Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 08/101/01. The contractual start date was in May 2009. The draft report began editorial review in April 2011 and was accepted for publication in June 2011. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2012. This work was produced by Hockenhull et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2012 Queen’s Printer and Controller of HMSO
Chapter 1 Background
It has been suggested that worldwide incidents of violence account for more than 1.6 million deaths each year. 1 However, the proportion of personal violence resulting in death is only a fraction of personal violence or of violent assaults overall. In this introductory chapter we consider what we mean when we use the term ‘violence’ and examine the extent of violence in both the world and, specifically, the British context. Finally, the nature of the association between violence and mental disorder is explored.
The definition of violence
In a general sense, many would consider violence to consist of the use of physical force that is intended to hurt or injure another person. 2 However, arguably this rather simplistic and limited conceptualisation ignores the more insidious effects of non-physical violence, such as threats, intimidation and the self-directed violence of suicidal behaviour. It has been suggested that there may be several approaches to the definition of violence,3 although at present there is no widely held agreement on which of these is most appropriate. In this document we have adopted the broad conception offered by the World Health Organization (WHO), which has defined violence as ‘The intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community, that either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment or deprivation’. 4
This definition includes threats, intimidation, neglect and physical, sexual and psychological abuse, as well as acts of self-harm and suicidal behaviour. Furthermore, it conceives of violence in terms of its outcomes on health and well-being rather than, for example, its characteristics as a construct that is purely culturally determined. 5
A number of attempts have been made to formulate a typology of violence. Krug et al. ,4 for example, suggested three broad categories: self-directed, interpersonal and collective violence. For our purposes here we propose to focus on only the second of these. This category, interpersonal violence, incorporates intimate partner violence, child abuse and stranger assaults, whether sexual or not. Excluded from this are acts of collective violence committed as a concomitant of war, terrorism or gang conflict.
The extent of violence
Determining the extent of serious violence at a global level is particularly problematic. Important among the range of obstacles to this is variation in the willingness and capacity of different governments and agencies to collect, and then make available, reliable data. The statistics that do exist indicate that global violence-related deaths in the year 2000 (the most recent year for which data exist) included 520,000 homicides, with rates being several times higher in low- to middle-income countries relative to high-income countries. 4 In absolute terms, death by homicide or suicide is considerably more likely among males, especially those aged 15–44 years, than among any other age/gender demographic grouping. 4 Comparable data for non-fatal violence are not available, as the true extent of this can be determined only by self-report, which is necessarily unreliable because much violence is likely to go unreported to the authorities or untreated by medical personnel. However, it seems reasonable to conclude that the true degree of violence will far outstrip nationally recognised figures for homicide. 6
In England and Wales, provisional data indicate that in the year 2008–9, 648 incidents of homicide were recorded in police figures, which represents the lowest level in 20 years. The most recent evidence from the British Crime Survey (BCS) and from police figures (crimes reported to the police) indicates that non-fatal violent crime remained essentially stable in the year 2008–9 compared with the previous year, with statistically non-significant reductions of between 4% and 6%. 7 In fact, BCS data suggest that the trend in all violence has gradually fallen year on year from a peak in 1995–6 to a current level that is 49% lower than this. 7 Nevertheless, the English Department of Health has identified the short-term management of violence as a key priority and supported development of clinical practice guidelines. 8
Perhaps ongoing public concern about the level of person-to-person violence serves to retain violence at the top of the political agenda, no doubt partly because acts of violence against the person account for approximately 20% of total crime, as recorded in police figures and reported by the BCS, respectively. 7 Domestic violence (DV) in particular has come to be regarded as a key priority of the British government, which recently set out its National Domestic Violence Delivery Plan for 2008–9. 9 This document makes it clear that in England and Wales in the year 2008–9 DV accounted for 14% of all violent incidents and had more repeat victims than any other crime. Violence towards staff working in the NHS has also come to be seen as a significant element in the government agenda, with 12% of staff reporting physical violence from patients or their relatives in the previous 12 months. 10 The government response to concerns about violence in adult psychiatric inpatient settings and hospital emergency departments has been to develop guidelines and other initiatives to improve the short-term management of this behaviour. 11
Although our focus in this document is principally on the perpetrators of violence, it is worth noting that, overall, 3% of adults in England and Wales have experienced a violent crime in the preceding year, with men being twice as likely as women to have been victims of some form of violence. 7 However, victim statistics are unlikely to present a true picture of the full extent of violence, as victim surveys tend to show lower rates of reporting for violence than for other types of crimes. 12,13
The association of violence with mental disorder
As many as 10 years ago it was observed that the number of homicides in England and Wales committed by persons with serious mental disorders had steadily declined over a 38-year period. 14 Despite this, acts of violence committed by people with mental illness remain a matter of continuing major concern to the public, as well as to service providers and policy-makers. 15
Recent large-scale reviews suggest that some diagnosed mental disorders, notably schizophrenia and other psychoses, are associated with an increased risk of violence. Fazel et al. 16 reviewed 20 studies with an aggregate sample of 18,423 individuals and, after discounting the influence of concurrent substance abuse, found an odds ratio (OR) of 2.1 for the relationship between active schizophrenia and violence. Douglas et al. 17 reviewed a total of 204 studies, subsuming 166 independent samples, and concluded that ‘… psychosis was reliably and significantly associated with an approximately 49–68% increase in the odds of violence relative to the odds of violence in the absence of psychosis’ (p. 687). Although this is clearly a substantial increase, it should also be noted that ‘the average effect size for psychosis … is comparable to numerous individual risk factors’ found in other research (p. 693). Furthermore, there was considerable heterogeneity in the findings surveyed. For example, approximately 25% of the effect sizes obtained were < 0 (with a mean OR of 0.73), whereas another 25% were large (above a mean OR of 3.30).
Violence reduction interventions
The mental health and criminal justice systems provide an important environment for the management and treatment of violence and for the prevention of future violence when the person is in the community. This review will examine the evidence base for a wide range of pharmacological, psychosocial and organisational interventions that have been used to deal with the problem of violence.
For the purpose of this report, an intervention is considered to be any explicitly defined action or set of actions taken by a practitioner with the aim of reducing the potential for violence by a specified individual. This definition incorporates a huge range of potential interventions18,19 with varying degrees of evidence supporting them, and a number of distinctions can be introduced in order to organise the field. One distinction is whether an intervention is based on a view of violence as secondary and symptomatic of an underlying problem or whether it is an intervention explicitly and primarily targeting violence as the problem. Most interventions designed to reduce antisocial personality disorder ‘globally’, for instance, would expect reductions in violent behaviour as a result of success in improving the person’s way of generally relating with the world. The review presented here includes both primary and secondary interventions, but includes only the former group when there is some assessment of violent behaviour as an outcome.
A further distinction must be drawn between short-term and long-term violence reduction interventions. Some interventions, such as rapid tranquillisation and verbal de-escalation, are designed for the prompt control and management of imminent violence involving highly aroused and disordered patients,11 whereas many others are delivered over longer time periods, up to a period of years for some milieu therapies, and are designed as treatments dealing with underlying causes rather than temporary or short-term symptom management. These long-term structured therapeutic interventions tend to be delivered in relatively low-arousal settings aimed at preventing future violence in inpatient, prison or community settings.
The range of factors underlying violent behaviour is very wide, ranging from genetic and biochemical influences to cultural forces, and the interplay between these factors in any particular act of violence is extremely complex. Given the complex causal pathways for any violent act, interventions have been developed to operate at numerous different levels ranging across neurological, psychological and social processes. Most studies consider an intervention operating at only one of these levels, whereas most health practice involves multimodal interventions where, for instance, drug treatment is combined with psychological techniques within a particular social milieu. This disparity between research and real world practice should be borne in mind when examining the evidence base.
With regard to pharmacological interventions, there are no drugs designed specifically to reduce violence per se. Haloperidol and lorazepam have been recommended for rapid tranquillisation in emergency situations11 and clozapine, among other second-generation antipsychotic drugs (e.g. olanzapine), has been reported to be effective in reducing violence associated with psychosis over longer time periods. 20 In the results of a systematic review,21 there is support for the use of benzodiazepines, combined, if necessary, with antipsychotic drugs, as part of a longer-term maintenance regime for people with mental health problems who are acting aggressively as part of their disorder.
Psychosocial interventions can be targeted at the individual or may be delivered as part of a therapeutic milieu. At the individual level, most interventions, and certainly most evidence-based interventions, are based on cognitive behavioural principles designed to change the person’s thinking style and interpretation of situations in which conflict may arise. The most well-articulated approaches within this family are Aggression Replacement Therapy22 and the variants of anger management. 23 Individual-level psychological interventions may also be based on psychodynamic or humanistic principles (e.g. Doctor and Nettleton24), but these are less well evaluated.
Beyond these individually targeted interventions, therapeutic communities and milieus have been used to generate therapeutic change through immersion of the violent individual into a particular culture that reinforces non-violent behaviour and encourages confrontation with antisocial behaviour. 25 Similarly, some interventions in traditional mental health units (i.e. outwith therapeutic communities) are environmental and cultural, in that their delivery is mediated through a third party. For instance, the human environment of a ward may be changed by training all staff in proactive de-escalation strategies26 or the physical environment may be adjusted. 27
An important methodological issue is deciding whether an intervention is a cause or an effect. Certain short-term management approaches (e.g. seclusion of an agitated person in a locked room) are interventions (i.e. an independent variable) as defined above but may also be a proxy measure (i.e. a dependent variable), as they may indicate the failure of more long-term interventions. As a general rule in this review, reactive management strategies – such as seclusion and restraint – are considered as dependent variables, whereas proactive strategies such as de-escalation are considered as interventions, even although they are equally short term. Part of the justification for this is that reactive strategies are often the target themselves of interventions designed to reduce reliance on them. 28 It is acknowledged, however, that this distinction is difficult to maintain with complete consistency.
A distinction can be drawn between complex and non-complex interventions. Non-complex interventions, such as pharmacological and dietary approaches, are relatively simple in terms of the relationship between exposure to the intervention and changes in behaviour. The drug is targeted at one specific physical system and if, all other things being equal, it changes behaviour then the causal mechanism and its efficacy can be more easily established. Complex interventions are considered to be those that consist of several components, each of which may make a contribution to the success of the intervention. 29 They are also recognised to be operating within the complex social system of a ward, prison or organisation. There is a growing recognition that traditional methods used to evaluate non-complex interventions and which prioritise the randomised controlled trials (RCTs) are severely limited in evaluating complex interventions.
Rationale for the review
The scope of the review presented here is deliberately wide. We have noted above the complexity of the phenomenon of violence, but there are benefits from casting the net as widely as possible and looking for consistent patterns across populations. Two populations are covered by the review as a reflection of the need to integrate the insights that can be gained from clinical and criminological research. These populations (people with an Axis 1 or 2 diagnosis and people who have committed an indictable offence, regardless of whether they have been found guilty or not) often overlap and often move between the criminal justice and mental health systems. 30 For similar reasons, the review encompasses interventions delivered both in institutions (i.e. hospitals, prisons and their variants) and outside in the community as part of an outpatient or community offender management programme.
After 20 years of sustained activity in this area, the primary research literature is now very large, yet the evidence base for making clinical and policy decisions is often bemoaned as inadequate. 31 The quality of the evidence base is certainly poor considering the vast number of studies and reviews that have been published in the last decade,32 largely because of a combination of methodological difficulties and lack of focus characteristic of the unusually rapid development of interest in the field. A number of systematic reviews have been conducted to summarise and integrate the findings from the literature and these provide evidence on a number of specific areas. However, inevitably these reviews tend to focus on a specific intervention, for example second-generation antipsychotic drugs33 and/or a specific outcome (e.g. reoffending) in various special populations (e.g. sex offenders). This review will instead adopt a more comprehensive approach by aiming to capture research on all interventions relating to a broad range of violence-related outcomes among a wide mental health and criminal justice population. In this way it is anticipated that the fragmented clinical and criminological literatures can be reintegrated to the mutual benefit of practitioners and researchers in both settings. 34
Other reviews
This review was conducted in the context of a number of other reviews of research on evaluations of violence reduction interventions by various teams around the world (for a survey of those pertaining to the field of criminal justice, see McGuire35,36). Given the breadth of the inclusion criteria adopted for the review here, 17 of these reviews are most relevant to the focus adopted here. However, these previous reviews cover specific populations and treat them distinctly, whereas the review reported below attempts to integrate the literature across these distinct groups. Four of the reviews focus exclusively on younger offenders in the age range of 12–21 years;37–40 seven address the problem of sexual offending;41–47 one deals with DV;48 one includes both adolescent and adult samples;49 and four are focused on studies of individuals diagnosed with personality disorders. 50–53
The broadest review was a meta-analysis (MA) by Dowden and Andrews. 49 This subsumed a range of studies that included mixed samples of adult and adolescent offenders and target offence behaviours, including general violence, sexual and domestic assaults. These authors found 34 evaluations of interventions to reduce violence, yielding 52 effect-size tests. Approximately 70% of the included studies focused primarily on work with adults. Unfortunately, they do not report separate outcome data for the two age groups. The overall mean effect size (r) was relatively low at +0.07, although there was enormous heterogeneity in the findings: effect sizes ranged from a low of –0.22 to a high of +0.63. The effect size for interventions based on the risk–need–responsivity model54 was better than the overall mean, at +0.12. This corresponds to recidivism rates of 44% for experimental and 56% for control groups. Possibly the most notable finding to emerge from this review was evidence of a close correspondence between the number of criminogenic needs targeted in interventions and the associated effect size: a correlation coefficient of 0.69 (p < 0.001).
Sexual offences
Regarding the specific phenomenon of sexual violence, to date a total of seven reviews have been reported; not surprisingly there is considerable overlap between these reviews, although they varied in their breadth of compass, their thoroughness and, in some cases, selected subdivisions of the field were the primary focus of interest. 41–47 The most comprehensive MA of this field46 synthesised findings from 69 studies, covering a cumulative sample of 22,181 participants, and included both medical and psychosocial treatments. From these findings Lösel and Schmucker46 were able to compute a total of 80 effect-size tests. A majority (60%) of the studies consisted of non-equivalent group designs, equivalence was assumed for a further 19, seven used statistical controls and six involved random allocation. Mean effect sizes across interventions, expressed as ORs, were +1.70 for reductions in sexual recidivism, equivalent to a 37% reduction relative to comparison samples; +1.90 for violent recidivism (44% reduction); and +1.67 for general recidivism (31% reduction). The largest effects were for physical treatments (surgical castration, eight studies, OR = 15.34; hormonal medication, six studies, OR = 3.08). Some psychosocial interventions achieved significant effects (behavioural, seven studies, OR = 2.19; cognitive behavioural, 35 studies, OR = 1.45), whereas others (insight-oriented and therapeutic community approaches) had ORs that were not significantly different from 1. The mean effect size for cognitive behavioural methods is lower than the OR of 1.67 found in another review of sex offender treatment that focused solely on psychologically based interventions. 44
Personality disorders
Personality disorder is a specific clinical phenomenon, which, in certain manifestations, can be relevant to violent behaviour. Two reviews have been reported of offenders with personality disorders, but neither is a systematic review nor has used statistical integration methods, because of the small number of studies that were located. Salekin50 reviewed a series of 42 outcome studies; however, only eight involved group comparison designs, and many others were single case reports, so although the latter may be clinically instructive, any firmer conclusions must remain tentative at present. Of those studies that could be regarded as more robust, there were five studies of cognitive behavioural therapy (CBT) incorporating a cumulative sample of 246 individuals. There were high-effect sizes on intermediate outcome variables for several therapeutic approaches, including CBT, personal construct therapy, and other approaches which ‘ addressed patients’ thoughts about themselves, others and society. Thus, they tended to directly treat some psychopathic traits’ (p. 93). 50 Salekin50 also observed that there was a strong association between effect size and duration and intensity of treatment: interventions lasting < 6 months were less likely to produce benefits than longer ones. Where attendance was maintained for > 1 year, or delivered at a rate of more than four sessions per week, a considerably higher fraction of the samples benefitted.
Addressing the controversial question of whether those individuals assessed as ‘psychopaths’ are untreatable, or (as reported by an earlier study) could potentially be made worse by treatment, Tanasichuk and Wormith51 found only three studies that compared treated and untreated samples. They located an initial total of 21 studies yielding 50 effect-size estimates (cumulative sample n = 5550). In comparisons between those designated as psychopaths and samples of non-psychopaths, the former consistently showed higher general, violent and sexual recidivism, more antisocial behaviour, higher levels of substance abuse, and spent significantly less time in treatment. In the three studies where comparisons were possible between treated and untreated psychopaths, there were no significant differences in general or violent recidivism; other types of comparisons were not feasible given the available data. However, contrary to the findings of some earlier research there was no evidence that treatment made psychopaths worse.
Recent National Institute for Health and Clinical Excellence (NICE) guidance (NICE. Antisocial personality disorder: treatment, management and prevention. NICE clinical guideline 77. 2009. URL: www.nice.or.uk/CG77) with regard to the management of antisocial personality disorder warns against the routine use of pharmacological interventions for the disorder overall or for aggression associated with it, and notes that there is insufficient evidence to justify the use of any specific medication, although appropriate medications may be used for treatment of comorbid conditions. To address problems such as impulsivity, interpersonal difficulties and antisocial behaviour associated with antisocial personality disorder, psychological interventions such as group-based CBT (e.g. ‘reasoning and rehabilitation’ programme) are recommended instead.
Borderline personality disorder (BPD) is a second major diagnostic category that has been seen as linked to an increased risk of violent behaviour. A recent Cochrane review52 of 27 pharmacotherapy trials indicated that pharmacotherapy had some beneficial but differential effects on all aspects of the disorder. The affective dysregulation element, for instance, which is clearly relevant to aggressive propensities, was improved through treatment with haloperidol, aripiprazole, olanzapine and mood stabilisers. Other attempts to synthesise the evidence in this area (e.g. Herpertz et al. 53) are inconclusive about the efficacy of pharmacotherapy on the specific aggressive aspects of BPD. As with antisocial personality disorder, recent NICE guidance (NICE. Antisocial personality disorder: treatment, management and prevention. NICE clinical guideline 77. 2009. URL: www.nice.or.uk/CG77) recommends avoiding pharmacological treatment for the core disorder or its associated behaviours (other than for short-term crisis management), while highlighting the potential benefits of psychological interventions. No specific theoretical approach is indicated as long as there is some explicit orientation to the therapy, which is shared with the service user.
Domestic violence/partner abuse
This review also included the specific phenomenon of DV in order to enable comparisons to be made between this and the related violence fields. There is one MA of methods or strategies designed to reduce DV, consisting (almost overwhelmingly) of assaults by males on female partners. Babcock et al. ,48 examined findings from 22 studies yielding (after elimination of outliers) 36 effect size tests; 17 of the studies were quasi-experiments and the remaining five were ‘true’ experimental designs. The overall conclusion of Babcock et al. 48 (p. 1044) was that ‘… there is great room for improvement in our batterers’ treatment interventions’ and it is widely recognised that this remains possibly the largest single area in which, to date, effective methods of intervention have not yet been firmly identified.
Young offenders
Although the focus below is on violence by adults (aged > 16 years) there is some overlap with previous reviews of young offenders as the definition of young offenders can include those up to the age of 21 years. The largest of the previous reviews focused on young offenders is that of Lipsey and Wilson,37 who integrated findings from a total of 200 studies, 117 of interventions based in the community and 83 of interventions based in residential or custodial settings. All of these studies were with adjudicated offenders or with young people with adjustment problems, but not diagnosed with mental disorders. Intervention programmes in the ‘most consistently effective’ category were found to have an average impact in reducing recidivism by 40% in community settings and 30% in custodial settings. 37
A later review by Garrido and Morales38 is essentially an updated version of portions of the Lipsey and Wilson37 review, combining studies carried out in the period up to 2006 but including only studies with ‘chronic delinquents’ detained in institutions. Covering a related but separate area of research, Wilson et al. 39 reviewed studies of methods designed to reduce aggression in schools. Addressing a more specific question, McCart et al. 40 compared the relative effectiveness of behavioural parent training and CBT in reducing aggression and other antisocial behaviour among young people < 18 years old; they found 41 studies of the former and 30 of the latter.
Findings from all of these reviews showed on average positive outcome effects and the authors report analyses of the relative effectiveness of different interventions and the roles of moderator variables where possible. However, in all of these reviews a majority of the studies that were included consisted of quasi-experimental designs, with only a fairly small proportion using randomisation.
Previous review
The review reported here is an update of one part of an existing review. In 2002 the Department of Health commissioned the Liverpool Violence Research Group (LiVio) to complete a broad-ranging systematic review of interventions and risk assessment strategies for the management of violence in a widely defined population (offenders, people with mental health problems and offenders with mental health problems). The aim was to provide a picture of the literature that was broad enough to inform future improvements in research, policy and clinical practice, while strictly adhering to the main criteria for high-quality reviews. The original review55 covered publications released between 1955 and 2001 (with partial update to 2004) on a population that consisted of (1) adult offenders (> 17 years) with or without a mental disorder; (2) adults with a diagnosable mental disorder but no offences; and (3) adults in the general population exhibiting indictable acts of aggression without actual indictment (e.g. DV). Substance abuse alone was not deemed sufficient to constitute a diagnosis of mental disorder. Any pharmacological, psychological or other intervention targeted at the individual patient/offender and delivered individually or in small groups was included. Organisational interventions (e.g. ward-level changes) that did not report individualised outcomes were excluded. Changes on any outcome measure that was an actual or proxy assessment of aggression (e.g. observed aggression, self-reported hostility) were included. There were no exclusions based on design, language or publication format.
Search strategy and selection of studies
The primary method used to identify studies meeting the above criteria was to conduct (1) a detailed search of 31 electronic databases from their point of inception to December 2004; (2) a hand-search of 42 specialist research journals covering the period January 1990 to December 2000; and (3) a consultation exercise with a specified list of 50 active international violence researchers.
In total, 228,182 citations of relevance to human aggression were retrieved. Of these, 41,886 citations related, broadly speaking, to risk or intervention. Of the material meeting the broad review inclusion criteria, just over 1000 citations reported on empirical research, with aggression being the sole or main focus for nearly 90% of the reported studies. In line with the rapid expansion noted in the literature, the majority of empirical studies identified (85%) were written or published from 1980 onwards. An executive summary of the findings from the review can be found at www.liv.ac.uk/fmhweb/MRD%2012%2034%20Final%20Report.doc.
The final report55 has had significant influence on national policy in England and was formerly flagged on the website of the Department of Health/Ministry of Justice (England) National Risk Management Programme. 56 It also formed the basis for a set of national best practice guidelines on risk management57 and national policy guidance on selection of risk assessment tools. 58
Update of the review
This update uses the same search strategy and the same databases were searched where possible. The four senior reviewers involved in the original review were also involved in this update and are referred to in this document as ‘expert reviewers’.
Owing to the size of the original review it was decided that the update would be split into two distinct elements: this intervention review and, secondly, a review of risk assessment approaches with the same population (to be published at a later date). It is important to emphasise that the two processes are closely linked. Estimates of predictive validity from a risk assessment tool are of little use on their own if they are not used to design and target effective interventions. The structured clinical (or professional) judgement approach59 is important in this context, as this approach is recognised as encouraging practitioners to focus on risk management and flexibility in choosing appropriate interventions.
Research question
Which interventions are the most effective in reducing violence and which key variables are associated with a significant outcome?
Chapter 2 Methods
This review was conducted by a large team of reviewers, with varying numbers working on the review at any particular stage. The searches were conducted by two reviewers, application of stage one inclusion criteria by 11 reviewers, stage two inclusion criteria by seven reviewers, data extraction and cross-checking by nine reviewers, extraction of statistical outcomes by five ‘expert’ reviewers (four of whom had been involved in the original review).
Search strategy
The search strategy (see example in Table 54) used in the original review was rerun on the 19 databases shown in Table 1. The first database to be searched was PsycINFO and the searches were run in April 2008. The last database to be searched was SIGLE (System for Information on Grey Literature In Europe) and the searches we carried out in November 2008. Where it was possible to limit searches, they were initially run without limits and then rerun limited to children or animals or editorials. These hits were then removed from the first run. This method was used so that papers that had not been indexed on a term, for example ‘humans’, were not missed when running the searches.
| Database | Limits used |
|---|---|
| PsycINFO (CSA) | Animals, editorials, childhood (birth to 12 years) |
| MEDLINE (Ovid) | (Animals or (“newborn infant (birth to 1 month)” or “infant (1 to 23 months)” or “preschool child (2 to 5 years)” or “child (6 to 12 years)”) or editorial) |
| CINAHL (Cumulative Index to Nursing and Allied Health Literature) | Animals or (“newborn infant (birth to 1 month)” or “infant (1 to 23 months)” or “preschool child (2 to 5 years)” or “child (6 to 12 years)”) or editorial) |
| AMED (Allied and Complementary Medicine Database) | None |
| British Nursing Index/Royal College of Nursing | None |
| IBSS (International Bibliography of the Social Sciences) | None |
| ERIC (Education Resources Information Center)/International ERIC | None |
| The Cochrane Library (Cochrane reviews, other reviews, clinical trials, methods studies, technology assessments, economic evaluations) | None |
| Web of Science [Science Citation Index Expanded (SCIE), Social Sciences Citation Index (SSCI), Art and Humanities Citation Index (A&HCI)] | Document type=(bibliography or editorial material or letter) |
| Sociological abstracts/SocioFile | None |
| Social Services Abstracts | None |
| EconLit (American Economic Association’s electronic bibliography) | None |
| British Humanities Index Online | None |
| Elsevier Science Direct | None |
| ProQuest (dissertations and theses) | None |
| ASLIB (index to theses) (searched on screen) | None |
| C2-SPECTR | None |
| Emerald Fulltext | None |
| SIGLE (searched on screen) | None |
As the searches were run, citations were imported into Endnote XIV® (Thomson Reuters, CA, USA) sequentially. Owing to the limitations of Endnote, duplicate references were deleted first electronically and then manually.
The reference lists of relevant reviews identified at inclusion were searched for additional relevant references.
Inclusion and exclusion criteria
The identified citations were assessed for inclusion through two stages. The criteria used were those used in the previous review and are shown in Table 2.
| Inclusion | Exclusion |
|---|---|
| Active diagnosis of mental illness, learning disability or personality disorder or | Participants are members of the general public, with no identified mental illness and no recorded violent offence and no evidence of having committed an act of violence that would constitute an indictable offence |
| Substance abuse (including alcohol abuse) in isolation from any other diagnosis of mental illness is not to be defined for the purposes of the review as an active diagnosis of mental illness | |
| Substance abuse (including and separately specified as alcohol abuse) is to be identified in relation to participant characteristics for the purposes of data extraction, as it is identified in primary studies | |
| Offender (person subject to penal sanction) or | |
| Person(s) known to have committed one or more acts of aggression constituting an indictable offence (whether or not an indictment has been made) | |
| Aged ≥ 17 years | Aged ≤ 16 years |
| Any intervention specifically identified as being evaluated with the intention of preventing violent behaviour or | Interventions focused solely on reducing or preventing target behaviours other than aggression towards others |
| Implemented with the immediate intention of preventing violent behaviour (e.g. ‘naturalistic’ evaluation in a clinical setting) | |
| Interventions must be targeted at the individual level | Studies that evaluate the impact of broad-based local or national population-level initiatives and which also fail to evaluate outcomes (compared with outcome criteria) at the individual level are to be excluded |
| Studies that have a focus on a main target behaviour which is not other-directed aggression (the target behaviour may be self-directed aggression), but which do include an evaluation of the association between exposure to an intervention and rates of other-directed aggression as a subsidiary focus are to be included | |
| Studies that evaluate the impact of broad-based local or national population-level initiatives and which also fail to evaluate outcomes (compared with outcome criteria) at the individual level are to be excluded | |
| For example, a study evaluating the impact of a binge drinking campaign on aggression, which evaluated outcomes purely by noting changes in population rates of violence across time would be excluded; a study evaluating the same intervention but reporting outcomes based on the same set of individuals with behaviour evaluated before and after the initiative would be included. The key point is that the specific individuals being assessed need to be evaluated at outcome | |
| Interventions may include, but are not restricted to, pharmacological, physical, psychological, environmental, or training initiatives | |
| Interventions include both ‘single dose’ and complex ‘multiple dose’ or ‘multifactorial’ interventions | |
| Studies that have a focus on a main target behaviour which is not other-directed aggression (the target behaviour may be self-directed aggression), but which do include an evaluation of the intervention on other-directed aggression as a subsidiary focus are to be included | Studies focused solely on self-directed aggression, including self-harm and suicidal behaviours are to be excluded |
| Any institutional setting/location | Setting/location of any study is not to be regarded as grounds for excluding that study |
| Any community setting/location | |
| Community-based ‘institutional’ settings, such as outpatient clinics, A&E, private practice clinics, etc., are also to be included | |
| Studies conducted at ‘remote’ locations, for example studies evaluating interventions conducted by telephone or in writing, are also to be included | |
| Any design explicitly measuring outcomes following an intervention meeting the above criteria | No attempt at any sort of empirical approach likely to elicit at least an association between dependent variables and outcomes should such exist |
| No clear identification of an intervention taken as either the main or as a subsidiary focus of the study | |
| Directly observed physical or verbal aggression by person(s) with an identified mental illness | No evaluation of outcomes |
| Aggressive behaviour (as defined for the population groups considered), not either a main or subsidiary outcome of the evaluation | |
| Directly observed physical aggression (meeting criteria for indictment) by members of the general public or current/previous offenders | |
| Proxy measures of the above (including but not restricted to: self or other report of the above categories of behaviour, including reports established via clinical records; official records of offence and conviction; psychometric and other scale-based outcomes of mentations or behaviours directly relevant to aggression, for example BPRS measures of ‘hostility’) | |
| Outcome evaluation must be based on individual-level data | Evaluations based on ‘non-attributable’ rates and other summary data are to be excluded: |
| ‘Collective’ acts of aggression, such as terrorism, ‘gang’ violence, organised violent crime, football violence, drug feuds, etc., are excluded from consideration by the review where the focus of the study is on the phenomenon as a collective behaviour; studies focused specifically on individual behaviour within these contexts should be included | |
| Evaluation of both imminent and non-imminent (future) violence is included within the review | Directly observed or proxy-evaluated aggressive behaviour (as defined for the population groups considered) is not either a main or subsidiary outcome of the evaluation |
Inclusion stage one
At stage one inclusion, six reviewers independently applied the inclusion criteria to 200 citations and a Cohen’s kappa (Fleiss–Cuzick extension) was calculated [κ = 0.63 (SE = 0.019), z (for k = 0) = 34.24, p < 0.0001]. Each new reviewer who joined the team was required to look at 100 citations that had previously been looked at by a reviewer and a > 80% agreement had to be reached. At this stage an ‘inclusive’ attitude was taken, i.e. where there was doubt a citation was included. Given the high level of agreement and the inclusive approach, further citations were screened by only 1 of the 11 reviewers.
If a citation was excluded then it was possible to mark the citation as either a review that needed the reference list checked (‘check’) or a paper of particular interest that should be obtained (‘obtain’).
Acquiring papers
Electronic copies of papers were then downloaded where possible by the University of Liverpool’s interlibrary loans team. Where electronic copies were not available, paper copies were either obtained from the University of Liverpool’s library or through interlibrary loans at the British Library.
Inclusion stage two
At stage two, the inclusion/exclusion criteria were applied to the full papers identified from stage one. To aid with this a Microsoft Access database (Microsoft Corporation, Redmond, WA, USA) was developed using a front page form with drop-down menus and tick boxes. It was at this stage that included papers were categorised into each of the two reviews: intervention or both risk and intervention. Furthermore, studies not reporting any statistical analysis, mainly due to qualitative designs, were excluded from the review though retained for future analysis.
As a quality control measure, all seven of the reviewers applied the inclusion criteria to 50 papers and a Kappa score was calculated [Cohen’s kappa (Fleiss–Cuzick extension): κ = 0.62 (standard error, SE = 0.032) z (for k = 0) = 19.46, p < 0.0001]. Investigation of individual pairs of inter-rater agreement (Table 3) revealed that one reviewer (G) had poorer reliability scores owing to being more inclusive than other reviewers. Therefore, it was decided that there was high enough agreement to continue with single reviewer application of inclusion criteria.
| A | B | C | D | E | F | G | |
|---|---|---|---|---|---|---|---|
| A | 1 | 0.618 | 0.86 | 0.753 | 0.66 | 0.711 | 0.55 |
| B | 1 | 0.537 | 0.702 | 0.685 | 0.57 | 0.421 | |
| C | 1 | 0.683 | 0.684 | 0.684 | 0.68 | ||
| D | 1 | 0.571 | 0.628 | 0.477 | |||
| E | 1 | 0.523 | 0.59 | ||||
| F | 1 | 0.355 | |||||
| G | 1 |
Quality assessment
Owing to the diverse nature of the papers included in this review, no appropriate methodological quality assessment tool was identified. Therefore, variables pertinent to quality assessment were extracted as part of the full data extraction process (see Data extraction) and frequencies calculated where appropriate. Where there were available data, the effect of the quality of studies was explored in MAs.
Data extraction
Data extraction was carried out independently by nine reviewers, with regular meetings to co-ordinate activity and to explicitly cross-check extracted data. Data from each study relating to study design, type of intervention and whether or not a statistically significant outcome was reported were extracted into a predefined Statistical Package for the Social Sciences (SPSS) (SPSS Inc., Chicago, IL, USA) database.
The Spss database was based on the one used in the original review and included both free-text variables, number variables and drop-down menus. The reviewers were then trained in its use and a pilot extraction conducted. Relevant changes were made and reviewers retrained. This process was repeated until the final version was agreed. Ongoing support was also given to reviewers in the form of a crib sheet covering each variable and an electronic forum was set up so that reviewers could post any queries that the expert reviewers could then answer.
Each paper was printed off and marked as data pertaining to the basic aspects of the study were extracted into the Spss database. The data extracted were then cross-checked by another reviewer using the marked paper and any disagreements were noted in a Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) spreadsheet. The two reviewers then discussed disagreements and where no consensus could be found a third reviewer adjudicated.
Papers included in the intervention review were then given to one of the expert reviewers to extract outcome data in an Excel spreadsheet. Intervention arm and resultant statistics were loaded, with multiple lines per study. In particular, specific data were extracted on dependent variable means and standard deviations (SDs) together with statistical test values, confidence intervals (CIs) and probability levels when study groups (treatment vs control and/or baseline vs end point) were compared. This level of analysis had not been attempted in the original review. Subgroup analyses were not extracted where an included full analysis was reported. The outcome extraction for any RCTs identified was then cross-checked and any discrepancies settled with a third party.
Descriptive data
Details of key variables pertaining to quality, trial characteristics, participant characteristics, and intervention characteristics are tabulated and are discussed in Chapter 3, along with comparisons of the characteristics of RCT and non-RCT studies. Where appropriate, differences between RCTs and non-RCTs were investigated with either a chi-squared test or Mann–Whitney U-test (kurtosis and skewness tests reported).
Statistical methods
In Chapter 4, the key variables, as discussed in the descriptive section above, are explored in terms of their role in explaining the variance in whether a study reported a statistical significant result or not. These subgroup analyses should be seen as hypothesis generating rather than providing conclusive answers.
Bivariate and multivariate analyses
Bivariate analyses
A series of bivariate analyses using either a chi-squared test (for dichotomous data) or Spearman’s rho test (for continuous data) were conducted to explore possible sources of variance in whether or not a study reported a statistically significant result.
Multivariate analyses
A binary logistic regression was conducted, with categorical variables coded as ‘dummy’ (0/1, with 0 as the baseline category) and ‘whether or not a statistically significant outcome in favour of the primary intervention arm was established’ as the dependent variable (also coded 0/1). With no specific direction of effect or composite weighting in mind, the ‘ENTER’ method of adding variables to the model was used.
Selection of studies for analyses
Studies were selected for inclusion in these analyses if they provided statistical data suited to extraction and statistical analyses and reported data on statistical significance.
Where an individual study contributed more than one comparison to the data set, we selected for inclusion the main comparison focused on by the authors or, where comparisons appeared to be of equal weight, the comparison which provided the most substantive evaluation of effect (e.g. the comparison using the longest follow-up interval). This ensured, as far as possible, independence between the data points included in the MAs.
Meta-analysis
Selection of studies for meta-analysis
Studies were selected for inclusion into the MAs if they followed a RCT design and reported data that could be converted into ORs or risk ratios. Where an individual study contributed more than one comparison to the data set, we selected for inclusion the main comparison focused on by the authors or, where comparisons appeared to be of equal weight, the comparison that provided the most substantive evaluation of effect (e.g. the comparison using the longest follow-up interval). This ensured, as far as possible, independence between the data points included in the MA. Details of studies and outcomes selected for each MA are outlined in Appendix 3.
Effect sizes
Where possible, metrics were converted to ORs using equations provided by Lipsey and Wilson. 60 To provide a context in which to evaluate the relative impact implied by the mean effect sizes presented, effect sizes based on the standardised mean differences are also reported.
For each MA, both an fixed-effects model and a random-effects model were fitted, rather than assuming a priori that either was most appropriate.
Heterogeneity
To identify the indicative variance existing within various groupings of studies used in MA, we calculated both Q statistic and I2 estimates of heterogeneity for each MA performed. The rationale for providing two tests in this context was that the Q-statistic, although generally a reliable test of heterogeneity, fails to provide an estimate of the extent of heterogeneity. The I2-statistic can be used to evaluate the extent of heterogeneity, which is useful in exploring the likely impact on outcomes.
Where heterogeneity was present, data were re-evaluated by modelling the impact of the potential modifiers on both observed heterogeneity and on effect size outcomes. The potential impact of each modifier was explored using metric-appropriate statistics (analysis of variance, logistic and linear regression). Further MAs focused on studies identified as similar in respect of these key characteristics were then carried out to explore the mean effect sizes generated for a range of interventions within relevantly similar groupings.
Subgroup analyses on the following were also conducted to investigate heterogeneity: (1) type of comparison, for example single group designs, active treatment versus treatment as usual (TAU); (2) broad intervention groups, i.e. pharmacological, psychological and ‘other’; and (3) specific intervention groupings.
The exploration of potential modifiers that may account for the variation in outcome between studies was restricted to the variables that were reliably reported by the included studies. Taking into account the likely relevance of these to clinical practice and policy, sensitivity analyses were carried out for (1) clinically relevant factors; mental health status, age, sex and ethnicity and the setting in which the study was conducted; (2) type of outcome measure; and (3) study quality indicators, namely sample size, number lost to follow-up, blinding, length of follow-up baseline equivalence and whether an intention-to-treat (ITT) analysis was used.
Publication bias
Publication bias was explored using a funnel plot,61 i.e. a scatterplot of effect size against sample size (or SE, which is expected to closely associate with sample size).
Advisory panel
As this review is part of a larger project Developing Evidence-based Guidelines for the Prevention of Violence in Mental Health Settings (EPOV) funded by the Department of Health, Research for Patient Benefit Programme (RfPB), the steering group for this larger project provided support and answered specific questions as the review progressed and commented on a draft of this report.
Chapter 3 Overview of the literature
Selection of included studies
As shown in Figure 1, the electronic searches identified 127,550 citations. After deduplication, both within and between the databases, 102,267 citations had the inclusion criteria applied at stage one. This resulted in 96,077 citations being excluded, 246 of which were reviews.
FIGURE 1.
Flow diagram of inclusion of studies.
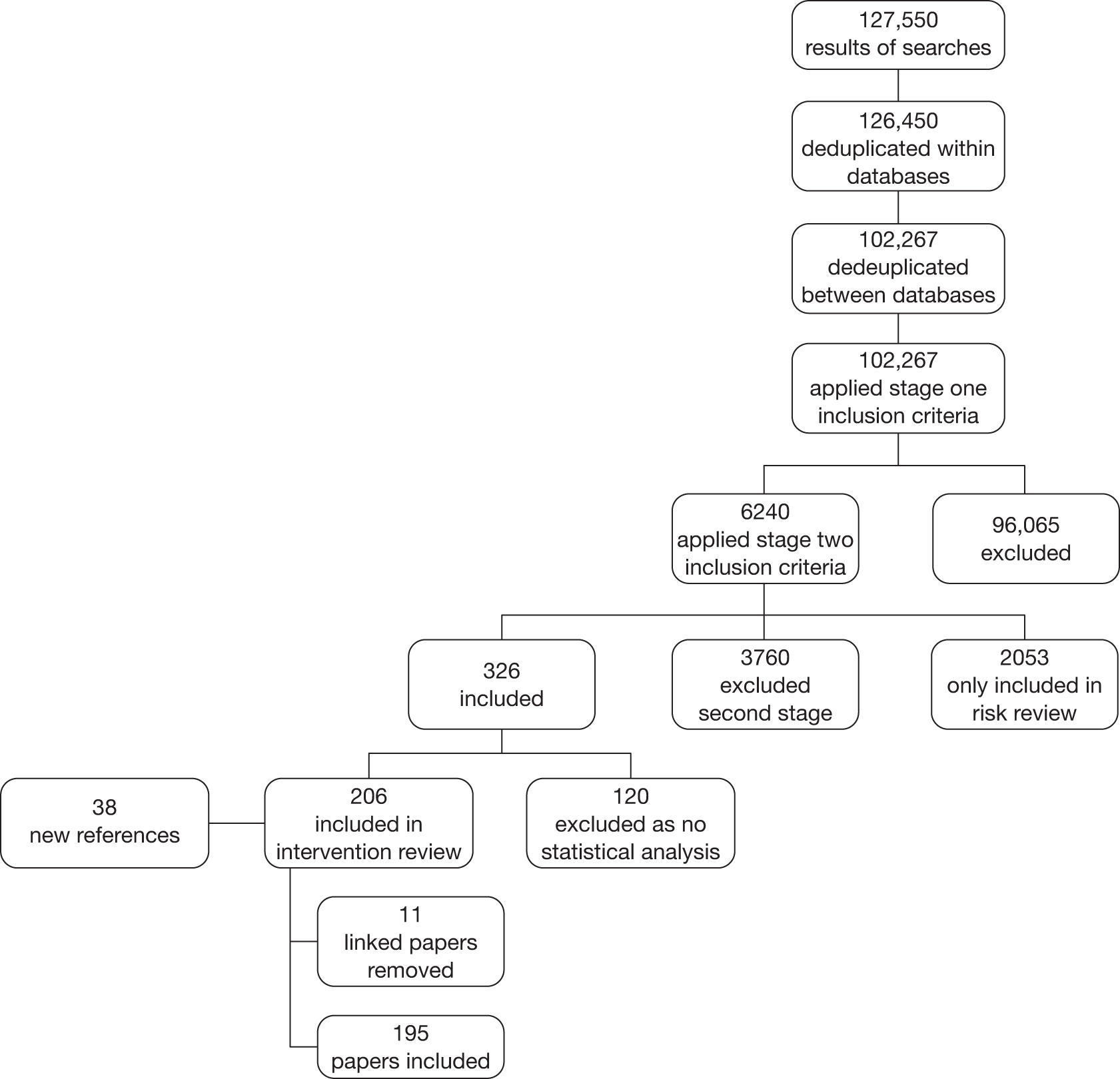
As a result of searching the reference lists of the 246 reviews, an additional 38 references were identified. Therefore, a total of 6240 papers had the inclusion criteria applied at stage two.
The process of applying stage two inclusion criteria resulted in 3760 references being excluded from both the intervention and risk reviews and a further 2053 being included in the risk review only. The remaining 326 papers met the inclusion criteria for the intervention review and data were extracted. At data extraction, 120 of the 326 papers were identified as not reporting any statistical analysis, mainly because of qualitative designs, and were therefore excluded from the review. A further 11 papers were identified as reporting data that were reported in other included papers. The primary paper for each study was retained, with any additional data reported in the linked paper combined, while the linked paper itself was excluded. A list of included papers is shown in Appendix 1, Table 55, and a list of excluded papers available on request.
Of the 195 included papers, three included more than one study, resulting in 198 studies being data extracted. All of the following analyses will be reported by study rather than by paper.
Different sections of the report require different selections of studies, as described throughout the report. However, Table 4 summarises the number of studies for each level of analysis.
| Chapter | Section | Description | No. of studies | No. of comparisons |
|---|---|---|---|---|
| 3 | Quality assessment; Study characteristics, Participant characteristics, Intervention characteristics | Descriptives | 198 | 728 |
| 3 | RCTs | RCTs | 51 | NA |
| 3 | Non-RCTs | 147 | NA | |
| 4 | Bivariate/multivariate analyses | 179 | 195 | |
| 5 | MAs | 40 | NA |
Quality assessment
Design of studies
Of 198 studies, 51 (25.8%) were RCTs, one-third (33.3%) were concurrent/cross-sectional group comparisons and 68 (34.3%) were before/after study comparisons. The remaining 13 studies were crossover comparisons, correlational studies and experimental case studies (Table 5).
| Study design | n | % |
|---|---|---|
| RCT | 51 | 25.8 |
| Concurrent/cross-sectional group comparison | 66 | 33.3 |
| Crossover comparison (n > 1) | 2 | 1 |
| Before-/after-study comparison (n > 1) | 68 | 34.3 |
| Correlational/single group no comparator | 8 | 4 |
| Experimental case study (n = 1 or set of Ns = 1) | 3 | 1.5 |
| Total | 198 | 100 |
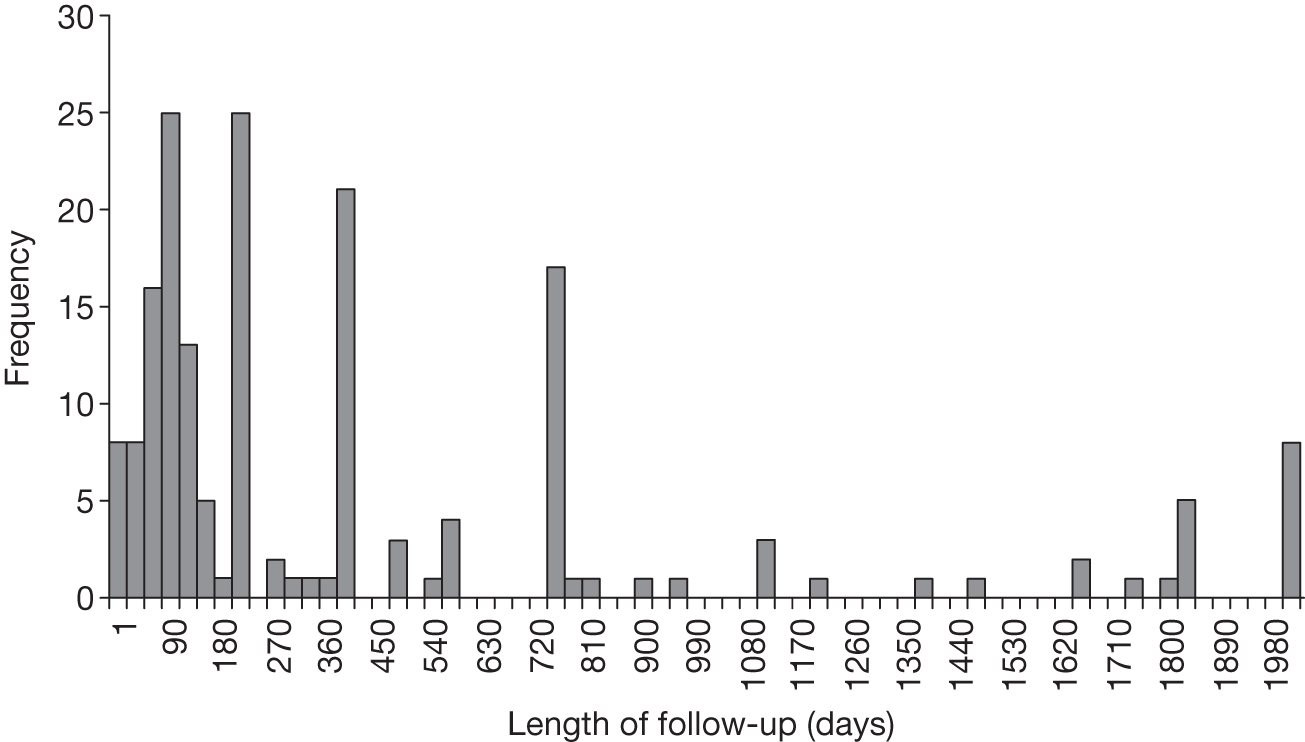
Length of follow-up
The maximum length of follow-up was reported by 179 studies and ranged from half an hour to 14 years, with the average length of follow-up being: mean = 524.26 days, median = 183.40 days and mode = 365 days (Figure 2).
FIGURE 2.
Total length of follow-up in days.
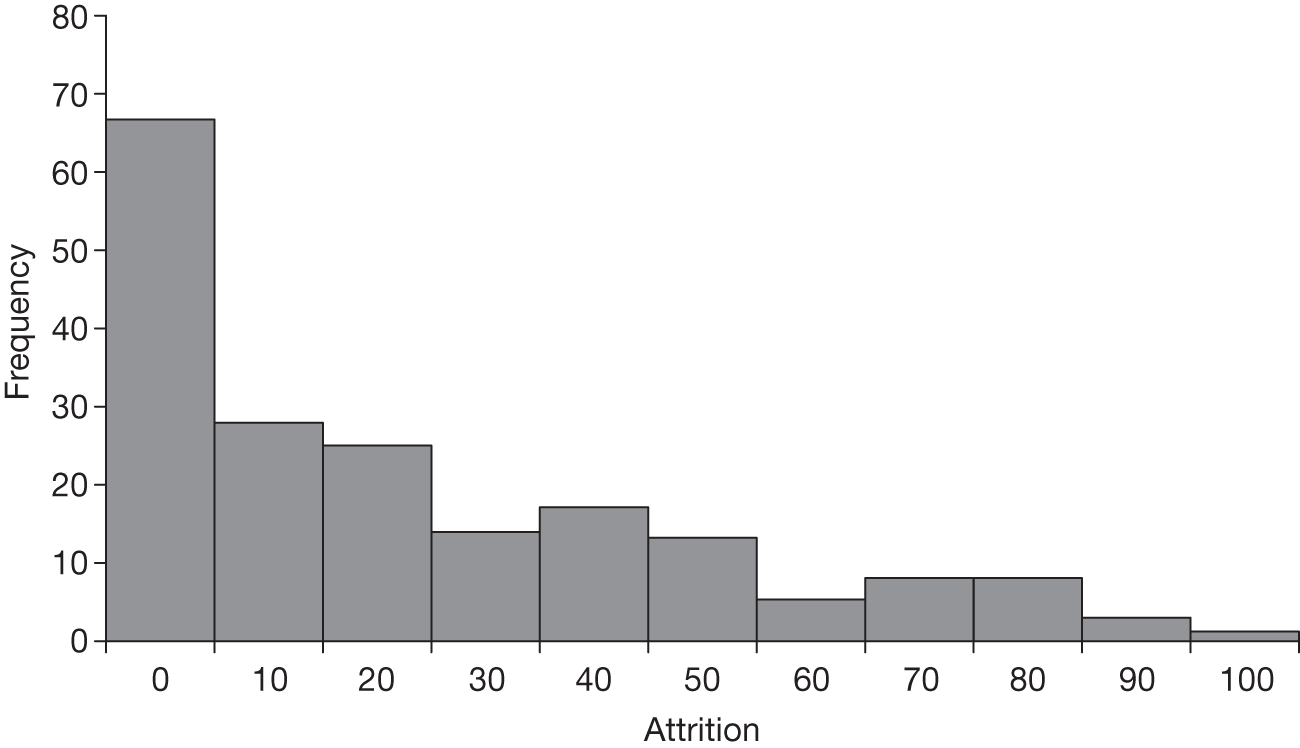
Attrition
Attrition was calculable for 189 of the studies: 67 (35.4%) reported no attrition and four (2.1%) more than 80% attrition (Figure 3). The mean attrition was 20.0% and the median was 9.9%.
FIGURE 3.
Attrition rates.
Intention to treat
The 198 studies included in the review reported on 728 comparisons. Of these, 31.9% were analysed on an ITT basis, 59.1% were not analysed on an ITT basis and 9.1% did not state whether they were ITT analysis or not (Table 6).
| ITT analysis | n | % |
|---|---|---|
| No | 430 | 59.1 |
| Yes | 232 | 31.9 |
| Not stated | 66 | 9.1 |
| Total | 728 | 100 |
Baseline equivalence
Of the 120 studies comparing different study groups, equivalent baseline measures of aggression were reported for 51 (42.5%) studies. A further 11 reported equivalence on some measures of aggression and 16 (13.3%) reported non-equivalence. Twenty studies reported the baseline levels of aggression for each group but did not compare them statistically and 22 (18.3%) did not report any baseline measure of aggression (Table 7).
| Equivalence of baseline measures of aggression | n | % |
|---|---|---|
| Yes, for all aggression outcome variables | 51 | 42.5 |
| Yes, for some aggression outcome variables | 11 | 9.2 |
| No | 16 | 13.3 |
| Unsure, no p-values stated | 20 | 16.7 |
| Not stated/unclear | 22 | 18.3 |
| Total | 120 | 100.0 |
Blinding
Given the nature of many of these studies it is not surprising that blinding was not stated in the majority of papers, as for practical reasons this is impossible to achieve when evaluating psychosocial interventions. Where it was stated, it was most frequently reported for patients and the interventionist, with 10.1% of patients not being blinded and 14.6% being blinded, and interventionists not being blinded in 12.1% of studies and blinded in 12.6% of studies (Table 8).
| Blinding | Patient | Interventionist | Assessor | Analyst | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| No | 20 | 10.1 | 24 | 12.1 | 4 | 2 | 1 | 0.5 |
| Yes, i.e. explicitly stated | 29 | 14.6 | 25 | 12.6 | 16 | 8.1 | 3 | 1.5 |
| Partial | 0 | 0 | 0 | 0 | 4 | 2 | 176 | 88.9 |
| Not stated/unclear | 126 | 63.6 | 128 | 64.6 | 156 | 78.8 | 17 | 8.6 |
| Not applicable | 23 | 11.6 | 21 | 10.6 | 18 | 9.1 | 1 | 5 |
| Total | 198 | 100 | 198 | 100 | 198 | 100 | 198 | 100 |
| 198 | 99.9 | 198 | 99.9 | 198 | 100 | 198 | 100 | |
Study characteristics
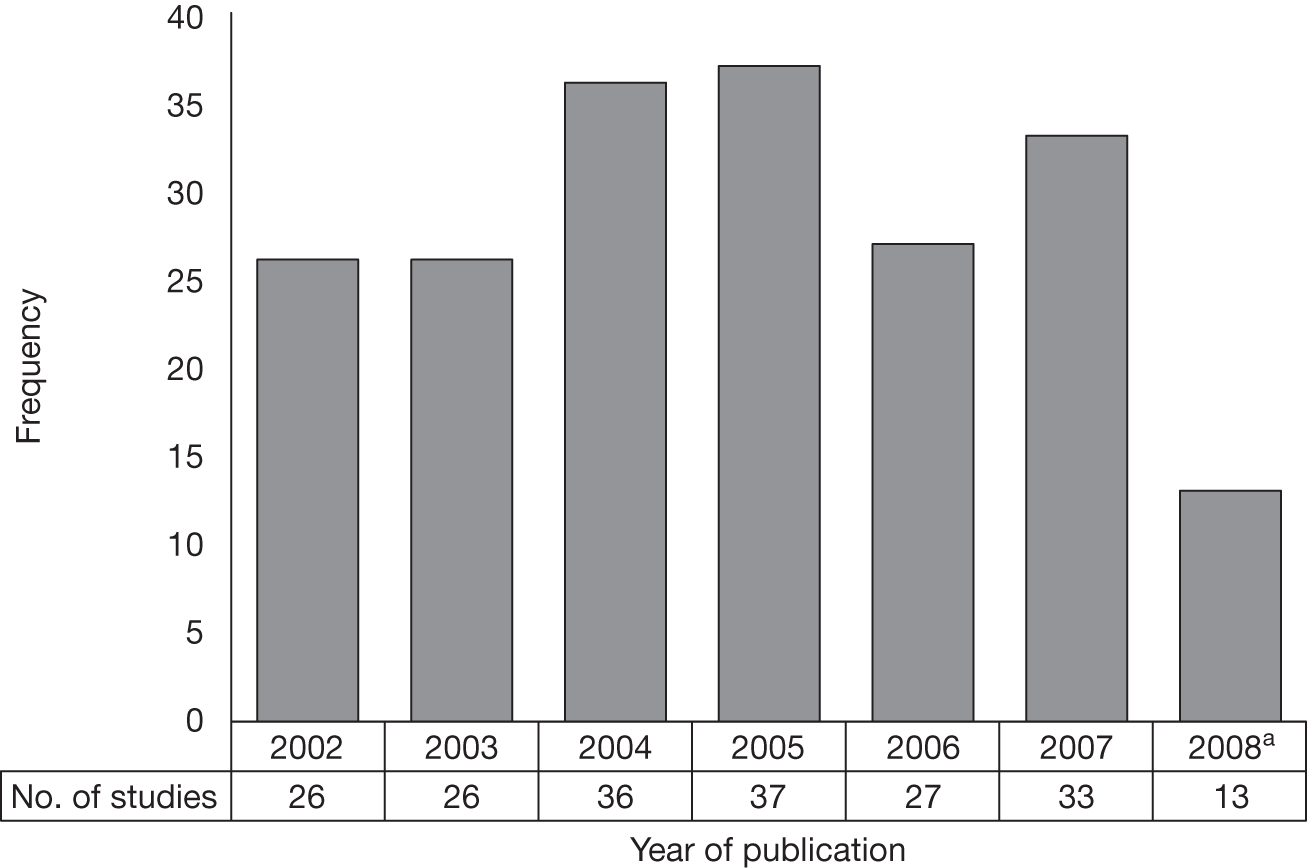
Number of studies
The number of studies published was relatively steady across the years, with an average of 32 papers being published each full year (Figure 4).
FIGURE 4.
Number of studies by year of publication. a, The year 2008 was a partial year.
Country in which studies were conducted
Studies were conducted in 21 different countries, with only three studies being multinational, i.e. participants from more than one country. The majority of studies were conducted in the USA (55.1%), with the UK being the second most common location (10.6%), followed by Canada (6.6%) (Table 9).
| Country | n | % |
|---|---|---|
| USA | 109 | 55.1 |
| UK | 21 | 10.6 |
| Canada | 13 | 6.6 |
| Australia | 8 | 4.0 |
| Netherlands | 4 | 2.0 |
| Italy | 3 | 1.5 |
| Spain | 3 | 1.5 |
| Brazil | 2 | 1.0 |
| Germany | 2 | 1.0 |
| India | 2 | 1.0 |
| Israel | 2 | 1.0 |
| New Zealand | 2 | 1.0 |
| South Korea | 2 | 1.0 |
| Sweden | 2 | 1.0 |
| Belgium | 1 | 0.5 |
| China | 1 | 0.5 |
| Finland | 1 | 0.5 |
| Japan | 1 | 0.5 |
| Norway | 1 | 0.5 |
| Switzerland | 1 | 0.5 |
| Taiwan | 1 | 0.5 |
| Multinational | 3 | 1.5 |
| Not stated/unclear | 13 | 6.6 |
| Total | 198 | 100 |
Participant characteristics
Details of the characteristics of people included in the studies are shown below (see Tables 10–14 and Figures 5–7).
| Variable | n | Lower value (years) | Upper value (years) |
|---|---|---|---|
| Mean age | 158 | 19.0 | 80.9 |
| SD | 118 | 1 | 15.9 |
| Median age | 8 | 29 | 43 |
| Minimum age | 71 | 13 | 65 |
| Maximum age | 70 | 32 | 97 |
| Population | n | % |
|---|---|---|
| Mental disorder | 75 | 38 |
| Offender | 70 | 35 |
| Indictable offences | 29 | 15 |
| Forensic | 24 | 12 |
| Total | 198 | 100 |
| Diagnostic group | Mental disorder | Forensic | Total | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Schizophrenia or schizoaffective disorder only | 10 | 13.3 | 1 | 4.2 | 11 | 11.1 |
| Dementia only | 4 | 5.3 | 0 | 0.0 | 4 | 4.0 |
| Personality disorder only | 18 | 24.0 | 2 | 8.3 | 20 | 20.2 |
| Other single mental health grouping | 25 | 33.3 | 9 | 37.5 | 34 | 34.3 |
| Mixed diagnostic groups | 17 | 22.7 | 11 | 45.8 | 28 | 28.3 |
| No specific diagnoses given | 0 | 0.0 | 1 | 4.2 | 1 | 1.0 |
| Not stated/unclear | 1 | 1.3 | 0 | 0.0 | 1 | 1.0 |
| Total | 75 | 100 | 24 | 100 | 99 | 100 |
| Type of offence | Offender | Forensic | Indictable | Total | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| General violence | 3 | 4.3 | 1 | 4.2 | 3 | 10.3 | 7 | 5.7 |
| Domestic violence | 31 | 44.3 | 0 | 0.0 | 19 | 65.5 | 50 | 40.7 |
| Sex offending | 16 | 22.9 | 7 | 29.2 | 0 | 0.0 | 23 | 18.7 |
| Mixed group of offences | 20 | 28.6 | 10 | 41.7 | 0 | 0.0 | 30 | 24.4 |
| Not stated/unclear | 0 | 0.0 | 5 | 20.8 | 0 | 0.0 | 5 | 4.1 |
| Other indictable offences | 0 | 0.0 | 1 | 4.2 | 7 | 24.1 | 8 | 6.5 |
| Total | 70 | 100 | 24 | 100 | 29 | 100 | 123 | 100 |
| Type of substance abuse | n | % | % of studies reporting on substance abuse (n = 86) |
|---|---|---|---|
| No substance abuse identified | 21 | 10.6 | 24.4 |
| Illicit drug use identified | 5 | 2.5 | 5.8 |
| Alcohol abuse identified | 3 | 1.5 | 3.5 |
| Both illicit drug use and alcohol abuse identified | 33 | 16.7 | 38.4 |
| Substance not specified | 24 | 12.1 | 27.9 |
| Not stated or unclear | 112 | 56.6 | NA |
| Total | 198 | 100 | 100 |
FIGURE 5.
Number of participants in complete data set.
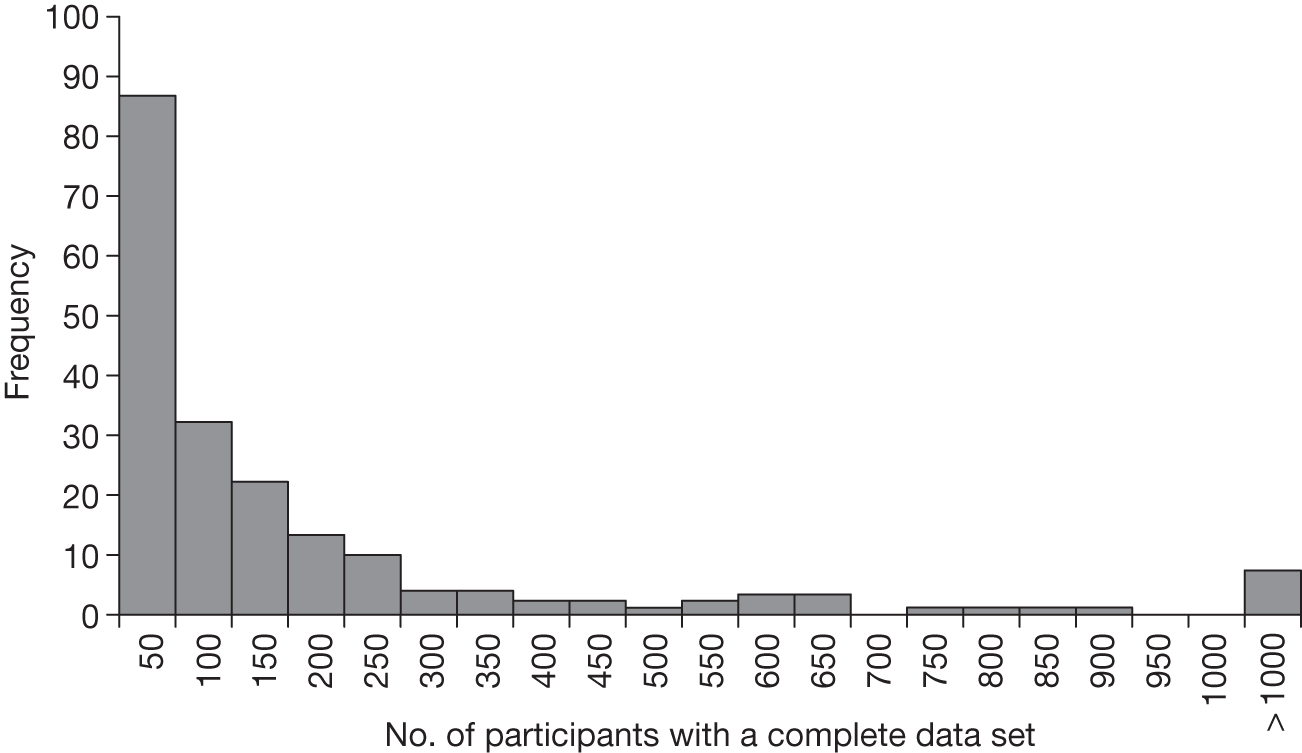
FIGURE 6.
Percentage of participants who were male.
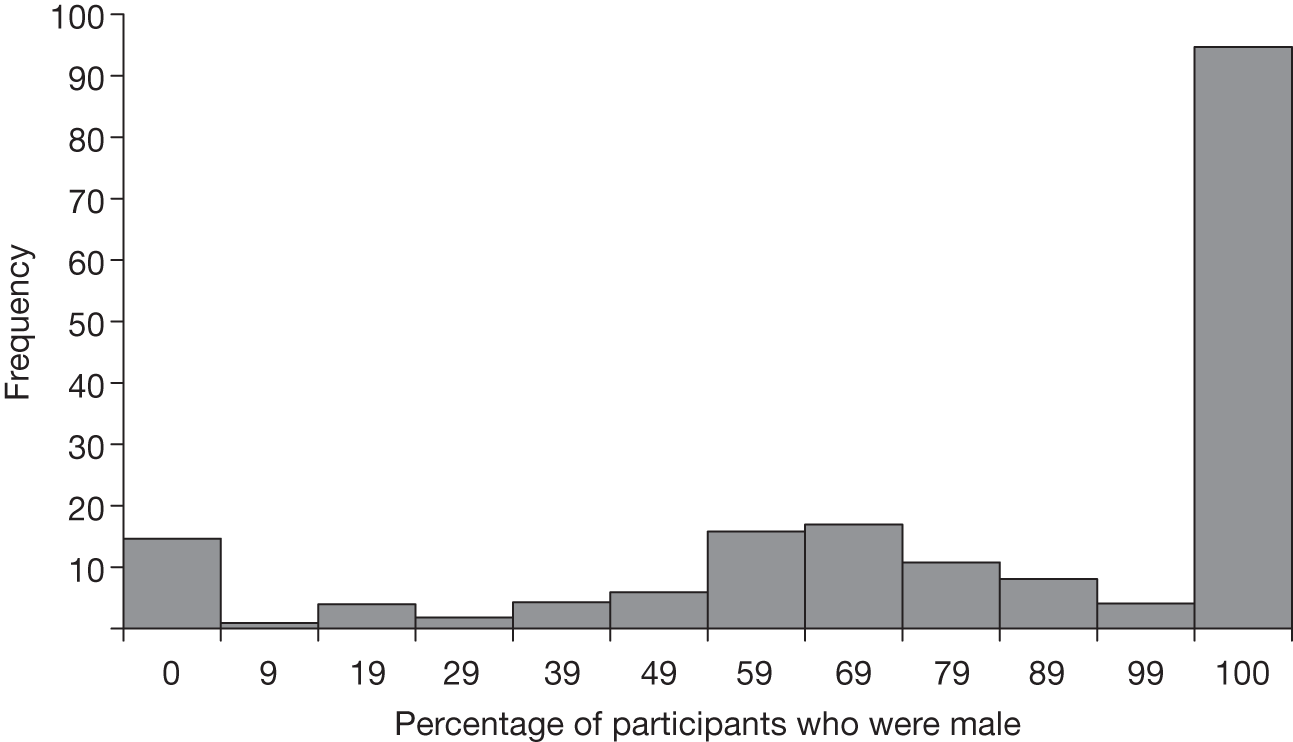
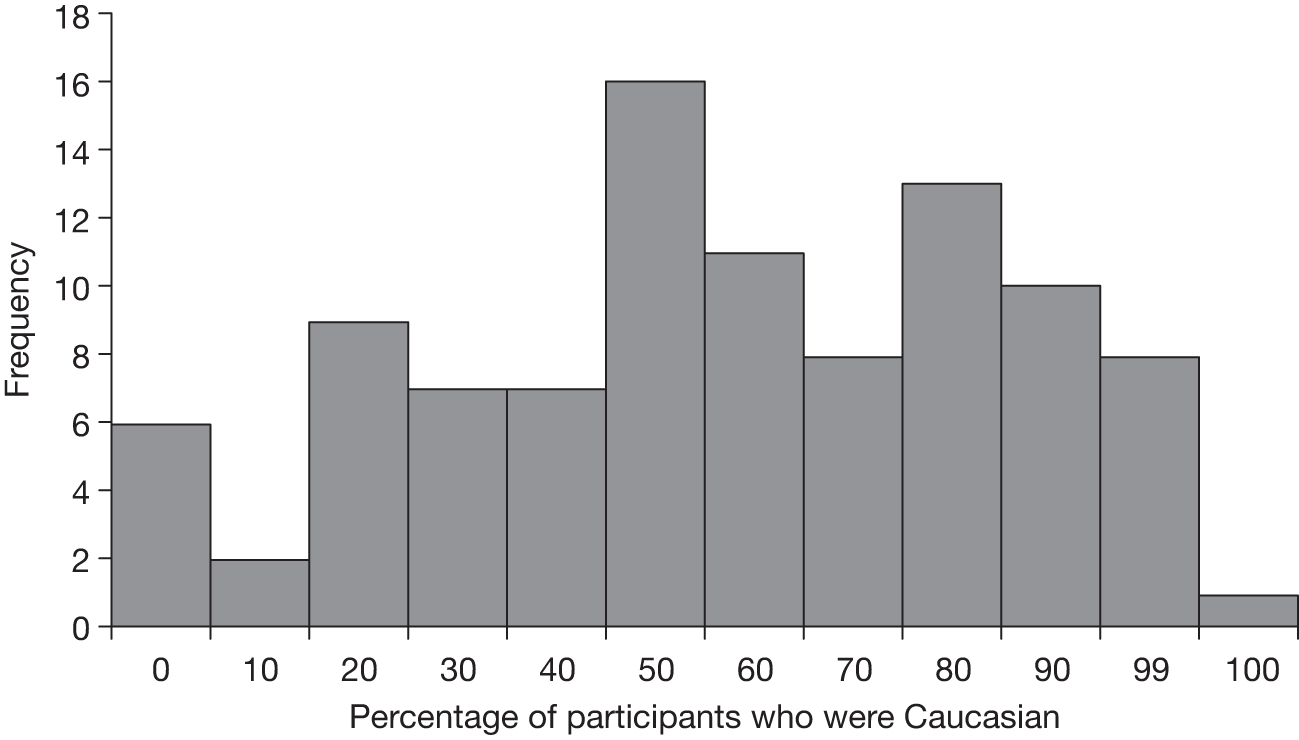
FIGURE 7.
Percentage of participants who were Caucasian.
Number of participants
The number of people approached to take part in the studies was reported in 94 (47.4%) of studies and ranged from 1 to 8325. The number of participants enrolled was reported in 191 (96.5%) of studies and ranged from 1 to 10,753. The number of participants at the end point of the study was reported in 196 (99.0%) of studies meaning that two studies failed to report the final number of participants in their study.
The studies reporting the final number of participants described a total of 51,258 individuals, the smallest study having one participant and the largest 10,753 participants (Figure 5). The majority (60%) of studies included ≤ 100 people.
Demographics of participants
The sex of participants was reported in 183 (92.4%) studies, with 95 (52%) studies including only males and 15 (8%) including only females. The percentage of males in the remaining studies ranged from 8% to 95% (Figure 6).
The average age of participants was reported in 166 studies (158 reported the mean age, four reported the median age and four reported both the mean and median age). The mean age ranged from 19 to 80.9 years, with SDs (reported by 118 studies) ranging from 1 to 15.9 years. The range of ages was reported by 70 studies (an additional study reported minimum age only). The minimum age of participants ranged from 13 and 65 years and the maximum age ranged from 32 to 97 years. Therefore, the youngest participant was 13 years and the oldest was 97 years (Table 10).
The percentage of participants who were described as Caucasian was reported in 98 studies, with six (6%) studies not including any Caucasian participants, and one study (1%) including only Caucasian participants. The percentage of Caucasian participants in the remaining studies ranged from 6% to 99% (Figure 7).
Population
Populations included in the review were either participants with a diagnosis of mental disorder, offenders, indictable offenders (i.e. those having committed indictable offences but not having been charged) or forensic participants (i.e. those with a diagnosis of mental disorder and offender/indictable offender status). The numbers of studies looking at each of these population types are shown in Table 11. Participants were mainly people with a mental disorder (38%) or offenders (35%), with those reported to have committed an indictable offence being studied in 15% of studies and offenders with a mental disorder (forensic) being included in 12% of cases.
Studies reporting on individuals with a diagnosis of a mental disorder (including forensic groups) reported a range of diagnostic groups, with patients defined as having an ‘other’ single mental health grouping being the most frequently reported (34%), followed by participants with a ‘mixed diagnosis’ (28%). Participants with personality disorders only were studied in 20% of the studies and participants with a diagnosis of schizophrenia or schizoaffective disorder only were studied in 11% of the studies (Table 12).
There were differences between the diagnosis of participants in the mental disorder group and the forensic group. Almost half of the studies investigating forensic participants reported mixed diagnoses, and a further 37.5% reported participants with an ‘other single mental health grouping’. Participants with a specific mental health diagnosis were reported in only 3 out of the 24 forensic studies (12.5%), whereas 32 out of the 75 studies (42.6%) examining participants with just a mental disorder reported investigating participants with specific mental disorder diagnoses.
The index offences that participants had committed differed greatly between the three groups. Offender participants had been charged with predominantly DV (44.3%), followed by mixed group of offences (28.6%) and sex offending (22.9%). For studies including forensic participants, mixed groups of offences were more frequently reported (41.7%), followed by sex offending (29.2%). A further 20.8% of studies did not report what offences participants had committed.
As expected, in the indictable group, DV was the most reported offence type (65.5%), with other indictable offences being reported in 24.1% of studies (Table 13).
Substance abuse
Substance abuse by participants was poorly reported in most studies, with only 43.4% (86) of papers reporting whether current substance abuse was or was not identified. Of the 86 studies reporting on substance abuse, 21 (24.4%) reported no substance abuse, five (5.8%) identified drug abuse, three identified (3.5%) alcohol abuse and 33 (38.4%) both alcohol and drug abuse. A further 24 (27.9%) studies identified some form of substance abuse, but did not report on the nature, i.e. whether it was drugs or alcohol (Table 14).
Intervention characteristics
Types of interventions
Of the 198 studies, 74 (37.37%) were single-group designs and 124 (62.6%) compared two or more groups. Of the 124 using a comparator group, 29.8% compared two different types of treatment (head-to-head comparisons), 24.2% TAU, 14.5% a placebo, 12.9% compared subgroups of one treatment (e.g. completers vs non-completers) and 8.9% no treatment. The remaining seven studies used a historical control (3.2%) or self as a control (2.4%) (Table 15).
| Type of comparison | n | % |
|---|---|---|
| Head to head | 37 | 29.6 |
| Historical control | 5 | 4.0 |
| Placebo | 18 | 14.4 |
| Self as control | 3 | 2.4 |
| Subgroup | 16 | 12.8 |
| TAU | 30 | 24.0 |
| No treatment | 11 | 8.8 |
| WL | 5 | 4.0 |
The types of intervention studied are shown in Tables 16 and 17. Half of included studies used a psychological intervention (50.5%) as the primary intervention, one-quarter used a pharmacological intervention (23.7%) and one-quarter another form of intervention (25.8%). The specific categories of intervention by comparison type are shown in Table 16 and the comparators used in head-to-head studies in Table 17.
| Primary intervention | Comparator group: n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Single group | Historical control | Placebo | Self as control | Subgroup | TAU | No treatment | WL | Head to head | |
| Behavioural/cognitive | 30 (40.5) | 1 (33.3) | 8 (50) | 10 (33.3) | 5 (45.5) | 4 (80) | 10 (27.0) | ||
| Other psychological therapy | 4 (5.4) | 1 (6.3) | 1 (9.1) | 2 (5.4) | |||||
| Substance abuse therapy | 2 (2.7) | ||||||||
| Domestic violence/batterer programmes | 10 (13.5) | 3 (18.8) | 3 (10) | 1 (20) | 1 (2.7) | ||||
| Case management model | 1 (20) | 2 (6.7) | |||||||
| Legal | 1 (1.4) | 2 (40) | 4 (13.3) | 1 (9.1) | 1 (2.7) | ||||
| Clozapine | 3 (8.1) | ||||||||
| Divalproex | 1 (1.4) | 2 (11.1) | 1 (6.3) | ||||||
| Fluoxetine | 2 (11.1) | ||||||||
| Fluvoxamine | 1 (1.4) | 1 (5.6) | |||||||
| Haloperidol | 1 (5.6) | 1 (2.7) | |||||||
| Lamotrigine | 1 (1.4) | 1 (5.6) | |||||||
| Lorazepam | 1 (5.6) | 1 (2.7) | |||||||
| Midazolam | 1 (2.7) | ||||||||
| Nefalzone | 1 (1.4) | ||||||||
| Olanzapine | 1 (5.6) | 4 (10.8) | |||||||
| Quetiapine | 2 (2.7) | ||||||||
| Risperidone | 2 (11.1) | 2 (5.4) | |||||||
| Topiramate | 4 (22.2) | ||||||||
| Ziprasidone | 1 (1.4) | 1 (2.7) | |||||||
| Zuclopenthixol | 1 (2.7) | ||||||||
| Other pharmacological | 4 (5.4) | 3 (16.7) | 1 (9.1) | 2 (5.4) | |||||
| Therapeutic communities | 1 (3.3) | ||||||||
| Multimodal programme | 7 (9.5) | 2 (40) | 5 (16.7) | 3 (27.3) | 3 (8.1) | ||||
| Other form of intervention | 9 (12.2) | 2 (66.7) | 3 (18.8) | 5 (16.7) | 4 (10.8) | ||||
| Total studies | 74 (100) | 5 (100) | 18 (100) | 3 (100) | 16 (100) | 30 (100) | 11 (100) | 5 (100) | 37 (100) |
| Primary intervention | Comparator group: n (%) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Behavioural/cognitive | Other psychological therapy | Community therapy | Legal intervention | Multi-modal programme | Clozapine | Fluoxetine | Haloperidol | Olanzapine | Topiramine | Zuclopenthixol | Other pharmacological | Other form of intervention | Total | |
| Behavioural/cognitive | 3 (30.0) | 2 (20.0) | 1 (10.0) | 1 (10.0) | 3 (30.0) | 10 (100) | ||||||||
| Other psychological therapy | 1 (50.0) | 1 (50.0) | 2 (100) | |||||||||||
| Domestic violence/batterer programmes | 1 (100.0) | 1 (100) | ||||||||||||
| Legal | 1 (100) | 1 (100) | ||||||||||||
| Clozapine | 3 (100) | 3 (100) | ||||||||||||
| Haloperidol | 1 (100) | 1 (100) | ||||||||||||
| Lorazepam | 1 (100) | 1 (100) | ||||||||||||
| Midazolam | 1 (100) | 1 (100) | ||||||||||||
| Olanzapine | 1 (25) | 1 (25) | 2 (50) | 4 (100) | ||||||||||
| Risperidone | 1 (50) | 1 (50) | 2 (100) | |||||||||||
| Ziprasidone | 1 (100) | 1 (100) | ||||||||||||
| Zuclopenthixol | 1 (100) | 1 (100) | ||||||||||||
| Other pharmacological | 1 (50) | 1 (50) | 2 (100) | |||||||||||
| Multimodal programme | 1 (33.3) | 1 (33.3) | 3 (100) | |||||||||||
| Other form of intervention | 4 (100) | 4 (100) | ||||||||||||
| Total | 5 (13.5) | 4 (10.8) | 1 (2.7) | 1 (2.7) | 1 (2.7) | 1 (2.7) | 1 (2.7) | 1 (2.7) | 4 (10.8) | 1 (2.7) | 1 (2.7) | 7 (18.9) | 9 (24.3) | 37 (100) |
Psychological studies were more likely to use single-group comparisons and pharmacological studies head-to-head or placebo comparators. Where head-to-head studies were used, the same categories of intervention were compared, i.e. psychological interventions compared with another psychological intervention, and pharmacological interventions compared with another pharmacological intervention.
Setting
The start and end settings are shown in Table 18. The term ‘setting’ here refers to the location where the intervention is conducted and in the case of ‘community’ under what conditions, i.e. a probation order, or under the supervision of a mental health practitioner or neither (e.g. a person concerned about their propensity for violence who is offered a self-help intervention). The most frequently reported setting was community with people on probation (18.7%), followed by penal institutions (16.2%), community (14.6%) and community mental health (12.1%). The majority of studies (87.9%) had the same start and end setting. Of the 24 studies reporting different start and end settings, 12 were studies that started in penal institutions but ended in either the community or in mixed settings.
| Setting started in: | Setting follow-up ended in: | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Forensic mental health | Penal institution, e.g. prison | Open inpatient hospital ward | Secure non-forensic inpatient ward | Nursing home | Community | Community: probation | Community mental health | A&E or psychiatric emergency service | Mixed settings | Other | Not stated or unclear | Total: n (%) | |
| Forensic mental health | 11 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 12 (6.1) |
| Penal institution, e.g. prison | 0 | 20 | 0 | 0 | 0 | 6 | 1 | 0 | 0 | 5 | 0 | 0 | 32 (16.2) |
| Open inpatient hospital ward | 0 | 0 | 14 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 16 (8.1) |
| Secure non-forensic inpatient ward | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 (1.5) |
| Nursing home | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 (1.5) |
| Community | 0 | 0 | 0 | 0 | 0 | 28 | 0 | 0 | 0 | 1 | 0 | 0 | 29 (14.6) |
| Community: probation | 0 | 0 | 0 | 0 | 0 | 0 | 33 | 0 | 0 | 3 | 0 | 1 | 37 (18.7) |
| Community mental health | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 24 | 0 | 0 | 0 | 0 | 24 (12.1) |
| A&E or psychiatric emergency service | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 | 0 | 0 | 7 (3.5) |
| Mixed settings | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 12 | 0 | 2 | 15 (7.6) |
| Other | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 10 | 0 | 10 (5.1) |
| Not stated or unclear | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 9 | 10 (5.1) |
| Total n | 11 (5.6) | 20 (10.1) | 14 (7.1) | 3 (1.5) | 3 (1.5) | 36 (18.2) | 34 (17.2) | 25 (12.6) | 7 (3.5) | 22 (11.1) | 11 (5.6) | 12 (6.1) | 198 (100) |
When start settings for the interventions are examined by intervention type (Table 19), it can be seen that studies in a forensic mental health setting mainly studied behavioural and cognitive therapies (75.0%), as did penal institutions (56.3%), community (44.8%), mixed settings (33.3%) and other settings (40.0%), whereas community probation settings used DV programmes. Pharmacological interventions were the focus of the majority of studies in community mental health settings (58.0%), accident and emergency (A&E) settings (100%), mixed settings (33.3%) and studies where the setting was unclear or not stated (40.0%).
| Start setting | Intervention type | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pharmacological | Behavioural and cognitive therapies | Therapeutic community | DV programme | Other psychological intervention | Substance abuse | Case management | Legal | Multimodal | Other | Total | |
| Forensic mental health | 0 | 9 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 12 |
| Penal institution, e.g. prison | 1 | 18 | 1 | 0 | 1 | 0 | 0 | 3 | 3 | 5 | 32 |
| Open inpatient hospital ward | 6 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 6 | 16 |
| Secure non-forensic inpatient ward | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 3 |
| Nursing home | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3 |
| Community | 4 | 13 | 0 | 4 | 1 | 1 | 0 | 1 | 4 | 1 | 29 |
| Community: probation | 1 | 10 | 0 | 11 | 3 | 0 | 1 | 3 | 5 | 3 | 37 |
| Community mental health | 14 | 5 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 2 | 24 |
| A&E or psychiatric emergency service | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 7 |
| Mixed settings | 5 | 5 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 1 | 15 |
| Other | 2 | 4 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 10 |
| Not stated or unclear | 4 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 3 | 1 | 10 |
| Total | 47 | 67 | 1 | 18 | 8 | 2 | 3 | 9 | 20 | 23 | 198 |
Level of intervention
The levels of interventions for each of the types of intervention are shown in Table 20. Pharmacological interventions were by design at an individual level, whereas the psychological interventions were generally at the small group level.
| Type of intervention | Level of intervention | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Individual | Small group | Ward or team | Hospital or institution | Population | Other | Mixed | Not stated/unclear | Total | |
| Behavioural and cognitive therapies | 5 | 45 | 1 | 4 | 0 | 0 | 8 | 4 | 67 |
| Therapeutic community | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| DV programme | 1 | 13 | 0 | 0 | 0 | 0 | 2 | 2 | 18 |
| Other psychological intervention | 1 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 8 |
| Substance abuse | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| Case management | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 3 |
| Legal | 6 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 9 |
| Multimodal | 4 | 9 | 0 | 3 | 0 | 0 | 3 | 1 | 20 |
| Pharmacological | 47 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 47 |
| Other | 12 | 2 | 5 | 2 | 1 | 0 | 1 | 0 | 23 |
| Total | 78 | 78 | 6 | 12 | 1 | 1 | 14 | 8 | 198 |
Randomised controlled trials
In total, 51 RCTs, reporting on 197 comparisons between active interventions and/or active interventions plus placebo or other inactive control, were identified in the literature. These studies represent 25.8% of all intervention studies identified as meeting our inclusion criteria.
Predictably, studies meeting the design criteria of prospective RCTs were also not entirely representative of the empirical literature as a whole. The differences between the RCTs and the other studies are outlined below.
Quality
On variables used to assess methodological quality of studies, the RCTs reflected what was found in the whole data set (see Quality assessment) for baseline equivalence [χ2 = 2.347, degrees of freedom (df) = 3, p = 0.504] (Table 21), and sample attrition (Mann–Whitney U-test, p = 0.568) (Table 22). However, the total length of follow-up reported in studies was significantly longer in the non-RCTs (mean 629 days, SD 932, median 364 days) than in the RCTs (mean 253 days, SD 731, median 84 days) (Mann–Whitney U-test, p < 0.0001) (see Table 22) and the number of studies using some form of blinding to the intervention was far higher in the RCT data set (58.8%) than in the non-RCTs (6.1%) (χ2 = 66.486, df = 1, p < 0.0001) (see Table 21). Of the 197 comparisons conducted in the RCT studies, 53.3% used an ITT analysis, whereas only 27.2% of the 464 comparisons reporting whether an ITT analysis was used in the non-RCT data set used an ITT analysis (χ2 = 41.578, df = 1, p < 0.0001) (see Table 21).
| Categorical variable | Group | RCT | Non-RCT | p-value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Baseline equivalence | No | 5 | 9.8 | 11 | 15.5 | 0.504 |
| Yesa | 26 | 45.1 | 36 | 39.4 | ||
| Unsure: no p-values stated | 11 | 21.6 | 9 | 12.7 | ||
| Not stated/unclear | 9 | 17.6 | 15 | 21.1 | ||
| Blind | No | 21 | 41.2 | 138 | 93.9 | < 0.0001 |
| Yes | 30 | 58.8 | 9 | 6.1 | ||
| ITT | No | 92 | 46.7 | 338 | 72.8 | < 0.0001 |
| Yes | 105 | 53.3 | 127 | 27.2 | ||
| Not stated | 0 | 0.0 | 66 | 12.4 | ||
| Variable | Statistical test | RCT | Non-RCT | p-value | |
|---|---|---|---|---|---|
| Attrition (%) | Mean | 16.78 | 21.07 | 0.568 | |
| SD | 18.8 | 25.8 | |||
| Kurtosis | Statistic | 2.216 | 0.019 | ||
| SE | 0.668 | 0.407 | |||
| Skewness | Statistic | 1.575 | 1.079 | ||
| SE | 0.34 | 0.205 | |||
| Length of follow-up (days) | Mean | 253 | 629 | < 0.0001 | |
| SD | 731 | 932 | |||
| Kurtosis | Statistic | 41.754 | 41.754 | ||
| SE | 0.662 | 0.662 | |||
| Skewness | Statistic | 6.251 | 6.251 | ||
| SE | 0.337 | 0.337 | |||
Trial and participant characteristics
The distribution of the number of papers being published in each year was the same for RCTs and non-RCTs (χ2 = 3.629, df = 6, p = 0.774) (Table 23), as was the distribution of the number of participants in the studies (Mann–Whitney U-test, p = 0.422), mean age (Mann–Whitney U-test, p = 0.084), proportion of sample who were Caucasian (Mann–Whitney U-test, p = 0.436) (Table 24), the reporting of substance abuse (χ2 = 2.347, df = 3, p = 0.05) and the types of offences offenders had committed (statistical analyses not appropriate) (see Table 23) (see Study characteristics and Participants characteristics for description of whole sample).
| Categorical variable | Group | RCT | Non-RCT | p-value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Year of publication | 2002 | 8 | 15.7 | 18 | 12.2 | 0.774 |
| 2003 | 6 | 11.8 | 20 | 13.6 | ||
| 2004 | 8 | 15.7 | 28 | 19.0 | ||
| 2005 | 8 | 15.7 | 29 | 19.7 | ||
| 2006 | 9 | 17.6 | 18 | 12.2 | ||
| 2007 | 7 | 13.7 | 26 | 17.7 | ||
| 2008 | 5 | 9.8 | 8 | 5.4 | ||
| Substance abuse | No substance abuse identified in sample | 10 | 19.6 | 11 | 7.5 | 0.05 |
| Substance use identified in sample | 16 | 31.4 | 49 | 33.3 | ||
| ■ Illicit drug use identified in sample | 2 | 3.9 | 3 | 2.0 | NA | |
| ■ Alcohol abuse identified in sample | 1 | 2.0 | 2 | 1.4 | ||
| ■ Both illicit drug use and alcohol abuse identified in sample | 5 | 9.8 | 28 | 19.0 | ||
| ■ Substance not specified | 8 | 15.7 | 16 | 10.9 | ||
| Not stated or unclear | 25 | 49.0 | 87 | 59.2 | ||
| Types of offences | General violence | 2 | 11.8 | 5 | 4.7 | NA |
| Domestic violence | 6 | 35.3 | 44 | 41.5 | ||
| Sex offending | 1 | 5.9 | 22 | 20.8 | ||
| Mixed group of offences | 5 | 29.4 | 25 | 23.6 | ||
| Not stated/unclear | 0 | 0.0 | 5 | 4.7 | ||
| Other single type of indictable offence | 3 | 17.6 | 5 | 4.7 | ||
| Country study conducted | US | 29 | 56.9 | 80 | 54.8 | NA |
| UK | 2 | 3.9 | 19 | 13.0 | ||
| Canada | 0 | 0.0 | 13 | 8.9 | ||
| Sweden | 0 | 0.0 | 2 | 1.4 | ||
| Finland | 0 | 0.0 | 1 | 0.7 | ||
| India | 2 | 3.9 | 0 | 0.0 | ||
| Brazil | 2 | 3.9 | 0 | 0.0 | ||
| Multinational | 2 | 3.9 | 1 | 0.7 | ||
| Norway | 0 | 0.0 | 1 | 0.7 | ||
| Netherlands | 1 | 2.0 | 3 | 2.1 | ||
| Belgium | 0 | 0.0 | 1 | 0.7 | ||
| Israel | 0 | 0.0 | 2 | 1.4 | ||
| Japan | 0 | 0.0 | 1 | 0.7 | ||
| Spain | 1 | 2.0 | 2 | 1.4 | ||
| Italy | 1 | 2.0 | 2 | 1.4 | ||
| Australia | 0 | 0.0 | 8 | 5.5 | ||
| New Zealand | 0 | 0.0 | 2 | 1.4 | ||
| Switzerland | 0 | 0.0 | 1 | 0.7 | ||
| Germany | 2 | 3.9 | 0 | 0.0 | ||
| China | 0 | 0.0 | 1 | 0.7 | ||
| South Korea | 1 | 2.0 | 1 | 0.7 | ||
| Not stated/unclear | 8 | 15.7 | 5 | 3.4 | ||
| Population | Mental | 34 | 66.7 | 41 | 27.9 | NA |
| Offender | 9 | 17.6 | 60 | 40.8 | ||
| Forensic | 1 | 2.0 | 24 | 16.3 | ||
| Indictable offender | 7 | 13.7 | 22 | 15.0 | ||
| Diagnostic group | Schizophrenia or schizoaffective only | 4 | 11.8 | 7 | 10.8 | NA |
| Dementia only | 2 | 5.9 | 2 | 3.1 | ||
| Personality disorder only | 13 | 38.2 | 7 | 10.8 | ||
| Other single mental health grouping | 9 | 26.5 | 25 | 38.5 | ||
| Mixed diagnostic groups | 5 | 14.7 | 23 | 35.4 | ||
| No specific diagnoses given | 0 | 0.0 | 1 | 1.5 | ||
| Not stated/unclear | 1 | 2.9 | 0 | 0.0 | ||
| Variable | Statistical test | RCT | Non-RCT | p-value | |
|---|---|---|---|---|---|
| No. of participants | Mean | 131.06 | 305.01 | 0.422 | |
| SD | 135.67 | 1,095.19 | |||
| Kurtosis | Statistic | 2.495 | 65.042 | ||
| SE | 0.668 | 0.397 | |||
| Skewness | Statistic | 1.562 | 7.627 | ||
| SE | 0.34 | 0.2 | |||
| % male | Mean | 55.02 | 83 | < 0.0001 | |
| SD | 38.76 | 26.06 | |||
| Kurtosis | Statistic | –1.435 | 1.748 | ||
| SE | 0.681 | 0.413 | |||
| Skewness | Statistic | –0.341 | –1.535 | ||
| SE | 0.347 | 0.208 | |||
| Mean age (years) | Mean | 35.98 | 36.67 | 0.084 | |
| SD | 12.84 | 7.31 | |||
| Kurtosis | Statistic | 5.42 | 6.554 | ||
| SE | 0.724 | 0.437 | |||
| Skewness | Statistic | 2.172 | 1.663 | ||
| SE | 0.369 | 0.22 | |||
| % Caucasian | Mean | 56.7 | 51.33 | 0.436 | |
| SD | 28.61 | 28 | |||
| Kurtosis | Statistic | –0.903 | –0.846 | ||
| SE | 0.953 | 0.545 | |||
| Skewness | Statistic | –0.514 | –0.125 | ||
| SE | 0.491 | 0.276 |
The country in which studies were conducted appeared to differ between RCTs and non-RCTs (see Table 23), most notably the proportion of RCTs that were conducted in the UK (3.9%) was lower than non-RCTs (13.0%) and RCTs were more likely to fail to report where the study was conducted than non-RCTs (13.7% vs 3.4%, respectively). RCTs also reported a lower percentage of males (mean 55.02%, SD 38.76) than non-RCTs (mean 83.0%, SD 26.06) (Mann–Whitney U-test, p < 0.0001) (see Table 24).
The populations in the studies also appeared different in the RCTS and non-RCTS (see Table 23). RCTs focused primarily on participants with mental disorder (66.7%) compared with non-RCTs (27.9%), whereas non-RCTs included offenders in 40.8% of studies compared with 17.6% of RCTs. Only one (2.0%) RCT included forensic patients, whereas 16.3% of non-RCTs included forensic patients.
The diagnoses of participants in studies investigating a population of people with a mental disorder seemed to differ between RCTs and non-RCTs (see Table 23), with RCTs focusing on participants with a personality disorder (38.2%) and non-RCT studies participants with other single mental health grouping (38.5%).
Intervention characteristics
As expected, the types of comparisons differed between RCTs and non-RCTs, with nearly half of the non-RCTs reporting single group comparisons (49.3%) (Table 25).
| Categorical variable | Group | RCT | Non-RCT | p-value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Type of comparisona | Head to head | 18 | 36.0 | 18 | 12.8 | NA |
| Placebo | 17 | 34.0 | 1 | 0.7 | ||
| TAU | 13 | 26.0 | 17 | 11.5 | ||
| No treatment | 1 | 2.0 | 10 | 6.8 | ||
| WL | 1 | 2.0 | 3 | 2.7 | ||
| No comparator | 1 | 2.0 | 73 | 49.3 | ||
| Historical control | NA | NA | 4 | 2.7 | ||
| Self as control | NA | NA | 4 | 2.7 | ||
| Subgroup | NA | NA | 16 | 10.8 | ||
| Broad category of primary intervention | Psychological | 11 | 21.6 | 89 | 60.5 | < 0.0001 |
| Pharmacological | 29 | 56.9 | 18 | 12.2 | ||
| Other | 11 | 21.6 | 40 | 27.2 | ||
| Specific category of primary intervention where broad category is psychological | Behavioural/cognitive | 8 | 72.7 | 59 | 66.3 | NA |
| Therapeutic communities | 0 | 0 | 1 | 1.1 | ||
| DV/batterer programmes | 2 | 18.2 | 16 | 18.0 | ||
| Other psychological therapy | 1 | 9.1 | 7 | 7.9 | ||
| Substance abuse therapy | 0 | 0 | 1 | 1.1 | ||
| Multimodal programme | 0 | 0 | 5 | 5.6 | ||
| Specific category of primary intervention where broad category is pharmacological | Clozapine | 1 | 3.4 | 2 | 11.1 | NA |
| Divalproex | 2 | 6.9 | 2 | 11.1 | ||
| Fluoxetine | 2 | 6.9 | 0 | 0 | ||
| Fluvoxamine | 1 | 3.4 | 1 | 5.6 | ||
| Haloperidol | 2 | 6.9 | 0 | 0 | ||
| Lamotrigine | 1 | 3.4 | 1 | 5.6 | ||
| Lorazepam | 1 | 3.4 | 1 | 5.6 | ||
| Midazolam | 1 | 3.4 | 0 | 0 | ||
| Nefalzone | 0 | 0 | 1 | 5.6 | ||
| Olanzapine | 4 | 13.8 | 1 | 5.6 | ||
| Quetiapine | 0 | 0 | 2 | 11.1 | ||
| Risperidone | 4 | 13.8 | 0 | 0 | ||
| Topiramate | 4 | 13.8 | 0 | 0 | ||
| Ziprasidone | 0 | 0 | 2 | 11.1 | ||
| Zuclopenthixol | 1 | 3.4 | 0 | 0 | ||
| Other pharmacological | 5 | 17.2 | 5 | 27.8 | ||
| Specific category of primary intervention where broad category is other somatic | Other form of intervention | 0 | 0 | 1 | 100.0 | NA |
| Specific category of primary intervention where broad category is other form of intervention | Substance abuse therapy | 0 | 0 | 1 | 2.6 | NA |
| Case management model | 2 | 18.2 | 1 | 2.6 | ||
| Legal intervention | 1 | 9.1 | 8 | 20.5 | ||
| Multimodal programme | 6 | 54.5 | 9 | 23.1 | ||
| Other form of intervention | 2 | 18.2 | 20 | 51.3 | ||
| Setting study started in | Forensic mental health | 1 | 2.0 | 11 | 7.5 | NA |
| Penal institution, e.g. prison | 3 | 5.9 | 29 | 19.7 | ||
| Open inpatient hospital ward | 3 | 5.9 | 13 | 8.8 | ||
| Secure non-forensic inpatient ward | 0 | 0 | 3 | 2.0 | ||
| Nursing home | 2 | 3.9 | 1 | 0.7 | ||
| Community | 10 | 19.6 | 19 | 12.9 | ||
| Community: probation | 4 | 7.8 | 33 | 22.4 | ||
| Community mental health | 10 | 19.6 | 14 | 9.5 | ||
| A&E or psychiatric emergency service | 5 | 9.8 | 2 | 1.4 | ||
| Mixed settings | 3 | 5.9 | 12 | 8.2 | ||
| Other | 4 | 7.8 | 6 | 4.1 | ||
| Not stated or unclear | 6 | 11.8 | 4 | 2.7 | ||
| Level of intervention | Individual | 34 | 67 | 44 | 30 | NA |
| Small group | 11 | 22 | 67 | 46 | ||
| Ward or team | 0 | 0 | 6 | 4 | ||
| Hospital or institution | 2 | 4 | 10 | 7. | ||
| Population | 0 | 0 | 1 | 1. | ||
| Other | 0 | 0 | 1 | 1. | ||
| Mixed | 1 | 2 | 13 | 9. | ||
| Not stated/unclear | 3 | 6 | 5 | 3 | ||
As shown in Table 25, the type of primary intervention being tested in the studies also differed between RCTs and non-RCTs (χ2 = 43.611, df = 2, p < 0.0001), with 56.9% (n = 29) of RCTs evaluating pharmacological intervention alone, and only 21.6% of studies (n = 11) evaluating a psychological intervention. This compares with 12.2% of non-RCTs testing a pharmacological intervention and 60.5% a psychological intervention. Within each of the four broad categories of primary interventions, the specific groupings of primary interventions had too few studies for statistical analyses.
The setting that interventions were started in appeared to differ between RCTs and non-RCTs. RCTs were more likely to fail to report the type of setting (11.8%) compared with non-RCTs (2.7%), and were more likely to be conducted in community mental health settings (RCTs 19.6%, non-RCTS 9.5%). In contrast, non-RCTs were more likely than RCTs to be conducted in a penal institution (non-RCTs 19.7%, RCT 5.9%) or on community probation (non-RCTs 22.4%, RCTs 7.8%) (see Table 25).
The level the intervention was conducted on also appeared to differ between RCTs and non-RCTs. RCTs were primarily conducted at the individual level (67%), probably reflecting the focus on pharmacological interventions, whereas non-RCTs were more frequently conducted in small groups (46%) (see Table 25).
Chapter 4 Results of bivariate and multivariate analyses
Overview
Of the 198 studies identified 188 (94.9%) provided statistical data suited to extraction and statistical analyses. The 10 analyses that did not report data suitable for statistical analyses included six non-RCT analyses62–67 and four RCT analyses. 68–71 A further five analyses72–76 were excluded from the analyses in this chapter as they did not report data on statistical significance (the dependent variable in all following analyses). Raveendran et al. ,75 Huf72 and Huf et al. 73 presented only figures for relative risk (RR); Marques et al. 74 reported change in absolute proportions only and Villari et al. 76 presented mean/mean change data only. This resulted in 183 studies reporting on a total of 655 separate statistical analyses. Of the 655 separate analyses, 331 (50.5%) reported an outcome that was not statistically significant. A further 315 (48.1%) reported a statistically significant outcome in favour of the intervention that was the primary focus of the study, whereas only five (< 1%) analyses reported an outcome in favour of an active comparator and only four (< 1%) in favour of a placebo or other inactive comparator.
In order to maintain independence of samples, only studies reporting on different groups of participants are included in the remainder of the analyses. Whereas for the most part any overlap between populations occurred within studies, two studies77,78 were excluded entirely, as the data they reported on overlapped with data included in other studies, which provided greater detail in respect of outcomes. A further two analyses79,80 were subsequently excluded because of concerns over the correct interpretation of the analyses they presented (both studies presented summative figures only). Given the above, the final selection of outcomes to be included in the analyses outlined here comprised 195 analyses taken from 179 studies.
Bivariate associations
Analyses by broad intervention groupings
Significant bivariate associations between broad category of intervention and the statistical significance of an analysis were not observed for either pharmacological or psychological interventions (60.8% of pharmacological and 57.3% of psychological intervention analyses found in favour of the primary intervention arm vs its comparator). Where an impact on outcomes was shown, was in the case of analyses focused on ‘other’ forms of intervention. Analyses focused on such interventions were less likely than analyses focused either on pharmacological or on psychological interventions to result in a statistically significant outcome in favour of the primary intervention arm of the analysis (n = 195, χ2 = 6.006, p = 0.011) (Table 26).
| Intervention grouping | n | Favours treatment (%) | Does not favour treatment (%) | Chi-squared | p-value | |
|---|---|---|---|---|---|---|
| Pharmacological | Yes | 51 | 31 (60.8) | 20 (39.2) | 0.975 | 0.205 |
| No | 144 | 76 (52.8) | 68 (47.2) | |||
| Psychological | Yes | 110 | 63 (57.3) | 47 (42.7) | 0.587 | 0.267 |
| No | 85 | 44 (51.8) | 41 (48.2) | |||
| Other | Yes | 50 | 20 (40.0) | 30 (60.0) | 6.006 | 0.011 |
| No | 145 | 87 (60.0) | 58 (40.0) | |||
Population
Mental health status
The broad population group chosen for evaluation did have an impact on outcomes. Analyses focused on people with a mental disorder were overall more likely to find in favour of the primary intervention arm than those not focused on a general mental health population (64.5% vs 48.7%, n = 195, χ2 = 4.377, p = 0.022). In contrast, analyses that focused on offending populations were far less likely to report outcomes favouring the primary intervention arm (44.1% vs 60.6%, n = 195, χ2 = 4.876, p = 0.02). Analyses focused on interventions for people who have committed indictable acts of aggression but who have not yet been convicted of such were, overall, more likely to find in favour of the primary intervention arm (59.3% vs 54.2%), but this distinction failed to reach statistical significance (n = 195, χ2 = 0.244, p = 0.390) (Table 27).
| Population | n | Favours treatment (%) | Does not favour treatment (%) | Chi-squared | p-value | |
|---|---|---|---|---|---|---|
| Mental disorder only | Yes | 76 | 49 (64.5) | 27 (35.5) | 4.637 | 0.022 |
| No | 119 | 58 (48.7) | 61 (51.3) | |||
| Offenders only | Yes | 68 | 30 (44.1) | 38 (55.9) | 4.876 | 0.020 |
| No | 127 | 77 (60.6) | 50 (39.4) | |||
| Forensic patients | Yes | 28 | 14 (50.0) | 14 (50.0) | 0.313 | 0.360 |
| No | 16 | 93 (55.7) | 74 (44.3) | |||
| Indictable offenders only | Yes | 27 | 16 (59.3) | 11 (40.7) | 0.244 | 0.390 |
| No | 168 | 91 (54.2) | 77 (45.8) | |||
Demographics
No statistically significant association was found between outcomes favouring the primary intervention arm and the demographic variables mean age, proportion of males and proportion of participants who were Caucasian (Table 28).
| Variable | Output | Statistical significance of finding in favour of primary intervention or not | Mean age (years) | % male | % Caucasian |
|---|---|---|---|---|---|
| Statistical significance finding in favour of primary intervention or not | Pearson’s correlation | 1 | 0.027 | –0.141 | 0.065 |
| Significance (two tailed) | 0.738 | 0.060 | 0.534 | ||
| n | 195 | 160 | 180 | 93 | |
| Mean age of all participants in the study (years) | Pearson’s correlation | 0.066 | 0.270a | ||
| Significance (two tailed) | 0.419 | 0.014 | |||
| n (mean years) | 154 | 83 | |||
| % of sample who are male | Pearson’s correlation | –0.168 | |||
| Significance (two tailed) | 0.113 | ||||
| n (mean) | 90 | ||||
| % of sample who are Caucasian | Pearson’s correlation | ||||
| Significance (two tailed) | |||||
| n |
The mean age of participants in the analyses was 36.6 years and showed no significant association with statistically significant outcomes favouring the primary intervention (n = 160, r = 0.027, p = 0.738) (see Table 28).
The mean proportion of males within the analyses was 76.4% and again showed no association with statistically significant outcomes favouring the primary intervention (n = 180, r = –0.141, p = 0.06) (see Table 28).
Across the analyses, 53.9% of the sample were reported as being Caucasian although once again this showed no association with statistically significant outcomes favouring the primary intervention (n = 93, r = 0.065, p = 0.534) (see Table 28).
The only significant association between these demographic variables was a positive association between the percentage of participants in the sample who were Caucasian and increasing mean age of the participants (n = 83, Pearson’s r = 0.27, p = 0.014) (see Table 28).
Setting
The ‘setting’ of a study can be categorised in a number of ways (e.g. start setting, end setting, change between start and end, settings based on usual transition through the health-care system, etc.). Based both on outcomes from a previous review55 and the analysis numbers available within each context in this review, we chose to simplify the comparisons drawn here to reflect the initial choice of broad outcome setting identified in the analyses at their start point (categorised into mental health, offenders’ institution, community and ‘other’). Categorised in this way, there were no statistically significant differences with respect to the outcomes for the primary intervention based on setting (Table 29).
| Setting | n | Favours treatment n % | Does not favour treatment n % | Chi-squared | p-value | |
|---|---|---|---|---|---|---|
| Mental health (including forensic) | Yes | 34 | 18 (52.9) | 16 (47.1) | 0.062 | 0.475 |
| No | 161 | 89 (55.3) | 72 (44.7) | |||
| Penal institution (excluding forensic) | Yes | 33 | 17 (51.5) | 16 (48.5) | 0.181 | 0.406 |
| No | 162 | 90 (55.6) | 72 (44.4) | |||
| Community | Yes | 87 | 49 (56.3) | 38 (43.7) | 0.133 | 0.413 |
| No | 108 | 58 (53.7) | 50 (46.3) | |||
| Other | Yes | 28 | 14 (50.0) | 14 (50.0) | 0.313 | 0.360 |
| No | 167 | 93 (55.7) | 74 (44.3) | |||
Outcome measure
As the majority of studies in the literature use a scale-based outcome measure the impact of this choice on outcomes for the primary intervention was investigated. Although a trend was observed for scale-based outcomes to favour the primary intervention arm (58.1% of scale-based outcomes showed statistical significance in favour of the primary arm in contrast with 48.5% of non-scale-based outcomes), this trend did not reach statistical significance (n = 195, χ2 = 1.644, p = 0.129) (Table 30).
| Outcome measure | n | Favours treatment n % | Does not favour treatment n % | Chi-squared | p-value |
|---|---|---|---|---|---|
| Scale | 129 | 75 (58.1) | 54 (41.9) | 1.644 | 0.129 |
| Non-scale | 66 | 32 (48.5) | 34 (51.5) |
Study quality indicators
Perhaps unexpectedly, none of the ‘design-quality’ variables, including whether or not a RCT design was used in a study, showed a statistically significant association with whether or not the primary intervention arm was favoured in terms of outcome (Table 31).
| Variable | n | Favours treatment n % | Does not favour treatment n % | Chi-squared | p-value | |
|---|---|---|---|---|---|---|
| Blinding used | Yes | 34 | 20 (58.8) | 14 (41.2) | 0.260 | 0.376 |
| No | 161 | 87 (54.0) | 74 46.0) | |||
| Same baseline measure of aggression | Yes | 48 | 27 (56.3) | 21 (43.8) | 0.049 | 0.480 |
| No | 147 | 80 (54.4) | 67 (45.6) | |||
| ITT analysis | Yes | 66 | 42 (63.6) | 24 (36.4) | 3.095 | 0.54 |
| No | 129 | 65 (60.4) | 64 (49.6) | |||
| Within groups or between group analyses | Within | 78 | 55 (70.5) | 23 (29.5) | 12.843 | 0.000 |
| Between | 117 | 52 (44.4) | 65 (55.5) | |||
| RCT design | Yes | 42 | 20 (47.6) | 22 (52.4) | 1.137 | 0.186 |
| No | 153 | 87 (56.9) | 66 (43.1) | |||
| Head to head | Yes | 50 | 20 (40.0) | 30 (60.0) | 6.006 | 0.011 |
| No | 145 | 87 (60.0) | 58 (40.0) | |||
| Active vs TAU | Yes | 31 | 11 (35.5) | 20 (64.5) | 5.595 | 0.015 |
| No | 164 | 96 (58.5) | 68 (41.5) | |||
| Active vs placebo, WL or no intervention | Yes | 36 | 21 (58.3) | 15 (41.7) | 0.214 | 0.393 |
| No | 159 | 86 (54.1) | 73 (45.9) |
Although direct measures of study quality did not show any association with outcomes, measures that can be seen as indicating the ‘strength’ of the evaluation being made did show such an association. Specifically, both the nature of the comparator (if any) against which the primary intervention was tested and whether the analysis focused on a within- (e.g. single group pre/post) or between-group evaluation showed a statistically significant association with outcomes (see Table 31).
Comparisons involving head-to-head contrasts between two active interventions were significantly less likely to favour the ‘primary’ intervention being evaluated (n = 195, χ2 = 6.06, p = 0.01). Similarly, comparisons against TAU were less likely to favour the intervention being evaluated (n = 195, χ2 = 5.59, p = 0.01). No significant difference was observed between analyses comparing the primary intervention with ‘no treatment’ [placebo, waiting list control (WL) or no intervention at all] and analyses drawing a comparison with an active comparator or TAU.
Analyses comparing two groups (one allocated to the primary intervention and one to a placebo, TAU or an active comparator) were substantially less likely to show favourable outcomes for the primary intervention than analyses relying on a single within-group comparison (e.g. pre/post evaluations) (n = 195, χ2 = 12.84, p = 0.000) (see Table 31).
Blinding
Studies that used some element of blinding were more likely to show outcomes in favour of the primary intervention arm (60.5% vs 54.1% of analyses), although this did not reach statistical significance (n = 195, χ2 = 0.260, p = 0.376) (Table 32).
| Variable | Output | Statistically significant finding in favour of primary intervention or not | No. in sample at initial recruitment | % dropout | Total length of follow-up (days) |
|---|---|---|---|---|---|
| Statistically significant finding in favour of primary intervention or not | Pearson’s correlation | 1 | –0.071 | –0.043 | –0.013 |
| Significance (two tailed) | 0.333 | 0.557 | 0.865 | ||
| n (median) | 195 | 188 | 185 | 178 | |
| No. in sample at initial recruitment | Pearson’s correlation | 0.004 | 0.098 | ||
| Significance (two tailed) | 0.953 | 0.199 | |||
| n (median) | 185 | 172 | |||
| % dropout | Pearson’s correlation | –0.127 | |||
| Significance (two tailed) | 0.101 | ||||
| n (median) | 169 | ||||
| Total length of follow-up (days) | Pearson’s correlation | ||||
| Significance (two tailed) | |||||
| n (median) |
Baseline evaluation
Least variance was shown by the variable indicating whether or not there was an equivalence in aggression between comparators at baseline (n = 195, χ2 = 0.049, p = 0.48) (see Table 32). This is particularly unexpected, as baseline equivalence is a variable noted to be of considerable theoretical importance within the violence literature as a whole. It may be accounted for by the hypothesis that where baselines have been recorded it is more likely that they show equivalence. This may be worth further exploration in future research.
Intention-to-treat analysis
Whether the analysis was an ITT or not had no statistically significant association with whether the results favoured the primary treatment or not (n = 195, χ2 = 3.095, p = 0.54) (see Table 32).
Design
Studies following a RCT design were less likely to report analyses in favour of the primary treatment (47.6% vs 52.4% of analyses) but this did not reach statistical significance (n = 195, χ2 = 1.137, p = 0.186) (see Table 32).
Sample size and loss to follow-up
The median sample size at recruitment was 87.5. This also showed no significant association with whether an analysis favoured the primary intervention or not (n = 188, r = –0.07, p = 0.33) (see Table 32).
The median dropout rate was 10.14% and was not associated with whether an analysis favoured the primary treatment or not (n = 185, r = –0.43, p = 0.557) (see Table 32).
Length of follow-up
The median length of follow-up in days was 182.4. This was not associated with whether an analysis favoured the primary intervention or not (n = 178, r = –0.013, p = 0.865) (see Table 32).
Summary of bivariate associations
Only six variables showed a significant bivariate association with outcomes based on the key dichotomised variable coding whether or not a study (based on its strongest measure) recorded a significant finding in favour of the primary intervention arm. These were:
-
whether the primary intervention was something other than a pharmacological or psychological intervention (outcome is less likely to be positive)
-
whether or not the study was carried out in a general mental health population (outcome more likely to be positive)
-
whether or not the intervention was carried out in an offenders’ institution (outcome is less likely to be positive)
-
whether or not the study design involved a head-to-head comparison between the primary intervention and another active intervention (outcome less likely to be positive if comparator is active intervention)
-
whether or not the study design involved comparison against TAU (outcome less likely to be positive if comparator is TAU)
-
whether the analysis was within or between groups (outcome less likely to be positive for between-groups analyses).
In addition to the above, one potential confounder in respect of analysis outcomes was identified in respect of associations between the demographic and study design variables. This was:
-
proportion of participants who were Caucasian (increasing proportions associated with increasing age and decreasing likelihood of ethnic minority participants).
The very limited bivariate associations between key variables noted above fails to justify substantive multivariate analysis. To explore the extent of variation explained in respect of the central dependent variable (whether or not a significant outcome in favour of the primary intervention was established) we carried out a single regression analysis based around the above modifiers. The likely impact of the one potential confounding variable was not considered sufficiently strong to justify inclusion in the model.
Multivariate analyses
A binary logistic regression was conducted with ‘whether or not a statistically significant outcome in favour of the primary intervention arm was established’ as the dependent variable. The variation attributable to the model in attempting to account for outcomes was not large (Cox and Snell R2 = 0.12), but also not insignificant given the small number of variables included.
The relative weight of each independent variable in accounting for variation within this model is given in Table 33 below.
| Variable | Beta | SE | df | Significance |
|---|---|---|---|---|
| Intervention is ‘other’ | –0.552 | 0.384 | 1 | 0.150 |
| Mental disorder only | 0.650 | 0.423 | 1 | 0.125 |
| Offenders only | –0.143 | 0.404 | 1 | 0.723 |
| Within- or between-group analyses | –0.797 | 0.457 | 1 | 0.081 |
| Head to head | –0.583 | 0.458 | 1 | 0.203 |
| Active vs TAU | –0.275 | 0.576 | 1 | 0.632 |
| Constant | 0.827 | 0.337 | 1 | 0.014 |
As indicated in Table 33, the impact of most of the modifiers on outcome is not strong. Their relative weight in contributing to the model suggests that, all else being equal, the use of a within-groups analysis and a focus on evaluating outcomes in the context of general mental health are the attributes of a study most likely to ensure positive outcomes for the primary intervention being evaluated.
Further exploration of variance
In an attempt to explore further potential modifying variables accounting for variation in outcome in the data set, we divided the broad intervention (‘pharmacological/psychological/other’) and outcome measure (‘scale/not scale’) categories into smaller component groups. In line with the ‘scattergun’ approach for this literature, the range of both interventions and outcome measures was entirely disproportionate to the number of analyses included. Within the 195 analyses included above, there were a total of 94 distinct types of intervention and 55 different types of outcome measure.
The only individual categories with numbers approaching sufficient for any further consideration were as follows.
Primary intervention
-
Anger management (all programmes defined as such and not elsewhere categorised), n = 13.
-
Batterer Intervention Programme (BIP) (broadly defined as any such programme), n = 22.
-
Cognitive behavioural therapy (broadly defined as any such programme), n = 29.
Outcome measure
-
Conflict Tactics Scale (CTS) (any subscale), n = 14.
-
‘Hostility’ (measured by observation or self-report), n = 2.
-
Overt Aggression Scale (OAS) or Modified OAS (M-OAS), n = 11.
-
Reassault (defined as any observed or otherwise objectively reported), n = 67.
-
State-Trait Anger Inventory (STAXI) (any subscale), n = 25.
Of the above subcategories, all but one (‘hostility’) contained sufficient numbers for bivariate analysis with the dependent variable (‘whether or not a statistically significant outcome in favour of the primary intervention arm was established’). However, none of the analyses carried out on these potential modifiers showed any significant associations with the dependent variable. Furthermore, the only observable trends within the data were a slight tendency for analyses using CBT as the primary intervention, to be more likely to report statistically significant outcomes in favour of this intervention and for analyses using reassault, but not using OAS/M-OAS (a scale-based observer measure of assault) as an outcome measure to identify significant findings in favour of the primary intervention. Table 34 summarises the outcomes for this further exploratory analysis.
| Intervention type/outcome measure | n | Favours treatment n (%) | Does not favour treatment n (%) | Chi-squared | p-value | |
|---|---|---|---|---|---|---|
| Anger management | Yes | 13 | 6 (46.2) | 7 (53.8) | 0.428 | 0.355 |
| No | 182 | 101 (55.5) | 81 (44.5) | |||
| BIP | Yes | 22 | 11 (50.0) | 11 (50.0) | 0.238 | 0.396 |
| No | 173 | 96 (55.5) | 77 (44.5) | |||
| CBT | Yes | 29 | 107 (54.9) | 88 (45.1) | 0.713 | 0.262 |
| No | 166 | 89 (53.6) | 77 (46.4) | |||
| CTS | Yes | 14 | 8 (57.1) | 6 (42.9) | 0.031 | 0.543 |
| No | 181 | 99 (54.7) | 82 (45.3) | |||
| Hostility | Yes | 2 | 0 (0.0) | 2 (100) | 2.457 | 0.202 |
| No | 193 | 107 (55.4) | 86 (44.6) | |||
| OAS/M-OAS | Yes | 11 | 4 (36.4) | 7 (63.6) | 1.613 | 0.169 |
| No | 184 | 103 (56.0) | 81 (44.0) | |||
| Reassault | Yes | 67 | 40 (59.7) | 27 (40.3) | 0.961 | 0.204 |
| No | 128 | 67 (52.3) | 61 (47.7) | |||
| STAXI | Yes | 25 | 14 (56.0) | 11 (44.0) | 0.015 | 0.539 |
| No | 170 | 93 (54.7) | 77 (45.3) | |||
Chapter 5 Results of meta-analyses
All randomised controlled trials
In order to explore the general profile of the RCT data, we first carried out an exploratory MA. This analysis included all 40 analyses for which metrics suited to conversion to ORs were available (see Chapter 2, Meta-analysis). The number of ‘risk ratio’ analyses was too small to be meaningfully combined for this purpose.
Meta-analysis of all randomised controlled trials
Figure 8 summarises the outcomes for this initial exploratory analysis of the RCT data. Both on the assumption of a fixed- and random-effects model, the overall mean effect tends to slightly favour the intervention of interest rather than the placebo or active comparator. A diversity of interventions contribute to this profile, with studies evaluating psychological (e.g. Cavanaugh81), pharmacological (e.g. Krakowski et al. 82) and ‘other’ (e.g. Lasley83) interventions all showing positive outcomes for the primary intervention of interest. For the majority of studies favouring the primary intervention, the CIs are also reasonably small, indicating that the sample outcomes are likely to be representative of the actual population profile. Pooled effect size estimates based on the standardised mean difference (see Table 35) suggest that, overall, interventions for violent behaviour can be expected to show a small to moderate impact.
FIGURE 8.
Meta-analysis of all RCTs. For a full explanation of the comparisons included see Appendix 3, Table 56. BPD, borderline personality disorder; CB, cognitive behavioural; CBT, dialectical behaviour therapy; CMAI, Cohen-Mansfield Agitation Inventory; F, female; M, male; PANSS, Positive and Negative Syndrome Scale; PSE, present state examination; SCL-90, Symptom-Checklist-90.

| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 40 | 40 | |
| Effect size | 0.59 | 0.35 | |
| 95% CI | Lower | 0.53 | 0.26 |
| Upper | 0.65 | 0.49 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –9.86 | –6.29 |
| p-score | 0.0001 | 0.0001 | |
| Estimates of heterogeneity | Q | 278.95 | |
| df Q | 39 | ||
| p-score | 0.0001 | ||
| I 2 | 86.02% | ||
| Effect size estimates based on standardised mean difference | –0.29 | –0.57 | |
| 95% CI | Lower | –0.35 | –0.75 |
| Upper | –0.23 | –0.39 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –9.86 | –6.29 |
| p-score | 0.0001 | 0.0001 | |
Heterogeneity
Table 35 summarises the outcome of heterogeneity estimates and the effect sizes for this overall combination of RCTs. Although the likely general profile of outcomes for interventions evaluated in the literature can legitimately be drawn from an overview of this exploratory MA, it is important to recognise that we are combining across a very diverse range of studies. It is readily apparent from the estimates in Table 35 that the RCT analyses in this literature are hugely variable. An I2 of 86% is extremely large, indicating that from a statistical viewpoint the ‘averaged’ estimates contained in the MA are not robust. They should therefore be taken, at best, as an indicator of potential outcomes. Subsequent MAs, outlined below, demonstrate that this variance is not a simple function of either intervention or outcome type. Before moving on to explore this variability further, it is worth noting that three studies contributing to the MA have particularly large CIs,84–86 suggesting that these studies’ estimates of likely effect size are unlikely to be wholly representative of the potential outcomes in the population of interest. Studies reporting analyses with larger CIs are also not restricted to the smallest sample sizes, implying that levels of uncertainty are not purely the consequence of sampling error. The impact of study focus and study quality is explored further later on in the report. Removing the three studies reporting notably wide CIs from the analysis did not, however, serve to substantially reduce the observed heterogeneity (Q = 260.88, I2 = 89.6%) relative to that reported in Table 35. Neither did the removal of all analyses with CIs wider than the average for this group of analyses (the above three analyses plus Volavka et al. ,87 Nickel et al. 88 and Brown University89) (Q = 232.19, I2 = 89.66%).
Taking note of the likely unreliability of this exploratory analysis in respect of results, we calculated effect sizes based on standardised mean differences across all included analyses (see Table 35). The aim of this very broad estimate was to provide an initial indication of the potential efficacy of violence reduction interventions as such. Under a fixed-effects model, the mean effect size was –0.29 and under a random-effects model the effect size increased to –0.57. Although these figures are subject to substantial caveats, as outlined above, they indicate the potential for small to moderate decreases in violent behaviour as a result of some intervention, with the potential for greater gain where modifying factors, such as population group, are taken into account (as the random-effects model identified a larger effect size than the fixed-effects model).
Analyses by comparison types
The first step in exploring the heterogeneity present in the overall MA was to analyse by the type of comparison conducted, i.e. comparison of two active treatments, comparison of an active treatment and TAU and comparison against a true control, for example placebo or no treatment (Figures 9–11).
FIGURE 9.
Meta-analysis of RCTs comparing two active treatments. For a full explanation of the comparisons included see Appendix 3, Table 56. CMAI, Cohen-Mansfield Agitation Inventory; DBT, dialectical behaviour therapy; PANSS, Positive and Negative Syndrome Scale.
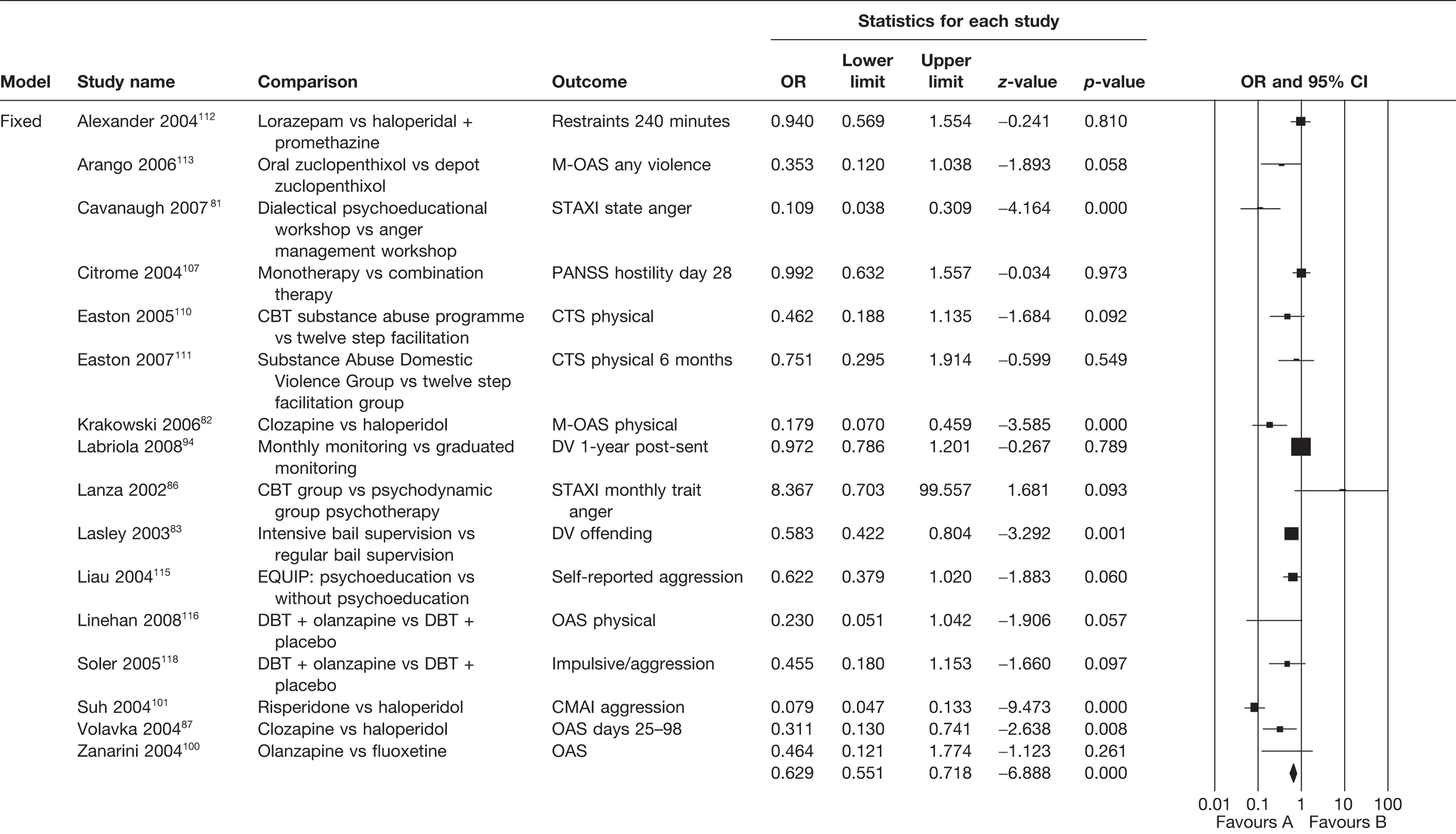
FIGURE 10.
Meta-analysis of RCTs comparing an active treatment to TAU. For a full explanation of the comparisons included see Appendix 3, Table 56. CB, cognitive bahavioural; F, female; M, male.
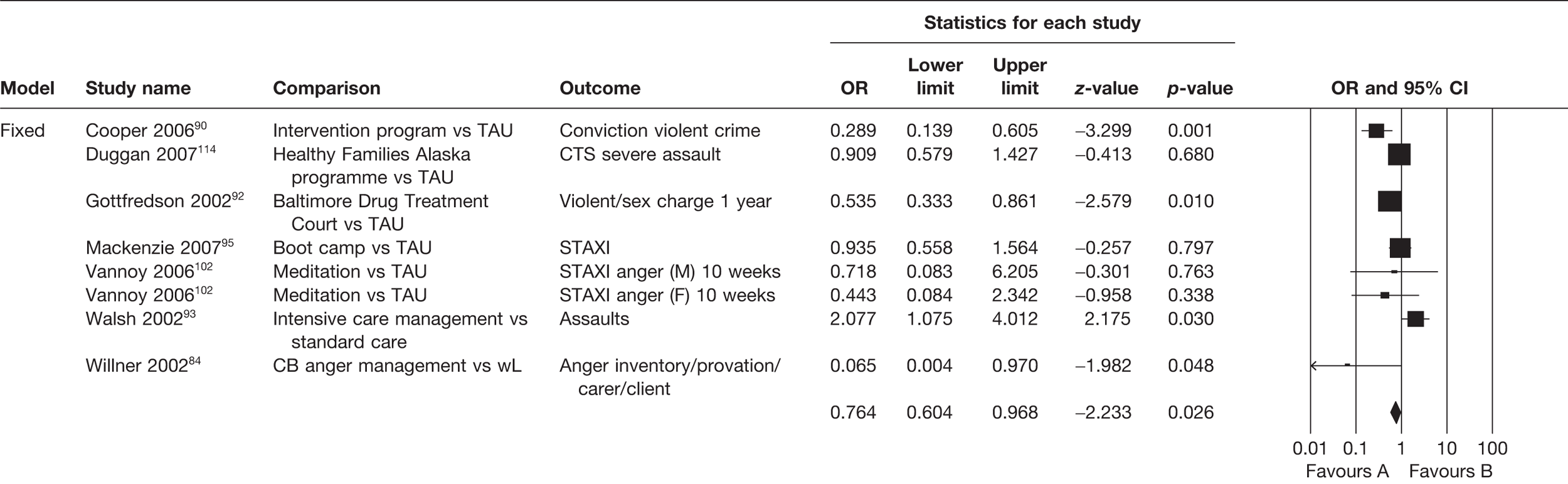
FIGURE 11.
Meta-analysis of RCTs comparing an active treatment to a true control. For a full explanation of the comparisons included see Appendix 3, Table 56. BPD, borderline personality disorder; PSE, present state examination; SCL-90, Symptom-Checklist-90.
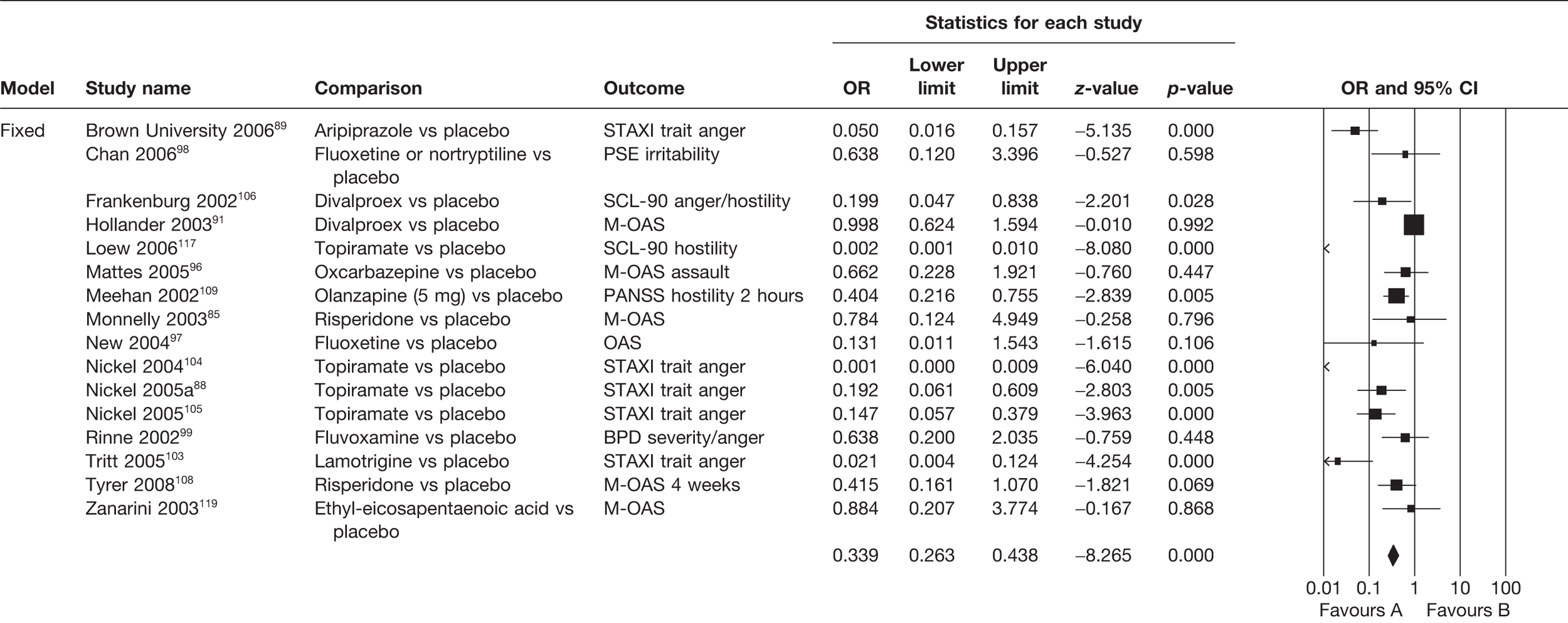
Head-to-head comparisons
Although in the broader range of studies included in the bivariate analyses head-to-head comparisons were significantly less likely to favour the primary intervention, this is not the case for the RCT studies included in the MA (Figure 9). Here, again, both fixed-effects models and, to a lesser extent, random-effects models showed outcomes slightly in favour of the primary intervention. As for the general evaluation outlined above, favourable outcomes ranged across diverse intervention types. For all but one small study, CIs were acceptably small. The one exception to this was a small study86 that also presented as something of an outlier in respect of the general trend, in favouring the comparative intervention (‘psychodynamic psychotherapy’) over the primary intervention being evaluated (CBT). As with the general model above, effect size estimates (Table 36) suggested a likely small-to-moderate impact on violence of the interventions taken as a whole, with some potential for further gains if population groups particularly responsive to the intervention could be identified (fixed-effects model effect size –0.26, random-effects model effect size –0.44).
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 16 | 16 | |
| Effect size | 0.63 | 0.45 | |
| 95% CI | Lower | 0.55 | 0.29 |
| Upper | 0.72 | 0.68 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –6.89 | –3.71 |
| p-value | 0.0001 | 0.0001 | |
| Estimates of heterogeneity | Q | 111.21 | |
| df Q | 15 | ||
| p-value | 0.0001 | ||
| I 2 | 86.51% | ||
| Effect size estimates based on standardised mean difference | –0.26 | –0.44 | |
| 95% CI | Lower | 0.04 | 0.12 |
| Upper | –0.33 | –0.68 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –0.18 | –0.21 |
| p-value | 0.0001 | 0.0001 | |
Restricting the MA to ‘head-to-head’ comparisons had no impact on estimated heterogeneity between studies. With I2 remaining at 86%, the outcomes for the analysis must be regarded with caution, as, despite their similar focus on drawing a direct comparison between interventions, the studies included clearly remain very diverse in other respects.
Active treatment versus treatment as usual
A smaller range of studies compared the primary intervention with ‘treatment as usual’ (Figure 10). Predictably, observed heterogeneity for this smaller group of studies, all but one of which (Willner et al. ,84 focusing on CBT anger management) focused on ‘other’ interventions, was less extreme than for the ‘head-to-head’ analyses. Nevertheless, with an I2 of 68% (Table 37) overall outcomes for this MA still need to be regarded with caution. In addition, it should be noted that the studies included within this analysis vary quite considerably both in size (with larger studies carrying a greater weighting with respect to model outcomes) and in the length of their CIs. Taken as they stand, the fixed- and random-effects models show comparable outcomes, slightly favouring the primary intervention. Again, this is in contrast with the outcome observed for the broader range of studies included in the bivariate analysis. However, the suggested likely impact, based on the observed standardised mean difference, is very small and is also primarily driven by outcomes from one moderately sized study90 that focused on an individually tailored intervention delivered in a hospital setting.
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 8 | 8 | |
| Effect size | 0.76 | 0.7 | |
| 95% CI | Lower | 0.6 | 0.43 |
| Upper | 0.97 | 1.14 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –2.23 | –1.43 |
| p-value | 0.03 | 0.15 | |
| Estimates of heterogeneity | Q | 22.45 | |
| df Q | 7 | ||
| p-value | 0.002 | ||
| I 2 | 68.82% | ||
| Effect size estimates based on standardised mean difference | –0.15 | –0.2 | |
| 95% CI | Lower | –0.28 | –0.5 |
| Upper | –0.02 | 0.07 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –2.23 | –1.4 |
| p-value | 0.03 | 0.15 | |
Active treatment versus true control
The number of studies included in our MA of ‘active versus true control’ evaluations was larger (n = 16) than that in the ‘head-to-head’ evaluation and again showed very high levels of heterogeneity (I2 = 87%, Table 38) despite the fact that all of the studies in this category focused on pharmacological intervention. The majority of RCTs in this category found in favour of the primary intervention (primarily antidepressant drugs and novel antipsychotic drugs). The main exception to this trend was one large study91 which found no significant difference between divalproex (Depakote, Sanof-Aventis, UK) and placebo. The outcome of this study notwithstanding, the overall effect size based on standardised mean difference (see Table 38) suggest a likely moderate-to-large impact on violence for the interventions combined in this MA (fixed effects –0.60, random effects –0.98), with potential additional gains to be made by tailoring the intervention to specific population groups.
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 16 | 16 | |
| Effect size | 0.34 | 0.17 | |
| 95% CI | Lower | 0.26 | 0.08 |
| Upper | 0.44 | 0.37 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –8.26 | –4.39 |
| p-value | 0.0001 | 0.0001 | |
| Estimates of heterogeneity | Q | 121.85 | |
| df Q | 15 | ||
| p-value | 0.0001 | ||
| I 2 | 87.69% | ||
| Effect size estimates based on standardised mean difference | –0.60 | –0.98 | |
| 95% CI | Lower | –0.74 | –1.42 |
| Upper | –0.45 | –0.54 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –8.26 | –4.39 |
| p-value | 0.0001 | 0.0001 | |
Analyses by broad intervention groupings
In order to explore further potential sources of heterogeneity, we next compared results for each of the three main groups of interventions: pharmacological interventions, psychological therapies and the combined category of ‘other’ interventions. Note that none of the available RCTs sought to directly compare across these distinct modes of intervention (e.g. pharmacological vs psychotherapeutic). This is disappointing, and also further indicates the potential benefits of drawing on a broader range of analyses than purely RCTs in order to identify analyses that include such comparisons.
Pharmacological interventions
Figure 12 summarises the outcomes of a MA combining all RCTs with calculated ORs comparing a pharmacological product with either an active or placebo comparator.
FIGURE 12.
Meta-analysis of RCTs comparing pharmacological products with either an active or placebo comparator. For a full explanation of the comparisons included see Appendix 3, Table 56. BPD, borderline personality disorder; CMAI, Cohen-Mansfield Agitation Inventory; DBT, dialectical behaviour therapy; PANSS, Positive and Negative Syndrome Scale; PSE, present state examination; SCL-90, Symptom-Checklist-90.
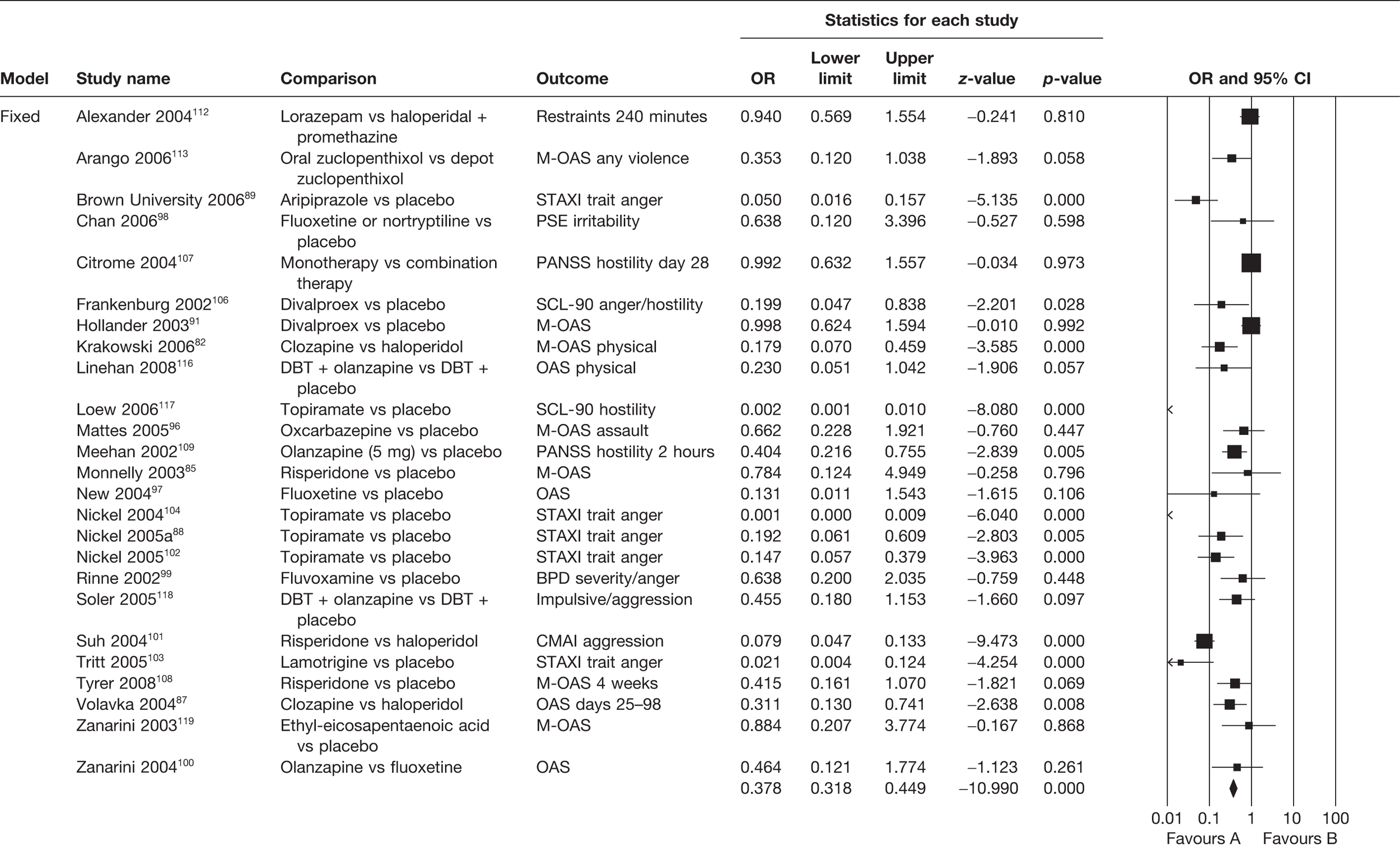
Given that evaluations of pharmacological interventions formed the bulk of the RCT data, it is not surprising that outcomes for the data for pharmacological interventions alone broadly track those for the overall data set. For the same reason, they also track the outcomes reported above for studies comparing an intervention with a ‘true control’. Specifically, the combined effect sizes tend to provide support for the likely efficacy of the main intervention rather than the active or placebo comparator. Estimates of overall outcome (pooled standardised mean difference using a fixed-effects model –0.54, using a random-effects model –0.81) suggest moderate-to-large impacts on aggressive behaviour with a likely significant benefit of fitting the intervention to appropriate populations, settings or other clinically relevant potential modifiers. Again, however, this implied profile needs to be considered cautiously, as estimates of heterogeneity (Table 39) for these studies, all focused on a single mode of intervention, remain very high (I2 = 87%).
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 25 | 25 | |
| Effect size | 0.38 | 0.23 | |
| 95% CI | Lower | 0.32 | 0.14 |
| Upper | 0.45 | 0.39 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –10.99 | –5.46 |
| p-value | 0.0001 | 0.0001 | |
| Estimates of heterogeneity | Q | 190.22 | |
| df Q | 24 | ||
| p-value | 0.0001 | ||
| I 2 | 87.38% | ||
| Effect size estimates based on standardised mean difference | –0.54 | –0.81 | |
| 95% CI | Lower | –0.63 | –1.10 |
| Upper | –0.44 | –0.52 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –10.99 | –5.46 |
| p-value | 0.0001 | 0.0001 | |
Psychological interventions
Outcomes for the combined RCT data for psychological interventions taken as a whole (Figure 13) were slightly less optimistic overall than the combined outcomes for pharmacological intervention. Estimated potential reductions in aggression were towards the low end of the scale (pooled standardised mean differences based on a fixed-effects model –0.26, based on a random-effects model –0.35) with less promise of improvement to be gained by targeting relevant population groups or other modifiers.
FIGURE 13.
Meta-analysis of RCTs comparing psychological interventions. For a full explanation of the comparisons included see Appendix 3, Table 56. CB, cognitive behavioural; F, female; M, male.
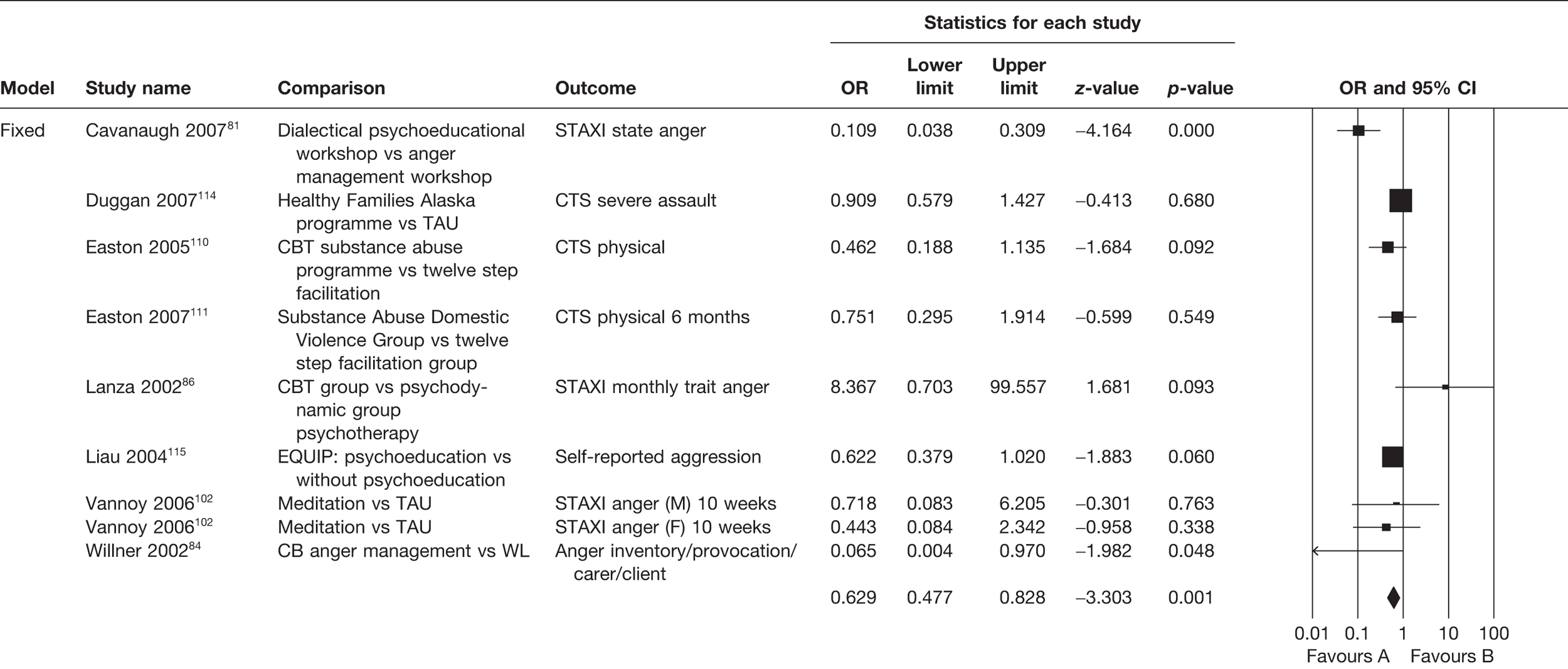
Although the overall effect sizes observed were less than those observed for the model for pharmacological interventions, the outcomes of the MA for psychological interventions are more robust, as there is less observed heterogeneity among the psychological studies, so the observed outcomes are more likely to be ‘real’ than the result of artefact. Significant heterogeneity was still observed within this group of studies (I2 = 65%, Table 40), but to a moderate rather than an extreme degree. It is therefore reasonably, if not wholly, safe to conclude that psychological interventions do have the potential for making a small impact on violent behaviour. Given the range of approaches included within this category and the lack of a large and consistent body of work evaluating any single type of psychological intervention, further exploration is clearly needed to establish which form of psychological intervention may be most promising.
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 9 | 9 | |
| Effect size | 0.63 | 0.53 | |
| 95% CI | Lower | 0.48 | 0.31 |
| Upper | 0.83 | 0.93 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –3.30 | –2.22 |
| p-value | 0.001 | 0.03 | |
| Estimates of heterogeneity | Q | 21.10 | |
| df Q | 8 | ||
| p-value | 0.007 | ||
| I 2 | 62.09% | ||
| Effect size estimates based on standardised mean difference | –0.26 | –0.35 | |
| 95% CI | Lower | –0.41 | –0.65 |
| Upper | –0.10 | –0.04 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –3.30 | –2.22 |
| p-value | 0.001 | 0.03 | |
That the number of RCTs available in this context is so low is unfortunate, as the error margin entailed by this degree of variance cannot be adequately accounted for by dividing analyses into comparable smaller groupings. In the absence of any forthcoming additional RCT data in this area, any conclusions about the effect of psychological interventions will need to be informed by the existing non-RCT analyses to a greater degree than is the case for pharmacological intervention.
Other interventions
The available prospective RCT data for evaluations of interventions other than either pharmacological or psychological intervention are extremely limited. Within this already limited field, only five of the available analyses contributed data suited to MAs based around ORs (Figure 14). These analyses addressed quite distinct forms of intervention, albeit all compared against TAU. Gottfredson and Exum92 compared a drug treatment court approach with TAU, Walsh et al. 93 compared intensive case management with TAU, Labriola et al. 94 and Lasley83 compared intensified bail supervision with other forms of bail supervision, and MacKenzie et al. 95/Mitchell and MacKenzie77 compared a multimodal ‘boot camp’ approach with TAU.
FIGURE 14.
Meta-analysis of RCTs comparing other active or TAU interventions. For a full explanation of the comparisons included see Appendix 3, Table 56.

Given the diversity in focus, it is not surprising that the analyses showed substantial heterogeneity (I2 = 77%; Table 41). In contrast with both pharmacological intervention and psychological intervention, the averaged effect size of these ‘alternative’ forms of intervention is also very low, clustering around an outcome of no significant difference in aggression between treatment and TAU (pooled standardised mean differences based on fixed-effects model –0.09, based on random-effects model –0.08; see Table 41).
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 5 | 5 | |
| Effect size | 0.84 | 0.86 | |
| 95% CI | Lower | 0.72 | 0.59 |
| Upper | 0.98 | 1.24 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –2.17 | –0.82 |
| p-value | 0.03 | 0.41 | |
| Estimates of heterogeneity | Q | 17.65 | |
| df Q | 4 | ||
| p-value | 0.001 | ||
| I 2 | 77.34% | ||
| Effect size estimates based on standardised mean difference | –0.09 | –0.08 | |
| 95% CI | Lower | –0.18 | –0.29 |
| Upper | –0.009 | 0.119 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –2.17 | –0.82 |
| p-value | 0.03 | 0.41 | |
Although the overall MAs for the three primary modes of intervention suggest more promising outcomes for pharmacological intervention than for either psychological intervention or ‘other’ forms of intervention, it is important to note that, overall, the sets of data analysed here display either significant amounts of heterogeneity between analyses or, in the case of ‘other’ interventions, numbers too small to be suited to the further exploration of possible outcome modifiers. Additional appropriately large RCTs of psychological and ‘other’ interventions would be needed to allow any direct comparison between outcomes for pharmacological interventions and outcomes for other forms of intervention. Evaluation of pharmacological intervention is a well-established research field, while the evaluation of other modes of intervention for violent behaviour is, relatively speaking, in its infancy.
Analyses for specific comparator groupings
Pharmacological analyses
Sufficient studies were available to analyse three pharmacological groupings in separate meta-analyses: anticonvulsant drugs against placebo, selective serotonin reuptake inhibitor (SSRI) antidepressants against placebo and atypical antipsychotic drugs against haloperidol or placebo.
Anticonvulsant drugs against placebo
As shown in Figure 15 the majority of analyses evaluating anticonvulsant drugs against placebo reported statistically significant outcomes in favour of the active medication (Hollander et al. ,91 Mattes and Mattes96 being the exceptions). Mean effect sizes suggested a substantive potential reduction in aggression, again notably if treatment can be appropriately applied within relevant populations or other modifier subgroups (pooled standardised mean differences based on fixed-effects model –0.62, based on random-effects model –1.47, Table 42).
| Heterogenity estimates and effect sizes of all included RCTs | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 8 | 8 | |
| Effect size | 0.32 | 0.07 | |
| 95% CI | Lower | 0.23 | 0.01 |
| Upper | 0.45 | 0.32 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –6.56 | –3.45 |
| p-value | 0.0001 | 0.001 | |
| Estimates of heterogeneity | Q | 105.82 | |
| df Q | 7 | ||
| p-value | 0.0001 | ||
| I 2 | 93.38% | ||
| Effect size estimates based on standardised mean difference | –0.62 | –1.47 | |
| 95% CI | Lower | –0.81 | –2.3 |
| Upper | –0.44 | –0.63 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –6.56 | –3.45 |
| p-value | 0.0001 | 0.001 | |
FIGURE 15.
Meta-analysis of RCTs comparing anticonvulsant drugs to placebo. For a full explanation of the comparisons included Appendix 3, Table 56. SCL-90, Symptom-Checklist-90.
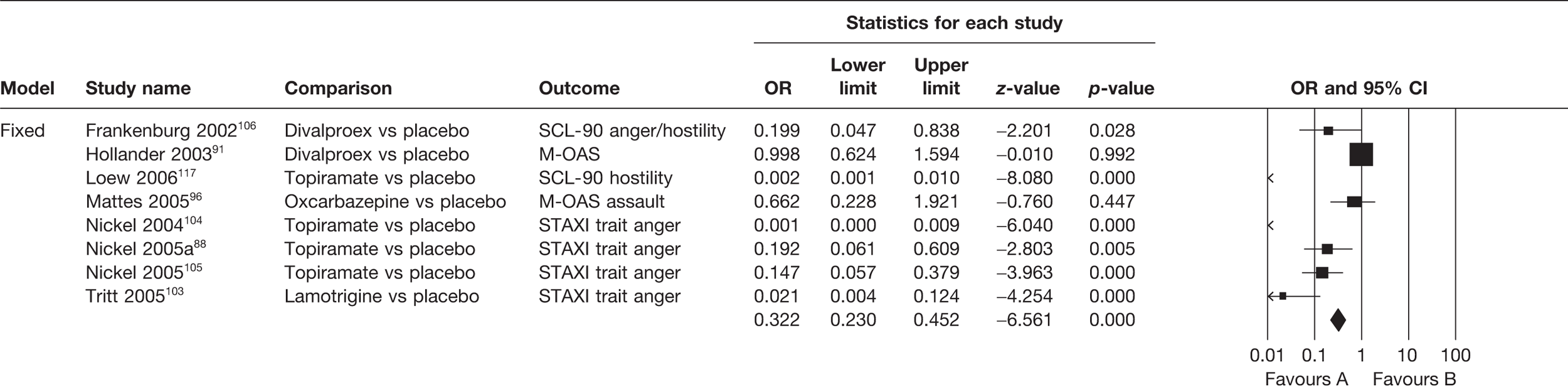
Unfortunately, despite the evident similarities between the analyses in this category, very substantial heterogeneity remained apparent in this combined analysis (see Table 42). As previously, therefore, the promising mean effect sizes cannot be considered robust and should be regarded as indicative at best.
Selective serotonin reuptake inhibitor antidepressant against placebo
A second smaller grouping of analyses97–100 compared three types of SSRI antidepressant (fluoxetine; fluoxetine or nortriptyline and fluvoxamine, respectively) primarily against placebo (against olanzapine in the case of Zanarini et al. 100).
Figure 16 summarises the outcome of this MA. Both fixed- and random-effects models report an equivalently small mean effect size in favour of the primary intervention (pooled standardised mean differences based on fixed-effects model –0.12, based on random-effects model –0.15). The equivalence in outcomes for the two models implies that targeting specific populations or other modifiers is unlikely to result in additional gains.
FIGURE 16.
Meta-analysis of RCTs comparing SSRI antidepressant to placebo/olanzapine. For a full explanation of the comparisons included see Appendix 3, Table 56. BPD, borderline personality disorder; PSE, present state examination.
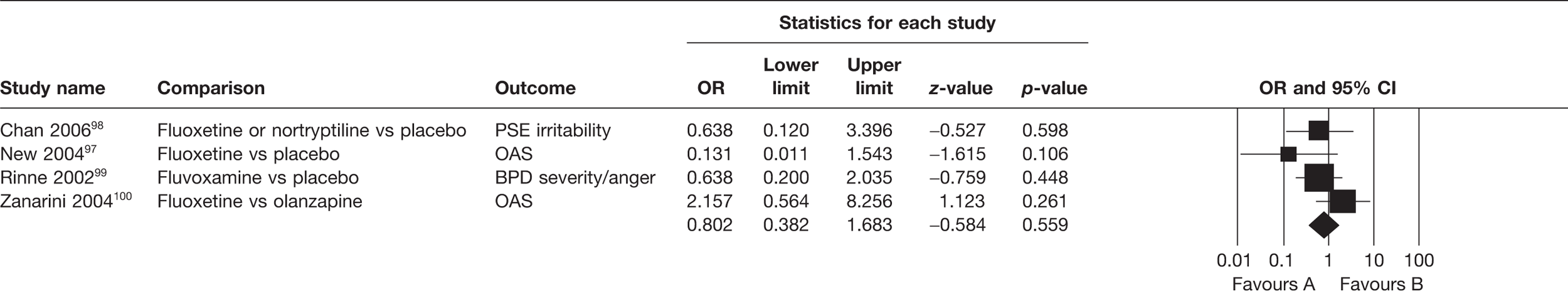
Unlike the previous analyses, heterogeneity analyses failed to identify any important variances between these analyses (Table 43).
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 4 | 4 | |
| Effect size | 0.80 | 0.76 | |
| 95% CI | Lower | 0.38 | 0.30 |
| Upper | 1.68 | 1.93 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –0.58 | –0.58 |
| p-value | 0.57 | 0.56 | |
| Estimates of heterogeneity | Q | 4.38 | |
| df Q | 3 | ||
| p-value | 0.22 | ||
| I 2 | 31.55% | ||
| Effect size estimates based on standardised mean difference | –0.12 | –0.15 | |
| 95% CI | Lower | –0.63 | –0.67 |
| Upper | 0.29 | 0.36 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –0.58 | –0.58 |
| p-value | 0.56 | 0.56 | |
Atypical antipsychotic drugs against haloperidol or placebo
A final grouping of pharmacological analyses with sufficient commonality for evaluation via MA compared a number of atypical antipsychotic drugs (risperidone, aripiprazole, olanzapine, quetiapine and clozapine) with either haloperidol, fluoxetine or placebo. Figure 17 summarises the outcome of this MA. The majority of comparisons drawn found in favour of the active atypical comparator. Mean effect size estimates were very high and roughly comparable between fixed- and random-effects models (pooled standardised mean differences based on fixed-effects model –0.86, based on random-effects model –0.78), suggesting a potentially large impact on aggressive behaviour for these drugs. One characteristic of note is the large effect reported by Suh et al. 101 This study differs from other studies included in the analysis in that it was conducted in a nursing home, with the mean age of patients being 81 years.
FIGURE 17.
Meta-analysis of RCTs comparing atypical antipsychotic drugs to haloperidol or placebo. For a full explanation of the comparisons included see Appendix 3, Table 56. CMAI, Cohen-Mansfield Agitation Inventory; DBT, dialectical behaviour therapy; PANSS, Positive and Negative Syndrome Scale.
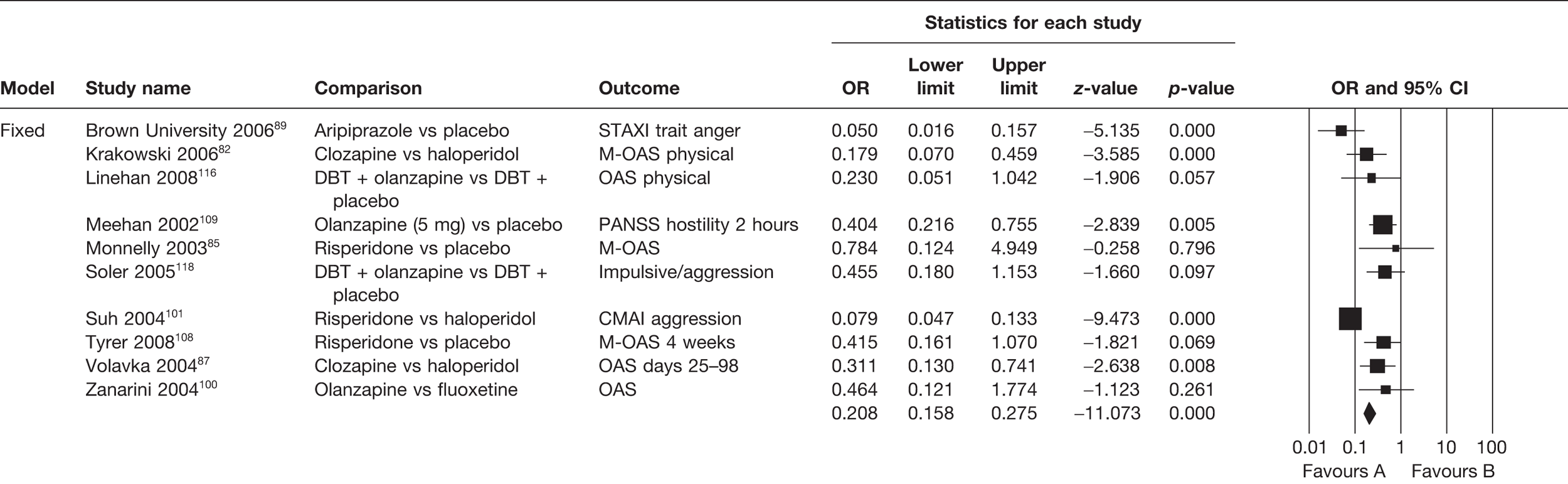
As indicated in Table 44, outcomes from this MA were again undermined by the presence of substantial heterogeneity, despite the small number of analyses included and their comparative similarity. No other combination of pharmacological analyses showed sufficient comparability in focus to justify MA.
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 10 | 10 | |
| Effect size | 0.21 | 0.24 | |
| 95% CI | Lower | 0.16 | 0.14 |
| Upper | 0.27 | 0.43 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –11.07 | –4.87 |
| p-value | 0.0001 | 0.0001 | |
| Estimates of heterogeneity | Q | 32.4 | |
| df Q | 9 | ||
| p-value | 0.0001 | ||
| I 2 | 72.23% | ||
| Effect size estimates based on standardised mean difference | –0.86 | –0.78 | |
| 95% CI | Lower | –1.02 | –1.09 |
| Upper | –0.71 | –0.46 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –11.07 | –4.87 |
| p-value | 0.0001 | 0.0001 | |
Psychological analyses
The only set of psychological analyses with sufficient comparability to combine in a within-groupings MA was a broad set of analyses all comparing CBT (of diverse types) against a range of active and waiting list comparators (prison, anger management, psychotherapy and related interventions). One study102 that focused on meditation is included in this MA, as the approach taken to meditation was relevantly similar to more usual forms of CBT (broadly defined as per the range of approaches taken by this group of studies). Figure 18 sets out the results of this MA and Table 45 explores the degree of heterogeneity within this group of analyses.
FIGURE 18.
Meta-analysis of RCTs comparing CBT to a range of active and waiting list comparators. For a full explanation of the comparisons included see Appendix 3, Table 56. CB, cognitive behavioural; F, female; M, male.
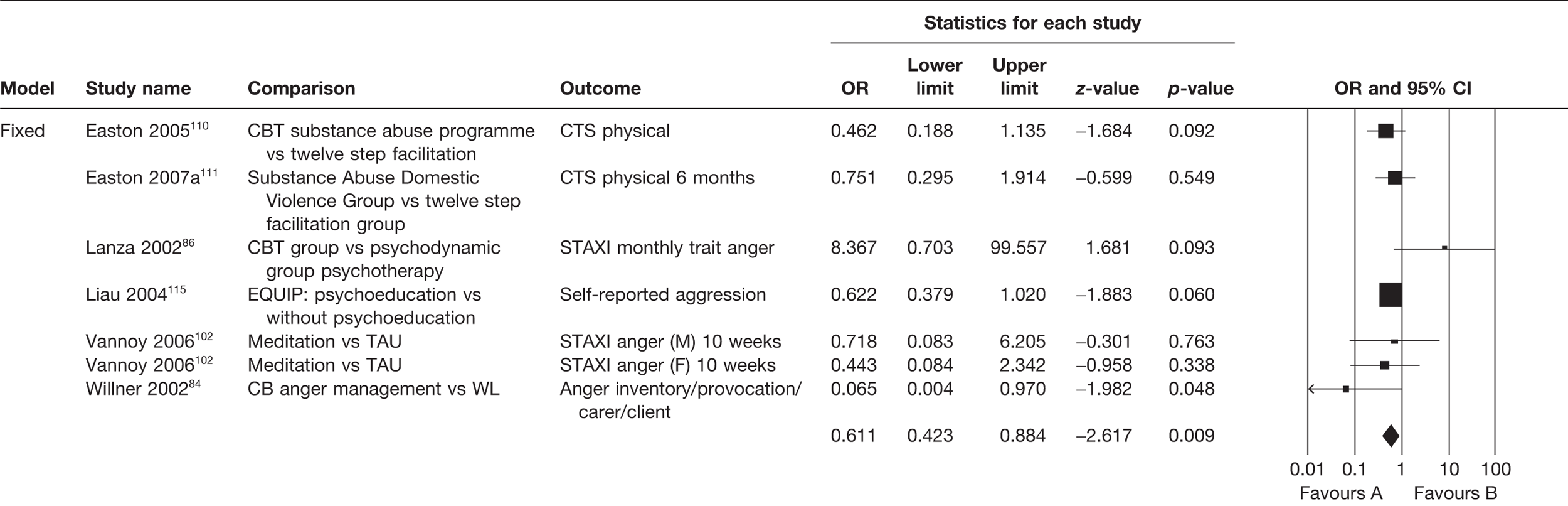
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 7 | 7 | |
| Effect size | 0.61 | 0.61 | |
| 95% CI | Lower | 0.42 | 0.37 |
| Upper | 0.88 | 0.99 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –2.62 | –1.97 |
| p-value | 0.009 | 0.05 | |
| Estimates of heterogeneity | Q | 7.65 | |
| df Q | 6 | ||
| p-value | 0.26 | ||
| I 2 | 21.62% | ||
| Effect size estimates based on standardised mean difference | –0.27 | –0.27 | |
| 95% CI | Lower | –0.47 | –0.54 |
| Upper | –0.07 | –0.001 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –2.62 | –1.97 |
| p-value | 0.009 | 0.05 | |
Although the majority of individual analyses within this group were unable to report statistically significant findings in favour of CBT, the combined effect sizes, both fixed and random, indicated a small potential decrease in aggression by applying the CBT model (pooled standardised mean differences based on fixed-effects model –0.27, based on random-effects model –0.27). The size of effect being equivalent between fixed and random models again implied that increases in effectiveness are unlikely to be gained by targeting specific populations or other modifiers.
The outcomes of this MA, indicating a small effect of CBT, are likely to be robust. No significant degree of heterogeneity is indicated in the analysis set out in Table 45 and the number of analyses although small is adequate for the exploration of heterogeneity. This type of intervention would therefore be a promising one to explore further in future RCTs. One caveat here is the need to define the intervention more tightly than has been done to date in the literature. The approaches to ‘CBT’ vary so widely that they could be considered very distinct interventions and it is of substantial importance to be able to identify which components of these diverse interventions actually contribute to the relative ‘success’ of CBT in impacting on aggressive behaviour.
Analyses of ‘other’ interventions
The number of analyses in this final grouping is small, as indicated previously, and the focus of the comparisons is diverse. No further benefit could be gained by attempting to partition these data further in additional MAs.
Exploring the impact of potential modifiers
The majority of the MAs outlined above exhibited substantial amounts of heterogeneity between analyses. Although random-effects models found a significant fit within these data, allowing the assumption that heterogeneity may be distributed randomly rather than indicating systematic differences between analyses, ideally we should aim to identify the causes of variation between analyses. In the absence of such identified causes the pooled estimates of effect size drawn from these potentially quite distinct analyses are inevitably subject to question. In an attempt to account for variation, we explored the association between individual analysis effect size and a number of key factors of clinical and statistical significance with respect to study design.
The associations between effect size and categorical variables are set out in Table 46; the impact of these variables on heterogeneity is outlined in Table 47. The associations between continuous variables and effect size are set out in Table 48, with the potential impact on heterogeneity discussed later in this chapter.
| Variable | Group | n analyses | Pooled standardised mean: fixed effects | z | p-value | Pooled standardised mean: random effects | z | p-value |
|---|---|---|---|---|---|---|---|---|
| Population | Indictable | 3 | –0.22 | –2.10 | 0.04 | –0.44 | –1.32 | 0.19 |
| Mental health status | 28 | –0.47 | –10.04 | 0.0001 | –0.73 | –5.00 | 0.0001 | |
| Offend | 9 | –0.17 | –0.49 | 0.0001 | –0.25 | –3.20 | 0.001 | |
| Start setting | Community | 20 | 0.64 | –6.15 | 0.000 | 0.23 | –5.50 | 0.0001 |
| Open ward | 3 | 0.36 | –3.20 | 0.001 | 0.36 | –3.20 | 0.001 | |
| Prison | 9 | 0.45 | –7.48 | 0.0001 | 0.52 | –1.91 | 0.06 | |
| Other or mixed | 3 | 0.34 | –0.58 | 0.56 | 0.34 | –0.58 | 0.56 | |
| Scale-based outcome measures | Not scale | 7 | –0.13 | –3.21 | 0.001 | –0.17 | –1.77 | 0.08 |
| Scale | 33 | –0.48 | –11.02 | 0.0001 | –0.71 | –5.72 | 0.0001 | |
| Blinding | Not blinded/unstated | 16 | –0.15 | –4.03 | 0.0001 | –0.23 | –2.65 | 0.008 |
| Blinded (any type) | 26 | –0.52 | –10.91 | 0.0001 | –0.81 | –5.49 | 0.0001 | |
| Baseline aggression | Different baseline or not stated | 19 | 0.57 | –6.35 | 0.0001 | 0.43 | –3.80 | 0.0001 |
| Same baseline | 21 | 0.60 | –7.56 | 0.0001 | 0.30 | –4.89 | 0.0001 | |
| ITT | Not ITT | 22 | 0.36 | –6.55 | 0.0001 | 0.48 | –3.70 | 0.0001 |
| ITT | 16 | 0.33 | –8.97 | 0.0001 | 0.21 | –5.07 | 0.0001 |
| Variable | Group | n analyses | Q | df Q | p-value | I 2 (%) |
|---|---|---|---|---|---|---|
| Population | Indictable | 3 | 13.47 | 2 | 0.001 | 85.15 |
| Mental health status | 28 | 221.69 | 27 | 0.0001 | 87.82 | |
| Offender | 9 | 19.16 | 8 | 0.01 | 58.25 | |
| Start setting | Community | 20 | 126.38 | 19 | 0.0001 | 84.85 |
| Open ward | 3 | 0.56 | 2 | 0.76 | 0.0001 | |
| Prison | 9 | 69.57 | 8 | 0.0001 | 86.57 | |
| Other or mixed | 3 | 0.73 | 2 | 0.69 | 0.0001 | |
| Scale-based outcome measures | Not scale | 7 | 26.45 | 6 | 0.0001 | 77.31 |
| Scale | 33 | 217.97 | 32 | 0.0001 | 85.32 | |
| Blinding | Not blinded/unstated | 16 | 49.03 | 14 | 0.0001 | 71.45 |
| Blinded (any type) | 26 | 192.12 | 24 | 0.0001 | 87.50 | |
| Baseline aggression | Different baseline or not stated | 19 | 66.78 | 18 | 0.0001 | 79.02 |
| Same baseline | 21 | 192.96 | 20 | 0.0001 | 89.63 | |
| ITT | Not ITT | 22 | 132.46 | 21 | 0.0001 | 84.15 |
| ITT | 16 | 112.81 | 15 | 0.0001 | 86.70 |
| Mixed-Effects regression model (maximum likelihood) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Q model | df Q | Q Residual | df Q | Q Total | df Q | p-value (model) | p-value (residual) | p-value (total) |
| Mean age | 0.19 | 1 | 38.28 | 32 | 38.46 | 33 | 0.66 | 0.20 | 0.23 |
| Sex (% male) | 8.63 | 1 | 43.95 | 36 | 52.60 | 37 | 0.003 | 0.17 | 0.05 |
| Ethnicity (% Caucasian) | 0.11 | 1 | 7.54 | 16 | 7.88 | 17 | 0.73 | 0.35 | 0.41 |
| Initial sample size | 6.40 | 1 | 48.53 | 38 | 54.92 | 39 | 0.01 | 0.12 | 0.05 |
| Dropout (% lost to follow-up) | 3.24 | 1 | 42.85 | 36 | 46.09 | 37 | 0.07 | 0.20 | 0.15 |
| Follow-up (total in days) | 2.99 | 1 | 45.09 | 36 | 48.06 | 37 | 0.08 | 0.14 | 0.10 |
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 4 | 4 | |
| Effect size | 0.07 | 0.03 | |
| 95% CI | Lower | 0.04 | 0.005 |
| Upper | 0.15 | 0.24 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –7.41 | –3.39 |
| p-value | 0.0001 | 0.001 | |
| Estimates of heterogeneity | Q | 20.21 | |
| df Q | 3 | ||
| p-value | 0.0001 | ||
| I 2 | 85.16% | ||
| Effect size estimates based on standardised mean difference | –1.44 | –1.88 | |
| 95% CI | Lower | –0.47 | –0.54 |
| Upper | –1.82 | –2.97 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –1.06 | –0.79 |
| p-value | –7.41 | –3.39 | |
Table 58 in Appendix 4 outlines the values for each of these potential modifier variables. Where data are missing for an analysis, the analysis itself will have been excluded from the analysis focused on that particular variable.
Although in the context of the broader range of studies included in our bivariate analyses, design characteristics of the included studies appeared to have little impact on outcomes, in the context of this more tightly defined set of RCTs design features did show a significant impact, both on effect sizes and associated levels of heterogeneity between studies.
Clinically relevant factors
Focus
The potential ‘modifier’ of choice of intervention (pharmacological vs psychological vs other) has been discussed previously in this chapter. As discussed, the more numerous pharmacological analyses produced relatively large effect sizes, but with concomitantly high levels of heterogeneity. Psychological analyses showed a more equivocal profile, with low-to-moderate effect sizes and slightly less heterogeneity. ‘Other’ forms of intervention provided the most equivocal outcomes but also the lowest level of heterogeneity, despite their very diverse range of interventions.
Population
Mental health status
As indicated in Table 47, the mental health status of the population group included within an analysis showed a statistically significant association with the effect size, under both fixed and random models. Overall, interventions targeted at people with a mental health problem were more likely to succeed than interventions targeted at non-mental health offender groups (convicted offenders and those known to have offended but not as yet indicted). However, analyses for studies focused on the general mental health population also showed the greatest degree of heterogeneity, indicating less robust outcomes (see Table 48). RCTs focused on forensic populations were too few in number (n = 1) to provide useable data in this context.
Demographics
Three demographic factors were coded for data extraction, namely age, sex and ethnicity. To take account of the diverse range of ways in which these characteristics were recorded in the analysis papers, we coded each as a continuous variable indicating, respectively, the proportion of groupings included within a study (% male, % Caucasian) and the mean age of the sample (a small number of studies recorded only median age and these have been excluded from analysis here). As indicated in Table 48, the only demographic characteristic showing a statistically significant association with the effect size for an analysis was sex, with analyses including a higher proportion of males tending to report more positive outcomes for the target intervention. Although statistically significant, it should be noted that the association is not a particularly strong one.
Setting
Four settings provided sufficient data for analysis, namely community settings (pooled between distinct types of community setting), open wards, prisons and the eclectic combined group of ‘other or mixed’ settings. As noted previously, the number of identified RCTs carried out in forensic settings is disappointingly small (n = 1). Overall, analyses focused on community settings that were most likely to produce comparatively large effect sizes (see Table 46), under both fixed- and random-effects models. The relatively greater pooled effect size for fixed than for random effect sizes relating to community settings suggests that there is unlikely to be a benefit to further targeting within this broad category.
Outcome measures
In the context of the RCT analyses, there was considerable consistency in the choice of outcome measure, with the vast majority of included analyses favouring scale-based measures. Contrasting scale versus non-scale (generally behavioural) measures (Tables 46 and 47), scale-based measures tended to be associated with better outcomes under both fixed- and random-effects models, with non-scale-based analyses showing non-significant pooled effect sizes. Both types of grouping showed large heterogeneity between analyses, although the diversity (in all likelihood because of analysis numbers) was smaller between analyses not using scale-based outcomes.
Study quality indicators
Clearly, the studies used for these analyses had been selected on the basis of perceived ‘study quality’, following the accepted gold standard of the prospective RCT. This notwithstanding, they of course differed in other aspects of study design and a number of these have implications for the likely reliability and validity of analysis outcomes. The ‘quality modifiers’, for which we have sufficient data for analysis, are explored below.
Sample size and loss to follow-up
An agreed ‘cut-off’ mark for partitioning sample size is not readily available, since virtually no studies reported power calculations. However, a natural split within the data appeared between studies recording up to 100 participants (generally substantially less) and studies recording rather more than this figure. Larger sample sizes (see Table 48) were, predictably, associated with larger individual effect sizes and hence with a greater likelihood of positive outcome.
The proportion of a given sample lost to follow-up, in contrast, did not quite reach statistical significance with regard to the potential association with analysis effect size. This is possibly because of the quite constrained nature of the RCTs identified. Unlike the more ‘real-world’ studies contained within the non-RCT data, loss to follow-up in the RCT setting was, overall, quite small, ranging, in the main, from 0% to around 15%.
Blinding
A number of distinct aspects of blinding were considered in our analysis (blinding of the participants, persons carrying out the intervention and persons collating and analysing the data). Aside from the blinding of participants, however, papers for the studies showed poor attention to detail in recording these various options. In the current analysis, therefore, of necessity, we combined across the various measures to define a combined ‘blinded or not’ variable. Although both design options (see Table 46) showed a positive association with analysis effect size, analyses that reported one or more methods of blinding showed a substantially stronger association with positive outcomes. Studies without blinding showed less heterogeneity than studies with blinding (see Table 47).
Length of follow-up
Surprisingly, length of follow-up (recorded in days) showed no statistically significant association with effect size (see Table 48). The range in timescale for the RCTs was substantially more varied than that recorded for the data overall. The consequent lack of any smooth distribution may have impacted on outcomes here.
Baseline evaluation
Baseline similarities/differences in the core aggression variables were poorly reported overall in the identified violence literature. Poor reporting of this highly significant moderating variable in the RCT data was particularly disappointing. To explore potential associations with effect size, we therefore contrasted analyses reporting equivalent aggression baselines for comparator groups at study outset, with analyses either recording differing baselines or analyses failing to record any attempt to measure relevant baselines. In the event, there was little difference in the level of association with outcomes shown by either grouping (see Table 46). Levels of heterogeneity between analyses in either grouping remained substantive (see Table 47).
Intention-to-treat analysis
There was comparatively little difference in effect size for studies evaluating interventions with an ITT or with a non-ITT approach (notably under the fixed-effects model). The extent of heterogeneity within analyses in the two groupings remained very high despite taking this characteristic into account (see Table 47).
Meta-analytic models incorporating identified modifiers
In an attempt to explore potentially more robust estimates of outcomes for subgroups of analyses selected with regard to both their intervention focus and with regard to potential modifiers highlighted as being associated with effect size, we outline below a final set of MAs.
Taking into account those modifiers now known to be associated with effect size (e.g. design characteristics such as sample size and demographic characteristics such as sex or population group) we identified subgroups of analyses with comparable characteristics on key features. Subdividing the data in this way led to four meta-analytic models with the potential to provide non-heterogeneous data for a more robust evaluation of outcomes. All but one of these comparisons focused on pharmacological interventions. In the event, only two of the models resulted in MAs with non-heterogeneous outcomes. This is a further indication of the substantial degree of variance that exists within this literature.
The models set out below each combine data from the studies within a given category (e.g. pharmacological interventions), which show the greatest degree of overall similarity of the range of key potential modifiers outlined above. Specifically, we looked for studies that focused on the same (or at least broadly similar) comparisons between interventions, which were also similar in profile on all, or most, of the following:
-
population
-
outcome measure (whether scale based or not)
-
sex (all male, all female, mixed group of participants)
-
setting study started in (prison, community, general mental health, forensic mental health, ‘other/mixed’)
-
number of participants at start of trial
-
whether or not any form of blinding was used in the study.
The number of studies available for each analysis is inevitably small and the ‘equivalence’ of the studies on the range of modifiers identified will vary between models. The main aim here is to see whether or not heterogeneity can be reduced by excluding studies that vary considerably on key features such as population, proportion of males included and so forth. None of the studies will show perfect equivalence on these features, as design diversity is a characteristic of this literature, but it was hoped that the models might provide an indication of how heterogeneity could be reduced and more robust outcomes identified via MA.
Model 1: anticonvulsant drugs versus placebo
Four studies were included in this model. 103–106 All four studies focused on an exclusively female, general mental health population. All studies took place in a community setting and used some form of blinding. Sample sizes at the outset ranged from 30 to 64 participants and outcomes for all four studies were scale based. Frankenburg and Zanarini106 evaluated the efficacy of divalproex sodium, Nickel et al. 104,105 evaluated the efficacy of topiramate and Tritt et al. 103 evaluated the efficacy of lamotrigine (Figure 19).
FIGURE 19.
Meta-analysis model 1. For a full explanation of the comparisons included see Appendix 3, Table 56. SCL-90, Symptom-Checklist-90.
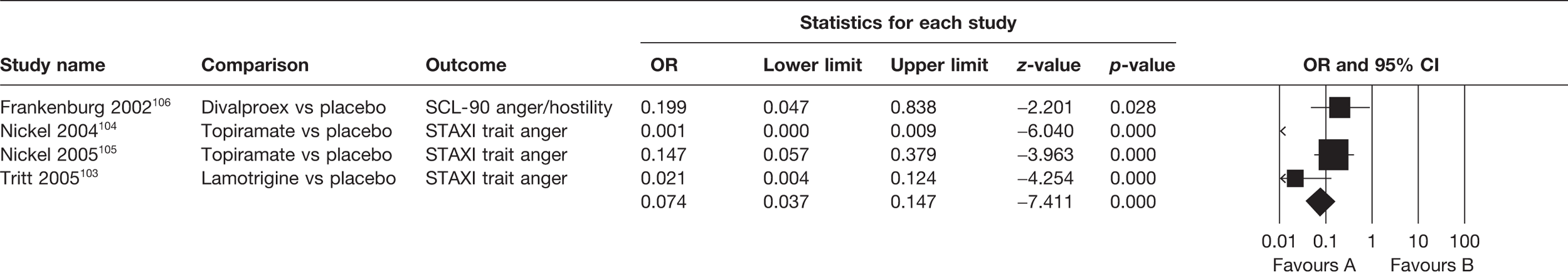
Despite the similarities between these studies both in respect of their main focus and in respect of relevant modifiers, substantive heterogeneity was observed (Q = 20.21, p = 0.0001, I2 = 85.16%) (Table 49). Although the model could be viewed as suggesting a potential impact of anticonvulsant medication on violent behaviour, it is consequently not advisable to draw this conclusion because of the substantial heterogeneity observed.
Model 2: atypical antipsychotic drugs versus any active comparator
Three studies were included in this model. 82,101,107 All three focused again on a general mental health population. Participants in all three studies included both males and females, with the proportion of male participants ranging from 25% to 83.8%. Settings were not specified for two of the studies82,107 and the setting for Suh et al. 101 fell into the ‘other/mixed’ category. Some form of blinding was used in all three studies and outcomes for all three were scale based. Citrome et al. 107 compared monotherapy with either risperidone or olanzapine to combination therapy with either of these drugs plus divalproex sodium. Krakowski et al. 82 compared clozapine with haloperidol and Suh et al. 101 compared risperidone with haloperidol (Figure 20).
FIGURE 20.
Meta-analysis model 2. For a full explanation of the comparisons included see Appendix 3, Table 56. PANSS, Positive and Negative Syndrome Scale.
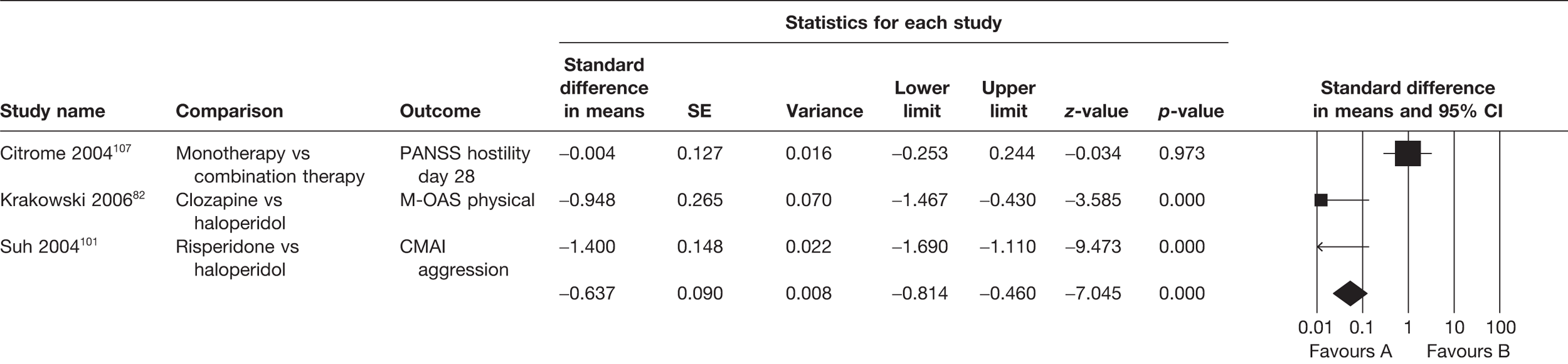
Again, despite selecting studies for apparent similarities in respect of focus and potential modifiers, a significant degree of heterogeneity was observed in this model (Q = 52.96, p = 0.0001, I2 = 96.22%) (Table 50). The promising outcomes suggested for atypical antipsychotic drugs therefore fall prey to the unreliability generated within the model by characteristics of the studies that we have yet to identify.
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 3 | 3 | |
| Effect size | 0.31 | 0.24 | |
| 95% CI | Lower | 0.23 | 0.04 |
| Upper | 0.43 | 1.43 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –7.04 | –1.56 |
| p-value | 0.0001 | 0.12 | |
| Estimates of heterogeneity | Q | 52.96 | |
| df Q | 2 | ||
| p-value | 0.0001 | ||
| I 2 | 96.22% | ||
| Effect size estimates based on standardised mean difference | –0.64 | –0.78 | |
| 95% CI | Lower | –0.81 | –1.75 |
| Upper | –0.46 | 0.2 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –7.04 | –1.56 |
| p-value | 0.0001 | 0.12 | |
Model 3: atypical antipsychotic drugs versus placebo
Three studies were included in this model. 89,108,109 Again, all three focused on a general mental health population. Participants in all three studies included both males and females, with the proportion of male participants ranging from 19.23% to 59%. Two of the studies took place in community settings,89,108 and the setting for Meehan et al. 109 fell into the ‘other/mixed’ category. Some form of blinding was used in all three studies and outcomes for all three were scale based. Sample sizes ranged from 52 to 272. Brown University89 evaluated the efficacy of aripiprazole, Tyrer et al. 108 evaluated the efficacy of risperidone, and Meehan et al. 109 evaluated the efficacy of olanzapine (Figure 21).
FIGURE 21.
Meta-analysis model 3. For a full explanation of the comparisons included see Appendix 3, Table 56. PANSS, Positive and Negative Syndrome Scale.
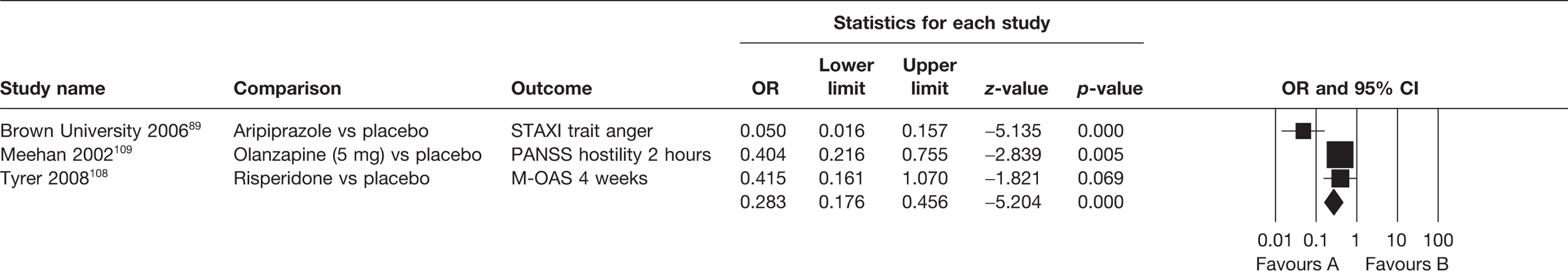
This model follows a very similar pattern to the model 2, with promising outcomes undermined by significant heterogeneity in the data (Q = 10.67, p = 0.0001, I2 = 81.26%) (Table 51) despite apparent similarities between the studies with respect to focus and key modifiers.
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 3 | 3 | |
| Effect size | 0.28 | 0.22 | |
| 95% CI | Lower | 0.18 | 0.07 |
| Upper | 0.46 | 0.71 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –5.2 | –2.51 |
| p-value | 0.0001 | 0.01 | |
| Estimates of heterogeneity | Q | 10.67 | |
| df Q | 2 | ||
| p-value | 0.005 | ||
| I 2 | 81.26% | ||
| Effect size estimates based on standardised mean difference | –0.69 | –0.84 | |
| 95% CI | Lower | –0.96 | –1.49 |
| Upper | –0.43 | –0.18 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –5.2 | –2.51 |
| p-value | 0.0001 | 0.01 | |
Model 4: cognitive behavioural therapy versus any active comparator
Three studies were included in this model. 86,110,111 All three studies focused exclusively on male participants, none of the studies used any form of blinding, outcomes for all three studies were scale based and sample sizes ranged from 42 to 78. All studies took place in either community111 or ‘other/mixed’ settings. This group of studies were more varied in respect of their target participant group than studies included in the above three models. Lanza et al. 86 focused on a general mental health population, Easton110 on an offender population, and Easton et al. 111 on a group of participants who had committed acts of violence but as yet had not been indicted for these acts (Figure 22).
FIGURE 22.
Meta-analysis model 4. For a full explanation of the comparisons included see Appendix 3, Table 56.
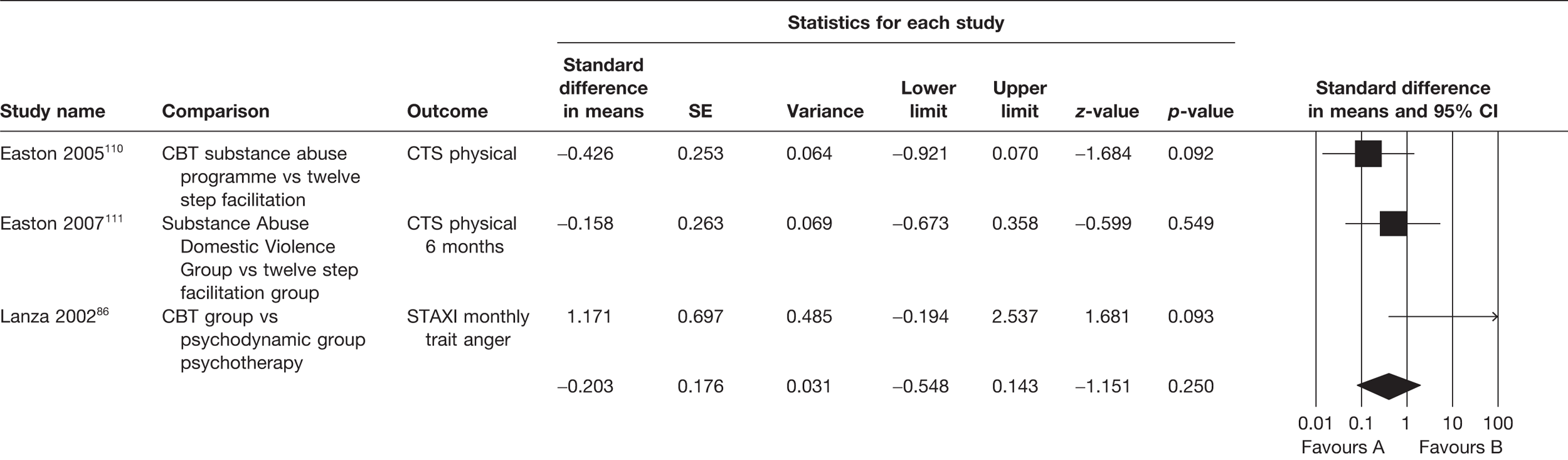
Despite the clear differences in population focus, this model generated the least heterogeneity (Q = 4.70, p = 0.09, I2 = 57.4%) (Table 52).
| Heterogeneity estimates and effect sizes | Model | ||
|---|---|---|---|
| Fixed | Random | ||
| n analyses | 3 | 3 | |
| Effect size | 0.69 | 0.86 | |
| 95% CI | Lower | 0.37 | 0.29 |
| Upper | 1.29 | 2.55 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –1.15 | –0.26 |
| p-value | 0.25 | 0.79 | |
| Estimates of heterogeneity | Q | 4.7 | |
| df Q | 2 | ||
| p-value | 0.09 | ||
| I 2 | 57.43% | ||
| Effect size estimates based on standardised mean difference | –0.2 | –0.08 | |
| 95% CI | Lower | –0.55 | –0.68 |
| Upper | 0.14 | 0.52 | |
| Two-tailed test of null hypothesis (homogeneous data) | z | –1.15 | –0.26 |
| p-value | 0.25 | 0.79 | |
Publication bias
Figure 23 presents a funnel plot of the analyses included in the overall MA. The asymmetric distribution apparent in Figure 23 is suggestive of publication bias. The pattern is consistent with, in particular, the rejection of smaller analyses with negative outcomes. This would be consistent with biases observed in other literatures and would not be an unexpected finding, notably in the context of a comprehensive search of the literature such as the one carried out here. Although the possibility of publication bias is therefore worth bearing in mind, it is important to note that a similar distribution could result from systematic associations between sample size and other analysis characteristics that impact on outcome.
FIGURE 23.
Funnel plot of SE by logs, OR and all included RCTs.
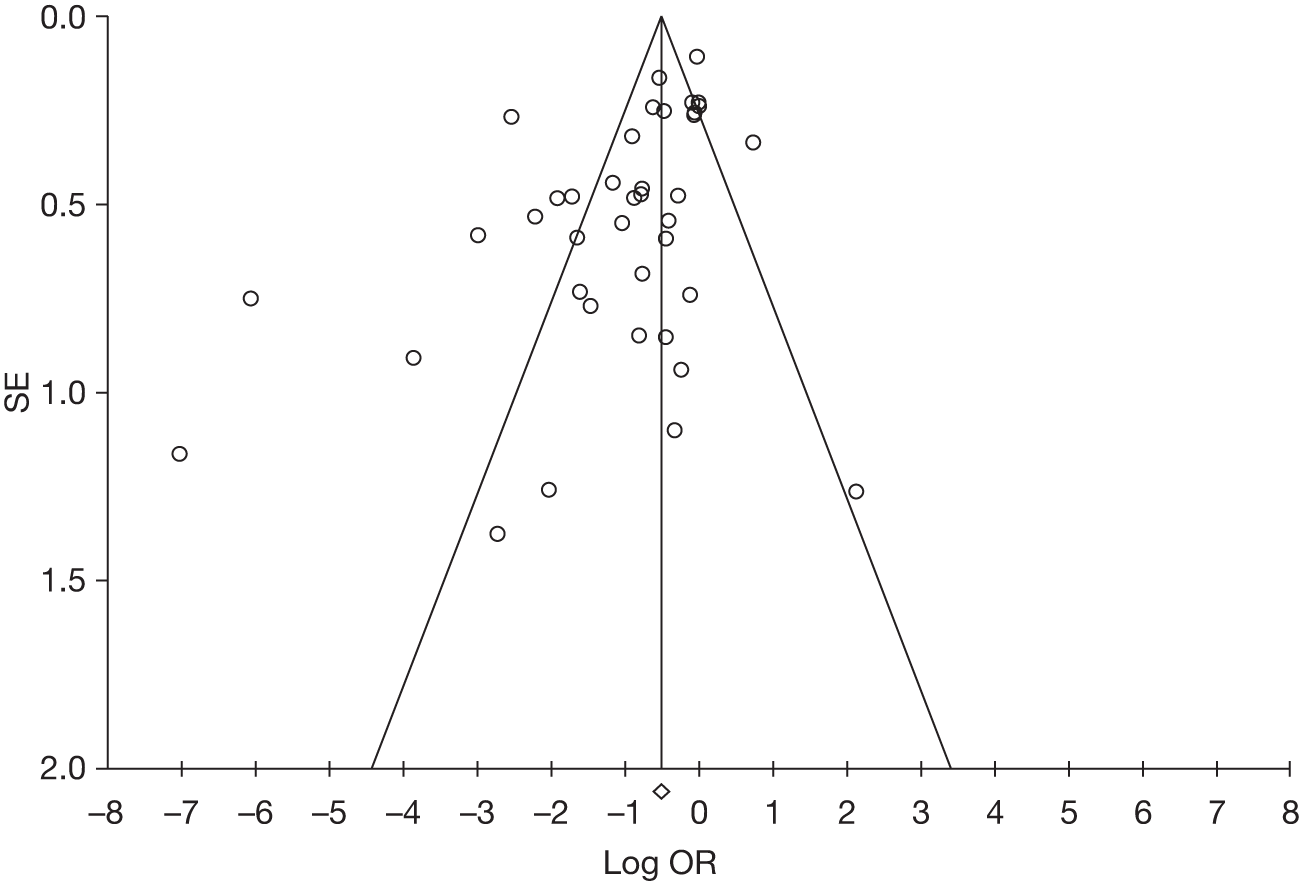
Summary
It is evident from the summary data presented in Table 53 that the ‘scattergun’ approach to empirical evaluation of interventions to prevent or reduce aggressive behaviour has produced a literature in the main that is unsuited to MA. This having been said, the MAs as set out serve both to provide a profile of the available ‘high-quality’ (RCT) data available and to provide some indicators of likely effect modifiers that are informative for the design of future studies. On the assumption that the observed variation can be accounted for by non-systematic differences between the analyses included in any given analysis (an assumption in part supported by the effect size models), the pooled outcome data can be taken as likely indicators of outcome for the intervention groupings evaluated.
| Variable | n | Fixed-effects model | Random-effects model | Heterogeneity | |||||
|---|---|---|---|---|---|---|---|---|---|
| Effect size (95% CI) | p-value | Effect size (95% CI) | p-value | Q | df Q | p-value | I 2 (%) | ||
| All RCTs | 40 | 0.59 (0.53 to 0.65) | 0.00001 | 0.35 (0.26 to 0.49) | 0.00001 | 279 | 39 | 0.0001 | 86 |
| Two active treatments | 16 | 0.63 (0.55 to 0.72) | 0.0001 | 0.45 (0.29 to 0.68) | 0.0001 | 111.2 | 15 | 0.0001 | 86.5 |
| Active treatment vs TAU | 8 | 0.76 (0.60 to 0.97) | 0.03 | 0.70 (0.43 to 1.14) | 0.15 | 22.4 | 7 | 0.002 | 68.8 |
| Active treatment vs true control | 16 | 0.34 (0.26 to 0.44) | 0.0001 | 0.17 (0.08 to 0.37) | 0.0001 | 121.9 | 15 | 0.0001 | 87.7 |
| Pharmacological intervention | 25 | 0.38 (0.32 to 0.45) | 0.0001 | 0.23 (0.14 to 0.39) | 0.0001 | 190.2 | 24 | 0.0001 | 87.4 |
| Anticonvulsant drugs | 8 | 0.32 (0.23 to 0.45) | 0.0001 | 0.07 (0.01 to 0.32) | 0.001 | 105.8 | 7 | 0.0001 | 93.4 |
| SSRIs | 4 | 0.80 (0.38 to 1.68) | 0.57 | 0.76 (0.30 to 1.93) | 0.56 | 4.38 | 3 | 0.22 | 31.6 |
| Atypical antipsychotic drugs | 10 | 0.21 (0.16 to 0.27) | 0.0001 | 0.24 (0.14 to 0.43) | 0.0001 | 32.4 | 9 | 0.0001 | 72.2 |
| Psychological intervention | 9 | 0.63 (0.48 to 0.83) | 0.001 | 0.53 (0.31 to 0.93) | 0.03 | 21.1 | 8 | 0.007 | 62.1 |
| CBT | 7 | 0.61 (0.42 to 0.88) | 0.009 | 0.61 (0.37 to 0.99) | 0.05 | 7.65 | 6 | 0.26 | 21.6 |
| Other intervention | 5 | 0.84 (0.72 to 0.98) | 0.03 | 0.86 (0.59 to 1.24) | 0.41 | 17.7 | 4 | 0.001 | 77.3 |
| Model 1: anticonvulsant drugs vs placebo | 4 | 0.07 (0.04 to 0.15) | 0.0001 | 0.03 (0.01 to 0.24) | 0.001 | 20.2 | 3 | 0.0001 | 85.2 |
| Model 2: atypical antipsychotic drugs vs any active comparator | 3 | 0.31 (0.23 to 0.43) | 0.0001 | 0.24 (0.04 to 1.43) | 0.12 | 53.0 | 2 | 0.0001 | 96.2 |
| Model 3: atypical antipsychotic drugs vs placebo | 3 | 0.28 (0.18 to 0.46) | 0.0001 | 0.22 (0.07 to 0.71) | 0.01 | 10.7 | 2 | 0.005 | 81.3 |
| Model 4: CBT vs any comparator | 3 | 0.69 (0.37 to 1.29) | 0.25 | 0.86 (0.29 to 2.55) | 0.79 | 4.7 | 2 | 0.09 | 57.4 |
Combining together this relatively large group of ‘gold standard’ analyses is particularly useful for gaining insight, as above, into the nature of the literature openly available. However, it is of rather less value in establishing a robust estimate of the likely impact of intervening to reduce violent behaviour using the combined range of interventions evaluated to this standard to date.
Chapter 6 Discussion and conclusions
Strengths and limitations of the review
This review offers a number of advantages over previous work in this area. The key strength is an attempt to combine breadth of scope in terms of widely defining aggression and relevant populations with rigour in terms of the depth to which each study was analysed. The review set out to encompass not only the highest-quality empirical studies, but also all relevant quantitative studies. RCTs are regarded, of course, as the gold standard for empirical evaluation. However, such trials emphasise internal validity over external validity and so are frequently constrained in a way that departs substantively from the reality of intervention in the clinical context. Having collated data from all available empirical studies, we have been able to contextualise the findings of RCTs by exploring the outcomes suggested by more pragmatic studies. Another benefit of this broad approach has been the identification of studies focusing on the head-to-head comparison of pharmacological and psychotherapeutic interventions. The approach also reflects the varied clinical reality faced by practitioners in mental health and criminal justice settings working with violent people. We are confident, therefore, that the review offers the most comprehensive account of the recent research literature to date with regard to the effectiveness of interventions to prevent or manage violence in mental health settings.
It is clear that the research literature on both violence risk assessment and treatment has grown enormously during the period of study, but at the same time the focus of research has shown no strong indication of a coalescence into the development of a common focus in design, treatment approach or outcome measurement. There is no obvious co-ordinated programmatic approach to the problem across different countries or even within specific countries. In consequence the heterogeneity noted above in many areas inhibits both robust MA and the clear application of findings to establishing improvements in clinical practice. Nevertheless a number of noteworthy trends are emerging, which are discussed below.
Summary of key findings
We deal first with aspects of the literature itself, then with the findings on effectiveness obtainable from the regression and MA of data extracted from it.
Characteristics of the overall literature
The descriptive analysis in the review provides a summary of the overall literature. Approximately 25–30 new studies are published each year and 70% of these are conducted in three countries (USA, UK and Canada). Inevitably, this restricts the generalisability of findings to less developed and/or non-English-speaking countries. The median length of follow-up is 6 months, with an average attrition rate of 10%. Given the intractability of the propensity to violence compared with more acute problems such as active psychosis and its lifelong nature for many people, this follow-up is not much more than a snapshot of the potential for change or otherwise. A third of the literature focuses on three diagnostic groups exclusively (schizophrenia, dementia and personality disorder). Half of the studies are conducted on males only, with < 10% conducted on female-only populations, and there is a disproportionate emphasis on non-Caucasian populations (i.e. half of the studies have samples in which the majority of participants are non-Caucasian). As, for instance, rates of violence by women with some types of mental health problem are not very different from those for similar men,120 this could be taken to suggest that there is an emphasis on certain groups in society that does not reflect the actual scale of the problem.
Methodologically speaking, it is clear that there are comparatively few RCTs in this research area (51/198, 26%: see Table 53). Compared with the number of trials in many other areas of health care, the proportion is very small. 121 The proportion is smaller still within the psychosocial intervention literature. Possible reasons for this are familiar from other research reviews and include the impracticality of achieving formal randomisation in service delivery settings, within interventions that entail individual contact or of using appropriate placebos, and the absence of means of checking against multiple treatment interference. On the other hand, it is worth noting that, across both literatures, non-RCTs had much longer follow-up periods than RCTs so that gains in causal inference from improved design quality in RCTs have to be weighed against losses in terms of tracking the persistence of an effect. Taken together, these issues reflect the complexity of the violence phenomenon and make it difficult to address the issue of effectiveness with any simplicity.
Within the located studies there are relatively few that focus on measured or recorded aggressive or violent behaviour as outcomes. The majority define outcome in non-behavioural terms, such as hostility or anger (e.g. the STAXI instrument), which can be detected only through self-report. Although these types of outcome measure obviously have value in some respects, they are only ever a proxy or risk factor for the main problem of actual aggressiveness as recorded, for example, on the basis of inpatient ward incident reports or of criminal reconvictions. Much of the literature can therefore provide evidence of effectiveness in terms of only a relatively subjective aspect of the problem.
Finally, a funnel plot of the data set, as a whole, is indicative of the possibility of there being some publication bias within the studies analysed. This is despite significant efforts having been undertaken to secure unpublished studies via extensive search for dissertations. Although this requires the exercise of caution when interpreting the findings, the number of studies conducted and the extent of the review team’s contact with other researchers active in the field, thus ensuring inclusion of a substantial number of unpublished studies, suggests that this bias does not distort the findings as much as in other reviews. It is important to note that the distribution observed here could result from systematic association between sample size and other study characteristics that impact on outcome and that the absence of funnel plot asymmetry does not rule out the possibility of publication bias anyway so the impact of funnel plots should not be exaggerated. Nevertheless, it must be acknowledged that the presence of such funnel asymmetry indicates that the MA results could well be overestimates of the effectiveness of interventions and that the literature is more suited to informing future research strategies than answering clinical questions at this stage.
Regression analysis of the overall literature: correlates of effectiveness
The regression analysis of all 198 studies (RCTs and non-RCTs) was aimed at establishing the design and population factors associated with a statistically significant effect (p < 0.05) in favour of the active intervention, and highlighted a number of issues of interest.
In terms of intervention types, ‘other’ interventions were less likely than psychological or pharmacological interventions to be associated with an effective outcome.
Two population variables showed a significant association with effectiveness. Offender-focused studies were significantly less likely to be effective, whereas mental health-focused studies were more likely to be effective. However, it is worth noting that analysis based on settings rather than populations showed that application in either mental health or offender settings was not relevant to outcome. This gives grounds for optimism with mentally ill samples whether they are located in general mental health or offender settings, but conversely highlights difficulties in implementing therapeutic interventions with offender populations wherever they are located. Furthermore, three design variables were associated with a reduced likelihood of demonstrated effectiveness: head-to-head comparisons, comparison against TAU, and between-groups comparisons.
Further (multivariate) analysis was then conducted to explore the extent of variation explained by outcomes in favour of the primary intervention arm. None of the selected factors had a significant relationship to effectiveness but, in population terms, the relative advantage noted above of studies focused on a mental illness sample over those focused on an offender sample was maintained. The relative disadvantage of ‘other’-type interventions was also maintained. Methodologically, only the use of a within-groups design approached significance in this analysis. Further analysis may help to identify if the lack of effect for evaluations of ‘other’ interventions and those conducted in penal institutions are due to design issues (e.g. insufficient power), implementation issues (e.g. lack of protocols) or the actual inapplicability of these approaches.
Meta-analysis
Heterogeneity became a particular problem when conducting the MA. This underpinned our decision to conduct the above preliminary regression analysis of variables associated with a significant outcome and, when considering the more stringent formal MA, indicates that great caution should be used when interpreting the results. Q-statistics for a series of comparisons in the MA, for instance, were as follows: for all pharmacological interventions comparing two active treatments Q = 111.21 (p < 0.0001), and for all psychological interventions, Q = 21.1 (p < 0.007). I2 estimates are similarly large and statistically significant. The exception to this is the comparison between SSRI antidepressants and placebo, for which across four studies Q was exceptionally low, at 4.38 (p = 0.22), suggesting relatively low heterogeneity in this particular set of comparisons. The relatively high heterogeneity overall is a function of the comprehensive scope of the review but does again indicate the absence of a programmatic approach to violence research in which there is consistency in outcome measurement. Also, with regard to non-pharmacological interventions, it indicates a failure to specify the treatment approaches adopted. Even ‘CBT interventions’, supposedly drawing on a consistent theoretical model, adopt a range of different techniques. Although this high degree of heterogeneity limits the conclusiveness of the overall review, the estimation of the size of heterogeneity is an important step in itself in bringing some order to the violence research field.
Notwithstanding the heterogeneity issue, across the data set as a whole there is evidence from the MA of a positive outcome of intervention, and this emerges from both fixed-effect and random-effects analyses of the results. Discussion of mean effects across this entire data set is not, however, likely to be especially informative, given (1) the variability of intervention methods (both with respect to different principal categories, e.g. pharmacological vs psychosocial) and the combinations within those categories and (2) the mixed range of outcome measures used. Comparisons between the same method applied to different populations, in different settings, or using different outcome measures is simply not possible. The exception to this is the set of seven studies of CBT84,86,102,110,111,198 (which are based on a common theoretical model and possess similar operational characteristics). Using Lipsey’s60 ‘rule of thumb’, which, in turn, drew on conventions proposed by Cohen,122 small-to-moderate effects (combined with relatively low heterogeneity) are found for CBT, for all psychological interventions combined and larger effects for atypical antipsychotic drugs. Caution must be exercised when interpreting all results, however, as 95% CIs are relatively wide and sometimes include zero, particularly in the random-effects models.
Analysis of the modifier variables provides some evidence that interventions targeted at mental health populations, and particularly male groups in community settings, are more likely to achieve stronger effects. In terms of future research design, high-quality features such as blinding and ITT analysis are likely to be associated with larger effects, which indicates the detection of a ‘true’ effect. However, the low-quality marker of baseline non-equivalence of comparison groups was also associated with such effects. It is nonetheless encouraging to note that in a review of cognitive behavioural programmes for offenders, examining criminal recidivism as the principal outcome variable, the mean OR effect size for studies with ‘best practice’ design features was considerably higher than that for the collection of studies overall. 123
Scale-based measurement was also associated with stronger effects but we have noted above that these provide only a proxy for actual aggression and thus interventions aimed at such behaviour should include observational measures as well, which may reduce the effect size estimate. It is of course legitimate to study such proxies as anger in their own right using validated scales, as they are likely to be predictive of subsequent violence.
There was evidence, although again not emerging in a clear or entirely consistent pattern, for larger effects to be found in community than in institutional settings, a finding obtained in a number of previous MAs in criminal justice. 123,124 Similarly, larger effects sizes were not from smaller samples, reinforcing the impression that emerges from large-scale dissemination exercises that effects are attenuated possibly because of compromises in integrity of treatment or service delivery. 125
The findings obtained from the present review tailor reasonably well with the trends noted in previous reviews summarised earlier (see Chapter 1, Other reviews), given that, being mainly sited in criminal justice settings, they also focused on aggression and violent behaviour (including sexual assault) rather than adopting a diagnostic approach. Thus, there is further support for the use of cognitive and behavioural interventions. The principal residual difficulty arises from the heterogeneity of specific methods used; thus, although theoretically grounded in the cognitive social learning model there is still insufficient evidence regarding any single treatment programme to identify a ‘treatment of choice’ or make firm selective recommendations. The evidence of effectiveness found here for some forms of pharmacotherapy does not fit well with the recommendations made by NICE against routine use of such treatments for aggression associated with antisocial or BPD, and could be an opportunity to reopen some aspects of this question. The effect observed in this review, for instance, could reflect the general tranquillising or suppressing effect on acting-out behaviour. It does support the conclusions to the Cochrane review52 with regard to the role of antipsychotic drugs with BPD symptoms associated with aggression (e.g. affective dysregulation) and some of the individual studies of neuroleptics cited by Herpertz et al. 53 Nevertheless, the latter review overall was, like NICE, inconclusive with regard to pharmacotherapy and aggression in antisocial personality disorder. On the other hand, the effectiveness of psychological interventions, including CBT, observed here for reducing aggression reinforces the recommendations made by NICE for the role of such interventions in the overall treatment of borderline and antisocial personality disorder.
Conclusions and implications for research
-
There is evidence that interventions targeted at mental health populations, and particularly male groups in community settings, are well supported, as they are more likely to achieve stronger effects than interventions with the other groups.
-
Improvements are needed in the design quality of future research studies. Of particular note is the paucity of RCTs in all areas, but especially in the evaluation of non-pharmacological interventions. Furthermore, RCTs themselves should be improved by extending the study follow-up period wherever possible so that it more closely matches that for non-RCTs. The quality and rigour of research in the field could be improved by more consistent attention to the protocols that have been published with respect to the reporting of both randomised and quasi-experimental designs [e.g. for RCTs, the Consolidated Standards of Reporting Trials (CONSORT) statement;126,127 for non-randomised designs, the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement128]. Researchers should identify a single primary outcome variable against which effectiveness is judged to avoid the impression of trawling for significant results across multiple outcome variables.
-
Any approach that could increase the homogeneity of research in this field will be welcomed. Greater homogeneity in study design, the interventions applied and outcome measures used would all be beneficial, especially if actual aggression or violence were to be adopted as an outcome rather than some proxy for these. With reference to outcome evaluation methods for example, a recent review has identified those measures that have the firmest evidence for these purposes in forensic mental health. 129 Were the best-validated measures to be more widely used, it would strengthen internal validity and also facilitate comparability across studies for review purposes.
-
Small-to-moderate effects are found for CBT and for all psychological interventions combined and larger effects for atypical antipsychotic drugs and this occurs in the context of relatively low heterogeneity.
-
A programme of research funded and co-ordinated at a national or international level should be developed as this would improve the capacity to conduct robust MAs and increase our confidence in their results. The review has revealed the extensive literature that exists, especially in the past few years, but coupled with relatively low design quality. Much of the research is conducted opportunistically by practitioners on the basis of what is possible within their clinical setting. Although this is laudable as a contribution to the principle of evidence-based practice, without adequate resources to improve study design, the cumulative evidence base will never produce knowledge that is generalisable beyond specific local settings.
-
Some treatment approaches are particularly lacking in evidence-based interventions, such as psychosocial treatments other than CBT. A greater focus on improving the quantity and quality of research here is likely to prove very beneficial.
-
Psychosocial and other non-pharmacological interventions should be defined more clearly so that the theoretical elements they are testing is made explicit. In this way, the key components that make up a broad intervention such as CBT will be identified and examined for effectiveness.
Acknowledgements
About the Assessment Group
The Assessment Group was based on a partnership between two research groups within the University of Liverpool.
The Liverpool Reviews and Implementation Group (LRiG) was established at The University of Liverpool in April 2001. It is a multidisciplinary research group whose purpose, in the first instance, is to conduct Health Technology Assessments (HTAs) commissioned by the HTA programme.
The LiVio is a multidisciplinary partnership of academics and clinicians with a commitment to both qualitative and quantitative research approaches and their application to problems of violence and self-harm linked to mental health issues in real-world settings. It has received funding from the Department of Health since 2002 to run both primary research studies in secondary mental health service settings and to conduct the preceding stage of this systematic review.
Administrative support
Ms Janet Atkinson, University of Liverpool’s Inter-Library Loan team and all members of the review team.
Advisory Panel members (provided feedback to the team during the review process)
-
Dr Joy Duxbury, Reader in Mental Health Nursing, Faculty of Health and Social Care, University of Central Lancashire.
-
Ms Kathryn Harney, Associate Director of Research, Greater Manchester West Mental Health Trust.
-
Ms Sue Imlack, patient representative.
-
Dr Caroline Logan, Consultant Forensic and Clinical Psychologist, Edenfield Centre.
-
Ms Ruth Sayers, patient representative.
-
Professor Jenny Shaw, Professor of Forensic Psychiatry, School of Medicine, University of Manchester.
Contributions of authors
Ms Juliet Hockenhull Review co-ordination, literature searches, data management, methods, and input into all aspects of review.
Professor Richard Whittington Project management and input into all aspects of the of the review.
Dr Maria Leitner Data analysis, advice and assistance in all aspects of review.
Dr Wally Barr Advice and assistance in all aspects of the review.
Professor James McGuire Advice and assistance in all aspects of the review.
Ms M Gemma Cherry Application of inclusion criteria, data extraction and input into all aspects of review.
Ms R Flentje Application of inclusion criteria and data extraction.
Ms B Quinn Application of inclusion criteria and data extraction.
Dr Yenal Dundar Literature searches.
Ms Rumona Dickson Advice and assistance in all aspects of the review.
All authors read and commented on draft versions of the Assessment Group report.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- World Health Organization . Violence and Injury Prevention and Disability 2009. www.who.int/violence_injury_prevention/violence/en/.
- Wright S, Gray R, Parkes J, Gournay K. The recognition, prevention and therapeutic management of violence in acute in-patient psychiatry: a literature review and evidence-based recommendations for good practice. London: United Kingdom Central Council for Nursing, Midwifery and Health Visiting; 2002.
- Jackson SL, Brownstein HH, Zahn MA, Brownstein HH, Jackson SL. Violence: from theory to research. Cincinnati, OH: LexisNexis/Anderson Publishing; 2004.
- Krug E, Dahlberg L, Mercy J, Zwi A, Lozano R. World Report on Violence and Health 2002.
- Walters R, Parke R, Berkowitz L. Advances in experimental social psychology. New York, NY: Academic Press; 1964.
- Mcguire J. A review of effective interventions for reducing aggression and violence. Phil Trans 2008;363:2577-97.
- Walker A, Flatley J, Kershaw C, Moon D. Crime in England and Wales 2008/09 volume 1: findings from the British crime survey and police recorded crime. London: Home Office; 2009.
- National Institute for Health and Clinical Excellence (NICE) . Clinical Practice Guidelines for the Violence: the Short Term Management of Disturbed Violent Behaviour in Psychiatric in-Patient Settings and Emergency Departments 2005.
- Home Office . National Domestic Violence Delivery Plan: Annual Progress Report 2008–09 2009.
- Healthcare Commission . National NHS Staff Survey 2008: Summary of Key Findings 2009.
- National Institute for Health and Clinical Excellence (NICE) . Violence: The Short-Term Management of Disturbed Violent Behaviour in in-Patient Psychiatric Settings and Emergency Departments 2005.
- Del Frate AA. The voice of victims of crime: estimating the true level of conventional crime. Forum Crime Soc 2003;3:127-40.
- Van Kesteren JN, Mayhew P, Nieuwbeerta P. Criminal victimisation in seventeen industrialised countries: key findings from the 2000 International Crime Victims Survey. The Hague, The Netherlands: Ministry of Justice, WODC; 2000.
- Taylor PJ, Gunn J. Homicides by people with mental illness: myth and reality. Br J Psychiatry 1999;174:9-14.
- Windfuhr K, Swinson N, Whittington R, Logan C. Self-harm and violence: towards best practice in managing risk in mental health services. Chichester: Wiley; 2011.
- Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PLoS Med 2009;6.
- Douglas KS, Guy LS, Hart SD. Psychosis as a risk factor for violence to others: a meta-analysis. Psychol Bull 2009;135:679-706.
- Hodgins S. Violence and the mentally ill. Effective treatments and management strategies. Dordrecht: Kluwer Academic Publishers; 2000.
- Hollin C. The essential handbook of offender assessment and treatment. London: Wiley-Blackwell; 2003.
- Whittington R, McGuire J, Steinert T, Quinn B, Whittington R, Logan C. Self-harm and violence: towards best practice in managing risk. Oxford: Wiley-Blackwell; 2011.
- Goedhard LE, Stolker JJ, Heerdink ER, Nijman HLI, Olivier B, Egberts TCG. Pharmacotherapy for the treatment of aggressive behaviour in general adult psychiatry: a systematic review. J Clin Psychiatr 2006;67:1013-24.
- Goldstein AP, Nensen R, Dalefold B, Kalt M. New perspectives on aggression replacement therapy. Practice, research and application. Chichester: Wiley; 2004.
- Naeem F, Clarke I, Kingdon D. A randomized controlled trial to assess an anger management group programme. Cogn Behav Therapist 2009;2:20-31.
- Doctor R, Nettleton S. Dangerous patients: a psychodynamic approach to risk assessment and management. London: Karnac Books; 2003.
- Legget K, Hirons B, Parker MA, Gunn J. Dynamic security: the democratic therapeutic community in prison. London: Jessica Kingsley; 2007.
- Jonikas JA, Cook JA, Rosen C, Laris A, Kim JB. A program to reduce use of physical restraint in psychiatric inpatient facilities. Psychiatr Serv 2004;55:818-20.
- Vaaler AE, Morken G, Linaker OM. Effects of different interior decorations in the seclusion area of a psychiatric acute ward. Nordic J Psychiatr 2005;59:19-24.
- Gaskin C, Elsom S, Happell B. Interventions for reducing the use of seclusion in psychiatric facilities: review of the literature. Br J Psychiatr 2007;191:298-303.
- Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455-9.
- Priebe S, Badesconyi A, Fioritti A, Hansson L, Kilian R, Torres-Gonzales F, et al. Reinstitutionalisation in mental health care: comparison of data on service provision from six European countries. BMJ 2005;330:123-6.
- Department of Health . Public Health White Paper. Reforming the Mental Health Act. Part III: High Risk Patients 2000.
- Cure S, Chua W, Duggan L, Adams C. Randomised controlled trials relevant to aggressive and violent people, 1955–2000: a survey. Br J Psychiatr 2005;186:185-9.
- Bhana N, Foster R, Olney R, Plosker G. Olanzapine: an updated review of its use in the management of schizophrenia. Drugs 2001;61:111-61.
- Hollin C. Evaluating offending behaviour programmes. Criminol Crim Justice 2008;8:89-106.
- McGuire J. A review of effective interventions for reducing aggression and violence. Phil Trans R Soc B 2008:363-97.
- McGuire J, Hodgins S, Viding E, Plodowski A. The neurobiological basis of violence: science and rehabilitation. Oxford: Oxford University Press; 2009.
- Lipsey MW, Wilson DB, Loeber R, Farrington DP. Serious & violent juvenile offenders: risk factors and successful interventions. Thousand Oaks, CA: Sage Publications; 1998.
- Garrido V, Morales LA. Serious (violent and chronic) juvenile offenders: a systematic review of treatment effectiveness in secure corrections. Philadelphia, PA: The Campbell Collaboration Reviews of Intervention and Policy Evaluations (C2-RIPE); 2007.
- Wilson SJ, Lipsey MW, Derzon JH. The effects of school-based intervention programs on aggressive behaviour: a meta-analysis. J Consult Clin Psychol 2003 n.d.;71:136-49.
- McCart MR, Priester PE, Davies WH, Azen R. Differential effectiveness of behavioural parent-training and cognitive-behavioral therapy for antisocial youth: a meta-analysis. J Abnorm Child Psychol 2006 n.d.;34:527-43.
- Alexander MA. Sexual offender treatment efficacy revisited. J Child Sex Abuse 1999;11:101-16.
- Gallagher CA, Wilson DB, Hirschfield P, Coggeshall MB, MacKenzie DL. A quantitative review of the effects of sexual offender treatment on sexual reoffending. Correct Manag Q 1999;3:19-2.
- Hall GCN. Sexual offender recidivism revisited: a meta-analysis of recent treatment studies. J Consult Clin Psychol 1995;63:802-9.
- Hanson RK, Gordon A, Harris AJR, Marques JK, Murphy W, Quinsey VL, et al. First report of the Collaborative Outcome Data Project on the effectiveness of psychological treatment for sex offenders. Sex Abuse J Res Treat 2002;14:169-94.
- Kenworthy T, Adams C, Bilby C, Brooks-Gordon B, Fenton M. Psychological interventions for those who have sexually offended or at risk of offending. Cochrane Database Syst Rev 2004;3.
- Lösel F, Schmucker M. The effectiveness of treatment for sexual offenders: a comprehensive meta-analysis. J Exp Criminol 2005;1:117-46.
- Polizzi DM, MacKenzie DL, Hickman LJ. What works in adult sex offender treatment? A review of prison- and non-prison-based treatment programs. Int J Offender Ther Comp Criminol 1999;43:357-74.
- Babcock JC, Green CE, Robie C. Does batterers’ treatment work? A meta-analytic review of domestic violence treatment. Clin Psychol Rev 2004;23:1023-53.
- Dowden C, Andrews DA. Effective correctional treatment and violent reoffending: a meta-analysis. Can J Criminol Crim Justice 2000;42:449-67.
- Salekin RT. Psychopathy and therapeutic pessimism: clinical lore or clinical reality?. Clin Psychol Rev 2002;22:79-112.
- Tanasichuk CL, Wormith JS. Does Treatment Makes Psychopaths Worse? A Meta-Analytic Review n.d.
- Lieb K, Vollm B, Rucker G, Timmer A, Stoffers JM. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatr 2010;196:4-12.
- Herpertz S, Zanarini M, Schulz SZ, Siever L, Lieb K, Moller H, et al. World Federation of Societies of Biol Psychiatr (WFSBP) guidelines for biological treatment of personality disorders. World J Biol Psychiatr 2007;8:212-44.
- Andrews DA, Bonta J, Wormith SJ. The recent past and near future of risk and/or need assessment. Crime Delinquen 2006;52:7-27.
- Leitner M, Barr W. Systematic Review of Prevention Strategies for the Forensic Mental Health Population at High Risk of Engaging in Violent Behaviour. Final Report to National Forensic Mental Health R&Amp;D Programme 2006.
- Lipsey MW, Cullen FT. The effectiveness of correctional rehabilitation: a review of systematic reviews. Ann Rev Law Soc Sci 2007 n.d.;3:297-320.
- Department of Health (DoH) . Best Practice in Managing Risk: Principles and Evidence for Best Practice in the Assessment and Management of Risk to Self and Others in Mental Health Services 2007.
- Leitner M. An Evaluation of Six Risk Assessment Tools. Report to the Department of Health National Risk Management Programme 2006.
- Pedersen L, Rasmussen K, Elass P. Risk assessment: the value of structured professional judgments. Int J Forensic Ment Health 2010;9:74-81.
- Lipsey MW, Wilson DB. Practical meta-analysis. Thousand Oaks, CA: Sage Publications; 2001.
- Elvik R. Evaluating the statistical conclusion validity of weighted mean results in meta-analysis by analysing funnel graph diagrams. Accid Anal Prev 1998;30:255-66.
- Estelle LM. Assessment of child abuse potential in spouse abusive men. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2002.
- Huss MT, Ralston A. Do batterer subtypes actually matter? Treatment completion, treatment response, and recidivism across a batterer typology. Crim Justice Behav 2008;35:710-24.
- Jones AS, D’Agostino RB, Gondolf EW, Heckert A. Assessing the effect of batterer program completion on reassault using propensity scores. J Interpers Violence 2004;19:1002-20.
- Murphy CM, Taft CT, Eckhardt CI. Anger problem profiles among partner violent men: differences in clinical presentation and treatment outcome. J Counsel Psychol 2007;54:189-200.
- Schweitzer R, Dwyer J. Sex crime recidivism: evaluation of a sexual offender treatment program. J Interpers Violence 1292;18:1292-310.
- Williamson P, Day A, Howells K, Bubner S, Jauncey S. Assessing offender readiness to change problems with anger. Psychol Crime Law 2003;9:295-307.
- Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: a multiwave study. Am J Psychiatry 2007;164:922-8.
- Galovski TE, Blanchard EB. The effectiveness of a brief psychological intervention on court-referred and self-referred aggressive drivers. Behav Res Ther 2002;40:1385-402.
- Houston RJ, Stanford MS. Characterization of aggresive behaviour and phenytoin response. Aggress Behav 2006;32:38-43.
- Theall KP, Elifson KW, Sterk CE, Stewart EA. Criminality among female drug users following an HIV risk-reduction intervention. J Interpers Violence 2007;22:85-107.
- Huf G. Rapid tranquillisation for agitated patients in emergency psychiatric rooms: a randomised trial of midazolam versus haloperidol plus promethazine. BMJ 2003;327:708-13.
- Huf G, Coutinho ESF, Adams CE, Group TC. Rapid tranquillisation in psychiatric emergency settings in Brazil: pragmatic randomised controlled trial of intramuscular haloperidol versus intramuscular haloperidol plus promethazine. BMJ 2007;335.
- Marques JK, Wiederanders M, Day DM, Nelson C, Van Ommeren A. Effects of a relapse prevention program on sexual recidivism: final results from California’s Sex Offender Treatment and Evaluation Project (SOTEP). J Child Sex Abuse 2005;17:79-107.
- Raveendran NS, Tharyan P, Alexander J, Adams CE. Rapid tranquillisation in psychiatric emergency settings in India: PRAGMATIC randomised controlled trial of intramuscular olanzapine versus intramuscular haloperidol plus promethazine. BMJ 2007;335.
- Villari V, Rocca P, Fonzo V, Montemagni C, Pandullo P, Bogetto F. Oral risperidone, olanzapine and quetiapine versus haloperidol in psychotic agitation. Progr Neuro Psychopharmacol Biol Psychiatr 2008;32:405-13.
- Mitchell O, MacKenzie DL. The stability and resiliency of self-control in a sample of incarcerated offenders. Crime Delinquen 2006;52:432-49.
- Rempel M, Labriola M, Davis RC. Does judicial monitoring deter domestic violence recidivism? Results of a quasi-experimental comparison in the Bronx. Violence Against Women 2008;14:185-207.
- Berry S. Stopping violent offending in New Zealand: is treatment an option?. NZ J Psychol 2003;32:92-100.
- Timmer SG, Urquiza AJ, Zebell NM, McGrath JM. Parent-child interaction therapy: application to maltreating parent-child dyads. Child Abuse Neglect 2005;29:825-42.
- Cavanaugh MM. An exploration of the feasibility and utility of the Dialectical Psychoeducational Workshop (DPEW) as a preventative intervention for males at potential risk of intimate partner violence. Dissertation Abstracts International Section A: Humanities and Social Sciences; 2007.
- Krakowski MI, Czobor P, Citrome L, Bark N, Cooper TB. Atypical antipsychotic agents in the treatment of violent patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatr 2006;63:622-9.
- Lasley J. The effect of intensive bail supervision on repeat domestic violence offenders. Pol Stud J 2003;31:187-20.
- Willner P, Jones J, Tams R, Green G. A randomized controlled trial of the efficacy of a cognitive-behavioural anger management group for clients with learning disabilities. J Appl Res Intellect Disabil 2002;15:224-35.
- Monnelly EP, Ciraulo DA, Knapp C, Keane T, Monnelly EP, Ciraulo DA, et al. Low-dose risperidone as adjunctive therapy for irritable aggression in posttraumatic stress disorder. J Clin Psychopharmacol 2003;23:193-6.
- Lanza ML, Anderson J, Boisvert CM, Leblanc A, Fardy M, Steel B. Assaultive behavior intervention in the veterans administration: psychodynamic group psychotherapy compared to cognitive behavioural therapy. Perspect Psychiatr Care 2002;38:89-97.
- Volavka J, Czobor P, Nolan K, Sheitman B, Lindenmayer JP, Citrome L, et al. Overt aggression and psychotic symptoms in patients with schizophrenia treated with clozapine, olanzapine, risperidone, or haloperidol. J Clin Psychopharmacol 2004;24:225-8.
- Nickel MK, Nickel C, Kaplan P, Lahmann C, Muhlbacher M, Tritt K, et al. Treatment of aggression with topiramate in male borderline patients: a double-blind, placebo-controlled study. Biol Psychiatr 2005;57:495-9.
- Brown University Psychopharmacology Update . Aripiprazole for treating borderline personality disorder. Brown Univ Psychopharmacol Update 2006;17:5-6.
- Cooper C, Eslinger DM, Stolley PD. Hospital-based violence intervention programs work. J Trauma 2006;61:534-40.
- Hollander E, Tracy KA, Swann AC, Coccaro EF, McElroy SL, Wozniak P, et al. Divalproex in the treatment of impulsive aggression: efficacy in cluster B personality disorders. Neuropsychopharmacology 2003;28:1186-97.
- Gottfredson DC, Exum ML. The Baltimore City Drug Treatment Court: one year results from a randomized study. J Res Crime Delinquen 2002;39:337-56.
- Walsh E, Leese M, Byford S, Gilvarry C, Samele C, Tyrer P, et al. Do violent patients benefit from intensive case management?. Schizophr Res 2002;53.
- Labriola M, Rempel M, Davis RC. Do batterer programs reduce recidivism? Results from a randomized trial in the Bronx. JQ 2008;25:252-82.
- MacKenzie DL, Bierie D, Mitchell O. An experimental study of a therapeutic boot camp: Impact on impulses, attitudes and recidivism. J Exp Criminol 2007;3:221-46.
- Mattes JA, Mattes JA. Oxcarbazepine in patients with impulsive aggression: a double-blind, placebo-controlled trial. J Clin Psychopharmacol 2005;25:575-9.
- New AS, Buchsbaum MS, Hazlett EA, Goodman M, Koenigsberg HW, Lo J, et al. Fluoxetine increases relative metabolic rate in prefrontal cortex in impulsive aggression. Psychopharmacology 2004;176:451-8.
- Chan KL, Campayo A, Moser DJ, Arndt S, Robinson RG. Aggressive behaviour in patients with stroke: association with psychopathology and results of antidepressant treatment on aggression. Arch Phys Med Rehabil 2006;87:793-8.
- Rinne T, Van Den Brink W, Wouters L, Van Dyck R, Rinne T, Van Den Brink W, et al. SSRI treatment of borderline personality disorder: a randomized, placebo-controlled clinical trial for female patients with borderline personality disorder. Am J Psychiatry 2002;159:2048-54.
- Zanarini MC, Frankenburg FR, Parachini EA, Zanarini MC, Frankenburg FR, Parachini EA. A preliminary, randomized trial of fluoxetine, olanzapine, and the olanzapine-fluoxetine combination in women with borderline personality disorder. J Clin Psychiatr 2004;65:903-7.
- Suh G-H, Son HG, Ju Y-S, Jcho KH, Yeon BK, Shin YM, et al. A randomized, double-blind, crossover comparison of risperidone and haloperidol in Korean dementia patients with behavioral disturbances. Am J Geriatr Psychol 2004;12:509-16.
- Vannoy SD. Evaluating the impact of a meditation curriculum on anger, hostility, and egoism with incarcerated adults. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2006.
- Tritt K, Nickel C, Lahmann C, Leiberich PK, Rother WK, Loew TH, et al. Lamotrigine treatment of aggression in female borderline-patients: a randomized, double-blind, placebo-controlled study. J Psychopharmacol 2005;19:287-91.
- Nickel MK, Nickel C, Mitterlehner FO, Tritt K, Lahmann C, Leiberich PK, et al. Topiramate treatment of aggression in female borderline personality disorder patients: a double-blind, placebo-controlled study. J Clin Psychiatr 2004;65:1515-19.
- Nickel C, Lahmann C, Tritt K, Muehlbacher M, Kaplan P, Kettler C, et al. Topiramate in treatment of depressive and anger symptoms in female depressive patients: a randomized, double-blind, placebo-controlled study. J Affect Disord 2005;87:243-52.
- Frankenburg FR, Zanarini MC. Divalproex sodium treatment of women with borderline personality disorder and bipolar II disorder: a double-blind placebo-controlled pilot study. J Clin Psychiatr 2002;63:442-6.
- Citrome L, Casey D, Daniel D, Wozniak P, Kochan L, Tracy K. Adjunctive divalproex and hostility among patients with schizophrenia receiving olanzapine or risperidone. Psychiatr Serv 2004;55:290-4.
- Tyrer P, Oliver-Africano PC, Ahmed Z, Bouras N, Cooray S, Deb S, et al. Risperidone, haloperidol, and placebo in the treatment of aggressive challenging behaviour in patients with intellectual disability: a randomised controlled trial. Lancet 2008;371:57-63.
- Meehan KM, Wang H, David SR, Nisivoccia JR, Jones B, Beasley CM, et al. Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: a double blind, randomised study in acutely agitated patients with dementia. Neuropsychopharmacology 2002;26:494-50.
- Easton CJ. Treatment Outcome Among Substance-Dependent Offenders of Intimate Partner Violence: A Randomized Clinical Trial n.d.
- Easton CJ, Mandel DL, Hunkele KA, Nich C, Rounsaville BJ, Carroll KM. A cognitive behavioral therapy for alcohol-dependent domestic violence offenders: an integrated Substance Abuse-Domestic Violence Treatment Approach (SADV). Am J Addict 2007;16:24-31.
- Alexander J, Tharyan P, Adams C, John T, Mol C, Philip J. Rapid tranquillization of violent or agitated patients in a psychiatric emergency setting: pragmatic randomised trial of intramuscular lorazepam v. haloperidol plus promethazine. Br J Psychiatr 2004;185:63-9.
- Arango C, Bombin I, Gonzalez-Salvador T, Garcia-Cabeza I, Bobes J. Randomised clinical trial comparing oral versus depot formulations of zuclopenthixol in patients with schizophrenia and previous violence. Eur Psychiatr 2006;21:34-40.
- Duggan A, Caldera D, Rodriguez K, Burrell L, Rohde C, Crowne SS. Impact of a statewide home visiting program to prevent child abuse. Child Abuse Neglect 2007;31:801-27.
- Liau AK, Shively R, Horn M, Landau J, Barriga A, Gibbs JC. Effects of psychoeducation for offenders in a community correctional facility. J Community Psychol 2004;32:543-58.
- Linehan MM, McDavid JD, Brown MZ, Sayrs JHR, Gallop RJ. Olanzapine plus dialectical behaviour therapy for women with high irritability who meet criteria for borderline personality disorder: a double-blind, placebo-controlled pilot study. J Clin Psychiatr 2008;69:999-1005.
- Loew TH, Nickel MK, Muehlbacher M, Kaplan P, Nickel C, Kettler C, et al. Topiramate treatment for women with borderline personality disorder: a double-blind, placebo-controlled study. J Clin Psychopharmacol 2006;26:61-6.
- Soler J, Pascual JC, Campins J, Barrachina J, Puigdemont D, Alvarez E, et al. Double-blind, placebo-controlled study of behavioural therapy olanzapine for borderline personality disorder. Am J Psychiatry 2005;162:1221-4.
- Zanarini MC, Frankenburg FR, Zanarini MC, Frankenburg FR. Omega-3 fatty acid treatment of women with borderline personality disorder: a double-blind, placebo-controlled pilot study. Am J Psychiatry 2003;160:167-9.
- Brunette M, Drake R. Gender differences in patients with schizophrenia and substance abuse. Compr Psychiatr 1997;38:109-16.
- Lambert MJ, Ogles BM, Lambert MJ. Bergin and Garfield’s handbook of psychotherapy and behavior change. New York, NY: Wiley; 2004.
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
- Lipsey MW, Landenberger NA, Wilson SJ. Effects of cognitive-behavioral programs for criminal offenders. Philadelphia, PA; 2007.
- Redondo S, Sanchez-Meca J, Garrido V. The influence of treatment programmes on the recidivism of juvenile and adult offenders: an European meta-analytic review. Psychol Crime Law 1999;5:251-2.
- Raynor P, Bottoms A, Rex S, Robinson G. Alternatives to prison. Cullompton: Willan; 2004.
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Med Res Meth 2001;1.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLOS Med 2010;7.
- Des Jarlais DC, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health 2004;94:361-6.
- Yiend J, Chambers JC, Burns T, Doll H, Fazel S, Kaur A, et al. Outcome measurement in forensic mental health research: an evaluation. Psychol Crime Law 2011;17:277-92.
- Afaq I, Riaz J, Sedky K, Chung DJ, Vanina Y, El-Mallakh R, et al. Divalproex as a calmative adjunct for aggressive schizophrenic patients. J KY Med Assoc 2002;100:17-22.
- Barnes AD. The Role of Male-Male Relationships in Partner Violence Treatment Groups: The Effects of Improving Same-Sex Relationships on Attachment 2007.
- Belaga I. Domestic violence: typology of batterers and effectiveness of treatment. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005.
- Belfrage H, Fransson G, Strand S. Management of violent behaviour in the correctional system using qualified risk assessments. Leg Criminol Psychol 2004;9:11-22.
- Bennett LW, Stoops C, Call C, Flett H. Program completion and re-arrest in a batterer intervention system. Res Soc Work Pract 2007;17:42-54.
- Bitter I, Czobor P, Dossenbach M, Volavka J. Effectiveness of clozapine, olanzapine, quetiapine, risperidone, and haloperidol monotherapy in reducing hostile and Aggress Behav in outpatients treated for schizophrenia: a prospective naturalistic study (IC-SOHO). Eur Psychiatr 2005;20:403-8.
- Booth BD, Fedoroff JP, Curry SD, Douglass AB. Sleep apnea as a possible factor contributing to aggression in sex offenders. J Forensic Sci 2006;51:1178-81.
- Bowen E, Gilchrist EA, Beech AR. An examination of the impact of community-based rehabilitation on the offending behaviour of male domestic violence offenders and the characteristics associated with recidivism. Leg Criminol Psychol 2005;10:189-20.
- Bradbury KE, Clarke I. Cognitive behavioural therapy for anger management: effectiveness in adult mental health services. Behav Cognit Psychother 2007;35:201-8.
- Brodaty H, Ames D, Snowdon J, Woodward M, Kirwan J, Clarnette R, et al. A randomized placebo-controlled trial of risperidone for the treatment of aggression, agitation and psychosis of dementia. J Clin Psychiatr 2003;64:134-43.
- Broner N, Mayrl DW, Landsberg G. Outcomes of mandated and nonmandated New York City jail diversion for offenders with alcohol, drug, and mental disorders. Prison Journal 2005;85:18-49.
- Burke HC. Psychopathy and treatment outcome in incarcerated violent offender program participants. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2004.
- Burns M, Bird D, Leach C, Higgins K. Anger management training: the effects of a structured programme on the self-reported anger experience of forensic inpatients with learning disability. J Psychiatr Ment Health Nurs 2003;10:569-77.
- Buttell FP, Pike CK. Investigating the differential effectiveness of a batterer treatment program on outcomes for African American and Caucasian batterers. Res Soc Work Pract 2003;13:675-92.
- Buttell FP, Carney MM. A multidimensional assessment of a batterer treatment program: an alert to a problem?. Res Soc Work Pract 2004;14:93-101.
- Buttell FP, Carney MM. Do batterer intervention programs serve African American and Caucasian batterers equally well? An investigation of a 26-week program. Res Soc Work Pract 2005;15:19-28.
- Buttell FP, Carney MM. A large sample evaluation of a court-mandated batterer intervention program: investigating differential program effect for African American and Caucasian men. Res Soc Work Pract 2006;16:121-31.
- Carney MM, Buttell FP. An evaluation of a court-mandated batterer intervention program: investigating differential program effect for African American and white women. Res Soc Work Pract 2006;16:571-81.
- Carney MM, Buttell FP. A multidimensional evaluation of a treatment program for female batterers: a pilot study. Res Soc Work Pract 2004;14:249-58.
- Chan H-Y, Lu R-B, Tseng C-L, Chous K-R. Effectiveness of the anger-control program in reducing anger expression in patients with schizophrenia. Arch Psychiatr Nurs 2003;17:88-95.
- Chan KL. Group therapy for male batterers: a Chinese experience. Social Work With Groups 2003;26:79-90.
- Childs A, Price L. Cranial electrotherapy stimulation reduces aggression in violent neuropsychiatric patients. Prim Psychiatr 2007;14:50-6.
- Choi Y-J, Lee K-J. Evidence-based nursing: effects of a structured nursing program for the health promotion of Korean women with Hwa-Byung. Arch Psychiatr Nurs 2007;21:12-6.
- Cohen-Mansfield J, Parpura-Gill A. Bathing: a framework for intervention focusing on psychosocial, architectural and human factors considerations. Arch Gerontol Geriatr 2007;45:121-35.
- Combs DR, Adams SD, Penn DL, Roberts D, Tiegreen J, Stem P. Social Cognition and Interaction Training (SCIT) for inpatients with schizophrenia spectrum disorders: preliminary findings. Schizophr Res 2007;91:112-16.
- Craissati J, Falla S, McClurg G, Beech A. Risk, reconviction rates and pro-offending attitudes for child molesters in a complete geographical area of London. J Sex Aggress 2002;8:22-38.
- Davis MA. Effects treatment length has on recidivism of domestic violence perpetrators. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2002.
- Dietz EF, O’Connell DJ, Scarpitti FR. Therapeutic communities and prison management: an examination of the effects of operating an in-prison therapeutic community on levels of institutional disorder. Int J Offender Ther Comp Criminol 2003;47:210-23.
- Easton CJ, Mandel D, Babuscio T, Rounsaville BJ, Carroll KM. Differences in treatment outcome between male alcohol dependent offenders of domestic violence with and without positive drug screens. Addict Behav 2007;32:2151-63.
- Echeburua E, Fernandez-Montalvo J, Amor PJ. Psychological treatment of men convicted of gender violence: a pilot study in Spanish prisons. Int J Offender Ther Comp Criminol 2006;50:57-70.
- Erickson SK. Outpatient commitment in New York: examining violence, compliance and demographic characteristics of the seriously mentally ill under Kendra’s Law. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2004.
- Evershed S, Tennant A, Boomer D, Rees A, Barkham M, Watson A. Practice-based outcomes of dialectical behaviour therapy (DBT) targeting anger and violence, with male forensic patients: a pragmatic and non-contemporaneous comparison. Crim Behav Mental Health 2003;13:198-213.
- Feder L, Dugan L. A test of the efficacy of court-mandated counselling for domestic violence offenders: the Broward Experiment. JQ 2002;19:343-75.
- Fhager B, Meiri IM, Sjogren M, Edman A. Treatment of aggressive behaviour in dementia with the anticonvulsant topiramate: a retrospective pilot study. Int Psychogeriatr 2003;15:307-9.
- Forbes D, Hawthorne G, Elliott P, McHugh T, Biddle D, Creamer M, et al. A concise measure of anger in combat-related posttraumatic stress disorder. J Trauma Stress 2004;17:249-56.
- Friendship C, Mann RE, Beech AR. Evaluation of a national prison-based treatment program for sexual offenders in England and Wales. J Interpers Violence 2003;18:744-59.
- Gelkopf M, Gonen B, Kurs R, Melamed Y, Bleich A. The effect of humorous movies on inpatients with chronic schizophrenia. J Nerv Ment Dis 2006;194:880-3.
- Gerra G, Di Petta G, D’Amore A, Iannotta P, Bardicchia F, Falorni F, et al. Effects of olanzapine on aggressiveness in heroin dependent patients. Progr Neuro Psychopharmacol Biol Psychiatr 2006;30:1291-8.
- Gershater-Molko RM, Lutzker JR, Wesch D. Using recidivism data to evaluate Project Safecare: teaching bonding, safety, and health care skills to parents. Child Maltreat 2002;7:277-85.
- Gondolf E. Outcomes of case management for African-American men in batterer counseling. J Fam Violence 2008;23:173-81.
- Gordon JA, Moriarty LJ. The effects of domestic violence batterer treatment on domestic violence recidivism: the Chesterfield County experience. Crim Justice Behav 2003;30:118-34.
- Gossop M, Trakada K, Stewart D, Witton J. Reductions in criminal convictions after addiction treatment: 5-year follow-up. Drug Alcohol Depend 2005;79:295-302.
- Gregory CR. Assessing amenability to treatment in community corrections: creating a valid and reliable instrument for male batterers. Dissertation Abstracts International Section A: Humanities and Social Sciences; 2004.
- Grubin D, Madsen L, Parsons S, Sosnowski D, Warberg B. A prospective study of the impact of polygraphy on high-risk behaviors in adult sex offenders. Sex Abuse J Res Treat 2004;16:209-22.
- Hanson RK, Bloom I, Stephenson M. Evaluating community sex offender treatment programs: a 12-year follow-up of 724 offenders. Can Behav J Sci 2004;36:87-96.
- Harkins L, Beech AR. Examining the impact of mixing child molesters and rapists in group-based cognitive-behavioral treatment for sexual offenders. Int J Offender Ther Comp Criminol 2008;52:31-45.
- Henderson CE. A study of competing treatment models for the dually diagnosed: chemical dependency programs versus mental health. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2007.
- Hendricks B, Werner T, Shipway L, Turinetti GJ. Recidivism among spousal abusers: predictions and program evaluation. J Interpers Violence 2006;21:703-16.
- Hensley C, Koscheski M, Tweksbury R. Does participation in conjugal visitations reduce prison violence in Mississippi? An exploratory study. Crim Justice Rev 2002;27:52-65.
- Hilton NZ, Harris GT, Rice ME. The effect of arrest on wife assault recidivism: controlling for pre-arrest risk. Crim Justice Behav 2007;34:1334-44.
- Hornsveld RHJ, Nijman HLI, Kraaimaat FW. Aggression control therapy for violent forensic psychiatric patients: first results. Psychol Crime Law 2008;14:1-18.
- Hornsveld RHJ. Evaluation of aggression control therapy for violent forensic psychiatric patients. Psychol Crime Law 2005;11:403-10.
- Hough WG, O’Brien KP. The effect of community treatment orders on offending rates. Psychiatr Psychol Law 2005;12:411-23.
- Howells K, Day A, Williamson P, Bubner S, Jauncey S, Parker A, et al. Brief anger management programs with offenders: outcomes and predictors of change. J Forensic Psychiatr Psychol 2005;16:296-311.
- Ireland JL. Anger management therapy with young male offenders: an evaluation of treatment outcome. Aggress Behav 2004;30:174-85.
- Janowsky DS, Shetty M, Barnhill J, Elamir B, Davis JM. Serotonergic antidepressant effects on aggressive, self-injurious and destructive/disruptive behaviours in intellectually disabled adults: a retrospective, open-label, naturalistic trial. Int J Neuropsychopharmacol 2005;8:37-48.
- Johansen TM. Predicting treatment outcomes of an anger management treatment program using the stages of change model. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2006.
- Johnson DR, Fontana A, Lubin H, Corn B, Rosenheck R. Long-term course of treatment-seeking Vietnam veterans with posttraumatic stress disorder: mortality, clinical condition, and life satisfaction. J Nerv Ment Dis 2004;192:35-41.
- Johnson S. Male domestic violence treatment programs: effect on attitudes towards women and intimate relationships. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2007.
- Keeling JA, Rose JL, Beech AR. An investigation into the effectiveness of a custody-based cognitive-behavioural treatment for special needs sexual offenders. J Forensic Psychiatr Psychol 2006;17:372-92.
- Keeling JA, Rose JL, Beech AR. Comparing sexual offender treatment efficacy: mainstream sexual offenders and sexual offenders with special needs. J Intellect Dev Disabil 2007;32:117-24.
- Kerne PA. Domestic violence group counseling impact on abusiveness potential and conflict resolution styles. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2007.
- Kunselman JC, Vito GF. Questioning mandatory sentencing efficiency: a case study of persistent felony offender rapists in Kentucky. Am J Crim Justice 2002;27:53-68.
- Labinsky EB. Evaluating a group treatment program for male batterers. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2002.
- Labriola M, Rempel M, Davis RC. Testing the effectiveness of batterer programs and judicial monitoring: results from a randomized trial at the Misdemeanor Domestic Violence Court. New York, NY: National Institute of Justice of the US Department of Justice; 2005.
- Lauretti JM. A study of the therapeutic working alliance, client motivation for therapy and subsequent self-reported changes in abusive behavior among a sample of male batterers from the abuse ceases today program. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2003.
- Lavey R, Sherman T, Mueser KT, Osborne DD, Currier M, Wolfe R. The effects of yoga on mood in psychiatric inpatients. Psychiatr Rehabil J 2005;28:399-402.
- Lawson DM, Barnes AD, Madkins JP, Francois-Lamonte BM. Changes in male partner abuser attachment styles in group treatment. Psychother Theor Res Pract Train 2006;43:232-7.
- Lawson WB, Nanos J. Effects of divalproex on disruptive behavior of jail inmates. Progr Neuro Psychopharmacol Biol Psychiatr 2008;32:909-10.
- Lee MY, Uken A, Sebold J. Accountability for change: solution-focused treatment with domestic violence offenders. Families in Society 2004;85:463-76.
- Levesque D, Driskell M, Castle P, Greene N, Prochaska J, Prochaska J. Efficacy of a Computerized Stage-Matched Intervention for Domestic Violence Offenders: Preliminary Findings n.d.
- Lewis K. The relationship between the URICA and correctional treatment in a sample of violent male offenders. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2004.
- Ley LF. A study of domestic violence recidivism following treatment among incarcerated men who batter. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2006.
- Lindsay WR, Allan R, Parry C, MacLeod F, Cottrell J, Overend H, et al. Anger and aggression in people with intellectual disabilities: treatment and follow-up of consecutive referrals and a waiting list comparison. Clin Psychol Psychother 2004;11:255-64.
- MacVaugh GS. Outcomes of court intervention and diversionary programs for domestically violent offenders. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005.
- Mammen OK, Pilkonis PA, Chengappa KNR, Kupfer DJ. Anger attacks in bipolar depression: predictors and response to citalopram added to mood stabilizers. J Clin Psychiatr 2004;65:627-33.
- McCue RE, Urcuyo L, Lilu Y, Tobias T, Chambers MJ. Reducing restraint use in a public psychiatric inpatient service. J Behav Health Serv Res 2004;31:217-24.
- McGrath RJ, Cumming G, Livingston JA, Hoke SE. Outcome of a treatment program for adult sex offenders: from prison to community. J Interpers Violence 2003;18:3-17.
- McGrath RJ, Cumming GF, Hoke SE, Bonn-Miller MO. Outcomes in a community sex offender treatment program: a comparison between polygraphed and matched non-polygraphed offenders. Sex Abuse J Res Treat 2007;19:381-93.
- McGregor M, Tutty LM, Babins-Wagner R, Gill M. The long term impacts of group treatment for partner abuse. Can J Community Ment Health 2002;21:67-84.
- McKee SA, Harris GT, Rice ME, Silk L. Effects of a Snoezelen Room on the behavior of three autistic clients. Res Dev Disabil 2007;28:304-16.
- McNiel DE, Binder RL. Effectiveness of a mental health court in reducing criminal recidivism and violence. Am J Psychiatry 2007;164:1395-403.
- Megna JL, Devitt PJ, Sauro MD, Dewan MJ, Megna JL, Devitt PJ, et al. Gabapentin’s effect on agitation in severely and persistently mentally ill patients. Ann Pharmacother 2002;36:12-6.
- Mischoulon D, Dougherty DD, Bottonari KA, Gresham RL, Sonawalla SB, Fischman AJ, et al. An open pilot study of nefazodone in depression with anger attacks: relationships between clinical response and receptor binding. Psychiatr Res Neuroimaging 2002;116:151-61.
- Miyaoka T, Furuya M, Yasuda H, Hayashia M, Inagaki T, Horiguchi J. Yi-gan san for the treatment of borderline personality disorder: an open-label study. Progr Neuro Psychopharmacol Biol Psychiatr 2008;32:150-4.
- Monson CM, Rodriguez BF, Warner R. Cognitive-behavioral therapy for PTSD in the real world: do interpersonal relationships make a real difference?. J Clin Psychol 2005;61:751-61.
- Morrel TM, Elliott JD, Murphy CM, Taft CT. Cognitive behavioral and supportive group treatments for partner-violent men. Behav Ther 2003;34:77-95.
- Muftic LR, Bouffard JA. An evaluation of gender differences in the implementation and impact of a comprehensive approach to domestic violence. Violence Against Women 2007;13:46-69.
- Murphy CM, Stosny S, Morrel TM. Change in self-esteem and physical aggression during treatment for partner violent men. J Fam Violence 2005;20:201-10.
- Taft CT, Murphy CM, King DW, Musser PH, Dedeyn JM. Process and treatment adherence factors in group cognitive-behavioral therapy for partner violent men. J Consult Clin Psychol 2003;71:812-20.
- Murphy D. The Effects of Ethnic Match and Length of Treatment on Anger and Aggression in Male Batterers 2007.
- Murphy G, Powell S, Guzman A-M, Hays S-J. Cognitive-behavioural treatment for men with intellectual disabilities and sexually abusive behaviour: a pilot study. J Intellect Disabil Res 2007;51:902-12.
- Needham I, Abderhalden C, Meer R, Dassen T, Haug HJ, Halfens RJG, et al. The effectiveness of two interventions in the management of patient violence in acute mental inpatient settings: report on a pilot study. J Psychiatr Ment Health Nurs 2004;11:595-601.
- Nickel MK, Loew TH. Treatment of aggression with topiramate in male borderline patients, part II: 18-month follow-up. Eur Psychiatr 2008;23:115-17.
- Norman ME. The Rosenzweig Picture Frustration Study ‘extra-aggression’ Score As an Indicator of Progress in Cognitive Restructuring Therapy for Male Perpetrators of Domestic Violence 2002.
- O’Farrell TJ, Murphy CM, Stephan SH, Fals-Stewart W, Murphy M. Partner violence before and after couples-based alcoholism treatment for male alcoholic patients: the role of treatment involvement and abstinence. J Consult Clin Psychol 2004;72:202-17.
- O’Farrell TJ, Fals-Stewart W, Murphy M, Murphy CM. Partner violence before and after individually based alcoholism treatment for male alcoholic patients. J Consult Clin Psychol 2003;7:92-102.
- Ong ALY. Hispanic batterers: describing a profile and treatment outcomes. Loma Linda, CA: Loma Linda University; 2003.
- Pake DR. Usefulness of the Trait Anger, Anger Control and Anger Out Subscale Scores of the State-Trait Anger Expression Inventory–2 for Assessing the Efficacy of Anger Management Training in Reducing Aggressive Behaviour Associated With the Expression of Anger 2006.
- Pascual JC, Oller S, Soler J, Barrachina J, Alvarez E, Perez V. Ziprasidone in the acute treatment of borderline personality disorder in psychiatric emergency services. J Clin Psychiatr 2004;65:1281-3.
- Patel K, Khalid F, Cree A, Sainz-Fuertes R, Shortt M, Mak T, et al. Specific antipsychotic medications-a treatment for aggressive behaviour in schizophrenia?. Eur Neuropsychopharmacol 2008;18:s73-4.
- Paul JD, Arruabarrena I. Evaluation of a treatment program for abusive and high-risk families in Spain. Child Welfare 2003;82:413-42.
- Perrella C, Carrus D, Costa E, Schifano F. Quetiapine for the treatment of borderline personality disorder; an open-label study. Progr Neuro Psychopharmacol Biol Psychiatr 2007;31:158-63.
- Phillips KA, Siniscalchi JM, McElroy SL. Depression, anxiety, anger, and somatic symptoms in patients with body dysmorphic disorder. Psychiatr Q 2004;75:309-20.
- Pietras CJ, Lieving LM, Cherek DR, Lane SD, Tcheremissine OV, Nouvion S. Acute effects of lorazepam on laboratory measures of aggressive and escape responses of adult male parolees. Behav Pharmacol 2005;16:243-51.
- Polaschek DLL, Wilson NJ, Townsend MR, Daly LR. Cognitive-behavioral rehabilitation for high-risk violent offenders: an outcome evaluation of the violence prevention unit. J Interpers Violence 2005;20:1611-27.
- Porporino FJ, Robinson D, Millson B, Weekes JR. An outcome evaluation of prison-based treatment programming for substance users. Subst Use Misuse 1047;37:8-10.
- Porter A. Cognitive processing patterns associated with completion of treatment for domestic violence. Dissertation Abstracts International Section B: The Sciences and Engineering; 2004.
- Preston GA, Marchant BK, Reimherr FW, Strong RE, Hedges DW. Borderline personality disorder in patients with bipolar disorder and response to lamotrigine. J Affect Disord 2004;79:297-303.
- Preval H, Klotz SG, Southard R, Francis A. Rapid-acting IM ziprasidone in a psychiatric emergency service: a naturalistic study. Gen Hosp Psychiatr 2005;27:140-4.
- Ricci RJ, Clayton CA, Shapiro F. Some effects of EMDR on previously abused child molesters: theoretical reviews and preliminary findings. J Forensic Psychiatr Psychol 2006;17:538-62.
- Rose J, Loftus M, Flint B, Carey L. Factors associated with the efficacy of a group intervention for anger in people with intellectual disabilities. Br J Clin Psychol 2005;44:305-17.
- Sartin RM. Characteristics associated with domestic violence perpetration: an examination of factors related to treatment response and the utility of a batterer typology. Dissertation Abstracts International Section B: The Sciences and Engineering; 2005.
- Savage T, Crawford I, Nashed Y. Decreasing assault occurrence on a psychogeriatric ward: an agitation management model. J Gerontol Nurs 2004;30:30-7.
- Scalora MJ, Garbin C. A multivariate analysis of sex offender recidivism. Int J Offender Ther Comp Criminol 2003;47:309-23.
- Schiff M, Katz K. Therapeutic components and differential treatment outcomes among clients of Israeli services for substance abusers. Res Soc Work Pract 2007;17:19-2.
- Schmitz MJ. An Outcome Study to Determine the Clinical Effectiveness of an Anger Management Program in an Adult, Rural Minnesota Sample 2005.
- Schober JM, Kuhn PJ, Kovacs PG, Earle JH, Byrne PM, Fries RA. Leuprolide acetate suppresses pedophilic urges and arousability. Arch Sex Behav 2005;34:691-705.
- Scott SD. Anger experience in violent and non-violent male offenders. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005.
- Seager JA, Jellicoe D, Dhaliwal GK. Refusers, dropouts, and completers: measuring sex offender treatment efficacy. Int J Offender Ther Comp Criminol 2004;48:600-12.
- Shepard MF, Falk DR, Elliott BA. Enhancing coordinated community responses to reduce recidivism in cases of domestic violence. J Interpers Violence 2002;17:551-69.
- Siddle R, Jones F, Awenat F. Group cognitive behaviour therapy for anger: a pilot study. Behav Cognit Psychother 2003;31:69-83.
- Simpson LE, Atkins DC, Gattis KS, Christensen A. Low-level relationship aggression and couple therapy outcomes. J Fam Psychol 2008;22:102-11.
- Skeem JL, Monahan J, Mulvey EP. Psychopathy, treatment involvement, and subsequent violence among civil psychiatric patients. Law Hum Behav 2002;26:577-603.
- Smedley MET. Sell v. United States: effects on institutional violence and forensic hospital practice. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2006.
- Stevenson J, Meares R, D’Angelo R. Five-year outcome of outpatient psychotherapy with borderline patients. Psychol Med 2005;35:79-87.
- Stuart GL, Ramsey SE, Moore TM, Kahler CW, Farrell LE, Recupero PR, et al. Reductions in marital violence following treatment for alcohol dependence. J Interpers Violence 2003;18:1113-31.
- Summerhill RR. Assessing diagnostic and treatment effectiveness of a sex offender population. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005.
- Swanson JW, Swartz MS, Elbogen EB. Effectiveness of atypical antipsychotic medications in reducing violent behavior among persons with schizophrenia in community-based treatment. Schizophrenia Bull 2004;30:3-20.
- Swanson JW, Swartz MS, Elbogen EB, Van Dorn RA. Reducing violence risk in persons with schizophrenia: olanzapine versus risperidone. J Clin Psychiatr 2004;65:1666-73.
- Taylor JL, Thorne I, Robertson A, Avery G. Evaluation of a group intervention for convicted arsonists with mild and borderline intellectual disabilities. Crim Behav Ment Health 2002;12:282-93.
- Taylor JL, Novaco RW, Gillmer BT, Robertson A, Thorne I. Individual cognitive-behavioural anger treatment for people with mild-borderline intellectual disabilities and histories of aggression: a controlled trial. Br J Clin Psychol 2005;44:367-82.
- Taylor JL, Novaco RW, Guinan C, Street N. Development of an imaginal provocation test to evaluate treatment for anger problems in people with intellectual disabilities. Clin Psychol Psychother 2004;11:233-46.
- Ternowski DR. Sex offender treatment: an evaluation of the Stave Lake Correctional Centre program (British Columbia). Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005.
- Thomas MK. Assessment of the effectiveness of anger management treatment in Vietnam veterans with posttraumatic stress disorder. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2004.
- Timmerman IGH, Emmelkamp PMG. The effects of cognitive-behavioral treatment for forensic inpatients. Int J Offender Ther Comp Criminol 2005;49:590-606.
- Trappler B, Newville H. Trauma healing via cognitive behavioural therapy in chronically hospitalized patients. Psychiatr Q 2007;78:317-25.
- Vaaler AE, Morken G, Flovig JC, Iversen VC, Linaker OM. Effects of a psychiatric intensive care unit in an acute psychiatric department. Nordic J Psychiatr 2006;60:144-9.
- Van Den Eynde F, Senturk V, Naudts K, Vogels C, Bernagie K, Thas O, et al. Efficacy of quetiapine for impulsivity and affective symptoms in borderline personality disorder. J Clin Psychopharmacol 2008;28:147-55.
- Van Nieuwenhuizen C. A treatment programme for sexually violent forensic psychiatric inpatients: development and first results. Psychol Crime Law 2005;11:467-77.
- Vannoy SD, Hoyt WT. Evaluation of an anger therapy intervention for incarcerated adult males. J Offend Rehabil 2004;39:39-57.
- Webster SD, Akhtar S, Bowers LE, Mann RE, Rallings M, Marshall WL. The impact of the prison service sex offender treatment programme on minority ethnic offenders: a preliminary study. Psychol Crime Law 2004;10:113-24.
- Williams F, Wakeling H, Webster S. A psychometric study of six self-report measures for use with sexual offenders with cognitive and social functioning deficits. Psychol Crime Law 2007;13:505-22.
- Willner P, Tomlinson S. Generalization of anger-coping skills from day-service to residential settings. J Appl Res Intellect Disabil 2007;20:553-62.
- Willner P, Brace N, Phillips J. Assessment of anger coping skills in individuals with intellectual disabilities. J Intellect Disabil Res 2005;49:329-39.
- Wong SCP, Veen SV, Leis TA, Parrish H, Gu D, Liber EU, et al. Reintegrating seriously violent and personality-disordered offenders from a supermaximum security institution into the general offender population. Int J Offender Ther Comp Criminol 2005;49:362-75.
- Wooldredge J. Convicting and incarcerating felony offenders of intimates assault and the odds of new assault charges. J Crim Justice 2007;35:379-89.
- Yocum R, Anderson J, Davigo T, Lee S. Direct-supervision and remote-supervision jails: a comparative study of psychosocial factors. J Appl Soc Psychol 2006;36:1790-812.
Appendix 1 Search strategies
| # | Searches | Results |
|---|---|---|
| 1 | ((Homicid* or murder* or manslaughter* or infanticid* or parricid* or assault* or ((bodily and (harm or assault)) or assail* or bugger* or sodom* or molest* or pedophil* or paedophil* or sadis* or sadomasochis* or sado-masochis* or anger* or cruel* or rapist* or (rape* and offend*) or physical abus* or spouse abus* or partner abus* or sexual abus*) or (((dangerous* and (behavior* or behaviour* or histor* or conduct*)) or violen*) and (risk* or predict* or anteced* or assess* or cause* or reason* or interven* or prevention* or preventing* or controlling* or manage* or treatment* or treating* or reduction* or reducing* or stop* or mental* or forensic* or psychiatric* or offend* or Axis 1 or Axis 2 or criminal* or detain* or insan* or NGRI or retard* or (learning disab* or learning-disab*) or acquit* or (child abus* or elder abus* or hostil* or killing* or attack* or aggress*)) and (mental* or forensic* or psychiatric* or offend* or axis 1 or axis 2 or criminal* or detain* or insan* or NGRI or retard* or (learning disab* or learning-disab*) or acquit* or disorder*))) not (cancer* or cancer or tumo* or tumour or heart* or heart)).mp. | 22,934 |
| 2 | limit 1 to ((100 childhood <birth to age 12 yrs> or 120 neonatal <birth to age 1 mo> or 140 infancy <age 2 to 23 mo> or 160 preschool age <age 2 to 5 yrs> or 180 school age <age 6 to 12 yrs> or 200 adolescence <age 13 to 17 yrs>) and yr=”2002 - 2008”) | 5631 |
| 3 | Limit 1 to (animals and yr=”2002 - 2008”) | 235 |
| 4 | Limit 1 to (editorial and yr=”2002 - 2008”) | 332 |
| 5 | 2 or 3 or 4 | 6198 |
| 6 | 1 not 5 | 16,736 |
Appendix 2 Included studies
| 130Afaq I, Riaz J, Sedky K, Chung DJ, Vanina Y, El-Mallakh R, et al. Divalproex as a calmative adjunct for aggressive schizophrenic patients. J KY Med Assoc 2002;100:17–22. |
| 112Alexander J, Tharyan P, Adams C, John T, Mol C, Philip J. Rapid tranquillization of violent or agitated patients in a psychiatric emergency setting: pragmatic randomised trial of intramuscular lorazepam v. haloperidol plus promethazine. Br J Psychiatr 2004;185:63–9. |
| 113Arango C, Bombin I, Gonzalez-Salvador T, Garcia-Cabeza I, Bobes J. Randomised clinical trial comparing oral versus depot formulations of zuclopenthixol in patients with schizophrenia and previous violence. Eur Psychiatr 2006;21:34–40. |
| 131Barnes AD. The role of male-male relationships in partner violence treatment groups: the effects of improving same-sex relationships on attachment. PhD thesis. College Station; TX: Texas A&M University; 2007. |
| 132Belaga I. Domestic violence: typology of batterers and effectiveness of treatment. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005. |
| 133Belfrage H, Fransson G, Strand S. Management of violent behaviour in the correctional system using qualified risk assessments. Leg Crim Psychol 2004;9:11–22. |
| 134Bennett LW, Stoops C, Call C, Flett H. Program completion and re-arrest in a batterer intervention system. RSWP 2007;17:42–54. |
| 79Berry S. Stopping violent offending in New Zealand: is treatment an option? NZ J Psychol 2003;32:92–100. |
| 135Bitter I, Czobor P, Dossenbach M, Volavka J. Effectiveness of clozapine, olanzapine, quetiapine, risperidone, and haloperidol monotherapy in reducing hostile and aggressive behaviour in outpatients treated for schizophrenia: a prospective naturalistic study (IC-SOHO). Eur Psychiatr 2005;20:403–8. |
| 136Booth BD, Fedoroff JP, Curry SD, Douglass AB. Sleep apnea as a possible factor contributing to aggression in sex offenders. J Forensic Sci 2006;51:1178–81. |
| 137Bowen E, Gilchrist EA, Beech AR. An examination of the impact of community-based rehabilitation on the offending behaviour of male domestic violence offenders and the characteristics associated with recidivism. Leg Criminol Psychol 2005;10:189–209. |
| 138Bradbury KE, Clarke I. Cognitive behavioural therapy for anger management: effectiveness in adult mental health services. Behav Cognit Psychother 2007;35:201–8. |
| 139Brodaty H, Ames D, Snowdon J, Woodward M, Kirwan J, Clarnette R, et al. A randomized placebo-controlled trial of risperidone for the treatment of aggression, agitation and psychosis of dementia. J Clin Psychiatr 2003;64:134–43. |
| 140Broner N, Mayrl DW, Landsberg G. Outcomes of mandated and nonmandated New York City jail diversion for offenders with alcohol, drug, and mental disorders. Prison Journal 2005;85:18–49. |
| 141Burke HC. Psychopathy and treatment outcome in incarcerated violent offender program participants. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2004. |
| 142Burns M, Bird D, Leach C, Higgins K. Anger management training: the effects of a structured programme on the self-reported anger experience of forensic inpatients with learning disability. J Psychiatr Ment Health Nurs 2003;10:569–77. |
| 143Buttell FP, Carney MM. A large sample evaluation of a court-mandated batterer intervention program: investigating differential program effect for African American and Caucasian men. Res Soc Work Pract 2006;16:121–31. |
| Linked paper 144Buttell FP, Carney MM. A multidimensional assessment of a batterer treatment program: an alert to a problem? Res Soc Work Pract 2004;14:93–101. |
| Linked paper 145Buttell FP, Carney MM. Do batterer intervention programs serve African American and Caucasian batterers equally well? An investigation of a 26-week program. Res Soc Work Pract 2005;15:19–28. |
| 146Buttell FP, Pike CK. Investigating the differential effectiveness of a batterer treatment program on outcomes for African American and Caucasian batterers. Res Soc Work Pract 2003;13:675–92. |
| 147Carney MM, Buttell FP. An evaluation of a court-mandated batterer intervention program: investigating differential program effect for African American and white women. Res Soc Work Pract 2006;16:571–81. |
| Linked paper 148Carney MM, Buttell FP. A multidimensional evaluation of a treatment program for female batterers: a pilot study. Res Soc Work Pract 2004;14:249–58. |
| 81Cavanaugh MM. An exploration of the feasibility and utility of the Dialectical Psychoeducational Workshop (DPEW) as a preventative intervention for males at potential risk of intimate partner violence. Dissertation Abstracts International Section A: Humanities and Social Sciences; 2007. |
| 149Chan H-Y, Lu R-B, Tseng C-L, Chous K-R. Effectiveness of the anger-control program in reducing anger expression in patients with schizophrenia. Arch Psychiatr Nurs 2003;17:88–95. |
| 150Chan KL. Group therapy for male batterers: a Chinese experience. Soc Work Groups 2003;26:79–90. |
| 98Chan KL, Campayo A, Moser DJ, Arndt S, Robinson RG. Aggressive behaviour in patients with stroke: association with psychopathology and results of antidepressant treatment on aggression. Arch Phys Med Rehabil 2006;87:793–8. |
| 151Childs A, Price L. Cranial electrotherapy stimulation reduces aggression in violent neuropsychiatric patients. Prim Psychiatr 2007;14:50–6. |
| 162Choi Y-J, Lee K-J. Evidence-based nursing: effects of a structured nursing program for the health promotion of Korean women with Hwa-Byung. Arch Psychiatr Nurs 2007;21:12–16. |
| 107Citrome L, Casey D, Daniel D, Wozniak P, Kochan L, Tracy K. Adjunctive divalproex and hostility among patients with schizophrenia receiving olanzapine or risperidone. Psychiatr Serv 2004;55:290–4. |
| 68Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: a multiwave study. Am J Psychiatry 2007;164:922–8. |
| 153Cohen-Mansfield J, Parpura-Gill A. Bathing: a framework for intervention focusing on psychosocial, architectural and human factors considerations. Arch Gerontol Geriatr 2007;45:121–35. |
| 154Combs DR, Adams SD, Penn DL, Roberts D, Tiegreen J, Stem P. Social Cognition and Interaction Training (SCIT) for inpatients with schizophrenia spectrum disorders: preliminary findings. Schizophr Res 2007;91:112–16. |
| 90Cooper C, Eslinger DM, Stolley PD. Hospital-based violence intervention programs work. J Trauma 2006;61:534–40. |
| 155Craissati J, Falla S, McClurg G, Beech A. Risk, reconviction rates and pro-offending attitudes for child molesters in a complete geographical area of London. J Sex Aggress 2002;8:22–38. |
| 156Davis MA. Effects treatment length has on recidivism of domestic violence perpetrators. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2002. |
| 157Dietz EF, O’Connell DJ, Scarpitti FR. Therapeutic communities and prison management: an examination of the effects of operating an in-prison therapeutic community on levels of institutional disorder. Int J Offender Ther Comp Criminol 2003;47:210–23. |
| 114Duggan A, Caldera D, Rodriguez K, Burrell L, Rohde C, Crowne SS. Impact of a statewide home visiting program to prevent child abuse. Child Abuse Neglect 2007;31:801–27. |
| 110Easton CJ. Treatment outcome among substance-dependent offenders of intimate partner violence: a randomized clinical trial. Proceedings of the 67th Annual Scientific Meeting of the College on Problems of Drug Dependence, Orlando, FL, 19–23 June 2005. |
| 111Easton CJ, Mandel DL, Hunkele KA, Nich C, Rounsaville BJ, Carroll KM. A cognitive behavioral therapy for alcohol-dependent domestic violence offenders: an integrated Substance Abuse-Domestic Violence Treatment Approach (SADV). Am J Addict 2007;16:24–31. |
| Linked paper 158Easton CJ, Mandel D, Babuscio T, Rounsaville BJ, Carroll KM. Differences in treatment outcome between male alcohol dependent offenders of domestic violence with and without positive drug screens. Addict Behav 2007;32:2151–63. |
| 159Echeburua E, Fernandez-Montalvo J, Amor PJ. Psychological treatment of men convicted of gender violence: a pilot study in Spanish prisons. Int J Offender Ther Comp Criminol 2006;50:57–70. |
| 160Erickson SK. Outpatient commitment in New York: examining violence, compliance and demographic characteristics of the seriously mentally ill under Kendra’s Law. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2004. |
| 62Estelle LM. Assessment of child abuse potential in spouse abusive men. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2002. |
| 161Evershed S, Tennant A, Boomer D, Rees A, Barkham M, Watson A. Practice-based outcomes of dialectical behaviour therapy (DBT) targeting anger and violence, with male forensic patients: a pragmatic and non-contemporaneous comparison. Crim Behav Mental Health 2003;13:198–213. |
| 162Feder L, Dugan L. A test of the efficacy of court-mandated counselling for domestic violence offenders: the Broward Experiment. JQ 2002;19:343–75. |
| 163Fhager B, Meiri IM, Sjogren M, Edman A. Treatment of aggressive behaviour in dementia with the anticonvulsant topiramate: a retrospective pilot study. Int Psychogeriatr 2003;15:307–9. |
| 164Forbes D, Hawthorne G, Elliott P, McHugh T, Biddle D, Creamer M, et al. A concise measure of anger in combat-related posttraumatic stress disorder. J Trauma Stress 2004;17:249–56. |
| 106Frankenburg FR, Zanarini MC. Divalproex sodium treatment of women with borderline personality disorder and bipolar II disorder: a double-blind placebo-controlled pilot study. J Clin Psychiatr 2002;63:442–6. |
| 165Friendship C, Mann RE, Beech AR. Evaluation of a national prison-based treatment program for sexual offenders in England and Wales. J Interpers Violence 2003;18:744–59. |
| 69Galovski TE, Blanchard EB. The effectiveness of a brief psychological intervention on court-referred and self-referred aggressive drivers. Behav Res Ther 2002;40:1385–402. |
| 166Gelkopf M, Gonen B, Kurs R, Melamed Y, Bleich A. The effect of humorous movies on inpatients with chronic schizophrenia. J Nerv Ment Dis 2006;194:880–3. |
| 167Gerra G, Di Petta G, D’Amore A, Iannotta P, Bardicchia F, Falorni F, et al. Effects of olanzapine on aggressiveness in heroin dependent patients. Progr Neuro Psychopharmacol Biol Psychiatr 2006;30:1291–8. |
| 168Gershater-Molko RM, Lutzker JR, Wesch D. Using recidivism data to evaluate Project Safecare: teaching bonding, safety, and health care skills to parents. Child Maltreat 2002;7:277–85. |
| 169Gondolf E. Outcomes of case management for African-American men in batterer counseling. J Fam Violence 2008;23:173–81. |
| 170Gordon JA, Moriarty LJ. The effects of domestic violence batterer treatment on domestic violence recidivism: the Chesterfield County experience. Crim Justice Behav 2003;30:118–34. |
| 171Gossop M, Trakada K, Stewart D, Witton J. Reductions in criminal convictions after addiction treatment: 5-year follow-up. Drug Alcohol Depend 2005;79:295–302. |
| 92Gottfredson DC, Exum ML. The Baltimore City Drug Treatment Court: one year results from a randomized study. J Res Crime Delinquen 2002;39:337–56. |
| 172Gregory CR. Assessing amenability to treatment in community corrections: creating a valid and reliable instrument for male batterers. Dissertation Abstracts International Section A: Humanities and Social Sciences 2004;65:1992-a. |
| 173Grubin D, Madsen L, Parsons S, Sosnowski D, Warberg B. A prospective study of the impact of polygraphy on high-risk behaviors in adult sex offenders. Sex Abuse J Res Treat 2004;16:209–22. |
| 174Hanson RK, Bloom I, Stephenson M. Evaluating community sex offender treatment programs: a 12-year follow-up of 724 offenders. Can Behav J Sci 2004;36:87–96. |
| 175Harkins L, Beech AR. Examining the impact of mixing child molesters and rapists in group-based cognitive-behavioral treatment for sexual offenders. Int J Offender Ther Comp Criminol 2008;52:31–45. |
| 176Henderson CE. A study of competing treatment models for the dually diagnosed: chemical dependency programs versus mental health. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2007. |
| 177Hendricks B, Werner T, Shipway L, Turinetti GJ. Recidivism among spousal abusers: predictions and program evaluation. J Interpers Violence 2006;21:703–16. |
| 178Hensley C, Koscheski M, Tweksbury R. Does participation in conjugal visitations reduce prison violence in Mississippi? An exploratory study. Crim Justice Rev 2002;27:52–65. |
| 179Hilton NZ, Harris GT, Rice ME. The effect of arrest on wife assault recidivism: controlling for pre-arrest risk. Crim Justice Behav 2007;34:1334–44. |
| 91Hollander E, Tracy KA, Swann AC, Coccaro EF, McElroy SL, Wozniak P, et al. Divalproex in the treatment of impulsive aggression: efficacy in cluster B personality disorders. Neuropsychopharmacology 2003;28:1186–97. |
| 180Hornsveld RHJ, Nijman HLI, Kraaimaat FW. Aggression control therapy for violent forensic psychiatric patients: first results. Psychol Crime Law 2008;14:1–18. |
| Linked paper 181Hornsveld RHJ. Evaluation of aggression control therapy for violent forensic psychiatric patients. Psychol Crime Law 2005;11:403–10. |
| 182Hough WG, O’Brien KP. The effect of community treatment orders on offending rates. Psychiatr Psychol Law 2005;12:411–23. |
| 70Houston RJ, Stanford MS. Characterization of aggressive behaviour and phenytoin response. Aggress Behav 2006;32:38–43. |
| 183Howells K, Day A, Williamson P, Bubner S, Jauncey S, Parker A, et al. Brief anger management programs with offenders: outcomes and predictors of change. J Forensic Psychiatr Psychol 2005;16:296–311. |
| 72Huf G. Rapid tranquillisation for agitated patients in emergency psychiatric rooms: a randomised trial of midazolam versus haloperidol plus promethazine. BMJ 2003;327:708–13. |
| 73Huf G, Coutinho ESF, Adams CE, Group TC. Rapid tranquillisation in psychiatric emergency settings in Brazil: pragmatic randomised controlled trial of intramuscular haloperidol versus intramuscular haloperidol plus promethazine. BMJ 2007;335:869. |
| 63Huss MT, Ralston A. Do batterer subtypes actually matter? Treatment completion, treatment response, and recidivism across a batterer typology. Crim Justice Behav 2008;35:710–24. |
| 184Ireland JL. Anger management therapy with young male offenders: an evaluation of treatment outcome. Aggress Behav 2004;30:174–85. |
| 185Janowsky DS, Shetty M, Barnhill J, Elamir B, Davis JM. Serotonergic antidepressant effects on aggressive, self-injurious and destructive/disruptive behaviours in intellectually disabled adults: a retrospective, open-label, naturalistic trial. Int J Neuropsychopharmacol 2005;8:37–48. |
| 186Johansen TM. Predicting treatment outcomes of an anger management treatment program using the stages of change model. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2006. |
| 187Johnson DR, Fontana A, Lubin H, Corn B, Rosenheck R. Long-term course of treatment-seeking Vietnam veterans with posttraumatic stress disorder: mortality, clinical condition, and life satisfaction. J Nerv Ment Dis 2004;192:35–41. |
| 188Johnson S. Male domestic violence treatment programs: effect on attitudes towards women and intimate relationships. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2007. |
| 64Jones AS, D’Agostino RB, Gondolf EW, Heckert A. Assessing the effect of batterer program completion on reassault using propensity scores. J Interpers Violence 2004;19:1002–20. |
| 189Keeling JA, Rose JL, Beech AR. An investigation into the effectiveness of a custody-based cognitive-behavioural treatment for special needs sexual offenders. J Forensic Psychiatr Psychol 2006;17:372–92. |
| 190Keeling JA, Rose JL, Beech AR. Comparing sexual offender treatment efficacy: mainstream sexual offenders and sexual offenders with special needs. J Intellect Dev Disabil 2007;32:117–24. |
| 191Kerne PA. Domestic violence group counseling impact on abusiveness potential and conflict resolution styles. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2007. |
| 82Krakowski MI, Czobor P, Citrome L, Bark N, Cooper TB. Atypical antipsychotic agents in the treatment of violent patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatr 2006;63:622–9. |
| 192Kunselman JC, Vito GF. Questioning mandatory sentencing efficiency: a case study of persistent felony offender rapists in Kentucky. Am J Crim Justice 2002;27:53–68. |
| 193Labinsky EB. Evaluating a group treatment program for male batterers. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2002. |
| 94Labriola M, Rempel M, Davis RC. Do batterer programs reduce recidivism? Results from a randomized trial in the Bronx. JQ 2008;25:252–82. |
| Linked paper 194Labriola M, Rempel M, Davis RC. Testing the effectiveness of batterer programs and judicial monitoring: results from a randomized trial at the Misdemeanor Domestic Violence Court: National Institute of Justice of the US Department of Justice; 2005. |
| 86Lanza ML, Anderson J, Boisvert CM, Leblanc A, Fardy M, Steel B. Assaultive behavior intervention in the veterans administration: psychodynamic group psychotherapy compared to cognitive behavior therapy. Perspect Psychiatr Care 2002;38:89–97. |
| 83Lasley J. The effect of intensive bail supervision on repeat domestic violence offenders. Pol Stud J 2003;31:187–207. |
| 195Lauretti JM. A study of the therapeutic working alliance, client motivation for therapy and subsequent self-reported changes in abusive behavior among a sample of male batterers from the abuse ceases today program. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2003. |
| 196Lavey R, Sherman T, Mueser KT, Osborne DD, Currier M, Wolfe R. The effects of yoga on mood in psychiatric inpatients. Psychiatr Rehabil J 2005;28:399–402. |
| 197Lawson DM, Barnes AD, Madkins JP, Francois-Lamonte BM. Changes in male partner abuser attachment styles in group treatment. Psychother Theor Res Pract Train 2006;43:232–7. |
| 198Lawson WB, Nanos J. Effects of divalproex on disruptive behavior of jail inmates. Progr Neuro Psychopharmacol Biol Psychiatr 2008;32:909–10. |
| 199Lee MY, Uken A, Sebold J. Accountability for change: solution-focused treatment with domestic violence offenders. Fam Soc J 2004;85:463–76. |
| 200Levesque D, Driskell M, Castle P, Greene N, Prochaska J, Prochaska J, editors. Efficacy of a computerized stage-matched intervention for domestic violence offenders: Preliminary findings. 133rd Annual Meeting & Exposition of the American Public Health Association; Philadelphia, MA, 2005. |
| 201Lewis K. The relationship between the URICA and correctional treatment in a sample of violent male offenders. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2004. |
| 202Ley LF. A study of domestic violence recidivism following treatment among incarcerated men who batter. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2006. |
| 115Liau AK, Shively R, Horn M, Landau J, Barriga A, Gibbs JC. Effects of psychoeducation for offenders in a community correctional facility. J Community Psychol 2004;32:543–58. |
| 203Lindsay WR, Allan R, Parry C, MacLeod F, Cottrell J, Overend H, et al. Anger and aggression in people with intellectual disabilities: treatment and follow-up of consecutive referrals and a waiting list comparison. Clin Psychol Psychother 2004;11:255–64. |
| 116Linehan MM, McDavid JD, Brown MZ, Sayrs JHR, Gallop RJ. Olanzapine plus dialectical behavior therapy for women with high irritability who meet criteria for borderline personality disorder: a double-blind, placebo-controlled pilot study. J Clin Psychiatr 2008;69:999–1005. |
| 117Loew TH, Nickel MK, Muehlbacher M, Kaplan P, Nickel C, Kettler C, et al. Topiramate treatment for women with borderline personality disorder: a double-blind, placebo-controlled study. J Clin Psychopharmacol 2006;26:61–6. |
| 95MacKenzie DL, Bierie D, Mitchell O. An experimental study of a therapeutic boot camp: Impact on impulses, attitudes and recidivism. J Exp Criminol 2007;3:221–46. |
| 204MacVaugh GS. Outcomes of court intervention and diversionary programs for domestically violent offenders. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005. |
| 205Mammen OK, Pilkonis PA, Chengappa KNR, Kupfer DJ. Anger attacks in bipolar depression: predictors and response to citalopram added to mood stabilizers. J Clin Psychiatr 2004;65:627–33. |
| 74Marques JK, Wiederanders M, Day DM, Nelson C, Van Ommeren A. Effects of a relapse prevention program on sexual recidivism: final results from California’s Sex Offender Treatment and Evaluation Project (SOTEP). J Child Sex Abuse 2005;17:79–107. |
| 96Mattes JA, Mattes JA. Oxcarbazepine in patients with impulsive aggression: a double-blind, placebo-controlled trial. J Clin Psychopharmacol 2005;25:575–9. |
| 206McCue RE, Urcuyo L, Lilu Y, Tobias T, Chambers MJ. Reducing restraint use in a public psychiatric inpatient service. J Behav Health Serv Res 2004;31:217–24. |
| 207McGrath RJ, Cumming G, Livingston JA, Hoke SE. Outcome of a treatment program for adult sex offenders: from prison to community. J Interpers Violence 2003;18:3–17. |
| 208McGrath RJ, Cumming GF, Hoke SE, Bonn-Miller MO. Outcomes in a community sex offender treatment program: a comparison between polygraphed and matched non-polygraphed offenders. Sex Abuse J Res Treat 2007;19:381–93. |
| 209McGregor M, Tutty LM, Babins-Wagner R, Gill M. The long term impacts of group treatment for partner abuse. Can J Community Ment Health 2002;21:67–84. |
| 210McKee SA, Harris GT, Rice ME, Silk L. Effects of a Snoezelen Room on the behavior of three autistic clients. Res Dev Disabil 2007;28:304–16. |
| 211McNiel DE, Binder RL. Effectiveness of a mental health court in reducing criminal recidivism and violence. Am J Psychiatry 2007;164:1395–403. |
| 109Meehan KM, Wang H, David SR, Nisivoccia JR, Jones B, Beasley CM, et al. Comparison of rapidly acting intramuscular olanzapine, lorazepam, and placebo: a double blind, randomised study in acutely agitated patients with dementia. Neuropsychopharmacology 2002;26:494–504. |
| 212Megna JL, Devitt PJ, Sauro MD, Dewan MJ, Megna JL, Devitt PJ, et al. Gabapentin’s effect on agitation in severely and persistently mentally ill patients. Ann Pharmacother 2002;36:12–16. |
| 213Mischoulon D, Dougherty DD, Bottonari KA, Gresham RL, Sonawalla SB, Fischman AJ, et al. An open pilot study of nefazodone in depression with anger attacks: relationships between clinical response and receptor binding. Psychiatr Res Neuroimaging 2002;116:151–61. |
| 75Mitchell O, MacKenzie DL. The stability and resiliency of self-control in a sample of incarcerated offenders. Crime Delinquen 2006;52:432–49. |
| 214Miyaoka T, Furuya M, Yasuda H, Hayashia M, Inagaki T, Horiguchi J. Yi-gan san for the treatment of borderline personality disorder: an open-label study. Progr Neuro Psychopharmacol Biol Psychiatr 2008;32:150–4. |
| 85Monnelly EP, Ciraulo DA, Knapp C, Keane T, Monnelly EP, Ciraulo DA, et al. Low-dose risperidone as adjunctive therapy for irritable aggression in posttraumatic stress disorder. J Clin Psychopharmacol 2003;23:193–6. |
| 215Monson CM, Rodriguez BF, Warner R. Cognitive-behavioral therapy for PTSD in the real world: do interpersonal relationships make a real difference? J Clin Psychol 2005;61:751–61. |
| 216Morrel TM, Elliott JD, Murphy CM, Taft CT. Cognitive behavioral and supportive group treatments for partner-violent men. Behav Ther 2003;34:77–95. |
| 217Muftic LR, Bouffard JA. An evaluation of gender differences in the implementation and impact of a comprehensive approach to domestic violence. Violence Against Women 2007;13:46–69. |
| 65Murphy CM, Stosny S, Morrel TM. Change in self-esteem and physical aggression during treatment for partner violent men. J Fam Violence 2005;20:201–10. |
| 218Murphy CM, Taft CT, Eckhardt CI. Anger problem profiles among partner violent men: differences in clinical presentation and treatment outcome. J Counsel Psychol 2007;54:189–200. |
| Linked paper 219Taft CT, Murphy CM, King DW, Musser PH, Dedeyn JM. Process and treatment adherence factors in group cognitive-behavioral therapy for partner violent men. J Consult Clin Psychol 2003;71:812–20. |
| 220Murphy D. The effects of ethnic match and length of treatment on anger and aggression in male batterers. PsyD thesis. La Verne, CA: University of La Verne; 2007. |
| 221Murphy G, Powell S, Guzman A-M, Hays S-J. Cognitive-behavioural treatment for men with intellectual disabilities and sexually abusive behaviour: a pilot study. J Intellect Disabil Res 2007;51:902–12. |
| 222Needham I, Abderhalden C, Meer R, Dassen T, Haug HJ, Halfens RJG, et al. The effectiveness of two interventions in the management of patient violence in acute mental inpatient settings: report on a pilot study. J Psychiatr Ment Health Nurs 2004;11:595–601. |
| 97New AS, Buchsbaum MS, Hazlett EA, Goodman M, Koenigsberg HW, Lo J, et al. Fluoxetine increases relative metabolic rate in prefrontal cortex in impulsive aggression. Psychopharmacology 2004;176:451–8. |
| 105Nickel C, Lahmann C, Tritt K, Muehlbacher M, Kaplan P, Kettler C, et al. Topiramate in treatment of depressive and anger symptoms in female depressive patients: a randomized, double-blind, placebo-controlled study. J Affect Disord 2005;87:243–52. |
| 104Nickel MK, Nickel C, Kaplan P, Lahmann C, Muhlbacher M, Tritt K, et al. Treatment of aggression with topiramate in male borderline patients: a double-blind, placebo-controlled study. Biol Psychiatr 2005;57:495–9. |
| 88Nickel MK, Nickel C, Mitterlehner FO, Tritt K, Lahmann C, Leiberich PK, et al. Topiramate treatment of aggression in female borderline personality disorder patients: a double-blind, placebo-controlled study. J Clin Psychiatr 2004;65:1515–19. |
| Linked paper 223Nickel MK, Loew TH. Treatment of aggression with topiramate in male borderline patients, part II: 18-month follow-up. Eur Psychiatr 2008;23:115–17. |
| 224Norman ME. The Rosenzweig Picture Frustration Study ‘extra-aggression’ score as an indicator of progress in cognitive restructuring therapy for male perpetrators of domestic violence. PhD thesis. Cincinnati: OH: Union Institute and University; 2002. |
| 225O’Farrell TJ, Murphy CM, Stephan SH, Fals-Stewart W, Murphy M. Partner violence before and after couples-based alcoholism treatment for male alcoholic patients: the role of treatment involvement and abstinence. J Consult Clin Psychol 2004;72:202–17. |
| Linked paper 226O’Farrell TJ, Fals-Stewart W, Murphy M, Murphy CM. Partner violence before and after individually based alcoholism treatment for male alcoholic patients. J Consult Clin Psychol 2003;7:92–102. |
| 227Ong ALY. Hispanic batterers: describing a profile and treatment outcomes. PsyD and DrPH theses. Loma Linda, CA: Loma Linda University; 2003. |
| 228Pake DR, Jr. Usefulness of the Trait Anger, Anger Control and Anger Out subscale scores of the State-Trait Anger Expression Inventory–2 for assessing the efficacy of anger management training in reducing aggressive behaviour associated with the expression of anger. PsyD thesis. Chicago, IL: Adler School of Professional Psychology; 2006. |
| 229Pascual JC, Oller S, Soler J, Barrachina J, Alvarez E, Perez V. Ziprasidone in the acute treatment of borderline personality disorder in psychiatric emergency services. J Clin Psychiatr 2004;65:1281–3. |
| 230Patel K, Khalid F, Cree A, Sainz-Fuertes R, Shortt M, Mak T, et al. Specific antipsychotic medications-a treatment for aggressive behaviour in schizophrenia? Eur Neuropsychopharmacol 2008;18:s73–4. |
| 231Paul JD, Arruabarrena I. Evaluation of a treatment program for abusive and high-risk families in Spain. Child Welfare 2003;82:413–42. |
| 232Perrella C, Carrus D, Costa E, Schifano F. Quetiapine for the treatment of borderline personality disorder; an open-label study. Progr Neuro Psychopharmacol Biol Psychiatr 2007;31:158–63. |
| 233Phillips KA, Siniscalchi JM, McElroy SL. Depression, anxiety, anger, and somatic symptoms in patients with body dysmorphic disorder. Psychiatr Q 2004;75:309–20. |
| 234Pietras CJ, Lieving LM, Cherek DR, Lane SD, Tcheremissine OV, Nouvion S. Acute effects of lorazepam on laboratory measures of aggressive and escape responses of adult male parolees. Behav Pharmacol 2005;16:243–51. |
| 235Polaschek DLL, Wilson NJ, Townsend MR, Daly LR. Cognitive-behavioral rehabilitation for high-risk violent offenders: an outcome evaluation of the violence prevention unit. J Interpers Violence 2005;20:1611–27. |
| 236Porporino FJ, Robinson D, Millson B, Weekes JR. An outcome evaluation of prison-based treatment programming for substance users. Subst Use Misuse 1047;37:8–10. |
| 237Porter A. Cognitive processing patterns associated with completion of treatment for domestic violence. Dissertation Abstracts International Section B: The Sciences and Engineering; 2004. |
| 238Preston GA, Marchant BK, Reimherr FW, Strong RE, Hedges DW. Borderline personality disorder in patients with bipolar disorder and response to lamotrigine. J Affect Disord 2004;79:297–303. |
| 239Preval H, Klotz SG, Southard R, Francis A. Rapid-acting IM ziprasidone in a psychiatric emergency service: a naturalistic study. Gen Hosp Psychiatr 2005;27:140–4. |
| 75Raveendran NS, Tharyan P, Alexander J, Adams CE. Rapid tranquillisation in psychiatric emergency settings in India: pragmatic randomised controlled trial of intramuscular olanzapine versus intramuscular haloperidol plus promethazine. BMJ 2007;335:865. |
| 78Rempel M, Labriola M, Davis RC. Does judicial monitoring deter domestic violence recidivism? Results of a quasi-experimental comparison in the Bronx. Violence Against Women 2008;14:185–207. |
| 240Ricci RJ, Clayton CA, Shapiro F. Some effects of EMDR on previously abused child molesters: theoretical reviews and preliminary findings. J Forensic Psychiatr Psychol 2006;17:538–62. |
| 99Rinne T, Van Den Brink W, Wouters L, Van Dyck R, Rinne T, Van Den Brink W, et al. SSRI treatment of borderline personality disorder: a randomized, placebo-controlled clinical trial for female patients with borderline personality disorder. Am J Psychiatry 2002;159:2048–54. |
| 241Rose J, Loftus M, Flint B, Carey L. Factors associated with the efficacy of a group intervention for anger in people with intellectual disabilities. Br J Clin Psychol 2005;44:305–17. |
| 242Sartin RM. Characteristics associated with domestic violence perpetration: an examination of factors related to treatment response and the utility of a batterer typology. Dissertation Abstracts International Section B: The Sciences and Engineering; 2005. |
| 243Savage T, Crawford I, Nashed Y. Decreasing assault occurrence on a psychogeriatric ward: an agitation management model. J Gerontol Nurs 2004;30:30–7. |
| 244Scalora MJ, Garbin C. A multivariate analysis of sex offender recidivism. Int J Offender Ther Comp Criminol 2003;47:309–23. |
| 245Schiff M, Katz K. Therapeutic components and differential treatment outcomes among clients of israeli services for substance abusers. Res Soc Work Pract 2007;17:19–29. |
| 246Schmitz MJ. An outcome study to determine the clinical effectiveness of an anger management program in an adult, rural Minnesota sample. PhD thesis. Minneapolis, MN: Capella University; 2005. |
| 247Schober JM, Kuhn PJ, Kovacs PG, Earle JH, Byrne PM, Fries RA. Leuprolide acetate suppresses pedophilic urges and arousability. Arch Sex Behav 2005;34:691–705. |
| 66Schweitzer R, Dwyer J. Sex crime recidivism: evaluation of a sexual offender treatment program. J Interpers Violence 1292;18:1292–310. |
| 248Scott SD. Anger experience in violent and non-violent male offenders. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005. |
| 249Seager JA, Jellicoe D, Dhaliwal GK. Refusers, dropouts, and completers: measuring sex offender treatment efficacy. Int J Offender Ther Comp Criminol 2004;48:600–12. |
| 250Shepard MF, Falk DR, Elliott BA. Enhancing coordinated community responses to reduce recidivism in cases of domestic violence. J Interpers Violence 2002;17:551–69. |
| 251Siddle R, Jones F, Awenat F. Group cognitive behaviour therapy for anger: a pilot study. Behav Cognit Psychother 2003;31:69–83. |
| 252Simpson LE, Atkins DC, Gattis KS, Christensen A. Low-level relationship aggression and couple therapy outcomes. J Fam Psychol 2008;22:102–11. |
| 253Skeem JL, Monahan J, Mulvey EP. Psychopathy, treatment involvement, and subsequent violence among civil psychiatric patients. Law Hum Behav 2002;26:577–603. |
| 254Smedley MET. Sell v. United States: effects on institutional violence and forensic hospital practice. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2006. |
| 118Soler J, Pascual JC, Campins J, Barrachina J, Puigdemont D, Alvarez E, et al. Double-blind, placebo-controlled study of dialectical behaviour therapy plus olanzapine for borderline personality disorder. Am J Psychiatry 2005;162:1221–4. |
| 255Stevenson J, Meares R, D’Angelo R. Five-year outcome of outpatient psychotherapy with borderline patients. Psychol Med 2005;35:79–87. |
| 256Stuart GL, Ramsey SE, Moore TM, Kahler CW, Farrell LE, Recupero PR, et al. Reductions in marital violence following treatment for alcohol dependence. J Interpers Violence 2003;18:1113–31. |
| 101Suh G-H, Son HG, Ju Y-S, Jcho KH, Yeon BK, Shin YM, et al. A randomized, double-blind, crossover comparison of risperidone and haloperidol in Korean dementia patients with behavioral disturbances. Am J Geriatr Psychol 2004;12:509–16. |
| 257Summerhill RR. Assessing diagnostic and treatment effectiveness of a sex offender population. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005. |
| 258Swanson JW, Swartz MS, Elbogen EB. Effectiveness of atypical antipsychotic medications in reducing violent behavior among persons with schizophrenia in community-based treatment. Schizophr Bull 2004;30:3–20. |
| Linked paper 259Swanson JW, Swartz MS, Elbogen EB, Van Dorn RA. Reducing violence risk in persons with schizophrenia: olanzapine versus risperidone. J Clin Psychiatr 2004;65:1666–73. |
| 260Taylor JL, Novaco RW, Gillmer BT, Robertson A, Thorne I. Individual cognitive-behavioural anger treatment for people with mild-borderline intellectual disabilities and histories of aggression: a controlled trial. Br J Clin Psychol 2005;44:367–82. |
| 261Taylor JL, Novaco RW, Guinan C, Street N. Development of an imaginal provocation test to evaluate treatment for anger problems in people with intellectual disabilities. Clin Psychol Psychother 2004;11:233–46. |
| 262Taylor JL, Thorne I, Robertson A, Avery G. Evaluation of a group intervention for convicted arsonists with mild and borderline intellectual disabilities. Crim Behav Ment Health 2002;12:282–93. |
| 263Ternowski DR. Sex offender treatment: an evaluation of the Stave Lake Correctional Centre program (British Columbia). Dissertation Abstracts International. Section B: The Sciences and Engineering; 2005. |
| 71Theall KP, Elifson KW, Sterk CE, Stewart EA. Criminality among female drug users following an HIV risk-reduction intervention. J Interpers Violence 2007;22:85–107. |
| 264Thomas MK. Assessment of the effectiveness of anger management treatment in Vietnam veterans with posttraumatic stress disorder. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2004. |
| 80Timmer SG, Urquiza AJ, Zebell NM, McGrath JM. Parent-child interaction therapy: application to maltreating parent-child dyads. Child Abuse Neglect 2005;29:825–42. |
| 265Timmerman IGH, Emmelkamp PMG. The effects of cognitive-behavioral treatment for forensic inpatients. Int J Offender Ther Comp Criminol 2005;49:590–606. |
| 266Trappler B, Newville H. Trauma healing via cognitive behaviour therapy chronically hospitalized patients. Psychiatr Q 2007;78:317–25. |
| 103Tritt K, Nickel C, Lahmann C, Leiberich PK, Rother WK, Loew TH, et al. Lamotrigine treatment of aggression in female borderline-patients: a randomized, double-blind, placebo-controlled study. J Psychopharmacol 2005;19:287–91. |
| 108Tyrer P, Oliver-Africano PC, Ahmed Z, Bouras N, Cooray S, Deb S, et al. Risperidone, haloperidol, and placebo in the treatment of aggressive challenging behaviour in patients with intellectual disability: a randomised controlled trial. Lancet 2008;371:57–63. |
| 267Vaaler AE, Morken G, Flovig JC, Iversen VC, Linaker OM. Effects of a psychiatric intensive care unit in an acute psychiatric department. Nordic J Psychiatr 2006;60:144–9. |
| 268Van Den Eynde F, Senturk V, Naudts K, Vogels C, Bernagie K, Thas O, et al. Efficacy of quetiapine for impulsivity and affective symptoms in borderline personality disorder. J Clin Psychopharmacol 2008;28:147–55. |
| 269Van Nieuwenhuizen C. A treatment programme for sexually violent forensic psychiatric inpatients: development and first results. Psychol Crime Law 2005;11:467–77. |
| 102Vannoy SD. Evaluating the impact of a meditation curriculum on anger, hostility, and egoism with incarcerated adults. Dissertation Abstracts International. Section B: The Sciences and Engineering; 2006. |
| Linked paper 270Vannoy SD, Hoyt WT. Evaluation of an anger therapy intervention for incarcerated adult males. J Offend Rehabil 2004;39:39–57. |
| 76Villari V, Rocca P, Fonzo V, Montemagni C, Pandullo P, Bogetto F. Oral risperidone, olanzapine and quetiapine versus haloperidol in psychotic agitation. Progr Neuro Psychopharmacol Biol Psychiatr 2008;32:405–13. |
| 87Volavka J, Czobor P, Nolan K, Sheitman B, Lindenmayer JP, Citrome L, et al. Overt aggression and psychotic symptoms in patients with schizophrenia treated with clozapine, olanzapine, risperidone, or haloperidol. J Clin Psychopharmacol 2004;24:225–8. |
| 93Walsh E, Leese M, Byford S, Gilvarry C, Samele C, Tyrer P, et al. Do violent patients benefit from intensive case management? Schizophr Res 2002;53:234. |
| 271Webster SD, Akhtar S, Bowers LE, Mann RE, Rallings M, Marshall WL. The impact of the prison service sex offender treatment programme on minority ethnic offenders: a preliminary study. Psychol Crime Law 2004;10:113–24. |
| 272Williams F, Wakeling H, Webster S. A psychometric study of six self-report measures for use with sexual offenders with cognitive and social functioning deficits. Psychol Crime Law 2007;13:505–22. |
| 67Williamson P, Day A, Howells K, Bubner S, Jauncey S. Assessing offender readiness to change problems with anger. Psychol Crime Law 2003;9:295–307. |
| 273Willner P, Brace N, Phillips J. Assessment of anger coping skills in individuals with intellectual disabilities. J Intellect Disabil Res 2005;49:329–39. |
| 84Willner P, Jones J, Tams R, Green G. A randomized controlled trial of the efficacy of a cognitive-behavioural anger management group for clients with learning disabilities. J Appl Res Intellect Disabil 2002;15:224–35. |
| 274Willner P, Tomlinson S. Generalization of anger-coping skills from day-service to residential settings. J Appl Res Intellect Disabil 2007;20:553–62. |
| 275Wong SCP, Veen SV, Leis TA, Parrish H, Gu D, Liber EU, et al. Reintegrating seriously violent and personality-disordered offenders from a supermaximum security institution into the general offender population. Int J Offender Ther Comp Criminol 2005;49:362–75. |
| 276Wooldredge J. Convicting and incarcerating felony offenders of intimates assault and the odds of new assault charges. J Crim Justice 2007;35:379–89. |
| 277Yocum R, Anderson J, Davigo T, Lee S. Direct-supervision and remote-supervision jails: a comparative study of psychosocial factors. J Appl Soc Psychol 2006;36:1790–812. |
| 100Zanarini MC, Frankenburg FR, Parachini EA, Zanarini MC, Frankenburg FR, Parachini EA. A preliminary, randomized trial of fluoxetine, olanzapine, and the olanzapine-fluoxetine combination in women with borderline personality disorder. J Clin Psychiatr 2004;65:903–7. |
| 119Zanarini MC, Frankenburg FR, Zanarini MC, Frankenburg FR. Omega–3 fatty acid treatment of women with borderline personality disorder: a double-blind, placebo-controlled pilot study. Am J Psychiatry 2003;160:167–9. |
Appendix 3 Selection of data for meta-analyses
| Study ID | Line | Comparators | Outcome | Metric |
|---|---|---|---|---|
| Alexander 2004112 | I | Lorazepam vs haloperidol + promethazine | In physical restraints at 60 minutes | OR |
| II | Lorazepam vs haloperidol + promethazine | In physical restraints at 15 minutes | OR | |
| III | Lorazepam vs haloperidol + promethazine | In physical restraints at 30 minutes | OR | |
| IV | Lorazepam vs haloperidol + promethazine | In physical restraints at 120 minutes | OR | |
| Va | Lorazepam vs haloperidol + promethazine | In physical restraints at 240 minutes | OR | |
| Arango 2006113 | I | Oral zuclopenthixol vs depot zuclopenthixol | No. of months from baseline to first violent episode (M-OAS) | OR |
| II | Oral zuclopenthixol vs depot zuclopenthixol | Severity of violence (using M-OAS) | OR | |
| III | Oral zuclopenthixol vs depot zuclopenthixol | Violence during follow-up: yes/no (using M-OAS) | OR | |
| IV | Oral zuclopenthixol vs depot zuclopenthixol | Violence frequency (M-OAS) | OR | |
| Brodaty 2003139 | Risperidone vs placebo | Cohen-Mansfield Agitation Inventory – aggressive behaviour subscale | NSD | |
| Brown University 200689 | I | Aripiprazole vs placebo | STAXI – anger in | OR |
| II | Aripiprazole vs placebo | STAXI – anger control | OR | |
| III | Aripiprazole vs placebo | SCL-90-R aggressiveness/hostility subscale | OR | |
| IV | Aripiprazole vs placebo | STAXI – state anger | OR | |
| V | Aripiprazole vs placebo | STAXI – anger out | OR | |
| VI | Aripiprazole vs placebo | STAXI – trait anger | OR | |
| Cavanaugh 200781 | I | Dialectical psychoeducational workshop vs anger management workshop | STAXI – state anger feelings | OR |
| II | Dialectical psychoeducational workshop vs anger management workshop | STAXI – state anger verbal | OR | |
| III | Dialectical psychoeducational workshop vs anger management workshop | STAXI – state anger physical | OR | |
| IV | Dialectical psychoeducational workshop vs anger management workshop | STAXI – trait anger temperament | OR | |
| V | Dialectical psychoeducational workshop vs anger management workshop | STAXI – trait anger reactions | OR | |
| VI | Dialectical psychoeducational workshop vs anger management workshop | STAXI – anger expressions out | OR | |
| VII | Dialectical psychoeducational workshop vs anger management workshop | STAXI – anger expressions in | OR | |
| VIII | Dialectical psychoeducational workshop vs anger management workshop | STAXI – anger control out | OR | |
| IX | Dialectical psychoeducational workshop vs anger management workshop | STAXI – anger control in | OR | |
| X | Dialectical psychoeducational workshop vs anger management workshop | Risk of Eruptive Violence Scale | OR | |
| Chan 200698 | Fluoxetine or nortriptyline vs placebo | Present State Examination irritability | OR | |
| Citrome 2004107 | I | Combination therapy: (olanzapine or risperidone + divalproex sodium) vs monotherapy: (olanzapine or risperidone) + placebo | PANSS hostility: change to day 7 | OR |
| II | Combination therapy: (olanzapine or risperidone + divalproex sodium vs monotherapy: (olanzapine or risperidone + placebo | PANSS hostility: change to day 3: | OR | |
| III | Combination therapy: (olanzapine or risperidone) + divalproex sodium vs monotherapy: (olanzapine or risperidone + placebo | PANSS hostility: change to day 5: | OR | |
| IV | Combination therapy: (olanzapine or risperidone) + divalproex sodium vs monotherapy: (olanzapine or risperidone) + placebo | PANSS hostility: change to day 14 | OR | |
| V | Combination therapy: (olanzapine or risperidone) + divalproex sodium vs monotherapy: (olanzapine or risperidone) + placebo | PANSS hostility: change to day 10 | OR | |
| VI | Combination therapy: (olanzapine or risperidone) + divalproex sodium vs monotherapy: (olanzapine or risperidone) + placebo | PANSS Hostility: change to day 21 | OR | |
| VII | Monotherapy: (olanzapine or risperidone) + placebo vs combination therapy: (olanzapine or risperidone) + divalproex sodium | PANSS Hostility: change to day 28 | OR | |
| Clarkin 200768 | DBT vs transference focused psychotherapy | NSD | ||
| Cooper 200690 | Ia | Violence Intervention Program vs standard medical treatment | Convicted for violent crime | OR |
| II | Violence Intervention Program vs standard medical treatment | Ever arrested violent crime | OR | |
| Duggan 2007114 | I | Healthy Families Alaska Program – positive parenting, etc. vs TAU | CTS – extreme physical punishment | OR |
| II | Healthy Families Alaska Program – positive parenting, etc. vs TAU | CTS – corporal/verbal punishment | OR | |
| III | Healthy Families Alaska Program – positive parenting, etc. vs TAU | CTS – hit with object | OR | |
| IV | Healthy Families Alaska Program – positive parenting, etc. vs TAU | CTS – severe assault | OR | |
| V | Healthy Families Alaska Program – positive parenting, etc. vs TAU | CTS – common corporal punishment | OR | |
| VI | Healthy Families Alaska Program – positive parenting, etc. vs TAU | CTS – mild physical assault | OR | |
| VII | Healthy Families Alaska Program – positive parenting, etc. vs TAU | CT – psychological aggression | OR | |
| Easton 2005110 | CBT substance abuse program vs twelve-step facilitation | CTS – physical | OR | |
| Easton 2007111 | I | Substance Abuse Domestic Violence Group vs twelve-step facilitation | CTS – physical violence frequency at 12 weeks | OR |
| II | Substance Abuse Domestic Violence Group vs twelve-step facilitation | CTS – physical violence % at 12 weeks | OR | |
| III | Substance Abuse Domestic Violence Group vs twelve-step facilitation group | CTS – physical violence frequency at 6 months | OR | |
| Frankenburg 2002106 | I | Divalproex vs placebo | SCL-90 anger/hostility subscale | OR |
| II | Divalproex vs placebo | M-OAS | OR | |
| Galovski 200269 | Cognitive behavioural psychological intervention vs self-monitoring of symptoms only | NSD | ||
| Gottfredson 200292 | Baltimore Drug Treatment Court vs TAU | % with violent or sex charge at 1 year | OR | |
| Hollander 200391 | Divalproex vs placebo | M-OAS (median) | OR | |
| Houston 200670 | NSD | |||
| Huf 200372 | Midazolam vs haloperidol + promethazine | % not needing restraints at 120 minutes | RR | |
| Midazolam vs haloperidol + promethazine | % no further aggression at 24 hours | RR | ||
| Huf 200773 | Haloperidol vs haloperidol plus promethazine | No other episodes of aggression at 24 hours | RR | |
| Haloperidol vs haloperidol plus promethazine | Restraints not needed at 120 minutes | RR | ||
| Krakowski 200682 | I | Clozapine vs haloperidol | M-OAS physical aggression | OR |
| II | Clozapine vs olanzapine | M-OAS physical aggression | OR | |
| III | Olanzapine vs haloperidol | M-OAS physical aggression | OR | |
| IV | Clozapine vs haloperidol | M-OAS verbal aggression | OR | |
| V | Clozapine vs olanzapine | M-OAS verbal aggression | OR | |
| VI | Olanzapine vs haloperidol | M-OAS verbal aggression | OR | |
| Labriola 200894 | I | Batterer programme vs no TAU | Any rearrest for domestic violence at 1-year post-sentence | OR |
| II | Batterer programme vs no TAU | Any rearrest for domestic violence at 18-months post-sentence | OR | |
| III | Batterer programme vs no TAU | Any rearrest for domestic violence at 1-year post-monitoring | OR | |
| IV | Batterer programme vs no TAU | Victim report of any type of new abuse | OR | |
| V | Batterer programme vs no TAU | Victim report new physical abuse | OR | |
| VI | Batterer programme vs no TAU | Victim report new threats | OR | |
| VII | Batterer programme vs no TAU | Victim report other abuse | OR | |
| VIII | Monthly monitoring vs graduated monitoring | Any rearrest for domestic violence at 1-year post-sentence | OR | |
| IX | Monthly monitoring vs graduated monitoring | Any rearrest for domestic violence at 18-months post-sentence | OR | |
| X | Monthly monitoring vs graduated monitoring | Any rearrest for domestic violence at 1-year post-monitoring | OR | |
| XI | Monthly monitoring vs graduated monitoring | Victim report of any type of new abuse | OR | |
| XII | Monthly monitoring vs graduated monitoring | Victim report new physical abuse | OR | |
| XIII | Monthly monitoring vs graduated monitoring | Victim report new threats | OR | |
| XIV | Monthly monitoring vs graduated monitoring | Victim report other abuse | OR | |
| Lanza 200286 | I | CBT group vs psychodynamic group psychotherapy | Monthly STAXI trait anger change | OR |
| II | CBT group vs psychodynamic group psychotherapy | OAS | OR | |
| III | CBT group vs psychodynamic group psychotherapy | Weekly STAXI anger control change | OR | |
| IV | CBT group vs psychodynamic group psychotherapy | Weekly STAXI state anger change | OR | |
| Lasley 200383 | Intensive bail supervision vs regular bail supervision | Repeat DV offending | OR | |
| Levesque 2005200 | I | Computerised stage-matched intervention for DV offenders adjunctive to traditional batterer programme vs traditional batterer programme | Beat up partner | NSD |
| II | Computerised stage-matched intervention for DV offenders adjunctive to traditional batterer programme vs traditional batterer programme | Slapped | NSD | |
| III | Computerised stage-matched intervention for DV offenders adjunctive to traditional batterer programme vs traditional batterer programme | Physical aggression | NSD | |
| IV | Computerised stage-matched intervention for DV offenders adjunctive to traditional batterer programme vs traditional batterer programme | Psychological aggression | NSD | |
| Liau 2004115 | Psychoeducational component of the EQUIP program vs EQUIP without psychoeducational component | Self-reported aggression | OR | |
| Linehan 2008116 | I | DBT plus olanzapine vs DBT plus placebo | OAS – irritability | OR |
| II | DBT plus olanzapine vs DBT plus placebo | OAS – physical aggression | OR | |
| III | DBT plus olanzapine vs DBT plus placebo | OAS – verbal aggression | OR | |
| Loew 2006117 | Topiramate vs placebo | SCL-90 hostility subscale | OR | |
| MacKenzie 200795 | Boot camp vs prison | STAXI | OR | |
| Marques 200574 | I | Relapse prevention vs volunteer control | Sexual reoffence | NSD |
| II | Relapse prevention vs non-volunteer control | Sexual reoffence | NSD | |
| III | Relapse prevention vs volunteer control | Violent reoffence | NSD | |
| IV | Relapse prevention vs non-volunteer control | Violent reoffence | NSD | |
| Mattes 200596 | I | Oxcarbazepine vs placebo | Change in BPRS hostility rating | OR |
| II | Oxcarbazepine vs placebo | M-OAS – global (change in score) | OR | |
| IV | Oxcarbazepine vs placebo | M-OAS verbal aggression (change in score) | OR | |
| VI | Oxcarbazepine vs placebo | M-OAS – assault against others (change in score) | OR | |
| Meehan 2002109 | I | Olanzapine (5 mg) vs placebo | Change PANSS hostility item: 2 hours | OR |
| II | Lorazepam vs placebo | Change PANSS hostility item: 2 hours | OR | |
| III | Olanzapine (2.5 mg) vs placebo | Change PANSS hostility item: 2 hours | OR | |
| Mitchell 200677 | Boot camp vs traditional correctional facility | Self-control scale – temper | Linked with MacKenzie95 | |
| Monnelly 200385 | Risperidone vs placebo | M-OAS – aggression subscale | OR | |
| New 200497 | Fluoxetine vs placebo | OAS – aggression | OR | |
| Nickel 2004104 | I | Topiramate vs placebo | STAXI – anger control | OR |
| II | Topiramate vs placebo | STAXI – anger out | OR | |
| III | Topiramate vs placebo | STAXI – state anger | OR | |
| IV | Topiramate vs placebo | STAXI – trait anger | OR | |
| V | Topiramate vs placebo | STAXI – anger in | OR | |
| Nickel 200588 | I | Topiramate vs placebo | Anger symptoms – anger in | OR |
| II | Topiramate vs placebo | Anger symptoms – anger control | OR | |
| III | Topiramate vs placebo | Anger symptoms – anger out | OR | |
| IV | Topiramate vs placebo | Anger symptoms – state anger | OR | |
| V | Topiramate vs placebo | Anger symptoms – trait anger | OR | |
| Nickel 2005105 | I | Topiramate vs placebo | Anger symptoms – anger control | OR |
| II | Topiramate vs placebo | Anger symptoms – anger in | OR | |
| III | Topiramate vs placebo | Anger symptoms – anger out | OR | |
| IV | Topiramate vs placebo | Anger symptoms – state anger | OR | |
| V | Topiramate vs placebo | Anger symptoms – trait anger | OR | |
| Raveendran 200775 | I | Olanzapine vs haloperidol plus promethazine | In restraints at 120 minutes | RR |
| II | Olanzapine vs haloperidol plus promethazine | In restraints at 15 minutes | RR | |
| III | Olanzapine vs haloperidol plus promethazine | In restraints at 240 minutes | RR | |
| IV | Olanzapine vs haloperidol plus promethazine | In restraints at 30 minutes | RR | |
| V | Olanzapine vs haloperidol plus promethazine | In restraints at 60 minutes | RR | |
| Rinne 200299 | Fluvoxamine vs placebo | Borderline Personality Disorder Severity Index – anger subscale | OR | |
| Soler 2005118 | DBT plus olanzapine vs DBT plus placebo | Impulsivity/aggressive behaviour (bi-weekly reports) | OR | |
| Suh 2004101 | I | Risperidone vs haloperidol | Cohen-Mansfield Agitation Inventory – aggressive behaviour subscale | OR |
| II | Risperidone vs haloperidol | Behavioural Pathology in Alzheimer’s Disease Rating Scale – aggressiveness subscale | OR | |
| Theall 200771 | Four-session motivated focused condition vs four-session negotiation-focused condition (TAU) National Institute on Drug Abuse (NIDA) | NSD | ||
| Tritt 2005103 | I | Lamotrigine vs placebo | STAXI – anger control | OR |
| II | Lamotrigine vs placebo | STAXI – anger out | OR | |
| III | Lamotrigine vs placebo | STAXI – state anger | OR | |
| IV | Lamotrigine vs placebo | STAXI – trait anger | OR | |
| V | Lamotrigine vs placebo | STAXI – anger in | OR | |
| Tyrer 2008108 | I | Risperidone vs placebo | M-OAS 4 weeks | OR |
| II | Haloperidol vs placebo | M-OAS 4 weeks | OR | |
| III | Risperidone or haloperidol vs placebo | M-OAS 4 weeks | OR | |
| Vannoy 2006102 | RCTI | Anger control based on Buddhist meditation vs TAU | STAXI anger (males) 1-week post-treatment | OR |
| RCTII | Anger control based on Buddhist meditation vs TAU | AQ anger (males) 1-week post-treatment | OR | |
| RCTIII | Anger control based on Buddhist meditation vs TAU | AQ hostility (males) 1-week post-treatment | OR | |
| RCTIV | Anger control based on Buddhist meditation vs TAU | CM hostility (males) 1-week post-treatment | OR | |
| RCTV | Anger control based on Buddhist meditation vs TAU | STAXI anger (females) 1-week post-treatment | OR | |
| RCTVI | Anger control based on Buddhist meditation vs TAU | AQ anger (females) 1-week post-treatment | OR | |
| RCTVII | Anger control based on Buddhist meditation vs TAU | AQ hostility (females) 1-week post-treatment | OR | |
| RCTVIII | Anger control based on Buddhist meditation vs TAU | CM hostility (females) 1-week post-treatment | OR | |
| RCTIX | Anger control based on Buddhist meditation vs TAU | STAXI anger (males) 10-weeks post-treatment | OR | |
| RCTX | Anger control based on Buddhist meditation vs TAU | AQ anger (males) 10-weeks post-treatment | OR | |
| RCTXI | Anger control based on Buddhist meditation vs TAU | AQ hostility (males) 10-weeks post-treatment | OR | |
| RCTXII | Anger control based on Buddhist meditation vs TAU | CM hostility (Males) 10-weeks post-treatment | OR | |
| RCTXIII | Anger control based on Buddhist meditation vs TAU | STAXI anger (females) 10-weeks post-treatment | OR | |
| RCTIX | Anger control based on Buddhist meditation vs TAU | AQ anger (females) 10-weeks post-treatment | OR | |
| RCTXV | Anger control based on Buddhist meditation vs TAU | AQ hostility (Females) 10-weeks post-treatment | OR | |
| RCTXVI | Anger control based on Buddhist meditation vs TAU | CM hostility (Females) 10-weeks post-treatment | OR | |
| Villari 200876 | I | Risperidone vs olanzapine | BPRS hostility | NSD |
| II | Risperidone vs quetiapine | BPRS hostility | NSD | |
| III | Risperidone vs haloperidol | BPRS hostility | NSD | |
| IV | Olanzapine vs quetiapine | BPRS hostility | NSD | |
| V | Olanzapine vs haloperidol | BPRS hostility | NSD | |
| VI | Quetiapine vs haloperidol | BPRS hostility | NSD | |
| VII | Risperidone vs olanzapine | M-OAS verbal aggression | NSD | |
| VIII | Risperidone vs quetiapine | M-OAS verbal aggression | NSD | |
| IX | Risperidone vs haloperidol | M-OAS verbal aggression | NSD | |
| X | Olanzapine vs quetiapine | M-OAS verbal aggression | NSD | |
| XI | Olanzapine vs haloperidol | M-OAS verbal aggression | NSD | |
| XII | Quetiapine vs haloperidol | M-OAS verbal aggression | NSD | |
| XIII | Risperidone vs olanzapine | M-OAS physical aggression | NSD | |
| XIV | Risperidone vs quetiapine | M-OAS physical aggression | NSD | |
| XV | Risperidone vs haloperidol | M-OAS physical aggression | NSD | |
| XVI | Olanzapine vs quetiapine | M-OAS physical aggression | NSD | |
| XVII | Olanzapine vs haloperidol | M-OAS physical aggression | NSD | |
| XVIII | Quetiapine vs haloperidol | M-OAS physical aggression | NSD | |
| XIX | Risperidone or olanzapine or quetiapine vs haloperidol | BPRS hostility | NSD | |
| XX | Risperidone or olanzapine or quetiapine vs haloperidol | M-OAS verbal aggression | NSD | |
| XXI | Risperidone or olanzapine or quetiapine vs haloperidol | M-OAS physical aggression | NSD | |
| Volavka 200487 | I | Clozapine vs olanzapine | Incident of aggression during 14-week study (OAS) | OR |
| II | Clozapine vs risperidone | Incident of aggression during 14-week study (OAS) | OR | |
| III | Clozapine vs haloperidol | Incident of aggression during 14-week study (OAS) | OR | |
| IV | Olanzapine vs risperidone | Incident of aggression during 14-week study (OAS) | OR | |
| V | Olanzapine vs haloperidol | Incident of aggression during 14-week study (OAS) | OR | |
| VI | Risperidone vs haloperidol | Incident of aggression during 14-week study (OAS) | OR | |
| VII | Clozapine vs olanzapine | Incident of aggression during 14-week study (OAS) | OR | |
| VIII | Clozapine vs risperidone | Incident of aggression during 14-week study (OAS) | OR | |
| IX | Clozapine vs haloperidol | Incident of aggression during 14-week study (OAS) | OR | |
| X | Olanzapine vs risperidone | Incident of aggression during days 25–98 of study (OAS) | OR | |
| XI | Olanzapine vs haloperidol | Incident of aggression during days 25–98 of study (OAS) | OR | |
| XII | Risperidone vs haloperidol | Incident of aggression during days 25–98 of study (OAS) | OR | |
| Walsh 200293 | Intensive care management vs standard care | More assaults | OR | |
| Willner 200284 | I | CB anger management vs WL | Anger Inventory – client ratings | OR |
| II | CB anger management vs WL | Composite score of anger inventory and provocation index both clients and carers | OR | |
| III | CB anger management vs WL | Composite score of anger inventory and provocation index clients ratings | OR | |
| IV | CB anger management vs WL | Provocation Index – client ratings | OR | |
| V | CB anger management vs WL | Composite score of anger inventory and provocation index carer ratings | OR | |
| VI | CB anger management vs WL | Provocation Index – carer ratings | OR | |
| VII | CB anger management vs WL | Anger Inventory – carer ratings | OR | |
| Zanarini 2003119 | Ethyl-eicosapentaenoic acid vs placebo | M-OAS | OR | |
| Zanarini 2004100 | I | Olanzapine vs fluoxetine | OAS (change) | OR |
| II | Olanzapine vs olanzapine + fluoxetine combined | OAS (change) | OR | |
| III | Fluoxetine vs olanzapine + fluoxetine combined | OAS (change) | OR |
Appendix 4 Selection of data for meta-analyses
| Study ID | MA overall | MA head to head | MA active vs TAU | MA active vs true | MA all pharma | MA all psych | MA all other | MA anticonvulsant drugs | MA SSRI | MA atypical | MA CBT | MA model 1 | MA model 2 | MA model 3 | MA model 4 | MA model 5 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alexander 2004112 | Yes | Yes | Yes | |||||||||||||
| Arango 2006113 | Yes | Yes | Yes | Yes | ||||||||||||
| Brown University 200689 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Cavanaugh 200781 | Yes | Yes | Yes | |||||||||||||
| Chan 2006150 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Citrome 2004107 | Yes | Yes | Yes | Yes | ||||||||||||
| Cooper 200690 | Yes | Yes | Yes | |||||||||||||
| Duggan 2007114 | Yes | Yes | Yes | |||||||||||||
| Easton 2005110 | Yes | Yes | Yes | Yes | ||||||||||||
| Easton 2007111 | Yes | Yes | Yes | Yes | ||||||||||||
| Frankenburg 2002106 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Gottfredson 200292 | Yes | Yes | Yes | |||||||||||||
| Hollander 200391 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Krakowski 200682 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Labriola 200894 | Yes | Yes | Yes | |||||||||||||
| Lanza 200286 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Lasley 200383 | Yes | Yes | Yes | |||||||||||||
| Liau 2004115 | Yes | Yes | Yes | Yes | ||||||||||||
| Linehan 2008116 | Yes | Yes | Yes | Yes | ||||||||||||
| Loew 2006117 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| MacKenzie 200795 | Yes | Yes | Yes | |||||||||||||
| Mattes 200596 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Meehan 2002109 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Monnelly 200385 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| New 200497 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Nickel 2004104 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Nickel 200588 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Nickel 2005105 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Rinne 200299 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Soler 2005118 | Yes | Yes | Yes | Yes | ||||||||||||
| Suh 2004101 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Tritt 2005103 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Tyrer 2008108 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Vannoy 2006102 | Yes | Yes | Yes | Yes | ||||||||||||
| Vannoy 2006102 | Yes | Yes | Yes | Yes | ||||||||||||
| Volavka 200487 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Walsh 200293 | Yes | Yes | Yes | |||||||||||||
| Willner 2002274 | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Zanarini 2003119 | Yes | Yes | Yes | Yes | ||||||||||||
| Zanarini 2004100 | Yes | Yes | Yes | Yes | Yes | Yes |
Appendix 5 Modifier data for meta-analyses
| Study ID | Primary focus | Specific focus | Population | Scale | Sex | Start setting | Start n | Blinding | |
|---|---|---|---|---|---|---|---|---|---|
| Arm A | Arm B | ||||||||
| MacKenzie 200795 | Other | Boot camp | TAU | Offend | Yes | Male | Prison | 234 | No/ns |
| Gottfredson 200292 | Other | Drug court | TAU | Offend | No | Mix | Commun | 235 | No/ns |
| Lasley 200383 | Other | Intensive monitoring | Active | Offend | No | Female | Othmix | 552 | No/ns |
| Walsh 200293 | Other | Intensive | TAU | Mental | No | 122 | No/ns | ||
| Labriola 200894 | Other | Monthly monitoring | Active | Offend | No | Male | Commun | 420 | No/ns |
| Cooper 200690 | Other | Intervention programme | TAU | Offend | No | Mix | Commun | 100 | No/ns |
| Vannoy 2006102 | Other | Meditation | TAU | Offend | Yes | Male | Prison | 11 | No/ns |
| Vannoy 2006102 | Other | Meditation | TAU | Offend | Yes | Female | Prison | 21 | No/ns |
| Loew 2006117 | Pharma | Anticonvulsant | Placebo | Mental | Yes | Female | 56 | Yes | |
| Frankenburg 2002106 | Pharma | Anticonvulsant | Placebo | Mental | Yes | Female | Commun | 30 | Yes |
| Hollander 200391 | Pharma | Anticonvulsant | Placebo | Mental | Yes | Mix | Commun | 246 | Yes |
| Nickel 2004109 | Pharma | Anticonvulsant | Placebo | Mental | Yes | Female | Commun | 31 | Yes |
| Nickel 200568 | Pharma | Anticonvulsant | Placebo | Mental | Yes | Female | Commun | 64 | Yes |
| Nickel 2005105 | Pharma | Anticonvulsant | Placebo | Mental | Yes | Male | Commun | 44 | Yes |
| Tritt 2005103 | Pharma | Anticonvulsant | Placebo | Mental | Yes | Female | Commun | 27 | Yes |
| Mattes 200596 | Pharma | Anticonvulsant | Placebo | Mental | Yes | Mix | Othmix | 48 | Yes |
| New 200497 | Pharma | Antidepressant | Placebo | Mental | Yes | Mix | Commun | 20 | Yes |
| Chan 2006150 | Pharma | Antidepressant | Placebo | Mental | Yes | Mix | Open | 92 | Yes |
| Rinne 200299 | Pharma | Antidepressant | Placebo | Mental | Yes | Female | Othmix | 38 | Yes |
| Citrome 2004107 | Pharma | Atypical antipsychotic | Active | Mental | Yes | Mix | 249 | Yes | |
| Krakowski 200682 | Pharma | Atypical antipsychotic | Active | Mental | Yes | Mix | 110 | Yes | |
| Suh 2004101 | Pharma | Atypical antipsychotic | Active | Mental | Yes | Mix | Othmix | 120 | Yes |
| Brown University 200689 | Pharma | Atypical antipsychotic | Placebo | Mental | Yes | Mix | Commun | 52 | Yes |
| Tyrer 2008108 | Pharma | Atypical antipsychotic | Placebo | Mental | Yes | Mix | Commun | 86 | Yes |
| Zanarini 2004100 | Pharma | Atypical antipsychotic | Placebo | Mental | Yes | Female | Commun | 45 | Yes |
| Volavka 200487 | Pharma | Atypical antipsychotic | Placebo | Mental | Yes | Mix | Open | 167 | Yes |
| Meehan 2002109 | Pharma | Atypical antipsychotic | Placebo | Mental | Yes | Mix | Othmix | 272 | Yes |
| Monnelly 200385 | Pharma | Atypical antipsychotic | Placebo | Mental | Yes | Male | Othmix | 16 | Yes |
| Soler 2005118 | Psych | Atypical antipsychotic | Placebo | Mental | Yes | Mix | 60 | Yes | |
| Linehan 2008116 | Psych | Atypical antipsychotic | Placebo | Mental | Yes | Female | Commun | 44 | Yes |
| Alexander 2004112 | Pharma | Benzodiazepine | Active | Mental | No | Mix | Othmix | 200 | No/ns |
| Zanarini 2003119 | Pharma | E-EPA | Placebo | Mental | Yes | Female | Commun | 30 | Yes |
| Arango 2006113 | Pharma | Typical antipsychotic | Active | Mental | Yes | Mix | Open | 46 | Yes |
| Lanza 200286 | Psych | CBT | Active | Mental | Yes | Male | Othmix | 42 | No/ns |
| Easton 2005110 | Psych | CBT | Active | Offend | Yes | Male | Othmix | 64 | No/ns |
| Easton 2007111 | Psych | CBT | Active | Indict | Yes | Male | Commun | 78 | No/ns |
| Willner 2002274 | Psych | CBT | Wait list | Mental | Yes | Mix | Commun | 16 | No/ns |
| Duggan 2007114 | Other | CBT | TAU | Indict | Yes | Female | Commun | 325 | Yes |
| Cavanaugh 200781 | Psych | DiaPsyEd | Active | Indict | Yes | Male | Commun | 55 | No/ns |
| Liau 2004115 | Psych | PsyEd EQUIP | Active | Offend | No | Mix | Commun | 316 | No/ns |
Appendix 6 Protocol
List of abbreviations
- A&E
- accident and emergency
- BCS
- British Crime Survey
- BIP
- Batterer Intervention Programme
- BPD
- borderline personality disorder
- CBT
- cognitive behavioural therapy
- CI
- confidence interval
- CTS
- Conflict Tactics Scale
- df
- degrees of freedom
- DV
- domestic violence
- ITT
- intention to treat
- LiVio
- Liverpool Violence Research Group
- MA
- meta-analysis
- M-OAS
- Modified Overt Aggression Scale
- NICE
- National Institute for Health and Clinical Excellence
- OAS
- Overt Aggression Scale
- OR
- odds ratio
- RCT
- randomised controlled trial
- RR
- relative risk
- SD
- standard deviation
- SE
- standard error
- SSRI
- selective serotonin reuptake inhibitor
- STAXI
- State-Trait Anger Inventory
- TAU
- treatment as usual
- WL
- waiting list control
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
Prioritisation Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Imti Choonara, Professor in Child Health, Academic Division of Child Health, University of Nottingham
Chair – Pharmaceuticals Panel
-
Dr Bob Coates, Consultant Advisor – Disease Prevention Panel
-
Dr Andrew Cook, Consultant Advisor – Intervention Procedures Panel
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Dr Nick Hicks, Consultant Adviser – Diagnostic Technologies and Screening Panel, Consultant Advisor–Psychological and Community Therapies Panel
-
Ms Susan Hird, Consultant Advisor, External Devices and Physical Therapies Panel
-
Professor Sallie Lamb, Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick
Chair – HTA Clinical Evaluation and Trials Board
-
Professor Jonathan Michaels, Professor of Vascular Surgery, Sheffield Vascular Institute, University of Sheffield
Chair – Interventional Procedures Panel
-
Professor Ruairidh Milne, Director – External Relations
-
Dr John Pounsford, Consultant Physician, Directorate of Medical Services, North Bristol NHS Trust
Chair – External Devices and Physical Therapies Panel
-
Dr Vaughan Thomas, Consultant Advisor – Pharmaceuticals Panel, Clinical
Lead – Clinical Evaluation Trials Prioritisation Group
-
Professor Margaret Thorogood, Professor of Epidemiology, Health Sciences Research Institute, University of Warwick
Chair – Disease Prevention Panel
-
Professor Lindsay Turnbull, Professor of Radiology, Centre for the MR Investigations, University of Hull
Chair – Diagnostic Technologies and Screening Panel
-
Professor Scott Weich, Professor of Psychiatry, Health Sciences Research Institute, University of Warwick
Chair – Psychological and Community Therapies Panel
-
Professor Hywel Williams, Director of Nottingham Clinical Trials Unit, Centre of Evidence-Based Dermatology, University of Nottingham
Chair – HTA Commissioning Board
Deputy HTA Programme Director
HTA Commissioning Board
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
-
Department of Public Health and Epidemiology, University of Birmingham
-
Professor of Clinical Pharmacology, Director, NIHR HTA programme, University of Liverpool
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Peter Brocklehurst, Professor of Women’s Health, Institute for Women’s Health, University College London
-
Professor Jenny Donovan, Professor of Social Medicine, University of Bristol
-
Professor Jonathan Green, Professor and Acting Head of Department, Child and Adolescent Psychiatry, University of Manchester Medical School
-
Professor John W Gregory, Professor in Paediatric Endocrinology, Department of Child Health, Wales School of Medicine, Cardiff University
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Freddie Hamdy, Professor of Urology, Head of Nuffield Department of Surgery, University of Oxford
-
Professor Allan House, Professor of Liaison Psychiatry, University of Leeds
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor Irwin Nazareth, Professor of Primary Care and Head of Department, Department of Primary Care and Population Sciences, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norrie, Chair in Clinical Trials and Biostatistics, Robertson Centre for Biostatistics, University of Glasgow
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Martin Underwood, Professor of Primary Care Research, Warwick Medical School, University of Warwick
-
Professor Marion Walker, Professor in Stroke Rehabilitation, Associate Director UK Stroke Research Network, University of Nottingham
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Dr Tom Foulks, Medical Research Council
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
HTA Clinical Evaluation and Trials Board
-
Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick and Professor of Rehabilitation, Nuffield Department of Orthopaedic, Rheumatology and Musculoskeletal Sciences, University of Oxford
-
Professor of the Psychology of Health Care, Leeds Institute of Health Sciences, University of Leeds
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Keith Abrams, Professor of Medical Statistics, Department of Health Sciences, University of Leicester
-
Professor Martin Bland, Professor of Health Statistics, Department of Health Sciences, University of York
-
Professor Jane Blazeby, Professor of Surgery and Consultant Upper GI Surgeon, Department of Social Medicine, University of Bristol
-
Professor Julia M Brown, Director, Clinical Trials Research Unit, University of Leeds
-
Professor Alistair Burns, Professor of Old Age Psychiatry, Psychiatry Research Group, School of Community-Based Medicine, The University of Manchester & National Clinical Director for Dementia, Department of Health
-
Dr Jennifer Burr, Director, Centre for Healthcare Randomised trials (CHART), University of Aberdeen
-
Professor Linda Davies, Professor of Health Economics, Health Sciences Research Group, University of Manchester
-
Professor Simon Gilbody, Prof of Psych Medicine and Health Services Research, Department of Health Sciences, University of York
-
Professor Steven Goodacre, Professor and Consultant in Emergency Medicine, School of Health and Related Research, University of Sheffield
-
Professor Dyfrig Hughes, Professor of Pharmacoeconomics, Centre for Economics and Policy in Health, Institute of Medical and Social Care Research, Bangor University
-
Professor Paul Jones, Professor of Respiratory Medicine, Department of Cardiac and Vascular Science, St George‘s Hospital Medical School, University of London
-
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, Queen Mary, University of London
-
Professor Richard J McManus, Professor of Primary Care Cardiovascular Research, Primary Care Clinical Sciences Building, University of Birmingham
-
Professor Helen Rodgers, Professor of Stroke Care, Institute for Ageing and Health, Newcastle University
-
Professor Ken Stein, Professor of Public Health, Peninsula Technology Assessment Group, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Jonathan Sterne, Professor of Medical Statistics and Epidemiology, Department of Social Medicine, University of Bristol
-
Mr Andy Vail, Senior Lecturer, Health Sciences Research Group, University of Manchester
-
Professor Clare Wilkinson, Professor of General Practice and Director of Research North Wales Clinical School, Department of Primary Care and Public Health, Cardiff University
-
Dr Ian B Wilkinson, Senior Lecturer and Honorary Consultant, Clinical Pharmacology Unit, Department of Medicine, University of Cambridge
-
Ms Kate Law, Director of Clinical Trials, Cancer Research UK
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, University of Manchester
-
Mr Angus S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital, Birmingham
-
Dr Diana Baralle, Consultant and Senior Lecturer in Clinical Genetics, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Diane Eccles, Professor of Cancer Genetics, Wessex Clinical Genetics Service, Princess Anne Hospital
-
Dr Trevor Friedman, Consultant Liason Psychiatrist, Brandon Unit, Leicester General Hospital
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Public contributor
-
Professor Anthony Robert Kendrick, Associate Dean for Clinical Research and Professor of Primary Medical Care, University of Southampton
-
Dr Nicola Lennard, Senior Medical Officer, MHRA
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee, London
-
Mr David Mathew, Public contributor
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mrs Una Rennard, Public contributor
-
Dr Stuart Smellie, Consultant in Clinical Pathology, Bishop Auckland General Hospital
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr Allison Streetly, Programme Director, NHS Sickle Cell and Thalassaemia Screening Programme, King’s College School of Medicine
-
Dr Matthew Thompson, Senior Clinical Scientist and GP, Department of Primary Health Care, University of Oxford
-
Dr Alan J Williams, Consultant Physician, General and Respiratory Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Joanna Jenkinson, Board Secretary, Neurosciences and Mental Health Board (NMHB), Medical Research Council
-
Professor Julietta Patrick, Director, NHS Cancer Screening Programme, Sheffield
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Disease Prevention Panel
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook, Clinical Programmes Director, Bazian Ltd, London
-
Dr Colin Greaves, Senior Research Fellow, Peninsula Medical School (Primary Care)
-
Mr Michael Head, Public contributor
-
Professor Cathy Jackson, Professor of Primary Care Medicine, Bute Medical School, University of St Andrews
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Julie Mytton, Consultant in Child Public Health, NHS Bristol
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Dr Richard Richards, Assistant Director of Public Health, Derbyshire County Primary Care Trust
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Dr Kenneth Robertson, Consultant Paediatrician, Royal Hospital for Sick Children, Glasgow
-
Dr Catherine Swann, Associate Director, Centre for Public Health Excellence, NICE
-
Mrs Jean Thurston, Public contributor
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust
-
Reader in Wound Healing and Director of Research, University of Leeds
-
Professor Bipin Bhakta, Charterhouse Professor in Rehabilitation Medicine, University of Leeds
-
Mrs Penny Calder, Public contributor
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol
-
Mrs Anthea De Barton-Watson, Public contributor
-
Professor Nadine Foster, Professor of Musculoskeletal Health in Primary Care Arthritis Research, Keele University
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester
-
Professor Christine Norton, Professor of Clinical Nursing Innovation, Bucks New University and Imperial College Healthcare NHS Trust
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham
-
Dr Kate Radford, Senior Lecturer (Research), University of Central Lancashire
-
Mr Jim Reece, Public contributor
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton
-
Dr Pippa Tyrrell, Senior Lecturer/Consultant, Salford Royal Foundation Hospitals’ Trust and University of Manchester
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Interventional Procedures Panel
-
Professor of Vascular Surgery, University of Sheffield
-
Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Mrs Isabel Boyer, Public contributor
-
Mr Sankaran Chandra Sekharan, Consultant Surgeon, Breast Surgery, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Ms Leonie Cooke, Public contributor
-
Mr Seumas Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor Sam Eljamel, Consultant Neurosurgeon, Ninewells Hospital and Medical School, Dundee
-
Dr Adele Fielding, Senior Lecturer and Honorary Consultant in Haematology, University College London Medical School
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Fiona Lecky, Senior Lecturer/Honorary Consultant in Emergency Medicine, University of Manchester/Salford Royal Hospitals NHS Foundation Trust
-
Dr Nadim Malik, Consultant Cardiologist/Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Professor Jon Moss, Consultant Interventional Radiologist, North Glasgow Hospitals University NHS Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Dr Matthew Wilson, Consultant Anaesthetist, Sheffield Teaching Hospitals NHS Foundation Trust
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Dr Martin Ashton-Key, Medical Advisor, National Commissioning Group, NHS London
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr James Gray, Consultant Microbiologist, Department of Microbiology, Birmingham Children’s Hospital NHS Foundation Trust
-
Dr Jurjees Hasan, Consultant in Medical Oncology, The Christie, Manchester
-
Dr Carl Heneghan, Deputy Director Centre for Evidence-Based Medicine and Clinical Lecturer, Department of Primary Health Care, University of Oxford
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Maria Kouimtzi, Pharmacy and Informatics Director, Global Clinical Solutions, Wiley-Blackwell
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Ms Amanda Roberts, Public contributor
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Professor Donald Singer, Professor of Clinical Pharmacology and Therapeutics, Clinical Sciences Research Institute, CSB, University of Warwick Medical School
-
Mr David Symes, Public contributor
-
Dr Arnold Zermansky, General Practitioner, Senior Research Fellow, Pharmacy Practice and Medicines Management Group, Leeds University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick, Coventry
-
Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Public contributor
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Peter Langdon, Senior Clinical Lecturer, School of Medicine, Health Policy and Practice, University of East Anglia
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician and Cardiologist, County Durham and Darlington Foundation Trust
-
Dr Richard Neal, Clinical Senior Lecturer in General Practice, Cardiff University
-
Mr John Needham, Public contributor
-
Ms Mary Nettle, Mental Health User Consultant
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry and Warwickshire Partnership Trust
-
Dr Lesley Stockton, Lecturer, School of Health Sciences, University of Liverpool
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Expert Advisory Network
-
Professor Douglas Altman, Professor of Statistics in Medicine, Centre for Statistics in Medicine, University of Oxford
-
Professor John Bond, Professor of Social Gerontology & Health Services Research, University of Newcastle upon Tyne
-
Professor Andrew Bradbury, Professor of Vascular Surgery, Solihull Hospital, Birmingham
-
Mr Shaun Brogan, Chief Executive, Ridgeway Primary Care Group, Aylesbury
-
Mrs Stella Burnside OBE, Chief Executive, Regulation and Improvement Authority, Belfast
-
Ms Tracy Bury, Project Manager, World Confederation of Physical Therapy, London
-
Professor Iain T Cameron, Professor of Obstetrics and Gynaecology and Head of the School of Medicine, University of Southampton
-
Professor Bruce Campbell, Consultant Vascular & General Surgeon, Royal Devon & Exeter Hospital, Wonford
-
Dr Christine Clark, Medical Writer and Consultant Pharmacist, Rossendale
-
Professor Collette Clifford, Professor of Nursing and Head of Research, The Medical School, University of Birmingham
-
Professor Barry Cookson, Director, Laboratory of Hospital Infection, Public Health Laboratory Service, London
-
Dr Carl Counsell, Clinical Senior Lecturer in Neurology, University of Aberdeen
-
Professor Howard Cuckle, Professor of Reproductive Epidemiology, Department of Paediatrics, Obstetrics & Gynaecology, University of Leeds
-
Professor Carol Dezateux, Professor of Paediatric Epidemiology, Institute of Child Health, London
-
Mr John Dunning, Consultant Cardiothoracic Surgeon, Papworth Hospital NHS Trust, Cambridge
-
Mr Jonothan Earnshaw, Consultant Vascular Surgeon, Gloucestershire Royal Hospital, Gloucester
-
Professor Martin Eccles, Professor of Clinical Effectiveness, Centre for Health Services Research, University of Newcastle upon Tyne
-
Professor Pam Enderby, Dean of Faculty of Medicine, Institute of General Practice and Primary Care, University of Sheffield
-
Professor Gene Feder, Professor of Primary Care Research & Development, Centre for Health Sciences, Barts and The London School of Medicine and Dentistry
-
Mr Leonard R Fenwick, Chief Executive, Freeman Hospital, Newcastle upon Tyne
-
Mrs Gillian Fletcher, Antenatal Teacher and Tutor and President, National Childbirth Trust, Henfield
-
Professor Jayne Franklyn, Professor of Medicine, University of Birmingham
-
Mr Tam Fry, Honorary Chairman, Child Growth Foundation, London
-
Professor Fiona Gilbert, Consultant Radiologist and NCRN Member, University of Aberdeen
-
Professor Paul Gregg, Professor of Orthopaedic Surgical Science, South Tees Hospital NHS Trust
-
Bec Hanley, Co-director, TwoCan Associates, West Sussex
-
Dr Maryann L Hardy, Senior Lecturer, University of Bradford
-
Mrs Sharon Hart, Healthcare Management Consultant, Reading
-
Professor Robert E Hawkins, CRC Professor and Director of Medical Oncology, Christie CRC Research Centre, Christie Hospital NHS Trust, Manchester
-
Professor Richard Hobbs, Head of Department of Primary Care & General Practice, University of Birmingham
-
Professor Alan Horwich, Dean and Section Chairman, The Institute of Cancer Research, London
-
Professor Allen Hutchinson, Director of Public Health and Deputy Dean of ScHARR, University of Sheffield
-
Professor Peter Jones, Professor of Psychiatry, University of Cambridge, Cambridge
-
Professor Stan Kaye, Cancer Research UK Professor of Medical Oncology, Royal Marsden Hospital and Institute of Cancer Research, Surrey
-
Dr Duncan Keeley, General Practitioner (Dr Burch & Ptnrs), The Health Centre, Thame
-
Dr Donna Lamping, Research Degrees Programme Director and Reader in Psychology, Health Services Research Unit, London School of Hygiene and Tropical Medicine, London
-
Professor James Lindesay, Professor of Psychiatry for the Elderly, University of Leicester
-
Professor Julian Little, Professor of Human Genome Epidemiology, University of Ottawa
-
Professor Alistaire McGuire, Professor of Health Economics, London School of Economics
-
Professor Neill McIntosh, Edward Clark Professor of Child Life and Health, University of Edinburgh
-
Professor Rajan Madhok, Consultant in Public Health, South Manchester Primary Care Trust
-
Professor Sir Alexander Markham, Director, Molecular Medicine Unit, St James’s University Hospital, Leeds
-
Dr Peter Moore, Freelance Science Writer, Ashtead
-
Dr Andrew Mortimore, Public Health Director, Southampton City Primary Care Trust
-
Dr Sue Moss, Associate Director, Cancer Screening Evaluation Unit, Institute of Cancer Research, Sutton
-
Professor Miranda Mugford, Professor of Health Economics and Group Co-ordinator, University of East Anglia
-
Professor Jim Neilson, Head of School of Reproductive & Developmental Medicine and Professor of Obstetrics and Gynaecology, University of Liverpool
-
Mrs Julietta Patnick, Director, NHS Cancer Screening Programmes, Sheffield
-
Professor Robert Peveler, Professor of Liaison Psychiatry, Royal South Hants Hospital, Southampton
-
Professor Chris Price, Director of Clinical Research, Bayer Diagnostics Europe, Stoke Poges
-
Professor William Rosenberg, Professor of Hepatology and Consultant Physician, University of Southampton
-
Professor Peter Sandercock, Professor of Medical Neurology, Department of Clinical Neurosciences, University of Edinburgh
-
Dr Philip Shackley, Senior Lecturer in Health Economics, Sheffield Vascular Institute, University of Sheffield
-
Dr Eamonn Sheridan, Consultant in Clinical Genetics, St James’s University Hospital, Leeds
-
Dr Margaret Somerville, Director of Public Health Learning, Peninsula Medical School, University of Plymouth
-
Professor Sarah Stewart-Brown, Professor of Public Health, Division of Health in the Community, University of Warwick, Coventry
-
Dr Nick Summerton, GP Appraiser and Codirector, Research Network, Yorkshire Clinical Consultant, Primary Care and Public Health, University of Oxford
-
Professor Ala Szczepura, Professor of Health Service Research, Centre for Health Services Studies, University of Warwick, Coventry
-
Dr Ross Taylor, Senior Lecturer, University of Aberdeen
-
Dr Richard Tiner, Medical Director, Medical Department, Association of the British Pharmaceutical Industry
-
Mrs Joan Webster, Consumer Member, Southern Derbyshire Community Health Council
-
Professor Martin Whittle, Clinical Co-director, National Co-ordinating Centre for Women’s and Children’s Health, Lymington