Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the HTA programme on behalf of NICE as project number 08/31/01. The protocol was agreed in January 2009. The assessment report began editorial review in August 2009 and was accepted for publication in October 2010. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2012. This work was produced by Rogers et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2012 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Description of underlying health problem
Leukaemia is a form of cancer affecting the blood and can be classified as lymphoid or myeloid [depending on the type of white blood cell (WBC) affected] and as either acute or chronic (depending on the speed at which the disease progresses if left untreated). Chronic myeloid leukaemia (CML) is characterised by excessive proliferation of WBCs, mainly, but not exclusively, of the granulocytic series, in the bone marrow (BM) and circulating blood. In its initial stages, CML evolves very slowly.
Molecular mechanism
The molecular hallmark of CML is the presence of an acquired breakpoint cluster region (BCR)–Abelson oncogene (ABL) fusion gene in multipotent stem cells. More than 90% of individuals diagnosed with CML have an acquired (non-inherited) chromosomal abnormality caused by a reciprocal translocation between chromosomes 9 and 22 in an individual stem cell. The result is a shortened 22q, which is called the Philadelphia chromosome. 1,2 More specifically, the ABL gene, which is located on chromosome 9, translocates to the BCR gene on chromosome 22. The result is a fusion gene, BCR–ABL, and its corresponding protein, a constitutively active BCR–ABL tyrosine kinase. BCR–ABL tyrosine kinase is not controlled by normal cellular mechanisms and its presence leads to enhanced cell proliferation, resistance to apoptosis (programmed cell death) and altered adhesion. These are key features in the pathophysiology of CML. 3,4 Approximately 10% of people with CML do not have a demonstrable Philadelphia chromosome, but have a complex of different translocations that still results in the formation of the BCR–ABL gene and its product. 5
Diagnosis
Chronic myeloid leukaemia is diagnosed by the presence of a characteristic pattern of cells in the blood and BM in conjunction with specific cytogenetic and molecular abnormalities.
At presentation, patients typically have an enlarged spleen and a raised WBC count, with a higher than normal number of immature WBCs. BM biopsy typically shows very little fat present and the BM space is occupied entirely with large numbers of leukaemia cells.
The presence of the Philadelphia chromosome is important both in terms of diagnosis and for monitoring responses to treatment. It is usually demonstrated by cytogenetic techniques which involve examining BM cells in mitosis under a microscope to allow visualisation of metaphase chromosomes. This test can also identify additional clonal chromosomal abnormalities in Philadelphia-positive cells (Ph+) (clonal cytogenetic evolution, CCE), which may be important indicators of prognosis. The technique requires at least 20–30 BM cells in mitosis which can be difficult to achieve. There are considerable sampling errors because of the relatively small number of cells examined and the infrequency of measurement because BM examination is a relatively invasive though minor procedure. The sensitivity is approximately 5% if 20 metaphases are examined. 5
Fluorescence in situ hybridisation (FISH) is a sensitive and quantitative method used to detect specific chromosomal aberrations not only in cells undergoing metaphase, but in interphase nuclei as well. It uses specific fluorescent probes to map the chromosomal location of genes and identify other genetic abnormalities. In the case of CML, the probe looks for the BCR–ABL fusion gene in BM or peripheral blood (PB) cells. FISH can therefore detect BCR–ABL in the absence of the Philadelphia chromosome. This test is usually performed in addition to the conventional cytogenetic test and uses approximately 200 cells. The limit of detection is between 1% and 5% abnormal cells.
Reverse transcriptase-polymerase chain reaction (RT-PCR) to detect BCR–ABL transcripts is also sometimes used to provide confirmation of diagnosis in CML. In this technique, a defined piece of a ribonucleic acid (RNA) molecule is first reverse transcribed into its deoxyribonucleic acid (DNA) homologue, followed by amplification of the resulting complementary DNA (cDNA) using PCR. This qualitative technique is a simplified version of real-time quantitative PCR (qPCR) which is used to detect and quantify the level of BCR–ABL transcripts in a sample and can be used to monitor disease progression and response to treatment more closely.
Natural history and clinical presentation
With the advent of a new class of drugs for the treatment of CML, of which imatinib (Glivec®, Novartis) was the first (see Medical treatment), the natural history of the disease has been markedly changed. The original studies of imatinib are still ongoing, but current evidence suggests that patients whose disease responds favourably to treatment with imatinib may remain essentially symptom free for at least 10 years. The following paragraphs describe the natural history of the disease in the absence of imatinib treatment.
Traditionally, CML has been regarded as a progressive disease that evolves through three phases. The initial chronic phase (CP) during which the disease is stable and slow to progress is followed after a variable interval by progression through an accelerated phase (AP) to a rapidly fatal BC. In approximately one-third of patients there is no demonstrable AP, with the disease progressing directly from the CP to the BC. Transition between the phases may be gradual or rapid.
Chronic phase
Most people (approximately 90%) are diagnosed during the CP. Symptoms tend to be mild and non-specific and may include tiredness, anaemia, a feeling of ‘fullness’ or a tender lump on the left side of the abdomen caused by enlargement of the spleen, night sweats and weight loss. Approximately 40% of patients are asymptomatic and are diagnosed as a result of a routine blood test. 6
Hydroxycarbamide [Hydrea®, Bristol-Myers Squibb (BMS)] can be used to control the WBC count, but does not alter the natural history of the disease. In patients treated with hydroxycarbamide, the CP typically lasts between 3 and 5 years, during which time the patient is well with stable WBC counts.
Accelerated phase
The AP lasts for up to 6 months, during which progression is more rapid. The AP is associated with increases in the percentage of immature blast cells seen in blood and BM rather than fully differentiated cells. Evidence of cytogenetic abnormalities in addition to the Philadelphia chromosome (clonal evolution) is also an indication of disease progression. 7 New symptoms such as bruising or bleeding and infections may become apparent together with a worsening of additional symptoms. 8
Blast crisis
Also known as the blast phase, the BC is usually fatal within 3–6 months of onset. This phase is characterised by the rapid expansion of a population of differentiation-arrested blast cells. So much of the BM becomes replaced with immature cells that the other blood cells are prevented from functioning. An increased proportion of blast cells are found in the blood and BM, and blast cells may also spread to tissues and organs beyond the BM (extramedullary blast involvement). The BC may be associated with significant symptoms including fever, sweats, pain, weight loss, hepatosplenomegaly, enlarged lymph nodes and extramedullary disease. 6,8,9
Multiple genetic abnormalities are a feature of blastic transformation. The BC is of myeloid phenotype [myeloid blast crisis (MBC)] in approximately two-thirds of patients and lymphoid phenotype [lymphoid blast crisis (LBC)] in most other cases, with occasionally patients having an undifferentiated or a mixed-lineage phenotype. 10
Although the three phases of CML are clinically well recognised, there are several descriptions of defining criteria available in the literature. Varying definitions have been used in clinical studies. In 2001, the World Health Organization (WHO) proposed a new classification system with the intention to refine the criteria for AP and BC. The fourth edition of this document was released in October 2008. Table 1 describes the criteria used to define the AP and BC recommended by the WHO and those used in recent clinical studies. The implication is that none of these criteria are met in CP.
| WHO criteria | Criteria used in recent studies11–13 |
|---|---|
| AP | |
| Blast cells in blood or BM 10–19% | Blast cells in blood or BM 15–29%; blast cells plus promyelocytes in blood or BM > 30% with < 30% blast cells |
| Basophils in blood 20% or more | Basophils in blood 20% or more |
| Persistent thrombopenia (platelet count < 100 × 109/l) uncontrolled by therapy | Persistent thrombopenia (platelet count < 100 x 109/l) unrelated to therapy |
| Thrombocytosis (platelet count > 1000 × 109/l) unrelated to therapy | Not included |
| Increasing spleen size and increasing WBC count unresponsive to therapy | Not included |
| Cytogenetic evidence of clonal evolution (the appearance of additional genetic abnormalities that were not present at the time of diagnosis) | |
| BC | |
| Percentage of blast cells in blood or BM (≥ 20%) | Percentage of blast cells in blood or BM (≥ 30%) or |
| Extramedullary blast proliferation or large foci or clusters of blasts in the BM biopsy | Extramedullary blast involvement |
Epidemiology of chronic myeloid leukaemia
Incidence
The Haematological Malignancy Research Network (HMRN), based in Yorkshire, estimates that 560 cases of CML are newly diagnosed in the UK each year: an annual age-standardised rate of 1.2 per 100,000 for men and 0.7 per 100,000 for women.
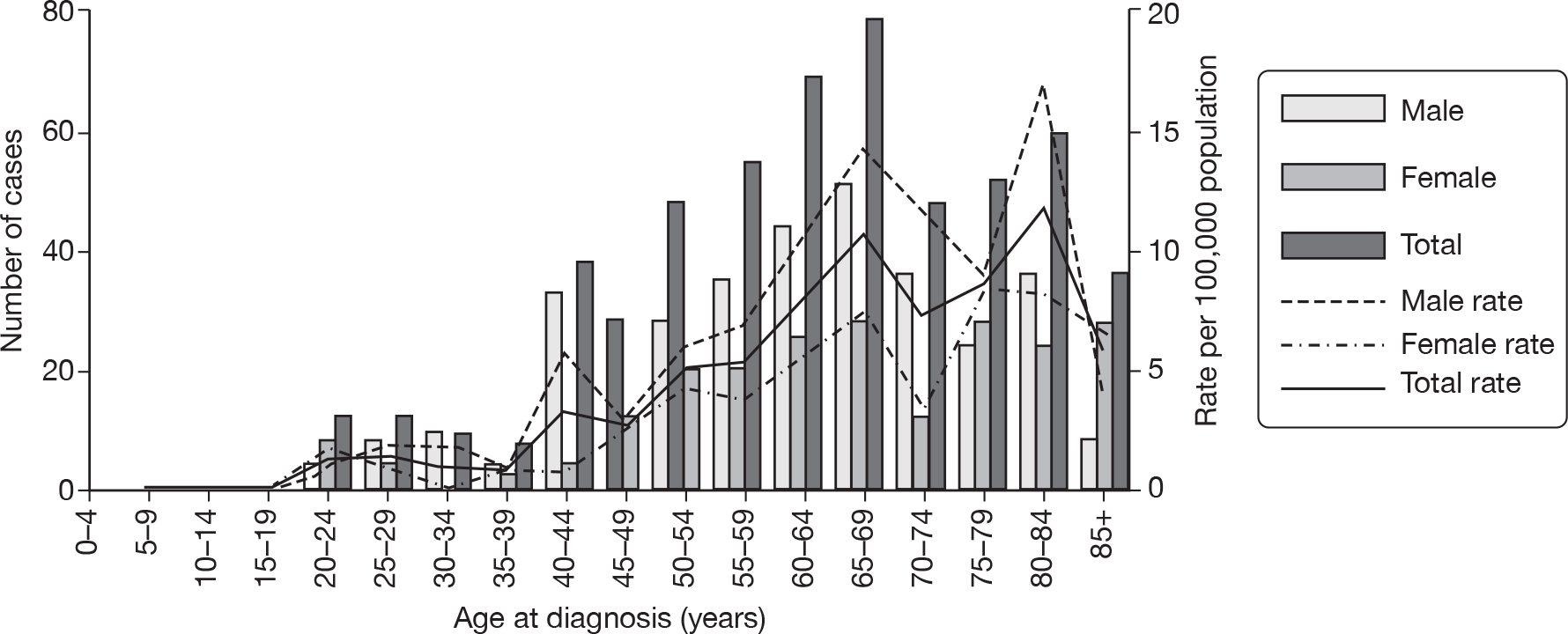
Figure 1 shows the annual estimated incidence of CML in the UK with age and gender distributions. The data are extrapolated from those collected within the HMRN regions whose population of 3.7 million is broadly representative of the UK as a whole. Approximately 60% of those diagnosed with CML are male. CML occurs in all age groups, although it is uncommon in those below the age of 30 years; the median age at diagnosis is 60 years. 14
FIGURE 1.
Annual estimated incidence in the UK, with age and gender distribution. Reproduced from Smith et al. 14 with permission from The Haematological Malignancy Research Network (www.hmrn.org/Statistics/Incidence.aspx).
Prognosis
There are two prognostic staging scores for CML in common practice – the Sokal score15 and the Euro or Hasford score. 16 Both scores are used to determine if a patient is at a low, intermediate or high risk of death and may also predict response to treatment. Both must be applied at diagnosis, prior to any treatment. The Sokal score is based on age, spleen size, and platelet and PB blast count. The Hasford score also includes data on eosinophil and basophil counts. Both scores were developed prior to the introduction of tyrosine kinase inhibitors (TKIs) [the Hasford score in response to improvements in survival seen with interferon-α (IFN) treatment], but they appear to have some value in predicting response to treatment with imatinib (see Medical treatment).
At the 18-month follow-up of the International Randomized Study of Interferon versus STI571 (IRIS), 49%, 67% and 76% of people with high-, intermediate- and low-risk scores, respectively, had achieved a complete cytogenetic response (CCyR). 17 This relationship was maintained at the 48-month update, with patients with a high Sokal score having a 69% probability of achieving a CCyR (see Disease monitoring), compared with 84% and 91% for patients with intermediate and low scores, respectively. 18 A similar relationship was seen with molecular responses (see Disease monitoring) at 12 months; 38% of patients in the high-risk group had a reduction from baseline of at least 3 log in BCR–ABL transcripts, compared with 45% in the intermediate-risk group and 66% of those in the low-risk group (p = 0.007). 19
Details of how the scores are calculated are shown in Table 2.
| Calculation using the Hasford score16 | Calculation using the Sokal score15 | |
|---|---|---|
| Relative riska | ||
| Low | ≤ 780 | < 0.8 |
| Intermediate | 781–1480 | 0.8–1.2 |
| High | > 1480 | > 1.2 |
| Age | 0.666 when age ≥ 50 years | 0.116 × (age – 43.4 years) |
| Spleenb | 0.042 × spleen | 0.0345 × (spleen – 7.51) |
| Platelet count (× 109/l) | 1.0956 when platelet count ≥1500 × 109/l | 0.188 × [(platelet count ÷ 700)2 – 0.563] |
| Blood myeloblasts (%) | 0.0584 × myeloblasts | 0.0887 × (myeloblasts – 2.10) |
| Blood basophils (%) | 0.20399 when basophils > 3% | NA |
| Blood eosinophils (%) | 0.0413 × eosinophils | NA |
Survival
The most recently available survival statistics for leukaemia in the UK are based on data collected from 1950 to 1999, prior to the introduction of imatinib. 20 Over this period, the clinical classifications of leukaemia have been revised as knowledge has increased and these revisions have been gradually incorporated into the International Classification of Diseases for Oncology (ICD-O), on which the encoding of data from cancer registries is based. As a result of difficulties with aligning older data with more specific recent categories, Rachet et al. 20 chose to group the data for all types of leukaemia together and were unable to present any survival data for CML alone.
A recently published analysis of survival among CML patients in the USA, derived from the 1973–2004 limited-use database of the Surveillance, Epidemiology and End Results (SEER) Program of the US National Cancer Institute, suggests a dramatic recent increase in long-term survival for people with CML since the introduction of imatinib into routine clinical practice. Improvements in both 5- and 10-year relative survival were greatest in the younger age groups. For all age groups combined, 5-year relative survival increased from 27.1% in 1990–2 to 48.7% in 2002–4 (p < 0.0001 for the trend). In the age groups 15–44 years and 45–54 years, about 90% and 80%, respectively, of patients surviving the first 5 years could expect to survive another 5 years – this compares with about 40% and 30%, respectively, in 1990–2. There were indications from the data of improvements in long-term survival in the older age groups, but long-term prognosis remained poor and essentially unchanged for the oldest patients. 21
Disease monitoring
Disease monitoring plays a key role in assessing response to therapy and detecting early relapse. Several measures of disease status are used for monitoring: blood counts [haematological response (HR)], the proportion of Philadelphia chromosomes in BM aspirate [cytogenetic response (CyR)] and the presence or absence (qualitative molecular response) and number (quantitative molecular response) of BCR–ABL transcripts in PB and BM using PCR technology. In clinical studies, CyRs are variously defined as complete, partial, overall, major and minor, and the definitions vary according to the phase of the disease in which a patient is diagnosed.
The following definitions are commonly used to describe response in chronic disease.
Haematological response
Classification of HR varies widely between studies. An example of the definition of a complete haematological response (CHR) is (1) WBC count no more than the upper limit of normal; (2) absolute neutrophil count (ANC) at least 1 × 109/l; (3) platelet count < 450 × 109/l and no more than the institutional upper limit of normal; (4) no blasts or promyelocytes in PB; (5) < 2% basophils in PB; and (6) no extramedullary involvement, with all of these being maintained for 4 weeks. 11 Other studies have used variations of this definition including some or all of the elements.
Cytogenetic response
The definition of a CyR appears to be fairly standard across most studies and is split into complete, partial, minor, minimal and none (Table 3). A CCyR is defined as the absence of the Philadelphia chromosome among at least 20 cells in metaphase in a BM aspirate. 11 A commonly used additional term is major cytogenetic response (MCyR), which encompasses complete and partial.
| Cytogenetic response | Percentage of Ph+ chromosomes in metaphase in BM |
|---|---|
| Complete | None |
| Partial | 1–35 |
| Major | ≤ 35 |
| Minor | 36–65 |
| Minimal | 66–95 |
| None | > 95 |
Molecular response
In people with a CCyR, quantitative PCR techniques can be used to monitor the level of BCR–ABL transcripts in PB (and sometimes BM). A complete molecular response (CMR) has been defined as undetectable levels of BCR–ABL transcripts in an assay that can detect a reduction from baseline of at least 4.5 logs. A major molecular response (MMR) is a standardised BCR–ABL/ABL ratio of < 0.10%, which is equivalent to a 3 log reduction from the 100% baseline for untreated patients. 13,19
Disease progression
Typically, disease progression describes the process in which the disease develops into the AP or to BC. Differences in the definition of AP have resulted in the use of more specific definitions of disease progression. The definition of progression used in several of the studies in this assessment22–24 relies on participants meeting any one of the four criteria:
-
development of CML in AP (CML-AP) or CML in BC (CML-BC)
-
loss of CHR
-
loss of MCyR
-
increasing WBC count (recorded by the investigator as a doubling from lowest value to > 20,000/mm3 or an increase by > 50,000/mm3 on two assessments performed at least 2 weeks apart).
Treatment
Allogeneic stem cell transplant
Currently, the only known curative treatment for CML is allogeneic haematopoietic stem cell transplantation (SCT), from either a matched related or unrelated donor. 25,26 Patient age, disease phase and duration, the degree of mismatch between patient and donor, and therapy before transplantation all influence the outcome. Younger patients in CP receiving a transplant from a matched sibling donor soon after diagnosis have the best prognosis. 27 Two studies have shown similar outcomes for transplantation in patients with CML in CP (CML-CP) using either a fully matched related or unrelated donor, with 5-year survival rates > 70% for people aged 50 years and younger who undergo transplantation within a year of diagnosis. 28,29 Results are less promising for those patients in AP and BC phases. 26
The morbidity and mortality of allogeneic transplant is considerable; transplant-related mortality ranges from 15% to 40%. 30
Allogeneic SCT is not a treatment option for many people, either for reasons related to age at diagnosis (the median age at diagnosis of CML is 60 years, and many patients are considered to be unsuitable for a transplant at diagnosis) or because of the lack of a suitable donor.
Medical treatment
Imatinib
Imatinib [originally STI571; Gleevec® (USA), Novartis or Glivec® (Europe/Australia/Latin America)] is an orally administered TKI specifically designed to inhibit the BCR–ABL fusion protein by occupying the adenosine 5′-triphosphate (ATP)-binding pocket of the ABL-kinase domain. This prevents a change in conformation of the protein to the active form of the molecule. 4 By blocking the ATP-binding site, imatinib reduces cell proliferation and stops disease progression. The recommended dose of imatinib is 400 mg every day (q.d.) for those in CP and 600 mg q.d. for those in AP and BC. Imatinib is administered orally q.d. with a meal and a large glass of water.
In chronic phase
The efficacy data for imatinib are based on a large, open-label, randomised controlled trial (RCT; IRIS) in which a total of 1106 people with newly diagnosed CML-CP received either imatinib or IFN plus low-dose cytarabine. 17 After a median follow-up of 19 months, the estimated rate of a MCyR at 18 months was 87.1% in the imatinib group and 34.7% in the control group (p < 0.001). Corresponding figures for a CCyR were 76.2% and 14.5% (p < 0.001), respectively. 17
Patients who received imatinib continue to be followed up; after a median follow-up of 60 months, the Kaplan–Meier estimate of cumulative best rate of CCyR was 87%. An estimated 7% of patients had progressed to CML-AP or CML-BC and the estimated overall survival (OS) of patients who received imatinib as initial therapy was 89%. 18
The most recently published update reports no disease progression to AP or BC during the sixth year of treatment and 63% of all patients randomised to receive imatinib and still on study treatment showing a CCyR at the last assessment. The estimated OS at 6 years was 88%, or 95% when only CML-related deaths were considered. 31
Commonly experienced adverse events (AEs) associated with imatinib treatment include superficial oedema, nausea, muscle cramps and rashes (reported by 56%, 44%, 38% and 34% of patients, respectively, in the IRIS study17). In the IRIS study,17 grades 3 or 4 AEs included musculoskeletal pain, abdominal pain, neutropenia, thrombopenia and anaemia. These occurred in approximately 3% of patients, but had diminished over time by the 5-year follow-up. 17,18
In accelerated phase and blast crisis
Imatinib is clinically less active in people with advanced CML. In one study,32 in which a total of 253 patients with CML (181 with confirmed AP) received imatinib (400 or 600 mg q.d.), 34% experienced a CHR and 17% a CCyR. The estimated 12-month OS was 74%. Long-term follow-up results of a Phase II study of imatinib (600 mg q.d.) in people with CML-AP have recently been published. 33 A total of 111 people were enrolled into the study and initial results indicate that 71% (n = 79) achieved a CHR. At the latest follow-up (median 82 months) of the remaining 41 living patients, four (4%) were alive in complete remission after allogeneic transplant, 16 (14%) had switched to a second-generation TKI and 21 (19%) patients were alive on imatinib therapy. 33
Imatinib resistance
Resistance to imatinib is well documented. People may initially be refractory to imatinib (primary resistance) or may develop resistance during treatment (acquired resistance), particularly during AP and BC. In the IRIS study,17 24% of participants failed to achieve a CCyR after 18 months, which has been attributed to primary resistance. At 5-year follow-up, 7% of participants had progressed to the advanced disease and 17% had relapsed disease, presumably because of acquired resistance to imatinib. 18
Imatinib resistance has been variously defined. In a recent clinical study of dasatinib [Sprycel®, Brystol-Myers Squibb (BMS)], imatinib resistance was defined as a lack of CHR after 3 months of imatinib treatment, a lack of any CyR after 6 months of treatment, a lack of a MCyR (Ph+ cells > 35%) after 12 months of treatment, an increasing WBC count on at least two consecutive occasions or a relapse after a CHR or MCyR. 11 A European LeukemiaNet panel of experts reviewed the management of CML in 2006 and proposed a set of definitions of failure and suboptimal response to imatinib in CP (Table 4) which is now widely accepted. 34
| Time | ||||||
|---|---|---|---|---|---|---|
| Diagnosis | 3 months after diagnosis | 6 months after diagnosis | 12 months after diagnosis | 18 months after diagnosis | Any time | |
| Failure | NA | No HR (stable disease or disease progression) | Less than CHR, no CCyR (Ph+ > 95%) | Less than PCyR (Ph+ > 35%) | Less than CCyR | Loss of CHR, loss of CCyR, mutations |
| Suboptimal response | NA | Less than CHR | Less than PCyR (Ph+ > 35%) | Less than CCyR | Less than MMR | Additional chromosomal abnormalities in Ph+ cells, loss of MMR, mutations |
| Warnings | High-risk patients, additional chromosomal abnormalities in Ph+ cells, chromosome 9q + deletions | NA | NA | Less than MMR | NA | Any rise in transcript level, other chromosome abnormalities in Ph+ cells |
Molecular basis of imatinib resistance
Point mutations in the ABL-kinase domain which preclude the binding of imatinib have been identified as a major underlying cause of imatinib resistance, developing in between 35% and 70% of people displaying clinical resistance. 35,36 Over 50 point mutations have been identified to date; the most frequently mutated region of BCR–ABL is the ATP-binding loop (P-loop) of the ABL-kinase domain, accounting for 36–48% of all mutations. 35,36 The frequency of P-loop mutations has been shown to increase in the AP and BC, and with disease duration, and is associated with a poor prognosis. 36,37 Some mutations can be overcome by dose escalation; others, e.g. T315I, which is present in approximately 15% of imatinib-resistant (ImR) patients,38 confer a much greater level of resistance requiring higher plasma concentrations of imatinib than are clinically possible. 34,39
Imatinib resistance is likely to be multifactorial and the involvement of many other mechanisms has been debated, including overexpression and amplification of the BCR–ABL gene locus,40,41 activation of BCR–ABL-independent pathways such as members of the SRC kinase family,42 clonal evolution,7 binding of imatinib to serum α1-acid glycoprotein43,44 and increased drug efflux through the multidrug resistance gene. 45–47
Imatinib intolerance is frequently defined as at least grade 3 non-haematological toxicity, or grade 4 haematological toxicity persisting for > 7 days, related to imatinib at any dose. 11 In the IRIS study,17 0.7% of patients (n = 4) crossed over to the alternative treatment because of intolerance of imatinib; the proportion of patients who withdrew from the study as a result of intolerance to imatinib is not clear. A review of medical and pharmacy claims in the Healthcore Managed Care Database concluded that discontinuation and dose modification of imatinib as a result of AEs occur frequently in clinical practice. 48
Residual disease
In approximately 95% of people who achieve a CCyR with imatinib, residual BCR–ABL-positive cells remain and it is postulated that imatinib is not able to completely eradicate the leukaemic stem cell population. 19 These long-term stem/progenitor cells are resistant to imatinib treatment and may therefore contribute to disease progression at a later date. Rising levels of BCR–ABL transcripts are an early indicator of loss of response to imatinib and the need to re-evaluate treatment. 49,50
The proportion of patients with a CMR to imatinib in the IRIS study17 appears to be increasing, suggesting a time-dependent decrease in residual disease. After 1 year, levels of BCR–ABL transcripts had fallen by 3 log in 66 of 124 patients (53%); this had increased to 80% (99 of 124 patients, p < 0.001) at the 4-year follow-up. 18 In a small study of 12 patients with undetectable residual disease for > 2 years, cessation of imatinib treatment resulted in an early molecular relapse (positive qPCR results within 6 months) in six patients; the remainder were still in molecular remission after a median follow-up of 18 months. The authors explored various factors associated with remission, but no significant differences between relapsing and non-relapsing patients were identified. 51
Treatment options in people with imatinib resistance and imatinib intolerance
Allogeneic SCT remains an important treatment option in young patients with a matched sibling or unrelated donor. A large retrospective study comparing the transplant outcomes of 223 people who had not received imatinib before transplantation with 145 who had various exposures to imatinib found no significant differences in death, relapse rate and non-relapse mortality between groups. 52
A frequently used strategy in patients with imatinib resistance is dose escalation. Clinical responses can be achieved by increasing the dose of imatinib to 600 mg or 800 mg q.d. In a retrospective analysis, 54 patients with CML-CP with haematological resistance or CyR or relapse on 400 mg q.d. of imatinib were subsequently treated with either 600 mg or 800 mg q.d. of imatinib. In 20 people with haematological resistance, 65% achieved a CHR and 56% (n = 34) of those with CyR or relapse achieved a CCyR. 53 In a retrospective analysis, a CyR was obtained in 42% of the subset of patients in the IRIS study who began treatment on 400 mg q.d. and who subsequently underwent dose escalation to either 600 mg or 800 mg q.d. 54 Some mutations can be overcome by dose escalation; others, e.g. T315I, which is present in approximately 15% of ImR patients,38 are fully resistant to imatinib. 34,39
Interferon-α was the mainstay of treatment for CML prior to the introduction of imatinib and, although it remains a treatment option for people in CP and AP who are intolerant to imatinib, it is currently little used in England and Wales. IFN is administered daily by subcutaneous injection. The evidence-based analysis of the effect of IFN in treating CML-CP, published by the American Society of Hematology (ASH) in 1999, concluded that, despite methodological limitations in the design and conduct of some of the clinical studies, IFN improves survival in CP patients with favourable prognostic features (e.g. no or minimal prior treatment, relatively normal haemoglobin levels and platelet counts, < 10% blasts in the blood and beginning treatment within 6 months of diagnosis) compared with other treatment options including busulfan (Myleran®, GlaxoSmithKline; Busulfex IV®, PDL BioPharma, Inc.) and hydroxycarbamide. Meta-analysis suggests that the pooled 5-year survival rate is 57% for IFN compared with 42% for chemotherapy (p < 0.0001), with most of this advantage a result of delaying progression to BC phase. Compared with busulfan and hydroxycarbamide, IFN increases life expectancy by a median of 20 months. 30 The most recent updates of the main IFN studies reported a 9- or 10- year OS ranging from 27% to 53%. 34 Almost all patients who receive IFN experience some side effects of treatment, the most common being flu-like symptoms, fever and chills, fatigue and malaise. Toxicity-related treatment discontinuation is necessary for between 4% and 18% of patients. 30
Once people develop a myeloid or lymphoid blastic transformation, acute leukaemia-type chemotherapy can be used as a debulking or cytoreductive treatment prior to treatment with other agents including SCT; this therapy generally produces a HR in the region of 40%. 55
Quality of life
Assessment of health-related quality of life (HRQoL) has become an important feature of cancer studies, enabling evaluation of treatment effectiveness from the perspective of the person with the condition and facilitating improved clinical decision making.
There are several general HRQoL instruments for people with cancer that can be used to assess quality of life (QoL) both in research studies and in clinical practice, e.g. the Functional Assessment of Cancer Therapy (FACT) scale and the European Organisation for Research and Treatment of Cancer (EORTC) quality of life questionnaire (QLQ-C30). Disease-specific instruments for CML appear not to have been widely used in clinical studies.
A recent systematic review of HRQoL in leukaemia highlighted the relative paucity of research in this area compared with solid tumours; three RCTs including HRQoL evaluation were identified in patients with CML. 56 HRQoL was not reported in any of the clinical studies of dasatinib or nilotinib (Tasigna®, Novartis). Assessment of QoL in CML is further discussed in Chapter 5, Valuation of outcomes (utilities).
Current service provision
The National Institute for Health and Clinical Excellence (NICE) manual on improving outcomes in haematological cancers was published in 2003 and does not contain detailed recommendations for the treatment of individuals resistant to or intolerant of imatinib. 57 Recommendations from an expert panel on behalf of the European LeukemiaNet, published in 2006, proposed that the first choice of treatment in ImR patients should be allogeneic SCT or dose escalation of imatinib to 600 mg or 800 mg q.d. provided that 400 mg q.d. is tolerated and that resistance to imatinib was not associated with a BCR–ABL mutation with a high level of insensitivity to imatinib. 34
Description of new interventions
Increased understanding of the mechanisms responsible for imatinib resistance (see Medical treatment) has led to the development of alternative therapies designed to overcome imatinib resistance. This assessment is concerned with two alternative, rationally designed agents: dasatinib and nilotinib. There is some evidence to suggest differential activity between the new agents against particular point mutations, with dasatinib being more active against P-loop mutations than nilotinib. 58 Neither agent is active against the T315I mutation. 59 There is also evidence to suggest that neither intervention is able to completely eradicate disease cells and residual disease may continue to be an issue. 60,61
Dasatinib
Dasatinib is a second-generation TKI.
Pharmacology
Dasatinib is a highly potent, orally active inhibitor of SRC and the SRC-family kinases. 62 The SRC family of tyrosine kinases modulates multiple intracellular signal transduction pathways involved in cell growth, differentiation, migration and survival, many of which are involved in oncogenesis, tumour metastasis and angiogenesis. Dasatinib is an inhibitor of FYN and YES, which are ubiquitously expressed, and of FGR, HCK, LCK and LYN, which are found mainly in haematopoietic cells. Dasatinib is also a potent BCR–ABL kinase inhibitor and has additional activity against the KIT, PDGFR and ephrin receptor tyrosine kinases. Dasatinib has been shown to directly inhibit 21 out of 22 mutant forms of BCR–ABL resistant to imatinib. 63–65
In pre-clinical comparisons with imatinib, dasatinib was 325 times more potent than imatinib against cells expressing wild-type BCR–ABL. 65 This may be due in part to the ability of dasatinib to bind to both the active and inactive conformations of ABL. 66
A series of Phase II clinical studies called the START (SRC/ABL Tyrosine kinase inhibition Activity: Research Trials of dasatinib) programme are under way to assess the efficacy of dasatinib in people with CML (resistant or intolerant to the effects of imatinib) by phase of disease. Further details are provided in Chapter 2, Identification of evidence.
Licensing
In the UK, dasatinib is licensed for the treatment of adults with AP, CML-AP or CML-BC with resistance or intolerance to prior therapy including imatinib. Dasatinib has also received accelerated approval for this indication by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA). The Scottish Medicines Consortium (SMC) has also accepted dasatinib for restricted use in adults with ImR or imatinib intolerant (ImI) CML. Dasatinib has orphan drug status.
Special populations
There are no pharmacokinetic data in people with impaired renal or hepatic function. No paediatric pharmacokinetic studies have been published. 67 Dasatinib is contraindicated during pregnancy and breastfeeding, and female patients are advised to use adequate contraception during treatment.
Adverse events
The AEs of dasatinib treatment are reported in detail in Chapter 2, Adverse events. The most common (seen in more than 1 in 10 patients) reported side effects in the studies are headache, pleural effusion, shortness of breath, cough, diarrhoea, nausea, vomiting, abdominal pain, skin rash, musculoskeletal pain, infections, haemorrhage, superficial oedema (swelling), fatigue, fever, neutropenia (low WBC counts), thrombopenia (low blood platelet counts) and anaemia (low red blood cell counts). 67
Dose
For CP patients, the recommended dose is 100 mg taken q.d. For AP or BC the recommended dose is 70 mg twice daily (b.i.d.). The dose can be altered based on patient response.
Cost
According to the current edition of the British National Formulary (BNF), the cost of treatment with dasatinib at a dose of 100 mg q.d. is £86.85 per day. 68
Nilotinib
Nilotinib is a second-generation TKI.
Pharmacology
Nilotinib is an orally active phenylaminopyrimidine derivative of imatinib developed using rational drug design based on the crystal structures of inhibitors in complexes with ABL. Nilotinib is approximately 30 times more potent than imatinib at inhibiting BCR–ABL. Nilotinib does not inhibit the SRC family of tyrosine kinases. Studies performed in vitro suggest that nilotinib inhibits 32 of 33 mutant BCR–ABL forms resistant to imatinib at physiologically relevant concentrations. 65,69
Nilotinib, like imatinib, binds to the inactive conformation of ABL, but with a slightly better topographical fit. 9
The clinical effectiveness data for nilotinib are discussed more fully in Chapter 2, Effectiveness of nilotinib.
Licensing
Nilotinib is indicated for the treatment of adults with CP and AP Ph+ CML with resistance or intolerance to prior therapy including imatinib. Nilotinib is not licensed for use in the BC. Nilotinib has also been approved by the FDA and the EMA for a similar indication. The SMC has accepted nilotinib for restricted use within NHS Scotland for adults with ImR or ImI CML in CP. Nilotinib has orphan drug status.
Special populations
Nilotinib is contraindicated in pregnant and/or breastfeeding women. Female patients are advised to use adequate contraception during treatment.
Nilotinib prolongs the QT interval and is therefore contraindicated in patients with hypokalaemia, hypomagnesaemia or long QT syndrome.
Nilotinib has not been studied in a paediatric population or in people with impaired renal or hepatic function. 70
Adverse events
A full description of the AEs experienced during treatment with nilotinib can be found in Chapter 2, Adverse events. The most common side effects with nilotinib (reported by more than one patient in 10) are thrombopenia (low blood platelet counts), neutropenia (low WBC counts), anaemia (low red blood cell counts), headache, nausea, constipation, diarrhoea, rash, pruritus (itching), fatigue (tiredness) and increased blood levels of lipase (an enzyme produced by the pancreas) and bilirubin. 70 The FDA has stipulated that nilotinib carry a ‘black box’ warning for possible heart problems that may lead to an irregular heart beat and possibly sudden death. 68
Dose
The recommended starting dose for CP or CML-AP is 400 mg b.i.d. 68
Cost
According to the current edition of the BNF, the cost of nilotinib at a dose of 400 g mg b.i.d. is £86.89 q.d. Further discussion of the cost of nilotinib can be found in Chapter 5, Drug prices.
Current use of new interventions in the NHS
Anecdotal evidence suggests that dasatinib and nilotinib are currently widely used in the NHS in England and Wales following failure of treatment with imatinib.
Definition of the decision problem
The purpose of this report is to assess the clinical effectiveness and cost-effectiveness of dasatinib and nilotinib in the treatment of people with ImR and ImI CML.
Interventions
The two interventions are considered in accordance with their marketing authorisations:
-
dasatinib
-
nilotinib.
Populations including subgroups
The relevant population is people with CML who are either unable to tolerate imatinib because of AEs (ImI) or who have failed to respond to treatment with imatinib (ImR).
For the assessment of dasatinib, people may be in CP, AP or BC.
For the assessment of nilotinib, people may be in CP or AP.
Where possible we have considered populations who are ImI and ImR separately.
Relevant comparators
The interventions are compared with current standard treatments.
There are several possible alternative treatments available for people who are intolerant or resistant to imatinib [e.g. high-dose imatinib (HDI), IFN, hydroxycarbamide, acute leukaemia chemotherapy and best supportive care]. Owing to the paucity of available evidence to support their use, we have restricted the choice of comparators to those considered by our Expert Advisory Group to be most commonly used in the UK. The relevant comparators are therefore as follows.
For people with imatinib-resistant chronic myeloid leukaemia
The interventions are compared with each other (where appropriate), and with:
-
HDI (800 mg q.d.).
It is clear from discussion with clinical experts that IFN is used in only a minority of cases, and that second-generation TKIs have, in some areas, become the mainstay of treatment in this population. However, it is also clear that IFN was the most recent and widely accepted treatment prior to the introduction of imatinib. Its inclusion as a comparator, albeit that it is not widely used, seems therefore appropriate. However, in recognition of the limited current use of this alternative, we have not included IFN as a comparator in our main economic evaluation of the new TKIs, instead presenting the analysis against IFN as an appendix to the main assessment.
For people with imatinib-intolerant chronic myeloid leukaemia
The interventions are compared with each other (where appropriate), and with:
-
IFN (except in BC).
Outcomes
Dasatinib and nilotinib are assessed in terms of the following outcomes:
-
treatment response rates (including haematological, cytogenetic and molecular responses)
-
time to response
-
duration of response
-
progression-free survival (PFS)
-
OS
-
adverse effects of treatment
-
HRQoL.
Overall aims and objectives of the assessment
This assessment reviews available evidence for the clinical effectiveness and cost-effectiveness of dasatinib and nilotinib in the treatment of people with ImR and ImI CML according to their marketing authorisations. The assessment draws together the relevant evidence to determine what, if any, is the clinical effectiveness and cost-effectiveness of the interventions compared with current treatments.
More fully, the policy questions addressed are:
-
In CP:
-
– In those patients who have ImR disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib or treatment with nilotinib, using HDI as a comparator?
-
– In those patients who have ImI disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib or treatment with nilotinib, using IFN as a comparator?
-
-
In AP:
-
– In those patients who have ImR disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib or treatment with nilotinib, using HDI as a comparator?
-
– In those patients who have ImI disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib or treatment with nilotinib, using hydroxycarbamide as a comparator?
-
-
In BC:
-
– In those patients who have ImR disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib following initial cytoreductive treatment, using HDI as a comparator?
-
Chapter 2 Assessment of clinical effectiveness
Methods for reviewing effectiveness
The clinical effectiveness of dasatinib and nilotinib was assessed by a systematic review of published evidence. The review was undertaken in line with the general principles published by the NHS Centre for Reviews and Dissemination (CRD). 71
Identification of studies
MEDLINE (including MEDLINE In-Process & Other Non-Indexed Citations), EMBASE, (ISI Web of Science) Conference Proceedings Citation Index, (ISI Web of Science) Science Citation Index Expanded (SCIE), Database of Abstracts of Reviews of Effects (DARE), NHS Economic Evaluation Database (NHS EED) and the Health Technology Assessment (HTA) were searched for systematic reviews of RCTs, single RCTs and other clinical studies in January 2009. Bibliographies of included studies were searched for further relevant studies. Individual conference proceedings from 2008 and 2009 [American Society of Clinical Oncology (ASCO) and ASH] were searched using their online interface. All searches were rerun in June 2009. Full details of the search strategies are presented in Appendix 2. All references were managed using Reference Manager 11 (Thomson ISI Research Soft, New York, NY, USA) and Microsoft Access 2003 (Microsoft Corporation, Redmond, WA, USA) software.
Relevant studies were identified in two stages. One reviewer (GR) examined all titles and abstracts, with a sample checked by a second (JTC). Full texts of any potentially relevant studies were obtained. The relevance of each paper was assessed independently by two reviewers (GR and JTC) according to the inclusion and exclusion criteria, and any discrepancies resolved by discussion.
Inclusion and exclusion criteria
Studies were included if they compared any of the interventions (see Chapter 1, Interventions) with any of the comparators detailed in Chapter 1, Relevant comparators, in participants with ImI or ImR CML. The primary outcomes were molecular, CyR and HR rates. Secondary outcomes were time to response, duration of response, PFS, OS, adverse effects of treatment and HRQoL. Only studies which reported at least one of the primary outcomes were included in the review. The use of data from Phase II studies and non-randomised studies were considered only where there was insufficient evidence from good-quality RCTs. Conference abstracts were included if there was sufficient detail to assess quality or if they reported updated results of included studies.
Data extraction strategy
Data were extracted by one reviewer (GR) using a standardised data extraction form in Microsoft Access 2003 and checked independently by a second (ZL or JTC). Disagreements were resolved by discussion, with involvement of a third reviewer if necessary. Data extraction forms for each included study are included in Appendix 3.
Quality assessment strategy
The methodological quality of RCTs was assessed according to criteria specified by the CRD. 71 Assessment of the methodological quality of observational studies was performed using a structured checklist which included various aspects of internal and external validity. Quality was assessed by one reviewer (ZL) and judgements were checked by a second (GR or JTC). Any disagreement was resolved by discussion, with involvement of a third reviewer if necessary.
Methods of data synthesis
Details of the extracted data and quality assessment for each individual study are presented in structured tables and as a narrative description. Where presented, the 95% confidence intervals (CIs) of proportions arising from dichotomous data are calculated by the Clopper–Pearson method. 72 Any possible effects of study quality on the effectiveness data are discussed.
Where appropriate, we have used meta-analysis to estimate summary measure of effect on relevant outcomes based on intention-to-treat (ITT) analyses. We used random-effects meta-analysis (DerSimonian and Laird model73) only, in view of the known clinical heterogeneity between studies, regardless of any statistical evidence of inter-study homogeneity.
In instances where zero frequencies complicated the calculation of standard errors (SEs) required to calculate meta-analytical weights, correction factors of 0.5 and 1.0 were added to the numerator and denominator, respectively, of affected calculations. This procedure – common in pair-wise meta-analyses – is suggested by Einarson;74 however, the author notes that it will introduce a bias towards higher event rates (because the correction is not balanced in a comparator arm, as it is in the pair-wise scenario).
All selected articles have been scanned for short- and long-term adverse effects of treatment and data from included studies is presented in tables and as a narrative discussion.
Handling company submissions to NICE
All clinical effectiveness data included in the pharmaceutical company submissions to NICE were assessed. Where they met the inclusion criteria and have not already been identified from published sources, they were included in the systematic review of clinical effectiveness.
This report contains reference to confidential information provided as part of the NICE appraisal process. This information has been removed from the report, and the results, discussions and conclusions of the report do not include the confidential information. These sections are clearly marked in the report.
Results
Identification of evidence
From screening the 1221 references identified by our searches and additional sources, we included 15 studies in the review. The process is illustrated in detail in Figure 2. In assessing full-text papers for inclusion, agreement between the two reviewers was reasonable (κ = 0.79), with disagreements easily resolved by consensus.
FIGURE 2.
Identification of published evidence for review.
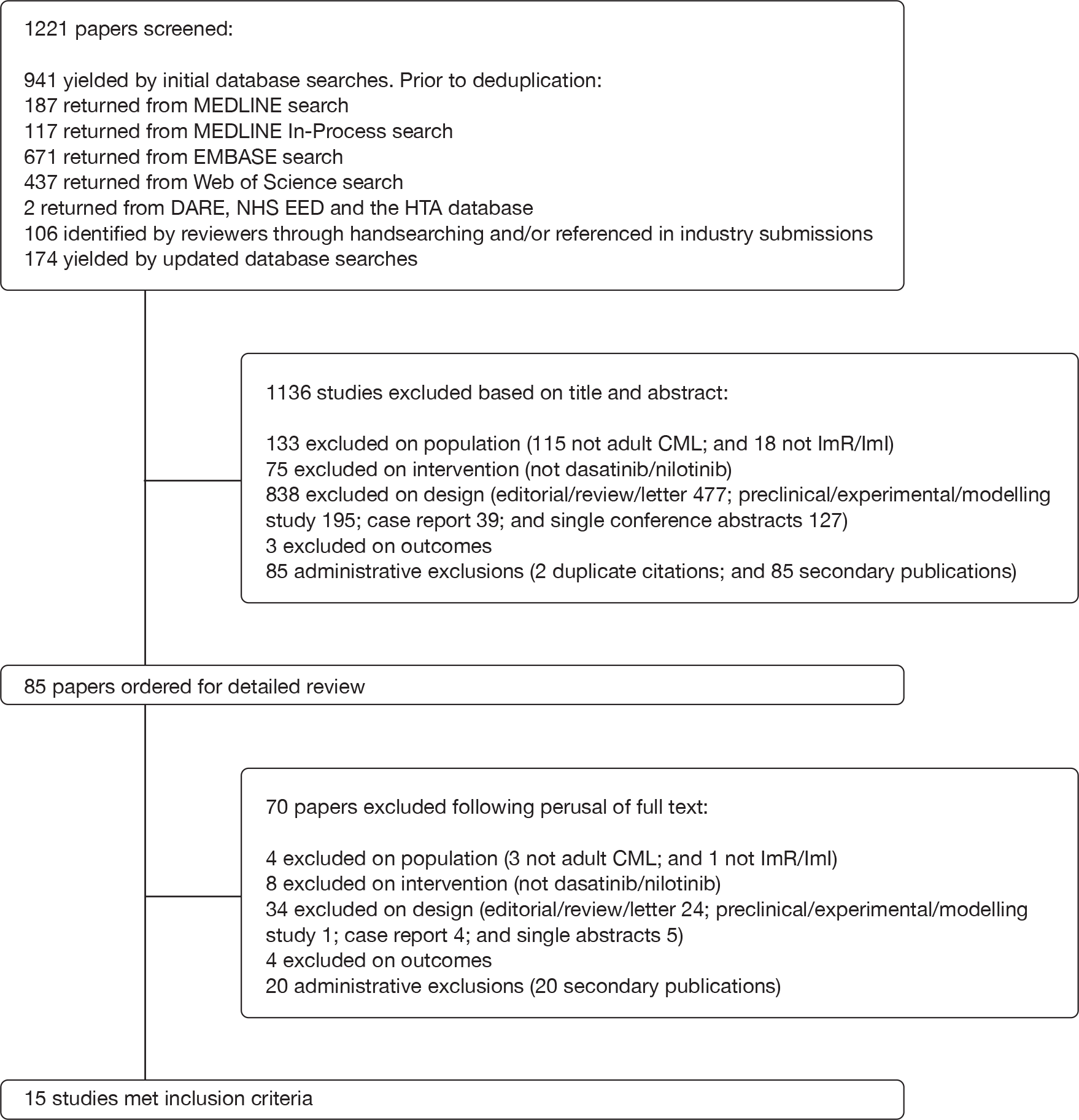
A number of case series reporting experience from a single institution were identified that met our inclusion criteria. However, in most cases, these studies contained a clear statement that some or all of the cases reported were also included in larger, multicentre studies (which are also included in our review). Therefore, to avoid double-counting of data, we excluded such case series75–78 from the review. Two similar single-unit case series were also identified that did not make any reference to the submission of participant data to multicentre studies. 79,80 It is possible that the problem of duplicate reporting applies in these cases. However, in the absence of explicit evidence to confirm that individuals from the case series also appear in the aggregated data in multicentre studies, these publications are included in the review.
Design and characteristics of included studies
Three of the included studies had a randomised controlled design. 22,23,81 Details of the interventions administered in each of these trials are provided in Table 5 and details of study design are presented in Table 6. The remaining 12 studies were observational in nature. 11–13,38,79,80,103–109 Intervention and design details are tabulated in Tables 7 and 8, respectively.
| Study | Arm no. | Drug | Dosage notes | Notes |
|---|---|---|---|---|
| Kantarjian et al. (2007)23 | 1 | Dasatinib |
70 mg b.i.d. Escalated to 180 mg b.i.d for participants with inadequate response at 12 weeks or progression Reduced to 100 mg or 80 mg b.i.d for participants experiencing toxicity |
Crossover to the alternative treatment was permitted after confirmed progression, lack of MCyR at the week 12 cytogenetic evaluation or intolerance |
| 2 | Imatinib |
400 mg b.i.d. Reduction to 600 mg b.i.d was permitted for toxicity in participants who had not previously received 600 mg b.i.d imatinib |
This is study 017 in the BMS submission184 to NICE | |
| Shah et al. (2008)22 | 1 | Dasatinib |
100 mg q.d. Escalation to 140 mg q.d. allowed for suboptimal response Reduction to 80 mg q.d. allowed for toxicity |
This is study 034 in the BMS submission184 to NICE |
| 2 | Dasatinib |
50 mg b.i.d. Escalation to 70 mg b.i.d. allowed for suboptimal response Reduction to 40 mg b.i.d. allowed for toxicity |
||
| 3 | Dasatinib |
140 mg q.d. Escalation to 180 mg q.d. allowed for suboptimal response Reduction to 80 mg q.d. allowed for toxicity |
||
| 4 | Dasatinib |
70 mg b.i.d. Escalation to 90 mg b.i.d. allowed for suboptimal response Reduction to 40 mg b.i.d. allowed for toxicity |
||
| Kantarjian et al. (2009)81 | 1 | Dasatinib |
140 mg q.d. Escalation to 180 mg q.d. was allowed for inadequate response (rising percentage of blasts or loss of HR in two consecutive assessments at least 1 week apart; absence of CHR, NEL, or minor HR within 4 weeks; no MCyR after 3 months or no CCyR after 6 months) Interruption or reduction to 80 mg q.d. was allowed in cases of drug toxicity (grade 2 or greater, non-haematological toxicity considered related to dasatinib; ANC 0.5 × 109/l and/or platelets < 100 × 109/l for > 6 weeks with BM cellularity < 10% with blasts < 5% or BM cellularity > 10% with blasts > 5%; or febrile neutropenia with signs of septicaemia) |
This is study 035 in the BMS submission184 to NICE |
| 2 | Dasatinib |
70 mg b.i.d. Escalation to 90 mg b.i.d. or reduction to 40 mg b.i.d. permitted; criteria as per arm 1 |
| Study | Additional publications | CP | AP | BC | Country | No. of centres | Inclusion criteria | Exclusion criteria | Method of allocation | Blinding | Therapy common to all participants | Notes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kantarjian et al. (2007)23 |
Shah et al. (2006)82 Shah et al. (2006)83 Cannell (2007)84 Kantarjian et al. (2007)85 Martinelli et al. (2007)86 Schiffer (2007)87 Rousselot et al. (2008)88 Rousselot et al. (2008)89 |
✓ | Not stated (n = 23); authors are from the USA, Brazil, France, Poland, Thailand, Poland, Russian Federation, Hungary and Australia | 58 | Patients with CML-CP and primary or acquired resistance to conventional doses of imatinib (400–600 mg q.d.), dasatinib-naive, at least 18 years of age and have adequate hepatic and renal function. CP was defined by the presence of < 15% blasts, < 20% basophils and < 30% blasts plus promyelocytes in PB or BM and a platelet count of at least 100,000 per cubic millimetre, with no extramedullary involvement. Primary resistance to imatinib was defined as a lack of CHR after 3 months of imatinib treatment, a lack of any CyR after 6 months of treatment or a lack of a MCyR (Ph+ cells > 35%) after 12 months of treatment. Relapse after a HR or MCyR was considered as secondary or acquired resistance | Patients who had received imatinib in the 7 days before the study were ineligible, as were patients who had received imatinib at doses in excess of 600 mg q.d. Patients with known specific BCR–ABL mutations (with high resistance to imatinib) before study entry were excluded | 2 : 1 randomisation (no details of methods used) | Open-label | Not reported | |||
| Shah et al. (2008)22 |
Hochhaus et al. (2006)90 Hochhaus et al. (2007)91 Shah et al. (2007)92 Hochhaus et al. (2008)93 Hochhaus et al. (2008)94 Nicaise et al. (2008)95 Porkka et al. (2008)96 Shah et al. (2008)97 Wang et al. (2008)98 |
✓ | Not stated; authors are from the USA, Republic of South Korea, France, Brazil, Argentina, Mexico, Russian Federation, Australia and Germany | 139 | Patients at least 18 years of age with Ph+ CML-CP and primary or acquired haematological resistance or intolerance to imatinib were enrolled. Patients were required to have < 15% blasts in PB or BM, < 30% blasts and promyelocytes in PB or BM, < 20% basophils in PB, equal to 100,000/µl platelets (or less if related to prior drug therapy), and no extramedullary involvement (except liver or spleen). Primary resistance to imatinib (400–800 mg q.d.) was defined as no decrease in WBC count after 4 weeks of treatment, no complete HR after 3 months, no MCyR after 6 months and no CCyR after 12 months. Acquired resistance was defined as loss of MCyR (equal to 30% absolute increase in the percentage of Ph+ metaphases), loss of molecular response (concomitant with a 10% Ph+ metaphases at cytogenetic analysis), evidence of a new mutation in the BCR–ABL-kinase domain, or loss of a confirmed CHR (WBC count > 10,000/μl on all assessments over at least a consecutive 2-week period). Intolerance to imatinib was defined as grade 3 or worse toxicity which led to discontinuation of therapy. Patients who tolerated 400 mg q.d. imatinib, but who did not achieve a CCyR and subsequently did not tolerate doses of 600 mg q.d. were considered to be resistant to imatinib | Included but not limited to: treatment with imatinib, IFN, cytarabine therapy or any targeted small-molecule anticancer agent within 7 days of initiation; uncontrolled or significant cardiovascular disease; history of a significant bleeding disorder unrelated to CML; eligibility for immediate autologous or allogeneic SCT; or concurrent incurable malignancy other than CML | A permuted block design was used to assign participants randomly with a 1 : 1 : 1 : 1 ratio | Open-label | Therapies other than dasatinib were prohibited, except hydroxycarbamide (limited to a period of 2 weeks) for treatment of elevated WBC counts (> 50 × 109/l). Administration of myeloid growth factors or recombinant erythropoietin was permitted at the discretion of the investigator. Patients were supported with platelet transfusions as required |
NCT00123474 CA 180–034 |
||
| Kantarjian et al. (2009)81 |
Kantarjian et al. (2006)99 Pasquini et al. (2007)100 Kantarjian et al. (2008)101 Saglio et al. (2008)102 |
✓ | (n = 30) Argentina, Australia, Austria, Belgium, Brazil, Canada, Czech Republic, Denmark, Finland, France, Germany, Hungary, Ireland, Israel, Italy, the Netherlands, Norway, Peru, Philippines, Poland, Republic of Korea, Russian Federation, Singapore, South Africa, Spain, Switzerland, Taiwan, Thailand, the UK and the USA | 97 | Participants with CML-AP (PB or BM counts of 15–30%); blasts, ≥ 30% blasts plus promyelocytes, but with < 30% blasts alone; ≥ 20% basophils, and platelet counts < 100 × 109/l unrelated to drug therapy; patients with clonal evolution or with prior CML-AP (except those defined by elevated basophil count only) who achieved a HR and subsequently progressed were included even if they did not reach the threshold values of percentage of blasts in PB or BM for AP, who had stopped treatment with imatinib following resistance or intolerance. Resistance to imatinib was defined as no HR to imatinib after at least 4 weeks of treatment or a 50% increase in PB blasts after 2 weeks’ treatment at 600 mg q.d.; achieved a HR and subsequently no longer met the criteria consistently on all assessments over a consecutive 2-week period while receiving imatinib 600 mg q.d.; or patients initially diagnosed with CML-CP who progressed to CML-AP while receiving imatinib at any dose. Intolerance to imatinib was defined as having grade 3 or greater non-haematological toxicity or grade 4 or greater haematological toxicity lasting for > 2 weeks while on imatinib ≥ 600 mg q.d. that led to discontinuation of therapy or to dose decrease to ≤ 400 mg q.d. with loss of HR | Eastern Cooperative Oncology Group (ECOG) performance status > 2; inadequate hepatic or renal function; treatment with imatinib, INF, cytarabine or any targeted small molecule anticancer agent within 7 days of initiation; uncontrolled or significant cardiovascular disease; history of a significant bleeding disorder unrelated to CML; or any concurrent incurable malignancy other that CML | Randomisation (no detail of methods) was stratified by phase and type of disease and imatinib status (resistant or intolerant) | Open-label | CML therapies other than dasatinib were prohibited during the study, with the exception of hydroxycarbamide for elevated WBC counts. Colony-stimulating factors and recombinant erythropoietin were permitted at the discretion of the investigator, according to institutional guidelines. Patients were supported with platelet transfusions as required | CA180–035 |
| Study | Arm no. | Drug | Dosage | Concurrent treatment | Notes |
|---|---|---|---|---|---|
| Kantarjian et al. (2006)103 | 1 | Nilotinib | Nine dose cohorts, ranging from 50 mg to 1200 mg q.d. and from 400 mg to 600 mg b.i.d. | During the first cycle of therapy or at times of worsening disease before intrapatient dose escalation, patients were allowed to receive cytoreductive therapy (leucaphereses and hydroxycarbamide) to control elevated counts of blasts, platelets or both | Multiple arms with different dosage levels; however, outcomes of interest for effectiveness only reported for all enrolled participants |
| Talpaz et al. (2006)104 | 1 | Dasatinib |
Dose escalation study (15–240 mg q.d.) The study protocol permitted progression to the administration of continuous daily doses of dasatinib and dose escalation |
Unclear | |
| Cortes et al. (2007)38 | 1 | Dasatinib | Not reported | Unclear | |
| 2 | Nilotinib | Not reported | Unclear | ||
| Cortes et al. (2007)13 | 1 | Dasatinib | 70 mg b.i.d.; after 4 weeks of treatment, dose escalation to 100 mg b.i.d. was permitted for participants with suboptimal response | No treatment for CML other than dasatinib was permitted during the study – except anagrelide and hydroxycarbamide for treatment of elevated platelet counts (higher than 700 × 109/l) and WBC counts (higher than 50 × 109/l), respectively. Use of hydroxycarbamide was limited to a period of 2 weeks. Administration of colony-stimulating factors and recombinant erythropoietin was permitted at the discretion of the investigator | |
| Fabarius et al. (2007)79 | 1 | Dasatinib | Started at a dose of 100–140 mg q.d. (2 × 50 mg q.d. or 2 × 70 mg q.d.) | Not clear. Only stated that five patients received allogeneic SCT | |
| Guilhot et al. (2007)12 | 1 | Dasatinib |
Starting dose 70 mg b.i.d. After 4 weeks of treatment, dose escalation to 100 mg b.i.d. was permitted for participants with suboptimal response |
No treatment for CML other than dasatinib was permitted during the study – except anagrelide and hydroxycarbamide for treatment of elevated platelet counts (higher than 700 × 109/l) and WBC counts (higher than 50 × 109/l), respectively. Use of hydroxycarbamide was limited to a period of 2 weeks | |
| Hochhaus et al. (2007)11,105 | 1 | Dasatinib |
70 mg b.i.d.; escalation to 90 mg b.i.d. permitted for patients with suboptimal response Interruptions or reduction to 50 mg or 40 mg b.i.d. in response to toxicity |
No treatment for CML other than dasatinib was permitted during the study – except anagrelide and hydroxycarbamide for treatment of elevated platelet counts (higher than 700 × 109/l) and WBC counts (higher than 50 × 109/l), respectively. Use of hydroxycarbamide was limited to a period of 2 weeks. Administration of colony-stimulating factors and recombinant erythropoietin was permitted at the discretion of the investigator | |
| Kantarjian et al. (2007)106 | 1 | Nilotinib | 400 mg b.i.d.; escalation to 600 mg b.i.d. allowed if suboptimal response and no safety concerns | Unclear | |
| le Coutre et al. (2008)107 | 1 | Nilotinib |
800 mg (400 mg b.i.d.) Escalation to 1200 mg (600 mg b.i.d.) was permitted for suboptimal response in the absence of toxicity Reductions to 400 mg daily and subsequently 200 mg daily were permitted for the management of toxicity |
Treatment with chemotherapy other than hydroxycarbamide was not permitted within 1 week of starting therapy with nilotinib | |
| Kim et al. (2009)80 | 1 | Dasatinib | Starting dose 70 mg b.i.d. | Not reported | |
| Tojo et al. (2009)108 | 1 | Nilotinib |
800 mg (400 mg b.i.d.) Reductions to 400 mg daily and subsequently 200 mg daily were permitted for the management of toxicity |
Not reported | |
| Sakamaki et al. (2009)109 | 1 | Dasatinib |
Phase I: dose escalation at 50 mg b.i.d., 70 mg b.i.d., 90 mg b.i.d. Unclear which participants took which doses Phase two: starting dose 140 mg q.d. (70 mg b.i.d.) Reduction (amount not reported) was permitted for participants with toxicity Escalation (amount not reported) was permitted for participants with suboptimal response |
No other anticancer therapy other than ≤ 14 days of hydroxycarbamide for WBC > 50 × 109/l | Presented results conflate Phase I (dose escalation) and Phase II (dose steady) results into a single cohort |
| Study | Additional publications | Design | CP | AP | BC | Country | No. of centres | Inclusion criteria | Exclusion criteria | Notes |
|---|---|---|---|---|---|---|---|---|---|---|
| Kantarjian et al. (2006)103 |
Giles et al. (2005)110 Singer et al. (2007)111 La et al. (2008)112 |
Case series (prospective) | ✓ | ✓ | ✓ | Unclear (authors from the USA and Germany) | Three |
Patients with Ph+ ImR CML or ALL, at least 18 years of age and have an adequate performance status and normal hepatic, renal and cardiac function. Patients with ImR CML-CP were enrolled in the study after the first four dose cohorts. Imatinib resistance was defined as a lack of complete haematological response after 3 months of imatinib treatment, a lack of any CyR (Ph+ cells > 95%) after 6 months of treatment, a lack of a substantial CyR (Ph+ cells > 35%) after 12 months of treatment or a relapse after a HR or a substantial CyR Note: 13 (11%) of the patients were Ph+ ALL |
Patients who had received imatinib therapy 7 days before or hydroxycarbamide 2 days before the study began were not eligible to participate | NCT00109707 |
| Talpaz et al. (2006)104 |
Chu et al. (2006)113 Sawyers et al. (2006)114 Cortes et al. (2008)115 |
Case series (prospective) | ✓ | ✓ | ✓ | USA | Two |
Patients who were at least 14 years of age, had Ph+ CML (CP or AP or BC) or Ph+ ALL, and haematological resistance or intolerance to imatinib. CP was defined by the presence of < 15% blasts, < 20% basophils and < 30% blasts plus promyelocytes in PB or BM and a platelet count of at least 100,000 per cubic millimetre, with no extramedullary involvement. BC was defined by the presence of at least 30% blasts in PB or BM or extramedullary infiltrates of leukaemic cells (other than the spleen or liver). AP patients were defined if they did not fulfill criteria for CP or BC, but did meet any of the following criteria: the presence of at least 15% (but < 30% blasts) in PB or BM, the presence of at least 20% basophils in PB or BM, the presence of at least 30% blasts plus promyelocytes (but < 30% blasts) in PB or BM or a platelet count of < 100,000 per cubic millimetre unrelated to therapy. Patients with AP disease or BC who had met the criteria for CP disease at the time of entry were enrolled as having CML-CP. Patients with Ph+ ALL had at least 30% lymphoblasts in PB or BM without previous evidence of CML-CP Haematological resistance to imatinib was classified as primary (a lack of adequate response) or acquired (a relapse after an initial response). Patients with cytogenetic or molecular resistance, but without haematological resistance to imatinib were not eligible. Patients were considered to be unable to tolerate imatinib if they had discontinued treatment as a result of non-haematological toxic effects of any grade |
Not reported | NCT00064233 |
| Cortes et al. (2007)38 | Cohort study (retrospective) | ✓ | ✓ | ✓ | USA | One | Not clearly reported. Between June 2003 and February 2006, 217 patients with CML who failed therapy with imatinib were treated with second-generation TKIs. Mutational analysis by direct sequencing was performed in all patients after imatinib failure and prior to the start of therapy with the second TKI. Mutational analysis was also performed after treatment with another TKI in 112 patients who had failure to imatinib therapy. These patients with mutation analysis before and after treatment with second TKI constitute the focus of the report | Not reported | Eighteen patients (five CP, nine AP and four myeloid BC) received a third TKI; most were in the advanced phase of CML; 15 of them received dasatinib after having failed imatinib and nilotinib | |
| Cortes et al. (2007)13 |
Ottmann et al. (2005)116 Talpaz et al. (2005)117 Chromik et al. (2006)118 Cortes et al. (2006)119 Martinelli et al. (2006)120 Soverini et al. (2006)77 Ganibacoiti et al. (2007)121 Ottmann et al. (2007)122 Soverini et al. (2007)78 Cortes et al. (2008)123 Porkka et al. (2008)124 Saglio et al. (2008)125 |
Case series (prospective) | ✓ | The USA, Switzerland, Germany, Argentina, Australia, Austria, Belgium, Israel, France, Italy, the Netherlands, Brazil, Canada, Finland, Republic of Korea, the Philippines, Sweden, Taiwan, Thailand and the UK | Multicentre, but number not reported |
Patients 18 years of age and older were eligible for inclusion if they had CML in MBC or LBC and were resistant to or intolerant of imatinib therapy. CML-BC was defined as > 30% blasts (myeloid or lymphoid) in PB or BM or extramedullary leukaemic infiltrates (other than in spleen or liver) with PB blast (myeloid or lymphoid) cell morphology Imatinib resistance was defined as progression from CP to BC while receiving 400 mg q.d. or more imatinib or from AP to BC while receiving 600 mg q.d. or more imatinib (or 400–600 mg q.d. if the patient was intolerant of 600 mg q.d. or more). Patients initially diagnosed in BC were classified as having ImR CML if they met the criteria for BC after 4 or more weeks (2 weeks for patients whose disease progressed rapidly) on imatinib 600 mg q.d. or more). Imatinib intolerance was defined as discontinuation of therapy because of toxicity considered at least possibly related to an imatinib dose of 400 mg q.d. or less or to an inability to tolerate imatinib doses higher than 400 mg q.d. For inclusion in the study, patients were required to have adequate hepatic and renal function and an Eastern cooperative Oncology Group (ECOG) performance score of 2 or lower |
Exclusion criteria included previous dasatinib therapy, imatinib therapy within 7 days of initiation, uncontrolled or significant cardiovascular disease, or history of a significant bleeding disorder unrelated to CML |
START-B START-L #CA180006 #CA180015 |
||
| Fabarius et al. (2007)79 | Case series (prospective) | ✓ | ✓ | ✓ | Germany | Not clearly defined, other than ‘patients with Ph+ and BCR–ABL-positive CML after imatinib failure’ | Not reported | |||
| Guilhot et al. (2007)12 |
Guilhot et al. (2005)126 Cortes et al. (2006)127 Talpaz et al. (2006)128 Guilhot et al. (2007)129 O’Brien (2007)130 Rea et al. (2008)131 Rea et al. (2008)132 |
Case series (prospective) | ✓ | The USA, Switzerland, Germany, Argentina, Australia, Austria, Belgium, Israel, France, Italy, the Netherlands, Singapore, Sweden, Taiwan, the UK, Brazil and Norway | 40 |
Male and female patients, aged 18 years or older, were eligible for inclusion if they had Ph+ or BCR–ABL-positive CML-AP with primary or acquired haematological resistance or intolerance to imatinib therapy, and had adequate hepatic function. CML-AP was defined as the occurrence of one or more of the following (1) at least 15–30% blasts in PB or BM; (2) at least 30% blasts plus promyelocytes (summed) in blood or BM (but with < 30% blasts alone); (3) at least 20% basophils in blood or BM; or (4) platelet counts < 100 × 109/l unrelated to drug therapy The definition of resistance to imatinib differed depending on the initial CML diagnosis Patients with an initial diagnosis of CML-CP were defined as having resistant disease if (1) progression to CML-AP occurred while receiving imatinib 400 mg q.d. or more; or (2) no HR was achieved after at least 4 weeks (or 2 weeks for patients who progressed rapidly) of imatinib 600 mg q.d.) Patients with an initial diagnosis of CML-AP or -BC who had experienced a HR were defined as having resistant disease if progression to CML-AP occurred while receiving imatinib 600 mg q.d. or more (or 400–600 mg q.d. if the patient was intolerant of ≥ 600 mg q.d.) Patients were defined as having ImI CML-AP if they had toxicity which led to a discontinuation of therapy and was considered to be possibly related to imatinib at a dose of ≯ 400 mg q.d. or if they could only tolerate imatinib doses < 400 mg q.d. |
Patients who had an ECOG performance status of grade 3 or greater, uncontrolled or significant cardiovascular disease, or a history of a significant bleeding disorder unrelated to CML |
#CA180005 START-A |
||
| Hochhaus et al. (2007)11,105 |
Hochhaus et al. (2005)133 Baccarani et al. (2006)134 Hochhaus et al. (2006)135 Hochhaus et al. (2006)136 Guilhot et al. (2007)137 Mueller et al. (2007)138 Stone et al. (2007)139 Baccarani et al. (2008)140 Cervantes et al. (2008)141 Goldman and Druker (2001)142 Cortes et al. (2008)143 Deininger et al. (2008)144 Hochhaus et al. (2008)145 Hochhaus et al. (2008)105 Hochhaus et al. (2008)146 Mauro et al. (2008)147 |
Case series (prospective) | ✓ | (n = 20) Australia, Belgium, Canada, Denmark, Finland, France, Germany, Ireland, Israel, Italy, Republic of Korea, the Netherlands, Peru, Singapore, Spain, Sweden, Switzerland, the UK and the USA | 75 |
Patients aged at least 18 years who had ImR or ImI CML in CP. CML-CP was defined as < 15% blasts in PB and BM, < 20% basophils in PB, < 30% blasts plus promyelocytes in PB and BM, platelets at least 100 × 109/l unless thrombopenia was because of recent therapy and no extramedullary involvement other than in liver or spleen The ImI population included patients with progressive CML-CP on imatinib > 600 mg q.d. or those who had resistance to imatinib ≯ 600 mg q.d. and BCR–ABL mutations associated with high-level imatinib resistance ImR was defined as a lack of complete HR after 3 months of imatinib treatment, a lack of any CyR after 6 months of treatment, a lack of an MCyR (Ph+ cells > 35%) after 12 months of treatment, an increasing WBC count on at least two consecutive occasions, or a relapse after a CHR or MCyR. ImI was defined as at least grade 3 non-haematological toxicity or grade 4 haematological toxicity persisting for > 7 days, related to imatinib at any dose |
Patients with prior AP or CML-BC; prior dasatinib therapy; imatinib therapy within 7 days of initiation; an ECOG performance status > 1; uncontrolled or significant cardiovascular disease; or a history of a significant bleeding disorder unrelated to CML |
CA180013 START-C |
||
| Kantarjian et al. (2007)106 |
Kantarjian et al. (2006)148 le Coutre et al. (2006)149 Cortes et al. (2007)150 Hochhaus et al. (2007)151 Hughes et al. (2007)152 Cortes et al. (2007)153 Martinelli et al. (2007)154 Mueller et al. (2007)155 Rosti et al. (2007)156 Rosti et al. (2007)157 Hochhaus et al. (2008)158 Jabbour et al. (2008)159 Kantarjian et al. (2008)160 Kantarjian et al. (2008)161 Lipton et al. (2008)162 Radich et al. (2008)163 Saglio et al. (2008)164 Clark et al. (2009)165 |
Case series (prospective) | ✓ | Not stated (n = 15); authors from the USA, Germany, Italy, the Netherlands, France, the UK and Spain | 63 | Patients with Ph+CML-CP aged at least 18 years who had ImR or ImI, adequate performance status (a WHO performance score of 2), and normal hepatic, renal and cardiac functions. Patients with had ImR had to have been treated with a dose of at least 600 mg q.d. for 3 months | Patients in BC and patients who had received treatment with imatinib for 7 days and with hydroxycarbamide for 2 days prior to nilotinib, were excluded. Potassium and magnesium levels had to be greater than or equal to the lower limit or normal or corrected to within normal range. Patients receiving concomitant medications known to prolong the QT interval or inhibit Cytochrome P4503A4 were excluded if alternative treatments were not possible. ImR was defined as failure to achieve CHR after 3 months or loss of a HR or CyR at any time during treatment with imatinib. Entry criteria for ImI included patients with intolerant symptoms (but who also had never achieved a MCyR with imatinib) and haematological toxicity of grade 4 severity persisting for > 7 days. ImI patients who had previously demonstrated sensitivity to imatinib, as evidenced by a prior MCyR, were excluded from participation in the study | NCT00109707 (same as 425, but hard to see connection) | ||
| le Coutre et al. (2008)107 |
le Coutre et al. (2007)166 le Coutre et al. (2007)167 le Coutre et al. (2007)168 Saglio et al. (2007)169 Alexander and le Coutre (2008)170 Apperley et al. (2008)171 Kantarjian et al. (2008)172 le Coutre et al. (2008)173 le Coutre et al. (2008)174 le Coutre et al. (2008)175 |
Case series (prospective) | ✓ | Not stated (n = 10); authors are from Germany, the USA, South Korea, the UK, Italy, Poland, France, China and Australia |
Patients at least 18 years of age and with ImR or ImI CML in AP. Patients were also required to have a WHO performance status score of 2 or lower and normal serum electrolytes as well as normal hepatic, renal and pancreatic function ImR was defined by one of the following criteria during treatment with imatinib at least 600 mg q.d. (1) disease progression from CP to AP occurring during imatinib therapy; (2) disease progression defined as at least a 50% increase in peripheral WBC count, blast count, basophils or platelets during imatinib therapy for AP; or (3) lack of HR in the BM following a minimum of 4 weeks of imatinib therapy for AP ImI was defined as the discontinuation of imatinib therapy because of any of the following: grades 3 or 4 AEs that persisted in spite of optimal supportive care measures, or grade 2 AEs related to imatinib therapy in spite of optimal supportive care measures that persisted for at least 1 month or that recurred more than three times whether or not the dose was reduced or discontinued. The protocol definition of ImI required the lack of an MCyR with imatinib |
Patients who had evidence of abnormal cardiac function or cardiac conduction, including individuals who had a myocardial infarction within the previous 12 months, individuals with left ventricular ejection fractions of 45% or less by echocardiogram or multiple-gated acquisition scan and individuals with a history of congenital long QT syndrome or a corrected QT interval of > 450 milliseconds on screening electrocardiogram using QT correction formula (QTcF) | NCT00384228 | |||
| Kim et al. (2009)80 | Case series (retrospective) | ✓ | ✓ | ✓ | Canada | One | CML patients treated with dasatinib at a single unit, March 2005 to October 2007 [seven with PB large granular lymphocyte (LGL) lymphocytosis]; not explicitly stated whether or not all such patients are included | No | The experience of one participant with Ph+ ALL is also reported in this publication, but has been excluded from consideration here | |
| Tojo et al. (2009)108 | Case series (prospective) | ✓ | ✓ | ✓ | Japan | Multicentre, but number of centres not reported (authors are from 16 different centres, including one in Australia) |
Japanese patients with ImR or ImI ImR defined according to phase: CP, failure to achieve CHR after 3 months/CyR after 6 months/MCyR after 12 months or loss of HR or CyR following ≥ 3 months of imatinib at ≥ 600 mg q.d. AP/BC, progression to AP/BC during imatinib (≥ 600 mg q.d.) in CP; ≥ 50% increase in WBC, blasts, basophils, or platelets during imatinib in AP/BC; lack of HR after ≥ 4 weeks imatinib in AP/BC In addition, participants receiving < 600 mg q.d. imatinib were eligible if named BCR–ABL mutations detected ImI defined as discontinuation of imatinib because of grade 3–4 AEs or grade 2 AEs lasting ≥ 1 month or recurring more than three times |
Performance status score > 2; hepatic, renal or cardiac dysfunction Participants meeting criteria for ImI were excluded if they had achieved an MCyR to imatinib |
The experience of seven participants with Ph+ ALL is also reported in this publication, but has been excluded from consideration here | |
| Sakamaki et al. (2009)109 | Case series (prospective) | ✓ | ✓ | ✓ | Japan | Appears to be multicentre (authors come from 22 separate centres), though not explicitly stated |
Adult CML aged 20–75 years ImR defined according to phase. CP, in individuals treated with imatinib at ≥ 400 mg q.d.: WBC greater or equal to a twofold increase from nadir to > 20 × 109/l or increase from nadir to ≥ 50 × 109/l; failure to achieve CHR after 3 months/CyR after 6 months/MCyR after 12 months or loss of CHR or MCyR; named BCR–ABL mutations suggestive of ImR detected. AP: progression to BC; progression to AP after HR to imatinib (≥ 400 mg q.d.) in CP; lack of HR after ≥ 4 weeks imatinib (≥ 600 mg q.d.) in AP BC: progression to BC after HR to imatinib (≥ 600 mg q.d.); BC persisted after ≥ 4 weeks imatinib ImI defined according to phase. CP, discontinuation of imatinib because of grade 3–4 non-haematological AEs or grade 4 haematological AEs persisting ≥ 7 days. AP/BC, any toxicity leading to discontinuation of imatinib or dose kept < 400 mg q.d. |
None reported | The experience of 13 participants with Ph+ ALL is also reported in this publication, but has been excluded from consideration here |
Table 9 gives a summary of evidence identified for this review. It shows that the preponderance of identified evidence relates to dasatinib: all three randomised studies – two comparing different dosages of dasatinib in CP22 and AP,81 and one comparing dasatinib with HDI23 – and 811–13,38,79,80,104,105,109 of 1211–13,38,79,80,103–109 observational studies investigated dasatinib. Most of this research addresses the efficacy of dasatinib in CML-CP: two of the three RCTs22,23 and six of the eight observational studies11,38,79,80,104,109 are, in whole or in part, set in this population. However, among the 11 separate treatment arms across these studies, only one – Shah et al. ’s dose optimisation RCT22 – explicitly adopts the UK licensed dosage of 100 mg q.d. Most other studies use the previously recommended regimen of 70 mg b.i.d. (i.e. total daily dose of 140 mg).
| Intervention | CP | AP | BC | Total | ||||
|---|---|---|---|---|---|---|---|---|
| RCT | Obs | RCT | Obs | RCT | Obs | RCT | Obs | |
| Dasatinib | 2 | 6 | 1 | 6 | 0 | 6 | 3 | 8a |
| Nilotinib | 0 | 4 | 0 | 4 | NA | NA | 0 | 5b |
One of the RCTs81 and one multicentre observational study12 concentrate on dasatinib in AP (both feature cohorts taking the UK recommended dose of 70 mg q.d.), and both single-centre case series79,80 and one small Japanese multicentre study109 report the experience of some individuals in AP taking dasatinib at the recommended dose. The Phase I dose escalation study104 also includes some participants in AP, but dasatinib was given at a wide variety of dosages, with no report of influence of dosage on results. Finally, Cortes et al. ’s retrospective cohort study38 features some participants in CML-AP, although the dosage at which they took dasatinib is not reported.
We identified a single multicentre observational study focusing exclusively on dasatinib in CML-BC. 13 Again, those case series that report experience across all disease phases79,80,109 feature some individuals in BC taking dasatinib at the recommended dose and Cortes et al. ’s retrospective cohort study38 includes some participants in BC, although the dosage at which they took dasatinib is not reported. The Phase I dose escalation study104 also includes some participants in BC, but dasatinib was given at a wide variety of dosages, with no report of influence of dosage on results.
Only five of the identified studies investigated nilotinib: a Phase I dose-ranging study in all phases of CML;104 Phase II multicentre studies in CP106 and AP;107 one small Japanese multicentre study across all phases of the disease;109 and one retrospective study relating experience with both dasatinib and nilotinib. 38
Eligibility criteria were broadly similar in included studies, with two important and related exceptions:
-
The definition of ImI varied between industry-sponsored studies of dasatinib and analogous studies of nilotinib. In dasatinib studies, intolerance was solely judged on the occurrence of persistent AEs during imatinib therapy; in nilotinib studies, ImI participants were only recruited if, alongside intolerable toxicity, they had shown no CyR to imatinib. This additional criterion is not quite the same as requiring that participants should be ImR as well as ImI, because no time limit is placed on failure to respond (ImR individuals must show failure to respond over a specified period – generally 12 months in CP studies); however, all such participants should have had non-responder status.
-
The definition of ImR in dasatinib studies generally included criteria (e.g. failure to achieve CCyR over a given period on imatinib) that would enable the recruitment of participants in MCyR. In contrast, nilotinib studies tended explicitly to exclude such participants.
These differences combine to make it more likely that participants taking dasatinib would enter the study having already achieved target CyR; those in nilotinib studies should not have had this status.
Table 10 details baseline characteristics of participants in the included studies. It is notable that, in line with the eligibility criteria discussed above, a lower proportion of participants were in MCyR in studies of nilotinib than in those that investigated dasatinib, where reported. This variability may also apply to CHR at baseline (perhaps as a result of the wider inclusion of dasatinib studies).
| Study | Arm no.a | Subgroup | n | Median age (years) | Gender (% male) | Imatinib failure | Duration of CML median (months) | BCR–ABL mutation (%) | MCyR at baseline (%) | CHR at baseline (%) | WBC × 109/l median | Platelets × 109/l median | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intolerance (%) | Resistance (%) | ||||||||||||
| Cortes et al. (2007)38 | See footnote b | All | 112 | 51 (range 17–96) | 4.5 | 96.4 | 54.5 | ||||||
| Cortes et al. (2007)13 | 1 | LBC | 42 | 47 (range 19–72) | 52.4 | 11.9 | 88.1 | 28.0 (range 2.0–186.0) | 7.7 (range 0.6–443.1) | 33 (range 6–423) | |||
| MBC | 74 | 55 (range 21–71) | 55.4 | 8.1 | 91.9 | 49.0 (range 3.0–216.0) | 17 (range 0.4–191.6) | 51 (range 10–2121) | |||||
| Fabarius et al. (2007)79 | 1 | All | 71 | 58 (range 28–78) | 56.3 | 59.0 (range 6.0–216.0) | |||||||
| Guilhot et al. (2007)12,176 | 1 | All | 107 | 57 (range 23–86) | 51.4 | 7.5 | 92.5 | 90.9 | 16.8 (range 1–243.4) | 165 (range 8–3580) | |||
| ImI | 8 | 67 (range 54–74) | 25.0 | 68.7 | 5.6 (range 3.2–68.4) | 166 (range 54–1463) | |||||||
| ImR | 99 | 57 (range 23–86) | 53.5 | 91.2 | 17.5 (range 1–243.4) | 165 (range 8–3580) | |||||||
| All – 14 months’ FU | 174 | 57 (range 22–86) | 55.2 | 7.5 | 92.5 | 82.0 (range 4.0–359.0) | 56.4 | ||||||
| ImI – 14 months’ FU | 13 | 61(range 29–80) | 30.8 | 91.0 (range 4.0–206.0) | 9.1 | ||||||||
| ImR – 14 months’ FU | 161 | 56 (range 22–86) | 57.1 | 82.0 (range 4.0–359.0) | 60.0 | ||||||||
| Hochhaus et al. (2007)11,105 | 1 | All – 8 months’ FU | 186 | 59 (range 24–79) | 46.2 | 31.7 | 68.3 | 64.0 | 9.9 (range 0.4–196.5) | 290 (range 24–1912) | |||
| ImI – 8 months’ FU | 59 | 59 (range 24–79) | 44.1 | 26.0 | 7.4 (range 2.0–182.7) | 254 (range 61–1165) | |||||||
| ImR – 8 months’ FU | 127 | 59 (range 24–79) | 47.2 | 77.0 | 11.9 (range 0.4–196.5) | 300 (range 24–1912) | |||||||
| All – 15 months’ FU | 387 | 58 (range 21–85) | 49.4 | 25.6 | 74.4 | 60.7 (range 2.8–250.5) | 40.3 | 10.6 | 39.8 | ||||
| ImI – 15 months’ FU | 99 | 57 (range 24–79) | 42.4 | 26.3 (range 3.2–144.5) | 12.1 | 23.2 | 51.5 | ||||||
| ImR – 15 months’ FU | 288 | 58 (range 21–85) | 51.7 | 74.4 (range 2.8–250.5) | 50.4 | 6.3 | 35.8 | ||||||
| Kantarjian et al. (2006)103 | 1 | All | 119 | 60 (range 15–83) | 47.9 | 100.0 | 45.1 | 9.4 | |||||
| CP | 17 | 100.0 | 59.7 (range 12.9–167.4) | 29.4 | |||||||||
| AP (all) | 56 | 100.0 | 90.6 (range 7.2–226.9) | 8.9 | |||||||||
| LBC | 9 | 100.0 | 19.4 (range 3.2–82.9) | 0.0 | |||||||||
| MBC | 24 | 100.0 | 49.9 (range 3.8–186.9) | 0.0 | |||||||||
| Kantarjian et al. (2007)23 | 1 | All | 101 | 51 (range 24–85) | 52.5 | 100.0 | 64.0 (range 6.0–166.0) | 40.6 | 5.9 | 50.5 | 7.5 (range 2.0–153.0) | 256 (range 55–1903) | |
| 2 | All | 49 | 51 (range 24–80) | 44.9 | 100.0 | 52.0 (range 14.0–133.0) | 22.4 | 0.0 | 55.1 | 7.4 (range 2.0–133.0) | 248 (range 80–2318) | ||
| Kantarjian et al. (2007)106 | 1 | All | 280 | 58 (range 21–85) | 51.4 | 30.7 | 69.3 | 57.0 (range 5.0–275.0) | 42.3 | ≥ 2.9c | 43.2 | 9.9 (range 0.9–372.0)– | 309 (range 28–2000) |
| Kim et al. (2009)80 | 1 | All | 17 | 11.8 | 88.2 | ||||||||
| le Coutre et al. (2008)107 | 1 | All | 119 | 57 (range 22–79) | 56.3 | 19.3 | 80.7 | 71.0 (range 2.0–298.0) | 4.2 | 12.7 (range 0.4–277.0) | 203 (range 4–3044) | ||
| Shah et al. (2008)22 | 1 | All | 167 | 56 (range 20–78) | 50.3 | 25.7 | 74.3 | 55.0 (range 1.6–251.0) | 34.0 | 20.4 | 50.9 | ||
| 2 | All | 168 | 55 (range 21–84) | 50.6 | 26.2 | 73.8 | 51.0 (range 4.4–212.0) | 41.4 | 13.7 | 41.7 | |||
| 3 | All | 167 | 54 (range 20–84) | 41.9 | 26.3 | 73.7 | 56.0 (range 0.9–227.0) | 37.0 | 16.8 | 41.3 | |||
| All | All | 168 | 55 [range 18–83] | 45.8 | 24.4 | 75.6 | 53.0 (range 1.2–246.0) | 31.5 | 18.5 | 38.1 | |||
| Talpaz et al. (2006)104 | 1 | All | 84 | 56 (range 15–79) | 56.0 | 14.3 | 85.7 | 71.0 (range 5.0–216.0) | 71.4 | 23.0 (range < 1.0–243.0) | 216 (range 4–2166) | ||
| AP | 11 | 63 (range 40–73) | 27.3 | 18.2 | 81.8 | 67.0 (range 22.0–139.0) | 72.7 | 21.0 (range 1.0–108.0) | 279 (range 4–1710) | ||||
| CP | 40 | 61 (range 28–79) | 52.5 | 20.0 | 80.0 | 90.0 (range 13.0–207.0) | 82.5 | 33.0 (range 3.0–243.0) | 310 (range < 1–2166) | ||||
| LBC/Ph+ ALL | 10 | 50 (range 15–73) | 90.0 | 10.0 | 90.0 | 26.0 (range 9.0–70.0) | 60.0 | 12.0 (range 1.0–198.0) | 40 (range 22–375) | ||||
| MBC | 23 | 53 (range 30–70) | 60.9 | 4.3 | 95.7 | 44.0 (range 5.0–216.0) | 56.5 | 20.0 (range < 1.0–117.0) | 39 (range 7–1057) | ||||
| Kantarjian et al. (2009)81 | 1 | All | 158 | 56 (range 17–81) | 55.7 | 25.9 | 74.1 | 74.3 (range 5.1–326.8) | 46.8 | 9.5 | 10.1 | ||
| 2 | All | 159 | 56 (range 19–84) | 59.1 | 27.0 | 73.0 | 70.1 (range 2.5–199.7) | 46.4 | 7.5 | 19.5 | |||
| Tojo et al. (2009)108 | 1 | CP | 16 | 57 (range 30–83) | 56.3 | 75.0 | 25.0 | See footnote d | |||||
| AP | 7 | 61 (range 30–74) | 71.4 | 42.9 | 57.1 | See footnote e | |||||||
| BC | 4 | 53 (range 29–70) | 50.0 | 0.0 | 100.0 | See footnote f | |||||||
| Sakamaki et al. (2009)107 | 1 | CP | 30 | See footnote g | 40.0 | 60.0 | See footnote h | 16.7 | |||||
| AP/BC | 11 | 57 (range 31–73) | 27.3 | 72.7 | 1.6 (range 0.0–14.0) | 18.2 | |||||||
Otherwise, there appears to be little obvious heterogeneity in the baseline characteristics of study participants. The median age of studied cohorts tends to be in the mid- to late-50s age group, although one or two small subgroups diverge somewhat from this (range of median ages in studies: 50–67 years). Similarly, most groups are fairly well balanced for gender (though, again, small subgroups provide extreme values).
Including the two studies that enrolled only ImR individuals by design,23,103 there was invariably a majority of ImR participants compared with ImI samples, with most cohorts falling into the range 70–90% ImR (the one exception is Tojo et al. ’s small Japanese nilotinib study,108 in which three-quarters of the CP cohort were ImI).
Unsurprisingly, duration of CML history prior to dasatinib/nilotinib therapy varied according to the phase of disease, with CP cohorts tending to have an average CML duration in the range 50–70 months and AP 70–90 months. Individuals in BC tended to have a fairly short previous CML history (20–50 months) and were also relatively young; this suggests that study participants were not necessarily representative of a general population arriving at BC following a prolonged disease course but, rather, represented a selected group of individuals with relatively aggressive disease. This is probably because of the need to identify a cohort of individuals who have failed regular-dose imatinib at a late phase in the disease development.
As might be expected, in the few instances where separate baseline details are provided, ImI populations have always entered studies with a shorter history of CML than their ImR counterparts.
It is also predictable that average platelet counts would be lower in AP cohorts and a lot lower in BC populations.
Table 11 details therapy received by study participants prior to study entry. In ImI groups, most individuals will have failed imatinib rapidly, taking it for < 1 year, although a proportion (10–25%) may have a history of > 3 years’ exposure. ImR cohorts are more likely to have a prolonged duration of imatinib therapy, with 40–70% extending over 3 years.
| Study | Arm no.a | Subgroup | n | Time on imatinib (%) | Highest imatinib dose (mg q.d.) (%) | Prior therapy (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 1 year | 1– 3 years | > 3 years | < 400 | 400–599 | 600–799 | ≥ 600 | ≥ 800 | Chemotherapy | HU | IFN | SCT | ||||
| Cortes et al. 200738 | See footnote b | All | 112 | 61.6 | |||||||||||
| Cortes et al. 200713 | 1 | LBC | 42 | 47.6 | 28.6 | 23.8 | 2.4 | 45.2 | 52.4 | 78.6 | 47.6 | 33.3 | |||
| MBC | 74 | 14.9 | 37.8 | 47.3 | 0.0 | 51.4 | 48.6 | 66.2 | 55.4 | 12.2 | |||||
| Fabarius et al. 200779 | 1 | All | 71 | 15.5c | 67.6 | 69.0 | |||||||||
| Guilhot et al. 200712,176 | 1 | All | 107 | 7.5 | 24.3 | 69.2 | 41.1 | 59.8 | 68.2 | 75.7 | 17.8 | ||||
| ImI | 8 | 50.0 | 25.0 | 25.0 | 62.5 | 37.5 | 50.0 | 50.0 | 25.0 | ||||||
| ImR | 99 | 4.0 | 24.2 | 72.7 | 39.4 | 61.6 | 69.7 | 77.8 | 17.2 | ||||||
| All – 14 months’ FU | 174 | 31.0 | 9.8 | 59.2 | 76.9 | 51.7 | 59.2 | 94. | 71.8 | 13.2 | |||||
| ImI – 14 months’ FU | 13 | 38.5 | 46.2 | 15.4 | 48.3 | 23.1 | 46.2 | 92.3 | 61.5 | 15.4 | |||||
| ImR – 14 months’ FU | 161 | 29.8 | 6.8 | 62.7 | 44.7 | 55.3 | 60.2 | 93.8 | 73.3 | 13.0 | |||||
| Hochhaus et al. 200711,105 | 1 | All – 8 months’ FU | 186 | 19.9d | 25.8d | 53.8d | 47.8d | 52.2d | 41.9d | 69.9d | 9. d | ||||
| ImI – 8 months’ FU | 59 | 54.2d | 30.5d | 15.3d | 93.2d | 6.8d | 25.4d | 54.2d | 6.8d | ||||||
| ImR – 8 months’ FU | 127 | 4.7d | 23.6d | 71.7d | 26.8d | 73.2d | 50.4d | 77.2d | 10.2d | ||||||
| All – 15 months’ FU | 387 | 19.1 | 27.6 | 53.2 | 0.3 | 44.4 | 55.3 | 34.9 | 65.1 | 9.8 | |||||
| ImI – 15 months’ FU | 99 | 57.6 | 30.3 | 12.1 | 0.0 | 91.9 | 8.1 | 18.2 | 46.5 | 7.1 | |||||
| ImR – 15 months’ FU | 288 | 5.9 | 26.7 | 67.4 | 0.3 | 28.1 | 71.5 | 40.6 | 71.5 | 10.8 | |||||
| Kantarjian et al. 2006103 | 1 | All | 119 | ||||||||||||
| AP (all) | 56 | ||||||||||||||
| LBC | 9 | ||||||||||||||
| MBC | 24 | ||||||||||||||
| CP | 17 | ||||||||||||||
| Kantarjian et al. 200723 | 1 | All | 101 | 11.9 | 43.6 | 44.6 | 64.4e | 38.6 | 96.0f | 73.3 | 6.9 | ||||
| 2 | All | 49 | 10.2 | 59.2 | 30.6 | 71.4e | 36.7 | 93.9f | 67.3 | 4.1 | |||||
| Kantarjian et al. 2007106 | 1 | All | 280 | 27.5g | 32.5 | 39.6 | 25.4h | 83.2 | 65.7 | 7.9i | |||||
| Kim et al. 200980 | 1 | All | |||||||||||||
| le Coutre et al. 2008107 | 1 | All | 119 | 17.6j | 33.6j | 48.7j | 26.1h | 91.6 | 58.0 | 7.6 | |||||
| Shah et al. 200822 | 1 | All | 167 | 21.6 | 32.9 | 45.5 | 36.5 | 23.4 | 52.1 | 6.0 | |||||
| 2 | All | 168 | 23.8 | 40.5 | 35.7 | 32.7 | 31.0 | 51.8 | 7.7 | ||||||
| 3 | All | 167 | 23.6k | 35.2k | 41.2k | 32.9 | 24.6 | 55.7 | 3.0 | ||||||
| 4 | All | 168 | 22.0 | 35.7 | 42.3 | 33.3 | 25.6 | 48.8 | 4.2 | ||||||
| Talpaz et al. 2006104 | 1 | All | 84 | 14.3 | 22.6l | 63.1 | 59.5 | 71.4 | 14.3m | ||||||
| AP | 11 | 9.1 | 27.3l | 63.6 | 36.4 | 81.8 | 0.0m | ||||||||
| CP | 40 | 17.5 | 17.5l | 65.0 | 55.0 | 92.5 | 5.0m | ||||||||
| LBC/Ph+ ALL | 10 | 10.0 | 20.0l | 70.0 | 90.0 | 20.0 | 50.0m | ||||||||
| MBC | 23 | 13.0 | 30.4l | 56.5 | 65.2 | 52.2 | 21.7m | ||||||||
| Kantarjian et al. 200981 | 1 | All | 158 | 14.6 | 32.3 | 53.2% | 43.0 | 44.3 | 53.8 | 12.0n | |||||
| 2 | All | 159 | 15.1 | 34.0 | 50.3% | 45.9 | 44.0 | 54.7 | 5.7n | ||||||
| Tojo et al. (2009)108 | 1 | CP | 16 | See footnote o | |||||||||||
| AP | 7 | See footnote p | |||||||||||||
| BC | 4 | See footnote q | |||||||||||||
| Sakamaki et al. (2009)109 | 1 | CP | 30 | 23.3 | 23.3 | 53.3 | 90.0r | 10.0s | 70.0 | 50.0 | 3.3 | ||||
| AP/BC | 11 | 18.2 | 54.5 | 27.3 | 45.5r | 54.5s | 81.8 | 27.3 | 27.3 | ||||||
Where reported, ImI individuals appear to have been relatively unlikely to have been exposed to imatinib at 600 mg q.d. or higher. In ImR or mixed cohorts, the majority of participants tend to have some history of imatinib therapy at an escalated dosage (i.e. above 400 mg q.d.).
Incidence of prior chemotherapy is fairly heterogeneous across all included studies, with rates ranging from 15% to 90%. Concentrating on the main multicentre studies and considering disease phase introduces a little more consistency, in CP populations, 20–40% of participants have had prior chemotherapy, in AP, 25–70% and in BC, 65–90%.
In most included evidence, the majority of participants have previous exposure to interferon, mostly in the 50–75% range (again, higher rates can be seen in AP). SCT is seen less commonly, mostly falling in the range 5–20%, although studies in CML-BC have featured subgroups with up to 50% having prior SCT.
Critical appraisal of included evidence
Summary indicators of the internal validity of included randomised and observational studies are presented in Tables 12 and 13, respectively.
| Kantarjian et al. (2007)23 | Shah et al. (2008)22 | Kantarjian et al. (2009)81 | |
|---|---|---|---|
| Is a power calculation provided? | No | No | No |
| Is the sample size adequate? | NR | NR | NR |
| Was ethical approval obtained? | Yes | Yes | Yes |
| Were the study eligibility criteria specified? | Yes | Yes | Yes |
| Were the eligibility criteria appropriate? | Yes | Yes | Yes |
| Were patients recruited prospectively? | Yes | Yes | Yes |
| Was assignment to the treatment groups really random? | Unknown | Unknown | Unknown |
| Were groups stratified? | No | Yesa | Yesb |
| Was the treatment allocation concealed? | Noc | Noc | Noc |
| Are adequate baseline details presented? | Yes | Yes | Yesd |
| Are the participants representative of the population in question? | Yes | Yes | Yes |
| Are groups similar at baseline? | Partiale | Yes | Partialf |
| Are any differences in baseline adequately adjusted for in the analysis? | Yesg | NA | No |
| Are outcome assessors blind? | No | No | No |
| Was the care provider blinded? | Noc | Noc | Noc |
| Are outcome measures relevant to research question? | Yes | Yes | Yes |
| Are data collection tools shown or known to be valid for the outcome of interest? | Yes | Yes | Yes |
| Is compliance with treatment adequate? | Unclear | Unclear | Unclearh |
| Are withdrawals/dropouts adequately described? | Yes | Yes | Yes |
| Are all patients accounted for? | Yes | Yes | Yes |
| Is the number randomised reported? | Yes | Yes | Yes |
| Are protocol violations specified? | No | No | Partiali |
| Are data analyses appropriate? | Yes | Partialj | Partialj |
| Is analysis conducted on an ITT basis? | Yes | Yes | Yes |
| Are missing data appropriately accounted for? | NR | NR | Yes |
| Were any subgroup analyses justified? | Yes | Yes | No |
| Are the conclusions supported by the results? | Nok | Partiall | Partialm |
| Generalisability | Lown | Partial | High |
| Inter-centre variability | NR | NR | NR |
| Conflict of interest declared? | Yeso | Yesp | Yesq |
| Kantarjian et al. (2006)103 | Talpaz et al. (2006)104 | Cortes et al. (2007)38 | Cortes et al. (2007)13 | Fabarius et al. (2007)79 | Guilhot et al. (2007)12 | Hochhaus et al. (2007)11 | Kantarjian et al. (2007)106 | le Coutre et al. (2008)107 | Kim et al. (2009)80 | Sakamaki et al. (2009)109 | Tojo et al. (2009)108 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Is the hypothesis/aim/objective of the study clearly described? | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No | No | Yes |
| Were the case series collected at more than one centre? | Single centre | Multicentre | Single centre | Multicentrea | Single centre | Multicentre | Multicentre | Multicentre | Multicentre | Single centre | Multicentreb | Multicentre |
| Was the main outcome independently assessed? | No | No | Unclear | No | No | No | No | No | No | No | Unclear | Unclear |
| Are patient characteristics adequately described? | Noc | Nod | No | Yes | Yes | Yes | Yes | Yes | Yes | No | Noe | Nof |
| How easy is it to assess generalisability of the results? | Low | Low | Low | Medium | Low | High | High | Medium | High | Low | Lowg | Lowh |
| Are inclusion and exclusion criteria clearly reported? | Yesi | Yes | No | Yes | No | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Were data collected prospectively? | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | No | Yes | Yes |
| Were patients recruited consecutively? | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | No | Unclear | Noj |
| Did all the participants receive the same intervention? | Yesk | Nol | Unclearm | Yesk | Yesk | Yesk | Yesk | Yesk | Yesk | Unclear | Unclear | Yesk |
| Is the use of any concurrent therapies adequately described? | Unclear | Unclear | Unclear | Yesn | Unclear | Unclear | Yesn | Unclear | Unclear | Unclear | Yeso | Unclear |
| Was an ITT analysis performed? | No | Yes | NAp | Noq | Yes | Yes | Noq | Yesr | Yes | NAp | Noq | Yes |
| Are dropouts from the study adequately described? | Yes | Yes | NAp | Yes | Unclear | Yes | Yes | Yes | Yes | NAp | Unclear | Yes |
Randomised studies
The three included RCTs are all substantially flawed, most notably owing to their open-label designs and ambiguous allocation methods.
None of the RCTs report methods of allocation concealment. Concealment of allocation has been shown to be an important determinant of study bias, with clear evidence that studies in which allocation methods are inadequate or unclear tend to overestimate treatment effect. 177–180 Bias of this type arises because, if treatment allocation methods are suboptimal, investigators may preferentially select participants with certain characteristics (including, most notably, better prognosis) for their preferred treatment. 181 Subverting randomisation is made easier in open-label studies, such as the three in question here (see below).
Despite the potential for selection bias, there is little evidence of systematically different baseline characteristics between the arms of included RCTs. On the basis of reported baseline characteristics, the two dose optimisation studies22,81 appear to have well-balanced arms, with the exception that significantly more participants in the 70 mg q.d. arm of the advanced-phase RCT81 were in CHR at study entry (p = 0.029 by chi-squared test with Yates’s correction). It may, in any case, be unlikely that investigators would have a bias in favour of a particular dosing regimen, compared with a preference for a given treatment. Accordingly, Kantarjian et al. ’s RCT,23 in which dasatinib was compared with HDI, may have been more susceptible to this kind of bias. We note that, in this study, all five participants who were in MCyR at baseline were allocated to the dasatinib treatment. Although a small imbalance like this is not inconsistent with purely random treatment allocation (p = 0.283 by chi-squared test with Yates’s correction), if there were systematic selection bias in favour of dasatinib, one would expect to see it manifested in baseline asymmetries such as this. However, the only other reported inter-arm imbalance in this RCT – an excess of participants with BCR–ABL mutations in the dasatinib arm – is most likely to bias against dasatinib (if it has any influence on outcomes at all). Regrettably, no indication is provided of the participants’ clinical status at study entry (e.g. WHO performance status, Sokal score).
Similarly, all three included RCTs had an open-label design, meaning that neither participants nor investigators were blinded to treatment allocation. As with inadequate concealment of treatment allocation, absence of double-blind methods has been associated with exaggerated estimates of treatment effect. 177,180
Traditionally, the supposed mechanisms of bias in open-label studies have related to (1) preferential provision of supplementary therapy in treatment arms favoured by investigators (co-intervention, performance bias); and/or (2) inconsistent outcome assessment, with knowledge of treatment allocation influencing measurement in favour of a preferred comparison group (detection bias). In addition to these dangers, the absence of blinding may have led to an additional mechanism of bias in the present assessment; we believe that, in the context of an open-label design, treatment crossovers present a very substantial threat to study validity. Any preference, on the part of investigators, for one treatment over the alternative(s) is very likely to result in premature discontinuation of treatment for those randomised to receive the less favoured option.
In Kantarjian et al. ’s RCT,23 crossover to the alternative treatment was permitted after confirmed progression, loss of CHR or MCyR, lack of MCyR at the week 12 cytogenetic evaluation, or intolerance. Of the 49 participants who had been randomised to receive HDI, 39 (79.6%) crossed over to dasatinib therapy after a median treatment duration of 13 weeks, despite the fact that rates of MCyR were not significantly different between treatments at the initial (12-week) analysis. Median time to CyR with HDI in individuals who had previously failed standard-dose imatinib has been reported to be 9 months. 182 This suggests that the duration of HDI therapy in Kantarjian et al. ’s RCT,23 in which a sizeable majority of participants randomised to HDI abandoned the treatment within a few weeks of starting it, was substantially too short to evaluate the likelihood of response.
This has to be seen as a considerable potential bias in favour of dasatinib and – in the context of an open-label study sponsored by the manufacturers of dasatinib, with a 2 : 1 randomisation ratio in favour of dasatinib – it is difficult to avoid the conclusion that investigators were, in some way, systematically favouring the newer treatment.
The included RCTs seem to be of a higher standard in observing ITT principles; hence, attrition bias does not appear to have affected reported results.
None of the RCTs provided a power calculation, which may mean that they were underpowered to detect a difference between groups (i.e. susceptible to type II error).
Observational studies
It is challenging to provide meaningful critical appraisal of the 11 prospective case series and one retrospective cohort study we have identified, because it is in the nature of such evidence to present partial information that is difficult to assess and generalise. The criteria detailed in Table 13 reflect aspects of study design that may be associated with more credible research.
The Phase I and Phase II industry-sponsored studies were all conducted across multiple centres, and all appeared to feature consecutive, prospective recruitment of participants. Such features might be expected to enhance the accuracy and generalisability of the research (although the empirical basis for this proposition is ambiguous, at best183). None of the included case series reported any steps taken to blind outcome assessors to the technology under scrutiny, which might help to provide an unbiased estimate of treatment effect. 183
In most cases, we can be relatively confident that all reported participants received the same intervention (including, in most cases, objective rules for escalation, reduction, or interruption of therapy) and the prospective Phase II studies were generally good at reporting fully on the recruited cohort, in line with ITT principles.
Relationship of identified evidence to research questions
None of the evidence we have identified enables us to address any of our research questions directly (see Chapter 1, Overall aims and objectives of the assessment). Only one study attempts to compare either of the technologies under review with a relevant alternative (Kantarjian et al. ’s randomised comparison of dasatinib and HDI). 23 However, as has been discussed, there are very substantial flaws in the methods of this study, most notably the open-label design with permitted crossover, leading to arguably premature discontinuations of therapy among those randomised to HDI. Because of the overwhelming number of such events, we conclude that the results of this study provide limited meaningful evidence of the relative effectiveness of dasatinib and HDI in the context of this assessment. The relevance of data from this study is further compromised by the fact that the dose of dasatinib administered was different to the currently licensed UK dosage (70 mg b.i.d. compared with 100 mg q.d.).
In the absence of robust comparative effectiveness evidence on the technologies under review, we have been limited to reviewing the absolute treatment effects reported in the literature. In the following sections, we present a review of available evidence on the efficacy of each technology, with data drawn from the studies we have identified (because, by and large, our reservations about Kantarjian et al. ’s RCT23 relate to the meaningfulness of its HDI arm, data from the dasatinib arm are presented among other non-comparative evidence, below). We look at dasatinib first (see Effectiveness of dasatinib) and then at nilotinib (see Effectiveness of nilotinib). We have chosen to present these sequentially, rather than in parallel, to emphasise that all the data discussed here have been drawn from completely different sources. We strongly caution against a naive comparison between estimates of the efficacy of dasatinib and estimates of the efficacy of nilotinib. As has been explained, there are substantial differences in the design, methods, outcomes and analysis of the available evidence. In the absence of any experimental comparison between the two technologies, any head-to-head comparison of results may lead to grossly misleading conclusions.
Effectiveness of dasatinib
Cytogenetic response
Chronic phase
Table 14 provides a summary of the available data detailing CyR to dasatinib in CML-CP. All included studies reported CCyR, partial cytogenetic response (PCyR) and MCyR rates (or provided enough information to enable the deduction of each). Minor and minimal responses were less commonly reported. The definitions of each category of response appeared consistent across all included studies, with complete response corresponding to an absence of the Philadelphia chromosome among at least 20 cells in metaphase in a BM aspirate, partial response corresponding to a Ph+ rate of 1–35% and major response representing the sum of these two categories (i.e. ≤ 35% Ph+). One exception is found in Fabarius et al. ’s case series,79 in which 1–35% Ph+ is labelled as a ‘major’ response in the study. This definition corresponds exactly to a partial response in other studies, so we have included it as such in our review, regardless of the language used to report it in the paper.
| Study | Length of follow-up | Dose | IMF | Complete (n/N) | Partial (n/N) | Major (n/N) | Minor (n/N) | Minimal (n/N) | Overall (n/N) |
|---|---|---|---|---|---|---|---|---|---|
| Talpaz et al. (2006)104 | > 12.0 monthsa,b | Mixed/NR | ImR/ImI | 14/40 = 35.0% | 4/40 = 10.0% | 18/40 = 45.0% | 0/40 = 0.0% | 7/40 = 17.5% | 25/40 = 62.5% |
| Cortes et al. (2007)38 | 17.0 monthsa | Mixed/NR | ImR/ImI | 8/24 = 33.3% | 4/24 = 16.7% | 12/24 = 50.0% | 15/24 = 62.5% | ||
| Fabarius et al. (2007)79 | 8.6 monthsa | Mixed/NR | ImR/ImI | 22/50 = 44.0% | 7/50 = 14.0%c | 29/50 = 58.0%d | |||
| Hochhaus et al. (2007)11,105 | 8.0 monthse | 70 mg b.i.d. | ImI | 38/59 = 64.4% | 9/59 = 15.3% | 47/59 = 79.7% | 1/59 = 1.7% | 1/59 = 1.7% | |
| ImR | 35/127 = 27.6% | 15/127 = 11.8% | 50/127 = 39.4% | 6/127 = 4.7% | 15/127 = 11.8% | ||||
| 15.2 monthsa | 70 mg b.i.d. | ImI | 74/99 = 74.7% | 5/99 = 5.1% | 79/99 = 79.8% | ||||
| ImR | 115/288 = 39.9% | 36/288 = 12.5% | 151/288 = 52.4% | ||||||
| 24.0 monthsf,g | 70 mg b.i.d. | ImI | 77/99 = 77.8% | 4/99 = 4.0% | 81/99 = 81.8% | ||||
| ImR | 127/288 = 44.1% | 31/288 = 10.8% | 158/288 = 54.9% | ||||||
| Kantarjian et al. (2007)23 | 15.0 monthsa | 70 mg b.i.d. | ImR | 40/101 = 39.6% | 13/101 = 12.9% | 53/101 = 52.5% | |||
| 24.0 monthsf,g | 70 mg b.i.d. | ImR | 44/101 = 43.6% | ||||||
| Shah et al. (2008)22 | 6.0 monthse | 100 mg q.d. | ImI | 27/43 = 62.8% | 5/43 = 11.6% | 32/43 = 74.4% | |||
| ImR | 42/124 = 33.9% | 24/124 = 19.4% | 66/124 = 53.2% | ||||||
| 50 mg b.i.d. | ImI | 27/44 = 61.4% | 5/44 = 11.4% | 32/44 = 72.7% | |||||
| ImR | 43/124 = 34.7% | 15/124 = 12.1% | 58/124 = 46.8% | ||||||
| 140 mg q.d. | ImI | 30/44 = 68.2% | 1/44 = 2.3% | 31/44 = 70.5% | |||||
| ImR | 44/123 = 35.8% | 18/123 = 14.6% | 62/123 = 50.4% | ||||||
| 70 mg b.i.d. | ImI | 25/41 = 61.0% | 3/41 = 7.3% | 28/41 = 68.3% | |||||
| ImR | 50/127 = 39.4% | 15/127 = 11.8% | 65/127 = 51.2% | ||||||
| 24.0 monthse,h | 100 mg q.d. | ImR/ImI | 84/167 = 50.3% | 21/167 = 12.6% | 105/167 = 62.9% | ||||
| 50 mg b.i.d. | ImR/ImI | 84/168 = 50.0% | 18/168 = 10.7% | 102/168 = 60.7% | |||||
| 140 mg q.d. | ImR/ImI | 84/167 = 50.3% | 21/167 = 12.6% | 105/167 = 62.9% | |||||
| 70 mg b.i.d. | ImR/ImI | 91/168 = 54.2% | 11/168 = 6.5% | 102/168 = 60.7% | |||||
| Updatei | 100 mg q.d. | ImI | 29/43 = 67.4% | 4/43 = 9.3% | 33/43 = 76.7% | ||||
| ImR | 54/124 = 43.5% | 19/124 = 15.3% | 73/124 = 58.9% | ||||||
| 50 mg b.i.d. | ImI | 32/44 = 72.7% | 2/44 = 4.5% | 34/44 = 77.3% | |||||
| ImR | 52/124 = 41.9% | 17/124 = 13.7% | 69/124 = 55.6% | ||||||
| 140 mg q.d. | ImI | 32/44 = 72.7% | 2/44 = 4.5% | 34/44 = 77.3% | |||||
| ImR | 52/123 = 42.3% | 19/123 = 15.4% | 71/123 = 57.7% | ||||||
| 70 mg b.i.d. | ImI | 29/42 = 69.0% | 2/42 = 4.8% | 31/42 = 73.8% | |||||
| ImR | 61/126 = 48.4% | 11/126 = 8.7% | 72/126 = 57.1% | ||||||
| Kim et al. (2009)80 | NR | 70 mg b.i.d. | ImR/ImI | 9/13 = 69.2% | 1/13 = 7.7% | 10/13 = 76.9% | |||
| Sakamaki et al. (2009)109 | 6.0 monthse | 70 mg b.i.d.j | ImI | 8/12 = 66.7% | 2/12 = 16.7% | 10/12 = 83.3% | 1/12 = 8.3% | 1/12 = 8.3% | |
| ImR | 5/18 = 27.8% | 1/18 = 5.6% | 6/18 = 33.3% | 3/18 = 16.7% | 3/18 = 16.7% |
It is important to recognise that some of the participants in the industry-sponsored Phase II multicentre studies (those reported by Hochhaus et al. ,11,105 Kantarjian et al. 23 and Shah et al. 22) already had some degree of CyR at entry to the studies. In Shah et al. ’s dose-ranging RCT,22 all four arms featured a notable proportion of participants in MCyR at study entry, with the highest proportion (34/167 = 20.4%) in the 100 mg q.d. arm (i.e. the current UK licensed dosage). In Hochhaus et al. ’s population,11,105 the overall proportion was a little lower (41/387 = 10.6%); however, most of these participants were in the (smaller) ImI subgroup, leading to a high proportion of MCyR at baseline among those individuals (23/99 = 23.2%). In Kantarjian et al. ’s23 randomised comparison of dasatinib and HDI (in which all participants were ImR), a much smaller proportion of individuals had this characteristic (6/101 = 5.9%).
Complete cytogenetic response was consistently defined in the evidence base as 0% Ph+ chromosomes in metaphase in BM. Table 15 presents details of response rates in ImI, ImR and mixed populations, with meta-analytical subtotals for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImI | |||||
| aHochhaus et al. (2007)11,105 | 70 mg b.i.d. | 99 | 74 | 74.7 | 65.0% to 82.9% |
| Shah et al. (2008)22 | 100 mg q.d. | 43 | 27 | 62.8 | 46.7% to 77.0% |
| 50 mg b.i.d. | 44 | 27 | 61.4 | 45.5% to 75.6% | |
| 70 mg b.i.d. | 41 | 25 | 61.0 | 44.5% to 75.8% | |
| 140 mg q.d. | 44 | 30 | 68.2 | 52.4% to 81.4% | |
| Sakamaki et al. (2009)109 | 70 mg b.i.d. | 12 | 8 | 66.7 | 34.9% to 90.1% |
| Subtotal [heterogeneity: Q = 4.56 (p on 5 df = 0.471); I2 = 0.0%; τ2 = 0.000] | 68.1 | 62.7% to 73.5% | |||
| ImR | |||||
| aHochhaus et al. (2007)11,105 | 70 mg b.i.d. | 288 | 115 | 39.9 | 34.2% to 45.8% |
| Kantarjian et al. (2007)23 | 70 mg b.i.d. | 101 | 40 | 39.6 | 30.0% to 49.8% |
| Shah et al. (2008)22 | 100 mg q.d. | 124 | 42 | 33.9 | 25.6% to 42.9% |
| 50 mg b.i.d. | 124 | 43 | 34.7 | 26.4% to 43.7% | |
| 140 mg q.d. | 123 | 44 | 35.8 | 27.3% to 44.9% | |
| 70 mg b.i.d. | 127 | 50 | 39.4 | 30.8% to 48.4% | |
| Sakamaki et al. (2009)109 | 70 mg b.i.d. | 18 | 5 | 27.8 | 9.7% to 53.5% |
| Subtotal [heterogeneity: Q = 3.25 (p on 6 df = 0.777); I2 = 0.0%; τ2 = 0.000] | 37.4 | 34.2% to 40.5% | |||
| ImR and/or ImI | |||||
| Talpaz et al. (2006)104 | Mixed/NR | 40 | 14 | 35.0 | 20.6% to 51.7% |
| Cortes et al. (2007)38 | Mixed/NR | 24 | 8 | 33.3 | 15.6% to 55.3% |
| Fabarius et al. (2007)79 | Mixed/NR | 50 | 22 | 44.0 | 30.0% to 58.7% |
| Kim et al. (2009)80 | 70 mg b.i.d. | 13 | 9 | 69.2 | 38.6% to 90.9% |
| Subtotal [heterogeneity: Q = 6.28 (p on 3 df = 0.099); I2 = 52.2%; τ2 = 0.008] | 43.1 | 30.5% to 55.7% | |||
| Overall pooled estimate | 47.8 | 40.6% to 55.0% | |||
|
Heterogeneity: Q = 107.77 (p on 16 df = 0.000); I2 = 85.2%; τ2 = 0.018 Heterogeneity between intolerant and resistant strata: z = 9.65 (p = 0.000) |
|||||
As noted above, Shah et al. ’s dose-ranging RCT22 includes a notable proportion of participants in MCyR at study entry. The BMS submission184 provides a subanalysis, referenced to unpublished study data, suggesting that, among the 100 mg q.d. participants who had no MCyR at baseline (n = 133), a complete response to dasatinib was seen in 44% of all cases (no data were presented for ImR and ImI subgroups).
This analysis provides clear evidence of superior response rates in ImI populations compared with ImR groups. Although there is strong evidence of heterogeneity in the data set as a whole, results in the ImI and ImR strata individually were strongly suggestive of a homogeneous treatment effect.
In contrast, there was no convincing evidence of dose-related variation in effectiveness; in a stratified meta-analysis (not shown), evidence for a null hypothesis of homogeneity between 100 mg q.d. and 140 mg q.d. strata was estimated at p = 0.087 and p = 0.113 in ImR and ImI populations, respectively.
Figure 3, which plots response rate against daily dose, clearly shows both these findings. The data points representing ImI cohorts are clustered at a higher response rate than the collection of points showing ImR populations, but there is no apparent influence of dose on response.
FIGURE 3.
Complete cytogenetic response rates relative to daily dose of dasatinib. Dose categories include totals of once-daily and twice-daily administrations; the area of the bubbles is inversely proportional to the variance of each estimate.
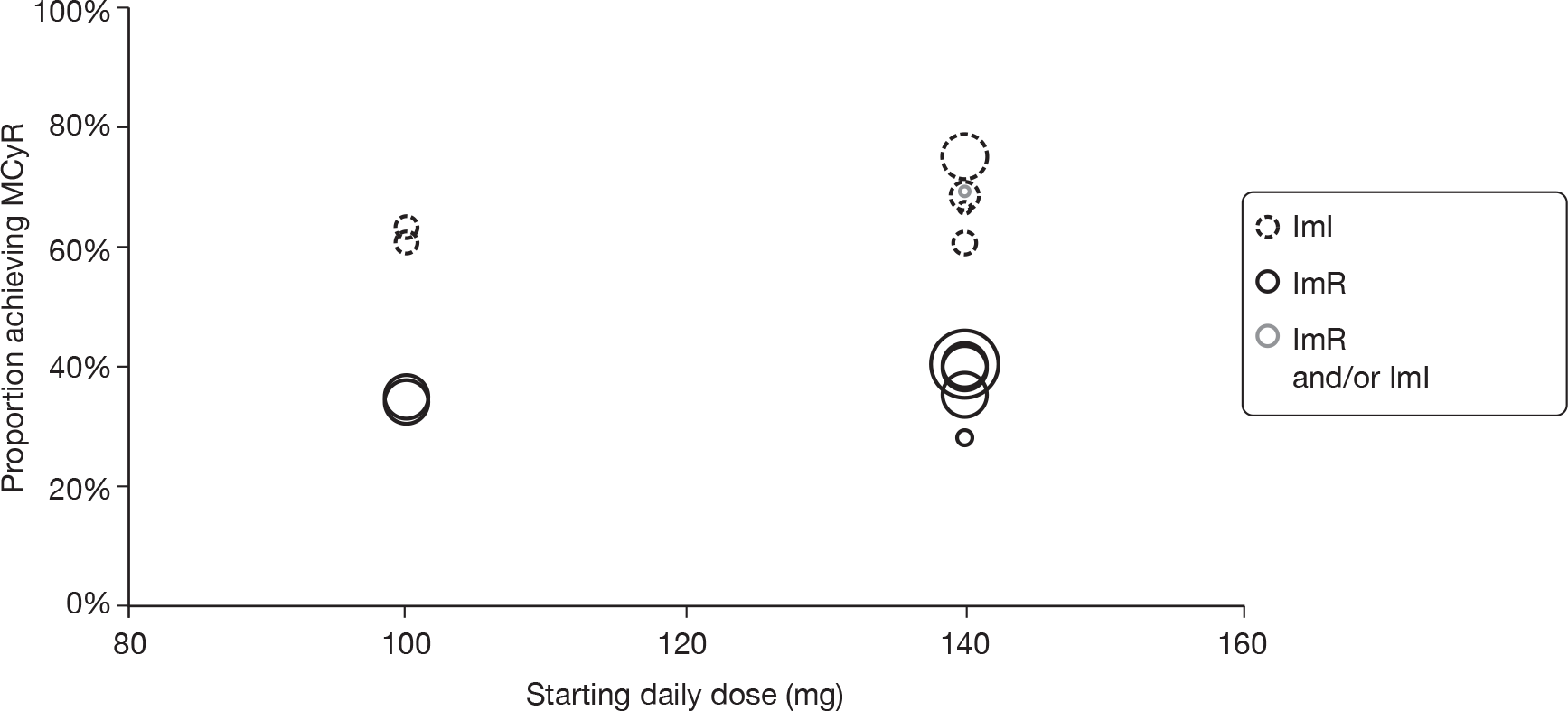
Major cytogenetic response is defined as the number of participants experiencing either CCyR or PCyR (i.e. ≤ 35% Ph+) and is reported in all included studies. Table 16 presents details of response rates in ImI, ImR and mixed populations, with meta-analytical subtotals for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImI | |||||
| aHochhaus et al. (2007)11,105 | 70 mg b.i.d. | 99 | 79 | 79.8 | 70.5% to 87.2% |
| Shah et al. (2008)22 | 100 mg q.d. | 43 | 32 | 74.4 | 58.8% to 86.5% |
| 50 mg b.i.d. | 44 | 32 | 72.7 | 57.2% to 85.0% | |
| 140 mg q.d. | 44 | 31 | 70.5 | 54.8% to 83.2% | |
| 70 mg b.i.d. | 41 | 28 | 68.3 | 51.9% to 81.9% | |
| Sakamaki et al. (2009)109 | 70 mg b.i.d. | 12 | 10 | 83.3 | 51.6% to 97.9% |
| Subtotal [heterogeneity: Q = 3.38 (p on 5 df = 0.641); I2 = 0.0%; τ2 = 0.000] | 75.5 | 70.5% to 80.5% | |||
| ImR | |||||
| aHochhaus et al. (2007)11,105 | 70 mg b.i.d. | 288 | 151 | 52.4 | 46.5% to 58.3% |
| Kantarjian et al. (2007)23 | 70 mg b.i.d. | 101 | 53 | 52.5 | 42.3% to 62.5% |
| Shah et al. (2008)22 | 100 mg q.d. | 124 | 66 | 53.2 | 44.1% to 62.2% |
| 50 mg b.i.d. | 124 | 58 | 46.8 | 37.8% to 55.9% | |
| 140 mg q.d. | 123 | 62 | 50.4 | 41.2% to 59.5% | |
| 70 mg b.i.d. | 127 | 65 | 51.2 | 42.2% to 60.1% | |
| Sakamaki et al. (2009)109 | 70 mg b.i.d. | 18 | 6 | 33.3 | 13.3% to 59.0% |
| Subtotal [heterogeneity: Q = 4.0 (p on 6 df = 0.676); I2 = 0.0%; τ2 = 0.000] | 50.9 | 47.6% to 54.1% | |||
| ImR and/or ImI | |||||
| Talpaz et al. (2006)104 | Mixed/NR | 40 | 18 | 45.0 | 29.3% to 61.5% |
| Cortes et al. (2007)38 | Mixed/NR | 24 | 12 | 50.0 | 29.1% to 70.9% |
| Fabarius et al. (2007)79 | Mixed/NR | 50 | 29 | 58.0 | 43.2% to 71.8% |
| Kim et al. (2009)80 | 70 mg b.i.d. | 13 | 10 | 76.9 | 46.2% to 95.0% |
| Subtotal [heterogeneity: Q = 5.56 (p on 3 df = 0.135); I2 = 46.0%; τ2 = 0.007] | 56.0 | 44.1% to 67.9% | |||
| Overall pooled estimate | 59.5 | 53.4% to 65.7% | |||
|
Heterogeneity: Q = 79.24 (p on 16 df = 0.000); I2 = 79.8%; τ2 = 0.012 Heterogeneity between intolerant and resistant strata: z = 8.11 (p = 0.000) |
|||||
As noted above, Shah et al. ’s dose-ranging RCT22 includes a notable proportion of participants who were already in MCyR at study entry. The BMS submission184 provides a subanalysis, referenced to unpublished study data, suggesting that, among the 100 mg q.d. participants who had no MCyR at baseline (n = 133), a major response to dasatinib was seen in 57% of cases (across ImI and ImR strata).
In Hochhaus et al. ’s updated report of their multicentre assessment of dasatinib at 70 mg b.i.d.,105 MCyR results are reported separately for those participants who were in MCyR at study entry. When such participants are excluded, response rates decrease in both the ImI (58/76 = 76.3%) and ImR (137/270 = 50.7%) subgroups.
There was clear evidence of superior response rates in ImI populations compared with ImR groups. This is to be expected, in view of the similar finding in CCyRs (which are, of course, a subset within this measure). As in that case, homogeneous discrete strata combine to form a heterogeneous-looking data set.
Again, there was no evidence of dose-related variation in effectiveness: in a stratified meta-analysis (not shown), evidence for a null hypothesis of homogeneity between 100 mg q.d. and 140 mg q.d. strata was estimated at p = 0.323 and p = 0.372 in the ImR and ImI populations, respectively.
Figure 4, which plots response rate against daily dose, clearly shows both these findings: the data points representing ImI cohorts are clustered at a higher response rate than the collection of points showing ImR populations, but there is no apparent influence of dose on response.
FIGURE 4.
Major cytogenetic response rates relative to daily dose of dasatinib. Dose categories include totals of once-daily and twice-daily administrations; the area of the bubbles is inversely proportional to the variance of each estimate.
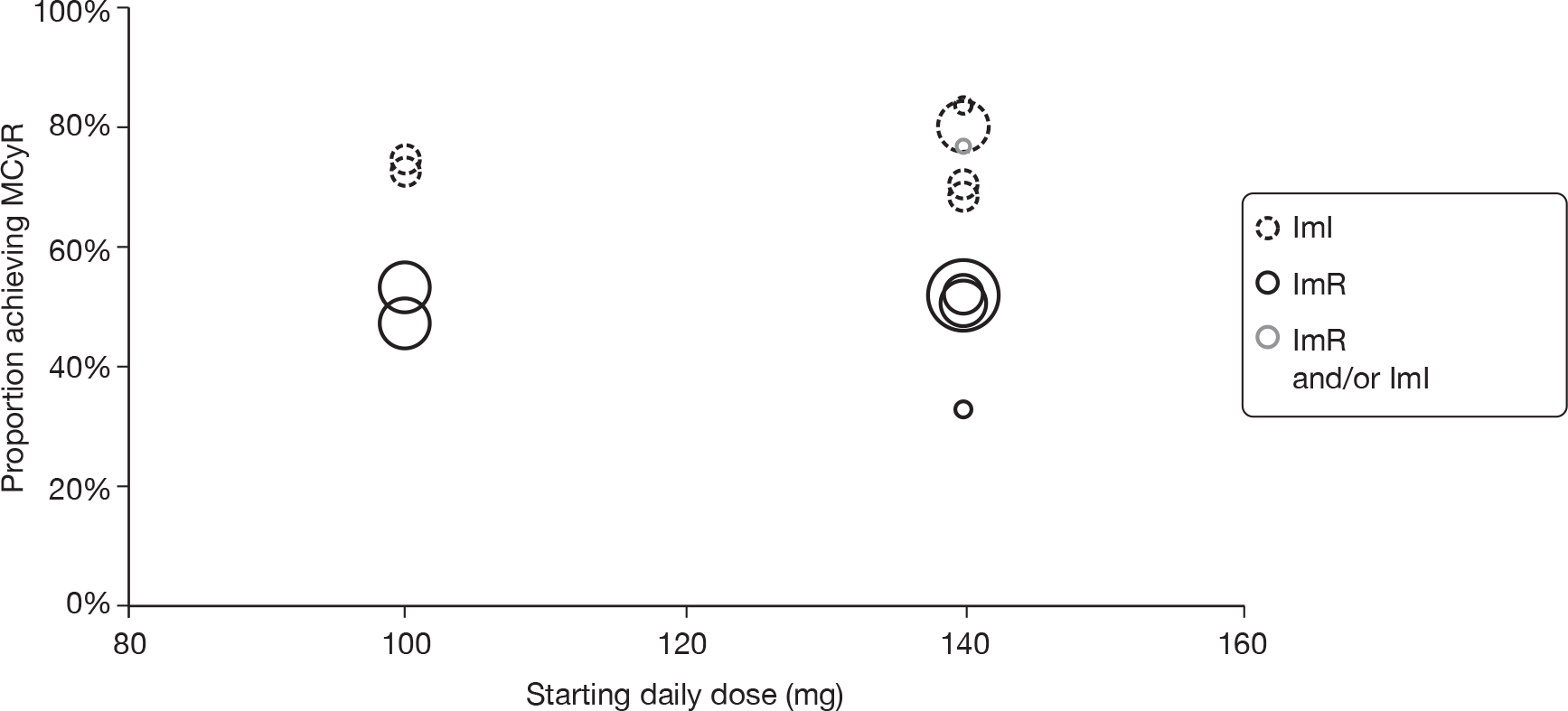
Three manufacturer-sponsored multicentre studies investigating the effectiveness of dasatinib in CML-CP report duration of MCyR, although length of follow-up is, in each case, relatively short. Across these three studies, the probability of maintained major response 6 months after that response was achieved is estimated at a median of 0.97 (range 0.88–1.00). The longest follow-up is provided by Kantarjian et al. ’s RCT;23 the probability of a maintained response at 1 year is 0.98 in their cohort. A conference abstract97 updating results from the dose optimisation RCT reported by Shah et al. 22 reports that, across ImI and ImR groups combined, 24-month MCyR maintenance probabilities ranged from 0.68 to 0.88, with the four dosage regimens under assessment. In the arm investigating what is now the UK licensed dose (100 mg q.d.), the figure was 0.87.
Hochhaus et al. ’s Phase II study11,105 is the only study to report ImI and ImR populations separately. They find a more durable response in the ImI group; response maintenance probability at 14 months was 0.98 compared with a maintenance probability of 0.755 among ImR participants. A conference abstract140 presenting updated results from this study reports that, 24 months after achieving MCyR, the probability of response maintenance was 0.97 and 0.84 in the ImI and ImR individuals, respectively (note that the latter figure is somewhat higher than was estimated for less mature follow-up).
Accelerated phase
Table 17 provides a summary of the available data detailing CyR to dasatinib in CML-AP. We have not included data from Sakamaki et al. ’s case series,109 because it conflates results from AP and BC participants. Otherwise, all included studies reported CCyR, PCyR and MCyR rates (or provided enough information to enable the deduction of each). Definitions are consistent with those noted in CP results (see Chronic phase). As in CP results, we have counted the ‘major’ responses from Fabarius et al. ’s case series79 as partial responses.
| Study | Length of follow-up | Dose | IMF | Complete (n/N) | Major (n/N) | Partial (n/N) | Minor (n/N) | Minimal (n/N) | Overall (n/N) |
|---|---|---|---|---|---|---|---|---|---|
| Talpaz et al. (2006)104 | > 12 monthsa,b | Mixed/NR | Mixed | 2/11 = 18.2% | 3/11 = 27.3% | 1/11 = 09.1% | 0/11 = 00.0% | 1/11 = 09.1% | 4/11 = 36.4% |
| Cortes et al. (2007)38 | 17 monthsa | Mixed/NR | Mixed | 3/22 = 13.6% | 4/22 = 18.2% | 1/22 = 04.5% | 5/22 = 22.7% | ||
| Fabarius et al. (2007)79 | 9 monthsa | Mixed/NR | Mixed | 0/6 = 00.0% | 0/6 = 00.0% | 0/6 = 00.0% | |||
| Guilhot et al. (2007)12 | 8 monthsc | 70 mg b.i.d. | ImI | 1/8 = 12.5% | 1/8 = 12.5% | 0/8 = 00.0% | 0/8 = 00.0% | 3/8 = 37.5% | 4/8 = 50.0% |
| ImR | 25/99 = 25.3% | 34/99 = 34.3% | 9/99 = 09.1% | 6/99 = 06.1% | 17/99 = 17.2% | 57/99 = 57.6% | |||
| 14 monthsa,d | 70 mg b.i.d. | ImI | 5/13 = 38.5% | 5/13 = 38.5% | 0/13 = 00.0% | 0/13 = 00.0% | |||
| ImR | 50/161 = 31.1% | 62/161 = 38.5% | 12/161 = 07.5% | 10/161 = 06.2% | |||||
| Kantarjian et al. (2009)81 | 15 monthsa | 140 mg q.d. | ImI | 17/41 = 41.5% | 19/41 = 46.3% | 2/41 = 04.9% | |||
| ImR | 34/117 = 29.1% | 42/117 = 35.9% | 8/117 = 06.8% | ||||||
| 70 mg b.i.d. | ImR | 14/43 = 32.6% | 19/43 = 44.2% | 5/43 = 11.6% | |||||
| ImI | 38/116 = 32.8% | 49/116 = 42.2% | 11/116 = 09.5% |
Eligibility criteria of included studies did not exclude individuals meeting criteria for CyR. It is likely that, as with studies in CP, a proportion of participants will have already attained target response; however, details of any such individuals are not provided in the study reports.
Table 18 presents details of CCyR rates in ImI, ImR and mixed populations, with meta-analytical subtotals for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImI | |||||
| aGuilhot et al. (2007)12 | 70 mg b.i.d. | 13 | 5 | 38.5 | 13.9% to 68.4% |
| Kantarjian et al. (2009)81 | 70 mg b.i.d. | 43 | 14 | 32.6 | 19.1% to 48.5% |
| Kantarjian et al. (2009)81 | 140 mg q.d. | 41 | 17 | 41.5 | 26.3% to 57.9% |
| Subtotal [heterogeneity: Q = 0.73 (p on 2 df = 0.693); I2 = 0.0%; τ2 = 0.000] | 36.9 | 27.3% to 46.5% | |||
| ImR | |||||
| aGuilhot et al. (2007)12 | 70 mg b.i.d. | 161 | 50 | 31.1 | 24.0% to 38.8% |
| Kantarjian et al. (2009)81 | 70 mg b.i.d. | 116 | 38 | 32.8 | 24.3% to 42.1% |
| Kantarjian et al. (2009)81 | 140 mg q.d. | 117 | 34 | 29.1 | 21.0% to 38.2% |
| Subtotal [heterogeneity: Q = 0.38 (p on 2 df = 0.829); I2 = 0.0%; τ2 = 0.000] | 30.9 | 26.4% to 35.5% | |||
| ImR and/or ImI | |||||
| Kim et al. (2009)80 | 70 mg b.i.d. | 3 | 3 | 100.0 | 29.2% to 100.0% |
| Talpaz et al. (2006)104 | Mixed/NR | 11 | 2 | 18.2 | 2.3% to 51.8% |
| Fabarius et al. (2007)79 | Mixed/NR | 6 | 0 | 0.0 | 0.0% to 45.9% |
| Cortes et al. (2007)38 | Mixed/NR | 22 | 3 | 13.6 | 2.9% to 34.9% |
| Subtotal [heterogeneity: Q = 19.18 (p on 3 df = 0.000); I2 = 84.4%; τ2 = 0.060] | 28.5 | 2.1% to 54.9% | |||
| Overall pooled estimate | 30.3 | 22.8% to 37.7% | |||
|
Heterogeneity: Q = 26.91 (p on 9 df = 0.001); I2 = 66.6%; τ2 = 0.008 Heterogeneity between intolerant and resistant strata: z = 1.11 (p = 0.134) |
|||||
A curious feature of the meta-analytical pooling of data is that the estimated overall rate is lower than that estimated for each stratum of the analysis. This comes about because of variation in the random-effects terms calculated for each of the subanalyses (in a fixed-effects model, this feature disappears).
In contrast to the findings for CML-CP (see Complete cytogenetic response: chronic phase, above), there is no evidence of a difference in efficacy between ImR and ImI populations, with comparable rates of response in all cases.
Because two of the four estimates in the mixed resistant–intolerant stratum contain no counts, it may be more accurate to perform a simple aggregation of all data to provide an overall raw average. 74 Doing so for that stratum confirms that the continuity-corrected meta-analysis may overestimate treatment effect: 8/42 = 19.0% (95% CI 8.6% to 34.1%). However, applying the same approach to the whole data set results in a slight increase in the estimated response rate: 166/533 = 31.1% (95% CI 27.2% to 35.3%).
Where reported, all cohorts received the same daily starting dose (140 mg q.d.), so it was not necessary to investigate the impact of dosage on outcome.
As in the evidence base relating to CML-CP, MCyR (≤ 35% Ph+) is reported in all included studies. Table 19 presents details of the response rates in ImI, ImR and mixed populations, with meta-analytical subtotals for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImI | |||||
| aGuilhot et al. (2007)12 | 70 mg b.i.d. | 13 | 5 | 38.5 | 3.9% to 68.4% |
| Kantarjian et al. (2009)81 | 70 mg b.i.d. | 43 | 19 | 44.2 | 29.1% to 60.1% |
| 140 mg q.d. | 41 | 19 | 46.3 | 30.7% to 62.6% | |
| Subtotal [heterogeneity: Q = 0.26 (p on 2 df = 0.880); I2 = 0.0%; τ2 = 0.000] | 44.3 | 34.4% to 54.2% | |||
| ImR | |||||
| Guilhot et al. (2007)12 | 70 mg b.i.d. | 161 | 62 | 38.5 | 31.0% to 46.5% |
| Kantarjian et al. (2009)81 | 140 mg q.d. | 117 | 42 | 35.9 | 27.2% to 45.3% |
| 70 mg b.i.d. | 116 | 49 | 42.2 | 33.1% to 51.8% | |
| Subtotal [heterogeneity: Q = 1.0 (p on 2 df = 0.607); I2 = 0.0%; τ2 = 0.000] | 38.8 | 34.0% to 43.6% | |||
| ImR and/or ImI | |||||
| Talpaz et al. (2006)104 | Mixed/NR | 11 | 3 | 27.3 | 6.0% to 61.0% |
| Cortes et al. (2007)38 | Mixed/NR | 22 | 4 | 18.2 | 5.2% to 40.3% |
| Fabarius et al. (2007)79 | Mixed/NR | 6 | 0 | 0.0 | 0.0% to 45.9% |
| Kim et al. (2009)80 | 70 mg b.i.d. | 3 | 3 | 100.0 | 29.2% to 100.0% |
| Subtotal [heterogeneity: Q = 18.3 (p on 3 df < 0.001); I2 = 83.6%; τ2 = 0.065] | 32.3 | 4.8% to 59.9% | |||
| Overall pooled estimate | 36.8 | 28.8% to 44.9% | |||
|
Heterogeneity: Q = 28.31 (p on 9 df = 0.001); I2 = 68.2%; τ2 = 0.010 Heterogeneity between intolerant and resistant strata: z = 0.98 (p = 0.163) |
|||||
No evidence was identified to estimate the rate of response in individuals who are already in MCyR at the commencement of treatment.
As was the case for CCyR rates, the difference in efficacy between ImR and ImI populations that is evident in CML-CP disappears in the AP population, with comparable rates of response in all cases. Apparently homogeneous results are reported in the ImI and ImR strata.
Because two of the four estimates in the mixed resistant–intolerant stratum contain no counts, it may be more accurate to perform a simple aggregation of all data to provide an overall raw average. 74 Doing so for that stratum confirms that the continuity-corrected meta-analysis may overestimate treatment effect: 10/42 = 23.8% (95% CI 12.1% to 39.5%). However, applying the same approach to the whole data set results in an increase in the estimated response rate: 206/533 = 38.6% (95% CI 34.5% to 42.9%).
Where reported, all cohorts received the same daily starting dose (140 mg q.d.), so it was not necessary to investigate the impact of dosage on outcome.
Both included industry-sponsored multicentre studies report duration of MCyR in participants with CML-AP. In Guilhot et al. ’s single-arm study,12 as updated by Apperley et al. ,176 the probability of the maintained response 12 months after that response was achieved is estimated at 0.865 across all participants, with an 18-month response maintenance of 0.855. In Kantarjian et al. ’s dose optimisation RCT,81 12-month response maintenance probability is estimated at 0.905 in the 140 mg q.d. arm and 0.815 in the 70 mg q.d. arm, and the 24-month response maintenance probabilities are 0.625 and 0.745, respectively.
Blast crisis
Table 20 provides a summary of the available data detailing CyR to dasatinib in CML-BC. All included studies reported CCyR, PCyR and MCyR rates (or provided enough information to enable the deduction of each). In this population, minor and minimal responses were more commonly reported.
| Study | Length of follow-up | Dose | IMF | Subgroup | Complete (n/N) | Major (n/N) | Partial (n/N) | Minor (n/N) | Minimal (n/N) | Overall (n/N) |
|---|---|---|---|---|---|---|---|---|---|---|
| Talpaz et al. (2006)104 | > 12 monthsa,b | Mixed/NR | Mixed | LBC | 3/10 = 30.0% | 8/10 = 80.0% | 5/10 = 50.0% | 1/10 = 10.0% | 0/10 = 00.0% | 9/10 = 90.0% |
| MBC | 6/23 = 26.1% | 8/23 = 34.8% | 2/23 = 08.7% | 2/23 = 08.7% | 2/23 = 08.7% | 12/23 = 52.2% | ||||
| Cortes et al. (2007)38 | 17 monthsa | Mixed/NR | Mixed | – | 4/10 = 40.0% | 4/10 = 40.0% | 0/10 = 00.0% | 4/10 = 40.0% | ||
| Cortes et al. (2007)13 | 8 monthsc | 70 mg b.i.d. | Mixed | LBC | 18/42 = 42.9% | 21/42 = 50.0% | 3/42 = 07.1% | 0/42 = 00.0% | 3/42 = 07.1% | 24/42 = 57.1% |
| MBC | 20/74 = 27.0% | 23/74 = 31.1% | 3/74 = 04.1% | 2/74 = 02.7% | 7/74 = 09.5% | 32/74 = 43.2% | ||||
| 12 monthsc,d | 70 mg b.i.d. | ImI | LBC | 67%e | 67%e | |||||
| MBC | 20%e | 20%e | ||||||||
| ImR | LBC | 43%e | 50%e | |||||||
| MBC | 26%e | 34%e |
Table 21 presents details of CCyR rates in CML-BC, with a meta-analytical subtotal estimating the average overall effect.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImR and/or ImI | |||||
| Cortes et al. (2007)13 – MBC | 70 mg b.i.d. | 74 | 20 | 27.0 | 17.4% to 38.6% |
| Cortes et al. (2007)13 – LBC | 70 mg b.i.d. | 42 | 18 | 42.9 | 27.7% to 59.0% |
| Kim et al. (2009)80 | 70 mg b.i.d. | 1 | 1 | 100.0 | 2.5% to 100.0% |
| Talpaz et al. (2006)104 – MBC | Mixed/NR | 23 | 6 | 26.1 | 10.2% to 48.4% |
| Talpaz et al. (2006)104 – LBC | Mixed/NR | 10 | 3 | 30.0 | 6.7% to 65.2% |
| Fabarius et al. (2007)79 | Mixed/NR | 15 | 4 | 26.7 | 7.8% to 55.1% |
| Cortes et al. (2007)38 | Mixed/NR | 10 | 4 | 40.0 | 12.2% to 73.8% |
| Overall pooled estimate (random-effects model) | 31.5 | 24.7% to 38.3% | |||
| Heterogeneity: Q = 5.82 (p on 6 df = 0.443); I2 = 0.0%; τ2 = 0.000 | |||||
Notably, the pooled response rate is slightly higher than the average seen in the evidence base for CML-AP (see Complete cytogenetic response: accelerated phase). CCyRs in subgroups in MBC appear somewhat lower than in LBC; however, these results are insufficient to establish a conclusive difference in response.
Where reported, all cohorts received the same daily starting dose (140 mg q.d.), so it was not necessary to investigate the impact of dosage on outcome.
As in the evidence base relating to other phases of CML, MCyR (≤ 35% Ph+) is reported in all included studies. Table 22 presents details of response rates, with a meta-analytical subtotal estimating the average overall effect.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImR and/or ImI | |||||
| Talpaz et al. (2006)104 – MBC | Mixed/NR | 23 | 8 | 34.8 | 16.4% to 57.3% |
| Talpaz et al. (2006)104 – LBC | Mixed/NR | 10 | 8 | 80.0 | 44.4% to 97.5% |
| Cortes et al. (2007)38 | Mixed/NR | 10 | 4 | 40.0 | 12.2% to 73.8% |
| Cortes et al. (2007)13 – MBC | 70 mg b.i.d. | 74 | 23 | 31.1 | 20.8% to 42.9% |
| Cortes et al. (2007)13 – LBC | 70 mg b.i.d. | 42 | 21 | 50.0 | 34.2% to 65.8% |
| Fabarius et al. (2007)79 | Mixed/NR | 15 | 4 | 26.7 | 7.8% to 55.1% |
| Kim et al. (2009)80 | 70 mg b.i.d. | 1 | 1 | 100.0 | 2.5% to 100.0% |
| Overall pooled estimate (random-effects model) | 44.0 | 30.5% to 57.5% | |||
| Heterogeneity: Q = 17.37 (p on 6 df = 0.008); I2 = 65.5%; τ2 = 0.019 | |||||
Again, the response rates reported are higher than those seen in the equivalent evidence base for CML-AP (see Major cytogenetic response: accelerated phase). MCyRs in subgroups in MBC are fewer than they are for those in LBC [a stratified meta-analysis (not shown) estimates evidence for a null hypothesis of homogeneous strata at p = 0.022].
Where reported, all cohorts received the same daily starting dose (140 mg q.d.), so it was not necessary to investigate the impact of dosage on outcome.
No included studies report duration of CyR in participants with CML-BC.
Haematological response
Chronic phase
Table 23 provides a summary of the available data detailing HR to dasatinib in CML-CP. All included studies report CHR; subtotal responses are very seldom reported in CP populations.
| Study | Length of follow-up | Dose | IMF | Complete (n/N) | Major (n/N) | Minor | NEL | Overall (n/N) |
|---|---|---|---|---|---|---|---|---|
| Talpaz et al. (2006)104 | > 12.0 monthsa,b | Mixed/NR | Mixed | 37/40 = 92.5% | 37/40 = 92.5% | |||
| Cortes et al. (2007)38 | 17.0 monthsa | Mixed/NR | Mixed | 20/24 = 83.3% | 21/24 = 87.5% | |||
| Hochhaus et al. (2007)11,105 | 8.0 monthsc | 70 mg b.i.d. | ImI | 57/59 = 96.6% | ||||
| ImR | 111/127 = 87.4% | |||||||
| 15.2 monthsa | 70 mg b.i.d. | ImI | 93/99 = 93.9% | |||||
| ImR | 258/288 = 89.6% | |||||||
| Kantarjian et al. (2007)23 | 15.0 monthsa | 70 mg b.i.d. | ImR | 94/101 = 93.1% | ||||
| Shah et al. (2008)22 | 6.0 monthsc | 100 mg q.d. | ImI | 43/43 = 100.0% | ||||
| ImR | 107/124 = 86.3% | |||||||
| 50 mg b.i.d. | ImI | 41/44 = 93.2% | ||||||
| ImR | 113/124 = 91.1% | |||||||
| 140 mg q.d. | ImI | 38/44 = 86.4% | ||||||
| ImR | 105/123 = 85.4% | |||||||
| 70 mg b.i.d. | ImI | 35/41 = 85.4% | ||||||
| ImR | 111/127 = 87.4% | |||||||
| 24.0 monthsd | 100 mg q.d. | ImR/ImI | 154/167 = 92.2% | |||||
| 50 mg b.i.d. | ImR/ImI | 155/168 = 92.3% | ||||||
| 140 mg q.d. | ImR/ImI | 145/167 = 86.8% | ||||||
| 70 mg b.i.d. | ImR/ImI | 148/168 = 88.1% | ||||||
| Updatee | 100 mg q.d. | ImI | 43/43 = 100.0% | |||||
| ImR | 110/124 = 88.7% | |||||||
| 50 mg b.i.d. | ImI | 41/44 = 93.2% | ||||||
| ImR | 114/124 = 91.9% | |||||||
| 140 mg q.d. | ImI | 39/44 = 88.6% | ||||||
| ImR | 106/123 = 86.2% | |||||||
| 70 mg b.i.d. | ImI | 36/42 = 85.7% | ||||||
| ImR | 112/126 = 88.9% | |||||||
| Sakamaki et al. (2009)109 | 6.0 monthsc | 70 mg b.i.d.f | ImI | 12/12 = 100.0% | ||||
| ImR | 15/18 = 83.3% |
As is the case with CyR, it should be remembered that some participants entered dasatinib studies already exhibiting target response, in this case CHR (indeed, proportions are much higher). In Shah et al. ’s dose-ranging RCT,22 all four arms featured a notable proportion of participants in CHR at study entry, with the highest proportion (85/167 = 50.9%) in the 100 mg q.d. arm (i.e. the current UK licensed dosage). Among those randomised to dasatinib therapy in Kantarjian et al. ’s RCT,23 versus HDI, the number of participants who met the criteria for CHR at baseline was similar (51/101 = 50.5%). In Hochhaus et al. ’s population,11,105 the overall proportion was a little lower (154/387 = 39.8%); however, a disproportionate number of these participants were in the ImI subgroup, leading to a high proportion of CHR at baseline among those individuals (23/99 = 51.5%).
Definitions of CHR were similar in all included studies. In their dose optimisation RCT, Shah et al. 22 explicitly refer the reader to two other included studies – Hochhaus et al. 11 and Kantarjian et al. 23 – although the latter contains no original definition of CHR; in turn, it directs readers to a third source (Talpaz et al. 104). There are minor differences between the definition in that source and in Hochhaus et al. 11 (the latter specifies a minimum ANC and sets an upper limit of 20% on basophils in PB compared with 2% in the former). The full definitions are summarised in Table 24.
| Study | Definition |
|---|---|
| Shah et al. (2008)22 | As defined in Kantarjian et al.23 and Hochhaus et al.11,105 |
| Kantarjian et al. (2007)23 | As defined in Talpaz et al.104 |
| Hochhaus et al. (2007)11,105 |
WBC ≤ institutional ULN ANC ≥ 1 × 109/l Platelet count < 450 × 109/l and no more than the institutional ULN No blasts or promyelocytes in PB < 5% myelocytes plus metamyelocytes in PB < 2% basophils in PB No extramedullary involvement (including no hepatomegaly or splenomegaly) Haematological responses were required to be maintained for at least 4 weeks |
| Talpaz et al. (2006)104 |
WBC ≤ institutional ULN Platelets < 450 × 109/l No blasts or promyelocytes in PB < 5% myelocytes plus metamyelocytes in PB < 20% basophils in PB No extramedullary involvement (including no hepatomegaly or splenomegaly) |
| Cortes et al. (2007)38 |
WBC count < 10 × 109/l Platelet count < 450 × 109/l No immature cells (blasts, promyelocytes or myelocytes) in the PB Disappearance of all signs and symptoms related to leukaemia (including palpable splenomegaly) |
| Sakamaki et al. (2009)109 |
WBC ≤ institutional ULN Platelet count < 450 × 109/l and no more than the institutional ULN No blasts or promyelocytes in PB < 5% myelocytes plus metamyelocytes in PB < 20% basophils in PB No extramedullary involvement (including no hepatomegaly or splenomegaly) |
Table 25 presents details of CHR rates in ImI, ImR and mixed populations, with meta-analytical subtotals for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImI | |||||
| aHochhaus et al. (2007)11,105 | 70 mg b.i.d. | 99 | 93 | 93.9 | 87.3% to 97.7% |
| Shah et al. (2008)22 | 100 mg q.d. | 43 | 43 | 100.0 | 91.8% to 100.0% |
| 50 mg b.i.d. | 44 | 41 | 93.2 | 81.3% to 98.6% | |
| 140 mg q.d. | 44 | 38 | 86.4 | 72.6% to 94.8% | |
| 70 mg b.i.d. | 41 | 35 | 85.4 | 70.8% to 94.4% | |
| Sakamaki et al. (2009)110 | 70 mg b.i.d. | 12 | 12 | 100.0 | 73.5% to 100.0% |
| Subtotal [heterogeneity: Q = 11.66 (p on 5 df = 0.040); I2 = 57.1%; τ2 = 0.001] | 93.7 | 89.5% to 97.9% | |||
| ImR | |||||
| aHochhaus et al. (2007)11,105 | 70 mg b.i.d. | 288 | 258 | 89.6 | 85.5% to 92.9% |
| Kantarjian et al. (2007)23 | 70 mg b.i.d. | 101 | 94 | 93.1 | 86.2% to 97.2% |
| Shah et al. (2008)22 | 100 mg q.d. | 124 | 107 | 86.3 | 79.0% to 91.8% |
| 50 mg b.i.d. | 124 | 113 | 91.1 | 84.7% to 95.5% | |
| 140 mg q.d. | 123 | 105 | 85.4 | 77.9% to 91.1% | |
| 70 mg b.i.d. | 127 | 111 | 87.4 | 80.3% to 92.6% | |
| Sakamaki et al. (2009)109 | 70 mg b.i.d. | 18 | 15 | 83.3 | 58.6% to 96.4% |
| Subtotal [heterogeneity: Q = 6.11 (p on 6 df = 0.411); I2 = 1.8%; τ2 = 0.000] | 89.2 | 87.2% to 91.3% | |||
| ImR and/or ImI | |||||
| Talpaz et al. (2006)104 | Mixed/NR | 40 | 37 | 92.5 | 79.6% to 98.4% |
| Cortes et al. (2007)38 | Mixed/NR | 24 | 20 | 83.3 | 62.6% to 95.3% |
| Subtotal [heterogeneity: Q = 1.12 (p on 1 df = 0.291); I2 = 10.5%; τ2 = 0.000] | 90.1 | 82.3% to 98.0% | |||
| Overall pooled estimate | 90.7 | 88.1% to 93.4% | |||
|
Heterogeneity: Q = 37.01 (p on 14 df = 0.001); I2 = 62.2%; τ2 = 0.001 Heterogeneity between intolerant and resistant strata: z = 1.87 (p = 0.031) |
|||||
As noted above, all three Phase II studies include a notable proportion of participants who were already in CHR at study entry.
-
In Hochhaus et al. ’s updated report of their multicentre assessment of dasatinib at 70 mg b.i.d.,105 CHR results are reported separately to account for those participants who were in CHR at study entry. When such participants are excluded, response rates decrease in both the ImI (44/48 = 91.7%) and ImR (158/185 = 85.4%) subgroups.
-
With respect to the dose-ranging RCT reported in the peer-reviewed literature by Shah et al. ,22 the BMS submission184 provides a subanalysis, referenced to unpublished study data, suggesting that, among the 100 mg q.d. participants who had no CHR at baseline (n = 81), a complete response to dasatinib was seen in 67 (82.7%) cases. Similar results were reported in the study arms representing alternative dosage regimens: 86/97 = 88.7%, 77/98 = 78.6% and 87/102 = 85.3% for 50 mg b.i.d., 140 mg q.d. and 70 mg b.i.d., respectively. No separate results are reported for ImI and ImR strata.
-
Kantarjian et al. ’s randomised comparison of dasatinib and HDI23 is also supplemented by additional information in the BMS submission. 184 This suggests that, among those who had no CHR at baseline, the complete response rate was 43/50 = 86.0% (note that in this study all participants were ImR).
Response rates are all high, ranging from 835% to 100%. Within ImR and mixed strata, evidence for a homogeneous treatment effect appears fairly strong; the ImI stratum has a more heterogeneous appearance.
Higher response rates are reported for ImI populations compared with ImR groups and, in the stratified meta-analysis, evidence is sufficient to reject a null hypothesis of homogeneous strata at conventional levels of significance.
As was seen in the analysis of CyR rates, there was no evidence of dose-related variation in effectiveness in the ImR population; in a stratified meta-analysis (not shown), heterogeneity between 100 mg q.d. and 140 mg q.d. strata was estimated at p = 0.537. The same technique in the ImI population gave p = 0.063 and, as some have argued that tests for heterogeneity are underpowered and that p-values < 0.1 should be considered significant,185 this may be considered sufficient evidence to reject a null hypothesis of homogeneity between strata. However, it should be noted that it is the lower-dose stratum that apparently provides the better response. In view of the less than conclusive p-value and the relatively small number of data points, a type I error might be inferred.
Figure 5, which plots response rate against daily dose, shows both these findings; the data points representing the ImI cohorts are mostly at a higher response rate than the points showing ImR populations, but there is no very clear influence of dose on response, even in the ImI subgroup.
FIGURE 5.
Complete haematological response rates relative to daily dose of dasatinib. Dose categories include totals of once-daily and twice-daily administrations; the area of the bubbles is inversely proportional to the variance of each estimate.
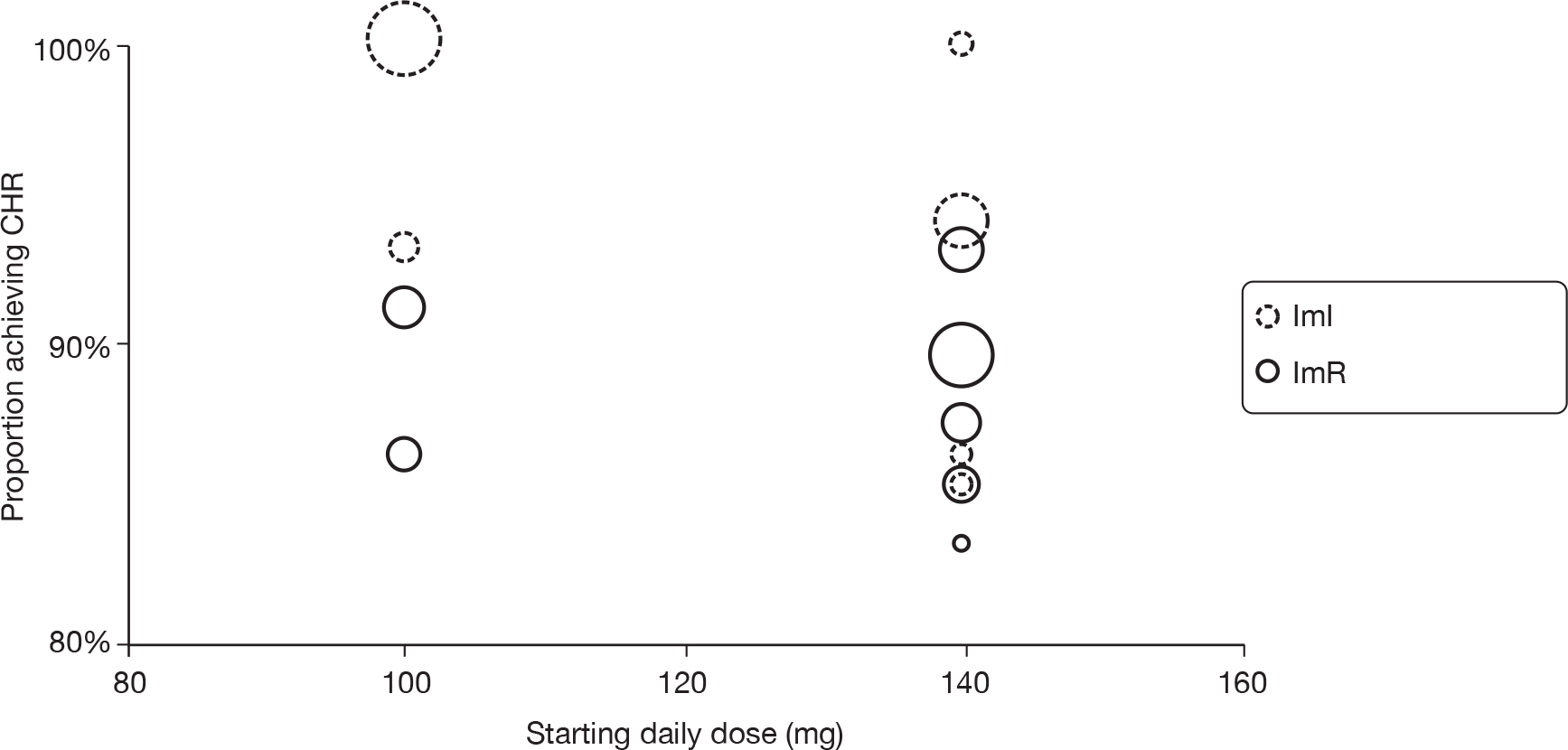
Accelerated phase
Table 26 provides a summary of the available data detailing HR to dasatinib in CML-AP. We have not included data from Sakamaki et al. ’s case series,109 because it conflates results from AP and BC participants. Otherwise, all included studies report CHR; subtotal responses are also more commonly reported in this population.
| Study | Length of follow-up | Dose | IMF | Complete (n/N) | Major (n/N) | Minor (n/N) | NEL (n/N) | Overall (n/N) |
|---|---|---|---|---|---|---|---|---|
| Talpaz et al. (2006)104 | > 12 monthsa,b | Mixed/NR | Mixed | 5/11 = 45.5% | 9/11 = 81.8% | 0/11 = 00.0% | 4/11 = 36.4% | |
| Cortes et al. (2007)38 | 17 monthsa | Mixed/NR | Mixed | 14/22 = 63.6% | 16/22 = 72.7% | |||
| Guilhot et al. (2007)12 | 8 monthsc | 70 mg b.i.d. | ImI | 3/8 = 37.5% | 5/8 = 62.5% | 2/8 = 25.0% | 2/8 = 25.0% | 7/8 = 87.5% |
| ImR | 39/99 = 39.4% | 64/99 = 64.6% | 16/99 = 16.2% | 25/99 = 25.3% | 80/99 = 80.8% | |||
| 14 monthsa,d | 70 mg b.i.d. | ImI | 6/13 = 46.2% | 9/13 = 69.2% | 3/13 = 23.1% | 12/13 = 92.3% | ||
| ImR | 72/161 = 44.7% | 102/161 = 63.4% | 30/161 = 18.6% | 126/161 = 78.3% | ||||
| Kantarjian et al. (2009)81 | 15 monthsa | 140 mg q.d. | ImI | 16/41 = 39.0% | 31/41 = 75.6% | 15/41 = 36.6% | 36/41 = 87.8% | |
| ImR | 59/117 = 50.4% | 74/117 = 63.2% | 15/117 = 12.8% | 83/117 = 70.9% | ||||
| 70 mg b.i.d. | ImR | 23/43 = 53.5% | 29/43 = 67.4% | 6/43 = 14.0% | 34/43 = 79.1% | |||
| ImI | 59/116 = 50.9% | 79/116 = 68.1% | 20/116 = 17.2% | 83/116 = 71.6% |
There are some (fairly minor) differences between the definitions of CHR adopted by the included studies. In the two Phase II studies,12,81 definitions are identical and, in turn, very similar to the initial, Phase I definition104 (with the exception that the upper limit for basophils in PB was substantially reduced from 20% to 2%). Cortes et al. ’s retrospective analysis of experience in their unit38 adopts a different – though broadly comparable – definition. The full definitions are summarised in Table 27.
| Study | Definition |
|---|---|
| Talpaz et al. (2006)104 |
WBC ≤ institutional ULN ANC ≥ 1 × 109/l Platelets ≥ 100 × 109/l No blasts or promyelocytes in PB BM blasts ≤ 5% Myelocytes plus metamyelocytes in PB < 5% Basophils in PB < 20% No extramedullary involvement (including no hepatomegaly or splenomegaly) |
| Cortes et al. (2007)38 |
WBC count < 10 × 109/l Platelet count < 450 × 109/l No immature cells (blasts, promyelocytes or myelocytes) in the PB Disappearance of all signs and symptoms related to leukaemia (including palpable splenomegaly) |
| Guilhot et al. (2007)12 |
WBC count ≤ institutional ULN ANC ≥ 1 × 109/l Platelet count ≥ 100 x 109/l No blasts or promyelocytes in PB BM blasts ≤ 5% Myelocytes plus metamyelocytes in PB < 5% Basophils in PB < 2% and basophils in BM < 2% No extramedullary involvement (including no hepatomegaly or splenomegaly) |
| Kantarjian et al. (2009)81 |
As defined in Guilhot et al. 12 Confirmed if all criteria were met consistently for subsequent assessments for at least 28 days – two consecutive assessments showing non-response were interpreted as response not achieved, whereas a single non-response between two assessments qualifying for CHR did not preclude a response being achieved |
Table 28 presents details of CHR rates in ImI, ImR and mixed populations, with meta-analytical subtotals for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImI | |||||
| aGuilhot et al. (2007)12 | 70 mg b.i.d. | 13 | 6 | 46.2 | 19.2% to 74.9% |
| Kantarjian et al. (2009)81 | 70 mg b.i.d. | 41 | 16 | 39.0 | 24.2% to 55.5% |
| 140 mg q.d. | 43 | 23 | 53.5 | 37.7% to 68.8% | |
| Subtotal [heterogeneity: Q = 1.81 (p on 2 df = 0.406); I2 = 0.0%; τ2 = 0.000] | 46.3 | 36.4% to 56.1% | |||
| ImR | |||||
| Guilhot et al. (2007)12 | 70 mg b.i.d. | 161 | 72 | 44.7 | 36.9% to 52.7% |
| Kantarjian et al. (2009)81 | 70 mg b.i.d. | 117 | 59 | 50.4 | 41.0% to 59.8% |
| 140 mg q.d. | 116 | 59 | 50.9 | 41.4% to 60.3% | |
| Subtotal [heterogeneity: Q = 1.35 (p on 2 df = 0.509); I2 = 0.0%; τ2 = 0.000] | 48.2 | 43.3% to 53.1% | |||
| ImR and/or ImI | |||||
| Talpaz et al. (2006)104 | Mixed/NR | 11 | 5 | 45.5 | 16.7% to 76.6% |
| Cortes et al. (2007)38 | Mixed/NR | 22 | 14 | 63.6 | 40.7% to 82.8% |
| Subtotal [heterogeneity: Q = 1.0 (p on 1 df = 0.317); I2 = 0.0%; τ2 = 0.000] | 57.9 | 41.3% to 74.4% | |||
| Overall pooled estimate | 48.5 | 44.2% to 52.7% | |||
|
Heterogeneity: Q = 5.59 (p on 7 df = 0.589); I2 = 0.0%; τ2 = 0.000 Heterogeneity between intolerant and resistant strata: z = –0.35 (p = 0.636) |
|||||
In their dose optimisation RCT, Kantarjian et al. 81 provide a limited breakdown of CHR rates according to HR status at baseline. Across both dose arms, 47 (14.8%) participants were in CHR at study entry: 28/233 (12.0%) ImR and 19/84 (22.6%) ImI. When these individuals are excluded from analysis, CHR rates decreased: 97/205 = 47.3% for the ImR subgroup and 25/65 = 38.5% for those who are ImI. Analogous data were not available in the other studies reported here.
This was a very homogeneous data set, with all estimates both within and between strata falling in a fairly narrow range either side of 50%. In contrast to the findings for CML-CP (see Complete haematological response: chronic phase), there is no evidence of a difference in efficacy between the ImR and ImI populations, with comparable rates of response in all cases.
Where reported, all cohorts received the same daily starting dose (140 mg q.d.), so it was not necessary to investigate the impact of dosage on outcome.
Guilhot et al. 12 report a 12-month major haematological response (MHR) maintenance probability of 0.81 in all participants and 0.79 in the ImR subgroup (no separate data were provided for ImI individuals). In Apperley et al. ’s updated results (including expanded enrolment),176 12-month MHR maintenance across all participants was a fraction higher (0.84) and an 18-month response maintenance probability of 0.78 was reported.
In Kantarjian et al. ’s dose optimisation RCT,81 a 12-month MHR maintenance probability was estimated at 0.855 in the 140 mg q.d. arm and 0.805 in the 70 mg q.d. arm, and 24-month response maintenance probabilities are 0.645 and 0.600, respectively.
Blast crisis
In the Phase II studies,13 the definition of CHR is very similar to the initial, Phase I definition104 (with the exception that the upper limit for basophils in PB was substantially reduced, from 20% to 2%). Cortes et al. ’s retrospective analysis of experience in their unit38 adopts a different – though broadly comparable – definition. The full definitions are summarised in Table 29.
| Study | Definition |
|---|---|
| Talpaz et al. (2006)104 |
WBC ≤ institutional ULN ANC ≥ 1 × 109/l Platelets ≥ 100 × 109/l No blasts or promyelocytes in PB BM blasts ≤ 5% Myelocytes plus metamyelocytes in PB < 5% Basophils in PB < 20% No extramedullary involvement (including no hepatomegaly or splenomegaly) |
| Cortes et al. (2007)38 |
WBC count < 10 × 109/l Platelet count < 450 × 109/l No immature cells (blasts, promyelocytes or myelocytes) in the PB Disappearance of all signs and symptoms related to leukaemia (including palpable splenomegaly) |
| Cortes et al. (2007)13 |
WBC ≤ institutional ULN ANC ≥ 1 × 109/l Platelets ≥ 100 × 109/l Marrow blasts ≤ 5% or less with no peripheral blasts or promyelocytes Myelocytes plus metamyelocytes in PB < 5% Basophils in PB < 2% No evidence of extramedullary involvement |
Table 30 provides a summary of the available data detailing HR to dasatinib in CML-BC. All included studies reported complete response rates; subtotal responses were also often available.
| Study | Length of follow-up | Dose | Subgroup | IMF | Complete | Major | Minor | NEL | Overall |
|---|---|---|---|---|---|---|---|---|---|
| Talpaz et al. (2006)104 | > 12 monthsa,b | Mixed/NR | LBC | Mixed | 7/10 = 70.0% | 8/10 = 80.0% | 0/10 = 00.0% | 1/10 = 10.0% | |
| MBC | Mixed | 8/23 = 34.8% | 14/23 = 60.9% | 4/23 = 17.4% | 6/23 = 26.1% | ||||
| Cortes et al. (2007)38 | 17 monthsa | Mixed/NR | Mixed | 4/10 = 40.0% | 6/10 = 60.0% | ||||
| Cortes et al. (2007)13 | 8 monthsc | 70 mg b.i.d. | LBC | Mixed | 11/42 = 26.2% | 13/42 = 31.0% | 2/42 = 04.8% | 2/42 = 04.8% | 15/42 = 35.7% |
| MBC | Mixed | 19/74 = 25.7% | 25/74 = 33.8% | 14/74 = 18.9% | 6/74 = 08.1% | 39/74 = 52.7% | |||
| 12 monthsc,d | 70 mg b.i.d. | ImI | LBC | 33%e | |||||
| MBC | 20%e | ||||||||
| ImR | LBC | 36%e | |||||||
| MBC | 35%e |
Table 31 presents details of CHR rates in CML-BC, with a meta-analytical subtotal estimating the average overall effect.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImR and/or ImI | |||||
| Talpaz et al. (2006)104 – MBC | Mixed/NR | 23 | 8 | 34.8 | 16.4% to 57.3% |
| Talpaz et al. (2006)104 – LBC | Mixed/NR | 10 | 7 | 70.0 | 34.8% to 93.3% |
| Cortes et al. (2007)38 | Mixed/NR | 10 | 4 | 40.0 | 12.2% to 73.8% |
| Cortes et al. (2007)13 – MBC | 70 mg b.i.d. | 74 | 19 | 25.7 | 16.2% to 37.2% |
| Cortes et al. (2007)13 – LBC | 70 mg b.i.d. | 42 | 11 | 26.2 | 13.9% to 42.0% |
| Overall pooled estimate (random-effects model) | 34.7 | 22.5% to 46.9% | |||
| Heterogeneity: Q = 9.3 (p on 4 df = 0.054); I2 = 57.0%; τ2 = 0.010 | |||||
These data sets were heterogeneous in appearance, although the small sample sizes for each data point could be expected to contribute to variability. CHR rates in subgroups in MBC appear somewhat lower than they are for those in LBC; however, these results are insufficient to establish a conclusive difference in response.
Where reported, all cohorts received the same daily starting dose (140 mg q.d.), so it was not necessary to investigate the impact of dosage on outcome.
One included study, Cortes et al. ,13 provides data on duration of MHR to dasatinib in CML-BC. For participants in MBC, the probability of maintaining a response at 10 months is estimated at 0.84. For those in LBC, the same probability appears much lower, at 0.36 [although this estimate was based on a smaller number of individuals (13) achieving MHR].
Progression-free survival
Chronic phase
In the industry-sponsored multicentre studies, the definition of disease progression appears relatively consistent (indeed, the report of the dose optimisation RCT22 explicitly directs the reader to the single-arm study11 and the comparative RCT23 for its definition of disease progression). In each case, the definition relies on participants meeting any one of four criteria:
-
development of CML-AP or CML-BC
-
loss of CHR
-
loss of MCyR
-
increasing WBC count (recorded by the investigator as a doubling from lowest value to > 20,000/mm3 or an increase by > 50,000/mm3 on two assessments performed at least 2 weeks apart).
The BMS submission184 gives the full protocol definitions adopted in two of the studies22,23 (see Appendix 5). These are reproduced in Table 32.
| Kantarjian et al. (2007)23 | Shah et al. (2008)22 |
|---|---|
|
Progression of disease as reported by the investigator defined as the first occurrence of any of the following: Death Discontinuation of treatment owing to progression prior to crossover |
Achieved a CHR and subsequently no longer met the criteria consistently over a consecutive 2-week period after starting maximum dose of dasatinibDeath Discontinuation of treatment owing to progression |
Table 33 summarises reported PFS data. After follow-up of up to 3 years, none of the reported cohorts have yet reached median survival. Estimated PFS probabilities suggest that at least three-quarters of individuals treated with dasatinib in CML-CP can expect to survive without disease progression for 2 years or more.
| Study | Dose | Length of follow-up | Imatinib | n | 6 months (years) | 12 months (years) | 18 months (years) | 24 months (years) | 36 months (years) |
|---|---|---|---|---|---|---|---|---|---|
| Talpaz et al. (2006)104 | Mixed/NR | ImR/ImI | 40 | 1 | 1 | 1 | |||
| Hochhaus et al. (2007)11 | 70 mg b.i.d. | 8 months | ImI | 59 | 1 | ||||
| ImR | 127 | 0.91 | |||||||
| ImR/ImI | 186 | 0.94 | |||||||
| 15 months | ImI | 99 | 0.995 | 0.985 | 0.955 | ||||
| ImR | 288 | 0.92 | 0.88 | 0.805 | |||||
| ImR/ImI | 387 | 0.94 | 0.905 | 0.845 | |||||
| Kantarjian et al. (2007)23 | 70 mg b.i.d. | ImR | 101 | 0.975 | 0.925 | 0.925 | 0.86b | ||
| Shah et al. (2008)22 | 100 mg q.d. | ImR/ImI | 167 | 0.95 | 0.89 | 0.80c | 0.73d | ||
| ImI | 43 | 0.87e | |||||||
| ImR | 124 | 0.77e | |||||||
| 50 mg b.i.d. | ImR/ImI | 168 | 0.94 | 0.815 | 0.75c | 0.72d | |||
| 140 mg q.d. | ImR/ImI | 167 | 0.93 | 0.89 | 0.76c | 0.60d | |||
| 70 mg b.i.d. | ImR/ImI | 168 | 0.93 | 0.78 | 0.76c | 0.67d |
Accelerated phase
In the single-arm study reported by Guilhot et al. ,12 progression was defined as loss of HR or no decrease from baseline levels in percentage of blasts in PB or BM on all assessments over a 4-week period after receiving the maximum dose of dasatinib. In Kantarjian et al. ’s dose optimisation RCT,81 the definition of progression is similar, with the addition of three extra criteria: (1) absolute increase of at least 50% in PB blasts over a 2-week period; (2) development of CML-BC at any time after initiation of therapy; and (3) development of extramedullary disease sites other than the spleen or liver. The BMS submission184 gives the full protocol definition (see Appendix 5).
Table 34 tabulates PFS results from the relevant studies. Although only Kantarjian et al. ’s dose optimisation RCT81 has sufficient follow-up to estimate median PFS, it appears that individuals taking dasatinib in CML-AP can, on average, expect a little over 2 years’ PFS.
| Study | Dose | Length of follow-up | Imatinib | n | 6 months (years) | 12 months (years) | 18 months (years) | 24 months (years) | 30 months (years) | Median (months) |
|---|---|---|---|---|---|---|---|---|---|---|
| Talpaz et al. (2006)104 | Mixed/NR | ImR/ImI | 11 | 0.715 | 0.715 | |||||
| Guilhot et al. (2007)12 | 70 mg b.i.d. | 8 monthsa | ImR | 99 | 0.800 | 0.555 | ||||
| ImR/ImI | 107 | 0.805 | 0.615 | |||||||
| 14 monthsb,c | ImR/ImI | 174 | 0.795 | 0.660 | 0.610 | |||||
| Kantarjian et al. (2009)81 | 140 mg q.d. | ImR/ImI | 158 | 0.795 | 0.695 | 0.610 | 0.510 | 0.410 | 25.2 | |
| 70 mg b.i.d. | ImR/ImI | 159 | 0.825 | 0.700 | 0.635 | 0.550 | 0.490 | 26.1 |
Blast crisis
In Cortes et al. ’s study,13 progression was defined as loss of HR or no decrease from baseline levels in percentage of blasts in PB or BM on all assessments over a 4-week period after receiving the maximum dose of dasatinib. In Talpaz et al. ’s study,104 the disease of participants with BC was considered to have progressed if the number of blasts in PB or BM increased despite at least 4 weeks of treatment.
Table 35 details the PFS achieved in the relevant studies. Disease progression is clearly much more rapid, in this population, than that seen in CP or AP, with most study participants achieving no more than a few months’ PFS.
| Study | Dose | Imatinib | Subgroup | n | 6 months (years) | 12 months (years) | Median (months) |
|---|---|---|---|---|---|---|---|
| Cortes et al. (2007)13 | 70 mg b.i.d. | ImR/ImI | LBC | 42 | 0.200 | 2.80 | |
| MBC | 74 | 0.500 | 0.42 | 5.00 | |||
| Talpaz et al. (2006)104 | Mixed/NR | ImR/ImI | LBC or Ph+ ALL | 10 | 0.235 | 3.85 | |
| MBC | 23 | 0.450 | 5.80 |
In an abstract presenting updated results from the START-B (MBC) study (including additional enrolment to that reported by Cortes et al. 13), median PFS is reported as 3.1 months for participants in LBC and 5.6 months for those in MBC. 125
Overall survival
Chronic phase
Table 36 presents observed survival of individuals in CML-CP taking dasatinib. It appears that around only 10% of people are expected to die within 2 years of commencing treatment and, according to the one study with sufficient follow-up,22 more than four-fifths of the population should survive for at least 3 years.
| Study | Length of follow-up | Dose | Imatinib | n | 6 months (years) | 12 months (years) | 18 months (years) | 24 months (years) | 36 months (years) |
|---|---|---|---|---|---|---|---|---|---|
| Hochhaus et al. (2007)11 | 15 months | 70 mg b.i.d. | ImI | 99 | 1.000 | 1.000 | 1.000 | ||
| ImR | 288 | 0.975 | 0.955 | 0.945 | |||||
| ImR/ImI | 387 | 0.980 | 0.965 | 0.960 | |||||
| Shah et al. (2008)22 | 100 mg q.d. | ImR/ImI | 167 | 0.975 | 0.970 | 0.91b | 0.87c | ||
| ImI | 43 | 0.95d | |||||||
| ImR | 124 | 0.89d | |||||||
| 50 mg b.i.d. | ImR/ImI | 168 | 0.970 | 0.930 | 0.90b | 0.84c | |||
| 140 mg q.d. | ImR/ImI | 167 | 0.990 | 0.960 | 0.94b | 0.84c | |||
| 70 mg b.i.d. | ImR/ImI | 168 | 0.960 | 0.890 | 0.88b | 0.80c |
Accelerated phase
Table 37 tabulates OS results from the relevant studies. Although only Kantarjian et al. ’s dose optimisation RCT81 has sufficient follow-up to estimate median OS, it appears that individuals taking dasatinib in CML-AP can, on average, expect a little over 2.5 years’ OS. Somewhere in the region of two-thirds to three-quarters can expect to survive for 2 years or more.
| Study | Dose | Imatinib | n | 6 months (years) | 12 months (years) | 18 months (years) | 24 months (years) | 30 months (years) | Median (months) |
|---|---|---|---|---|---|---|---|---|---|
| Guilhot et al. (2007)12 | 70 mg b.i.d. | ImR/ImI | 174 | 0.905a | 0.825a | 0.790a | |||
| Kantarjian et al. (2009)81 | 140 mg q.d. | ImR/ImI | 158 | 0.870 | 0.775 | 0.725 | 0.635 | 0.54 | |
| 70 mg b.i.d. | ImR/ImI | 159 | 0.930 | 0.840 | 0.790 | 0.730 | 0.67 | 30.75 |
Blast crisis
None of the full-length publications in the assembled evidence base report OS in CML-BC treated with dasatinib. However, limited information is available in a conference abstract presenting updated results from the START-B (MBC) study (including additional enrolment to that reported in the main publication13), which reports a 24-month survival probability of 0.26 for participants in LBC and 0.38 for those in MBC. 125
Adverse events
Most included studies (including all industry-sponsored, Phase I and II, multicentre studies) reported incidence of AEs during therapy with dasatinib. All assessed toxicities according to the National Cancer Institute’s Common Toxicity Criteria v3.0. 186
Chronic phase
The most notable toxicities of dasatinib are haematological. Table 38 details the incidence of grade 3–4 cytopenias reported in the included studies. In most included evidence, neutropenia and thrombopenia each affect in the order of 50% ± 10% of individuals taking dasatinib. However, it should be noted that most of this evidence relates to a 70 mg b.i.d. dosing schedule, which has now been replaced, in UK practice, by a recommended regimen of 100 mg q.d. In the one group in our review that took this dose, incidence of cytopenias is somewhat lower; in particular, there was a significant reduction in the likelihood of thrombopenia compared with the 70 mg b.i.d. arm of the same study (22% vs 36%; p = 0.006 by chi-squared test with Yates’s correction).
| Adverse event | Talpaz et al.,104 ImR/ImI, Mixed/NR | Hochhaus et al.,11 ImR/ImI, 70 mg b.i.d. | Hochhaus et al.,11 18 months follow-upa ImR/ImI, 70 mg b.i.d. | Kantarjian et al.,23 ImR, 70 mg b.i.d. | Shah et al.,22 ImR/ImI, 100 mg q.d. | Shah et al.,22 ImR/ImI, 50 mg b.i.d. | Shah et al.,22 ImR/ImI, 140 mg q.d. | Shah et al.,22 ImR/ImI, 70 mg b.i.d. | Sakamaki et al.,109 ImR/ImI, 70 mg b.i.d. |
|---|---|---|---|---|---|---|---|---|---|
| n | 40 | 186 | 387 | 101 | 167 | 168 | 167 | 168 | 30 |
| Anaemia (%) | 21.5 | 21.4 | 9.6 | 16.1 | 16.8 | 16.1 | 16.7 | ||
| Leucopenia (%) | 24.7 | 26.9 | 16.2 | 25.0 | 19.8 | 22.6 | 26.7 | ||
| Neutropenia (%) | 45.0 | 49.5 | 48.6 | 61.4 | 32.9 | 42.9 | 40.7 | 40.5 | 46.7 |
| Thrombopenia (%) | 35.0 | 47.3 | 48.3 | 56.4 | 22.2 | 31.0 | 38.3 | 36.3 | 50.0 |
Incidence of non-haematological AEs is summarised in Table 39 (all grades) and Table 40 (grade 3–4). Sakamaki et al. 109 only report non-haematological AEs across all phases of disease, so we have not included their results (which are broadly comparable with those collected according to the disease phase, here and in the following sections).
| Adverse event | Talpaz et al.,104 ImR/ImI, Mixed/NR | Hochhaus et al.,11 ImR/ImI, 70 mg b.i.d. | Hochhaus et al.,11 18 months follow-up,a ImR/ImI, 70 mg b.i.d. | Kantarjian et al.,23 ImR, 70 mg b.i.d. | Shah et al.22 ImR/ImI, 100 mg q.d. | Shah et al.,22 ImR/ImI, 50 mg b.i.d. | Shah et al.,22 ImR/ImI, 140 mg q.d. | Shah et al.,22 ImR/ImI, 70 mg b.i.d. |
|---|---|---|---|---|---|---|---|---|
| n | 40 | 186 | 387 | 101 | 167 | 168 | 167 | 168 |
| Anorexia (%) | 12.9 | 12.9 | ||||||
| Asthenia (%) | 19.9 | 14.2 | 12.9 | |||||
| CHF/cardiac dysfunction (%) | 0.0 | 1.2 | 1.2 | 3.0 | ||||
| Cough (%) | 13.2 | |||||||
| Diarrhoea (%) | 17.5 | 30.1 | 37.0 | 34.7 | 23.4 | 23.8% | 22.8 | 21.4 |
| Dyspnoea (%) | 27.4 | 30.2 | 20.8 | 10.2 | 14.9% | 14.4 | 11.3 | |
| Dyspnoea or pulmonary oedema (%) | 10.0 | |||||||
| Elevated activity of ALAT (%) | 51.6 | |||||||
| Elevated activity of ASAT (%) | 59.7 | |||||||
| Elevated bilirubin (%) | 14.0 | |||||||
| Face oedema (%) | 4.0 | |||||||
| Fatigue (%) | 7.5 | 28.0 | 31.3 | 29.7 | 19.8 | 13.1 | 17.4 | 16.1 |
| Flushing (%) | 0.0 | |||||||
| Gastrointestinal haemorrhage (%) | 10.0 | |||||||
| Generalised oedema (%) | 5.0 | |||||||
| Headache (%) | 10.0 | 33.9 | 32.3 | 24.8 | 29.3 | 19.0 | 25.7 | 27.4 |
| Muscle spasms (%) | 2.0 | |||||||
| Myalgia (%) | 11.4 | 3.0 | 11.4 | 6.0 | ||||
| Nausea (%) | 5.0 | 19.4 | 24.5 | 23.8 | 15.0 | 17.9 | 18.0 | 25.0 |
| Pain in extremity (%) | 6.9 | |||||||
| Pericardial effusion (%) | 2.5 | 0.6 | 1.2 | 3.0 | 1.2 | |||
| Periorbital oedema (%) | 5.0 | |||||||
| Peripheral oedema (%) | 17.5 | 17.7 | 17.8 | 9.9 | 9.6 | 5.4 | 5.4 | 10.1 |
| Pleural effusion (%) | 12.5 | 18.8 | 27.4 | 16.8 | 7.2 | 11.3 | 14.4 | 15.5 |
| Pulmonary hypertension (%) | 0.0 | 0.0 | 0.0 | 1.2 | ||||
| Pulmonary oedema (%) | 0.0 | 0.6 | 0.0 | 1.2 | ||||
| Pyrexia (%) | 15.5 | 13.9 | 3.0 | 7.1 | 12.0 | 7.1 | ||
| Rash (%) | 2.5 | 22.0 | 26.1 | 16.8 | 11.4 | 14.9 | 19.2 | 16.1 |
| Superficial oedema (%) | 14.9 | 13.8 | 12.5 | 11.4 | 13.7 | |||
| Tumour lysis syndrome (%) | 0.0 | |||||||
| Vomiting (%) | 0.0 | 10.9 | 8.9 | 5.4 | 7.1 | 7.8 | 10.1 | |
| Weight increase (%) | 5.0 |
| Adverse event | Talpaz et al.,104 ImR/ImI, Mixed/NR | Hochhaus et al.,11 ImR/ImI, 70 mg b.i.d. | Hochhaus et al.,11 18 months follow-up,, ImR/ImI, 70 mg b.i.d. | Kantarjian et al.,23 ImR, 70 mg b.i.d. | Shah et al.,22 ImR/ImI, 100 mg q.d. | Shah et al.,22 ImR/ImI, 50 mg b.i.d. | Shah et al.,22 ImR/ImI, 140 mg q.d. | Shah et al.,22 ImR/ImI, 70 mg b.i.d. |
|---|---|---|---|---|---|---|---|---|
| n | 40 | 186 | 387 | 101 | 167 | 168 | 167 | 168 |
| Anorexia (%) | 0.0 | 0.0 | ||||||
| Asthenia (%) | 1.6 | 1.0 | 0.0 | |||||
| CHF/cardiac dysfunction (%) | 0.0 | 0.6 | 0.6 | 2.4 | ||||
| Cough (%) | 0.0 | |||||||
| Diarrhoea (%) | 0.0 | 2.2 | 2.8 | 2.0 | 0.6 | 2.4 | 1.8 | 3.6 |
| Dyspnoea (%) | 3.2 | 5.2 | 4.0 | 1.2 | 4.2 | 4.8 | 3.0 | |
| Dyspnoea or pulmonary oedema (%) | 0.0 | |||||||
| Elevated activity of ALAT (%) | 1.6 | |||||||
| Elevated activity of ASAT (%) | 2.2 | |||||||
| Elevated bilirubin (%) | 0.0 | |||||||
| Face oedema (%) | 0.0 | |||||||
| Fatigue (%) | 2.5 | 1.1 | 2.1 | 2.0 | 1.2 | 0.0 | 2.4 | 3.0 |
| Flushing (%) | 0.0 | |||||||
| Gastrointestinal haemorrhage (%) | 5.0 | |||||||
| Generalised oedema (%) | 0.0 | |||||||
| Headache (%) | 0.0 | 1.1 | 1.0 | 2.0 | 0.6 | 0.0 | 1.2 | 3.0 |
| Muscle spasms (%) | 0.0 | |||||||
| Myalgia (%) | 0.0 | 0.0 | 0.6 | 0.6 | ||||
| Nausea (%) | 0.0 | 1.1 | 0.8 | 0.0 | 0.6 | 0.6 | 0.6 | 0.6 |
| Pain in extremity (%) | 0.0 | |||||||
| Pericardial effusion (%) | 0.0 | 0.0 | 0.6 | 0.6 | 0.6 | |||
| Periorbital oedema (%) | 0.0 | |||||||
| Peripheral oedema (%) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Pleural effusion (%) | 0.0 | 3.2 | 6.2 | 4.0 | 1.2 | 1.8 | 2.4 | 1.2 |
| Pulmonary hypertension (%) | 0.0 | 0.0 | 0.0 | 0.6 | ||||
| Pulmonary oedema (%) | 0.0 | 0.0 | 0.0 | 0.6 | ||||
| Pyrexia (%) | 1.0 | 0.0 | 0.6 | 0.6 | 0.0 | 0.6 | ||
| Rash (%) | 0.0 | 0.5 | 0.5 | 0.0 | 1.2 | 0.6 | 0.0 | 1.2 |
| Superficial oedema (%) | 0.0 | 0.0 | 0.0 | 0.6 | 0.0 | |||
| Tumour lysis syndrome (%) | 0.0 | |||||||
| Vomiting (%) | 0.0 | 0.5 | 0.0 | 0.6 | 1.2 | 1.2 | 0.0 | |
| Weight increase (%) | 0.0 |
The most commonly reported AEs of any grade were diarrhoea, dyspnoea, fatigue, headache, nausea, pleural effusion and rash, each of which was reported at a frequency in the range 10–40%. Grade 3–4 AEs appear to be fairly rare, with only dyspnoea and pleural effusion occurring in > 5% of any of the reported cohorts. Alongside these two toxicities, the most consistently reported events were diarrhoea and nausea.
As with haematological AEs, the dose optimisation RCT reported by Shah et al. 22 is thought to provide evidence of a superior toxicity profile for the 100 mg q.d. regimen when compared with the previously recommended 70 mg b.i.d. approach. In particular, incidence of pleural effusion (all grades) was significantly lower in the 100 mg q.d. arm (7% vs 15%; p = 0.026 by chi-squared test with Yates’s correction). It should also be noted that, although AE rates look rather lower in Talpaz et al. ’s study,104 this was an initial, dose-ranging investigation, in which some participants took very low doses of dasatinib.
Reported rates of treatment discontinuation because of intolerable AEs range from approximately 5% to 15% (Table 41). Note that the lowest reported withdrawal rate is in the one included group taking dasatinib at its UK recommended dosage of 100 mg q.d.
| Study | Length of follow-up | Dose | Imatinib | Discontinuations |
|---|---|---|---|---|
| Talpaz et al. (2006)104 | > 12 monthsa,b | Mixed/NR | ImR/ImI | 58/387 = 15.0%c |
| Hochhaus et al. (2007)11,105 | 8 monthsd | 70 mg b.i.d. | ImR/ImI | 58/387 = 15.0%e |
| Kantarjian et al. (2007)23 | 15 monthsa | 70 mg b.i.d. | ImR | 16/101 = 15.8% |
| Shah et al. (2008)22 | 6 monthsd | 100 mg q.d. | ImR/ImI | 8/167 = 4.8%f |
| 50 mg b.i.d. | ImR/ImI | 13/168 = 7.7%g | ||
| 140 mg q.d. | ImR/ImI | 15/167 = 9.0%h | ||
| 70 mg b.i.d. | ImR/ImI | 23/168 = 13.7%i |
Accelerated phase
Again, in the AP population, by far the most frequently reported AEs are cytopenias. Details of the reported rates are provided in Table 42. In all included evidence, a notable majority of individuals experienced grade 3–4 neutropenia and thrombopenia, and anaemia and leucopenia were almost as prevalent.
| Adverse event | Talpaz et al.,104 ImR/ImI, Mixed/NR | Guilhot et al.,12 ImI, 70 mg b.i.d. | Guilhot et al.,12 ImR, 70 mg b.i.d. | Guilhot et al.,12 14 months follow-upa ImI, 70 mg b.i.d. | Guilhot et al.,12 14 months follow-upa ImR, 70 mg b.i.d. | Kantarjian et al.,81 ImR/ImI, 140 mg q.d. | Kantarjian et al.,81 ImR/ImI, 70 mg b.i.d. |
|---|---|---|---|---|---|---|---|
| n | 11 | 8 | 99 | 13 | 161 | 155 | 159 |
| Anaemia (%) | 87.5 | 67.7 | 84.6 | 64.0 | 47.7 | 42.8 | |
| Leucopenia (%) | 75.0 | 59.6 | 84.6 | 56.5 | 44.5 | 40.9 | |
| Neutropenia (%) | 81.8 | 100.0 | 75.8 | 100.0 | 73.3 | 58.7 | 68.6 |
| Thrombopenia (%) | 81.8 | 87.5 | 81.8 | 76.9 | 81.4 | 63.9 | 67.3 |
Incidence of non-haematological AEs is summarised in Table 43 (all grades) and Table 44 (grade 3–4). The most commonly reported AEs of any grade were diarrhoea, dyspnoea, fatigue, headache, nausea, pleural effusion and rash, each of which tended to be reported at a frequency in the range 20–40%, although incidence of diarrhoea was reported at over 50% in some studies. Although less uncommon than in the CP population, grade 3–4 AEs remain relatively rare. The only toxicities reported at a frequency of > 10% in any of the included evidence were diarrhoea, febrile neutropenia and fluid retention. In addition, there was consistent evidence of a non-trivial rate of grade 3–4 dyspnoea, fatigue and pyrexia.
| Adverse event | Talpaz et al.,104 ImR/ImI, Mixed/NR | Guilhot et al.,12 ImR/ImI, 70 mg b.i.d. | Guilhot et al.,12 14 months follow-up,a ImI, 70 mg b.i.d. | Guilhot et al.,12 14 months follow-up,a ImR, 70 mg b.i.d. | Kantarjian et al.,81 ImR/ImI, 140 mg q.d. | Kantarjian et al.,81 ImR/ImI, 70 mg b.i.d. |
|---|---|---|---|---|---|---|
| n | 11 | 107 | 13 | 161 | 157 | 159 |
| Abdominal pain (%) | 11.2 | 15.4 | 10.6 | |||
| Anorexia (%) | 13.1 | 15.4 | 15.5 | |||
| Arthralgia (%) | 10.3 | 0.0 | 13.7 | 9.6 | 8.2 | |
| Asthenia (%) | 18.7 | 15.4 | 13.7 | |||
| Cough (%) | 0.0 | 11.2 | 7.6 | 11.3 | ||
| Diarrhoea (%) | 45.5 | 49.5 | 69.2 | 50.3 | 31.2 | 31.4 |
| Dizziness (%) | 11.2 | 7.7 | 10.6 | |||
| Dyspnoea (%) | 15.9 | 23.1 | 21.1 | 20.4 | 23.3 | |
| Dyspnoea or pulmonary oedema (%) | 27.3 | |||||
| Epistaxis (%) | 11.2 | |||||
| Fatigue (%) | 0.0 | 23.4 | 30.8 | 26.1 | 19.1 | 20.1 |
| Febrile neutropenia (%) | 3.8 | 10.1 | ||||
| Fluid retention (%) | 33.8 | 48.4 | ||||
| Fluid retention (other) (%) | 4.5 | 15.1 | ||||
| Flushing (%) | 27.3 | |||||
| Gastrointestinal haemorrhage (%) | 0.0 | 11.2 | 8.3 | 13.2 | ||
| Generalised oedema (%) | 9.1 | |||||
| Haemorrhage (non-GI) (%) | 19.1 | 20.8 | ||||
| Headache (%) | 27.3 | 28.0 | 15.4 | 30.4 | 27.4 | 23.3 |
| Infection (%) | 10.2 | 10.7 | ||||
| Musculoskeletal pain (%) | 11.5 | 14.5 | ||||
| Myalgia (%) | 10.3 | 7.7 | 11.8 | 7.0 | 13.2 | |
| Nausea (%) | 9.1 | 22.4 | 23.1 | 28.0 | 19.1 | 17.6 |
| Pain in extremity (%) | 14.0 | 7.7 | 12.4 | |||
| Pericardial effusion (%) | 0.0 | |||||
| Periorbital oedema (%) | 9.1 | |||||
| Peripheral oedema (%) | 27.3 | 22.4 | 30.8 | 21.7 | ||
| Petechiae (%) | 15.4 | 13.7 | ||||
| Pleural effusion (%) | 0.0 | 23.4 | 23.1 | 27.3 | 19.7 | 39.0 |
| Pyrexia (%) | 23.4 | 30.8 | 23.6 | 11.5 | 11.3 | |
| Rash (%) | 45.5 | 15.0 | 23.1 | 20.5 | 14.6 | 18.2 |
| Superficial oedema (%) | 17.8 | 20.1 | ||||
| Tumour lysis syndrome (%) | 0.0 | |||||
| Vomiting (%) | 9.1 | 15.9 | 46.2 | 18.0 | 11.5 | 15.1 |
| Adverse event | Talpaz et al.,104 ImR/ImI, Mixed/NR | Guilhot et al.,12 ImR/ImI, 70 mg b.i.d. | Guilhot et al.,12 14 months follow-upa ImI, 70 mg b.i.d. | Guilhot et al.,12 14 months follow-up,a ImR, 70 mg b.i.d. | Kantarjian et al.,81 ImR/ImI, 140 mg q.d. | Kantarjian et al.,81 ImR/ImI, 70 mg b.i.d. |
|---|---|---|---|---|---|---|
| n | 11 | 107 | 13 | 161 | 157 | 159 |
| Abdominal pain (%) | 0.0 | 0.0 | 0.0 | |||
| Anorexia (%) | 0.9 | 0.0 | 0.6 | |||
| Arthralgia (%) | 0.0 | 0.0 | 0.0 | 0.0 | 1.3 | |
| Asthenia (%) | 3.7 | 0.0 | 2.5 | |||
| Cough (%) | 0.0 | 0.0 | ||||
| Diarrhoea (%) | 0.0 | 5.6 | 15.4 | 6.8 | 2.5 | 3.1 |
| Dizziness (%) | 0.0 | 0.0 | 0.0 | |||
| Dyspnoea (%) | 3.7 | 0.0 | 4.3 | 3.2 | 6.9 | |
| Dyspnoea or pulmonary oedema (%) | 0.0 | |||||
| Epistaxis (%) | 0.0 | |||||
| Fatigue (%) | 0.0 | 3.7 | 7.7 | 3.7 | 1.9 | 3.1 |
| Febrile neutropenia (%) | 3.8 | 10.1 | ||||
| Fluid retention (%) | 7.6 | 10.7 | ||||
| Fluid retention (other) (%) | 1.3 | 5.0 | ||||
| Flushing (%) | 0.0 | |||||
| Gastrointestinal haemorrhage (%) | 0.0 | 8.4 | 5.7 | 6.3 | ||
| Generalised oedema (%) | 0.0 | |||||
| Haemorrhage (non-GI) (%) | 1.9 | 1.3 | ||||
| Headache (%) | 0.0 | 0.9 | 0.0 | 0.6 | 1.3 | 0.6 |
| Infection (%) | 5.7 | 1.9 | ||||
| Musculoskeletal pain (%) | 0.0 | 1.9 | ||||
| Myalgia (%) | 0.9 | 0.0 | 0.6 | 0.6 | 1.9 | |
| Nausea (%) | 0.0 | 0.0 | 0.0 | 0.6 | 0.6 | 1.9 |
| Pain in extremity (%) | 0.0 | 0.0 | 0.0 | |||
| Pericardial effusion (%) | 0.0 | |||||
| Periorbital oedema (%) | 0.0 | |||||
| Peripheral oedema (%) | 0.0 | 0.0 | 0.0 | 0.6 | ||
| Petechiae (%) | 0.0 | 1.2 | ||||
| Pleural effusion (%) | 0.0 | 2.8 | 0.0 | 5.0 | 7.0 | 6.3 |
| Pyrexia (%) | 3.7 | 7.7 | 3.7 | 1.9 | 1.3 | |
| Rash (%) | 0.0 | 0.9 | 0.0 | 1.2 | 0.0 | 0.6 |
| Superficial oedema (%) | 0.6 | 0.0 | ||||
| Tumour lysis syndrome (%) | 0.0 | |||||
| Vomiting (%) | 0.0 | 0.9 | 0.0 | 2.5 | 0.6 | 1.3 |
As in CP, a dose optimisation RCT has suggested that incidence of pleural effusion may be lower at an alternative dosage (140 mg q.d. rather than 70 mg b.i.d.), with around half the incidence of all-grade events with the once-daily regimen (20% vs 39%; p < 0.001 by chi-squared test with Yates’s correction). In addition, events classified as ‘fluid retention (other)’ were significantly less common in the 140 mg q.d. group (4% vs 15%; p = 0.003 by chi-squared test with Yates’s correction).
Reported rates of treatment discontinuation because of intolerable AEs encompass a broad range, from 0% to 30% (Table 45).
| Study | Length of follow-up | Dose | IMF | Discontinuations (n/N) |
|---|---|---|---|---|
| Talpaz et al. (2006)104 | > 12 monthsa,b | Mixed/NR | ImR/ImI | 0/11 = 0.0% |
| Guilhot et al. (2007)12 | 14 monthsa,c | 70 mg b.i.d. | ImI | 2/13 = 15.4%d |
| ImR | 16/161 = 9.9%e | |||
| Kantarjian et al. (2009)81 | 15 monthsa | 140 mg q.d. | ImR/ImI | 41/158 = 25.9%f |
| 70 mg b.i.d. | ImR/ImI | 46/159 = 28.9%g |
Blast crisis
Table 46 collects evidence of grade 3–4 haematological AEs in people taking dasatinib in CML-BC. As in AP, it appears that a substantial majority of individuals receiving dasatinib can expect to experience cytopenias meeting the criteria for grade 3–4 AEs. There is no clear evidence that individuals in MBC fare better or worse than those in LBC in this respect.
| Adverse event | Talpaz et al.,104 ImR/ImI, Mixed/NR, CML with LBC or Ph+ ALL | Talpaz et al.,104 ImR/ImI, Mixed/NR, CML with MBC | Cortes et al.,13 ImR/ImI, 70 mg b.i.d., LBC | Cortes et al.,13 ImR/ImI, 70 mg b.i.d., MBC |
|---|---|---|---|---|
| n | 10 | 23 | 42 | 74 |
| Anaemia (%) | 52.4 | 67.6 | ||
| Leucopenia (%) | 69.0 | 63.5 | ||
| Neutropenia (%) | 80.0 | 95.7 | 78.6 | 82.4 |
| Thrombopenia (%) | 70.0 | 82.6 | 88.1 | 83.8 |
Incidence of non-haematological AEs (all grades) is summarised in Table 47. Diarrhoea appears to be the most commonly reported AE, with somewhere between one-fifth and one-third of individuals experiencing it. There are also notable incidences of dyspnoea, fatigue, nausea, peripheral oedema, pleural effusion, pyrexia, rash, and vomiting. Frequency of some events – notably, pleural effusion – appears to be greater in MBC than in LBC, although numbers are too small to be confident of a genuine difference.
| Adverse event | Talpaz et al.,104 ImR/ImI, Mixed/NR, CML with LBC or Ph+ ALL | Talpaz et al.,104 ImR/ImI, Mixed/NR, CML with MBC | Cortes et al.,13 ImR/ImI, 70 mg b.i.d., LBC | Cortes et al.,13 ImR/ImI, 70 mg b.i.d., MBC |
|---|---|---|---|---|
| n | 10 | 23 | 42 | 74 |
| Anorexia (%) | 4.8 | 10.8 | ||
| Arthralgia (%) | 4.8 | 10.8 | ||
| Asthenia (%) | 9.5 | 14.9 | ||
| Diarrhoea (%) | 20.0 | 21.7 | 31.0 | 36.5 |
| Dyspnoea (%) | 11.9 | 17.6 | ||
| Dyspnoea or pulmonary oedema (%) | 10.0 | 8.7 | ||
| Epistaxis (%) | 2.4 | 12.2 | ||
| Fatigue (%) | 10.0 | 0.0 | 28.6 | 12.2 |
| Febrile neutropenia (%) | 14.3 | 4.1 | ||
| Flushing (%) | 0.0 | 4.3 | ||
| Gastrointestinal haemorrhage (%) | 0.0 | 13.0 | 0.0 | 12.2 |
| Generalised oedema (%) | 10.0 | 0.0 | ||
| Headache (%) | 0.0 | 4.3 | 14.3 | 8.1 |
| Nausea (%) | 10.0 | 17.4 | 23.8 | 16.2 |
| Pericardial effusion (%) | 0.0 | 13.0 | ||
| Periorbital oedema (%) | 10.0 | 8.7 | ||
| Peripheral oedema (%) | 10.0 | 21.7 | 11.9 | 18.9 |
| Pleural effusion (%) | 20.0 | 34.8 | 14.3 | 28.4 |
| Pyrexia (%) | 19.0 | 16.2 | ||
| Rash (%) | 10.0 | 8.7 | 16.7 | 12.2 |
| Tumour lysis syndrome (%) | 0.0 | 8.7 | ||
| Vomiting (%) | 10.0 | 8.7 | 23.8 | 16.2 |
Table 48 summarises reported grade 3–4 AEs. Pleural effusion occurred in > 10% of both MBC groups. It may be that serious AEs are generally less common in participants in LBC than in those in MBC (indeed, no grade 3–4 AEs at all were reported in the small LBC subgroup of Talpaz et al. ’s dose-ranging study104).
| Adverse event | Talpaz et al.,104 ImR/ImI, Mixed/NR, CML with LBC or Ph+ ALL | Talpaz et al.,104 ImR/ImI, Mixed/NR, CML with MBC | Cortes et al.,13 ImR/ImI, 70 mg b.i.d., LBC | Cortes et al.,13 ImR/ImI, 70 mg b.i.d., MBC |
|---|---|---|---|---|
| n | 10 | 23 | 42 | 74 |
| Anorexia (%) | 4.8 | 1.4 | ||
| Arthralgia (%) | 0.0 | 2.7 | ||
| Asthenia (%) | 2.4 | 2.7 | ||
| Diarrhoea (%) | 0.0 | 4.3 | 0.0 | 8.1 |
| Dyspnoea (%) | 0.0 | 6.8 | ||
| Dyspnoea or pulmonary oedema (%) | 0.0 | 8.7 | ||
| Epistaxis (%) | 0.0 | 1.4 | ||
| Fatigue (%) | 0.0 | 0.0 | 4.8 | 1.4 |
| Febrile neutropenia (%) | 11.9 | 4.1 | ||
| Flushing (%) | 0.0 | 0.0 | ||
| Gastrointestinal haemorrhage (%) | 0.0 | 13.0 | 0.0 | 8.1 |
| Generalised oedema (%) | 0.0 | 0.0 | ||
| Headache (%) | 0.0 | 0.0 | 2.4 | 0.0 |
| Nausea (%) | 0.0 | 0.0 | 0.0 | 4.1 |
| Pericardial effusion (%) | 0.0 | 8.7 | ||
| Periorbital oedema (%) | 0.0 | 0.0 | ||
| Peripheral oedema (%) | 0.0 | 0.0 | 0.0 | 0.0 |
| Pleural effusion (%) | 0.0 | 13.0 | 2.4 | 13.5 |
| Pyrexia (%) | 2.4 | 5.4 | ||
| Rash (%) | 0.0 | 0.0 | 4.8 | 0.0 |
| Tumour lysis syndrome (%) | 0.0 | 8.7 | ||
| Vomiting (%) | 0.0 | 0.0 | 2.4 | 1.4 |
Reported rates of treatment discontinuation because of intolerable AEs ranged from 0% to 15% (Table 49).
| Study | Length of follow-up | Dose | IMF | Subgroup | Discontinuations (n/N) |
|---|---|---|---|---|---|
| Talpaz et al. (2006)104 | > 12 monthsa,b | Mixed/NR | ImR/ImI | LBC | 1/42 = 2.4% |
| MBC | 10/74 = 13.5%c | ||||
| Cortes et al. (2007)13 | 8 monthsd | 70 mg b.i.d. | ImR/ImI | LBC | 0/10 = 0.0% |
| MBC | 0/23 = 0.0% |
Additional reports of adverse events
In addition to the safety data extracted from studies presenting efficacy results, we have identified the following evidence relating to dasatinib toxicity.
-
As noted above, the most frequent adverse responses to dasatinib are haematological:
-
– A conference abstract presented by Quintas-Cardama et al. 187 from the Anderson Cancer Center, Houston, TX, USA details their experience with cytopenias among individuals receiving dasatinib in CML-CP. Of 122 such people, 38 (31%) developed at least one episode of grades 2–4 neutropenia and/or thrombopenia.
-
– Neutropenia occurred in 29 patients (24%; grade 3–4 in 23). Median time to the development of neutropenia was 59 days (range 2–149 days).
-
– Thrombopenia occurred in 33 patients (27%; grade 3–4 in 25). Median time to the development of thrombopenia was 28 days (range 11–368 days).
-
– Grade 3–4 neutropenia and/or thrombopenia necessitated dasatinib interruption at some point in 34 patients (28%).
-
– Anaemia was observed in most of those patients who had neutropenia and/or thrombopenia.
-
– Therapy reported was granulocyte-colony stimulating factor for neutropenia (seven cases), interleukin 11 for thrombopenia (three cases), and EPO (erythropoietin) for anaemia (15 cases). Each of these additional therapies enabled maintenance of dasatinib in most cases.
-
-
– In their preliminary report on the potential of interleukin 11 as therapy for TKI-induced thrombopenia, Aribi et al. 188 describe three individuals who were treated while taking dasatinib.
-
-
In line with the significant incidence of dyspnoea, cough and pleural effusion reported in efficacy studies (see Tables 47 and 48), respiratory AEs have received some attention in the literature:
-
– Bergeron et al. 189 present a series of nine individuals with dasatinib-related respiratory AEs: six had pleural effusions and seven had lung parenchyma changes (four had both). Symptoms resolved when therapy was interrupted and reintroduction of dasatinib at a reduced dose was possible in some cases. Immune-mediated pathogenesis of pleural effusion is posited.
-
– Quintas-Cardama et al. , from the Anderson Cancer Center, Houston, TX, USA, have detailed their experience with dasatinib-related pleural effusion in all phases of CML. 190,191 In the sample of 138 people treated at the unit, 48 (31%) experienced pleural effusion (grade 3–4 in 23). Median time from start of therapy to development of pleural effusion was 5 weeks (range 1–107 weeks). Effusion was more frequent among those patients receiving daily doses ≥ 140 mg than in those patients treated at < 140 mg. Dasatinib was interrupted in 40 patients (83%) and dose reduced in 34 patients (71%); permanent discontinuation was necessary in only three individuals (2%). Effusion was managed with diuretics in 71%, steroids in 27% and thoracocentesis in 19%. In a multivariate analysis, prior cardiac history, hypertension and a twice-daily dasatinib schedule were associated with an increased risk of pleural effusion.
-
– Another single unit’s experience of dasatinib-related pleural effusion is presented by de Lavallade et al. 192,193 Seventeen of 62 consecutive cases were affected (14 grade 2 events and three of grade 3). CML-BC, previous history of cardiac disease, hypertension and hypercholesterolaemia appeared to be risk factors for development of pleural effusion. Histories of autoimmune disease and/or skin rashes during dasatinib (or prior imatinib) therapy were also strongly predictive of subsequent pleural effusion, adding weight to the hypothesis that this form of toxicity has an immune-mediated origin.
-
– At Rousselot et al. ’s centre,194 pleural effusion and/or pulmonary manifestations were seen in 9 of 40 (22.5%) individuals receiving dasatinib in CML-CP. All except one patient were able to tolerate dasatinib at a reduced dose.
-
-
Quintas-Cardama et al. , from the Anderson Cancer Center, Houston, TX, USA, have detailed the incidence of bleeding episodes associated with dasatinib therapy among individuals receiving dasatinib across all phases of CML. 195,196 Among 138 such individuals, 37 bleeding episodes occurred in 32 patients (23%; seven grade 1, 16 grade 2, and nine grade 3). Median time to development of bleeding was 6 weeks (range 0.5–38.0 weeks). Most bleeding episodes occurred in the gastrointestinal tract (81%); gingival and vaginal bleeding, and epistaxis were also reported. Bleeding led to transient dasatinib interruptions in 15 patients (47%). Episodes were more frequent among patients treated at daily doses ≥ 140 mg compared with those treated at ≤ 100 mg (p = 0.001). Bleeding was not necessarily related to thrombopenia.
-
A single case of dasatinib-related renal failure is reported by Holstein et al. 197 The patient in question, who was in CML-AP, became dialysis dependent although, when switched to nilotinib, briefly recovered renal function before death due to progressive disease.
-
Immunosuppressive/infective illness has been the subject of a few reports:
-
– García-Muñoz et al. present a case report of an individual receiving dasatinib who developed extensive infective illness. 198 The authors conclude that dasatinib therapy was a cause of immunosuppression, leading to reactivation of a latent viral infection.
-
– Radaelli et al. report a case of dasatinib-related alveolar pneumonia that resolved after discontinuation of dasatinib and treatment with corticosteroids. 199
-
– Rea et al. report the case of a 74-year-old woman diagnosed with dasatinib-related lupus with symptoms including fever, arthralgia, fatigue, hepatosplenomegaly and pleuro-pericardial effusions. 200 Dasatinib was discontinued and nilotinib commenced, with a resolution of symptoms.
-
-
Dermatological complications are well recognised. Two cases of panniculitis believed to be caused by dasatinib are reported by Assouline et al. 201
-
A single case of acute hepatitis that may have been induced by dasatinib is reported by Bonvin et al. 202 Liver function returned to normal following discontinuation of dasatinib.
-
A single case of dasatinib-induced gynaecomastia in a 70-year-old man with ImI CML-CP is reported by Caocci et al. 203 Dasatinib therapy was continued and tamoxifen introduced, with reportedly good effect in reducing tissue enlargement and discomfort.
-
Preliminary results suggest that prior dasatinib therapy causes no increase in transplant-related complications among individuals undergoing salvage SCT. 204
Summary of effectiveness of dasatinib
A summary of the evidence identified in this review estimating the clinical effectiveness of dasatinib is given below. Findings relating to CML-CP, -AP, and CML-BC are summarised in Boxes 1–3, respectively.
CCyR is shown by about half of all study participants:
-
around two-thirds of ImI individuals achieved a CCyR
-
around 30–40% of ImR individuals achieved a CCyR
MCyR is shown by about 60% of all study participants:
-
around three-quarters of ImI individuals achieved or maintained an MCyR
-
around half of ImR individuals achieved or maintained an MCyR
-
75% or more of those patients achieving an MCyR will maintain it for at least 2 years (ImI individuals probably have a better response maintenance rate than ImR groups)
CHR was achieved or maintained in around 90% of cases
Three-quarters or more can expect PFS of 2 years or more
For OS, only around 10% of people are expected to die within 2 years of commencing treatment and more than four-fifths of the population survive for at least 3 years
Haematological AEs are common:
-
grade 3–4 neutropenia and thrombopenia each affect in the order of 50 ± 10% of individuals taking dasatinib, although rates may be lower (20–30%) in the currently recommended dosage of 100 mg q.d.
Non-haematological AEs are also reported:
-
diarrhoea, dyspnoea, fatigue, headache, nausea, pleural effusion and rash were most commonly reported; frequencies in the range 10–40% at any grade
-
grade 3–4 AEs appear to be fairly rare, with only dyspnoea and pleural effusion occurring in > 5% of any of the reported cohorts
-
approximately 5–15% of study participants discontinued dasatinib therapy because of AEs, with the lowest withdrawal rate (4.8%) in the currently recommended dosage of 100 mg q.d.
CCyR is shown by about one-third of all study participants, with no evidence of a difference in efficacy between ImR and ImI populations.
MCyR is shown by 35–45% of all study participants, with no evidence of a difference in efficacy between ImR and ImI populations.
80–90% of those achieving an MCyR will maintain it for at least 1 year.
CHR was achieved or maintained in around 50% of cases, with no evidence of a difference in efficacy between ImR and ImI populations.
80–90% of those achieving a MHR will maintain it for at least 1 year; in over 60% of cases the response will last for 2 years or more.
Average PFS is a little over 2 years.
Average OS is a little over 2.5 years. Two-thirds to three-quarters of individuals can expect to survive for 2 years or more.
Haematological AEs are extremely common:
-
the majority of individuals experience grade 3–4 neutropenia and thrombopenia; anaemia and leucopenia are almost as prevalent.
Non-haematological AEs are also reported:
-
diarrhoea, dyspnoea, fatigue, headache, nausea, pleural effusion, and rash were most commonly reported; frequencies in the range 20–50% at any grade.
-
the grade 3–4 toxicities reported at a frequency of > 10% were diarrhoea, febrile neutropenia and fluid retention.
-
up to 30% of study participants discontinued dasatinib therapy due to AEs.
CCyR is shown by about one-third of all study participants.
MCyR is shown by around 45% of all study participants on average, though there is huge variability in reported rates:
-
MCyRs in subgroups in MBC are less common than they are for those in LBC.
CHR was achieved or maintained in around one-third of cases.
Most study participants achieve ≯ 3–6 months’ PFS.
Only one-quarter to one-third of individuals can expect OS of > 2 years.
Haematological AEs are nearly inevitable:
-
a substantial majority of individuals experience multiple cytopenias meeting the criteria for grade 3–4 AEs.
Non-haematological AEs are also reported:
-
diarrhoea, dyspnoea, fatigue, nausea, peripheral oedema, pleural effusion, pyrexia, rash and vomiting were most commonly reported; frequencies in the range 10–40% at any grade
-
grade 3–4 pleural effusion occurred in > 10% of participants in MBC; gastrointestinal haemorrhage and febrile neutropenia were also reported at frequencies > 10%
-
serious AEs may be less common in participants in LBC
-
0–15% of study participants discontinued dasatinib therapy because of AEs.
Effectiveness of nilotinib
Cytogenetic response
Chronic phase
Table 50 provides a summary of the available data detailing CyR to nilotinib in CML-CP. All included studies reported CCyR, PCyR and MCyR rates (or provided enough information to allow calculation of each). Minor and minimal responses were less commonly reported.
| Study | Dose | Length of follow-up | IMF | Complete (n/N) | Partial (n/N) | Major (n/N) | Minor (n/N) | Minimal (n/N) | Overall (n/N) |
|---|---|---|---|---|---|---|---|---|---|
| Kantarjian et al. (2006)103 | Mixed/NR | NR | ImR | 6/17 = 35.3% | 0/17 = 00.0% | 6/17 = 35.3% | 0/17 = 00.0% | 3/17 = 17.6% | 9/17 = 52.9% |
| Cortes et al. (2007)38 | Mixed/NR | 17 monthsa | ImR/ImI | 2/13 = 15.4% | 2/13 = 15.4% | 4/13 = 30.8% | 6/13 = 46.2% | ||
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 6 monthsb | ImI | 30/86 = 34.9% | 10/86 = 11.6% | 40/86 = 46.5% | 6/86 = 07.0% | 14/86 = 16.3% | |
| ImR | 58/194 = 29.9% | 36/194 = 18.6% | 94/194 = 48.5% | 16/194 = 08.2% | 25/194 = 12.9% | ||||
| Updatec | ImI | 47/93 = 50.5%d | 12/93 = 12.9%d | 59/93 = 63.4%d | |||||
| ImR | 89/228 = 39.0%d | 39/228 = 17.1%d | 128/228 = 56.1%d | ||||||
| Tojo et al. (2009)108 | 400 mg b.i.d. | 12 monthsb | ImR/ImI | 11/16 = 68.8% | 4/16 = 25.0% | 15/16 = 93.8% | 0/16 = 0.0% | 1/16 = 6.3% | 16/16 = 100.0% |
It is important to emphasise that the entry criteria for the large, multicentre study106 were such that participants were enrolled only as ImR if they had either (1) never had an MCyR to imatinib or (2) lost their CyR during imatinib therapy. In addition, participants were excluded from enrolment if they met the criteria for imatinib intolerance, but had achieved a prior MCyR to imatinib. According to these principles, it should be the case that no participants were experiencing MCyR at study entry. However, Kantarjian et al. 106 report at least five participants who entered the study with a CCyR and at least three who entered the study in PCyR. It is difficult to account for the enrolment of such individuals according to the stated eligibility criteria. In their submission (p. 35), Novartis explicitly states that ‘patients with MCyR at baseline were not eligible for the study’. 205 It is not absolutely clear whether or not the eight participants mentioned above are the only ones to have breached this principle; if so, the level of contamination may be perceived to be fairly minor (8/280 = 2.9%). It is entirely unclear to what extent this issue further distorts results published in conference abstracts as long-term follow-up.
It is notable that the response rates from Tojo et al. ’s small Japanese case series108 tend to be somewhat higher than those from other studies. The outlying nature of this data source may reflect differences in the cohort reported. In particular, we note that participants were only enrolled on successful completion of a 3-month preliminary phase, which suggests that they may have been disproportionately likely to respond to treatment in the main study.
Complete cytogenetic response was consistently defined in the evidence base as 0% Ph+ chromosomes in metaphase in BM. Table 51 presents details of response rates in ImI, ImR and mixed populations, with meta-analytical subtotals, where appropriate, for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImI | |||||
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 86 | 30 | 34.9 | 24.9% to 45.9% |
| ImR | |||||
| Kantarjian et al. (2006)103 | Mixed/NR | 17 | 6 | 35.3 | 14.2% to 61.7% |
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 194 | 58 | 29.9 | 23.5% to 36.9% |
| Subtotal [heterogeneity: Q = 0.2 (p on 1 df = 0.654); I2 = 0.0%; τ2 = 0.000] | 30.3 | 24.1% to 36.5% | |||
| ImR and/or ImI | |||||
| Cortes et al. (2007)38 | Mixed/NR | 13 | 2 | 15.4 | 1.9% to 45.4% |
| Tojo et al. (2009)108 | 400 mg b.i.d. | 16 | 11 | 68.8 | 41.3% to 89.0% |
| Subtotal [heterogeneity: Q = 12.15 (p on 1 df = 0.000); I2 = 91.8%; τ2 = 0.131] | 41.7 | 0.0% to 94.0% | |||
| Overall pooled estimate | 35.1 | 23.6% to 46.6% | |||
|
Heterogeneity: Q = 13.61 (p on 4 df = 0.009); I2 = 70.6%; τ2 = 0.011 Heterogeneity between intolerant and resistant strata: z = 0.76 (p = 0.224) |
|||||
This issue of CyR rates being complicated by target response status at baseline in the main multicentre study106 is difficult to unpick, as the evidence as presented in the published report is somewhat ambiguous. Five participants are noted to have entered the study with a CCyR and, alongside three whose baseline CyR status was unknown, they are not counted as complete responders in the published rates (i.e. these individuals are included in the denominator, but not the numerator of the calculation). If these individuals were included in the numerator as well as the denominator of this proportion (this is how such calculations are presented in the evidence base relating to dasatinib), the CCyR rate would become 96/280 = 34.3% across both ImI and ImR groups. Another method of calculation would be to exclude these individuals from both the denominator and the numerator of the calculation; this would lead to an estimated CCyR rate of 80/272 = 29.4%.
It should also be noted that the evidence from the main multicentre study106 included here is comparatively immature. Lengthier follow-up (including expanded enrolment) is available in a conference abstract (for details, see Table 50), but is not included in Table 51, because it has yet to be made available in a full-length publication which can be assessed for methodological validity.
On the basis of this small sample, there seems to be little heterogeneity in this evidence base, with the exception of one apparently outlying estimate provided by Tojo et al. 108 (excluding this single data point, heterogeneity drops considerably: p = 0.360; I2 = 6.7%). One consequence of this apparent homogeneity is that there seems to be little evidence of a difference in efficacy between ImI and ImR subgroups [although more recent follow-up172 of Kantarjian et al. ’s 2007 multicentre series106 suggests that the difference between the two cohorts has widened to 50.5% vs 39.0% in ImI and ImR groups, respectively (p = 0.077 by chi-squared test with Yates’s correction)].
Major cytogenetic response – defined as the number of participants experiencing either CCyR or PCyR (i.e. ≤ 35% Ph+) – is reported in all included studies. Table 52 presents details of the response rates in ImI, ImR and mixed populations, with meta-analytical subtotals, where possible, for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImI | |||||
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 86 | 40 | 46.5 | 35.7% to 57.6% |
| ImR | |||||
| Kantarjian et al. (2006)103 | Mixed/NR | 17 | 6 | 35.3 | 14.2% to 61.7% |
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 194 | 94 | 48.5 | 41.2% to 55.7% |
| Subtotal [heterogeneity: Q = 1.18 (p on 1 df = 0.278); I2 = 15.0%; τ2 = 0.001] | 46.5 | 37.3% to 55.7% | |||
| ImR and/or ImI | |||||
| Cortes et al. (2007)38 | Mixed/NR | 13 | 4 | 30.8 | 9.1% to 61.4% |
| Tojo et al. (2009)108 | 400 mg b.i.d. | 16 | 15 | 93.8 | 69.8% to 99.8% |
| Subtotal [heterogeneity: Q = 19.79 (p on 1 df = 0.000); I2 = 94.9%; τ2 = 0.188] | 63.3 | 1.6% to 125.0% | |||
| Overall pooled estimate | 52.3 | 31.5% to 73.0% | |||
|
Heterogeneity: Q = 53.29 (p on 4 df = 0.000); I2 = 92.5%; τ2 = 0.049 Heterogeneity between intolerant and resistant strata: z = 0.0 (p = 0.499) |
|||||
In the main multicentre study,106 eight participants are noted to have entered the study with a CCyR and, alongside three whose baseline CyR status was unknown, they are not counted as major responders in the published rates (i.e. these individuals are included in the denominator, but not the numerator of the calculation). If these individuals were included in the numerator as well as the denominator of this proportion (this is how such calculations are presented in the evidence base relating to dasatinib), the MCyR rate would become 145/280 = 51.8% across both ImI and ImR groups. Another method of calculation would be to exclude these individuals from both the denominator and the numerator of the calculation; this would lead to an estimated CCyR rate of 123/269 = 45.7%.
[Commercial-in-confidence (CiC) information (or data) removed.]
Again, a single data point from Tojo et al. ’s small Japanese case series108 appears to be inconsistent with an otherwise very homogeneous picture (excluding this single estimate removes all significant heterogeneity from the data set: p = 0.434; I2 = 0.0%).
There appears to be little evidence of a difference in the efficacy between ImI and ImR subgroups [although, once more, more recent follow-up of Kantarjian et al. ’s multicentre series106 suggests that the gap between the two cohorts has widened to 63.4% vs 56.1% in ImI and ImR groups, respectively (p = 0.281 by chi-squared test with Yates’s correction)].
One included study106 reports duration of MCyR to nilotinib in CML-CP, in a mixed population of ImI and ImR participants, estimating a 12-month maintenance probability of 0.96. A subsequent conference presentation updating results from this study states that 84% of patients maintained their MCyR at 18 months. 172
Accelerated phase
Table 53 provides a summary of the available data detailing CyR to nilotinib in CML-AP. All included studies reported CCyR, PCyR and MCyR rates (or provided enough information to enable the deduction of each).
| Study | Length of follow-up | Dose | IMF | Complete (n/N) | Partial (n/N) | Major (n/N) | Minor (n/N) | Minimal (n/N) | Overall (n/N) |
|---|---|---|---|---|---|---|---|---|---|
| Kantarjian et al. (2006)103 | NR | Mixed/NR | ImR | 8/56 = 14.3% | 7/56 = 12.5% | 15/56 = 26.8% | 5/56 = 08.9% | 11/56 = 19.6% | 31/56 = 55.4% |
| Cortes et al. (2007)38 | 17 monthsa | Mixed/NR | ImR/ImI | 8/31 = 25.8% | 2/31 = 6.5% | 10/31 = 32.3% | 13/31 = 41.9% | ||
| le Coutre et al. (2008)107 | 6 monthsb | 400 mg b.i.d. | ImR/ImI | 19/119 = 16.0% | 16/119 = 13.4% | 35/119 = 29.4% | 16/119 = 13.4% | 28/119 = 23.5% | |
| Tojo et al. (2009)108 | 12 monthsb | 400 mg b.i.d. | ImR/ImI | 1/7 = 14.3% | 0/7 = 0.0% | 1/7 = 14.3% | 0/7 = 0.0% | 3/7 = 42.9% | 4/7 = 57.1% |
Discussing findings in CP, above, we noted that a small number of study participants were in MCyR at enrolment, despite this apparently contradicting the study eligibility criteria. A very similar picture is seen in the main multicentre study of nilotinib in CML-AP. 107 It is reported that ‘one patient with a CCyR and four patients with a PCyR at baseline were entered in to the study’. In this instance, however, entry criteria only explicitly exclude potential participants in MCyR in the ImI group, although it is difficult to imagine participants in MCyR meeting the criteria for imatinib resistance (disease transformation or progression during imatinib therapy or absence of HR). It should be emphasised that – even if these cases do represent a violation of entry criteria – absolute numbers (5/119 = 4.2%) are small.
It should be noted that the reservations about Tojo et al. ’s study108 expressed above (see Chronic phase) do not apply in AP disease, because the preliminary study phase was only necessary for CP participants.
Table 54 presents details of CCyR rates in ImR and mixed populations, with meta-analytical subtotals, where appropriate. As noted above, one participant in le Coutre et al. ’s multicentre study107 met the criteria for CCyR at study entry.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImR | |||||
| Kantarjian et al. (2006)103 | Mixed/NR | 56 | 8 | 14.3 | 6.4% to 26.2% |
| ImR and/or ImI | |||||
| Cortes et al. (2007)38 | Mixed/NR | 31 | 8 | 25.8 | 11.9% to 44.6% |
| le Coutre et al. (2008)107 | 400 mg b.i.d. | 119 | 19 | 16.0 | 9.9% to 23.8% |
| Tojo et al. (2009)108 | 400 mg b.i.d. | 7 | 1 | 14.3 | 0.4% to 57.9% |
| Subtotal [heterogeneity: Q = 1.38 (p on 2 df = 0.501); I2 = 0.0%; τ2 = 0.000] | 17.3 | 11.4% to 23.2% | |||
| Overall pooled estimate | 16.4 | 11.5% to 21.4% | |||
| Heterogeneity: Q = 1.68 (p on 3 df = 0.642); I2 = 0.0%; τ2 = 0.000 | |||||
There is good agreement between this small sample of estimates and little evidence that response rates systematically differ according to imatinib failure status (note, however, that no estimates are available for an exclusively ImI population).
As in the evidence base relating to CML-CP, MCyR (≤ 35% Ph+) is reported in all included studies. Table 55 presents details of response rates in ImR and mixed populations, with meta-analytical subtotals, where appropriate. As noted above, five participants in le Coutre et al. ’s multicentre study107 met the criteria for MCyR at study entry.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImR | |||||
| Kantarjian et al. (2006)103 | Mixed/NR | 56 | 15 | 26.8 | 15.8% to 40.3% |
| ImR and/or ImI | |||||
| Cortes et al. (2007)38 | Mixed/NR | 31 | 10 | 32.3 | 16.7% to 51.4% |
| le Coutre et al. (2008)107 | 400 mg b.i.d. | 119 | 35 | 29.4 | 21.4% to 38.5% |
| Tojo et al. (2009)108 | 400 mg b.i.d. | 7 | 1 | 14.3 | 0.4% to 57.9% |
| Subtotal [heterogeneity: Q = 1.4 (p on 2 df = 0.498); I2 = 0.0%; τ2 = 0.000] | 28.8 | 21.8% to 35.9% | |||
| Overall pooled estimate | 28.3 | 22.2% to 34.3% | |||
| Heterogeneity: Q = 1.48 (p on 3 df = 0.687); I2 = 0.0%; τ2 = 0.000 | |||||
The MCyR rates collected, here, are closely comparable (as reflected in very low estimates of heterogeneity in meta-analytical calculations). Rates appear to be approximately two-thirds of the level seen in a CP population (see Major cytogenetic response: chronic phase).
Haematological response
Chronic phase
Table 56 provides a summary of the available data detailing HR to nilotinib in CML-CP. All included studies report CHR; subtotal responses are seldom reported in a CP population.
| Study | Dose | Length of follow-up | IMF | Complete (n/N) | Overall (n/N) |
|---|---|---|---|---|---|
| Kantarjian et al. (2006)103 | Mixed/NR | NR | ImR | 11/12 = 91.7% | 11/12 = 91.7% |
| Cortes et al. (2007)38 | Mixed/NR | 17 monthsa | ImR/ImI | 10/13 = 76.9% | 10/13 = 76.9% |
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 6 monthsb | ImI | 45/50 = 90.0%c | |
| ImR | 92/135 = 68.1%d | ||||
| Updatee | ImR/ImI | 158/206 = 76.7%f | |||
| Tojo et al. (2009)108 | 400 mg b.i.d. | 12 monthsb | ImR/ImI | 6/16 = 37.5% |
| Study | Definition |
|---|---|
| Kantarjian et al. (2006)103 |
WBC count < 10 × 109/l Platelet count < 450 × 109/l < 5% myelocytes plus metamyelocytes < 20% basophils Absence of blasts and promyelocytes in PB Absence of extramedullary involvement |
| Cortes et al. (2007)38 |
WBC count < 10 × 109/l Platelet count < 450 × 109/l No immature cells (blasts, promyelocytes or myelocytes) in the PB Disappearance of all signs and symptoms related to leukaemia (including palpable splenomegaly) |
| Kantarjian et al. (2007)106 | As defined in Kantarjian et al. (2006)103 |
| Tojo et al. (2009)108 | As defined in Kantarjian et al. (2006)103 |
In both the Phase I dose-ranging study,103 and the Phase II multicentre study,106 response rates are presented only for participants who did not meet criteria for CHR at baseline.
Definitions of CHR were similar in all included studies (indeed, in their Phase II multicentre study,106 Kantarjian et al. 103 explicitly refer the reader to the earlier, Phase I study for a full definition of CHR). The full definitions are summarised in Table 24.
Table 58 presents details of response rates in ImI, ImR and mixed populations, with meta-analytical subtotals, where appropriate, for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImI | |||||
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 50 | 45 | 90.0 | 78.2% to 96.7% |
| ImR | |||||
| Kantarjian et al. (2006)103 | Mixed/NR | 12 | 11 | 91.7 | 61.5% to 99.8% |
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 135 | 92 | 68.1 | 59.6% to 75.9% |
| Subtotal [heterogeneity: Q = 6.94 (p on 1 df = 0.008); I2 = 85.6%; τ2 = 0.024] | 78.9 | 55.9% to 100.0% | |||
| ImR and/or ImI | |||||
| Cortes et al. (2007)38 | Mixed/NR | 13 | 10 | 76.9 | 46.2% to 95.0% |
| Tojo et al. (2009)108 | 400 mg b.i.d. | 16 | 6 | 37.5 | 15.2% to 64.6% |
| Subtotal [heterogeneity: Q = 5.49 (p on 1 df = 0.019); I2 = 81.8%; τ2 = 0.064] | 57.3 | 18.7% to 96.0% | |||
| Overall pooled estimate | 74.6 | 59.1% to 90.1% | |||
|
Heterogeneity: Q = 28.17 (p on 4 df = 0.000); I2 = 85.8%; τ2 = 0.025 Heterogeneity between intolerant and resistant strata: z = 0.89 (p = 0.186) |
|||||
Five out of the 19 CP participants in the Phase I dose-ranging study103 and 95 out of the 280 participants in the Phase II multicentre case series are excluded from reported HR rates because they were in CHR at study entry.
There is a noticeable degree of variation in this data set, as reflected in estimates of substantial heterogeneity in the meta-analytical calculations. The inclusion of data from the Phase I dose-ranging study103 may serve to mask a distinct difference between ImI and ImR subgroups in the Phase II study (p = 0.005 by chi-squared test with Yates’s correction). 106
Accelerated phase
Table 59 provides a summary of the available data detailing HR to nilotinib in CML-AP. All included studies report CHR; subtotal responses are more sparsely reported.
| Study | Length of follow-up | Dose | IMF | Complete | Return to CP | Marrow response | Major or NEL | Overall |
|---|---|---|---|---|---|---|---|---|
| Kantarjian et al. (2006)103 | NR | Mixed/NR | ImR | 26/31 = 83.9% | 26/31 = 83.9% | |||
| Cortes et al. (2007)38 | 17 monthsa | Mixed/NR | ImR/ImI | 26/51 = 51.0% | 9/51 = 17.6% | 3/51 = 5.9% | 38/51 = 74.5% | |
| le Coutre et al. (2008)107 | 6 monthsb | 400 mg b.i.d. | ImR/ImI | 31/119 = 26.1% | 14/119 = 11.8% | 11/119 = 9.2% | 56/119 = 47.1% | |
| Updatec | 400 mg b.i.d. | ImI | 14/25 = 56.0% | |||||
| ImR | 55/104 = 52.9% | |||||||
| Tojo et al. (2009)108 | 400 mg b.i.d. | 12 monthsb | ImR/ImI | 1/7 = 14.3% | 1/7 = 14.3% | 3/7 = 42.9% |
In the Phase I dose-ranging study,103 at least 5 out of 46 AP participants were in CHR at study entry; these individuals are excluded from the publication’s calculation of HR. We have been unable to ascertain what proportion of participants in the Phase II study107 also met the criteria for CHR at baseline. We assume that the number must be greater than zero, for at least three reasons: (1) entry criteria do not explicitly exclude such individuals; (2) a small number of participants are known to have had MCyR at baseline (see Major cytogenetic response: accelerated phase), and it is unlikely that this response could be achieved without a simultaneous CHR; and (3) the large proportion of participants with CHR at baseline in analogously designed industry-sponsored studies of nilotinib in CP populations.
There are some notable differences between the definitions of CHR adopted by, on the one hand, the two studies reported by Kantarjian et al. 103 and Cortes et al. 38 (which use relatively similar definitions) and, on the other, the Phase II multicentre study of le Coutre et al. 107 Instead of overall WBC count, the latter concentrates on neutrophils in particular, gives a lower – rather than upper – bound for platelets and has a much lower limit for basophils (5% as opposed to 20%). The full definitions are summarised in Table 60.
| Study | Definition |
|---|---|
| Kantarjian et al. (2006)103 |
WBC count < 10 × 109/l Platelet count < 450 × 109/l < 5% myelocytes plus metamyelocytes < 20% basophils Absence of blasts and promyelocytes in PB Absence of extramedullary involvement |
| Cortes et al. (2007)38 |
WBC count < 10 × 109/l Platelet count < 450 × 109/l No immature cells (blasts, promyelocytes or myelocytes) in the PB Disappearance of all signs and symptoms related to leukaemia (including palpable splenomegaly) |
| le Coutre et al. (2008)107 |
Marrow blasts < 5% No blasts in PB Neutrophils > 1.5 × 109/l Platelets > 100 × 109/l Basophils < 5% No extramedullary disease |
| Tojo et al. (2009)108 | As defined in Kantarjian et al. (2006)103 |
Table 61 presents details of response rates in ImR and mixed populations, with meta-analytical subtotals, where appropriate, for each stratum.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| ImR | |||||
| Kantarjian et al. (2006)103 | Mixed/NR | 51 | 26 | 51.0 | 36.6% to 65.2% |
| ImR and/or ImI | |||||
| Cortes et al. (2007)38 | Mixed/NR | 31 | 26 | 83.9 | 66.3% to 94.5% |
| le Coutre et al. (2008)107 | 400 mg b.i.d. | 119 | 31 | 26.1 | 18.4% to 34.9% |
| Tojo et al. (2009)108 | 400 mg b.i.d. | 7 | 1 | 14.3 | 0.4% to 57.9% |
| Subtotal [heterogeneity: Q = 59.91 (p on 2 df = 0.000); I2 = 96.7%; τ2 = 0.138] | 42.1 | 0.0% to 85.2% | |||
| Overall pooled estimate | 44.6 | 14.6% to 74.6% | |||
| Heterogeneity: Q = 61.93 (p on 3 df = 0.000); I2 = 95.2%; τ2 = 0.087 | |||||
This evidence is very heterogeneous, with the three data points predicting CHR rates anywhere between one-seventh and over five-sixths. It is noticeable that the second lowest reported rate comes from the largest individual study population; however, it should be remembered that the duration of follow-up, in this data source, was short (6 months) compared with much other evidence reviewed here.
Progression-free survival
Progression-free survival is very sparsely reported in the published literature; in particular, no Kaplan–Meier curves are presented in the peer-reviewed journal articles we have identified. A small amount of information can be gleaned from alternative sources, as summarised below.
Chronic phase
We were unable to identify a published source of estimates of PFS with nilotinib in CML-CP. In its submission, Novartis205 provides unpublished data from the Phase II multicentre study of nilotinib at 400 mg b.i.d.;106 data extracted from the Kaplan–Meier graph that Novartis presents is tabulated in Table 62. Although no explicit information is provided, the reference given by Novartis suggests that these data relate to the extended follow-up cohort172 [with additional enrolment (n = 321) to that reported in the journal publication106 (n = 280)].
| Study | Dose | Length of follow-up | Imatinib | n | 6 months (years) | 12 months (years) | 18 months (years) | 24 months (years) | 36 months (years) |
|---|---|---|---|---|---|---|---|---|---|
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | ? updatea | ImR/ImI | 321 | 0.925 | 0.84 | 0.73 | 0.64 | 0.575 |
| NRb | ImI | NR | 0.95 | 0.91 | 0.84 | ||||
| ImR | NR | 0.86 | 0.77 | 0.63 | |||||
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | ? updatec | ImR/ImI | 321 | 0.925 | 0.84 | 0.73 | 0.64 | 0.575 |
In the submission, progression is defined simply as ‘progression to AP or blastic phase, loss of CHR, loss of MCyR or death’ (p. 20). 205 [CiC information (or data) removed.]
The single published data source suggests that the majority of individuals receiving nilotinib for CML-CP can expect > 3 years’ PFS. No separate data were available from published sources for ImI and ImR subgroups. However, a limited number of data of this type are available within the cost-effectiveness model provided by Novartis as part of its submission to NICE. This suggests that PFS is much greater in the ImI subgroup, with more than twice the likelihood of progression or death in the ImR cohort at follow-up times up to 18 months.
Accelerated phase
The relevant outcome in the Phase II multicentre study of nilotinib in CML-AP107 is referred to as time to progression (TTP). This label is sometimes given to a selective measure of progression, in which deaths unrelated to disease progression are censored. However, in this instance, the measure is explicitly defined as representing ‘time from study start to disease progression or death’ and, in the absence of any further qualification, we have to assume the outcome can be considered synonymous with PFS. In the main study publication, TTP is only presented for a subgroup of participants achieving a HR to nilotinib (in this group, 1-year probability is given as 0.73).
In two conference abstracts updating follow-up from this study, the 12-month probability of remaining progression free is given as 0.57173 and median TTP for the whole cohort is reported at 16 months. 175 A full Kaplan–Meier curve is provided in the Novartis submission. 205 Data extracted from this source are presented in Table 63.
| Study | Length of follow-up | Dose | Imatinib | n | 6 months (years) | 12 months (years) | 18 months (years) | Median (months) |
|---|---|---|---|---|---|---|---|---|
| le Coutre et al. (2008)107 | Updatea | 400 mg b.i.d. | ImR/ImI | 129 | 0.69 | 0.56 | 0.425 | 16 |
In the study publication107 and in the submission, progression is not defined for the AP population. [CiC information (or data) removed.]
In this single source, average PFS appears to lie in the range 12–18 months. No separate data were available for ImI and ImR subgroups.
Overall survival
Chronic phase
We found a single published source of estimates of OS with nilotinib in CML-CP: the main multicentre study of nilotinib at 400 mg b.i.d.,106 supplemented in a subsequent conference abstract. 172 In its submission, Novartis205 provides unpublished data updating this experience further; data extracted from this source is also presented in Table 64.
| Study | Dose | Length of follow-up | Imatinib | n | 6 months (years) | 12 months (years) | 18 months (years) | 24 months (years) | 30 months (years) |
|---|---|---|---|---|---|---|---|---|---|
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 6 monthsa | ImR/ImI | 280 | 0.995 | 0.95 | 0.95 | ||
| Updateb | ImR/ImI | 321 | 0.95 | 0.91 | |||||
| Further updatec | ImR/ImI | 321 | 0.995 | 0.95 | 0.91 | 0.88 | 0.88 | ||
| NRd | ImI | NR | 1.000 | 0.989 | 0.955 | 0.908 | 0.908 | ||
| ImR | NR | 0.987 | 0.937 | 0.894 |
It appears that only 5–10% or so of people are expected to die within 2 years of commencing treatment. No separate data were available from published sources for ImI and ImR subgroups. However, a limited number of data of this type were available within the cost-effectiveness model provided by Novartis as part of their submission to NICE. This suggests that < 5% of ImI people are expected to die within 18 months of commencing treatment, with the corresponding proportion in the ImR population a little over 10%.
Accelerated phase
Table 65 presents OS data from the main multicentre study of nilotinib in CML-AP. Data presented in the full study publication107 were supplemented by extended follow-up extracted from the manufacturer’s submission. 205
| Study | Dose | Length of follow-up | Imatinib | n | 6 months (years) | 12 months (years) | 18 months (years) | 24 months (years) | 30 months (years) |
|---|---|---|---|---|---|---|---|---|---|
| le Coutre et al. (2008)107 | 400 mg b.i.d. | 6 monthsa | ImR/ImI | 129 | 0.91 | 0.79 | 0.72 | ||
| 11 monthsa,b | ImR/ImI | 129 | 0.82 | 0.72 | 0.67 | 0.645 |
On the basis of this sparse data set, it would be estimated that around two-thirds of individuals taking nilotinib in CML-AP can expect to survive for ≥ 2 years. No separate data were available for ImI and ImR subgroups.
Adverse events
Most included studies (including all industry-sponsored, Phase I and II, multicentre studies) reported incidences of AEs during therapy with nilotinib. All assessed toxicities according to the National Cancer Institute’s Common Toxicity Criteria v3.0. 186
All relevant evidence is reproduced in Table 66. Figures from included publications are supplemented by safety data from the expanded access programme, as reported in Novartis’s submission. It should be noted that one included study (Kantarjian et al. ’s Phase I dose escalation study103) presents safety results aggregated across all phases of CML only.
| CP | AP | All phases | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All grades | Grade 3–4 | All grades | Grade 3–4 | All grades | Grade 3–4 | ||||||||
| Kantarjian et al.,106 ImR/ImI, 400 mg b.i.d. | Expanded access programmea | Kantarjian et al.,106 ImR/ImI, 400 mg b.i.d. | Expanded access programmea | Tojo et al.,108 ImR/ImI, 400 mg b.i.d. | le Coutre et al.,107 ImR/ImI, 400 mg b.i.d. | Expanded access programmea | le Coutre et al.,107 ImR/ImI, 400 mg b.i.d. | Expanded access programmea | Tojo et al.,108 ImR/ImI, 400 mg b.i.d. | Tojo et al.,108 ImR/ImI, 400 mg b.i.d. | Kantarjian et al.,103 ImR, Mixed/NR | Tojo et al.,108 ImR/ImI, 400 mg b.i.d. | |
| n | 280 | 1217 | 280 | 1217 | 16 | 119 | 157 | 119 | 157 | 7 | 34 b | 119 | 34 b |
| Haematological AEs | |||||||||||||
| Anaemia (%) | 3.0 | 18.8c | 12.6 | 12.0 | 57.1c | 5.0 | |||||||
| Leucopenia (%) | 31.3d | 42.9d | |||||||||||
| Neutropenia (%) | 28.9 | 11.0 | 37.5e | 21.0 | 25.0 | 71.4e | 10.9 | ||||||
| Thrombopenia (%) | 28.9 | 18.0 | 18.8f | 35.3 | 15.0 | 42.9f | 16.8 | ||||||
| Non-haematological AEs | |||||||||||||
| Abdominal pain (%) | 6.7 | 0.8 | |||||||||||
| Alopecia (%) | 18.4 | 0.0 | 0.0 | ||||||||||
| Anorexia (%) | 5.9 | 0.0 | 14.7 | 0.0 | |||||||||
| Arthralgia (%) | 5.0 | 0.0 | |||||||||||
| Back pain (%) | 11.8 | 2.9 | |||||||||||
| Chest pain (%) | 11.8 | 0.0 | |||||||||||
| Constipation (%) | 12.1 | 6.0 | 0.0 | < 1.0 | 10.9 | 1.0 | 0.0 | 0.0 | 11.8 | 0.0 | 0.0 | ||
| Diarrhoea (%) | 11.4 | 2.1 | 19.2 | 0.8 | |||||||||
| Dry skin (%) | 0.0 | ||||||||||||
| Eczema (%) | 14.7 | 0.0 | |||||||||||
| Erythema (%) | 11.8 | 0.0 | |||||||||||
| Fatigue (%) | 18.6 | 8.0 | 1.1 | < 1.0 | 10.1 | 6.0 | 0.8 | < 1.0 | 0.8 | ||||
| Headache (%) | 18.6 | 16.0 | 1.8 | 2.0 | 10.1 | 11.0 | 0.8 | < 1.0 | 32.4 | 5.9 | |||
| Hepatic dysfunction (%) | 14.7 | 0.0 | |||||||||||
| Malaise (%) | 14.7 | 0.0 | |||||||||||
| Muscle spasms (%) | 19.2 | 0.0 | 11.8 | 0.0 | |||||||||
| Myalgia (%) | 8.2 | 1.1 | 19.2 | 0.8 | |||||||||
| Nausea (%) | 23.6 | 12.0 | 1.1 | < 1.0 | 10.1 | 14.0 | 0.8 | 0.0 | 32.4 | 2.9 | |||
| Nausea and/or vomiting (%) | 0.0 | ||||||||||||
| Pain in extremity (%) | 4.6 | 0.7 | 5.0 | 0.0 | |||||||||
| Peripheral oedema (%) | 5.0 | 0.0 | |||||||||||
| Pruritus (%) | 23.9 | 12.0 | 1.1 | < 1.0 | 20.2 | 5.0 | 0.0 | 0.0 | 11.8 | 1.7 | 0.0 | ||
| Pyrexia (%) | 18.4 | 0.8 | 23.5 | 0.0 | |||||||||
| Rash (%) | 28.2 | 24.0 | 3.2 | 3.0 | 21.8 | 17.0 | 0.0 | 2.0 | 50.0 | 1.7 | 2.9 | ||
| Stomach pain (%) | 11.8 | 0.0 | |||||||||||
| Upper abdominal pain (%) | 5.0 | 0.0 | |||||||||||
| Vomiting (%) | 10.7 | 7.0 | 0.7 | < 1.0 | 8.0 | < 1.0 | 29.4 | 0.0 | |||||
Grade 3–4 haematological toxicities were seen at frequencies of roughly 15–30% in both CP and AP (although neutropenia was somewhat less common than that in the large CP population in the expanded access programme and noticeably higher rates are provided by the small Japanese case series108). With the exception of anaemia, it does not appear that cytopenias are any more common in AP than in CP. Leucopenia is not reported separately from neutropenia in any of the evidence we have identified.
Similarly, there does not appear to be much difference between CP and AP in the incidence of non-haematological AEs. Among all-grade toxicities, constipation, diarrhoea, fatigue, headache, nausea/vomiting, pruritus and rash appear most common, with between one-tenth and one-quarter of participants experiencing such events. Grade 3–4 AEs appear rare, with only rash exceeding a 3% incidence in any of the identified evidence.
It should be noted that, although rates for all types of AEs may appear rather low in the combined-phase results reported by Kantarjian et al. ,103 this was a Phase I dose escalation study, in which some participants took very low doses of nilotinib.
Rates of withdrawal because of AEs were between 5% and 15%: 42/280 = 15.0% in the Phase II CP study106 [CiC information (or data) removed] and 8/119 = 6.7% in the cross-phase dose-ranging study.
Additional reports of adverse events
There are relatively few sources of additional evidence on the adverse effects of nilotinib treatment.
-
Although there was no academically published evidence on the issue, there was concern about nilotinib’s cardiac toxicity:
-
– The summary of product characteristics (SPC) approved by the FDA carries a ‘black box warning’ alerting patients and physicians to the association between nilotinib and QT prolongation and sudden death. According to the SPC, nilotinib ‘has been shown to prolong cardiac ventricular repolarization as measured by the QT interval on the surface electrocardiogram in a concentration-dependent manner’. 206 No published source is given for this finding; however, it is stated that, in a clinical efficacy study (this appears to be the study reported by Kantarjian et al. 106), ‘the maximum mean QTcF change from baseline at steady state was 10 milliseconds. Increase in QTcF > 60 milliseconds from baseline was observed in 2.1% of the patients and QTcF of > 500 milliseconds was observed in three patients (< 1%)’. 206 Importantly, no episodes of torsade de pointes (the most life-threatening electrocardiogram manifestation related to QT prolongation) were observed in clinical studies.
-
– Additional unpublished data from the SPC reveal that five sudden deaths have been reported in individuals receiving nilotinib in ‘an on-going study (n = 867)’ and that a ‘similar incidence was also reported in the expanded access program’. 206 It is speculated that ventricular repolarisation abnormalities ‘may have contributed to their occurrence’. 206
-
– Recommendations are made to minimise the risk of cardiac toxicity (e.g. regular electrocardiograms; careful monitoring of electrolytes, especially hypokalaemia and hypomagnesaemia; avoidance of concomitant medications known to prolong QT interval).
-
-
The common haematological side effects of nilotinib have received a certain amount of attention in published literature:
-
– In their preliminary report on the potential of interleukin 11 as therapy for TKI-induced thrombopenia, Aribi et al. describe two individuals who were treated while taking nilotinib. 188
-
– In a paper detailing a subset of participants from the Phase I dose escalation study of nilotinib, Singer et al. 103 report that nilotinib is frequently associated with hyperbilirubinaemia [especially in the presence of the (TA)7/(TA)7 UGT1A1 genotype]. 111 The clinical significance of this finding is unclear; effects tended to be manageable and only two study participants were forced to discontinue nilotinib for this reason.
-
– The possibility that nilotinib may disturb glycaemia function is investigated by Breccia et al. 207 They studied nine individuals taking nilotinib in various disease phases and found that fasting glucose level rose in those who had a CCyR (though not in those who did not). The clinical significance of this finding is unclear.
-
-
As with dasatinib (and in line with the high incidence of rash noted in the efficacy studies) dermatological complications are also a subject of interest:
-
– Nilotinib-induced bullous Sweet syndrome is described by Kaune et al. 208 This syndrome is closely associated with cytopenias of the type seen in many people receiving nilotinib.
-
Summary of clinical effectiveness of nilotinib
A summary of the evidence identified in this review relating to the clinical effectiveness of nilotinib is given below. Box 4 summarises our findings for CML-CP; Box 5 provides similar information relating to CML-AP.
CCyR is shown by about one-third of all study participants, with no evidence of a difference in efficacy between ImI and ImR subgroups.
MCyR is shown by a little under half of all study participants, with little evidence of a difference in efficacy between ImI and ImR subgroups:
-
around 85% of those patients achieving an MCyR may maintain it for at least 18 months.
CHR was achieved in around 80% of cases:
-
ImI participants may have had a higher likelihood of CHR.
The majority of individuals receiving nilotinib for CML-CP can expect > 3 years’ PFS; a little under two-thirds have PFS of 2 years or more.
For OS, only around 10% of people are expected to die within 2 years of commencing treatment.
Haematological AEs are common:
-
grade 3–4 neutropenia and thrombopenia each affected around 30% of individuals taking nilotinib in the published study; rates were lower (< 20%) in the expanded access programme.
Non-haematological AEs are also reported:
-
constipation, diarrhoea, fatigue, headache, nausea/vomiting, pruritus and rash were most common among all-grade toxicities, with between one-tenth and one-quarter of participants experiencing such events
-
grade 3–4 AEs appear rare, with only rash exceeding a 3% incidence in any of the identified evidence
-
15% of study participants discontinued nilotinib therapy owing to AEs.
CCyR is shown by about one-sixth of all study participants, with no evidence of a difference in efficacy between ImR and ImI populations.
MCyR is shown by approximately 30% of all study participants, with no evidence of a difference in efficacy between ImR and ImI populations.
Evidence on CHR is very heterogeneous: on average, CHR was achieved in around half of cases; however, the CHR rate was only one-quarter in the largest individual study population.
Average PFS is a little under 1.5 years.
Around two-thirds of individuals can expect OS of 2 years or more.
Haematological AEs are common:
-
grade 3–4 neutropenia and thrombopenia each affected approximately 20–35% of individuals taking nilotinib in the published study; rates were slightly lower (15–25%) in the expanded access programme.
Non-haematological AEs are also reported:
-
alopecia, constipation, diarrhoea, fatigue, headache, muscle spasms, myalgia, nausea/vomiting, pruritus, pyrexia and rash were most common among all-grade toxicities, with between 10% and 20% of participants experiencing such events
-
grade 3–4 AEs appear very rare, with only rash exceeding a 1% incidence in any of the identified evidence
-
10% of study participants discontinued nilotinib therapy due to AEs.
Summary of review of clinical effectiveness
We were unable to identify any published evidence with direct relevance to any of our research questions (see Chapter 1, Definition of the decision problem). Only one included study assesses either of the technologies under review against a relevant comparator: Kantarjian et al. ’s randomised comparison of dasatinib and HDI. 23 Although the dasatinib arm of this study provides some additional data on the efficacy of that drug, it is impossible to draw any inference about the relative effectiveness of the interventions, because of the overwhelming extent of premature crossover from the HDI arm (80% swapped therapy after a median of 13 weeks).
The remainder of the identified evidence provides a heterogeneous collection of observational data (although two dose optimisation studies22,81 have a randomised design, they are, for the purposes of this review, essentially observational, as randomisation was not designed to address any of the research questions under review).
As emphasised in Design and characteristics of included studies and Critical appraisal of included evidence, the studies investigating dasatinib and nilotinib are heterogeneous in design, population, implementation and analysis. Among the most notable sources of variation are the following.
-
Differences in eligibility criteria:
-
– In nilotinib studies, ImI participants were also required to be non-responders; this restriction did not apply in dasatinib studies.
-
– In nilotinib studies, most participants with an ongoing MCyR to imatinib at study baseline were excluded from studies; in dasatinib studies, entry criteria were broader, in this respect (see Design and characteristics of included studies, Chronic phase, Accelerated phase, Complete cytogenetic response: chronic phase and Complete cytogenetic response: accelerated phase).
-
-
Differences in baseline characteristics:
-
– In line with the eligibility criteria discussed above, a lower proportion of participants were in MCyR in studies of nilotinib than in those that investigated dasatinib, where reported. Up to 20% of participants were in MCyR in dasatinib studies; the analogous proportion in nilotinib studies may have been 5% or lower.
-
– A concomitant variability in CHR at baseline was seen, with greater proportions tending to feature in the dasatinib studies than in the nilotinib studies.
-
-
Differences in outcome definitions:
-
– There is heterogeneity in the studies’ definition of CHR. A minimum ANC is specified in some cases, but not others; some studies impose a constant limit for WBC counts whereas others rely on the ranges adopted by participating institutions; and the upper limit for basophils in PB varies between 2% and 20%. There does not appear to be systematic differences according to the technology under assessment.
-
– Definitions of PFS vary quite substantially between industry-sponsored studies of dasatinib and nilotinib (see Progression-free survival). [CiC information (or data) removed.]
-
-
Differences in outcome reporting:
-
– In assessing the comparability of reported outcome data, length of follow-up is a very significant concern, especially with regard to CyR and HR rates. Some studies reported such data after participants had been receiving treatment for as little as 6 months; others give outcomes based on 2 years’ follow-up or more. Because response rates are based on best ever status on treatment (as opposed to current status at the time of analysis), they cannot decrease – and are very likely to increase – as additional follow-up accrues. The upward tendency of response rates reported in consecutive updates from single studies confirms this. Accordingly, studies based on lengthier follow-up will appear to report a higher likelihood of response, even if the technology under assessment is no more effective than those assessed after less time. The substantial variation in follow-up times in the evidence base identified here is therefore bound to introduce additional heterogeneity and uncertainty to reported outcomes.
-
– Nilotinib studies tend to report HRs and CyRs only for the subset of participants who did not meet the criteria for the target response at study entry; dasatinib studies include all participants regardless of baseline status (and, in those instances, it is not entirely clear at what stage participants who were in response at baseline are considered to have maintained their response with the new drug).
-
– For both dasatinib and nilotinib, we have identified a certain number of data estimating CyR rates in participants with and without target response at baseline; however, this information is not available in all cases, and is often partial (for example, it may not distinguish between ImR and ImI cohorts). As a result, it is challenging to deduce response rates that are comparable between different studies.
-
The potential impact of these differences – along with inevitable additional variation in population due to unacknowledged or occult factors – may be easily sufficient to overwhelm any differences in results attributable to the underlying effectiveness of the technologies themselves. We have no confidence that a well-conducted randomised study of dasatinib versus nilotinib would produce results comparable to those seen in the assortment of observational data collected in this review. It is entirely possible that one technology would be seen to produce superior results to the other; equally, it might be that a similar effectiveness profile would be demonstrated. The evidence we have identified does not enable us to predict which of these outcomes is most likely. Similarly, the relative effectiveness of either of the technologies under review, when assessed against any other relevant comparator, can only be a matter of conjecture.
Chapter 3 Cost-effectiveness: introduction
The following four sections present an assessment of the cost-effectiveness of dasatinib and nilotinib. The analysis of cost-effectiveness comprises a systematic review of available literature on the cost-effectiveness of these drugs for CML (see Chapter 5), an assessment of the cost-effectiveness of dasatinib and nilotinib in CP (see Chapter 6) and in AP (see Chapter 7), and an assessment of the cost-effectiveness of dasatinib in BC (see Chapter 8).
Our assessment of cost-effectiveness in CP includes a review and critique of the manufacturer submissions to NICE and an independent economic model and analysis of cost-effectiveness carried out by the Peninsula Technology Assessment Group (PenTAG). The assessment of cost-effectiveness in AP and BC is undertaken through a review and critique of the manufacturer submissions to NICE, including exploration of the economic models they contain.
We have not produced a de novo economic model to estimate the cost-effectiveness of the interventions in AP and BC as we were unable to identify suitable effectiveness data for the comparator treatments in these populations with which to populate the model. Cost-effectiveness estimates for ImR comparisons provided in the manufacturer submissions rely on data generated in studies in which individuals with imatinib-naive CML received treatment with standard-dose imatinib (400 mg q.d.). We were unable to find any evidence to suggest that the response to standard dose imatinib in imatinib-naive individuals could be used to inform the expected response to HDI in individuals either resistant or intolerant to standard-dose imatinib. We were, therefore, unable to perceive a benefit in building an additional model based on these data as all potential models face the same fundamental problem. We therefore provide a review and critique of the manufacturer submissions and have explored the sponsor models through, where appropriate, the use of alternative parameter values and with limited threshold analyses.
Following the systematic review of existing cost-effectiveness studies, this section of our assessment of dasatinib and nilotinib is organised according to the three phases of CML, considering cost-effectiveness in CP, AP and BC in turn.
Chapter 4 Cost-effectiveness: systematic review
Methods
We undertook a systematic literature search to identify economic evaluations of dasatinib and nilotinib which were carried out in line with the scope of the current assessment. Appendix 2 outlines in detail the search strategy used and databases searched. Manufacturer submissions to NICE were reviewed to identify additional studies.
All titles and abstracts were examined. The relevance of each paper was assessed according to the inclusion and exclusion criteria. The review was carried out by one researcher (MH).
Results
Our literature search did not identify any published full economic evaluations meeting the inclusion criteria. However, we identified nine abstracts which met the specified inclusion criteria209–217 and two reports from the SMC. 218,219 Six studies reported on dasatinib209–213,219 and three reported on nilotinib. 214,215,218 All cost-effectiveness studies considered HDI as the only comparator.
There is insufficient detail in the abstracts or reports to undertake a detailed critical appraisal of the methods used. However, a summary of study characteristics and results is given below (Table 67).
| Study/characteristics | SMC219 | Sambrook et al. (2007)209 | Logman et al. (2007)210 | Juarez-Garcia et al. (2008)211 | Brosa et al. (2007)212 | Quissak et al. (2008)213 | SMC218 | Jewitt et al. (2008)214 | Pilgrim et al. (2007)215 |
|---|---|---|---|---|---|---|---|---|---|
| Dasatinib or nilotinib | Dasatinib 70 mg b.i.d. | Dasatinib | Dasatinib 140 mg q.d. | Dasatinib | Dasatinib 140 mg q.d. | Dasatinib | Nilotinib 400 mg b.i.d. | Nilotinib | Nilotinib |
| Comparator | Imatinib | Imatinib 800 mg q.d. | Imatinib 800 mg q.d. | Imatinib | Imatinib 800 mg q.d. | Imatinib | HDI | HDI (800 mg) | HDI (800 mg) |
| Patient population | Resistant to 400–600 mg imatinib | Resistant to imatinib | Resistant to 400–600 mg imatinib | Resistant and intolerant to imatinib | Resistant to imatinib | Resistant and intolerant to imatinib | Unknown | Resistant to imatinib | Resistant to imatinib |
| Analysis by CML stage | CP, AP and BC | CP, AP and BC | CP | CP, AP and BC | CP | CP, AP and BC | CP | CP | CP |
| Model type | Markov | Markov | Markov | Markov | Markov | Markov | Unknown | Markov | Markov |
| Time horizon | Lifetime | Unknown | Lifetime | Lifetime | Unknown | Lifetime | Lifetime | Lifetime | Lifetime |
| Perspective | Scotland | Canada | Austria | Mexico | Spain | Brazil | Scotland | UK | UK |
| Effectiveness data | Phase two non-comparative studies | Unknown | Kantarjian et al. (2007)23 | Unknown | Kantarjian et al. (2007)23 | Unknown | One non-comparative study | Interim data from Phase II nilotinib study CAMN107A2101, subgroup of IRIS study | Interim data from Phase II nilotinib study CAMN107A2101, subgroup of IRIS study |
| Base-case results | Dasatinib dominated imatinib in CP. ICERs in AP and BC: £44,456/QALY; £63,727/QALY | Dasatinib dominated imatinib in CP. ICERs in AP and BC: CAN$88,098/QALY; CAN$173,922/QALY | Dasatinib dominated imatinib | Dasatinib dominated imatinib in CP. ICERs in AP and BC: US$36,366/LYG; US$205,405/LYG | Dasatinib dominated imatinib | ICERs in CP, AP and BC: R$80,000/QALY; R$91,000/QALY, R$123,000/QALY | Nilotinib dominated imatinib | Nilotinib dominated imatinib | ICER is £22,000/QALY |
Summary: cost-effectiveness literature
All studies considered patients either resistant to, or intolerant of, imatinib. In some, it was not clear whether the population was resistant to imatinib, intolerant or both. Most studies of dasatinib modelled the cost-effectiveness of patients starting in the CP, AP and BC separately, whereas all the studies of nilotinib modelled the cost-effectiveness of patients starting in only CML-CP. Not all the studies state the type of model used, but those which did used a Markov approach with a lifetime time horizon. The studies were performed from a range of national perspectives with four from a UK perspective. 214,215,218,219
Not all studies stated the source of clinical effectiveness data, but those which did cited the Phase II studies of dasatinib and nilotinib. Two studies214,215,217 used a subgroup of the IRIS study (imatinib vs interferon) to project long-term OS for dasatinib and nilotinib.
The studies of dasatinib concluded that the drug is most cost-effective when started in the CP, followed by the AP and least cost-effective for patients when starting in the BC. Five209–212,219 of the six studies of dasatinib concluded that dasatinib dominates (i.e. is more effective and less costly) HDI for people starting in the CP. Two214,218 of the three nilotinib studies concluded that nilotinib dominates HDI for patients starting in the CP, with the third215 estimating cost-effectiveness of £22,000 per quality-adjusted life-year (QALY) gained.
In the absence of more complete methodological details, it was difficult to provide guidance on the validity of these studies and, therefore, the extent to which the results may be considered reliable.
Chapter 5 Cost-effectiveness: chronic myeloid leukaemia in chronic phase
Review of manufacturer submissions to NICE
Methods
The cost-effectiveness models reported in the manufacturer submissions were assessed against the NICE reference case220 and are critically appraised using the framework presented by Phillips et al. ,221 who synthesised the literature on evaluating decision-analytic models in health technology assessment to present guidelines for good reporting practice.
Nilotinib (manufacturer analysis/model)
Appendix 4 presents a summary review of the nilotinib manufacturer submissions against the main items in the NICE reference case requirements and the criteria set out by Philips et al. 221
Summary of Novartis’s cost-effectiveness analysis
Comparators, patient groups
Novartis present two discrete cost-effectiveness analyses of nilotinib for patients starting treatment in CML-CP: one simulating individuals with demonstrated resistance to normal-dose imatinib (ImR) and the other representing a subgroup of people intolerant to normal-dose imatinib (ImI) who had also shown no MCyR while on therapy. In line with the Phase II study which informs the nilotinib arm of the analysis (as discussed in Chapter 2, Design and characteristics of included studies),106 the second subgroup is referred to as ‘intolerant as well as resistant’ in the submission. This is not strictly accurate; in order to qualify as ImR, participants had to show a long-term lack (or loss) of response to imatinib, whereas ImI individuals were enrolled so long as they had not achieved MCyR over a period of therapy which may have been much shorter. It is therefore more accurate to think of this group as ‘intolerant as well as (at least initially) unresponsive’.
In the ImR population, nilotinib is compared with HDI. In the ImI population, nilotinib is compared with hydroxycarbamide. Nilotinib was not compared with IFN in either population; this is justified on the basis that no suitable data were found on the use of IFN following failure of normal-dose imatinib. Nilotinib was not compared with dasatinib in either population; it is argued that different patient entry requirements make study data incomparable, especially with regard to differences in studies of the two drugs according to the presence of response at baseline and definitions of ImR and ImI, which, it is contended, are more restrictive in nilotinib studies than in dasatinib studies (see further discussion in Review of Novartis’s chronic phase submission).
Model structure
The model is a Markov cost-effectiveness model, written in Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). It assumes that patients start second-line treatment aged 57 years, with a 50 : 50, male–female ratio, consistent with the main Phase II study of nilotinib. 106 Patients are modelled until age 100 years, implying a lifetime horizon of 43 years. The model cycle length is 3 months. A half-cycle correction is not applied.
The models take a UK NHS perspective, and all costs and benefits are discounted at 3.5%. 222
The model comprises the following health states: CP, AP, BC and death (Figure 6). Patients enter the model in CP, progress to AP, then to BC, and then finally to death from CML causes. Patients may also die in the CP and AP states from non-CML causes (data from life tables). On progression to AP, all patients, independent of treatment arm, are assumed to receive the same therapy options, either conventional hospital-based chemotherapy, hydroxycarbamide or SCT.
FIGURE 6.
Structure of Novartis’s CP model. Reproduced with permission from Novartis’s submission, Figure 11, p. 37. 205
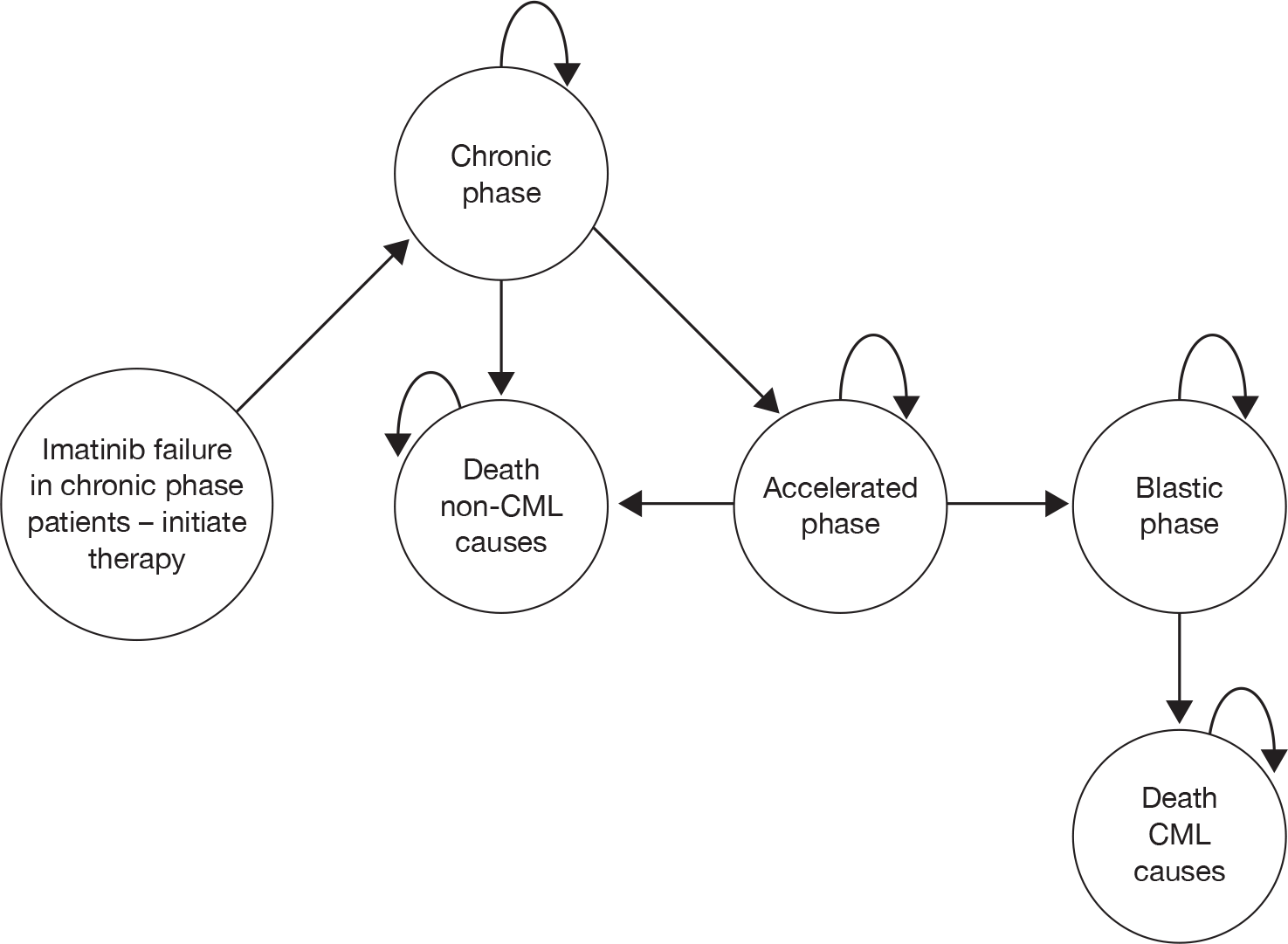
Time spent in AP and BC was assumed to be independent of treatment arm and independent of TTP, and is taken from the same data source used to parameterise the ImI model’s hydroxycarbamide arm. 223
Overall survival and PFS were both assumed to follow exponential distributions. OS was calculated as PFS plus time spent in AP plus time spent in BC.
Clinical effectiveness
No details are provided of the review methods by which data sources were identified (other than a statement that a ‘literature search was carried out to identify all relevant papers’ without further details of methods or results).
Nilotinib effectiveness data were taken from the single-arm, Phase II nilotinib study reported by Kantarjian et al. 106 (see Chapter 2, Effectiveness of nilotinib).
High-dose imatinib effectiveness data were taken from a study reporting a subgroup of participants in the IRIS study who underwent dose escalation having shown – or developed – resistance to normal-dose imatinib. 54 Novartis claim that these data offer unbiased results from the largest sample of comparable patients to those in the nilotinib study. Novartis identified three other studies of HDI, which were rejected as candidate data sources for a variety of reasons: small number of patients,224 problems with allowance for dose escalation and early discontinuation owing to crossover to alternative treatment23 and differences in patient population from the nilotinib study, including some patients starting HDI with a PCyR. 182
For the ImI subgroup, the hydroxycarbamide arm is parameterised with effectiveness data taken from a retrospective analysis of therapy following imatinib failure at a single institution. 223 Novartis acknowledges that there are several serious limitations with these data, including the fact that only 12 (19.7%) of the 61 individuals whose experience is reported actually received hydroxycarbamide [the others received a variety of treatments including tipifarnib (Zarnestra, Johnson & Johnson), lonafarnib (Sarasar, Schering–Plough), decitabine (Dacogen, MGI Pharma), cytarabine, homoharringtonine (Stratgen France SAS) and IFN].
As explained above, the critical effectiveness input to the model is PFS (with OS calculated as a function of this distribution). For nilotinib, PFS is estimated using an extrapolation of results from the Phase II study (unpublished data with additional follow-up from the published report106 is used). For HDI, empirical PFS data were not used directly, on the grounds that they were not comparable with nilotinib PFS data. Novartis states that the published curves in the preferred data source54 exclude death from non-CML causes, although the publication in question explicitly states that ‘death from any cause’ was treated as an event in PFS calculations (in addition, we have substantial reservations about this data source – see Progression-free survival: high-dose imatinib). Instead, PFS is estimated using OS from the selected data sources,54,223 and is then adjusted so that the ‘relative risk of PFS to OS’ is the same as that observed in ‘the nilotinib data of the relevant patient population’ (presumably, the relevant subgroup of the Phase II study106). Similarly, for hydroxycarbamide in the ImI model, empirical PFS data were not used directly, on the grounds the data were not available from the preferred data source,223 and the same OS-based method of estimating PFS was adopted.
Overall survival for each treatment was then calculated as the sum of the modelled PFS, plus time in AP, plus time in BC.
Time in AP for all comparators was estimated as 9.14 months and time in BC for all comparators was estimated as 9.89 months. These estimates were calculated on the basis of OS curves for participants not receiving dasatinib, nilotinib or SCT in Kantarjian et al. ’s retrospective analysis of survival following imatinib failure (the same data source used to parameterise the ImI model’s hydroxycarbamide arm223). Exponential curves were fitted to empirical OS in AP and BC. Time in BC was estimated directly as the area under the BC curve and time in AP was estimated as the difference between the two curves (i.e. expectation of survival for those starting in AP minus expectation of survival for those starting in BC).
Resource use
The following costs were modelled: drug acquisition, hospital appointments for administration and monitoring and treatment for grade 3–4 AEs.
Modelled patients were assumed to take 800 mg of nilotinib q.d., 800 mg (high-dose) of imatinib q.d. or 2 g of hydroxycarbamide q.d. Drug costs were not reduced for dose intensities below 100%.
To estimate duration of therapy, patients are assumed to continue drug treatment until they progress (according to the structure of the model, this equates to transition to AP) or discontinue owing to serious AEs. Discontinuation rates are drawn from the literature for nilotinib and HDI (15%106 and 2%,54 respectively), and assumed to be 0% for hydroxycarbamide. It is assumed that patients experience serious AEs only in the first 6 months of treatment. It is further stated that not all patients who experience serious AEs stop treatment; however, this is not captured in the Novartis model. In the absence of an evidence-based source to estimate subsequent disease course following discontinuation, Novartis assumes that 10% of all patients who stop treatment owing to AEs will progress from CP to AP in each 3-month cycle.
It is assumed that patients have outpatient monitoring appointments, the frequency of which depends on the phase of the disease. The costs of BM tests are absorbed within the cost of outpatient visits. Costs of treatment-related grade 3–4 AEs in CP were considered. The average monthly cost of treating AEs from nilotinib and HDI was estimated as £45 and £42 per patient, respectively, during the first 6 months.
Once progressed to AP, patients also incur the cost of hydroxycarbamide (89.9% of patients; 2 g/day) and/or chemotherapy (50% in the first 3-month cycle only) and/or SCT (23.5% in the first cycle only). A round of chemotherapy is assumed to comprise daunorubicin (50 mg/m2/day for 3 days), cytarabine (100 mg/m2/day for 10 days) and thioguanine (2.5 mg/kg/day for 10 days), at a cost of £918.22, to which is added a further cost to reflect inpatient care for the duration of therapy (30 × £300 = £9000). It was assumed that this regimen would induce remission sufficient to make SCT viable in 47% of patients, for 43% of whom a suitable donor would be available. In sum, 10% are assumed to receive SCT at a unit cost of £47,565. These assumptions combine to a state cost of just over £10,000 for the first quarter of AP and around £650 for each 3-month cycle thereafter.
For BC, it was assumed that all patients receive hydroxycarbamide (2 g/day) and require four outpatient appointments per month, to give a state cost of £1269.30 per 3-month cycle. Finally, it was assumed that patients require 10 days of inpatient stay as end-of-life care, regardless of cause of death (10 × £300 = £3000).
Valuation of outcomes (utilities)
Utilities were taken from the IRIS study of standard-dose imatinib, taken from European Quality of Life-5 Dimensions (EQ-5D) responses, as reported by Reed et al. :225 CP = 0.854, AP and BC = 0.595. Novartis assumes that these underlying utilities are independent of treatment. Next, disutilities corresponding to grade 3–4 AEs were modelled for nilotinib and HDI (again, it is assumed that hydroxycarbamide induces no serious AEs). Novartis assumes that serious AEs would occur during the first 6 months of treatment. The treatment-specific disutilities were calculated from the sum, over all AEs, of the product of the disutility, the duration of the AEs and the proportion of patients who experience the AE for each treatment. Based on these assumptions, the average utilities of patients in CP receiving nilotinib, HDI and hydroxycarbamide during the first 6 months of treatment were defined as 0.805, 0.827 and 0.854, respectively.
Summary of Novartis’s cost-effective analysis results
The base-case deterministic results of Novartis’s model are given in Tables 68 and 69.
| Drug therapy | Costs (£) | LYs | QALYs | Incremental cost per LYG | Incremental cost per QALY gained |
|---|---|---|---|---|---|
| HDI | 136,797 | 4.62 | 3.53 | ||
| Nilotinib | 117,705 | 4.93 | 3.79 | Nilotinib dominates | Nilotinib dominates |
| Drug therapy | Costs (£) | LYs | QALYs | Incremental cost per LYG | Incremental cost per QALY gained |
|---|---|---|---|---|---|
| Hydroxycarbamide | 20,111 | 4.14 | 3.12 | ||
| Nilotinib | 231,156 | 8.25 | 6.72 | £51,308 | £58,590 |
Nilotinib dominates HDI for all one-way sensitivity analyses investigated by Novartis (varying utilities, costs of AEs, PFS and time horizon). The incremental cost-effectiveness ratio (ICER) for nilotinib versus hydroxycarbamide varies between £50,000 and £60,000 per QALY for virtually all scenario analyses investigated by Novartis.
The probabilistic sensitivity analysis indicates that nilotinib can be expected to be cost-effective compared with HDI at all willingness-to-pay (WTP) thresholds and to be cost-effective compared with hydroxycarbamide for WTP thresholds above approximately £59,000 per QALY.
Review of Novartis’s chronic phase submission
Comparators, patient groups
A summary of our review of the Novartis CP model is shown in Box 6. Novartis did not attempt to estimate the incremental cost-effectiveness of nilotinib compared with dasatinib. It was argued that study data for the two technologies were incomparable owing to different patient entry requirements. In particular, Novartis asserts that the ImI cohorts are excessively dissimilar. They state that 12–41% of the ‘intolerant’ patients in the dasatinib studies had baseline MCyR responses, whereas none of the ImI patients in the nilotinib study had an MCyR at baseline. It was contended that this implies superior baseline prognosis for dasatinib patients compared with nilotinib patients who were intolerant to imatinib.
-
Novartis has not used systematic methods to identify the data on which their economic analysis is based.
-
Novartis has incorrectly assumed that PFS is identical to time in CP. Consequently, OS has been underestimated for all treatments, probably to a substantial extent. It is not possible to establish which comparators are most greatly influenced by this error, or the extent of the bias it introduces.
-
Novartis has not used CyR rates in their estimation of OS, even though CyR rates are well established as surrogate measures of OS.
-
All treatments are always assumed to be taken at the recommended dose. Using dose intensities quoted from the studies would have a substantial impact on ICERs (nilotinib vs HDI changes from –£76,755 to £25,267 per QALY and the ICER for nilotinib vs hydroxycarbamide changes from £58,491 to £51,139 per QALY).
-
We are concerned about the very large degree of extrapolation of PFS, in particular for the ImI subgroup. This makes all cost-effectiveness results highly uncertain.
-
The hydroxycarbamide clinical effectiveness data have serious limitations – most notably that only a small minority of the study participants actually received hydroxycarbamide.
The proportions quoted may exaggerate the true discrepancy between the populations; we believe that 12–41% represents the number of participants who had achieved an MCyR at any time during imatinib therapy and that the proportion of participants who met the criteria for MCyR at baseline was around half that level (6–23%; see Chapter 2, Design and characteristics of included studies). Clearly, asymmetry in prior response – whether maintained at baseline or not – might introduce important bias into a head-to-head economic evaluation, although we find it difficult to predict the direction of that bias. On the one hand, previous MCyR to normal-dose imatinib may bode well for the prospects of a response to an alternative TKI; on the other hand, individuals who have already been through successful imatinib treatment are likely to have a longer history of therapy and, accordingly, may have progressed further within the natural history of CML. Novartis also contends that, in the nilotinib study,106 the definition of ImI required ‘sustained, recurrent and persistent AEs in spite of optimal supportive care’ whereas, in the dasatinib studies, the definitions of intolerance would be ‘considered by UK experts as very relaxed entry criteria by comparison’ (Novartis, appendix 5).
Where ImR populations are concerned, Novartis emphasises that participants in the nilotinib study106 were required to have received prior therapy with dose-escalated imatinib (≥ 600 mg q.d.) for a minimum of 3 months (unless they met the criteria for ImI or had a P-loop mutation), meaning that the ‘resistant’ status of this population had been firmly established. In contrast, participants in dasatinib studies were classified as ImR if they had met the criteria for primary or secondary resistance, regardless of whether dose escalation had been undertaken.
Novartis did not compare nilotinib with IFN in either population. Its justification for this decision was that no suitable data were found on the use of IFN following failure of normal-dose imatinib. We are not convinced that, in order to undertake a cost-effectiveness analysis of IFN in this population, it is essential to rely on data specifically relating to those with demonstrated imatinib failure before IFN therapy. IFN has a different mechanism of action to TKIs and we are unaware of any evidence suggesting that ImI or ImR populations respond to IFN in a systematically different way. Accordingly, we suggest that relying on data drawn from an imatinib-naive population (of which there are many to choose from) would be no more egregious an assumption than several others adopted in Novartis’s model (for instance, that it is acceptable to estimate HDI PFS on the basis of a ratio derived from a study of nilotinib).
Model structure
The model cycle length of 3 months seems reasonable given the large uncertainty in model structure and data, and given that patients live for several years. For the same reasons, it seems reasonable not to model a half-cycle correction. Patients were modelled for life, from age 57 to 100 years, which is appropriate.
We disagree with Novartis’s calculation of OS in the model. OS was calculated as PFS plus time spent in AP, plus time spent in BC. This definition would be correct only if progression were defined as progression from CP to AP. However, progression may also occur for other reasons, including loss of MCyR or loss of CHR (see Chapter 2, Progression-free survival). As a result, average PFS will always be of a shorter duration than time in CP. Therefore, it appears that Novartis has seriously underestimated OS. There is good evidence that ImR patients may spend several years in CP after failure of second-line HDI treatment (figure 2, Jabbour et al. 182) and most patients who fail second-line dasatinib treatment remain in CP after progression. 143 All comparators are susceptible to this shortcoming although, in the absence of an estimate of time spent in post-progression CP, it is difficult to estimate whether or not some are more affected than others and, if so, to what degree. This is an important consideration when comparing the results of the three cost-effectiveness analyses (BMS, PenTAG and Novartis) as discussed in Comparison of results of PenTAG and manufacturer cost-effective analysis.
We are concerned that Novartis has made no use of the CyR rates reported in the single-arm studies, because they are known to be important correlates of OS, although we recognise that the approach they have taken, with progression through each of the phases of CML being inferred directly, rather than via a surrogate relationship, is not necessarily invalid (and forms the basis for most previous models of CML).
Clinical effectiveness data
There is no evidence that the data used to parameterise the model were identified using systematic techniques, so we cannot be certain that all evidence relevant to the decision problems has been found. However, it does not appear that Novartis failed to consider any major sources of clinical effectiveness data identified in our own systematic review (see Chapter 2, Identification of evidence).
The HDI effectiveness data for the ImR patient subgroup were taken from the IRIS study. 54
Of the alternative candidate data sources, we agree that it was reasonable to reject Zonder et al. ’s study224 (owing to the very small number of patients reported) and the HDI arm from Kantarjian et al. ’s randomised comparison with dasatinib23 (most importantly, because of the bias introduced by premature crossover from HDI to dasatinib; see our analysis of this study in Chapter 2, Randomised studies). We are less convinced by Novartis’s reasons for rejecting Jabbour et al. ’s study,182 for which two main arguments are advanced.
First, it is argued that participants were more likely to respond to treatment because a proportion of them had been receiving a suboptimal dosage of imatinib (300 mg q.d.) prior to dose escalation. Although we acknowledge this, only a relatively small proportion of individuals were affected in this way (14%) and there was no evidence to support (and quantify) Novartis’s contention that treatment effect would be likely to be exaggerated because of it.
Second, Novartis suggests that it was significant that a proportion of participants in Jabbour et al. ’s study182 met the criteria for MCyR at study entry (13/84 = 15%), contrasting this with the study used to estimate the efficacy of nilotinib,106 in which ‘patients with MCyR at baseline were not eligible for the study’. This latter statement is, as already discussed (Chapter 2, Chronic phase), incorrect. For participants with ImR, there was no such restriction in the nilotinib study and it is reported that at least eight individuals were in MCyR at baseline. If it is assumed that, per eligibility criteria, all such participants must have been in the ImR subgroup, this means that ≥ 4% of that cohort benefited from this status; this is probably fewer than in the HDI study, but removes the objection that the populations were fundamentally incomparable on this issue. By the same token, it might be argued that Novartis’s decision to adopt a source for HDI data which excluded participants in MCyR (the per-protocol subgroup of the IRIS dose escalation study54) confers an advantage on the nilotinib arm of the model, which is parameterised using a study in which some participants had baseline MCyR).
Set against these considerations, it is also important to recognise the areas in which Jabbour et al. ’s study182 may be considered superior to the IRIS subgroup analysis used by Novartis. 54 First, it is based on more than twice as many participants – 84 as opposed to 39 (Novartis relies on the per-protocol analysis of the IRIS paper). Second, because Novartis considers that the definition of PFS in the IRIS publication renders it inappropriate for incorporation in its model, it is compelled to adopt a very uncertain method to estimate PFS for HDI (see below). In contrast, Jabbour et al. ’s study182 reports PFS in a way that could have been used directly in the model, thereby obviating the need for the less robust methods adopted by Novartis. On a balance of these considerations, we consider that it would have been at least as appropriate to base HDI efficacy parameters on Jabbour et al. ’s study. 182
The estimation of PFS on the basis of reported OS adjusted according to a PFS–OS ratio derived from an unrelated data source (the nilotinib study) introduces an additional uncertainty to the estimated efficacy of HDI. It is impossible to guess whether or not this method produces accurate results and, if not, whether HDI PFS is underestimated or overestimated. Another solution would have been to model PFS for HDI by fitting model OS to the empirical curve and subtracting constant time in AP and BC to provide an estimate of PFS (i.e. the reverse of the method used to estimate OS where a reliable estimate of PFS was available).
We are concerned that, as Novartis acknowledges, the model appears to underestimate OS for HDI when plotted against the empirical data from the IRIS study (Figure 7). This may be a reflection of the uncertain derivation of PFS but, in any case, it is consistent with our criticism that Novartis has underestimated OS for all treatments.
FIGURE 7.
Novartis’s CP model: modelled OS for nilotinib and imatinib, and compared with empirical OS from studies. Reproduced with permission from Novartis’s submission, figure 13, p. 39. 205
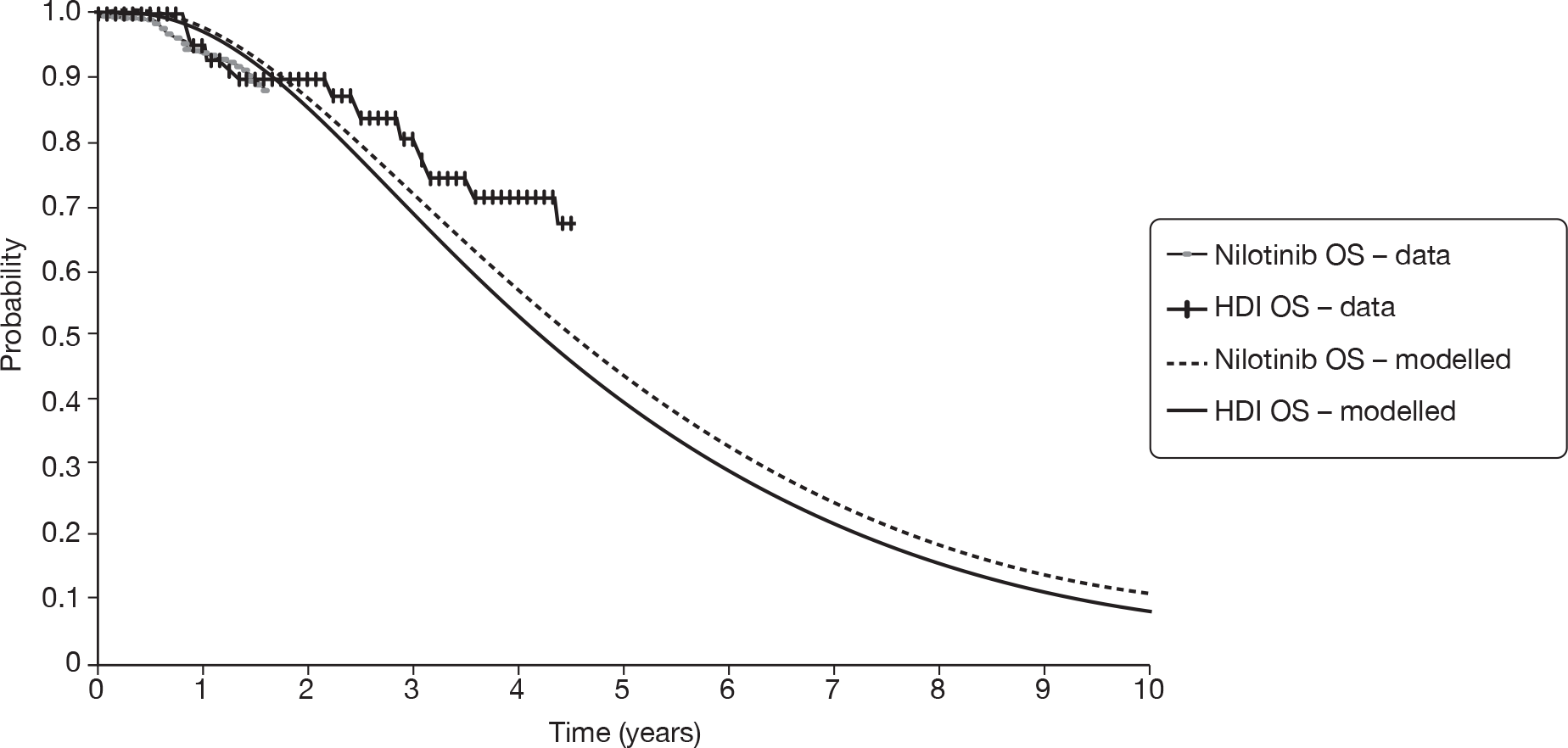
Hydroxycarbamide effectiveness data for ImI patients were taken from a retrospective analysis of therapy following imatinib failure at a single institution. 223 Novartis acknowledges that there are several serious limitations with these data. In particular, only 12 of the 61 patients in this treatment arm actually received hydroxycarbamide and that the study does not distinguish between participants who failed imatinib owing to resistance and those who could not tolerate it.
Time spent in the AP and BC is taken from the same data source used to estimate the effectiveness of hydroxycarbamide. 223 Novartis calculates that the mean time patients spend in AP is 9.14 months and in BC 9.89 months. We are satisfied with these values, especially since they do not affect cost-effectiveness greatly, given that they are independent of treatment.
We are concerned about the very large degree of extrapolation of PFS; for the ImR subgroup, many years’ experience is estimated on the basis of follow-up of only 19 months, with the result that PFS is dependent on supposition for around two-thirds of the simulated cohort. The ImI PFS curve is even more immature, with over 80% of the distribution undefined empirically. This adds further to the uncertainty in the cost-effectiveness results.
We note that cost-effectiveness is insensitive to the allowance for general mortality, i.e. the cost-effectiveness results change only marginally when general mortality is or is not incorporated.
Resource use
In order to estimate duration of therapy, participants are assumed to continue drug treatment until they progress or discontinue owing to serious AEs. Despite our reservations about the use of PFS to estimate total time in CP, this approach is appropriate for the calculation of resource use, as drug therapy will be discontinued in the post-progression, pre-AP period that is missing from the Novartis model.
An alternative, and superior, method of modelling total drug costs would have been to use the empirical data on time to discontinuation of treatment. A Kaplan–Meier curve for time to discontinuation of nilotinib in the Phase II study is given in appendix 6 (p. 89) of Novartis’s report, but is not used in its analysis. However, these data presumably represent all patients in the nilotinib study combined; it would be necessary to have had these data split by ImR and ImI subgroups in order to inform the economic analyses.
Novartis has correctly implemented reductions in drug costs for patients stopping treatment owing to serious AEs in its models, as described in its report. However, we note that its assumption that 10% of all patients who stop treatment owing to AEs progress from CP to AP each quarter-year is not fully justified (although we appreciate that the data for this parameter may not be readily available). However, we believe that cost-effectiveness outputs are relatively insensitive to this parameter.
The medical management costs, such as outpatient appointments, costs of chemotherapy, SCTs and costs of treating AEs, affect cost-effectiveness only very marginally.
Novartis acknowledges that, in the studies of nilotinib and HDI, participants experienced dose interruptions, reductions and escalations. However, such variations are not accounted for in the model. Patients were modelled to take 800 mg of nilotinib every day and 800 mg (high dose) of imatinib every day until disease progression or serious AEs. Instead, it is more accurate to model the cost of nilotinib and imatinib corresponding to the doses actually received in the studies.
In the single-arm study of nilotinib,205 dose intensity was defined as the cumulative dose divided by the cumulative duration of exposure, where duration of exposure was defined as the time between the date of last dose and the date of first dose (i.e. including periods of dose interruptions). The mean dose intensity of nilotinib was [CiC information (or data) removed] and the median dose intensity was 800 mg q.d. for both resistant and intolerant patients combined. For the economic model, the mean was required, not the median dose intensity. Therefore, for consistency with the clinical outcomes from this study, we believe that the cost of nilotinib for the CP model should be based on approximately [CiC information (or data) removed] of nilotinib q.d., a cost of [CiC information (or data) removed] per quarter year, not £7928 as assumed by Novartis.
In the IRIS HDI subgroup,54 approximately half of the patients took 600 mg imatinib q.d. and half took 800 mg of imatinib q.d. When allowing for dose interruptions, the median dose intensity was 604 mg of imatinib q.d. 54 Mean dose intensity is not reported. Assuming the same ratio of mean to median dose intensities as in the nilotinib study, the mean dose intensity in the IRIS HDI study is estimated as 604 × {[CiC information (or data) removed]/800} = 529 mg q.d., a cost of [CiC information (or data) removed] per quarter-year, in contrast to £9758 as used by Novartis.
Revising drug costs in this way is likely to have a substantial effect on model outputs. According to our calculations, when applying these corrections to Novartis’s model, the ICER for nilotinib versus HDI changes from –£76,755 (nilotinib dominates) to £25,267 per QALY, and the ICER for nilotinib versus hydroxycarbamide changes from £58,491 to £51,139 per QALY.
Valuation of outcomes (utilities)
It was appropriate for Novartis to source utilities from the IRIS study of standard-dose imatinib,225 because this study included a relatively large sample of patients and because the utilities were obtained using EQ-5D responses, which are preferred in the NICE reference case. 222 Utilities from IRIS were also reported by Dalziel et al. 226 and are slightly different in this source: CP 0.854, AP 0.73 and BC 0.52. This discrepancy arises because Reed et al. 225 chose to adopt a pooled utility of 0.595 for AP and BC, because there was no statistically significant difference between the values of 0.73 (SE = 0.20) in AP and 0.52 (SE = 0.42) in BC. However, given that parameter uncertainty may be incorporated in the model through probabilistic analysis, we believe that it may be more appropriate to the use phase-specific utilities despite their imprecision. It should be acknowledged, however, that using the utilities quoted by Dalziel et al. 226 changes the estimates of cost-effectiveness only very marginally, because time spent in AP and BC is constant across all modelled treatments.
The treatment-specific disutilities due to AEs appear reasonable. We note that the disutilities have only marginal impact on cost-effectiveness.
Dasatinib (manufacturer analysis/model)
Appendix 4 presents a summary review of the dasatinib manufacturer submissions against the main items in the NICE reference case requirements and against criteria set out by Philips et al. 221
Summary of industry submission (chronic phase)
The manufacturer of dasatinib presents cost-effectiveness analyses in CML-CP in pair-wise comparisons as follows:
-
dasatinib compared with HDI (600 mg or 800 mg q.d.) in people with ImR disease
-
dasatinib compared with nilotinib in a mixed population of people with ImR and ImI disease.
Model structure
The analysis uses a Markov model to estimate cost-effectiveness. The model was written in Microsoft Excel with Crystal Ball® (Oracle) software used to implement the probabilistic sensitivity analysis.
The model takes a UK NHS perspective.
The modelled population was based on participants in the BMS 034 study, published in the peer-reviewed literature by Shah et al. ,22 which also forms the basis for assumptions regarding progression. The starting age of the cohort was therefore 56 years, with a 50 : 50 male–female ratio and 36% of patients having taken > 600 mg of imatinib q.d. prior to dasatinib treatment (the remaining two-thirds failed imatinib at 400–600 mg q.d.).
The model commences after an individuals’ best initial response (no response, CHR, PCyR or CCyR) to treatment has been achieved on each treatment (Figure 8). For dasatinib, response categories are assessed as mutually exclusive from raw study data. For comparators, CyR rates were calculated by subtraction from CHR in included studies to prevent double counting.
FIGURE 8.
Structure of BMS’s CP model. Reproduced wth permission from BMS’s submission, figure 3, p. 93. 184
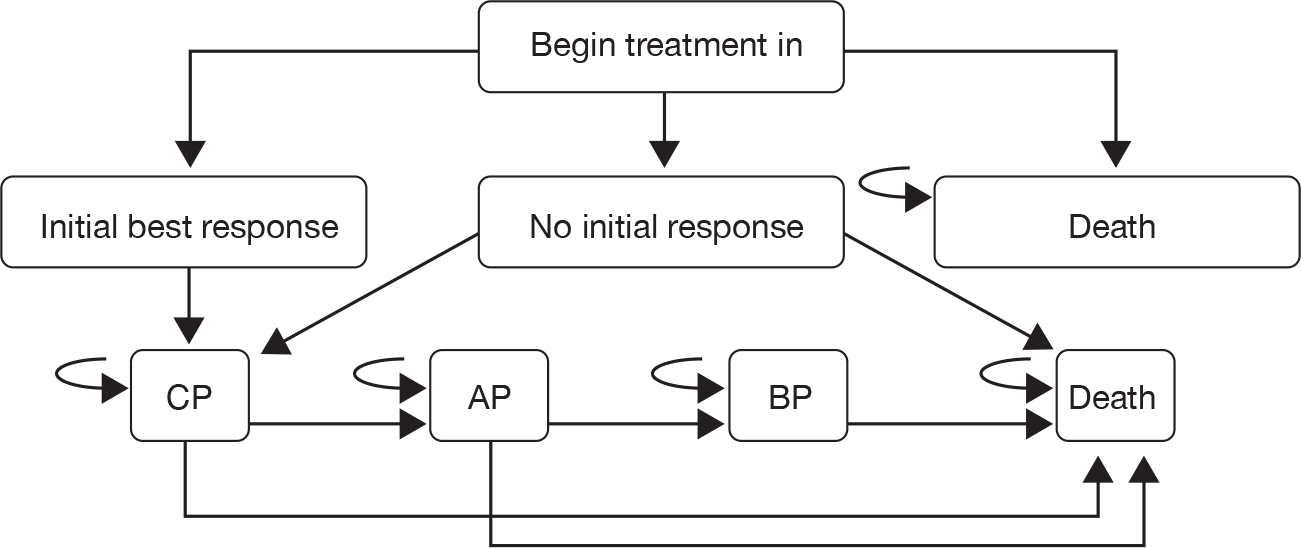
Given the ‘best response’ assumed at the outset of the model, individuals may then progress through three disease phases (CP, AP or BC) to death. Mortality from non-CML causes was modelled from life tables.
Disease progression is modelled as contingent on response status and disease phase, and independent of treatment. This is determined by extrapolation of PFS and OS data from the 100 mg q.d. dose arm of the 034 study (Shah et al. , dose-ranging RCT22) for patients with imatinib resistance (n = 124) according to responses at 3 months. A scenario analysis was also carried out, with progression based on the experience of people with ImR with responses measured at 24 months. In the base-case analysis of dasatinib versus nilotinib, progression was calculated based on responses shown in Shah et al. 22 (study 034) for all patients (i.e. ImR and ImI).
The modelling assumes that individuals receive treatment until disease progression or intolerable toxicity, after which they receive post-failure treatment.
As already noted, progression may be variously defined; definitions include loss of response and increasing white blood cell counts, which may occur during CP disease, as well as progression to accelerated disease. In the BMS model, ‘progression’ describes movement from CP to AP in CML and was calculated from data ‘on file’ for the study (BMS 034, published by Shah et al. 22) contingent on response category. Progression was calculated separately for the first and subsequent years, using 1-year (short-term) and 2-year (long-term) data from Shah et al. 22 After 1 year, progression rates are assumed to remain as per the 2-year data throughout the remaining duration of the model.
The model uses a lifetime horizon (modelled as 100 years) and a model cycle of 1 month. No additional subgroup analyses were presented. A half-cycle correction was employed.
Clinical effectiveness
Response rates for dasatinib and HDI were calculated from Kantarjian et al. 23 and Shah et al. ,22 with data at 3 and 24 months informing base-case and scenario analyses. Response data for nilotinib were taken from Kantarjian et al. 106 Table 70 reports the response data employed in the CP analyses. Note that in all cases the transition probabilities which are contingent on these response rates are calculated from the ImR population in the BMS 034/Shah et al. 22 study as described in the previous section.
| Treatment | Best response | Sourcea | |||
|---|---|---|---|---|---|
| NR | CHR | PCyR | CCyR | ||
| Base-case 1: dasatinib vs imatinib 800 mg (ImI and ImR) | |||||
| Dasatinib 100 mg q.d. (70 mg b.i.d. data) | 0.079 | 0.574 | 0.139 | 0.208 | Kantarjian et al. (2007)23 (3 months’ data) |
| Imatinib 800 mg q.d. | 0.184 | 0.531 | 0.204 | 0.082 | Kantarjian et al. (2007)23 (3 months’ data) |
| Base-case 2: dasatinib vs imatinib (ImR) | |||||
| Dasatinib 100 mg q.d. | 0.121 | 0.508 | 0.129 | 0.242 | Shah et al. (2008)22 (3 months’ data) |
| Imatinib 800 mg q.d. | 0.184 | 0.531 | 0.204 | 0.082 | Kantarjian et al. (2007)23 (3 months’ data) |
| Base-case 3: dasatinib vs nilotinib (ImR and ImI) | |||||
| Dasatinib 100 mg q.d. | 0.060 | 0.305 | 0.138 | 0.497 | Shah et al. (2008)22 (24 months’ data) |
| Nilotinib 800 mg q.d. | 0.059 | 0.352 | 0.150 | 0.439 | Kantarjian et al. (2007)106 (24 months’ data) |
| Scenario 1: dasatinib vs imatinib (ImR; 24-month data) | |||||
| Dasatinib 100 mg q.d. | 0.069 | 0.396 | 0.099 | 0.436 | Kantarjian et al. (2007)23 (24 months’ data) |
| Imatinib 800 mg q.d. | 0.184 | 0.496 | 0.143 | 0.184 | Kantarjian et al. (2007)23 (24 months’ data) |
| Scenario 2: dasatinib vs imatinib (ImR; 24-month data) | |||||
| Dasatinib 100 mg q.d. | 0.081 | 0.331 | 0.153 | 0.435 | Shah et al. (2008)22 (24 months’ data – ImR only) |
| Imatinib 800 mg q.d. | 0.184 | 0.490 | 0.143 | 0.184 | Kantarjian et al. (2007)23 (24 months’ data – ITT) |
The categories of response following treatment are mutually exclusive, i.e. the PCyR category includes only people who reached this level of response but who did not proceed to CCR at any point. The CHR category includes people who achieved a CHR, but did not achieve partial or CCyR, i.e. this category includes people who showed a minor CyR.
Adverse events are modelled for each of the treatments investigated using data from the relevant studies. 22,23,106 AEs are incorporated by adjusting the costs and utility for health states according to the impact of AEs and their incidence. AEs are assumed to occur only during the first 3 months of treatment (because of the absence of long-term data). However, duration was taken into account when modelling impact of AEs on costs. It was not clear whether AE disutility was handled similarly.
Treatment discontinuation as a result of AEs was not included explicitly in the model, although it was asserted that this was partly reflected in the progression rates used.
Resource use and costs
Resource use associated with the management of CML was estimated predominantly from the opinions of a panel of UK clinical experts. This addressed routine management resources (e.g. primary and secondary care use, outpatient attendances, disease monitoring and diagnostic costs, resources used in management of AEs and the nature of post-failure treatment). Resource use was estimated separately for responders and non-responders for each stage of CML. The estimation of resource use was stratified by time in the model, with all management resources considered separately for the first 3 months and subsequent time in the model.
The clinical experts consulted by BMS estimated post-failure treatment pathways, which are applied in the model independent of prior treatment. These included:
-
BM transplant (in mean 31% of patients, range 20–50%).
-
Chemotherapy [a wide range of possibilities was suggested for, on average, 50% of patients, including use of dasatinib combination therapy (17% of patients) and alternative TKI regimens (mean 35% of patients, range 0–90%). The most common post-failure treatment was judged to be hydroxycarbamide (39%, and 7.4% of patients (range 0–20%) were considered potential candidates for interferon therapy].
-
In-hospital palliative care, which was estimated to be used by around 20% of patients and included in-patient stays, clinic visits, anti-infective agents (antibiotics and antifungals), blood tests, radiological investigation [computerised tomography (CT) and magnetic resonance imaging], blood transfusions and BM aspiration.
Costs of managing serious adverse treatment effects were included in the analysis, again based on resource use estimates from a panel of clinicians, based on the frequency of outpatient visits and inpatient spells (including duration), investigations and medication. Mean and ranges of estimates are reported for each item considered by the expert panel. The cost of treating AEs was modelled as a weighted average by the proportion of patients affected, and was applied for the expected duration of events, although the incidence of AEs was constrained to the first 3 months of the lifetime model.
Resource use was valued by applying NHS reference costs and tariffs to estimates from the BMS clinical panel. The base year for costs was 2008 (2006–7 national costs were inflated using rates reported by the Personal Social Services Research Unit, i.e. Pay Cost and Health Service Cost Indices),227 except for drug costs which were priced in 2009 terms.
Drug costs were based on recommended doses from SPCs for the three comparators being considered, using the lowest cost approach to delivering the appropriate dose. Doses were not adjusted for dose intensity from clinical study data. Pack prices for drugs were obtained from the latest version of the Monthly Index of Medical Specialities (MIMS). 228 Unit costs assumed for the main comparators are shown in Table 71.
| Drug | Cost per montha (£) |
|---|---|
| Dasatinib 100 mg q.d. (CP) | 2541.48 |
| Dasatinib 140 mg q.d. (AP and BC) | 2541.48 |
| Imatinib 300 mg b.i.d. (CP) | 2441.21 |
| Imatinib 400 mg b.i.d. | 3254.95 |
| Nilotinib 400 mg b.i.d. | 2644.64 |
Costs were discounted at 3.5% in line with the NICE reference case. 222
Valuation of outcomes (utilities)
Outcomes which were valued in terms of utility and therefore inform the estimates of QALYs associated with each treatment option were response to treatment, disease progression (i.e. CML phase) and serious treatment-related AEs.
Based on the justification that ‘no relevant estimates of health utility in CML patients were available’, BMS commissioned a cross-sectional study among members of the UK general population unaffected by CML to calculate utility values for the economic analysis. The submission reports that this study used the ‘time trade off technique and the EQ-5D instrument’. Six health states, corresponding to the three phases of CML, each according to whether or not a response to treatment was shown were valued.
The manufacturer submission indicates that full details of the methods employed in this study are given in the cited study report. 229 Although this report was not included in the submission, some details of what may be presumed to be the same study are available from a poster presentation. 230
The UK arm of the study by Levy et al. ,229 which we presume informs the current analysis, was carried out with 100 respondents. The average age of the whole study population (Australia, Canada and the UK) was 46 years and 54% of respondents were female. In common with many studies of this nature, the population was disproportionately highly educated. The report of methods, if this is the same study as informed the BMS submission, contradicts the BMS report in that no mention is made of the EQ-5D. Instead, it appears that respondents valued written health-state descriptions developed using ‘clinical expert consultation’ directly using the time trade-off method. The health-state descriptions are not available for review.
The health-state valuation study addressed seven health states: those noted above (CML phase by response/no response) and a further state of ‘withdrawal of treatment due to serious AEs’ which was not incorporated in the BMS economic evaluation. Generalised linear modelling showed that age, gender and country were significant predictors of mean utility and, therefore, values adjusted for these factors were reported. The values reported in the poster presentation by Levy et al. 230 for the UK sample are slightly different from those reported in the BMS submission (Table 72).
| Health state | Mean utility | |
|---|---|---|
| BMS submission | aLevy et al. (2008)229 | |
| CP – responder | 0.85 | 0.80 |
| CP – non-responder | 0.68 | 0.66 |
| AP – responder | 0.79 | 0.78 |
| AP – non-responder | 0.50 | 0.51 |
| BC – responder | 0.50 | 0.50 |
| BC – non-responder | 0.31 | 0.32 |
The disutility associated with AEs was separately applied in the BMS model, with values obtained from a NICE single technology appraisal of erlotinib (Tarceva®, Roche) for non-small cell lung cancer for a range of events (diarrhoea, rash, fatigue, nausea and neutropenia). 231 This permitted more specific modelling than would have been possible using the single value for treatment withdrawal reported by Levy et al. 229 (0.47). However, utility estimates could not be found for many potential AEs. In these cases the model arbitrarily applied an utility decrement of 0.05.
As noted earlier, the incidence of AEs was modelled only during the first 3 months of therapy, with disutility and additional costs applied to health states in proportion to the expected occurrence of events. Although the duration of additional resource consumption as a result of AEs was allowed to extend over more than one model cycle, it was not clear whether disutilities were handled in the same way.
Benefits (QALYs) were discounted at 3.5%, consistent with NICE’s reference case requirements. 222
Analysis of uncertainty in Bristol-Myers Squibb’s evaluation
A range of analyses were carried out in the BMS submission to explore the considerable uncertainty present in the analysis. Two aspects of structural uncertainty were explored: the time horizon (set at 5 and 15 years from 100 years in the base case) and the starting age of the cohort (± 10% from base case of 56 years in CP).
One-way sensitivity analyses were carried out on most parameters, as reported in Table 73.
| Parameter | Base case | Values tested | Source | |
|---|---|---|---|---|
| Progression rates | NA | –20% | + 20% | Assumption |
| Probability of BMT for patients failing treatment | 30.8% | 0% | NA | Assumption |
| Costs | ||||
| Cost of dasatinib (per month) | £2541.48 | £2033.00 | £3050.00 | ± 20% |
| Cost of nilotinib (per month) | £2644.64 | £2116.00 | £3174.00 | ± 20% |
| Cost of imatinib (per month) | £3254.95 | £2604.00 | £3906.00 | Lower value used reflects 600 mg imatinib cost. Higher value is + 20% |
| Cost of post-failure treatment | £1648.39 | £1319.00 | £1978.00 | ± 20% |
| Cost of blood transfusion | £100.08 | £80.00 | £120.00 | ± 20% |
| Cost of BM transplant | £52,638.00 | £42,111.00 | £63,166.00 | ± 20% |
| All resource use costs | NA | –20% | + 20% | Assumption |
| SAE costs | NA | –20% | + 20% | Assumption |
| Utilities | ||||
| Chronic (no response) | 0.68 | 0.54 | 0.82 | ± 20% |
| Chronic (with response) | 0.85 | 0.68 | 1.00 | ± 20% |
| Accelerated (no response) | 0.50 | 0.40 | 0.60 | ± 20% |
| Accelerated (with response) | 0.79 | 0.63 | 0.95 | ± 20% |
| Blast (no response) | 0.31 | 0.25 | 0.37 | ± 20% |
| Blast (with response) | 0.50 | 0.40 | 0.60 | ± 20% |
| SAE utilities | NA | –20% | + 20% | Assumption |
| Other | ||||
| Starting age (years) | ||||
| CP | 56 | 50.4 | 61.6 | ± 20% |
| AP | 56 | 50.4 | 61.6 | ± 20% |
| BC | 48 | 43.2 | 52.8 | ± 20% |
| Time horizon of model (years) | Lifetime (20) | 5 | 15 | Assumption |
| Discounting | ||||
| Costs = 0%, benefits = 0% | 3.5%, 3.5% | NA | NA | Assumption |
| Costs = 6%, benefits = 1.5% | 3.5%, 3.5% | NA | NA | Assumption |
| Costs = 6%, benefits = 6% | 3.5%, 3.5% | NA | NA | Assumption |
In addition, probabilistic sensitivity analysis was carried out to take account of parameter uncertainty in the analysis. Methods for the probabilistic sensitivity analysis are reported comprehensively and includes initial responses to treatments, disease progression rates, management costs and utilities. In all cases, mean values were varied in 10,000 model runs with values drawn from appropriate distributions (beta for probabilities, gamma for costs, and beta for response and progression rates). Distributions were characterised using the standard deviation (SD) of the base-case mean values, with these reduced proportionately to represent monthly rates.
Results of Bristol-Myers Squibb’s chronic phase economic evaluation
Dasatinib versus high-dose imatinib
As described, BMS carried out two base-case analyses of the cost-effectiveness of dasatinib compared with HDI (Table 74). In the first, based on response data originating from the comparative RCT (BMS study 017 published as Kantarjian et al. 23), treatment with dasatinib dominates HDI.
| Result | Kantarjian et al. (2007)23 (3 months) | Differences | Shah et al. (2008)22 (3 months) | Kantarjian et al. (2007)23 (3 months) | Differences | |
|---|---|---|---|---|---|---|
| Dasatinib (70 mg b.i.d.) |
Imatinib (400 mg b.i.d.) | Dasatinib (100 mg q.d.) |
Imatinib (400 mg b.i.d.) | |||
| LYs | 7.21 | 7.02 | 0.19 | 7.13 | 7.02 | 0.11 |
| QALYs | 5.76 | 5.56 | 0.19 | 5.70 | 5.56 | 0.13 |
| Drug cost (£) | 195,808 | 243,129 | –47,321 | 194,716 | 243,129 | –48,413 |
| Other health-care cost (£) | 66,624 | 66,874 | –250 | 64,742 | 66,874 | –2131 |
| Total cost (£) | 262,432 | 310,003 | –47,571 | 259,459 | 310,003 | –50,545 |
| Incremental cost/LY | Dominant | Dominant | ||||
| Incremental cost/QALY | Dominant | Dominant | ||||
| Mean survival (undiscounted) | 9.71 | 9.65 | 0.06 | 9.61 | 9.65 | –0.04 |
| Median survival (undiscounted) | 6.33 | 5.75 | 0.58 | 6.25 | 5.75 | 0.50 |
| Median time on treatment | 4.75 | 4.08 | 0.67 | 4.67 | 4.08 | 0.58 |
Dasatinib results in an additional 0.19 QALYs and life-years gained. The costs for dasatinib were approximately £47,000 less than the costs for HDI, primarily as a result of the lower per patient monthly cost of dasatinib.
The second base-case analysis (using data from two separate sources – Shah et al. 22 for dasatinib and 3-month data from the imatinib arm of Kantarjian et al. 23) also concludes that dasatinib dominates HDI. Treatment with dasatinib is expected to improve mean discounted OS by 0.11 years (5.7 weeks) or 0.13 QALYs (6.8 quality-adjusted weeks). Costs were approximately £50,000 less than treatment with HDI, again predominantly due to the difference in drug acquisition costs.
The one-way sensitivity analyses, performed only on the base case which employed data from Kantarjian et al. 23 and Shah et al. 22 in people with ImR, showed little influence on estimated cost-effectiveness. Dasatinib remained dominant in all analyses with the exception of when the cost of imatinib was based on 600 mg q.d. (£2441 per month vs £2541 in the base case for dasatinib) which gave an ICER for dasatinib of £68,605 per QALY.
The probabilistic sensitivity analysis reports a very high probability (99.9%) that treatment with dasatinib would be considered cost-effective compared with HDI at WTP thresholds of both £20,000 per QALY and £30,000 per QALY.
Two scenario analyses were outlined in the BMS methods (section 7.2.7.1 of the submission) to explore the impact of using a longer term response and prognosis data (Table 75). These used progression data at 24 months from (a) Kantarjian et al. 23 for both agents or (b) the imatinib arm of Kantarjian et al. 23 and the 100-mg arm of Shah et al. 22 for dasatinib. This scenario explored only the ImR population. Note, that we have not been able to reproduce these results using the BMS model. When attempting to replicate the analysis in the BMS model we found that dasatinib dominates HDI in both scenario analyses.
| Result | Kantarjian et al. (2007)23 (3 months) | Differences | Shah et al. (2008)22 (3 months) | Kantarjian et al. (2007)23 (3 months) | Differences | |
|---|---|---|---|---|---|---|
| Dasatinib (70 mg b.i.d.) |
Imatinib (400 mg b.i.d.) | Dasatinib (100 mg q.d.) |
Imatinib (400 mg b.i.d.) | |||
| LYs | 7.15 | 5.63 | 1.53 | 7.41 | 5.63 | 1.79 |
| QALYs | 5.71 | 4.35 | 1.37 | 5.94 | 4.35 | 1.59 |
| Drug cost (£) | 193,752 | 184,012 | 9740 | 202,209 | 184,012 | 18,197 |
| Other health-care cost (£) | 66,807 | 67,108 | –301 | 66,934 | 67,108 | –174 |
| Total cost (£) | 260,559 | 251,120 | 9439 | 269,143 | 251,120 | 18,023 |
| Incremental cost/LY (£) | 6182 | 10,092 | ||||
| Incremental cost/QALY (£) | 6905 | 11,315 | ||||
| Mean survival (undiscounted) | 9.49 | 7.19 | 2.31 | 9.91 | 7.19 | 2.72 |
| Median survival (undiscounted) | 6.50 | 4.67 | 1.83 | 6.83 | 4.67 | 2.17 |
| Median time on treatment | 4.92 | 3.00 | 1.92 | 5.33 | 3.00 | 2.33 |
In both scenarios dasatinib costs more than imatinib overall, although non-drug costs are very slightly less. The incremental benefits are greater in these scenarios than in the base case, with gains of more than 1 QALY estimated (1.37 QALYs in scenario 1 and 1.59 QALYs in scenario 2). Incremental costs of dasatinib are, however, considerably higher than in the base case, leading to positive ICERs although these are estimated to be considerably less than the NICE threshold range at around £7000 and £11,000 per QALY. No probabilistic sensitivity analyses were carried out in relation to these scenarios.
Dasatinib versus nilotinib
The BMS model suggests that treatment with dasatinib can be expected to increase OS by 0.53 years (0.30 QALYs) compared with nilotinib, with overall costs being greater by £2532. Again, drug costs predominate in the cost comparison and non-drug costs are expected to be slightly less with dasatinib than nilotinib. The base-case analysis estimates a cost per life-year gained of £7627 and cost per QALY of £8507 (Table 76). Again, it has not been possible to replicate these results using the BMS model; instead we found that dasatinib dominates nilotinib.
| Shah et al. (2008)22 (24 months) Dasatinib (100 mg q.d.) |
Kantarjian et al. (2007)106 (24 months) Nilotinib (400 mg b.i.d.) |
Differences | |
|---|---|---|---|
| LYs | 7.74 | 7.40 | 0.33 |
| QALYs | 6.21 | 5.91 | 0.30 |
| Drug cost (£) | 211,359 | 208,235 | 3123 |
| Other health-care cost (£) | 69,261 | 69,852 | –591 |
| Total cost (£) | 280,619 | 278,087 | 2532 |
| Incremental cost/LY (£) | 7627 | ||
| Incremental cost/QALY (£) | 8507 | ||
| Mean survival (undiscounted) | 10.42 | 9.89 | 0.53 |
| Median survival (undiscounted) | 7.33 | 6.75 | 0.58 |
| Median time on treatment | 5.75 | 5.17 | 0.58 |
The one-way sensitivity analysis, as in the comparison with imatinib, shows that drug costs are the parameter with the greatest impact on the ICER within the ranges explored. Indeed, the sensitivity appears rather greater than in the case of imatinib. The sensitivity analysis on drug costs varied input values by ± 20%. When the cost of dasatinib is reduced by 20% this option dominates in the analysis, whereas if the cost is increased by the same proportion the ICER becomes £150,000. When the costs of nilotinib are varied by the same proportions, the ICER for dasatinib varies between £148,000 and £36,000. The second of these results is counterintuitive in that the base case predicts greater cost for dasatinib, therefore suggesting that increasing the cost of nilotinib (and therefore decreasing the incremental cost) should reduce the ICER for dasatinib.
The probabilistic sensitivity analysis predicts probabilities of 73.4% and 98.2% that dasatinib is cost-effective compared with nilotinib at WTP thresholds of £20,000 and £30,000 per QALY, respectively.
Review of Bristol-Myers Squibb’s chronic phase submission
A summary of our review of the BMS CP model is shown in Box 7. As noted in the BMS submission, the economic evaluation in CP has a number of strengths:
-
appropriate structure reflecting progression through the phases of CML, including lifetime horizon
-
comprehensive investigation of the sensitivity of the chosen structure and inputs within a reasonably wide range of possible values
-
probabilistic sensitivity analysis.
-
The data used to estimate the effectiveness of HDI in an ImR population were compromised owing to patient crossover from imatinib to dasatinib at 3 months.
-
All treatments are always assumed to be taken at the recommended dose. Using the dose intensity of 76% for HDI from the IRIS dose escalation study54 has an important impact on the cost-effectiveness of dasatinib vs HDI, as dasatinib changes from dominating HDI to an ICER of £58,000 per QALY.
-
BMS has incorrectly assumed that PFS is identical to time in AP. It has therefore assumed that treatment continues through the whole of the CP.
-
The BMS submission does not include an assessment of the management of people who are ImI.
-
Very immature OS data were extrapolated over many years. This makes all cost-effectiveness results highly uncertain.
However, we do have a number of concerns about the analysis, some resulting from the considerable degree of uncertainty inherent in the available evidence base informing this assessment.
Populations and comparators
The BMS comparison of dasatinib with HDI in CP was restricted to patients with ImI. Therefore an element of the NICE scope was not addressed, i.e. the treatment of patients in CP with ImI.
In the comparison of dasatinib against nilotinib, a mixed population was considered, on the grounds that both TKIs are options. However, there may be concerns about the applicability of the clinical effectiveness evidence in this economic analysis given the mix of resistant and intolerant patients in the separate studies used to carry out the analysis, and the evidence that people with a history of intolerance or resistance may respond differently to the different TKIs. The case for holding this view about dasatinib may be stronger than for nilotinib as its mode of action may be more different from that of imatinib, though this line of argument is speculative.
In the comparison of the two new TKIs, Novartis (nilotinib manufacturer) argues that dasatinib and nilotinib should not be compared because of differences in the way that intolerance and resistance were defined in the relevant studies. It is further asserted that the ImI cohort for dasatinib had a higher proportion of patients who had previously shown a response to imatinib than in the Kantarjian et al. 106 study of nilotinib, and that this is likely to lead to bias which would undermine any comparison carried out. The BMS submission presents some evidence (table 10, p. 43), drawn from the final report of their study of dasatinib versus HDI in CML-CP, that people who had previously experienced a response to imatinib may show a greater response to the new drug than those who have not (CCyR at 24 months; 50% vs 33% for those with vs without any previous CCyR). This suggests that a preponderance of patients with a previous response may bias a comparison of response rates, although any difference in baseline responses was likely to be relatively small and the direction of any influence in the longer term was not easy to predict.
The BMS model starts at age 56 years, which was close to the reported median age at diagnosis of CML. However, patients who fail first-line imatinib therapy, particularly those with resistance, are likely to be older and therefore the age group modelled appears somewhat younger than might be expected in routine practice. The influence of starting age was explored in the BMS evaluation and does not change the central results, although the extent to which dasatinib dominates HDI was attenuated to some extent.
The BMS model uses HR and CyR as surrogates for PFS and OS, based on the relationship shown in the 100-mg arm of Shah et al. 22 for dasatinib. This was a strength of the analysis in that the analysis was based on the currently licensed dose of dasatinib. However, there are weaknesses in this approach. Firstly, the study was of short duration and contained only 167 people. Secondly, although all types of response category, correctly made mutually exclusive, are considered to influence progression according to the relationship seen in the limited data from this cohort, it may be that there are differences in the way which different responses influence progression in the longer term. This is in addition to the uncertainty inherent in the assumption that response results in changes in progression that are equivalent on different drugs, though we acknowledge that this assumption is unavoidable and that the empirical approach taken by BMS for dasatinib provides novel estimates of the relationship between response for one of the new TKIs. Thirdly, and again unavoidably, the influence of response on progression is assumed to remain constant throughout the model, i.e. extrapolation from 2 to 20 years (lifetime). The BMS model was validated by comparing the modelled prediction of survival and progression with that reported by Shah et al. 22 for dasatinib and it was found that these broadly agree (p. 134 BMS report). In fact, in CP, the model underpredicts progression and OS for dasatinib by 6% and 7% at the 2-year point. How much these differences influence the model in the longer term is not explored. Furthermore, how well the model predicts PFS and OS for studies of imatinib, which are available over a longer term, is not clear.
A further important structural uncertainty arises from differences in the definition of progression between the studies included in the model. For example, a ‘> 30% increase in Ph+ metaphases’ counts as progression in Shah et al. ,22 but not in Kantarjian et al. 23 This is important because different definitions of progression may lead to different proportions of people in whom progression was, in fact, due to development of CML-AP as opposed to haematological changes while remaining in the CP, which we believe is common. As the assumption in the BMS model is that progression means ‘change of phase’ in all cases, then bias may arise in comparisons between treatments. This assumption is important because higher probabilities of death and possible development of BC apply to people once they have moved into the AP of disease. It is also important because treatment is ceased at progression, and therefore results in lower drug acquisition costs, which is particularly important in the incremental analysis.
Related to the use of multiple response categories and the heterogeneous meaning of progression, the BMS model does not incorporate loss of response as a reason for progression despite these data being available at an individual patient level and utilities being available for response. It is unclear what influence this more sophisticated approach would have on the analysis, although the value of such an approach given the considerable and intractable uncertainty inherent in the analysis from other causes is questionable.
Clinical effectiveness
A central issue with all economic evaluations in this assessment (including our own) is the absence of comparative data, with the notable exception of Kantarjian et al.’s23 study of dasatinib versus HDI, which informs the base-case analyses carried out by BMS. However, as noted, this study is limited in value by the crossover from imatinib to dasatinib that was allowed to occur at 3 months, which confounds the 24-month data. Therefore, the analysis relies on 3-month responses which, as seen from the increasing proportion in the dasatinib arm showing responses by 24 months, is likely to underestimate effectiveness. What is not clear is whether or not the group taking imatinib showed similarly increased responses over the longer term, in which case the necessary restriction of the analysis at the 3-month point may bias the analysis in favour of dasatinib. We have already noted this significant concern with Kantarjian et al. 23 and that the median time to response in second-line imatinib treatment has been reported elsewhere as 9 months (see Major cytogenetic response to high-dose imatinib).
The comparison of dasatinib with nilotinib is carried out in a mixed population, comparing arms from two separate studies. Unfortunately, the study by Kantarjian et al. ,106 which provides estimates of the effects of nilotinib on response rates did not report results separately for the ImR and ImI populations. It is therefore not possible to consider the possible influence of different proportions of these subgroups on results and this must therefore be considered another source of uncertainty in the analysis.
Some of the transition probabilities which are used in the CP model and displayed in tables 45 and 46 (pp. 103–4) of the BMS submission, seem open to question. In particular, for ImR and ImI patients combined (24 months’ data), there is a higher probability of death from CML than progression to AP from the no response and CCyR best response groups (see Table 45). This is surprising because the disease process in CML generally moves from CP to AP to BC and finally to death. A further example is that in ImR patients only (3 months’ data), there was a higher probability of progression to AP from CCyR than from PCyR in the longer term, which was surprising given clinician beliefs regarding the relationship between depth of response on disease progression.
The BMS model appropriately incorporates treatment-related AEs, though these data were taken from only one study, which limits the precision of the analysis. It is clear, however, that the frequency and consequences of such events are not particularly influential in the results of the analysis.
Resource use and utility
In general, the modelling of resource use in the BMS model is appropriate. The base year is 2008 for all items except drug prices (2009) and costs are inflated using the NICE reference case value of 3.5%. 222
Estimates for resource use associated with the management of CML and adverse effects of treatment were provided by a group of clinical experts. The range of reported post-failure treatments demonstrates considerable variation in practice, which adds further to uncertainty in the analysis, although it is clear that, as such costs fall equally on all treatment comparisons, there was little influence on the overall results. We note that clinical experts reported that a further TKI would be chosen as post-failure treatment in around one-third of patients. This highlights the extent to which TKIs are in common use and the absence of evidence supporting sequential use, which is outside the scope of this assessment.
Drug acquisition costs are a very important driver of the BMS model’s results and relatively small changes in the cost of agents results in substantial changes in expected cost-effectiveness. Dose intensity was not taken into account in the BMS model, which affects costs and therefore cost-effectiveness as follows. If a dose intensity of 76% for HDI (taken from the IRIS dose-escalation study54) is applied within the BMS model, then for the comparison of dasatinib with HDI in patients resistant to imatinib, the incremental total cost per patient increases substantially from –£50,545 to £7806, i.e. dasatinib no longer dominates HDI. The costs and QALYs for dasatinib and HDI are very similar and the ICER for dasatinib versus imatinib changes to £58,000 per QALY.
Also, MIMS was used to provide costs of drugs rather than the BNF, which suggests slightly lower prices.
Duration of treatment was particularly influential on the costs modelled in comparisons between TKIs. BMS assumes that treatment was continued throughout the whole of the CP, which we believe was not necessarily true; many patients ‘progress’ while remaining in the CP. We return to this point in more detail in the context of the comparison between economic evaluations reported in Comparison of results of PenTAG and manufacturer cost-effective analyses. However, it should be noted that different estimates of the duration of treatment, in particular the assumption of a period in CP without treatment, may give rise to enormously different estimates of incremental cost-effectiveness between treatment options.
It was not clear whether the BMS model captures drug costs in the period from the start of drug treatment until the assessment of treatment response. In particular, p. 92 of the BMS report states: ‘following the assessment of response to treatment at the beginning of the analysis, the Markov process starts and in each subsequent cycle the patient’s disease may…’. We believe that such drug costs should be captured in the model. If not, it was not clear whether correction of this issue would result in substantial differences in expected cost-effectiveness.
A survey of members of the general public was carried out to inform quality adjustment of time spent in the main health states of CML. It was unclear why this was considered necessary as a range of estimates were already available, as reported elsewhere in this assessment. Limited details are given of the utility study and it is unclear whether or how the EQ-5D instrument was used in describing relevant health states as implied in the BMS submission. It seems more likely, from our identification of what appears to be a conference poster reporting the study that a range of health-state descriptions were developed by clinicians. We note the considerable increments in utility associated with response in all phases of CML, although without further details of the methods used to develop and value these states it is not possible to comment on their validity. However, given the influence of other more important drivers of the BMS model (response rates and duration of treatment), QALY weights appear of limited importance in the analyses.
The PenTAG cost-effectiveness analysis: methods
Scope of economic evaluation
The economic evaluation presented here is restricted to patients with ImR or ImI CML in CP. Of the decision problems identified for this assessment, and noted in Chapter 1, Definition of the decision problem, our economic evaluation seeks to estimate the cost-effectiveness, in terms of incremental cost per QALY, of dasatinib and nilotinib against relevant comparators, as follows:
-
for people in CML-CP who develop resistance to imatinib, dasatinib or nilotinib compared with HDI and
-
for people in CML-CP who are intolerant of imatinib, dasatinib or nilotinib compared with IFN.
The following section describes the approach taken to the cost-effectiveness analysis and model structure. Subsequent sections provide further detail on the parameterisation of the model, and are followed by a summary of model inputs and an outline of the approach to uncertainty analyses.
Analytic approach
The cost-effectiveness model was implemented in Microsoft Excel. Two separate models were implemented: one simulating a cohort of individuals that have shown (or developed) resistance to normal-dose imatinib (ImR) and one representing individuals who have been unable to continue imatinib treatment owing to AEs (ImI).
The model was structured using five health states to represent progression of CML in, and following, the CP:
-
CP on treatment (in this state, the population was divided between patients who achieve an MCyR and those who do not achieve an MCyR)
-
CP following discontinuation of the treatment under simulation (in this state, the population was divided between patients who achieved an MCyR and those who never achieved an MCyR)
-
CML-AP
-
CML-BC
-
death.
The structure of the model is shown in Figure 9 and was informed by a review of the available literature, clinical guidelines for treatment of CML and expert opinion on the clinical progression of the disease.
FIGURE 9.
Influence diagram for the PenTAG CML cost-effectiveness model.
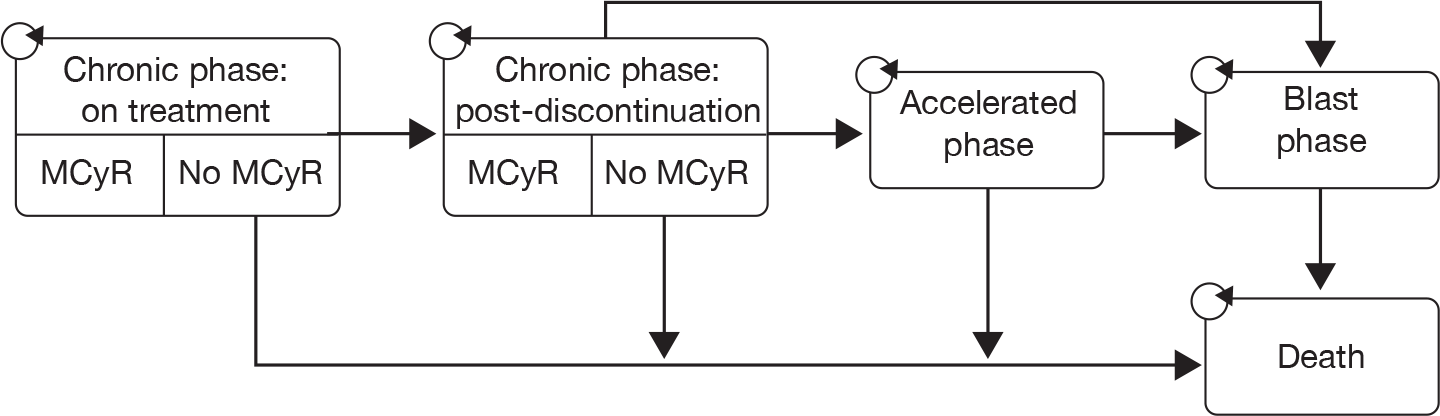
In Figure 9, boxes represent health states and arrows represent the possible transitions between the states. Circular arrows denote that patients can remain in a state at the end of each cycle. During each cycle, a patient is assumed to be in one of the states. Patients are assumed to move between states once at the end of each cycle. For example, if a patient is in post-discontinuation CP then, at the end of the cycle, they can either stay in this state or move to the AP, BC or die.
Although this model closely resembles a Markov state-transition approach, it differs in that an ‘area under the curve’ method is used to determine state populations at each cycle of the model (rather than using transition probabilities). In this method, the number of patients in each state of the model is determined by using survival curve data to apportion the overall cohort population between the states at each successive cycle of the model. This approach is illustrated in Figure 10, which shows how, at each cycle, state populations in the model are calculated from a ‘time slice’ across the survival curves for each disease state.
FIGURE 10.
Illustrative example of how state populations are determined at each model cycle in the ‘area under the curve’ approach. A = OS; B = time in CP plus time in AP; C = time in CP; D = time in CP and on treatment.
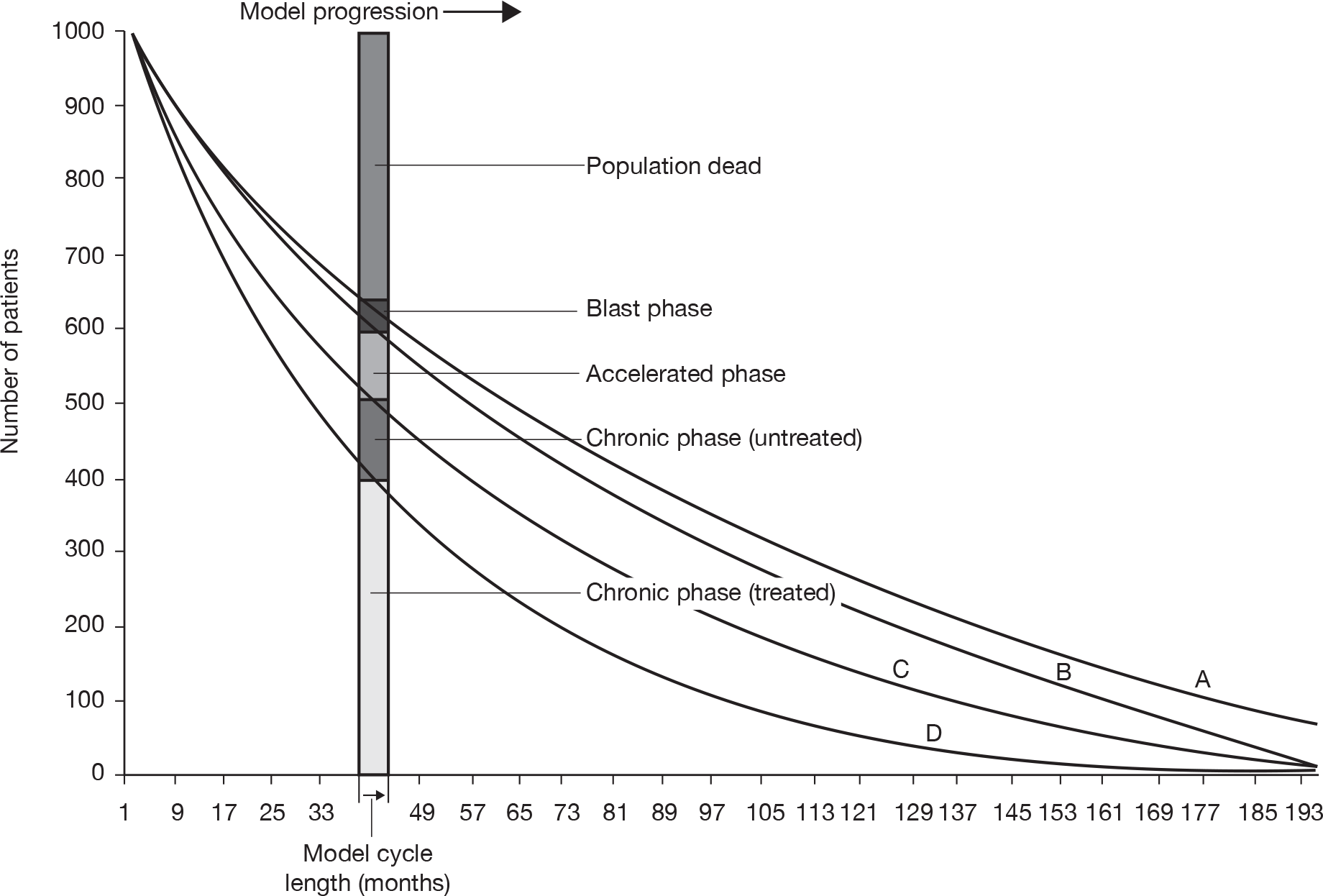
Using this method, it can be seen that there was no requirement to calculate the probabilities of transition between health states (depicted by the arrows in Figure 9), as estimates of populations for each health state are derived directly from the survival curve data.
Within the model, time between treatment discontinuation and death is calculated as a single meta-state, comprising post-discontinuation CP, AP and BC. This means that, in terms of its internal logic, the model only has three states: one representing CP on treatment, one representing death and one encompassing all time in between. Once occupancy of these states has been calculated, the post-discontinuation–pre-death period is split into three parts: first, a period estimating time in BC is deducted, then time in AP is calculated in the same way and, finally, time in post-discontinuation CP is estimated as the remainder. For simplicity, for the purposes of discounting, it was assumed that all patients enter the AP and BC just before the mean OS time for each treatment.
The model was initialised with a cohort of 1000 patients with an assumed age of 56 years who all enter the model in CP on treatment. Disease progression through the five defined CML states was then modelled as described above, where differences in treatment effectiveness between comparators are represented by the differences between survival curves (and, hence, the populations of each disease state at each successive cycle of the model). Estimates of cost and utility are assigned to each health state and these provide an aggregated output over the modelled time horizon for the overall costs and utility for each treatment. The model therefore provides a cost per QALY analysis of the different treatment options.
A cycle length of 2 months was used with a time horizon of 44 years (after which virtually all the cohort – by then, aged 100 years – had died), to ensure that lifetime outcomes are accounted for in the analysis. A half-cycle correction was applied in the model.
Future costs and benefits were discounted at 3.5% per annum from the perspective of the NHS and Personal Social Services in accordance with the NICE reference case. 16
The following subsections provide a detailed description of the methods by which the various survival curves were calculated.
Method of estimating overall survival
In a terminal condition, predicted OS will always be a key driver of cost-effectiveness outputs, so it is important to adopt the most robust method possible of estimating this parameter. Given the short-term follow-up available from studies of dasatinib and nilotinib (see Chapter 2, Design and characteristics of included studies) and the long duration of CML-CP, an approach based on empirical OS data was currently not feasible. We have therefore developed a model of CML-CP based on the development of MCyR and the relationship between this surrogate marker and OS (see Appendix 5). Although this constraint on modelling OS does not apply as strongly to the comparators of HDI and IFN (for which longer term data were available), we have used the MCyR surrogate approach for all comparators for reasons of consistency. The validity of this method was explored by comparing predicted OS with such empirical estimates as were available for each comparator.
The method enables estimation of an OS curve for any combination of people with an MCyR (responders) compared with people without an MCyR (non-responders). It was carried out in the following stages:
-
Weibull curves were specified for CML-cause mortality for responders and non-responders, based on an assumption of constant hazard ratio which was derived from a review of the relevant study data (see Overall survival: hazard ratio for people achieving an MCyR versus people who do not achieve an MCyR).
-
These curves were adjusted to account for the force of general mortality (see Method of incorporating mortality from non-CML causes).
-
Survival data from a published study in which the responder proportion is known were used to calibrate these OS curves.
For the point of calibration referred to in stage 3, we used OS data from Jabbour et al. ’s182 retrospective study of the long-term efficacy of dose-escalated imatinib in a population that had failed normal-dose imatinib. This source was selected because it provided the longest available estimates of OS for responders and non-responders in a population taking a TKI.
A more detailed technical account of the method used to determine OS curves for the model is given in Appendix 6.
It was important to recognise that this method assumes that the OS experience of a cohort can be predicted as a function of MCyR rate alone and, by extension, that the relationship between MCyR rate and OS is identical for each comparator. This assumption has important implications: in effect, our method overlooks any inter-treatment heterogeneity that may be present in issues such as timing of response, depth of response and duration of response. We acknowledge that, if any of our modelled treatments was superior to its comparators with respect to one or all of these factors, and if that superiority can be expected to translate to long-term OS advantage, our model underestimate the effectiveness of the technology in question.
Method of incorporating mortality from non-chronic myeloid leukaemia causes
In addition to deaths caused by CML within the model, it was important to account for expected mortality due to other causes. Although OS and PFS curves from study data include general mortality, the model needs to account for the increasing contribution of general mortality as the cohort population ages.
In order to adjust for the increasing impact of ‘background’ mortality in our curve fitting for OS and PFS, data from UK life tables232 were used to provide an estimate of deaths due to other causes at each model cycle within the time horizon. A full description of the method used to integrate general mortality within the model is provided in Appendix 6.
Figure 11 illustrates graphically the impact of integrating both these mortality causes on the overall combined survival curve.
FIGURE 11.
Example survival curves showing the effects of mortality due to CML, general causes and combined mortality curve when these are integrated in the model.
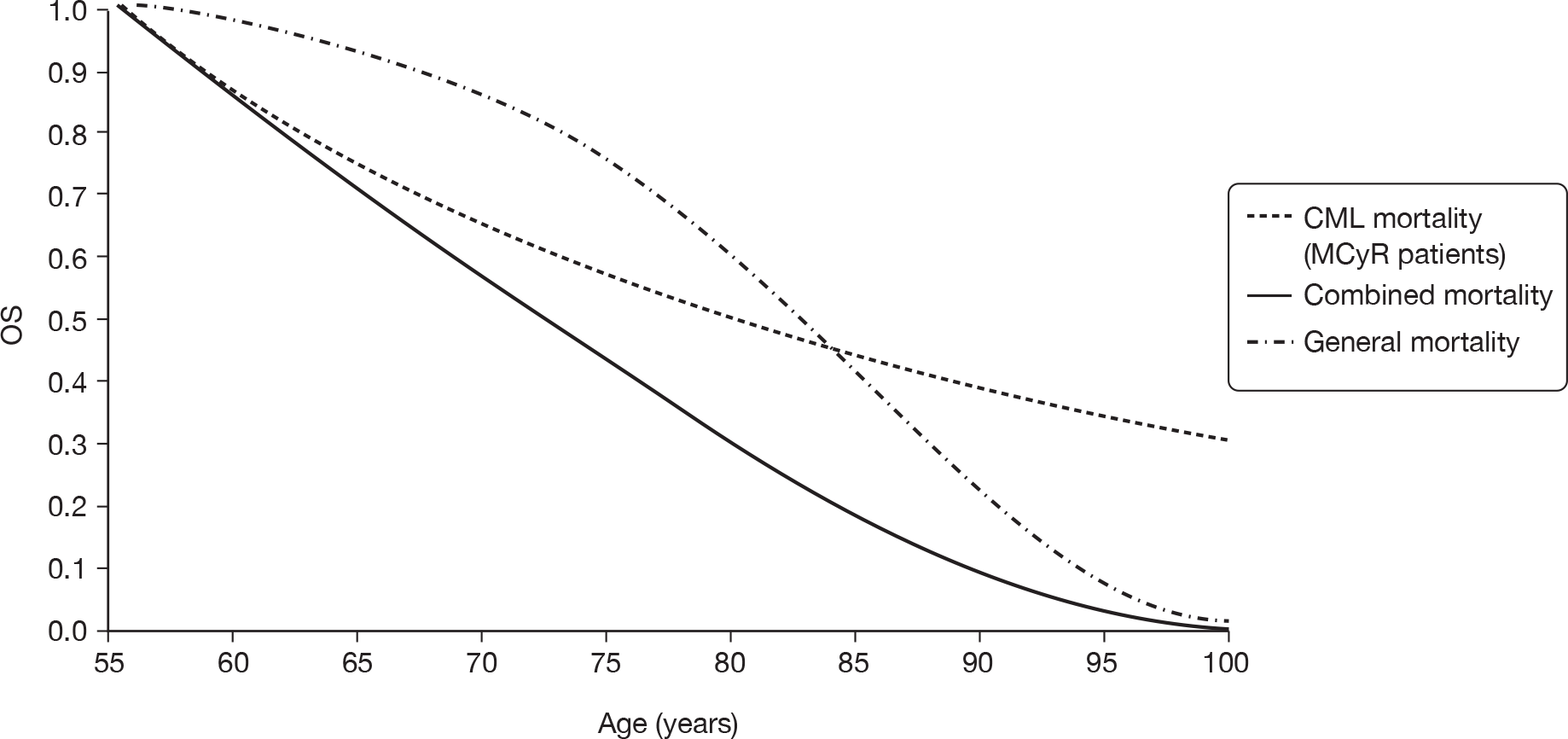
Method of estimating time on treatment in chronic phase
Clearly, the duration of treatment was a key input for the costs of the technologies simulated in our model. Sadly, there was no direct evidence on the length of time for which these medications are taken. Although some of the studies of dasatinib and nilotinib that we have identified report a median duration of treatment during the study, these data are reported as a single data point, and do not appear to account for right-censoring (this explains why the median treatment durations reported appear extremely low – at approximately 8 months – when, according to clinical opinion, treatment is likely to last for considerably longer). Accordingly, such point estimates do not provide a suitable basis on which to estimate treatment duration in our model.
We have therefore adopted a three-stage method of estimating time on treatment. First, we have identified the best available estimate of PFS for each technology. Because the drugs are intended to be taken until disease progression or death, this gives a baseline estimate of treatment duration. However, not all individuals are able to take the drugs in question for the full intended course; a proportion will discontinue for a variety of reasons other than progression or death, most commonly the development of intolerable AEs. Accordingly, as a second step, we estimate the experience of such people. In order to do so, we require an estimate of the treatment-specific rates of premature discontinuation (which can be drawn from published literature) and two additional parameters: an estimate of when they discontinued treatment and a basis for simulating their experience between discontinuation and progression. With these parameters, we estimate the overall profile of individuals who prematurely discontinue treatment. Finally, by subtracting the experience of such people from basic PFS, we arrive at an estimate of the amount of time for which the whole cohort was exposed to the technology. A schematic illustration of this process is given in Figure 12.
FIGURE 12.
Calculation of treatment duration in the PenTAG model.
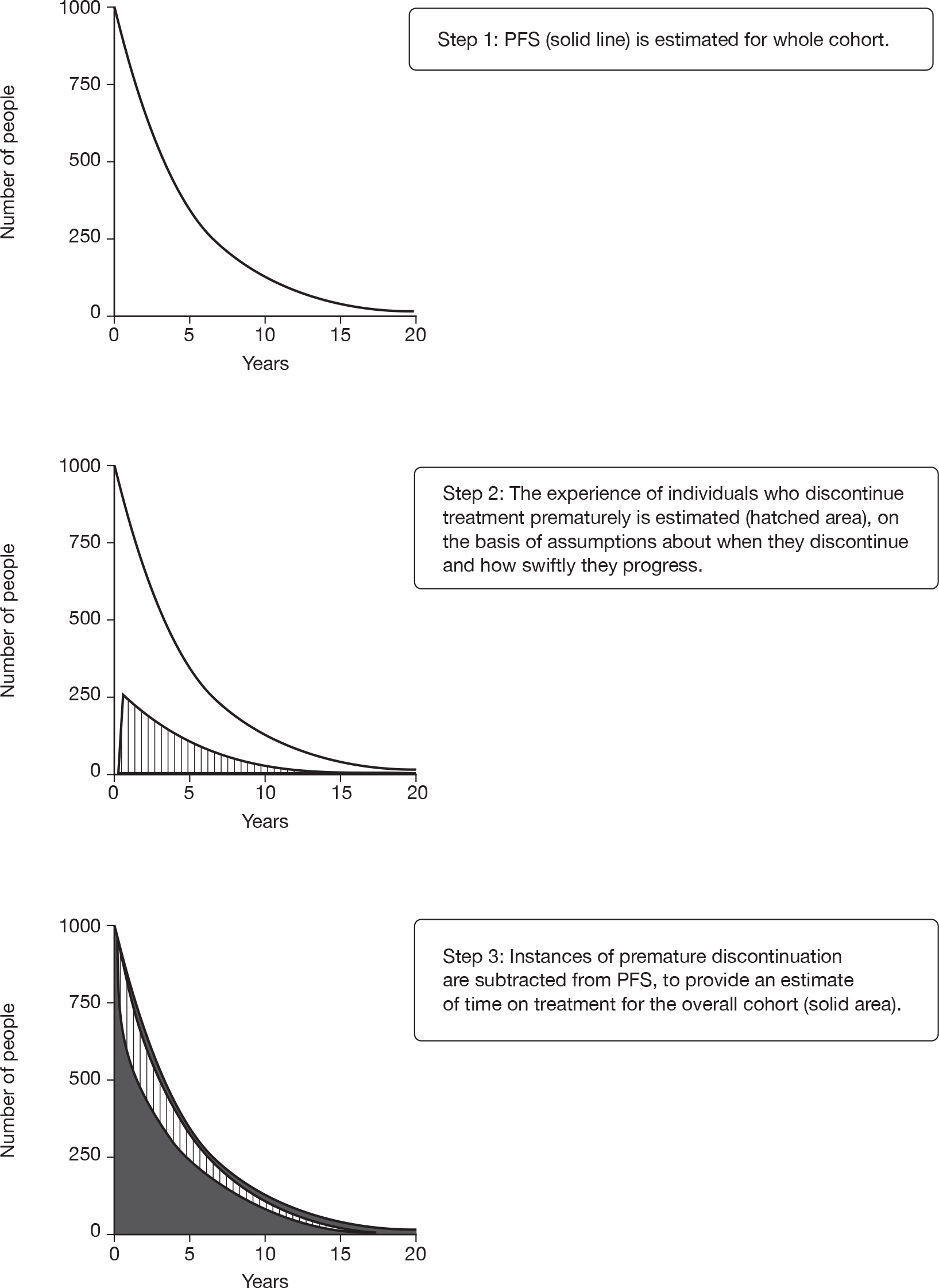
We were unable to find a suitable published source for estimating the time at which discontinuations take place. Following consultation with our expert advisors, we adopted the assumption that discontinuations would take place an average of 3 months after treatment commenced. This value was chosen on the basis that the majority of withdrawals result from serious AEs and that these are likely to manifest relatively early in treatment (although this assumption may not apply in the case of IFN – see Premature discontinuations from interferon-α).
We were also unable to identify a published source directly estimating post-discontinuation–pre-progression experience for individuals who discontinue treatment prematurely. Owing to the availability of alternative treatments, it is possible that many patients in the UK would move to alternative progression-delaying treatment(s) after discontinuing the technologies under review. However, in the absence of any evidence on the likely course of such individuals, we have adopted the simplifying assumption that the PFS curve for premature discontinuations follows the profile of the least effective intervention in the assembled evidence base: that of interferon. Because interferon is more effective than no treatment whatsoever, it was likely that we overestimated the length of time it would take individuals who prematurely discontinue treatment and remain untreated to reach progressive disease; in turn, this means we may somewhat underestimate treatment duration and, hence, drug costs.
Method of estimating time in accelerated phase and blast crisis
We found no data on the time patients spend in the AP and BC following CP treatment with dasatinib, nilotinib and HDI. This was not surprising, as these drugs are relatively new agents, and patients typically take many years from diagnosis to reach these health states. We therefore used generic epidemiological literature to derive values for the mean time patients spend in these health states. In common with other models of the cost-effectiveness of treatment for CML,225,233–235 we have assumed that time spent in AP and BC is independent of treatment arm. This assumption seems reasonable, given that treatment typically stops several years before people enter these health states and we have found no clear argument that earlier treatments influence disease course when patients are diagnosed as being in these later stages of disease.
Method of estimating time in post-discontinuation chronic phase
The survival time in post-discontinuation CP is derived as a residual once the other state durations have been assigned in the model. This duration is therefore calculated as the OS of the patient minus the time on treatment (in CP) minus the time in AP minus the time in BC.
Accounting for severe adverse events
As explained in Method of incorporating mortality from non-CML causes, severe AEs may lead to premature discontinuation of any drug and, to reflect this, we have adjusted our estimate of treatment duration (and, hence, drug costs). However, in the base case, the costs of treating AEs and the disutility associated with their incidence are not included. We have adopted this simplifying assumption for the following three reasons. First, the incidence of serious AEs on HDI, dasatinib and nilotinib appears to be relatively low (see Chapter 2, Adverse events). Second, clinical opinion suggests that the cost of treating patients with these AEs was also likely to be low. Third, given that there was substantial structural and parameter uncertainty in the model, we believe that modelling the costs of treating patients with AEs may introduce spurious accuracy.
It should be emphasised that, in reflection of its notable incidence of AEs, the utility value adopted during CP on treatment with IFN was empirically lower than that used for other treatments [see Valuation of outcomes (utilities)]. However, we have not included additional costs to reflect this.
Sensitivity analysis was carried out to explore the effect of changing assumptions regarding incidence and timing of AEs and incorporating their projected costs (see Costs associated with adverse events).
Model parameter inputs
The following section describes the approach taken to parameterise the model, covering data sources and values chosen from among alternatives.
Ideally, we would have drawn our parameter inputs from randomised studies directly comparing the various treatments simulated in our model. In the absence of any such evidence, we were compelled to rely on estimates taken from a heterogeneous collection of observational studies with single arms (or single relevant arms). Our overarching rationale for the derivation of model inputs from this kind of evidence was as follows:
-
The data chosen should be as representative as possible of the UK population, of UK licensing and of UK health-care provision for the technologies being simulated.
-
We have a strong preference for parameters drawn from published, peer-reviewed data sources; data drawn from other types of evidence (e.g. conference abstracts, industry submissions to NICE) were adopted only in the absence of an appropriate fully published data source.
-
Publications identified as part of our clinical effectiveness review (Chapter 2) are considered on the basis of our appraisal of that evidence and the biases to which it may be subject.
-
In reflection of the likely correlations between the various inputs, we have a strong preference for deriving as many parameters as possible from the same source for a given comparator (within-comparator consistency).
-
Parameters influencing individual comparators should be selected on as consistent a basis as the choice set allows (between-comparator consistency).
-
Wherever possible, separate parameter inputs for ImR and ImI populations should be obtained; a single estimate should be applied to both subgroups only in the absence of suitable status-specific data sources.
-
Where other things are considered equal, we prefer a data source that reports a larger sample size.
-
Where other things are considered equal, we prefer a data source that reports longer follow-up.
-
Where more than one candidate of equal validity was available, consideration was given to pooling the available estimates using meta-analysis or other appropriate methods.
The model synthesises data in a variety of categories which are described in turn. These are grouped as clinical effectiveness, health-state utilities and costs.
Clinical effectiveness
Overall survival: hazard ratio for people achieving an MCyR compared with people who do not achieve an MCyR
We have assumed that the OS hazard ratio for those who achieve an MCyR compared with those who do not achieve an MCyR was the same for all treatments and equal to that shown in studies of imatinib at standard dose. This approach was chosen on the basis of availability of long-term follow-up in a population exposed to TKIs, although uncertainty about the assumed transferability between different treatments was acknowledged and necessarily considerable.
Three studies were identified in which OS data for imatinib at standard dose were presented for individuals who achieve an MCyR and those who do not (Figure 13). 236–238 All three are large studies of patients with CML-CP:
-
a retrospective analysis of early chronic disease in 279 individuals236
-
a combined analysis of 261 individuals from a Phase II study and an expanded access study,237 and
-
a retrospective analysis of the imatinib arm of the IRIS study (n = 551). 238
FIGURE 13.
Data sources for OS hazard ratio of people who achieve an MCyR versus those who do not achieve an MCyR. a, Based on MCyR versus weighted average of minor and ‘other’ responses after 6 months’ follow-up.
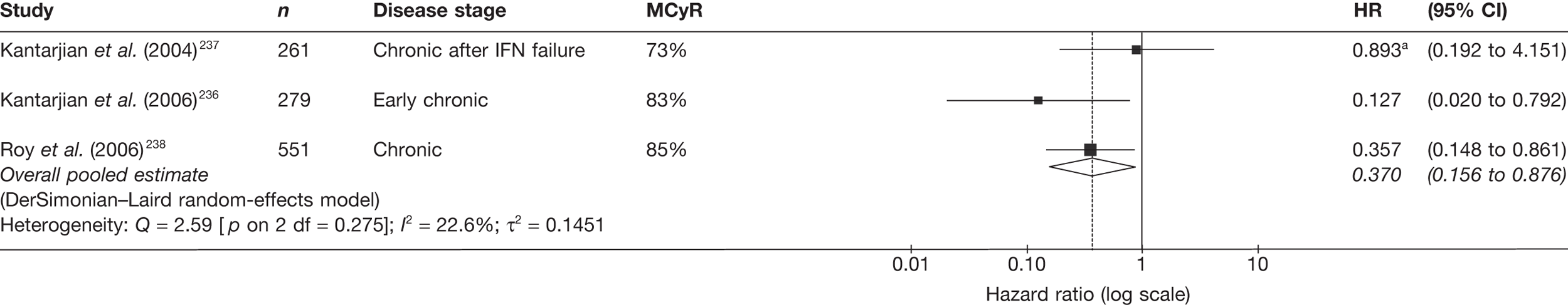
To reduce the uncertainty surrounding this parameter, and in the absence of a strong rationale for preferring one of these data sources in particular, we calculated a pooled hazard ratio for use in our model. Hazard ratios for each data source were based on data extracted from Kaplan–Meier curves in each study, calculated using the method described by Parmar et al. ,239 with the aid of a spreadsheet provided as an online supplement by Tierney et al. 240 In the retrospective analysis of 261 individuals reported by Kantarjian in 2004,237 survival data were provided according to CyR status at 3 months’ follow-up (denoted by ‘A’ in the table) and at 6 months’ follow-up (denoted by ‘B’ in the table). We used the second, more mature, data set. In this graph, data were provided in three categories: people who achieved a MCyR, a minor CyR and ‘other’ CyR. We therefore calculated a hazard ratio for MCyR versus non-MCyR using, on the one hand, the reported OS for those achieving an MCyR and, on the other, an average of the minor and ‘other’ cohorts weighted according to the size of the subgroups at baseline. The estimates provided by this data set appear to be much higher than those in the other two sources, although there was substantial uncertainty around the point estimate. In all three studies, relatively few events were reported over the duration of follow-up, which leads to considerable uncertainty in the data.
The pooled estimate was fairly close to that provided in the largest single source. 238 However, it can also be seen that there was little gain in terms of the precision of the estimate (CIs are similar), because the random-effects model estimates fairly high between-study variance.
Major cytogenetic response rates
The following sections describe the choices of values for MCyR on each treatment. These are used to weight the generic MCyR and non-MCyR OS curves, to provide a comparator-specific OS curve for each modelled treatment.
There may be important sources of heterogeneity between the MCyR rates reported in published literature. Where possible, we report two factors that may be significant in the evidence summary tables in the following sections: proportion of study participants in MCyR at study baseline and duration of follow-up.
Although the impact of MCyR status at baseline may be important, it was not straightforward to deduce the direction of bias. On the one hand, prior response to a TKI may augur well for increased likelihood of response to an alternative technology; on the other, participants who have achieved and then lost a CCyR to normal-dose imatinib (as will be the case in many individuals who meet the criteria for MCyR at study entry) may be in a more mature phase of CML progression and those who have achieved a PCyR, but never progressed to CCyR may be subject to a degree of primary resistance that means they will fare no better under a different regimen. Accordingly, this factor may have unpredictable effects, but is clearly a source of heterogeneity between the populations reported in the evidence base.
In contrast, duration of follow-up has a predictable effect on response rates. It was important to recognise that MCyR rates reflect best ever status on treatment (as opposed to current status at the time of analysis). This means that, as follow-up is extended, response rates can only go up. Accordingly, studies based on lengthier follow-up will appear to report a higher likelihood of response, even if the technology under assessment is no more effective than those assessed after less time. Because of this, we took the view that it was imperative to maintain inter-comparator consistency by parameterising the model with MCyR rates that represent likelihood of response at a single, uniform juncture. On scrutiny of the evidence base, we selected 12 months as the follow-up time that could most accurately be derived or approximated for each of the comparators for ImR CML; for ImI CML, a 6-month follow-up provided a more complete picture.
Our systematic review of clinical effectiveness data identified a number of clinical studies in which MCyR to dasatinib in CML-CP was reported (see Chapter 2,Major cytogenetic response: chronic phase). Data relating to ImR and ImI CML are reproduced in Tables 77 and 78. We had a strong preference for using the values originating in the study reported by Shah et al. ,22 as these form the only estimates of MCyR rate achieved with the recommended dose of dasatinib (100 mg once a day). A 12-month response rate was available in data provided by BMS as part of the NICE consultation process and, although we would have preferred to rely on validated, peer-reviewed data, the imperative of maintaining a consistent follow-up juncture across all comparators dictated that we adopt this data point. For the ImI stratum, a published 6-month MCyR rate was available from the optimal study arm, so it was a straightforward decision to use this.
| Study | Length of follow-up | Dose | MCyR at baseline (%) | n | MCyR | % | 95% CI |
|---|---|---|---|---|---|---|---|
| Selected parameter | |||||||
| Shah et al. (2008)22 | 12.0 monthsa,b | 100 mg q.d. | 20.4c | 124 | 72 | 58.1 | 48.9% to 66.9% |
| Rejected alternatives | |||||||
| Hochhaus et al. (2007)11,105 | 15.2 monthsd | 70 mg b.i.d. | 6.3 | 288 | 151 | 52.4 | 46.5% to 58.3% |
| Kantarjian et al. (2007)23 | 15.0 monthsd | 70 mg b.i.d. | 5.9 | 101 | 53 | 52.5 | 42.3% to 62.5% |
| Shah et al. (2008)22 | 6.0 months | 100 mg q.d. | 20.4 | 124 | 66 | 53.2 | 44.1% to 62.2% |
| 50 mg b.i.d. | 13.7c | 124 | 58 | 46.8 | 37.8% to 55.9% | ||
| 140 mg q.d. | 16.8c | 123 | 62 | 50.4 | 41.2% to 59.5% | ||
| 70 mg b.i.d. | 18.5c | 127 | 65 | 51.2 | 42.2%, to 60.1% | ||
| Sakamaki et al. (2009)109 | 6.0 monthsa | 70 mg b.i.d. | NR | 18 | 6 | 33.3 | 13.3% to 59.0% |
| Study | Length of follow-up | Dose | MCyR at baseline (%) | n | MCyR | % | 95% CI |
|---|---|---|---|---|---|---|---|
| Selected parameter | |||||||
| Shah et al. (2008)22 | 6.0 monthsa | 100 mg q.d. | 20.4b | 43 | 32 | 74.4 | 58.8% to 86.5% |
| Rejected alternatives | |||||||
| Hochhaus et al. (2007)11,105 | 15.2 monthsc | 70 mg b.i.d. | 23.2 | 99 | 79 | 79.8 | 70.5% to 87.2% |
| Shah et al. (2008)22 | 6.0 monthsa | 50 mg b.i.d. | 13.7b | 44 | 32 | 72.7 | 57.2% to 85.0% |
| 140 mg q.d. | 16.8b | 44 | 31 | 70.5 | 54.8% to 83.2% | ||
| 70 mg b.i.d. | 18.5b | 41 | 28 | 68.3 | 51.9% to 81.9% | ||
| Sakamaki et al. (2009)109 | 6.0 monthsa | 70 mg b.i.d. | NR | 12 | 10 | 83.3 | 51.6% to 97.9% |
We had a strong preference for using the values originating in the study reported by Shah et al. ,22 as these form the only estimates of MCyR rate achieved with the recommended dose of dasatinib (100 mg once a day). A 12-month response rate was available in data provided by BMS as part of the NICE consultation process and, although we would have preferred to rely on validated, peer-reviewed data, the imperative of maintaining a consistent follow-up juncture across all comparators dictated that we adopt this data point. For the ImI stratum, a published 6-month MCyR rate was available from the optimal study arm, so it was a straightforward decision to use this.
Of the possible data sources identified in our systematic review of clinical effectiveness data relating to CML-CP (see Chapter 2, Major cytogenetic response: chronic phase), only two studies provided an estimate of MCyR rate to nilotinib in ImR CML and only one provided separate data for an ImI subgroup. Details are reproduced in Tables 79 and 80, respectively. The dose escalation study reported by Kantarjian et al. in 2006103 includes only a small number of people with CP disease (n = 17), taking a variety of doses of nilotinib. We therefore had a strong preference for using the values provided in the larger, Phase II open-label study of nilotinib at recommended dose reported by Kantarjian et al. in 2007. 106 However, the 12-month MCyR rate for this study was unavailable so, for the ImR stratum of our model, we estimated the parameter by interpolating 6-month and 19-month rates, assuming a linear trend between the known data points. To do this, we interpolated both the numerator and the denominator of the proportion of responders (note that the longer follow-up includes expanded access, with the ImR sample growing from 194 to 228), which also enabled valid calculation of the error of the estimate. For the ImI model, we were again able to use the reported response rate for our preferred follow-up time (6 months) directly from this study.
| Study | Length of follow-up | Dose | MCyR at baseline (%) | n | MCyR | % | 95% CI |
|---|---|---|---|---|---|---|---|
| Selected parameter | |||||||
| Kantarjian et al. (2007)106 | 12 months estimatea | 400 mg b.i.d. | ≥ 4.1b,c | 210 | 110 | 52.4 | 45.4% to 59.3% |
| Rejected alternatives | |||||||
| Kantarjian et al. (2007)106 | 6 monthsd | 400 mg b.i.d. | ≥ 4.1b,c | 194 | 94 | 48.5 | 41.2% to 55.7% |
| 19 monthsd,e | 228 | 128 | 56.1 | 49.4% to 62.7% | |||
| Kantarjian et al. (2006)103 | NR | Mixed/NR | NR | 17 | 6 | 35.3 | 14.2% to 61.7% |
| Study | Length of follow-up | Dose | MCyR at baseline (%) | n | MCyR | % | 95% CI |
|---|---|---|---|---|---|---|---|
| Selected parameter | |||||||
| Kantarjian et al. (2007)106 | 6 monthsa | 400 mg b.i.d. | 0b | 86 | 40 | 46.5 | 35.7% to 57.6% |
Literature searches revealed four potential sources for an estimate of MCyR rate to HDI in CP patients (Table 81). We do not include the paper reporting a subgroup from the IRIS study that underwent dose escalation following failure of normal-dose imatinib,54 because it was not possible to deduce how many of the participants achieved an MCyR (subgroups of participants are reported separately according to various categories of imatinib failure, with separate target outcomes for each).
| Study | Length of follow-up | Daily dose | MCyR at baseline (%) | n | MCyR | % | 95% CI |
|---|---|---|---|---|---|---|---|
| Selected parameter | |||||||
| Jabbour et al. (2009)182 | 12 monthsa | 800 mg | 15.5 | 84 | 37b | 44.0 | 33.2% to 55.3% |
| Rejected alternatives | |||||||
| Kantarjian et al. (2003)53 | > 8 monthsc | 600 mg or 800 mg | 0.0d | 54 | 13 | 24.1 | 13.5% to 37.6% |
| Zonder et al. (2003)224 | 14 monthsc | 600 mg or 800 mg | 0.0e | 12 | 4 | 33.3 | 9.9% to 65.1% |
| Kantarjian et al. (2007)23 | 15 monthsc | 800 mg | 0.0 | 49 | 16 | 32.7 | 19.9% to 47.5% |
| Jabbour et al. (2009)182 | 61 monthsc | 800 mg | 15.5 | 84 | 44 | 52.4 | 41.2% to 63.4% |
Most of the identified data sources are small studies reporting the experiences of fewer than 50 individuals. Because it was the largest sample reported, because it presented data enabling us to deduce a 12-month response rate and because it allowed us to draw a variety of parameters from the same source, we have used the estimate reported by Jabbour et al. in our model. 182 Calculating a 12-month MCyR rate from this source was not straightforward. It was reported that 35 participants had achieved a MCyRs after 12 months of follow-up. However, although the number of 12-month responses reported includes participants with PCyR at the time of imatinib dose escalation who achieved CCyR, it excludes an unknown number of additional participants who maintained their baseline PCyR (and it was important to recognise that analogous cases appear to have been included in published response rates from studies of dasatinib). We infer, from figures reported elsewhere in Jabbour et al. ’s paper, that there were probably two such cases. [Note, among participants who discontinued normal-dose imatinib owing to cytogenetic failure, the number of CCyRs among the 50 participants with no MCyR at baseline was calculable as 22 (30 MCyRs minus 8 PCyRs), and the number of CCyRs among all participants was stated to be 33; therefore, it could be deduced that the number of CCyRs among participants with baseline MCyR was 11. We also know that there were a total of 13 participants with MCyR at baseline, so we can infer that only two of them failed to achieve a CCyR to HDI.] Accordingly, we can conclude that, when calculated according to the same principles used in the calculation of dasatinib MCyR rates, the 12-month MCyR rate for Jabbour et al. ’s HDI cohort would be 37/84 = 44.0%.
We note that this was a relatively high estimate, in comparison with the other identified data sources. However, it should also be remembered that the alternative data sources are subject to notable shortcomings. In particular, we believe that the estimate derived from the randomised comparison with dasatinib23 was very likely to underestimate the true likelihood of MCyR to HDI owing to that study’s bias in favour of its comparator (see Chapter 2, Randomised studies).
On a balance of these considerations, we conclude that our chosen data point was unlikely to represent a gross distortion of the likelihood of MCyR to HDI. In our sensitivity analyses, we vary the parameter across the range of the 95% CI for the estimate, to explore the impact on the model of assuming a greater or lesser probability of response. These analyses provide an opportunity to monitor model outputs that would be expected using an alternative source for this parameter.
We have used the estimate of MCyR rate to IFN in CP reported in the control arm of the IRIS study of imatinib. 17 The IRIS study represents the most recent, large study of IFN in the treatment of CML. The study also brings the further methodological benefit of providing data to inform the other clinical parameters for IFN treatment needed for the model, ensuring consistency across data sources.
The estimate for the proportion of people with a MCyR to IFN from the IRIS study was 22%. This was measured after a minimum follow-up of 18 months, which exceeds our target follow-up of 6 months. However, in view of the methodological advantages of relying on this study and the relatively low rate of responses overall, we concluded that it was reasonable to compromise our ideal data requirements and rely on this data point.
A previous health technology assessment by PenTAG of imatinib for the treatment of CML includes a systematic review of the clinical effectiveness of IFN in CP disease. 241 As there has been little research on the treatment of CML with IFN since 2002, we believe that this review appropriately summarises the evidence base without the need to be updated. In the review, 24 studies of treatment with IFN in CML-CP were identified. MCyR rates varied from 0% to 54.5% with median response being 20%. This suggests that our chosen data point provides a representative estimate of the efficacy of IFN.
No details were provided to estimate the proportion of participants who met the criteria for MCyR at baseline in this study; however, as it primarily reflects first-line treatment, it was unlikely that the proportion was much (if at all) above zero.
Mean time spent in accelerated phase and blast crisis
As explained above, we have assumed that time spent in AP and BC is independent of treatment arm; hence, a single estimate of mean time in each phase was needed to apply to all model comparators. We have assumed a mean time in AP of 9.64 (SE 0.69) months and a mean time in BC of 13.12 (SE 0.94) months. These values were taken from a previous cost-effectiveness analysis225 in CML in which the authors derived time spent in AP and BC by calculating the area under the curve from published survival curves. 242,243
Valuation of outcomes (utilities)
A review of the literature identified six sources of utility values for CML (Table 82). From these, we chose the values shown in Table 83. These data were collected during the IRIS study, as reported by Reed et al. 225,235 and used by Dalziel et al. in a previous health technology assessment of imatinib for CML. 226 These data were drawn from a large sample of patients using the EQ-5D, which was preferred in the NICE reference case. 220
| Disease stage | Drug | Gordois et al. (2003);244 Warren et al. (2004)233 | Reed et al. (2004);225 Reed et al. (2008)235 | Dalziel et al. (2005)226 | Kattan et al. (1996)234 | Liberato et al. (1997)245 | BMS (2009)184 |
|---|---|---|---|---|---|---|---|
| Method | EQ-5D | EQ-5D | EQ-5D | Not stated | Not stated | EQ-5D | |
| Elicited from | Six clinicians | Patients in IRIS RCT | Patients in IRIS RCT | Clinicians | 10 clinicians | 100 lay people | |
| CP (CyR and no CyR) | Imatinib | 0.90 | 0.854 (SE 0.004) | 0.854 (SD 0.19) |
0.85 responding to treatment, 0.68 not responding Plus treatment-related AE disutility |
||
| Hydroxycarbamide | 0.90 | 0.90 (SD = 0.2) | |||||
| IFN + cytarabine | 0.710 (SE 0.008) | 0.710 (SD 0.27) | 0.90 | 0.875 | |||
| AP (no CyR) | Imatinib | 0.58 | 0.595 (SE 0.077) | 0.729 (SD 0.204) | 0.50 plus treatment-related AE disutility | ||
| IFN + cytarabine | 0.595 (SE 0.077) | 0.729 (SD 0.204) | 0.50 | ||||
| BC (no CyR) | Imatinib | 0.38 | 0.595 (SE 0.077) | 0.524 (SD 0.424) | 0.31 plus treatment-related AE disutility | ||
| IFN + cytarabine | 0.595 (SE 0.077) | 0.524 (SD 0.424) | 0.50 | 0.500 |
| Disease stage | Dasatinib | Nilotinib | Imatinib | IFN |
|---|---|---|---|---|
| CP (on treatment) | 0.85 (SE 0.004) | 0.85 (SE 0.004) | 0.85 (SE 0.004) | 0.71 (SE 0.008) |
| CP (post-discontinuation) | 0.85 (SE 0.004) | |||
| AP | 0.73 (SE 0.06) | |||
| BC | 0.52 (SE 0.08) |
It was necessary to estimate utility values for people taking dasatinib and nilotinib in CP because no values were cited in the literature. We set these values equal to the value for HDI in CP based on similarity of the incidence of AEs by treatment and clinical opinion.
We did not locate a utility value for patients in CP who were not on treatment. We considered using a value of 0.90, based on data from a group taking hydroxycarbamide, which was considered relatively free of adverse effects (Table 83). However, this value appears counterintuitive in the context of a patient who has lost a response to treatment and is therefore likely to suffer additional anxiety and depression about the future. Therefore, we have assumed a value equal to that of people on TKIs (0.85) during CP.
The utilities for AP and BC reported by Reed et al. 225 are slightly different from those quoted by Dalziel et al. ,226 although both were originally taken from the IRIS study. 17 In Reed et al. ’s225 analysis, no difference was assumed between accelerated and BC as the observed difference in values was not statistically significant. We believe this problem was substantially overcome in the context of probabilistic analysis, which takes account of relevant parameter uncertainty. We have therefore used the utility values cited by Dalziel et al. 226
Decrements in utility associated with AEs have not been modelled separately in the base-case analysis, as the data used refer to the experience of people on treatment and therefore include treatment-related AEs which did not result in treatment discontinuation. Disutility associated with treatment-related AEs which occurred in the first 3 months of treatment, resulting in cessation of therapy (see Accounting for severe events), has not been included in the model.
Costs
Cost estimates in the economic evaluation include drug costs, administration costs of IFN and cytarabine, outpatient visits, BM tests, radiographs, CT scans, blood transfusions and inpatient terminal care. Drug prices are taken from the BNF. 246 All costs were inflated to 2009–10 values where appropriate. 68
In addition to drug acquisition prices, drug costs must also take account of dose intensity and treatment duration; our approach to these issues is described in subsequent sections.
Drug prices
Table 84 presents the drug prices, which have been taken from the BNF (No. 58). 246 Given that we used the clinical outcomes for IFN (with cytarabine) from the IRIS study,17 we have also used this study for the dosing regimen and dose intensity of the IFN regimen.
| Drug | Brand | Dose and frequency | Pricea | Cost per 2-month cycle (£) |
|---|---|---|---|---|
| Dasatinib | Sprycel | 100 mg once q.d. | 50 mg, 56-tab pack = £2337.97 | 5080.00 |
| Nilotinib | Tasigna | 400 mg twice q.d. | 200 mg, 112-cap pack = £2432.85 | 5286.00 |
| HDI | Glivec | 400 mg twice q.d. | 400 mg, 30-tab pack = £1604.08 | 6505.00 |
| IFN | Roferon-A®, Roche | Target dose: 5 million units per square metre body surface area q.d. = 8.65 milion units per person q.d. (1.73 m2 body area)b | 0.5-ml (4.5 million units) prefilled syringe = £22.60 | 2643.00 |
| Cytarabine (used with IFN) | 20 mg per m2 body q.d. for 10 days per monthb | 20 mg/ml, 5-ml vial = £4.00 | 28.00 |
Drug costs: dose intensity
For consistency between the costs of the drugs and the clinical outcomes, it was necessary to model the amounts of the drugs actually taken while on treatment in the relevant clinical studies. The dose intensity of a drug was defined as the amount of drug administered in a clinical study as a proportion of the amount that would have been administered if there had been no dose reductions or dose interruptions. Note, that this does not include, for the cohort, people who withdrew from treatment owing to AEs.
Ideally, we would use mean dose intensities in our model. Unfortunately, we were unable to identify estimates of mean dose intensity from the studies. We have therefore used the median estimates taken from the primary clinical effectiveness studies for dasatinib and nilotinib (Table 85). The impact of changing both the absolute values for dose intensity and the relative dose intensities between treatments was explored in sensitivity analyses (see Deterministic sensitivity).
| Treatment | Median dose intensity | Source |
|---|---|---|
| Dasatinib | 100% [100 mg q.d. (range 18–150)] | Shah et al. (2008)106 |
| Nilotinib | 99.7% [797 mg q.d. (range 151–1112)] | Kantarjian et al. (2007)54 |
| HDI | 92.3% (average dose of 738 mg q.d., calculated as a weighted average of the dose data in figure 5, taking interpolated averages over the specified intervals, and then weighting according to the average proportion of participants in PFS over each period) | Jabbour et al. (2009)182 |
| IFN | 55.5% (median dose = 4.8 million units q.d.) | IRIS RCT: O’Brien et al. (2003)17 |
| Cytarabine | Not reported in the IRIS RCT17 but 29% never received cytarabine |
Drug costs and drug costs adjusted for dose intensity are shown in Figure 14.
FIGURE 14.
Drug costs and drug costs adjusted for dose intensity.
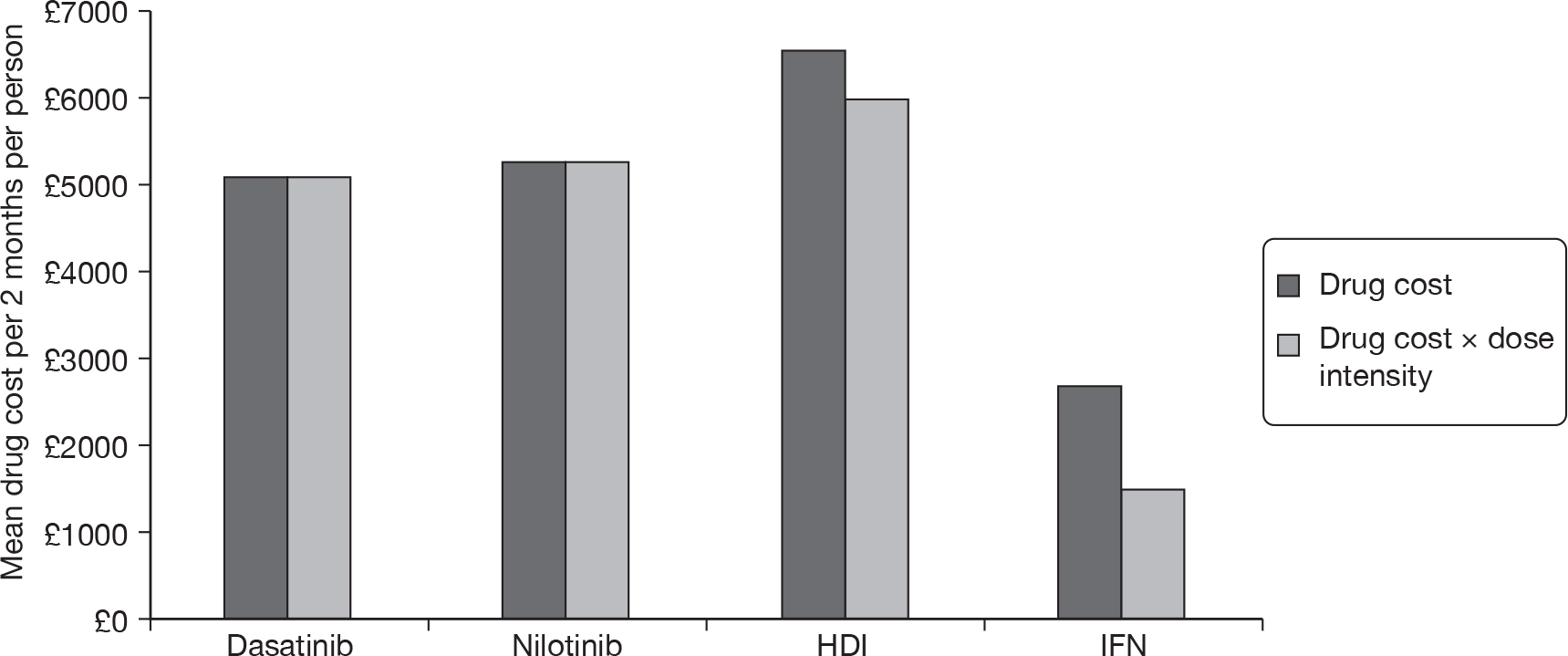
Drug administration costs
Dasatinib, nilotinib and HDI are all taken orally, and therefore incur no administration costs. IFN dose and administration schedule are taken from the IRIS study, with the assumption (based on clinical opinion) that IFN will be taken at home. We assume that 75% of patients administer IFN themselves, or with the help of a carer, and in 25% of cases administration is carried out by district nurses.
The cost of a single district nurse visit in 2006–7 is quoted as £24 (Schema 9.1 Community nurse). 227 Inflating this value to 2009–10 prices,184 gives £27 per visit. This implies an average cost per 2-month model cycle of £409.
We do not adjust the cost of administration according to dose intensity of IFN, because doses tend to be reduced, rather than omitted completely, so administration costs will continue to be incurred.
Treatment duration
As explained in Method of incorporating mortality from non-CML causes, our method for estimating time on treatment was dependent on two evidence-based parameters: PFS and an estimate of the proportion of individuals who prematurely discontinued treatment (i.e. prior to progression or death).
It was important to emphasise that this was the only purpose for which PFS was used in our model; these estimates do not underpin any estimates of health-state transition (i.e. effectiveness) which, as described above, was simulated purely as a function of MCyR rates (as translated into OS).
In our clinical effectiveness review, we identified estimates of PFS in several studies of dasatinib in CML-CP, including the one from which we have drawn our effectiveness estimate22 (see Chapter 2, Progression-free survival). However, for the purposes of our model, it was imperative to have access to separate estimates of PFS for ImR and ImI subgroups, because these different cohorts are assumed to have quite different efficacy profiles. Unfortunately, no such data relating to Shah et al. ’s study22 were available in the published literature. However, single data points corresponding to 24-month PFS probability in the same study are provided in the submission made by BMS to NICE; it was estimated that the likelihood of PFS was 0.87 in ImI individuals and 0.77 in the ImR subgroup. 184 Although we would rather rely on (1) a fully published, peer-reviewed data source and (2) a complete PFS curve, rather than a single estimate from a single time point, we have adopted these values in our model because of the crucial importance of maintaining consistency between data sources as far as possible in a limited evidence base and the need for separate estimates according to imatinib failure status. In the absence of information on the shape of the PFS curves in this study, we simply fitted exponential curves to the single data points (with an allowance made for non-CML mortality).
In an identical way to that described above, we found no published evidence on PFS with nilotinib in CML-CP that was subdivided according to imatinib-failure status (see our clinical effectiveness review, Chapter 2, Progression-free survival), but we did note that the data we required were available in the relevant industry submission to NICE. PFS probability at 6, 12 and 18 months was 0.864, 0.769 and 0.632, and 0.951, 0.906 and 0.845 in the ImR and ImI subgroups, respectively. Although, in this case, complete status-specific PFS curves were available, we found that these were adequately modelled using an exponential distribution (as did Novartis, in their model; see Summary of Novartis’s cost-effective analysis). Again, the curve was modified to account for non-CML mortality.
A full Kaplan–Meier curve showing PFS for follow-up extending, in the longest cases, over 7 years is available from Jabbour et al. ’s single-centre study,182 the same data source was used to provide efficacy parameters for our model. Accordingly, we have used these data in our model. Because of the additional maturity of this data source, we were able to achieve a precise fit to the empirical data using a Weibull distribution (λ = 0.22; γ = 1.16).
Table 86 provides summary data from our chosen parameter source and compares them with results from other studies. It was immediately noticeable that PFS from the dose escalation subgroup of the IRIS study54 was substantially superior to that reported elsewhere. This may be because the study used a narrower definition of disease progression (limited to death, progression to AP or BC, or loss of an MCyR) than that adopted elsewhere. Confusingly, however, PFS is seen to exceed OS according to the curves in this publication; it was hard to explain this finding without questioning the authors’ explicit assurance that deaths ‘from any cause’ were counted as events in the PFS analysis. Consequently, we are unsure how to interpret this data set. The remaining source of data for this parameter was Kantarjian et al. ’s randomised comparison of HDI and dasatinib. 23 This was a comparatively immature data set, which may be badly distorted as a result of an overwhelming level of early crossover from HDI to the comparator arm.
| Study | Dose | n | 6 months (years) | 12 months (years) | 18 months (years) | 24 months (years) | 36 months (years) | 48 months (years) | 60 months (years) |
|---|---|---|---|---|---|---|---|---|---|
| Selected parameter | |||||||||
| Jabbour et al. (2009)182 | 800 mg | 84 | 0.865 | 0.81 | 0.71 | 0.57 | 0.47 | 0.29 | 0.24 |
| Rejected alternatives | |||||||||
| Kantarjian et al. (2007)23 | 800 mg | 49 | 0.73 | 0.73 | 0.65a | ||||
| Kantarjian et al. (2009)54 | 600 mg or 800 mg | 103b | 0.95 | 0.935 | 0.935 | 0.92 | 0.885 | 0.85 | 0.85 |
Treatment duration was assumed to follow PFS as reported for the control arm of the IRIS study,17 our source for other parameters for this arm. Summary details are shown in Table 87.
| Study | n | 6 months (years) | 12 months (years) | 18 months (years) | 24 months (years) |
|---|---|---|---|---|---|
| Selected parameter | |||||
| O’Brien et al. (2003)17 | 553 | 0.925 | 0.805 | 0.735 | 0.705 |
Table 88 summarises the available evidence on premature discontinuation rates in studies of dasatinib for CML-CP. None of the evidence distinguishes between ImR and ImI populations, so we have had to assume that the overall withdrawal rates apply equally to both subgroups.
| Study | Dose | n | Premature discontinuations | % | 95% CI |
|---|---|---|---|---|---|
| Selected parameter | |||||
| Shah et al. (2008)22 | 100 mg q.d. | 167 | 17 | 10.2 | 6.0% to 15.8% |
| Rejected alternatives | |||||
| Hochhaus et al. (2007)11 | 70 mg b.i.d. | 186 | 86 | 22.2 | 18.2% to 26.7% |
| Kantarjian et al. (2007)23 | 70 mg b.i.d. | 101 | 16a | 15.8 | 9.3% to 24.4% |
| Shah et al. (2008)22 | 50 mg b.i.d. | 168 | 22 | 13.1 | 8.4% to 19.2% |
| 140 mg q.d. | 167 | 21 | 12.6 | 8.0% to 18.6% | |
| 70 mg b.i.d. | 168 | 31 | 18.5 | 12.9% to 25.2% | |
In our base-case model, we have adopted the estimate provided in the 100 mg q.d. arm of Shah et al. ’s dose optimisation RCT, from which the primary clinical effectiveness data for the model and the PFS curve that forms the baseline for our calculation of treatment duration were also taken. 22 It was essential for us to maintain consistency between these parameters, where possible, so that our model corresponds to directly observed experience. Moreover, in this instance, it was particularly important to reflect the lower dosage presently recommended for UK use, as the primary rationale for the adoption of this regimen was the expectation that fewer AEs will result without any significant loss of effectiveness (see Chapter 2, Effectiveness of dasatinib). As intolerable AEs are the most common reason for premature discontinuation, it would be anticipated that lower rates would be seen in this group and, indeed, it can be seen in Table 88 that the selected parameter reflects the lowest withdrawal rate reported.
We note that, in its model, BMS does not include any treatment discontinuations, on the grounds that ‘discontinuation due to AEs are already included within the overall PFS… and OS… study survival data’, with the result that ‘including an additional probability of discontinuation due to AEs would lead to double counting’. 184 In our chosen model structure, this conclusion does not apply, as we were not making use of PFS to predict health-state transitions (i.e. it was not an effectiveness parameter, in our model). However, it was important for us to account for pre-progression withdrawals in estimating the time for which dasatinib was likely to be taken and, as none of the studies in question included treatment discontinuation as an event in their PFS calculations (see Chapter 2, Chronic phase), it was appropriate for us to deduct such cases from our estimate.
The two available sources for this parameter for nilotinib are shown in Table 89. None of the evidence distinguishes between ImR and ImI populations, so we have had to assume that the overall withdrawal rates apply equally to both subgroups.
| Study | Dose | n | Premature discontinuations | % | 95% CI |
|---|---|---|---|---|---|
| Selected parameter | |||||
| Kantarjian et al. (2007)106 | 400 mg b.i.d. | 280 | 65 | 23.2 | 18.4% to 28.6% |
| Rejected alternatives | |||||
| Kantarjian et al. (2006)103 | Nine cohorts ranging from 50 mg q.d. to 1200 mg q.d. | 17 | 0 | 0.0 | 0.0% to 19.5% |
For our base-case model input, we have chosen to use the estimate of 23.2% from the larger Phase II study. 106 Again, this enables us to rely on a single, consistent source for our simulated cohort. In any case, the only alternative source of data (the initial dose escalation study103) was far from ideal; only a small number of patients with chronic disease were reported, the doses of nilotinib taken varied widely, and did not reflect current practice.
Of the five identified sources of data on treatment with HDI,23,53,54,182,224 three23,53,54 provide estimates of the proportion of patients who discontinued treatment for reasons other than progression or death. Results are summarised in Table 90.
| Study | Dose | n | κ | % | 95% CI |
|---|---|---|---|---|---|
| Kantarjian et al. (2003)53 | 600 mg or 800 mg | 54 | 0 | 0.0 | 0.0% to 6.6% |
| Zonder et al. (2003)224 | 600 mg or 800 mg | 16 | NR | ||
| Kantarjian et al. (2007)23 | 800 mg | 49 | 10 | 20.4 | 10.2% to 34.3% |
| Jabbour et al. (2009)182 | 800 mg | 84 | NRa | ||
| Kantarjian et al. (2009)54 | 800 mg | 106 | 21 | 19.8 | 12.7% to 28.7% |
| Simple pooled estimate | 209 | 31 | 14.8 | 10.3% to 20.4% |
Unfortunately, the clinical study from which we have taken the majority of parameter estimates for HDI (Jabbour et al. ’s 2009 publication182) does not provide details on treatment discontinuation, so we were unable to maintain consistency between inputs, as we have for the technologies under review. Because we had no strong reason for preferring any of the other candidate data sources, we have pooled the data from all available sources, giving an estimate of 14.8% for the analysis (as per the recommendations of Einarson,74 we did not attempt to synthesise these results in a meta-analysis as, in a single-arm meta-analysis, there was no validated way of dealing with zero frequencies – as seen in one data point, here – without introducing bias).
In order to maintain consistency across data sources used in the model, we have taken our input value from the control arm of the IRIS study. 17 This gives a parameter estimate of 55.5% [307/553 (95% CI 51.3% to 59.7%)]. It should be noted that this value is much higher than that seen for the other comparators; this is probably an appropriate reflection of IFN’s known susceptibility to a variety of unpleasant side effects.
Anecdotal evidence suggests that the time frame over which AEs may be tolerated with IFN before treatment is discontinued may be longer and subject to much variation. In the base-case analysis, however, withdrawals from IFN are modelled as for other treatments (i.e. assumed to occur within the first 3 months of therapy). We have explored the impact of varying the time at which withdrawal occurs in sensitivity analyses.
Post-discontinuation chronic phase treatment
Because we estimate OS for all treatments on the basis of empirical OS drawn from Jabbour et al. ’s study of HDI,182 it was important to acknowledge that the participants in that study received life-prolonging therapies (including BM transplants). Accordingly, it was necessary to account for the costs associated with this phase of the disease. To do so, we made use of data provided by BMS, in its submission to NICE. 184 On the basis of a survey of UK clinical experts, BMS estimated that likely treatment costs for patients in disease phases analogous to this one would be £1039.53 per month. Therefore, in our model, time in post-discontinuation CP incurs an additional cost of £2079.06 per 2-month cycle.
General medical management costs
Table 91 presents the frequency, unit cost and cost per 2-month model cycle for all medical management resource use.
| Item | Population | Frequency | Cost | Cost per 2-month model cycle (£) |
|---|---|---|---|---|
| Consultant outpatient visits | CP treated | Four visits/year | £121 per visita | 81 |
| CP post-discontinuation | Four visits/year | 81 | ||
| AP | One visit/month | 243 | ||
| BC | Two visits/month | 486 | ||
| BM tests | CP treated | Two tests/year | £615 per testb | 205 |
| CP post-discontinuation | None | None | ||
| AP | None | None | ||
| BC | None | None | ||
| Radiography | CP treated | None | £29 per visitc | None |
| CP post-discontinuation | None | None | ||
| AP | None | None | ||
| BC | Three/month | 175 | ||
| CT scans | CP treated | None | £103 per scand | None |
| CP post-discontinuation | None | None | ||
| AP | None | None | ||
| BC | 0.5/month | 103 | ||
| Blood transfusions | CP treated | None | £490/transfusione | None |
| CP post-discontinuation | None | None | ||
| AP | None | None | ||
| BC | One/month | 981 | ||
| Inpatient terminal care | CP treated | None | £119 q.d.f | None |
| CP post-discontinuation | None | None | ||
| AP | None | None | ||
| BC | One stay/month, each stay 3 days | 715 |
Costs associated with adverse events
As explained in Accounting for severe adverse events, we have not modelled the costs of treating patients with AEs. To test the impact of this assumption, costs of treating AEs are modelled in sensitivity analyses, using data reported by the two manufacturers, BMS and Novartis, in their submissions to NICE. 184,205
Parameter estimates: summary
Tables 92 and 93 summarise the clinical effectiveness parameter estimates employed in the PenTAG models of CML-CP in ImR and ImI populations, respectively.
| Parameter | Estimate | Source | Justification |
|---|---|---|---|
| MCyR rate – dasatinib | 58.1% | Shah et al. (2008)22 | Only available estimate at currently recommended dose of dasatinib |
| MCyR rate – nilotinib | 52.4% | Kantarjian et al. (2007)106 | Only available estimate |
| MCyR rate – HDI | 44.0% | Jabbour et al. (2009)182 | Estimates of OS, PFS and MCyR rate all originate from the same study |
| Proportion of patients who discontinue dasatinib prematurely | 10.2% | Shah et al. (2008)22 | Only available estimate at currently recommended dose of dasatinib |
| Proportion of patients who discontinue nilotinib prematurely | 23.2% | Kantarjian et al. (2007)106 | Only available estimate |
| Proportion of patients who discontinue HDI prematurely | 14.8% | Pooled estimate | Pooled from all available data |
| OS hazard ratio between people who achieve a MCyR to imatinib and those who do not | 0.370 | Pooled estimate | Pooling all data sources reduces the uncertainty in the data |
| Mean time spent in AP | 0.80 years |
Reed et al. (2004)225 Derived from survival curves published in Cervantes et al. (1996)243 |
Large, relevant data source |
| Mean time spent in BC | 1.09 years |
Reed et al. 2004225 Derived from survival curves published in Kantarjian et al. (2001)249 |
Large, relevant data source |
| Parameter | Estimate | Source | Justification |
|---|---|---|---|
| MCyR rate – dasatinib | 74.4% | Shah et al. (2008)22 | Only available estimate at currently recommended dose of dasatinib |
| MCyR rate – nilotinib | 46.5% | Kantarjian et al. (2007)106 | Only available estimate |
| MCyR rate – IFN | 22.0% | O’Brien et al. (2003)17 |
Recent, large study Estimates of OS, PFS and MCyR rate all originate from the same study |
| Proportion of patients who discontinue dasatinib prematurely | 10.2% | Shah et al. (2008)22 | Only available estimate at currently recommended dose of dasatinib |
| Proportion of patients who discontinue nilotinib prematurely | 23.2% | Kantarjian et al. (2007)106 | Only available estimate |
| Proportion of patients who discontinue IFN prematurely | 55.5% | O’Brien et al. (2003)17 |
Recent, large study Estimates of OS, PFS and MCyR rate all originate from the same study |
| OS hazard ratio between people who achieve a major cytogenetic response to imatinib and those who do not | 0.370 | Pooled estimate | Pooling all data sources reduces the uncertainty in the data |
| Mean time spent in AP | 0.80 years |
Reed et al. (2004)225 Derived from survival curves published in Cervantes et al. (1996)243 |
Large, relevant data source |
| Mean time spent in BC | 1.09 years |
Reed et al. (2004)225 Derived from survival curves published in Kantarjian et al. (2001)249 |
Large, relevant data source |
Deterministic one-way sensitivity analysis
In order to explore key aspects of the model, a wide range of deterministic one-way sensitivity analyses were performed, in which single model parameters were varied to investigate the model’s sensitivity to uncertainty associated with particular input values.
Probabilistic sensitivity analysis
Probabilistic sensitivity analysis was carried out to incorporate parameter uncertainty in the cost-effectiveness analysis.
In this approach, values for each parameter in a given run of the cost-effectiveness model are drawn at random from a specified distribution. The cost-effectiveness model was run 1000 times to generate a range of cost-effectiveness estimates. These are plotted on a cost-effectiveness plane and used to construct a cost-effectiveness acceptability curve, which shows the probability that a technology will be considered cost-effective given a particular WTP for an additional QALY.
Table 94 reports the values used to define the probabilistic sensitivity analysis and includes the mean values employed in the deterministic analysis described earlier. Note, that we did not model uncertainty in the dose intensity of cytarabine for two reasons: first, because these data were unavailable and, second, because the very low cost of cytarabine makes this variable a limited source of uncertainty.
| Parameter type | Parameter | Comparator | Mean (unless otherwise stated) (SE) | Statistical distribution |
|---|---|---|---|---|
| Utilities | CP | Dasatinib | 0.85 (0.004) | Beta |
| Nilotinib | 0.85 (0.004) | |||
| HDI | 0.85 (0.004) | |||
| IFN |
0.71 (0.008) on treatment 0.85 (0.004) post discontinuation |
|||
| AP | All | 0.73 (0.06) | ||
| BC | All | 0.52 (0.08) | ||
| Costs (£) | District nurse visit for administration of IFN | All | 27 (3)a | Gamma |
| Consultant outpatient visits | 121 (12) per visita | |||
| BM tests | 615 (62) per testa | |||
| Radiographs | 29 (2) per visitb | |||
| CT scans | 103 (3) per scanb | |||
| Blood transfusions | 490 (49) per transfusiona | |||
| Inpatient terminal care | 119 (7) q.d.b | |||
| Dose intensities | Dasatinib |
100% (100 mg q.d.) (18–150) SE = 2.0%c |
Normal | |
| Nilotinib |
99.7% (797 mg q.d.) (151–1112) SE = 1.3%c |
|||
| HDI |
92.3% (738 mg q.d.) SE = 1.3% |
|||
| IFN | 55.5% (median dose = 4.8 MU q.d.) (0.6–11.3 MU q.d.) SE = 0.9%c | |||
| Cytarabine | Not reported in IRIS RCT,17 but 29% never received cytarabine. SE = 0%d | |||
| PFS | ImR | Dasatinib | At 2 years, 0.77 (0.038)e | |
| Nilotinib | At 1.58 years, 0.626 (0.035)e | |||
| HDI | At 5 years, 0.24 (0.047)e,f | |||
| ImI | Dasatinib | At 2 years, 0.87 (0.051)e | ||
| Nilotinib | At 1.59 years, 0.829 (0.041)e | |||
| ImR or ImI | IFN | At 1.75 years, 0.71 (0.038)e | ||
| OS | Calibration point from HDI study | All | At 5 years, 0.675 (0.051)e | Beta |
| MCyR rates | ImR | Dasatinib | 58.1% (4.4%) | Normal |
| Nilotinib | 52.4% (3.6%) | |||
| HDI | 44.0% (5.4%) | |||
| ImI | Dasatinib | 74.4% (6.7%) | ||
| Nilotinib | 46.5% (5.4%) | |||
| ImR or ImI | IFN | 22.1% (1.8%) | ||
| Hazard ratio responders vs non-responders | All | 0.370 (95% CI 0.156 to 0.876) | Log-normal |
Uncertainty in PFS for all treatments was modelled by considering the uncertainty in PFS at a certain single time point. This uncertainty was estimated from Peto’s formula. 250 For all treatments except HDI, uncertainty in PFS was modelled by allowing the parameter of the exponential distribution to vary in such a way that the PFS probability at the single time point varied as a beta distribution. For HDI, the same method was adopted, but fixing the parameter gamma of the Weibull distribution and varying the parameter lambda.
Uncertainty in OS for all treatments was modelled in the following ways. First, the CyR rates for all treatments were varied according to a normal distribution. Second, the hazard ratio between responders and non-responders was varied as a log-normal distribution. Third, uncertainty in the empirical OS data for HDI was modelled by considering the uncertainty in OS at a certain single time point, again estimated from Peto’s formula. 250 In this case, the parameter gamma of the Weibull distribution was fixed and the parameter lambda was allowed to vary in such a way that the OS probability at the single time point varied as a beta distribution.
Summary of model assumptions
Box 8 provides a summary of the key assumptions adopted in our model.
OS can be predicted on the basis of MCyR; and
-
the relationship between MCyR and OS is the same for all treatments
-
timing, duration and depth of CyR do not modify the relationship
-
the relative difference (hazard ratio) in OS related to MCyR seen in studies of first-line therapy with normal-dose imatinib was transferable to the treatments under review in the second-line setting
-
the OS experience of ImR individuals taking HDI can be used to calibrate the surrogate relationship between MCyR and OS for all comparators in ImR and ImI CML
-
the hazard ratio between responders and non-responders remains constant over time; and
-
MCyR rates for each treatment, measured in differing populations in differing observational studies, can be treated as a homogeneous measure of treatment effect.
Duration of treatment can be estimated on the basis of PFS with a deduction to account for premature discontinuations; and
-
premature discontinuations typically occur 3 months after commencement of treatment
-
time from premature discontinuation to disease progression can be estimated by PFS seen in individuals taking the least effective treatment in the evidence base (IFN)
-
PFS, measured according to differing criteria in differing populations in differing observational studies, can be treated as a homogeneous measure of time on treatment; and
-
it is reasonable to extrapolate very immature PFS data many years into the future.
Following disease transformation, time spent in AP and BC is independent of CP treatment, so is identical between comparators.
Treatment-related AEs incur no utility decrement and no additional costs.
Utility values estimated for individuals taking normal-dose imatinib in a first-line setting are transferable to those taking dasatinib, nilotinib or HDI following failure of normal-dose imatinib.
Utility for post-discontinuation CP is the same as that for CP on treatment (except for IFN).
The PenTAG cost-effectiveness analysis: results
The following section presents the cost-effectiveness results from the PenTAG model and is divided into two parts. A summary of the cost–utility results for the ImR CP CML model is shown in Box 9. First, we present the model outputs for individuals who are resistant to normal-dose imatinib and, second, the outputs for those who are intolerant of normal-dose imatinib. For each of these, we first present and discuss the base-case results, show validation analysis for the model and then describe the sensitivity analyses carried out.
Our deterministic and probabilistic results make it appear unlikely that dasatinib would be considered to provide an acceptable cost–utility balance.
In our base-case deterministic analysis:
-
our model predicts that dasatinib will typically be taken for far longer than the other technologies under review, so incurs much higher drug acquisition costs; however,
-
this additional expenditure was not counterbalanced by an equivalent effectiveness gain, with dasatinib providing ≯ 3 extra quality-adjusted months compared with nilotinib; accordingly,
-
dasatinib was estimated to have a very high cost–utility ratio, costing over a £250,000 for every additional QALY gained.
-
One-way sensitivity analyses suggest that it was difficult to explain this finding on the basis of the uncertainty attached to single parameters alone, with the exception that, if dasatinib was assumed to be taken for a similar amount of time as was predicted for its comparators, it would dominate HDI.
Dasatinib provided the best value for money in a very small proportion of our probabilistic simulations, and only then when high levels of WTP were assumed.
Results for nilotinib suggest that it is likely to be considered good value for money.
In our base-case deterministic analysis:
-
we estimate that nilotinib dominates HDI; and
-
one-way sensitivity analyses suggest that this preliminary finding was subject to little parameter uncertainty. However, if treatment duration was assumed to be much longer, as it was with dasatinib, nilotinib’s ICER compared with HDI rises to over £100,000 per QALY.
In our probabilistic analysis:
-
both nilotinib and dasatinib are predicted to be more effective than HDI in a substantial majority of simulations; however,
-
it seems clear that dasatinib was predicted to cost more than HDI, whereas nilotinib was invariably estimated to cost less.
-
As a result, according to our model predictions, nilotinib was most likely to be the most cost-effective option at all investigated WTP thresholds.
However, the above sensitivity analyses only encompass parameter uncertainty. In addition, our model was subject to very substantial structural uncertainty. Moreover, it was necessarily parameterised on the basis of a heterogeneous collection of observational data, in which the outcome measures on which we rely have been defined and measured in different ways, at different times and in different populations.
It was very noticeable that estimated treatment duration was absolutely crucial in determining cost–utility outputs. When any of the technologies being compared are assumed to have dasatinib’s long treatment period, they do not appear cost-effective; when they are assumed to be taken for shorter periods of time – as our model predicts for nilotinib – they tend to suggest good value for money.
In view of the paucity of data available and the many assumptions made in our analysis (see Analytic approach and Summary of model assumptions), we would caution at the outset that the analysis should been seen as exploratory rather than definitive.
Imatinib-resistant chronic myeloid leukaemia
Below, we present the results of our model for ImR CML. Three treatments are considered: dasatinib, nilotinib and HDI. Our model also estimates the costs and effects of an older standard-of-care treatment (IFN + cytarabine) in this population; however, because our advice has been that IFN is not a realistic comparator in clinical practice, we have not presented our results here. The outputs of our model including IFN are shown separately in Appendix 8.
Base-case model outputs for imatinib-resistant chronic myeloid leukaemia
Table 95 presents the aggregated totals for the base-case model results for the three treatments. Outputs are shown for total-life years (undiscounted) and total discounted QALYs and costs for each treatment over the time horizon of the model.
| Parameter | Dasatinib | Nilotinib | HDI |
|---|---|---|---|
| Life-years (mean) (undiscounted) | |||
| CP treated | 6.50 | 2.44 | 2.68 |
| CP post discontinuation | 5.00 | 8.65 | 7.79 |
| AP | 0.80 | 0.80 | 0.80 |
| BC | 1.09 | 1.09 | 1.09 |
| Total (mean) | 13.40 | 12.98 | 12.37 |
| Total (median) | 10.76 | 10.21 | 9.45 |
| QALYs (mean) (discounted) | |||
| CP treated | 4.50 | 1.89 | 2.10 |
| CP post discontinuation | 2.62 | 5.00 | 4.46 |
| AP | 0.37 | 0.38 | 0.38 |
| BC | 0.36 | 0.36 | 0.37 |
| Total | 7.85 | 7.63 | 7.31 |
| Costs (mean) (discounted) (£) | |||
| Drug costs | 161,432 | 70,143 | 88,883 |
| Drug administration | 0 | 0 | 0 |
| Monitoring OP appointment | 6818 | 6728 | 6597 |
| BM tests | 6518 | 2732 | 3038 |
| Radiographs | 726 | 736 | 752 |
| CT scans | 428 | 434 | 444 |
| Blood transfusions | 4058 | 4117 | 4205 |
| Third-line CP treatment | 38,386 | 73,436 | 65,429 |
| Inpatient palliative care | 2960 | 3003 | 3067 |
| Total (£) | 221,325 | 161,330 | 172,415 |
The model estimates that all three treatments result in relatively similar survival gains, with median OS ranging from 9.45 years for HDI to 10.76 years for dasatinib, with nilotinib predicted to lie between the two new technologies. This order of OS reflects the relative proportion of patients with a MCyR for each treatment (see Major cytogenetic response rates). Once expected lifespan is quality adjusted and discounted, the difference is minimised further, with only around 6 quality-adjusted months separating all three comparators. Notwithstanding the similarity in predicted OS, there is substantial heterogeneity in the constituent elements of the predicted lifespans. In particular, the amount of time each cohort is expected to spend in pre-progression CP varies notably; individuals taking dasatinib are predicted to spend an average of 6.5 years before progression, whereas those taking either nilotinib or HDI spend less than half as long in the same state. This difference is counterbalanced by time in post-progression CP, which is predicted to last an average of 5 years for the dasatinib cohort, compared with around 8 years for those taking either nilotinib or HDI. As per the model assumptions (see Method of estimating time in accelerated phase and blast crisis), time in AP and BC is essentially the same across all comparators (although very small discrepancies in QALYs may result from the discounting process).
These results are illustrated in Figure 15, which shows the relative proportions of patients in each health state for each treatment throughout the time horizon of the model. The total duration in each health state for each treatment (as reported in Table 95) is represented in these graphs by the area under each curve. Accordingly, the duration for patients receiving treatment in CP is represented by the area underneath the dotted line, and the area between the dotted line and the solid OS curve represents the sum of post-progression CP, AP and BC. As would be expected, virtually all patients are predicted to have died by 40 years from start of treatment (i.e. by age 96 years), regardless of treatment. Notice that the predicted time on treatment falls steeply at 3 months for nilotinib and HDI, because of the large numbers of patients who stop treatment owing to serious AEs.
FIGURE 15.
Base-case cohort composition over time by treatment: ImR.
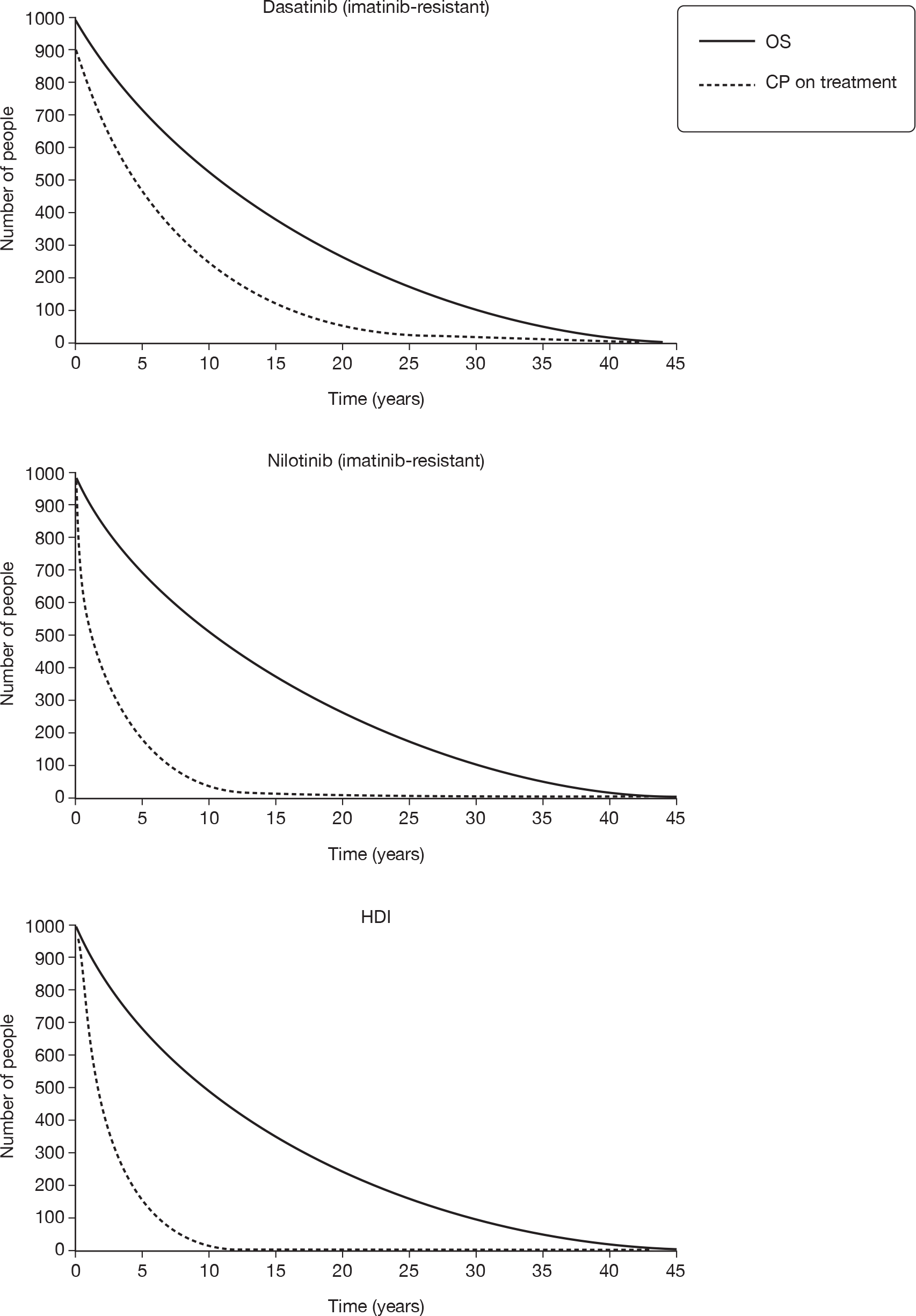
It can also be seen that, as explained above, the proportion of time that individuals are predicted to spend in CP taking dasatinib (i.e. prior to discontinuation) is substantially greater than the equivalent period for nilotinib and HDI. Note, however, that the expected time on treatment is highly uncertain owing to the extensive extrapolation of PFS (see sensitivity analyses in Deterministic sensitivity analysis).
The impact of this discrepancy can be seen in the predicted costs shown in Table 95. The nilotinib and HDI arms accrue costs a little over £160,000 and £170,000, respectively, per simulated patient over the course of the model, but treatment with dasatinib was estimated to incur lifetime costs around £50,000–60,000 higher than this. This situation arises because, in line with the time in pre-progression CP discussed above, our model predicts that individuals tend to take dasatinib for twice as long as nilotinib or HDI. Accordingly, in the breakdown in Table 95, it can be seen that the overall heterogeneity in costs is almost entirely ascribable to differences in (a) the acquisition costs of the drugs themselves over the time they are taken and (b) the cost of post-discontinuation–pre-transformation therapy.
Figure 16 shows the OS curves for each of the three treatments overlaid, as well as showing the generic OS curves for patients with a MCyR versus those with no response. The general survival curve for the equivalent aged non-CML population is also shown. The OS curves for dasatinib, nilotinib and HDI are represented by an asterisk, and can be seen to be very closely aligned.
FIGURE 16.
Predicted OS for ImR people by treatment and for responders and non-responders.* OS curves for dasatinib, nilotinib and HDI.
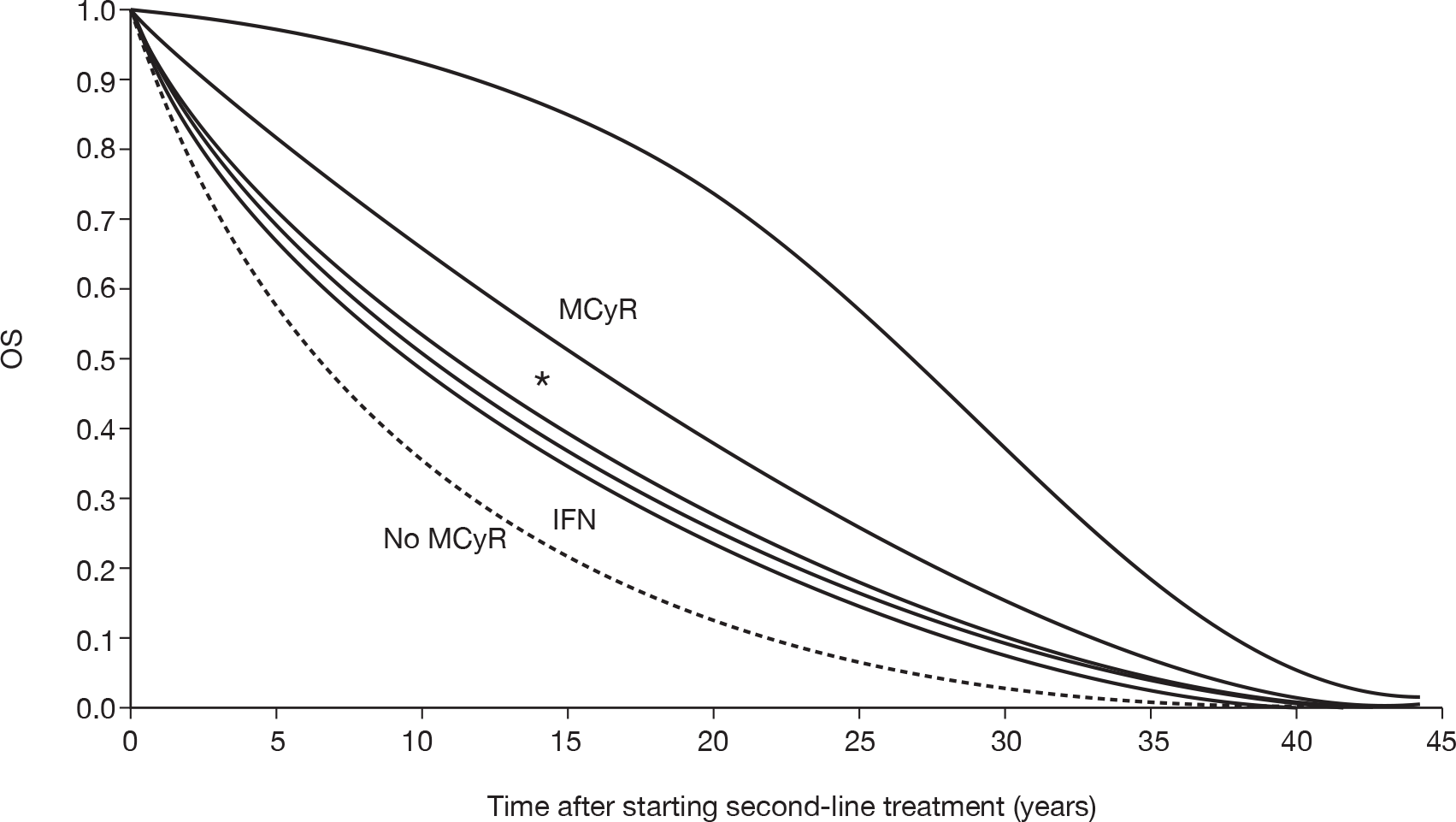
Base-case deterministic cost–utility results
The incremental cost–utility of dasatinib, nilotinib and HDI as estimated in our model is shown in Table 96, with the results depicted on the cost–utility plane in Figure 17.
| Drug | Cost (£)a | Utility (QALY) | Incremental cost (£) | Incremental utility (QALY) | Incremental £/QALY (ICER)b |
|---|---|---|---|---|---|
| Nilotinib | 161,300 | 7.630 | |||
| HDI | 172,400 | 7.311 | 11,100 | –0.318 | HDI dominated by nilotinib |
| Dasatinib | 221,300 | 7.846 | 60,000 | 0.216 | 277,698 |
FIGURE 17.
Deterministic base-case incremental cost–utility for ImR CML: cost–utility plane. C-E, cost-effectiveness.
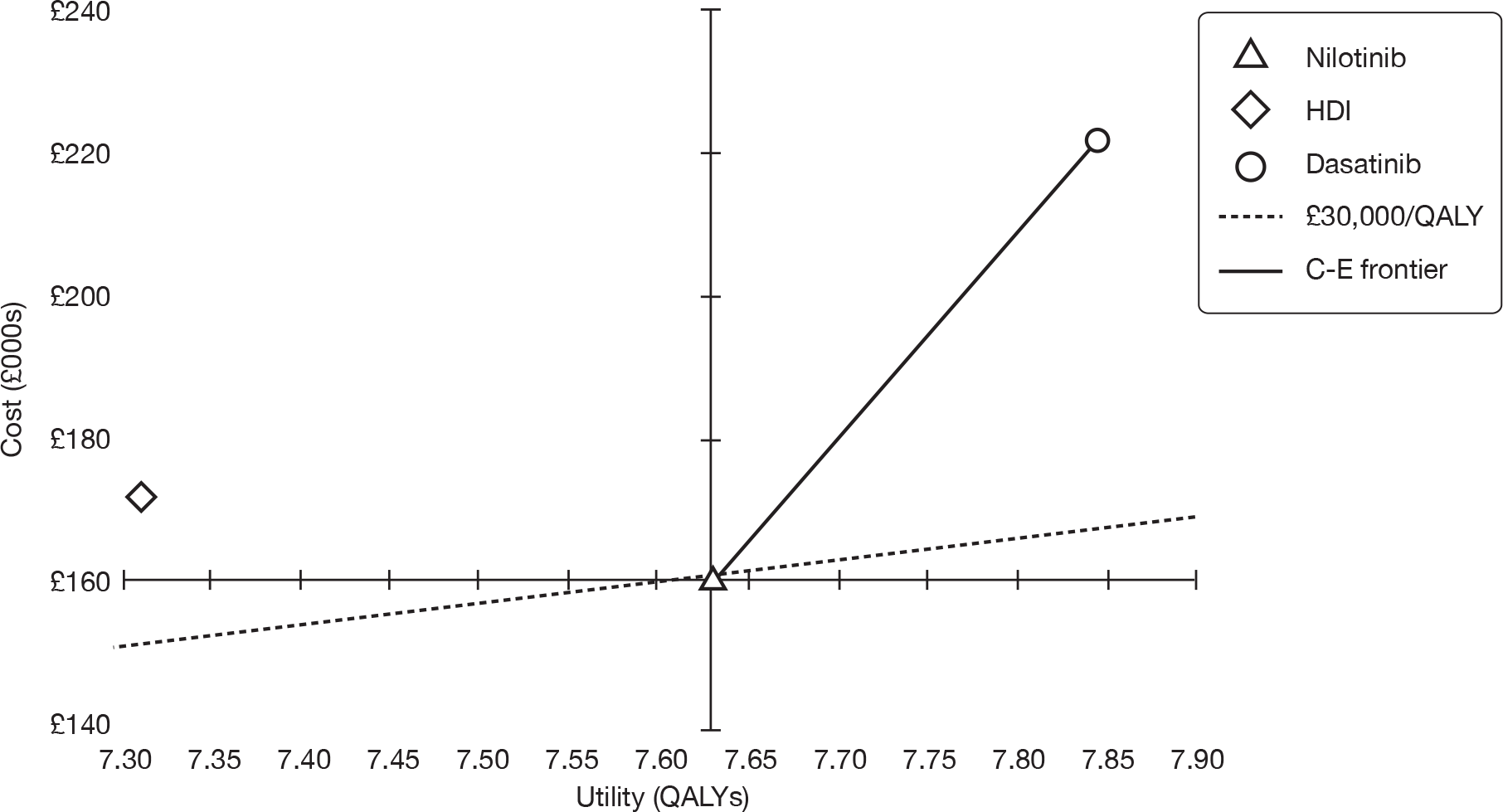
Because it was the least costly of the available alternatives, nilotinib was considered to be the base option. HDI was not predicted to be a viable option, because it was both more costly and less effective than nilotinib (i.e. it was dominated). In comparison with nilotinib, dasatinib was predicted to provide a small QALY gain (equivalent to around 80 days in perfect health). However, substantial additional costs of £60,000 per patient were also estimated, with the result that dasatinib was predicted to provide incremental benefit at a cost of over £250,000 per QALY (as reflected in the steep gradient in Figure 17).
Model validation: model outputs compared with study data
Progression-free survival
Figure 18 shows the actual data for PFS versus the fitted model curve for each of the three modelled treatments. From this it can be seen that our model, in general, achieves a relatively close fit between the study data and the fitted curves in the model.
FIGURE 18.
Empirical versus predicted PFS (ImR).
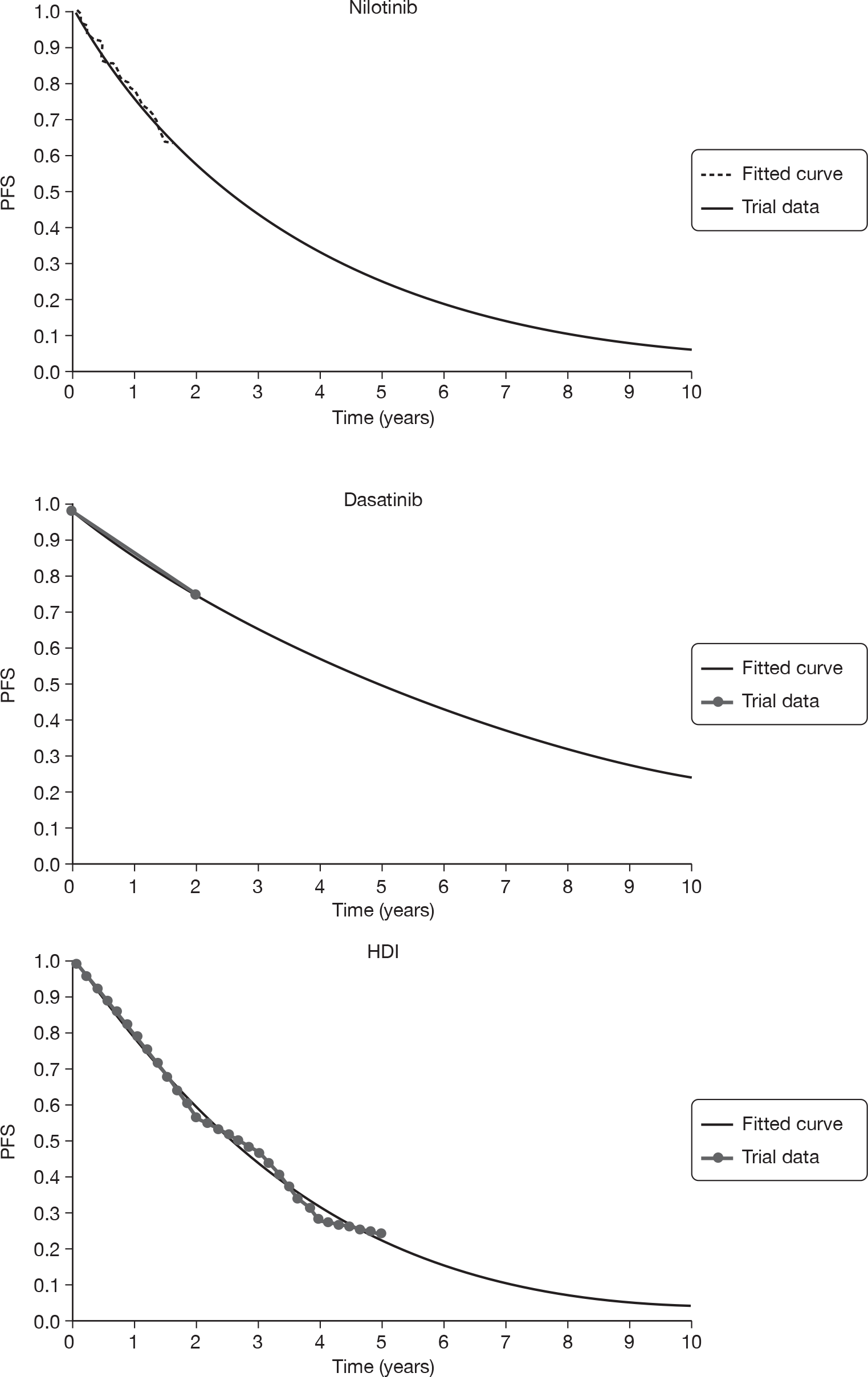
Overall survival
Figure 19 shows the actual data for OS versus the fitted model curve for each of the three modelled treatments. The modelled OS for HDI was fitted to empirical study data, so a very close fit between the actual and the predicted OS for HDI was obtained. The predicted OS for dasatinib and nilotinib, however, was modelled completely independently of the empirical OS for these treatments (because the empirical OS data set was very immature). Despite this, however, we found that the OS curves from our model predict the empirical data well for the short period of the study follow-up.
FIGURE 19.
Empirical versus predicted OS (ImR).
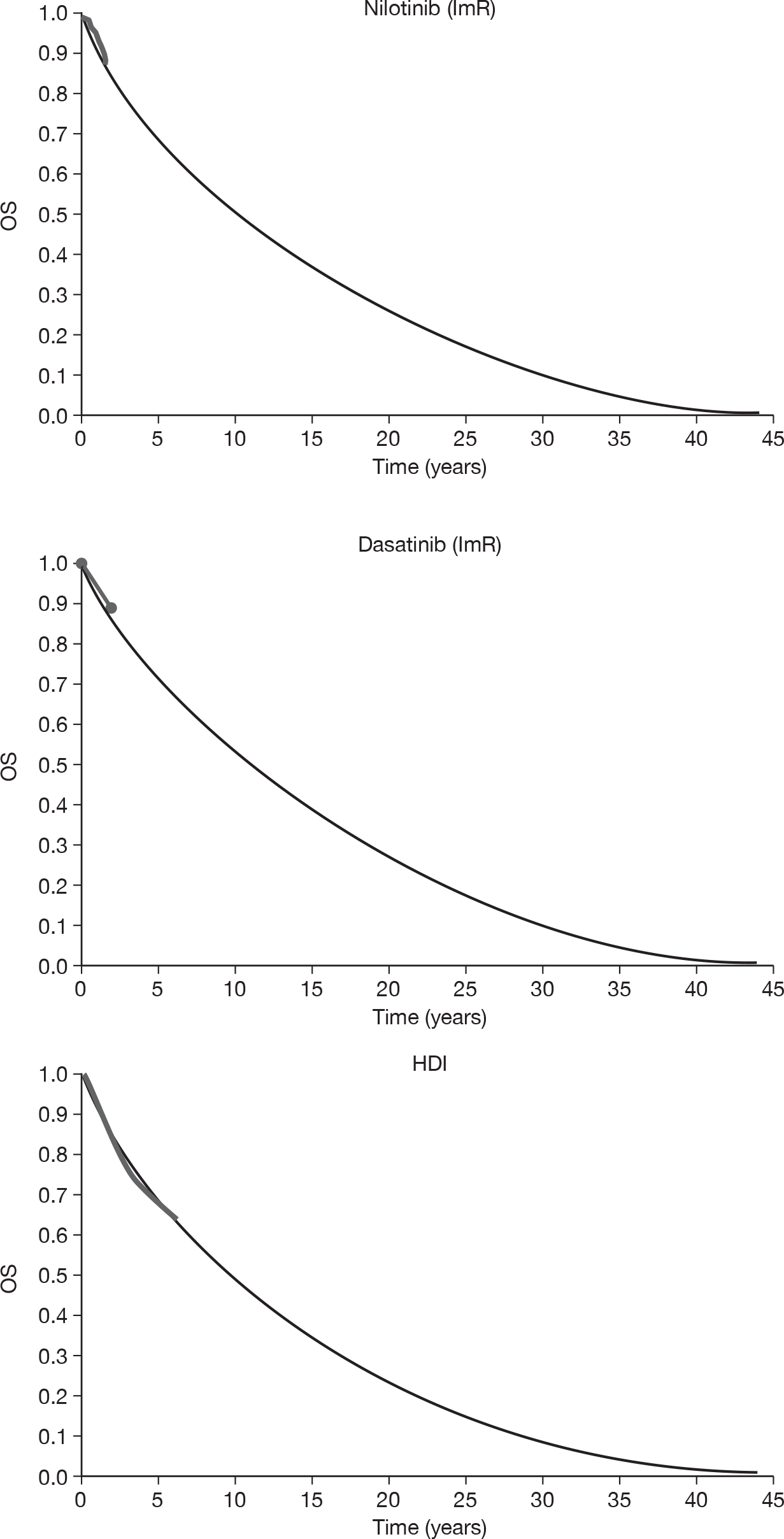
Deterministic sensitivity analysis
Nilotinib versus high-dose imatinib
One-way deterministic sensitivity analyses for nilotinib versus HDI are reported in Table 97, which shows the impact on the deterministic ICER of various specified alterations in model parameters. The same information is presented in a tornado diagram in Figure 20, but these data were presented in terms of incremental net (monetary) benefit (INB). This was a more stable metric than the ICER, when differences between comparators are small, so it provides a more consistent basis on which to visualise the model’s sensitivity to parameter alterations. INB values > £0 indicate that the technology would be considered to provide a positive balance of costs and benefits, assuming a given WTP threshold (which, for the purposes of this analysis, is fixed at £30,000 per QALY). Negative values show that the technology would be considered to incur excessive costs, for the additional benefit it provides.
| Parameter | Base case | Sensitivity analysis | ICER |
|---|---|---|---|
| Base case | NA | NA | Nilotinib dominates |
| General | |||
| Discounting | 3.5% p.a. costs and benefits | 0% p.a. costs and benefits | Nilotinib dominates |
| Effectiveness | |||
| Time in post-progression survival | 9.7 years HDI, 10.5 years nilotinib | Nilotinib and HDI value equal to HDI | £113,861a |
| Dose intensity | HDI 92%, nilotinib 100% | HDI 100%, nilotinib 100% | Nilotinib dominates |
| HDI 72%, nilotinib 80% (both reduced by 20%) | Nilotinib dominates | ||
| MCyR rates | Nilotinib 52.4% | Nilotinib 45.4% (lower 95% CI) | Nilotinib dominates |
| Nilotinib 59.4% (upper 95% CI) | Nilotinib dominates | ||
| HDI 44.0% | HDI 33.4% (lower 95% CI) | Nilotinib dominates | |
| HDI 54.6% (upper 95% CI) | £201,854a | ||
| HDI 24.1% [lowest estimate identified: Kantarjian et al. (2003)53] | £407 | ||
| Nilotinib 52.4%, HDI 44% | Nilotinib 48.5%, HDI 52.4% | £121,575a | |
| OS HDI at 5 years | 0.675 | 0.575 (lower 95% CI) | Nilotinib dominates |
| 0.775 (lower 95% CI) | Nilotinib dominates | ||
| Hazard ratio responders vs non-responders | 0.370 (pooled mean) | 0.127 [lowest estimate identified: Kantarjian et al. (2006)236] | Nilotinib dominates |
| 0.156 (lower 95% of pooled estimate) | Nilotinib dominates | ||
| 0.876 (upper 95% of pooled estimate) | Nilotinib dominates | ||
| 0.893 [highest estimate identified: Kantarjian et al. (2004)251] | Nilotinib dominates | ||
| Time in AP and BC | 0.8 years AP, 1.1 years BC | Half: 0.4 years AP, 0.5 years BC | Nilotinib dominates |
| Double: 1.6 years AP, 2.2 years BC | Nilotinib dominates | ||
| Age starting second-line treatment | 56 years | 52 years | Nilotinib dominates |
| 60 years | Nilotinib dominates | ||
| Costs | |||
| PFS | Nilotinib PFS probability at 1.58 years = 0.63 | 0.56 (lower 95% CI) | Nilotinib dominates |
| 0.69 (upper 95% CI) | Nilotinib dominates | ||
| Equal to dasatinib PFS | £127,899 | ||
| Equal to HDI PFS | Nilotinib dominates | ||
| HDI lambda = 0.22 | HDI lambda = 0.15 (lower 95% CI) | Nilotinib dominates | |
| HDI lambda = 0.30 (upper 95% CI) | £11,298 | ||
| Premature discontinuation rate | 23.2% nilotinib, 14.8% HDI | 0% nilotinib, 0% HDI | Nilotinib dominates |
| Time treatment stops for patients who discontinue prematurely | 3 months | 1 month | Nilotinib dominates |
| 5 months | Nilotinib dominates | ||
| Medical management costs | Half all unit costs or frequencies of use | Nilotinib dominates | |
| Double all unit costs or frequencies of use | Nilotinib dominates | ||
| Third-line treatment cost | £1040/month | Zero | Nilotinib dominates |
| AE costs | None | (£279 per patient HDI, £238 nilotinib) Novartis’s assumption | Nilotinib dominates |
| Health-state utilities | |||
| CP on treatment | 0.85 for nilotinib and HDI | 0.76 nilotinib, 0.76 HDI (BMS 0.85 response, 0.68 no response) | Nilotinib dominates |
| CP no treatment | 0.85 | 0.70 | Nilotinib dominates |
| AP | 0.73 | 0.60 | Nilotinib dominates |
| BC | 0.52 | 0.40 | Nilotinib dominates |
FIGURE 20.
Tornado diagram: nilotinib versus HDI for ImR patients.
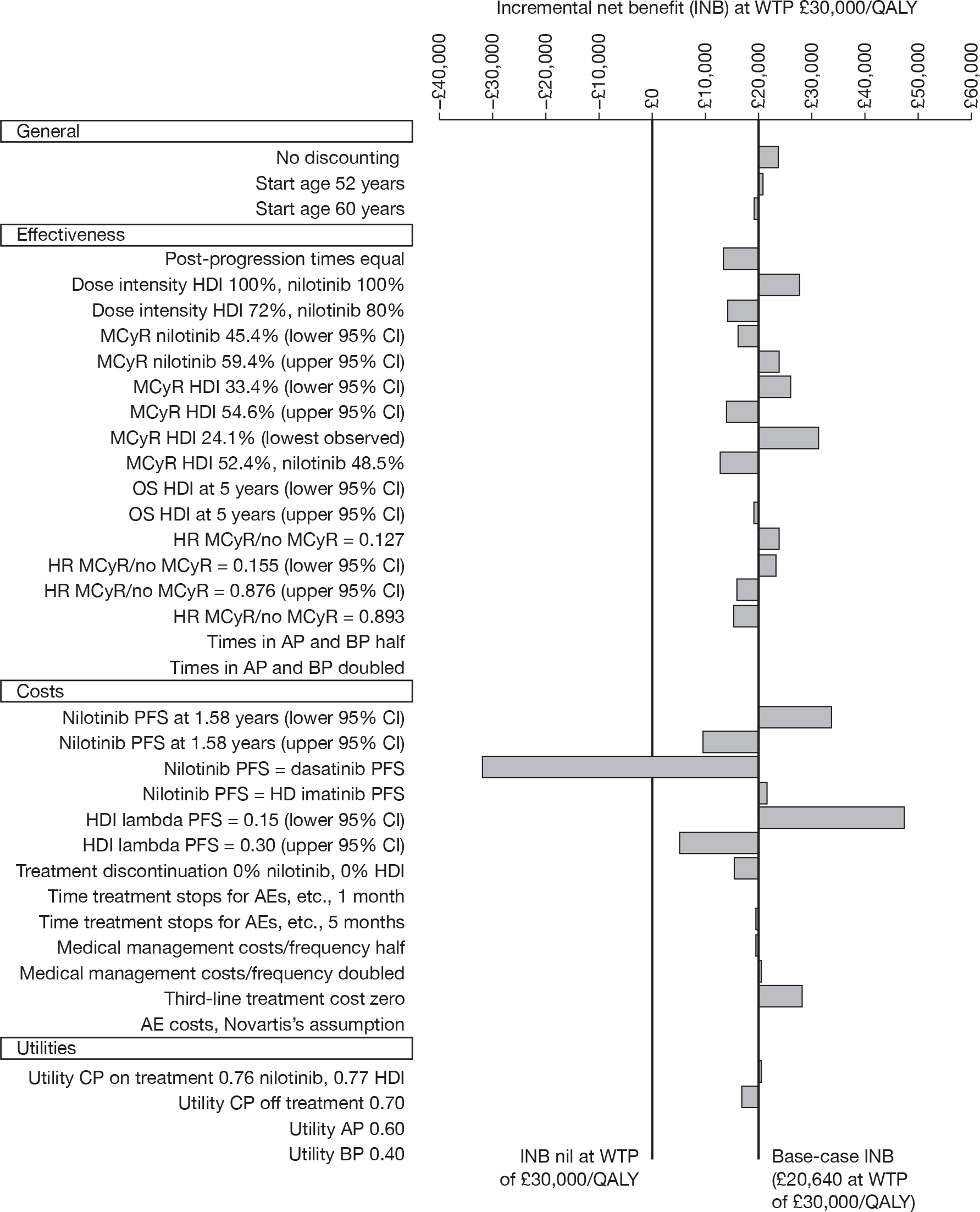
In the majority of cases, parameter alterations did not influence nilotinib’s dominance of HDI. There were six exceptions. In three instances, nilotinib was estimated to be both less costly and less effective than HDI (i.e. in the south-west quadrant of the cost–utility plane). In each case, the cost saving was substantially greater than the QALY loss (assuming conventional levels of WTP), so nilotinib would still be considered to provide good value for money, if normal decision-making rules can be assumed to apply. Three further analyses resulted in nilotinib being estimated to be more expensive than HDI. In two of these cases, an effectiveness benefit that would normally be considered to outweigh the marginal cost increase was also seen (i.e. ICERs < £12,000). Only in one analysis was the ICER increased to a level that would not meet conventional cost-per-QALY thresholds. This was where we assumed PFS with nilotinib was identical to that with dasatinib, thereby making treatment duration approximately equal. It was unsurprising that this alteration has a very substantial influence on the estimated cost–utility of nilotinib, in view of the base-case model outputs, in which duration of treatment (and, hence, the cost of treatment) is very much longer for dasatinib than for the other comparators (see Base-case model outputs for imatinib-resistant CML).
Dasatinib versus high-dose imatinib
One-way deterministic sensitivity analyses for dasatinib versus HDI are reported in Table 98, which shows the impact on the deterministic ICER of various specified alterations in the model parameters. The same information is presented in a tornado diagram in Figure 21 (again, as INB assuming WTP of £30,000 per QALY).
| Parameter | Base case | Sensitivity analysis | ICER (£) |
|---|---|---|---|
| Base case | NA | NA | 91,499 |
| General parameters | |||
| Discounting | 3.5% p.a. costs and benefits | 0% p.a. costs and benefits | 81,899 |
| Effectiveness | |||
| Time in post-progression survival | 9.7 years HDI, 6.9 years dasatinib | Dasatinib and HDI value equal to HDI | 43,174 |
| Dose intensity | HDI 92%, dasatinib 100% | HDI 100%, dasatinib 100% | 77,530 |
| HDI 72%, dasatinib 80% (both reduced by 20%) | 67,599 | ||
| Dasatinib clinical data | Shah et al. (2008)22 | Kantarjian et al. (2007) comparative study236 | 322,764 |
| Hochhaus et al. (2007)11,105 | 161,862 | ||
| MCyR rates | Dasatinib 58.1% | Dasatinib 49.4% (lower 95% CI) | 213,713 |
| Dasatinib 66.8% (upper 95% CI) | 62,450 | ||
| Dasatinib 100% (maximum possible) | 34,474 | ||
| HDI 44.0% | HDI 33.4% (lower 95% CI) | 59,734 | |
| HDI 54.6% (upper 95% CI) | 318,492 | ||
| HDI 24.1% [lowest estimate identified: Kantarjian et al. (2003)53] | 48,332 | ||
| Dasatinib 58.1%, HDI 44% | Dasatinib 53.2%, HDI 52.4% | 1,340,016 | |
| OS for HDI at 5 years | 0.675 | 0.575 (lower 95% CI) | 89,251 |
| 0.775 (lower 95% CI) | 106,036 | ||
| Hazard ratio responders vs non-responders | 0.370 (pooled mean) | 0.127 [lowest estimate identified: Kantarjian et al. (2006)238] | 57,446 |
| 0.156 (lower 95% of pooled estimate) | 60,534 | ||
| 0.876 (upper 95% of pooled estimate) | 559,519 | ||
| 0.893 [highest estimate identified: Kantarjian et al. (2004)251] | 651,700 | ||
| Time in AP and BC | 0.8 years AP, 1.1 years BC | Half: 0.4 years AP, 0.5 years BC | 92,312 |
| Double: 1.6 years AP, 2.2 years BC | 90,028 | ||
| Age starting second-line treatment | 56 years | 52 years | 87,436 |
| 60 years | 96,213 | ||
| Costs | |||
| PFS | Dasatinib PFS probability at 2 years = 0.77 | 0.70 (lower 95% CI) | 46,664 |
| 0.84 (upper 95% CI) | 158,503 | ||
| Equal to nilotinib PFS | Dasatinib dominates | ||
| Equal to HDI PFS | Dasatinib dominates | ||
| HDI lambda = 0.22 | HDI lambda = 0.15 (lower 95% CI) | 39,804 | |
| HDI lambda = 0.30 (upper 95% CI) | 118,969 | ||
| Premature discontinuation rate | 10.2% dasatinib, 14.8% HDI | 0% dasatinib, 0% HDI | 78,899 |
| Time treatment stops for patients who discontinue prematurely | 3 months | 1 month | 92,010 |
| 5 months | 90,973 | ||
| Medical management costs | Half all unit costs or frequencies of use | 88,315 | |
| Double all unit costs or frequencies of use | 97,867 | ||
| Third-line treatment cost | £1040/month | Zero | 142,090 |
| AE costs | None | £279 per patient HDI, £296 dasatinib (BMS assumption) | 91,527 |
| Health-state utilities | |||
| CP on treatment | 0.85 for dasatinib and HDI | 0.77 dasatinib, 0.76 HDI (BMS 0.85 response, 0.68 no response) | 146,879 |
| CP no treatment | 0.85 | 0.70 | 56,890 |
| AP | 0.73 | 0.60 | 91,091 |
| BC | 0.52 | 0.40 | 90,987 |
FIGURE 21.
Tornado diagram: dasatinib versus HDI for ImR patients.
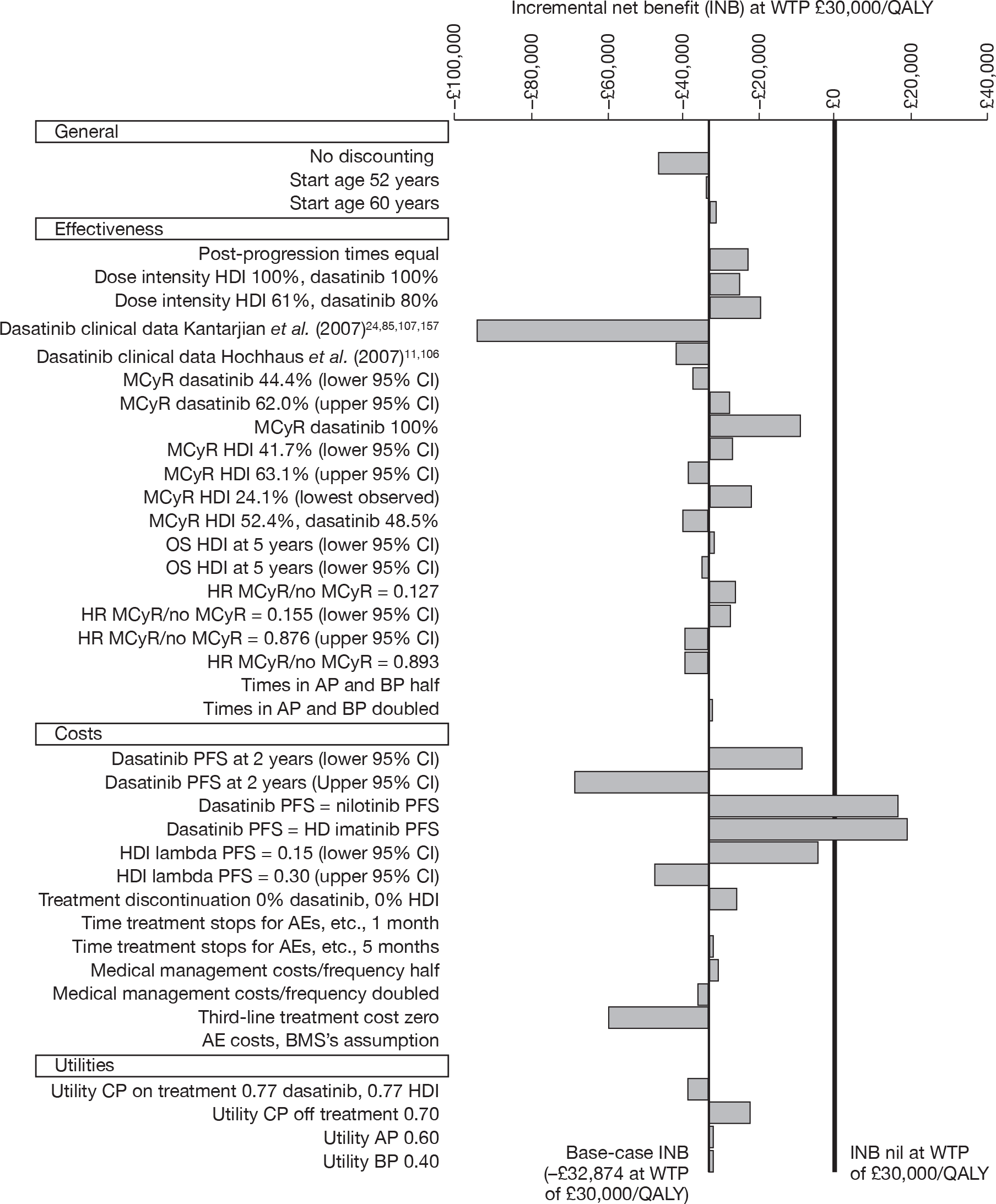
It can be seen that most of the parameter variations resulted in model outputs that would fail to meet conventional standards of acceptable balance between costs and QALYs for dasatinib, as would be evident in the ICER versus HDI falling below £30,000 per QALY (and, concomitantly, the INB becoming positive). There were two exceptions; when we assumed that PFS with dasatinib was identical to that seen with either nilotinib or HDI (and, therefore, that treatment duration was similar for all modelled treatments, and much shorter than our base-case estimate for dasatinib), model outputs were overturned, and dasatinib was predicted to dominate HDI.
In addition, testing the upper limit of estimated PFS for HDI (lower 95% CI of lambda of fitted Weibull curve) resulted in an ICER of just < £40,000. Again, this is in keeping with our finding that incremental cost–utility is overwhelmingly driven by differences in estimated treatment duration. By assuming that individuals take HDI for longer, the difference between comparators was diminished, and the ICER falls from a very high level to one that approaches conventional standards of reasonable costs per QALY gained.
Finally, when we assumed that every single individual taking dasatinib achieved an MCyR, the ICER fell to £34,474, which suggests that any underestimate of treatment effect for dasatinib – while important – was not, on its own, quite enough to bring our estimate of cost–utility below the £30,000 per QALY threshold.
We chose to use clinical data for dasatinib from Shah et al. 22 because patients in this study took dasatinib at the correct dose of 100 mg q.d. (see Chapter 2, Design and characteristics of included studies). However, when we take all the dasatinib clinical effectiveness data from the two other studies of dasatinib, in which patients took dasatinib at 140 mg q.d. (Kantarjian et al. 11,105 and Hochhaus et al. 17), the ICER becomes even less favourable to dasatinib.
Probabilistic sensitivity analyses
We ran 1000 Monte-Carlo simulations, varying model input parameters simultaneously, to estimate the impact of parameter uncertainty on estimated cost–utility. In each iteration, parameters are randomly sampled from pre-defined distributions reflecting the precision of each input value (for effectiveness parameters, this was usually defined in terms of the 95% CI around data drawn from the literature).
The scatterplot shown in Figure 22(a) depicts the results of each simulation, in terms of the incremental cost–utility of dasatinib (+s) and nilotinib (×s) compared with HDI. Data points appearing on the right-hand side of the y-axis represent simulations in which the technology in question was predicted to be more effective than HDI, those appearing on the left generated fewer QALYs. Similarly, the area above the plot’s x-axis represents simulations in which the technologies were estimated to cost more than HDI, and data points appearing below the line are predicted to be cost-saving, when compared with HDI.
FIGURE 22.
Probabilistic sensitivity analyses: incremental cost–utility (ImR CML). a, Cost–utility plane, showing incremental cost–utility of dasatinib and nilotinib compared with a common baseline of HD in 1000 iterations of probabilistic sensitivity analysis. b, CEAC, showing probability that each treatment is the most cost-effective (delivers highest net monetary benefit).
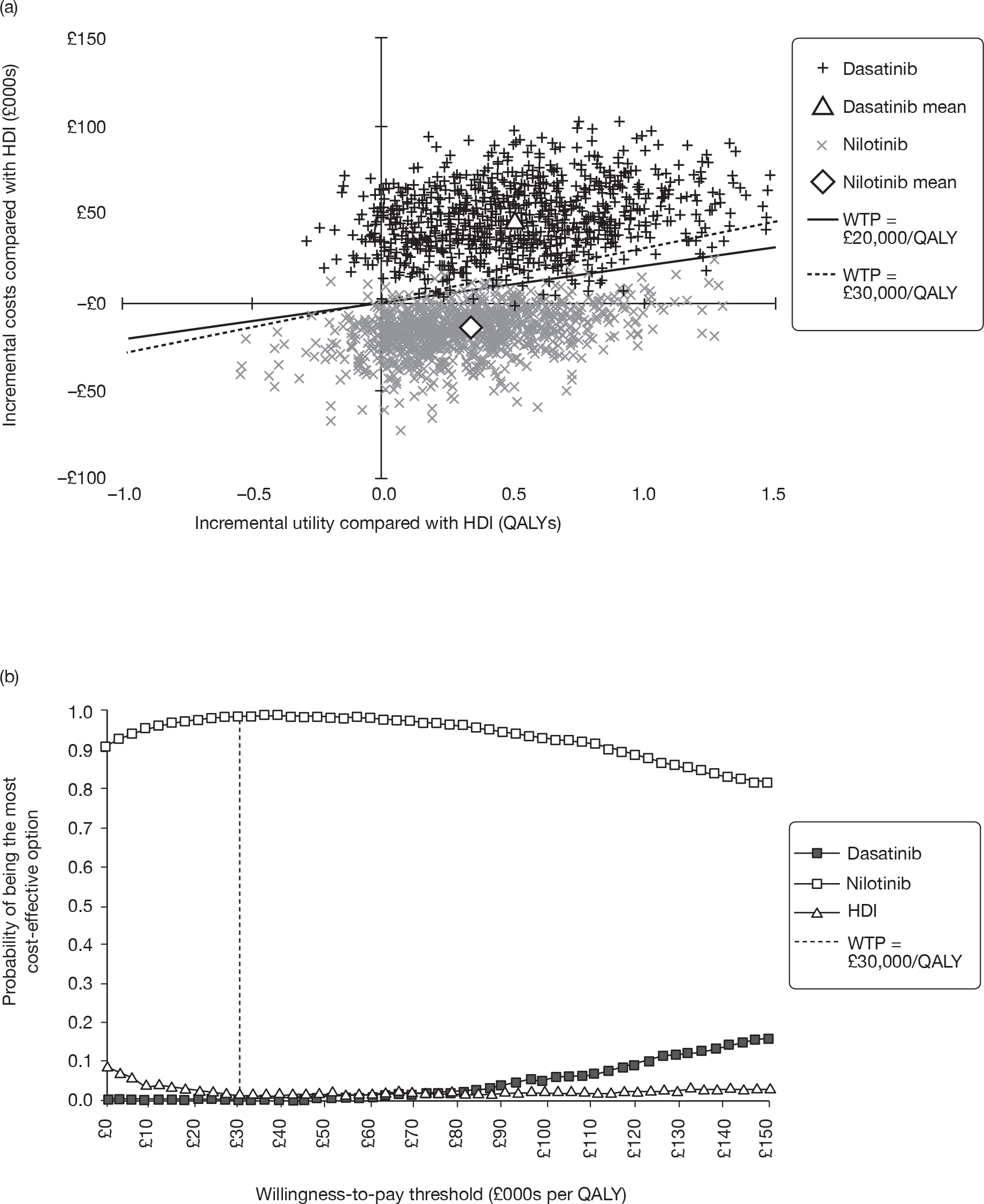
It can be seen that, in terms of parameter uncertainty alone, there was reasonably robust evidence of the superior effectiveness of the new technologies. Dasatinib generated more QALYs than HDI in 95% of the simulations and nilotinib was predicted to have greater utility than HDI in 90% of cases. Overall, dasatinib generated most QALYs in 80% of the simulations; HDI in 3%, nilotinib in 16%.
The predicted costs of dasatinib are clear, despite uncertainty attaching to resource use parameters, the lifetime costs of the dasatinib cohort were greater than those of the HDI arm in 99% of simulations. The reverse was true in nilotinib’s case. It was predicted to be less expensive than HDI in a substantial majority of cases, with only 9% of simulations resulting in a higher total cost for nilotinib.
Figure 22(b) shows a cost-effectiveness acceptability curve (CEAC) for the three comparators, predicting the probability that each would be considered to provide best value for money, given a range of different societal WTP thresholds. Our model predicts that there are almost no circumstances under which HDI would be considered the best option: even when WTP was assumed to be very low, the probability of HDI providing the best value for money remains under 10%. The probability of dasatinib being considered the most cost-effective option was very small, until WTP rises to very high levels and, even at a threshold of £150,000 per QALY, does not exceed 20%. In contrast, nilotinib was most likely to provide the greatest value for money at all WTP thresholds; the probability of it being the best option always exceeds 80%.
Imatinib-intolerant chronic myeloid leukaemia
As per our specified research questions (see Chapter 1, Overall aims and objectives of the assessment), our economic analysis of ImI CML compares the technologies under review to IFN plus cytarabine. For convenience, this comparator is referred to as IFN in the following analysis; however, it should be remembered that the model arm was parameterised using study data from a cohort in which the majority of participants had also received cytarabine and the costs of this additional treatment are included in all analyses. A summary of the results of the PenTAG cost–utility model for ImI CP CML is shown in Box 10.
In all analyses, the ICERs for dasatinib and nilotinib vs IFN are high.
-
The acquisition costs of the new technologies are substantially greater than those of IFN plus cytarabine; our model predicts that the discounted costs of treating an individual with ImI CML with nilotinib are, on average, £123,000 greater than the costs of using IFN, and the equivalent figure for dasatinib vs IFN was over £184,000 per patient.
-
Although the utility gains predicted by our model are also substantial, they are not sufficient to counterbalance these very high costs, unless it can be assumed that society was willing to pay an extremely high premium for such health gains (over £80,000 per QALY).
-
None of our one-way sensitivity analyses provide evidence that uncertainty attaching to any single parameter can account for the poor balance of costs and utility predicted by our model for both new technologies.
-
Once all parameter uncertainty was accounted for in probabilistic analysis, our best estimate of the likelihood that IFN provides better value for money than nilotinib or dasatinib at a conventional WTP threshold of £30,000 per QALY was 100%.
However, we emphasise that our model is reliant on an array of major assumptions. In particular:
-
substantial structural uncertainty was associated with the methods by which we have predicted both costs and QALYs, in the absence of direct evidence of either; and
-
there are notable differences between the populations reported in each of the observational studies on which we rely; and
-
the critical outcome measures – above all, MCyR and PFS – used as model inputs have been defined in different ways and measured at different times.
Base-case model outputs for imatinib-intolerant chronic myeloid leukaemia
Table 99 presents the base-case aggregated totals for dasatinib, nilotinib and IFN in ImI CML-CP. Outputs are shown for total life-years (undiscounted), and total discounted QALYs and costs for each treatment over the time horizon of the model.
| Parameter | Dasatinib | Nilotinib | IFN |
|---|---|---|---|
| Life-years (mean) (undiscounted) | |||
| CP treated | 10.77 | 6.79 | 2.04 |
| CP post discontinuation | 1.94 | 3.87 | 6.82 |
| AP | 0.80 | 0.80 | 0.80 |
| BC | 1.09 | 1.09 | 1.09 |
| Total (mean) | 14.60 | 12.55 | 10.75 |
| Total (median) | 12.47 | 9.67 | 7.75 |
| QALYs (mean) (discounted) | |||
| CP treated | 6.83 | 4.57 | 1.27 |
| CP post discontinuation | 0.93 | 2.09 | 4.16 |
| AP | 0.35 | 0.38 | 0.41 |
| BC | 0.34 | 0.37 | 0.39 |
| Total | 8.46 | 7.41 | 6.23 |
| Costs (mean) (discounted) (£) | |||
| Drug costs) | 244,926 | 169,771 | 15,936 |
| Drug administration | 0 | 0 | 4390 |
| Monitoring OP appointment | 7077 | 6636 | 6259 |
| BM tests | 9889 | 6612 | 2199 |
| Radiographs | 697 | 748 | 795 |
| CT scans | 411 | 441 | 469 |
| Blood transfusions | 3894 | 4179 | 4445 |
| Post-discontinuation CP treatment | 13,709 | 30,658 | 61,083 |
| Inpatient palliative care | 2840 | 3048 | 3242 |
| Total (£) | 283,441 | 222,092 | 98,818 |
The model predicts fairly large differences in OS, with individuals taking dasatinib, nilotinib and IFN predicted to live for a median of approximately 12½, 9⅔, and 7¾ years, respectively. Once expected lifespan is quality-adjusted and discounted, the difference reduces a little, with mean OS of somewhat over 8, 7 and 6 years, respectively. There are also substantial differences in the breakdown of these predicted lifespans. Individuals taking dasatinib spend the majority of their lives in pre-progression CP; those on nilotinib also spend a substantial amount of time in this phase, but somewhat longer in post-progression CP (over one-third of the total predicted duration of CP); those on IFN spend only a little over 2 years, on average, in pre-progression CP, before an extended post-progression–pre-AP phase encompassing the majority of their predicted lifespan. As per the model assumptions (see Method of estimating time in accelerated phase and blast crisis), time in AP and BC was essentially the same across all comparators (the very slight discrepancy between some QALY totals was a result of the discounting process).
These results are illustrated in Figure 23, which shows the relative proportions of patients in each health state for each treatment throughout the time horizon of the model. The features discussed above – with time on treatment in CP taking up the majority of predicted survival time for dasatinib, somewhat less for nilotinib, and a small minority for IFN – are clearly seen. Once again, the predicted time on treatment falls steeply at 3 months for nilotinib and IFN because of the large numbers of patients who stop treatment owing to causes other than progression or death (most notably, serious AEs).
FIGURE 23.
Base-case cohort composition over time by treatment for ImI patients.
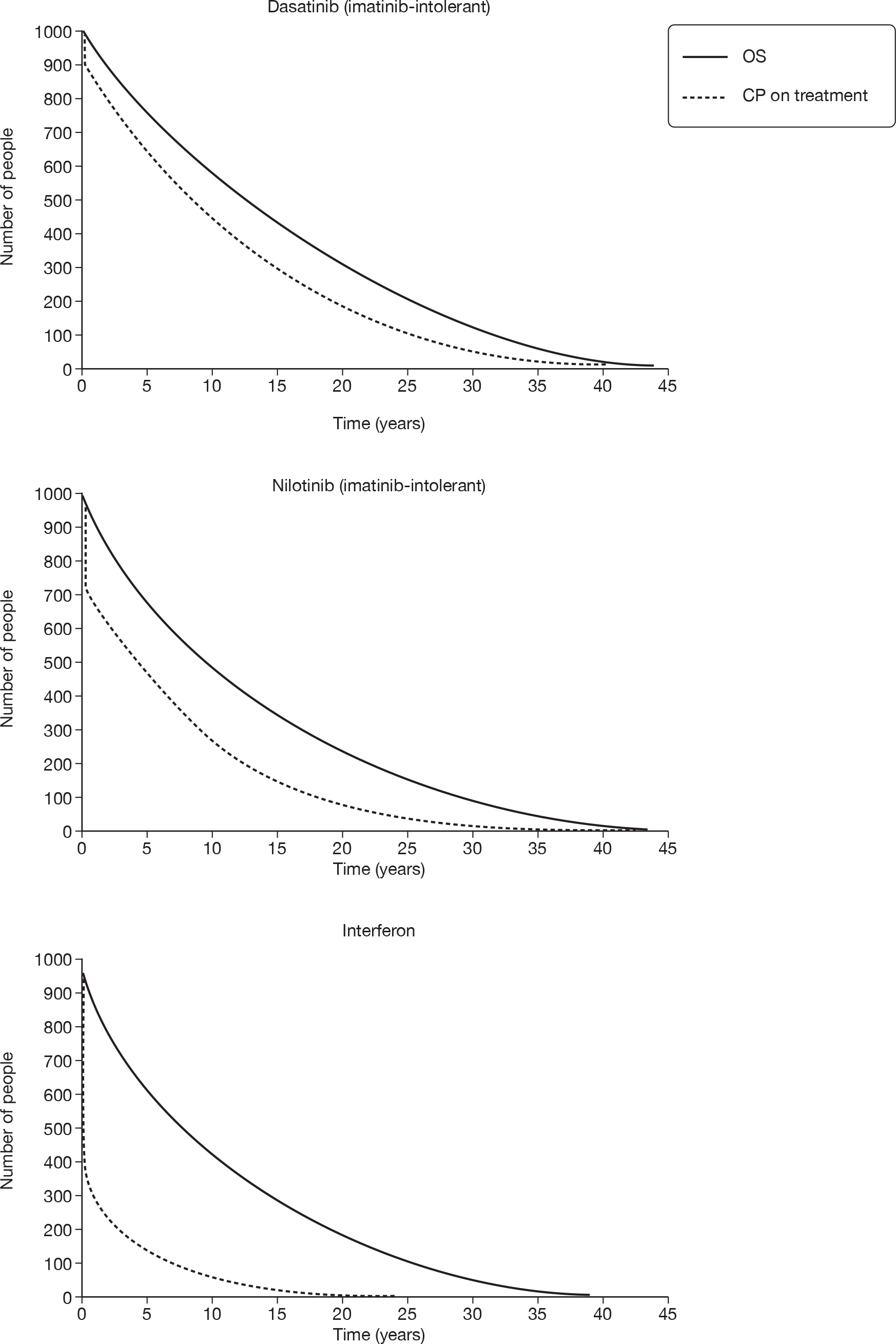
As in ImR CML, drug costs (Table 99) constitute by far the largest single cost item. Note, that costs of post-discontinuation treatment are – broadly speaking – inversely proportional to costs of the technologies under investigation. This is because the model predicts a longer dwell-time in the CP post-discontinuation state for technologies in which the CP treated state is shortest. The cost of administration of IFN was comparatively small. Whereas some of the medical management costs are large (for example, blood transfusions), they are fairly consistent across comparators, and are dwarfed by acquisition costs for the technologies themselves.
Figure 24 shows the OS curves for each of the three treatments, as well as showing the generic OS curves for patients with an MCyR versus those with no response. The general survival curve for the equivalent-aged non-CML population is also shown. With all treatments, virtually all patients are predicted to have died by 40 years from the start of treatment, i.e. by age 96 years.
FIGURE 24.
Predicted OS for ImI people by treatment and for responders and non-responders.
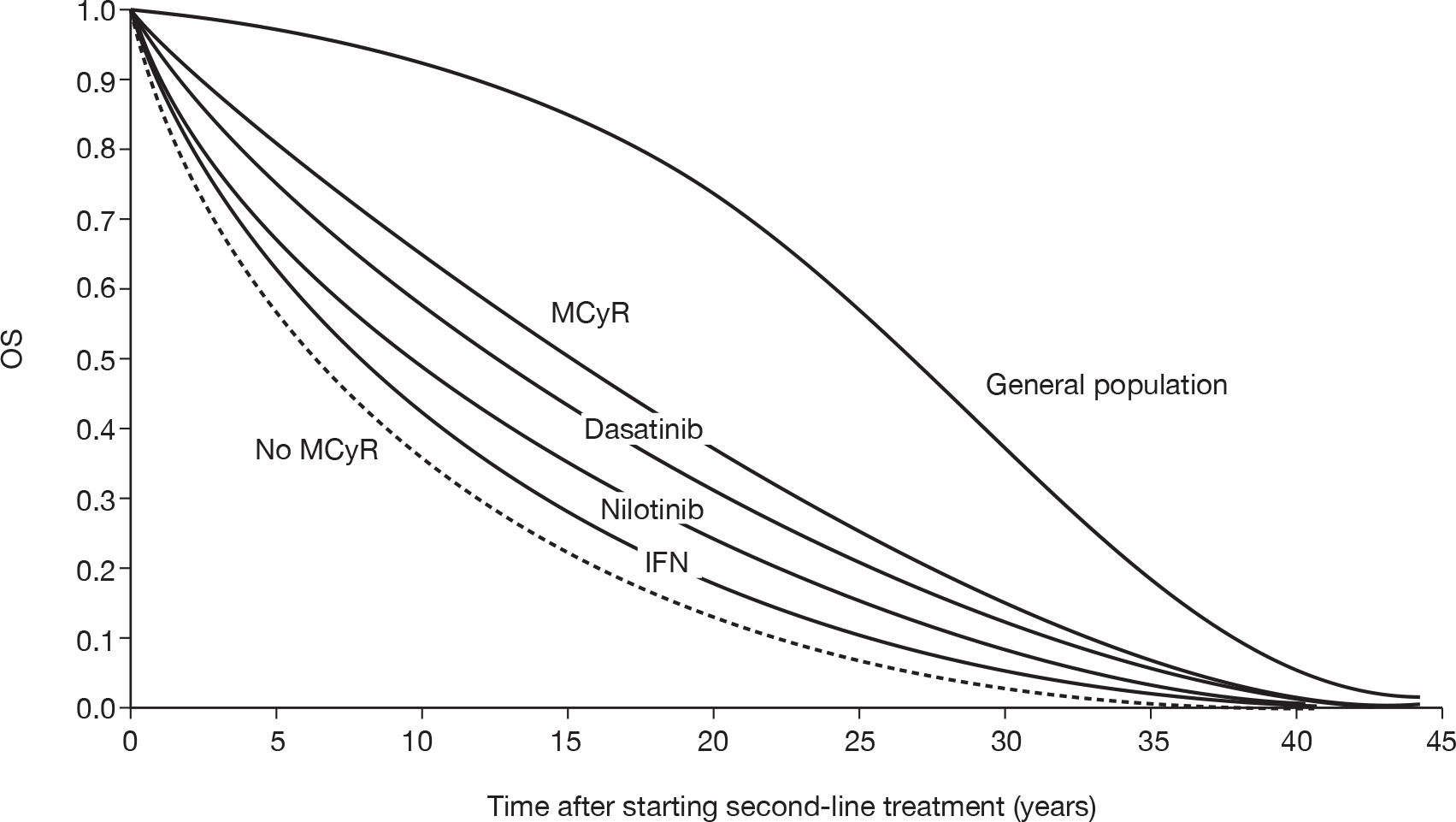
The ranking of comparators – with dasatinib providing greatest OS, followed by nilotinib, with IFN the least effective – was a direct reflection of the MCyR rates used to estimate survival. Very nearly three-quarters of individuals receiving dasatinib are expected to achieve an MCyR; under half of the simulated patients taking nilotinib will achieve a response and the analogous response rate for those receiving IFN is under one-quarter (for full details, see Major cytogenetic response rates).
Base-case deterministic cost–utility results
The incremental cost–utility of dasatinib, nilotinib and IFN as estimated in our model is shown in Table 100, with the results depicted on the cost–utility plane in Figure 25.
| Drug | Cost (£)a | Utility (QALY) | Incremental cost (£) | Incremental utility (QALY) | Incremental £/QALY (ICER)b |
|---|---|---|---|---|---|
| IFN | 98,800 | 6.229 | |||
| Nilotinib | 222,100 | 7.406 | 123,300 | 1.177 | Extendedly dominated by IFN and dasatinib |
| Dasatinib | 283,441 | 8.463 | 184,623 | 2.235 | £82,600 |
FIGURE 25.
Deterministic base-case incremental cost–utility for ImI CML: cost–utility plane. C-E, cost-effectiveness.
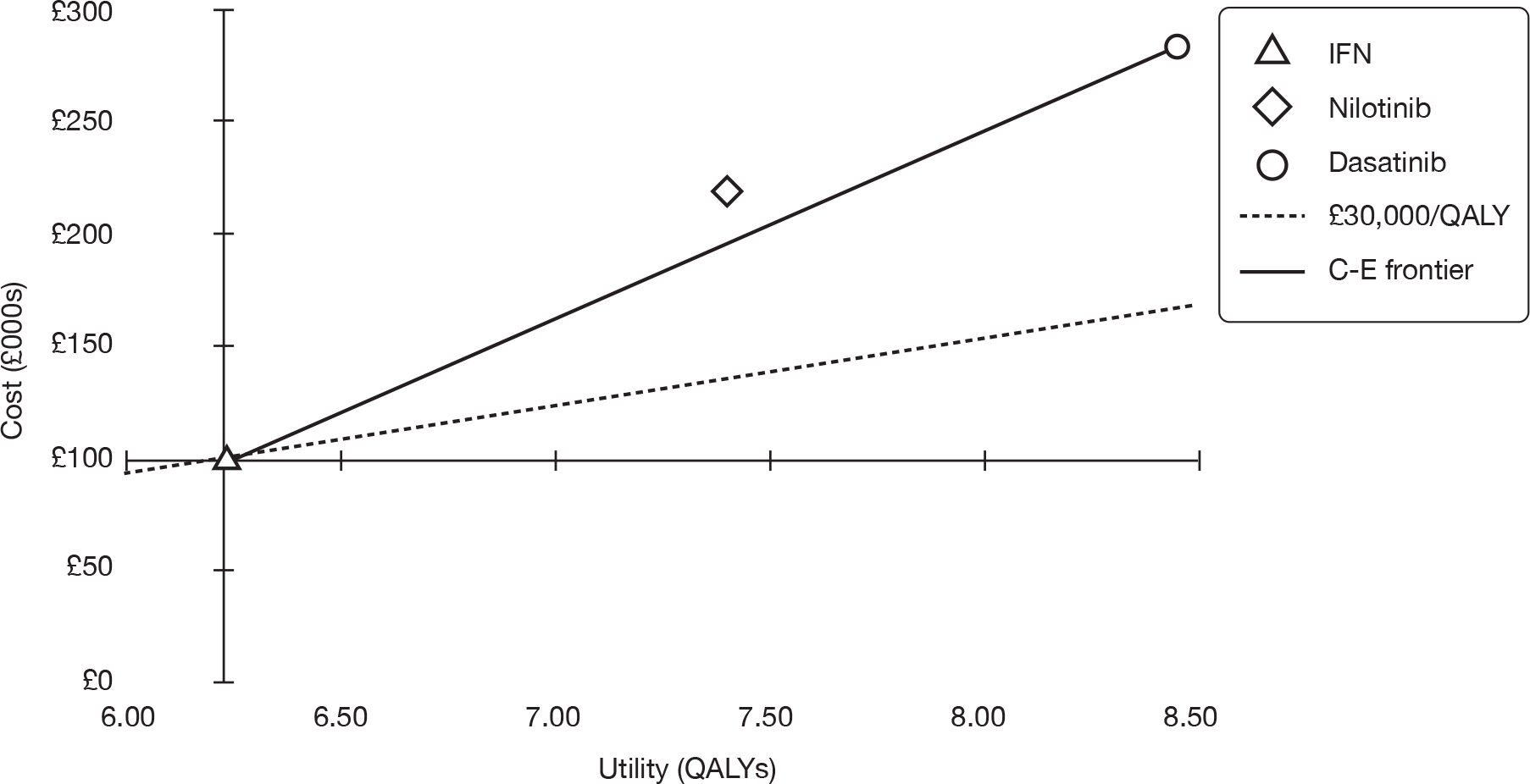
It was estimated that, in comparison with IFN, nilotinib will provide an additional 1.2 QALYs, but cost almost £125,000 extra; this would equate to an ICER of £104,700 per QALY. However, in an incremental analysis, nilotinib would not be considered a viable option, because it was extendedly dominated by IFN and dasatinib. This means that greater health gain could be achieved by providing a mixture of IFN and dasatinib (for example, if 100 people received nilotinib, our model would predict an aggregate of 741 QALYs to accrue; if, instead, 66 people received dasatinib and 34 received IFN, the health gain would be 770 QALYs at an identical cost).
When compared with IFN, dasatinib produces 2.2 extra QALYs at an additional cost of around £185,000, equating to a cost–utility ratio of a little over £80,000 per QALY.
Model validation: model outputs compared with study data
Progression-free survival
Figure 26 below shows the actual data for PFS versus the fitted model curve for each of the three modelled treatments. From this it can be seen that the PFS curves of our model in general fit the study data well.
FIGURE 26.
Progression-free survival for ImI people by treatment.
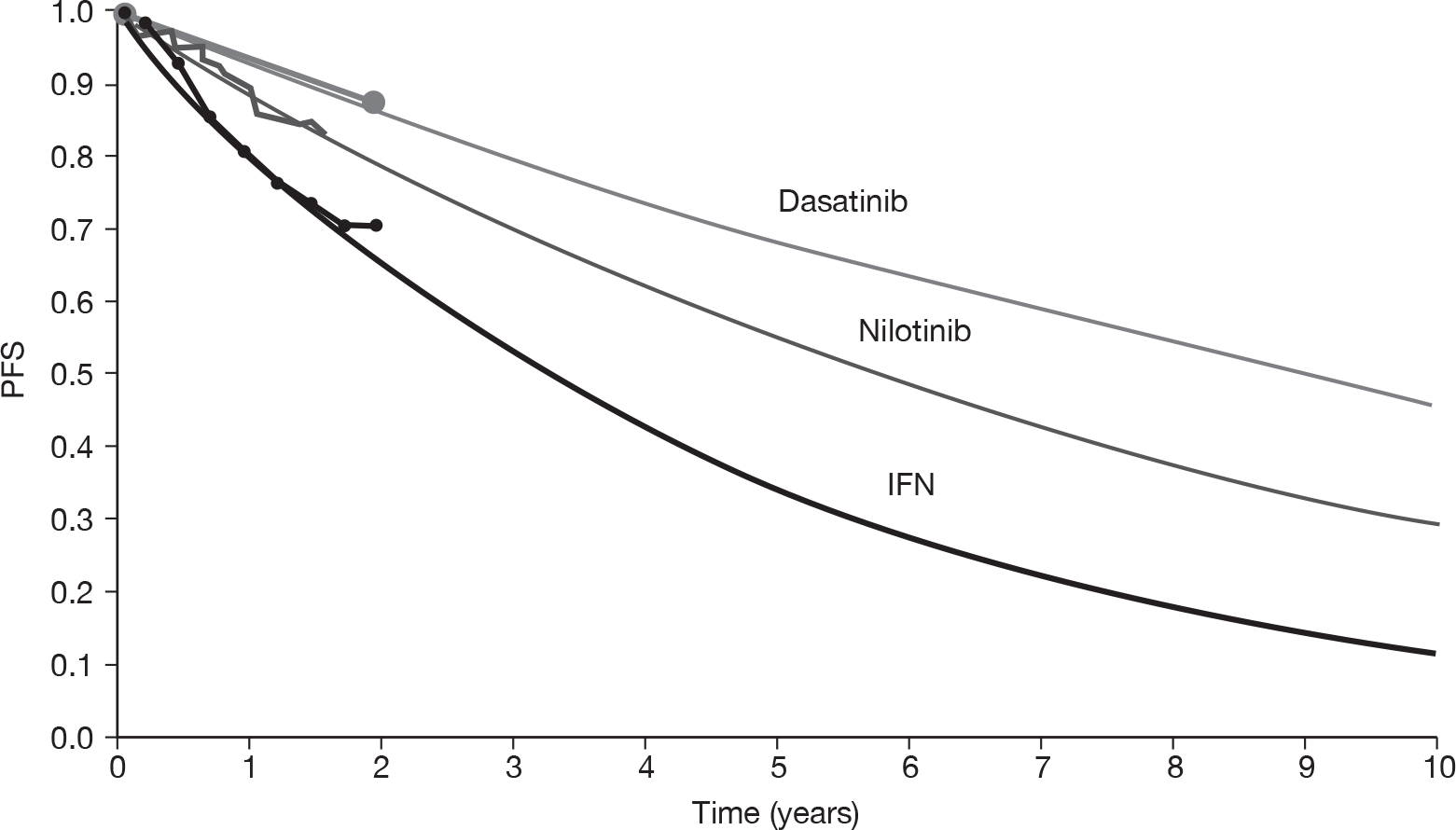
Overall survival
Figure 26 shows the OS curves as modelled for the three compared treatments for ImI CML. This shows that the predicted OS is lower for all treatments than the empirical OS.
The poor fit to the empirical IFN OS in our model may be because the empirical data present first-line treatment, whereas the predicted data were for second-line treatment; there was also the problem that the study from which our IFN data were drawn11,105 featured substantial crossover from the IFN arm to the alternative treatment (imatinib), with the likely consequence of exaggerated OS.
The lack of fit for dasatinib and nilotinib was harder to explain, but may be because we calibrated OS (for any given response rate) to the empirical OS for HDI for patients resistant to normal-dose imatinib. However, the empirical OS presented in Figure 27 corresponds to patients not resistant to, but intolerant of, imatinib. Nonetheless, any underestimation of OS for ImI CML applies to all drugs being compared, and therefore the incremental OS, which drives cost-effectiveness, may be relatively accurate.
FIGURE 27.
Actual versus predicted OS for ImI people by treatment.
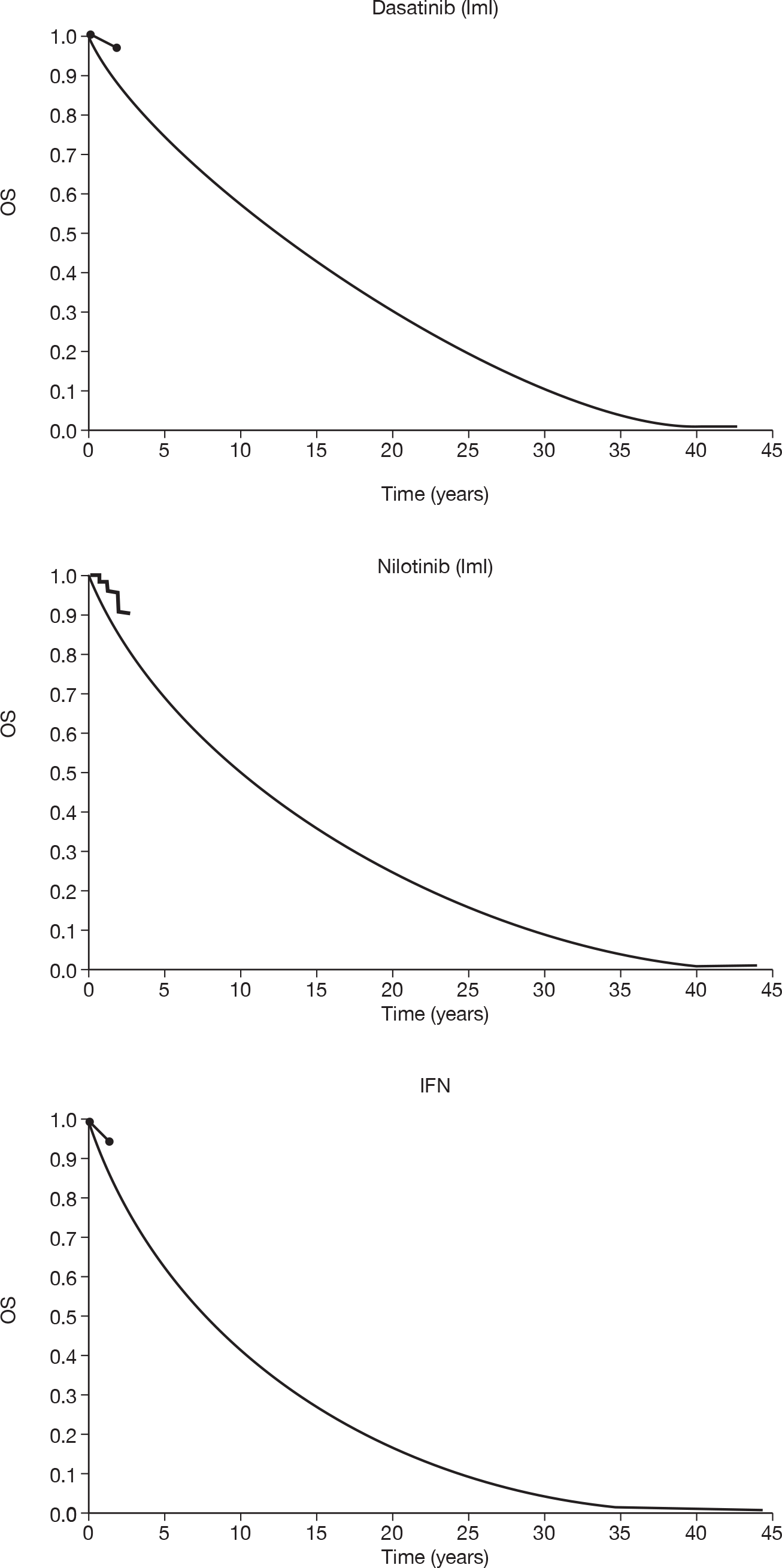
To address this lack of fit, we performed a sensitivity analysis in which we adopted an alternative method of calibrating OS (i.e. stage 3 in the methods detailed in Method of estimating overall survival). In our base case, we used the survival data in Jabbour et al. ’s study of HDI182 as our point of calibration; this study has the advantage of being substantially more mature than any other data available to us, but it has the disadvantage of relating to an ImR cohort. In our sensitivity analysis, we instead calibrated OS to the most mature data available in an ImI-specific population, which was found in the study on which we rely for our nilotinib data. 106 This was much less mature (2.9 years’ follow-up; over 90% of participants right-censored) and, hence, much more uncertain, but it does have the advantage of relating directly to an ImI cohort.
Adopting this approach, the modelled OS for ImI people closely fits the empirical OS for not just nilotinib (as would be expected), but all treatments (see Appendix 9). However, there was no critical change in estimated cost–utility; the ICER for dasatinib versus IFN increases to £107,594 per QALY, and the ICER for nilotinib versus IFN increases to £132,936 per QALY. These results come about because, although additional survival was predicted for nilotinib and dasatinib, a similar gain was seen for IFN, which means that incremental cost–utility was not greatly altered. This suggests that, if our model does indeed suffer from suboptimal prediction of OS in the ImI setting, any inaccuracy does not have a decisive impact on outputs.
Deterministic sensitivity analysis
Dasatinib versus interferon
One-way deterministic sensitivity analyses for dasatinib versus IFN for ImI CML patients are reported in Table 101, which shows the impact on the deterministic ICER of various specified alterations in model parameters. The same information is presented in a tornado diagram in Figure 28. For consistency with previous analyses (see Nilotinib versus high-dose imatinib), the data were presented in terms of INB (assuming WTP of £30,000 per QALY).
| Parameter | Base case | Sensitivity analysis | ICER (£) |
|---|---|---|---|
| Base case | NA | NA | 82,619 |
| General | |||
| Discounting | 3.5% p.a. costs and benefits | 0% p.a. costs and benefits | 72,156 |
| Effectiveness | |||
| Time in post-progression survival | 8.7 years IFN, 3.8 years dasatinib | Dasatinib and IFN value equal to IFN value | 54,335 |
| Dose intensity | IFN 55.5%, dasatinib 100% | IFN 100%, dasatinib 100% | 76,901 |
| Dasatinib clinical data | Shah et al. (2008)22 | Hochhaus et al. (2007)11,105 (Note, patients took dasatinib at 140 mg q.d. in this study) | 95,278 |
| MCyR rates | Dasatinib 74.4% | Dasatinib 61.4% (lower 95% CI) | 101,738 |
| Dasatinib 87.4% (upper 95% CI) | 70,430 | ||
| Dasatinib 100% (maximum possible) | 62,249 | ||
| IFN 22.1% | IFN 18.6% (lower 95% CI) | 78,883 | |
| IFN 25.5% (upper 95% CI) | 86,820 | ||
| OS HDI at 5 years | 0.675 | 0.575 (lower 95% CI) | 80,847 |
| 0.775 (lower 95% CI) | 93,636 | ||
| Hazard ratio responders vs non-responders | 0.370 (pooled mean) | 0.127 [lowest estimate identified: Kantarjian et al. (2006)236] | 54,491 |
| 0.156 (lower 95% of pooled estimate) | 57,261 | ||
| 0.876 (upper 95% of pooled estimate) | 300,258 | ||
| 0.893 [highest estimate identified: Kantarjian et al. (2004)251] | 323,776 | ||
| Time in AP and BC | 0.8 years AP, 1.1 years BC | Half: 0.4 years AP, 0.5 years BC | 83,209 |
| Double: 1.6 years AP, 2.2 years BC | 81,469 | ||
| Age starting second-line treatment | 56 years | 52 years | 79,381 |
| 60 years | 86,566 | ||
| Costs | |||
| PFS | Dasatinib PFS probability at 2 years = 0.87 | 0.77 (lower 95% CI) | 58,948 |
| 0.97 (upper 95% CI) | 101,442 | ||
| IFN PFS probability at 1.75 years = 0.71 | 0.63 (lower 95% CI) | 85,170 | |
| 0.78 (upper 95% CI) | 78,417 | ||
| Premature discontinuation rate | 10.2% dasatinib, 55.3% IFN | 0% dasatinib, 0% IFN | 75,405 |
| Time treatment stops for patients who discontinue prematurely | 3 months | 1 month | 82,947 |
| 5 months | 82,285 | ||
| Medical management costs | Half all unit costs or frequencies of use | 81,946 | |
| Double all unit costs or frequencies of use | 83,965 | ||
| Third-line treatment cost | £1040/month | Zero | 103,819 |
| Health-state utilities | |||
| CP on treatment | 0.85 dasatinib, 0.71 IFN | 0.81 dasatinib, (BMS 0.85 response, 0.68 no response), 0.71 IFN | 96,499 |
| CP no treatment | 0.85 | 0.70 | 65,836 |
| AP | 0.73 | 0.60 | 82,289 |
| BC | 0.52 | 0.40 | 82,205 |
FIGURE 28.
Tornado diagram: dasatinib versus IFN for ImI patients.
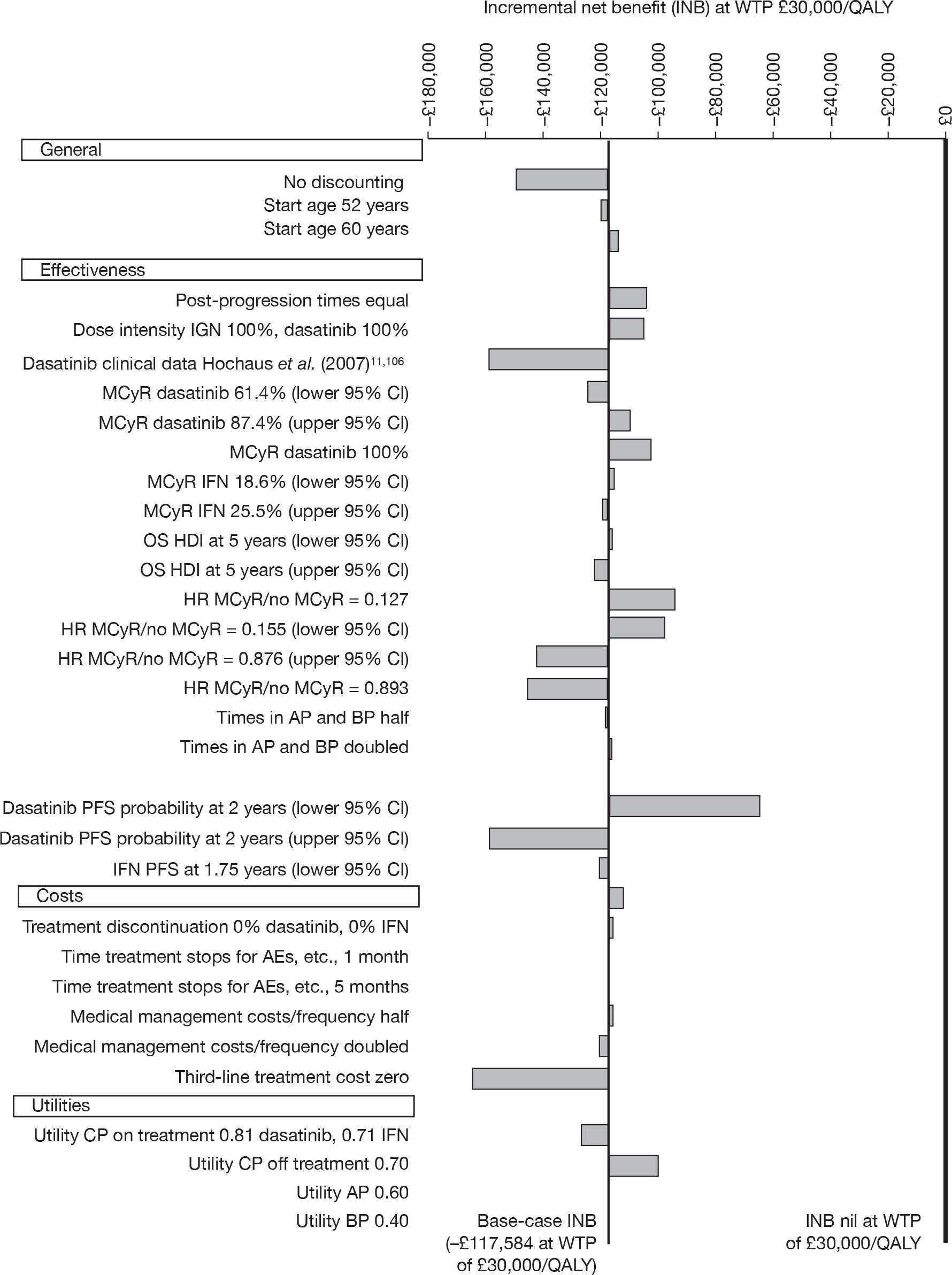
It can be seen that none of the parameter variations on their own resulted in model outputs that might conventionally be considered to represent an acceptable balance of costs and QALYs for nilotinib, as would be evident in the ICER versus HDI falling below £30,000 per QALY (and, concomitantly, the INB becoming positive). Individual sensitivity analyses are discussed below.
Nilotinib versus interferon
One-way deterministic sensitivity analyses for nilotinib versus IFN for CML patients intolerant to imatinib are reported in Table 102, which shows the impact on the deterministic ICER of various specified alterations in model parameters. The same information was presented in a tornado diagram in Figure 29. For consistency with previous analyses (see Nilotinib versus high-dose imatinib), the data were presented in terms of INB (assuming WTP of £30,000 per QALY).
| Parameter | Base case | Sensitivity analysis | ICER (£) |
|---|---|---|---|
| Base case | NA | NA | 104,698 |
| General | |||
| Discounting | 3.5% p.a. costs and benefits | 0% p.a. costs and benefits | 88,863 |
| Effectiveness | |||
| Time in post-progression survival | 8.7 years IFN, 5.8 years nilotinib | Nilotinib and IFN value equal to IFN value | 60,313 |
| Dose intensity | IFN 55.5%, nilotinib 100% | IFN 100%, nilotinib 100% | 93,846 |
| MCyR rates | Nilotinib 46.5% | Nilotinib 36.0% (lower 95% CI) | 150,683 |
| Nilotinib 57.0% (upper 95% CI) | 82,034 | ||
| Nilotinib 100% (maximum possible) | 48,132 | ||
| IFN 22.1% | IFN 18.6% (lower 95% CI) | 95,730 | |
| IFN 25.5% (upper 95% CI) | 115,915 | ||
| OS HDI at 5 years | 0.675 | 0.575 (lower 95% CI) | 102,595 |
| 0.775 (lower 95% CI) | 117,441 | ||
| Hazard ratio responders vs non-responders | 0.370 (pooled mean) | 0.127 [lowest estimate identified: Kantarjian et al. (2006)236] | 69,906 |
| 0.156 (lower 95% of pooled estimate) | 73,485 | ||
| 0.876 (upper 95% of pooled estimate) | 292,414 | ||
| 0.893 [highest estimate identified: Kantarjian et al. (2004)251] | 306,842 | ||
| Time in AP and BC | 0.8 years AP, 1.1 years BC | Half: 0.4 years AP, 0.5 years BC | 105,419 |
| Double: 1.6 years AP, 2.2 years BC | 103,292 | ||
| Age starting second-line treatment | 56 years | 52 years | 100,099 |
| 60 years | 110,273 | ||
| Costs | |||
| PFS | Nilotinib PFS probability at 1.59 years = 0.83 | 0.75 (lower 95% CI) | 72,771 |
| 0.91 (upper 95% CI) | 152,763 | ||
| IFN PFS probability at 1.75 years = 0.71 | 0.63 (lower 95% CI) | 112,457 | |
| 0.78 (upper 95% CI) | 92,576 | ||
| Premature discontinuation rate | 23.2% nilotinib, 55.3% IFN | 0% nilotinib, 0% IFN | 95,255 |
| Time treatment stops for patients who discontinue prematurely | 3 months | 1 month | 105,174 |
| 5 months | 104,218 | ||
| Medical management costs | Half all unit costs or frequencies of use | 104,756 | |
| Double all unit costs or frequencies of use | 104,582 | ||
| Third-line treatment cost | £1040/month | Zero | 130,539 |
| Health-state utilities | |||
| CP on treatment | 0.85 nilotinib, 0.71 IFN |
0.76 nilotinib, (BMS 0.85 response, 0.68 no response) 0.71 IFN |
177,667 |
| CP no treatment | 0.85 | 0.70 | 79,878 |
| AP | 0.73 | 0.60 | 104,315 |
| BC | 0.52 | 0.40 | 104,217 |
FIGURE 29.
Tornado diagram: nilotinib versus IFN for ImI patients. BP, blast phase.
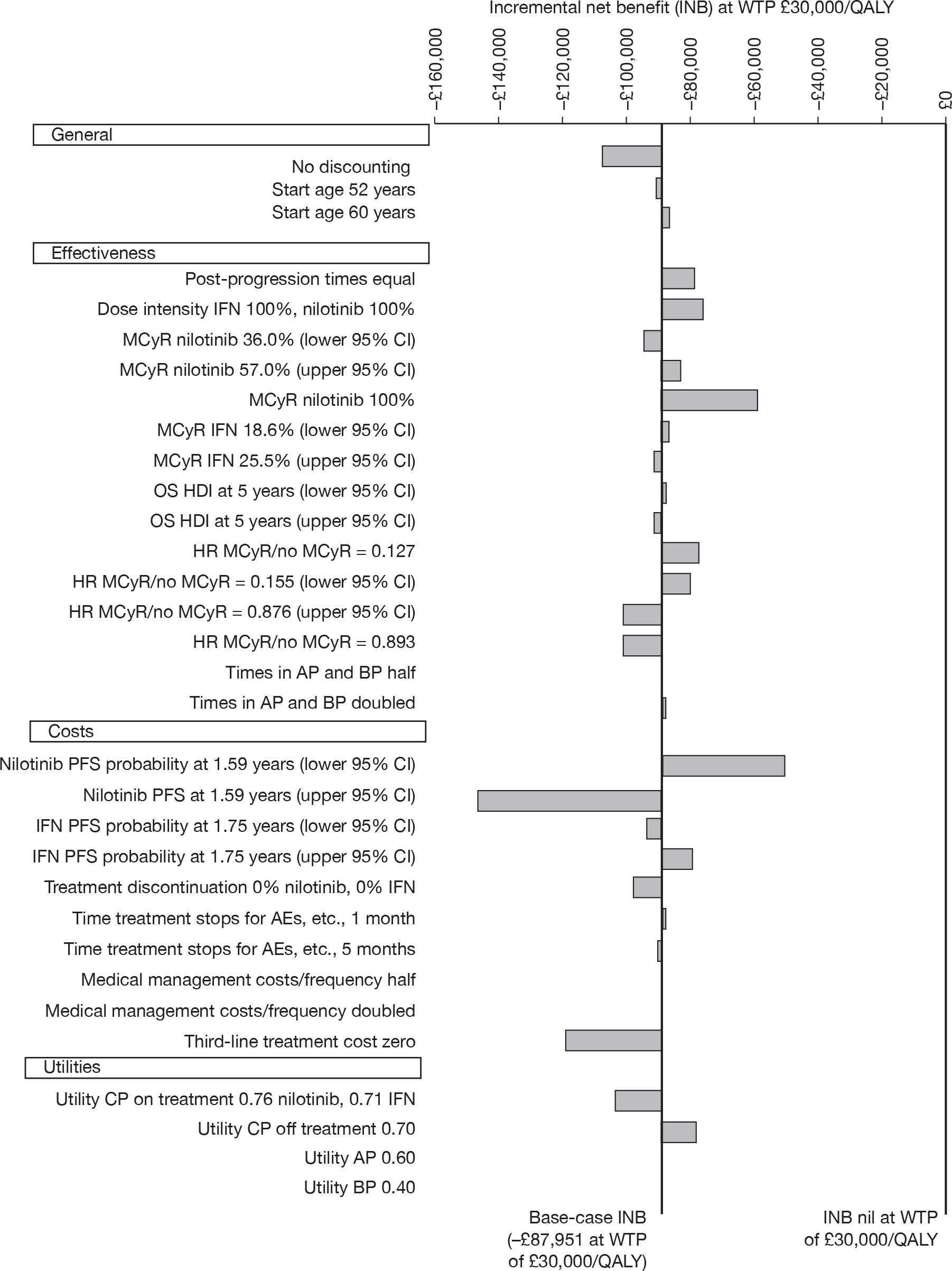
It can be seen that none of the parameter variations on their own resulted in model outputs that might conventionally be considered to represent an acceptable balance of costs and QALYs for nilotinib.
Probabilistic sensitivity analyses
The scatterplot shown in Figure 30a depicts the results of 1000 Monte-Carlo simulations, varying model input parameters simultaneously, in terms of the incremental cost–utility of dasatinib (+s) and nilotinib (×s) compared with IFN.
FIGURE 30.
Probabilistic sensitivity analyses: incremental cost–utility (ImI CML). (a) Cost–utility plane, showing incremental cost–utility of dasatinib and nilotinib compared with a common baseline of IFN in 1000 iterations of probabilistic sensitivity analysis. (b) CEAC, showing probability that each treatment was most cost-effective (delivers highest net monetary benefit).
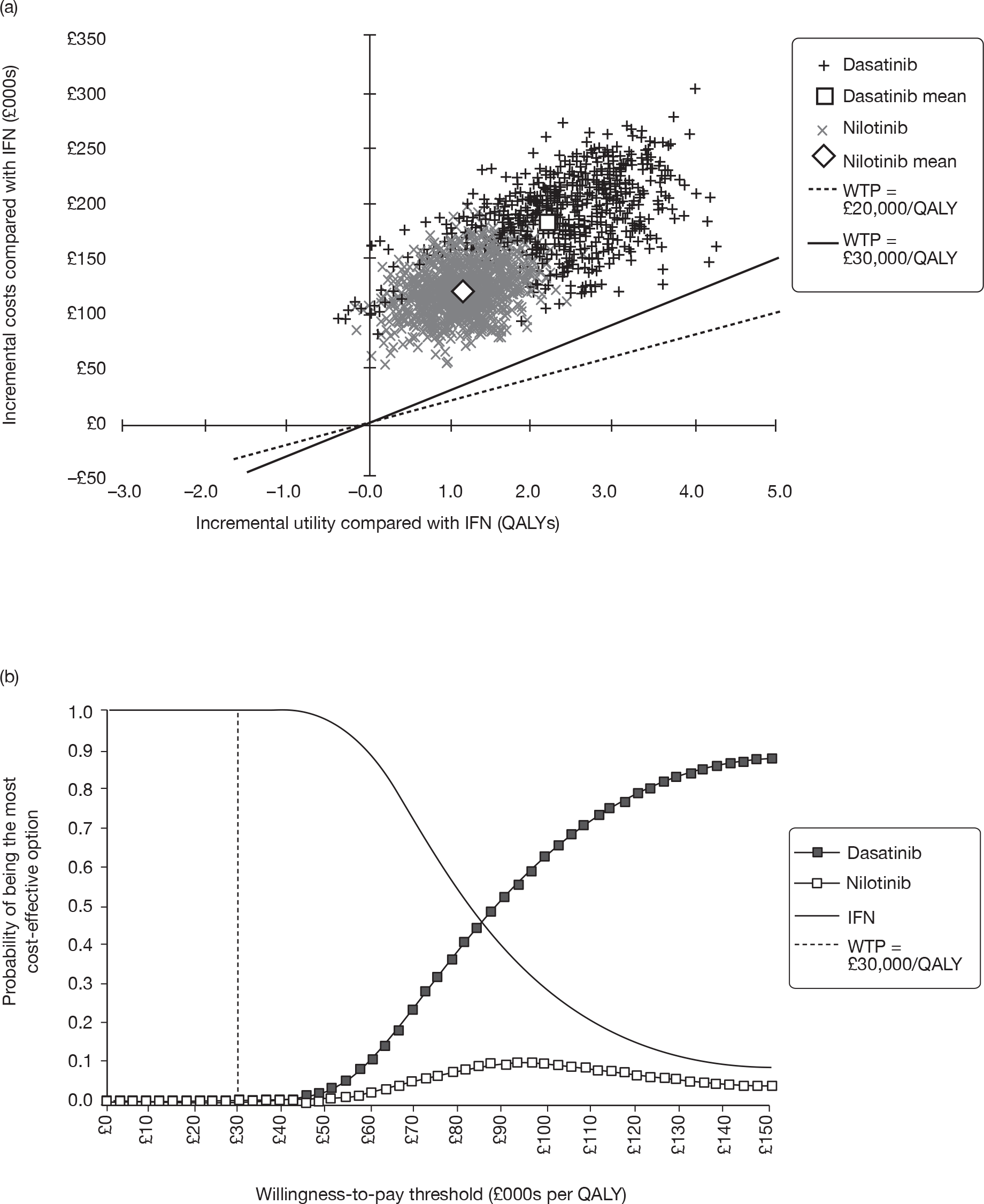
It can be seen that parameter uncertainty does not impinge on the general direction of results; both nilotinib and dasatinib are always predicted to incur greater lifetime costs than IFN and, with the exception of a very small number of outlying estimates, the new technologies are also predicted to be more effective in terms of additional QALY yield. It appears that there was greater uncertainty around the effectiveness of dasatinib (with incremental QALY gains ranging from 0.0 to 4.5 QALYs) than there was for nilotinib (for which estimates are more tightly clustered around approximately 1 ± 1 additional QALY). This discrepancy arises because the published ImI cohorts from which dasatinib effectiveness inputs were drawn were half the size (n = 43)106 of the nilotinib cohorts (n = 86), leading to a greater level of uncertainty around the estimated likelihood of an MCyR to dasatinib (see Major cytogenetic response rates).
Figure 30b shows a CEAC for the three comparators, predicting the probability that each would be considered to provide best value for money, given a range of different societal WTP thresholds.
Our model predicts that, despite its inferior effectiveness profile, IFN would be considered to provide best value for money at all but the highest levels of WTP. At a conventional threshold of £30,000 per QALY, it appears certain that best value for money was provided by IFN. Societal WTP would have to exceed £80,000 per QALY before one of the new technologies (dasatinib) would be considered the best option. At any level of WTP, nilotinib appears very unlikely to provide the greatest cost–utility. This situation arises because, in most simulations, the model predicts that the extent to which dasatinib was estimated to be more effective than nilotinib outweighs the extent to which nilotinib is estimated to be cheaper than dasatinib. This was consistent with the extended dominance of nilotinib in the deterministic base case (see Base-case deterministic cost–utility results).
Comparison of results of the PenTAG and manufacturer cost-effective analyses
In the preceding sections, we have presented a summary of the cost-effectiveness analyses (CEAs) of BMS, the manufacturer of dasatinib, Novartis, the manufacturer of nilotinib, and of PenTAG. In this section, differences in the results produced by these three analyses for people starting in CML-CP are described and explored. In particular, the reasons for the dramatically different predictions of cost-effectiveness from the PenTAG and BMS models of dasatinib are explored, i.e. that dasatinib may be very poor value for money (PenTAG) or excellent value for money (BMS). With respect to nilotinib, we explore why the PenTAG analysis predicts similar per patient costs and benefits for nilotinib and HDI for patients resistant to normal-dose imatinib, whereas Novartis predicts that nilotinib dominates HDI.
No comparison of the estimates for the cost-effectiveness of dasatinib and nilotinib for patients intolerant to imatinib was possible. This was because BMS did not carry out an analysis for this population and Novartis assumed a different comparator treatment (hydroxycarbamide).
Imatinib-resistant chronic myeloid leukaemia
In this section, the results of the BMS and PenTAG models are first compared for dasatinib versus HDI in people with imatinib resistance, followed by a comparison of the PenTAG and Novartis evaluations of nilotinib in the same population.
Comparison of PenTAG and Bristol-Myers Squibb evaluations in imatinib-resistant chronic phase chronic myeloid leukaemia
A summary of the results from the PenTAG and BMS models is given in Table 103, and PFS and OS plots from both models are displayed in Figure 31 (dasatinib) and Figure 32 (HDI).
| Result | PenTAG | BMS |
|---|---|---|
| Dasatinib | ||
| Years on treatment (undiscounted, mean) | 6.5 | 8.8 |
| Years in CP (undiscounted, mean) | 10.5 | 8.8 |
| OS (undiscounted, mean) | 13.4 | 9.7 |
| Drug cost (£) (discounted, mean) | 161,000 | 195,000 |
| Dose intensity (%) (median) | 100 | 100 |
| HDI | ||
| Years on treatment (undiscounted, mean) | 2.7 | 8.8 |
| Years in CP (undiscounted, mean) | 10.5 | 8.8 |
| OS (undiscounted, mean) | 12.4 | 9.8 |
| Drug cost (£) (discounted, mean) | 88,900 | 243,000 |
| Dose intensity (%) (median) | 92 | 100 |
| Incremental results | ||
| Incremental total costs (£) (discounted) | 48,900 | –50,545 |
| Incremental total QALYs (discounted) | 0.54 | 0.13 |
| ICER (£/QALY) | 91,500 | Dasatinib dominates HDI |
FIGURE 31.
The BMS and PenTAG predictions of time on treatment and OS for ImR CML on dasatinib.
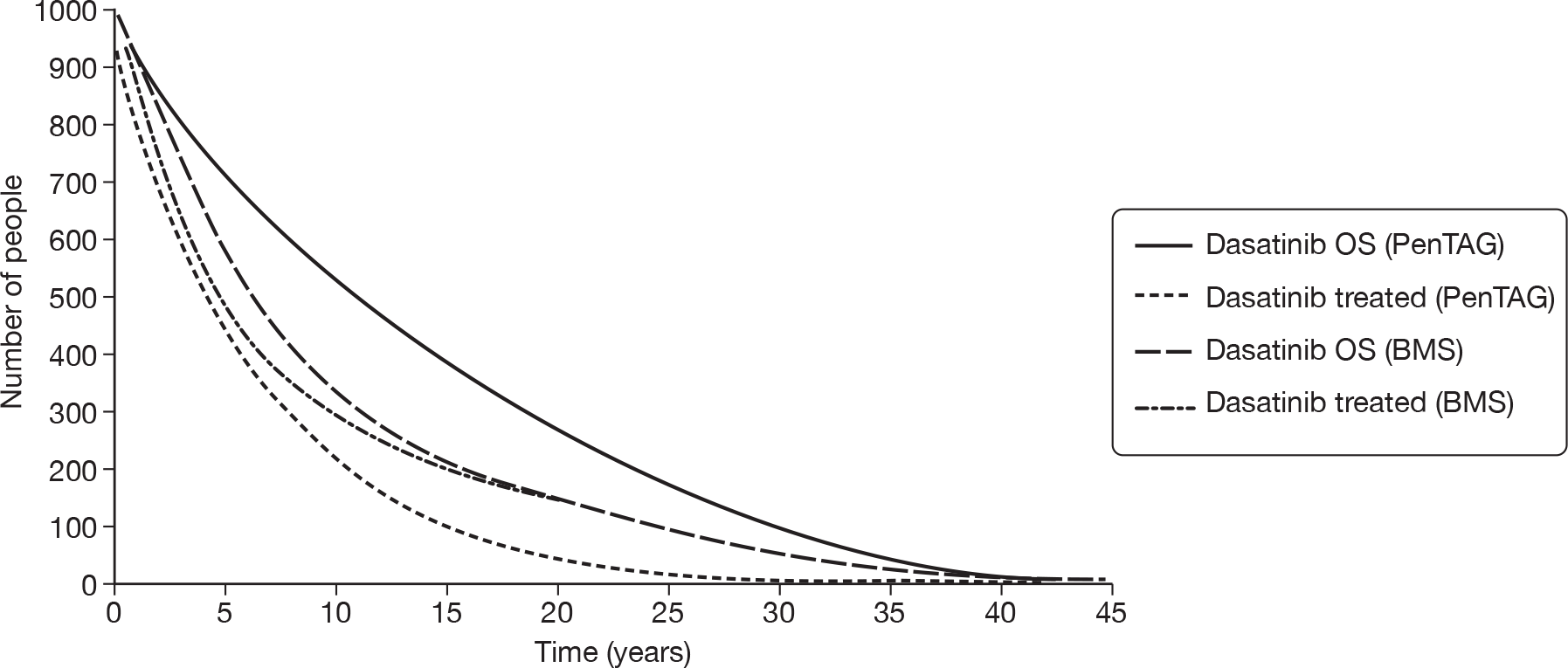
FIGURE 32.
The BMS and PenTAG predictions of time on treatment and OS for HDI in ImR CML.
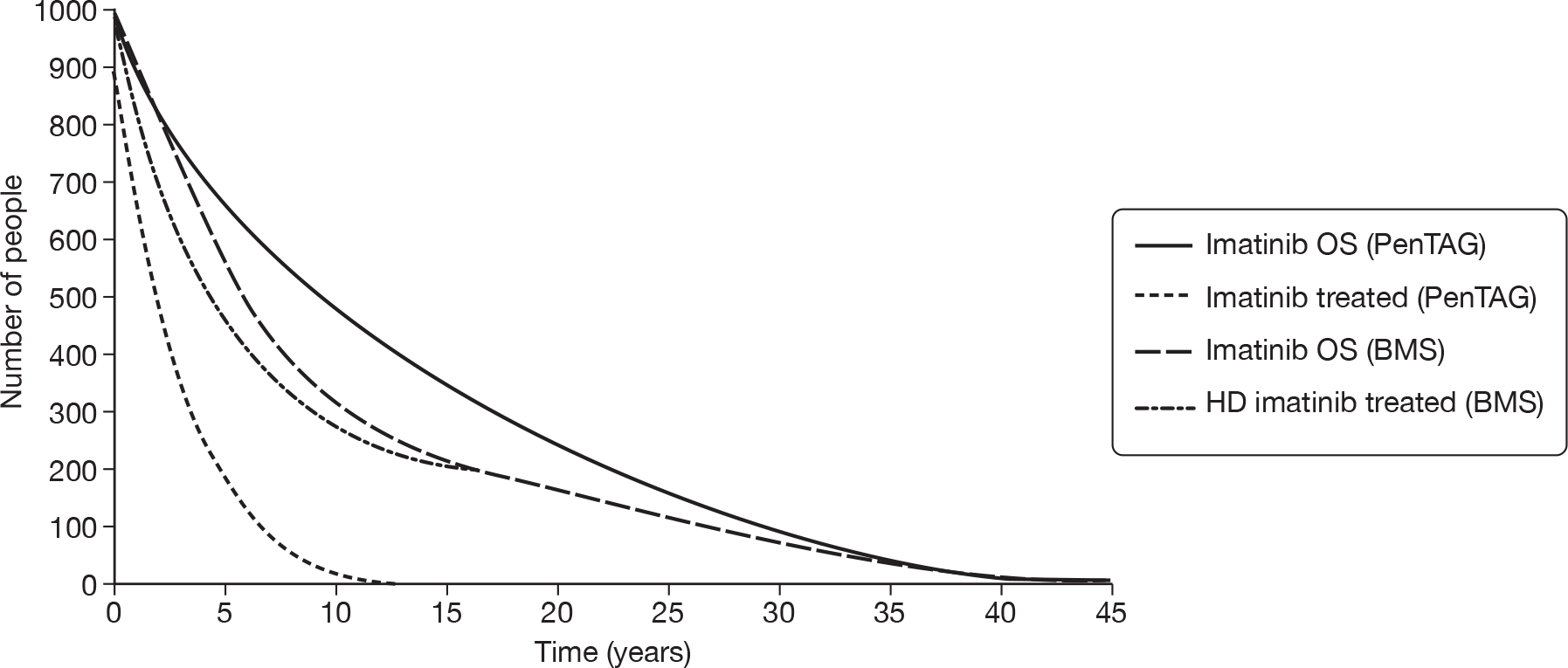
The ICERs of dasatinib versus HDI are clearly very different between PenTAG (£91,500 per QALY) and BMS (dasatinib dominates HDI). This difference in the cost-effectiveness of dasatinib was substantially explained by issues relating to cost in the BMS model. These are (1) the greater time on HDI treatment predicted in the BMS model (8.8 years) compared with the PenTAG model (2.7 years), and consequently the higher per patient discounted cost of imatinib acquisition (PenTAG £89,000 and BMS £243,000); and (2) the dose intensity used for imatinib (100% in the BMS model vs 92% in the PenTAG model).
However, before examining differences in assumptions between the BMS and PenTAG analyses which influence incremental costs, it was worth noting some important similarities between the studies in relation to modelling of effectiveness.
With respect to OS, similarities in the PenTAG and BMS modelling approaches include:
-
Both models predict OS independent of treatment.
-
Both allow for non-CML mortality.
-
More fundamentally, in both models OS is modelled contingent on best response (for BMS: CHR, PCyR, CCyR, no response; for PenTAG: MCyR or no MCyR).
However, the BMS approach differs in that time-independent transition probabilities are assumed, whereas the PenTAG model effectively assumes time-dependent transition probabilities, based on fitted Weibull curves.
Although both models base their OS predictions on the same empirical data (published as Shah et al. 22), predicted OS is higher in the PenTAG model than in the BMS model (see Figure 31). The difference is a consequence of the methods used to calculate OS. PenTAG estimated OS for responders and non-responders using the hazard ratio for OS following MCyR versus no response with HDI reported in Jabbour et al. 182 This approach has the benefit that the surrogate relationship which drives the model of OS was based on relatively long follow-up in a RCT of a TKI (imatinib). However, a disadvantage was the corollary assumption that the influence of response (MCyR) on OS was transferable between TKIs. The BMS approach was to extrapolate OS from the 034 study (published as Shah et al. 22), with the obvious advantage of specificity for dasatinib, but the important shortcoming of short follow-up and relatively low number of events. It should be noted that, overall, the differences in expected survival for dasatinib and nilotinib are similar.
The approach to modelling PFS was similar in both models in that time-independent transitions probabilities were assumed (explicitly for BMS by taking probabilities directly from the 034 clinical study, and implicitly by PenTAG through fitting an exponential distribution). However, the approaches to modelling PFS are different in that the BMS models PFS according to best response (independent of treatment), whereas PenTAG extrapolates PFS separately for each treatment, irrespective of best response (% MCyR).
It is important to note that, in the PenTAG approach, PFS does not contribute directly to the model of disease progression, but rather it was used as a proxy for treatment duration. Relatedly, the BMS model equates disease progression to advancing from CP to AP, whereas in the PenTAG model patients typically remain in CP for several years after disease progression. In other words, PFS in the BMS model was a driver for disease process and costs, whereas in the PenTAG model it was only a driver of costs. Both models allow for further decay in PFS due to non-CML mortality.
Figure 31 shows that the BMS model predicts that dasatinib would be taken almost until death, whereas the PenTAG model predicts a long period after progression, during which people would not be treated with dasatinib.
Given that both models use the same effectiveness data for PFS (Shah et al. 22), it was not surprising that predictions of time on dasatinib treatment are similar up to about 7 years (see Figure 31). However, thereafter, the BMS evaluation predicts a longer time on dasatinib treatment, which results in the higher per patient cost of dasatinib drug treatment for BMS compared with PenTAG.
Our model predicts a long period, approximately 8 years, in the CP after ‘progression’, during which people are not treated with HDI (see Figure 32). Note, that the definition of progression in the relevant study included a range of haematological changes as well as the diagnosis of CML-AP and that clinical advice confirms that patients may spend considerable time in the CP after progression has occurred.
From Figure 32, it can also be seen that predictions for time on HDI treatment are very different between the PenTAG and BMS models (mean 2.7 years PenTAG vs 8.8 years BMS). This difference arises because different clinical effectiveness data were used for HDI. The PenTAG model uses Jabbour et al. ,182 whereas the BMS model uses Kantarjian et al. 23 This was the strongest factor which explains the large difference in per-patient discounted costs for imatinib (£89,000 PenTAG vs £243,000 BMS). Indeed, if the BMS figure for treatment cost of HDI was assumed, then the PenTAG model also predicts that dasatinib dominates HDI.
A further explanation of the difference in cost estimates for imatinib lies in the different assumptions made about treatment dose intensity. The PenTAG model assumes dose intensity of 92% (taken from the Jabbour et al. 182 study), whereas the BMS model assumes 100% dose intensity for imatinib. If the BMS model was run with a dose intensity of 92% for HDI, then the incremental total cost per patient increases from –£50,545 to –£31,100.
In summary, therefore, there are a number of similarities between the PenTAG and BMS models regarding approaches to the effectiveness of dasatinib, i.e. the relationship between response and OS. Although the BMS model also includes PFS as a driver of disease progression, which has some face validity, there must be concerns about whether this approach was valid given the heterogeneous definition of ‘progression’ in the underlying studies.
However, the main reasons why the ICERs for dasatinib in the ImR population are so different relate to assumptions which influence incremental costs. We believe that the assumptions made by BMS regarding the dose intensity and duration of imatinib treatment are open to question and, where alternative and plausible assumptions are made instead, the ICER for dasatinib in this population can be demonstrated to be highly labile.
Comparison of the PenTAG and the Novartis evaluations in imatinib-resistant chronic phase chronic myeloid leukaemia
Headline results from the PenTAG and Novartis models are given in Table 104.
| Result | PenTAG | Novartis |
|---|---|---|
| Nilotinib | ||
| Years on treatment (undiscounted, mean) | 2.4 | 3.4 |
| Years in CP (undiscounted, mean) | 11.1 | 3.8 |
| OS (undiscounted, mean) | 13.0 | 5.5 |
| Drug cost (£) (discounted, mean) | 70,100 | 96,300 |
| Dose intensity (%) (median) | 100 | 100 |
| HDI | ||
| Years on treatment (undiscounted, mean) | 2.7 | 3.3 |
| Years in CP (undiscounted, mean) | 10.5 | 3.3 |
| OS (undiscounted, mean) | 12.4 | 5.1 |
| Drug cost (£) (discounted, mean) | 88,900 | 116,700 |
| Dose intensity (%) (median) | 92 | 100 |
| Incremental results | ||
| Incremental total costs (£) (discounted) | –11,100 | –20,700 |
| Incremental total QALYs (discounted) | 0.32 | 0.27 |
| ICER (£/QALY) | Nilotinib dominates HDI | Nilotinib dominates HDI |
In both the PenTAG and Novartis models, the two main drivers of cost-effectiveness are drug costs (estimated using PFS) and OS. These are displayed in Figure 33 (nilotinib) and Figure 34 (HDI). In both models, non-drug resource use has less impact on cost-effectiveness.
FIGURE 33.
The Novartis and PenTAG predictions of time on treatment and OS for ImR CML on nilotinib.
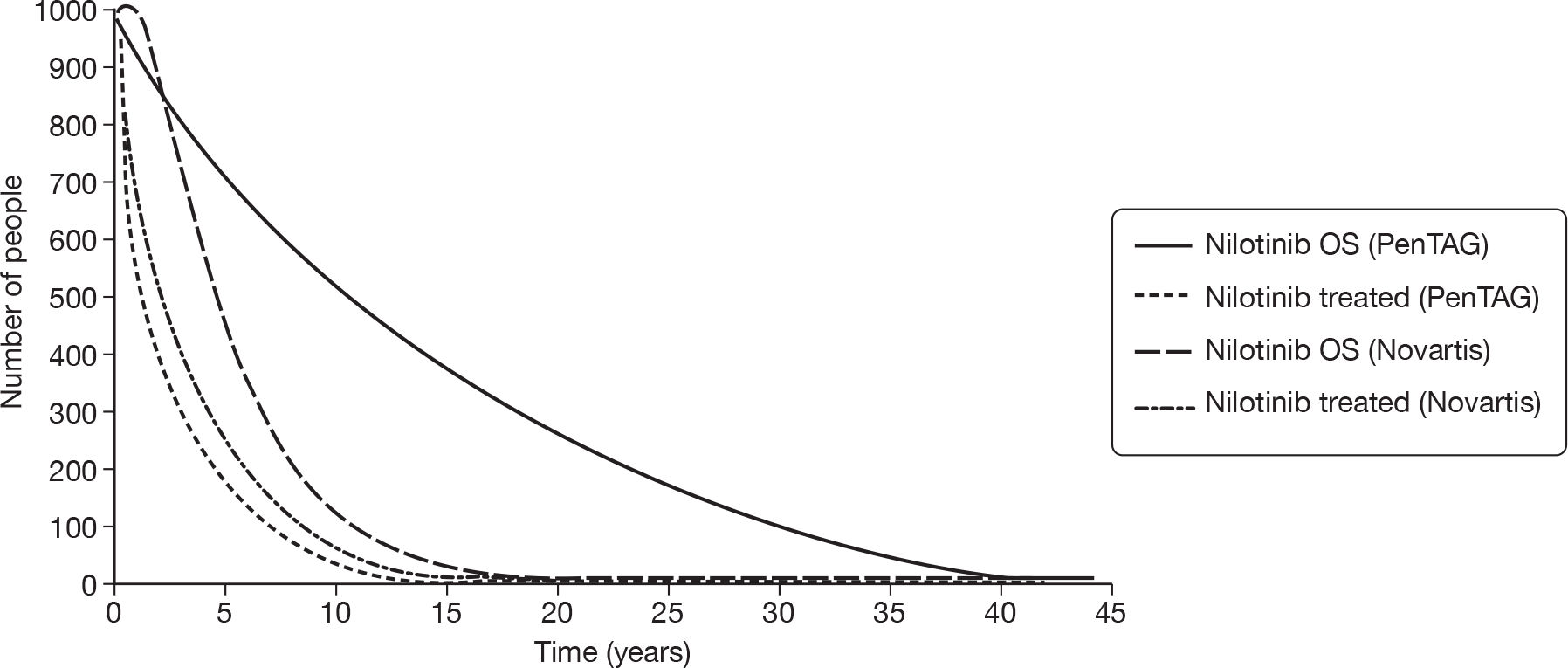
FIGURE 34.
The Novartis and PenTAG predictions of time on treatment and OS for HDI in ImR CML.
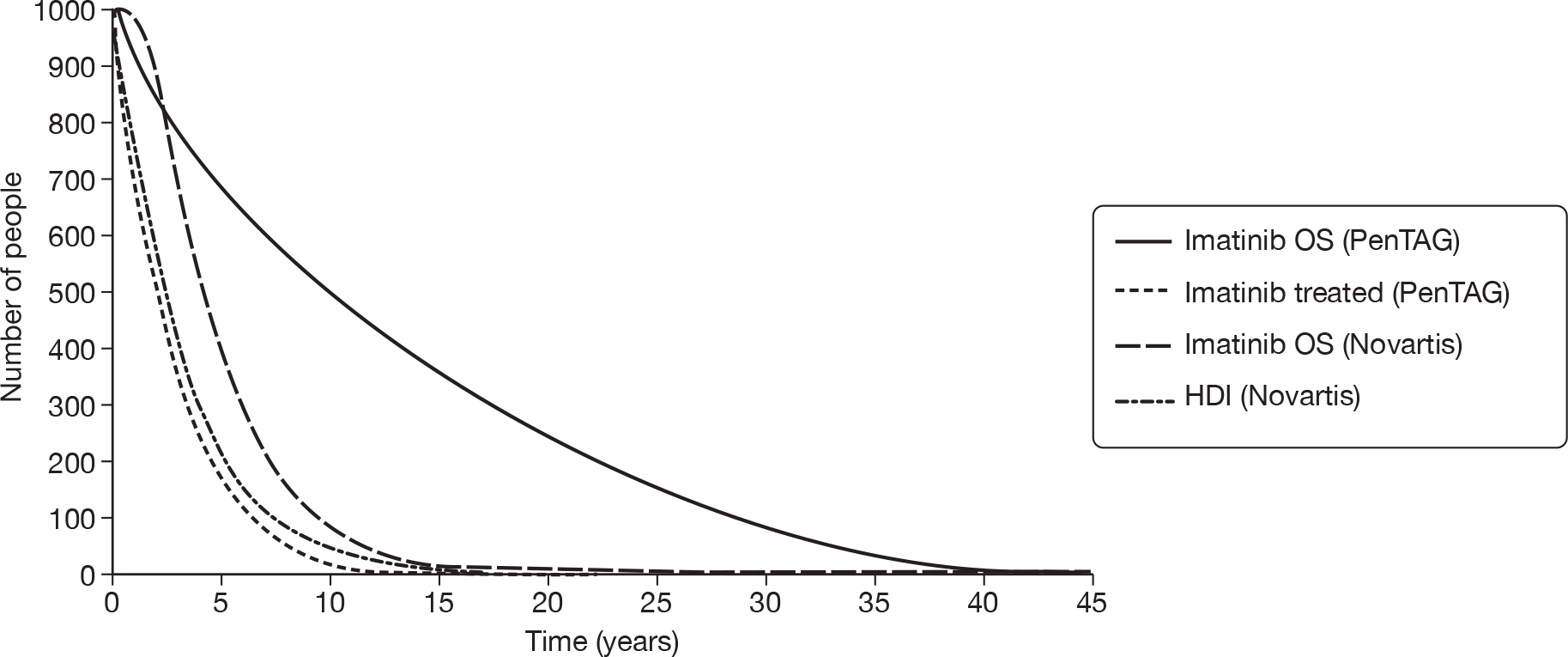
Despite important differences between the models, both predict that nilotinib dominates HDI.
The Novartis approach to modelling PFS for nilotinib was very similar to that taken by PenTAG. In particular, the same PFS Kaplan–Meier data for nilotinib were used, and both models extrapolate PFS using an exponential distribution, which was further eroded by non-CML mortality (taken from life tables). This explains why estimates of time on nilotinib treatment are similar (see Figure 33). The Novartis estimate of time on nilotinib treatment was slightly longer because a lower proportion of patients is assumed to discontinue treatment (15% vs 23% in the PenTAG model). This explains the slightly higher per-patient discounted cost of nilotinib according to Novartis (£96,300) compared with PenTAG (£70,100). The 15% represents the proportion of patients discontinuing treatment owing to serious AEs, whereas the 23% represents these patients plus those patients who withdrew for other reasons.
In contrast to PFS, the approaches to modelling OS for both treatments are completely different between the models. Our model uses MCyR to estimate OS, calibrated according to OS for HDI taken from empirical data. In contrast, Novartis calculates OS as TTP plus time in AP plus time in BC. We believe this approach was flawed because (1) the definition of progression included criteria other than development of CML-AP; and (2) it was clear from clinical experience that people may spend several years still in CP after developing signs of ‘progression’ which result in treatment cessation [Nilotinib (manufacturer analysis/model)]. Unfortunately, the precise time spent in CP following progression was impossible to estimate because of the multiple criteria that are used to define progression.
Our model estimates that patients typically spend less than half of the total time in CP on nilotinib treatment (2.4 years on treatment compared with 11.1 years in CP). It was therefore unsurprising that the estimates of mean OS for nilotinib are very different (13.0 years PenTAG vs 5.5 years Novartis) (see Table 104). Novartis’s estimate was shorter at least partly because the time patients spend in post-discontinuation CP was not modelled.
Novartis based its estimate of PFS for HDI on the IRIS dose escalation study,54 whereas the PenTAG model uses the Jabbour et al. 182 study. As stated in Nilotinib (manufacturer analysis/model), although Novartis based its estimate of PFS for HDI on the IRIS dose escalation study,54 it did not use the empirical PFS data from this study. Instead it estimated PFS from OS from the IRIS dose escalation study,54 and the relative risk between PFS and OS from the nilotinib study. Given that Novartis and PenTAG have used very different data to estimate PFS for HDI, it was interestingly coincidental that similar times on treatment are predicted (see Table 104 and Figure 34).
Despite similar predicted times on HDI treatment, the predicted per-patient discounted cost of imatinib drug treatment was higher when estimated by Novartis (£116,700 Novartis vs £88,900 PenTAG). This was because Novartis assumes an imatinib dose intensity of 100%, whereas we assume 92%. Indeed, were the Novartis model to incorporate 92% dose intensity, the predicted imatinib drug cost falls to £107,400, which was closer to our estimate of £88,900. Using this adjustment, Novartis’s model still predicts that nilotinib dominates HDI.
The PenTAG model predicts a far longer OS for patients taking HDI than the Novartis model (see Table 104 and Figure 34). This was mostly because Novartis has not modelled the period in post-discontinuation CP, which our model predicts will be around 8 years. Furthermore, as acknowledged by the analysts, the Novartis model underestimates empirical OS from the IRIS dose escalation population [Nilotinib (manufacturer analysis/model)], the study from which HDI clinical data were drawn.
We argue that Novartis’s QALY estimates, which are far lower than our estimates for both treatments, are questionable because their calculation of OS as TTP plus time in AP plus time in BC appears to contradict the definition of progression in the relevant studies. Nonetheless, both models estimate similar difference in QALYs between the treatments (0.32 for PenTAG versus 0.27 for Novartis).
Imatinib-intolerant chronic myeloid leukaemia
The results of the PenTAG model of dasatinib for people who are ImI cannot be compared with either of the manufacturers’ models because (1) Novartis did not model this population taking dasatinib and (2) BMS did not model separately people taking dasatinib who are ImI. Instead, the BMS model considers people taking dasatinib who are ImR and ImI.
However, it was possible to compare our results for ImI people taking nilotinib with the results from the Novartis model (Table 105).
| Result | PenTAG | Novartis |
|---|---|---|
| Nilotinib | ||
| Years on treatment (undiscounted, mean) | 6.8 | 8.5 |
| Years in CP (undiscounted, mean) | 10.7 | 8.9 |
| OS (undiscounted, mean) | 12.6 | 10.4 |
| Drug cost (£) (discounted, mean) | 169,800 | 213,400 |
| Dose intensity (%) (median) | 100 | 100 |
The Novartis approach to modelling nilotinib PFS for ImI people was very similar to our approach. In particular, both models use the same PFS Kaplan–Meier data for nilotinib, and both extrapolate PFS by an exponential distribution, which was further eroded by non-CML mortality (taken from life tables). It was therefore not surprising that estimates of time on nilotinib treatment are similar (Table 105 and Figure 35). The Novartis estimate was slightly greater because a lower proportion of patients discontinuing treatment is assumed (15% vs 23% in PenTAG model). The difference in proportions is due to patients discontinuing treatment for reasons other than AEs. This goes some way towards explaining the slightly higher per-patient discounted cost of nilotinib according to Novartis (£213,400) compared with PenTAG (£169,800).
FIGURE 35.
The Novartis and PenTAG predictions of time on treatment and OS for ImI CML on nilotinib.
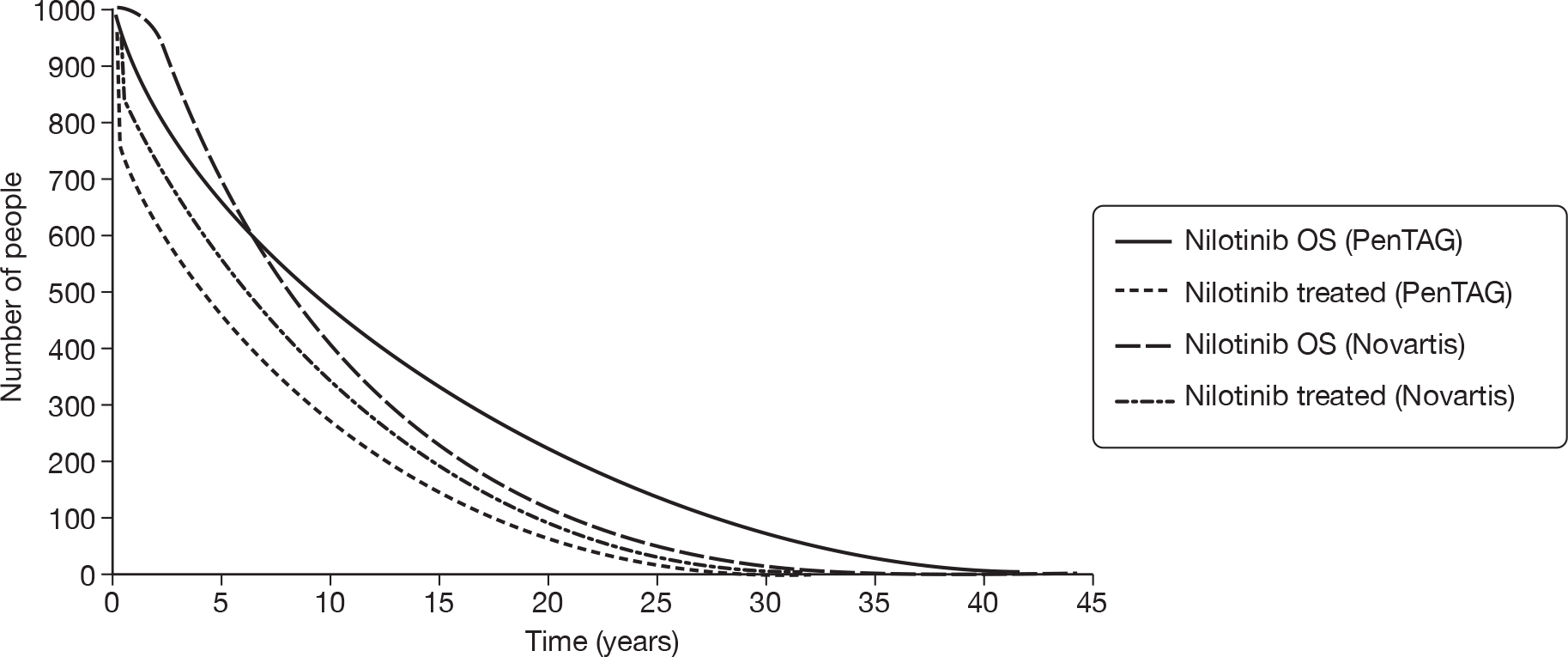
On the other hand, as explained in the discussion of ImR people, the PenTAG and Novartis approaches to modelling OS are notably different. To reiterate, our model uses MCyR rates to estimate OS, calibrated according to OS for HDI taken from empirical data, whereas Novartis calculates OS as TTP plus time in AP, plus time in BC, which we believe is flawed [Nilotinib (manufacturer analysis/model)].
It was therefore not surprising that our estimates of OS for nilotinib are different (12.6 years vs 10.4 years Novartis) (Table 105 and Figure 35). Novartis’s estimate was shorter at least partly because it did not model the time patients spend in post-discontinuation CP.
Chapter 6 Cost-effectiveness: chronic myeloid leukaemia in accelerated phase
As explained earlier (see Chapter 3), we have not produced a de novo model of CML-AP because of the lack of clinical effectiveness data for comparator treatments. As an alternative, in this section, we provide a review, critical appraisal and exploration of the cost-effectiveness analyses contained within the manufacturer submissions made to NICE.
Review of manufacturer submissions to NICE
Methods
The cost-effectiveness models reported in the manufacturer submissions were assessed against the NICE reference case220 and are critically appraised using the framework presented by Phillips et al. ’s guidelines for good practice in decision-analytic modelling for health technology assessment. 221 A summary of the reviews is presented below, with additional detail provided in Appendix 4. More in-depth exploration of the models was performed by, for example, substituting alternative parameter values, assessing the impact on the model outputs and exploring the sensitivity of the model outputs to changes in key parameter inputs.
Nilotinib (manufacturer analysis/model)
Appendix 4 presents a summary review of the nilotinib manufacturer submissions against the main items in the NICE reference case requirements220 and against the criteria set out by Philips et al. 221
Summary of Novartis’s cost-effective analysis
Comparators, patient groups
Novartis presents two discrete cost-effectiveness analyses of nilotinib for patients starting treatment in CML-AP, one simulating individuals with demonstrated resistance to normal-dose imatinib (ImR) and the other representing a subgroup of those intolerant to normal-dose imatinib (ImI) who had also shown no MCyR while on therapy. As a reflection of the Phase II study informing the nilotinib arm of the analysis,107 the second subgroup was referred to as ‘intolerant as well as resistant’ in the submission. This was not strictly accurate, in order to qualify as ImR, participants had to show long-term lack (or loss) of response to imatinib, whereas ImI individuals were enrolled so long as they had not achieved MCyR over a period of therapy which may have been much shorter. Therefore, it was more accurate to think of this group as ‘intolerant as well as (at least initially) unresponsive’.
In the ImR population, nilotinib was compared with HDI. In the ImI population, nilotinib was compared with hydroxycarbamide. Nilotinib was not compared with IFN in either population. This was not justified with specific reference to the AP model; however, the CP model excludes this comparator on the grounds that no suitable data were found on the use of IFN following failure of normal-dose imatinib (see Summary of Novartis’s cost-effective analysis).
Nilotinib was not compared with dasatinib in either population; it was briefly contended that different patient entry requirements make study data incomparable, although no analysis of such differences was presented with particular reference to AP studies, which was in contrast to the detailed argument for CP (see Summary of Novartis’s cost-effective analysis).
Model structure
The model was a Markov cost-effectiveness model, written in Microsoft Excel. It assumed that patients start second-line treatment aged 57 years, with a 50 : 50 male – female ratio, consistent with the main Phase II study of nilotinib in AP. 107 Patients were modelled until age 100 years, implying a lifetime horizon of 43 years. The model cycle length was 3 months. A half-cycle correction was not applied.
The models take a UK NHS perspective and all costs and benefits were discounted at 3.5%. 222
Both models comprise the following health states: AP, BC and death (Figure 36). Patients enter the model in AP, progress to BC and then finally may die from CML causes. Patients may also die in the AP and BC states from non-CML causes (data from life tables). On progression to BC, all patients, independent of treatment arm, are assumed to receive the same therapy (hydroxycarbamide).
FIGURE 36.
Structure of Novartis’s AP model. Reproduced with permission from Novartis’s submission, Figure 18, p. 46. 205
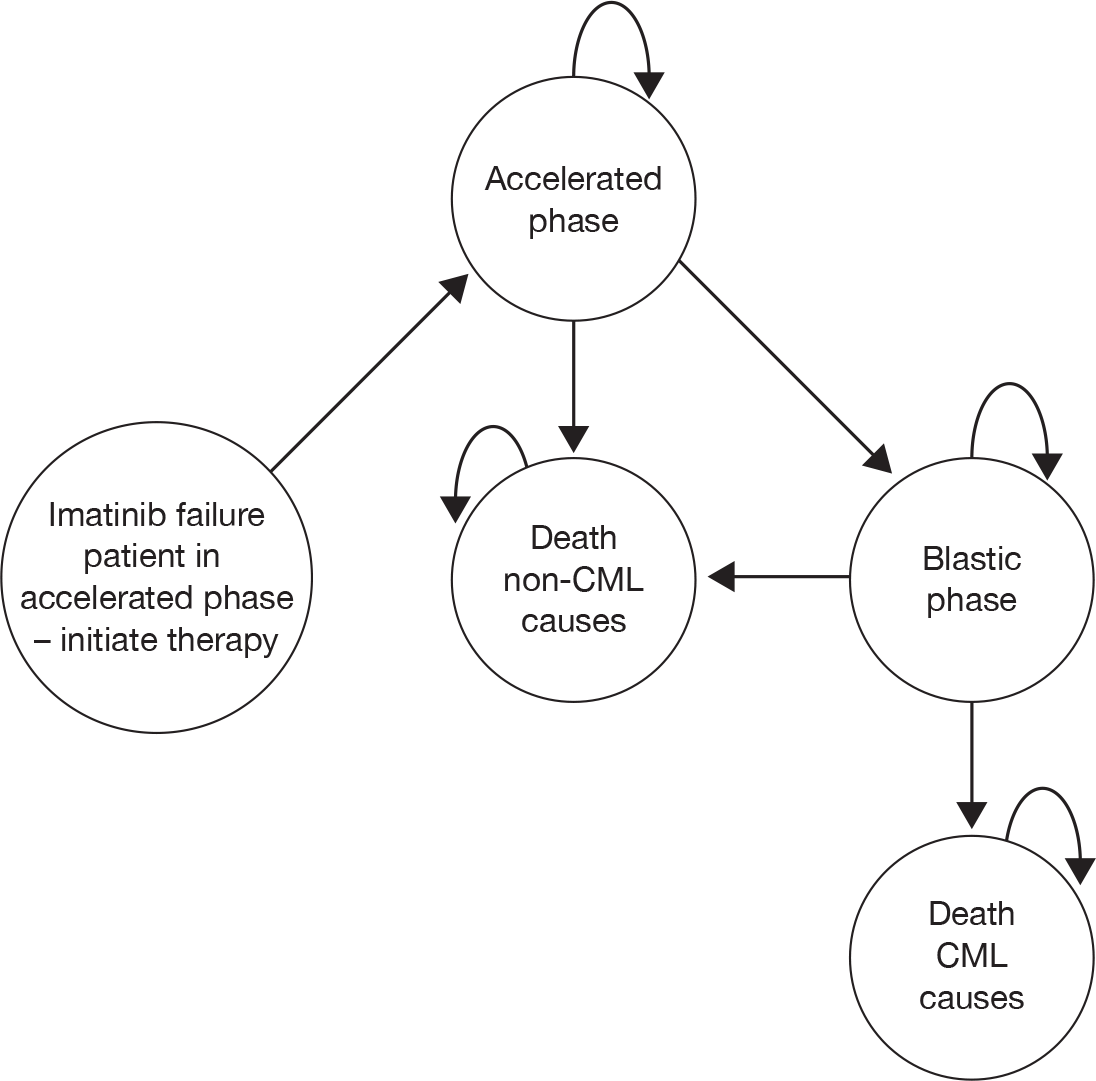
Overall survival and PFS were both assumed to follow exponential distributions. OS was calculated as PFS plus time spent in BC. Time spent in BC was assumed to be independent of treatment arm and independent of TTP.
Clinical effectiveness
No details were provided of the review methods by which data sources were identified (other than a simple statement that a ‘literature search was carried out to identify all relevant papers’ without further details of methods or results).
Nilotinib effectiveness data were taken from the single-arm Phase II study of nilotinib in AP reported by le Coutre et al. 107 (see our review of this evidence in Chapter 2, Effectiveness of nilotinib).
Novartis found no data on the efficacy of HDI following failure of normal-dose imatinib in AP patients. Nonetheless, it presents a model of HDI for ImR patients in AP, using data taken from a multicentre study of normal-dose imatinib in an imatinib-naive population. 32 These data have serious limitations, as described in Review of Novartis’s cost-effective analysis.
For the ImI subgroup, the hydroxycarbamide arm was parameterised with effectiveness data taken from a retrospective analysis of therapy following imatinib failure at a single institution. 223 Novartis acknowledges that there were several serious limitations to these data (see Review of Novartis’s cost-effective analysis).
As explained above, the critical effectiveness input to the model was PFS (with OS calculated as a function of this). For nilotinib, PFS was estimated using an extrapolation of results from the Phase II study (using unpublished data with additional follow-up from the published report107). Similarly, the HDI arm in the ImR model was parameterised using an extrapolation of reported PFS data from the preferred data source. 32 For hydroxycarbamide in the ImI model, empirical PFS data were unavailable in the preferred data source. 223 Instead, PFS was estimated using OS from the study, which was then adjusted so that the ‘relative risk of PFS to OS’ was the same as that observed in ‘the nilotinib data of the relevant patient population’ (presumably, this would be the ImI subgroup of the Phase II study107 although, as this method was not specifically presented in discussion of the AP model, it was possible that relative risk from the CP study106 was used instead).
Overall survival for each treatment was then calculated as the sum of modelled PFS plus time in BC. Time in BC for all comparators was estimated as 9.89 months, calculated on the basis of BC OS curves for participants in Kantarjian et al. ’s retrospective analysis of survival following imatinib failure (the same data source used to parameterise the ImI model’s hydroxycarbamide arm223). An exponential curve was fitted to empirical OS in BC, based on data collected to 5 years, at which point 91% of the cohort had died. Time in BC was estimated as the area under the curve.
Resource use
The following costs were modelled: drug acquisition, hospital appointments for administration and monitoring and treatment for grade 3–4 AEs.
Modelled patients were assumed to take 800 mg of nilotinib q.d., 800 mg (high dose) of imatinib q.d. or 2 g of hydroxycarbamide q.d. Drug costs were not reduced for dose intensities below 100%.
To estimate the duration of therapy, patients were assumed to continue drug treatment until they progressed or discontinued owing to serious AEs. Discontinuation rates were drawn from the literature for nilotinib (10%)107 and assumed to be 0% for hydroxycarbamide. For HDI, a discontinuation rate of 0% was adopted, on the basis that treatment discontinuation was counted as an event in PFS analyses in the study from which efficacy data had been drawn32 (i.e. to include an additional reduction would amount to double-counting).
It was assumed that patients experience serious AEs only in the first 6 months of treatment (and not all patients who experience serious AEs stop treatment). In the absence of an evidence-based source to estimate subsequent disease course following discontinuation, Novartis assumed that 80% of all patients who stop treatment owing to AEs would progress from AP to BC in each 3-month cycle.
It was assumed that patients have outpatient monitoring appointments, the frequency of which depends on the phase of disease. The costs of BM tests were absorbed within the cost of outpatient visits. The costs of grade 3–4 AEs were considered. The average monthly cost of AE treatment for nilotinib and HDI was estimated as £112 and £98 per patient, respectively, for the first 6 months. It was assumed that hydroxycarbamide induces no serious AEs.
Once progression to BC had taken place, it was assumed that all patients receive hydroxycarbamide (2 g/day) and require four outpatient appointments per month, to give a state cost of £1269.30 per 3-month cycle. Finally, it was assumed that patients require 10 days of inpatient stay as end-of-life care, regardless of cause of death (10 × £300 = £3000).
Valuation of outcomes (utilities)
Utilities were taken from the IRIS study of standard-dose imatinib, taken from EQ-5D responses, as reported by Reed et al. :225 CP = 0.854, AP and BC = 0.595. Novartis assumed that these underlying utilities are independent of treatment. Next, disutilities corresponding to grade 3–4 AEs were modelled for nilotinib and HDI (again, it was assumed that hydroxycarbamide induces no serious AEs). Novartis assumed that serious AEs would occur during the first 6 months of treatment. The treatment-specific disutilities were calculated from the sum over all AEs of the product of the disutility, the duration of the AEs and the proportion of patients that experience the AE for each treatment. Based on these assumptions, the average utilities of patients in AP receiving nilotinib, HDI and hydroxycarbamide during the first 6 months of treatment were defined 0.571, 0.545 and 0.595, respectively.
Summary of Novartis’s cost-effective analysis results
The base-case deterministic results of Novartis’s model are given in Tables 106 and 107.
| Drug therapy | Costs (£) | LYs | QALYs | Incremental cost per LY gained (£) | Incremental cost per QALY gained (£) |
|---|---|---|---|---|---|
| HDI | 53,144 | 2.00 | 1.17 | ||
| Nilotinib | 57,571 | 2.38 | 1.41 | 11,577 | 18,541 |
| Drug therapy | Costs (£) | LYs | QALYs | Incremental cost per LY gained (£) | Incremental cost per QALY gained (£) |
|---|---|---|---|---|---|
| Hydroxycarbamide | 9448 | 1.67 | 0.99 | ||
| Nilotinib | 100,414 | 3.60 | 2.13 | 47,071 | 79,914 |
The ICER for nilotinib versus HDI varied between £16,000 and £20,000 per QALY for all one-way sensitivity analyses investigated by Novartis (varying utilities, costs of AEs, PFS and time horizon). The ICER for nilotinib versus hydroxycarbamide varied between £72,000 and £96,000 per QALY for all scenario analyses.
The probabilistic sensitivity analysis indicated that nilotinib was cost-effective compared with HDI for WTP thresholds above approximately £19,000 per QALY, and nilotinib was cost-effective compared with hydroxycarbamide for WTP thresholds above approximately £80,000 per QALY.
Review of Novartis’s cost-effective analysis
Comparators, patient groups
A summary of our review of the Novartis AP model is shown in Box 11. Novartis did not attempt to estimate the incremental cost-effectiveness of nilotinib compared with dasatinib, arguing that study data for the two technologies were incomparable owing to different patient entry requirements. However, no detail was provided to assess this issue in relation to the AP evidence base in particular; instead, the reader was referred to a previous discussion of dissimilarities between studies in CP.
Novartis has not used systematic methods to identify the data on which its economic analysis was based.
Novartis has incorrectly assumed that PFS was identical to time in AP. Consequently, it may have underestimated OS for all treatments.
Novartis has not used CyR rates in their estimation of OS, even though CyR rates are well established as surrogate measures of OS
The data used to estimate the effectiveness of HDI in an ImR population were very seriously flawed:
-
the study investigates normal-dose and low-dose imatinib
-
the study was based on an imatinib-naive population; and
-
the key effectiveness parameter (PFS) has mistakenly been drawn from the wrong survival curve (400 mg q.d., rather than 600 mg q.d.).
When the model is reparameterised using the correct data, it predicts that nilotinib was less effective and less costly than HDI, saving around £100,000 per QALY lost.
All treatments are always assumed to be taken at the recommended dose. Using dose intensities quoted from the studies would have a substantial impact on ICERs (nilotinib vs HDI changes from £18,704 to £57,441 per QALY and nilotinib vs hydroxycarbamide changes from £79,984 to £67,669 per QALY).
We are concerned about the very large degree of extrapolation of PFS, in particular for the ImI subgroup. This makes all cost-effectiveness results highly uncertain.
The hydroxycarbamide clinical effectiveness data have serious limitations: it was likely that a small minority of the study participants actually received hydroxycarbamide, and the data were not specific to an ImI population
One of the major discrepancies emphasised in the CP evidence base was that a significant proportion of ImI individuals in the dasatinib studies had baseline MCyR responses, whereas none of the participants in the analogous nilotinib study had an MCyR at baseline. In the AP population, it was not clear whether – and, if so, to what extent – this asymmetry applied. It appears that eligibility criteria were, in this respect, similar to those adopted in the CP studies, with the Phase II nilotinib study107 explicitly excluding participants with previous MCyR to imatinib from its ImI cohort, whereas no such restriction applied in AP dasatinib studies. 12,81 However, this difference may not have had a very substantial impact in practice. There were two multicentre studies investigating the efficacy of dasatinib in AP specifically (see Chapter 2, Design and characteristics of included studies): a single-arm Phase II study reported by Guilhot et al. 12 and a dose optimisation RCT by Kantarjian et al. 81 (Novartis does not appear to have identified the latter, probably because its publication post-dates Novartis’s literature searches.) Only Kantarjian et al. 81 report the number of study participants who met the criteria for MCyR at baseline and they do not provide a breakdown of these figures according to ImI and ImR subgroups. Nevertheless, we note that, across ImI and ImR populations combined, the proportion of participants who were in MCyR at baseline was not significantly different between either dosage group of this study81 and the study used to parameterise the nilotinib arm of Novartis’s AP model107 [15/158 vs 5/119 (p = 0.147) and 12/159 vs 5/119 (p = 0.369) for 140 mg q.d. and 70 mg b.i.d. arms, respectively; p by chi-squared test with Yates’s correction]. Accordingly, it might be argued that this difference was unlikely to substantially influence study outcomes.
Moreover, we found it difficult to predict the direction of any bias that might be introduced by asymmetry in prior response. On the one hand, previous MCyR to normal-dose imatinib may bode well for the prospects of response to an alternative TKI; on the other, individuals who have already been through successful imatinib treatment are likely to have a longer history of therapy and, accordingly, may have progressed further within the natural history of CML.
Another objection to the comparison of nilotinib and dasatinib in the CP setting was that the definition of ImI was ‘very relaxed’ in the dasatinib studies compared with the nilotinib study (see Chapter 5, Summary of Novartis’s cost-effective analysis). This issue may also apply in AP. In the Phase II nilotinib study,107 ImI was defined as ‘discontinuation of imatinib therapy due to… grade 3 or 4 AEs that persisted in spite of optimal supportive care measures, or grade 2 AEs related to imatinib therapy in spite of optimal supportive care measures that persisted for at least 1 month or that recurred more than three times whether the dose was reduced or discontinued’. In dasatinib studies, the corresponding definitions were, in Hochhaus et al. ’s study,12 ‘if they had toxicity which led to a discontinuation of therapy and was considered to be possibly related to imatinib at a dose of ≯ 400 mg q.d., or if they could only tolerate imatinib doses < 400 mg q.d.’ and, in Kantarjian et al. ’s dose optimisation RCT,81 ‘grade 3 or greater non-haematologic toxicity or grade 4 or greater haematologic toxicity lasting for > 2 weeks while on imatinib ≥ 600 mg q.d. that led to discontinuation of therapy, or to dose decrease to ≤ 400 mg q.d. with loss of HR’.
It was not clear to us that these definitions suggest classification of ImI was most stringent in the nilotinib study. On one hand, we note the explicit requirement for ‘optimal supportive care’ and specific stipulations regarding minimum duration of some AEs for nilotinib participants; on the other, it was notable that dosages of imatinib were not specified and some grade 2 AEs were sufficient to indicate ImI in the nilotinib study, whereas one or both dasatinib studies were more prescriptive in these regards. As a result, we believe it was less easy to argue that the cohorts were too dissimilar to compare.
Finally, when discussing dissimilarities between CP cohorts, Novartis emphasised that ImR participants in the nilotinib study were mostly required to have received extended prior therapy with dose-escalated imatinib, whereas participants in dasatinib studies were classified as ImR regardless of whether or not imatinib dose escalation had been undertaken (see Chapter 5, Summary of Novartis’s cost-effective analysis). In the AP evidence base, this objection may be somewhat less justified. Although the relevant Phase II nilotinib study107 was, once more, clear that a history of imatinib at ≥ 600 mg q.d. was (in the absence of ImI or named P-loop mutations) a necessary criterion for ImR, there was no requirement that dose-escalated treatment should have spanned a minimum duration (as there is in the CP study106). In addition to these slightly relaxed entry criteria for nilotinib study, analogous dasatinib studies12,81 appear to have had slightly more stringent criteria (with a history of ≥ 600 mg q.d. imatinib required for those taking imatinib in AP although, unlike the nilotinib study, those who qualify through progression from CP to AP despite imatinib therapy could have been taking it at 400 mg q.d.).
The net result of these considerations may be to bring studies of the two technologies closer together than was seen in the CP evidence base (on which Novartis bases its objection to comparing the two technologies). Although we acknowledge that non-trivial dissimilarities exist between the two populations, it was not clear to us that these differences exceed those seen between comparators that Novartis were prepared to model in AP. By extension, it was arguable that an economic analysis based on such data could, if well performed, be as valid as any presented in submission.
Novartis did not compare nilotinib with IFN in either population. This was justified on the grounds of (1) an absence of suitable data on the use of IFN following failure of normal-dose imatinib and (2) expert clinical opinion suggesting that ImI individuals are more likely to receive hydroxycarbamide rather than IFN. We have also been informed by our expert advisory group that IFN was unlikely to be considered as a therapeutic option in CML-AP because of its poor toxicity profile.
Model structure
The model cycle length of 3 months seems reasonable given the large uncertainty in model structure and data and, although expected survival was substantially shorter than for patients presenting in CP, the model still extends for a number of years. For the same reasons, it seems reasonable not to model a half-cycle correction. Patients were modelled for life, from age 57 to 100 years, which was appropriate.
Overall survival was calculated as PFS plus time spent in BC. This definition would be correct if progression were defined as progression from AP to BC. However, for some comparators, progression may also be deemed to have occurred for other reasons [CiC information (or data) removed] (see Chapter 2, Accelerated phase). As a result, it was likely that PFS would be of somewhat shorter duration than time in AP. Novartis’s failure to account for this distinction was likely to result in an underestimation of OS for all treatments. However, because definitions of progression were less wide-ranging, it was probably unlikely model outputs would be affected in the dramatic way we believe applies in the CP model (see Chapter 5, Review of Novartis’s chronic phase submission).
Clinical effectiveness data
There was no evidence that the data used to parameterise the model were identified using systematic techniques, so we cannot be certain that all evidence relevant to the decision problems have been found. With the exception of Kantarjian et al. ’s dose optimisation RCT for dasatinib81 (which is a recent publication that may post-date Novartis’s literature searches), it does not appear that Novartis failed to consider any major sources of clinical effectiveness data identified in our own systematic review (see Chapter 2, Identification of evidence).
The parameterisation of the nilotinib arm appears reasonable. However, when the outputs of the Novartis model were compared with empirical data, the fit of predicted to observed OS for nilotinib (Figure 37) was not especially convincing; it appears that survival was overestimated in the early part of the curve, but became underestimated as follow-up extended beyond the first year.
FIGURE 37.
Novartis’s CP model: modelled OS for nilotinib and imatinib, compared with empirical OS from studies. Reproduced with permission from Novartis’s submission, Figure 20, p. 47. 205
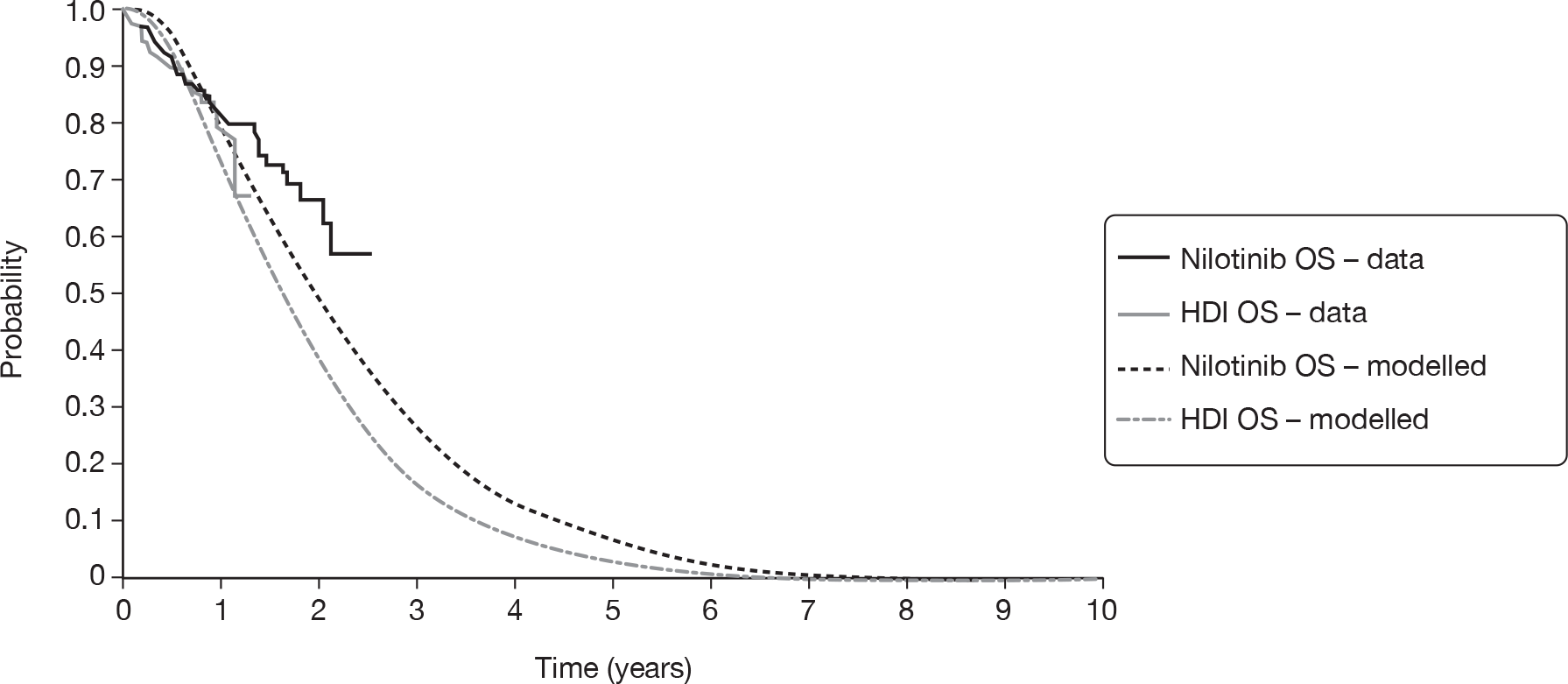
The data used by Novartis to model the efficacy of HDI following failure of normal-dose imatinib in AP patients32 were very seriously flawed. We have three over-riding concerns with the appropriateness of this study:
-
Participants in the study were imatinib naive at baseline. Although an unknown proportion of individuals went on to receive dose escalation in response to primary or secondary resistance to imatinib, these participants were not reported separately in the publication. The relevance of these data to a decision problem founded on an ImR population was extremely limited.
-
Starting doses of imatinib do not qualify as high dose. In the first part of the study, participants received 400 mg q.d.; subsequently, the starting dose was raised to 600 mg q.d. However, neither of these doses amounts to HDI which, in an AP population, would be 800 mg q.d. As noted above, an unknown proportion of study participants went on to receive imatinib at 800 mg q.d.; however, this subgroup was not reported separately in the publication. Again, the relevance of these data is disputed.
-
Even allowing for the reservations expressed above, it appears that Novartis has mistakenly extracted data relating to the wrong cohort for the PFS parameter of ‘HDI’ arm. It was stated in the submission that PFS was drawn from the 600 mg q.d. subgroup of the study. Although it was still less than the 800 mg q.d. (high-dose) regimen supposedly being simulated, we agree that the 600 mg q.d. (normal dose for AP) cohort can be expected to provide a slightly more appropriate estimate of efficacy than the 400 mg q.d. (suboptimal dose for AP) group that was also reported in the paper. However, data used in the model relate to this low-dose group. The graph in the publication is poorly reproduced, making it difficult to identify which of the two PFS curves relates to which group. However, only one of the curves extends beyond the 50% level on the y-axis (i.e. median survival), and it was explicitly stated in the text of the article that ‘median TTP… had not been reached at the time of analysis for patients in the 600-mg dose group’. Therefore, it was clear that the 600 mg q.d. group provided the PFS curve with better survival. However, the data used in the Novartis’s model had been taken from the 400 mg q.d. curve, which shows substantially shorter PFS. The mistake was illustrated in Figure 38, which overlays empirical PFS from the imatinib study (figure 4 of Talpaz et al. ’s publication32) with the curves representing the inputs and outputs of Novartis’s model (figure 19 of Novartis’s submission).
FIGURE 38.
Empirical and modelled PFS for nilotinib and imatinib in Novartis’s AP model.
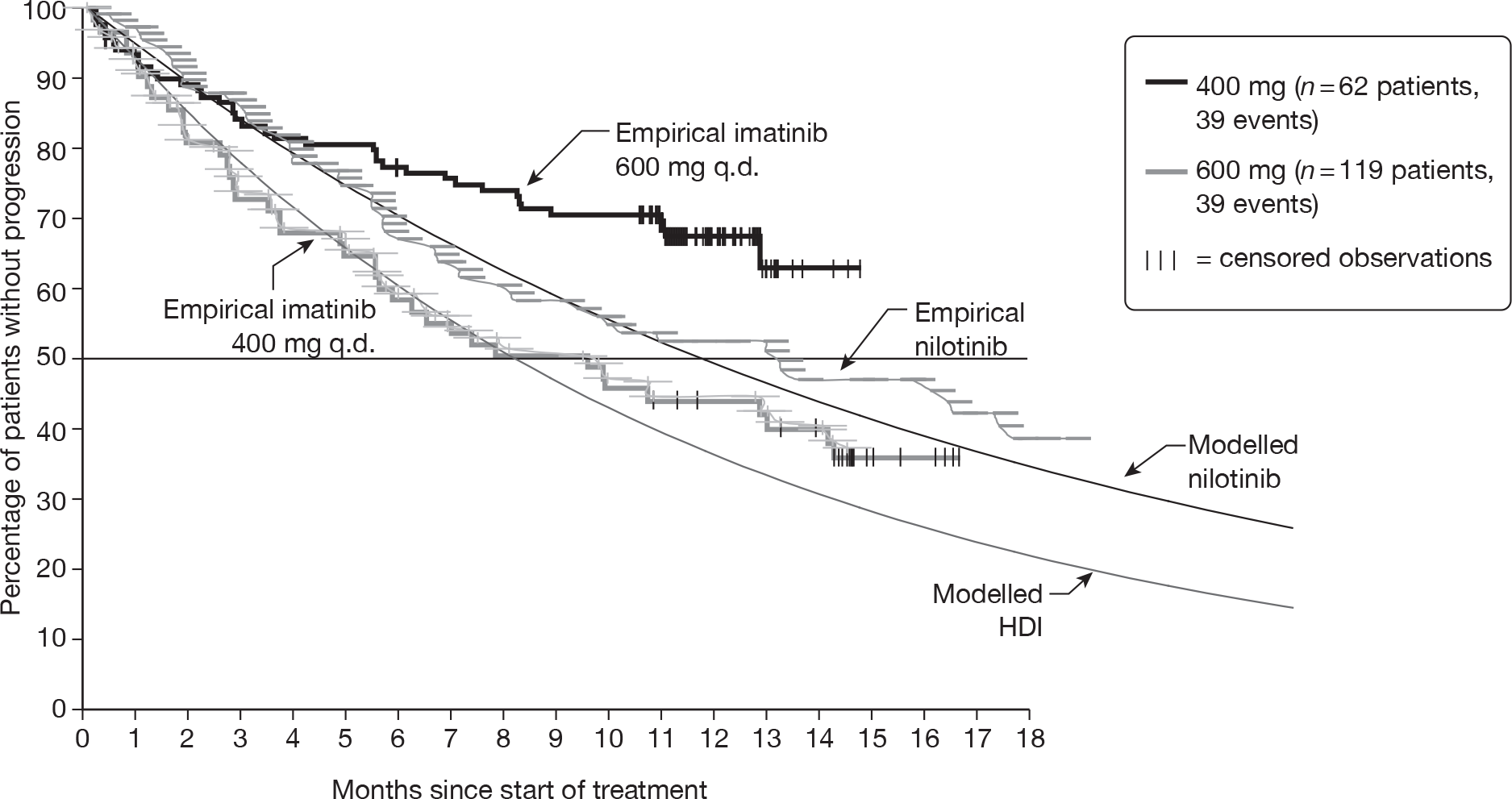
These three problems combine to render any estimates of the cost-effectiveness of nilotinib compared with HDI of extremely dubious validity. To accept Novartis’s results as they stand, one has to assume that the effectiveness of 800 mg q.d. of imatinib in an ImR population was, by nothing more than coincidence, identical to the effectiveness of 400 mg q.d. in an imatinib-naive population.
Substituting the ‘correct’ PFS data for HDI would result in a substantial increase in estimated efficacy of HDI (note that the 600 mg q.d. curve was some way above the empirical nilotinib PFS). Because costs would rise along with estimated effectiveness, it was not possible to guess what impact this would have on the cost-effectiveness outputs.
We investigated the implications of this error by substituting the ‘correct’ PFS data for HDI for the data in Novartis’s model. Figure 39 shows the extrapolated PFS curves from Novartis’s model as submitted, together with the study data on which they were based. Figure 40 shows the same data for the revised model. It can be seen that, in the revised model, in contrast to Novartis’s model as submitted, HDI was predicted to achieve longer PFS than nilotinib (note, that the nilotinib curves are unaffected by this revision).
FIGURE 39.
Empirical and modelled PFS for nilotinib and imatinib in Novartis’s AP model as submitted. Reproduced with permission from Novartis’s submission to NICE, figure 19, p. 47. 205
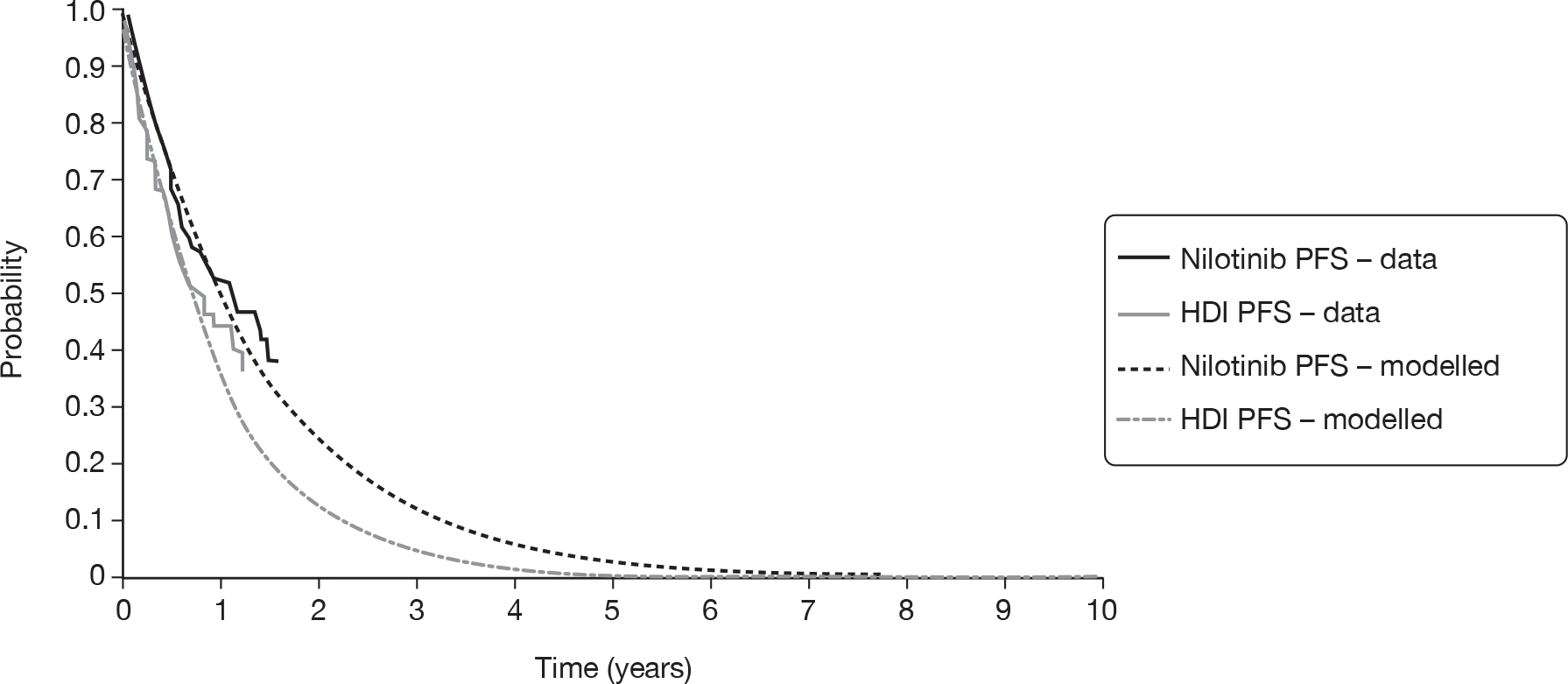
FIGURE 40.
Empirical and modelled PFS for nilotinib and imatinib in the corrected version of Novartis’s AP model.
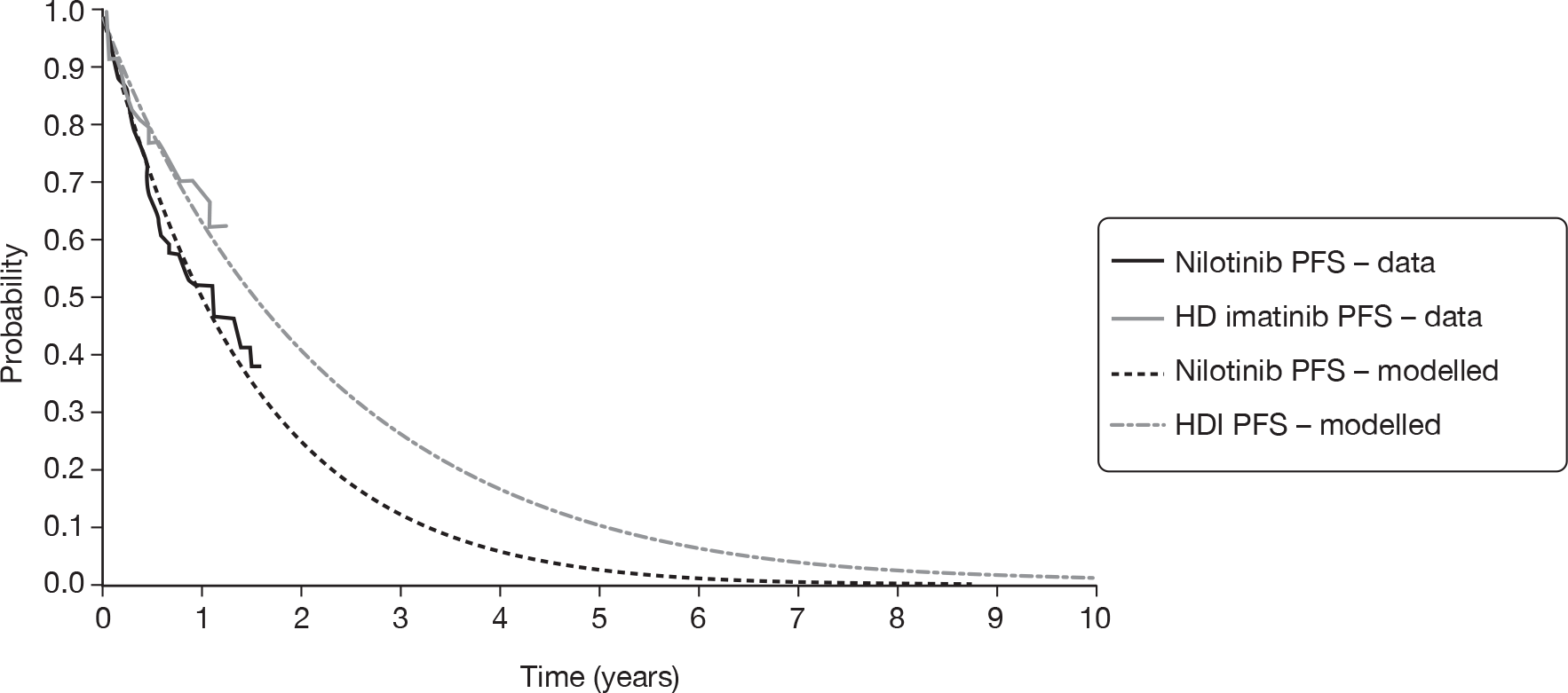
Analogous data for OS are shown in Figure 41 (cf. outputs of model as submitted in Figure 37). It should be remembered that the model was not directly fitted to study data for OS, so the correspondence between simulated and empirical data was a matter of model validation, rather than accuracy of fit.
FIGURE 41.
Empirical and modelled OS for nilotinib and imatinib in the corrected version of Novartis’s AP model.
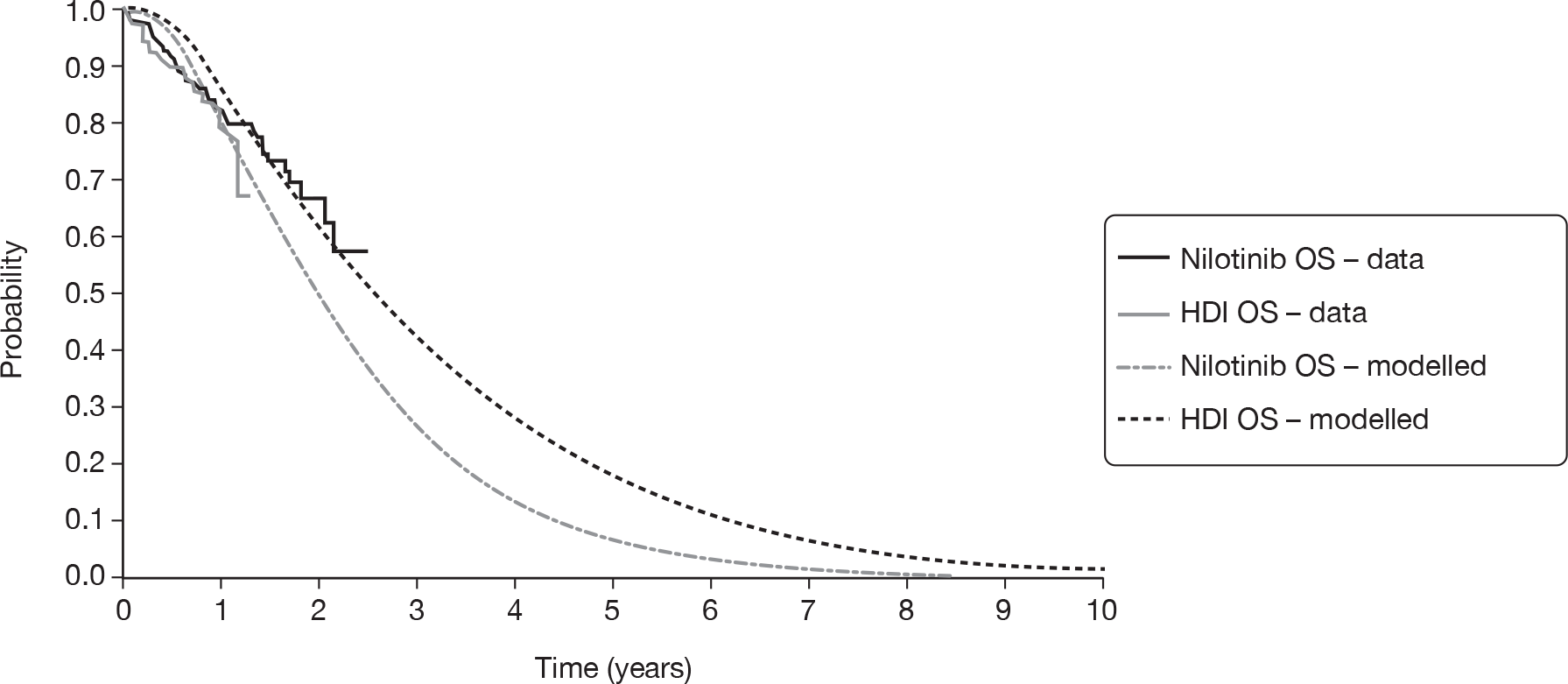
Again, it was immediately obvious that HDI was predicted to achieve longer OS than nilotinib in the revised curves, in contrast to Novartis’s model as submitted. The fit of the simulated HDI cohort to the published curve was visually extremely unconvincing; it appears that the model substantially overestimates OS in this group. As noted above, the fit of predicted to observed OS for nilotinib was also suboptimal.
It can be seen that, in the study data informing the revised model, PFS was substantially superior for HDI than for nilotinib but, when it comes to OS, the comparators are similar, with any slight advantage favouring nilotinib. This suggests that the assumption of treatment-independent post-progression experience (i.e. uniform time in BC) was at odds with the study data used in the model. However, because the model relies on this assumption, it predicts that HDI’s PFS advantage will translate into superior OS.
There are multiple ways to explain the finding that, in the two studies informing the model, there was a large difference in post-progression survival. It was possible that the technologies themselves confer different survival profiles in the post-progression period (i.e. after discontinuation), in which case it would be inappropriate to assume identical post-progression survival, as Novartis’s model does. Alternatively, there may have been systematic differences in aspects of care other than the drugs under investigation. Although neither study provides detail of therapy beyond the technology of interest, we note that Talpaz et al. ’s imatinib study32 was published in 2002, and reflects experience from 1999 to 2001, whereas le Coutre et al. ’s nilotinib study107 was from 2008, with a data cut-off in 2007. As a result, it might be expected that the more recent cohort had access to a superior standard of care following discontinuation of nilotinib, perhaps including other second-generation TKIs, which would not have been available at the time of the imatinib study. If this conjecture was true, it was to be expected that the nilotinib cohort would appear to benefit from superior post-progression survival, irrespective of any difference in treatment effect between the technologies in question. Under these circumstances, it would be appropriate to resolve this asymmetry by assuming uniform post-progression experience, as was the case in Novartis’s model (although this will have the effect of emphasising the difference between model-predicted OS and that observed in the studies).
The cost-effectiveness outputs of the revised model are shown in Table 108. It was important to emphasise that the revised model predicts that nilotinib was both less effective and less costly than HDI (that was, it appeared in the ‘south-west quadrant’ of the cost-effectiveness plane). Therefore, the ICER represents incremental saving per QALY lost; it was predicted that, were nilotinib adopted in place of HDI, the net saving to the health-care system would be a little over £100,000 per QALY lost.
| Drug therapy | Costs (£) | LYs | QALYs | Incremental saving per LY lost (£) | Incremental saving per QALY lost (£) |
|---|---|---|---|---|---|
| HDI | 98,935 | 3.08 | 1.81 | ||
| Nilotinib | 57,676 | 2.39 | 1.41 | 59,866 | 103,847 |
It was important to emphasise that the revised model does not necessarily present a more accurate estimate of the cost-effectiveness of nilotinib in ImR CML-AP. Instead, we believe that the corrected model draws attention to the fundamental inadequacy of the chosen HDI model inputs, an inadequacy that may be in danger of being overlooked, if the outputs of the model as submitted were considered more superficially plausible. If Talpaz et al. ’s imatinib study32 was to be used to estimate the efficacy of HDI in this population, then it must be predicted that nilotinib was a substantially inferior technology, in terms of QALY gain.
Given that we have strong reservations about the use of the clinical effectiveness data from Talpaz et al. 32 for the effectiveness of HDI, we investigated the sensitivity of the ICER to varying assumptions about the clinical effectiveness of HDI. In particular, the median time in AP was varied using Novartis’s model. Technically, this was achieved by varying the quarterly transition probability from AP to BC.
As the median time in AP increases, the ICER for nilotinib versus HDI decreases quickly (Figure 42). This was because imatinib is assumed to be taken for a longer time (while in AP), and therefore incurs higher costs of imatinib acquisition. When the median time in AP was more than about 7.4 months (implying median OS > 1.5 years), Novartis’s model predicts that the ICER was < £30,000 per QALY. Conversely, when median time in AP was less than about 7.4 months (and median OS is < 1.5 years), the ICER was > £30,000 per QALY. Novartis’s base-case scenario is indicated by the dotted line in Figure 42.
FIGURE 42.
Sensitivity of the ICER of nilotinib versus HDI to the median time in AP for people taking HDI.
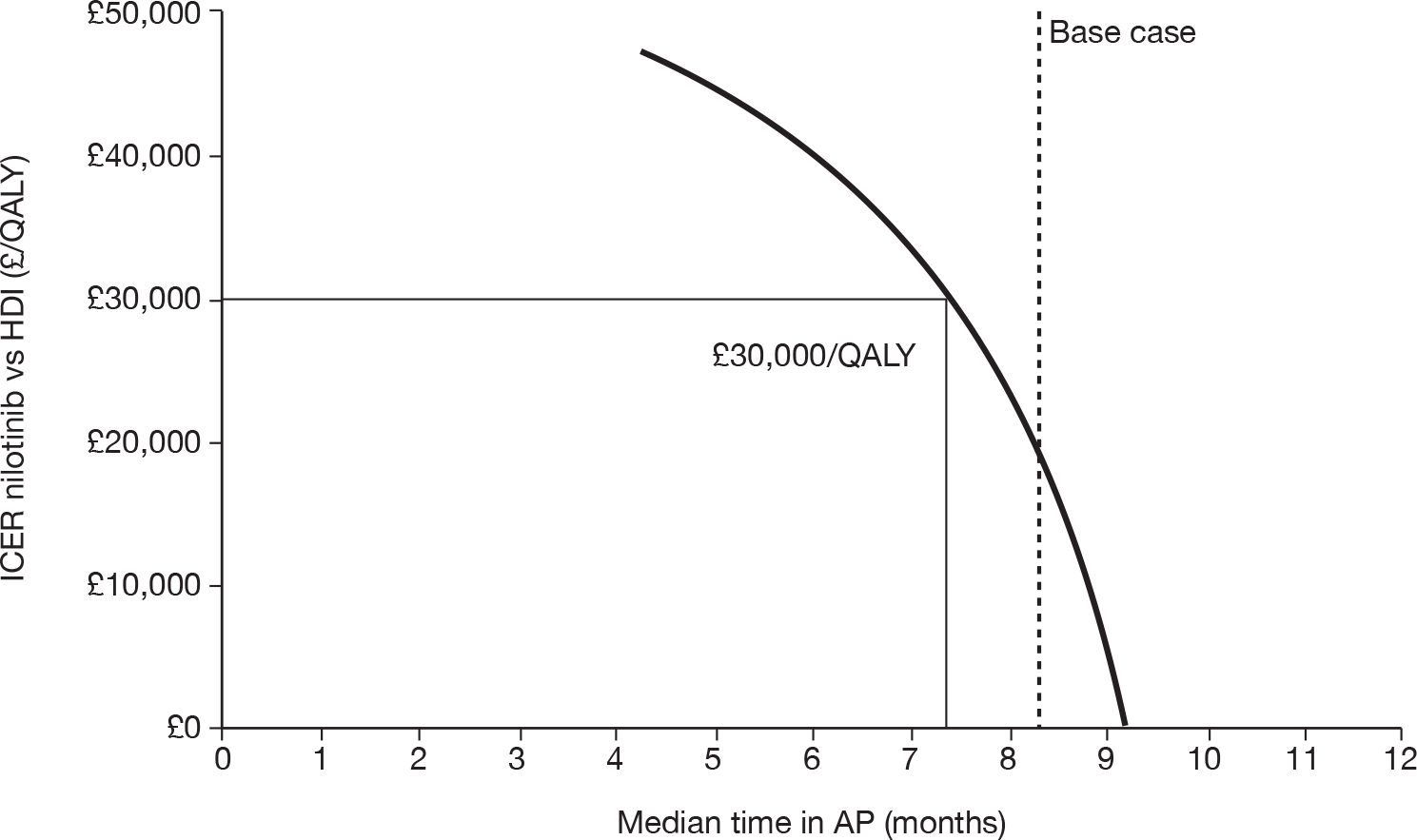
Note that in this analysis, only the time HDI patients spend in AP was varied. Other shortcomings in the model (in particular, failure to account for dose intensity; see below) were not addressed.
For the ImI decision problem, nilotinib was compared with hydroxycarbamide, effectiveness data for which were taken from a retrospective analysis of therapy following imatinib failure at a single institution. 223 Novartis acknowledges that there are several serious limitations with these data. The study arm, from which parameters are drawn, comprises participants receiving a variety of therapies (all treatments other than dasatinib, nilotinib or SCT), but the study does not provide details of the number of participants, if any, who took hydroxycarbamide in AP (only 20% of individuals whose experience in CP was reported in the same paper received hydroxycarbamide; see Chapter 5, Summary of Novartis’s cost-effective analysis). Additionally, the study does not distinguish between participants who failed imatinib owing to resistance and those who were intolerant.
As we are not aware of any evidence suggesting that those who have failed imatinib respond to hydroxycarbamide in a systematically different way to those taking it as a first-line therapy, it may have been preferable to parameterise this arm using a historical, well-powered study describing experience with hydroxycarbamide alone in an imatinib-naive population.
Time spent in BC was assumed to be independent of treatment arm and independent of TTP and was taken from the same data source used to estimate the effectiveness of hydroxycarbamide. 223 Novartis calculated that the mean time in BC was 9.89 months. We are satisfied with this assumption, which was applied independent of treatment and does not greatly affect cost-effectiveness.
We are concerned about the very large degree of extrapolation of PFS, in particular for the ImI subgroup. This makes the cost-effectiveness results highly uncertain.
We note that cost-effectiveness was insensitive to the allowance for general mortality, i.e. the cost-effectiveness results change only marginally when we allow for no general mortality.
Resource use
In order to estimate duration of therapy, participants are assumed to continue drug treatment until they progress or discontinue owing to serious AEs. Despite our reservations about the use of PFS to estimate total time in AP, this approach was appropriate for the calculation of resource use, as drug therapy would be discontinued in the post-progression–pre-BC period that was missing from Novartis’s model.
An alternative, and superior, method of modelling total drug costs would have been to use empirical data on time to discontinuation of treatment. A Kaplan–Meier curve for time to discontinuation of nilotinib in the Phase II study is given in appendix 7 of Novartis’s report, but was not used in its analysis. However, as these data presumably represent all patients in the nilotinib study combined, it would be necessary to use these data split into ImR and ImI subgroups in order to make use of them in the economic model.
We are satisfied that Novartis has implemented the reduction in drug costs for patients stopping treatment as a result of serious AEs in its models as it has described in its report. However, we note that Novartis’s assumption that 80% of all patients who stop treatment because of AEs progress from AP to BC each quarter-year is not fully justified (although we appreciate that the data for this parameter may not be readily available). However, we believe that cost-effectiveness outputs are relatively insensitive to this parameter.
Medical management costs, such as outpatient appointments, costs of chemotherapy, SCTs and costs of treating AEs, appear reasonable. Changes to these parameters affect cost-effectiveness outputs only very marginally.
When discussing its CP model, Novartis acknowledges that, in the studies of nilotinib and HDI, participants experienced dose interruptions, dose reductions and dose escalations. However, such variations are not accounted for in the CP or AP model. Patients were modelled to take 800 mg of nilotinib every day and 800 mg (high dose) of imatinib every day until disease progression or serious AEs. Instead, it was more accurate to model the cost of nilotinib and imatinib corresponding to the doses actually received in the studies.
In the single-arm study of nilotinib,107 the mean dose intensity of nilotinib was [CiC information (or data) removed] and the median dose intensity was 797 mg q.d. for both ImR and ImI patients combined. Therefore, for consistency with the clinical outcomes from this study, we believe that the cost of nilotinib for the AP model should be based on approximately [CiC information (or data) removed] of nilotinib, a cost of [CiC information (or data) removed] per patient per 3-month cycle, not £7928 as assumed by Novartis.
In the ‘HDI’ study,32 the median dose intensity was 578 mg q.d. of imatinib for patients in the 600-mg dose group32 and the mean dose intensity was not reported. Assuming the same ratio of mean to median-dose intensities as in the nilotinib study, we estimate the mean dose intensity in the HDI study as 578 × {[CiC information (or data) removed]/800} = [CiC information (or data) removed] mg q.d., amounting to a cost of [CiC information (or data) removed] per patient per 3-month cycle, not £9758 as used by Novartis.
Assuming a cost of [CiC information (or data) removed] per patient per cycle for nilotinib, and [CiC information (or data) removed] per cycle for HDI, the ICER for nilotinib versus HDI changes from £18,704 to £57,441 per QALY, and the ICER for nilotinib versus hydroxycarbamide changes from £79,984 to £67,669 per QALY.
Valuation of outcomes (utilities)
We believe it was appropriate to source utilities from the IRIS study of standard-dose imatinib,225 because it was based on a large sample of patients and because the utilities were taken from EQ-5D responses, which are preferred in the NICE reference case. 222 Utilities from IRIS were also reported by Dalziel et al. ,226 and are slightly different in this source: AP 0.73, BC 0.52. This discrepancy arises because Reed et al. 225 chose to adopt a pooled utility of 0.595 for AP and BC, because there was no significant difference between the utilities of 0.73 (SE = 0.20) in AP and 0.52 (SE = 0.42) in BC. However, given that uncertainty within model inputs is accounted for in probabilistic analysis, we believe that it may be more appropriate to the use the phase-specific utilities. Doing so changes the estimates of cost-effectiveness a little in nilotinib’s favour: the ICER for nilotinib versus HDI drops to £14,759 per QALY and the ICER for nilotinib versus hydroxycarbamide becomes £64,733 per QALY.
It was notable that, because of different AE profiles, nilotinib was predicted to benefit from a higher utility than HDI, which was the reverse of the finding in CP (see Chapter 5, Summary of Novartis’s cost-effective analysis). It was possible that this was a reflection of the dubious relevance of the data source used to parameterise the HDI arm; as an ImR population has already tolerated normal-dose imatinib, participants are perhaps less likely to experience a toxic response to HDI than imatinib-naive individuals are to have AEs when receiving normal-dose imatinib. However, we note that the disutilities appear to have only a marginal impact on cost-effectiveness outputs.
Dasatinib (manufacturer analysis/model)
Appendix 4 presents a summary review of the dasatinib manufacturer’s submissions against the main items in the NICE reference case requirements and against criteria set out by Philips et al. 221
Summary of industry submission
Comparators, patient groups
Bristol-Myers Squibb, the manufacturer of dasatinib, presents a three-way cost-effectiveness analysis for dasatinib compared with HDI (800 mg q.d.) and nilotinib for patients who failed prior imatinib therapy because of resistance or intolerance.
Model structure
The submission uses a Markov model to estimate cost-effectiveness. The model was written in Microsoft Excel; Crystal Ball® software was used to implement the probabilistic sensitivity analysis.
The model takes a UK NHS perspective, and all costs and benefits are appropriately discounted at 3.5%. 222
The structural assumptions of the AP model are similar to those for the CP model, described in Chapter 5, Summary of industry submission (chronic phase). On entry into the model, an individual’s best initial response (no response, CHR, PCyR or CCyR) to treatment was assessed (Figure 43). As with the CP model, the efficacy of each treatment was represented by the specific mix of patients in each response category. Individuals may then enter one of two disease phases (AP or BC) or death. At each subsequent cycle, individuals may remain in the same phase or progress to a more severe disease state or die. Death may or may not be related to CML. Death unrelated to CML was taken from life tables.
FIGURE 43.
Structure of BMS’s AP model. Reproduced with permission from BMS’s submission, figure 3, p. 94. 184
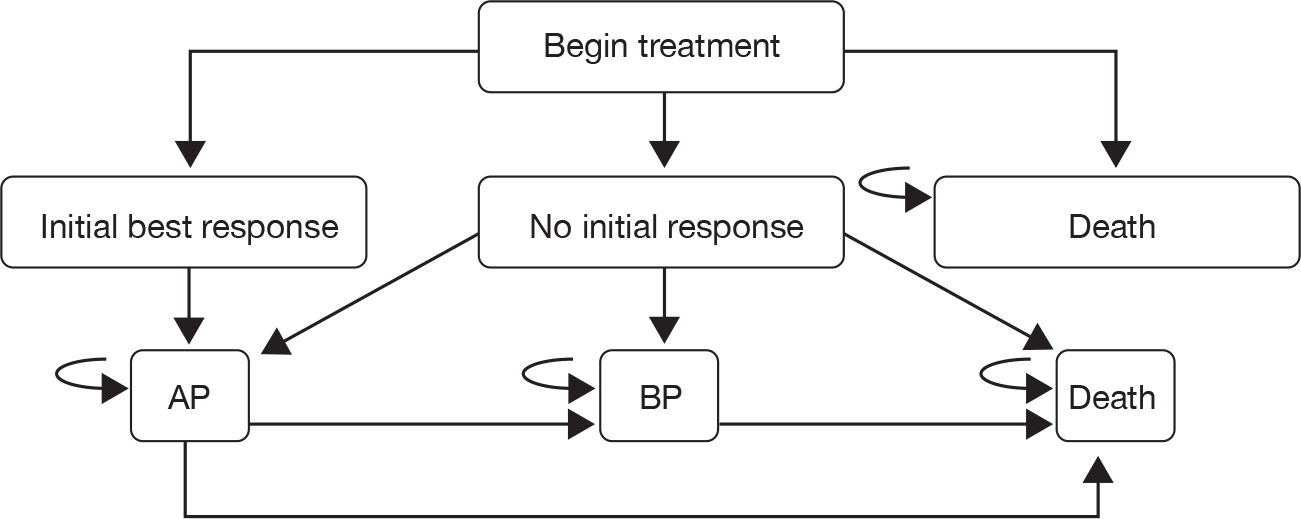
The levels of response to treatment used at the start of the analysis (i.e. NR, CHR, PCyR and CCyR) can be considered comparable to baseline risks as they, together with the phase of CML, determine the probability of disease progression for the rest of the analysis, with different rates of disease progression applied for each level of response. The proportion of patients in each response category represents the efficacy of the treatment.
The model uses a lifetime horizon (100 years) and a model cycle of 1 month. A half-cycle correction was applied. No subgroup analyses were presented. Patients were assumed to enter the model aged 56 years.
Clinical effectiveness
The clinical data for dasatinib were taken from a single-arm clinical study, Guilhot et al. ,12 and for nilotinib from a single-arm study reported by le Coutre et al. 107 BMS found no data on the efficacy of HDI following failure of normal-dose imatinib in AP patients. Nonetheless, BMS took the data for HDI from a multicentre study of normal-dose imatinib in an imatinib-naive population in AP (Talpaz et al. ). 32 These data have serious limitations (see Review of industry submission). Table 109 reports the response data used in the model.
| Treatment and dose | Best response | Source | |||
|---|---|---|---|---|---|
| No response | CHR | PCyR | CCyR | ||
| Dasatinib 140 mg q.d. | 0.278 | 0.335 | 0.063 | 0.323 | Guilhot et al. (2007)12 |
| Imatinib 800 mg q.d. | 0.900 | 0.100 | 0.000 | 0.000 | Talpaz et al. (2002)32 |
| Nilotinib 800 mg q.d. | 0.686 | 0.000 | 0.117 | 0.197 | le Coutre et al. (2008)107 |
As explained in our critique of BMS’s CP model (Chapter 5, Review of BMS’s chronic phase submission), the categories of best response are mutually exclusive, e.g. the PCyR category includes only people who reached this level of response, but did not proceed to CCyR.
Monthly rates of disease progression were calculated from individual patient data from the dasatinib clinical study and applied in the model regardless of treatment. Two sets of transition probabilities were estimated, short-term rates (for the first year) based on PFS and OS by response type at 12 months, and long-term rates (for use after the first year) based on the 24-month PFS and OS data.
Individuals are assumed to receive treatment until disease progression (progression to BC, loss of CHR or MCyR, or increasing WBC count) or intolerable toxicity, after which they receive post-failure treatment (chemotherapy, BM transplant or alternative TKIs).
Resource use
Health-care resources used to treat CML were estimated by UK clinical experts. As for the CP model, the resource-use data covered prescription drugs, outpatient visits, inpatient visits, monitoring tests (i.e. blood tests, chest radiographs and BM tests) and treatment for serious AEs. Resource use was estimated separately for responders and non-responders, and separately before and after the first 3 months. Resource use was valued by applying NHS reference costs and tariffs to estimates from the BMS clinical panel. The base year for costs was 2008 (2006–7 national costs were inflated using rates reported by the Personal Social Services Research Unit, i.e. Pay cost and health service cost indices),227 except for drug costs, which were priced in 2009 terms.
Patients were assumed to take 800 mg of nilotinib q.d., 140 mg of dasatinib q.d. or 800 mg of imatinib (high dose) q.d. Drug costs were taken from the MIMS. 228 Dasatinib was assumed to cost £2541 per month, HDI £3255 per month and nilotinib £2645 per month. Drug costs were not reduced for dose intensities below 100%.
To estimate duration of therapy, patients are assumed to continue drug treatment until they progress or discontinue because of serious AEs.
Adverse events were modelled for each treatment using data from the relevant clinical study. They were incorporated by adjusting the costs and utilities for health states according to their impact and incidence. AEs were assumed to occur only during the first 3 months of treatment. The cost of treating AEs was modelled as a weighted average by the proportion of patients affected and was applied for the duration of events. The average per-patient total cost of treating serious AEs was £444 for imatinib, £0 for dasatinib and £694 for nilotinib.
Valuation of outcomes (utilities)
We have discussed BMS’s choice of utilities in detail in our critique of its CP model (Chapter 5, Review of BMS’s chronic phase submission). In summary, utility values were elicited from a representative sample of 100 unaffected individuals in the UK using the time trade-off method and, possibly, the EQ-5D instrument. Utilities were dependent on response: AP (no response) 0.50, AP (response) 0.79, BC (no response) 0.31, BC (response) 0.50. Disutilities due to serious AEs were modelled, with values obtained from a NICE single technology appraisal of erlotinib for non-small cell lung cancer for a range of events (diarrhoea, rash, fatigue, nausea and neutropenia). 231 However, utility estimates could not be found for many potential AEs. In these cases, the model arbitrarily applied an utility decrement of 0.05.
Analysis of uncertainty
One-way sensitivity analyses, several scenario analyses and probabilistic sensitivity analysis to address parameter uncertainty are presented. In the probabilistic sensitivity analysis, all probabilities of disease progression and the proportions of patients in each best response category were sampled from beta distributions and all costs were sampled from gamma distributions. For the initial response to treatment, the parameter alpha of the beta distribution was set as the number of patients who achieved the specific response and the parameter beta was set as the number who did not respond. For cost data, given that no estimates of uncertainty were available, BMS arbitrarily set the SD equal to 10% of the mean.
Summary of cost-effective analysis results
The base-case deterministic estimates of cost-effectiveness are given in Table 110. Compared with HDI, treatment with dasatinib increases OS by 1.88 years, QALYs by 1.62 years and total costs by £57,000. Compared with nilotinib, treatment with dasatinib increases OS by 0.93 years, QALYs by 0.82 years and total costs by £30,000.
| Drug therapy | Costs (£) | LYs | QALYs | Incremental cost per LY gained vs HDI (£) | Incremental cost per QALY gained vs HDI (£) | Incremental cost per LY gained vs nilotinib (£) | Incremental cost per QALY gained vs nilotinib (£) |
|---|---|---|---|---|---|---|---|
| HDI | 78,190 | 1.29 | 0.65 | 28,495 | 33,772 | ||
| Nilotinib | 105,545 | 2.25 | 1.46 | 28,495 | 33,772 | ||
| Dasatinib | 135,570 | 3.17 | 2.28 | 30,462 | 35,319 | 32,392 | 36,778 |
The one-way sensitivity analyses had little effect on the estimates of cost-effectiveness for dasatinib versus HDI. The probabilistic sensitivity analysis predicts a low level of certainty (11.9%) that treatment with dasatinib was cost-effective compared with HDI at a WTP threshold of £20,000 per QALY, but 63.4% that dasatinib was more cost-effective at a WTP threshold of £30,000 per QALY. The probabilistic sensitivity analysis predicts a 8.2% probability that dasatinib was cost-effective compared with nilotinib at a WTP threshold of £20,000 per QALY and a probability of 30% at a WTP threshold of £30,000 per QALY.
Review of industry submission
A summary of our review of the BMS AP model is shown in Box 12. As noted in the BMS submission, the economic evaluation in AP has a number of strengths:
-
appropriate structure reflecting progression through the phases of CML, including lifetime horizon
-
comprehensive investigation of the sensitivity of the chosen structure and inputs within a reasonably wide range of possible values
-
probabilistic sensitivity analysis.
The data used to estimate the effectiveness of HDI in an ImR population were very seriously flawed:
-
the study investigates normal-dose and low-dose imatinib.
-
the study was based on an imatinib-naive population.
It was not possible to estimate the direction of bias for the cost-effectiveness of dasatinib vs HDI, because the first flaw biased cost-effectiveness in favour of dasatinib, whereas the second flaw biased cost-effectiveness in favour of HDI.
All treatments are always assumed to be taken at the recommended dose. Using dose intensities quoted from the studies had an important impact on the cost-effectiveness of dasatinib vs HDI, as the ICER increased from £35,300 per QALY to £42,100 per QALY.
BMS predicts far shorter-tailed OS for HDI and nilotinib than was experienced in the studies. All other matters equal, this suggested that BMS had underestimated the ICERs for dasatinib vs HDI and dasatinib vs nilotinib.
BMS predicted shorter-tailed PFS and OS for dasatinib than was experienced in the study. It was not possible to say how this biased cost-effectiveness.
BMS has taken the cost of dasatinib from MIMS,230 which was 4% lower than the cost quoted in the BNF. 68 Assuming the cost of dasatinib from the BNF,68 and the dose intensities quoted from the studies, the ICER for dasatinib vs HDI increased from £35,300 per QALY to £44,300 per QALY, and the ICER for dasatinib vs nilotinib increased from £36,800 per QALY to £41,100 per QALY.
We do, however, have a number of concerns about the analysis. These are considered under the same sections as the description of the model.
Comparators, patient groups
The BMS comparison of dasatinib with HDI in AP was presented for patients with ImR and ImI combined. Therefore, an element of the NICE scope was not addressed: treatment of patients in AP: with imatinib resistance separately from those with ImI.
Differences in the baseline characteristics of individuals in the single-arm studies of dasatinib, nilotinib and HDI may limit the accuracy of the model results, but these differences are not explored. For example, in the study of dasatinib,12 all patients had previously been treated with imatinib, whereas, in the study of imatinib,32 no patients had previously been treated with imatinib. This factor alone might be expected to bias response rates in favour of imatinib. However, contrary to this, in the imatinib study,32 normal- and low-dose imatinib was used, whereas BMS models HDI. Therefore, the response rates from the study of imatinib may underestimate the response rates if HDI had been used.
There may also be concerns about the applicability of the clinical effectiveness evidence given the different mix of ImR and ImI patients in the three studies used to carry out the analysis since patients with a history of intolerance or resistance may respond differently to the different TKIs. Moreover, further uncertainty must relate to the fact that separate studies are used to inform comparisons.
Model structure
The model cycle length of 1 month was easily short enough to capture the natural history of the disease. Patients are appropriately modelled for life.
Patients are modelled to take drug treatment until transferring to BC. This would be correct if progression were defined as progression from AP to BC. However, progression may also be deemed to have occurred for other reasons, such as loss of MCyR. As a result, it was likely that PFS would be of shorter duration than time in AP. Failure to account for this distinction was likely to result in an overestimation of treatment duration for all treatments. However, because the expected time in AP was far shorter than the expected time in CP, it was unlikely that this issue was as influential in AP as it appeared to be in the BMS CP evaluation.
People were assumed to enter the model aged 56 years. This seems rather young, given that BMS has also assumed a starting age of 56 for patients in its CP model and patients typically spend several years in CML-CP.
The influence of response on progression was assumed to remain constant over time. This generates an unknown amount of structural uncertainty in the analysis.
Clinical effectiveness data
Bristol-Myers Squibb and Novartis used the same study to model the clinical effectiveness of HDI. 32 As stated in our critique of Novartis’s AP model [Dasatinib (manufacturer analysis/model)], we have two very serious concerns with these data. In summary, they are that:
-
Participants in the study were imatinib naive at baseline.
-
The starting doses of imatinib do not qualify as high dose. In the first part of the study, participants received 400 mg q.d.; subsequently, the starting dose was raised to 600 mg q.d. However, neither of these doses amounts to HDI which, in an AP population, would be 800 mg q.d.
Indeed, BMS acknowledges that the AP model cost-effectiveness estimates are ‘associated with more uncertainty’ (compared with the results from the CP model) ‘due to a lack of comparative efficacy data’ (p. 83, BMS’s submission). These problems combine to render any estimates of the cost-effectiveness of dasatinib and nilotinib compared with HDI somewhat dubious. To accept BMS’s results as they stand, one has to assume that the effectiveness of 800 mg q.d. imatinib in an ImR population was identical to the effectiveness of 400 mg q.d. in an imatinib-naive population.
Turning to the clinical effectiveness data for nilotinib, we were concerned that the BMS model underestimates OS for nilotinib because it predicted an OS rate of 0.54 at 1 year, whereas the published empirical value was 0.79. 107
We have a similar criticism of predicted OS for HDI from the BMS model. The BMS model predicted far shorter-tailed OS than was experienced in the study of HDI. 32 For example, at 0.5 years, BMS predicts an OS of 0.62, whereas the empirical study value was approximately 0.90 (patients taking 600 mg imatinib), and at 1 year BMS predicts an OS of 0.38, whereas the study value was approximately 0.79. All other matters equal, these observations on nilotinib and imatinib suggest that BMS has underestimated the ICERs for dasatinib versus HDI and nilotinib.
Finally, the BMS AP model was validated by comparing the modelled prediction of PFS and OS for dasatinib with that seen in the dasatinib clinical study. BMS reports that these broadly agree. In fact, the model substantially underpredicts these quantities: PFS by 10% and OS by 15% at the 2-year point. It was not possible to say how this may bias cost-effectiveness.
A further important structural uncertainty arises from differences in the definition of progression between the studies included in the model. For example, ‘at least a 50% in peripheral WBC count, blast count, basophils or platelets’ counts as progression in le Coutre et al. ,107 but not in Guilhot et al. 12 This was important because treatment stops at progression, and therefore affects drug acquisition costs, which are particularly important for cost-effectiveness.
Given that we have strong reservations about the use of the clinical effectiveness data from Talpaz et al. 32 for the effectiveness of HDI, the sensitivity of the ICER to the assumption for the clinical effectiveness of HDI was investigated. Specifically, we varied the proportion of people who experience a CHR for HDI (the remainder were assumed to have no response), using BMS’s model.
As the proportion achieving a CHR increases, the ICER for dasatinib versus HDI decreases (Figure 44). This was because imatinib was assumed to be taken for a longer time (while in AP), and therefore incurs higher costs for imatinib acquisition. When the response rate was more than about 40% (median OS more than about 1.0 year), BMS’s model predicts an ICER < £30,000 per QALY. Conversely, when the response rate was less than about 40% (median OS less than about 1.0 year), the ICER was > £30,000 per QALY. The BMS base-case scenario for HDI is indicated by the dotted line in Figure 44. The base-case split of best response for dasatinib is 28% no response, 34% CHR, 6% PCyR and 32% CCyR.
FIGURE 44.
Sensitivity of the ICER of dasatinib versus HDI to the proportion of people taking HDI who experience a CHR.
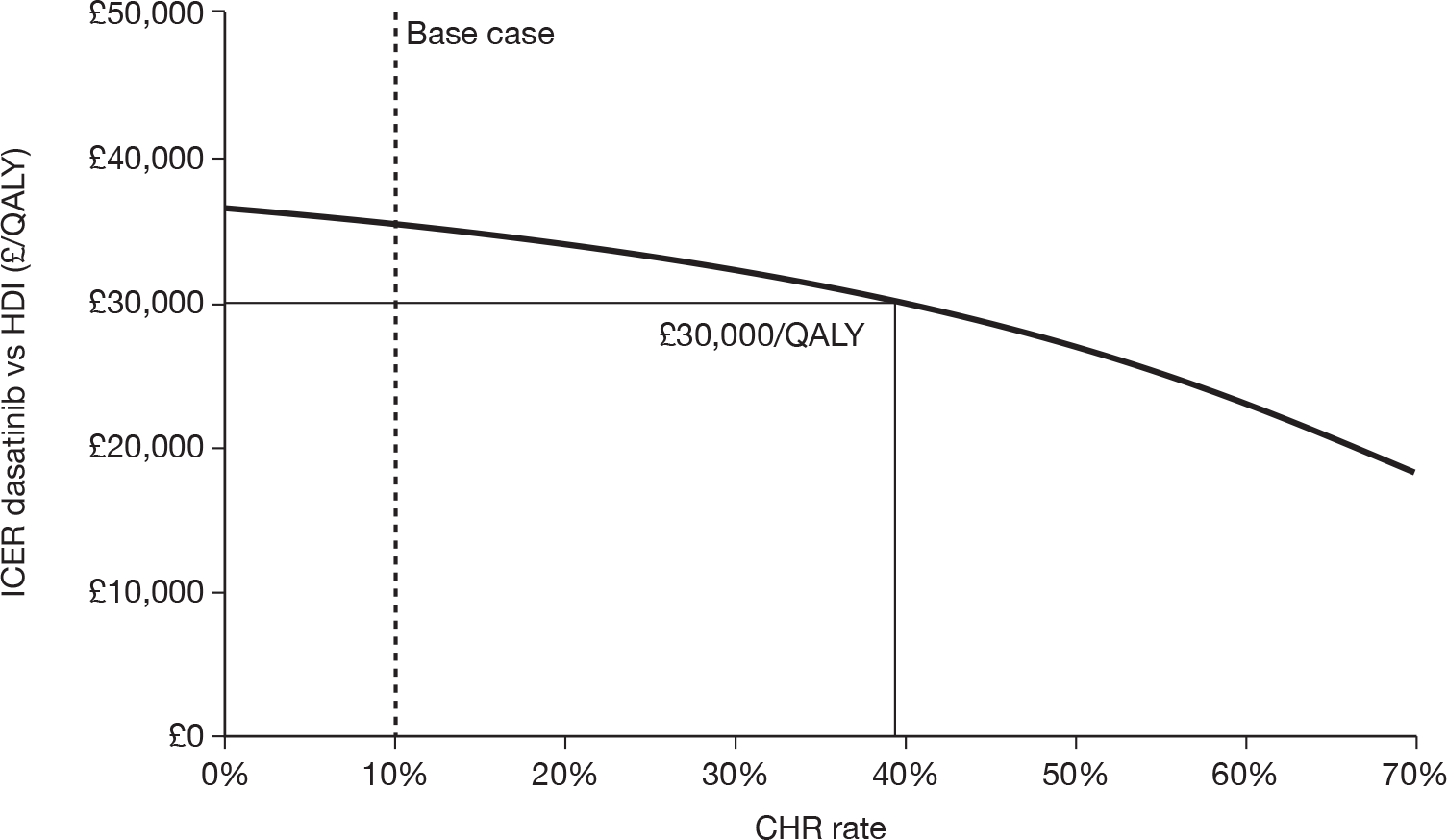
Note that, in this analysis, we varied only the proportion of people taking HDI who experience a CHR. Other shortcomings in the model (in particular, failure to account for dose intensity) are not addressed.
Resource use
Participants are assumed to continue drug treatment until they progress or develop serious AEs. Despite our reservations about the use of PFS to estimate total time in AP (see Box 12), this approach was appropriate for the calculation of resource use, as drug therapy would be discontinued in the post-progression–pre-BC period that was missing from the BMS model.
Medical management costs, such as outpatient appointments, chemotherapy and SCTs, appear reasonable. Changes to these parameters affect cost-effectiveness only slightly. The range of reported post-failure treatments demonstrates considerable variation in practice, which adds further to uncertainty in the analysis, although it was clear that, as such costs fall equally on all treatment comparisons, there was little influence on cost-effectiveness.
The costs of treating serious AEs for patients taking imatinib and nilotinib appear reasonable. However, it seemed unlikely that the cost of treating AEs for patients taking dasatinib would be zero. Nonetheless, changes to these parameters affect cost-effectiveness only slightly.
Drug acquisition costs were a very important driver of the BMS model’s results. Patients were assumed to take 800 mg of nilotinib q.d., 140 mg of dasatinib q.d. or 800 mg of imatinib (high dose) q.d. Instead, it was more accurate to model the costs of these drugs corresponding to the doses actually received in the studies.
In the single-arm study of nilotinib,107 the median dose was 797 mg q.d. for both ImR and ImI patients combined, which corresponds to a median dose intensity of 100%. In the HDI study,32 the median dose intensity was 578 mg q.d. for patients in the 600-mg dose group, corresponding to a median dose intensity of 72% (relative to the modelled dose of 800 mg q.d.). This equates to £2344 per patient per month, compared with £3255 as assumed by BMS.
The median dose intensity of patients in the dasatinib study for patients starting in AP was not published. 12 However, the cost of dasatinib was relatively insensitive to the dose, because the cost of 100 mg of dasatinib was the same as the cost of 140 mg. 68 Therefore, a dose intensity of 100% for dasatinib seemed reasonable.
Using these revised dose intensities, the ICER for dasatinib versus HDI increased from £35,300 per QALY to £42,100 per QALY and the ICER for dasatinib versus nilotinib remained unchanged.
BMS has taken the cost of all drugs from MIMS. 228 The drug costs from this source were the same as the costs cited in the BNF,68 except for dasatinib (£2643 per patient per month in BNF vs £2541 in MIMS, a difference of 4%). When the higher cost of dasatinib, quoted in the BNF,68 was used in the BMS model, the ICER for dasatinib versus HDI increased from £35,300 per QALY to £37,500 per QALY, and the ICER for dasatinib versus nilotinib increased from £36,800 per QALY to £41,100 per QALY.
When both the slightly higher cost of dasatinib cited in the BNF68 and the revised dose intensities were modelled, the ICER for dasatinib versus HDI increased from £35,300 per QALY to £44,300 per QALY, and the ICER for dasatinib versus nilotinib increased from £36,800 per QALY to £41,100 per QALY.
It is important to emphasise that the amended ICERs do not necessarily present a more accurate estimate of the cost-effectiveness of dasatinib versus HDI because they are still based on flawed clinical effectiveness data for HDI.
Valuation of outcomes (utilities)
We have discussed BMS’s choice of utilities in detail in our critique of its CP model (Chapter 5, Review of BMS’s chronic phase submission). A survey of members of the general public was carried out to inform quality adjustment of time spent in the main health states of CML. It was unclear why this was considered necessary as a range of estimates were already available, as reported elsewhere in this report. The survey included differences in utility according to response status, although this seemed to influence the model to a very limited extent. Nonetheless, the values obtained seem reasonable and those for responders are very similar to those reported in the IRIS RCT.
Chapter 7 Cost-effectiveness: chronic myeloid leukaemia in blast crisis
As explained in Chapter 3, we have not produced a de novo model of CML-BC because of the lack of clinical effectiveness data for comparator treatments. In this section we provide a review, critique and exploration of the cost-effectiveness analysis provided in the manufacturer submission of dasatinib.
Review of manufacturer submissions to NICE
Methods
The cost-effectiveness models reported in the manufacturer submissions were assessed against the NICE reference case,220 and are critically appraised using the framework presented by Phillips et al. ,221 who have synthesised the literature on the evaluation of decision-analytic models in a health technology context to present guidelines for good practice. A summary of the reviews is presented below, with additional details provided in Appendix 4. More in-depth exploration of the models was performed by, for example, substituting alternative parameter values and assessing the impact on the model outputs, and exploring the sensitivity of the model outputs to changes in key parameter inputs.
Dasatinib (manufacturer analysis/model)
Appendix 4 presents a summary review of the dasatinib manufacturer submissions against the main items in the NICE reference case requirements and against criteria set out by Philips et al. 221
Summary of industry submission
Comparators, patient groups
Bristol-Myers Squibb, the manufacturer of dasatinib, presents a cost-effectiveness analysis for dasatinib compared with HDI (800 mg q.d.) for patients in whom prior imatinib therapy has failed because of resistance or intolerance.
Model structure
The submission uses a Markov model to estimate cost-effectiveness. The model was written in Microsoft Excel; Crystal Ball® software was used to implement the probabilistic sensitivity analysis.
The model takes a UK NHS perspective and all costs and benefits are discounted at 3.5%. 222
The structural assumptions of the BC model are similar to those of the CP and AP models, which were described in Chapter 5, Dasatinib (manufacturer analysis/model) and Chapter 6, Dasatinib (manufacturer analysis/model). On entry into the model, an individual’s best initial response (no response, CHR, PCyR or CCyR) to treatment was assessed (Figure 45). The efficacy of each treatment was represented by the specific mix of patients in each response category. At each subsequent cycle, individuals may remain in BC or die. Death may or may not be related to CML. Death unrelated to CML was taken from life tables.
FIGURE 45.
Structure of BMS’s BC model. Reproduced with permission from BMS’s submission, figure 3, p. 94. 184
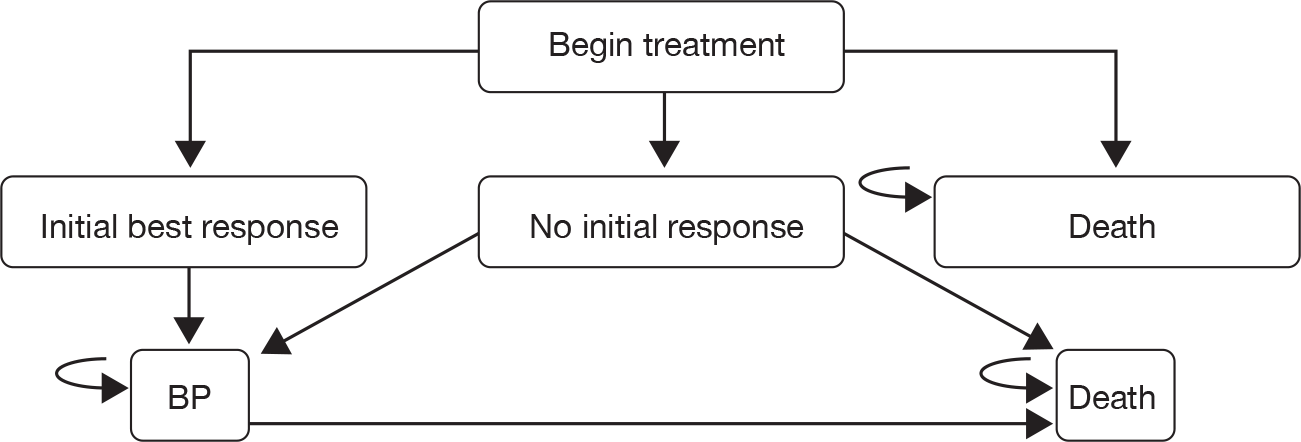
As in the CP and AP models, the levels of response to treatment used at the start of the analysis (i.e. NR, CHR, PCyR and CCyR) can be considered comparable to baseline risks as they, together with the phase of CML, determine the probability of disease progression for the rest of the analysis, with different rates of disease progression applied for each level of response. The proportion of patients in each response category represents the efficacy of the treatment.
The model uses a lifetime horizon (100 years) and a model cycle of 1 month. A half-cycle correction was applied. No subgroup analyses were presented. Patients were assumed to enter the model aged 48 years, with a 50 : 50 male–female ratio.
Clinical effectiveness
The clinical data for dasatinib were taken from a single-arm clinical study by Cortes et al. ,13 sponsored by BMS (study CA180–035). BMS found no data on the efficacy of HDI following failure of normal-dose imatinib in BC patients. Nonetheless, BMS took the data for HDI from a multicentre study of normal-dose imatinib in an imatinib-naive population in BC. 252 These data have serious limitations (see Review of industry submission below). Table 111 reports the response data used in the model.
| Treatment | Best response | Source | |||
|---|---|---|---|---|---|
| No response | CHR | PCyR | CCyR | ||
| Dasatinib 140 mg | 0.444 | 0.204 | 0.111 | 0.241 | Cortes et al. (2007)13 |
| Imatinib 800 mg | 0.938 | 0.062 | 0.000 | 0.000 | Sawyers et al. (2002)252 |
As explained in the critiques of the BMS CP and AP models, the categories of best response are mutually exclusive, e.g. the PCyR category includes only people who reached this level of response, but did not proceed to CCyR.
Monthly rates of disease progression were calculated from individual patient data from the dasatinib clinical study and applied in the model regardless of treatment. Two sets of transition probabilities were estimated, short-term rates (for the first year) based on PFS and OS by response type at 12 months, and long-term rates (for use after the first year), based on the 24-month PFS and OS data.
Individuals were assumed to receive treatment until disease progression (loss of CHR or MCyR, or increasing WBC count) or intolerable toxicity, after which no further treatment was assumed.
Resource use
As in the BMS CP and AP models, health-care resources used to treat CML were estimated by UK clinical experts. Also, as in the CP and AP models, resource-use data covered prescription drugs, outpatient visits, inpatient visits, monitoring tests (i.e. blood tests, chest radiographs and BM tests) and treatment for serious AEs. Resource use was estimated separately for responders and non-responders, and separately before and after the first 3 months. Resource use was valued by applying NHS reference costs and tariffs to estimates from the BMS clinical panel. The base year for costs was 2008 (2006–7 national costs were inflated using rates reported by the Personal Social Services Research Unit, i.e. Pay cost and health service cost indices),227 except for drug costs, which were priced in 2009 terms.
Patients were assumed to take 140 mg of dasatinib q.d. or 800 mg of imatinib (high dose) q.d. Drug costs were taken from the MIMS. 228 Dasatinib was assumed to cost £2541 per month and HDI £3255 per month. Drug costs were not reduced for dose intensities below 100%.
To estimate duration of therapy, patients are assumed to continue drug treatment until they progress or discontinue owing to serious AEs.
Adverse events were modelled for each treatment using data from the relevant clinical study. They were incorporated by adjusting the costs and utilities according to their impact and incidence. AEs were assumed to occur only during the first 3 months of treatment. The cost of treating AEs was modelled as a weighted average by the proportion of patients affected and was applied for the duration of events. The average per-patient total cost of treating serious AEs was £482 for imatinib and £0 for dasatinib.
Valuation of outcomes (utilities)
We have discussed BMS’s choice of utilities in detail in our critique of its CP model (Chapter 5, Review of BMS’s chronic phase submission). In summary, utility values were elicited from a representative sample of 100 unaffected individuals in the UK using the time trade-off method. Although the EQ-5D was mentioned in the BMS submission, it was not clear whether or not or how this was used in the study, for which very limited methodological detail was reported. Utilities were dependent on response: BC (no response) 0.31, BC (response) 0.50. Disutilities due to serious AEs were modelled, with values obtained from a NICE single technology appraisal of erlotinib for non-small cell lung cancer for a range of events (diarrhoea, rash, fatigue, nausea and neutropenia). 231 However, utility estimates could not be found for many potential AEs. In these cases, the model arbitrarily applied an utility decrement of 0.05.
Analysis of uncertainty
One-way sensitivity analyses, several scenario analyses and probabilistic sensitivity analysis to address parameter uncertainty are presented. In the probabilistic sensitivity analysis, all probabilities of disease progression and the proportions of patients in each best response category were sampled from beta distributions and all costs were sampled from gamma distributions. For the initial response to treatment, the parameter alpha of the beta distribution was set as the number of patients who achieved the specific response and the parameter beta was set as the number who did not respond. For cost data, given that no estimates of uncertainty were available, BMS arbitrarily set the SD equal to 10% of the mean.
Summary of cost-effective analysis results
The base-case deterministic estimates of cost-effectiveness are given in Table 112. Compared with HDI, treatment with dasatinib increases OS by 0.45 years and QALYs by 0.28 years and decreases total costs by £11,000.
| Drug therapy | Costs (£) | LYs | QALYs | Incremental cost per LY gained | Incremental cost per QALY gained |
|---|---|---|---|---|---|
| HDI | 99,367 | 0.56 | 0.19 | ||
| Dasatinib | 88,181 | 1.01 | 0.46 | Dasatinib dominates HDI | Dasatinib dominates HDI |
The one-way sensitivity analyses had little effect on the estimates of cost-effectiveness; in all cases dasatinib dominated HDI. The probabilistic sensitivity predicted a high level of certainty (100%) that treatment with dasatinib was cost-effective compared with HDI at WTP thresholds of £20,000 and £30,000 per QALY.
Review of industry submission
A summary of our review of the BMS BC model is shown in Box 13. As noted in the BMS submission, the economic evaluation in BC had a number of strengths:
-
appropriate structure reflecting the progression of CML, including lifetime horizon
-
comprehensive investigation of the sensitivity of the chosen structure and inputs within a reasonably wide range of possible values
-
probabilistic sensitivity analysis.
The data used to estimate the effectiveness of HDI in an ImR population were very seriously flawed:
-
the study investigates normal-dose and low-dose imatinib; and
-
the study was based on an imatinib-naive population.
It was not possible to estimate the direction of bias for the cost-effectiveness of dasatinib vs HDI, because the first flaw biased cost-effectiveness in favour of dasatinib, whereas the second flaw biased cost-effectiveness in favour of HDI.
Both treatments are always assumed to be taken at the recommended do se. Using dose intensities quoted from the studies, the expected per patient costs of dasatinib and HDI were similar, but dasatinib still dominated HDI.
BMS predicted far shorter-tailed OS for HDI than was experienced in the study. All other matters equal, this suggests that BMS have underestimated the ICER for dasatinib vs HDI.
BMS has taken the cost of dasatinib from MIMS,230 which was 4% lower than the cost quoted in the BNF. 68
We do, however, have a number of concerns about the analysis. These are considered under the same sections as the description of the model.
Comparators, patient groups
The BMS comparison of dasatinib with HDI in BC was presented for patients with ImR and ImI combined. Therefore, an element of the NICE scope was not addressed: treatment of patients in BC with ImR, separately from those with ImI.
Differences in the baseline characteristics of individuals in the single-arm studies of dasatinib and HDI may limit the accuracy of the model results, but these differences are not explored. For example, in the study of dasatinib,13 all patients had previously been treated with imatinib, whereas, in the study of imatinib,252 no patients had previously been treated with imatinib. This factor alone might be expected to bias response rates in favour of imatinib. However, contrary to this, in the imatinib study,252 normal- and low-dose imatinib was used, whereas the BMS model used HDI. Therefore, the response rates from the study of imatinib may underestimate the response rates if HDI had been used.
There may be concerns about the applicability of the clinical effectiveness evidence given the different mix of ImR and ImI patients in the two studies used to carry out the analysis, as patients with a history of ImI or ImR may respond differently to the different TKIs.
Model structure
The model cycle length of 1 month was easily short enough to capture the natural history of the disease. Patients were appropriately modelled for life.
Patients were assumed to enter the model aged 48 years. This appeared to be too young, given that BMS assumes a starting age of 56 years for patients in its CP and AP models, and patients typically spend several years in CML-CP. Indeed, we would expect patients to start BC several years after they start CML-CP.
The influence of response on progression was assumed to remain constant over time. This generates structural uncertainty in the model.
Clinical effectiveness data
We have two very serious concerns with the data that BMS used to model the clinical effectiveness of HDI. 252 These concerns are the same as those regarding the clinical effectiveness data for HDI that BMS and Novartis use in their AP models. In summary, these are that:
-
Participants in the study were imatinib-naive at baseline.
-
The doses of imatinib do not qualify as high dose.
Indeed, BMS acknowledges that the BC model cost-effectiveness estimates are ‘associated with more uncertainty’ (compared with the results from the CP model) ‘due to a lack of comparative efficacy data’. These problems combine to render any estimates of the cost-effectiveness of dasatinib compared with HDI of limited validity. To accept the BMS results as they stand, one has to assume that the effectiveness of 800 mg q.d. of imatinib in an ImR population was identical to the effectiveness of 400 mg q.d. in an imatinib-naive population.
The predicted OS for dasatinib patients from the BMS model appears consistent with that reported in the study by Cortes et al. 123 For example, at 12 months, the BMS model predicts an OS of 0.36, whereas the study value for myeloid BC patients was approximately 0.50 and for lymphoid BC patients approximately 0.25. 123
However, we are concerned about the predicted OS for HDI. The BMS model predicts shorter-tailed OS than was experienced in the study of HDI. 252 For example:
-
At 9 months, BMS predicts an OS of 0.24, whereas the empirical study value was 0.43.
-
At 12 months, BMS predicts an OS of 0.15, whereas the study value was 0.32.
-
At 18 months, BMS predicts an OS of 0.10, whereas the study value was 0.20.
All other matters equal, this suggests that BMS has underestimated the ICER for dasatinib versus HDI.
Given that we have strong reservations about the use of the clinical effectiveness data from Sawyers et al. 252 for the effectiveness of HDI, we investigated the sensitivity of the ICER to alternative assumptions for the clinical effectiveness of HDI. BMS’s base case for the best response for HDI was 94% of patients with no response and 6% with a CHR. The proportion of people who experienced a CHR for HDI was varied (the remainder were assumed to have no response). By contrast, the base-case split of best response for dasatinib was 44% no response, 20% CHR, 11% PCyR and 24% CCyR.
As the proportion achieving a CHR increased, the cost-effectiveness of dasatinib deteriorated. When the proportion achieving a response was ≤ 0.5 (median OS less than about 0.49 years), dasatinib dominated HDI. When the proportion was ≥ 0.6 (median OS > ∼0.51 years), the ICER of dasatinib versus HDI was > £30,000 per QALY. This would represent a substantial improvement in OS for HDI compared with what was assumed in BMS’s base case. When the proportion was ≥ 0.9 (median OS > ∼0.67 years), imatinib dominates dasatinib.
Note that, in this analysis, only the proportion of people taking HDI who experience a CHR was varied. In the next section, further concerns are raised about the dose intensity for HDI used by BMS.
Resource use
Medical management costs, such as outpatient appointments, chemotherapy and SCTs, appear reasonable. Unlike in the BMS CP and AP models, these costs have a significant impact on the cost-effectiveness of dasatinib versus imatinib. Non-drug costs on dasatinib treatment were predicted to be £20,000 per patient lower than on imatinib treatment. If we ignore all non-drug costs, then dasatinib no longer dominates imatinib. Instead, the ICER of dasatinib versus imatinib becomes £33,000 per QALY. The range of reported post-failure treatments demonstrates considerable variation in practice, which adds further to uncertainty in the analysis, although it was clear that, as such costs fall equally on all treatment comparisons, there was little influence on cost-effectiveness.
The cost of treating serious AEs for patients taking imatinib appears reasonable. However, it seemed unlikely that the costs of treating AEs for patients taking dasatinib would be zero. Nonetheless, changes to these parameters affect cost-effectiveness only slightly.
Drug acquisition costs are a very important driver of the BMS model’s results. Patients are assumed to take 140 mg of dasatinib q.d. or 800 mg of imatinib (high-dose) q.d. However, it was more accurate to model the costs of these drugs corresponding to the doses actually received in the studies.
In the HDI study,252 the median dose intensity was 600 mg q.d. for patients in the 600-mg dose group and 400 mg q.d. for patients in the 400-mg dose group. Given that most (86%) patients were in the 600 mg q.d. group, it would be preferable to assume a median dose of 600 mg q.d. for the whole study, which corresponds to a dose intensity of 75% (relative to the modelled dose of 800 mg q.d.). This equated to a cost of £2441 per patient per month, compared with £3255 as assumed by BMS.
The median dose intensity of patients in the dasatinib study for patients starting in BC was approximately 138 mg q.d.,123 which corresponded to a dose intensity of approximately 100%.
Using these revised dose intensities, the expected per-patient costs of dasatinib and HDI were similar (imatinib costs £6000 per person more than dasatinib), but dasatinib still dominated HDI.
Bristol-Myers Squibb has taken the cost of all drugs from MIMS. 228 The drug costs from this source are the same as the costs cited in the BNF,68 except for dasatinib (£2643 per patient per month in BNF vs £2541 in MIMS, a difference of 4%). When the higher cost of dasatinib, quoted in the BNF,68 was used, dasatinib still dominated HDI.
When both the slightly higher cost of dasatinib cited in the BNF68 and the revised dose intensities were used, dasatinib still dominated HDI.
It is important to emphasise that the amended estimates of cost-effectiveness do not necessarily present a more accurate estimate of the cost-effectiveness of dasatinib versus HDI, because they are still based on flawed clinical effectiveness data for HDI.
Valuation of outcomes (utilities)
We have discussed BMS’s choice of utilities in detail in our critique of its CP model (Chapter 5, Review of BMS’s chronic phase submission). A survey of members of the general public was carried out to inform quality adjustment of time. It is unclear why this was considered necessary as a range of estimates are already available, as reported elsewhere in this report. The survey included differences in utility according to response status, although this seemed to have influenced the model to a very limited extent. Nonetheless, the utilities seemed reasonable and the values for responders are very similar to those measured in the IRIS RCT.
Chapter 8 Discussion
The principal finding of this assessment was the paucity of comparative clinical studies in which the effects of treatment with dasatinib or nilotinib have been compared with any other treatment in people with ImR or ImI CML. The lack of appropriate available data has had a significant impact on our ability to assess either the effectiveness or the cost-effectiveness of the interventions. In this section, we first discuss the issues surrounding and relating to available clinical data and then, for each of the three phases of CML, the discussion is structured as follows:
-
We present a summary of the findings of the systematic review of clinical effectiveness followed by an overview of the results from the PenTAG economic evaluation in relation to the considered policy questions.
-
Key factors and uncertainties influencing the results are then explored and discussed, including in the context of those presented by the manufacturers.
-
The strengths and limitations of the assessment of clinical effectiveness and cost-effectiveness for each disease phase and their potential impact on the results are considered.
Finally, we provide an overall discussion of the strengths and limitations of the assessment and present a summary of our conclusions and current priorities for further research.
Quantity and quality of available clinical evidence
The evidence presented and summarised in the review of clinical effectiveness comes predominantly from small, observational, open-label, single-arm studies. Owing to differences in the definitions of eligibility criteria, baseline characteristics and outcomes including progression, and the methods and timing of reporting outcomes, the results from the evidence base were heterogeneous in terms of design, population and analysis. The potential impact of these differences on reported measures of effectiveness was unclear and these factors preclude any sensible comparison between interventions. Using estimates from separate clinical sources in economic evaluations requires an assumption that the same treatment-specific results for outcomes, notably CyR rate and PFS, would be obtained if all treatments had been included in the same randomised clinical study. We have little confidence that this was an appropriate assumption given the differences between the data sources. Evidence to support several of the cost estimates in the economic model was also sparse with few available data to inform key parameters, e.g. treatment duration or dose intensity. The uncertainties that necessarily and irrevocably exist in the data available to assess the new TKIs combine to give an evidence base which does not fully inform the decision problems faced by policy-makers, was difficult to interpret and which provided little opportunity for valid synthesis.
Two particularly important sources of uncertainty which cannot readily be accommodated in economic evaluations of the new TKIs are the meaning of ‘progression’ across studies and the importance of the surrogate relationship assumed to exist between CyR to treatment and OS.
Definition of progression
Progression has been defined in a variety of ways in the included clinical studies of dasatinib and nilotinib. Within each definition there was a range of possible criteria which need to be met prior to a patient being deemed to have progressed, e.g. disease transformation to AP or increase in WBC count. Comparison between studies in terms of assessing differences in progression was therefore highly problematic. None of the studies provide detail of the proportion of individuals meeting each criterion. Whether all the criteria are clinically relevant and would result in equivalent treatment decisions outside of a clinical study setting was also unclear.
Use of a surrogate outcome
Where survival data have been reported in clinical studies, the length of follow-up was such that all available OS data were very immature. Fortunately, there was ample evidence within the literature to suggest a surrogate relationship between CyR and OS, and this relationship has been demonstrated for several different treatment regimens, including standard-dose imatinib, although it has not as yet been demonstrated for any of the second-generation TKIs. The relationship has been utilised in the BMS economic model submitted to NICE (based on short-term data and multiple response categories) and in the de novo economic model in CP developed by PenTAG (based on longer term data, but confined to imatinib).
Although the assumption and specification of a surrogate relationship has enabled economic models to be built and has reduced the impact of confounding often seen where extensive extrapolation of data was necessary, other assumptions have been required which may not be appropriate. For example, in the PenTAG model, it was assumed that the relationship seen between MCyR and OS during imatinib treatment also exists for dasatinib, nilotinib and HDI treatment and was identical to that seen during imatinib treatment.
The remainder of this section is divided according to phase of disease: CP, AP and BC. In each section we discuss findings against each research questions defined in Chapter 1, Overall aims and objectives of the assessment. The bulk of the discussion is centred on the assessment of the clinical effectivness and cost-effectiveness of the interventions in CP. This reflects the relative size of the population of individuals diagnosed with CML-CP and the size and relative value of the available evidence base for comparator treatments.
Chronic phase
We have considered two policy questions in CP, relating to two important subgroups of patients considered for second-line TKI therapy in CML:
-
In those patients who have ImR disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib or treatment with nilotinib, using HDI as a comparator?
-
In those patients who have ImI disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib or treatment with nilotinib, using IFN as a comparator?
We considered that it was important, as far as possible, to use standard current treatment as the comparator for all research questions. From discussions with the clinical community, we understand that dasatinib and nilotinib are readily available in the UK and have been used for some time as second- (and possibly third-) line treatment in CP. It was therefore difficult to determine clinically relevant treatments for comparison. For the ImR population, we have compared treatment with dasatinib or nilotinib with treatment with HDI. Clinical opinion suggested that, in the absence of dasatinib and nilotinib, hydroxycarbamide might be considered the treatment of choice. However, opinion was divided on this point; we believe that, as IFN is more effective than hydroxycarbamide, it would be considered a suitable alternative to HDI in this situation and we therefore present an alternative analysis including IFN as a comparator in Appendix 8.
The results of our assessment of clinical effectiveness and cost-effectiveness in CP are discussed in more detail below. Issues of general relevance to all CP populations are considered first; ImR and ImI subgroups are discussed in detail subsequently.
Systematic review of clinical effectiveness evidence
We identified 11 studies investigating the efficacy of dasatinib and/or nilotinib in CML-CP (two RCTs and nine observational studies). The majority of evidence relates to dasatinib (both RCTs and six observational studies, reporting in total the experience of 1315 individuals with CML-CP). Evidence relating to nilotinib was more limited (four observational studies, with a total of 326 participants).
Generally, all of the included studies have low internal validity, demonstrated by the lack of appropriate comparators, lack of blinding, insufficient follow-up and evidence that entry criteria have not been strictly enforced. Although, the one available comparative RCT of two separate agents (dasatinib vs HDI) was conducted in CP, the study had serious methodological flaws, notably early crossover from imatinib to dasatinib (see Chapter 2, Critical appraisal of included evidence). All remaining clinical data originated from single-arm observational studies, necessitating the presentation of absolute rather than relative effectiveness estimates for dasatinib and nilotinib.
One feature of the assembled evidence that may be important was that, in most studies, the majority of participants had prior exposure to a range of previous therapies aside from imatinib. Where reported, most patients had taken IFN and/or hydroxycarbamide, and a proportion had received chemotherapy or SCT. In effect, then, the evidence base relates to a population taking dasatinib or nilotinib as third- or fourth-line treatment. This may be a historical situation, reflecting populations that had been initially diagnosed in the pre-imatinib era. In the current UK setting, it is much more likely that newly diagnosed individuals will receive first-line imatinib, so anyone failing normal-dose imatinib and, hence, falling into the population of interest for this review, is likely to be a candidate for dasatinib or nilotinib therapy as a second-line option. Such individuals may be younger, and have a less extensive history of CML than those in the studies, which may imply improved prognosis. It was also possible that prior exposure to other therapies, in itself, has (positive or negative) consequences for long-term outcome that may not be repeated in future practice. We also note that, in ImR populations, a majority of participants had some experience of dose-escalated imatinib prior to failure. As HDI was a specified comparator in this review, it may be important that, in the evidence relating to dasatinib and nilotinib, a substantial proportion of participants have already demonstrated resistance to HDI.
Economic evaluation
We conceive of our model as an exploratory analysis of uncertainty in the available evidence, rather than a comprehensive and robust evaluation of cost–utility. Starting from the heterogeneous collection of observational data available, substantial structural assumptions have been necessary to construct an economic model. Over and above this, a large amount of parameter uncertainty, which was more amenable to incorporation in the analysis, was acknowledged.
In order to estimate the cost–utility of any technology in a way that conforms to the NICE reference case,220 it was necessary to calculate the lifetime costs and benefits that can be expected to accrue with it and its comparators. This was particularly challenging in the case of dasatinib and nilotinib, for which empirical data were patchy and immature.
To begin with, our model requires a method of estimating the likely OS of people receiving the technologies under assessment in CML-CP following imatinib failure. There was no direct source of such evidence, even at the most recent follow-up in all identified evidence, < 20% of any cohort had died (in most cases, attrition was only around 10%). Moreover, we can assume that the necessary data will remain unavailable for several years, because of the relatively long natural history of CML-CP. To circumvent this problem, the model structure we have adopted derives its estimate of treatment efficacy from the most commonly and consistently reported outcome measure in the evidence base (CyR). The surrogate relationship we have described between MCyR and OS was based on a strong association that was well established in literature discussing first-line use of normal-dose imatinib (see Appendix 5). However, we have no evidence for assuming that this relationship was transferable to the technologies under review in a post-imatinib-failure setting. Moreover, in assuming a simple relationship between CyR and OS, we necessarily overlook any inter-treatment heterogeneity that may be present in issues such as timing of response, depth of response and duration of response.
In addition to a method of estimating OS (i.e. the potential overall benefits of treatment), our model required a basis on which to calculate the duration for which each drug would be taken (i.e. the main component of the costs of treatment). Again, no direct estimate of this parameter could be drawn from the assembled evidence, so it was necessary to approximate likely treatment duration on the basis of the available data. We have done so by using reported PFS to define the length of time for which the drug in question should have been taken, and then applying a deduction to reflect the experience of those who discontinue treatment prematurely, for reasons such as drug toxicity. This was an imperfect way of estimating treatment duration, because it relied on an outcome measure (PFS) that was not only sparsely reported (in imatinib failure status-specific cohorts), but was also defined in different ways in the studies informing the different comparators. Additionally, this method required non-evidence-based assumptions about the experience of those prematurely discontinuing treatment.
Imatinib-resistant chronic myeloid leukaemia
Clinical effectiveness
Of the published evidence we identified, only one study purported to provide data that applied directly to our research questions: Kantarjian et al. ’s randomised comparison of dasatinib (70 mg b.i.d.) and HDI. 23 However, we have taken the view that this open-label study was unable to estimate the relative efficacy of the two interventions, for at least two reasons. Firstly, the dose of dasatinib used in the study was greater than the licensed dose which was the subject of the assessment (notwithstanding the demonstration of similar results for 70 mg b.i.d. and 100 mg q.d.), and, secondly, the HDI arm was compromised by the overwhelming extent of premature crossover to the alternative treatment arm (a substantial majority of the participants who were randomised to receive HDI discontinued treatment a few weeks into the study). No other evidence was identified that attempts a direct comparison between the two technologies under assessment or any that compares them with any other treatments.
Accordingly, the evidence base was limited to a heterogeneous collection of observational evidence (or – amounting to the same thing, from the perspective of this review – data drawn from studies which, though randomised, do not address the questions at issue here).
For dasatinib, four studies11,22,23,105,109 reported some or all outcomes in imatinib failure status-specific subgroups, enabling us to deduce results for a total of 905 ImR participants in CML-CP. This was a substantially larger population than can be extracted from the nilotinib evidence base, in which 211 ImR individuals in two studies were available. 103,106
There were some consistent differences in eligibility criteria between industry-sponsored studies of each technology. Most notably, in nilotinib studies, most participants with an ongoing MCyR to imatinib at baseline were excluded whereas, in dasatinib studies, entry criteria were broader in this respect. These differences are reflected in reported baseline characteristics. In dasatinib studies, up to 20% of participants met the criteria for MCyR at baseline; the proportion of such individuals appears to have been a good deal lower in the nilotinib studies (although it was not possible to specify figures accurately with confidence).
Cytogenetic response rates were defined and measured in a relatively consistent way across all included evidence. Evidence suggests that an MCyR was achieved by around half of all ImR individuals taking dasatinib or nilotinib; roughly two-thirds to three-quarters of these would qualify as CCyRs. Response rates may be confounded by the proportion of participants who had some degree of CyR at entry to the studies.
We found homogeneous evidence that a CHR to dasatinib can be expected in about 90% of cases, but these figures included participants who met the criteria for CHR at study entry. For nilotinib, the one reasonably sized study reporting relevant data suggested that the proportion of CHRs was rather lower, a little less than 70%. In this case, however, study participants with a CHR at baseline were excluded from reported results. For this reason (among others), it was difficult to infer whether superior response rates could be expected with the new TKIs. Moreover, although there did not appear to be systematic variation according to the technology under assessment, there was a degree of heterogeneity in different studies’ definition of levels of HR.
The value of time-to-event data was limited by the short duration of follow-up available, in the context of a disease with a relatively protracted natural history.
Progression-free survival was seldom presented on an imatinib failure status-specific basis in the assembled evidence base. To the extent that it was possible to disentangle results for ImR individuals in particular, it appears that around three-quarters of people taking dasatinib could be expected to survive 2 years without disease progression. Evidence was even sparser for nilotinib, the only available source of relevant data was that contained in the cost-effectiveness model provided by Novartis as part of its submission to NICE. This suggests that over one-third of participants are expected to progress or die within 18 months of commencing treatment. A variety of definitions of progression were adopted in different studies and industry-sponsored studies of dasatinib and nilotinib vary quite substantially. [CiC information (or data) removed.] It should also be emphasised that, in each case, progression could be deemed to have occurred for a range of reasons (e.g. disease transformation to AP/BC, or loss of CHR, or loss of MCyR, or specified alterations in laboratory parameters, or death). However, in no case do we have access to data specifying the proportion of participants who were classified as progressed for each reason. It was possible that there were differences between treatments in the breakdown of types of progression observed; if so, this may have important consequences for long-term prognosis that cannot be deduced from the available data.
Overall survival data were subject to some of the same limitations. Unverified data from Novartis’s cost-effectiveness model suggest that around 10% of ImR people taking nilotinib in CML-CP can be expected to die within 18 months of commencing treatment. For dasatinib, a single data point in BMS’s submission suggests a similar rate of attrition at 24 months.
PenTAG economic evaluation
Summary of results: dasatinib
For dasatinib, our deterministic and probabilistic results make it appear highly unlikely that, when compared with HDI, dasatinib would be considered to provide benefits with an acceptable cost–utility ratio. Given that dasatinib was cheaper per patient q.d. (at the intended doses) and was predicted to give greater life expectancy, one might expect it to dominate HDI. This was not the case for two main reasons. First, our model predicts that dasatinib was typically taken for far longer than HDI (a mean of 6.5 vs 2.7 years in the deterministic base case), thus incurring far greater drug costs. Second, the dose intensity for HDI was, according to the imperfect evidence on which we base our model inputs, lower than for dasatinib (92.3% vs 100%). As a result, acquisition costs for dasatinib were typically almost twice as much as those estimated for HDI (in the deterministic base case, the values are £161,000 and £89,000, respectively) and, although this discrepancy was to a minor extent counterbalanced by higher post-discontinuation costs in the HDI arm, a substantial difference in overall lifetime costs was estimated. This additional expenditure was not counterbalanced by an equivalent effectiveness gain, according to our model, with dasatinib providing around 0.5 extra QALYs compared with HDI in the base case. The net result was that dasatinib was estimated to have a high cost–utility ratio, costing approximately £91,000 for every additional QALY gained.
Our sensitivity analyses suggest that it was difficult to explain this finding on the basis of the uncertainty associated with single parameters alone. None of the one-way deterministic analyses resulted in an ICER that would conventionally be considered to represent an acceptable balance of costs and QALY gains. For example, although the ICER for the comparison between dasatinib and HDI fell substantially when we substituted a lower estimate of MCyR to HDI, it remained at a level that would conventionally be thought to represent an unreasonable price for the extra benefits achieved (£48,000 per QALY gained).
There was one very notable exception to this pattern. When we assumed that PFS – and, hence, treatment duration – was identical between dasatinib and HDI, the model suggested that dasatinib could be expected to dominate HDI.
Dasatinib provided best value for money in only a tiny proportion of our probabilistic simulations (incorporating the uncertainty associated with all model parameters), and only then when high levels of WTP for a QALY were assumed. We acknowledge that this finding may reflect a degree of spurious confidence in the probability distributions from which each sample was drawn. A probability density function derived from the mean and variance of a sample can be said to capture true parameter uncertainty only if the sample in question is assumed to provide an unbiased estimate of the parameter in the population under simulation. This assumption was difficult to maintain in the case in hand, in which it was known that the evidence base informing the simulations was subject to substantial limitations. For example, 95% of the values our model draws to represent the MCyR rate associated with HDI, in any one of its probabilistic simulations, will lie within the 95% CI of the observed rate in our chosen data source; what is more, the model was most likely to draw a value close to the mean of that distribution. In fact, we may have little confidence that this source provides a reliable estimate of the true likelihood of response to HDI; rather, it has been chosen as the most appropriate (or it may be more accurate to say ‘least inappropriate’) estimate from a selection of arguably flawed data sources (see Chapter 5, Major cytogenetic response to high-dose imatinib). Accordingly, it may be plausible that the ‘true’ values of several parameters lies beyond the ranges adopted in our Monte Carlo simulations.
We also reiterate that, above and beyond parameter uncertainty, our model was reliant on an array of substantial assumptions which made it extremely difficult to draw conclusions with any degree of confidence. The most critical shortcoming was that our model was necessarily parameterised on the basis of a heterogeneous collection of observational data, in which the outcome measures on which we rely – above all, MCyR and PFS – have been defined and measured in different ways, at different times and in different populations. It was feasible that a well-conducted randomised comparison of the alternatives would produce entirely different results to those on which we have been forced to rely and a completely different cost–utility picture would be very likely to result.
Summary of results: nilotinib
In our base-case deterministic analysis, we estimate that nilotinib provides incremental QALY gains, compared with HDI, and it was also predicted to be cost-saving (in other words, it dominates that comparator).
Our sensitivity analyses demonstrate that, in terms of parameter uncertainty alone, the deterministic base case was relatively robust. In most cases, the finding that nilotinib dominates HDI was maintained and, with only one exception, nilotinib was always predicted to provide good value for money (assuming WTP of £12,000 per QALY or greater) when compared with HDI. The single exception comes when nilotinib PFS, and, therefore, treatment duration, was set to be equal to that seen in dasatinib.
Discussion of results
In the base case, the three TKIs were predicted to have relatively similar effectiveness profiles, with only around 6 quality-adjusted months separating all three. The major difference between the simulated alternatives lies in our prediction of likely costs. More specifically, the discrepancy was found in the estimated acquisition costs of the technologies during the course of simulated treatment. Given that there were no notable differences in per-patient daily drug costs, this could be largely attributed to the estimated length of time for which the model predicts that drugs would be taken. For nilotinib and HDI, undiscounted time in CP on treatment was estimated to average in the region of 2.5 years; for dasatinib, the equivalent figure was 6.5 years. This difference arose as a result of the PFS distributions we have adopted to underpin our calculation of treatment duration.
As shown in Chapter 5, Progression-free survival, our model benefits from an excellent fit to the empirical PFS data. However, it should be recognised that the PFS data on which we have relied was likely to be unreliable and/or inconsistent. PFS for HDI was most reliable; the data were relatively mature (5 years’ follow-up; < 30% of participants censored) and have been drawn from a fully published, peer-reviewed data source. In contrast, estimation of PFS for dasatinib was based on a single data point, representing fairly short follow-up, that had been taken from the manufacturer’s written submission to NICE. Because, in an immature time-to-event analysis, relatively few participants have experienced the event in question, estimates would be relatively unstable. Although this uncertainty was reflected in our probabilistic analyses, it should be recognised that fuller follow-up might provide an importantly different estimate of likely PFS. Moreover, in the absence of detailed information about the distribution of event times, we have adopted an exponential curve to model PFS; it was possible that a different distribution would fit the (unknown) actual data more accurately, and this might have led to quite different results. Finally, without access to a published report, it was not possible for us to appraise the appropriateness of the methods by which this single data point was derived. Despite these misgivings, we note that the data we have derived accord very well with the only published source of evidence on PFS with dasatinib in ImR CML-CP, the single-arm study of dasatinib 70 mg b.i.d. reported by Hochhaus et al. 11,105 (though that too was a very immature data set). For nilotinib, the data on which we rely have the advantage of being based on a full Kaplan–Meier curve (which we found was adequately approximated by an exponential function). Once more, however, the data were immature (just 18 months’ follow-up), and were not drawn from a published, peer-reviewed source (in fact, in this instance, the data in question were not even reported in the written submission; as we took the data from raw numbers included in Novartis’s model).
Sensitivity analyses provide strong corroboration of the importance of this factor. Above all, the crucial importance of PFS inputs (which dictate the estimated costs of the comparators under review) was demonstrated. It was worth emphasising the implications of this finding.
-
If it was assumed that – as per the best published evidence currently available – PFS was distinctly longer with dasatinib than with nilotinib, then it was very likely that nilotinib would be considered to provide good value for money, and extremely unlikely that dasatinib would achieve the same status.
-
If, on the other hand, it was assumed that PFS for dasatinib was likely to be about the same length as that for nilotinib (as the anecdotal evidence of some of our expert advisors has suggested), then both technologies would be on a similar footing. Under those circumstances, it would be crucially important to determine which of the PFS distributions was the ‘correct’ one.
-
– If PFS was assumed to be the same as it was for nilotinib for both technologies, each was predicted to provide good value for money versus HDI.
-
– If PFS was assumed to be the same as it was for dasatinib for both technologies, neither was likely to be considered good value for money, with ICERs higher than £90,000 per QALY.
-
– If PFS was assumed to be the same as it was for HDI for both technologies, each was predicted to provide good value for money versus HDI.
-
The impact of our reliance on an assumed relationship between OS and MCyR was tested in a sensitivity analysis in which the surrogate approach was discarded and, instead, OS was calculated as observed PFS plus a constant amount of post-progression survival for all comparators (this was similar to the approach adopted by Novartis, in the model it has submitted to NICE). This made important differences for both nilotinib and dasatinib, when each was compared with HDI. Nilotinib was estimated to be the less effective than HDI, although it remained cheaper to a degree that, conventionally, would be considered to provide better value for money than its comparator (with the additional benefit of HDI coming at a cost in excess of £100,000 per QALY). For dasatinib, assuming identical post-progression survival halved the ICER compared with HD imatininb, although it remained over £40,000 per QALY; the outputs of this analysis contrast with our base-case model, because the much longer PFS seen with dasatinib was directly reflected in OS whereas, in our base-case model, the two are modelled independently.
Comparison of PenTAG results with manufacturers’ submissions
The very notable discrepancy between the ICER generated in the PenTAG model of dasatinib versus HDI (£91,500 per QALY) and that calculated in the BMS analysis (dasatinib dominates) was, in the main, attributable to differences in the modelled experience of people taking HDI. The models’ dasatinib arms are not identical, but they have several features in common, and the differences between them cannot, by themselves, account for the large differences in the incremental outputs (costs, in particular). Above all, simulated treatment duration for individuals taking HDI was critical. BMS predicts an average of almost 9 years whereas, in the PenTAG model, the equivalent figure was < 3 years. This, coupled with BMS’s failure to account for dose intensities < 100%, explains the very large difference in costs outputs. PenTAG estimates that, over an average individual’s lifetime, costs associated with HDI were approximately £50,000 lower than those with dasatinib. BMS suggests that they were £50,000 higher.
The gap in PenTAG’s simulated HDI cohort between, on the one hand, relatively short PFS and, on the other, relatively long OS may appear counterintuitive. However, we believe that these parameters are empirically sound, because predicted PFS was a direct fit to our chosen data source for HDI (Jabbour et al. 182) and because this study has been used as the point of calibration for predicted OS for all treatments; our model also benefits from an optimal fit to the empirical OS data for HDI. According to this evidence, there was clearly a substantial period between disease progression and death. Moreover, it was clear that most of this time was spent in post-progression–pre-transformation CP (time to transformation was also recorded in this study); this important phase of disease was overlooked in the BMS model. We therefore believe that the profile predicted in the PenTAG model was a realistic one (within the limits imposed by a sparse, low-quality evidence base).
It was notable that the Novartis model predicts much shorter life expectation for nilotinib than those models developed by PenTAG and BMS. Before quality adjustment and discounting, the Novartis model predicts typical OS of just 5.5 years for those taking nilotinib, whereas BMS estimates 9.9 years, and PenTAG 13 years. At least in part, this discrepancy arises because Novartis assumes that disease progression is synonymous with transition to AP (i.e. it does not model post-progression CP), which was a substantial shortcoming in their model (see Chapter 5, Review of Novartis’s chronic phase submission). Additionally, Novartis’s failure to account for dose intensity accounts for some of the discrepancy between model outputs.
Imatinib-intolerant chronic myeloid leukaemia
Clinical effectiveness
For dasatinib, three studies reported some or all outcomes in imatinib failure status-specific subgroups, enabling us to deduce results for a total of 283 ImI participants in CML-CP. The nilotinib evidence base was limited to a single study, in which 86 ImI individuals are reported.
There were important differences between studies in entry criteria for ImI participants. In the nilotinib study, ImI participants were recruited only if, alongside intolerable toxicity, they had shown no CyR to imatinib; this restriction did not apply in dasatinib studies. One corollary of this dissimilarity was that, although a proportion of ImI participants in dasatinib studies met the criteria for MCyR at study entry, the nilotinib study excluded all such individuals.
These differences may contribute to our finding that, although CyR rates were defined and measured in a relatively consistent way across all included evidence, there were apparent differences in reported rates of response. In particular, in studies of dasatinib, there was clear evidence that the rate of CCyR and MCyR to dasatinib was greater in ImI individuals than in the ImR population. In contrast, the people who were defined as ImI in the nilotinib study appear to have no higher chance of CyR than their ImR counterparts.
For both dasatinib and nilotinib, CHR rates appear to be approximately 90% (although 100% CHRs were seen in more than one population taking dasatinib).
As in the ImR population, PFS findings were limited by the short duration of follow-up available, a paucity of imatinib failure status-specific data, interstudy differences in definitions of progression, and the absence of evidence specifying types of progression observed. Such evidence as was available appears to suggest that PFS was somewhat longer in ImI individuals than was seen in ImR populations, with approximately 5–15% of individuals dying or progressing within 18–24 months of commencing treatment. In view of the very sparse data and considerable differences between cohorts and the definitions of progression used, we do not consider that it was currently possible to draw any inferences about the relative efficacy of the two technologies under review with respect to this outcome measure.
Overall survival data were similarly patchy and uncertain. As far as can be ascertained, < 10% of ImI participants can be expected to die within 2 years of commencing treatment with either nilotinib or dasatinib.
PenTAG economic evaluation
Because of the dissimilarities between eligibility criteria for nilotinib and dasatinib studies described above, it was questionable whether or not our model can be thought of as estimating analogous cost–utility results across comparators. In particular, our necessary reliance on reported data for nilotinib in ImI populations dictates that we were unable to provide an estimate of the cost–utility of nilotinib for people who show a CyR to imatinib, but develop intolerable toxicity. It was not clear to us what impact the inclusion of such individuals in the ImI population (as in the equivalent dasatinib study) would have on model outputs.
We have used IFN as a comparator for this population, on the assumption that it was the most effective treatment available if imatinib could not be tolerated and the technologies under review are assumed to be unavailable. Our expert advisors were not unanimous on this point, with some arguing that hydroxycarbamide would be as appropriate a comparator. However, IFN was the standard of care for this population prior to the development of TKIs (as corroborated by its use as comparator in the landmark study of effectiveness of first-line, normal-dose imatinib17). In any event, because IFN and hydroxycarbamide are both relatively inexpensive treatments with limited relative effectiveness, the results of our model’s IFN arm might be thought of as representing a generic, older standard of care and, to some extent, whether this arm was labelled IFN or hydroxycarbamide was immaterial.
In all our analyses, the ICERs for dasatinib and nilotinib versus IFN were high. This was because the QALY gains predicted by our model, although considerable, were insufficient to outweigh the very high estimated costs of the new technologies.
The acquisition costs of the new technologies were substantially greater than those of IFN plus cytarabine; both nilotinib and dasatinib were far more expensive than IFN per patient q.d. and, in addition, were predicted to be taken typically for far longer. Before discounting was applied, our model predicts that, for the average ImI individual, lifetime drug acquisition costs of dasatinib would be over £325,000; for nilotinib, the equivalent figure was just less than £215,000. As a consequence, our model predicts that the discounted costs of treating an individual with ImI CML with nilotinib were, on average, £123,000 greater than the costs of using IFN, and the equivalent figure for dasatinib versus IFN was over £185,000 per patient. In our probabilistic analyses, there were multiple individual simulations in which the estimated discounted lifetime costs of individuals taking nilotinib or dasatinib were > £250,000 greater than those for the IFN cohort (in one instance, dasatinib costs exceeded IFN by over £370,000 per patient).
Although the utility gains predicted by our model were also substantial, they were not sufficient to counterbalance these very high costs, unless it could be assumed that society was willing to pay an extremely high premium for such health gains (over £80,000 per QALY). Our best estimate of the probability that IFN provides best value for money at a conventional WTP threshold of £30,000 per QALY was 99.9%.
As in our ImR model, our estimation of treatment duration was substantially reliant on PFS data, with regard to which we have substantial misgivings: (1) the data were immature; (2) where dasatinib and nilotinib are concerned, the data were unpublished; and (3) for dasatinib, a single data point alone was relied on. Similarly, dose intensity was imperfectly captured and may have had an influence on results. However, in this instance, our deterministic sensitivity analyses did not suggest that such issues had a critical impact on model outputs.
We acknowledge that, in its base case, our ImI model had an unconvincing fit to empirical OS data (see Chapter 5, Overall survival). However, when we performed a sensitivity analysis in which an alternative method of calibrating modelled OS was adopted, a very good fit to empirical OS was achieved, and it was demonstrated that cost–utility results were not especially sensitive to any inaccuracy that may have resulted from our base-case methods (see Chapter 5, Overall survival and Appendix 9).
Despite evidence that, in general terms, the outputs of our model were robust to uncertainty in the individual parameters that inform it, it must be remembered that our model was also reliant on an array of substantial, untested structural and methodological assumptions. Accordingly, any conclusions drawn from it must be seen as speculative. We reiterate that a robust model of the decision problems under assessment would have relied on at least one randomised comparison of some or, ideally, all of the relevant comparators. We have very little confidence that such a source of evidence could be expected to produce identical, or even similar, results to those seen in the heterogeneous collection of observational data used to inform the model presented here. There were notable differences between the populations reported in each of the studies on which we rely; moreover, the critical outcome measures – above all, MCyR and PFS – have been defined and measured in different ways and at different times. It was feasible that a well-conducted randomised comparison of the alternatives would have produced entirely different results to those on which we have been forced to rely, and a completely different cost–utility picture would have been be very likely to result.
Comparison of PenTAG results with manufacturers’ submissions
Bristol-Myers Squibb does not present an estimate of the cost–utility of dasatinib in ImI populations. Consequently, PenTAG’s model provides the only available economic analysis of dasatinib in this subgroup.
Novartis’s model of nilotinib in ImI CML-CP was subject to the limitations of its ImR model (see PenTAG economic evaluation). In addition, the comparator arm for this subgroup purports to simulate the experience of individuals receiving hydroxycarbamide; however, only 12 (19.7%) of the 61 individuals in the publication used to parameterise this cohort223 actually received hydroxycarbamide, which makes findings uncertain. Furthermore, we note that the clinical efficacy of nilotinib was predicted in Novartis’s model, as a function of observed PFS, which was an extremely immature data set (over 80% of the distribution was undefined empirically), making results extremely speculative regardless of other shortcomings in the analysis.
Summary of assessment in chronic phase chronic myeloid leukaemia
Strengths
Our analysis was an independent assessment of nilotinib and dasatinib. It was the first complete cost–utility study of either drug to have been undertaken in a UK setting. Moreover, it was the first to consider both technologies together; this was clearly appropriate as they are mutually exclusive options for the same indications.
Our model structure makes use of the information that was most certain in the evidence base (CyR rates) to predict long-term outcomes. Moreover, we have estimated the surrogate relationship based on data from a synthesis of RCTs carried out over a relatively long period. One advantage of this surrogate-based approach was that it was not susceptible to confounding by co-intervention in the period following treatment with the technology under assessment. Whereas empirical data showing the long-term OS of individuals receiving nilotinib or dasatinib in CML-CP would provide a useful basis on which to model lifetime outcomes, such data sources are invariably subject to a degree of uncertainty owing to the variable provision of treatments later in the disease course. By assuming that OS was a simple function of CyR, we remove this problem, which enabled us to provide, at least in theory, a less biased estimate of the efficacy of the comparators.
Our model predicted empirical data well, the fit with PFS distributions was good (see Chapter 5, Progression-free survival) and, although the empirical data against which we validated model-predicted OS was partial and immature, our ImR model provided an excellent fit to such information as was available (see Chapter 5, Overall survival). Our ImI model had a less convincing fit to empirical OS data (see Chapter 5, Overall survival); however, when we performed a sensitivity analysis in which an alternative method of calibrating modelled OS was adopted, a very good fit to empirical OS was achieved, and it was demonstrated that cost–utility results were not especially sensitive to any inaccuracy that may result from our base-case methods (see Chapter 5, Overall survival and Appendix 9).
Limitations
Although definitions of MCyR appear consistent across the assembled evidence base, important heterogeneity may be introduced by differences in populations (perhaps especially as regards the proportion of participants meeting the criteria for MCyR before treatment commenced). The duration of follow-up may also be important, MCyR rates reflect best ever status on treatment (as opposed to current status at the time of analysis) so, as follow-up extends, response rates can only go up. Accordingly, studies based on lengthier follow-up will appear to report a higher likelihood of response, even if the technology under assessment was no more effective than those assessed after less time.
Because of this problem, we sought to rely on MCyR rates at a single, consistent time point for both strata of our model. For ImR CML, 12-month rates were used or approximated, for ImI CML, it was preferable to use 6-month rates because of data availability. Additional uncertainty was introduced by the methods that were necessary to approximate MCyR rates for the juncture in question when such data were not empirically available. However, all our one-way sensitivity analyses examining the impact of varied MCyR inputs suggested that our base-case results are, in broad terms, insensitive to this parameter. In ImR CML, no plausible alterations to MCyR rates overturned our finding that, compared with HDI, nilotinib appeared to provide a conventionally acceptable cost–utility balance, whereas dasatinib was unlikely to achieve the same. In ImI CML, neither of the technologies under assessment could be made to appear good value for money, compared with IFN, by varying MCyR rates.
Furthermore, even if we could suppose that MCyR rates had been perfectly and consistently captured for each comparator, a fair degree of uncertainty was associated with the use to which they were put in our model. Above all, we assumed that the relationship between MCyR rate and OS was identical for each comparator. This may be a reasonable assumption: when Kantarjian et al. compared experience with first-line imatinib with historical results for IFN-based regimens, they found that, whereas OS was significantly superior with imatinib, OS within each CyR category was similar with imatinib or IFN, suggesting that the survival benefit was achieved through improving CyR. 236 However, if this assumption was not entirely accurate, it might be important that our method effectively overlooked any differences between treatments that may be present as a result of timing of response, depth of response or duration of response.
We are aware that there was ambiguous evidence about whether an early CCyR does253 or does not254–256 predict long-term outcome in studies of normal-dose imatinib. Evidence regarding the impact of timing of MCyR in second-line treatment was difficult to identify. However, if there were positive implications to an early or late MCyR, and one of the comparators in our model could be shown to benefit from a superior profile in this regard, the effectiveness of the technology in question would be underestimated in our model (which, because it treats MCyRs as a homogeneous event, was unable to reflect such complexities).
Similarly, our model assumes that, beyond the threshold of MCyR, depth of response has no impact on OS. Taken to its extreme, this assumption would dictate that a cohort with 50% non-responders and 50% showing PCyR would have an identical OS profile, in our model, to one comprising 50% non-responders and 50% complete molecular responders. In literature investigating the prognostic significance of CyR to first-line imatinib, there was good evidence that a deeper response predicts a longer response,257–259 and may also be associated with greater PFS. 19,260,261 However, it has not been demonstrated that any such benefit translates into longer OS; in particular, studies show no significant difference in OS between complete responders who achieve MMRs and those who do not. 236,259,260,262 However, we emphasise that, if there are systematic differences between comparators in CyR level (beyond the MCyR threshold), and if these have implications for the OS profile of individuals receiving each treatment, such complexities are not captured in our model.
Finally, duration of response was unaccounted for in our model structure. Again, this may be a factor that mediates the relationship between MCyR and OS, and it was possible that the typical duration of MCyRs achieved with the various comparators in our model differed. For example, it has been suggested that CyRs to HDI may be relatively short-lived263 (although this assertion contrasts with the findings of others182). Assuming, for the moment, that MCyRs on HDI are truly less durable than those achieved with other treatments, our model would overestimate the effectiveness of HDI, so long as it could also be assumed that a more durable response would translate into tangible benefit in terms of OS. However, we note that, as far as limited evidence so far shows, duration of response does appear to be associated with long-run differences in OS, as might be assumed. 260
In any case, with reference to the example cited here, it is worth emphasising that, in the study used to parameterise the HDI arm of our model, MCyR maintenance probabilities (approximately 0.93 at 18 months and 0.85 at 24 months)182 compare quite favourably with MCyR durability seen with dasatinib (0.87 at 24 months; see Chapter 2, Duration of major cytogenetic response) and nilotinib (0.84 at 18 months; see Chapter 2, Duration of major cytogenetic response), especially if it is recognised that these figures relate to combined ImR/ImI populations, whereas the HDI arm gains no benefit from the inclusion of a proportion of ImI individuals.
All investigations into the dynamics of our model suggested that cost–utility outputs are overwhelmingly sensitive to inputs reflecting treatment duration. This parameter was not available in the empirical data available to us; instead, we estimated treatment duration using a method that predominantly relies on reported PFS for each comparator. This was an imperfect way of approximating a crucial parameter, which was further compromised by heterogeneity in definitions of PFS among data sources. It was notable, in particular, that the poor cost–utility profile predicted for dasatinib in ImR CML comes about because our model estimates that, in order to achieve undiscounted OS gains of 0.5–1.0 years compared with nilotinib and HDI, it was necessary to take dasatinib for around 4 years longer than was estimated for the comparators. Our expert advisors have expressed doubt at the clinical validity of this finding and, although there was no published evidence to substantiate the assumption that treatment duration should be similar for all three drugs, we acknowledge that, if this assumption was to be preferred, a very different cost–utility picture emerged.
Because they are both defined by the available evidence on nilotinib in ImI populations (in which people who had shown a response to imatinib were excluded), neither our model nor Novartis’s was able to provide an estimate of the cost–utility of nilotinib for people who show a CyR to imatinib but cannot tolerate it. It was not clear to us how large this population might be, nor was it clear whether or not it might be expected to have a cost–utility profile that resembles either ImR or ImI cohorts.
Accelerated phase
We have considered two policy questions in AP:
-
In those patients who have ImR disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib or treatment with nilotinib, using HDI as a comparator?
-
In those patients who have ImI disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib or treatment with nilotinib, using hydroxycarbamide as a comparator?
As with the research questions defined for CP, we struggled to identify clinically relevant treatments with which to compare treatment with dasatinib and treatment with nilotinib. Anecdotal clinical opinion suggests that dasatinib and nilotinib are already widely used in this population and that treatment regimens other than these would rarely be considered; although it is worth remembering that few patients are diagnosed with ImR or intolerant CML in AP.
We were unable to identify any relevant clinical data for the treatment of ImR CML in AP with HDI or hydroxycarbamide. The manufacturer submissions contained analyses using data from studies of standard-dose imatinib in patients with imatinib-naive disease. We felt that further economic modelling based on such obviously flawed data would not assist the decision-making process and have therefore not produced a de novo model in AP. Our assessment of the cost-effectiveness of treatment with dasatinib and treatment with nilotinib was therefore based on a review, critique and exploration of the models provided in the manufacturer submissions to NICE.
The results of our assessment of the clinical effectiveness of treatment with dasatinib and treatment with nilotinib in AP are discussed in more detail in the next section.
Clinical effectiveness
All available data originated from observational, single-arm studies. As discussed in Chapter 2, Design and characteristics of included studies, there were considerable, and potentially important, differences in baseline characteristics, e.g. previous and ongoing response to imatinib, the criteria used to define disease progression and the definition, timing and reporting of outcome measures. These seriously undermine any process for making meaningful comparison between treatment with dasatinib and nilotinib.
A summary of the results of the included studies of dasatinib can be found in Box 2. A MCyR was observed in between 34% and 45% of participants, with 80–90% maintaining this response for at least 1 year. Average PFS was a little over 1 year and average OS was a little over 2.5 years. Haematological AEs were common in studies of dasatinib, with the majority of individuals experiencing grade 3–4 neutropenia and thrombopenia. The most frequently reported non-haematological grade 3–4 toxicities were diarrhoea, febrile neutropenia and fluid retention. Up to 30% of individuals discontinued dasatinib therapy because of AEs.
In the included studies of nilotinib, a MCyR was observed in approximately 30% of all individuals, with no reported evidence of a difference between ImR and ImI populations. Average PFS was a little under 1.5 years and about two-thirds of individuals could expect OS for 2 years or more. Haematological AEs were common; grade 3–4 neutropenia and thrombopenia each affected approximately 20–35% of individuals taking nilotinib in the published study. Rates were slightly lower (15–25%) in the expanded access programme. Common non-haematological AEs included alopecia, rash, constipation, diarrhoea and fatigue, although grade 3–4 AEs were rarely reported. Approximately 10% of study participants discontinued nilotinib therapy because of AEs.
Cost-effectiveness
Our assessment of the cost-effectiveness of dasatinib and nilotinib in AP was based on the manufacturer submissions to NICE.
Nilotinib
Novartis presented two cost-effectiveness analyses for individuals starting treatment in AP: one in ImR individuals in which nilotinib was compared with HDI and one in ImI individuals in which nilotinib was compared with hydroxycarbamide. The analyses were performed using a Markov model with three health states: AP, BC and death.
In ImR patients, compared with HDI, the Novartis economic analysis predicted an incremental benefit to patients receiving nilotinib of 0.38 life-years at an incremental cost of £4427. When QoL is taken into account, the base-case cost per QALY for dasatinib compared with HDI was £18,541. The probabilistic sensitivity analysis indicates that nilotinib was likely to be considered cost-effective compared with HDI in ImR individuals for WTP thresholds above £19,000 per QALY.
The analyses in both subgroups (ImR and ImI) are reviewed and critiqued in Chapter 5, Nilotinib (manufacturer analysis/model), and the major concerns with the analyses are summarised in Box 6. The over-riding concern was that the clinical effectiveness data used to populate the model for both HDI and hydroxycarbamide were seriously flawed.
Data for the ImR population came from a population who were imatinib naive and treated with doses of imatinib which were lower (400 mg and 600 mg) than the 800 mg ‘high’ dose. Furthermore, it appeared that Novartis did not, in fact, use the higher of the doses used in this study (600 mg), which the imatinib study predicted would result in better PFS for HDI than for nilotinib (the key parameter driving the model).
Novartis also made the assumption that progression equates to the development of BC which, again, was not how this parameter was defined in the studies. Progression may have occurred for a variety of reasons including, but not confined to, the onset of BC.
Finally, dose intensity of treatments was not taken into account. As the dose intensity for imatinib was lower than that for dasatinib, this factor resulted in a bias in incremental costs which favoured nilotinib.
Clearly, the fact that the data sources for the drugs being compared come from separate studies introduces a range of possible reasons why such differences are shown, aside from the effectiveness of the agents themselves, and these cannot readily be explored. We have, however, investigated the impact of using data for PFS on the higher dose of imatinib in the Novartis model. This resulted in lower costs and fewer benefits on nilotinib, with an ICER of £100,000 saved per QALY lost. This finding was sensitive to the amount of time spent in PFS on treatment and, taking into account the separate sources for these parameter, should be regarded with extreme caution.
When values for the dose intensity of imatinib reported in the relevant study were applied in the Novartis model, the ICER for nilotinib obtained in the Novartis base case increased from £18,704 to £57,441 per QALY.
In ImI patients, compared with hydroxycarbamide, the Novartis economic analysis predicts an incremental benefit of 1.14 QALYs at an incremental cost of £90,966, giving a base-case ICER of £79,914 per QALY. The probabilistic sensitivity analysis suggests that nilotinib would be considered cost-effective compared with hydroxycarbamide only at WTP thresholds above £80,000 per QALY.
The data on hydroxycarbamide were particularly problematic in this evaluation. A major weakness in the underlying study was that only a minority of participants actually took hydroxycarbamide and available data were not specific to the ImI (as opposed to resistant) population. In our judgement this makes it extremely difficult for the analysis to meaningfully inform any policy decision. Uncertainties include the long extrapolation of PFS and the definitional problem with ‘progression’ that has already been described.
The overarching problem, however, in both analyses of nilotinib in AP was the absence of comparative data on the effectiveness arising from an appropriately defined and conducted study in which more than one agent was evaluated. The potential confounding factors in the analyses carried out by Novartis, notwithstanding the problem with defining and handling progression, are many and their influence was difficult to predict even in terms of the direction of possible biases that may be present. Taking these into account to generate a robust quantitative analysis was, in our view, not currently possible.
Dasatinib
Bristol-Myers Squibb presented a three-way cost-effectiveness analysis for dasatinib compared with HDI (800 mg q.d.) and nilotinib for patients who have failed prior imatinib therapy as a result of resistance or intolerance.
The analysis used a Markov model to estimate cost-effectiveness, using the observed relationship between response and progression (defined for the model as development of BC, though this did not follow the study definition) and OS.
We note that BMS has provided an analysis of dasatinib versus nilotinib in this phase of CML, whereas Novartis has argued that this comparison would be rendered uninformative because of differences in the proportion of patients who had had a previous CyR at baseline. However, this argument appears less convincing in AP than in CP. Although it was very difficult to predict the size and direction of bias introduced by this and other differences in definitions used in the studies (e.g. of imatinib intolerance) and the baseline characteristics of participants, we believe that the analysis carried out by BMS was no more likely to be subject to invalidating influences than that carried out by Novartis. Essentially, we believe that both analyses in AP are deeply flawed.
In the BMS evaluation, treatment with dasatinib was expected to increase OS, compared with HDI, by 1.88 years with total costs increased by £57,000. When QoL was incorporated, treatment with dasatinib results in a little over 1.5 additional QALYs compared with treatment with HDI, i.e. an ICER of £35,319 per QALY. Compared with nilotinib, treatment with dasatinib increases OS by 0.93 years and total costs by £30,000. The corresponding increase in QALYs was a little under 1 year (0.82 QALYs), i.e. an ICER of £36,778.
The probabilistic sensitivity analysis predicted a reasonable level of certainty (63.4%) that treatment with dasatinib would be likely to be considered cost-effective compared with treatment with HDI at a WTP threshold of £30,000 per QALY, although we note that this certainty was not implied by the deterministic ICER, which was > £30,000 per QALY. Compared with treatment with nilotinib, the BMS analysis predicted a low certainty (30%) that treatment with dasatinib would be considered cost-effective at a WTP threshold of £30,000 per QALY.
Both Novartis and BMS used the same study as the basis for modelling the effectiveness of HDI and, as already noted, this appears fundamentally flawed. Because the biases arising from the imatinib-naive nature of the population and the non-HDI used operate in opposite directions, it was not possible to predict and control for their possible influence on cost-effectiveness.
The BMS model predicts poorer OS for both comparators than was reported in their clinical studies, suggesting a bias in favour of dasatinib. We explored the influence of HDI effectiveness (CHR rate) in sensitivity analysis using the BMS model. This showed that the ICER for dasatinib was sensitive to this parameter, though cost-effectiveness of dasatinib would be enhanced by greater response to CHR as this would, more importantly from the cost-effectiveness point of view, result in longer time on HDI treatment and therefore HDI costs would increase.
Bristol-Myers Squibb used the price quoted in MIMS for dasatinib, which was slightly lower than that given in the BNF. Drawing all prices from the BNF increased the ICERs for dasatinib, which were expressed in pair-wise terms against each comparator: from £35,300 to £44,300 against HDI and from £36,800 to £41,100 against nilotinib.
Dose intensity was also important in the comparison with HDI. When the values reported in studies were used, the ICER for dasatinib increases from £35,300 to £42,100. We would expect the ICER when both dose intensity and price are adjusted to increase yet further.
Although we have not produced a de novo analysis of the new TKIs in AP, by reviewing and exploring the models provided in the manufacturer submissions we have highlighted the considerable and, to a large extent, intractable problems with the evidence which was available to inform such analyses. The results obtained from the two manufacturer analyses, which both consider nilotinib versus HDI, are very different. Furthermore, the changes to cost-effectiveness estimates which are shown following corrections or plausible adjustment of the key input parameters in both manufacturer submissions make it clear, in our view, that assessment of the new TKIs in this phase of CML is fraught with difficulty, and calls into question whether the currently available evidence base is fit for the purpose of policy-making.
Blast crisis
There was only one policy question in CML-BC:
-
In those patients who have ImR disease, what is the clinical effectiveness and cost-effectiveness of treatment with dasatinib following initial cytoreductive treatment, using HDI as a comparator?
Again, we struggled to identify clinically relevant treatments with which to compare treatment with dasatinib in CML-BC. We identified no clinical studies in which treatment with dasatinib in patients with ImR or ImI CML in BC was compared with any other treatment. We also failed to identify any studies of HDI in this patient group or to find any suitable comparator in ImI individuals. Clinical advice has suggested that it is relatively unusual for individuals to be diagnosed with ImR or ImI CML in BC, and that incident CML meeting these criteria is likely to be considered as acute leukaemia and treated accordingly.
Again, we have not developed a de novo economic model of BC because of the lack of available clinical data and the belief that any model created on the basis of the available data would be flawed. In preference, we chose to review and explore the model provided in the BMS manufacturer submission of dasatinib in this phase of CML.
Clinical effectiveness
All available data originated from observational, single-arm studies. As discussed in Chapter 2, Design and characteristics of included studies, there were considerable differences in baseline characteristics, e.g. previous and ongoing response to imatinib, criteria used to define disease progression and the definition, timing and reporting of outcome measures, precluding any meaningful comparison between treatment with dasatinib and treatment with nilotinib.
A summary of the review of clinical effectiveness of treatment of CML in BC with dasatinib can be found in Box 3. There was a huge variability in the reported rates of MCyR between studies, though on average around 45% of participants showed a MCyR. Most study participants achieved ≯ 3–6 months’ PFS and only one-quarter to one-third of individuals could expect OS of > 2 years. A substantial majority of individuals experienced multiple grade 3–4 cytopenias. Non-haematological AEs were also relatively common, with grade 3–4 pleural effusion occurring in > 10% of participants in MBC. Gastrointestinal haemorrhage and febrile neutropenia were also reported at frequencies > 10%.
Cost-effectiveness
Our assessment of the cost-effectiveness of dasatinib in BC was based on the manufacturer submission to NICE.
Bristol-Myers Squibb presented a cost-effectiveness analysis for dasatinib compared with HDI (800 mg q.d.) for patients in whom prior imatinib treatment has failed owing to ImR or ImI. Cost-effectiveness was estimated using a Markov model with similar structural assumptions to those used in the BMS models of the CP and APs of CML.
Compared with HDI, treatment with dasatinib increased OS by 0.45 years and decreased total costs by £11,000. The corresponding increase in survival when QoL was taken into account amounted to a total of 0.28 QALYs. In all cases, the base case and all identified one-way sensitivity analyses, dasatinib were shown to dominate HDI. The probabilistic sensitivity analysis predicted a high level of certainty (100%) that treatment with dasatinib would be considered good value for money compared with treatment with HDI at WTP thresholds of £20,000 and £30,000 per QALY.
The analysis was reviewed and critiqued in Chapter 7, Review of manufacturer submissions to NICE, and the main concerns with the model are summarised in Box 13. Concerns were similar to those raised with the models of AP and centre around the inappropriate clinical effectiveness data for HDI and the assumption that all treatments were used at recommended doses. In addition, we note that the BMS analysis was based on a mixed population of people with ImI and ImR, adding further uncertainty in relation to the policy question noted above.
As before, our major concern with the HDI data source was that it refered to a different population taking a non-high dose of the drug. The extent to which it could form the basis for a comparison with dasatinib is therefore open to considerable doubt. In addition, the BMS model appeared to under estimate the values for OS quoted in the study of HDI, such that a bias appeared present which may favour dasatinib.
In addition to concerns about effectiveness data in BC, we note that BMS has applied 100% dose intensity for HDI. When this was adjusted to better reflect the conduct of the underlying study, dasatinib continued to dominate HDI. Given the large and pervasive uncertainty regarding the relative effectiveness of dasatinib and HDI, for the reasons stated, it has not been possible to identify a less inappropriate estimate of effectiveness with improved drug cost data. Despite this apparent robustness, caution should be exercised at this point. Firstly, we know close to nothing on the effectiveness and tolerability of HDI in this population. Secondly, and perhaps more importantly, it seems unlikely that many (if any) patients would arrive at the BC stage of CML without exposure to one or other of the new TKIs given what we know about current clinical practice. Therefore, several further questions become relevant: what sequence of treatments across CP, AP and BC should be preferred? Are there differences in responses, PFS and OS, according to whether or not a response has been shown in an earlier stage of disease?
The work carried out by BMS into the cost-effectiveness of dasatinib in BC was greatly constrained by the quality of available data on comparators. It was therefore not surprising that parameter uncertainty appeared to be relatively less important in the analysis than the underlying differences in populations and treatments being compared, which arise as a disappointing consequence of the limited available evidence at that time. Until further data are available, we do not believe it is possible to reach a robust conclusion on the clinical effectiveness and cost-effectiveness of new agents in this stage of CML.
Strengths of the health technology assessment
This was the first independent analysis of the clinical effectiveness and cost-effectiveness of dasatinib and nilotinib in ImR and ImI CML to inform policy in the UK NHS setting.
Comprehensive, explicit and systematic literature searches, including hand searching of conference proceedings, were performed to locate evidence both for the review of clinical effectiveness and to inform the economic modelling study.
A major finding of this assessment was the lack of relevant clinical data to inform the policy questions. Careful consideration of the flaws in the evidence base and consequently the conclusions that may be drawn from the evidence has allowed us both to make sensible conclusions as to the clinical effectiveness of the interventions and to highlight the areas of priority for further study. Economic modelling has been necessarily constrained by the lack of evidence and has necessitated careful reflection on possible model structure. We have endeavoured to build a suitably and meaningful model which was no more complex than the data allowed.
The PenTAG model, as others, relies on the surrogate relationship between MCyR and OS. The data underlying this relationship were taken from several large randomised clinical studies.
Acknowledging the large degree of uncertainty in both the parameter inputs and the structural assumptions underlying the model, considerable exploration and analyses of uncertainty including one-way, multiway and probabilistic sensitivity analyses have been carried out.
Limitations of the assessment
Model-based cost-effectiveness analyses are an inevitable consequence of the need to integrate a range of information about a wide variety of factors to support policy decisions on new technologies. These relate to the natural history of the disease, the efficacy and effectiveness of the interventions, the treatment pathway and the resultant life expectancy and QoL in different disease states and with different treatments.
We have already described several important limitations of this work, including the constraint imposed by the lack of comparative clinical effectiveness data for the interventions and their comparators and the lack of long-term survival data. This final point leads to a need for modelling to be based on a surrogate relationship. Major differences in the design and reporting of the included clinical studies, particularly in the differing definitions of disease progression used in the studies and the baseline characteristics of participants’, further increase uncertainty.
We were not able to identify data to inform on all the potential policy questions identified for this assessment, e.g. clinical effectiveness data for HDI in AP and BC. As a result of this we have been unable to fully inform the policy questions.
We are aware that a patient demonstrating signs of disease progression during treatment with one of the interventions, e.g. dasatinib, would be likely to receive treatment with an alternative TKI, e.g. nilotinib. As dictated by the scope of this assessment, and with no relevant clinical data, it was not possible to model any specific sequences of treatment. However, it seems clear that to address issues of therapy sequencing would be complex and would require more and better data than are currently available from studies of the new TKIs. As clinical effectiveness data become available on the use of dasatinib and nilotinib as third- and subsequent-line treatments, the complexities of the treatment pathway may warrant further evaluation.
As the assessment of the mutational status of individuals becomes more commonplace in the care of patients with CML, targeting of dasatinib and nilotinib to those subgroups who may respond better to treatment is likely to become possible. In light of the extreme lack of good-quality data to inform the clinical effectiveness of the interventions in the wider population of individuals with CML, further consideration of mutational status in this assessment was inappropriate. However, as further clinical effectiveness data become available, consideration of mutational status in any additional evaluation will become a priority.
Other relevant patient subgroups which have not been considered in this assessment because of the lack of data include those with a previous response to imatinib versus those without. This would appear to be a clinically relevant division of the patient population, as those who have an existing response to imatinib or a history of such a response on entry into a study may be expected to achieve a better response to related treatment with second-generation TKIs than those who have never achieved a response to imatinib.
One of the potential roles for dasatinib and nilotinib may be to act as disease-stabilising agents for people awaiting BM transplant. This aspect of treatment has not been considered.
Conclusions
Chronic myeloid leukaemia in chronic phase
Effectiveness data are limited, but dasatinib and nilotinib appear efficacious in terms of obtaining CyR and HR in both ImR and ImI populations. The extent to which greater frequency and/or degrees of response may impact on long-term outcomes is more difficult to conclude given the limited nature of the evidence base. In particular, only one study has compared either agent (dasatinib) with HDI. The findings of this open-label study – that higher proportions of patients experience positive responses to dasatinib than HDI – are importantly confounded by substantial crossover at an early point in follow-up.
In terms of cost-effectiveness, it was extremely difficult to reach any conclusions regarding either agent in the ImR population. All three models (Novartis, PenTAG and BMS) were seriously flawed in one way or another, again as a consequence of the paucity of data appropriate to construct robust decision-analytic models with currently available data.
The economic picture is similar for people who are ImI, for whom even fewer data exist, and this comparison is made more difficult in structural terms by the lack of clarity about what constitutes the appropriate comparator in current practice.
The findings of the effectiveness studies suggest, perhaps unsurprisingly, that better responses are shown in people for whom second-line therapy was indicated as a consequence of intolerance than in those who were resistant to first-line imatinib. However, reflecting the uncertainty about duration of therapy in particular, this ranking seems reversed in our economic analyses.
Chronic myeloid leukaemia in accelerated phase and blast crisis
The economic evaluations carried out by the manufacturers of nilotinib and dasatinib were seriously undermined by the absence of evidence on HDI in these populations. In response to this, both models assume that the effectiveness of imatinib therapy can be adduced from evidence obtained in an imatinib-naive population using normal-dose imatinib. In addition to this factor, problems exist in all evaluations with respect to cost estimates, and only in the BC analysis of dasatinib (in which the new TKI dominates) do findings appear robust to changes in parameter assumptions.
Suggested research priorities
Appendix 10 summarises the ongoing clinical studies identified through a search of the controlled studies meta-register. There are several randomised clinical studies of the interventions under way. It is perhaps surprising, given the oral nature of the interventions and thus the relative ease of blinding of a study, that these are all open studies. We feel that a three-way, double-blind RCT of dasatinib, nilotinib and HDI would be the most useful addition to the scant existing evidence base.
Acknowledgements
We would like to acknowledge the help of Jo Perry, Sue Whiffin, Jenny Lowe and Virginia Webb for their administrative support.
We would particularly like to thank the Expert Advisory Group for their help throughout the project. The views expressed in this report are those of the authors and not necessarily those of the Expert Advisory Group nor those of the NIHR HTA programme. Any errors are the responsibility of the authors.
Contributions of authors
Gabriel Rogers contributed to the design of the assessment, performed data extraction of clinical effectiveness data, managed the reference database, performed the systematic review of clinical effectiveness and the critique of industry submissions, and contributed to the design and implementation of the economic model, to the interpretation of results, and to the writing and editing of the report.
Jo Thompson Coon provided overall project management, wrote the protocol, assessed abstracts for inclusion and exclusion, checked the data extraction of clinical effectiveness data and contributed to the critique of industry submissions, to the cost-effectiveness analysis, to the interpretation of results, and to the writing and editing of the report.
Martin Hoyle contributed to the design and implementation of the economic model, to the critique of industry submissions, to the interpretation of results, and to the writing and editing of the report.
Tiffany Moxham carried out literature searches for the systematic reviews and identification of model parameters.
Zulian Liu contributed to the review of clinical effectiveness.
Martin Pitt contributed to the design and implementation of the economic model, to the critique of the industry submissions, and to the writing and editing of the report.
Ken Stein contributed to the design of the assessment and to the design and development of the cost-effectiveness analysis including the critique of industry submissions, to the interpretation of the results, and to the writing and editing of the report.
About the Peninsula Technology Assessment Group
The Peninsula Technology Assessment Group is part of the Institute of Health Service Research at the Peninsula Medical School. PenTAG was established in 2000 and carries out independent Health Technology Assessments for the UK National Institute for Health Research (NIHR) and other local and national research funding bodies and policy-makers. The group is multidisciplinary and draws on individuals’ backgrounds in public health, health services research, computing and decision analysis, systematic reviewing, statistics and health economics. The Peninsula Medical School is part of the Peninsula College of Medicine and Dentistry, a school of the Universities of Plymouth and Exeter. The Institute of Health Research is made up of discrete, but methodologically-related research groups. Health Technology Assessment is a strong and recurring theme in the Institute’s work, in terms of both primary research and evidence synthesis.
Expert Advisory Group
Professor Jane Apperley: Chair of the Department of Haematology, Imperial College, London, UK
Catherine Chapman: Haematology Nurse Specialist, Royal Bournemouth Hospital, Bournemouth, UK
Professor Charles Craddock: Professor of Haematolo-oncology, Queen Elizabeth Hospital, Birmingham, UK
Dr Mark Drummond: Gartnavel General Hospital, Glasgow, UK
Professor John Goldman: Emeritus Professor of Haematology, Imperial College, London, UK
Professor Tessa Holyoake: Professor of Experimental Haematology, University of Glasgow, Gartnavel General Hospital, Glasgow, UK
Dr Claudius Rudin: Department of Haematology, Royal Devon and Exeter Hospital, Exeter, UK
Dr Andrew Walker: Health Economist, University of Glasgow, Glasgow, UK.
Competing interests of Expert Advisory Group
Professor Jane Apperley has received honoraria from Novartis and BMS for participating in educational events, almost entirely speaking in satellite symposia at medical meetings.
Catherine Chapman: none declared.
Professor Charles Craddock has received honoraria from Novartis and BMS for lectures and advisory boards. He was also involved in the preparation of the BMS submission to NICE.
Dr Mark Drummond has received honoraria and advisory board payments from Novartis and BMS.
Professor John Goldman has been asked to speak at meetings organised by Novartis, BMS and other companies that make TKIs. These are normally, but not always, paid with honoraria in the range of US$1000.
Professor Tessa Holyoake: has had research funding from Novartis and BMS. She has had honoraria payments from Novartis and BMS.
Dr Claudius Rudin: none declared.
Dr Andrew Walker: Novartis, which makes imatinib and nilotinib, has commissioned various pieces of work from Dr Walker over the last few years including seminars to NHS staff on health economics, internal seminars on the data requirements of the SMC, and so on. He has also described the principles behind SMC appraisals at meetings on breast cancer in Prague, Lisbon and Berlin (Novartis’s product letrozole) and age-related macular degeneration in Edinburgh (ranibizumab).
None of this work related to imatinib, dasatinib and CML, except in so far as these are among the 500-plus pieces of guidance issued by the SMC. Payment for these pieces of work would usually go to Glasgow University, although on a few occasions an honorarium has been accepted. In the system we in use at the SMC he has both personal, non-specific and non-personal conflicts of interest.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Nowell P, Hungerford D. A minute chromosome in human chronic granulocytic leukemia. Science 1960;132.
- Rowley J. Letter: a new consistent chromosomal abnormality in chronic myelogenous leukaemia identified by quinacrine fluorescence and Giemsa staining. Nature 1973;243:290-3.
- Deininger MW, Goldman JM, Melo JVS. The molecular biology of chronic myeloid leukemia. Blood 2000;96:3343-56.
- Druker BJ. Translation of the philadelphia chromosome into therapy for CML. Blood 2008;112:4808-17.
- O’Brien S, Berman E, Bhalla K, Copelan EA, Devetten MP, Emanuel PD, et al. Chronic myelogenous leukemia. J Natl Compr Canc Netw 2007;5:474-96.
- Sawyers CL. Chronic myeloid leukemia. N Engl J Med 1999;340:1330-40.
- O’Dwyer ME, Mauro MJ, Blasdel C, Farnsworth M, Kurilik G, Hsieh YC, et al. Clonal evolution and lack of cytogenetic response are adverse prognostic factors for hematologic relapse of chronic phase CML patients treated with imatinib mesylate. Blood 2004;103:451-5.
- Calabretta B, Perrotti D. The biology of CML blast crisis. Blood 2004;103:4010-22.
- Heaney NB, Holyoake TL. Therapeutic targets in chronic myeloid leukaemia. Hematol Oncol 2007;25:66-75.
- Kurzrock R, Gutterman JU, Talpaz M. The molecular genetics of philadelphia chromosome-positive leukemias. N Engl J Med 1988;319:990-8.
- Hochhaus A, Kantarjian HM, Baccarani M, Lipton JH, Apperley JF, Druker BJ, et al. Dasatinib induces notable hematologic and cytogenetic responses in chronic-phase chronic myeloid leukemia after failure of imatinib therapy. Blood 2007;109:2303-9.
- Guilhot F, Apperley J, Kim DW, Bullorsky EO, Baccarani M, Roboz GJ, et al. Dasatinib induces significant hematologic and cytogenetic responses in patients with imatinib-resistant or -intolerant chronic myeloid leukemia in accelerated phase. Blood 2007;109:4143-50.
- Cortes J, Rousselot P, Kim DW, Ritchie E, Hamerschlak N, Coutre S, et al. Dasatinib induces complete hematologic and cytogenetic responses in patients with imatinib-resistant or -intolerant chronic myeloid leukemia in blast crisis. Blood 2007;109:3207-13.
- Smith A, Roman E, Howell D, Jones R, Patmore R, Jack A, et al. The Haematological Malignancy Research Network (HMRN): a new information strategy for population based epidemiology and health service research. Br J Haematol 2010;148:739-53.
- Sokal JE, Baccarani M, Russo D, Tura S. Staging and prognosis in chronic myelogenous leukemia. Semin Hematol 1988;25:49-61.
- Hasford J, Pfirrmann M, Hehlmann R, Allan NC, Baccarani M, Kluin-Nelemans JC, et al. A new prognostic score for survival of patients with chronic myeloid leukemia treated with interferon alfa. Writing Committee for the Collaborative CML Prognostic Factors Project Group. J Natl Cancer Inst 1998;90:850-8.
- O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F, et al. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 2003;348:994-1004.
- Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarijan H, Gatterman N, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med 2006;355:2408-17.
- Hughes TP, Kaeda J, Branford S, Rudzki Z, Hochhaus A, Hensley ML, et al. Frequency of major molecular responses to imatinib or interferon alfa plus cytarabine in newly diagnosed chronic myeloid leukemia. N Engl J Med 2003;349:1423-32.
- Rachet B, Mitry E, Shah A, Cooper N, Coleman MP. Survival from adult leukaemia in England and Wales up to 2001. Br J Cancer 2008;99:S116-18.
- Brenner H, Gondos A, Pulte D. Recent trends in long-term survival of patients with chronic myelocytic leukemia: disclosing the impact of advances in therapy on the population level. Haematologica 2008;93:1544-9.
- Shah NP, Kantarjian HM, Kim DW, Rea D, Dorlhiac-Llacer PE, Milone JH, et al. Intermittent target inhibition with dasatinib 100 mg qd preserves efficacy and improves tolerability in imatinib-resistant and -intolerant chronic-phase chronic myeloid leukemia. J Clin Oncol 2008;26:3204-12.
- Kantarjian H, Pasquini R, Hamerschlak N, Rousselot P, Holowiecki J, Jootar S, et al. Dasatinib or high-dose imatinib for chronic-phase chronic myeloid leukemia after failure of first-line imatinib: a randomized phase 2 study. Blood 2007;109:5143-50.
- Hochhaus A. Dasatinib induces notable hematologic and cytogenetic responses in chronic-phase chronic myeloid leukemia after failure of imatinib therapy. Blood 2007;110.
- Goldman JM, Apperley JF, Jones L, Marcus R, Goolden AW, Batchelor R, et al. Bone marrow transplantation for patients with chronic myeloid leukemia. N Engl J Med 1986;314:202-7.
- Clift RA, Buckner CD, Thomas ED, Bryant E, Anasetti C, Bensinger WI, et al. Marrow transplantation for patients in accelerated phase of chronic myeloid leukemia. Blood 1994;84:4368-73.
- Goldman JM, Szydlo R, Horowitz MM, Gale RP, Ash RC, Atkinson K, et al. Choice of pretransplant treatment and timing of transplants for chronic myelogenous leukemia in chronic phase. Blood 1993;82:2235-8.
- Davies SM, DeFor TE, McGlave PB, Miller JS, Verfaillie CM, Wagner JE, et al. Equivalent outcomes in patients with chronic myelogenous leukemia after early transplantation of phenotypically matched bone marrow from related or unrelated donors. Am J Med 2001;110:339-446.
- Hansen JA, Gooley TA, Martin PJ, Appelbaum F, Chauncey TR, Clift RA, et al. Bone marrow transplants from unrelated donors for patients with chronic myeloid leukemia. N Engl J Med 1998;338:962-8.
- Silver RT, Woolf SH, Hehlmann R, Appelbaum F, Anderson J, Bennett C, et al. An evidence-based analysis of the effect of busulfan, hydroxyurea, interferon, and allogeneic bone marrow transplantation in treating the chronic phase of chronic myeloid leukemia: developed for the American Society of Hematology. Blood 1999;94:1517-36.
- Hochhaus A, O’Brien SG, Guilhot F, Druker BJ, Branford S, Foroni L, et al. Six-year follow-up of patients receiving imatinib for the first-line treatment of chronic myeloid leukemia. Leukemia 2009;23:1054-61.
- Talpaz M, Silver RT, Druker BJ, Goldman JM, Gambacorti-Passerini C, Guilhot F, et al. Imatinib induces durable hematologic and cytogenetic responses in patients with accelerated phase chronic myeloid leukemia: results of a phase 2 study. Blood 2002;99:1928-37.
- Palandri F, Castagnetti F, Alimena G, Testoni N, Breccia M, Luatti S, et al. The long-term durability of cytogenetic responses in patients with accelerated phase chronic myeloid leukemia treated with imatinib 600 mg: the GIMEMA CML Working Party experience after a 7-year follow-up. Haematologica 2009;94:202-12.
- Baccarani M, Saglio G, Goldman J, Hochhaus A, Simonsson B, Appelbaum F, et al. Evolving concepts in the management of chronic myeloid leukemia: recommendations from an expert panel on behalf of the European LeukemiaNet. Blood 2006;108:1809-20.
- Jabbour E, Kantarjian H, Jones D, Talpaz M, Bekele N, O’Brien S, et al. Frequency and clinical significance of BCR–ABL mutations in patients with chronic myeloid leukemia treated with imatinib mesylate. Leukemia 2006;20:1767-73.
- Branford S, Rudzki Z, Walsh S, Parkinson I, Grigg A, Szer J, et al. Detection of BCR–ABL mutations in patients with CML treated with imatinib is virtually always accompanied by clinical resistance, and mutations in the ATP phosphate-binding loop (P-loop) are associated with a poor prognosis. Blood 2003;102:276-83.
- Soverini S, Martinelli G, Rosti G, Bassi S, Amabile M, Poerio A, et al. ABL mutations in late chronic phase chronic myeloid leukemia patients with up-front cytogenetic resistance to imatinib are associated with a greater likelihood of progression to blast crisis and shorter survival: a study by the GIMEMA working party on chronic myeloid leukemia. J Clin Oncol 2005;23:4100-9.
- Cortes J, Jabbour E, Kantarjian H, Yin CC, Shan J, O’Brien S, et al. Dynamics of BCR–ABL-kinase domain mutations in chronic myeloid leukemia after sequential treatment with multiple tyrosine kinase inhibitors. Blood 2007;110:4005-11.
- Deininger MWN. Novel agents for chronic myeloid leukemia: from imatinib to dasatinib and nilotinib: overcoming resistance. Commun Oncol 2006;3:519-23.
- Gorre ME, Mohammed M, Ellwood K, Hsu N, Paquette R, Rao PN, et al. Clinical resistance to STI-571 cancer therapy caused by BCR–ABL gene mutation or amplification. Science 2001;293:876-80.
- Hochhaus A, Kreil S, Corbin AS, La Rosee P, Muller MC, Lahaye T, et al. Molecular and chromosomal mechanisms of resistance to imatinib (STI571) therapy. Leukemia 2002;16:2190-6.
- Donato NJ, Wu JY, Stapley J, Gallick G, Lin H, Arlinghaus RB, et al. BCR–ABL independence and LYN kinase overexpression in chronic myelogenous leukemia cells selected for resistance to STI571. Blood 2003;101:690-8.
- Gambacorti-Passerini C, Barni R, le Coutre P, Zucchetti M, Cabrita G, Cleris L, et al. Role of alpha1 acid glycoprotein in the in vivo resistance of human BCR–ABL(+) leukemic cells to the abl inhibitor STI571. J Natl Cancer Inst 2000;92:1641-50.
- Jorgensen HG, Elliott MA, Allan EK, Carr CE, Holyoake TL, Smith KD. Alpha1-acid glycoprotein expressed in the plasma of chronic myeloid leukemia patients does not mediate significant in vitro resistance to STI571. Blood 2002;100:367-8.
- Thomas J, Wang L, Clark RE, Pirmohamed M. Active transport of imatinib into and out of cells: implications for drug resistance. Blood 2004;104:3739-45.
- Illmer T, Schaich M, Platzberger U, Freiberg-Richter J, Oelschlagel U, von Bonin M, et al. P-glycoprotein-mediated drug efflux is a resistance mechanism of chronic myelogenous leukemia cells to treatment with imatinib mesylate. Leukemia 2004;18:401-8.
- Dulucq S, Bouchet S, Turcq B, Lippert E, Etienne G, Reiffers J, et al. Multidrug resistance gene (MDR1) polymorphisms are associated with major molecular responses to standard-dose imatinib in chronic myeloid leukemia. Blood 2008;112:2024-7.
- Hamdan MY, Sanders L, Oliveria S, Campbell U, Willey V, Hiji I, et al. Discontinuation and dose modification of imatinib in clinical practice. J Clin Oncol 2007;25.
- Apperley JF. Part I: mechanisms of resistance to imatinib in chronic myeloid leukaemia. Lancet Oncol 2007;8:1018-29.
- Apperley JF. Part II: management of resistance to imatinib in chronic myeloid leukaemia. Lancet Oncol 2007;8:1116-28.
- Rousselot P, Huguet F, Rea D, Legros L, Cayuela JM, Maarek O, et al. Imatinib mesylate discontinuation in patients with chronic myelogenous leukemia in complete molecular remission for more than 2 years. Blood 2007;109:58-60.
- Oehler V, Gooley TA, Snyder DS, Johnston L, Lin A, Cummings CC, et al. The effects of imatinib mesylate treatment before allogeneic transplantation for chronic myeloid leukemia. Blood 2007;109:1782-9.
- Kantarjian HM, Talpaz M, O’Brien S, Giles F, Garcia-Manero G, Faderl S, et al. Dose escalation of imatinib mesylate can overcome resistance to standard-dose therapy in patients with chronic myelogenous leukemia. Blood 2003;101:473-5.
- Kantarjian HM, Larson RA, Guilhot F, O’Brien SG, Mone M, Rudoltz M, et al. Efficacy of imatinib dose escalation in patients with chronic myeloid leukemia in chronic phase. Cancer 2009;115:551-60.
- Schiffer CA, Hehlmann R, Larson R. Perspectives on the treatment of chronic phase and advanced phase CML and philadelphia chromosome positive ALL. Leukemia 2003;17:691-9.
- Efficace F, Kemmler G, Vignetti M, Mandelli F, Molica S, Holzner B. Health-related quality of life assessment and reported outcomes in leukaemia randomised controlled trials – a systematic review to evaluate the added value in supporting clinical decision making. Eur J Cancer 2008;44:1497-506.
- National Institute for Health and Clinical Excellence (NICE) . Improving Outcomes in Haematological Cancers: The Manual 2003.
- Cang S, Liu D. P-loop mutations and novel therapeutic approaches for imatinib failures in chronic myeloid leukemia. J Hematol Oncol 2008;1.
- Deininger MWN, Druker BJ. Circumventing imatinib resistance. Cancer Cell 2004;6:108-10.
- Copland M, Hamilton A, Elrick LJ, Baird JW, Allan EK, Jordanides N, et al. Dasatinib (BMS-354825) targets an earlier progenitor population than imatinib in primary CML but does not eliminate the quiescent fraction. Blood 2006;107:4532-9.
- Jorgensen HG, Allan EK, Jordanides NE, Mountford JC, Holyoake TL. Nilotinib exerts equipotent antiproliferative effects to imatinib and does not induce apoptosis in CD34 + CML cells. Blood 2007;109:4016-19.
- Das J, Chen P, Norris D, Padmanabha R, Lin J, Moquin RV, et al. 2-Aminothiazole as a novel kinase inhibitor template. Structure-activity relationship studies toward the discovery of N-(2-chloro-6-methylphenyl)-2-[[6-[4-(2-hydroxyethyl)-1-piperazinyl]-2-methyl-4-pyrimidinyl]amino]-1, 3-thiazole-5-carboxamide (Dasatinib, BMS-354825) as a potent pan-Src kinase inhibitor. J Med Chem 2006;49:6819-32.
- Shah NP, Tran C, Lee FY, Chen P, Norris D, Sawyers CL. Overriding imatinib resistance with a novel ABL kinase inhibitor. Science 2004;305:399-401.
- Burgess MR, Skaggs BJ, Shah NP, Lee FY, Sawyers CL. Comparative analysis of two clinically active BCR–ABL kinase inhibitors reveals the role of conformation-specific binding in resistance. Proc Natl Acad Sci USA 2005;102:3395-400.
- O’Hare T, Walters DK, Stoffregen EP, Jia TP, Manley PW, Mestan J, et al. In vitro activity of Bcr-Abl inhibitors AMN107 and BMS-354825 against clinically relevant imatinib-resistant Abl kinase domain mutants. Cancer Res 2005;65:4500-5.
- Tokarski JS, Newitt JA, Chang CYJ, Cheng JD, Wittekind M, Kiefer SE, et al. The structure of dasatinib (BMS-354825) bound to activated ABL-kinase domain elucidates its inhibitory activity against imatinib-resistant ABL mutants. Cancer Res 2006;66:5790-7.
- European Medicines Agency . EPARS for Authorised Medicinal Products for Human Use. Sprycel: European Public Assessment Report n.d. www emea europa eu/humandocs/Humans/EPAR/sprycel/sprycel htm (accessed 26 March 2009).
- British Medical Association and Royal Pharmaceutical Society of Great Britain . British National Formulary 2009.
- Weisberg E, Manley P, Mestan J, Cowan-Jacob S, Ray A, Griffin JD. AMN107 (nilotinib): a novel and selective inhibitor of BCR–ABL. Br J Cancer 2006;94:1765-9.
- European Medicines Agency . EPARs for Authorised Medicinal Products for Human Use. Tasigna: European Public Assessment Report n.d. www.emea.europa.eu/humandocs/Humans/EPAR/tasigna/tasigna.htm (accessed 26 March 2009).
- NHS Centre for Reviews and Dissemination . Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care 2009.
- Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the bionmial. Biometrika 1934;26:404-13.
- DerSimonian R, Laird N. Meta-analysis in clinical studies. Control Clin Trials 1986;7:177-88.
- Einarson TR. Pharmacoeconomic applications of meta-analysis for single groups using antifungal onychomycosis lacquers as an example. Clin Ther 1997;19:559-69.
- Khorashad JS, Milojkovic D, Mehta P, Anand M, Ghorashian S, Reid AG, et al. In vivo kinetics of kinase domain mutations in CML patients treated with dasatinib after failing imatinib. Blood 2008;111:2378-81.
- Nicolini FE, Chabane K, Tigaud I, Michallet M, Magaud JP, Hayette S. BCR–ABL mutant kinetics in CML patients treated with dasatinib. Leuk Res 2007;31:865-8.
- Soverini S, Martinelli G, Colarossi S, Gnani A, Castagnetti F, Rosti G, et al. Presence or the emergence of a F317L BCR–ABL mutation may be associated with resistance to dasatinib in philadelphia chromosome-positive leukemia. J Clin Oncol 2006;24:e51-e52.
- Soverini S, Colarossi S, Gnani A, Castagnetti F, Rosti G, Bosi C, et al. Resistance to dasatinib in Philadelphia-positive leukemia patients and the presence or the selection of mutations at residues 315 and 317 in the BCR–ABL-kinase domain. Haematologica 2007;92:401-4.
- Fabarius A, Haferlach C, Muller MC, Erben P, Lahaye T, Giehl M, et al. Dynamics of cytogenetic aberrations in Philadelphia chromosome positive and negative hematopoiesis during dasatinib therapy of chronic myeloid leukemia patients after imatinib failure. Haematologica 2007;92:834-7.
- Kim DH, Kamel-Reid S, Chang H, Sutherland R, Jung CW, Kim HJ, et al. Natural killer or natural killer/T cell lineage large granular lymphocytosis associated with dasatinib therapy for philadelphia chromosome positive leukemia. Haematologica 2009;94:135-9.
- Kantarjian H, Cortes J, Kim DW, Dorlhiac-Llacer P, Pasquini R, DiPersio J, et al. Phase III study of dasatinib 140 mg qd versus 70 mg twice daily in patients with chronic myeloid leukemia in accelerated phase resistant or intolerant to imatinib: 15-month median follow-up. Blood 2009;113:6322-9.
- Shah N, Pasquini R, Rousselot P, Jootar S, Holowiecki J, Countouriotis A, et al. Dasatinib (SPRYCEL (R)) vs escalated dose of imatinib (im) in patients (pts) with chronic phase chronic myeloid leukemia (CP-CML) resistant to imatinib: results of the CA180-017 START-R randomized study. Blood 2006;108.
- Shah NP, Rousselot P, Pasquini R, Hamerschlak N, Holowiecki J, Gerard B, et al. Dasatinib (D) vs high dose imatinib (IM) inpatients (pts) with chronic phase chronic myeloid leukemia (CP-CML) resistant to imatinib. Results of CA180017 START-R randomized study. J Clin Oncol 2006;24.
- Cannell E. Dasatinib is effective in imatinib-resistant CML. Lancet Oncol 2007;8.
- Kantarjian HM, Rousselot P, Pasquini R, Hamerschlak N, Holowiecki J, Dejardin D, et al. Dasatinib or high-dose imatinib for patients with chronic-phase chronic myeloid leukemia resistant to standard-dose imatinib: 2-year follow-up data from START-R (CA180-017). Blood 2007;110.
- Martinelli G, Rousselot P, Robak T, Masszi T, Skotnicki A, Hellmann A. Comparison of dasatinib to high-dose imatinib in patients who experience imatinib failure: results from a randomized, phase-II study (CA180017, START-R). Haematologica 2007;92.
- Schiffer CA. What if conventional-dose imatinib fails?. Blood 2007;109:5068-9.
- Rousselot P, Corm S, Paquette R, Bleickardt E, Dejardin D, Kantarjian HM, et al. Dasatinib compared with high-dose imatinib in patients with chronic myelogenous leukemia in chronic phase (Cml-Cp) after failure of standard-dose imatinib – a two-year update of the Start-R study. Haematologica 2008;93.
- Rousselot PH, Facon T, Paquette R, Bleickardt E, Dejardin D, Kantarjian HM. Dasatinib or high-dose imatinib for patients with chronic myelogenous leukemia chronic-phase (CML-CP) resistant to standard-dose imatinib: 2-year follow-up data from START-R. J Clin Oncol 2008;26.
- Hochhaus A, Kim DW, Rousselot P, Dorlhiac-Llacer PE, Milone J, Francis S, et al. Dasatinib (SPRYCEL (R)) 50 mg or 70 mg BID versus 100 mg or 140 mg QD in patients with chronic myeloid leukemia in chronic phase (CML-CP) resistant or intolerant to imatinib: results of the CA180-034 study. Blood 2006;108.
- Hochhaus A, Kim DW, Rousselot P, Kantarjian H, Charbonnier A, Heim D. Dasatinib dose and schedule optimization in chronic-phase CML resistant or intolerant to imatinib: results from a randomized phase-III study (CA180034). Haematologica 2007;92.
- Shah NP, Kim DW, Kantarjian HM, Rousselot P, Dorlhiac-Llacer PE, Milone JH, et al. Dasatinib 50 mg or 70 mg BID compared to 100 mg or 140 mg QD in patients with CML in chronic phase (CP) who are resistant or intolerant to imatinib: one-year results of CA180034. J Clin Oncol 2007;25.
- Hochhaus A, Mueller M, Cortes JE, Kim D, Matlob Y, Ploughman L, et al. Dasatinib efficacy by dosing schedule across individual baseline BCR–ABL mutations in chronic phase chronic myelogenous leukemia (CML-CP) after imatinib failure. J Clin Oncol 2008;26.
- Hochhaus A, Muller MC, Cortes J, Kim DW, Matloub Y, Ploughman L, et al. Dasatinib efficacy after imatinib failure by dosing schedule and baseline Bcr-Abl mutation status in patients with chronic myeloid leukemia in chronic phase (Cml-Cp). Haematologica 2008;93.
- Nicaise C, Wang X, Roy A, Pfister M, Chen TT, Bleickardt E, et al. Dasatinib pharmacokinetics and exposure-response (E-R): relationships to efficacy and safety in patients with chronic myelogenous leukemia in chronic phase (Cml-Cp). Haematologica 2008;93.
- Porkka K, Khoury HJ, Paquette R, Matloub Y, Liu D, Sinha R, et al. Dasatinib 100 mg qd (QD) maintains long-term efficacy and minimizes the occurrence of pleural effusion: an analysis of 24-month data in patients with resistance, suboptimal response, or intolerance to imatinib (CA180-034). Blood 2008;112.
- Shah NP, Kim DW, Kantarjian HM, Rousselot P, Dorlhiac-Llacer P, Milone J, et al. Dasatinib dose-optimization in chronic phase chronic myeloid leukemia (CML-CP): two-year data from CA180-034 show equivalent long-term efficacy and improved safety with 100 mg qd dose. Blood 2008;112.
- Wang X, Hochhaus A, Kantarjian HM, Agrawal S, Roy A, Pfister M, et al. Dasatinib pharmacokinetics and exposure-response (E-R): relationship to safety and efficacy in patients (pts) with chronic myeloid leukemia (CML). J Clin Oncol 2008;26.
- Kantarjian H, Ottmann O, Pasquini R, Goh YT, Kim DW, Van Tornout J, et al. Dasatinib (SPRYCEL (R)) 140 mg qd (QD) vs 70 mg twice daily (BID) in patients (pts) with advanced phase chonic myeloid leukemia (ABP-CML) or ph(+) ALL who are resistant or intolerant to imatinib (im): results of the CA180-035 study. Blood 2006;108.
- Pasquini R, Ottmann OG, Goh YT, Kim D, Dorlhiac Llacer PE, DiPersio JF, et al. Dasatinib 140 mg QD compared to 70 mg BID in advanced-phase CML or Ph(+) ALL resistant or intolerant to imatinib: one-year results of CA180-035. J Clin Oncol 2007;25.
- Kantarjian HM, Kim DW, Dorlhiac-Llacer P, Pasquini R, Khoroshko N, DiPersio JF, et al. Dasatinib 140 mg qd (QD) demonstrates equivalent efficacy and improved safety compared with 70 mg twice daily (BID) in patients with accelerated phase chronic myeloid leukemia (CML-AP): 2-year follow-up data from CA180-035. Blood 2008;112.
- Saglio G, Kantarjian HM, Hochhaus A, Goh YT, Masszi T, Pasquini R, et al. Dasatinib 140 mg qd (QD) demonstrates equivalent efficacy and improved safety compared with 70 mg twice daily (BID) in patients with chronic myeloid leukemia in blast phase (CML-BP): 2-year data from CA180-035. Blood 2008;112.
- Kantarjian H, Giles F, Wunderle L, Bhalla K, O’Brien S, Wassmann B, et al. Nilotinib in imatinib-resistant CML and Philadelphia chromosome-positive ALL. N Engl J Med 2006;354:2542-51.
- Talpaz M, Shah NP, Kantarjian H, Donato N, Nicoll J, Paquette R, et al. Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med 2006;354:2531-41.
- Hochhaus A, Baccarani M, Deininger M, Apperley JF, Lipton JH, Goldberg SL, et al. Dasatinib induces durable cytogenetic responses in patients with chronic myelogenous leukemia in chronic phase with resistance or intolerance to imatinib. Leukemia 2008;22:1200-6.
- Kantarjian HM, Giles F, Gattermann N, Bhalla K, Alimena G, Palandri F, et al. Nilotinib (formerly AMN107), a highly selective BCR–ABL tyrosine kinase inhibitor, is effective in patients with Philadelphia chromosome-positive chronic myelogenous leukemia in chronic phase following imatinib resistance and intolerance. Blood 2007;110:3540-6.
- le Coutre CP, Ottmann OG, Giles F, Kim DW, Cortes J, Gattermann N, et al. Nilotinib (formerly AMN107), a highly selective BCR–ABL tyrosine kinase inhibitor, is active in patients with imatinib-resistant or -intolerant accelerated-phase chronic myelogenous leukemia. Blood 2008;111:1834-9.
- Tojo A, Usuki K, Urabe A, Maeda Y, Kobayashi Y, Jinnai I, et al. A Phase I/II study of nilotinib in Japanese patients with imatinib-resistant or -intolerant Ph+ CML or relapsed/refractory Ph+ ALL. Int J Hematol 2009;89:679-88.
- Sakamaki H, Ishizawa K, Taniwaki M, Fujisawa S, Morishima Y, Tobinai K, et al. Phase I/2 clinical study of dasatinib in Japanese patients with chronic myeloid leukemia or Philadelphia chromosome-positive acute lymphoblastic leukemia. Int J Hematol 2009;89:332-41.
- Giles FG, Ottmann OT, Cortes J, Wassmann B, Bhalla K, Jones D, et al. AMN107, a novel aminopyrimidine inhibitor of Bcr-Abl, has significant activity in imatinib-resistant Bcr-Abl positive chronic myeloid leukemia (CML). Br J Haematol 2005;129.
- Singer JB, Shou Y, Giles F, Kantarjian HM, Hsu Y, Robeva AS, et al. UGT1A1 promoter polymorphism increases risk of nilotinib-induced hyperbilirubinemia. Leukemia 2007;21:2311-15.
- La RP, Holm-Eriksen S, Konig H, Hartel N, Ernst T, Debatin J, et al. Phospho-CRKL monitoring for the assessment of BCR–ABL activity in imatinib-resistant chronic myeloid leukemia or Ph+ acute lymphoblastic leukemia patients treated with nilotinib. Haematologica 2008;93:765-9.
- Chu SC, Tang JL, Li CC. Dasatinib in chronic myelogenous leukemia. N Engl J Med 2006;355:1062-3.
- Sawyers CL, Talpaz M, Bleickardt E. Dasatinib in chronic myelogenous leukemia – reply. N Engl J Med 2006;355:1063-4.
- Cortes J, Sawyers CL, Kantarjian HM, Shah NP, Paquette R, Bleickardt E, et al. Dasatinib is associated with durable treatment responses in chronic phase chronic myeloid leukemia: long-term follow-up from the phase I trial (Ca180002). Haematologica 2008;93.
- Ottmann OG, Martinelli G, Dombret H, Kantarjian H, Hochhaus A, Simonsson B, et al. A phase II study of dasatinib in patients with chronic myeloid leukemia (CML) in lymphoid blast crisis or philadelphia-chromosome positive acute lymphoblastic leukemia (Ph plus ALL) who are resistant or intolerant to imatinib: the ‘START-L’ CA180015 study. Blood 2005;106.
- Talpaz M, Rousselot P, Kim DW, Guilhot F, Corm S, Bleickardt E, et al. A phase II study of dasatinib in patients with chronic myeloid leukemia (CML) in myeloid blast crisis who are resistant or intolerant to imatinib: first results of the CA180006 ‘START-B’ study. Blood 2005;106.
- Chromik J, Pfeifer H, Wunderle L, Schoch N, Wassmann B, Brueck P, et al. Sustained molecular responses to dasatanib (SPRYCEL (R)) in patients with Philadelphia chromosome-positive (Ph(+)) acute lymphoblastic leukemia (ALL) or lymphoid blast phase (LyBP) chronic myeloid leukemia after imatinib (IM) failure: a single-center experience. Blood 2006;108.
- Cortes JE, Kim DW, Rosti G, Rousselot P, Bleickardt E, Zink R, et al. Dasatinib (D) in patients (pts) with chronic myelogenous leukemia (CML) in myeloid blast crisis (MBC) who are imatinib-resistant (IM-R) or IM-intolerant (IM-I): results of the CA180006 ‘START-B’ study. J Clin Oncol 2006;24.
- Martinelli G, Hochhaus A, Coutre S, Apperley JF, Shah N, Gollerkeri A, et al. Dasatinib (SPRYCEL (R)) efficacy and safety in patients (pts) with chronic myelogenous leukemia in lymphoid (CML-LB) or myeloid blast (CML-MB) phase who are imatinib-resistant (Im-r) or -intolerant (Im-i). Blood 2006;108.
- Ganibacoiti C, Cortes J, Kim DW, Dombret H, Zhu C, Van Tornout JMA, et al. Efficacy and safety of dasatinib in patients with chronic myeloid leukemia in blast phase whose disease is resistant or intolerant to imatinib: 2-year follow-up data from the START program. Blood 2007;110.
- Ottmann O, Dombret H, Martinelli G, Simonsson B, Guilhot F, Larson RA, et al. Dasatinib induces rapid hematologic and cytogenetic responses in adult patients with Philadelphia chromosome positive acute lymphoblastic leukemia with resistance or intolerance to imatinib: interim results of a phase 2 study. Blood 2007;110:2309-15.
- Cortes J, Kim DW, Raffoux E, Martinelli G, Ritchie E, Roy L, et al. Efficacy and safety of dasatinib in imatinib-resistant or -intolerant patients with chronic myeloid leukemia in blast phase. Leukemia 2008;22:2176-83.
- Porkka K, Koskenvesa P, Lundan T, Rimpilainen J, Mustjoki S, Smykla R, et al. Dasatinib crosses the blood-brain barrier and is an efficient therapy for central nervous system philadelphia chromosome-positive leukemia. Blood 2008;112:1005-12.
- Saglio G, Dombret H, Rea D, Corm S, Cortes J, Kim DW, et al. Dasatinib efficacy in patients with imatinib-resistant/-intolerant chronic myeloid leukemia in blast phase: 24-month data from the Start Program. Haematologica 2008;93.
- Guilhot F, Apperley JF, Shah N, Kim DW, Grigg A, Cheng S, et al. A phase II study of dasatinib in patients with accelerated phase chronic myeloid leukemia (CML) who are resistant or intolerant to imatinib: first results of the CA180005 ‘START-A’ study. Blood 2005;106.
- Cortes J, Kim DW, Guilhot F, Rosti G, Silver RT, Gollerkeri A, et al. Dasatinib (SPRYCEL (R)) in patients (pts) with chronic myelogenous leukemia in accelerated phase (AP-CML) that is imatinib-resistant (im-r) or -intolerant (im-i): updated results of the CA180-005 ‘START-A’ phase II study. Blood 2006;108.
- Talpaz M, Apperley JF, Kim DW, Silver RT, Bullorsky EO, Cheng S, et al. Dasatinib (D) in patients with accelerated phase chronic myeloid leukemia (AP-CML) who are resistant or intolerant to imatinib: results of the CA180005 ‘START-A’ study. J Clin Oncol 2006;24.
- Guilhot F, Apperley JF, Kim DW, Kosti G, Yuan X, Van Tomout JMA, et al. Efficacy of dasatinib in patients with accelerated-phase chronic myelogenous leukemia with resistance or intolerance to imatinib: 2-year follow-up data from START-A (CA180-005). Blood 2007;110.
- O’Brien S. Dasatinib in accelerated phase. Blood 2007;109.
- Rea D, Dombret H, Kim DW, Rosti G, Roy L, Garzon FT, et al. Dasatinib efficacy in patients with imatinib-resistant/-intolerant chronic myeloid leukemia in accelerated phase: 24-month data from START-A. Haematologica 2008;93.
- Rea D, Dombret H, Kim DW, Rosti G, Roy L, Garzon FT, et al. Dasatinib efficacy in patients with imatinib-resistant/-intolerant chronic myeloid leukemia in accelerated phase: 24-month data from Start-A. Haematologica 2008;93.
- Hochhaus A, Baccarani M, Sawyers C, Nagler A, Facon T, Goldberg SL, et al. Efficacy of dasatinib in patients with chronic phase Philadelphia chromosome-positive CML resistant or intolerant to imatinib: first results of the CA180013 ‘START-C’ phase II study. Blood 2005;106.
- Baccarani M, Kantarjian HM, Apperley JF, Lipton JH, Druker B, Countouriotis A, et al. Efficacy of dasatinib (SPRYCEL (R)) in patients (pts) with chronic phase chronic myelogenous leukemia (CP-CML) resistant to or intolerant of imatinib: updated results of the CA180013 ‘START C’ phase II study. Blood 2006;108.
- Hochhaus A, Kantarjian H, Baccarani M, Cervantes F, Facon T, Goldberg S, et al. Dasatinib in patients with chronic phase chronic myeloid leukemia (CP-CML) who are resistant or intolerant to imatinib: results of the CA180013 ‘START-C’ Study. J Clin Oncol 2006;24.
- Hochhaus A, Kantarjian H, Baccarani M, Cervantes F, Facon T, Goldberg S, et al. Dasatinib in patients with chronic phase chronic myeloid leukemia (CP-CML) who are resistant or intolerant to imatinib: results of the CA180013 ‘START-C’ Study. J Clin Oncol 2006;24.
- Guilhot F, Apperley J, Facon T, Niederwieser D, Gambacorti C, Fischer T, et al. Dasatinib induces durable cytogenetic responses in patients with chronic-phase CML with resistance or intolerance to imatinib: updated results of the CA180013 (START-C) study. Haematologica 2007;92.
- Mueller MC, Erben P, Ernst T, Giehl M, Schenk T, Hoffmann J, et al. Molecular response according to type of preexisting BCR–ABL mutations after second Line dasatinib therapy in chronic phase CML patients. Blood 2007;110.
- Stone RM, Kantarjian HM, Baccarani M, Lipton JH, Hughes T, Ezzeddine R, et al. Efficacy of dasatinib in patients with chronic-phase chronic myelogenous leukemia with resistance or intolerance to imatinib: 2-year follow-up data from START-C (CA180-013). Blood 2007;110.
- Baccarani M, Rosti G, Saglio G, Cortes J, Stone R, Niederwieser DW, et al. Dasatinib time to and durability of major and complete cytogenetic response (MCyR and CCyR) in patients with chronic myeloid leukemia in chronic phase (CML-CP). Blood 2008;112.
- Cervantes F, Baccarani M, Lipton J, Matloub Y, Sinha S, Stone R, et al. Dasatinib long-term efficacy in patients with chronic myeloid leukemia in chronic phase (CML-CP) with resistance or intolerance to imatinib: a 2-year update of the START-C Study. Haematologica (EHA Annual Meeting Abstracts) 2008;93.
- Goldman JM, Druker BJ. Chronic myeloid leukemia: current treatment options. Blood 2001;98:2039-42.
- Cortes J, Mauro M, O’Brien S, Borthakur G, Wierda W, Matloub Y, et al. The vast majority of CML-CP patients treated with dasatinib (70 mg BID) who progress after long-term follow-up (24 mo) remain in chronic-phase. Blood 2008;112.
- Deininger MWN, Mauro MJ, Matloub Y, Sinha R, Ploughman L, Liu D, et al. Prevalence of T315I, dasatinib-specific resistant mutations (F317L, V299L, and T315A), and nilotinib-specific resistant mutations (P-loop and F359) at the time of imatinib resistance in chronic-phase chronic myeloid leukemia (CP-CML). Blood 2008;112.
- Hochhaus A, Baccarani M, Deininger M, Apperley JF, Lipton JH, Goldberg SL, et al. Dasatinib induces durable cytogenetic responses in patients with chronic myelogenous leukemia in chronic phase with resistance or intolerance to imatinib. Leukemia 2008;22:1200-6.
- Hochhaus A, Muller MC, Radich J, Branford S, Hanfstein B, Rousselot P, et al. Dasatinib-associated major molecular responses are rapidly achieved in patients with chronic myeloid leukemia in chronic phase (CML-CP) following resistance, suboptimal response, or intolerance on imatinib. Blood 2008;112.
- Mauro MJ, Baccarani M, Cervantes F, Lipton JH, Matloub Y, Sinha R, et al. Dasatinib 2-year efficacy in patients with chronic-phase chronic myelogenous leukemia (CML-CP) with resistance or intolerance to imatinib (START-C). J Clin Oncol 2008;26.
- Kantarjian HM, Gattermann N, O’Brien SG, Bhalla K, Hochhaus A, Cervantes F, et al. A phase II study of AMN107, a novel inhibitor of Bcr-Abl, administered to imatinib resistant and intolerant patients (pts) with chronic myelogenous leukemia (CML) in chronic phase (CP). J Clin Oncol 2006;24.
- le Coutre P, Bhalla K, Giles F, Baccarani M, Ossenkoppele GJ, Hochhaus A, et al. A phase II study of nilotinib, a novel tyrosine kinase inhibitor administered to imatinib-resistant and -intolerant patients with chronic myelogenous leukemia (CML) in chronic phase (CP). Blood 2006;108.
- Cortes J, Jabbour E, Hochhaus A, le Coutre P, Baccarani M, Bhalla KN, et al. Nilotinib is associated with minimal cross intolerance to imatinib in patients with imatinib-intolerant philadelphia-positive (Ph+) chronic myelogenous leukemia (CML) in either chronic phase (CP) or accelerated phase (AP). Blood 2007;110.
- Hochhaus A, Giles FJ, le Coutre P, Baccarani M, Gattertnann N, Bhalla KN, et al. Safety, and efficacy of nilotinib dose escalation 600 mg BID in patients (pts) with imatinib-resistant or -intolerant chronic myeloid leukemia (CML) in chronic phase (CP). Blood 2007;110.
- Hughes T, Saglio G, Martinelli G, Kim DW, Soverini S, Mueller M, et al. Responses and disease progression in CML-CP patients treated with nilotinib after imatinib failure appear to be affected by the BCR–ABL mutation status and types. Blood 2007;110.
- Kantarjian HM, Hochhaus A, Cortes J, Martinelli G, Bhalla KN, Giles FJ, et al. Nilotinib is highly active and safe in chronic phase chronic myelogenous leukemia (CML-CP) patients with imatinib-resistance or intolerance. Blood 2007;110.
- Martinelli G, Rosti G, le Coutre P, Bhalla K, Giles F, Ossenkoppele G, et al. A phase II study of nilotinib, a novel tyrosine kinase inhibitor administered to imatinib-resistant and -intolerant patients with Philadelphia-positive chronic myelogenous leukemia in chronic phase. Haematologica 2007;92.
- Mueller MC, Branford S, Radich J, Kim DW, Martinelli G, Saglio G, et al. Response dynamics to nilotinib depend on the type of BCR–ABL mutations in patients with chronic myelogenous leukemia (CML) after imatinib failure. J Clin Oncol 2007;25.
- Rosti G, Hochhaus A, le Coutre P, Baccarani M, Bhalla K, Ossenkoppele G, et al. Nilotinib isassociated with minimal cross intoleranceto imatinib in patients with imatinib-intolerant Philadelphia-positive chronic myelogenous leukemia in either chronic phase or accelerated phase. Haematologica 2007;92.
- Rosti G, le Coutre P, Bhalla K, Giles F, Ossenkoppele G, Hochhaus A, et al. A phase II study of nilotinib administered to imatinib resistant and intolerant patients with chronic myelogenous leukemia (CML) in chronic phase (CP). J Clin Oncol 2007;25.
- Hochhaus A, Kantarjian HM, Baccarani M, le Coutre P, Haque A, Gallagher N, et al. Minimal cross-intolerance between nilotinib and imatinib in patients with imatinib-intolerant chronic myelogenous leukaemia (Cml) in chronic phase (Cp) or accelerated phase (Ap). Haematologica 2008;93.
- Jabbour E, Kantarjian HM, Baccarani M, le Coutre PD, Haque A, Gallagher NJ, et al. Minimal cross-intolerance between nilotinib and imatinib in patients with imatinib-intolerant chronic myeloid leukemia in chronic phase (CML-CP) or accelerated phase (CML-AP). Blood 2008;112.
- Kantarjian HM, Giles FJ, Bhalla KN, Larson RA, Gatterman N, Ottmann OG, et al. Nilotinib in chronic myelogenous leukaemia in chronic phase (Cml-Cp) patients with imatinib-resistance or intolerance: updated phase 2 results. Haematologica 2008;93.
- Kantarjian HM, Giles FJ, Hochhaus A, Bhalla KN, Ossenkoppele GJ, Gattermann N, et al. Nilotinib in patients with imatinib-resistant or -intolerant chronic myelogenous leukemia in chronic phase (CML-CP): updated phase II results. J Clin Oncol 2008;26.
- Lipton JH, le Coutre PD, Wang J, Yang M, Szczudlo T, Giles F. Nilotinib in elderly chronic myeloid leukemia patients in chronic phase (CML-CP) with imatinib resistance or intolerance: efficacy and safety analysis. Blood 2008;112.
- Radich J, Kim DW, Martinelli G, Soverini S, Branford S, Mueller M, et al. Response to nilotinib in chronic myelogenous leukemia patients in chronic phase (Cml-Cp) according to Bcr-Abl mutations at baseline. Haematologica 2008;93.
- Saglio G, Radich J, Kim D, Martinelli G, Branford S, Mueller M, et al. Response to nilotinib in chronic myelogenous leukemia patients in chronic phase (CML-CP) according to BCR–ABL mutations at baseline #7060. J Clin Oncol 2008;26.
- Clark R, le Coutre P, Giles FJ, Hocchaus A, Haque A, Gallagher N, et al. Nilotinib in chronic myeloid leukaemia patients in chronic phase (CML-CP) with imatinib resistance or intolerance: follow-up results of a phase 2 study. Br J Haematol 2009;145.
- le Coutre P, Gattermann N, Hochhaus A, Larson R, Weitzman A, Haque A, et al. A phase II study of nilotinib administered to imatinib resistant or intolerant patients with chronic myelogenous leukemia (CML) in accelerated phase (AP). J Clin Oncol 2007;25.
- le Coutre P, Giles FJ, Apperley J, Ottmann OG, Gattermann N, O’Brien SG, et al. Nilotinib is safe and effective in accelerated phase chronic myelogenous leukemia (CML-AP) patients with imatinib resistance or intolerance. Blood 2007;110.
- le Coutre P, Larson R, Kantarjian H, Gattermann N, Hochhaus A, Haque A, et al. A phase II study of nilotinib,a noveltyrosine kinase inhibitor administered to imatinib-resistant or -intolerant patients with Philadelphia positive chronic myelogenous leukemia in accelerated phase. Haematologica 2007;92.
- Saglio G, Kim DW, Hochhaus A, Soverini S, Erben P, Branford S, et al. Correlation of clinical response to nilotinib with BCR–ABL mutation status in advanced phase chronic myelogenous leukemia (CML-AP) patients with imatinib-resistance or intolerance. Blood 2007;11.
- Alexander W, le Coutre CP. American Society of Hematology 49th Annual Meeting: nilotinib (Tasigna) in chronic myelogenous leukemia. P and T 2008;33:113-7.
- Apperley J, le Coutre P, Giles FJ, Ottmann OG, Larson RA, Haque A, et al. Nilotinib in accelerated phase chronic myelogenous leukaemia (CML-AP) patients with imatinib-resistance or -intolerance: update of a phase 2 study. Br J Haematol 2008;141.
- Kantarjian HM, Giles F, Bhalla KN, Larson RA, Gattermann N, Ottmann OG, et al. Nilotinib in chronic myeloid leukemia patients in chronic phase (CMLCP) with imatinib resistance or intolerance: 2-year follow-up results of a phase 2 study. Blood 2008;112.
- le Coutre P, Giles FJ, Apperley J, Ottmann OG, Larson RA, Haque A, et al. Nilotinib in accelerated phase chronic myelogenous leukemia (CML-AP) patients with imatinib-resistance or -intolerance: update of a phase II study. J Clin Oncol 2008;26.
- le Coutre P, Giles FJ, Hochhaus A, Apperley J, Ossenkoppele G, Haque A, et al. Nilotinib in imatinib-resistant or -intolerant patients with chronic myelogenous leukaemia in accelerated phase (Cml-Ap): update of a phase 2 study. Haematologica 2008;93.
- le Coutre PD, Giles F, Hochhaus A, Apperley JF, Ossenkoppele G, Haque A, et al. Nilotinib in chronic myeloid leukemia patients in accelerated phase (CML-AP) with imatinib resistance or intolerance: 2-year follow-up results of a phase 2 study. Blood 2008;112.
- Apperley JF, Cortes JE, Kim DW, Roy L, Roboz GJ, Rosti G, et al. Dasatinib in the treatment of chronic myeloid leukemia in accelerated phase after imatinib failure: the START A trial. J Clin Oncol 2009;27:3472-9.
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled studies. JAMA 1995;273:408-12.
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, et al. Does quality of reports of randomised studies affect estimates of intervention efficacy reported in meta-analyses?. Lancet 1998;352:609-13.
- Kjaergard LL, Villumsen J, Gluud C. Quality of Randomised Clinical Studies Affects Estimates of Intervention Efficacy. Abstracts for Workshops and Scientific Sessions n.d.
- Juni P, Altman DG, Egger M. Systematic reviews in health care: assessing the quality of controlled clinical studies. BMJ 2001;323:42-6.
- Schulz KF. Subverting randomization in controlled studies. JAMA 1995;274.
- Jabbour E, Kantarjian HM, Jones D, Shan J, O’Brien S, Reddy N, et al. Imatinib mesylate dose escalation is associated with durable responses in patients with chronic myeloid leukemia after cytogenetic failure on standard-dose imatinib therapy. Blood 2009;113:2154-60.
- Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L. Do the findings of case series studies vary significantly according to methodological characteristics?. Health Technol Assess 2005;9.
- Bristol-Myers Squibb Pharmaceuticals Ltd . Dasatinib (Sprycel) for the Treatment of Adults With Chronic, Accelerated or Blast Phase CML With Resistance or Intolerance to Prior Therapy Including Imatinib 2009.
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34.
- National Cancer Institute’s Common Toxicity Criteria v3.0 2006. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm (accessed December 2008).
- Quintas-Cardama A, Kantarjian HM, Nicaise C, Garcia-Manero G, O’Brien S, Ravandi F, et al. Cytopenias in patients (pts) with chronic myelogenous leukemia (CML) in chronic phase (CP) treated with dasatinib (SPRYCEL (R)): clinical features and management, including outcome after hematopoietic growth factor therapy. Blood 2006;108.
- Aribi A, Kantarjian H, Koller C, Thomas D, Faderl S, Garcia-Manero G, et al. The Effect of interleukin 11 on thrombopenia associated with tyrosine kinase inhibitor therapy in patients with chronic myeloid leukemia. Cancer 2008;113:1338-43.
- Bergeron A, Rea D, Levy V, Picard C, Meignin V, Tamburini J, et al. Lung abnormalities after dasatinib treatment for chronic myeloid leukemia: a case series. Am J Respir Crit Care Med 2007;176:814-18.
- Quintas-Cardama A, Kantarjian H, O’Brien S, Borthakur G, Bruzzi J, Munden R, et al. Pleural effusion in patients with chronic myelogenous leukemia treated with dasatinib after imatinib failure. J Clin Oncol 2007;25:3908-14.
- Quintas-Cardama A, Kantarjian HM, Munden R, Talpaz M, Bruzzi J, O’Brien S, et al. Pleural effusion in patients (pts) with chronic myelogenous leukemia (CML) treated with dasatinib after imatinib failure. Blood 2006;108.
- de Lavallade H, Punnialingam S, Milojkovic D, Bua M, Khorashad JS, Gabriel IH, et al. Pleural effusions in patients with chronic myeloid leukaemia treated with dasatinib may have an immune-mediated pathogenesis. Br J Haematol 2008;141:745-7.
- Punnialingam S, De Lavallade H, Milojkovic D, Marco B, Khorashad JS, Goldman JM, et al. Pleural effusions associated with use of dasatinib in chronic myeloid leukemia may have an auto-immune pathogenesis. Blood 2007;110.
- Rousselot PH, Bergeron A, Rea D, Levy V, Picard C, Meignin V, et al. Pleural and pulmonary events in patients treated with dasatinib for chronic myeloid leukemia in chronic phase. Haematologica 2007;92.
- Quintas-Cardama A, Kantarjian H, Ravandi F, O’Brien S, Thomas D, Vidal-Senmache G, et al. Bleeding diathesis in patients with chronic myelogenous leukemia receiving dasatinib therapy. Cancer 2009;115:2482-90.
- Quintas-Cardama A, Kantarjian H, Ravandi F, Burger J, Borthakur G, Cortes J. Bleeding diathesis in patients (pts) with chronic myelogenous leukemia receiving dasatinib therapy. Blood 2007;110.
- Holstein SA, Stokes JB, Hohl RJ. Renal failure and recovery associated with second-generation Bcr-Abl kinase inhibitors in imatinib-resistant chronic myelogenous leukemia. Leuk Res 2009;33:344-7.
- Garcia-Munoz R, Galar A, Moreno C, Rodriguez-Otero P, Panizo-Morgado E, Ponz-Sarvise M, et al. Parvovirus B19 acute infection and a reactivation of cytomegalovirus and herpesvirus 6 in a chronic myeloid leukemia patient during treatment with dasatinib (BMS-354825). Leuk Lymphoma 2007;48:2461-4.
- Radaelli F, Bramanti S, Fantini N, Fabio G, Greco I, Lambertenghi-Deliliers G. Dasatinib-related alveolar pneumonia responsive to corticosteroids. Leuk Lymphoma 2006;47:1180-1.
- Rea D, Bergeron A, Fieschi C, Bengoufa D, Oksenhendler E, Dombret H. Dasatinib-induced lupus. Lancet 2008;372:713-14.
- Assouline S, Laneuville P, Gambacorti-Passerini C. Panniculitis during dasatinib therapy for imatinib-resistant chronic myelogenous leukemia. N Engl J Med 2006;354:2623-4.
- Bonvin A, Mesnil A, Nicolini FE, Cotte L, Michallet M, Descotes J, et al. Dasatinib-induced acute hepatitis. Leuk Lymphoma 2008;49:1630-2.
- Caocci G, Atzeni S, Orru N, Azzena L, Martorana L, Littera R, et al. Gynecomastia in a male after dasatinib treatment for chronic myeloid leukemia. Leukemia 2008;22:2127-8.
- Leiba M, Shimoni A, Guilhot F, Martineau G, Renaud M, Francois S, et al. No evidence for increased transplant related complications in Ph plus chronic myelogenous leukemia and acute lymphoblastic leukemia with prior treatment with Dasatinib. Blood 2006;108.
- Novartis Pharmaceuticals UK Ltd . Nilotinib for the Treatment of Adults With Chronic Myeloid Leukaemia in the Chronic Phase or Accelerated Phase With Resistance or Intolerance As Well As Resistance to Prior Therapy, Including Imatinib 2009.
- Food and Drug Administration . Tasigna® (nilotinib) Capsules n.d. www.accessdata.fda.gov/drugsatfda_docs/label/2007/022068lbl.pdf (accessed 15 December 2009).
- Breccia M, Muscaritoli M, Gentilini F, Latagliata R, Carmosino I, Fanelli FR, et al. Impaired fasting glucose level as metabolic side effect of nilotinib in non-diabetic chronic myeloid leukemia patients resistant to imatinib. Leuk Res 2007;31:1770-2.
- Kaune KM, Baumgart M, Gesk S, Mitteldorf C, Baesecke J, Glass B, et al. Bullous sweet syndrome in a patient with t(9;22)(q34;q11)-positive chronic myeloid leukemia treated with the tyrosine kinase inhibitor nilotinib: interphase cytogenetic detection of BCR–ABL-positive lesional cells. Arch Dermatol 2008;144:361-4.
- Sambrook JC, Zou D, Taylor MJ, Davis CC, Joyeux A, Levy AR. Cost-effectiveness analysis in Canada of dasatinib versus imatinib for the treatment of chronic myelogenous leukemia in patients with imatinib resistance. Blood 2007;110.
- Logman JFS, Taylor MJ, Neumann K, Kutikova L, Cerri KH, Van Houc BA, et al. Cost–utility analysis of dasatinib in patients after first-line failure of imatinib in chronic myeloid leukemia (CML) in Austria. Value Health 2007;10.
- Juarez-Garcia A, Zapata L, Vega G, Idrovo J, Rivas R, Kramis JL, et al. The cost and cost effectiveness of dasatinib (Sprycel) therapy for the management of imatinib resistant and intolerant patients with chronic myeloid leukemia (CML) in Mexico. Value Health 2008;11.
- Brosa M, Taylor MJ, Staginnus U, Meno Duran A, Cerri KH, Cervantes F. Cost-effectiveness of dasatinib vs imatinib 800 mg qd in patients with imatinib-resistant chronic myeloid leukemia in Spain. Value Health 2007;10.
- Quissak C, Litalien G, Alves MR. Cost-effectiveness analysis of dasatinib for the treatment of imatinib resistant or intolerant CML patients in Brazil. Value Health 2008;11.
- Jewitt K, Pilgrim H, Ward S. A cost–utility analysis of nilotinib for CML patients who have become resistant to imatinib. Br J Haematol 2008;141.
- Pilgrim H, Jewitt K, Ward S. A cost–utility analysis of nilotinib for CML patients who have become resistant to imatinib. Blood 2007;110.
- Mataveli FD, Feng W, Calabro A, Mendes W, Hungria VS. The treatment cost to achieve a complete cytogenetic response in imatinib resistant chronic phase (CP) chronic myelogenous leukemia (CML) patients: nilotinib vs. dasatinib. Blood 2007;110.
- Botteman M, Stephens J, Carpiuc K, Feng W. Projecting the long-term quality-adjusted. survival of patients with imatinib-resistant chronic myelogenous leukemia in chronic phase receiving nilotinib, dasatinib dose escalation imatinib, or palliative care: an essential element for cost-effectiveness analysis. Blood 2007;110.
- Scottish Medicines Consortium . Nilotinib, 200 Mg Capsules (Tasigna) 2008. www.scottishmedicines.org.uk/files/nilotinib_200mg_capsules_Tasigna_FINAL_Feb_2008_amended_May_2008_for_Website.pdf (accessed December 2008).
- Scottish Medicines Consortium . Dasatinib, 20 Mg, 50 Mg, 70 Mg Tablets (Sprycel) 2007. www.scottishmedicines.org.uk/files/dasatanib__Sprycel__CML_FINAL_April_2007__amended_010507__for_website.pdf (accessed December 2008).
- National Institute for Health and Clinical Excellence . Guide to the Methods of Technology Appraisal 2004.
- Philips Z, Bojke L, Sculpher M, Claxton K, Golder S. Good practice guideliens for decision analytic modelling in health technology assessment: a review and consolidation of quality assessment. Pharmacoeconomics 2006;24:355-71.
- National Institute for Health and Clinical Excellence . Guide to the Methods of Technology Appraisal 2008.
- Kantarjian H, O’Brien S, Talpaz M, Borthakur G, Ravandi F, Faderl S, et al. Outcome of patients with philadelphia chromosome-positive chronic myelogenous leukemia post-imatinib mesylate failure. Cancer 2007;109:1556-60.
- Zonder JA, Pemberton P, Brandt H, Mohamed AN, Schiffer CA. The effect of dose increase of imatinib mesylate in patients with chronic or accelerated phase chronic myelogenous leukemia with inadequate hematologic or cytogenetic response to initial treatment. Clin Cancer Res 2003;9:2092-7.
- Reed SD, Anstrom KJ, Ludmer JA, Glendenning GA, Schulman KA. Cost-effectiveness of imatinib versus interferon-alpha plus low-dose cytarabine for patients with newly diagnosed chronic-phase chronic myeloid leukemia. Cancer 2004;101:2574-83.
- Dalziel K, Round A, Garside R, Stein K. Cost effectiveness of imatinib compared with interferon-alpha or hydroxycarbamide for first-line treatment of chronic myeloid leukaemia. Pharmacoeconomics 2005;23:515-26.
- Curtis L. Unit Costs of Health and Social Care 2007. www.pssru.ac.uk/pdf/uc/uc2007/uc2007.pdf (accessed December 2008).
- MIMS 2009. www.mims.co.uk (accessed December 2008).
- Levy A. Utility Values for Health States for Chronic Myelogenous Leukemia from Laypersons in the United States, Australia, United Kingdom and Canada 2008.
- Levy A, Szaba SM, Taberrer M, Davis C. Utility values for health states for chronic myelogenous leukaemia (CML): estimates from laypersons in Australia, the United Kingdom (UK) and Canada. Dublin: ISPOR; 2007.
- McLeod C, Bagust A, Boland A, Hockenhull J, Dundar Y, Proudlove C, et al. Erlotinib for the treatment of relapsed non-small cell lung cancer. Health Technol Assess 2009;13:41-7.
- Government Actuary’s Department . Life Tables n.d. www.gad.govsuk/Demography%20Data/Life%20Tables/index.html (accessed 2 February 2009).
- Warren E, Ward S, Gordois A, Scuffham P. Cost-utility analysis of imatinib mesylate for the treatment of chronic myelogenous leukemia in the chronic phase. Clin Ther 2004;26:1924-33.
- Kattan MW, Inoue Y, Giles FJ, Talpaz M, Ozer H, Guilhot F, et al. Cost-effectiveness of interferon-alpha and conventional chemotherapy in chronic myelogenous leukemia. Ann Intern Med 1996;125:541-8.
- Reed SD, Anstrom KJ, Li Y, Schulman KA. Updated estimates of survival and cost effectiveness for imatinib versus interferon-alpha plus low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukaemia. Pharmacoeconomics 2008;26:435-46.
- Kantarjian HM, Talpaz M, O’Brien S, Jones D, Giles F, Garcia-Manero G, et al. Survival benefit with imatinib mesylate versus interferon-alpha-based regimens in newly diagnosed chronic-phase chronic myelogenous leukemia. Blood 2006;108:1835-40.
- Kantarjian HM, Cortes JE, O’Brien S, Luthra R, Giles F, Verstovsek S, et al. Long-term survival benefit and improved complete cytogenetic and molecular response rates with imatinib mesylate in Philadelphia chromosome-positive chronic-phase chronic myeloid leukemia after failure of interferon-alpha. Blood 2004;104:1979-88.
- Roy L, Guilhot J, Krahnke T, Guerci-Bresler A, Druker BJ, Larson RA, et al. Survival advantage from imatinib compared with the combination interferon-alpha plus cytarabine in chronic-phase chronic myelogenous leukemia: historical comparison between two phase 3 studies. Blood 2006;108:1478-84.
- Parmar MKB, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 1998;17:2815-34.
- Tierney J, Stewart L, Ghersi D, Burdett S, Sydes M. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007;8.
- Garside R, Round A, Dalziel K, Stein K, Royle P. The effectiveness and cost-effectiveness of imatinib in chronic myeloid leukaemia: a systematic review. Health Technol Assess 2002;6.
- Kantarjian H, Cortes J. BCR–ABL tyrosine kinase inhibitors in chronic myeloid leukemia: using guidelines to make rational treatment choices. J Natl Compr Canc Netw 2008;6:S43-S44.
- Cervantes F, Lopez-Guillermo A, Bosch F, Terol MJ, Rozman C, Montserrat E. An assessment of the clinicohematological criteria for the accelerated phase of chronic myeloid leukemia. Eur J Haematol 1996;57:286-91.
- Gordois A, Scuffham P, Warren E, Ward S. Cost-utility analysis of imatinib mesilate for the treatment of advanced stage chronic myeloid leukaemia. Br J Cancer 2003;89:634-40.
- Liberato NL, Quaglini S, Barosi G. Cost-effectiveness of interferon alfa in chronic myelogenous leukemia. J Clin Oncol 1997;15:2673-82.
- British Medical Association and Royal Pharmaceutical Society of Great Britain . British National Formulary 2009.
- Department of Health 2007. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4127649 (accessed December 2009).
- Department of Health . NHS Reference Costs 2006 07 2008.
- Kantarjian HM, Shan J, Smith T, Talpaz M, Kozuch P, Rios MB, et al. Response to therapy is independently associated with survival prolongation in chronic myelogenous leukemia in blastic phase. Cancer 2001;92:2501-7.
- Collett D. Modelling survival data in medical research. Boca Raton, FL: Chapman & Hall/CRC; 2003.
- Kantarjian H, O’Brien S, Cortes J, Giles F, Shan J, Rios MB, et al. Survival advantage with imatinib mesylate therapy in chronic-phase chronic myelogenous leukemia (CML-CP) after IFN-{alpha} failure and in late CML-CP, comparison with historical controls. Clin Cancer Res 2004;10:68-75.
- Sawyers CL, Hochhaus A, Feldman E, Goldman JM, Miller CB, Ottmann OG, et al. Imatinib induces hematologic and cytogenetic responses in patients with chronic myelogenous leukemia in myeloid blast crisis: results of a phase II study. Blood 2002;99:3530-9.
- Piazza RG, Magistroni V, Franceschino A, Andreoni F, Tornaghi L, Colnaghi F, et al. The achievement of durable complete cytogenetic remission in late chronic and accelerated phase patients with CML treated with Imatinib mesylate predicts for prolonged response at 6 years. Blood Cells Mol Dis 2009;37:111-15.
- Palandri F, Iacobucci I, Martinelli G, Amabile M, Poerio A, Testoni N, et al. Long-term outcome of complete cytogenetic responders after imatinib 400 mg in late chronic phase, philadelphia-positive chronic myeloid leukemia: the GIMEMA Working Party on CML. J Clin Oncol 2008;26:106-11.
- Iacobucci I, Rosti G, Amabile M, Poerio A, Soverini S, Cilloni D, et al. Comparison between patients with philadelphia-positive chronic phase chronic myeloid leukemia who obtained a complete cytogenetic response within 1 year of imatinib therapy and those who achieved such a response after 12 months of treatment. J Clin Oncol 2006;24:454-59.
- Guilhot F, Larson RA, O’Brien SG, Gathmann I, Druker BJ. Time to complete cytogenetic response (CCyR) does not affect long-term outcomes for patients on imatinib therapy. Blood 2007;110.
- Cortes J, Talpaz M, O’Brien S, Jones D, Luthra R, Shan J, et al. Molecular responses in patients with chronic myelogenous leukemia in chronic phase treated with imatinib mesylate. Clin Cancer Res 2005;11:3425-32.
- Iacobucci I, Saglio G, Rosti G, Testoni N, Pane F, Amabile M, et al. Achieving a major molecular response at the time of a complete cytogenetic response (CCgR) predicts a better duration of CCgR in imatinib-treated chronic myeloid leukemia patients. Clin Cancer Res 2006;12:3037-42.
- Marin D, Milojkovic D, Olavarria E, Khorashad JS, de Lavallade H, Reid AG, et al. European LeukemiaNet criteria for failure or suboptimal response reliably identify patients with CML in early chronic phase treated with imatinib whose eventual outcome is poor. Blood 2008;112:4437-44.
- Kantarjian H, O’Brien S, Shan J, Huang X, Garcia-Manero G, Faderl S, et al. Cytogenetic and molecular responses and outcome in chronic myelogenous leukemia. Cancer 2008;112:837-45.
- Press RD, Love Z, Tronnes AA, Yang R, Tran T, Mongoue-Tchokote S, et al. BCR–ABL mRNA levels at and after the time of a complete cytogenetic response (CCR) predict the duration of CCR in imatinib mesylate-treated patients with CML. Blood 2006;107:4250-6.
- de Lavallade H, Apperley JF, Khorashad JS, Milojkovic D, Reid AG, Bua M, et al. Imatinib for newly diagnosed patients with chronic myeloid leukemia: incidence of sustained responses in an intention-to-treat analysis. J Clin Oncol 2008;26:3358-63.
- Marin D, Goldman JM, Olavarria E, Apperley JF, Cortes J, Kantarjian H. Transient benefit only from increasing the imatinib dose in CML patients who do not achieve complete cytogenetic remissions on conventional doses. Blood 2003;102:2702-3.
- Kantarjian HM, Cortes J, O’Brien S, Giles FJ, Albitar M, Rios MB, et al. Imatinib mesylate (STI571) therapy for philadelphia chromosome-positive chronic myelogenous leukemia in blast phase. Blood 2002;99:3547-53.
- Kantarjian HM, Smith T, O’Brien S, Beran M, Pierce S, Talpaz M, et al. Prolonged survival in chronic myelogenous leukemia after cytogenetic response to interferon-α. Ann Intern Med 1995;122:254-61.
- Steegman JL, Odriozola J, Rodriguez-Salvanes F, Giraldo P, Garcia-Larana J, Ferro MT, et al. Stage, percentage of basophils at diagnosis, hematologic response within six months, cytogenetic response in the first year: the main prognostic variables affecting outcome in patients with chronic myeloid leukemia in chronic phase treated with interferon-alpha. Results of the CML89 study of the Spanish Collaborative Group on interferon-alpha2a and CML. Haematologica 1999;84:978-87.
- Bonifazi F, de Vivo A, Rosti G, Guilhot F, Trabacchi E, Hehlmann R, et al. Chronic myeloid leukemia and interferon-alpha: a study of complete cytogenetic responders. Blood 2001;98:3074-81.
- Hehlmann R, Hochhaus A, Berger U, Reiter A. Current trends in the management of chronic myelogenous leukemia. Ann Hematol 2000;79:345-54.
- Guilhot F, Chastang C, Michallet M, Guerci A, Harousseau JL, Maloisel F, et al. Interferon alfa-2b combined with cytarabine versus interferon alone in chronic myelogenous leukemia. French Chronic Myeloid Leukemia Study Group. N Engl J Med 1997;337:223-9.
- Mahon F-X, Delbrel X, Cony-Makhoul P, Faberes C, Boiron JM, Barthe C, et al. Follow-up of complete cytogenetic remission in patients with chronic myeloid leukemia after cessation of interferon alfa. J Clin Oncol 2002;20:214-20.
- Schrover RJ, Adena MA, Lourenco RD, Prince HM, Seymour JF, Wonder MJ. Development of a predictive population survival model according to the cytogenetic response rate for patients with chronic myeloid leukemia in the chronic phase. Leuk Lymphoma 2006;47:1069-81.
- Taylor RS, Elston J. The use of surrogate outcomes in model-based cost-effectiveness analyses: a survey of UK Health Technology Assessment reports. Health Technol Assess 2009;13.
- Quintas-Cardama A, Kantarijan H, Jones D, Shan J, Borthakur G, Thomas D, et al. Delayed achievement of cytogenetic and molecular response is associated with increased risk of progression among patients with chronic myeloid leukemia in early chronic phase receiving high-dose or standard-dose imatinib therapy. Blood 2009;113:6315-21.
- Anstrom KJ, Reed SD, Allen AS, Glendenning GA, Schulman KA. Long-term survival estimates for imatinib versus interferon-alpha plus low-dose cytarabine for patients with newly diagnosed chronic-phase chronic myeloid leukemia. Cancer 2004;101:2584-92.
Appendix 1 Review protocol
Technology Assessment Report commissioned by the NIHR HTA programme on behalf of NICE
Final protocol
19 January 2009
Project title: Dasatinib and nilotinib for imatinib-resistant or -intolerant chronic myeloid leukaemia
Plain English summary
Chronic myeloid leukaemia is a type of leukaemia in which granulocytes (a type of WBC) start growing out of control. It is a progressive disease that evolves through three phases. Most (85%) people find out that they have the disease when it is in the CP, which lasts between 4 and 6 years. The disease then progresses into an AP before entering a terminal BC. Only a small number of people (about 35%) diagnosed with CML survive for more than 5 years after diagnosis.
Chronic myeloid leukaemia is a rare disease. In England and Wales, around 600 people are diagnosed with CML each year.
The usual treatment for CML in the UK is a drug called imatinib. Imatinib works to block the effects of an enzyme produced in CML and slow down the uncontrolled growth of WBCs. However, doctors believe that between 10% and 40% of people with CML become resistant to the effects of imatinib, which means that the treatment does not work as well. Some people also develop side-effects which force them to stop taking imatinib. In both cases, other therapies are needed to control the disease.
This assessment will review the clinical effectiveness and cost-effectiveness of two new drugs for treating ImR CML; dasatinib (also known as Sprycel®) and nilotinib (also known as Tasigna®). Both these drugs work in a similar way to imatinib.
The assessment will systematically draw together all the relevant evidence about these drugs compared with current standard treatments for CML after imatinib has stopped working. It will focus on differences in response to treatment, time to and duration of response, PFS and OS, side effects of treatment and HRQoL. The assessment will also consider whether the treatments are likely to be considered good value for money for the NHS.
Decision problem
Purpose
The purpose of this technology assessment is to appraise the clinical effectiveness and cost-effectiveness of dasatinib and nilotinib in the treatment of people with ImR CI.
The interventions
Dasatinib (Sprycel®, BMS) and nilotinib (Tasigna®, Novartis) are oral TKIs which inhibit several kinases including BCR–ABL kinase. BCR–ABL kinase is an enzyme produced by leukaemia cells in CML which makes them multiply uncontrollably and, by inhibiting its action, dasatinib and nilotinib may reduce this uncontrolled growth.
For CP CML the recommended starting dose of dasatinib is 100 mg once a day. For AP or BC CML the recommended dose of dasatinib is 70 mg twice a day. The dose of dasatinib may be increased or decreased depending on the patient’s response to the treatment. Nilotinib is administered at a recommended starting dose of 400 mg twice daily for CP and AP. The dose of nilotinib may be reduced or treatment interrupted if significant side effects occur.
The place of dasatinib and nilotinib in the management of imatinib-resistant chronic myeloid leukaemia
Dasatinib has a marketing authorisation for the treatment of adults with CP, AP or BC CML with resistance or intolerance to prior therapy including imatinib mesylate.
Nilotinib has a marketing authorisation for the treatment of adults with CP and AP, Ph+ CML with resistance or intolerance to prior therapy including imatinib.
Population
For the assessment of dasatinib, the population will be adults with CP, AP or BC CML, resistant to or intolerant of prior therapy including imatinib.
For the assessment of nilotinib, the population will be adults with CP or AP, Ph+ CML, resistant to or intolerant of prior therapy including imatinib.
Comparators
The current treatment options for ImR CML depend on the phase of the disease (i.e. CP, AP and BC) and include HDI, hydroxycarbamide, IFN, acute leukaemia chemotherapy and best supportive care.
Where evidence allows, and for each phase of the disease, the Technology Assessment Report (TAR) team will endeavour to make comparisons between the interventions and current standard therapy in line with marketing authorisations. However, preliminary scoping has highlighted a paucity of published data in which the new interventions are directly compared with any other therapy.
Where randomised head-to-head comparison data are not available, the TAR team will investigate the validity of performing indirect comparisons between the interventions and appropriate comparators using suitable methodology. If evidence allows, a comparison of the clinical effectiveness and cost-effectiveness of dasatinib and nilotinib will also be considered.
All comparisons (direct and indirect) are contingent on the availability of good-quality data.
Outcomes to be examined
If possible, outcome measures will include:
-
treatment response rates (including molecular response, CyR and HRs)
-
time to response
-
duration of response
-
PFS
-
OS
-
adverse effects of treatment
-
HRQoL.
Subgroups to be examined
Depending on the availability and quality of data the following subgroups may be considered:
-
people who are ImI
-
people who are ImR
-
people with Ph– (Philadelphia negative cell) CML who may respond to TKIs (for dasatinib only).
Methods of synthesis of evidence of clinical effectiveness
The assessment report will include a systematic review of the evidence for clinical effectiveness of dasatinib and nilotinib in the treatment of ImR CI. The review will be undertaken following the general principles published by the NHS CRD. 1
Search strategy
Refer to Appendix 1 for details of the sources to be searched and the draft search strategy for MEDLINE.
The search strategy will comprise the following main elements:
-
searching of electronic databases, including MEDLINE, PREMEDLINE In-Process & Other Non-Indexed Citations and EMBASE
-
scrutiny of bibliographies of included studies
-
contact with experts in the field
-
searching of major conference proceedings, e.g. ASCO, ASH and European Hematology Association (EHA)
-
current research will be identified through searching the Current Controlled Trials Register and the Medical Research Council (MRC) Clinical Trials Register.
In addition, any industry submissions to NICE, as well as any relevant systematic reviews identified by the search strategy, will be scrutinised in order to identify additional relevant studies.
Study selection criteria and procedures
Types of study to be included
Systematic reviews of RCTs and single RCTs will be included. These study design criteria may be relaxed to include other controlled and uncontrolled study designs depending on the availability of more methodologically robust evidence.
Studies will only be included if they are of dasatinib or nilotinib in the treatment of ImR CI, have used relevant comparators (see Comparators) and report relevant outcomes (see Outcomes to be examined).
Types of study to be excluded
-
Non-RCTs (unless there are insufficient RCTs).
-
Uncontrolled studies (unless there are insufficient RCTs or controlled studies).
-
Animal models.
-
Pre-clinical and biological studies.
-
Narrative reviews, editorials and opinions.
-
Reports published as meeting abstracts only, where insufficient methodological details are reported to allow critical appraisal of study quality.
-
Studies not available in the English language.
Study selection
The abstracts and titles of references retrieved by the electronic searches will be screened for relevance. Full paper copies of potentially relevant studies will be obtained. The retrieved articles will be assessed for inclusion by one reviewer and independently checked by a second, using the pre-specified inclusion/exclusion criteria. Discrepancies will be resolved by discussion, with involvement of a third reviewer, where necessary. All duplicate papers will be double checked and excluded.
Quality assessment strategy
The quality of individual studies will be assessed by one reviewer and checked by a second reviewer. Any disagreement will be resolved by consensus and if necessary a third reviewer will arbitrate.
The quality of the clinical effectiveness studies will be assessed according to criteria suggested by NHS CRD Report No. 4, according to study type. 1
Data extraction strategy
Data will be extracted from included studies by one reviewer into a bespoke database and checked by another reviewer. Discrepancies will be resolved by discussion, with the involvement of a third reviewer if necessary.
Methods of analysis/synthesis
Data will be tabulated and discussed in a narrative review. Where appropriate, meta-analysis will be employed to estimate summary measures of effect on relevant outcomes, based on ITT analyses.
If meta-analysis is conducted it will be carried out using fixed- and random-effects models, using bespoke software and Stata. Heterogeneity will be explored through consideration of the study populations, methods and interventions, by visualisation of results and, in statistical terms, by the chi-squared test for homogeneity and I2 statistic and, where appropriate, using meta-regression. Small-study effects (including publication bias) will be visually assessed using funnel plots and quantified using Egger’s statistic.
Where randomised head-to-head comparison data are not available, the TAR team will investigate the validity of performing indirect comparisons between the interventions using appropriate methodology. All comparisons (direct and indirect) are contingent on the availability of good-quality data.
All selected articles will be scanned for short- and long-term adverse effects of treatment. Data will be extracted from the included studies and presented as a narrative discussion.
Technology Assessment Report team economic evaluation
The TAR team will endeavour to perform an independent economic evaluation from the perspective of the UK NHS and Personal Social Services (PSS), consistent with the methods recommended in the NICE reference case. 2 Any deviation from the NICE reference case will be identified and discussed as appropriate.
Systematic review of cost-effectiveness studies
A systematic review of economic evaluations of dasatinib and nilotinib in the treatment of ImR CML will be undertaken. Full economic evaluations will be included where they meet the inclusion criteria set out for the review of clinical effectiveness (see Study selection criteria and procedures). [Note: CRD NHS Economic Evaluation Database handbook3 defines full economic evaluations as studies in which a comparison of two or more alternatives is undertaken and costs and outcomes are examined for each alternative. They are classified as cost-benefit analysis, cost-utility analysis or cost-effectiveness analysis (including cost-consequences analysis).] The sources to be searched will be similar to those in the clinical effectiveness review (see Search strategy). Searches will be limited to English-language sources.
Economic evaluations identified in the search will be critically assessed using accepted frameworks, such as the consensus-developed list of criteria developed by Evers et al. 4 and Drummond et al. 5,6 For included economic evaluations based on decision models, critical appraisal of these studies will make use of guidelines for good practice in decision-analytic modelling in HTA. 7
Methods and findings from included economic evaluations will be summarised in a tabular format and synthesised in a narrative review. Economic evaluations carried out from the perspective of the UK NHS and PSS perspective will be presented in greater detail.
Systematic literature search for other data related to cost-effectiveness
A search of the broader literature on ImR CML will be undertaken to identify the evidence base on HRQoL (i.e. health state values), resource use and costs for treatment and side effects, and the methods available for the modelling of CML to inform cost-effectiveness analyses. The search strategies employed will be reported, and findings from these explorative searches will be presented in summary format, using a tabular approach and narrative text.
These searches, and any additional searches to identify data to inform the TAR team cost-effectiveness analyses (e.g. to populate a decision model), will be based on the methodological discussion paper ‘Methods for establishing parameter values for decision analytic models’ commissioned by the UK Department of Health and produced by InterTASC (January 2005).
Economic modelling
Our preliminary scoping of the topic suggests that there is very little comparative data available in the literature for either intervention. If no further data is located during the assessment, the extent to which de novo economic modelling to inform an independent cost-effectiveness analysis can be performed is unclear.
However, if data allows, an economic model will be constructed either by adapting an existing model or developing a new model using available evidence, and following guidance on good practice in decision-analytic modelling for HTA. 7
The structure of any model will be determined on the basis of research evidence and clinical expert advice about:
-
the natural history of ImR CML
-
the main treatment pathways in a UK NHS context
-
the disease states and/or events that are most relevant in determining the clinical outcome of patients, HRQoL, and resource use and costs.
All assumptions applied in the modelling framework will be clearly stated. All data inputs and their source will be clearly identified.
Where appropriate and if data allows, sensitivity analyses will be undertaken to explore uncertainty. These may include one-way and multiway sensitivity analyses, and use of probabilistic sensitivity analyses where modelling permits. The use of probabilistic sensitivity analysis involves sampling of parameter inputs from distributions that characterise uncertainty in the mean estimate of the parameter. Probabilistic sensitivity analysis is used to characterise uncertainty in a range of parameter inputs simultaneously, to consider the combined implications of uncertainty in parameters.
Where probabilistic modelling is undertaken, results will be presented using the cost-effectiveness plane and CEACs.
Handling the company submissions
All data submitted by the manufacturers/sponsors will be considered if received by the TAR team no later than 7 May 2009. Data arriving after this date will not be considered.
If the data meet the inclusion criteria for the review they will be extracted and quality assessed in accordance with the procedures outlined in this protocol. Any economic evaluations included in the company submission will be assessed against NICE’s guidance on the methods of technology appraisal2 and will also be assessed for clinical validity, reasonableness of assumptions and appropriateness of the data used. Where the TAR team have undertaken further analyses, using models submitted by manufacturers/sponsors or via de novo modelling and cost-effectiveness analysis, a comparison will be made of the alternative models used for the analysis.
Any ‘commercial in confidence’ data taken from a company submission will be underlined and highlighted in the assessment.
Additional considerations
We will collate the available relevant material necessary to inform an assessment of the applicability of the end-of-life criteria.
If the evidence allows, the cost and impact of analysis for mutations known to be resistant to imatinib and second-generation TKIs will be considered.
The TAR team cannot guarantee to consider any data or information relating to the technologies if received after 7 May 2009.
Competing interests of authors
None.
References
- NHS Centre for Reviews and Dissemination . Undertaking Systematic Reviews of Research on Effectiveness 2001.
- National Institute for Clinical Excellence . Guide to the Methods of Technology Appraisal 2008.
- NHS Centre for Reviews and Dissemination . NHS Economic Evaluation Database Handbook 2007.
- Evers S, Goossens M, de Vet H, van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care 2005;21:240-54.
- Drummond MF. Guidelines for authors and peer reviewers of economic submissions to the BMJ. BMJ 1996;313:275-83.
- Drummond MF, Sculpher M, Torrance GW, O’Brien B, Stoddart GL. Methods for the economic evaluation of health care programmes. New York, NY: Oxford University Press; 2005.
- Philips Z, Ginnelly L, Sculpher M, Claxton K, Golder S, Riemsma R, et al. Review of guidelines for good practice in decision-analytic modelling in health technology assessment. Health Technol Assess 2004;8.
Sample search strategy
MEDLINE
Interface: Ovid Web
-
myeloid$leuk?emia$.mp.
-
myelogenous$leuk?emia$.mp.
-
myelocytic$leuk?emia$.mp.
-
exp leukemia, myelogenous, chronic, bcr-abl positive/or leukemia, myeloid, chronic-phase/or exp leukemia, myeloid, chronic, atypical, bcr-abl negative/or exp leukemia, myelomonocytic, chronic/
-
Leukemia, Myeloid/
-
5
-
limit 6 to yr=“1974 – 1988”
-
3 or 2 or 4 or 7 or 1
-
nilotinib.mp.
-
tasigna.mp.
-
((amn107 or amn-107 or amn) adj “107”).mp.
-
11 or 10 or 9
-
dasatinib.mp.
-
sprycel.mp.
-
(BMS354825 or BMS 354825 or BMS-354825).mp.
-
13 or 14 or 15
-
8 and 12
-
8 and 16
-
18 or 17
-
(animals not human).sh.
-
19 not 20
-
limit 21 to english language
-
Randomized controlled study.pt.
-
randomized controlled study/
-
(random$or placebo$).ti,ab,sh.
-
((singl$or double$or triple$or treble$) and (blind$or mask$)).tw,sh.
-
or/1-4
-
“controlled clinical study”.pt.
-
(retraction of publication or retracted publication).pt.
-
6 or 7 or 5
-
22 AND 30
Appendix 2 Search strategies
In January 2009, searches were initially carried out to find papers that included the desired population of CML and looked at the interventions, dasatinib and nilotinib, without restriction for study design. These searches were then rerun on 8 June 2009. An additional set of searches were carried out in April 2009 to look for utility information for the desired intervention (CML). All database searches were run from their inception until the search date, and a human and English-language filter applied where possible.
Individual conference proceedings from 2008 and 2009 (ASCO and ASH) were searched using their online interface. Ongoing studies were searched for on ClinicalTrials.gov (www.clinicalstudies.gov) and on the Current Controlled studies [Meta Register of Controlled studies (mRCT) database (www.controlled-studies.com/)].
Numbers in brackets denote number of database hits.
Ovid MEDLINE(R) 1950 to week 3 November 2008
Search date: 8 January 2009
-
myeloid$leuk?emia$.mp. (22,684)
-
myelogenous$leuk?emia$.mp. (11,189)
-
myelocytic$leuk?emia$.mp. (2344)
-
exp leukemia, myelogenous, chronic, bcr-abl positive/or leukemia, myeloid, chronic-phase/or exp leukemia, myeloid, chronic, atypical, bcr-abl negative/or exp leukemia, myelomonocytic, chronic/ (12,440)
-
Leukemia, Myeloid/ (21,451)
-
5 (21,451)
-
limit 6 to yr = “1974 - 1988” (7523)
-
Philadelphia Chromosome/ (1797)
-
(Philadelphia adj Chromosome).mp. (3699)
-
3 or 2 or 4 or 7 or 1 or 8 or 9 (44,230)
-
nilotinib.mp. (141)
-
“4-methyl-N-(3-(4-methylimidazol-1-yl)-5-(trifluoromethyl)phenyl)-3-((4-pyridin-3-ylpyrimidin-2-yl)amino)benzamide”.mp. [mp = title, original title, abstract, name of substance word, subject heading word] (122)
-
tasigna.mp. (7)
-
((amn107 or amn-107 or amn) adj “107”).mp. (4)
-
14 or 13 or 11 or 12 (186)
-
dasatinib.mp. (291)
-
sprycel.mp. (15)
-
(BMS354825 or BMS 354825 or BMS-354825).mp. (57)
-
16 or 17 or 18 (298)
-
10 and 15 (137)
-
10 and 19 (226)
-
21 or 20 (272)
-
(animals not human).sh. (4,410,095)
-
22 not 23 (202)
-
limit 24 to english language (187)
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations
Search date: 8 January 2009
-
myeloid$leuk?emia$.mp. (1935)
-
myelogenous leuk?emia$.mp. (566)
-
myelocytic$leuk?emia$.mp. (55)
-
(Philadelphia adj Chromosome).mp. (151)
-
1 or 2 or 3 or 4 (2546)
-
nilotinib.mp. (83)
-
“4-methyl-N-(3-(4-methylimidazol-1-yl)-5-(trifluoromethyl)phenyl)-3-((4-pyridin-3-ylpyrimidin-2-yl)amino)benzamide”.mp. (0)
-
tasigna.mp. (5)
-
((amn107 or amn-107 or amn) adj “107”).mp. (1)
-
6 or 7 or 8 or 9 (83)
-
dasatinib.mp. (139)
-
sprycel.mp. (11)
-
(BMS354825 or BMS 354825 or BMS-354825).mp. (15)
-
11 or 12 or 13 (144)
-
10 or 14 (176)
-
5 and 15 (123)
-
limit 16 to english language (117)
EMBASE 1980 to week 1 2009 (via Ovid interface)
Search date: 8 January 2009
-
myeloid$leuk?emia$.mp. (31,757)
-
myelogenous$leuk?emia$.mp. (9259)
-
myelocytic$leuk?emia$.mp. (1473)
-
chronic myeloid leukemia/or myeloid leukemia/ (19,599)
-
Philadelphia 1 Chromosome/ (3678)
-
1 or 2 or 3 or 4 or 5 (37,643)
-
nilotinib.mp. (629)
-
tasigna.mp. (119)
-
(amn107 or amn-107 or (amn adj “107”)).mp. (301)
-
9 or 8 or 7 (641)
-
dasatinib.mp. (1016)
-
sprycel.mp. (245)
-
(BMS354825 or BMS 354825 or BMS-354825).mp. (357)
-
11 or 12 or 13 (1024)
-
((animal$or nonhumans) not human$).sh,hw. (1,985,421)
-
10 or 14 (1193)
-
6 and 16 (767)
-
17 not 15 (754)
-
limit 18 to english language (671)
Web of Science
Conference Proceedings Citation Index: Science (CPCI-S) 1990–present
Science Citation Index Expanded (SCI-EXPANDED) 1900–present
Via ISI Web of Knowledge online
Search date: 14 January 2009
-
# 9 437 #8 AND Language=(English)
-
Databases=SCI-EXPANDED, CPCI-S Timespan=All Years
-
# 8 448 #7 AND #4
-
Databases=SCI-EXPANDED, CPCI-S Timespan=All Years
-
# 7 733 #6 OR #5
-
Databases=SCI-EXPANDED, CPCI-S Timespan=All Years
-
# 6 548 TS=(dasatinib) OR TS=(sprycel) OR TS=(BMS354825) OR TS=(BMS 354825) OR TS=(BMS-354825)
-
Databases=SCI-EXPANDED, CPCI-S Timespan=All Years
-
# 5 317 TS=(nilotinib) OR TS=(tasigna) OR TS=(amn107) OR TS=(amn-107) OR TS=(amn adj “107”)
-
Databases=SCI-EXPANDED, CPCI-S Timespan=All Years
-
# 4 54,363 #3 OR #2 OR #1
-
Databases=SCI-EXPANDED, CPCI-S Timespan=All Years
-
# 3 2,771 TS=(myelocytic* leukaemia*) OR TS=(myelocytic* leukemia*)
-
Databases=SCI-EXPANDED, CPCI-S Timespan=All Years
-
# 2 43,276 TS=(myeloid* leukaemia*) OR TS=(myeloid* leukemia*)
-
Databases=SCI-EXPANDED, CPCI-S Timespan=All Years
-
# 1 20,888 TS=(myelogenous* leukemia*) or TS=(myelogenous* leukaemia*)
-
Databases=SCI-EXPANDED, CPCI-S Timespan=All Years
DARE, NHS EED, HTA via CRD databases online
Search date: 14 January 2009
-
# 1 myelogenous* AND leukemia* (17)
-
# 2 myelogenous* AND leukaemia* (12)
-
# 3 myeloid* AND leukemia* (38)
-
# 4 myeloid* AND leukaemia* (44)
-
# 5 myelocytic* AND leukemia* (0)
-
# 6 myelocytic* AND leukaemia* (2)
-
# 7 nilotinib (1)
-
# 8 tasigna (0)
-
# 9 amn107 (0)
-
# 10 amn-107 (1)
-
# 11 dasatinib (1)
-
# 12 sprycel (0)
-
# 13 BMS354825 (0)
-
# 14 BMS AND 354825 (1)
-
# 15 BMS-354825 (1)
-
# 16 BMS-354825 (1)
-
# 17 BMS-354825 (1)
-
# 18 #1 or #2 or #3 or #4 or #5 or #6 (83)
-
# 19 #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 (2)
-
# 20 #18 AND #19 (2)
Additional utilities searches
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) 1950–present
Search date: 17 April 2009
-
myeloid$leuk?emia$.mp. (23,694)
-
myelogenous leuk?emia$.mp. (11,464)
-
myelocytic$leuk?emia$.mp. (2341)
-
(Philadelphia adj Chromosome).mp. (3776)
-
1 or 2 or 3 or 4 (37,636)
-
6 nilotinib.mp. (199)
-
“4-methyl-N-(3-(4-methylimidazol-1-yl)-5-(trifluoromethyl)phenyl)-3-((4-pyridin-3-ylpyrimidin-2-yl)amino)benzamide”.mp. (141)
-
tasigna.mp. (8)
-
((amn107 or amn-107 or amn) adj “107”).mp. (6)
-
6 or 7 or 8 or 9 (249)
-
dasatinib.mp. (434)
-
sprycel.mp. (21)
-
(BMS354825 or BMS 354825 or BMS-354825).mp. (71)
-
11 or 12 or 13 (444)
-
10 or 14 (538)
-
5 and 15 (338)
-
(animals not human).sh. (4,356,049)
-
16 not 17 (261)
-
limit 18 to english language (244)
-
“Quality of Life”/ (73,701)
-
“Value of Life”/ (5023)
-
(life adj2 qualit$3).tw. (87,933)
-
quality-adjusted life years/ (3780)
-
(disabilit$3 adj2 life).tw. (1010)
-
daly.tw. (423)
-
Health Status Indicators/ (13,813)
-
(sf36 or sf 36 or short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirstysix or shortform thirty six or short form thirty six or short form thirtysix or short form thirty six).tw. (9296)
-
(sf6 or sf 6 or short form 6 or shortform 6 or sf six or sfsix or shortform six or short form six).tw. (921)
-
(sf12 or sf 12 or short form 12 or shortform 12 or sf twelve of sftwelve or shortform twelve or short form twelve).tw. (1311)
-
(sf16 or sf 16 or short form 16 or shortform 16 or sf sixteen or sfsixteen or shortform sixteen or short form sixteen).tw. (16)
-
(sf20 or sf 20 or short form 20 or shortform 20 or sf twenty of sftwenty or shortform twenty of short form twenty).tw. (284)
-
(euroqol or euro qol or eq5d or eq 5d).tw. (1671)
-
(euroqol or euro qol or eq5d or eq 5d).tw. (1671)
-
(hye or hyes).tw. (48)
-
health$year$equivalent$.tw. (34)
-
health utilit$.ab. (578)
-
hui$1.tw. (738)
-
disutil$.tw. (114)
-
rosser.tw. (65)
-
quality of well being.tw. (236)
-
quality of wellbeing.tw. (2)
-
qwb.tw. (131)
-
willingness to pay.tw. (1180)
-
standard gamble$.tw. (536)
-
(time trade off or time tradeoff).tw. (628)
-
(health adj3 (utilit$3 or value$2 or preference$2)).tw. (4391)
-
(visual analog$3 scale or VAS).tw. (24,685)
-
(health adj2 (utilit$3 or value$2 or preference$2)).tw. (2804)
-
patient preference$2.tw. (2949)
-
or/20-49 (166,395)
-
50 and 5 (249)
-
51 not 17 (243)
-
limit 52 to (english language and yr=“1990 -Current”) (196)
-
from 53 keep 1-196 (196)
-
exp Economics/ (400,716)
-
exp “Costs and Cost Analysis”/ (140,550)
-
exp Cost-benefit Analysis/ (45,031)
-
“Value of Life”/ (5023)
-
exp Models, Economic/ (6398)
-
exp “Fees and Charges”/ (23,936)
-
exp Budgets/ (10,067)
-
(economic$or price$or pricing or financ$or fee$or pharmacoeconomic$or pharma economic$).tw. (407,483)
-
(cost$or costly or costing$or costed).tw. (239,491)
-
(cost$adj2 (benefit$or utilit$or minim$or effective$)).tw. (61,728)
-
(expenditure$not energy).tw. (12,993)
-
(value adj2 (money or monetary)).tw. (788)
-
(economic adj2 burden).tw. (2142)
-
“resource use”.ti,ab. (2726)
-
or/55-68 (884,540)
-
or/1-3 (36,277)
-
69 and 70 (595)
-
71 not 17 (524)
-
limit 72 to english language (479)
NHS EED via CRD databases online
-
# 1 myelogenous* AND leukemia* 17
-
# 2 myelogenous* AND leukaemia* 12
-
# 3 myeloid* AND leukemia* 38
-
# 4 myeloid* AND leukaemia* 44
-
# 5 myelocytic* AND leukemia* 0
-
# 6 myelocytic* AND leukaemia* 2
-
#7 #1 or #2 or #3 or #4 or #5 or #6
EconLit via FirstSearch
The following individual terms were searched within the database:
-
Myeloid leukaemia
-
myeloid leukemia
-
myelogenous leukaemia 0
-
myelogenous leukaemia 0
-
myelocytic leukaemia
-
myelocytic leukemia
Appendix 3 Systematic review of clinical effectiveness: data extraction forms
| Study details | Population | Arms | Outcomes | |||||
|---|---|---|---|---|---|---|---|---|
|
Study: Cortes et al. (2007)38 Design: cohort study (prospective) CP: yes AP: yes BC: yes Country: USA Number of centres: one Notes Eighteen patients (five CP, nine AP and four myeloid BC) received a third TKI; most were in the advanced phase of CML; 15 of them received dasatinib after having failed imatinib and nilotinib |
Inclusion criteria: not clearly reported. Between June 2003 and February 2006, 217 patients with CML who failed therapy with imatinib were treated with second-generation TKIs. Mutational analysis by direct sequencing was performed in all patients after imatinib failure and prior to the start of therapy with the second TKI. Mutational analysis was also performed after treatment with another TKI in 112 patients who had failure to imatinib therapy. These patients with mutation analysis before and after treatment with second TKI constitute the focus of the report Exclusion criteria: not reported |
Arm 1 dasatinib n: 56 Drug: dasatinib Starting daily dose (mg): not reported Dosage details: not reported Concurrent treatment: not clear Arm 2 nilotinib n: 54 Drug: nilotinib Starting daily dose (mg): not reported Dosage details: not reported Concurrent treatment: not clear |
CyR: judged by standard cytogenetic analysis in 20 metaphases on BM aspiration; FISH (dual-fusion probe on PB) was used only when routine cytogenetic analysis was un-analysable (i.e. insufficient metaphases) CCyR (0% Ph+) PCyR [1–35% Ph+ metaphases in BM (calculated by reviewer as MCyR – CCyR)] MCyR [CCyR + PCyR (35% Ph+)] Overall CyR (not defined; assumed to be CCyR + PCyR + Minor CyR) HR: overall HR (not defined) CHR [WBC count < 10 × 109/l, platelet count < 450 × 109/l, no immature cells (blasts, promyelocytes or myelocytes) in the PB, and disappearance of all signs and symptoms related to leukaemia (including palpable splenomegaly)] |
|||||
| All study participants | ||||||||
| n | κ | Mean | ||||||
| Baseline characteristics | ||||||||
| Demographics | ||||||||
| Age (years) (median) | 112 | 51 (range 17–96) | ||||||
| Imatinib failure | ||||||||
| Intolerance | 111 | 5 | 4.5% | |||||
| Resistance | 111 | 107 | 96.4% | |||||
| Prior therapy | ||||||||
| Best response to imatinib – CHR | 112 | 58 | 51.8% | |||||
| Best response to imatinib – CCyR | 112 | 29 | 25.9% | |||||
| Best response to imatinib – MCyR | 112 | 41 | 36.6% | |||||
| Duration of response to imatinib (months) (median) | 112 | 24 range 2–68 | ||||||
| Time on imatinib (months) (median) | 112 | 32 range 2–70 | ||||||
| Prior interferon | 112 | 69 | 61.6% | |||||
| Imatinib failure | ||||||||
| BCR–ABL mutation | 112 | 61 | 54.5% | |||||
| Results | ||||||||
| Dasatinib | Nilotinib | Δ | p-value | |||||
| n | κ | Mean % | n | κ | Mean % | |||
| CP | 0.432a | |||||||
| CyR | ||||||||
| CCyR | 24 | 8 | 33.3 | 13 | 2 | 15.4 | ||
| PCyR | 24 | 4 | 16.7 | 13 | 2 | 15.4 | ||
| MCyR | 24 | 12 | 50.0 | 13 | 4 | 30.8 | 0.436a | |
| Overall CyR | 24 | 15 | 62.5 | 13 | 6 | 46.2 | 0.541a | |
| HR | 0.714a | |||||||
| Overall HR | 24 | 21 | 87.5 | 13 | 10 | 76.9 | ||
| CHR | 24 | 20 | 83.3 | 13 | 10 | 76.9 | 0.972a | |
| AP | 0.464a | |||||||
| CyR | ||||||||
| CCyR | 22 | 3 | 13.6 | 31 | 8 | 25.8 | ||
| PCyR | 22 | 1 | 4.5 | 31 | 2 | 6.5 | ||
| MCyR | 22 | 4 | 18.2 | 31 | 10 | 32.3 | 0.407a | |
| Overall CyR | 22 | 5 | 22.7 | 31 | 13 | 41.9 | 0.246a | |
| HR | 0.521a | |||||||
| Overall HR | 22 | 16 | 72.7 | 31 | 26 | 83.9 | ||
| CHR | 22 | 14 | 63.6 | 31 | 26 | 83.9 | 0.173a | |
| BC/ALL | 1.000a | |||||||
| CyR | ||||||||
| CCyR | 10 | 4 | 40.0 | 10 | 3 | 30.0 | ||
| PCyR | 10 | 0 | 0.0 | 10 | 0 | 0.0 | ||
| MCyR | 10 | 4 | 40.0 | 10 | 3 | 30.0 | 1.000a | |
| Overall CyR | 10 | 4 | 40.0 | 10 | 3 | 30.0 | 1.000a | |
| HR | 1.000a | |||||||
| Overall HR | 10 | 6 | 60.0 | 10 | 5 | 50.0 | ||
| CHR | 10 | 4 | 40.0 | 10 | 5 | 50.0 | 1.000a | |
| Quality appraisal | ||||||||
| 1 General | ||||||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? Yes | ||||||||
| 1.2 Were the case series collected at more than one centre? Single centre | ||||||||
| 1.3 Was the main outcome independently assessed? Unclear | ||||||||
| 1.4 Are patient characteristics adequately described? No | ||||||||
| 1.5 How easy is it to assess generalisability of the results? Low | ||||||||
| 2 Assessment of selection bias | ||||||||
| 2.1 Are inclusion and exclusion criteria clearly reported? No | ||||||||
| 2.2 Were data collected prospectively? Yes | ||||||||
| 2.3 Were patients recruited consecutively? Yes | ||||||||
| 3 Assessment of performance bias | ||||||||
| 3.1 Did all the participants receive the same intervention? Uncertain, e.g. dosage not reported | ||||||||
| 3.2 Is the use of any concurrent therapies adequately described? Uncertain | ||||||||
| 4 Assessment of attrition bias | ||||||||
| 4.1 Was an ITT analysis performed? Yes. Seems no dropouts | ||||||||
| 4.2 Were dropouts from the study adequately described? Yes? Seems no dropouts | ||||||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Cortes et al. (2007)13 Secondary publications: Chromik et al. (2006),118 Cortes et al. (2008),123 Cortes et al. (2006),119 Ganibacoiti et al. (2007),121 Martinelli et al. (2006),120 Ottmann et al. (2007),122 Ottmann et al. (2005),116 Porkka et al. (2008),124 Soverini et al. (2006),77 Soverini et al. (2007),78 Talpaz et al. (2005),117 Saglio et al. (2008)125 Design: case series (prospective) CP: no AP: no BC: yes Country: USA, Switzerland, Germany, Argentina, Australia, Austria, Belgium, Israel, France, Italy, the Netherlands, Brazil, Canada, Finland, Republic of Korea, Philippines, Sweden, Taiwan, Thailand and the UK Note: there were more than one centre, but number of centres were not reported Trial code(s): START-B START-L #CA180006 #CA180015 NCT00108719 NCT00110097 |
Inclusion criteria: patients 18 years of age and older were eligible for inclusion if they had CML in MBC or LBC and were resistant to or intolerant of imatinib therapy. CML-BC was defined as 30% or greater blasts (myeloid or lymphoid) in PB or BM or extramedullary leukaemic infiltrates (other than in spleen or liver) with PB blast (myeloid or lymphoid) cell morphology Imatinib resistance was defined as progression from CP to BC while receiving 400 mg q.d. or more imatinib or from AP to BC while receiving 600 mg q.d. or more imatinib (or 400 mg to less than 600 mg q.d. if the patient was intolerant of 600 mg q.d. or more). Patients initially diagnosed in BC were classified as having ImR CML if they met the criteria for BC after 4 or more weeks (2 weeks for patients whose disease progressed rapidly) on imatinib 600 mg q.d. or more. Imatinib intolerance was defined as discontinuation of therapy because of toxicity considered at least possibly related to an imatinib dose of 400 mg q.d. or less or to an inability to tolerate imatinib doses higher than 400 mg q.d. For inclusion in the study, patients were required to have adequate hepatic and renal function and an Eastern Cooperative Oncology Group (ECOG) performance score of 2 or lower Exclusion criteria: exclusion criteria included previous dasatinib therapy, imatinib therapy within 7 days of initiation, uncontrolled or significant cardiovascular disease, or history of a significant bleeding disorder unrelated to CML |
Arm 1 dasatinib n: 116 Drug: dasatinib Starting daily dose (mg): 140 Dosage details: 70 mg b.i.d.; after 4 weeks of treatment, dose escalation to 100 mg b.i.d. was permitted for participants with suboptimal response Concurrent treatment: no treatment for CML other than dasatinib was permitted during the study – except anagrelide and hydroxycarbamide for treatment of elevated platelet counts (higher than 700 × 109/l) and WBC counts (higher than 50 × 109/l), respectively. Use of hydroxycarbamide was limited to a period of 2 weeks. Administration of colony-stimulating factors and recombinant erythropoietin was permitted at the discretion of the investigator |
CyR: evaluated by once-monthly BM aspirates (at least 20 metaphases)/biopsies for the first 3 months and every 3 months thereafter CCyR (0% Ph+) PCyR (1–35% Ph+) MCyR (complete or partial remission) Minor CyR (36–65% Ph+) Minimal CyR (66–95% Ph+) Overall CyR (complete, partial or minor remission) HR: patients were monitored with once-weekly CBCs. Confirmed HRs were required to be maintained for a minimum of 4 weeks, and no concomitant anagrelide or hydroxycarbamide was to be used during this interval Overall HR (CHR, no evidence of leukaemia or minor HR) CHR (WBC count less than or equal to the institutional upper limit of normal; ANC 1.0 × 109/l or higher; platelet count 100 × 109/l or higher; marrow blasts 5% or less with no peripheral blasts or promyelocytes; peripheral myelocytes + metamyelocytes < 5%; basophils in PB < 2%; and no evidence of extramedullary involvement) Major HR (CHR or no evidence of leukaemia) No evidence of leukaemia [CHR without full recovery of platelets and neutrophils (platelet count 20–100 × 109/l and ANC 0.5–1.0 × 109/l)] Minor HR (blasts < 15% and blasts + promyelocytes < 30%; PB basophils < 20%, blasts < 15%, and blasts + promyelocytes < 30%; no extramedullary disease other than in spleen and liver) Duration of HR (measured from the first day the criteria were met until progression or death; censored at the last haematological assessment for patients who discontinued for reasons other than progression or death) Duration of major HR Study medication: duration of study therapy (months) Average daily dose (mg q.d.) Survival: PFS (no decrease from baseline levels in percentage blasts in PB or BM on all assessments over a 4-week period after start of the maximum dasatinib dose; following documented response, progression was defined as loss of response on all assessments over a consecutive 2-week period after starting their maximum dasatinib dose) Participant disposition: withdrawal because of AEs AEs (grades 1–4): study drug toxicities were assessed continuously. In particular, a targeted physical examination for assessment of AEs, including assessment of skin and mucosa, was conducted weekly for the first 2 months and every other week thereafter. AEs were evaluated according to NCI CTC Version 3.0186 |
|
| Dasatinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| MBC | ||||
| Demographics | ||||
| Age (years) (median) | 74 | 55 (range 21–71) | ||
| Gender (n male) | 74 | 41 | 55.4% | |
| Imatinib failure | ||||
| Intolerance | 74 | 6 | 8.1% | |
| Resistance | 74 | 68 | 91.9% | |
| Prior therapy | ||||
| Time on imatinib < 1year | 74 | 11 | 14.9% | |
| Time on imatinib 1–3 years | 74 | 28 | 37.8% | |
| Time on imatinib > 3 years | 74 | 35 | 47.3% | |
| Highest imatinib dose < 400 mg q.d. | 74 | 0 | 0.0% | |
| Highest imatinib dose 400–600 mg q.d. | 74 | 38 | 51.4% | |
| Highest imatinib dose > 600 mg q.d. | 74 | 36 | 48.6% | |
| Prior chemotherapy | 74 | 49 | 66.2% | |
| Prior interferon | 74 | 41 | 55.4% | |
| Prior transplantation | 74 | 9 | 12.2% | |
| Disease history | ||||
| Duration of CML (months) (median) | 74 | 49 (range 3–216) | ||
| Laboratory parameters | ||||
| WBC × 109/l (median) | 74 | 17 (range 0.4–191.6) | ||
| WBC – 20 × 109/l or more | 74 | 35 | 47.3% | |
| BM blasts (%) (median) | 74 | 40 (range 0–95) | ||
| Peripheral blasts (%) (median) | 74 | 39 (range 0–99) | ||
| Peripheral blasts – 30% or more | 74 | 29 | 39.2% | |
| Platelets × 109/l (median) | 74 | 51 (range 10–2121) | ||
| Platelets – below 100 × 109/l | 74 | 53 | 71.6% | |
| LBC | ||||
| Demographics | ||||
| Age (years) (median) | 42 | 47 (range 19–72) | ||
| Gender (n male) | 42 | 22 | 52.4% | |
| Imatinib failure | 42 | 5 | 11.9% | |
| Intolerance | ||||
| Resistance | 42 | 37 | 88.1% | |
| Prior therapy | 42 | 20 | 47.6% | |
| Time on imatinib < 1 year | ||||
| Time on imatinib 1–3 years | 42 | 12 | 28.6% | |
| Time on imatinib > 3 years | 42 | 10 | 23.8% | |
| Highest imatinib dose < 400 mg q.d. | 42 | 1 | 2.4% | |
| Highest imatinib dose 400–600 mg q.d. | 42 | 19 | 45.2% | |
| Highest imatinib dose > 600 mg q.d. | 42 | 22 | 52.4% | |
| Prior chemotherapy | 42 | 33 | 78.6% | |
| Prior interferon | 42 | 20 | 47.6% | |
| Prior transplantation | 42 | 14 | 33.3% | |
| Disease history | ||||
| Duration of CML (months) (median) | 42 | 28 (range 2–186) | ||
| Laboratory parameters | ||||
| WBC × 109/l (median) | 42 | 7.7 (range 0.6–443.1) | ||
| WBC – 20 × 109/l or more | 42 | 14 | 33.3% | |
| BM blasts (%) (median) | 42 | 82 (range 0–100) | ||
| Peripheral blasts (%) (median) | 42 | 31 (range 0–82) | ||
| Peripheral blasts – 30% or more | 42 | 15 | 35.7% | |
| Platelets × 109/l (median) | 42 | 33 (range 6–423) | ||
| Platelets – below 100 × 109/l | 42 | 33 | 78.6% | |
| Results | ||||
| MBC | ||||
| CyR | ||||
| CCyR | 74 | 20a | 27.0% | |
| PCyR | 74 | 3a | 4.1% | |
| MCyR | 74 | 23a | 31.1% | |
| Minor CyR | 74 | 2a | 2.7% | |
| Minimal CyR | 74 | 7a | 9.5% | |
| Overall CyR | 74 | 32a | 43.2% | |
| HR | 74 | 39a | 52.7% | |
| Overall HR | ||||
| CHR | 74 | 19a | 25.7% | |
| Major HR | 74 | 25a | 33.8% | |
| No evidence of leukaemia | 74 | 6a | 8.1% | |
| Minor HR | 74 | 14a | 18.9% | |
| Duration of major HR | 25 | 1.00 | ||
| Duration of major HR | 0.96 | |||
| Duration of major HR | 0.92 | |||
| Duration of major HR | 0.92 | |||
| Duration of major HR | 0.84 | |||
| Duration of major HR | 0.84 | |||
| Study medication | ||||
| Duration of study therapy (months) (median) | 74 | 3.5 (range 0.03–12.00) | ||
| Average daily dose (mg q.d.) (median) | 74 | 137 | ||
| Survival | ||||
| PFS – 0 months | 74 | 1.00 | ||
| PFS – 2 months | 53 | 0.74 | ||
| PFS – 4 months | 37 | 0.54 | ||
| PFS – 6 months | 31 | 0.50 | ||
| PFS – 8 months | 25 | 0.45 | ||
| PFS – 10 months | 8 | 0.42 | ||
| PFS – 12 months | 1 | 0.42 | ||
| Participant disposition | ||||
| Withdrawal because of AEs | 74 | 10b | 13.5% | |
| AEs – grades 1–4 | 74 | 8 | 10.8% | |
| Anorexia | ||||
| Arthralgia | 74 | 8 | 10.8% | |
| Asthenia | 74 | 11 | 14.9% | |
| Diarrhoea | 74 | 27 | 36.5% | |
| Dyspnoea | 74 | 13 | 17.6% | |
| Epistaxis | 74 | 9 | 12.2% | |
| Fatigue | 74 | 9 | 12.2% | |
| Febrile neutropenia | 74 | 3 | 4.1% | |
| Gastrointestinal haemorrhage | 74 | 9 | 12.2% | |
| Headache | 74 | 6 | 8.1% | |
| Nausea | 74 | 12 | 16.2% | |
| Peripheral oedema | 74 | 14 | 18.9% | |
| Pleural effusion | 74 | 21 | 28.4% | |
| Pyrexia | 74 | 12 | 16.2% | |
| Rash | 74 | 9 | 12.2% | |
| Vomiting | 74 | 12 | 16.2% | |
| AEs – grade 3–4 | 74 | 62 | 83.8% | |
| Thrombopenia | ||||
| Anaemia | 74 | 50 | 67.6% | |
| Neutropenia | 74 | 61 | 82.4% | |
| Leucopenia | 74 | 47 | 63.5% | |
| Anorexia | 74 | 1 | 1.4% | |
| Arthralgia | 74 | 2 | 2.7% | |
| Asthenia | 74 | 2 | 2.7% | |
| Diarrhoea | 74 | 6 | 8.1% | |
| Dyspnoea | 74 | 5 | 6.8% | |
| Epistaxis | 74 | 1 | 1.4% | |
| Fatigue | 74 | 1 | 1.4% | |
| Febrile neutropenia | 74 | 3 | 4.1% | |
| Gastrointestinal haemorrhage | 74 | 6 | 8.1% | |
| Headache | 74 | 0 | 0.0% | |
| Nausea | 74 | 3 | 4.1% | |
| Peripheral oedema | 74 | 0 | 0.0% | |
| Pleural effusion | 74 | 10 | 13.5% | |
| Pyrexia | 74 | 4 | 5.4% | |
| Rash | 74 | 0 | 0.0% | |
| Vomiting | 74 | 1 | 1.4% | |
| LBC | ||||
| CyR | ||||
| CCyR | 42 | 18a | 42.9% | |
| PCyR | 42 | 3a | 7.1% | |
| MCyR | 42 | 21a | 50.0% | |
| Minor CyR | 42 | 0a | 0.0% | |
| Minimal CyR | 42 | 3a | 7.1% | |
| Overall CyR | 42 | 24a | 57.1% | |
| HR | ||||
| Overall HR | 42 | 15a | 35.7% | |
| CHR | 42 | 11a | 26.2% | |
| Major HR | 42 | 13a | 31.0% | |
| No evidence of leukaemia | 42 | 2a | 4.8% | |
| Minor HR | 42 | 2a | 4.8% | |
| Duration of major HR | 13 | 1.00 | ||
| Duration of major HR | 0.82 | |||
| Duration of major HR | 0.455 | |||
| Duration of major HR | 0.36 | |||
| Duration of major HR | 0.36 | |||
| Study medication | ||||
| Duration of study therapy (months) (median) | 42 | 2.8 (range 0.1–9.2) | ||
| Average daily dose (mg q.d.) (median) | 42 | 140 | ||
| Survival | 42 | 1.00 | ||
| PFS – 0 months | ||||
| PFS – 2 months | 26 | 0.63 | ||
| PFS – 4 months | 13 | 0.37 | ||
| PFS – 6 months | 8 | 0.20 | ||
| PFS – 8 months | 3 | 0.17 | ||
| Participant disposition | 42 | 1 | 2.4% | |
| Withdrawal because of AEs | ||||
| AEs – grades 1–4 | 42 | 2 | 4.8% | |
| Anorexia | ||||
| Arthralgia | 42 | 2 | 4.8% | |
| Asthenia | 42 | 4 | 9.5% | |
| Diarrhoea | 42 | 13 | 31.0% | |
| Dyspnoea | 42 | 5 | 11.9% | |
| Epistaxis | 42 | 1 | 2.4% | |
| Fatigue | 42 | 12 | 28.6% | |
| Febrile neutropenia | 42 | 6 | 14.3% | |
| Gastrointestinal haemorrhage | 42 | 0 | 0.0% | |
| Headache | 42 | 6 | 14.3% | |
| Nausea | 42 | 10 | 23.8% | |
| Peripheral oedema | 42 | 5 | 11.9% | |
| Pleural effusion | 42 | 6 | 14.3% | |
| Pyrexia | 42 | 8 | 19.0% | |
| Rash | 42 | 7 | 16.7% | |
| Vomiting | 42 | 10 | 23.8% | |
| AEs – grade 3–4 | ||||
| Thrombopenia | 42 | 37 | 88.1% | |
| Anaemia | 42 | 22 | 52.4% | |
| Neutropenia | 42 | 33 | 78.6% | |
| Leucopenia | 42 | 29 | 69.0% | |
| Anorexia | 42 | 2 | 4.8% | |
| Arthralgia | 42 | 0 | 0.0% | |
| Asthenia | 42 | 1 | 2.4% | |
| Diarrhoea | 42 | 0 | 0.0% | |
| Dyspnoea | 42 | 0 | 0.0% | |
| Epistaxis | 42 | 0 | 0.0% | |
| Fatigue | 42 | 2 | 4.8% | |
| Febrile neutropenia | 42 | 5 | 11.9% | |
| Gastrointestinal haemorrhage | 42 | 0 | 0.0% | |
| Headache | 42 | 1 | 2.4% | |
| Nausea | 42 | 0 | 0.0% | |
| Peripheral oedema | 42 | 0 | 0.0% | |
| Pleural effusion | 42 | 1 | 2.4% | |
| Pyrexia | 42 | 1 | 2.4% | |
| Rash | 42 | 2 | 4.8% | |
| Vomiting | 42 | 1 | 2.4% | |
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? No. The report presents data from two Phase II clinical trails of dasatinib in patients with ImR or ImI CML-BC. | ||||
| 1.2 Were the case series collected at more than one centre? Multicentre. No. of centres not reported | ||||
| 1.3 Was the main outcome independently assessed? No | ||||
| 1.4 Are patient characteristics adequately described? Yes | ||||
| 1.5 How easy is it to assess generalisability of the results? Medium | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? Yes | ||||
| 2.2 Were data collected prospectively? Yes | ||||
| 2.3 Were patients recruited consecutively? Yes | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? No. Different dosage | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Yes. No treatment for CML other than dasatinib – except anagrelide and hydroxycarbamide for treatment of elevated platelet counts and WBC counts (threshold reported for both). Use of hydroxycarbamide was limited to a period of 2 weeks. | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? No. Only patients who received at least one dose of study drug were included in the analysis | ||||
| 4.2 Were dropouts from the study adequately described? Yes | ||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Sakamaki et al. (2009)109 Design: case series (prospective) CP: yes AP: yes BC: yes Country: Japan Appears to be multicentre (authors come from 22 separate centres), though not explicitly stated Trial code(s): NCT00227454 |
Inclusion criteria: adult CML aged 20–75 years ImR defined according to phase CP: in individuals treated with imatinib at 400 mg q.d.; WBC two-fold increase from nadir to > 20 × 109/l or increase from nadir to 50 × 109/l; failure to achieve CHR after 3 months/CyR after 6 months/MCyR after 12 months, or loss of CHR or MCyR; named BCR–ABL mutations suggestive of ImR detected AP: progression to BC; progression to AP after HR to imatinib (400 mg q.d.) in CP; lack of HR after 4 weeks of imatinib (600 mg q.d.) in AP BC: progression to BC after HR to imatinib (600 mg q.d.); BC persisted after 4 weeks of imatinib ImI defined according to phase CP: discontinuation of imatinib because of grade 3–4 non-haematological AEs or grade 4 haematological AEs persisting for 7 days AP/BC: any toxicity leading to discontinuation of imatinib or dose kept < 400 mg q.d. Exclusion criteria: none reported |
Arm 1 dasatinib n: 41 Drug: dasatinib Starting daily dose (mg): 140 Dosage details: Phase I: dose escalation at 50 mg b.i.d., 70 mg b.i.d. and 90 mg b.i.d.. Unclear which participants took which doses Phase II: starting dose 140 mg q.d. (70 mg b.i.d.). Reduction (amount not reported) was permitted for participants with toxicity. Escalation (amount not reported) was permitted for participants with suboptimal response Concurrent treatment: no other anticancer therapy other than 14 days of hydroxycarbamide for WBC > 50 × 109/l Notes: presented results conflate Phase I (dose escalation) and Phase II (dose steady) results into a single cohort |
CyR CCyR PCyR MCyR Minor CyR Minimal CyR HR CHR Major HR No evidence of leukaemia Minor HR |
|
| Dasatinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| CP (all) | ||||
| Demographics | ||||
| Age (years) | 30 | See footnote a | ||
| Imatinib failure | ||||
| Intolerance | 30 | 12 | 40.0% | |
| Resistance | 30 | 18 | 60.0% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 30 | 7 | 23.3% | |
| Time on imatinib 1–3 years | 30 | 7 | 23.3% | |
| Time on imatinib > 3 years | 30 | 16 | 53.3% | |
| Highest imatinib dose 400–600 mg q.d. | 30 | 27 | 90.0% | |
| Highest imatinib dose > 600 mg q.d. | 30 | 3 | 10.0% | |
| Prior chemotherapy | 30 | 21 | 70.0% | |
| Prior interferon | 30 | 15 | 50.0% | |
| Prior transplantation | 30 | 1 | 3.3% | |
| Disease history | ||||
| Duration of CML (months) | 30 | See footnote b | ||
| Baseline status | ||||
| BCR–ABL mutation | 30 | 5 | 16.7% | |
| AP or BC (all) | ||||
| Demographics | ||||
| Age (years) (median) | 11 | 57 (range 31–73) | ||
| Imatinib failure | ||||
| Intolerance | 11 | 3 | 27.3% | |
| Resistance | 11 | 8 | 72.7% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 11 | 2 | 18.2% | |
| Time on imatinib 1–3 years | 11 | 6 | 54.5% | |
| Time on imatinib > 3 years | 11 | 3 | 27.3% | |
| Highest imatinib dose 400–600 mg q.d. | 11 | 5 | 45.5% | |
| Highest imatinib dose > 600 mg q.d. | 11 | 6 | 54.5% | |
| Prior chemotherapy | 11 | 9 | 81.8% | |
| Prior interferon | 11 | 3 | 27.3% | |
| Prior transplantation | 11 | 3 | 27.3% | |
| Disease history | ||||
| Duration of CML (months) (median) | 11 | 1.6 (range 0–14) | ||
| Baseline status | ||||
| BCR–ABL mutation | 11 | 2 | 18.2% | |
| Results | ||||
| AEs – grades 1–4 | ||||
| Anorexia | 54 | 10 | 18.5% | |
| Arthralgia | 54 | 6 | 11.1% | |
| Constipation | 54 | 11 | 20.4% | |
| Cough | 54 | 10 | 18.5% | |
| Diarrhoea | 54 | 18 | 33.3% | |
| Generalised oedema | 54 | 17 | 31.5% | |
| Headache | 54 | 22 | 40.7% | |
| Malaise | 54 | 16 | 29.6% | |
| Nausea | 54 | 11 | 20.4% | |
| Pain in extremity | 54 | 6 | 11.1% | |
| Pleural effusion | 54 | 14 | 25.9% | |
| Pyrexia | 54 | 18 | 33.3% | |
| Rash | 54 | 17 | 31.5% | |
| Stomatitis | 54 | 7 | 13.0% | |
| Vomiting | 54 | 6 | 11.1% | |
| Weight increase | 54 | 14 | 25.9% | |
| Weight loss | 54 | 7 | 13.0% | |
| AEs – grade 3–4 | ||||
| Anorexia | 54 | 0 | 0.0% | |
| Arthralgia | 54 | 0 | 0.0% | |
| Constipation | 54 | 0 | 0.0% | |
| Cough | 54 | 0 | 0.0% | |
| Diarrhoea | 54 | 1 | 1.9% | |
| Generalised oedema | 54 | 0 | 0.0% | |
| Malaise | 54 | 0 | 0.0% | |
| Nausea | 54 | 0 | 0.0% | |
| Pain in extremity | 54 | 1 | 1.9% | |
| Pleural effusion | 54 | 1 | 1.9% | |
| Pyrexia | 54 | 0 | 0.0% | |
| Rash | 54 | 1 | 1.9% | |
| Stomatitis | 54 | 0 | 0.0% | |
| Vomiting | 54 | 0 | 0.0% | |
| Weight increase | 54 | 0 | 0.0% | |
| Weight loss | 54 | 0 | 0.0% | |
| CP (all) | ||||
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 30 | 15 | 50.0% | |
| Anaemia | 30 | 5 | 16.7% | |
| Neutropenia | 30 | 14 | 46.7% | |
| Leucopenia | 30 | 8 | 26.7% | |
| CP (ImI) | ||||
| CyR | ||||
| CCyR | 12 | 8 | 66.7% | |
| PCyR | 12 | 2 | 16.7% | |
| MCyR | 12 | 10 | 83.3% | |
| Minor CyR | 12 | 1 | 8.3% | |
| Minimal CyR | 12 | 1 | 8.3% | |
| HR | ||||
| CHR | 12 | 12 | 100.0% | |
| CP (ImR) | ||||
| CyR | ||||
| CCyR | 18 | 5 | 27.8% | |
| PCyR | 18 | 1 | 5.6% | |
| MCyR | 18 | 6 | 33.3% | |
| Minor CyR | 18 | 3 | 16.7% | |
| Minimal CyR | 18 | 3 | 16.7% | |
| HR | ||||
| Complete HR | 18 | 15 | 83.3% | |
| AP or BC (all) | ||||
| Haematological AEs – grades 3-4 | ||||
| Thrombopenia | 11 | 7 | 63.6% | |
| Anaemia | 11 | 2 | 18.2% | |
| Neutropenia | 11 | 8 | 72.7% | |
| Leucopenia | 11 | 5 | 45.5% | |
| AP or BC (ImI) | ||||
| CyR | ||||
| CCyR | 3 | 0 | 0.0% | |
| PCyR | 3 | 0 | 0.0% | |
| MCyR | 3 | 0 | 0.0% | |
| Minor CyR | 3 | 0 | 0.0% | |
| Minimal CyR | 3 | 1 | 33.3% | |
| HR | ||||
| CHR | 3 | 0 | 0.0% | |
| Major HR | 3 | 2 | 66.7% | |
| No evidence of leukaemia | 3 | 2 | 66.7% | |
| Minor HR | 3 | 0 | 0.0% | |
| AP or BC (ImR) | ||||
| CyR | ||||
| CCyR | 8 | 1 | 12.5% | |
| PCyR | 8 | 2 | 25.0% | |
| MCyR | 8 | 3 | 37.5% | |
| Minor CyR | 8 | 2 | 25.0% | |
| Minimal CyR | 8 | 1 | 12.5% | |
| HR | ||||
| CHR | 8 | 2 | 25.0% | |
| Major HR | 8 | 5 | 62.5% | |
| No evidence of leukaemia | 8 | 3 | 37.5% | |
| Minor HR | 8 | 1 | 12.5% | |
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? No | ||||
| 1.2 Were the case series collected at more than one centre? Unclear. Appears to be multicentre (authors from 22 separate centres), but not explicitly stated | ||||
| 1.3 Was the main outcome independently assessed? Unclear | ||||
| 1.4 Are patient characteristics adequately described? No. Baseline characteristics split by phase of study; outcomes are not; hence, impossible to cross-reference the two | ||||
| 1.5 How easy is it to assess generalisability of the results? Low. Impossible to tell what dosages were taken in Phase I, results for which are not presented separately | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? Yes | ||||
| 2.2 Were data collected prospectively? Yes | ||||
| 2.3 Were patients recruited consecutively? Unclear | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? Uncertain | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Yes. Hydroxycarbamide allowed in prescribed circumstances | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? No. One participant registered but not included in results, because did not take study medication | ||||
| 4.2 Were dropouts from the study adequately described? Unclear | ||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Fabarius et al. (2007)79 Design: case series (prospective) CP: yes AP: yes BC: yes Country: Germany (no. of centres not reported, although all authors are from a single unit) |
Inclusion criteria: not clearly defined, other than ‘patients with Ph+ and BCR–ABL-positive CML after imatinib failure’ Exclusion criteria: not reported |
Arm 1 dasatinib n: 71 Drug: dasatinib Starting daily dose (mg): 5 Dosage details: started at a dose of 100–140 mg q.d. (2 × 50 mg q.d. or 2 × 70 mg q.d.) Concurrent treatment: not clear. Only stated that five patients received allogeneic SCT |
CyR: cytogenetic analyses of BM were made and interpreted according to the International System for Human Cytogenetic Nomenclature CCyR (0% Ph+) PCyR [1–35% Ph+ (labelled as ‘major’ response in study; however, definition corresponds to partial response in other studies)] MCyR [complete + ’major’ (partial) response] |
|
| Dasatinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| Demographics | ||||
| Age (years) (median) | 71 | 58 (range 28–78) | ||
| Gender (n male) | 71 | 40 | 56.3% | |
| Prior therapy | ||||
| Prior hydroxycarbamide | 71 | 50 | 70.4% | |
| Prior chemotherapy | 71 | 11a | 15.5% | |
| Prior interferon | 71 | 49 | 69.0% | |
| Disease history | ||||
| Duration of CML (months) (median) | 71 | 59 (range 6–216) | ||
| Results | ||||
| CP | ||||
| CyR | ||||
| CCyR | 50 | 22 | 44.0% | |
| PCyR | 50 | 7b | 14.0% | |
| MCyR | 50 | 29 | 58.0% | |
| AP | ||||
| CyR | ||||
| CCyR | 6 | 0 | 0.0% | |
| PCyR | 6 | 0b | 0.0% | |
| MCyR | 6 | 0 | 0.0% | |
| BC | ||||
| CyR | ||||
| CCyR | 15 | 4 | 26.7% | |
| PCyR | 15 | 0b | 0.0% | |
| MCyR | 15 | 4 | 26.7% | |
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? Yes | ||||
| 1.2 Were the case series collected at more than one centre? Single centre | ||||
| 1.3 Was the main outcome independently assessed? No | ||||
| 1.4 Are patient characteristics adequately described? Yes | ||||
| 1.5 How easy is it to assess generalisability of the results? Low | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? No | ||||
| 2.2 Were data collected prospectively? Unclear | ||||
| 2.3 Were patients recruited consecutively? Unclear | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? No. Dosage ranged | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Uncertain | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? Yes | ||||
| 4.2 Were dropouts from the study adequately described? Unclear | ||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Guilhot et al. (2007)12 Secondary publications: Cortes et al. (2006),127 Guilhot et al. (2005),126 Guilhot et al. (2007),129 O’Brien (2007),130 Talpaz et al. (2006),128 Rea et al. (2008),131 Rea et al. (2008)132 Design: case series (prospective) CP: no AP: yes BC: no Country: USA, Switzerland, Germany, Argentina, Australia, Austria, Belgium, Israel, France, Italy, the Netherlands, Singapore, Sweden, Taiwan, the UK, Brazil, and Norway Number of centres: 40 Trial code(s): #CA180005 START-A |
Inclusion criteria: male and female patients, aged 18 years or older, were eligible for inclusion if they had Ph+ or BCR–ABL-positive CML-AP with primary or acquired haematological resistance or intolerance to imatinib therapy, and had adequate hepatic function. CML-AP was defined as the occurrence of one or more of the following (1) at least 15% to less than 30% blasts in PB or BM; (2) at least 30% blasts plus promyelocytes (summed) in blood or BM (but with < 30% blasts alone); (3) at least 20% basophils in blood or BM; or (4) platelet counts < 100 × 109/l unrelated to drug therapy The definition of resistance to imatinib differed depending on the initial CML diagnosis Initial diagnosis of CML-CP was defined as having resistant disease if (1) progression to CML-AP occurred while receiving imatinib ≥ 400 mg q.d. or (2) no HR was achieved after at least 4 weeks (or 2 weeks for patients who progressed rapidly of imatinib 600 mg q.d.) Patients with an initial diagnosis of CML-AP or BC who had experienced a HR were defined as having resistant disease if progression to CML-AP occurred while receiving imatinib 600 mg q.d. or more (400–600 mg q.d. if the patient was intolerant of 600 mg q.d.) Exclusion criteria: patients who had an Eastern Cooperative Oncology Group (ECOG) performance status of grade 3 or greater, uncontrolled or significant cardiovascular disease or a history of a significant bleeding disorder unrelated to CML |
Arm 1 dasatinib n: 107 Drug: dasatinib Starting daily dose (mg): not reported Dosage details: starting dose 70 mg b.i.d. After 4 weeks of treatment, dose escalation to 100 mg b.i.d. was permitted for participants with suboptimal response Concurrent treatment: no treatment for CML other than dasatinib was permitted during the study – except anagrelide and hydroxycarbamide for treatment of elevated platelet counts (higher than 700 × 109/l) and WBC counts (higher than 50 × 109/l), respectively. Use of hydroxycarbamide was limited to a period of 2 weeks |
CyR: evaluated by once-monthly BM aspirates/biopsies for the first 3 months and every 3 months thereafter; calculated from the percentage of Ph+ cells in metaphase in the BM sample CCyR (0% Ph+) PCyR (1–35% Ph+) MCyR (complete plus partial) Minor CyR (36–65% Ph+) Minimal CyR (66–95% Ph+) Overall CyR (complete, partial, minor, or minimal) Duration of MCyR HR: determined by assessment of once-weekly CBCs Overall HR (major or minor response) CHR [WBC count no more than institutional ULN; ANC ≥ 1 × 109/l; platelet count ≥ 100 × 109/l; no blasts or promyelocytes in PB; BM blasts ≤ 5%; < 5% myelocytes plus metamyelocytes in PB; basophils in PB < 2% and basophils in the BM < 2%; no extramedullary involvement (including no hepatomegaly or splenomegaly)] Major HR (CHR or NEL) No evidence of leukaemia [WBC count no more than institutional ULN; no blasts or promyelocytes in PB; BM blasts < 5%; < 5% myelocytes plus metamyelocytes in PB; no extramedullary involvement (including no hepatomegaly or splenomegaly); basophils in PB < 2%; at least one of the following: platelets between 20 and 100 × 109/l and/or ANC between 0.5 and 1.0 × 109/l] Minor HR (< 15% blasts in BM and in PB; < 30% blasts plus promyelocytes in BM and < 30% blasts plus promyelocytes in PB; < 2% basophils in PB; no extramedullary involvement other than spleen and liver) Duration of major HR Study medication: duration of study therapy (months) Average daily dose (mg q.d.) Survival: PFS (in all patients: no decrease from baseline levels in percentage of blasts in PB or BM on all assessments over a 4-week period after receiving the maximum dose of dasatinib; in patients who had achieved a major HR or minor HR: failure to meet the criteria for a major HR or minor HR, respectively, on all assessments over a consecutive 2-week period after receiving the maximum dose of dasatinib) OS Participant disposition: withdrawal because of AEs Haematological AEs – grades 1–4: anaemia; neutropenia; thrombopenia; leucopenia AEs – grades 1–4: safety information was assessed for patients who received at least one dose of dasatinib. Patients were assessed by physical examination, performance status, vital signs, and 12-lead electrocardiogram at baseline. AEs were evaluated throughout the study and graded according to the NCI CTC Version 3.0186 |
|
| Dasatinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| Demographics | ||||
| Age (years) (median) | 107 | 57 (range 23–86) | ||
| Gender (n male) | 107 | 55 | 51.4% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 107 | 9 | 8.4% | |
| Time on imatinib 1–3 years | 107 | 26 | 24.3% | |
| Time on imatinib > 3 years | 107 | 73 | 68.2% | |
| Highest imatinib dose 400–600 mg q.d. | 107 | 44 | 41.1% | |
| Highest imatinib dose > 600 mg q.d. | 107 | 63 | 58.9% | |
| Prior chemotherapy | 107 | 72 | 67.3% | |
| Prior interferon | 107 | 80 | 74.8% | |
| Prior transplantation | 107 | 19 | 17.8% | |
| Disease history | ||||
| Duration of CML (months) (median) | 107 | 90.9 | ||
| Grade 3–4 leucopenia at baseline | 107 | 5 | 4.7% | |
| Grade 3–4 thrombopenia at baseline | 107 | 25 | 23.4% | |
| Grade 3–4 neutropenia at baseline | 107 | 7 | 6.5% | |
| Grade 3–4 anaemia at baseline | 107 | 5 | 4.7% | |
| Laboratory parameters | ||||
| WBC × 109/l (median) | 107 | 16.8 (range 1.0–243.4) | ||
| WBC – 20 × 109/l or more | 107 | 45 | 42.1% | |
| BM blasts (%) (median) | 107 | 9 | ||
| BM blasts – 15% or more | 107 | 35 | 32.7% | |
| Peripheral blasts (%) (median) | 107 | 2.5 | ||
| Peripheral blasts – 15% or more | 107 | 14 | 13.1% | |
| Platelets × 109/l (median) | 107 | 165 (range 8–3580) | ||
| Platelets – below 100 × 109/l | 107 | 44 | 41.1% | |
| Basophils – 20% or more | 107 | 20 | 18.7% | |
| ImR | ||||
| Demographics | ||||
| Age (years) (median) | 99 | 57 (range 23–86) | ||
| Gender (n male) | 99 | 53 | 53.5% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 99 | 4 | 4.0% | |
| Time on imatinib 1–3 years | 99 | 24 | 24.2% | |
| Time on imatinib > 3 years | 99 | 72 | 72.7% | |
| Highest imatinib dose 400–600 mg q.d. | 99 | 39 | 39.4% | |
| Highest imatinib dose > 600 mg q.d. | 99 | 61 | 61.6% | |
| Prior chemotherapy | 99 | 69 | 69.7% | |
| Prior interferon | 99 | 77 | 77.8% | |
| Prior transplantation | 99 | 17 | 17.2% | |
| Disease history | ||||
| Duration of CML (months) (median) | 99 | 91.2 | ||
| Grade 3–4 leucopenia at baseline | 99 | 5 | 5.1% | |
| Grade 3–4 thrombopenia at baseline | 99 | 25 | 25.3% | |
| Grade 3–4 neutropenia at baseline | 99 | 7 | 7.1% | |
| Grade 3–4 anaemia at baseline | 99 | 5 | 5.1% | |
| Laboratory parameters | ||||
| WBC × 109/l (median) | 99 | 17.5 (range 1.0–243.4) | ||
| WBC – 20 × 109/l or more | 99 | 42 | 42.4% | |
| BM blasts (%) (median) | 99 | 8.9 | ||
| BM blasts – 15% or more | 99 | 31 | 31.3% | |
| Peripheral blasts (%) (median) | 99 | 2 | ||
| Peripheral blasts – 15% or more | 99 | 13 | 13.1% | |
| Platelets × 109/l (median) | 99 | 165 (range 8–3580) | ||
| Platelets – below 100 × 109/l | 99 | 40 | 40.4% | |
| Basophils – 20% or more | 99 | 20 | 20.2% | |
| ImI | ||||
| Demographics | ||||
| Age (years) (median) | 8 | 67 (range 54–74) | ||
| Gender (n male) | 8 | 2 | 25.0% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 8 | 4 | 50.0% | |
| Time on imatinib 1–3 years | 8 | 2 | 25.0% | |
| Time on imatinib > 3 years | 8 | 2 | 25.0% | |
| Highest imatinib dose 400–600 mg q.d. | 8 | 5 | 62.5% | |
| Highest imatinib dose > 600 mg q.d. | 8 | 3 | 37.5% | |
| Prior chemotherapy | 8 | 4 | 50.0% | |
| Prior interferon | 8 | 4 | 50.0% | |
| Prior transplantation | 8 | 2 | 25.0% | |
| Disease history | ||||
| Duration of CML (months) (median) | 8 | 68.7 | ||
| Grade 3–4 leucopenia at baseline | 8 | 0 | 0.0% | |
| Grade 3–4 thrombopenia at baseline | 8 | 0 | 0.0% | |
| Grade 3–4 neutropenia at baseline | 8 | 0 | 0.0% | |
| Grade 3–4 anaemia at baseline | 8 | 0 | 0.0% | |
| Laboratory parameters | ||||
| WBC × 109/l (median) | 8 | 5.6 (range 3.2–68.4) | ||
| WBC – 20 × 109/l or more | 8 | 3 | 37.5% | |
| BM blasts (%) (median) | 8 | 15 | ||
| BM blasts – 15% or more | 8 | 4 | 50.0% | |
| Peripheral blasts (%) (median) | 8 | 7 | ||
| Peripheral blasts – 15% or more | 8 | 1 | 12.5% | |
| Platelets × 109/l (median) | 8 | 166 (range 54–1463) | ||
| Platelets – below 100 × 109/l | 8 | 4 | 50.0% | |
| Basophils – 20% or more | 8 | 0 | 0.0% | |
| 14 months’ follow-up (all) | ||||
| Demographics | ||||
| Age (years) (median) | 174 | 57 (range 22–86) | ||
| Gender (n male) | 174 | 96a | 55.2% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 174 | 17 | 9.8% | |
| Time on imatinib 1–3 years | 174 | 54 | 31.0% | |
| Time on imatinib > 3 years | 174 | 103a | 59.2% | |
| Highest imatinib dose 400–600 mg q.d. | 174 | 84a | 48.3% | |
| Highest imatinib dose > 600 mg q.d. | 174 | 90 | 51.7% | |
| Prior hydroxycarbamide | 174 | 164b | 94.3% | |
| Prior chemotherapy | 174 | 103a | 59.2% | |
| Prior interferon | 174 | 125a | 71.8% | |
| Prior transplantation | 174 | 23a | 13.2% | |
| Prior radiotherapy | 174 | 7 | 4.0% | |
| Disease history | ||||
| Duration of CML (months) (median) | 174 | 82 (range 4–359) | ||
| Splenomegaly at study entry | 174 | 37a | 21.3% | |
| Baseline status | ||||
| BCR–ABL mutation | 156 | 88 | 56.4% | |
| 14 months’ follow-up (ImR) | ||||
| Demographics | ||||
| Age (years) (median) | 161 | 56 (range 22–86) | ||
| Gender (n male) | 161 | 92a | 57.1% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 161 | 11a | 6.8% | |
| Time on imatinib 1–3 years | 161 | 48a | 29.8% | |
| Time on imatinib > 3 years | 161 | 101a | 62.7% | |
| Highest imatinib dose 400–600 mg q.d. | 161 | 72a | 44.7% | |
| Highest imatinib dose > 600 mg q.d. | 161 | 89a | 55.3% | |
| Prior hydroxycarbamide | 161 | 151a | 93.8% | |
| Prior chemotherapy | 161 | 97a | 60.2% | |
| Prior interferon | 161 | 118a | 73.3% | |
| Prior transplantation | 161 | 21 | 13.0% | |
| Prior radiotherapy | 161 | 6a | 3.7% | |
| Disease history | ||||
| Duration of CML (months) (median) | 161 | 82 (range 4–359) | ||
| Splenomegaly at study entry | 161 | 34a | 21.1% | |
| Baseline status | ||||
| BCR–ABL mutation | 145 | 87 | 60.0% | |
| 14 months’ follow-up (ImI) | ||||
| Demographics | ||||
| Age (years) (median) | 13 | 61 (range 29–80) | ||
| Gender (n male) | 13 | 4 | 30.8% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 13 | 6 | 46.2% | |
| Time on imatinib 1–3 years | 13 | 5 | 38.5% | |
| Time on imatinib > 3 years | 13 | 2 | 15.4% | |
| Highest imatinib dose 400–600 mg q.d. | 13 | 10 | 76.9% | |
| Highest imatinib dose > 600 mg q.d. | 13 | 3 | 23.1% | |
| Prior hydroxycarbamide | 13 | 12 | 92.3% | |
| Prior chemotherapy | 13 | 6 | 46.2% | |
| Prior interferon | 13 | 8 | 61.5% | |
| Prior transplantation | 13 | 2 | 15.4% | |
| Prior radiotherapy | 13 | 1 | 7.7% | |
| Disease history | ||||
| Duration of CML (months) (median) | 13 | 91 (range 4–206) | ||
| Splenomegaly at study entry | 13 | 4 | 30.8% | |
| Baseline status | ||||
| BCR–ABL mutation | 11 | 1 | 9.1% | |
| Results | ||||
| CyR | ||||
| CCyR | 107 | 26c | 24.3% | |
| PCyR | 107 | 9c | 8.4% | |
| MCyR | 107 | 35c | 32.7% | |
| Minor CyR | 107 | 6c | 5.6% | |
| Minimal CyR | 107 | 20c | 18.7% | |
| Overall CyR | 107 | 61c | 57.0% | |
| HR | ||||
| Overall HR | 107 | 87c | 81.3% | |
| CHR | 107 | 42c | 39.3% | |
| Major HR | 107 | 69c | 64.5% | |
| No evidence of leukaemia | 107 | 27c | 25.2% | |
| Minor HR | 107 | 18c | 16.8% | |
| Duration of major HR – 0 months | 107 | 1 | ||
| Duration of major HR – 2 months | 1 | |||
| Duration of major HR – 4 months | 0.95 | |||
| Duration of major HR – 6 months | 0.93 | |||
| Duration of major HR – 8 months | 0.805 | |||
| Duration of major HR – 10 months | 0.805 | |||
| Duration of major HR – 12 months | 0.805 | |||
| Study medication | ||||
| Duration of study therapy (months) (median) | 107 | 8.3 (range 0.2–12.9)d | ||
| Survival | ||||
| PFS – 0 months | 107 | 1 | ||
| PFS – 2 months | 0.94 | |||
| PFS – 4 months | 0.875 | |||
| PFS – 6 months | 0.805 | |||
| PFS – 8 months | 0.755 | |||
| PFS – 10 months | 0.74 | |||
| PFS – 12 months | 0.615 | |||
| PFS – 14 months | 107 | |||
| AEs – grades 1–4 | ||||
| Abdominal pain | 107 | 12 | 11.2% | |
| Anorexia | 107 | 14 | 13.1% | |
| Arthralgia | 107 | 11 | 10.3% | |
| Asthenia | 107 | 20 | 18.7% | |
| Diarrhoea | 107 | 53 | 49.5% | |
| Dizziness | 107 | 12 | 11.2% | |
| Dyspnoea | 107 | 17 | 15.9% | |
| Epistaxis | 107 | 12 | 11.2% | |
| Fatigue | 107 | 25 | 23.4% | |
| Gastrointestinal haemorrhage | 107 | 12 | 11.2% | |
| Headache | 107 | 30 | 28.0% | |
| Myalgia | 107 | 11 | 10.3% | |
| Nausea | 107 | 24 | 22.4% | |
| Pain in extremity | 107 | 15 | 14.0% | |
| Peripheral oedema | 107 | 24 | 22.4% | |
| Pleural effusion | 107 | 25 | 23.4% | |
| Pyrexia | 107 | 25 | 23.4% | |
| Rash | 107 | 16 | 15.0% | |
| Vomiting | 107 | 17 | 15.9% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 107 | 88 | 82.2% | |
| Anaemia | 107 | 74 | 69.2% | |
| Neutropenia | 107 | 83 | 77.6% | |
| Leucopenia | 107 | 65 | 60.7% | |
| AEs – grade 3–4 | ||||
| Abdominal pain | 107 | 0 | 0.0% | |
| Anorexia | 107 | 1 | 0.9% | |
| Arthralgia | 107 | 0 | 0.0% | |
| Asthenia | 107 | 4 | 3.7% | |
| Diarrhoea | 107 | 6 | 5.6% | |
| Dizziness | 107 | 0 | 0.0% | |
| Dyspnoea | 107 | 4 | 3.7% | |
| Epistaxis | 107 | 0 | 0.0% | |
| Fatigue | 107 | 4 | 3.7% | |
| Gastrointestinal haemorrhage | 107 | 9 | 8.4% | |
| Headache | 107 | 1 | 0.9% | |
| Myalgia | 107 | 1 | 0.9% | |
| Nausea | 107 | 0 | 0.0% | |
| Pain in extremity | 107 | 0 | 0.0% | |
| Peripheral oedema | 107 | 0 | 0.0% | |
| Pleural effusion | 107 | 3 | 2.8% | |
| Pyrexia | 107 | 4 | 3.7% | |
| Rash | 107 | 1 | 0.9% | |
| Vomiting | 107 | 1 | 0.9% | |
| ImR | 99 | 25 | 25.3% | |
| CyR | ||||
| CCyR | ||||
| PCyR | 99 | 9 | 9.1% | |
| MCyR | 99 | 34 | 34.3% | |
| Minor CyR | 99 | 6 | 6.1% | |
| Minimal CyR | 99 | 17 | 17.2% | |
| Overall CyR | 99 | 57 | 57.6% | |
| HR | 99 | 80 | 80.8% | |
| Overall HR | ||||
| CHR | 99 | 39 | 39.4% | |
| Major HR | 99 | 64 | 64.6% | |
| No evidence of leukaemia | 99 | 25 | 25.3% | |
| Minor HR | 99 | 16 | 16.2% | |
| Duration of major HR – 0 months | 99 | 1 | ||
| Duration of major HR – 2 months | 1 | |||
| Duration of major HR – 4 months | 0.94 | |||
| Duration of major HR – 6 months | 0.92 | |||
| Duration of major HR – 8 months | 0.79 | |||
| Duration of major HR – 10 months | 0.79 | |||
| Duration of major HR – 12 months | 0.79 | |||
| Survival | 99 | 1 | ||
| PFS – 0 months | ||||
| PFS – 2 months | 0.93 | |||
| PFS – 4 months | 0.86 | |||
| PFS – 6 months | 0.8 | |||
| PFS – 8 months | 0.755 | |||
| PFS – 10 months | 0.74 | |||
| PFS – 12 months | 0.555 | |||
| Haematological AEs – grade 3–4 | 99 | 81 | 81.8% | |
| Thrombopenia | ||||
| Anaemia | 99 | 67 | 67.7% | |
| Neutropenia | 99 | 75 | 75.8% | |
| Leucopenia | 99 | 59 | 59.6% | |
| ImI | 8 | 1 | 12.5% | |
| CyR | ||||
| CCyR | ||||
| PCyR | 8 | 0 | 0.0% | |
| MCyR | 8 | 1 | 12.5% | |
| Minor CyR | 8 | 0 | 0.0% | |
| Minimal CyR | 8 | 3 | 37.5% | |
| Overall CyR | 8 | 4 | 50.0% | |
| HR | 8 | 7 | 87.5% | |
| Overall HR | ||||
| CHR | 8 | 3 | 37.5% | |
| Major HR | 8 | 5 | 62.5% | |
| No evidence of leukaemia | 8 | 2 | 25.0% | |
| Minor HR | 8 | 2 | 25.0% | |
| Haematological AEs – grade 3–4 | 8 | 7 | 87.5% | |
| Thrombopenia | ||||
| Anaemia | 8 | 7 | 87.5% | |
| Neutropenia | 8 | 8 | 100.0% | |
| Leucopenia | 8 | 6 | 75.0% | |
| 14 months’ follow-up (all) | ||||
| CyR | ||||
| CCyR | 174 | 55 | 31.6% | |
| PCyR | 174 | 12 | 6.9% | |
| MCyR | 174 | 67 | 38.5% | |
| Minor CyR | 174 | 10 | 5.7% | |
| Duration of MCyR – 0 months | 174 | 1 | ||
| Duration of MCyR – 2 months | 0.925 | |||
| Duration of MCyR – 4 months | 0.895 | |||
| Duration of MCyR – 6 months | 0.88 | |||
| Duration of MCyR – 8 months | 0.88 | |||
| Duration of MCyR – 10 months | 0.855 | |||
| Duration of MCyR – 12 months | 0.855 | |||
| Duration of MCyR – 14 months | 0.855 | |||
| Duration of MCyR – 16 months | 0.855 | |||
| Duration of MCyR – 18 months | 0.855 | |||
| HR | ||||
| Overall HR | 174 | 138 | 79.3% | |
| CHR | 174 | 78 | 44.8% | |
| Major HR | 174 | 111 | 63.8% | |
| No evidence of leukaemia | 174 | 33 | 19.0% | |
| Minor haematological response | 174 | |||
| Duration of major HR – 0 months | 174 | 1 | ||
| Duration of major HR – 2 months | 0.99 | |||
| Duration of major HR – 4 months | 0.94 | |||
| Duration of major HR – 6 months | 0.925 | |||
| Duration of major HR – 8 months | 0.87 | |||
| Duration of major HR – 10 months | 0.84 | |||
| Duration of major HR – 12 months | 0.84 | |||
| Duration of major HR – 14 months | 0.8 | |||
| Duration of major HR – 16 months | 0.8 | |||
| Duration of major HR – 18 months | 0.78 | |||
| Study medication | ||||
| Duration of study therapy (months) | 174 | |||
| Average daily dose (mg q.d.) (median) | 174 | 126 (range 32–196) | ||
| Survival | ||||
| PFS – 0 months | 174 | 1 | ||
| PFS – 3 months | 149 | 0.89 | ||
| PFS – 6 months | 130 | 0.795 | ||
| PFS – 9 months | 111 | 0.715 | ||
| PFS – 12 months | 91 | 0.66 | ||
| PFS – 15 months | 52 | 0.605 | ||
| PFS – 18 months | 4 | 0.605 | ||
| OS – 0 months | 174 | 1 | ||
| OS – 3 months | 163 | 0.965 | ||
| OS – 6 months | 143 | 0.905 | ||
| OS – 9 months | 122 | 0.87 | ||
| OS – 12 months | 102 | 0.825 | ||
| OS – 15 months | 62 | 0.8 | ||
| OS – 18 months | 4 | 0.785 | ||
| Participant disposition | ||||
| Withdrawal because of AEs | 174 | 18e | 10.3% | |
| Haematological AEs – grades 1–4 | ||||
| Anaemia | 174 | 172 | 98.9% | |
| Neutropenia | 174 | 159 | 91.4% | |
| Thrombopenia | 174 | 167 | 96.0% | |
| Leucopenia | 174 | 152 | 87.4% | |
| AEs – grades 1–4 | ||||
| Abdominal pain | 174 | 19 | 10.9% | |
| Anorexia | 174 | 27 | 15.5% | |
| Arthralgia | 174 | 22 | 12.6% | |
| Asthenia | 174 | 24 | 13.8% | |
| Cough | 174 | 18 | 10.3% | |
| Diarrhoea | 174 | 90 | 51.7% | |
| Dizziness | 174 | 18 | 10.3% | |
| Dyspnoea | 174 | 37 | 21.3% | |
| Fatigue | 174 | 46 | 26.4% | |
| Headache | 174 | 51 | 29.3% | |
| Myalgia | 174 | 20 | 11.5% | |
| Nausea | 174 | 48 | 27.6% | |
| Pain in extremity | 174 | 21 | 12.1% | |
| Peripheral oedema | 174 | 39 | 22.4% | |
| Petechiae | 174 | 24 | 13.8% | |
| Pleural effusion | 174 | 47 | 27.0% | |
| Pyrexia | 174 | 42 | 24.1% | |
| Rash | 174 | 36 | 20.7% | |
| Vomiting | 174 | 35 | 20.1% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 174 | 141 | 81.0% | |
| Anaemia | 174 | 120 | 69.0% | |
| Neutropenia | 174 | 131 | 75.3% | |
| Leucopenia | 174 | 102 | 58.6% | |
| AEs – grade 3–4 | ||||
| Abdominal pain | 174 | 0 | 0.0% | |
| Anorexia | 174 | 1 | 0.6% | |
| Arthralgia | 174 | 0 | 0.0% | |
| Asthenia | 174 | 4 | 2.3% | |
| Diarrhoea | 174 | 13 | 7.5% | |
| Dizziness | 174 | 0 | 0.0% | |
| Dyspnoea | 174 | 7 | 4.0% | |
| Fatigue | 174 | 7 | 4.0% | |
| Headache | 174 | 1 | 0.6% | |
| Myalgia | 174 | 1 | 0.6% | |
| Nausea | 174 | 1 | 0.6% | |
| Pain in extremity | 174 | 0 | 0.0% | |
| Peripheral oedema | 174 | 1 | 0.6% | |
| Petechiae | 174 | 2 | 1.1% | |
| Pleural effusion | 174 | 8 | 4.6% | |
| Pyrexia | 174 | 7 | 4.0% | |
| Rash | 174 | 2 | 1.1% | |
| Vomiting | 174 | 4 | 2.3% | |
| 14 months’ follow-up (ImR) | ||||
| CyR | ||||
| CCyR | 161 | 50 | 31.1% | |
| PCyR | 161 | 12 | 7.5% | |
| MCyR | 161 | 62 | 38.5% | |
| Minor CyR | 161 | 10 | 6.2% | |
| HR | ||||
| Overall HR | 161 | 126 | 78.3% | |
| CHR | 161 | 72 | 44.7% | |
| Major HR | 161 | 102 | 63.4% | |
| No evidence of leukaemia | 161 | 30 | 18.6% | |
| Study medication | ||||
| Duration of study therapy (months) | 161 | |||
| Average daily dose (mg q.d.) (median) | 161 | 127 (range 32–196) | ||
| Participant disposition | ||||
| Withdrawal because of AEs | 161 | 16f | 9.9% | |
| Haematological AEs – grades 1–4 | ||||
| Anaemia | 161 | 159 | 98.8% | |
| Neutropenia | 161 | 146 | 90.7% | |
| Thrombopenia | 161 | 155 | 96.3% | |
| Leucopenia | 161 | 140 | 87.0% | |
| AEs – grades 1–4 | ||||
| Abdominal pain | 161 | 17 | 10.6% | |
| Anorexia | 161 | 25 | 15.5% | |
| Arthralgia | 161 | 22 | 13.7% | |
| Asthenia | 161 | 22 | 13.7% | |
| Cough | 161 | 18 | 11.2% | |
| Diarrhoea | 161 | 81 | 50.3% | |
| Dizziness | 161 | 17 | 10.6% | |
| Dyspnoea | 161 | 34 | 21.1% | |
| Fatigue | 161 | 42 | 26.1% | |
| Headache | 161 | 49 | 30.4% | |
| Myalgia | 161 | 19 | 11.8% | |
| Nausea | 161 | 45 | 28.0% | |
| Pain in extremity | 161 | 20 | 12.4% | |
| Peripheral oedema | 161 | 35 | 21.7% | |
| Petechiae | 161 | 22 | 13.7% | |
| Pleural effusion | 161 | 44 | 27.3% | |
| Pyrexia | 161 | 38 | 23.6% | |
| Rash | 161 | 33 | 20.5% | |
| Vomiting | 161 | 29 | 18.0% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 161 | 131 | 81.4% | |
| Anaemia | 161 | 103 | 64.0% | |
| Neutropenia | 161 | 118 | 73.3% | |
| Leucopenia | 161 | 91 | 56.5% | |
| AEs – grade 3–4 | ||||
| Abdominal pain | 161 | 0 | 0.0% | |
| Anorexia | 161 | 1 | 0.6% | |
| Arthralgia | 161 | 0 | 0.0% | |
| Asthenia | 161 | 4 | 2.5% | |
| Diarrhoea | 161 | 11 | 6.8% | |
| Dizziness | 161 | 0 | 0.0% | |
| Dyspnoea | 161 | 7 | 4.3% | |
| Fatigue | 161 | 6 | 3.7% | |
| Headache | 161 | 1 | 0.6% | |
| Myalgia | 161 | 1 | 0.6% | |
| Nausea | 161 | 1 | 0.6% | |
| Pain in extremity | 161 | 0 | 0.0% | |
| Peripheral oedema | 161 | 1 | 0.6% | |
| Petechiae | 161 | 2 | 1.2% | |
| Pleural effusion | 161 | 8 | 5.0% | |
| Pyrexia | 161 | 6 | 3.7% | |
| Rash | 161 | 2 | 1.2% | |
| Vomiting | 161 | 4 | 2.5% | |
| 14 months’ follow-up (ImI) | 13 | 5 | 38.5% | |
| CyR | ||||
| CCyR | ||||
| PCyR | 13 | 0 | 0.0% | |
| MCyR | 13 | 5 | 38.5% | |
| Minor CyR | 13 | 0 | 0.0% | |
| HR | 13 | 12 | 92.3% | |
| Overall HR | ||||
| CHR | 13 | 6 | 46.2% | |
| Major HR | 13 | 9 | 69.2% | |
| No evidence of leukaemia | 13 | 3 | 23.1% | |
| Study medication | 13 | |||
| Duration of study therapy (months) | ||||
| Average daily dose (mg q.d.) (median) | 13 | 110 (range 49–140) | ||
| Participant disposition | 13 | 2g | 15.4% | |
| Withdrawal because of AEs | ||||
| Haematological AEs – grades 1–4 | 13 | 13 | 100.0% | |
| Anaemia | ||||
| Neutropenia | 13 | 13 | 100.0% | |
| Thrombopenia | 13 | 12 | 92.3% | |
| Leucopenia | 13 | 12 | 92.3% | |
| AEs – grades 1–4 | 13 | 2 | 15.4% | |
| Abdominal pain | ||||
| Anorexia | 13 | 2 | 15.4% | |
| Arthralgia | 13 | 0 | 0.0% | |
| Asthenia | 13 | 2 | 15.4% | |
| Cough | 13 | 0 | 0.0% | |
| Diarrhoea | 13 | 9 | 69.2% | |
| Dizziness | 13 | 1 | 7.7% | |
| Dyspnoea | 13 | 3 | 23.1% | |
| Fatigue | 13 | 4 | 30.8% | |
| Headache | 13 | 2 | 15.4% | |
| Myalgia | 13 | 1 | 7.7% | |
| Nausea | 13 | 3 | 23.1% | |
| Pain in extremity | 13 | 1 | 7.7% | |
| Peripheral oedema | 13 | 4 | 30.8% | |
| Petechiae | 13 | 2 | 15.4% | |
| Pleural effusion | 13 | 3 | 23.1% | |
| Pyrexia | 13 | 4 | 30.8% | |
| Rash | 13 | 3 | 23.1% | |
| Vomiting | 13 | 6 | 46.2% | |
| Haematological AEs – grade 3–4 | 13 | 10 | 76.9% | |
| Thrombopenia | ||||
| Anaemia | 13 | 11 | 84.6% | |
| Neutropenia | 13 | 13 | 100.0% | |
| Leucopenia | 13 | 11 | 84.6% | |
| AEs – grade 3–4 | 13 | 0 | 0.0% | |
| Abdominal pain | ||||
| Anorexia | 13 | 0 | 0.0% | |
| Arthralgia | 13 | 0 | 0.0% | |
| Asthenia | 13 | 0 | 0.0% | |
| Diarrhoea | 13 | 2 | 15.4% | |
| Dizziness | 13 | 0 | 0.0% | |
| Dyspnoea | 13 | 0 | 0.0% | |
| Fatigue | 13 | 1 | 7.7% | |
| Headache | 13 | 0 | 0.0% | |
| Myalgia | 13 | 0 | 0.0% | |
| Nausea | 13 | 0 | 0.0% | |
| Pain in extremity | 13 | 0 | 0.0% | |
| Peripheral oedema | 13 | 0 | 0.0% | |
| Petechiae | 13 | 0 | 0.0% | |
| Pleural effusion | 13 | 0 | 0.0% | |
| Pyrexia | 13 | 1 | 7.7% | |
| Rash | 13 | 0 | 0.0% | |
| Vomiting | 13 | 0 | 0.0% | |
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? Yes | ||||
| 1.2 Were the case series collected at more than one centre? Multicentre | ||||
| 1.3 Was the main outcome independently assessed? No | ||||
| 1.4 Are patient characteristics adequately described? Yes | ||||
| 1.5 How easy is it to assess generalisability of the results? High | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? Yes | ||||
| 2.2 Were data collected prospectively? Yes | ||||
| 2.3 Were patients recruited consecutively? Yes | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? No. Treatment was reduced or interrupted in response to haematological or non-haematological toxicity | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Uncertain | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? Yes | ||||
| 4.2 Were dropouts from the study adequately described? Yes | ||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Hochhaus et al. (2007)11 Secondary publications: Baccarani et al. (2006),134 Hochhaus et al. (2006),135 Hochhaus et al. (2008),105 Stone et al. (2007),139 Mauro et al. (2008),147 Hochhaus et al. (2005),133 Hochhaus et al. (2008),146 Deininger et al. (2008),144 Cortes et al. (2008),143 Mueller et al. (2007),138 Cervantes et al. (2008),141 Hochhaus et al. (2008),145 Baccarani et al. (2008),140 Guilhot et al. (2007),140 Hochhaus et al. (2006),136 Cervantes et al. (2008)142 Design: case series (prospective) CP: yes AP: no BC: no Country: (n = 20) Australia, Belgium, Canada, Denmark, Finland, France, Germany, Ireland, Israel, Italy, Republic of Korea, the Netherlands, Peru, Singapore, Spain, Sweden, Switzerland, the UK, and the USA Number of centres: 75 Trial code(s): CA180013 START-C |
Inclusion criteria: patients, aged at least 18 years and who had ImR or ImI CML in CP. CP CML was defined as < 15% blasts in PB and BM, < 20% basophils in PB, < 30% blasts plus promyelocytes in PB and BM, platelet at least 100 × 109/l unless thrombopenia was because of recent therapy, and no extramedullary involvement other than in liver or spleen The ImR population included patients with progressive CML-CP on imatinib > 600 mg q.d. or those who had resistance to imatinib ≯ 600 mg q.d. and BCR–ABL mutations associated with high-level imatinib resistance ImR was defined as a lack of CHR after 3 months of imatinib treatment, a lack of any CyR after 6 months of treatment, a lack of an MCyR (Ph+ cells > 35%) after 12 months of treatment, an increasing WBC count on at least two consecutive occasions, or a relapse after a CHR or MCyR. ImI was defined as at least grade 3 non-haematological toxicity, or grade 4 haematological toxicity persisting for > 7 days, related to imatinib at any dose Exclusion criteria: patients with prior CML-AP or -BC; prior dasatinib therapy; imatinib therapy within 7 days of initiation; an Eastern Cooperative Oncology Group (ECOG) performance status > 1; uncontrolled or significant cardiovascular disease; or a history of a significant bleeding disorder unrelated to CML |
Arm 1 dasatinib n: 186 Drug: dasatinib Starting daily dose (mg): 140 Dosage details: 70 mg b.i.d.; escalation to 90 mg b.i.d. permitted for patients with suboptimal response interruptions or reduction to 50 mg or 40 mg b.i.d. in response to toxicity Concurrent treatment: no treatment for CML other than dasatinib was permitted during the study; except anagrelide and hydroxycarbamide for treatment of elevated platelet counts (higher than 700 × 109/l) and WBC counts (higher than 50 × 109/l), respectively. Use of hydroxycarbamide was limited to a period of 2 weeks. Administration of colony-stimulating factors and recombinant erythropoietin was permitted at the discretion of the investigator |
CyR: based on the prevalence of Ph+ metaphases among at least 20 metaphase cells in BM aspirates or biopsies (conducted every 12 weeks) CCyR (0% Ph+) PCyR (1–35% Ph+) MCyR (complete + partial) Minor CyR (36–65% Ph+) Minimal CyR (66–95% Ph+) Duration of MCyR HR: monitored by CBCs (once weekly for the first 12 weeks, and every 3 months thereafter) CHR [WBC count no more than the institutional upper limit of normal; ANC at least 1 × 109/l; platelet count < 450 × 109/l and no more than the institutional upper limit of normal; no blasts or promyelocytes in PB; > 5% myelocytes plus metamyelocytes in PB; > 2% basophils in PB; no extramedullary involvement (including no hepatomegaly or splenomegaly). Haematological responses were required to be maintained for at least 4 weeks] Duration of CHR Study medication: duration of study therapy (months) Average daily dose (mg q.d.) Survival: PFS (progression = development of CML-AP or -BC; loss of MCyR; loss of CHR; or an increasing WBC count) OS Participant disposition: withdrawal because of AEs AEs – grades 1–4: assessment of study drug toxicities was continuous and included a physical examination to monitor AEs, conducted weekly for the first month and every 4 weeks thereafter, with AEs graded according to the NCI CTC Version 3.0186 |
|
| Dasatinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| Demographics | ||||
| Age (years) (median) | 186 | 59 (range 24–79) | ||
| Gender (n male) | 186 | 86a | 46.2% | |
| Prior therapy | ||||
| Time on imatinib > 1 year | 186 | 37a | 19.9% | |
| Time on imatinib 1–3 years | 186 | 48a | 25.8% | |
| Time on imatinib > 3 years | 186 | 100a | 53.8% | |
| Highest imatinib dose 400–600 mg q.d. | 186 | 89a | 47.8% | |
| Highest imatinib dose > 600 mg q.d. | 186 | 97a | 52.2% | |
| Prior chemotherapy | 186 | 78a | 41.9% | |
| Prior interferon | 186 | 130a | 69.9% | |
| Prior transplantation | 186 | 17a | 9.1% | |
| Disease history | ||||
| Duration of CML (months) (median) | 186 | 64 | ||
| Laboratory parameters | ||||
| WBC × 109/l (median) | 186 | 9.9 (range 0.4–196.5) | ||
| WBC – 20 × 109/l or more | 186 | 56a | 30.1% | |
| Platelets × 109/l (median) | 186 | 290 (range 24–1912) | ||
| Basophils in PB (%) (median) | 186 | 2 (range 0–20) | ||
| ImR | ||||
| Demographics | ||||
| Age (years) (median) | 127 | 59 (range 24–79) | ||
| Gender (n male) | 127 | 60a | 47.2% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 127 | 6a | 4.7% | |
| Time on imatinib 1–3 years | 127 | 30a | 23.6% | |
| Time on imatinib > 3 years | 127 | 91a | 71.7% | |
| Highest imatinib dose 400–600 mg q.d. | 127 | 34a | 26.8% | |
| Highest imatinib dose > 600 mg q.d. | 127 | 93a | 73.2% | |
| Prior chemotherapy | 127 | 64a | 50.4% | |
| Prior interferon | 127 | 98a | 77.2% | |
| Prior transplantation | 127 | 13a | 10.2% | |
| Disease history | ||||
| Duration of CML (months) (median) | 127 | 77 | ||
| Laboratory parameters | ||||
| WBC × 109/l (median) | 127 | 11.9 (range 0.4–196.5) | ||
| WBC – 20 × 109/l or more | 127 | 48a | 37.8% | |
| Platelets × 109/l (median) | 127 | 300 (range 24–1912) | ||
| Basophils in PB (%) (median) | 127 | 3 (range 0–18) | ||
| ImI | ||||
| Demographics | ||||
| Age (years) (median) | 59 | 59 (range 24–79) | ||
| Gender (n male) | 59 | 26a | 44.1% | |
| Prior therapy: | ||||
| Time on imatinib < 1 year | 59 | 32a | 54.2% | |
| Time on imatinib 1–3 years | 59 | 18a | 30.5% | |
| Time on imatinib > 3 years | 59 | 9a | 15.3% | |
| Highest imatinib dose 400–600 mg q.d. | 59 | 55a | 93.2% | |
| Highest imatinib dose > 600 mg q.d. | 59 | 4a | 6.8% | |
| Prior chemotherapy | 59 | 15a | 25.4% | |
| Prior interferon | 59 | 32a | 54.2% | |
| Prior transplantation | 59 | 4a | 6.8% | |
| Disease history | ||||
| Duration of CML (months) (median) | 59 | 26 | ||
| Laboratory parameters | ||||
| WBC × 109/l (median) | 59 | 7.4 (range 2.0–182.7) | ||
| WBC – 20 × 109/l or more | 59 | 8a | 13.6% | |
| Platelets × 109/l (median) | 59 | 254 (range 61–1165) | ||
| Basophils in PB (%) (median) | 59 | 1 (range 0–20) | ||
| 18 months’ follow-up (all) | ||||
| Demographics | ||||
| Age (years) (median) | 387 | 58 (range 21–85) | ||
| Gender (n male) | 387 | 191 | 49.4% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 387 | 74 | 19.1% | |
| Time on imatinib 1–3 years | 387 | 107 | 27.6% | |
| Time on imatinib > 3 years | 387 | 206 | 53.2% | |
| Highest imatinib dose < 400 mg q.d. | 387 | 1 | 0.3% | |
| Highest imatinib dose 400–600 mg q.d. | 387 | 172 | 44.4% | |
| Highest imatinib dose > 600 mg q.d. | 387 | 214 | 55.3% | |
| Prior chemotherapy | 387 | 135 | 34.9% | |
| Prior interferon | 387 | 252 | 65.1% | |
| Prior transplantation | 387 | 38b | 9.8% | |
| Prior radiotherapy | 387 | 9 | 2.3% | |
| Disease history | ||||
| Duration of CML (months) (median) | 387 | 60.7 (range 2.8–250.5) | ||
| Previous CHR to imatinib | 387 | 318 | 82.2% | |
| Previous CCyR to imatinib | 387 | 75 | 19.4% | |
| Previous MCyR to imatinib | 387 | 143 | 37.0% | |
| Baseline status | ||||
| Splenomegaly | 387 | 21 | 5.4% | |
| Hepatomegaly | 387 | 4 | 1.0% | |
| Lymph node | 387 | 0 | 0.0% | |
| ECOG performance status 0 | 384 | 276 | 71.9% | |
| ECOG performance status 1 | 384 | 105 | 27.3% | |
| ECOG performance status 2 | 384 | 3 | 0.8% | |
| CHR at study entry | 387 | 154 | 39.8% | |
| MCyR at study entry | 387 | 41 | 10.6% | |
| BCR–ABL mutation | 345 | 139 | 40.3% | |
| 18 months’ follow-up (ImR) | ||||
| Demographics | ||||
| Age (years) (median) | 288 | 58 (range 21–85) | ||
| Gender (n male) | 288 | 149 | 51.7% | |
| Prior therapy | ||||
| Time on imatinib < 1 year | 288 | 17 | 5.9% | |
| Time on imatinib 1–3 years | 288 | 77 | 26.7% | |
| Time on imatinib > 3 years | 288 | 194 | 67.4% | |
| Highest imatinib dose < 400 mg q.d. | 288 | 1 | 0.3% | |
| Highest imatinib dose 400–600 mg q.d. | 288 | 81 | 28.1% | |
| Highest imatinib dose > 600 mg q.d. | 288 | 206 | 71.5% | |
| Prior chemotherapy | 288 | 117 | 40.6% | |
| Prior interferon | 288 | 206 | 71.5% | |
| Prior transplantation | 288 | 31b | 10.8% | |
| Prior radiotherapy | 288 | 6 | 2.1% | |
| Disease history | ||||
| Duration of CML (months) (median) | 288 | 74.4 (range 2.8–250.5) | ||
| Previous CHR to imatinib | 288 | 242 | 84.0% | |
| Previous CCyR to imatinib | 288 | 48 | 16.7% | |
| Previous MCyR to imatinib | 288 | 100 | 34.7% | |
| Baseline status | ||||
| Splenomegaly | 288 | 20 | 6.9% | |
| Hepatomegaly | 288 | 4 | 1.4% | |
| Lymph node | 288 | 0 | 0.0% | |
| ECOG performance status 0 | 285 | 205 | 71.9% | |
| ECOG performance status 1 | 285 | 77 | 27.0% | |
| ECOG performance status 2 | 285 | 3 | 1.1% | |
| CHR at study entry | 288 | 103 | 35.8% | |
| MCyR at study entry | 288 | 18 | 6.3% | |
| BCR–ABL mutation | 254 | 128 | 50.4% | |
| 18 months’ follow-up (ImI) | 99 | 57 (range 24–79) | ||
| Demographics | ||||
| Age (years) (median) | ||||
| Gender (n male) | 99 | 42 | 42.4% | |
| Prior therapy | 99 | 57 | 57.6% | |
| Time on imatinib < 1 year | ||||
| Time on imatinib 1–3 years | 99 | 30 | 30.3% | |
| Time on imatinib > 3 years | 99 | 12 | 12.1% | |
| Highest imatinib dose < 400 mg q.d. | 99 | 0 | 0.0% | |
| Highest imatinib dose 400–600 mg q.d. | 99 | 91 | 91.9% | |
| Highest imatinib dose > 600 mg q.d. | 99 | 8 | 8.1% | |
| Prior chemotherapy | 99 | 18 | 18.2% | |
| Prior interferon | 99 | 46 | 46.5% | |
| Prior transplantation | 99 | 7b | 7.1% | |
| Prior radiotherapy | 99 | 3 | 3.0% | |
| Disease history | 99 | 26.3 (range 3.2–144.5) | ||
| Duration of CML (months) (median) | ||||
| Previous CHR to imatinib | 99 | 76 | 76.8% | |
| Previous CCyR to imatinib | 99 | 27 | 27.3% | |
| Previous MCyR to imatinib | 99 | 43 | 43.4% | |
| Baseline status | 99 | 1 | 1.0% | |
| Splenomegaly | ||||
| Hepatomegaly | 99 | 0 | 0.0% | |
| Lymph node | 99 | 0 | 0.0% | |
| ECOG performance status 0 | 99 | 71 | 71.7% | |
| ECOG performance status 1 | 99 | 28 | 28.3% | |
| ECOG performance status 2 | 99 | 0 | 0.0% | |
| CHR at study entry | 99 | 51 | 51.5% | |
| MCyR at study entry | 99 | 23 | 23.2% | |
| BCR–ABL mutation | 91 | 11 | 12.1% | |
| Results | ||||
| CyR | 186 | 73c | 39.2% | |
| CCyR | ||||
| PCyR | 186 | 24c | 12.9% | |
| MCyR | 186 | 97c | 52.2% | |
| Minor CyR | 186 | 7c | 3.8% | |
| Minimal CyR | 186 | 16c | 8.6% | |
| Duration of MCyR – 0 months | 186 | 1 | ||
| Duration of MCyR – 1 months | 1 | |||
| Duration of MCyR – 2 months | 0.99 | |||
| Duration of MCyR – 3 months | 0.99 | |||
| Duration of MCyR – 4 months | 0.99 | |||
| Duration of MCyR – 5 months | 0.99 | |||
| Duration of MCyR – 6 months | 0.96 | |||
| HR | ||||
| CHR | 186 | 168c | 90.3% | |
| Study medication | ||||
| Duration of study therapy (months) (median) | 186 | 8.3 (range 0.03–11) | ||
| Average daily dose (mg q.d.) (median) | 186 | 101 (range 18–149) | ||
| Survival | ||||
| PFS – 0 months | 186 | 1 | ||
| PFS – 2 months | 0.98 | |||
| PFS – 4 months | 0.96 | |||
| PFS – 6 months | 0.94 | |||
| PFS – 8 months | 0.92 | |||
| PFS – 10 months | 0.87 | |||
| AEs – grades 1–4 | ||||
| Asthenia | 186 | 37 | (19.9%) | |
| Diarrhoea | 186 | 56 | 30.1% | |
| Dyspnoea | 186 | 51 | 27.4% | |
| Elevated activity of ALAT | 186 | 96 | 51.6% | |
| Elevated activity of ASAT | 186 | 111 | 59.7% | |
| Elevated bilirubin | 186 | 26 | 14.0% | |
| Fatigue | 186 | 52 | 28.0% | |
| Headache | 186 | 63 | 33.9% | |
| Nausea | 186 | 36 | 19.4% | |
| Peripheral oedema | 186 | 33 | 17.7% | |
| Pleural effusion | 186 | 35 | 18.8% | |
| Rash | 186 | 41 | 22.0% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 186 | 88 | 47.3% | |
| Anaemia | 186 | 40 | 21.5% | |
| Neutropenia | 186 | 92 | 49.5% | |
| Leucopenia | 186 | 46 | 24.7% | |
| AEs – grade 3–4 | ||||
| Asthenia | 186 | 3 | 1.6% | |
| Diarrhoea | 186 | 4 | 2.2% | |
| Dyspnoea | 186 | 6 | 3.2% | |
| Elevated activity of ALAT | 186 | 3 | 1.6% | |
| Elevated activity of ASAT | 186 | 4 | 2.2% | |
| Elevated bilirubin | 186 | 0 | 0.0% | |
| Fatigue | 186 | 2 | 1.1% | |
| Headache | 186 | 2 | 1.1% | |
| Nausea | 186 | 2 | 1.1% | |
| Peripheral oedema | 186 | 0 | 0.0% | |
| Pleural effusion | 186 | 6 | 3.2% | |
| Rash | 186 | 1 | 0.5% | |
| ImR | ||||
| CyR | ||||
| CCyR | 127 | 35c | 27.6% | |
| PCyR | 127 | 15c | 11.8% | |
| MCyR | 127 | 50c | 39.4% | |
| Minor CyR | 127 | 6c | 4.7% | |
| Minimal CyR | 127 | 15c | 11.8% | |
| Duration of MCyR – 0 months | 127 | 1 | ||
| Duration of MCyR – 1 months | 1 | |||
| Duration of MCyR – 2 months | 0.975 | |||
| Duration of MCyR – 3 months | 0.975 | |||
| Duration of MCyR – 4 months | 0.975 | |||
| Duration of MCyR – 5 months | 0.975 | |||
| Duration of MCyR – 6 months | 0.915 | |||
| HR | 127 | 111c | 87.4% | |
| CHR | ||||
| Survival | 127 | 1 | ||
| PFS – 0 months | ||||
| PFS – 2 months | 0.975 | |||
| PFS – 4 months | 0.94 | |||
| PFS – 6 months | 0.91 | |||
| PFS – 8 months | 0.89 | |||
| PFS – 10 months | 0.84 | |||
| ImI | 59 | 38c | 64.4% | |
| CyR | ||||
| CCyR | ||||
| PCyR | 59 | 9c | 15.3% | |
| MCyR | 59 | 47c | 79.7% | |
| Minor CyR | 59 | 1c | 1.7% | |
| Minimal CyR | 59 | 1c | 1.7% | |
| Duration of MCyR – 0 months | 59 | 1 | ||
| Duration of MCyR – 1 months | 1 | |||
| Duration of MCyR – 2 months | 1 | |||
| Duration of MCyR – 3 months | 1 | |||
| Duration of MCyR – 4 months | 1 | |||
| Duration of MCyR – 5 months | 1 | |||
| HR | 59 | 57c | 96.6% | |
| CHR | ||||
| Survival | 59 | 1 | ||
| PFS – 0 months | ||||
| PFS – 2 months | 1 | |||
| PFS – 4 months | 1 | |||
| PFS – 6 months | 1 | |||
| PFS – 8 months | 1 | |||
| PFS – 10 months | 0.955 | |||
| 18 months’ follow-up (all) | 387 | 189 | 48.8% | |
| CyR | ||||
| CCyR | ||||
| PCyR | 387 | 41 | 10.6% | |
| MCyR | 387 | 230 | 59.4% | |
| Duration of MCyR – 0 months | 387 | 1 | ||
| Duration of MCyR – 2 months | 0.995 | |||
| Duration of MCyR – 4 months | 0.995 | |||
| Duration of MCyR – 6 months | 0.975 | |||
| Duration of MCyR – 8 months | 0.975 | |||
| Duration of MCyR – 10 months | 0.96 | |||
| Duration of MCyR – 12 months | 0.96 | |||
| Duration of MCyR – 14 months | 0.87 | |||
| HR | ||||
| CHR | 387 | 351 | 90.7% | |
| Duration of CHR – 0 months | 387 | 1 | ||
| Duration of CHR – 2 months | 0.995 | |||
| Duration of CHR – 4 months | 0.98 | |||
| Duration of CHR – 6 months | 0.97 | |||
| Duration of CHR – 8 months | 0.955 | |||
| Duration of CHR – 10 months | 0.94 | |||
| Duration of CHR – 12 months | 0.93 | |||
| Duration of CHR – 14 months | 0.92 | |||
| Duration of CHR – 16 months | 0.885 | |||
| Study medication | ||||
| Duration of study therapy (months) (median) | 387 | 13.8 (range 1.0–18.4) | ||
| Average daily dose (mg q.d.) (median) | 387 | 101 (range 11–171) | ||
| Survival | ||||
| PFS – 0 months | 387 | 1 | ||
| PFS – 2 months | 362 | 0.985 | ||
| PFS – 4 months | 344 | 0.96 | ||
| PFS – 6 months | 328 | 0.94 | ||
| PFS – 8 months | 312 | 0.925 | ||
| PFS – 10 months | 300 | 0.91 | ||
| PFS – 12 months | 270 | 0.905 | ||
| PFS – 14 months | 169 | 0.89 | ||
| PFS – 16 months | 61 | 0.865 | ||
| PFS – 18 months | 2 | 0.845 | ||
| OS – 0 months | 387 | 1 | ||
| OS – 2 months | 377 | 0.99 | ||
| OS – 4 months | 361 | 0.985 | ||
| OS – 6 months | 349 | 0.98 | ||
| OS – 8 months | 331 | 0.975 | ||
| OS – 10 months | 319 | 0.975 | ||
| OS – 12 months | 298 | 0.965 | ||
| OS – 14 months | 208 | 0.96 | ||
| OS – 16 months | 85 | 0.96 | ||
| OS – 18 months | 7 | 0.96 | ||
| Participant disposition | ||||
| Withdrawal because of AEs | 387 | 58d | 15.0% | |
| AEs – grades 1–4 | ||||
| Anorexia | 387 | 50 | 12.9% | |
| Asthenia | 387 | 55 | 14.2% | |
| Cough | 387 | 51 | 13.2% | |
| Diarrhoea | 387 | 143 | 37.0% | |
| Dyspnoea | 387 | 117 | 30.2% | |
| Fatigue | 387 | 121 | 31.3% | |
| Headache | 387 | 125 | 32.3% | |
| Nausea | 387 | 95 | 24.5% | |
| Peripheral oedema | 387 | 69 | 17.8% | |
| Pleural effusion | 387 | 106 | 27.4% | |
| Pyrexia | 387 | 60 | 15.5% | |
| Rash | 387 | 101 | 26.1% | |
| Vomiting | 387 | 42 | 10.9% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 387 | 187 | 48.3% | |
| Anaemia | 387 | 83 | 21.4% | |
| Neutropenia | 387 | 188 | 48.6% | |
| Leucopenia | 387 | 104 | 26.9% | |
| AEs – grade 3–4 | ||||
| Anorexia | 387 | 0 | 0.0% | |
| Asthenia | 387 | 4 | 1.0% | |
| Cough | 387 | 0 | 0.0% | |
| Diarrhoea | 387 | 11 | 2.8% | |
| Dyspnoea | 387 | 20 | 5.2% | |
| Fatigue | 387 | 8 | 2.1% | |
| Headache | 387 | 4 | 1.0% | |
| Nausea | 387 | 3 | 0.8% | |
| Peripheral oedema | 387 | 0 | 0.0% | |
| Pleural effusion | 387 | 24 | 6.2% | |
| Pyrexia | 387 | 4 | 1.0% | |
| Rash | 387 | 2 | 0.5% | |
| Vomiting | 387 | 2 | 0.5% | |
| 18 months’ follow-up (ImR) | ||||
| CyR | ||||
| CCyR | 288 | 115 | 39.9% | |
| PCyR | 288 | 36 | 12.5% | |
| MCyR | 288 | 151 | 52.4% | |
| Duration of MCyR – 0 months | 288 | 1 | ||
| Duration of MCyR – 2 months | 0.995 | |||
| Duration of MCyR – 4 months | 0.995 | |||
| Duration of MCyR – 6 months | 0.97 | |||
| Duration of MCyR – 8 months | 0.97 | |||
| Duration of MCyR – 10 months | 0.945 | |||
| Duration of MCyR – 12 months | 0.945 | |||
| Duration of MCyR – 14 months | 0.755 | |||
| HR | ||||
| CHR | 288 | 258 | 89.6% | |
| Duration of CHR – 0 months | 288 | 1 | ||
| Duration of CHR – 2 months | 0.995 | |||
| Duration of CHR – 4 months | 0.98 | |||
| Duration of CHR – 6 months | 0.96 | |||
| Duration of CHR – 8 months | 0.935 | |||
| Duration of CHR – 10 months | 0.925 | |||
| Duration of CHR – 12 months | 0.91 | |||
| Duration of CHR – 14 months | 0.91 | |||
| Duration of CHR – 16 months | 0.855 | |||
| Study medication | ||||
| Average daily dose (mg q.d.) (median) | 288 | 101 [range 18–171] | ||
| Survival | ||||
| PFS – 0 months | 288 | 1 | ||
| PFS – 2 months | 269 | 0.985 | ||
| PFS – 4 months | 255 | 0.95 | ||
| PFS – 6 months | 240 | 0.92 | ||
| PFS – 8 months | 226 | 0.9 | ||
| PFS – 10 months | 216 | 0.885 | ||
| PFS – 12 months | 196 | 0.88 | ||
| PFS – 14 months | 122 | 0.87 | ||
| PFS – 16 months | 43 | 0.835 | ||
| PFS – 18 months | 1 | 0.805 | ||
| OS – 0 months | 288 | 1 | ||
| OS – 2 months | 281 | 0.99 | ||
| OS – 4 months | 268 | 0.98 | ||
| OS – 6 months | 257 | 0.975 | ||
| OS – 8 months | 244 | 0.97 | ||
| OS – 10 months | 233 | 0.965 | ||
| OS – 12 months | 216 | 0.955 | ||
| OS – 14 months | 146 | 0.945 | ||
| OS – 16 months | 56 | 0.945 | ||
| OS – 18 months | 5 | 0.945 | ||
| 18 months’ follow-up (ImI) | ||||
| CyR | ||||
| CCyR | 99 | 74 | 74.7% | |
| PCyR | 99 | 5 | 5.1% | |
| MCyR | 99 | 79 | 79.8% | |
| Duration of MCyR – 0 months | 99 | 1 | ||
| Duration of MCyR – 2 months | 0.995 | |||
| Duration of MCyR – 4 months | 0.995 | |||
| Duration of MCyR – 6 months | 0.98 | |||
| Duration of MCyR – 8 months | 0.98 | |||
| Duration of MCyR – 10 months | 0.98 | |||
| Duration of MCyR – 12 months | 0.98 | |||
| Duration of MCyR – 14 months | 0.98 | |||
| HR | ||||
| CHR | 99 | 93 | 93.9% | |
| Duration of CHR – 0 months | 99 | 1 | ||
| Duration of CHR – 2 months | 1 | |||
| Duration of CHR – 4 months | 1 | |||
| Duration of CHR – 6 months | 1 | |||
| Duration of CHR – 8 months | 1 | |||
| Duration of CHR – 10 months | 0.975 | |||
| Duration of CHR – 12 months | 0.975 | |||
| Duration of CHR – 14 months | 0.96 | |||
| Duration of CHR – 16 months | 0.96 | |||
| Study medication | ||||
| Average daily dose (mg q.d.) (median) | 99 | 104 [range 11–140] | ||
| Survival | ||||
| PFS – 0 months | 99 | 1 | ||
| PFS – 2 months | 93 | 0.995 | ||
| PFS – 4 months | 89 | 0.995 | ||
| PFS – 6 months | 88 | 0.995 | ||
| PFS – 8 months | 86 | 0.995 | ||
| PFS – 10 months | 84 | 0.985 | ||
| PFS – 12 months | 74 | 0.985 | ||
| PFS – 14 months | 47 | 0.955 | ||
| PFS – 16 months | 18 | 0.955 | ||
| PFS – 18 months | 1 | 0.955 | ||
| OS – 0 months | 99 | 1 | ||
| OS – 2 months | 96 | 1 | ||
| OS – 4 months | 93 | 1 | ||
| OS – 6 months | 92 | 1 | ||
| OS – 8 months | 87 | 1 | ||
| OS – 10 months | 86 | 1 | ||
| OS – 12 months | 82 | 1 | ||
| OS – 14 months | 62 | 1 | ||
| OS – 16 months | 29 | 1 | ||
| OS – 18 months | 2 | 1 | ||
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? Yes. The report presented the reslults of a Phase II study evaluating dasatinib efficacy and safety | ||||
| 1.2 Were the case series collected at more than one centre? Multicentre | ||||
| 1.3 Was the main outcome independently assessed? No | ||||
| 1.4 Are patient characteristics adequately described? Yes | ||||
| 1.5 How easy is it to assess generalisability of the results? High | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? Yes | ||||
| 2.2 Were data collected prospectively? Yes | ||||
| 2.3 Were patients recruited consecutively? Yes | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? No. Could be interrupted or reduced in response to haematological toxicity of at least grade 3 or some non-haematological toxicity events of at least grade 2 | ||||
| 3.2 Is the use of any concurrent therapies adequately described? No. No treatment for CML other than dasatinib; except anagrelide and hydroxycarbamide for treatment of elevated platelet counts and WBC counts (threshold reported for both). Usage was limited to a period of 2 weeks. | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? No. Analysis of efficacy parameters was performed for all patients receiving at least one dose of dastinib | ||||
| 4.2 Were dropouts from the study adequately described? Yes | ||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Kantarjian et al. (2006)103 Secondary publications: Giles et al. (2005),110 La et al. (2008),112 Singer et al. (2007)111 Design: cohort study (prospective) CP: yes AP: yes BC: yes Country: unclear (authors from the USA and Germany) Number of centres: 3 Trial code(s): NCT00109707 |
Inclusion criteria: patients with Ph+ ImR CML or ALL who are at least 18 years of age and have an adequate performance status and normal hepatic, renal, and cardiac function. Patients with ImR CML-CP were enrolled in the study after the first four dose cohorts. Imatinib resistance was defined as a lack of CHR after 3 months of imatinib treatment, a lack of any CyR (Ph+ cells, > 95%) after 6 months of treatment, a lack of a substantial CyR (Ph+ cells > 35%) after 12 months of treatment, or a relapse after a HR or a substantial CyR Note: 13 (11%) of the patients were Ph+ ALL Exclusion criteria: patients who had received imatinib therapy 7 days before or hydroxycarbamide 2 days before the study began were not eligible to participate |
Arm 1 nilotinib n: 119 Drug: nilotinib Starting daily dose (mg): not reported Dosage details: nine dose cohorts, ranging from 50 mg to 1200 mg q.d. and from 400 mg to 600 mg b.i.d. Concurrent treatment: during the first cycle of therapy or at times of worsening disease before intrapatient dose escalation, patients were allowed to receive cytoreductive therapy (leucapheresis and hydroxycarbamide) to control elevated counts of blasts, platelets, or both Notes: multiple arms with different dosage levels; however, outcomes of interest for effectiveness only reported for all enrolled participants |
CyR: BM assessments were done on days 15 and 28 of the first cycle and on day 28 of every even-numbered cycle CCyR (0% Ph+) PCyR (1–35% Ph+) MCyR (complete + partial) Minor CyR (36–65% Ph+) Minimal CyR (66–95% Ph+) Overall CyR (major + minor + minimal) HR: CBCs and biochemical analysis were obtained weekly for the first 8 weeks and then every other week Overall HR CHR (WBC count < 10 × 109/l; a platelet count < 450 × 109/l; < 5% myelocytes plus metamyelocytes, < 20% basophils; absence of blasts and promyelocytes in PB; absence of extramedullary involvement) Return to CP (< 15% blasts in the blood and BM; < 30% blasts plus promyelocytes in the blood or BM; < 20% peripheral basophils; > 100,000 platelets/mm3) Marrow response (unclear; the reader is directed to a series of other publications for definitions, one of which264 appears to classify this outcome as < 5% blasts in marrow) Study medication: duration of study therapy (months) Haematological AEs – grades 1–2: neutropenia, thrombopenia, anaemia AEs – grade 1–2: safety assessments included an evaluation of AEs, haematological and cardiac enzyme assessment, biochemical testing, urinalysis, electrocardiography, and physical examination. Toxic effects were graded according to the NCI CTC Version 3.0186 |
|
| Nilotinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| Demographics | ||||
| Age (years) (median) | 119 | 60 (range 15–83) | ||
| Gender (n male) | 119 | 57 | 47.9% | |
| Disease history | ||||
| Splenomegaly at study entry | 119 | 32 | 26.9% | |
| Imatinib failure | ||||
| BCR–ABL mutation | 91 | 41 | 45.1% | |
| Laboratory parameters | ||||
| Haemoglobin – below 10 g/dl | 119 | 40 | 33.6% | |
| WBC – 50 × 109/l or more | 119 | 41 | 34.5% | |
| Platelets – below 100 × 109/l | 119 | 98 | 82.4% | |
| CP | ||||
| Prior therapy | ||||
| Highest imatinib dose (median) | 17 | 600 (range 400–800) | ||
| Disease history | ||||
| Duration of CML (months) (median) | 17 | 59.7 (range 12.9–167.4) | ||
| AP (all) | ||||
| Prior therapy | ||||
| Highest imatinib dose (median) | 56 | 800 (range 400–1000) | ||
| Disease history | ||||
| Duration of CML (months) (median) | 56 | 90.6 (range 7.2–226.9) | ||
| AP (clonal evolution) | ||||
| Prior therapy | ||||
| Highest imatinib dose (median) | 10 | 600 (range 400–800) | ||
| Disease history | ||||
| Duration of CML (months) (median) | 10 | 59 (range 8.1–126.7) | ||
| BC (myeloid) | ||||
| Prior therapy | ||||
| Highest imatinib dose (median) | 24 | 600 (range 400–800) | ||
| Disease history | ||||
| Duration of CML (months) (median) | 24 | 49.9 (range 3.8–186.9) | ||
| BC (lymphoid) | ||||
| Prior therapy | ||||
| Highest imatinib dose (median) | 9 | 600 (range 400–800) | ||
| Disease history | ||||
| Duration of CML (months) (median) | 9 | 19.4 (range 3.2–82.9) | ||
| Results | ||||
| AEs – grades 1–2 | ||||
| Neutropenia | 119 | 1 | 0.8% | |
| Thrombopenia | 119 | 1 | 0.8% | |
| Anaemia | 119 | 3 | 2.5% | |
| Alopecia | 119 | 6 | 5.0% | |
| Constipation | 119 | 8 | 6.7% | |
| Dry skin | 119 | 12 | 10.1% | |
| Elevated ALT and/or AST | 119 | 1 | 0.8% | |
| Elevated bilirubin | 119 | 5 | 4.2% | |
| Elevated conjugated bilirubin | 119 | 2 | 1.7% | |
| Elevated lipase level | 119 | 0 | 0.0% | |
| Fatigue | 119 | 5 | 4.2% | |
| Nausea and/or vomiting | 119 | 8 | 6.7% | |
| Pruritus | 119 | 15 | 12.6% | |
| Rash | 119 | 20 | 16.8% | |
| AEs – grade 3–4 | ||||
| Thrombopenia | 119 | 20 | 16.8% | |
| Anaemia | 119 | 6 | 5.0% | |
| Neutropenia | 119 | 13 | 10.9% | |
| Alopecia | 119 | 0 | 0.0% | |
| Constipation | 119 | 0 | 0.0% | |
| Dry skin | 119 | 0 | 0.0% | |
| Elevated ALT and/or AST | 119 | 3 | 2.5% | |
| Elevated bilirubin | 119 | 3 | 2.5% | |
| Elevated lipase levels | 119 | 5 | 4.2% | |
| Elevated unconjugated bilirubin | 119 | 4 | 3.4% | |
| Fatigue | 119 | 1 | 0.8% | |
| Nausea and/or vomiting | 119 | 0 | 0.0% | |
| Pruritus | 119 | 2 | 1.7% | |
| Rash | 119 | 2 | 1.7% | |
| CP | ||||
| CyR | ||||
| CCyR | 17 | 6 | 35.3% | |
| PCyR | 17 | 0 | 0.0% | |
| MCyR | 17 | 6 | 35.3% | |
| Minor CyR | 17 | 0 | 0.0% | |
| Minimal CyR | 17 | 3 | 17.6% | |
| Overall CyR | 17 | 9 | 52.9% | |
| HR | ||||
| Overall HR | 12 | 11 | 91.7% | |
| CHR | 12 | 11 | 91.7% | |
| Study medication | ||||
| Duration of study therapy (months) (median) | 17 | 4.9 (range 1.4–9.3) | ||
| AP (all) | ||||
| CyR | ||||
| CCyR | 56 | 8 | 14.3% | |
| PCyR | 56 | 7 | 12.5% | |
| MCyR | 56 | 15 | 26.8% | |
| Minor CyR | 56 | 5 | 8.9% | |
| Minimal CyR | 56 | 11 | 19.6% | |
| Overall CyR | 56 | 31 | 55.4% | |
| HR | ||||
| Overall HR | 51 | 38 | 74.5% | |
| CHR | 51 | 26 | 51.0% | |
| Return to CP | 51 | 9 | 17.6% | |
| Marrow response | 51 | 3 | 5.9% | |
| Study medication | ||||
| Duration of study therapy (months) (median) | 56 | 5.1 (range 0.3–12.6) | ||
| AP (clonal evolution) | ||||
| Study medication | ||||
| Duration of study therapy (months) (median) | 10 | 5 (range 0.1–9.6) | ||
| BC (all) | ||||
| CyR | ||||
| CCyR | 33 | 2 | 6.1% | |
| PCyR | 33 | 4 | 12.1% | |
| MCyR | 33 | 6 | 18.2% | |
| Minor CyR | 33 | 2 | 6.1% | |
| Minimal CyR | 33 | 1 | 3.0% | |
| Overall CyR | 33 | 9 | 27.3% | |
| HR | ||||
| Overall HR | 33 | 13 | 39.4% | |
| CHR | 33 | 2 | 6.1% | |
| Return to CP | 33 | 8 | 24.2% | |
| Marrow response | 33 | 3 | 9.1% | |
| BC (myeloid) | ||||
| Study medication | ||||
| Duration of study therapy (months) (median) | 24 | 2.9 (range 0.4–10.7) | ||
| BC (lymphoid) | ||||
| Study medication | ||||
| Duration of study therapy (months) (median) | 9 | 1.4 (range 0.9–9.7) | ||
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? Yes | ||||
| 1.2 Were the case series collected at more than one centre? Single centre | ||||
| 1.3 Was the main outcome independently assessed? No | ||||
| 1.4 Are patient characteristics adequately described? No. Not by dose group | ||||
| 1.5 How easy is it to assess generalisability of the results? Low | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? Yes. But only stated that patients with Ph+ ImR CML or ALL were eligible. Clearly? | ||||
| 2.2 Were data collected prospectively? Yes | ||||
| 2.3 Were patients recruited consecutively? Yes | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? No | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Uncertain | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? No | ||||
| 4.2 Were dropouts from the study adequately described? Yes | ||||
| Study details | Population | Arms | Outcomes | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
Study: Kantarjian et al. (2007)23 Secondary publications: Cannell (2007),84 Kantarjian et al. (2007),85 Schiffer (2007),87 Shah et al. (2006),82 Shah et al. (2006),83 Rousselot et al. (2008),89 Martinelli et al. (2007),86 Rousselot et al. (2008)88 CP: yes AP: no BC: no Country: not stated (n = 23); authors are from the USA, Brazil, France, Poland, Thailand, Russian Federation, Hungary and Australia Number of centres: 58 |
Inclusion criteria: patients with CML-CP with primary or acquired resistance to conventional doses of imatinib (400–600 mg), dastinib naive, at least 18 years of age and have adequate hepatic and renal function. CP was defined by the presence of < 15% blasts, < 20% basophils, and < 30% blasts plus promyelocytes in PB or BM and a platelet count of at least 100,000 per cubic millimetre, with no extramedullary involvement. Primary resistance to imatinib was defined as a lack of CHR after 3 months of imatinib treatment, a lack of any CyR after 6 months of treatment or a lack of a MCyR (Ph+ cells > 35%) after 12 months of treatment. Relapse after a HR or MCyR was considered as secondary or acquired resistance Exclusion criteria: patients who had received imatinib in the 7 days before the study were ineligible, as were patients who had received imatinib at doses in excess of 600 mg q.d. Patients with known specific BCR–ABL mutations (with high resistance to imatinib) before study entry were excluded Method of allocation: 2 : 1 randomisation (no details of methods used) Blinding: open-label Therapy common to all participants: not reported |
Arm 1 dasatinib n: 101 Drug: dasatinib Starting daily dose (mg): 140 Dosage details: 70 mg b.i.d. escalated to 180 mg for participants with inadequate response at 12 weeks or progression reduced to 100 mg or 80 mg for participants experiencing toxicity Notes: crossover to the alternate treatment was permitted after confirmed progression, lack of MCyR at the week 12 cytogenetic evaluation, or intolerance Arm 2 HDI n: 49 Drug: imatinib Starting daily dose (mg): 800 Dosage details: 400 mg b.i.d. Reduction to 600 mg was permitted for toxicity in participants who had not previously received 600 mg imatinib Notes: crossover to the alternative treatment was permitted after confirmed progression, lack of MCyR at the week 12 cytogenetic evaluation or intolerance |
CyR: evaluated through BM aspirates every 12 weeks CCyR (0% Ph+) PCyR (1–35% Ph+) MCyR (complete + partial) Duration of MCyR HR: weekly blood counts for the first 12 weeks of treatment and every 2 weeks thereafter CHR [WBC ≤ institutional ULN; platelets < 450 × 109/l; no blasts or promyelocytes in PB; < 5% myelocytes plus metamyelocytes in PB; < 20% basophils in PB; no extramedullary involvement (including no hepatomegaly or splenomegaly)] Molecular response: MMR (not defined in paper or in study referenced as providing definitions of response;22 usually defined as a reduction in BCR–ABL transcript levels of at least 3 log19) Study medication: duration of study therapy (months) Average daily dose (mg q.d.) Survival: time to treatment failure [time from randomisation to progression (see PFS) or end of treatment (lack of response, study drug intolerance, or off treatment for any reason); subjects still on treatment were censored as of their last day of dosing] PFS [time from randomisation until disease progression (AP disease, BC, loss of CHR or MCyR, or increasing WBC count), death, or discontinuation of treatment because of progression prior to crossover] Participant disposition: withdrawal because of AEs AEs – grades 1–4: assessed continuously and graded according to the NCI CTC Version 3.0. 186 Specific focus was given to cases of myelosuppression and fluid retention |
||||||
| Dasatinib | HDI | Δ | p-value | ||||||
| n | κ | Mean | n | κ | Mean | ||||
| Baseline characteristics | |||||||||
| Demographics | |||||||||
| Age (years) (median) | 101 | 51 (range 24–85) | 49 | 51 (range 24–80) | |||||
| Gender (n male) | 101 | 53 | 52.5% | 49 | 22 | 44.9% | 0.486a | ||
| Imatinib failure | |||||||||
| Resistance – loss of MCyR | 101 | 21 | 20.8% | 49 | 14 | 28.6% | 0.395a | ||
| Resistance – loss of CHR | 101 | 24 | 23.8% | 49 | 15 | 30.6% | 0.485a | ||
| Resistance – increasing WBC count | 101 | 4 | 4.0% | 49 | 2 | 4.1% | 0.683a | ||
| Resistance – no CHR after 3 months | 101 | 3 | 3.0% | 49 | 2 | 4.1% | 0.897a | ||
| Resistance – no CyR after 6 months | 101 | 39 | 38.6% | 49 | 16 | 32.7% | 0.596a | ||
| Resistance – no MCyR after 12 months | 101 | 39 | 38.6% | 49 | 24 | 49.0% | 0.303a | ||
| Prior therapy | |||||||||
| Best response to imatinib – CHR | 101 | 93 | 92.1% | 49 | 47 | 95.9% | 0.593a | ||
| Best response to imatinib – CCyR | 101 | 15 | 14.9% | 49 | 4 | 8.2% | 0.372a | ||
| Best response to imatinib – PCyR | 101 | 13 | 12.9% | 49 | 10 | 20.4% | 0.337a | ||
| Time on imatinib < 1 year | 101 | 12 | 11.9% | 49 | 5 | 10.2% | 0.977a | ||
| Time on imatinib 1–3 years | 101 | 44 | 43.6% | 49 | 29 | 59.2% | 0.105a | ||
| Time on imatinib > 3 years | 101 | 45 | 44.6% | 49 | 15 | 30.6% | 0.145a | ||
| Highest imatinib dose > 400 mg q.d. | 101 | 65 | 64.4% | 49 | 35 | 71.4% | 0.498a | ||
| Prior hydroxycarbamideb | 101 | 97 | 96.0% | 49 | 46 | 93.9% | 0.860a | ||
| Prior chemotherapy | 101 | 39 | 38.6% | 49 | 18 | 36.7% | 0.966a | ||
| Prior interferon | 101 | 74 | 73.3% | 49 | 33 | 67.3% | 0.576a | ||
| Prior transplantation | 101 | 7 | 6.9% | 49 | 2 | 4.1% | 0.747a | ||
| Disease history | |||||||||
| Duration of CML (months) (median) | 101 | 64 (range 6–166) | 49 | 52 (range 14–133) | |||||
| CHR at study entry | 101 | 51 | 50.5% | 49 | 27 | 55.1% | 0.722a | ||
| Baseline status | |||||||||
| CHR at study entry | 101 | 51 | 50.5% | 49 | 27 | 55.1% | 0.722a | ||
| Disease history | |||||||||
| MCyR at study entry | 101 | 6 | 5.9% | 49 | 0 | 0.0% | 0.283a | ||
| Baseline status | |||||||||
| MCyR at study entry | 101 | 6 | 5.9% | 49 | 0 | 0.0% | 0.283a | ||
| Imatinib failure | |||||||||
| BCR–ABL mutation | 101 | 41 | 40.6% | 49 | 11 | 22.4% | 0.045a | ||
| Baseline status | |||||||||
| BCR–ABL mutation | 101 | 41 | 40.6% | 49 | 11 | 22.4% | 0.045a | ||
| Laboratory parameters | |||||||||
| WBC × 109/l (median) | 101 | 7.5 (range 2–153) | 49 | 7.4 (range 2–133) | |||||
| WBC – 20 × 109/l or more | 101 | 11 | 10.9% | 49 | 7 | 14.3% | 0.740a | ||
| Platelets × 109/l (median) | 101 | 256 (range 55–1903) | 49 | 248 (range 80–2318) | |||||
| Results | |||||||||
| CyR | |||||||||
| CCyR | 101 | 40 | 39.6% | 49 | 8 | 16.3% | 0.007c | ||
| PCyR | 101 | 13 | 12.9% | 49 | 8 | 16.3% | 0.748c | ||
| MCyR | 101 | 53 | 52.5% | 49 | 16 | 32.7% | 0.035c | ||
| Duration of MCyR – 0 months | 53 | 1 | 16 | 1 | |||||
| Duration of MCyR – 12 months | 7 | 0.98 | 0 | 0.425 | |||||
| Duration of MCyR – 4 months | 44 | 0.98 | 9 | 0.835 | |||||
| Duration of MCyR – 8 months | 37 | 0.98 | 6 | 0.835 | |||||
| HR | |||||||||
| CHR | 101 | 94 | 93.1% | 49 | 40 | 81.6% | 0.065c | ||
| Molecular response | |||||||||
| MMR | 101 | 16 | 15.8% | 49 | 2 | 4.1% | 0.070c | ||
| Study medication | |||||||||
| Duration of study therapy (months) (median) | 101 | 13.7 (range 0.2–19.3) | 49 | 3.1 (range 0.2–15.6) | |||||
| Average daily dose (mg q.d.) (median) | 101 | 103 (range 38–175) | 49 | 796 (range 358–800) | |||||
| Survival | |||||||||
| Time to treatment failure – 0 months | 101 | 1 | 49 | 1 | |||||
| Time to treatment failure – 12 months | 66 | 0.74 | 9 | 0.205 | |||||
| Time to treatment failure – 15 months | 17 | 0.715 | 0 | 0.155 | |||||
| Time to treatment failure – 18 months | 4 | 0.715 | |||||||
| Time to treatment failure – 3 months | 95 | 0.935 | 36 | 0.735 | |||||
| Time to treatment failure – 6 months | 86 | 0.845 | 10 | 0.205 | |||||
| Time to treatment failure – 9 months | 79 | 0.78 | 10 | 0.205 | |||||
| PFS – 0 months | 101 | 1 | 49 | 1 | |||||
| PFS – 12 months | 66 | 0.925 | 9 | 0.73 | |||||
| PFS – 15 months | 17 | 0.925 | 0 | 0.545 | |||||
| PFS – 18 months | 4 | 0.925 | |||||||
| PFS – 3 months | 95 | 0.99 | 36 | 0.87 | |||||
| PFS – 6 months | 86 | 0.975 | 10 | 0.73 | |||||
| PFS – 9 months | 79 | 0.94 | 10 | 0.73 | |||||
| Participant disposition | |||||||||
| Withdrawal because of AEsd | 101 | 16 | 15.8% | 49 | 9 | 18.4% | |||
| AEs – grades 1–4 | |||||||||
| Anorexia | 101 | 13 | 12.9% | 49 | 4 | 8.2% | 0.748c | ||
| Asthenia | 101 | 13 | 12.9% | 49 | 2 | 4.1% | 0.563c | ||
| Diarrhoea | 101 | 35 | 34.7% | 49 | 14 | 28.6% | 0.008c | ||
| Dyspnoea | 101 | 21 | 20.8% | 49 | 2 | 4.1% | 0.087c | ||
| Face oedema | 101 | 4 | 4.0% | 49 | 5 | 10.2% | 0.003c | ||
| Fatigue | 101 | 30 | 29.7% | 49 | 11 | 22.4% | 0.099c | ||
| Headache | 101 | 25 | 24.8% | 49 | 5 | 10.2% | 0.701c | ||
| Muscle spasms | 101 | 2 | 2.0% | 49 | 6 | 12.2% | < 0.001c | ||
| Nausea | 101 | 24 | 23.8% | 49 | 16 | 32.7% | < 0.001c | ||
| Pain in extremity | 101 | 7 | 6.9% | 49 | 5 | 10.2% | 0.030c | ||
| Peripheral oedema | 101 | 10 | 9.9% | 49 | 10 | 20.4% | < 0.001c | ||
| Pleural effusion | 101 | 17 | 16.8% | 49 | 0 | 0.0% | 0.009c | ||
| Pyrexia | 101 | 14 | 13.9% | 49 | 5 | 10.2% | 0.431c | ||
| Rash | 101 | 17 | 16.8% | 49 | 7 | 14.3% | 0.147c | ||
| Superficial oedema | 101 | 15 | 14.9% | 49 | 21 | 42.9% | < 0.001c | ||
| Vomiting | 101 | 9 | 8.9% | 49 | 12 | 24.5% | < 0.001c | ||
| Weight increase | 101 | 5 | 5.0% | 49 | 5 | 10.2% | 0.008c | ||
| Haematological AEs – grade 3–4 | |||||||||
| Thrombopenia | 101 | 57 | 56.4% | 49 | 7 | 14.3% | |||
| Neutropenia | 101 | 62 | 61.4% | 49 | 19 | 38.8% | |||
| AEs – grade 3-4 | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Anorexia | |||||||||
| Asthenia | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Diarrhoea | 101 | 2 | 2.0% | 49 | 1 | 2.0% | 0.835c | ||
| Dyspnoea | 101 | 4 | 4.0% | 49 | 0 | 0.0% | 0.533c | ||
| Face oedema | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Fatigue | 101 | 2 | 2.0% | 49 | 2 | 4.1% | 0.171c | ||
| Headache | 101 | 2 | 2.0% | 49 | 1 | 2.0% | 0.835c | ||
| Muscle spasms | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Nausea | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Pain in extremity | 101 | 0 | 0.0% | 49 | 1 | 2.0% | 0.209c | ||
| Peripheral oedema | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Pleural effusion | 101 | 4 | 4.0% | 49 | 0 | 0.0% | 0.533c | ||
| Pyrexia | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Rash | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Superficial oedema | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Vomiting | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Weight increase | 101 | 0 | 0.0% | 49 | 0 | 0.0% | 0.482c | ||
| Quality appraisal | |||||||||
| 1. Is a power calculation provided? No | |||||||||
| 2. Is the sample size adequate? Not reported | |||||||||
| 3. Was ethical approval obtained? Yes | |||||||||
| 4. Were the study eligibilty criteria specified? Yes | |||||||||
| 5. Were the eligibility criteria appropriate? Yes | |||||||||
| 6. Were patients recruited prospectively? Yes | |||||||||
| 7. Was assignment to the treatment groups really random? Unknown | |||||||||
| 8. Were groups stratified? No | |||||||||
| 9. Was the treatment allocation concealed? Unknown | |||||||||
| 10. Are adequate baseline details presented? Yes | |||||||||
| 11. Are the participants representative of the population in question? Yes | |||||||||
| 12. Are groups similar at baseline? Yes. Well balanced with one exception; approximately twice as many patients in the dasatinib treatment arm (45%) had a BCR–ABL mutation as in the HDI group (22%) | |||||||||
| 13. Are any differences in baseline adequately adjusted for in the analysis? Yes | |||||||||
| 14. Are outcome assessors blind? Not clear | |||||||||
| 15. Was the care provider blinded? No. Open-label | |||||||||
| 16. Are outcome measures relevant to research question? Yes | |||||||||
| 17. Are data collection tools shown or known to be valid for the outcome of interest? Yes | |||||||||
| 18. Is compliance with treatment adequate? Unclear | |||||||||
| 19. Are withdrawals/dropouts adequately described? Yes | |||||||||
| 20. Are all patients accounted for? Yes | |||||||||
| 21. Is the number randomised reported? Yes | |||||||||
| 22. Are protocol violations specified? No | |||||||||
| 23. Are data analyses appropriate? Yes | |||||||||
| 24. Is analysis conducted on an ITT basis? Yes | |||||||||
| 25. Are missing data appropriately accounted for? Not reported | |||||||||
| 26. Were any subgroup analyses justified? Yes | |||||||||
| 27. Are the conclusions supported by the results? No. Open-label; relatively small sample size; lack of power calculation; unplanned crossover; results from subgroup analyses were based on small sample size | |||||||||
| 28. Generalisability: flaws in the study methodology impaired the internal validity of the study results | |||||||||
| 29. Inter-centre variability: not taken into account | |||||||||
| 30. Conflict of interest declared? Yes | |||||||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Kantarjian et al. (2007)106 Secondary publications: Hochhaus et al. (2007),151 Cortes et al. (2007),150 Kantarjian et al. (2006),148 Kantarjian et al. (2007),153 le Coutre et al. (2006),149 Martinelli et al. (2007),154 Rosti et al. (2007),156 Rosti et al. (2007),157 Mueller et al. (2007),155 Kantarjian et al. (2008),161 Saglio et al. (2008),164 Hughes et al. (2007),152 Jabbour et al. (2008),159 Lipton et al. (2008),162 Clark et al. (2009),165 Radich et al. (2008),163 Hochhaus et al. (2008),158 Kantarjian et al. (2008)160 Design: cohort study (prospective) CP: yes AP: no BC: no Country: not stated (n = 15); authors from the USA, Germany, Italy, the Netherlands, France, the UK and Spain Number of centres: 63 Trial code(s): NCT00109707 ***same as 425, but hard to see connection*** |
Inclusion criteria: patients with Ph+CML-CP aged at least 18 years, and who had imatinib resistance or intolerance, adequate performance status (WHO performance score 2), and normal hepatic, renal and cardiac functions. Patients with ImR had to have been treated with a dose of at least 600 mg q.d. for 3 months Exclusion criteria: patients in BC or patients who had received treatment with imatinib for 7 days and with hydroxycarbamide for 2 days prior to nilotinib, were excluded. Potassium and magnesium levels had to be greater than or equal to the lower limit of normal or corrected to within normal range. Patients receiving concomitant medications known to prolong the QT interval or inhibit CYP3A4 were excluded if alternative treatments were not possible. ImR was defined as failure to achieve CHR after 3 months or loss of a HR or CyR at any time during treatment with imatinib. Entry criteria for ImI included patients with intolerant symptoms (but who also had never achieved a MCyR with imatinib), and haematological toxicity of grade 4 severity persisting for > 7 days. ImI patients who had previously demonstrated sensitivity to imatinib, as evidenced by a prior MCyR, were excluded from participation in the study |
Arm 1 nilotinib n: 280 Drug: nilotinib Starting daily dose (mg): 800 Dosage details: 400 mg b.i.d.; escalation to 600 mg b.i.d. allowed if suboptimal response and no safety concerns Concurrent treatment: unclear |
CyR: based on the percentage of Ph+ metaphases among 20 or more metaphase cells in each BM sample. BM assessments were done on day 28 of cycle 1 and every 3 months. Cytogenetic studies on BM samples were performed at baseline and repeated every 3 months in responding patients. FISH studies to document CyR were accepted if routine cytogenetic studies were not successful or not available at a particular analysis time CCyR (0% Ph+) PCyR (1–35% Ph+) MCyR (complete + partial) Minor CyR (36–65% Ph+) Minimal CyR (66–95% Ph+) Duration of MCyR (measured from date of response until the date treatment was discontinued for progression or death; patients who discontinued for other reasons were censored at date of last treatment and patients still on treatment at data cut-off date) HR: CBC and biochemistries were obtained weekly for the first 8 weeks, and thereafter every 2 weeks CHR (WBC count < 10 × 109/l; a platelet count < 450 × 109/l; < 5% myelocytes plus metamyelocytes, < 20% basophils; absence of blasts and promyelocytes in PB; absence of extramedullary involvement) Study medication: duration of study therapy (months) Average daily dose (mg q.d.) Survival: OS (dated from start of nilotinib therapy until death from any cause and censored at last follow-up for patients who were alive) Participant disposition: withdrawal because of AEs AEs – grades 1–4: safety assessments included evaluation of AEs, haematological assessment, biochemical testing, urinalysis, cardiac enzyme assessment, serial electrocardiogram evaluation and physical examination. AEs were graded according to NCI CTC Version 3.0186 |
|
| Nilotinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| Demographics | ||||
| Age (years) (median) | 280 | 58 (range 21–85) | ||
| Gender (n male) | 280 | 144 | 51.4% | |
| Imatinib failure | ||||
| Resistance | 280 | 194 | 69.3% | |
| Prior therapy | ||||
| Best response to imatinib CHR | 280 | 88 | 31.4% | |
| Highest imatinib dose < 600mg q.d. | 280 | 77 | 27.5% | |
| Highest imatinib dose 600–800 mg q.d. | 280 | 91 | 32.5% | |
| Highest imatinib dose > 800 mg q.d. | 280 | 111 | 39.6% | |
| Prior hydroxycarbamide | 280 | 233 | 83.2% | |
| Prior chemotherapy | 280 | 71a | 25.4% | |
| Prior interferon | 280 | 184 | 65.7% | |
| Prior transplantation | 280 | 22b | 7.9% | |
| Disease history | ||||
| Duration of CML (months) (median) | 280 | 57 (range 5–275) | ||
| Splenomegaly at study entry | 280 | 48 | 17.1% | |
| Chromosomal abnormalities other than Ph+ | 280 | 72 | 25.7% | |
| Imatinib failure | ||||
| BCR–ABL mutation | 182 | 77 | 42.3% | |
| Laboratory parameters | ||||
| Haemoglobin – g/l (median) | 280 | 120 (range 77–172) | ||
| WBC × 109/l (median) | 280 | 9.9 (range 0.9–372) | ||
| Platelets × 109/l (median) | 280 | 309 (range 28–2000) | ||
| Results | ||||
| CyR | ||||
| CCyR | 280 | 88c | 31.4% | |
| PCyR | 280 | 46d | 16.4% | |
| MCyR | 280 | 134 | 47.9% | |
| Minor CyR | 280 | 22 | 7.9% | |
| Minimal CyR | 280 | 39 | 13.9% | |
| Duration of MCyR – 0 months | 280 | 1 | ||
| Duration of MCyR – 2 months | 1 | |||
| Duration of MCyR – 4 months | 0.99 | |||
| Duration of MCyR – 6 months | 0.965 | |||
| Duration of MCyR – 8 months | 0.955 | |||
| Duration of MCyR – 10 months | 0.955 | |||
| Duration of MCyR – 12 months | 0.955 | |||
| HR | ||||
| CHR | 185 | 137e | 74.1% | |
| Study medication | ||||
| Duration of study therapy (months) (median) | 280 | 8.05 | ||
| Average daily dose (mg q.d.) (median) | 280 | 797 (range 151–1112) | ||
| Survival | ||||
| OS – 0 months | 280 | 1 | ||
| OS – 6 months | 0.995 | |||
| OS – 12 months | 0.95 | |||
| OS – 18 months | 0.95 | |||
| Participant disposition | ||||
| Withdrawal because of AEs | 280 | 42 | 15.0% | |
| AEs – grades 1–4 | ||||
| Constipation | 280 | 34 | 12.1% | |
| Diarrhoea | 280 | 32 | 11.4% | |
| Fatigue | 280 | 52 | 18.6% | |
| Headache | 280 | 52 | 18.6% | |
| Myalgia | 280 | 23 | 8.2% | |
| Nausea | 280 | 66 | 23.6% | |
| Pain in extremity | 280 | 13 | 4.6% | |
| Pruritus | 280 | 67 | 23.9% | |
| Rash | 280 | 79 | 28.2% | |
| Vomiting | 280 | 30 | 10.7% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 280 | 81f | 28.9% | |
| Neutropenia | 280 | 81f | 28.9% | |
| AEs – grade 3–4 | ||||
| Constipation | 280 | 0 | 0.0% | |
| Diarrhoea | 280 | 6 | 2.1% | |
| Fatigue | 280 | 3 | 1.1% | |
| Headache | 280 | 5 | 1.8% | |
| Myalgia | 280 | 3 | 1.1% | |
| Nausea | 280 | 3 | 1.1% | |
| Pain in extremity | 280 | 2 | 0.7% | |
| Pruritus | 280 | 3 | 1.1% | |
| Rash | 280 | 9 | 3.2% | |
| Vomiting | 280 | 2 | 0.7% | |
| ImR | ||||
| CyR | ||||
| CCyR | 194 | 58 | 29.9% | |
| PCyR | 194 | 36 | 18.6% | |
| MCyR | 194 | 94 | 48.5% | |
| Minor CyR | 194 | 16 | 8.2% | |
| Minimal CyR | 194 | 25 | 12.9% | |
| Duration of MCyR – 0 months | 194 | |||
| Duration of MCyR – 2 months | 194 | |||
| Duration of MCyR – 4 months | 194 | |||
| Duration of MCyR – 6 months | 194 | |||
| Duration of MCyR – 8 months | 194 | |||
| Duration of MCyR – 10 months | 194 | |||
| Duration of MCyR – 12 months | 194 | |||
| HR | ||||
| CHR | 135 | 92e | 68.1% | |
| Survival | ||||
| OS – 0 months | 194 | |||
| OS – 6 months | 194 | |||
| OS – 12 months | 194 | |||
| OS – 18 months | 194 | |||
| ImI | ||||
| CyR | ||||
| CCyR | 86 | 30 | 34.9% | |
| PCyR | 86 | 10 | 11.6% | |
| MCyR | 86 | 40 | 46.5% | |
| Minor CyR | 86 | 6 | 7.0% | |
| Minimal CyR | 86 | 14 | 16.3% | |
| Duration of MCyR – 0 months | 86 | |||
| Duration of MCyR – 2 months | 86 | |||
| Duration of MCyR – 4 months | 86 | |||
| Duration of MCyR – 6 months | 86 | |||
| Duration of MCyR – 8 months | 86 | |||
| Duration of MCyR – 10 months | 86 | |||
| Duration of MCyR – 12 months | 86 | |||
| HR | ||||
| CHR | 50 | 45e | 90.0% | |
| Survival | ||||
| OS – 0 months | 86 | |||
| OS – 6 months | 86 | |||
| OS – 12 months | 86 | |||
| OS – 18 months | 86 | |||
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? Yes | ||||
| 1.2 Were the case series collected at more than one centre? Multicentre | ||||
| 1.3 Was the main outcome independently assessed? No | ||||
| 1.4 Are patient characteristics adequately described? Ye | ||||
| 1.5 How easy is it to assess generalisability of the results? Medium | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? Yes | ||||
| 2.2 Were data collected prospectively? Yes | ||||
| 2.3 Were patients recruited consecutively? Yes | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? No. Dose of nilotinib could be escalated | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Uncertain | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? Yes. Aimed to report results of interim analyses of 280 of the total enrolled (318) and analyses were based on all the 280 patients | ||||
| 4.2 Were dropouts from the study adequately described? Yes | ||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Kim et al. (2009)80 Design: case series (retrospective) CP: yes AP: yes BC: yes Country: Canada Number of centres: 1 |
Inclusion criteria: not clearly defined. May represent all CML patients treated with dasatanib at a single unit, March 2005–October 2007 [seven with PB large granular lymphocyte (LGL) lymphocytosis] Exclusion criteria: none reported |
Arm 1 dasatinib n: 17 Drug: dasatinib Starting daily dose (mg): 140 Dosage details: starting dose 70 mg b.i.d. Concurrent treatment: not reported |
CyR: CCyR [number of participants achieving a CCyR (not defined), or complete or a MMR (not defined), summed by reviewer] PCyR (not defined) MCyR (complete + partial) Study medication: duration of study therapy (months) |
|
| Notes | ||||
| The experience of one participant with Ph+ ALL is also reported in this publication, but has been excluded from consideration here | ||||
| Baseline characteristics | ||||
| Dastinib | ||||
| n | κ | Mean | ||
| Imatinib failure | ||||
| Intolerance | 17 | 15 | 88.2% | |
| Resistance | 17 | 2 | 11.8% | |
| Results | ||||
| CyR | ||||
| CCyR | 17 | 13 | 76.5% | |
| PCyR | 17 | 1 | 5.9% | |
| MCyR | 17 | 14 | 82.4% | |
| Study medication | ||||
| Duration of study therapy (months) (median) | 17 | 23 (range 5–25) | ||
| CP | ||||
| CyR | ||||
| CCyR | 13 | 9 | 69.2% | |
| PCyR | 13 | 1 | 7.7% | |
| MCyR | 13 | 10 | 76.9% | |
| Study medication | ||||
| Duration of study therapy (months) (median) | 13 | 22.5 (range 7.5–23.5) | ||
| AP | ||||
| CyR | ||||
| CCyR | 3 | 3 | 100.0% | |
| PCyR | 3 | 0 | 0.0% | |
| MCyR | 3 | 3 | 100.0% | |
| Study medication | ||||
| Duration of study therapy (months) (median) | 3 | 24 (range 5–25) | ||
| BC | ||||
| CyR | ||||
| CCyR | 1 | 1 | 100.0% | |
| PCyR | 1 | 0 | 0.0% | |
| MCyR | 1 | 1 | 100.0% | |
| Study medication | ||||
| Duration of study therapy (months) (median) | 1 | 23.5 | ||
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? No. Report of a series of eight patients | ||||
| 1.2 Were the case series collected at more than one centre? Single centre | ||||
| 1.3 Was the main outcome independently assessed? No | ||||
| 1.4 Are patient characteristics adequately described? No | ||||
| 1.5 How easy is it to assess generalisability of the results? Low | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? No | ||||
| 2.2 Were data collected prospectively? No | ||||
| 2.3 Were patients recruited consecutively? No | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? Uncertain | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Uncertain | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? NA. Report of a series of eight patients | ||||
| 4.2 Were dropouts from the study adequately described? NA. Report of a series of eight patients | ||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: le Coutre et al. (2008)107 Secondary publications: Alexander and le Coutre (2008),170 Apperley et al. (2008),171 le Coutre et al. (2007),167 le Coutre et al. (2007),168 Saglio et al. (2007),169 le Coutre et al. (2007),166 le Coutre et al. (2008),173 Kantarjian et al. (2008),172 le Coutre et al. (2008),175 le Coutre et al. (2008)174 Design: cohort study (prospective) CP: no AP: yes BC: no Country: not stated (n = 10); authors are from Germany, the USA, Republic of Korea, the UK, Italy, Poland, France, China and Australia Number of centres: 36 Trial code(s): NCT00384228 |
Inclusion criteria: patients at least 18 years of age and with ImR or ImI CML in AP. Patients were also required to have a WHO performance status score of 2 or lower and normal serum eletolytes as well as normal hepatic, renal and pancratic function Definition of ImR was defined by one of the following criteria during treatment with imatinib at least 600 mg q.d. (1) disease progression from CP to AP occurring during imatinib therapy; (2) disease progression defined as at least a 50% increase in peripheral WBC count, blast count, basophils or platelets during imatinib therapy for AP; or (3) lack of HR in the BM following a minimum of 4 weeks of imatinib therapy for AP ImI was defined as the discontinuation of imatinib therapy because of any of the following: grade 3–4 AEs that persisted in spite of optimal supportive care measures or grade 2 AEs related to imatinib therapy in spite of optimal supportive care measures that persisted for at least 1 month or that recurred more than three times whether the dose was reduced or discountued. The protocol definiton of ImI required the lack of an MCyR with imatinib Exclusion criteria: patients who had evidence of abnormal cardiac function or cardiac conduction, including individuals who had a myocardial infarction within the previous 12 months, individuals with left ventricular ejection fractions of 45% or less by echocardiogram or multiple-gated acquisition scan, and individuals with a history of congenital long QT syndrome or a corrected QT interval of > 450 milliseconds on screening ECG using QTcF |
Arm 1 nilotinib n: 119 Drug: nilotinib Starting daily dose (mg): not reported Dosage details: 800 mg (400 mg b.i.d.) escalation to 1200 mg (600 mg b.i.d.) was permitted for suboptimal response in the absence of toxicity reductions to 400 mg daily and subsequently 200 mg daily were permitted for the management of toxicity Concurrent treatment: treatment with chemotherapy other than hydroxycarbamide was not permitted within 1 week of starting therapy with nilotinib |
CyR: based on assessment of Ph+ cells in at least 20 metaphases. Where cytogenetic evaluation failed, assessment by FISH was permitted CCyR (0% Ph+) PCyR (1–35% Ph+) MCyR Minor CyR [36–85% Ph+ (NB 65% is the normal upper limit for this category, and minimal response is defined as > 65%, suggesting that 85% may be a typographical error)] Minimal CyR (86–95% Ph+) HR: assessed on the basis of (1) CBC collected weekly for the first 8 weeks and every 2 weeks thereafter; and (2) BM aspirate and/or biopsy performed on days 28, 56 and 84, and every 84 days thereafter Overall HR (complete, NEL or return to chronic) CHR (marrow blasts < 5%; no blasts in PB; neutrophils > 1.5 × 109/l; platelets > 100 × 109/l; basophils < 5%; no extramedullary disease) MHR or no evidence of leukaemia No evidence of leukaemia (marrow blasts < 5%; no blasts in PB; neutrophils > 1.0 × 109/l; platelets 20 × 109/l; no extramedullary disease) Return to CP [< 15% blasts in marrow and PB; < 30% blasts plus promyelocytes in marrow and PB; < 20% basophils; and no extramedullary disease (with the exception of liver or spleen enlargement)] Study medication: duration of study therapy (months) Average daily dose (mg q.d.) Survival: TTP [for patients achieving an HR, time from study start to disease progression or death; definition of ‘progression’ not entirely clear – in inclusion criteria (i.e. as regards failure of imatinib), progression is defined as ≥ 50% increase in peripheral WBC, blast count, basophils, or platelets during imatinib therapy for AP] |
|
| Nilotinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| Demographics | ||||
| Age (years) (median) | 119 | 57 (range 22–79) | ||
| Gender (n male) | 119 | 67 | 56.3% | |
| Imatinib failure | ||||
| Intolerance | 119 | 23 | 19.3% | |
| Resistance | 119 | 96 | 80.7% | |
| Prior therapy | ||||
| Time on imatinib (months) (median) | 119 | 32.1 (range 0.1–71.1) | ||
| Highest imatinib dose 400–600 mg q.d. | 119 | 21a | 17.6% | |
| Highest imatinib dose 600–800 mg q.d. | 119 | 40a | 33.6% | |
| Highest imatinib dose > 800 mg q.d. | 119 | 58a | 48.7% | |
| Prior hydroxycarbamide | 119 | 109 | 91.6% | |
| Prior chemotherapy | 119 | 31b | 26.1% | |
| Prior interferon | 119 | 69 | 58.0% | |
| Prior transplantation | 119 | 9 | 7.6% | |
| Disease history | ||||
| Duration of CML (months) (median) | 119 | 71 (range 2–298) | ||
| Chromosomal abnormalities other than Ph+ | 119 | 35 | 29.4% | |
| Laboratory parameters | ||||
| WBC × 109/l (median) | 119 | 12.7 (range 0.4–277.0) | ||
| WBC – 50 × 109/l or more | 119 | 25 | 21.0% | |
| BM blasts (%) (median) | 119 | 10.5 (range 0–28) | ||
| BM blasts – 15% or more | 119 | 42 | 35.3% | |
| Peripheral blasts (%) (median) | 119 | 0.4 (range 0–33) | ||
| Peripheral blasts – 15% or more | 119 | 15 | 12.6% | |
| Platelets × 109/l (median) | 119 | 203 (range 4–3044) | ||
| Platelets – below 50 × 109/l | 119 | 25 | 21.0% | |
| Basophils in PB (%) (median) | 119 | 4 (range 0–62) | ||
| Basophils – 20% or more | 119 | 15 | 12.6% | |
| Results | ||||
| CyR | ||||
| CCyR | 119 | 19 | 16.0% | |
| PCyR | 119 | 16 | 13.4% | |
| MCyR | 119 | 35 | 29.4% | |
| Minor CyR | 119 | 16 | 13.4% | |
| Minimal CyR | 119 | 28 | 23.5% | |
| HR | ||||
| Overall HR | 119 | 56 | 47.1% | |
| CHR | 119 | 31 | 26.1% | |
| MHR or no evidence of leukaemia | 119 | 11 | 9.2% | |
| Return to CP | 119 | 14 | 11.8% | |
| Study medication | ||||
| Duration of study therapy (months) (median) | 119 | 6.637 (range 0.066–20.074) | ||
| Average daily dose (mg q.d.) (median) | 119 | 790 (range 180–1149) | ||
| Survival | ||||
| TTP – 0 months | 119 | 1 | ||
| TTP – 2 months | 1 | |||
| TTP – 4 months | 0.96 | |||
| TTP – 6 months | 0.825 | |||
| TTP – 8 months | 0.76 | |||
| TTP – 10 months | 0.76 | |||
| TTP – 12 months | 0.73 | |||
| TTP – 14 months | 0.64 | |||
| TTP – 16 months | 0.64 | |||
| TTP – 18 months | 0.56 | |||
| OS – 0 months | 119 | 1 | ||
| OS – 2 months | 0.97 | |||
| OS – 4 months | 0.945 | |||
| OS – 6 months | 0.91 | |||
| OS – 8 months | 0.84 | |||
| OS – 10 months | 0.82 | |||
| OS – 12 months | 0.79 | |||
| OS – 14 months | 0.76 | |||
| OS – 16 months | 0.72 | |||
| OS – 18 months | 0.72 | |||
| OS – 20mo | 0.72 | |||
| AEs – grades 1–4 | 119 | 8 | 6.7% | |
| Abdominal pain | ||||
| Alopecia | 119 | 10 | 8.4% | |
| Anorexia | 119 | 7 | 5.9% | |
| Arthralgia | 119 | 6 | 5.0% | |
| Constipation | 119 | 13 | 10.9% | |
| Diarrhoea | 119 | 11 | 9.2% | |
| Fatigue | 119 | 12 | 10.1% | |
| Headache | 119 | 12 | 10.1% | |
| Muscle spasms | 119 | 11 | 9.2% | |
| Myalgia | 119 | 11 | 9.2% | |
| Nausea | 119 | 12 | 10.1% | |
| Pain in extremity | 119 | 6 | 5.0% | |
| Peripheral oedema | 119 | 6 | 5.0% | |
| Pruritus | 119 | 24 | 20.2% | |
| Pyrexia | 119 | 10 | 8.4% | |
| Rash | 119 | 26 | 21.8% | |
| Upper abdominal pain | 119 | 6 | 5.0% | |
| AEs – grade 3–4 | 119 | 42 | 35.3% | |
| Thrombopenia | ||||
| Anaemia | 119 | 15 | 12.6% | |
| Neutropenia | 119 | 25 | 21.0% | |
| Abdominal pain | 119 | 1 | 0.8% | |
| Alopecia | 119 | 0 | 0.0% | |
| Anorexia | 119 | 0 | 0.0% | |
| Arthralgia | 119 | 0 | 0.0% | |
| Constipation | 119 | 0 | 0.0% | |
| Diarrhoea | 119 | 1 | 0.8% | |
| Fatigue | 119 | 1 | 0.8% | |
| Headache | 119 | 1 | 0.8% | |
| Muscle spasms | 119 | 0 | 0.0% | |
| Myalgia | 119 | 1 | 0.8% | |
| Nausea | 119 | 1 | 0.8% | |
| Pain in extremity | 119 | 0 | 0.0% | |
| Peripheral oedema | 119 | 0 | 0.0% | |
| Pruritus | 119 | 0 | 0.0% | |
| Pyrexia | 119 | 1 | 0.8% | |
| Rash | 119 | 0 | 0.0% | |
| Upper abdominal pain | 119 | 0 | 0.0% | |
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? Yes | ||||
| 1.2 Were the case series collected at more than one centre? Multicentre | ||||
| 1.3 Was the main outcome independently assessed? No | ||||
| 1.4 Are patient characteristics adequately described? Yes | ||||
| 1.5 How easy is it to assess generalisability of the results? High | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? Yes | ||||
| 2.2 Were data collected prospectively? Yes | ||||
| 2.3 Were patients recruited consecutively? Yes | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? No. Dose escalation and reduction were permitted | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Uncertain | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? Yes | ||||
| 4.2 Were dropouts from the study adequately described? Yes | ||||
| Study details | Population | Arms | Outcomes | |||
|---|---|---|---|---|---|---|
|
Study: Shah et al. (2008)22 Secondary publications: Hochhaus et al. (2006),90 Shah et al. (2007),92 Hochhaus et al. (2008),93 Wang et al. (2008),98 Shah et al. (2008),97 Porkka et al. (2008),96 Hochhaus et al. (2007),91 Nicaise et al. (2008),95 Hochhaus et al. (2008)94 Trial code: NCT00123474 CA 180–034 CP: yes AP: no BC: no Country: not stated; authors are from the USA, Republic of Korea, France, Brazil, Argentina, Mexico, Russia, Australia, and Germany Number of centres: 139 |
Inclusion criteria: patients at least 18 years of age with Ph+ CML-CP and primary or acquired HR or intolerance to imatinib were enrolled. Patients were required to have < 15% blasts in PB or BM, < 30% blasts and promyelocytes in PB or BM, < 20% basophils in PB 100,000/µl platelets (or less if related to prior drug therapy), and no extramedullary involvement (except liver or spleen). Primary resistance to imatinib (400–800 mg q.d.) was defined as no decrease in WBC count after 4 weeks of treatment, no CHR after 3 months, no MCyR after 6 months and no CCyR after 12 months. Acquired resistance was defined as loss of MCyR (30% absolute increase in the percentage of Ph+ metaphases), loss of molecular response (concomitant with a 10% Ph+ metaphases at cytogenetic analysis), evidence of a new mutation in the BCR–ABL-kinase domain or loss of a confirmed CHR (WBC count > 10,000/µl on all assessments over at least a consecutive 2-week period). ImI was defined as grade 3 or worse toxicity which led to discontinuation of therapy. Patients who tolerated 400 mg q.d. imatinib but who did not achieve a CCyR and subsequently did not tolerate doses of 600 mg q.d. were considered to be resistant to imatinib Exclusion criteria: included but not limited to treatment with imatinib, IFN, cytarabine therapy or any targeted small-molecule anticancer agent within 7 days of initiation; uncontrolled or significant cardiovascular disease; history of a significant bleeding disorder unrelated to CML; eligibility for immediate autologous or allogeneic SCT; or concurrent incurable malignancy other than CML Method of allocation: a permuted block design was used to assign participants randomly with a 1 : 1 : 1 : 1 ratio Blinding: open-label Therapy common to all participants: therapies other than dasatinib were prohibited, except hydroxycarbamide (limited to a period of 2 weeks) for treatment of elevated WBC counts (> 50 × 109/l). Administration of myeloid growth factors or recombinant erythropoietin was permitted at the discretion of the investigator. Patients were supported with platelet transfusions as required |
Arm 1 dasatinib 100 mg q.d. n: 167 Drug: dasatinib Starting daily dose (mg): 100 Dosage details: 100 mg q.d. escalation to 140 mg q.d. allowed for suboptimal response reduction to 80 mg q.d. allowed for toxicity Arm 2 dasatinib 50 mg b.i.d. n: 168 Drug: dasatinib Starting daily dose (mg): 100 Dosage details: 50 mg b.i.d. escalation to 70 mg b.i.d. allowed for suboptimal response reduction to 40 mg b.i.d. allowed for toxicity Arm 3 dasatinib 140 mg q.d. n: 167 Drug: dasatinib Starting daily dose (mg): 140 Dosage details: 140 mg q.d. escalation to 180 mg q.d. allowed for suboptimal response reduction to 80 mg q.d. allowed for toxicity Arm 4 dasatinib 70 mg b.i.d. n: 168 Drug: dasatinib Starting daily dose (mg): 70 Dosage details: 70 mg b.i.d. escalation to 90 mg b.i.d. allowed for suboptimal response reduction to 40 mg b.i.d. allowed for toxicity |
CyR: CCyR (0% Ph+ metaphases in BM) PCyR [1–35% Ph+ metaphases in BM (calculated by reviewer as MCyR – CCyR)] MCyR (0–35% Ph+ metaphases in BM) Duration of MCyR HR: CHR [WBC count no more than the institutional upper limit of normal; ANC at least 1 × 109/l; platelet count < 450 × 109/l and no more than the institutional upper limit of normal; no blasts or promyelocytes in PB; < 5% myelocytes plus metamyelocytes in PB; < 2% basophils in PB; no extramedullary involvement (including no hepatomegaly or splenomegaly). HRs were required to be maintained for at least 4 weeks] Study medication: average daily dose (mg q.d.) Survival: PFS [progression defined as confirmed AP or BC disease; loss of a previous CHR or MCyR; ≥ 30% increase in Ph+ metaphases; increasing WBC count (recorded by the investigator as a doubling from lowest value to > 20,000/µl or an increase by > 50,000/µl on two assessments performed at least 2 weeks apart); or death from any cause] OS Participant disposition: withdrawal because of AEs AEs – grades 1–4: NCI CTC Version 3.0. 186 Monitoring for pleural effusions included scheduled chest radiography. Classifications of pleural effusions were as follows: grade 1, asymptomatic; grade 2, symptomatic, with intervention such as diuretics or up to two therapeutic thoracocenteses indicated; grade 3, symptomatic and supplemental oxygen, more than two therapeutic thoracenteses, tube drainage, or pleurodesis indicated; and grade 4, life-threatening (e.g. causing haemodynamic instability or ventilatory support indicated) |
|||
| Dasatinib 100 mg q.d. | Dasatinib 50 mg b.i.d. | |||||
| n | κ | Mean | n | κ | Mean | |
| Baseline characteristics | ||||||
| Demographics | 167 | 56 (range 20–78) | 168 | 55 (range 21–84) | ||
| Age (years) (median) | ||||||
| Gender (n male) | 16 | 84 | 50.3% | 168 | 85 | 50.6% |
| Imatinib failure | 167 | 75 | 44.9% | 168 | 88 | 52.4% |
| Resistance – primary | ||||||
| Resistance – acquired | 167 | 49 | 29.3% | 168 | 36 | 21.4% |
| Prior therapy | 167 | 136 | 81.4% | 168 | 146 | 86.9% |
| Best response to imatinib – CHR | ||||||
| Best response to imatinib – MCyR | 167 | 76 | 45.5% | 168 | 65 | 38.7% |
| Time on imatinib < 1 year | 167 | 36 | 21.6% | 168 | 40 | 23.8% |
| Time on imatinib 1–3 years | 167 | 55 | 32.9% | 168 | 68 | 40.5% |
| Time on imatinib > 3 years | 167 | 76 | 45.5% | 168 | 60 | 35.7% |
| Highest imatinib dose > 800 mg q.d. | 167 | 61 | 36.5% | 168 | 55 | 32.7% |
| Prior chemotherapy | 167 | 39 | 23.4% | 168 | 52 | 31.0% |
| Prior interferon | 167 | 87 | 52.1% | 168 | 87 | 51.8% |
| Prior transplantation | 167 | 10 | 6.0% | 168 | 13 | 7.7% |
| Disease history | 167 | 55 (range 1.6–251.0) | 168 | 51 (range 4.4–212.0) | ||
| Duration of CML (months) (median) | ||||||
| Baseline status | 167 | 85 | 50.9% | 168 | 70 | 41.7% |
| CHR at study entry | ||||||
| MCyR at study entry | 167 | 34 | 20.4% | 168 | 23 | 13.7% |
| BCR–ABL mutation | 144 | 49 | 34.0% | 145 | 60 | 41.4% |
| Dasatinib 140 mg q.d. | Dasatinib 70 mg b.i.d. | |||||
| n | κ | Mean | n | κ | Mean | |
| Baseline characteristics | ||||||
| Demographics | 167 | 54 (range 20–84) | 168 | 55 (range 18–83) | ||
| Age (years) (median) | ||||||
| Gender (n male) | 167 | 70 | 41.9% | 68 | 77 | 45.8% |
| Imatinib failure | 167 | 78 | 46.7% | 168 | 82 | 48.8% |
| Resistance – primry | ||||||
| Resistance – acquired | 167 | 45 | 26.9% | 168 | 45 | 26.8% |
| Prior therapy | 167 | 138 | 82.6% | 168 | 141 | 83.9% |
| Best response to imatinib – CHR | ||||||
| Best response to imatinib – MCyR | 167 | 71 | 42.5% | 168 | 66 | 39.3% |
| Time on imatinib < 1 year | 165 | 39a | 23.6% | 168 | 37 | 22.0% |
| Time on imatinib 1–3 years | 165 | 58a | 35.2% | 168 | 60 | 35.7% |
| Time on imatinib > 3 years | 165 | 68a | 41.2% | 168 | 71 | 42.3% |
| Highest imatinib dose > 800 mg q.d. | 167 | 55 | 32.9% | 168 | 56 | 33.3% |
| Prior chemotherapy | 167 | 41 | 24.6% | 168 | 43 | 25.6% |
| Prior interferon | 167 | 93 | 55.7% | 168 | 82 | 48.8% |
| Prior transplantation | 167 | 5 | 3.0% | 168 | 7 | 4.2% |
| Disease history | 167 | 56 (range 0.9–227.0) | 168 | 53 (range 1.2–246.0) | ||
| Duration of CML (months) (median) | ||||||
| Baseline status | 167 | 69 | 41.3% | 168 | 64 | 38.1% |
| CHR at study entry | ||||||
| MCyR at study entry | 167 | 28 | 16.8% | 168 | 31 | 18.5% |
| BCR–ABL mutation | 138 | 51 | 37.0% | 143 | 45 | 31.5% |
| Dasatinib 100 mg q.d. | Dasatinib 50 mg b.i.d. | |||||
| n | κ | Mean | n | κ | Mean | |
| Results | ||||||
| CyR | 167 | 69 | 41.3% | 168 | 70 | 41.7% |
| CCyRb | ||||||
| PCyRb | 167 | 29 | 17.4% | 168 | 20 | 11.9% |
| MCyRb | 167 | 98 | 58.7% | 168 | 90 | 53.6% |
| Duration of MCyR – 0 months | 167 | 1 | 168 | 1 | ||
| Duration of MCyR – 2 months | 1 | 0.98 | ||||
| Duration of MCyR – 4 months | 1 | 0.98 | ||||
| Duration of MCyR – 6 months | 1 | 0.98 | ||||
| Duration of MCyR – 8 months | 0.89 | 0.98 | ||||
| HR | 167 | 150 | 89.8% | 168 | 154 | 91.7% |
| CHRb | ||||||
| Study medication | 167 | 100 (range 18–150) | 168 | 93 (range 21–158) | ||
| Average daily dose (mg q.d.) (median) | ||||||
| Survival | 167 | 1 | 168 | 1 | ||
| PFS – 0 months | ||||||
| PFS – 10 months | 40 | 0.91 | 42 | 0.93 | ||
| PFS – 12 months | 5 | 0.89 | 6 | 0.815 | ||
| PFS – 14 months | 167 | 1 | 0.815 | |||
| PFS – 2 months | 163 | 0.99 | 161 | 0.99 | ||
| PFS – 4 months | 160 | 0.97 | 153 | 0.975 | ||
| PFS – 6 months | 133 | 0.95 | 132 | 0.94 | ||
| PFS – 8 months | 98 | 0.91 | 98 | 0.93 | ||
| OS – 0 months | 167 | 1 | 168 | 1 | ||
| OS – 10 months | 49 | 0.97 | 51 | 0.965 | ||
| OS – 12 months | 9 | 0.97 | 12 | 0.93 | ||
| OS – 14 months | 1 | 0.93 | ||||
| OS – 2 months | 165 | 1 | 164 | 0.99 | ||
| OS – 4 months | 165 | 1 | 160 | 0.99 | ||
| OS – 6 months | 156 | 0.975 | 150 | 0.97 | ||
| OS – 8 months | 113 | 0.97 | 108 | 0.965 | ||
| Participant disposition | 167 | 8c | 4.8% | 168 | 13d | 7.7% |
| Withdrawal because of AEs | ||||||
| Haematological AEs – grades 1–4 | 167 | 147 | 88.0% | 168 | 151 | 89.9% |
| Anaemia | ||||||
| Neutropenia | 167 | 105 | 62.9% | 168 | 124 | 73.8% |
| Thrombopenia | 167 | 100 | 59.9% | 168 | 110 | 65.5% |
| Leucopenia | 167 | 98 | 58.7% | 168 | 119 | 70.8% |
| AEs – grades 1–4 | ||||||
| CHF/cardiac dysfunction | 167 | 0 | 0.0% | 168 | 2 | 1.2% |
| Diarrhoea | 167 | 39 | 23.4% | 168 | 40 | 23.8% |
| Dyspnoea | 167 | 17 | 10.2% | 168 | 25 | 14.9% |
| Fatigue | 167 | 33 | 19.8% | 168 | 22 | 13.1% |
| Headache | 167 | 49 | 29.3% | 168 | 32 | 19.0% |
| Myalgia | 167 | 19 | 11.4% | 168 | 5 | 3.0% |
| Nausea | 167 | 25 | 15.0% | 168 | 30 | 17.9% |
| Pericardial effusion | 167 | 1 | 0.6% | 168 | 2 | 1.2% |
| Peripheral oedema | 167 | 16 | 9.6% | 168 | 9 | 5.4% |
| Pleural effusion | 167 | 12 | 7.2% | 168 | 19 | 11.3% |
| Pulmonary hypertension | 167 | 0 | 0.0% | 168 | 0 | 0.0% |
| Pulmonary oedema | 167 | 0 | 0.0% | 168 | 1 | 0.6% |
| Pyrexia | 167 | 5 | 3.0% | 168 | 12 | 7.1% |
| Rash | 167 | 19 | 11.4% | 168 | 25 | 14.9% |
| Superficial oedema | 167 | 23 | 13.8% | 168 | 21 | 12.5% |
| Vomiting | 167 | 9 | 5.4% | 168 | 12 | 7.1% |
| Haematological AEs – grade 3–4 | ||||||
| Thrombopenia | 167 | 37 | 22.2% | 168 | 52 | 31.0% |
| Anaemia | 167 | 16 | 9.6% | 168 | 27 | 16.1% |
| Neutropenia | 167 | 55 | 32.9% | 168 | 72 | 42.9% |
| Leucopenia | 167 | 27 | 16.2% | 168 | 42 | 25.0% |
| AEs – grade 3–4 | ||||||
| CHF/cardiac dysfunction | 167 | 0 | 0.0% | 168 | 1 | 0.6% |
| Diarrhoea | 167 | 1 | 0.6% | 168 | 4 | 2.4% |
| Dyspnoea | 167 | 2 | 1.2% | 168 | 7 | 4.2% |
| Fatigue | 167 | 2 | 1.2% | 168 | 0 | 0.0% |
| Headache | 167 | 1 | 0.6% | 168 | 0 | 0.0% |
| Myalgia | 167 | 0 | 0.0% | 168 | 0 | 0.0% |
| Nausea | 167 | 1 | 0.6% | 168 | 1 | 0.6% |
| Pericardial effusion | 167 | 0 | 0.0% | 168 | 1 | 0.6% |
| Peripheral oedema | 167 | 0 | 0.0% | 168 | 0 | 0.0% |
| Pleural effusion | 167 | 2 | 1.2% | 168 | 3 | 1.8% |
| Pulmonary hypertension | 167 | 0 | 0.0% | 168 | 0 | 0.0% |
| Pulmonary oedema | 167 | 0 | 0.0% | 168 | 0 | 0.0% |
| Pyrexia | 167 | 1 | 0.6% | 168 | 1 | 0.6% |
| Rash | 167 | 2 | 1.2% | 168 | 1 | 0.6% |
| Superficial oedema | 167 | 0 | 0.0% | 168 | 0 | 0.0% |
| Vomiting | 167 | 1 | 0.6% | 168 | 2 | 1.2% |
| ImR | ||||||
| CyR | ||||||
| CCyRb | 124 | 42 | 33.9% | 124 | 43 | 34.7% |
| PCyRb | 124 | 24 | 19.4% | 124 | 15 | 12.1% |
| MCyRb | 124 | 66 | 53.2% | 124 | 58 | 46.8% |
| HR | ||||||
| CHRb | 124 | 107 | 86.3% | 124 | 113 | 91.1% |
| ImI | ||||||
| CyR | ||||||
| CCyRa | 43 | 27 | 62.8% | 44 | 27 | 61.4% |
| PCyRb | 43 | 5 | 11.6% | 44 | 5 | 11.4% |
| MCyRb | 43 | 32 | 74.4% | 44 | 32 | 72.7% |
| HR | ||||||
| CHRb | 43 | 43 | 100.0% | 44 | 41 | 93.2% |
| 2-year follow-up (all)e | ||||||
| CyR | ||||||
| CCyR | 167 | 84 | 50.3% | 168 | 84 | 50.0% |
| PCyR | 167 | 21 | 12.6% | 168 | 18 | 10.7% |
| MCyR | 167 | 105 | 62.9% | 168 | 102 | 60.7% |
| HR | ||||||
| CHR | 167 | 154 | 92.2% | 168 | 155 | 92.3% |
| Dasatinib 140 mg q.d. | Dasatinib 70 mg b.i.d. | |||||
| n | κ | Mean | n | κ | Mean | |
| CyR | ||||||
| CCyRf | 167 | 74 | 44.3% | 168 | 75 | 44.6% |
| PCyRf | 167 | 19 | 11.4% | 168 | 18 | 10.7% |
| MCyRf | 167 | 93 | 55.7% | 168 | 93 | 55.4% |
| Duration of MCyR – 0 months | 167 | 1 | 168 | 1 | ||
| Duration of MCyR – 2 months | 0.98 | 0.98 | ||||
| Duration of MCyR – 4 months | 0.94 | 0.92 | ||||
| Duration of MCyR – 6 months | 0.88 | 0.92 | ||||
| Duration of MCyR – 8 months | 0.88 | 0.92 | ||||
| HR | ||||||
| CHRf | 167 | 143 | 85.6% | 168 | 146 | 86.9% |
| Study medication | ||||||
| Average daily dose (mg q.d.) (median) | 167 | 126 (range 42–166) | 168 | 108 (range 13–167) | ||
| Survival | ||||||
| PFS – 0 months | 167 | 1 | 168 | 1 | ||
| PFS – 10 months | 30 | 0.89 | 38 | 0.86 | ||
| PFS – 12 months | 9 | 0.89 | 10 | 0.78 | ||
| PFS – 14 months | 2 | 0.78 | ||||
| PFS – 2 months | 155 | 0.98 | 155 | 0.975 | ||
| PFS – 4 months | 146 | 0.965 | 148 | 0.95 | ||
| PFS – 6 months | 115 | 0.93 | 125 | 0.93 | ||
| PFS – 8 months | 86 | 0.92 | 93 | 0.89 | ||
| OS – 0 months | 167 | 1 | 168 | 1 | ||
| OS – 10 months | 42 | 0.96 | 48 | 0.94 | ||
| OS – 12 months | 11 | 0.96 | 10 | 0.89 | ||
| OS – 14 months | 3 | 0.89 | ||||
| OS – 2 months | 160 | 0.99 | 163 | 0.98 | ||
| OS – 4 months | 155 | 0.99 | 159 | 0.965 | ||
| OS – 6 months | 142 | 0.99 | 150 | 0.96 | ||
| OS – 8 months | 106 | 0.99 | 107 | 0.94 | ||
| Participant disposition | ||||||
| Withdrawal because of AEs | 167 | 15g | 9.0% | 168 | 23h | 13.7% |
| Haematological AEs – grades 1–4 | ||||||
| Anaemia | 167 | 146 | 87.4% | 168 | 154 | 91.7% |
| Neutropenia | 167 | 119 | 71.3% | 168 | 121 | 72.0% |
| Thrombopenia | 167 | 122 | 73.1% | 168 | 122 | 72.6% |
| Leucopenia | 167 | 116 | 69.5% | 168 | 114 | 67.9% |
| AEs – grades 1–4 | ||||||
| CHF/cardiac dysfunction | 167 | 2 | 1.2% | 168 | 5 | 3.0% |
| Diarrhoea | 167 | 38 | 22.8% | 168 | 36 | 21.4% |
| Dyspnoea | 167 | 24 | 14.4% | 168 | 19 | 11.3% |
| Fatigue | 167 | 29 | 17.4% | 168 | 27 | 16.1% |
| Headache | 167 | 43 | 25.7% | 168 | 46 | 27.4% |
| Myalgia | 167 | 19 | 11.4% | 168 | 10 | 6.0% |
| Nausea | 167 | 30 | 18.0% | 168 | 42 | 25.0% |
| Pericardial effusion | 167 | 5 | 3.0% | 168 | 2 | 1.2% |
| Peripheral oedema | 167 | 9 | 5.4% | 168 | 17 | 10.1% |
| Pleural effusion | 167 | 24 | 14.4% | 168 | 26 | 15.5% |
| Pulmonary hypertension | 167 | 0 | 0.0% | 168 | 2 | 1.2% |
| Pulmonary oedema | 167 | 0 | 0.0% | 168 | 2 | 1.2% |
| Pyrexia | 167 | 20 | 12.0% | 168 | 12 | 7.1% |
| Rash | 167 | 32 | 19.2% | 168 | 27 | 16.1% |
| Superficial oedema | 167 | 19 | 11.4% | 168 | 23 | 13.7% |
| Vomiting | 167 | 13 | 7.8% | 168 | 17 | 10.1% |
| Haematological AEs – grade 3–4 | ||||||
| Thrombopenia | 167 | 64 | 38.3% | 168 | 61 | 36.3% |
| Anaemia | 167 | 28 | 16.8% | 168 | 27 | 16.1% |
| Neutropenia | 167 | 68 | 40.7% | 168 | 68 | 40.5% |
| Leucopenia | 167 | 33 | 19.8% | 168 | 38 | 22.6% |
| AEs – grade 3–4 | ||||||
| CHF/cardiac dysfunction | 167 | 1 | 0.6% | 168 | 4 | 2.4% |
| Diarrhoea | 167 | 3 | 1.8% | 168 | 6 | 3.6% |
| Dyspnoea | 167 | 8 | 4.8% | 168 | 5 | 3.0% |
| Fatigue | 167 | 4 | 2.4% | 168 | 5 | 3.0% |
| Headache | 167 | 2 | 1.2% | 168 | 5 | 3.0% |
| Myalgia | 167 | 1 | 0.6% | 168 | 1 | 0.6% |
| Nausea | 167 | 1 | 0.6% | 168 | 1 | 0.6% |
| Pericardial effusion | 167 | 1 | 0.6% | 168 | 1 | 0.6% |
| Peripheral oedema | 167 | 0 | 0.0% | 168 | 0 | 0.0% |
| Pleural effusion | 167 | 4 | 2.4% | 168 | 2 | 1.2% |
| Pulmonary hypertension | 167 | 0 | 0.0% | 168 | 1 | 0.6% |
| Pulmonary oedema | 167 | 0 | 0.0% | 168 | 1 | 0.6% |
| Pyrexia | 167 | 0 | 0.0% | 168 | 1 | 0.6% |
| Rash | 167 | 0 | 0.0% | 168 | 2 | 1.2% |
| Superficial oedema | 167 | 1 | 0.6% | 168 | 0 | 0.0% |
| Vomiting | 167 | 2 | 1.2% | 168 | 0 | 0.0% |
| ImR | ||||||
| CyR | ||||||
| CCyRf | 123 | 44 | 35.8% | 127 | 50 | 39.4% |
| PCyRf | 123 | 18 | 14.6% | 127 | 15 | 11.8% |
| MCyRf | 123 | 62 | 50.4% | 127 | 65 | 51.2% |
| HR | ||||||
| CHRf | 123 | 105 | 85.4% | 127 | 111 | 87.4% |
| ImI | ||||||
| CyR | ||||||
| CCyRf | 44 | 30 | 68.2% | 41 | 25 | 61.0% |
| PCyRf | 44 | 1 | 2.3% | 41 | 3 | 7.3% |
| MCyRf | 44 | 31 | 70.5% | 41 | 28 | 68.3% |
| HR | ||||||
| CHRf | 44 | 38 | 86.4% | 41 | 35 | 85.4% |
| 2-year follow-up (all)i | ||||||
| CyR | ||||||
| CCyR | 167 | 84 | 50.3% | 168 | 91 | 54.2% |
| PCyR | 167 | 21 | 12.6% | 168 | 11 | 6.5% |
| MCyR | 167 | 105 | 62.9% | 168 | 102 | 60.7% |
| HR | ||||||
| CHR | 167 | 145 | 86.8% | 168 | 148 | 88.1% |
| Quality appraisal | ||||||
| 1. Is a power calculation provided? No | ||||||
| 2. Is the sample size adequate? Not reported | ||||||
| 3. Was ethical approval obtained? Yes | ||||||
| 4. Were the study eligibilty criteria specified? Yes | ||||||
| 5. Were the eligibility criteria appropriate? Yes | ||||||
| 6. Were patients recruited prospectively? Yes | ||||||
| 7. Was assignment to the treatment groups really random? Unknown | ||||||
| 8. Were groups stratified? Yes. Stratified by imatinib resistance or intolerance | ||||||
| 9. Was the treatment allocation concealed? Unknown | ||||||
| 10. Are adequate baseline details presented? Yes | ||||||
| 11. Are the participants representative of the population in question? Yes | ||||||
| 12. Are groups similar at baseline? Yes | ||||||
| 13. Are any differences in baseline adequately adjusted for in the analysis? Yes | ||||||
| 14. Are outcome assessors blind? Not clear | ||||||
| 15. Was the care provider blinded? No | ||||||
| 16. Are outcome measures relevant to research question? Yes | ||||||
| 17. Are data collection tools shown or known to be valid for the outcome of interest? Yes | ||||||
| 18. Is compliance with treatment adequate? Unclear | ||||||
| 19. Are withdrawals/dropouts adequately described? Yes | ||||||
| 20. Are all patients accounted for? Yes | ||||||
| 21. Is the number randomised reported? Yes | ||||||
| 22. Are protocol violations specified? No | ||||||
| 23. Are data analyses appropriate? Yes | ||||||
| 24. Is analysis conducted on an ITT basis? Yes | ||||||
| 25. Are missing data appropriately accounted for? Not reported | ||||||
| 26. Were any subgroup analyses justified? Yes | ||||||
| 27. Are the conclusions supported by the results? Partial. Open-label; lack of power calculation; dose escalation was allowed | ||||||
| 28. Generalisability: Partial | ||||||
| 29. Inter-centre variability: Not reported | ||||||
| 30. Conflict of interest declared? Yes. Study supported by BMS; authorship includes individuals who are employed by, consult for, receive research funding from and/or own stock in BMS. Consultancy for and research funding from Novartis also declared | ||||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Talpaz et al. (2006)104 Secondary publications: Chu et al. (2006),113 Sawyers et al. (2006),114 Cortes et al. (2008)115 Design: cohort study (prospective) CP: yes AP: yes BC: yes Country: USA Number of centres: 2 Trial code(s): NCT00064233 |
Inclusion criteria: patients who were at lest 14 years of age, had Ph+ CML (CP or AC or BC phase) or Ph+ ALL, and haematological resistance or intolerance to imatinib. CP was defined by the presence of < 15% blasts, < 20% basophils and < 30% blasts plus promyelocytes in PB or BM and a platelet count of at least 100,000 per cubic millimetre, with no extramedullary involvement. BC was defined by the presence of at least 30% blasts in PB or BM or extramedullary infiltrates of leukaemic cells (other than the spleen or liver). AP patients were defined if they did not fulfilling criteria for CP or BC, but did meet any of the following criteria: the presence of at least 15% (but < 30% blasts) in PB or BM, the presence of at least 20% basophils in PB or BM, the presence of at least 30% blasts plus promyelocytes (but < 30% blasts) in PB or BM, or a platelet count of < 100,000 per cubic millimetre unrelated to therapy. Patients with AP disease or BC who had met the criteria for CP disease at the time of entry were enrolled as having CML-CP. Patients with Ph+ ALL had at least 30% lymphoblasts in PB or BM without previous evidence of CML-CP Haematological resistance to imatinib was classified as primary (a lack of adequate response) or acquired (a relapse after an initial response). Patients with cytogenetic or molecular resistance, but without haematological resistance, to imatinib were not eligible. Patients were considered to be unable to tolerate imatinib if they had discontinued treatment as a result of non-haematological toxic effects of any grade Exclusion criteria: not reported |
Arm 1 dasatinib n: 84 Drug: dasatinib Starting daily dose (mg): not reported Dosage details: dose escalation study (15–240 mg q.d.) The study protocol permitted progression to the administration of continuous daily doses of dasatinib and dose escalation Concurrent treatment: unclear |
CyR: morphological and cytogenetic analyses of BM were performed every 3 months or more frequently in patients with CML-AP, CML-BC, or Ph+ ALL if such analysis was clinically indicated CCyR (0% Ph+) PCyR (1–35% Ph+) MCyR (complete + partial) Minor CyR (36–65% Ph+) Minimal CyR (66–95% Ph+) Overall CyR (major + minor + minimal) HR: complete and differential blood counts were obtained twice weekly for the first 12 weeks, every 2 weeks for 12 weeks and every 6 weeks thereafter CHR [CML-CP: WBC ≤ institutional ULN; platelets < 450 × 109/l; no blasts or promyelocytes in PB; < 5% myelocytes plus metamyelocytes in PB; < 20% basophils in PB; no extramedullary involvement (including no hepatomegaly or splenomegaly). CML-AP/CML-BC/Ph+ ALL: WBC ≤ institutional ULN; ANC ≥ 1 × 109/l; platelets ≥ 100 × 109/l; no blasts or promyelocytes in PB; ≤ 5% BM blasts; < 5% myelocytes plus metamyelocytes in PB; < 20% basophils in PB; no extramedullary involvement (including no hepatomegaly or splenomegaly)] Major HR (CML-CP; CHR only. CML-CP/CML-BC/Ph+ ALL; CHR or NEL) No evidence of leukaemia [CML-CP: N/A. CML-AP/CML-BC/Ph+ALL: WBC ≤ institutional ULN; no blasts or promyelocytes in PB; ≤ 5% BM blasts; < 5% myelocytes plus metamyelocytes in PB; < 20% basophils in PB; no extramedullary involvement (including no hepatomegaly or splenomegaly); either platelets 20–100 × 109/l or ANC 0.5–1.0 × 109/l] Minor HR [CML-CP: N/A. CML-AP/CML-BC/Ph+ALL: < 30% blasts plus promyelocytes in PB; < 15% blasts in BM and in PB; < 20% basophils in PB; no extramedullary involvement (other than hepatomegaly or splenomegaly)] Survival: PFS (definitions of progression in CML-CP: AP disease or BC or an inability to maintain a complete response even with dose escalation; in CML-AP: loss of major or minor response during a 2 week period or BC; CML-BC/Ph+ ALL: increasing blasts in PB or BM despite at least 4 weeks of treatment) Participant disposition: withdrawal because of AEs AEs – grades 1–4: patients were seen weekly for the first 12 weeks, monthly for the next 12 weeks, and then every 3 months. AEs were graded according to NCI CTC Version 3.0186 |
|
| Dasatinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| Demographics | ||||
| Age (years) (median) | 84 | 56 (range 15–79) | ||
| Gender (n male) | 84 | 47 | 56.0% | |
| Imatinib failure | ||||
| Intolerance | 84 | 12 | 14.3% | |
| Resistance | 84 | 72 | 85.7% | |
| Resistance – primary | 84 | 16a | 19.0% | |
| Resistance – acquired | 84 | 54a | 64.3% | |
| Prior therapy | ||||
| Highest imatinib dose 400-600 mg q.d. | 84 | 12 | 14.3% | |
| Highest imatinib dose 600 mg q.d. | 84 | 19 | 22.6% | |
| Highest imatinib dose > 600mg q.d. | 84 | 53 | 63.1% | |
| Prior chemotherapy | 84 | 50 | 59.5% | |
| Prior interferon | 84 | 60 | 71.4% | |
| Prior transplantation | 84 | 12b | 14.3% | |
| Disease history | ||||
| Duration of CML (months) (median) | 84 | 71 (range 5–216) | ||
| Previous CHR to imatinib | 84 | 62 | 73.8% | |
| Previous CyR to imatinib | 84 | 32c | 38.1% | |
| Imatinib failure | ||||
| BCR–ABL mutation | 84 | 60 | 71.4% | |
| Laboratory parameters | ||||
| WBC × 109/l (median) | 84 | 23 (range 1–243)d | ||
| Platelets × 109/l (median) | 84 | 216 (range 4–2166) | ||
| CP | ||||
| Demographics | ||||
| Age (years) (median) | 40 | 61 (range 28–79) | ||
| Gender (n male) | 40 | 21 | 52.5% | |
| Imatinib failure | ||||
| Intolerance | 40 | 8 | 20.0% | |
| Resistance | 40 | 32 | 80.0% | |
| Resistance – primary | 40 | 8e | 20.0% | |
| Resistance – acquired | 40 | 23e | 57.5% | |
| Prior therapy | 40 | 7 | 17.5% | |
| Highest imatinib dose 400-600 mg q.d. | ||||
| Highest imatinib dose 600 mg q.d. | 40 | 7 | 17.5% | |
| Highest imatinib dose > 600 mg q.d. | 40 | 26 | 65.0% | |
| Prior chemotherapy | 40 | 22 | 55.0% | |
| Prior interferon | 40 | 37 | 92.5% | |
| Prior transplantation | 40 | 2b | 5.0% | |
| Disease history | 40 | 90 (range 13–207) | ||
| Duration of CML (months) (median) | ||||
| Previous CHR to imatinib | 40 | 30 | 75.0% | |
| Previous CyR to imatinib | 40 | 20c | 50.0% | |
| Imatinib failure | 40 | 33 | 82.5% | |
| BCR–ABL mutation | ||||
| Laboratory parameters | 40 | 33 (range 3–243) | ||
| WBC × 109/l (median) | ||||
| Platelets × 109/l (median) | 40 | 310 (range 52–2166)f | ||
| AP | 11 | 63 (range 40–73) | ||
| Demographics | ||||
| Age (years) (median) | ||||
| Gender (n male) | 11 | 3 | 27.3% | |
| Imatinib failure | 11 | 2 | 18.2% | |
| Intolerance | ||||
| Resistance | 11 | 9 | 81.8% | |
| Resistance – primary | 11 | 1 | 9.1% | |
| Resistance – acquired | 11 | 8 | 72.7% | |
| Prior therapy | 11 | 1 | 9.1% | |
| Highest imatinib dose 400–600 mg q.d. | ||||
| Highest imatinib dose 600 mg q.d. | 11 | 3 | 27.3% | |
| Highest imatinib dose > 600 mg q.d. | 11 | 7 | 63.6% | |
| Prior chemotherapy | 11 | 4 | 36.4% | |
| Prior interferon | 11 | 9 | 81.8% | |
| Prior transplantation | 11 | 0b | 0.0% | |
| Disease history | 11 | 67 (range 22–139) | ||
| Duration of CML (months) (median) | ||||
| Previous CHR to imatinib | 11 | 8 | 72.7% | |
| Previous CyR to imatinib | 11 | 4c | 36.4% | |
| Imatinib failure | 11 | 8 | 72.7% | |
| BCR–ABL mutation | ||||
| Laboratory parameters | 11 | 21 (range 1–108) | ||
| WBC × 109/l (median) | ||||
| Platelets × 109/l (median) | 11 | 279 (range 4–1710) | ||
| CML with MBC | 23 | 53 (range 30–70) | ||
| Demographics | ||||
| Age (years) (median) | ||||
| Gender (n male) | 23 | 14 | 60.9% | |
| Imatinib failure | 23 | 1 | 4.3% | |
| Intolerance | ||||
| Resistance | 23 | 22 | 95.7% | |
| Resistance – primary | 23 | 6e | 26.1% | |
| Resistance – acquired | 23 | 15e | 65.2% | |
| Prior therapy | 23 | 3 | 13.0% | |
| Highest imatinib dose 400–600 mg q.d. | ||||
| Highest imatinib dose 600 mg q.d. | 23 | 7 | 30.4% | |
| Highest imatinib dose > 600 mg q.d. | 23 | 13 | 56.5% | |
| Prior chemotherapy | 23 | 15 | 65.2% | |
| Prior interferon | 23 | 12 | 52.2% | |
| Prior transplantation | 23 | 5b | 21.7% | |
| Disease history | 23 | 44 (range 5–216) | ||
| Duration of CML (months) (median) | ||||
| Previous CHR to imatinib | 23 | 15 | 65.2% | |
| Previous CyR to imatinib | 23 | 5c | 21.7% | |
| Imatinib failure | 23 | 13 | 56.5% | |
| BCR–ABL mutation | ||||
| Laboratory parameters | 23 | 20 (range 1–117)d | ||
| WBC × 109/l (median) | ||||
| Platelets × 109/l (median) | 23 | 39 (range 7–1057) | ||
| CML with LBC or Ph+ ALL | 10 | 50 (range 15–73) | ||
| Demographics | ||||
| Age (years) (median) | ||||
| Gender (n male) | 10 | 9 | 90.0% | |
| Imatinib failure | 10 | 1 | 10.0% | |
| Intolerance | ||||
| Resistance | 10 | 9 | 90.0% | |
| Resistance – primary | 10 | 1 | 10.0% | |
| Resistance – acquired | 10 | 8 | 80.0% | |
| Prior therapy | 10 | 1 | 10.0% | |
| Highest imatinib dose 400–600 mg q.d. | ||||
| Highest imatinib dose 600 mg q.d. | 10 | 2 | 20.0% | |
| Highest imatinib dose > 600 mg q.d. | 10 | 7 | 70.0% | |
| Prior chemotherapy | 10 | 9 | 90.0% | |
| Prior interferon | 10 | 2 | 20.0% | |
| Prior transplantation | 10 | 5b | 50.0% | |
| Disease history | 10 | 26 (range 9–70) | ||
| Duration of CML (months) (median) | ||||
| Previous CHR to imatinib | 10 | 9 | 90.0% | |
| Previous CyR to imatinib | 10 | 3c | 30.0% | |
| Imatinib failure | 10 | 6 | 60.0% | |
| BCR–ABL mutation | ||||
| Laboratory parameters | 10 | 12 (range 1–198) | ||
| WBC × 109/l (median) | ||||
| Platelets × 109/l (median) | 10 | 40 (range 22–375) | ||
| Results | ||||
| CyR | 84 | 25 | 29.8% | |
| CCyR | ||||
| PCyR | 84 | 12g | 14.3% | |
| MCyR | 84 | 37 | 44.0% | |
| Minor CyR | 84 | 3 | 3.6% | |
| Minimal CyR | 84 | 10 | 11.9% | |
| Overall CyR | 84 | 50 | 59.5% | |
| HR | ||||
| CHR | 84 | 57h | 67.9% | |
| Major HR | 84 | 68 | 81.0% | |
| No evidence of leukaemia | 44 | 11i | 25.0% | |
| Minor HR | 44 | 4i | 9.1% | |
| Participant disposition | ||||
| Withdrawal because of AEs | 84 | 0 | 0.0% | |
| AEs – grades 1–4 | ||||
| Diarrhoea | 84 | 19 | 22.6% | |
| Dyspnoea or pulmonary oedema | 84 | 10 | 11.9% | |
| Fatigue | 84 | 4 | 4.8% | |
| Flushing | 84 | 4 | 4.8% | |
| Gastrointestinal haemorrhage | 84 | 7 | 8.3% | |
| Generalised oedema | 84 | 4 | 4.8% | |
| Headache | 84 | 8 | 9.5% | |
| Nausea | 84 | 8 | 9.5% | |
| Pericardial effusion | 84 | 4 | 4.8% | |
| Periorbital oedema | 84 | 6 | 7.1% | |
| Peripheral oedema | 84 | 16 | 19.0% | |
| Pleural effusion | 84 | 15 | 17.9% | |
| Rash | 84 | 9 | 10.7% | |
| Tumour lysis syndrome | 84 | 2 | 2.4% | |
| Vomiting | 84 | 4 | 4.8% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 84 | 49 | 58.3% | |
| Neutropenia | 84 | 57 | 67.9% | |
| AEs – grade 3–4 | ||||
| Diarrhoea | 84 | 1 | 1.2% | |
| Dyspnoea or pulmonary oedema | 84 | 2 | 2.4% | |
| Fatigue | 84 | 1 | 1.2% | |
| Flushing | 84 | 0 | 0.0% | |
| Gastrointestinal haemorrhage | 84 | 5 | 6.0% | |
| Generalised oedema | 84 | 0 | 0.0% | |
| Headache | 84 | 0 | 0.0% | |
| Nausea | 84 | 0 | 0.0% | |
| Pericardial effusion | 84 | 2 | 2.4% | |
| Periorbital oedema | 84 | 0 | 0.0% | |
| Peripheral oedema | 84 | 0 | 0.0% | |
| Pleural effusion | 84 | 3 | 3.6% | |
| Rash | 84 | 0 | 0.0% | |
| Tumour lysis syndrome | 84 | 2 | 2.4% | |
| Vomiting | 84 | 0 | 0.0% | |
| CP | ||||
| CyR | ||||
| CCyR | 40 | 14 | 35.0% | |
| PCyR | 40 | 4 | 10.0% | |
| MCyR | 40 | 18 | 45.0% | |
| Minor CyR | 40 | 0 | 0.0% | |
| Minimal CyR | 40 | 7 | 17.5% | |
| Overall CyR | 40 | 25 | 62.5% | |
| HR | ||||
| CHR | 40 | 37h | 92.5% | |
| Major HR | 40 | 37 | 92.5% | |
| Survival | ||||
| PFS – 0 months | 40 | 1 | ||
| PFS – 2 months | 1 | |||
| PFS – 4 months | 1 | |||
| PFS – 6 months | 1 | |||
| PFS – 8 months | 1 | |||
| PFS – 10 months | 1 | |||
| PFS – 12 months | 1 | |||
| PFS – 14 months | 1 | |||
| PFS – 16 months | 1 | |||
| PFS – 18 months | 1 | |||
| Participant disposition | ||||
| Withdrawal because of AEs | 40 | 0 | 0.0% | |
| AEs – grades 1–4 | ||||
| Diarrhoea | 40 | 7 | 17.5% | |
| Dyspnoea or pulmonary oedema | 40 | 4 | 10.0% | |
| Fatigue | 40 | 3 | 7.5% | |
| Flushing | 40 | 0 | 0.0% | |
| Gastrointestinal haemorrhage | 40 | 4 | 10.0% | |
| Generalised oedema | 40 | 2 | 5.0% | |
| Headache | 40 | 4 | 10.0% | |
| Nausea | 40 | 2 | 5.0% | |
| Pericardial effusion | 40 | 1 | 2.5% | |
| Periorbital oedema | 40 | 2 | 5.0% | |
| Peripheral oedema | 40 | 7 | 17.5% | |
| Pleural effusion | 40 | 5 | 12.5% | |
| Rash | 40 | 1 | 2.5% | |
| Tumour lysis syndrome | 40 | 0 | 0.0% | |
| Vomiting | 40 | 0 | 0.0% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 40 | 14 | 35.0% | |
| Neutropenia | 40 | 18 | 45.0% | |
| AEs – grade 3–4 | ||||
| Diarrhoea | 40 | 0 | 0.0% | |
| Dyspnoea or pulmonary oedema | 40 | 0 | 0.0% | |
| Fatigue | 40 | 1 | 2.5% | |
| Flushing | 40 | 0 | 0.0% | |
| Gastrointestinal haemorrhage | 40 | 2 | 5.0% | |
| Generalised oedema | 40 | 0 | 0.0% | |
| Headache | 40 | 0 | 0.0% | |
| Nausea | 40 | 0 | 0.0% | |
| Pericardial effusion | 40 | 0 | 0.0% | |
| Periorbital oedema | 40 | 0 | 0.0% | |
| Peripheral oedema | 40 | 0 | 0.0% | |
| Pleural effusion | 40 | 0 | 0.0% | |
| Rash | 40 | 0 | 0.0% | |
| Tumour lysis syndrome | 40 | 0 | 0.0% | |
| Vomiting | 40 | 0 | 0.0% | |
| AP | ||||
| CyR | ||||
| CCyR | 11 | 2 | 18.2% | |
| PCyR | 11 | 1 | 9.1% | |
| MCyR | 11 | 3 | 27.3% | |
| Minor CyR | 11 | 0 | 0.0% | |
| Minimal CyR | 11 | 1 | 9.1% | |
| Overall CyR | 11 | 4 | 36.4% | |
| HR | ||||
| CHR | 11 | 5 | 45.5% | |
| Major HR | 11 | 9 | 81.8% | |
| No evidence of leukaemia | 11 | 4 | 36.4% | |
| Minor HR | 11 | 0 | 0.0% | |
| Survival | ||||
| PFS – 0 months | 11 | 1 | ||
| PFS – 2 months | 1 | |||
| PFS – 4 months | 1 | |||
| PFS – 6 months | 0.715 | |||
| PFS – 8 months | 0.715 | |||
| PFS – 10 months | 0.715 | |||
| PFS – 12 months | 0.715 | |||
| Participant disposition | ||||
| Withdrawal because of AEs | 11 | 0 | 0.0% | |
| AEs – grades 1–4 | ||||
| Diarrhoea | 11 | 5 | 45.5% | |
| Dyspnoea or pulmonary oedema | 11 | 3 | 27.3% | |
| Fatigue | 11 | 0 | 0.0% | |
| Flushing | 11 | 3 | 27.3% | |
| Gastrointestinal haemorrhage | 11 | 0 | 0.0% | |
| Generalised oedema | 11 | 1 | 9.1% | |
| Headache | 11 | 3 | 27.3% | |
| Nausea | 11 | 1 | 9.1% | |
| Pericardial effusion | 11 | 0 | 0.0% | |
| Periorbital oedema | 11 | 1 | 9.1% | |
| Peripheral oedema | 11 | 3 | 27.3% | |
| Pleural effusion | 11 | 0 | 0.0% | |
| Rash | 11 | 5 | 45.5% | |
| Tumour lysis syndrome | 11 | 0 | 0.0% | |
| Vomiting | 11 | 1 | 9.1% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 11 | 9 | 81.8% | |
| Neutropenia | 11 | 9 | 81.8% | |
| AEs – grade 3–4 | ||||
| Diarrhoea | 11 | 0 | 0.0% | |
| Dyspnoea or pulmonary oedema | 11 | 0 | 0.0% | |
| Fatigue | 11 | 0 | 0.0% | |
| Flushing | 11 | 0 | 0.0% | |
| Gastrointestinal haemorrhage | 11 | 0 | 0.0% | |
| Generalised oedema | 11 | 0 | 0.0% | |
| Headache | 11 | 0 | 0.0% | |
| Nausea | 11 | 0 | 0.0% | |
| Pericardial effusion | 11 | 0 | 0.0% | |
| Periorbital oedema | 11 | 0 | 0.0% | |
| Peripheral oedema | 11 | 0 | 0.0% | |
| Pleural effusion | 11 | 0 | 0.0% | |
| Rash | 11 | 0 | 0.0% | |
| Tumour lysis syndrome | 11 | 0 | 0.0% | |
| Vomiting | 11 | 0 | 0.0% | |
| CML with MBC | ||||
| CyR | ||||
| CCyR | 23 | 6 | 26.1% | |
| PCyR | 23 | 2 | 8.7% | |
| MCyR | 23 | 8 | 34.8% | |
| Minor CyR | 23 | 2 | 8.7% | |
| Minimal CyR | 23 | 2 | 8.7% | |
| Overall CyR | 23 | 12 | 52.2% | |
| HR | ||||
| CHR | 23 | 8 | 34.8% | |
| Major HR | 23 | 14 | 60.9% | |
| No evidence of leukaemia | 23 | 6 | 26.1% | |
| Minor HR | 23 | 4 | 17.4% | |
| Survival | ||||
| PFS – 0 months | 23 | 1 | ||
| PFS – 2 months | 0.89 | |||
| PFS – 4 months | 0.715 | |||
| PFS – 6 months | 0.45 | |||
| PFS – 8 months | 0.375 | |||
| PFS – 10 months | 0.25 | |||
| Participant disposition | ||||
| Withdrawal because of AEs | 23 | 0 | 0.0% | |
| AEs – grades 1–4 | ||||
| Diarrhoea | 23 | 5 | 21.7% | |
| Dyspnoea or pulmonary oedema | 23 | 2 | 8.7% | |
| Fatigue | 23 | 0 | 0.0% | |
| Flushing | 23 | 1 | 4.3% | |
| Gastrointestinal haemorrhage | 23 | 3 | 13.0% | |
| Generalised oedema | 23 | 0 | 0.0% | |
| Headache | 23 | 1 | 4.3% | |
| Nausea | 23 | 4 | 17.4% | |
| Pericardial effusion | 23 | 3 | 13.0% | |
| Periorbital oedema | 23 | 2 | 8.7% | |
| Peripheral oedema | 23 | 5 | 21.7% | |
| Pleural effusion | 23 | 8 | 34.8% | |
| Rash | 23 | 2 | 8.7% | |
| Tumour lysis syndrome | 23 | 2 | 8.7% | |
| Vomiting | 23 | 2 | 8.7% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 23 | 19 | 82.6% | |
| Neutropenia | 23 | 22 | 95.7% | |
| AEs – grade 3–4 | ||||
| Diarrhoea | 23 | 1 | 4.3% | |
| Dyspnoea or pulmonary oedema | 23 | 2 | 8.7% | |
| Fatigue | 23 | 0 | 0.0% | |
| Flushing | 23 | 0 | 0.0% | |
| Gastrointestinal haemorrhage | 23 | 3 | 13.0% | |
| Generalised oedema | 23 | 0 | 0.0% | |
| Headache | 23 | 0 | 0.0% | |
| Nausea | 23 | 0 | 0.0% | |
| Pericardial effusion | 23 | 2 | 8.7% | |
| Periorbital oedema | 23 | 0 | 0.0% | |
| Peripheral oedema | 23 | 0 | 0.0% | |
| Pleural effusion | 23 | 3 | 13.0% | |
| Rash | 23 | 0 | 0.0% | |
| Tumour lysis syndrome | 23 | 2 | 8.7% | |
| Vomiting | 23 | 0 | 0.0% | |
| CML with LBC or Ph+ ALL | ||||
| CyR | ||||
| CCyR | 10 | 3 | 30.0% | |
| PCyR | 10 | 5g | 50.0% | |
| MCyR | 10 | 8 | 80.0% | |
| Minor CyR | 10 | 1 | 10.0% | |
| Minimal CyR | 10 | 0 | 0.0% | |
| Overall CyR | 10 | 9 | 90.0% | |
| HR | ||||
| CHR | 10 | 7 | 70.0% | |
| Major HR | 10 | 8 | 80.0% | |
| No evidence of leukaemia | 10 | 1 | 10.0% | |
| Minor HR | 10 | 0 | 0.0% | |
| Survival | ||||
| PFS – 0 months | 10 | 1 | ||
| PFS – 2 months | 0.75 | |||
| PFS – 4 months | 0.47 | |||
| PFS – 6 months | 0.235 | |||
| PFS – 8 months | 0 | |||
| PFS – 10 months | 0 | |||
| PFS – 12 months | 0 | |||
| PFS – 14 months | 0 | |||
| PFS – 16 months | 0 | |||
| PFS – 18 months | 0 | |||
| Participant disposition | ||||
| Withdrawal because of AEs | 10 | 0 | 0.0% | |
| AEs – grades 1–4 | ||||
| Diarrhoea | 10 | 2 | 20.0% | |
| Dyspnoea or pulmonary oedema | 10 | 1 | 10.0% | |
| Fatigue | 10 | 1 | 10.0% | |
| Flushing | 10 | 0 | 0.0% | |
| Gastrointestinal haemorrhage | 10 | 0 | 0.0% | |
| Generalised oedema | 10 | 1 | 10.0% | |
| Headache | 10 | 0 | 0.0% | |
| Nausea | 10 | 1 | 10.0% | |
| Pericardial effusion | 10 | 0 | 0.0% | |
| Periorbital oedema | 10 | 1 | 10.0% | |
| Peripheral oedema | 10 | 1 | 10.0% | |
| Pleural effusion | 10 | 2 | 20.0% | |
| Rash | 10 | 1 | 10.0% | |
| Tumour lysis syndrome | 10 | 0 | 0.0% | |
| Vomiting | 10 | 1 | 10.0% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 10 | 7 | 70.0% | |
| Neutropenia | 10 | 8 | 80.0% | |
| AEs – grade 3–4 | ||||
| Diarrhoea | 10 | 0 | 0.0% | |
| Dyspnoea or pulmonary oedema | 10 | 0 | 0.0% | |
| Fatigue | 10 | 0 | 0.0% | |
| Flushing | 10 | 0 | 0.0% | |
| Gastrointestinal haemorrhage | 10 | 0 | 0.0% | |
| Generalised oedema | 10 | 0 | 0.0% | |
| Headache | 10 | 0 | 0.0% | |
| Nausea | 10 | 0 | 0.0% | |
| Pericardial effusion | 10 | 0 | 0.0% | |
| Periorbital oedema | 10 | 0 | 0.0% | |
| Peripheral oedema | 10 | 0 | 0.0% | |
| Pleural effusion | 10 | 0 | 0.0% | |
| Rash | 10 | 0 | 0.0% | |
| Tumour lysis syndrome | 10 | 0 | 0.0% | |
| Vomiting | 10 | 0 | 0.0% | |
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? Yes | ||||
| 1.2 Were the case series collected at more than one centre? Multicentre | ||||
| 1.3 Was the main outcome independently assessed? No | ||||
| 1.4 Are patient characteristics adequately described? No. By CML phase only, not by drug dose | ||||
| 1.5 How easy is it to assess generalisability of the results? Low | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? Yes | ||||
| 2.2 Were data collected prospectively? Yes | ||||
| 2.3 Were patients recruited consecutively? Yes | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? No | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Uncertain | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? Yes | ||||
| 4.2 Were dropouts from the study adequately described? Yes | ||||
| Study details | Population | Arms | Outcomes | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
Study: Kantarjian et al. (2009)81 Secondary publications: Kantarjian et al. (2006),99 Pasquini et al. (2007),100 Saglio et al. (2008),102 Kantarjian et al. (2008)101 Trial code: CA180–035 CP: no AP: yes BC: no Country: (n = 31) Argentina, Australia, Austria, Belgium, Brazil, Canada, the Czech Republic, Denmark, Finland, France, Germany, Hungary, Ireland, Israel, Italy, the Netherlands, Norway, Peru, the Philippines, Poland, Republic of Korea, Russian Federation, Singapore, South Africa, Spain, Sweden, Switzerland, Taiwan, Thailand, the UK, and the USA Number of centres: 97 |
Inclusion criteria: participants with CML-AP [PB or BM counts of 15–30% blasts; ≥ 30% blasts plus promyelocytes but with < 30% blasts alone; ≥ 20% basophils, and platelet counts < 100 × 109/l unrelated to drug therapy; patients with clonal evolution or with prior CML-AP (except those defined by elevated basophil count only) who achieved a HR and subsequently progressed were included even if they did not reach the threshold values of percentage of blasts in PB or BM for AP]. Participants who had stopped treatment with imatinib following resistance or intolerance. ImR was defined as no HR to imatinib after at least 4 weeks of treatment or a 50% increase in PB blasts after 2 weeks treatment at 600 mg q.d.; achieved a HR and subsequently no longer met the criteria consistently on all assessments over a consecutive 2-week period while receiving imatinib 600 mg q.d.; or patients initially diagnosed with CML-CP who progressed to CML-AP while receiving imatinib at any dose. ImI was defined as having grade 3 or greater non-haematological toxicity or grade 4 or greater haematological toxicity lasting for > 2 weeks while on imatinib ≥ 600 mg q.d. that led to a discontinuation of therapy or to dose decrease to ≤ 400 mg q.d. with loss of HR Exclusion criteria: Eastern Cooperative Oncology Group (ECOG) performance status > 2; inadequate hepatic or renal function; treatment with imatinib, IFN, cytarabine or any targeted small molecule anticancer agent within 7 days of initiation; uncontrolled or significant cardiovascular disease; history of a significant bleeding disorder unrelated to CML; or any concurrent incurable malignancy other that CML Method of allocation: randomisation (no detail of methods) was stratified by phase and type of disease and imatinib status (ImR or ImI) Blinding: open-label Therapy common to all participants: CML therapies other than dasatinib were prohibited during the study, with the exception of hydroxycarbamide for elevated WBC counts. Colony-stimulating factors and recombinant erythropoietin were permitted at the discretion of the investigator, according to institutional guidelines. Patients were supported with platelet transfusions as required |
Arm 1 dasatinib 140 mg q.d. n: 158 Drug: dasatinib Starting daily dose (mg): 140 Dosage details: 140 mg q.d. escalation to 180 mg q.d. was allowed for inadequate response (rising percentage of blasts or loss of HR in two consecutive assessments at least 1 week apart; absence of CHR, NEL or minor HR within 4 weeks; no MCyR after 3 months; or no CCyR after 6 months) Interruption or reduction to 80 mg q.d. was allowed in cases of drug toxicity (grade 2 or greater non-haematological toxicity considered related to dasatinib; ANC 0.5 × 109/l and/or platelets < 100 × 109/l for > 6 weeks with BM cellularity < 10% with blasts < 5% or BM cellularity > 10% with blasts > 5%; or febrile neutropenia with signs of septicaemia) Arm 2 dasatinib 70 mg q.d. n: 159 Drug: dasatinib Starting daily dose (mg): 140 Dosage details: 70 mg b.i.d. escalation to 90 mg b.i.d. or reduction to 40 mg b.i.d. permitted; criteria as per arm 1 |
CyR: Cytogenetic assessment of BM metaphases was performed within 4 weeks and subsequently at the end of months 1, 2, 3, 6, 9 and 12 CCyR (0% Ph+) PCyR (1–35% Ph+) MCyR (complete + partial) Duration of MCyR HR: Haematological assessment was performed on all patients within 72 hours of initiating treatment, weekly during weeks 1–6, at weeks 8 and 12 and monthly thereafter Overall HR [major or minor (< 15% blasts in BM and in PB; < 30% blasts plus promyelocytes in BM and < 30% blasts plus promyelocytes in PB; < 2% basophils in PB; no extramedullary involvement other than spleen and liver) response] CHR [WBC count no more than institutional ULN; ANC ≥ 1 × 109/l; platelet count ≥ 100 × 109/l; no blasts or promyelocytes in PB; BM blasts ≤ 5%; < 5% myelocytes plus metamyelocytes in PB; basophils in PB < 2% and basophils in the BM < 2%; no extramedullary involvement (including no hepatomegaly or splenomegaly); confirmed if all criteria were met consistently for subsequent assessments for at least 28 days – two consecutive assessments showing non-response were interpreted as response not achieved, whereas a single non-response between two assessments qualifying for CHR did not preclude a response being achieved] Major HR (CHR or NEL) No evidence of leukaemia (normalisation of PB counts, WBC < 10 × 109/l, platelets 20–100 × 109/l, ANC 0.5–1.0 × 109/l) Duration of major HR Study medication: duration of study therapy (months) Average daily dose (mg q.d.) Survival: PFS (progression defined by the first occurrence after administration of maximum dasatinib dose of any of the following: initial HR but subsequent failure to consistently meet HR criteria over a consecutive 2-week period; no decrease from on-study baseline for percentage blasts in PB or BM on all assessments over a 4-week period; absolute increase of at least 50% in PB blasts over a 2-week period; development of CML-BC at any time after initiation of therapy; or development of extramedullary disease sites other than the spleen or liver. Patients who died without progressing were considered to have progressed at the time of death) OS Participant disposition: withdrawal because of AEs Haematological AEs – grades 1–4: assessed using the NCI CTC Version 3.0186 |
||||||
| Dasatinib 140 mg q.d. | Dasatinib 70 mg q.d. | Δ | p-value | ||||||
| n | κ | Mean | n | κ | Mean | ||||
| Baseline characteristics | |||||||||
| Demographics | |||||||||
| Age (years) (median) | 158 | 56 (range 17–81) | 159 | 56 (range 19–84) | |||||
| Gender (n male) | 158 | 88 | 55.7% | 159 | 94 | 59.1% | 0.615a | ||
| Imatinib failure | |||||||||
| Intolerance | 158 | 41 | 25.9% | 159 | 43 | 27.0% | 0.925a | ||
| Resistance | 158 | 117 | 74.1% | 159 | 116 | 73.0% | 0.925a | ||
| Prior therapy | |||||||||
| Best response to imatinib – CHR | 158 | 121 | 76.6% | 159 | 119 | 74.8% | 0.818a | ||
| Best response to imatinib – MCyR | 158 | 48 | 30.4% | 159 | 44 | 27.7% | 0.684a | ||
| Time on imatinib < 1 year | 158 | 23 | 14.6% | 159 | 24 | 15.1% | 0.981a | ||
| Time on imatinib 1–3 years | 158 | 51 | 32.3% | 159 | 54 | 34.0% | 0.842a | ||
| Time on imatinib > 3 years | 158 | 84 | 53.2% | 159 | 80 | 50.3% | 0.693a | ||
| Highest imatinib dose > 600 mg q.d. | 158 | 68 | 43.0% | 159 | 73 | 45.9% | 0.688a | ||
| Prior chemotherapy | 158 | 70 | 44.3% | 159 | 70 | 44.0% | 0.950a | ||
| Prior interferon | 158 | 85 | 53.8% | 159 | 87 | 54.7% | 0.959a | ||
| Prior transplantationb | 158 | 19 | 12.0% | 159 | 9 | 5.7% | 0.072a | ||
| Disease history | |||||||||
| Duration of CML (months) (median) | 158 | 74.3 (range 5.1–326.8) | 159 | 70.1 (range 2.5–199.7) | |||||
| Demographics | |||||||||
| ECOG performance status 0–1 | 158 | 148 | 93.7% | 159 | 143 | 89.9% | 0.314a | ||
| Baseline status | |||||||||
| ECOG performance status 0–1 | 158 | 148 | 93.7% | 159 | 143 | 89.9% | 0.314a | ||
| CHR at study entry | 158 | 16 | 10.1% | 159 | 31 | 19.5% | 0.029a | ||
| Disease history | |||||||||
| CHR at study entry | 158 | 16 | 10.1% | 159 | 31 | 19.5% | 0.029a | ||
| Baseline status | |||||||||
| CCyR at study entry | 158 | 1 | 0.6% | 159 | 3 | 1.9% | 0.619a | ||
| MCyR at study entry | 158 | 15 | 9.5% | 159 | 12 | 7.5% | 0.675a | ||
| Results | |||||||||
| CyR | |||||||||
| CCyR | 158 | 51 | 32.3% | 159 | 52 | 32.7% | 0.969c | ||
| PCyR | 158 | 10 | 6.3% | 159 | 16 | 10.1% | 0.314c | ||
| MCyR | 158 | 61 | 38.6% | 159 | 68 | 42.8% | 0.523c | ||
| Duration of MCyR – 0 months | 158 | 1 | 159 | 1 | |||||
| Duration of MCyR – 12 months | 0.905 | 0.815 | |||||||
| Duration of MCyR – 15 months | 0.86 | 0.795 | |||||||
| Duration of MCyR – 18 months | 0.805 | 0.77 | |||||||
| Duration of MCyR – 21 months | 0.705 | 0.745 | |||||||
| Duration of MCyR – 24 months | 0.625 | 0.745 | |||||||
| Duration of MCyR – 27 months | 0.585 | ||||||||
| Duration of MCyR – 3 months | 0.96 | 0.92 | |||||||
| Duration of MCyR – 6 months | 0.96 | 0.895 | |||||||
| Duration of MCyR – 9 months | 0.945 | 0.87 | |||||||
| HR | |||||||||
| Overall HR | 158 | 119 | 75.3% | 159 | 120 | 75.5% | 0.922c | ||
| CHR | 158 | 75 | 47.5% | 159 | 82 | 51.6% | 0.536c | ||
| Major HR | 158 | 105 | 66.5% | 159 | 108 | 67.9% | 0.874c | ||
| No evidence of leukaemia | 158 | 30 | 19.0% | 159 | 26 | 16.4% | 0.640c | ||
| Duration of major HR – 0 months | 158 | 1 | 159 | 1 | |||||
| Duration of major HR – 12 months | 0.855 | 0.805 | |||||||
| Duration of major HR – 15 months | 0.765 | 0.745 | |||||||
| Duration of major HR – 18 months | 0.74 | 0.7 | |||||||
| Duration of major HR – 21 months | 0.705 | 0.685 | |||||||
| Duration of major HR – 24 months | 0.645 | 0.6 | |||||||
| Duration of major HR – 27 months | 0.585 | 0.57 | |||||||
| Duration of major HR – 3 months | 0.98 | 0.965 | |||||||
| Duration of major HR – 6 months | 0.92 | 0.905 | |||||||
| Duration of major HR – 9 months | 0.885 | 0.875 | |||||||
| Study medication | |||||||||
| Duration of study therapy (months) (median) | 158 | 15.4 (range 0.03–31.15) | 159 | 12 (range 0.39–28.8) | |||||
| Average daily dose (mg q.d.) (median) | 158 | 138 (range 20–216) | 159 | 110 (range 20–178) | |||||
| Survival | |||||||||
| PFS – 0 months | 158 | 1 | 159 | 1 | |||||
| PFS – 12 months | 0.695 | 0.7 | |||||||
| PFS – 15 months | 0.665 | 0.66 | |||||||
| PFS – 18 months | 0.61 | 0.635 | |||||||
| PFS – 21 months | 0.565 | 0.59 | |||||||
| PFS – 24 months | 0.51 | 0.55 | |||||||
| PFS – 27 months | 0.48 | 0.49 | |||||||
| PFS – 3 months | 0.91 | 0.895 | |||||||
| PFS – 30 monthso | 0.41 | 0.49 | |||||||
| PFS – 6 months | 0.795 | 0.825 | |||||||
| PFS – 9 months | 0.72 | 0.78 | |||||||
| OS – 0 months | 158 | 1 | 159 | 1 | |||||
| OS – 12 months | 0.775 | 0.84 | |||||||
| OS – 15 months | 0.76 | 0.8 | |||||||
| OS – 18 months | 0.725 | 0.79 | |||||||
| OS – 21 months | 0.68 | 0.755 | |||||||
| OS – 24 months | 0.635 | 0.73 | |||||||
| OS – 27 months | 0.595 | 0.67 | |||||||
| OS – 3 months | 0.925 | 0.955 | |||||||
| OS – 30 monthso | 0.54 | 0.67 | |||||||
| OS – 33 months | 0.54 | ||||||||
| OS – 6 months | 0.87 | 0.93 | |||||||
| OS – 9 months | 0.83 | 0.88 | |||||||
| Participant disposition | |||||||||
| Withdrawal because of AEs | 158 | 41d | 25.9% | 159 | 46e | 28.9% | 0.639c | ||
| Haematological AEs – grades 1–4 | |||||||||
| Anaemia | 155 | 154 | 99.4% | 159 | 158 | 99.4% | 0.489c | ||
| Neutropenia | 155 | 130 | 83.9% | 159 | 141 | 88.7% | 0.282c | ||
| Thrombopenia | 155 | 137 | 88.4% | 159 | 148 | 93.1% | 0.214c | ||
| Leucopenia | 155 | 127 | 81.9% | 159 | 136 | 85.5% | 0.477c | ||
| AEs – grades 1–4 | |||||||||
| Arthralgia | 157 | 15 | 9.6% | 159 | 13 | 8.2% | 0.816c | ||
| Cough | 157 | 12 | 7.6% | 159 | 18 | 11.3% | 0.356c | ||
| Diarrhoea | 157 | 49 | 31.2% | 159 | 50 | 31.4% | 0.939c | ||
| Dyspnoea | 157 | 32 | 20.4% | 159 | 37 | 23.3% | 0.628c | ||
| Fatigue | 157 | 30 | 19.1% | 159 | 32 | 20.1% | 0.931c | ||
| Febrile neutropenia | 157 | 6 | 3.8% | 159 | 16 | 10.1% | 0.050c | ||
| Fluid retention | 157 | 53 | 33.8% | 159 | 77 | 48.4% | 0.011c | ||
| Fluid retention (other) | 157 | 7 | 4.5% | 159 | 24 | 15.1% | 0.003c | ||
| Gastrointestinal haemorrhage | 157 | 13 | 8.3% | 159 | 21 | 13.2% | 0.218c | ||
| Haemorrhage (non-GI) | 157 | 30 | 19.1% | 159 | 33 | 20.8% | 0.822c | ||
| Headache | 157 | 43 | 27.4% | 159 | 37 | 23.3% | 0.476c | ||
| Infectionf | 157 | 16 | 10.2% | 159 | 17 | 10.7% | 0.969c | ||
| Musculoskeletal pain | 157 | 18 | 11.5% | 159 | 23 | 14.5% | 0.531c | ||
| Myalgia | 157 | 11 | 7.0% | 159 | 21 | 13.2% | 0.101c | ||
| Nausea | 157 | 30 | 19.1% | 159 | 28 | 17.6% | 0.843c | ||
| Pleural effusion | 157 | 31 | 19.7% | 159 | 62 | 39.0% | < 0.001c | ||
| Pyrexia | 157 | 18 | 11.5% | 159 | 18 | 11.3% | 0.891c | ||
| Rash | 157 | 23 | 14.6% | 159 | 29 | 18.2% | 0.479c | ||
| Superficial oedema | 157 | 28 | 17.8% | 159 | 32 | 20.1% | 0.707c | ||
| Vomiting | 157 | 18 | 11.5% | 159 | 24 | 15.1% | 0.433c | ||
| Haematological AEs – grade 3–4 | |||||||||
| Thrombopenia | 155 | 99 | 63.9% | 159 | 107 | 67.3% | 0.603c | ||
| Anaemia | 155 | 74 | 47.7% | 159 | 68 | 42.8% | 0.440c | ||
| Neutropenia | 155 | 91 | 58.7% | 159 | 109 | 68.6% | 0.090c | ||
| Leucopenia | 155 | 69 | 44.5% | 159 | 65 | 40.9% | 0.591c | ||
| AEs – grade 3–4 | |||||||||
| Arthralgia | 157 | 0 | 0.0% | 159 | 2 | 1.3% | 0.569c | ||
| Cough | 157 | 0 | 0.0% | 159 | 0 | 0.0% | 0.320c | ||
| Diarrhoea | 157 | 4 | 2.5% | 159 | 5 | 3.1% | 0.985c | ||
| Dyspnoea | 157 | 5 | 3.2% | 159 | 11 | 6.9% | 0.209c | ||
| Fatigue | 157 | 3 | 1.9% | 159 | 5 | 3.1% | 0.734c | ||
| Febrile neutropenia | 157 | 6 | 3.8% | 159 | 16 | 10.1% | 0.050c | ||
| Fluid retention | 157 | 12 | 7.6% | 159 | 17 | 10.7% | 0.457c | ||
| Fluid retention (other) | 157 | 2 | 1.3% | 159 | 8 | 5.0% | 0.113c | ||
| Gastrointestinal haemorrhage | 157 | 9 | 5.7% | 159 | 10 | 6.3% | 0.977c | ||
| Haemorrhage (non-GI) | 157 | 3 | 1.9% | 159 | 2 | 1.3% | 0.989c | ||
| Headache | 157 | 2 | 1.3% | 159 | 1 | 0.6% | 0.991c | ||
| Infectionf | 157 | 9 | 5.7% | 159 | 3 | 1.9% | 0.135c | ||
| Musculoskeletal pain | 157 | 0 | 0.0% | 159 | 3 | 1.9% | 0.320c | ||
| Myalgia | 157 | 1 | 0.6% | 159 | 3 | 1.9% | 0.624c | ||
| Nausea | 157 | 1 | 0.6% | 159 | 3 | 1.9% | 0.624c | ||
| Pleural effusion | 157 | 11 | 7.0% | 159 | 10 | 6.3% | 0.976c | ||
| Pyrexia | 157 | 3 | 1.9% | 159 | 2 | 1.3% | 0.989c | ||
| Rash | 157 | 0 | 0.0% | 159 | 1 | 0.6% | 0.993c | ||
| Superficial oedema | 157 | 1 | 0.6% | 159 | 0 | 0.0% | 0.993c | ||
| Vomiting | 157 | 1 | 0.6% | 159 | 2 | 1.3% | 0.991c | ||
| ImI | |||||||||
| CyR | |||||||||
| CCyR | 41 | 17 | 41.5% | 43 | 14 | 32.6% | 0.536c | ||
| PCyR | 41 | 2 | 4.9% | 43 | 5 | 11.6% | 0.469c | ||
| MCyR | 41 | 19 | 46.3% | 43 | 19 | 44.2% | 0.983c | ||
| HR | |||||||||
| Overall HR | 41 | 36 | 87.8% | 43 | 34 | 79.1% | 0.435c | ||
| CHR | 41 | 16 | 39.0% | 43 | 23 | 53.5% | 0.267c | ||
| Major HR | 41 | 31 | 75.6% | 43 | 29 | 67.4% | 0.557c | ||
| No evidence of leukaemia | 41 | 15 | 36.6% | 43 | 6 | 14.0% | 0.032c | ||
| ImR | |||||||||
| CyR | |||||||||
| CCyR | 117 | 34 | 29.1% | 116 | 38 | 32.8% | 0.639c | ||
| PCyR | 117 | 8 | 6.8% | 116 | 11 | 9.5% | 0.618c | ||
| MCyR | 117 | 42 | 35.9% | 116 | 49 | 42.2% | 0.391c | ||
| HR | |||||||||
| Overall HR | 117 | 83 | 70.9% | 116 | 83 | 71.6% | 0.967c | ||
| CHR | 117 | 59 | 50.4% | 116 | 59 | 50.9% | 0.948c | ||
| Major HR | 117 | 74 | 63.2% | 116 | 79 | 68.1% | 0.521c | ||
| No evidence of leukaemia | 117 | 15 | 12.8% | 116 | 20 | 17.2% | 0.447c | ||
| Quality appraisal | |||||||||
| 1. Is a power calculation provided? No | |||||||||
| 2. Is the sample size adequate? Not reported | |||||||||
| 3. Was ethical approval obtained? Yes | |||||||||
| 4. Were the study eligibilty criteria specified? Yes | |||||||||
| 5. Were the eligibility criteria appropriate? Yes | |||||||||
| 6. Were patients recruited prospectively? Yes | |||||||||
| 7. Was assignment to the treatment groups really random? Unknown | |||||||||
| 8. Were groups stratified? Yes. By phase and type of disease and imatinib status (ImR or ImI) | |||||||||
| 9. Was the treatment allocation concealed? No | |||||||||
| 10. Are adequate baseline details presented? Yes. More information about previous imatinib regimen might have been useful | |||||||||
| 11. Are the participants representative of the population in question? Yes | |||||||||
| 12. Are groups similar at baseline? Partial. Reported that groups ‘were comparable between the two treatment schedules’; however, significantly more participants in 70 mg b.i.d. arm were in CHR at study entry | |||||||||
| 13. Are any differences in baseline adequately adjusted for in the analysis? No | |||||||||
| 14. Are outcome assessors blind? No | |||||||||
| 15. Was the care provider blinded? No | |||||||||
| 16. Are outcome measures relevant to research question? Yes | |||||||||
| 17. Are data collection tools shown or known to be valid for the outcome of interest? Yes | |||||||||
| 18. Is compliance with treatment adequate? Unclear. One participant (140 mg q.d. arm) discontinued therapy because of protocol violation | |||||||||
| 19. Are withdrawals/dropouts adequately described? Yes | |||||||||
| 20. Are all patients accounted for? Yes | |||||||||
| 21. Is the number randomised reported? Yes | |||||||||
| 22. Are protocol violations specified? Yes. One participant reported; exact reasons not given | |||||||||
| 23. Are data analyses appropriate? Yes | |||||||||
| 24. Is analysis conducted on an ITT basis? Yes | |||||||||
| 25. Are missing data appropriately accounted for? Yes | |||||||||
| 26. Were any subgroup analyses justified? No | |||||||||
| 27. Are the conclusions supported by the results? Partial. No formal testing of differences in efficacy outcomes; just a statement that ‘the treatment groups were comparable’ and a conclusion that results demonstrate that ‘dasatinib 140 mg q.d. has similar efficacy to dasatinib 70 mg b.i.d.’ | |||||||||
| 28. Generalisability: High | |||||||||
| 29. Inter-centre variability: Not reported | |||||||||
| 30. Conflict of interest declared? Yes. All lead authors have received funding from manufacturers including BMS and Novartis | |||||||||
| Study details | Population | Arms | Outcomes | |
|---|---|---|---|---|
|
Study: Tojo et al. (2009)108 Design: case series (prospective) CP: yes AP: yes BC: yes Country: Japan Number of centres: multicentre, but number of centres not reported (authors are from 16 different centres, including one in Australia) |
Inclusion criteria: Japanese patients with ImR or ImI ImR defined according to phase: CP: failure to achieve CHR after 3 months/CyR after 6 months/MCyR after 12 months, or loss of HR or CyR following 3 months of imatinib at 600 mg q.d. AP/BC: progression to AP/BC during imatinib (600 mg q.d.) in CP; 50% increase in WBC, blasts, basophils, or platelets during imatinib in AP/BC; lack of HR after 4 weeks’ imatinib in AP/BC In addition, participants receiving < 600 mg q.d. imatinib were eligible if named BCR–ABL mutations detected ImI defined as discontinuation of imatinib because of grade 3–4 AEs or grade 2 AEs lasting 1 month or recurring more than three times Exclusion criteria: WHO performance status > 2; hepatic, renal or cardiac dysfunction Participants meeting criteria for imatinib intolerance were excluded if they had achieved an MCyR to imatinib |
Arm 1 nilotinib n: 27 Drug: nilotinib Starting daily dose (mg): 800 Dosage details: 400 mg b.i.d. Reductions to 400 mg daily and subsequently 200 mg daily were permitted for the management of toxicity Concurrent treatment: not reported |
CyR: CCyR PCyR MCyR Minor CyR Minimal CyR Overall CyR HR: CHR No evidence of leukaemia Return to CP AEs – grades 1–4 |
|
| Nilotinib | ||||
| n | κ | Mean | ||
| Baseline characteristics | ||||
| CP | ||||
| Demographics | ||||
| Age (years) (median) | 16 | 57 (range 30–83) | ||
| Gender (n male) | 16 | 9 | 56.3% | |
| Imatinib failure | ||||
| Intolerance | 16 | 12 | 75.0% | |
| Resistance | 16 | 4 | 25.0% | |
| Prior therapy | ||||
| Highest imatinib dose | 16 | 519 (SD 210) | ||
| Disease history | ||||
| Duration of CML < 6 months | 16 | 2 | 12.5% | |
| Duration of CML 6 months to < 1 year | 16 | 2 | 12.5% | |
| Duration of CML 1–2 years | 16 | 3 | 18.8% | |
| Duration of CML 2–5 years | 16 | 3 | 18.8% | |
| Duration of CML 5 years | 16 | 6 | 37.5% | |
| Baseline status | ||||
| WHO performance status 0 | 16 | 16 | 100.0% | |
| WHO performance status 1 | 16 | 0 | 0.0% | |
| WHO performance status 2 | 16 | 0 | 0.0% | |
| WHO performance status > 2 | 16 | 0 | 0.0% | |
| AP | ||||
| Demographics | ||||
| Age (years) (median) | 7 | 61 (range 30–74) | ||
| Gender (n male) | 7 | 5 | 71.4% | |
| Imatinib failure | ||||
| Intolerance | 7 | 3 | 42.9% | |
| Resistance | 7 | 4 | 57.1% | |
| Prior therapy | ||||
| Highest imatinib dose | 7 | 686 (SD 159) | ||
| Disease history | ||||
| Duration of CML < 6 months | 7 | 0 | 0.0% | |
| Duration of CML 6 months to < 1 year | 7 | 0 | 0.0% | |
| Duration of CML 1–2 years | 7 | 2 | 28.6% | |
| Duration of CML 2–5 years | 7 | 0 | 0.0% | |
| Duration of CML 5 years | 7 | 5 | 71.4% | |
| Baseline status | ||||
| WHO performance status 0 | 7 | 4 | 57.1% | |
| WHO performance status 1 | 7 | 2 | 28.6% | |
| WHO performance status 2 | 7 | 1 | 14.3% | |
| WHO performance status > 2 | 7 | 0 | 0.0% | |
| BC | ||||
| Demographics | ||||
| Age (years) (median) | 4 | 53 (range 29–70) | ||
| Gender (n male) | 4 | 2 | 50.0% | |
| Imatinib failure | ||||
| Intolerance | 4 | 0 | 0.0% | |
| Resistance | 4 | 4 | 100.0% | |
| Prior therapy | ||||
| Highest imatinib dose | 4 | 700 (SD 115) | ||
| Disease history | ||||
| Duration of CML < 6 months | 4 | 0 | 0.0% | |
| Duration of CML 6 months to < 1 year | 4 | 0 | 0.0% | |
| Duration of CML 1–2 years | 4 | 1 | 25.0% | |
| Duration of CML 2–5 years | 4 | 1 | 25.0% | |
| Duration of CML 5 years | 4 | 2 | 50.0% | |
| Baseline status | ||||
| WHO performance status 0 | 4 | 2 | 50.0% | |
| WHO performance status 1 | 4 | 2 | 50.0% | |
| WHO performance status 2 | 4 | 0 | 0.0% | |
| WHO performance status > 2 | 4 | 0 | 0.0% | |
| Results | ||||
| AEs – grades 1–4 | ||||
| Anorexia | 34 | 5 | 14.7% | |
| Back pain | 34 | 4 | 11.8% | |
| Chest pain | 34 | 4 | 11.8% | |
| Constipation | 34 | 4 | 11.8% | |
| Eczema | 34 | 5 | 14.7% | |
| Erythema | 34 | 4 | 11.8% | |
| Headache | 34 | 11 | 32.4% | |
| Hepatic function abnormal | 34 | 5 | 14.7% | |
| Malaise | 34 | 5 | 14.7% | |
| Muscle spasms | 34 | 4 | 11.8% | |
| Nausea | 34 | 11 | 32.4% | |
| Pruritus | 34 | 4 | 11.8% | |
| Pyrexia | 34 | 8 | 23.5% | |
| Rash | 34 | 17 | 50.0% | |
| Stomach pain | 34 | 4 | 11.8% | |
| Vomiting | 34 | 10 | 29.4% | |
| AEs – grade 3–4 | ||||
| Anorexia | 34 | 0 | 0.0% | |
| Back pain | 34 | 1 | 2.9% | |
| Chest pain | 34 | 0 | 0.0% | |
| Constipation | 34 | 0 | 0.0% | |
| Eczema | 34 | 0 | 0.0% | |
| Erythema | 34 | 0 | 0.0% | |
| Headache | 34 | 2 | 5.9% | |
| Hepatic function abnormal | 34 | 0 | 0.0% | |
| Malaise | 34 | 0 | 0.0% | |
| Muscle spasms | 34 | 0 | 0.0% | |
| Nausea | 34 | 1 | 2.9% | |
| Pruritus | 34 | 0 | 0.0% | |
| Pyrexia | 34 | 0 | 0.0% | |
| Rash | 34 | 1 | 2.9% | |
| Stomach pain | 34 | 0 | 0.0% | |
| Vomiting | 34 | 0 | 0.0% | |
| CP | ||||
| CyR | ||||
| CCyR | 16 | 11 | 68.8% | |
| PCyR | 16 | 4 | 25.0% | |
| MCyR | 16 | 15 | 93.8% | |
| Minor CyR | 16 | 0 | 0.0% | |
| Minimal CyR | 16 | 1 | 6.3% | |
| Overall CyR | 16 | 16 | 100.0% | |
| HR | ||||
| CHR | 16 | 6 | 37.5% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 16 | 3a | 18.8% | |
| Anaemia | 16 | 3b | 18.8% | |
| Neutropenia | 16 | 6c | 37.5% | |
| Leucopenia | 16 | 5d | 31.3% | |
| AP | ||||
| CyR | ||||
| CCyR | 7 | 1 | 14.3% | |
| PCyR | 7 | 0 | 0.0% | |
| MCyR | 7 | 1 | 14.3% | |
| Minor CyR | 7 | 0 | 0.0% | |
| Minimal CyR | 7 | 3 | 42.9% | |
| Overall CyR | 7 | 4 | 57.1% | |
| HR | ||||
| CHR | 7 | 1 | 14.3% | |
| No evidence of leukaemia | 7 | 3e | 42.9% | |
| Return to CP | 7 | 1 | 14.3% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 7 | 2a | 28.6% | |
| Anaemia | 7 | 4b | 57.1% | |
| Neutropenia | 7 | 5c | 71.4% | |
| Leucopenia | 7 | 3d | 42.9% | |
| BC | ||||
| CyR | ||||
| CCyR | 4 | 2 | 50.0% | |
| PCyR | 4 | 0 | 0.0% | |
| MCyR | 4 | 2 | 50.0% | |
| Minor CyR | 4 | 1 | 25.0% | |
| Minimal CyR | 4 | 0 | 0.0% | |
| Overall CyR | 4 | 3 | 75.0% | |
| HR | ||||
| CHR | 4 | 1 | 25.0% | |
| No evidence of leukaemia | 4 | 0e | 0.0% | |
| Return to CP | 4 | 1 | 25.0% | |
| Haematological AEs – grade 3–4 | ||||
| Thrombopenia | 4 | 2a | 50.0% | |
| Anaemia | 4 | 4b | 100.0% | |
| Neutropenia | 4 | 2c | 50.0% | |
| Leucopenia | 4 | 3d | 75.0% | |
| Quality appraisal | ||||
| 1 General | ||||
| 1.1 Is the hypothesis/aim/objective of the study clearly described? Yes | ||||
| 1.2 Were the case series collected at more than one centre? Multicentre | ||||
| 1.3 Was the main outcome independently assessed? Unclear | ||||
| 1.4 Are patient characteristics adequately described? Yes | ||||
| 1.5 How easy is it to assess generalisability of the results? Low. It appears that population is subset of those recruited for Phase I study who tolerated initial treatment; hard to tell how this relates to clinical population without additional details | ||||
| 2 Assessment of selection bias | ||||
| 2.1 Are inclusion and exclusion criteria clearly reported? Yes | ||||
| 2.2 Were data collected prospectively? Yes | ||||
| 2.3 Were patients recruited consecutively? No. Seems that some participants failing Phase I were not eligible for the main study (as reported here) | ||||
| 3 Assessment of performance bias | ||||
| 3.1 Did all the participants receive the same intervention? Yes | ||||
| 3.2 Is the use of any concurrent therapies adequately described? Uncertain | ||||
| 4 Assessment of attrition bias | ||||
| 4.1 Was an ITT analysis performed? Yes | ||||
| 4.2 Were dropouts from the study adequately described? Yes | ||||
Appendix 4 Appraisal of economic evaluations in industry submissions: checklists
| NICE reference case requirement | Criteria met? | Reviewer comment | |
|---|---|---|---|
| Decision problem | As per the scope developed by NICE (especially technologies and patient group) | Yes |
Treatment with dasatinib of adults with CML ImR or ImI to previous treatment including imatinib ImI patients were not considered separately |
| Comparator | Alternative therapies routinely used in the UK NHS | Yes |
Imatinib (600 mg q.d. and 800 mg q.d.) and nilotinib Other comparators included in the scope (hydroxycarbamide, IFN and acute leukaemia chemotherapy) were not included in the analysis as not considered relevant |
| Perspective on costs | NHS and PSS | Yes | |
| Perspective on outcomes | All health effects on individuals | Yes | |
| Type of economic evaluation | Cost-effectiveness analysis | Yes | |
| Synthesis of evidence on outcomes | Based on a systematic review | Yes | |
| Measure of health benefits | QALYs | Yes | Life-years gained were also measured |
| Description of health states for QALY calculations | Use of a standardised and validated generic instrument | Yes | A cross-sectional study was commissioned to calculate utility values. The impact of serious AEs on health utility was identified from non-CML literature |
| Method of preference elicitation for health-state values | Choice-based method (e.g. time trade-off, standard gamble, not rating scale) | Yes | Values were elicited from a representative sample of 100 unaffected individuals in the UK using the time trade-off method and the EQ-5D instrument |
| Source of preference data | Representative sample of the UK public | Yes | |
| Discount rate | 3.5% per annum for costs and health effects | Yes | |
| Dimension of quality | Criteria met? | Comments | |
|---|---|---|---|
| Structure | |||
| S1 | Statement of decision problem/objective | Yes | Cost-effectiveness modelling of treatment with dasatinib vs treatment with HDI or nilotinib in adults with CML-CP resistant or intolerant to previous therapy including imatinib. NICE is the primary decision-maker |
| S2 | Statement of scope/perspective | Yes | NHS perspective. Model inputs are consistent with the perspective. Scope of the model stated and justification given. Outcomes consistent with perspective and scope of the model |
| S3 | Rationale for structure | Yes | Model structure has been described and is largely consistent with the progression of CML. The model uses the relationship between response to treatment and long-term survival to estimate long-term benefits. Sources of data used to develop the model structure are specified. Other model structures were considered |
| S4 | Structural assumptions | Yes | Model assumptions were stated and justified |
| S5 | Strategies/comparators | Yes |
A clear definition of the comparators is provided and justified. Not all the comparators identified in the scope are evaluated – the analysis is limited to those believed to be most relevant Differences in the baseline characteristics of individuals in the single-arm studies of dasatinib, nilotinib and HDI may render comparison invalid; these differences are not explored |
| S6 | Model type | Yes | The model type is appropriate for this type of decision problem |
| S7 | Time horizon | Yes | The time horizon is lifetime (100 years), which is appropriate to capture differences between treatment options. Treatment is continued until disease progression or until no longer tolerated. Owing to the extensive data extrapolation needed to model a 100-year time horizon and a sensitivity analysis with a 5-year time horizon is also included |
| S8 | Disease states/pathways | Yes | The disease states reflect the biological pathway of the disease (CP, AP, BC and death) and the level of response on initiating treatment (initial best response and no initial response). Progression within CP prior to progressing to AP does not appear to be captured in the model |
| S9 | Cycle length | Yes | The cycle length is defined (monthly) and is justified in terms of the natural history of the disease and the frequency of follow-up of CML patients |
| Data | |||
| D1 | Data identification | Yes | Data identification methods are described. The data for the main clinical parameters have been taken from single-arm clinical studies. Data choices have been justified. The quality of the data has not been assessed. The use of health-care resources in the treatment of CML and the management of serious AEs was estimated by UK clinical experts; the methods of data collection are described. Health-state utilities were elicited in a cross-sectional study; the methods are described |
| D2 | Pre-model data analysis | Yes | Costs of health-care resource use. Utility values for serious AEs |
| D2a | Baseline data | Partial |
All data are derived from single-arm studies. Data for dasatinib are sourced from data on file; data for HDI and nilotinib are sourced from the systematic literature review The model does not use a baseline risk of disease progression or baseline treatment strategy directly. Levels of response to treatment are considered comparable to baseline risk as they determine the probability of disease progression for the rest of the analysis Monthly rates of progression were calculated from the dasatinib clinical studies and applied in the model regardless of treatment A half-cycle correction was used in the model; it is not clear whether or not this was applied to both costs and outcomes |
| D2b | Treatment effects | Partial |
All data are derived from single-arm studies ImR and ImI populations were not considered separately The model uses the relationship between attainment of a MCyR and OS seen with imatinib and assumes that the relationship will also be true for dasatinib and nilotinib Survival at 24 months is used for dasatinib and nilotinib and survival at 3 months for HDI. Methods of data extrapolation are not described, but disease progression is assumed to occur at a constant monthly rate The model assumes that individuals move directly from CP to AP, which may not be an accurate reflection of clinical reality. The literature suggests that individuals may progress within CP without meeting the criteria for AP. This is not captured in the model Progression rates based on molecular response are assumed to be the same as CCyR owing to the lack of available data Data used to derive treatment effects are likely to be subject to a large amount of uncertainty due to the range of sources from which they have been elicited and the length of extrapolation necessary to inform a 100-year model |
| D2c | QoL weights (utilities) | Yes | The methods of utility derivation are described. Utilities were commissioned in a cross-sectional study of 100 representative unaffected individuals in the UK using the time trade-off method and the EQ-5D instrument. The impacts of serious AEs on health utility were taken from non-CML literature. The values used for CP/response are similar to those collected in the IRIS study of imatinib |
| D3 | Data incorporation | Yes |
Data incorporated into the model are referenced and generally well described. For the probabilistic sensitivity analysis, the input parameters and choice of distribution are described All effectiveness data used in the model are derived from single-arm studies; although this is described, the impact of the uncertainty associated with these methods is not explored |
| D4 | Assessment of uncertainty | Partial | All types of uncertainty have been discussed, although only parameter uncertainty is explored to any extensive degree (through probabilistic sensitivity analysis) |
| D4a | Methodological | No | Other modelling methods were considered possible; however, a Markov model was considered to be the most appropriate and alternative modelling approaches were not developed |
| D4b | Structural | Partial | This model is subject to a large amount of structural uncertainty that has not been discussed. Only the effect of differing time horizons was explored; the model has been run with two time horizons, 100 years (lifetime) and 5 years |
| D4c | Heterogeneity | Yes | No subgroup analyses were conducted; given the data available this is reasonable |
| D4d | Parameter | Yes | One-way and probabilistic sensitivity analyses have been performed |
| Consistency | |||
| C1 | Internal consistency | Yes | The report states that the internal validity of the model was tested by using extreme values in the input parameters |
| C2 | External consistency | Partial | The report states that results of the model have been compared with those of other published economic analyses and against study data. However, it is also agreed that given the limited details available for previously published studies meaningful comparisons are difficult to perform. Few details of validation against study data are provided |
| NICE reference case requirement | Criteria met? | Reviewer comment | |
|---|---|---|---|
| Decision problem | As per the scope developed by NICE (especially technologies and patient group) | Yes |
Treatment with dasatinib of adults with CML resistant or intolerant to previous treatment including imatinib ImR and ImI patients were not considered separately |
| Comparator | Alternative therapies routinely used in the UK NHS | Yes |
Imatinib (800 mg q.d.) and nilotinib Other comparators included in the scope (hydroxycarbamide, IFN and acute leukaemia chemotherapy) were not included in the analysis as not considered relevant |
| Perspective on costs | NHS and PSS | Yes | |
| Perspective on outcomes | All health effects on individuals | Yes | |
| Type of economic evaluation | Cost-effectiveness analysis | Yes | |
| Synthesis of evidence on outcomes | Based on a systematic review | Yes | |
| Measure of health benefits | QALYs | Life-years gained were also measured | |
| Description of health states for QALY calculations | Use of a standardised and validated generic instrument | A cross-sectional study was commissioned to calculate utility values. The impact of serious AEs on health utility was identified from non-CML literature | |
| Method of preference elicitation for health-state values | Choice-based method (e.g. time trade-off, standard gamble, not rating scale) | Values were elicited from a representative sample of 100 unaffected individuals in the UK using the time trade-off method and the EQ-5D instrument | |
| Source of preference data | Representative sample of the UK public | Yes | |
| Discount rate | 3.5% per annum for costs and health effects | Yes | |
| Dimension of quality | Criteria met? | Comments | |
|---|---|---|---|
| Structure | |||
| S1 | Statement of decision problem/objective | Yes | Cost-effectiveness modelling of treatment with dasatinib vs treatment with HDI or nilotinib in adults with CML-AP resistant or intolerant to previous therapy including imatinib. NICE is the primary decision-maker |
| S2 | Statement of scope/perspective | Yes | NHS perspective. Model inputs are consistent with the perspective. Scope of the model stated and justification given. Outcomes consistent with perspective and scope of the model |
| S3 | Rationale for structure | Yes | Model structure has been described and is largely consistent with the progression of CML. The model uses the relationship between response to treatment and long-term survival to estimate long-term benefits. Sources of data used to develop the model structure are specified. Other model structures were considered |
| S4 | Structural assumptions | Yes | Model assumptions were stated and justified |
| S5 | Strategies/comparators | Yes |
A clear definition of the comparators is provided and justified. Not all the comparators identified in the scope are evaluated; the analysis is limited to those believed to be most relevant Differences in the baseline characteristics of individuals in the single-arm studies of dasatinib, nilotinib and HDI may render comparison invalid; these differences are not explored |
| S6 | Model type | Yes | The model type is appropriate for this type of decision problem |
| S7 | Time horizon | Yes |
The model uses a lifetime time horizon (20 years) which may be unnecessarily long for those entering the model in AP Treatment is continued until disease progression or until no longer tolerated Owing to the extensive data extrapolation needed to model a 20-year time horizon and a sensitivity analysis with a 5-year time horizon is also included |
| S8 | Disease states/pathways | Yes | The disease states reflect the biological pathway of the disease (AP, BC and death) and the level of response on initiating treatment (initial best response and no initial response) |
| S9 | Cycle length | Yes | The cycle length is defined (monthly) and is justified in terms of the natural history of the disease and the frequency of follow-up of CML patients |
| Data | |||
| D1 | Data identification | Yes | Data identification methods are described. Data choices have been justified. All data are derived from single-arm studies. The quality of the data has not been assessed. The use of health-care resources in the treatment of CML and the management of serious AEs was estimated by UK clinical experts; the methods of data collection are described. Health-state utilities were elicited in a cross-sectional study; the methods are described |
| D2 | Pre-model data analysis | Yes | Costs of health-care resource use. Utility values for serious AEs |
| D2a | Baseline data | No |
All data are derived from single-arm studies. Data for dasatinib are sourced from data on file; data for nilotinib are sourced from a conference abstract identified in the systematic literature review; there are no available data for HDI in this population, data are therefore taken from a study of standard-dose imatinib in patients not displaying ImR. The likelihood of treatment effects between these two populations being interchangeable is unclear and not discussed or explored The model does not use a baseline risk of disease progression or baseline treatment strategy directly. Levels of response to treatment are considered comparable to baseline risk as they determine the probability of disease progression for the rest of the analysis Monthly rates of progression were calculated from the dasatinib clinical studies and applied in the model regardless of treatment A half-cycle correction was used in the model; it is not clear whether or not this was applied to both costs and outcomes |
| D2b | Treatment effects | No |
All data are derived from single-arm studies ImR and ImI populations were not considered separately The model uses the relationship between attainment of a MCyR and OS seen with imatinib and assumes that the relationship will also be true for dasatinib and nilotinib There are no available data on the treatment effects of HDI in ImR or ImI patients in CML-AP. The model therefore uses data from a study of standard-dose imatinib in first-line treatment of CML-AP. It is unlikely that these two scenarios are comparable Survival at 24 months is used for dasatinib and nilotinib and survival at 3 months for HDI. Methods of data extrapolation are not described, but disease progression is assumed to occur at a constant monthly rate Progression rates based on molecular response were assumed to be the same as that for patients with CCyR owing to lack of available data Data used to derive treatment effects are likely to be subject to a large amount of uncertainty due to the range of sources from which they have been elicited and the length of extrapolation necessary to inform a 20-year model |
| D2c | QoL weights (utilities) | Yes | The methods of utility derivation are described. Utilities were commissioned in a cross-sectional study of 100 representative, unaffected individuals in the UK using the time trade-off method and the EQ-5D instrument. The impacts of serious AEs on health utility were taken from non-CML literature. The values used for AP/response are similar to those collected in the IRIS study of imatinib |
| D3 | Data incorporation | Yes |
Data incorporated into the model are referenced and generally well described. For the, the input parameters and choice of distribution are described All effectiveness data used in the model are derived from single-arm studies; although this is described, the impact of the uncertainty associated with these methods is not explored Dose intensities of drugs have not been considered |
| D4 | Assessment of uncertainty | Yes | All types of uncertainty have been discussed |
| D4a | Methodological | No | Other modelling methods were considered possible; however, a Markov model was considered to be the most appropriate and alternative modelling approaches were not developed |
| D4b | Structural | Partial | This model is subject to a large amount of structural uncertainty that has not been discussed. Only the effect of differing time horizons was explored; the model has been run with two time horizons, 20 years (lifetime) and 5 years |
| D4c | Heterogeneity | Yes | No subgroup analyses were conducted; given the data available this is reasonable |
| D4d | Parameter | Yes | One-way and probabilistic sensitivity analyses have been performed |
| Consistency | |||
| C1 | Internal consistency | Yes | The report states that the internal validity of the model was tested by using extreme values in the input parameters |
| C2 | External consistency | Partial | The report states that results of the model have been compared with those of other published economic analyses and against study data. However, it is also agreed that given the limited details available for previously published studies meaningful comparisons are difficult to perform. Few details of validation against study data are provided |
| NICE reference case requirement | Criteria met? | Reviewer comment | |
|---|---|---|---|
| Decision problem | As per the scope developed by NICE (especially technologies and patient group) | Yes |
Treatment with dasatinib of adults with CML resistant or intolerant to previous treatment including imatinib ImR and ImI patients were not considered separately |
| Comparator | Alternative therapies routinely used in the UK NHS | Yes |
Imatinib (800 mg q.d.) Other comparators included in the scope (hydroxycarbamide, IFN and acute leukaemia chemotherapy) were not included in the analysis as not considered relevant |
| Perspective on costs | NHS and PSS | Yes | |
| Perspective on outcomes | All health effects on individuals | Yes | |
| Type of economic evaluation | Cost-effectiveness analysis | Yes | |
| Synthesis of evidence on outcomes | Based on a systematic review | Yes | |
| Measure of health benefits | QALYs | Yes | Life-years gained were also measured |
| Description of health states for QALY calculations | Use of a standardised and validated generic instrument | A cross-sectional study was commissioned to calculate utility values. The impact of serious AEs on health utility was identified from non-CML literature | |
| Method of preference elicitation for health-state values | Choice-based method (e.g. time trade-off, standard gamble, not rating scale) | Values were elicited from a representative sample of 100 unaffected individuals in the UK using the time trade-off method and the EQ-5D instrument | |
| Source of preference data | Representative sample of the UK public | Yes | |
| Discount rate | 3.5% per annum for costs and health effects | Yes | |
| Dimension of quality | Criteria met? | Comments | |
|---|---|---|---|
| Structure | |||
| S1 | Statement of decision problem/objective | Yes | Cost-effectiveness modelling of treatment with dasatinib vs treatment with HDI in adults with CML-BC resistant or intolerant to previous therapy including imatinib. NICE is the primary decision maker |
| S2 | Statement of scope/perspective | Yes | NHS perspective. Model inputs are consistent with the perspective. Scope of the model stated and justification given. Outcomes consistent with perspective and scope of the model |
| S3 | Rationale for structure | Yes | Model structure has been described and is largely consistent with the progression of CML. The model uses the relationship between response to treatment and long-term survival to estimate long-term benefits. Sources of data used to develop the model structure are specified. Other model structures were considered |
| S4 | Structural assumptions | Yes | Model assumptions were stated and justified |
| S5 | Strategies/comparators | Yes |
A clear definition of the comparators is provided and justified. Not all the comparators identified in the scope are evaluated; the analysis is limited to those believed to be most relevant Differences in the baseline characteristics of individuals in the single-arm studies of dasatinib and nilotinib may render comparison invalid; these differences are not explored |
| S6 | Model type | Yes | The model type is appropriate for this type of decision problem |
| S7 | Time horizon | Yes |
The time horizon used is lifetime (20 years), which may be unnecessarily long for people entering the model in BC Treatment is continued until disease progression or until no longer tolerated Owing to the extensive data extrapolation needed to model a 20-year time horizon and a sensitivity analysis with a 5-year time horizon is also included |
| S8 | Disease states/pathways | Yes | The disease states reflect the biological pathway of the disease (BC and death) and the level of response on initiating treatment (initial best response and no initial response) |
| S9 | Cycle length | Yes | The cycle length is defined (monthly) and is justified in terms of the natural history of the disease and the frequency of follow-up of CML patients |
| Data | |||
| D1 | Data identification | Yes |
Data identification methods are described. Data choices have been justified All data are derived from single-arm studies. The quality of the data has not been assessed The use of health-care resources in the treatment of CML and the management of serious AEs was estimated by UK clinical experts; the methods of data collection are described Health-state utilities were elicited in a cross-sectional study; the methods are described |
| D2 | Pre-model data analysis | Yes | Costs of health-care resource use. Utility values for serious AEs |
| D2a | Baseline data | No |
All data are derived from single-arm studies Data for dasatinib are sourced from data on file. There are no available data for HDI in this population; data are therefore taken from a study of standard-dose imatinib in patients not displaying ImR. The likelihood of treatment effects between these two populations being interchangeable is unclear and is not discussed or explored The model does not use a baseline risk of disease progression or baseline treatment strategy directly. Levels of response to treatment are considered comparable to baseline risk as they determine the probability of disease progression for the rest of the analysis Monthly rates of progression were calculated from the dasatinib clinical studies and applied in the model regardless of treatment A half-cycle correction was used in the model; it is not clear whether or not this was applied to both costs and outcomes |
| D2b | Treatment effects | No |
All data are derived from single-arm studies ImR and ImI populations were not considered separately The model uses the relationship between attainment of a MCyR and OS seen with imatinib and assumes that the relationship will also be true for dasatinib and nilotinib There are no available data on the treatment effects of HDI in ImR or ImI patients in CML-BC. The model therefore uses data from a study of standard-dose imatinib in first-line treatment of CML-AP. It is unlikely that these two scenarios are comparable Survival at 24 months is used for dasatinib and nilotinib and survival at 3 months for HDI. Methods of data extrapolation are not described, but disease progression is assumed to occur at a constant monthly rate Progression rates based on molecular response were assumed to be the same as that for patients with CCyR owing to lack of available data Data used to derive treatment effects are likely to be subject to a large amount of uncertainty due to the range of sources from which they have been elicited and the length of extrapolation necessary to inform a 20-year model |
| D2c | QoL weights (utilities) | Yes | The methods of utility derivation are described. Utilities were commissioned in a cross-sectional study of 100 representative unaffected individuals in the UK using the time trade-off method and the EQ-5D instrument. The impacts of serious AEs on health utility were taken from non-CML literature. The values used for AP/response are similar to those collected in the IRIS study of imatinib |
| D3 | Data incorporation | Yes |
Data incorporated into the model are referenced and generally well described. For the probabilistic sensitivity analysis, the input parameters and choice of distribution are described All effectiveness data used in the model are derived from single-arm studies; although this is described, the impact of the uncertainty associated with these methods is not explored |
| D4 | Assessment of uncertainty | Yes | All types of uncertainty have been discussed |
| D4a | Methodological | No | Other modelling methods were considered possible; however, a Markov model was considered to be the most appropriate and alternative modelling approaches were not developed |
| D4b | Structural | Partial | This model is subject to a large amount of structural uncertainty that has not been discussed. Only the effect of differing time horizons was explored; the model has been run with two time horizons, 20 years (lifetime) and 5 years |
| D4c | Heterogeneity | Yes | No subgroup analyses were conducted; given the data available, this is reasonable |
| D4d | Parameter | Yes | One-way and probabilistic sensitivity analyses have been performed |
| Consistency | |||
| C1 | Internal consistency | Yes | The report states that the internal validity of the model was tested by using extreme values in the input parameters |
| C2 | External consistency | Partial | The report states that results of the model have been compared with those of other published economic analyses and against study data. However, it is also agreed that given the limited details available for previously published studies meaningful comparisons are difficult to perform. Few details of validation against study data are provided |
| NICE reference case requirement | Criteria met? | Reviewer comment | |
|---|---|---|---|
| Decision problem | As per the scope developed by NICE (especially technologies and patient group) | Partial |
Treatment with nilotinib of adults with CML resistant to treatment with imatinib In line with the main study informing the model,106 ImI individuals were only considered if they were also non-responders to imatinib. These individuals are referred to as ‘intolerant as well as resistant’ in the submission, which is not strictly accurate; in order to qualify as ImR, participants had to show long-term lack (or loss) of response to imatinib, whereas ImI individuals were enrolled so long as they had not achieved MCyR over a period of therapy, which may have been much shorter. Accordingly, the analysis is not able to provide an estimate of the cost-effectiveness of nilotinib for people who show a CyR to imatinib but cannot tolerate it ImR and ImI patients were considered separately |
| Comparator | Alternative therapies routinely used in the UK NHS | Partial |
ImR: nilotinib is compared with high-dose (800 mg q.d.) imatinib ImI: hydroxycarbamide (2 g/day) No comparisons are presented for nilotinib vs dasatinib in either population. It is argued that differences in study populations (especially definitions of imatinib intolerance) render such a comparison impossible No comparisons are presented for nilotinib vs IFN in either population, because no evidence was identified for IFN as a second-line therapy following failure of standard-dose imatinib |
| Perspective on costs | NHS and PSS | Yes | The models take a UK NHS and PSS perspective |
| Perspective on outcomes | All health effects on individuals | Yes | |
| Type of economic evaluation | Cost-effectiveness analysis | Yes | |
| Synthesis of evidence on outcomes | Based on a systematic review | No |
Simple statement that a ‘literature search was carried out to identify all relevant papers’ without further details of methods or results Some (e.g. imatinib failure status-specific PFS) drawn from unpublished data from main study No synthesis performed; all inputs based on single data sources |
| Measure of health benefits | QALYs | Yes | QALYs and life-years are reported |
| Description of health states for QALY calculations | Use of a standardised and validated generic instrument | Partial | No intervention-specific estimates: EQ-5D from Phase II study of standard-dose imatinib adopted for baseline utility for all comparators. Technology-specific weightings were then added to reflect assumed incidence of AEs; however, the utility of AE states was ‘in general’ not based on EQ-5D data |
| Method of preference elicitation for health-state values | Choice-based method (e.g. time trade-off, standard gamble, not rating scale) | Yes | |
| Source of preference data | Representative sample of the UK public | Yes | |
| Discount rate | 3.5% per annum for costs and health effects | Yes | All costs and health effects are discounted at 3.5% per annum |
| Dimension of quality | Criteria met? | Comments | |
|---|---|---|---|
| Structure | |||
| S1 | Statement of decision problem/objective | Yes | ‘To evaluate the cost-effectiveness of nilotinib for the treatment of adult CML patients who are resistant and/or intolerant to prior therapy in… CP.’ NICE is the primary decision-maker |
| S2 | Statement of scope/perspective | Yes | NHS and PSS perspective. Model inputs are consistent with the perspective. Scope of model stated and justification given. Outcomes consistent with perspective and scope of model |
| S3 | Rationale for structure | Yes | Model structure is stated to be ‘based on published data where available’ and expert opinion where not. None of the evidence informing model structure is explicitly discussed. The structure of the model – based on three disease states (CP, AP, BC) and death – is consistent with a well-established theory of CML. There is no record that any competing theories regarding model structure were considered |
| S4 | Structural assumptions | Partial | The structural assumptions of the model are clearly described and, for the most part, are reasonable. The assumption that disease progression is equivalent to disease transformation (transition from CP to AP) is not justified and is contrary to available evidence. The assumption that PFS can be used as a surrogate for OS is an ostensibly reasonable solution to the problem of absent long-term OS data; however, the assumption is not justified or tested |
| S5 | Strategies/comparators | Yes |
The options under evaluation are clearly defined In line with the main study informing the model,106 ImI individuals were only considered if they were also non-responders to imatinib. These individuals are referred to as ‘intolerant as well as resistant’ in the submission, which is not strictly accurate; in order to qualify as ImR, participants had to show long-term lack (or loss) of response to imatinib, whereas ImI individuals were enrolled so long as they had not achieved MCyR over a period of therapy which may have been much shorter. Accordingly, the analysis is not able to provide an estimate of the cost-effectiveness of nilotinib for people who show a CyR to imatinib but cannot tolerate it In ImR population, nilotinib is compared with HDI (800 mg q.d.). In ImI population, nilotinib is compared with hydroxycarbamide (2 g/day). No comparisons are presented for nilotinib vs dasatinib in either population. It is argued that differences in study populations (especially definitions of imatinib intolerance) render such a comparison impossible. No comparisons are presented for nilotinib vs IFN in either population, because no evidence was identified for IFN as a second-line therapy following failure of standard-dose imatinib |
| S6 | Model type | Yes | Markov model. Theoretically appropriate, although problems with parameterisation in practice (see S8) |
| S7 | Time horizon | Yes | Lifetime horizon used with 5-year time horizon in sensitivity analysis |
| S8 | Disease states/pathways | ? | States are theoretically appropriate for disease pathway; however, transition from CP to AP is difficult to parameterise from available evidence and chosen solution (use of PFS) is inadequate |
| S9 | Cycle length | Yes | 3-month cycle length, based on expert clinical opinion. Appears reasonable for a chronic condition with few disease states |
| Data | |||
| D1 | Data identification | Partial | No details of review methods by which data sources were identified (simple statement that a ‘literature search was carried out to identify all relevant papers’ without further details of methods or results). Single data sources are used for each comparator: nilotinib, Kantarjian et al.;23 HDI, Kantarjian et al.;54 hydroxycarbamide, Kantarjian et al.223 The choice of each is justified. No critical appraisal of the nilotinib data source; the validity of sources for other comparators is considered solely in terms of how well the populations compare to the nilotinib study. Expert opinion is cited as a source of some resource-use parameters; the methods by which such views were elicited are not described |
| D2 | Pre-model data analysis | ||
| D2a | Baseline data | Partial | Population is assumed to comprise equal proportions of male and female patients aged 57 years at the time of entry into the model, based on the demographics of the patients in the nilotinib study.106 No half-cycle correction ‘due to the short-cycle lengths’ |
| D2b | Treatment effects | Partial |
No synthesis performed; all inputs based on separate, single, observational studies Time in CP is assumed to be equal to PFS. For nilotinib, PFS is projected by way of an exponential curve fitted to maximum empirical follow-up (19 months, additional unpublished follow-up from the Phase II study106). For HDI and hydroxycarbamide, the modellers were unwilling to use any identified PFS data, so a curve was fitted to empirical OS data [HDI: 5-year follow-up from Kantarjian et al. ;54 hydroxycarbamide: 5-year follow-up from Kantarjian et al. ]223 and adjusted using an estimate of the ratio between PFS and OS (calculated on the basis of nilotinib data) to provide an estimated PFS curve OS was calculated by adding a treatment-independent estimate of time spent in AP and BC to each estimated PFS curve, with an additional deduction for background mortality, based on age-specific mortality rates taken from published government life tables No alternative assumptions were explored through sensitivity analysis |
| D2c | QoL weights (utilities) | Yes | No intervention-specific estimates; EQ-5D from Phase II study of standard-dose imatinib adopted for baseline utility for all comparators. Technology-specific weightings were then added to reflect assumed incidence of AEs; however, the utility of AE states was ‘in general’ not based on EQ-5D data. Methods are clear and sources referenced |
| D3 | Data incorporation | Yes |
All data incorporated into the model have been described and referenced in sufficient detail (note that nilotinib PFS is based on unpublished additional follow-up) Mutually inconsistent data have been used extensively (note different methods for estimating time in CP across comparators). In addition, there are some differences between the populations in the studies from which data has been drawn (e.g. up to 20% of participants in the HDI study may have been in MCyR at baseline; only around 3% in the nilotinib study were). It is emphasised that data used to estimate the effectiveness of hydroxycarbamide are drawn from a study in which a variety of other therapies were administered, as well as or instead of hydroxycarbamide. Where justified, such inconsistencies are seen as a function of paucity of suitable data The process of data incorporation is clearly described Where used for probabilistic sensitivity analysis, distributions for each parameter have been specified but not justified. Choices appear reasonable All effectiveness data used in the model are derived from single-arm studies. Although this is described, the impact of the uncertainty associated with these methods is not explored |
| D4 | Assessment of uncertainty | ||
| D4a | Methodological | No | There is no evidence that methodological uncertainties have been addressed by running alternative versions of the model with different methodological assumptions |
| D4b | Structural | No | A single sensitivity analysis was performed adopting a 5-year time horizon. Otherwise, there is no evidence that the – very considerable – structural uncertainties inherent in the model have been addressed via sensitivity analysis |
| D4c | Heterogeneity | Yes | The provision of separate models for ImI and ImR populations helps to address heterogeneity owing to distinct subgroups |
| D4d | Parameter | Partial |
A limited number of one-way sensitivity analyses were performed, with PFS, OS, utility and cost parameters varied, generally within the range of each parameter’s 95% CI. Effectiveness parameters were varied simultaneously for each comparator, so relative differences remain constant and it is not possible to deduce to what extent the model is sensitive to uncertainty in individual effectiveness parameters Probabilistic sensitivity analysis is reported, with outputs shown in CEACs (no scatterplots provided) |
| Consistency | |||
| C1 | Internal consistency | No | There is no evidence that internal consistency has been evaluated (e.g. by testing expected behaviour when setting parameters to extreme or null values) |
| C2 | External consistency | Partial |
The conclusions presented are a fair reflection of model outputs, and a degree of caution is expressed, in view of the numerous sources of uncertainty within the model. It is suggested that results are most uncertain in the ImI subgroup, owing to weak evidence on the effectiveness of hydroxycarbamide. A considerable amount of uncertainty attaches to all other outputs – especially in view of untested structural and methodological assumptions – but these are not given emphasis in discussion It is suggested that uncertain effectiveness of comparator technologies is likely to result in an overestimate of OS for HDI and hydroxycarbamide and that, as a result, ICERs are likely to underestimate cost-effectiveness of nilotinib. This is not necessarily the case (shorter OS would be associated with lower benefits, but also lower costs, and it is impossible to predict how the model would respond to more certain input data) Model-predicted OS is shown against empirical OS for nilotinib, HDI and hydroxycarbamide. In the ImR subgroup, in particular, the fit between predicted and observed OS is visually unconvincing (with nilotinib OS apparently overestimated and HDI OS apparently underestimated); however, the modellers emphasise that ‘the difference in OS between HDI and nilotinib at 19 months is supported within the extrapolation of the data’ It does not appear that the results of the model have been compared with those of any previous models |
| NICE reference case requirement | Criteria met? | Reviewer comment | |
|---|---|---|---|
| Decision problem | As per the scope developed by NICE (especially technologies and patient group) | Partial |
Treatment with nilotinib of adults with CML resistant to treatment with imatinib In line with the main study informing the model,107 ImI individuals were considered only if they were also non-responders to imatinib. These individuals are referred to as ‘intolerant as well as resistant’ in the submission, which is not strictly accurate; in order to qualify as ImR, participants had to show long-term lack (or loss) of response to imatinib, whereas ImI individuals were enrolled so long as they had not achieved MCyR over a period of therapy which may have been much shorter. Accordingly, the analysis is not able to provide an estimate of the cost-effectiveness of nilotinib for people who show a CyR to imatinib but cannot tolerate it ImR and ImI patients were considered separately |
| Comparator | Alternative therapies routinely used in the UK NHS | Partial |
ImR: nilotinib is compared with a theoretical comparator of high-dose (800 mg q.d.) imatinib, although the data used to parameterise the comparator arm have not been drawn from a source reporting HDI use in an ImR population ImI: hydroxycarbamide (2 g/day) No comparisons are presented for nilotinib vs dasatinib in either population. It is argued that differences in study populations (especially definitions of ImI) render such a comparison impossible No comparisons are presented for nilotinib vs IFN in either population, because no evidence was identified for IFN as a second-line therapy following failure of standard-dose imatinib |
| Perspective on costs | NHS and PSS | Yes | The models take a UK NHS and PSS perspective |
| Perspective on outcomes | All health effects on individuals | Yes | |
| Type of economic evaluation | Cost-effectiveness analysis | Yes | |
| Synthesis of evidence on outcomes | Based on a systematic review | No |
Simple statement that a ‘literature search was carried out to identify all relevant papers’ without further details of methods or results Some (e.g. imatinib-failure status-specific PFS) drawn from unpublished data from main study No synthesis performed; all inputs based on single data sources |
| Measure of health benefits | QALYs | Yes | QALYs and life-years are reported |
| Description of health states for QALY calculations | Use of a standardised and validated generic instrument | Partial | No intervention-specific estimates: EQ-5D from Phase II study of standard-dose imatinib adopted for baseline utility for all comparators. Technology-specific weightings were then added to reflect assumed incidence of AEs; however, the utility of AE states was ‘in general’ not based on EQ-5D data |
| Method of preference elicitation for health-state values | Choice-based method (e.g. time trade-off, standard gamble, not rating scale) | Yes | |
| Source of preference data | Representative sample of the UK public | Yes | |
| Discount rate | 3.5% per annum for costs and health effects | Yes | All costs and health effects are discounted at 3.5% per annum |
| Dimension of quality | Criteria met? | Comments | |
|---|---|---|---|
| Structure | |||
| S1 | Statement of decision problem/objective | Yes | ‘To evaluate the cost-effectiveness of nilotinib for the treatment of adult CML patients who are resistant and/or intolerant to prior therapy in… AP.’ NICE is the primary decision-maker |
| S2 | Statement of scope/perspective | Yes | NHS and PSS perspective. Model inputs are consistent with the perspective. Scope of model stated and justification given. Outcomes consistent with perspective and scope of model |
| S3 | Rationale for structure | Partial | Model structure is stated to be ‘based on published data where available’ and expert opinion where not. None of the evidence informing model structure is explicitly discussed. The structure of the model – based on two disease states (AP, BC) and death – is consistent with a well-established theory of CML. There is no record that any competing theories regarding model structure were considered |
| S4 | Structural assumptions | Partial | The structural assumptions of the model are clearly described and, for the most part, are reasonable. However, the assumption that disease progression is equivalent to disease transformation (transition from AP to BC) is not justified and may be inappropriate. The assumption that PFS can be used as a surrogate for OS is an ostensibly reasonable solution to the problem of absent long-term OS data; however, the assumption is not justified or tested. In particular, the use of alternative surrogates (e.g. CyR) is not explored |
| S5 | Strategies/comparators | Yes |
The options under evaluation are clearly defined In line with the main study informing the model,107 ImI individuals were considered only if they were also non-responders to imatinib. These individuals are referred to as ‘intolerant as well as resistant’ in the submission, which is not strictly accurate; in order to qualify as ImR, participants had to show long-term lack (or loss) of response to imatinib, whereas ImI individuals were enrolled so long as they had not achieved MCyR over a period of therapy which may have been much shorter. Accordingly, the analysis is not able to provide an estimate of the cost-effectiveness of nilotinib for people who show a CyR to imatinib but cannot tolerate it In ImR population, the theoretical comparator for nilotinib is HDI (800 mg q.d.) (although no source of data was found to parameterise this comparator; see below). In ImI population, nilotinib is compared with hydroxycarbamide (at a theoretical dose of 2 g/day). No comparisons are presented for nilotinib vs dasatinib in either population. It is argued that differences in study populations (especially definitions of ImI) render such a comparison impossible. No comparisons are presented for nilotinib vs IFN in either population, because no evidence was identified for IFN as a second-line therapy following failure of standard-dose imatinib |
| S6 | Model type | Yes | Markov model. Theoretically appropriate, although possible problems with parameterisation in practice (see S8) |
| S7 | Time horizon | Yes | Lifetime horizon used with 5-year time horizon in sensitivity analysis |
| S8 | Disease states/pathways | Partial | States are theoretically appropriate for disease pathway; however, transition from AP to BC is not directly reported in available evidence and the chosen solution (use of PFS) may not be appropriate |
| S9 | Cycle length | Yes | 3-month cycle length, based on expert clinical opinion. Appears reasonable for a chronic condition with few disease states |
| Data | |||
| D1 | Data identification | Partial |
No details of review methods by which data sources were identified (simple statement that a ‘literature search was carried out to identify all relevant papers’ without further details of methods or results). Single data sources are used for each comparator: nilotinib = le Coutre et al. ;107 HDI = Talpaz et al. ;32 hydroxycarbomide = Kantarjian et al. 223 The choice of each is justified. It is noted that the ‘HDI’ data derived from Talpaz et al. 32 relates to predominantly first-line use of imatinib (i.e. in a population that was neither ImR nor ImI) at doses which were commonly < 800 mg q.d. (i.e. less than ‘high dose’), and that these inconsistencies make the data source ‘less than ideal’. Moreover, although it is stated in the submission that the model uses PFS estimates from a subgroup of participants receiving 600 mg q.d., the data adopted are, in fact, from the 400 mg q.d. subgroup, who are even less representative of the treatment being simulated, and in whom time to disease progression was much swifter than in the 600 mg q.d. cohort. The latter group appear to benefit from PFS which is markedly superior to that seen with nilotinib; however, it must be remembered that, in contrast to the nilotinib cohort, they do not have an extended history of prior failed treatment with imatinib There is no critical appraisal of the nilotinib data source. Expert opinion is cited as a source of some resource-use parameters; the methods by which such views were elicited are not described |
| D2 | Pre-model data analysis | ||
| D2a | Baseline data | Partial | Population is assumed to comprise equal proportions of male and female patients aged 57 years old at the time of entry into the model, based on the demographics of the patients in the nilotinib study.107 No half-cycle correction ‘due to the short-cycle lengths’ |
| D2b | Treatment effects | Partial |
No synthesis performed; all inputs based on separate, single, observational studies Time in AP is assumed to be equal to PFS. For nilotinib and HDI, PFS is projected by way of an exponential curve fitted to maximum empirical follow-up [nilotinib: 19 months, additional unpublished follow-up from the Phase II study;106 HDI: 15 months from 400 mg q.d. subgroup of Talpaz et al. 32]. For hydroxycarbamide, the modellers did not identify any PFS data suitable for their purposes, so a curve was fitted to empirical OS data [5-year follow-up from Kantarjian et al. 223] and adjusted using an estimate of the ratio between PFS and OS (calculated on the basis of nilotinib data) to provide an estimated PFS curve OS was calculated by adding a treatment-independent estimate of time spent in BC to each estimated PFS curve, with an additional deduction for background mortality, based on age-specific mortality rates taken from published government life tables No alternative assumptions were explored through sensitivity analysis |
| D2c | QoL weights (utilities) | Yes | No intervention-specific estimates: EQ-5D from Phase II study of standard-dose imatinib adopted for baseline utility for all comparators. Technology-specific weightings were then added to reflect assumed incidence of AEs; however, the utility of AE states was ‘in general’ not based on EQ-5D data |
| D3 | Data incorporation | Yes |
All data incorporated into the model has been described and referenced in sufficient detail (note that nilotinib PFS is based on unpublished additional follow-up) Mutually inconsistent data have been used extensively, note different methods for estimating PFS (time in AP) across comparators. In addition, there are overwhelming differences between the populations in the studies from which ImR data have been drawn. The cohort reported in Talpaz et al. ’s study32 had not previously failed imatinib; hence, they are not only non-comparable with the nilotinib population, but entirely beyond the scope of the review. For ImI, it is emphasised that data used to estimate the effectiveness of hydroxycarbamide are drawn from a study in which a variety of other therapies were administered, as well as or instead of hydroxycarbamide. Where justified, such inconsistencies are seen as a function of paucity of suitable data The process of data incorporation is clearly described Where used for probabilistic sensitivity analysis, distributions for each parameter have been specified but not justified All effectiveness data used in the model are derived from single-arm studies; while this is described, the impact of the uncertainty associated with these methods is not explored |
| D4 | Assessment of uncertainty | ||
| D4a | Methodological | Partial | A single sensitivity analysis was performed adopting a 5-year time horizon. Otherwise, there is no evidence that methodological uncertainties have been addressed by running alternative versions of the model with different methodological assumptions |
| D4b | Structural | No | There is no evidence that the – very considerable – structural uncertainties inherent in the model have been addressed via sensitivity analysis |
| D4c | Heterogeneity | Yes | The provision of separate models for ImI and ImR populations helps to address heterogeneity |
| D4d | Parameter | Partial |
A limited number of one-way sensitivity analyses were performed, with PFS, OS, utility and cost parameters varied, generally within the range of each parameter’s 95% CI. Effectiveness parameters were varied simultaneously for each comparator, so it is not possible to deduce the extent to which the model is sensitive to uncertainty in individual parameters Probabilistic sensitivity analysis is reported, with outputs shown in CEACs (no scatterplots provided) |
| Consistency | |||
| C1 | Internal consistency | No | There is no evidence that internal consistency has been evaluated (e.g. by testing expected behaviour when setting parameters to extreme or null values) |
| C2 | External consistency | No |
The results presented are subject to a degree of uncertainty that overwhelms any credible conclusions. In particular, it was impossible to draw any inferences regarding the cost-effectiveness of nilotinib in comparison to HDI in ImR AP, when the ‘high-dose’ imatinib arm is parameterised with data from a study investigating standard-dose imatinib in an imatinib-naive population (and, even then, has mistakenly been based on the wrong subgroup of this data source) Results are almost as uncertain in the ImI subgroup, because of very weak evidence on the effectiveness of hydroxycarbamide Aside from inadequacies in the data sources informing the models, a considerable amount of uncertainty attaches to untested structural and methodological assumptions underpinning the model, but these are not given emphasis in discussion Model-predicted OS is shown against empirical OS for nilotinib, HDI and a hydroxycarbamide. In the ImR subgroup, in particular, the fit between predicted and observed OS is visually unconvincing. For all follow-up up to around 14 months, empirical OS for nilotinib and ‘HDI’ appear very similar, although there is a slight divergence in nilotinib’s favour in the very unstable tail of the distribution. This is not matched in the simulated cohorts, with a notable survival gain predicted for nilotinib throughout. This inconsistency is probably due to the fact that OS is modelled as a function of PFS, and ‘HDI’ PFS appears to have been mistakenly drawn from the wrong (400 mg q.d.) cohort of Talpaz et al. ’s study32 (see D1). The fit to empirical OS in the ImI subgroup is somewhat more credible It does not appear that the results of the model been compared with those of any previous models |
Appendix 5 Surrogate outcomes in chronic myeloid leukaemia
Assessment of the clinical effectiveness and cost-effectiveness of a health technology is most meaningful when based on unambiguous patient-based outcomes such as death, myocardial infarction, stroke or changes in HRQoL. However, our review of the clinical evidence has revealed very little information on the long-term effects of treatment with dasatinib and nilotinib. Although there are indications that treatment with dasatinib and nilotinib may delay progression and, hence, improve PFS (see Chapter 2, Progression-free survival), the clinical studies currently provide no direct evidence of a survival benefit associated with dasatinib or nilotinib treatment.
The majority of identified studies provide data on the proportion of people attaining a CyR, reported as either a CCyR or a MCyR or both. Therefore, we considered the validity of using the achievement of a MCyR as a surrogate for OS on which to base our economic evaluation of the new agents.
The largest body of evidence in support of such a surrogate relationship in CML comes from studies of IFN. 30,142,265–270 However, it has been postulated that as the achievement of a MCyR signifies a substantial reduction in the number of Ph+ cells, any surrogate relationship may be independent of the drug used to achieve the response. Preliminary evidence suggests that a relationship exists for treatments other than IFN, e.g. allogeneic BM transplant268 and imatinib,17–19 although we are not aware of an explicit exploration of the wider evidence base.
Schrover et al. 271 used the data from seven randomised clinical studies of drugs used to treat patients with CML in the CP (mainly IFN compared with other chemotherapy, e.g. busulphan or hydroxycarbamide) to explore the association between a MCyR and survival using landmark survival analysis and regression analysis. As a MCyR occurs some time after the initiation of treatment, an analysis of survival that did not take into account the time taken to achieve the response would overestimate the survival of patients with a response compared with those without, as patients with a CyR must have survived long enough for that response to occur. Therefore, an analysis was performed which assesses survival after the landmark time, for patients classified by their best CyR achieved at or before the landmark time. The difference in survival (from the landmark point) between responders and non-responders was calculated for each of the treatment groups described in each study. A comparison of the landmark survival for responders and non-responders clearly demonstrated that the achievement of a MCyR was associated with improved OS. Further modelling using regression analysis supports the use of MCyR rate in patients with CML-CP to predict overall long-term survival. The estimated weighted odds ratio for the survival of those who achieved a MCyR compared with those who did not was 7 (95% CI 5 to 11) at 2 years and 5 (95% CI 3 to 8) at 4 years. Based on data from the included studies, the long-term survival model predicts that median survival may be increased by 1.8 years for every 25 percentage points increase in MCyR rate. However, the authors caution that, as the proportion of responders in a study increases, the quality of those responses in terms of their implications for survival may improve and, although achievement of a MCyR is a major predictor of survival, there is evidence that other factors, e.g. baseline risk profiles, may also have significant influence on OS.
A recently published report from the NIHR Health Technology Assessment programme272 reviewed the literature on the use of surrogate outcomes in health technology assessment and proposed the following hierarchy of evidence for surrogacy validation:
-
level 1: evidence demonstrating treatment effects on the surrogate correspond to effects on the patient-related outcome obtained from RCTs
-
level 2: evidence demonstrating a consistent association between surrogate outcomes and final patient-related outcome obtained from epidemiological/observational studies
-
level 3: evidence supporting the biological plausibility of a surrogate relationship.
The authors recommend that an economic evaluation should only be based on a surrogate outcome where there is levels 1 or 2 validation evidence. From the available evidence, we believe that there is sufficient evidence to support the proposition that achievement of a MCyR is a valid surrogate for OS in CML-CP and we use this relationship in the development of our economic evaluation. Although it appears reasonable to assume that the surrogate relationship will exist for treatment with dasatinib and nilotinib, there is no direct evidence to support this assumption. The issue of transferability of a surrogate relationship between analyses of different technologies has received, apparently, little attention in the literature, though it must be that Schrover’s271 words of caution about the multifactorial determinants of OS might be germane. Against that is the evidence that, in the context of CML, the surrogate relationship appears to hold across several treatments.
Therefore, we have assumed that the relationship between MCyR rate and OS is identical for each comparator in the model and, moreover, is identical to that estimated from the pooled analysis of three identified studies in which OS was reported according to MCyR status (see Chapter 5, Overall survival, hazard ratio for people achieving an MCyR vs people who do not achieve an MCyR). 236–238 We chose to base the surrogate relationship on this evidence base, rather than IFN, in recognition of the possibility that response may not be entirely independent of treatment and that, therefore, it would be better to model surrogacy based on data arising from an agent in the same class as the principal focus of the assessment (i.e. the new TKIs).
Note, however, that the implementation of the surrogate relationship between response and OS in our model does not take into account any influence on OS from the timing, depth and duration of response.
We were unable to identify evidence specifically on the significance of the timing of the achievement of a MCyR in terms of effects on OS. There is debate within the literature as to the prognostic importance of the early achievement of a CCyR. Initial reports suggested that the time to response correlated with outcome where an early response predicted the best long-term outcome,17,257 but the 5-year update of the IRIS study suggests that the risk of disease progression is decreased among individuals who achieve a CCyR regardless of whether this was achieved at 12, 18 or 24 months. 18 However, an analysis of the probability of achieving a CCyR, MMR and progression in 258 participants with CML-CP treated with normal-dose imatinib found that individuals not in CCyR after 12 months have a higher risk of progression and that molecular analysis reveals that this risk is discernible as early as 3 months after starting treatment with imatinib. 273
Depth of CyR is potentially more troublesome to our assumption that the surrogate relationship is identical between treatments. There is good evidence in the literature that a deeper response predicts a longer response257–259 and may also be associated with greater PFS,19,260,261 although whether or not these differences translate into effects on long-term survival has not yet been demonstrated.
Our model also assumes that, in the relationship between response and OS, duration of response does not influence OS. There is suggestion within the literature that responses to HDI are less durable than those achieved with other interventions, although the evidence is scant and conflicting. 182,260,263
Appendix 6 Estimation of overall survival by treatment in the PenTAG model
Overall survival curves for each treatment were generated in the following four-stage process.
Stage 1 – estimation of survival owing to chronic myeloid leukaemia-related deaths for responders and non-responders
Cytogenetic response has been shown to be a useful predictor of OS and has been used in other models of cost-effectiveness for CML. 274 In particular, MCyR, as opposed to CCyR, has been shown to provide a good surrogate outcome for OS. 271 Further discussion of this surrogate relationship is provided in Appendix 5.
We define ‘responders’ as those patients who achieve an MCyR while on treatment, and ‘non-responders’ as those patients who do not achieve an MCyR. Two separate Weibull curves, SRESPCML(t) for responders and SNON-RESPCML(t) for non-responders, are used to fit OS owing to CML-related deaths, where OS is better for responders than for non-responders.
In common with another cost-effectiveness model for CML,274 we assumed a constant hazard ratio (λ) between the OS because of CML-related deaths for responders versus non-responders, i.e.:
A literature search was undertaken to find those studies that reported OS for patients on normal-dose imatinib according to whether they were responders or non-responders. Trials of imatinib (rather than IFNα were preferred because, according to our clinical experts, OS given a certain response for dasatinib and nilotinib is most likely to be similar to OS for imatinib given its mode of action. A meta-analysis of studies of imatinib concluded that λ = 0.370.
Stage 2 – estimation of overall survival (chronic myeloid leukaemia- and non-chronic myeloid leukaemia-related deaths) for responders and non-responders
Next, the OS curves for responders and non-responders, SRESPoverall(t) and SNON-RESPoverall(t), allowing for CML- and non-CML-related mortality combined, were calculated as follows. First, the rate of CML-related mortality at time t was calculated as:
for responders and non-responders, respectively.
Next, the general background mortality rate at time t, rgeneral(t) was taken from UK life tables. 232 Then, the OS for responders and non-responders was calculated allowing for the sum of the rates of CML-related and general mortality;
where
For consistency with the studies of the drugs for second-line treatment, the male : female ratio was assumed to be 50 : 50 and in the base case, all patients in the model were assumed to be aged 56 years at the start of second-line therapy.
Stage 3 – estimation of overall survival for all treatments
If the proportion of responders for a given treatment is denoted by MCyR%, then the OS for that treatment at time t, OS(t), owing to all deaths is:
Stage 4 – calibration to empirical overall survival
So far, we have not specified the parameters of the CML-related survival for responders and non-responders, SRESPCML(t) and SNON-RESPCML(t), except that they are related by Equation 1. These parameters were estimated by calibration by regressing expected OS for HDI, OS(t), to the empirical OS for HDI from Jabbour et al. 182 This empirical data were chosen for two reasons. First, this is the most mature OS for treatment after normal-dose imatinib failure that we are aware of. Second, the response rate is quoted in this study, which allows us to specify precisely the expected OS curve, OS(t).
Appendix 7 Estimation of treatment duration in the PenTAG model
Unlike OS, we did not split PFS according to responders and non-responders.
Progression-free survival for HDI was estimated as follows. First, PFS excluding general mortality was assumed to follow a Weibull curve. Similar to the estimation of OS above (see Appendix 6, Equation 3), overall PFS, i.e. including general mortality, was calculated from the rate of decay of PFS excluding general mortality and the rate of general mortality. Then, the parameters of the Weibull curve for PFS excluding general mortality (and, hence, overall PFS) were estimated by regressing the expected PFS against the empirical PFS from Jabbour et al. 182
Progression-free survival for all other drugs was estimated slightly differently. For simplicity, given that the follow-up for the empirical PFS for these drugs is very short (up to 2 years), we assumed that the empirical PFS was unaffected by general mortality over this period and that we could model the PFS excluding general mortality by an exponential curve. Therefore, we estimated PFS excluding general mortality by regressing an exponential curve to the empirical PFS. Overall PFS, including general mortality, was then calculated similar to Equation 3 (see Appendix 6), by allowing for the rate of decay of PFS, excluding general mortality and the rate of general mortality.
The empirical PFS and therefore estimated PFS for each treatment included those patients who stopped treatment because of serious AEs or other causes. Therefore, to estimate the treatment duration survival curve, a key model input, the PFS for those patients who stopped treatment because of serious AEs or other causes was subtracted from the overall PFS (Figure 46). The rates of treatment discontinuation were taken from the clinical studies. In the base case, we assumed that treatment stopped at the end of 3 months for those patients who suffered severe AEs, based on expert opinion. Given that treatment stops at the time of serious AEs, and that we do not model third lines of treatment, ideally we would assume that the PFS curve for those patients who stopped treatment because of serious AEs follows the PFS survival curve for no active treatment. However, given that such data were unavailable, we assumed that the PFS curve for those patients who stopped treatment because of serious AEs or other causes follows the modelled overall PFS for IFN, where we assumed that IFN delays progression only slightly compared with no drug treatment.
FIGURE 46.
Overall PFS, time on treatment and PFS for patients who stop treatment because of serious AEs or other causes for the example of nilotinib (ImI patients).
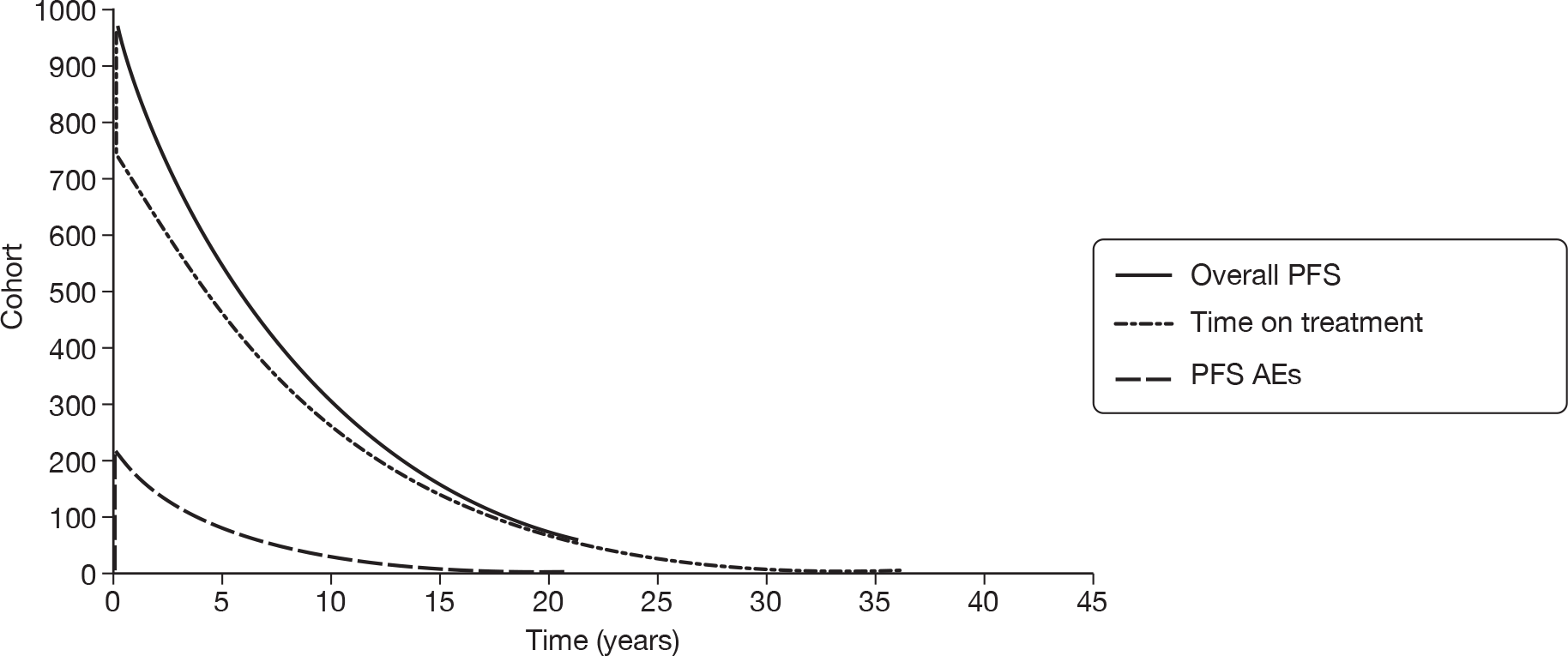
Appendix 8 Cost-effectiveness in imatinib-resistant chronic myeloid leukaemia in chronic phase (including interferon)
This supplementary analysis presents results for ImR CML-CP in a decision space that includes an older standard-of-care treatment as a comparator (IFN plus cytarabine). For convenience, this comparator is referred to as IFN in the following analysis; however, it should be remembered that the model arm was parameterised using study data from a cohort in which the majority of participants had also received cytarabine, and the costs of this additional treatment are included in all analyses.
Base-case model outputs for imatinib-resistant chronic myeloid leukaemia
Table 123 presents the aggregated totals for the base-case model results for the four treatments. Outputs are shown for total life-years (undiscounted) and total discounted QALYs and costs for each treatment over the time horizon of the model.
| Dasatinib | Nilotinib | HDI | IFN | |
|---|---|---|---|---|
| Life-years (mean) (undiscounted) | ||||
| CP treated | 6.50 | 2.44 | 2.68 | 2.04 |
| CP post-discontinuation | 5.00 | 8.65 | 7.79 | 6.82 |
| AP | 0.80 | 0.80 | 0.80 | 0.80 |
| BC | 1.09 | 1.09 | 1.09 | 1.09 |
| Total (mean) | 13.40 | 12.98 | 12.37 | 10.75 |
| Total (median) | 10.76 | 10.21 | 9.45 | 7.75 |
| QALYs (mean) (discounted) | ||||
| CP treated | 4.50 | 1.89 | 2.10 | 1.27 |
| CP post-discontinuation | 2.62 | 5.00 | 4.46 | 4.16 |
| AP | 0.37 | 0.38 | 0.38 | 0.41 |
| BC | 0.36 | 0.36 | 0.37 | 0.39 |
| Total | 7.846 | 7.630 | 7.311 | 6.23 |
| Costs (£) (mean) (discounted) | ||||
| Drug costs | 161,432 | 70,143 | 88,883 | 15,936 |
| Drug administration | 0 | 0 | 0 | 4390 |
| Monitoring OP appointment | 6818 | 6728 | 6597 | 6259 |
| BM tests | 6518 | 2732 | 3038 | 2199 |
| Radiography | 726 | 736 | 752 | 795 |
| CT scans | 428 | 434 | 444 | 469 |
| Blood transfusions | 4058 | 4117 | 4205 | 4445 |
| Post-discontinuation treatment | 38,386 | 73,436 | 65,429 | 61,083 |
| Inpatient palliative care | 2960 | 3003 | 3067 | 3242 |
| Total | 221,325 | 161,330 | 172,415 | 98,818 |
The model estimates that both dasatinib and nilotinib produce median survival of over 10 years, whereas the HDI cohort has median OS of 9.5 years, and the equivalent figure for IFN is 7.75 years. This order of OS reflects the relative proportion of patients with a MCyR for each treatment (see Chapter 5, Major cytogenetic response rates). Once expected lifespan is quality adjusted and discounted, the difference between dasatinib, nilotinib and HDI is minimised, with only around 6 quality-adjusted months separating all three comparators. IFN is predicted to provide at least 1 QALY fewer.
Notwithstanding the similarity in predicted OS between dasatinib, nilotinib and HDI, there is substantial heterogeneity in the constituent elements of the predicted lifespans. In particular, the amount of time each cohort is expected to spend in pre-progression CP varies notably; individuals taking dasatinib are predicted to spend an average of 6.5 years before progression, whereas those taking either nilotinib or HDI spend less than half as long in the same state. This difference is counterbalanced by time in post-progression CP, which is predicted to last a mean of 5 years for the dasatinib cohort, compared approximately 8 years for those taking either nilotinib or HDI. For IFN, a comparatively short period of pre-progression CP is followed by a more extended post-progression CP phase; in total, however, the cohort is predicted to spend a mean of 2 or more years fewer in CP than those taking the three other comparators.
As per the model assumptions (see Chapter 5, Method of estimating time in accelerated phase and blast crisis), time in AP and BC is essentially the same across all comparators (the very slight discrepancies in numbers are a result of the discounting process).
These results are illustrated in Figure 47, which shows the relative proportions of patients in each health state for each treatment throughout the time horizon of the model. The total duration in each health state for each treatment (as reported in Table 123) is represented in these graphs by the area under each curve. Accordingly, the duration for patients receiving treatment in CP is represented by the area underneath the dotted line, and the area between the dotted line and the solid OS curve represents the sum of post-progression CP, AP and BC. As would be expected, virtually all patients are predicted to have died by 40 years from start of treatment (i.e. by age 96 years), regardless of treatment. Notice that the predicted time on treatment falls fairly steeply at 3 months for nilotinib and HDI, because of the large numbers of patients who stop treatment because of serious AEs. The decline is even more dramatic in the IFN cohort, in which over 50% of participants are predicted to withdraw because of AEs.
FIGURE 47.
Base-case cohort composition over time by treatment: ImR.
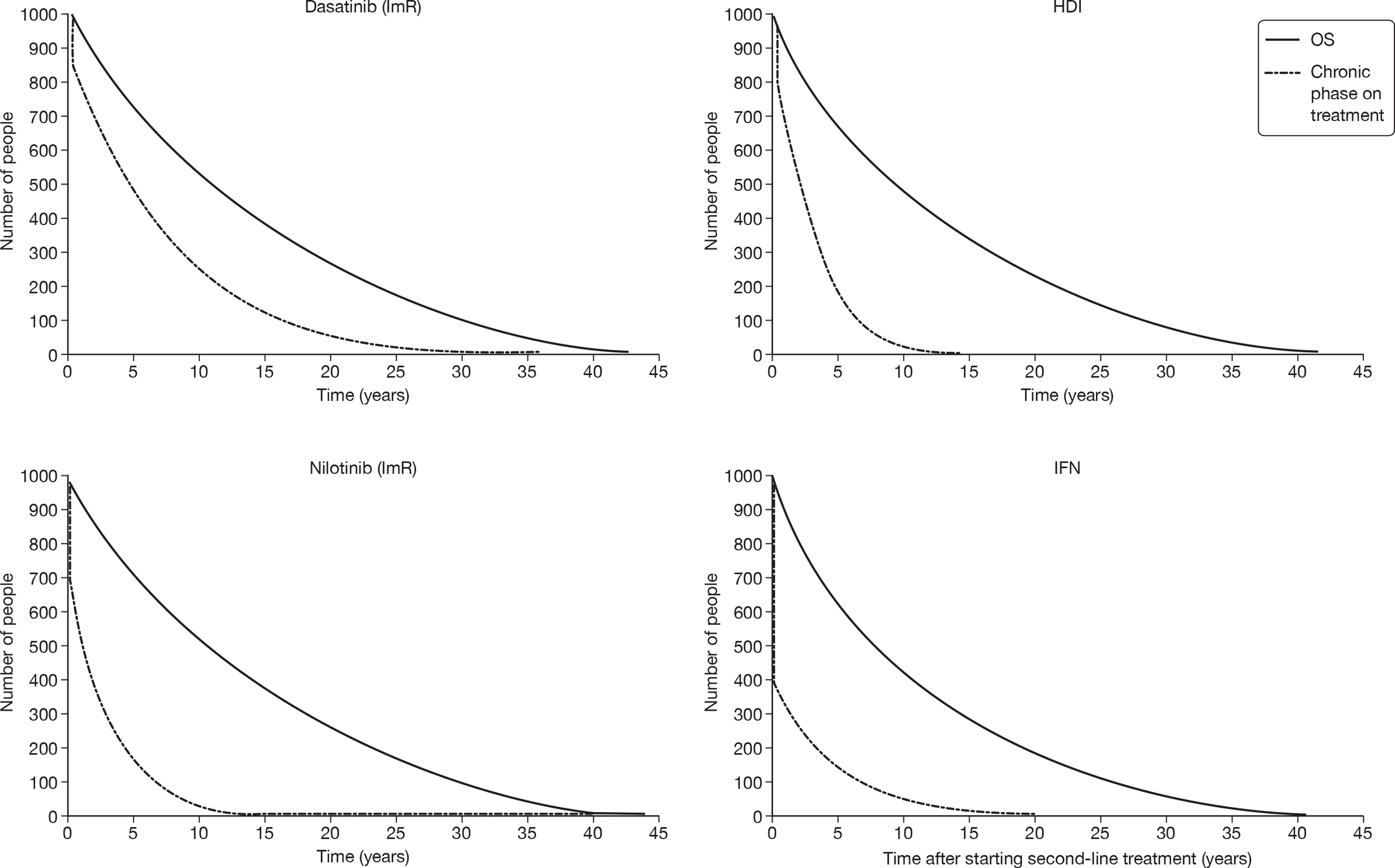
It can also be seen that, as explained above, the proportion of time that individuals taking dasatinib are predicted to spend in CP on treatment (i.e. prior to disease progression) is substantially greater than the equivalent period for the other comparators. It should be remembered, however, that the expected time on treatment is highly uncertain because of the extensive extrapolation of PFS (see sensitivity analyses in Executive summary, Results).
The impact of this discrepancy can be seen in the predicted costs shown in Table 123. Nilotinib and HDI are estimated to accrue lifetime costs of approximately £160,000 and £170,000, respectively, per simulated patient over the course of the model, but treatment with dasatinib is estimated to incur lifetime costs of at least £50,000 more. This situation arises because, in line with the time in pre-progression CP discussed above, our model predicts that it is necessary to take dasatinib for twice as long as nilotinib or HDI. Accordingly, in the breakdown in Table 123, it can be seen that the overall heterogeneity in costs is dominated by differences in the acquisition costs of the drugs themselves. As expected, owing to its relatively low unit cost, IFN is by far the cheapest comparator, although – in contrast to the other three comparators, which are delivered orally – it is also subject to some administration costs.
Figure 48 shows the OS curves for each of the four treatments overlaid, as well as showing the generic OS curves for patients with a MCyR compared with those with no response. The general survival curve for the equivalent aged non-CML population is also shown. The OS curves for dasatinib, nilotinib and HDI are represented by an asterisk, and can be seen to be very closely aligned. As expected, OS on IFN is estimated to be clearly lower, and only slightly better than would be achieved if a 0% MCyR rate could be assumed.
FIGURE 48.
Predicted OS for ImR people by treatment and for responders and non-responders.
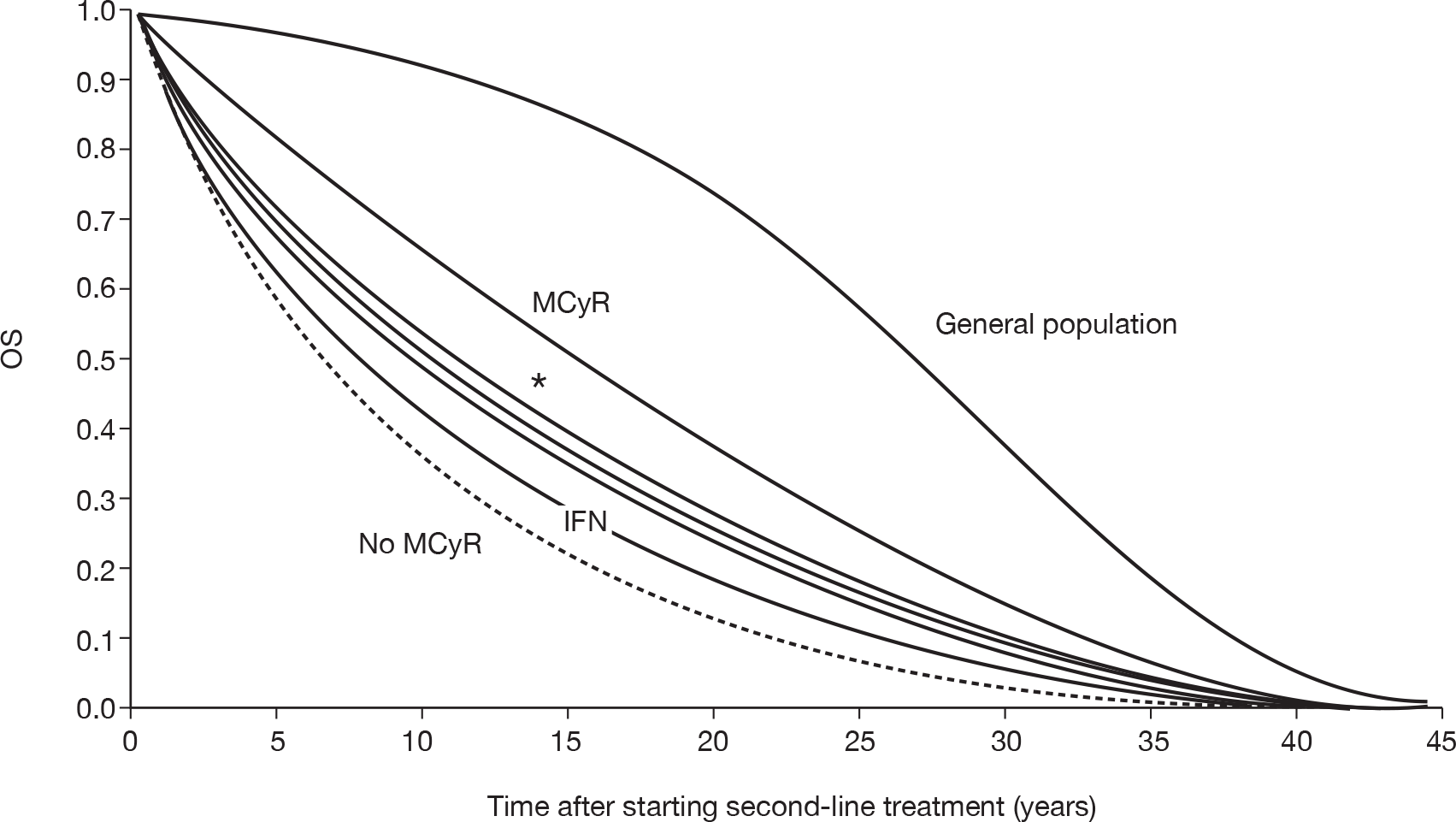
Base-case deterministic cost–utility results
The incremental cost–utility of dasatinib, nilotinib, HDI and IFN as estimated in our model is shown in Table 124, with the results depicted on the cost–utility plane in Figure 49.
| Cost (£)a | Utility (QALY) | Incremental cost (£) | Incremental utility (QALY) | Incremental £/QALY (ICER)b | |
|---|---|---|---|---|---|
| IFN | 98,800 | 6.23 | |||
| Nilotinib | 161,300 | 7.63 | 62,500 | 1.40 | 44,600 |
| HDI | 172,400 | 7.31 | 11,100 | 0.32 | Dominated by nilotinib |
| Dasatinib | 221,300 | 7.85 | 60,000 | 0.22 | 277,700 |
FIGURE 49.
Deterministic base-case incremental cost–utility for ImR CML: cost–utility plane. C-E, cost-effectiveness.
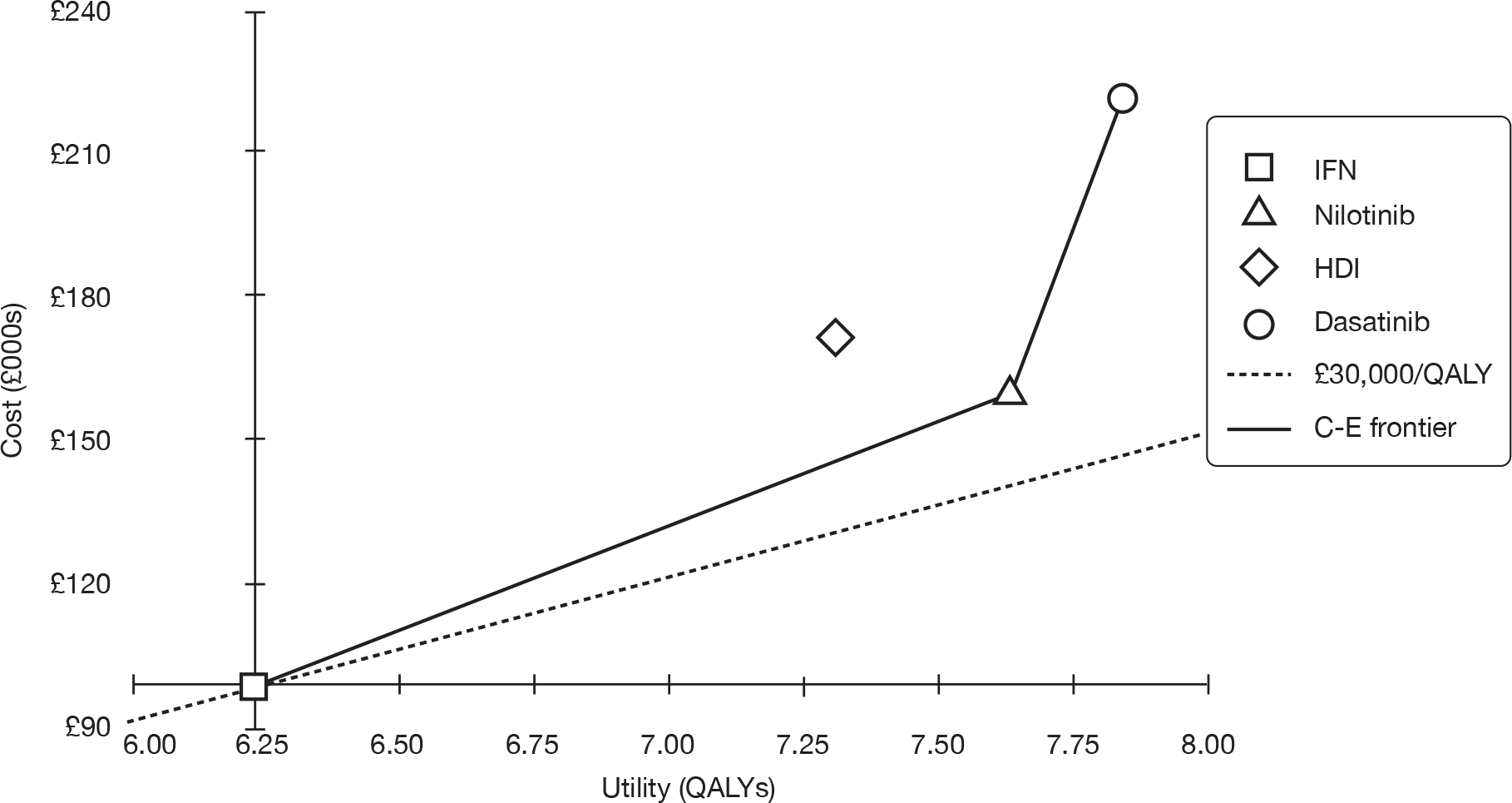
Because is it is the least costly of the available alternatives, IFN is considered to be the base option. It is estimated that, in comparison with IFN, the second cheapest comparator (nilotinib) will provide an additional 1.4 QALYs and cost an extra £62,500, equating to a cost–utility ratio of £44,600 per QALY. HDI is dominated by nilotinib (i.e. nilotinib is predicted to be both cheaper and more effective), so it would not be considered a viable option. When compared with nilotinib, dasatinib is predicted to provide a small utility gain of around 80 quality-adjusted days at substantial extra cost (approaching £100,000). As a result, it has a high cost–utility ratio (as reflected in the steep gradient in Figure 49), so it is likely to be considered to provide poor value for money.
Model validation: model outputs compared with study data
Progression-free survival
Figure 50 shows the actual data for PFS versus the fitted model curve for each of the four modelled treatments. From this, it can be seen that our model in general uses a relatively close fit between the study data and the fitted curves in the model.
FIGURE 50.
Curve fit for PFS for ImR patients by treatment.
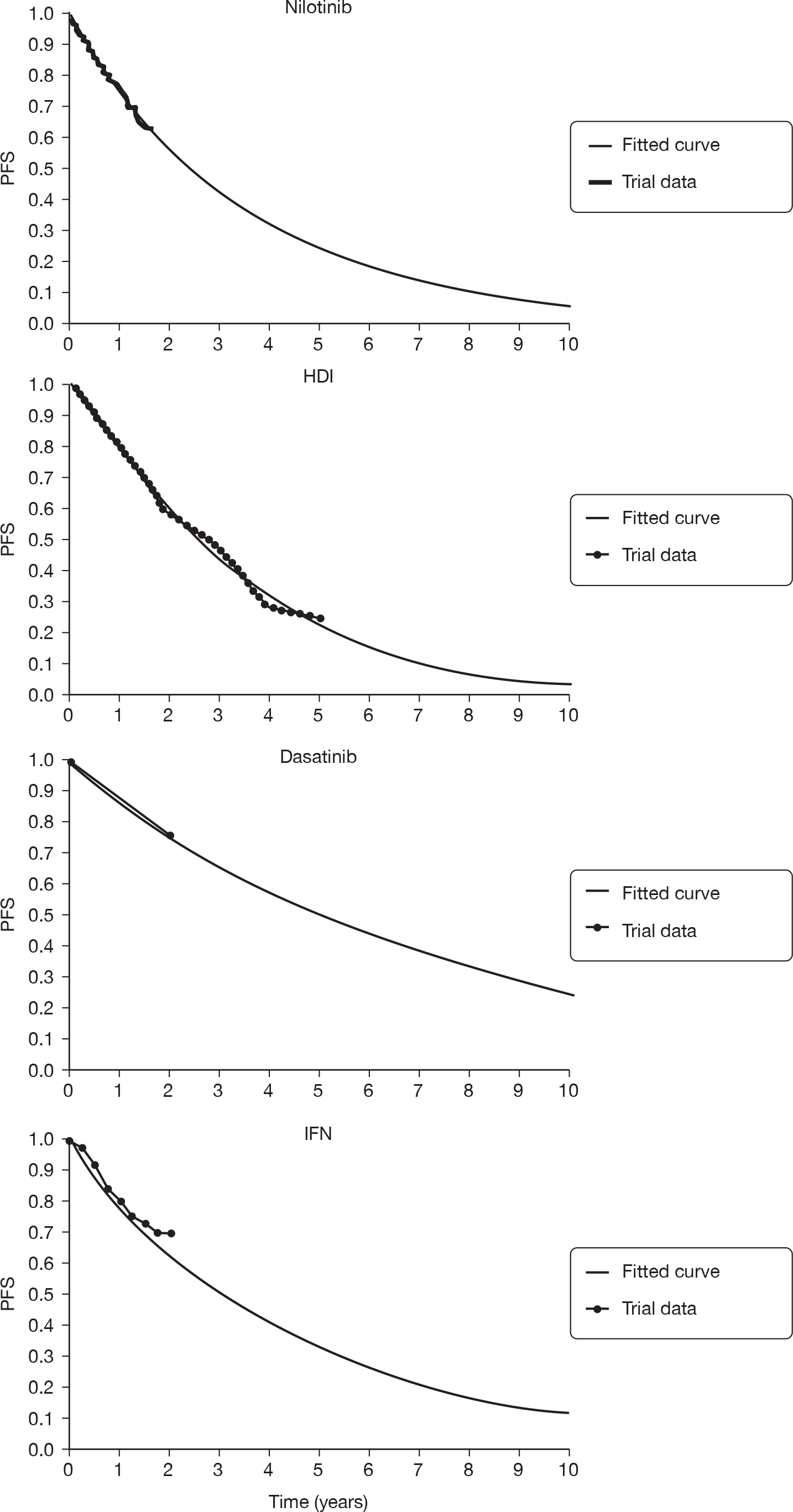
Overall survival
Figure 51 shows the actual data for OS versus the fitted model curve for each of the four modelled treatments. The modelled OS for HDI was fitted to empirical study data, so a very close fit between actual and predicted OS for HDI was obtained. The predicted OS for dasatinib and nilotinib, however, was modelled completely independently of the empirical OS for these treatments (because the empirical OS data set is very immature). Despite this, however, we found that the OS curves from our model predict the empirical data well for the short period of the study follow-up. The curve fit for the empirical IFN OS does not appear especially accurate. This may be because the empirical data present first-line treatment, whereas the predicted data were for second-line treatment. There is also the problem that the study from which our IFN data were drawn17 featured substantial crossover from the IFN arm to the alternative treatment (imatinib), with the likely consequence of exaggerated OS. Finally, any disparity may also be exaggerated because we have a single data point against which to validate the model’s prediction. A more complete survival curve might have a less discrepant appearance.
FIGURE 51.
Curve fit for OS for ImR patients by treatment.
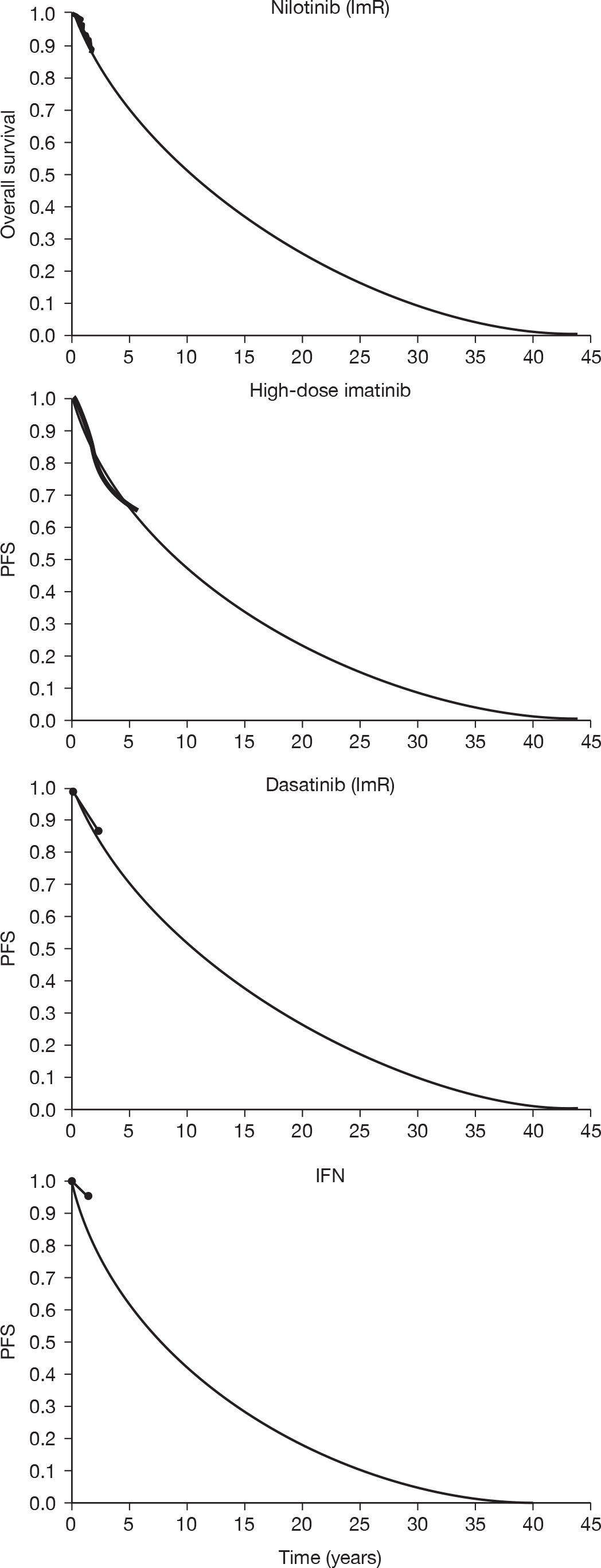
Deterministic sensitivity analysis
We have not undertaken separate deterministic sensitivity analyses for decision problems including IFN; for an indication of model dynamics please refer to the relevant section in the main text.
Probabilistic sensitivity analyses
We ran 1000 Monte Carlo simulations, varying model input parameters simultaneously, to estimate the impact of parameter uncertainty on estimated cost–utility. In each iteration, parameters are randomly sampled from pre-defined distributions reflecting the precision of each input value (for effectiveness parameters, this is usually defined in terms of the 95% CI around data drawn from the literature).
The scatterplot shown in Figure 52a depicts the results of each simulation, in terms of the incremental cost–utility of dasatinib (+s), nilotinib (×s), and HDI (circles) compared with IFN.
FIGURE 52.
Probabilistic sensitivity analyses: incremental cost–utility (ImR CML). (a) Cost–utility plane, showing incremental cost–utility of dasatinib, nilotinib and HDI compared with a common baseline of IFN in 1000 iterations of probabilistic sensitivity analyses. (b) CEAC showing probability that each treatment is most cost-effective (delivers highest net monetary benefit).
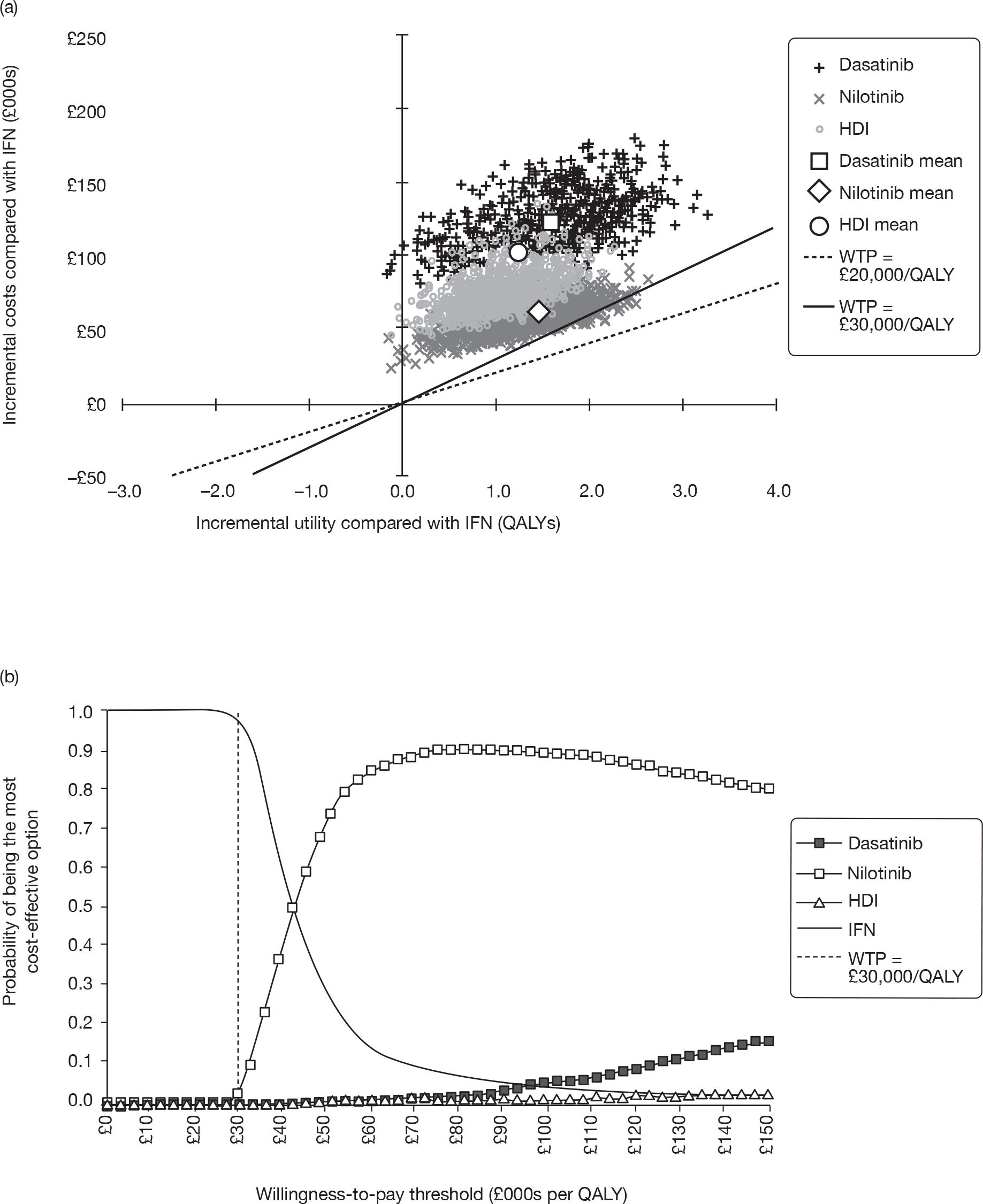
It can be seen that there is very little uncertainty about the relationship between IFN and the three other comparators. The TKIs are always more expensive and, with the exception of a tiny number of outlying simulations, always more effective than IFN.
In contrast, there is substantial uncertainty about the effectiveness of the TKIs. Dasatinib generated more QALYs than HDI in 95% of the simulations, whereas nilotinib was predicted to have greater utility than HDI in 90%. (Overall, dasatinib generated most QALYs in 80% of the simulations; HDI in 3%, nilotinib in 16% and IFN in fewer than 1%.)
The estimated costs for nilotinib and HDI are relatively similar, although nilotinib was predicted to be less expensive than HDI in all except 9% of simulations. The cost implications of dasatinib are clear: despite uncertainty attaching to resource use parameters, the lifetime costs of the dasatinib cohort were greater than those of the HDI arm in all 1000 simulations.
Figure 52b shows a CEAC for the four comparators, predicting the probability that each would be considered to provide best value for money, given a range of different societal WTP thresholds. Because IFN is substantially the cheapest comparator, it is predicted to provide best value for money if WTP is assumed to be low; as WTP rises, the probability that nilotinib would provide best cost–utility becomes higher. At a conventional WTP threshold of £30,000 per QALY, our model estimates the probability of IFN providing optimal cost–utility at 97%, with corresponding likelihoods for nilotinib, HDI and dasatinib of 3%, 0% and 0%, respectively. At a threshold of around £45,000 per QALY, it becomes unlikely that IFN provides the best balance of costs and utility. From this value onwards, nilotinib is predicted to be the optimal choice.
Our model predicts that it is unlikely that dasatinib would be considered the best option; even when WTP approaches £150,000 per QALY, the probability of dasatinib providing the best value for money is under 20%.
Discussion: imatinib-resistant chronic myeloid leukaemia
Dasatinib
For dasatinib, our deterministic and probabilistic results make it appear unlikely that the technology would be considered to provide an acceptable cost–utility balance. Given that dasatinib is cheaper per patient q.d. (at the intended doses) and is predicted to give greater life expectancy, one might expect dasatinib to dominate HDI. This is not the case for two main reasons. First, we predict that dasatinib is typically taken for far longer than HDI (a mean of 6.5 years vs 2.7 years in the deterministic base case), thus incurring far greater drug costs. Second, the dose intensity for HDI is lower than for dasatinib (76% vs 100%). As a result, acquisition costs for dasatinib are typically more than twice as much as those estimated for HDI (in the deterministic base case, the values are £169,000 and £74,000, respectively), which leads to a similar discrepancy in overall lifetime costs. This additional expenditure is not counterbalanced by an equivalent effectiveness gain, according to our model, with dasatinib providing no more than a few extra quality-adjusted days of life compared with HDI in the base case. The net result is that dasatinib is estimated to have an extremely high cost–utility ratio, costing millions of pounds for every additional QALY gained.
Our sensitivity analyses suggest that it is difficult to explain this finding on the basis of parameter uncertainty alone. Dasatinib provided best value for money in only a tiny proportion of our probabilistic simulations, and only then when high levels of WTP for a QALY were assumed.
However, we reiterate that – above and beyond parameter uncertainty – our model is reliant on an array of substantial assumptions, which make it extremely difficult to draw conclusions with any degree of confidence. The most critical shortcoming is that our model is necessarily parameterised on the basis of a heterogeneous collection of observational data, in which the outcome measures on which we rely – above all, MCyR and PFS – have been defined and measured in different ways, at different times, in different populations. It is feasible that a well-conducted randomised comparison of the alternatives would produce entirely different results to those on which we have been forced to rely and a completely different cost–utility picture would be very likely to result.
Nilotinib
Results for nilotinib are subject to an overwhelming amount of uncertainty. In our base-case deterministic analysis, we estimate that nilotinib is extendedly dominated by IFN and HDI. However, we note that the costs and QALYs estimated for nilotinib and HDI are very similar, with only £2000 in lifetime costs and 0.15 QALYs separating the comparators.
As would be expected, then, our sensitivity analyses demonstrate that our base-case deterministic finding is subject to very substantial uncertainty. Our analyses suggest that it is extremely difficult to conclude whether the average individual taking nilotinib accrues higher or lower costs than one taking HDI. Although nilotinib is cheaper than HDI per patient q.d. at the intended doses (800 mg q.d. each), the total expected per-patient drug acquisition costs of nilotinib and HDI are very similar. This is because our model assumes that the dose intensity for HDI is lower than for nilotinib (76% vs 100% in the deterministic base case). Once additional uncertainty around resource use and health-state transition is accounted for in probabilistic analysis, there is no consistent evidence to identify one or other technology as the least expensive.
Similarly, it is entirely unclear whether or not higher or lower quality-adjusted life expectation follows the use of nilotinib or HDI. Our base-case estimate suggests that HDI may benefit from an effectiveness advantage of a little less than 2 quality-adjusted months; however, that result is very easily reversed when parameters are varied within plausible ranges (see one-way sensitivity analyses in Probabilistic sensitivity analyses). Once all parameter uncertainty is accounted for in probabilistic analysis, the identity of the technology with the superior effectiveness profile becomes very uncertain.
Unsurprisingly, therefore, it is extremely challenging to estimate whether or not nilotinib provides an acceptable balance of cost–utility. Our best estimate is that there is somewhere in the order of a 28% chance that it would be considered to provide reasonable value for money, assuming a societal WTP threshold of £30,000 per QALY.
Appendix 9 Modelled versus empirical overall survival: alternative calibration for imatinib intolerant people
Figure 53 shows the modelled OS curves for ImI people when we calibrate OS to the OS for nilotinib (see Chapter 5, Overall survival).
FIGURE 53.
Actual versus predicted OS for ImI people when OS is calibrated to observed OS for nilotinib.
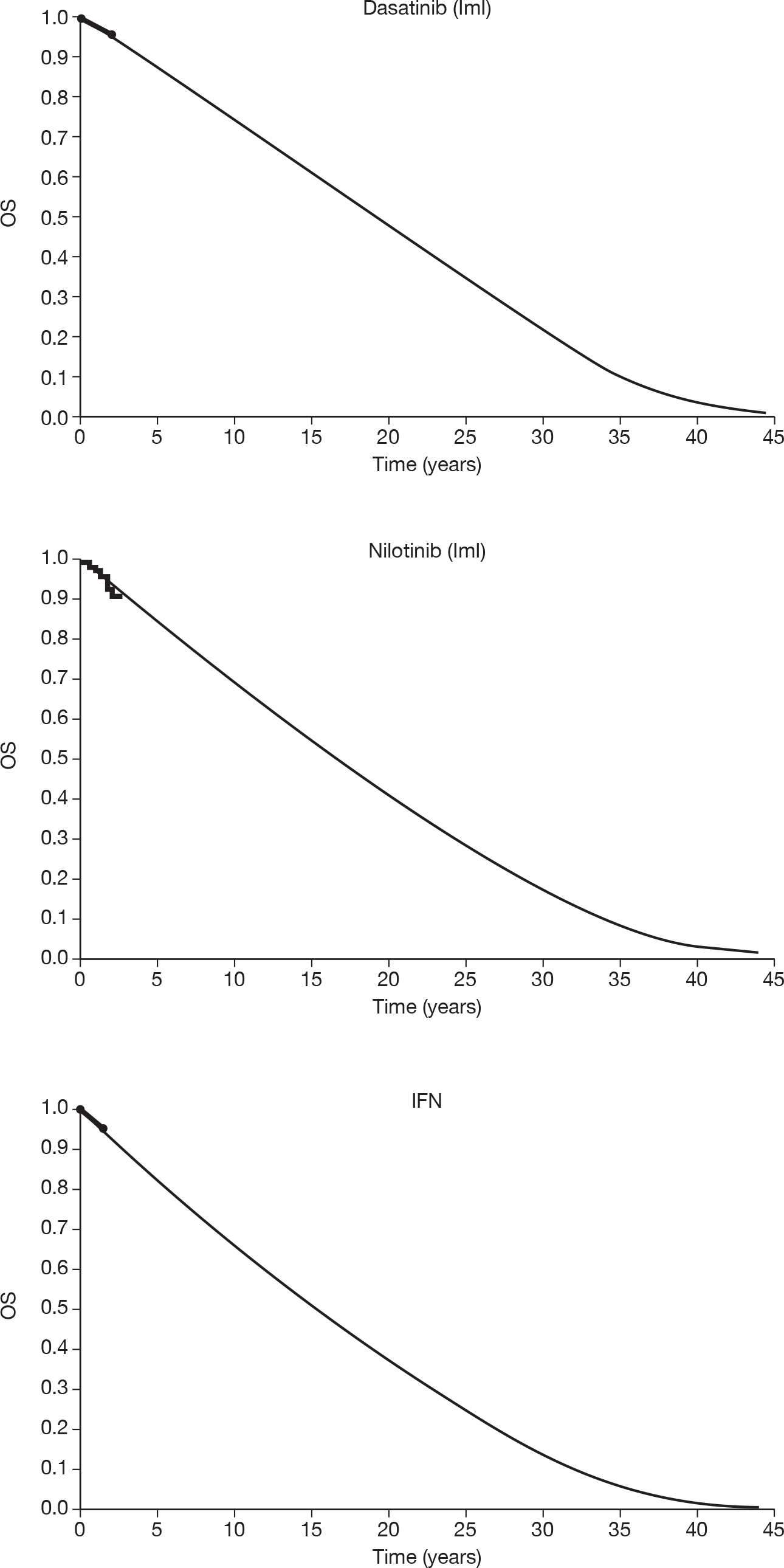
Appendix 10 Ongoing studies
| Official title | Sponsors/collaborators | Start date | Expected completion date | Study IDs/link |
|---|---|---|---|---|
| A randomized multi-center open label study of BMS-354825 v. imatinib mesylate (Gleevec) 800 mg q.d. in subjects with chronic phase philadelphia chromosome-positive chronic myeloid leukemia who have disease that is resistant to imatinib at a dose at 400–600 mg q.d. | BMS | February 2005 |
March 2008 Status: completed |
CA180-017 |
| An open-label, randomized study of dasatinib v. high-dose (800 mg) imatinib in the treatment of subjects with chronic phase chronic myeloid leukemia who have had a suboptimal response after at least 3 months of therapy with 400 mg Imatinib | BMS | August 2006 | September 2010 |
CA180-043; EUDRACT number: 2005-005153-22 |
| Therapy of early chronic phase chronic myelogenous leukemia (CML) with dasatinib (BMS-354825) | M.D. Anderson Cancer Center, BMS | November 2005 | September 2010 |
2005-0422 |
| Randomized, open label study of dasatinib (100 mg q.d.) v. high-dose imatinib (600 mg) in patients with chronic phase CML who have had suboptimal response after 3–18 months of therapy with imatinib (400 mg) | Pusan National University Hospital | Not stated | Not stated |
CA180-257; KCML02 |
| A randomized two-by-two, multicenter-open-label Phase II study of BMS-354825 administered orally at a dose of 50 mg or 70 mg twice daily or 100 mg or 140 mg q.d. in subjects with chronic phase philadelphia chromosome or BCR–ABL positive chronic myelogenous leukemia who are resistant or intolerant to imatinib mesylate (Gleevec) | BMS | July 2005 | April 2011 |
CA180-034 |
| A randomized, multicenter, open-label Phase II study of dasatinib (BMS-354825) administered orally at a dose of 50 mg twice daily or 100 mg q.d. in subjects with chronic phase philadelphia chromosome positive chronic myeloid leukemia who are resistant or intolerant to imatinib | BMS | May 2007 | May 2009 status: completed |
CA180-138 |
| A randomized multi-center open label study of BMS-354825 vs imatinib mesylate (Gleevec®) 800 mg q.d. in subjects with chronic phase philadelphia chromosome-positive chronic myeloid leukemia who have disease that is resistant to imatinib at a dose of 400–600 mg q.d. | Jonsson Comprehensive Cancer Center, National Cancer Institute (NCI) | March 2005 |
Date not stated Status: active, not recruiting |
CDR0000428457; UCLA-0501047-01; BMS-CA180017; EUDRACT-2004-004450-96 |
| An open-label randomized Phase II study of dasatinib v. high-dose (600 mg) imatinib mesylate in the treatment of subjects with chronic phase philadelphia chromosome-positive chronic myeloid leukemia who are imatinib failures or who have had a suboptimal response after 3–18 months of therapy with 400 mg imatinib | BMS | April 2007 |
September 2012 Status: terminated |
CA180-044 |
| An open-label, randomized, multicenter Phase II trial comparing the depletion of malignant stem cells with dasatinib v. imatinib in patients with newly diagnosed chronic phase chronic myeloid | Norwegian University of Science and Technology |
March 2009 Status: recruiting |
December 2011 |
2008-004106-13 |
| A randomized two-arm, multicenter, open-label Phase II study of BMS-354825 administered orally at a dose of 70 mg twice daily or 140 mg q.d. in subjects with chronic myeloid leukemia in accelerated phase or in myeloid or lymphoid blast crisis or with philadelphia chromosome positive acute lymphoblastic leukemia who are resistant or intolerant to imatinib mesylate (Gleevec) | BMS | June 2005 |
March 2011 Status: active, not recruiting |
CA180-035 |
| A Phase II study of molecular responses to imatinib at standard or increased doses or dasatinib (NSC-732517) for previously untreated patients with chronic myelogenous leukemia (CML) in chronic phase | Southwest Oncology Group National Cancer Institute (NCI) Eastern Cooperative Oncology Group | August 2004 |
Date not given (5-year follow-up) Status: active, not recruiting |
CDR0000334588; SWOG-S0325; ECOG-S0325 |
| An open-label, randomized, multicenter Phase II trial of dasatinib (SPRYCEL®) v. standard dose imatinib (400 mg) in the treatment of subjects with newly diagnosed chronic phase philadelphia chromosome positive chronic myeloid leukemia | BMS | September 2007 | June 2010 |
CA180-056 |
| STI571 prospective international randomised trial 2: a Phase II, prospective randomised comparison of imatinib (STI571, Glivec®/Gleevec®) 400 mg daily versus dasatinib (Sprycel®) 100 mg daily in patients with newly-diagnosed chronic phase chronic myeloid leukaemia |
Funder: BMS (USA) Sponsor: Newcastle-upon-Tyne Hospitals NHS Foundation Trust (UK) |
Anticipated start date: 30 June 2008 | Anticipated end date: 30 June 2016 |
ISRCTN54923521 |
| A Phase II randomized, open-label multi-center study of nilotinib versus imatinib in adult patients with Ph+ chronic myelogenous leukemia in chronic phase (CML-CP) who have a suboptimal cytogenetic response (CyR) on imatinib | Novartis Pharmaceuticals | October 2007 | Completed |
CAMN107A2302 |
| Randomized Phase III study of imatinib dose optimization compared with nilotinib in patients with chronic myelogenous leukemia and suboptimal response to standard-dose imatinib | Novartis Pharmaceuticals | May 2009 | Status: recruiting |
CAMN107A2404 |
| An open-label, randomized study of nilotinib v. standard imatinib (400/600 mg QD) comparing the kinetics of complete molecular response for CML-CP patients with evidence of persistent leukemia by RQ-PCR | Novartis Pharmaceuticals | April 2009 | Not yet recruiting |
CAMN107A2405 |
| A Phase II multi-center, open-label, randomized study of imatinib versus nilotinib in adult patients with newly diagnosed philadelphia chromosome positive (Ph+) chronic myelogenous leukemia in chronic phase (CML-CP) | Novartis Pharmaceuticals | July 2007 | Status: active, not recruiting |
CAMN107A2303 |
| Extension study to a Phase II multi-center, open-label, randomized study of imatinib versus nilotinib in adult patients with newly diagnosed philadelphia chromosome positive (Ph+) chronic myelogenous leukemia in chronic phase (CML-CP) | Novartis Pharmaceuticals | April 2008 | Status: active, not recruiting |
CAMN107A2303E1 |
| Phase I/II study of the adjunctive use of nilotinib in patients undergoing reduced intensity allogeneic transplantation for ImR or intolerant CML (TRICE) |
Funding source: Novartis Pharmaceuticals (UK) Sponsor source: University of Birmingham (UK) |
3 November 2008 | Anticipated end: 29 October 2010 |
ISRCTN12974558 |
Glossary
- Abelson oncogene (ABL)
- An oncogene is a cancer-causing gene. The ABL gene is located on part of chromosome 9 that translocates to chromosome 22 in chronic myeloid leukaemia (CML).
- Allogeneic transplant
- A bone marrow (BM) or stem cell transplant (SCT) using marrow from another person.
- Basophilia
- An excess number of basophils, a rare type of white blood cell (WBC) found in the peripheral blood (PB).
- Blast cells
- Immature cells found in and produced by the BM. Not normally found in the PB.
- BCR–ABL
- An oncogene fusion protein consisting of breakpoint cluster region (BCR) and ABL.
- Bone marrow (BM)
- The soft substance that fills bone cavities. It is composed of mature and immature blood cells and fat. Red and WBCs and platelets are formed in the BM.
- Breakpoint cluster region (BCR)
- The region of on a chromosome where breaks cluster. In the case of CML, it is the narrow part of chromosome 22 where the translocation to chromosome 9 occurs which includes the ABL (BCR–ABL). The BCR–ABL protein product results in the excessive proliferation of a tyrosine kinase.
- Bone marrow transplant
- A procedure in which a patient’s BM is replaced by healthy BM. The BM to be replaced may be deliberately destroyed by high doses of chemotherapy and/or radiation therapy. The replacement marrow may come from another person or it may have been previously harvested from the patient’s own marrow.
- Chemotherapy
- The treatment of a disease by chemicals to destroy cancer cells. Chemotherapy can affect the whole body.
- Cytogenetic response (CyR)
- A response to treatment at the level of chromosomal abnormalities. In the case of CML, assessed by counting the number of Philadelphia-positive (Ph+) cells in metaphase (usually 20 metaphases are analysed). A complete response generally means no Ph+ cells, a partial response leaves up to 35% Ph+ cells evident and with a minor response from 35% to 95% Ph+ cells are still evident.
- Cytopenia
- A reduction in the number of cells circulating in the blood.
- CRKL
- An adapter protein that becomes tyrosine phosphorylated by BCR–ABL.
- European Quality of Life-5 Dimensions (EQ-5D)
- A European quality of life questionnaire containing five physical and psychological dimensions.
- Extramedullary disease
- Disease occurring outside the BM.
- Haematological response (HR)
- A HR refers to the normalisation of blood cell counts. CML causes overproliferation of WBCs, which treatments aims to lower and categories of response indicate the extent to which this occurs. Typically, the HR is classified as complete if the WBC count is < 10 × 109/l, platelet count is < 450 × 109/l, there are no immature cells in the PB with normal differential count, and there is a disappearance of symptoms and signs.
- Hydroxycarbamide
- Hydroxycarbamide (Hydrea®, Bristol-Myers Squibb) is a drug used in the treatment of CML which inhibits deoxyribonucleic acid (DNA) synthesis.
- Incremental cost-effectiveness ratio (ICER)
- Demonstrates the total additional cost per quality-adjusted life-year (QALY) gained of one alternative over another. There is no particular point at which an alternative is said to be ‘cost-effective’ as this will be a policy decision. The larger the ICER, the less likely the treatment is to be cost-effective.
- Interferon-α (IFN)
- Interferon is a protein derived from human cells. It has a role in fighting viral infections by preventing virus multiplication in cells. IFN-α is made by leucocytes. It is often used as a first-line therapy in CML.
- Landmark analysis
- A form of survival analysis that includes only patients who have survived for a specified period of time.
- Leucocytes
- WBCs which are responsible for fighting infections.
- Leukapheresis
- A process of removing excess WBCs from the PB.
- Leucopenia
- A reduced number of WBCs in the blood – it may affect a single cell type or all WBCs.
- Metaphase
- The second phase of mitosis (cell division). Cells in this phase of division are used for cytogenetic analysis in CML to identify the proportion of Ph+ chromosomes.
- Mitosis
- A division of cells which consists of four phases: prophase, metaphase, anaphase and telophase.
- Myelocytes
- Committed progenitor cells produced by, and found in, the BM which develop into mature leucocytes.
- Neutropenia
- A decrease in neutrophils (WBCs) circulating in the blood.
- Peripheral blood (PB)
- In this report PB refers to blood in the circulatory system.
- Promyelocytes
- Committed progenitor cells produced by and found in the BM which develop into myelocytes.
- SRC
- A non-receptor protein tyrosine kinase.
- Stem cells
- Very early progenitor cells which divide and mature to become all the types of cells which make up the blood and the immune system.
- Thrombocytes
- Platelets (fragments of BM cells) found in the blood which help to form clots and control bleeding.
- Thrombopenia
- A reduced number of thrombocytes (platelets) in the blood.
- Toxicity
- The quality of being poisonous. The National Cancer Institute grades toxicity levels of treatments as: 1 = mild, 2 = moderate, 3 = severe and 4 = life-threatening.
- Tyrosine kinase
- An enzymatic protein which adds phosphate residues to other proteins in the cell. In CML, the abnormal tyrosine kinase, BCR–ABL, phosphorylates proteins which cause cellular proliferation.
- Weibull curve
- A mathematical function which is often used in modelling to describe survival times and in which the chance of survival varies with time.
List of abbreviations
- ABL
- Abelson oncogene
- AE
- adverse event
- ALL
- acute lymphoblastic leukaemia
- ANC
- absolute neutrophil count
- AP
- accelerated phase
- ASCO
- American Society of Clinical Oncology
- ASH
- American Society of Hematology
- ATP
- adenosine 5′-triphosphate
- b.i.d.
- twice daily
- BC
- blast crisis
- BCR
- breakpoint cluster region
- BM
- bone marrow
- BMS
- Bristol-Myers Squibb
- BNF
- British National Formulary
- CCE
- clonal cytogenetic evolution
- CCyR
- complete cytogenetic response
- CEAC
- cost-effectiveness acceptability curve
- CHR
- complete haematological response
- CI
- confidence interval
- CiC
- commercial-in-confidence
- CML
- chronic myeloid leukaemia
- CML-AP
- chronic myeloid leukaemia in accelerated phase
- CML-BC
- chronic myeloid leukaemia in blast crisis
- CML-CP
- chronic myeloid leukaemia in chronic phase
- CMR
- complete molecular response
- CRD
- Centre for Reviews and Dissemination
- CP
- chronic phase
- CT
- computerised tomography
- CyR
- cytogenetic response
- DARE
- Database of Abstracts of Reviews of Effects
- EMA
- European Medicines Agency
- EQ-5D
- European Quality of Life-5 Dimensions
- FDA
- the US Food and Drug Administration
- FISH
- fluorescence in situ hybridisation
- HDI
- high-dose imatinib
- HMRN
- Haematological Malignancy Research Network
- HR
- haematological response
- HRQoL
- health-related quality of life
- ICD-O
- International Classification of Diseases for Oncology
- ICER
- incremental cost-effectiveness ratio
- IFN
- interferon-α
- ImI
- imatinib intolerance/intolerant
- ImR
- imatinib resistance/resistant
- INB
- incremental net benefit
- IRIS
- International Randomized Study of Interferon versus STI571
- ITT
- intention to treat
- LBC
- lymphoid blast crisis
- MBC
- myeloid blast crisis
- MCyR
- major cytogenetic response
- MHR
- major haematological response
- MIMS
- Monthly Index of Medical Specialities
- MMR
- major molecular response
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Clinical Excellence
- OS
- overall survival
- PB
- peripheral blood
- PCR
- polymerase chain reaction
- PCyR
- partial cytogenetic response
- PenTAG
- Peninsula Technology Assessment Group
- PFS
- progression-free survival
- Ph+
- Philadelphia-positive
- PSS
- Personal Social Services
- QALY
- quality-adjusted life-year
- q.d.
- every day
- QoL
- quality of life
- qPCR
- real-time quantitative PCR
- RCT
- randomised controlled trial
- RT-PCR
- reverse transcriptase-polymerase chain reaction
- SCT
- stem cell transplantation
- SD
- standard deviation
- SE
- standard error
- SEER
- Surveillance, Epidemiology and End Results
- SMC
- Scottish Medicines Consortium
- SPC
- summary of product characteristics
- START
- SRC/ABL Tyrosine kinase inhibition Activity: Research Trials of dasatinib
- TKI
- tyrosine kinase inhibitor
- TTP
- time to progression
- WBC
- white blood cell
- WHO
- World Health Organization
- WTP
- willingness to pay
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
NoteThis monograph is based on the Technology Assessment Report produced for NICE. The full report contained a considerable number of data that were deemed commercial-in-confidence. The full report was used by the Appraisal Committee at NICE in their deliberations. The full report with each piece of commercial-in-confidence data removed and replaced by the statement ‘commercial-in-confidence information (or data) removed’ is available on the NICE website: www.nice.org.uk.
The present monograph presents as full a version of the report as is possible while retaining readability, but some sections, sentences, tables and figures have been removed. Readers should bear in mind that the discussion, conclusions and implications for practice and research are based on all the data considered in the original full NICE report.
Notes
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
Prioritisation Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Imti Choonara, Professor in Child Health, Academic Division of Child Health, University of Nottingham
Chair – Pharmaceuticals Panel
-
Dr Bob Coates, Consultant Advisor – Disease Prevention Panel
-
Dr Andrew Cook, Consultant Advisor – Intervention Procedures Panel
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Dr Nick Hicks, Consultant Adviser – Diagnostic Technologies and Screening Panel, Consultant Advisor–Psychological and Community Therapies Panel
-
Ms Susan Hird, Consultant Advisor, External Devices and Physical Therapies Panel
-
Professor Sallie Lamb, Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick
Chair – HTA Clinical Evaluation and Trials Board
-
Professor Jonathan Michaels, Professor of Vascular Surgery, Sheffield Vascular Institute, University of Sheffield
Chair – Interventional Procedures Panel
-
Professor Ruairidh Milne, Director – External Relations
-
Dr John Pounsford, Consultant Physician, Directorate of Medical Services, North Bristol NHS Trust
Chair – External Devices and Physical Therapies Panel
-
Dr Vaughan Thomas, Consultant Advisor – Pharmaceuticals Panel, Clinical
Lead – Clinical Evaluation Trials Prioritisation Group
-
Professor Margaret Thorogood, Professor of Epidemiology, Health Sciences Research Institute, University of Warwick
Chair – Disease Prevention Panel
-
Professor Lindsay Turnbull, Professor of Radiology, Centre for the MR Investigations, University of Hull
Chair – Diagnostic Technologies and Screening Panel
-
Professor Scott Weich, Professor of Psychiatry, Health Sciences Research Institute, University of Warwick
Chair – Psychological and Community Therapies Panel
-
Professor Hywel Williams, Director of Nottingham Clinical Trials Unit, Centre of Evidence-Based Dermatology, University of Nottingham
Chair – HTA Commissioning Board
Deputy HTA Programme Director
HTA Commissioning Board
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
-
Department of Public Health and Epidemiology, University of Birmingham
-
Professor of Clinical Pharmacology, Director, NIHR HTA programme, University of Liverpool
-
Professor Ann Ashburn, Professor of Rehabilitation and Head of Research, Southampton General Hospital
-
Professor Judith Bliss, Director of ICR-Clinical Trials and Statistics Unit, The Institute of Cancer Research
-
Professor Peter Brocklehurst, Professor of Women’s Health, Institute for Women’s Health, University College London
-
Professor David Fitzmaurice, Professor of Primary Care Research, Department of Primary Care Clinical Sciences, University of Birmingham
-
Professor John W Gregory, Professor in Paediatric Endocrinology, Department of Child Health, Wales School of Medicine, Cardiff University
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, University College Hospital, London
-
Professor Angela Harden, Professor of Community and Family Health, Institute for Health and Human Development, University of East London
-
Dr Martin J Landray, Reader in Epidemiology, Honorary Consultant Physician, Clinical Trial Service Unit, University of Oxford
-
Dr Joanne Lord, Reader, Health Economics Research Group, Brunel University
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor Dion Morton, Professor of Surgery, Academic Department of Surgery, University of Birmingham
-
Professor Gail Mountain, Professor of Health Services Research, Rehabilitation and Assistive Technologies Group, University of Sheffield
-
Professor Irwin Nazareth, Professor of Primary Care and Head of Department, Department of Primary Care and Population Sciences, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norrie, Chair in Clinical Trials and Biostatistics, Robertson Centre for Biostatistics, University of Glasgow
-
Dr Rafael Perera, Lecturer in Medical Statisitics, Department of Primary Health Care, University of Oxford
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Peter Tyrer, Professor of Community Psychiatry, Centre for Mental Health, Imperial College London
-
Professor Martin Underwood, Professor of Primary Care Research, Warwick Medical School, University of Warwick
-
Professor Caroline Watkins, Professor of Stroke and Older People’s Care, Chair of UK Forum for Stroke Training, Stroke Practice Research Unit, University of Central Lancashire
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Dr Tom Foulks, Medical Research Council
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
HTA Clinical Evaluation and Trials Board
-
Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick and Professor of Rehabilitation, Nuffield Department of Orthopaedic, Rheumatology and Musculoskeletal Sciences, University of Oxford
-
Professor of the Psychology of Health Care, Leeds Institute of Health Sciences, University of Leeds
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Keith Abrams, Professor of Medical Statistics, Department of Health Sciences, University of Leicester
-
Professor Martin Bland, Professor of Health Statistics, Department of Health Sciences, University of York
-
Professor Jane Blazeby, Professor of Surgery and Consultant Upper GI Surgeon, Department of Social Medicine, University of Bristol
-
Professor Julia M Brown, Director, Clinical Trials Research Unit, University of Leeds
-
Professor Alistair Burns, Professor of Old Age Psychiatry, Psychiatry Research Group, School of Community-Based Medicine, The University of Manchester & National Clinical Director for Dementia, Department of Health
-
Dr Jennifer Burr, Director, Centre for Healthcare Randomised trials (CHART), University of Aberdeen
-
Professor Linda Davies, Professor of Health Economics, Health Sciences Research Group, University of Manchester
-
Professor Simon Gilbody, Prof of Psych Medicine and Health Services Research, Department of Health Sciences, University of York
-
Professor Steven Goodacre, Professor and Consultant in Emergency Medicine, School of Health and Related Research, University of Sheffield
-
Professor Dyfrig Hughes, Professor of Pharmacoeconomics, Centre for Economics and Policy in Health, Institute of Medical and Social Care Research, Bangor University
-
Professor Paul Jones, Professor of Respiratory Medicine, Department of Cardiac and Vascular Science, St George‘s Hospital Medical School, University of London
-
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, Queen Mary, University of London
-
Professor Richard J McManus, Professor of Primary Care Cardiovascular Research, Primary Care Clinical Sciences Building, University of Birmingham
-
Professor Helen Rodgers, Professor of Stroke Care, Institute for Ageing and Health, Newcastle University
-
Professor Ken Stein, Professor of Public Health, Peninsula Technology Assessment Group, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Jonathan Sterne, Professor of Medical Statistics and Epidemiology, Department of Social Medicine, University of Bristol
-
Mr Andy Vail, Senior Lecturer, Health Sciences Research Group, University of Manchester
-
Professor Clare Wilkinson, Professor of General Practice and Director of Research North Wales Clinical School, Department of Primary Care and Public Health, Cardiff University
-
Dr Ian B Wilkinson, Senior Lecturer and Honorary Consultant, Clinical Pharmacology Unit, Department of Medicine, University of Cambridge
-
Ms Kate Law, Director of Clinical Trials, Cancer Research UK
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, University of Manchester
-
Mr Angus S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital, Birmingham
-
Dr Diana Baralle, Consultant and Senior Lecturer in Clinical Genetics, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Diane Eccles, Professor of Cancer Genetics, Wessex Clinical Genetics Service, Princess Anne Hospital
-
Dr Trevor Friedman, Consultant Liason Psychiatrist, Brandon Unit, Leicester General Hospital
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Public contributor
-
Professor Anthony Robert Kendrick, Associate Dean for Clinical Research and Professor of Primary Medical Care, University of Southampton
-
Dr Nicola Lennard, Senior Medical Officer, MHRA
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee, London
-
Mr David Mathew, Public contributor
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mrs Una Rennard, Public contributor
-
Dr Stuart Smellie, Consultant in Clinical Pathology, Bishop Auckland General Hospital
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr Allison Streetly, Programme Director, NHS Sickle Cell and Thalassaemia Screening Programme, King’s College School of Medicine
-
Dr Matthew Thompson, Senior Clinical Scientist and GP, Department of Primary Health Care, University of Oxford
-
Dr Alan J Williams, Consultant Physician, General and Respiratory Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Joanna Jenkinson, Board Secretary, Neurosciences and Mental Health Board (NMHB), Medical Research Council
-
Professor Julietta Patrick, Director, NHS Cancer Screening Programme, Sheffield
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Disease Prevention Panel
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook, Clinical Programmes Director, Bazian Ltd, London
-
Dr Colin Greaves, Senior Research Fellow, Peninsula Medical School (Primary Care)
-
Mr Michael Head, Public contributor
-
Professor Cathy Jackson, Professor of Primary Care Medicine, Bute Medical School, University of St Andrews
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Julie Mytton, Consultant in Child Public Health, NHS Bristol
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Dr Richard Richards, Assistant Director of Public Health, Derbyshire County Primary Care Trust
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Dr Kenneth Robertson, Consultant Paediatrician, Royal Hospital for Sick Children, Glasgow
-
Dr Catherine Swann, Associate Director, Centre for Public Health Excellence, NICE
-
Mrs Jean Thurston, Public contributor
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust
-
Reader in Wound Healing and Director of Research, University of Leeds
-
Professor Bipin Bhakta, Charterhouse Professor in Rehabilitation Medicine, University of Leeds
-
Mrs Penny Calder, Public contributor
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol
-
Mrs Anthea De Barton-Watson, Public contributor
-
Professor Nadine Foster, Professor of Musculoskeletal Health in Primary Care Arthritis Research, Keele University
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester
-
Professor Christine Norton, Professor of Clinical Nursing Innovation, Bucks New University and Imperial College Healthcare NHS Trust
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham
-
Dr Kate Radford, Senior Lecturer (Research), University of Central Lancashire
-
Mr Jim Reece, Public contributor
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton
-
Dr Pippa Tyrrell, Senior Lecturer/Consultant, Salford Royal Foundation Hospitals’ Trust and University of Manchester
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Interventional Procedures Panel
-
Professor of Vascular Surgery, University of Sheffield
-
Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Mrs Isabel Boyer, Public contributor
-
Mr Sankaran Chandra Sekharan, Consultant Surgeon, Breast Surgery, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Ms Leonie Cooke, Public contributor
-
Mr Seumas Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor Sam Eljamel, Consultant Neurosurgeon, Ninewells Hospital and Medical School, Dundee
-
Dr Adele Fielding, Senior Lecturer and Honorary Consultant in Haematology, University College London Medical School
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Fiona Lecky, Senior Lecturer/Honorary Consultant in Emergency Medicine, University of Manchester/Salford Royal Hospitals NHS Foundation Trust
-
Dr Nadim Malik, Consultant Cardiologist/Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Professor Jon Moss, Consultant Interventional Radiologist, North Glasgow Hospitals University NHS Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Dr Matthew Wilson, Consultant Anaesthetist, Sheffield Teaching Hospitals NHS Foundation Trust
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Dr Martin Ashton-Key, Medical Advisor, National Commissioning Group, NHS London
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr James Gray, Consultant Microbiologist, Department of Microbiology, Birmingham Children’s Hospital NHS Foundation Trust
-
Dr Jurjees Hasan, Consultant in Medical Oncology, The Christie, Manchester
-
Dr Carl Heneghan, Deputy Director Centre for Evidence-Based Medicine and Clinical Lecturer, Department of Primary Health Care, University of Oxford
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Maria Kouimtzi, Pharmacy and Informatics Director, Global Clinical Solutions, Wiley-Blackwell
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Ms Amanda Roberts, Public contributor
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Professor Donald Singer, Professor of Clinical Pharmacology and Therapeutics, Clinical Sciences Research Institute, CSB, University of Warwick Medical School
-
Mr David Symes, Public contributor
-
Dr Arnold Zermansky, General Practitioner, Senior Research Fellow, Pharmacy Practice and Medicines Management Group, Leeds University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick, Coventry
-
Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Public contributor
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Peter Langdon, Senior Clinical Lecturer, School of Medicine, Health Policy and Practice, University of East Anglia
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician and Cardiologist, County Durham and Darlington Foundation Trust
-
Dr Richard Neal, Clinical Senior Lecturer in General Practice, Cardiff University
-
Mr John Needham, Public contributor
-
Ms Mary Nettle, Mental Health User Consultant
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry and Warwickshire Partnership Trust
-
Dr Lesley Stockton, Lecturer, School of Health Sciences, University of Liverpool
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health