Brown R. A poetic for sociology. New York, NY: Cambridge University Press; 1977.
- Martin G. Language, truth and poetry. Edinburgh: Edinburgh University Press; 1975.
- House ER. Coherence and credibility: the aesthetics of evaluation. Educ Eval Pol Anal 1979;1:5-17.
- Doyle LH. Synthesis through meta-ethnography: paradoxes, enhancements, and possibilities. Qual Res 2003;3:321-44.
- Stewart A, Sandercock J, Bryan S, Hyde C, Barton PM, Fry-Smith A, et al. The clinical and cost-effectiveness of riluzole for motor neuron disease: a rapid and systematic review. Health Technol Assess 2001.
- Barbour RS, Barbour M. Evaluating and synthesizing qualitative research: the need to develop a distinctive approach. J Eval Clin Pract 2003;9:179-86.
Appendix 1 Appraisal form
Paper ID
Theoretical perspectives
(To help with Q7e)
| Research tradition | Focus | Data | Analysis |
|---|---|---|---|
| 1. Phenomenology | Understanding social phenomena/actions in terms of multiple perspectives | Primarily interviews, but increasing use of observation and focus groups | Constant comparison to describe/develop explanations (discourse analysis and CA) |
| 2. Grounded theory | Developing a substantive theory | Theoretical sampling. Multiple sources of data | Well defined procedures to develop theory |
| 3. Ethnography |
Study of a cultural system or group in terms of behaviour, customs and way of life OR Case study (in-depth study of bounded system, e.g. hospital ward, school) |
Extensive fieldwork and time in field. Multiple sources of data As above |
‘Thick’ narratives |
| 4. Action research | Participation of those being researched as equals and negotiation of research design | Interviews and observation | Data collection and analysis iterative (responses to research are data). ‘Thick’ narrative |
Appendix 2 Protocol
Systematic appraisal and synthesis of qualitative research: evaluating meta ethnography.
Dr Rona Campbell, University of Bristol.
Objectives
-
To conduct, using the meta ethnographic method, systematic appraisal and synthesis of quantitative research studies in 2 areas:
-
patient experiences of living with rheumatoid arthritis and
-
lay beliefs about medicine taking in chronic disease.
-
-
To test our modified version of the CASP criteria for appraising qualitative research for their appropriateness, ease of use and inter reviewer agreement.
-
To evaluate the meta ethnographic method of synthesis including its reproducibility.
-
To complete our review of the methods available for appraising and synthesising qualitative research.
-
To document the effectiveness of the different elements of the search strategy in identifying relevant qualitative research studies.
Design
Systematic appraisal and synthesis of qualitative research.
Search Strategy
The strategy will include electronic searches of specialist databases and databases of grey literature, hand searching of key journals and collections of qualitative studies published in book form, contacting other qualitative health researchers in relevant areas, searching reference lists of studies retrieved.
Review strategy
The study will test our modified version of the CASP criteria for appraising qualitative research for their appropriateness, ease of use and inter reviewer agreement. The two syntheses will be undertaken using the meta ethnographic method which will be evaluated overall and for its reproducibility.
Expected output of research
-
Report containing:
-
a review of methods available for synthesis,
-
results of the summative evaluation of our modified CASP criteria for appraising qualitative research,
-
two qualitative research syntheses,
-
an evaluation of the syntheses and a discussion of the contribution qualitative research synthesis could make to HTA.
-
-
Two papers on each of the syntheses and a methodology paper concerned with the processes of appraisal and synthesis of qualitative research to be published in peer reviewed journals.
-
Presentations of the synthesis findings to different audiences.
Expertise in team
Every member of the research team is a senior social scientist and an experienced qualitative researcher. The research team will be supported by a steering group whose multi-disciplinary membership is drawn from cognate subject areas including public health, epidemiology, anthropology, health economics and rheumatology.
List of abbreviations
- ADR
- adverse drug reactions
- AZT
- azidothymidine (zidovudine)
- CASP
- Critical Appraisal Skills Programme
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CIS
- critical interpretive synthesis
- ESRC
- Economic and Social Research Council
- HIV
- human immunodeficiency virus
- HTA
- health technology assessment
- NatCen
- National Centre for Social Research
- PPI
- proton pump inhibitor
- RA
- rheumatoid arthritis
- RCT
- randomised controlled trial
- WHO
- World Health Organization
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
Prioritisation Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Imti Choonara, Professor in Child Health, Academic Division of Child Health, University of Nottingham
Chair – Pharmaceuticals Panel
-
Dr Bob Coates, Consultant Advisor – Disease Prevention Panel
-
Dr Andrew Cook, Consultant Advisor – Intervention Procedures Panel
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Dr Nick Hicks, Consultant Adviser – Diagnostic Technologies and Screening Panel, Consultant Advisor–Psychological and Community Therapies Panel
-
Ms Susan Hird, Consultant Advisor, External Devices and Physical Therapies Panel
-
Professor Sallie Lamb, Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick
Chair – HTA Clinical Evaluation and Trials Board
-
Professor Jonathan Michaels, Professor of Vascular Surgery, Sheffield Vascular Institute, University of Sheffield
Chair – Interventional Procedures Panel
-
Professor Ruairidh Milne, Director – External Relations
-
Dr John Pounsford, Consultant Physician, Directorate of Medical Services, North Bristol NHS Trust
Chair – External Devices and Physical Therapies Panel
-
Dr Vaughan Thomas, Consultant Advisor – Pharmaceuticals Panel, Clinical
Lead – Clinical Evaluation Trials Prioritisation Group
-
Professor Margaret Thorogood, Professor of Epidemiology, Health Sciences Research Institute, University of Warwick
Chair – Disease Prevention Panel
-
Professor Lindsay Turnbull, Professor of Radiology, Centre for the MR Investigations, University of Hull
Chair – Diagnostic Technologies and Screening Panel
-
Professor Scott Weich, Professor of Psychiatry, Health Sciences Research Institute, University of Warwick
Chair – Psychological and Community Therapies Panel
-
Professor Hywel Williams, Director of Nottingham Clinical Trials Unit, Centre of Evidence-Based Dermatology, University of Nottingham
Chair – HTA Commissioning Board
Deputy HTA Programme Director
HTA Commissioning Board
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
-
Department of Public Health and Epidemiology, University of Birmingham
-
Professor of Clinical Pharmacology, Director, NIHR HTA programme, University of Liverpool
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Peter Brocklehurst, Professor of Women’s Health, Institute for Women’s Health, University College London
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Jonathan Green, Professor and Acting Head of Department, Child and Adolescent Psychiatry, University of Manchester Medical School
-
Professor John W Gregory, Professor in Paediatric Endocrinology, Department of Child Health, Wales School of Medicine, Cardiff University
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, Head of Nuffield Department of Surgery, University of Oxford
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor Irwin Nazareth, Professor of Primary Care and Head of Department, Department of Primary Care and Population Sciences, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norrie, Chair in Clinical Trials and Biostatistics, Robertson Centre for Biostatistics, University of Glasgow
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Martin Underwood, Professor of Primary Care Research, Warwick Medical School, University of Warwick
-
Professor Marion Walker, Professor in Stroke Rehabilitation, Associate Director UK Stroke Research Network, University of Nottingham
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Dr Tom Foulks, Medical Research Council
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
HTA Clinical Evaluation and Trials Board
-
Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick and Professor of Rehabilitation, Nuffield Department of Orthopaedic, Rheumatology and Musculoskeletal Sciences, University of Oxford
-
Professor of the Psychology of Health Care, Leeds Institute of Health Sciences, University of Leeds
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Keith Abrams, Professor of Medical Statistics, Department of Health Sciences, University of Leicester
-
Professor Martin Bland, Professor of Health Statistics, Department of Health Sciences, University of York
-
Professor Jane Blazeby, Professor of Surgery and Consultant Upper GI Surgeon, Department of Social Medicine, University of Bristol
-
Professor Julia M Brown, Director, Clinical Trials Research Unit, University of Leeds
-
Professor Alistair Burns, Professor of Old Age Psychiatry, Psychiatry Research Group, School of Community-Based Medicine, The University of Manchester & National Clinical Director for Dementia, Department of Health
-
Dr Jennifer Burr, Director, Centre for Healthcare Randomised trials (CHART), University of Aberdeen
-
Professor Linda Davies, Professor of Health Economics, Health Sciences Research Group, University of Manchester
-
Professor Simon Gilbody, Prof of Psych Medicine and Health Services Research, Department of Health Sciences, University of York
-
Professor Steven Goodacre, Professor and Consultant in Emergency Medicine, School of Health and Related Research, University of Sheffield
-
Professor Dyfrig Hughes, Professor of Pharmacoeconomics, Centre for Economics and Policy in Health, Institute of Medical and Social Care Research, Bangor University
-
Professor Paul Jones, Professor of Respiratory Medicine, Department of Cardiac and Vascular Science, St George‘s Hospital Medical School, University of London
-
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, Queen Mary, University of London
-
Professor Richard J McManus, Professor of Primary Care Cardiovascular Research, Primary Care Clinical Sciences Building, University of Birmingham
-
Professor Helen Rodgers, Professor of Stroke Care, Institute for Ageing and Health, Newcastle University
-
Professor Ken Stein, Professor of Public Health, Peninsula Technology Assessment Group, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Jonathan Sterne, Professor of Medical Statistics and Epidemiology, Department of Social Medicine, University of Bristol
-
Mr Andy Vail, Senior Lecturer, Health Sciences Research Group, University of Manchester
-
Professor Clare Wilkinson, Professor of General Practice and Director of Research North Wales Clinical School, Department of Primary Care and Public Health, Cardiff University
-
Dr Ian B Wilkinson, Senior Lecturer and Honorary Consultant, Clinical Pharmacology Unit, Department of Medicine, University of Cambridge
-
Ms Kate Law, Director of Clinical Trials, Cancer Research UK
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, University of Manchester
-
Mr Angus S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital, Birmingham
-
Dr Diana Baralle, Consultant and Senior Lecturer in Clinical Genetics, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Diane Eccles, Professor of Cancer Genetics, Wessex Clinical Genetics Service, Princess Anne Hospital
-
Dr Trevor Friedman, Consultant Liason Psychiatrist, Brandon Unit, Leicester General Hospital
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Public contributor
-
Professor Anthony Robert Kendrick, Associate Dean for Clinical Research and Professor of Primary Medical Care, University of Southampton
-
Dr Nicola Lennard, Senior Medical Officer, MHRA
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee, London
-
Mr David Mathew, Public contributor
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mrs Una Rennard, Public contributor
-
Dr Stuart Smellie, Consultant in Clinical Pathology, Bishop Auckland General Hospital
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr Allison Streetly, Programme Director, NHS Sickle Cell and Thalassaemia Screening Programme, King’s College School of Medicine
-
Dr Matthew Thompson, Senior Clinical Scientist and GP, Department of Primary Health Care, University of Oxford
-
Dr Alan J Williams, Consultant Physician, General and Respiratory Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Joanna Jenkinson, Board Secretary, Neurosciences and Mental Health Board (NMHB), Medical Research Council
-
Professor Julietta Patrick, Director, NHS Cancer Screening Programme, Sheffield
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Disease Prevention Panel
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook, Clinical Programmes Director, Bazian Ltd, London
-
Dr Colin Greaves, Senior Research Fellow, Peninsula Medical School (Primary Care)
-
Mr Michael Head, Public contributor
-
Professor Cathy Jackson, Professor of Primary Care Medicine, Bute Medical School, University of St Andrews
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Julie Mytton, Consultant in Child Public Health, NHS Bristol
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Dr Richard Richards, Assistant Director of Public Health, Derbyshire County Primary Care Trust
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Dr Kenneth Robertson, Consultant Paediatrician, Royal Hospital for Sick Children, Glasgow
-
Dr Catherine Swann, Associate Director, Centre for Public Health Excellence, NICE
-
Mrs Jean Thurston, Public contributor
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust
-
Reader in Wound Healing and Director of Research, University of Leeds
-
Professor Bipin Bhakta, Charterhouse Professor in Rehabilitation Medicine, University of Leeds
-
Mrs Penny Calder, Public contributor
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol
-
Mrs Anthea De Barton-Watson, Public contributor
-
Professor Nadine Foster, Professor of Musculoskeletal Health in Primary Care Arthritis Research, Keele University
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester
-
Professor Christine Norton, Professor of Clinical Nursing Innovation, Bucks New University and Imperial College Healthcare NHS Trust
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham
-
Dr Kate Radford, Senior Lecturer (Research), University of Central Lancashire
-
Mr Jim Reece, Public contributor
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton
-
Dr Pippa Tyrrell, Senior Lecturer/Consultant, Salford Royal Foundation Hospitals’ Trust and University of Manchester
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Interventional Procedures Panel
-
Professor of Vascular Surgery, University of Sheffield
-
Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Mrs Isabel Boyer, Public contributor
-
Mr Sankaran Chandra Sekharan, Consultant Surgeon, Breast Surgery, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Ms Leonie Cooke, Public contributor
-
Mr Seumas Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor Sam Eljamel, Consultant Neurosurgeon, Ninewells Hospital and Medical School, Dundee
-
Dr Adele Fielding, Senior Lecturer and Honorary Consultant in Haematology, University College London Medical School
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Fiona Lecky, Senior Lecturer/Honorary Consultant in Emergency Medicine, University of Manchester/Salford Royal Hospitals NHS Foundation Trust
-
Dr Nadim Malik, Consultant Cardiologist/Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Professor Jon Moss, Consultant Interventional Radiologist, North Glasgow Hospitals University NHS Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Dr Matthew Wilson, Consultant Anaesthetist, Sheffield Teaching Hospitals NHS Foundation Trust
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Dr Martin Ashton-Key, Medical Advisor, National Commissioning Group, NHS London
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr James Gray, Consultant Microbiologist, Department of Microbiology, Birmingham Children’s Hospital NHS Foundation Trust
-
Dr Jurjees Hasan, Consultant in Medical Oncology, The Christie, Manchester
-
Dr Carl Heneghan, Deputy Director Centre for Evidence-Based Medicine and Clinical Lecturer, Department of Primary Health Care, University of Oxford
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Maria Kouimtzi, Pharmacy and Informatics Director, Global Clinical Solutions, Wiley-Blackwell
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Ms Amanda Roberts, Public contributor
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Professor Donald Singer, Professor of Clinical Pharmacology and Therapeutics, Clinical Sciences Research Institute, CSB, University of Warwick Medical School
-
Mr David Symes, Public contributor
-
Dr Arnold Zermansky, General Practitioner, Senior Research Fellow, Pharmacy Practice and Medicines Management Group, Leeds University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick, Coventry
-
Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Public contributor
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Peter Langdon, Senior Clinical Lecturer, School of Medicine, Health Policy and Practice, University of East Anglia
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician and Cardiologist, County Durham and Darlington Foundation Trust
-
Dr Richard Neal, Clinical Senior Lecturer in General Practice, Cardiff University
-
Mr John Needham, Public contributor
-
Ms Mary Nettle, Mental Health User Consultant
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry and Warwickshire Partnership Trust
-
Dr Lesley Stockton, Lecturer, School of Health Sciences, University of Liverpool
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation of Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Professor Bruce Campbell, Consultant Vascular & General Surgeon, Royal Devon & Exeter Hospital, Wonford
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Neill McIntosh, Edward Clark Professor of Child Life and Health, University of Edinburgh
-
Professor Rajan Madhok, Consultant in Public Health, South Manchester Primary Care Trust
-
Professor Sir Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, Director, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Philip Shackley, Senior Lecturer in Health Economics, Sheffield Vascular Institute, University of Sheffield
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Dr Nick Summerton, GP Appraiser and Codirector, Research Network, Yorkshire Clinical Consultant, Primary Care and Public Health, University of Oxford
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Dr Ross Taylor, Senior Lecturer, University of Aberdeen
-
Dr Richard Tiner, Medical Director, Medical Department, Association of the British Pharmaceutical Industry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington