Notes
Article history
The research reported in this issue of the journal was commissioned by the National Coordinating Centre for Research Methodology (NCCRM), and was formally transferred to the HTA programme in April 2007 under the newly established NIHR Methodology Panel. The HTA programme project number is 07/63/03. The contractual start date was in January 2009. The draft report began editorial review in June 2009 and was accepted for publication in November 2011. The commissioning brief was devised by the NCCRM who specified the research question and study design.The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2012. This work was produced by Liu et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to NETSCC. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2012 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background and overview
There is now a considerable body of evidence revealing that some ethnic minority groups in the UK experience disproportionate levels of morbidity and mortality compared with the majority white European-origin population. 1–4 These patterns have also been documented in most economically developed countries and are particularly pronounced for a range of long-term conditions. 5,6 In an attempt to better understand the reasons underlying these ethnic variations in incidence and outcomes, attention has turned to describing the prevalence of underlying risk factors for these conditions, and also the access to and quality of care. Although relative social and economic disadvantages, which are legacies of long-standing social, structural and historical factors, are major contributors to these marked and persistent health inequalities,7 behavioural patterns also affect the day-to-day health experiences for individuals and communities and these are potentially more amenable to change.
Reducing health inequalities is a declared national priority in many economically developed countries. 8 Across these countries, health promotion approaches are increasingly seen as the long-term strategies most likely to prove clinically effective and cost-effective for preventing disease and improving health outcomes in those with established disease. For many of the key chronic diseases, such as diabetes, cardiovascular disease (CVD) and cancers, the main preventable risk factors are behaviours such as smoking, physical inactivity and unhealthy eating, and tackling these behaviours therefore represents the focus of the majority of health promotion interventions internationally. There is hence a considerable body of completed research and work in progress seeking to identify the ways in which to tackle these risk factors, whether individually or collectively.
A key assumption underpinning the work in this report is that health promotion interventions found to be effective in the general population are also, if appropriately adapted, likely to prove effective in ethnic minority populations. 9 Building on this premise we began our research by first identifying health promotion interventions that have been shown to be effective in promoting smoking cessation, increasing physical activity and improving healthy eating in the general population, and in turn identifying what evidence, if any, was available in high-level evidence syntheses (guidelines and systematic reviews) on the effectiveness of these interventions for ethnic minority populations and, in particular, for African-, Chinese- and South Asian-origin populations, which constitute the populations of interest in our enquiry. Adding to this foundation we then systematically identified, critically reviewed, and interpreted the evidence on adapted interventions targeting these same modifiable risk factors in the three target populations. In-depth qualitative interviews with researchers and health promoters with experience of developing, delivering and evaluating adapted interventions for our target populations further supplemented this systematic review of adapted interventions. This body of quantitative and qualitative evidence was then synthesised in order to distil overarching findings for future research. Our work and approach was informed throughout by ongoing engagement with likely end users of this research.
Concepts and terminology
Ethnicity
Ethnicity is a complex and contested concept. Definitions of ethnicity vary, for example, across nations, as does the nomenclature that is used. For example, in the USA, ‘race’ and ‘ethnicity’ are often used interchangeably, whereas in much of Europe, ‘migrant’ is the preferred term, this term encompassing a diverse group of people such as students, labourers and asylum seekers. 10 In the UK, ethnicity often encompasses ‘race’, whereas in other countries ethnicity is a concept of cultural affiliation and is therefore distinct from race. Despite these important differences, there is emerging scientific consensus on the preferential usage of the term ‘ethnicity’. A recent analysis of MEDLINE indexed articles, for example, showed that the use of ‘ethnicity’ has now surpassed the use of ‘race’, both in the USA and worldwide. 11 Given this movement and indeed our own substantial contributions to this debate, we preferentially use the term ‘ethnicity’ in this report. 4,12–24
Furthermore, the particular terminology used to describe broader ethnic groups may also differ between countries. In the UK, for example, the label ‘Asian’ is often used to refer to Bangladeshi-, Indian- and Pakistani-origin populations. Conversely, in the USA, ‘Asian’ is more commonly used to describe people of Chinese, Korean and Japanese origin. In other countries, nationality, citizenship, name, country of birth, parents’/grandparents’ country of birth and religion are used either alone or in combination as proxies for ethnicity. 25 A definition of the term ‘ethnicity’ as used in public health16 is found in Box 1 along with the ethnic categories and definitions,16,26 we employed when conducting this work.
One dominant definition in public health defines ethnicity as:
-
(a) a multifaceted quality that refers to the group to which people belong, and/or are perceived to belong, as a result of certain shared characteristics, including geographical and ancestral origins, but particularly cultural traditions and languages. The characteristics that define ethnicity are not fixed or easily measured, so ethnicity is imprecise and fluid. Ethnicity differs from race, nationality, religion, and migrant status, sometimes in subtle ways, but may include facets of these other concepts16
In the present study we opted to apply the following ethnic categories and definitions outlined by Bhopal16 and Bhopal and Agyemang26 to our populations of interest:
African: Person with ancestral origins who self-identifies, or is identified, as African, and excludes other ancestral origins. This term is the preferred description for more specific categories, e.g. African American
African American: Person with ancestral origins who self-identifies, or is identified, as African American. The term most applies to those with origins in sub-Saharan Africa. Most African Americans are descendants of slavery and are different from those coming from Africa or the Caribbean in the twentieth and twenty-first centuries (distant and recent ancestry)
Afro-Caribbean/African Caribbean: Person with ancestral origins in Africa, with history of familial settlement in the Caribbean prior to emigrating, who self-identifies, or is identified, as Afro-Caribbean
Asian: Person with ancestral origins in the Asian continent; however, this definition differs by country. In the UK it usually refers to persons with ancestral origins in the Indian subcontinent, whereas in the USA it refers to persons with ancestral origins in East Asia, e.g. China, Japan, Thailand
Bangladeshi: Person with ancestral origins in the Indian subcontinent who self-identifies, or is identified, as Bangladeshi
Black: Person with ancestral origins in Africa who self-identifies, or is identified, as black, African or Afro-Caribbean
Black and minority ethnic: This term originated and is limited to use in the UK and encompasses non-white (and often non-migrant) persons
Chinese: Person with ancestral origins in China who self-identifies, or is identified, as Chinese
Ethnic minority group: Usually refers to a non-white population, often used interchangeably with minority ethnic group
Indian: Person with ancestral origins in the Indian subcontinent who self-identifies, or is identified, as Indian
Pakistani: Person with ancestral origins in the Indian subcontinent who self-identifies, or is identified, as Pakistani
South Asian: Person with ancestry in countries of the Indian subcontinent, including India, Pakistan, Bangladesh and Sri Lanka
White European: Person with ancestral origins in Europe, who self-identifies, or is identified, as white
Although we have chosen a particular approach to dealing with nomenclature-related issues, we recognise that the use of the term ‘ethnicity’ is contingent on history, politics and geography. Who belongs and who does not and how someone identifies himself or herself or how he or she is identified are context and situation dependent. As public health and its related fields, such as epidemiology and the social sciences, strive to detect and address patterns of disease within populations,16 ‘ethnicity’ (usefully) remains a contested term as an outcome of its location amid the tension between the search for similarities and differences. 27 Consequently, ethnicity and its derivatives, such as ‘ethnic groups’, have, we appreciate, been conceptualised in many ways.
Overwhelmingly, the contemporary literature gives primacy to self-identified ethnicity, and, although this is ethically appealing and likely to best approximate ‘ethnicity’, it is worth bearing in mind that this seemingly personal ‘choice’ is a balance of preference, identification (by others) and (self-)identity, as we rarely classify ourselves in a vacuum. Therefore, in the present study, ‘ethnicity’ is emphasised as an intersubjective activity that is contingent on a range of contextual considerations. Furthermore, conventions and self-identified ethnicity can change over time. For example, in the UK, ‘black and minority ethnic’ is a relatively new term used to include all visible and invisible minorities (including the Irish, for example). 28 However, there have been more recent moves away from using ‘ethnic minority’ and its derivatives altogether, opting instead for terms such as ‘multicultural’, ‘pluralistic’ and ‘diverse’. 28 This can be contrasted with the use of a more ‘racialised ethnicity’ in the USA, where demarcation is more likely to be based on ‘white’ versus ‘non-white’, and ‘people of colour’ is an institutionally acceptable term. 28 Similarly, colour parameters to define populations are used in Canada, where ‘visible minorities’ is a widely employed substitute for ‘race’. 28 The fact that groups of people can be moved in and out of these categories gives credence to the highly contextual nature of ‘ethnicity’; for example, Aboriginal people were once included among Canada’s ‘visible minorities’28 whereas now the term refers only to non-white immigrants.
Using the term ‘ethnicity’ without reference to the context in which it was conceptualised or the method by which the term was assigned is thus problematic and limits its analytical value28 in research. Often related to or synonymous with ethnicity is ‘culture’, which has, to an extent, now replaced ‘race’ to describe sets of seemingly innate and immutable characteristics,29 or is otherwise differentiated from ‘race’ by rather indistinct criteria. 2,9,30 Irrespective of the terminology used, there is furthermore a tendency towards ‘groupism’, in which ‘ethnically, racially and nationally named populations continue to be construed as entities and cast as actors’. 30 Groupism is evident in health-care research given how commonplace it is to compare the health of ethnic minority groups and/or describe their raised incidence or prevalence of a particular disease. 29 This tendency towards groupism, when compounded by an equal propensity to locate ill-health in individuals and their bodies31 and their cultures, suggests that we have not moved far from ‘race’ in the entrenchment of concepts and ideas associated with particular ethnic minority populations.
In this study we hoped to progress the concept of ‘ethnicity’ to one that shifts the focus from defining what an ethnic group is to defining how ethnicity is enacted,30 or, in other words, moving away from characterising ethnic groups as is towards describing ethnicity-mediated effects in different contexts, which requires an active engagement with more process-focused definitions. Furthermore, we sought to encourage thinking on culture away from it being either a liability or an asset, as this view maintains the concept of culture within the framework of immutable traits, akin to previous conceptions of race. Instead, we hoped to situate culture as one dimension alongside, for example, politics and economy, environment and context, to explain observed advantages and disadvantages. Such approaches will, we hope, contribute to advancing ethnicity as a useful analytical concept in health.
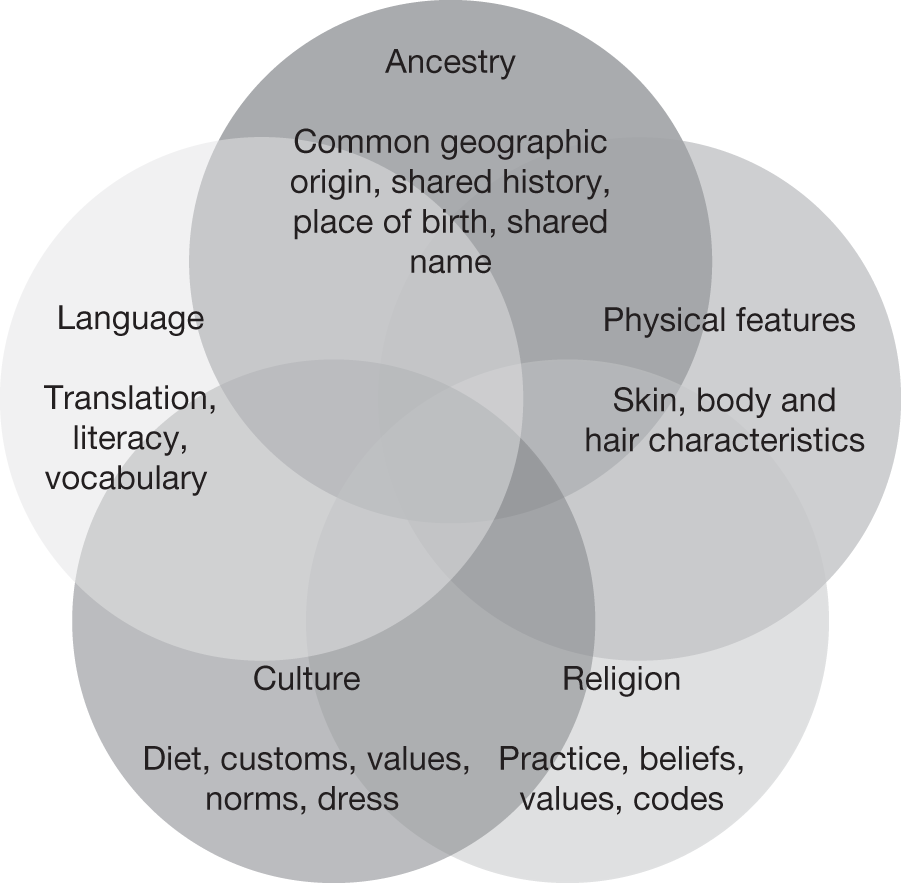
In this study we use the term ‘ethnicity’ in a generic sense to encompass a few, some, or all of the following dimensions: ancestry, culture, language, physical features and religion. 12 Figure 1 provides examples for each of the more traditional dimensions of ethnicity and illustrates how these five dimensions of ethnicity overlap to constitute ‘ethnicity’.
FIGURE 1.
Dimensions contributing to the definition of ethnicity.
Health promotion interventions
The goal of health promotion is to enhance positive health and reduce the risk of ill health by encouraging the pursuit of a number of actions;32 these actions are commonly classified as health education or prevention. An inclusive definition of disease prevention was used in this study to encompass strategies that seek to limit the manifestation of disease through risk reduction, but also to manage its consequences and/or improve prognosis when disease is present. 33 Similarly, a broad definition of education can include communication strategies to improve health literacy: knowledge, attitudes and beliefs and skills relating to health. 33 Health promotion interventions are therefore conscious and planned actions towards achieving these goals. 33 Health promotion interventions may encompass initiatives at various levels, ranging from individual-, organisational- and institutional-level initiatives34 to environmental- and policy-based initiatives. Although we were open to any approaches to health promotion interventions, the body of evidence we uncovered focused on individual-centred health education and prevention approaches as it is in relation to these approaches that the evidence is currently best developed. We acknowledge that, in the UK at least, the term ‘health promotion’ has, over recent years, largely been replaced by the term ‘health improvement’ as one of the three main activities in the public health domain.
Adaptation of health promotion interventions for ethnic minority populations
Adapting an intervention for ethnic minority populations should involve an explicit set of methods and processes that can be used to increase its appropriateness or salience. 35 Adaptation can take place at any step along the intervention pathway and is aimed at improving access to, engagement in, participation with and sustainability of an intervention. Adaptation of interventions is, for example, important to improve access to health services or promote health-enhancing behaviours for ethnic minority populations when there are major language barriers. However, a more fundamental rationale for undertaking adaptation is that the body of work underpinning the entire field of health promotion has been undertaken primarily in white European-origin populations, with ethnic minority populations rarely being studied or considered. Aspects of health promotion interventions may not therefore be optimised, suitable or even appropriate for ethnic minority populations. The fact that there exist substantial and persistent inequalities in health outcomes and status represents an additional important argument for the need to adapt interventions.
Adaptation is referred to by a wide variety of other terms, including ‘culturally appropriate’, ‘culturally sensitive’, ‘culturally tailored’, ‘culturally targeted’ or ‘modified’. The degree to which an intervention is determined to be adapted or culturally sensitive is measured by ‘the extent to which ethnic/cultural characteristics, experiences, norms, values, behavioural patterns and beliefs of a target population as well as relevant historical, environmental and social forces are incorporated in the design, delivery, and evaluation of targeted health promotion materials and program’. 35 In this study we opted for the terms ‘adapted’ or ‘modified’, as opposed to using a term prefixed by ‘culturally’, as we have defined culture as being a part of ethnicity, but not its only constituent (see Figure 1); we were thereby seeking to recognise that ethnicity can influence health through aspects other than culture. In addition, terms such as ‘targeted’ and ‘tailored’ are also sometimes used to convey the purpose of increasing appropriateness. Definitions have been proposed to clearly differentiate between these two terms, with ‘targeted’ reserved for adaptations made for a ‘defined population subgroup that takes into account characteristics shared by the subgroup’s members’, and ‘tailored’ being ‘intended to reach one specific person, based on characteristics . . . derived from an individual assessment’. 36 Although we were interested only in targeted interventions, we recognised that there may be unclear and inconsistent usage in terminology and we therefore gave consideration to interventions that may have been ‘tailored’ to an individual. Furthermore, although adaptation usually excludes interventions developed from scratch, for example through community-based participatory research, we included these interventions when there was support from UK guidelines and international systematic reviews for the underlying intervention. Therefore, adaptation can refer to an adaptation of a specific or generic intervention programme. Adapted interventions in this study can refer to a range of interventions as well, from individual to community based.
Increasing ethnic diversity
Ethnic diversity is now a feature of urban centres in most economically developed societies and this demographic trend is expected to continue. The 2001 UK census (including England, Northern Ireland, Wales and Scotland) reported 4.6 million people (7.9% of the population) who identified themselves as belonging to a black or other ethnic minority group. 37 Around half of the ethnic minority population were South Asians of Bangladeshi, Indian, Pakistani or other Asian origin; a further quarter were black of black Caribbean, black African or other black origin; 15% were from the mixed ethnic group; and < 1% were of Chinese origin. 37 The number of people identifying with an ethnic minority group increased by 53% between 1991 and 2001. 37 The UK has recently completed the 2011 census, which will provide more contemporary data on the ethnic composition of the nation. It is projected that, by 2051, 20% of the population will identify with an ethnic minority group. 38
Parts of Western Europe share similar degrees of ethnic diversity to the UK; for example, in 2005, Europe was the destination for 34% of the global migrant population. 39 There are, however, some difficulties in compiling ethnicity data on populations in Europe for multiple reasons, including the heterogeneity in terminology used and the availability of census data. Data collected can contain combinations of different parameters, such as country of birth of parents, country of birth, citizenship, nationality, ethnicity, language and religion. 40 The importance of collecting reliable and valid ethnicity data for health-care research that can be comparable between European countries has been recognised by projects such as the Migrant and Ethnic minority Health Observatory project (MEHO). 41
In the USA, the census and the American Community Survey provide population demographics. 42,43 Data from the American Community Survey indicate that approximately 26% of the US population are from non-white ethnic groups. 42 Similarly, the 2000 US census reported that 22.9% of the population identified themselves as ‘non-white’, this group comprised of 12.9% black or African Americans, 4.2% Asians, 1.5% American Indians or Alaskan Natives, 0.3% Native Hawaiians or other Pacific Islanders and 6.6% from other ‘races’ or a mixture of races. 43
The 2006 Canadian census documented over 200 minority populations within the country. ‘Visible minorities’ accounted for 16.2% of Canada’s total population in 2006, up from 13.4% in 2001 and 11.2% in 1996. 44 Between 2001 and 2006, Canada’s visible minority population increased by 27.2%, a rate five times faster than the 5.4% growth rate of the total population. 44 South Asians became Canada’s largest visible minority group in 2006, surpassing the Chinese-origin population for the first time in history. Filipino (8.1%), Latin American (6.0%), Arab (5.2%), South-East Asian (4.7%), West Asian (3.1%), Korean (2.8%) and Japanese (1.6%) people represented some of the other visible minority groups. There was also a small proportion (4.0%) of individuals who belonged to more than one visible minority group or to other visible minorities such as Pacific Islanders. 44
In New Zealand the largest ethnic minority population is the indigenous New Zealand Maori population (14.6%). 45 However, Asian (Chinese, Korean, Indian, Filipino, Japanese, Sri Lankan and Cambodian) and Pacific populations increased by almost 50% and 14.7%, respectively, from the 2001 census to the 2006 census. 45 Middle Eastern, Latin American and African groups totalled 0.9% of the population. 45
In Australia the census data do not capture self-identified ethnicity per se, but cover a range of proxy indicators including parents’ country of birth, country of birth, ancestry, Australian citizenship, indigenous status, language spoken at home, proficiency in spoken English and religious affiliation. 46 In the 2006 census, 30% of Australian residents were born outside of Australia, this representing a slight increase from 2001. 47 Of people born overseas, the most common countries of birth were England, New Zealand, China, Italy and Vietnam. 47 In the same census, 2.3% of the population identified themselves as being of Aboriginal and/or Torres Strait Islander origin. 48
These data demonstrate the effects of globalisation on population demographics: ‘never before in history has the movement of diverse racial, cultural, ethnic, religious, and linguistic groups within and across nation states been so extensive, so rapid’. 49 Although each of these (and other) nations have their own unique history of diversity that may include indigenous populations, colonisation and unique pathways of migration,50 they share a common challenge of responding to the changing needs of their populations in a just and equitable manner. A key first step in this process is to reliably capture data on the ethnic composition of the population in order to assess population needs and identify inequalities. These data can then be used to develop approaches and monitor progress with respect to achieving delivery of appropriate and equitable health services for all sections of the population.
Justification for focusing on African-, Chinese- and South Asian-origin populations
Our focus on these three broad ethnic groupings was a conscious decision supported by the demographics presented in the preceding section. African-, Chinese- and South Asian-origin people account for the majority of the diversity documented within the UK, and also documented in other economically developed countries – albeit in differing proportions in different countries. Given the differences noted above in terminology used across economically developed countries to describe their ethnic populations, we opted for terminology that would capture a broad range of ethnicities. For example, ‘African origin’ can refer to an Afro-Caribbean population in the UK, an African American population in the USA and also an African population in New Zealand, as different migratory histories have dictated the varying representation of these ethnic groups in their respective countries. For ‘Chinese-origin’ populations the definition is used more or less consistently across countries, describing a population with origins in mainland China or Hong Kong. Sometimes Chinese-origin people are grouped along with other ‘Asian’ populations, although this is more commonly observed in the USA than elsewhere. For this reason we have a distinct ‘South Asian’-origin term, which encompasses people with origins in Bangladesh, India, Pakistan and Sri Lanka (see Box 1).
Inequalities in health
Chronic disease in economically developed societies
Chronic or non-communicable disease represents the largest disease burden worldwide. These long-term conditions prominently include diabetes, CVD [including ischaemic heart disease (IHD)], respiratory diseases and cancers, and they have come to surpass communicable disease as the leading causes of death. Chronic disease is estimated to account for 35 million deaths per year, representing 60% of all deaths worldwide, while 20% of chronic disease deaths occur in high-income countries. 51 Chronic disease, therefore, presents one of the biggest health challenges in these economically developed nations.
Although the prevalence of and deaths from chronic disease appear overall to be increasing in low-income nations, and in many contexts surpassing the rates of communicable disease such as human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS), tuberculosis and malaria,51 the trend is less consistent in economically developed societies. Sharp decreases in age-standardised mortality rates from IHD from a high in the 1960s, for example, have been documented across countries such as Australia, Canada, New Zealand, the UK and the USA. 52 Within countries, for example in the USA, the age-adjusted incidence of cancer at all sites has also significantly declined in recent years (1999–2006). 53
The numbers of people diagnosed with diabetes has been seen to increase. The USA, for example, has experienced an upward trend from 5.6 to 18.1 million cases from 1980 to 2008,54 with projections of the number of people diagnosed or undiagnosed with diabetes by 2030 being between 37.7 and 47.3 million; however, these estimates differ significantly depending on the model used. 55 In the UK there were 2.6 million people with diagnosed diabetes in 2009, representing an average prevalence of 4%. 56 We know that chronic disease increases the risk of premature death and decreases quality of life. Furthermore, having one chronic disease increases susceptibility to and risk of another, for example CVD is the main cause of mortality and morbidity for people with diagnosed diabetes, accounting for 52% of deaths among people with diagnosed type 2 diabetes. 56 The cost of chronic disease extends beyond health outcomes as it has implications for health-care systems and for families and communities. 51
Overweight and obesity, defined as having a body mass index (BMI) of 25–29.9 kg/m2 and ≥ 30kg/m2 in white European-origin populations, respectively, is inextricably linked with the above-mentioned chronic diseases and will therefore be considered alongside these key long-term conditions. Furthermore, there is debate about whether or not these BMI cut-offs should be lowered for people of South Asian origin, given their increased risk of disease at lower BMI cut-points. 57 The prevalence of adult obesity has been on the rise in many countries, albeit at different rates. In England, the prevalence of obesity is 24.5% in adults aged ≥ 16 years. 58 In the USA, the age-adjusted prevalence of obesity was found to be 33.8% in adults aged ≥ 20 years. 59 Although the prevalence of obesity is lower in Canada than in the USA, obesity prevalence has nonetheless increased on average 10 percentage points over the past 20 years. 60
Ethnic variations in rates of chronic diseases and underlying risk factors
Within economically developed nations with a large proportion of ethnic minority populations, it is recognised that members of some ethnic groups experience an elevated risk of disease in comparison with the general population and relative to other ethnic groups. For example, 10-year CVD61 and type 2 diabetes62 risks were estimated using the QRISK2 and QDScore prediction algorithms, respectively. Both algorithms were developed and validated using routinely collected data from 531 general practices across England and Wales. 61,62 QRISK2 identified risk of CVD among South Asian men and women after adjusting for deprivation, diabetes and family history,61 whereas QDScore found a significant elevated risk of type 2 diabetes by ethnicity after adjusting for factors such as age, BMI, deprivation and family history of diabetes. 62 Significant heterogeneity was observed, with Bangladeshi-origin men and women at the greatest risk for diabetes, with an adjusted hazard ratio of 4.07 [95% confidence interval (CI) 3.24 to 5.11] for women and 4.53 (95% CI 3.67 to 5.59) for men. Pakistani-origin women and men had adjusted hazard ratios of 2.15 (95% CI 1.84 to 2.52) and 2.54 (95% CI 2.20 to 2.83), respectively,62 and both Bangladeshi- and Pakistani-origin men had a significantly higher risk than Indian-origin men. Black African-origin men and Chinese-origin women were also reported to be at increased risk compared with the white reference group. 62 Lower risk was also observed: black African-origin women had an adjusted hazard ratio of 0.81 (95% CI 0.66 to 0.98) and black Caribbean-origin women an adjusted hazard ratio of 0.80 (95% CI 0.70 to 0.92). 62
Different levels of risk are therefore apparent when ethnic groups are examined independently. Identifying or belonging to an ethnic group can be associated with both better and worse health, depending on the outcome considered, and this has been highlighted by health departments and government organisations around the world.
In the UK, the Health survey for England 2004: the health of minority ethnic groups6 (HSE) represents a key document outlining the existing health inequalities for the major health outcomes and their modifiable factors. As the HSE provides survey data, the information is self-reported and actual disease rates may vary. In the USA, the Centers for Disease Control and Prevention (CDCP) Health disparities and inequalities report – United States, 20115 represents a similar effort to capture differences in health outcomes for the main chronic diseases. These documents, along with others, have captured overall trends, including the relative disadvantage of the black population in the USA. For example, black people have been noted to have the highest rate of new cases of all-cause cancer compared with white, American Indian/Alaskan Native, Hispanic and Asian/Pacific Islander populations (1992–2006), despite an observed overall decrease in new cases of cancer. 53,63
In the UK, a different distribution of cancers emerges among ethnic minority populations. Overall, ethnic minority populations are reported to have a lower risk of all-cause cancer, with increased risk for certain types of cancers, for example prostate cancer for black men; liver cancer for Asian men and women; oral and cervical cancer for Asian women aged ≥ 65 years of age; cancers of the stomach, liver and myeloma for both black men and women; and cervical cancer for black women aged ≥ 65 years. 64 Although overall rates of cancer were reported to be lower for ethnic minority populations in England, health promotion and services must acknowledge the cancer types and risk factors that are most relevant to ethnic minority as well as mainstream populations in order to deliver a more equitable health-care system.
In the USA, the age-adjusted mortality rate for coronary heart disease (CHD) was higher for black men and women than for men and women from other ethnic groups (white, Asian/Pacific Islander, American Indian/Alaskan Native). 5 In the UK, a different trend was observed. For any CVD (including IHD/CHD/coronary artery disease and stroke), black African men had the lowest prevalence and Irish men the highest; for women, those from the general population had the highest prevalence and Bangladeshi women had the lowest. 6 For IHD only, South Asian (Bangladeshi-, Indian- and Pakistani-origin) people had higher mortality rates than the general population, and black Caribbean- and black African-origin people had lower mortality rates than the general population. 6 Within the South Asian-origin population, further differences and disparities were observed. 6
For obesity, black females aged ≥ 5 years consistently have had the highest prevalence of obesity in the USA from 1988 to 2008. 5 Furthermore, higher obesity rates persisted across income classes for black females whereas an inverse relationship between obesity rates and family income was observed for white and Mexican populations (2005–8). 5 In the UK, black Caribbean- and Irish-origin men were more likely to be obese and Bangladeshi- and Chinese-origin men were less likely to be obese than men in the general population. Black Caribbean-, black African- and Pakistani-origin women had a higher prevalence of obesity than the general population, whereas Chinese-origin people had a much lower prevalence. 6
In the USA, differences in the prevalence of diabetes between black and Hispanic populations and the white population were observed,5 with black females having the highest age-specific prevalence of diabetes. 65 In the UK, similar health disparities were observed, with diabetes prevalence higher in Bangladeshi- and Pakistani-origin men than in general population men. Similarly, Pakistani-origin women had a higher prevalence of diabetes than general population women. 6
From the above summary of ethnic differences in health outcomes and risk factors it is clear that ethnic health disparities have been documented and compared in many economically developed countries. Documenting and comparing trends represents an initial essential step towards the goal of improving the health of the entire population. In striving to reduce these disparities it is vital to capitalise on the opportunities presented by preventive health approaches to chronic disease, which have the potential to greatly improve health outcomes and reduce health inequalities for present and future generations.
Responding to ethnic health inequalities in chronic disease
Justification for focusing on smoking cessation, physical activity and healthy eating
Chronic diseases can to a large extent be prevented and once present managed through the modification of shared risk factors, in particular unhealthy diet, physical inactivity, tobacco use and alcohol abuse. 66 These are commonly referred to as individual ‘lifestyle factors’. Controlling for these risk factors, for example, has the potential to eliminate 80% of CVD and type 2 diabetes and 40% of cancers. 51 The potential health gains of a preventive approach provide the justification to focus on smoking cessation, physical activity and healthy eating in our study. Alcohol abuse was not within the scope of this study (see Study scope).
These lifestyle risk factors, however, operate within the complexity of everyday life, in which food choices, living conditions, educational achievement and access to health services51 may not be entirely within the control of the ‘at-risk’ individual. Where an individual or group finds themselves in relation to these social determinants, among other determinants such as income, social status, gender and culture,26 can increase their susceptibility or enhance their resiliency to these modifiable risk factors. One significant factor is ‘ethnicity’, which can, as noted above, encompass dimensions of ancestry, culture, language, physical features and religion (see Figure 1). 12 The broad reach of ethnicity and its intersection with social and contextual factors that can enable or constrain behaviour needs to be taken into consideration when planning health promotion interventions aiming to prevent the onset of or minimise the impact of chronic diseases.
Prioritising preventive health care
A preventive health approach is warranted given that the underlying causes of chronic disease are to a large extent avoidable through the elimination of shared risk factors such as smoking, physical inactivity and unhealthy eating. 66 Consequently, international, national and local responses have been initiated to support a preventive health-care approach. The World Health Organization (WHO), for example, produced the 2008–2013 Action plan for the global strategy for the prevention and control of noncommunicable diseases,66 along with the creation of the NCDnet (global Noncommunicable Disease Network), a voluntary collaboration comprising United Nations agencies, intergovernmental organisations, academic institutions, research centres, non-governmental organisations and the private sector working towards the prevention and control of long-term conditions. 66
At a national level, countries have responded to the WHO agenda and created strategies to combat chronic disease. The CDCP describes chronic disease as the ‘public health challenge of the 21st Century’67 and highlights the huge demand that chronic disease places on the US economy, for example estimated annual expenditures of US$313.8B (2009), US$89.0B (2007) and US$116B (2007) for CVD, cancer and diabetes, respectively. 67 The CDCP actively promotes the preventive approach, with a focus on obesity (physical activity and healthy eating), smoking and alcohol as the most effective and cost-effective methods to tackle chronic disease. 67
Similarly, in England (2002), the direct cost of treating obesity was estimated to be between £45.8M and £49.0M, and between £945M and £1075M for treating the consequences of obesity,68 which included CVD and diabetes. For the Scottish population, the equivalent costs were estimated as £175M to NHS Scotland,69 the majority of the costs being associated with the consequences of obesity, most notably type 2 diabetes (£48M) and hypertension (£38M). Primary prevention is thus rightly a priority strategy for the tackling of chronic disease in the UK,69,70 given that almost a quarter of adults in England aged ≥ 16 years have been classified as obese, with only one-quarter of men and women reporting meeting the government’s ‘5-a-day’ guideline of consuming five or more portions of fruit and vegetables a day. 70 Other economically developed countries, including Canada,71 New Zealand72–74 and Australia,75 are similarly making the prevention of chronic disease a health policy priority. In Canada, an investment of C$300M over 5 years has been made towards disease prevention. 71 Equally, in European countries, recognition of the health and economic burden of chronic disease and the importance of a co-ordinated preventive health approach76 has led to the establishment of the European Chronic Disease Alliance77 to influence the policies of European member states towards a unified prevention approach to chronic disease. A corresponding alliance was formed in Australia to monitor and advocate for a national preventive health strategy. 78
The majority of these strategies, in reflection of the broader literature, also recognise the contribution of chronic disease to inequalities in health. 77,79–83 The CDCP, for example, underscores how chronic disease disproportionately affects ethnic minority populations and has called for equity in the provision of health promotion programmes that are accessible and target the social determinants of health. 67 Creating effective, appropriate preventive health/health promotion programmes for ethnic minority groups is thus now seen as a key strategy in reducing ethnic disparities in health.
Evidence of effective preventive health care for ethnic minority populations
The preventive health approach includes health promotion campaigns, interventions and services to decrease tobacco use, increase physical activity and improve diet to reduce and control chronic diseases and the approaches adopted are often steered by international guidelines and national health policies. General recommendations for type, dose and duration of physical activity to improve health are usually made without specific recommendations for gender, ethnicity or income group. Evidence-based UK guidelines, for example, include four methods to increase physical activity for the population,79 although a new framework has been established to drive local physical activity activities84 (see Chapter 4). Despite these strategies there is low adherence to recommended levels of physical activity for health85 in most ethnic minority groups compared with adherence in the general population, except for the black Caribbean-origin population. 6 Low prevalence of physical activity has most strikingly been noted in Bangladeshi- and Pakistani-origin women compared with the general population. 6 Given that a higher prevalence of obesity and diabetes clusters within these South Asian-origin groups, a more concerted effort is required to determine the differential needs of, and identify approaches to increasing physical activity in, these population groups. 85
A review of the effectiveness of interventions to promote healthy eating in people from ethnic minority groups80 found limited research in the UK; the majority of evidence came from the USA. A more recent review of the healthy eating of UK South Asians81 reported that there had been an increase in research that could help develop effective interventions, but with little attempt to synthesise this evidence for use by health practitioners. The Welsh Assembly Government undertook a review of the health promotion evidence base for ethnic minority groups and, regarding healthy eating, concluded that the messages may not be appropriate or understood by a high percentage of the population. 82 Recent evidence-based UK guidelines on preventing type 2 diabetes, including increasing physical activity and improving healthy eating in high-risk groups, have demonstrated some consideration for ethnic minority populations. 83
In the USA, a main driving force directing preventive strategies is the Healthy people 201086 initiative, now superseded by Healthy people 2020. 87 Although emphasising that additional effort is needed to reach subgroups according to age, gender, socioeconomic position and ethnicity, there is also acknowledgement that the evidence is lacking to inform more definitive recommendations for what works in these subpopulations. Federal initiatives such as a National Tobacco Quitline network and public–private initiatives such as insurance coverage for tobacco treatment have been proposed to promote smoking cessation,88,89 while evidence-based guidance provides key recommendations for the treatment of tobacco dependence. 90 There remain, however, health disparities in tobacco-related health outcomes, as indicated by the differential prevalence of current smokers. 86 Although prevalence is comparable between white (non-Hispanic) and black (non-Hispanic) populations, prevalence is low among the Asian (non-Hispanic) population. 91 For those reporting multiple ‘races’, however, the prevalence is higher than in the white (non-Hispanic) population. 91 Beyond disparities in prevalence, there are other pronounced differences in usage, environmental contact, commencement, treatment and health outcomes related to tobacco use. 92
In the UK, the NHS Stop Smoking Service is the primary vehicle for delivering cessation services. There is, however, documented evidence of lower use of the Stop Smoking Service by ethnic minority groups, which may be a consequence of these services not being linguistically or culturally appropriate or sensitive. 93 Guidance that highlights best practice in tobacco prevention and cessation for ethnic minority communities can help to support Stop Smoking Service managers working at the front line within their catchments, as it is commonly believed that the services need to be made more accessible, rather than tailored per se. 93,94 These additional efforts are needed to address smoking health disparities, particularly among Bangladeshi-origin men who have the highest prevalence of cigarette smoking in England, followed by white Irish-origin men and women and Pakistani-origin men and black Caribbean-origin women. 6 All of these groups have higher smoking prevalence than the general population. 6 Among Bangladeshi-origin women, chewing tobacco is much more prevalent than cigarette smoking6 and potentially represents a gap in the current services as smokeless tobacco falls outside the official scope of stop smoking programmes. Therefore, in the case of smokeless tobacco cessation, targeted services may be appropriate based on a local needs assessment, as there may be potential difficulties with access. 93
When determining whether adapted mainstream services or specially developed, culturally sensitive services would be most appropriate, needs assessments are essential to draw out local knowledge and attitudes towards health, as well as draw on local assets and resources. In particular, how ethnicity relates to eating practices, physical activity and smoking is contingent on many inter-related factors such as age, gender, culture, education, income, family structure and immigration status, in the context of the local environment. Insight into these issues and its application to preventive services is likely to increase successful uptake and implementation of health promotion activities and strategies. 95
Furthermore, even if services were believed to be culturally sensitive, the reasons for their underuse are multifaceted and may include aspects such as location and available hours of services; appropriateness to language, gender, culture and religious norms; and preferences for and linkages with other community services and institutions. Overall, research suggests that, if services demonstrated appreciation for the importance of diversity without reverting to stereotypes, provided respectful and supportive staff, increased accessibility to information on services and created a safe environment without discrimination, they were reported as being acceptable by ethnic minority people. 96
Study rationale
In view of the burden of long-term conditions experienced by ethnic minority populations in the UK (and indeed in many other economically developed countries) and the associated lack of evidence on how best to provide preventive health care to these large and increasing subsections of the population, there is a pressing need to identify optimal approaches to health promotion interventions for ethnic minority populations. This evidence should ideally be pursued through primary research, but evidence shows that ethnic minority populations tend to be marginalised from much of this research, let alone its focus. 21,22,97–101 This body of evidence is therefore likely to take many years if not decades to accrue. In the meantime, it is, we believe, important to undertake parallel work on identifying approaches to promoting health that have proven effectiveness in the general population. We hypothesise that, when these effective approaches are appropriately adapted and made culturally relevant, they too can be effective for ethnic minority populations. 9
Our study builds and expands on the work by Netto et al. ,13 which extracted five common principles of adaptation for CHD-reducing health promotion interventions for Chinese-, Indian- and Pakistani-origin populations studied in relation to smoking cessation, physical activity and healthier diets, through the addition of an additional ethnic group (African origin). The five principles include (1) drawing on community resources for promotion and increasing accessibility; (2) identifying barriers to access and participation; (3) developing language- and format-appropriate strategies; (4) utilising cultural and/or religious values strategies that promote change; and (5) accommodating for different levels of cultural identification. These principles elaborate on how cultural communities should be engaged. We also drew on a substantially larger body of theoretical and empirical evidence. For example, secondary health promotion interventions, using physical activity and dietary activities to improve outcomes for diabetes, as well as community-wide intervention studies for smoking cessation, increasing physical activity and improving healthy eating have been studied. Given the lack of direct evidence and the pressing need to improve the health of all populations, including the reduction of health disparities, we cast a wide net to capture all of the available evidence on adapted interventions for smoking cessation, increasing physical activity and improving healthy eating in order to determine the effectiveness of adapted health promotion interventions for ethnic minority populations.
Study scope
The field of ethnicity and health is broad and far-reaching, as has been illustrated by the above introductory note. In the context of this report, we will henceforth be focusing on the three main populations of interest to this study, that is, African-, Chinese- and South Asian-origin populations, along with the three areas of health promotion important for the prevention and/or reduction of chronic diseases, namely, smoking cessation, increasing physical activity and improving healthy eating. Literature on other ethnic populations, such as the Hispanic population in the USA and the indigenous populations in the USA, Canada, New Zealand and Australia, although important and potentially very useful in informing learning about adapting interventions, was not within the remit of this particular piece of work. Furthermore, as noted above, although alcohol is another modifiable risk factor salient for chronic disease prevention and control, it was purposefully excluded, as there is a lack of consensus across countries and communities as to what constitutes an acceptable/unacceptable alcohol intake and how this differs from high-risk alcohol use. On the other hand, the recommendations for smoking, physical activity and healthy eating and their associated health outcomes are relatively clear-cut and agreed upon.
Furthermore, the primary purpose of this report and its research components is to support a conceptual and methodological study of the issue of adapting interventions to meet the needs of ethnic minority populations. This purpose is in direct response to an Health Technology Assessment (HTA) commissioning brief (see Appendix 1) that sought research on how to adapt interventions to meet the needs of ethnic minority groups. The brief works with the assumption that adaptation should be pursued as the best way forward to reduce the observed inequities for some health conditions among particular ethnic minority populations. 9
Structure of the remainder of this report
Chapter 2 summarises the aims and objectives of this work and describes how the various research components complemented and inter-related with each other. Chapter 3 provides a description of the two user engagement conferences held to launch the study and discuss our preliminary findings. The four major components of this study each have their own dedicated chapter (Chapters 4–7). Chapter 4 provides evidence on effective smoking cessation, physical activity and healthy eating health promotion interventions from UK guidelines and international systematic reviews for the general population; Chapter 5 considers the description of ethnicity in UK guidelines and international systematic reviews; Chapter 6 reports on our systematic review of adapted health promotion interventions for ethnic minority populations; and Chapter 7 presents the findings from the qualitative interviews with researchers and health promoters who have adapted health promotion interventions for ethnic minority populations. Chapters 4–7 can be read as self-contained studies, each with their own abstract, background context, research questions, methods, results and discussion sections. Chapter 8 synthesises the results from the preceding chapters using a realist framework derived from principles outlined by Pawson and Tilley. 102 In the final chapter (see Chapter 9) we critically reflect on the strengths and limitations of this research and seek to place our findings within the broader body of work; we conclude by offering recommendations for future research.
In view of the recognition that some readers may read only certain chapters, we spell out abbreviations in full at first mention in each chapter.
Chapter 2 Aims, objectives and overview of research methods
Aims
We aimed to identify, describe, appraise and interpret research on the processes and procedures employed to maximise the cross-cultural validity, utility and effectiveness of health promotion interventions. As discussed in the previous chapter, we focused on health behaviours known to be associated with considerable morbidity and mortality. Specifically, we undertook a phased programme of research to study the cultural adaptation of three key health promotion areas – smoking cessation, physical activity and healthy eating – that are potentially applicable to African-, Chinese- and South Asian-origin populations. These groups represent the major ethnic minority groupings in the UK and the USA and feature prominently in the diverse populations of, for example, Canada, New Zealand and Australia (discussed in Chapter 1).
Research objectives
This programme of work included three phases, described in the following sections.
Phase 1 objectives
-
A. To identify and summarise information on health promotion interventions for smoking cessation, physical activity and healthy eating that are of proven effectiveness for use in populations at large.
-
B. To assess to what degree ethnic minority populations are considered within the evidence base for smoking cessation, physical activity and healthy eating health promotion interventions known to be effective in populations at large.
-
C. To identify health promotion interventions for smoking cessation, increasing physical activity, and improving healthy eating that have been adapted to meet the needs of African-, Chinese- and South Asian-origin ethnic minority populations, describe the adaptation approaches used and assess the clinical effectiveness, cost-effectiveness, feasibility, acceptability and equity of these adapted approaches.
Phase 2 objective
-
D. To understand the rationale for and processes and experiences of adapting health promotion interventions for ethnic minority populations and to summarise lessons learned.
Phase 3 objective
-
E. To identify which adapted interventions are ready for implementation and establish which interventions require further research.
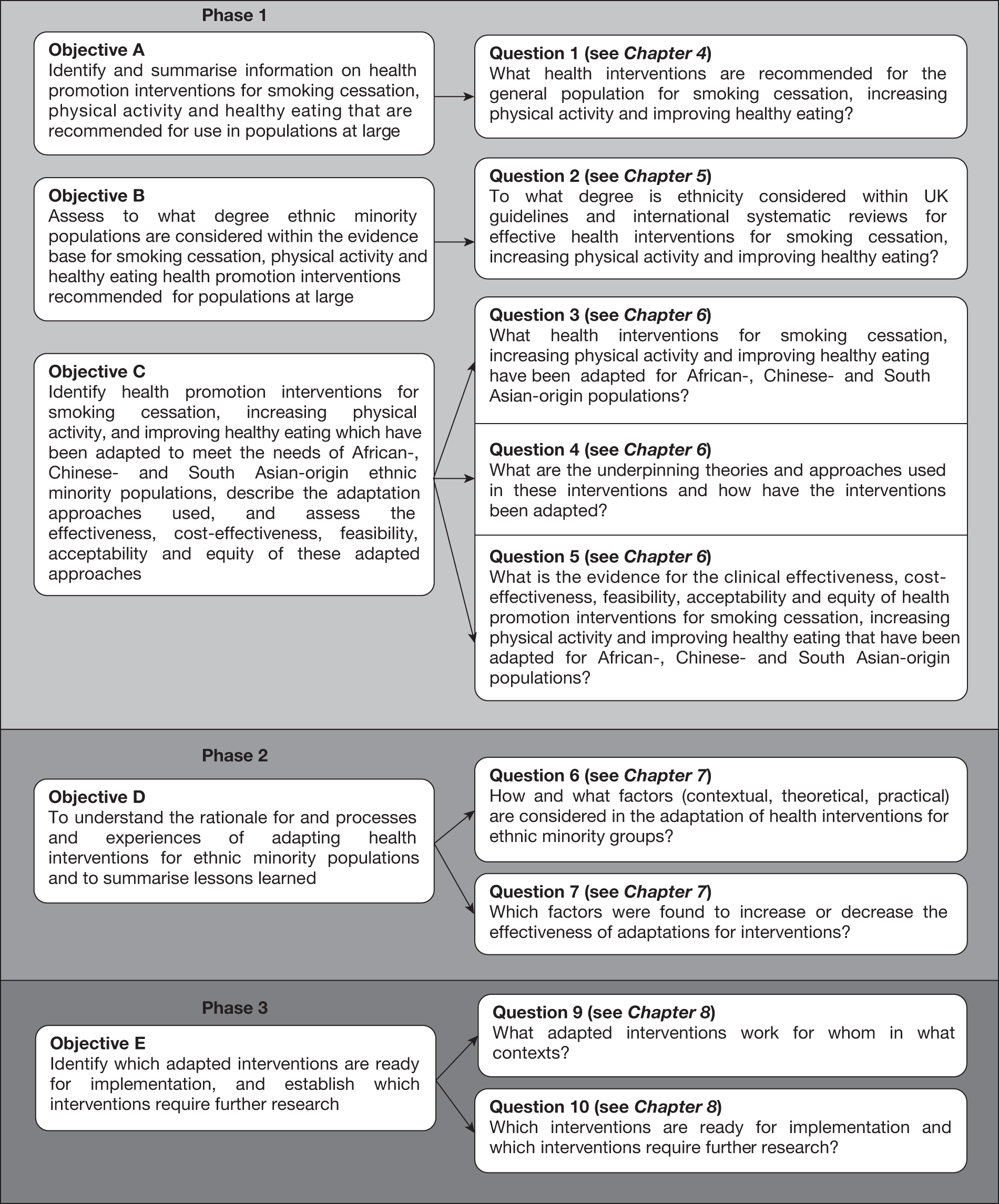
The research questions arising from these objectives are discussed in subsequent chapters (see Chapters 4–8). Figure 2 outlines the relationship between the three phases, five objectives (A–E) and 10 questions and maps them onto the chapter(s) in which they are discussed in more detail.
FIGURE 2.
Relationship between project phases, objectives and questions.
The original scientific rationale for this study is included in Appendix 2. The relatively few amendments made to aspects of work outlined in the original scientific rationale are detailed in Appendix 3. These in the main reflected our responses to the unexpectedly large volume of literature identified.
Overview of methods
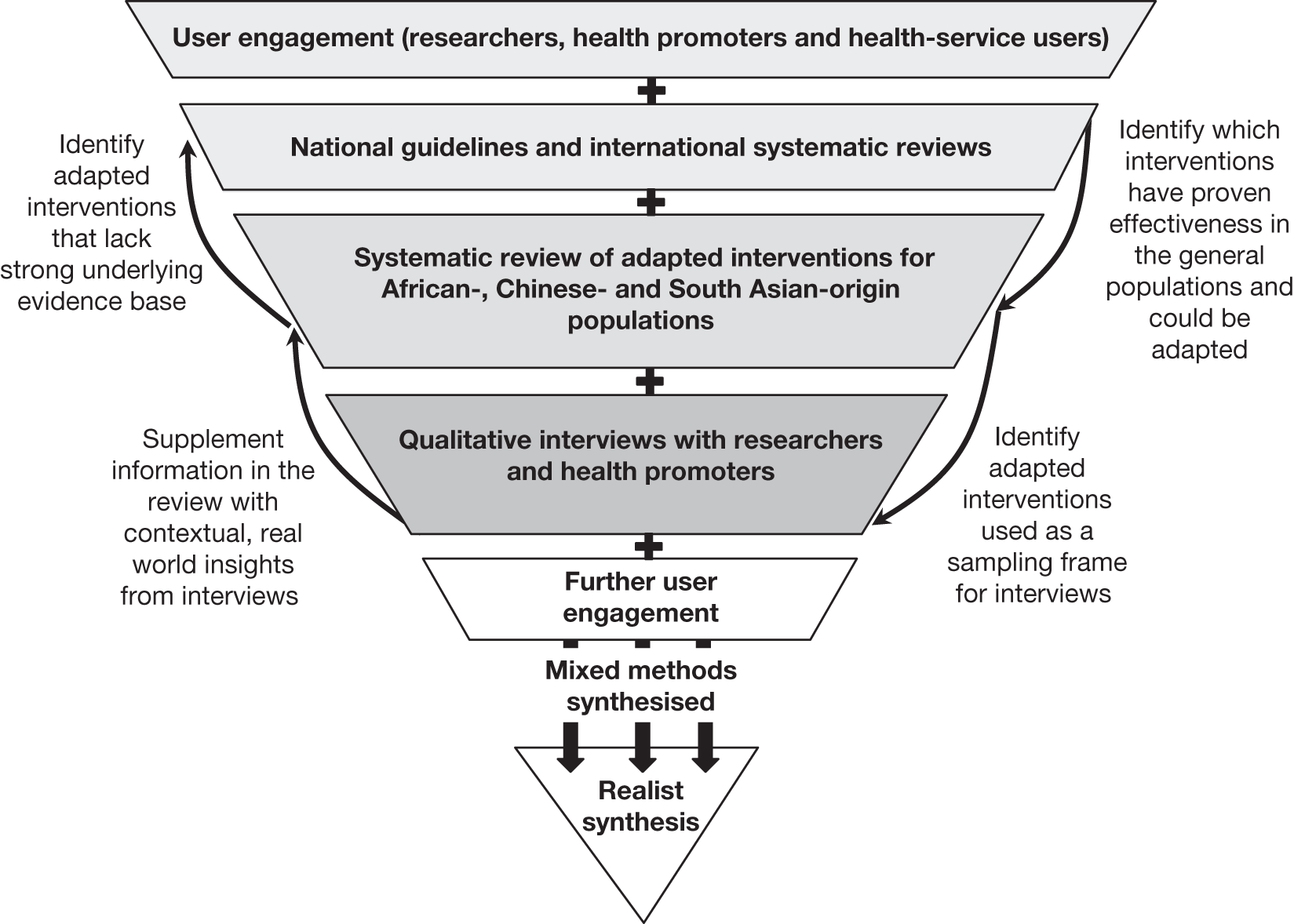
A mixed-methods approach was employed to collate and synthesise data from multiple sources. Our methods included a review of UK guidelines and international systematic reviews to identify evidence on health promotion interventions for the general population; a systematic review of interventions adapted for ethnic minority populations; qualitative interviews with researchers and health promoters developing, delivering and evaluating adapted interventions; and, finally, a realist synthesis of the results from each of the preceding components. We provide below a brief overview of the methods used for orientation purposes; more detailed information is contained in subsequent chapters (see Chapters 3–8). Figure 3 summarises the relationships linking the methods used in the study.
FIGURE 3.
Overview of study methods and the relationships linking the methods.
User engagement
User engagement was undertaken throughout our project through the inclusion of lay members on our Independent Project Steering Committee; in addition, we held two user conferences, one to launch the study and one to share and discuss our preliminary findings. The details of our user engagement approach and conferences are found in Chapter 3.
UK guidelines and international systematic reviews
Our review of UK guidelines and international systematic reviews was designed to examine what health promotion interventions have proven effectiveness in the general population for smoking cessation, increasing physical activity and improving healthy eating. Details of effectiveness for the general population were extracted from guidelines and systematic reviews and a summary framework of effective interventions was created for behaviour change in general and for each of the health promotion topics of interest (see Chapter 4). These frameworks were further compared with the adapted interventions to identify where there was overlap and to identify research gaps in which promising evidence-based interventions for the general population have not yet been adapted for ethnic minority populations (see Chapter 8).
This same body of literature was also searched to determine whether or not recommendations and interventions made by UK guidelines and international systematic reviews were equally applicable to ethnic minority populations (see Chapter 5).
Systematic review of adapted interventions
We then conducted a systematic review of health promotion interventions to identify smoking cessation, physical activity and healthy eating interventions that have been adapted for African-, Chinese- and South Asian-origin populations. From the included studies we identified the adaptation approaches utilised in these interventions (see Chapter 6). The included studies were also assessed for clinical effectiveness and cost-effectiveness in relation to health behaviour change and associated outcomes.
Qualitative interviews
In parallel with the systematic review we carried out qualitative interviews with key researchers and health promoters who had been involved in developing, delivering and evaluating adapted health promotion interventions to supplement the systematic review of published literature. In-depth semi-structured interviews were conducted either by telephone or face-to-face and were recorded and transcribed. Transcripts were coded and thematically analysed to identify overarching themes (see Chapter 7).
Realist synthesis
Finally, we synthesised the findings from the above phases of work – that is, the user engagement conferences, the review of UK guidelines and international systematic reviews, the systematic review of adapted interventions and qualitative interviews with researchers and health promoters – using the explanatory framework offered by realistic evaluation102 to understand better how adapted interventions work and to identify interventions ready for implementation and prioritise future research (see Chapter 8).
Ethics
Ethical considerations were outlined in the original scientific rationale (see Appendix 2) and an application was submitted to the School of Health in Social Science Research Ethics Committee for the qualitative interviews (see Appendix 4).
Chapter 3 User engagement
Approaches to user engagement
The value and importance of involving service users in research was explicitly recognised from the outset of this study and a commitment was made to the approaches advocated by INVOLVE,103 a UK public engagement in health research advisory group funded by the National Institute for Health Research. The term ‘service users’ carried a dual meaning in this study as it was used to represent both users of health services and users of health research. It was felt important to involve research users such as academics and health service providers (at governmental, non-governmental and community level) and bridge the gap between research and the delivery of interventions from the outset. Several approaches were therefore employed to integrate public perspectives into the research study phases. Particular attention was paid to ensuring the representation of the views of diverse ethnic minority communities while recognising the risk of exploiting or exhausting their ability to contribute. Our approaches to user involvement thus included:
-
representation of the Expert Patient Panel of the Leicester Centre for Ethnic Health Research on the Independent Project Steering Committee
-
an Ethnicity and Health launch conference designed to engage users and obtain feedback on the research proposal and methods
-
a second Ethnicity and Health dissemination conference to present and discuss preliminary findings from our work
-
a project website (www.chs.med.ed.ac.uk/ethnicity-and-health/) to facilitate interaction with service users that made available contact details of the project team, relevant study materials and the presentations from the two study conferences discussed below.
We consider the two project conferences in more detail in the following sections.
Launch conference
This conference was held in London, England in June 2009. Speakers included members of the project team and international experts in ethnicity and health research from the UK, the USA and Europe. A total of 81 delegates attended the conference from a wide variety of stakeholder organisations. Interactive workshops allowed smaller group discussion of topics pertinent to the research methods, including approaches to multiple behaviour change; the role of culture/acculturation in interventions for ethnic minority communities; reflecting on community-adapted programmes; and adaptation in non-health contexts. The programme for this conference is available in Appendix 5. This conference was reported in the British Medical Journal (www.bmj.com/content/338/bmj.b2326.extract).
Conference findings and recommendations
Overall the conference was very well evaluated (see Appendix 6). The main feedback from this conference emphasised the importance of incorporating ecological models of health promotion and not limiting the study focus to individual health behaviours. Delegates also suggested that there should be a greater consideration of a variety of intervention contexts, for example those outside of traditional health-care delivery, to include health promotion delivered by commercial organisations and social marketing strategies. There was also a shared feeling that greater linkages were required between people working in ethnic minority health to better facilitate the exchange of research findings. This concern stemmed from the observation that, although there appeared to be substantial work accumulating internationally, there was little integration of this work, which could potentially result in an unnecessary duplication of effort.
Actions
We undertook the following actions in response to these user recommendations:
-
active consideration of all health promotion interventions including community-level and ecological interventions and also health promotion programmes delivered by commercial organisations and through social marketing strategies (see Chapters 4, 6 and 8)
-
development of an Ethnicity and Health website on the University of Edinburgh’s server as a platform for ongoing user engagement (www.chs.med.ed.ac.uk/ethnicity-and-health/)
-
dissemination of a list of attendees to facilitate collaborative working and communication
-
liaison with researchers and others who attended the conference to share relevant papers.
Dissemination conference
Our second user engagement event was a project dissemination conference held in Edinburgh, Scotland in February 2011. This event was held towards the end of the project and provided us with the opportunity to share, discuss and debate our preliminary conclusions, and refine these in the light of participant feedback. A total of 71 delegates attended the conference from a wide variety of stakeholder organisations – some of the participants were attendees at the first conference. In addition to the presentation of project findings, interactive workshops allowed smaller group discussion and feedback on the project outputs including methodological reflections on complex systematic reviews; theoretical considerations on the principles of adaptation; translation of study research findings into practice; and identifying key future research themes. The programme for the conference can be found in Appendix 7.
Conference findings and recommendations
This conference was also very well evaluated (see Appendix 8). The main recommendations from the conference were for a greater consideration of the effects of socioeconomic status (SES) in the identified adapted intervention literature and greater recognition that SES may be confounding the findings attributed to ethnicity. It was noted that adaptations made for culture may consciously or inadvertently also address SES and the effects of each need to be more clearly delineated. It was recommended that SES should be recorded when possible and independently considered in relation to intervention outcomes.
It was also noted that other factors that contribute to the heterogeneity of the population should be captured; these included intergenerational issues, age, gender and education. These factors should, it was suggested, be considered when interpreting the studies and they should also be taken into account, as well as SES, in any statistical analyses.
There was considerable discussion of theoretical considerations, including the possibility of developing a theory of adaptation. Suggestions for theory development were proposed, along with preliminary discussion on how to differentiate between theories of behaviour change and theories of adaptation, and perhaps reframing adaptations by their function rather than categorising them by types. Six suggested functions (i.e. accessibility, comprehension, identification, engagement, motivation and activation) and the five principles generated by Netto et al. 13 (i.e. community resources, barriers, sensitive communication strategies, cultural or religious values, and cultural identification) were raised as potential candidates to begin generating a theory for adaptation (Table 1).
| Functions | Five principles of adaptation | ||||
|---|---|---|---|---|---|
| Community resources | Barriers | Sensitive communication strategies | Cultural or religious values | Cultural identification | |
| Accessibility | |||||
| Comprehension | |||||
| Identification | |||||
| Engagement | |||||
| Motivation | |||||
| Activation | |||||
Finally, it was suggested that we should apply and test the principles/adaptations that are conceptualised in practice with ethnic minority communities as it was considered to be equally important to build experience-based practice as well as evidence-based practice.
Actions
The following actions were taken to incorporate these recommendations into this body of work:
-
we extracted and recorded details relating to the heterogeneity of the populations (SES, age, education, gender) (see Appendix 15)
-
we undertook further analyses and theory generation, which are being pursued through planned publications; in addition, testing the principles/adaptations in practice will, we anticipate, be pursued through follow-on studies (see Chapter 9).
Chapter 4 Summarising evidence on effective health promotion interventions from guidelines and systematic reviews
Abstract
Background
A key assumption underpinning this project is that health promotion interventions found to be effective in the general population are, if appropriately adapted, likely to also prove effective in ethnic minority populations. We therefore began our work by seeking evidence-based recommendations for health promotion interventions found to be effective in the general population.
Objectives
We sought to identify and summarise information on health promotion interventions for smoking cessation, increasing physical activity and improving healthy eating that are recommended for use in populations at large.
Methods
We undertook a systematic review of the evidence for health promotion interventions for smoking cessation, increasing physical activity and improving healthy eating in UK guidelines and these searches were supplemented by additional scrutiny of international systematic reviews. Relevant guidelines were identified from the Clinical Evidence, National Institute for Health and Clinical Excellence (NICE) and Scottish Intercollegiate Guidelines Network (SIGN) databases. We also searched for international systematic reviews from established databases of evidence, namely The Campbell Collaboration, The Cochrane Library, the Database of Abstracts of Reviews of Effects (DARE) and the National Institute for Health Research Health Technology Assessment (NIHR HTA) databases, in order to identify additional and more recent evidence that had not yet been incorporated into the guidelines. Two reviewers independently searched for and identified the literature and extracted data on recommended interventions for the general population. We created summary tables of the evidence identified according to health promotion topic and also a table for behaviour change interventions in general (not specific to any topic). These tables were then further categorised by six Tannahill-based intervention ‘strategies and activities’ (i.e. environment, policy, setting based, techniques, provider and resource).
Results
We identified 15 relevant guidelines and 111 systematic reviews. Most of the evidence we identified was targeted at individuals. There were considerably stronger recommendations for smoking cessation than for interventions aiming to increase physical activity and/or improve healthy eating. The strongest evidence and guidance in relation to smoking cessation was for pharmacological treatments and approaches aiming to promote the use of these pharmacological therapies. In contrast, there was relatively little in the way of strong or consistent guidance in relation to interventions that were successful for promoting changes in diet and exercise patterns that were sustained over time, or those directed at societal level-mediated change.
Conclusions
We have identified a number of guidelines and systematic reviews that have summarised and sought to provide guidance on how best to promote smoking cessation, increase physical activity and improve healthy eating. This evidence is strongest and most consistent in relation to pharmacological treatments for smokers and approaches aimed at increasing use of these products. Based on this work we suggest the need for improved communication between guideline developers and research commissioners with a view to catalysing research into finding effective and sustainable interventions for promoting physical activity and improving healthy eating. There is, in particular, a need for more evidence on the providers and resources that can meaningfully increase physical activity and improve healthy eating, and, more generally, for policy- and environmental-based interventions for smoking cessation, increasing physical activity and improving healthy eating.
Introduction
Health promotion is fundamental in the drive to reduce the growing burden of chronic disease worldwide66,67 and to address the considerable and persistent health inequalities now seen in many economically developed countries (see Chapter 1). 5,6 Inequalities in morbidity and mortality attributable to, for example, CVD and diabetes are observed among a number of ethnic minority populations. 6,65 It is therefore widely accepted that increasing access to and participation in health promotion interventions represents an important component of strategies aiming to reduce health inequalities with respect to ethnicity (see Chapter 1). 67,69,72–75 Foremost among these preventive efforts are finding effective and cost-effective ways of promoting smoking cessation, increasing physical activity and improving healthy eating – the key modifiable risk factors for the majority of chronic diseases. 51
As with any intervention, the recommendations for these health promotion interventions should be based on the most rigorous evidence available104 and on studies that are at low risk of bias. 105 Ideally, this evidence would be derived from randomised controlled trials (RCTs) and systematic reviews of RCTs because of their unique ability to control for known and unknown confounders. 106 For public health practice, technical issues may, however, limit investigators’ ability to undertake the simpler RCT designs, as interventions aimed at promoting behavioural change are more often than not ‘complex’ – that is, they have multiple interacting components. 107 Interventions aimed at the level of the household, school/workplace, community or indeed any other grouping of individuals should ideally be studied using cluster RCT designs to reduce contamination,108 but this may not prove possible, in which case other experimental designs may need to be employed. 108 Given the ethical and methodological challenges that are inherent to developing a rigorous and comprehensive evidence base for public health interventions, it is perhaps unsurprising that there are at times differing and/or conflicting conclusions drawn with regards to the most effective health promotion interventions,109 including interventions for smoking cessation, increasing physical activity and improving healthy eating. There is therefore a need to develop a detailed overview of the current state of evidence for promoting sustainable changes in relation to these key risk factors.
A key assumption underpinning the call for research (see Appendix 1) and our approach was that health promotion interventions of proven effectiveness for use in the general population are also, if appropriately adapted, likely to be effective in ethnic minority populations (see Chapter 1). 9 Our formative work therefore sought to develop a detailed, evidence-based and up-to-date overview of the evidence for health promotion interventions aimed at promoting smoking cessation, increasing physical activity and improving healthy eating in the general population.
Research question
The research question we addressed in this chapter arose from Phase 1A of our study (see Chapter 2), namely:
-
What health interventions are recommended for the general population for smoking cessation, increasing physical activity and improving healthy eating?
Methods
Overview of methods
The UK has some of the most well-established and respected guideline development procedures in the world. These guidelines therefore represented the principal source of evidence that we sought to identify and scrutinise. Because of their lengthy and rigorous development processes, guidelines, however, inevitably remain a step behind the evidence and are thus less likely to contain as up-to-date information as is contained within the systematic review literature on which they predominantly draw. We therefore supplemented our guideline-based searches with data derived from international systematic reviews of evidence.
Searches for guidelines and systematic reviews
We searched for and retrieved any pertinent guidelines on interventions for smoking cessation, increasing physical activity and improving healthy eating in the Clinical Evidence, NICE and SIGN databases using the following broad key search terms:
-
diet
-
exercise
-
healthy eating
-
obesity
-
physical activity
-
smoking
-
tobacco.
We also conducted searches in The Campbell Collaboration (Campbell), The Cochrane Library (Cochrane), the DARE databases and the NIHR HTA database for systematic reviews and health technology assessments (HTAs) of interventions for smoking cessation, increasing physical activity and improving healthy eating from January 1950 to April 2009 using the same broad search terms detailed above. HTA reports use systematic methods110 to provide independent research information about the effectiveness, costs and broader impact of health-care treatments and tests for those who plan, provide or receive care in the NHS and henceforth in this report will be referred to under systematic reviews.
Selection of eligible guidelines and systematic reviews
Two researchers (JJL and ED) independently screened and selected guidelines and systematic reviews based on predefined inclusion/exclusion criteria (Table 2), first by scrutinising titles and then, if necessary, the abstracts and full text of manuscripts. Disagreements regarding inclusion/exclusion of papers were resolved through discussion. If consensus could not be reached a third reviewer (AS) was consulted. The full text of all eligible records was retrieved; 12 full-text papers were translated into English from Danish, French, Norwegian, Spanish and Swedish.
| Population |
General population adults and children (any age), non-clinical (exclude hypertension, diabetes, CVD, obese, hospitalised), non-special (exclude pregnant, menopausal, lower SES, or if focused on any specific ethnicity, religion or gender) Aim was not focused on any of the special populations; however, reviews or guidelines were not excluded if they contained individual studies that included special populations |
| Intervention | Any health promotion intervention (individual, community, population, policy level) promoting smoking cessation, physical activity and healthy eating |
| Outcomes |
Any outcomes related to smoking cessation, improving healthy eating and increasing physical activity Included: interventions that report evidence of effectiveness. Interventions must measure one or more of the three outcomes. For example, if the intervention is focused on weight loss, it must report an outcome relating to either physical activity or inactivity and/or healthy eating. Reviewers must comment on physical activity or healthy eating if they are secondary outcomes Excluded: interventions with no evidence, lack of quality evidence or no evidence of effect; drug and surgical interventions; fall functions; adherence to or maintenance of behaviour change |
| Date | Published between January 1950 and April 2009 |
| Language | No language restriction |
| Study design | Guidelines and systematic reviews |
Data extraction and synthesis
We extracted relevant evidence from the guidelines and systematic reviews onto a customised data extraction form (see Appendix 9). We extracted statements pertaining to the effectiveness of smoking cessation, increasing physical activity and improving healthy eating interventions, the quality of the evidence (when reported) and the quality assessment tool used (when reported). These evidence statements were compiled in two tables (see Appendix 10) where they remain attributed to the guideline(s) or systematic review(s) from which they were derived. The tables of evidence statements therefore incorporated two levels of evidence – guidelines that have been developed through a collaborative scrutiny of the evidence, as in the case of NICE and SIGN guidelines, and systematic reviews, which have been subject to quality control by peer reviewers and journal editors.
Subsequently, the evidence statements were organised in a summary framework of effective interventions according to the health promotion topic: health behaviour in general (not specific to one health promotion topic), smoking cessation, increasing physical activity and improving healthy eating (see Tables 3–6). We adapted the revised Tannahill model of health promotion (Box 2)111 to categorise the evidence statements according to six broad categories of ‘strategies and activities’ (Box 3).
| Categories of ‘strategies and activities’ | |||||
|---|---|---|---|---|---|
| Environment | Policy | Setting based | Technique | Provider | Resources |
|
Build partnerships112 Remove barriers112 Advertising and mass media campaigns112 Health-enhancing environments112 |
Fiscal and legislative interventions112 |
Primary care113 |
Biomarker feedback115 Tailored to individuals112,116 Face-to-face care116 |
Nothing reported |
Web-based interventions117 Computer-generated116 |
| Categories of ‘strategies and activities’ | |||||
|---|---|---|---|---|---|
| Environment | Policy | Setting based | Technique | Provider | Resources |
|
Campaigns120 Health coalitions122 |
Workplace smoke-free policy118,120 Increases in tobacco prices118 Decreased cost of cessation therapies118 |
Primary care128 |
Group-based counselling and therapy120,131–133 Individual counselling120,130,131 Telephone counselling118,120,131,134–136 Counselling,129 + pharmacotherapy,134 + self-help,134 + support120 Brief or intensive advice137,138 Individual tailored advice120,130,139 Auricular acupuncture141 |
Family physicians/GPs134,139,143–146 Physician brief advice131,147,148 Nurses120,131,139,143,145,146,149,150 Dentists120,145 providing counselling151 Trained counsellors143 Telephone quitline counsellors120,127 Midwives120 Pharmacists120 All health professionals120 All health professionals make referrals139 |
Pharmacotherapy118,120,139,151–153 NRTs,118,120,131,134,137,143,148,154,155,157–159 NRT-supported reduction142 NRTs + providers146 Bupropion hydrochloride120,131,134,137,158,159,164 Nortriptyline165 Self-help materials,120,140,143 self-help + pharmacotherapy134 Education129 Telephone quit-lines,120 advice143 Mobile telephone texts and calls169 |
| Categories of ‘strategies and activities’ | |||||
|---|---|---|---|---|---|
| Environment | Policy | Setting based | Technique | Provider | Resource |
|
Public parks and facilities172 National campaign for children and young people172 Walking/cycling routes174 Linkage of walking and cycling routes to schools and workplaces173 Stair use173 Build partnerships172 Address concerns of local people112 Prioritise pedestrians and cyclists173 |
Schools114,172,173,174,177–181,210,214 Multicomponent school based with family or community involvement172,177,201 Leisure centre182 Health-care settings for older adults (aged > 50 years)183 Primary care based184 Nurseries and childcare facilities174 |
Exercise on prescription,189,192 walking prescriptions187,193,194 Exercise referral scheme;182,195 only as part of research studies79 Active transport for adults,197 children173,198 Reducing sedentary behaviour174,199,212 Regular follow-up;193,194 by telephone191 Ongoing support (in person, by telephone, by mail or through internet support112) Booster interventions189 Tailored to individuals174,184,202 Formal172,201 and informal activities172,201 Occupational and leisure time activities137 Activity intensity: low,199 moderate, 137,193,194 high137 Delivered to individuals,202 households202 groups202,203,211 Stage-based interventions196 Goal setting213 |
Health-care professionals201,204 Primary care practitioners79 Involving children/young people in the design, planning and delivery of interventions172 |
Education;172,173,203 print or technological189 Computer tailored207 Pedometer;208 recommended only as part of research studies79 Written materials:79,184,211 written follow-up,191 signs175,176 Personalised travel plans174 |
|
| Categories of ‘strategies and activities’ | |||||
|---|---|---|---|---|---|
| Environment | Policy | Setting based | Technique | Provider | Resources |
|
Food subsidisation217 Health-enhancing environment218 Address concerns of local people174 Partner with food vendors to promote healthy choices174 |
Improve access to healthy foods through point of sales initiatives112 Workplace point of purchase216 University point of purchase216 |
Nurseries and childcare facilities174 Religious settings,227 e.g. churches226 Primary care222 Health-care settings for older adults (aged > 50 years)183 |
Face-to-face counselling228 Telephone counselling186,228,231 One-to-one contact232 Intensive/more contacts233 Social support229 Ongoing support174 Advice234 Tailored to individuals174 Motivational interviewing + education235 Goal setting213 |
Parents and carers174,220,233,236 |
Monetary incentives237 Clear messages233 Chronic disease messages232 |
Sustainable fostering of positive health and prevention of ill health through policies, strategies and activities in the overlapping areas of:
-
social, economic, physical and environmental factors
-
equity and diversity
-
education and learning
-
services, amenities and products
Environment: Intervention that alters the social, economic and physical space, with the potential to affect a more general population
Policy: Policy intervention at any level, e.g. national, local, organisational
Setting based: Specific places for an intervention, e.g. targeting and involving a more specific, often ‘captive’ community
Technique: Types and formats of interventions including education and learning; also behavioural techniques and other elements to enhance the effectiveness of an intervention
Provider: A specific resource referring to the specialised personnel or services used for intervention delivery
Resource: Intervention materials, amenities or products given to participants
Environment applied to interventions that alter the social, economic and physical space (as opposed to place), with the potential to affect a more general population. Policy included organisational, local or national policies. Setting based represented specific places or communities identified as effective locations to deliver an intervention, and which often target ‘captive audiences’, such as children at schools or employees at worksites. Techniques described the wide-ranging types and formats of interventions that have been found to be effective, including education and learning, but it also captured behavioural techniques and other elements that can enhance the effectiveness of a variety of interventions. Provider also included persons singled out as important partners in the intervention delivery process. Resource encompassed the materials or products given to participants as the intervention. Unlike in the Tannahill model, provider represented a specific type of resource, referring to the specialised personnel or services designated for intervention delivery.
These categories referred to the ‘strategies and activities’ utilised in health promotion interventions (not to the interventions themselves) and are overlapping and additive in that combinations of ‘strategies and activities’ may be used in any one intervention. These categories facilitated the examination, and cross-comparison, of such a large and diverse body of evidence for smoking cessation, increasing physical activity and improving healthy eating.
Results
We identified 189 records from NICE, of which 10 were included. We were unable to search SIGN and Clinical Evidence using keywords and instead manually searched these databases using the provided topic headings related to our health topics of interest and identified three and two additional relevant guidelines, respectively. Therefore, from the three guideline databases, 15 guidelines satisfied our inclusion/exclusion criteria (Figure 4). Although these guidelines were the products of different processes of evidence evaluation, from the descriptions of the methods used, they appeared to have undergone a broadly comparable approach to identifying studies and extracting evidence.
FIGURE 4.
Study selection process for guidelines and systematic reviews. CE, Clinical Evidence.
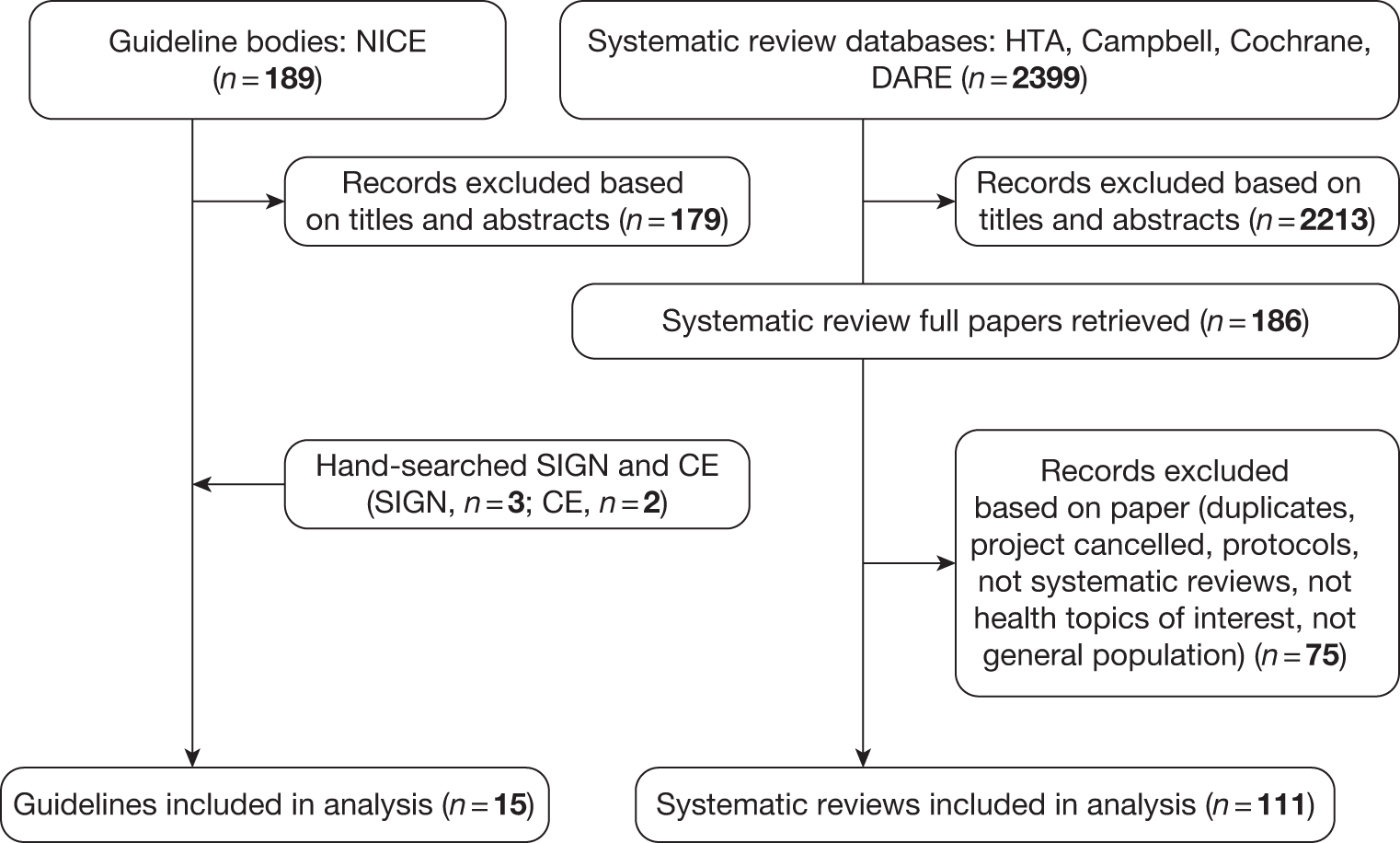
From Cochrane, Campbell, DARE and NIHR HTA we identified 2399 potentially relevant systematic reviews. Of these, 111 records satisfied our inclusion criteria and provided data on effective interventions. We included only strong evidence of effectiveness for smoking cessation, but strong/moderate evidence of effectiveness for physical activity and healthy eating (see Figure 4). The reasoning behind including moderate evidence for physical activity and healthy eating was that, in general, this body of evidence was at an earlier stage of development than the literature on smoking cessation.
Summary framework of effective ‘strategies and activities’
The evidence statements extracted from these included guidelines and systematic reviews were compiled in tables (see Appendix 10) and then synthesised into our summary framework according to health topic and the six categories of health promotion ‘strategies and activities’ discussed above. The following four tables represent the summary framework to guide behaviour change in general (see Table 3), smoking cessation (see Table 4), increasing physical activity (see Table 5) and improving healthy eating (see Table 6). Each table will be described in turn.
Behaviour change in general
There was minimal information on effective ‘strategies and activities’ for behaviour change in general, which was not specific to any particular health promotion topic and was aimed at individuals and/or populations (Table 3). This evidence was therefore separately examined and summarised. The majority of information in this area was concentrated in the environment category. Evidence of effective environmental approaches included working in partnership and in collaboration to develop programmes; reducing or removing barriers (e.g. social, financial and environmental); holding national and local advertising and mass media campaigns; and developing health-enhancing social, physical and service environments. 112 Policy wise, fiscal and legislative interventions were reported to be effective for behaviour change. 112 Setting-based evidence highlighted two main sites for interventions: brief counselling held in primary care113 and longer-term, multicomponent interventions held in schools. 112,114 Techniques included feedback on individual biomarkers for disease risk,115 face-to-face interventions116 and the recommendation that interventions should be tailored to individuals. 112,116 For biomarkers the evidence indicated that this strategy was most effective if multiple biomarkers were used, or if one biomarker was used at more than one time point, as well as if biomarker feedback was delivered in conjunction with other treatments. 115 Resources included web-based117 and computer-generated messages as interventions. 116
Smoking cessation
Evidence on effective ‘strategies and activities’ for smoking cessation was primarily concentrated in the resource, provider and technique categories, with comparatively fewer ‘strategies and activities’ in the environment, policy and setting-based categories (Table 4). Environment strategies included mass media118–121 and other campaigns120 to promote cessation. Mass media interventions were, however, felt to be less effective when directed at young people and were highlighted as requiring further research. 119 Health coalitions,122 defined as partnerships among three or more organisations or constituencies, could further enhance the environment for behaviour change. Policy initiatives included workplace smoke-free policies,118,120 increases in tobacco prices118 and decreases in the cost of cessation therapies. 118
Setting based included the workplace123–127 to provide information and onsite services as well as to tailor support and treatment to the needs and preferences of employees,127 along with primary care to provide advice for nicotine replacement therapy (NRT) and brief structured counselling. 128 Smoke-free workplaces were reported to show reductions in smoking prevalence of 3.8% [95% confidence interval (CI) 2.8% to 4.7%] and lower cigarette consumption by those who continued to smoke. 125
Techniques included counselling129 in a variety of formats: individual based,120,130,131 group based120,131–133 and telephone counselling118,120,131,134–136 as well as counselling129 alongside pharmacotherapy,134 self-help134 and support. 120 Intensive individual counselling was reported to have no significantly greater effect than brief individual counselling. 130 Advice, whether brief or intensive,137,138 was recommended, along with tailored advice,120,130,139 that is, advice sensitive to individual’s ‘preferences, needs and circumstances’. 112 There was, for example, some evidence that self-help materials were more effective if tailored for the individual smoker. 140 Auricular acupuncture141 was also recommended, although acupuncture in general was not shown to be effective in another review. 171
A range of providers were recommended for delivering smoking cessation interventions – family physicians/general practitioners134,139,143–146 providing brief advice,131,147,148 psychologists,146,148 nurses,120,131,139,143,145,146,149,150 dentists120,145 providing counselling,151 trained counsellors,143 telephone quit-line counsellors,120,127 midwives,120 pharmacists120 – in essence, all health professionals. 120 Brief advice by physicians delivered in a single routine consultation was reported to have a quit rate of approximately 2% (95% CI 1% to 3%) with no relapse at 1 year,147 and physicians were reported to be the most effective provider of brief advice, although perhaps not the most cost-effective. 145 Furthermore, community-based clinicians, nurses, dentists, pharmacists, community workers and hospital physicians were recommended to make referrals to more intensive cessation programmes. 139
Resources for cessation included pharmacotherapy,118,120,139,151–153 such as NRT,118,120,131,134,137,143,148,154,155,157–159 for example patches,156,160–162 antidepressants,143,163 including bupropion hydrochloride (Zyban®, GSK)120,131,134,137,158,159,164 and nortriptyline (Allegron®, King),165 and varenicline (Champix®, Pfizer). 120,159,166–168 NRT used independently, with no additional support, was reported in one review to increase the rate of quitting by 50–70%. 154 A review that specifically looked at long-term follow-up (average 4.3 years) found that the addition of NRT to brief advice or behavioural support contributed to a 70–90% increase in the cessation rate achieved without NRT; however, although this appears to be successful, the long-term quit rate without NRT was relatively small and so even with a 70–90% increase, the overall number of participants who managed to quit long term was still just 7% of those attempting to quit. 155 If quit status was maintained for 3 years post intervention, these effects appear to be sustained. 155 NRT was usually delivered by health-care providers such as physicians, psychologists and nurses, and these providers can be effective in providing smoking cessation interventions without NRT; however, NRT was again found to result in a twofold increase in the quit rates achieved by most of these providers. 146 For other pharmacotherapies, varenicline compared with placebo was reported at ≥ 6 months to have a pooled risk ratio for continuous abstinence of 2.33 (95% CI 1.95 to 2.80),167 and antidepressants (nortriptyline and bupropion hydrochloride) were reported as having similar efficacy to NRT. 163 Use of NRT prior to quitting156,170 and NRT-supported reduction (e.g. ‘cut down to quit’) are additional strategies;142 however, the latter has been recommended only as part of research studies. 120
Education was recommended as another effective resource,129 which could be given as part of an intervention, as were self-help materials120,140,143 and self-help materials given along with pharmacotherapy. 134 Telephone quit-lines120 providing cessation advice143 were found to be effective, with some evidence of a dose-dependent response with three or more calls increasing the chances of success. 136 Mobile telephone texts and calls, sometimes combined with internet/e-mail delivery, were reported to show effectiveness in the short term (results from relatively small literature on four trials). 169
Physical activity
Evidence on effective ‘strategies and activities’ for increasing physical activity was reasonably abundant for the categories of resource, environment and technique but relatively sparse for the category of provider compared with the smoking cessation literature (Table 5).
All of the environmental recommendations were made by NICE, which included the provision of public parks and facilities,172 national campaigns for children and young people (minimum duration of 5 years),172 increased access to walking or cycling routes112 and linking these routes to schools and workplaces173 and the development and maintenance of space to encourage stair use. 173 The concerns of local people with regard to the costs, expectations, dangers and misinformation174 surrounding physical activity should also be addressed, as well as the prioritisation of pedestrians and cyclists when developing/maintaining infrastructure. 173 Removing barriers,172,174 building partnerships172 and maximising opportunities for exercise172,174 were also recommended.
The policy recommendations included policies to increase opportunities for physical activities174,175 and, more specifically, workplace/organisational policies174,176 that would increase the level of physical activity of employees.
Setting-based recommendations included use of schools114,172,173,174,177–181,210,214 to promote physical activity and education during school hours,172 as well as during school break periods,172 and to encourage active transport173 to and from school. It was recommended that schools provide a playground that would allow for varied physical activities. 173,177,179 Multicomponent school-based interventions with family or community involvement172,177,201 were also thought to be effective. Even school-based strategies with a minimum of printed educational materials and changes to the school curriculum were found to result in positive changes in activity levels. 178 It was noted that there was ‘very limited but good evidence’ that children exposed to these settings would go on to lead active adult lives. 181 Physical activity strategies were also found to be effective when delivered in the home,174,178,187–189 at leisure centres,182 at nurseries174 and childcare facilities174 and, for older adults (> 50 years), in health-care settings183 such as primary care-based counselling184 and brief interventions. Finally, worksite interventions185 that promoted active travel,174 supported incentive schemes and provided education and promotion programmes174 and were multicomponent in nature174,176 demonstrated effect in increasing physical activity levels.
Techniques was a category for physical activity that contained a wide range of ‘strategies and activities’. Counselling, including telephone counselling,186,187 was recommended for the general population. Counselling143,188–191 was recommended to increase the intensity of physical activity for those who are active191 and also to increase the activity levels of sedentary people. 212 Goal setting,213 exercise on prescription189,192 and walking prescriptions187,193,194 along with exercise referral schemes182,195 and stage-based interventions196 were also recommended; however, walking and cycling schemes were only recommended as part of research studies by one NICE guideline. 79 Walking advice193,194 and active transport for adults197 and children173,198 were recommended, along with the reduction of sedentary behaviour to increase activity levels. 174,199 It was recommended that sedentary people be targeted to increase walking, along with other behaviours. 202 Regular follow-ups193,194 by telephone191 and the provision of ongoing support in person, by telephone, by mail or via the internet174 were also recommended. As with smoking cessation there was a dose–response reported with telephone interventions with a longer duration and higher number of calls, characteristics associated with more positive outcomes. 186 Similarly, booster interventions were suggested for longer-term effectiveness. 189 Whether recommended activities were formal172 and structured201 or informal and unsupervised,172,201 and taking place within an occupational role or during leisure time,137 guidelines suggested enhanced effect if they were tailored to individuals174 – to their needs,174,202 characteristics,184 preferences and circumstances. 174 Furthermore, the recommended intensity of activity ranged from low199 to moderate137,193,194 to increasing activity levels to high if already active,137 and these activities could be delivered to individuals,202 households202 or groups. 202,203,211
Providers included health-care professionals in general to deliver advice, support and counselling201,204 and, more specifically, primary care practitioners to identify, advise and monitor and to consider individuals’ needs, preferences and circumstances. 79 No other providers were recommended in the guidelines or systematic reviews. The remainder of the recommendations suggested involving parents and carers172–174 in supportive roles to help plan school-based interventions174 and for monitoring television/video use,173,179 and involving children and young people in the design, planning and delivery of interventions. 172 Finally, a few guidelines encouraged adults (parents and carers) to set an example for their children in terms of being physically active, and encouraged them to be active along with their children. 172
Resources included education,172,173,203 either through print or through technology,189 such as the internet205,206 or computer-tailored207 materials. Interventions including written materials79,184 were recommended in guidelines and appeared to be associated with increased effectiveness. These written materials,211 which included follow-up191 as well as, for example, specific signs that encouraged increased stair use,175,176 were reported to have evidence of effectiveness. The provision by local authorities of personalised travel plans for active travel174 was also recommended, and this was sometimes observed within specific settings, as suggested above. Pedometers were reported to increase users’ physical activity by almost a third over baseline. 208 One guideline, however, advised that pedometers should be recommended only for use as part of research studies. 79 Finally, education and monitoring of television/video use179,200,209 was thought to decrease sedentary behaviour, particularly in children.
Overall, the body of evidence for physical activity promotion was weak in terms of providing evidence for interventions with longer-term effectiveness215 and maintenance of behaviour changes. In addition, it was unclear if these behaviour changes translated into gains in health status. Finally, for some interventions, the evidence was predominately from the USA and thus the generalisability of the evidence to other countries was unclear.
Improving healthy eating
There were relatively fewer resources and providers recommended for interventions to improve healthy eating compared with smoking cessation and, as was the case for interventions to increase physical activity, the bulk of the evidence comes under setting-based and technique-oriented ‘strategies and activities’ (Table 6). Policies such as workplace and university point-of-purchase policies216 and other point of sales initiatives were recommended to improve access to healthy foods. 174 Environmental changes of interest included food subsidies to increase general access to healthier foods,217 as well as working with caterers, shops, supermarkets, restaurants, cafes and voluntary community services to promote healthy choices through signs, posters, pricing and positioning of healthier food products. 174 It was highlighted that, in creating a health-enhancing environment,218 the concerns of local people, for example costs, expectations, dangers and misinformation,174 also needed to be addressed.
Setting-based approaches included focusing on nurseries and childcare facilities174 as well as on schools174,219–224 to promote healthy eating and increase fruit and vegetable intake in children through activities and education; these approaches were found to be particularly effective for young women. 224 Workplaces were also noted as being settings that could effectively promote fruit and vegetable intake and fat reduction222,225,226 as they could accommodate incentive schemes and education and promotion programmes. 174 Religious settings227 such as churches,226 primary care settings222 and health-care settings for older adults (aged > 50 years)183 were all recommended as effective sites to deliver interventions. Sites located in the community222,228 and within the family174,229 were also felt to be effective in making changes to dietary behaviours.
Techniques such as counselling,129,218,230 whether face-to-face228 or by telephone,186,228,231 were shown to be effective. A dose-dependent effect was observed for healthy eating counselling by telephone. 186 Counselling contact can be one-to-one232 or group based211,229,232 and can be intensive, involving more contacts,233 representing both social229 and ongoing support. 174 Goal setting213 advice,234 particularly when tailored to individuals,174 was noted as being helpful. Motivational interviewing was recommended, but only alongside education. 235
There were few suggestions on who should be the provider of healthy eating interventions. The guidelines did recommend, however, that parents and carers174,220,233,236 should be involved in planning school-based interventions174 and family-based interventions,112 although there was no definitive evidence that this was effective.
In terms of resources, monetary incentives to influence purchases and consumption behaviours,237 along with education,129,218,228 written material211,232 and perhaps computer-tailored interventions,207,228 were suggested as being effective for changing behaviours associated with healthy eating. Clear messages,233 particularly about people’s risk of chronic disease,232 were also thought to be effective. Several reviews suggested that, in general, interventions delivered to those who were at risk of, or diagnosed with, disease were more effective than those delivered to low-risk populations. 229–232
As with physical activity interventions there was a lack of long-term evidence for many of the included healthy eating interventions, with few studies examining behaviour change for longer than a year. Studies of longer duration had difficulties with participants maintaining changes in behaviour. 222 Furthermore, for changes in diet and healthy eating, the actual changes in lifestyle were often quite small,212 for example one review reported an average increase in fruit and vegetable intake of 0.6 servings a day229 and another review reported a change from seven effective studies ranging from +0.3 to +1.0 servings a day. 220 Whether or not these changes are sufficient to prevent disease remain unclear.
Discussion
An examination of the summary tables (see Tables 3–6) and evidence statements (see Appendix 10) revealed that there was a difference in the strength of evidence for interventions for smoking cessation in the general population compared with evidence for interventions to increase physical activity or improve healthy eating. Guidance on smoking cessation interventions was on the whole reasonably well developed, described and supported by the systematic review literature (particularly in relation to pharmacological treatments). In contrast, interventions for promoting physical activity and improving healthy eating in the general population were less likely to be underpinned by robust evidence.
Overall, smoking cessation interventions were well represented in the categories of resources, providers and techniques, which suggests that we have strong evidence available on the resources that work and which can be delivered easily, with a range of defined providers of those resources. These three categories reflect individual-oriented ‘strategies and activities’ in which a provider and resource (usually pharmacotherapy) are employed to help an individual achieve cessation. Once successfully smoke free, that is, abstinent for 3 years post intervention,155 individuals are unlikely to relapse, although they may always be vulnerable to smoking. Therefore, it appears that relatively short-term, didactic and resource-dependent interventions can successfully affect behaviour change for smoking cessation.
On the other hand, evidence of effectiveness for increasing physical activity and improving healthy eating were featured more prominently under the ‘strategies and activities’ categories of setting based, techniques and environment, with less definitive evidence underpinning recommendations on what resources can be delivered easily and who would be best positioned to provide them. These categories, in contrast to individual-oriented ‘strategies and activities’ observed for smoking, are relatively more immersive and interactive, and may reflect the nature of the health issues themselves. Engaging in physical activity and improving healthy eating present lifelong challenges, and may require immersion in health-enhancing settings and environments along with techniques that engage the individual to make and maintain healthy behaviour changes, through educational but also experiential and practical opportunities.
These findings could also be related to the nature of the health issue, whereby smoking cessation represents the reduction of a particular behaviour, and increasing physical activity represents the addition of behaviours. Meanwhile, improving healthy eating can involve both reduction and addition behaviours. These characteristics appear to relate to intervention design, with interventions for a reduction of a behaviour, such as smoking cessation, mapping onto ‘strategies and activities’ generally undertaken at an individual level and, conversely, the ‘strategies and activities’ for promoting the addition of behaviours, such as increased exercise or fruit and vegetable intake, generally undertaken at a community or population level. 238
The work undertaken in this chapter has allowed us to investigate our underpinning rationale, that is, to focus on adapting those interventions for which we have the strongest evidence of effects in the general population. If we pursued this line of thinking we would predominantly target individual-level interventions for smoking cessation and, to an extent, setting-based, interactive interventions for increasing physical activity and improving healthy eating. A blind pursuit of this task would, however, be at odds with one of the key recommendations to emerge from our launch user engagement conference (see Chapter 3). Overwhelmingly, our research users highlighted the need to pay more attention to environmental and structural-level interventions.
The work undertaken in this chapter to identify effective interventions has also illuminated how six different categories of ‘strategies and activities’ may have potentially varying scope for adaptation. For example, governmental policy and whole population-level environmental interventions can represent immersive conditions, which may be difficult to adapt for specific population groups. Within these immersive conditions, then, it is essential to consider possible differential impact and, in response, to have a clear commitment to ensuring equality – these then may involve more targeted individual- or community-level modifications. On the other hand, organisational policy, setting-based interventions, and techniques can provide more interactive conditions to catalyse behaviour change. These interventions may be relatively more readily available to modify and cater for specific population groups, therefore providing a much greater scope for adaptation. Providers are also more amenable than policy or environmental conditions. Through matching, for example, or utilising lay health workers and peer providers, an intervention can be made more acceptable for a particular ethnic minority group. Lastly, resources have perhaps the greatest scope for adaptation, as they involve the relatively straightforward (but not always) task of, for example, translating educational materials or piloting the appropriate incentives for a particular population. The exception for the resources category is of course pharmacotherapy, although engagement of the population and the acceptability of drug treatment remain areas for consideration for modification within pharmacotherapy.
Challenged by these initial findings and feedback, we developed a model (Figure 5) to begin thinking about the relationship between intervention ‘strategies and activities’, the levels of health promotion interventions best suited to affect behaviour change and the scope for adaptation for ethnic minority populations.
FIGURE 5.
’Strategies and activities’ in health promotion interventions and their relationship to intervention level and scope for adaptation.
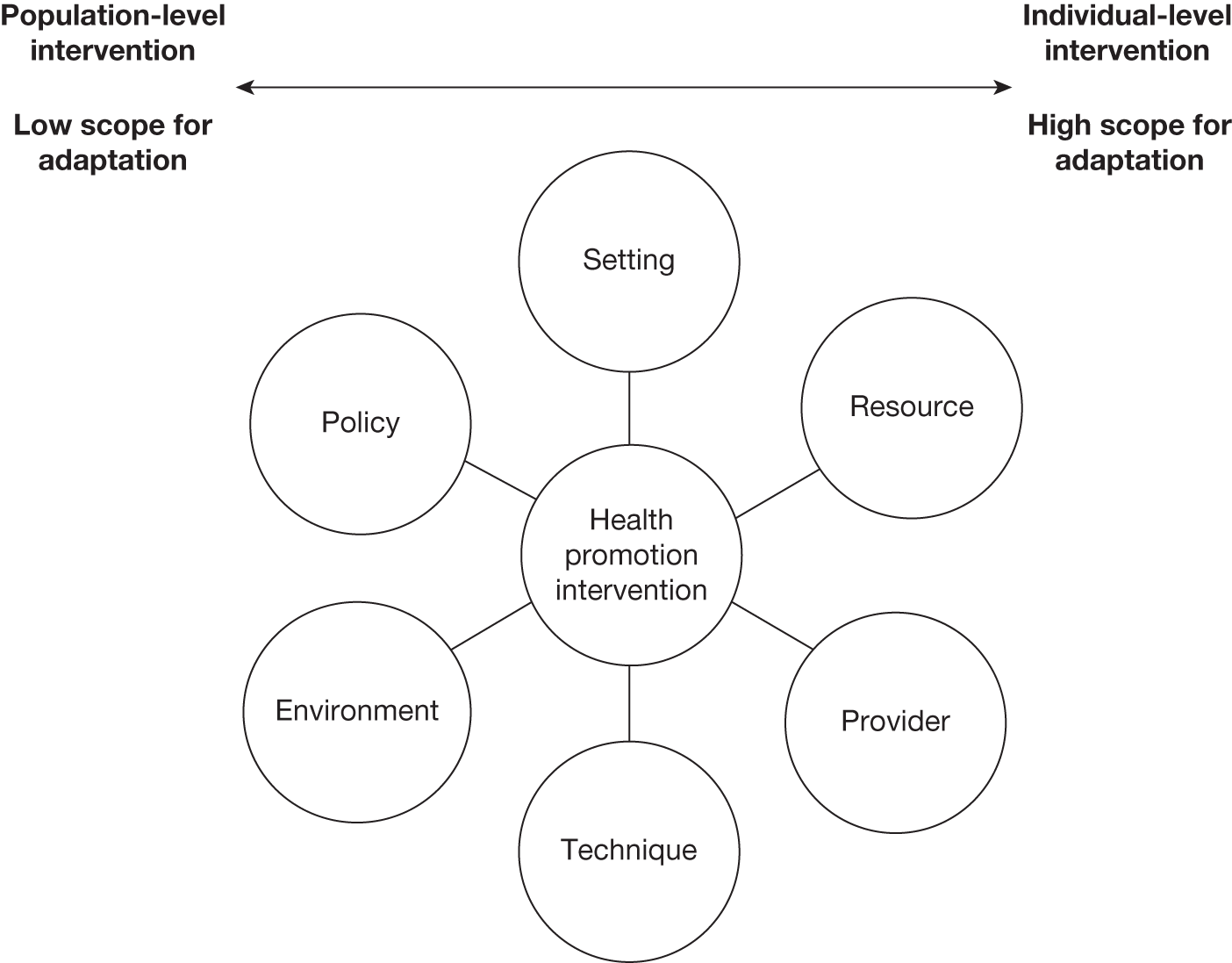
By distinguishing between different health promotion intervention ‘strategies and activities’ according to the six categories, while at the same time recognising their overlapping and additive nature, we were able to demonstrate their distribution across the differing levels of interception – from individual to population level. We were also able to identify where there were gaps in the literature and where, in particular, evidence needs to be pursued. For example, noticeably absent were designated specialist providers to deliver physical activity and healthy eating interventions. Guidelines and systematic reviews may recommend who should be involved, such as parents and carers, but more clarity is needed on who should be delivering these interventions. There was also a lack of long-term studies for physical activity and healthy eating interventions that were able to demonstrate changes in behaviour that are sufficient in magnitude and sustained to the extent that they can meaningfully alter risk factors for disease. Although evidence for effective interventions for increasing physical activity and improving healthy eating is, as yet, wanting, the patterns observed possibly point to the need for different approaches for different health issues.
Strengths and limitations
The four summary tables (see Tables 3–6) succinctly summarise the current evidence available for effective ‘strategies and activities’ for behaviour change in general, smoking cessation, increasing physical activity and improving healthy eating. In the systematic reviews we searched for compelling evidence of effectiveness that had not yet found its way into the guideline literature; in contrast, we deliberately excluded interventions that have not yet accumulated a sufficient body of evidence of effect. Thus, for example, we excluded a review of nicotine vaccines239 and cytisine240 for smoking cessation, a review of eHealth interventions for physical activity and/or diet241 and a review of clinical counselling for increasing physical activity. 242 The summary tables have therefore captured the most up-to-date and relevant evidence for smoking, physical activity and healthy eating health promotion interventions.
Because of the large volume of evidence identified, and the fact that this was one part of a much larger mixed-methods study (see Chapter 2), we were unable independently to quality appraise each guideline and systematic review and instead relied on the quality control measures in place for producing and publishing guidelines and systematic reviews. When reported we extracted whether or not the quality of the evidence and the recommendations was appraised and the appraisal tool used (see Appendix 10). To an extent this approach represented a limitation. In the case of contradictory evidence statements (e.g. if an intervention was reported as effective in one systematic review and not effective in another), we were unable to investigate the reasons underpinning this difference in evidence. In such cases we opted to describe both evidence statements.
Our review of guidelines was limited to UK-based bodies, which is a further potential limitation. The above described ‘strategies and activities’ thus provide a detailed and comprehensive overview of the UK recommendations; however, as the UK guidelines draw on international evidence and because, in addition, we identified international systematic reviews, the state of the evidence described should also on the whole reflect the international evidence base in relation to these three areas of enquiry. In the absence of also interrogating guidelines from other countries (which we were unable to do because of resource constraints), however, we cannot be sure.
The definition of health promotion adopted for this study111 was adapted to produce the six categories of ‘activities and strategies’; this has a potential limitation in that the categories are overlapping and not mutually exclusive. In addition, not all interventions could easily be assigned directly to a level of health promotion intervention. For example, policies can be implemented at the organisational or population level and providers could deliver interventions individually or in groups. In support of this approach these categories are placed across a spectrum, from individual- to population-level ‘strategies and activities’, which loosely corresponds to their scope for adaptation. Despite these potential limitations it was overall still helpful to have an organising framework to describe these strategies and actions to allow the examination, and cross-comparison, of such a large and diverse body of evidence.
Conclusions
In this review of UK guidelines and international systematic reviews we have assessed and aggregated the evidence for interventions for smoking cessation, increasing physical activity and improving healthy eating, and created a summary framework of effective interventions as a potential basis for those interested in developing adapted health promotion interventions for ethnic minority populations. The strength of evidence on interventions for smoking cessation in the general population was greater than that on interventions to increase physical activity or improve healthy eating. Examining these effective interventions according to the six categories (i.e. environment, policy, setting based, technique, provider and resource) has helped to clarify which ‘strategies and activities’ have accrued more evidence and which areas remain sparsely populated. These categories, although overlapping, reflect levels of health promotion intervention from individual to population level and demonstrate important relationships between the health topic and the level and nature of the intervention.
Overall, there was considerably more evidence of clinically important effects for individual-centred pharmacologically based smoking cessation interventions and approaches aimed at increasing access to and use of these treatments, but only moderately supportive guidance for setting-based immersive and interactive interventions for increasing physical activity and improving healthy eating. In terms of health promotion interventions for ethnic minority populations, we have argued that there is perhaps less need and scope for adaptations of individual-focused drug interventions than of the more provider- and setting-based approaches to improve access to these drugs. Similarly, there is considerable scope for adaptation of population-level and setting-based interventions of the kind that are being studied in the context of promoting physical activity and healthy eating. We further explore the extent to which these guidelines and systematic reviews provide clarity on the effectiveness of these interventions for ethnic minority populations in the following chapter (see Chapter 5) and consider in more detail how suited various ‘strategies and activities’ of health promotion interventions are for adaptation, for ethnic minority populations, and how this may influence prioritisation in terms of implementation and further research in Chapter 8.
Chapter 5 Consideration of ethnicity in guidelines and systematic reviews
Abstract
Background
A number of interventions have been developed to aid smoking cessation, promote physical activity and improve healthy eating for use in the general population. The effectiveness of these interventions in improving health outcomes for ethnic minority populations is, however, unclear.
Objectives
We sought to assess to what degree ethnic minority populations are considered within the evidence base for smoking cessation, physical activity and healthy eating health promotion interventions known to be effective in populations at large.
Methods
Two reviewers independently searched UK guidelines and international systematic reviews of interventions for smoking cessation, increasing physical activity and improving healthy eating. Guidelines were identified from the Clinical Evidence, National Institute for Health and Clinical Excellence (NICE) and Scottish Intercollegiate Guidelines Network (SIGN) databases. Systematic reviews were identified from The Campbell Collaboration, The Cochrane Library, the Database of Abstracts of Reviews of Effects (DARE) and the National Institute for Health Research Health Technology Assessment (NIHR HTA) database. We searched the guidelines and systematic reviews using predefined terms relating to ethnicity. Two reviewers independently extracted the statements made in relation to ethnicity, initially grouping these according to shared meaning and/or concept; these data were then thematically analysed.
Results
We identified 15 guidelines and 111 systematic reviews that fulfilled our eligibility criteria. A total of 12 (87%) guidelines and 66 (59%) systematic reviews had one or more terms relating to ethnicity. All 12 of these guidelines containing key terms made statements relating to ethnicity; however, only 41 of the 66 systematic reviews with key terms made any informative statements relating to ethnicity and none of the systematic reviews conducted subgroup analyses by ethnic group. Five main themes emerged from the thematic analysis of statements: (1) acknowledging diversity; (2) identifying evidence gaps; (3) observing differential effects of interventions; (4) taking action to adapt interventions; and (5) improving research, reporting and analysis.
Conclusions
UK guidelines and international systematic reviews provided little specific guidance with regard to which health promotion interventions are effective (or ineffective) for ethnic minority populations or how interventions with proven effectiveness in the general population can be adapted to be effective for ethnic minority populations. There is a need to consider more explicitly the evidence in relation to ethnic minority populations in the context of guidelines and systematic reviews of key health promotion interventions.
Introduction
A key component of our work was first developing a detailed appreciation of which health promotion interventions are of proven effectiveness for the general population (see Chapter 4). 9 We can in turn build on this understanding to develop a theoretically informed and empirically grounded approach to promoting the health of ethnic minority populations. 9 Our study has focused on identifying and assessing the evidence for effective interventions promoting smoking cessation, increasing physical activity and improving healthy eating (see Chapter 1). Evidence from guidelines, and to a lesser extent systematic reviews, usually represents the first point of access for such information on effectiveness, which increasingly underpins key decisions in health-care delivery and prioritisation. As such, it is imperative that guidelines and systematic reviews present not only evidence of effect for the general population, but also evidence of differential effects by age, gender, socioeconomic status (SES), disability and ethnicity, as these other subgroupings are likely to be associated with differential effectiveness of an intervention. In this chapter we report on our evaluation of UK guidelines and international systematic reviews to assess the degree to which ethnic minority populations – specifically African-, Chinese- and South Asian-origin populations – were considered in the evidence.
Research questions
The research question arises from Phase 1B of our study (see Chapter 2):
-
To what degree is ethnicity considered within UK guidelines and international systematic reviews on effective health interventions for smoking cessation, increasing physical activity and improving healthy eating?
Methods
The method for the identification of the guidelines and systematic reviews that we drew on is outlined in Chapter 4 (see Methods). To explore the consideration of ethnicity in UK guidelines and international systematic reviews reporting on effective interventions for smoking cessation, increasing physical activity and improving healthy eating for the general population we searched the identified guidelines and systematic reviews for any evidence statements specifically addressing ethnicity. In addition, we searched the systematic reviews for subgroup analysis by ethnic group.
We searched the full text either electronically or by eye if electronic versions were unavailable using a set of predefined key terms16 relating to our ethnic groups of interest, adopting a definition of ethnicity that included race, ethnic origin or nationality. 22 The key terms used were as follows (the asterisk indicates the truncated version to encompass variations of the term, e.g. searching for Cultur* would include culture, cultures and cultural):
-
African
-
Afro*
-
Asian
-
Bangladeshi
-
Black
-
Caribbean
-
Chinese
-
Cultur*
-
Ethnic*
-
Indian
-
Minorit*
-
Rac*
-
Pakistani
-
South Asian.
The data extraction process was independently undertaken by two sets of researchers (SK and JJL for guidelines and SK and UY for systematic reviews) who recorded on the customised data extraction form (see Appendix 9) whether a guideline or systematic review included any of the key terms. The text was scrutinised and the details of the population(s) studied were recorded, including the methods used to assess ethnicity, as well as any recommendations made. A third reviewer (ED) checked for accuracy of extracted information. The systematic reviews were subsequently categorised as having either undertaken subgroup analyses or not; if they had, we aimed to record whether or not the intervention was more/equally/less likely to be effective for the ethnic minority population than for the general population considered. Evidence statements pertaining to ethnicity were recorded by ED, JJL, UY and SK. The evidence statements relating to ethnicity extracted from the guidelines were grouped according to shared meaning and/or concept and given a generic statement to illustrate this shared meaning and/or concept. The generic statements were then further categorised under themes. Evidence statements from the systematic reviews were related to these generic statements where applicable.
Results
Through our searches we identified 15 relevant UK guidelines and 2399 international systematic reviews, which were assessed for eligibility. In total, 15 guidelines and 111 systematic reviews met the inclusion criteria (see Table 2).
Figure 6 illustrates the screening process for key terms. The evidence statements from the UK guidelines are summarised in Table 7 while the evidence statements from the international systematic reviews are included in Appendix 11.
FIGURE 6.
Identification of key terms and statements on ethnicity in UK guidelines and international systematic reviews. CE, Clinical Evidence.
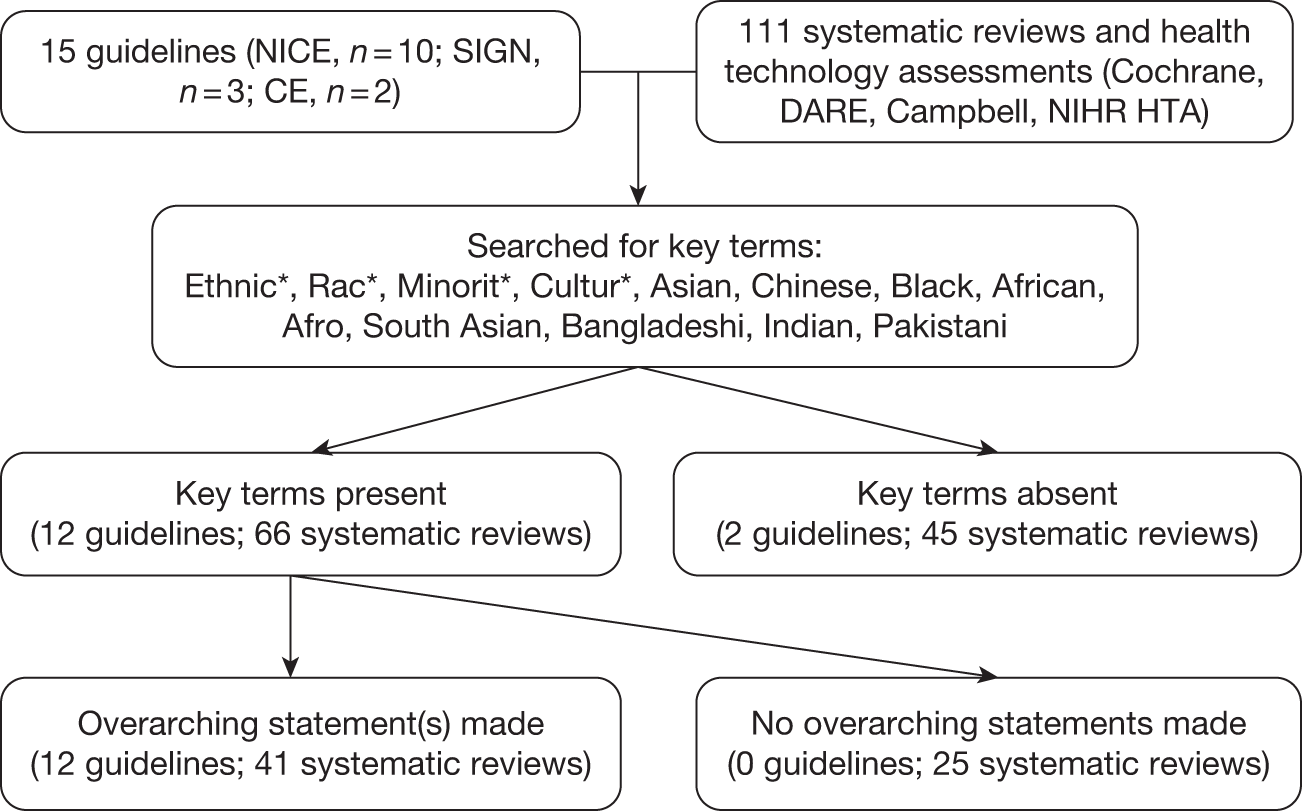
| Source | Evidence statements |
|---|---|
| NICE | |
|
PH1 Brief interventions and referral for smoking cessation in primary care and other settings139 2006 |
Ethnic*, Minorit* Differences in risk between diverse populations. Despite a reduction in smoking prevalence, some groups such as ethnic minority groups and deprived communities retain a high prevalence Smoking cessation advice and support should be targeted to high-risk population groups including ethnic minorities and focus on their needs There are unique risk behaviours for some ethnic minority groups, such as chewing tobacco, which are not provided for by current service provision and need to be addressed |
|
PH10 Smoking cessation services in primary care, pharmacies, local authorities and workplaces, particularly for manual working groups, pregnant women and hard to reach communities120 2008 |
Ethnic*, Minorit* NHS Stop Smoking Services should target ethnic minority communities Ensure that smoking cessation interventions are tailored and language appropriate for ethnic minority communities – both for individual services and public education and communications campaigns Ethnic minority and disadvantaged groups should be treated by smoking cessation services at least in proportion to their representation in the local population of tobacco users |
|
PH13 Workplace health promotion: how to encourage employees to be physically active176 2008 |
Ethnic* Queried the differential effect of interventions according to contexts including ethnicity Lack of evidence of how workplace interventions for physical activity are influenced by wider contexts such as ethnicity |
|
PH6 Behaviour change at population, community and individual levels112 2007 |
Ethnic*, Minorit*, Cultur* Awareness that different groups (including ethnicity) react differently to health promotion messages, e.g. ‘fear’ messages Need to target and tailor interventions to the needs of populations to be effective, with the goal of health equity Service user views may be helpful when planning interventions and needs assessment is a method to gather information to inform the appropriate development and tailoring of interventions The cultural acceptability and value of behaviours varies according to contexts, including ethnicity, and it is important not to stereotype or stigmatise groups of people because of these differences; working with communities and addressing prejudice and discrimination in professional practice is recommended Some ‘negative’ health behaviours may provide positive benefits (psychological, social or physical) for individuals in certain social and cultural contexts and these contexts, plus economic considerations, must be taken into consideration to develop effective interventions (account for diversity) Lack of high-quality evidence (RCTs) and cost-effectiveness data for interventions concerning specific subgroups including ethnic groups and a lack of research that considers health inequalities in relation to cultural differences Recommend research always takes ethnic minority groups into consideration and that there is improved reporting on differences in access, recruitment and uptake according to contextual variables including ethnicity Recommend research that takes into account the social and cultural contexts of behaviour and behaviour change, including SES, income levels, environmental characteristics of neighbourhoods and work-related factors |
|
CG43 Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children174 2006 |
Ethnic*, Minorit*, Cultur*, Asian Black Recommend tailoring of advice for different populations and vulnerable groups, particularly black and minority ethnic groups, and considering barriers (such as cost, personal tastes, availability, time, views of family and community members) Engagement with communities is important to assess barriers to physical activity and healthy eating, and these barriers may vary according to different contexts, including ethnicity, such that specific needs assessment is required Advice, treatment and care should be non-discriminatory, culturally appropriate and accessible to people who do not read or speak English Acknowledge that some ethnic backgrounds may be at greater risk of obesity and have different beliefs and attitudes regarding weight and weight management Information should be delivered in the appropriate language and be conscious of people’s culture and ethnicity Lack of evidence for multicomponent obesity interventions for particular subgroups including ethnic minority groups Recommend future research and the collation of data that consider the effectiveness of interventions for different subgroups, including how it varies by ethnicity |
|
PH8 Promoting and creating built or natural environments that encourage and support physical activity173 2008 |
Ethnic*, Minorit*, Cultur* Shortage of evidence on the differential effectiveness of environmental interventions for physical activity for different groups, including how effectiveness varies with ethnicity and culture, and therefore it is unclear how these interventions affect health inequalities. Must take into account health inequalities when implementing recommendations Cycling interventions in both urban and rural areas can be effective in increasing participation in cycling and could be considered with modification for cultural issues |
|
PH2 Four commonly used methods to increase physical activity: brief interventions in primary care, exercise referral schemes, pedometers and community-based exercise programmes for walking and cycling79 2006 |
Ethnic*, Minorit*, Cultur*, Asian, Chinese, Bangladeshi A difference in participation in physical activity between ethnic groups was reported by the health of ethnic minority groups survey – it found that South Asian and Chinese people of both genders were much less likely to participate in physical activity of any kind (whether it was sport and exercise, walking, heavy housework or DIY). Bangladeshi men and women were the most inactive, being almost twice as likely as the general population to be classified as sedentary There are gaps in the evidence for interventions for physical activity for effectiveness and cost-effectiveness, long-term outcomes and the differential effect of interventions according to varying contexts including ethnicity When developing services and infrastructure for the promotion of physical activity, particular attention needs to be given to the needs of disadvantaged and hard-to-reach communities, including ethnic minority groups Physical activity is an important factor in a number of government Public Service Agreement targets. These include targets to tackle obesity, increase cultural and sporting opportunities and improve the quality of the built environment |
|
PH17 Promoting physical activity, active play and sport for pre-school and school-age children and young people in family, pre-school, school and community settings172 2009 |
Ethnic*, Minorit*, Cultur*, Rac*, Asia*, Chines*, Black, India*, Bangladesh*, Pakistan*, Afric* Levels of physical activity vary according to many contextual factors including ethnicity. There was little reported difference between boys and girls in the main ethnic minority group in terms of participation in sports and exercise. Bigger differences were reported between Indian, Pakistani, Bangladeshi, and Chinese children when compared with the general population in terms of participation in sports and exercise. Active consultation is required to determine the best method of delivery of messages including the appropriate language for different groups (including different ethnic groups, among many other variables) Actively involve all children and young people, including those from different socioeconomic and ethnic minority groups, in physical activity initiatives; all groups should have the opportunity to be involved Ensure physical activity facilities are suitable for all children and young people, particularly those from ethnic minority groups with specific cultural requirements Recognise the need to tailor to individuals, including being sensitive to culture and gender issues, yet also encourage people to explore a variety of options for involvement in physical activity Lack of evidence on how to engage children and young people in physical activity who are the least likely to be active, including children and young people from certain ethnic minority groups or traveller and refugee communities Need to determine the most effective and cost-effective interventions to increase and maintain increased levels of physical activity in subgroups of children and young people (taking account of age, culture, ethnicity, disability, gender, geographic area, e.g. inner city, urban, rural, and religion or SES, and giving particular attention to disadvantaged groups) Establish continuing professional development programmes for people involved in carrying out physical activity interventions to assist them in understanding practical issues and barriers to involvement, including cultural appropriateness Evaluations of physical activity interventions should be undertaken regularly and should measure uptake by different groups, including people from different ethnic backgrounds |
|
PH5 Workplace health promotion: how to help employees to stop smoking127 2007 |
Ethnic*, Minorit*, Cultur* Intervention materials may be aimed at a particular subgroup of the population, including certain ethnic groups A tailored intervention study in the USA reported effectiveness in promoting behaviour change in a working-class multiethnic population There are gaps in the evidence and research is required to uncover what the most effective and cost-effective interventions are for smoking cessation for different sectors of the workforce, including ethnic minority groups |
| SIGN | |
|
SIGN 69 Management of obesity in children and young people200 2003 |
Ethnic*, Cultur*, African* Interested in differential risk among ethnic populations in the UK Evidence searched for ‘culture’ only in relation to the UK Studies that included African American or Far Eastern patients perceived not to apply or were not relevant to the Scottish population |
|
SIGN 8 Obesity in Scotland236 1996 |
Ethnic*, Indian* Age-specific BMI cut-offs provided in the annex for ethnic-origin UK children Increased likelihood of abdominal fat deposits with weight gain, which increased susceptibility to glucose intolerance, diabetes and CHD over that of Caucasians |
|
SIGN 97 Risk estimation and the prevention of cardiovascular disease137 2007 |
Ethnic* There are differences in the baseline population risk for different ethnic groups Ethnicity should be considered as a risk factor in CVD risk assessment Scotland’s ethnic minority population is at present small but increasing (ethnic minorities represent 2% of the 5 million population of Scotland) INTERHEART study reported on nine risk factors for CVD and observed that risk was consistent for men and women by ethnic group Current risk prediction algorithms are unable to accurately predict risk profiles for different ethnic groups and cultures and may underpredict risk in Chinese populations Mentions that risk prediction tools including waist measurement and BP may require different cut off points for different ethnic groups ASSIGN CVD prediction tool includes social deprivation and family history as a proxy for ethnic susceptibility; however, tool not validated and may underestimate risk for South Asians, for example Prevalence of smoking or effectiveness of interventions for ethnic minorities have not been reliably measured in Scotland; therefore, report on research from England No evidence found for relevant interventions with ethnic minority groups A mapping exercise identified some evidence of target smoking cessation materials but, in general, tobacco services were not attracting ethnic minority populations Optimal dose and intensity of physical activity has not been addressed in terms of how it relates to or varies for different populations including ethnic minority groups |
Of the 15 guidelines identified, 12 contained one or more key search terms and 12 made recommendations or evidence statements relating to ethnicity (see Table 7). Of the 111 systematic reviews identified, 66 (59%) contained one or more key search terms; however, 41 (62%) of the 66 systematic reviews made evidence statements relating to ethnicity (see Appendix 11). The remaining 25 systematic reviews contained the key term without any further information. None of the 66 systematic reviews conducted subgroup meta-analysis to pool the ethnic-specific results and assess differential effect sizes according to ethnicity.
Themes relating to ethnicity in UK guidelines and international systematic reviews
The evidence statements from the 12 guidelines were grouped under 16 generic statements (Table 8). From the generic statements, five themes were identified and these are summarised in Box 4. No new themes emerged from the evidence statements extracted from the systematic reviews that were not already encompassed under the five themes. Table 8 therefore represents these two sources of evidence.
Theme 1: Acknowledging diversity
Theme 2: Identifying evidence gaps
Theme 3: Observing differential effects of interventions
Theme 4: Taking action to adapt interventions
Theme 5: Improving research design, analysis and reporting
| Generic statements | Themes |
|---|---|
| Importance of ethnicity in health | 1. Acknowledging diversity |
| Awareness of differential risks for/rates of disease and unique health risks | |
| Awareness of differing health beliefs, values and attitudes | |
| Gap in/lack of evidence on the effectiveness of interventions according to ethnicity/comparing different ethnic groups | 2. Identifying evidence gaps |
| Gap in/lack of evidence on cost-effectiveness of interventions for ethnic minority populations | |
| Awareness of varying effectiveness for recommendations and interventions according to ethnicity | 3. Observing differential effects of interventions |
| Some interventions and materials reach ethnic minority populations and demonstrate some effect or no clear evidence of effect | |
| Tools to assess risk should consider risk in terms of ethnicity | |
| Awareness of a need to adapt interventions and services for ethnic minority groups and that adaptated interventions may be effective for behaviour change | 4. Taking action to adapt interventions |
| Ensure interventions are appropriately adapted for psychological, social, cultural and economic determinants | |
| Examine how gender, age and SES intersect with ethnicity | |
| Ensure that interventions are appropriately adapted by working with communities and families | |
| Address inequalities and avoid discrimination and stereotyping | |
| Recommend better representation of ethnic minority populations in research, and more research, because of increasing ethnic minority populations | 5. Improving research design, analysis and reporting |
| Recommend more syntheses of existing data and trends involving ethnic minority populations | |
| Recommend better data collection and reporting of ‘differences in access, recruitment and uptake according to ethnicity’ |
Theme 1: acknowledging diversity
The guidelines and systematic reviews recognised ethnicity as an important factor in health promotion interventions. 215 There was acknowledgement of the variation in disease patterns and risk factors137,200,221,227 between different ethnic groups,137,200 for example smoking,137,139 stress,137,215 physical inactivity79,173 and diseases such as obesity174 and cardiovascular disease,221 and awareness that some health issues may in fact be unique to certain ethnic groups. Diversity in beliefs, values and attitudes was also identified, for example perceptions of weight and overweight,174 and consequently the need to involve ethnic groups in formative work for interventions. 179
Theme 2: identifying evidence gaps
The second theme related to gaps in the evidence base for health promotion interventions for ethnic minority populations. These gaps were discussed in terms of a lack of high-quality studies and randomised controlled trials79,112,137,172–174,204 and a lack of studies examining whether or not intervention strategies known to be effective in the general population are also effective for ethnic minority populations (e.g. incentives201,237 and workplace127,176 settings). 188,222 There was poor-quality analysis and reporting of studies involving ethnic minority populations. 215 There were also studies that did not report results according to ethnic subgroups223 or which statistically adjusted for ethnicity but did not analyse their results according to ethnicity. 209,219 Not surprisingly, considering the general lack of quality studies, there was also a major gap in cost-effectiveness evidence reported in the guidelines. 112,170
Theme 3: observing differential effects of interventions
There was awareness of the differential effects of interventions on different ethnic groups and also across ethnic groups in various settings112,118,121,172,177,178,181,182,204,211,214,215,223,230,232 and contexts (e.g. different countries200). How recommendations for practice may impact on the health of specific ethnic minority groups and how effective interventions are for the health of ethnic minority groups were generally not known. 112,172,182,204 Even within those populations for which significant evidence has accrued, such as within the African American population in the USA, there was still a lack of clear evidence despite interventions and/or materials reportedly demonstrating increased reach and better utilisation. 172 Some guidelines and reviews presented evidence of interventions carried out in ethnic minority populations and there was mixed effectiveness found for these interventions, with no definitive conclusions reported. 136,172,201,232 It was recommended that, in addition to interventions, there may also be differential effectiveness of the tools used to assess risk of ill-health and that ethnicity should be taken into consideration when assessing risk (e.g. body mass index,236 waist circumference137 and blood pressure137 measurements) to avoid inaccurate predictions. 137
Theme 4: taking action to adapt interventions
There was also awareness that action needed to be taken to address the gaps in evidence and to adapt interventions139,211,229 and services120 to be more appropriate for diverse populations and to produce interventions and services that are equally effective for all populations. Adaptations were discussed for ethnic minority groups182,210 (e.g. language120,172,174) with the evidence suggesting that adapted interventions may be effective for behaviour change. 127,136,153,183,189,198,207,216,218,227,228,229 In addition to adapting for ethnicity, the guidelines and reviews suggested that interventions should examine how other factors such as gender,172,179 age172 and SES intersect with ethnicity112,201 to influence health outcomes and affect health intervention successes. They should also adapt for psychological, social, cultural and economic determinants, this recognising the effects of the wider contexts of health in relation to health promotion for ethnic minority populations. 112,172,173,176,217,232 Avoiding discrimination and stereotyping112,172 were other important considerations that were raised. The guidelines proposed that a way to ensure that interventions were appropriately adapted was by working with communities and families (e.g. conduct initial needs assessments, address barriers). 79,112,122,172,174,227
Theme 5: improving research design, analysis and reporting
Improved representation of ethnic minority populations in research, along with more well-designed research studies, was recommended as a response to the observed increasing ethnic diversity. 120,218,221,223,229,237 It was suggested that research should focus on filling in the gaps in evidence on, for example, effectiveness of physical activity and dietary counselling delivered in health-care settings. 183 The need for research to address past and current levels of under-representation of, for example, African Americans and Asian Americans218 in studies on physical activity199 and healthy eating223 was also emphasised. It was recommended that ethnic minority groups should be proportionally represented in research in terms of their risk or rate of disease stemming from, for example, tobacco use. 120 Furthermore, better collection182 and reporting214,215,223 of interventions in relation to ‘differences in access, recruitment and uptake according to . . . ethnicity’112 were recommended. Finally, more syntheses of existing data for ethnic minority health were also recommended,174,180 making use of the existing empirical studies and providing stronger evidence for researchers and health practitioners on which to base future interventions.
Discussion
An in-depth analysis of national guidelines and systematic reviews developed for populations in general has not contributed substantially to our knowledge base of which health promotion interventions work for ethnic minority populations for smoking cessation, increasing physical activity or improving healthy eating. Most guidelines (12/15) made statements regarding ethnicity whereas approximately one-third of the systematic reviews (41/111) contained such statements, which suggested that the other two-thirds did not factor ethnicity into their review process.
When ethnic minority groups were mentioned, a lack of reporting and synthesis of data for these groups further contributed to a shortage in evidence of effectiveness for ethnic minority populations, for example there were no subgroup analyses of the effects of the intervention according to ethnicity identified in these high-level syntheses of evidence. We were thus limited in our ability to detect whether there were potential differences in intervention effectiveness attributable to ethnicity or whether adapted interventions were effective.
Summarising the evidence statements provided a starting point to make sense of the guidelines and systematic reviews. The statements acknowledged diversity within populations and differential effects of interventions for different ethnic groups. They also identified gaps in our knowledge base with regard to which interventions are effective for ethnic minority populations and that action should be taken to adapt interventions. Lastly, they recommended improved research design, analysis and reporting as a response to the gaps in the evidence (see Table 8).
A search for evidence pertaining to ethnic minority populations in guidelines and systematic reviews for the general population has demonstrated that there is as yet little clarity from the existing body of evidence to guide those planning and implementing health promotion interventions for diverse populations. We hypothesise that there is a gap in the cycle of evidence in translating empirical evidence, of the health, lifestyle and life circumstances of ethnic minority populations, into national guidelines (Figure 7).
FIGURE 7.
Cycle of evidence for health promotion interventions.
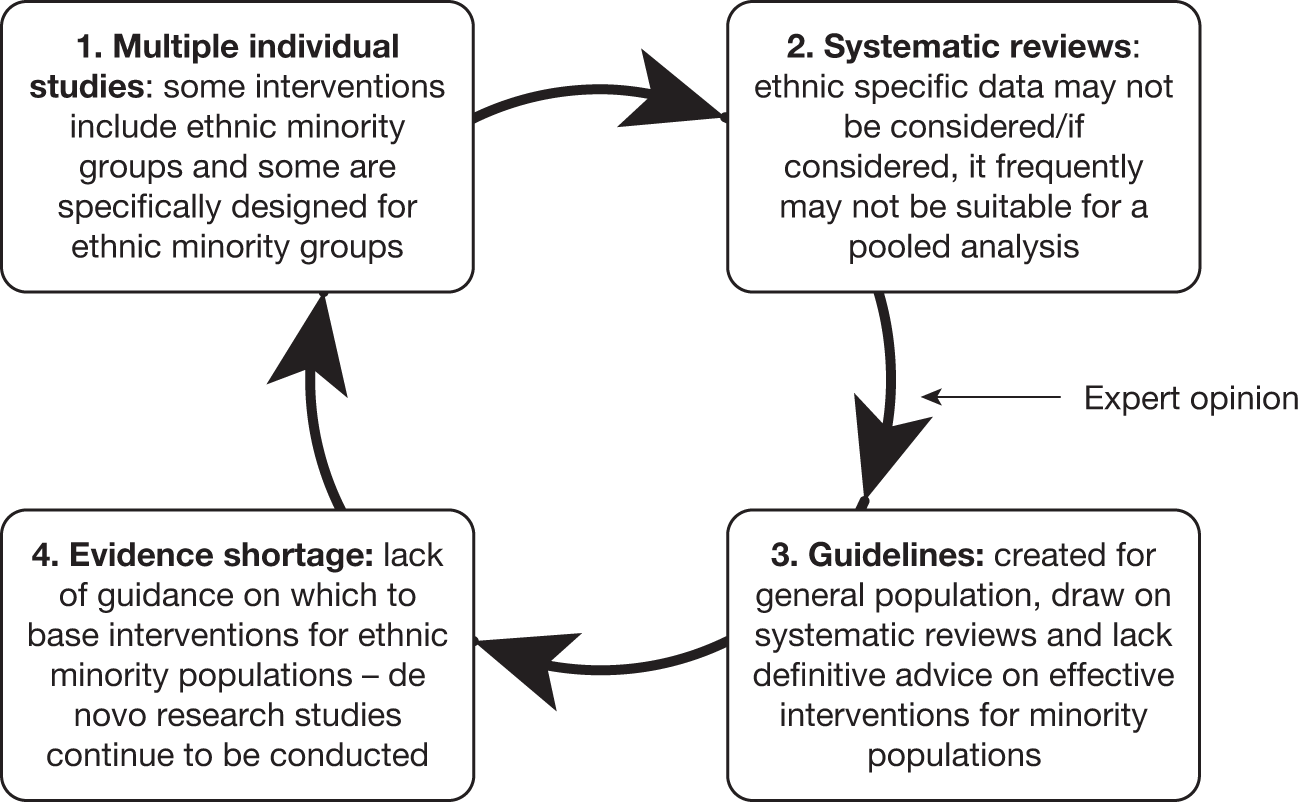
Currently, individual intervention studies, some that may have included ethnic minority groups and others that were specifically designed for ethnic minority groups, may be identified for inclusion in systematic reviews (Step 1 in Figure 7). However, these studies may be unavailable or are possibly not considered of importance to the review question at hand and are thus excluded (Step 2). Even when data from these studies are analysed, they may be discounted from the systematic review for reasons of study quality or other issues, including, for example, the diversity of ethnic groups, the small number of ethnic minority participants and different outcome measures used, all of which would prevent the pooling of ethnicity-specific data. Meanwhile, guidelines generally draw on systematic reviews as their main source of information and supplement this with expert opinion and consensus (Step 3). The latter process may introduce greater consideration of ethnicity in guidelines than was apparent in the systematic reviews drawn upon. Guidelines, for example, acknowledge diversity and research gaps and propose that these issues be addressed (see themes identified in Box 4). However, because of the lack of systematic review data, there is an absence of a solid evidence base on which to make recommendations as to whether interventions are effective for ethnic minority populations, or how to adapt interventions for ethnic minority populations. Consequently, new empirical studies are conducted with limited guidance and the cycle is perpetuated (Step 4).
Strengths and limitations
A key strength was our systematic approach to assessing what consideration has been taken of ethnic minority populations in the high-level evidence and recommendations for health promotion interventions for smoking cessation, increasing physical activity and improving healthy eating. To our knowledge, this is the first time such an endeavour has ever been undertaken with the inclusion of international systematic review.
The 2 years between the literature search (April 2009) and the production of this report (June 2011) mean that additional guidelines and systematic reviews are likely to have been published or updated during this time and this is therefore a potentially important limitation. For example, the two SIGN guidelines (SIGN 8236 and 69200) that have been included in this study have since been superseded by a newer guideline (SIGN 115243). Similarly, other reviews, such as the recently published interventions to reduce pre-diabetes risk factors for ethnic minority populations,244 have been used by NICE to develop Public Health Guidelines. An examination of these recent reviews has not, however, revealed any definitive evidence on how to improve the health of ethnic minority populations that has not already been included in systematic reviews identified in this study.
Conclusions
There exists little detailed guidance/summary evidence on how to adapt interventions to best meet the needs of ethnic minority populations. Although some individual studies may report and focus on ethnicity, this information is unlikely to be synthesised in systematic reviews, resulting in a lack of evidence from which guideline developers can develop recommendations. A two-pronged solution is needed: better reporting and synthesis of studies that include ethnic minority participants; and the development of more systematic reviews and guidelines with the specific aim of searching for and synthesising evidence of effective interventions for ethnic minority populations. In the next chapter we report on our systematic review of adapted health promotion interventions for ethnic minority populations (i.e. African-, Chinese- and South Asian-origin populations) for smoking cessation, increasing physical activity and improving healthy eating.
Chapter 6 Systematic review of adapted health promotion interventions
Abstract
Background
Health promotion interventions are potentially important strategies to reduce the morbidity and mortality associated with smoking, physical inactivity and poor diet. Adaptation of interventions with proven effectiveness in the general population may help to increase their acceptability to and effectiveness in ethnic minority populations.
Objectives
We sought to identify health promotion interventions for smoking cessation, increasing physical activity, and improving healthy eating that have been adapted to meet the needs of African-, Chinese- and South Asian-origin ethnic minority populations; describe the adaptation approaches used; and assess the clinical effectiveness, cost-effectiveness, feasibility, acceptability and equity of these adapted approaches.
Methods
We systematically searched Applied Social Sciences Index and Abstracts (ASSIA), BIOSIS, The Campbell Collaboration, Cumulative Index to Nursing and Allied Health Literature (CINAHL), The Cochrane Library, EMBASE, ISI Web of Science, Latin American and Caribbean Health Sciences Literature (LILACS), MEDLINE, PsycINFO and NHS Evidence Specialist Collection for Ethnicity and Health (SCEH) to identify relevant conceptual work, systematic reviews and empirical investigations of adapted interventions. Study quality was independently assessed by two reviewers using the Critical Appraisal Skills Program (CASP) and Effective Public Health Practice Project (EPHPP) tools. Study findings were descriptively summarised and then thematically synthesised.
Results
Our searches identified a total of 48,740 potentially eligible studies, of which 173 reports satisfied our inclusion criteria. We identified 12 theoretical papers, seven systematic reviews and 107 empirical investigations (reported in 154 papers). The majority of adapted intervention studies took place in the USA and were conducted with African American populations, predominantly women. All studies conducted with Chinese-origin populations took place in the USA while studies with South Asian-origin populations were conducted in Australia, New Zealand and the UK. Multicomponent interventions targeting physical activity and healthy eating were the most common focus of attention, followed by smoking cessation interventions. We were able to describe and classify a spectrum of approaches used to adapt these interventions for ethnic minority populations. Of the 107 experimental studies identified, only nine directly compared an adapted intervention with a standard approach. One of these nine studies found evidence in support of the adapted intervention; five studies reported no differences; one study was in favour of the standard approach; and the remaining two studies reported no difference for some outcomes with other outcomes favouring the standard intervention. No studies reported a cost-effectiveness analysis. Through studying the adapted approaches we were able to describe the range of methods employed and use this to construct a 46-item Typology of Adaptation. These adaptation approaches were then mapped on to different stages of the research cycle to produce an eight-stage Programme Theory of Adapted Health Promotion Interventions.
Conclusions
We identified a large body of studies predominantly from the USA examining adapted interventions in African American populations, but relatively little evidence in relation to other ethnic minority populations. This body of evidence has been used to develop a novel 46-item Typology of Adaptation and eight-stage Programme Theory of Adapted Health Promotion Interventions, which will, we hope, assist researchers in more systematically reflecting on approaches that can be employed to adapt interventions and also support the improved reporting of these studies of adapted interventions. There is at present a small inconclusive body of evidence examining the effectiveness of adapted compared with standard intervention approaches. Further studies of well-theorised adapted compared with standard interventions are needed and it is important that these trials assess long-term outcomes and cost-effectiveness considerations.
Introduction
There is increasing recognition that members of a number of ethnic minority groups in the UK and other economically developed countries experience disproportionate levels of risk of disease and mortality associated with a range of long-term conditions (see Chapter 1). 1–4 Although preventive approaches are increasingly being pursued in the UK and elsewhere in an attempt to reduce the incidence of long-term conditions,67,69,70,73–76 there is evidence that these health promotion interventions may be relatively underutilised by ethnic minority groups. 85,93 The complex and multifaceted reasons for these disparities are summarised in Chapter 1. Culturally adapting interventions to increase their salience and acceptability to ethnic minority populations may increase access to and the effectiveness of health promotion interventions and thereby help reduce these inequalities. 9 Given the substantial risks associated with smoking, physical inactivity and unhealthy diets,51,66 we sought to describe the approaches to adapting health promotion interventions tackling these risk factors in African-, Chinese- and South Asian-origin populations and to assess the strength of evidence in support of such adapted interventions.
Research questions
We sought to answer the following questions, which relate to Phase 1C of our project (see Chapter 2):
-
What health interventions for smoking cessation, increasing physical activity and improving healthy eating have been adapted for African-, Chinese- and South Asian-origin populations?
-
What are the underpinning theories and approaches used in these interventions and how have the interventions been adapted?
-
What is the evidence for the effectiveness and cost-effectiveness, feasibility, acceptability and equity of health interventions for smoking cessation, increasing physical activity and improving healthy eating that have been adapted for African-, Chinese- and South Asian-origin populations?
Methods
Search strategy
We searched the following 11 databases for literature on health promotion interventions for smoking cessation, increasing physical activity and improving healthy eating for African-, Chinese- and South Asian-origin populations: ASSIA, BIOSIS, The Campbell Collaboration, CINAHL, Cochrane Central Register of Controlled Trials, published in The Cochrane Library, EMBASE, ISI Web of Science, LILACS, MEDLINE, PsycINFO and NHS Evidence SCEH.
We used the search terms and strategy described in Appendix 12; a more detailed specimen search strategy for the MEDLINE database is provided in Appendix 13. The terms and search strategies used were adapted accordingly for each database. There were no restrictions placed on the language of publication. The searches were carried out between March and June 2009 and included literature dating from 1950.
A grey literature search was conducted using Google, Google Scholar and NHS Evidence (the first five pages), along with ClinicialTrials.gov and current controlled trials (www.controlled-trials.com) for ongoing trials. Additional grey literature was referred to us by the experts who we contacted for our qualitative interviews.
Inclusion and exclusion criteria
Summarised below are the review inclusion and exclusion criteria in relation to the populations, interventions, outcomes and types of studies.
Conceptual/theoretical reports
For the theoretical/conceptual literature identified we applied inclusion/exclusion criteria based on population and health topic (discussed below). Identified studies needed to discuss the populations and health areas of interest. Furthermore, we only included theoretical papers with an explicit stated aim of developing theories, conceptual frameworks and models that were sensitive to the preferences and needs of ethnic minority populations.
Systematic reviews
For the systematic reviews identified we applied inclusion/exclusion criteria based on population, interventions and outcomes to ensure that we captured reviews that synthesised relevant evidence (discussed below). At least 50% of the primary studies included in the reviews had to be health promotion interventions for smoking cessation, increasing physical activity and improving healthy eating for African-, Chinese- and South Asian-origin populations that were explicitly adapted for these populations. For the primary studies included in these reviews, if the subject of the review was a disease state such as diabetes or cardiovascular disease (CVD) (either primary or secondary prevention), we required the review to have examined the interventions of interest (smoking cessation, increasing physical activity or improving healthy eating) in at least 50% of the studies included in the review.
Empirical investigations
Populations
The populations ‘at risk’ (targeted by interventions) included children and (non-pregnant) adults of African, Chinese and South Asian origin. The definition of ethnicity used and the dimensions of ethnicity incorporated within this definition are discussed in Chapter 1. Care was taken when interpreting any studies utilising broad classifications such as South Asian when more specific identifiers, that is, Bangladeshi or Indian, were preferable. When the study report permitted it, a thorough documentation of the description of ethnicity, how this was assessed and any within-group heterogeneity or acculturation was undertaken (see Chapter 1).
We excluded any study that was described as ‘multiethnic’ but did not report the percentage of the specific ethnic groups. We also excluded studies that were ‘multiethnic’ and which reported the percentage of ethnic groups, but in which the ethnic group(s) of interest constituted < 90% of the total study population and reported outcomes were not disaggregated by ethnicity. Exclusion criteria such as these have been applied in other systematic reviews of this nature245,246 and were used to minimise the effect of possible confounders and to focus more closely on the effects of ethnicity.
Interventions
Studies of any health promotion interventions that aimed to aid smoking cessation, promote physical activity and/or modify healthy eating to improve the health and well-being of ethnic minority people were eligible for inclusion. We considered all types of study designs, including experimental studies (controlled and uncontrolled studies), observational studies (prospective cohort studies) and evaluation studies using qualitative methods. Interventions at any level, ranging from individual to organisational, institutional and environmental, were eligible for inclusion (see Chapter 3). Primary or secondary health promotion interventions were also included, the latter referring to interventions for populations with already diagnosed conditions such as diabetes or heart disease. Secondary interventions were included only if they had at least one intervention component directly intervening in smoking, physical activity or healthy eating behaviours and they reported outcomes related to these components (e.g. a study that reported on increased physical activity as opposed to improved blood glucose). Furthermore, given our focus on identifying adapted interventions (see Chapter 1), we included only studies that clearly described the adaptations that were undertaken, rather than merely stating that an intervention was adapted without any further elaboration. When the nature of ‘adaptation’ was unclear, agreement was reached through discussion among reviewers on whether or not the study yielded important enough insights in relation to adaptation to warrant inclusion.
Outcome measures
We included studies that reported on primary, secondary and tertiary outcome measures of interest to the aims of this systematic review. The primary outcomes related to smoking cessation (e.g. quit attempts, quit rates, abstinence, number of cigarettes smoked – both validated and self-reported measures), improved healthy eating (e.g. calories, fat, per cent calories from fat, fruit and vegetable intake) and increased physical activity (e.g. cardiorespiratory fitness, time spent in physical activity, number of steps taken). Secondary outcomes were body weight, body mass index (BMI) and waist-to-hip ratio. The tertiary outcomes were changes in knowledge, beliefs and attitudes.
Types of studies
No restrictions were set according to study design. We thus included systematic reviews, experimental studies [e.g. randomised controlled trials (RCTs), clinical controlled trials (CCTs), controlled before-and-after studies, interrupted time series, before-and-after studies and pilot intervention studies] and also qualitative studies. These studies were all eligible for inclusion as long as they reported on one or more of the primary, secondary or tertiary outcomes described in the previous section. As discussed above we also included relevant theoretical literature.
Data extraction strategy
Two reviewers (JJL and ED) independently screened all titles and abstracts identified by the search strategy to assess inclusion/exclusion. Full papers of potentially eligible studies were retrieved and assessed by the same two reviewers based on the above criteria. Any differences of opinion between the two reviewers were resolved by discussion or, when necessary, by a third reviewer (AS). Reasons for exclusion were documented and the list of excluded studies is located in Appendix 14.
Two reviewers (either JJL/ED for physical activity and healthy eating studies or JJL/CW for smoking cessation studies) independently extracted data using a tailored data extraction form (see Appendix 15). Data were extracted on:
-
country of study and study setting (urban, rural, community, school)
-
study design, inclusion/exclusion criteria
-
participant demographics [sample number, age, gender, socioeconomic status (SES)]
-
ethnicity and how ethnicity was assessed
-
description of intervention – level of intervention (population, group, individual), type of intervention (focus – health risk/disease, duration, setting), selection criteria, sampling, randomisation, characteristics of comparison groups or control groups (as relevant to study design)
-
type of adaptation(s) used
-
outcome measures (these varied considerably according to the study design and focus)
-
analytical techniques (where relevant)
-
outcomes
-
relevant process evaluations
-
conclusions.
The extracted data were summarised in data tables and checked for discrepancies by a third reviewer (SK), and then further checked and edited by the original reviewers (JJL and ED). Discrepancies were resolved through discussion.
Quality assessment strategy
Two authors (either JJL/ED or JJL/CW or ED/SK) independently assessed the methodological quality of included studies using a suite of appropriate assessment tools appropriate to the study design. As recommended by the Cochrane Public Health Group in their Guidelines for Systematic Reviews of Health Promotion and Public Health Interventions,247 we used the CASP checklist for reviews to assess the quality of adapted systematic reviews;248 the quality appraisal tool developed by the EPHPP to assess intervention and observational studies;249 and the CASP checklist for qualitative research for qualitative studies. 250 Disagreements were resolved by discussion and, if necessary, with the involvement of a third reviewer (AS).
Methods of analysis and synthesis
Both quantitative and qualitative data were extracted to assess how interventions were designed and adapted, and to assess feasibility, acceptability, clinical effectiveness, cost-effectiveness and equity.
Because of the wide range of health promotion topics, populations, interventions, time frames and outcome measures studied, it was neither desirable nor possible to undertake meta-analyses. Instead, the findings of each study were descriptively summarised and then this body of work was thematically synthesised.
Given the focus of this work, specific attention was given to extracting the behaviour change theories and adaptations employed in the interventions. When studies reported using a specific theory, this information was extracted; however, many papers did not report the use of a theory or, when they did report this, it was unclear how theory had informed the study design, intervention content or study outcomes.
Results
Summary of the literature identified
A total of 48,740 records were identified. A breakdown of the number of records identified from each of the 11 databases is provided in Table 9. The bulk of the records was identified from MEDLINE and EMBASE.
| Database | Records |
|---|---|
| MEDLINE | 22,768 |
| EMBASE | 21,460 |
| ASSIA | 167 |
| PsycINFO | 756 |
| CINAHL | 469 |
| BIOSIS | 1005 |
| The Cochrane Library | 376 |
| ISI Web of Science | 1643 |
| LILACS | 16 |
| The Campbell Collaboration | 15 |
| SCEH | 65 |
| Total | 48,740 |
After deduplication, 36,047 records remained. Titles were screened and 35,422 records were subsequently excluded as not relevant. Abstracts and full-text articles were obtained and assessed for the remaining 625 records. A further 452 records, after being assessed for eligibility according to our inclusion/exclusion criteria, were subsequently excluded as they were not relevant to the interventions, populations, health promotion topics or outcomes of interest, or they were not deemed to contain sufficient information on adaptation. A total of 12 conceptual/theoretical papers, 7 systematic reviews and 154 reports of 107 empirical investigations were included in the final review (Figure 8).
FIGURE 8.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram to identify literature on adapted health promotion interventions.
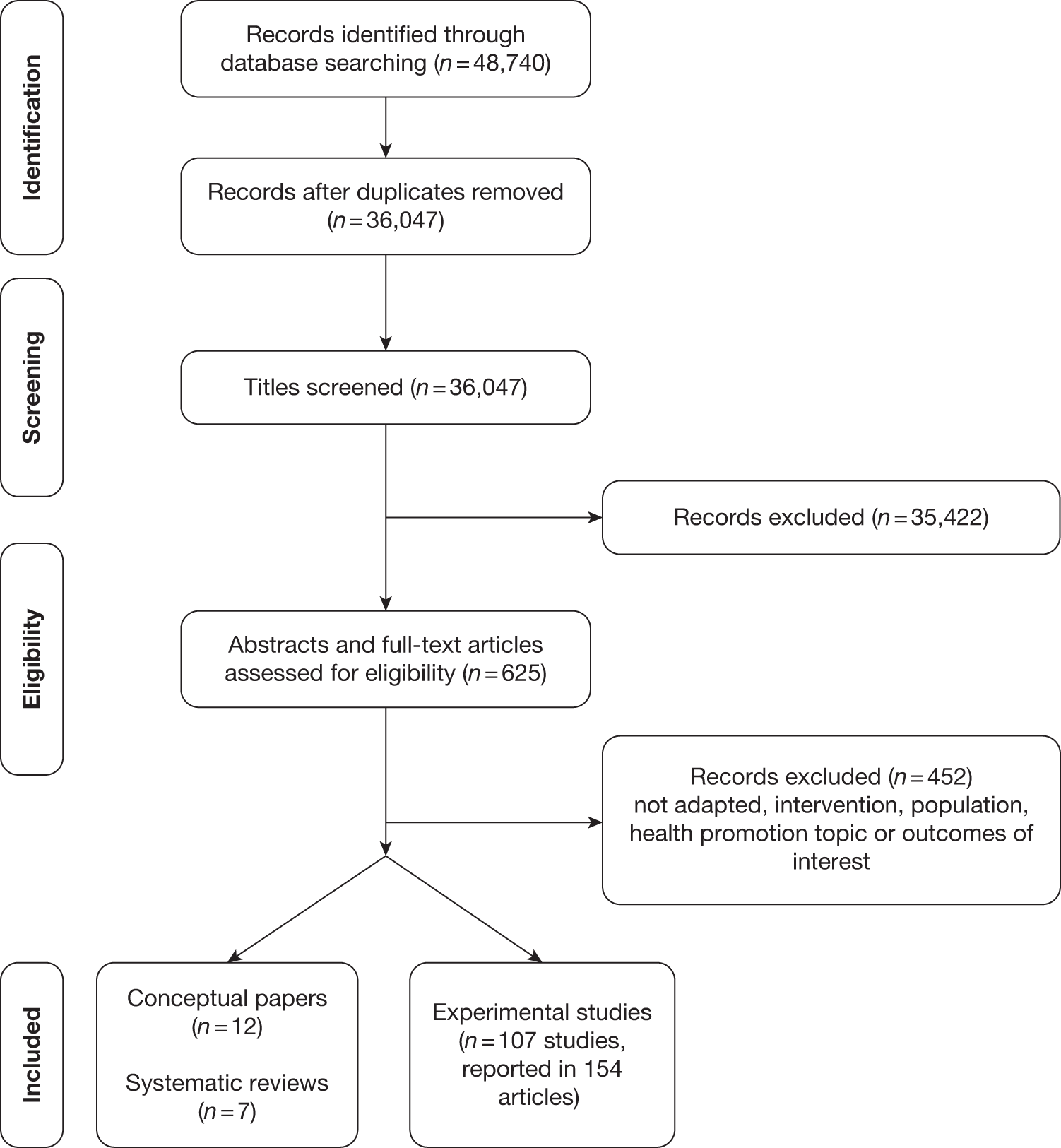
Summary of conceptual/theoretical papers
It is suggested that theory-based interventions are in general more effective than interventions that are not underpinned by theory. 251 ‘Theories’ are broadly defined here as hypotheses, models or frameworks to help clarify thinking about situated realities. 252 A theory can help explain and/or predict outcomes by explicating the relationships between variables posited to be important,251 for example why some people do or do not make health behavioural changes. A theory is characterised by abstraction rather than specificity for any context and should allow for testing in different contexts. 251 A theory can be broadly categorised as either explanatory- or change-oriented, posited to either understand or model how change takes place, although these are not mutually exclusive. 251
Theory in public health interventions has been usefully classified along a continuum, that is, studies that are informed by theory, by applying a theory, by testing theory and by building/creating theory. 253 The use of ‘theory’, however, has been variable, with few studies applying or testing theories,253 which represents the foundation work before theory building can occur, and this thus reveals a gap in the field. 251 Although theories for behaviour change dominate the health promotion literature, our focus here was more directed as we gave consideration to the ‘theoretical’ literature in the sense that the studies discussed a model, framework or approach to adapting health promotion interventions for ethnic minority populations. Each theory was first briefly summarised (see Table 10) and the overarching themes are presented in Box 5; in this, we highlight the different points of emphasis between the health promotion for ethnic minority populations and that for the general population.
-
Communication strategies used to deliver health messages focus on oral delivery and group format whereas written materials are more commonly used in health messages delivered to the general population. Experiential learning is also emphasised for ethnic minority populations
-
The focus of interventions is at the level of the family, defined to include extended and adopted family members as opposed to nuclear families, or at the level of communities, whereas individuals are usually the target of health promotion interventions for the general population
-
Women are central figures as targets of behaviour change and as agents of change because of their role in the family (e.g. role-modelling, care-taking), whereas this emphasis is less apparent in health promotion interventions in the general population
-
The goals for behaviour change for ethnic minority groups are framed around psychological, community and family gains as benefits of behaviour change compared with more individual and aesthetic-focused goals to motivate behaviour change in the general population – this is particularly apparent for weight loss. Furthermore, many health goals are seen to represent mainstream or dominant discourses and behaviour change may be perceived as assimilation, and this was contrasted with maintaining traditional practices as resistance
-
Day-to-day lived experiences, particularly stressors, and competing priorities are perceived as barriers to change for ethnic minority populations. Although these factors are acknowledged in health promotion interventions for the general population, they appear to be more substantive barriers for ethnic minority populations
-
Culture is constituted as a protective asset rather than a pathology and framed as an important factor in both risk and resilience. Culture is rarely discussed in health promotion interventions for the general population
-
Degrees of acculturation, ethnic identity and religious affiliation should be measured to better adapt interventions for ethnic minority populations; these factors are not considerations that are evident in health promotion interventions for general populations
| Study | Theory/concept | Population | Description |
|---|---|---|---|
| Airhihenbuwa 1994255 | Empowerment education as a health education and prevention model | African American | Model promotes group education, efficacy and action |
| Appel et al. 2005269 | Rational choice theory | African American | Contextual factors, social incongruency and social isolation lead to increased opportunity costs to engage in protective health behaviours |
| Ashley 1999259 | Framework for health promotion and disease prevention | African American | Framework to guide the assessment, planning, implementation and evaluation of health promotion and disease prevention interventions |
| Burnet et al. 2002270 | Conceptual model for prevention of type 2 diabetes in high-risk minority youth | African American | Model situates behaviour change as constrained by barriers such as knowledge and beliefs, attitudes, social norms and the environment |
| Davis et al. 1999254 | Afrocentric systems approach to treat obese/overweight women | African American | Guideline to integrate cultural strength and supports into the development of interventions for weight management |
| Davis et al. 2005258 | Tool kit for health and resilience in vulnerable environments (THRIVE) | Ethnic minority communities | THRIVE is a community assessment tool to understand and prioritise factors that can help improve health and reduce disparities |
| Fitzgibbon and Sánchez-Johnsen 2004263 | Recruitment, retention, development and implementation | African American and Latino | Considerations at recruitment, retention, development and implementation stages |
| Hugo 2000257 | Grading model for health education communication strategies | Ethnic minority groups | Grading model for media appropriateness and cultural sensitivity of communication strategies used in health education |
| James 2004262 | PEN-3 model: three dimensions: health education diagnosis, educational diagnosis of health behaviour, cultural appropriateness of health behaviour | African American | Framework for health promotion with culture at the centre of health promotion and disease prevention |
| Keller et al. 2005265 | Treatment theory to address recruitment and retention | Ethnic minority groups, with examples from African American and Latino communities | Theory to address issues of recruitment and retention of ethnic minority women in obesity reduction intervention |
| Resnicow et al. 199935 | Deep/surface level | African American | Framework to guide development of health promotion and disease prevention programmes that are culturally sensitive |
| Sorensen et al. 2003268 | Social ecological conceptual model for behaviours and their sociocontextual moderators and mediators | Working-class, multiethnic populations | Conceptual model that links the pathways between risk-related behaviours and sociocontextual factors and proposes where along the pathway interventions should take place |
Davis et al. 254 proposed an Afrocentric approach for therapists to treat obese and overweight African American women. This approach incorporates cultural strengths with recognition and address of multiple oppressions (e.g. racism, sexism and stigma of obesity and overweight). The framework promotes developing trust, treating the client as the expert, taking personal histories, tailoring treatment and considering cultural components, such as tapping into social support networks and recognising potential strengths in the clients’ environment. Davis et al. 254 posit that African American women are likely to operate outside of mainstream ideals of thinness and, as such, identification with African American culture may offer protections against, for example, stigma in African American women who are overweight or obese, while greater acculturation may be harmful in this respect. When framing weight loss interventions for African American women, it is thus posited that weight loss for aesthetic reasons should not be emphasised as the main goal. Furthermore, individual-oriented activities promoted by interventions such as healthy eating or lifestyle changes may be perceived to detract from family activities (in which the definition of ‘family’ includes adopted and extended family members, as well as the nuclear family). Furthermore, the type of communication strategy used could influence what is deemed appropriate; for example, a preference for improvisation and oral communication (compared with written) could render interventions with a self-monitoring component unsuccessful. Recognition of the importance of biculturalism, acculturation and degree of black identity and their moderating effects on the enablers and barriers are also acknowledged in this approach.
Airhihenbuwa255 presented empowerment education for a health education and prevention model, with group education, efficacy and action at the core of this theory. Empowerment here goes beyond controlling environmental forces and draws on Freire’s notion256 of empowerment to engage both the interventionist and the target groups in the joint production of meaning, value and knowledge as a central aim of the health promotion intervention. A ‘failure to involve communities in the production of knowledge based on their own cultures, histories, and experiences doomed an otherwise logical health promotion strategy’. For example, utilising storytelling for health promotion draws on African oral tradition; however, applying this technique requires a consideration of both the storyteller(s) and the listener(s), with both groups being equally important to the meaning-making process. The educational and cultural background of both members engaged in the dialogue needs clarification, as the reasons why storytelling is effective may be a function of strong cultural traditions, or a function of social inequalities producing low literacy levels.
Hugo257 proposed a model for grading media appropriateness and cultural sensitivity of communication strategies used in health education for a culturally diverse community. As health education is largely reliant on the success of messages, the message needs to reflect ‘relevancy of information, the particular sociocultural context in which communication takes place, as well as the suitability of media used in message transfer’. It is therefore the method or type of technology used in context that is thought to produce effective communication and generate the appropriate response (i.e. behaviour change). Furthermore, media acculturation, defined as modifying the communication message to increase acceptability and reduce confusion, is another crucial aspect, bearing in mind that ‘appropriateness by nature is not at all a fixed quality’. The proposed method assesses both the appropriateness of the media and sociocultural sensitivity and can contribute to the design of health education materials. The programme outcome, whether the learning concept is abstract or concrete, media preferences of instructor and learners, current level of knowledge, preferred ‘media codes’ (e.g. showing colour, motion) and potential resource limitations are considered when developing communication strategies.
Davis et al. 258 described a tool kit for health and resilience in vulnerable environments (THRIVE) to aid communities to identify and increase health-improving factors and reduce ethnic disparities. The tool kit underscores the contribution of oppression and racism and addresses these factors by directing attention to both risk and resilience. Risk describes the ‘characteristics or circumstances that increase the likelihood that people within the community will experience poor health and safety outcomes’, whereas resilience describes the ‘ability to thrive despite the presence of risk factors’. Health promotion has, it is argued, overemphasised risk reduction while neglecting to see that resilience can buffer the negative effects of risk factors. Even when resilience is explored, it is usually considered as an individual quality rather than a potential community attribute. THRIVE assesses risk and resilience at four levels: built environment (e.g. safety, availability of spaces, accessibility to transportation), social capital (e.g. trust, community engagement and behaviour and gender norms), services and institutions (e.g. availability of public and community-based services) and structural factors (e.g. employment and advertising).
Ashley259 presented a framework to guide the needs assessment, programme planning and implementation and evaluation of health promotion and disease prevention interventions for African American communities. At the needs assessment stage, the framework recommends building relationships, involving community members throughout the intervention process, collaborating with formal and informal community leaders and working with community organisations such as churches to help access the community and form a planning committee to understand residents’ health needs. Data collection instruments should be pre-tested with a target group, culturally appropriate and matched for both language and literacy level. During planning a detailed account of the historical, economic, political and traditional or culture-specific issues for the community should be collected. Furthermore, it is important to assess whether there are competing priorities or socially sanctioned or acceptable norms, such as bigger body sizes (discussed above). Interventions should be based on scientific theories that have been tested in the target population, such as social learning theory260 and theory of planned behaviour change261 in African American communities. During implementation interventions should be pilot tested to determine cultural appropriateness and acceptability. Furthermore, given the difficulty of retention, ‘non-traditional sites and captive audiences . . . [such as] churches, Laundromats, nail shops, beauty salons, barber shops, family and class reunions, social clubs and organisations’ should be considered, as well as the use of a small group discussion format, which has been found to be effective. Evaluation and dissemination should be presented in clear, jargon-free language.
Resnicow et al. 35 introduced a framework for developing culturally sensitive interventions using the concepts of surface and deep structures. Surface structures are the ‘observable, “superficial” characteristics of target population’, while deep structures are the cultural, social, historical, environmental and psychological forces. Addressing surface structures is perceived to increase ‘receptivity’ and ‘acceptance’ and is achieved by delivering messages and programmes through appropriate channels and settings, using people, places, language, music, food brands, locations and clothing preferred by or familiar to the target population. On the other hand, addressing deep structures is thought to increase ‘salience’ and efficacy. For African American communities, for example, deep structures can include religion/spiritualism, expressiveness, preference for verbal communication, connection to ancestors and history, centrality of community and family and their potential use as motivators, and intuition and experience over empiricism, as well as stressors and responses to these stressors. Addressing deep structures is likely to require pre-testing and involve directed questions on perceived differences between the target group and the mainstream group and preferences for intervention content and format while being simultaneously aware of within-group differences. For example, for African Americans, promoting the spiritual or psychological benefits of weight loss may be effective. Resnicow et al. 35 suggested that an important means of articulating whether surface or deep structures are relevant is to determine individuals’ degree of ethnic identity. Therefore, even Afrocentric programmes may actually be culturally insensitive depending on participants’ ethnic identity, and therefore what constitutes an ‘adapted’ baseline intervention is unknown. Although the framework was developed for African American and Hispanic/Latino populations, it is suggested that this may be equally applicable to other populations.
James262 proposed the PEN-3 health education model that places culture as the central focus for both health promotion and disease prevention, such that culture is both an explanatory model and an action model. The PEN-3 model has three central dimensions: a ‘diagnosis’ of who should be targeted for health education and the most appropriate channel to reach that target group; a ‘diagnosis’ of target groups’ perception of health information, barriers and enablers; and the identification of the enabling and constraining culturally appropriate health behaviours. The PEN-3 model utilises findings from a focus group study about food with African Americans to illustrate the application of the model. In this study, women were identified as central targets for dietary change. Differing responsibilities among these women (i.e. with or without children) translated into different experiences and relationships with their weight and food. Discussion of dietary changes focused on ‘Soul Food’, a traditional form of African American cuisine. The women concluded that the food items themselves were not unhealthy, rather, it was the methods of food preparation that increased the fat content, for example. Although individuals recognised that Soul Food may be unhealthy, they also articulated the difficulty in changing such a historically and contemporarily significant cultural artefact. Furthermore, Soul Food was sometimes perceived as resistance to mainstream culture and connected with feelings of belonging, comfort and tradition. Mainstream guidance, such as the food guide, was perceived not to be applicable to the African American population. In light of this work, James proposed that health behaviours should be examined according to whether they are ‘long term’, that is, rooted in tradition (e.g. Soul Food), or ‘short term’, that is, more recent manifestations of cultural and/or socioeconomic idiosyncrasies (e.g. consumption of fast food). Making a distinction between eating healthy food as giving up tradition and eating healthy food to reduce fast food consumption was one recommended approach to dietary change. The PEN-3 model emphasised that ‘culture’ is an ever-changing dynamic force in individuals’ lives.
Fitzgibbon and Sánchez-Johnsen263 described successful strategies for low-income African American women for CVD and cancer risk reduction and the development of culturally competent programmes to address their specific needs. They recommended the stages of change model,264 a model originally designed to address addictive behaviours such as smoking cessation, but increasingly used for dietary modification and in programmes targeting ethnic minority populations. They suggested that ‘dietary change interventions present unique challenges to researchers because their main focus is replacement and modification, not cessation, as in smoking or drug abuse’. Their discussions also encompassed logistical considerations for encouraging recruitment: having safe and easily accessible settings in familiar locations and developing relationships with trusted, community and peer leaders, as well as considering the importance of the extended rather than the nuclear family. These strategies were important in the context of multiple recruitment challenges, including fear of exploitation by researchers and various obligations, roles and day-to-day stressors that may render health-care important only when there is presence of symptoms. As programmes are developed and implemented, a range of cultural factors should be considered, including acculturation, ethnic identity and religion. Focus groups should be conducted to determine the preferred intervention format, cultural norms and literacy and educational levels (not just reading level, but also the amount of material that could be read/digested). For dietary programmes ethnic foods should be encouraged. Programme retention presented unique challenges such as transient populations, gang activity and poverty-related stress. To address these challenges, retention strategies such as weekly contact calls, multiple incentives (monetary more effective than vouchers/coupons), the use of peer leaders and tracking participants by obtaining multiple telephone numbers and the contact details of close friends and family can be employed.
Keller et al. 265 used treatment theory to address issues of recruitment and retention of minority women participants in an exercise programme to reduce obesity. They identified the Harvard Matching Model of Recruitment266 and a model by Levkoff et al. ,267 which assessed matching at three levels: macro (community agencies vs academic institutions), mediator (gatekeepers vs research team) and micro (participants vs interviewers). These papers were more focused on recruitment whereas the present paper considered retention, which can be improved by considering critical inputs, mediating processes and substantive participant characteristics in intervention design. Treatment theory looks for the causal mechanism between the intervention and its outcomes. It further highlights the significant variables and proposes a way to measure them and control sources of external influences. The critical inputs for increased retention were identified as convenience, supportive surroundings and cognitive factors such as self-efficacy. Mediating processes included, for example, recognition that caring for their family was contingent on their own positive health status. Three types of participant characteristics were posited to influence intervention outcomes: personal characteristics, which were the measurable features such as demographics; cognitive processes and health knowledge, attitudes and beliefs – either illness or health related, such as degree of illness and associated symptoms or disabilities; and personal resources, such as social support and coping mechanisms.
Sorensen et al. 268 developed a conceptual model that tackled the interconnected pathways between risk-related behaviours leading to increased cancer morbidity and mortality and the complex sociocontextual factors mediating these behaviours. The model includes sociodemographic characteristics (e.g. social class, ethnicity, gender) as inputs into a larger social context, which includes interpersonal, organisational, neighbourhood/community and societal factors. These sociocontextual factors, which are modifiable, are in turn mediated by sociocontextual mechanisms, such as social norms, social support and organisational environment, as well as by individual factors, such as self-efficacy, intentions to perform behaviour and skills. This model therefore targets interventions at the level of mediating mechanisms that are amenable and actionable. Interventions are thus targeted at multiple risk factors while being sensitive to the sociodemographic characteristics of participants and their broader social contexts. This model attempts to draw out the salient characteristics of these multilayered sociocontextual factors as they relate to ethnicity and integrate them into intervention design. For example, one intervention study sought to target modifying factors salient to low-income, multiethnic populations, such as barriers to physical activity, by, for example, providing free gym passes, working to create walking paths with employers and creating opportunities to access community resources. Social support was further enhanced by working with employers to maintain healthy and safe working environments.
Appel et al. 269 addressed the disproportionate mortality and morbidity burden of African American women and developed a model that takes into account the wide variety of daily contextual factors influencing the health status of this population. The model is structured on ‘the interrelationship between contextual risk factors, rational choice theory, and opportunity cost’. Contextual risk factors were defined as those circumstances outside the control of women and could lead to both social isolation – a lack of access to health-care information and hesitancy to interact with the health-care system – and social incongruence – ‘an inconsistency between individuals’ social, educational, lifestyle, and monetary status they were able to achieve’. Appel et al. 269 argued that contextual factors become risk factors when they conflict with women’s capacity to modify cardiovascular risk factors. This model suggested that rational choice theory is useful for understanding how women make particular choices that can negatively impact on their health outcomes. Rational choice theory has four main factors that impact on African American women’s health choices, including a hierarchy of preferences (lifestyle, beliefs, attitudes, habits that shape behaviour); opportunity costs that encourage unhealthy choices (such as difficult access to healthy foods); and institutional constraints (such as a lack of culturally competent African American physicians). The fourth factor is an aggregation mechanism that proposes the replication of these factors in a given population – when faced with similar experiences and needs there is a tendency to make similar choices. These risk factors then create increased opportunity costs for African American women wanting to engage in healthier behaviours. Advanced practice nurses will, it is envisaged, play important roles in implementing interventions for communities living in this socially isolated environment of scarcity. The central role of the advanced practice nurses is, it is suggested, to work with community leaders to reduce opportunity costs and institutional constraints and provide education. Reducing these costs and constraints can be achieved through projects such as providing childcare, bus passes and car pools. Minimising opportunity costs within a community-based framework is proposed to empower women to make positive health choices.
Burnet et al. 270 developed a theoretical model focused on preventing diabetes in high-risk minority youth. This model situated behaviour change as constrained by a number of barriers including knowledge and beliefs (e.g. perceived difficulties in modifying cooking to include lower fat methods), attitudes (e.g. enjoyment in eating unhealthy foods), social norms (e.g. acceptance of larger body sizes) and the environment (e.g. a lack of safe recreational areas). Minority populations such as African Americans face difficulty in accessing health care, have little experience with research as few studies are directed at them and may distrust the medical community because of past abuses, which affects participation in health programmes. Taking stock of these factors, Burnet’s model is based on an underlying conceptual framework that situates positive behavioural skills as most effectively emerging from experienced-based learning to cultivate self-efficacy. Behaviours are cognitively targeted by social learning theory,260 which hypothesises that individuals must believe that their current behaviours are detrimental to their health and that changing them will lead to a positive outcome expectation. In addition, the individual must feel able to make those changes, and value the incentives for changing. The health belief model271 contributes to this modelling and suggests that behavioural change must also be considered subjectively acceptable. The broader environmental conditions influencing behaviour are also considered in the form of the theory of planned behaviour272 and the ecological model. 273,274 Within interventions, self-efficacy should be promoted through achievable performance goals and verbal encouragement. Normative beliefs that hinder self-efficacy must be targeted through community members and leaders. Thus, interventions must target both cognitive and environmental conditions of minority populations, within community contexts to increase self-efficacy.
Table 10 summarises the salient features of these explanatory theories and models.
It can be seen from this summary that the theoretical literature on how to modify health promotion interventions to meet the needs and preferences of ethnic minority populations is rather piecemeal, and contains a mixture of both explanatory and predictive theories, featuring some, but not all, of the three ethnic minority populations of interest to our current study. Whether different approaches apply to different ethnic groups or whether there are consistent principles that can apply across ethnic groups is still under investigation. Nonetheless, overall this body of work directs our attention to some overarching themes or messages for practice that may be relevant across ethnic groups, and are summarised in Box 5. Furthermore, as most of these papers do not present theories per se, there is room to develop a more all-encompassing approach, drawing on both these themes identified here and the findings from the critique of systematic reviews and primary studies presented in the remainder of this chapter.
Summary of systematic reviews
The seven systematic reviews that met our eligibility criteria covered various health topics including smoking cessation,246,275 physical activity/fitness,245,276 obesity,277 diabetes278 and CVD. 279 Most of the reviews undertook narrative analysis and synthesis of the included studies; however, two reviews had sufficient data to undertake meta-analyses. The studies are summarised in Table 11 and are discussed in this chapter by health topic. More detailed descriptions of these systematic reviews are found in Appendix 16, while quality assessments are included in Appendix 17.
| Review | No. of studies and time period | Population | Health issue | Intervention | Synthesis approach | Conclusions/recommendations |
|---|---|---|---|---|---|---|
| Banks-Wallace and Conn 2002245 |
18 studies 1984–2000 |
African American women | No particular health issue, looking at increasing physical activity for all health reasons | Any intervention increasing physical activity | Narrative | The findings of this study suggest that culturally relevant strategies are effective for promoting physical activity and dietary changes among African American women. Study design and measurement issues meant that it was not possible to draw any firm conclusions on what particular components of adaptation are effective and further, well-designed research is required |
| Chen and Tang 2007275 |
4 studies 1995–2005 |
Asian American | Smoking | Smoking cessation interventions | Narrative | The existing research is very limited and, although it shows some promise, it was suggested that more research is needed. Care must also be taken not to generalise results across different Asian populations |
| Hawthorne et al. 2008278 |
11 studies No publication year restrictions |
Ethnic minority groups in upper-middle- and high-income countries (4 African American studies and 3 South Asian) | Type 2 diabetes | Culturally appropriate health education | Narrative with meta-analysis when outcome measures were sufficiently similar and subgroup analyses including by ethnicity | Significant effect observed for culturally adapted interventions over the control groups for all ethnic groups. Authors recommended that culturally appropriate interventions should be the ‘gold standard’ for health education programmes for ethnic minority populations (how they were adapted or what features of adaptation may relate to effectiveness was not assessed) |
| Hudson 2008277 |
6 studies 1997–2007 |
African American children | Obesity | Obesity prevention interventions | Narrative | Almost all of the experimental studies identified had culturally tailored interventions; however, several of these studies had only preliminary data and, as limited research exists in this area, further well-designed intervention studies are required to shed light on effective strategies for this population |
| Shaya et al. 2006279 |
10 studies 1966–2004 |
African American | CVD | Interventions focused on improving CVD-related health behaviours, adherence to treatment and access to health care | Narrative | Cultural adaptations are discussed for the individual studies included; however, there is a lack of evidence, particularly of any long-term effects. More research is needed, along with more sustainable approaches, possibly through community-level initiatives |
| Webb 2008246 |
20 studies 1984–2006 |
African American | Smoking | Smoking cessation | Meta-analysis | Cultural specificity of the intervention was one of the factors that moderated the treatment effect, increasing the effectiveness in the short term but having less effect than the culturally non-specific intervention in the long term |
| Whitt-Glover and Kumanyika 2009276 |
29 studies in adults and 14 in children 1985–2006 |
African American | No particular health issue, looking at increasing physical activity for all health reasons | Interventions to increase physical activity or fitness | Narrative | Mixed results on effectiveness. Adult studies were more effective than those in children. Studies with cultural adaptations did not appear to result in significantly better outcomes. Further high-quality studies are required to advance understanding in this area |
Smoking cessation
Chen and Tang275 undertook a review of the smoking cessation research in Asian American populations (including South-East Asian, Chinese, Korean and Vietnamese populations). Their search included studies from 1995 to 2005 and identified two clusters of controlled studies and two uncontrolled intervention studies. Cultural adaptations included adapting intervention materials for language and cultural specificity, the use of lay health workers and utilising community events for health promotion presentations. The authors commented that the interventions had differing degrees of success and they related this in some cases to levels of acculturation within the population. They concluded that further research is needed in this area and also cautioned that, because of the high degree of heterogeneity within the Asian American population, intervention results are not readily generalisable.
Webb246 conducted a systematic review and meta-analysis of the treatment of tobacco dependence among African Americans. This review identified 20 published and unpublished studies. Eleven of these studies had adaptations for cultural specificity, which included tailored print materials and the use of church settings for the delivery of the intervention. When the culturally specific intervention results were pooled, the odds ratio (OR) was 1.47 post treatment [95% confidence interval (CI) 1.12 to 1.91] compared with an OR of 1.34 (95% CI 0.99 to 1.82) for the standard intervention. However, the author reported that the culturally specific interventions were not effective at follow-up whereas the standard interventions retained a significant effect. The authors concluded that both culturally adapted and standard interventions are effective, but that adaptation was particularly effective in the short term (perhaps in relation to increasing enrolment and reducing attrition) and the effect then declined with time.
Physical activity
Two reviews focused on physical activity among African Americans. 245,276 Whitt-Glover and Kumanyika276 identified 29 physical activity studies in adults and 14 in children. Of the 43 studies, 40 were adapted. Adaptations included utilising African American music and dance, cognisance of cultural, social, historical and environmental perspectives, utilising church settings for interventions and using an interactive format of intervention delivery. Only three studies directly compared an adapted intervention with a standard intervention and none of these showed a statistically significant advantage of the adapted intervention over the same intervention without adaptation. The authors concluded that culturally adapted interventions may not increase effectiveness and that further research is required.
The review by Banks-Wallace and Conn245 identified 18 studies, of which four focused on physical activity with the remainder also including a dietary component. In total, 14 of these studies mentioned some form of cultural adaptation. The adaptations ranged from community consultations and focus groups contributing to the design of the intervention to the choice of location and the content of the intervention. Only one study examined the effectiveness of adaptation and this suggested that the strategies they included were effective.
Obesity
Hudson277 reviewed obesity prevention interventions adapted for African Americans. Twenty-eight studies were included; six of these were experimental studies (one of these six was not explicitly adapted, but all six studies included physical activity and healthy eating components). The six experimental studies included preliminary data and therefore the authors were unable to draw any definitive conclusions.
Cardiovascular disease
Shaya et al. 279 reviewed community interventions addressing cardiovascular disparities. They identified 10 studies, of which five were conducted in African American populations, focusing on physical activity and/or healthy eating, and described some form of cultural adaptation. Four of these studies were church-based interventions. Churches were identified as a focal point of the African American community, especially for older women, and therefore an acceptable setting for health promotion interventions. Lay health workers and culturally appropriate recruitment strategies were also discussed. Although the adaptations were described, no conclusions were offered on the effectiveness of adaptation for health promotion strategies.
Diabetes
A Cochrane review by Hawthorne et al. 278 on culturally appropriate health education for type 2 diabetes mellitus identified 11 studies. Four of these studies focused on culturally adapted interventions for African Americans and another three on culturally adapted interventions for South Asian populations. Subgroup meta-analyses were performed to assess the effect of the culturally adapted interventions for each population group and for a variety of intervention outcomes. Outcomes relevant to this work included healthy eating knowledge, feelings of empowerment to make dietary changes, and BMI. Knowledge increase was significant post intervention at the 3-, 6- and 12-month follow-ups, but no significant changes in health outcomes such as BMI were identified. Despite this the authors concluded that adapted interventions produce better outcomes than those that are unadapted and should be the ‘gold standard’ for ethnic minority populations.
Overall, there were mixed results from systematic reviews on the topic of adapted interventions for smoking cessation, increasing physical activity and improving healthy eating in African-, Chinese- and South Asian-origin populations. The majority of the authors recommended further research in this area. There was also a recurrent comment with regard to the physical activity- and healthy eating-based interventions that the intervention data were on the whole short term and that longer-term outcomes were unknown and needed further exploration. 245,276,278,279 The lack of definitive evidence also justified the need for a more thorough investigation of adapted empirical studies.
Summary of empirical studies of adapted interventions
In total, 107 studies (reported in 154 papers) met our inclusion/exclusion criteria and were fully extracted and quality appraised. A summary of the distribution of these papers across ethnic minority populations and health promotion topics is outlined in Table 12. The bulk of the included studies focused on African-origin populations for physical activity and healthy eating (n = 50) and smoking cessation (n = 19). Detailed one-page summaries of all 107 studies are included in Appendix 18. A summary of the quality scores of the included studies is reported in Appendix 19. We first use the entire corpus of 107 studies to consider the feasibility, acceptability and equity of adapted interventions. In-depth discussion of direct comparison studies, adapted studies with additional components and studies reporting cost information is presented later in this chapter. These studies have the potential to inform deliberations on the effectiveness of adapted interventions.
| Population origin | Smoking | Smoking + physical activity | Physical activity | Physical activity + healthy eating | Healthy eating | All three | Total |
|---|---|---|---|---|---|---|---|
| African | 19 | 0 | 7 | 50 | 14 | 1 | 91 |
| Chinese | 4 | 0 | 1 | 2 | 0 | 0 | 7 |
| South Asian | 0 | 0 | 1 | 5 | 2 | 0 | 8 |
| Multiethnic | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Total | 23 | 0 | 10 | 57 | 16 | 1 | 107 |
Typology of adaptation
We extracted the adaptations reported by each study. We then compared and contrasted these adaptations and identified 46 mutually exclusive types of adaptation. Collectively, these 46 adaptations represent the breadth and depth of adaptations undertaken in the 107 included studies, which span all three health promotion topics and three ethnic populations of interest (Table 13). The number of adaptations used within each study varied and different combinations of adaptations were apparent. The main adaptations undertaken in each study are described in the one-page study summaries (see Appendix 18) and are also summarised in Appendix 20 to allow for comparison of adaptations used across studies.
| Adaptation | Example | |
|---|---|---|
| 1 | Exploratory phase with target population (same group as intervention group) | Adaptations based on previous relevant (qualitative) research |
| 2 | Exploratory phase with target population (different group from intervention group or unknown) | Adaptations based on focus groups from a previous study |
| 3 | Exploratory phase with community leaders | Needs assessment |
| 4 | Ethnically matched intervention staff or facilitators (with qualifications) | Dietician, exercise instructor, programme staff; knowledge of culture and religion |
| 5 | Ethnically matched peer role models or peer education | Lay health advisors with the same background, age, ethnicity |
| 6 | Ethnically matched facilitators and peer role models who have successfully changed their behaviour (both ethnically and behaviourally matched) | Lay health advisors who themselves are ex-smokers |
| 7 | Ethnically matched high-level/respected individuals to increase salience of programme goals | Former surgeon general (African American) to deliver a message, spokesperson |
| 8 | Ethnically matched high-level/respected individuals and community members throughout planning, directing, reviewing and implementing stages | Steering group all Chinese |
| 9 | Ethnically matched leadership within the study | Principal investigator is South Asian |
| 10 | Utilise local/respected religious/spiritual leaders | Church pastors, church pastors’ wives |
| 11 | Collaboration with ethnic-specific institutions and professional organisations (formal) | For example the National Black Leadership Initiative on Cancer; hold intervention at local tutoring programme |
| 12 | Material depicts individuals from target population | Posters with appropriate models, e.g. of same ethnicity and age |
| 13 | Material (video, booklet, skits, handouts, games) in target population’s language | Translation, bilingual, interpretation |
| 14 | Reflect target population’s language (usage – concepts, vocabulary) | Figurative language: ‘Dear Sister’ |
| 15 | Match reading level and literacy | Consider matching text with graphics, or fifth- to sixth-grade reading level for populations with low literacy; assistance with questions |
| 16 | Reflect target population’s preferred method of communication | Storytelling, poetry and literature; hands-on/interactive learning; testimonials; face-to-face |
| 17 | Material presents ethnic-specific data | Statistics for heart disease among African Americans |
| 18 | Material depicts appropriate graphics and scenarios (this can be heterogeneous) | Foods, clothing, logos, artwork |
| 19 | Material/guidance based on preferences of target population | Foods, recipes, flavourings |
| 20 | Material developed specifically for target population (by project investigators, expert opinion, tools) | KIS II Quit Smoking Guide – 36-page booklet developed for African American light smokers developed by investigators, expert feedback and cultural relevance analysis using the suitability of assessment materials (SAMS); recipe books |
| 21 | Material created by members of the target population | African American-owned advertising company produced campaign media spots |
| 22 | Intervention content targets population’s social and cultural values | Spiritual themes, prayers, inclusion of kinship, collectivism; cultural traditions; family commitments; connection to history |
| 23 | Intervention goals and outcomes are culturally appropriate | Focus on reducing fat and not on losing weight when weight loss is not a priority for the population; emphasis on personal health improvement as a means of assisting the family or community |
| 24 | Intervention delivered in culturally appropriate or preferred format | Joint counselling sessions for Chinese smoker’s physician and family |
| 25 | Consider target population’s employment situations | Caretaker, night-shift worker, taxi driver |
| 26 | Intervention addresses health behaviour patterns found in target population | Modal smoking patterns of African American smokers (low daily smoking rate, menthol, high tar/nicotine cigarettes) |
| 27 | Dietary issues unique to their context | Church meals; food at social gatherings |
| 28 | Utilise resources from target population | Recipes provided by participants used in direct instruction |
| 29 | Utilise appropriate incentives and timing of programme | Held in evenings rather than daytime; use of small gifts given at intervals during the study found to enhance retention of rural African Americans |
| 30 | Utilise and addresses appropriate norms | BMI cut-offs, normative frameworks, body image |
| 31 | Address concerns with medical programmes, procedures and medication | Medicine may be perceived as too strong; giving blood |
| 32 | Utilise appropriate evaluation instruments and tools | Regionally and culturally specific foods added to Food Frequency Questionnaire (FFQ) |
| 33 | Located in ethnically/culturally appropriate/familiar location | Black-owned commercial gym; community-based clinic that serves predominantly low-income African American patients |
| 34 | Utilise ethnically/culturally appropriate media sources | Chinese-language newspaper |
| 35 | Utilise ethnically/culturally appropriate formal and informal networks | Community groups, lay health educator networks |
| 36 | Provide ethnically/culturally appropriate food/activities/music | Serve culturally appropriate foods and dishes; African dance |
| 37 | Present a pro-ethnic/race approach | Asian pride |
| 38 | Address emotional barriers and stressors | Stress (of inner city life) |
| 39 | Address physical/financial (structural) barriers to participation | Access to transport, time restrictions, safe locations, financial constraints addressed (providing compensation/suggesting alternatives); childcare |
| 40 | Teach appropriate communication skills | Asian youth learned to communicate their smoking cessation needs to parents and elders while maintaining harmony and respect |
| 41 | Encourage/involve social support | Joint or family counselling (contrast this with no. 23, emphasising family in messages, e.g. quit smoking for the kids); invited families and friends to sessions |
| 42 | Purposefully maintaining an exclusive or open intervention environment | African American only (non-African American research members asked to leave); targeted to African American churchgoers, but open to all churchgoers |
| 43 | Maintaining cultural significance of food | Encourage different preparation rather than avoidance of food |
| 44 | Cross-cultural training for all study personnel | Cultural competency training |
| 45 | Address discrimination and mistrust | Address oppressions such as racism and stigma |
| 46 | Gender considerations | Women-only sessions |
Assessing the feasibility, acceptability and equity of adapted interventions
Explicit discussions of the feasibility, acceptability and equity of adapted interventions were limited in the systematic reviews discussed earlier (see Summary of systematic reviews). In addition, therefore, we searched the primary studies for relevant insights.
Feasibility
The review of UK guidelines and systematic reviews identified that some health promotion topics and levels of health promotion interventions were more feasible to conduct in the adapted form, in terms of having identified evidence of effect and also scope for applying adaptations (see Chapter 4). For example, smoking cessation interventions using pharmacotherapy had less scope for adaptation than settings-based interventions for physical activity or healthy eating. The main additional insights from this review of empirical studies relate to the practicalities of successfully delivering research interventions and health promotion interventions. We found that the feasibility of interventions was primarily dependent on resources, including both funding and infrastructure (workforce, materials and venues). In some cases the resources were required for the underlying intervention and in other cases the resources were required for adaptation and were related to the degree of adaptation undertaken.
Examples of interventions for which the resource requirements may have affected feasibility include an internet-delivered weight loss intervention in which all participants were provided with part funding for the purchase of home computers. 280–282 Other such resource-intensive interventions involved subsidised gym membership283 or children’s camps. 284 The feasibility of delivering these interventions in other contexts, or to larger numbers, may be challenged by the cost of these resources. Examples of other costly interventions were the national VERB campaign in the USA285–287 (US$194M) and the Charlotte REACH multicomponent intervention (US$7M for a population of 20,000). 288–289 Although resource intensive, these costs need to be weighed up against the possible health gains, but with no high-quality health economic studies available this could not be assessed. The most feasible studies appeared to be those that professed to require few health-care resources and minimal technology. 290,291 An example of this was an intervention for African American adults with diabetes conducted through five group meetings delivered by family health advocates in community locations. 290,291 Topics of discussion included stress reduction, increasing physical activity and encouraging the consumption of fruit and vegetables. This intervention encouraged the participation of family and friends and demonstrated significant improvements in healthy eating practices. 290,291
In terms of the adaptation of interventions, feasibility may be limited by the amount of additional work required to adapt. Several adapted interventions developed individualised intervention materials that were tailored on the basis of participants’ survey data; this included tailoring for participants’ cultural perspectives,292,293 levels of cultural affiliation,294,295 ethnic identity,296 health risks297 and stage of readiness for change. 298,299 The most sophisticated tailored intervention catered for 16 degrees of ethnic identity. 296 This level of adaptation may limit the feasibility in terms of the resources required to both develop the materials and assess each individual’s ethnic identity.
Feasibility appeared to be enhanced when an existing organisation or setting was used for the adapted intervention. Churches, for example, were frequently used as intervention sites300,301 to encourage participation and reduce resource requirements. Reasons for increased feasibility included having a structure and network of people with existing relationships, the support of community leaders302 and access to existing community resources. 303–304 One challenge to the feasibility of delivering an adapted intervention in partnership with existing organisations is the necessary negotiations involved on how the intervention is delivered and how to maintain the integrity of the intervention. 303–305
Even when the resource demands are low, a lack of funding can limit the feasibility of sustaining or evaluating an adapted intervention,302 which was apparent in the case of a physical activity intervention aimed at South Asian Muslims. 302 The funding was insufficient to meet the need and demand for the intervention in this population.
Acceptability
Increasing acceptability was frequently cited as a rationale for undertaking adaptation. The adapted interventions were often rated by participants as more appropriate306 and measurements of perceived cultural relevance of the intervention were shown to be associated with programme satisfaction and attendance. 298,307 However, other elements contributing to acceptability also emerged including study and intervention design, incentives, costs and relationships with the target community.
A randomised study design was, for example, often not perceived to be acceptable, particularly with African American populations, because of a history of research abuse and mistrust of research involvement. 290,291,308,309 However, this is an issue relevant to research rather than delivering health promotion programmes per se. Similarly, when control groups were used in research with an African American population, it was sometimes not acceptable for the control group to receive a minimal intervention. The control groups therefore usually received either an equivalent intervention (attention control) or a condition with some adaptation, and this may have diluted intervention effects. 296
Study researchers attempting multiple behaviour changes observed reduced acceptability as the complexity (e.g. more than one behaviour targeted) of the intervention increased. 294,295 High-intensity programmes were also observed to reduce acceptability, for example one programme required classes to be held in a school 5 days a week and it was uncertain whether or not this would be acceptable to teachers if they had to deliver this on an ongoing basis. 310 Gradually introducing intervention components, in terms of the expected behaviour change and behaviour change goals, may have increased acceptability. 312 In contrast, internet-based interventions delivered in the home, for example, required less commitment in terms of attendance and tended to be acceptable in the beginning. The acceptability in this case, however, appeared to relate to the novelty factor and once this wore off, and in light of competing internet content, the participation rates decreased. 280–282,313,314 Even when interventions were not complex, competing priorities315,316 reduced the acceptability of participation in an intervention, for example life stresses317 or even other intervention programmes (e.g. ‘Welfare to Work’ programmes). 315,316
Interventions that were designed to allow more freedom and flexibility for participants were found to be acceptable. This flexibility allowed for the intervention to be altered to suit the participants,318 or the participants to choose the degree of participation,319 or an organisation to decide which components to take up in their setting. 320 One intervention relaxed their requirements for participating in sessions as a result of low attendance; they found that people wanted to exercise without having to attend all of the counselling and educational sessions. 321,322 The data suggested that interventions required a balance between flexibility/acceptability and effectiveness. One intervention with a strict vegan diet, although perhaps effective for weight loss, was not very acceptable,323 whereas another intervention that evaluated a decision-making framework without any such structured diet was in retrospect felt by the researchers to be too flexible, thus rendering it ineffective. 284,324
Incentives were also used to increase acceptability and featured in many US studies. Incentives were given to either individuals or to partner organisations (e.g. churches) to increase the acceptability for both individual and institutional participants. 292,294,295,325,326 In one study incentives were reported to be important for class attendance for half of the participants;327,328 however, in another study, despite offering a number of incentives, including monetary rewards, prizes and gifts, the attendance remained low. 321,322 It is therefore unclear to what extent incentives increase the acceptability of an intervention; this is likely to vary across different populations and population contexts. Interventions for which participants had to pay to participate, even at a subsidised level, may also have reduced acceptability. 323 Convenience in terms of transport, particularly for young participants,329,330 provision of childcare and low-cost parking331 and fitting in with work commitments332 increased acceptability of the intervention. Convenience and low cost were motivators for 70% of participants in another intervention. 297
Lastly, a collaborative approach was reported to increase acceptability,298 particularly when the target community was involved in developing the intervention materials333 and prioritising intervention objectives. 334 Relationships that were long-standing and felt to respect the cultures, health concerns and needs of the population297 increased acceptability. A study of physical activity and healthy eating delivered to an African American population through a day-care centre increased acceptability when a long-term relationship was developed based on culturally appropriate strategies. Participation rose from 26% in the first year to 73% once this relationship was established. 297 Both cultural relevance of an intervention and cultural competence of staff were felt to be key elements for programme satisfaction. 298,307
Equity
Specific settings were often used to deliver adapted interventions. In the review of UK guidelines and international systematic reviews (see Chapter 4), we identified setting-based ‘strategies and activities’ as having good scope for adaptation; however, it should to be noted that such adaptations may prove to be restrictive in who they can cater to by the very nature of being more attractive to selected populations. Religious settings were often used to deliver adapted interventions292,299,308,325,334,335,336 – the literature we identified focused on US African American churches as either venues for or providers of the interventions. These interventions may be less accessible to or appropriate for non-faith populations or those who are spiritual but do not attend church, particularly if the intervention is also held in or delivered by the church. Churches with a high degree of organisation, such as those having an existing and established health ministry,334 were often chosen to deliver health interventions and this may further exacerbate inequalities through non-enrolment of perhaps smaller, less organised churches serving more deprived/marginalised populations.
Schools were another setting where interventions were often delivered; however, some participants may have been disadvantaged if their school was unable to provide the required intervention resources. 337 Furthermore, within school settings, there were observed gender differences in access to recreational facilities. 337 Gender differences were observed as the majority of adapted interventions targeted female participants exclusively.
Access to interventions was also limited by study design when children’s participation was contingent on parental involvement. Children with less motivated or less interested parents were sometimes unable to participate. 319
In addition, interventions that did not have adequate funding were observed to have raised awareness but then denied access to interested people. 302 In other cases, people allocated to a wait-list control group had to wait a long time for the resources to become available and this negatively affected their results. 338–340
The materials used to deliver an intervention also made an impact on access and equity. Interventions that were internet based disadvantaged those without computers or internet access or those who have limited experience with computers. 313 In one intervention, participants had to contribute funding for a home computer in order to access the intervention,280–282,314 as this was part of the eligibility criteria. Some interventions excluded potential participants if they had no home address or access to a telephone or video cassette player,341 which disadvantaged people from lower-income strata. Furthermore, attrition from interventions was often related to difficulties in tracking or maintaining contact342–345 as a consequence of participants losing access to their telephone lines. Getting multiple contact numbers from participants’ friends and family members was a suggested method to decrease such attrition.
Some interventions were unable to reach their target groups, for example low education groups306,307 or populations with lower literacy or health literacy levels,346 or the intervention worked better for groups who were physically fitter and with higher educational attainment,312 which suggested that education level was important to monitor in terms of equitable access and participation in interventions.
Finally, it emerged that adapting interventions can positively contribute to equity as the transferability of an intervention developed for one ethnic minority population (Native Americans) was successfully demonstrated for other ethnic minority populations (African American and Latino populations);290,291 this was also the case for an intervention originally developed for Latino populations and later adapted for African American populations. 310
Effectiveness
The vast majority of the 107 studies had effective outcomes. This is including studies that reported effectiveness for any of the outcomes measured, at any time point and sometimes within subgroups of the participants. These findings are encouraging; however, the design of these studies does not allow any assessment of the extent to which the adaptation contributes to their effectiveness. To determine whether or not adapted interventions are effective for ethnic minority populations we therefore identified the studies that directly compared an adapted approach with a non-adapted intervention. These studies were mostly RCTs or CCTs, as a control group was essential to draw conclusions on the comparative effectiveness of adapted interventions. The hypothesis was that interventions that had been adapted would be more effective than interventions that had not been adapted (i.e. standard or usual care).
Direct comparison of adapted with non-adapted interventions
Nine studies (reported in eleven papers) were identified that directly compared an adapted intervention group with a non-adapted control group. 293–295,306,341,347–352 Four of these studies (reported in six papers) were included in the seven systematic reviews that we identified. 294,295,306,347,350,352 The comparison conditions were near equivalent in terms of duration, intensity and materials/methods used, although slight variations were allowed as long as both reviewers (JJL and ED) felt that the comparison conditions were similar enough. There were four smoking cessation studies, one physical activity study, one healthy eating study and three combined physical activity and healthy eating studies. The study quality was variable; five studies were rated ‘strong’, three were rated ‘moderate’ and one was rated ‘weak’. These studies are summarised in Table 14 and an exemplar study is outlined in Box 6.
This RCT was one of the few studies we identified that directly examined an intervention with and without a component of cultural adaptation. The study population was lower-income African American women (n = 1227) and the health promotion topic was mammography in the older population (aged 40–65 years) and increasing fruit and vegetable intake in the younger population (aged 18–39 years); we focused on the latter group
This was a four-arm study with three intervention groups and a control group. The intervention arms were delivered through a women’s health magazine and the magazine was developed with BCT, CRT or both (BCT + CRT). Each magazine contained 10 items focusing on fruit and vegetable intake and four items on general topics that were chosen according to the demographics of the women to increase the magazine’s appeal. The control group received no materials during the intervention but were sent a full set of the magazines once the intervention was completed
The BCT was based on diet-related knowledge, self-efficacy for change, perceived barriers to eating fruit and vegetables, perceived importance of eating fruit and vegetables, levels of interest in starting to eat more fruit and vegetables and actual dietary practice
AdaptationThe CRT was based on four cultural concepts identified in the formative work as being pertinent to African American women. These concepts were:
-
religiosity (a range of dimensions from church attendance and prayer to participation in religious ceremonies, spirituality and beliefs about God as a causal agent)
-
collectivism (belief that the basic unit of society is a family or group and not the individual)
-
racial pride (holding positive attitudes about one’s race)
-
time orientation (related to a person’s tendency to think and act according to consequences that are primarily immediate or primarily distal)
The CRT elements were measured in a baseline questionnaire to determine the tailoring and the magazine was tailored on the two cultural constructs on which the women scored the highest. This approach takes into account the individual in terms of how relevant the cultural concepts are to them, which may alter according to people’s priorities and perceptions and their level of acculturation. This study demonstrates a degree of specificity to the individual’s culture and cultural expression that was not observed in many of the included studies
In terms of adaptation the magazines also contained artwork from local African American artists and stories of local African American history. Extensive consultation was carried out in the development and formative evaluation of the materials with the population of interest
Outcomes and insightsThe results showed that women who received BCT + CRT magazines were more likely than those in the BCT, CRT and control groups to have greater increases in the number of fruit and vegetable servings consumed daily. This suggests that the CRT required behavioural constructs to be effective and also that messages based on BCT alone were effective for some participants only when placed in certain cultural contexts. The authors suggest that there is an important link between culture, behaviour and communication that needs to be investigated and pursued further
| Study | Setting | Health topic | Population | Intervention and comparison | Effecta |
|---|---|---|---|---|---|
|
Ma et al. 2004349 Quality: weak |
USA | Smoking cessation | Chinese | Compared 10 sessions of a culturally adapted group programme with a standard programme for smoking cessation in Chinese male adolescents (aged 14–19 years) |
=/– Adapted intervention did not improve quit rates over standard intervention; number of cigarettes smoked at the 3-month follow-up was lower among participants in the standard programme |
|
Nollen et al. 2007341 Quality: strong |
USA | Smoking cessation | African American | Compared culturally targeted video and guide with standard video and guide. Both groups received nicotine replacement patches and reminder calls and postcards |
= No significant differences were detected between groups for any smoking outcomes (7-day PPA, smoking reduction and readiness to quit) |
|
Quality: moderate |
USA | Smoking cessation | African American | Compared culturally tailored counselling and tailored guide with standard counselling and standard guide for smoking cessation |
= At the 6-month follow-up, 1-week abstinence and quit rates were not statistically different between the two groups |
|
Webb 2008351 Quality: strong |
USA | Smoking cessation | African American | Compared a culturally adapted self-help guide for smoking with a standard guide |
– Adapted guide did not improve 24-hour PPA at the 3-month follow-up; participants who were less acculturated (i.e. more traditional) and received the standard intervention were more likely to report 24-hour PPA |
|
Newton and Perri 2004350 Quality: moderate |
USA | Physical activity | African American | Compared 10 standard group counselling sessions over 6 weeks (mixed ethnicity groups; group leader not African American; located within hospital; standard material) with 10 culturally sensitive group counselling sessions (all African American groups; African American group leader; located in African American community; material adapted) |
= No statistically significant differences were detected in improvements in cardiovascular fitness and reported physical activity between the culturally sensitive and standard conditions |
|
Kreuter et al. 2005293 Quality: strong |
USA | Healthy eating | African American | Compared intervention of six magazines to increase fruit and vegetable consumption. Four arms: magazine stories were tailored to behaviour (BCT), culture (CRT), behaviour + culture (BCT + CRT) or control (delayed intervention) |
=/– Median changes in daily fruit and vegetable servings were significantly greater for women in the BCT + CRT group than for women in the CRT group, but not significantly greater than for those in the BCT or control group |
|
Ard et al. 2008348 Quality: strong |
USA | Physical activity + healthy eating | African American | Compared all African American group sessions with mixed race group sessions for weight loss |
= Significant weight loss was reported for both groups (mean weight loss 4.2 kg) with no effect (adherence, fruit and vegetable intake, physical activity or weight loss outcomes) attributable to group composition |
|
Quality: strong |
USA | Physical activity + healthy eating | African American | Compared three church-delivered interventions: standard education materials vs culturally adapted education materials vs culturally adapted education materials and four motivational interviewing telephone counselling calls |
+ Participants who received the culturally adapted education materials with and without the motivational interviewing calls increased fruit and vegetable intake and minutes of physical activity at the 1-year follow-up compared with participants receiving standard education materials |
|
Yanek et al. 2001352 Quality: moderate |
USA | Physical activity + healthy eating | African American | Compared three church-based interventions: standard group sessions vs standard group sessions and spiritual/culturally adapted component vs non-spiritual self-help materials |
= At the 1-year follow-up there were no differences in outcomes (dietary nutrient intake, physical activity and BMI) detected between the different conditions |
Smoking cessation interventions
A self-help intervention trial conducted by Orleans et al. 306,347 for African American adult smokers (n = 1422) compared those who received tailored counselling and a targeted guide with those who received standard counselling and a guide. The tailored guide was called Pathways to Freedom: Winning the Fight against Tobacco and was written at a sixth-grade reading level and featured only images of African American smokers and quitters. It presented information matched to the pattern of smoking observed in African American populations (low daily smoking rate, smoking mentholated and/or high tar/nicotine cigarettes) and addressed unique barriers faced by African American smokers. The control group received standard quit smoking counselling and a guide called Clearing the Air (produced by the National Cancer Institute). This guide was written at an eighth-grade reading level and featured images of ethnically diverse smokers and quitters. The one-off counselling offered to the comparison group was standard stage-based counselling, whereas the tailored counselling utilised an interactive style, reflecting a communication preference of African Americans. At 6 months, significantly more quit attempts (p = 0.007), a greater reduction in the number of cigarettes smoked (p = 0.002), more quit dates set (p < 0.001), greater switching to a lower nicotine brand of cigarettes (p < 0.001) and greater use of pre-quitting strategies (p < 0.05) were observed among participants who received the tailored intervention than among those who received the standard intervention. However, differences in self-reported 1-week abstinence (16.2% tailored vs 14.4% standard) and quit rates (10.1% tailored vs 9.1% standard) were not statistically significant between the two groups. A subset of participants was selected for follow-up at 12 months and those in the tailored group reported higher self-quit rates than those in the comparison group, and this difference was significant (25.0% tailored vs 15.4% standard, p = 0.034). This difference, however, was detected only in a much smaller, opportunistic cohort and must therefore be interpreted with caution.
Webb352 conducted a RCT with African American adult smokers (n = 260) comparing a culturally sensitive (adapted) smoking cessation guide compared with a standard guide. The guide was the same Pathways to Freedom used in the Orleans et al. trial,306,347 which featured statistics specific to African Americans and emphasised collectivism, African American history and religious and spiritual elements. In contrast to the Orleans et al. trial,306,347 however, the comparison group received the same guide, but with all of the culturally sensitive elements removed and replaced with more generic messages and images (e.g. cartoon images; race-neutral images instead of African American images; motivational quotations instead of cultural or religious quotations; epidemiological information for the general population rather than specifically addressing African American smoking issues; discussion of light cigarettes instead of menthol cigarettes; and with no emphasis on African American history). Participants completed an African American Acculturation Scale prior to the intervention. At 3 months’ follow-up and following an intention-to-treat analysis, the 24-hour self-reported point prevalence abstinence (PPA) was 13.7% adapted compared with 14.7% standard, and the 7-day PPA was 10.7% adapted compared with 9.4% standard. Surprisingly, those who were less acculturated (i.e. greater ethnic group affiliation or identification) and received the standard, generic intervention were more likely to report 24-hour PPA, whereas those who were less acculturated and received the adapted intervention were less likely to report 24-hour PPA. Despite those who were less acculturated reporting a preference for the adapted guide and greater readiness to quit, this was not reflected in 24-hour PPA at the 3-month follow-up.
The third study conducted by Ma et al. 349 was a small RCT to help Chinese male adolescents (aged 14–19 years, n = 31) quit smoking. The trial compared a 10-session (one session per week) culturally modified (adapted) programme with a standard programme. The adapted programme was conducted at a community-based organisation and addressed themes that were thought to be relevant to Asian populations, such as collectivism and harmony, persistence and hard work, Asian pride and social norms. The standard programme also consisted of 10 sessions (one session per week), but it was poorly described. At the 3-month follow-up the quit rate was comparable among participants in the adapted programme and those in the standard programme (18.2% adapted vs 23.1% standard). Among continued smokers there was a difference in the reported number of cigarettes smoked between participants in the adapted programme and those in the standard programme (mean 13.9 cigarettes on weekdays and 20.8 at the weekend for those who received the adapted intervention vs mean 7.4 weekdays and 10 weekend for those who received the standard intervention; p < 0.05).
The fourth study was a RCT (n = 500) conducted by Nollen et al. 341 for African American smokers. At randomisation, both groups received 8 weeks of nicotine replacement patches. Intervention participants received a culturally targeted smoking cessation programme with a video (The Harlem Health Connection’s Kick-It!) and print guide (Pathways to Freedom). Both materials were developed by and for African Americans, with an emphasis on communalism, religion/spirituality and African American ancestry and history, along with appropriate graphics and an orientation towards a communication style of experience-based storytelling. Standard care participants received a video tape (How to Quit) produced by the American Medical Association and a print guide (Freedom from Smoking) produced by the American Lung Association. Both included images of African Americans but neither was specifically designed for use with African American smokers. Both groups received reminder telephone calls and postcards. At the 6-month follow-up, intervention participants reported greater usage of the targeted guide (68.8% vs 59.6%, p < 0.05); however, this did not translate into improved outcomes. No significant differences were detected between groups for any smoking outcomes (7-day PPA, smoking reduction and readiness to quit). Although not significant, there was an indication that the adapted intervention material was more effective for African Americans who scored highly on a racial identity scale (higher scores suggesting greater Afrocentricity).
Physical activity interventions
Newton and Perri350 conducted a RCT comparing three home-based exercise promotion interventions for African American adults (n = 90). Participants were first randomised to one of five interventions (four intervention conditions that differed in intensity and frequency of prescribed exercise and one physician advice) and then further randomised to one of three conditions differing on cultural adaptation. The three adaptation conditions were standard behavioural exercise counselling, culturally sensitive exercise counselling and a physician advice group. Standard counselling participants received 10 group sessions over 6 months; group sessions were with predominantly white European (‘Caucasian’) members and ‘Caucasian’ group leaders (this study was part of a larger study) in a hospital setting, utilising standard materials. Culturally sensitive counselling groups received the same programme as the standard counselling with the exception that the group sessions included only African American members, sessions were led by African American counsellors, sessions took place at a site within the African American community and the programme used materials that addressed the sociocultural concerns of African Americans. At the 6-month follow-up, participants in all three streams reported increases in their physical activity; however, no statistically significant differences were detected in improvements in cardiovascular fitness and reported physical activity between the culturally sensitive and the standard conditions. The authors also reported that acculturation, as measured by the African American Acculturation Scale, did not moderate the observed relationship between group assignment and outcomes. They hypothesised that the majority of the participants were ‘bicultural’ and therefore it was likely that both the culturally tailored and the standard information would be salient to them.
Healthy eating interventions
Kreuter et al. 293 conducted a cancer prevention RCT (n = 1227) for African American women. The study compared the effectiveness of six health magazines, delivered over an 18-month period, to increase fruit and vegetable intake in women between 18 and 39 years of age. The four approaches were behavioural construct tailoring (BCT), culturally relevant tailoring (CRT), BCT + CRT and control. Each magazine featured 10 tailored stories (six of which were on the health topic). Cultural tailoring was based on four constructs – religiosity, collectivism, racial pride and time orientation – thought to be related to health behaviours in African American women. Behavioural tailoring was based on diet-related knowledge and identified barriers. BCT + CRT magazines featured equal numbers of BCT and CRT stories. The control was a delayed intervention upon completion of the study. At 18 months, the median increase in daily fruit and vegetable servings for all women was +0.57 servings per day. Increases in daily fruit and vegetable servings were largest for women who received BCT + CRT magazines, compared with those who received BCT, CRT and no magazines (control) (+0.96 vs +0.43 vs +0.25 vs +0.59, respectively). Median changes in daily fruit and vegetable servings were significantly greater for women in the BCT + CRT group than for those in the CRT group (p < 0.05), but not significantly greater than for those in the BCT or control group. The study therefore did not find evidence of effectiveness of culturally tailored messages alone, but only when combined with behaviourally tailored messages.
Physical activity and healthy eating interventions
Resnicow et al. 294,295 conducted a three-group cluster RCT (16 churches, 1056 participants) to increase fruit and vegetable consumption and physical activity among black church attendees. Group 1 received standard education material, a health fair at baseline, individualised results feedback, a project newsletter, an aerobic video and health education brochures. Group 2 received culturally targeted self-help healthy eating and physical activity material (including a healthy eating video Forgotten Miracles, an Eat for Life cookbook, a 20-minute Healthy Body Healthy Spirit exercise video and guide and an audio cassette featuring workouts set to gospel music) along with a pedometer to encourage physical activity. Group 3 received the same culturally targeted self-help material and pedometer as group 2 and in addition received four telephone counselling calls based on motivational interviewing principles. Only the comparison between groups 1 and 2 is discussed in this section; comparison between groups 2 and 3 is discussed in the following section (Comparison of adapted plus an additional component intervention). At the 1-year follow-up, the authors reported significant changes in both fruit and vegetable intake and physical activity for groups 2 and 3 compared with group 1 (p < 0.05). The mean of the three Food Frequency Questionnaires (FFQs) demonstrated a change of 0.44 servings for group 2 and 0.17 servings for group 1 and an increase in total minutes of physical activity. A relatively larger effect was observed for fruit and vegetable than for physical activity. The authors conclude that churches are appropriate settings to deliver health promotion programmes.
The second direct comparison study in this category was by Yanek et al. ,352 this being another group RCT aiming to increase physical activity and improve healthy eating for African Americans, with delivery through the church (16 churches). Three interventions were compared. Group 1 received standard group sessions on healthy eating and physical activity for 1 year. Group 2 received the same standard group sessions on healthy eating and physical activity and in addition a spiritual and cultural component. Group 3 received a control programme of non-spiritual self-help intervention that included materials from the American Heart Association on healthy eating and physical activity. At the 1-year follow-up there were no differences in outcomes (dietary nutrient intake, physical activity and BMI) detected between the different approaches. There is a possibility that the group effect may have diluted the effect of the spiritual and cultural components.
The third direct comparison was an observational study (n = 377) conducted by Ard et al. 348 as part of a larger weight loss maintenance trial. In this study, African Americans were assigned to either an all-African American weight loss maintenance intervention group or mixed race groups. All of the sessions on weight loss (through calorie reduction, changes in diet and increases in physical activity) were the same except for the racial composition of the group sessions and the ethnicity of the group leader. Only groups (all African American or mixed) led by the same interventionists were compared. Significant weight loss was reported for both groups (mean weight loss 4.2 kg) with no effects (whether for adherence, fruit and vegetable intake, physical activity or weight loss outcomes) attributable to group composition. The authors suggested that the large number of African Americans in the mixed group may have resulted in a critical mass effect.
Summary of adapted compared with standard approaches
In summary, the nine studies that compared an adapted intervention with a non-adapted or standard approach did not show increased effectiveness in favour of the adapted version (see Table 14). Only one study294,295 reported increased effectiveness with the use of adapted self-help material compared with standard materials; however, this study was the least equivalent in terms of materials received (the culturally tailored group also received pedometers as cues to walking) and detectable differences in fruit and vegetable intake also differed depending on the FFQ used. Five studies306,341,347,348,350,352 were unable to detect increased effectiveness of a tailored intervention compared with a standard intervention. As many of the outcomes were evaluated through self-reports, the authors have suggested that social desirability may have biased the reported outcomes. Two studies further reported some outcomes for which there was no differential effect and other outcomes for which the increased effect was in the opposite direction of the stated hypothesis. 293,349 One study reported outcomes that supported the effectiveness of the standard intervention over the culturally adapted intervention. 351 These studies highlight the complexity surrounding adaptation for ethnic minority groups, in which dimensions such as ethnic identity, acculturation and behavioural components appear to moderate the salience of the adaptations undertaken. The relationships are not straightforward as bicultural identity,344,345 ethnic identity335 and level of acculturation306,347 appeared to interact with targeted intervention materials in perhaps unexpected ways. There is the possibility that these ethnic identity dimensions may also have been related to income and social class. The same appeared to be true for behavioural components293 and future studies need to account for these complexities.
It is worthwhile noting that the two smoking studies with ‘strong’ quality scores341,351 demonstrated that, although adapted intervention materials were appropriate, particularly for those with higher degrees of ethnic identification, these preferences did not necessarily improve smoking cessation outcomes for participants in the intervention group. The healthy eating study with a ‘strong’ quality score293 provides compelling evidence suggesting that adaptation alone is insufficient to change behaviour, and that an intervention component that explicitly addresses behaviour in conjunction with tailored information is needed. The only study to demonstrate a behaviour change from adaptation and with a ‘strong’ quality score is a church-based physical activity and healthy eating intervention. 294,295 It should be noted that both the standard and the adapted conditions were delivered in a church context and may therefore already incorporate an element of cultural appropriateness.
Adaptations featured in adapted compared with unadapted/standard interventions
The nine studies comparing adapted with unadapted interventions covered 39 of the 46 adaptations identified from the entire body of 107 studies (Table 15). Although the number of adaptations used is high, seven adaptations were not utilised. These adaptations include ethnically matched leadership (adaptation 9), material in the target population’s language (adaptation 13), materials reflect target population’s language (adaptation 14), consideration of target population’s employment situation (adaptation 25), address concerns with medical programmes, procedures and medication (adaptation 31), maintain cultural significance of food (adaptation 43) and gender considerations (adaption 46). It is surprising that adapting materials for language was not featured among these studies, as it is probably an adaptation that one would intuitively consider first. More likely, these particular adaptations were perhaps not relevant to the interventions, for example maintaining the cultural significance of food for smoking cessation interventions, or adapting for language when the population consists of second-generation populations. These findings suggest that selecting adaptations may not be an additive process, in which more is better; rather, it requires a careful consideration of the needs of the population, balanced with the needs of the study. A calculation of the mean number of adaptations further illustrates this point. The mean number of adaptations was 11.3 for the 9 head-to-head studies and 9.2 for the other 98 studies. A t-test did not show this difference to be statistically significant.
| Study | Setting | Health topic | Population | Adaptations (see Table 13) |
|---|---|---|---|---|
| Ma et al. 2004349 | USA | Smoking cessation | Chinese | 2, 6, 18, 19, 22, 24, 37, 38, 40, 41 |
| Nollen et al. 2007341 | USA | Smoking cessation | African American | 8, 12, 15, 16, 20, 22, 26, 29, 38, 41, 45 |
| Orleans et al. 1998306,347 | USA | Smoking cessation | African American | 2, 10, 12, 15, 17, 18, 20, 21, 22, 23, 26, 30, 34, 38, 39 |
| Webb 2008351 | USA | Smoking cessation | African American | 11, 12, 15, 16, 17, 18, 20, 22, 26 |
| Newton and Perri 2004350 | USA | Physical activity | African American | 4, 12, 18, 22, 24, 33 |
| Kreuter et al. 2005293 | USA | Healthy eating | African American | 1, 2, 3, 8, 18, 20, 21, 22, 29, 32, 37 |
| Ard et al. 2008348 | USA | Physical activity + healthy eating | African American | 2, 4, 8, 24, 42, 44 |
| Resnicow et al. 2005294,295 | USA | Physical activity + healthy eating | African American | 2, 5, 7, 11, 12, 15, 18, 19, 20, 22, 26, 27, 28, 29, 30, 32, 33, 34, 35, 36, 38, 39 |
| Yanek et al. 2001352 | USA | Physical activity + healthy eating | African American | 2, 4, 5, 8, 10, 21, 22, 33, 34, 35, 36, 41 |
Comparison of adapted with adapted plus an additional component interventions
Examining studies that adapted for both control and intervention as a baseline and included an additional component for the intervention yielded further insights into the effectiveness of adaptation and whether or not the additional component would enhance effectiveness. A total of 16 studies with an ‘additional component’ were identified; one353 of these studies was included in the systematic reviews that we identified. Studies have been categorised according to the type of component under review and summarised. These components included additional cultural adaptation, additional behavioural modification, additional resources and altered intervention delivery. A summary of the studies is provided in Table 16 and an exemplar study is discussed in Box 7.
This RCT was designed to test the addition of individual tailoring to an adapted intervention promoting fruit and vegetable intake in an African American adult population (n = 560)
Both the intervention and the control groups received a set of three newsletters over 3 months promoting behaviour change for improved nutrition. Topics addressed in the newsletters included food and vegetable preferences, social roles for shopping, barriers to fruit and vegetable intake and dietary limitations
Participants were recruited from two integrated health-care delivery systems, one in Detroit and one in Atlanta. Participants were randomly selected from health-care lists and health-care centre attendees in the two sites, respectively. One-third of the participants were randomised to the control group and two-thirds to the intervention. This 2 : 1 design was employed to ensure that enough people received all of the 16 types of newsletters that were developed for the intervention
AdaptationThe newsletters were tailored to demographic and social cognitive variables for both the intervention and the control groups. The control group newsletters were designed for a ‘general Black American audience with a slight Afrocentric focus’ and contained untailored ethnically neutral graphics that did not contain any people or other ethnic cues
The intervention group received additional individual tailoring to their ethnic identity. Ethnic identity was measured using an assessment of newsletter preference (e.g. would you prefer a newsletter designed for black people in America, black and white Americans, people of various races and cultures) and also through the Black Identity Classification Scale (BICS). The BICS assigned participants to 16 types of ethnic identity ranging, for example, from ‘Assimilated’ to ‘Afrocentric/Multicultural with Cultural Mistrust’. The adapted newsletters were therefore tailored to have messages and graphics (from a large database of images) that were appropriate to the 16 types of ethnic identity. For some participants this would mean that their newsletters were more adapted than the control newsletters, which were already targeted to a degree, and for others it would mean that they may be less adapted, that is, newsletters featuring both black and white Americans
Outcomes and insightsA follow-up survey was administered by telephone at approximately 3 months post intervention. A total of 468 participants (83.6%) provided 3-month follow-up data. The intervention group increased their fruit and vegetable intake by 1.1 servings per day compared with 0.8 servings for the control group. This difference was not statistically significant. A subsequent analysis compared only the participants assessed to be highly ‘Afrocentric’ in both the intervention and control groups and demonstrated a significant difference in intake of 1.4 servings per day compared with 0.43 servings per day, respectively (p < 0.05)
This was one of the few studies that measured ethnic identity and attempted to adapt according to this measure. Although overall there was no significant difference between groups, the subsequent analysis suggested that an adapted intervention was most successful for participants with strong cultural affiliations (the ‘Afrocentric’ group). It may be most beneficial to target adapted interventions to those who are most receptive to such an approach. Furthermore, the effects of the adaptation may have been diluted as the control newsletter was already adapted with a ‘slight Afrocentric focus’
| Study | Setting | Health topic | Population | Intervention and comparison | Effecta |
|---|---|---|---|---|---|
| Ahluwalia et al. 1998355,356 | USA | Smoking cessation | African American | Culturally adapted behavioural support programme with the addition of NRT patches in the intervention group and placebo for the control group |
+ (short term) The addition of NRT patches was effective in the short term (10 weeks), but not at 6 months |
| Ahluwalia et al. 2002342–345 | USA | Smoking cessation | African American | Culturally adapted counselling and resources with the addition of bupropion slow release for the intervention group and placebo for the control group |
+ The addition of bupropion slow release was effective at 7 and 26 weeks |
| Ahluwalia et al. 2006361–364 | USA | Smoking cessation | African American | Culturally adapted motivational interviewing or health education plus nicotine gum for the intervention groups and placebo gum for the control groups |
= The addition of nicotine gum had no significant effect on the intervention |
| Li et al. 1984357 | USA | Smoking cessation | African American | Culturally adapted media intervention with the addition of physician brief advice |
+ The addition of physician brief advice significantly increased the effectiveness of the intervention |
| Lipkus et al. 1999358 | USA | Smoking cessation | African American | Health-care provider prompting and tailored print communications plus tailored telephone counselling for the intervention group |
= There was no significant effect of the addition of tailored telephone counselling over the effect of the baseline intervention |
| Campbell et al. 1999326 | USA | Healthy eating | African American | An adapted church bulletin that was further adapted for either spiritual or expert (control) content |
= Both the intervention and the control groups increased their fruit and vegetable intake but there was no significant difference in outcomes between the groups |
| Resnicow et al. 2001325,335 | USA | Healthy eating | African American | Culturally adapted self-help nutritional intervention with the addition of telephone counselling based on motivational interviewing |
+ The addition of motivational interviewing appeared to increase fruit and vegetable intake significantly over that in the control group |
| Resnicow et al. 2009296 | USA | Healthy eating | African American | An adapted newsletter promoting fruit and vegetable intake further adapted according to levels of participant ethnic identity |
+ (subgroup) Further adaptation according to levels of ethnic identity appears to have a significant effect only in some groups of the African American population |
| Befort et al. 2008317 | USA | Physical activity + healthy eating | African American | Culturally adapted weight loss programme with the addition of motivational interviewing (vs health education as an attention control) |
= There was no significant effect demonstrated through the addition of motivational interviewing |
| Djuric et al. 2009354 | USA | Physical activity + healthy eating | African American | Culturally adapted diet and exercise counselling with the addition of spiritual counselling |
+ (healthy eating) = (weight) The addition had no effect on weight loss but significantly improved some elements of dietary intake |
| Fitzgibbon et al. 2005353 | USA | Physical activity + healthy eating | African American | Culturally adapted weight loss intervention with the addition of a faith component |
= There was no significant difference in outcome between the faith group and the control group |
| Nothwehr et al. 2001312 | USA | Physical activity + healthy eating | African American | Culturally adapted healthy eating and exercise sessions delivered sequentially in one order for one group and in the reverse order for the other group |
= There was no significant difference in outcomes according to the sequence of delivery of the intervention |
| Resnicow et al. 2005324 | USA | Physical activity + healthy eating | African American | Culturally adapted physical activity and healthy eating intervention with the addition of a high-intensity vs a low-intensity intervention |
= Alteration of the intervention intensity did not significantly affect the outcomes |
| Resnicow et al. 2005294,295 | USA | Physical activity + healthy eating | African American | Culturally adapted self-help intervention with the addition of telephone counselling |
+ (healthy eating) = (physical activity) The addition of telephone counselling is effective for healthy eating outcomes, but not for physical activity outcomes |
| Thompson et al. 2008359,360 | USA | Physical activity + healthy eating | African American | Culturally adapted internet intervention with the incentive sequence to be given either immediately or at the end of the programme |
= The alteration of the incentive sequencing did not significantly alter the log-on rates for the intervention |
| Williamson 2006280–282,314 | USA | Physical activity + healthy eating | African American | Culturally adapted internet-based health education with the addition of internet-based counselling for the intervention group |
+ (short term) The addition of the counselling to create a more interactive intervention had a significant effect on fat loss at 6 months, but no significant effect at the 18-month follow-up |
Additional cultural adaptation
To increase effectiveness, some studies trialled the addition of a discrete adaptation. For example, a healthy eating intervention conducted by Resnicow et al. 296 for an African American population (n = 560) utilised a RCT design to assess the addition of a heightened degree of cultural adaptation to an intervention that was already adapted for this population. Participants were randomised to receive magazines promoting fruit and vegetable intake over a 3-month period. The control group newsletters targeted a general ‘black American’ audience with minimal Afrocentric focus and the graphics were untailored and ethnically neutral (e.g. no people featured). The intervention newsletters were specifically adapted to 16 levels of ethnic identity as assessed by the Black Identity Classification Scale. The intervention group slightly increased their daily mean fruit and vegetable intake compared with those assessed to be the most ‘Afrocentric’ in the control group and this was not statistically significant. However, when participants who were assessed to be the most Afrocentric in the intervention group were compared with the control group, the increase was statistically significant (p < 0.05). The authors concluded that the additional effort of adjusting an adapted intervention for varying degrees of ethnic identity might be an effective strategy for some African American groups.
Several studies examined the addition of a religious or spiritual component to an already culturally adapted intervention. 325,353,354 For example, in the Lifestyle Improvement with Food and Exercise (LIFE)348 weight loss trial for African American women (n = 31), all participants (obese breast cancer survivors) received individualised dietary and exercise counselling for an initial 6 months. At 6 months they were then randomised to receive additional spiritual (non-denominational) counselling or to continue with individualised counselling. The added spiritual component had no significant effect on weight loss, but it did appear to significantly improve fruit intake and healthy eating scores (p < 0.05 for both measures).
Similarly, Fitzgibbon et al. 353 conducted a randomised trial called ‘Faith on the Move’ for African American overweight/obese women (n = 59) in which all participants received a culturally tailored weight loss intervention with one group receiving an additional faith component. The baseline intervention emphasised oral communication skills (e.g. sharing ‘stories’ about unhealthy eating practices using historical figures to increase salience) and offered childcare to alleviate some of the women’s family obligations. The additional faith component included the addition of scriptures to the intervention. At 12 weeks’ follow-up, both groups lost weight and decreased their dietary fat intake. The average weight loss was 2.6 kg in the faith group and 1.6 kg in the group that did not receive spiritual counselling. However, despite these trends, there were no significant differences between the two groups at 12 weeks [BMI change: p = 0.37; weight change (kg): p = 0.34; weight change (%): p = 0.41].
The third study with an added spiritual component was conducted by Campbell et al. 326 with a rural African American population. The study was part of a larger study called Black Churches United for Better Health (BCUBH), which delivered a multilevel, multicomponent healthy eating intervention. A total of 10 counties320 (with 50 churches) were pair matched and randomised to receive either the intervention or the delayed intervention. The intervention included computer-tailored bulletins, healthy eating teams and lay health advisors, education sessions and cooking classes. Environmental modifications were also made to increase fruit and vegetable availability within the churches and at point of purchase in the community. For this study, the 25 churches (n = 2519) initially randomised to the intervention group were further randomised to receive a spiritual or pastor-oriented bulletin or an expert-oriented bulletin to test the effect of the spiritual component (n = 459). Both bulletins were designed to promote fruit and vegetable intake and were tailored to participants according to their baseline assessments for factors including stages of change, perceived risk and barriers and social support. Each bulletin was also tailored to the participant’s church name and contained a traditional African American fruit and vegetable recipe. The spiritual bulletin included a message from the pastor, a photo of the pastor, a ‘five-a-day’ grace, spiritual language, biblical references and articles written by church members. The expert bulletin referenced healthy eating research. At follow-up, message recall was good for both groups, but message trust was higher for the spiritual bulletin group (p < 0.05). Both groups increased fruit and vegetable consumption significantly (4.9 daily servings at follow-up for the spiritual group and 4.8 servings for the expert group) compared with the control group (p < 0.05), but there were no significant differences detected in outcomes between the spiritual and the expert groups. The results need to be interpreted with caution as it is difficult to know what changes in behaviour were attributed to the bulletin and what could be a result of the broader interventions in place.
Additional behavioural modification
Instead of additional adapted components, some studies trialled the addition of behavioural components to culturally adapted interventions to detect possible enhanced effectiveness. In the adapted Lifestyle Balance programme, Befort et al. 317 conducted an adapted behavioural weight loss programme for African American women (n = 44). Women were randomised to receive either additional sessions of motivational interviewing or health education delivered as the comparator intervention. Adaptations in the baseline intervention included guidance about food and physical activity relevant to cultural practices, the recognition of preferences for larger body sizes and the use of peer mentors who had been successful in weight loss. After the 16-week programme, both groups were successful in achieving significant dietary changes and weight loss but there were no significant differences between the groups (p-values not reported).
Motivational interviewing was also added to an adapted intervention by Resnicow et al. 325,335 The Eat 4 Life trial (14 churches, n = 1011) was a healthy eating intervention for an African American church-attending population. Churches were randomly assigned to receive a culturally adapted self-help intervention with one telephone cue call or a culturally adapted self-help intervention with one cue call and three counselling calls based on motivational interviewing. Adaptations included targeted intervention materials, the involvement of an African American advisory board, the use of biblical and spiritual themes and the use of recipes from church members. At 1 year of follow-up, a significantly higher effect was detected for fruit and vegetable intake for the group who received motivational interviewing (net difference between motivational interviewing group and self-help group was 1.14 fruit and vegetable servings per day as measured by a 36-item FFQ; p < 0.05). The authors concluded that motivational interviewing was a promising strategy for improving dietary behaviours in this population and setting.
The Healthy Body/Healthy Spirit trial (16 churches, n = 1056) by Resnicow et al. 294,295 assessed the addition of motivational interviewing by telephone counselling to an adapted intervention. This intervention was again focused on an African American church-attending population to address healthy eating and physical activity. Telephone counselling was delivered in addition to a culturally targeted self-help healthy eating and physical activity intervention, and this was compared with the self-help intervention delivered alone. At 1 year of follow-up there was a statistically significant effect observed on fruit and vegetable intake (p < 0.05) with the addition of telephone counselling (measured using a composite FFQ), but not for the physical activity outcomes. It should be noted that the statistically significant increase in fruit and vegetable intake varied with the FFQ used, with several versions used in the assessment.
Additional resources
Five smoking cessation studies were identified that examined the addition of a resource; the resources were most often, although not exclusively, pharmaceutical adjuncts to smoking cessation. Ahluwalia et al. 355,356 conducted a randomised double-blind placebo-controlled trial among an inner-city African American population (n = 410). An adapted behavioural support programme for smoking cessation was offered as the baseline intervention with the added component of nicotine replacement therapy (NRT) in the intervention group. The adapted programme utilised a culturally sensitive smoking cessation guide, had flexible session times and catered for differing literacy levels. Both programmes proved effective at follow-up with quit rates of 21.5% and 13.7% at 10 weeks and 17.1% and 11.7% at 6 months in the intervention and control groups, respectively. The addition of the NRT patch was found to significantly increase the effectiveness of the culturally adapted intervention at 10 weeks both before and after adjusting for the baseline differences in age and education (p = 0.03, adjusted p = 0.04), but not at 6 months (p = 0.08, adjusted p = 0.14). The authors concluded that NRT patches were a useful adjunct to a culturally tailored behavioural support programme in the short term.
A later study by Ahluwalia et al. 342–345 again used a randomised double-blind placebo-controlled trial to assess the effect of bupropion slow release as an addition to counselling sessions for smoking cessation among an African American population (n = 600). The counsellors were all African American and a smoking cessation resource specifically developed for African American populations was provided for all participants. The addition of bupropion slow release to this adapted intervention was found to significantly increase the effectiveness of the intervention both after 7 weeks of treatment (36% vs 19% quit rates; p < 0.001) and at 26 weeks’ follow-up (21% vs 14% quit rates; p = 0.02) and this was therefore recommended as an effective addition to the culturally adapted counselling.
A third two-by-two factorial RCT conducted by Ahluwalia et al. 361–364 assessed the effectiveness of nicotine gum as an addition to a culturally adapted intervention for smoking cessation in an African American population of ‘light smokers’ (n = 755). All participants were given a culturally sensitive smoking cessation guide developed specifically for African American light smokers and were randomised to either motivational interviewing plus gum or placebo, or health education plus gum or placebo. At 6 months there was no significant increase in effectiveness of nicotine gum over placebo in conjunction with either motivational interviewing or health education on 7-day quit rates (14.2% vs 11.1%; p = 0.23); however, health education was reported to be significantly more effective than motivational interviewing for this population (16.7% vs 8.5%; p < 0.001) at all time points (1, 8 and 26 weeks).
Li et al. 357 conducted a smoking cessation trial with African American women (n = 1179) set in three family planning waiting rooms. Four conditions were compared: baseline questionnaire; baseline questionnaire and media programme; baseline questionnaire and physician message; and baseline questionnaire and media programme and physician message. The media intervention featured age- and ethnically appropriate models encouraging people to stop smoking. The additional resource delivered to the intervention group was physician brief advice to stop smoking (comparing the second and fourth interventions only). The findings showed that the brief advice increased cessation rates significantly over the culturally appropriate media intervention (quit rates of 12.9% vs 6.4% at 3 months; no p-values reported).
A smoking cessation randomised trial by Lipkus et al. 358 compared a baseline health-care provider prompting intervention for African Americans (n = 266 enrolled) with the addition of culturally appropriate, individually tailored print communications. A third group received both tailored print communications and tailored telephone counselling. Of the 160 participants who completed the study, 35 (21.8%) had quit smoking at the 16-month follow-up. Participants who received tailored print communications had a statistically significant higher quit rate than those with health-care prompting alone (32.7% vs 13.2%; p < 0.05); however, the addition of tailored telephone counselling to this adapted intervention did not increase the effectiveness significantly (19.2% vs 13.2%; no p-values reported).
Altered intervention delivery
The final type of study identified altered the delivery of the intervention. The Health Improvement Program for Teens (HIP Teens) was a RCT conducted by Williamson280–282 investigating an internet-based physical activity and healthy eating intervention delivered to African American adolescent girls (n = 57) and their parents (56 mothers and 1 father). Participants were randomised to either a culturally specific website that was interactive with internet-based counselling or a culturally specific website that provided education only (passive learning). All participants received four face-to-face counselling sessions in the first 12 weeks of the programme. The interactive intervention was significantly more effective at decreasing body fat in the adolescent participants and body weight in the parents at the 6-month follow-up (p < 0.05); however, in the following 18 months, parents and adolescents in both groups gained weight and at 2 years there were no significant differences between the two groups.
A trial called Go Girls! conducted by Resnicow et al. 324 delivered a culturally adapted intervention at either a moderate or a high intensity to African American adolescent girls (n = 123). Sessions consisted of half an hour of physical activity and preparation/tasting of healthy foods. The moderate-intensity intervention included six sessions, whereas the high-intensity intervention included 20–26 sessions. The high-intensity group girls also received four to six telephone counselling calls. The girls were recruited through 10 churches and there was extensive formative research within the African American community to develop this intervention and church involvement in intervention development and as a setting for the intervention. Outcomes were measured at 6 months and 1 year and no significant differences in BMI between the two groups were observed at either time point (p = 0.2 at 6 months, p = 0.76 at 1 year); however, when examining only high attendees (i.e. attended > 75% of sessions) a trend emerged for weight for the high-intensity intervention at 6 months (p = 0.07) and there were significantly better results for BMI, hip circumference and percentage body fat. Despite this, the authors conclude that the high-intensity intervention did not have an effect on adiposity.
Nothwehr et al. 312 carried out a RCT in which African American women (n = 23) were randomly assigned to either 10 weekly healthy eating sessions followed by six weekly exercise sessions or the reverse sequence. Sessions consisted of small group discussions and physical activity or food tasting. An African American Young Men’s Christian Association employee facilitated the intervention and the healthy eating education included culturally relevant dishes and methods of food preparation. Participants were followed up at 4 months and 1 year. Irrespective of the sequencing, both groups showed a significant increase in physical activity (4 months: p = 0.0002; 1 year: p = 0.0001) and vegetable intake (1 year: increase of 0.5 servings a day, p = 0.02) and a significant decrease in the per cent of calories from fat (4 months: p = 0.05), but with no significant weight loss. There was no significant differences attributable to intervention sequencing.
Thompson et al. 359,360 conducted an internet-based intervention for physical activity and healthy eating with 8- to 10-year-old African American girls (n = 80) at risk of obesity. The only difference between the conditions was the incentives given to participants to encourage logging on. Girls were randomised to receive immediate (weekly) incentives or to receive their incentives at the end of the 8-week programme. Incentives consisted of small amounts of money, t-shirts and pens. The baseline intervention was adapted for the participant population through the use of materials/comics with culturally appropriate images and the format of the intervention as an affiliated activity/club, which was a preferred format among these girls. After the 8-week programme a higher log-on rate was observed in the immediate incentive group (79% vs 70%), but this difference was not significant (p = 0.12). Irrespective of the incentive schedule, however, statistically significant improvements were observed in self-reported fruit, juice and vegetable consumption (p = 0.002) and usual physical activity (p = 0.001).
Overall, there were mixed findings from the addition of components to existing culturally adapted interventions. Half of the studies312,317,324,326,353,358–364 showed no difference in outcomes between the adapted intervention and the adapted intervention with an added component. In three studies the added component demonstrated an effect (the addition of physician brief advice for smoking cessation,357 bupropion for smoking cessation342–345 and motivational interviewing for fruit and vegetable intake325,335). Two studies showed short-term effects (smoking cessation355,356 and weight loss280–282,314). Finally, three studies showed some effect of the additional component either for a subgroup of the population296 or for selected outcomes. 294,295,354
Cost-effectiveness
Thirteen studies reported on cost data and one study conducted a cost–utility analysis. A summary of these studies is provided in Table 17. The level of detail and degree of formal economic evaluation differed across these studies. Two of these 13 studies reported on the cost of recruitment and the remaining 11 on the cost of intervention materials and delivery. No studies carried out a cost-effectiveness analysis.
| Study | Setting | Health topic | Population | Cost reporting | Costs |
|---|---|---|---|---|---|
| Ahluwalia et al. 2002342–345 | USA | Smoking cessation | African American | Cost of recruitment | Proactive vs reactive recruitment strategies US$159 per enrolee vs US$22 per enrolee, respectively |
| Stolley et al. 2009365–368 | USA | Physical activity + healthy eating | African American | Cost of recruitment | Active vs passive recruitment; only lowest cost option of e-mail recruitment reported (US$14 per person) |
| Lipkus et al. 1999358 | USA | Smoking cessation | African American | Cost of intervention | Cost approximately US$12.50 per tailored print communication, including material development costs |
| Carroll et al. 2002302 | UK | Physical activity | South Asian | Cost of intervention | Total intervention cost £3000 for a 6-week exercise programme |
| Huhman et al. 2007285–287 | USA | Physical activity | Multi (African American, Chinese) | Cost of intervention | US$194M to develop and implement a mass media campaign |
| Netto et al. 2007368–370 | UK | Physical activity | South Asian | Cost of intervention | Total intervention cost £50,000 per year |
| Anderson-Loftin et al. 2005371 | USA | Healthy eating | African American | Cost of intervention | Intervention cost US$384 per person |
| Agurs-Collins et al. 1997372 | USA | Physical activity + healthy eating | African American | Cost of intervention | Intervention cost US$150 per person |
| Anderson et al. 2007327,328 | USA | Physical activity + healthy eating | African American | Cost of intervention | Two-year total direct cost US$292 per person |
| Ard et al. 2000323 | USA | Physical activity + healthy eating | African American | Cost of intervention | Intervention cost US$106 per person |
| Davis-Smith et al. 2007334,373 | USA | Physical activity + healthy eating | African American | Cost of intervention | Total cost of materials for a six-session intervention US$1075 |
| Thrasher et al. 2004292,299 | USA | Physical activity + healthy eating | African American | Cost of intervention | Intervention materials cost US$20 per person |
| Plescia et al. 2008288,289 | USA | Smoking cessation, physical activity + healthy eating | African American | Cost of intervention | Cost of US$7M over 7 years for a multicomponent intervention for a community population of 20,000 people |
| McBride et al. 2002374 | USA | Smoking cessation | African American | Cost–utility | Incremental cost-effectiveness of biomarker feedback US$1629 per QALY saved |
Cost of recruitment
The RCT conducted by Ahluwalia et al. 342–345 compared bupropion slow release with placebo for smoking cessation among an African American population; only the cost of proactive compared with reactive recruitment strategies (US$159 per enrolee vs US$22 per enrolee, respectively) was reported. Proactive strategies included in-person efforts for recruitment. Proactive strategies alone were insufficient to generate enough participants and subsequent reactive strategies, which included disseminating information to call the study hotline. More potential participants were recruited through reactive than proactive strategies, and they were more likely to be eligible (OR = 4.8) and more likely to be enrolled (OR = 4.2). There were, however, significant differences between the participants recruited, with those recruited through reactive strategies having higher educational attainment, higher income and better health measures than those recruited through proactive strategies. Buproprion slow release was shown to be effective for smoking cessation compared with placebo.
Similarly, the Obesity Reduction Black Intervention Trial (ORBIT) by Stolley et al. 365–368 reported recruitment costs for their weight loss (diet and physical activity) intervention, as formal economic analysis was not possible. They too compared active with passive recruitment strategies and reported that active, in-person recruitment was the most expensive, followed by placing flyers at appropriate sites in the community; no figures were reported for either method of recruitment. E-mail recruitment was reported to be the least expensive at a cost of US$14 per person; however, e-mail recruitment also produced the highest percentage of participants who were ineligible for participation in the study. The intervention was successful as 25% of women in the intervention group lost > 5% of their initial weight over 6 months compared with only 5% in the control group.
Cost of interventions
One smoking cessation study reported the cost of the intervention. A RCT by Lipkus et al. 358 conducted with an African American population at a community health centre reported a cost of approximately US$12.50 per tailored print communication, including the developmental costs. This per item cost would have been reduced with a higher volume of production. The full intervention arm involved a health-care provider prompting intervention with tailored print communications and tailored telephone counselling; however, the costs of these components were not reported.
Three physical activity interventions reported on intervention costs. Carroll et al. 302 and Netto et al. 368,370 both delivered physical activity interventions for South Asian-origin populations and reported only total intervention cost. Carroll et al. 302 reported the cost to be £3000 for a 6-week exercise programme. The intervention was reported to be effective; however, it was difficult to quantify as only qualitative outcomes were provided. Netto et al. 368,370 made reference to supplementary paper369 which reported the costs of their Khush Dil coronary heart disease prevention and control programme to be £50,000 per year. The programme offered healthy eating workshops, healthy cooking workshops, exercise groups and health promotion events and was reported to be effective in reducing mean body weight and BMI.
Huhman et al. 285–287 conducted a prospective, longitudinal, quasi-experimental mass media campaign called VERB to promote physical activity for multiethnic children (3120 parent–child dyads evaluated). The campaign cost US$194M to develop and implement. Professional services were used to produce advertisements for media channels (television, radio and print). The authors concluded that the campaign was successful in raising awareness and that they detected a dose-dependent response whereby more reported views of VERB messages were associated with greater reported engagement in physical activity and positive attitudes towards physical activity at the 2-year follow-up. Children who were aware of VERB reported significantly more physical activity than children who were unaware of VERB.
The only healthy eating study that reported on cost was the Soul Food Light intervention, a longitudinal experimental study with a pre–post test control group conducted by Anderson-Loftin et al. 371 for African Americans with type 2 diabetes (n = 97). The study included four weekly dietary education classes, five monthly group discussions and weekly follow-up telephone calls. The reported cost of the intervention was US$384 per person. The cost included 12 hours a week for a nurse case manager and a hospital-based dietician to deliver the intervention, as well as the materials (e.g. African American food models, diabetes food pyramid, standard curriculum, balance scales, telephone calling cards, stove for diabetes centre, food and laboratory costs). The intervention was reported to be successful at reducing BMI and dietary fat behaviours at the 6-month follow-up compared with a usual care group, who received referrals to a standard diabetes education class.
The following five physical activity and healthy eating studies reported on the costs of their respective interventions. The Duke University Rice Diet was modified by Ard et al. 323 and delivered as a randomised weight loss study to an African American population (n = 56). The 8-week intervention included the provision of food for the first week along with daily counselling on diet and physical activity and group support. The reported cost of the programme was US$106 per person, which was discounted for the participants as they were university employees. The original cost of the programme would have been US$170 per person. At the 8-week follow-up the intervention was successful in reducing BMI and body weight; however, it was unclear whether or not the caloric restriction strategy could be sustained over the long term.
Agurs-Collins et al. 372 reported cost estimates of a 6-month weight loss intervention for African Americans diagnosed with non-insulin dependent diabetes mellitus to be US$150 (not including research-related costs and laboratory tests). This cost included the salaries for a dietician and an exercise physiologist, as well as support staff, the cost of supplies and approximately US$35 per patient worth of education materials. The authors suggested that there might have been changes in direct health-care costs but this was not reported. Weight reduction was statistically significant for women after 6 months, but not for men.
The Healthy Eating and Lifestyle Program (HELP) weight loss intervention conducted by Anderson et al. 327,328 reported the 2-year total direct cost to be US$292 per person. This cost included 10 classes led by healthy eating and physical activity behaviour change specialists (inclusive of their preparation and delivery time) and six individual assessment and counselling sessions. Sustained weight loss was reported at the 18-month follow-up; however, the difference between treatment conditions was not statistically significant.
The Wellness for African Americans Through Churches (WATCH) was a 2 × 2 randomised trial conducted by Thrasher et al. 292,299 comparing tailored print and video material with lay health advisor support for a physical activity and healthy eating programme. Process evaluation suggested that the personalised newsletters might have had a larger impact than the other materials. Together these materials cost approximately US$20 per person. This figure did not factor in the developmental cost of the materials. The intervention did not show differential effects in the comparison conditions.
The Lifestyle Balance church Diabetes Prevention Program (DPP) study was a six-session, volunteer-led feasibility pilot study conducted by Davis-Smith et al. 334,373 The total cost reported for materials was US$1075, which included paper handouts, food, scales, supplies and postage. The cost did not include the salary for the research assistant. Session leaders volunteered their time and the church donated the space for the sessions. Sustained weight loss was reported at the 12-month follow-up.
The final study that reported on costs was a community-based intervention addressing smoking, physical activity and healthy eating issues with an African American population. 288,289 A number of activities were undertaken, including a community coalition, a lay health advisor programme, a farmers’ market and advocacy for raising tobacco taxes and smoking bans. The cost of this multicomponent intervention was US$7M over 7 years for a community population of 20,000 people. Four thousand, seven hundred and thirty people were surveyed in total within the intervention population and statistical significant improvements for all three health behaviours were reported compared with state-wide trends (smoking among women: p = 0.03; decreasing physical inactivity among middle-aged adults: p = 0.01; increasing fruit and vegetable intake: p < 0.001).
Cost–utility
Only one study374 provided a cost–utility analysis of the intervention. A RCT for African American smokers provided feedback on susceptibility to lung cancer based on a test for a particular genetic biomarker. 374 Participants were also given an adapted self-help guide (Pathways to Freedom) along with nicotine patches (where appropriate). This experimental condition was compared with a control of provider advice and referral to a smoking cessation specialist. Genetic feedback of high susceptibility to lung cancer was found to increase smoking cessation rates at 6 months (p = 0.03), but not at 12 months (p = 0.34). Using an intention-to-treat effectiveness measure at 6 months, the average cost of the genetic biomarker feedback was US$1719 (cost per quit). The incremental cost-effectiveness of the genetic biomarker feedback compared with the control (cost per additional quit above usual care) was US$3210. Under the assumption that 1.97 quality-adjusted life-years (QALYs) were saved per quitter, the authors suggested that the incremental cost-effectiveness of biomarker feedback is US$1629 per QALY saved. As the experimental group received both the biomarker feedback and an adapted self-help guide, it was difficult to separate the degree to which they each contributed to the 6-month successful cessation rate.
Discussion
Although a substantial body of literature was identified on adapted interventions for smoking cessation, increasing physical activity and improving healthy eating among African-, Chinese- and South Asian-origin populations, there is little clear evidence on whether or not adaptation is effective. Findings from the 12 theoretical/conceptual reviews suggested that adaptation was important, but the findings from the seven systematic reviews were inconclusive. Although we identified 107 adapted interventions, only nine were designed such that we could directly compare the effectiveness of adaptation as distinct from the effectiveness of the intervention as a whole. The other identified studies ranged from pilot and feasibility studies to pre–post test studies, controlled studies and RCTs with non-equivalent comparison groups.
Only one294,295 of the nine studies comparing the effectiveness of an adapted intervention with that of an unadapted/standard intervention showed a greater effect of the adapted intervention in terms of behaviour change. There are many possibilities for this apparent lack of effect of adaptation. For instance, there may be an inability to detect effect when interventions are conducted with a population identifying with one ethnic group, particularly in group sessions, where a critical mass effect may be overwhelmingly positive, creating an adapted environment in itself. In addition, there are many ethical considerations and feedback from communities that prevent trials from using a strict control, particularly when an adapted intervention may have greater likelihood of improving health behaviours. Researchers, in turn, used attention control groups that offer some health-enhancing activities, which were not related to the outcomes of the study, or used delayed intervention strategies; therefore, there are far fewer ‘direct’ comparisons as some comparator conditions may inevitably involve some degree of adaptation. Issues of contamination are another important consideration, particularly in rural and/or tight-knit communities. Another possible reason for not detecting effects is that the adaptation may be quite sophisticated and irreducible to its component parts. Furthermore, adaptation may need targeting to the ethnic group as well as tailoring to the individual. 36,375 This latter approach is likely to involve more specialised assessment tools to measure the ethnic identity of individuals, the degree of preference and the need for such an adapted approach, and, finally, how ethnic identity and preferences/needs are related. In cases such as these, delivering an adapted intervention for an acculturated group may actually be considered inappropriate. 35
Findings from the 16 studies with a baseline adapted intervention testing the effects of an additional component were also inconclusive. Eight studies reported an increased effect from the added component; however, two were short-term effects and a further two were effective only for some outcomes, and another study was effective only when a subgroup analysis was conducted. Many studies hypothesised that the reason why they were unable to detect any effect was that available tools may not be sensitive enough to detect further difference. In addition, given that the tailored intervention already produced positive outcomes in many cases, the additional effort may not be able to produce any further gains. The latter can be interpreted as a positive finding of this review – that an effect may be reproducible with minimal resources – for example, in two studies, neither the intensive intervention with telephone counselling358 or the addition of motivational interviewing317 produced an additional effect to the baseline adapted intervention. Of the eight studies that detected an effect from the addition of an extra component, five of these studies reported that the effects were either short-lived or for subgroups of the populations or outcomes. It therefore remains to be determined what are the necessary and sufficient conditions under which adaptations can operate optimally, taking into account needs, preferences and resource (time and money) considerations. Finally, only 13 studies reported on the costs of recruitment and intervention materials and personnel, and one study performed a cost–utility analysis. We were therefore unable to draw any definitive conclusions on the effectiveness or cost-effectiveness of adapted interventions compared with standard interventions for ethnic minority populations.
Programme Theory of Adapted Health Promotion Interventions
The purpose of this strand of work was first to synthesise the available evidence on whether or not adapted interventions were more effective than non-adapted intervention, and then to assess whether or not adaptation was cost-effective for uptake by health services. Although no definitive evidence supports the assumption that adapted interventions are more effective for ethnic minority populations, this is likely to be because of the infancy of the evidence base. What is clear is that more studies are needed that compare an adapted intervention with a standard intervention of comparable frequency, intensity and materials/methods used. Given that we identified only nine (out of 107) studies that used a comparative design this suggests that we still lack a sufficient body of evidence and we are therefore unable to provide conclusive recommendations for or against adapted interventions for ethnic minority populations. Overall, the body of identified studies suggests that adaptation increases acceptability of the intervention within the targeted population, measured by process outcomes such as trust in the health message, programme satisfaction and increased programme usage. The onus is therefore on researchers and target populations alike to develop more sophisticated health promotion interventions and programmes that are better evaluated so that we are able to discern the effect of the basic interventions from that of the adaptations. For improved evaluation we also need better outcome measurement tools to differentiate between the lack of effect of adaptations compared with the lack of sensitive measures to detect difference.
One way forward in the pursuit of a rigorous evidence base for adapted interventions and programmes and development of the means to be able to detect difference is the adoption of a standardised approach, which would increase comparability between interventions. Given the diverse range of studies we have identified, it is imperative that future studies be reported in such a way that they can be discussed in a systematic and comparative manner. Thus, from the body of literature we have analysed, we propose a generic Programme Theory of Adapted Health Promotion Interventions (Figure 9) as one strategy to facilitate comparison. The theory is in no way prescriptive and it is certainly not intended to be followed without critical reflection; however, it does provide an initial scaffold to support one’s thinking on how to develop and report on adapted health promotion interventions as a primary goal, and also to further the undertaking of comparative work. Clearly, not all programmes can incorporate study designs with control groups, but being able to discuss findings in a way that can be compared and contrasted with findings from other intervention conditions, in other studies, can generate learning principles across the spectrum of health promotion topics and ethnic minority groups. This theory represents the health promotion intervention cycle as a generic model, which is likely to capture some (if not all) of the steps usually undertaken in a wide range of health promotion interventions. Given that it has been developed using a specific body of identified literature used for this review, we will restrict our current discussion of the theory to interventions that target smoking, physical activity and healthy eating behaviours, although it is likely to have wider applicability.
FIGURE 9.
Programme Theory of Adapted Health Promotion Interventions.
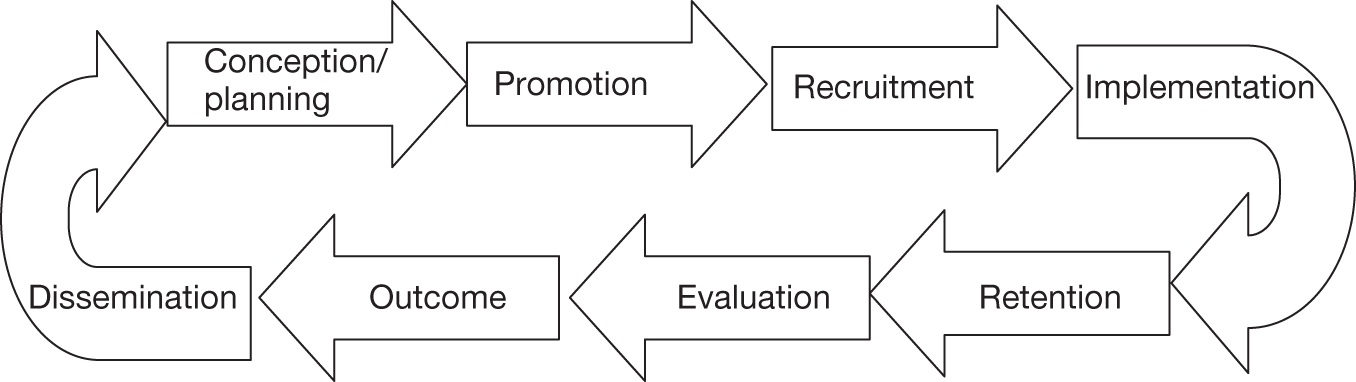
In addition to prompting thinking on improving the reporting of studies, this programme theory can also be viewed as an approach to improve the development of interventions. Other work in this area of ethnicity and health has highlighted the need to examine every stage of an intervention pathway for potential intervention-generated inequalities. 376 This present programme theory offers a possible way to address, then, those potential inequalities. From the 46 items outlined in our Typology of Adaptation (see Table 13) we can begin identifying which of these adaptations may be required when developing an intervention for a particular population and health topic and subsequently map these adaptations onto the Programme Theory of Adapted Health Promotion Interventions to help with study planning. Figure 10 provides a schematic representation of some of the possible adaptations mapped onto the appropriate stages of the intervention. This method represents both a systematic and a transparent way to plan as well as report on adapted interventions, as many of the studies we reviewed often lacked clarity on whether a particular action represented a conscious effort to adapt or an artefact of working with specific ethnic populations. To be able to detect these differences it is necessary first to identify the adapted techniques and strategies that are effective for health promotion. A more comprehensive mapping of the 46 items onto the Programme Theory of Adapted Health Promotion Interventions is offered in Table 18. This is by no means exhaustive or definitive; however, it does draw on the synthesised literature and should be used as a working document that requires further testing. Furthermore, discussion of how to consider adaptations at each stage along the intervention pathway is provided in Chapter 8.
FIGURE 10.
Programme Theory of Adapted Health Promotion Interventions with examples of adaptations at each stage.
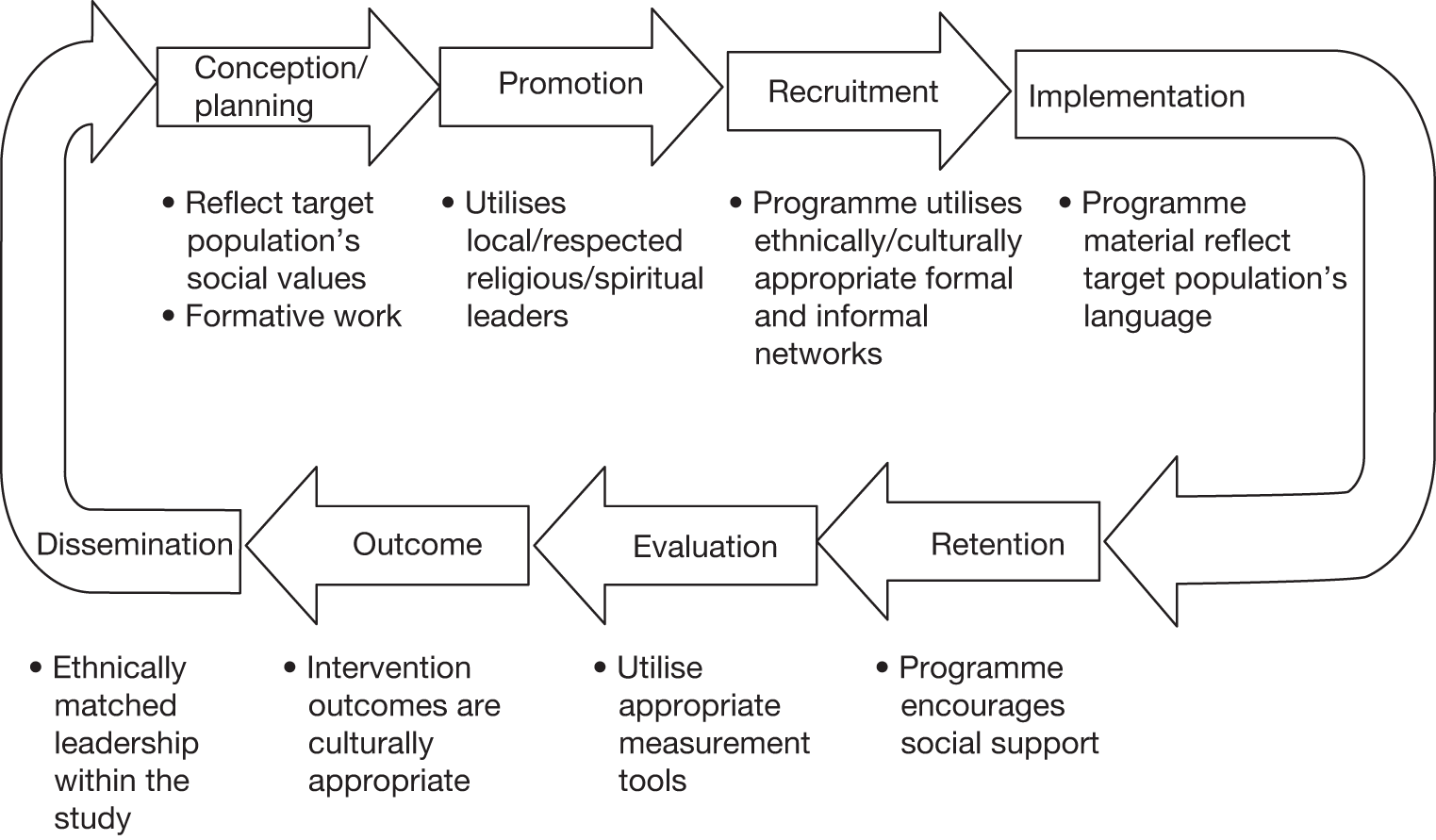
| Stage in programme theory | Adaptations relevant at each stage of the programme theory |
|---|---|
| Conception/planning | 1. Exploratory phase with target population (same group as intervention group) |
| 2. Exploratory phase with target population (different group from intervention group) | |
| 3. Exploratory phase with community leaders | |
| 7. Ethnically matched high-level/respected individuals to increase salience of programme goals | |
| 8. Ethnically matched high-level/respected individuals and community members throughout planning, directing, reviewing and implementing stages | |
| 9. Ethnically matched leadership within the study | |
| 10. Utilise local/respected religious/spiritual leaders | |
| 11. Collaboration with ethnic-specific institutions and professional organisations | |
| 20. Material developed specifically for target population (by project investigators, expert opinion, tools) | |
| 21. Material created by members of the target population | |
| 31. Address concerns with medical programmes, procedures and medication | |
| 35. Utilise ethnically/culturally appropriate formal and informal networks | |
| 42. Purposefully maintaining an exclusive or open intervention environment | |
| 44. Cross-cultural training for all study personnel | |
| 45. Address discrimination and mistrust | |
| 46. Gender considerations | |
| Promotion | 4. Ethnically matched intervention staff or facilitators |
| 7. Ethnically matched high-level/respected individuals to increase salience of programme goals | |
| 8. Ethnically matched-high level/respected individuals and community members throughout planning, directing, reviewing and implementing stages | |
| 9. Ethnically matched leadership within the study | |
| 10. Utilise local/respected religious/spiritual leaders | |
| 11. Collaboration with ethnic-specific institutions and professional organisations | |
| 14. Reflect target population’s language (usage – concepts, vocabulary) | |
| 16. Reflect target population’s preferred method of communication | |
| 22. Intervention content targets population’s social and cultural values | |
| 23. Intervention goals and outcomes for participants are culturally appropriate | |
| 28. Utilise resources from target population | |
| 30. Utilise and address appropriate norms | |
| 33. Located in ethnically/culturally appropriate/familiar location | |
| 34. Utilise ethnically/culturally appropriate media sources | |
| 35. Utilise ethnically/culturally appropriate informal networks | |
| 45. Address discrimination and mistrust | |
| 46. Gender considerations | |
| Engagement/recruitment | 4. Ethnically matched intervention staff or facilitators |
| 7. Ethnically matched high-level/respected individuals to increase salience of programme goals | |
| 8. Ethnically matched high-level/respected individuals and community members throughout planning, directing, reviewing and implementing stages | |
| 9. Ethnically matched leadership within the study | |
| 10. Utilise local/respected religious/spiritual leaders | |
| 11. Collaboration with ethnic-specific institutions and professional organisations | |
| 14. Reflect target population’s language (usage – concepts, vocabulary) | |
| 16. Reflect target population’s preferred method of communication | |
| 22. Intervention content targets population’s social and cultural values | |
| 25. Consider target population’s employment situations | |
| 28. Utilise resources from target population | |
| 29. Utilise appropriate incentives and timing of programme | |
| 30. Utilise and address appropriate norms | |
| 31. Address concerns with medical programmes, procedures and medication | |
| 33. Located in ethnically/culturally appropriate/familiar location | |
| 34. Utilise ethnically/culturally appropriate media sources | |
| 35. Utilise ethnically/culturally appropriate formal and informal networks | |
| 36. Provide ethnically/culturally appropriate food/activities/music | |
| 39. Address physical/financial (structural) barriers to participation | |
| 45. Address discrimination and mistrust | |
| 46. Gender considerations | |
| Implementation/delivery | 4. Ethnically matched intervention staff or facilitators |
| 5. Ethnically matched peer role models or peer education | |
| 6. Ethnically matched facilitators and peer role models who have successfully changed their behaviour | |
| 7. Ethnically matched high-level/respected individuals to increase salience of programme goals | |
| 8. Ethnically matched high-level/respected individuals and community members throughout planning, directing, reviewing and implementing stages | |
| 9. Ethnically matched leadership within the study | |
| 10. Utilise local/respected religious/spiritual leaders | |
| 11. Collaboration with ethnic-specific institutions and professional organisations | |
| 12. Material depicts individuals from target population | |
| 13. Material (video, booklet, skits, handouts, games) in target population’s language | |
| 14. Reflect target population’s language (usage – concepts, vocabulary) | |
| 15. Match reading level and literacy | |
| 16. Reflect target population’s preferred method of communication | |
| 17. Material presents ethnic-specific data | |
| 18. Material depicts appropriate graphics and scenarios (this can be heterogeneous) | |
| 19. Material/guidance based on preferences of target population | |
| 20. Material developed specifically for target population (by project investigators, expert opinion, tools) | |
| 22. Intervention content targets population’s social and cultural values | |
| 24. Intervention delivered in culturally appropriate or preferred format | |
| 25. Consider target population’s employment situations | |
| 26. Intervention addresses health behaviour patterns found in target population | |
| 27. Dietary issues unique to their context | |
| 28. Utilise resources from target population | |
| 29. Utilise appropriate incentives and timing of programme | |
| 30. Utilise and address appropriate norms | |
| 31. Address concerns with medical programmes, procedures and medication | |
| 33. Located in ethnically/culturally appropriate/familiar location | |
| 35. Utilise ethnically/culturally appropriate informal networks | |
| 36. Provide ethnically/culturally appropriate food/activities/music | |
| 37. Present a pro-ethnic/race approach | |
| 38. Address emotional barriers and stressors | |
| 39. Address physical/financial (structural) barriers to participation | |
| 40. Teach appropriate communication skills | |
| 41. Encourage/involve social support | |
| 42. Purposefully maintaining an exclusive or open intervention environment | |
| 43. Maintaining cultural significance of food | |
| 45. Address discrimination and mistrust | |
| 46. Gender considerations | |
| Retention | 4. Ethnically matched intervention staff or facilitators |
| 5. Ethnically matched peer role models or peer education | |
| 6. Ethnically matched facilitators and peer role models who have successfully changed their behaviour | |
| 7. Ethnically matched high-level/respected individuals to increase salience of programme goals | |
| 8. Ethnically matched high-level/respected individuals and community members throughout planning, directing, reviewing and implementing stages | |
| 9. Ethnically matched leadership within the study | |
| 10. Utilise local/respected religious/spiritual leaders | |
| 11. Collaboration with ethnic-specific institutions and professional organisations | |
| 16. Reflect target population’s preferred method of communication | |
| 22. Intervention content targets population’s social and cultural values | |
| 25. Consider target population’s employment situations | |
| 28. Utilise resources from target population | |
| 29. Utilise appropriate incentives and timing of programme | |
| 30. Utilise and address appropriate norms | |
| 38. Address emotional barriers and stressors | |
| 39. Address physical/financial (structural) barriers to participation | |
| 41. Encourage/involve social support | |
| 42. Purposefully maintaining an exclusive or open intervention environment | |
| 46. Gender considerations | |
| Evaluation | 8. Ethnically matched high-level/respected individuals and community members throughout planning, directing, reviewing and implementing stages |
| 9. Ethnically matched leadership within the study | |
| 22. Intervention content targets population’s social and cultural values | |
| 23. Intervention goals and outcomes for participants are culturally appropriate | |
| 25. Consider target population’s employment situations | |
| 30. Utilise and address appropriate norms | |
| 32. Utilise appropriate evaluation instruments and tools | |
| Outcome | 8. Ethnically matched high-level/respected individuals and community members throughout planning, directing, reviewing and implementing stages |
| 9. Ethnically matched leadership within the study | |
| 23. Intervention goals and outcomes for participants are culturally appropriate | |
| 30. Utilise and address appropriate norms | |
| 32. Utilise appropriate evaluation instruments and tools | |
| Dissemination | 8. Ethnically matched high-level/respected individuals and community members throughout planning, directing, reviewing and implementing stages |
| 9. Ethnically matched leadership within the study |
Strengths and limitations
A key strength of the systematic review presented in this chapter is its comprehensiveness; we examined a wide range of population groups and health promotion topics to identify the most contemporaneous research on the adaptation of interventions for ethnic minority populations. Our search strategy was not restricted by language and we included interventions from any nation. One limitation observed was the unequal geographical spread of the literature as the vast majority of studies originated from the USA and focused on African American populations. This reflects the state of the research and was thus out of our control; the concern is that this offers little in the way of direct evidence in relation to non-African American populations.
We were also limited by the quality of the studies. Because we did not limit the study type, many interventions were adapted but the studies did not tell us about the relative effectiveness of adapted interventions as there was no comparison group. The inclusion of diverse study designs added to the heterogeneity observed in the study populations, topics and techniques such that we were unable to meta-analyse any results. Furthermore, the quality of reporting of adaptations or adapted components varied dramatically across studies and subsequently, for some studies, it was difficult to extract this information. Information on equity and SES was also not often reported or linked with intervention findings; we were therefore unable to explore these factors further within the scope of our study.
There was also heterogeneity between health promotion interventions that were related to additive behaviours (e.g. increasing physical activity and improving healthy eating) and those promoting subtractive behaviours (e.g. smoking cessation), which posed difficulties in conceptualising how best to compare and analyse these health promotion interventions. Smoking cessation also differs in that once achieved for a number of years it appears easier to maintain, whereas increasing physical activity and improving healthy eating require more ongoing effort to sustain behaviour change; it is therefore a cause for concern that there is a lack of long-term studies to assess the sustainability of physical activity and healthy eating interventions.
Lastly, the review is limited to the search dates and we recognise that since the search was undertaken further reviews in this area have been published. This more recent literature includes, for example, the review by Netto et al. 13 on principles for adapting health promotion interventions for ethnic minority populations and the review from the National Institute for Health and Clinical Excellence on interventions to reduce risk factors for pre-diabetes among UK adults from black and minority ethnic groups. 244 Studying this more recent literature, however, suggests that the evidence has not progressed in any major way and thus we believe that the material presented in this chapter continues to provide a comprehensive overview of the state of the current evidence.
Conclusions
From this systematic review of adapted health promotion interventions for smoking cessation, increasing physical activity and improving healthy eating for African-, Chinese- and South Asian-origin populations we identified 12 theoretical papers that provided some preliminary insights into the kinds of adaptations and considerations recommended for working with ethnic minority populations (see Box 5). We further identified seven systematic reviews that yielded mixed evidence regarding whether or not adaptation increases the effectiveness of health promotion interventions. Our own review of the empirical literature identified 107 adapted empirical studies (reported on in 154 papers) focusing on the three populations and three topics of interest. Overall, these studies suggested that adaptation could increase the salience and acceptability of studies, this translating into improved recruitment. However, many studies showing positive outcomes lacked comparable conditions and relied on self-reported measures. Of the 107 studies, only nine were designed to directly compare the effectiveness of adaptations for interventions and these too yielded mixed findings. Equally, there was no direct evidence found for the cost-effectiveness of adapted interventions with only a handful of studies reporting on cost data and none carrying out formal cost-effectiveness analyses.
Some of our conclusions support those of other research groups; for example, the systematic review by Chen and Tang275 also found varying degrees of success of adapted interventions related to the degree of acculturation within the population. The overarching themes from the review of the relevant theoretical literature (see Box 5) were observed in the kinds of adaptations undertaken and are reflected in our 46-item Typology of Adaptation. Adaptations such as ‘Intervention goals and outcomes for participants are culturally appropriate’ (number 23) suggest that the goals for behaviour change for ethnic minority groups should be framed around psychological community and family gains, rather than individual personal gains. Adaptations such as ‘Present a pro-ethnic/race approach’ (number 37) and ‘Maintaining cultural significance of food’ (number 43) emphasise that cultural elements are protective assets rather than pathologies.
In this chapter we have proposed a novel approach to facilitate the conduct of studies that would be more conducive to detailed interrogation and synthesis, which if followed should enable the development of a more directly comparable evidence base. Our Programme Theory of Adapted Health Promotion Interventions, if used alongside the 46-item Typology of Adaptation, can, we suggest, help to conceptualise and develop adapted interventions as well as assist in improving the reporting of adapted interventions to facilitate comparative analysis.
Most of the evidence identified originated from the USA and was specifically related to African American populations. Although there is clearly learning to be drawn from these experiences, specific interventions developed for this population are not necessarily, nor easily, generalisable to other ethnic minority populations. We believe, therefore, that there is a need for more primary research in countries such as the UK where ethnic minority populations have their own distinct histories, contexts and experiences, and where there are also major differences (and similarities) between the majority (and indeed African American) population and ethnic minority populations in relation to factors such as religion, language and diet. This issue is discussed further in Chapters 8 and 9.
Chapter 7 Qualitative interviews with researchers and health promoters who have adapted interventions for ethnic minority populations
Abstract
Background
Because of the space limitations of many journal publications and the tendency to report normative accounts of research studies, much of the information on the process of adapting health promotion interventions for ethnic minority populations may not be accessible through published reports. This information may, however, be more forthcoming from detailed discussions with researchers and health promoters with particular experience of working with ethnic minority populations. Qualitative research is especially useful to understand processes and experiences and to gather in-depth knowledge to get beneath public accounts. The rationale for this qualitative component was to extend our understanding of how adapted interventions are delivered and why they were successful (or not) for smoking cessation, increasing physical activity and improving healthy eating for African-, Chinese- and South Asian-origin ethnic minority populations.
Objectives
To understand the processes and experiences of, as well as the rationale for, adapting health promotion interventions for ethnic minority populations and to summarise lessons learned.
Methods
We conducted semi-structured interviews with researchers and health promoters adapting health promotion interventions for smoking cessation, increasing physical activity and improving healthy eating aimed at African-, Chinese- and South Asian-origin ethnic minority groups around the world. Interviews were transcribed and two researchers independently coded the interview transcripts using NVivo 8 (QSR International, Doncaster, Australia). Thematic analysis was undertaken, this being informed by the literature reviewed in earlier phases of the work while also remaining open to more emergent issues.
Results
Twenty-six interviews were conducted. Findings both complemented and extended the existing literature on adapting interventions for ethnic minority populations. Participants discussed how adaptations to promote healthy behaviours for ethnic minority populations could occur at every stage of the research process, from conceptualisation to dissemination, but they in particular highlighted the importance of sustainability considerations. Newer insights emerged including the need for a greater recognition of the lived dimensions of ethnicity, these including dynamic relationships with particular spaces and places, intergroup heterogeneity and previous experience with other health interventions that impacted on how new adapted interventions were received. These insights are generally unaccounted for in conventional descriptions of ethnicity. Recognition of what we have framed as the ‘contextual elements of ethnicity’ can facilitate process-oriented thinking on ethnicity and its potential impact on health behaviour. Finally, interviewees discussed the benefits of informal research networks, which constrained or enabled access to unpublished findings and ‘lessons learned’, these being readily available in the USA but less available elsewhere.
Conclusions
Researchers have employed a broad array of approaches in adapting health promotion interventions for ethnic minority populations, these mapping onto the Typology of Adaptation and the Programme Theory of Adapted Health Promotion Interventions we have developed. In developing and delivering these interventions, participants emphasised the need to understand and work with a range of relevant contextual considerations, and, given the complexity of this task, the need to be able to draw on the experiences of colleagues is critical. This engagement was more easily achieved in the USA, where critical mass of researchers appeared to exist, in contrast to, for example, Australia, where researchers and health promoters felt more isolated.
Introduction
Within economically developed nations with large proportions of ethnic minority populations it is now well recognised that members of some ethnic groups experience elevated risk of disease in comparison to the general population and relative to other ethnic groups (see Chapter 1); this has, for example, been demonstrated for chronic diseases such as cardiovascular disease and diabetes mellitus. 61,62 A preventive health approach has been adopted in the UK and increasingly elsewhere to address the constellation of underlying causes of these chronic diseases, which are, to a large extent, potentially avoidable through the elimination of a core set of risk factors such as smoking, physical inactivity and unhealthy eating. 66 The preventive health approach is, as discussed at length in earlier chapters (see Chapters 1 and 4–6), increasingly multifaceted, with intervention approaches ranging from those that are individually centred to more population-based approaches. The bulk of the evidence on effective interventions to date, whether for the general population or for ethnic minority communities, relates predominantly to approaches aiming to change individual behaviours or risk factors, rather than changing settings or environments (see Chapters 4–6).
In tackling these shared risk factors, ‘ethnicity’, along with other demographic characteristics including education, income, social status and gender,31 have all been identified as important in enhancing either susceptibility or resiliency to disease. 258,377 ‘Ethnicity’ was, in the framework of this project, conceptualised as encompassing the dimensions of ancestry, culture, language, physical features and religion (see Figure 1). 12 These dimensions, however, offer only limited insight into how to operationalise ‘ethnicity’ in preventive health approaches, hence the need for detailed work with experienced investigators. When planning this work we anticipated that there might be little in the way of description in the published accounts of why or how interventions had been adapted, and what lessons had been learned from this process, and this was to a large extent verified from our systematic review (see Chapter 6).
Building on the systematic review (see Chapter 6), in which we identified and analysed the evidence on adapted health promotion interventions for smoking cessation, increasing physical activity and improving healthy eating for African-, Chinese- and South Asian-origin groups, we wished to better appreciate some of the experiences and lessons learned in delivering these adapted interventions. We had hypothesised that these accounts were unlikely to be documented in the very public peer-reviewed literature accounts.
Research questions
The following research questions addressed in this chapter relate to Phase 2D of the project proposal (see Chapter 2):
-
How and what factors (contextual, theoretical, practical) are considered in the adaptation of health promotion interventions for ethnic minority groups?
-
Which factors were found to increase or decrease the effectiveness of adaptations for interventions?
Methods
Ethics
Ethical approval was obtained from the School of Health in Social Science Research Ethics Committee at the University of Edinburgh (see Appendix 4).
Sampling
We employed purposive, maximum diversity sampling aiming to recruit 20–30 participants; based on our previous experience with undertaking a number of related qualitative studies, we anticipated that these numbers of interviews would allow us to achieve saturation on the issues at the heart of our enquiry. We primarily wished to sample researchers delivering and evaluating innovative interventions for smoking cessation, physical activity and healthy eating for African-, Chinese- and South Asian-origin groups. We were, in addition, also interested in hearing the perspectives of individuals involved in delivering the intervention, such as counsellors and health educators/promoters. To ensure that we had a maximum variation sample we devised a three-by-three recruitment approach (Figure 11), which was used to inform sampling and recruitment decisions. Participants with different roles in health promotion interventions and programmes were approached for interviews with the explicit aim of capturing a range of opinions and perspectives.
FIGURE 11.
Sampling matrix for qualitative interviews.
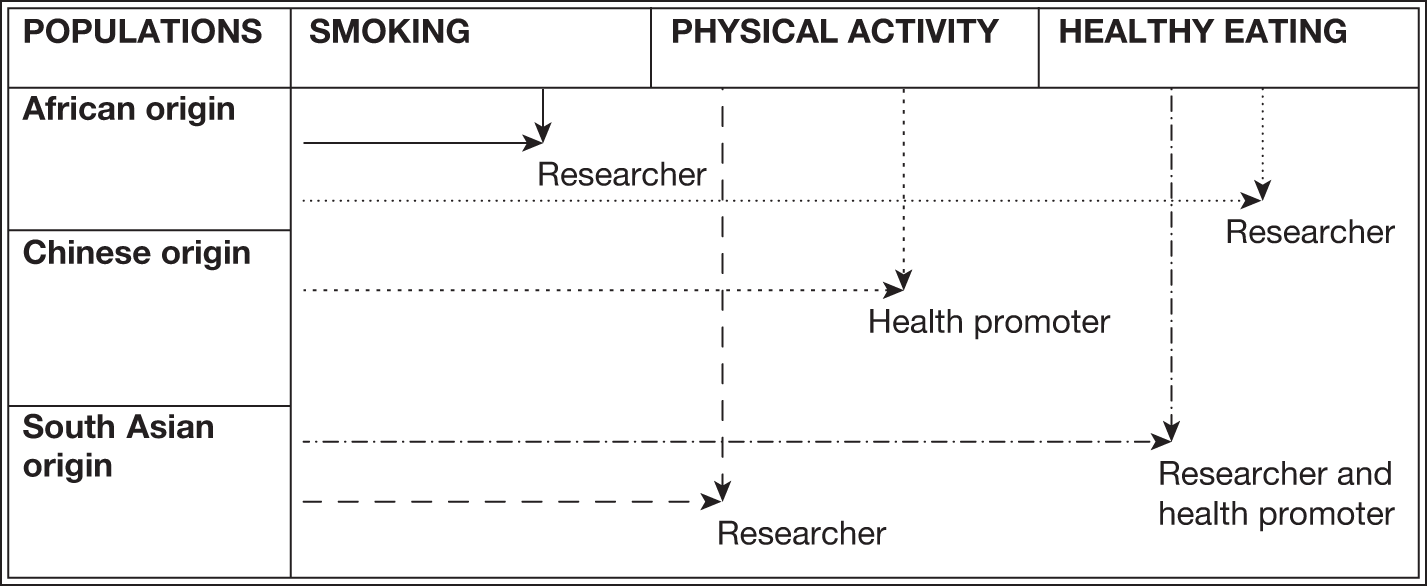
Participant selection and recruitment
Guided by the sampling matrix (see Figure 11) we initiated four interview recruitment waves. Each wave satisfied a different sampling goal, namely piloting, generating interest, maximising diversity and ensuring representativeness. A description of the recruitment waves and the corresponding numbers of participants approached and who participated is presented in Table 19. Recruitment wave two was particularly innovative as participants were recruited from a sampling frame derived from studies included in the systematic review (see Chapter 6). We continued to interview until we reached saturation,378 that is, when additional interview data no longer generated any major new insights. Although no formal assessment for saturation was used, saturation became apparent as we iteratively coded interview transcripts, such that no new NVivo codes were generated with the last few interviews.
| Wave | Description and rationale | Number of interviews requested | Number of interviews completed |
|---|---|---|---|
| 1 | Recruited from intervention studies known to the project team and three electronic mailing lists with a focus on ethnicity and health (Minority Ethnic Health Listserv, The Migrant Health of the European Public Health Association Listserv and CLAStalk-list) | 8 | 8 |
| 2 | Recruited from sampling frame populated with studies identified to have met our inclusion/exclusion criteria in our systematic literature review (see Chapter 6). The frame was restricted to studies published since 2005. This date was selected to optimise the recall of project content and salient information, and also to maximise the relevance to current project contexts. Studies published before 2005 are subject to different milieus of social, political and economic contexts that may be more or less salient at present. Furthermore, changes in migration patterns, government health polices and costs of living are less likely to align with current conditions | 25 | 15 |
| 3 | Recruited from additional papers identified during the analysis of the systematic review and additional contacts suggested during the preceding waves | 2 | 1 |
| 4 | Boosted sampling to match the large volume of literature on African-origin (particularly African American) populations and targeted sampling to compensate for minimal literature on Chinese-origin populations | 2 | 2 |
| Total | 37 | 26 |
We supplied an information sheet explaining the purpose of the study (see Appendix 21) to all potential participants and allowed them sufficient time to consider participation and ask questions. We provided a link to our project website (www.chs.med.ed.ac.uk/ethnicity-and-health/) and our contact details should those approached wish to request more information, and also contact details for someone outside of our project should they have questions they wished to ask an independent person. Written consent (see Appendix 22) was obtained from all consenting participants (both researcher and participant signed the consent form) and all participants completed a demographics questionnaire (see Appendix 23).
Data generation
Semi-structured interviews with participants were conducted either by telephone or face-to-face. Semi-structured interviews provided an opportunity to build rapport, elicit detailed accounts and explore new topics as they arose while keeping focus on the topic of interest. The interviews were structured around an interview guide, which was first piloted and refined through expert consultation (see Appendix 24). Interviews were conducted in English by either JJL or ED or jointly by both researchers and were digitally recorded and transcribed by the project secretary (FA). All transcripts were subsequently checked for accuracy and completeness by one of the two researchers (JJL, ED).
Data analysis
Analysis was comparative and iterative to synthesise the body of included studies. 379,380 A coding frame was developed drawing on both the theoretical concepts and emerging information and applied to the corpus of data for thematic extraction (and the subsequent realist evaluation, discussed in Chapter 8). The identified themes from the theoretical literature (see Box 5) were key concepts framing this analysis. As these themes were mirrored in the empirical literature, we therefore anticipated that they would also be apparent in the interviews and thus they informed the development of some of the deductive codes. Furthermore, the systematic review (see Chapter 6) gave rise to 46 adaptations derived from the empirical studies – these too further informed our deductive code generation. These findings together and along with the discussion of ethnicity in Chapter 1 constituted what we knew on this topic before conducting the interventions. We anticipated being able to locate and follow some of these common threads in the interview data; this was expected given that our sampling frame was in part populated by authors of the empirical studies included in our systematic review (see Chapter 6). We therefore anticipated uncovering some of these earlier discussed ideas. These qualitative findings were further important to contextualise and illustrate how adaptations and intervention stages work under the realist framework introduced and discussed in Chapter 8.
The coding frame (see Appendix 25) included both deductive codes generated through familiarity with the body of literature12,13,16,26,35,254,255,257–259,262,263,265,268–270 as described above (see Chapters 5 and 6) and inductive codes generated from an initial read-through of interview data. This hybrid approach381 has the potential to yield a rigorous thematic analysis as new insights and emerging themes are accommodated alongside themes already identified from the literature. The coding frame was independently piloted by two coders (JJL and ED) and disagreements were resolved by discussion or, when necessary, a third coder (AS). The two authors independently coded all transcripts using the NVivo 8 qualitative data analysis software. Multiple independent coding allowed for discussion of new and emerging insights and, importantly, the transparent documentation of how analysis developed. 382
The two coders grouped and mapped the identified codes with attention to how and what factors were considered to be important in the adaptation of health promotion intervention for ethnic minority groups. Thematic analysis383 was used to analyse text: 65 inductive and deductive codes were generated from the five topic areas and were grouped into conceptual clusters (see Appendix 26). These clusters formed 24 basic themes, which were further grouped into 11 organising themes. In light of our overall study question, namely ‘How can interventions be adapted to be more effective for ethnic minority groups?’, these themes were further abstracted into three global themes to answer this central question. The organisation of the codes into this hierarchical thematic network is described more fully in Appendix 26. This systematic method of building up the themes was grounded in the text-linked codes and helped to identify consensus or conflict across themes, as well as the absence of expected themes,384 to explore how adapted interventions worked or were thought to work.
Reflexive considerations
Our interest in interviewing researchers and health promoters with considerable experience in delivering adapted interventions meant that we were, in some instances, ‘studying up’. Research, and particularly interviews, usually take place between people of unequal socioeconomic status (SES). Participants in health-care studies, for example, are usually patients or subjects in trials, while those conducting the research are health professionals with institutionally sanctioned degrees. In contrast, ‘studying up’ refers to conducting research with participants who have a higher social/economic status and/or are members of bureaucratic or institutional bodies. ‘Studying up’ can help uncover the logic behind how and why interventions are designed and delivered, as well as help deconstruct the ideologies that both enable and constrain the success of adapted interventions. 385
The background of the team, with wide-ranging interests and expertise, aided recruitment as members initially reached out to those in their networks. This multidisciplinary and multiethnic research team provided thoughtful suggestions in grouping the deductive and inductive codes, cautioning against generalisations, and particularly in illuminating the boundaries of an analysis focused on ethnicity, to suggest considerations of SES, age and education.
The ethnic positionings of the two interviewers (JJL identifies as a Chinese Canadian who has also lived and worked in Asia, Africa and Europe, and ED identifies as Celtic European who has lived and worked in New Zealand for the past 10 years) positively facilitated identification and familiarity with the researchers interviewed. However, as the majority of our interviews were with researchers identifying as African American, although we were able to appreciate the historical situated experiences they were drawing on, we were largely unable to grasp the gravity of such a history that has been compounded by contemporary health-care and structural issues. At times these unfamiliarities widened our social distance and perhaps prevented us from ‘digging deeper’.
In analysis, our collective backgrounds in social sciences and public health framed our approach and likely directed our attention to the influence of social, structural and environmental factors on ethnicity and health over, for example, cognitive factors. Furthermore, there was a tension between two of the researchers (JJL and ED) over the use of the term ‘community’, with one opting for a more critical perspective and the other for a more practical perspective. This tension is likely apparent in our use and disuse of ‘community’ and who it can represent in our research.
Results
We approached 37 participants and 27 agreed to be interviewed (see Table 19). The majority of declines were implicit, as the participant did not respond to our request. Those who responded to our e-mail request cited time constraints as the reason why they were unable to participate; some of these people referred us to their colleagues. We therefore conducted 26 semi-structured interviews with researchers and health promoters delivering adapted health promotion interventions to African-, Chinese- and South Asian-origin ethnic minority groups around the world. The qualitative data were first independently analysed (this chapter) and then synthesised with findings from the other components of this mixed-methods study using a framework of realist synthesis (see Chapter 8).
Our maximum diversity sampling captured a wide range of participants of varying ages and occupations and working with different populations around the world (Table 20). The largest group of participants (35%) was aged between 46 and 55 years. Participants were located in the USA (n = 14; one interview included two participants), the UK (n = 7), Australia (n = 2), New Zealand (n = 2), Norway (n = 1) and China (n = 1). The participants’ occupations included community outreach workers and consultants (n = 5) and research associates (n = 4), with the majority being university professors (n = 17). Participant 25 did not return a demographics form and thus we have no information to report except to researcher-identify him as ‘male’. It should be noted that a participant’s self-identified ethnicity was not always matched to the ethnicity of the target group with whom the researcher had previous working experiences. This diverse sample allowed us to explore the process of adapting health promotion interventions in a broad range of sociopolitical contexts.
| Interview number | Wave | Age range (years) | Sex | Self-identified ethnicity | Location |
|---|---|---|---|---|---|
| 1 | 1 | 46–55 | F | Scottish | UK |
| 2 | 1 | ≤ 25 | F | Bangladeshi | UK |
| 3 | 1 | 46–55 | F | Indian | UK |
| 4 | 1 | 36–45 | M | Bangladeshi | UK |
| 5 | 1 | ≥ 56 | M | White | UK |
| 6 | 1 | 26–35 | F | Bangladeshi | UK |
| 7 | 1 | 36–45 | F | New Zealand European | New Zealand |
| 8 | 1 | 46–55 | F | White | UK |
| 9 | 2 | 46–55 | F | Pakistani | Australia |
| 10 | 2 | 46–55 | F | Chinese | USA |
| 11 | 2 | ≥ 56 | F | Black American | USA |
| 12 | 2 | 36–45 | M | Caucasian | Australia |
| 13 | 2 | 46–55 | F | African American | USA |
| 14 | 2 | 46–55 | F | Caucasian | USA |
| 15 | 2 | 36–45 | F | White | USA |
| 16 | 2 | 46–55 | F | White | USA |
| 17 | 2 | ≥ 56 | F | New Zealand European | New Zealand |
| 18 | 2 | 46–55 | F | Caucasian | USA |
| 19 | 2 | ≥ 56 | F | Norwegian | Norway |
| 20 | 2 | 36–45 | F | Asian Chinese | USA |
| 21 | 2 | ≥ 56 | F | Chinese | USA |
| 22 | 2 | ≥ 56 | F | White/Caucasian | USA |
| 23a | 2 | ≥ 56 | F | African American | USA |
| 23b | 2 | ≥ 56 | F | African American | USA |
| 24 | 4 | ≥ 56 | F | Caucasian | USA |
| 25 | 4 | Not specified | M | Not specified | China |
| 26 | 3 | 26–35 | F | Caucasian | USA |
In the following summary we first present an overview of the findings from the qualitative interviews and then, in subsequent sections, we elaborate and provide more detailed descriptions with illustrative quotes as well as a discussion of how these findings add to the existing literature that we reviewed in the previous chapter (see Chapter 6).
Overview of findings
We identified three main ‘global’ themes: constructing ethnicity, adapting interventions and sustaining adapted interventions.
Constructing ethnicity emerged as a new insight in terms of broadening the thinking on ethnicity from its more conventional dimensions (i.e. religion, language, culture, physical features and ancestry) as described in Chapter 1. Furthermore, although demographic variables such as age, gender and SES interact with ethnicity, these distinctions were maintained so as to retain the utility of ‘ethnicity’ as a concept and not render it all encompassing. We found that expanding the concept of ‘ethnicity’ to also include contextual elements (e.g. social environments, physical space, past exposures to health research and services, diverse life experiences including stress) was particularly valuable for consideration on how to adapt interventions for ethnic minority populations.
The theme of adapting interventions discussed the kinds of adaptations undertaken and considerations around implementing the adapted intervention. These adaptations and considerations reinforced the adaptations identified in the systematic review (see Table 13). This was expected as many of the interview participants were, as noted above, recruited from a sampling frame derived from studies included in the systematic review. Many of the identified themes complemented what was already known about working with ethnic minority populations, for example the importance of community engagement and building trusting relationships,97 providing incentives to individuals or organisations for recruitment and retention,386 adapting messages and materials,35 matching personnel and using preferred methods to deliver messages and materials257 and, finally, building linkages with existing organisations. 387
The final global theme, namely sustaining adapted interventions, was an unexpected finding as we did not anticipate the degree of in-depth discussion in relation to the practicalities of delivering adapted interventions and sustaining this field of research (e.g. funding, formalising the intervention, recognition of work, staff safety and capacity building).
More detailed findings on each of these overarching themes are presented in the following sections in which each of the three global themes is elaborated on and discussed in turn by drawing on its constitutive organising and basic themes (italicised). A schematic diagram precedes each global theme to outline the hierarchical and associated relationships between these themes. Verbatim quotes are provided to further illustrate and support the three overarching themes [the speaker is identified by their participant (P) number, e.g. P1]. In the following sections we use the term ‘researchers’ to refer to the participants of this study, and the term ‘participants’ to refer to those for whom the intervention was delivered.
Global theme 1: constructing ethnicity
The process of constructing ethnicity incorporated commonly used population demographics such as age, gender and socioeconomic factors, which were, generally speaking, acknowledged to intersect with ethnicity in both expected and sometimes surprising ways. Constructing ethnicity also drew on familiar dimensions of ethnicity such as ‘culture’, food, language, religion/spirituality and ancestry, which were discussed in Chapter 1. Finally, in considering ethnicity in the practice of delivering adapted interventions for ethnic minority groups, constructing ethnicity also stimulated discussions of participants’ exposure to health care and research, setting-based considerations in which space and place are prominently featured, participants’ social environment and researchers’ recognition and acknowledgement of differences. Consequently, population demographics, conventional ethnicity and contextual ethnicity represent the three organising themes contributing to the global theme of constructing ethnicity (Figure 12). Together, these three subthemes have the potential to shed light on ethnicity as a dynamic process rather than a limited set of immutable characteristics.
FIGURE 12.
Global theme 1: constructing ethnicity.
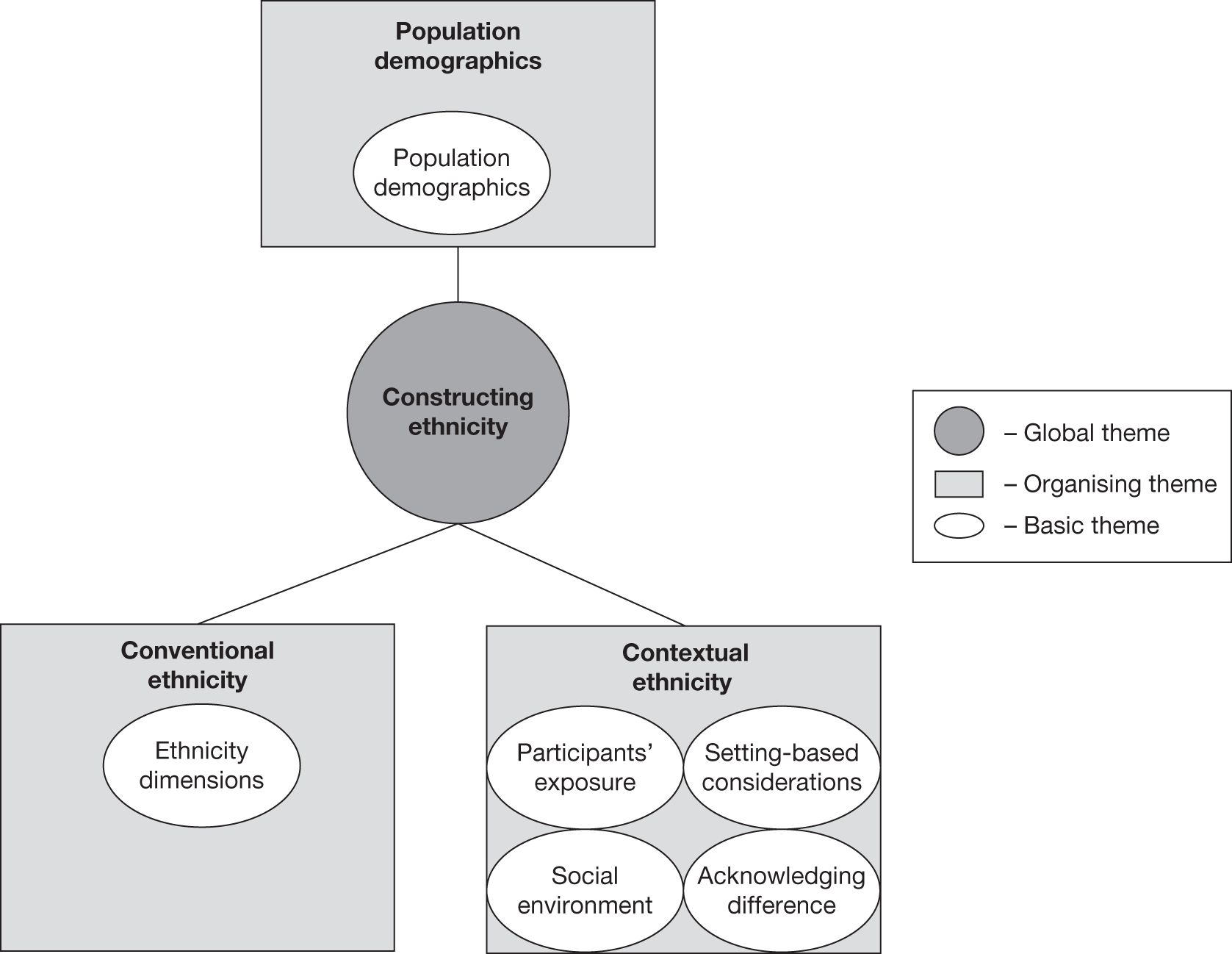
Population demographics
In the theme of population demographics, age, gender and SES, for example, were reported as common factors considered alongside ethnicity. These factors can intersect with and mediate how ethnicity is experienced.
Age-associated preferences were recognised to interact with ethnicity:
We have the facilitators and the experts. All of them are black women in mid-life. It was just as important to these women in, in the focus groups when we started, they said now don’t bring in here as our fitness expert a 20 year old that weighs 110 lb and is perky right. They don’t understand what we’re going through with our back problems, our knee problems.
(P23, general health, USA)
Gender, like age, appeared to intersect with ethnicity as women and men were observed to have different health problems, health concerns, levels of participation and ability to participate in interventions:
Women couldn’t get them on their saris, the saris not the best thing for a pedometer so they were trying their knickers and, and things like that. The men of course had no trouble on their belts. And the men would go out for a walk and their wives would be at home cooking dinner.
(P8, healthy eating, UK)
Different approaches to health behaviour change were also apparent:
The Chinese population prefer, the men, the men like to become smoke free and then celebrate it back with their family so they won’t lose face if they relapse.
(P7, smoking, New Zealand)
Socioeconomic status was another factor that intersected with ethnicity. In many cases, these interventions took place in lower socioeconomic settings:
Sure em the area in which we did the, em where we had where our offices were located was in a low socio economic em area [okay]. Em most em of our participants were em low em poverty level or below, em most of my clients did not ah have jobs or were between jobs, em, very transient sort of lifestyles. Eh we did have a few that were em you know middle class em that I can remember, eh most did not have any sort of em college experience, a lot of them did not em graduate from high school. Em so you know we were working with a very relatively low educated low income population.
(P26, smoking, USA)
Conventional ethnicity
The theme of conventional ethnicity encompassed the ethnicity dimensions, which were presented and discussed in Chapter 1.
‘Culture’, food, language, religion/spirituality and ancestry represent some of the ethnicity dimensions already discussed in Chapter 1. Broadly speaking, in the interviews ‘culture’ was discussed with a focus on shared qualities and understandings. ‘Culture’ was perceived to be particularly significant for dietary behaviours. Researchers felt that, despite their participants’ expressed willingness to change, behaviours surrounding food in social situations were quite durable and difficult to alter.
They view within their home that healthy food isn’t acceptable, either to themselves or their family, or visitors, they come over and say oh those were horrible cause we know we recommend for instance bake your samosas and the women are like oh wait a minute, I would be considered a horrible hostess, if I did that, if I didn’t offer them a [mithai] you know the Indian sweets whenever people were there then I would be a horrible hostess, and the pressure is so strong it would make them feel, you know, in a sense that they were ostracised from their community.
(P8, healthy eating, UK)
Language was another important dimension of ethnicity that was identified and a prime objective of these adapted interventions was to ensure the availability of language-appropriate materials, that is, that translations were accurate and/or that these reflected the literacy level of the target population. Interestingly, in one intervention, English versions of written intervention materials were perceived by the participants as providing an opportunity to learn English. In other interventions, written materials were eschewed in favour of pictorial information, as this was felt to be more accessible.
The role of religion and religious leaders in interventions varied. Interventions delivered for African American populations were more likely to embrace the role of religion and spirituality in assisting behaviour change, whereas interventions delivered to Muslim populations generated a mixed reception – for example some participants advocated behaviour change during Ramadan whereas others felt that it should be reserved for faith-based activities only.
Finally, ancestral ties were observed to affect health practices and behaviours, cutting across the many other aspects of ethnicity:
Where they come from influence what they eat, but not the location and the cities in United States . . . where they came from, from their original country, is it China but if they, they came from Hong Kong eh they like certain food, and from Taiwan they like a certain different kind of food, so it would be different.
(P21, healthy eating, USA)
We can’t do it in groups, again for confidentiality issues because if a community is quite close-knit, so you have to make sure that they don’t you know they’re not in a group where somebody knows them from Bangladesh back home so there’s a lot of village ties, so they don’t really want, somebody older wouldn’t want somebody younger than them knowing about their personal issues and why they smoke.
(P6, smoking, UK)
Interestingly, discrimination was not mentioned or raised by any of the interview participants, even though it is often cited in the literature to play an important role in determining health status. 258 Historical discrimination was, however, mentioned in the context of discussions on trust when attempting to engage African American populations.
Contextual ethnicity
The theme of contextual ethnicity discussed processes related to the concept of ethnicity relevant to the participants in the interventions or programmes. These processes included participants’ health-care/research exposure, considerations of their settings and their social environment and researchers’ acknowledging differences within the target groups.
Participants’ exposure to and past experiences with health care or health research affected the way that they perceived the intervention and influenced their level of interest and participation, particularly if their previous experiences with research projects or researchers were negative. Degree of exposure to information and services was identified as potentially hampering or increasing participation. For example, information on smoke-free environments was advertised through mainstream media and thus was perceived to represent a systematic exclusion of a group of Chinese-origin people from accessing the same health information:
P: Back in 2003 New Zealand em brought in the eh smoke-free environments legislation.
I: Yes, yes. So one of the leaders in the world weren’t they?
P: That legislation came in but of course most of the promotion and everything was done in the mainstream profession and what we found is that a lot of the em communities that weren’t accessing mainstream media [mm mhm] weren’t getting those messages across about to take the smoke outside and about the fact that it was now em you know legislated against em smoking in public places, bars, restaurants and things like that, so there was a whole section of the New Zealand population that kind of missed that message.
(P7, smoking, New Zealand)
Setting based included researchers’ observations of factors related to space and place and are thought to effect intervention outcomes, for example immigration status, availability of cheap and illegal tobacco products, migration influxes and movements in and out of the city, as well as changes in practice over time, such as increased dining out:
P: Em but it, it, there was a, just a complete lack of understanding from the business owners’ perspective of why they should care less about this.
I: Mm mhm. Em why, why were they suspicious of the pro, of the programme?
P: I think it’s because there’s a lot of suspicion, again I, you know, this is, you’re in Edinburgh and the United States, I mean you have to under, it, it, there’s all kinds of issues around immigration now in the United States [mmm], there’s a lot of ah fear and you know that people are gonna be accused of hiring illegal workers.
(P18, smoking, USA)
Migration, for example, was observed as a salient stressor, particularly in the context of providing for the family and dealing with family concerns ‘back home’ (this was particularly relevant for Bangladeshi-origin populations). Immigration status was another source of stress, which appeared to be prevalent within ethnic communities (more relevant for recent migrant Chinese- and South Asian-origin populations).
We tried to talk of you know discuss issues that were more relevant to men, other race-related issues that might be relevant such as the stress of dealing with you know recent immigration or other immigration-related issues, trying to find a job, trying to be able to support one’s family and things of that nature.
(P20, smoking, USA)
These stressors were widely acknowledged by researchers as inhibitors to intervention success, and therefore stress-reduction strategies featured prominently in smoking cessation interventions, for example for Chinese and African American populations:
The first thing to do for white women, now of course this is a broad generalisation, but in general if you ensure . . . that they are also involved in weight reduction plans, because if young white women, as a group, start to gain weight, when they stop smoking, they’re going to go back to smoking. If you’re trying to stop black women from smoking and you don’t have a stress management programme in place they, are going to go back to smoking when they get stressed.
(P23, general health, USA)
Where the intervention was delivered was another important setting-based consideration. Holding the intervention in a location and physical environment that was perceived to be relevant to the target ethnic group was thought to increase participation and salience. The implicit assumption made by researchers was that there were, in general, stronger spatial ties, particularly for recent immigrants. Community centres, schools, churches, libraries, mosques, homes, cultural centres and ethnic enclaves were all enthusiastically cited as convenient locations, and this was generally accompanied by a wholesale avoidance of academic institutions as sites of intervention.
There was a mixture of settings [mmm]. Em the initial meetings quite often were actually held em at the university, em although that tended to, that was in the early days of the intervention, because the participants in terms of transport sometimes had issues with that, not all the women drove and I, I suspected they didn’t feel as comfortable in that setting. We had access to a em community centre and some of the meetings occurred there and particularly once the intervention was rolling, so the initial meetings might be at the university or community centre, I would suggest that the community centre was preferable, em the women from what I can gather appeared to be more comfortable there [mmm] eh but the subsequent meetings say over the 12 weeks of the intervention quite often would end up being at one of the participants em homes and the meeting would occur there.
(P12, physical activity and healthy eating, Australia)
A consideration of physical environment also captured the effect of population density and spread, with less dispersed populations having a greater opportunity for participation in interventions. Therefore, the type of ethnic groups captured by intervention efforts appeared to be tied to the spaces they occupied.
I think the individuals we recruited in our group tended to be ah, some of the Korean American participants ah probably were less underserved than the Chinese American participants, if that makes sense [mm mhm]. Em the, a lot more of the Korean community sites that we recruit from, they tend to ah actually sprawl out into the suburbs, suburban regions. Em whereas the Chinese American communities that we’ve been working with have been a little bit more concentrated around the [city name] area.
(P20, smoking, USA)
Related to physical space, the social environment also shaped participants’ relationships with family and friends, and determined the kinds of social support one could receive, or be expected to receive. For healthy eating and physical activity interventions for women (South Asian and African American), for example, the family was often seen as a pivotal motivator for health improvement:
But then of course as these are women, we always hook it into if you don’t change your behaviour you’re going to see in your grandchildren the statistics of women dying prematurely from preventable deaths. So we really try to do both, I mean we, we focus on expanding their sense of responsibility to themselves in terms of health but we always link it to how, if they change, it can help in terms of their community, in terms of their family and, and the rest of their community.
(P23, general health, USA)
The family was also a strong motivator in smoking cessation interventions for men (of Chinese and South Asian origin):
I think and a lot of it would have to do with coming back to the family . . . we would say you know try to bear in mind that you know your children really want you to stop smoking and you know you, you’ve moved to this country to help your children have a better life and you know they really want you to, to be here with them for a long time and you’re doing this, you’ve done all these other things for your children you can do this one more thing too.
(P20, smoking, USA)
Another aspect of the social environment was social support, which was well documented in the interviews. Overall, the idea of organic social support was thought to be more effective than purposefully formed support groups; however, the use of the term ‘organic’ differed across interviews. In some cases it referred to friends and family as the support provider:
I mean peer support is likely to be successful if it’s done well. Even though we, we didn’t find this an effect, I’m not sure that that really means that that isn’t successful. But yes for sure, I think organic social support would be even better and that’s why we’ve, we’ve created the third study the way it’s designed.
(P14, physical activity and healthy eating, USA)
At other times, organic support referred to the groups that formed in the interventions:
In the intervention group you know changed more initially but then those changes washed out faster, and even reversed in some cases, versus the control group that changed more slowly without all the handholding but you know made use of the social support of you know the other women in their, in their classes, and they were actually able to make a more sustainable change in terms of being able to stabilise their waist circumference.
(P13, physical activity, USA)
Therefore, it remains unclear which kinds of organic support were considered to be effective, as this has been defined or interpreted differently across interviews. Furthermore, social support was also contingent on opportunity; for women who may not have received support at home for physical activity, for instance, an intervention may have acted as the catalyst for these women to form activity groups, which in turn provided support during and well after the end of the formal intervention period.
Lastly, researchers acknowledged differences that exist among supposedly similar intervention group members. In many cases, intervention effectiveness was difficult to determine because of the heterogeneity of participants. This heterogeneity was often related to factors such as educational attainment, gender and age, as discussed earlier, while degree of acculturation also contributed to heterogeneity:
There are those older people as well they would say . . . oh yeah I only eat a baked potato because my granddaughter makes this so I eat that as well, you know eh so before they were never eating but now with time eh there’s been a cultural shift and there even if it is pasta or so they could be cooking eh the pasta with eh Asian touch to it so there is, yes acculturation definitely there.
(P3, healthy eating, UK)
Global theme 2: adapting interventions
We classified researchers’ descriptions of implementing adapted interventions for ethnic minority groups (regardless of the ethnic group targeted) into the following six organising themes: development, engagement, materials, methods, description and linkages (Figure 13). Not all researchers provided insights for each theme as some tended to focus on, for example, engagement, whereas others more readily discussed materials and methods. These themes contributed to the global theme of adapting interventions. The interviews interpreted together revealed the additional considerations and frequent negotiations that required attention at different stages of the intervention. These considerations and negotiations shaped and mediated what adaptations and programme components were feasible and acceptable and, therefore, ultimately possible to deliver.
FIGURE 13.
Global theme 2: adapting interventions.
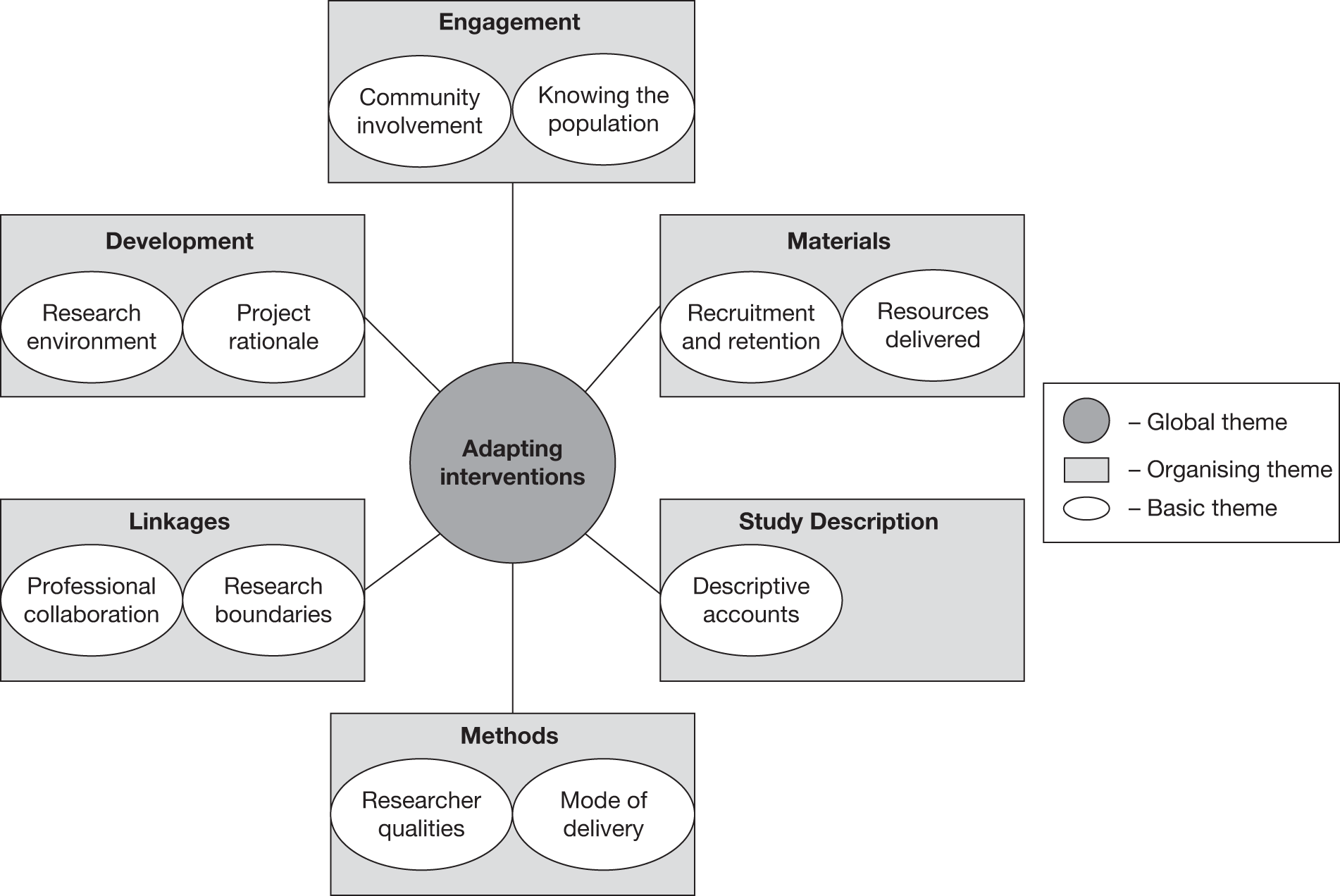
Development
The theme of programme development encompassed both political considerations (research environment) and personal factors (project rationale).
The initial steps of intervention development required a consideration of the research environment. This sometimes meant aligning the intervention with government policies but also ensuring that these policies, for example smoke-free policies, are understood and comprehended by ethnic communities; and sometimes delivering interventions for a group that had been largely overlooked by government health promotion policies. However, funding for these activities was often tied to government-prioritised areas, and when priorities changed, earmarked funding became scarce and determined the kinds of activities that could be undertaken.
We just didn’t have the resources to promote it the way we had hoped to promote that one, that, that event and that was partly because of the turnover at the City Health Department and the commissioner who had committed funds to this intervention left and the new commissioner came in and had his own agenda.
(P18, smoking, USA)
The researchers’ own backgrounds were usually the main driving force behind the project rationale for the intervention, sometimes aided by PhD students who had identified hitherto unexplored areas. Their past experiences usually influenced the adaptation rationale, as well as the kinds of intervention theory they were likely to adopt. For many US-based researchers, their research background and experiences allowed them to tap into a network of researchers working in this emerging field, and thus they were able simultaneously to draw on their collective knowledge regarding adaptation rationale and intervention theory in the development of the project.
Engagement
The theme of engagement involved two equally important steps: engagement with the targeted ethnic group or community (community involvement) and engagement with the characteristics of the targeted community (knowing the population).
Approaching the community and assessing their needs and considerations at the outset received near unanimous support from almost all of the interview participants. Community involvement was further improved when community advisory or steering groups were convened for the purpose of the intervention to advise on numerous issues, including appropriateness of incentives as well as health messages. Other times, pre-existing and established community organisations or leaders were approached to guide the interventions, and this was particularly evident at the recruitment stage.
The second kind of engagement required the researchers to know the population through various methods, including formative work, which encompassed focus groups, interviews, surveys and literature reviews. This was important to understand the community as a shifting, changing entity and to avoid inappropriate characterisation. This appreciation of the community continued throughout the lifecycle of projects through, among other things, participant feedback. For example, a weight loss intervention was developed to be culturally sensitive for an African American population, incorporating appropriate goals and motivators:
This is a journey this is a long process this is not a diet that you go on for a short period of time. A journey, but also for your best body so it, it’s for you to look and feel better but not necessarily to be thin, and we conveyed a lot about how you really can’t be there to take care of your family if you yourself are the one who is disabled or ill because stemming at least partly because of your weight.
(P14, physical activity and healthy eating, USA)
During the actual intervention recruitment period, participants also fed back to researchers, for example one group felt it was discriminatory within the church context to have an intervention for the exclusive use of one ethnicity:
Well I think some women who were not African American wanted to participate and felt excluded. Other women just felt that that was ridiculous that their friends were being excluded purely based on the colour of their skin, I mean it really is racially discriminatory against women who are not African American or black. And so and it was by design because the higher risk group is African American or black women, but within the context of the church that, that health risk is, is really immaterial.
(P14, physical activity and healthy eating, USA)
Materials
The theme of materials represented the practical strategies employed for recruitment and retention and included consideration of the resources delivered to participants.
In the USA, incentives were commonly used as motivators to improve recruitment and retention. The types of incentives employed included both direct financial rewards (money and travel costs) and indirect benefits (ranging from free toothbrushes to gym memberships). The value of the incentive was largely dependent on project funding.
There was mixed opinion on whether or not incentives improved individual-level participation. There was more support for providing incentives to organisations to enhance their participation, which was thought, in turn, to facilitate participation by its members. Providing incentives to established organisations was seen as an effective strategy to increase participation.
The resources delivered included materials and messages, which were targeted to the participants for language and message format, for example, and this was not surprising given our topic of enquiry. What was surprising was that some participants mentioned that these resources should be ‘evidence based’ and this was perceived to be an important criterion for those delivering the intervention as well as for some participants receiving the intervention.
So there may be a higher level of sort of sophistication and em and this, people feel that if it’s delivered through the church that’s enough you know but they want the information to be high quality and not necessarily delivered by a pastor anymore, they want it to be delivered by a health professional. So there seems to be a shift taking place, or it may be more of an urban rural shift, we’re not really sure.
(P22, healthy eating, USA)
Methods
The theme of methods described how intervention components were delivered (mode of delivery) and important researcher qualities that enhanced or constrained effective delivery of intervention components.
There was great emphasis on researcher qualities, particularly their ability to develop relationships. Relationships, although perceived as time-consuming pursuits, were also described as an absolute necessity.
One of the kind of ways of you know building trust and building partnership really have to do with spending time, going to the services, being there for events, listening.
(P22, healthy eating, US)
Perseverance was felt to be necessary to develop relationships with the target community, but also a necessary quality for researchers to secure resources for the community:
So it took me about 2 years to get permission to open up the swimming pool for these women at eh on the weekly basis, for few hours, which was just women only, and I had to go through many many steps.
(P9, physical activity and healthy eating, Australia)
Researchers also needed to be flexible within their roles and strike a balance between delivering a research project and responding to the target population, such that sometimes research components needed to be modified, for example translation of documents, timing of sessions or even completely dropping some component of the work if necessary:
One of the things that we found was that kids just abhorred having their fingers stuck, these are you know African American and Latino kids and so we just dropped the the serum glucose measure because . . . we were losing too many of our research participants you know even though they had parental consent and they had originally signed [consent] after the first round of data collection.
(P13, physical activity, USA)
The mode of delivery was often described as more important than the message itself; strategies such as peer educators or peer counsellors were seen to be appropriate for ethnic minority communities, although reasons were not always provided. Often interventions were delivered in group settings, and one motivation for this was that there may have been transferable modelling skills that could be shared with children or other family members who may be present during the intervention, or that could be taken home after the intervention.
So we knew that we had their attention, that was one main reason cause they’re a major target group because of their own health, and that’s what we emphasised. But number two we also know that a woman in that age group, and certainly African American women, we know are the matriarchs of their families, so they are influencing not only their adult children but their grandchildren, their great grandchildren, their churches, their workplaces, they are very influential [mmm]. And so if we can change the lifestyle of one single woman, just one single woman in that age group, we have a major ripple effect that’s going to impact on their entire community.
(P23, general health, USA)
Beyond the family there was thought to be potential peer modelling effects within tight-knit communities:
But, but the, the, the eh the and the higher risk group persons, at least some of them, very successful in eh change their behaviour, started to walk eh in the district every, every evening eh every afternoon or evening, attend the classes eh walking classes which walked in the district and, and eh some of them lose weight so that anyone could, anybody could see that. Eh and they became very important role models for the others.
(P19, physical activity, Norway)
Across the interviews, staff and staff characteristics were reported as contributing to successful uptake and delivery of the intervention. Having someone who was of the same gender, who spoke the same language were some of the practical attributes described:
Of the same culture . . . South Asian and . . . struggled with obesity herself.
(P8, healthy eating, UK)
Having an ethnically matched staff member was preferable; however, this was not always possible. It was felt that a person who was not from the same ethnicity (or background) would still be able to deliver the intervention if they were enthusiastic; however, they could be perceived by participants as not understanding their particular situation. It was also seen to be useful if the staff were well known in their community and respected. These were generally more nebulous characterisations, but the justification given was that:
Qualifications for working in those fields you know, we could teach the skills but we couldn’t teach the community connectiveness, that’s either there or it’s not.
(P7, smoking, New Zealand)
Description
The theme of study description encompassed descriptive accounts of the programme or intervention. Across the interviews an eclectic mix of approaches, various settings and multiple activities and actors were reported. Participants were similarly diverse, with a mix of generations, genders and ethnicities reported. Groups ranged from 10 participants in small pilot studies to thousands of participants in a citywide survey. There was no obvious model intervention for adaptation considerations.
Linkages
The theme of linkages described both the limits of collaboration and project scope (research boundaries) as well as the benefits of collaboration with other professionals and institutions (professional collaborations).
Health interventions delivered for ethnic minority populations often drew clear boundaries around health and social issues, which were outside of their remit. Although some projects acted as a link between services, they did not, for example, deal with mental health or abuse cases. In these situations they made referrals to the appropriate services. On the other hand, some interventions were purposefully involved in related services for their population, for example pregnancy services. There did not appear to be a clear pattern in determining research boundaries, as responsibilities were continuously negotiated:
You know again in some ways we were sort of battling [partner organisation] sometimes as well, wanting to do something that wasn’t just standard.
(P8, healthy eating, UK)
Overall, professional collaboration with existing institutions, services and professionals was reported to positively enhance the intervention. However, linkages with some organisations required more complex manoeuvring than others, and this feature was largely dependent on the characteristics of the organisation, for example the church and its religious leader:
There’s also a lot of differences between churches and denominations in terms of the governance and the structure and some denominations have, like a Baptist denomination, has a consistent pastor that will be there for many years and so if they commit to working with you they’re gonna stay with you, whereas other denominations like the AME [African Methodist Episcopal] we found they rotate pastors every couple of years and so you start into it and once the new pastor comes in they may have a different priority eh and may decide not to, that they’re not so enthused about working with you [laughs]. So that has been a problem in terms of you know often if, if a church, quits in the middle it’s usually because there’s a change in leadership [okay] so that was one thing in terms of working with an organization.
(P22, healthy eating, USA)
Global theme 3: sustaining adapted interventions
Sustaining an adapted intervention involved interpreting intervention findings, reflecting on what was learned and what could be taken forward, and fostering the capacity of the workforce as steps towards continuity. The three organising themes of evaluation, insights and strengthening the workforce thus contributed to the global theme of sustaining adapted interventions (Figure 14). Discussions of how to disseminate project findings, sustain the programme of research and manage project personnel demonstrated the constraints and challenges faced by the researchers we interviewed as well as revealing the rewards and motivators for continuing their work.
FIGURE 14.
Global theme 3: sustaining adapted interventions.
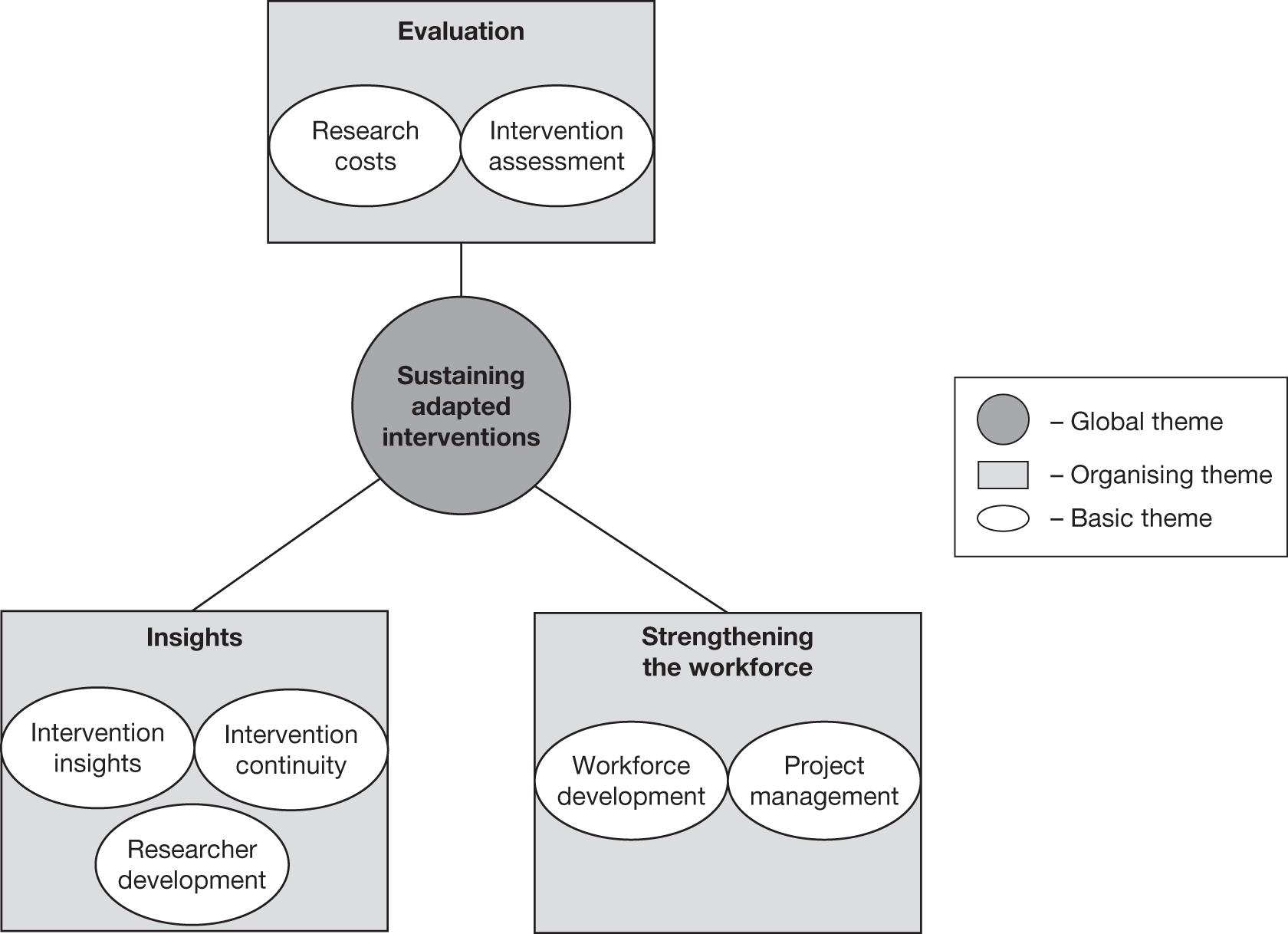
Evaluation
The theme of evaluation discussed issues relating to intervention cost (research costs) and effectiveness (intervention assessment).
Additional research costs were felt to be necessary, particularly for community engagement, and particularly justified when carrying out work with ethnic minority populations.
The truth is that any time you’re gonna do a, whether we were in the black community, Hispanic community, we, we were gonna have to fund community organisations to do this work because you can’t do this work unless you’re in the community. So I don’t think, I think doing any kind of tailoring or creating you know tailored programmes is a little, adds an expense to the existing programme, but then if you want to be effective in your, if you’re in a city like [city name] you, you don’t really even think about it that way because it’s the cost of doing business, it’s, it’s not a question of should we do this, its, you have to do it you know.
(P18, smoking, USA)
At times, researchers felt that funders had little understanding of these additional research costs (P10), which added to the difficulty of accessing sufficient funding for research or for sustaining interventions beyond the research phase. A lack of funding, as well as the lack of personnel and overlapping project phases, meant that many interventions were not formally evaluated, even though they had been delivered. It was, however, suggested that reporting in the usual peer-reviewed journals might not always be the preferred route for communicating results:
Dissemination in the community can be much more important than producing a peer-reviewed publication as far as being effective goes.
(P17, physical activity and healthy eating, New Zealand)
When the intervention assessment was published, the outcomes and results were not always straightforward and often raised more questions than answers in relation to the components that were likely to be effective in promoting behaviour change:
The structure is, is very critical. But what we, what we don’t know is really one site different from another? Another thing we think we know, we haven’t documented it, is the facilitator the key person to the success of the outcome?
(P23, general health, USA)
When ‘successes’ were mentioned, this was usually discussed anecdotally, as the evaluation either was carried out informally or had yet to be published:
I: So would you consider this intervention that you ran to be quite successful?
P: Oh without a doubt, yeah. No, it, it, in terms of, we did some informal, I mean, more informal follow-up and that would say for example the fact that the swimming sessions continued on you know a number of the ladies who, we, we got some data on that eh who had participated in the pilot study and so some of them we collected bloods most probably 18 months down the track, after they’d finished and again yeah we most probably had you know in the pilot I think we ended up with nearly 20 women, and of those I would think most probably 50% had actually made a positive change in terms of their lifestyle. And we had, and that, that was with no active intervention since we eh we started the pilot.
(P12, physical activity and healthy eating, Australia)
Insights
The theme of insights discussed growth experienced by the researchers (researcher development), confirmation and correction of initial research assumptions and new findings generated in the research (intervention insights), and how these understandings were translated into strategies to sustain health promotion actions (intervention continuity).
Researcher development was something that occurred over the intervention period. Researchers reflected on their own experiences by discussing personal growth and reward, and how this incentivised them to continue to work delivering and implementing adapted interventions and programmes. Other researchers used their work as a springboard to study ethnicity and health at a systems level.
Intervention insights were often derived from unexpected findings and through reflection on initial assumptions about the target community. Identifying and sharing their own insights on effective strategies and then relaying their lessons learned to other researchers were cited as reasons for participating in this present qualitative study. One participant was adamantly against maintaining anonymity because she wanted everyone to know about her programme:
I don’t have any problem if we are identified in your research because the whole thing as I see it is about sharing and caring so it was quite interesting when I went down to my boss and I said oh look I really don’t think I’ll sign off on this part where it says here, the your point number 6 where it says I understand you won’t put anything in your report that could be used to identify me and, and [name] says oh well scrub that out and oh no identify away.
(P7, smoking, New Zealand)
Widely publicising and marketing a programme was a reported method for increasing sustainability and intervention continuity. Formalising the intervention through ‘manualisation’ (developing manuals or guides on how to deliver the intervention) or the development of project logos appeared to coincide with the longevity of the intervention. Furthermore, continuity was also reported to require, on some level, a continued presence or advocacy on the part of the researchers. Developing training centres with set materials and teaching methods to facilitate the consistency of the intervention for participants in a broad geographical area was a model for sustainability reported in one intervention:
We said we’re gonna look at [name of a fast food chain] and see how they do it [laughs], a [name of a fast food chain] hamburger in [city name] is the same as the one in Edinburgh. But anyway, so the quality, one of the ways to maintain our quality em because we know it works and, and there are many ways, reasons that we know it works is to really eh be in charge of the training of future facilitators and community health leaders so that’s a real important piece of what we’re doing.
(P23, general health, USA)
Strengthening the workforce
The theme of strengthening the workforce discussed the management of a positive and safe working environment for these staff members (project management) and the training of intervention staff and recognition of their work (workforce development).
Project management largely involved facilitating positive working environments for staff, particularly a group of multiethnic staff working across sectors:
I mean our common goal was to provide an intervention that was going to support the population. Em and you know so we did have some disagreements, or should I say some very, very robust debates, but em getting everybody on the same page, it did take some time but once we did we just steamrolled, we really steamrolled . . . because of the robust discussions we had we forged such strong alliances out of them em and really paved the way for other tri-party initiatives to be able to happen a lot faster.
(P7, smoking, New Zealand)
Project management also involved the responsibility of ensuring the safety of staff, particularly in the context of delivering interventions in the community and through home visits, which were common for some ethnic minority groups:
Well as a manager of a multi-site project my concerns are safety, as I said we had a homicide last week we were with, we’re experiencing a lot of shootings and, and you know violence in the neighbourhoods and to have outsiders come in, especially when we first go in its, it’s alarming.
(P16, smoking, USA)
Staff, personnel and principal investigators working on interventions for ethnic minority health tended to originate from the target population. Across interviews the importance of this feature of the workforce was emphasised and that, for example, it was more appropriate to:
[take] lay people and [upskill] them rather than taking people and trying to skill them in the community.
(P7, smoking, New Zealand)
Thus, workforce development involved training in technical health promotion skills, rather than softer social skills already presumed to be held by staff members. Along with skills development, recognition of their work was also cited to strengthen the workforce:
It was a big buzz for the team to realise you know that they were, they were this important, that they should have this priority placed upon them and resource, resources spent on them.
(P5, smoking, UK)
Discussion
By naming the first global theme constructing ethnicity we have deliberately sought to invoke ‘ethnicity’ as a concept that has been built up and deconstructed over decades of discussion and debate, with boundaries around what it can encompass, for example the boundaries explicated by the five dimensions of ethnicity that we considered earlier (see Chapter 1), as well as ‘ethnicity’ as a concept that remains an unfinished process. In turn, the insights drawn from the theme of constructing ethnicity alert one to different kinds of ‘ethnicity’ at work and discussed when adapting interventions. The conventional elements of ethnicity relate to the five dimensions of ethnicity discussed in Chapter 1, which capture, more or less, the common sense usages and the commonly used definitions prevalent in health-care research. The contextual elements of ethnicity, as illustrated by the above data, extend our thinking around ethnicity, in particular by taking into account past health-care and research exposures and experiences, relationships with spaces and places, the significance of social dynamics and the inherent heterogeneity within the target group. These process-focused dimensions of ethnicity can offer a more dynamic conceptualisation of ethnicity beyond descriptive characteristics attributed to persons or groups, which at times appear entrenched and immutable (see Chapter 1).
The contextual elements of ethnicity can further offer a platform from which to consider ethnicity when adapting health promotion interventions. Ethnicity when considered in context can involve a mapping process that captures both conventional elements, such as religion, language, culture, physical features and ancestry, as well as demographic variables, such as age, gender and SES, and also the relationships that members of these ethnic groups have and share with their social groupings and their physical space as well as their diverse experiences. Mapping these processes and relationships has both practical applicability and analytical value for both intervention delivery and analysis. Ethnicity therefore interacts with a number of factors that affect behaviour change and understanding the complex nature of these interactions is useful in advancing the concept of ethnicity itself as well as the extent to which we can adapt health promotion interventions. These elements of conventional and contextual ethnicity represent a preliminary effort to reconceptualise a definition of ethnicity with greater utility for practice and theory.
The second and third global themes of adapting interventions and sustaining adapted interventions suggest that considerations for adapting interventions appear at every step of the intervention process, from initial thinking about funding and political and personal factors to community involvement, incentives for recruitment and retention, professional and institutional linkages and researchers’ qualities. The third global theme in particular indicates that fostering intervention and programme continuity requires an additional set of considerations, which include conducting formal and informal evaluation, sharing insights, formalising intervention/programme strategies and strengthening the workforce. These findings echo the Programme Theory of Adapted Health Promotion Interventions derived from empirical intervention studies (see Chapter 6, Figure 9), while the strategies for adaptation map onto those identified in the 46-item Typology of Adaptation (see Chapter 6, Table 13). These qualitative findings can help to contextualise and illustrate how adaptations and intervention stages work.
Finally, reflecting on this study as a whole, we observed that the majority of the researchers who were available for interview (i.e. identified from the sampling frame) were based in the USA and as such this revealed a geopolitical imbalance in the area of research on ethnicity and health, particularly for adapted interventions. For example, researchers working at institutions along the east coast of the USA identified an informal network that they accessed to share ideas and collaborate on projects. More importantly, this informal network was likely to facilitate the sharing of findings from projects. As we uncovered, projects may go unevaluated and unpublished, leaving those outside of the informal networks without access to this information. In essence, many of the lessons learned from these projects would be invaluable to other researchers in developing future interventions and this ‘lost’ knowledge hampers a sustained growth of evidence in this field.
Internationally, particularly in Australia and New Zealand, there was little connection to this emergent informal network in the USA and the researchers interviewed reported working within smaller groups with less government-financed and collegiate support. In Europe, connections between people and projects from the UK and continental Europe were reported and observed. Conspicuously absent were reports of an organic global network of researchers, as geography appeared to dictate the limits of collaboration and sharing, despite the wide availability of communication resources such as the internet. It was encouraging to hear that identifying effective strategies and relaying lessons learned for other researchers and the potential for generalisability were cited as reasons for participating in the qualitative interviews and this willingness to share insights could contribute to sustained work in this area.
Strengths and limitations
This qualitative component was developed alongside an extensive and rigorous systematic review (see Chapter 6). Included studies from the review published after 2005 were used to create a sampling frame to recruit participants for interviews. This integration represents an effort to link up the two separate components; it proved to be particularly fruitful in identifying a maximum diversity sample and therefore represented a particular strength of this component. However, despite the implementation of a cut-off date of 2005, some of the papers reported on studies that were conducted 10 years previously and consequently project recall was understandably poor. In the future, a later cut-off date might be used. The risk of such a strategy, however, is that forthcoming projects may not yet have analysed their data, or researchers may be unwilling to share data before publication, which was the case in one of our interviews.
A further limitation is that the majority of participants were researchers based in academic institutions. Although we made attempts to find projects developed within the community, this was not always possible as they tend not to be evaluated or written up for publication. This introduces a bias in our sampling towards university- and health professional-conceived interventions, rather than perhaps de novo community interventions. It is, however, worth bearing in mind that we did interview some community workers and that some academics are very much embedded in the communities they work with, and that the dichotomy between university led and community led may be less apparent. Widening the sampling frame and employing a longer search period for participants may mitigate this bias, but, more importantly, may enrich the accounts of adaptation.
The qualitative interviews themselves provided access to information that was not published or in some cases to information that may never be published. This was particularly important and necessary to learn about the processes associated with adapting interventions, of which there are few papers in the published literature. This access provided unique insights far beyond what a reader (ourselves included) could glean from accessing only peer-reviewed journal articles on the same study.
Another strength of this component of the research was the opportunity to speak to those delivering and implementing programmes; this was because they were ideally positioned to provide practical insights on adapting health promotion interventions for ethnic minority groups. On the other hand, speaking only to researchers and health educators about adapting health promotion interventions without supplementary interviews with the participants of those interventions was a limitation of this qualitative component. Therefore, we tried to exercise caution when interpreting interview participants’ views on ethnic groups, particularly when presenting the target community’s acceptance and satisfaction with the intervention, as these opinions were filtered through the lens of their own values and thinking.
Overall, the interview participants did not shy away from discussing aspects of their interventions that were ineffective or that simply did not work. Participants were willing to share some of their shortcomings, as well as their successes, with the explicit goal of advancing the field.
Conclusions
Qualitative studies undertaken alongside systematic reviews, and other linked studies of this nature, are important in teasing out the processes and thinking that underpin adapting interventions for ethnic minority populations. Our findings indicate that a process-oriented concept of ‘ethnicity’, encompassing both conventional and contextual elements of ethnicity, may be helpful to understand the factors and interactions that affect behaviour change and therefore to better adapt health promotion interventions for ethnic minority populations. Furthermore, our qualitative findings confirm many of the main findings from our systematic review of empirical intervention studies, which led to the development of our Programme Theory of Adapted Health Promotion Interventions (see Chapter 6). The programme theory illustrates that adaptations can take place throughout the entire intervention process, from conception to dissemination. Synthesis of these research components will be discussed in greater depth in the following chapter.
Chapter 8 Realist synthesis: prioritisation for implementation and future research
Abstract
Background
Increasing ethnic diversity and the persistence of health inequalities in the UK and elsewhere challenges health systems to produce evidence-based guidelines for effective health promotion interventions for ethnic minority populations. Relevant evidence should ideally come from randomised controlled trials (RCTs) of health promotion interventions in the target population, but adaptation of existing health promotion interventions that have been found to be effective in the general population offers a potential short- to medium-term solution to fill the current evidence void.
Objectives
In the context of promoting smoking cessation, physical activity and healthy eating in African-, Chinese- and South Asian-origin populations, we sought to identify which adapted interventions are ready for implementation and establish which interventions require further research.
Methods
We undertook a realist synthesis of our earlier phases of work, that is, the discussion groups in the two user engagement conferences, the review of guidelines and systematic reviews for health promotion interventions in the general population, the systematic review of adapted interventions and the in-depth interviews with academics and health promoters with experience of working with relevant ethnic minority populations. Explanatory frameworks to interpret and synthesise this body of work were sought by two researchers independently searching for and considering recurring patterns or demi-regularities in the evidence, and then reaching consensus through discussion. In particular, we aimed to describe which intervention contexts moderated adaptation mechanisms to impact on intervention outcomes. We utilised the six categories of ‘strategies and activities’ used in health promotion interventions to compare the findings from our review of UK guidelines and international systematic reviews in relation to the general population with those from our systematic review of adapted interventions. From this comparative work we identified which ‘strategies and activities’ were advocated by both guidelines and international systematic reviews, and which also featured in interventions adapted for ethnic minority populations. Through explicating this evidence base and interpreting it through the construction of context–mechanism–outcome (CMO) configurations, we reflected on interventions that are potentially ready for implementation in ethnic minority populations and those that require further research.
Results
We were able to identify contexts that either enhanced or diminished the effectiveness of adaptations at each stage of the Programme Theory of Adapted Health Promotion Interventions. Four exemplary in-depth case studies on group-based interventions, communication strategies, behaviour patterns and pharmacotherapy, and social support were derived to illustrate what adaptation approaches are likely to be effective for whom and in which circumstances. There was no clear evidence that any adapted intervention approach is ready for rolling out, but the ‘lowest hanging fruit’ in this respect was found to be in relation to pharmacotherapy-based interventions for promoting smoking cessation, which are likely to be effective for ethnic minority populations if the salience and acceptability to target populations can be increased. This effort could, we hypothesised, be achieved through paying close attention to underlying beliefs and values, the potential impact on family members and the provision of appropriate linguistic and peer-to-peer support, emphasising the benefits of relatively short-term drug therapy. There is also the need to create greater opportunities for incorporating exercise and active lifestyles into everyday life through interventions that alter the built inner-city environments in which many ethnic minority populations tend to be most concentrated; this may involve more easily accessible (by walking) amenities and safe locations for individuals, families and communities to increase physical activity. Interventions should also test changing the availability of foods served at community organisations and religious institutions as well as ensuring that any dietary modification or recommendation should prioritise substitution rather than avoidance of commonly consumed and perhaps culturally relevant foods. Furthermore, use of peer and lay advisors/educators and appropriately trained dietitians working with families, and in particular household cooks, has the potential to effect sustained changes in healthy eating habits. The RESET (relevance, evidence base, stages of intervention, ethnicity and trends) decision-making tool developed from this work will, we hope, aid the planning of this future research.
Conclusions
The appropriate adaptation of health promotion interventions is a complex undertaking with an, as yet, inadequate evidence base. This in part stems from the fact that, apart from a few notable exceptions, we still know relatively little about how best to effect clinically important and sustained lifestyle changes in the general population, let alone for ethnic minority populations. Relatively simple adaptations to improve the salience, acceptability, trust and use of smoking cessation therapies are likely to yield important benefits in the short to medium term, but, given the current paucity of evidence in relation to ethnic minority populations, this work needs to proceed in an evaluative context. Effecting sustained changes in exercise and healthy eating is likely to prove challenging, involving, among other things, environmental-level interventions that have been developed through a detailed understanding of the values, practices and aspirations of the target population.
Introduction
Select findings from the earlier phases of work, namely the two national user conferences, the review of UK guidelines and international systematic reviews of relevant health promotion interventions for the general population, our systematic review of adapted interventions and the qualitative interviews with researchers and health promoters who have experience delivering adapted health promotion interventions to the target populations (see Chapters 3–7 and Box 8 for a summary of the main findings) were reanalysed to identify areas for implementation and future research priorities. This was complicated by the limited evidence of effectiveness in relation to physical activity and healthy eating interventions for the general population (see Chapter 4) and the lack of direct evidence comparing adapted with standard health promotion interventions (see Chapter 6). What also became clearer from the qualitative work was the extent to which researchers needed to make sense of, draw on and balance a range of relevant contextual considerations in order to develop interventions that were likely to prove relevant, acceptable and effective, while also allowing rigorous evaluation (see Chapter 7).
Chapter 3: Discussions with researchers, health promoters and health service users with experience of working with ethnic minority populations highlighted the need to think beyond behavioural interventions and focus more on community- and ecological-level interventions. A focus at community or population level would thus take into account the effects of contextual factors such as level of education and socioeconomic status (SES). They further expressed the wish that our research team facilitate collaborations among individuals and groups who, although often grappling with similar issues, were isolated and unsupported. The need for the work being pursued was emphasised as many people recognised that they were working from a relatively weak evidence base, but an emphasis was placed on the generation of evidence that both had a sound theoretical basis and offered practical tools and techniques that could be used out in the field
Chapter 4: Our review of UK guidelines and international systematic reviews provided evidence on the limited numbers of interventions that have proven effectiveness for the general population. These ‘strategies and activities’, in the main, relate to drug-based interventions for promoting smoking cessation and to modest short-term improvements in diet and exercise associated with setting-based approaches. From this work we were able to identify which intervention ‘strategies and activities’ have accumulated relatively more evidence (i.e. individual centred) and which areas remain sparse (i.e. more population-level approaches)
Chapter 5: UK guidelines and international systematic reviews were further scrutinised for evidence of effect of recommended interventions according to ethnicity. We found that ethnicity was not always considered and, when it was considered, this was typically done rather nominally. It was therefore not possible from these highlevel evidence syntheses to determine whether these health promotion interventions are equally as or more or less likely to be effective for ethnic minority populations
Chapter 6: Our systematic review of adapted health promotion interventions identified a range of theoretical arguments for the importance of adaptation and the factors that should be taken into consideration. Despite identifying and critically reviewing a large body of (predominantly US-based) evidence, we found little clear evidence of whether or not adapted interventions were likely to be more effective than standard interventions, and no relevant evidence on cost-effectiveness. We were, however, able to derive from this body of work a novel 46-item Typology of Adaptations and develop a Programme Theory of Adapted Health Promotion Interventions
Chapter 7: Thematic analysis of qualitative interviews generated three new key themes that emphasised the importance of broadening thinking on ethnicity to understand situational contingencies, reinforcement of relevant adaptations used for interventions, and contextualisation of the practicalities of culturally adapting health-promoting interventions
Making sense of this large and somewhat heterogeneous body of evidence was thus challenging. 388 This is illustrated, for example, by the range of permutations that can arise through combining the multiple Tannahill-derived ‘strategies and activities’ of health promotion interventions we identified in Chapter 4 with the 46-item Typology of Adaptations and the Programme Theory of Adapted Health Promotion Interventions we proposed in Chapter 6. This combination generates multiple possible adapted interventions for evaluation, with multiple populations targeted and health topics promoted. These combinations are further complicated by the conceptual and practical considerations identified from the interview data presented in Chapter 7. Considering this complexity, there are clearly likely to be many different answers to the question of whether adaptations are effective or not. The challenge was thus to recognise and encompass this complexity, but still be able to generate meaningful insights that could contribute to identifying adapted interventions that were ready for implementation and also prioritising future research into adapted interventions for ethnic minority populations.
Research questions
The following research questions addressed in this chapter related to Phase 3E of the project (see Chapter 2):
-
What adapted interventions work for whom in what contexts?
-
Which interventions are ready for implementation and which interventions require further research?
Methods
Rationale and overview of the realist approach
We adopted a realist approach to synthesise the large and heterogeneous body of evidence from the preceding phases of work (see Chapters 3–7) in an attempt to understand which adaptation approaches are most likely to be effective in which populations, in what circumstances and why. We sought to develop a rich, multiperspective, contextualised interpretation and synthesis of our mixed-methods data.
Realist evaluation has previously been used in health research as a method for systematically reviewing primary studies (often in the context of studying complex interventions). These reviews have, for example, synthesised large and disparate bodies of evidence on internet-based medical education389 and provided a parallel analysis to a Cochrane review on the efficacy of school feeding programmes. 390 These reviews accommodated and often sought out heterogeneous studies (in design, population and topic, for example) for analysis. By searching for underlying theory in interventions and focusing on explaining the ‘demi-regularities’ or patterns observed in the body of evidence, it is often possible to generate important new insights into underlying explanatory mechanisms. 391 There is also the potential to elaborate on a body of evidence ‘to create an abstract model of how and why programmes work, which then can be used to provide advice on implementation and targeting of any novel incarnation of the intervention’. 392 Articulating how interventions are thought to work and how they actually work can thus help in contributing to the building of an evidence base that is sensitive to contextual considerations and, therefore, more likely to approximate ‘real-life’ circumstances and generate practical and applicable conclusions for research, practice and policy. 393 Data generated during the earlier stages of this project (see Chapters 3–7) were thus purposefully selected and used to derive a number of CMO configurations (illustrated in Figure 15: the mechanisms were the adapted interventions that we examined in different contexts to consider how their likely effectiveness was enhanced or diminished).
FIGURE 15.
Mapping the data generated from the different research methods to a realist CMO configuration.
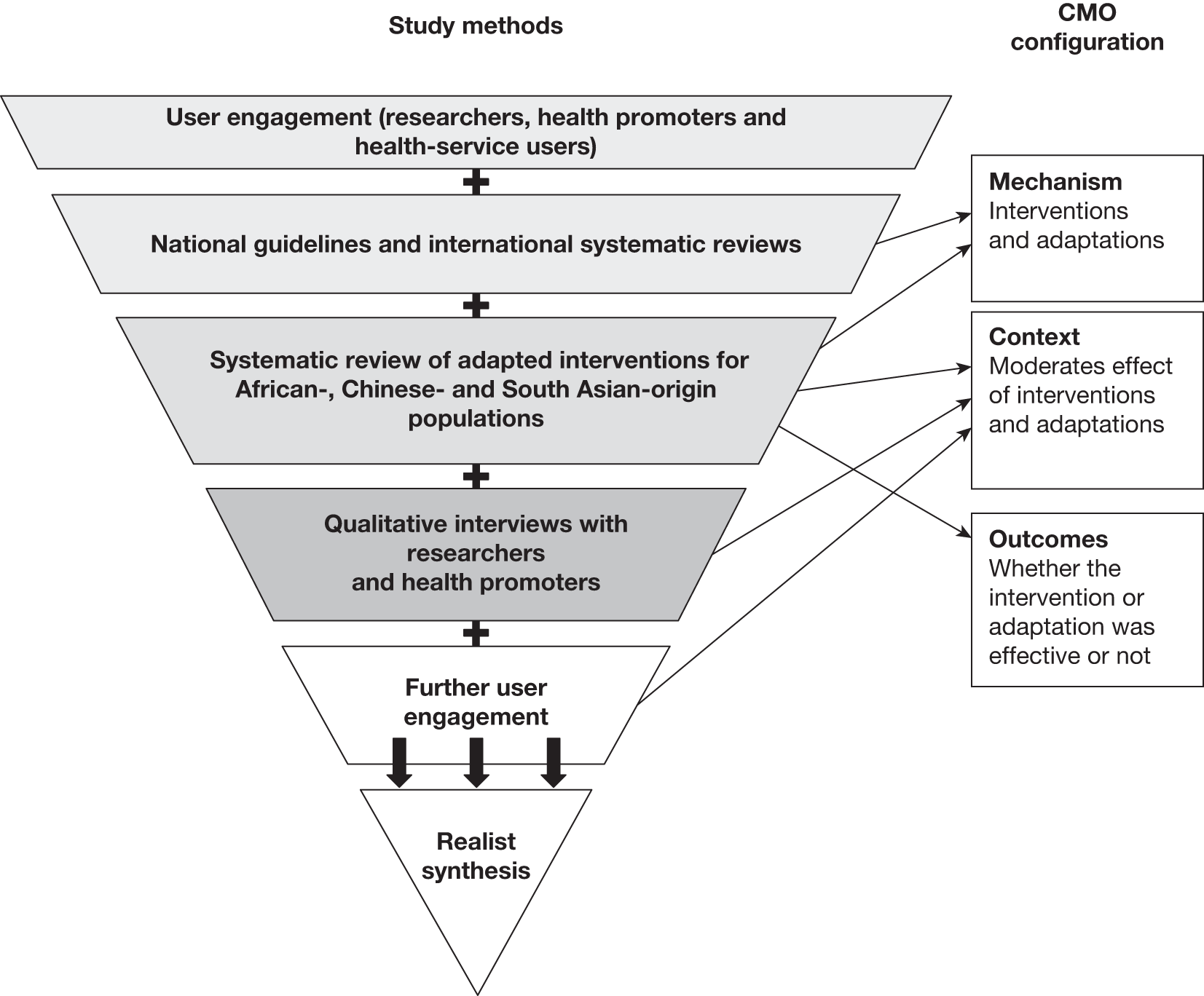
Realist framework
A realist approach to data is not a review technique but a review logic,394 meaning that it is driven by an underlying framework rather than by set procedures. Each review will therefore require its own specific methods in line with the key steps of identifying and testing key theories and uncovering the likely mechanisms of interventions to hypothesise and test how interventions might work (or not). The key overall steps in this process are outlined in Box 9. A central goal is to maximise learning using the most appropriate methods available. We therefore modified these key steps as the original steps were developed for the synthesis of primary studies and we required steps to synthesise data generated from multiple method sources. Our adapted framework for realist synthesis is outlined in Box 10.
-
Clarify scope:
-
identify the review question
-
refine the purpose of the review
-
articulate key theories to be explored
-
-
Search for the evidence:
-
exploratory background search to ‘get a feel’ for the literature
-
progressive focusing to identify key programme theories, refining inclusion criteria in the light of emerging data
-
purposive sampling to test a defined subset of these theories, with additional ‘snowball’ sampling to explore new hypotheses as they emerge
-
final search for additional studies when review near completion
-
-
Appraise primary studies and extract data:
-
use judgement to supplement formal critical appraisal checklists, and consider ‘fitness for purpose’: relevance – does the research address the theory under test?; rigour – does the research support the conclusions drawn from it by the researchers or the reviewers?
-
develop ‘bespoke’ set of data extraction forms and notation devices
-
extract different data from different studies to populate evaluative framework with evidence
-
-
Synthesise the evidence and draw conclusions:
-
synthesise data to achieve refinement of programme theory – that is, to determine what works for whom, how and under what circumstances
-
allow purpose of review (see Step 1b) to drive the synthesis process
-
use ‘contradictory’ evidence to generate insights about the influence of context
-
present conclusions as a series of contextualised decision points of the general format ‘If A, then B’ or ‘In the case of C, D is unlikely to work’
-
-
Disseminate, implement and evaluate:
-
draft and test out recommendations and conclusions with key stakeholders, focusing especially on levers that can be pulled in here-and-now policy contexts
-
work with practitioners and policy-makers to apply recommendations in particular contexts
-
evaluate in terms of extent to which programmes are adjusted to take account of contextual influences revealed by the review
-
the ‘same’ programme might be expanded in one setting, modified in another and abandoned in another
-
To answer the question ‘Does the adapted intervention work and which adaptations work particularly well for which populations, in what settings?’ We identified two key programme theories: the six ‘activities and strategies’ used in health promotion interventions (see Chapter 4, Box 3) and our Typology of Adaptations mapped onto the eight stages of a programme theory for adaptation (see Chapter 6, Figure 9)
2. Search for relevant evidenceWe searched for relevant evidence across all of our study data (see Box 8). This incorporated different study types (guidelines, systematic reviews, RCTs, quasi-experimental, pre–post test, qualitative studies and qualitative interviews), study topics (smoking cessation, physical activity and healthy eating) and study populations (African-, Chinese- and South Asian-origin populations). With progressive focusing we used data to guide the realist synthesis (user consultation), develop our programme theory (UK guidelines, international systematic reviews and empirical studies), identify realist insights of why adapted interventions work or not (empirical studies) and to test and explore new insights (qualitative interviews)
3. Appraise the quality of the evidence and extract the dataTwo researchers (JJL and ED) assessed the quality of the 107 empirical studies to see if they were ‘fit for purpose’, that is, whether or not they were relevant to the programme theory being tested. This realist approach also allowed us to draw on some of the studies ‘excluded’ from our traditional systematic review (see Appendix 14), which were, in some instances, useful for providing complementary insights. For the empirical studies, customised data extraction forms were used to record each study component (see below), with a dedicated section for realist insights and comments. The same two researchers (JJL and ED) extracted details on the intervention and adaptations; the study’s context including the population demographics, setting and past experiences with research; any explanations provided by the authors on the success or failure of the intervention; and information on the feasibility, acceptability and equity of the intervention
For the qualitative interviews, two researchers (JJL and ED) transcribed and independently coded the interview transcripts using NVivo 8. Interview data were revisited to identify realist insights relevant to the programme theory that confirmed or refuted what had been elicited from the empirical studies
4. Synthesise the evidenceWe actively constructed CMO configurations in tables (see Box 8 for relationship of methods to CMO configuration) to examine what factors and settings (context) moderated adapted interventions (mechanism) and to elucidate the configurations underpinning both success and failure (outcomes). These CMO configurations are included in Appendix 27. We presented the findings in the format of, for example, ‘If A, then B’ or ‘In the case of C, D is unlikely to work’ or ‘although E is effective, it may not be acceptable in light of F and G’ to illustrate the nuances of adaptations uncovered through a realist perspective
5. Framing recommendations and disseminating findingsPreliminary conclusions and recommendations were made in consultation with stakeholders, who reorganised priorities and recognised other important contextual factors
Data extraction and analysis relating to the different methods are discussed more fully in their appropriate chapters (see Chapters 3–7) and only a summary is offered here. In addition to the usual data extraction methods outlined for each specific chapter, two reviewers independently extracted any additional significant or ‘realist insights’. This means, for example, that when the reviewers extracted data from empirical studies for the systematic review (in Chapter 6), traditional information such as population, study type and outcome measures were recorded, as well as additional insights reported by the authors on why their intervention was thought to be successful or not. Synthesis of these data was achieved through repeated discussion among the same two researchers (JJL and ED) who searched, reviewed, interviewed, coded, extracted and analysed the datasets from the preceding chapters.
Reflexive considerations
Given the large amount of data collected over the course of the project, we frequently discussed the additional insights, or ‘nuggets’, found in the datasets; this process was facilitated by the close working proximity of the principal researchers and their complementary academic and practical backgrounds (social science and public health) and regular discussions with a third researcher (AS). Early in the project, insights discovered were discrete and fleeting and as such we struggled to detect initial patterns. Towards the end of the systematic review of adapted interventions (see Chapter 6), however, patterns began to emerge from the data. Only after the interview data (see Chapter 7) were coded and discussed did these patterns take on more tangible forms as the interview data helped to direct our attention to what the researchers working in this field perceived as significant to their work. Uncovering realist insights thus involved an iterative process – returning to the same piece of data with a slightly different perspective each time.
When initial CMO configurations (such as the ones presented in the examples, Boxes 11–14) were presented and discussed among the investigators and at the second user conference (see Chapter 3) they were generally well received. The research users felt that the example presented at the conference (see Box 11) offered valuable contextual information that was grounded in the evidence, but without being prescriptive. They did, however, caution an interpretation exclusively focused on ethnicity and suggested that SES might be an important confounder. This feedback broadened our perspective; however, determining whether SES or not was indeed a salient factor, or whether it acted alone or in concordance with ethnicity,376 was beyond the scope of the study.
The review of UK guidelines and international systematic reviews (see Chapter 4) found that there was some evidence that group-based interventions were effective for smoking cessation, increasing physical activity and improving healthy eating
The systematic review of adapted interventions (see Chapter 6) revealed that group delivery was a common adaptation and this was extracted and contributed to the Typology of Adaptation (number 41: encourage/involve social support, e.g. joint counselling, family counselling, families and friends invited to sessions)
Context and related outcome – systematic reviewRealist evaluation of the systematic review of adapted interventions highlighted two contextual considerations (see Appendix 27):
-
A group- and individual-based diabetes management intervention for African Americans held in a rural setting revealed that group-based programmes were not always appropriate as there were sometimes competing cultures of openness (facilitated by churches) and privacy (rural traditions)
-
A pictorial one-on-one diabetes education intervention to improve nutrition for South Asian populations reported participant preference for one-to-one health education at clinics rather than organised single-sex group sessions. Participants wanted to keep their diabetes status private and did not wish to discuss their food choices in public
The qualitative interviews (see Chapter 7) added other contextual considerations such as ethnicity, age and gender that may make group formats less acceptable:
-
(a) the younger people prefer that support from one another whereas the older people want to be able to . . . have a good go within the family environment with that support, although in saying that the Chinese population prefer, the men, the men they like to become smoke free and then celebrate it back with their family so they won’t lose face if they relapse
-
(P7, smoking, New Zealand)
-
-
(b) we provide one-to-one support to each memb, person that comes to us. We can’t do it in groups, again for confidentiality issues because if a community is quite close knit, so you have to make sure that they don’t you know they’re not in a group where somebody knows them from Bangladesh back home so there’s a lot of village ties, so they don’t really want, somebody older wouldn’t want somebody younger than them knowing about their personal issues and why they smoke
-
(P6, smoking, UK)
-
The majority of effective interventions identified from the UK guidelines and international systematic reviews (see Chapter 4) were communication based, whether delivered one-on-one, by telephone, via the internet or using written materials
The systematic review of adapted interventions (see Chapter 6) revealed that adaptation for language involved either having communication materials in the target population’s language (Typology of Adaptation number 13) or reflecting the target population’s language usage in terms of concepts and vocabulary (Typology of Adaptation number 14)
Context and related outcome – systematic reviewRealist evaluation of the systematic review of adapted interventions provided additional contextual considerations (see Appendix 27):
-
A group-based diabetes management programme (physical activity and healthy eating) for a Chinese-origin population observed that participants more openly discussed and interacted when classes included only Mandarin or only Cantonese speakers, suggesting that, even with similar writing (traditional Chinese), speaking a different dialect may provide an additional barrier to interaction and participation during the intervention. Furthermore, some participants were reluctant to reveal their reading comprehension abilities
The qualitative interviews (see Chapter 7) contributed further contextual considerations relating to age/generation/acculturation and the mode of delivery that may affect the outcome of adapted communication for the target population:
-
(a) if it was younger smokers it was usually English, for older smokers I think for older Bengali smokers in particular [mmm] that um they would use um Bengali to converse with them
-
(P5, smoking, UK)
-
-
(b) They had resources, they had Chinese language operators and they promoted it like crazy [mm mhm] call, and it wasn’t eve, you know, this was really a helpful quit line . . . and they said nobody called the number and that was their experience that people just like the human touch, if they come in you know and they want to meet with someone
-
(P18, smoking, USA)
-
Interventions with pharmacotherapy, including NRTs, were identified from the UK guidelines and international systematic reviews (see Chapter 4)
The systematic review of adapted interventions (see Chapter 6) provided evidence that an adapted intervention should address health behaviour patterns found in the target population (Typology of Adaptation number 26)
Context and related outcomeRealist evaluation of the systematic review of adapted interventions provided additional contextual considerations (see Appendix 27):
-
Smoking cessation interventions using NRT and tailored materials have been specially designed to target smoking patterns observed among African American populations, for example light smoking and menthol cigarette smoking
-
A smoking cessation intervention delivered with a smoking cessation manual and brief counselling and NRT or placebo for African Americans observed that lower than expected quit rates may be influenced by environmental factors, daily life stressors and aggressive targeted advertising – all aspects that may not be measured but may influence successful quitting
The qualitative interviews (see Chapter 7) contributed further contextual considerations relating to some ethnic minority populations’ perception of NRTs:
-
(a) Well you have to pay $20 out of pocket and the health plan insurance will pay the rest, but $20 for a lot of people is still a lot of money [mm mhm]. Em so we thought, and also because they don’t know where to go get these drugs, so some of the intervention is you know we deal we, we took care, we took care of the co-payment, we took care of free drugs, we make sure they get it, we mail it to them, you know and so on and so on but the rate of use is very very low you know small [interesting]. And sometime people say well they, they believe that ah Western medicine is too strong for them you know so a lot of time we, we, it’s possible because of the nicotine metabolism that we talked about, so we started very low like normally half 7 mg rather than 14 [mm mhm] em you know but we had nothing to compare with. So even though we were surprised that the rate of use is so small after they agreed to use it, it may still be higher than control you know, so we gotta look at it that way, it just didn’t meet my expectation, I want everybody to be using it if we gave it to them
-
(P10, smoking, USA)
-
The UK guidelines and international systematic reviews (see Chapter 4) recommended the involvement of parents and carers as providers and the family/home as settings for interventions for physical activity and healthy eating
The systematic review of adapted interventions (see Chapter 6) suggested that adapted interventions should encourage or involve social support (Typology of Adaptation number 41) and that gender is an important consideration (Typology of Adaptation number 46)
The theoretical literature (see Chapter 6) situated women as both targets and agents of change and therefore argued that they played a central part in role modelling change for their family and the wider community
Context and related outcome – systematic reviewRealist evaluation of the systematic review of adapted interventions provided additional contextual considerations (see Appendix 27):
-
In one intervention for physical activity and healthy eating, African American girls were specifically taught communication skills to help advocate for healthy changes within the home; however, the family involvement was not very successful as parents were not supportive of their daughters in attending sessions or making changes in the home environment
-
Home visitations may be carried out for convenience but they were also important to engage the support of male members of the family and build family support in an intervention for physical activity and healthy eating with an African American population; in these circumstances it was important for the public health educator to be male. Similarly, a concern among South Asian-origin women in a healthy eating intervention was whether or not changes would be approved by spouses and whether or not spouses would prevent them from making changes
-
In a diabetes intervention with Bangladeshi-origin adults, peer discussion and support were valued, but gender differences were observed as women were more interested in the social support and the men were more focused on the information elements
The qualitative interviews (see Chapter 7) contributed further contextual considerations relating to social support and gender:
-
(a) very mixed group there were you know Muslim, Sikh, Hindu em across age ranges as well, but they were all women (mm mhm), em there were no men involved in this, and em basically found things like em you know barriers, predominantly, are always the family demands on the women’s time, lack of childcare or even if a crèche is available sometimes their kids don’t wanna go there, they still wanna stay with the parent. Em a lot of family disapproval about being active where they felt where it wasn’t safe or appropriate for this person to go and be active em which means maybe they were supposed to do it at home but there’s really no space in the home to do it em and like I said it came up a lot, the mixed sex environment is just not acceptable for Muslim women, it’s just not gonna happen for them
-
(P8, healthy eating, UK)
-
-
(b) Pakistani ladies or the Muslim women in the, in the area were feeling comfortable enough to go to the pool and exercise, but you had women of various ages, so these ladies were going there with their children, their teenage girls, they felt comfortable and there were other ladies who you know were from you know different ethnic backgrounds you know just felt more comfortable in being able to be in that environment, being able to go for a swim and exercise and, and, and felt comfortable doing that
-
(P12, physical activity and healthy eating, Australia)
-
Results
What adapted interventions work for whom and in what contexts?
Our realist synthesis drew on data from 15 UK guidelines and 111 international systematic reviews of relevant health promotion interventions for the population in general; our systematic review of adapted interventions, which comprised 12 theoretical papers, seven reviews and 107 empirical studies of adapted interventions; 26 in-depth qualitative interviews with experts in adapting health promotion interventions; and seven discussion groups with research and health service users to identify, test and explore how adapted interventions work or not in the form of CMO configurations. A full list of the identified CMO configurations is included in Appendix 27. The findings presented should be considered a ‘work in progress’ of CMO configurations hypothesising which adaptations are likely to be effective for whom and in what circumstances. As evidence emerges we will be better placed to further test and, if necessary, refine these CMO configurations. Exerts from Appendix 27 are included in Tables 21–25 and are discussed below to illustrate some of the configurations identified for each adaptation mechanism at different stages of the Programme Theory of Adapted Health Promotion Interventions (see Chapter 6). Some of the eight proposed stages have been combined to facilitate more coherent discussion than might otherwise have been achieved.
| Adaptation (mechanism) | Context + outcome (systematic review) | Context + outcome (qualitative interviews) |
|---|---|---|
| 2. Exploratory phase with target population (different group from intervention group) | Discussions with community for a community-based group healthy eating intervention for African American population revealed that there were many competing community-based research activities, which may limit interest in the present intervention315,316 | ‘So all that’s to say that and, and you know the kind of research that’s valued in the academy tends to be you know working with secondary data sets you know behind your desk or you know doing the more rigorous kinds of studies that you can do in a university context, so, so the type of research that engages these populations is not highly valued, because you have to develop these relationships, many of which have been, have been broken by years of em exploitation or if not active exploitation at least em kind of neglect’ (P13, physical activity, USA) |
| 3. Exploratory phase with community leaders | Community-based outreach intervention for smoking cessation and physical activity for an African American population noted the importance of speaking to community members about participation, and not just limiting discussion to community advisory groups, as low participation in the health activities was observed398 | |
| 20. Material developed specifically for target population (by project investigators, expert opinion, tools) |
Targeted material for smoking cessation intervention which was pilot tested with African Americans in New York may not be equally salient to an African American population in Georgia as intervention participants were observed to be more responsive to surface-level targeting (e.g. materials) and less so to deep-structure targeting341 Utilising specified models of behaviour change in the development of the intervention was found in some cases to improve effectiveness;293,324,335 however, some behavioural theories were suggested to be more appropriate than others, e.g. social cognitive theory was salient for the personal life experiences of African American women in terms of prevailing against formidable obstacles399 |
|
| 31. Address concerns with medical programmes, procedures and medication |
Exploratory phase indicated that randomisation to a no-treatment control for a physical activity and healthy eating intervention for an African American population was not acceptable to participants and was therefore not utilised in study design290,291,395,396 Other studies also have reiterated that randomisation was inappropriate in church settings,308,397 particularly when interest was low315,316 The background tailoring of control groups may remove the effect of the intervention in terms of assessing the effectiveness of adaptation; however, not tailoring for the control group was often unacceptable to the participants296 |
P: ‘Randomisation is, is a hard thing with community groups in general, they don’t understand randomisation. I mean one thing we found in our project that was that, this design where you don’t have a real control group but you give the comparison churches a different intervention that they’re equally happy with [right] actually worked really well, they were very, the community was much happier with that than, you are the control group and you are the intervention group. And em and yet some of the funders don’t like that cause they think there’s gonna be some you know contamination doing anything with the comparison churches so we have to do some education around that [laughter] I think’ I: ‘For the funders or for the community?’ P: ‘Yeah for the people that review the grants, I mean this whole idea that you can maintain a sort of peer control groups doesn’t go over very well, when you get out to the community nobody wants to be in the no intervention control group [mm mhm]. Em so those are some of the big challenges’ (P22, healthy eating, USA) |
| Adaptation (mechanism) | Context + outcome (systematic review) | Context + outcome (qualitative interviews) |
|---|---|---|
| 4. Ethnically matched intervention staff or facilitators |
Half of the African American smokers contacted were unwilling to speak with the recruiters as they were identified over the telephone as not being black (exercised caution in talking with outsiders)404 Although matching of recruitment staff has been suggested in a physical activity and healthy eating intervention for an African American population, the recruiter’s experience and sensitivity was perhaps more important, particularly when demonstrating flexibility for scheduling interviews365–367 |
|
| 16. Reflect target population’s preferred method of communication |
For a physical activity and healthy eating intervention, the majority of African American participants learned about the intervention through brochures, family/friends and mass e-mails in equal proportions. However, those who responded to e-mail and brochure were more likely to be eligible than those referred by family/friends365–367 Recruitment through personal contact (i.e. active strategy) for a smoking cessation intervention for African Americans tended to attract participants who said that they would participate but then did not or who participated but then dropped out. Reactive strategies, however, were more likely to recruit higher socioeconomic groups of African Americans342–345 |
|
| 33. Located in ethnically/culturally appropriate/familiar location |
Recruitment of African Americans to a smoking cessation intervention was more successful in churches (81%) and health-care settings (78%) than in housing developments (59%), as measured by the number of participants willing to provide a telephone number, which suggests that more interpersonal contacts are needed to persuade people to disclose their telephone numbers in low-income settings397,401 Community-based group Tai Chi exercise programme for a Chinese population was popular because of the recruitment site, which was in the local community and linked in with other activities popular with women such as playing mah-jong and buying vegetables402,403 |
‘Em the second study with the programme, the participants were supposed to be there for healthy eating education but we, after we got into the study we found that the nutritionists were basically depending on the pamphlet and sending them off with their food vouchers [right], so to spend a half an hour doing a DVD was actually a lot more time than they were expecting. So that you know hurt us in terms of recruitment because some, a lot of people didn’t wanna wait and do it’ (P22, healthy eating, USA) |
| Adaptation (mechanism) | Context + outcome (systematic review) | Context + outcome (qualitative interviews) |
|---|---|---|
| 4. Ethnically matched intervention staff or facilitators | Matching intervention staff for ethnicity was important but matching other characteristics, including having intervention staff with diabetes, was also raised as important for a Bangladeshi population with diabetes409 | |
| 5. Ethnically matched peer role models or peer education | Church-based group physical activity and healthy eating intervention for African Americans reported for the self-help arm that women wanted the sessions to be led by professional leaders rather than their peers; this was supported by the observed drop in attendance when sessions were taken over by trained lay leaders352 | |
| 20. Material developed specifically for target population (by project investigators, expert opinion, tools) |
Smoking cessation intervention for African Americans comparing a culturally sensitive guide with a standard guide found that participants with reported lower levels of acculturation preferred the culturally sensitive guide and displayed a greater readiness to quit; however, they had higher rates of 24-hour abstinence when they received the standard guide. It was hypothesised that mismatched content can encourage greater information processing351 Tailored newsletters used in a healthy eating intervention for African Americans had a stronger impact for individuals who were better matched in terms of their ethnic identity and the degree of Afrocentricness of the newsletter296 For a smoking cessation intervention delivered to an African American population it may be necessary to match the intervention not only to participants’ apparent racial/ethnic identity but also to their degree of membership to a particular racial/ethnic group341 |
|
|
A pictorial one-on-one diabetes education intervention to improve healthy eating for a South Asian population reported participant preference for one-to-one health education at clinics rather than in organised single-sex group sessions. Participants wanted to keep their diabetes status private and felt unable to announce their food choices in public407 Churchwide smoking cessation intervention for an African American population reported that some church members were embarrassed by their smoking status and did not want to be identified, whereas others were not interested in programmes delivered by peers300,301 Group- and individual-based diabetes management intervention for African Americans held in a rural setting revealed that group-based programmes may not have been appropriate as there were competing cultures of openness (facilitated by churches) and privacy (rural traditions)408 |
‘In the Chinese community especially em if the man was trying to give up smoking [yes] he wanted also the opportunity em to give up outside of the family environment so that when he went back in he had actually managed to succeed and was smoke free and it could be celebrated, but if he relapsed he didn’t wanna lose face’ (P7, smoking, New Zealand) ‘So their normal situation would have been those that actually drove em would have driven the sch, the, the children to school or they, or the, the children would have been picked up by eh another, another friend and taken to school. Now that actually evolved to the point where they were taking the children to school, very often walking the children to school or if they got into em being part of the, the trial and they would meet other women who were also part of the trial at the school and so instead of, where uh once they were in the trial they would’ve walked the children to or from school em and that would’ve been the only em activity they would have possibly had outside the house [mmm], it evolved, and this was the completely on the participants em doing, they would walk to the school, they would meet other women who were part of the trial, by coincidence, and instead of walking straight back home, some of them actually lived within 500 m of the school for example [mmm], em they would then as a group go for a walk around em the streets in the area. So they would have a circuit set up from what I can gather and the fact that they would walk past one of their houses and one of them would stop there, and the other two or three would continue on home and drop the others off so to speak as they went on their walk’ (P12, physical activity and healthy eating, Australia) |
|
| 29. Utilise appropriate incentives and timing of programme | A group-based diabetes management programme (physical activity and healthy eating) for a Chinese population experienced attrition as participants travelled for Chinese New Year and did not complete the programme, although they returned for follow-up evaluation346 | ‘So they, people will put it off until the first Ramadan to set a quit date, then those will be, then Ramadan is such a busy month, everybody’s focused on the spiritual aspect of fasting, and family life. And then you’ve got Eid and then people will say well we’ll do it after Ramadan, give me the patches’ (P6, smoking, UK) |
| 33. Located in ethnically/culturally appropriate/familiar location |
Churches were sites rather than partners in a physical activity intervention for African American women. As such, women did not receive health-related or targeted messages from church officials and therefore it may not have affected deep-level structures397 Community-based group weight loss intervention for African American women initially was held at community locations that were familiar and close; however, there was not enough space for exercise and childcare and lack of continuity of room availability forced relocation. The second cohort was relocated to a space on campus that offered parking. This was mainly conducted with a middle-class cohort405 |
‘Em the oh in the, we tended to, there was a mixture of settings [mmm]. Em the initial meetings quite often were actually held em at the university, em although that tended to, that was in the early days of the intervention, because the participants in terms of transport sometimes had issues with that, not all the women drove and I, I suspected they didn’t feel as comfortable in that setting. We had access to a em community centre and some of the meetings occurred there and particularly once the intervention was rolling, so the initial meetings might be at the university or community centre, I would suggest that the community centre was preferable, em the women from what I can gather appeared to be more comfortable there [mmm] eh but the subsequent meetings say over the 12 weeks of the intervention quite often would end up being at one of the participants em homes and the meeting would occur there’ (P12, physical activity and healthy eating, Australia) |
| 41. Encourage/involve social support |
Diabetes self-care telephone intervention for African American population reported that ‘eating healthfully’ was seen as participants giving up their food heritage, and family members may be quite negative towards participants if they deviate from traditional food406 Family members can be a barrier to weight gain prevention interventions for African American girls as their mothers encouraged weight gain395,396 Social support from within the intervention group was valuable for African American participants in a physical activity and healthy eating intervention, but other social influences outside the intervention, such as family pressures and resistance to change, were observed to have a negative impact365–367 Encouraging family participation was built into some interventions but in a study with African Americans for physical activity and healthy eating only female adults participated despite male members of the family being encouraged to participate319 |
‘And what we found out was that … it, it mattered how much the partner participated, regardless of whether we had assigned participation so, so being together in the groups didn’t make any difference. Which was I mean a clear finding because only one group was together in the groups and being the people who were together in the groups they didn’t lose any more, any more em they didn’t … lose more weight than the people who didn’t have their partner in the groups [mm mhm] and they didn’t maintain any better. But, the people whose partners attended more of those personal sessions … lost more weight, you know so if, if, if your partner was interested enough to come in with you to those sessions your weight loss was greater’ (P11, physical activity and healthy eating, USA) |
| 45. Address discrimination and mistrust | ‘Interview showed that it was particularly important to the women that they had a culturally “safe” place to exercise, not just for themselves but also for the integrity of their whole community’ (p. 93). Furthermore, in this physical activity intervention delivered for South Asian women, the notion of ‘safe’ space operated under a different logic such that walking and playing sports after dark in an empty field behind a school was perceived to be safe whereas walking on the sidewalk during the daytime was felt to attract derogatory comments as they would be more visible283 |
| Adaptation (mechanism) | Context + outcome (systematic review) | Context + outcome (qualitative interviews) |
|---|---|---|
| 33. Located in ethnically/culturally appropriate/familiar location |
Community-based group Tai Chi exercise programme for Chinese population reported high adherence as classes were held at a convenient local community centre where other Cantonese-speaking seniors congregate for other activities, such as eating lunch and grocery shopping402,403 Group physical activity and healthy eating intervention delivered to participants during their regular community group meeting405 |
|
| 39. Address physical/financial (structural) barriers to participation |
Monthly self-addressed stamped postcards and a toll-free telephone number to update contact details may be good retention strategies for a parent-led healthy eating intervention for African Americans303–305 Low implementation rates of booster calls to African American participants in a smoking cessation intervention (31%). Telephone-assisted strategies may not be feasible as they depend on the ability to obtain telephone numbers. The intervention was not effective for smoking cessation400,401 Genetic biomarker feedback smoking cessation intervention with telephone counselling and NRT for African Americans lost 21% of participants, with the primary reason being that participants no longer had telephone access374 Community-based after-school intervention programmes can reduce barriers to transportation for a physical activity and healthy eating intervention for African American girls410 In a related study of African American girls, when transportation was provided from school to the community centre, 70% attended on average at least 2 days per week. When transportation was not provided, only 33% attended on average at least 2 days per week329,330 |
‘If they had to travel we have given them a little bit of taxi vouchers or we have brought them to the where they have to go [mmm] and we have provided them little bit of em [family support?] sort of thing, little bit of em childcare and all these things where woman is free and they felt responsible that, ok, we are eh sharing all the responsibility with them, we are helping them and they want, they really do get help as well, and really do participate’ (P9, physical activity and healthy eating, Australia) |
| Adaptation (mechanism) | Context + outcome (systematic review) | Context + outcome (qualitative interviews) |
|---|---|---|
| 23. Intervention goals and outcomes for participants are culturally appropriate |
A community-based group education healthy eating intervention for African Americans reported that there were discrepancies between intervention goals and participant goals, for example one incentive for participants was to receive documentation of achieving healthy eating-related education and competencies for potential jobs in the food service industry, as this was a largely unemployed cohort315,316 Group-based weight loss intervention for African Americans observed a difference between participants and investigators in interpreting intervention success. Participants were happy with their 3% weight loss whereas investigators were aiming for 7% (which is considered to be clinically significant by the National Heart, Lung, and Blood Institute)412 |
|
| 38. Address emotional barriers and stressors |
A smoking cessation intervention delivered with a guide and brief counselling plus NRT or placebo for African Americans observed that lower than expected quit rates may be influenced by environmental factors, daily life stressors and aggressive targeted advertising – all aspects that may not be measured but may influence successful quitting355,356 In a group-based behavioural weight loss programme for African Americans, the addition of motivational interviewing did not increase attendance, change dietary intake or physical activity levels or result in weight loss compared with health education only. Motivational interviewing may not enhance the effectiveness of an already culturally adapted intervention or motivate behaviour change among participants who face socioenvironmental barriers or life stressors, as motivational interviewing assissted only with the discussion of these barriers but did not help to reduce them317 |
|
| 23. Intervention goals and outcomes are culturally appropriate |
In a group-based healthy eating education intervention for African Americans, weight loss was unlikely to be for aesthetic reasons; health improvements were found to hold more significance as an outcome than weight change323 An effective intervention outcome for the community was strong community partnership and environmental/community changes such as the development of new and better recreational facilities and opportunities and not the outcomes that the study had specified413 |
‘she went back in November, like 3 months later and measured them to see the sustainability of the weight loss and if any of them could keep the weight off [mm mhm] and there was still a significant loss of weight, you know they didn’t lose anything in addition, they sustained their weight losses, so their weight loss was still significant compared to base line, but it wasn’t lower than it had been, so at least they maintained, they sustained over those kind of 3 months, over the feast fast period’ (P8, healthy eating, UK) |
Conception/planning
Adaptations such as exploratory phases with target populations and community leaders indicated that intervention study designs involving cluster randomisation are often challenging for community-based interventions in ethnic minority populations (Table 21). 290,291,395,396 In church settings, in particular, participants have reiterated the unacceptability of randomisation to a comparison condition with seemingly low benefits. 308,315,316,397 A comparison condition could be perceived as divisive within communities where the maintenance of a collective presence and voice is felt to be important.
When randomisation was perceived to be an absolute necessity by the researchers, a comparison condition with near-equivalent benefits was often negotiated (interview, P22). Similarly, not undertaking any adaptation of the control intervention was sometimes considered unacceptable and so, at times, the control group would also receive some degree of adaptation, thereby diluting comaprisons. 296 The opportunity to make meaningful inference of the impact of the adapted intervention compared with the standard approach was therefore limited. These study conditions potentially increased the study sample size required to demonstrate significant differences, thereby compounding the recruitment problems for researchers working with ethnic minority populations.
An exploratory phase with community leaders to increase effectiveness was an often-cited adaptation; however, it was also suggested that speaking to community members was equally important as they are ultimately the participants in interventions and were more often than not only loosely affiliated with the ‘leaders’. 398 These community discussions also revealed that some communities have been inundated with research activities, such that interventions (on various topics) may be in competition with other study invitations. 315,316 This current concentration of interest could reflect years of being exploited or neglected or both (interview, P13).
Furthermore, it was noted that focus groups or pilot testing undertaken with an ethnic minority population in one part of a country might generate materials inappropriate to a population in another part of a country341 who were perceived by the researchers to share the same ethnic background. Therefore, although adaptations for conventional dimensions of ethnicity such as language or religion may be applicable, more contextual elements, such as geographic location, may diverge and further influence preferences. 341
In the development of adapted interventions, the use of specific behavioural models was found to increase intervention effectiveness. 293,324,335 Some models were particularly salient; for example, social cognitive theory was appropriate for African American women in terms of their life experiences and their need to deal with life stressors and obstacles. 399
Promotion and engagement/recruitment
Interventions were promoted through different channels, and many adaptations were used to raise awareness and engage the population (Table 22). Associations between the approach to promotion (methods used) and eligibility were observed, and, at later stages of the programme theory, between promotion channels and recruitment and retention rates. For example, African Americans who learned about a physical activity and healthy eating intervention through family and friends were less likely to be eligible than those who responded to e-mail or promotional material. 365–367 Similarly, recruitment through personal contact for a smoking cessation intervention for an African American population attracted people who were interested and said they would participate but who then tended to not show up or to drop out. 342–345 On the other hand, reactive strategies were more successful at recruitment and retention; however, those recruited through reactive strategies tended to be from higher socioeconomic backgrounds. 342–345
Recruitment may also depend on the recruitment site chosen for different ethnic groups; for example, churches (81%) and health-care settings (78%) were found to be more successful than housing developments (59%) in a smoking cessation intervention for an African American population, as measured by the number of people who provided their telephone number. 400,401 The authors suggested that, in low-income housing developments, more interpersonal contacts are needed to boost recruitment. 400,401 A community-based group Tai Chi exercise programme for a Chinese population was popular with the target population because of the recruitment site, which was in the local community and linked in with other activities such as playing mah-jong and buying vegetables. 402,403 However, even when the recruitment took place in an appropriate location, for example a church, if the recruitment process was perceived to be too time-consuming this could still hinder uptake (interview, P22).
Ethnically matching facilitators was seen to be important in a smoking cessation intervention in which half of the African American smokers contacted were unwilling to speak with the recruiters over the telephone as the recruiters were perceived not to be black. 404 The authors suggested that this population was particularly cautious and unwilling to share information with outsiders. On the other hand, a recruiter’s experience and sensitivity may be equally as important as matching on ethnicity. 365–367 Successful recruitment discussed here appears to coincide less with participants’ preferred communication formats and more with the importance of sites used for recruitment.
Implementation/delivery
We found many examples of how context moderated the effectiveness of adaptations at the implementation stage (Table 23). Appropriate timing and location of the intervention were important adaptations to consider; for example, learning to avoid holding interventions during significant holidays as this was when people were travelling346 or participating in religious observance and were therefore unable to participate fully in an intervention (interview, P6).
Furthermore, holding an intervention in an appropriate location, such as a community centre or church, was generally viewed as a positive adaptation (interview, P12). Although these sites may have positive effects on intervention reach and sustainability, they may not be effectively used if acting only as sites (especially churches). 397 Moreover, although community centres may be convenient, they may disrupt the continuity of the programme if room and space availability present potential barriers. 405 Sometimes the location for an intervention may be preferred because it is felt to be more ‘culturally safe’, for example a group of South Asian-origin women ‘preferred’ to exercise in a poorly lit school field in the evenings rather than walking along the sidewalk during the day. However, this ‘preference’ was in response to their perception that they would attract derogatory comments if they were visible during the day. 283
Intervention adaptations that encourage social support may be faced with support that is counter to the interventionist’s desired behaviour change for the participant. Social support from the family, for example, was often cited as an important consideration in delivering health promotion interventions for ethnic minority populations (interview, P11); however, families were sometimes not supportive of behaviour change365–367 that contradicted social norms, such as decreasing body size,395,396 or traditions, such as abstaining from certain foods. 406 Furthermore, active family participation as part of an intervention may not have the intended effects, as was the case in a study for increasing physical activity and healthy eating with an African American population in which only female adults were observed to participate despite male members of the family being encouraged to engage. 319
Delivering interventions in culturally appropriate or preferred formats, such as in group formats, was encouraged and found to be successful, for example when utilised in a walking programme for Pakistani women (interview, P12). Group-based interventions, however, may not be appropriate for every health issue under study for ethnic minority populations. In some cases encouraging group-based programmes may be inappropriate, for example it was observed that men in the Chinese community ‘wanted also the opportunity em to give up outside of the family environment so that when he went back in he had actually managed to succeed and was smoke free and it could be celebrated, but if he relapsed he didn’t wanna lose face’ (interview, P7). Similarly, social support in the form of group sessions and discussions was not always desirable, for example with participants who wished to keep private their diabetes status, which jarred against the openness of some of the intervention formats. Such tensions arose in the context of a diabetes education intervention for a South Asian population,407 a diabetes management intervention for African Americans408 and a church-based smoking cessation intervention for African Americans. 300,301
Another important mechanism was targeted intervention materials, which were found to be more effective when they matched not only with participants’ identities, but also with their degree of affiliation with their ethnic identities. 296,341 Conversely, the opposite effect was also observed among participants, with reportedly lower levels of acculturation (more likely to have stronger ethnic affiliation) having better short-term quit rates with a standard guide than with an adapted guide. 351 Matching of intervention staff ethnicity was perceived to be important; however, matching for other characteristics such as having diabetes409 or gender and age was equally salient (interview, P23). In terms of using ethnically matched peer facilitators, it appeared for some that professional leaders were preferred (interview, P22) and an associated drop in attendance was observed when sessions were taken over by trained lay leaders. 352
Retention
Addressing structural barriers, such as access to transport and financial constraints, was identified as an important adaptation (Table 24). Telephone follow-up strategies appeared to be effective, for example a toll-free telephone number was successfully used in a church-based physical activity and healthy eating intervention for an African American population. 303–305 On the other hand, when telephone numbers were difficult to obtain, low implementation of booster calls (31%) to African American participants in a smoking cessation intervention was observed. 400,401 In another smoking cessation intervention for African Americans involving genetic biomarker feedback plus telephone and nicotine replacement therapy (NRT), 21% of participants were lost at follow-up and the primary reason cited was that participants no longer had telephone access. 374 Therefore, telephone-assisted strategies appeared to be successful for follow-up when there was consistent access to a telephone, otherwise they were observed to hinder retention.
Provision of transportation was another adaptation used to address physical and financial barriers to participation. This was observed to be salient for younger people who have limited access to different modes of transport to reach intervention sites. 410 A difference in retention associated with transportation provision was observed in a related study for African American girls. When transportation was provided after school, 70% attended an average of at least 2 days per week. 329,330 In another area where transportation was not provided, only 33% attended an average of at least 2 days per week. 329,330 Providing vouchers for taxis or childcare was also viewed to alleviate some of the barriers to participation (interview, P9). Holding the intervention at a convenient local community centre, for example where participants would congregate anyway for other activities such as eating and grocery shopping,402,403 or delivering the intervention during regular community group meetings411 were proposed as additional ways of addressing transportation issues.
From the user conferences we were alerted to the possible mediating or moderating effects of income in relation to interventions with ethnic minority populations, as it would appear that structural barriers such as inconsistent telephone ownership and limited access to transportation are likely related more to income than to ethnicity per se.
Evaluation and outcomes
Adaptation mechanisms at this stage suggest that participants’ life circumstances and goals should be taken into consideration when undertaking programme evaluation (Table 25). Considerations such as participants’ positive view of smoking in light of other life stressors, and participants’ critique of intervention strategies, such as motivational interviewing, that only discussed, rather than reduced or removed, barriers. In a group-based behavioural weight loss programme for an African American population, the addition of motivational interviewing did not increase attendance, change dietary intake or physical activity levels or result in weight loss compared with receiving only health education. Motivational interviewing may not enhance the effectiveness of an already culturally adapted intervention or provide additional motivation for behaviour change among participants who face overwhelming socioenvironmental barriers or life stressors, as motivational interviewing assisted only with the articulation of these barriers, but did not appear to help participants to overcome them. 317
Furthermore, participants’ reasons for engagement in interventions can differ from those established by the interventionists, and these outcomes need to be acknowledged. For example, African American women enrolled in a healthy eating intervention to earn qualifications to work in the food industry rather than to improve their healthy eating. 315,316 Goals for weight loss and body size, particularly among African American women and girls, for example, differed from the interventionists’ goals and perceptions of success. Women in one study were satisfied with their 3% weight loss, even though this was short of the 7% weight loss goal set by the investigators (and considered to be clinically significant by the National Heart, Lung, and Blood Institute in the USA). 412 Similarly, weight maintenance over a period of feasting was perceived to be an acceptable outcome for a group of Muslim women engaged in a healthy eating intervention (interview, P8).
Moreover, African American women were less likely to engage in weight loss for aesthetic reasons; health improvements and psychological benefits were perceived as more meaningful outcomes. 323 On a community level, a successful outcome may be increased community cohesion or improved community facilities as opposed to behaviour changes per se. 413
Dissemination
Few adaptation mechanisms were proposed for the dissemination stage; however, user engagement discussions suggested that greater linkages were required between people working in ethnic minority health to better facilitate the exchange of research findings. The absence of insights at this stage echoed the concerns raised at the event – although there might be substantial work accumulating internationally, there is little integration and sharing of this work. This concern was best articulated by one of our interview participants:
I don’t have any problem if em we are identified in your research because the whole thing as I see it is about sharing and caring so it was quite interesting when I went down to my boss and I said oh look I really don’t think I’ll sign off on this part where it says here [mm mhm], em the your point number 6 where it says I understand you won’t put anything in your report that could be used to identify me and, and [name] says oh well scrub that out and oh no identify away . . . Why keep reinventing em what’s been done out there cause it, I mean we piloted this and I mean it’s a bit of blood, sweat and tears when you’re piloting something and then you want to put those learnings into practice and you know it is a lot of work and if you’ve got something that could be adapted for use within your community then why not.
(P7, smoking, New Zealand).
Contextualised ‘real-world’ examples of how adapted interventions work
We developed a few illustrative examples to exemplify the main issues that have emerged from the above analysis, and to offer contextual richness to the main focus of this report.
Discussion of group-based interventions
The first example (Box 11) illustrates the competing priorities and desires at work when participants consider involvement in group-based interventions. This particular example suggests that group-based activities may be more appropriate for physical activity interventions than for healthy eating interventions, particularly in relation to diabetes education, and smoking cessation. Privacy appears to be the main concern raised in the context of group-based healthy eating interventions when providing diabetes education and smoking cessation activities. Group-based physical activity interventions were supported by both the evidence gathered from the systematic review and the qualitative interviews. A reanalysis of the empirical studies revealed that the health topic being addressed and issues of privacy may moderate the effectiveness of interventions.
Discussion of communication strategies
The second example (Box 12) illustrates that, although adapting the various communication strategies for language is an important consideration when delivering health promotion interventions for ethnic minority populations, there are often nuanced considerations of dialect, age and preference that can alter the effectiveness of adapted communication strategies. It appears that further stratification, or, taking a term from social marketing,414 ‘audience segmentation’, may be required to optimise the intervention effect. Although the evidence from the systematic review suggested that adapted communication strategies are crucial, these insights proposed that interventions should work even better when the targeted group share a greater number of characteristics and preferences.
Discussion of behaviour patterns and pharmacotherapy
The third example (Box 13) illustrates that, although NRT has been recommended by all UK guidelines and international systematic reviews, findings from the systematic review suggest that interventions should still accommodate for different health behaviour patterns. For example, African Americans are likely to engage in light smoking behaviour and smoke mentholated cigarettes. Interventions targeted to these smoking behaviour patterns in African Americans have been trialled. Despite the overall success rate of NRTs, the lower than expected quit rates observed in ethnic minority populations may be influenced by environmental factors, stressors and targeted advertising – aspects that can decrease quit rates. Furthermore, from the qualitative interviews, NRTs may be perceived to be ‘too strong’, and this potentially can act as a barrier to NRT uptake rather than, for example, prohibitive pricing.
Discussion of social support
The fourth example (Box 14) illustrates that, although family-/home-based interventions are recommended by guidelines and systematic reviews, the systematic review findings showed the importance of considering the different ways that social support and gender can intersect and interact. The insights generated suggested that home environments may not always be supportive, particularly for women, as they are faced with competing priorities and face barriers to change. Women may find better support systems outside of a home setting to support, for example, physical activity. Furthermore, there appeared to be gender-based preferences according to the type of intervention strategy: women expressed more interest in social support than men, who were more interested in obtaining information. Interestingly, these contextual considerations are set against a background discourse of women as central targets and agents in health promotion intervention. Particularly for ethnic minority women, who were seen as the change agents and role models for their family, it would appear that, for some, securing support in the family was the foremost barrier.
Interventions that are ready for implementation and interventions that need more research
We drew on the six categories of ‘strategies and activities’ derived from the Tannahill definition of health promotion interventions111 (see Chapter 4) to compare the findings from the review of UK guidelines and international systematic reviews with the findings from our systematic review (see Chapter 6).
Adapted interventions that are ready for implementation
Given that our review of guidelines and systematic reviews for the general population (see Chapter 4) found relatively little robust evidence in support of interventions effecting clinically important and sustained behavioural changes in relation to exercise and diet in the general population, there is understandably at present little clear evidence in relation to ethnic minority populations (see Chapter 5). Our systematic review of adapted interventions reported in Chapter 6 similarly found no clear evidence of how best to impact on these lifestyle factors in relation to our target populations. Therefore, based on this work, there is no clear evidence of any intervention for promoting exercise or healthy eating that is ready for widespread implementation in UK ethnic minority populations.
Although the overall evidence base is more encouraging for interventions aiming to promote smoking cessation in the general population (see Chapter 4) – particularly in relation to individual support and drug-based interventions – there is still uncertainty about how best to adapt interventions in a clinically effective and cost-effective way in relation to ethnic minority populations (see Chapters 5 and 6) and so here too, we contend, there is at present no adapted intervention approach that is ready for rolling out throughout the NHS.
Adapted interventions for research
Although there are no adapted interventions that are ready for implementation, there are a number of important and promising areas in need of further research; these are considered below. Interventions were considered candidates for research if they had evidence of effect in the general population but had not been identified as having been trialled in an adapted form for our populations of interest; in addition, interventions that we did identify as adapted in our review and which had demonstrated evidence of effect from ‘strong’ quality studies were considered suitable for pursuing with further study.
Smoking
Workplace policies and workplace interventions were both conspicuously absent from the adapted intervention literature. Some reasons for this were provided by the findings from the qualitative interviews in which researchers suggested that, although they actively tried to engage ‘typical’ workplaces for immigrant populations, for example restaurants, in their community-based activities, they were often met with resistance. The reasons for this resistance were not necessarily rooted in a disinterest in smoking cessation initiatives; rather, many of the owners and workers did not have legal status in the country and effectively did not want to draw unnecessary attention to themselves. On the other hand, workplaces with ethnic minority owners with longer histories in the country did express an interest in workplace smoke-free and/or cessation activities. Overall, there may be less scope to adapt workplace policies or interventions specifically for ethnic minority populations unless there are workplaces where the majority of workers are from ethnic minority groups, and this, as it has been suggested, may be challenging.
The other ‘strategies and activities’ that were not identified in the adapted studies were the use of the broader range of providers such as dentists, psychologists, pharmacists and midwives, as recommended for the general population (see Chapter 4). This finding may in part be because of the increased use of community-based lay workers or peer educators as the providers of health promotion interventions for ethnic minority populations. There is likely high scope for adaptation and collaboration with this broader range of providers, particularly because, as suggested in the realist analysis (implementation/delivery section), there may be a preference for health professional-delivered services in addition to or instead of peer- or lay-delivered interventions.
There were also no studies that trialled mobile telephone texts, although mobile telephone calls had been used, along with pagers, in adapted interventions. Finally, we did not find any studies that had carried out adapted interventions with antidepressants, such as nortriptyline, or varenicline as an aid to smoking cessation. These pharmacotherapies, however, have low scope for adaptation in terms of the product itself, but high scope for adaptation in terms of implementation as they are individually oriented and delivery can be readily modified. Parallel examples of implementation can be found in adapted NRT studies.
There were only two adapted smoking cessation interventions that were of high quality and had effective outcomes (excluding outcomes related to knowledge, beliefs and attitudes, and outcomes that were not sustained). 342–345 One of these interventions utilised bupropion as an adjunct to a culturally adapted intervention involving motivational counselling and the Pathways to Freedom culturally sensitive smoking cessation guide; the other was a provider prompting intervention (Ask–Advise–Assist–Arrange follow-up model) with tailored print materials/birthday cards providing stage-based behavioural messages. The latter intervention also examined the added effect of telephone counselling and, interestingly, the telephone counselling element had no significant added effect. These were both interventions with African American populations and would need to be further adapted for other ethnic populations to be trialled in the UK context.
Physical activity
Workplace/organisational policies were absent among adapted interventions for increasing physical activity for ethnic minority populations. However, in the excluded literature there were workplace policy ‘strategies and activities’ implemented for multiethnic workforces (these were excluded as they did not report the ethnic composition of the workforce, or the majority ethnic group was not of African, Chinese or South Asian origin). Workplace interventions415 were found to increase physical activity as well as productivity and therefore implementation could be acceptable for employees, if feasible for employers, as a strategy to increase physical activity for a larger population.
Although no adapted interventions identified in our systematic review (see Chapter 6) implemented environmental strategies to increase physical activity, there was evidence of walking/cycling route use by ethnic minorities reported from the interviews (P19, physical activity, Norway), as well as short bouts of ‘flash mob’ group activities in public places initiated through social networking devices (P13, physical activity, USA). This would be one way to combine the mobile texts and telephone calls discussed above with environmental strategies, facilitated by a potential preference for physical activities in social settings. Furthermore, walking, in general, appeared to be an activity supported by other researchers conducting physical activity interventions, particularly when informal walking circuits were created within participants’ own neighbourhoods (P12, physical activity and healthy eating, Australia). On the other hand, one study from the systematic review suggested that walking on the sidewalk was perceived to be unsafe and was less likely to be adopted. 283 These findings provide preliminary support for environmental interventions that create walking routes, personalised travel plans and short bouts of activity, noting the cultural and contextual considerations in each circumstance. Although there may be low scope for adapting the built environment, there may be opportunities for modifying how that built environment is used and the social activities that can take place within it.
Healthy eating
Overall there was a good degree of coherence between ‘strategies and activities’ recommended for the general population and those that have also been adapted for ethnic minority populations. Only two ‘strategies and activities’ had not been tested in an adapted form: food subsidisation and workplace point of purchase. Both activities have low scope for adaptation unless there are ethnic-specific or -exclusive workplaces willing to take up such strategies, and there may be difficulties in engaging with these sites, as discussed above for smoking cessation (see Smoking).
The high-level evidence syntheses contributed little information on appropriate providers for the delivery of healthy eating interventions. It is likely that many different providers have been trialled, but evidence of effect may not have reached the stage of inclusion in guidelines. In the case of healthy eating interventions, the adapted literature may shed light on potentially effective providers, such as peer educators, lay advisors/educators, dieticians and family physicians.
Furthermore, the high-level evidence syntheses were relatively uninformative on what techniques may be effective, and this deficit could potentially be informed by findings from the adapted interventions literature. For example, techniques that drew on spiritual themes or were faith based (and not necessarily held at a religious site) and cooking clubs constituted interactive activities that were acceptable and feasible for ethnic minority populations and, hence, may also prove to be promising for the general population. These potentially interactive techniques require further research and testing.
Thirty-one adapted studies were identified for physical activity and healthy eating that had a ‘strong’ quality rating (see Appendix 19). Out of these studies we examined only those that reported effective outcomes, excluding outcomes related to knowledge, beliefs and attitudes; outcomes that were not sustained; outcomes that were specific to a disease state, for example diabetes care; and, finally, outcomes in which the adapted intervention was not significantly better than the control (see Appendix 18). The common ‘strategies and activities’ across these interventions were setting based, group based or with social support, and used adapted materials. Common settings were churches, an after-school programme and a Parents as Teachers organisation. These provided trusted settings with established social networks. 320 It should be noted that the high number of church-based interventions is partly a product of the literature we identified, which was dominated by interventions for African American populations.
Social support was often a component of these settings or was introduced through a group-based design, parent-and-child interventions and/or family involvement. Adapted materials included newsletters, videos, recipe books and exercise tapes. In five interventions materials were also tailored to measure individual baseline data, such as knowledge, motivators and stages of change. These studies used behavioural techniques and motivational interviewing to tailor interventions; there was mixed evidence of whether this enhanced the effect of the intervention.
The adaptations most commonly used in these studies (numbered according to the Typology of Adaptation; see Chapter 6) were: conducting an exploratory phase with the target population (number 2); use of ethnically matched peer role models or peer education (number 5); use of material that depict appropriate graphics and scenarios (number 18); intervention content that targets population’s social and cultural values (number 22); and addressing dietary issues unique to their context (number 27).
Although these interventions, much like the smoking interventions, were conducted with African American populations, they again provided us with insights on strategies, activities and adaptations that can be taken forward for further evaluation.
Prioritisation of research
All three health promotion topic areas need further investigation through UK studies:
-
Smoking cessation represents the ‘lowest hanging fruit’ as we have effective drugs that may not, at present, be used to their best effect – adapted interventions therefore need to increase awareness about these, challenge erroneous beliefs and increase access to and use of these products, potentially utilising a greater range of providers alongside peer or lay providers.
-
Diet and exercise present bigger challenges both in the minority populations and more generally because appreciable changes are needed that are then sustained over time; this is difficult for most to achieve, let alone resource-constrained populations. There is, in particular, a need for intensive personalised or group-based support (depending on the health status of the targeted population) and, in the context of exercise, group-based initiatives along with setting-based and structural/environmental solutions.
-
Researchers and reviewers need to learn lessons from previous failings, particularly poorly theorised interventions, lack of clearly thought through or explicitly reported approaches to adaptation, the failure to justify assumptions (e.g. willingness of churches to be randomised) and the absence of high-quality studies, preferably of standard compared with appropriately adapted interventions. Taking these lessons forward will provide a steer for research examining the effectiveness of adapted interventions.
-
The necessary and sufficient conditions under which adaptations can operate optimally, and at low cost, remain to be determined. Therefore, cost-effectiveness studies need to be conducted and cost-effectiveness established for adapted interventions.
RESET (relevance, evidence base, stages of intervention, ethnicity and trends) decision-making tool
In our final synthesis we distilled the principal findings from our user engagement, the review of UK guidelines and international reviews, the systematic review of empirical studies and the qualitative interviews together with the insights from the realist synthesis to develop a tool to assist researchers and health promoters in the development of adapted interventions. This decision-making tool, called RESET (i.e. relevance, evidence base, stages of intervention, ethnicity and trends), is described in more detail in Box 15.
The RESET decision-making tool is aimed at researchers and health promoters who have already identified a health topic and target population, and is designed to assist with the health promotion intervention/programme adaptation process
Relevance: Is this health promotion topic relevant to the target population?
-
Is the topic of sufficient concern that action is required?
-
Are there competing priorities for this population that would lessen their engagement with this intervention?
Evidence base: What is the best intervention to address this health topic within this population?
-
Is there evidence of intervention effect within the general population?
-
Is there evidence of intervention effect within the target population?
Stage of intervention: What stage(s) of the intervention programme theory should be adapted?
-
What stages need adaptation for this population? (Adaptation may not be needed at every stage, e.g. English is appropriate as the language of intervention delivery for African Americans)
-
What stages can be adapted in this intervention? (Little adaptation can be undertaken with pharmacotherapy, e.g. NRT)
-
What stages are able to be adapted? (There may not be resources available to undertake all of the desired adaptations and therefore adaptations require prioritisation)
Ethnicity: What elements of ethnicity are most important to consider for this population?
-
What are the conventional elements that are important to consider in adaptation? (e.g. religion, language, culture, physical features, ancestry, age, gender and SES)
-
What are the contextual elements that are important to consider in adaptation? (social environments, physical space, past exposures to health research and services, and diverse life experiences including stress)
-
What degree of heterogeneity is present within the target population and is it possible to assess heterogeneity (i.e. measure ethnic identity, cultural affiliation or acculturation) and adapt the intervention appropriately at a subgroup level?
Trends: What are the shifting trends within this population?
-
Are there shifting patterns and trends in behaviours within this population?
-
Can we monitor the patterns and trends in population characteristics, preferences and contexts and revise the adaptation(s) to maintain relevancy over time?
The RESET tool can be used alone but is recommended for use along with other key outputs from this research, including the Typology of Adaptation (see Table 13) and the Programme Theory of Adapted Health Promotion Interventions (see Figure 9). The question posed by ‘Relevance’ (Is this health promotion topic relevant to the target population?) is derived from an engagement with the qualitative interviews in their entirety and the significant overall message of ‘knowing your population’. Answering the question posed by ‘Evidence base’ (What is the best intervention to address this health topic within this population?), with reference to the evidence for activities and strategies ready for implementation and those needing more research, can help adjudicate between the kinds of potential activities and strategies (for smoking cessation see Table 4, physical activity see Table 5 and healthy eating see Table 6). To answer the question posted by ‘Stages of intervention’ [What stage(s) of the intervention programme theory should be adapted?], the Programme Theory of Adapted Health Promotion Interventions (see Figure 9) should be used alongside the Typology of Adaptation (see Table 13) to consider which stage(s) of an intervention to modify. To answer the question posed by ‘Ethnicity’ (What elements of ethnicity are most important to consider for this population?), a reading of the qualitative interviews (see Chapter 7, particularly Global theme 1: constructing ethnicity) on ‘constructing ethnicity’ and the discussion on conventional and contextual ethnicity can be helpful in thinking about the dimensions of ethnicity important to the target population in the context of the potential intervention; furthermore, this realist chapter provides additional examples of how context may moderate the interventions, illustrated by CMO configurations (see Tables 21–25 and Boxes 11–14). Finally, ‘Trends’ (What are the shifting trends within this population?), like ‘Relevance’, were derived from an engagement with the qualitative interviews.
This is a preliminary tool built from the different research components undertaken in this volume of work and in due course we hope to test it and if necessary refine it further before making it available online.
Discussion
Across this body of evidence we found that multiple adaptations were used at all stages of the intervention process in an attempt to increase the acceptability and effectiveness of interventions; however, the effectiveness of these adaptations was highly context dependent. Table 22 summarises the CMO configurations that we identified which link the adaptations to context, which either enhances or diminishes their effectiveness. The table represents a working document to aid intervention development and context consideration. The utility of this document (a fuller version is provided in Appendix 27) will increase as further research is conducted and further configurations are tested. We have answered the questions of what adapted interventions work for whom and in what contexts, but perhaps not the overarching question of why adaptations work. Finding an answer to this question would help underpin and bring together the contextual findings generated; an explanatory theory as searched for in realist reviews. 389,390 A realist synthesis is both strengthened and complicated by the sheer volume of data and number of CMO configurations possible. Our synthesis suggested that the Programme Theory of Adapted Health Promotion Interventions developed in Chapter 6, in addition to providing a way of categorising adaptations, can act as a preliminary explanatory theory for how adaptation works (i.e. how adaptations work at each stage of the intervention process). Another principle, ubiquitous to the CMO configurations and operating at every stage in the intervention process, was ‘knowing the population’. We recommend that researchers know the population they are working with well enough to be able to select which adaptations to apply in developing the intervention. This principle is further encompassed in the second ‘E’ and ‘T’ of the RESET decision tool.
Strengths and limitations
The strengths of our approach were the ability to integrate and synthesise data from disparate bodies of literature, derived using different methods. Using CMO configurations to drive understanding we were able to uncover the contextual influences on adaptation mechanisms, which were perceived to either enhance or diminish the effectiveness of interventions. Although this method for synthesis was useful, we were limited by the reporting of the interventions themselves, and we noted a greater number of negative cases (how contexts negatively affected intended outcomes) than positive cases. We attributed the increased reporting of negative cases as a result of the tendency for authors to provide more explanations for why interventions did not work than for why they did work.
Furthermore, as our line of questioning sought clarification of underlying explanations for why an adaptation worked or not, we were able to better tackle the complexity inherent in an evaluation examining three different health topics within three ethnic populations. Our four illustrative examples (see Boxes 11–14) show how consideration at every level, from guideline recommendations to contextual issues, shapes the trajectory of adapted interventions. It should be noted that these examples are based on select evidence pulled together to present a coherent story of how and why interventions might work or not. They are by no means definitive pathways, as a realist orientation alerts to many possible pathways. We hope that the examples, along with consideration of CMO configurations along each stage of the intervention pathway, have demonstrated the explanatory power of a realist framework applied to complex data. Lastly, Appendix 27 is intended as a work in progress that will grow as further adapted interventions are conducted, evaluated and tested in a variety of contexts with different populations. We further hope it can act as a resource for researchers and health promoters involved in adapting health promotion interventions.
Realist evaluation explicitly rejects a hierarchy of evidence and this rationale is well suited to the body of evidence we identified, which is, for example, a mix of RCTs and quasi-experimental, pre–post and qualitative studies. It should be noted that, although interventions identified in the systematic review tend to be individually oriented, the interventions discussed by qualitative interview participants tend to be community based. This discrepancy could signal a trend that researchers are moving away from individual-centred interventions, or it may simply reflect their preference for community-based interventions. This somewhat limits the comparability of our two sets of data.
The evidence was assessed based on its ‘relevance’ and ‘rigour’. The definitions for these terms deviate from how they are usually applied in ‘traditional’ reviews. ‘Relevance’ refers to whether a study was able to address the theories being tested rather than strictly adhering to the topic of review, whereas ‘rigour’ refers to whether or not the insights and inferences drawn by the original intervention researchers were able to contribute to theory testing. Quality assurance is more concerned with the explicitness and reflexivity of the reviewers than with formal quality appraisal checklists such as whether or not the data are ‘fit for purpose’. This approach may not be conventional, but it allowed us to synthesise a rich and varied body of evidence and produce findings that we hope are insightful if not prescriptive.
Conclusions
The construction of CMO configurations using the data from earlier discussion groups with research and health service users (see Chapter 3), the review of relevant guidelines and systematic reviews (see Chapters 4 and 5), reviews, theoretical literature and empirical studies of adapted interventions (see Chapter 6) and the in-depth qualitative interviews (see Chapter 7) enabled us to suggest what adapted interventions work for whom, in what contexts and why (see Tables 21–25). The different CMO configurations are presented for each of the eight stages of an intervention lifecycle. Four illustrative examples were provided to demonstrate how data from preceding methods contributed to producing CMO configurations, which ultimately represent the contextual ‘real-life’ trajectory of adapted interventions.
In terms of prioritising the implementation of these interventions and future research, we compared the ‘strategies and activities’ recommended for the general population for smoking cessation, increasing physical activity and improving healthy eating with the ‘strategies and activities’ used in adapted interventions. Using insights from the preceding study components, and evidence of effectiveness, we concluded that at present there are no adapted intervention approaches that are ready for rolling out throughout the NHS; however, we provided preliminary guidance on which interventions should be prioritised for further research.
Lastly, we utilised this accumulated knowledge to develop the RESET decision tool, which presents a practical way for researchers and health promoters to utilise our findings when implementing or researching adapted health promotion interventions.
Chapter 9 Discussion
Summary of main findings
Overall, this body of work suggests that it is both possible and important to consider adapting existing health promotion interventions for ethnic minority communities; however, this finding should not be interpreted to mean that adapted interventions are simplistic undertakings that are amenable to any formulaic approaches. Rather, decisions on adaptation need to be based on a detailed understanding of the target community and an appreciation of the mechanism(s) through which the adapted intervention is likely to exert its effects. Furthermore, adaptation needs to be considered at all stages of the research process. Such tailoring of interventions to the target population is likely to increase salience of the study to the target population, translating into improved recruitment, acceptability and retention. As yet, however, there is insufficient evidence to determine whether or not such improvements in process measures result in improved clinical end points and whether or not they are cost-effective. However, given the substantial and increasing disease burden associated with lifestyle disorders – which tend to disproportionately affect ethnic minority communities – there is a pressing need for further work to investigate the comparative effectiveness and cost-effectiveness of appropriately adapted with standard health promotion interventions in ethnic minority populations.
The key assumption underpinning the work in this report was that health promotion interventions found to be effective in the general population are also likely to prove effective in ethnic minority populations if appropriately adapted. As discussed below, throughout each phase of work (see Chapters 3–8) we have generated evidence that both tests and supports this key assumption.
User engagement
In Chapter 3 we discussed our experiences with user engagement through, among other things, national launch and dissemination conferences. Members of the project team and invited international experts in ethnicity and health research spoke at, and led on, workshops at the initial 1-day launch conference. This conference was attended by a variety of stakeholders from government and community organisations. The main feedback emphasised the importance of incorporating ecological models of health promotion and the need to expand our breadth of vision beyond individual factors contributing to health. Delegates suggested, for example, that we should consider interventions delivered outside of traditional health-care settings and examine those delivered by commercial organisations. In response to this suggestion we ensured that we remained alert to potentially relevant evidence on policy, resource-based and environmental interventions, even if evidence in these areas was less robust than that for individual-focused behavioural interventions (see Chapter 4).
Delegates also expressed their wish for us to foster linkages among them as they felt that there was much that could be gained through sharing of local, national and international experience. This was pursued through the creation of a project website (www.chs.med.ed.ac.uk/ethnicity-and-health/), which allowed the sharing of project materials and presentations through circulating contact details of interested participants, and the creation of an informal network in relation to health promotion for ethnic minority communities. The network and relationships that developed served as a welcome source of information and advice that we were able to draw on during subsequent phases of the research.
Our dissemination conference was held towards the end of the project and facilitated the sharing and discussion of our preliminary conclusions. Delegates were encouraged to reflect on, challenge and debate our findings. Although there was considerable support to further develop this field of enquiry, delegates cautioned against drawing simplistic conclusions from the available evidence, pointing to, for example, the need to thoroughly consider the effects of socioeconomic status (SES) and reflect on the possible impact of unmeasured, confounding influences. In the realist synthesis presented in the preceding chapter (see Chapter 8) we took on board the feedback received, highlighting how attempts at interventions need to stem from a detailed appreciation of the target community, the heterogeneity within communities and the ways in which interventions are likely to be received and interpreted. The idea of developing a theory of adaptation was also raised and initial encouraging discussions on how to take this forward took place in one of the workshops (see Table 1).
Extracting evidence on effective health promotion interventions from UK guidelines and international systematic reviews
In Chapter 4 we identified the evidence on effective health promotion interventions for the population as a whole for behavioural change in general and, more specifically, for smoking cessation, increasing physical activity and improving healthy eating. We then created summary frameworks of the effective ‘strategies and activities’ for each health promotion topic (see Tables 3–6). These summary frameworks were organised according to six categories, which spanned the spectrum of health promotion intervention levels, from an individual to a population level, with corresponding variations in scope for adaptation (see Figure 5). These summary frameworks enabled us to identify both saturated and sparser areas of evidence across the health promotion topics of interest and approaches used. The evidence base identified was considerably stronger for smoking cessation than it was for either promoting physical activity or changing dietary practices, for which there is still considerable uncertainty as to how best to promote clinically relevant changes that can be sustained over any length of time. In particular, there was a lack of empirical evidence from studies investigating the effectiveness of population-based interventions such as food pricing policy or environmental modifications (e.g. introducing cycling routes). There is an obvious tension here as the latter are far more difficult to evaluate using rigorous designs of the kind that guideline developers and systematic reviewers preferentially draw on.
Individual-centred behavioural approaches thus dominated the body of evidence we identified. The strongest and most consistent evidence of effectiveness was for smoking cessation interventions, which tended to be individual-level strategies, such as resource provision and provider interactions, aiming to increase uptake of and compliance with pharmacological interventions. In contrast, the as yet minimal evidence on activities and strategies associated with promoting physical activity and healthy eating was more likely to draw on population-level strategies, such as enacting environmental changes. We hypothesised that this difference in focus is related to the differing needs of interventions attempting to reduce a particular behaviour for a relatively short period of time (e.g. tackling the nicotine cravings associated with smoking cessation) compared with interventions seeking to stimulate particular behaviours (i.e. increasing physical activity and changing healthy eating) over a sustained period of time. This insight, together with the feedback received from our launch stakeholder conference, resulted in a continued search for evidence and experiences of adaptation of population-level interventions for promoting physical activity and health eating (see Figure 5). We believe that this approach was justified and appropriate as the need for clear evidence on the effectiveness of adapted interventions is, from a public health and clinical perspective, particularly important in relation to non-pharmacological interventions.
Consideration of ethnicity in UK guidelines and international systematic reviews
The high-level evidence synthesis of UK guidelines and international systematic reviews was then further scrutinised in Chapter 5 to assess the extent to which the particular needs of ethnic minority populations were considered within the evidence base for smoking cessation, physical activity and healthy eating health promotion interventions that are known to have some evidence of effectiveness and, consequently, are recommended for use in the general population. Although most of the UK guidelines (12 of 15 guidelines) and just under two-thirds of the international systematic reviews (66 of 111 reviews) made at least some reference to ethnicity and its related terms, acknowledging the existence (and by implication the needs) of ethnic minority populations (see Table 7), none of the guidelines or systematic reviews reported sufficient evidence to determine whether recommended interventions were more or less effective for ethnic minority populations. Consequently, it is at present not possible to determine from such evidence syntheses whether interventions of proven effectiveness and recommended for the general population are equally, more or less effective for ethnic minority populations.
The 12 guidelines and 66 systematic reviews commenting on ethnicity were further probed to extract the evidence statements made in relation to ethnic minority groups. All 12 guidelines and only 41 of 66 systematic reviews made evidence statements pertaining to ethnicity in the context of the health promotion topics of interest. These statements were grouped according to shared meaning and/or concept and then thematically analysed to identify five overarching themes: the acknowledgment of diversity within populations; identifying gaps in the evidence of which interventions are effective for ethnic minority populations; observing differential effects of interventions for different ethnic groups; reporting that action should be taken to adapt interventions; and, lastly, recommending improved research, reporting and analysis as a response to the absence of definitive evidence for interventions that are effective for ethnic minority populations (see Table 7). Importantly, we found no guidance in these high-level syntheses on how best to adapt the health promotion interventions being recommended to ensure that they were acceptable to and effective in ethnic minority populations.
Systematic review of adapted health promotion interventions
To complement the summary and critique of the guidelines and systematic review literature (see Chapters 4 and 5), we conducted a systematic review to identify and analyse the evidence for smoking cessation, physical activity and healthy eating health promotion interventions that had been adapted for African-, Chinese- and South Asian-origin populations (see Chapter 6). We identified and separately analysed three types of evidence in our review: theoretical/conceptual literature on adapted health promotion interventions for our health topics; systematic reviews of adapted health promotion interventions for the ethnic minority populations of interest to us; and relevant primary studies investigating the effectiveness of adapted health promotion interventions.
We identified 12 theoretical studies35,249–259,262,263,265,268–271 that offered concepts and models/theories in relation to adapting health promotion interventions for African-, Chinese- and South Asian-origin populations (see Table 10). These studies provided seven important contributions to frame our thinking around the similarities and differences between interventions adapted for ethnic minority groups and interventions for the general population (see Box 5). One contribution suggested that women were identified as central figures for behaviour change as both targets and agents of change, and this insight suggested an important and possibly greater need to consider gender influences when planning health promotion for ethnic minority populations compared with health promotion for the general population. 253,262,263,265,269 It was also suggested that the goals underpinning or motivating behaviour change in ethnic minority populations should account for the role of individuals within the context of families and communities to a greater degree than is often considered when planning health promotion interventions for the general population. 35 The development of communication strategies to better match the needs and preferences of ethnic minority populations was also emphasised, although this approach has increasingly been recognised as an important strategy in health promotion interventions for the general population. 254,255,257
These and the other overarching themes from the theoretical studies discussed in Chapter 6 provided a comparative foundation from which to reflect on the systematic reviews and primary studies we identified (discussed below). These themes also yielded helpful insights in relation to understanding the context–mechanism–outcome (CMO) pathways that we constructed in the context of our realist synthesis of the evidence uncovered (discussed in Chapter 8 and below).
We identified seven systematic reviews245,246,275–279 of adapted health promotion interventions for ethnic populations, of which the majority (six of seven reviews)245,246,276–279 reported on interventions delivered for African American populations (see Table 11). Findings from these systematic reviews were largely inconclusive, revealing mixed effects. Two reviews245,278 suggested that adaptation of interventions increased their effectiveness, but they were unable to identify which specific adaptations were associated with this improved effectiveness. On the other hand, a review on smoking cessation246 suggested that adaptation increased the effectiveness of health promotion interventions in the short term, but with no demonstrated effects in the longer term. The remaining four reviews275–277,279 did not report on whether or not adapted interventions increased effectiveness, attributing this to the lack of available primary research and the preliminary nature of some of the included studies, which were still ongoing at the time that the review was conducted. There was therefore no conclusive evidence from systematic reviews specifically focusing on adapted interventions for African-, Chinese- and South Asian-origin populations on whether adaptation increases the effectiveness of health promotion interventions or indeed which adaptations are most important to undertake for promoting the health of ethnic minority populations.
In addition, we identified 107 empirical intervention studies (reported on in 154 papers) on smoking cessation, physical activity and healthy eating health promotion interventions adapted for African-, Chinese- and South Asian-origin populations (see Appendix 18). Overwhelmingly, the majority of these interventions (91 of 107 studies) were delivered for African American populations (see Table 12). From these studies we were able to extract the range of approaches to adaptation reported to create a novel 46-item Typology of Adaptations (see Table 13), developed to code all reported adaptations in these studies.
Although 107 studies were identified, only nine studies293–295,306,341,347–352 directly compared an adapted intervention with an unadapted version of the same intervention (see Table 14). These relatively few studies offered the most direct evidence on the effectiveness of adaptation. Eight293–295,306,341,347,348,350–352 of these nine intervention studies were conducted with African American populations (the ninth was with Chinese-origin people). The results of these direct comparison studies were mixed, providing no conclusive evidence of whether or not adaptation increased the effectiveness of health promotion interventions. To further test the assumption that adaptation increases the effectiveness of interventions for ethnic minority populations, we used our Typology of Adaptations (see Table 13) in subsequent realist synthesis to broadly detect which adaptations were used more often in effective interventions.
Given the absence of definitive evidence on whether or not adaptation(s) increased the effectiveness of interventions, we then looked to the entire body of studies to examine the feasibility, acceptability, related process measures and equity of the included adapted interventions. We found that resource-intensive interventions, interventions that required additional individual tailoring and interventions with limited/inadequate funding tended to reduce the feasibility of successfully delivering the adapted intervention. In contrast, the use of and/or linkages with existing organisations or familiar settings were, overall, found to increase the feasibility of delivering adapted interventions. In terms of acceptability, interventions developed in collaboration with the targeted community and interventions that offered a degree of flexibility in their structure and delivery were found to be the most acceptable, whereas randomised controlled designs, interventions perceived to be too complex, competing priorities and costs to participate were all found to decrease acceptability. Intervention settings (e.g. churches and schools), criteria for participation (e.g. parental participation) and resources required for participation (e.g. computers and telephone access) were reported to influence the equity of access to adapted interventions.
There was limited reporting of costs associated with conducting adapted interventions in the 107 studies identified in the systematic review and an absence of rigorous economic evaluation of interventions. Only 13 studies285–289,292,299,302,323,327,328,334,342–345,358,365–373 reported cost data and only one study374 performed a cost–utility analysis; no studies reported on cost-effectiveness (see Table 17).
Finally, these adaptations were observed to occur throughout the stages of an intervention, from development to dissemination, and we correspondingly developed an eight-stage Programme Theory of Adapted Health Promotion Interventions (see Figure 9), which is designed to be used alongside the Typology of Adaptations (see Figure 10). This Typology of Adaptations (see Table 13) was further mapped onto the eight intervention stages identified in the Programme Theory of Adapted Health Promotion Interventions (see Table 18). Our Programme Theory of Adapted Health Promotion Interventions aims to provide a tool for the systematic and transparent consideration of approaches to planning and reporting on adapted interventions.
Qualitative interviews with researchers and health promoters who have adapted interventions for ethnic minority populations
We supplemented the findings of the systematic review with 26 in-depth interviews with purposively selected researchers and health promoters involved in adapting and delivering health promotion interventions (see Chapter 7). A thematic analysis identified three main themes: constructing ethnicity within adapted interventions; considering how interventions are adapted; and sustaining these adapted interventions. Constructing ethnicity represented a new insight in terms of broadening thinking on ethnicity from its more conventional dimensions (i.e. religion, language, culture, physical features and ancestry), as well as demographic variables such as age, gender and SES, to include contextual elements (e.g. the influence of social environments, particularly, in recent immigrant communities, physical spaces that facilitated or hindered participation, past experiences with health research and services and diverse life experiences including stress) (see Figure 12). The theme of adapting interventions (see Figure 13) identified many of the adaptations extracted from the empirical studies examined in the systematic review in Chapter 6, which were subsequently incorporated into the Typology of Adaptations (see Table 13). The reinforcement of adaptations identified in the systematic review in the qualitative interviews was somewhat expected as a number of the interview participants were recruited from a sampling frame derived from studies included in the systematic review, but we also found that our typology featured more recent approaches that have yet to gain traction within the wider literature, for example the use of peer leaders who are not only ethnically matched but also matched in terms of having successfully changed their behaviour (adaptation number 6); interventions that address health behaviour patterns found in the target populations (adaptation number 26); and purposefully maintaining an open intervention environment (adaptation number 42). The last theme, namely sustaining adapted interventions (see Figure 14), was an unexpected finding as we did not anticipate the in-depth discussions in relation to the practicalities of delivering adapted interventions and sustaining this field of research (e.g. in terms of funding, formalising the intervention, getting recognition for the work, ensuring staff safety and capacity building) (see Appendix 26). Finally, we observed a potential geographical variation in the support networks available to researchers delivering adapted interventions for ethnic minority populations. Researchers in the USA, in particular, identified an informal network accessible for sharing ideas and collaborating on projects, whereas researchers in other geographical areas such as New Zealand and Australia reported less access to support and interactions, and tending to work somewhat in isolation. UK researchers were somewhere between these extremes.
Realist synthesis
In Chapter 8, our realist synthesis drew on data from seven group discussions with research and health service users attending our conferences; 15 UK guidelines; 111 international systematic reviews; a review of 12 theoretical papers, seven systematic reviews and 107 empirical studies on adapted interventions; and a further 26 qualitative interviews to identify, test and explore realist insights of how adapted interventions work or do not work in the form of CMO configurations. Data from each of the preceding phases of work contributed to the context, mechanism and/or outcome constituents of a CMO configuration. Using the Programme Theory of Adapted Health Promotion Interventions, along with the 46 adaptations mapped onto to the relevant stages of intervention (see Table 18), we constructed CMO configurations relating to the different adaptations in order to describe how adaptations function as mechanisms in different contexts to produce varying outcomes.
Through this analysis we began to uncover why interventions work in different contexts and what factors may moderate their effectiveness. At the initial stages of intervention conception and planning, taking stock of appropriate study designs and behaviour change models as well as conducting exploratory work with a wide range of target community members were highlighted. At the intervention promotion and engagement/recruitment stages it was noted that interventions promoted through a target community’s preferred method of communication showed mixed results in terms of success; participants’ preferred formats for communication may have facilitated uptake but not necessarily increased retention. Recruiting from appropriate settings, however, appeared to be more successful. This was owing, in part, to the existence of established social networks and existing activities. There was also evidence in support of the ethnic matching of research facilitators to the target population; however, in some instances the recruiter’s experience and sensitivity were perhaps more important than their ethnicity.
The majority of CMO configurations were linked to the implementation/delivery stage and highlighted how adaptations needed to accommodate the ‘lived experiences’ of ethnic minority participants, for example acknowledging travel patterns, the timing and location of interventions and preference for different kinds of facilitators. Furthermore, the CMO configurations revealed that social support, derived from family and friends or group-based formats, was far more complex than anticipated, with preliminary findings suggesting that the preference for social support may be contingent on a participant’s health status (e.g. diabetes) and desire for privacy. Culturally matched intervention materials were another often cited adaptation for ethnic minority populations. In the studies we examined, the effectiveness of these materials was observed to differ in relation to participants’ perceived ethnic identity and, as such, required a greater accommodation of the heterogeneity that exists within these populations. For retention, telephone follow-up was reported to be effective if access to a telephone was consistent and continuous. The provision of transportation to the intervention site, or locating the intervention site in an already familiar and convenient location, was also associated with successful retention. For evaluation and outcome stages, external factors such as life stressors, social networks and substantive barriers (e.g. employment priorities) were all reported to moderate intervention effect. Additionally, during evaluation, ensuring the appropriateness and importance of the outcomes to the target population was a critical consideration.
Following this examination of what adaptations work for whom and in what circumstances, four illustrative examples provided the contextual ‘real-life’ trajectory of adapted interventions. These examples elaborated on the CMO configurations underpinning potential successes and failures for group-based interventions, communication strategies, behaviour patterns and pharmacotherapy, and social support-oriented interventions (see Boxes 11–14).
We then compared the ‘strategies and activities’ recommended for the general population for smoking cessation, increasing physical activity and improving healthy eating (see Chapter 4) with the ‘strategies and activities’ used in adapted interventions (see Chapter 6) to consider which interventions are ready for implementation and which interventions require further research. At present there are no adapted intervention approaches that are ready for rolling out throughout the NHS; however, we have been able to suggest which interventions should be prioritised for further research. These research priorities include increasing awareness of, access to and use of effective pharmacotherapies and potentially utilising a greater range of providers alongside peer or lay providers for smoking cessation interventions; personalised or group-based support (depending on the health status of the targeted participants) for diet and exercise interventions; and, in the context of exercise, group-based initiatives with an emphasis on social and health benefits along with setting-based (e.g. religious sites, community organisations, established institutions) solutions.
Finally, we extracted the principal findings from this synthesis and developed a tool to assist researchers and health promoters in the development of adapted interventions. This decision-making tool, called RESET (i.e. Relevance, Evidence base, Stages of intervention, Ethnicity and Trends), is described in more detail in Box 15. The RESET decision-making tool can be used alone but is recommended for use along with other key outputs from this research, namely the 46-item Typology of Adaptation and the eight-item Programme Theory of Adapted Health Promotion Interventions. For example, one could take an intervention that has been recommended for more research and then use the RESET tool to decide if this would be an appropriate intervention to deliver for a particular target population and, if so, consider how best to adapt it. Although we have begun to validate this through the qualitative work with an international group of experts (see Chapter 7), it should be noted that this is, at present, still a preliminary tool built up from the different research components undertaken in this report; we hope in due course to formally test and if necessary refine this further before making it available online for widespread use (see Chapter 8).
Strengths and limitations of this study
We have discussed the strengths and limitations of individual strands of work in earlier chapters (see Chapters 4–8); here we provide a broader reflection on the overall body of research undertaken. Our study had a number of strengths, including our undertaking of a theoretically driven mixed-methods phased programme of work that built progressively on previous steps. This phased programme allowed us to remain receptive to the findings from preliminary stages of work and modify and adapt our approach as necessary. The utilisation of a realist framework to synthesise this broad body of evidence has helped us to produce a rich, nuanced account that will, we hope, prove useful to policy-makers, commissioners of research, academics and clinicians. We anticipate that the novel frameworks and tools developed – namely a comprehensive Typology of Adaptations, the Programme Theory of Adapted Health Promotion Interventions and the RESET instrument – will be of considerable benefit in ensuring the improved theorising, delivery and reporting of future studies seeking to extend and build the evidence base in this important area of research. Finally, we were able to achieve what we aimed to do – explicate the evidence base for general health promotion interventions, and, in particular, health promotion interventions that have been adapted for ethnic minority groups. This undertaking was enhanced by the skill mix of the research team, which allowed reflection from a range of disciplinary perspectives, including ethnicity and health, social sciences, epidemiology, public health, clinical trials and health economics. This expertise was augmented by the very helpful practice- and theory-oriented contributions and support from members of our Independent Project Steering Committee that oversaw this work.
The lack of robust evidence of effectiveness for physical activity and healthy eating interventions in the general population identified at the outset limited the comparative synthesis work we could undertake in the latter phases. In our systematic review we identified existing systematic reviews and these proved to be largely uninformative in relation to effectiveness considerations; this was largely also true of the empirical studies reviewed. Although our searches were wide-ranging, there is the possibility that we may have missed some relevant guidelines, systematic reviews and primary studies because of their poor indexation in medical databases. Also of note is that, although we identified over 100 empirical studies, the majority of studies were conducted with African American populations; this then raises important questions about the generalisability of findings to, for example, a UK context and other ethnic minority groups. It should be noted that, despite the overall volume of evidence reviewed, there were surprisingly few studies that directly compared an adapted intervention with a near equivalent unadapted approach to allow for an assessment of relative effectiveness. This therefore represents an important gap in the literature that urgently needs to be filled in order to move this field of enquiry forward.
By limiting the scope of our research to the three health topics of smoking cessation, increasing physical activity and improving healthy eating we inevitably excluded many studies of adapted interventions for other health topics (e.g. reduction of alcohol intake and promoting improved oral hygiene and dental care). Similarly, our focus on African-, Chinese- and South Asian-origin populations was also likely to have excluded potentially valuable learning opportunities from other populations, as our searches identified a number of potentially important and interesting reports of health promotion interventions with Hispanic/Latino populations and for the indigenous populations of the USA, Australia, Canada and New Zealand. That said, we believe that the range of interventions and populations studied has enabled the generation of a number of important insights that are potentially transferable to other health promotion areas, including with other ethnic minority communities. Moreover, the instruments we have developed and presented in this work need to be seen as preliminary until they have been formally tested in a broader range of subject areas and populations.
Another possible limitation is that the entire study, as a response to a commissioning brief, was framed by the assumption that, when effective health promotion approaches are appropriately adapted and made culturally relevant, they too can be effective for ethnic minority populations. 9 Although we were able to engage more fully in debate on whether adapted or targeted approaches are desirable, we do however acknowledge that this approach may have its own share of pitfalls, including possible discrimination or stereotyping as a consequence of trying to identify culture and categorise its components. These concerns need to be balanced with the need for interventions that engage an often marginalised section of the population.
Research findings in the context of the broader literature
Adapting health promotion interventions for ethnic minority populations
Over the past two decades, support for adapting health promotion interventions for ethnic minorities has been gathering momentum. 9,13 The rationale for conducting this body of work is the assumption that adapted or culturally sensitive (or culturally tailored, based or adapted)35 interventions will be more effective for ethnic minority populations than mainstream interventions. 9 Although culture is commonly invoked to explain health inequalities, it is seldom operationalised, and its pathways and mechanisms rarely explicated. 416 Greater testing of culturally sensitive interventions to demonstrate health benefits for ethnic minority populations has therefore been championed. 35 Reducing health disparities for ethnic minority populations requires considerable thinking around the complex issues of culture, context and theory. 251 More specifically, the role of culture must itself be tested. In this work, ‘ethnicity’, which was conceptualised as encompassing culture, was tested as an operationalisable feature of adapted interventions.
There have been previous attempts to synthesise the available evidence on adapted health promotion interventions for ethnic minority populations. 245,246,275–279 Although these reviews have varied in the populations and health topics considered, they have predominantly originated from the USA with a focus on African American populations. The findings of our systematic review echoed the larger evidence base such that the majority of the studies we identified (91 of 107 studies) were undertaken with African American populations.
In earlier work that informed the current research, Netto et al. 13 identified five common principles of adaptation for health promotion for Chinese-, Indian- and Pakistani-origin populations. The principles proposed were using community resources to publicise the interventions and increase accessibility; identifying and addressing barriers to access and participation; developing communication strategies sensitive to language use and information requirements; working with cultural or religious values that promote or hinder attitudinal and behavioural change; and accommodating various degrees of cultural identification. This study has built and expanded on the earlier work through the addition of African-origin populations, which dramatically increased the number of studies included for systematic review and also allowed us to draw on a far more diverse body of quantitative and qualitative evidence.
Through this work we have been able to elaborate on these five principles of adaptation by producing a much richer typology of approaches to adaptation, which will, we hope, assist researchers and health promoters to identify the specific adaptations that they might wish to consider. The five principles outlined by Netto et al. 13 map onto some of the adaptations presented in Table 13, and sometimes onto more than one adaptation mechanism. For example, the first principle, using community resources to publicise the interventions and increase accessibility, maps onto adaptation number 10 (utilise local/respected religious/spiritual leaders) and adaptation number 11 (collaboration with ethnic-specific institutions and professional organisations). The third principle, developing communication strategies sensitive to language use and information requirements, encompasses adaptation numbers 12–21 (see Table 13) as they all deal with modifying communication materials. One main difference between the two adaptation resources is that, although the five principles of adaptation provide a rationale for each action, for example using community resources ‘to publicise the interventions and increase accessibility’,13 the 46 adaptations developed in this study are not necessarily associated with a particular purpose, and these can therefore potentially be used at any stage of an intervention. In this flexible format, these adaptations relate to a Programme Theory of Adapted Health Promotion Interventions to assist in deciding at what stage of the intervention one needs to consider and undertake these adaptations.
Conclusions
Economically developed societies face an increasing burden of potentially preventable lifestyle-related disorders and diseases. The majority of these long-term conditions can be prevented and controlled through the modification of shared risk behaviours such as smoking, physical inactivity and unhealthy diets. As such, attention is increasingly focusing on health promotion efforts to address these behaviours. At present, the evidence in the population as a whole is reasonably strong in relation to individual-centred interventions for smoking cessation; in contrast, we know far less about how to promote physical activity and healthy diets in a sustainable manner. As economically developed societies are also becoming increasing ethnically diverse, there is an ethical and legal imperative to ensure that health care, including preventive strategies, is equitable for all sections of the population. Adapting health promotion interventions with established evidence of effect in the general population for ethnic minority populations is therefore a potentially central concern.
Despite the importance of this subject area we have found that available guidelines and systematic reviews tend to have little or nothing to say on whether or not ‘strategies and activities’ recommended for the general population are equally effective for ethnic minority populations. Our more detailed review of the empirical literature has shown that the absence of such information in guidelines and systematic reviews is at least in part owing to the lack of clear evidence on the effectiveness of many health promotion interventions in ethnic minority populations. We have furthermore shown that little progress has been made in establishing a scientific foundation for the adaptation of interventions to maximise their likely effectiveness in ethnically diverse populations. This dearth of evidence is compounded by confusion as to what constitutes an adaptation or why or how these adaptations have been decided on, and how these adaptations are best described, evaluated and reported on. Our work here contributes to improving the theorising on, undertaking of and reporting on adapted interventions. There remains, however, an urgent need for high-quality studies of carefully considered adapted interventions compared with standard interventions together with robust cost-effectiveness assessments of clinical outcomes.
Most of the empirical work in this report has been based in the USA, undertaken among the African American population, who have a longer history of settlement in North America and who are familiar with the English language, in contrast to other ethnic minority groups. Consequently, work carried out to adapt interventions for African American populations has in the main focused on addressing structural injustices, a history of mistrust of institutions and socioeconomic disparities. By contrast, even though over the last 50 years Europe has been a major focus for inward migration, including migration by populations with diverse cultures and languages, as evidenced by this work, European research on this topic remains sparse. Few syntheses of the principles for adaptation exist, and fewer still are research based. Given that these populations in Europe have different migration histories, and experiences of and interactions with social and economic institutions, evidence specific to these populations is vital to complement what is already known for the African American population.
This work has built upon and substantially extended the principles published by Netto et al. ,13 which were derived from a more limited evidence base. Our work has also extended the principles from a number of (mainly North American) practice-based guidelines on the adaptation of health promotion programmes. 54,417–420 Although in many respects the general conclusions are similar (itself a reassuring finding), our work has emphasised that the empirical scientific evidence is unfortunately limited. Nonetheless, our findings, and those of others, provide a coherent direction that practitioners can take pending new, more rigorous and larger-scale evaluations, which are now needed if we are to provide more equitable health care for all.
Recommendations for further research
Through this work we have been able to identify a number of priority areas for future research:
-
Guideline developers and systematic reviewers of health promotion interventions should be encouraged to make clearer the population from which the evidence is derived so that those wishing to apply the evidence can assess it for relevancy; it is important that any areas of caution/evidence gaps are highlighted so that these can be filled.
-
There is currently a lack of evidence-based models and tools to guide researchers and practitioners on how to best adapt health promotion interventions and, thus, the models and tools we have developed here should be tested and, if necessary, refined.
-
A key research recommendation is the need for more high-quality research that compares, for example, carefully adapted interventions for promoting exercise with near equivalent standard approaches to facilitate assessment of the effectiveness of the adaptation(s). Furthermore, there should be improved reporting of the intervention and any adaptation undertaken.
-
There is also a need for cost-effectiveness to be studied, possibly using mathematical modelling techniques such as Markov modelling, to examine the real end points of interest and link these with the costs of the interventions.
-
As noted above we have uncovered a body of work on other populations (e.g. Hispanic and indigenous populations) that could usefully be synthesised to inform more international deliberations. If pursued, it would then be useful to synthesise this body of work with the findings in this report.
-
We suggest that all multiethnic societies need to be contributing to this important research agenda, particularly as work in one geographical area is unlikely to be easily exportable elsewhere. Over-reliance on research in the USA is likely to undermine the initiation of appropriate scholarship and research elsewhere.
-
Our qualitative work revealed that there are many researchers and practitioners breaking new ground and that, in view of the uncertainties in the evidence base and challenges inherent in undertaking this work, they would value peer support of the kind that is now available in the USA. A UK-based academic network could readily meet this need for the UK and indeed possibly also many European academics. Further, links should be established between this network and US-based networks that have a longer history of working on adapted interventions.
-
Finally, given that the prevalence of long-term conditions is projected to soar and populations are likely to become increasingly ethnically diverse, it is crucial that this evidence synthesis on adapted health promotion interventions for ethnic minority populations is periodically updated as we strive to deliver equitable health services and outcomes for all.
Acknowledgements
We thank our Independent Project Steering Committee members, Dr Laurence Gruer (Chair), Professor Susan Michie, Dr Ash Samanta and Asma Sader, who provided helpful guidance and support throughout the project. In addition, we acknowledge the assistance of Dr Cecile Wabnitz, Dr Geoff Wong, Dr Umar Yousuf, Smitha Kakde, Fiona Adams and Anna Wierzoch for their contributions to this work and for their invaluable support. Furthermore, we would like to acknowledge the support from Diane Clay and Marshall Dozier for their invaluable help with searching the electronic databases.
We are very grateful to Dr Wayne Giles, Dr Anne Karen Jenum and Professor Mike Kelly for presenting at our first user engagement conference. In addition, we would also like to express our gratitude to the many academics and health service providers and users who participated in our qualitative interviews and our user engagement conferences, without whom this project would not have been possible.
Contribution of authors
Aziz Sheikh was the principal investigator for the project and as such was involved in all aspects of the project. He, along with Raj Bhopal, conceived this project, led the writing of the research grant, managed the researchers, led the Investigators Group and oversaw all aspects of the work, including the writing and editing of this report.
Jing Jing Liu (Research Associate) and Emma Davidson (Research Fellow) contributed to all aspects of the project and the design and writing of the report.
Raj Bhopal, Martin White, Mark Johnson, Gina Netto and Mark Deverill were involved in the development and oversight of the project in their role as the Investigators Group; they also contributed to reviewing and editing of the report.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Nazroo J. The health of Britain’s ethnic minorities. London: Policy Studies Institute; 1997.
- Acheson D. Independent Enquiry into Inequalities in Health. Report of the Scientific Advisory Group 1998.
- Johnson M, Owen D, Blackburn C. Black and minority ethnic groups in England: the second health and lifestyles survey. London: Health Education Authority; 2000.
- Johnson M, Killoran A, Swann C, Kelly M. Public health evidence: changing the health of the public. Oxford: University Press; 2006.
- Centers for Disease Control and Prevention (CDC), Epidemiology and Analysis Program Office; Surveillance, Epidemiology, and Laboratory Services . Health Disparities and Inequalities Report – United States, 2011 2011.
- Sproston K, Mindell J. Health Survey for England 2004: The Health of Minority Ethnic Groups 2004. www.ic.nhs.uk/pubs/hse04ethnic (accessed 6 June 2011).
- Wild S, Fischbacher C, Brock A, Griffiths C, Bhopal R. Mortality from all causes and circulatory disease by country of birth in England and Wales 2001–2003. J Public Health (Oxf) 2007;29:191-8.
- Crisp N. Race equality action plan. London: Department of Health; 2004.
- Bhopal R. Health education and ethnic minorities. BMJ 1991;302.
- Mladovsky P. A framework for analysing migrant health policies in Europe. Health Policy 2009;93:55-63.
- Afshari R, Bhopal RS. Ethnicity has overtaken race in medical science: MEDLINE-based comparison of trends in the USA and the rest of the world, 1965–2005. Int J Epidemiol 2010;39:1682-3.
- Davidson E, Liu JJ, Sheikh A. The impact of ethnicity on asthma care. Prim Care Respir J 2010;19:202-8.
- Netto G, Bhopal R, Lederle N, Khatoon J, Jackson A. How can health promotion interventions be adapted for minority ethnic communities? Five principles for guiding the development of behavioural interventions. Health Promot Int 2010;25:248-57.
- Bhopal R. Race and ethnicity: responsible use from epidemiological and public health perspectives. J Law Med Ethics 2006;34:500-7.
- Bhopal R. The public health agenda and minority ethnic health: a reflection on priorities. J R Soc Med 2006;99:58-61.
- Bhopal R. Glossary of terms relating to ethnicity and race: for reflection and debate. J Epidemiol Community Health 2004;58:441-5.
- Senior PA, Bhopal R. Ethnicity as a variable in epidemiological research. BMJ 1994;309:327-30.
- Sheikh A, Gatrad R, Dhami S. Consultations for people from minority groups. BMJ 2008;337:51-3.
- Sheikh A, Wallia S. Ramadan fasting and diabetes. BMJ 2007;335:613-14.
- Sheikh A. Should Muslims have faith based health services?. BMJ 2007;334.
- Sheikh A. Why are ethnic minorities under-represented in US research studies?. PLoS Med 2006;3.
- Sheikh A, Netuveli G, Kai J, Panesar SS. Comparison of reporting of ethnicity in US and European randomised controlled trials. BMJ 2004;329:87-8.
- Sheikh A. Dealing with ethics in a multicultural world. Western J Med 2001;174:87-8.
- Bhopal R, White M, Ahmad W. ‘Race’ and health in contemporary Britain. Buckingham: Open University Press; 1993.
- Rafnsson SB, Bhopal RS. Large-scale epidemiological data on cardiovascular diseases and diabetes in migrant and ethnic minority groups in Europe. Eur J Public Health 2009;19:484-91.
- Agyemang C, Bhopal R, Bruijnzeels M. Negro, Black, Black African, African Caribbean, African American or what? Labelling African origin populations in the health arena in the 21st century. J Epidemiol Community Health 2005;59:1014-18.
- Billinger MS. Another look at ethnicity as a biological concept: moving anthropology beyond the race concept. Crit Anthropol 2007;27.
- Aspinall PJ. Collective terminology to describe the minority ethnic population: the persistence of confusion and ambiguity in usage. Sociology 2002;36:803-16.
- Ahmad WIU, Bradby H. Locating ethnicity and health: exploring concepts and contexts. Sociol Health Illn 2007;29:795-810.
- Brubaker R. Ethnicity, race and nationalism. Annu Rev Sociol 2009;35:21-42.
- Weber L, Fore ME, Vera H, Feagin JR. Handbook of the sociology of racial and ethnic relations. New York, NY: Springer; 2007.
- Downie R, Tannahill C, Tannahill A. Health promotion: models and values. Oxford: Oxford University Press; 1996.
- World Health Organization . Health Promotion Glossary 1998. www.who.int/hpr/NPH/docs/hp_glossary_en.pdf.
- Swerissen H, Crisp BR. The sustainability of health promotion interventions for different levels of social organization. Health Promot Int 2004;19:123-30.
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis 1999;9:10-21.
- Kreuter MW, Skinner CS. Tailoring: what’s in a name?. Health Educ Res 2000;15:1-4.
- UK Office for National Statistics . Focus on Ethnicity and Identity 2005. www.ons.gov.uk/ons/rel/ethnicity/focus-on-ethnicity-and-identity/focus-on-ethnicity-and-identity-summary-report/index.html.
- Rees P, Raymer J, Willekens F. International migration in Europe: data, models and estimates. Chichester: John Wiley; 2008.
- United Nations . International Migration Facts and Figures 2006. www.un.org/esa/population/migration/hld/Text/Migration_factsheet.pdf.
- Simon P. ‘Ethnic’ Statistics and Data Protection in the Council of Europe Countries: Study Report: European Commission Against Racism and Intolerance (ECRI) 2007.
- Nielsen SS, Krasnik A, Rosano A. Registry data for cross-country comparisons of migrants’ healthcare utilization in the EU: a survey study of availability and content. BMC Health Serv Res 2009;9:210-21.
- US Census Bureau . 2005–2009 American Community Survey 5-Year Estimates 2009. http://factfinder.census.gov/servlet/DTTable?_bm=y%26-geo_id=01000US%26-ds_name=ACS_2009_5YR_G00_%26-redoLog=false%26-mt_name=ACS_2009_5YR_G2000_B02001.
- US Census Bureau . Census 2000 Summary File 1 (SF 1) 100-Percent Data 2009. http://factfinder.census.gov/servlet/QTTable?_bm=y%26-geo_id=01000US%26-qr_name=DEC_2000_SF1_U_QTP5%26-ds_name=DEC_2000_SF1_U.
- Statistics Canada . Canada’s Ethnocultural Mosaic, 2006 Census 2008. www12.statcan.ca/census-recensement/2006/as-sa/97-562/pdf/97-562-XIE2006001.pdf.
- Statistics New Zealand . QuickStats about Culture and Identity: 2006 Census: Statistics New Zealand 2006. http://search.stats.govt.nz/search?w=Ethnicity.
- Australian Bureau of Statistics . Cultural Diversity Overview 2006. www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/C724250359785DC6CA25754C0013DC0A/$File/20700_cultural_overview.pdf.
- Australian Bureau of Statistics . 2006 Census QuickStats: Australia 2007. www.censusdata.abs.gov.au/ABSNavigation/prenav/ViewData?method=Place%20of%20Usual%20Residence%26subaction=-1%26producttype=QuickStats%26areacode=0%26action=401%26collection=Census%26textversion=false%26breadcrumb=PL%26period=2006%26javascript=true%26navmapdisplayed=true%26.
- Australian Bureau of Statistics . Experimental Estimates and Projections, Aboriginal and Torres Strait Islander Australians, 1991 to 2021 2009. www.abs.gov.au/ausstats/abs@.nsf/Products/946D4BC28DB92E1BCA25762A001CBF38?opendocument.
- Banks J. Diversity, group identity, and citizenship education in a global age. Educ Res 2008;37:129-39.
- Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann NY Acad Sci 2010;1186:69-101.
- World Health Organization . Preventing Chronic Diseases: A Vital Investment: WHO Global Report 2005. www.who.int/chp/chronic_disease_report/full_report.pdf.
- Harper S, Lynch J, Smith GD. Social determinants and the decline of cardiovascular diseases: understanding the links. Annu Rev Public Health 2011;32:39-6.
- National Cancer Institute . Cancer Trends Progress Report – 2009 2010 Update 2010. http://progressreport.cancer.gov/.
- Centers for Disease Control and Prevention . Racial and Ethnic Approaches to Community Health 2008. www.cdc.gov/reach/about.htm.
- Wild S, Forouhi N. What is the scale of the future diabetes epidemic, and how certain are we about it?. Diabetologia 2007;50:903-5.
- Diabetes UK. Diabetes in the UK 2009: Key Statistics on Diabetes 2009. www.diabetes.org.uk/Documents/Reports/DiabetesintheUK2009_Dec-09.pdf.
- World Health Organization . Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157-63.
- NHS Information Centre for Health and Social Care . Health Survey for England, 2008: Physical Activity and Fitness 2009.
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA 2010;303:235-41.
- Shields M, Carroll M, Ogden C. Adult obesity prevalence in Canada and the United States. Hyattsville, MD: National Center for Health Statistic; 2011.
- Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:1475-82.
- Hippisley-Cox J, Coupland C, Robson J, Sheikh A, Brindle P. Predicting risk of type 2 diabetes in England and Wales: prospective derivation and validation of QDScore. BMJ 2009;338.
- National Cancer Institute . Cancer Trends Progress Report – 2009 2010 Update 2010. http://progressreport.cancer.gov.
- Cancer Research UK . Cancer Incidence and Survival by Major Ethnic Group, England, 2002–2006 2009. www.ncin.org.uk/view.aspx?rid=75.
- Centers for Disease Control and Prevention . Data & Trends – Prevalence of Diabetes 2011. www.cdc.gov/diabetes/statistics/prev/national/figbyage.htm.
- World Health Organization . 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases 2008. http://whqlibdoc.who.int/publications/2009/9789241597418_eng.pdf.
- Centers for Disease Control and Prevention . The Power of Prevention. Chronic Disease . . . The Public Health Challenge of the 21st Century 2009. www.cdc.gov/chronicdisease/pdf/2009-Power-of-Prevention.pdf.
- NHS Information Centre . Statistics on Obesity, Physical Activity and Diet: England, 2006 2006.
- Scottish Government . Preventing Overweight and Obesity in Scotland: A Route Map towards Healthy Weight 2010.
- Department of Health . Healthy Lives, Healthy People: Our Strategy for Public Health in England 2010. www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_127424.pdf.
- Public Health Agency of Canada . Integrated Strategy on Healthy Living and Chronic Disease 2005. www.phac-aspc.gc.ca/media/nr-rp/2005/2005_37bk1-eng.php.
- New Zealand Ministry of Health . New Zealand Health Strategy 2000. www.moh.govt.nz/moh.nsf/pagesmh/2285/$File/newzealandhealthstrategy.pdf.
- New Zealand Ministry of Health . Clearing the Smoke: A Five-Year Plan for Tobacco Control in New Zealand (2004–2009) 2004.
- New Zealand Ministry of Health . Healthy Eating – Healthy Action. Oranga Kai – Oranga Pumau: A Strategic Framework 2003 2003.
- Australian National Preventative Health Taskforce . Australia: The Healthiest Country by 2010 – National Preventative Health Strategy – the Roadmap for Action 2009.
- Busse R, Blümel M, Scheller-Kreinsen D, Zentner A. Tackling chronic disease in Europe: strategies, interventions and challenges. Geneva: World Health Organization; 2010.
- European Chronic Disease Alliance . A Unified Prevention Approach the Case for Urgent Political Action to Reduce the Social and Economic Burden of Chronic Disease through Prevention n.d.
- Australian Chronic Disease Prevention Alliance . Submission to National Preventative Health Taskforce 2008. www.cancer.org.au/File/ACDPA/ACDPA-NPHTF-final-submission.pdf (accessed 9 May 2012).
- National Institute for Health and Clinical Excellence (NICE) . Four Commonly Used Methods to Increase Physical Activity: Brief Interventions in Primary Care, Exercise Referral Schemes, Pedometers and Community-Based Exercise Programmes for Walking and Cycling 2006.
- White M, Carlin L, Rankin J. Effectiveness of interventions to promote healthy eating in people from minority ethnic groups: a review. London: Health Education Authority; 1998.
- Szczepura A. Nutrition in an ethnically diverse society: what are some of the key challenges?. Proc Nutr Soc 2011;70:252-62.
- Aspinall P. Enhancing the health promotion evidence base on minority ethnic groups, asylum seekers/refugees and gypsy travellers. Cardiff: Health ASERT Programme Wales, Welsh Assembly Government; 2006.
- National Institute for Health and Clinical Excellence (NICE) . Preventing Type 2 Diabetes: Population and Community-Level Interventions in High-Risk Groups and the General Population 2011.
- Department of Health . Be Active, Be Healthy: A Plan for Getting the Nation Moving 2009.
- Department of Health . At Least Five a Week: Evidence on the Impact of Physical Activity and Its Relationship to Health 2004.
- US Department of Health and Human Services . Healthy People 2010 2000;2.
- US Department of Health and Human Services . Healthy People 2020 – Framework. The Vision, Mission, and Goals of Healthy People 2020 2010. www.healthypeople.gov/2020/Consortium/HP2020Framework.pdf.
- Subcommittee on Cessation, Interagency Committee on Smoking and Health . Preventing 3 Million Premature Deaths, Helping 5 Million Smokers Quit, a National Action Plan for Tobacco Cessation 2003. www.ctri.wisc.edu/Researchers/NatActionPlan%2002-04.pdf.
- Frieden T, Mostashari F, Kerker B, Miller N, Hajat A, Frankel M. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002–2003. Am J Public Health 2005;95:1016-23.
- US Department of Health and Human Services . Treating Tobacco Use and Dependence: 2008 Update 2008.
- Centers for Disease Control and Prevention . Vital signs: current cigarette smoking among adults aged ≥ 18 years – United States, 2009. MMWR Morb Mortal Wkly Rep 2010;59:1135-40.
- Buchting FO. Lesbians, Gays, Bisexuals, and Transgenders of Color Sampling Methodology: Strategies for Collecting Data in Small, Hidden, or Hard-to-Reach Groups to Reduce Tobacco-Related Health Disparities 2009. http://dccps.nci.nih.gov/tcrb/trend/lgbt/docs/LGBTReport508.pdf.
- Crosier A, McNeill A. Mapping black and minority ethnic tobacco prevention resources. London: Health Development Agency; 2003.
- Rafnsson S, Bhopal R. Migrant and ethnic health research: report on the European public health association conference 2007. J R Inst Public Health 2008;122:532-4.
- Department of Health . Healthy Weight, Healthy Lives: Consumer Insight Summary 2008.
- Commission for Social Care Inspection . Putting People First: Equality and Diversity Matters 2 2008.
- Rooney LK, Bhopal R, Halani L, Levy ML, Partridge MR, Netuveli G, et al. Promoting recruitment of minority ethnic groups into research: qualitative study exploring the views of South Asian people with asthma. J Public Health 2011;33:604-15.
- Sheikh A. Recruitment of ethnic minorities to asthma studies. Thorax 2004;59.
- Bhopal R. Ethical issues in health research on ethnic minority populations: focusing on inclusion and exclusion. Res Ethics 2008;4:15-9.
- Bhopal R. Review of prevalence data and evaluation of methods for cross-cultural adaptation of UK surveys on tobacco and alcohol in ethnic minority groups. BMJ 2004;328:76-80.
- Rankin J, Bhopal R. Understanding of heart disease and diabetes in a South Asian community: cross sectional study testing the ‘snowball’ sample method. Public Health 2001;115:253-60.
- Pawson R, Tilley N. Realistic evaluation. London: Sage; 1997.
- National Institute for Health Research . INVOLVE: Supporting Public Involvement in NHS, Public Health and Social Care Research, Operational Plan, 2011–2012 2007. http://www.invo.org.uk/wp-content/uploads/2011/11/Final-Operational-Plan-2011-2012-April-2010-190511-040511.pdf.
- Rychetnik L, Wise M. Advocating evidence-based health promotion: reflections and a way forward. Health Promot Int 2004;19:247-57.
- Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health 2009;30:175-201.
- Rosen L, Manor O, Engelhard D, Zucker D. In defense of the randomized controlled trial for health promotion research. Am J Public Health 2006;96:1181-6.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:979-83.
- Bonell CP, Hargreaves J, Cousens S, Ross D, Hayes R, Petticrew M, et al. Alternatives to randomisation in the evaluation of public health interventions: design challenges and solutions. J Epidemiol Community Health 2009;65:582-7.
- Petticrew M. Why certain systematic reviews reach uncertain conclusions. BMJ 2003;326:756-8.
- National Institute for Health Research . About the HTA Programme 2010. www.hta.ac.uk/about/HTAaboutfinalleaflet.pdf.
- Tannahill A. Health promotion: the Tannahill model revisited. Public Health 2008;122:1387-91.
- National Institute for Health and Clinical Excellence (NICE) . Behaviour Change at Population, Community and Individual Levels 2007.
- Elford RW, MacMillan HL, Wathen CN. Counseling for risky health habits: a conceptual framework for primary care practitioners. London, ON: Canadian Task Force on Preventive Health Care (CTFPHC); 2001.
- Resnicow K, Robinson TN. School-based cardiovascular disease prevention studies: review and synthesis. Ann Epidemiol 1997;7:S14-31.
- McClure JB. Are biomarkers useful treatment aids for promoting health behavior change: an empirical review. Am J Prev Med 2002;22:200-7.
- Revere D, Dunbar PJ. Review of computer-generated outpatient health behavior interventions: clinical encounters ‘in absentia’. J Am Med Inform Assoc 2001;8:62-79.
- Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of web-based vs. non-web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res 2004;6.
- Hopkins DP, Briss PA, Ricard CJ, Husten CG, Carande-Kulis VG, Fielding JE, et al. Reviews of evidence regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. Am J Prev Med 2001;20.
- Friend K, Levy DT. Reductions in smoking prevalence and cigarette consumption associated with mass-media campaigns. Health Educ Res 2002;17:85-98.
- National Institute for Health and Clinical Excellence (NICE) . Smoking Cessation Services in Primary Care, Pharmacies, Local Authorities and Workplaces, Particularly for Manual Working Groups, Pregnant Women and Hard to Reach Communities 2008.
- Bala M, Strzeszynski L, Cahill K. Mass media interventions for smoking cessation in adults. Cochrane Database Syst Rev 2008;1.
- Kuhn M, Doucet C, Edwards N. Effectiveness of coalitions in heart health promotion, tobacco use reduction, and injury prevention: a systematic review of the literature 1990–1998. Dundas, ON: Ontario Ministry of Health, Region of Hamilton-Wentworth, Social and Public Health Services Division; 1999.
- Cahill K, Moher M, Lancaster T. Workplace interventions for smoking cessation. Cochrane Database Syst Rev 2008;4.
- Eriksen MP, Gottlieb NH. A review of the health impact of smoking control at the workplace. Am J Health Promot 1998;13:83-104.
- Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behavior: systematic review. BMJ 2002;325:188-91.
- Smedslund G, Fisher KJ, Boles SM, Lichtenstein E. The effectiveness of workplace smoking cessation programmes: a meta-analysis of recent studies. Tob Control 2004;13:197-204.
- National Institute for Health and Clinical Excellence (NICE) . Workplace Health Promotion: How to Help Employees to Stop Smoking 2007.
- Cohen D, Eliasson M, Eriksson C, Gilljam H, Hedin A, Hellnius M-L, et al. Smoking cessation methods. Stockholm: Swedish Council on Technology Assessment in Health Care (SBU); 1998.
- Mullen PD, Simons-Morton DG, Ramirez G, Frankowski RF, Green LW, Mains DA. A meta-analysis of trials evaluating patient education and counseling for three groups of preventive health behaviors. Patient Educ Couns 1997;32:157-73.
- Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev n.d.;2005.
- Van den Bruel A, Cleemput I, Van Linden A, Schoefs D, Ramaekers D, Bonneux L. Effectiveness and cost-effectiveness of treatments for smoking cessation. Brussels: Belgian Health Care Knowledge Centre (KCE); 2004.
- Manske S, Miller S, Moyer C, Phaneuf MR, Cameron RC. Best practice in group-based smoking cessation: results of a literature review applying effectiveness, plausibility, and practicality criteria. Am J Health Promot 2004;18:409-23.
- Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev 2005;2.
- Gorgojo Jimenez L, Gonzalez Enriquez J, Salvador Llivina T. Efficacy, Effectiveness and Cost-Effectiveness of Interventions for Smoking Cessation. IPE-03 40 (public Report) 2003.
- Pan W. Proactive telephone counseling as an adjunct to minimal intervention for smoking cessation: a meta-analysis. Health Educ Res 2006;21:416-27.
- Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev 2006;3.
- Scottish Intercollegiate Guidelines Network (SIGN) . Risk Estimation and the Prevention of Cardiovascular Disease. A National Clinical Guideline 2007.
- Ashenden R, Silagy C, Weller D. A systematic review of the effectiveness of promoting lifestyle change in general practice. Fam Pract 1997;14:160-75.
- National Institute for Health and Clinical Excellence (NICE) . Brief Interventions and Referral for Smoking Cessation in Primary Care and Other Settings 2006.
- Lancaster T, Stead LF. Self-help interventions for smoking cessation. Cochrane Database Syst Rev 2005;3.
- White A, Moody R. The effects of auricular acupuncture on smoking cessation may not depend on the point chosen: an exploratory meta-analysis. Acupunct Med 2006;24:149-56.
- Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D. ‘Cut down to quit’ with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis. Health Technol Assess 2008;12.
- Thorogood M, Hillsdon M, Summerbell C. Changing behaviour. Clin Evid 2006;8:203-19.
- Ritvo PG, Irvine MJ, Lindsay EA, Kraetschmer N, Blair N, Shnek ZM. A critical review of research related to family physician-assisted smoking cessation interventions. Cancer Prev Control 1997;1:289-303.
- Gorin SS, Heck JE. Meta-analysis of the efficacy of tobacco counseling by health care providers. Cancer Epidemiol Biomarkers Prev 2004;13:2012-22.
- Mojica WA, Suttorp MJ, Sherman SE, Morton SC, Roth EA, Maglione MA, et al. Smoking-cessation interventions by type of provider: a meta-analysis. Am J Prev Med 2004;26:391-40.
- Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev 2008;2.
- Law M, Tang JL. An analysis of the effectiveness of interventions intended to help people stop smoking. Arch Intern Med 1995;155:1933-41.
- Rice VH. Nursing intervention and smoking cessation: a meta-analysis. Heart Lung 1999;28:438-54.
- Rice VH, Stead LF. Nursing interventions for smoking cessation. Cochrane Database Syst Rev 2008;1.
- Brothwell DJ. Should the use of smoking cessation products be promoted by dental offices: an evidence-based report. J Can Dent Assoc 2001;67:149-55.
- Eisenberg MJ, Filion KB, Yavin D, Belisle P, Mottillo S, Joseph L, et al. Pharmacotherapies for smoking cessation: a meta-analysis of randomized controlled trials. Can Med Assoc J 2008;179:135-44.
- Ranney L, Melvin C, Lux L, McClain E, Morgan L, Lohr KN. Tobacco use: prevention, cessation, and control. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ); 2006.
- Stead LF, Perera R, Bullen C, Mant D, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev 2008;1.
- Etter JF, Stapleton JA. Nicotine replacement therapy for long-term smoking cessation: a meta-analysis. Tob Control 2006;15:280-5.
- Shiffman S, Ferguson SG. Nicotine patch therapy prior to quitting smoking: a meta-analysis. Addiction 2008;103:557-63.
- Hughes JR, Shiffman S, Callas P, Zhang J. A meta-analysis of the efficacy of over-the-counter nicotine replacement. Tob Control 2003;12:21-7.
- Woolacott NF, Jones L, Forbes CA, Mather LC, Sowden AJ, Song FJ, et al. The clinical effectiveness and cost-effectiveness of bupropion and nicotine replacement therapy for smoking cessation: a systematic review and economic evaluation. Health Technol Assess 2002;6.
- Wu P, Wilson K, Dimoulas P, Mills EJ. Effectiveness of smoking cessation therapies: a systematic review and meta-analysis. BMC Public Health 2006;6.
- Fiore MC, Smith SS, Jorenby DE, Baker TB. The effectiveness of the nicotine patch for smoking cessation: a meta-analysis. JAMA 1994;271:1940-7.
- Gourlay S. The pros and cons of transdermal nicotine therapy. Med J Aust 1994;160:152-9.
- Myung SK, Yoo KY, Oh SW, Park SH, Seo HG, Hwang SS, et al. Meta-analysis of studies investigating one-year effectiveness of transdermal nicotine patches for smoking cessation. Am J Health Syst Pharm 2007;64:2471-6.
- Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev 2007;1.
- Holmes S, Zwar N, Jimenez-Ruiz CA, Ryan PJ, Browning D, Bergmann L, et al. Bupropion as an aid to smoking cessation: a review of real-life effectiveness. Int J Clin Pract 2004;58:285-91.
- Wagena EJ, Knipschild P, Zeegers MP. Should nortriptyline be used as a first-line aid to help smokers quit: results from a systematic review and meta-analysis. Addiction 2005;100:317-26.
- National Institute for Health and Clinical Excellence (NICE) . Varenicline for Smoking Cessation 2007.
- Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst Rev 2008;1.
- Kerr JL, Timpe EM, Karpinski JP. Varenicline: a novel nicotinic receptor partial agonist for smoking cessation. J Pharm Technol 2007;23:23-9.
- Whittaker R, Borland R, Bullen C, Lin R, McRobbie H, Rodgers A. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev 2007;4.
- McRobbie H, Whittaker R, Bullen C. Using nicotine replacement therapy to assist in reducing cigarette consumption before quitting: another strategy for smoking cessation?. Dis Manag Health Outcomes 2006;14:335-40.
- White AR, Resch KL, Ernst E. A meta-analysis of acupuncture techniques for smoking cessation. Tob Control 1999;8:393-7.
- National Institute for Health and Clinical Excellence (NICE) . Promoting Physical Activity, Active Play and Sport for Pre-School and School-Age Children and Young People in Family, Pre-School, School and Community Settings 2009.
- National Institute for Health and Clinical Excellence (NICE) . Promoting and Creating Built or Natural Environments That Encourage and Support Physical Activity 2008.
- National Institute for Health and Clinical Excellence (NICE) . Obesity: Guidance on the Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children 2006.
- Foster C, Hillsdon M. Changing the environment to promote health-enhancing physical activity. J Sport Sci 2004;22:755-69.
- National Institute for Health and Clinical Excellence (NICE) . Workplace Health Promotion: How to Encourage Employees to Be Physically Active 2008.
- van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ 2007;335.
- Jago R, Baranowski T. Non-curricular approaches for increasing physical activity in youth: a review. Prev Med 2004;39:157-63.
- Brunton G, Harden A, Rees R, Kavanagh J, Oliver S, Oakley A. Children and physical activity: a systematic review of barriers and facilitators. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2003.
- Dobbins M, De Corby K, Robeson P, Husson H, Tirilis D. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6–18. Cochrane Database Syst Rev 2009;1.
- Dobbins M, Lockett D, Michel I, Beyers J, Feldman L, Vohra J, et al. The effectiveness of school-based interventions in promoting physical activity and fitness among children and youth: a systematic review. Ottawa: Health Canada; 2001.
- Morgan O. Approaches to increase physical activity: reviewing the evidence for exercise-referral schemes. Public Health 2005;119:361-70.
- Wilcox S, Parra-Medina D, Thompson-Robinson M, Will J. Nutrition and physical activity interventions to reduce cardiovascular disease risk in health care settings: a quantitative review with a focus on women. Nutr Rev 2001;59:197-214.
- Eakin EG, Glasgow RE, Riley KM. Review of primary care-based physical activity intervention studies: effectiveness and implications for practice and future research. J Fam Pract 2000;49:158-68.
- Proper KI, Koning M, van der Beek AJ, Hildebrandt VH, Bosscher RJ, van Mechelen W. The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med 2003;13:106-17.
- Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change: a systematic review. Am J Prev Med 2007;32:419-34.
- Williams DM, Matthews CE, Rutt C, Napolitano MA, Marcus BH. Interventions to increase walking behavior. Med Sci Sport Exerc 2008;40:S567-73.
- Breckon JD, Johnston LH, Hutchison A. Physical activity counseling content and competency: a systematic review. J Phys Act Health 2008;5:398-417.
- Müller-Riemenschneider F, Reinhold T, Nocon M, Willich SN. Long-term effectiveness of interventions promoting physical activity: a systematic review. Prev Med 2008;47:354-68.
- Petrella RJ, Lattanzio CN. Does counseling help patients get active: systematic review of the literature. Can Fam Physician 2002;48:72-80.
- Stensel D. Primary prevention of CVD: physical activity. Clin Evid 2009;6.
- Sorensen JB, Skovgaard T, Puggaard L. Exercise on prescription in general practice: a systematic review. Scand J Prim Health Care 2006;24:69-74.
- Hillsdon M, Thorogood M, Anstiss T, Morris J. Randomised controlled trials of physical activity promotion in free living populations: a review. J Epidemiol Community Health 1995;49:448-53.
- Hillsdon M, Thorogood M. A systematic review of physical activity promotion strategies. Br J Sport Med 1996;30:84-9.
- Williams N, Hendry M, France B, Lewis R, Wilkinson C. Effectiveness of exercise-referral schemes to promote physical activity in adults: systematic review. Br J Gen Pract 2007;57:979-86.
- Adams J, White M. Are activity promotion interventions based on the transtheoretical model effective: a critical review. Br J Sport Med 2003;37:106-14.
- Ogilvie D, Egan M, Hamilton V, Petticrew M. Promoting walking and cycling as an alternative to using cars: a systematic review. BMJ 2004;329:763-6.
- Clemmens D, Hayman LL. Increasing activity to reduce obesity in adolescent girls: a research review. J Obstet Gynecol Neonatal Nurs 2004;33:801-8.
- Dishman RK, Buckworth J. Increasing physical activity: a quantitative synthesis. Med Sci Sport Exerc 1996;28:706-19.
- Scottish Intercollegiate Guidelines Network (SIGN) . Management of Obesity in Children and Young People. A National Clinical Guideline 2003.
- Swedish Council on Technology Assessment in Health Care . Methods of Promoting Physical Activity – a Systematic Review 2007.
- Ogilvie D, Foster CE, Rothnie H, Cavill N, Hamilton V, Fitzsimons CF, et al. Interventions to promote walking: systematic review. BMJ 2007;334.
- van der Bij AK, Laurant MG, Wensing M. Effectiveness of physical activity interventions for older adults: a review. Am J Prev Med 2002;22:120-33.
- Foster C, Hillsdon M, Thorogood M. Interventions for promoting physical activity. Cochrane Database Syst Rev 2005;1.
- van den Berg MH, Schoones JW, Vliet Vlieland TP. Internet-based physical activity interventions: a systematic review of the literature. J Med Internet Res 2007;9.
- Vandelanotte C, Spathonis KM, Eakin EG, Owen N. Website-delivered physical activity interventions: a review of the literature. Am J Prev Med 2007;33:54-6.
- Kroeze W, Werkman A, Brug J. A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviours. Ann Behav Med 2006;31:205-23.
- Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, et al. Using pedometers to increase physical activity and improve health: a systematic review. JAMA 2007;298:2296-304.
- DeMattia L, Lemont L, Meurer L. Do interventions to limit sedentary behaviours change behaviour and reduce childhood obesity: a critical review of the literature. Obes Rev 2007;8:69-81.
- Salmon J, Booth ML, Phongsavan P, Murphy N, Timperio A. Promoting physical activity participation among children and adolescents. Epidemiol Rev 2007;29:144-59.
- Blue CL, Black DR. Synthesis of intervention research to modify physical activity and dietary behaviors. Res Theory Nurs Pract 2005;19:25-61.
- Kamath CC, Vickers KS, Ehrlich A, McGovern L, Johnson J, Singhal V, et al. Behavioral interventions to prevent childhood obesity: a systematic review and metaanalyses of randomized trials. J Clin Endocrinol Metab 2008;93:4606-15.
- Shilts MK, Horowitz M, Townsend MS. Goal setting as a strategy for dietary and physical activity behavior change: a review of the literature. Am J Health Promot 2004;19:81-93.
- Thomas H, Ciliska D, Micucci S, Wilson-Abra J, Dobbins M. Effectiveness of physical activity enhancement and obesity prevention programs in children and youth. Hamilton, ON: Effective Public Health Practice Project; 2004.
- Holtzman J, Schmitz K, Babes G, Kane RL, Duval S, Wilt TJ, et al. Effectiveness of behavioral interventions to modify physical activity behaviors in general populations and cancer patients and survivors. Rockville, MD: Agency for Healthcare Research and Quality; 2004.
- Seymour JD, Lazarus Yaroch A, Serdula M, Blanck HM, Khan LK. Impact of nutrition environmental interventions on point-of-purchase behavior in adults: a review. Prev Med 2004;39:S108-36.
- Faith MS, Fontaine KR, Baskin ML, Allison DB. Toward the reduction of population obesity: macrolevel environmental approaches to the problems of food, eating, and obesity. Psychol Bull 2007;133:205-26.
- Contento I, Balch GI, Bronner YL, Lytle LA, Maloney SK, Olson CM, et al. The effectiveness of nutrition education and implications for nutrition education policy, programs, and research: a review of research. J Nutr Educ 1995;27:277-418.
- Howerton MW, Bell BS, Dodd KW, Berrigan D, Stolzenberg-Solomon R, Nebeling L. School-based nutrition programs produced a moderate increase in fruit and vegetable consumption: meta and pooling analyses from 7 studies. J Nutr Educ Behav 2007;39:186-96.
- Knai C, Pomerleau J, Lock K, McKee M. Getting children to eat more fruit and vegetables: a systematic review. Prev Med 2006;42:85-9.
- McArthur DB. Heart healthy eating behaviors of children following a school-based intervention: a meta-analysis. Issues Compr Pediatr Nurs 1998;21:35-48.
- Roe L, Hunt P, Bradshaw H, Rayner M. Health promotion interventions to promote healthy eating in the general population: a review. London: Health Education Authority; 1997.
- Thomas J, Sutcliffe K, Harden A, Oakley A, Oliver S, Rees R, et al. Children and healthy eating: a systematic review of barriers and facilitators. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2003.
- Shepherd J, Harden A, Rees R, Brunton G, Garcia J, Oliver S, et al. Young people and healthy eating: a systematic review of research on barriers and facilitators. London: EPPI-Centre Report, Social Science Research Unit, Institute of Education, University of London; 2001.
- Engbers LH, van Poppel MN, Chin A Paw MJ, van Mechelen W. Worksite health promotion programs with environmental changes: a systematic review. Am J Prev Med 2005;29:61-70.
- Thorogood M, Simera I, Dowler E, Summerbell C, Brunner E. A systematic review of population and community dietary interventions to prevent cancer. Nutr Res Rev 2007;20:74-88.
- Coruh B, Ayele H, Pugh M, Mulligan T. Does religious activity improve health outcomes: a critical review of the recent literature. Explore 2005;1:186-91.
- Pomerleau J, Lock K, Knai C, McKee M. Interventions designed to increase adult fruit and vegetable intake can be effective: a systematic review of the literature. J Nutr 2005;135:2486-95.
- Ammerman A, Lindquist C, Hersey J, Jackman AM, Gavin NI, Garces C, et al. The Efficacy of Interventions to Modify Dietary Behavior Related to Cancer Risk. Volume 1: Evidence Report and Appendices 2001.
- Ammerman A, Pignone M, Fernandez L, Lohr K, Jacobs AD, Nester C, et al. Counseling to promote a healthy diet. Rockville, MD: Agency for Healthcare Research and Quality; 2002.
- VanWormer JJ, Boucher JL, Pronk NP. Telephone-based counseling improves dietary fat, fruit, and vegetable consumption: a best-evidence synthesis. J Am Diet Assoc 2006;106:1434-44.
- Brunner E, Rees K, Ward K, Burke M, Torogood M. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst Rev 2007;17.
- Ciliska D, Miles E, O’Brien MA, Turl C, Tomasik HH, Donovan U, et al. The effectiveness of community interventions to increase fruit and vegetable consumption in people four years of age and older. J Nutr Educ Behav 2000;32:341-52.
- Brunner E, White I, Thorogood M, Bristow A, Curle D, Marmot M. Can dietary interventions change diet and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Am J Public Health 1997;87:1415-22.
- VanWormer JJ, Boucher JL. Motivational interviewing and diet modification: a review of the evidence. Diabetes Educ 2004;30:404-16.
- Scottish Intercollegiate Guidelines Network (SIGN) . Obesity in Scotland. Integrating Prevention With Weight Management 1996.
- Wall J, Mhurchu CN, Blakely T, Rodgers A, Wilton J. Effectiveness of monetary incentives in modifying dietary behavior: a review of randomized, controlled trials. Nutr Rev 2006;64:518-31.
- Jepson RG, Harris FM, Platt S, Tannahill C. The effectiveness of interventions to change six health behaviours: a review of reviews. BMC Public Health 2010;10.
- Canadian Agency for Drugs and Technologies in Health . Nicotine Vaccines for Smoking Cessation 2007.
- Etter JF. Cytisine for smoking cessation: a literature review and a meta-analysis. Arch Intern Med 2006;166:1553-9.
- Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med 2007;33:336-45.
- Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. Clinical counseling and physical activity. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ); 2002.
- Scottish Intercollegiate Guidelines Network (SIGN) . Management of Obesity 2010.
- Johnson M, Everson-Hock E, Jones R, Woods HB, Baxter S, Goyder E, et al. Prevention of type 2 diabetes: interventions to reduce risk factors for pre-diabetes among UK adults from black and minority ethnic groups. Sheffield: ScHARR Public Health Collaborating Centre; 2010.
- Banks-Wallace J, Conn V. Interventions to promote physical activity among African American women. Public Health Nurs 2002;19:321-35.
- Webb MS. Treating tobacco dependence among African Americans: a meta-analytic review. Health Psychol 2008;27:S271-82.
- Armstrong R, Waters E. Guidelines for systematic reviews of health promotion and public health interventions. Australia: Melbourne University; 2007.
- NHS Solutions for Public Health . Critical Appraisal Skills Programme Tool for Systematic Reviews n.d. www.sph.nhs.uk/what-we-do/public-health-workforce/resources/critical-appraisals-skills-programme.
- Effective Public Health Practice Project (EPHPP) . Quality Assessment Tool for Quantitative Studies n.d. www.ephpp.ca/Tools.html.
- NHS Solutions for Public Health . Critical Appraisal Skills Programme Tool for Qualitative Studies n.d. www.sph.nhs.uk/what-we-do/public-health-workforce/resources/critical-appraisals-skills-programme.
- Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annu Rev Public Health 2010;31:399-418.
- Alderson P. The importance of theories in health care. BMJ 1998;317:1007-10.
- Painter J, Borba C, Hynes M, Mays D, Glanz K. The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med 2008;35.
- Davis N, Clance P, Gailis A. Treatment approaches for obese and overweight African American women: a consideration of cultural dimensions. Psychotherapy 1999;36:27-35.
- Airhihenbuwa CO. Health promotion and the discourse on culture: implications for empowerment. Health Educ Q 1994;21:345-53.
- Freire P. Education for critical consciousness. London: Continuum; 1973.
- Hugo J. A grading model for media appropriateness and cultural sensitivity in health education. J Audiov Media Med 2000;23:103-9.
- Davis R, Cook D, Cohen L. A community resilience approach to reducing ethnic and racial disparities in health. Am J Public Health 2005;95:2168-73.
- Ashley M, Huff R, Kline M. Promoting health in multicultural populations: a handbook for practitioners. Thousand Oaks, CA: Sage; 1999.
- Bandura. A. Social learning theory. Englewood Cliffs, NJ: Prentice Hall; 1977.
- Ajzen I. The theory of planned behaviour. Organ Behav Hum Decis Process 1991;50:179-211.
- James DC. Factors influencing food choices, dietary intake, and nutrition-related attitudes among African Americans: application of a culturally sensitive model. Ethn Health 2004;9:349-67.
- Fitzgibbon ML, Sánchez-Johnsen L, Camic PM, Knight S. Clinical handbook of health psychology. Seattle, WA: Hogrefe & Huber; 2004.
- Prochaska JD, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol 1992;47:1102-14.
- Keller CS, Gonzales A, Fleuriet KJ. Retention of minority participants in clinical research studies. Western J Nurs Res 2005;27:292-306.
- Hazuda HP, Gerety M, Williams JW, Lawrence V, Calmbach W, Mulrow C, et al. Recruitment and retention in minority populations. New York, NY: Springer; 2000.
- Levkoff SE, Prohaska TR, Weitzman PF, Ory MG. Recruitment and retention in minority populations. New York, NY: Springer; 2000.
- Sorensen G, Emmons K, Hunt MK, Barbeau E, Goldman R, Peterson K, et al. Model for incorporating social context in health behavior interventions: applications for cancer prevention for working-class, multiethnic populations. Prev Med 2003;37:188-97.
- Appel SJ, Giger JN, Davidhizar RE. Opportunity cost: the impact of contextual risk factors on the cardiovascular health of low-income rural southern African American women [reprint in J Natl Black Nurses Assoc 2008; 19: 42–51]. J Cardiovasc Nurs 2005;20:315-24.
- Burnet D, Plaut A, Courtney R, Chin MH. A practical model for preventing type 2 diabetes in minority youth. Diabetes Educ 2002;28:779-95.
- Rosenstock I. Historical origins of the health belief model. Health Educ Q 1974;2:328-35.
- Ajzen I, Kuhl J, Beckman J. Action control: from cognition to behavior. New York, NY: Springer-Verlag; 1985.
- McLeroy K, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q 1988;15:351-77.
- Brofenbrenner U. Toward an experimental ecology of human development. Am Psychol 1977;32:513-31.
- Chen MS, Tang H. Review of smoking cessation research among Asian Americans: the state of the research. Nicotine Tob Res 2007;9.
- Whitt-Glover MC, Kumanyika SK. Systematic review of interventions to increase physical activity and physical fitness in African-Americans. Am J Health Promot 2009;23:S33-56.
- Hudson CE. An integrative review of obesity prevention in African American children. Issues Compr Pediatr Nurs 2008;31:147-70.
- Hawthorne K, Robles Y, Cannings-John R, Edwards AG. Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database Syst Rev 2008;3.
- Shaya FT, Gu A, Saunders E. Addressing cardiovascular disparities through community interventions. Ethn Dis 2006;16:138-44.
- White MA, Martin PD, Newton RL, Walden HM, York-Crowe EE, Gordon ST, et al. Mediators of weight loss in a family-based intervention presented over the internet. Obes Res 2004;12:1050-9.
- Williamson DA, Martin PD, White MA, Newton R, Walden H, York-Crowe, et al. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eat Weight Disord 2005;10:193-20.
- Williamson DA, Walden HM, White MA, York-Crowe E, Newton RL, Alfonso A, et al. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity 2006;14:1231-43.
- Guerin PB, Diiriye RO, Corrigan C, Guerin B. Physical activity programs for refugee Somali women: working out in a new country. Women Health 2003;38:83-99.
- Resnicow K, Yaroch AL, Davis A, Wang DT, Carter S, Slaughter L, et al. GO GIRLS!: results from a nutrition and physical activity program for low-income, overweight African American adolescent females. Health Educ Behav 2000;27:616-31.
- Huhman M, Potter LD, Wong FL, Banspach SW, Duke JC, Heitzler CD. Effects of a mass media campaign to increase physical activity among children: year-1 results of the VERB campaign. Pediatrics 2005;116:e277-84.
- Huhman ME, Potter LD, Duke JC, Judkins DR, Heitzler CD, Wong FL. Evaluation of a national physical activity intervention for children: VERB campaign, 2002–2004 [erratum appears in Am J Prev Med 2007; 32: 455]. Am J Prev Med 2007;32:38-43.
- Huhman M, Berkowitz J, Wong F, Prosper E, Gray M, Prince D, et al. The VERB campaign’s strategy for reaching African-American, Hispanic, Asian, and American Indian children and parents. Am J Prev Med 2008;34:S194-209.
- Plescia M, Herrick H, Chavis L. Improving health behaviors in an African American community: the Charlotte Racial and Ethnic Approaches to Community Health project. Am J Public Health 2008;98:1678-84.
- DeBate R, Plescia M, Joyner D, Spann L. A qualitative assessment of Charlotte REACH: an ecological perspective for decreasing CVD and diabetes among African Americans. Ethn Dis 2004;14:S77-82.
- Two Feathers J, Kieffer EC, Palmisano G, Anderson M, Janz N, Spencer MS, et al. The development, implementation, and process evaluation of the REACH Detroit partnership’s diabetes lifestyle intervention. Diabetes Educ 2007;33:509-20.
- Two Feathers J, Kieffer EC, Palmisano G, Anderson M, Sinco B, Janz N, et al. Racial and Ethnic Approaches to Community Health (REACH) Detroit partnership: improving diabetes-related outcomes among African American and Latino adults. Am J Public Health 2005;95:1552-60.
- Thrasher JF, Campbell MK, Oates V. Behavior-specific social support for healthy behaviors among African American church members: applying optimal matching theory. Health Educ Behav 2004;31:193-205.
- Kreuter MW, Sugg-Skinner C, Holt CL, Clark EM, Haire-Joshu D, Fu Q, et al. Cultural tailoring for mammography and fruit and vegetable intake among low-income African-American women in urban public health centers. Prev Med 2005;41:53-62.
- Resnicow K, Jackson A, Blissett D, Wang T, McCarty F, Rahotep S, et al. Results of the Healthy Body Healthy Spirit trial. Health Psychol 2005;24:339-48.
- Resnicow K, Jackson A, Braithwaite R, Dilorio C, Blisset D, Rahotep S, et al. Healthy Body/Healthy Spirit: a church-based nutrition and physical activity intervention. Health Educ Res 2002;17:562-73.
- Resnicow K, Davis R, Zhang N, Tolsma D, Alexander G, Wiese C, et al. Tailoring a fruit and vegetable intervention on ethnic identity: results of a randomized study. Health Psychol 2009;28:394-403.
- Williams A, Mason A, Wold J. Cultural sensitivity and day care workers. Examination of a worksite based cardiovascular disease prevention project. AAOHN J 2001;49:35-43.
- Auslander W, Haire-Joshu D, Houston C, Rhee CW, Williams JH. A controlled evaluation of staging dietary patterns to reduce the risk of diabetes in African-American women. Diabetes Care 2002;25:809-14.
- Campbell MK, James A, Hudson MA, Carr C, Jackson E, Oakes V, et al. Improving multiple behaviors for colorectal cancer prevention among African American church members. Health Psychol 2004;23:492-50.
- Voorhees CC, Stillman FA, Swank RT, Heagerty PJ, Levine DM, Becker DM. Heart, body, and soul: impact of church-based smoking cessation interventions on readiness to quit. Prev Med 1996;25:277-85.
- Stillman FA, Bone LR, Rand C, Levine DM, Becker DM. Heart, body, and soul: a church-based smoking-cessation program for urban African Americans. Prev Med 1993;22:335-49.
- Carroll R, Ali N, Azam N. Promoting physical activity in South Asian Muslim women through ‘exercise on prescription’. Health Technol Assess 2002;6.
- Haire-Joshu D, Brownson RC, Nanney MS, Houston C, Steger-May K, Schechtman K, et al. Improving dietary behavior in African Americans: the Parents as Teachers High 5, Low Fat Program. Prev Med 2003;36:684-91.
- Haire-Joshu D, Brownson RC, Schechtman K, Nanney MS, Houston C, Auslander W. A community research partnership to improve the diet of African Americans. Am J Health Behav 2001;25:140-6.
- Eyler AA, Haire-Joshu D, Brownson RC, Nanney MS. Correlates of fat intake among urban, low income African Americans. Am J Health Behav 2004;28:410-17.
- Boyd NR, Sutton C, Orleans CT, McClatchey MW, Bingler R, Fleisher L, et al. Quit Today! A targeted communications campaign to increase use of the cancer information service by African American smokers. Prev Med 1998;27:S50-60.
- Williams J, Auslander WF, de Groot M, Robinson AD, Houston C, Haire-Joshu D. Cultural relevancy of a diabetes prevention nutrition program for African American women. Health Promot Pract 2006;7:56-67.
- Whitt-Glover MC, Hogan PE, Lang W, Heil DP. Pilot study of a faith-based physical activity program among sedentary blacks. Prev Chronic Dis 2008;5.
- Anderson RM, Funnell MM, Nwankwo R, Gillard M, Oh M, Fitzgerald JT. Evaluating a problem-based empowerment program for African Americans with diabetes: results of a randomized controlled trial. Ethn Dis 2005;15:671-8.
- Shaw-Perry M, Horner C, Trevino RP, Sosa ET, Hernandez I, Bhardwaj A. NEEMA: a school-based diabetes risk prevention program designed for African-American children. J Natl Med Assoc 2007;99:368-75.
- Rimmer JH, Silverman K, Braunschweig C, Quinn L, Liu Y. Feasibility of a health promotion intervention for a group of predominantly African American women with type 2 diabetes. Diabetes Educ 2002;28:571-80.
- Nothwehr FK, Guare J, Marrero DG, Hoen H. Sequencing diet and exercise programs for African American women with diabetes. Diabetes Educ 2001;27:245-51.
- Cullen KW, Thompson D. Feasibility of an 8-week African American web-based pilot program promoting healthy eating behaviors: Family Eats. Am J Health Behav 2008;32:40-51.
- Kennedy BM, Newton RL, York-Crowe E, Walden HM, Ryan DH, White MA, et al. Recruiting African American girls and parents for a secondary weight gain prevention study. J Cult Divers 2008;15:181-6.
- Shankar S, Klassen AC, Garrett-Mayer E, Houts PS, Wange T, McCarthy M, et al. Evaluation of a nutrition education intervention for women residents of Washington,DC, public housing communities. Health Educ Res 2007;22:425-37.
- Klassen AC, Garrett-Mayer E, Houts PS, Shankar S, Torio CM. The relationship of body size to participation and success in a fruits and vegetables intervention among low-income women. J Community Health 2008;33:78-89.
- Befort CA, Nollen N, Ellerbeck EF, Sullivan DK, Thomas JL, Ahluwalia JS. Motivational interviewing fails to improve outcomes of a behavioral weight loss program for obese African American women: a pilot randomized trial. J Behav Med 2008;31:367-77.
- Lasco RA, Curry RH, Dickson VJ, Powers J, Menes S, Merritt RK. Participation rates, weight loss, and blood pressure changes among obese women in a nutrition-exercise program. Public Health Rep 1989;104:640-6.
- Engels HJ, Gretebeck RJ, Gretebeck KA, Jimenez L. Promoting healthful diets and exercise: efficacy of a 12-week after-school program in urban African Americans. J Am Diet Assoc 2005;105:455-9.
- Campbell MK, Demark-Wahnefried W, Symons M, Kalsbeek WD, Dodds J, Cowan A, et al. Fruit and vegetable consumption and prevention of cancer: the Black Churches United for Better Health project. Am J Public Health 1999;89:1390-6.
- Baranowski T, Simons-Morton B, Hooks P, Henske J, Tiernan K, Dunn JK, et al. A center-based program for exercise change among black-American families. Health Educ Q 1990;17:179-96.
- Baranowski T, Henske J, Simons-Morton B, Palmer J, Tiernan K, Hooks PC, et al. Dietary change for cardiovascular disease prevention among black-American families. Health Educ Res 1990;5:433-43.
- Ard JD, Rosati R, Oddone EZ. Culturally-sensitive weight loss program produces significant reduction in weight, blood pressure, and cholesterol in eight weeks. J Natl Med Assoc 2000;92:515-23.
- Resnicow K, Taylor R, Baskin M, McCarty F. Results of Go Girls: a weight control program for overweight African-American adolescent females. Obes Res 2005;13:1739-48.
- Resnicow K, Jackson A, Wang T, De AK, McCarty F, Dudley WN, et al. A motivational interviewing intervention to increase fruit and vegetable intake through Black churches: results of the Eat for Life trial. Am J Public Health 2001;91:1686-93.
- Campbell MK, Bernhardt JM, Waldmiller M, Jackson B, Potenziani D, Weathers B. Varying the message source in computer-tailored nutrition education. Patient Educ Couns 1999;36:157-69.
- Anderson CAM, Kumanyika SK, Shults J, Kallan MJ, Gans KM, Risica PM. Assessing change in dietary-fat behaviors in a weight-loss program for African Americans: a potential short method. J Am Diet Assoc 2007;107:838-42.
- Kumanyika SK, Shults J, Fassbender J, Whitt MC, Brake V, Kallan MJ, et al. Outpatient weight management in African-Americans: the Healthy Eating and Lifestyle Program (HELP) study [erratum appears in Prev Med 2006; 42: 397]. Prev Med 2005;41:488-502.
- Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis 2003;13:S65-77.
- Robinson TN, Kraemer HC, Matheson DM, Obarzanek E, Wilson DM, Haskell WL, et al. Stanford GEMS phase 2 obesity prevention trial for low-income African-American girls: design and sample baseline characteristics. Contemp Clin Trials 2008;29:56-69.
- D’Eramo-Melkus G, Spollett G, Jefferson V, Chyun D, Tuohy B, Robinson T, et al. A culturally competent intervention of education and care for black women with type 2 diabetes. Appl Nurs Res 2004;17:10-2.
- Fang CY, Ma GX, Miller SM, Tan Y, Su X, Shive S. A brief smoking cessation intervention for Chinese and Korean American smokers. Prev Med 2006;43:321-4.
- Royce JM, Ashford A, Resnicow K, Freeman HP, Caesar AA, Orlandi MA. Physician- and nurse-assisted smoking cessation in Harlem. J Natl Med Assoc 1995;87:291-300.
- Davis-Smith YM, Davis-Smith M, Boltri JM, Seale JP, Shellenberger S, Blalock T, et al. Implementing a diabetes prevention program in a rural African-American church. J Natl Med Assoc 2007;99:440-6.
- Resnicow K, Wallace DC, Jackson A, Digirolamo A, Odom E, Wang T, et al. Dietary change through African American churches: baseline results and program description of the Eat for Life trial. J Cancer Educ 2000;15:156-63.
- Kumanyika SK, Charleston JB. Lose weight and win: a church-based weight loss program for blood pressure control among black women. Patient Educ Couns 1992;19:19-32.
- Frenn M, Malin S, Bansal N, Delgado M, Greer Y, Havice M, et al. Addressing health disparities in middle school students’ nutrition and exercise. J Community Health Nurs 2003;20:1-14.
- Yancey AK, McCarthy WJ, Harrison GG, Wong WK, Siegel JM, Leslie J. Challenges in improving fitness: results of a community-based, randomized, controlled lifestyle change intervention. J Womens Health 2006;15:412-29.
- Yancey AK, Miles OL, McCarthy WJ, Sandoval G, Hill J, Leslie JJ, et al. Differential response to targeted recruitment strategies to fitness promotion research by African-American women of varying body mass index. Ethn Dis 2001;11:115-23.
- McCarthy WJ, Yancey AK, Harrison GG, Leslie J, Siegel JM. Fighting cancer with fitness: dietary outcomes of a randomized, controlled lifestyle change intervention in healthy African-American women. Prev Med 2007;44:246-53.
- Nollen N, Ahluwalia JS, Mayo MS, Richter K, Choi WS, Okuyemi KS, et al. A randomized trial of targeted educational materials for smoking cessation in African Americans using transdermal nicotine. Health Educ Behav 2007;34:911-27.
- Harris K, Okuyemi K, Catley D, Mayo MS, Ge B, Ahluwalia JS. Predictors of smoking cessation among African-Americans enrolled in a randomized controlled trial of bupropion. Prev Med 2004;38:498-502.
- Manning BK, Catley D, Harris KJ, Mayo MS, Ahluwalia JS. Stress and quitting among African American smokers. J Behav Med 2005;28:325-33.
- Harris KJ, Ahluwalia JS, Catley D, Okuyemi KS, Mayo MS, Resnicow K. Successful recruitment of minorities into clinical trials: the Kick It at Swope project. Nicotine Tob Res 2003;5:575-84.
- Ahluwalia J, Harris K, Catley D, Okuyemi KS, Mayo MS. Sustained-release bupropion for smoking cessation in African Americans: a randomized controlled trial. JAMA 2002;288:468-74.
- Wang C-Y, Chan SMA. Culturally tailored diabetes education program for Chinese Americans: a pilot study. Nurs Res 2005;54:347-53.
- Orleans C, Boyd N, Bingler R, Sutton C, Fairclough D, Heller D, et al. A self-help intervention for African American smokers: tailoring cancer information service counseling for a special population. Prev Med 1998;27:S61-70.
- Ard JD, Kumanyika S, Stevens VJ, Vollmer WM, Samuel-Hodge C, Kennedy B, et al. Effect of group racial composition on weight loss in African Americans. Obesity 2008;16:306-10.
- Ma GX, Shive SE, Tan Y, Thomas P, Man VL. Development of a culturally appropriate smoking cessation program for Chinese-American youth. J Adolesc Health 2004;35:206-16.
- Newton RL, Perri MG. A randomized pilot trial of exercise promotion in sedentary African-American adults. Ethn Dis 2004;14:548-57.
- Webb MS. Does one size fit all African American smokers? The moderating role of acculturation in culturally specific interventions. Psychol Addict Behav 2008;22:592-6.
- Yanek L, Becker D, Moy T, Gittelsohn J, Koffman DM. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep 2001;116:68-81.
- Fitzgibbon ML, Stolley MR, Ganschow P, Schiffer L, Wells A, Simon N, et al. Results of a faith-based weight loss intervention for black women. J Natl Med Assoc 2005;97:1393-402.
- Djuric Z, Mirasolo J, Kimbrough L, Brown DR, Heilbrun LK, Canar L, et al. A pilot trial of spirituality counseling for weight loss maintenance in African American breast cancer survivors. J Natl Med Assoc 2009;101:552-64.
- Ahluwalia J, McNagny S, Clark W. Smoking cessation among inner-city African Americans using the nicotine transdermal patch. J Gen Intern Med 1998;13:1-8.
- Ahluwalia JS, Resnicow K, Clark WS. Knowledge about smoking, reasons for smoking, and reasons for wishing to quit in inner-city African Americans. Ethn Dis 1998;8:385-93.
- Li VC, Coates TJ, Spielberg LA, Ewart CK, Dorfman S, Huster WJ. Smoking cessation with young women in public family planning clinics: the impact of physician messages and waiting room media. Prev Med 1984;13:477-89.
- Lipkus IM, Lyna PR, Rimer BK. Using tailored interventions to enhance smoking cessation among African-Americans at a community health center. Nicotine Tob Res 1999;1:77-85.
- Thompson D, Baranowski T, Cullen K, Watson K, Liu Y, Canada A, et al. Food, fun, and fitness internet program for girls: pilot evaluation of an e-Health youth obesity prevention program examining predictors of obesity. Prev Med 2008;47:494-7.
- Thompson D, Baranowski T, Cullen K, Watson K, Canada A, Bhatt R, et al. Food, fun and fitness internet program for girls: influencing log-on rate. Health Educ Res 2008;23:228-37.
- Ahluwalia JS, Okuyemi K, Nollen N, Choi WS, Kaur H, Pulvers K, et al. The effects of nicotine gum and counseling among African American light smokers: a 2 × 2 factorial design. Addiction 2006;101.
- Nollen NL, Mayo MS, Sanderson Cox L, Okuyemi KS, Choi WS, Kaur H, et al. Predictors of quitting among African American light smokers enrolled in a randomized, placebo-controlled trial. J Gen Intern Med 2006;21:590-5.
- Okuyemi KS, Cox LS, Nollen NL, Snow TM, Kaur H, Choi W, et al. Baseline characteristics and recruitment strategies in a randomized clinical trial of African-American light smokers. Am J Health Promot 2007;21:183-91.
- Okuyemi KS, Faseru B, Sanderson Cox L, Bronars CA, Ahluwalia JS. Relationship between menthol cigarettes and smoking cessation among African American light smokers. Addiction 2007;102:1979-86.
- Fitzgibbon ML, Stolley M, Schiffer L, Sharp LK, Singh V, Van Horn L, et al. Obesity Reduction Black Intervention Trial (ORBIT): design and baseline characteristics. J Womens Health 2008;17:1099-110.
- Stolley MR, Fitzgibbon ML, Schiffer L, Sharp LK, Singh V, Van Horn L, et al. Obesity Reduction Black Intervention Trial (ORBIT): six-month results. Obesity 2009;17:100-6.
- Sharp LK, Fitzgibbon ML, Schiffer L. Recruitment of obese black women into a physical activity and nutrition intervention trial. J Phys Act Health 2008;5:870-81.
- Netto G, McCloughan L, Bhatnagar A. Effective heart disease prevention: lessons from a qualitative study of user perspectives in Bangladeshi, Indian and Pakistani communities. Public Health 2007;121:177-86.
- Mathews G, Alexander J, Rahemtulla T, Bhopal R. Impact of a cardiovascular risk control project for South Asians (Khush Dil) on motivation, behaviour, obesity, blood pressure and lipids. J Public Health 2007;29:388-97.
- Farooqi A, Bhavsar M. Project Dil: a co-ordinated primary care and community health promotion programme for reducing risk factors of coronary heart disease amongst the South Asian community of Leicester – experiences and evaluation of the project. Ethn Health 2001;6:265-70.
- Anderson-Loftin W, Barnett S, Bunn P, Sullivan P, Hussey J, Tavakoli A. Soul food light: culturally competent diabetes education. Diabetes Educ 2005;31:555-63.
- Agurs-Collins TD, Kumanyika SK, Ten Have TR, Adams-Campbell LL. A randomized controlled trial of weight reduction and exercise for diabetes management in older African-American subjects. Diabetes Care 1997;20:1503-11.
- Atkinson MJ, Boltri JM, Davis-Smith M, Seale JP, Shellenberger S, Gonsalves D. A qualitative inquiry into the community and programmatic dimensions associated with successful implementation of church-based diabetes prevention programs. J Public Health Manag Pract 2009;15:264-73.
- McBride CM, Bepler G, Lipkus IM, Lyna P, Samsa G, Albright J, et al. Incorporating genetic susceptibility feedback into a smoking cessation program for African-American smokers with low income. Cancer Epidemiol Biomarkers Prev 2002;11:521-8.
- Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav 2003;27:S227-32.
- White M, Adams J, Heywood P, Babones S. Health, inequality and society. Bristol: Policy Press; 2009.
- Bambra C, Gibson M, Sowden A, Wright K, Whitehead M, Petticrew M. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J Epidemiol Community Health 2010;64:284-91.
- Bauer M, Aarts B, Bauer M, Gaskell G. Qualitative research with text, image and sound. London: Sage; 2000.
- Noblit G, Hare R. Meta-ethnography: synthesizing qualitative studies. Newbury Park, CA: Sage; 1988.
- Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000;320:114-16.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5.
- Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog?. BMJ 2001;322:1115-17.
- Attride-Stirling J. Thematic networks: an analytical tool for qualitative research. Qual Res 2001;1:385-40.
- de-Graft Aikins A. Strengthening quality and continuity of diabetes care in rural Ghana: a critical social psychological approach. J Health Psychol 2004;9:295-309.
- Nader L, Hymes D. Reinventing anthropology. New York, NY: Pantheon Books; 1972.
- Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health 2006;27:1-28.
- Yancey AK, Miles O, Jordan AD. Organizational characteristics facilitating initiation and institutionalization of physical activity programs in a multiethnic urban community. J Health Educ 1999;30:S44-51.
- Ogrinc G, Batalden P. Realist evaluation as a framework for the assessment of teaching about the improvement of care. J Nurs Educ 2009;48:661-7.
- Wong G, Greenhalgh T, Pawson R. Internet-based medical education: a realist review of what works, for whom and what circumstances. BMC Med Educ 2010;10.
- Greenhalgh T, Kristjansson E, Robinson V. Realist review to understand the efficacy of school feeding programmes. Brit Med J 2007;335:858-61.
- Sheppard S, Lewin S, Straus S, Clarke M, Eccles MP, Fitzpatrick R, et al. Can we systematically review studies that evaluate complex interventions?. PloS Med 2009;6.
- Pawson R. Evidence-based policy: a realist perspective. London: Sage; 2006.
- Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health 2002;56:119-27.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review – a new method of systematic review designed for complex policy interventions. J Health Serv Res Policy 2005;10:21-34.
- Klesges RC, Obarzanek E, Klesges LM, Stockton MB, Beech BM, Murray DM, et al. Memphis Girls health Enrichment Multi-site Studies (GEMS): phase 2: design and baseline. Contemp Clin Trials 2008;29:42-55.
- Beech BM, Klesges RC, Kumanyika SK, Murray DM, Klesges L, McClanahan B, et al. Child- and parent-targeted interventions: the Memphis GEMS pilot study. Ethn Dis 2003;13:S40-53.
- Young DR, Stewart KJ. A church-based physical activity intervention for African American women. Fam Community Health 2006;29:103-17.
- Doyle E, Smith CA, Hosokawa MC. A process evaluation of a community-based health promotion program for a minority target population. Health Educ 1989;20:61-4.
- Gaston M, Porter G, Thomas V. Prime Time Sister Circles®: evaluating a gender-specific, culturally relevant health intervention to decrease major risk factors in mid-life African-American women. J Natl Med Assoc 2007;99:428-38.
- Resnicow K, Royce J, Vaughan R, Orlandi MA, Smith M. Analysis of a multicomponent smoking cessation project: what worked and why. Prev Med 1997;26:373-81.
- Resnicow K, Vaughan R, Futterman R, Weston RE, Royce J, Parms C, et al. A self-help smoking cessation program for inner-city African Americans: results from the Harlem Health Connection Project. Health Educ Behav 1997;24:201-17.
- Taylor-Piliae RE, Haskell WL, Stotts NA, Froelicher ES. Improvement in balance, strength, and flexibility after 12 weeks of Tai chi exercise in ethnic Chinese adults with cardiovascular disease risk factors. Altern Ther Health Med 2006;12:50-8.
- Taylor-Piliae RE, Haskell WL, Froelicher ES. Hemodynamic responses to a community-based Tai Chi exercise intervention in ethnic Chinese adults with cardiovascular disease risk factors. Eur J Cardiovasc Nurs 2006;5:165-74.
- Jason LA, Tait E, Goodman D, Buckenberger L, Gruder CL. Effects of a televised smoking cessation intervention among low-income and minority smokers. Am J Community Psychol 1988;16:863-76.
- Fitzgibbon ML, Stolley MR, Schiffer L, Sanchez-Johnsen LA, Wells AM, Dyer A. A combined breast health/weight loss intervention for black women. Prev Med 2005;40:373-83.
- Amoako E, Skelly AH, Rossen EK. Outcomes of an intervention to reduce uncertainty among African American women with diabetes. Western J Nurs Res 2008;30:928-42.
- Hawthorne K, Tomlinson S. One-to-one teaching with pictures: flashcard health education for British Asians with diabetes. Br J Gen Pract 1997;47:301-4.
- Utz SW, Williams IC, Jones R, Hinton I, Alexander G, Yan G, et al. Culturally tailored intervention for rural African Americans with type 2 diabetes. Diabetes Educ 2008;34:854-65.
- Choudhury SM, Brophy S, Fareedi MA, Zaman B, Ahmed P, Williams R. Examining the effectiveness of a peer-led education programme for type 2 diabetes and cardiovascular disease in a Bangladeshi population. Diabet Med 2009;26:40-4.
- Story M, Sherwood NE, Himes JH, Davis M, Jacobs DR, Cartwright Y, et al. An after-school obesity prevention program for African-American girls: the Minnesota GEMS pilot study. Ethn Dis 2003;13:S54-64.
- Rush EC, Chandu V, Plank LD. Reduction of abdominal fat and chronic disease factors by lifestyle change in migrant Asian Indians older than 50 years. Asia Pac J Clin Nutr 2007;16:671-6.
- Stolley MR, Sharp LK, Oh A, Schiffer L. A weight loss intervention for African American breast cancer survivors, 2006. Prev Chronic Dis 2009;6.
- Stewart AL, Gillis D, Grossman M, Castrillo M, Pruitt L, McLellan B, et al. Diffusing a research-based physical activity promotion program for seniors into diverse communities: CHAMPS III. Prev Chronic Dis 2006;3.
- Kreuter MW, McClure SM. The role of culture in health communication. Annu Rev Public Health 2004;25:439-55.
- Yancey AK, McCarthy WJ, Taylor WC, Merio A, Gewa C, Weber MD, et al. The Los Angeles Lift Off: a sociocultural environmental change intervention to integrate physical activity into the workplace. Prev Med 2004;38:848-56.
- Hruschka DJ. Culture as an explanation in population health. Ann Hum Biol 2009;36:235-47.
- Bronheim S, Sockalingam S. A guide to choosing and adapting culturally and linguistically competent health promotion materials. Washington, DC: National Center for Cultural Competence, Georgetown University Center for Child and Human Development; 2003.
- Centre for Addiction and Mental Health . Culture Counts: A Roadmap to Health Promotion 2008. www.camh.net/About_CAMH/Health_Promotion/Community_Health_Promotion/Culture_Counts_Guide/index.html.
- Nova Scotia Department of Health . Messages for All Voices: Integrating Cultural Competence and Health Literacy in Health Materials, Forms, and Signage 2010.
- Centers for Disease Control and Prevention . REACHing across the Divide: Finding Solutions to Health Disparities 2007.
- EPOC 2006. Effective Practice, Organisation of Care . Including Interrupted Time Series (ITS) Designs in an EPOC Review n.d. www.epoc.uottawa.ca/inttime.pdf (accessed 1 December 2006).
- Higgins JPT, Green S. Cochrane handbook for systematic reviews on interventions. Chichester: John Wiley & Son; 2006.
- Thomas H, Ciliska D, Dobbins M, Micucci S. A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldview Evid Based Nurs 2004;1:176-84.
- Chalmers I, Enkin M, Keirse MJNC. Effective Care in Pregnancy and Childbirth. Oxford: Oxford University Press; 1985.
- Sidani, S, Braden CJ. Evaluating nursing interventions: A theory-driven approach. Thousand Oaks, CA: Sage; 1998.
- Goldbloom R, Battista RN. The Periodic Health Examination: 1. Introduction. CMAJ 1986;134:721-3.
- Canadian Medical Journal guidelines . How to read clinical journals IV: to determine etiology or causation. Can Med Assoc J 1981;124:985-90.
- Canadian Medical Journal guidelines . How to read clinical journals V: to distinguish useful from useless or even harmful therapy. Can Med Assoc J 1981;124:1156-62.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary?. Contr Clin Trials 1996;17:1-12. 10.1016/0197-2456(95)00134-4.PMID8721797.
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322-7.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6. Chichester: John Wiley & Sons Ltd; 2006.
- Van Tulder MW, Assendelft WJJ, Koes BW, Bouter LM. Method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group for spinal disorders. Spine 1997;22:2323-30.
- National Heart, Lung and Blood Institute . The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults 2000.
- EPI-Centre . EPI-Centre Review Guidelines 1996.
- Briss PA, Zaza S, Pappaioanou M, Fielding J, Wright-De Agüero L, Truman BI, et al. Developing an evidence-based Guide to Community Preventive Services: methods. The Task Force on Community Preventive Services. Am J Prev Med 2000;18:35-43.
- Chalmers I, Adams M, Dickersin K, Hetherington J, Tarnow-Mordi W, Meinert C, et al. A cohort study of summary reports of controlled trials. JAMA 1990;263:1401-5.
- Khan K, Riet Gt, Glanville J, Sowden A, Kleijnen J. Undertaking Systematic Reviews of Research on Effectiveness. CRD’s Guidance for Those Carrying Out or Commissioning Reviews 2001.
- Ciliska D, Miles E, O’Brien M, Turl C, Tomasik H, Donovan U, et al. The Effectiveness of Community Interventions to Increase Fruit and Vegetable Consumption in People Four Years of Age and Older. ON: Ministry of Health, Public Health Research, Education and Development Program; 1999.
- Clarke M, Oxman AD. Cochrane Reviewers Handbook 4.1.5. Chichester: John Wiley & Sons Ltd; 2002.
- Scottish Intercollegiate Guidelines Network (SIGN) . SIGN 50: A Guideline developer’s Handbook 2001.
- Harbour, R, Miller, J. A new system for grading recommendations in evidence based guidelines. BMJ 2001;323:334-6.
- Mulrow CD, Oxman AD. Cochrane collaboration handbook. Oxford; 1997.
- Peersman G, Oliver S, Oakley A. EPPI-Centre Review Guidelines. London: EPPI-Centre; 1997.
- Oakley A, Dawson MF, Holland J, Arnold S, Cryer C, Doyle Y, et al. Preventing falls and subsequent injury in older people. Qual Health Care 1996;5:243-9.
- Peersman G. A Descriptive Mapping of Health Promotion Studies in Young People. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 1996.
- Peersman G, Harden A, Oliver S. Effectiveness of Health Promotion Intervention in the Workplace: A review. London: Health Education Authority; 1998.
- Van Tulder M, Furlan A, Bombardier C, Bouter L. For Editorial Board of the Cochrane Collaboration Back Review Group . Updated method guidelines for systematic reviews in the Cochrane Collaboration back review group. Spine 2003;28:1290-9.
- Davidson MB. American Diabetes Association: Clinical practice recommendations. Diabetes Care 2003;26:S1-156.
- Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, Bouter LM, et al. 1998) The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J Clin Epidemiol 1998;51:1235-41.
- National Health Service Centre for Reviews and Dissemination (CRD) . CRD’s Guidance for Those Carrying Out or Commissioning Reviews. Undertaking Systematic Reviews of Research on Effectiveness 2001.
- Haynes B, Taylor WD. Compliance in health care. Baltimore, MD; 1979.
- Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med 2001;20:21-35.
- Lacey LS, Tukes LS, Manfredi C, Warnecke RB. Use of lay health educators for smoking cessation in a hard-to-reach urban community. J Commun Health 1991;16:269-82.
- Ahijevych K, Wewers ME. Low-intensity smoking cessation intervention among African-American women cigarette smokers: a pilot study. Am J Health Promot 1995;9:337-9.
- Prochaska J, DiClemente C. Stages and processes of self-change in smoking: toward an integrative model of change. J Consult Clin Psychol 1983;5:390-5.
- Schorling JB, Roach J, Siegel M, Baturka N, Hunt DE, Guterbock TM, et al. A trial of church-based smoking cessation interventions for rural African Americans. Prev Med 1997;26:92-101.
- Darity WA, Chen TTL, Tuthill RW, Buchanan DR, Winder AE, Stanek E, et al. A multi-city community based smoking research intervention project in the African-American population. Int Q Community Health Educ 2006;26:323-36.
- Prochaska JO, Redding CA, Evers KE, Glanz K, Lewis FM, Rimer BK. Health Behavior and Health Education, Theory, Research and Practice. San Francisco, CA: Jessey-Bass; 1997.
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, NY: Guilford Press; 1991.
- Miller SM. Prim Care Cancer; 2000.
- Andrews JO, Bentley G, Crawford S, Pretlow L, Tingen MS. Using community-based participatory research to develop a culturally sensitive smoking cessation intervention with public housing neighborhoods. Ethn Dis 2007;17:331-7.
- Andrews JO, Felton G, Ellen Wewers M, Waller J, Tingen M. The effect of a multi-component smoking cessation intervention in African American women residing in public housing. Res Nurs Health 2007;30:45-60.
- Fiore MC, Bailey W, Cohen S, Dorfman S, Goldstein M, Gritz E, et al. Treating tobacco use and dependence. Rockville, MD: US Department of Health and Human Services; 2000.
- Freire P. Pedagogy of the oppressed. New York, NY: Seabury Press; 1970.
- Shelley D, Fahs M, Yemeni R, Das D, Nguyen N, Hung D, et al. Effectiveness of tobacco control among Chinese Americans: a comparative analysis of policy approaches versus community-based programs. Prev Med 2008;47:530-6.
- Wong CC, Tsoh JY, Tong EK, Horn FB, Cooper B, Chow EA. The Chinese community smoking cessation project: a community sensitive intervention trial. J Commun Health 2008;33:363-73.
- Larson CO, Schlundt DG, Patel K, Wang H, Beard K, Hargreaves MK. Trends in smoking among African-Americans: a description of Nashville’s REACH 2010 initiative. J Commun Health 2009;34:311-20.
- Andersen RE, Franckowiak SC, Zuzak KB, Cummings ES, Bartlett SJ, Crespo CJ. Effects of a culturally sensitive sign on the use of stairs in African American commuters. Soz Praventivmed 2006;51:373-80.
- Banks-Wallace J, Enyart J, Johnson C. Recruitment and entrance of participants into a physical activity intervention for hypertensive African American women. Adv Nurs Sci 2004;27:102-16.
- Banks-Wallace J, Conn V. Changes in steps per day over the course of a pilot walking intervention. ABNF J 2005;16:28-32.
- Banks-Wallace J. Outcomes from Walk the Talk: a nursing intervention for black women. ABNF J 2007;18:19-24.
- Wilbur J, McDevitt JH, Wang E, Dancy BL, Miller AM, Briller J, et al. Outcomes of a home-based walking program for African-American women. Am J Health Promot 2008;22:307-17.
- Campbell MK, Motsinger BM, Ingram A, Jewell D, Makarushka C, Beatty B, et al. The North Carolina Black Churches United for Better Health Project: intervention and process evaluation. Health Educ Behav 2000;27:241-53.
- Kristal AR, Shattuck AL, Patterson RE. Differences in fat-related dietary patterns between black, Hispanic and white women: results from the Women’s Health Trial Feasibility Study in Minority Populations. Public Health Nutr 1999;2:253-62.
- Snowdon W. Asian cookery clubs: a community health promotion intervention. Promot Educ 1999;37:135-6.
- Resnicow K, Campbell MK, Carr C, McCarty F, Wang T, Periasamy S, et al. Body and soul. A dietary intervention conducted through African-American churches. Am J Prev Med 2004;27:97-105.
- Fuemmeler BF, Masse LC, Yaroch AL, Resnicow K, Campbell MK, Carr C, et al. Psychosocial mediation of fruit and vegetable consumption in the Body and Soul effectiveness trial. Health Psychol 2006;25:474-83.
- Campbell MK, Resnicow K, Carr C, Wang T, Williams A. Process evaluation of an effective church-based diet intervention: Body & Soul. Health Educ Behav 2007;34:864-80.
- Glasgow RE, Bull SS, Gillette C, Klesges LM, Dzewaltowski DA. Behavior change intervention research in health care settings: A review of recent reports with emphasis on external validity. Am J Prevent Med 2002;23:62-9.
- Glasgow RE, McKay HG, Piette JD. The RE-AIM framework for evaluating interventions: What can it tell us about approaches to chronic illness management?. Patient Educ Couns 2001;44:119-27.
- Goodman J, Blake J. Nutrition education: a computer-based education program. J Health Care Poor Underserved 2005;16:118-27.
- Sullivan J, Carter JP. A nutrition-physical fitness intervention program for low-income black parents. J Natl Med Assoc 1985;77:39-43.
- Kanders BS, Ullmann-Joy P, Foreyt JP, Heymsfield SB, Heber D, Elashoff RM, et al. The Black American Lifestyle Intervention (BALI): the design of a weight loss program for working-class African-American women. J Am Diet Assoc 1994;94:310-12.
- Wallace P, Awan A, Talbot J. Health advice for Asian women with diabetes. Prof Nurse 1996;11:794-6.
- McNabb W, Quinn M, Kerver J, Cook S, Karrison T. The PATHWAYS church-based weight loss program for urban African-American women at risk for diabetes. Diabetes Care 1997;20:1518-23.
- Quinn MT, McNabb WL. Training lay health educators to conduct a church-based weight-loss program for African American women. Diabetes Educ 2001;27:231-8.
- Stolley MR, Fitzgibbon ML. Effects of an obesity prevention program on the eating behavior of African American mothers and daughters. Health Educ Behav 1997;24:152-64.
- Pender NJ. Health Promotion in Nursing Practice. Stamford, CT: Appleton & Lange; 1996.
- Pender NJ, Walker SN, Sechrist KR. Predicting health promotion lifestyles in the workplace. Nurs Res 1990;39:326-32.
- Karanja N, Stevens J, Hollis JF, Kumanyika SK. Steps to soulful living (steps): a weight loss program for African-American women. Ethn Dis 2002;12:363-71.
- Kumanyika SK, Morssink CB, Dalton S. Overweight and Weight Management. Gaithersburg, MD: Aspen Publishers; 1997.
- Keyserling TC, Ammerman AS, Samuel-Hodge CD, Ingram AF, Skelley AH, Elasy TA, et al. A diabetes management program for African American women with type 2 diabetes. Diabetes Educ 2000;26:796-805.
- Keyserling TC, Samuel-Hodge CD, Ammerman AS, Ainsworth BE, Henriquez-Roldan CF, Elasy TA, et al. A randomized trial of an intervention to improve self-care behaviors of African-American women with type 2 diabetes: impact on physical activity. Diabetes Care 2002;25:1576-83.
- Baranowski T, Baranowski JC, Cullen KW, Thompson DI, Nicklas T, Zakeri IE, et al. The Fun, Food, and Fitness Project (FFFP): the Baylor GEMS pilot study. Ethn Dis 2003;13:S30-9.
- Prochaska JO, Velicer WF, Rossi JS, Goldstein, MG, Marcus, BH, Rakowski, W, et al. Stages of change and decisional balance for 12 problem behaviours. Health Psychol 1994;13:39-46.
- Kelley MA. Culturally appropriate breast health educational intervention program for African-American women. J Natl Black Nurses Assoc 2004;15:36-47.
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215.
- Bandura A. The social foundations of thoughts and actions: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
- Bandura A. Self-efficacy: The exercise of control. New York, NY: WH Freeman; 1997.
- Williams A, Wold J, Dunkin J, Idleman L, Jackson C. CVD prevention strategies with urban and rural African American women. Appl Nurs Res 2004;17:187-94.
- Adult Treatment Panel III . The Third Report of the Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults 2001.
- Cormier WH, Cormier LS. Interviewing strategies for helpers. Monterey, CA: Brooks/Cole; 1991.
- Joint National Committee on Prevention, Detection, and Treatment of High Blood Pressure . The Sixth Report of the Joint National Committee on Prevention, Detection and Treatment of High Blood Pressure (JNC VI) 1997.
- Fitzgibbon ML, Stolley MR, Dyer AR, Van Horn L, KauferChristoffel K. A community-based obesity prevention program for minority children: rationale and study design for Hip-Hop to Health Jr. Prev Med 2002;34:289-97.
- Stolley MR, Fitzgibbon ML, Dyer A, Van Horn L, KauferChristoffel K, Schiffer L. Hip-Hop to Health Jr., an obesity prevention program for minority preschool children: baseline characteristics of participants. Prev Med 2003;36:320-9.
- Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Two-year follow-up results for Hip-Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr 2005;146:618-25.
- Mishel MH. Uncertainty in illness. J Nurs Scholarsh 1988;20:225-32.
- Eagan G. The skilled helper. Pacific Grove, CA: Brooks/Cole; 1998.
- Boltri JM, Davis-Smith YM, Seale JP, Shellenberger S, Okosun IS, Cornelius ME. Diabetes prevention in a faith-based setting: results of translational research. J Public Health Manag Pract 2008;14:29-32.
- Chen JL, Weiss S, Heyman MB, Vittinghoff E, Lustig R. Pilot study of an individually tailored educational program by mail to promote healthy weight in Chinese American children. J Spec Pediatr Nurs 2008;13:212-22.
- Davison KK, Birch LL. Childhood overweight: A contextual model and recommendations for future research. Obes Rev 2001;2:159-71.
- Kim KH, Linnan L, Campbell MK, Brooks C, Koenig HG, Wiesen C. The WORD (wholeness, oneness, righteousness, deliverance): a faith-based weight-loss program utilizing a community-based participatory research approach. Health Educ Behav 2008;35:634-50.
- Kousar R, Burns C, Lewandowski P. A culturally appropriate diet and lifestyle intervention can successfully treat the components of metabolic syndrome in female Pakistani immigrants residing in Melbourne, Australia. Metabolism 2008;57:1502-8.
- Martin PD, Dutton GR, Rhode PC, Horswell RL, Ryan DH, Brantley PJ. Weight loss maintenance following a primary care intervention for low-income minority women. Obesity 2008;16:2462-7.
- Murrock CJ, Gary FA. A culturally-specific dance intervention to increase functional capacity in African American women. J Cult Divers 2008;15:168-73.
- Murrock CJ, Madigan E. Self-efficacy and social support as mediators between culturally specific dance and lifestyle physical activity. Res Theory Nurs Pract 2008;22:192-204.
Appendix 1 Commissioning brief
NIHR Health Technology Assessment Programme HTA no 07/63/03
Modifying health promotion interventions to meet the needs of ethnic minority groups
Introduction
The aim of the HTA programme is to ensure that high quality research information on the costs, effectiveness and broader impact of health technologies is produced in the most efficient way for those who use, manage, provide care in or develop policy for the NHS. Topics for research are identified and prioritised to meet the needs of the NHS. Health technology assessment forms a substantial portfolio of work within the National Institute for Health Research and each year about fifty new studies are commissioned to help answer questions of direct importance to the NHS. The studies include both primary research and evidence synthesis.
Question
What is the effectiveness of different ways of modifying health promotion interventions to meet the needs of ethnic minority groups?
Technology: Health promotion interventions that have been modified to meet the needs of ethnic minority groups (i.e. to be culturally competent). Health promotion interventions addressing physical activity, diet and smoking cessation are of particular interest and researchers should justify their choice.
Patient group: Any ethnic minority group. Researchers wishing to focus on particular groups should carefully justify their choice.
Setting: Any setting in which health promotion interventions are employed. Researchers will need to consider how to relate evidence from other countries and decades to the present-day UK.
Control or comparator treatment: Standard health promotion interventions that are effective in the wider population.
Design: Evidence synthesis is required to summarise what is known about how health promotion interventions can be made culturally competent. This should include (a) examples of good practice in the UK; (b) a systematic review of the relevant qualitative literature; (c) a systematic review of how process and short-term outcomes can be modified in different ethnic groups; (d) modelling of longer-term health benefits and costs; with (e) recommendations for the HTA programme on the most appropriate research question for future primary research.
Outcomes: Better uptake of health promotion interventions, greater impact on health behaviours; cultural sensitivity and acceptability; longer-term effectiveness and cost-effectiveness.
Background to commissioning brief
Ethnicity contributes powerfully, both directly and indirectly, to health inequalities. Increasing the cultural competence of the health-care system and the individuals that work within it has been suggested as one mechanism for reducing health inequalities by improving the quality of services across racial/ethnic groups.
Evidence synthesis is therefore needed to summarise what is known about how health promotion interventions can be made culturally competent. The effectiveness of culturally appropriate models of health promotion should be explored in a UK context and researchers should make recommendations for the HTA programme on the most appropriate research question for future primary research.
Timescale
There are no fixed limits on the duration or funding of this project. However, there is a pressing need within the NHS for the information, so the research would normally be expected to be completed as soon as possible – however it is for applicants to justify the duration and costs proposed.
Making an application
If you wish to submit a proposal on this topic, please complete the NIHR Methodology Panel electronic application form and return it, along with a detailed project description, to the HTA Commissioning Manager at the National Coordinating Centre for Health Technology Assessment, Mailpoint 728, Boldrewood, University of Southampton, Southampton SO16 7PX by Wednesday 8 August 2007.
Your full proposal will be assessed by designated NIHR Methodology Panel members, alongside other applications submitted in the same topic area.
Applications received after 1300 hours on the due date will not be considered.
Appendix 2 Protocol
1. TITLE: Modifying smoking cessation, physical activity and nutrition health promotion interventions to meet the needs of UK ethnic minority groups
2. Planned investigation
2.1 Research aims and objectives
We aim to identify, describe, appraise, interpret and highlight research (and lack of it), in relation to the processes and procedures employed to maximise the cross-cultural validity, utility and effectiveness of health promotion interventions. 1 We will focus on health behaviours known to be associated with considerable morbidity and mortality in UK ethnic minority groups. Specifically, we will undertake a phased programme of research that will study the cultural adaptation of the three key areas highlighted in the brief – i.e. smoking cessation, physical activity and dietary health promotion interventions – that are potentially applicable to South Asian, Black and Chinese ethnic minority groups, these representing the major ethnic minority groupings in the UK. 2 This phased programme of work will involve:
Phase 1
-
Identifying evidence-based smoking cessation, physical activity and dietary health promotion interventions that are known to be effective in the general population and which have subsequently been modified (i.e. to be culturally competent and sensitive) to meet the needs of one or more of these ethnic minority groups.
-
Describing the theoretical considerations3 and empirical evidence4 drawn upon, and the approaches used, to modify5 these interventions.
-
Developing databases of effective and adapted interventions and a typology of approaches used to culturally adapt these interventions.
Phase 2
-
Assessing the feasibility, acceptability, equity, effectiveness (relating to impact on knowledge, attitudes, behaviours and health outcomes) and cost-effectiveness of these modified interventions.
-
Placing each culturally modified intervention on the spectrum described by the Medical Research Council framework for complex interventions;6;7 and identifying which are ready for widespread implementation, and which require further research.
Phase 3
-
Outlining future primary research that needs to be undertaken and prioritising this work by considering issues such as anticipated health benefits, likely effectiveness and cost-effectiveness, and the feasibility of conducting high quality research in this area. 8
Given the range of interventions and populations under study, we anticipate that this work will generate important transferable lessons both to the study of other health promotion interventions and other UK ethnic minority groups.
2.2 Existing research
Ethnic diversity is now a prominent feature of most economically developed societies and given recent demographic trends this heterogeneity is expected to increase substantially. The 2001 UK census, which provides the most reliable assessment of the ethnic profile for the UK, revealed that 7.9% of the population classified themselves as belonging to a Black or other minority ethnic group. Of these, 50% were of South Asian (Indian, Pakistani, Bangladeshi, and ‘other’) origin, 25% were Black (of Caribbean and African) origin and 5% were of Chinese origin; the remaining 20% were of various origins including ‘Mixed’ (i.e. dual heritage) backgrounds, and ‘Others’ (including Arab and other groups which are not separately identified). 2;9
There is now a considerable body of evidence showing that in general minority ethnic groups experience disproportionate levels of morbidity and mortality when compared with the majority White population. 10–13 Relative social and economic disadvantage are major contributors to these marked and persistent health inequalities, these in turn resulting from a variety of historical and structural factors. 14
Reducing health inequalities is a long-standing declared national priority for the NHS,15 but progress has unfortunately been very slow in this respect. 16 Again, the reasons for this are complex, but contributing to this impasse has been the systematic exclusion of minority ethnic communities from research,17;18 when in actual fact, what is needed is an increased focus of research on these marginalised populations so as to allow a critical evaluation of the impact of health promotion (and other) interventions on all sections of the population. 19
A review of health promotion interventions targeted at minority ethnic communities that we conducted as part of a wider review revealed that the forms of cultural adaptations most commonly employed are those designed to ensure the effective transmission of health messages by overcoming communication barriers. 20 These have largely involved the matching of intervention materials and messages to observable, superficial characteristics of the target population by using people, places, languages and locations familiar or preferred by the target population. 21 Specific methods employed included providing forums for open discussion in safe and familiar settings, employing bilingual workers, meeting the target groups’ preferences for the ethnicity, gender and age of health workers, disseminating translated material on identified areas of concern, conducting outreach work and liaising with minority ethnic agencies. However, other studies, some of which have been built on anthropological and sociological theory, have suggested that more considered adaptations informed by knowledge of the target groups’ cultural beliefs, knowledge and understanding are required to effect health-related behavioural changes. It has, for instance, been argued that while interventions which match interventions to superficial, observable characteristics such as language will increase the ‘receptivity’ of these messages, it is only interventions which engage with the cultural, social, historical, environmental and psychological forces that influence health behaviour that will affect behavioural change. 22 Consistent with this, others have argued that in order to be effective health education must be responsive to culturally related differences in health beliefs between ethnic groups. 23
Emphasising the importance of user beliefs and perspectives, it has been argued that rather than designing education programmes to rectify ‘deficiencies’ in knowledge or ‘incorrect’ behaviour, health promotion programmes should attempt to build on the beliefs, attitudes and behaviours that already exist within the target group to promote healthier lifestyles, improve quality of life and address practical barriers to positive health. 24 In support of this view, Netto et al. ’s study of user perspectives of a targeted coronary heart disease intervention illustrated the multiple factors acting at individual, community and societal levels that influence behavioural change. 25 This involved an examination of the complex interplay between limited knowledge of disease, risk factors and preventive measures, ingrained health beliefs and attitudes relating to the disease, social deprivation, lifestyle and environmental changes following migration to the UK, adherence to community norms, threats to traditional values and racial hostility. The longitudinal nature of this study illustrated the persistent nature of cultural beliefs and attitudes, community norms, socio-economic circumstances, and structural forces that act as barriers to change in ‘at-risk’ communities, indicating that unless attention is focused on these factors, efforts to reduce the disease in ‘high risk’ groups are destined to be limited. The findings from this work concurs with other studies in arguing that although greater understanding of the nature of disease on the part of ‘at-risk’ groups is a necessary precursor to behavioural change, the most important predictors of outcome and compliance are users’ beliefs about the cause and course of their disease, and the ways that the cultural milieu impact on health behaviour. 26;27 In the course of this study, we will rigorously appraise the qualitative and quantitative evidence for these, and other emergent views on effective health promotion interventions.
2.3 Overview of research methods
We will draw on and build on our considerable collective body of completed and ongoing relevant theoretical, primary research (involving sociological, qualitative, descriptive and experimental work), evidence synthesis and policy-based work in relation to adaptation of key health promotion interventions (see CVs for details). This proposed phased programme of work, which is informed by the MRC complex intervention framework,6;7 will culminate in the production of a rigorous state-of-the-art synthesis of the disparate and somewhat eclectic evidence base in this area. An overview of our proposed approach is detailed below and this is then followed by a detailed discussion of the methods to be used.
Phase 1: Identifying and describing evidence-based interventions that have been culturally modified
This work will begin by identifying interventions already found to be effective in modifying smoking cessation, physical activity and dietary health promotion interventions in any population. This will involve searching for key evidence-based systematic overviews such as SIGN and NICE guidelines, and Clinical Evidence and HTA reviews. If necessary, this will be supplemented by also searching the Cochrane Library, Campbell Collaboration and DARE for relevant systematic reviews. For interventions for which there is strong evidence of effectiveness, we will, in relation to ethnicity, using previously developed techniques,17;18 undertake a careful assessment of the inclusion criteria, details of the populations studied, as reported in these reviews and trials, and any subgroup analyses undertaken to ascertain whether these interventions are more/equally/less likely to be effective than for the majority White population.
From our previous work, we are well aware that the majority of publications relating to cultural modification are discursive, descriptive or anecdotal and promote views (or recommendations) of ‘best practice’ or lay out proposed approaches, rather than formally evaluating the effectiveness of these approaches or the interventions thereby developed in effecting behavioural changes. This important preliminary work will nonetheless allow us to develop a detailed familiarity with the current state of the relevant literature and develop an understanding of the types of interventions that are being employed in these areas and which interventions are effective in the general population. The assumption underpinning our approach is that interventions already found to be effective in the majority population are, if appropriately adapted, likely to also prove effective in minority ethnic populations. 28
Focusing on these interventions, we will then conduct a systematic search of the peer-reviewed and grey literature, and search for work in progress, to ascertain which of these interventions have been/are being culturally modified and, if so, how. It is anticipated that in order to answer this latter question we may, as is common in many systematic reviews of this kind, contact relevant research teams, practitioners and policy makers to seek clarity on the descriptions contained in the identified papers and also for obtaining further details on related work in progress.
This first phase of work will culminate in the production of databases of smoking cessation, physical activity and dietary health promotion interventions that are known to be effective in the general population and a detailed understanding of which of these have been formally studied with respect to cultural adaptation and the relevant maturity of the evidence in relation to this. This will also result in the development of an appreciation of the range of approaches used to modify these interventions, which we will collect in a separate database, and based on which we will develop an initial typology of adaptation approaches, which is informed by the relevant theoretical and empirical literature.
Phase 2: Assessing the feasibility, acceptability, equity, effectiveness and cost-effectiveness of modified health promotion interventions
This literature will be critically appraised to try and assess the feasibility, acceptability, equity, effectiveness and cost-effectiveness of these identified modified interventions. We are aware that this field is still in its infancy and much of the published research is likely to prove challenging to understand and synthesise. We therefore believe it is important to supplement our analysis of formal published reports with detailed discussions with those who have undertaken these adaptations, this being particularly important given the anticipated high yield of qualitative, descriptive and pilot work likely to be identified. We will undertake this by engaging, in a purposive fashion on the basis of disease/behaviour area of study, ethnic groups of particular interest and approach used to adaptation, with key members of the respective teams responsible for developing these adapted interventions, through a combination of email, telephone and face-to-face discussions. We anticipate discussions with between 20–30 research teams to reach saturation.
This literature review and associated discussions with research teams will allow us to access relevant data with which to understand the approaches used in adaptation, why any particular approaches have been used and the feasibility, acceptability, equity, effectiveness and cost-effectiveness of the approaches to adaptation taken. Synthesis of the findings from these first two phases of work will allow us to identify for which adapted interventions there is strong evidence of effectiveness and which also have the potential to synchronise well with existing UK health policy initiatives. Studies fulfilling both these criteria are most likely to be implemented and prove sustainable and will therefore be judged to be amenable to widespread implementation. This work will allow us to further refine the typology of adaptation approaches begun in Phase 1 and, furthermore, allow some assessment of which of these approaches are most likely to maximise the cross-cultural validity, utility and ultimately effectiveness of these interventions.
Phase 3: Highlighting further research that needs to be undertaken
We expect to find relatively few interventions that are ready for widespread implementation, but we do expect to identify a number of adapted health promotional interventions that might fulfil the above described criteria and thus fit this bill if further primary work was to be strategically commissioned. Our aim from this final phase of work will therefore be to identify the range of methodological and intervention specific research that needs to be undertaken, but also to suggest a prioritisation for this work, basing this assessment on anticipated health gains and whether or not it is likely to prove feasible for research teams to mount definitive experimental studies in the short- to medium-term. 8 When considering future primary work we will also, based on the data uncovered, reflect on whether adaptation of existing interventions is indeed the appropriate course (as this could be criticised as being ethnocentric on the European model), or whether there is a need to develop more grounded interventions that are cognizant of underlying health belief models, practices and norms of different ethnic minority groups of interest.
2.4 Systematic review of the qualitative and quantitative literature
Members of our research team have considerable experience with undertaking systematic reviews of experimental, epidemiological, and qualitative studies and also in synthesising data from reviews of these different study types. We will use the principles advocated by the Cochrane and Campbell Collaborations and adapt these for the much broader range of study designs likely to be of interest in relation to evaluating health promotion interventions in general and in particular the cultural adaptation field. 1;3;4;29
Criteria for considering studies for this review
Types of studies: We plan to include the full range of experimental (e.g. randomised controlled trials, controlled clinical trials, controlled before and after studies, interrupted time series, before and after, and pilot intervention studies), epidemiological (e.g. case control, cohort, ecological, descriptive and case series) and qualitative (e.g. interview, focus group and ethnographic) study designs. We are also very interested in the relevant theoretical literature.
Types of participants: We are interested in all studies internationally that will provide insights on how to apply interventions effectively to our prime target populations i.e. people (children and adults) and populations from South Asian, Black and Chinese backgrounds in the UK. In relation to: South Asians, this will include people tracing their ancestral origins to India, Pakistan or Bangladesh; for ‘Black’ this will include people tracing their ancestral origins to Sub-Saharan Africa or the Caribbean; and for Chinese those people tracing their ancestral origins to China. 9 Clearly, studies focusing on these populations will be of specific and special interest. This does not however preclude studies done on other populations e.g. the Turkish population of Holland or the Vietnamese in the USA, where the studies offer insights that can be generalised to our target populations. It should be noted that the notion of ‘race’ and religion are subsumed within our working definition of ethnicity. 9
Types of interventions: We are interested in any health promotion interventions aiming to facilitate smoking cessation, promote physical activity and facilitate dietary modifications to reduce health risks, aimed either at individuals or populations.
Types of outcome measures: We are interested in all relevant clinical, process (including beliefs, knowledge, attitudes and healthcare utilisation), and methodological outcome measures in relation to either the behaviours of interest or conditions for which smoking, physical activity and exercise are known to be aetiologically important.
Search methods for identification of studies
This will involve searching for published peer-reviewed work, grey literature and work in progress. Searches will be conducted from the time of inception of these databases to the present time.
Peer-reviewed literature: We will search the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library); MEDLINE; EMBASE; CINAHL; BIOSIS; Campbell Collaboration; ISI Web of Knowledge; LILACS; HealthPromise (National Health Promotion Database for England), HEAPS (Health Promotion Database); and the Specialist Library for Ethnicity and Health SLEH. A specimen provisional search strategy for use in MEDLINE based on the above is detailed in Appendix 1. Our detailed search terms will be adapted for the various databases as appropriate, but will in general terms be based on the following concepts:
-
Ethnic minority (i.e. South Asian OR Indian OR Pakistani OR Bangladeshi OR Black OR African OR Caribbean OR Chinese) groups OR culture (i.e. cultural OR multicultural OR transcultural OR racial or immigrant OR refugee OR asylum seeker) OR religion (i.e. Hindu or Muslim OR Sikh OR Christian OR Buddhist) AND
-
Health promotion (i.e. smoking cessation OR dietary modification OR physical activity) intervention OR health education.
Grey literature: There is likely to be a considerable body of relevant information contained within the grey literature. We plan to search for this by searching the Internet (using Google Scholar and Google), specialist libraries (e.g. HTA, HEA, NICE and King’s Fund), our own personal libraries, and contacting expert organisations (e.g. National Resource Centre on Ethnic Minorities) and experts in the field through posting email requests onto specialist academic ethnicity e-mail discussion lists (e.g. Jiscmail).
Research in progress: It is also important that this review uncovers relevant work in progress and to do this we intend to search the UK’s National Research Register and search the following websites listing ongoing trials: http://clinicaltrials.gov/ and http://www.controlledtrials.com/ and http://www.actr.org.au/ and to write to authors of eligible studies.
Language: There will be no restriction on the language of publication. Articles in major European and South Asian languages which refer to communities significantly represented in the UK (in our target ethnic categories) will have their titles and abstracts translated and then, if judged to be relevant, the full text of the papers/reports will be professionally translated.
Methods of the review
Selection of studies: Two authors will independently review titles and abstracts from the literature searches and select possible relevant studies. These potentially eligible studies will then be reviewed in full and assessed using the inclusion criteria detailed above. In the case of any disagreements between reviewers, this will be resolved by discussion; in the case of consensus not being reached, a third reviewer will become involved and, if necessary, arbitrate. To ensure transparency, this process will be described in a modified QUORUM flow diagram.
Data extraction: Two authors will independently extract data using a customised data extraction form. We will resolve any disagreements by discussion between reviewers; in the case of consensus not being reached, a third reviewer will become involved and, if necessary, arbitrate.
Assessment of methodological quality of included studies: We plan to assess and document the methodological quality of qualitative studies using the approach advocated by the Cochrane Qualitative Research Methods Group. This will involve using the CASP approach to study assessment which emphasises the importance of assessing the adequacy of study design, recruitment, data generation, reflexivity and analysis. 31
We plan to assess and document the methodological quality of included epidemiological studies using the MOOSE guidelines for meta-analysis and systematic reviews of observational studies which emphasises the importance of assessing for bias, confounding, regression, heterogeneity and modelling techniques employed. 32
We plan to assess and document the methodological quality of included intervention studies following the Cochrane approach using the methods detailed in section six of the Cochrane Handbook for Systematic Reviews of Interventions. 33 For these studies, we propose to concentrate on using the following five parameters to assess quality: allocation concealment, method of allocation to treatment, documentation of exclusions, completeness of follow-up, methods of documentation of complications. We plan to grade each parameter of trial quality: A – low risk of bias; B – moderate risk of bias; C – high risk of bias and an overall assessment for each controlled trial using the same three criteria will be made.
Following the inclusion criteria developed by the NHS SLEH (www.library.nhs.uk/ethnicity) and the glossary described by Bhopal,9 we shall also assess research against the degree to which the ethnic groups of interest are described and included at a fine level of detail, so that articles and interventions aimed at undifferentiated ‘South Asian’ or ‘black’ groups, without reference to language, religion or cultural background, may be reviewed critically to assess the degree of ‘fit’.
We plan to assess the agreement of reviewers on methodological quality assessment. Disagreements will be resolved by discussion and, if necessary, with the involvement of a third reviewer.
Data analysis
Most studies identified are likely to yield qualitative/descriptive data and these will be summarised, as noted above, in databases identifying which interventions are most effective in the general population and approaches used to adaptation. The email, telephone and face-to-face discussions will, with permission, be recorded and subjected to thematic analysis, which will be informed by the relevant conceptual and theoretical literature and the initial typology constructed. Analysis will be iterative and will guide further data generation. 34
In the event of finding suitable data, we propose to use Review Manager (RevMan 4.2) for quantitative data analysis and synthesis. For dichotomous data, we plan to calculate individual and pooled statistics as relative risks (RR) with 95% confidence intervals (95% CI). For continuous data, we plan to calculate individual and pooled statistics as mean differences (MD) and/or standardised means differences with 95% CI. We will consider the appropriateness of meta-analyses in the presence of significant clinical or statistical heterogeneity. We will assume significant heterogeneity if the I2 is greater than 40% (i.e. more than 40% of the variability in outcome between trials is not explained by sampling variation). We will undertake meta-analysis using a fixed-effects model in the absence of statistical heterogeneity and a random-effects model if such heterogeneity is present. We plan to explore any statistical or clinical heterogeneity by using sensitivity or subgroup analysis (see below). We plan to undertake quantitative analyses of outcomes, wherever possible, on an intention to treat basis. Evidence of publication bias will be sought graphically using Funnel plots and statistically using Begg and Egger tests. 35;36
Our main subgroup analyses of interest are analysing results for different health promotion interventions by ethnic minority group, age and gender. Sensitivity analyses will be undertaken on the basis of study design by excluding studies judged to be at high risk of bias and assessing what impact, if any, this has on the robustness of findings.
We plan to systematically identify and extract all health economic data – whether from the perspective of the patient or the healthcare provider, or ideally both – as reported in studies identified through conducting our searches. These data will be extracted onto a customised data extraction sheet and quality appraised using published criteria. 37;38;39 Any relevant data identified from individual studies will be presented in a summary table, together with an assessment of study quality and key contextual considerations that may be of importance in assessing the generalisability of the findings from these studies. 40 These data will then be synthesised with the broader body of work being undertaken.
Synthesis of data from qualitative studies will be undertaken using a thematic meta-narrative approach. This thematic framework will be informed by the above quantitative literature review and will continue to evolve as the data extraction and synthesis proceed. As subsequent papers are reviewed, new themes identified will be incorporated into our thematic framework and existing themes refined until no further new themes emerge. 37
2.5 Qualitative interviews
This strand of work will employ robust qualitative techniques for data generation, analysis and interpretation. Interviews will be recorded and transcribed together with accompanying field notes. Interview data and field notes will be analysed with the help of NVivo 7 software and will be ongoing to allow emerging themes to be fed back into future rounds of data collection. Transcripts will be read repeatedly and coded to include both anticipated and unanticipated themes. A coding framework will be drawn up by the research team as the themes emerge. Constant comparison will ensure that the thematic analysis represents all perspectives and negative cases will actively be sought.
2.6 Thematic meta-analysis and synthesis of data
Based on our previous experiences of undertaking methodologically similar work, thematically synthesising data from the likely disparate studies uncovered by our literature review and qualitative work will prove challenging, but this synthesis is an important and necessary step if we are to generate meaningful findings that will promote academic thinking and clinical practice in this nascent field. To this end, in addition to the proposed taxonomies and summary framework discussed above, we have also included a qualitative dimension to this work, which will entail discussions with key researchers in this field with a view to allow greater depth of perspective to emerge than is often possible when one relies solely on written reports. In particular, we will be keen to understand relevant contextual considerations that led to one approach to cultural adaptation being chosen over another, and also in relation to interpreting findings. This qualitative work will contribute to our overall thematic synthesis of these data, which we propose to undertake using the explanatory framework offered by realistic evaluation. A main strength of realistic evaluation is the attempt to link the specific contexts and mechanisms in a way that has perhaps not been considered in the past. What works in one population and under certain circumstances will not necessarily work in other contexts. The main issue is thus not only whether a culturally adapted intervention worked (as outcomes), but also how did it do so or, conversely, why it failed to work when logic dictated otherwise. Results of conducting evaluations in a realistic way should be that the contexts (structures) that trigger certain mechanisms are identified providing useful knowledge for future initiatives. This can thus help to inform what works for whom and in what circumstances and also to guide future research.
2.7 Ethical arrangements
The literature review is unlikely to raise any major ethical issues. The discussions with research teams, although not requiring formal NHS ethics review, will nonetheless be conducted in accordance with regard to respecting the autonomy and confidentiality of participants. Participants will therefore be provided with an information sheet, time to reflect on the invitation to participate and informed consent will be obtained in all cases. Participants will be informed that they have the right to withdraw from the study at any time without the need to give reasons to explain their decision. All data will be anonymised and stored in locked filing cabinets at the University of Edinburgh and on password protected desk-based PCs. Care will be taken to ensure that participants will not be identifiable in any research reports resulting from this work. Data will be archived for at least five years after the completion of the study.
3. PROJECT MANAGEMENT AND GOVERNANCE
The PI will be responsible for all aspects of managing this study. The study researchers will meet with the PI on at least a weekly basis and more often as and when the need arises. All co-applicants, who will comprise the study Steering Group (SG), will meet quarterly to assess progress against the agreed research questions and study milestones.
Based on our positive experiences of convening an independent international advisory team for an evidence synthesis review of this sort, we propose to convene an external Project Steering Committee (IPSC), which will include members with experience of conducting complex systematic reviews, epidemiological and qualitative expertise, a lay representative and a representative from the HTA. It is envisaged that this Committee will convene (either by conference call or face-to-face) on a six monthly basis for the duration of this project. All necessary administrative support for the SG and IPSC meetings will be provided by the University of Edinburgh team.
4. PROJECT TIMETABLE AND MILESTONES
The proposed start date for this 24 month project is September 2008.
Months Activity
0–3: Set up phase: recruit and train staff; develop search strategy and protocol; one day launch conference for service users and academics
4–7: Phase 1: literature review of health promotion interventions and development of databases and typology
8–18: Phase 2: detailed literature review and synthesising findings
19–21: Phase 3: highlighting research gaps, prioritising research and developing study briefs
22–24: Writing up of final report and abstracts/papers for publication; one day conference to disseminate findings to funding bodies, policy makers, academics and service users.
5. EXPERTISE
Our research team has considerable expertise in the fields of ethnicity, public health, and health promotion and also has considerable experience with conducting evidence synthesis work of this kind. Aziz Sheikh is an epidemiologist and Professor of Primary Care Research & Development at the University of Edinburgh; he has 10 years experience of conducting systematic reviews and conducting qualitative, epidemiological and more recently experimental work in relation to minority ethnic groups. He is currently PI on a pilot multi-centre cluster randomised controlled trial of an adapted smoking cessation intervention for Pakistanis and Bangladeshis and PI on an evidence synthesis review for Connecting for Health. As PI he will oversee all aspects of managing this project. Raj Bhopal is Professor of Public Health at the University of Edinburgh, Honorary Consultant in Public Health at NHS Lothian, and Chairman of the Steering Committee of the National Resource Centre for Ethnic Minority Health, Scotland. He has been involved in scholarship, research and NHS policy/planning in relation to ethnicity and health for 23 years. This work has included theoretical and conceptual work on developing effective health promotion interventions for ethnic minority groups, developing and evaluating interventions, and undertaking clinical trials (currently, he is the principal investigator of a randomised trial to evaluate an adapted household-based dietary modification and physical exercise intervention to prevent diabetes and obesity in South Asians (PODOSA). Martin White is Professor of Public Health at the University of Newcastle and has longstanding experience in the fields of public health, health promotion and ethnicity and health, with over 70 relevant research publications. He has conducted systematic reviews of interventions for ethnic minorities, as well as epidemiological studies, qualitative studies and trials in these groups. He has experience of complex data synthesis1–6 and is co-applicant on a similar project recently commissioned by HTA on evaluating health trainers. Mark Deverill is a health economist from the University of Newcastle with a particular research interest in methods of economic evaluation of health technology interventions. Mark Johnson is Clinical Lead for the NHS Specialist Library for Ethnicity & Health (NHS SLEH) and Director of the UK Centre for Evidence in Ethnicity Health and Diversity at the Mary Seacole Research Centre, De Montfort University in Leicester. He has considerable experience of conducting systematic reviews, health promotion research, and working with minority communities to assess the cultural competence and quality of translation of health information materials. He will take a lead in managing the systematic review search strategy and liaison with Black and minority ethnic ‘user’ communities. Gina Netto is a Research Fellow at the School of the Built Environment, Heriot Watt University, who has led and contributed to a number of academic and policy-oriented studies related to ethnicity in the fields of health, housing and social care over the last 11 years. She is currently leading on a review of health promotion interventions funded by NHS Health Scotland related to the main causes of mortality in Pakistani, Indian and Chinese communities. This work includes an examination of knowledge/beliefs, attitudes and behaviour related to risk factors including smoking, physical behaviour and diet, as well as an evaluation of the effectiveness of targeted interventions for minority ethnic groups.
6. SERVICE USERS
The team recognise the value and importance of involving service users in research, and are committed to the approaches advocated by INVOLVE in a number of ways. We shall be working closely with representative bodies from minority communities, such as Afiya Trust, but in view of the broad definition of a potential user of health promotion materials and the need to ensure representation of the views of a diversity of minority ethnic communities, it is difficult to identify individuals who could represent a ‘user voice’ without running the risk of exploiting or exhausting their ability to contribute. To overcome this, we will convene a one day conference for service users from a range of ethnic minority groups at the outset of the project and also at the conclusion of the project to disseminate findings. The later stages of the project will include more direct contact with user representative bodies, and initially we shall also make use of the Expert Patient Panel of the Leicester Centre for Ethnic Health Research, (an NHS initiative associated with the Mary Seacole Research Centre), who are supportive of the need for this study.
7. JUSTIFICATION OF SUPPORT REQUIRED
Staff: Funding is requested for a part-time (0.3WTE) post-doc researcher to lead the review, qualitative data collection and evidence synthesis, with support from a full-time research fellow. We request funding for a 50% study secretary, who will help organise meetings, populate databases, organise interviews and transcribe data from interviews. We also request 10% costs for six months from the NHS SLEH librarian to help with formulating and refining searches, retrieving published papers, reports and grey literature and organising translations. Staff equipment and training: Funding is requested for two PCs and a dictaphone and NVIVO software license. Research staff will be eligible to attend the University of Edinburgh’s MSc Public Health Research systematic review module free of charge and other in-house training opportunities; a small training budget is requested in case of additional training needs to attend the University of York or Oxford systematic review courses. Literature retrieval and translation: We envisage the need to obtain a large amount of grey literature, which may only be available in hard copy format and will therefore need to be purchased; some funds are also requested to cover inter-library loans and professional translations of key papers/reports that are not published in English. Meetings: We have requested costs to cover travel costs, subsistence and refreshments for members of the SG and IPSC to attend relevant meetings. Two conferences for service users/academics are also planned: one at the beginning of the study to raise awareness and encourage engagement and a second at the end of the project to share findings. Dissemination: We are also very keen to disseminate our findings at national and international conferences and costs are requested to support travel to and attendance at these meetings to present our work.
8. FLOW DIAGRAM
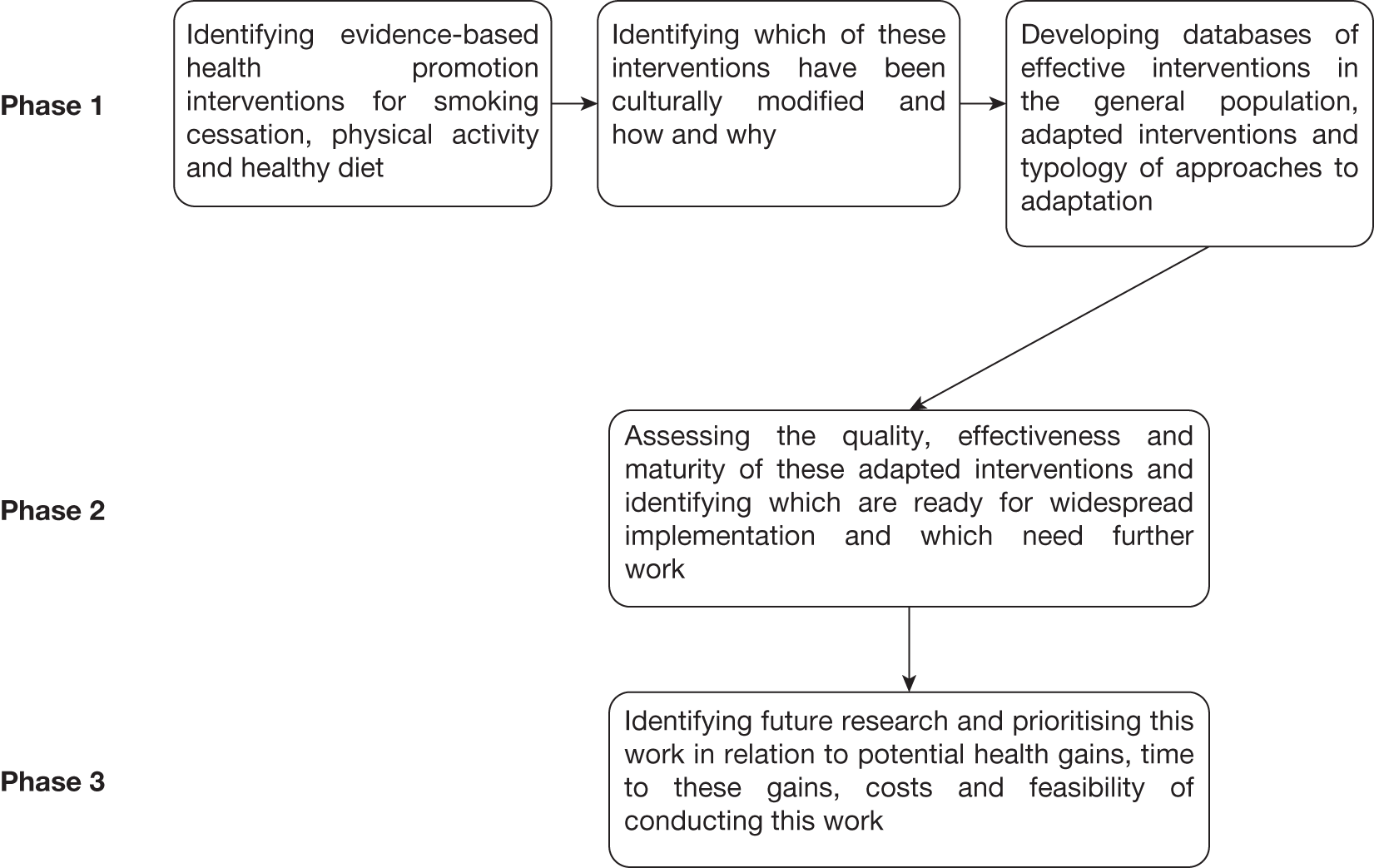
9. KEY REFERENCES
- Bhopal RS. Ethnicity, race, and health in multicultural societies; foundations for better epidemiology, public health, and health care. Oxford: Oxford University Press; 2007.
- National Statistics . Ethnicity n.d. URL: http://www.statistics.gov.uk/cci/nugget.asp?id=273 (accessed 6 August 2007).
- Davies M, Macdowall W. Health promotion theory. Berkshire: Open University Press; 2006.
- Macdowell W, Bonell C, Davies M. Health promotion practice. Berkshire: Open University Press; 2006.
- Bhopal R S, White M, Ahmad W. ‘Race’ and health in contemporary Britain. Buckingham, Open University Press; 1993.
- Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ 2000;321:694-96.
- Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455-59.
- Bhopal RS. The public health agenda and minority ethnic health: a reflection on priorities. J Roy Soc Med 2006;99:58-61.
- Bhopal R. Glossary of terms relating to ethnicity and race: for reflection and debate. J Epidemiol Comm Hlth 2004;58:441-45.
- Nazroo JY. The health of Britain’s ethnic minorities. London: Policy Studies Institute; 1997.
- Acheson Report . Independent Enquiry into Inequalities in Health. Report of the Scientific Advisory Group. London 1998.
- Johnson MRD, Owen D, Blackburn C. Black and minority ethnic groups in England: the second health and lifestyles survey. London: Health Education Authority; 2000.
- Johnson MRD, Killoran A, Swann C, Kelly M. Public health evidence: changing the health of the public. Oxford: University Press; 2006.
- Wild SH, Fischbacher C, Brock A, Griffiths C, Bhopal R. Mortality from all causes and circulatory disease by country of birth in England and Wales 2001–2003. J Public Health (Oxf) 2007;29:191-98.
- Crisp N. Race Equality Action Plan n.d. URL: http://www.dh.gov.uk/en/PublicationsAndStatistics/Bulletins/DH_4072494 (accessed 6 August 2007).
- McNaught A. Health policy and race equality: an illusion of progress?. J Roy Soc Med 2004;97:579-81.
- Ranganathan M, Bhopal R. Exclusion and inclusion of nonwhite ethnic minority groups in 72 North American and European cardiovascular cohort studies. PLoS Med 2006;3.
- Sheikh A, Netuveli G, Kai J, Panesar SS. Comparison of reporting of ethnicity in US and European randomised controlled trials. BMJ 2004;329:87-8.
- Sheikh A. Why are ethnic minorities under-represented in US research studies?. PLoS Med 2006;3.
- Netto G, Arshad R, de Lima P, Almeida Diniz F, Patel V, Syed R. Audit of research on minority ethnic issues from a ‘race’ perspective. Edinburgh: Scottish Executive; 2001.
- Johnson MRD, Samanta A, Hudson N, Culley L, Guo F, Rauf A. Evaluation of patient information resources on osteomalacia in Asian languages. Leicester: MSRC (for Arthritis Research Campaign); 2007.
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite R. Cultural sensitivity in public health: defined and demystified. Ethn Dis 1999;9:10-21.
- McAllister G, Farquhar M. Health beliefs: a cultural division?. J Adv Nurs 1992;17:1447-54.
- Greenhalgh T, Helman C, Chowdury AM. Health beliefs and folk models of diabetes in British Bangladeshis: a qualitative study. BMJ 1998;316:978-83.
- Netto G, McLouughan L, Bhatnagar A. Effective health disease prevention: lessons from a qualitative study of user perspectives in Bangladeshi, Indian and Pakistani communities. Pub Hlth 2007;121:177-86.
- Lewin B, Robertson IH, Cay EL, Irving JB, Campbell M. Effects of self-help post-myocardial infarction rehabilitation on psychological adjustment and use of health services. Lancet 1992;339:1036-40.
- Kelly M, Patel KC, Shah A. Prevention, treatment and rehabilitation of cardiovascular disease in South Asians. Birmingham: South Asian Foundation; 2005.
- Bhopal RS. Health education and ethnic minorities. BMJ 1991;302.
- Health Education Board for Scotland . Research for a Healthier Scotland: The Research Strategy of the Health Education Board for Scotland 1999.
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet 1999;354:1896-900.
- Critical Appraisal Skills Programme . Qualitative Research n.d. URL: http://www.phru.nhs.uk/Pages/PHD/CASP.htm (accessed 6 August 2007).
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12.
- Higgins JPT, Green S. Cochrane Handbook for systematic reviews of interventions 4.2.5. Chichester: John Wiley; 2005.
- Ritchie J, Spencer L, O’Connor W, Ritchie J, Lewis J. Qualitative research practice: a guide for social science students and researchers. London: SAGE Publications; 2003.
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-101.
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34.
- Pope C, Ziebland S, Mays N. Analysing qualitative data. BMJ 2000;320:114-16.
Appendix 3 Amendments to protocol
The following minor amendments were made to the original scientific rationale:
Overall project
The review of national guidelines and international systematic reviews, the systematic review and the qualitative interviews were carried out in parallel, instead of sequentially as proposed, in order to accommodate the large amount of literature identified in each component. This meant that the systematic review search was not limited to interventions which had been found to have high level evidence of efficacy in the national guidelines and international systematic reviews. However, this amendment allowed the inclusion of a greater body of literature in the systematic review and permitted recommendations for research to be generated in a reciprocal manner, i.e. also highlighting adapted studies utilising health promotion interventions outside of the evidence identified as effective in national guidelines and international systematic reviews provided scope to re-examine this evidence to consider whether these interventions, although not recommended for general populations, may actually be effective for ethnic minority populations (see Chapter 6).
The project team applied for a no-cost extension and was granted an additional four months to allow sufficient time to analyse the large volume of literature identified in the systematic review. This extended the project completion date from the end of December 2010 to the end of May 2011.
Systematic review
All study types were included in the search for the systematic review, as specified in the original scientific rationale. Epidemiological studies were rarely included for further analysis as they did not relate to the relevant interventions or outcomes of interest.
The literature included in the systematic review was limited to the populations of interest (African-, Chinese- and South Asian-origin) owing to the large body of literature identified with the initially specified populations, and therefore did not include other populations from which findings could be generalised, as suggested in the original scientific rationale.
The Health Education and Promotion System (HEAPS) and HealthPromise databases which were listed as literature sources in the original scientific rationale are no longer available for use and so were not able to be used. Owing to the volume of literature retrieved from the initial searches a more limited ‘grey literature’ search was undertaken primarily involving personal libraries and contacting expert organisations (e.g. National Resource Centre on Ethnic Minorities) and experts in the field through specialist academic ethnicity e-mail lists (e.g. Jiscmail). Searches were also carried out in Google, Google Scholar, controlledtrials.com and clinicaltrials.gov. The bibliographies of retrieved references were used to search for further relevant publications.
The outcome measures in the systematic review were further refined prior to commencing the literature searching. The outcomes were limited to defined primary, secondary and tertiary outcomes, which are outlined in the systematic review methods section (see Chapter 6).
To quality appraise the studies included in the systematic review, the Effective Public Health Practice Project (EPHPP), Critical Appraisal Skills Programme (CASP) and Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) tools were purposefully selected over the generic Cochrane quality appraisal approach originally specified.
In addition to considering the theoretical underpinnings of an adapted study, we have simultaneously analysed whether or not adapted studies drew on any behaviour change theories. This analysis was done using behaviour change techniques (Michie et al. in press), which are derived from a synthesis of different behaviour change theories commonly used in health promotion. Example behaviour change techniques such as goal setting, stress reduction and relapse prevention capture features of several health behaviour change theories.
Reporting of the behaviour change techniques identified in each study was planned. Also, a quantitative analysis to detect possible patterns arising from the number and type of behaviour change techniques or adaptations observed in the included studies and how they relate to intervention effectiveness was intended, but neither of these planned activities could be undertaken within the scope of the project.
Qualitative interviews
No changes were made.
Data synthesis
Realist approach was used to synthesis the data from the studies in the systematic review instead of a thematic or narrative approach in order to fit with the overall realist synthesis.
Appendix 4 Ethics application submitted for qualitative interviews
Appendix 5 Launch conference programme
Appendix 6 Launch conference feedback, 4 June 2009
-
Eighty-one delegates registered before the conference.
-
Eighty-one delegates attended the conference (a few delegates cancelled last minute; however, other delegates attended in their place).
-
Forty-four delegates (54%) completed a conference feedback form.
Summary of feedback scores (n = 44 delegates)
| How would you assess the following? | Excellent | Good | Average | Poor | Very poor | Total (%) |
|---|---|---|---|---|---|---|
| Pre-conference registration procedures | 73 | 27 | 0 | 0 | 0 | 100 |
| Conference information and documents | 64 | 34 | 2 | 0 | 0 | 100 |
| Registration procedures at the conference | 73 | 27 | 0 | 0 | 0 | 100 |
| Venue, food and refreshments | 80 | 20 | 0 | 0 | 0 | 100 |
| Presentations | 68 | 30 | 2 | 0 | 0 | 100 |
| Workshops and general discussions | 34 | 50 | 16 | 0 | 0 | 100 |
| Length of time allocated to presentations, workshops | 39 | 52 | 9 | 0 | 0 | 100 |
| Conference facilities including poster exhibition | 50 | 39 | 9 | 2 | 0 | 100 |
| How well did the conference meet your expectations? | 52 | 43 | 5 | 0 | 0 | 100 |
| Overall satisfaction with the conference? | 57 | 41 | 2 | 0 | 0 | 100 |
Summary points
-
Overall, the delegates who responded felt that the conference met their expectations and were satisfied with the conference.
-
The venue, food and registration process were well regarded.
-
The presentations by the speakers were also highly rated.
-
The workshops and general discussion could be improved as well as the length of time allocated to them.
Overall strengths of the conference
-
Wide range of speakers, delegates and topics of discussion:
-
– wide range of speakers on interesting topics
-
– relevant, engaging, practical and challenging
-
– excellent, high profile speakers with an international perspective
-
– the conference was a place for researchers, health-care professionals and community workers to come together, I think that is very important to bring different sections of public health together.
-
Room for improvement
-
More time required to look at posters, to network and for breaks:
-
– more time to look at posters, not just during lunch
-
– more time for networking.
-
-
Workshops were too big and unstructured:
-
– more time in workshops and time for feedback
-
– longer time for discussion within smaller groups
-
– unsure what the purpose of the workshop was.
-
Most useful session
-
Many delegates found Dr Wayne Giles’ presentation to be the most useful as it provided examples from projects outside the UK:
-
– very clear, practical, clear outcomes.
-
-
Others found all of the sessions to be equally useful:
-
– can’t pick one – all equally useful and complemented each other well.
-
Topics of interest for future ethnicity and health events
-
More examples of successful interventions, particularly those that make links between good practice and health outcomes:
-
– more on best practice examples, both in communities and in regards to research.
-
-
More community involvement and its role in research:
-
– how do research and community projects, which already exist, can come together?
-
-
More on topics that intersect with ethnicity:
-
– ethnicity and social care, palliative care, end of life care
-
– sociological determinants of behaviour
-
– institutionalised racism.
-
Reasons for attending the conference
-
To further professional capacity, network and learn:
-
– to see how other interventions/studies could be learnt from and applied to my work area.
-
Additional comments
Thank you – these types of discussion needs to take place within the mainstream as a regular ‘agenda’ item.
Appendix 7 Dissemination conference programme
Appendix 8 Dissemination conference feedback, 2 February 2011
-
Sixty-four delegates registered before the conference.
-
Fifty-seven delegates attended the conference.
-
Forty delegates (70%) completed a conference feedback form.
Summary of feedback scores (n = 40 delegates)
| How would you assess the following? | Excellent | Good | Average | Poor | Very poor | Total (%) |
|---|---|---|---|---|---|---|
| Pre-conference registration procedures | 54 | 39 | 5 | 2 | 0 | 100 |
| Conference information and documents | 62 | 33 | 5 | 0 | 0 | 100 |
| Registration procedures at the conference | 69 | 31 | 0 | 0 | 0 | 100 |
| Venue, food and refreshments | 87 | 13 | 0 | 0 | 0 | 100 |
| Presentations | 58 | 40 | 0 | 2 | 0 | 100 |
| Workshops and general discussions | 36 | 54 | 8 | 2 | 0 | 100 |
| Length of time allocated to presentations, workshops | 40 | 55 | 5 | 0 | 0 | 100 |
| Conference facilities including poster exhibition | 55 | 30 | 13 | 2 | 0 | 100 |
| How well did the conference meet your expectations? | 43 | 49 | 8 | 0 | 0 | 100 |
| Overall satisfaction with the conference? | 60 | 33 | 7 | 0 | 0 | 100 |
Summary points
-
The venue, food and registration process were well regarded.
-
The presentations received mixed feedback: some felt that they were too detailed; others felt that they were a concise summary of the project findings.
-
The workshops and general discussion could be improved as well as the length of time allocated to them (longer workshops and shorter general discussions).
Overall strengths of the conference
-
Mix of participants, good discussion and user involvement.
-
Presentation of findings was informative and concise.
Room for improvement
-
Presentations were too long and detailed.
Most useful session
-
Different sessions found to be useful, in particular, workshops on translation of research findings and theoretical considerations.
Topics of interest for future ethnicity and health events
-
More focus on policy-making and policy changes.
-
More focus on psychological aspects, or on work from psychosocial fields.
-
More information about the actual interventions used, working interventions.
Reasons for attending the conference
-
Many people working in this field (researchers, practitioners).
-
Networking.
Additional comments
-
Circulate delegates list.
Appendix 9 Extraction form for review of UK guidelines and international systematic reviews
| 1 | Paper number |
| 2 | Author |
| 3 | Year |
| 4 | Title |
| 5 | Journal |
| 6 | Study type – is it a systematic review? (predefined search terms and databases?) – if yes, continue on to question 7; if no, stop and exclude this study |
| 7 | List all recommendations/conclusions from the review and the strength of evidence provided by the authors (data used for Chapter 4, questions 8–18 used for Chapter 5) |
| 8 | Key terms search (full text) – systematically scan paper for terms equivalent to (Ethnic*, Rac*, Minorit*, Cultur*, Asian, Chinese, Black, African, Afro, Caribbean, South Asian, Bangladeshi, Indian, Pakistani). * denotes variants of the term, for example ethnic* = ethnicity, ethnicities. Record yes or no for each term (if it appears in the study or not) – if yes, continue to question 9; if no, stop |
| 9 | Population [record the population(s) included in the study; report for each ethnic group included after performing the key terms search] |
| 10 | For each ethnic group, record age, gender and n (questions 11, 12, 13): |
| 11 | Age |
| 12 | Gender |
| 13 | Number |
| 14 | Ethnicity criteria (record how ethnicity was determined? language, self-defined?) |
| 15 | Subgroup analysis – does the paper/review include subgroup meta-analysis providing pooled measures of effectiveness according to ethnicity? Yes/no. If yes, please describe the subgroup analysis and its findings (questions 16, 17); if no, proceed to question 18 |
| 16 | Intervention effective for ethnic minority group |
| 17 | Differential effect sizes for pooled results between ethnic minority and general population? |
| 18 | ‘Overarching comments’ – does the paper include any overarching statement on ethnicity (e.g. ethnicity should be considered in research)? Yes/no. If yes, please list the overarching statement (in the original language and in English if possible) |
Appendix 10 Tables of evidence statements extracted from guidelines and systematic reviews
Table of extracted guideline evidence statements
| Source | Evidence | Strength of evidence (grade) | Method of grading |
|---|---|---|---|
| SIGN | |||
| SIGN 8 Obesity in Scotland236 | Household involvement to increase compliance with dietary changes | A (level Ib) | SIGN |
| Behavioural modification techniques for diet and physical activity | A (level Ib) | SIGN | |
| SIGN 69 Management of obesity in children and young people200 | Reducing physical inactivity (e.g. television, computer games) to an average of < 2 hours/day or 14 hours/week | D | SIGN |
| SIGN 97 Risk estimation and the prevention of cardiovascular disease137 | Occupational and/or leisure time physical activity of moderate intensity should be taken | B | SIGN |
| NRTs or bupropion as part of smoking cessation programme | A | SIGN | |
| All smokers should receive advice to stop smoking and be offered support | |||
| Clinical Evidence | |||
| Primary prevention of CVD: physical activity 191 | Counselling can increase physical activity compared with no advice. Written materials and telephone follow-up can aid the increase | Likely to be beneficial | |
| Counselling to increase intensity of physical activity programme | Likely to be beneficial | ||
| Changing behaviour 143 | Physician and trained counsellors advise to quit smoking | Beneficial | |
| Antidepressants (bupropion or nortriptyline) for smoking cessation | Beneficial | ||
| NRTs for smoking cessation | Likely to be beneficial | ||
| Nurse advise on smoking cessation | Likely to be beneficial | ||
| Counselling for sedentary people to increase physical activity | Likely to be beneficial | ||
| Self-help materials for people looking to quit smoking | Likely to be beneficial | ||
| Telephone advice for smoking cessation | Likely to be beneficial | ||
| NICE | |||
| PH6 Behaviour change at population, community and individual levels112 | Work in partnership (individuals, communities, organisations, populations) and in collaboration in planning and development of programmes and interventions to change health behaviour | N/R | N/R |
| Remove or reduce barriers to behaviour change when possible (social, financial, environmental) | N/R | N/R | |
| Point-of-sale promotions and/or interventions to promote healthy eating | N/R | N/R | |
| Key life stages e.g. starting or leaving school | N/R | N/R | |
| National and local advertising and mass media campaigns for positive health behaviours | N/R | N/R | |
| Fiscal and legislative interventions for enhancing health | N/R | N/R | |
| Tailor interventions to individuals, address barriers and consider individuals’ social contexts | N/R | N/R | |
| Develop supportive health-enhancing social, physical and service environments | N/R | N/R | |
| PH2 Four commonly used methods to increase physical activity: brief interventions in primary care, exercise referral schemes, pedometers and community-based exercise programmes for walking and cycling79 | Brief interventions in primary care (opportunistic advice, discussion, negotiation or encouragement) for physical activity | N/R | N/R |
| Primary care practitioners to identify (using validated tool, e.g. Department of Health’s physical activity questionnaire) and advise inactive adults (30 minutes, moderate, 5 days a week); follow-up over 3- to 6-month periods | N/R | N/R | |
| Primary care practitioners to provide written information about the benefits of physical activity and local opportunities for physical activity | N/R | N/R | |
| Primary care practitioners to consider individual’s needs, preferences and circumstances when providing advice on physical activity; assist in goal setting | N/R | N/R | |
| Exercise referral schemes recommended only as part of research studies | N/R | N/R | |
| Pedometers and walking and cycling schemes (defined as organised walks or rides) recommended only as part of research studies | N/R | N/R | |
| PH17 Promoting physical activity, active play and sport for pre-school and school-age children and young people in family, pre-school, school and community settings172 | Deliver a national campaign to promote physical activity for children and young people (minimum 5 years) | N/R | N/R |
| Consult children, young people and their parents regarding media messages and appropriate language for physical activity | N/R | N/R | |
| Message should encourage a variety of formal and informal activities; fun, enjoyable and sociable, should become a regular part of daily life | N/R | N/R | |
| Adults, especially parents and carers, should set an example for physical activity; support families in promoting physical activity | N/R | N/R | |
| Local strategy to ensure safe and accessible local indoor and outdoor opportunities for physical activity (e.g. schools) | N/R | N/R | |
| Partnerships with and within community networks to provide physical activities for children and young people | N/R | N/R | |
| Education and advice to increase awareness of benefits of physical activity | N/R | N/R | |
| Active transport/travel to school for children and young people; mapping safe routes to school; reduce or remove barriers to active transport | N/R | N/R | |
| Involve children and young people in design, planning and delivery of physical activity opportunities; involve families and local communities on barriers (accessibility, preferences, needs identified through research, local consultation); particularly involve girls and young women | N/R | N/R | |
| Facilities for physical activity should meet the diversity of needs of children and young people | N/R | N/R | |
| Multicomponent physical activity programmes developed by schools (involving family and community-based activities) | N/R | N/R | |
| Promote public parks and facilities for physical activity; open spaces and outdoor facilities that encourage physical activity and are accessible (close to walking and cycling routes) | N/R | N/R | |
| Remove barriers to physical activity: facilities, accessibility, privacy for changing, dress policy | N/R | N/R | |
| Provide daily opportunities for physical activity for children, as well as after school, extracurricular, at weekends and during holidays; structured and unstructured play | N/R | N/R | |
| Provide advice on self-monitoring and individualised tailored feedback | N/R | N/R | |
| TA123 Varenicline for smoking cessation166 | Varenicline can aid smoking cessation | N/R | N/R |
| PH5 Workplace health promotion: how to help employees to stop smoking127 | Workplaces should publicise effective interventions and make available information on local services for smoking cessation | N/R | N/R |
| Telephone counselling and quitlines | N/R | N/R | |
| Workplaces, where feasible, should provide on-site smoking cessation services | N/R | N/R | |
| Workplaces should allow staff to attend smoking cessation services during work hours without loss of wages | N/R | N/R | |
| Workplaces should develop smoking cessation policy in partnership with staff, in addition to a smoke-free workplace policy | N/R | N/R | |
| Workplaces should tailor support and treatment to needs and preferences of employees | N/R | N/R | |
| PH8 Promoting and creating built or natural environments that encourage and support physical activity173 | Linkage of routes from workplace, schools, etc. to walking and cycling networks and other modes of active transport | N/R | N/R |
| Provide information and advice on benefits of physical activity | N/R | N/R | |
| Encourage parents and carers to be active along with their children; incorporate physical activity into daily life; parents and carers to encourage active travel | N/R | N/R | |
| Pedestrians, cyclists and users of other modes of transport should be prioritised when developing or maintaining infrastructure (streets and roads) | N/R | N/R | |
| Develop and maintain spaces to encourage stair use (signage, well lit) | N/R | N/R | |
| School playgrounds should be designed to encourage varied physical activities | N/R | N/R | |
| Planning and development should consider maximising opportunities for physical activity and conduct health impact assessments | N/R | N/R | |
| PH10 Smoking cessation services in primary care, pharmacies, local authorities and workplaces, particularly for manual working groups, pregnant women and hard to reach communities120 | Behavioural counselling, group therapy, pharmacotherapy or a combination of treatments for smoking cessation | N/R | N/R |
| Provide tailored advice, counselling and support, particularly to clients from minority ethnic and disadvantaged groups (service in language of choice) | N/R | N/R | |
| Telephone quit lines should offer a ‘rapid, positive and authoritative response’ (service in language of choice) | N/R | N/R | |
| NRTs, varenicline or bupropion to support smoking cessation, but not together in any combination | N/R | N/R | |
| Nicotine patches and another form of NRT (such as gum, inhalator, lozenge or nasal spray) for those with high level of nicotine dependence | N/R | N/R | |
| Advice, encouragement and support, and referrals to NHS Stop Smoking Services | N/R | N/R | |
| Brief interventions, individual behavioural counselling, group behaviour therapy, pharmacotherapies, self-help materials, telephone counselling and quit lines, mass media | N/R | N/R | |
| Varenicline and bupropion should not be offered to young people < 18 years or to pregnant or breastfeeding women | N/R | N/R | |
| Nicotine-assisted reduction to stop (NARS) strategy should be provided only as part of research studies | N/R | N/R | |
| Health-care professionals should identify and advise patients who smoke on health benefits and give brief advice on stopping tobacco use and refer to local services; for those refusing referrals, brief advice and support should be given, and pharmacotherapy if appropriate | N/R | N/R | |
| Advice and referral scheme applies to young people; professional judgement to decide whether to offer NRT to those > 12 years; behavioural support to help young people of 12–17 years to quit + NRT | N/R | N/R | |
| Doctors, nurses, midwives, pharmacists, dentists and telephone quit-line counsellors should provide brief advice on smoking cessation | N/R | N/R | |
| Workplace smoke-free policy | N/R | N/R | |
| Smoking cessation campaigns that are extensive and sustained; involve community pharmacies, dentists, fire services and voluntary groups | N/R | N/R | |
| PH13 Workplace health promotion: how to encourage employees to be physically active176 | Organisational policy to encourage employees to be more physically active and policy linkages with other internal, local and national policies | N/R | N/R |
| Multicomponent, organisational programmes to support employees to be physically active (e.g. active travel, disseminate information, advice, support incentive schemes, tailor to needs) | N/R | N/R | |
| Encourage goal setting; signs to encourage walking up stairs instead of using a lift; opportunities to be active at work | N/R | N/R | |
| Encourage active transport (to and from work; at work) | N/R | N/R | |
| PH1 Brief interventions and referral for smoking cessation in primary care and other settings139 | Stop smoking advice should be sensitive to individual’s ‘preferences, needs and circumstances’ | N/R | N/R |
| GPs should advise all patients who smoke to quit during consultations. GPs to make referrals to stop smoking services. If not ready to quit or unwilling, offer pharmacotherapy and additional support | N/R | N/R | |
| Nurses in primary and community care should provide stop smoking cessation advice and make referrals to intensive support service | N/R | N/R | |
| Community workers should refer those who smoke to intensive support services | N/R | N/R | |
| All health professionals, e.g. hospital clinicians, pharmacists and dentists, should make referrals to intensive stop smoking services | N/R | N/R | |
| CG43 Obesity: guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children174 | Assessing readiness to change is important to decide when and how to intervene | N/R | N/R |
| Barriers to lifestyle change should be explored, e.g. cost, safety, time, social and environmental factors | N/R | N/R | |
| Advice needs to be tailored to different groups, e.g. according to ethnicity, life stage and/or SES | N/R | N/R | |
| Needs to be a cross-sectorial approach to creating more safe spaces for incidental and planned physical activity | N/R | N/R | |
| Should take a settings approach including health promotion through nurseries, schools, workplaces, commercial and community settings | N/R | N/R | |
| Parents and carers to monitor children’s time spent watching TV to reduce exposure to advertisements and other inappropriate content | N/R | N/R | |
| Activities for physical activity should be tailored to people’s preferences, needs and circumstances; people should be supported in person, by telephone, by mail, through the internet | N/R | N/R | |
| For physical activity, improve people’s belief in their own ability to change (e.g. by verbal persuasion, modelling exercise behaviour and discussing positive effects) | N/R | N/R | |
| Improving diet and increasing activity levels in children should involve parents and carers | N/R | N/R | |
| Local authorities and health professionals should work with local shops, supermarkets, restaurants, caterers, cafes and voluntary community services to promote healthy eating choices and promote availability and accessibility of healthy food and drinks (signs, posters, pricing, positioning) | N/R | N/R | |
| Health professionals should promote community initiatives that increase access to physical activity, e.g. walking or cycling routes | N/R | N/R | |
| Family programmes to improve diet or increase physical activity should provide ongoing tailored support, incorporate behaviour change techniques | N/R | N/R | |
| Local authorities to provide personalised travel plans | N/R | N/R | |
| Community programmes for improving diet and increasing activity levels should address concerns of local people: availability of services, costs, expectations, dangers, mixed media messages | N/R | N/R | |
| Local authorities to work with industry and voluntary organisations to create safe spaces for incidental and planned physical activity | N/R | N/R | |
| Local policies should improve access to healthy foods and opportunities for physical activities | N/R | N/R | |
| At schools, nurseries and childcare facilities, children should eat regular meals in pleasant, sociable environments, supervised | N/R | N/R | |
| Schools in partnership with organisations and professionals to promote physical activity | N/R | N/R | |
| Longer-term multicomponent interventions in schools rather than one-off events (general health) | N/R | N/R | |
| Nurseries and childcare facilities should be involved in improving children’s diet and activity levels | N/R | N/R | |
| Whole-school approach (recreation space, catering, curriculum, active transport) to improve healthy eating and physical activity | N/R | N/R | |
| Views and preferences of children and young people should be considered for improving nutrition | N/R | N/R | |
| Involve parents and carers in planning school-based interventions for physical activity and improving nutrition (e.g. lunch menus, after-school activities). Involve parents and children in diet and physical activity interventions for children | N/R | N/R | |
| Workplaces should promote active travel | N/R | N/R | |
| Workplaces to support incentive schemes (food and drink provision and prices, gym memberships) and education and promotion programmes for improving diet and increasing physical activity | N/R | N/R | |
Table of extracted systematic review evidence statements
| Source | Evidence statements | Quality reported (yes or no/unclear) | Method of quality assessment |
|---|---|---|---|
| Cochrane | |||
| Bala et al. 2008121 | There is evidence that comprehensive tobacco control programmes that include mass media campaigns can be effective in changing smoking behaviour in adults |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported [Cochrane Effective Practice and Organisation of Care Group (EPOC 2006)421] |
| Brunner et al. 2007232 | Dietary advice appears to be effective in bringing about modest beneficial changes in diet (longer-term effects are not known) |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Cahill et al. 2008167 | Varenicline increased the chances of successful long-term smoking cessation |
Recommendations: no Evidence: yes |
Included only RCTs Recommendations: no Evidence: criteria reported (Cochrane handbook for systematic reviews on interventions422) |
| Cahill et al. 2008123 | Workplace interventions including individual counselling, group counselling and pharmacological treatment are effective |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Dobbins et al. 2009180 | There is good evidence that school-based physical activity interventions have a positive impact on four of the nine outcome measures. Specifically, positive effects were observed for duration of physical activity, television viewing and VO2max |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (a previously developed and tested quality assessment tool423) |
| Foster et al. 2005204 | Results are indicative that professional advice and guidance with continued support can encourage people to be more physically active in the short to mid-term. Conclusions about the effectiveness of individual aspects of interventions must be interpreted with caution as studies were heterogeneous |
Recommendations: no Evidence: yes |
Included RCTs only Recommendations: no Evidence: criteria reported (descriptive) |
| Hughes et al. 2007163 | The antidepressants bupropion and nortriptyline aid long-term smoking cessation (evidence suggests that they are of similar efficacy to nicotine replacement) |
Recommendations: no Evidence: yes |
Included RCTs only Recommendations: no Evidence: criteria reported (descriptive – reported to be consistent with Cochrane methods) |
| Lancaster and Stead 2005130 | Individually delivered smoking cessation counselling can assist smokers to quit. Did not detect a greater effect with intensive counselling compared with brief counselling |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Lancaster and Stead 2005140 | Standard self-help materials may increase quit rates compared with no intervention, but the effect is likely to be small. Absolute effect size that tailored materials are more effective than untailored materials was small |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Rice and Stead 2008150 | Reasonable evidence of potential benefits of smoking cessation advice and/or counselling provided by nurses to patients; the effect was weaker when nurse providers’ main role was not health promotion or smoking cessation |
Recommendations: no Evidence: yes |
Included RCTs only Recommendations: no Evidence: criteria reported (Cochrane methods) |
| Stead and Lancaster 2005133 | Group therapy is effective for helping people stop smoking. There is insufficient evidence to support the use of any specific psychological components and insufficient evidence whether or not group counselling is more effective than intensive counselling |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Stead et al. 2006136 | Proactive telephone counselling helps smokers interested in quitting to quit. Evidence of dose–response: one or two calls may be insufficient; three or more calls increase likelihood of quitting. This is compared with minimal intervention, i.e. standard self-help materials, brief advice or pharmacotherapy alone |
Recommendations: no Evidence: yes |
Included RCTs or quasi-RCTs Recommendations: no Evidence: criteria reported (descriptive) |
| Stead et al. 2008154 | All of the commercially available forms of NRT (gum, transdermal patch, nasal spray, inhaler and sublingual tablets/lozenges) can help people who make a quit attempt to increase their chances of successfully stopping smoking. NRTs increase the rate of quitting by 50–70% regardless of setting. The effectiveness of NRT appears to be largely independent of the intensity of the additional support provided |
Recommendations: no Evidence: yes |
Included RCTs only Recommendations: no Evidence: criteria reported (descriptive) |
| Stead et al. 2008147 | Physician-provided brief advice has a small effect on smoking cessation: it can increase quitting by 1–3% over the assumed unassisted quit rate of 2–3%. There is a small additional benefit from more intensive intervention compared with brief intervention |
Recommendations: no Evidence: yes |
Included only RCTs Recommendations: no Evidence: criteria reported (Cochrane Handbook422) |
| Whittaker et al. 2007169 | Mobile telephone (any intervention via mobile telephone delivery) interventions have been shown to have short-term effectiveness only; no long-term outcomes. Meta-analysis of text message programme trials demonstrated a significant increase in short-term self-reported quitting (RR 2.18, 95% CI 1.80 to 2.65). When data from the internet and mobile telephone programmes were pooled it significantly increased both short- and long-term self-reported quitting (RR 2.03, 95% CI 1.40 to 2.94) |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Database of Abstracts of Reviews of Effects | |||
| Adams and White 2003196 | Transtheoretical model-based activity promotion programmes are effective in promoting adoption of physical activity in the short term; long-term evidence is limited but likely not promising |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Ammerman et al. 2001229 | Components such as social support, group delivery and family are associated with increasing fruit and vegetable consumption (greater increases in fruit than vegetable). Average increase in fruit and vegetable intake reported was 0.6 servings per day, along with consistent decreases in intake of total fat and saturated fat. The mean change in total fat intake estimated as a 7.3% reduction in the percentage of calories from fat. Interventions appeared to be more successful for those at risk or diagnosed with disease than for healthy populations. Difficult to draw conclusions because of heterogeneity; unclear long-term sustainability |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (developed own quality rating form) |
| Ammerman et al. 2002230 | Counselling patients can improve dietary behaviours, including reduction in dietary total and saturated fat and increases in fruit and vegetable intake. More intensive counselling and counselling directed to higher-risk patients have generally produced larger changes than less intensive interventions delivered to low-risk populations. Common feature: goal setting and self-monitoring |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Ashenden et al. 1997138 |
For smoking cessation, meta-analysis showed that providing smoking cessation advice, brief or intensive, in primary care increased the odds of stopping smoking (OR 1.32, 95% CI 1.18 to 1.48); intensive-only advice improves this by a small amount (OR 1.46 compared with 1.27) – meta-analysis studies showed no significant difference between brief and intensive advice (OR 1.07, 95% CI 0.88 to 1.29). General practice-based lifestyle intervention may be promising but no evidence so far of substantial changes No definite conclusions for diet and exercise |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (simplified version of Chalmers et al. 424) |
| Blue and Black 2005211 | There is evidence that physical activity and dietary interventions which include educational components, including written materials; involving group sessions; and utilising behaviour change theory are successful in improving physical activity and dietary outcomes |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive according to methods of Sidani and Braden425) |
| Bravata et al. 2007208 | Pedometer use increases physical activity. In RCTs pedometer users significantly increased their physical activity by 2491 steps per day compared with control participants (95% CI 1098 to 3885 steps per day, p = 0.001). Among observational studies, pedometer users significantly increased their physical activity by 2183 steps per day over baseline (95% CI 1571 to 2796 steps per day, p < 0.0001). Overall, pedometer users increased their physical activity by 26.9% over baseline. An important predictor of increased physical activity was having a step goal such as 10,000 steps per day (p = 0.001). When data from all studies were combined, pedometer users significantly decreased their BMI by 0.38 (95% CI 0.05 to 0.72, p = 0.03). This decrease was associated with older age (p = 0.001) and having a step goal (p = 0.04) |
Recommendations: no Evidence: no |
Recommendations: no Evidence: some criteria reported (descriptive) |
| Breckon et al. 2008188 | Counselling can result in behavioural change and increased physical activity |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported although criteria were mentioned |
| Brothwell 2001151 | There is good evidence to recommend oral health professionals provide cessation counselling. Separately, there is good evidence to recommend the use of smoking cessation adjuncts, including NRT patches and gum and bupropion |
Recommendations: yes Evidence: yes |
Recommendations: there is good evidence to recommend that oral health professionals provide cessation counselling for all patients who use tobacco [level of recommendation A, level of evidence I (meta-analysis and systematic reviews) and III (case series)]; there is good evidence to recommend the use of smoking cessation adjuncts (nicotine patches, gum and bupropion) [level of recommendation A, level of evidence I (meta-analysis and systematic reviews)] Evidence: criteria reported (Canadian Task Force on the Periodic Health Examination426) |
| Brunner et al. 1997234 | Dietary advice can lead to dietary change and modest risk reduction (changes in blood pressure and serum cholesterol) among healthy adults. Longest study was 18 months |
Recommendations: no Evidence: no |
Randomised (or systematically allocated) studies only Recommendations: no Evidence: no explicit measure of quality of evidence reported |
| Brunton et al. 2003179 | For physical activity, the following have been demonstrated to be effective in one or more studies: education and provision of monitoring equipment for television or video game use; engaging parents in supporting or encouraging their children’s physical activity and providing opportunities for family participation; and multicomponent, multisite interventions using a combination of education in the classroom, improvements in school PE and home-based activities. Unclear if consistent association or which are the essential components |
Recommendations: no Evidence: no |
Recommendations: no Evidence: criteria reported (methods used reported in previous EPPI-Centre health promotion reviews; only five evaluations judged to be methodologically sound – recommendations are based on these five evaluations) |
| Ciliska et al. 2000233 | Of the 18 studies that were rated strong or moderate in quality, the most effective interventions were clear messages about increasing fruit and vegetable consumption; longer, more intensive interventions rather than one or two contacts; involved family members; had a greater impact on those with lower baseline values for knowledge and intake |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Clemmens and Hayman 2004198 | School-based, multicomponent interventions designed to decrease sedentary behaviour were also effective in increasing physical activity |
Recommendations: no Evidence: no |
RCTS and quasi-experimental designs only Recommendations: no Evidence: no explicit method reported |
| Contento et al. 1995218 | Multifaceted, sustained, ongoing nutrition education, goal oriented with supportive educational strategies. Successful elements include motivating communications and group educational strategies, strategies for behavioural change, active involvement of both the individual and the community and building health-enhancing environments |
Recommendations: no Evidence: unclear |
Recommendations: no Evidence: some criteria reported (descriptive) |
| Coruh et al. 2005227 | Religion/religious setting, faith-based partnerships, collaboration with churches may improve fruit and vegetable intake – although all of the studies this was based on were in African American populations |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (investigators independently reviewed abstracts and used a modified Delphi to reach consensus; RCTs evaluated using CONSORT guidelines; other studies used guidelines published in the Canadian Medical Journal427,428) |
| DeMattia et al. 2007209 | Decreasing sedentary behaviours, as measured by self-reported television/video use and improved weight measures |
Recommendations: no Evidence: no |
Only controlled intervention studies included Recommendations: no Evidence: criteria reported (validity assessed with items from the Jadad scale429) |
| Dishman and Buckworth 1996199 | Behaviour modification for healthy people – larger effect observed when exercise is group based, unsupervised or when the emphasis is on leisure activities and is low intensity |
Recommendations: no Evidence: no |
Strict inclusion criteria for meta-analysis Recommendations: no Evidence: no explicit method reported |
| Dobbins et al. 2001181 | Limited but good evidence that school-based physical interventions are effective in increasing physical activity rates and duration in children and adolescents |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (developed own) |
| Eakin et al. 2000184 | Primary care-based counselling for physical activity was found to be moderately effective in the short term, although heterogeneous studies. Tailoring to participant characteristics and provision of written materials have larger effects |
Recommendations: no Evidence: yes |
RCTs or quasi-experimental studies with comparison group Recommendations: no Evidence: criteria reported (based on the RE-AIM model430) |
| Eakin et al. 2007186 | Telephone interventions are effective for physical activity and nutrition; positive factors include length of intervention and the number of calls, with interventions lasting 6–12 months and those including ≥ 12 calls producing the most favourable outcomes |
Recommendations: no Evidence: yes |
RCTs prioritised for inclusion Recommendations: no Evidence: Cochrane guidelines431 |
| Eisenberg et al. 2008152 | Pharmacotherapy (varenicline, bupropion and five other NRTs) was more efficacious than placebo for smoking abstinence at 6 and 12 months |
Recommendations: no Evidence: no |
Only included double-blind, placebo-controlled RCTs with biochemically validated outcomes Recommendations: no Evidence: no explicit method reported |
| Engbers et al. 2005225 | Strong evidence of effect for worksite programmes on dietary intake; inconclusive for physical activity |
Recommendations: no Evidence: yes |
Only RCTs/controlled trials included Recommendations: no Evidence: criteria reported (checklist by Cochrane Back Review Group432) |
| Eriksen and Gottlieb 1998124 | Smoking cessation worksite programmes found to be more effective than minimal treatment programmes. Tobacco worksite policies also reduced cigarette consumption at work |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Etter and Stapleton 2006155 | NRT is effective for smoking cessation; addition of NRT to brief advice or behavioural support has OR of 2, representing a 70–90% increase in cessation rate without NRT |
Recommendations: no Evidence: no |
RCTs only included Recommendations: no Evidence: no explicit method reported |
| Faith et al. 2007217 | Strong evidence that subsidisation influences food purchases (but not necessarily food consumption or body weight). Ease of food access may influence food purchases, and possibly food intake and body weight. Policies at organisational level (e.g. schools and universities) |
Recommendations: yes Evidence: yes |
Recommendations: yes Evidence: criteria reported (NHLIBI 2000 criteria433) |
| Fichtenburg and Glantz 2002125 | Smoke-free workplaces protect non-smokers and encourage smokers to quit or reduce consumption |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Fiore et al. 1994160 | NRT patch is an effective aid to quitting smoking across different patch-use strategies |
Recommendations: no Evidence: no |
Included only double-blind, placebo-controlled nicotine patch studies with random assignment of subjects and biochemical validation of abstinence Recommendations: no Evidence: no explicit method reported |
| Foster and Hillsdon 2004175 | Changing environment or creating ‘point of choice’ educational materials show small increases for physical activity (before-and-after studies), e.g. stimulus for stair climbing shows consistent, small and short-term effects |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Friend and Levy 2002119 | Mass media campaigns for smoking cessation targeting the general population (state level) along with comprehensive tobacco control programmes are associated with reduced smoking rates. More mixed results observed in youth-targeted interventions |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Gorin and Heck 2004145 | Provider for increased smoking cessation: physicians > multiprovider > dentists and nurses (in order of effectiveness) |
Recommendations: no Evidence: no |
Only included RCTs or quasi-experimental studies Recommendations: no Evidence: no explicit method reported |
| Gourlay 1994161 | Transdermal nicotine therapy is an effective smoking cessation therapy for motivated, nicotine-dependent smokers |
Recommendations: no Evidence: no |
Only included randomised double-blind trials Recommendations: no Evidence: no explicit method reported |
| Hillsdon and Thorogood 1996194 | Home-based moderate-intensity walking with regular follow-up increased physical activity. Home-based walking more successful than attendance-based structured exercise sessions |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported, although EPPI-Centre review guidelines434 used |
| Hillsdon et al. 1995193 | Home-based physical activity intervention targeting sedentary subjects. Techniques associated with high levels of participation include unsupervised, informal or frequent professional contact, walking and moderate intensity |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Holmes et al. 2004164 | There is a growing body of evidence supporting the effectiveness of bupropion slow release as an aid to smoking cessation; 6-month point prevalence smoking cessation rates ranged from 25% to 49% |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Holtzman et al. 2004215 | Behavioural interventions for physical activity provided evidence for short-term effect only |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (Guide to community preventive services by Briss et al. 435 and scale developed by Chalmers et al. 436) |
| Hopkins et al. 2001118 |
Setting/policy: smoking bans in the workplace reduce exposure Environment: increasing tobacco prices; mass media to reduce tobacco use; reducing cost of cessation therapies Providers: multicomponent health-care systems with provider reminders and education with or without self-help materials Resources: telephone cessation services combined with other components such as self-help materials as a minimum |
Recommendations: yes Evidence: yes |
Recommendations and evidence: community guide method (Briss et al.435) |
| Howerton et al. 2007219 | School-based nutrition interventions produced a moderate increase in fruit and vegetable intake among children |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Hughes et al. 2003157 | Over-the-counter NRT is pharmacologically efficacious and produces modest quit rates similar to those seen in real-world prescription practice |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Jago and Baranowski 2004178 | Physical activity can be increased during school break periods; can be increased by 17–60% through existing youth organisations, summer day camps and active transportation |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Kamath et al. 2008212 | Paediatric obesity prevention programmes (physical activity and nutrition) caused small changes in target behaviours such as increasing physical activity, decreasing sedentary activity and decreasing unhealthy dietary behaviours. Trials of duration 6+ months and trials with post-intervention outcomes showed slightly larger effects |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Kerr et al. 2007168 | Varenicline shown to increase cessation rates compared with placebo (and possibly bupropion slow release). Limited safety concerns |
Recommendations: no Evidence: no |
Only included RCTs Recommendations: no Evidence: no explicit method reported |
| Knai et al. 2006220 | The evidence is strongest in favour of multicomponent interventions to increase fruit and vegetable consumption in children |
Recommendations: no Evidence: unclear |
Recommendations: no Evidence: criteria reported [a quality assessment tool (www.lshtm.ac.uk/ecohost/projects/interventions-fruit-veg.htm) was designed based on those of previous reviews by the Centre for Reviews and Dissemination of the University of York, UK437,438] |
| Kroeze et al. 2006207 | Overall, there seems to be potential for the application of computer tailoring for promoting healthy diets |
Recommendations: no Evidence: no |
Only included RCTs with pre-test and post-test Recommendations: no Evidence: criteria reported (study protocol based on the Cochrane Handbook439) |
| Kuhn et al. 1999122 | Health coalitions for tobacco reduction; decrease in smoking prevalence of 7% (10% for women < 35 years of age) among low socioeconomic neighbourhoods in a large city compared with 1% in comparable neighbourhoods in another city |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (Quality assessment tool for quantitative studies developed for the EPHPP249) |
| Law and Tang 1995148 | Physician advice, behavioural modification techniques (relaxation, rewards and punishment, avoiding ‘trigger’ situations, etc.) used in group or individual sessions led by a psychologist and NRT are all effective for smoking cessation. Among those who seek help in cessation, the effect is greater in those who are nicotine dependent |
Recommendations: no Evidence: unclear |
Only included RCTs Recommendations: no Evidence: no explicit method reported |
| Manske et al. 2004132 | Multicomponent behavioural interventions and pharmacological treatment (NRT, bupropion) are effective for group-based smoking cessation programmes. Successful components include behavioural skills, information about smoking, self-monitoring, social support and four or more sessions of 60–90 minutes. Results did not differ between worksite or community interventions |
Recommendations: yes Evidence: yes |
Recommendations: criteria reported (descriptive – effective, plausible and practical) Evidence: criteria reported (developed own – RCTs and quasi-experimental received high rating if met three or more quality criteria) |
| McArthur 1998221 | School-based interventions are effective for improving healthy eating behaviours of students; overall effect size was 0.24 (95% CI 0.17 to 0.30) |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (seven items for 18 points, higher score = higher quality) |
|
McClure 2002115 (general behaviour change) |
Biomarkers (biological information) can produce behaviour change (motivation, intent, change) for diet, physical activity and tobacco use compared with control group (did not receive biomarker feedback). Using multiple biomarkers or one biomarker at more than one time point increased detection of behaviour change |
Recommendations: no Evidence: no |
Only included published randomised trials Recommendations: no explicit method reported Evidence: no explicit method reported |
| McRobbie et al. 2006170 |
Using NRT to assist in reducing cigarette consumption before quitting Use of NRTs prior to quitting can reduce number of cigarettes smoked before quitting Five published, randomised, placebo-controlled trials with sample size of 2138 excluded no-treatment arm. Pooled results at 6–12 months: 16% using NRT vs 9% using placebo sustained reduction of ≥ 50% of baseline levels at 1 year. No meta-analysis owing to heterogeneity. 8% using NRT stopped smoking 6–12 months post randomisation vs 4% using placebo (OR 2.50; 95% CI 1.69 to 3.68) |
Recommendation: no Evidence: unclear |
Recommendation: no Evidence: no criteria reported |
| Mojica et al. 2004146 | Physicians, counsellors/psychologists, nurses and self-help without NRT are effective for smoking cessation. Effectiveness with NRT is doubled for most providers |
Recommendations: no Evidence: unclear |
Recommendations: no Evidence: criteria reported (quality of the study based on study design: RCT > CCT; blinding not considered a factor) |
| Morgan 2005182 | Exercise referral schemes can increase physical activity in certain populations [not sedentary/slightly active, older adults, overweight (but not obese)] in the short term. Long-term sustainability unknown |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported [SIGN framework (rating)440] |
| Mullen et al. 1997129 | Behavioural techniques, especially self-monitoring, with multiple communication channels, e.g. media + personal, can increase behaviour change for smoking/nutrition groups |
Recommendations: no Evidence: unclear |
Recommendations: no Evidence: no explicit method reported |
| Müller-Riemenschneider et al. 2008189 | Additional exercise prescription strategies, counselling and provision of materials and booster interventions by telephone or mail can facilitate long-term increases in physical activity behaviour. Unclear most effective and efficient delivery mode of booster messages. Information technologies used for booster interventions may be equally as effective as print materials |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (SIGN framework440) |
| Myung et al. 2007162 | Nicotine patches effective for smoking abstinence at 1 year compared with placebo group: OR 1.79 (95% CI 1.55 to 2.08) |
Recommendations: no Evidence: yes |
Only RCT studies with 1 year of follow-up, abstinence biochemically validated, OR as outcome measure included Recommendations: no Evidence: criteria reported (Jadad scale429) |
| Ogilvie et al. 2004197 | Evidence that targeted behaviour change programmes to increase walking and cycling over using cars can produce behaviour change in motivated subgroups (short-term benefits). No good evidence on health effects of intervention at population level |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Ogilvie et al. 2007202 | Interventions that cater to people’s needs, targeted at either the most sedentary or the most motivated at the individual level (brief advice, supported use of pedometers, telecommunications), can increase walking in the short term; increase an average of 30–60 minutes/week |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (validity score between 1 and 7) |
| Pan 2006135 | Proactive telephone counselling as an additional component to minimal intervention is effective for smoking cessation for particular subgroups (younger, male, light smokers) |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Petrella and Lattanzio 2002190 | Positive associations found between counselling and adoption of physical activity, stage of change and change in physical activity level |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Pomerleau et al. 2005228 | Positive effects on fruit and vegetable intake observed with face-to-face education or counselling, as well as with telephone contacts or computer-tailored information and community-based multicomponent interventions. Larger effects for those with pre-existing health disorders |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (based on tools used in previous reviews; studies of poor quality excluded) |
|
Proper et al. 2003185 (some general health behaviour but mostly physical activity) |
Worksite physical activity programmes can increase physical activity. No evidence for physical fitness, general health |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (Cochrane Back Review Group432) |
| Resnicow and Robinson 1997114 | School setting interventions are effective |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no (effect ratios reported instead) |
|
Revere and Dunbar 2001116 (general health behaviour) |
Computer-generated health behaviour interventions are effective when used as an adjunct to face-to-face patient care, e.g. tailored interventions had positive effects on health behaviour change compared with targeted, personalised and generic interventions. Computer-generated health behaviour interventions as extensions of face-to-face patient care in ambulatory settings are effective |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (created own system, 10 points maximum, minimum 5 for inclusion) |
| Rice 1999149 | Nurses as intervention provider can increase smoking cessation. Modest effects at 6 months or longer; no evidence that intensiveness of intervention made any difference to effect |
Recommendations: no Evidence: yes |
Only RCTs included Recommendations: no Evidence: criteria reported (Cochrane Handbook442) |
| Ritvo et al. 1997144 | Family physician/practice setting can enhance smoking cessation; NRT can double effect of physician intervention alone |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Roe et al. 1997222 |
Interventions in school, workplace, primary care and the community with diet only or diet and exercise showed sustained effect on diet-related outcomes, e.g. reduction of dietary fat as a percentage of total energy intake Behavioural theories and goals rather than information alone, personal contact with individuals or groups, degree of personalisation, feedback, multiple contacts and social support were features of effective healthy eating interventions |
Recommendations: no Evidence: yes |
In most settings, only included controlled experimental and quasi-experimental studies Recommendations: no Evidence: criteria reported (descriptive – more weight given to well-designed and well-conducted studies) |
| Salmon et al. 2007210 | School setting can increase physical activity for children and adolescents by focusing on physical education, activity breaks and family strategies. Family settings demonstrated weak positive effects |
Recommendations: no Evidence: unclear |
Sample size of > 16; RCT, group randomised trial or quasi-experimental study design Recommendations: no Evidence: criteria reported (methodological limitations described) |
| Seymour et al. 2004216 | Workplace and university point-of-purchase interventions can affect behaviour change (e.g. food choices). Grocery stores were the least effective setting. Interventions in ‘limited access’ sites (i.e. with fewest choices for food) had greatest effect |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (research design rated using published rating schemes; studies with serious methodological limitations excluded) |
| Shepherd et al. 2001224 | ‘Whole school’ approach can promote healthy eating; this includes availability of health foods and classroom activities with information on nutrition. These may be effective, particularly among young women |
Recommendations: no Evidence: Evidence: criteria reported (EPPI-Centre Review Guidelines443) |
Recommendations: no Evidence: criteria reported (Jadad scale429) |
| Shiffman and Ferguson 2008156 | Nicotine patch use before quitting smoking compared with starting on quit day is effective for cessation. Patches double the odds of quitting at 6 weeks (pooled OR 1.96, 95% CI 1.31 to 2.93) and 6 months (pooled OR 2.17, 95% CI 1.46 to 3.22) |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Shilts et al. 2004213 | Goal setting shows some positive effects for promoting dietary and physical activity behaviour change in adults, whereas evidence of effect in adolescents and children was limited |
Recommendations: no Evidence: yes |
Experimental, quasi-experimental or pre-experimental studies were included Recommendations: no Evidence: criteria reported (grading – methodological quality rated with four-letter rating system designating research qualities) |
| Smedslund et al. 2004126 | Workplace settings for smoking cessation are effective in the short term; however, effects decrease over time and are not sustained beyond 12 months. The adjusted random effects OR was 2.03 (95% CI 1.42 to 2.90) at 6 months’ follow-up, 1.56 (95% CI 1.17 to 2.07) at 12 months’ follow-up and 1.33 (95% CI 0.95 to 1.87) at > 12 months’ follow-up |
Recommendations: no Evidence: no |
Studies analysed according to randomised and non-randomised. The non-randomised studies show a much stronger effect (OR 4.65) than the randomised ones (OR 1.74) Recommendations: no Evidence: no explicit method reported |
| Sorensen et al. 2006192 | Exercise on prescription can increase physical activity levels compared with control groups (the level of physical activity was significantly increased for patients in half of the studies reviewed). Limited effectiveness evidence on intensive vs less intensive interventions; unknown if sustainable for everyday use in general practice |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (studies rated high, medium or low quality; all studies included) |
| Thomas et al. 2003223 | Schools can promote healthy eating (hands-on learning, parent/teacher involvement) for children aged 4–10 years. Fruit consumption easier to increase than vegetable consumption; important that health benefits were not emphasised; interventions focused on fruits and vegetables only |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported [EPPI-Centre health promotion review criteria (four factors)444–446] |
| Thomas et al. 2004214 | Schools can be effective in increasing physical activity of children by balancing aerobic activity and skill development. Actual differences and clinical significance unknown. Involving parents had mixed results. Teachers’ skills need addressing |
Recommendations: no Evidence: unclear |
RCTs and cohort studies included Recommendations: no Evidence: criteria reported (methodological limitations assessed, only strong studies described) |
| Thorogood et al. 2007226 | Workplaces and churches can reduce fat intake and increase fruit and vegetable intake (small positive effects). Community-based interventions showed little effect. Short-term effects may not be sustained |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (own method for assessing methodological quality) |
| Vandelanotte et al. 2007206 | Website-delivered physical activity interventions can increase physical activity. Better outcomes with five or more contacts and short follow-up times. Effects were small and only short term |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| van den Berg et al. 2007205 | Internet-based physical activity interventions tailored to individuals may be effective compared with waiting list control. Self-monitoring and feedback used; longer-term effects unknown |
Recommendations: no Evidence: yes |
Only RCTs included Recommendations: no Evidence: criteria reported (rating – list based on Cochrane Back Review Group447) |
| van der Bij et al. 2002203 | Home-based, group-based and educational physical activity interventions can increase physical activity, but effect was small and short term |
Recommendations: no Evidence: unclear |
Only RCTs included Recommendations: no Evidence: methodological rigour evaluated but not reported |
| van Sluijs et al. 2007177 | School-based interventions with involvement of family or community and multicomponent interventions can increase physical activity in adolescents |
Recommendations: no Evidence: unclear |
Recommendations: no Evidence: criteria reported (only studies with high methodological quality included) |
| VanWormer and Boucher 2004235 | Motivational interviewing plus education moderately effective for diet behaviour change compared with education alone. Reduced fat and sodium intake and increased fruit and vegetable intake; longer-term maintenance unknown |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (simplified version of the American Diabetes Association evidence grading system448) |
| VanWormer et al. 2006231 | Telephone-based counselling can increase fruit and vegetable consumption and reduce dietary fat intake compared with usual care; effects particularly evident among women with (or at high risk for developing) cancer. Not enough evidence to recommend over other forms of dietary counselling; best used as adjunct to clinical care |
Recommendations: no Evidence: yes |
Only RCTs included Recommendations: no Evidence: criteria reported (American Diabetes Association evidence grading system448) |
| Wagena et al. 2005165 | Nortriptyline is effective for smoking cessation compared with placebo. Higher prolonged abstinence rates after at least 6 months (RR 2.4, 95% CI 1.7 to 3.6; RD 0.11, 95% CI 0.07 to 0.15). Lower cost than bupropion |
Recommendations: no Evidence: yes |
Only RCTs included Recommendations: no Evidence: criteria reported (score between 7 and 11; items from the Delphi list449 + Jadad criteria429) |
| Wall et al. 2006237 | Four trials showed that monetary incentives on food purchases, food consumption or weight loss had a positive effect; goal was to reduce financial barriers or reward behaviour change (e.g. farmers’ market coupons, payment for weight loss) |
Recommendations: no Evidence: yes |
Only RCTs included Recommendations: no Evidence: criteria reported |
| Wang et al. 2008142 | NRT-supported reduction in smoking can result in long-term (12-month) abstinence. The 12-month sustained abstinence success rate was approximately 5.3% with NRT vs 2.6% with placebo. |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (quality appraisal guidelines in Report No. 4 of the NHS Centre for Reviews and Dissemination450) |
|
Wantland et al. 2004117 (general behaviour) |
One time web-based intervention can improve positive outcomes for knowledge and behaviour change compared with non-web-based interventions. Studies demonstrated heterogeneity |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (quality appraisal from Haynes et al. 451) |
| White and Moody 2006141 | Auricular acupuncture may be effective for smoking cessation compared with control interventions (OR 2.24, 95% CI 1.61 to 3.10); effect may not depend on point location |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (reviewer developed points system) |
| Wilcox et al. 2001183 | Health-care settings can improve outcomes for physical activity, dietary fat, BMI or weight, albeit these are modest changes. Effects larger for older adults (> 50 years) and for studies with shorter follow-up times (< 6 months) |
Recommendations: no Evidence: no |
Majority were RCTs Recommendations: no Evidence: no explicit method reported |
| Williams et al. 2007195 | Exercise referral schemes can increase physical activity in sedentary people. A statistically significant increase was observed in the proportion of participants doing moderate exercise (combined RR 1.20, 95% CI 1.06 to 1.35) |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive and scored out of a maximum of 34 on quality scale) |
| Williams et al. 2008187 | Telephone counselling (brief and intensive) can increase physical activity, especially when tailored and theory based; individual studies support walking prescriptions to increase walking; mass media campaigns can increase knowledge and awareness but unclear if they can initiate individual behaviour change |
Recommendations: no Evidence: no |
Only RCTs Recommendations: no Evidence: no explicit method reported |
| Woolacott et al. 2002158 | NRT and bupropion are effective for smoking cessation |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported |
| Wu et al. 2006159 | NRT, bupropion and varenicline can assist smoking cessation; hierarchy varenicline > bupropion > NRTs (gum, patch) > placebo |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported [(descriptive) quality of studies described] |
| National Institute for Health Research Health Technology Assessment | |||
| Cohen et al. 1998128 | Brief structured counselling in primary care settings and dental services followed by clear recommendations to stop smoking and advice on NRTs is cost-effective when performed routinely |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (descriptive) |
| Elford et al. 2001113 (general health behaviours) | Brief counselling in primary care setting |
Recommendations: no Evidence: no |
Recommendations: no Evidence: no explicit method reported |
| Gorgojo Jimenez et al. 2003134 | Bupropion and NRT plus medical advice and support are effective and cost-effective for smoking cessation. Medical practitioners to advise and support cessation |
Recommendations: no Evidence: no |
Recommendations: no Evidence: criteria reported (descriptive – high-quality interventions included) |
| Ranney et al. 2006153 | Self-help alone is not effective in smoking cessation; however, counselling and pharmacotherapy, either alone or combined with each other, are effective in smoking cessation |
Recommendations: yes Evidence: yes |
Recommendations: criteria reported [strength of evidence using categories (strong, sufficient, insufficient) based on criteria from the Task Force on Community Preventive Services452] Evidence: criteria reported (US Preventive Services Task Force435 and the NHS Centre for Reviews and Dissemination450) |
| Swedish Council on Technology Assessment in Health Care 2007201 | Advice and counselling by health-care professionals can increase physical activity by 12–50% for at least 6 months after the counselling session; more frequent, intensive counselling can additionally increase physical activity; counselling plus prescribed physical activity, diaries, pedometers and information brochures also increase physical activity; lifestyle-focused interventions reinforce the increase in activity; multicomponent school interventions, theory-based behavioural interventions and structured exercise programmes increase physical activity compared with usual care |
Recommendations: yes Evidence: yes |
Recommendations: criteria reported (evidence grades 1, 2 and 3) Evidence: criteria reported (weak, medium, strong) |
| Van den Bruel et al. 2004131 |
For smoking, recommended brief interventions – doctor or nurse (for every 50 smokers advised, one will stop smoking); individual counselling (for every 25 people, one will stop smoking); group counselling; telephone counselling (for every 40 people, one will stop smoking); NRT and bupropion (effective and cost-effective). Group counselling > self-help; group counselling < individual counselling; group counselling + NRT = group counselling alone Self-help found not to be effective Not enough evidence for aversion therapy, exercise therapy, hypnotherapy or acupuncture |
Recommendations: no Evidence: yes |
Recommendations: no Evidence: criteria reported (Cochrane based) |
Appendix 11 Table of extracted evidence statements on ethnicity from the 40 international systematic reviews
| Source | Overarching statement |
|---|---|
| Cochrane | |
| Bala et al. 2008121 |
No consistent relationship seen between campaign effectiveness and age, education, ethnicity or gender Highest smoking prevalence reported for African Americans |
| Brunner et al. 2007232 |
Dietary change may depend as much on wider determinants (access and availability of foods) as on information and motivation Reduction in fat intake shown for minority ethnic group in one trial |
| Dobbins et al. 2009180 |
Additional subgroup analysis of differences in physical activity by gender, age and ethnicity is required Research is needed to assess impact of strategies to increase physical activity that account for barriers and facilitators among children and adolescents of various ethnicities |
| Foster et al. 2005204 | Included studies that did not examine the effect of intervention on participants from various ethnic groups (effectiveness of interventions in ethnic groups unknown) |
| Stead et al. 2006136 |
Targeted advertising may increase calls to smoking quit lines from ethnic groups Did not detect a significant increased benefit from either counselling or materials designed for African Americans |
| Database of Abstracts of Reviews of Effects | |
| Adams and White 2003196 | Innovative strategies are required to recruit and retain hard-to-reach participants, such as those from ethnic minority groups |
| Ammerman et al. 2001229 |
Few studies were designed to allow for examination of the efficacy of intervention for ethnic subgroups (limited) Lacking good-quality research on dietary interventions for minority populations Few studies designed to be culturally or ethnically specific Studies that were designed to be culturally or ethnically specific (five studies) reported significant decreases in fat intake compared with studies that were not culturally or ethnically specific (magnitude unknown as insufficient number of studies to explore this) |
| Ammerman et al. 2002230 | Sodium intake reduction interventions show greater effects in African Americans |
| Blue and Black 2005211 |
Discusses the importance of cultural tailoring and how culture influences people’s health experiences and choices and calls for greater attention to account for these differences when interventions are designed. Intervention choices should include factors such as ‘settings, culture, spirituality/religion affiliations and primary language’ Discuss one included study aimed at native Hawaiians which did undertake cultural tailoring Reported that there were differential findings of interventions according to demographic factors including race in those studies which undertake this examination Focusing on particular demographic segments of the populations including racial/ethnic groups may also help to minimise attrition |
| Breckon et al. 2008188 | Trials with ‘perfect fidelity’ for physical activity may not be adaptable across different cultures and therefore lack applicability in clinical practice |
| Brunton et al. 2003179 |
Ethnicity was not often reported compared with age and sex of children for physical activity interventions Views of children from minority ethnic groups are needed Little is known about how different social factors, such as gender, social class and ethnicity, interact and where and how to intervene successfully Girls and children from minority ethnic groups more restricted in their use of public space |
| Clemmens et al. 2004198 |
Interventions should be culturally sensitive and more context specific to the population Largest effect on reduction of television viewing hours was among African American girls (for reduction in obesity) |
| Contento et al. 1995218 |
More research needed to reach disadvantaged groups, e.g. non-white, with regard to diet Nutrition education should be tailored to the audience; segmentation should take into account under-represented populations, e.g. African Americans, Asian Americans Offering bilingual programmes may be effective; in some cases more extensive cultural adaptation may be necessary Ethnic and cultural differences in motivators need more investigation to build a culturally competent agenda |
| Coruh et al. 2005227 |
African Americans who attend church once a week have a greater life expectancy Faith-based collaborations may improve health outcomes in the African American community, e.g. fruit and vegetable intake |
| DeMattia et al. 2007209 | Ethnicity was adjusted in determining intervention effect (statistical adjustment) (intervention to limit sedentary behaviours) |
| Dishman and Buckworth 1996199 | Racial and ethnic minorities are under-represented in past research studies on physical activity |
| Dobbins et al. 2001181 |
Research is needed to assess the impact of physical activity strategies among children and adolescents, particularly those from various ethnic backgrounds Black girls found to be less active than white girls |
| Faith et al. 2007217 | The availability of a supermarket in African American communities was associated with meeting dietary recommendations for fruit and vegetable intake, total fat intake and saturated fat intake |
| Foster and Hillsdon 2004175 | Ethnicity may mediate the observed effect on stair use in one of the included studies |
| Hillsdon and Thorogood 1996194 | Brisk walking holds potential for increasing activity levels as it is most likely to be adopted by a range of ethnic groups |
| Holtzman et al. 2004215 |
Questions of the review specifically considered to what extent these interventions had been delivered to ethnic minority populations, whether or not the efficacy differed for these populations and what factors mediated the effectiveness Included studies which compared ethnic minority and general population participants Quality assessment included whether or not the studies described the population participating well, including race/ethnicity; commented that in the studies where it was reported, all but two of the studies had majority white populations Advised that improved reporting of who the participants were, including their race/ethnicity, would help greatly in assessing the external validity of the results Proposed a model where cultural factors can be one of three targets for creating behaviour change |
| Hopkins et al. 2001118 |
Florida campaign provided evidence on the effectiveness of mass media campaigns among black populations Two studies found black adolescents more responsive to produce pricing (smoking) |
| Howerton et al. 2007219 | Statistically adjusted for race, sex and duration of intervention |
| Jago and Baranowski 2004178 | Five-a-day achievement badges led to increase in fruit and vegetable intake among African American boy scouts |
| Kroeze et al. 2006207 | No significant differences in effects between different tailored interventions for African Americans |
| Kuhn et al. 1999122 |
Work with minority groups may require coalitions as a prerequisite for delivering health promotion strategies for smoking cessation Failure to work with community advisory groups can leave the community feeling that the project is not relevant to their culture and context |
| McArthur 1998221 |
Lack of research focused on ethnic minorities African Americans are at a greater risk than Caucasians for CVD |
| Morgan 2005182 | Few studies collected information on ethnicity; results unlikely to apply to all populations. Some groups (e.g. Muslim women) may need different opportunities or settings for exercise |
| Müller-Riemenschneider et al. 2008189 | Cultural adaptation of materials seems to increase effectiveness |
| Pomerleau et al. 2005228 |
Studies targeting smaller, specific communities including African American churches had larger effects on fruit and vegetable intake than general population interventions One intervention showed that culturally sensitive multicomponent self-help materials plus telephone motivational interviewing was more effective than standard nutrition education materials |
| Roe et al. 1997222 |
Limited evidence of interventions targeted at ethnic minority groups Further effort needed to develop and evaluate healthy eating interventions in ethnic minority populations in different settings |
| Salmon et al. 2007210 | Further tailoring of physical activity for children from different ethnic backgrounds may be necessary |
| Seymour et al. 2004216 | One study showed increased fruit and vegetable intake for members of African American churches in a multicomponent intervention |
| Thomas et al. 2003223 |
Children from ethnic minority groups were not well represented in healthy eating studies looking at barriers and facilitators Studies said little about reducing health inequalities Results not reported according to different subgroups This represents an area for further research Unclear how findings can be applicable to children from ethnic minority groups because of lack of reporting on ethnicity Relative impact of interventions unknown because not reported on in primary studies |
| Thomas et al. 2004214 |
Noted that few studies report the effect of factors, including culture, on the outcomes of interventions and acknowledges that these factors can result in differential outcomes Recommends that all studies should include analysis according to contextual factors, including culture, when determining their impact |
| van Sluijs et al. 2007177 |
No intervention effect was found for interventions targeting girls or ethnic minority groups Inconsistent evidence on association between ethnicity and physical activity in children, even though a third of the studies were targeted at ethnic groups Levels of physical activity tend to be lower in non-white ethnic groups, yet no interventions were identified that targeted adolescents from minority ethnic groups Research should focus on filling the gaps, i.e. the lack of studies among adolescent ethnic minority populations and preschool children, and interventions outside the school setting |
| Wall et al. 2006237 |
No studies to date have assessed the effects of incentives on dietary behaviour according to ethnic group, or measured cost-effectiveness Need for further RCTs to measure effectiveness of pricing strategies for dietary modification in ethnically diverse populations (who often experience higher rates of nutrition-related diseases) |
| Wilcox et al. 2001183 |
Interventions targeted to a population can produce significant effects More studies need to address the effectiveness of physical activity and dietary counselling delivered in health-care settings with ethnically diverse individuals |
| Williams et al. 2008187 | Comparable results were found between an individually tailored, theory-based intervention and one that was not individually tailored among racial ethnic minority women |
| National Institute for Health Research Health Technology Assessment database | |
| Hellenius 2007201 |
Future research should take into consideration the ethical and social aspects, including the relationship between gender and ethnic background and physical activity No study has been designed to detect differences in effect with regard to ethnicity and the different methods suited to promote physical activity with various ethnic groups |
| Ranney et al. 2006153 |
Smokers from members of minority groups achieved higher rates of abstinence with a nasal spray A review of interventions specifically designed for particular racial or ethnic groups demonstrated the efficacy of a variety of smoking cessation interventions for minority populations Members of racial and ethnic minorities should be provided with effective treatments as an earlier review showed that smoking cessation treatments are effective across different racial and ethnic minorities |
Appendix 12 Search strategy
-
ethnic minorit*
-
(BME or black ethnic minorit* or black minorit* ethnic*)
-
asylum seeker*
-
(migrant* or immigrant*)
-
mixed race*
-
cultur*
-
(multicultural or multi-cultural)
-
(cross-cultural or crosscultural)
-
(trans-cultural or transcultural)
-
(multi-rac* or multirac*)
-
(multiethnic or multi-ethnic)
-
refugee*
-
(multi-lingu* or multilingu*)
-
(ethno-cultur* or ethnocultur*)
-
(socio-cultural or sociocultural)
-
(divers* or diverse population* or cultural diversity)
-
(south asian* or bangladeshi* or pakistani* or indian* or sri lankan*)
-
(asian* or east asian* or chinese or taiwanese or vietnamese or korean* or japanese)
-
(afro-caribbean* or african-caribbean* or caribbean or african* or black* or afro*)
-
(islam* or hindu* or Sikh* or buddhis* or muslim* or moslem* or christian* or catholic*
-
or jew*)
-
exp Ethnic Groups/or ethnic group*
-
((ethnic or linguistic) adj diversity)
-
(transient adj (group* or population*))
-
acculturation
-
(faith* or belief* or religion*)
-
or/1–26
-
(health promotion or health promotion intervention* or promot* health)
-
((intervention* adj5 health) or (health adj5 intervention*) or interven*)
-
Health education.mp. or exp Health Education/
-
prevention
-
public health.mp. or exp Public Health/
-
community intervention*
-
((community-level or community level) adj5 intervention*)
-
(health* adj (behaviour or behavior))
-
or/28–35
-
((physical adj5 activit*) or exercise*)
-
((weight adj5 (management or control)) or weight)
-
(diet* or diet* modification or diet* change* or nutrition* or food*)
-
(smoking or smoking cessation or stop smoking or smoking reduction)
-
exp Life Style/
-
lifestyle*
-
(fruit* or vegetable*)
-
(activit* or inactivit*)
-
(food habit* or healthy eat*)
-
exp Obesity/
-
(obes* or overweight)
-
or/37–47
-
(adapt* or modif* or sensitiv* or target* or chang* or alter*)
-
27 and 36 and 48
-
limit 50 to (English language and humans)
-
51 and 49
Appendix 13 MEDLINE search results
Search carried out at Warwick University via OvidSP.
Ovid MEDLINE(R) 1950 to August week 3 2009.
| # | Searches | Results |
|---|---|---|
| 1 | (ethnic or minorit*).ab,ti. | 59,443 |
| 2 | (BME or black ethnic minorit* or black minorit* ethnic*).mp. | 416 |
| 3 | asylum seeker*.ab,ti. | 484 |
| 4 | (migrant* or immigrant*).ab,ti. | 17,079 |
| 5 | race*.mp. or racial.ab,ti. [mp=title, original title, abstract, name of substance word, subject heading word] | 70,580 |
| 6 | cultur*.ab,ti. | 648,829 |
| 7 | (multicultural or multi-cultural).ab,ti. | 1407 |
| 8 | (cross-cultural or crosscultural).ab,ti. | 4767 |
| 9 | (trans-cultural or transcultural).ab,ti. | 1258 |
| 10 | (multi-rac* or multirac*).ab,ti. | 438 |
| 11 | (multiethnic or multi-ethnic).ab,ti. | 2384 |
| 12 | refugee*.ab,ti. | 4487 |
| 13 | (multi-lingu* or multilingu*).ab,ti. | 441 |
| 14 | (ethno-cultur* or ethnocultur*).ab,ti. | 262 |
| 15 | (socio-cultural or sociocultural).ab,ti. | 5313 |
| 16 | (divers* or diverse population* or cultural diversity).ab,ti. | 164,741 |
| 17 | (south asian* or bangladeshi* or pakistani* or indian* or sri lankan*).mp. | 53,496 |
| 18 | (asian* or east asian* or chinese or taiwanese or vietnamese or korean* or japanese).mp. | 185,631 |
| 19 | (afro-caribbean* or african-caribbean* or caribbean or african* or black* or afro*).mp. | 156,091 |
| 20 | (islam* or hindu* or Sikh* or buddhis* or muslim* or moslem* or christian* or catholic* or jew*).ab,ti. | 20,204 |
| 21 | ethnic group*.mp. | 45,506 |
| 22 | ((ethnic or linguistic) adj diversity).ab,ti. | 422 |
| 23 | (transient adj (group* or population*)).ab,ti. | 182 |
| 24 | acculturation.ab,ti. | 1925 |
| 25 | (faith* or belief* or religion*).ab,ti. | 44,497 |
| 26 | or/1–25 | 1,292,357 |
| 27 | intervention*.ab,ti. | 329,760 |
| 28 | (health promotion or promot* health).ab,ti. | 14,093 |
| 29 | Health education.mp. or exp Health Education/ | 119,536 |
| 30 | prevent*.ab,ti. | 666,010 |
| 31 | (health* adj (behaviour or behavior)).ab,ti. | 3979 |
| 32 | or/27–31 | 1,042,442 |
| 33 | ((physical adj5 activit*) or exercise*).ab,ti. | 170,662 |
| 34 | ((weight adj5 (management or control)) or weight).ab,ti. | 429,181 |
| 35 | (diet* or diet* modification or diet* change* or nutrition* or food*).ab,ti. | 514,000 |
| 36 | (smoking or smoking cessation or stop smoking or smoking reduction).ab,ti. | 103,809 |
| 37 | exp Life Style/ | 46,770 |
| 38 | lifestyle*.ab,ti. | 28,886 |
| 39 | (fruit* or vegetable*).ab,ti. | 44,821 |
| 40 | (activit* or inactivit*).ab,ti. | 1,676,639 |
| 41 | (food habit* or healthy eat*).ab,ti. | 2309 |
| 42 | exp Obesity/ | 95,073 |
| 43 | (obes* or overweight).ab,ti. | 110,076 |
| 44 | or/33–43 | 2,699,951 |
| 45 | 26 and 32 and 44 | 36,106 |
| 46 | limit 45 to animals | 11,378 |
| 47 | 45 not 46 | 24,728 |
| 48 | limit 47 to humans | 22,759 |
Appendix 14 Excluded studies
Excluded systematic reviews
-
Appel LJ, Gauvey-Kern ME, Anderson CAM. Weight loss interventions to control blood pressure in an increasingly overweight, multi-ethnic society, in cardiovascular disease in racial and ethnic minorities. In Ferdinand KC, Armani A, editors. Contemporary cardiology: cardiovascular disease in racial and ethnic minorities. New York, NY: Humana Press; 2009. pp. 151–91.
-
Bronner Y, Boyington JEA. Developing weight loss interventions for African-American women: elements of successful models. J Natl Med Assoc 2002;94:224–35.
-
Connell P, Wolfe C, McKevitt C. Preventing stroke: a narrative review of community interventions for improving hypertension control in black adults. Health Soc Care Comm 2008;16:165–87.
-
Crook ED, Bryan NB, Hanks R, Slagle ML, Morris CG, Ross MC, et al. A review of interventions to reduce health disparities in cardiovascular disease in African Americans [summary for patients in Ethn Dis 2009;19:221]. Ethn Dis 2009;19:204–8.
-
Davis AM, Vinci LM, Okwuosa TM, Chase AR, Huang ES. Cardiovascular health disparities: a systematic review of health care interventions. Med Care Res Rev 2007;64(Suppl. 5):29S–100S.
-
DeHaven M, Hunter I, Wilder L, Walton J, Berry J. Health programs in faith-based organizations: are they effective? Am J Public Health 2004;94:1030–6.
-
Doolan DM, Froelicher ES. Efficacy of smoking cessation intervention among special populations: review of the literature from 2000 to 2005. Nurs Res 2006;55(Suppl. 4):S29–37.
-
Eakin EG, Bull SS, Glasgow RE, Mason M. Reaching those most in need: a review of diabetes self-management interventions in disadvantaged populations. Diabetes Metab Res 2002;18:26–35.
-
Jones PR. African American tobacco control organizations taking action: building the tobacco control capacity of African American communities. San Francisco, CA: University of California, San Francisco; 2006.
-
Krummel DA, Koffman DM, Bronner Y, Davis J, Greenlund K, Tessaro I, et al. Cardiovascular health interventions in women: what works? J Womens Health Gend Based Med 2001;10:117–36.
-
Lawrence D, Graber JE, Mills SL, Meissner HI, Warnecke R. Smoking cessation interventions in US racial/ethnic minority populations: an assessment of the literature. Prev Med 2003;36:204–16.
-
Lee RE, McGinnis KA, Sallis JF, Castro CM, Chen AH, Hickmann SA. Active vs. passive methods of recruiting ethnic minority women to a health promotion program. Ann Behav Med 1997;19:378–84.
-
Main C, Thomas S, Ogilvie D, Stirk L, Petticrew M, Whitehead M, et al. Population tobacco control interventions and their effects on social inequalities in smoking: placing an equity lens on existing systematic reviews. BMC Public Health 2008;8:178.
-
Meininger JC. School-based interventions for primary prevention of cardiovascular disease: evidence of effects for minority populations. Annu Rev Nurs Res 2000;18:219–44.
-
Pederson LL, Ahluwalia JS, Harris KJ, McGrady GA. Smoking cessation among African Americans: what we know and do not know about interventions and self-quitting. Prev Med 2000;31:23–38.
-
Robles GI, Singh-Franco D, Ghin HL. A review of the efficacy of smoking-cessation pharmacotherapies in nonwhite populations. Clin Ther 2008;30:800–12.
-
Sanchez-Johnsen LAP. Smoking cessation, obesity and weight concerns in black women: a call to action for culturally competent interventions. J Natl Med Assoc 2005;97:1630–8.
-
Satterfield DW, Volansky M, Caspersen CJ, Engelgau MM, Bowman BA, Gregg EW, et al. Community-based lifestyle interventions to prevent type 2 diabetes. Diabetes Care 2003;26:2643–52.
-
Seo D, Sa J. A meta-analysis of psycho-behavioral obesity interventions among US multiethnic and minority adults. Prev Med 2008;47:573–82.
-
Taylor WC, Baranowski T, Young DR. Physical activity interventions in low-income, ethnic minority, and populations with disability. Am J Prev Med 1998;15:334–43.
-
Yancey AK, Kumanyika SK, Ponce NA, McCarthy WJ, Fielding JE, Leslie JP, et al. Population-based interventions engaging communities of color in healthy eating and active living: a review. Prev Chronic Dis 2004;1:A09.
Excluded theoretical papers
-
Base-Smith V, Campinha-Bacote J. The culture of obesity. J Natl Black Nurses Assoc 2003;14:52–6.
-
Hyman I, Guruge S. A review of theory and health promotion strategies for new immigrant women. Can J Public Health 2002;93:183–7.
-
Kumanyika S, Bonner M. Toward a lower-sodium lifestyle in black communities. J Natl Med Assoc 1985;77:969–75.
-
Magnus MH. What’s your IQ on cross-cultural nutrition counseling? Diabetes Educ 1996;22:57–60.
-
Middleton JL. A proposed new model of hypertensive treatment behavior in African Americans. J Natl Med Assoc 2009;101:12–17.
-
Peterson J, Atwood JR, Yates B. Key elements for church-based health promotion programs: outcome-based literature review. Public Health Nurs 2002;19:401–11.
-
Robinson T. Applying the socio-ecological model to improving fruit and vegetable intake among low-income African Americans. J Community Health 2008;33:395–406.
-
Scisney-Matlock M, Bosworth HB, Giger JN, Strickland OL, Harrison RV, Coverson D, et al. Strategies for implementing and sustaining therapeutic lifestyle changes as part of hypertension management in African Americans. Postgrad Med 2009;121:147–59.
Excluded empirical studies
Excluded based on health topic
-
Adler S. Pluralism, relevance, and language intervention for culturally different children. Asha 1971;13:719–23.
-
Bental T, Gersten R, Alkan M. Health education for the Ethiopian community in the Negev. Isr J Med Sci 1993;29:429–37.
-
Burgi D. Health promotion and prevention in foreign populations in Switzerland: step-by-step progress. Praxis 1997;86:906–10.
-
Griffiths T. British Diabetic Association (BDA) initiatives for black and Indo-Asian peoples. Pract Diabetes Int 2000;17:S1–2.
-
Kumanyika S, Bonner M. Toward a lower-sodium lifestyle in black communities. J Natl Med Assoc 1985;77:969–75.
-
Kumanyika SK, Story M, Beech BM, Sherwood NE, Baranowski JC, Powell TM, et al. Collaborative planning for formative assessment and cultural appropriateness in the Girls health Enrichment Multi-site Studies (GEMS): a retrospection. Ethn Dis 2003;13(Suppl. 1): S15–29.
-
Kumpfer KL. Effectiveness of a culturally tailored, family-focused substance abuse program: the Strengthening Families Program. National Conference on Drug Abuse Prevention Research: Presentations, Papers, and Recommendations, September 1996.
-
Levine DM, Becker DM, Bone LR, Stillman FA, Tuggle MB II, Prentice M, et al. A partnership with minority populations: a community model of effectiveness research. Ethn Dis 1992;2:296–305.
-
Middleton JL. A proposed new model of hypertensive treatment behavior in African Americans. J Natl Med Assoc 2009;101:12–17.
-
Muñoz RF, Mendelson T. Toward evidence-based interventions for diverse populations: the San Francisco General Hospital prevention and treatment manuals. J Consult Clin Psych 2005;73:790–9.
-
Orlandi MA. Community-based substance abuse prevention: a multicultural perspective. J Sch Health 1986;56:394–401.
-
Parker MW, Bellis JM, Bishop P, Harper M, Allman RM, Moore C, et al. A multidisciplinary model of health promotion incorporating spirituality into a successful aging intervention with African American and white elderly groups. Gerontologist 2002;42:406–15.
-
Plescia M, Groblewski M, Chavis L. A lay health advisor program to promote community capacity and change among change agents. Health Promot Pract 2008;9:434–9.
-
Pullen-Smith B, Carter-Edwards L, Leathers KH. Community health ambassadors: a model for engaging community leaders to promote better health in North Carolina. J Public Health Manag Pract 2008;14(Suppl.):S73–81.
-
Rochon J, Klesges RC, Story M, Robinson TN, Baranowski T, Obarzanek E, et al. Common design elements of the Girls health Enrichment Multi-site Studies (GEMS). Ethn Dis 2003;13(Suppl. 1):S6–14.
-
Sherwood NE, Beech BM, Klesges LM, Story M, Killen J, McDonald T, et al. Measurement characteristics of weight concern and dieting measures in 8–10-year-old African-American girls from GEMS pilot studies. Prev Med 2004;38(Suppl.):S50–9.
-
Sherwood NE, Taylor WC, Treuth M, Klesges LM, Baranowski T, Zhou A, et al. Measurement characteristics of activity-related psychosocial measures in 8- to 10-year-old African-American girls in the Girls Health Enrichment Multisite Study (GEMS). Prev Med 2004;38(Suppl.):S60–8.
-
Story M, Sherwood NE, Obarzanek E, Beech BM, Baranowski JC, Thompson NS, et al. Recruitment of African-American pre-adolescent girls into an obesity prevention trial: the GEMS pilot studies. Ethn Dis 2003;13(Suppl. 1):S78–87.
-
Swerissen H, Belfrage J, Weeks A, Jordan L, Walker C, Furler J, et al. A randomised control trial of a self-management program for people with a chronic illness from Vietnamese, Chinese, Italian and Greek backgrounds. Patient Educ Couns 2006;64:360–8.
Excluded based on population
-
Albright CL, Bruce B, Howard-Pitney B, Winkleby MA, Fortmann SP. Development of a curriculum to lower dietary fat intake in a multiethnic population with low literacy skills. J Nutr Educ 1997;29:215–23.
-
Anderko L, Bartz C, Lundeen S. Wellness for a lifetime: improving lifestyle behaviors of low-income, ethnically diverse populations. Ann Fam Med 2005;3(Suppl. 2):S35–6.
-
Baruth M, Wilcox S, Laken M, Bopp M, Saunders R. Implementation of a faith-based physical activity intervention: insights from church health directors. J Community Health 2008;33:304–12.
-
Beckham S, Bradley S, Washburn A. One health center’s response to the obesity epidemic: an overview of three innovative, culturally appropriate, community-based strategies. Hawaii Med J 2005;64:151–5.
-
Bekker FJ, Hentschel U, Fujita M. Basic cultural values and differences in attitudes towards health, illness and treatment preferences within a psychosomatic frame of reference. Psychother Psychosom 1996;65:191–8.
-
Bibeau WS, Moore JB, Caudill P, Topp R. Case study of a transtheoretical case management approach to addressing childhood obesity. J Pediatr Nurs 2008;23:92–100.
-
Brenner B. Implementing a community intervention program for health promotion. Soc Work Health Care 2002;35:359–75.
-
Brug J. Determinants of healthy eating: motivation, abilities and environmental opportunities. Fam Pract 2008;25(Suppl. 1):i50–5.
-
Brug J, van Lenthe FJ, Kremers SPJ. Revisiting Kurt Lewin: how to gain insight into environmental correlates of obesogenic behaviors. Am J Prev Med 2006;31:525–9.
-
Buller DB, Morrill C, Taren D, Aickin M, Sennott-Miller L, Buller MK, et al. Randomized trial testing the effect of peer education at increasing fruit and vegetable intake. J Natl Cancer Inst 1999;91:1491–500.
-
Buller DB, Woodall WG, Zimmerman DE, Heimendinger J, Rogers EM, Slater MD, et al. Formative research activities to provide web-based nutrition education to adults in the Upper Rio Grande Valley. Fam Community Health 2001;24:1–12.
-
Campbell MK, Honess-Morreale L, Farrell D, Carbone E, Brasure M. A tailored multimedia nutrition education pilot program for low-income women receiving food assistance. Health Educ Res 1999;14:257–67.
-
Chen MS Jr. The status of tobacco cessation research for Asian Americans and Pacific Islanders. Asian Am Pac Isl J Health 2001;9:61–5.
-
Colby SE, Haldeman L. Peer-led theater as a nutrition education strategy. J Nutr Educ Behav 2007;39:48–9.
-
Collins R, Lee RE, Albright CL, King AC. Ready to be physically active? The effects of a course preparing low-income multiethnic women to be more physically active. Health Educ Behav 2004;31:47–64.
-
Cox RH, Parker GG, Watson AC, Robinson SH, Simonson CJ, Elledge JC, et al. Dietary cancer risk of low-income women and change with intervention. J Am Diet Assoc 1995;95:1031–4.
-
Cramer JS, Sibley RF, Bartlett DP, Kahn LS, Loffredo L. An adaptation of the diabetes prevention program for use with high-risk, minority patients with type 2 diabetes. Diabetes Educ 2007;33:503–8.
-
Davies SL, Kohler CL, Fish L, Taylor BE, Foster GE, Annang L. Evaluation of an intervention for hospitalized African American smokers. Am J Health Behav 2005;29:228–39.
-
Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 2002;25:2165–71.
-
Dornelas EA, Stepnowski RR, Fischer EH, Thompson PD. Urban ethnic minority women’s attendance at health clinic vs. church based exercise programs. J Cross Cult Gerontol 2007;22:129–36.
-
Edwards N, Ciliska D, Halbert T, Pond M. Health promotion and health advocacy for and by immigrants enrolled in English as a second language classes. Can J Public Health 1992;83:159–62.
-
Eicher-Miller HA, Mason AC, Abbott AR, McCabe GP, Boushey CJ. The effect of Food Stamp Nutrition Education on the food insecurity of low-income women participants. J Nutr Educ Behav 2009;41:161–8.
-
El Fakiri F, Hoes AW, Uitewaal PJM, Frenken RAA, Bruijnzeels MA. Process evaluation of an intensified preventive intervention to reduce cardiovascular risk in general practices in deprived neighbourhoods. Eur J Cardiovasc Nurs 2008;7:296–302.
-
Emmons KM, Stoddard AM, Gutheil C, Suarez EG, Lobb R, Fletcher R. Cancer prevention for working class, multi-ethnic populations through health centers: the healthy directions study. Cancer Causes Control 2003;14:727–37.
-
Fardy P, Azzollini A, Tekverk L, Agin D, McDermott K. Physical activity and teenage health. A program to improve cardiovascular fitness, health behavior, and coronary disease risk factors in multiethnic teenagers. Ann NY Acad Sci 1997;817:356–8.
-
Fernandez S, Scales KL, Pineiro JM, Schoenthaler AM, Ogedegbe G. A senior center-based pilot trial of the effect of lifestyle intervention on blood pressure in minority elderly people with hypertension. J Am Geriatr Soc 2008;56:1860–6.
-
Flores R. Dance for health: improving fitness in African American and Hispanic adolescents. Public Health Rep 1995;110:189–93.
-
Frable PJ, Dart L, Bradley PJ. The Healthy Weigh/El Camino Saludable: a community campus partnership to prevent obesity. J Interprof Care 2004;18:447–9.
-
Garvin CC, Cheadle A, Chrisman N, Chen R, Brunson E. A community-based approach to diabetes control in multiple cultural groups. Ethn Dis 2004;14(Suppl. 1):S83–92.
-
Grey M, Berry D, Davidson M, Galasso P, Gustafson E, Melkus G. Preliminary testing of a program to prevent type 2 diabetes among high-risk youth. J Sch Health 2004;74:10–15.
-
Hagberg JM, Park JJ, Brown MD. The role of exercise training in the treatment of hypertension: an update. Sports Med 2000;30:193–206.
-
Hampton K. Communicating health messages to marginalised communities – a culture sensitive approach. Int J Health Promot Educ 2000;38:40–6.
-
Hannon PA, Bowen DJ, Christensen CL, Kuniyuki A. Disseminating a successful dietary intervention to faith communities: feasibility of using staff contact and encouragement to increase uptake. J Nutr Educ Behav 2008;40:175–80.
-
Hosper K, Deutekom M, Stronks K. The effectiveness of ‘exercise on prescription’ in stimulating physical activity among women in ethnic minority groups in the Netherlands: protocol for a randomized controlled trial. BMC Public Health 2008;8:406.
-
Irvine AB, Ary DV, Grove DA, Gilfillan-Morton L. The effectiveness of an interactive multimedia program to influence eating habits. Health Educ Res 2004;19:290–305.
-
Jayasinghe SR. Yoga in cardiac health (a review). Eur J Cardiovasc Prev Rehabil 2004;11:369–75.
-
Jenum AK, Lorentzen C, Anderssen SA, Birkeland KI, Holme I, Lund-Larsen PG, et al. Promoting physical activity in a multi-ethnic district – methods and baseline results of a pseudo-experimental intervention study. Eur J Cardiovasc Prev Rehabil 2003;10:387–96.
-
Jenum AK, Anderssen SA, Birkeland KI, Holme I, Graff-Iversen S, Lorentzen C, et al. Promoting physical activity in a low-income multiethnic district: effects of a community intervention study to reduce risk factors for type 2 diabetes and cardiovascular disease: a community intervention reducing inactivity. Diabetes Care 2006;29:1605–12.
-
Jolly K, Taylor R, Lip GY, Greenfield S, Raftery J, Mant J, et al. The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence. Health Technol Assess 2007;11(35).
-
Kennedy C, Floriani V. Translating research on healthy lifestyles for children: meeting the needs of diverse populations. Nurs Clin North Am 2008;43:397–417.
-
Khare MM, Huber R, Carpenter RA, Balmer PW, Bates NJ, Nolen KN, et al. A lifestyle approach to reducing cardiovascular risk factors in underserved women: design and methods of the Illinois WISEWOMAN Program. J Womens Health 2009;18:409–19.
-
Khunti K, Stone MA, Bankart J, Sinfield P, Pancholi A, Walker S, et al. Primary prevention of type-2 diabetes and heart disease: action research in secondary schools serving an ethnically diverse UK population. J Public Health 2008;30:30–7.
-
Klug C, Toobert DJ, Fogerty M. Healthy changes for living with diabetes: an evidence-based community diabetes self-management program. Diabetes Educ 2008;34:1053–61.
-
Komesaroff PA, Thomas S. Combating the obesity epidemic: cultural problems demand cultural solutions. Intern Med J 2007;37:287–9.
-
Kriska A. Striving for a more active community: lessons from the diabetes prevention program and beyond. Am J Prev Med 2002;22(Suppl. 1):6–7.
-
Kromhout D, Menotti A, Kesteloot H, Sans S. Prevention of coronary heart disease by diet and lifestyle: evidence from prospective cross-cultural, cohort, and intervention studies. Circulation 2002;105:893–8.
-
Leslie J, Yancy A, McCarthy W, Albert S, Wert C, Miles O, et al. Development and implementation of a school-based nutrition and fitness promotion program for ethnically diverse middle-school girls. J Am Diet Assoc 1999;99:967–70.
-
Luzzi AF, Gibney M, Sjoestroem M. Nutrition and diet for healthy lifestyles in Europe: the EURODIET evidence [erratum appears in Public Health Nutr 2001;4:1306]. Public Health Nutr 2001;4:437–739.
-
Maddock J, Choy LB, Nett B, McGurk MD, Tamashiro R. Increasing access to places for physical activity through a joint use agreement: a case study in urban Honolulu. Prev Chronic Dis 2008;5:A91.
-
Mansky P, Sannes T, Wallerstedt D, Ge A, Ryan M, Johnson LL, et al. Tai chi chuan: mind-body practice or exercise intervention? Studying the benefit for cancer survivors. Integr Cancer Ther 2006;5:192–201.
-
Mayer-Davis EJ, D’Antonio AM, Smith SM, Kirkner G, Levin Martin S, Parra-Medina D, et al. Pounds off With Empowerment (POWER): a clinical trial of weight management strategies for black and white adults with diabetes who live in medically underserved rural communities. Am J Public Health 2004;94:1736–42.
-
Nimmon LE. Within the eyes of the people: using a photonovel as a consciousness-raising health literacy tool with ESL-speaking immigrant women. Can J Public Health 2007;98:337–40.
-
Peerbhoy D, Majumdar A, Wightman N, Brand V. Success and challenges of a community healthy lifestyles intervention in Merseyside (UK) to target families at risk from coronary heart disease. Health Educ J 2008;67:134–47.
-
Perez-Rodrigo C, Wind M, Hildonen C, Bjelland M, Aranceta J, Klepp K-I, et al. The pro children intervention: applying the intervention mapping protocol to develop a school-based fruit and vegetable promotion programme. Ann Nutr Metab 2005;49:267–77.
-
Peters RM. Theoretical perspectives to increase clinical effectiveness of lifestyle modification strategies in diabetes. Ethn Dis 2004;14:S2–17–22.
-
Qian Y, Zhang J, Lin Y, Dong M, Xu M, Qian Y, et al. A tailored target intervention on influence factors of quality of life in Chinese patients with hypertension. Clin Exp Hypertens 2009;31:71–82.
-
Queral CB. The impact of a nutrition education program on nutrition knowledge and attitudes, as well as food selection, in a cohort of migrant and seasonal farm worker children. Diss Abstr Int B 2008;68(12-B).
-
Resnick B, Luisi D, Vogel A. Testing the Senior Exercise Self-efficacy Project (SESEP) for use with urban dwelling minority older adults. Public Health Nurs 2008;25:221–34.
-
Rickard K, Farnum S. Food for fun and thought: nutrition education in a children’s hospital. J Am Diet Assoc 1974;65:294–7.
-
Rimmer JH, Silverman K, Braunschweig C, Quinn L, Liu Y. Feasibility of a health promotion intervention for a group of predominantly African American women with type 2 diabetes. Diabetes Educ 2002;28:571–80.
-
Risica P, Strolla L, Fournier L, Kirtania U, Upegui D, Zhao J, et al. Effectiveness of different methods for delivering tailored nutrition education to low income, ethnically diverse adults. Int J Behav Nutr Phys Act 2009;6:24.
-
Roberts E, Takenaka JI, Ross CJ, Chong EH, Tulang JI, Napps SE. Hawaii Asian-American response to the Staying Healthy After Fifty program. Health Educ Q 1989;16:509–27.
-
Robison J, Putnam K, McKibbin L. Health At Every Size: a compassionate, effective approach for helping individuals with weight-related concerns – part II. AAOHN J 2007;55:185–92.
-
Scanlan D, Wyatt M. Tools for nutrition and preventive dental counselling for South East Asian refugees. Can Dent Hyg 1980;14:60–2.
-
Scardella P, Piombo L, Spada R, Morrone A. ‘A table in the Mediterranean: one diet, many cultures’. A project for schools in the city of Rome. Riv Sci Aliment 2006:35;17–24.
-
Schensul JJ, Trickett E. Introduction to multi-level community based culturally situated interventions. Am J Commun Psychol 2009;43:232–40.
-
Schlegel-Matthies K. Changing eating habits. Med Welt 2005;56:135–8.
-
Schmidt M, Absalah S, Nierkens V, Stronks K. Which factors engage women in deprived neighbourhoods to participate in exercise referral schemes? BMC Public Health 2008;8:371.
-
Shah M, Coyle Y, Kavanaugh A, Adams-Huet B, Lipsky PE. Development and initial evaluation of a culturally sensitive cholesterol-lowering diet program for Mexican and African American patients with systemic lupus erythematosus. Arthritis Care Res 2000;13:205–12.
-
Shah M, Kavanaugh A, Coyle Y, Adams-Huet B, Lipsky P. Effect of a culturally sensitive cholesterol lowering diet program on lipid and lipoproteins, body weight, nutrient intakes, and quality of life in patients with systemic lupus erythematosus. J Rheumatol 2002;29:2122–8.
-
Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working-class, multiethnic workers: results of the healthy directions–small business study. Am J Public Health 2005;95:1389–95.
-
Tak NI, Te Velde SJ, Brug J. Ethnic differences in 1-year follow-up effect of the Dutch Schoolgruiten Project – promoting fruit and vegetable consumption among primary-school children. Public Health Nutr 2007;10:1497–507.
-
Thompson SC, Schwankovsky L, Pitts J. Counselling patients to make lifestyle changes: the role of physician self-efficacy, training and beliefs about causes. Fam Pract 1993;10:70–5.
-
Weintraub DL, Tirumalai EC, Haydel KF, Fujimoto M, Fulton JE, Robinson TN. Team sports for overweight children: the Stanford Sports to Prevent Obesity Randomized Trial (SPORT). Arch Pediatr Adolesc Med 2008;162:232–7.
-
White JA, Drechsel J, Johnson J. Faithfully fit forever: a holistic exercise and wellness program for faith communities. J Holist Nurs 2006;24:127–31.
-
Whitehead D, Bodenlos JS, Cowles ML, Jones GN, Brantley PJ. A stage-targeted physical activity intervention among a predominantly African-American low-income primary care population. Am J Health Promot 2007;21:160–3.
-
Will JC, Farris RP, Sanders CG, Stockmyer CK, Finkelstein EA. Health promotion interventions for disadvantaged women: overview of the WISEWOMAN projects. J Womens Health (Larchmt) 2004;13:484–502.
-
Yancey AK, McCarthy WJ, Taylor WC, Merlo A, Gewa C, Weber MD, et al. The Los Angeles Lift Off: a sociocultural environmental change intervention to integrate physical activity into the workplace. Prev Med 2004;38:848–56.
-
Yancey AK, Lewis LB, Guinyard JJ, Sloane DC, Nascimento LM, Galloway-Gilliam L, et al. Putting promotion into practice: the African Americans building a legacy of health organizational wellness program. Health Promot Pract 2006;7(3 Suppl.):233–46S.
-
Zinkovskiy AK. [The School for Health based on a healthy, balanced and civilized life style – a new direction for psychohygienic health education] [in French]. Sante Publique (Bucur) 1989;32:263–70.
Excluded based on intervention
-
Aponte J, Nickitas DM. Community as client: reaching an underserved urban community and meeting unmet primary health care needs. J Community Health Nurs 2007;24:177–90.
-
Assaf A, Coccio E, Gans K, Lasater T. Community-based approaches with implications for hypertension control in blacks. Ethn Dis 2002;12:S27–33.
-
Barer-Stein T. Multiculturalism and nutrition counselling. J Can Diet Assoc 1979;40:112–16.
-
Barnett A. Dyslipidaemia in ethnic populations: special considerations. Br J Cardiol 2005;12:118–22.
-
Barnett A. Cardiometabolic risk in the South Asian community. Cardiometab Risk Weight Manage 2007;2:9–13.
-
Bauer KW, Patel A, Prokop LA, Austin SB. Swimming upstream: faculty and staff members from urban middle schools in low-income communities describe their experience implementing nutrition and physical activity initiatives. Prev Chronic Dis 2006;3:A37.
-
Beaven DW. Failure of school health education: cultural neglect or political rigidity? N Z Med J 1981;94:268–70.
-
Bediako SM, Kwate NOA, Rucker R. Dietary behavior among African Americans: assessing cultural identity and health consciousness. Ethn Dis 2004;14:527–32.
-
Bere E, Klepp K. Moderators of environmental intervention effects on diet and activity in youth. Am J Prev Med 2007;33:163–72.
-
Bertorelli AM. Nutrition counseling: meeting the needs of ethnic clients with diabetes. Diabetes Educ 1990;16:285–9.
-
Blocker DE, Freudenberg N. Developing comprehensive approaches to prevention and control of obesity among low-income, urban, African-American women. J Am Med Womens Assoc 2001;56:59–64.
-
Boardman S. The Apnee Sehat (our health) Project. Cardiometab Risk Weight Manage 2006;1:17.
-
Botvin GJ, Batson HW, Witts-Vitale S, Bess V, Baker E, Dusenbury L. A psychosocial approach to smoking prevention for urban black youth. Public Health Rep 1989;104:573–82.
-
Brown A. Patient, system and clinician level interventions to address disparities in diabetes care. Curr Diabetes Rev 2007;3:244–8.
-
Brudenell I. Parish nursing: nurturing body, mind, spirit, and community. Public Health Nurs 2003;20:85–94.
-
Brugge D, Dejong W, Hyde J, Le Q, Shih C-S, Wong A, et al. Development of targeted message concepts for recent Asian immigrants about secondhand smoke. J Health Commun 2002;7:25–37.
-
Bunge C, Meyer-Nurnberger M, Kilian H. [Health promoting interventions for migrants. Analysis of the database ‘Health Promotion for the Socially Disadvantaged’] [in German]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2006;49:893–7.
-
Burden M, Woghiren O, Burden A. Diabetes in African Caribbean, and Indo-Asian ethnic minority people. J R Coll Physicians Lond 2000;34:343–6.
-
Carlini BH, Zbikowski SM, Javitz HS, Deprey TM, Cummins SE, Zhu S-H. Telephone-based tobacco-cessation treatment: re-enrollment among diverse groups. Am J Prev Med 2008;35:73–6.
-
Carnethon MR. Diabetes prevention in US ethnic minorities: role of the social environment. J Am Diet Assoc 2008;108:942–4.
-
Centers for Disease Control and Prevention (CDCP). Improvement in lipid and glycated hemoglobin control among black adults with diabetes – Raleigh and Greensboro, North Carolina, 1997–2004. MMWR Morb Mortal Wkly Rep 2006;55:1248–51.
-
Chen MS Jr. Cardiovascular health among Asian Americans/Pacific Islanders: an examination of health status and intervention approaches. Am J Health Promot 1993;7:199–207.
-
Chowdhury T, Grace C, Kopelman P. Preventing diabetes in south Asians. Br Med J 2003;327:1059–60.
-
Clark DO. Physical activity efficacy and effectiveness among older adults and minorities. Diabetes Care 1997;20:1176–82.
-
Clark L. Primary prevention of cardiovascular disease in high-risk patients: physiologic and demographic risk factor differences between African American and white American populations. Am J Med 1999;107(Suppl. 1):22–4.
-
Coleman E, Tyll L, Lacroix A, Allen C, Leveille S, Wallace J, et al. Recruiting African-American older adults for a community based health promotion intervention: which strategies are effective? Am J Prev Med 1997;13(Suppl.):51–6.
-
Corbie-Smith G, Ammerman AS, Katz ML, St George DMM, Blumenthal C, Washington C, et al. Trust, benefit, satisfaction, and burden: a randomized controlled trial to reduce cancer risk through African-American churches. J Gen Intern Med 2003;18:531–41.
-
Cornell C, Littleton M, Greene P, Pulley L, Brownstein J, Sanderson B, et al. A community health advisor program to reduce cardiovascular risk among rural African-American women. Health Educ Res 2009;24:622–33.
-
Crespo C. Encouraging physical activity in minorities: eliminating disparities by 2010. Physician Sportsmed 2000;28:36–51.
-
Daly J, Davidson P, Chang E, Hancock K, Rees D, Thompson DR. Cultural aspects of adjustment to coronary heart disease in Chinese-Australians: a review of the literature [erratum appears in J Adv Nurs 2002;40:486]. J Adv Nurs 2002;39:391–9.
-
Davachi S, Flynn M, Edwards A. A health region/community partnership for type 2 diabetes risk factor screening in Indo-Asian communities. Can J Diabetes 2005;29:87–94.
-
Davies JA, Damani P, Margetts BM. Intervening to change the diets of low-income women. Proc Nutr Soc 2009;68:210–15.
-
Davis B. Lack of access to good healthcare & obese African-American women. J Natl Med Assoc 2003;95:405–6.
-
Davis PG, Durstine JL, Thompson RW, Drowatzky KL, Velliquette RA, Ainsworth BE. Race, exercise, and cardiovascular risk factors – relationships with plasma endothelin-1: the cross-cultural activity participation study. Med Sci Sports Exerc 2000;32(Suppl.):S173.
-
Deedwania P, Singh V. Coronary artery disease in south Asians: evolving strategies for treatment and prevention. Indian Heart J 2005;57:617–31.
-
De Groot MK. The relationship of ethnicity to diabetes self-care and medical outcomes in African-Americans with type 2 diabetes mellitus. Diss Abstr Int B 2000;61(1–B):526.
-
Demark-Wahnefried W, Hoben KP, Hars V, Jennings J, Miller MW, McClelland JW. Utility of produce ratios to track fruit and vegetable consumption in a rural community, church-based 5 a day intervention project. Nutr Cancer 1999;33:213–17.
-
Demark-Wahnefried W, McClelland JW, Jackson B, Campbell MK, Cowan A, Hoben K, et al. Partnering with African American churches to achieve better health: lessons learned during the Black Churches United for Better Health 5 a day project. J Cancer Educ 2000;15:164–7.
-
Dhami S, Sheikh A. Health promotion: reaching ethnic minorities. Pract Nurse 2008;36:21–5.
-
Diabetes Prevention Program Group. The Diabetes Prevention Program: recruitment methods and results. Control Clin Trials 2002;23:157–71.
-
Dieser RB. A cross-cultural critique of newer therapeutic recreation practice models: the Self-Determination and Enjoyment Enhance model, Aristotelian Good Life model, and the Optimizing Lifelong Health Through Therapeutic Recreation model. Ther Recreation J 2002;36:352–68.
-
Dietz W. Focus group data pertinent to the prevention of obesity in African Americans [republished from Am J Med Sci 2001;322:275–8]. Am J Med Sci 2001;322:286–9.
-
Dodani S, Kramer MK, Williams L, Crawford S, Kriska A. Fit body and soul: a church-based behavioral lifestyle program for diabetes prevention in African Americans [summary for patients in Ethn Dis 2009;19:219]. Ethn Dis 2009;19:135–41.
-
Donaldson S, Klien D. Creating healthful work environments for ethnically diverse employees working in small and medium-sized businesses: a non-profit industry/community/university collaboration model. Empl Assist Q 1997;13:17–32.
-
Doyle E, Smith CA, Hosokawa MC. A process evaluation of a community-based health promotion program for a minority target population. Health Educ 1989;20:61–4.
-
Dutton GR, Johnson J, Whitehead D, Bodenlos JS, Brantley PJ. Barriers to physical activity among predominantly low-income African-American patients with type 2 diabetes. Diabetes Care 2005;28:1209–10.
-
Dwyer JJM, Hansen B, Barrera M, Allison K, Ceolin-Celestini S, Koenig D, et al. Maximizing children’s physical activity: an evaluability assessment to plan a community-based, multi-strategy approach in an ethno-racially and socio-economically diverse city. Health Promot Int 2003;18:199–208.
-
Ejidokum O, Ramaiah S, Singh R. Places of worship and health education. Lancet 1997;350:223.
-
el-Askari G, Freestone J, Irizarry C, Kraut KL, Mashiyama ST, Morgan MA, et al. The Healthy Neighborhoods Project: a local health department’s role in catalyzing community development. Health Educ Behav 1998;25:146–59.
-
Epps R. A comprehensive national minority intervention in tobacco control. Cancer 1998;83(8 Suppl.):1793–5.
-
Evenson K, Aytur S. Modifying physical activity in a multiethnic sample of low-income women: one-year results from the IMPACT (increasing motivation for physical ACTivity) project. Am J Health Promot 2007;21:286–7.
-
Fagerli RA, Lien ME, Wandel M. Experience of dietary advice among Pakistani-born persons with type 2 diabetes in Oslo. Appetite 2005;45:295–304.
-
Fallon EA, Wilcox S, Laken M. Health care provider advice for African American adults not meeting health behavior recommendations. Prev Chronic Dis 2006;3:A45.
-
Farren C, Naidoo J. Smoking cessation programmes targeted at black and minority ethnic communities. Br J Cancer Suppl 1996;29:S78–80.
-
Fleury J, Lee SM. The social ecological model and physical activity in African American women. Am J Community Psychol 2006;37:129–40.
-
Fleury J, Sedikides C, Donovan K. Possible health selves of older African Americans: toward increasing the effectiveness of health promotion efforts. Top Geriatr Rehabil 2002;18:52–8.
-
Floyd M, Spengler J, Maddock J, Gobster P, Suau L. Park-based physical activity in diverse communities of two US cities. An observational study. Am J Prev Med 2008;34:299–305.
-
Furness S. Shifting sands: developing cultural competence. Practice 2005;17:247–56.
-
Gans KM, Kumanyika SK, Lovell HJ, Risica PM, Goldman R, Odoms-Young A, et al. The development of SisterTalk: a cable TV-delivered weight control program for black women. Prev Med 2003;37:654–67.
-
Gans KM, Risica PM, Kirtania U, Jennings A, Strolla LO, Steiner-Asiedu M, et al. Dietary behaviors and portion sizes of black women who enrolled in SisterTalk and variation by demographic characteristics. J Nutr Educ Behav 2009;41:32–40.
-
Garcia-Lascurain M, Kicklighter J, Jonnalagadda S, Boudolf E, Duchon D. Effect of a nutrition education program on nutrition-related knowledge of English-as-second-language elementary school students: a pilot study. J Immigr Minor Health 2006;8:57–65.
-
Genkinger JM, Jehn ML, Sapun M, Mabry I, Young DR. Does weight status influence perceptions of physical activity barriers among African-American women? Ethn Dis 2006;16:78–84.
-
Gerber JC, Stewart DL. Prevention and control of hypertension and diabetes in an underserved population through community outreach and disease management: a plan of action. J Assoc Acad Minor Phys 1998;9:48–52.
-
Ghouri N. Health fair in a mosque: putting policy into practice. Public Health 2005;119:197–201.
-
Giachello AL, Arrom JO, Davis M, Sayad JV, Ramirez D, Nandi C, et al. Reducing diabetes health disparities through community-based participatory action research: the Chicago Southeast Diabetes Community Action Coalition. Public Health Rep 2003;118:309–23.
-
Giarratano G, Bustamante-Forest R, Carter C. A multicultural and multilingual outreach program for cervical and breast cancer screening. J Obstet Gynecol Neonatal Nurs 2005;34:395–402.
-
Ginne M. Physicians’ attitudes and practices with patients who smoke: a multicultural analysis. Diss Abstr Int B 1993;54(5–B).
-
Granner ML, Liguori G, Kirkner GJ, Ainsworth BE. Health care provider counseling for physical activity among black and white South Carolinians. J S C Med Assoc 2001;97:338–41.
-
Greene EL, Thomas CR Jr. Minority health and disparities-related issues: part I. Med Clin North Am 2005;89:721–912.
-
Greene EL, Thomas CR Jr. Minority health and disparities-related issues: part II. Med Clin North Am 2005;89:921–1057.
-
Greenhalgh T, Collard A, Begum N. Sharing stories: complex intervention for diabetes education in minority ethnic groups who do not speak English. BMJ 2005;330:628–31.
-
Gregg E, Narayan K, Kumanyika S, Agurs-Collins T. Culturally appropriate lifestyle interventions in minority populations. Diabetes Care 1998;21:875–7.
-
Griffiths C, Motlib J, Azad A, Ramsay J, Eldridge S, Feder G, et al. Randomised controlled trial of a lay-led self-management programme for Bangladeshi patients with chronic disease. Br J Gen Pract 2005;55:831–7.
-
Hardoff D, Nudelman A, Chigier E. Changes in the eating habits of Ethiopian adolescent immigrants. Int J Adolesc Med Health 1999;11:39–45.
-
Harley AE, Buckworth J, Katz ML, Willis SK, Odoms-Young A, Heaney CA. Developing long-term physical activity participation: a grounded theory study with African American women. Health Educ Behav 2009;36:97–112.
-
Harrison GG, Kagawa-Singer M, Foerster SB, Lee H, Pham Kim L, Nguyen T-U, et al. Seizing the moment: California’s opportunity to prevent nutrition-related health disparities in low-income Asian American population. Cancer 2005;104(12 Suppl.):2962–8.
-
Hatch JW, Cunningham AC, Woods WW, Snipes FC. The Fitness Through Churches project: description of a community-based cardiovascular health promotion intervention. Hygie 1986;5:9–12.
-
Herman WH, Thompson TJ, Visscher W, Aubert RE, Engelgau MM, Liburd L, et al. Diabetes mellitus and its complications in an African-American community: project DIRECT. J Natl Med Assoc 1998;90:147–56.
-
Herreria J. ‘Control your diabetes’ campaign encourages a healthy lifestyle. National Diabetes Education Program. Profiles Healthc Mark 1999;15:23–6.
-
Hinkle AJ. Community-based nutrition interventions: reaching adolescents from low-income communities. Ann N Y Acad Sci 1997;817:83–93.
-
Horowitz CR, Goldfinger JZ, Muller SE, Pulichino RS, Vance TL, Arniella G, et al. A model for using community-based participatory research to address the diabetes epidemic in East Harlem. Mt Sinai J Med 2008;75:13–21.
-
Hyman I, Guruge S, Makarchuk M-J, Cameron J, Micevski V. Promotion of healthy eating among new immigrant women in Ontario. Can J Diet Pract Res 2002;63:125–9.
-
Ilett S, Freeman A. Improving the diet of toddlers of Pakistani origin: a study of intensive dietary health education. J Fam Health Care 2004;14:16–19.
-
Izquierdo-Porrera A, Powell C, Reiner J, Fontaine K. Correlates of exercise adherence in an African American church community. Cultur Divers Ethnic Minor Psychol 2002;8:389–94.
-
Jabbour S, Fouad FM. Religion-based tobacco control interventions: how should WHO proceed? Bull World Health Organ 2004;82:923–7.
-
Jackson F, Chu K, Garcia R. Special Populations Networks – how this innovative community-based initiative affected minority and underserved research programs. Cancer 2006;107(8 Suppl.):1939–44.
-
Jackson FLC. Ethnogenetic layering (EL): an alternative to the traditional race model in human variation and health disparity studies [erratum appears in Ann Hum Biol 2008;35:362]. Ann Hum Biol 2008;35:121–44.
-
Jennings GE. Foods and nutrition in a Black Studies program. J Am Diet Assoc 1974;65:661–3.
-
Johnson CA, Unger JB, Ritt-Olson A, Palmer PH, Cen SY, Gallaher P, et al. Smoking prevention for ethnically diverse adolescents: 2-year outcomes of a multicultural, school-based smoking prevention curriculum in Southern California. Prev Med 2005;40:842–52.
-
Kaufman FR, Hirst K, Linder B, Baranowski T, Cooper DM, Foster GD, et al. Risk factors for type 2 diabetes in a sixth-grade multiracial cohort: the HEALTHY study. Diabetes Care 2009;32:953–5.
-
Kaufman JS, Jason LA, Sawlski LM, Halpert JA. A comprehensive multi-media program to prevent smoking among black students. J Drug Educ 1994;24:95–108.
-
Kennedy BM, Ard JD, Harrison L Jr, Conish BK, Kennedy E, Levy EJ, et al. Cultural characteristics of African Americans: implications for the design of trials that target behavior and health promotion programs. Ethn Dis 2007;17:548–54.
-
King TK, Borrelli B, Black C, Pinto BM, Marcus BH. Minority women and tobacco: implications for smoking cessation interventions. Ann Behav Med 1997;19:301–13.
-
Krall LP. The history of diabetes lay associations. Patient Educ Couns 1995;26:285–91.
-
Kriska A, Rexroad A. The role of physical activity in minority populations. Womens Health Issues 1998;8:98–103.
-
Kumanyika SK. Can hypertension be prevented? Applications of risk modifications in black populations: US populations. Ethn Dis 1997;7:72–7.
-
Kumanyika SK, Adams-Campbell L, Van Horn B, Ten Have TR, Treu JA, Askov E, et al. Outcomes of a cardiovascular nutrition counseling program in African-Americans with elevated blood pressure or cholesterol level. J Am Diet Assoc 1999;99:1380–91.
-
LaMonte MJ, Durstine JL, DuBose KD, Yanowitz FG, Irwin ML, Bopp CM, et al. Physical activity, physical fitness, and C-reactive protein: the cross-cultural activity participation study. Med Sci Sports Exerc 2002;34(Suppl.):S228.
-
Laverentz ML, Cox CC, Jordan M. The Nuer Nutrition Education Program: breaking down cultural barriers. Health Care Women Int 1999;20:593–601.
-
Lee MM, Huang S. Immigrant women’s health: nutritional assessment and dietary intervention. West J Med 2001;175:133–7.
-
Lee SM. Physical activity among minority populations: what health promotion practitioners should know – a commentary. Health Promot Pract 2005;6:447–52.
-
Lesley ML. Social problem solving training for African Americans: effects on dietary problem solving skill and DASH diet-related behavior change. Patient Educ Couns 2007;65:137–46.
-
Levine DM, Becker DM, Bone LR. Narrowing the gap in health status of minority populations: a community–academic medical center partnership. Am J Prev Med 1992;8:319–23.
-
Lewis CE, Raczynski JM, Heath GW, Levinson R, Cutter GR. Physical activity of public housing residents in Birmingham, Alabama. Am J Public Health 1993;83:1016–20.
-
Lopes AA, James SA, Port FK, Ojo AO, Agodoa LY, Jamerson KA. Meeting the challenge to improve the treatment of hypertension in blacks. J Clin Hypertens 2003;5:393–401.
-
Lubell A. Can exercise help treat hypertension in black Americans? Physician Sportsmed 1988;16:165–8.
-
Ma GX, Chu KC, Jackson FE, Tsou W. The Asian Tobacco Education, Cancer Awareness and Research’s role in tobacco and cancer control efforts in Asian American communities. Asian Am Pac Isl J Health 2003;10:25–39.
-
Malik P. Creating a fitness culture. Can J Cardiol 2005;21:243.
-
Maras ML, Adolphi CL. Ethnic tailoring improves dietary compliance. Diabetes Educ 1985;10:47–50.
-
Massaro E, Claiborne N. Effective strategies for reaching high-risk minorities with diabetes. Diabetes Educ 2001;27:820–6.
-
Mazas CA, Wetter DW. Smoking cessation interventions among African Americans: research needs. Cancer Control 2003;10(Suppl.):87–9.
-
Melnyk B. The latest evidence on smoking cessation interventions with diverse populations. Worldviews Evid Based Nurs 2005;2:12–16.
-
Meyer K. Prevention of obesity and physical inactivity – a socio-cultural challenge. J Public Health 2008;16:1–2.
-
Middelkoop BJ, van der Wal G. Culture-specific diabetes care for Surinam South Asians with a low socio-economic position: who benefits? Patient Educ Couns 2004;53:353–8.
-
Mirenda R, Brooks AB. International food festival – a community action program. Am J Public Health 1973;63:40–2.
-
Nestle M, Cowell C. Health promotion for low-income minority groups: the challenge for nutrition education. Health Educ Res 1990;5:527–33.
-
Nimmon L. Photonovela to educate on nutrition: ESL speakers create copy that is easy to understand. Patient Educ Manag 2008;15:112–13.
-
Nollen NL, Catley D, Davies G, Hall M, Ahluwalia JS. Religiosity, social support, and smoking cessation among urban African American smokers. Addict Behav 2005;30:1225–9.
-
Office of Minority Health. Pocket guide to minority health resources. Washington, DC: US Department of Health and Human Services, Public Health Service; 2001.
-
Palmer TA, Jaworski CA. Exercise prescription for underprivileged minorities. Curr Sports Med Rep 2004;3:344–8.
-
Pella D, Thomas N, Tomlinson B, Singh RB. Prevention of coronary artery disease: the south Asian paradox. Lancet 2003;361:79.
-
Peters J, Jackson M. Accessibility and use of touchscreens by black and ethnic minority groups in the three cities project. Ethn Health 2005;10:199–211.
-
Peterson D, Govindji A. Giving dietary advice to Asian diabetic patients. Diabet Med 1988;5:683–6.
-
Prohaska T, Walcott-Mcquigg J, Peters K, Li M. Recruitment of older African Americans into church-based exercise programs. J Ment Health Aging 2000;6:53–66.
-
Punzalan C, Paxton KC, Guentzel H, Bluthenthal RN, Staunton AD, Mejia G, et al. Seeking community input to improve implementation of a lifestyle modification program. Ethn Dis 2006;16(1 Suppl. 1):S79–88.
-
Rankins J, Wortham J, Brown L. Modifying soul food for the Dietary Approaches to Stop Hypertension diet (DASH) plan: implications for metabolic syndrome (DASH of Soul). Ethn Dis 2007;17(Suppl. 4):S4–7–12.
-
Robinson L, Klesges R, Levy M, Zbikowski S. Preventing cigarette use in a bi-ethnic population: results of the Memphis Smoking Prevention Program. Cogn Behav Pract 1999;6:136–43.
-
Rogers ME, Sherwood HS, Rogers NL, Bohlken RM. Effects of dumbbell and elastic band training on physical function in older inner-city African-American women. Women Health 2002;36:33–41.
-
Ruffing-Rahal MA. Evaluation of group health promotion with community-dwelling older women. Public Health Nurs 1994;11:38–48.
-
Schulz AJ, Zenk S, Odoms-Young A, Hollis-Neely T, Nwankwo R, Lockett M, et al. Healthy eating and exercising to reduce diabetes: exploring the potential of social determinants of health frameworks within the context of community-based participatory diabetes prevention. Am J Public Health 2005;95:645–51.
-
Sloane DC, Diamant AL, Lewis LB, Yancey AK, Flynn G, Nascimento LM, et al. Improving the nutritional resource environment for healthy living through community-based participatory research. J Gen Intern Med 2003;18:568–75.
-
Taylor VM, Cripe SM, Acorda E, Teh C, Coronado G, Do H, et al. Development of an ESL curriculum to educate Chinese immigrants about physical activity. J Immigr Minor Health 2008;10:379–87.
-
Thampy R. Therapeutic diets for Asians. J Hum Nutr 1977;31:256–8.
-
Thomas J. Nutrition intervention in ethnic minority groups. Proc Nutr Soc 2002;61:559–67.
-
Thompson D, Jago R, Baranowski T, Watson K, Zakeri I, Cullen KW, et al. Covariability in diet and physical activity in African-American girls. Obes Res 2004;12(Suppl.):46–54S.
-
Tong E, Tang H, Tsoh J, Wong C, Chen MS Jr. Smoke-free policies among Asian-American women. Comparisons by education status. Am J Prev Med 2009;37(Suppl.):S144–50.
-
Treuth M, Sherwood N, Baranowski T, Butte N, Jacobs D Jr, McClanahan B, et al. Physical activity self-report and accelerometry measures from the Girls health Enrichment Multi-site Studies. Prev Med 2004;38(Suppl.):S43–9.
-
Tung WC, Hsu CH. Assessing transcultural validity of the transtheoretical model with Chinese Americans and physical activity. J Transcult Nurs 2009;20:286–95.
-
Unger JB, Chou C-P, Palmer PH, Ritt-Olson A, Gallaher P, Cen S, et al. Project FLAVOR: 1-year outcomes of a multicultural, school-based smoking prevention curriculum for adolescents. Am J Public Health 2004;94:263–5.
-
Ursin G, Henderson BE. Breast cancer prevention in African-American women. J Natl Cancer Inst 1996;88:1332–3.
-
Vyas A, Haidery AZ, Wiles PG, Gill S, Roberts C, Cruickshank JK. A pilot randomized trial in primary care to investigate and improve knowledge, awareness and self-management among South Asians with diabetes in Manchester. Diabet Med 2003;20:1022–6.
-
Ward J, Collins G, Walmsley J. A model for implementing Healthy People 2000 objectives in African-American communities in California. Ethn Dis 1993;3:158–68.
-
Washington CR. Community-based hypertension control programs. N C Med J 1995;56:138–40.
-
Webb M, Francis J, Hines B, Quarles F. Health disparities and culturally specific treatment: perspectives and expectancies of African American smokers. J Clin Psychol 2007;63:567–83.
-
Webb MS. Focus groups as an intervention for low-income African American smokers to promote participation in subsequent intervention studies. Res Nurs Health 2008;31:141–51.
-
Wenger NK. Diet and exercise for perimenopausal women lifestyle interventions can decrease cardiovascular risk. J Am Coll Cardiol 2004;44:586–7.
-
Wiist WH, Flack JM. A church-based cholesterol education program. Public Health Rep 1990;105:381–8.
-
Williams E. Cooking with soul: a look into faith-based wellness programs: interview conducted by Tony Peregrin. J Am Diet Assoc 2006;106:1016–20.
-
Xu Y, Crane P, Ryan R. School nursing in an underserved multiethnic Asian community: experiences and outcomes. J Community Health Nurs 2002;19:187–98.
-
Yancey A, McCarthy WJ, Leslie J. Recruiting African-American women to community-based health promotion research. Am J Health Promot 1998;12:335–8.
-
Yancey A, Ory M, Davis S. Dissemination of physical activity promotion interventions in underserved populations. Am J Prev Med 2006;31(Suppl.):82–91.
-
Yancey AK, Miles O, Jordan AD. Organizational characteristics facilitating initiation and institutionalization of physical activity programs in a multiethnic urban community. J Health Educ 1999;30:S44–51.
-
Yancey AK, Jordan A, Bradford J, Voas J, Eller TJ, Buzzard M, et al. Engaging high-risk populations in community-level fitness promotion: ROCK! Richmond. Health Promot Pract 2003;4:180–8.
-
Yancey AK, Lewis LB, Sloane DC, Guinyard JJ, Diamant AL, Nascimento LM, et al. Leading by example: a local health department-community collaboration to incorporate physical activity into organizational practice. J Public Health Manag Pract 2004;10:116–23.
-
Yancey AK, Tomiyama AJ. Physical activity as primary prevention to address cancer disparities. Semin Oncol Nurs 2007;23:253–63.
-
Yates T, Khunti K, Davies M. Preventing type 2 diabetes: making the evidence work for migrant Indian populations. Indian J Med Res 2009;130:495–7.
-
Zaidi Q. Breaking barriers: health promotion initiatives in places of worship. Pract Cardiovasc Risk Manag 2006;4:8–10.
-
Zanchetta M, Poureslami I. Health literacy within the reality of immigrants’ culture and language. Can J Public Health 2006;97(Suppl. 2):S26–30.
-
Zhang J, Wang Z. Factors associated with smoking in Asian American adults: a systematic review. Nicotine Tob Res 2008;10:791–801.
-
Zhu SH, Anderson CM, Johnson CE, Tedeschi G, Roeseler A. A centralised telephone service for tobacco cessation: the California experience. Tob Control 2000;9:48–55.
-
Zunker C, Cox TL, Wingo BC, Knight BN, Jefferson WK, Ard JD. Using formative research to develop a worksite health promotion program for African American women. Women Health 2008;48:189–207.
Excluded based on adaptation
-
Batik O, Phelan EA, Walwick JA, Wang G, LoGerfo JP. Translating a community-based motivational support program to increase physical activity among older adults with diabetes at community clinics: a pilot study of Physical Activity for a Lifetime of Success (PALS). Prev Chronic Dis 2008;5:A18.
-
Batts ML, Gary TL, Huss K, Hill MN, Bone L, Brancati FL. Patient priorities and needs for diabetes care among urban African American adults. Diabetes Educ 2001;27:405–12.
-
Bayne-Smith M, Fardy PS, Azzollini A, Magel J, Schmitz KH, Agin D. Improvements in heart health behaviors and reduction in coronary artery disease risk factors in urban teenaged girls through a school-based intervention: the PATH program. Am J Public Health 2004;94:1538–43.
-
Bean MKVO. Physical activity in elementary school girls: implementation and theory-based evaluation of Girls on the Run. Diss Abstr Int B 2006;67(4–B).
-
Becker D, Yanek L, Johnson W Jr, Garrett D, Moy T, Reynolds S, et al. Impact of a community-based multiple risk factor intervention on cardiovascular risk in black families with a history of premature coronary disease. Circulation 1298;111:1298–304.
-
Beresford SA, Farmer EM, Feingold L, Graves KL, Sumner SK, Baker RM. Evaluation of a self-help dietary intervention in a primary care setting. Am J Public Health 1992;82:79–84.
-
Berry D, Grey M, Melkus G, Savoye M. Preliminary testing of an intervention for multiethnic overweight and obese parents of obese children. Annual Scientific Meeting of the North American Association for the Study of Obesity (NAASO), Vancouver, BC, Canada, 2005.
-
Bhargava A, Guthrie JF. Unhealthy eating habits, physical exercise and macronutrient intakes are predictors of anthropometric indicators in the Women’s Health Trial: Feasibility Study in Minority Populations. Br J Nutr 2002;88:719–28.
-
Bhargava A, Hays J. Behavioral variables and education are predictors of dietary change in the Women’s Health Trial: Feasibility Study in Minority Populations. Prev Med 2004;38:442–51.
-
Bray P, Thompson D, Wynn JD, Cummings DM, Whetstone L. Confronting disparities in diabetes care: the clinical effectiveness of redesigning care management for minority patients in rural primary care practices. J Rural Health 2005;21:317–21.
-
Bruening K, Gilbride J, Passannante M, McClowry S. Dietary intake and health outcomes among young children attending 2 urban day-care centers. J Am Diet Assoc 1529;99:1529–35.
-
Campbell MK, Carbone E, Honess-Morreale L, Heisler-Mackinnon J, Demissie S, Farrell D. Randomized trial of a tailored nutrition education CD-ROM program for women receiving food assistance. J Nutr Educ Behav 2004;36:58–66.
-
Castro CM, Sallis JF, Hickmann SA, Lee RE, Chen AH. A prospective study of psychosocial correlates of physical activity for ethnic minority women. Psychol Health 1999;14:277–93.
-
Cene C, Yanek L, Moy T, Levine D, Becker L, Becker D. Sustainability of a multiple risk factor intervention on cardiovascular disease in high-risk African American families. Ethn Dis 2008;18:169–75.
-
Chen AHW. The effectiveness of a home-based intervention to promote walking in ethnic minority women. Diss Abstr Int B 1996;57(2–B).
-
Clark DO, Stump TE, Damush TM. Outcomes of an exercise program for older women recruited through primary care. J Aging Health 2003;15:567–85.
-
Clarke KK, Freeland-Graves J, Klohe-Lehman DM, Bohman TM. Predictors of weight loss in low-income mothers of young children. J Am Diet Assoc 2007;107:1146–54.
-
Cotton B, Smith A, Hansen I, Davis C, Doyle A, Walsh A. Physician-directed primary care intervention to reduce risk factors for type 2 diabetes in high-risk youth. Am J Med Sci 2006;332:108–11.
-
Covelli MM. Efficacy of a school-based cardiac health promotion intervention program for African-American adolescents. Appl Nurs Res 2008;21:173–80.
-
Cullen KW, Baranowski T, Baranowski J, Warnecke C, de Moor C, Nwachokor A, et al. ‘5 A Day’ achievement badge for urban boy scouts: formative evaluation results. J Cancer Educ 1998;13:162–8.
-
Curry S, Ludman E, Graham E, Stout J, Grothaus L, Lozano P. Pediatric-based smoking cessation intervention for low-income women: a randomized trial. Arch Pediatr Adolesc Med 2003;157:295–302.
-
Damush T, Stump T, Saporito A, Clark D. Predictors of older primary care patients’ participation in a submaximal exercise test and a supervised, low-impact exercise class. Prev Med 2001;33:485–94.
-
Davies M, Tringham J, Troughton J, Khunti K. Prevention of type 2 diabetes mellitus. A review of the evidence and its application in a UK setting. Diabet Med 2004;21:403–14.
-
Davis Martin P, Rhode PC, Dutton GR, Redmann SM, Ryan DH, Brantley PJ. A primary care weight management intervention for low-income African-American women. Obesity (Silver Spring) 2006;14:1412–20.
-
Dennison CR, Post WS, Kim MT, Bone LR, Cohen D, Blumenthal RS, et al. Underserved urban African American men: hypertension trial outcomes and mortality during 5 years. Am J Hypertens 2007;20:164–71.
-
Dollahite J, Olson C, Scott-Pierce M. the impact of nutrition education on food insecurity among low-income participants in EFNEP. Fam Consum Sci Res J 2003;32:127–39.
-
Domel S, Alford B, Cattlett H, Gench B. Weight control for black women. J Am Diet Assoc 1992;92:346–8.
-
Drayton-Brooks S, White N. Health promoting behaviors among African American women with faith-based support. ABNF J 2004;15:84–90.
-
Dunn MZ. Psychosocial mediators of a walking intervention among African American women. J Transcult Nurs 2008;19:40–6.
-
Dunton GF, Robertson TP. A tailored internet-plus-email intervention for increasing physical activity among ethnically-diverse women. Prev Med 2008;47:605–11.
-
Dutton GR, Martin PD, Brantley PJ. Ideal weight goals of African American women participating in a weight management program. Body Image 2004;1:305–10.
-
Dutton GR, Davis Martin P, Welsch MA, Brantley PJ. Promoting physical activity for low-income minority women in primary care. Am J Health Behav 2007;31:622–31.
-
Ebbeling CB, Pearson MN, Sorensen G, Levine RA, Hebert JR, Salkeld JA, et al. Conceptualization and development of a theory-based healthful eating and physical activity intervention for postpartum women who are low income. Health Promot Pract 2007;8:50–9.
-
Economos CD, Hyatt RR, Goldberg JP, Must A, Naumova EN, Collins JJ, et al. A community intervention reduces BMI z-score in children: Shape Up Somerville first year results. Obesity (Silver Spring) 2007;15:1325–36.
-
Eliassen AH, Colditz GA, Peterson KE, Furtado JD, Fay ME, Sorensen G, et al. Biomarker validation of dietary intervention in two multiethnic populations. Prev Chronic Dis 2006;3:A44.
-
Emmons KM, Stoddard AM, Fletcher R, Gutheil C, Suarez EG, Lobb R, et al. Cancer prevention among working class, multiethnic adults: results of the healthy directions-health centers study. Am J Public Health 2005;95:1200–5.
-
Fardy PS, White RE, Haltiwanger-Schmitz K, Magel JR, McDermott KJ, Clark LT, et al. Coronary disease risk factor reduction and behavior modification in minority adolescents: the PATH program. J Adolesc Health 1996;18:247–53.
-
Feldman RH, Damron D, Anliker J, Ballesteros RD, Langenberg P, DiClemente C, et al. The effect of the Maryland WIC 5-A-Day promotion program on participants’ stages of change for fruit and vegetable consumption. Health Educ Behav 2000;27:649–63.
-
Fisher E, Musick J, Scott C, Miller J, Gram R, Richardson V, et al. Improving clinic- and neighborhood-based smoking cessation services within federally qualified health centers serving low-income, minority neighborhoods. Nicotine Tob Res 2005;7(Suppl. 1):S45–56.
-
Fisher EB, Auslander WF, Munro JF, Arfken CL, Brownson RC, Owens NW. Neighbors for a smoke free north side: evaluation of a community organization approach to promoting smoking cessation among African Americans. Am J Public Health 1998;88:1658–63.
-
Ford BS, McDonald TE, Owens AS, Robinson TN. Primary care interventions to reduce television viewing in African-American children. Am J Prev Med 2002;22:106–9.
-
Fouad MN, Kiefe CI, Bartolucci AA, Burst NM, Ulene V, Harvey MR. A hypertension control program tailored to unskilled and minority workers. Ethn Dis 1997;7:191–9.
-
Fox PJ, Breuer W, Wright JA. Effects of a health promotion program on sustaining health behaviors in older adults. Am J Prev Med 1997;13:257–64.
-
Frenn M, Malin S, Bansal NK. Stage-based interventions for low-fat diet with middle school students. J Pediatr Nurs 2003;18:36–45.
-
Frenn M, Malin S, Brown RL, Greer Y, Fox J, Greer J, et al. Changing the tide: an internet/video exercise and low-fat diet intervention with middle-school students. Appl Nurs Res 2005;18:13–21.
-
Frieden T, Mostashari F, Kerker B, Miller N, Hajat A, Frankel M. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002–2003. Am J Public Health 1016;95:1016–23.
-
Fries EA, Ripley JS, Figueiredo MI, Thompson B. Can community organization strategies be used to implement smoking and dietary changes in a rural manufacturing work site? J Rural Health 1999;15:413–20.
-
Fu SS, Okuyemi KS, Partin MR, Ahluwalia JS, Nelson DB, Clothier BA, et al. Menthol cigarettes and smoking cessation during an aided quit attempt. Nicotine Tob Res 2008;10:457–62.
-
Germann J, Kirschenbaum D, Rich B. Use of an orientation session may help decrease attrition in a pediatric weight management program for low-income minority adolescents. J Clin Psychol Med Settings 2006;13:169–79.
-
Germann J, Kirschenbaum D, Rich B, O’Koon J. Long-term evaluation of multi-disciplinary treatment of morbid obesity in low-income minority adolescents: La Rabida Children’s Hospital’s FitMatters Program. J Adolesc Health 2006;39:553–61.
-
Gortmaker SL, Cheung LW, Peterson KE, Chomitz G, Cradle JH, Dart H, et al. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: eat well and keep moving. Arch Pediatr Adolesc Med 1999;153:975–83.
-
Griffith J. Assessing childhood obesity programs in low-socioeconomic and diverse communities. J Natl Med Assoc 2009;101:421–9.
-
Gutin B, Cucuzzo N, Islam S, Smith C, Moffatt R, Pargman D. Physical training improves body composition of black obese 7- to 11-year-old girls. Obes Res 1995;3:305–12.
-
Gutin B, Cucuzzo N, Islam S, Smith C, Stachura ME. Physical training, lifestyle education, and coronary risk factors in obese girls. Med Sci Sports Exerc 1996;28:19–23.
-
Hanna S, Walker P, Walker J, Claes J, Stewart C, Swank A, et al. A smoking cessation project for African American women: implications for relational research. Fam Syst Health 2003;21:383–95.
-
Harrington KF, Franklin FA, Davies SL, Shewchuk RM, Binns MB. Implementation of a family intervention to increase fruit and vegetable intake: the Hi5+ experience. Health Promot Pract 2005;6:180–9.
-
The HEALTHY Study Group. HEALTHY study rationale, design and methods: moderating risk of type 2 diabetes in multi-ethnic middle school students. Int J Obes 2009;33:S4–20.
-
Heisler M, Blumenthal D, Rust G, Dubois A. The Second Annual Primary Care Conference – programming to eliminate health disparities among ethnic minority populations: an introduction to proceedings. Ethn Dis 2003;13(Suppl. 3):S3–1–5.
-
Hoffman AM, Redding CA, Goldberg D, Anel D, Prochaska JO, Meyer PM, et al. Computer expert systems for African-American smokers in physicians offices: a feasibility study. Prev Med 2006;43:204–11.
-
Holland CA, Everitt P, Johnson A, Devi R. The ‘healthy passport’ intervention with older people in an English urban environment: effects of incentives and peer-group organisers in promoting healthy living. Ageing Soc 2008;28:525–49.
-
Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, et al. Weight loss during the intensive intervention phase of the weight-loss maintenance trial. Am J Prev Med 2008;35:118–26.
-
Hughes AR, McLaughlin R, McKay J, Lafferty K, McKay T, Mutrie N. The B’Active programme for overweight primary school children in Glasgow: determining the prevalence of overweight and obesity and piloting an activity intervention. Br J Nutr 2007;97:204–9.
-
Hunt MK, Stoddard AM, Barbeau E, Goldman R, Wallace L, Gutheil C, et al. Cancer prevention for working class, multiethnic populations through small businesses: the healthy directions study. Cancer Cause Control 2003;14:749–60.
-
Hunt MK, Stoddard AM, Kaphingst KA, Sorensen G. Characteristics of participants in a cancer prevention intervention designed for multiethnic workers in small manufacturing worksites. Am J Health Promot 2007;22:33–7.
-
Islam N, Kwon SC, Ahsan H, Senie RT. New York AANCART: using participatory research to address the health needs of South Asian and Korean Americans in New York City. Cancer 2005;104(Suppl.):2931–6.
-
Jacobs AD, Ammerman AS, Ennett ST, Campbell MK, Tawney KW, Aytur SA, et al. Effects of a tailored follow-up intervention on health behaviors, beliefs, and attitudes. J Womens Health 2004;13:557–68.
-
Jeffries S, Choi W, Butler J, Harris K, Ahluwalia J. Strategies for recruiting African-American residents of public housing developments into a randomized controlled trial. Ethn Dis 2005;15:773–8.
-
Jennings-Sanders A. Using health fairs to examine health promotion behaviors of older African Americans. ABNF J 2003;14:13–16.
-
Johnson C, Nicklas T, Arbeit M, Franklin F, Cresanta J, Harsha D, et al. Cardiovascular risk in parents of children with elevated blood pressure. ‘Heart Smart’ – family health promotion. J Clin Hypertens 1987;3:559–66.
-
Jordan KC, Freeland-Graves JH, Klohe-Lehman DM, Cai G, Voruganti VS, Proffitt JM, et al. A nutrition and physical activity intervention promotes weight loss and enhances diet attitudes in low-income mothers of young children. Nutr Res 2008;28:13–20.
-
Kalenderian E, Pegus C, Francis C, Goodwin N, Jacques H, Lasa D. Cardiovascular disease urban intervention: baseline activities and findings. J Community Health 2009;34:282–7.
-
Kaphingst KA, Lobb R, Fay ME, Hunt MK, Suarez EG, Fletcher RH, et al. Impact of intervention dose on cancer-related health behaviors among working-class, multiethnic, community health center patients. Am J Health Promot 2007;21:262–6.
-
Karanja N, Lancaster KJ, Vollmer WM, Lin P-H, Most MM, Ard JD, et al. Acceptability of sodium-reduced research diets, including the Dietary Approaches To Stop Hypertension diet, among adults with prehypertension and stage 1 hypertension. J Am Diet Assoc 2007;107:1530–8.
-
Kaul L, Nidiry JJ. Management of obesity in low-income African Americans. J Natl Med Assoc 1999;91:139–43.
-
Kennedy BM, Paeratakul S, Champagne CM, Ryan DH, Harsha DW, McGee B, et al. A pilot church-based weight loss program for African-American adults using church members as health educators: a comparison of individual and group intervention. Ethn Dis 2005;15:373–8.
-
Kennedy BM, Champagne CM, Ryan DH, Newton R Jr, Conish BK, Harsha DW, et al. The ‘Rolling Store’: an economical and environmental approach to the prevention of weight gain in African American women. Ethn Dis 2009;19:7–12.
-
King A, Sanchez-Johnsen L, Van Orman S, Cao D, Matthews A. A pilot community-based intensive smoking cessation intervention in African Americans: feasibility, acceptability and early outcome indicators. J Natl Med Assoc 2008;100:208–17.
-
Klebanoff R, Muramatsu N. A community-based physical education and activity intervention for African American preadolescent girls: a strategy to reduce racial disparities in health. Health Promot Pract 2002;3:276–85.
-
Klinedinst NJ. Effects of a nutrition education program for urban, low-income, older adults: a collaborative program among nurses and nursing students. J Community Health Nurs 2005;22:93–104.
-
Klohe-Lehman DM, Freeland-Graves J, Anderson ER, McDowell T, Clarke KK, Hanss-Nuss H, et al. Nutrition knowledge is associated with greater weight loss in obese and overweight low-income mothers. J Am Diet Assoc 2006;106:65–75, quiz 76–9.
-
Klohe-Lehman DM, Freeland-Graves J, Clarke KK, Cai G, Voruganti VS, Milani TJ, et al. Low-income, overweight and obese mothers as agents of change to improve food choices, fat habits, and physical activity in their 1-to-3-year-old children. J Am Coll Nutr 2007;26:196–208.
-
Kumanyaka S, Obarzanek E, Stevens V, Hebert P, Whelton P. Weight-loss experience of black and white participants in NHLBI-sponsored clinical trials. Am J Clin Nutr 1991;53(Suppl.): 1631–8S.
-
Kumanyika SK, Hebert PR, Cutler JA, Lasser VI, Sugars CP, Steffen-Batey L, et al. Feasibility and efficacy of sodium reduction in the Trials of Hypertension Prevention, phase I. Trials of Hypertension Prevention Collaborative Research Group. Hypertension 1993;22:502–12.
-
Lang JE, Mercer N, Tran D, Mosca L. Use of a supermarket shelf-labeling program to educate a predominately minority community about foods that promote heart health. J Am Diet Assoc 2000;100:804–9.
-
Langenberg P, Ballesteros M, Feldman R, Damron D, Anliker J, Havas S. Psychosocial factors and intervention-associated changes in those factors as correlates of change in fruit and vegetable consumption in the Maryland WIC 5 A Day Promotion Program. Ann Behav Med 2000;22:307–15.
-
Lee RE, Goldberg JH, Sallis JF, Hickmann SA, Castro CM, Chen AH. A prospective analysis of the relationship between walking and mood in sedentary ethnic minority women. Women Health 2001;32:1–15.
-
Levin-Zamir D, Lipsky D, Goldberg E, Melamed Z. Health education for Ethiopian immigrants in Israel, 1991–92. Isr J Med Sci 1993;29:422–8.
-
Lewis CE, Raczynski JM, Heath GW, Levinson R, Hilyer JC Jr, Cutter GR. Promoting physical activity in low-income African-American communities: the PARR project. Ethn Dis 1993;3:106–18.
-
Lobb R, Gonzalez Suarez E, Fay ME, Gutheil CM, Hunt MK, Fletcher RH, et al. Implementation of a cancer prevention program for working class, multiethnic populations. Prev Med 2004;38:766–76.
-
Long JD, Armstrong ML, Amos E, Shriver B, Roman-Shriver C, Feng D, et al. Pilot using World Wide Web to prevent diabetes in adolescents. Clin Nurs Res 2006;15:67–79.
-
Low A, Grothe K, Wofford T, Bouldin M. Addressing disparities in cardiovascular risk through community-based interventions. Ethn Dis 2007;17:S2–55–9.
-
Macey L, Sternberg A, Muzundar H. The Downstart Program: a hospital-based weight-loss program. Ethn Dis 2005;15(Suppl. 4):S4–58.
-
Magnus MH. What’s your IQ on cross-cultural nutrition counseling? Diabetes Educ 1996;22:57–60.
-
Martin PD, Dutton GR, Brantley PJ. Self-efficacy as a predictor of weight change in African-American women. Obes Res 2004;12:646–51.
-
McKay RB, Levine DM, Bone LR. Community organization in a school health education program to reduce sodium consumption. J Sch Health 1985;55:364–6.
-
McNeill LH, Viswanath K, Bennett GG, Puleo E, Emmons KM. Feasibility of using a web-based nutrition intervention among residents of multiethnic working-class neighborhoods. Prev Chronic Dis 2007;4:A55.
-
Moore SM, Charvat J. Promoting health behavior change using appreciative inquiry: moving from deficit models to affirmation models of care. Fam Community Health 2007;30(Suppl.):S64–74.
-
Motl RW, Dishman RK, Ward DS, Saunders RP, Dowda M, Felton G, et al. Examining social-cognitive determinants of intention and physical activity among black and white adolescent girls using structural equation modeling. Health Psychol 2002;21:459–67.
-
Motl RW, Dishman RK, Ward DS, Saunders RP, Dowda M, Felton G, et al. Comparison of barriers self-efficacy and perceived behavioral control for explaining physical activity across 1 year among adolescent girls. Health Psychol 2005;24:106–11.
-
Murray RP, Connett JE, Skeans MA, Tashkin DP. Menthol cigarettes and health risks in Lung Health Study data. Nicotine Tob Res 2007;9:101–7.
-
Nanney M, Haire-Joshu D, Elliott M, Hessler K, Brownson R. Evaluating changeability to improve fruit and vegetable intake among school aged children. Nutr J 2005;4:34.
-
Nicklas BJ, Dennis KE, Berman DM, Sorkin J, Ryan AS, Goldberg AP. Lifestyle intervention of hypocaloric dieting and walking reduces abdominal obesity and improves coronary heart disease risk factors in obese, postmenopausal, African-American and Caucasian women. J Gerontol A Biol Sci Med Sci 2003;58:181–9.
-
Nine SL, Lakies CL, Jarrett HK, Davis BA. Community-based chronic disease management program for African Americans. Outcomes Manag 2003;7:106–12.
-
Obarzanek E, Sacks F, Vollmer W, Bray G, Miller IE, Lin P, et al. Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) trial. Am J Clin Nutr 2001;74:80–9.
-
Oexmann MJ, Ascanio R, Egan BM. Efficacy of a church-based intervention on cardiovascular risk reduction. Ethn Dis 2001;11:817–22.
-
Paschal AM, Lewis RK, Martin A, Dennis-Shipp D, Simpson DS. Baseline assessment of the health status and health behaviors of African Americans participating in the activities-for-life program: a community-based health intervention program. J Community Health 2004;29:305–18.
-
Patterson RE, Kristal A, Rodabough R, Caan B, Lillington L, Mossavar-Rahmani Y, et al. Changes in food sources of dietary fat in response to an intensive low-fat dietary intervention: early results from the Women’s Health Initiative. J Am Diet Assoc 2003;103:454–60.
-
Perman JA, Young TL, Stines E, Hamon J, Turner LM, Rowe MG. A community-driven obesity prevention and intervention in an elementary school. J Ky Med Assoc 2008;106:104–8.
-
Piane G. A comparison of the effect of a hypertension education program among black and white participants. J Health Care Poor Underserved 1990;1:243–53.
-
Pratt CA, Hurst R, Williams KP, Martin J. Evaluating cardiovascular disease prevention programs in African American communities. J Public Health Manag Pract 1999;5:81–90.
-
Prokhorov A, Kelder S, Shegog R, Murray N, Peters Jr, Agurcia-Parker C, et al. Impact of A Smoking Prevention Interactive Experience (ASPIRE), an interactive, multimedia smoking prevention and cessation curriculum for culturally diverse high school students. Nicotine Tob Res 1477;10:1477–85.
-
Qian J, Wang B, Dawkins N, Gray A, Pace R. Reduction of risk factors for cardiovascular diseases in African Americans with a 12-week nutrition education program. Nutr Res 2007;27:252–7.
-
Rankins J, Sampson W, Brown B, Jenkins-Salley T. Dietary Approaches to Stop Hypertension (DASH) intervention reduces blood pressure among hypertensive African American patients in a neighborhood health care center. J Nutr Educ Behav 2005;37:259–64.
-
Resnicow K, Davis RE, Zhang G, Konkel J, Strecher VJ, Shaikh AR, et al. Tailoring a fruit and vegetable intervention on novel motivational constructs: results of a randomized study. Ann Behav Med 2008;35:159–69.
-
Reusser ME, McCarron DA. Reducing hypertensive cardiovascular disease risk of African Americans with diet: focus on the facts. J Nutr 2006;136:1099–102.
-
Reynolds KD, Franklin FA, Leviton LC, Maloy J, Harrington KF, Yaroch AL, et al. Methods, results, and lessons learned from process evaluation of the high 5 school-based nutrition intervention. Health Educ Behav 2000;27:177–86.
-
Rimmer JH, Braunschweig C, Silverman K, Riley B, Creviston T, Nicola T. Effects of a short-term health promotion intervention for a predominantly African-American group of stroke survivors. Am J Prev Med 2000;18:332–8.
-
Rimmer JH, Nicola T, Riley B, Creviston T. Exercise training for African Americans with disabilities residing in difficult social environments. Am J Prev Med 2002;23:290–5.
-
Robbins LB, Gretebeck KA, Kazanis AS, Pender NJ. Girls on the move program to increase physical activity participation. Nurs Res 2006;55:206–16.
-
Rodriguez JE, Burg JR, Brown LS. Mobile health unit for minority obesity education: local residents’ attitudes and perceptions. J Natl Med Assoc 2006;98:1792–6.
-
Rothert K, Strecher VJ, Doyle LA, Caplan WM, Joyce JS, Jimison HB, et al. Web-based weight management programs in an integrated health care setting: a randomized, controlled trial. Obesity 2006;14:266–72.
-
Rothman R, Malone R, Bryant B, Sequist T. A pharmacist-driven intervention improves diabetes care. J Clin Outcomes Manag 2005;12:188–9.
-
Royce J, Hymowitz N, Corbett K, Hartwell T, Orlandi M. Smoking cessation factors among African Americans and whites. Am J Public Health 1993;83:220–6.
-
Royce JM, Corbett K, Sorensen G, Ockene J. Gender, social pressure, and smoking cessations: the Community Intervention Trial for Smoking Cessation (COMMIT) at baseline. Soc Sci Med 1997;44:359–70.
-
Samuel-Hodge CD, Keyserling TC, France R, Ingram AF, Johnston LF, Pullen Davis L, et al. A church-based diabetes self-management education program for African Americans with type 2 diabetes. Prev Chronic Dis 2006;3:A93.
-
Scisney-Matlock M, Glazewki L, McClerking C, Kachorek L. Development and evaluation of DASH diet tailored messages for hypertension treatment. Appl Nurs Res 2006;19:78–87.
-
Singh R, Dubnov G, Niaz M, Ghosh S, Rastogi S, Manor O, et al. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): a randomised single-blind trial. Lancet 2002;360:1455–61.
-
Skelly AH, Carlson JR, Leeman J, Holditch-Davis D, Soward ACM. Symptom-focused management for African American women with type 2 diabetes: a pilot study. Appl Nurs Res 2005;18:213–20.
-
Skoro-Kondza L, Tai SS, Gadelrab R, Drincevic D, Greenhalgh T. Community based yoga classes for type 2 diabetes: an exploratory randomised controlled trial. BMC Health Serv Res 2009;9:33.
-
Sohn AJ, Hasnain M, Sinacore JM. Impact of exercise (walking) on blood pressure levels in African American adults with newly diagnosed hypertension. Ethn Dis 2007;17:503–7.
-
Sorensen G, Barbeau EM, Stoddard AM, Hunt MK, Goldman R, Smith A, et al. Tools for health: the efficacy of a tailored intervention targeted for construction laborers. Cancer Causes Control 2007;18:51–9.
-
Staffileno BA, Minnick A, Coke LA, Hollenberg SM. Blood pressure responses to lifestyle physical activity among young, hypertension-prone African-American women. J Cardiovasc Nurs 2007;22:107–17.
-
Steinhardt MA, Mamerow MM, Brown SA, Jolly CA. A resilience intervention in African American adults with type 2 diabetes: a pilot study of efficacy. Diabetes Educ 2009;35:274–84.
-
Stephens MB, Wentz SW. Supplemental fitness activities and fitness in urban elementary school classrooms. Fam Med 1998;30:220–3.
-
Stephens Q, Kirby T, Buckworth J, Devor S, Hamlin R. Aerobic exercise improves cardiorespiratory fitness but does not reduce blood pressure in prehypertensive African American women [summary for patients in Ethn Dis 2007;17:176]. Ethn Dis 2007;17:55–8.
-
Stern M, Mazzeo S, Porter J, Gerke C, Bryan D, Laver J. Self-esteem, teasing and quality of life: African American adolescent girls participating in a family-based pediatric overweight intervention. J Clin Psychol Med Settings 2006;13:217–28.
-
Sternberg A, Muzumdar H, Dinkevich E, Quintos J, Austin-Leon G, Owens T, et al. The Downstart Program: a hospital-based pediatric healthy lifestyle program for obese and morbidly obese minority youth. Pediatr Endocrinol Rev 2006;3(Suppl. 4):584–9.
-
Stewart AL, Grossman M, Bera N, Gillis DE, Sperber N, Castrillo M, et al. Multilevel perspectives on diffusing a physical activity promotion program to reach diverse older adults. J Aging Phys Act 2006;14:270–87.
-
Strecher V, Wang C, Derry H, Wildenhaus K, Johnson C. Tailored interventions for multiple risk behaviors. Health Educ Res 2002;17:619–26.
-
Sunseri AJ, Alberti JM, Kent ND, Schoenberger JA, Dolecek TA. Ingredients in nutrition education: family involvement, reading and race. J Sch Health 1984;54:193–6.
-
Tan E, Xue Q, Li T, Carlson M, Fried L. Volunteering: a physical activity intervention for older adults – the Experience Corps program in Baltimore. J Urban Health 2006;83:954–69.
-
Tan EJ, Rebok GW, Yu Q, Frangakis CE, Carlson MC, Wang T, et al. The long-term relationship between high-intensity volunteering and physical activity in older African American women. J Gerontol B Psychol Sci Soc Sci 2009;64:304–11.
-
Tuomilehto J, Lindstrom J. The major diabetes prevention trials. Curr Diab Rep 2003;3:115–22.
-
Tuuri G, Zanovec M, Silverman L, Geaghan J, Solmon M, Holston D, et al. ‘Smart Bodies’ school wellness program increased children’s knowledge of healthy nutrition practices and self-efficacy to consume fruit and vegetables. Appetite 2009;52:445–51.
-
Tyers S. Using the ‘english as a second language’ class as a medium for nutrition education to immigrant groups. J Hum Nutr 1981;35:375–8.
-
Vachon G, Ezike N, Brown-Walker M, Chhay V, Pikelny I, Pendergraft T. Improving access to diabetes care in an inner-city, community-based outpatient health center with a monthly open-access, multistation group visit program. J Natl Med Assoc 1327;99:1327–36.
-
Walter HJ. Primary prevention of chronic disease among children: the school-based ‘Know Your Body’ intervention trials. Health Educ Q 1989;16:201–14.
-
Walter HJ, Wynder EL. The development, implementation, evaluation, and future directions of a chronic disease prevention program for children: the ‘Know Your Body’ studies. Prev Med 1989;18:59–71.
-
Wang Y, Tussing L, Odoms-Young A, Braunschweig C, Flay B, Hedeker D, et al. Obesity prevention in low socioeconomic status urban African-American adolescents: study design and preliminary findings of the HEALTH-KIDS Study. Eur J Clin Nutr 2006;60:92–103.
-
Warnecke RB, Flay BR, Kviz FJ, Gruder CL, Langenberg P, Crittenden KS, et al. Characteristics of participants in a televised smoking cessation intervention. Prev Med 1991;20:389–403.
-
Watkins SA, Hoffman A, Burrows R, Tasker F. Colorectal cancer and cardiac risk reduction using computer-assisted dietary counseling in a low-income minority population. J Natl Med Assoc 1994;86:909–14.
-
Watson K, Jamerson K. Therapeutic lifestyle changes for hypertension and cardiovascular risk reduction. J Clin Hypertens 2003;5(Suppl 1):32–7.
-
Williams AE, Vogt TM, Stevens VJ, Albright CA, Nigg CR, Meenan RT, et al. Work, Weight, and Wellness: the 3W Program: a worksite obesity prevention and intervention trial. Obesity 2007;15(Suppl. 1):16–26S.
-
Wilson DB, Porter JS, Parker G, Kilpatrick J. Anthropometric changes using a walking intervention in African American breast cancer survivors: a pilot study. Prev Chronic Dis 2005;2:A16.
-
Wilson DK, Ampey-Thornhill G. The role of gender and family support on dietary compliance in an African American adolescent hypertension prevention study. Ann Behav Med 2001;23:59–67.
-
Wilson DK, Evans AE, Williams J, Mixon G, Sirard JR, Pate R. A preliminary test of a student-centered intervention on increasing physical activity in underserved adolescents. Ann Behav Med 2005;30:119–24.
-
Wilson DK, Kitzman-Ulrich H, Williams JE, Saunders R, Griffin S, Pate R, et al. An overview of ‘The Active by Choice Today’ (ACT) trial for increasing physical activity. Contemp Clin Trials 2008;29:21–31.
-
Winett RA, Anderson ES, Wojcik JR, Winett SG, Bowden T. Guide to health: nutrition and physical activity outcomes of a group-randomized trial of an internet-based intervention in churches. Ann Behav Med 2007;33:251–61.
-
Winnick JJ, Gaillard T, Schuster DP. Resistance training differentially affects weight loss and glucose metabolism of white and African American patients with type 2 diabetes mellitus. Ethn Dis 2008;18:152–6.
-
Wolf RL, Lepore SJ, Vandergrift JL, Basch CE, Yaroch AL. Tailored telephone education to promote awareness and adoption of fruit and vegetable recommendations among urban and mostly immigrant black men: a randomized controlled trial. Prev Med 2009;48:32–8.
-
Wong WW, Abrams SH, Mikhail C, Terrazas NL, Wilson TA, Arceo D, et al. An innovative summer camp program improves weight and self-esteem in obese children. J Pediatr Gastr Nutr 2009;49:493–7.
-
Zemel M. Dietary pattern and hypertension: the DASH study. Nutr Rev 1997;55:303–5.
-
Ziemer DC, Berkowitz KJ, Panayioto RM, El-Kebbi IM, Musey VC, Anderson LA, et al. A simple meal plan emphasizing healthy food choices is as effective as an exchange-based meal plan for urban African Americans with type 2 diabetes. Diabetes Care 2003;26:1719–24.
Appendix 15 Extraction form for primary studies
| Study reference | Country, setting | Ethnicity | Inclusion criteria | Study type | n, sex, age, education, socioeconomic status | Description of intervention and control | Theory, behavioural construct tailoring | Approach/es to adaptation | Quality |
|---|---|---|---|---|---|---|---|---|---|
| Study reference | Outcome measures | Main results | Author and reviewer conclusions | Comments (limitations, etc.) | Implications and learnings |
|---|---|---|---|---|---|
Appendix 16 Summaries of included systematic reviews of adapted interventions
| Study reference | |
|---|---|
| Whitt-Glover and Kumanyika 2009276 | |
| Title | |
| Systematic review of interventions to increase physical activity and physical fitness in African-Americans | |
| Aim of/objectives of/questions addressed in the review | |
| To identify characteristics of effective interventions designed to increase physical activity or fitness among African Americans | |
| Number of studies included in the review | |
| Twenty-nine studies with African American adults | |
| Fourteen studies with African American children | |
| Design of included studies | |
| Controlled trials and RCTs | |
| Interventions included | |
| Physical activity and fitness | |
| Settings included | |
|
For adults: churches and other community locations such as YMCAs, community centres or public housing projects chosen for convenience for African Americans; health-care settings – primary care, hospitals and medical centres For children: schools, community centres, churches, summer camps, internet programmes, neighbourhood clinics, medical centres, etc. |
|
| Population included | Date |
| African American | 1985–2006 |
| Key findings | |
| This systematic review focused on increasing physical activity among African American adults and children. In total, 40 of the 43 studies indicated some degree of cultural adaptation. There is evidence that physical activity and dietary interventions which include educational components, including written materials; involving group sessions; and utilising behaviour change theory are successful in improving physical activity and dietary outcomes. The most minimal degree of adaptation was a deliberate recruitment of an African American-only study population. Other adaptations included the use of specific music, e.g. African music, gospel; dancing, e.g. hip-hop, ‘afrobics’; direct attempts to change ideas and attitudes about exercise among African American participants; consideration of cultural, social, historical, environmental and psychological factors that had been found to influence physical activity among African Americans. Intervention settings were also an important part of cultural adaptation, e.g. utilising churches. Some studies conducted focus groups and discussions before tailoring the interventions to suit the specific populations included in the study | |
| Although these studies were adapted, it is unclear how cultural adaptations affected intervention results. Only three studies evaluated the effect of utilising a culturally tailored programme compared with the same programme with no or fewer adaptations. The results from these studies indicted that none of the studies showed statistically significant differences between culturally adapted or unadapted interventions | |
| Conclusions | |
| The findings of this review suggest that explicit cultural adaptations do not necessarily result in better physical activity outcomes. The review identifies factors that could have influenced the intervention findings, including the use of the randomised controlled design, implementation of structured exercise programmes and the measures used to assess physical activity. The influence of these factors on the findings, including the influence of culturally adapted strategies, is unclear and requires further research | |
| Comments | |
| The limited number of studies with long-term follow-up suggests that, although various physical activity interventions might increase activity levels in short-term controlled circumstances, there is no evidence that these changes are sustainable. Further high-quality studies of adapted interventions are required to assess if adaptation results in significantly better outcomes | |
| Study reference | |
|---|---|
| Hawthorne et al. 2008278 | |
| Title | |
| Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups | |
| Aim of/objectives of/questions addressed in the review | |
| To assess the effects of culturally appropriate health education interventions for people with type 2 diabetes mellitus in ethnic minority groups | |
| Number of studies included in the review | |
| There were 11 studies in this review, all of which focused on culturally appropriate health interventions for individuals with type 2 diabetes mellitus | |
| Design of included studies | |
| RCTs | |
| Interventions included | |
| Culturally adapted type 2 diabetes mellitus health education interventions | |
| Settings included | |
| Most studies were set in deprived areas, either in rural or in inner city urban settings | |
| Population included | Date |
| Individuals of ethnic minority communities with type 2 diabetes mellitus of any duration of diagnosis, with or without complications of diabetes. With regard to the populations of interest to this review, there were four studies with African American-origin populations and three with South Asian-origin populations | Until August 2007 |
| Key findings | |
| This review considered the effects of culturally appropriate health education interventions for ethnic minority populations with type 2 diabetes mellitus. Of the three primary outcome measures, blood pressure and quality of life measures showed no significant improvements, whereas glycaemic control [as measured by HbA1c (glycated haemoglobin) levels] showed improvement at 3 and 6 months; however, there was no effect at 12 months post intervention | |
| Of the secondary measures, knowledge scores improved significantly at 3, 6 and 12 months post intervention but there was no change in total cholesterol levels, high-density lipoprotein or low-density lipoprotein between the intervention and control groups at 3 and 6 months post intervention | |
| Conclusions | |
| There is a lack of high-quality data on the effectiveness of culturally appropriate diabetic health education programmes for ethnic minority groups, and the data that do exist are difficult to standardise and compare in a formal meta-analysis. However, it does appear that this type of intervention is effective in improving glycaemic control and knowledge about diabetes in the short to mid-term. There is a need for long-term, well-designed multicentre RCTs that examine a range of different types of health education intervention involving different combinations of educators, link workers or advocates in a number of differing ethnic minority groups | |
| Comments | |
| Of the 11 studies included in the review, four included African American populations and three South Asian populations. This review suggests that culturally adapted interventions may be successful among these ethnic minority populations; however, the outcomes measured in each study varied and this made assimilation of results difficult. The authors recommend that culturally appropriate interventions should be the ‘gold standard’ for health education programmes for ethnic minority populations. The strategies used for cultural adaptations ranged from tailoring education material based on levels of knowledge in the target population to using recognised theoretical models, and having suitable individuals deliver health education interventions using appropriate language when necessary | |
| Study reference | |
|---|---|
| Hudson 2008277 | |
| Title | |
| An integrative review of obesity prevention in African American children | |
| Aim of/objectives of/questions addressed in the review | |
| To examine attitudes and perceptions of African American children and parents, and lifestyle behaviours in African American children aged from 2 to 18 years | |
| Number of studies included in the review | |
| A total of 28 studies were included, of which six were experimental RCTs, 14 were cross-sectional, two were longitudinal, five were qualitative and one was mixed | |
| Design of included studies | |
| Qualitative and quantitative studies were included | |
| Interventions included | |
| Obesity prevention interventions, including nutrition and physical activity | |
| Settings included | |
| Any | |
| Population included | Date |
| African American | 1997–2007 |
| Key findings | |
| Although the review mentions culturally appropriate methods used in various studies there is not much detail in relation to qualitative and non-experimental studies. Almost all of the six RCTs were culturally adapted and included the use of dance; involved families in interventions; modified diet; used culturally appropriate newsletters, lectures and comic books; and ran day camps as well as culturally appropriate family interventions, etc. The findings of the planet health study were interesting as they demonstrated a large effect in African American females (compared with control subjects) on reducing obesity prevalence (OR 0.14, 95% CI 0.04 to 0.48), although this study did not have ethnically targeted content | |
| Conclusions | |
| The existing research on obesity prevention that targets African American children and adolescents is limited. Most studies were pilot studies and had insufficient power because of their small sample size and short-term intervention and follow-up. The author states that, although the findings of preliminary RCTs appear to be promising, the final results are still pending | |
| Comments | |
| Although the results of this review highlight the importance of the attitudes and perceptions of the African American population for successfully adapting interventions, more research is needed because of the limited number of RCTs reporting interventions for obesity prevention among African American children and adolescents | |
| Study reference | |
|---|---|
| Webb 2008246 | |
| Title | |
| Treating tobacco dependence among African Americans: a meta-analytic review | |
| Aim of/objectives of/questions addressed in the review | |
| To evaluate the overall efficacy of smoking cessation interventions among African American adults and to examine specific study characteristics and methods that influence treatment outcome | |
| Number of studies included in the review | |
| A total of 20 published and unpublished studies evaluating the efficacy of smoking cessation interventions among African Americans | |
| Design of included studies | |
| RCTs | |
| Interventions included | |
| Smoking cessation | |
| Settings included | |
| Any – ranging from clinics to churches, community locations, inpatient hospitals, mail, telephone, etc. | |
| Population included | Date |
| African American | 984–2006 |
| Key findings | |
| Studies conducted in a clinic setting by a paraprofessional yielded a treatment effect of OR 1.48 (95% CI 1.09 to 2.01) at post test whereas the effect for studies conducted in a church context was of a slightly larger magnitude: OR 1.69 (95% CI 1.08 to 2.65). However, a contrast analysis indicated that this difference was not statistically significant (contrast 1.23, 95% CI 0.73 to 3.19, z = 0.76, p = 0.22). The treatment effect for studies testing a culturally specific intervention was OR 1.47 (95% CI 1.12 to 1.91) at the post-treatment assessment. The effect of standard interventions was OR 1.34 (95% CI 0.99 to 1.82). At follow-up the effect for standard interventions was significant (OR 1.35, 95% CI 1.02 to 1.78); however, the effect for culturally specific interventions was not | |
| Conclusions | |
| The findings suggest that a positive relationship exists between smoking cessation interventions and abstinence among African American adults. Results support the overall efficacy of smoking cessation treatment targeting African Americans. The clinical benefit is meaningful in both the short and the longer term. The odds of short-term smoking cessation varied according to seven of the 11 moderators investigated (treatment type, setting, control group, cultural specificity, unit of analysis, outcome measure and biochemical verification). In the longer term, these variables did not differentially affect treatment effects. Optimal treatment conditions include paraprofessional contact and behavioural counselling conducted in either a clinic or a church setting. Treatment effects were also maximised compared with attention placebos or minimal contact controls, and when defined as 7-day PPA or abstinence at the time of assessment. The odds of abstinence were also greatest when evaluated from both the community and individual levels, and when biochemically verified | |
| Comments | |
| Homogeneity tests were not significant and variability in effect size was attributed to sampling errors. The primary treatment modalities included nicotine replacement, bupropion, individual counselling, group counselling, counsellor telephone calls, targeted or tailored print materials, community outreach, video and radio media or a combination of these formats. The ORs for culturally specific interventions do not seem to be much different from those of the standard interventions, although they seemed to have some advantage in the short term | |
| Study reference | |
|---|---|
| Chen and Tang 2007275 | |
| Title | |
| Review of smoking cessation research among Asian Americans: the state of the research | |
| Aim of/objectives of/questions addressed in the review | |
| To provide an analytical review of population-based efforts to measure smoking prevalence levels among Asian Americans and peer-reviewed smoking cessation research targeting Asian Americans | |
| Number of studies included in the review | |
| Four studies were included; however, the authors supplemented the review by compiling an example of resources available for population-level tobacco survey data for Asian Americans in California | |
| Design of included studies | |
| Two quasi-experimental, one experimental and one non-experimental | |
| Interventions included | |
| Smoking cessation | |
| Settings included | |
| Any | |
| Population included | Date |
| Asian American | 1986–2005 |
| Key findings | |
|
This review focuses on smoking cessation interventions among Asian Americans. All four studies were culturally adapted. Two studies were large-scale interventions conducted among Vietnamese, using similar culturally adapted interventions, one resulting in a positive finding and the other showing no effect. Of the other studies included, individuals in the intervention groups had better cessation rates, quit rates and abstinence rates. p-values were reported only for one study, which showed that intervention subjects engaged in more quit attempts (p = 0.0001) and smoking cessation rates of 17% in the intervention group vs 1% in the control group The cultural adaptations implemented in these interventions were in language- and culturally specific print media, billboard postings, television programmes, counselling, health education materials, etc. |
|
| Conclusions | |
| There is very limited documented evidence of smoking cessation interventions for Asian American-origin populations. The interventions identified suggest that scientifically valid, culturally tailored and language-specific interventions are both potentially and practically effective in reducing tobacco usage among ethnically specific Asian American populations. There is a need for additional research on the effectiveness of these interventions. In addition, care must be taken not to generalise these findings to different Asian populations | |
| Comments | |
| Although this review focused on Asian Americans the majority of the included population was Vietnamese | |
| Study reference | |
|---|---|
| Shaya et al. 2006279 | |
| Title | |
| Addressing cardiovascular disparities through community interventions | |
| Aim of/objectives of/questions addressed in the review | |
| To identify the components and impact of intervention programmes aimed at reducing cardiovascular disparities | |
| Number of studies included in the review | |
| A total of 10 studies were included and all of them focused on cardiovascular disparities among African Americans | |
| Design of included studies | |
| Not reported; however, studies appear to be a mix of RCTs and quasi-experimental studies | |
| Interventions included | |
| CVD | |
| Settings included | |
| Any | |
| Population included | Date |
| African American | 1966–2004 |
| Key findings | |
|
This systematic review was a descriptive review of interventions to reduce CVD among African Americans. All of the included studies showed positive results and the interventions were either culturally tailored or individually tailored. The strategies that were used for cultural tailoring included the location of the intervention – church-based interventions, barber shops, beauty salons, etc. – and liaising with the community and training lay individuals from the community to deliver health programmes. One study used the Healthier People Health Risk Appraisal (HPHRA) as a culturally appropriate recruitment strategy Among the studies included only one had a comparison group to evaluate the effectiveness of cultural tailoring and this showed positive effects of cultural tailoring The studies that used culturally adapted interventions found significant improvements in BMI, waist circumference, dietary fat, exercise, blood pressure, etc. |
|
| Conclusions | |
| The review concluded that these programmes are short term and their impact is short-lived. This highlights the need for sustainable programmes possibly implemented through community partnerships | |
| Comments | |
| The review focuses on CVD among African Americans; the findings are positive when the intervention is culturally tailored. It appears that the intervention setting and community involvement are important aspects of cultural tailoring | |
| Study reference | |
|---|---|
| Banks-Wallace and Conn 2002245 | |
| Title | |
| Interventions to promote physical activity among African American women | |
| Aim of/objectives of/questions addressed in the review | |
| To review interventions designed to promote physical activity among African American women | |
| Number of studies included in the review | |
| There were 18 studies included in the review, all of which focused on increasing physical activity among African Americans | |
| Design of included studies | |
| Clinical trials – seven RCTs and eight pre–post designs and three studies that compared various experimental groups with each other | |
| Interventions included | |
| Physical activity | |
| Settings included | |
| Any – three neighbourhood recreation centres, three churches and clinics or hospitals | |
| Population included | Date |
| Originally intended to focus only on African American women but because of the paucity of research the authors decided to include studies in which African American women comprised at least 35% of the sample (range 41–98%) | 1984–2000 |
| Key findings | |
| This study focused on increasing physical activity among African American women. Of the 18 studies, 12 were culturally adapted and nine of these 12 studies reported positive findings with regard to physical activity, weight loss or BMI. Although the results were descriptive, the findings suggest that African American women increase their physical activity in response to culturally adapted interventions; however, the sustainability is questionable | |
| Conclusions | |
| Although the number of studies designed to promote activity among African American women is growing, the study designs and measurement limitations combined with inadequate replication of intervention components prevent the existing evidence from forming a solid base for practice. Further research is needed to illuminate which components are critical for efficacious interventions among this population | |
| Comments | |
| This review addresses interventions to promote physical activity among African American women. The findings of the review suggest that culturally relevant strategies are effective for promoting physical activity and dietary changes in this population. The strategies for cultural adaptation focused heavily on factors related to the delivery of interventions, recruitment and choice of location, whereas minimal attention was devoted to ensure the cultural relevance of retention strategies, data collection instruments and methods of evaluation | |
Appendix 17 Quality assessment of included systematic reviews of adapted interventions (Critical Appraisal Skills Programme)
| Study | Clearly focused question? | Right type of study? | Tried to identify all relevant studies? | Assessed quality of studies? | Are results combined and, if so, was it reasonable? | How are the results presented (OR/RR, etc.) and what is the main result? | How precise are the results? (CIs, p-values) | Can the results be applied to the local population? | Were all important outcomes considered? | Should policy change as a result of the evidence? |
|---|---|---|---|---|---|---|---|---|---|---|
| Whitt-Glover and Kumanyika 2009276 | Yes | Yes | Unclear | Yes | Not combined | Narrative (see Table 11) | N/R | Results are relevant to our study populations | Yes | Not enough evidence |
| Hawthorne et al. 2008278 | Yes | Yes | Yes | Yes | Yes | Weighted mean difference (see Table 11) | 95% CIs and p-values reported and some significant results | Yes, UK-relevant ethnic minority groups and others relevant to study | Yes | Yes – recommends cultural adaptation as a good standard for ethnic minority groups |
| Hudson 2008277 | Yes | Yes | Unclear | Unclear | Not combined | Narrative (see Table 11) | N/R | Results are relevant to our study populations | Yes | Not enough evidence |
| Webb 2008246 | Yes | Yes | Yes | Yes | Yes | OR (see Table 11) | 95% CIs reported and some significant results | Results are relevant to our study populations | Yes | Not enough evidence |
| Chen and Tang 2007275 | Yes | Yes | Unclear | Unclear | Not combined | Narrative (see Table 11) | N/R | Results are relevant to our study populations | Yes | Not enough evidence |
| Shaya et al. 2006279 | Yes | Yes | Unclear | Unclear | Not combined | Narrative (see Table 11) | N/R | Results are relevant to our study populations | Yes | Not enough evidence |
| Banks-Wallace and Conn 2002245 | Yes | Yes | Unclear | Unclear | Not combined | Narrative (see Table 11) | N/R | Results are relevant to our study populations | Yes | Not enough evidence |
Appendix 18 One-page summaries of the 107 included empirical studies
Adapted smoking cessation interventions
| Study reference |
|---|
| Li et al. 1984357 |
| Setting |
| USA; Baltimore City Health Department Family Planning Services |
| Inclusion criteria |
| Women smokers invited to participate. Women completed a baseline questionnaire and confirmed if the film had been viewed or physician message received (depending on condition) |
| Study type |
| RCT (however, treatment groups were formed post intervention) |
| Description of population |
|
Ethnicity: 91% black; not reported how ethnicity assessed Age (years): Mean: 22.24 ± 5.56 n: 1179 Sex: 100% female Income: Not reported Other: On average smoked 10.23 ± 7.36 cigarettes per day |
| Description of intervention and control |
|
Smoking cessation intervention comparing four conditions: (1) baseline questionnaire, (2) baseline questionnaire + media programme, (3) baseline questionnaire + physician message and (4) baseline questionnaire + media programme + physician message Baseline questionnaire: Targeted heightened awareness and could have also had a motivational function; 9th- to 11th-grade reading level Media programme: Delivered without interference with clinic activities. A movie called The Feminine Mistake was played continuously in the clinic waiting room. A physician message was also delivered, which was brief, was easy to deliver and required minimal training. Physician made individual risk assessment and, using a protocol, gave advice to stop smoking. Message took 3–5 minutes to deliver, provided information about the health hazards of smoking and elicited a commitment to take steps towards quitting (think about quitting, set a target date, enlist help of family and friends and throw away all cigarettes) |
| Theory: Both media programme and physician message based on social learning principles of behaviour change |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: 3- and 12-month follow-up Quit rates: Self-reported cessation rates in the two physician message conditions were three times greater than those in conditions 1 and 2 after adjusting for loss to follow-up and cotinine readings (cessation rates were 3.1, 4.8, 9.9 and 9.9 for conditions 1, 2, 3 and 4, respectively). Cotinine-verified cessation rates were 0.09%, 2.4%, 3.7% and 2.1% for conditions 1, 2, 3 and 4, respectively. A total of 12.9% of women who received the physician message reported to have stopped smoking at 3 months, compared with 6.4% in the control conditions |
| Conclusions |
|
Authors: A message from a physician or nurse-midwife about quitting and instruction on how to quit produced cessation rates two to three times higher than spontaneous quit rates. The media programme alone had a clinically but not statistically significant impact. After adjusting for confounding, the two conditions with a physician message had significant effects. Although the quit rates are conservative, participants’ success in quitting is not attributable to a desire to seek help to quit as they were recruited and entered into the study incidentally at a family planning clinic. This study also showed that self-reported behaviour may overestimate treatment effects; future studies need to incorporate biological validation. Physician anti-smoking messages warrant further investigation Reviewers: This intervention showed greater effectiveness for the physician message than for the other conditions. This suggests that this is an area for potential development |
| Comments and limitations |
| Forty-four per cent of those reporting to be non-smokers and 24% of those reporting to be still smokers refused to provide saliva samples for validation. The authors did not explore the reasons why people did not want to provide saliva samples |
| Study reference |
|---|
| Jason et al. 1988404 |
| Setting |
| USA; West Garfield area, Chicago, IL |
| Inclusion criteria |
| Smoker; resident in West Garfield area, Chicago |
| Study type |
| RCT |
| Description of population |
|
Ethnicity: 96% black in experimental group; 91% black in control group; not reported how ethnicity assessed Age (years): Mean: experimental group: 41.8; control group: 43.2 n: 218 interested, pre- and post-intervention data available for 78 experimental and 87 control participants Sex: 55% female Income: Not reported |
| Description of intervention and control |
|
Experimental group: Television smoking cessation programme broadcast for 20 days on the mid-day and 9 pm news; distribution of self-help manuals, weekly support meetings and supportive telephone calls. Television programme consisted of 2- to 4-minute broadcasts. Programme was discussed on weekend newscasts. Manuals entitled Freedom from Smoking in 20 Days were mailed out. Supportive telephone calls were made urging individuals to follow the manual and the television programme and to come to support groups. Calls lasted from 30 seconds to 15 minutes. The self-help group was co-led by a community member and psychology graduate and was designed to provide social support and to encourage use of the manual and the television programme. Group meetings were held at a neighbourhood health centre three times during the 20-day programme Control group: Television smoking cessation programme only. Could pick up a manual or request it but were not alerted to the manual by the project staff; 100,000 manuals were distributed free to requesters in True Value Hardware stores |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: Immediately following the end of the televised intervention and at 4 months Quit rates: 4 months: 20% of experimental participants were abstinent compared with 9% of control participants (p < 0.06) Number of cigarettes smoked per day: Of those who were still smoking, the experimental participants smoked significantly fewer cigarettes post test than the control participants (mean 10.83 vs 14.43, p < 0.01), and directionally fewer cigarettes at follow-up (mean 12.45 vs 14.57) [F(1,116) = 41.18] |
| Conclusions |
|
Authors: An intensive outreach effort in combination with a large-scale media-based smoking cessation intervention was successful in achieving abstinence rates of 8% at post intervention and 20% at 4 months’ follow-up. Without the outreach intervention, only 1% of control participants quit by post intervention and 9% by the follow-up. Intensive supplementary opportunities enhanced the participation of low-income smokers in a media smoking programme. Many of the residents of these neighbourhoods will not actively participate in such programmes unless active outreach efforts are initiated, and, when they are, they can increase the chances of successful quitting Reviewers: The intervention was successful; however, it did not feature many culturally tailored components except for the black news reporter. The authors did acknowledge that they used a television programme because it was a preferred format for the low-income African American population. We agree with the authors that it is difficult to determine exactly what accounted for the quit rate in the control group, who received minimal contact, did not receive a manual and watched fewer programmes. However, it would appear that active outreach is required to increase rates of quitting |
| Comments and limitations |
| Not all residents had telephones so the sample might not have been representative. High attrition and differences in pre-intervention motivation levels may explain the difference in cessation rates; however, it could be due to social desirability given the greater contact that experimental participants had with the investigators. There was no biochemical confirmation of the results. About half of the smokers contacted were not willing to talk about the project, as the authors hypothesised, because telephone interviewers were identified as not black. The authors suggested that residents were cautious about talking to strangers on the telephone because their neighbourhood is frequently visited by outsiders (e.g. social workers, police) who are often viewed with suspicion by the community |
| Study reference |
|---|
| Lacey et al. 1991453 |
| Setting |
| USA; Chicago, IL, four low-income housing developments |
| Inclusion criteria |
| Black women aged 18–39 years living in four Chicago Housing Authority low-income public housing projects |
| Study type |
| Pre–post |
| Description of population |
|
Ethnicity: Black; not reported how ethnicity assessed Age (years): Range 18–39, but older people were allowed to participate n: 235 Sex: Classes: women 46, men 15 (61 registered, but only 56 completed by attending at least one class – five men did not attend); visitations: women 117, men 57 Income: Not reported |
| Description of intervention and control |
| Intervention was part of a large 20-week televised smoking cessation programme conducted in Chicago from 1986 to 1989. Interested viewers were asked to register and a manual was provided. The supplemental intervention’s key objective was to establish interpersonal contact with the target population using women from the community employed as lay health educators to liaise with community organisations and disseminate information about the times of televised segments and the location of supplemental intervention classes. Residents were recruited door to door and encouraged to register. Two intervention strategies were devised: a reminder visitation programme and smoking cessation classes. Reminder visitations were carried out in all four housing developments and classes in three of them. The visitation programme consisted of weekly visits during the course of the television series (over 20 weeks). Reminder cards were left with participants to watch the television programme. The six smoking cessation classes were based on a curriculum that followed the television programme but with population-specific content |
| Theory: Theoretical support for the use of community members as lay health educators came from innovation diffusion theory and was most fully developed in the health communication–behaviour change model. The basic tenet is that the effectiveness of health institutions as change agents can be enhanced when their message is communicated by influential local members of the target group |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: Pre and post intervention (time frame not clear) Quit rates: Of 56 participants in smoking cessation classes, three quit by the end of the intervention. Of 174 allocated for visitation, 85 participated. None of the women in the reminder group quit smoking immediately after the intervention |
| Conclusions |
|
Authors: The intervention was successful at a community level as indicated by the active involvement and acceptance of the programme by community organisations, groups and prominent individuals; the recruiting of lay health educators; effective dissemination of the programme; and integration of the programme into existing health promotion activities within nurse-run Health Promotion Centres of housing developments in target communities. This approach can be replicated in communities with similar characteristics. At an individual level results were less conclusive or clear-cut. The quit rate was small. Baseline data indicated this population was not motivated to quit Reviewers: We appreciate the fact that the authors have commented on community and individual successes separately. Having someone personally solicit you to attend a class is much more personal, especially if you can relate to them. It appears that one of the main problems, as described by the authors, is that the population was, in fact, not motivated to quit smoking in light of their competing interests and the fact that smoking is regarded quite positively within their community |
| Comments and limitations |
| Central to lay health workers’ ability to perform this bridging function is their position as local experts on a relevant topic in naturally occurring social networks. In this position, a locally influential individual is able to facilitate learning and to influence community residents to accept changes. Importantly, focus groups found that smoking is not perceived as a major health threat for this population; rather, smoking had a positive value as it is associated with positive life experiences in general life. The results of this study suggest that in this type of community the lay health educator may be well suited for active, close community contact that can eventually address the motivation issues. Social influences are barriers to smoking cessation, e.g. targeted marketing, etc. |
| Study reference |
|---|
| Ahijevych and Wewers 1995454 |
| Setting |
| USA; Ohio, urban |
| Inclusion criteria |
| African American women, cigarette smokers |
| Study type |
| RCT |
| Description of population |
|
Ethnicity: African origin; not reported how ethnicity assessed Age (years): Mean: 39 n: 64 Sex: 100% women Income: 48% income < US$20,000 Other: 52% high school education |
| Description of intervention and control |
| The intervention group (n = 21) received weekly mailings (four in total) of printed smoking cessation materials (including Quit for Life, Freedom from Smoking for You and Your Family and Don’t Let Your Dreams Go up in Smoke). A lay African American facilitator and ex-smoker also contacted participants to clarify information and provide them with encouragement (four calls over the 4-week period). There were two control groups: in one participants (n = 22) received ‘one-time’ advice only in which a nurse investigator advised individuals to make an effort to stop smoking in the next 6 weeks and in the other participants (n = 21) were informed that further information would be collected in 6 weeks time |
| Theory: The authors do not specifically discuss theory but do say that homogeneity in economic, cultural and social characteristics between client and provider has been identified as important in increasing the success of quit smoking programmes and this influenced the approach they undertook |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: Baseline to 6 weeks and 12 weeks Number of cigarettes smoked per day: The intervention group reported a decrease in the average number of cigarettes smoked per day (13.6, 11.4 and 9.9 at baseline and 6 and 12 weeks, respectively) that neared significance (p = 0.08) |
| Conclusions |
|
Authors: The authors felt that the intervention had some success. Although there were non-significant trends in the average number of cigarettes smoked in the intervention and advice groups, and in mean cotinine levels in all three groups, it was the participation in the research that may have increased smoking awareness in everyone. These women were in the early stages of change and slight shifts in behaviour accompanied by setting a quit date in the next 3 months showed some success Reviewers: It is difficult to judge the success of this intervention. There were no significant differences demonstrated but there was positive qualitative feedback on the intervention content and delivery on the exit interview. The lay facilitator was thought to be helpful and more input would have been favourable. The materials were deemed suitable and people looked forward to the programme materials being delivered. Perhaps a more intensive delivery of this type of intervention would have proven successful |
| Comments and limitations |
| As commented on by the authors, the group may not have been at the readiness to quit stage: 56% were very interested in quitting at the baseline assessment whereas the rest were somewhat or not interested The lay facilitator was not always able to contact participants and only 13 received the weekly telephone call, only two received two telephone calls and five were not reached at all during the intervention (there were no notes written by the lay facilitator about the other intervention participant). There was a 9% attrition rate from baseline to final data collection, with the intervention group dropping from 21 to 16, the advice only group dropping from 22 to 21 and the control group dropping from 21 to 20 |
| Study reference |
|---|
| Royce et al. 1995333 (Harlem Health Connection Project) |
| Setting |
| USA; Harlem, NY; Sydenham health provider |
| Inclusion criteria |
| Patient’s eligibility assessed from recruitment card: currently smoking cigarettes, aged > 18 years, African American self-identification. Approached patient to request an on-the-spot interview |
| Study type |
| Pre–post |
| Description of population |
|
Ethnicity: African American (sample predominantly African American, 91.4%); self-identification Age (years): Median: 37 n: 153 Sex: 63% women Income: Not reported |
| Description of intervention and control |
|
Aimed to increase smoking cessation rates, quit attempts and cutting down among low-income African Americans using brief clinician advice and socioculturally appropriate self-help cessation/relapse prevention materials Intervention: Smokers received a personal copy of a project-designed self-help smoking cessation video and companion manual (Kick It! Stop Smoking Guide) as well as newsletters with smoking cessation/relapse prevention tips and monthly mailings inviting participation in stop smoking contests. The stop smoking contest format was used to send monthly ‘booster reminders’ and award prizes to winners of quit date raffles. There were ‘Quit and Win’ contests for study participants who remained smoke-free for 30 days, which was carbon monoxide validated. Participants received a distinctive bag with the project logo and a ‘quit kit’ (containing stress tips, sugarless gum and American Cancer Society headless matches). Participants were instructed to turn in their tracking sheet after their appointment. They were reminded of the exit interview and given associated incentives – 10-pack of transit tokens or a money order for US$12.50 |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: Baseline interview and 7 months (actual ranges from 6–8 months) Quit rates: Intervention group reported 21% cessation rate at follow-up Quit attempts: 66% made at least one quit attempt Number of cigarettes smoked per day: 27% decreased the number of cigarettes smoked per day |
| Conclusions |
|
Authors: This study found that appropriate smoking cessation/relapse prevention materials and approaches effectively reached low-income African American women and men. Smokers reported a 21% abstinence rate at 7–8 months post intervention. Designating a quit date with clinician or interviewer encouragement at baseline and being employed played a significant role in cessation. For the additional 27% of smokers who decreased cigarette intake by at least 50% there was evidence that physician advice and materials had an impact. Clinician smoking advice for every patient is said to be warranted Reviewers: This study was able to show an effect on smoking cessation and a decrease in cigarette intake by 50% in those who did not quit. This is the predecessor to the Resnicow et al. 401 RCT by the same name, which showed no effect. However, in that intervention, physician advice was not included in the trial (booster call instead) |
| Comments and limitations |
| Incentives for completing recruitment card included a US$250 cash draw and access to a freephone Harlem Health Connection telephone number that offered information about Harlem health and social service organisations. Limitations include the pre–post design without comparison group and the fact that smoking status was not biochemically validated. The sample, although not a probability sample, is representative of the population of Harlem but has limited transferability to other dissimilar populations. Accuracy of patient reports of clinician advice vs clinician reports of giving advice is unknown |
| Study reference |
|---|
| Stillman et al. 1993;301 Voorhees et al. 1996300 (Heart, Body and Soul Programme) |
| Setting |
| USA; East Baltimore, MD |
| Inclusion criteria |
| African American churchgoers from 22 churches attending baseline health fair |
|
Study type: Cluster RCT |
| Description of population |
|
Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean: intensive 46 (standard deviation 11.5), minimal 47 (standard deviation 13.5) n: 22 churches randomly assigned, one dropped out (11 intensive culturally specific intervention; 10 minimal self-help intervention), n = 350 (n = 199 intensive, n = 93 minimal, n = 48 lost to follow-up); n = 802 in community reference population survey Sex: Intensive 68.9% female, minimal 75.3% female Income: Not reported Other: Baptist church most common denomination (intensive 78% Baptist, minimal 74% Baptist) |
| Description of intervention and control |
|
Intensive culturally specific intervention compared with a minimal self-help intervention for smoking cessation Intensive: Between one and four pastoral sermons given on smoking, had testimony during church services from individuals going through the quit process, training of volunteers as lay smoking cessation counsellors, access to individual or group support supplemented with spiritual audiotapes containing gospel music, and baseline and follow-up health fairs. Evaluation of cardiovascular risk status including feedback about exhaled carbon monoxide levels, cholesterol levels, blood pressure and degree of overweight. Intervention contained elements for individuals in all stages of change and individuals were given tailored quit pamphlets through the churches Minimal: Participants received identical baseline health fair with the same feedback about health status and were given tailored quit pamphlets through the churches |
| Theory: Stages of change (Prochaska and DiClemente455) and social learning theory and a community wide social action model (described in Stillman et al.301 only) |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: Baseline and 1 year Quit rates: (Self-reported, quitters’ saliva cotinine and carbon monoxide validated, smoke free = carbon monoxide < 6 ppm and cotinine < 20 ng/ml). Between groups the quit rates were not significantly different (p = 0.32). Both intensive (27.13%, χ2 = 1322, p < 0.0001) and minimal (21.50%, χ2 = 63.29, p < 0.0001) differed significantly from secular trends among churchgoers in the community reference population (2.87%), assessed through a cross-sectional random digit dialling telephone survey |
| Conclusions |
|
Authors: This study provides evidence that the intensive intervention was more effective in producing positive progress when controlling for demographic and baseline smoking variables. An additional positive effect was seen for Baptist churches receiving the intensive intervention. The intervention was not stage targeted but included elements for participants at every stage. Although quit rates are not statistically significantly different between the two conditions, they are clinically significant. Strong social norms and sanctions against smoking in Baptist religious organisations may explain why an intensive spiritually oriented intervention was more effective in this group Reviewers: This study did not show a statistically significant difference between groups for smoking cessation. Smoking cessation rates for both groups were significantly increased compared with a community survey population. A church social support system may have contributed to similar cessation rates in both conditions |
| Comments and limitations |
| Up to 1 year of follow-up, all smokers in both churches were offered the opportunity to obtain a small gift at the follow-up health fair. Method of recruitment more likely to yield a greater number of pre-contemplators (community recruitment strategies). No study limitations offered by authors. Low attrition rate possibly due to strong social networks in the church and ability to track study participants through friends |
| Study reference |
|---|
| Resnicow et al. 1997;400 Resnicow et al. 1997401 (Harlem Health Connection Project – Kick It!) |
| Setting |
| USA; Manhattan Island, Central Harlem, NY; sites selected from three institutional settings (channels) within the Harlem community: six health-care facilities, four large public housing developments and 16 churches |
| Inclusion criteria |
| Sites serving a predominantly (> 80%) low-income African American population considered. Before recruiting individuals, sites were randomly assigned to either treatment or comparison. Inclusion criteria were African American, aged ≥ 18 years, self-reported smokers, provided address or telephone number within five boroughs of New York City and completed an information card during the recruitment period. Participants were later contacted by telephone or through a personal visit and asked to complete a home interview |
| Study type |
| Cluster randomisation |
| Description of population |
|
Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean: intervention 44, comparison 46.4 (range 20–94) n: 9311 recruited, ~3000 African American smokers; 1244 (703 intervention and 541 control) completed home interview and were included in the study, follow-up interviews obtained for 1154 (93%) Sex: Intervention: 58% female, comparison: 65% female Income: Not reported |
| Description of intervention and control |
|
Culturally sensitive, low-intensity smoking cessation intervention for low SES African Americans Intervention: Multicomponent with self-help cessation kit including cessation guide, companion video and several quit aids. The 6-month intervention phase included bimonthly mailings related to smoking and other health concerns. Participants were scheduled to receive one booster call. The cessation guide, a self-help booklet written at fifth-grade level, was entitled Kick It! The Kick It! video comprised two parts: (1) ‘A Message from the Ancestors’ – a fictional story about two Harlem smokers who, in a dream sequence, are summoned by a tribunal of figures from black history, (2) a well-known local internist and media personality providing instruction (and modelling) on how to quit, how to maintain quit status and how to start over for relapsers Control: Health education materials not directly addressing tobacco use but, instead, substance use, HIV/AIDS (human immunodeficiency virus/acquired immune deficiency syndrome), diet, heart disease and cancer and a 10-minute cholesterol education video were developed for African Americans. Booster calls were made encouraging the use of the materials and brief motivational counselling provided dependent on participants’ stage of change |
| Theory: Each chapter of the booklet corresponds to one of the major stages of change delineated by Prochaska and Diclemente455 |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: Baseline interview and 6 months post intervention Quit rates: Primary outcome: point prevalence quit rate at 6 months post test: 11.2% intervention group vs 7.9% control group; not statistically significant Quit attempts: Secondary outcome: quit attempts in past 6 months – did not differ significantly between the intervention and the control groups Stages of change: Calculated using three items asked at baseline: (1) Do you plan on making any changes in your smoking habits in the next 6 months? (2) How much do you want to quit smoking in the next 6 months? (3) How many times in the past year have you been able to stay off cigarettes for at least 24 hours? |
| Conclusions |
|
Authors: Results were mixed. No significant effects observed for the entire treatment cohort at 6 months’ follow-up Reviewers: This study did not show a significant difference in quit rates or quit attempts between the two groups (see limitations) |
| Comments and limitations |
| Low completion rate for booster call and design limitations, follow-up data collected only at 6 months post test, point prevalence only was assessed. Longer-term follow-up would have provided a more comprehensive assessment. Quit rates determined by self-report and not validated |
| Study reference |
|---|
| Schorling et al. 1997456 |
| Setting |
|
USA; two rural Virginia counties: Buckingham County – intervention community, Louisa County – control community Each county has about 35 churches that were identified as primarily serving black residents |
| Inclusion criteria |
| Considered if they had smoked at least 100 cigarettes in their lifetime (current smokers were those who had smoked at least one cigarette per day for the past 7 days, occasional smokers were classified as smoking intermittently but less than one cigarette per day for the past 7 days), African American, > 17 years |
| Study type |
| Two-group pre–post test, population survey |
| Description of population |
|
Ethnicity: African American; how ethnicity assessed not reported Age (years): Mean: Louisa: 41.5, Buckingham: 40.1 n: 3744, all adult members of each sampled household; 965 smokers identified, 898 selected for interview, 652 (73%) completed baseline survey. Louisa: n = 304, Buckingham: n = 344; n = 648 personally interviewed Sex: Louisa: 56.3% male, Buckingham: 53.5% male Other: 90% Baptist; Louisa: employed 56.8%, high school graduate 46.3%; Buckingham: employed 59.9%, high school graduate 46.4% |
| Description of intervention and control |
|
Community-based smoking cessation project with smoking cessation intervention delivered through a coalition of black churches Intervention: Core smoking cessation programme: one-on-one counselling, self-help materials and community-wide activities provided by two smoking cessation counsellors trained from participating churches. Counsellors were also asked to discuss the programme with the congregation at large. Self-help programme designed by project staff with assistance from coalition members (Call It Quits) – based on a calendar-style handout, each page contains a goal for 1 day with 7 days preparing to quit and seven pages relevant to 7 days after quitting. Each page can be torn off and carried as a reminder of the day’s task. Counsellors trained to give brief active follow-up counselling. Guide can be used alone as a self-help guide as well. Coalitions were formed consisting of community leaders. Additional smoking cessation programmes were developed to address other local priorities, including church booklets, Gospel quit nights, educational contests in schools and an annual community-wide cessation contest Control: Community chose to address hypertension (they were not allowed to choose smoking). Smoking was not addressed by the volunteers or by any coalition activities |
| Theory: Guided by principles of community empowerment |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: Baseline and 18 months, door-to-door survey, population-based cohorts of smokers in each county; n = 452 (70%) Primary: Whether or not smoking cessation interventions would increase smoking cessation rate of church members exposed to intervention (direct impact). Intervention effects measured at population level; church attendance used as proxy for exposure Secondary: Whether or not community-wide smoking cessation rate among African Americans would also increase (indirect impact) Quit rates: Self-reported 1-month continuous abstinence. In text, smoking cessation rate reported as 9.6% vs 6.2% (difference 3.4%, 95% CI –1.5% to 8.4%). Elsewhere reported as 9.6% vs 5.4% (p = 0.18). Among church attendees (at least once a month), quit rate was 10.5% vs 5.9% (p = 0.20); for less frequent attendees, quit rate was 8.8% vs 6.4% (difference 1.8%, 95% CI –5.4% to 9.0%). Trend in intervention county observed for church attendees, but not significant. Adjusted OR of quitting was 1.64 (95% CI 0.79 to 3.40) Stages of change: Progress along the stages of change in the intervention vs control group was significant. Progress in each county approached significance (p = 0.06) Knowledge: Similar proportions of the population had heard of the church coalition in both counties; there was greater awareness of the smoking cessation programme in the intervention county than in the control county |
| Conclusions |
|
Authors: Smoking cessation interventions can be implemented with success through a church coalition. Intervention was associated with significant progress along the stages of change. A higher quit rate in the intervention county compared with the control county was not significant. Individuals who attended church were more likely to quit than those who did not attend; however, this too was not significant Reviewers: Agree with the authors’ conclusions. Authors noted the pattern of smoking to be late onset, low rate and high menthol. Programme reported to be active after 12 months. Coalition of churches helped with development and implementation. Counties were randomised to either smoking cessation intervention or not; this health issue was determined before community engagement |
| Comments and limitations |
| Baseline survey initially designed to be carried out by telephone with a supplementary in-person interview for those without a telephone; however, this pilot study failed and in-person surveys were carried out instead. Follow-up was only 70%; tracking those in rural communities was difficult, about a quarter did not have a telephone. No biochemical validation |
| Study reference |
|---|
| Darity et al. 2006457 |
| Setting |
| USA; four sites in the north-eastern and south-eastern parts of the USA |
| Inclusion criteria |
| Black adult smokers |
| Study type |
| CCT (community intervention with control sites) |
| Description of population |
|
Ethnicity: African American; not reported how ethnicity assessed Age (years): Not reported n: 2544 reported in abstract/2644 reported in body of paper; n = sample of 520 for 6 months’ follow-up, n = sample of 490 for 12 months’ follow-up (the 6-month sample was randomly taken from the baseline cohort and the 12-month cohort was another random sample from the cohort excluding those who had participated in the 6 month follow-up), n = sample of 1344 for 18 months’ follow-up; unknown how many were in the control and intervention conditions Sex: Not reported Income: Not reported |
| Description of intervention and control |
|
Community-based smoking cessation intervention in which both active intervention and passive control areas were exposed to a mass media campaign designed to promote readiness to quit smoking Active intervention sites: Community organising + mass media. Special area-based intervention activities. Direct interpersonal educational activities: 14 workshops involving 108 participants held. Neighbourhood Health Advocates were recruited and trained to distribute educational materials and to host formal discussion meetings. Professional Advisory Committees were set up in each active site to gain support and cooperation of key professionals. Project staff made presentations to organised social groups and held informal small-group discussion meetings Passive control sites: Mass media only |
| Theory: Health belief and diffusion of innovation models |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: Baseline and 6 months, 12 months and 18 months after baseline Quit rates: Absolute difference of 4.9%; 41.5% greater point prevalence rate of non-smoking in the active vs the passive group (p = 0.012) Quit attempts: 6-month period prevalence of quit attempts was 33.8% in the active group and 26.2% for the passive group, with an absolute difference of 7.6% which was statistically significant (p = 0.003) Number of cigarettes smoked per day: There was a difference in the decrease in number of cigarettes smoked between the active and passive groups, with an absolute difference of 1.6 fewer cigarettes smoked daily in the intervention group (p=0.004); this represents a 400% greater reduction in cigarettes smoked in the active intervention group |
| Conclusions |
|
Authors: Analysis of process variables strongly suggests that, within this African American community, ‘hands-on’ or ‘face-to-face’ approaches combined with mass media, mailings and other less personal approaches were more effective in reducing personal smoking behaviour than mass media, mailings and other impersonal approaches alone Reviewers: The study suggests that more active contacts with study participants can increase cessation rates. It would be beneficial to have more information about the informal meetings to determine whether it was the way in which communities were engaged that increased cessation rates rather than any personal contact alone. Furthermore, cohort retrospective analysis showed increasing effect of the intervention on cessation rates (6, 12 and 18 months, with little effect at 6 or 12 months), which suggests that sustained community intervention (18 months) may be necessary to increase cessation rates. Need to compare with other long-term community-based studies |
| Comments and limitations |
| Very minimal cultural tailoring in this case, with only media outlets being contacted where appropriate. Three other analyses were performed and reported (but are not extracted here): cohort retrospective analysis (trend of little effect in first 6 months, appreciable in second 6-month period and important additional effect for final 6 months), a sequential cross-sectional analysis and several validity comparisons |
| Study reference |
|---|
| Ahluwalia et al. 1998;355 Ahluwalia et al. 1998356 |
| Setting |
| USA; Atlanta, GA; inner-city hospital serving a low-income, predominantly African American population |
| Inclusion criteria |
| Self-report of being African American, having smoked a minimum of 10 cigarettes per day continuously for at least the past year, at least one previous quit attempt, a home address, a telephone number and weight > 100 lb, and if they reported being self-motivated to quit |
| Study type |
| RCT (double blind, placebo controlled) |
| Description of population |
|
Ethnicity: African American; self-reported Age (years): Patch group: 48.7, placebo group: 46.7 n: 410 randomised, 205 into each arm of the study Sex: 65% female (patch 65.9% female, placebo 64.4% female) Income: Not reported |
| Description of intervention and control |
|
Double-blind, placebo-controlled RCT to evaluate efficacy of nicotine patch as an adjunct to brief counselling and education in an inner-city population Placebo/transdermal nicotine patches with following schedule: 21 mg/day for 6 weeks, 14 mg/day for 2 weeks and 7 mg/day for 2 weeks (10 weeks total); these three doses provided an average steady-state plasma nicotine concentration of 17, 12 and 6 ng/ml. Patients who relapsed to smoking were advised to discontinue using the patch and to set another quit date. At randomisation, patients received an initial 2 weeks of 21 mg/day patches and 1 hour-long visit with a counsellor for instructions on the use of the patch and brief education about the risks of smoking and the benefits. All patients received a bag with the programme logo and clinic telephone number; the bag also contained additional material (one-page patch tip sheet written at sixth-grade reading level with pictures, and a diary for everyday recording). Patients received a written guide, The 6–2–2 Committed Quitters’ Programme: How to Quit Smoking Using Nicoderm (seventh-grade reading level). At follow-up visits, issues related to relapse were discussed, compliance was encouraged, it was determined if participants had any adverse reactions and participants’ diaries were reviewed. Placebo: pharmacologically irrelevant amount of nicotine in the drug reservoir to mimic the odour of active systems; delivered < 1 mg of nicotine in 21 hours |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: 1, 2, 6 and 10 weeks after quit day; final visit at 6 months Quit rates: 10-week quit rates were 21.5% in the patch group and 13.7% in the placebo group (p = 0.03); at 6 months, self-reported quit rates were 17.1% in the patch group and 11.7% in the placebo group (p = 0.08) |
| Conclusions |
|
Authors: Using Pathways to Freedom, a guide specifically designed for low literate African American smokers, was thought to be comparable in terms of use to the manufacturer’s product guide. This study highlights that poor, inner-city African American smokers were interested in smoking cessation. The patch significantly improved 10-week smoking cessation rates, but more relapse prevention is needed to ensure abstinence to 6 months and beyond. With the placebo patch, 10-week quit rates were two to three times higher than national quit rates Reviewers: The 6-month quit rate was not significantly different with and without an intention-to-treat analysis. Follow-up was low. The authors state that this may be because of a disenfranchised population, but it may also be a result of too frequent follow-up. A good point is made by the authors that reduction in the number of cigarettes smoked should also be recorded; smoking cessation (reduction) not a discrete event |
| Comments and limitations |
| Lack of biochemical verification. 6-month follow-up rather than 1 year. Did not assess the literacy level of patients or ability to comprehend the intervention materials. Use of one-sided statistical analysis limits reporting of risk ratios with 95% CIs. Only outcome measured was total abstinence. Smoking should be viewed as a dynamic process rather than a discrete event. Any reduction in the number of cigarettes smoked may reduce harm |
| Study reference |
|---|
| Orleans et al. 1998;347 Boyd et al. 1998306 |
| Setting |
| USA; four communities: Durham, NC, Philadelphia, PA, Houston, TX and Birmingham, AL |
| Inclusion criteria |
| African American, smoker or recent quitter (past 30 days), ≥ 20 years, no previous use of Pathways to Freedom guide, consent to 6 months’/12 months’ telephone follow-up |
| Study type |
| RCT |
| Description of population |
|
Ethnicity: African American; not reported how ethnicity assessed Age (years): > 20 (62% 20–39, 26% 40–49, 12% ≥ 50) n: 1422 (n = 445 at 12 months) Sex: Both sexes; however, percentages of men and women not reported Income: Not reported |
| Description of intervention and control |
|
Targeted communications campaign: radio and television advertisements and some community outreach to increase telephone call volume from African American smokers to the Cancer Information Service (CIS) for smoking cessation Intervention: ‘Tailored’ counselling and guide, Pathways to Freedom Control: ‘Standard’ CIS quit smoking counselling and guide, Clearing the Air |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
|
Follow-up: 1 week, 6 months and 1 year Quit rates: 6 months: no significant difference in self-reported abstinence – 9.1% control vs 10.1% intervention; 12 months (n = 445): significantly higher quite rate – 15.4% control vs 25% intervention Quit attempts: At 6 months more participants had set a quit date, made quit attempts and undertaken pre-quitting behaviours, e.g. reduction in number of cigarettes per day |
| Conclusions |
|
Authors: Paid targeted advertising, using radio as a primary channel, is an effective method of reaching African American smokers to increase call volume to a smoking cessation helpline. Results show some promise for a culturally tailored approach to boost quit attempts in African American smokers: there were more quit attempts and greater use of pre-quitting strategies, and significantly higher self-reported quit rates at opportunistic follow-up at 12 months in the tailored intervention group (although no differences in self-reported 1-week abstinence at 6 months) Reviewers: Paid targeted advertisements were hugely successful in increasing call volumes to CIS by African American smokers (radio > television) and the advertisements had a very high reach (> 88%) – despite this, overall the uptake was still low (0.1–0.2%), especially in lower socioeconomic groups. Promising results of a tailored telephone smoking cessation counselling intervention for African American smokers; follow-up at 12 months in a subgroup showed significant differences in self-reported quitting rates |
| Comments and limitations |
| Gender was reported at baseline for only half of the participants. Half of smokers were in contemplation stage or had recent quit attempts (< 30 days), which reduced chances of successful quit attempt; 85% smoked within 30 minutes of awakening suggesting high level of nicotine addiction – yet NRT was not a direct part of the study (used by ~25%). Young group (62% in 20–39 years age group) – possibly not generalisable to other/older age groups. Results relied on self-reported abstinence, which is less reliable than biochemical verification. Adaptations were mostly personalised rather than culturally adapted |
| Study reference |
|---|
| Lipkus et al. 1999358 |
| Setting |
| USA; Durham, NC |
| Inclusion criteria |
| Random sample of 3490 adult patients of Lincoln Community Health Center, aged ≥ 18 years, who visited the centre within the 18 months up to November 1993. Final sample consisted of 1318 men and women at baseline, 266 were African American smokers of whom, 160 were able to be contacted and completed the final interview |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): 18–49 |
| n: 160; 266 were recruited, 257 were alive at the time of follow-up and 160 completed the final interview |
| Sex: 46% male |
| Income: Not reported |
| Description of intervention and control |
| Provider prompting intervention: The Medical Record (TMR) is a comprehensive computer system with a computerised health maintenance tracking system that generated printed physician prompts to provide patients with stage-based behavioural messages. Providers were trained and asked to follow the Ask–Advise–Assist–Arrange follow-up model developed by the National Cancer Institute to promote smoking cessation |
| Tailored print communications (TPCs) were sent to patients around the time of their birthdays (an oversized tailored birthday card with a picture of the clinic staff on the cover and a personalised ‘Healthy Birthdays’ newsletter). Both were written for fifth-grade reading level |
| Tailored telephone counselling: Men received one call per year, women could receive two calls if they were due for breast or cervical cancer screening and were also smokers; female counsellors |
| Three arms: Provider prompting alone, prompting + TPC, and prompting + TPC + tailored telephone counselling |
| Theory: Research guided by the transtheoretical or stages of change model458 |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 16 months after last intervention |
| Quit rates: Of 160 participants, 35 (21.9%) quit smoking. Provider prompting + TPC group was more likely to result in quitting at follow-up (n = 18, 32.7%, p < 0.05) than provider prompting alone (n = 7, 13.2%) or prompting + TPC + tailored telephone counselling (n = 10, 19.2%, p < 0.05) |
| Conclusions |
| Authors: Overall, the results provide encouraging support for the use of TPCs with African Americans. Compared with the provider prompting intervention alone (least intensive intervention) or those who received all three intervention components (most intensive intervention), smokers in the provider prompting intervention group who also received TPCs were more likely to report having quit at follow-up (32.7% quit rate). The effects of the provider prompting intervention with TPCs remained significant after controlling for different variables. Stage of change was most powerfully related to quitting at follow-up. Contemplators at baseline were eight times more likely to report having quit at follow-up than pre-contemplators. When stage of change and intervention group were both included in the multivariate model, the OR for the tailored print intervention arm was even higher (OR = 6.56). It is unclear why the addition of telephone counselling did not increase cessation rates above those achieved in the group that received the provider prompting intervention and TPCs |
| Reviewers: Although the authors did not report findings from an intention-to-treat perspective, 21.9% had quit at follow-up. The quit rate of 32.7% using TPCs is, according to the authors, comparable to results of recent studies using tailored interventions with African American smokers. The findings indicate that smokers who received provider prompting with TPCs were more likely to report having quit than smokers who received the provider intervention alone. It appears that there is value here and, promisingly, that this is a cost-effective method of increasing quit rates (vs telephone counselling) |
| Comments and limitations |
| Unclear as to the precise mechanisms whereby, and situations in which, TPCs may be effective. Compliance rate was 48%. Approximately one-third were lost to follow-up (reflects difficulty of conducting intervention with low-income, transient African American populations; however, refusal rate of 3% low) |
| Study reference |
|---|
| Ahluwalia et al. 2002;345 Harris et al. 2003;344 Harris et al. 2004;342 Manning et al. 2005343 (Kick It at Swope) |
| Setting |
| USA; community-based health-care centres |
| Inclusion criteria |
| African American or black, at least 18 years of age, smoked at least 10 cigarettes per day, interested in quitting in the next 30 days, speaks English and had a permanent home address with working telephone. Only one smoker per household allowed to enrol |
| Study type |
| RCT |
| Description of population |
| Ethnicity: Black American; self-described |
| Age (years): mean 44; bupropion: 44 (SD 10.9), placebo: 44.4 (SD 11.3) |
| n: 600; bupropion 300, placebo 300 |
| Sex: 70% female; bupropion 70.7%, placebo 69.3% |
| Other: ≤ high school graduate: bupropion 50.3%, placebo 49.7% |
| Description of intervention and control |
| Trial to compare a sustained-release form of bupropion (bupropion SR) with placebo for smoking cessation among African Americans. Both groups received eight in-person 45-minute brief motivational counselling sessions [at baseline, quit day, weeks 1 and 3, end of treatment (week 6) and by telephone at day 3 and weeks 5 and 7]. In general, counselling was provided by the same person. Dose was 150 mg of bupropion SR or placebo twice daily for 7 weeks. Participants were instructed to continue taking pills for the full 7 weeks regardless of smoking status |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Weeks 6 and 26 following quit day |
| Quit rates: At week 26, quit rates were 21.0% in the treatment group and 13.7% in the placebo group (7.3% point difference, 95% CI 1.0 to 13.7%, p = 0.02). Continuous abstinence was significantly higher for the bupropion SR group at weeks 1, 3 and 6 (p < 0.001) and 26 (p < 0.01) |
| Number of cigarettes smoked per day: At week 26, reduction in number of cigarettes smoked per day was 8.3 (SD 10.3) vs 7.9 (SD 8.8) (p = 0.61) for the treatment group vs the placebo group |
| Conclusions |
| Authors: Bupropion SR was effective for smoking cessation among African Americans and may be useful in reducing health disparities associated with smoking. Difficulty in locating participants within an acceptable time frame, combined with counting those lost to follow-up as smokers, may underestimate the actual quit rate. Alternatively, may have had higher relapse rates due to the high stress associated with lower-income populations. However, quit rates in the placebo group were comparable with those in other studies. This is the largest treatment-based trial of smoking cessation in any ethnic minority conducted to date |
| Reviewers: From the primary paper,345 the study showed an effect on smoking cessation for the bupropion group compared with the placebo group. The intervention was equitable; however, difficulty in locating participants for participation and follow-up may exclude some who may not have a permanent telephone/mailing address. The intervention was feasible; however, additional behavioural/motivational counselling requires additions that ‘regular care’ practices may not be able to sustain |
| Comments and limitations |
| Limitations: Findings cannot be generalised to all African Americans and although community based it remains a single-site study. The majority of participants were women and this may result in a lower overall quit rate in the study population because African American women appear to have lower quit rates in the short and long term. Smokers are self-selected who are motivated to quit |
| Study reference |
|---|
| McBride et al. 2002374 |
| Setting |
| USA; inner-city community health clinic (Lincoln Community Health Center) in an urban county in North Carolina; serves low-income residents and African Americans comprise 83% of patients |
| Inclusion criteria |
| Self-identified as African American and smoked at least one cigarette per day in the previous 7 days. Would consider genetic testing |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; self-identified |
| Age (years): Mean (SD): 44.5 (12.3) |
| n: 557 smokers identified; 185 enhanced usual care, 372 biomarker feedback |
| Sex: 40% male |
| Income: Not reported |
| Other: 64% had one or more chronic illness |
| Description of intervention and control |
| A multicomponent intervention with feedback about genetic susceptibility to lung cancer to increase risk perceptions and rates of smoking cessation compared with a standard intervention. All smokers received a self-help manual and, if appropriate, nicotine patches; refills were provided as needed |
| Biomarker feedback: Offered blood test for genotyping the glutathione S-transferase 3 (GST3) gene (GSTM1) as well as a tailored feedback booklet (eight pages, fifth-grade reading level) about genetic susceptibility to lung cancer. Those who refused testing were sent the same booklet. Participants received telephone counselling (up to four times) with a health educator over a 12-week period. The first call discussed their results and the importance of cessation; calls two to four encouraged steps towards quitting and reinforced the test results |
| Enhanced usual care: Received provider advice to quit smoking and referred to smoking specialist who assessed stage of readiness to quit and whether NRT was appropriate |
| Theory: Mentions social cognitive theory training for callers |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 6 and 12 months |
| Quit rates: Smoking cessation (prevalent abstinence) was significantly greater for the biomarker feedback arm than the enhanced usual care arm (19% vs 10%, p < 0.006) at 6 months but not at 12 months (15% vs 10%, p = 0.12) (unadjusted). After adjustment for desire to quit, chronic illness and smoking within 30 minutes of waking, the difference in the 6-month cessation rate between the groups was still significant (p = 0.03) and the 12-month difference was still not significant (p = 0.34) |
| Quit attempts: Not reported |
| Conclusions |
| Authors: Smokers agreed to genetic feedback as part of the multicomponent cessation programme. Although the short-term cessation rate in the biomarker feedback arm was increased compared with standard intervention, genetic feedback of susceptibility may not benefit smokers with high baseline risk perceptions |
| Reviewers: This study compared a genetic feedback arm with an arm that cannot be considered ‘standard’. This study was not effective in sustaining long term (12 months) the cessation that was observed at 6 months. There is the potential for ceiling effects in this older population, with 64% having at least one chronic disease |
| Comments and limitations |
| Feedback from the pilot study may not have had powerful impact because 45% of smokers did not fully understand the test results. Low education level of target group warranted need for follow-up telephone counselling. However, in pilot study this figure was unchanged following telephone calls. Future studies should evaluate other graphical approaches for communicating results |
| Study reference |
|---|
| Ma et al. 2004349 |
| Setting |
| USA; Delaware Valley region of Pennsylvania and New Jersey |
| Inclusion criteria |
| Male, Chinese, between 14 and 19 years and in the summer youth programme recruited from community-based Asian-American organisations that participated in an Asian Community Cancer coalition |
| Study type |
| Pre–post quasi-experimental |
| Description of population |
| Ethnicity: Chinese American; not reported how ethnicity assessed |
| Age (years): 14–19, mean (SD): 17.7 (2.2) |
| n: 17 standard intervention; 14 culturally modified intervention |
| Sex: Male |
| Income: Not reported |
| Other: Approximately 67% of participants were in grades 9–12 |
| Description of intervention and control |
| Smoking cessation for Chinese American adolescents |
| Culturally modified programme [Asian Adolescents Choose Tobacco-Free (ACT)]: Conducted through a community-based organisation that served high-risk youth. Used a buddy system (participants received monetary rewards if they brought their buddies); additional incentives (t-shirts, gift certificates) if they continued to attend the sessions – 10 sessions (one session per week) lasting 50 minutes |
| Standard smoking cessation curriculum (SC): First recruited into a 6-week summer programme. All joined the SC programme: one 50-minute session each week for 10 weeks |
| In total, 17 of 17 in the SC group and 9 of 14 in the ACT group completed the programme |
| Theory: Not reported |
| Approaches to adaptation |
ACT applied principles of:
|
| Outcome measures and results |
| Follow-up: Baseline, post intervention, 3 months |
| Quit rates: 23.1% cessation rate among the SC group and 18.2% among the ACT group (χ2 = 0.09) |
| Number of cigarettes smoked per day: The ACT group showed a greater reduction in typical weekday (mean 6.7, SD 5.9) and weekend (mean 6.0, SD 6.5) tobacco use than the SC group |
| Conclusions |
| Authors: Given the positive results among this high-risk group, ACT programme needs to be tested among a larger population of Chinese Americans. Major challenge to increasing parental involvement is that youth are reluctant to participate in a smoking cessation programme because they do not want their parents to know that they smoke. In the ACT programme parental consent is requested and Asian adults were used to conduct the programme. Cultural modification programmes for Asian American youth are complicated because youth are bicultural and identify with two cultures. The ACT programme was evaluated to be as effective. Further research addressing culturally relevant factors that enhance the efficacy of ACT and the curriculum needs to be implemented among a larger and more representative Asian American group |
| Reviewers: Based on self-reported quit rates, at 3 months the quit rates for ACT and SC are comparable. We question the value of the culturally tailored intervention if the SC programme worked just as well, or even better in this case. The authors provide a comprehensive list citing the factors that Asian adolescents perceive to be important in helping them quit; however, many of these factors are cited for both the ACT and the SC groups. This intervention was effective in increasing quit rates, but the culturally tailored intervention did not show added value |
| Comments and limitations |
| Adolescents were selected from a community-based organisation setting and not from a school setting. Many adolescents were at high risk socially and economically. Small sample size. Higher-risk group than is typical of Asian American youth. The facilitator characteristics most important to smokers in the ACT programme included caring about students, confidentiality, trustworthiness, being non-judgemental; and are likely transferable to other programmes |
| Study reference |
|---|
| Ahluwalia et al. 2006;361 Nollen et al. 2006;362 Okuyemi et al. 2007;363 Okuyemi et al. 2007;364 (Kick It at Swope II) |
| Setting |
| USA, KS; Kansas City metropolitan area |
| Inclusion criteria |
| Self-identified African American or black, at least 18 years old, smoked ≤ 10 cigarettes per day for at least 6 months prior to enrolment, smoked at least 25 of the last 30 days, interested in quitting in the next 2 weeks, speaking English, with a permanent home address and working telephone |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African-American; self-identified |
| Age (years): Mean: 45 (range 19–81); nicotine gum + motivational interviewing (MI): 45.2 (SD 10.7), nicotine gum + health education (HE): 43.5 (SD 11.8), placebo gum + MI: 46.5 (SD 10.0), placebo gum + HE: 45.2 (SD 10.0) |
| n: 755 light smokers |
| Sex: Female: nicotine gum + MI: 66.1%, nicotine gum + HE: 68.3%, placebo gum + MI: 65.1%, placebo gum + HE: 68.1% |
| Income: Not reported |
| Description of intervention and control |
| An 8-week double-blind placebo-controlled smoking cessation intervention for African Americans. At randomisation, participants were assigned to an 8-week supply of either active 2 mg nicotine gum or placebo. Instructions given for gum usage depended on the number of cigarettes smoked at baseline. In general, participants received counselling from the same person for all six counselling sessions (three in person, three by telephone, 20 minutes each). Participants were encouraged to set a quit date for the day following their randomisation visit |
| HE: Standard counselling approach based on current treatment guidelines that focus on providing information and advice. Trained counsellors used the KIS II Quit Smoking Guide |
| MI: Counsellors followed scripts that discussed pros/cons of smoking/quitting, motivation and confidence to quit |
| Theory: Theories of HE and MI; values clarification strategy of Miller and Rollnick459 |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Weeks 1, 3, 6, 8 and 26 |
| Quit rates: 194 participants reported quitting at week 26 across all four groups; of these, 95 were confirmed quitters (salivary cotinine ≤ 20 ng/ml) Quit rates for nicotine gum were no better than for the placebo group (14.2% vs 11.1%, p = 0.232) at 6 months; however, a counselling effect emerged, with HE performing significantly better than MI (16.7% vs 8.5%, p < 0.001). These results were consistent across time points (weeks 1, 8 and 26) |
| Conclusions |
| Authors: The nicotine gum was not effective for smoking cessation in this sample of African American light smokers. Failure to detect an effect of the gum may be a result of inadequate dosing or underdosing: 2 mg was used as opposed to 4 mg and it was prescribed for a maximum of 10 pieces per day. African American light smokers randomised to HE were more likely to return for counselling visits than those randomised to MI. Those in the HE group had higher quit rates than those in the MI group. HE was perceived as more relevant. MI was better with a population who are resistant, whereas this population was highly motivated |
| Reviewers: Interesting conclusion, seemingly validated in other studies, that HE is more effective in highly motivated participants than MI, which works better among people who are resistant/angry/poorly motivated. The integrity of the respective counselling protocols was maintained and each session was tape-recorded to maintain fidelity and consistency |
| Comments and limitations |
| Randomisation and follow-up occurred at a single community health centre and participants were required to have a home address and telephone. Participants were all highly motivated to quit. Study staff did not begin to document the various recruitment sources until 5 months into the study |
| Study reference |
|---|
| Fang et al. 2006332 |
| Setting |
| USA; south-eastern Pennsylvania |
| Inclusion criteria |
| Smokers were eligible if they were of Chinese or Korean ancestry, had smoked at least one puff of one cigarette in the past 7 days (i.e. 7-day point prevalence), were ≥ 18 years and possessed a telephone |
| Study type |
| RCT |
| Description of population |
| Ethnicity: Chinese and Korean; not reported how ethnicity assessed |
| Age (years): Mean (SD) (range): intervention: 43.97 (17.21) (18–77), control: 48.35 (16.47) (19–83) |
| n: 66; intervention 34 (Chinese 56%), control 32 (Chinese 53%) |
| Sex: Intervention: 9% female, control: 0% female |
| Income: Not reported |
| Description of intervention and control |
| Theory-based smoking cessation intervention + NRT |
| Intervention: One in-person session (90–120 minutes) and targeted cognitive-affective reactions to smoking and cessation. Participants were encouraged to explore their risk perceptions for cancer and other smoking-related diseases, probed for their beliefs about quitting and asked about their values and goals (e.g. reasons for quitting). Past smoking cessation efforts, identification of personal smoking triggers and cultural barriers to quitting were also discussed |
| Control: General health counselling (nutrition, exercise and the harmful effects of tobacco) + NRT as a time and attention control |
| Theory: Cognitive-social health information processing (C-SHIP) model460 |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Follow-up assessments were conducted by telephone at 1 week, 1 month and 3 months post counselling |
| Quit rates: 38% reported quitting at 3 months’ follow-up |
| Conclusions |
| Authors: No difference in cessation rates by ethnic group at each time point. Quit rates were relatively high in both the intervention and control groups. At 1 month, a significantly higher proportion of intervention participants (56% or 19/34) reported having quit smoking than control participants (31% or 10/32) (χ2(1) = 4.06, p < 0.05). At 3 months, 47% (16/34) of intervention participants and 28% (9/32) of control participants had quit smoking but this difference was not statistically significant [χ2(1) = 2.51, p = 0.11]. Because of the characteristics of this population (e.g. long work hours, often 7 days a week) it was important to develop an intervention that was brief and time-efficient for it to be acceptable to the targeted condition. The intervention increased self-efficacy and decreased negative attitudes towards quitting. Self-efficacy was the only significant predictor of smoking status. The intervention may have been successful in motivating individuals to make a quit attempt but not in preventing smoking relapse, particularly among Chinese smokers. A brief culturally adapted intervention can yield changes in smoking-related cognitions among low-income, hard-to-reach Chinese and Korean smokers |
| Reviewers: The intervention did not produce sustained quit rates at 3 months. The trend among Chinese participants was different from that observed for Korean participants; the authors do not comment but there may be more subtle cultural differences that could be explored |
| Comments and limitations |
| Quit rates may have been high because participants were recruited through community organisations and networks in which an informal support system was already in place. Limited by self-reported smoking status, small sample size and including predominately men. A longer follow-up period (6–12 months) would have been preferred. Future interventions need additional support during the critical period following initial abstinence. Research on factors that contribute to smoking cessation among Asian American women is needed |
| Study reference |
|---|
| Andrews et al. 2007;461 Andrews et al. 2007462 |
| Setting |
| USA; Augusta-Richmond County, GA; two subsidised housing developments |
| Inclusion criteria |
| Non-pregnant/non-breastfeeding African American women, > 18 years, current daily smoker, planning to quit smoking within the next 6 months, resident of the intervention or control community or a female relative or close friend of a resident of these communities |
| Study type |
| Quasi-experimental repeated measures design with comparison group |
| Description of population |
| Ethnicity: African American; how ethnicity assessed not reported |
| Age (years): Mean (range): 40.2 (18–85) |
| n: 103; 51 intervention, 52 comparison |
| Sex: 100% female |
| Description of intervention and control |
| Community smoking cessation intervention for African American women with three major components |
| Nurse-delivered weekly behavioural/empowerment group counselling for 6 weeks (1 hour) with a booster session at weeks 12 and 24. Participants who progressed to the preparation stage were assisted to set a quit date (week 2) |
| Free NRTs for 6 weeks |
| Community health worker (CHW) made personal weekly contact (face-to-face or by telephone) outside of group sessions for 24 weeks to enhance smoking cessation self-efficacy and provide social support and spiritual well-being |
| Comparison participants received self-help written material, You Can Quit Smoking, at baseline and group attention during the study period – group education from a nurse on self-image, exercise, hypertension, smoking cessation; groups had 10–12 participants and lasted about 1 hour |
| Theory: Curriculum for group behavioural counselling was adapted from the US Public Health Service (PHS) treating tobacco dependence guideline463 and empowerment educational principles from Freire256,464 |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to weeks 6, 12 and 24 |
| Quit rates: 6-month continuous abstinence: 27.5% and 5.7% in the intervention and comparison groups respectively; OR of quitting was 6.18 (95% CI 1.65 to 23.01) |
| Stages of change: Measured by stages of change questionnaire |
| Conclusions |
| Authors: Women who received the Sister to Sister intervention were six times more likely to quit than women who received group attention and minimum self-help written materials. A total of 27.5% of the women in the intervention group maintained abstinence for a 6-month period as validated by exhaled carbon monoxide measurements. A key finding was that changes in social support predicted cessation. Smoking cessation self-efficacy improved over time and mediated cessation outcomes indicating that building confidence in quitting may explain how the intervention group participants were able to quit. Spiritual well-being was not associated with 6-month continuous abstinence and did not mediate 6-month continuous abstinence |
| Reviewers: The intervention was successful in showing a difference of effect between the intervention and control groups. The quit rate was significantly higher for the intervention group. However, the use of two communities limits generalisability and there may be potential confounders (as mentioned by the authors) |
| Comments and limitations |
| The intervention group differed from the control group: intervention participants were older, had higher monthly incomes and were more likely to have completed high school. The retention rate was 87.4% during the 6-month study period (attrition was seven participants out of the comparison group and six participants out of the intervention group) |
| Study reference |
|---|
| Nollen et al. 2007341 |
| Setting |
| USA; Atlanta, GA |
| Inclusion criteria |
| African American, > 18 years, wanting to quit smoking in the next 30 days to 6 months (preparation/contemplation stage of change), smoking > 10 cigarettes per day, weight > 100 lb, having a home address and access to a telephone and video cassette recorder (VCR) |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; self-identified |
| Age (years): Mean: 43 |
| n: 500 |
| Sex: 55–65% female |
| Income: Not reported |
| Description of intervention and control |
| Intervention: Culturally targeted videotape and print guide (The Harlem Health Connection’s Kick It! video and Pathways to Freedom: Winning the Fight against Tobacco) |
| Standard care: Videotape (How to Quit) and print guide (Freedom from Smoking) |
| Both groups: NRT: 8 weeks of nicotine patches, reminder telephone calls during the first week and at 1 and 3 months; postcards at 3 and 5.5 months |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Week 4 and 6 months |
| Quit rates: No significant differences in smoking outcomes |
| Conclusions |
| Authors: Study highlights the importance of greater audience segmentation and individual tailoring to better match intervention materials to the target population, particularly with regards to racial/ethnic identity. Materials (video and guide) had been tested and evaluated in Harlem and Philadelphia but not in Atlanta – the results suggest heterogeneity within the African American population |
| Reviewers: Homogeneity within African American populations cannot be assumed and interventions need to be piloted in the target population, including assessment of their cultural identification |
| Comments and limitations |
| The study considered Netto’s fifth principle regarding cultural identification. Alternatively, any effect of the targeted intervention may have been overwhelmed by the success of the nicotine patch. The current study enrolled only motivated smokers (contemplation or preparation stages). There was also potential for cross-contamination between the two groups. Other limitations included the single-blind design, the necessity for participants to have a home address, telephone and access to a VCR and basing quit rates on self-report and carbon monoxide assessments |
| Study reference |
|---|
| Shelley et al. 2008465 |
| Setting |
| USA; Flushing, Queens (intervention); Sunset Park, Brooklyn (comparison), NY |
| Inclusion criteria |
| Households obtained from the White Pages using a list of 867 unique spellings from 622 native surnames identified in consultation with Chinese linguists |
| Study type |
| Pre–post quasi-experimental design |
| Description of population |
| Ethnicity: Chinese; ethnicity assigned by surnames (unclear if confirmed by participants themselves) |
| Age (years): 18–34: 27.9%, 35–44: 25.6%, 45–54: 25.8%, > 55: 20.7% |
| n: 2537 at baseline, 1384 at follow-up interview; 617 from Flushing and 767 from Sunset park |
| Sex: 56.1% male |
| Income: Not reported |
| Description of intervention and control |
| Smoking cessation for a Chinese population |
| Intervention: Distribution of bilingual posters and Chinese-language educational materials to local businesses, community organisations, health settings. Access to language-specific smoking cessation resources: (1) physician education and distribution of tools kits to 99 physicians in 42 practices; (2) distribution of 305 6-week courses of free NRT patches through two community organisations; (3) implementation of three free Chinese-language smoking cessation programmes that included free pharmacotherapy; (4) a quit and win contest; and (5) smoking cessation workshops. No intervention activities were directed specifically at individuals. Advertised the free nicotine patch programme in Chinese newspapers in both communities |
| Control: Tobacco control public policy only |
| Theory: Behavioural theory and evidence-based smoking cessation programmes; community-based participatory research |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Not reported |
| Quit rates: Between 2002 and 2006, overall smoking prevalence declined from 17.7% to 13.6% (23.2% relative decline, p < 0.01); Flushing 19.5% to 13.7% (relative decline 29.7%, p < 0.01) and Sunset Park 16.9% to 13.5% (20.1% relative decline, p < 0.01) |
| Conclusions |
| Authors: A community-based tailored intervention may increase the impact of population approaches to tobacco control. Documented an additional 2.8% decline in prevalence over a 2-year period in the intervention community beyond the overall 3.3% decrease across Chinese communities attributable to Department of Health policies and programmes. This study builds on two areas: that tailoring programme content and delivery methods may enhance the effectiveness of interventions when trying to engage non-English-speaking immigrant populations and that citywide policy can be generalisable and effective among an immigrant population. Additional targeted efforts in immigrant populations may enhance general population-based policy approaches. Research is needed to develop an evidence base of cost-effective approaches for reaching subgroups who are at greatest risk |
| Reviewers: This intervention was successful in that an additional effect was demonstrated in the intervention community; however, high dropout may have biased the findings. The authors did calculate non-response adjustment factors applied to base weights to derive the non-response adjusted follow-up weight |
| Comments and limitations |
| Self-reported smoking cessation data and high dropout rate at follow-up. No smokers from Sunset Park enrolled in the free nicotine patch programme. All indices showed trends in differences in favour of the intervention community. Chinese-language community-level social marketing campaigns appeared to have the greatest penetration (intervention receipt index 1.48, 95% CI 1.15 to 1.81) |
| Study reference |
|---|
| Webb et al. 2008351 |
| Setting |
| USA; home |
| Inclusion criteria |
| Self-identified as African American, smoked at least five cigarettes per day, could read English, wanted to quit smoking, not enrolled in a smoking cessation treatment and between 18 and 65 years of age |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; self-identified |
| Age (years): Mean: standard intervention: 43 (SD 9.80), culturally sensitive (CS) intervention: 44 (SD 10.79) |
| n: 260; 128 standard, 132 CS; n = 182 completed follow-up |
| Sex: Female: standard 64%, CS 52% |
| Income: < US$10,000: standard 49%, CS 44% |
| Other: Smoking: cigarettes per day: standard: 16 (SD 8.87), CS: 17 (SD 9.42); years smoking: standard: 23 (SD 11.04), CS: 22 (SD 12.13) |
| Description of intervention and control |
| CS intervention: Pathways to Freedom: Winning the Fight against Tobacco, a smoking cessation guide designed for African American smokers, written at sixth-grade reading level, which discusses how smoking impacts African Americans, provides cessation advice and strategies and encourages community organisations to work against the tobacco industry |
| Standard: Culturally sensitive aspects of the CS book were modified to create a generic intervention. Modifications: replacing most of the African American images with cartoons, Caucasians or race-neutral smoking-related pictures; replacing religious and cultural quotations with motivational quotations; using epidemiological data used that addressed the general population; discussion of tobacco marketing for multiple populations, including adolescents and women; replacing the discussion of menthol cigarettes with one of light cigarettes; and no emphasis on history |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 3 months |
| Quit attempts: Under intention to treat, 14.2% of participants in the sample reported 24-hour smoking abstinence, including 13.7% of the CS group and 14.7% of the standard group. A total of 10% of the sample reported 7-day PPA, including 10.7% of the CS group and 9.4% of the standard group; 39% reported making an attempt to quit |
| Conclusions |
| Authors: It is very important to acknowledge the intra-ethnic heterogeneity and differing influences of acculturation. These findings suggest that individual differences in levels of acculturation to the dominant culture affect receptivity to culturally sensitive written interventions. Acculturation had a moderating effect on smoking status but not in the hypothesised direction |
| Reviewers: The authors do not delve too much into whether the intervention was successful or not, as the moderating effect on smoking status was not in the hypothesised direction, such that less acculturated smokers were more likely to achieve 24-hour abstinence if they received the standard materials. No other outcomes were significant. This is a very interesting finding and the reasons given by the authors warrant further analysis |
| Comments and limitations |
| Findings may not generalise to African Americans of higher income or who are in other geographical locations. Follow-up duration was too short. Smoking status not biochemically verified |
| Study reference |
|---|
| Wong et al. 2008466 |
| Setting |
| USA; San Francisco Bay Area, CA |
| Inclusion criteria |
| Participants who reported using a cigarette, cigar or tobacco pipe during the 3 months preceding the baseline interview were considered smokers. Speaking either English or Chinese, not engaging in other assisted smoking cessation efforts and not cognitively impaired |
| Study type |
| RCT |
| Description of population |
| Ethnicity: Chinese American; not reported how ethnicity assessed |
| Age (years): Mean: 58.3 ± 16 |
| n: 464 |
| Sex: 8.6% female |
| Other: 57.9% < high school education, 30.6% high school/trade/some college, 11.4% bachelor/master/doctorate |
| Description of intervention and control |
| Smoking cessation intervention for Chinese American population |
| Intensive intervention (2.5–3 hours of contact): physician advice, 45-minute bedside nurse counselling including video and self-help manual, five telephone contacts within 90 days (at 2, 7, 21, 45 and 90 days), each 10 minutes in length, with NRT and one repeat relapse counselling session with one additional telephone contact for individuals who relapsed. Community collaboration throughout all phases of work. Victory over Smoking manual was recommended. Telephone calls: messages about proper nutrition, physical activity and also enlisting support from family members and friends |
| Minimal intervention (30 minutes of contact): a strong message to quit smoking from primary care physician and/or research nurse, self-help manual with information on pharmacotherapies and a list of smoking cessation programmes available in the San Francisco Bay Area |
| Theory: Social learning theory. Based on social learning theory, the intervention included self-efficacy with three additional resources: (1) information about the health risks of smoking delivered by a nurse or a physician, emphasising the benefit of quitting for the smoker’s particular medical condition, (2) practical information about ways to stop smoking, (3) coping skills to deal with stressful situations to prevent relapse |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: 6, 12 and 24 months |
| Quit rates: Unpublished: self-reported abstinence at 12 months: outpatient (n = 196) intensive arm 34 (SD 0.30) (p < 0.05); outpatient minimal arm 27 (SD 0.25) (p < 0.05); inpatient (n = 89) intensive arm 22 (SD 0.46), inpatient minimal arm 24 (SD 0.48); overall abstinence rates appeared higher at 12 months than at 6 months among outpatients: 28% vs 20% (in both arms) |
| Conclusions |
| Authors: The intensive intervention outperformed the minimal condition at both 6 and 12 months for outpatient but not for inpatient smokers. In contrast to other smoking cessation treatment studies in which abstinence rates decreased over time, the overall abstinence rates appeared to be higher at 12 months than at 6 months, particularly among outpatients [28% vs 20% (in both arms)]. In contrast to previous smoking cessation studies in which 1-year abstinence rates were reported as approximately 25%, the self-reported 1-year abstinence rates in this study were approximately 35% (will need to be verified with saliva cotinine levels) |
| Reviewers: The self-reported abstinence would suggest that the intervention was successful for outpatients in the intensive arm at 6 and 12 months; however, this was not validated with saliva cotinine levels. It also seems that the analysis has been separated by inpatients and outpatients as a post hoc analysis. It appears that the intensive intervention did not show effect when comparing both inpatients and outpatients in the intensive group with inpatients and outpatients in the minimal group. These preliminary study data are currently being analysed; they have not been peer reviewed and were supplied by the authors through personal contact |
| Comments and limitations |
| Paid US$40 for completing baseline interview as well as 6- and 12-month telephone assessments of smoking. Additional US$20 paid for completing a 24-month telephone assessment |
| Study reference |
|---|
| Larson et al. 2009467 (REACH Nashville) |
| Setting |
| USA; Nashville, TN |
| Inclusion criteria |
| African American residents of North Nashville, TN and African American and white residents of Tennessee who were > 18 years |
| Study type |
| Observational study |
| Description of population |
| Ethnicity: African American (97–100% between 2001 and 2005); not reported how ethnicity assessed |
| Age (years): 18–24: 23.5%, 23–54: 37.5%, 55+: 39.0% |
| n: 4578 |
| Sex: 60.9% female (range 59.0–64.0%) |
| Income: Not reported |
| Description of intervention and control |
| Nashville’s REACH 2010 initiative developed community partnerships to promote awareness, education and participatory programmes to prevent and decrease smoking among residents |
| Community-level strategies to increase awareness and knowledge about the effects of smoking; messaging campaigns, including presentations, seminars and documentary-dramas at community centres, senior citizen facilities, neighbourhood association meetings, churches, public schools, universities and medical centres. (1) Physical cues placed in the environment: ‘dump a pack’ garbage cans to encourage people to throw away their cigarettes as a first step toward quitting, (2) initiatives to include awareness of second-hand smoke exposure at work sites including clinics, day-care centres and at public places, (3) ‘never take another puff’ referral cards for smoking cessation classes distributed at businesses and community events |
| Individual-level strategies to enlist and train community members to become advocates, lead smoking cessation classes and encourage current smokers in quit attempts. (1) Recruitment and training of volunteers from businesses and profit and non-profit organisations to facilitate and lead smoking cessation classes, (2) ‘readiness to quit’ seminars for smokers held at local businesses, clinics and community centres to discuss the pros and cons of smoking cessation to facilitate readiness to change. Youth-based strategies that included individual cessation and prevention pledges and contracts |
| Strategies directed to changing policy through education and partnership building; impacting policies at the business or organisational level |
| Theory: Socioecological model |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Each year for 5 consecutive years |
| Number of cigarettes smoked per day: Significant decreasing trend in daily smoking (p < 0.02) and smoking uptake (p < 0.03) in North Nashville. In contrast to the North Nashville community, an increasing trend was observed for quitting smoking (p < 0.01) in Tennessee |
| Conclusions |
| Authors: This study suggests that consistent, cumulative, multiple and multilevel strategies targeted to an African American community may impact smoking behaviours, such as reducing the level of smoking. African Americans in North Nashville may have reduced their cigarette use and fewer residents initiated smoking over the study period; these findings were found for men but not for women. The cumulative frequency of community-based tobacco control initiatives over the 5-year study period corresponded to the linear trends observed. The decline in everyday smoking and differences observed in occasional smoking combined with the decreasing trend of those who reported that they have ever smoked suggests a possible ‘dose–response’ effect of the intervention to decrease heavy smoking and prevent the initiation of smoking. Prevalence of quitting increased among both white men and women in Tennessee whereas no trend of smoking cessation was found in Nashville overall. The existence of the anti-tobacco community campaign for several years in our geographical area suggests a contributory effect on reducing smoking among our population |
| Reviewers: Developing an intervention with strategies at the policy, community and individual level may help to promote smoking cessation and smoking reduction and prevent smoking uptake in African American smokers |
| Comments and limitations |
| Analysis here does not allow for causal interpretation. No countrywide data. Small sample size of African Americans state-wide reduced the statistical power to detect any differences over time. Self-reported data may have been affected by social desirability. Telephone surveys exclude certain populations (institutionalised individuals and those without landlines) |
Adapted physical activity interventions
| Study reference |
|---|
| Carroll et al. 2002302 |
| Setting |
| UK; Leeds, urban |
| Inclusion criteria |
| Women were to be in the contemplation or pre-contemplation stage of behaviour change, to be South Asian, Muslim and living in the Beeston area of Leeds and to have confirmation from their GP that they were fit enough to participate |
| No other inclusion or exclusion criteria are given |
| Study type |
| Qualitative |
| Description of population |
| Ethnicity: South Asian; not reported how ethnicity assessed |
| Age (years): Not reported |
| n: 15 |
| Sex: Not reported |
| Income: Not reported |
| Description of intervention and control |
| Exercise to Health’s pilot project targeted South Asian women at high risk of heart disease and diabetes. It was adapted from the successful Heart Watch and Diabetes Watch programmes. Exercise programmes were twice weekly, with a moderate type of exercise and suitable equipment, and the intervention was located in a church hall in the heart of the community. The hall could be sealed off so that women had exclusive access. All but two women attended five or more sessions |
| Theory: Action research framework |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Measurements were taken at baseline and at 6 and 14 weeks |
| Psychological measures (questionnaire was not repeated at 6 weeks as it was considered too short a time): The follow-up interviews showed that women felt healthier, lost weight, had made positive behavioural changes and had a positive outlook to continuing exercise |
| Conclusions |
| Authors: Women were happy with the scheme and the results and were willing to let other people know about it and to recommend it to others. None of the women experienced any difficulties accessing the programme with regard to the points of view of their families. There was much more demand for the programme than could be provided and this was a missed opportunity. The project appeared to be a success, not just from the point of view of the women but also from the perspectives of the scheme providers |
| Reviewers: A lot of formative work and preparation went into this project and it seemed to have been acceptable to the population. It is unfortunate that the funding ceased and this prevented further intervention and further evaluation. It is particularly unfortunate that none of the physiological measurements is presented as this prevents any assessment of effect |
| Comments and limitations |
| This was a pilot programme and the period of 6 weeks was too short, but it was not possible to continue because there was no more funding. The behavioural and psychological measures were not repeated because 6 weeks was felt too short a time for change. The physiological measures were said to have been repeated at 6 weeks but there was no documentation on the results and therefore we were unable to comment. Further tests are needed of the tools that were used as measures as they had been adapted for this population. There was no comparison group |
| Study reference |
|---|
| Guerin et al. 2003283 |
| Setting |
| New Zealand; Hamilton |
| Inclusion criteria |
| Somali women living in Hamilton, New Zealand; no other explicit criteria given (for the gym membership it was given on a first-come first-served basis) |
| Study type |
| Qualitative |
| Description of population |
| Ethnicity: Somali; not reported how ethnicity assessed |
| Age (years): Average (range): 33 (17–67) |
| n: 37 |
| Sex: 100% female |
| Income: Majority were unemployed and on government benefits |
| Description of intervention and control |
| Three exercise programmes were delivered: an exercise class at a community centre, a 3-month trial membership to a fitness centre with a women-only facility and a walking/sport group. The three classes were delivered independently at different times of the year |
| Community centre classes were held in a facility that had been altered to be culturally appropriate with windows painted over so that the women could not be seen exercising. Between 8 and 40 women attended each session; sessions lasted for 6 weeks (16 classes) and concluded at the start of Ramadan |
| Gym membership was provided for 20 women (first come first served) and was highly subsidised so that it cost only NZ$5 for 3 months |
| The walking/sport group was organised twice a week weather permitting. The women met at a sports field after dark and would walk, jog, play various ball games and participate in other exercises |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: The data were from interviews, observations and casual conversations with women over a year during which these activities were provided |
| Changes in physical activity: Women stated that they would like to have more exercise available to help them be more physically active. It was found that engaging in physical activity was helping to decrease weight gain among this population and improve their physical health (no data reported) |
| Conclusions |
| Authors: Overall, the authors found many benefits for the Somali women in the opportunities provided for increasing physical activity. In working with the women of the Somali community they found that identification of their needs contributed to the success of the programmes. They also found that ongoing communication with the women was the best way to provide opportunities to identify and meet their needs |
| Reviewers: The study is limited by its design/reporting in terms of the conclusions that can be drawn about its effectiveness. However, it provides interesting insights into the adaptation of interventions for a refugee population and some of the unique features that should be taken into consideration |
| Comments and limitations |
| This study is limited by its design and there is limited evaluation of the effectiveness of the interventions |
| Study reference |
|---|
| Newton and Perri 2004350 |
| Setting |
| USA; Florida |
| Inclusion criteria |
| Between 30 and 69 years, sedentary lifestyle (defined as < 1 hour per week of leisure time over the previous 12 months) and good health status (absence of significant medical illnesses and orthopaedic problems that would interfere with walking) |
| Study type |
| RCT (part of a wider RCT) |
| Description of population |
| Ethnicity: African American; self-classified |
| Age (years): 30–69 |
| n: 90 |
| Sex: 81% female |
| Income: 75% had a personal income of at least US$25,000 per year |
| Other: 92% had some college education or more |
| Description of intervention and control |
| Compared effects of three home-based exercise promotion interventions for improving cardiorespiratory fitness and physical activity in sedentary African American adults |
| Physician advice (PA): Minimal treatment corresponding to the recommended exercise guidelines that a health-care provider would typically give to a sedentary individual. After the initial meeting, participants were invited to monthly physician-led meetings in which various health topics were discussed (all health topics were unrelated to altering exercise or eating habits) |
| Standard behaviour exercise counselling (SB): Received 10 group sessions over 6 months. Sessions held weekly during month 1, biweekly during months 2–3 and monthly during months 4–6. Sessions were led by counsellors with graduate training in exercise science and/or behavioural science. Standard written materials were related to key behavioural components; however, materials were not tailored to address issues of particular concern to African Americans |
| Culturally sensitive exercise counselling (CS): Identical to the SB programme with the exception of four key elements: (1) all group members were African American; (2) the sessions were led by African American counsellors; (3) the sessions were conducted at a site located in the African American community; and (4) the programme included materials that were designed to address sociocultural concerns of African Americans regarding exercise |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 6 months post treatment |
| Changes in fitness: Post hoc tests showed significant differences between the SB and PA conditions (p = 0.006) and between the CS and PA groups (p = 0.034). Both exercise counselling groups had greater changes in fitness than the PA group |
| Conclusions |
| Authors: Participants in all three conditions reported an increase in exercise participation; however, only participants in the SB and CS counselling groups demonstrated significant improvements in cardiorespiratory fitness. Participants in the CS intervention reported significantly higher social support for exercise than the other two groups. The CS group was more satisfied with the programme than the other groups. Despite significant changes in fitness in the SB and CS counselling groups, there were no group differences in physical activity. It was hypothesised that those in the PA group were subject to ‘demand characteristics’ and self-reported increases in physical activity while demonstrating decreased fitness levels |
| Reviewers: Improvements in fitness and in physical activity did not differ significantly between the CS and SB groups. Rates of attendance and adherence were also equivalent. It is possible that the CS group may not have included cultural elements of sufficient salience to produce a greater effect than the SB intervention, e.g. the use of testimonials or ‘testifying’, which is a common form of communication among African Americans. CS may have made it easier to obtain social support such as ‘a buddy’ for exercising resulting in increased satisfaction. It is unclear which aspects of cultural tailoring were related to change in social support and participant satisfaction. Acculturation did not moderate the relationship between the intervention groups and outcome measures. This could be because there was not enough variation in acculturation between the participants – the majority were ‘bicultural’ and consequently receptive to information presented from both a culturally tailored and a standard orientation |
| Comments and limitations |
| The majority were highly educated, which may limit the generalisability to a less educated population. Self-reported data. Small sample size limits generalisability and its power to detect between-group differences |
| Study reference |
|---|
| Andersen et al. 2006468 |
| Setting |
| USA; Baltimore, MD |
| Inclusion criteria |
| Adult commuters in the subway station were included; people were excluded if they were carrying items larger than a briefcase, were carrying a baby or child or were judged to be < 18 years of age |
| Study type |
| Observational |
| Description of population |
| Ethnicity: African American, Caucasian or other categories but these were assigned by observers not self-assigned; 8477 were classified as African American, 6689 as Caucasian and 869 as ‘others’ |
| Age (years): 14–31% of the African American participants were > 40 years age in the five different data sets |
| n: 540 people were observed in the pilot phase; 16,035 adult commuters were observed in the study |
| Sex: Not reported |
| Income: Not reported |
| Description of intervention and control |
| Adult commuters in an urban subway station (of a university hospital in Baltimore) were observed while taking the escalators or stairs |
| Pilot phase: People were observed for 1 week and then a sign was put up that encouraged people to use the stairs and people were observed for the following week. This was carried out at one subway stop only |
| Study phase: A culturally sensitive sign was developed. People were observed for 2 weeks before the sign was put up. People were then observed for 2 weeks with the sign present and for a further 2 weeks after the sign was taken down. Data were once again recorded for one week without the sign present at week 7. Finally, the last phase of the study involved putting the sign up once again at week 8 and recording stair use. Data were collected unobtrusively from a distant point above |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: See study phase above |
| Changes in physical activity: African American people increased their stair use when the sign was displayed, from 10.3% (95% CI 9% to 11.5%) to 16.4% (95% CI 15.1% to 17.7%; NNT = 16). Stair use remained elevated 1 week after the sign was removed but returned to baseline levels 3 weeks after removal, and overall stair use did not differ from baseline to 4 weeks after the display of the sign |
| Conclusions |
| Authors: A low-cost culturally sensitive sign can significantly increase the proportion of African American commuters who use the stairs rather than an adjacent escalator in an urban subway station. Given that stair use may be an efficient way to add physical activity into a daily routine, these findings have important public health implications |
| Reviewers: This is an observational study and so it is difficult to draw causal associations. The sample included different people with different age and weight distributions, and all of the variables – ethnicity, age and weight – were judged by observation only. However, observationally, it did appear that significantly more people chose to use the stairs when the sign was in situ |
| Comments and limitations |
| The greatest limitation to this study is that the data collection was carried out by estimating people’s ethnicity, weight and age. The authors comment that there was good agreement between investigators in their judgement, but this does not alter the fact that there was likely a large margin of error in terms of people’s true demographics and particularly their self-assigned ethnicity |
| Study reference |
|---|
| Stewart et al. 2006413 (CHAMPS III) |
| Setting |
| USA; San Francisco, CA |
| Inclusion criteria |
| No explicit inclusion criteria |
| Study type |
| Pre–post |
| Description of population |
| Ethnicity: African American (90%), Asian (2%) and white (8%); not reported how ethnicity assessed |
| Age (years): 97% of African American participants were > 60 years |
| n: 321; 53 participants completed the 6-month follow-up |
| Sex: Not reported |
| Income: Not reported |
| Description of intervention and control |
| Community Health Activities Model Programme for Seniors, CHAMPS II, was diffused to lower-income and minority groups |
| Intervention: A choice-based individually tailored programme providing information, skills training, support and problem-solving through personal planning, regular telephone follow-up, group workshops, newsletters, activity diaries and functional fitness assessments |
| Theory: Social cognitive theory |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Process evaluation was conducted with staff, volunteers, and directors every 6–12 months while the programme was running; participant outcomes were measured at the end of each cohort’s 6-month intervention |
| Changes in calories: 53 participants who completed to 6 months showed an increased expenditure of calories per week of 481 (SD 1939) |
| Changes in physical activity: Increase in hours of physical activity per week of 1.9 (SD 8.0) |
| Conclusions |
| Authors: The project enabled community organisations to implement physical activity promotion programmes. The overarching challenge was to retain the original programme features within each organisation’s resources yet for it to be sustainable. Although the programmes differed from the original research programme they were a catalyst for numerous community-level changes. The findings were said to be able to guide similar projects to reach underserved older adults |
| Reviewers: This intervention did not show any significant effect in terms of increased physical activity although there were trends in this direction. There was a strong community partnership in the intervention. The successes that occurred were the environmental/community changes in the development of new and better recreational facilities and opportunities. This infrastructure has been sustained to 1.5 years by the community |
| Comments and limitations |
| This study has a relatively small sample that completed to 6 months. There is no comparison group. The recruitment was self-referral and prone to bias |
| Study reference |
|---|
| Taylor-Piliae et al. 2006;402 Taylor-Piliae et al. 2006403 |
| Setting |
| USA; San Francisco, CA, urban |
| Inclusion criteria |
| Chinese, ≥ 45 years with at least one major CVD risk factor living in the San Francisco Bay Area, Cantonese or English speaker, not practising Tai Chi in the last 6 months and willing to give written informed consent |
| Study type |
| Quasi-experimental |
| Description of population |
| Ethnicity: Chinese; not reported how ethnicity assessed |
| Age (years): 66 ± 8.3 |
| n: 39 |
| Sex: 69% female |
| Income: The majority reported an income of < US$35,000 per year |
| Other: Most were Cantonese speakers. The majority reported ≤ 12 years of education |
| Description of intervention and control |
| Recruitment occurred through flyers, posters, brochures and newspaper advertisements. Intervention was a 12-week community-based Tai Chi exercise programme in a community centre. The subjects were recruited to cohorts of a maximum of 20 per group and had 60-minute sessions three times a week. Yang Style 24 posture Tai Chi was used, which is thought to have an intensity equal to brisk walking. Each session had a 20-minute warm-up, 30 minutes of Tai Chi and then a 10-minute cool down. Subjects were encouraged to practice at home at least two other days a week and on completion of the 12 weeks they received a CD-ROM of the Master performing the sequence |
| Theory: Minimal theory as was exercise only |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 6 and 12 weeks |
| Changes in physical activity: Subjects were sedentary at baseline but had a significant increase in aerobic endurance over time (p = 0.001) |
| Conclusions |
| Authors: This innovative culturally relevant community-based 12-week Tai Chi exercise intervention appealed to Chinese adults with CVD risk factors and resulted in significant improvements in aerobic endurance. This intervention has the potential to reduce expenditure associated with CVD by facilitating a lifestyle that promotes physical activity while remaining a low-tech, low-cost alternative to exercise |
| Reviewers: This intervention appears to have been highly acceptable to the population and had positive effects on aerobic endurance. A prolonged effect or any effects on weight or other health factors are yet to be demonstrated. This has limited generalisability although it shows that using a form of exercise that is traditional to a population is acceptable and feasible |
| Comments and limitations |
| Possible selection bias – may have included only people interested in Tai Chi and may not be generalisable within this population. No control group and small sample size. Unknown if there is a longer term effect/sustainability |
| Study reference |
|---|
| Young and Stewart 2006397 |
| Setting |
| USA; Baltimore City and Baltimore County, MD |
| Inclusion criteria |
| African American woman, attended study churches or had friends who were church members or lived in the neighbourhood, between 25 and 75 years, did not engage in moderate-intensity activity more than three times a week and indicated willingness to increase their level of physical activity |
| Study type |
| RCT (randomised by church) |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean: active intervention: 48.0 ± 2.2, control: 48.4 ± 2.3 |
| n: 196 |
| Sex: 100% female |
| Income: Not reported |
| Other: Prevalence of obesity (BMI ≥ 30 kg/m2) was 65% |
| Description of intervention and control |
| Participants were randomised to an aerobic exercise or a Stretch N Health intervention |
| Intervention: 1-hour weekly exercise class led by certified aerobics instructors from the African American community who served as role models. An emphasis was placed on optimising social support, and women were paired with a buddy and encouraged to contact them regularly for support. Information handouts and monthly newsletters were given out. Volunteers were trained so that the classes could continue once the trial was over |
| Stretch N Health condition: Free, alternating, weekly low-intensity stretching classes and health lectures. Certified aerobics instructors from African American community led classes. Member of the African American community led the health lectures. Participants were given a list from which to choose relevant topics: healthy eating, stress management, time management skills, meal planning for children and families, and natural herbal remedies. Newsletters with general health messages provided. At the end of 6 months of classes, 1 month of aerobic exercise classes was provided |
| Theory: Resnicow et al.’s two dimensions of cultural sensitivity;35 social cognitive theory |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Not reported |
| Changes in physical activity: Prevalence of no physical activity declined to 32% in the intervention group and 31% in the comparison group. Physical activity measures, estimated daily energy expenditure, kcal/kg/day; activity summary score did not differ between the two groups (p = 0.3) |
| Conclusions |
| Authors: Church-based aerobic exercise intervention did not increase habitual physical activity levels more than a Stretch N Health lecture intervention. Both treatment groups reduced their degree of physical inactivity, although this was not a focus of this trial and may have implications for obesity reduction. From other studies it appears that secondary trials are better at retaining participants than primary prevention trials. Shorter-term intervention and follow-up (3–4 months), brief (< 1 hour) assessments and conducting assessment procedures at convenient community locations are suggested for future studies. Qualitative work was also recommended to understand the values that surround African American women and their attitudes towards physical activity |
| Reviewers: This study was not successful in demonstrating a significant difference in improving physical activity levels when comparing the aerobic intervention with the stretching intervention. However, we agree with the author that results are limited because of low participation. They noted that both groups decreased physical inactivity; however, this is to be expected in an intervention with a physical activity component (as in both conditions). The authors have raised a credible suggestion for further interventions that could reduce attrition – conducting assessment procedures at convenient community locations. Low participation may need to be addressed by increasing social support components, as the authors suggest that baseline levels of social support predicted change in physical activity |
| Comments and limitations |
| Low participation contributed to a lack of significance between group differences in activity levels. Churches were sites rather than true partners in the research process and lacked ownership of the programme; therefore, women were not receiving tailored messages from the pastor or church officials. Authors suggest that the adaptations made in this intervention may not have met the deep structure-level adaptations needed. Trial did not use a true control group. Only 117 (60%) completed the 6-month follow-up physical activity assessment (61% active and 58% comparison). The reasons for this were being unable to schedule, having no interest, not participating in the intervention, being unwilling to be measured, being unable to locate |
| Study reference |
|---|
| Banks-Wallace et al. 2004;469 Banks-Wallace and Conn 2005;470 Banks-Wallace 2007471 (Walk the Talk: a nursing intervention for black women) |
| Setting |
| USA; Mid-Missouri |
| Inclusion criteria |
| African American women, self-reported engagement in non-work- or non-chore-related physical activity for at most 20 minutes per day, no more than 2 days per week, ≥ 18 years, expressed a desire to increase physical activity and either currently treated for hypertension or been notified by a health-care provider that they have hypertension |
| Study type |
| Pilot pre–post single-group design |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean: 50.3 |
| n: 21 |
| Sex: 100% female |
| Income: Not reported |
| Other: All had completed high school |
| Description of intervention and control |
| Pilot 12-month group intervention to increase physical activity among sedentary hypertensive African American women: 3-hour monthly meeting with an at-home walking component. Involved professional and personal storytelling, interactive learning, group physical activity and walking partners, with the aim of enhancing problem-solving skills and social support for walking for cardiovascular health |
| Monthly group sessions: (1) Brief sharing of current life situation by both participants and research team members; (2) professional storytelling; (3) interactive learning about cardiovascular health promotion; (4) group physical activity; (5) debriefing period; and (6) informal visiting while sharing a heart-healthy snack |
| Women walked together during the session, initially for 5 minutes and increasing gradually to 40 minutes. Line dancing was used as a substitute when the weather prevented walking. Participants were instructed to select a walking partner from the group to walk 2 days a week to promote social support. Each woman was given a Stanford Walking Kit to develop a personalised walking outline over a 6-week period |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline, 12-month intervention with 6-month follow-up (18 months) |
| Changes in physical activity: Mean (SD) steps per day taken by participants: baseline (n = 21): 3857.2 (2578.0); 12 months (n = 13): 4059.7 (2721.6), change of +5%; 18 months (n = 15): 5281.6 (3257.0), change of +37% |
| Weight: Mean (SD) weight: baseline (n = 21): 206.1 lb (28.8 lb); 12 months (n = 13): 187.5 lb (29.6 lb), change of –10%; 18 months (n = 15): 213.3 lb (60.2 lb), change of +4% |
| Conclusions |
| Authors: Results from this pilot study are encouraging with respect to the potential of group-level interventions as a strategy for promoting cardiovascular health among hypertensive African American women. Maintained decreases in systolic blood pressure and further decreases in diastolic blood pressure despite regaining weight during the follow-up period. Negligible change in steps taken per day at the end of the 12-month intervention; however, during the 6-month follow-up, walking behaviour increased a mean of 37% over baseline. A follow-on study with a larger sample size and control is needed |
| Reviewers: Longer follow-up allowed detection of sustained/increased walking behaviour after the intervention period. Women were not able to sustain weight change and gained weight from baseline. Effectiveness was difficult to determine because of the small sample size and low follow-up rates. A lot of effort was put into recruitment of 21 participants |
| Comments and limitations |
| Single-group design and small sample size make it impossible to accurately evaluate the clinical effectiveness of the intervention with respect to decreasing CVD risk factors. Intended to triangulate walking diaries, pedometers and CAPSPAQ but implausible physical activity reports on CAPSPAQ and failure to record information on walking calendars forced elimination of these outcome measures. Because of the variability among individual participants across data collection periods and the overall small sample size, more appropriate to discuss trends rather than statistical significance |
| Compensation: US$10 for competing data assessments. Personal pampering items, books by African American authors, candles and note cards were raffled off every 3 months to encourage participation in intervention meetings |
| Pedometers do not provide information about activity intensity or duration – proposed using accelerometers along with pedometers in future studies to measure walking intensity and duration along with changes in steps per day |
| Study reference |
|---|
| Huhman et al. 2005;285 Huhman et al. 2007;286 Huhman et al. 2008287 (the VERB campaign) |
| Setting |
| USA; national |
| Inclusion criteria |
| Children aged 9–13 years |
| Study type |
| Prospective longitudinal quasi-experimental study |
| Description of population |
| Ethnicity: Multiethnic: African American, Asian American, American Indian, Hispanic; not reported how ethnicity assessed |
| Age (years): Not reported |
| n: 3120 parent–child dyads in the initial survey and 2257 in the second evaluation |
| Sex: Not reported |
| Income: Not reported |
| Description of intervention and control |
| VERB was a campaign to promote physical activity to ‘tweens’ in the USA by delivering messages to a general audience and then to ‘tweens’ in various racial or ethnic groups. Messages were marketed on television, in print, on billboards, through a website and through school and community promotions. A portion of the marketing was directed at parents. Six advertising agencies were employed to undertake the general and targeted messages |
| The African American programme started sponsorships with music groups and developed a theme urging parental involvement; it also utilised sponsored music events and sports events to deliver the messages. The Asian American programme shifted the focus to parents promoting the benefits of daily exercise; they encouraged parents to be active with their children and marketed the messages at cultural events |
| Theory: Theory of planned behaviour and social cognitive theory were used in planning this intervention |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to years 2 and 4 |
| Changes in physical activity: An association between increasing awareness and increasing activity was not initially found and the marketing was reviewed and intensified; by 2 and 4 years there were increases in activity associated with increased awareness |
| Knowledge: Outcomes for African American ‘tweens’ showed that, although the initial reach of the programme was not as large as for white or Hispanic tweens, there were no significant differences after 4 years when levels of awareness were 72%. Awareness among Asian Americans was 45% and 63% at 2 and 4 years, respectively |
| Conclusions |
| Authors: The VERB campaign continued to positively influence children’s attitudes to physical activity and their physical activity patterns. With adequate and sustained investment, health marketing shows promise to affect the attitudes and behaviour of children |
| Reviewers: This study shows some positive effects of a national media campaign for physical activity that was targeted to specific ethnic minority groups. However the study design has inherent limitations |
| Comments and limitations |
| All data in the longitudinal study were self-reported. Reverse causation could mean that physically active children noticed the messages more than non-active children. The response rate to the telephone survey was 32% after 2 years |
| It is interesting that this paper talks about health media campaigns and how, generally, only one message is developed, which, if tailoring at all, will be translated and include ethnic-specific characters in the advertising. The authors felt that this was not enough and that there needed to be a separate approach, formative evaluation and campaigns which, although true to the original message, were also developed specifically for the target populations |
| Study reference |
|---|
| Whitt-Glover et al. 2008308 |
| Setting |
| USA; suburban community in North Carolina |
| Inclusion criteria |
| Self-identified as black, ≥ 18 years, not currently meeting recommendations for moderate or vigorous physical activity [self-report of < 30 minutes of moderate physical activity on ≤ 5 days per week, ≤ 20 minutes of vigorous physical activity on ≤ 3 days per week or carrying out recommended moderate and physical activity but in bouts lasting < 10 minutes (assessed using a modified International Physical Activity Questionnaire)], responding ‘no’ to all questions on the Physical Activity Readiness Questionnaire |
| Study type |
| Pre–post intervention, single-group design |
| Description of population |
| Ethnicity: Black; self-identified |
| Age (years): 52 ± 14 (range 20–83) |
| n: 87 |
| Sex: 89% female |
| Other: 96% had high school education or higher |
| Description of intervention and control |
| A 3-month faith-based physical activity intervention to determine the effect of daily walking and moderate- and vigorous-intensity physical activity among sedentary black participants (particularly in bouts lasting 10+ minutes) |
| A total of eight group sessions focused on behavioural strategies. Weekly sessions included 30 minutes of moderate physical activity and a 60-minute discussion session. Group leaders led weekly intervention sessions at churches |
| Certified fitness instructor conducted the 30-minute moderate physical activity session and provided an opportunity to practice. Participants kept weekly logs of pedometer step counts to self-monitor walking. Weekly summary to track progress given to participants. Incentives were used to encourage an increase in daily moderate physical activity to at least 30 minutes by engaging in moderate-intensity walking. Each church pastor acted as a liaison and was paid a modest honorarium. They received a group leader training manual and all session materials to facilitate continued implementation after completion of the study |
| Theory: Social cognitive theory |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and after 3 months |
| Changes in physical activity: Self-reported increase in minutes per week of moderate physical activity was 66.9 ± 77.6 or 251% (p < 0.01) and in minutes per week of vigorous physical activity was 43.8 ± 66.4 or 438% (p < 0.01) |
| BMI: BMI remained stable over 12-week intervention |
| Weight: Weight remained stable over 12-week intervention |
| Conclusions |
| Authors: Statistically significant increases were demonstrated in the number of steps per day after 4 weeks and after 12 weeks, and significant changes in moderate physical activity and vigorous physical activity were seen after 12 weeks. This study suggests that a faith-based programme was successful in increasing physical activity levels over a 3-month period among sedentary black adults. It is surprising that weight did not change; however, the increase in steps may have prevented excess weight gain. Changes in steps per day did not reach the recommended 10,000 steps per day. It remains unclear how big an increase in steps per day is necessary for significant changes in clinical outcomes |
| Reviewers: Although there were significant increases in steps per day, and increases in physical activity, there were no observed changes in weight and BMI. Agree with the authors that the increase in steps per day may not have been enough to result in clinically meaningful changes (e.g. in weight); however, weight maintenance would also be an appropriate objective. With regard to collaborative research with churches, randomisation may not be appropriate in churches |
| Comments and limitations |
| Lack of a control group because this was a pilot study and reluctance of some faith-based communities to be a part of a randomised study. Small sample size – study had a large enough sample to test for meaningful differences in daily walking as assessed by pedometers. No objective data for participation in moderate physical activity and vigorous physical activity (tried to use accelerometers but encountered adherence issues and were therefore unable to use data for analyses). Generalisability of findings may be limited in the general population (e.g. those who do not attend church) |
| In community church-based interventions, high retention and participation are often reported, for example in this study the participation rate was 6.2 ± 1.8 of 8 sessions |
| Study reference |
|---|
| Wilbur et al. 2008472 |
| Setting |
| USA; Midwestern urban; centres in predominantly African American communities |
| Inclusion criteria |
| 40–65 years |
| Study type |
| Quasi-experimental design |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean (SD): 48.6 (6.0) |
| n: 156 intervention, 125 control |
| Sex: Not reported |
| Income: Not reported |
| Description of intervention and control |
| A 12-month trial of a home-based walking intervention enhanced by behavioural strategies targeted and tailored to African American women for the intervention group. A 24-week intensive adoption phase followed by a 24-week maintenance phase for the intervention group. Weight loss not a focus of the intervention |
| All participants: Individualised orientation and tailored walking prescription (walk three times a week within target heart range with gradual progression to 20–30 minutes). Places and times to walk determined by women. All received heart monitors to wear during walking, log books, toll-free telephone number, coupon to buy walking shoes and newsletters with walking tips |
| Intervention: Four targeted workshops held at community health centre, 6 to 10 women per workshop, 60 minutes long, followed by weekly tailored telephone calls over 24 weeks [weekly for 3 weeks, then every other week for 14 weeks and monthly during maintenance phase (weeks 25–48)]. Women reported walking frequency via an automated telephone system |
| Theory: Intervention guided by the client–professional interaction component of the interaction model of client health behaviour (health information, decisional control, social support); previously successful strategies based on social cognitive theory and the transtheoretical model incorporated into this intervention to move women from contemplation into the preparation and action stages of motivational readiness |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 24 and 48 weeks |
| Changes in physical activity: Intervention group: increase from 19.5% to 44.2% at 24 weeks and 41.6% at 48 weeks; control group: increase from 23.3% to 41.8% at 24 weeks and 34.9% at 48 weeks |
| BMI: No significant changes in BMI from baseline to 24 weeks and 48 weeks for either treatment group – BMI stable |
| Conclusions |
| Authors: Using objective monitoring and self-monitoring (heart rate monitors, walking logs and automated telephone response reporting) provided multiple sources of data for more accurate indication of adherence. Self-reported improvements in physical activity were found, but no difference was detected between the treatment groups. Both groups maintained BMI for the duration of the study and did not gain any weight. This suggests a positive effect of exercise |
| Reviewers: Significant increase in fitness suggests that this intervention was successful even though the women did not meet the recommended time spent walking at moderate intensity. It appears that group support was important for adherence and booster workshops (in addition to or instead of telephone calls) may be helpful in further interventions. The automated telephone response system is novel and may suggest a new way of getting women to self-report at their convenience. In other populations (with computers) online reporting may be a promising next step. Because the objective was weight maintenance, a result of maintained BMI can be considered successful |
| Comments and limitations |
| Self-report measures might not be sensitive enough to detect differences between treatment groups for physical activity. In addition, women may have provided socially desirable responses as they may have connected personally with their respective intervention staff. All women reported walking every week via a toll-free number accessible at any time. The correlations between the telephone response system and heart rate monitor data with the walking log were 0.79 and 0.73 respectively. Women assumed not to be walking if no data were reported; thus, walks may be under-reported. Adoption phase: intervention group attended an average of 2.4 of the 4 workshops and received an average of 7.2 tailored calls. Another change was the movement from telephone landlines to mobile phones, which may have caused under-reporting if women were limiting their mobile telephone minutes. US$50 was given after each data collection |
Adapted nutrition interventions
| Study reference |
|---|
| Hawthorne and Tomlinson 1997407 |
| Setting |
| UK; Manchester, hospital outpatient clinic or diabetic clinics in 10 general practices |
| Inclusion criteria |
| Pakistani patients with type 2 diabetes mellitus attending Manchester Diabetes Centre and 10 neighbouring general practices were entered into the study |
| Study type |
| RCT |
| Description of population |
| Ethnicity: Pakistani Muslim; not reported how ethnicity assessed |
| Age (years): Mean (range): intervention: 52 (50–54), control: 54 (51–58) |
| n: 201; 112 intervention, 89 control |
| Sex: 56% female |
| Income: Not reported |
| Description of intervention and control |
| RCT of pictorial flashcard one-to-one education to improve knowledge about diabetes, increase self-caring behaviour and affect attitudes to diabetes |
| A total of 10 coloured photographs produced by a dietician, link worker and professional photographer were enlarged to A3 and laminated. Each card covered one or more teaching objectives. Interviews were used alongside the flashcards and were videotaped. Interviews (20 minutes) took place in the hospital clinic, at GP surgeries or at the participants’ homes, in the language that they felt most comfortable using |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 6 months |
| Knowledge: All outcomes measuring knowledge increased in the intervention group, e.g. increase in knowledge about individual food value scores from 71% to 84% (% correct) (analysis of variance adjusted difference in knowledge scores +7.8%, 95% CI +4.9% to +10.7%). Between groups: at 6 months, intervention group showed significant improvements in knowledge scores, increased self-caring behaviours and some changes in attitudes to diabetes and diabetes service. Few changes in control group over the 6 months |
| Conclusions |
| Authors: Health education programmes can empower Asian people with diabetes to take control of their diets, learn to monitor and interpret glucose results and understand the implications of poor glycaemic control for diabetic complications. Low literacy levels and inexperience of formal education did not stop patients from learning about diabetes and how to control it. For this group, health education needs to be delivered in a combination of ways (flashcards, one-to-one interviews and reinforcement) |
| Reviewers: This study is poorly described and the significant results reported often do not include the percentage change and significance level. The study showed significant changes in knowledge regarding foods in the intervention group. More description of the control group is needed as it is unclear what they were receiving |
| Comments and limitations |
| Acceptability: patients were positive about the education received and felt empowered. Few people suggested improvements to the teaching method. Flashcard showing pictures of foods one could eat with diabetes and another showing sites of diabetic complications were the most popular |
| The control was not described and it was unclear what happened with the control group. Many patients did not want others to know that they were diabetic and they felt unable to dictate their food choices publicly and found it difficult to refuse food in social situations. Education level needs to be accounted for when designing health education programmes (culturally acceptable and appropriate to literary skills). Patients preferred one-to-one opportunistic health education at clinics rather than organised group sessions, even if these were single sex (this is in opposition to other diabetes education studies in which group formats were thought to be acceptable as well) |
| Study reference |
|---|
| Campbell et al. 1999326 |
| Setting |
| USA; eastern North Carolina |
| Inclusion criteria |
| Participants were a one-eighth random subsample of the sample in the Black Churches United for Better Health (BCUBH) project. The criteria for that study were that participants were members of African American churches in 10 rural counties. Members had to be active adult members – defined as those who participated in worship services or church activities at least once per month |
| Study type |
| RCT (part of a larger study, the BCUBH project) |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): ≤ 50 years for 44.7% EXP (expert) group, 49% SPIR (spiritual) group, 44.7% control group |
| n: 459 participants; 109 in the expert (EXP) group, 108 in the spiritual (SPIR) group, 242 control group |
| Sex: EXP group: 74% female, SPIR group: 73% female |
| Income: In both groups about 64% had a household income of < US$20,000 a year |
| Other: 60.5% and 48.3% in the EXP and SPIR groups, respectively, had a high school education or more |
| Description of intervention and control |
| This intervention compared two different computer-tailored messages designed to promote fruit and vegetable intake among African American church members, who were part of a bigger multicomponent trial. Both sets of messages were tailored to the same baseline variables, were formatted similarly to resemble church bulletins and incorporated cultural themes such as African American recipes and artwork; however, one set was generated by nutrition experts and used scientific research as the source (EXP) whereas the other set was put together by pastors and referenced God and scripture (SPIR). Both of these groups were evaluated and compared with a delayed intervention control group who during the intervention did not receive any bulletins |
| For the bulletins there were 20 different personalised messages drawn from a library of several hundred messages and chosen based on responses to the baseline questionnaire. Tailored feedback included text and graphics showing the participant’s current fruit and vegetable intake and responses to their perceived risk of cancer, perceived benefits of eating fruit and vegetables, stages of change, perceived barriers and social support. They were also tailored to the person’s name and church title (Sister or Brother). Each bulletin also contained one of several randomly chosen low-fat recipes for a traditional African American fruit or vegetable dish |
| The EXP bulletins stated that they were based on the latest research and had messages about social support, the top three barriers to eating fruit and vegetables, artwork depicting families and an article on ‘Why Doctors Want You to Eat Healthy’. The bookmark in the EXP included the statement ‘Eat 5 servings of fruit and vegetables a day for better health’ |
| The SPIR bulletins began with a message form the pastor and his photograph. They included church-oriented artwork, a five-a-day grace and messages with spiritual and biblical themes. There was an article on ‘Why God Wants You to Be Healthy’ and a bookmark with a passage from the book of Genesis |
| Theory: Bulletins tailored to stages of change |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Surveys were undertaken at baseline, 1 year (subsample) and 2 years |
| Fruit and vegetable consumption (7-day FFQ validated in subsample with 3-day food records): Fruit and vegetable consumption at 2 years had increased for the two intervention groups compared with the control group. The EXP group consumed an average of 4.8 daily servings, the SPIR group consumed an average of 4.9 daily servings and the control group consumed 3.8 daily servings. This difference was significant (p < 0.005). There was no significant difference at follow-up between the EXP and SPIR intervention groups |
| Conclusions |
| Authors: The authors conclude that this intervention was successful for both groups, but that the effect of the tailored bulletin cannot be separated out from the other components of the BCUBH intervention as a whole. Although there was no significant difference between the two intervention groups in terms of fruit and vegetable consumption, there was a finding that the SPIR bulletin was perceived as significantly more trustworthy than the EXP bulletin |
| Reviewers: This was a very interesting study as it added an additional adaptation to an already adapted intervention to see if either expert or additional spiritual content would enhance the intervention |
| Comments and limitations |
| Included the use of self-reported data. Also, there was a delay between the completion of the survey data and the delivery of the bulletins and this may have reduced their relevance as information may have changed over that time. The effect of the bulletin cannot be separated out from the effect of the overall study |
| Study reference |
|---|
| Campbell et al. 1999320,473 [Black Churches United for Better Health Project (BCUCH)] |
| Setting |
| USA; eastern North Carolina, rural |
| Inclusion criteria |
| Members of African American churches in 10 rural counties. Members had to be active adult members – defined as those who participated in worship services or church activities at least once per month |
| Study type |
| RCT (randomised by county) |
| Description of population |
| Ethnicity: 98% African American with 1% multiracial and 1% ‘other’; not reported how ethnicity assessed |
| Age (years): Mean: 53.8 |
| n: 2519 |
| Sex: 73% female |
| Income: 59% reported household incomes < US$20,000 per year |
| Other: 67% had at least a high school education |
| Description of intervention and control |
| Churches in the five intervention counties received a planned five-a-day intervention programme and the other churches did not receive any programme activities until after the completion of the 2-year follow-up survey |
| As well as being culturally tailored, the materials were individually tailored with people receiving personalised messages and feedback based on survey information regarding their intake of fruit and vegetables, their stage of change, barriers, beliefs and social support. The church was also supplied with monthly packets of materials including brochures, posters, banners, bulletin board materials, idea sheets and church bulletin inserts |
| Activities included gardening; educational sessions (including modifying cooking methods and classes on canning and freezing produce); cookbook and recipe tasting (cookbooks put together from members’ recipes modified to include five-a-day and given to all members); serving more fruit and vegetables at church functions; lay health advisors who attended training sessions on topics such as providing social support and helping members to advance stages of change; community coalitions that met to plan community events; pastor support (encouraged to promote the project from the pulpit); grocer–vendor involvement (materials designed to promote locally grown produce such as recipe cards, coupons and farmers’ market posters were distributed to the church members and also to local grocery stores); church-initiated activities |
| Theory: Used an ecological framework targeting activities at the individual, social network and community levels. Also used stages of change transtheoretical model, social cognitive theory and social support models and the PRECEDE–PROCEED model |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 2 years |
| Changes in fruit and vegetable consumption: There was an increase in fruit and vegetable consumption in the intervention group to 4.45 servings compared with 3.60 servings in the delayed intervention group (difference of 0.85 servings, p < 0.0001) |
| Knowledge: OR of 1.8 for the intervention group vs the delayed group for an increase in knowledge that five or more daily servings are needed for health |
| Conclusions |
| Authors: This RCT of a five-a-day intervention in black churches showed a positive result in achieving dietary behaviour change. The observed effect size (0.85 servings) was greater than the half-serving increase projected in the study design and is impressive considering that all eligible subjects were included regardless of their level of participation in the project activities. In this project the institutional support and social networks of the church provided an effective avenue for diffusion of the five-a-day message. Also, partnering with the churches results in the potential for long-term maintenance and institutionalisation of the programme |
| Reviewers: This intervention appears to have been successful within the church setting with changes observed in knowledge and behaviour. If the programme was to be continued it would be interesting to see if there was ultimately any change in anthropomorphic measures or in health status |
| Comments and limitations |
| Limitations included findings being based on self-reported information, which is subject to response bias. Biomarkers that could have been used to validate the findings, such as carotenoid levels, were not assessed in this study. Anthropomorphic measures such as weight and height were also not determined |
| Study reference |
|---|
| Kristal et al. 1999474 [Women’s Health Trial: Feasibility Study in Minority Populations (WHT: FSMP] |
| Setting |
| USA; Atlanta, GA, Birmingham, AL and Miami, FL |
| Inclusion criteria |
| 50–79 years, postmenopausal and consumed at least 36% of energy from fat as estimated from a FFQ administered during screening |
| Study type |
| RCT |
| Description of population |
| Ethnicity: Black, Hispanic and white; self-identified |
| Age (years): Mean: 59.6 ± 6.7 |
| n: 1702 of whom 530 were black |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| Low-fat diet intervention with group sessions: met weekly for 6 weeks, biweekly for 6 weeks and monthly for 9 months. Didactic nutrition education and activities to provide motivation for sustained dietary change |
| Nutrition intervention delivered in group sessions led by centrally trained registered dieticians. Sessions integrated both nutritional and behavioural topics and consisted of problem-solving, role-playing, sharing experiences and food tasting. Each participant received a personal goal for fat intake based on their height and estimated energy intake determined from a FFQ at baseline. Self-monitored by self-administered and scored ‘fat scan’. Participants selected the specific changes in food choices and food preparation methods that best fit their own eating patterns, preferences and lifestyle |
| No information reported for control condition |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 6 months post randomisation |
| Changes in dietary fat: No differences across race/ethnic groups in overall intervention effects on total grams of fat consumed. Compared with the white group, intervention effects were significantly larger among the black group for consuming poultry (–2.5 g, p < 0.001) and fish (–1.0 g, p < 0.001), and smaller for added fat (–8.9 g, p < 0.05), dairy foods (–1.3 g, p < 0.05) and baked goods (–2.8 g, p < 0.05) |
| The authors interpreted a difference in intervention effects between race/ethnic groups of 10 as meaningful (although not statistically significant) but this corresponds to 1.3 percentage points in per cent of energy from fat |
| Conclusions |
| Authors: The study demonstrated that, if properly designed, a single nutrition intervention programme can work well even in groups with culturally diverse dietary patterns. The largest decreases in all race/ethnic groups between baseline and 6 months were in fat from added fats, red meat and baked fats. There were only modest differences across race/ethnic groups in sources of fat, which suggests that the intervention was effective in lowering fat from all food groups |
| Reviewers: This intervention was successful in lowering fat intake in all ethnic groups, which suggests that a more inclusive programme that is sensitive to multicultural values and practices can be successful. Reasons why the intervention was successful include that it was broadly inclusive of culturally diverse dietary and lifestyle patterns and it was designed to accommodate individual dietary patterns and food preferences rather than prescribe specific foods or menus. People are likely to utilise different practices and are not limited to their own ‘cultural’ practices |
| Comments and limitations |
| The specific aim of this study was to test whether a single nutrition intervention programme would be effective among women with markedly different culturally associated dietary patterns. It is difficult to comment on the intervention in terms of cultural appropriateness when it was supposed to appeal to everyone. There were two substantial differences in sources of fat and dietary patterns. At baseline, the black group consumed more fat from meat, poultry and fish and used high-fat preparation methods such as frying, not removing skin from chicken and not trimming excess fat. The white group ate more fat added to foods as flavouring, e.g. fats added to vegetables or on bread. Consistent with these baseline differences, intervention effects were larger for the white group for avoiding fat as flavouring and for the black group for modifying meat to be lower in fat. Results in this paper are reported as the black group compared with the white group, rather than with the control group. This makes it difficult to determine whether there was an actual intervention effect |
| Limitations include that the intervention may not be generalisable and that participants had high fat intakes at baseline, were interested in nutrition and health and were highly motivated |
| Study reference |
|---|
| Snowdon 1999475 |
| Setting |
| UK; Luton, Bedfordshire |
| Inclusion criteria |
| No details of inclusion or exclusion criteria except that participants were women and were not recruited because of health needs |
| Study type |
| Qualitative |
| Description of population |
| Ethnicity: South Asian; not reported how ethnicity assessed |
| Age (years): Not reported |
| n: 20 |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| Practical cookery clubs held by trained community members to demonstrate to local women how to make their dishes in a healthier way without affecting the taste. Club leaders were active members of the local community who were trained and received resources and then were asked to recruit 10–12 women from the community (not particularly targeting those with health needs) who have a shared language. The club was run in a local community centre or suitable kitchen over three sessions each lasting 2 hours. During the sessions the women all prepared four or five dishes using healthier recipes from the pack; they worked in small groups under the guidance of the leader and then tasted and discussed all items prepared |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: 12–18 months |
| Knowledge: At the 12- to 18-month follow-up all of the women remembered the main messages of reducing fat, sugar and salt intake, felt that they had made changes in their diet since attending the club and gave examples of changes that included using less salt, less oil, oil instead of ghee and more fruit and vegetables and grilling more food |
| Conclusions |
| Authors: The evaluation of these starter clubs has demonstrated that this model of helping individuals to follow healthier diets was effective. All of the responding participants enjoyed attending the sessions and would recommend them to their friends. All had used the ideas in their homes and most reported positive responses from their families. Those who had not tried them had been worried about how the male members of their families would respond. The clubs subsequently have been run in Urdu-, Gujeranti-, Punjabi- and Bengali-speaking communities in Bedford and Luton. The impact on the participants as indicated by self-completed questionnaires has been similar |
| Reviewers: The sessions appear to have been effective but there are no objective measures. They appear feasible and acceptable in this population. There is relatively little detail of adaptations or any theory |
| Comments and limitations |
| This study includes a limited sample and there is no control group. The outcome measures are self-reported |
| Study reference |
|---|
| Resnicow et al. 2000;335 Resnicow et al. 2001325 (Eat for Life) |
| Setting |
| USA |
| Inclusion criteria |
| Individuals aged ≥ 18 years from Baptist and Methodist churches (including African Methodist Episcopal) were included |
| Study type |
| RCT (randomised by church) |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean (range): 44 (18–87) |
| n: 1011 were initially recruited from 14 churches and 861 were assessed at 1-year follow-up |
| Sex: 73.3% female |
| Income: Not reported |
| Description of intervention and control |
| A multicomponent intervention to increase fruit and vegetable intake among African Americans that was delivered through black churches |
| The churches were assigned to three groups. One group was a comparison, one was a self-help intervention with one telephone cue call and the last was a self-help intervention with one cue call and three counselling calls. The telephone counselling was based on motivational interviewing. The comparison group received standard nutrition education materials initially and culturally sensitive intervention materials 1 year post intervention |
| Theory: Motivational interviewing was central to the counselling |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: 1-year follow-up |
| Changes in fruit and vegetable consumption: The net differences between the motivational interviewing group and the comparison group were 1.38, 1.02 and 1.21 servings of fruit and vegetables per day for the 2-item, 7-item and 36-item FFQs, respectively. The net differences between the motivational interviewing group and the self-help group were 1.14, 1.10 and 0.97 servings for the three questionnaires, respectively |
| Changes in dietary fat: Low-fat preparation practices improved significantly in the motivational interviewing group |
| Conclusions |
| Authors: Motivational interviewing appears to be a promising strategy for modifying dietary behaviour, and black churches are an excellent setting to implement and evaluate health promotion |
| Reviewers: This study suggests that churches are a good setting for health promotion interventions for African American populations. It shows that it is not enough to adapt the materials if people are not motivated to use them, and the addition of motivational interviewing/or the additional contact with a counsellor appears to provide this motivation and produces a more effective intervention |
| Comments and limitations |
| Monetary incentives for the churches were donated according to the number of people who stayed in the intervention |
| Limited by the self-reported measures although the use of multiple measures will have improved reliability and validity and the correlation with serum carotenoids has added verification; however, this is still prone to social desirability bias. There may have been sampling bias as sampling occurred on a first-come fist-served basis in each church and it is unclear if these participants were representative of the wider church population. The improvement with motivational interviewing may be due to the additional contact with a counsellor and not the techniques involved; this needs further study with a group receiving the same contact but no motivational interviewing technique. There could have been a change in the reporting of intake that was due to learning about portion sizes rather than a real change; however, there was no change in knowledge of portion size, which tends to suggest that this would not have occurred |
| Study reference |
|---|
| Auslander et al. 2002;298 Williams et al. 2006307 [Eat Well Live Well (EWLW) nutrition programme] |
| Setting |
| USA; St. Louis, MO |
| Inclusion criteria |
| African American women aged 25–55 years and living in the intervention neighbourhood were eligible if they did not have diabetes, were not pregnant and were > 20% over the ideal body weight as determined by self-reported BMI (> 27 kg/m2) |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean: treatment group: 41.2 ± 7.8, control group: 40.2 ± 8.2 |
| n: 294 African American women; 138 treatment group, 156 control group |
| Sex: 100% female |
| Income: US$1367.8 ± US$1047 treatment group, US$1619.1 ± US$1206.7 control group per month |
| Other: 33% of the treatment group had a high school education or less compared with 43.6% of the control group |
| Description of intervention and control |
| Community-based dietary change programme for African American women at risk of diabetes. The primary focus was to reduce dietary fat intake and increase low-fat dietary practices by tailoring the intervention to participants’ readiness to make changes in their diet. Weight reduction was encouraged but the major emphasis was on lowering fat |
| Intervention: Peer educators were African American women from the community. The manual-based programme consisted of six group sessions (six to eight people per group) and six individual sessions with a peer educator integrated over the 3-month intervention |
| Control: Did not receive any intervention in the treatment or follow-up phases but were given a self-help workbook that reflected the content of the programme and offered a half-day workshop on healthy low-fat eating after their follow-up assessment |
| Theory: Stages of change, community organisation theory |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Evaluated at post test (3 months after baseline) and then at follow-up (6 months after baseline) |
| Changes in dietary fat: The treatment group reported significantly more low-fat dietary patterns (p < 0.0001) at both post test and follow-up. There was also a difference in dietary fat intake with the treatment group reporting significantly less fat intake (p < 0.0001) and this was maintained post test and at follow-up. The actual percentages were a reduction from 35.9% to 32.1% (post test) and 32.3% (follow-up) for the intervention group compared with 36% to 35.6% (post test) and 34.5% (follow-up) in the control group |
| Knowledge: At post test there was a significant difference between the groups in knowledge about fat in the diet (p < 0.0001) |
| Conclusions |
| Authors: The gathered data indicated that a stage-based intervention conducted by trained peer leaders in the community was effective in changing dietary patterns and reducing fat intake among low-income African American women. A peer-led approach with the collaboration of a community organisation that is located in the target neighbourhood holds promise for reducing the risk of diabetes among lower-income women |
| Reviewers: This study shows an effective intervention for reducing fat intake among African American women at risk of diabetes. The changes appear to be sustained for 3 months after the 3-month intervention ceased (6 months after baseline). This does not seem to translate into any change in weight or BMI, but may have other health benefits and, as the authors state, a reduction in weight was not a focus of the intervention. The intervention was not designed in a way to allow us to evaluate the effectiveness of the adaptation |
| Comments and limitations |
| There may have been some effect in the control group of completing the three 45-minute FFQs over the study that might have made them think more about their diet and make dietary changes and thereby reduce the difference between the intervention and the control groups. Measures were self-reported. This was a convenience sample of women and may not be generalisable |
| Study reference |
|---|
| Haire-Joshu et al. 2001;304 Haire-Joshu et al. 2003;303 Eyler et al. 2004305 (Hi 5, low fat) |
| Setting |
| USA; St Louis, MO, urban |
| Inclusion criteria |
| African American parents in the Parents as Teachers (PAT) programme who were considered to be high risk (single parents, low income, ethnic minority, living with stressors such as serious illness, recent divorce or death) |
| Study type |
| Group randomised nested cohort with parents as the unit of analysis |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean (range): 29 (16–77) |
| n: 738 |
| Sex: 98% female |
| Income: 40% of parents earned < US$20,000 per year |
| Description of intervention and control |
| Culturally appropriate dietary intervention developed in partnership with PAT, which is a national parent education programme free to all parents of children from birth to 3 years |
| There were six intervention and six control sites. Parent educators recruited high-needs African American parents to the study; these parents are entitled to additional visits funded by the state. These parents were sent a packet of materials including pictures of foods used to guide the estimation of portion sizes. There were five personal visits with instruction on assessing current food intake, reading and interpreting nutritional labels, comparison shopping, choosing low-fat foods when eating out and recipe modification. There was also a visit that taught the parents how to model dietary behaviours to their children |
| Theory: Guided by community organisation principles with an ecological approach; curriculum incorporated social cognitive theory (particularly observational learning, goal-setting and behavioural capability); the approach was also guided by the family strength model, consistent with an Afrocentric approach that recognises the resilience of African American families rather than focusing on potential deficits; adult learning theory was also employed |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Not reported |
| Changes in fruit and vegetable consumption: A higher percentage of the intervention group (53%) than the control group (41%) increased their fruit and vegetable intake (p = 0.002). The intervention group parents achieved an increase in fruit and vegetable intake of 0.53 (p = 0.03) |
| Changes in dietary fat: The intervention group’s fat intake decreased from 37.88% to 36.21%, a change of 1.7% calories from fat (p = 0.07) and they also improved their performance of dietary behaviours (p = 0.004). A higher proportion of intervention group parents reduced their intake of calories from fat to < 30% (p < 0.03) |
| Conclusions |
| Authors: This intervention was effective and is appropriate for national adoption by over 2000 PAT sites with the potential to impact the dietary intake of African American parents nationwide |
| Reviewers: This intervention appears effective in changing parental behaviour although perhaps not as effective as hoped in changing role modelling of dietary behaviours to their children. Its greatest advantage is the mode of delivery and ability to be disseminated widely throughout the existing PAT programme; however, this partnership involved negotiation and resulted in fluctuations of what elements of the programme were deliverable in different settings and with the sometimes competing interests of the existing programme |
| Comments and limitations |
| The study did not show a significant increase in parental modelling of healthy dietary behaviours to children but this may have been because the control group were also in the PAT programme, which has parental modelling as a core component, and therefore the parents were used to the importance of role modelling from the outset. A larger difference may have been seen if this had not been the case |
| There was also some lack of consistency of the intervention because, to be consistent with the philosophy of PAT, the intervention was delivered at teachable moments and not when there were other priority needs. Therefore, the course in its entirety was delivered to only 40% of the participants. This was due to the participatory nature of the research, which gave it more sustainability over time, and it is likely that over time more of the intervention would be delivered and greater efficacy observed. The study relied on self-reported information, which may be subject to reporting bias (to enhance accuracy everyone received information about portion sizes) |
| Because of the setting of this intervention it has the possibility to be extended to a very wide audience. The intervention considered dissemination and sustainability as key components in the design |
| Study reference |
|---|
| Resnicow et al. 2004;476 Fuemmeler et al. 2006;477 Campbell et al. 2007478 (Body and Soul) |
| Setting |
| USA; California, south-east (GA, NC, SC) and north-east (DE, VA) regions |
| Inclusion criteria |
| Churches recruited through local American Cancer Society (ACS) offices in California, south-east (GA, NC, SC) and north-east (DE, VA) regions. Individuals were recruited by liaisons on a first-come first-served basis |
| Study type |
| RCT (randomised by church) |
| Description of population |
| Ethnicity: African American, all churches had a predominantly African American membership; not reported how ethnicity assessed |
| Age (years): Mean (range): 50.6 (17–89) |
| n: 1022 |
| Sex: 74.4% female |
| Income: Not reported |
| Description of intervention and control |
| A 6-month dietary intervention conducted with African American churches |
| Intervention at two levels: Churchwide events, pastor support, policy changes and environmental changes aimed at the entire congregation, regardless of consent. Lay counselling delivered only to individuals who voluntarily enrolled in the study and provided active consent. Self-help print and video materials and motivational interviewing conducted by trained volunteer advisors. Two follow-up telephone calls |
| Control: Churchwide events only, no individual lay counselling |
| Theory: Process evaluation used the RE-AIM model479,480 emphasising the importance of both external validity (reach and adoption) and internal validity (efficacy and implementation) |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 6 months |
| Changes in fruit and vegetable consumption: Fruit and vegetable intake (servings per day): two-item measure: intervention 4.8 ± 0.12, control 4.1 ± 0.12, estimated effect size 0.39 (p < 0.05); 17-item measure: intervention 6.6 ± 0.39, control 5.2 ± 0.45, estimated effect size 0.18 (p < 0.05). Intervention group reported significantly greater consumption of fruit and vegetables than the control group. Adjusted post-test difference was 0.7 servings per day based on the two-item measure and 1.4 servings for the 17-item measure. Differences equate to standardised effect sizes. The change in fruit and vegetable intake comprised 0.4 and 0.9 servings from fruit and 0.2 and 0.5 servings from vegetables across the two-item and 17-item measures, respectively |
| Conclusions |
| Authors: This project demonstrated that a research-based intervention can be adapted and implemented under real-world conditions using volunteer staff and lay counsellors, and under these conditions positive effects on behaviour change can be achieved. Effect size for change in fruit and vegetable intake was smaller than that observed in parent efficacy trials but statistically significant. ‘These “dilutions” of implementation are consistent with the transition from efficacy to effectiveness’ (p. 103) |
| Reviewers: This intervention was successful in increasing fruit and vegetable consumption among the intervention group in a church setting. However, the group seemed to be a higher-income, higher-education group than in other African American studies. Furthermore, self-selection bias was possible as a result of non-random individual sampling. However, the point was to test the intervention in real-life conditions and the authors acknowledged that the effects would be diluted |
| Comments and limitations |
| Self-reported fruit and vegetable intake (however, the two measures have been validated against serum carotenoids among African American populations suggesting partial validity). Quota sampling framework (first come first served); therefore, participants may not be representative of the entire church population. Programme exposure also self-reported. Unclear if effects due to counselling or motivational interviewing per se. RE-AIM framework applied post hoc to process analysis; may have weakened ability to fully utilise the predictive value of the model |
| Study reference |
|---|
| Anderson-Loftin et al. 2005371 |
| Setting |
| USA; diabetes education centre in a rural South Carolina county |
| Inclusion criteria |
| African American, medical diagnosis of type 2 diabetes, aged ≥ 18 years, no mental/physical limitations that would preclude participation in group activities and discussion and at least one of the following indicators of diabetic complications defined as high risk and modifiable by diet: (1) HbA1c (glycated haemoglobin) ≥ 8%; (2) cholesterol ≥ 100 mg/dl; (3) triglycerides ≥ 200 mg/dl; (4) low-density lipoprotein cholesterol ≥ 100 mg/dl; (5) weight ≥ 25 kg/m2; and (6) high-fat dietary patterns [score on the Food Habits Questionnaire (FHQ)] ≥ 2.5 |
| Study type |
| Longitudinal experimental pre–post test control group |
| Description of population |
| Ethnicity: African Americans; not reported how ethnicity assessed |
| Age (years): Mean (SD) (range): treatment group: 58.9 (10.1) (40–77), control group: 55.7 (12.1) (32–86) |
| n: 97; 49 intervention, 48 control |
| Sex: Intervention group 78% female, control group 75% female |
| Description of intervention and control |
| Intervention: Four weekly 90-minute educational classes in low-fat dietary strategies. Five monthly 1-hour peer-professional group discussions and weekly telephone follow-up by a nurse case manager. Participation of family members was encouraged not only to integrate black cultural traditions with food but also to capitalise on the value of family and to provide transportation – a common barrier in rural areas. Experiential teaching method was used, e.g. assisting with meal preparations, reading food labels and making food choices at a simulated church supper. Educational classes: taught to make healthy, low-fat food choices according to the Diabetes Food Pyramid and strategies for reducing fats and set individualised mutual goals. Because of low literacy, the intervention focused on one major dietary concept for improved chances of success |
| Control: Referral to a local 8-hour traditional diabetes class. Received instruction about diabetes and complications |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 6 months post intervention |
| Changes in dietary fat: The intervention group reduced high-fat dietary habits to moderate whereas the high-fat dietary habits of the control group remained unchanged |
| BMI: Intervention group BMI decreased by a mean of 0.81 kg/m2 at 6 months, control group BMI increased by 0.57 kg/m2; 1.38 kg/m2 difference between groups at 6 months (p = 0.009) |
| Weight: At 6 months, weight decreased by 1.8 kg for the intervention group and increased by 1.9 kg for the control group, a net difference of 3.7 kg |
| Conclusions |
| Authors: This study shows that a culturally competent self-management intervention can improve health outcomes for southern African Americans, especially those at risk because of a high-fat diet and a BMI ≥ 35 kg/m2. Statistically significant changes were seen for BMI and FHQ in the intervention group and between genders; men gained weight despite a decrease in significant dietary fat behaviours compared with women. Improved cultural competency can improve adherence; there was 78% retention for the intervention group and 56% for the control group. A larger RCT was proposed |
| Reviewers: This study was effective at reducing BMI and dietary fat behaviours, although findings were more pronounced for BMI. Because this study is well described in terms of the adaptations, it gives a good sense of why the programme may have worked. However, in the adapted arm there was also more contact (as the control group were referred to a diabetes programme and it is not known whether they attended or not). A more informative control would be a similar-intensity intervention without adaptations; however, it would be difficult to keep the fidelity of such a control if the health educator was also from a similar background |
| Comments and limitations |
| All participants received US$15 for attendance, a Soul Food Light sweatshirt, small token gifts and ‘door prizes’ at each intervention and testing session and when receiving the results of laboratory tests |
| Study reference |
|---|
| Goodman and Blake 2005481 |
| Setting |
| USA; church-based community setting |
| Inclusion criteria |
| Not reported |
| Study type |
| Pre–post test |
| Description of population |
| Ethnicity: African Americans; not reported how ethnicity assessed |
| Age (years): Range: 25–75 |
| n: 82 |
| Sex: Not reported |
| Income: Not reported |
| Description of intervention and control |
| Computer-based nutrition education programme for African Americans adults (church-based sample). Interactive multimedia was used to simulate situations that involve complex learned behaviour, skills, values and environment related to nutrition and health |
| Computer-based programme composed of a pre-test assessment module (knowledge about healthy diet and eating habits) and two sections each containing four modules and a food game. Based on an assessment score, the learner would complete the entire section on basic nutrition or proceed to the section on food and health. Section 1: healthy eating and basic food groups with examples; section 2: meal planning and food preparation methods; benefits of selecting healthy choices (grilled foods) and the risks associated with poor choices (fried foods). Entire programme takes approximately 30–45 minutes to complete. Graphics and voice narration. The use of the programme does not require previous experience with a computer or a reading level higher than sixth grade |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: 3 and 6 months |
| BMI: BMI was lower for participants who completed the programme compared with their initial screening scores and weight. There was a 7% increase in the number of people in the ‘normal’ category, a 2% decrease in the ‘overweight’ category and a 5% decrease in the ‘obese’ category |
| Conclusions |
| Authors: This study indicates that African Americans are responsive to culturally sensitive education programmes that focus on health and illness prevention. Individuals who received nutrition information by computer demonstrated a positive change in health-promoting nutrition behaviours and positive changes in BMI. The computer program appears to promote interest in nutrition and healthy eating and to capture the attention of the user. Health-promoting activities could be provided on a regular basis within the context of church-related activities and have the potential to promote lifestyle changes in food consumption and eating patterns |
| Reviewers: A poor-quality study in terms of reporting, in which recruitment and important demographics such as gender were not described. The study was successful in shifting patterns of BMI; however, it is unclear how and no measures of statistical significance are given for the reported findings |
| Comments and limitations |
| User-friendly format easy to use, even for those with limited computer abilities. Limitation: no indication of statistical analysis methods |
| Study reference |
|---|
| Kreuter et al. 2005293 |
| Setting |
| USA; St Louis, MO, 10 urban public health centres |
| Inclusion criteria |
| Women who were able to demonstrate reading ability and reading comprehension by completing a six-item self-administered questionnaire written at fifth-grade reading level that included one open-ended question requiring an appropriate written response |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean (range): 35.6 (18–65) |
| n: 1227 |
| Sex: 100% female |
| Income: Not reported |
| Other: Mean education of 12.3 years (range 2–20 years) |
| Description of intervention and control |
| Women were assigned to a usual care control group or to receive a series of six women’s health magazines with the content tailored to each individual. The magazines were generated from either BCT, CRT or both (BCT + CRT), and women receiving magazines were randomly assigned to one of these three groups |
| All women aged 40–65 years received magazines that promoted the use of mammography and all women aged 18–39 years received magazines that promoted fruit and vegetable intake. Each magazine contained 10 tailored stories – for the younger age group there were six stories addressing fruit and vegetable intake and four on general topics |
| Women in the control group were sent nothing during the intervention but were sent a full set of tailored magazines after the intervention |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: 1, 6 and 18 months post baseline |
| Changes in fruit and vegetable consumption: Women receiving BCT + CRT magazines were more likely than those in the BCT, CRT and control groups to have greater increases in daily fruit and vegetable servings (+0.96 servings vs +0.43 vs +0.25 vs +0.59, respectively) (and in the older age group to report getting a mammogram) |
| Conclusions |
| Authors: Systematically integrating culture into tailored cancer prevention and control interventions may enhance their effectiveness in diverse populations and certainly justifies further enquiry |
| Reviewers: This study shows that cultural tailoring combined with tailoring for behaviour change appears to be a more effective strategy for changing nutritional behaviours |
| Comments and limitations |
| Limitations include the self-reported measures of outcomes. The fact that the magazines for BCT + CRT contained more varied articles may also have contributed to their increased effect, although it is not possible to measure this in this study. Also, the findings may not be generalisable to other populations |
| This study explicitly set out to examine whether cultural tailoring had a greater effect than behavioural tailoring or no tailoring at all. This is the most beneficial type of study for our research hypothesis and suggested in this case that there is benefit from cultural tailoring in combination with behavioural tailoring. It is very interesting that the group receiving CRT magazines did not experience good levels of change; they never exceeded that of the control group and it was only when CRT was combined with BCT that there was an effect. The authors suggest that there is an important link between culture, behaviour and communication that needs to be investigated and pursued farther |
| Study reference |
|---|
| Resnicow et al. 2002;295 Resnicow et al. 2005294 (Healthy Body/Healthy Spirit) |
| Setting |
| USA; Atlanta, urban |
| Inclusion criteria |
| Members of 16 African American churches in a metropolitan area of Atlanta, ≥ 18 years |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean (SD): group 1: 46.3 (13.4), group 2: 45.9 (12.7), group 3: 46.6 (13.7) |
| n: 1056 |
| Sex: Group 1: 74.2% female, group 2: 76.1% female, group 3: 78% female |
| Income: 10.5%, 13.1% and 11.1% of groups 1, 2 and 3, respectively, had income < US$20,000 |
| Other: 30.6%, 21.7% and 26.7% had completed high school or vocational training in groups 1, 2 and 3, respectively |
| Description of intervention and control |
| Sixteen churches were randomly assigned to three conditions: group 1 (five churches) received a standard nutrition and physical activity intervention; group 2 (six churches) received a culturally targeted self-help nutrition and physical activity intervention; group 3 (five churches) received the same intervention as group 2 plus four telephone counselling calls based on motivational interviewing. Culturally tailored material included a cookbook and video developed for a previous trial (Eat for Life316), an exercise video, an exercise guide and an audio cassette for exercise. The advice was to undertake 30 minutes of exercise on most days of the week and that activity of greater intensity and duration will result in added health benefits. Group 1 (control) received an intervention of the same approximate intensity and type as group 2 and a health fair, a newsletter, an aerobics video and numerous educational health brochures. Motivational interviewing was delivered by telephone by psychologists; there were calls at 4, 12, 26 and 40 weeks |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Not reported |
| Changes in fruit and vegetable consumption: Fruit and vegetable intake change scores were 0.17, 0.44 and 1.13 servings, respectively, for groups 1, 2 and 3 |
| Changes in physical activity: Significantly bigger increases in activity for groups 2 and 3 than for group 1 for each of the three scores. Groups 2 and 3 did not vary significantly from each other on any of these scores |
| Conclusions |
| Authors: The two self-help groups were generally successful in inducing change in fruit and vegetable intake and physical activity. The impact of adding the motivational interviewing varied depending on the behaviour; for fruit and vegetable intake there was a clear additive effect but for physical activity there was no real difference. This may be because of differences in the delivery of the motivational interviewing for these two subjects or it may be that the self-help material for physical activity was better than that for fruit and vegetables and left little to be added. This effect could also be due to the fact that more people elected to work on their fruit and vegetable intake in the motivational interviewing sessions. The motivational interviewing group also appeared to have the greatest number of people making changes to both fruit and vegetable intake and physical activity at the same time (70%). Overall, churches appear to be an excellent setting to implement and evaluate culturally targeted interventions for the African American population and continued refinement and evaluation of such interventions appears warranted |
| Reviewers: This appears to be a successful intervention for nutrition and physical activity modification in a church setting for an African American population. There appears to be an advantage of a culturally tailored programme and perhaps an added benefit of adding motivational interviewing to this programme, certainly for the promotion of increased fruit and vegetable intake |
| Comments and limitations |
| Self-reported measures although they were validated with serum and exercise tests. May be sampling bias as was sampled on a first-come first-served basis and this may not be representative of the wider population, reducing external validity. Possible social desirability bias. Effects of motivational interviewing may be due to the added contact and not to the type of counselling itself |
| Study reference |
|---|
| Shankar et al. 2007;315 Klassen et al. 2008316 |
| Setting |
| USA; Washington DC, urban |
| Inclusion criteria |
| Women aged 20–50 years from 11 public housing communities |
| Study type |
| Pre–post |
| Description of population |
| Ethnicity: African-American; not reported how ethnicity assessed although study states that only American women whose parents and grandparents were born in the USA were included |
| Age (years): 19% aged 20–29 years, 37% aged 30–39 years, 44% aged 40–50 years |
| n: 212 |
| Sex: 100% female |
| Income: Not reported |
| Other: 39% had less than a high school level of education and 83% were currently not working |
| Description of intervention and control |
| The intervention was designed to be brief and low cost with the aim of being replicable in other low-income communities. Included 90-minute classes with a professional nutritionist, which were conducted twice a week for 3 weeks, followed by one 90-minute booster session held 6 weeks later. The sessions were led by a female African American registered dietician in small groups and took place in the community centre kitchen. Extensive formative work informed the intervention |
| Programme activities combined nutrition education and food-related skill development. To build self-efficacy for nutrition-related problem-solving, psychosocial tools such as goal-setting and planning were used. Social support was planned with techniques to encourage interaction within the class and also women were partnered and were encouraged to contact each other outside of class |
| Theory: Social ecological framework |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to weeks 4 and 20 weeks after enrolment |
| Changes in fruit and vegetable consumption: Baseline dietary recalls showed average daily consumption of 3.05 servings of fruit and vegetables. No improvements were seen in fruit and vegetable consumption at follow-up |
| Changes in calories: Statistically significant decreases in total calories and per cent calories from fat were seen at both the post-test and follow-up end points for the whole sample |
| Conclusions |
| Authors: The aggregate results demonstrated that the intervention produced dietary improvement in attendees and should be considered as a possible model for a nutrition intervention in low-resource households and communities |
| Reviewers: This study appears to show effect for the sample as a whole and some difference in effect dependent on attendance; however, further research is needed to truly evaluate effectiveness. There was quite a high degree of attrition in the study |
| Comments and limitations |
| There was quite a high loss to follow-up. Women enrolling were often at the extremes of ill health as otherwise they were busy with Welfare to Work programmes and therefore they were not a representative sample. There was no control group. There was relatively short-term evaluation |
| Study reference |
|---|
| Cullen and Thompson 2008313 |
| Setting |
| USA |
| Inclusion criteria |
| Families with 9- to 12-year-old African American girls who owned a home computer with internet access and had a parent or guardian willing to participate in the programme |
| Study type |
| Pre–post |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Not reported |
| n: 67 families (parent and 9- to 12-year-old daughter) (three recruitment groups) |
| Sex: Not reported |
| Income: Not reported |
| Other: Parental education was at college level or above for 92% of mothers and 60% of fathers |
| Description of intervention and control |
| An eight-session web-based programme for families of African American girls promoting healthy home food environments and positive parenting behaviours to increase fruit and vegetable intake. An existing web-based programme was used as a starting point – it had low log-on rates and interviews with African American mothers were used to alter it and identify factors that may explain how parents can influence their children’s diet. The new programme was called Family Eats. It included eight photonovella stories (maximum of 3 minutes) portraying real life-type situations regarding nutrition. There were a lot of pictures, activity pages, links to recipes, parenting tips and links to other fact-based websites. Grocery lists that could be saved to participants’ computers were added. Thoughts and quotes on modelling of fruit and vegetable consumption and getting children to eat fruit and vegetables were added. The website was designed to be accessed on a weekly basis; the structure remained the same but the content changed to take participants through a planned sequence of material |
| Theory: Social cognitive theory |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to weeks 1 and 8 |
| Changes in fruit and vegetable consumption: Significantly positive changes were reported in self-efficacy for fruit and vegetable availability (p < 0.05), and daughters reported parent modelling of fruit and vegetable consumption (p < 0.05) |
| Changes in dietary fat: Significantly positive changes were reported in modifying meat fat practices (p < 0.05) and marginally significant changes in fat substitution practices (p < 0.10) |
| Conclusions |
| Authors: An internet-delivered nutrition intervention for families was successful in achieving change in some mediating variables, with modest log-on rates. Further research should investigate the impact on dietary behaviours |
| Reviewers: There seem to be positive effects from this study perhaps as a result of targeting the family together, but it is limited by the requirement to have internet access at home and also because the log-on rate diminished considerably as the novelty value of the intervention wore off |
| Comments and limitations |
| Small sample size and lack of generalisability to other demographic populations in other regions or with less education or resources; being internet based, limits intervention to those with internet access and computer experience and this may limit the generalisability of this intervention, particularly in very-low-income groups. There was a novelty aspect to the intervention and, although it was accessible, once the novelty had worn off the log-on rates decreased; these low log-on rates minimise the effectiveness of the programme |
| Study reference |
|---|
| Utz et al. 2008408 |
| Setting |
| USA; rural county of central Virginia |
| Inclusion criteria |
| Pre-screened and enrolled if they were African American (self-identified), aged 18+, reported being diagnosed with type 2 diabetes mellitus, resident of a rural county and able to give informed consent (e.g. no evidence of dementia or mental illness during routine screening) |
| Study type |
| Quasi-experimental random design |
| Description of population |
| Ethnicity: African American; self-identified |
| Age (years): Mean: 60.2 ± 14.6 |
| n: 22 |
| Sex: 82% female |
| Income: Not reported |
| Other: 10/21 (47.7%) had less than high school completion |
| Description of intervention and control |
| A culturally tailored intervention for a rural African American population based on the seven areas of self-management identified by the American Association of Diabetes Educators in literature published at that time |
| Group diabetes management: Held weekly for 2 hours for 8 weeks: storytelling, hands-on activities and problem-solving |
| Individual diabetes management: Met with educator on three occasions over 8 weeks at the same time as the group sessions but in a separate room. The individual sessions were 10–15 minutes |
| Theory: Social cognitive theory |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Study conducted over a 6-month period. Outcomes measured at baseline and 10 weeks after baseline |
| Outcome measure: Daily actions for diabetes self-care measured – two-sample t-test using change scores from baseline to post intervention did not indicate significant differences in outcomes between the two groups. Median test and analysis of covariance controlling for baseline level of outcome and number of years since diagnosis obtained similar results of non-significance |
| Conclusions |
| Authors: Culturally tailored approach was well received by all participants. Group diabetes management tended to show improvements in difficult areas such as carbohydrate spacing and foot care compared with individual diabetes management, as well as higher self-efficacy, although these results were not significant. They provide a preliminary indication that the culturally tailored group approach may be more effective with rural African Americans with type 2 diabetes. Storytelling is a culturally appropriate education and empowerment strategy that was well received because of traditions of oral history, which value the teaching and community-building functions of storytelling |
| Reviewers: The conclusions drawn by the authors are slightly premature as this was a very small sample. However, storytelling may hold promise in this population as an intervention delivery strategy and should be further tested. Furthermore, as both intervention arms received culturally tailored information, the differences between the arms were group effect and greater contact with an educator. Focus groups or interviews would have been helpful at this formative stage to gauge the benefits of group vs individual delivery. Contamination is a possibility given that the interventions were held at the same time and place but in different rooms and because of the small tight-knit community. Different numbers were reported within the paper: 18 women, 4 men reported in recruitment and sample section; 16 women and 6 men reported in a table |
| Comments and limitations |
| Results limited by small sample size and brief follow-up of 10 weeks. Difference in the amount of time that educators spent with participants: group 16 hours total, individual time estimated at a total of 1–2 hours (which, although a lot less than the group, is more than was planned) |
| Study reference |
|---|
| Resnicow et al. 2009296 |
| Setting |
| USA; Detroit, MI and Atlanta, GA, urban |
| Inclusion criteria |
| Self-identifying as black or African American, living at least half of their life in the USA, not currently hospitalised or living in skilled care facilities, the absence of mental or physical conditions that would inhibit or be endangered by participation in the study and consuming < 10 servings of fruit and vegetables per day |
| Study type |
| RCT, 2 : 1 randomisation |
| Description of population |
| Ethnicity: African Americans; self-identified |
| Age (years): Mean: 49 |
| n: 560 |
| Sex: 73% female |
| Income: 60% earned at least US$40,000 per year |
| Other: 69% had at least some college education |
| Description of intervention and control |
| Intervention to test whether or not tailoring a print-based fruit and vegetable intervention on ethnic identity would enhance the programme effect |
| Participants were randomised to receive three newsletters focused on fruit and vegetable behaviour change over 3 months. One set was tailored only on demographic and social cognitive variables (control condition) whereas the other (intervention) was additionally tailored to ethnic identity. Both groups received newsletters once a month over 3 months and each contained two recipe cards with small bags of spices that corresponded to the recipes and a magnetised refrigerator notepad or magnet with fruit and vegetable serving sizes. Text for both groups was individualised with the participants’ names and tailored to sociobehavioural variables |
| The control group newsletters targeted a general black American audience with a slight Afrocentric focus (as this was most prevalent in the pilot study). In contrast, the intervention newsletters contained tailored messages designed to each of the 16 types of ethnic identity. Graphics were tailored to the ethnic identity types in the intervention group and for the control group they were ethnically neutral and therefore usually did not feature people or any other racial or ethnic cues |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 3 months post baseline |
| Changes in fruit and vegetable consumption: Intervention group increased daily mean fruit and vegetable intake by 1.1 servings compared with 0.8 servings in the control group (p = 0.13). Afrocentric experimental group participants showed a 1.4-serving increase in fruit and vegetable intake per day compared with a 0.43-serving increase among Afrocentric control participants (p < 0.05) |
| Conclusions |
| Authors: Although the overall between-group effects were not significant, tailoring dietary messages on ethnic identify may improve the impact for some African American subgroups. Perhaps a brief measure could be created and tested that could be applied in the health-care setting |
| Reviewers: This study stood alone as one that tested the hypothesis of ethnic identity and adjusting the degree of tailoring of material accordingly to see whether this affects efficacy. The overall hypothesis is not proven and reasons why, including the tailoring of the control group, etc., are given. However, for participants who are Afrocentric, a significant difference was demonstrated |
| Comments and limitations |
| It is suggested that three newsletters was perhaps an insufficient dose to obtain a significant effect. Another reason for limited differences between the two groups may have been the intensity of the background tailoring used in both groups and also the decision to culturally tailor the control group. Measures were self-reported and there could also be social desirability bias. The reliability of some of the subcategories of the ethnic identity scale was low. External validity was limited by the 31% participation rate of those contacted |
Adapted physical activity and nutrition interventions
| Study reference |
|---|
| Sullivan and Carter 1985482 |
| Setting |
| USA; New Orleans, LA |
| Inclusion criteria |
| Obese (body weight ≥ 20% over ideal) and overweight (body weight 10–20% above ideal) mothers attending a Parent Child Development Centre |
| Study type |
| Pre–post |
| Description of population |
| Ethnicity: Black; not reported how ethnicity assessed |
| Age (years): Mean (range): 25.2 (16–31) |
| n: 10 mothers |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| A 2-month programme to alter diet, weight and cardiovascular endurance implemented at a Parent Child Development Centre (designed to aid low-income inner-city mothers with children aged 0–3 years to become more effective parents) |
| Dietary recommendations were given to participants based on their food diaries and a nutritional assessment. The nutritionist taught the participants a food group plan. A Food Book created by the Dairy Council of California was used to illustrate food groups and serving sizes. Mothers were advised to lose no more than 2 lb a week and to decrease their usual amount of food and to eat in a place without a radio or television. Dance was chosen for aerobic exercise with the music adapted to be soul. One-hour sessions were conducted twice a week for 8 weeks while childcare was provided. This included 20 minutes of dance and callisthenics followed by nutrition education highlights including discussion |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Unclear, not reported |
| Changes in dietary fat: Significant reduction in the consumption of fat; significant decrease in body fat from 30.4% (range 22.1–40.0%) to 26.8% (range 23.0–33.2%) |
| Weight: No significant effect on weight loss |
| Conclusions |
| Authors: This programme is thought to be valuable as a preliminary study but the results cannot be considered representative for the general population because of the very small sample size. There was no significant weight loss but the pre and post analysis does demonstrate an improvement and modification of nutritional practices. There were also improvements in body fat composition and resting heart rates as a result of the aerobic exercise programme |
| Reviewers: This intervention appears to have been effective for the small number of mothers involved but is not generalisable and would need further study on a wider scale, as acknowledged by the authors |
| Comments and limitations |
| The findings are limited by the very small sample size |
| Study reference |
|---|
| Lasco et al. 1989318 (The Community Health Assessment and Promotion Project) |
| Setting |
| USA; Atlanta, GA |
| Inclusion criteria |
| Clinically diagnosed as obese, aged 18–59 years |
| Study type |
| Pre–post |
| Description of population |
| Ethnicity: Black; not reported how ethnicity assessed |
| Age (years): Not reported |
| n: 70 |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| Community coalition designed and directed a 10-week exercise and nutrition intervention. This consisted of an orientation session, attitudes assessment, selection of a specific exercise class and twice-weekly information session on nutrition and community resources. The programme used a wide range of strategies including individual consultations, reminder telephone calls and incentives and rewards and free transportation and childcare to encourage participation |
| The intervention was run from a clinic, a YMCA and a school, all of which were in an easily accessible area of the community. Meetings were on two week nights and each session lasted for 2 hours. The first session of the week had a nutrition focus for the first hour and the second session of the week had assessment, counselling and special interest session in the first hour. The second hour consisted of exercise |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 3 months post intervention |
| Weight: The most weight lost was 41 lb. The changes in weight were found to be significant (p = 0.0009). A total of 89% were also weighed 3 months after the end of the programme and 55% still weighed less than they did at the start of the programme. The average weight loss in this group was 2.8 lb (range +17 to –59 lb) |
| Conclusions |
| Authors: The results in terms of weight loss and blood pressure change indicated that a nutrition/exercise programme can lead to positive behavioural change in this population. The participation rates were also high. A comparison of the high and low participant groups indicated more family involvement, more family encouragement and less criticism from family and friends among the high participation group. The programme was subsequently run nine times with over 400 additional people participating. Community impetus for programme contributes to success of intervention; a community coalition was formed that led to the intervention |
| Reviewers: This intervention appears to have been effective for weight loss in this population. There is limited description of the adaptations; however, there is good evidence of the community involvement and of the elements of social support and family involvement and the strong use of incentives and rewards. The intervention appears to have been sustainable but no data are presented in this paper for the subsequent large number of participants |
| Comments and limitations |
| There was no control group. Some of the measures, e.g. food diaries and measures of family involvement, are self-identified measures and may be biased. Some test results (e.g. step test) were incomplete as the participants found them difficult to do (beta-blocker medication also made this invalid for a high proportion). One of the prime objectives was to minimise attrition and the following strategies were thought to be important: pre-screening – resulting in the enrolment of motivated people; home visitations by a male public health educator to discuss the programme with the husband and children and building family support |
| Study reference |
|---|
| Baranowski et al. 1990;322 Baranowski et al. 1990321 |
| Setting |
| USA; Texas, urban |
| Inclusion criteria |
| Sampling frame was a listing of all black American students in fifth, sixth or seventh grade in public or private school systems in the area |
| Study type |
| RCT (randomised by family) |
| Description of population |
| Ethnicity: Black American; self-identified |
| Age (years): Mean: adults: 31.8 experimental group, 32.9 control group; children: 10.6 experimental group, 10.0 control group |
| n: 96 families with 114 adults and 120 children |
| Sex: Adults: 79% female in the experimental group, 88.2% female in the control group; children: 51.6% female in the experimental group, 66.1% female in the control group |
| Income: Not reported |
| Other: Educational attainment: 12.9% of the experimental group and 26.5% of the control group reported to have less than a high school education |
| Description of intervention and control |
| Intervention: The intervention group was encouraged to participate in a programme with one education and two fitness sessions per week for 14 weeks. Educational sessions included individual family behavioural counselling (10–20 minutes) – the counsellor reviewed the weeks’ food and activity records and there was a monetary reward for completing the record; the counsellor also reviewed the achievement of specific behavioural goals set the previous week, elicited social reinforcement for accomplishing goals and counselled the family on problem-solving for unaccomplished goals; new goals were then set and negotiated with the family |
| Control: Both groups came to a baseline clinic for assessment and then no contact was made with the control group during the 14 weeks |
| Theory: Social learning: social support and adult education theories |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Not reported |
| Changes in calories: There were changes in the calories expended for both the experimental group and the control group adults, with the experimental group having consistently higher levels than the control group |
| Weight: A significant difference was detected between the groups in weight and body surface area (however, this was because two adult males lost a very significant amount of weight) |
| Changes in fitness: No significant differences were detected in cardiovascular fitness among the children or adults |
| Conclusions |
| Authors: As a result of low participation, no significant differences were detected between the intervention and control groups in indicators of cardiovascular fitness. It was concluded that, because of difficulties in attendance, centre-based programmes appear to have limited value as the sole modality for intervention in public health programmes for healthy low-income black American families with young children. More comprehensive community-based programs are likely to be needed |
| Reviewers: This study does not demonstrate any significant changes in outcomes. This may in part be due to high levels of attrition. The study incorporates a high degree of theory and adaptation and yet it was not successful. If people are not motivated or able to attend (have too many competing life demands) then, regardless of how adapted the intervention is, there will not be positive change |
| Comments and limitations |
| High attrition/low attendance and self-reported measures |
| Study reference |
|---|
| Kumanyika and Charleston 1992336 (Lose Weight and Win) |
| Setting |
| USA; Baltimore, MD |
| Inclusion criteria |
| The programme was open to men and women and was aimed at those who were moderately overweight (10–100% overweight). Having diabetes or being on anti-hypertensive medication did not preclude participation but physician approval was necessary in these cases |
| Study type |
| Pre–post |
| Description of population |
| Ethnicity: Black; not reported how ethnicity assessed |
| Age (years): Mean (range): 51 (18–81) |
| n: 184 black (3 white) |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| This was part of a bigger programme called the Baltimore Church High Blood Pressure Program (CHBPP). The core components of the weight control programme are based on the state health department’s ‘I Can … I Will …’ programme with adaptations to promote effectiveness in this population. Some changes were adding an exercise component, using individual and team competitions as incentives and using teams to facilitate mutual support for weight loss |
| Eight weekly 2-hour diet counselling/exercise sessions were provided. Meetings were held on the church property, usually early in the morning, and had as many as 30 individuals. Participants had a weigh-in, had a blood pressure check, talked with the dietician and participated in group behavioural modification activities. The latter included experience sharing, discussion and setting behavioural goals. The last 35–40 minutes were dedicated to exercise. There were two groups of participants – one group who were on anti-hypertensive medication and one group who were not on medication |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: At the end of the 8-week programme and at 3 and 6 months |
| Weight: Mean weight loss was 6 lb (range –14 to +13 lb) in both groups at 8 weeks (p < 0.005). Of participants who were on no medication, 89% lost weight; of participants who were on medication, 88% lost weight. The average number of sessions attended was five and weight loss was significantly associated with attendance. Follow-up weight measurements at 6 months showed that 65% of the women with data had maintained their weight or lost more weight |
| Conclusions |
| Authors: Weight control/exercise programmes such as Lose Weight and Win may help to limit weight gain that would otherwise occur among black women and also improve activity and physical fitness levels. The high receptivity to the exercise component suggested that a lack of convenient opportunities to exercise may be more of a barrier to increasing physical activity among black women than a lack of motivation |
| Reviewers: This study demonstrated significant weight loss following the 8-week intervention that appeared to be sustained at a 6-month follow-up. The intervention appears acceptable and effective but may not be transferable to other settings where there is not already existing support and relationships. The results also were not compared with a control group and would need further confirmation in a controlled trial. The development of alumni classes and training lay leaders were promising strategies to sustain the intervention in the community once the research was complete |
| Comments and limitations |
| This was a post hoc evaluation and there was no control group to be able to compare how these weight changes relate to the normal trends in this population. An external control was created from women who did not attend the programme but who had had their blood pressure measured; however, this control was carried out only for blood pressure results |
| The programme was based on the existence of an established church health awareness programme and therefore would not necessarily be feasible or have the same effect if implemented in a different setting. As part of this there were existing interpersonal relationships between the participants and an atmosphere of mutual support |
| The follow-up data may represent the women who were most successful in their behaviour change. There were no significant differences between the demographics of the women who were retained to follow-up and the demographics of those who did not carry on; however, it is likely that the women who were retained were in some way more motivated |
| Study reference |
|---|
| Kanders et al. 1994483 [Black American Lifestyle Intervention (BALI)] |
| Setting |
| USA; Boston, MA, and Houston, TX, multicentre |
| Inclusion criteria |
| Women, aged 40–64 years, BMI 30–40 kg/m2, earning US$1000–5000 monthly (working class), diastolic blood pressure (without medication) < 95 mmHg, serum cholesterol < 7.76 mmol/l and no history of diabetes |
| Study type |
| Pre–post |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean: 49 |
| n: 61 |
| Sex: 100% female |
| Income: Not reported |
| Other: 95% had completed a high school education |
| Description of intervention and control |
| A 10-week weight loss phase with culturally appropriate nutrient-balanced 1200-kcal diet in which two meals were replaced by meal replacement shakes (provided free of charge) |
| Intervention: 1-hour group sessions were provided, led by a female African American nutritionist. One-page handouts were distributed on nutrition, exercise and behaviour modification topics. These sessions were highly interactive and included goal-setting, problem identification and role-playing. Participants were given US$30 at weeks 5 and 10 in return for completing a programme evaluation. Exercise was advised in the form of three 15-minute walks per week and participants were also told to increase the frequency and duration of walks gradually until they reached 200 minutes walked weekly |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to weeks 5 and 10 |
| Weight: There was significant weight loss in participants (6.5 ± 5.3 lb, 3.5% of total body weight, p = 0.001) over the 10 weeks. Breaking down the results, 17 women lost ≥ 10 lb, 18 women lost 5.1–10 lb, 14 women lost 1–5 lb, eight women remained within 1 lb of baseline weight and four gained weight |
| Conclusions |
| Authors: The weight loss results are superior to most that are reported in minority groups and both this and the attendance supported the effectiveness of the intervention. This study was to be followed by a larger more sustained intervention |
| Reviewers: As commented by the authors, this intervention was a pilot study and had a small sample size and no control group and therefore the conclusions are limited in their significance and generalisability; however, the intervention showed promise and it would be interesting to see the results of any future work |
| Comments and limitations |
| Pilot study and lack of detail on recruitment. Could funding of shakes be sustained – what is the cost-effectiveness? |
| Study reference |
|---|
| Wallace et al. 1996484 |
| Setting |
| UK; St. John’s, Halifax |
| Inclusion criteria |
| Asian women selected from a practice database |
| Study type |
| Pre–post study with qualitative and quantitative measures |
| Description of population |
| Ethnicity: Asian; not reported how ethnicity assessed (provided Punjabi and Urdu translators) |
| Age (years): Not reported |
| n: 20 |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| Educational project to target a group of women with non-insulin-dependent diabetes mellitus (NIDDM) |
| Home visits by a district nurse accompanied by an interpreter to explain the purpose and objectives of the course. Women attended the surgery for a full medical examination. A 10-session course was delivered that was planned and facilitated collaboratively by a nursing team and a GP (topics included diet and diabetes, diet and the family, benefits of exercise). Talks were given by team members or professionals from outside the practice. Each session included a talk on one aspect of living with diabetes followed by questions and a general discussion. Each session included an exercise component led by a ‘Look After Yourself tutor’. Women were encouraged to continue exercises regularly at home. There was no control group |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Post course (quantitative and qualitative) and at 12 months |
| Changes in dietary fat: Cholesterol level: little change occurred |
| Changes in physical activity: Activity level increased in all women |
| Knowledge: Post course (qualitative): Everyone’s knowledge had increased |
| Conclusions |
| Authors: The benefits of a health education programme in a chronic condition such as NIDDM, which also has a genetic component, cannot be fully evaluated in the early stages and must be assessed after many years. Plan to involve whole families in the groups and to extend programme to Asian men and Caucasian patients |
| Reviewers: The intervention appeared to have changed knowledge; however, this was not quantified. The authors suggest that attitudes and beliefs also need to change, and that knowledge may not be enough as women are faced with significant barriers. Future interventions should include the family and/or men |
| Comments and limitations |
| Some women felt unable to make significant changes to their lifestyle as the barriers were too great and required modification of beliefs and attitudes. Women living in large extended families of three or more generations were influenced by the wishes and views of significant others and were expected to fulfil the roles of wife and mother in a traditional way (the women expressed desires to fulfil this). There was family pressure to provide what was perceived by Asian people living in the West as high-status food, with high calorie and fat content. Men usually do the family shopping. Unclear what exercises were carried out (not described) |
| Study reference |
|---|
| Agurs-Collins et al. 1997372 [Positive Outgoing Sexy Seniors Exercise Club (POSSE) study] |
| Setting |
| USA; Washington, DC, urban |
| Inclusion criteria |
| African American men and women aged ≥ 55 years with a diagnosis of non-insulin-dependent diabetes mellitus (NIDDM) by medical history were eligible if they had ≥ 120% of Metropolitan weight standards, had HbA1c (glycated haemoglobin) levels > 8%, were ambulatory and had no medical contraindications to programme participation |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American |
| Age (years): Mean: intervention group: 62.4, control group: 61 |
| n: 64 |
| Sex: Intervention group: 66% female, control group: 88% female |
| Income: Not reported |
| Other: Intervention group: 56.3% had completed a high school education and 59.4% were not employed; control group: 59.4% had completed a high school education and 56.2% were not employed |
| Description of intervention and control |
| Overweight African Americans with NIDDM were randomised to an intervention or control group |
| Intervention: 12 weekly group sessions (8 to 10 people per group) with 60 minutes of nutrition education followed by 30 minutes devoted to exercising in the physical therapy area of the clinic (participants also encouraged to exercise two additional days on their own); one individual session during this time for nutrition counselling; and six biweekly group sessions offered in the subsequent 3 months to provide additional information and support with less formal instruction and more sharing and problem-solving |
| Control: Minimal intervention approximating ‘usual care’, which was one class (within 3 weeks of enrolment) related to methods of glycaemic control and two informal mailings of nutritional information at 3 and 6 months |
| Theory: The behavioural component was social action theory |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 12 weeks post intervention, 3 months and 6 months |
| Changes in physical activity: Physical activity scores increased with a net increase at 3 months of 49.4 points (p < 0.001); women’s scores increased more to 54 points (p < 0.001) and men showed minimal differences when analysed separately. However, the changes in physical activity were not sustained and were no longer statistically significant at 6 months |
| Weight: After 12 weeks the intervention group mean weight decreased and the control group mean weight increased, with an overall net difference from baseline of –2 kg (p = 0.006), a 6-month net change of –1.3 kg (non-significant) and a 6-month net difference of –2.4 kg (p = 0.01). The results were different for men and women |
| Waist-to-hip ratio: This did not change during the intervention |
| Conclusions |
| Authors: This programme was successful in improving HbA1c levels, for knowledge and behavioural changes (although not sustained at 6 months) and for moderate weight reduction, which was achieved within the first 12 weeks. The intervention group showed a relative advantage, which was maintained at 6 months despite the decrease in frequency of intervention contacts |
| Reviewers: This appears to be a successful intervention and a suitable approach for this population, although it is unclear how long the effects would be sustained |
| Comments and limitations |
| The principal limitation is the duration of the study, which is insufficient to determine whether the effects can be sustained and what level of contact would need to be put in place to maintain these effects. Participant feedback forms suggested that a third of participants never developed sufficient motivation to change their behaviour |
| Per patient delivery cost of US$150 (exclusive of research expenses and laboratory costs; includes dietician salary, exercise physiologist, support staff, supplies and educational materials) – costs at this level are negligible compared with the potential savings if the programme effects can be sustained; per patient savings by avoiding the need for insulin, minimising emergency department visits and avoiding renal failure and dialysis, for example, have been estimated at US$7500–100,000 per year |
| Study reference |
|---|
| McNabb et al. 1997;485 Quinn and McNabb 2001486 (PATHWAYS programme) |
| Setting |
| USA; Chicago, IL |
| Inclusion criteria |
| African American women with a BMI between 30 and 45 kg/m2 and no known physical limitations that would prevent moderate physical activity. They also had to agree to random assignment to the intervention or control group, who were wait-listed to receive a delayed intervention |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Not reported |
| n: 39 were enrolled and 33 were available for post-treatment data collection |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| Intervention: Intervention group received a 14-week weight loss programme conducted by trained lay volunteers in the setting of African American churches. Each of the weekly sessions lasted for 90 minutes, was administered in a group format and was delivered through guided learning activities and small group instruction. The group leaders assisted and facilitated. Participants were given small hand-held calculators and food guides to analyse their food practices. They were then to develop their own plans to change their diet. The main aims were to reduce dietary fat and increase fibre intake and these changes were made gradually over time. An exercise regime was also integral to the programme – subjects were instructed to begin a home exercise programme; generally this took the form of recreational walking |
| Control: Control group subjects were put on a waiting list to receive the programme at the conclusion of the study period |
| Theory: Utilised ‘discovery learning’ in which participants identify their own dietary problems and with the assistance of the facilitator and their peers try to arrive at personally relevant solutions |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and at 1 week after the 14-week programme had been administered |
| BMI: BMI decreased by 1.4 kg/m2 in the intervention group and increased by 0.6 kg/m2 in the control group; this difference was significant (p < 0.0001) |
| Weight: The intervention group lost an average of 10 lb and the control group gained an average of 1.9 lb. The post-treatment difference in weight loss was statistically significant (p < 0.0001) |
| Conclusions |
| Authors: A weight loss programme delivered by trained lay volunteers was effective in producing significant and clinically meaningful weight loss among African American women who do not often benefit from typical weight loss interventions. Ongoing research is focusing on whether the weight loss can be maintained or enhanced through monthly reinforcement sessions |
| Reviewers: This study is well designed and describes an efficacious weight loss programme for African American women that is adapted for cultural salience and which also uses a facilitated discovery learning style that encourages people to assess their own dietary patterns and undergo problem-solving to develop personalised plans for behaviour change |
| Comments and limitations |
| Remains unknown whether weight loss can be maintained over time. The generalisability of the programme is unclear although it had also been run in a clinic setting and the authors suggest that the content is highly structured and could be successfully delivered in different settings. The programme appears to be effective and acceptable with very good attendance and minimal attrition. The adaptations appear to contribute to the success as does the discovery learning design, which motivates people through making them the agents of change in their lives so that they can assess their own needs and design an action plan |
| Study reference |
|---|
| Stolley and Fitzgibbon 1997487 |
| Setting |
| USA; Chicago’s inner city, IL |
| Inclusion criteria |
| Live in Chicago’s inner city and attend a local tutoring programme: (1) attendance at weekly 1-hour meetings for 12 consecutive weeks, followed by a meeting every 3 months for 15 months; (2) completion of a health screening with questionnaires; and (3) enrolment of daughters in the Cabrini-Green tutoring programme |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean (SD): intervention mothers: 31.5 (3.4), control mothers: 33.7 (6.8); intervention daughters: 9.9 (1.3), control daughters: 10 (1.5) |
| n: 65 African American mother–daughter dyads (62 mothers and 65 daughters, some mothers with more than one daughter involved); mothers: n = 32 intervention, n = 30 control |
| Sex: 100% female |
| Income: Intervention mothers: 56% unemployed, control mothers: 60% unemployed |
| Other: Intervention mothers: 79.1% single, control mothers: 70.0% single |
| Description of intervention and control |
| Culturally specific obesity prevention programme focused on adopting a low-fat, low-calorie diet and increasing activity |
| Intervention: Each week subjects met in small groups of 7 to 10 dyads led by either an advanced doctoral student in clinical psychology or a registered dietician (two African American women, one white woman and one Asian woman). A concept of the week was discussed followed by an activity that reinforced the information presented |
| Control: Attention placebo – general health programme was run like the intervention group, meeting in small groups with group leaders. The focus of each session was on general health topics such as communicable disease control, effective communication skills, relaxation techniques and stress reduction |
| 1-hour weekly meetings for 12 weeks |
| Theory: Based on the premise that the method of presentation would be as important as the curriculum in motivating participation |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Measurements taken at baseline and 12 weeks |
| Changes in dietary fat: Mothers had a significant decrease in intake of saturated fat (p < 0.05) and also calories from fat (p < 0.001) from pre to post intervention, and also the intervention group mothers had greater reductions in overall dietary fat than the control mothers (although not significant). Daughters also showed a decrease in the percentage of calories from fat (p < 0.05) over time but there were no significant differences between the two groups |
| Weight: No significant changes detected for either the intervention or control mothers |
| Behaviour: There was a significant increase in parental support in the intervention group compared with the control group |
| Conclusions |
| Authors: This study suggests that a culturally adapted intervention for African American mothers and daughters can have some initial effect on behaviour change in relation to nutrition. The increase in parental support may help these changes to continue to be maintained. Future research is needed on this type of study |
| Reviewers: This study is interesting in design with the mother–daughter dyads and the idea of creating support within the home and parental role-modelling for behavioural change |
| Comments and limitations |
| Limitations include self-reported measures, which are prone to social desirability bias; generalisability, as the results could not be generalised to other African American populations in other areas of the country or of other SES, or to men and boys; self-selection of subjects, as mothers and daughters had to have a certain level of interest and motivation to sign up and this may influence the findings; and the lack of follow-up data for sustainability of effect |
| Study reference |
|---|
| Ard et al. 2000323 |
| Setting |
| USA; Durham, NC |
| Inclusion criteria |
| All African American subjects interested in participating were eligible if they received clearance from their primary physician |
| Study type |
| Randomised modified cross-over study |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Not reported |
| n: 56 |
| Sex: Not reported |
| Income: Not reported |
| Description of intervention and control |
| Modified 1000 calorie per day version of the Rice Diet, 7% fat vegan vegetarian for first 2 weeks. Participants were randomly assigned to receive the intervention immediately or after a delay of 8 weeks. A fee was charged for the programme |
| Patients were educated on the usefulness of exercise in weight loss and weight maintenance and advised to increase their activity above baseline levels by whatever means they felt comfortable. Participants met twice weekly for support and educational sessions. Sessions lasted for 30–60 minutes with education on basic nutritional principles and healthful eating. Low-fat and low-salt cooking techniques were demonstrated and participants were taught how to modify recipes at home. As part of a motivational approach participants had their weight and blood pressure measured at each session |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: 8 weeks |
| BMI: Mean decreased from 37.8 kg/m2 to 35.3 kg/m2 (p < 0.01) |
| Weight: Average (SD) weight loss for the participants completing the intervention was 14.8 lb (6.8 lb) |
| Conclusions |
| Authors: Diet programmes can be successfully tailored to incorporate the needs of African Americans. Most importantly, these dietary programme changes can lead to significant improvements in clinical parameters; additional studies are needed to determine the permanence of these short-term changes |
| Reviewers: The cost of participation as well as recruitment of university employees may have meant that participants were of fairly high SES, education and income (these demographics are not provided) and perhaps the results are less generalisable to a wider population |
| Comments and limitations |
| Outcomes were monitored for 8 weeks only and there is no evidence of long-term effect. A highly motivated group was selected that included employees in the university or health centre, although it did show that this group was unable (although motivated) to lose weight on their own in the delay experienced by the control group. This study had an unusual design and approach and perhaps the results are less generalisable to a wider population |
| Study reference |
|---|
| Resnicow et al. 2000284 (Go Girls) |
| Setting |
| USA; city or state not reported |
| Inclusion criteria |
| Female, living in or near the public housing development, age 11–17 years, overweight based on BMI ≥ 85th percentile for age and sex or percentage body fat > 35% based on dual-emission X-ray absorptiometry or (if neither measurement available) visual inspection |
| Study type |
| Pre–post |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean: 13.5 |
| n: 57 |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| The programme was delivered to 8–14 adolescents at a time in a community space or apartment and was conducted in four 6-month cycles over 2 years. For the first 4 months, sessions were twice per week, and for the final 2 months they were weekly. There were also some field trips at the weekends and during school holidays |
| Each session had three elements – an education/behavioural activity, 30–60 minutes of physical activity and preparation/tasting of low-fat meals. Primary target behaviours were increased fruit and vegetable consumption, decreased fat intake, decreased fast food intake, decreased television watching, increased physical activity and communication skills to enhance participants’ ability to encourage parents to shop and prepare healthier foods. Experiential activities were designed to enhance skills, efficacy and outcome expectations. Messages emphasised the physical and health effects of changes rather than the aesthetic effects (based on focus group findings about body image) – emphasis on substitution, moderation and abstinence |
| Theory: Social cognitive theory |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and immediately post intervention |
| Changes in dietary fat: High attendees showed more favourable results at 6 months for most outcomes compared with low attendees, e.g. low-fat practices (p = 0.05), perceived changes in low-fat practices (p = 0.04) |
| Knowledge: High attendees showed more favourable results at 6 months compared with low attendees, e.g. nutrition knowledge (p = 0.001) |
| Conclusions |
| Authors: The authors concluded that the programme had a modest favourable impact on knowledge and some dietary behaviours and served as a maintenance programme, perhaps decelerating weight gain and the associated morbidities |
| Reviewers: This study has no control group and undertook a post hoc analysis. It appears to suggest some change in behaviour but no change in physical outcomes. Further evaluation is needed to see whether the intervention is effective |
| Comments and limitations |
| There was difficulty with attendance and retention and participants on average attended 43% of sessions and the dropout rate was 45%; this may have biased the sample. The analysis of low and high attendees was post hoc and the cut-off point of 50% was arbitrary. Most of the measures were self-reported and may have been influenced by social desirability bias. Some measures were developed for this intervention and had not been used previously. The relatively small sample size meant low statistical power. There was no real control group. There were budgetary limitations that limited the amount of outcome data collected |
| Study reference |
|---|
| Nothwehr et al. 2001312 |
| Setting |
| USA; Indianapolis, IN |
| Inclusion criteria |
| African American women aged 30–65 years with type 2 diabetes diagnosed for at least 1 year, BMI of ≥ 27 kg/m2, able to walk independently, not currently pregnant and able to provide informed consent. Also had to not have any major illness or history of heart disease that would prevent them from participation in regular exercise. They were all reviewed by an endocrinologist to check eligibility for the programme |
| Study type |
| RCT (pilot study) |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean: 49.4 |
| n: 23 |
| Sex: 100% female |
| Income: Predominantly low income |
| Other: 39% were married and 69.5% were unemployed |
| Description of intervention and control |
| Women were randomly assigned to either 10 weekly sessions about healthy eating followed by six weekly sessions about exercise or the reverse sequence. Sessions consisted of small group discussions (four to five people) and physical activity or food tasting. The sessions lasted for 90 minutes and were held in the local YMCA |
| Topics in the exercise sessions included group problem-solving regarding barriers to behaviour change, exercise safety, benefits of an active lifestyle, finding time to be active and relapse prevention. Handouts were given with the key messages. Participants were also given a year’s free membership to the YMCA and audiotapes and videotapes of chair-based exercises |
| Theory: Not reported |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 4 and 12 months post programme |
| Changes in fruit and vegetable consumption: There was a significant increase in vegetable intake (an increase of 0.5 servings a day at 1 year, p = 0.02) |
| Changes in calories: Significant decrease in the per cent of calories from fat (4 months, p = 0.05) |
| Changes in physical activity: Significant increase in minutes of activity (4 months, p = 0.0002, 1 year, p = 0.0001) in both groups |
| Weight: No significant change in weight over the year – both groups lost an average of 3 lb |
| Conclusions |
| Authors: This study does not provide definitive evidence of which sequence is best to bring about behaviour change, and the effects of sequencing difficult behaviour changes, such as diet modification and exercise, deserve further study |
| Reviewers: This study does not show a difference according to sequencing, which was the overall goal, but it does show overall improvements with the intervention for both groups, including increased exercise, improved nutrition and some weight loss (although the last was not significant). However, the fact that there was weight loss and not an overall weight gain is said by some to be reaching a goal in itself (reversing the usual trajectory). However, this was a pilot study with small numbers and needs further research. The adaptation was not a focus of the study and there is relatively little adaptation described but the intervention does appear to have been acceptable with good retention of participants |
| Comments and limitations |
| Limitations included that this was a small pilot study with a small sample size and no control group (a control group could have shown a greater effect of the intervention, particularly on weight, which may have had an upward trajectory for control participants over the year). The fact that the intervention retained for longer participants who were more educated and also somewhat fitter may limit its generalisability and affect its equity as it suggests that it was more sustainable for those participants who perhaps needed it less. The intervention offered free gym access and free exercise videos, which may have assisted participation levels, but it is hard to tell to what degree these incentives were important |
| Study reference |
|---|
| Williams et al. 2001297 |
| Setting |
| USA; city or state not reported |
| Inclusion criteria |
| Workers in a non-profit day-care centre with multiple sites |
| Study type |
| Pre–post |
| Description of population |
| Ethnicity: Black; not reported how ethnicity assessed |
| Age (years): Mean: 40 |
| n: 61 |
| Sex: Most were female (exact number not reported) |
| Income: Not reported |
| Other: Education varied from less than high school to graduate degrees |
| Description of intervention and control |
| Day-care centres were used as a site to develop a culturally sensitive intervention with on-site cardiovascular screening, informal interviews and discussion of behaviour change for better health |
| Intervention: The intervention aimed to assess the impact of the Healthier People Health Risk Appraisal (HPHRA) as a culturally appropriate recruitment strategy to involve workers at the day-care centre in screening and risk reduction. The HPHRA uses statistical actuarial software to perform an individual analysis of health risk, which facilitates individual health promotion and disease prevention intervention. The tool gives a report of positive life factors as well as risk factors. It can be a powerful tool for intervention but has been used in few studies with ethnic minority populations. Participants had counselling focusing on the integration of physical activity and healthy diet intake with their lifestyle and culture |
| Theory: The conceptual framework was the health promotion model (HPM) developed by Pender.488,489 The HPM is based on social cognitive theory with four components – cognition, affects, actions and environmental events – interacting to determine health behaviour |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 1 year post intervention |
| Changes in dietary fat: Positive changes in cholesterol but not statistically significant (p = 0.0589); the day-care workers reported eating less fat and more fibre |
| Changes in physical activity: The day-care workers reported participating more in physical activity |
| Conclusions |
| Authors: Participation rates in the project increased from 26% in the first year of the project to 73% when long-term relationships were built on culturally appropriate strategies. The project’s culturally sensitive educational intervention focused on individual risks and lifestyle. Statistical analysis of the outcomes of the intervention and personal interviews demonstrated the improvement of cardiovascular status in the day-care workers. This psychosocial approach can provide the foundation for culturally sensitive care in larger occupational and community settings |
| Reviewers: The authors considered this an effective intervention and there certainly appears to have been good engagement and also changes in behaviour/self-reported measures. However, there were no significant changes in blood values or weight and BMI. There needs to be further research to examine the effectiveness of this approach utilising comparison groups, preferably a RCT |
| Comments and limitations |
| This study is limited by having no control group and using self-reported measures, which can be prone to social desirability bias. This is also a very specific population and it is hard to assess the generalisability |
| Study reference |
|---|
| Yanek et al. 2001352 (Project Joy) |
| Setting |
| USA; inner-city churches in Baltimore, MD |
| Inclusion criteria |
| Urban core of Baltimore, primarily African American congregation (80%), high interest level and participation in local activities, average Sunday attendance of at least 150 people, no currently active programme in weight control, exercise or smoking cessation for women aged ≥ 40 years |
| Study type |
| Group RCT (randomisation later dropped) |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean: spiritual and cultural group (SP): 53.6 ± 9, standard group (SI): 51.9 ± 9, self-help group (SH): 53.9 ± 10 |
| n: 16 churches; n = 529 |
| Sex: 100% female |
| Other: 92.9%, 90.4% and 93.2% of the SP, SI and SH groups, respectively, completed high school |
| Description of intervention and control |
| Impact of a 20-week active nutrition and physical activity intervention on 1-year measures relating to lifestyle risk factors and CVD risk profiles compared with a self-help (control) group. Also, studied the impact of church culture on the intervention. Three intervention groups: (1) standard group method + weekly sessions (SI); (2) standard group method + spiritual and cultural component (SP); (3) non-spiritual, self-help intervention (SH) |
| SI: Weigh-in and group discussion; 30- to 45-minute nutrition education module with taste testing or cooking demonstration; 30 minutes of moderate-intensity aerobic activity. After 20 weeks, lay leaders offered weekly sessions |
| SP: Same sessions as SI with the addition of spiritual components and church contextual components. Telephone calls from lay leaders and word of mouth from other participants motivated attendance |
| SH: Included materials from the American Heart Association (AHA) on healthy eating, and physical activity and information targeted participants’ personal screening results and feedback |
| Theory: Social cognitive theory to enhance individual self-efficacy; interventions designed at the individual level to enhance self-efficacy but implemented through churches in group sessions to assure strong support |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 1 year |
| Changes in fruit and vegetable consumption: 38% of the active intervention groups consumed five or more servings of fruit and vegetables a day vs 44.6% of the control group (p = 0.0001) |
| Changes in calories: Mean change in energy intake of –117 kcal/day in the active intervention groups vs –7 kcal/day in the control group (p=0.0038) |
| Changes in dietary fat: Mean change in total fat of –8.1 g/day in the active intervention groups vs –2.3 g/day in the control group (p = 0.0250) |
| BMI: Mean change of –0.17 kg/m2 in the active intervention groups vs 0.14 kg/m2 in the control group (p < 0.0012) |
| Weight: Mean change of –1.1 lb in the active intervention groups vs 0.83 lb in the control group (p < 0.0008) |
| Conclusions |
| Authors: This study demonstrates significant improvements in anthropometric measures, blood pressure levels and diet and, to a lesser extent, physical activity at 1 year in the active intervention groups, although the magnitude of effect was modest. Follow-up was longer in this study and focused on globally healthy lifestyles as opposed to a single behavioural goal. A total of 10% of participants in the active church-based intervention achieved clinically significant improvements in CVD risk profiles (top decile for weight loss) 1 year post intervention. There were no differences in outcomes between the SI and SP churches. It is not possible to maintain a non-spiritual intervention within the African American church environment. There was a lack of interest in the self-help programme. Eight of nine active intervention churches held weekly sessions led by their own lay leaders |
| Reviewers: The self-help group is much smaller than the SI and SP groups. It is interesting to see that the results of the SI and SP groups are comparable, which suggests that it may be less the religious component and more the social support/group format that accounts for the success of the intervention compared with the self-help group |
| Comments and limitations |
| Authors do not present many limitations, except that the churches were not really willing to be randomised to the self-help condition. Randomisation was dropped later in the recruitment process. Despite aggressive recruitment, women from churches randomised to the self-help group were not interested in the self-help intervention. Women were avidly interested in active sessions and expressed a strong desire to receive directed assistance. For this reason, numbers recruited for self-help were lower. There were dropouts as a result of not seeing immediate results; follow-up calls were insufficient to motivate attendance. Anecdotally, churches with the strongest support from the pastor’s wife had the best attendance and vice versa |
| Study reference |
|---|
| Karanja et al. 2002490 |
| Setting |
| USA; Portland, OR |
| Inclusion criteria |
| Relatively good health as ascertained by the participants’ physicians and a desire to lose weight were the only criteria |
| Study type |
| Controlled before and after/pre–post |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean (SD): 44 (9) |
| n: 62 |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| A 6-month weight loss programme with 26 weekly group meetings with 15–25 participants and encouraged to attend weekly supervised exercise sessions held at a local community centre. During each group meeting the first 30 minutes was spent being weighed and providing other data such as food records and self-reported exercise activity for the preceding week. The group then shared a meal prepared by participants, who discussed how they reduced the fat content of each dish. The second hour of each session was spent discussing nutrition and behaviour modification topics |
| Nutrition: Modelled after Kaiser Permanente’s Freedom from Fat programme, which emphasises reducing energy consumption by reducing total fat intake |
| Exercise: Encouraged to increase physical activity gradually until exercising three to four times a week for ≥ 30 minutes. Professionally led exercise classes offered every Saturday at a local community centre; could choose between a water aerobics class, a beginners-level strength training class or a walking group. Classes were scheduled so that participants could attend two sessions on the same day. Classes created a social support system for exercise and provided demonstrations |
| Theory: Modelled after Kaiser Permanente’s Freedom from Fat programme. Relapse prevention training. Consistent with cultural/adaptation approaches suggested by Kumanyika and Morssink491 and Resnicow et al.35 |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 6 months |
| Changes in calories: Significant changes from baseline to follow-up in reported intake of total energy [9623 ± 4138 kJ to 8640 ± 3962 kJ (p = 0.02)] and dietary fat [102 ± 53 g to 80 ± 49 g (p = 0.001)] |
| Changes in physical activity: Average number of hours exercised increased significantly. Proportion of participants meeting the study goal of 1.5 hours also increased significantly |
| Weight: Participants attending at least 75% of group meetings lost a mean of 6.2 kg at 6 months; those who attended fewer meetings lost a mean of 0.9 kg. Mean weight loss at 26 weeks was 3.7 ± 5.1 kg (range 5–25 kg) for all participants at a mean rate of 0.14 kg per week |
| Conclusions |
| Authors: Relatively larger weight losses, particularly among participants with high attendance, than have usually been observed in culturally adapted programmes for African American women. Successful weight loss was ascribed to cultural adjustments made to the programme delivery. Difficult to compare results with other studies that have tested the effects of culturally adapted programmes on weight loss in African American women because they tend to be smaller, of a shorter time period and achieve weight loss ranging from 0.2 to 4.5 kg. Although the study did not test a hypothesis about the role of cultural adaptations in promoting weight loss, the impression is that the programme outcomes were greatly enhanced by the adaptations made |
| Reviewers: The intervention was successful in helping African American women lose weight. It appears that there was an intervention dose-dependent response in which participants who attended > 75% of the sessions lost the majority of the weight. The adaptations are thoroughly described |
| Comments and limitations |
| Did not collect data on SES, health status (presence/absence of comorbid conditions) or previous experience in weight loss programmes – may influence comparability with other programmes. Another factor that may have contributed to improved weight loss was the relatively high BMI range of these participants. |
| Sixty-six women attended the information session and were weighed, three dropped out after the first three of the 26 weekly sessions; 76% of women attended at least 50% of the 26 weekly sessions; 56% attended at least 75% of sessions (an intention-to-treat analysis was used in most analyses) |
| Study reference |
|---|
| Keyserling et al. 2000;492 Keyserling et al. 2002493 (New Leaf programme) |
| Setting |
| USA; North Carolina |
| Inclusion criteria |
| African American women aged ≥ 40 years with type 2 diabetes (defined as a diagnosis of diabetes at ≥ 20 years with no history of ketoacidosis) |
| Study type |
| RCT |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean: 59 |
| n: 219 |
| Sex: 100% female |
| Income: One-third reported a total annual household income of < US$10,000 |
| Other: Mean educational achievement was approximately 11 years in all groups |
| Description of intervention and control |
| Conducted at primary care practices. The intervention evolved from the Food for Heart programme. The intervention combined traditional clinic-based counselling with a co-ordinated community component using peer counsellors and it included physical activity to a cumulative time of 30 minutes a day; a dietary component designed to decrease total and saturated fat intake and to improve control and distribution of carbohydrates; and a diabetes care component addressing various aspects of self-care |
| Participants were assigned to one of three conditions: the clinic and community interventions (A), the clinic intervention only (B) or a minimal intervention (C). The clinic-based component included individual counselling visits at months 1, 2, 3 and 4. The community-based component included two group sessions and monthly telephone calls from a peer counsellor. The minimal intervention group were mailed pamphlets on staying active, healthy eating and diabetes |
| Theory: Transtheoretical model, social cognitive theory and basic behaviour modification principles |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 6 and 12 months |
| Changes in dietary fat: Percentage calories from saturated fats, dietary cholesterol intake and total energy intake decreased in all three groups but changes were not statistically significant |
| Changes in physical activity: Physical activity increased over 1 year; changes were significantly higher for group A compared with group C (p = 0.005) and for group B compared with group C (p = 0.029) |
| Weight: For all groups weight increased modestly although not significantly |
| Conclusions |
| Authors: The New Leaf intervention was associated with a statistically significant enhancement of physical activity energy expenditure as assessed by an accelerometer (p = 0.014). Group A on average were 15% more active than group C. The study was not designed to detect a difference between groups A and B but there appears to be a favourable effect of the additional community component. It was disappointing to observe that participants in all groups gained weight. Both the clinic and community components were acceptable to participants and feasible within the context of a research study. Overall, the programme was associated with a modest enhancement of physical activity compared with the minimal intervention, but whether this will translate to improved health outcomes is unknown |
| Reviewers: This study shows some effect on physical activity and appears acceptable and feasible. It does not tell us much about adaptation as there is no comparison with an unadapted intervention |
| Comments and limitations |
| Possible bias in physical activity measurements from differences in how much people wore the accelerometers. Also, measures were self-reported |
| Study reference |
|---|
| Baranowski et al. 2003494 [Baylor Girls health Enrichment Multisite Studies (GEMS) Fun, Food and Fitness Project (FFFP)] |
| Setting |
| USA; Houston, TX, summer day camp and homes |
| Inclusion criteria |
| 8-year-old African American girls with parents willing to be involved, ≥ 50th percentile for age- and gender-specific BMI (Centers for Disease Control growth charts), in possession of a home computer with internet access, informed and parental consent. Those with a medical condition, taking medication that affects growth or with a condition that would limit participation or measurement were excluded |
| Study type |
| Two-arm parallel group randomised pilot study (urn randomisation procedure) |
| Description of population |
| Ethnicity: African American; reported by parent(s) or legal guardian(s) |
| n: 35 girls and parents/caregivers; 19 treatment, 16 control |
| Sex: 100% female |
| Income: Majority earned ≥ US$40,000 a year with college education or postgraduate education |
| Description of intervention and control |
| Obesity prevention among healthy 8-year-old African American girls by increasing fruit and vegetable intake, lowering dietary fat, increasing water consumption and fibre intake and increasing physical activity to 60 minutes a day. Camps were subsidised. Different internet programmes for intervention girls, intervention parents/carers, control girls and control parents/carers |
| Intervention: 4-week summer day camp (regular + GEMS-FFFP) followed by 8-week home internet maintenance intervention for girls and parents. At camp there was a buddy system to increase physical activity; camp cheers as mnemonic devices for decision-making; problem-solving and communication skills to get parents to undertake physical activity with children; dance; games for increasing fruit and vegetable and juice intake; and food preparation. Also included education for parents and children for healthier lunches; a pedometer was also given. Girls had access to a comic book with characters who attended GEMS, problem-solving, goal-setting, a photo album, an ask the expert feature, links to other websites. Received weekly e-mails and telephone reminders to log on. Parents/carers also had a comic book linked to the children’s comic book with an ask the expert feature and links to other websites |
| Control: 4-week summer day camp (different from the intervention) followed by monthly home internet intervention with no GEMS-FFFP components. Girls had access to general health and homework websites for 8-year-old girls. Parents/carers had access to girls’ websites with information on general health issues and links |
| Theory: Social cognitive theory; this intervention explains how components of social cognitive theory are used throughout the intervention |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline, 4 weeks (BMI only measured) and 12 weeks; intention-to-treat analysis |
| Changes in fruit and vegetable consumption: At 12 weeks there was greater consumption of water, fruit and vegetables and juice and less consumption of sweetened beverages for intervention girls; the difference was not significant |
| Changes in calories: At 12 weeks, lower calories; the difference was not significant |
| Changes in dietary fat: At 12 weeks there was a lower percentage of calories from fat for intervention girls; the difference was not significant |
| BMI: No significant differences in BMI between treatment groups at any time point; at 4 weeks, girls in the intervention group who were heavier at baseline showed a trend (p < 0.08) towards lower BMI compared with similar girls in the control group (28.6 kg/m2 vs 29.3 kg/m2) |
| Log-on rates: Less than half of the intervention girls logged on to the website, which limited the intervention dose; weekly log-on was < 50% from the beginning for both girls and parents/carers. The control group had lower log-on rates but this was expected |
| Conclusions |
| Authors: This intervention did not lower BMI in the intervention compared with the control group at 12 weeks. The difference in BMI at baseline may have contributed to a lack of difference (even though adjusted for baseline). Trend towards lower BMI for heavier girls suggests that a camp may be useful for heavier African American girls (also observed in other studies). Summer day camp appeared to be useful for initiating behaviour; need more methods for enhancing log-on |
| Reviewers: Agree with authors’ conclusions. Furthermore, it is unclear how generalisable this study would be as it included a highly educated and middle-income cohort – perhaps may benefit a low-income group more. Authors suggest that the initial interest in the internet component eventually became a burden; thus, its use for this group was minimal |
| Comments and limitations |
| US$100 weekly lottery was run for 5 weeks to increase the log-on rates; they did not change from approximately 50%. There were incentives for completing the baseline and 12-week assessments (US$10 for children, US$25 for adults) |
| Study reference |
|---|
| Beech et al. 2003;396 Klesges et al. 2008395 |
| Setting |
| USA; Memphis, TN |
| Inclusion criteria |
| African American girls aged 8–10 years and their parents/caregivers were eligible to participate, girls with BMI ≥ 25th percentile of the Centers for Disease Control growth charts, able to participate in physical education classes at school |
| Study type |
| Pilot RCT |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean: children: 8.9 ± 0.8, parents: 35.5 ± 7.2 |
| n: 60 |
| Sex: Children 100% female; gender of parents/caregivers was not reported, unclear if all women |
| Income: 64% had a household income < $40,000 per year and almost one-quarter had a household income < $20,000 per year |
| Description of intervention and control |
| Content was focused on knowledge and behaviour change skills to promote healthy eating and increase physical activity |
| Child targeted: 90-minute session with 30 minutes of hip hop aerobics as the main activity; also taste testing and food preparation activities, food art, modified farmers’ market, basic label reading skills, healthy snacks and child-friendly recipes provided at each session |
| Parent targeted: 90-minute session with a physical activity component of dancing, a didactic nutrition segment and a segment alternating food preparation and nutrition-related games. Childcare provided with specific activities designed for the 9- to 10-year-old daughters that did not focus on nutrition or physical activity. Discussions regarding links between nutrition and parental concerns, suggestions and strategies to increase healthy family lifestyles, and cooking activities alternated with games. Culturally relevant print information to take home provided in both arms |
| Comparison: Focused on global self-esteem. Three monthly 90-minute sessions over a 12-week pilot period. Designed to enhance and prevent a decline in self-esteem among 8- to 10-year-old girls and to be neutral with respect to dietary practices and physical activity. Personalised greeting cards and general health information were mailed to participants bimonthly to maintain contact and build rapport |
| Theory: Social cognitive theory; theoretical and empirical evidence supporting the use of a family-based approach; and conceptualisation of family influences on children’s weight-related behaviours informed by family systems theory. Key foci in social cognitive theory interventions include developing knowledge and skills needed to change behaviour, expecting positive outcomes in association with behaviour change, developing self-efficacy in performing new behaviours and learning self-regulatory skills |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 12 weeks |
| Changes in physical activity: Girls in the active intervention groups increased their minutes of moderate to vigorous physical activity by 11.7% |
| BMI: Girls in both the child-targeted and parent-targeted interventions demonstrated a trend towards reduced BMI and waist circumference compared with girls in the comparison intervention |
| Conclusions |
| Authors: This pilot study demonstrated the feasibility, perceived acceptability and efficacy of culturally relevant obesity prevention interventions for pre-adolescent African American girls and their parents/caregivers. Both active interventions were associated with some level of behaviour change in the expected direction |
| Reviewers: This appears to be quite an innovative intervention in which both active groups showed trends in the hypothesised direction, even in the arm in which the girls were not intervened on themselves (in the parent-targeted group). This study is now in Phase 2, which is a 2-year RCT to evaluate the short- and long-term ability of the intervention to prevent obesity in pre-adolescent girls. Baseline data reported in Klesges et al.396 |
| Comments and limitations |
| The 12-week intervention period was insufficient to see significant changes in BMI. The comparison group included statistically significantly older caregivers than the treatment groups. Both the active and the comparison interventions had to be viewed as substantive and appealing to recruit and retain African American girls and their parents/caregivers. Randomisation to a ‘no treatment’ control was difficult for participants to accept |
| Study reference |
|---|
| Frenn et al. 2003337 |
| Setting |
| USA; Midwest |
| Inclusion criteria |
| Two urban low- to middle-income schools. Entire classrooms of students were enrolled in the intervention or control group to prevent diffusion of the intervention |
| Study type |
| Quasi-experimental |
| Description of population |
| Ethnicity: Mixed but some results presented stratified by ethnicity – African American, Hispanic, Asian, white, Native American |
| Age (years): Range: 12–15 |
| n: 130; 341 were sampled from and 130 included; 67 intervention group, 63 control group (of relevance to our study, there were 58 African American and 9 Asian participants included among the 130 participants) |
| Sex: Not reported |
| Income: Not reported |
| Description of intervention and control |
| An internet and video intervention to promote a low-fat diet and moderate and vigorous physical activity |
| The intervention was tailored to the students’ stage of change; those in the earlier stages focused on awareness of their current behaviours and overcoming barriers to change; those in the later stages were prepared as ‘peer models’ to lead healthy snack and exercise sessions with the help of senior nursing staff and faculty. The intervention took place in the computer lab and consisted of four internet sessions plus a healthy snack session and a gym class (one school only) of approximately 50 minutes (six sessions in total) |
| Theory: Transtheoretical model and tailored to stages of change and Penders Health Promotion model488,495 |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Not reported |
| Changes in dietary fat: For the African American population there was a significant reduction in fat intake (p = 0.018); for the Asian population there was a significant change in access to low-fat foods (p = 0.036) |
| Changes in physical activity: Both the intervention and control groups decreased their amounts of physical activity, although the decrease was significantly less in the intervention group (–8.58 minutes as opposed to –37.61 minutes, p = 0.024). When analysed by ethnicity and income levels there was a significant increase in physical activity for African American and Asian participants who were in the lowest income group. In addition, those who had the peer-led gym sessions increased their total physical activity, whereas those with only the internet and video intervention decreased their total physical activity, but not as much as those in the control group |
| Conclusions |
| Authors: This intervention was effective in increasing moderate and vigorous activity levels in particular groups. The internet content alone prevented a decrease in exercise to the degree that it occurred in the control group. Interventions delivered through the internet and by video may enable a reduction of health disparities in students by encouraging those most at risk to consume ≤ 30% of calories from fat and to engage in moderate and vigorous physical activity |
| Reviewers: This study appears to show some effect in changing diet and exercise behaviours in the populations of interest. However, conclusions are limited by the study design, missing data and the presentation of the results, which included graphs for ethnic-specific data and not the actual data |
| Comments and limitations |
| Limited by the number of students with missing data; there were a lot of data missing, including from different categories, which prevented analysis of both diet and exercise in the same equations, and there was low test–retest correlation |
| Study reference |
|---|
| Robinson et al. 2003;329 Robinson et al. 2008330 (Stanford GEMS pilot study) |
| Setting |
| USA; low-income neighbourhoods of Oakland and East Palo Alto, CA |
| Inclusion criteria |
| Aged 8–10 years, identified as African American or black by a parent or guardian, BMI ≥ 50th percentile for age and/or at least one overweight parent/guardian with BMI ≥ 25 kg/m2 |
| Study type |
| CCT |
| Description of population |
| Ethnicity: African American; identified by a parent or guardian |
| Age (years): Children 8–10 years and their parents |
| n: 61 |
| Sex: Not reported |
| Income: 1% < US$20,000 per year, 72% < US$40,000 per year |
| Other: 56% lived in female-headed households |
| Description of intervention and control |
| A 12-week programme to test the feasibility, acceptability and potential efficacy of after-school dance classes and a family-based intervention to reduce television watching and thereby reduce weight gain |
| GEMS Jewels dance class: After-school dance classes were held at three community centres, 5 days a week, in the target neighbourhood. Each daily session lasted for up to 2.5 hours (snack, homework period, 45–60 minutes of moderate to vigorous dance, 30 minutes of discussion). START (Sisters Taking Action to Reduce Television): A five-lesson intervention over 12 weeks, delivered in participants’ homes, to reduce television, videotape and video game use. Also five newsletters mailed to the participants |
| Active control: Newsletters (five to parents, 11 to girls) and monthly health education lectures promoting healthful diet and activity patterns by volunteers from African American task forces of the American Heart Association and American Diabetes Association. Content focused on reducing risk, especially among African American populations, and was age appropriate and included culturally targeted educational materials |
| Theory: Social cognitive model suggests that four processes are important in learning and adopting new behaviours: attention, retention, production and motivation. Intervention development and implementation was organised around these processes |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 12 weeks |
| Changes in calories: Small non-significant differences in the total calorie intake per day, favouring the control group |
| Changes in dietary fat: Non-significant differences in the percentage of calories derived from fat, favouring the treatment group |
| Changes in physical activity: Increased after-school physical activity (adjusted difference between treatment and control 55.1 counts/minute, 95% CI –115.6 to 225.8 counts/minute, d = 0.21 SD, p = 0.53) |
| BMI: Compared with girls in the control group, girls in the intervention group showed trends towards lower BMI (adjusted difference between treatment and control –0.32 kg/m2, 95% CI –0.77 to 0.12 kg/m2, Cohen’s d = 0.38 SD, p = 0.16) |
| Conclusions |
| Authors: This study confirmed the feasibility, acceptability and potential efficacy of using dance classes and a family-based intervention to reduce television viewing, thereby reducing weight gain in African American girls. Integrating the project into the community and designing the assessment and intervention methods to meet the needs of participants led to highly successful recruitment and retention. A major barrier was transportation to after-school dance classes; this could be overcome if the programme was implemented at the school itself. Standardised effect sizes of 0.38 for BMI and 0.25 for waist circumference over 12 weeks, although not definitive, are of clinical importance. Decrease in weight concerns counters the suggestion that an obesity prevention intervention might have promoted disordered eating attitudes |
| Reviewers: This study showed positive results and was quite innovative as it utilised both surface and deep level adaptations in the treatment and compared with an ‘active’ (somewhat adapted) control condition. Furthermore, the de-emphasis on obesity prevention was seen as important. The holistic after-school programme appeared to be an effective way of engaging girls; however, it was unclear how sustainable this would be without long-term funding |
| Comments and limitations |
| Interventions focused on weight are not highly motivating to African American girls and their families as they report heavier ideal/desired weights, more positive body image, etc.; therefore, the intervention must place more stress on physical activity as being good for health. The study was not powered to detect all clinically significant differences between groups. It is quite interesting that physical activity was measured after the intervention was complete, to observe residual effects, because if measured during the intervention it is likely that the treatment group would have increased physical activity compared with the control group |
| Study reference |
|---|
| Story et al. 2003410 (Minnesota GEMS) |
| Setting |
| USA; Minnesota, community based |
| Inclusion criteria |
| 8- to 10-year-old African American girls with BMI ≥ 25th percentile for age and sex, able to participate in physical education classes at school, having a primary caregiver fluent in English and not held back more than one grade in school |
| Study type |
| Pilot two-arm parallel group RCT |
| Description of population |
| Ethnicity: African American; not reported how ethnicity assessed |
| Age (years): Mean (SD): children 9.3 (0.9), parents/caregivers 36.8 (7.6) |
| Sex: 100% female |
| Income: 54% of parents reported incomes of < US$30,000 per year |
| Description of intervention and control |
| A 12-week after-school obesity prevention programme for African American girls. Included two sessions a week focused on increasing physical activity and healthy eating. Family component included |
| Family intervention: Weekly family packets sent home to parents; family night events; telephone calls from intervention staff to parents (to encourage them and to check progress); organised neighbourhood walks. Two family nights held during the second and ninth weeks of the intervention. An integral part of both family nights was a family goal-setting activity. Principles and techniques from motivational interviewing were used |
| Control: 12-week programme unrelated to nutrition and physical activity. Focused on promoting positive self-esteem and cultural enrichment. Participants attended monthly Saturday morning meetings (three meetings during the 12-week period) that included arts and crafts, self-esteem activities, creating memory books and a workshop on African percussion instruments. Transportation was provided for both groups as required |
| Theory: Intervention was based on social cognitive theory and targeted key constructs from three domains: environment factors, personal factors and behavioural factors. A youth development, resiliency-based approach was also employed, which acknowledged the importance of building on individual and family strengths |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline and 12 weeks |
| Changes in fruit and vegetable consumption: Fruit and vegetable servings per day were lower for the intervention group at follow-up than the control group (not significant) |
| Changes in calories: Intervention group girls had a lower calorie intake, lower per cent of calories derived from fat and more servings of water per day than control group girls |
| Changes in physical activity: Physical activity measures demonstrated consistently greater activity levels in the intervention group than in the control group |
| BMI: After adjustment for baseline level, follow-up BMI did not differ between the treatment groups |
| Knowledge: The intervention group reported significantly higher scores than the control group at follow-up on the healthy choice behavioural intentions (p = 0.001), diet knowledge (p = 0.001) and preferences for physical activity (p = 0.04) |
| Conclusions |
| Authors: An after-school obesity prevention programme for low-income African American girls is a promising model for future efforts. No between-group differences were observed for BMI, and only a few significant findings were seen for other variables. Differences are, however, in the hypothesised direction. Surprisingly, follow-up results showed a trend towards higher mean waist circumference among the intervention group compared with the control group, with an adjusted mean difference of 1.4 cm between groups; this could be because the intervention group included three of the heaviest girls in the study. The intervention group was more likely to report both moderate and less healthy weight concern behaviours at follow-up, e.g. taking on unhealthy behaviours such as skipping meals and fasting |
| Reviewers: No significant differences were reported in the main outcomes of interest but the intervention group showed a trend in the anticipated direction. The surprising findings are interesting to note, as they suggest that the intervention may not have been long enough or may have had adverse/opposite effects in terms of leading girls to develop excess concern with weight and shape |
| Comments and limitations |
| Small sample size and short duration – did not have the power to test for between-group differences in BMI or other key outcome measurements. Tests of statistical significance used as guides for interpretation, rather than as definitive inferential tests |
| Study reference |
|---|
| D’Eramo-Melkus et al. 2004331 |
| Setting |
| USA; general clinical research centre of a major university hospital located in the community from which the study sample was drawn |
| Inclusion criteria |
| Women, aged 18–60 years, having a primary care provider, diagnosed with type 2 diabetes mellitus (C-peptide levels ≥ 200 pmol/l) and English speaking |
| Study type |
| Controlled before and after; pilot feasibility testing. One-group, pre–post test experimental design |
| Description of population |
| Ethnicity: Black American; not reported how ethnicity assessed |
| Age (years): Mean (SD): 51.7 (SD 6.9) |
| n: 25 |
| Sex: 100% female |
| Income: Not reported |
| Description of intervention and control |
| A 6-week culturally competent, cognitive-behavioural intervention of education and care for black women with type 2 diabetes. Led by registered nurses trained in diabetes care |
| Intervention: Two groups of 7 to 10 women. Evening and Saturday sessions offered for convenience. Childcare and no-cost parking provided. Missed sessions could be made up. Presentation and discussion with the emphasis on problem-solving, counterconditioning, stimulus control and decision-making for goal attainment. Group context was used for support |
| Class 1: diabetes-related health risk for black American women; class 2: cultural barriers and beliefs that support or hinder dietary modification and desirable body weight; discussed social support systems/networks in the facilitation of behaviour change; class 3: caloric density of food and food density; class 4: monitoring glucose control and personal eating habits; class 5: activity/exercise and foot-care class; 6: identification of ways and means of reaching goals for diabetes self-care. Monthly diabetes care visits |
| Theory: Social learning theory, particularly self-efficacy and behaviour change. Transtheoretical model of behaviour change incorporates the personal and environmental variables of social learning theory that are modifiable, including expectancies of efficacy and outcome. Two main constructs are experiential and behavioural processes of change. These processes of change promote stage transitions |
| Approaches to adaptation |
|
| Outcome measures and results |
| Follow-up: Baseline to 3 months post intervention |
| BMI: Significant change in mean (SD) BMI from 32.1 kg/m2 (7.5 kg/m2) to 31.7 kg/m2 (7.8 kg/m2) (t = 3.1, p = 0.005) |
| Weight: Significant decrease in mean (SD) weight from 193.2 lb (10.3 lb) to 191.0 lb (10.5 lb) (t = 2.3, p = 0.03) |
| Conclusions |
| Authors: This study suggests that, when black women are given the opportunity to participate in a planned programme of culturally competent diabetes education and care that is acceptable and accessible, improved health outcomes can be attained |
| Reviewers: This intervention showed statistically significant changes in mean weight and correspondingly BMI; however, given that it is a convenience sample it is difficult to generalise. Furthermore, it is difficult to know how nutrition and physical activity were affected as there were no indicators measuring changes in these outcomes |
| Comments and limitations |
| The study design needs a control condition. Included a self-selected group of volunteers who may represent black women with T2DM who would benefit the most from a self-management intervention of diabetes education and care. Future testing with a larger sample and a two-group design is warranted. Furthermore, the authors suggest that this study provided data on how to design an intervention to empower participants with the knowledge and skills necessary to assume diabetes self-management; however, this is a bit of a leap because their self-efficacy scores were not significant. ‘Empowerment’ would likely be reflected in these types of scores; thus, we are unsure by what mechanisms this intervention achieved its successful reduction in weight and BMI. Long-term follow-up is needed to determine if outcomes could be maintained over time. It is difficult to know if the women with type 2 diabetes are more motivated than healthy women to take up physical activity or make nutritional changes because of their condition |
|
Study reference Kelley et al. 2004496 |
|
Setting USA; Mississippi |
|
Inclusion criteria African American women aged 20–40 years |
|
Study type Partially blinded CCT |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean: control group: 28.51, intervention group: 31.91 n: 159 enrolees; 70 intervention group, 89 control group Sex: 100% female Income: Not reported |
|
Description of intervention and control The intervention included education on decreasing stress levels with exercise, meditation, reading, music and behavioural modification with approximately 5 minutes spent on the demonstration of deep breathing exercises Intervention group in clusters of three to nine; women received education on breast cancer, breast self-examination, healthy eating, exercise and stress management Control group in clusters of three to eight; women received education on poison control in the home environment |
| Theory: Bandura’s social cognitive theory497–499 and Giger and Davidhizar’s transcultural assessment model.269 The latter was derived as a means to understand diversity through cultural expression and was used to assist the nurse in utilising culturally relevant information. Related and sometimes overlapping components of this are communication, space, social organisation, time, environmental control and biological variations |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Not reported Changes in dietary fat: No significant differences between the intervention and control groups in the amount of fat or fibre intake Changes in physical activity: No significant differences in the amount of physical activity |
|
Conclusions Authors: In this research study an examination of the cultural appropriateness of an intervention for breast cancer prevention has provided a greater understanding of the theoretical application of Bandura’s social cognitive theory and Giger and Davidhizar’s model of transcultural assessment. There was no statistical evidence that the programme had an effect on the behavioural risk factors of high fat intake, limited amounts of physical activity and low fibre intake Reviewers: This intervention was aimed at changing behaviours that are risk factors for breast cancer, including physical activity and nutrition, for African American women. There were no significant differences between the intervention and control groups post intervention |
|
Comments and limitations The sample may not be generalisable to other regions and populations. As the subjects volunteered for the study and were then randomised by groups the sample may not represent the target population. Measures are self-reported. There was quite a high number of dropouts |
|
Study reference Thrasher et al. 2004;293 Campbell et al. 2004300 [Wellness for African Americans Through Churches (WATCH)] |
|
Setting USA; five rural eastern North Carolina counties, 12 African American churches |
|
Inclusion criteria All active members (i.e. those attending the study church at least once per month) aged 18+ years were eligible |
|
Study type Randomised trial, 2 × 2 factorial research design |
|
Description of population Ethnicity: 99% African American; not reported how ethnicity assessed Age (years): Mean: 52 n: 850 (12 churches); n = 587 completed both the baseline and follow-up surveys Sex: 72% women Income: Not reported Other: Approximately 25% had some education beyond high school |
|
Description of intervention and control Comparing the effectiveness of two theory-based strategies to promote colorectal cancer (CRC)-preventive behaviours. Church-based research study aimed at improving nutrition, physical activity and CRC screening among rural African Americans. Compared a tailored print and video (TPV) intervention consisting of four individually tailored newsletters and targeted videotapes with a lay health advisor (LHA) intervention, these two interventions combined (TPV + LHA) and a control. Primary prevention message encouraged increased fruit and vegetable consumption, lowering of dietary fat and moderate to vigorous physical activity on most days of the week TPV intervention: Computer-generated tailored messages based on individuals’ survey data and tailored to their stage of change, beliefs, knowledge, barriers and motivators, and cultural and spiritual factors. Four personalised computer-tailored newsletters and four videotapes corresponding to the same behaviours delivered to individuals at home bimonthly for the first 6 months after baseline data collection and not dependent on participation in church activities LHA intervention: Used the same theoretical constructs to train lay advisors to diffuse health information while supporting the behaviour change among church members. Lay advisors were used to disseminate information and promote interactions and activities aimed at the interpersonal, social network and church levels of influence and support Control: Offered health education sessions and speakers on topics of their choice not directly related to the study objectives – two sessions. After data collection control group was given intervention materials including the LHA training manuals and sessions |
| Theory: Social cognitive theory, stages of change transtheoretical framework and health belief and social support model |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline and 1 year after baseline (approximately 3 months after all intervention components were delivered) Changes in fruit and vegetable consumption: TPV intervention significant improved fruit and vegetable consumption (0.6 servings over baseline) (p < 0.05) Changes in physical activity: TPV intervention significantly improved recreational physical activity (2.5 metabolic task equivalents per hour) compared with the control. When each intervention group was compared with the control group, the TPV-only group showed significant improvement in recreational exercise (p = 0.04) whereas the LHA-only group showed a marginally significant improvement (p = 0.07) and the combined TPV + LHA group showed no significant improvement |
|
Conclusions Authors: This study failed to confirm the original hypothesis that a multicomponent approach that combined a tailored and targeted home-based intervention with a lay helping, church-based intervention would be more effective than either intervention alone. This may be due to exposure – only 10% of those in the LHA churches recalled talking with a LHA – limited reach with some social networks not represented among chosen LHAs. Also, the content may not have been delivered in the same way as the professionally developed tailored materials and it may take longer for a health message to diffuse through a community using LHAs. In addition, as they may have shared with others outside of the church, the full impact of LHAs may be missed by assessing change in only one part of their network (e.g. the church) Reviewers: Compared with the control group, the TPV-only group showed a significant improvement in recreational exercise; no other outcomes were significant compared with the control group. The LHAs had limited reach |
|
Comments and limitations Non-respondents to follow-up survey were younger and consumed fewer fruit and vegetables at baseline. Self-reported data and the small number of clusters and factorial design limited the ability to detect significant between-group differences |
|
Study reference Williams et al. 2004500 |
|
Setting USA; Georgia |
|
Inclusion criteria Not reported |
|
Study type Controlled before and after; two-group pre–post test |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean: urban 34, rural 33 n: Convenience sample, n = 294; n = 160 from five rural companies, n = 134 from 17 urban companies Sex: 100% female Income: Not reported Other: Mean education: urban 12.0 years, rural 11.0 years |
|
Description of intervention and control The intervention aimed to compare CVD risk factors in rural low-income African American women (LAAW) and urban LAAW with national risk factor data for AAW; test a worksite CVD risk factor reduction intervention among LAAW based on identified individual risk. There was no control group Phase 1: During the diet and physical activity interview, participants received personal health risk assessment (HRA) reports based on self-reported baseline survey data. The intervention followed protocols established for single risk factor or multiple risk factor lifestyle modification (ATP III,501 2001;502 JNC VI, 1997503). Participants were referred for medical tests if abnormal measures were identified. Lifestyle support and/or management of barriers for diet and physical activity behaviour change were part of the intervention Phase 2: To complete the intervention with a reinforced diet and physical activity message, a follow-up letter was mailed 2 weeks after the on-site visit with a recalculated HRA report using objectively measured blood pressure, BMI, weight and total cholesterol values |
| Theory: Pender’s health promotion model488,489 |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Pre-test and 1 year post intervention Changes in dietary fat: At baseline, a significantly larger percentage of urban and rural LAAW exhibited high daily fat intake than the national sample (p < 0.01). At post test there was a significant decrease in the rural LAAW group in the percentage of participants with a high daily fat intake (70.5% pre-test vs 55.4% post-test, p < 0.01) BMI: no significant change in BMI for either group from pre- to post-test Changes in physical activity: no significant changes in self-reported physical activity in either group from pre- to post-test |
|
Conclusions Authors: This study showed that LAAW can be reached at the work site and that rural LAAW are responsive to a worksite CVD prevention intervention. Pre-test/post-test analysis showed that the intervention was effective with rural women for dietary fat intake reduction. It is thought that they are more responsive because they lack previous measurements of risk and previous access to prevention interventions in their geographical areas. Neither rural nor urban women had significant changes in physical activity levels. Different interventions or more intense/longer intervention periods may be needed for urban LAAW Reviewers: This study was a one-off risk factor identification and brief interview intervention with LAAW in rural and urban worksites. Agree with the author that the change observed in the rural group is likely due to the lack of previous access to interventions. Given that both groups have comparable levels of education, it seems that access is perhaps the key difference here. This study showed that one-off interventions may have some effect; this needs to be tested in a more rigorously recruited sample |
|
Comments and limitations Pre test, significantly smaller percentages of the urban LAAW group had elevated cholesterol or high daily dietary fat intake than the rural LAAW group. Limitations include that the study was confined to one state. Sample size was large enough; however, there was no control group. More research needs to be carried out at small companies because little is known about preventive strategies that can be effective in these settings. No inclusion criteria included (convenience sample) and there was a 10% attrition rate |
|
Study reference Anderson et al. 2005309 |
|
Setting USA; Detroit, MI, urban |
|
Inclusion criteria No explicit criteria given |
|
Study type RCT, pre–post test design with repeated measures |
|
Description of population Ethnicity: African Americans; not reported how ethnicity assessed Age (years): Mean (SD): 61 (11.4) n: 239; 125 intervention, 114 control Sex: 82% female Income: Not reported Other: The intervention and control groups did not differ in any baseline characteristics |
|
Description of intervention and control Problem-based empowerment intervention for African Americans with diabetes Intervention: Consisted of six weekly 2-hour group sessions held in convenient community-based locations. In the first session participants were given data on blood results and information on behaviours that would affect these results and then were to identify problems and solve them under the guidance of the facilitators. The subsequent sessions focused on discussion of the previous week’s experiences of self-management. The topics varied based on the individual needs and concerns of the participants Control: 6-week wait-listed control group |
| Theory: Empowerment behaviour change model |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Data collected at baseline, after the 6-week intervention period, after the 6-week control period and at 6 months and 1 year Weight: No significant difference in weight was demonstrated between the intervention and control groups over the 6 weeks of the study; however, there was weight loss in the overall group between pre and post intervention when examined at all time points. The difference between mean weight pre intervention and at 1 year was 2.9 lb (p = 0.024) Knowledge: Only the patients’ self-rated understanding of managing diabetes score was different between the intervention and control groups |
|
Conclusions Authors: Only one significant change was found between the control and intervention groups (this was a perceived understanding of diabetes mellitus); thus, the study was unable to show benefit from participating in the 6-week intervention; however, there were some significant pre–post improvements in measurements. We believe the results of this study can be attributed to volunteer bias, study effects (i.e. providing study data/blood results, etc. on several occasions to patients and physicians during the 1-year study period) and impact of the interventions; however, the study design does not allow us to examine the relative impact of these factors on the patient improvements seen over the 1-year study period. We believe that the best explanation for the findings is that we developed an effective intervention but employed a research design that did not allow the relative effect of the three forces at work in the study to be determined Reviewers: This study was not able to demonstrate much difference between the intervention and control groups and the authors have provided an explanation of why they felt this occurred. This represents the tension of study designs and what is acceptable and ethical for the community |
|
Comments and limitations This study is limited by the short duration of the comparison between the intervention and control groups. The authors discuss how they could not make the wait-list control longer as they felt that it was unethical, particularly for an underserved population. The self-referred sample is also open to bias |
|
Study reference Engels et al. 2005319 |
|
Setting USA; Detroit, MI |
|
Inclusion criteria Urban African American children and their parents/guardians – very little information on recruitment and inclusion criteria |
|
Study type Pre–post |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean (SD): 11.1 (1.3) n: 56 Sex: 69% female Income: Not reported |
|
Description of intervention and control Students and parents actively involved in the Being Fit programme. The programme was delivered as an after-school programme for 12 weeks to students and parents/guardians in an urban middle school. The aims were to increase participants’ fruit and vegetable intake and to affect their health-related fitness through dance and games and fitness activities. The programme was offered 4 days a week with 60- to 75-minute sessions Major components: Provision of supervised dance sessions, sports games, fitness activities, step pedometers, 5 a Day for Better Health Program nutrition learning activities, targeted educational handouts on nutrition and fitness and thematic poster board display at the school. A ‘Students and Parents Actively Involved in Being Fit’ passport was given out to record fruit and vegetable intake and steps taken on a daily basis. A well-known public figure made a motivational guest appearance in support of the programme goals. The school district waived the cost of community-use fees to lease the school’s gymnasium and dance rooms for the project |
| Theory: Combination of theories and approaches used in the intervention |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Before test and 12 weeks post intervention Changes in fruit and vegetable consumption: Adults’ fruit and vegetable intake remained relatively unchanged; children, in contrast, increased their fruit and vegetable intake Changes in dietary fat: Adults had reductions in body fat (1%, p = 0.004) Changes in physical activity: Adults showed improved fitness (4-minute reduction in walk/run time, p = 0.007) BMI: Adults had reductions in BMI (0.5 kg/m2, p = 0.002) |
|
Conclusions Authors: The findings indicate that after-school programmes such as this can potentially contribute to improved health levels in urban African Americans. The adults tended to gain more health-related outcomes and the children tended to show more dietary gains. Further larger studies are warranted to test this farther Reviewers: This study shows some promising results for both parents and children but the study design is not able to show if these are generalisable or sustainable. There is also limited detail or description of the adaptations undertaken |
|
Comments and limitations Findings are limited by the relatively small sample size, absence of control group and the short duration of 12 weeks. The dietary assessment tools, although validated for this population, may also have limitations and may overestimate intake. Good collaboration with the idea coming from the community but partnering with the school teacher, university and health promotion services. Utilised a wide variety of social, cognitive and behavioural strategies enveloped and delivered in a collective format. Had quite a free approach offering multiple activities and participants were allowed to choose what they participated in – less prescriptive than many interventions. Adapting the style of delivery for a teenage audience also requires significant consideration |
|
Study reference Fitzgibbon et al. 2002;504 Stolley et al. 2003;505 Fitzgibbon et al. 2005506 (Hip Hop to Health Jr) |
|
Setting USA; Chicago, IL |
|
Inclusion criteria All children at the sites were eligible to participate |
|
Study type RCT |
|
Description of population Ethnicity: African American, Latino and multiracial; not reported how ethnicity assessed Age: Mean (SD): intervention group: 48.6 (7.6) months, control group: 50.8 (SD 6.4) months Sex: Not reported n: 409 Income: Mean (SD) education parents: intervention group: 12.4 (SD 1.8) years, control group: 12.7 (SD 1.7) years |
|
Description of intervention and control The intervention took place in 12 Head Start preschool programmes; the 12 programmes were paired on class size and one member of each pair was assigned to the weight control intervention (WCI) and one to the general health intervention (GHI) Children in the WCI schools participated in a 14-week (40 minutes, three times weekly) healthy eating and exercise intervention. The two major components were a 20-minute lesson introducing a healthy eating and exercise concept with an activity and 20 minutes of ongoing physical activity. Parents in the WCI schools also received weekly newsletters with information mirroring the child’s curriculum Children in the GHI schools received a 14-week (20 minutes once a week) class in which they learned about a variety of general health concepts such as dental health, immunisation, seat belt safety and 911 procedures |
| Theory: Based on social learning theory, self-determination theory and the transtheoretical model including the stages of change |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline to years 1 and 2 post intervention Changes in dietary fat: Saturated fat intake was significantly lower in WCI children at year 1 (p = 0.002) but not at the 2-year follow-up BMI: Post-intervention BMI scores did not differ significantly between the two groups. At 1 year there was less of an increase in BMI in the WCI children than in the GHI children (0.02 kg/m2 vs 0.64 kg/m2, p = 0.002). At year 2 the mean increase in BMI was 0.65 kg/m2 higher in GHI children than in WCI children (1.14 kg/m2 and 0.48 kg/m2 respectively, p = 0.008) Weight: The mean increases in weight over this 2 year period were 7.95 kg for GHI children and 6.84 kg for WCI children |
|
Conclusions Authors: Hip Hop to Health Jr, a randomised controlled efficacy trial in minority preschool-age children, demonstrated success in reducing increases in BMI as children age, not only at the 1-year follow-up but also at the 2-year follow-up. This represents a promising approach to the prevention of overweight among minority children in the preschool years Reviewers: This intervention appears to slow weight gain in preschool children and could prove a promising approach. There needs to be further research to address whether or not it could be delivered consistently by teachers instead of trained educators and to see whether or not the effects are sustained beyond 2 years |
|
Comments and limitations This intervention may not be generalisable to other populations (it was designed for this population and it was delivered by specially trained educators and perhaps could not be delivered so enthusiastically by busy teachers). There may also be a dose–response as the WCI was delivered at a higher dose then the GHI |
|
Study reference Fitzgibbon et al. 2005353 (Faith on the Move) |
|
Setting USA; Chicago, IL |
|
Inclusion criteria Self-identified as African American or black, female, age ≥ 21 years, BMI ≥ 25 kg/m2, not currently pregnant or nursing, no current illegal drug use, reported consumption of no more than two alcoholic beverages per day, no medical problems that would restrict or prohibit moderate physical activity, no cancer that required treatment in the last 5 years (except skin cancers other than melanoma), agreed to randomisation, not planning to move from the Chicago area within the time frame of the classes and able to attend scheduled classes |
|
Study type RCT |
|
Description of population Ethnicity: African American or black; self-identified Age (years): Mean (SD): faith-based group: 47.8 (10.3), no faith element: 49.1 (11.6) n: 59 Sex: 100% female Income: Mean income US$20,500 per year in both groups Other: Mean (SD) education: faith-based group: 13.6 (2.3) years, no faith element: 12.9 (2.2) years |
|
Description of intervention and control A 12-week culturally tailored faith-based weight loss intervention vs a culturally tailored weight loss intervention with no faith component Culturally tailored intervention was underpinned by social cognitive theory. The intervention was delivered in a small group format; the group met twice weekly for 12 weeks. The first meeting of each week was divided into an interactive didactic component and an exercise component; the second meeting of each week was all exercise Faith-based intervention was identical to the culturally tailored one except that it also addressed faith and spirituality issues in a structured and systematic manner. This was done through incorporating scripture each week into the content of the intervention |
| Theory: Theoretical underpinning was social cognitive theory |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Unclear; study states that pre and post measures were taken but it is unclear when Changes in dietary fat: Decreases in both groups (significant with a Wilcoxon signed-rank test but not with a t-test) Changes in physical activity: Significant increase in physical activity in the control group but not in the faith-based weight loss group Weight: Overall 70% lost weight (78% in the faith-based group and 61% in the other group) with the average weight loss in the faith group being 2.6 kg and in the other group being 1.6 kg. None of the changes was significant between the two groups at 12 weeks [BMI change: p = 0.37; weight change (kg): p = 0.34; weight change (%): p = 0.41] |
|
Conclusions Authors: Overall, this study showed that there may be benefit to adding a faith component to our previously tested culturally based weight loss programme. Weight loss was expected to be modest in both groups given the relatively short duration of the pilot intervention. Overall, the magnitude of weight loss observed in our study in the faith-based intervention was comparable or somewhat better than that seen with other interventions of similar length designed specifically for black populations. Future adequately powered trials can provide more definitive results Reviewers: This study shows that a culturally adapted intervention for weight loss was effective but the study was not significantly powered to demonstrate if the addition of a religious element increased effectiveness. Larger studies are warranted to distinguish between the effects of cultural adaptation and the effects of specific religious adaptation |
|
Comments and limitations This was a pilot study and was underpowered to show any significant effects. Attendance was not different between the two groups but only 56% of the faith-based group and 60% of the weight loss group attended ≥ 75% of the sessions. There was no standard control group, which meant that any differences could not be compared with a group receiving no intervention at all. The findings may not be generalisable as this was a very specific population and there were also very strict eligibility criteria and very strict screening. The outcomes were based on self-reported information, which is subject to bias |
|
Study reference Fitzgibbon et al. 2005405 |
|
Setting USA; Chicago, IL, YMCA located in an ethically diverse area of Chicago |
|
Inclusion criteria Self-identified as African American or black, female, aged 35–65 years, BMI ≥ 25 kg/m2, not currently pregnant, nursing or anticipating a pregnancy, no current illegal drug use, reported consumption of no more than two alcoholic beverages per day, no medical problems that would restrict physical activity, no cancer that required treatment in the last 5 years (except skin cancer other than melanoma) and not planning to move from the Chicago area within the intervention time frame |
|
Study type Pilot RCT delivered in two cohorts |
|
Description of population Ethnicity: African American Age (years): Mean (SD): cohort 1 (n = 27): 44.4 (7.9), cohort 2 (n = 37): 45.1 (6.9) n: 64 Sex: 100% female Income: Median: cohorts 1 and 2 both US$42,500 Other: Education: cohort 1: 14.7 (SD 2.0) years, cohort 2: 14.9 (SD 2.6) years |
|
Description of intervention and control A combined breast health/weight loss intervention for 20 weeks (twice a week) [to decrease weight and dietary fat intake and increase physical activity and breast self-exam (BSE) proficiency]. Two cohorts: both cohorts were delivered in a small group format; the first 90-minute meeting included a 45-minute didactic component and 45 minutes of exercise – structured aerobic and walking; the second meeting was a 45-minute exercise session Cohort 1: Equal time spent on breast health and weight loss Cohort 2: 80% of time spent on weight loss, 20% on breast health Control: Identical for both cohorts – received weekly newsletters by mail for 20 weeks on general health topics, e.g. first aid, smoking cessation and screening for cancers other than breast cancer. The modified intervention and all intervention materials were offered to this group following the completion of the 20-week trial |
| Theory: Social cognitive theory and cultural competency – surface and deep tailoring |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: 20 weeks post intervention Cohort 1: No statistically significant differences were demonstrated between the intervention and control groups in change in BMI or weight. No difference for diet and physical activity outcomes Cohort 2: Per cent weight change (–4.0 vs 0.9, p < 0.01), weight change in kg (–3.4 vs 0.3, p < 0.01) and change in BMI (–1.3 vs 0.9 kg/m2, p < 0.09) were significantly larger in the intervention group than in the control group. Changes in frequency of regular physical activity in sessions per week [mean (SD) 2.4 (2.9) vs 0.1 (2.3), p < 0.05], duration of physical activity in minutes per session [mean (SD) 27.1 (38.3) vs 1.4 (29.9), p < 0.05] and intensity of physical activity measured on a 0–10 scale [mean (SD) 4.4 (4.8) vs 0.2 (3.5) p < 0.01] were significantly greater in the intervention group than in the control group. A non-significant difference in change in dietary fat consumption was observed between the intervention and control groups No significant difference was reported between the intervention and control groups in changes in television viewing for either cohort |
|
Conclusions Authors: In this study, only cohort 2 demonstrated improvements in weight and associated lifestyle changes; this was thought to be due to the increased allocation of time to weight loss in cohort 2 Reviewers: Interesting that cohort 2 showed effect in terms of body weight, physical activity and diet; shifting the time allocated to weight loss from 50% to 80% had a discernable effect (suggesting a dose–dependent relationship) |
|
Comments and limitations Self-reported data. The majority of the women were well educated and middle class and it is unclear whether or not this intervention would be generalisable to lower-income black populations |
|
Study reference Resnicow et al. 2005324 (Go Girls) |
|
Setting USA; Atlanta, metropolitan area |
|
Inclusion criteria Middle- and upper-income churches identified and contacted prior to randomisation; household income > US$40,000 confirmed, > 100 church members. Eligibility: 12- to 16-year-old girls, BMI > 90th percentile for age and gender |
|
Study type RCT |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean (SD): 13.6 (1.43) n: 10 churches; 5 treatment, 5 comparison; n = 123 girls Sex: 100% female Income: Middle- and upper-income churches |
|
Description of intervention and control Church-based obesity reduction intervention for middle and upper socioeconomic African American adolescent girls delivered through culturally tailored behavioural group sessions over 6 months. Each session included an experiential group activity, approximately 30 minutes of physical activity and preparation/tasting of healthy foods. Girls participated in every session and parents were invited to participate. Girls were taught principles of substitution, moderation and abstinence High intensity: 20–26 sessions (held weekly) and four to six motivational interviewing calls over 6 months lasting 20–30 minutes. Received a two-way pager to receive messages throughout the day and also participated in a retreat Moderate intensity: Six sessions (once a month); selected from topics delivered to high-intensity group, e.g. fat, physical activity barriers, benefits of physical activity, fad diets. No two-way pagers, motivational interviewing calls or retreat |
| Theory: None reported |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline, 6 months and 1 year (selected measurements only) BMI: At 6 months, net difference between the two groups was 0.5 BMI units but this was not significant (p = 0.2); 1-year outcomes were similar Weight: At 6 months, net difference between the two groups was 1.8 lb but this was not significant (p = 0.38); 1-year outcomes were similar Body fat: At 6 months, net difference between the two groups was 1.1% but this was not significant (p = 0.28); 1-year outcomes were similar In the high-intensity group, high attendees (> 75% of the sessions) had significantly reduced BMI (0.8 units for difference of 1.3 units, p = 0.01), percentage body fat (p = 0.01) and hip circumference (p = 0.01) compared with low attendees and also a trend for weight with high attenders losing 1.3 lb and low attenders gaining 3.7 lb (p = 0.07); 1-year outcomes similar Other: The intervention was generally well received by participants |
|
Conclusions Authors: The intervention was not effective in reducing adiposity but some positive effects were observed among high attendees. The moderate-intensity comparison may have reduced the ability to detect a difference; however, it was likely that there was a failure of the high-intensity condition, possibly because of the lack of a structured programme. High attendees had sustained effects at 1 year Reviewers: The intervention was not successful in showing effect. When comparing high attendees with low attendees the differences were significant, suggesting that either those who were particularly motivated to attend did better or there was a dose-dependent effect of the intervention |
|
Comments and limitations: Churches received an incentive of US$500 if 15 eligible participants completed the baseline assessment and an additional US$200 if 20 eligible participants completed the baseline assessment. There was difficulty recruiting as there were competing priorities at churches. Participants lost interest in pagers and the impact of motivational interviewing was mixed. Use of the moderate-intensity comparison group was needed to get buy-in from the churches |
|
Study reference Wang and Chan 2005346 |
|
Setting USA; Hawaii |
|
Inclusion criteria Previously diagnosed with type 2 diabetes and managing the diabetes with diet, oral hypoglycaemic agents or insulin or both, age 44–87 years, residents of Hawaii and speakers of Mandarin, Cantonese or Taiwanese |
|
Study type Pre–post |
|
Description of population Ethnicity: Chinese; not reported how ethnicity assessed Age (years): Mean (range): 68.8 (44–87) n: 40 Sex: 51.5% female Income: 75.8% retired, 81.8% combined monthly household income < US$1001 Other: 57.6% education level of high school graduate and higher |
|
Description of intervention and control Group sessions were delivered by the investigator and a registered nurse (certified diabetes instructor). Maximum of 10 people per session to enhance interaction. Sessions lasted 60 minutes and were held in a clinic in Chinatown Handouts of all lectures were given to all participants. Presentations included videos, hands-on activities and visual presentations. Topics included understanding the research programme and its components. Recipe books, exercise books and pamphlets on diabetes were also distributed Dietary patterns were explained and analysed, including recipes brought in by participants. Exercise, calories and medicines (Western and traditional) were all discussed. Skills for managing stress were outlined (meditation, Tai Chi and Chi-gong) Participants were asked to involve their families outside the classroom and strong peer–peer support was developed during the course. Activity log and pedometer were given to each participant |
| Theory: Guided by the ‘empowerment model’; this aims to help a patient explore and develop their inherent ability to manage their life and disease |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline, at the end of the intervention and 3 months post intervention Weight: 43.6% of participants lost more than 5 lb |
|
Conclusions Authors: Culturally tailored diabetes management may be effective for Chinese Americans with type 2 diabetes. Participants had improved outcomes and also found a strong support network through participation in this intervention. Further study with a larger sample and a control group is recommended Reviewers: This study showed the benefit of integrating culturally appropriate values and paradigms into a diabetes education programme and showed effective results for a preliminary study. However, the sample size was small. The cultural adaptations are well described |
|
Comments and limitations Small sample size and lack of control group. May not be generalisable to primary prevention. Also, the timing of the study in a holiday period when quite a few people travelled meant that some could not continue participation (programmes should not be held over Chinese New Year) |
|
Study reference White et al. 2004;280 Williamson et al. 2005;281 Williamson et al. 2006;282 Kennedy et al. 2008314 [Health Improvement Programme for Teens (HIP Teens)] |
|
Setting USA; city or state not reported |
|
Inclusion criteria African American girls aged from 11 to 15 years who were overweight (BMI > 85% for age and gender percentile) or obese and with at least one obese biological parent (BMI > 30 kg/m2) and one designated parent who was overweight (BMI > 27 kg/m2) who was willing to participate in the programme, the adolescent’s family was willing to pay US$300 out of pocket towards the purchase of a computer worth US$1000 and the family home had to have at least one functional telephone line and electricity |
|
Study type RCT |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean (SD): adolescents: 13.2 (1.4), parents: 43.2 (6.2) n: 57 Sex: Not reported Income: Not reported |
|
Description of intervention and control There were two arms, an interactive behaviour therapy group and a passive health education control group. The interventions were available continually for use over a 2-year period on the internet. There were four face-to-face counselling sessions for both groups. Because of the difficulties of disparity in access to the internet, low-cost computers and also free internet access were provided to participants in both groups. The participants were adolescents and they were randomly assigned The internet-based behavioural intervention included the provision of nutrition education plus an internet counselling behaviour modification programme that targeted lifestyle eating and physical activity habits of the adolescent and parent. The control condition included education on healthy nutrition and exercise but behavioural changes were not prescribed and internet counselling was not provided. Thus, the behavioural programme was highly interactive whereas the control was very passive |
| Theory: Based on family treatment methods |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline to months 6, 12, 18 and 24 BMI: Overall, the effect of treatment was significant for parental changes in BMI (p < 0.04). Post hoc comparisons of groups indicated that the difference was significant at months 6 and 12 but not at months 18 and 24 Weight: Compared with the control group, adolescents in the treatment group lost more body fat and parents in the treatment group lost significantly more body weight during the first 6 months. In the following 18 months, parents and adolescents in both groups gained weight and at 2 years the weight/fat of the two treatment groups did not differ |
|
Conclusions Authors: An internet-based behavioural intervention was found to be superior to internet-based health education because it yielded decreased body fat for adolescent girls and decreased body weight in parents after 6 months of treatment; however, these weight/fat losses were not maintained during the subsequent 18 months. The use of the website decreased dramatically after the first year of the study. Based on these observations we have recommended that internet-based weight management interventions should be integrated into other forums for supervised behaviour change, e.g. health classes in schools, and that they might best fit with goals of relatively low weight loss and weight gain prevention Reviewers: This intervention was effective at the 6-month mark but then had decreasing participation/interest and therefore decreasing effect so that any significant gains were lost by the 2-year mark. The authors’ suggestion seems appropriate that integrating the web-based approach with some other component may help sustain the use of the internet site and encourage ongoing behavioural change. They do not comment on how regularly the content of the site varied and perhaps changing the content would sustain interest. This study was not designed to be able to assess the advantage of adaptation over non-adaptation |
|
Comments and limitations Small sample size. Use of individual learning styles as opposed to co-operative learning styles, which are thought to be more appropriate for African American populations. African American populations make less use of the internet and as this possibly changes in the future this type of design may become better suited to this population |
|
Study reference Yancey et al. 2001;339 Yancey et al. 2006;338 McCarthy et al. 2007340 [African American Women Fight Cancer with Fitness (FCF)] |
|
Setting USA; Los Angeles, CA |
|
Inclusion criteria Self-identified as African American, female |
|
Study type RCT |
|
Description of population Ethnicity: African American; self-identified Age (years): Mean (SD): control group: 46.5 (10.10), intervention group: 44.56 (10.82) n: 393 Sex: 100% female Income: Moderate income Other: On average participants had completed 3 years of college |
|
Description of intervention and control Culturally targeted nutrition and physical activity educational and social support intervention to produce cancer-protective anthropometric, physiological, psychological and behavioural changes in African American women. Education was delivered in group sessions and targeted lifestyle changes at the individual level. A social support component was intended to influence social environments. Economic incentives were also provided with free gym membership for all participants (and for their social support person) Both intervention and control groups received eight weekly 2-hour sessions with ethnically matched community role models in a black-owned community health club. The intervention group focused on skills training to improve lifestyle changes. The control group sessions discussed current African American health topics |
| Theory: Social learning theory, social action theory and a social ecological perspective were imbedded in the intervention approach, with progressive goal setting. Physiological and psychosocial behaviour change strategies were used complementarily in the intervention |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: 2, 6 and 12 months Changes in physical activity: Physical activity levels increased significantly only among intervention participants (p < 0.0001 and p = 0.04 at 2 and 6 months, respectively) Weight: Longitudinal analysis revealed a trend towards weight stability in the intervention group at 2 months compared with the control group. Both groups were significantly heavier at 12 months (intervention group +1.37 kg/m2, p = 0.0001; control group +1.02 kg/m2, p = 0.001); at this time point, 42% of intervention women and 36% of control women had lost or maintained weight (p = 0.08) |
|
Conclusions Authors: The intervention showed significant but modest changes immediately post intervention with decay thereafter in time. Both intervention and control participants received benefit from participation, with intervention participants experiencing a broader spectrum of favourable changes in overall fitness than control participants, but control participants having better longer-term improvements. It was felt that the control condition actually delivered a more substantive social environmental intervention and therefore reduced the difference between the two groups. The findings underscore the need for multilevel social ecological interventions that address multiple barriers to active leisure participation Reviewers: The intervention could be considered as ineffective as the control group appeared to receive more benefit than the intervention group in the long term; however, the control in itself was an intervention and both showed some moderate success |
|
Comments and limitations The physical activity and sedentary behaviour measures were not very developed at this time and it was difficult to distinguish between the effects of sedentary behaviour vs physical activity and resistance vs aerobic training and to examine the amount that the gym was used. As the free gym membership was delivered to both groups the intervention did not test the effectiveness of the membership alone; however, it demonstrated that free membership and the intervention or control changes made only a very modest difference. There were delays in participants being scheduled for sessions. It was shown that those who waited longer had less successful outcomes than those who started sooner. This effect may have reduced the overall effectiveness but non-differentially |
|
Study reference |
|
Setting USA; Pennsylvania |
|
Inclusion criteria Age 25–70 years, BMI between 30 and 50 kg/m2, with a physician in the university health system and English speaking. Exclusions were for conditions or circumstances in which weight reduction would be contraindicated, inappropriate or unfeasible or that could confound data interpretation, e.g. pregnancy, active treatment for unstable depression or other psychiatric disorders, current use of antipsychotic medication, active chemotherapy or radiotherapy, alcoholism, eating disorders or being non-ambulatory. For CVD, diabetes or obesity-related comorbidities, the condition had to be stable and permission sought from their personal physician |
|
Study type RCT; permuted block randomisation in a 1 : 1 : 1 ratio |
|
Description of population Ethnicity: African American; self-identified Age (years): Mean (SD): phase 1: 43.4 (10.5), phase 2: 45.4 (10.2) n: 237 people were enrolled; 167 attended no classes or only the first phase 1 class, 134 provided phase 1 follow-up data and 128 were randomised in phase 2 with 87 of them providing final follow-up data (‘completers’). Of the completers there were 28 in the HELP classes, 28 in the self-HELP classes and 31 in the clinic visits only group Sex: Phase 1 89.9% female, phase 2 90.6% female Income: 50.5% and 56.2% had a professional occupation in phases 1 and 2, respectively Other: 63.5% and 70.2% had > 12 years of education in phases 1 and 2, respectively |
|
Description of intervention and control Recruited through outpatient practices in a family practice department of an urban university health system and delivered in the family practice conference room. The intervention had two phases. Phase 1 was a 10-week, weekly weight loss class/group counselling with the option of continuing on to phase 2. Participants were not given a specific diet but were advised on caloric intake per day and encouraged to set goals for gradual behaviour change in eating patterns, particularly tracking fat and caloric intake and substituting low calorie foods into their diet. They were also advised to increase their levels of physical activity and this advice was tailored to their ability and preferences. Phase 2 was for another 8–18 months in a randomised comparison of two intervention groups aimed at weight loss maintenance or additional weight loss and a control group. The intervention groups were the HELP group – further group counselling (classes less frequent: biweekly, then monthly) – and the staff-facilitated self-HELP group. These were compared with a ‘clinic visits only’ group that had no further intervention delivered Intervention classes were led by part-time nutrition exercise or behaviour change specialists usually working in pairs; four out of the nine were African American. The self-HELP group were given a kit with a personalised calendar, local resources for healthy eating and physical activity, a personal diary, a pedometer and ad hoc telephone support from an outreach worker. There were also some walks led for this group. All participants also received a seasonal study newsletter, small gifts as incentives and a video designed to motivate lifestyle changes for CVD risk reduction in African Americans |
| Theory: Not reported but HELP was adapted from a weekly programme used in the TONE weight loss interventions, which were based on well-established theoretical behaviour change approaches |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Follow-up visits in phase 2 every 6 months Weight: Mean weight changes for completers were –1.5 kg (p < 0.001), +0.3 kg (p = 0.47) and –1.2 kg (p = 0.04), respectively, for phase 1, phase 2 and overall (baseline to final visit was on average 18 months) There was no treatment effect of phase 2 (p = 0.55). The final study weight was < 5% below baseline for 25% of completers and was strongly predicted by phase 1 weight loss |
|
Conclusions Authors: There was a modest average weight loss after the programme in phase 1 that was reasonably sustained regardless of which arm people were assigned to in phase 2. About a quarter of the completers achieved a clinically significant weight loss over an overall average duration of 18 months Reviewers: This study seemed somewhat complex in the design and execution. There does appear to be a promising effect of the phase 1 intervention and some maintenance, which suggests that this approach may have merit and potential to develop as a longer-term intervention |
|
Comments and limitations The incentives were important for attendance for about half of the participants. There was considerable attrition in the study with only 60% and 36% of cohorts 1 and 2, respectively, attending the 6- and 12-month follow-ups and only 70% of cohorts 3 and 4 attending the 6-month follow-up. There was a significant difference in the duration of the intervention because of the time taken for enrolment and to start the intervention |
|
Study reference Davis-Smith et al. 2007;334 Atkinson et al. 2009373 [Lifestyle Balance Church Diabetes Prevention Programme (DPP)] |
|
Setting USA; Georgia |
|
Inclusion criteria All adults > 18 years were included |
|
Study type Pre–post |
|
Description of population Ethnicity: African American Age (years): Not reported n: 99 Sex: 97% female Income: Not reported |
|
Description of intervention and control This intervention was to determine the feasibility of implementing a diabetes prevention programme (DPP) in a rural African American church Intervention: A six-session DPP modelled after the National Institutes for Health was implemented with adult members of the church identified as being at high risk for diabetes, based on the results of a questionnaire and a fasting glucose test. The major goals were 7% weight loss and ≥ 150 minutes of exercise a week. The three aims were nutrition, physical activity and behaviour change. The materials were modified for the church setting to be group based. Each session was led by volunteer health-care professionals and handouts were given from the sessions. Diet and physical activity log books were reviewed by the leader and the leader guided the group discussion. After the presentation and discussion, individuals set goals for diet and exercise behaviour change for the subsequent week. A prayer concluded the session. Following the intervention there was no additional support provided |
| Theory: Not reported |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline to 6 and 12 months BMI: Average decrease in BMI was 1.9 kg/m2 at the 12-month follow-up Weight: Weight loss ranged from 0.5 to 27.2 lb after the 6-week intervention. Overall, the mean weight loss was 8.8 lb, 6.5 lb and 10.6 lb from baseline to immediately after the intervention, to the 6-month follow-up and to the 12-month follow-up, respectively |
|
Conclusions Authors: This pilot project suggests that a modified six-session DPP can be translated to a group format and successfully implemented in a church setting. Further randomisation studies are needed to determine the effectiveness of such an intervention Reviewers: This study demonstrated a successful translation of the National Institutes for Health DPP into a church setting. There were changes in weight and BMI and these appeared to be sustained to 12 months |
|
Comments and limitations Very small sample size (one church) and no control group. Finger-stick glucose sampling was used in lieu of plasma values Additional comments from supporting paper: A supporting paper373 looked at what factors helped the programme fit within the community and these were the initial alignment of the programme objectives with the church mission, the endorsement and continued participation of church leadership and community activities and support. Programme success is dependent on and magnified by the broader engagement of the church community so that people realise that the changes are not just for those involved in the programme but for the wider community. Partnership and integration within the community are emphasised. Sustainability may have been contributed to by the social support of the church and the fact that ongoing healthy behaviour changes occurred at a church level following the intervention and this may have helped people to continue the behaviours that they started under the programme |
|
Study reference Gaston et al. 2007399 [Prime Time Sister Circles (PTSC)] |
|
Setting USA; multisite: Illinois, Washington, DC, Florida and Maryland |
|
Inclusion criteria African American/black women aged > 35 years |
|
Study type Quasi-experimental study, pre–post |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean (SD): 54.4 (9.46) n: 134 women; 106 intervention, 28 comparison Sex: 100% female Income: Not reported |
|
Description of intervention and control 10 Prime Time Sister Circle (PTSC) groups and two comparison groups in 11 sites Intervention: The intervention was a curriculum-based approach that was low cost and short term – it incorporated a support group approach to address four key modifiable disease risk factors. A total of 8–13 women per intervention group met for 90 minutes for 10 weeks They signed a group contract and set a specific goal related to physical activity, nutrition and stress management. They were given educational material in the form of a book. The 10-week curriculum included stress, spirituality, self-esteem, prioritising themselves first, nutrition and exercise, CVD, diabetes, nutrition and exercise. Participants were taught cognitive behavioural strategies and skills to help develop and implement their health plan in the targeted areas Comparison: The comparison group received a copy of the book but no sessions, facilitator, expert consultants or stipend |
| Theory: Cognitive behavioural modality; social support and social circles; transtheoretical model; Person, Extended family, Neighbourhood (PEN) model that focused on health education, educational diagnosis of health behaviour and cultural sensitivity; based on information from focus groups |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline to 10 weeks and 6 and 12 months Change in calories: There was a significant increase in the number of nutritious foods eaten at 10 weeks but this was not significant at 6 and 12 months Changes in physical activity: Significant changes in physical activity: increased from participating in aerobic exercise on 1.91 days per week at baseline to 3.97 (p < 0.01), 2.48 (p < 0.05) and 3.21 (p < 0.01) days per week at 10 weeks and 6 and 12 months, respectively. Engaging in strength-building exercise also increased significantly at 10 weeks and 12 months Knowledge: At 10 weeks knowledge scores ranged from 85.1% to 93.5%; by 6 months all areas of knowledge had decreased to a range of 61.9–88.1% and at 12 months to a range of 73.1–82.7% |
|
Conclusions Authors: This study demonstrated the effectiveness of a culture- and gender-specific group intervention to modify certain high-risk behaviours in mid-life African American women. Significant improvements were seen at various intervals in stress management, physical activity and nutrition. The utilisation of an integrated approach and a group format were major factors in the study’s success Reviewers: This study demonstrated a significant effect of the intervention but it is unclear what contributes most to the effect – possibly it was the group support element. It is unclear how generalisable this would be to other populations as this is a very specific population in terms of gender, ethnicity and age and SES |
|
Comments and limitations Limitations included relatively small sample size, the quasi-experimental design of the study in multiple sites with no randomisation and the self-reported nature of the data (social desirability bias may have been increased by peer pressure in this intervention) |
|
Study reference Farooqi and Bhavsar 2001;370 Netto et al. 2007368 (Khush Dil) |
|
Setting UK; Edinburgh, UK |
|
Inclusion criteria People were self-referred or referred from voluntary organisations, GPs and other health-care workers. There were no exclusions |
|
Study type Pre–post, service evaluation |
|
Description of population Ethnicity: South Asian: Indian (23%), Pakistani (48%) and Bangladeshi (21%); not reported how ethnicity assessed Age (years): Mean (range): 44 (13–81) n: 304 Sex: 66.6% female Income: Not reported |
|
Description of intervention and control The intervention included a nurse-led community-based CVD risk clinic and nutrition workshops led by a dietician. Activities included cookery workshops, exercise classes and CHD/diabetes awareness sessions to encourage lifestyle change and reduce CHD risk. It also included stress management and participation in local Asian community events. Participants attended initially for a 30-minute screening visit and had blood taken and their CHD risk assessed and this was then discussed with the nurse along with goal-setting; there was a follow-up visit at 6 months |
| Theory: Transtheoretical model used to assess stages of change at screening visit |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Measures taken at baseline, follow-up interviews at 6 months post baseline Changes in dietary fat: 77.9% of women reported reducing the amount of oil they used in cooking and 57.5% reported healthier cooking methods such as baking, grilling and steaming; men also showed a significant decrease in consumption of fried meat Changes in physical activity: Women and men showed an increase in moderate exercise BMI: Significant improvements in BMI Weight: Significant improvements in weight |
|
Conclusions Authors: The Kush Dil intervention led to a reduction in cardiovascular risk in a South Asian population. In addition, participants reported a shift in their motivational status, increasing the likelihood that diet and lifestyle changes can be maintained Reviewers: This intervention provides an effective and culturally appropriate service for South Asian communities to reduce their cardiovascular risk |
|
Comments and limitations This was an in-service evaluation and not a research trial and therefore there is no control group for this intervention. Self-reported measures are prone to social desirability bias. It is not possible to say if the findings are generalisable to other settings and populations or to comment on sustainability |
|
Study reference Rush et al. 2007411 |
|
Setting New Zealand |
|
Inclusion criteria Asian Indians aged > 50 years and resident in the urban Auckland area were recruited by personal contact with community organisations |
|
Study type Controlled before and after/pre–post |
|
Description of population Ethnicity: Asian Indian; not reported how ethnicity assessed Age (years): Women: 59 ± 8, men: 62 ± 8 n: 41 Sex: 48.7% female Income: Not reported |
|
Description of intervention and control Monthly group diet and physical activity intervention that emphasised the importance of lifestyle changes to reduce risk factors for chronic disease. Participants visited the university laboratory three times. The intervention lasted for 5 months An initial group education session encouraged an increase in physical activity and improved diet and was delivered to two community groups at their regular meetings. Messages and handouts were given to everyone irrespective of their participation in the study. There were two booklets: Good Health Is in Your Hands! A Food Guide for Indian Adults in New Zealand, which included a Hindi translation, and Healthy Living, Putting the Squeeze on Lifestyle Disease for NZ Indian People (written by the study author). Following the initial session, monthly group sessions with handouts were held that included cooking demonstrations (substitute canola oil in place of other oils, remove fat from meat, increase fish consumption), a pedometer club and ‘weigh-ins’. Individually marked waist threads (to assess changes in girth), pedometers and diaries to record steps taken daily were given out |
| Theory: Not reported |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Two baseline measurements were taken, 1 month before and immediately before the intervention, the average taken and follow-up was at 5 months post intervention Changes in dietary fat: There were decreases in percentage body fat [–1.1% (SD 1.6%), p < 0.004] and abdominal fat [–0.14 kg (SD 0.22 kg), p < 0.006] – when stratified by gender there was a significant decrease in men (p < 0.006) whereas these changes were not statistically significant in women. Most popular reported changes were related to diet: changing cooking oil to canola, eating more cereals, removing skin from chicken before cooking and drinking water when thirsty Weight: Men: body weight, mean (SD): –1.5 kg (1.8 kg) (p < 0.001), weight of body fat, mean (SD): –1.1 kg (SD 1.4 kg) (p < 0.002); women: body weight, mean (SD): –1.2 kg (2.5 kg) (p = 0.06), weight of body fat, mean (SD): –1.0 kg (2.3 kg) (p = 0.06) |
|
Conclusions Authors: In a group of older Indian people, lifestyle changes mediated by group education and individual follow-up to modify diet resulted in a reduction in whole body and abdominal fat and improvements in lipid profile and therefore a reduced risk for CVD. Beneficial changes occurred in both women and men but tended to be greater in men. The nature of the group adds potential for changes made in a relatively short period of time to be sustained by the volunteers and the rest of the community and families without the involvement of the researchers Reviewers: The intervention showed significant changes for men but not for women. The authors suggest that, as eight women and four men had high fasting blood glucose, which would classify them as having impaired fasting glucose, their capacity for lifestyle change may be limited. This certainly could be one reason for the lack of significant changes in women; however, it would have been interesting to learn more about the intervention sessions, whether they catered for different genders, what kind of activities were performed and what were some of the challenges |
|
Comments and limitations This study does not report much detail of the intervention and thus it is difficult to pick out the active component; however, holding the intervention during times when the two community organisations regularly met would likely have helped engagement. It is unclear whether men and women participated in the study together or whether the two community groups were single sex Alcohol consumption decreased from baseline. Fish consumption increased in only three cases but this recommendation was not relevant to everyone as nine people were lacto-ovo vegetarian. This is important to consider when giving out advice – what people are already eating instead of generic advice. Anecdotally, changes were adopted by others in the community group and wider families. This community has continued to work together to maintain these changes The authors do not provide any limitations to this study; however, it is clear that the small convenience sample and having no control group are two limitations |
|
Study reference Shaw-Perry et al. 2007310 (NEEMA; meaning ‘wellness’ in Swahili) |
|
Setting USA; eastside of San Antonio, TX, San Antonio Independent School District |
|
Inclusion criteria Schools with 40% African American students and not alternative schools; fourth-grade students selected because children aged around 9 years. All students were allowed to participate in the four programme components but only students with assent and parental consent participated in data collection |
|
Study type Controlled before and after/pre–post |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): 10.54 ± 0.74 n: 68 Sex: 55.9% female Income: Low-income neighbourhoods |
|
Description of intervention and control A 14-week school-based diabetes prevention programme tailored for African American children. Programme implemented via four social networks/components: classroom, after school, home and school cafeteria. The intervention lasted for 7 weeks and there was no control group Health education and physical education (PE) class: 13 lessons covered nutrition, physical activity, self-esteem, self-control and diabetes. The PE curriculum was aimed at promoting moderate to vigorous physical activity. Health and PE classes were held for 45 minutes a day, 5 days a week: 1 day to teach health education and 4 days for physical activity Health club: 18 sessions to reinforce classroom learning and to promote leisure-time physical activity. Student participation was voluntary and parents were encouraged to attend with their children. Involved physical activity, aerobics, games, dancing, singing and arts and crafts. Health club meetings were held once a week, Monday to Friday, for 45 minutes during school or for 1 hour after school. A Family Fun Fair was conducted to promote healthy choices for the family School Food Service Program also run: seven cafeteria lesson plans to improve nutrition knowledge of food service staff and a lunch visit for students to encourage them to make healthy food choices |
| Theory: Not reported |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Week 3 – baseline (weeks 4–10 included the 7-week intervention) and week 11 – follow-up Changes in dietary fat: Per cent body fat decreased from 27.26% (SD 12.89%) to 26.68% (SD 11.67%) (p < 0.537) Changes in physical activity: Fitness laps increased from 16.40 (SD 9.8) to 23.72 (SD 14.79) (p < 0.000) BMI: Increased from 20.30 (SD 5.29) kg/m2 to 20.81 (SD 5.57) kg/m2 (p < 0.003) (this is in the opposite direction to hypothesised change) |
|
Conclusions Authors: This pilot study provided teacher feedback useful for revising the NEEMA health curricula. The aim of the study was to determine if the new NEEMA instructional manual was culturally appropriate for African American children. Feedback from teachers and comments expressed by the children were positive. There was a significantly positive impact of the NEEMA PE classes on children’s fitness and blood glucose levels. Teachers recommended more hands-on activities, smaller groups and the provision of more incentives to participate and more training hours for teachers. Future studies to determine efficacy should include a RCT, a larger sample of schools and a cluster analysis Reviewers: The study demonstrated that the intervention was culturally acceptable (although students were not themselves interviewed) and was able to produce positive effects on children’s fitness (although opposite effect with BMI). Success, however, could be attributed to the fact that familiar PE teachers delivered the intervention during school hours – unclear how this would work if voluntary and after school. No process data were reported, such as the number of sessions attended |
|
Comments and limitations Lack of a randomised control but, because this was a formative study, it involved small groups and biological measures were analysed at the individual level. Despite an increase in fitness there was an increase in BMI. This could be because, if fitness is increased in rapidly growing children, bone and muscle mass develop, producing greater increases in BMI. Students carried out two practice runs 1 day before the test – this may skew the results as students would have experience with the test and would likely strive to better their performance; thus, follow-up data may be inflated. Teachers reported that the NEEMA programme was supportive of school-based lifestyle interventions but emphasised constraints at home and school and that state action was required, e.g. food insufficiency at home (low cost of fast food and soft drinks is a cause for unhealthy behaviour) |
|
Study reference Two Feathers et al. 2005;291 Two Feathers et al. 2007290 (REACH Detroit) |
|
Setting USA; Detroit, MI, urban |
|
Inclusion criteria African American and Latino adults with physician-diagnosed type 2 diabetes, aged > 18 years, with insurance or receiving care from a federally qualified health centre, mentally able and residing in one of the six REACH Detroit zip codes |
|
Study type Pre–post [with comparison of data with an existing data set for HbA1c (glycated haemoglobin) results] |
|
Description of population Ethnicity: African American (64%) and Latino (36%); not reported how ethnicity assessed Age (years): African American: mean (SD): 60.9 (13.9) n: 377 (271 from 14 all-African American groups and 106 from eight mixed-race groups) Sex: 7.5% female Income: Not reported Other: For the African American population it is reported that 25.4% had a high school education, 22.5% had less than a high school education and 33.8% had attended college |
|
Description of intervention and control This intervention aimed to compare the effects of an intervention conducted with an African American only group of participants with one conducted with a mixed-ethnicity group of participants. The intervention was based on an intervention originally developed for Native Americans. The curriculum was adapted and was called ‘The Journey to Health’ for African American participants. It was designed to reduce risk factors associated with diabetes complications. The content was designed to help participants gain knowledge related to healthy eating, physical activity and stress reduction through five 2-hour group meetings delivered every 4 weeks by 10 Family Health Advocates (FHAs) in two community locations. Participants were encouraged to bring a family member or friend |
| Theory: Social cognitive theory was used with an emphasis on behavioural capability, self-control, emotional coping response and self-efficacy |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: 20 weeks Changes in fruit and vegetable consumption: African Americans showed a significant improvement in vegetable consumption, from 2.1 ± 1.4 servings a day to 2.7 ± 1.4 servings a day (p < 0.01) Knowledge: Significant increase in knowledge in those who followed a healthy eating plan 7 days a week, from 32.4% to 44.9% (p < 0.05) |
|
Conclusions Authors: These findings suggested that a culturally tailored, community-based healthy lifestyle intervention delivered by community residents over five sessions can significantly improve glycaemic control and reduce the risk factors associated with diabetic complications. It is also commented that there was limited evidence of interventions that have been successful for one group being replicated or adapted and being successful for another group. This intervention provided evidence of an intervention developed for and tested with Native Americans that can be adapted and be successful for African Americans and Latinos. It’s important to continue to develop our understanding of the critical components of successful interventions that encourage and sustain healthy lifestyle behaviours among populations at high risk from diabetes and its complications Reviewers: This study was interesting as it showed an intervention that has been successfully adapted and transferred from one population to another. The results are slightly limited in their power once stratified to individual ethnic groups and this may have limited the number of areas in which effectiveness could be demonstrated. It is also hard to say whether there was effect in terms of knowledge changes as values were compared only with baseline levels and there was no comparison group for the survey measurements (unlike the clinical measurements) |
|
Comments and limitations The survey data were limited by having no comparison group. Subgroup power may be limited by sample size. Measures were self-reported for the surveys and the small size of groups and relationships with the workers may have contributed to social desirability in the responses. There was quite a high degree of non-attendance and attrition at the sessions. The Hawthorne effect could have been operating |
|
Study reference Amoako et al. 2008406 |
|
Setting USA; Guilford County, NC |
|
Inclusion criteria English speaking, with access to a telephone. Recruitment: 14 clinics and physicians’ offices |
|
Study type Experimental design |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean (SD) (range): 61.0 (9.5) (49–83) n: 68 Sex: 100% female Income: 65% had incomes of ≤ US$1000 a month |
|
Description of intervention and control Telephone intervention for diabetes self-care (to reduce uncertainty) and psychosocial adjustment (physical activity and diet) Intervention: Once-a-week telephone semi-structured clinic interview with embedded intervention for 4 weeks. Self-care activities included diet, medication, foot care, exercise and blood sugar testing. Interview included open-ended questions, direct exploration and use of reflective comments. Four phases: warm up, assessment of problem, uncertainty appraisal and delivery of strategies to manage the uncertainty, closing. Calls (10–60 minutes) were recorded. Women could make calls to a 1-800 number as needed. Assertive communication skills taught. Printed information provided Control: Usual care, which included regular primary care and speciality visits as well as support group meetings and scheduled classes for diabetes management. Two telephone calls to keep in touch and remind participants of the final data collection period. At completion of the post-test data collection, women were offered one intervention telephone call: 15 accepted, 15 declined |
| Theory: Mishel’s uncertainty-in-illness theory;507 theories of counselling and behaviour change guided the interactive processes used in delivery of the intervention502,508 |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline and 6 weeks post baseline Changes in physical activity: Intervention group reported increased participation in exercise (self-care component; p < 0.001) |
|
Conclusions Authors: In this study, participants who experienced reduced uncertainty experienced a significantly greater improvement in psychosocial adjustment. Participants who experienced reduced uncertainty showed improvement that was significantly greater than that of the control group in the number of days per week that they participated in physical activity. Diet did not improve. Barriers included poor understanding of the relationship between disease and diet, poor psychosocial adjustment and denial of the seriousness of diabetes. Most of the improvements involved cognitive changes; however, they may precede behaviour change Reviewers: This study showed improvements in psychosocial adjustment and reduced uncertainty for diabetes care. Agree that this may be important as a predecessor of other more behavioural changes (the intervention group participants increased exercise levels but did not improve their diet in this study – however, this is to be expected as it may be easier to take up a behaviour than to alter long-standing dietary patterns and practices). Future studies should include greater cognitive components to motivate people |
|
Comments and limitations This was part of a larger study of a telephone intervention to manage uncertainty related to diabetes self-care. Limitations include not using HbA1c as an outcome to measure effectiveness and measuring the outcomes 2 weeks after the intervention. In future, multiple measurement points should be used. The authors state that, for African Americans with diabetes, modifying diet may be particularly difficult given the deeply rooted traditions surrounding food in their culture (they perceive ‘eating healthfully’ as having to give up part of their heritage). Family members may perceive deviations from traditional food experiences in a negative way, which can result in conflict for people with diabetes |
|
Study reference Ard et al. 2008348 |
|
Setting USA; multicentre trial |
|
Inclusion criteria Age ≥ 25 years, BMI 25–45 kg/m2, currently taking medication for hypertension and/or dyslipidaemia, not taking medication for diabetes, requiring a negative stress test if diabetic or with a history of CVD, no CVD event in the past 12 months and willing to lose 4 kg in phase 1 of the study (20 weeks) |
|
Study type Reanalysis of a multicentre RCT |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Average: 51.6 ± 9.3 n: 377 (271 from 14 all-African American groups and 106 from 8 mixed race groups) Sex: 73.4% female Income: 84.3% had income ≥ US$30,000 (50% in excess of US$60,000) Other: 92.5% had more than a high school education with 32.6% having a postgraduate qualification |
|
Description of intervention and control This intervention aimed to compare the effects of an intervention conducted with an African American only group of participants versus a mixed ethnicity group of participants. Participants met weekly in groups of 15–25 led by an interventionist who was of African American ethnicity (the mixed ethnicity groups that this was compared with also had interventionists who were of African American ethnicity). Weight loss was promoted through calorie reduction, change in dietary pattern and increased energy expenditure with physical activity. The DASH diet was used and physical activity was for 180 minutes a week. Key strategies included self-monitoring of diet and physical activity, reducing portion sizes, substituting foods and modifying foods to be lower in calories and fat, increasing fruit and vegetable and fibre intake, identifying problematic situations and undesired behaviours and rehearsing specific plans of action to deal with those situations and, lastly, developing food choice competencies |
| Theory: No theories explicitly stated |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: 20 weeks Changes in fruit and vegetable and fibre consumption: Increase in fruit and vegetable consumption by about three servings a day and in fibre consumption by about 3.5 g/day Changes in calories: Decrease in the percentage of calories from fat of about 7% Changes in physical activity: A doubling in the proportion of people reporting at least 180 minutes of vigorous activity per week Weight: Weight change of > 4 kg for 61.2% of the participants |
|
Conclusions Authors: There was a lack of a statistically significant effect of group composition on intervention attendance, the lifestyle change variables and weight loss. This suggests that special logistics to accommodate African Americans may not be worthwhile. Whether this holds true, or the importance of the group leader being African American or not, cannot be determined from these data. The results of this study suggest that, regardless of the ethnic mix of the groups, African Americans appear to respond positively to well-designed lifestyle change interventions designed to promote healthier eating and increase physical activity and weight loss Reviewers: This study was very interesting and attempted to examine the effectiveness of a single adaptation; however, this was hampered by the group composition of the mixed groups and the culturally appropriate approach also taken to the mixed groups that most likely diluted any effects that could have been observed |
|
Comments and limitations The negative findings between the African American and mixed groups could have been contributed to by this being a reanalysis and not a RCT itself and there being residual confounding in the analysis. Also, there were high numbers of African Americans in the mixed groups, which may have reached ‘critical mass’ to alter the environment and blur the contrast. The overall intervention had adaptations anyway in terms of a minority implementation committee charged with developing trial-wide procedures to enhance minority participation and success, and cross-cultural training for all study personnel that included specific instruction on cultural sensitivity and motivational interviewing techniques for study interventionists – this may have contributed to the fact that African Americans in the programme in general had better weight loss than usually reported in these types of studies and this may well have reduced the effect of having African American-only groups. In addition, the participants were recruited because they were at a particularly high risk of CVD and this may have made them more motivated than an average population |
|
Study reference Befort et al. 2008317 |
|
Setting USA; Kansas City, KS |
|
Inclusion criteria Women were eligible if they were ≥ 18 years, obese (BMI 30–50 kg/m2), not pregnant or intending to become pregnant within 6 months, not currently involved in any other weight loss treatments, free from psychiatric illness or substance abuse, able to walk continuously for at least 10 minutes, not planning to move out of the area in 6 months and able to obtain medical clearance from their medical practitioner |
|
Study type RCT |
|
Description of population Ethnicity: African American Age (years): Mean (SD): 44.3 (6.4) n: 44 women were recruited and randomised, but only 34 returned for post treatment assessment Sex: 100% female Income: Women were recruited from a community health centre serving predominantly lower-income people |
|
Description of intervention and control A 16-week culturally adapted behavioural weight loss programme with randomisation to receive either four sessions of motivational interviewing or four sessions of education (attention control) Intervention: The programme was adapted from the Lifestyle Balance programme and involved gradual, sustainable lifestyle changes using goal-setting and self-monitoring. Treatment goals were to decrease weight by 7%, decrease energy intake by 500–1000 calories a day (25% from fat), consume five to nine fruit and vegetable servings a day and exercise for 150 minutes per week. Participants received individual goals, charted their weekly weight and were instructed to self-monitor their daily food intake and physical activity |
| Theory: Not reported |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: 16 weeks Changes in fruit and vegetable consumption: Increase in fruit and vegetable consumption of 1.7 (SD 3) servings a day Changes in calories: Diet improved with a mean drop of 465 kcal/day (SD 696 kcal/day) and a drop in kcal from fat of 4.6% (SD 8.2%) Changes in physical activity: Increase in physical activity of 101 minutes (SD 350 minutes) and an increase of energy expenditure of 7 kcal/week/kg (SD 25.1 kcal/week/kg) Changes in dietary fat: No significant difference in outcomes between the two groups but both groups had an improved diet; mean weight loss 3 kg (SD 5.1 kg) Weight: No significant difference in outcomes between the two groups but both groups lost weight; BMI decrease 1.1 kg/m2 (SD 1.8 kg/m2) |
|
Conclusions Authors: Results showed that both groups lost a significant amount of weight, reduced their energy intake and per cent fat from calories and increased their fruit and vegetable intake, but adherence to the behavioural weight loss programme did not differ across the two groups. The authors suggest that further work is needed to dismantle the socioeconomic barriers from the sociocultural barriers that may limit the impact of motivational interviewing Reviewers: The study focus is on the effect of the addition of motivational interviewing to a culturally adapted intervention. This is a bit different to our focus of how culturally adapted interventions work, but the finding that the underlying intervention was successful was helpful; however, as adaptation was not the main focus there is perhaps less detail reported on this aspect |
|
Comments and limitations High attrition of 23% but this is consistent with other studies of this type Limited that the tools measured for self efficacy and motivation were not validated in this population |
|
Study reference Boltri et al. 2008509 |
|
Setting USA; area not reported, 100,000 inhabitants |
|
Inclusion criteria All churches attendees aged ≥ 18 years |
|
Study type Pre–post |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Not reported n: 50 Sex: Not reported Income: Not reported |
|
Description of intervention and control The purpose of this intervention was to translate the National Institutes of Health (NIH) Diabetes Prevention Program (DPP) to a church setting/African American Baptist church. Recruitment occurred through announcements in the church and in the Sunday bulletin for 2 weeks. During the church services a member of the research team also outlined the research and a survey was completed by church members on risk assessment for diabetes. High-risk people were then tested and those found to be at risk of pre-diabetes (eight) were included in the intervention There were 16 sessions lasting for 60–90 minutes in this individualised lifestyle programme. There was goals of 7% weight loss and 150 minutes of exercise per week. The sessions were designed to teach people how to improve their diet, lower fat intake, increase exercise and change behaviour to establish a lifelong healthy lifestyle. The programme was modified by changing it to group sessions and also adding in prayer. The intervention lasted for 4 months |
| Theory: Not reported |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: 6 months and 12 months post intervention BMI: decreased post intervention by a mean of –1.2 kg/m2, at 6 months it was raised by +0.3 kg/m2 and by 12 months it was raised again by +0.7 kg/m2 but still remained slightly lower than the starting BMI Weights: Mean weight decreased by –7.5 lb post intervention, the mean weight then increased at both the 6 month (+1.9 lb) and 12 month follow-up (+ 4.6 lb) |
|
Conclusions Authors: This study demonstrated successful translation of the 16-session NIH DPP into a church-based setting. Future studies should test this intervention in churches of different sizes and denominations Reviewers: This study is interesting as it shows successful translation of a DPP to a church setting for an African American population |
|
Comments and limitations Very small sample and no comparison group |
|
Study reference Chen et al. 2008510 |
|
Setting USA; San Francisco, CA |
|
Inclusion criteria Children aged 8–10 years who self-identified as Chinese American and their mothers |
|
Study type Pre–post |
|
Description of population Ethnicity: Chinese; self-identified Age (years): Mean (SD): children: 8.8 (0.8), mothers: (SD) 40 (7.1) n: 52 children completed to the 1-month follow-up and 42 to the 6-month follow-up Sex: 49.1% female Income: Not reported Other: Mean number of years of education of the mothers was 14 (SD 4.9) |
|
Description of intervention and control Initial data were collected for the mothers and children including height and weight. Questionnaires assessed mothers’ knowledge of children’s lifestyle and behaviours and also their levels of acculturation. Mothers then received information on whether their child was overweight or normal weight, their dietary intake and whether they were active or sedentary. They were also sent materials on nutrition, physical activity and healthy weight maintenance based on the baseline assessment. Parents were instructed to share the information with their children. There was a telephone consultation and follow-up 2 weeks after the mail out of the information |
| Theory: Based on the ecological model of childhood obesity prevention,511 which was derived from ecological system theory |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: 1 and 6 months Changes in physical activity: Statistically significant improvements were observed in time spent in physical activity BMI: BMI significantly declined among children who were overweight at baseline, and those who were not overweight at baseline appeared to gain weight more slowly than the usual annual increase in this population Knowledge: No significant changes in parental knowledge about their children’s nutrition and physical activity needs were noted as a result of the intervention |
|
Conclusions Authors: Results suggest that this intervention is feasible in the population. Some data suggested that the mail intervention is preferable to mothers as there is no need to keep appointments. There is also a lower cost to this than running education sessions, which means that it could be used to reach a larger population. However, this was a pilot/feasibility study and data from a RCT with a control group are needed to support the findings. This research suggests that health-care providers need to provide parents and children with specific recommendations regarding children’s weight status, dietary intake and levels of activity Reviewers: This intervention takes the approach of mailing information, which is less hands-on but perhaps more cost-effective. It did demonstrate effect but it is hard to know whether this would be sustainable or certainly whether this would be generalisable to other populations, particularly those who may not have such good health literacy or motivation or who may have competing life concerns. It is a feasibility study and, as stated by the researchers, evidence from a larger controlled trial is needed |
|
Comments and limitations This is limited by it being a pilot/feasibility study with a relatively small sample size and no control group. There are limited data on the changes occurring in the study to interpret them fully. There are limited data on adaptation other than the more superficial characteristics of the study such as language and researcher characteristics. This intervention is based on ecological systems theory, which emphasises the critical and important interaction between the individual’s characteristics and the environment in which a person is embedded and the context in which a person is situated. This is an interesting and perhaps cost-effective approach to reach a wide audience, although a cost-effective analysis has not been conducted |
|
Study reference Kim et al. 2008512 (The WORD) |
|
Setting USA; North Carolina |
|
Inclusion criteria Association with a participating church through membership or participation in a church activity, adult aged ≥ 18 years, African American |
|
Study type Two-group quasi-experimental delayed intervention design with the church as the unit of randomisation |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): ≥ 18 n: 73 Sex: 71% female Income: 41% of the treatment group had an annual income of < US$20,000 compared with 13% of the control group |
|
Description of intervention and control Community-based participatory research approach to develop a faith-based weight loss intervention for rural African American populations The intervention was an 8-week behaviourally focused weight loss programme in which participants met once a week for 2 hours in groups of 8–10 people led by a pair of trained community leaders who facilitated the groups. The intervention emphasised healthy nutrition, physical activity and faith’s connection with health |
| Theory: Community-based participatory research, social support theory, stages of change, transtheoretical model, social cognitive theory |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: 8-week follow-up Changes in physical activity: Treatment participants reported greater recreational physical activity from baseline to follow-up (p = 0.01) and there was a significant change in mean recreational physical activity over time within the treatment group (p < 0.05) Weight: Mean weight loss of the treatment group was 3.60 ± 0.64 lb compared with 0.59 ± 0.59 lb in the control group |
|
Conclusions Authors: The WORD intervention resulted in a significant difference in weight loss (3.00 ± 0.87 lb) from baseline to the 8-week follow-up between the intervention participants and the control participants. Although this weight loss is significant it is relatively modest compared with that seen with other weight loss interventions. The most critical factor relating to this may be the short duration of the intervention. The use of lay health advisors in this intervention increased the possibility of programme sustainability and built on social networks within the faith community in an economical way. This study offers promising preliminary results that a faith-based weight loss programme using a community-based participatory research approach is effective in a rural African American faith community Reviewers: This study showed promise for lifestyle change in African American faith populations. The study was not able to examine whether the intervention could result in sustained change and also was not designed in a way that could show how the adaptation contributed to intervention effectiveness |
|
Comments and limitations Limitations include the lack of randomisation and subsequent differences in baseline characteristics (although this was controlled for in the analysis). Also, the purposive sampling in one rural African American faith community limits the external validity of the study |
|
Study reference Kousar et al. 2008513 |
|
Setting Australia; Melbourne |
|
Inclusion criteria Pakistani-born women aged 20–60 years residing in Melbourne permanently and migrated to Australia over 5 years ago. Must have at least one component of metabolic syndrome (National Cholesterol Education Programme Adult Treatment Panel III criteria: elevated blood pressure, elevated blood glucose, obesity and increased waist circumference) |
|
Study type Cohort pre–post |
|
Description of population Ethnicity: Pakistani; not reported how ethnicity assessed Age (years): Mean: 37.6 n: 53 Sex: 100% female Income: Not reported |
|
Description of intervention and control Peer education delivering weekly modules on healthy diet and lifestyle over a 12-week period. Delivered individually by a female facilitator (a trained nutritionist with expertise in obesity management) for on average 4 hours per week (3 hours in person and 1 hour by telephone). Written materials also provided. Multifaceted goals included reducing overall energy intake and increasing physical activity. Modules aimed to increase the participants’ self-efficacy and self-regulation |
| Theory: Formulated on the principles of cultural competence |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline to weeks 12 and 24 Changes in physical activity: At 24 weeks there was a significant change in physical activity – an increase from 4000 (± 22.6) steps a day to 8617.4 (± 596.8) steps a day BMI: At 24 weeks there was a significant change in BMI from 29.2 (± 0.46) kg/m2 to 27.8 (± 0.45) kg/m2 |
|
Conclusions Authors: This was a successful intervention for the treatment of metabolic syndrome in a high-risk ethnic population in which the principles of cultural competence were applied to overcome the cultural barriers in place for Pakistani women to allow them to make the lifestyle changes necessary to lose weight and reduce the risk of metabolic syndrome Reviewers: This appears to have been a successful intervention, although conclusions and transferability are limited by the small sample size and lack of a control group |
|
Comments and limitations Limitations listed are the high-risk population; the sex bias as women only were included (justification given that women are primarily responsible for food preparation and influence the whole family); that long-term follow-up is required to assess sustainability; and that physical activity was limited by inappropriate leisure facilities and it was felt that better results could have been achieved with simultaneous environmental changes |
|
Study reference Martin et al. 2008514 |
|
Setting USA |
|
Inclusion criteria Women, 18–65 years, overweight or obese (BMI ≥ 25 kg/m2), classified as low income (< US$16,000 annual income), attendees of the primary care clinic for at least 1 year and free of serious or uncontrolled medical conditions (e.g. renal or hepatic failure, cancer, immunological disease, uncontrolled hypertension). Women with well-controlled chronic diseases such as hypertension, diabetes or hyperlipidaemia were included |
|
Study type RCT |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean: 41.8 ± 12.0 n: 144 enrolled, seven participants developed conditions so that they could not participate, and only 105 completed the 5-month programme Sex: 100% female Income: Not reported Other: 78% completed high school |
|
Description of intervention and control Weight loss maintenance of low-income African American women participating in a physician-delivered, primary care weight management intervention Tailored: 6-month weight loss intervention delivered by a primary care physician. Intervention derived from information provided during an initial assessment. Received five physician-counselled office visits on a monthly basis. Topics included information on weight loss, ways to decrease dietary fat, ways to increase physical activity, dealing with barriers to weight loss and healthy alternatives when eating out and shopping. There was a maintenance session at month 6 on the ways to stay motivated during weight loss. Each visit lasted for approximately 15 minutes (total approximately 90 minutes). Participants received both oral recommendations and handouts summarising the focus of each visit Standard care: Participants received no special instructions regarding weight loss and were seen as needed for regular medical care. Physicians provided usual obesity management conducted during a typical office visit |
| Theory: Not reported |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: 6 (post treatment), 9, 12 and 18 months following randomisation Weight: Weight loss of intervention participants (–1.52 ± 3.72 kg) was significantly greater than that of standard care participants (0.61 ± 3.37 kg) at month 9 (p = 0.01); however, no significant difference was detected between groups at 12 months [intervention group: 1.38 ± 3.69 kg vs standard care group: –0.16 ± 3.63 kg, F(1,6) = 3.80, p = 0.10] or 18 months [intervention group: –0.49 ± 3.33 kg vs standard care group: +0.07 ± 3.75 kg, F(1,6) = 0.85, p = 0.39] |
|
Conclusions Authors: Participants receiving a tailored weight loss intervention from physicians were able to maintain modest weight loss up to 3–6 months following treatment. Weight was regained at the 18-month follow-up suggesting that a more intensive follow-up in the primary care setting may be needed for long-term weight loss maintenance. Only a small minority achieved and maintained a weight loss of at least 5% at any follow-up, which did not differ from standard care values. Modest weight loss with brief treatment (approximately 15 minutes at each of six sessions) and prevention of weight gain can be helpful for chronic disease outcomes, i.e. hypertension and diabetes. More extended follow-up intervals are needed to determine the course of weight change Reviewers: This study managed to improve weight loss for the participants at 9 months but that effect was lost at the 12- and 18-month follow-ups. These findings are similar to those of other studies, which suggest that long-term sustained weight loss is difficult to achieve. It is noteworthy that weight gain was kept to a minimal, which is also thought to be helpful in addressing risk factors for chronic diseases |
|
Comments and limitations To decrease attrition, reimbursement was provided for potential barriers, e.g. transportation and childcare. Physicians were also reimbursed. However, there was still considerable attrition – 105 completed the 6-month programme (an attrition rate of 27%). Also, the attrition rates by the 9-month, 12-month, and 18-month follow-up assessments were 29, 35 and 37% respectively. Time constraints and reimbursement could make this intervention impractical for many clinical settings. Generalisability is limited because the focus is low-income African American populations; unclear what effects might be in obese adolescents or higher SES and other ethnic groups |
|
Study reference |
|
Setting USA; city or state not reported |
|
Inclusion criteria African American women aged ≥ 53 years, able to speak and read English, members of the church, not currently engaged in a physical activity programme, with written clearance from their physician and had signed the consent form |
|
Study type Quasi-experimental; randomised to intervention or control by church (although only two churches involved) |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Not reported n: 126 participants; 66 in the experimental group, 60 in the comparison group Sex: Not reported Income: Not reported |
|
Description of intervention and control Two churches were assigned to an intervention or control group by blind draw of sealed envelopes. The study was announced from the pulpit and advertised in the church bulletin of both churches and recruitment occurred over 1 month Intervention: Dance sessions were held twice a week for 8 weeks with each session lasting for 45 minutes and including a 5-minute warm-up, 30 minutes of dance and a 10-minute cool down. The dance was of moderate intensity. At the end of the 8 weeks the women were given a video of the dance to carry on the intervention at home Control: The comparison group continued their normal activities and were sent health information for African American women on heart disease, obesity, diabetes and hypertension. After the 18-week assessment they also received the free dance video so that they could carry out the exercise |
| Theory: Based on social cognitive theory |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline and 8 and 18 weeks Changes in physical activity: There was a significant improvement in functional capacity (this consisted of a 6-minute walk test in which the participants walked as far as possible around a pre-measured area of the church in 6 minutes; body fat was also measured using a segmental bioelectrical impedance arm-to-arm analyser). These changes occurred for both groups at 8 weeks (p < 0.001) and 18 weeks (p < 0.001); a significant difference between the groups was found only at 18 weeks (p = 0.04) |
|
Conclusions Authors: This study provided empirical data about a culturally specific dance intervention to improve functional capacity in African American women. The culturally specific dance intervention was within their own community and was taught by a respected member of their community to gospel music selected by the women. The dance steps were altered to match the age and health status of the women without reducing the health benefits. Culturally specific dance may be an initial step to encourage African American women to become more physically active and improve health outcomes Reviewers: This study showed the effect of a culturally specific dance intervention for African American women. A significant effect was seen at the 18-week follow-up point. The intervention appeared to be acceptable and was adapted for the population; however, the design did not permit comment on how the adaptation contributes to the effect |
|
Comments and limitations Randomisation of the churches, not the individuals, limited the generalisation of the results, even though the groups were matched on similar characteristics. The convenience sample of people volunteering may have been different from the people who did not or could not participate. As the study was carried out in one city and with only two churches it may not be generalisable and may not apply to women who are not church attendees. There was higher attrition in the experimental group than in the comparison group and this may have affected the results |
|
Study reference |
|
Setting USA; Houston |
|
Inclusion criteria African American girls aged 8–10 years with a BMI ≥ 50th percentile, with a home computer, internet access and an e-mail address |
|
Study type Randomised two-group design |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): 8–10 n: 80 Sex: 100% female Income: Not reported |
|
Description of intervention and control An 8-week internet-based intervention to change fruit, juice and vegetable consumption, physical activity and self-efficacy in youth at risk of obesity Treatment website was from a previous study with African American girls494 and was adapted to be a stand-alone internet programme by adding an introduction and a club member manual. Groups differed only on the incentive schedule (immediate, delayed). Participants’ weekly goals were to increase fruit, juice, and vegetable consumption (five servings) and water consumption (five glasses) and lifestyle physical activity (30 minutes). Weekly programming included role-modelling comics, problem-solving and goal-setting/review. Modules were designed to be completed in approximately 20 minutes each week and constituted the ‘required activities’. In addition, there was a ‘fun activities’ module |
| Theory: Social cognitive theory guided the content while elaboration likelihood guided character development, the storyline and the design framework |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Post-assessment data after completion of week 8 activities Changes in fruit, juice and vegetable consumption and physical activity: Statistically significant pre-to-post differences observed in fruit, juice and vegetable consumption with an increase of 1.01 servings (p = 0.002), increased physical activity-yesterday (p < 0.001), increased physical activity-usually (p = 0.001) and improved fruit, juice and vegetable self efficacy (p = 0.003) |
|
Conclusions Authors: A pilot study of a theory-based internet programme for girls indicated significant changes in fruit, juice and vegetable consumption and physical activity in an at-risk group of young girls. The current study achieved greater change in fruit, juice and vegetable consumption and physical activity than a previous study using the internet programme490 (also included in this systematic review), which may be explained by a greater programme dose in the current study and an exclusive internet approach rather than a mixed internet + camp approach, which may have attracted families more interested in a low-cost summer day camp than an internet programme. A full-scale RCT may be needed to more fully examine the impact of an internet-based e-Health programme on diet and physical activity. Incentives were tied to the programme dose (i.e. increased exposure) rather than to goal attainment or behaviour change. The use of multiple recruitment methods may influence generalisability Reviewers: This study compared the same treatment but with a different incentive schedule. The motivation for this was not entirely clear but the study showed that fruit, juice and vegetable consumption and physical activity increased in both groups and that immediate incentives encouraged greater log-on rates than delayed incentives, but this was not significant. Overall, the interesting finding came from participation based on the recruitment method (media vs church): those recruited through the media had higher log-on rates (although this was not statistically significant) |
|
Comments and limitations Strengths include a delivery channel that minimised differences in delivery, the low attrition rate (< 10%) and the reasonably high log-on rates (i.e. programme dose), suggesting that an acceptable dose was achieved (log-on rate averaged 74.5%). Log-on may have been enhanced compared with other studies because of the club format and staff computer support. Limitations include the small sample size, lack of a control group, self-reported measures with the possibility of socially desirable responses, the short study duration and the requirement to have a home computer with internet access, which likely excluded at-risk girls. Further, joining of sports groups, family vacations, holidays and chance or other events may have influenced fruit, juice and vegetable consumption and physical activity during the intervention |
|
Study reference Choudhury et al. 2009409 |
|
Setting UK; Swansea and Cardiff |
|
Inclusion criteria Bangladeshi adults living in and around Swansea and Cardiff with type 2 diabetes |
|
Study type Uncontrolled before-and-after study |
|
Description of population Ethnicity: Bangladeshi; not reported how ethnicity assessed Age (years): Not reported n: 72 Sex: 66.6% female Income: Not reported |
|
Description of intervention and control Recruitment was carried out through posters displayed in GP surgeries, pharmacies, the mosque and other community settings. Peer educators and the researcher also advertised the educational sessions to their contacts who were asked to spread the word. Announcements were also made at the mosque and these would have reached people in their homes. People who registered were all telephoned or visited at their homes the day before the course and were also telephoned on the morning of the course as a reminder. The venue was within walking distance of the homes of registered responders. The intervention consisted of one 4-hour session of a culturally adapted version of the X-PERT programme (utilising four of the original six sessions – carried out in one session) |
| Theory: No theories are explicitly stated |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Outcomes were measured after the course and a course assessment questionnaire was carried out Changes in dietary fat: The results of the questionnaire showed an increase in the time spent on self-management of general diet and specific diet of 0.3 days Changes in fitness: Exercise increased over the study period but not significantly – this may be related to the sample size as the sample only had 50% power to detect a 1-day improvement in self-care activities |
|
Conclusions Authors: The response in terms of registration was good; however, attendance was only 53% of those registered despite the extra reminders by telephone and home visits. The most valued things were information provided in a language that was understood and also the discussion of problems and solutions with others. The peer educators were the most important part of the course as they were well known to the community, had bilingual language ability, had the time to devote to the course, had diabetes themselves and had the ability to learn and deliver the course. Findings suggest that the 4-hour intensive course was a success and was well received and could be part of a strategy to improve outcomes for people with diabetes in the Bangladeshi community Reviewers: This intervention seems to be well accepted but it is difficult to interpret its success as it was short-lived and the study did not have sufficient power to detect a change in exercise and diet. There are interesting lessons in terms of the success of the social support aspect and a suggestion that results may have improved with a longer duration of the programme and a larger sample size to examine the effects |
|
Comments and limitations The course was kept to one intensive 4-hour session because in the pilot work it was felt that numbers would not be sustained over more than one session. However, it is hypothesised that because of the acceptability of the programme it may have been possible to sustain numbers and have a longer course with perhaps more significant results. The power of the study limited the analysis of the questionnaires. The issues of cost-effectiveness and equity were not addressed |
|
Study reference Djuric et al. 2009354 [Lifestyle Improvement with Food and Exercise (LIFE)] |
|
Setting USA; Detroit, MI |
|
Inclusion criteria Women who had been diagnosed with stage I, II or IIIA breast cancer within the last 10 years and who identified themselves as African American. Other eligibility criteria were BMI 30–45 kg/m2, completed chemotherapy or radiation therapy at least 3 months previously (with exception of tamoxifen), age 18–70 years, willing and able to follow a diet and exercise recommendations and having spiritual influences in their lives as determined from a spiritual index. Women with a recurrence, a second primary tumour or other history of malignant tumours were not eligible. Eligible women had to also not be presently on a special diet for a medical condition, e.g. type 2 diabetes, or currently participating in a formal weight loss programme |
|
Study type RCT |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Mean (SD): 56 (10) n: 31 Sex: 100% female Income: Mean household annual income: dietician group: 25% < US$30,000, spirituality arm: 25% < US$30,000 Other: Dietician group: 50% college graduates, spirituality arm: 67% college graduates |
|
Description of intervention and control Randomised culturally tailored clinical trial of spirituality counselling for weight management in African American breast cancer survivors. Both arms received individualised dietician-led dietary and exercise counselling by telephone combined with free Weight Watchers coupons for 18 months and at the 6-month time point the dietary counselling became less frequent and women were randomised to receive spiritual counselling (non-denominational) or not in addition to the standard programme. Exercise was for at least 30 minutes most days each week using participants’ preferred mode of exercise. A monthly newsletter was sent |
| Theory: Bandura’s social cognitive theory498 |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline to 6, 12 and 18 months Changes in fruit and vegetable consumption: Spirituality group had significant increases in fruit servings (p = 0.007) and in their healthy eating index (p = 0.036), and the fruit servings change was significantly different from that of the control group Changes in physical activity: Physical activity did not change significantly in either group Weight: Mean weight loss from baseline to 6 months was a modest 2% of baseline weight. From the 6- to 18-month assessment there was no further weight change in the spirituality arm and a gain of 0.7% in the dietician-only arm |
|
Conclusions Authors: Despite little effect on weight loss it did appear that spirituality counselling positively affected spiritual well-being scores and dietary quality. The spirituality framework therefore may be further refined and used for other health promotion studies with African American populations Reviewers: The study showed that spirituality counselling may have some added effect to a culturally adapted diet programme in this population in terms of weight change; however, the differences are small |
|
Comments and limitations Limitations include the small sample size and the fact that the sample was fairly well educated and may not be generalisable to other populations |
|
Study reference Stolley et al. 2009412 (Moving Forward) |
|
Setting USA; Chicago, IL |
|
Inclusion criteria At least 18 years old, self-identifying as African American/black, having a stage I, II or III breast cancer diagnosis, BMI ≥ 25 kg/m2, completed breast cancer treatment (except endocrine treatment) at least 6 months before baseline interview, having physician approval to participate in a moderate physical activity programme, not using prescription weight loss medication, not currently participating in an organised weight loss programme and willing to participate and able to complete the pre-intervention and post-intervention interviews and attend twice weekly classes for 6 months |
|
Study type Pre–post |
|
Description of population Ethnicity: African American/black; self-identified Age (years): Mean (SD) (range): 51.4 (8.9) (30.6–70.1) n: 23 Sex: 100% female Income: Not reported |
|
Description of intervention and control A 6-month culturally tailored weight loss intervention The intervention provided information to increase knowledge and improve attitudes about diet, physical activity and weight loss and their relationship to breast cancer prognosis and general health, an opportunity to enact positive behavioural changes and increase self-efficacy, an environment in which participants felt comfortable applying problem-solving skills, allowing them to confront barriers to change, and reinforcement and social support for making health behaviour changes. The intervention consisted of 6 months of two-weekly classes; the first class included 2 hours of discussion around barriers, knowledge, attitudes, facilitators, benefits and costs related to changes in diet, exercise and weight |
| Theory: The intervention was developed by integrating two health behaviour change theories: social cognitive theory and the health belief model |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline and 6 months Changes in fruit and vegetable consumption: Vegetable consumption increased significantly by 1.6 servings per day (p = 0.05) Changes in dietary fat: Fat consumption decreased significantly by 23.6 g (p = 0.03) although the decrease in percentage of energy from fat was not significant Changes in physical activity: Median time spent in physical activity increased significantly by 23.6 minutes per day (p = 0.02). Changes in moderate physical activity and all physical activity also increased but not significantly Weight: Mean weight loss was 5.6 lb (p = 0.001) and there was a decrease in BMI of 1 kg/m2 |
|
Conclusions Authors: Although a RCT is needed to establish efficacy, the positive results suggest that this weight loss intervention may be feasible for African American breast cancer survivors. Lifestyle interventions may reduce the disparities in breast cancer mortality rates Reviewers: This study had a very good formative component in its development in both theory of behaviour change considerations and adaptation. It has been shown to be effective, acceptable and feasible. As stated by the authors, a larger study is required to assess generalisability and to be able to truly assess effectiveness |
|
Comments and limitations Limitations include the small sample size, lack of a control group, the fact that recruitment was based on self-selection and may have been biased and the fact that measures of dietary intake and physical activity were self-reported and may be biased. Also, the study cannot be generalised to a wider population as it includes a very specific population and it is not clear how long these changes may be sustained for |
|
Study reference Sharp et al. 2008;367 Fitzgibbon et al. 2008;365 Stolley et al. 2009366 [Obesity Reduction Black Intervention Trial (ORBIT)] |
|
Setting USA; Chicago, IL |
|
Inclusion criteria Female, self-identified as African American or black, aged 30–65 years, BMI between 30 and 50 kg/m2, able to participate in a programme requiring 30 minutes of uninterrupted walking or other moderate activity, able to attend class at scheduled times and return of medical approval form signed by physician |
|
Study type RCT |
|
Description of population Ethnicity: African American or black; self-identified Age (years): 30–65 n: 213 Sex: 100% female Income: Not reported |
|
Description of intervention and control Culturally proficient 6-month weight loss intervention. Intervention targeted changes in diet and physical activity patterns. There was the opportunity for monthly motivational interviewing. Intervention groups were a valuable source of social support The weight loss intervention was conducted in a small group format and groups met twice weekly on the university campus. All participants were encouraged to adopt a low-fat high-fibre diet with increased fruit and vegetable intake and to increase their physical activity. Dietary objectives included reducing dietary fat to < 30% of total daily calories, increasing dietary fibre to a minimum of 25 g per day and increasing fruit and vegetable intake to a minimum of five servings a day. Exercise objectives were three to four times a week for at least 30 minutes. The intervention involved hands-on activities such as portion size, weighing and measuring, trips to grocery stores, label reading and creating weekly meal plans |
| Theory: Social cognitive theory |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Baseline and 6 months Changes in fruit and vegetable consumption: Women in the intervention group showed improvements in fruit intake (p < 0.01) and the Healthy Eating Index score (p < 0.001) compared with women in the control group Changes in physical activity: Women in the intervention group also showed improvements in moderate (p = 0.05) and vigorous (p < 0.001) physical activity compared with women in the control group Weight: Women in the intervention group lost an average of 3 kg (SD 4.9 kg) compared with a gain of 0.2 kg (SD 3.7 kg) in the control group (p < 0.001). However, weight change was variable within the groups with a maximum weight loss in the intervention group of 19.4% of initial body weight and a maximum weight gain in this same group of 6.4% of body weight (25% of women in the intervention group lost > 5% of their initial weight over 6 months compared with only 5% in the control group) |
|
Conclusions Authors: This study demonstrated that a culturally adapted programme can successfully promote weight loss in obese black women; however, average weight loss was relatively modest and weight change varied widely within the intervention group. Weight loss of 5% has been shown to alleviate the burden of many chronic diseases. Further research is needed to develop programmes that will allow more black women to achieve their weight loss goals Reviewers: This study showed an effect of a culturally adapted weight loss programme for African American women. The effects were varied within the groups, they were moderate in size and also it is unknown how long they could be sustained for. A maintenance study is under way. The study design does not tell us about the effectiveness of adaptation vs no adaptation |
|
Comments and limitations Self reported measures were used for diet and physical activity. Recruitment was voluntary and participants may be more motivated than the average population. Only BMI was used as a measure whereas other factors are also associated with chronic disease, such as fat distribution, and perhaps these other measures would have related to health outcomes more |
Adapted smoking cessation, physical activity and nutrition interventions
|
Study reference DeBate et al. 2004;289 Plescia et al. 2008288 (Charlotte REACH) |
|
Setting USA; north-west corridor of Charlotte, NC |
|
Inclusion criteria Resident of the study communities of Charlotte; men or women aged ≥ 18 years |
|
Study type Quasi-experimental evaluation design compared residents assessed by annual cross-sectional survey with African Americans across the state; community-based research |
|
Description of population Ethnicity: African American; not reported how ethnicity assessed Age (years): Charlotte REACH population: 18–34 years: 20.2%, 35–44 years: 17.3%, 45–54 years: 19.6%, 55–64 years: 16.2%, ≥ 65 years: 26.0%; state-wide Behavioral Risk Factor Surveillance System (BRFSS) population: 18–34 years: 33.1%, 35–44 years: 20.9%, 45–54 years: 19.0%, 55–64 years: 11.8%, ≥ 65 years: 14.4% n: Charlotte REACH 4730, state-wide BRFSS 9814 Sex: Charlotte REACH 63.4% female, state-wide BRFSS 55.8% female Income: Not reported |
|
Description of intervention and control Intervention in an African American community and its effect on three behavioural risk factors for heart disease and diabetes: low fruit and vegetable consumption, low physical activity and cigarette smoking Lay health advisor (LHA) programme: LHAs chosen by leaders of 14 neighbourhood associations and three community-based organisations (26 LHAs trained, all African American, 80% were aged > 50 years); they led community-based exercise classes, walking groups, smoking cessation classes and religion-based nutrition programmes A farmers’ market was held to improve access to fresh fruit and vegetables (operated 8 months per year); physical activity programmes were expanded into community settings; a culturally specific mass media campaign was conducted with a local African American-owned public relations firm; and health promotion changes were advocated for by contacting political leaders about the importance of raising state tax on tobacco products and banning smoking in restaurants and bars |
| Theory: Socioecological model – community and policy change were emphasised; logic model used to assess progress in addressing health disparities through five progressive stages; community-oriented primary care model; Charlotte REACH designed on an ecological model (see DeBate et al.289) |
|
Approaches to adaptation |
|
Outcome measures and results Follow-up: Annually for 5 years Quit rates: Smoking rates decreased in both populations but only northwest corridor women reached statistical significance (26.8% in 2001 vs 20.9% in 2005; p = 0.03) Changes in fruit and vegetable consumption: Fruit and vegetable consumption increased in northwest participants and decreased in state-wide participants Changes in physical activity: Improvements were statistically significant for physical activity in women (p = 0.02) and physical activity among middle-aged adults (p = 0.01) |
|
Conclusions Authors: Findings from this study supported the emerging role of policy and community environmental change and community participation as strategies to improve health behaviours in African American communities and to reduce health disparities. Statistically significant declines were demonstrated in physical inactivity and smoking among women and in physical inactivity among middle-aged adults. Decreases in physical inactivity and increases in fruit and vegetable consumption were significantly greater in the northwest corridor sample than in the state-wide African American sample. These findings are important as few well-designed studies have documented community-wide improvement in cardiovascular risk and protective behaviours among African Americans. Two factors were integral to the project’s success: community participation and environmental change. DeBate’s qualitative assessment: those who participated in REACH activities indicated that improvement in social health through fellowship was the main reason why they continued to participate. Observed interpersonal-level changes among target area residents who participated and changes in knowledge, attitudes and behaviours regarding CVD and diabetes prevention strategies Reviewers: It’s difficult to conclude whether the community-based activities are what contributed to the observed outcomes because of the study design (cross-sectional surveys); however, because the comparison was with the state-wide data (secular trend) it would suggest that the effects observed may be attributable to the intervention activities |
|
Comments and limitations The preferred profile for a LHA is female and aged > 50 years. Farmers’ markets in the north-west corridor can greatly promote fruit and vegetable consumption, particularly if this is categorised as a ‘food desert’. The legacy of racial discrimination in the southern community was a difficult issue in the collaborative process. As the project matured, some LHAs began to work in institutions such as churches and the local health centre |
Appendix 19 Quality assessment of the 107 included empirical studies (Effective Public Health Practice Project)
| Study | Strong | Moderate | Weak |
|---|---|---|---|
| Resnicow et al. 1997;400 Resnicow et al. 1997401 | ✗ | ||
| Wang and Chan 2005346 | ✗ | ||
| Cullen and Thompson 2008313 | ✗ | ||
| Sullivan and Carter 1985482 | ✗ | ||
| Gaston et al. 2007399 | ✗ | ||
| Yancey et al. 2001;339 Yancey et al. 2006;338 McCarthy et al. 2007340 | ✗ | ||
| Chen et al. 2008504 | ✗ | ||
| Kanders et al. 1994483 | ✗ | ||
| Ahijevych and Wewers 1995454 | ✗ | ||
| Kousar et al. 2008513 | ✗ | ||
| Ahluwalia et al. 2006;361 Nollen et al. 2006;362 Okuyemi et al. 2007;363 Okuyemi et al. 2007364 | ✗ | ||
| Andrews et al. 2007;461 Andrews et al. 2007462 | ✗ | ||
| Fang et al. 2006332 | ✗ | ||
| Engels et al. 2005319 | ✗ | ||
| Shelley et al. 2008453 | ✗ | ||
| Agurs-Collins et al. 1997372 | ✗ | ||
| Frenn et al. 2003337 | ✗ | ||
| Baranowski et al. 1990;322 Baranowski et al. 1990321 | ✗ | ||
| Kumanyika et al. 2005;328 Anderson et al. 2007327 | ✗ | ||
| Williams et al. 2001297 | ✗ | ||
| Nothwehr et al. 2001312 | ✗ | ||
| Djuric et al. 2009354 | ✗ | ||
| Guerin et al. 2003283 | ✗ | ||
| Thrasher et al. 2004;292 Campbell et al. 2004299 | ✗ | ||
| Stolley et al. 2009412 | ✗ | ||
| Anderson et al. 2005309 | ✗ | ||
| Fitzgibbon et al. 2005405 | ✗ | ||
| Shankar et al. 2007;315 Klassen et al. 2008316 | ✗ | ||
| Befort et al. 2008317 | ✗ | ||
| Resnicow et al. 2002;295 Resnicow et al. 2005294 | ✗ | ||
| Murrock and Gary 2008;515 Murrock and Madigan 2008516 | ✗ | ||
| Resnicow et al. 2000284 | ✗ | ||
| Kim et al. 2008512 | ✗ | ||
| Resnicow et al. 2005324 | |||
| Huhman et al. 2005;285 Huhman et al. 2007;286 Huhman et al. 2008287 | ✗ | ||
| Andersen et al. 2006468 | ✗ | ||
| Davis-Smith et al. 2007;334 Atkinson et al. 2009373 | ✗ | ||
| Fitzgibbon et al. 2008;365 Sharp et al. 2008;368 Stolley et al. 2009366 | |||
| Kelley et al. 2004496 | ✗ | ||
| Resnicow et al. 2000;335 Resnicow et al. 2001325 | ✗ | ||
| Resnicow et al. 2004;476 Fuemmeler et al. 2006;477 Campbell et al. 2007478 | |||
| Haire-Joshu et al. 2001;304 Haire-Joshu et al. 2003;303 Eyler et al. 2004305 | ✗ | ||
| Ahluwalia et al. 1998;355 Ahluwalia et al. 1998356 | ✗ | ||
| Orleans et al. 1998;347 Boyd et al. 1998306 | ✗ | ||
| Wong et al. 2008466 | ✗ | ||
| DeBate et al. 2004;289 Plescia et al. 2008288 | Observational | ||
| Robinson et al. 2003;329 Robinson et al. 2008330 | ✗ | ||
| Stolley and Fitzgibbon 1997487 | ✗ | ||
| Webb et al. 2008351 | ✗ | ||
| Newton and Perri 2004350 | ✗ | ||
| Story et al. 2003410 | ✗ | ||
| Campbell et al. 1999326 | ✗ | ||
| Schorling et al. 1997451 | ✗ | ||
| Lacey et al. 1991453 | ✗ | ||
| Stillman et al. 1993;301 Voorhees et al. 1996300 | ✗ | ||
| Banks-Wallace et al. 2004;469 Banks-Wallace and Conn 2005;470 Banks-Wallace 2007471 | ✗ | ||
| Ahluwalia et al. 2002;345 Harris et al. 2003;344 Harris et al. 2004;342 Manning et al. 2005343 | |||
| Royce et al. 1995333 | ✗ | ||
| Anderson-Loftin et al. 2005371 | ✗ | ||
| Martin et al. 2008514 | ✗ | ||
| Darity et al. 2006457 | ✗ | ||
| Li et al. 1984357 | ✗ | ||
| Wilbur et al. 2008472 | ✗ | ||
| Shaw-Perry et al. 2007310 | ✗ | ||
| Rush et al. 2007411 | ✗ | ||
| Utz et al. 2008408 | ✗ | ||
| Kristal et al. 1999474 | |||
| Yanek et al. 2001352 | ✗ | ||
| Young and Stewart 2006397 | ✗ | ||
| Whitt-Glover et al. 2008308 | ✗ | ||
| Larson et al. 2009467 | Observational | ||
| Nollen et al. 2007341 | ✗ | ||
| Beech et al. 2003;396 Klesges et al. 2008395 | ✗ | ||
| Thompson et al. 2008;359 Thompson et al. 2008360 | ✗ | ||
| Goodman and Blake 2005481 | ✗ | ||
| Baranowski et al. 2003494 | ✗ | ||
| Campbell et al. 1999;320 Campbell et al. 2000473 | ✗ | ||
| Resnicow et al. 2009296 | ✗ | ||
| Two Feathers et al. 2005;291 Two Feathers et al. 2007290 | ✗ | ||
| Farooqi and Bhavsar 2001;370 Netto et al. 2007368 | ✗ | ||
| White et al. 2004;280 Williamson et al. 2005;281 Williamson et al. 2006;282 Kennedy et al. 2008314 | ✗ | ||
| Taylor-Piliae et al. 2006;402 Taylor-Piliae et al. 2006403 | ✗ | ||
| McNabb et al. 1997;485 Quinn and McNabb 2001486 | ✗ | ||
| Snowdon 1999475 | Qualitative | ||
| Carroll et al. 2002302 | Qualitative | ||
| Fitzgibbon et al. 2002;504 Stolley et al. 2003;505 Fitzgibbon et al. 2005506 | ✗ | ||
| Kumanyika and Charleston 1992336 | ✗ | ||
| Auslander et al. 2002;298 Williams et al. 2006307 | ✗ | ||
| Boltri et al. 2008509 | |||
| Lasco et al. 1989318 | ✗ | ||
| Keyserling et al. 2000;492 Keyserling et al. 2002493 | ✗ | ||
| Fitzgibbon et al. 2005405 | ✗ | ||
| Ard et al. 2000323 | ✗ | ||
| Ard et al. 2008348 | ✗ | ||
| Choudhury et al. 2009409 | ✗ | ||
| Kreuter et al. 2005293 | ✗ | ||
| Stewart et al. 2006413 | ✗ | ||
| Wallace et al. 1996484 | ✗ | ||
| Hawthorne and Tomlinson 1997407 | ✗ | ||
| McBride et al. 2002374 | |||
| Amoako et al. 2008406 | ✗ | ||
| Lipkus et al. 1999358 | ✗ | ||
| Karanja et al. 2002490 | ✗ | ||
| Williams et al. 2004500 | ✗ | ||
| D’Eramo-Melkus et al. 2004331 | ✗ | ||
| Jason et al. 1988404 | ✗ | ||
| Ma et al. 2004349 | ✗ |
Appendix 20 Summary of adaptations used in included studies
| Study | Adaptation | Total | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 | 33 | 34 | 35 | 36 | 37 | 38 | 39 | 40 | 41 | 42 | 43 | 44 | 45 | 46 | ||
| Resnicow et al. 1997;400 Resnicow et al. 1997401 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Wang and Chan 2005346 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Cullen and Thompson 2008313 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Sullivan and Carter 1985482 | • | • | • | 3 | |||||||||||||||||||||||||||||||||||||||||||
| Gaston et al. 2007399 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Yancey et al. 2001;339 Yancey et al. 2006;338 McCarthy et al. 2007340 | • | • | • | 3 | |||||||||||||||||||||||||||||||||||||||||||
| Chen et al. 2008510 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Kanders et al. 1994483 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Ahijevych and Wewers 1995454 | • | • | 2 | ||||||||||||||||||||||||||||||||||||||||||||
| Kousar et al. 2008513 | • | • | • | • | • | • | • | • | • | • | • | • | 12 | ||||||||||||||||||||||||||||||||||
| Ahluwalia et al. 2006;361 Nollen et al. 2006;362 Okuyemi et al. 2007;363 Okuyemi et al. 2007364 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Andrews et al. 2007;461 Andrews et al. 2007462 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 18 | ||||||||||||||||||||||||||||
| Fang et al. 2006332 | • | • | • | • | • | 5 | |||||||||||||||||||||||||||||||||||||||||
| Engels et al. 2005319 | • | • | • | 3 | |||||||||||||||||||||||||||||||||||||||||||
| Shelley et al. 2008465 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Agurs-Collins et al. 1997377 | • | • | • | • | • | • | • | • | • | • | • | • | • | 13 | |||||||||||||||||||||||||||||||||
| Frenn et al. 2003337 | • | • | • | 3 | |||||||||||||||||||||||||||||||||||||||||||
| Baranowski et al. 1990;322 Baranowski et al. 1990321 | • | • | • | • | • | • | • | • | • | • | • | • | • | 13 | |||||||||||||||||||||||||||||||||
| Kumanyika et al. 2005;328 Anderson et al. 2007327 | • | • | • | • | • | • | • | • | • | • | • | • | • | 13 | |||||||||||||||||||||||||||||||||
| Williams et al. 2001297 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Nothwehr et al. 2001312 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Djuric et al. 2009354 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Guerin et al. 2003283 | • | • | • | • | • | • | • | • | • | • | • | • | • | 13 | |||||||||||||||||||||||||||||||||
| Thrasher et al. 2004;292 Campbell et al. 2004299 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 14 | ||||||||||||||||||||||||||||||||
| Stolley et al. 2009412 | • | • | • | • | • | • | • | • | • | • | • | • | 12 | ||||||||||||||||||||||||||||||||||
| Anderson et al. 2005309 | • | • | • | • | • | • | • | • | • | • | 10 | ||||||||||||||||||||||||||||||||||||
| Fitzgibbon et al. 2005405 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Shankar et al. 2007;315 Klassen et al. 2008316 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 15 | |||||||||||||||||||||||||||||||
| Befort et al. 2008317 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 16 | ||||||||||||||||||||||||||||||
| Resnicow et al. 2002;295 Resnicow et al. 2005294 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 22 | ||||||||||||||||||||||||
| Murrock and Gary 2008;515 Murrock and Madigan 2008516 | • | • | • | • | • | • | • | • | 8 | ||||||||||||||||||||||||||||||||||||||
| Resnicow et al. 2000284 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Kim et al. 2008512 | • | • | • | • | • | • | • | • | 8 | ||||||||||||||||||||||||||||||||||||||
| Resnicow et al. 2005324 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Huhman et al. 2005;285 Huhman et al. 2007;286 Huhman et al. 2008287 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Andersen et al. 2006468 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Haire-Joshu et al. 2001;304 Haire-Joshu et al. 2003;303 Eyler et al. 2004305 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Ahluwalia et al. 1998;355 Ahluwalia et al. 1998356 | • | • | • | • | • | • | • | • | 8 | ||||||||||||||||||||||||||||||||||||||
| Orleans et al. 1998;347 Boyd et al. 1998306 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 15 | |||||||||||||||||||||||||||||||
| Wong et al. 2008466 | • | • | • | • | • | • | • | • | • | • | • | • | • | 13 | |||||||||||||||||||||||||||||||||
| DeBate et al. 2004;289 Plescia et al. 2008288 | • | • | • | • | • | • | • | • | • | • | 10 | ||||||||||||||||||||||||||||||||||||
| Robinson et al. 2003;329 Robinson et al. 2008330 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Stillman et al. 1993;301 Voorhees et al. 1996300 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 19 | ||||||||||||||||||||||||||||
| Banks-Wallace et al. 2004;469 Banks-Wallace and Conn 2005;470 Banks-Wallace 2007471 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 22 | |||||||||||||||||||||||||
| Ahluwalia et al. 2002;345 Harris et al. 2003;344 Harris et al. 2004;342 Manning et al. 2005343 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Royce et al. 1995333 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Anderson-Loftin et al. 2005371 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 16 | ||||||||||||||||||||||||||||||
| Martin et al. 2008514 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Darity et al. 2006457 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Li et al. 1984357 | • | • | • | • | • | • | • | • | 8 | ||||||||||||||||||||||||||||||||||||||
| Wilbur et al. 2008472 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Shaw-Perry et al. 2007310 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Rush et al. 2007411 | • | • | • | • | • | 5 | |||||||||||||||||||||||||||||||||||||||||
| Utz et al. 2008408 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 16 | ||||||||||||||||||||||||||||||
| Kristal et al. 1999474 | • | • | • | • | 4 | ||||||||||||||||||||||||||||||||||||||||||
| Yanek et al. 2001352 | • | • | • | • | • | • | • | • | • | • | • | • | 12 | ||||||||||||||||||||||||||||||||||
| Young and Stewart 2006397 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 15 | |||||||||||||||||||||||||||||||
| Whitt-Glover et al. 2008308 | • | • | • | • | • | • | • | • | • | • | • | • | • | 13 | |||||||||||||||||||||||||||||||||
| Larson et al. 2009467 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Nollen et al. 2007341 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Beech et al. 2003;396 Klesges et al. 2008395 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Thompson et al. 2008;359 Thompson et al. 2008360 | • | • | • | • | • | 5 | |||||||||||||||||||||||||||||||||||||||||
| Goodman and Blake 2005481 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Baranowski et al. 2003494 | • | • | • | • | • | 5 | |||||||||||||||||||||||||||||||||||||||||
| Campbell et al. 1999;320 Campbell et al. 2000473 | • | • | • | • | • | • | • | • | • | • | • | • | 12 | ||||||||||||||||||||||||||||||||||
| Resnicow et al. 2009296 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Two Feathers et al. 2005;291 Two Feathers et al. 2007290 | • | • | • | • | • | • | • | • | 8 | ||||||||||||||||||||||||||||||||||||||
| Farooqi and Bhavsar 2001;370 Netto et al. 2007368 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| White et al. 2004;280 Williamson et al. 2005;281 Williamson et al. 2006;282 Kennedy et al. 2008314 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Taylor-Piliae et al. 2006;402 Taylor-Piliae et al. 2006403 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| McNabb et al. 1997;485 Quinn and McNabb 2001486 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Snowdon 1999475 | • | • | • | • | • | • | • | • | 8 | ||||||||||||||||||||||||||||||||||||||
| Carroll et al. 2002302 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 14 | ||||||||||||||||||||||||||||||||
| Fitzgibbon et al. 2002;504 Stolley et al. 2003;505 Fitzgibbon et al. 2005506 | • | • | • | • | • | • | • | • | • | • | • | • | • | 13 | |||||||||||||||||||||||||||||||||
| Kumanyika and Charleston 1992336 | • | • | • | • | 4 | ||||||||||||||||||||||||||||||||||||||||||
| Auslander et al. 2002;298 Williams et al. 2006307 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Boltri et al. 2008509 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Lasco et al. 1989318 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Keyserling et al. 2000;492 Keyserling et al. 2002493 | • | • | • | • | • | 5 | |||||||||||||||||||||||||||||||||||||||||
| Fitzgibbon et al. 2005405 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Ard et al. 2000323 | • | • | • | • | • | • | • | • | 8 | ||||||||||||||||||||||||||||||||||||||
| Ard et al. 2008348 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Choudhury et al. 2009409 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Kreuter et al. 2005293 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Stewart et al. 2006413 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Wallace et al. 1996484 | • | • | • | • | • | 5 | |||||||||||||||||||||||||||||||||||||||||
| Hawthorne and Tomlinson 1997407 | • | • | • | • | • | • | • | • | • | • | 10 | ||||||||||||||||||||||||||||||||||||
| McBride et al. 2002374 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Amoako et al. 2008406 | • | • | • | • | • | 5 | |||||||||||||||||||||||||||||||||||||||||
| Lipkus et al. 1999358 | • | • | • | • | • | • | • | • | • | • | • | 11 | |||||||||||||||||||||||||||||||||||
| Karanja et al. 2002490 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 17 | |||||||||||||||||||||||||||||
| Williams et al. 2004500 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| D’Eramo-Melkus et al. 2004331 | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | • | 18 | ||||||||||||||||||||||||||||
| Jason et al. 1988404 | • | • | • | • | • | 5 | |||||||||||||||||||||||||||||||||||||||||
| Ma et al. 2004349 | • | • | • | • | • | • | • | • | • | • | 10 | ||||||||||||||||||||||||||||||||||||
| Lacey et al. 1991453 | • | • | • | • | • | • | • | 7 | |||||||||||||||||||||||||||||||||||||||
| Stolley and Fitzgibbon 1997487 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Webb et al. 2008351 | • | • | • | • | • | • | • | • | • | 9 | |||||||||||||||||||||||||||||||||||||
| Newton and Perri 2004352 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Story et al. 2003410 | • | • | • | • | • | • | 6 | ||||||||||||||||||||||||||||||||||||||||
| Campbell et al. 1999326 | • | • | • | • | • | • | • | • | 8 | ||||||||||||||||||||||||||||||||||||||
| Resnicow et al. 2004;476 Fuemmeler et al. 2006;477 Campbell et al. 2007478 | • | • | • | • | • | • | • | • | 8 | ||||||||||||||||||||||||||||||||||||||
| Kelley et al. 2004496 | • | • | • | • | 4 | ||||||||||||||||||||||||||||||||||||||||||
| Davis-Smith et al. 2007;334 Atkinson et al. 2009373 | • | • | • | • | • | • | • | • | • | • | 10 | ||||||||||||||||||||||||||||||||||||
| Resnicow et al. 2000;335 Resnicow et al. 2001325 | • | • | • | • | • | • | • | • | • | • | • | 12 | |||||||||||||||||||||||||||||||||||
| Fitzgibbon et al. 2008;365 Sharp et al. 2008;368 Stolley et al. 2009366 | • | • | • | • | • | • | • | • | • | • | • | • | • | 13 | |||||||||||||||||||||||||||||||||
| Schorling et al. 1997456 | • | • | • | • | • | • | • | • | • | • | • | • | 12 | ||||||||||||||||||||||||||||||||||
Appendix 21 Information sheet for interview participants
Appendix 22 Consent form for participants
Appendix 23 Demographics questionnaire for participants
Appendix 24 Interview topic guide
Appendix 25 Coding frame for qualitative interviews
| Topic area | No. | Code | Description of code | Example quote |
|---|---|---|---|---|
| Description | 1 | Access to services and information | Lack of access for the population; hoping to increase access to services for population | ‘that legislation came in but of course most of the promotion and everything was done in the mainstream profession and what we found is that a lot of the communities that weren’t accessing mainstream media weren’t getting those messages across . . . so there was a whole section of the New Zealand population that kind of missed that message’ (P7, smoking, New Zealand) |
| 2 | Assumptions | Researchers’ assumptions about what cultural factors would be relevant or effective for the population | ‘I think about you know for, for African Americans or for groups that don’t have a very, don’t have a real obsession about being thin, you know the way that you talk about weight, the different terms that are used, the assumptions you make about whether people consider that their body size is problematic’ (P11, physical activity and healthy eating, USA) | |
| 3 | Awareness raising | Awareness-raising efforts/campaigns outside of the intervention, as a by-product of the intervention, as a direct result of the intervention | ‘they know from the school, they do lots of uh . . . health awareness about smoking and chewing stuff and we sort of do the . . . we do the . . . we working with the school’ (P4, smoking, UK) | |
| 4 | Background | Information on how the intervention developed (excluding pilot/formative work); researchers’ history and/or experience leading to the intervention | ‘I worked with Asian immigrant refugee populations for years and I worked with the South East Asian, Vietnamese Cambodian communities as well as the Chinese community. And we’ve done a lot of work around lay health intervention’ (P15, physical activity, USA) | |
| 5 | Community advisory or steering group | Needing or involving a community advisory or steering group formed for the purpose of the research, its benefits and the recommendations and actions stemming from the community advisory or steering group | ‘the other things were just small incentives to that that were, were cheap enough for us to afford and that the ah community advisor board thought would be appropriate’ (P26, smoking, USA) | |
| 6 | Community considerations | Discussion of what is in the community’s interest or active attempts to gauge this interest | ‘this is a journey, this is a long process, this is not a diet that you go on for a short period of time. A journey, but also for your best body so it, its for you to look and feel better but not necessarily to be thin and we conveyed a lot about how you really can’t be there to take care of your family if you yourself are the one who is disabled or ill because stemming at least partly because of your weight’ (P14, physical activity and healthy eating, USA) | |
| 7 | Community observations | Researchers’ description of people in the community and description of the community physical environment | ‘it also means in terms of um what I guess academics call the informal market, which is you bring a load of stuff back in your suitcase [laughter] yeah, because if it’s cheap here and chewing tobacco products are cheap, if it’s cheap here it is ridiculous, absolutely ridiculously cheap in Bangladesh’ (P5, smoking, UK) | |
| 8 | Community organisations or leaders | Needing or involving pre-existing community organisations or established leaders within the community; researchers discuss the benefits of this community advisory or steering group involvement, and recommendations and actions stemming from the involvement | ‘em what we did was we put out a request for proposals and we did fund ah organisations around the city, ah one was [name of organisation] and the [name of organisation] were the two Asian, the organisations who serve the Asian community that we gave grants to. Em and what we, our approach was that they would take the lead in creating a community advisory board and we really used community-based participatory research principles’ (P18, smoking, USA) | |
| 9 | Description of participants | Describing the intervention population | ‘we screened Indian and Pakistani people in [city] and [city], 35 years or older, with an oral glucose tolerance test to find those with impaired glucose levels [cough] and those people and members of their family were invited to take part in a [time] trial’ (P1, healthy eating, UK) | |
| 10 | Evidence based (I) | When ‘evidence-based’ interventions are specifically discussed (the term is usually used) | ‘So there may be a higher level of sort of sophistication and em and this, people feel that if it’s delivered through the church that’s enough you know but they want the information to be high quality and not necessarily delivered by a pastor anymore, they want it to be delivered by a health professional. So there seems to be a shift taking place, or it may be more of an urban–rural shift, we’re not really sure’ (P22, healthy eating, USA) | |
| 11 | Formative research | Research work undertaken to inform the intervention | ‘they also take up eh Chinese herbal [mm mhm] medicine and I open the channel, I just dialogue with em people in the Chinatown and talk about how can you treat this diabetes. Sometimes even they chew on some leaves when some people tell them it work. . . . open mind and talk with people and collect all the data, what they are doing in terms of the diabetes. There’s uh in the first of five years, I built all those kind of connection and, and data collection. Even before I have em a grant, before and I have all the connection set up already. The people know about me [mm mhm] so for five years’ (P21, healthy eating, USA) | |
| 12 | Heterogeneity | Documenting researchers’ observations of heterogeneity within the populations they are working with | ‘The other thing about Shanghai which might, it’s different probably than in, than the populations you’re looking into, is that it’s really quite a em multiethnic city in terms of the food offered [mmm] and so in fact the people that em, many people who dine out there really do sometimes have Italian and they will have Japanese so, so you really need ah to provide the different ethnic options em to them there, which might not be the, it’s not the same situation if you’re looking at for example the Chinese population in ca, in em San Francisco or so. Well maybe not, I mean I guess anytime you stay in a city for any length of time or in a new country you do slowly adapt some of the other food taste, hamburgers and so forth’ (P24, healthy eating, USA) | |
| 13 | Intervention attendance | Includes discussions on retention, attrition, attendance at sessions | ‘and other thing was fantastic was the attendance because normally you can call people and they do not turn up and then well it’s no use you know [mm mhm], it defeats the entire purpose for these people who are coming because they felt very much at home that the information was getting across to them because it was culturally tailored to them’ (P3, physical activity and healthy eating, UK) | |
| 14 | Intervention description | Description of intervention ethos; intervention aims and objectives and description of components (frequency, intensity) | ‘so the second show actually was em focused on em or the second intervention project em was focused on women with hypertension or who were at risk for hypertension [mm mhm] and they were women recruited from em clinic groups so em from a particular medical clinic or medical care provider’ (P14, physical activity and healthy eating, USA) | |
| 15 | Intervention outcomes and results | Outcome measures, measurement tools, results, evaluation | ‘What we ended up finding was, that the policy the, the smoking prevalence dropped significantly in both communities which we attributed to the smoke-free air law and the tax increase’ (P18, smoking, USA) | |
| 16 | Intervention recruitment | Discussions relating to recruitment, including challenges and descriptions | ‘Now another challenge we had was em we had originally only enrolled women who em call themselves African American or black [mm mhm]. The first two shows we did that, our first two programmes we did that. And then in the, the last one with the churches em many cultural or many churches in and around [name of city] and [name of city] em are not strictly African American churches em where they used to be much more racially segregated em a lot of churches in this area are very multicultural and so just having that em requirement that the participants em participate only if they’re African American or black or call themselves that em was a bit of an issue, I think it made people uncomfortable and I think it unnecessarily em caused a little bit of strife within some of the churches [mm mhm] and so we’ve decided for the last four churches anyway to remove that recruitment criteria. And we’re not, we don’t think that it’s gonna make a big difference, we’re still gonna probably get mostly African American women who are participating, but we think that it may make a big difference in terms of our relationship with those churches and also their comfort level with the recruitment process’ (P14, physical activity and healthy eating, USA) | |
| 17 | Link with existing institutions/services (I) | Collaboration/working together on any components of the intervention (only when working together, not for incentives) and challenges of working with institutions and services | ‘There’s also a lot of differences between churches and denominations in terms of the governance and the structure and some denominations have, like a Baptist denomination, has a consistent pastor that will be there for many years and so if they commit to working with you they’re gonna stay with you, whereas other denominations like the AME, we found they rotate pastors every couple of years and so you start into it and once the new pastor comes in they may have a different priority eh and may decide not to, that they’re not so enthused about working with you [laughs]. So that has been a problem in terms of you know often if, if a church, quits in the middle it’s usually because there’s a change in leadership [okay] so that was one thing in terms of working with an organisation’ (P22, healthy eating, USA) | |
| 18 | Link with professionals (I) | Collaboration/working together on any components of the intervention (only when working together, not for incentives) and challenges of working with professionals (GPs, dieticians, etc.) | ‘the interesting thing was that they, some of them said that their regular customers who came in for prescriptions and other things like that knew about their service whereas sort of they weren’t very good at getting new [mmm] customers [mm mhm] so um which was why some of them felt that having outreach workers in the community was a good thing [mmm] because it would target people who wouldn’t necessarily know [mmm] that there um [right] a chemist was there’ (P2, smoking, UK) | |
| 19 | Locations and physical environments (I) | In reference to a specific place for the intervention (type and geographical area); any challenges to the intervention associated with that place | ‘because I am living in [name of district] [mmm okay], they are living in [name of district] and then when we go to them, when we go to the local market then we will, we can see each other and they say hello, some people call me cigarette doctor [laughter], I always say I am not cigarette doctor, I am not doctor [laughter], somebody who is a cigarette doctor somebody is a doctor, I am not a doctor, I am a smoking advisor [mm mhm] and interesting things, one interesting things [long pause] like elderly people give up the smoking yeah and after six month they start again and he, he just saw me that passed the road and he’s his hand is smoking he’s just hiding smoking [laughter] like he’s, he’s seventy-year-old man but when he saw me just [laughter] [yeah] then say oh I’m sorry, sorry’ (P4, smoking, UK) | |
| 20 | Modelling | Intervention (educator, material) demonstrating or modelling health behaviours; participants modelling behaviour to peers and family members | ‘So we knew that we had their attention, that was one main reason cause they’re a major target group because of their own health, and that’s what we emphasised. But number two we also know that a woman in that age group, and certainly African American women, we know are the matriarchs of their families, so they are influencing not only their adult children but their grandchildren, their great grandchildren, their churches, their workplaces, they are very influential [mmm]. And so if we can change the lifestyle of one single woman, just one single woman in that age group, we have a major ripple effect that’s going to impact on their entire community’ (P23, general health, USA) | |
| 21 | Not involved with other activities (I) | Establishing boundaries around the intervention (in terms of scope and health areas covered) | ‘You know again in some ways we were sort of battling [partner organisation] sometimes as well, wanting to do something that wasn’t just standard’ (P8, healthy eating, UK) | |
| 22 | Outside influences (I) | Social, historical, ancestral influences on healthy or unhealthy behaviour (e.g. home country) | ‘Where they come from influence what they eat, but not the location and the cities in United States, have any influence on what they eat. . . . where they came from, from their original country, is it China but if they, they came from Hong Kong eh they like certain food, and from Taiwan they like a certain different kind of food, so it would be different’ (P21, healthy eating, USA) | |
| 23 | Participant feedback | Concerns relating to the intervention components (medication, ethics, randomisation, confidentiality, etc.); positive and negative feedback about the intervention; learning and experiences relayed from participants to researchers | ‘Well I think some women who were not African American wanted to participate and felt excluded. Other women just felt that that was ridiculous that their friends were being excluded purely based on the colour of their skin, I mean it really is racially discriminatory against women who are not African American or black. And so and it was by design because the higher risk group is African American or black women, but within the context of the church that, that health risk is, is really immaterial’ (P14, physical activity and healthy eating, USA) | |
| 24 | Participants’ experiences with health | Participants’ experiences with health and/or health care | ‘I mean we’ve only done a small amount of qualitative work but just generally people’s attitudes about research trials, diabetes, understanding prevention and risk rather than, it’s much easier to understand if you’ve got an illness and a disease and you get treatment. But to understand, well, you can actually prevent this happening I think is much harder, so I think that was quite complicated’ (P1, healthy eating, UK) | |
| 25 | Participants’ involvement with research | Past experiences with research or researchers | ‘No ah we didn’t ever get funding to evaluate whether changes occurred in the control churches after they received the intervention [mm mhm]. I would say from, from other research that we’ve done that a lot of times em even though you give training to the control group or the control organisations, somehow the teachable moment has passed and a lot of times they don’t implement it [laughs] [right] with the same enthusiasm and fidelity as the early intervention group does. So that is em one danger of you know assuming that the control group is going to go ahead and do it em sometimes they just don’t do it. But we don’t know that because we were not able to get funding to go longer and evaluate those churches’ (P22, healthy eating, USA) | |
| 26 | Political and/or policy environment | Anything concerning political will or the policy environment (enabling or inhibiting the intervention) |
I: ‘Is there any interest in doing interventions em like this one with the male population, the male em South Asian population?’ P: ‘Eh no not really em . . . no, there’s not. I mean we tried, I’ve tried to track extra funding eh to do this. Ah part of the issue is the majority of the, the migrants who fit within this group actually reside within eh lower socioeconomic suburbs of [name of city] [mm mhm]. And there’s another overlay that goes with that, those particular suburbs are safe em in terms of the political eh parties that always get voted in there, so there’s safe Labour seats so em which means that essentially not a lot is changing there, you don’t win votes by helping Pakistani women or men becoming healthier [mm mhm], and so funding, etc. that flows on there is limited’ (P12, physical activity and healthy eating, Australia) |
|
| 27 | Referrals to other services | Referrals to services for health or social problems outside of the intervention remit | ‘We make a lot of referrals, we refer to, to primary care clinics for blood pressure and other things that we identified, we refer to drug rehab programmes, em we refer for mental health; there’s lots of depression [mm mhm]. We, we make referrals based on the. . . we see’ (P16, smoking, USA) | |
| 28 | Social support | Relating to receiving support or not (within the intervention and outside of the intervention) | ‘the intervention group you know changed more initially but then those changes washed out faster, and even reversed in some cases, versus the control group that changed more slowly without all the handholding but you know made use of the social support of you know the other women in their, in their classes, and they were actually able to make a more sustainable change in terms of being able to stabilise their waist circumference’ (P13, physical activity, USA) | |
| 29 | SES | Any reference to SES of participants, or adaptations for SES | ‘the area in which we did the where we had where our offices were located was in a low socioeconomic area. Em most of our participants were low poverty level or below, most of my clients did not ah have jobs or were between jobs, very transient sort of lifestyles. Eh we did have a few that were you know middle class that I can remember, eh most did not have any sort of college experience, a lot of them did not graduate from high school. Em so you know we were working with a very relatively low-educated low-income population’ (P26, smoking, USA) | |
| 30 | Successes | When researchers/interviewees highlighted something that was particularly successful in the intervention |
I: ‘So would you consider this intervention that you ran to be quite successful?’ P: ‘Oh without a doubt, yeah. No, it, it, in terms of, we did some informal, I mean, more informal follow-up and that would say for example the fact that the swimming sessions continued on you know a number of the ladies who, we, we got some data on that eh who had participated in the pilot study and so some of them we collected bloods most probably 18 months down the track, after they’d finished and again yeah we most probably had you know in the pilot I think we ended up with nearly 20 women, and of those I would think most probably 50% had actually made a positive change in terms of their lifestyle. And we had, and that, that was with no active intervention since we eh we started the pilot’ (P12, physical activity and healthy eating, Australia) |
|
| 31 | Taking ownership | When the target community or community members or the intervention participants take ownership of the health promotion activities (or do not) | ‘And there is one more thing about the project which I should, I think I should mention. And that is that these physical activity groups are still ongoing, the project stopped in 2003 and now it’s seven or nearly eight years afterwards, so it’s a good, so that tells me that em eh there is something in the project that has been sustainable and without any eh pushing from me [yes] eh it mainly organised by the participants themselves but also with a little eh organised and financed, by a litt, small eh fee to pay eh em to attend but much cheaper than the commercial things’ (P19, physical activity, Norway) | |
| Adaptation | 32 | Acculturation | Describing the level of acculturation, how level of acculturation has affected health behaviour and how acculturation affects intervention success | ‘the more sort of legitimate business with acculturated owners were much more likely to wanna work with us on their worksite wellness, integrating cessation into their worksite wellness, or even had a worksite wellness you know programme, than these very small, very newly immigrant-owned businesses who just really, they just, they just didn’t get it, what we wanted to do’ (P18, smoking, USA) |
| 33 | Adaptation rationale | Thoughts behind carrying out the adaptation, why it is relevant to the population | ‘they had em lots of eh em information from em from the behaviour side for the US you know the US meetings we have certain [I wouldn’t?] call them meeting guides, I don’t know what they call them anymore, but you know some format for the leader to follow each week with some goal in mind as information that we want to share to help the, the person be successful in their weight loss. But there were cert, we certainly didn’t know how these would translate to the, China and that’s the kind of adaptation that, that were done by [name] and his group [okay]. So em but we were aware that there would be eh certainly some change is needed’ (P24, healthy eating, USA) | |
| 34 | Age | Consideration of age and generational issues within the population | ‘We also mentioned, as we said, we have the facilitators and the experts. All of them are black women in mid-life. It was just as important to these women in, in the focus groups when we started, they said now don’t bring in here as our fitness expert a 20 year old that weighs 110 lb and is perky right. They don’t understand what we’re going through with our back problems, our knee problems. So the issue is, age again is a very important piece of cultural competence’ (P23, general health, USA) | |
| 35 | ‘Culture’ | Consideration of ‘culture’ in relation to the population (not necessarily linked to adaptation, this represents more general discussion; where possible code text under ‘gender’, ‘religion’, ‘age’, ‘family’, ‘work’, ‘soioeconomic status’, ‘food’, ‘language’ as they are more specific codes) | ‘So, so the cultural adaptation is broadly defined in terms of something that would be appealing on the surface but also have some relevance to the context in which it, you know, permanent context in which people were living’ (P11, physical activity and healthy eating, USA) | |
| 36 | Family and friends | Consideration of family and friends of the population | ‘But then of course as these are women, we always hook it into if you don’t change your behaviour you’re going to see in your grandchildren the statistics of women dying prematurely from preventable deaths. So we really try to do both, I mean we, we focus on expanding their sense of responsibility to themselves in terms of health but we always link it to how, if they change, it can help in terms of their community, in terms of their family and, and the rest of their community’ (P23, general health, USA) | |
| 37 | Food | Any reference to food | ‘they view within their home that healthy food isn’t acceptable [mm mhm], either to themselves or their family, or visitors, they come over and say oh those were horrible cause we know we recommend for instance bake your samosas and the women are like oh wait a minute, I would be considered a horrible hostess, if I did that, if I didn’t offer them a [mithai] you know the Indian sweets whenever people were there then I would be a horrible hostess, and the pressure is so strong it would make them feel you know in a sense that they were ostracised from their community’ (P8, healthy eating, UK) | |
| 38 | Gender | Consideration of gender issues relevant to the population | ‘the women couldn’t get them on their saris, the saris not the best thing for a pedometer so they were trying their knickers and, and things like that. The men of course had no trouble on their belts. And the men would go out for a walk and their wives would be at home cooking dinner’ (P16, smoking, USA) | |
| 39 | Intervention health messages | The health message delivered or conveyed in the intervention, as told by the interviewees | ‘that was a scene that kept coming up in the focus groups, the smokers had said this is really hard, we don’t like people to tell us that you know, you just, why haven’t you quit it’s so easy you know. Em but what was funny is that its the same tagline that the National Cancer Institute or the National Institute of Health had come up with years ago’ (P18, smoking, USA) | |
| 40 | Intervention materials | Resources that researchers drew on or used or produced (booklets, pamphlets). Anything to do with lack of resources should be coded under ‘funding’ | ‘It was a picture of people who looked empowered, so that it was a group of Chinese Americans standing with sort of their arm crossed, a woman, a man and they looked healthy and, and in control of their lives [mm mhm] and that’s what they wanted to project that, that quitting smoking em is associated with you know, in the same way that, that the tobacco industry promotes smoking as being associated with being empowered and you know cool and you know healthful and you know be rich and famous. They, they wanted to project the same thing for quitting and so you have this, it looked like professionals, young professionals, and some older em and ah you know standing just up there and then with this’ (P18, smoking, USA) | |
| 41 | Language | Any reference to language or ability | ‘eh it would necessarily you know it would have to be available in the languages eh in which our participant would be most familiar. So we had the intervention materials adapted into Mandarin and Cantonese for our Chinese participants and Korean for our Korean participants, and they were also available in English for those participants who desired the English-language material’ (P20, smoking, USA) | |
| 42 | Peer education and counselling | Recruiting and utilising peer workers for intervention (delivery, implementation, experience) | ‘But, but the, the, the eh the and the higher risk group persons, at least some of them, very successful in eh change their behaviour, started to walk eh in the district every, every evening eh every afternoon or evening, attend the classes eh walking classes which walked in the district and, and eh some of them lose weight so that anyone could, anybody could see that. Eh and they became very important role models for the others’ (P19, physical activity, Norway) | |
| 43 | Population stressors | Sources of stress within the ethnic populations | ‘for other groups the stresses might be you know for example originally this was tailored to our low-income women, so for this group we tried to talk of you know discuss issues that were more relevant to men, other race-related issues that might be relevant such as the stress of dealing with you know recent immigration or other immigration-related issues, trying to find a job, trying to ah be able to support one’s family and things of that nature. So the content was modified in that to some degree along those lines’ (P20, smoking, USA) | |
| 44 | Preferences | Statements of general preference for intervention or health promotion techniques (where possible code text under ‘gender’, ‘religion’, ‘age’, ‘family’, ‘work’, ‘socioeconomic status’, ‘food’, ‘language’ as they are more specific codes) | ‘But getting back to their preferences, so they had a preference for em collectivism that we you know involved the whole neighbourhood, they had high preference for spirituality and in that all meetings were opened with prayer’ (P16, smoking, USA) | |
| 45 | Religion and spirituality | If the intervention has been integrated into a religious setting or uses religious/spiritual components then code here; if just in a church location, for example, code under ‘location’ | ‘Religiosity is they attend church services and you know read their Bible and, and, and, listen to Gospel music and spirituality is more of an intimate personal relationship with God’ (P16, smoking, USA) | |
| Theory | 46 | Intervention theory | Any mention of theory or concepts related to the intervention (rather than general discussion of theories) | ‘a group in Australia have developed, the ANGELO model, that is a useful grid for em kind of deconstructing macro and micro environments em physical economic em social cultural and policy eh and, and thinking through what might be different in communities of colour in order to you know what might be say excess risk factors compa, you know first of all what might be the risk factors or the influences but then which of these kind of em jump out at you as something that you know, where you know a comm, eh a community is worse off, and so that’s, that’s the kind of reasoning that would get us to looking at the food marketing environments for example’ (P11, physical activity and healthy eating, USA) |
| Practical | 47 | Being flexible (I) | How the intervention or the research process was/should be flexible | ‘but one of the things that we found was that kids just abhorred having their fingers stuck, these are you know African American and Latino kids and so we just dropped the the eh serum glucose measure because . . . we were losing too many of our research participants you know even though they had parental consent and they had originally signed [consent?] after the first round of data collection they didn’t wanna, they didn’t wanna come back. So we, we were, we dropped it in favour of the other measures in being able to retain a larger proportion of our sample’ (P13, physical activity, USA) |
| 48 | Cost/cost-effectiveness | Costs associated with running the intervention or hypothetical alternatives, excluding incentives, and costs to participants (e.g. low cost, free) | ‘The truth is that any time you’re gonna do a, whether we were in the black community, Hispanic community, we, we were gonna have to fund community organisations to do this work because you can’t do this work unless you’re in the community. So I don’t think, I think doing any kind of tailoring or creating you know tailored programmes is a little, adds an expense to the existing programme, but then if you want to be effective in your, if you’re in a city like [name of city] you, you don’t really even think about it that way because it’s the cost of doing business, it’s, it’s not a question of should we do this, its, you have to do it you know’ (P18, smoking, USA) | |
| 49 | Effective strategies | Identifying specific aspects of the intervention thought to enhance effectiveness | ‘So we had found from our process evaluation that there were some key components which included em churchwide events that made fruits and vegetables available, em pastor support, talking with other church members and em the tailored messages, tailored newsletters seemed to be the ones that people cited the most often’ (P22, healthy eating, USA) | |
| 50 | Funding (I) | Researchers’ experiences with securing funding or description of the funding environment | ‘We just didn’t have the resources to promote it the way we had hoped to promote that one, that, that event and that was partly because of the turnover at the City Health Department and the commissioner who had committed funds to this intervention left and the new commissioner came in and had his own agenda’ (P18, smoking, USA) | |
| 51 | Incentives | Incentives given during the intervention to increase participation or retention | ‘we actually we were having such a hard time with recruitment towards the end that the last appointment em we bumped up that voucher card to uh if they, we told them at the beginning if they would complete all their appointments that they would get $40 in gift cards, if they missed em one I think they would get $35, if they missed two appointments they’d get $30 and if they just showed up for the last em contact then they would get $20’ (P26, smoking, USA) | |
| 52 | Intervention issues raised | Challenges and issues within the actual intervention (delivery or components) | ‘The structure is, is very critical. But what we, what we don’t know is really is one site different from another. Another thing we think we know, but we haven’t documented it, is the facilitator is the key person to the success of the outcome of, of the and the effectiveness’ (P23, general health, USA) | |
| 53 | Personal experiences | This is in relation to the intervention under discussion, rather than past experiences – how the intervention has provided personal insights | ‘So me personally, no I’m not interested in doing, now granted if they want, if they did it the way I wanted, if they came to me and said we can give you £350,000 to do this intervention and you can pretty much do it the way you want and we’ll just pay for it, hell yeah [mm mhm]. You know but absolutely not in terms of the way I’ve seen them do business. And I don’t think it’s just [name of slimming programme], I think that would be true of any sort of slimming programme you know, I haven’t worked with them all, but in fact the others weren’t even interested at all, they didn’t even wanna tailor materials for anybody that wasn’t white British’ (P8, healthy eating, UK) | |
| 54 | Staff characteristics | Qualities that the staff possesses, e.g. skills or of the same ethnicity | ‘Of the same culture . . . South Asian and . . . struggled with obesity herself’ (P8, healthy eating, UK) | |
| 55 | Staff management | Managing people and staff | ‘We actually had a few difficulties or should I say the management had a few difficulties with one particular outreach worker um who it, the role was probably not suited to him’ (P2, smoking, UK) | |
| 56 | Staff safety (I) | Ensuring the safety of staff workers | ‘Well as a manager of a multisite project my concerns are safety, as I said we had a homicide last week we were with, we’re experiencing a lot of shootings and, and you know violence in the neighbourhoods and to have outsiders come in, especially when we first go in its, it’s alarming’ (P16, smoking, USA) | |
| 57 | Sustainability | If the intervention or any components/staff continue after the formal research period | ‘So now we are just we are just enter, just ending the first year, the first year of a 3-year contract [okay] which is which has given everybody a lot of stability, a lot of eh confidence about what they’re doing [mm mhm] and it’s also we’ve also had additional money so we now have um basically the equivalent of two full-time male workers and two full-time female workers’ (P5, smoking, UK) | |
| 58 | Unexpected findings (I) | Researchers reported surprising findings | ‘we tried to access eh em migrant I mean eh med, specific media channels but we don’t know how much eh access, how much that helped eh but eh em but the, the, the strange thing then is was to see the results but even with with that little em specific adaptation we had a kind of breakthrough in ethnic minority groups’ (P19, physical activity, Norway) | |
| Lessons | 59 | Developing relationships | Researcher relationships with community members and leaders and gaining access to the community | ‘it’s very time-consuming, one of the kind of ah ways of you know building trust and building partnership really have to do with spending time, going to the services, being there for events, listening. A lot of the things that go into community-based participatory research you know take a lot of time, so it’s not like you just go in and recruit the church today and they start tomorrow’ (P22, healthy eating, USA) |
| 60 | Formalising the intervention (I) | Setting quality standards, creating manuals and guides, creating a distinct logo or brand | ‘We said we’re gonna look at [name of a fast food chain] and see how they do it [laughs], a [name of a fast food chain] hamburger in New York is the same as the one in Edinburgh. But anyway, so the quality, one of the ways to maintain our quality em because we know it works and, and there are many ways, reasons that we know it works is to really eh be in charge of the training of future facilitators and community health leaders so that’s a real important piece of what we’re doing’ (P23, general health, USA) | |
| 61 | Generalisability | Potential for generalisability (whether or not participants think it could be generalisable or have identified aspects in their intervention that would promote generalisability) | ‘I don’t have any problem if we are identified in your research because the whole thing as I see it is about sharing and caring so it was quite interesting when I went down to my boss and I said oh look I really don’t think I’ll sign off on this part where it says here, the your point number 6 where it says I understand you won’t put anything in your report that could be used to identify me and, and [name] says oh well scrub that out and oh no identify away’ (P7, smoking, New Zealand) | |
| 62 | Learnings | Take-home messages, lessons to be shared with others | ‘Lessons em is engaging with the community to make sure that this is something that they see as a priority and that they want to do [mm mhm], that you engage them to em to help develop, to come up with solutions to help, to, they need to be part of, of developing em an intervention and they have be part of the delivery of the intervention and evaluation and dissemination of the intervention, so they feel [ownership?] to it. I think that’s the biggest lesson learned now’ (P16, smoking, USA) | |
| 63 | Perseverance (I) | Researchers’ perseverance with intervention or population | ‘it took me about 2 years to get eh permission to open up the swimming pool for these women at eh on the weekly basis, for few hours, which was just women only, and I had to go through many many steps because, because people who are, it’s, it’s very multicultural country but just eh when it comes to that sort of thing it was really really challenging, I had to go through various ah city councils and local eh government areas and all that just to get the permission for the women only because people eh it can eh classified as a discrimination against men and all, all, all that side of things. But finally because this, this part was taking so long but then’ (P9, physical activity and healthy eating, Australia) | |
| 64 | Recognition of work (I) | External recognition of the work | ‘I think it was a big buzz for the team to realise you know that they were, they were this important, that they should have this priority placed upon them and resource, resources spent on them’ (P5, smoking, UK) | |
| 65 | Staff capacity building (I) | Upskilling or training for staff | ‘taking lay people and upskilling them rather than taking people and trying to skill them in [out of?] the community I think would’ve been, I don’t know actually how we would do that’ (P7, smoking, New Zealand) |
Appendix 26 Organisation of the units of thematic analysis
| Code clusters | Description of basic theme | Basic theme | Organising theme | Global theme |
|---|---|---|---|---|
|
Funding (I) Political and/or policy environment |
The broader research environment is discussed in relation to the immediate intervention and usually centres on the funding climate or the (lack of) political will and policies in place to support the research initiatives | Research environment | Development | Adapting interventions |
|
Adaptation rationale Intervention theory Background |
The background of the researchers and involvement in past projects shape the development of the intervention; similarly, rationales for adaptation and theories applied to the intervention are explored | Project rationale | ||
|
Community advisory or steering group Community organisations or leaders Taking ownership |
The needs of the target community are a central concern before, during and after the intervention. Purposeful community advisory groups are established to steer the intervention; pre-existing community organisations and leaders are tapped to assist with the intervention. In some cases, intervention initiatives led to greater ownership of health promotion activities | Community involvement | Engagement | |
|
Formative research Participant feedback Community considerations |
Undertaking earlier work with the target population to gain insight for intervention development through focus groups, interviews, surveys and literature searching, as well as soliciting feedback from participations throughout the intervention | Knowing the population | ||
|
Intervention recruitment Intervention attendance Incentives |
Discussion of recruitment strategies, degree of attendance by participants and incentives used to increase recruitment and retention | Recruitment and retention | Materials | |
|
Evidence based (I) Intervention health messages Intervention materials |
Evidence-based approaches seen as desirable; intervention messages and materials were tailored in some way to the target population | Resources delivered | ||
|
Peer education and counselling Staff characteristics Modelling |
Peer educators used to deliver intervention components thought to increase saliency. The same rationale applied to choosing intervention staff, often matching for ethnicity and language. Emphasis on modelling behaviour of intervention participants to family members | Mode of delivery | Methods | |
|
Developing relationships Perseverance (I) Being flexible (I) |
Highlighted qualities including importance of developing relationships with target community members; persevering throughout the intervention; and being flexible during the intervention phase | Researcher qualities | ||
|
Intervention description Description of participants |
General descriptions of the intervention study, as well as characteristics of the participants | Descriptive accounts | Study description | |
|
Referrals to other services Not involved with other activities (I) |
Outlining what activities are within the remit of the intervention and what lie outside and need referral services; recognising that target population may have other associated issues | Research boundaries | Linkages | |
|
Link with existing institutions/services (I) Link with professionals (I) |
Forging connections with existing institutions, services or professional groups to deliver the intervention or enhance uptake and receptivity | Professional collaboration | ||
|
Age Gender Socioeconomic status |
Discussion of population demographics and how they come to shape health, health behaviour and health behaviour change | Population demographics | Population demographics | Constructing ethnicity |
|
‘Culture’ Food Language Religion and spirituality |
Discussion of the ‘traditional’ dimensions of ethnicity influences on health, health behaviour and health behaviour change. Dimensions include culture (including diet, norms), language, ancestry (common geographical origin, shared history, referred to as outside influences) and religion (practices, beliefs) | Ethnicity dimensions | Conventional ethnicity | |
|
Access to services and information Participants’ experiences with health Outside influences (I) Participants’ involvement with research Awareness raising |
Participants past and present experiences with health, health care and health promotion activities, along with their experiences with researchers and research activities | Participants’ health-care/research exposure | Contextual ethnicity | |
|
Locations and physical environment (I) Population stressors Community observations |
Influence of locations and physical environment on health and health promotion activities; exploring stressors common to target population and observations of changes within target community | Setting-based considerations | ||
|
Family and friends Social support |
Families and friends were often mentioned as motivators and barriers to successful behaviour change; importance of social support | Social environment | ||
|
Preferences Heterogeneity Acculturation |
Differences within target community evident through discussion of preferences, level of heterogeneity and degree of acculturation | Acknowledging difference | ||
| Cost/cost-effectiveness | Cost of conducting the intervention and considerations of cost-effectiveness | Research costs | Evaluation | Sustaining adapted interventions |
|
Intervention issues raised Intervention outcomes and results Successes |
Issues that were of concern during the intervention were discussed, as well as any outcomes or results, if available; successes of the intervention were highlighted | Intervention assessment | ||
|
Unexpected findings (I) Assumptions Effective strategies Learnings Generalisability |
Intervention insights derived from unexpected findings; correcting initial assumptions about the target community; identifying effective strategies and relaying lessons learned for other researchers; and potential for generalisability | Intervention insights | Insights | |
|
Formalising the intervention (I) Sustainability |
Steps taken to ‘manualise’ or ‘professionalise’ the health promotion activities and discussions around increasing sustainability of activities | Intervention continuity | ||
| Personal experiences | Reflections on personal experiences and growth | Researcher development | ||
|
Staff safety (I) Staff management |
Facilitating positive working environments for staff, particularly multiethnic staff, and putting in place safety measures for community workers | Project management | Strengthening the workforce | |
|
Staff capacity building (I) Recognition of work (I) |
Increasing training and up-skilling staff involved in the intervention, as well as recognition of their work (internal and external) | Workforce development |
Appendix 27 Context–mechanism–outcome configurations from the realist review
| Stage in Programme Theory of Adapted Health Promotion Interventions | Adaptation (mechanism) | Context + outcome |
|---|---|---|
| Conception/planning |
1. Exploratory phase with target population (same group as intervention group) 2. Exploratory phase with target population (different group from intervention group or unknown) 3. Exploratory phase with community leaders 7. Ethnically matched high-level/respected individuals to increase salience of programme goals 8. Ethnically matched high-level/respected individuals throughout planning, directing, reviewing and implementing stages 9. Ethnically matched leadership within the study 10. Utilise local/respected religious/spiritual leaders 11. Collaboration with ethnic-specific institutions and professional organisations 20. Material developed specifically for target population (by project investigators, expert opinion, tools) 21. Materials created by members of the target population 31. Address concerns with medical programmes, procedures and medication 35. Utilise ethnically/culturally appropriate formal and informal networks 42. Purposefully maintaining an exclusive or open intervention environment 44. Cross-cultural training for all study personnel 45. Address discrimination and mistrust 46. Gender considerations |
Exploratory phase indicated that randomisation to a no-treatment control for a physical activity and nutrition intervention for an African American population was not acceptable to participants and therefore not utilised in the study design. 91,92,95,96 Other studies also have reiterated that randomisation was inappropriate in church settings,308,397 particularly when interest was low315,316 The background tailoring of control groups may remove the effect of the intervention group in terms of assessing the effectiveness of adaptation, but it was found that not tailoring for the control group was often unacceptable296 Community-based outreach intervention for smoking cessation, physical activity and nutrition for an African American population observed that it was important to speak to actual community members about participation and not just limit discussion to the community advisory group as low participation in the health activities was observed398 Discussions with the community for a community-based group nutrition intervention for an African American population revealed that there were many competing community-based research activities, which may limit interest in the present intervention315,316 Parents in focus groups reported that they were attracted to a culturally specific programme that targeted only African American girls for physical activity and nutrition intervention; feedback from girls and parents suggested the same thing. There was high retention (98%) but, despite this, the intervention was ineffective for primary and secondary outcomes410 Targeted material for a smoking cessation intervention pilot tested with African Americans in New York may not be equally salient to an African American population in Georgia, as intervention participants were observed to be more responsive to surface level targeting (e.g. materials) and less so to deep structure targeting341 Black churches often include health in their overall mission and thus represent an established infrastructure for recruitment and retention; furthermore, they allow access to African Americans from middle and upper social economic strata, as they are often under-represented in research (Resnicow et al. 324) An open and flexible design for a physical activity intervention may suit South Asian women with multiple responsibilities that are perceived to be more important than physical activity; this includes open schedules for data collection although this may not always be feasible in terms of cost and time283 Utilising specified models of behaviour change in the development of the intervention was found in some cases to improve effectiveness,293,325,335 but some behavioural theories were suggested to be more appropriate for some communities than others, e.g. social cognitive theory was felt to be salient for the personal life experiences of African American women in terms of prevailing against formidable obstacles in life399 |
| Promotion |
4. Ethnically matched intervention staff or facilitators 7. Ethnically matched high-level/respected individuals to increase salience of programme goals 8. Ethnically matched high-level/respected individuals throughout planning, directing, reviewing and implementing stages 9. Ethnically matched leadership within the study 10. Utilise local/respected religious/spiritual leaders 11. Collaboration with ethnic-specific institutions and professional organisations 14. Reflect target population’s language (usage – concepts, vocabulary) 16. Reflect target population’s preferred method of communication 22. Intervention content targets population’s social and cultural values 23. Intervention goals and outcomes are culturally appropriate 28. Utilise resources from target population 30. Utilise and address appropriate norms 33. Located in ethnically/culturally appropriate/familiar location 34. Utilise ethnically/culturally appropriate media sources 35. Utilise ethnically/culturally appropriate formal and informal networks 45. Address discrimination and mistrust 46. Gender considerations |
For a physical activity and nutrition intervention, the majority of African American participants learnt about the intervention through brochures, family/friends and mass e-mails in equal proportions; however, those who responded to e-mails and brochures were more likely to be eligible than those referred by family/friends365–367 |
| Engagement/recruitment |
4. Ethnically matched intervention staff or facilitators 7. Ethnically matched high-level/respected individuals to increase salience of programme goals 8. Ethnically matched high-level/respected individuals throughout planning, directing, reviewing and implementing stages 9. Ethnically matched leadership within the study 10. Utilise local/respected religious/spiritual leaders 11. Collaboration with ethnic-specific institutions and professional organisations 14. Reflect target population’s language (usage – concepts, vocabulary) 16. Reflect target population’s preferred method of communication 22. Intervention content targets population’s social and cultural values 25. Consider target population’s employment situations 28. Utilise resources from target population 29. Utilise appropriate incentives and timing of programme 30. Utilise and address appropriate norms 31. Address concerns with medical programmes, procedures and medication 33. Located in ethnically/culturally appropriate/familiar location 34. Utilise ethnically/culturally appropriate media sources 35. Utilise ethnically/culturally appropriate formal and informal networks 36. Provide ethnically/culturally appropriate food/activities/music 39. Address physical/financial (structural) barriers to participation 45. Address discrimination and mistrust 46. Gender considerations |
Recruitment via personal contact (i.e. active strategy) for a smoking cessation intervention for African Americans tended to attract participants who said they would participate but then did not or who participated but then dropped out. Reactive strategies, however, were more likely to recruit higher socioeconomic groups of African Americans342–345 Recruitment of African Americans to a smoking cessation intervention was more successful in churches (81%) and health-care settings (78%) than in housing developments (59%), as measured by the numbers of participants willing to provide a telephone number, which suggests that more interpersonal contacts are needed to get people to disclose their telephone numbers in low-income settings400,401 Half of the African American smokers contacted were unwilling to speak with the recruiters as they were identified over the telephone as not being black (exercised caution in talking with outsiders)404 Although matching of recruitment staff has been suggested in a physical activity and nutrition intervention for an African American population, the recruiter’s experience and sensitivity was perhaps more important, particularly when demonstrating flexibility for scheduling interviews365–367 Initial recruitment through churches for African Americans for an internet-based intervention for physical activity and nutrition was expanded to the broader community and combined with media and non-media channels. Greater log-on rates were observed for African Americans recruited through the media rather than for those recruited through interpersonal channels as there may have been social pressure to sign up, despite a lack of interest. Those recruited through the media reported a 71% log-on rate for a follow-on internet-based intervention compared with 38% and 65% log-on rates for the two groups which were recruited through churches313 Recruitment of African Americans through churches and Historically Black Colleges and Universities for a computer-based nutrition intervention based in churches was successful in maintaining interest as participants were willing to wait for computers to use within the church environment481 A community-based group Tai Chi exercise programme for a Chinese population was popular because of the recruitment site, which was in the local community and linked in with other activities popular with women such as playing mah-jong and buying vegetables402,403 |
| Implementation/delivery |
4. Ethnically matched intervention staff or facilitators 5. Ethnically matched peer role models or peer education 6. Ethnically matched facilitators and peer role models who have successfully changed their behaviour 7. Ethnically matched high-level/respected individuals to increase salience of programme goals 8. Ethnically matched high-level/respected individuals throughout planning, directing, reviewing and implementing stages 9. Ethnically matched leadership within the study 10. Utilise local/respected religious/spiritual leaders 11. Collaboration with ethnic-specific institutions and professional organisations 12. Material depicts individuals from target population 13. Material (video, booklet, skits, handouts, games) in target population’s language 14. Reflect target population’s language (usage – concepts, vocabulary) 15. Match reading level and literacy 16. Reflect target population’s preferred method of communication 17. Material presents ethnic-specific data 18. Material depicts appropriate graphics and scenarios (this can be heterogeneous) 19. Material/guidance based on preferences of target population 20. Material developed specifically for target population (by project investigators, expert opinion, tools) 22. Intervention content targets population’s social and cultural values 24. Intervention delivered in culturally appropriate or preferred format 25. Consider target population’s employment situations 26. Intervention addresses health behaviour patterns found in target population 27. Dietary issues unique to their context 28. Utilise resources from target population 29. Utilise appropriate incentives and timing of programme 30. Utilise appropriate norms 31. Address concerns with medical programmes, procedures and medication 33. Located in ethnically/culturally appropriate/familiar location 35. Utilise ethnically/culturally appropriate formal and informal networks 36. Provide ethnically/culturally appropriate food/activities/music 37. Present a pro-ethnic/race approach 38. Address emotional barriers and stressors 39. Address physical/financial (structural) barriers to participation 40. Teach appropriate communication skills 41. Encourage/involve social support 42. Purposefully maintaining an exclusive or open intervention environment 43. Maintaining cultural significance of food 45. Address discrimination and mistrust 46. Gender considerations |
Matching intervention staff for ethnicity was important for a Bangladeshi population with diabetes but other characteristics, including having intervention staff with diabetes, were also raised as important409 A group-based diabetes management programme (physical activity and nutrition) for a Chinese population experienced attrition as participants travelled for Chinese New Year and did not complete the programme, although they returned for the follow-up evaluation346 Churches were sites rather than partners in a physical activity intervention for African American women and, as such, women did not receive health-related or targeted messages from church officials and therefore may not have affected deep-level structures397 Using familiar sites for an intervention can improve effectiveness, but some sites may be better than others. For a physical activity and nutrition intervention for an African American population, it was found that sites which people held membership to, as opposed to just community sites, produced better institutionalisation of the intervention387 Churches as a setting for African American populations can have a positive effect on the intervention over and above being an appropriate setting, such as spreading the intervention to a wider population (not just intervention participants) and creating intervention sustainability. This was particularly true if they had a pre-existing health ministry334 A community-based group weight loss intervention for African American women was initially held at community locations that were familiar and close by; however, the lack of space for exercise and childcare and lack of room availability forced relocation. The second cohort was relocated to a space on campus that offered parking. This was mainly conducted with a middle-class cohort405 A church-based group physical activity and nutrition intervention for African Americans reported that, for the self-help arm, women wanted the sessions to be led by professional leaders rather than their peers; this was supported by the observed drop in attendance when sessions were taken over by trained lay leaders A diabetes self-care telephone intervention for African Americans reported that ‘eating healthfully’ was seen as giving up their food heritage and that family members may be quite negative towards participants if they deviate from traditional foods406 Family members can be a barrier to weight gain prevention interventions for African American girls as their mothers encouraged weight gain395,396 In one intervention for physical activity and nutrition, African American girls were specifically taught communication skills to help advocate for healthy changes within the home; however, the family involvement was not very successful as parents were not supportive of their daughters in attending sessions or making changes in the home environment324 Social support from within the intervention group was valuable for African American participants in a physical activity and nutrition intervention but other social influences outside the intervention, such as family pressures and resistance to change, were observed to have a negative impact365–367 Encouraging family participation was built into some interventions, but in a study of a physical activity and nutrition intervention in an African American population only female adults participated despite male members of the family being encouraged to participate;319 this may affect uptake and role-modelling within the home. Social support was an explicit intention in an intervention for physical activity and nutrition for African American cancer survivors and this was to tap into an observation that kinship networks were strongly related to health decision-making in this community412 A pictorial one-on-one diabetes education intervention to improve nutrition for a South Asian population reported participant preference for one-to-one health education at clinics rather than organised single-sex group sessions. Participants wanted to keep their diabetes status private and felt unable to announce their food choices in public407 A churchwide smoking cessation intervention for an African American population reported that some church members were embarrassed by their smoking status and did not want to be identified, while others were not interested in programmes delivered by their peers300,301 A group- and individual-based diabetes management intervention for African Americans held in a rural setting revealed that group-based programmes may not have been appropriate as there were competing cultures of openness (facilitated by churches) and privacy (rural traditions)408 ‘Interview showed that it was particularly important to the women that they had a culturally “safe” place to exercise, not just for themselves but also for the integrity of their whole community’ (p. 93). Furthermore, in this physical activity intervention delivered for South Asian women, the notion of ‘safe’ space operated under a different logic such that walking and playing sports after dark in an empty field behind a school was perceived to be safe, whereas walking on the sidewalk during the daytime was felt to attract derogatory comments as they would be more visible283 For a smoking cessation intervention delivered to African Americans, it may be necessary to match the intervention not only to participants’ apparent racial/ethnic identity but also to their degree of membership to a particular racial/ethnic group341 Tailored newsletters used in a nutrition intervention for African Americans reported a stronger impact for individuals who were better matched in terms of their ethnic identity and the degree of Afrocentricness of the newsletter296 A smoking cessation intervention for African Americans comparing a culturally sensitive guide with a standard guide found that participants with reported lower levels of acculturation preferred the culturally sensitive guide and displayed a greater readiness to quit; however, they had higher rates of 24-hour abstinence when they received the standard guide. It was hypothesised that mismatched content can encourage greater information processing351 A group-based nutrition intervention compared the effect of group composition: an all-African American group vs groups of mixed ethnicities. The percentage of African Americans was high in the mixed groups and this may have created a group environment similar to that of the all-African American group, suggestive that there may have been a critical mass effect323 Acculturation did not moderate the relationship between a tailored experimental group and an outcome measure for a home-based physical activity intervention for African Americans and a likely explanation was that the majority of the participants were bicultural and therefore receptive to both tailored and standard material350 A group-based diabetes management programme (physical activity and nutrition) for a Chinese population observed that participants openly discussed and interacted when classes included only Mandarin or only Cantonese speakers, suggesting that, even with similar writing (traditional Chinese), different dialects provide an additional barrier to participation during intervention. Furthermore, some participants were reluctant to reveal their reading comprehension abilities346 A sign designed for African American women to increase their physical activity was culturally salient (featured African American women) but also addressed more generic concerns (lack of time for physical activity). This sign was effective in the short term for both men and women, although it targeted women only468 Home visitations may be carried out for convenience but they were also important to engage the support of male members of the family and build family support in an intervention for physical activity and nutrition with an African American population; in these circumstances it was important for the public health educator to be male. 318 Similarly, a concern among South Asian-origin women in a nutrition intervention was whether or not changes would be approved by spouses and whether or not spouses would prevent them from making changes475 A nutrition intervention delivered to an African American population demonstrated positive results, but the intervention was not successful for younger participants and males. Younger people considered the health topic less relevant to them and also had competing priorities in their lives that made dedicated participation more difficult, and the materials may not have been relevant for males (Campbell et al. 320). Therefore, both age and gender were observed to mediate intervention effects In a diabetes intervention with Bangladeshi adults, peer discussion and support were valued but gender differences were observed, as women were more interested in the social support and the men were more focused on the information elements409 |
| Retention |
4. Ethnically matched intervention staff or facilitators 5. Ethnically matched peer role models or peer education 6. Ethnically matched facilitators and peer role models who have successfully changed their behaviour 7. Ethnically matched high-level/respected individuals to increase salience of programme goals 8. Ethnically matched high-level/respected individuals throughout planning, directing, reviewing and implementing stages 9. Ethnically matched leadership within the study 10. Utilise local/respected religious/spiritual leaders 11. Collaboration with ethnic-specific institutions and professional organisations 16. Reflect target population’s preferred method of communication 22. Intervention content targets population’s social and cultural values 25. Consider target population’s employment situations 28. Utilise resources from target population 29. Utilise appropriate incentives and timing of programme 30. Utilise and address appropriate norms 38. Address emotional barriers and stressors 39. Address physical/financial (structural) barriers to participation 41. Encourage/involve social support 42. Purposefully maintaining an exclusive or open intervention environment 46. Gender considerations |
Monthly self-addressed stamped postcards and a toll-free telephone number to update contact details may be good retention strategies for a parent-led nutrition intervention for African Americans303–305 Low implementation rates (31%) of booster calls to African American participants in a smoking cessation intervention. Telephone-assisted strategies may not be feasible as they depend on the ability to obtain telephone numbers. The intervention was not effective for smoking cessation400,401 A genetic biomarker feedback smoking cessation intervention with telephone counselling and NRT for African Americans lost 21% of participants, with the primary reason being that participants no longer had telephone access374 Community-based after-school intervention programmes can reduce transportation barriers for a physical activity and nutrition intervention for African American girls. 411 In a related study with African American girls, when transportation was provided from school to the community centre, 70% attended on average at least 2 days a week. In another area where transportation was not provided, only 33% attended on average at least 2 days a week329,330 A community-based group Tai Chi exercise programme for a Chinese population reported high adherence as classes were held at a convenient local community centre where other Cantonese-speaking seniors congregate for other activities, such as eating lunch and grocery shopping402,403 A group physical activity and nutrition intervention was delivered to participants during their regular community group meeting411 |
| Evaluation |
8. Ethnically matched high-level/respected individuals throughout planning, directing, reviewing and implementing stages 9. Ethnically matched leadership within the study 22. Intervention content targets population’s social and cultural values 23. Intervention goals and outcomes for participants are culturally appropriate 25. Consider target population’s employment situations 30. Utilise and address appropriate norms 32. Utilise appropriate evaluation instruments and tools |
A dose-dependent response was observed after 2 years for both increased physical activity and positive attitudes about the benefits of physical activity for a multimedia campaign promoting physical activity for children. Children aware of the campaign reported greater engagement in physical activity than children unaware of the campaign. 285–287 Evidence of a dose-dependent response was also observed in other interventions,490 e.g. African Americans who reported reading more tailored newsletters also reported eating more fruit and vegetables, but no association was observed for video watching292,299 A smoking cessation intervention delivered with a guide and brief counselling plus NRT or placebo for African Americans observed that lower than expected quit rates may be influenced by environmental factors, daily life stressors and aggressive targeted advertising – all aspects that may not be measured but which may influence successful quitting355,356 A school-based diabetes prevention programme for African American children targeted the classroom, after-school activities, home and the school cafeteria; however, an unhealthy home environment in terms of food was countering gains made at school and a one-off health fair for families was not perceived to have lasting effects310 Lay advisors used in a church-based physical activity and nutrition intervention for African Americans have networks beyond the church and assessing changes in only one part of their network (e.g. churches) may miss documenting an impact in other parts of their network. Only 10% of church members reported speaking to a lay advisor; however, it was unknown if lay advisors were operating outside the church as well292,299 Consultation with community leaders and community members and pre-testing of intervention components for centre-based behavioural counselling for exercise and diet for African American families were unable to counter the disrupting effects of unstable employment, such that frequent job changes and changes from full-time to part-time work, day shift to night shift and employed to unemployed contributed to poor regular attendance at evening sessions321,322 Targeted approaches may be helpful for African American participants to initiate thinking about quitting smoking; however, individual approaches such as counselling may be needed once the quitting process has been initiated to facilitate quitting341 In a group-based behavioural weight loss programme for African Americans, the addition of motivational interviewing did not increase attendance, change dietary intake or physical activity or result in weight loss compared with health education only. Motivational interviewing may not enhance the effectiveness of an already culturally adapted intervention or motivate behaviour change among participants who face socioenvironmental barriers or life stressors, as in motivational interviewing barriers are only discussed317 |
| Outcome |
8. Ethnically matched high-level/respected individuals throughout planning, directing, reviewing and implementing stages 9. Ethnically matched leadership within the study 23. Intervention goals and outcomes for participants are culturally appropriate 30. Utilise and address appropriate norms 32. Utilise appropriate evaluation instruments and tools |
Lay health advisors used in a smoking cessation intervention for African Americans in a close-knit community environment were successful at gaining community support; however, individual quit rates were less clear-cut. The role of lay health advisors was to promote the programme to those ready to quit; however, the participants were not motivated (positive associations with smoking). Community leadership in recruitment and selection of lay health workers helped to effectively navigate the community and made them more credible453 A community-based group nutrition education intervention for African Americans reported that there were discrepancies between intervention goals and participant goals, e.g. one incentive for participants was that they received documentation of achieving nutrition-related education and competencies for potential jobs in the food service industry, as this was a largely unemployed cohort315,316 Concerns over sustainability of a group-based physical activity as African American participants indicated that the intervention for physical activity and nutrition itself was their solution for overcoming barriers to physical activity365–367 Group-based weight loss intervention for African Americans observed a difference between participants and investigators in interpreting intervention success. Participants were happy with their loss of 3% of initial weight whereas investigators were aiming for 7% (which is considered to be clinically significant by the National Heart, Lung and Blood Institute)412 For a group-based nutrition education intervention for African Americans, weight loss was unlikely for aesthetic reasons; improving health was found to hold more significance as an outcome than weight change323 Mothers’ concern was with their own weight rather than their daughters’ weight (majority were normal weight) and thinner mothers dropped out of the intervention at higher rates in an exercise and dietary education intervention for African American mother–daughter dyads as daughters’ behaviour change was minimal487 Weight-focused intervention did not appeal to African American girls and their parents/guardians as heavier weight was accepted or desired and a more positive body image. Instead, intervention emphasised the health benefits of physical activity329,330 An effective intervention outcome for the community was strong community partnership and environmental/community changes in the development of new and better recreational facilities and opportunities and not the outcomes that the study had specified413 |
| Dissemination |
8. Ethnically matched high-level/respected individuals throughout planning, directing, reviewing and implementing stages 9. Ethnically matched leadership within the study |
A community-based outreach intervention for smoking cessation, physical activity and nutrition for an African American population observed that there was little leadership within the community and lack of ownership of a health project, which may relate either to the ‘outside’ funding or to the fact that it addressed primary prevention (rather than an illness)398 |
List of abbreviations
- ASSIA
- Applied Social Sciences Index and Abstracts
- BCT
- behavioural construct tailoring
- BMI
- body mass index
- CASP
- Critical Appraisal Skills Programme
- CCT
- clinical controlled trial
- CDCP
- Centers for Disease Control and Prevention
- CHD
- coronary heart disease
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMO
- context–mechanism–outcome
- CRT
- culturally relevant tailoring
- CVD
- cardiovascular disease
- DARE
- Database of Abstracts of Reviews of Effects
- EPHPP
- Effective Public Health Practice Project
- FFQ
- Food Frequency Questionnaire
- HSE
- Health Survey for England
- HTA
- health technology assessment
- IHD
- ischaemic heart disease
- IPSC
- Independent Project Steering Committee
- LILACS
- Latin American and Caribbean Health Sciences Literature
- NICE
- National Institute for Health and Clinical Excellence
- NIHR
- National Institute for Health Research
- NIHR HTA
- National Institute for Health Research Health Technology Assessment
- NRT
- nicotine replacement therapy
- OR
- odds ratio
- PPA
- point prevalence abstinence
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RESET
- RESET (relevance, evidence base, stages of intervention, ethnicity and trends) decision-making tool
- RR
- risk ratio
- SCEH
- Specialist Collection for Ethnicity and Health
- SES
- socioeconomic status
- SIGN
- Scottish Intercollegiate Guidelines Network
- WHO
- World Health Organization
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, Department of Pharmacology and Therapeutics, University of Liverpool
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
Prioritisation Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, Department of Pharmacology and Therapeutics, University of Liverpool
-
Professor Imti Choonara, Professor in Child Health, Academic Division of Child Health, University of Nottingham
Chair – Pharmaceuticals Panel
-
Dr Bob Coates, Consultant Advisor – Disease Prevention Panel
-
Dr Andrew Cook, Consultant Advisor – Intervention Procedures Panel
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Dr Nick Hicks, Consultant Adviser – Diagnostic Technologies and Screening Panel, Consultant Advisor–Psychological and Community Therapies Panel
-
Ms Susan Hird, Consultant Advisor, External Devices and Physical Therapies Panel
-
Professor Sallie Lamb, Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick
Chair – HTA Clinical Evaluation and Trials Board
-
Professor Jonathan Michaels, Professor of Vascular Surgery, Sheffield Vascular Institute, University of Sheffield
Chair – Interventional Procedures Panel
-
Professor Ruairidh Milne, Director – External Relations
-
Dr John Pounsford, Consultant Physician, Directorate of Medical Services, North Bristol NHS Trust
Chair – External Devices and Physical Therapies Panel
-
Dr Vaughan Thomas, Consultant Advisor – Pharmaceuticals Panel, Clinical
Lead – Clinical Evaluation Trials Prioritisation Group
-
Professor Margaret Thorogood, Professor of Epidemiology, Health Sciences Research Institute, University of Warwick
Chair – Disease Prevention Panel
-
Professor Lindsay Turnbull, Professor of Radiology, Centre for the MR Investigations, University of Hull
Chair – Diagnostic Technologies and Screening Panel
-
Professor Scott Weich, Professor of Psychiatry, Health Sciences Research Institute, University of Warwick
Chair – Psychological and Community Therapies Panel
-
Professor Hywel Williams, Director of Nottingham Clinical Trials Unit, Centre of Evidence-Based Dermatology, University of Nottingham
Chair – HTA Commissioning Board
Deputy HTA Programme Director
HTA Commissioning Board
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
-
Professor of Bio-Statistics, Department of Public Health and Epidemiology, University of Birmingham
-
Professor of Clinical Pharmacology, Director, NIHR HTA programme, Department of Pharmacology and Therapeutics, University of Liverpool
-
Professor Zarko Alfirevic, Head of Department for Women’s and Children’s Health, Institute of Translational Medicine, University of Liverpool
-
Professor Judith Bliss, Director of ICR-Clinical Trials and Statistics Unit, The Institute of Cancer Research
-
Professor David Fitzmaurice, Professor of Primary Care Research, Department of Primary Care Clinical Sciences, University of Birmingham
-
Professor John W Gregory, Professor in Paediatric Endocrinology, Department of Child Health, Wales School of Medicine, Cardiff University
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, Department of Specialist Radiology, University College Hospital, London
-
Professor Angela Harden, Professor of Community and Family Health, Institute for Health and Human Development, University of East London
-
Dr Joanne Lord, Reader, Health Economics Research Group, Brunel University
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor Dion Morton, Professor of Surgery, Academic Department of Surgery, University of Birmingham
-
Professor Gail Mountain, Professor of Health Services Research, Rehabilitation and Assistive Technologies Group, University of Sheffield
-
Professor Irwin Nazareth, Professor of Primary Care and Head of Department, Department of Primary Care and Population Sciences, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norrie, Director, Centre for Healthcare Randomised Trials, Health Services Research Unit, University of Aberdeen
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Peter Tyrer, Professor of Community Psychiatry, Centre for Mental Health, Imperial College London
-
Professor Martin Underwood, Professor of Primary Care Research, Warwick Medical School, University of Warwick
-
Professor Caroline Watkins, Professor of Stroke and Older People’s Care, Chair of UK Forum for Stroke Training, Stroke Practice Research Unit, University of Central Lancashire
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Dr Tom Foulks, Medical Research Council
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
HTA Clinical Evaluation and Trials Board
-
Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick and Professor of Rehabilitation, Nuffield Department of Orthopaedic, Rheumatology and Musculoskeletal Sciences, University of Oxford
-
Professor of the Psychology of Health Care, Leeds Institute of Health Sciences, University of Leeds
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Keith Abrams, Professor of Medical Statistics, Department of Health Sciences, University of Leicester
-
Professor Martin Bland, Professor of Health Statistics, Department of Health Sciences, University of York
-
Professor Jane Blazeby, Professor of Surgery and Consultant Upper GI Surgeon, Department of Social Medicine, University of Bristol
-
Professor Julia M Brown, Director, Clinical Trials Research Unit, University of Leeds
-
Professor Alistair Burns, Professor of Old Age Psychiatry, Psychiatry Research Group, School of Community-Based Medicine, The University of Manchester & National Clinical Director for Dementia, Department of Health
-
Dr Jennifer Burr, Director, Centre for Healthcare Randomised trials (CHART), University of Aberdeen
-
Professor Linda Davies, Professor of Health Economics, Health Sciences Research Group, University of Manchester
-
Professor Simon Gilbody, Prof of Psych Medicine and Health Services Research, Department of Health Sciences, University of York
-
Professor Steven Goodacre, Professor and Consultant in Emergency Medicine, School of Health and Related Research, University of Sheffield
-
Professor Dyfrig Hughes, Professor of Pharmacoeconomics, Centre for Economics and Policy in Health, Institute of Medical and Social Care Research, Bangor University
-
Professor Paul Jones, Professor of Respiratory Medicine, Department of Cardiac and Vascular Science, St George‘s Hospital Medical School, University of London
-
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, Queen Mary, University of London
-
Professor Richard J McManus, Professor of Primary Care Cardiovascular Research, Primary Care Clinical Sciences Building, University of Birmingham
-
Professor Helen Rodgers, Professor of Stroke Care, Institute for Ageing and Health, Newcastle University
-
Professor Ken Stein, Professor of Public Health, Peninsula Technology Assessment Group, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Jonathan Sterne, Professor of Medical Statistics and Epidemiology, Department of Social Medicine, University of Bristol
-
Mr Andy Vail, Senior Lecturer, Health Sciences Research Group, University of Manchester
-
Professor Clare Wilkinson, Professor of General Practice and Director of Research North Wales Clinical School, Department of Primary Care and Public Health, Cardiff University
-
Dr Ian B Wilkinson, Senior Lecturer and Honorary Consultant, Clinical Pharmacology Unit, Department of Medicine, University of Cambridge
-
Ms Kate Law, Director of Clinical Trials, Cancer Research UK
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, University of Manchester
-
Mr Angus S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital, Birmingham
-
Dr Diana Baralle, Consultant and Senior Lecturer in Clinical Genetics, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Diane Eccles, Professor of Cancer Genetics, Wessex Clinical Genetics Service, Princess Anne Hospital
-
Dr Trevor Friedman, Consultant Liason Psychiatrist, Brandon Unit, Leicester General Hospital
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Public contributor
-
Professor Anthony Robert Kendrick, Associate Dean for Clinical Research and Professor of Primary Medical Care, University of Southampton
-
Dr Nicola Lennard, Senior Medical Officer, MHRA
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee, London
-
Mr David Mathew, Public contributor
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mrs Una Rennard, Public contributor
-
Dr Stuart Smellie, Consultant in Clinical Pathology, Bishop Auckland General Hospital
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr Allison Streetly, Programme Director, NHS Sickle Cell and Thalassaemia Screening Programme, King’s College School of Medicine
-
Dr Matthew Thompson, Senior Clinical Scientist and GP, Department of Primary Health Care, University of Oxford
-
Dr Alan J Williams, Consultant Physician, General and Respiratory Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Joanna Jenkinson, Board Secretary, Neurosciences and Mental Health Board (NMHB), Medical Research Council
-
Professor Julietta Patrick, Director, NHS Cancer Screening Programme, Sheffield
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Disease Prevention Panel
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook, Clinical Programmes Director, Bazian Ltd, London
-
Dr Colin Greaves, Senior Research Fellow, Peninsula Medical School (Primary Care)
-
Mr Michael Head, Public contributor
-
Professor Cathy Jackson, Professor of Primary Care Medicine, Bute Medical School, University of St Andrews
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Julie Mytton, Consultant in Child Public Health, NHS Bristol
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Dr Richard Richards, Assistant Director of Public Health, Derbyshire County Primary Care Trust
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Dr Kenneth Robertson, Consultant Paediatrician, Royal Hospital for Sick Children, Glasgow
-
Dr Catherine Swann, Associate Director, Centre for Public Health Excellence, NICE
-
Mrs Jean Thurston, Public contributor
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust
-
Reader in Wound Healing and Director of Research, University of Leeds
-
Professor Bipin Bhakta, Charterhouse Professor in Rehabilitation Medicine, University of Leeds
-
Mrs Penny Calder, Public contributor
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol
-
Mrs Anthea De Barton-Watson, Public contributor
-
Professor Nadine Foster, Professor of Musculoskeletal Health in Primary Care Arthritis Research, Keele University
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester
-
Professor Christine Norton, Professor of Clinical Nursing Innovation, Bucks New University and Imperial College Healthcare NHS Trust
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham
-
Dr Kate Radford, Senior Lecturer (Research), University of Central Lancashire
-
Mr Jim Reece, Public contributor
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton
-
Dr Pippa Tyrrell, Senior Lecturer/Consultant, Salford Royal Foundation Hospitals’ Trust and University of Manchester
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Interventional Procedures Panel
-
Professor of Vascular Surgery, University of Sheffield
-
Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Mrs Isabel Boyer, Public contributor
-
Mr Sankaran Chandra Sekharan, Consultant Surgeon, Breast Surgery, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Ms Leonie Cooke, Public contributor
-
Mr Seumas Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor Sam Eljamel, Consultant Neurosurgeon, Ninewells Hospital and Medical School, Dundee
-
Dr Adele Fielding, Senior Lecturer and Honorary Consultant in Haematology, University College London Medical School
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Fiona Lecky, Senior Lecturer/Honorary Consultant in Emergency Medicine, University of Manchester/Salford Royal Hospitals NHS Foundation Trust
-
Dr Nadim Malik, Consultant Cardiologist/Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Professor Jon Moss, Consultant Interventional Radiologist, North Glasgow Hospitals University NHS Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Dr Matthew Wilson, Consultant Anaesthetist, Sheffield Teaching Hospitals NHS Foundation Trust
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Dr Martin Ashton-Key, Medical Advisor, National Commissioning Group, NHS London
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr James Gray, Consultant Microbiologist, Department of Microbiology, Birmingham Children’s Hospital NHS Foundation Trust
-
Dr Jurjees Hasan, Consultant in Medical Oncology, The Christie, Manchester
-
Dr Carl Heneghan, Deputy Director Centre for Evidence-Based Medicine and Clinical Lecturer, Department of Primary Health Care, University of Oxford
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Maria Kouimtzi, Pharmacy and Informatics Director, Global Clinical Solutions, Wiley-Blackwell
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Ms Amanda Roberts, Public contributor
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Professor Donald Singer, Professor of Clinical Pharmacology and Therapeutics, Clinical Sciences Research Institute, CSB, University of Warwick Medical School
-
Mr David Symes, Public contributor
-
Dr Arnold Zermansky, General Practitioner, Senior Research Fellow, Pharmacy Practice and Medicines Management Group, Leeds University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick, Coventry
-
Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Public contributor
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Peter Langdon, Senior Clinical Lecturer, School of Medicine, Health Policy and Practice, University of East Anglia
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician and Cardiologist, County Durham and Darlington Foundation Trust
-
Dr Richard Neal, Clinical Senior Lecturer in General Practice, Cardiff University
-
Mr John Needham, Public contributor
-
Ms Mary Nettle, Mental Health User Consultant
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry and Warwickshire Partnership Trust
-
Dr Lesley Stockton, Lecturer, School of Health Sciences, University of Liverpool
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health